Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 09/1801/1055. The contractual start date was in October 2010. The final report began editorial review in December 2013 and was accepted for publication in August 2014. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Professor Rebecca Harris reports a grant from the Department of Health to her institution, the University of Liverpool, for work outside the submitted work, in relation to evaluating pilots of the new NHS dental contract.
Disclaimer
This report contains transcripts of interviews conducted in the course of the research and contains language that may offend some readers.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2015. This work was produced by Harris et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Positioning the study
Introduction and background
The use of contracts in health care
Contracts are defined as ‘voluntary agreements through which parties make legally binding commitments about their future behaviour’. 1 In the NHS quasi-market, contracts are the crucial means by which purchasers influence providers of health care.
New public management
New public management (NPM) is a loose term that encompasses several doctrinal elements which have taken root deeply in the UK in recent years, and inspired many aspects of reform to public services. 2 NPM has been particularly applied to health care because of growing expenditures due to technological advances and an ageing population. A key component of NPM is a greater reliance on market forces for the provision of public services and an opening up to competition at all levels. Competition is presumed to provide greater room for differentiation and thus open the way to a wide variety of delivery mechanisms, out of which the best ideas and the most efficient mechanisms for delivering public services can emerge. Deregulation and conversion of non-public goods from the public to the private sector is therefore a key mantra. 2 NPM also implies a shift in the perception of users, viewing beneficiaries of services much more like customers than passive recipients of public services. These theory-based reforms are intended therefore to be antihierarchical and antibureaucratic, although NPM can also be seen as a ‘bundle of managerial thoughts’ that focuses on application of managerial solutions as a remedy for a broken system of government. 2 NPM implementation continues to be debated, since reforms have often been found wanting, with core NPM values (competition, choice, service differentiation) often clashing with public values such as social and cultural equity, homogeneity and universality of service. 3
Quasi-markets in health care
New public management ideas and an emerging political philosophy based on a belief that a strong economy should take precedence over all other objectives culminated in the 1989 health care reforms where responsibilities for purchasing services were separated from the responsibility for providing them. 4,5 Under this structure an internal market in health care is created whereby, although most providers (and also purchasers) are still part of the public sector, purchasers are given a role to act on behalf of patients to buy what they consider to be appropriate health services which will best meet patients’ needs. Since patients do not pay at the point of consumption (in the same way as consumers of non-health-related goods and services do), nor do they act on their ‘preferences’, prices are not determined purely by supply and demand as in commercial markets. Purchasers procure services from providers at an agreed price and level of quality, the agreement being embodied in a contract. In theory, efficiency and quality gains are delivered, and transparency and decentralisation increased, because of competition between providers and the use of incentives embedded in the contract. 6
Contracts are the mechanism by which the internal market works. Transactions between purchaser and providers are governed by contractual agreements which specify the normal parameters of commercial intercourse (cost, volume, quality, timeliness and so forth),5 although some important differences exist between an internal market in health care and commercial markets. Regulation and strong management of health care markets is generally recommended because of a risk that, were providers completely free to pursue profit, this would compromise equity within the health-care system. 7 Controls are therefore built into the design of health-care markets to give the Secretary of State control over the degree of competitive behaviour that is allowed. The term ‘quasi-market’ is therefore often used interchangeably with the term ‘internal market’ to reflect the fact that in these systems the government retains control over the size and distribution of funds and this limits the capacity of the market to fully function in response to consumer demand.
Design and regulation of health-care contracts are key to whether or not the efficiency gains envisaged by the internal market are realised: an issue which continues to be hotly debated. Many commentators point to the surprising lack of empirical evidence underpinning the implementation of market-based reforms. 5,8,9 Critics argue that, since Enthoven’s ideas are rooted in ‘clean’ models of micro-economic theory and are based on assumptions that decision-making is entirely rational and there is no environmental uncertainty, they are insufficiently subtle to reflect the realities of the health-care contracting. Enthoven’s theory of managed competition carries other assumptions too: that information relating to the cost and quality of the service is readily available and consumer preferences are predetermined; conditions which are not often met in the health-care context. Despite this, the core beliefs that, in order to increase service quality and efficiency, the NHS must be freed from top-down management and that there are benefits in creating a competitive market are still key drivers of more recent organisational change in the NHS. 8
Evolution of quasi-markets
The rational choice perspective also underpins the economic theory of principal–agency (see Grand theories of health-care contracting). This grand theory is concerned with incentives and assumes that, where the principals’ and agents’ objectives differ, and where principals do not have full information about the circumstances and behaviour of agents, agents act to maximise their own self-interest at the expense of the principal’s interest. 10 Essentially people are viewed as opportunistic; given half a chance the spirit of the contract is broken (‘reinterpreted’). The scope for opportunism is enhanced by the complexity of the transaction and bounded rationality,11 characteristics which are especially pertinent to health-care contracting. Consequently, in health systems where services are obtained through a process of contracting, purchasers and government regulators are advised to ‘scrutinize contracts for possible ways in which opportunism may affect all parties’:12 are there opportunities to avoid high-risk groups? will the services be equitably distributed? and the like. The emphasis is on identifying and closing loopholes, and close monitoring of the agents’ behaviour, all of which add to transaction costs. Where opportunistic behaviour and transaction costs are extensive, the contract is widely seen as having failed.
Conventional micro-economic analysis and principal–agent theory can, however, be criticised as treating the organisation as a ‘black box’, and paying little attention to characteristics of organisations or organisational environments that affect structural or behavioural adaption. 13 Light14 instead outlines the more evolutionary view from institutional analysis, which arises from a theoretical cross-fertilisation between economics and sociology, where both the errors and the corrective mechanisms which occur in shaping contracts are understood to be defined by social context and institutional forces. He portrays behavioural responses to contracts as neither rational nor irrational, but interactional and contingent. Thus, using this perspective, practitioners’ responses to health-care contracts, often viewed merely as self-interested opportunism, are instead seen within a wider context of organisational resistance to institutional change. Studying the evolution of the organisational field, and looking beyond principal–agent dyads to wider forces concerned with change and resistance to change, gives a means to capture a more subtle understanding of providers’ responses to contracts.
Institutional theory provides a dynamic view of quasi-market contracting, since organisations and their responses to quasi-markets are viewed as not emerging fully formed, but undergoing processes of creation and evolution. 15 After the ‘big bang’ of creation, local ‘rules of the game’, learning and bargaining styles build incrementally over the first years of operation. Contracting is accepted as an iterative, learning process, with a series of unintended consequences, negotiations and amendments, and as a means by which social institutions arise and are shaped, rather than planned. Hughes et al. 13 describe the cycle of change in NHS contracting practice as resembling a macro–micro process model applied in institutional studies. First, the central department (government) creates or modifies a body of rules to which purchasers or providers must react. This may be differentially enforced and some differences in local implementation can be tolerated, but there is a general pressure towards compliance. Second, purchasers and providers arrive at a working understanding of the rules, adapting their practices accordingly, but selectively resisting some policies. Third, purchasers and providers respond to local problems of coordination and resource allocation by using permitted flexibility to adjust their contracting practice in novel ways, sometimes going against the ‘spirit’ of central policy. Fourth, under the influence of mimetic, coercive or normative processes as well as efficiency considerations, elements shared by most organisations in the field emerge. These practices produce distributional outcomes that disadvantage some players to the detriment of others and, because of conflictual outcomes and other emergent problems, are seen to require further adjustment. Finally, a new cycle is triggered by renewed central intervention, often as a response to disturbances in the system, but also to effect further strategic change.
Thus the NHS case is marked by the frequency of the cycles of contract implementation, revision and reform. Alongside this, periods of relative stability and incremental development of contracting policies are punctuated by more fundamental shifts in policy. 13 The macro–micro process model outlined above appears to reflect with remarkable accuracy the evolution of the dental practice organisational field (see The evolution of the dental practice organisational field).
Literature on health-care contracting theory
The study of health-care contracts stands at a crossroads of several disciplines: economics, organisational sociology, strategic management, sociolegal studies and political science. Increasingly, health-care contracting is viewed, not just as a technical task, but as a complex intervention influenced by a system of inter-related social networks, organisational forms, labour markets, political policies and institutions. 1 Theory is a way of simplifying complex reality. 16 Theories, therefore, are an important way to capture all the factors which may influence the processes and outcomes of health-care contracting. The theory of managed competition which underpins quasi-market approaches in health care is, as outlined above, only one of a number of theories relating to the use of contracts. As in other fields, different disciplines have contributed to furthering understanding in the area, with no one approach explaining all the complexities which are present.
It was noted in the referees’ comments on the original research proposal that there is considerable literature relating to the use of contracts more generally, and taking note of this would be helpful. We found, however, that previous literature reviews in this area were narrative reviews which were focused on describing macro-level or grand theories (broad in scope, attempting an overall explanation of social life, history or human experience), and there was relatively little synthesis between theories, particularly at the lower theory level, which outlines concepts and relationships. This is in spite of the fact that it is the synthesis of lower levels of theory which leads more readily to testable hypotheses. Micro-range theory, for example, links concrete concepts into a statement that can be examined in practice and research. We therefore approached the literature review, which was undertaken in phase 1 of our research, as a systematic review which was focused at not only obtaining an overview of macro-level theory in this area, but as a piece of work to generate a synthesis between theories culminating in a logic model identifying lower-level concepts and relationships between these concepts. We did this to enable a capturing and synthesis of lower-level theories and identification of concepts relevant to our study to be explored in our qualitative work.
Literature review methods
An electronic search of the literature was undertaken using Web of Science, Scopus and MEDLINE databases using the following search terms:
-
Web of Science: contract*AND “Health Service*”; quasi markets AND competition; “internal markets”; contract* AND “health care” AND market*
-
MEDLINE: Health care reform [medical subject heading (MeSH)] AND Contract Services (MeSH)
-
Scopus (excluding Physical Sciences, restricted to articles or reviews): contract* AND “health service*”(both in Title); contract* AND “health service*”AND “public sector”; contract* AND “health service*”AND “publicly funded”; contract* AND “health care” AND “public sector”; contract* AND “health care” AND “publicly funded”.
The search was limited to journal articles published in English from 1980 onwards. Books and other types of reports were not included because, if the theory was significant in the field, this would be cited and therefore identified in peer-reviewed academic publications. Since the use of ‘managed competition’ in health care has not been limited to England (policies in other countries moved in a similar direction at the same time, most notably New Zealand, Sweden and the Netherlands), the literature search was not limited by health-care system involved. Exclusion criteria were identified at the outset: articles not concerned with publicly funded health care were excluded. Health care was defined as the delivery of patient care by a clinically qualified provider and hence articles concerned with the provision of ancillary services such as cleaning were excluded. All articles not concerned with contracts were excluded, as well as those concerned with contracts with non-clinical workers, because this was not of central importance. Articles where theory could not be identified were also excluded.
In order to assess whether or not the article contained theory, Kerlinger’s definition of a theory was applied: a theory is an inter-related set of constructs, definitions and propositions that presents a systematic view of phenomena by specifying relationships between variables with the purpose of explaining natural phenomena. 17 Three primary criteria were therefore set that had to be satisfied in order for the material to be identified as a theory.
These widely recognised criteria were that (1) constructs had to be identified, (2) relationships among constructs had to be specified and (3) these relationships had to be falsifiable (testable). 18 Although there is some debate about whether typologies are theories or just simple classification systems, articles containing typologies were included provided these three features of a theory outlined were met.
The electronic search identified 1519 titles, which were then screened independently by two researchers for inclusion. Where there was disagreement, the abstract was obtained. The resulting 311 abstracts were then also screened by two researchers. Of the 131 papers remaining, a further 49 papers were excluded on reading. The 82 included papers were then grouped according to grand theory. For each paper, constructs and relationships between constructs were identified. Papers outlining the same theory were grouped together, and papers organised according to a hierarchy of theory types (macro-level or grand theory, and mid-range theory). In some cases mid-level theory could be associated with more than one grand theory, but was attributed to one only, for clarity. We have not also distinguished between mid-range and micro-theory because a range of levels of abstractions exists between the two which makes making reliable distinctions difficult.
Grand theories of health-care contracting
We identified five macro-theories, and organised mid-level theory under these themes. Details of mid-level theory with references are found in Appendix 1. Here we give five macro-level theory tables within which the 80 lower-level concepts we identified sit (outlined in bold print). The main features of each macro-theory are summarised briefly below: (1) the use of markets to increase efficiency, quality and consumer responsiveness; (2) the principal–agent model; (3) transaction cost economic theory (TCE); (4) relational contracts; (5) that markets are institutionally as well as socially embedded.
Use of markets to increase efficiency, quality and consumer responsiveness
This macro theory sets out the main theory in favour of internal markets: that, where health-care contracts are contestable, this results in a system which is more efficient, of higher quality and more responsive to consumers. Individual firms are set up to operate as productive units, which require that production costs are kept low if profits are to be maximised. To maintain the business in the long term in a competitive environment, firms also need to demonstrate that the services they provide represent a level of quality expected of that price. 19 One of the distinctive features of health-care markets is that consumers (patients) have relatively weak incentives to seek out low-cost producers and have little knowledge about the quality of care. Establishing public agencies to act as purchasers on behalf of consumers is seen as a way to shift power away from providers and moderate this asymmetry of information. 20
A range of economic theories have been generated which outline the relationship between competition between providers and the cost, price and quality of health-care services (see Appendix 1, Table 17). Where there are too few providers for effective competition (e.g. specialist hospital services), the benefit of the market may still exist if the contract is contestable. In other words, there need not be day-to-day competition within markets, but rather periodic competition for markets (review of contracts) to ensure that adequate competition puts pressure on providers. Mid-level theory outlines the circumstances where competition may not lead to reductions in costs (see Appendix 1, Table 17). The relationship between competition and cost is further complicated by the quality of services. Quality outcomes are predicted to vary according to what is measured as a performance indicator, and hence the availability of information, as well as price and market conditions.
The principal–agent model
The principal–agent model describes the relationship between a principal and an agent. The principal delegates an action to a single agent through a take-it-or-leave-it offer of a contract. 10 The principal compensates the agent for performing certain acts that are useful to the principal and costly to the agent. The contract is limited in not being able to define all future behaviour because the contract may involve a range of varied activities and some activity may be unforeseen. The model, based in the economic literature where behaviour is defined by rational choice, makes three assumptions: that goal conflicts exist between principals and agents; that agents have more information than their principals; and that human agents will always rationally evaluate and exploit situations in order to maximise personal gain (see Appendix 1, Table 18). Since the principal is not in a position to directly observe the agent doing the work, the agent may expend less effort than the principal might reasonably expect and yet still reap the full reward specified in the contract. Where one party exploits contract loopholes because of the limitation in the specificity of contract terms, this is known as opportunistic behaviour. Opportunism (defined by Williamson21 as ‘interest seeking with guile’; p. 255) may be used by principals too, for example by failing to reveal information to the agent concerning how difficult the work may be, resulting in the agent being undercompensated.
Opportunistic behaviour can occur when the contract is being set up (ex ante) or after it has been signed (ex post). Misrepresenting how difficult it would be to deliver the contract is an example of ex ante opportunism (termed adverse selection). Moral hazard (ex post opportunism) occurs when the party with more information about its actions or intentions has a tendency to behave inappropriately from the perspective of the party with less information, for example resulting in manipulation of events (such as the amount and type of treatment given to a patient) so that there are more rewards than would be expected given the effort applied, according to the spirit of the agreement.
Scope for opportunism depends upon the type of contract used. 12 The difficulty in foreseeing the number of patients demanding care and the extent of their needs means that, within the health-care context, problems arising from information asymmetry are complicated by uncertainty. The three basic types of contract [block, cost and volume, fee-for-item (FFI)], for as well as hybrid models, vary in whether the risk of a higher than expected demand falls on the purchaser or provider, or if it is shared. A range of mid-level economic theories exist which identify which contract type is optimal to manage situations of asymmetric information and stochastic patient demand, in order to minimise the scope for opportunism (see Appendix 1, Table 18).
Transaction cost economic theory
Transaction cost economic theory also offers insights into strategies to deal with opportunism in contractual situations. Williamson22 argues that transaction costs and therefore contractual characteristics are affected by two behavioural assumptions: a tendency towards opportunism; and that people are constrained in their ability to make rational decisions by their capacity to receive, process, store and retrieve information (bounded rationality). The issue central to TCE is whether it is more ‘efficient’ for transactions to proceed through the market or to be integrated within a hierarchical organisation15 (see Appendix 1, Table 19). Transaction costs include the costs of establishing contracts and acquiring the necessary information; of designing, negotiating, monitoring and enforcing contracts; and of avoiding and resolving conflict. TCE identifies the circumstances where transaction costs may outweigh any cost savings generated from using an internal market approach. 22
Transaction cost economic theory predicts that transaction costs will be particularly high where the product and its environment are complex; purchasers will find it more difficult and therefore costly to make precise stipulations about quality, quantity and even cost. Besides, where providers need specialised equipment, skills and premises to carry out the work (termed asset specificity) which purchasers may find difficult to source from another supplier, and which cannot be easily redeployed should a continuation of the contract not be forthcoming, this tends to lead to purchasers being ‘locked in’ to current providers, since changing providers under these conditions will be particularly costly. Transaction costs may be also higher when there is a frequent exchange of the product (with recurring transaction costs), where there is uncertainty in the level of demand and where purchasers lack sufficient information to make detailed specifications relating to performance and effort.
When transactions involve highly specific assets and are associated with considerable uncertainty and/or problems of measurement, contracts between purchasers and providers will tend to be incompletely specified and may therefore be open to opportunism. Because this increases transaction costs, TCE concludes that some sort of vertically integrated organisation is likely to be more efficient than markets. 22 Mid-level theory has sought to operationalise these high-level concepts. 23 Long-term contracts are considered more beneficial than short-term because, in situations where there is high asset specificity, a supplier may withhold cost-efficient investment if there is a risk of a discontinuation of the contract24 (see Appendix 1, Table 19).
Transaction cost economic theory derives from economic theory, albeit with fresh insights from organisational theory. However, this and previously outlined theories such as the principal–agent model have been criticised because of their under-representation of the importance of social relations in the transaction. Granovetter25 argues that economic transactions should be seen as much more ‘socially embedded’ (p. 490) than the transaction cost framework recognises. He argues that TCE overstates the role of governance systems and of hierarchy in regulating transactions, because trust between the parties involved in contracting can act as an economic asset in limiting opportunism and the need for highly specified, expensive contracts. Trust, however, is loosely defined here.
Moreover, both TCE and the principal–agent model assume that choices made by principals and agents are purely rational, arising from a set of sharply defined possibilities. Originating in classical economic theory also leads TCE to assume that markets and the internal structure of organisations are static, rather than the more messy reality where there is evolution over time. 15 The importance of social relations and the fact that not all decisions are rational are acknowledged in the fourth grand theory outlined, which attempts to extend economic analysis into other disciplines such as contract law, sociology and organisational theory.
Relational contracts
MacNeil26 distinguishes between classical, neoclassical and relational models of contracts in contract law. The classical model of the contract focuses on a single exchange between two parties. The contract is considered to be complete: all possible eventualities are specified and there is full advance allocation of risk (see Appendix 1, Table 20). Since everything can be measured and recorded, opportunism is irrelevant. However, in many situations parties expect to do business again and therefore there is an interest in maintaining a relationship. A contract which is relatively flexible, and allows unpredicted outcomes to be resolved by mutual agreement over the longer term, is therefore more appropriate (the neoclassical model). Approaches to disputes in the neoclassical model are by arbitration rather than litigation. MacNeil contends that contracts viewed in this way may actually foster co-operation, and in certain circumstances the contract itself performs an important trust-building function. 26
The concept of neoclassical contracts has been further developed using sociological theory to recognise the importance of social relations between the parties involved. How parties react during negotiation and contract performance is significantly influenced by the history of social relations between the parties and the social norms of trust and reciprocity. 15 The relational model of the contract identifies social norms such as trust, solidarity and reciprocity embedded in the contractual relationship as an alternative means of controlling opportunistic behaviour to the use of highly specified contracts (see Appendix 1, Table 20). The existence of ignorance and uncertainty is fundamental to the importance of trust, since trust can be defined as ‘levels of subjective probability with which one party assesses that another party will perform a particular action’. 27 A principal’s level of trust is likely to have been influenced by the agent’s previous behaviour, which gives rise to reputation, although, if the principal has no alternative agent with whom to contract, the relationship may be based more on dependency and hope than on trust. The calculative trust outlined by Goddard and Mannion28 represents a rational deliberation, although affective dimensions of trust (social trust) are also often involved (grounded on relationships and bonds generated through interaction, empathy and identification). 29
While TCE suggests a one-dimensional continuum of types of organisation form along which firms may place themselves, with hierarchies (with centralised decision-making and relatively little autonomy at lower levels) at one end and markets at another, relational theory offers a range of other possibilities such as strategic alliances and joint ventures. 23 Organisational forms described as networks or clans, formed through collaboration and interdependency, offer an alternative to the two extremes and are relatively common.
Donato30 gave an alternative view to the TCE approach of balancing organisational form against the costs involved in contracting. He suggested a resource-based view where organisational form is viewed as driven by capabilities development rather than cost considerations. This view focuses on close network relationships, in which trust plays an important role, and considers that such relationships enable firms to access a richer variety of resources than would be available to any one of them alone. Furthermore, by developing communication channels, parties can have access to vital information in a ‘freer’ and more timely way than if reliant on markets or hierarchical channels. Professions such as medicine display a strong network component and can shape the relational market and constrain opportunistic behaviour (see Appendix 1, Table 20).
Markets are institutionally as well as socially embedded
Social networks are increasingly considered important, not just at the micro level, but also at an institutional level31 (see Appendix 1, Table 21). Institutions such as the NHS and the professions are seento act as congealed social networks which play an important part in shaping health-care markets. Attitudes of the parties involved in the contract are not merely influenced by the relationships in which they are directly involved, but each party may have relationships with a wider network of people; this history and experience has an impact on their behaviour in the more immediate relationship. Each party in the contracting relationship may have other constituents (e.g. patients, the government, professional colleagues) to which they are also accountable. This perspective draws attention to the important influence on the contractual relationship of the wider institutional context in which an individual purchaser–provider relationship occurs. 31 This differs from TCE and the principal–agent model, which both conceptualise the relationship between purchaser and provider as dyadic. 32 Instead it recognises that a purchaser–provider relationship is not adequately conceptualised as a single principal–agent relationship, but is rather the product of a string of principal–agent relationships extending from the health-care system into the political arena.
This view of contracting is informed by political science, where the relationship between purchaser and provider is pictured as akin to international relations between states. Here the relationships are seen as ‘regimes’ which are based on ‘sets of principles, norms, rules and decision-making procedures around which actors’ expectations converge’. 32 Although there are some commonalities with the relational contract perspective, there is a greater emphasis here on purchasers being accountable to multiple constituents, including interest groups and the press. In order to insulate themselves from being accountable to so many different players, purchasers have a tendency to resort to complicated procedures and regulations.
While trust at an individual level (between purchaser and provider) is an important component in contractual relationships, decisions informed by an assessment of the risk involved in contracting may also be based on how generally sympathetic the actors feel towards the institutions involved. 29 Evidence also suggests that in market-led systems the extent of users’ affective trust in health-care institutions is relevant,29 and the media may have a role in forming such views (see Appendix 1, Table 21).
Synthesis of theory and a logic model of the theory of health-care contracting
Recent research synthesising public health theory and interventions has adopted a ‘logic model’ approach which elucidates the internal pathways of interventions. 33 Logic models (also known as logical frameworks) originating from the field of programme evaluation are typically diagrams or flow charts that convey the logical relationship between different elements which make up a programme or intervention, explaining how these work together to influence the end result. The underlying purpose of logic models is to postulate the ‘if–then’ causal relationships between the various elements, which can then be tested. This approach is particularly applicable to complex policy interventions, such as implementation of health-care contracts, where there are multifactorial outcomes, and the causal chain between the agent and the outcome is neither short nor simple. 33 Conceptual models (logic models) are thus useful in providing a structure for exploring the complex relationships between contextual factors, inputs, processes and outcomes. Figure 1 provides an aggregative synthesis in the form of a logic map of the various concepts and relationships we identified in our review of theory.
FIGURE 1.
A logic model of health-care contracting theory.

In the next section we provide the institutional background of general dental practice contracting, with a contrast with the general medical practice context. The logic map highlights the factors which we identified as particularly pertinent to our study.
The policy context: general dental and medical practice
General dental practitioners and general medical practitioners as independent contractors to the NHS: ownership of assets and modes of governance
When the NHS was created in 1948, general dental practitioners (GDPs), like general medical practitioners (GMPs), retained their status as independent contractors to the NHS, who offer their services to patients in exchange for a variety of fees and allowances paid from the general tax fund. 34 Neither single dentists nor partners obtain practice profits as personal income. This is described as a professional partnership model,35 whereby dentists do not just own the business and govern the firm, but also provide professional services. The terminology ‘principal’ (i.e. owner and contract holder, sometimes alternatively termed ‘provider’) and ‘performer’ (performing care under the contract) is used to distinguish between the two, often combined, roles. Among the 11,000 dental practices in the UK, a significant number (one-third) are solo practices, where just one principal dentist owns the practice and provides care. 36 The size and structure of general dental practice ownership is changing, though, with a steady reduction in these single-handed practices. Moreover, in recent years a relaxation of regulation has allowed practices to be owned by external commercial organisations (Dental Bodies Corporate, DBCs). There are now several large chains of bodies corporate, which trade on the stock market and own upwards of 300 practices each. In the case of dental practice, principals own the premises; employ their own staff [associate dentists (where there is a subcontracting arrangement to other dentists within the practice), nurses, hygienists, therapists, practice managers, etc.] and pay expenses (such as dental materials and laboratory bills for crowns, dentures and the like) from their income. The medical practice model is similar: single GMP owners, or groups of GMP partners, employ other staff: salaried GMPs, practice managers, practice nurses, community-based Allied Health Professionals and practice-based administrative staff.
General dental practitioners carry a greater financial burden concerned with owning practice assets than do GMPs. The government contributes to the cost of medical practice premises, but not for dental practice premises. Dental practice premises and facilities are generally owned by the principal(s)/body corporate as capital assets. The costs involved are then incorporated into the sum of practice overheads, and reimbursed through the dental remuneration scheme (e.g. FFI, etc.). The financial risk concerned with falling levels of property value rests solely with the GDP. If the practice is sold, the dental practice owner receives the value of the premises and (previous to the 2006 contractual arrangements) an amount for practice ‘goodwill’. ‘Goodwill’ represents a value attached to the size of the list of patients attending the practice, measured usually as a percentage of turnover. Prior to 2006, GDPs therefore worked to build up a loyal following of patients which was subsequently recognised in financial terms when their practice was sold. However, in 2006 the following clause was included in national model General Dental Service (GDS) contracts and Personal Dental Service (PDS) agreements:
The contractor shall not give, sell, assign or otherwise dispose of the benefit of any of its rights under this contract, save in accordance with the contract. The contract does not prohibit the contractor from subcontracting its obligations arising under the contract where such subcontracting is expressly permitted by the contract. 37
This statement was seen to prevent a NHS dental contract value from being transferred or sold, and was interpreted by GDPs as affecting the ‘goodwill’ of the practice and, therefore, its saleability in the future. While commissioners argued that this was not strictly true, they did acknowledge that, because NHS dental contracts were personal contracts between the parties, a successor contractor could not be assigned by the practice wishing to sell. Instead primary care trusts (PCTs) were to end one contract and decide whether or not to issue a new one in order to replace the lost dental workforce capacity (but this could be at a different level and location from the previous contract depending on local needs and priorities). 38 Rules for sharing accreditations and depreciations of capital assets, including human assets (patient lists) had therefore been redrawn, without recognition of value or alternative means of sharing financial risks. Selling medical practice ‘goodwill’, by contrast, has never been permitted.
In the medical practice model, capital assets are shared with purchasers. For medical partners who own their premises, borrowing costs (previously known as ‘Cost Rent’ reimbursement, notional rent and improvement grants) are provided as recurrent funding by the Department of Health (DH) and consolidated into their Baseline Allocation. 39 There are also increasingly other models whereby the premises are not owned by the medical practice partners, but a leasing arrangement is in place. Primary care organisations (PCOs), formerly PCTs, may, for example, take the head lease on premises owned by third-party developers, subletting to individual GMPs. Under the private finance initiative, medical practice premises may be developed by private sector consortia and leased to the PCO, with the consortium, not the NHS, retaining the ownership at the end of the lease.
Premises provision is inextricably linked with government policy and strategy in primary medical care. PCOs have explicit responsibilities to prepare a general statement of need for medical premises and a strategy for property management. Medical practitioners have to take account of their local PCO strategy on premises development, which may restrict their options about how and where to practice. Strategies, for example, concerned with offering a wide range of ‘integrated’ care within one centre imply a multidisciplinary primary care team where GMPs may even be in the majority39 – an evolution which is facilitated by the PCO’s financial involvement in premises provision. PCOs’ financial involvement in premises ownership is seen as a mechanism for retaining control over medical practice provision:
Some [PCOs] may use this opportunity to exert greater control over premises provision, thereby reducing the control of the GPs [general practitioners].
p. 439
Transformation of smaller traditional medical partnerships into larger multidisciplinary primary medical care teams is further facilitated by the structure of the General Medical Service (GMS) contract, which involves more of a mixture of payments and allowance than does the GDS contract (see Appendix 2). In 1966, a three-part payment system was introduced for GMPs, comprising a basic practice allowance, capitation fees and payments for designated items of service such as contraception and immunisation. Additional practice allowances included loans and grants for the construction and improvement of practice premises, reimbursement to the practice of costs for employing nursing or ancillary staff, and allowances to encourage GMPs to undertake vocational training and work together as groups. 40 These new contractual arrangements resulted in an expansion of the number of health centres, and larger medical practice teams with more employed practice staff such as practice nurses and receptionists. 41
Furthermore, financial arrangements between purchasers and medical practice owners also include elements beyond support for capital assets. Water rates for medical practices are reimbursed by commissioners, and the PCT owns and technically supports practice information technology systems. Through NHS Purchasing practices benefit from economies of scale across a wide range of products. By contrast, the same extent of financial support and ownership does not exist in dental practice.
The GDP contract in the 1960s, by contrast, remained a FFI contract, with no additional allowances paid to support development of premises or the team. Development of skill mix within dental practice teams has never been directly incentivised in association with additional allowances to any significant extent; instead, any broadening of the use of skill mix has been driven by some principal dentists adopting a team philosophy themselves, and using their general practice income and discretion over the employment of staff and task allocation to pursue this vision. 42 Likewise, only under recent local commissioning models have allowances been available to dental practices to allow development of premises and standards of surgeries’ facilities; and these have been relatively short term, ad hoc and locally determined.
Dental provision is particularly highly asset specific, with a significant investment of premises and equipment necessary for new entrants to the market, and this may raise a barrier to entry for smaller enterprises. The usual market response to asset specificity is the negotiation of longer-term contracts that include risk-sharing arrangements between both purchaser and provider43 – a mechanism which has not been used in the context of NHS dental contracting. Ownership is recognised as central to the normal workings of markets, with the providers’ share of the capital value of assets a powerful motivator for agents, although the full implications of the GMP model are far from clear. 12 Implications of the GDP model of asset ownership are equally uncertain. There are, though, indications that the extent to which GDPs have a financial interest in their premises is important, and probably an important distinction between GDPs and GMPs.
Independent contractor status is defined as where the payer has the right to control or direct the result of the work done, but not what will be done and how it will be done. 44 This suggests a purely transactional relationship between GDPs or GMPs, the fulcrum of which is the contract between either the state or the commissioner and the provider. However, while on the one hand the independent contractor status of GDP and GMPs may appear to represent a classical market-based mode of governance, the distinction between ‘markets’ and ‘hierarchies’, as Walsh et al. 45 suggest, is not easily drawn. In reality, although organisations (such as dental practices) have strong elements of contract, the contractor/client relationship may still look very much like an organisational relationship between employer and employee.
A structure with legitimate authority, with a manipulable incentive system for adjusting costs, quantities and process, with a structure with dispute resolution and with a set of standard operating relationships, works very much like a hierarchy, very little like a competitive market.
p. 12646
Given the quasi-market situation in which UK health care operates, together with a relative shift from a national contract to local contracts involving relationships with commissioners (see Contracts in general dental practice), we therefore did not assume that studying general dental practice contracts is confined solely to issues related to contractual governance and incentives. We considered the contract as a focus around which negotiation and discussion occurs, and not a means of governance and change which is limited to contract design issues. Walsh et al. 45 suggest that the contractor–client relationship is shaped by a range of factors such as risk, trust, observability of inputs and outputs, and the extent to which quality can be defined. We therefore considered that the extent to which hierarchical governance sits alongside market governance could be an important difference making general dental practice contracting distinct from GMP contracting.
Straddling public and private spheres
The independent contractor status of GDPs and GMPs has meant both types of practitioners have developed commercial and entrepreneurial as well as professional identities, although their relationship with the NHS has meant that they are distinct from private limited companies and thus straddle public and private spheres. 47 GDPs are not restricted in the extent to which they provide both NHS and private care. Some dentists accept only certain categories of patient (such as children only and/or adults who are exempt from charges because of low income, for instance) or carry out a limited range of treatment under the NHS, often providing a mixture of NHS and private dentistry in the same practice. Nevertheless, there are many GDPs for whom the NHS provides the bulk of their workload: 50% of GDPs nationally concentrate on NHS dentistry, based on figures where treatment was carried out on an NHS basis for 85% or more of patients. 48
Since the early 1990s there has been a steady reduction in the level of commitment of GDPs to NHS work. 49 For example, figures show practitioners earning 48% of their gross income from NHS work in 2004/5, down from 54% in the previous year. 50 It is this shift which has given rise to growing problems experienced by the public in getting access to an NHS dentist, particularly in some parts of the country. 51
Medical practices are also free to provide both NHS and private care to patients, but face a higher degree of restriction. GMPs are free to generate income from private practice or commercial contract work, provided (1) they meet their NHS commitments to provide the range of essential, enhanced and out-of-hours services the practice is contracted to deliver and (2) they do not charge their registered patients for services they may offer that are not available, or are available only in limited circumstances under the NHS (e.g. cosmetic procedures, some advanced dermatology procedures or osteopathy). 52 GMPs can also charge their registered patients for a limited range of services when requested to do so. These include (1) examinations and reports for medico-legal purposes (e.g. in connection with a claim for compensation by a patient, or at a police station in connection with possible criminal proceedings against the patient) and (2) a range of services for patients travelling overseas (e.g. prescriptions for treatment, immunisation not covered by the PCT or an opinion on fitness to travel). Until recently, conditions of PCO financial involvement with the costs of premises came with restrictions on NHS/private mix: if NHS staff or premises were used for private work, the practice could not earn more than 10% of total practice receipts privately, otherwise rent reimbursements from the PCT would be reduced on a sliding scale as the proportion of private work increased. This ‘10% rule’ has now been completely removed from the 2013 regulations, potentially allowing GMP practices to increase their level of private work on the site without financial penalty. 53
Dental patient copayment
The GDS is one of the few areas of the NHS where patients are involved in copayment, meaning that commercial and health-care concerns are intimately connected. Legislation allowing patient charges for dentures, which were roughly half of the total cost, was enacted in 1951, becoming the first charges of any kind to be levied for NHS care. 54 Only a year later a further Act extended dental charges to other types of treatment. This set a precedent for copayment, which has been a feature of NHS GDS care ever since; the proportion of care paid by the patient has grown steadily over subsequent years (although certain groups such as children, pregnant women and those on state benefits remain exempt). Currently, non-exempt patients contribute as much as 80% of the cost of their NHS dental care up to a ceiling limit. The government pays the remaining 20% and any additional sum over the ceiling limit, as well as the full cost of care for exempt groups.
Contracts in general dental practice
The evolution of the dental practice organisational field
Institutional work studies analyse organisations, fields and logics from the perspective of not just the service delivery level (e.g. what happens at the micro level of the dental practice) but also the field level (e.g. the negotiations, values and changes occurring at the level of government policy, professional associations, community groups, etc.). In doing so they often find that organisations are sites of struggle. Several logics (for definition see Chapter 3, Institutional logics and general dental practice as an organisational field) can coexist within an organisational field, although one is generally thought to be dominant. 55 Struggles are experienced as existing practices, beliefs and norms are challenged by breakdown events, new actors, shifts in leadership or new technologies, with established ways of doing things defended or amended. The following section outlines some of the key events which have prompted change and struggle within the dental practice organisational field (for a summary see Appendix 3). We start with the 1980s, since, from the 1980s onwards, professions faced challenges from a political era of NPM, with dentistry being no exception.
Between 1980 and 1990
By the end of the 1980s the government had instituted an internal market in the NHS, with attention focused on maximising efficiency, quality and consumer responsiveness. Although organisational restructuring associated with the implementation of an internal market did not affect dental practice directly at the time, the underpinning political philosophy and environment of budget restraint did have an impact in several ways. In 1987’s Promoting Better Health, a White Paper on primary health care,56 the government made clear its intention to use dental charges as a way of raising tax revenue. Free dental examinations were abolished. Providers saw this as a breakdown event, set against a background of improving dental health in the population, where numbers of dentists were out of proportion to need, and competition for patients was becoming a concern for dental practitioners. At the same time there was a growing voice of consumerism; rising patient charges, with media reports portraying dentists as overprescribing, culminated in the 1986 Schanschieff report into unnecessary dental treatment. 57 Government policy created further challenges to dental practice when relaxation of advertising constraints for opticians was followed by similar changes in dentistry.
Between 1990 and 2000
A new dental contract introducing an element of capitation to a previously exclusively FFI system of remuneration precipitated a haemorrhaging of practitioners from the NHS and a shift to private provision. 58 The new contract also required dentists to give fuller descriptions of treatment to patients in treatment plans, to use information leaflets and to guarantee rights of access to emergency care. There were reports of one in five dentists pulling out of the NHS for non-exempt patients, shifting the balance of their practice to private work. This skewing towards private provision became more pronounced in 1992, when, because of unexpected earnings under a newly instituted capitation arrangement, the Treasury instituted a 7% fee cut (initially proposed as 20%). Expansion of private dentistry, which required marketing and selling of dental services, and a consumer focus, meant many practices becoming overtly commercial.
Following a remuneration review by Kenneth Bloomfield,59 and an enquiry by the House of Commons Health Select Committee,60 the government published a response in 1994 outlining alternative options for remuneration that favoured setting up local purchasing systems sensitive to regional differences in needs. 61 A White Paper62 confirmed the government’s intention to pilot a system based on local purchaser/provider arrangements, and a new type of organisational structure was instituted called PDS. The previous FFI and capitation arrangements had both been administered centrally from a national budget, whereas PDS contract terms and monitoring of performance were undertaken locally and involved local purchasers. PDS pilot arrangements structurally changed the organisational field with the creation of a new central actor – the purchaser – set within quasi-market structures.
Between 2000 and 2012
Inclusion of purchasers was more widely instituted in the organisational field with the passing of the 2003 Health and Social Care Bill. 63 The previously centrally managed scheme of administering the dental budget was replaced with local contracts between practitioners and commissioners employed by PCTs. Budgets were devolved to a local level and PCT commissioners charged with procuring dental services to meet the needs of local populations. Practices were encouraged to transfer voluntarily from the GDS centrally managed system into local contracts with commissioners, until in 2006 the previous system was abolished and all remaining practitioners forced to transfer into the new arrangements. That year also brought a change in dental contract currency, with the FFI replaced with a system based on bands of activity: a new, previously untested arrangement which was widely contested. 42 The 2006 dental contract created a further watershed moment and around 10% of practitioners refused to sign the contract and effectively withdrew completely from providing a NHS service.
The emergence of local commissioning within the organisational field meant that, when a dental practice exited to the private sector, the contract could be recommissioned to another NHS provider, usually via a tendering process. This created new market opportunities for actors to expand practices or set up new practices in different areas. The government removal of restrictions on the number of DBCs in 2006 made market entry easier for organisations using commercialised models of delivering dentistry.
Different dental contract models: Personal Dental Service, Personal Dental Service Plus, nGDS, nPDS, new contract pilots
For a summary of the different models and comparison of key features see Appendix 4.
Personal Dental Service
The 1996 White Paper Choice and Opportunity62 and the NHS (Primary Care) Act64 provided the legislation to allow GDPs to move from the relatively autonomous position of FFI remuneration, administered centrally via GDS regulations, to locally negotiated contracts, or even salaried employment. PDS pilots were first introduced to test the efficacy of the policy65 and participation was voluntary. Fifteen pilots commenced in 1998/9, rising to 54 pilots following the third ‘wave’ in 2000/1. The purpose of the PDS pilots was to develop new ways of delivering NHS dentistry and to tailor services to meet local needs. Thus PDS pilots included a range of remuneration arrangements, some with a salaried model, others involving capitation arrangements or sessional payments. However, although PDS was broadly welcomed by the profession, treatment interventions fell and, because the system required the FFI arrangements for patient charges to remain in place during the pilots, income from patient charges fell alongside the reduction in treatment interventions, leaving a problem revenue shortfall. 66 Consequently the anticipated whole-system change from GDS to PDS type of contracting arrangements proved difficult and resulted in an entirely different contract currency, Units of Dental Activity (UDAs), being introduced.
nGDS and nPDS
General dental practitioners transferring from FFI remuneration to remuneration based on UDAs governed by a contract with PCT commissioners (nGDS) were guaranteed the same yearly gross fees as they had earned during a 12-month ‘reference period’ (2004–5) for the next three years (from 2006 until 2009). PCT dental allocations were ring-fenced during his period. Ring-fencing was later extended until 2011.
Contracts between commissioners and GDPs (usually with practice owners but occasionally with individual GDPs) were drawn up around an agreement to deliver a prescribed number of UDAs in a 12-month period for an agreed annual financial value. The provider had a contractual duty to provide all necessary care for an unspecified number of patients for which the provider was paid a certain number of UDAs. The targets of UDAs on which contracts were based were calculated on historical funding levels for that area, and this has led to a number of anomalies where, for example, UDA values varied between providers in different areas of the country (and not necessarily in association with deprivation indicators).
The UDA system condensed the 400 items of treatment associated with the previous FFI system into three bands according to the complexity of procedures: band 1 including examination and preventative work; band 2 including routine treatments such as fillings and extractions; and band 3 involving complex treatments, for example crowns and dentures. Each band is associated with a certain number of UDAs that are awarded to practitioners for the procedures they finish within that band in one course of treatment; 1 UDA is given for a band 1 treatment, 3 UDAs for a band 2 treatment and 12 UDAs for a band 3 treatment. A feature of this system is that the treatment bands take account of only the type of treatment but not the number of procedures undertaken. This means that the same number of UDAs is awarded regardless of how many procedures are done within the same band in a single course of treatment. A contract between the practice and the PCT stipulates a certain number of UDAs to be achieved within a 12-month period for an agreed contract value.
From April 2006 two new sets of regulations replaced the old-style GDS and the PDS: the NHS (General Dental Service Contracts; GDSCs) Regulations 2006 and the NHS (Personal Dental Service Agreements; PDSAs) Regulations 2006. The two sets of regulations are very similar to each other. The reason that two sets of regulations were necessary is that the GDSC regulations introduced nGDS and the PDSA regulations ratified the extant PDS schemes into something that looked more or less the same.
As well as a change in the system of remuneration, the biggest difference with the introduction of these new regulations was perhaps the intended recipients. In the old world, the regulations bore largely upon dentists themselves, with the PCTs and the Dental Practice Board acting only as enforcers of the Terms of Service for Dentists and the Statement of Dental Remuneration. The new regulations, by contrast, controlled the responsibilities and powers of the local bodies and dictated what they must provide by way of services and what contractual terms they could/could not/must include when contracting with dentists and dental practices. The 2006 dental contract also appeared to represent little room for negotiation between GDPs and local commissioners; Ward and Mehra67 observe that:
Within the text there are many areas that leave the practitioner bound and vulnerable, but with no corresponding benefits on his or her side. It is certainly the case that a commercial contract would never be as long or as demanding and it would be open for both parties to negotiate points to mutual advantage. This is very much a ‘take-it-or-leave-it’ contract. Under the regulations the PCTs are simply prohibited from softening any of the requirements as described. Consequently, all a prospective contractor can hope to do is understand what obligations are placed upon them and whether they are satisfied to be so bound.
p. 667
A key difference between nPDS and nGDS contracts is that nPDS contracts are time limited, although contractors holding a PDS-type contract have the right to serve notice that they intend to convert to a GDS-type contract, which is open-ended. GDS Regulation 13 states that ‘(1) Except in the circumstances specified in paragraph (2), a contract must provide for it to subsist until it is terminated in the accordance with the terms of the contract or the general law’. 37 Recently, therefore, GDPs have tended to move from nPDS to nGDS contracts to gain the greater level of security that the latter regulations afford.
Personal Dental Service Plus
The DH set up the Dental Access programme in March 2009 ‘to address the problem that whilst NHS dental access is good in some areas of the country it is worse in others’. 38 Several procurements of new dental services were set up with new money, and this came with central assistance in contract monitoring. These new procurements were set up based on a contract labelled ‘PDS+’ contracts.
The PDS+ contract was an addition to the standard NHS primary dental contract that was supplemented by DH guidance in the form of a user guide. This was drafted to take into account some of the recommendations from the independent review of NHS dental services,66 which suggested that there should be a shift away from a contract based mainly on activity measures (UDAs) to clearer incentives for improving health, improving access and improving quality. A ‘blended’ contract was foreseen with a mixture of contract currencies: an annual per patient payment to encourage continuing care, as well as more overt incentives for prevention and quality. No additional legislation was required to enact these changes to the dental contract, since PCTs were already free to use ‘baskets of indicators’ to monitor performance in ways that are deemed appropriate. Thus the regulations underpinning PDS+ contracts are the same that underpin nPDS agreements. The initial reaction of dental professional bodies to drafts of this new contract was not promising. The view of the General Dental Practice Committee was that this new contract is ‘unnecessarily complex, making it risky and inappropriate for dental practice’. 68 Within the draft PDS+ agreement there were nearly 50 pages and 17 schedules specifying contractual obligations, with many ‘controlling provisions’, leading to (in the view of the General Dental Practice Committee) ‘intrusive micromanagement by PCTs’. 68
The PDS+ contract incorporates a payment mechanism that comprises three types of payments: in relation to services, access and performance. The services payment is what dental commissioners know as the Negotiated Annual Agreement Value. The access payment encourages providers to increase access to patients who have not visited the contractor’s practice in the preceding 24 months, and is based on the number of ‘unique patients’ that the contractor treats. The performance payment element is linked to the contractor’s delivery on a number of key performance indicators (KPIs). Standard KPIs fall under the headings of ‘Effective Care’, ‘Health Promotion’ and ‘Patient Experience’. Remedies are included in the agreement should the contractor fail to meet certain KPIs, with, for example, failure to achieve a target twice for the same KPI in any 12-month period resulting in commissioners serving a breach or remedial notice on the contractor.
New contract pilots
Following the Steele review,66 proposals to test ingredients of a new dental contract were published in 2010. 69 Practices were invited to volunteer to be pilot practices, starting in April 2011. The 50 practices initially chosen were allocated to one of three pilot types: (1) a simulation model (receiving the same contract sum from commissioners as previously but practices are expected to follow evidence-based care pathways concerned with preventative dental care); (2) a weighted capitation and quality model (practices receive a capitation payment to cover all care: preventative, routine and complex); and (3) a weighted capitation model with a separately identified budget for higher-cost treatments within the contract value (practices receive a weighted capitation payment to cover all preventative and routine care only, with the remaining contract value attributed to cover more expensive and complex care, particularly of the type requiring a dental laboratory). After changes to the care pathway protocols in summer 2013, a further set of practices were recruited to join the new contract pilot (NCP) programme. The evaluation is currently ongoing and reform to the dental contract is expected in the next few years.
Chapter 2 Aims, objectives and research questions
The approach of our study
Institutional work theory rather than activity theory
It was noted in the referees’ comments on the original research proposal that there is considerable literature relating to the use of contracts more generally, and taking note of this would be helpful. We therefore undertook a systematic review of the literature related to the use of contracts in health care. This, together with stakeholder interviews which were undertaken alongside the literature review, influenced our decision to look at the use of contracts from an institutional theory perspective, rather than using activity theory,70 as had previously been proposed.
It became apparent, first through the extensive literature review undertaken at the outset of the project, and second through stakeholder interviews, that the theoretical framing of activity theory might prove too narrow in scope. Much of the literature discussed health-care provision generally and dental care specifically, using broad concepts associated with political, social and economic settings. While the term ‘norms’ covers these in activity theory, it does so only from the perspective of the human agent, and we wanted to engage with a broader perspective. It was also found that the dental practitioners themselves, although the focus of the study, worked in a broader community of actors, all of whom were involved, influencing the emergence of contractual forms in ways that became very difficult to distinguish using the activity theory triangles. It became increasingly artificial to separate one actor using one triangle. On both counts, moving towards institutional theory aided analysis, both from within the field and more broadly in dovetailing our studies with other studies where some form of institutional theory had been used.
Aims and objectives
Aims
We aimed to identify the factors which facilitate and hinder the use of contractual processes to manage and strategically develop General Dental Services. In particular the study aimed to investigate the relationship between commissioners and GDPs and how this relationship is affected by the differing needs and professional outlooks of both parties. A comparison with general medical practice commissioning will be used to highlight factors which are particular to dental practitioners.
Objectives
-
To understand what constitutes ‘success’ in contractual agreements from the different perspectives of GDPs and commissioners.
-
To understand the factors which influence successful (or unsuccessful) outcomes being reached in contractual negotiations between GDPs and commissioners.
-
To make recommendations of approaches that would facilitate the reaching of mutually agreeable contractual agreements between GDPs and commissioners, and help avoid the potential difficulties embedded in this contracting process.
Research questions
We framed our research questions around our study objectives.
Related to objective 1
-
What does ‘success’ mean to GDPs and PCT commissioners?
Related to objective 2
-
What are the institutional logics of GDPs and PCT commissioners, and the differences between these, that predispose the contracting process to success or failure?
-
To what extent do GDPs and PCT commissioners find it difficult to reconcile differences in managerial and professional perspectives?
-
To what extent does the issue of the balance of power between GDP and PCT commissioner create difficulties in reaching contractual agreements?
-
What role does trust play in the success or failure of contract negotiations, and how does trust become established?
-
Are there features of the relationship between GDPs and PCT commissioners which are unique to this contracting context, or do the same issues arise in similar scenarios, for example in the relationship between GMPs and PCT commissioners?
Related to objective 3
-
Under what circumstances are contractual agreements which are mutually acceptable to GDPs and PCT commissioners reached?
-
How can the contracting system be best structured and supported to optimise outcomes for both parties?
Chapter 3 Methods
Research design
We used both qualitative and quantitative methods in our study because it is recognised that a combination of both methods can overcome the bias inherent in any particular data source, investigator or particular method. 71 Convergence of findings stemming from two or more methods is said to ‘enhance our belief that the results are valid and not a methodological artefact’ (p. 268). 72 Indeed, Boring73 argues that ‘As long as a new construct has only a single operational definition, it is just a construct. When it gets two or more operational definitions, it is beginning to be validated’ (p. 182). We therefore tested hypotheses generated from qualitative data arising from stakeholder interviews (phase 1) and case studies (phase 2) using a questionnaire to GDPs (phase 3), which resulted in the refinement of our concepts. Collecting further qualitative data from commissioners and stakeholders towards the end of the study (phase 3) allowed us to further interpret, clarify, describe and validate our quantitative results. 74
Critics of the case study method argue that the study of a small number of cases gives no grounds to establish generality of findings and that the intense exposure to study of the case, biases findings. 75 By testing our findings emerging from the case studies using a questionnaire circulated to a wider group of dental practitioners, and undertaking further work with a wider group of commissioners, we were able to address these potential limitations. In circulating the questionnaire to a sampling frame inclusive of all GDPs in the areas selected, we also sought to avoid the elite bias inherent in studying practices willing to be involved in the relatively intense scrutiny associated with case study research.
Phase 1: literature review and stakeholder interviews
For literature review methods see Chapter 1, Literature review methods.
Alongside the literature review we undertook interviews with actors at the organisational field level, to provide a multilevel analysis of the factors influencing NHS dental contracting (see Chapter 3, Telephone interviews with commissioners), and to inform the topic guide used in interviews and observations made in dental and medical practices.
We started the interviews by selecting key people at the highest policy level [e.g. DH, British Dental Association (BDA)] and added breadth and numbers of key stakeholders interviewed as the study progressed. Rather than restrict stakeholder interviews to phase 1 as in the original proposal, we continued to undertake targeted stakeholder interviews throughout the 3-year study, to develop and test emerging findings. Interviews with stakeholders were audio-taped and transcribed, incorporated into the qualitative data set and analysed using grounded theory alongside data from the service delivery (dental and medical practice) level. Details and numbering of stakeholder interviews are included in Appendix 5.
Phase 2: case studies
Case studies as a methodological approach in the study of institutions
The case study is a research strategy which focuses on understanding the dynamics present within single settings. 76 It emphasises detailed contextual analysis of a number of events or conditions and relationships. Yin77 defines case studies as ‘an empirical enquiry that investigates a contemporary phenomenon within its real life context, when the boundary between the context and the phenomenon are not clearly evident’ (p. 13). He further elaborates that case studies cope with the technically distinctive situation where there are many more variables of interest than data points and therefore the method relies on a range of data collection methods (such as interviews, archives and observations), which act as multiple sources of evidence, with data converging in a triangulating way. These factors therefore differentiate case study research from experimental or quasi-experimental designs, which aim to divorce the phenomenon under study from its context, limit the number of variables under study and minimise the impact of both historical and current events. 78
Case study methodology is particularly suited to an institutional theory perspective, which emphasises change and continuity, and process as well as structure. The term ‘institution’ is not synonymous with the term ‘organisation’, for institutions are ‘sets of rules which structure interactions between actors’ whereas organisations are ‘collective actors who might be subject to institutional constraint’. 79 Organisations are therefore understood as the outcome or expression of the results of rule-governed action. The framework that constitutes the organisation is based upon the rules involved and the way they relate to each other. Action within organisations is seen as a set of ‘games’ that are governed by institutional rules, in the same way that mathematics and chess both operate to relatively simple sets of rules but have possibilities for extensive creative development. The nature of the rule system determines the extent to which new patterns of action can emerge from within the existing organisational framework.
Institutional rules are therefore seen to act as constraints (or conversely a lack of constraint) to action (e.g. in GDPs interpreting contract rules, or in commissioners applying financial penalties to GDPs failing to meet targets) because they express people’s fundamental understanding of the nature of social exchange (e.g. of the exchange involved in contracting). Although GDPs and commissioners are obviously key agents (with the capacity to affect somehow the social world) at the micro-institutional level, there are other agents too (such as other members of the dental practice team, patients, politicians, commissioning bodies, professional bodies, etc.), as well as meso-level institutions which influence how the GDPs behave (public policy agenda, health-and-safety procedures, market forces, etc.). Norms such as professionalism and affordability are also involved in defining actions and reactions in day-to-day work; all the above are set within the macro-institution operating at societal level, framing, for example, the way money operates.
Case studies are multiperspective analyses. This means that the researcher considers not just the voice and perspective of the actors, but also the relevant groups of actors and the interaction between them, which makes the methodology particularly suited to capturing the range of institutional forces influencing patterns of action and reaction within general dental practice. Supplementing our service-level data from case studies with data from stakeholders allows us to capture a range of institutional forces beyond the immediate dental practice environment (from legal representatives, professional bodies, policy-makers and the like), which nevertheless shape action at the micro-institutional level, since values, assumptions and practice in dental practices are shaped by a range of other influences outside their immediate environment; for example, by other institutions associated with the law (e.g. employment law, litigation systems) or politics (health policy, ruling parties).
This institutional perspective fosters analysis of the ways in which agents enact their environment and are similarly acted upon by the same environment, in everyday work settings,80 and accepts that institutional structures such professional ethics, profit-based market forces and prevailing ideas of ‘health’ have meaning outside any specific individual’s interpretation. To institutionalise, therefore, is to appreciate the values that pertain beyond the immediate technical requirements of tasks at hand. 81,82 For example, a patient’s decision to open his or her mouth while lying prostrate in a chair is possible only in a setting of habituated expectations concerning the competence and integrity of professionals, the desirability of healthy teeth, the probity of payment mechanisms and so on. Using qualitative methods (case studies and stakeholder interviewers) we therefore set out to make explicit the institutional rules governing general dental practice in order to explain both action and structure, encompassing change and continuity, and therefore responses and tensions concerned with dental practice contracting.
Institutional logics and general dental practice as an organisational field
Following DiMaggio and Powell,83 we identify dental practice as an organisational ‘field’ governed by prevailing logics, often tacitly expressed, that are beyond the gift of individuals to change, and which govern day-to-day work. A field is defined as a ‘common meaning system, where participants interact more frequently and fatefully with each other than with actors outside the field’84 (pp. 138–9) – in other words, the organisational field encompasses the whole range of actors and influences that shape dental practice work. Institutional logics are said to provide the organising principles for a field. 85 These logics describe the rules, many of which are unwritten but commonly understood, governing behaviours of GDPs, of commissioners and of GMPs, whom we used as a contrast group in order to identify aspects that are particularly distinct in dental practice. Thornton and Ocasio86 define institutional logics as ‘the socially constructed, historical patterns of material practices, assumptions, values, beliefs and rules by which individuals produce and reproduce their material subsistence, organise time and space, and provide meaning to their social reality’ (p. 804). Logics are then the predominating beliefs that create connections and a common purpose allowing those within a field a sense of grounding, orthodoxy and habituated normality.
It is through logics that organisation, actors and agency are woven into one another; when logics change, the rest also changes. Thus no sooner are institutional logics posited than their dynamic nature becomes apparent. 84 To explore institutional logics we therefore require a methodology able to capture the dynamic of the forming and evolution of logics, the action and interaction between various actors, and a whole range of other external influences which shape responses. Case study methodology, being focused on studying the dynamic nature of particular settings, is particularly suited to this task. We also incorporated a longitudinal aspect to the design, in studying cases over the course of a year, to examine in more detail how institutional logics of GDPs and commissioners were expressed and defined by changes in their environment, and their interaction with each other.
Institutional work studies often find that some fields and organisations have logics which are not in sympathy with each other. So rather than being constituted by a homogenous collection of actors, each behaving according to a set social script designed by their environment, organisational fields and organisations are seen as sites of struggle. Several logics may coexist within an organisational field and organisation, although one is generally dominant. Struggles are experienced as new practices or norms – perhaps prompted by breakdown events, new actors, shifts in leadership or new technologies – are advocated, and established ones defended, or amended. In the course of this, the meaning and priority of activities can change, with some becoming redundant or anachronistic, and others lying dormant, to be resurrected at a later time, all of which can lead in turn to increased variation within the field. How individual actors respond to institutional pressures also varies, and, in this process of struggle and resolution, actors are understood to gain skills and capital for future institutional involvement. 55,87 Of particular interest to us therefore was to understand how individual responses (e.g. of different GDPs) varied in response to the various institutional pressures acting on the dental practice organisational field.
In summary, therefore, in our qualitative work we sought to explicate institutional logics governing general dental practice and contrast this with commissioning logics to inform the nature of interaction concerned with the different parties involved in dental practice contracting. We also elucidated institutional logics which govern general medical practice in order to facilitate a deeper understanding of the institutional forces and tensions which are particular to the dental context.
Definition and selection of cases
Case studies can be undertaken using either a single case study or multiple case study design. Phase 2 involved a multiple case-study design. In multiple case-study designs, each case remains a single case, but conclusions are used as information contributing to the whole study. A multiple case-study design was employed to take advantage of both the replication logics of literal replication, the assumption that cases are similar and thus findings may be similar also, and theoretical replication, the assumption that cases may yield contrasting results. 77
In our case studies we wanted to examine our unit of analysis: the phenomenon of institutional logics governing general dental practice (as well as commissioning and our comparator, general medical practice), which included the expression of logics in interactions between GDPs and commissioners. To reflect the institutional perspective, which recognises layers of influence outside the immediate environment, it was necessary for us to construct our cases as reaching beyond the walls of each dental (or medical) practice. Thus data gathered from, for example, commissioners responsible for contract monitoring and negotiations with the practice were considered as part of that case, albeit providing a different perspective on events impacting on the practice that occurred during the study period. We were limited by time and resources, so in our data collection we did not include perspectives from the range of other actors (such as accountants, suppliers or people in the local community) interacting with the practice ‘more frequently and fatefully . . . than with actors outside the field’ (pp. 138–9),88 although we did include perspectives from patients attending for care. Although our ‘cases’ can be loosely equated to dental or medical practice settings, these cases should still be considered institutionally as a larger interconnected social system rather than in the more easily delineated sense of everything that is contained within each dental/medical practice as a distinct organisation.
Within both single and multiple case-study designs, the context in which the case is located is of interest as well as the case, although the boundaries between the case and context may be blurred. 78 Our cases (dental and medical practices) were set in a range of different contexts (different PCT areas). PCTs vary not only in a geographic sense but in a variety of other factors such as the level of dental manpower relative to the population and the socioeconomic characteristics of the population, along with corresponding differences in levels of oral disease and demand for care. Since commissioning policies are defined locally, strategies and culture as well as the personnel involved in commissioning were also likely to vary between PCTs.
Our selection of cases was undertaken in two stages: first selecting PCT contexts and then selecting dental and medical practices to be studied as cases within these areas. Case study methodology argues that cases in multiple case-study designs should be dependent on the theoretical framework that specifies conditions under which the phenomenon is likely to be found. 76 In other words, rather than looking to undertake a random sample of dental (and medical practices) we aimed to obtain a sample from which our particular phenomenon under investigation was likely to emerge. A typical or average case is often not the richest in information, and thus a purposive sample is preferable.
In the first stage of our sampling procedure, we aimed to reflect a range of different contexts, so that in our cross-case analysis we could draw analytical conclusions that would go beyond the immediate findings of each case and allow us to generalise about the impact of various case contexts89 – particularly across different approaches to commissioning, different levels of competition for provision of NHS dental care and different levels of population demand and need.
Selection of primary care trusts
Primary care trusts were first established in 2000. Of the 152 English PCTs, 24 were in the North West. Given the range of contexts represented in these 24 PCTs we were confident that, with careful sampling, we could mirror the national picture without incurring costs that would result from recruiting PCTs from a larger geographic area. We set out to purposively sample six of these 24 PCTs from where the sample of dental and medical practice cases would be drawn.
A four-stage hierarchical selection procedure was used to identify the six PCTs. First we aimed to identify PCTs which represented a range of approaches relating to dental commissioning and relationships with GDPs, and then after that we selected PCTs to obtain a balance across a range of sociodemographic factors (first looking at indicators reflecting the extent of urbanisation and then selecting PCTs reflecting a range of dental caries prevalence as measured by dental epidemiological studies of children). For the first stage of the sampling grid selection we used as our data source the results of a survey published in Dentistry magazine (a free publication circulated to registered GDPs) in March 2010. Although the methodology of the survey was not published, and neither was the number of responses from GDPs, the data did provide national statistics for each PCT according to a range of parameters including GDP perceptions of the PCT’s consistency in negotiations, overall quality of the relationship with commissioners, willingness to innovate and ease of communication. We used the proportion of GDPs in the PCT rating their overall quality of relationship on a 5-point scale (1 = very poor to 5 = very good) as our measure. The overall mean score nationally for the quality of the relationship was 1.97. We selected three PCTs rated as having a poor-quality relationship with GDPs (mean score 1.5 or less) and three PCTs rated as having a good-quality relationship with GDP (mean score 3.0 or more).
The second measure used in the sampling grid was data concerned with urbanisation sourced from the Rural Evidence Research Centre at Birkbeck College. 90 We selected two of the six PCTs to represent Major Urban Areas (defined as those PCTs with either 100,000 people or 50% of their population in urban areas with a population of more than 750,000), two PCTs to represent Other Urban Areas (defined as those with either fewer than 40,000 people or less than 26% of their population in rural settlements and larger market towns) and two PCTs to represent Rural Areas (defined as having at least 50% of the population in rural settlements and larger market towns).
The third measure concerned dental caries prevalence in children as measured by the National Dental Epidemiology Programme of 5-year-olds, data from 2007/8. The mean number of decayed, missing and filled primary teeth per child (dmft) for 5-year-olds in England in this data set was 1.11. We selected two PCTs with a mean dmft of 1.0 or less, two PCTs with a mean dmft of between 1.2 and 1.5 and two PCTs with a mean dmft of 1.75 or more.
The fourth measure we used was national data on patient access to NHS dentistry. National data were available for each PCT on the number of adult patients seen as an NHS patient in the previous 24 months. 91 We could compare proportions of the adult population by year going back to 2005, and therefore took as our measure the change in the percentage of patients accessing NHS care between 2005 and 2008/9. We took this to reflect changes in response to the implementation of the contested 2006 dental contract, which was possibly influenced by the way PCT commissioners handled relationships with GDPs, since, where commissioners’ relationships with GDPs were generally poor, practitioners had a tendency to withdraw from NHS provision following contractual changes, in clusters. We selected two PCTs that showed an increase in access between 2005 and 2008, two PCTs that had a slight decrease in access (between 1% and 3% fewer adults using NHS services in the last 24 months) and two PCTs that had a significant decrease in access (of 5% or more). Table 1 shows our sampling grid used to select the six PCTs.
| Area classification | PCTs with poor relationships with GDPs | PCTs with good relationships with GDPs |
|---|---|---|
| Rural | Medium dmft Significant decrease in access |
Low dmft Increase in access |
| Other urban | Low dmft Significant decrease in access |
High dmft Slight reduction in access |
| Major urban | High dmft Increase in access |
Medium dmft Slight reduction in access |
Selection of dental practices
We used the same principles of purposive sampling to reflect a range of contexts, to select dental practice cases in each PCT. We set out to have a sample of 16 dental practices, with at least two dental practices coming from each PCT. Within the sample we wanted to reflect a range of contrasting contexts of interest in order to explore our phenomenon more fully. Thus, within our sample we wanted to be able to contrast dental practices where the business comprised mainly NHS work (11 practices) with practices where the NHS contract was a only small part of the business (three practices) or where the business was fully private (two practices). We felt that including private and part-private practices within the study would allow us to capture why some practitioners had moved away from NHS to private work.
Likewise, because responses to NHS contracts were the phenomenon we wanted to explore, within our fully NHS case study practices we wanted to include a range of type of contract forms. In Chapter 1, Different dental contract models (summarised in Appendix 4), we described four current types of NHS dental contracts: nGDS, nPDS, PDS+ and NCP. To facilitate cross-case comparisons, we selected practices within the same PCT with a variety of contracts as well as representing corporate/partnership and single-handed models. Table 2 shows our sampling grid which guided the type of dental practices selected as case studies. Of the 11 fully or partly NHS practices, we selected three NCP practices, two PDS+ practices, four nGDS practices and two nPDS practices.
| PCT | Practice 1 | Practice 2 | Practice 3 |
|---|---|---|---|
| A | nPDS | GDS child only | PDS+ |
| B | nPDS | Private | NCP |
| C | nGDS child and exempt only | PDS+ (corporate) | NCP |
| D | Private | nGDS | – |
| E | nPDS child and exempt only | nGDS | NCP |
| F | nGDS (corporate) | nGDS | – |
We selected dental practices from lists of NHS dental practices together with contract type provided by each of the six participating PCTs. Fully private practices were identified through online searching within each of the six PCT geographical areas. Initial contact was made by phone, before further information was sent by post or e-mail as preferred. Follow-up phone calls were then made to ascertain if the practice would participate. When a practice declined to participate, another in the same area was approached and the procedure repeated until sufficient practices had been recruited.
Selection of medical practices
One medical practice was selected in each PCT, again from a list provided by each PCT. We set out to choose, where possible, a medical practice within the vicinity of one of the dental practices recruited in that area (to give us a similar range of patient characteristics for dental/medical practice cases). Recruitment of medical practices to the study proved to be more difficult than for dental practices. Through persistent approaches to numerous medical practices we recruited one medical practice case in five of the six PCTs. However, it proved impossible to recruit in the sixth PCT despite seeking assistance from Primary Care Research Network (PCRN) North West. We therefore selected a second medical practice in one of the other PCTs.
In a similar situation to dental practice, there are a number of different contract forms which coexist governing NHS medical practice. We provide a summary of some of these different types of contracts and the context outlining how these different models of contract arose, in Appendix 2. The contract types held by our six medical practice cases were GMS (two practices), Personal Medical Service (three practices) and Alternative Provider Medical Services (APMS) (one practice).
Data collection
Dental practice interviews
Over a 15-month period, from February 2011 to April 2012, successive rounds of semistructured interviews were undertaken. We started by undertaking interviews in all the dental practice cases, first with principal dentists and then strategically broadening the interviews undertaken with other members of the dental practice according to what appeared relevant to that case, gathering additional perspectives and triangulating accounts. In one dental practice (FD2; see Appendix 6 for coding scheme) we were not able to interview the principal because he felt under time pressure to complete his contract targets. We revisited and reinterviewed many participants during the case-study period to follow key events, such as contract reviews, interventions and disputes with the PCT, etc. In some practices the original respondent was reinterviewed (up to four times); in most practices other members of practice staff (managers, nurses, other practitioners) were also interviewed.
We also undertook patient interviews at seven of the 16 dental practices, where practices had the facilities to provide a private area for interviews and were willing for patient interviews to take place. Within the patient interview topic guide we included a question to prompt a comparison of dental and medical practices, so patient data were used in the analyses of both dental and medical practices. The number of interviews (not including patient interviews) undertaken in each dental practice ranged from one to five (see Appendix 7). We undertook 39 patient interviews in all.
Medical practice interviews
The number of interviews undertaken in each medical practice ranged from one to three. In all non-corporate cases a principal or partner was interviewed. Initial interviews with GMPs and practice managers were undertaken over a period of 14 months between March 2011 and April 2012 inclusive. Seven GMPs and three practice managers were interviewed, with a second interview undertaken with one of the GMPs almost a year after the first. A second round of interviews was undertaken between July and November 2013 involving two GMPs, one of which was a second interview, and one finance director (see Appendix 8). This allowed us to test and further explore emergent findings as well as describe cases in more detail.
Commissioners
At five PCTs, initial interviews were undertaken with the Head of Primary Care; at the sixth it was with the Dental Commissioning Lead. Successive PCT interviews involved some reinterviews and also interviews with dental and medical commissioning leads (with a variety of official job titles), a dental practice advisor and the chair of a GMP commissioning consortium. Typically a total of three or four interviews were conducted at each PCT, some lasting well over 2 hours (see Appendix 9).
Topic guides
Topic guides for the initial dental case studies are included in Appendix 10, and subsequent topic guides were developed specifically in relation to that case or to cover emergent issues from cross case analysis in more depth. Separate topic guides were prepared for first-round interviews with GDPs, GMPs and commissioners, the first two being very similar (see Appendix 10). Commencing with questions about the practice’s history, size and business structure and the nature of the contract, they went on to probe for the respondent’s views on success, competition and business management. A series of questions explored perceptions of the relationship with the PCT, the role of external bodies such as the DH, BDA/British Medical Association, Local Dental Committee (LDC)/Local Medical Committee and the sources of information used. We undertook several GDP interviews before any GMP was interviewed, and then included an extra section in the GMP topic guide to explore their responses to some of the ways GDPs had defined differences between themselves and GMPs.
Commissioner interviews were not conducted until interviews had taken place in at least two dental practices in the PCT (and in some cases also at the medical practice). This enabled efforts to be made to triangulate information received at practice level. Clearly this had to be handled sensitively in order to preserve practice anonymity; nevertheless in many cases it proved possible to get the commissioner perspective on events previously described by practitioners.
Interviews with commissioners began by exploring the structure of the dental commissioning team and practitioner input and how the PCT’s performance was managed and monitored, before going on to get a picture of the number and nature of dental contracts across the patch. A series of questions was asked about relationships with GDPs, and commissioners were encouraged to talk about those they had experienced as particularly good or difficult or which had notably changed over time. Ideas around trust and openness were explored as well as success, competition and sources of information. At various points commissioners were asked about differences or similarities between GDPs and GMPs.
Non-participant observation
In some PCTs face-to-contract meetings between GDPs and commissioners took place annually as routine, although not in all PCTs. It was difficult to maintain the anonymity of PCTs and practices and observe the meetings between the PCTs and the dental practice cases. There was also a possibility that observation by a researcher might influence proceedings. However, for two dental cases within the same PCT, where interviews had established that practitioners considered their relations with the PCT to be non-problematic, anonymity regarding the PCT was waived, with consent, and the annual contract review meetings were observed. An informal meeting of a group of local dentists with PCT commissioners in the PCT headquarters was also observed; in this case the anonymity of the participating dental practice case was preserved. For medical practices, contracts tend to be ‘in perpetuity’, rolling on year-on-year. Contract reviews with the PCT were therefore infrequent, generally ranging from 3 to 5 years, although one GMP reported that, during the 8 years he had been at the practice, no contract review had occurred. No meetings between commissioners and GMPs were therefore observed. Meetings observed were audio-taped and supplemented with the researcher’s observation notes.
Further into the study we also observed delivery of patient care at the dental chair side. We had identified some areas of the dental contract where there was a variation between GDPs and commissioners about how the contract was interpreted (e.g. what UDA band and therefore patient charge should be allocated in particular circumstances). We felt it would be helpful to look at particular instances in relation to treatment, to gain a better understanding of how GDPs made these types of decisions and the extent to which the patient was involved in this.
Documentary evidence
A variety of documentation was also collected during this phase of the study, including copies of contracts (i.e. the standard contracts plus the short addendum stipulating UDA rate and quantity); pro formas designed by PCTs for monitoring and evaluation purposes; standard monitoring documentation (i.e. the Vital Signs report, monthly and annual); Vital Signs Guidance for PCTs; published reports in the dental press and correspondence regarding a PCT action which entered the public domain during our study (details not provided to preserve PCT anonymity); written and e-mail correspondence between the PCT and particular case-study practices; and notes of three unrecorded phone calls with two practices in one PCT supplied by the dental practice cases. We also included within our data set for analysis both internal (waiting areas, notice boards, signage, branding) and external photographs of dental practices (marketing, signage, branding). We have limited references to some of these data in reporting in order to preserve anonymity.
Data collection processes
An information sheet was given to, and written consent obtained from, each participant at the time of his or her first interview. All interviews were digitally recorded and transcribed verbatim, as were the non-participant observations and patient interviews described above. Only one GDP requested that part of the interview be not recorded; in this case, notes were made. One follow-up interview with a commissioner was conducted by telephone; all other interviews in this phase of the study were conducted in person.
Data analysis
We used NVivo version 10.0 (QSR International, Warrington, UK) to organise different types of data (interview transcripts, documentary evidence, notes and transcripts of non-participant observations) into cases. We used a grounded theory approach to the analysis. Data were initially open coded before being recoded according to theoretical concepts and emergent categories. We wrote both case memos and conceptual memos to support the analysis. The process of analysis was iterative, with emerging themes discussed with a wider analysis team alongside further reading of the literature, leading to refinement of codes and categories. 92
Phase 3: questionnaire and commissioner interviews
Phase 1 studies provided detailed accounts of the reasons that individual GDPs, GMPs and commissioners engage with the commissioning processes in the ways that they do. This permits the development of a body of theory which then requires quantitative testing to establish the extent to which constructs are useful in explaining population-wide patterns of behaviour. The objectives of the empirical component were twofold: to use a factor-analytic approach to develop measures of the theoretical constructs, such as institutional logics, derived from phase 1 qualitative work, and to assess the capacity of these measure to predict outcomes pertaining to micro- and macro-level responses to commissioning. In phase 2 we incorporated a quantitative component to the study, as well as broadening geographically the PCTs included in the study. We added to our sample of six PCTs a further eight PCTs selected randomly from a list of the 152 PCTs in England, making a total of 14 PCTs involved in phase 3.
Questionnaire to general dental practitioners
The questionnaire was developed from our earlier qualitative work, and piloted to nine GDPs. The advisory group was also involved in refining the questionnaire. We posted the questionnaire with covering letter to a cluster sample of 924 named providers on the Care Quality Commission (CQC) national register of dental practices registered under the Health and Social Care Act 2012 (source: CQC database 3 January 2012) between 24 January 2013 and 24 April 2013. The list included providers ranging from fully NHS to fully private practices. We used a number of techniques recognised to be effective in increasing questionnaire response rates. We addressed the covering letter to an individual, handwriting the name. A stamped, addressed envelope was enclosed for reply. We used coloured ink in the questionnaire, which was printed as a booklet, and used brown instead of white envelopes. We sent a further two follow-up questionnaires to non-respondents. In order to try to maximise response rates, the covering letter was countersigned by a regional LDC representative as well as the chief investigator. For the third mail-out to non-respondents, those identified as corporate bodies were sent a revised cover letter directly addressing area/practice managers to highlight areas of the questionnaire they would be eligible to complete. We felt that the use of monetary incentives might contribute to response bias in a questionnaire involving exploration of commercial values, so incentives were not used.
Institutional logics were assessed using items developed directly from the qualitative work with GDPs. These were developed initially from GDPs’ verbatim descriptions of their beliefs and modified to fit a questionnaire context (removal of ambiguous or double-barrelled meanings). The questionnaire contained 47 items relating to institutional logics as well as sections relating to relationships to commissioners, approaches to interpreting grey areas of the dental contract, and macro-level approaches to commissioning such as a willingness to work co-operatively, as well as professional network links. We also included practice finance questions with Likert-type responses asking if the practice financial turnover had changed in the last 2 years (ranging from ‘reduced significantly’ to ‘increased significantly’), the extent of difficulty in sustaining business profits over the previous 5 years. A copy of the questionnaire is included in Appendix 11.
Micro-level (chair-side) behaviour in relation to grey areas of the dental contract
Case-study data indicated six areas where interpretation of the contract by practitioners could reveal differences in behaviour geared towards practitioners’ or patients’ interest and away from the interest of commissioners. The six areas were (1) whether or practitioners were willing to accept a patient for NHS care because the extent of work that was needed would mean that remuneration was insufficient to cover the cost of care, meaning that there was low or no profit for the practice (avoiding high-cost patients); (2) restriction of certain types of NHS treatment (e.g. root canal treatment) where remuneration was insufficient to cover practice costs (restricting high-cost treatment); (3) gearing treatments undertaken towards a higher complexity of treatment towards the end of the financial year in order to meet targets (over-representing patients’ diagnoses); (4) restricting access to NHS routine care for patients towards the end of the year when targets had already been met (inequitable care); (5) allocating payment claims for treatment to a lower band than should have appropriately been used, so that the patient contributed a lower charge (under-representing need for patients’ copayment); and (6) not adhering to national guidelines on the period of recall, which recommend that, for patients at low risk of dental disease, the period between check-ups should be between 12 months and 2 years (overallocation of treatment resources).
Behavioural responses to contract rules were measured in two ways: by asking a set of questions relating to each of the six ‘grey’ contract areas in relation to (1) past behaviour (how often they had engaged in that behaviour over a specified time period, e.g. the previous 2 years) – all 300 responses had sufficiently completed items – and (2) intended behaviour (phrased as intentions to make specific clinical decisions relating to gaming within the next 2 years assuming a hypothetical stability of contracts) – 294 practitioner responses were sufficiently complete to include in the analysis. We also assessed descriptive norms by asking how often dentists/practices in England would behave with respect to the six grey areas described. Response sets for intended and previous behaviours and descriptive norms were identical, using a five-category response set labelled ‘never’, ‘rarely’, ‘occasionally’, ‘often’ and ‘routinely’. Practitioners’ perceptions of injunctive norms were obtained by asking what proportion of dentists in England ‘might not approve’ of behaviour with respect to each of the six grey areas. The response set consisted of five categories labelled ‘none’, ‘less than 10%’, ‘about 10–50%’, ‘50–75%’ and ‘almost all’.
Macro-level behaviour of dentists in relation to approaches to commissioning
From our case study data we developed 15 items concerned with dentists’ approaches to commissioning, such as ‘Persisting in arguing with the PCT/commissioners to wear them down’ and ‘Work together to solve problems’. These approaches were measured in two ways: (1) past behaviour, assessed by asking how often they had engaged in the negotiating tactic over the previous 5 years; and (2) intentions to adopt the tactic in the future, phrased as intentions to use tactics during a specified time period. Past employment of each negotiating tactics was assessed by prefacing items with the phrase ‘During the past ___ how often have you . . .’, using a 4-point scale labelled ‘never’, ‘rarely’, ‘occasionally’ and ‘routinely’. Intention to engage each negotiating tactics was assessed by prefacing items with the phrase ‘During the next ___ how much do you intend to . . .’, using a 4-point response scale labelled ‘extremely unlikely’, ‘unlikely’, ‘likely’ and ‘very likely’.
Relationships with commissioners
Based on the qualitative work, we developed an 18-item scale to explore antecedents of trust: previous experiences of the PCT being honest (four items) and open with the practitioner (five items), distributive justice (fairness about allocations and outcomes e.g. placing unfair demands on the practice; four items) and interactional justice (fairness of interpersonal treatment during implementation; five items). Participants rated their experience of positive (e.g. ‘I have always found the PCT to be dependable’) or negative (e.g. ‘The PCT have rarely listened to my views’) events on a 5-point scale anchored by the terms ‘strongly disagree’ (1) to ‘strongly agree’ (5). Positive items were reversed and an average item score used. These items are items 1–19 of section 6 of the questionnaire (excluding item 18). We found all of these 18 items were so highly correlated that we used the items as a single scale (which we named negative experiences) rather than subscales relating to honesty, openness and fairness: a principal components analysis showed a single factor with an eigenvalue of 8.60 with a minimum item loading of 0.47. Cronbach’s alpha of the negative experiences scale was 0.93.
Trust
The measure of trust was future orientated. We used Fernandez’s93 four-item scale of interorganisational trust composed of three attributes (items 16, 26, 29 and 31 in section 6 of the questionnaire): (1) positive expectations that commissioners would act favourably (items 26 and 29); (2) a willingness to be vulnerable (item 31); and (3) dependability that commissioners would act in one’s own interest (item 16). We supplemented this with three additional items derived from our qualitative research: (1) ‘I assume that the things that the PCT tells me are right’ (item 27, vulnerability); (2) ‘I have no reason to think the PCT would treat me badly’ (item 24, positive expectations); and (3) ‘I am willing to share with commissioners information about my practice which I don’t have to share, such as business information’ (item 32, vulnerability). The response format for this measure was a 5-point scale ranging from ‘very unlikely’ (1) to ‘very likely’ (5). Thus, in all, we collected data on seven items in our measure of trust (items 16, 24, 26, 27, 29, 31 and 32). In our analysis, however, we did not include item 32 because it reduced Cronbach’s alpha. The scale alpha was 0.83, with a principal components analysis showing our trust data as a single factor with an eigenvalue of 2.81 and a minimum item loading of 0.66.
Both Cronbach’s alphas for the negative experiences and trust scales exceeded the scaling acceptability cut-off (normally considered to be 0.70), with the single-factor solutions from the factor analysis showing that the scales were best treated as being unidimensional.
Professional network links
We measured dentists’ connectedness with dental and other professionals in three different ways. The first reflected previous professional roles and membership of professional bodies (e.g. dental practice advisor, member of the BDA, foundation trainer, LDC committee member). The mean number of roles/membership held by respondents was 2.64 [standard deviation (SD) = 1.79]. The second reflected the frequency of respondents’ contacts outside their practices over the previous 6 months, in terms of attending (non-PCT or commissioning) professional meetings, having contact outside the practice regarding professional issues, or discussing clinical, practice management or commissioning issues (either face to face or through electronic or telephone forums). The response sets for these five items were ‘none’, ‘once’, ‘twice’, ‘3–6 times’ or ‘more than once per month’. Cronbach’s alpha for this scale was 0.70 with a mean of 2.03 (SD = 1.06). The third measure of connectedness was respondents’ willingness to discuss difficulties with PCT contracts, with the following: the chair of the LDC, other members of the LDC, family members, online GDP forums, fellow practitioners, family members with dental, legal or business backgrounds, a dental defence association or a solicitor. The response format for this measure was a 5-point scale ranging from ‘very unlikely’ (1) to ‘very likely’ (5). Cronbach’s alpha for this scale was 0.92 with a mean of 3.21 (SD = 0.80).
Questionnaire analysis and response rate
After three mailings, 393 questionnaires were returned (43%), 333 of these from practitioners involved in some NHS work.
Of the 333 practitioners involved in NHS work, 294 fulfilled the criteria of completing all of the chair-side decision (‘micro behaviours’) items and having no more than four missing data items over the 47 scale items used to measure institutional logics. Of the respondents used in the first analysis, 225 were male and 69 (21%) female. This reflects national figures, which show that only 23% of practitioners owning practices are female. 91 Practitioners had a mean age of 49.31 years (SD = 8.80 years) and a mean time in practice of 26.78 years (SD = 9.18 years). Fifty-eight (17.8%) were sole traders, 45 (13.8%) were in partnerships, 98 (30.1%) worked at sole trader practices with associates, 79 (24.2%) worked in partnerships with associates and 46 (14.1%) worked in corporate practices or limited liability companies. The median number of dentists working in each practice was 3 [interquartile range (IQR) 2–5]. The median percentage of NHS/private mix of work in the practice (based on patient numbers) was 75% (IQR 29–95) and private work 30% (IQR 5–75). Again, this was roughly comparable to national figures, which show that 57% of dentists spend 75% or more of their time on NHS dentistry. 94
There were sufficient data from 300 responses to use these in an analysis on logics items (having no more than four missing data items over the 47 scale items). Using an exploratory factor analysis, logics items were entered into a factor analysis using maximum likelihood extraction with oblique rotation. Scree plots were used to identify the optimal number of factors. To obtain items that independently contributed to the solution, those that did not have loadings over 0.30 on one or more of the four factors in the pattern matrix were discarded. This enabled identification of items that contributed uniquely to one or more factors. Factor scores were retained and used for later analyses. Confirmatory factor analysis could not be used because the sample size was inadequate for division into exploratory and confirmatory subsamples.
We used intended behaviour in the six grey areas of the contract over the coming 2 years as outcome variables. Examining intentions while controlling for current behaviour alleviates the methodological problem of reverse correlation that arises when past behaviour is used as an outcome variable. This creates a stringent test of the hypotheses because significance tests apply to the extent to which variables predict the criterion independently of each other; since the majority of variance in future intentions is explained by past behaviour, this leaves limited scope for other predictors. 95 Hypotheses were tested using two sets of regression analyses. The first set examined unique prediction of behavioural intentions by descriptive and injunctive norms and institutional logics. Significance testing of regression beta weightings was used to assess unique relationships between individual predictor and the outcome variables in each regression analysis.
Demographic, practice type and practice finance variables were entered into all analyses to serve as control variables. Significance testing of regression beta weightings was used to assess unique relationships between predictor and outcome variables in each regression analysis.
The second set of analyses involved moderated regressions examining interactions between negative views of relationships with commissioners and institutional logics in a subsample (n = 288) of practitioners who reported having had experience of negotiating with PCT commissioners (in dental practices with partnership arrangements, sometimes only some of the partners deal with commissioner negotiations on behalf of the others). This second set of analyses followed the same format as the other, but then added the negative views of experiences. It was predicted that any influence of institutional logics would become manifest if dentists viewed their relationships with commissioners negatively. Four interaction terms represented interactions between negative relationships with commissioners and the four logic factors. Interaction terms were computed from the product of centred experience scores and each of the saved logic factor scores, and entered into regression equations with main effect variables to behaviour in relation to the six grey areas of the contract.
A total of 268 dentists completed 12 or more of the 15 items relating to ‘macro behaviours’ in terms of their likely approaches to commissioners. Using an exploratory factor analysis, intended approaches to commissioning were entered into a factor analysis using maximum likelihood extraction with oblique rotation. Scree plots were used to identify the optimal number of factors. To obtain items that independently contributed to the solution, those that did not have loadings over 0.30 on one or more of the four factors in the pattern matrix were discarded. This enabled identification of items that contributed uniquely to one or more factors. Factor scores were retained and used for the analysis. Confirmatory factor analysis was not used because the sample size was inadequate for division into exploratory and confirmatory subsamples.
We saved the resultant factor scores to be used as the outcome variable in the set of analyses concerned with macro-level behaviour. Examining intentions while controlling for current behaviour alleviates the methodological problem of reverse correlation that arises when past behaviour is used as an outcome variable, for the same set of reasons as was pertinent to the analysis of micro-level behaviour. Hypotheses were tested using sets of regression analyses to identify variables that uniquely predicted intentions of engaging in these various types of macro-level behaviour.
Telephone interviews with commissioners
In our protocol we planned to conduct telephone interviews with commissioners in the 14 PCTs forming the sampling frame for our questionnaire. This was to further test our qualitative findings from the case study work, and also widen participation in the qualitative work to include other regions of England. However, since the telephone interviews were scheduled to be undertaken in 2013, reorganisation of commissioning meant that the structures had changed by the time we undertook this phase of data collection. By April 2013 the 14 PCTs which had given consent for commissioner participation in this phase of the study had been recently merged into larger NHS England Area Teams. This resulted in a revised total of 11 areas from which commissioners were sought to participate in phase 3. Of these 11, two commissioners declined to participate because of lack of capacity/high team workload. Of the nine commissioners interviewed in phase 3, only two were from the original sample of the six PCTs studied in depth in our case-study work, with just one of these still working as a commissioner in the same area.
We found the shift from PCT commissioning to NHS England Area Teams in 2013 had resulted in a turnover of dental commissioning team staff in the majority of the participating areas. Only two of the original commissioners remained in post, and one of these declined to participate. Commissioners selected for interview were those nearest in role to commissioners previously interviewed in phase 1. Several interview questions were designed to draw out differences between GMP and GDP commissioning, although this was dependent on the commissioning experience and role of the participants. While some had wide experience of commissioning in different primary care sectors, others had previous experience of only a dental commissioning role. The interviews were undertaken predominantly by telephone, and conducted over a 4-month period (April 2013 to July 2013). After each interview, the topic guide was refined in an iterative process by the research team to take account of the concurrent analysis and emerging themes. Alongside answering questions verbally, the commissioners were asked to answer the same questions on six grey areas of dental practice as had been put to GDPs in the postal questionnaire.
Research ethics
National research ethics approval (reference number 10/H1011/38) and NHS research governance approvals for all 14 PCT areas involved were obtained before the study commenced.
Chapter 4 Findings
Study findings are reported in two main sections: from qualitative work (phase 2 case studies and phase 3 commissioners/stakeholder interviews) in the first section of the chapter, and from quantitative work (phase 3 questionnaire) in the second section. In the final section we provide an overview of the integration between the qualitative and quantitative work streams.
Qualitative findings
A key focus of our qualitative work was the elucidation of institutional logics as the common meaning system of GDPs, commissioners and GMPs. Findings are therefore reported first as a typology of four general dental practice logics in Institutional logics in general dental practice. In Institutional logics of commissioners we move on to describe a typology of three NHS commissioner institutional logics. The contrasts and synergies between the various logics outlined are then drawn out and illustrated with further reference to data sources in Interacting institutional logics in general dental practice.
Next we give a similar description as a typology of five institutional logics governing general medical practice (Institutional logics in general medical practice), followed by a subsection expanding where various tensions and synergies exist between interacting logics governing general medical practice (Interacting institutional logics in general medical practice) and those of commissioners, which enables us to contrast dental and medical practice and identify the features which are distinct to dental practice contracting.
Our theoretical perspective from institutional theory leads us to understand that tensions between competing institutional logics are played out at various levels. We therefore report how the various actors react to and resolve some of these tensions in their daily work environment, first at the micro level, from the perspective of GDPs (interpreting contract rules at the chairside in dental practice, GDPs working with contract: micro-level chair-side behaviour) and from the perspective of commissioners (working with and interpreting contract rules in dealing with GDPs, Commissioners working with contract: dealing with general dental practitioners). Before moving on to describe tactics which operate at the macro level, some of which involve GDPs strategically co-operating with commissioners (General dental practitioners working with the contract: macro-level behaviour), we describe our findings relating to the role of relationships and trust between practitioners and commissioners as an antonym for opportunism (Trust as an antonym for opportunism and Relationships and trust).
Where findings are illustrated with quotes from interview and observation data, sources are anonymised using codes (see Appendix 6 for full details).
Institutional logics in general dental practice
We identified four distinct yet inter-relating logics: ownership responsibility; professional clinical values; population health managerialism; and entrepreneurial commercialism. Some logics appeared hesitant, others committed; some of these logics are more prevailing as well as more commonly experienced by all dental practices (e.g. ownership responsibility) than others. Population health managerialism in particular appears to be only an emergent logic in the field, and not dominant. At the service delivery level, certain logics appear more prominently in some practices than others. The logic of entrepreneurial commercialism, for example, appears to be a dominant principle guiding work in some practices (not all of them operating just in the private sector), but only a small influence in guiding day-to-day work in other dental practices. The typology of four dental practice logics is summarised in Table 3, where examples of various ways in which these various logics are expressed by dental practitioners are given.
| Ownership responsibility | Professional clinical values | Population health managerialism | Entrepreneurial commerciality |
|---|---|---|---|
| Composite principles | |||
| Authority and managerial responsibility for practice staff, reputation and servicing patients and the community | Clinical excellence, best interests of patients, patient advocacy, technical knowledge, professional responsibility and self-governance | Trace and explain public expenditure, govern good practice | Trading and opportunity with a focus on sustaining and developing a profitable business |
| Expressions | |||
| Try to sustain the business long term for the sake of staff and patients Close relationships with staff Subcontracting is risky Ownership is beyond just owning the enterprise it is about setting the ethos Sustain the business through reputation in the area Close relationships with patients ‘coal face’ built on family and friends Emphasis on ‘our’/’my’ patients |
Patients are treated according to ethical values – look patients in the eye Give the patients options and let them decide Gatekeeper role to police what is available on the NHS. Try not to think about charges when defining what is available Do your best for the patient – good quality care. Treat NHS and private patients the same Do what is in the patients’ best interests Make sure the patient is satisfied |
Patients are treated as a unit Be accountable via bureaucracy for what you’ve done and why Meet the required targets Feel part of the NHS Community orientated Subcontract to others Dispassionate decision-making Decision-making is not personal but issue based Funding decisions based on strategic priorities Hierarchical lines of accountability |
Patients are treated as a source of income Conscious of the market and place in market Happy to deal with demand Conscious of branding Range includes GDPs at other end with no interest or investment in the business, Business entrepreneurship Use managerial skills to manage a wider team |
Ownership responsibility
Dental practices are considered independent enterprises the viability of which is the responsibility of the partners. There is a palpable sense of the practice providing a livelihood for employees. It is separate from values, beliefs and rules related to clinical autonomy insofar as the expertise is managerial, it is close to leadership and the sense of duty is one better described as that of ownership, geared around sustaining the enterprise for the sake of staff and patients. There is a sense of solidarity within the practice in relations with the PCT. In these ways, the enterprise carries a sense of distinction that extends beyond its capacity to generate rents.
Same practice manager, the same partners but the partners were always silent because they felt they had to support [the former principal]. But they have a completely different relationship now with the PCT.
DC1
In dentistry both patient, the dentist and the staff . . . personal relationships are extremely strong.
CC2
. . . when it’s everyone in the building, and we are quite a tight-knit community . . .
CC3
I just work; I mean I feel part of the practice and my patients and staff. I don’t really feel a part of the NHS. I have meetings with the PCT once a year.
DD2
The ‘dental practice community’ is not just the small community of the dental team; it includes patients and their families too. Owners feel a responsibility to sustain a viable business for the sake of this wider community. These ties are expressed where GDPs talk frequently about ‘our patients’. Reputation is important in the local area, perhaps connected to the sustainability of the practice as an enterprise.
I think one thing here is we are a small community. You’ve got to remember that. That the people we see in the waiting room, a percentage of them are friends – you see them in the shops.
CD3
My problem with that is that I’m not going to send my children to another practice because I don’t want them to go to another practice because my children are used to coming here, and children need continuity of treatment.
AD2
We’re all, every day, I was asked this morning at school by one of the teachers, every day I’m asked by people ‘please can we join your practice?’
CC3
Ownership responsibility also involves a sense of entitlement to managerial autonomy from having invested financially in the business. The sense of independence that comes with independent contractor status is strong among practice owners.
We were at a meeting once and the guy, the [PCT] financial director said ‘We want our practices to do it this way’ and I said ‘What do you mean, your practices? It’s our practice; you haven’t put a penny into this practice. We subcontract and do treatments and you pay us. We bought the building, we put all the equipment in, we pay all the staff, how come it’s your practice?’
DD1
But I think, from a dental point of view, what a lot of dentists feel is that their business has been taken from them by these UDA activities, that they’re not managing anything and the [PCT A] are very much managing everything for them.
BC2
I don’t like the idea of being told what I can or can’t do by a third party . . . ‘Use this software’ or ‘You don’t do this’ even if it’s nothing to do with your clinical practice – I don’t like the idea of that.
ED1
He just wants to be left alone and he thinks if he reaches his UDA target everything’s fine, never mind all the other issues that go with it. He just wants to be left alone, he’s the dentist, his wife is the receptionist/dental nurse, end of story.
DC1
Autonomy is also expressed in a reluctance shown by some principals to employ others or subcontract work. To these GDPs subcontracting feels risky, and instead there is recourse to long-standing employees and family members. With ownership comes the ability to define ‘the way of doing things’, or the ‘ethos’ of the practice. Principals feel a responsibility for the ethics and practice of colleagues, particularly where they carry the ‘professional partnership’ role.
I would [like to take a lead on recruitment] because they’re working alongside me on my contract and I’d like to know what kind of person it is rather than somebody saying, this is the person working for you.
AD3
We are an independent contractor but I’m not removed from the practice, I’m not a corporate body where I’m sitting in an office who has several dental practices and working ‘on the coal face’ as they say.
BD3
I’m a little frightened of employing the younger generation, you know, as two of them were terrible. And I’m not very good at managing the unruly who would need a lot of time to put right.
DD2
But you weigh that up against the aggravation factor and if you get a good one they’re great, but then if they have problems you have the problems.
ED1A
The logic of ownership is expressed in the way principals establish the practice’s ‘way of doing things’. Approaches to interpreting contract rules can be made on a strategic basis as ‘ownership business decisions’. Practice policies are geared towards maintaining the business and also as a means to maintain harmony within the practice, for example extending to produce practice rules where clinical approaches of performers differ. While both dentists and commissioners respect the dental practice ownership role as involving ‘running the business’, there is a fuzzy boundary between aspects concerned with ‘running the business’ and the PCT‘s right to dictate ‘how things are done in the practice, and how the contract is interpreted’.
And when you go out and you start talking to them, again one of them I’ve got in hand at the minute, I said ‘I can’t tell you how to run your business but there is somebody running your business that you’re telling the staff to do treatment that is either (a) inappropriate or (b) at a higher banding than what it should be’.
BC1
We have a loose system. If the patient wants to have cosmetic improvement work then there is a rule of advice that if they want to have that sort of work done then it’s not available on the NHS so it won’t matter who they see, it won’t be available full stop. We don’t make any exception to that because otherwise it creates disharmony.
AD1
But obviously one has to look at things as perverse incentives, shall we say, which obviously it shouldn’t be the quality of care is done but then the funding is taken away from you. Because you don’t get it paid back to you, you pay and train the junior colleague. [PCT] don’t, basically don’t want to know about that, it’s not in their remit to be bothered. In fact they’re probably surprised if you say anything because they’re not interested in things like that.
AD1
The sense of a community of practice guided by the owner can give rise to tensions where individual clinicians guided by their own professional clinical values place different interpretations on the contract. In order to maintain harmony, dissent within the dental team (e.g. by performers not agreeing with the stance taken by the principal) may even be expressed by recourse to the PCT, but anonymously.
We’ve had anonymous letters from people saying ‘My boss is asking me to do inappropriate treatments’ and so on and so forth.
BC1
Professional clinical values
This is a long-standing and well-attested logic espoused as that the dentist always acts in the patients’ best interest, and according to professionally defined standards of care as judged by the individual clinician at the dental chair side. Working in the patients’ best interest is at the heart of professional clinical values.
I’d be at a loss to justify it, there was no justification. I’ve got my patients’ best interest as my best interest.
CD1
And it’s a bit of an old-fashioned view I suppose, but from a professional point of view it was impregnated into me from when I was a youngster that it was the patient who was the most important aspect of treatment provision, everything else was anecdotal to that.
AD1
To me it’s all, I look at it and to be honest sometimes I think I don’t really know what that percentage means and I don’t understand it. But to me I am not bothered about things like that. I mean I look at it and our patients are 100% satisfied with what treatment they are getting.
AD2
This underpins why many dentists want to provide the same quality of care for NHS and private patients, and private patients within the practice may subsidise care for NHS patients.
I’m in the privileged position of not being not fully committed to the NHS so I can provide that chrome denture for my NHS patient and accept that I’m not making any money on it; if I was treating an NHS patient or a private patient and you were sat as an observer, you wouldn’t notice the difference I hope. You wouldn’t be able to say ‘That’s definitely a private or NHS patient.’
CD1
I believe my standards are good enough for private dentistry, especially with some of the private dentistry I’ve seen. We produce private dentistry on the National Health Service and that basically is what they get.
BD1
It’s neither here nor there as long as we can maintain our standards and we don’t have to do things that we feel uncomfortable with.
DD1
My customer is the person who wants my services, that is my patient, NHS or private, I don’t differentiate the way I treat people.
ED1
Professional clinical values involve the dentist taking a role as patient advocate. By definition, being an advocate means completely representing someone’s wishes and position on his or her behalf – in other words, acting as an agent on behalf of the patient, but not altering what the patient is asking for in terms of care. To dentists, this means listening to what the patient wants and completely identifying their wishes in terms of appreciating what type of treatment they want to receive. This was expressed in the importance placed on, and daily practice of, giving patients choices of alternative treatment options (with costs). Moreover, GDPs recognise their role as gatekeeper to police the line between what the NHS can provide and what would be considered eligible as an option only on a privately funded basis. There is a perception, too, that, because dentists are involved in carrying out procedures themselves, rather than often referring to other members of the team or to secondary care, maintaining an honest and trustful relationship with patients is paramount. Though the logic of professionalism finds clinical expertise paramount and unimpeachable, many dentists in the sample discussed care as being engaged, relational, rather than the imposition of an expert view. Among many practices studied, there appeared an increasing affordance of the feelings of patients: their experience of problems and solutions carries weight; it is not simply the dental ‘look’ that counts. Talking through options with patients, discussing side effects, showing care as an array of possibilities (with differing price implications), in general being aware of care from the patient’s perspective, was very apparent. Agency within the field was conversational, accepting contingencies related to care as an unfolding process rather than the managed application of fixed responses.
I thought my patients deserved that sort of choice if you want. We still offer cheaper, patients still can have amalgams if they want them, patients can still have cheaper crowns if they want them, we still try even though we are private, we still offer a range where they can also have the more expensive option if they want to, they can get what they want.
AD2
And the guy came to me and I always give everybody all the options available to them. So if you’ve got a missing tooth I’ll say ‘There are three ways to replace it – denture, bridge or implant, OK? This is the advantage of this, this is the advantage of that, this is the cost. In your case you’ve got all these options, you make a decision.’
DD1
The difference between GPs [general practitioners] and dentists is the fact that we deal with patients and we also deal on them. Invariably GP medics only deal with patients, very rarely do they deal on them. Absolutely, they are a gatekeeper of a different nature. There’s a patient who will be quite happy to deal with anyone who is present, even if they just give you a prescription. It’s a totally different kettle of fish if they start getting an instrument in your mouth and start either drilling holes in your teeth or taking scalpel blades to your body, it would be totally different psyche for the patient and for the clinician.
AD1
I’m talking general doctors (and my own included), I don’t think they give you examinations that they used to when I was younger. You go in and they look at a computer and you give them the diagnosis of what you think’s wrong with you and they just sort of look at a computer and give you a prescription for whatever they think it is.
AD1P1
If you look at a classical customary meaning of customer is somebody who goes into a place and then takes an object out or purchases something or is getting a service. Actually physically doing care and treatment and we are going beyond that, we are going into the invasive territory of providing that sort of thing. Maybe it is a customer I mean, hairdressers and people like that call them customers or clients or things. I’d never call them customers, patients is a term that I use.
BD3
Having to face the patient is integral to GDPs’ work. Working at the coal face means being able to look the patient in the eye and justify the approaches taken. The fact that patient charges are involved makes this all the more difficult.
When you’re working in private practice and most of it is private practice, a patient comes in and they need six crowns and they run deep because like me they had a fairly grubby childhood, yes, I’ll look them straight in the face and say ‘That will be $6000’. It’s hard to say, well, I find it hard to say $6000.
BD1
The belief that each clinician is individually responsible for the care that he or she provides according to this threshold means that principals may be slow to challenge the clinical practice of others (such as associates) in their practice. This reluctance shows the esteem in which this logic is held; challenging the competence of a dentist is tantamount to challenging long-standing commitments to others’ well-being and to the demands of gaining technical expertise. The skills gained through apprenticeship are neither gained nor lost lightly.
Then actually you know standing up and being counted because . . . kind of very typically, they all kind of close ranks don’t they and don’t kind of shop their mates kind of thing you know, but it got so bad that they were like . . . this can’t go on any longer.
CC3
But anything else I am not in a position to comment on because we look after our own patients here, I don’t inspect other practices.
CD3
Population health managerialism
The logic of managerialism involves implementation of tight discipline which is driven by efficiency, external accountability and monitoring, and an emphasis on standards. Although discipline may be internal, PCT commissioners represent external imposition of control and expectation of accountability which is accepted to a greater or lesser extent.
I think it’s just the idea that the PCT is watching him and stopping him from being as independent as he’d like. I think that’s the main, I don’t think it’s actually personal. I think it’s more about what I stand for and to him I’m the face of the PCT and then the face of the Department of Health and saying this is how things work, which he doesn’t like.
AC2
Acceptance of working to (UDA) targets, with internal procedures implemented to monitor and achieve these, is an expression of managerialism. Focus on patient ‘numbers’ introduces language referring to patients as commodities rather than individual people. Managerialism also involves the use of technical metaphors and processes to manage performance, although these are often not readily adopted.
We handle it by keeping a close eye on our UDAs and we know when we’re coming up to the number and then we’ll stop seeing children.
AD2
We’ve got schedules every month saying how many have been achieved. So he’s going to send all them fortnightly to see how we’re getting on. And we’re going to have a meeting on a monthly basis; he’s going to do the figures fortnightly with the computers.
AD3
In order to improve the quality of care we had to shed some numbers.
CD1
There is a daily count and monthly count. And we’ll just know as we go along, and it just seems to work.
CD3
Well I’m more or less relieved when I’ve more or less achieved my stupid targets because that really would be the last straw really, if I didn’t. Which is sad. Well, it’s pointless. I mean, I don’t know what the point of worrying is (laughs). It’s not achieving anything other than trying to stay financially viable.
DD2
We’re looking after a lot more because we’ve pushed our recall right out and we’ve now got 13,000–14,000 patients at the practice. So for the size of the practice, we’re getting on for 3500 patients per dentist.
ED3
I’ve heard this from dentists before that they are not interested so much in the patient, you’ve got to hit your targets, never mind the NHS, private targets and everything else.
ED1
Information governance toolkit, I think someone should give me a car but never mind. Now, you have to sign up for the information governance toolkit on various levels, I think its zero, one and two, I’ll have a look into it. To be perfectly honest I just lost interest.
BD2
Population health managerialism logic captures an additional set of values to do with the efficient and effective use of scarce public resources shared equitably according to need among the wider population. Some GDPs studied had put themselves forward to work alongside commissioners to improve oral health at the population level.
So we’re working hand in hand with the PCT to do that, and that’s something that’s developed in the last year really. And the PCT will come and have a meeting in our room with other practitioners as well in the area so we’re not saying ‘This is us, closed ranks’. We’re very much into ‘Let’s go out into the community, let’s help the PCT achieve what they want to achieve’ because it benefits everybody to do that.
CD2
Access should be fair and equal. If you do have a health service they should be open to everybody. And I feel for all these people who were, who are currently in the shoes I was in. So I’m philosophically attached to the NHS.
BD1
But there are a good many dentists who see themselves as a subcontractor into the NHS, which is why they’ve got high commitment and that’s about personal conviction.
SKC
Many GDPs in the sample expressed a philosophical attachment to the principle of universal access to NHS care. However, at the same time, sometimes these principles were not demonstrated freely in their everyday practice. Commercial considerations and loyalty to existing patients of the practice constrained a motivation to work for the wider public good, as illustrated by the apparent contradictions between values and behaviour seen in case ED1. On the one hand he talks about wanting to put ‘something back into society’; on the other, he is not willing to offer universal access to just any member of the public needing NHS care (in the non-discriminatory way stipulated and intended by NHS regulations). Instead he manages his practice by fulfilling the NHS component of his contract by serving ‘his’ NHS patients who regularly come to the practice.
I never got rid of any of my NHS patients because I like putting something back into society.
ED1
I am not totally discriminatory because you’re not allowed to be. But there are ways of managing your patient practice and profile because I’ve worked that way from 1992.
ED1
Many GDPs studied appeared conscious of the public purse and contemptuous where they saw resources being wasted by commissioners. Against a backdrop of scarce resources, many viewed equity of provision important, and reporting and record keeping necessary to ensure transparency. However, managerialist approaches taken by commissioners were often felt to be wasteful in themselves.
But I could do the head if I wanted to without looking the patient in the eye and saying ‘That’ll be £3000’. That was fine with me, obviously it wasn’t fine with the Treasury but if the patient needed that treatment as a matter of demand, hitting the need and demand we’ve got a bit of a problem.
BD1
I also think they should not give the subsidy to everybody, which happens at the moment. It’s nonsense that the Queen could have a subsidy if she went to an NHS practice or anybody who’s loaded can go to an NHS practice and get £500 worth of treatment for £200. It’s nonsense, they shouldn’t be given that subsidy, they don’t need it. You could take that money and buy a very good NHS service from a practice like this for example . . .
DD1
They asked us to do a spider diagram last year, which we did, and I think we all had to go to a meeting just to finalise it and it turned out that half the people there hadn’t even started it. So it was just a waste of time me going when I could have been . . .
DD2
Entrepreneurial commercialism
There is growing awareness of dental care offering commercial opportunity. This suggests an understanding of the dental practice as a business entity: a commercial space in which different units perform differently, but each carries a supportive purpose. More entrepreneurial behaviours found practitioners looking for opportunities to expand (grow practice through acquisition or joint ventures), enter new areas of business (cosmetic services) and invest in marketing (advertising, sponsorship), and using creativity to push forward. They were happy to cater to patient demand, which provides an opportunity to expand provision.
I am a businessman and I initially thought of this contract on day 1 as a business. Trust me I’ll be a lot more rapid in terms of marketing but I didn’t want to peak the practice because it’s essential to be positioned.
AD3
We have the best opportunity to work one on one with anybody because they’re a captive audience. Sometimes it’s difficult for them to speak . . . That’s OK, that’s great, you can tell them whatever you like, they can’t argue. But you can get a point across. But if you really wanted to sell the opportunity, anybody else would grasp the opportunity we’ve got with two hands. You’ve got someone sitting in a chair one on one for half an hour. You should be able to sell them anything.
BD1
We have [xxx] who was just sitting in the corner there, she is our onsite business manager and she looks at turnover, our expenditure, keeping material costs sensible, finding the best deals on bills, services.
BD2
The public sector, maybe they don’t deal with the money side of it as much. I’m not really sure – because I sit and look at profitability of every single site on a monthly basis – whether a public sector servant does that.
CD2
It’s not limited in any way. The limit on what we do is what the patient is prepared to pay for as opposed to practical limitations.
DD1
Everybody out there, well it doesn’t even matter if they’ve got teeth or not (laughter). In fact the ones without teeth are good customers if you’re doing implants. So yes, everybody, our target audience is everybody. I do realise that some people can’t afford private dentistry, but we don’t ask people if they can afford it when they come, we publish our prices and we tell them the cost of the treatment. If they want to have it, they can have it.
DD1
Although branding provides a means of marketing, commercial GDPs recognise local reputation to be more important than advertising. The NHS brand (blue) logo is seen as giving the wrong sort of signal about the type of service (low quality) provided, and perceived more as a badge of public ownership.
There was a lot of trouble a few years ago, wasn’t there, about branded practices in the NHS when that little blue label came out and I can remember being at a Local Dental Committee meeting and I said ‘Why would you want to be part of a brand that doesn’t have a very good reputation?’ Boots, yeah (laughter), not NHS. It has got a brand problem, the NHS, if you ask me anyway.
DD1
We’re not big fans of advertising. We think the most powerful advertising is word of mouth anyway. Personal recommendation. We very rarely advertise in the local papers, once a year maybe if that. Not necessarily every year. Yes, we’ve just changed the signage, actually, specifically to make it more noticeable in fact; it’s where we spend the money (laughter).
DD1
Whereas dentists do have that option [GMPs don’t]. Yes if they’re aggrieved, if they don’t like the NHS brand, well bye bye.
2AC2
Summary: multiple logics in the dental practice field
Although they were woven together as threads running through everyday activity in dental practice, we identified four distinct institutional logics. First, we identified a set of principles concerned with the responsibility of owning an enterprise on which members of staff, patients and the wider community depend. This brings together managerial aspects of running the practice as a business, but contains a leadership focus rather than a focus on running an enterprise as a means of making a profit as an end in itself. Making money through running the practice is here a necessity to sustain the viability of the practice as an enterprise, as is maintaining a good reputation in the local community. Second, we identified a set of professional values usually recognised as core aspects of medical professionalism (acting in the patients’ best interest according to professionally defined standards of care). The ‘expert’ clinical view, however, was rarely imposed on patients and care provided on the basis of a relationship between the dentists and patient, usually cognisant of the patients’ perspective. Third, we observed a population health managerialism logic which described a concern for the prudent use of public money for the wider good, and with this an acceptance of procedures associated with external accountability of care involved with being a public servant. Finally, we described a set of values and practices associated with developing the commercial aspects of the practice (entrepreneurial commercialism).
Institutional logics of commissioners
Although commissioners’ logics can be described broadly as a population health managerialism logic as outlined in Institutional logics in general dental practice, in a more detailed look at the beliefs, goals, practices and values of commissioners gathered from qualitative data gathered in phase 1 (stakeholders), phase 2 (case studies) and phase 3 (commissioner follow-up interviews), we identified three parallel, interacting and sometimes competing logics defining commissioners’ work with dental and medical commissioners (Table 4).
| Bureaucracy | Managerialism | Public goods |
|---|---|---|
| Composite principles | ||
| Focus on management by rules and hierarchy | Focus on external accountability and power connected to state regulation importing management principles from the private sector | Duty of serving the public interest through publicly funded health care |
| Expression | ||
| Formal hierarchical structure: refer back to the centre, centralised planning Management by rules: do things correctly by policies, procedures, regulation, managing the contract ‘Up focused’ – serve the board or agency empowering it (DH) Unwilling to admit mistakes – attempt to shift blame to others Impersonal Little room for grey Focus on the transactional Inflexible |
Quasi-markets accepted Work to targets Monitoring of performance Focus on efficiency and effectiveness Procedural diligence Rationing of resources by effectiveness criteria Technical metaphors such as ‘engagement’ Surveillance of professional work Dispassionate decision-making: subcontract clinical work |
Promote patient choice Focus on negotiation Brand NHS Defend the public purse Consider exceptional cases for treatment/referral Quality matters and not just numbers, for example on access, dictated centrally Benefits for the population Aim for equity in the population Patient advocate |
Managerialism logic
Conceptions of ‘new managerialism’ originate from ideological approaches to managing public services connected to state regulation and power over such services and their employees. 96 This configuration of ideas and practices represents forms of administration and the way of running and regulating public services, often at the behest of government and government agencies. There is a heavy emphasis on importing ideas and practices from the private sector. Characteristics of ‘new managerialism’ in organisations include the erasure of bureaucratic rule-following procedures, emphasising management above all other activities and monitoring employees’ performance (and encouraging self-monitoring too). This can be expressed in the use of technical metaphors such as KPIs, ‘dashboards’, etc. Quasi-markets are accepted and developed; outsourcing of services is encouraged and includes partnerships with private providers. Labour-force restructuring is advocated to enable more team working and flexibility. There is a heavy emphasis on efficiency and effectiveness as well as on financial and other targets, with a widespread use of performance measures, league tables and benchmarking reinforcing imposed external accountability. 96
We found commissioners’ beliefs and practices driven by managerialism. Their goal is to implement what they see as effective means of managing dental and medical service delivery.
Yes, they’ve gone through [a practice managers’ course run by the PCT] and are well versed in what the requirements of a good organisation is.
DC1
Reviewing performance is part and parcel of their work with both dental and medical practices. Monitoring outputs according to UDA targets entirely fits with this ideology. This is a mechanism for performance and resource management driven from above the local level [from the Strategic Health Authority (SHA)]. This approach does not lend itself to flexibility in negotiations with service providers concerning problems with delivery.
When we performance manage a GP you don’t performance monitor based on the numbers of something being done like we do with a general dental practice. We performance manage them on a huge variety of stuff. All the QOF [Quality Outcomes Framework] stuff, erm, all the clinical governance stuff, there is just, it’s endless really. The stuff that we do. We do an annual review with the Medical Director to look at all the performances.
AC1
They’ve got their own pressures; particularly financial ones of them that they have to meet certain targets.
CM2
They [the SHA] monitor us on Units of Dental Activity so they will inform us if they’ve had information that if any of our dentists are underperforming and they want to know what we’ve done about it, basically in a nutshell. They want to know if we’ve clawed back the money or if we’ve just let them get away with it if you like, or what action plans we’ve got in place. So they want to see robust performance management in other words of our independent dentists.
AC1
You’ve got a [UDA] target, you’ve got a price, and you’ve got the framework if you like around that, which is really quite black and white. We know where our problem areas are and we evaluate what we’re doing each year and roll it forward. So in that respect it’s black and white . . . It’s tidy, it’s straightforward.
DC1
Benchmarking between practices is favoured as a means of monitoring and performance management, although currently used more often in the medical than the dental practice context.
Do you see yourself as being in a situation of competition?
With other practices you mean? I am sure that’s what the PCT want us to do. They are forever showing you how you are doing compared to other practices; they love that.
But in terms of bringing in comparative data, all we can do – we know for example the types of treatments that are going through our deprived areas and it would be useful really to compare some of that.
DC1
There is a ready acceptance of the principle of ‘outsourcing’ work, expressed in an approval of tendering and subcontracting of work. Commissioners accept that practices generate profits and that there is a mixed public–private health economy. Whether providers make a profit or not is not something of concern to commissioners, for issues to do with viability of businesses in a competitive environment and the extent of any profit are left to the market. Hence issues to do with problems related to delivery at the service level are not of interest. Why would commissioners therefore need a visit to the ‘coal face’? Managerialism logic, with its emphasis on patients as ‘commodities’, is also expressed in commissioners’ viewing subcontracting of work within dental practices as a pragmatic solution to the management of the organisation.
I have no problem with this profit idea as long as patients aren’t being forced down that route, or being misinformed and having to go down that private route. I’ve got no problems with that.
2AC2
Well you can’t prevent private work because it produces patient choice. You know for example the standard NHS treatment for a filling in a back tooth would be an amalgam filling. The patient might not want that, they might want a white one so there’s the option there to have a private white filling and you can’t remove that because you remove the patient choice.
2AC2
I’ve had an open invitation outstanding for two and a half years now for the Primary Care Trust personnel to come over and have a look and see what goes on for either half a day or a day. Oh no, it’s been an ongoing invitation but they’re all too busy I’m afraid. What would you need a coal face visit for?
AD1
I think they took the risk that they are reliant on an outside company, somebody they can’t control in effect . . . A lot of it is a big risk for them to, it’s a big ‘This is what we want but now we’re handing it to you to deliver it.’
CD1
This is where I get shouted at, your contract value is £186,000, your outgoings, your infrastructure and everything else is £86,000. If it was me I’d want to spend my £100,000. Fancy doing us a favour, come in and work 1 day a week while I go on holiday to Barcelona for 3 days – that’s what I would do.
BC1
Bureaucratic logic
In the 1980s and 1990s managerialism was introduced as an antithesis of bureaucracy, intending to bring an emphasis on decentralisation, operational flexibility and a more entrepreneurial approach to the organisation of public services. 97 Certainly the devolution of a large part of NHS budget to PCTs, who were charged with determining local care priorities and commission services against this, suggests that PCTs are geared towards this approach. 98 The intention appears to represent a significant shift away from the Weberian model of bureaucracy, which places a significant emphasis on management by hierarchy and rules. 99 Weber’s key characteristics of bureaucracy include a unity of command, a system of supervision and subordination, and reliance on application of consistent and complete rules. Often characterised as involving ‘red tape’ and inefficient administration, bureaucracy is generally used in a pejorative sense; the approach, however, has previously also been applied as a means of governing organisations according to calculable rules, which has brought benefits in introducing concepts such as fairness and equality of opportunity to the organisation of business affairs.
We found commissioners expressing several features of a bureaucratic logic. PCTs commissioners expressed an ‘up-focused’ approach to many aspects of their work.
What with the PCT who want to know what we’ve been demanded of the PCT from above.
2AC2
But we’re all into localities so there is a [XXX] locality, who, although supposedly are responsible for commissioning, I don’t feel can commission. They have to refer back to the Senate all the time. Is that because they haven’t got the expertise? No I think it’s because they haven’t been given the power.
CM1
Well I think the PCT behaved the way they did because of the Department of Health . . . those guys were under serious pressure, you could tell they were under serious pressure. And it had to come out somewhere.
DD1
I think one thing I’ll say about PCT managers, dog eat dog, they are responsible to their line . . . my PCT manager is responsible to A; A is responsible to B. And they have to do figures because if they don’t do figures or their PCT don’t do figures they get the rap from up and that’s all they are bothered about in the same way I’m bothered about doing my UDAs and that’s the problem with the whole system. If you don’t do points then someone will rap on them and even at the top of the PCT, the CEO [chief executive officer], he’s going to get it from the next level of management right up to the Minister for Health. OK, and that was the problem with the NHS, they are bothered about fulfilling their requirements whether it be points or . . .
ED1
What do you think that the PCT goals are? At the moment, saving money at all costs! Being absolutely frank, I think after various edicts that have come out of the NHS . . .
CM1
Decisions often could not be made at a local level, but had to be referred upwards in a chain of hierarchical command, thus reducing the amount of operational flexibility which was available. In our case studies we found examples where local commissioners were over-ruled by those working higher in the chain of command, sometimes with damaging consequences for relationships between the local commissioner and the practitioners who had been ‘dealing’ together.
We were told you can do anything with the contract as long as you give sufficient notice . . . well, you can’t with a dental contract. Unfortunately the dentists then thought that myself and [A] were involved with that, and you can understand, you know, you’re supposed to know about dentistry and yet you told your managers that . . .
BC2
I pointed out, [A] and I [dental commissioner and contract manager] both pointed out to the powers that be you can’t do this but they ran with it, rammed it through and we said ‘Fine’. It’s caused a lot of angst.
BC1
I dislike intensely what I call corridor conversations such as if I see a certain dentist come in and they nip in to see the Chief Exec, I don’t like that. Not that I’m paranoid but if I’m playing a straight bat and saying ‘No’, I’ve got good reason and I’ve explained it to you half a dozen times, don’t go behind my back and see somebody else.
BC1
In terms of the PCTs goals obviously you know they have people to answer to and at the same time they’ve got to show the numbers and the funds are being used in the right way and things like that – they are . . . it’s the bureaucracy.
AD3
The hierarchical structure of accountability extended upwards from the PCT to the SHA and beyond, reducing operational flexibility particularly around setting and achieving UDA targets. Achieving targets and implementing ‘claw-back’ was a rule which was increasingly inflexible in recent years as budget constraints grew tighter and targets were imposed from above; for example, in relation to access, targets were rigorously pursued.
[A] will get like a mailing say, say we need to reach 66% and then get the following year we need to up it to 68%, well then obviously that gets filtered down to me and what do we need to do to get this and that sort of thing.
DC2
On the back of some information we’d received we were told that we had to commission for 70% access over a 24-month period . . . I don’t think it’s anything more than 50, 60% to be honest with you. It was ridiculously high.
BC1
Before [A] left he wrote to them and said right, this is where it ends, this is the target. End of story. If you don’t achieve it, we’re going to take some money off you.
CC3
The SHA monitors us and gets us to provide information on the amount of UDAs for each practice. then they’ll regurgitate and reflect back to us that ‘You have said such and such a practice has done this number of UDAs, what have you done about it?’
AC1
Certainly last year the DH gave us a new target and they wanted, they actually have linked the GP satisfaction survey to dentistry and what they did was they basically said ‘Well when the GP survey goes out we’ll ask the questions on the member of the public “Have you tried to get a dentist, you know, what’s your level of satisfaction?”’ And I think we were achieving something like 95% satisfaction or whatever it is. Last year they said ‘Well if you’re not achieving and there are still people that are unsatisfied and can’t get a dentist then you’ve not met your need.’
DC1
But if we had to defend ourselves [from the SHA] would they turn round and say ‘Did you take the money back?’ ‘No?’ ‘Why not?’ ‘Well . . .’ and you are going to get hammered again.
BPCR
Decisions are made by committee and due process has to be followed, although this brings delays and again reduces operational flexibility. Forms, figures and procedures leave little room for ambiguity and capturing the complexity of patient care, but commissioners were shown to be tied to the procedures in place, with limited flexibility to adapt and recognise the nuances involved with patient care.
So we did report after report after report for two and a half years and nothing happened.
BD1
I don’t know what the term that the people use for us, or the public, is the sort of pen pushers isn’t it . . .
2IC1
It frustrates them [practitioners] I think, the bureaucracy quite often and the processes that we have to go to choose something in a correct fashion and it just frustrates them and I think it’s . . . oh I haven’t got time for this, you know. Yes we know in terms of as a commissioner, you know the policies, the procedures, the regulations, the contract that we have to manage.
2AC2
So it’s very much a tick box exercise even though she could stand there and say ‘I know exactly where you’re coming from, I know why you didn’t do it and I know that you can’t justify taking an X-ray, however this isn’t what my form says.’
CD2
They just bulk you down in bureaucracy, the amount of paperwork that comes out is just incredible. You know, proving and double proving and re-proving.
BM1
In general as I see it I think PCTs have been populated to a very large extent by a lot of pen pushers, bean counters and paper shufflers who in my mind do not necessarily serve a useful function.
FM1
There is a sense that the organisation is corporate and there is shared responsibility for decisions. No one person is accountable for his or her actions at the local commissioning level. It is difficult to find individuals to blame for mistakes and sometimes it is difficult to contact individuals at all. There are rarely apologies for mistakes. There is a sense of solidarity where commissioners ‘toe the party line’. Dental practice advisors were sometimes liable to be too open with practitioners, which could be a source of tension. GDPs’ ability to hold local commissioners to account was difficult, given the hierarchical and corporate nature of the organisation.
[B]ut the dentist who was on the PEC [Professional Executive Committee] . . . actually said all the right things corporately but then acted differently when he was with his dental colleagues.
DC1
It is about knowing sometimes that the direct commissioner that you are dealing with, they have a certain level of authority and beyond that authority is then down to the bigger heads and, you know, if you know that they are doing all that they can for yourself then you can’t really hold them to account, which has happened to us before.
BD3
They disappear if there’s conflict, you can’t get . . . you can’t talk to anyone, it’s nobody’s responsibility, it’s somebody else in a different department, they’re on holiday or they can’t decide anything until they have a committee meeting. The person you need to talk to isn’t there, the finance director can’t . . .
BM3
We were supposed to get an apology in another letter to clarify things. We got the other letter to clarify things . . . we didn’t get an apology (laughter).
BD1
Public goods logic
While the commissioners studied appeared to acknowledge and be driven by a set of rules around targets, with success evaluated in clearly demarcated processes which make accountability of care provision fully explicit, many also expressed a deeply held set of values concerned with their work having a duty to work for the public good. These commissioners recognise that individual patients do matter, and they hold to principles of promoting patient choice, considering exceptions for care and addressing patients’ complaints about their care. Commissioners therefore are not always merely concerned with catering at a population level, although they recognise the dilemma which exists in reconciling what is best for the whole population with what is best for an individual.
Oh now I would disagree that the PCT had a population health culture. Although we have targets and we’re driven by targets . . . We’re set to targets. That did not mean that we did not focus or address individual patients concerns and . . . treatments and requests for treatment at all. And that continues where a patient is considered to be an exceptional case then that is addressed appropriately.
2HC1
And the fact that we are able to discuss that very openly and acknowledge the dilemmas and the, the fact that ‘yes it can quite easily tip over to become a very strong [population] health culture’ . . . It’s trying to make sure that that balance is addressed correctly . . . and that we do focus, we are here for the patient after all as well . . . and that needs to be dealt with appropriately.
2HC1
Because I would say in the early days of the current contracts, the focus was on target delivery. Because that was what, what the focus was both for commissioners and from providers. I think increasingly that, whilst target delivery is still a factor, there is an increasing focus on looking at what’s been, what’s been delivered in terms of care for patients and the outcomes and benefits for patients.
2MC1
That practice was told in no uncertain terms . . . that’s your contracted activity, it’s your responsibility to deliver that over the year, not let’s get it done as quick as we can and then sit back because that’s not providing that service that we’ve bought for the patients and then . . .
CC3
The problem [with the DBCs] is they do tend to move on quickly and patients aren’t happy, they don’t feel they are as well understood as they could be.
AC2
I would be more comfortable justifying to my Chief Exec or the SHA a failure to meet a Vital sign rather than a practice which was delivering all its UDA targets but providing a poor-quality service. For me, my first priority will always be on the quality of the service.
CC1
Serving the public interest, and particularly representing what individual patients want/need, requires a more flexible approach than a mere monitoring and measuring of targets. Commissioners studied recognised that this is a softer issue and not easily represented with reference to figures, with issues of this kind addressed in face-to-face meetings between commissioners and practitioners.
We, the practitioners, the dental performers themselves, yes they do have targets but their main concern is making sure that they’re dealing with the treatment. They, they will, they are very aware of that dilemma or ensuring that they have that balance in place. And those discussions again are often expressed and brought into being at the contract review meetings . . . and often there’s another case where we have a patient complaint or a patient query about treatment undertaken . . . and the practitioners are desperate to ensure that they have that balance correct. So it’s openly expressed, openly discussed.
2AC2
This public duty is expressed where commissioners fiercely defend the ‘public purse’. They talk about the ‘public pot’. This appears to go beyond being driven to achieve financial targets, and is portrayed in indignation where they see waste of public funds. The public or practitioners may be the cause of waste, although commissioners acknowledge that PCT procedures and processes may represent waste in themselves.
But when a patient turns up in a lot of pain, you sort them out and you say ‘You’re going to need that level of treatment, come back in 2 weeks’ time and we’ll carry on’ and the little bugger doesn’t turn up. He’s wasted that time and money. And that’s bang out of order and I’ve said and I’ve tried really hard to re-educate the public here in [B].
BC1
It’s a contract that’s in place and, whether it’s liked or not, if you’re signed up to something and then you perform inappropriately and you provide a service in an inappropriate way the only person who is being penalised is the patient. You know . . . the public pot.
AC2
This is what we’re doing all the time because they do say that there’s a lot of money that’s being wasted through fraud.
B Informal LDC
But again the other thing about retendering at the minute it’s a massively expensive process. It’s not in the interests of the public purse really, is it?
B Informal LDC
If they’re turning round to me and saying that a clinical procedure is going to cost £3000 and I’ve only got £1000 then yes I am. But again, question, is that clinical procedure really really necessary? Patient would say yes, dentist would say yes, but I’ve only got £1000 Sarah.
BC1
Commissioners then were found to be conscious that NHS dental care is owned by the public, this being expressed particularly in NHS branding (the blue logo), representing public investment in services.
We had quite a push on NHS signage. Again we wanted the branding to be up there and we wanted public perception to be that we were investing in NHS dentistry in [A].
CC2
Obviously walking out the doors and talking to a lay person, you know, people say they can’t get an NHS dentist and patients do seem to make an association with that brand . . .
CD1
Summary: institutional logics of NHS commissioners
We identified three logics as strands woven into the work of commissioners. First, we found principles of managerialism clearly expressed in frequent use of jargon, reliance on procedural diligence, monitoring outputs and information intelligence focusing on patients as commodities. Here there is little room for the personal and an emphasis on outsourcing of work to maximise efficiency. Second, we observed a bureaucratic logic which focused on a strict adherence to rules and procedures laid down by those higher in the hierarchy. The focus here is clearly on the transaction rather than the relational, which influences the degree to which flexibility and innovation can be incorporated into their daily work. Third, we described a set of principles around being a custodian of public goods expressed as a duty to seek to optimise the use of public funds, looking for creative solutions to problems such as inequalities in care. In this context, patients and the public are seen not purely as commodities, but as people with needs, where quality of service is as important as quantity and cost.
These logics all simultaneously infuse the work of commissioners. None particularly predominates. Sometimes conflicts occur (e.g. between bureaucratic logic and the greater flexibility and relational stance demanded of public goods logic) giving rise to an ongoing negotiation as commissioning organisational structures change and evolve.
Interacting institutional logics in general dental practice
We found that the four general dental practice logics described earlier (see Institutional logics in general dental practice) interacted with each other, sometimes in competition, sometimes in synergy, in an ongoing dynamic between actors in the field and the environment in which they worked. This interaction we found quite explicitly in the practice of some dentists (BD3 for example), fully aware of the practice as a business, yet also avowing a status of public servant and resistant to the idea of his selling a service.
It is a business at the end of the day, you do have to ensure you’re getting the best costs when it comes to materials but as foremost I still [see] myself as a public [servant].
BD3
We found that some logics were less in conflict than others. For all dentists, the organisational field appears marbled with commercial logic. Commercialism resonates with, as much as it resists, aspects of professionalism and ownership responsibility. Commercialism appeared less compatible with population health managerialism, most notably the bureaucratic and inefficient structures detailing forms of apportioning of care, often with little regard for the ordinary experiences of patient need. Moreover, considering patients as numbers runs counter to logics of ownership and professional clinical values.
They wanted us to take more patients; they wanted us to release time in the day to do emergencies like they do now under the UDA system. And we were resistant to take on more patients because we thought we couldn’t provide the correct level of care to patients.
DD1
I don’t want to be put under pressure to meet targets and not be able to spend time with patients.
AD2
And if they’re not engaged at all of the points in the cycle, you get these . . . sides. One wondering what on earth you’re trying to do, what you’re trying to measure, them trying to deliver what they’ve set out to do for their individual patients, sometimes not recognising that there is a wider responsibility to a population than just the people who walk through their door. And once they . . . if you fully engage them and link with them and sometimes it’s taken them back to the basics of public health.
SKP1
Practitioner leaders recognise the institutional forces which have shaped the dental practice field since the 1980s. They observe the shift towards the commerciality of the private sector particularly in a cohort of older practitioners, and see this as a ‘push’ as well as a ‘pull’ away from the NHS. This older group of GDPs appear to have more in common with entrepreneurial commercialism than with the emerging logic of population health managerialism.
I think the profession has got, er, probably a larger number of older white male dentists who, er, who started practising in the late ’70s right the way through to the late ’80s. Erm, and they are the that sort of tranche of practitioners who received no state support at all, no granting, no payment of their business rates, no, er, had to buy their own premises, had to pay their own staff, had to buy their own materials, etc. And were to a large extent entrepreneurs. Er, totally subcontracted to the health service when they started for the most part but then due to this unique availability of dentists to move in and out of the public sector at will pretty much, erm, er, latterly probably part of a group that moved, has moved from the public sector into the private sector by virtue of the pressures which are pulling them from one side and pushing them from the other.
SKDR4
Commissioners’ managerialism and public goods logics, looking to maximise efficiency and effectiveness of NHS dental expenditure, and equitable provision of resources to the wider population, results in queries relating to the level of resources expended on individual patients. This presents a challenge to dentists’ professional clinical care and ownership logics.
The bigger thing is say for example if you’re providing one patient with multiple courses of treatment that could be provided under one course of treatment you are denying other patients access to that service because what’s happening is you’re eating through UDAs quickly by treating one group of patients when there’s other people out there who need access but can’t get it because we haven’t got the UDAs to do it.
AC2
I suppose the only thing I would say is it has to be a quality service delivered within the financial limit we can afford. We have had some, we had a practice who were delivering not even gold standard but probably platinum standard which was very very nice but completely unaffordable. And there has to be a balance because we’d love to do that.
CC2
Population health managerialism also comes into opposition with ownership logic where commissioners direct practices which patients to accept for NHS care. This cuts across the values integral to ownership logic, which places a greater importance on serving ‘our patients’. While it aims to improve equity of provision for the wider population, this can upset commercial sensitivities, for commercialism feeds into a sense of autonomy; dentists are increasingly aware of patients as the source of income from which their livelihood springs.
But I would much rather see 50 people come through the door, than 50 people ring up (from a PCT waiting list). Rather than say somebody who’s come through the door who’s not . . . who’s one of the people who is unpleasant and is rude and obnoxious and you wouldn’t see them for any other reason. And yet somebody who can present a letter saying ‘The PCT has told me to come to you’ and you’re thinking ‘I don’t really want you as a patient’. Standing next to my well-paid private professional who is paying over and above for a service with some oicks sat next to them, it’s difficult.
CD1
The commercial, though, can erode a commitment to provide the best possible care, forcing ability to pay onto the relationship, yet some dentists were found to acknowledge counterbalancing forces, for example an increased sensitivity to patient demand. Their expertise is negotiated in conversation with patients, as the criteria by which care is understood expand. They understand what is ‘wanted’ by patients in terms of specific services (whitening, straightening, filling colour) and bring in new actors (hygienists, technicians, machinery). For less commercially orientated practitioners, the emergence of new structures such as DBCs which organise care in ways involving an outsourcing business pressures and relinquishment of partnerships and enterprise, allows these practitioners to concentrate on clinical expertise.
Though many actors sustain commitments to a professional logic and, by implication, eschew overtly commercial ideas of care, in all of our cases they acknowledged a responsibility for sustaining viable enterprises. Moreover, where the GDPs studied discussed with commissioners approaches to using public funds wisely to expand access to NHS dentistry for the wider population, they often advocated expanding their own businesses or allocating resources for their local area. Commissioners studied, in contrast, often took a stance of a more dispassionate allocation of resources according to population need.
It is public money and . . . it would be sensible to actually enhance, as I’ve said before, enhance effectively the practices that are already here . . . let them expand if they can.
AD1A
There was disagreement over the new practice in [Area X] whereas the LDC felt . . . they agreed there was a need but they didn’t necessarily feel there was going to be any uptake there, they thought that they didn’t actually want the dentistry even though they might need it, whereas people in [Area Y] wanted the dentistry but in theory there isn’t any need in terms of the decay rates and stuff. So there was a dilemma there about investment in a poorer area of [Area X] and the LDC were not happy that a lot of resource was going into one area.
DC3
Whereas others on the LDC just focused on their own patch and couldn’t really see the logic in spending all the money.
DC3
Summary: competing multiple logics
While we identified various sets of socially constructed principles guiding the behaviour of dental practitioners and commissioners, these strands were woven together in a dynamic and sometimes uneasy way. Certain sets of principles (e.g. entrepreneurial commercialism) appeared to work synergistically with other sets of values (ownership, professional clinical values), but sit uneasily with an emerging logic of population health managerialism. When we explored the logics of commissioners, we also found some logics in conflict, for example where the bureaucratic logic inherent in a NHS hierarchical form maintains a focus on the transactional rather than the relational and resists the flexibility required to effectively realise public goods logics.
Institutional logics in general medical practice
Using qualitative data from stakeholder interviews, case studies of medical practices and interviews with commissioners, we also identified several logics (beliefs, values and rules which shape work) in general medical practice (Table 5). While there are some similarities to general dental practice, there are differences too. Ownership responsibility logic is evident in medical practices in a similar form as expressed in dental practices. Also, like dental practices, we identified a logic concerned with professional clinical values and named this ‘duty to patients’. Whereas in dental practice we identified a logic of population health managerialism, for medical practices we drew a distinction between managerialism logic and a logic of public goods. Finally, while in the dental context there was a strong sense of commerciality in the organisational field, this was more confined, although present, in the medical practice context. A logic of entrepreneurship in medical practice, though, was nevertheless important, and used as a means to meet other goals/beliefs associated with the logics of duty to patients and public goods. Entrepreneurial commercialism in medical practice appears to take a more ethical entrepreneurial focus than is apparent in dental practice, where the focus is predominantly on expanding profit in order to grow the business and increase income. Therefore, in all, we identified five medical practice logics: ownership responsibility, duty to patients, managerialism, public goods and entrepreneurial commercialism.
| Ownership responsibility | Duty to patients | Managerialism | Public goods | Entrepreneurial commercialism |
|---|---|---|---|---|
| Composite principles | ||||
| Keep the practice running for the sake of patients and staff; profit is secondary to that | Make the care of your patient your first concern – ‘the patient in front of you is always first’ | Accept external accountability and power connected to state regulation, and management principles from the private sector | Duty of serving the public interest through publicly funded health care | Use initiative and risk to expand opportunities with a focus on sustaining and developing a profitable business |
| Expression | ||||
| Maintain stability for the sake of the staff and service of the community Managerial autonomy Balance the books: live within the budgets you have been given Maintain a good working atmosphere in the practice team Work as a team and invest in the workforce Commercial aspects of running the business are a necessary evil |
Care for the person, not just the problem Keep your professional knowledge and skills up to date Work with colleagues in the ways that best serve patients’ interests – duty of partnership Treat patients as individuals and respect their dignity Act without delay if you believe that you or a colleague may be putting patients at risk Patient advocate: means listening to their concerns and representing them if you can meet what they want Provide a good standard of practice and care |
Work to and value targets Accept professional surveillance Procedural diligence Use targets strategically Accept rationing on effectiveness and efficiency criteria |
Managing services according to priorities Work at the level of health services to ensure ultimate benefits for patients Deliver effective health care in the best possible way Measurement by quality and outcomes, not processes Spend public money in the best way |
Seek and exploit opportunities and drive forward – adventurism Look carefully and monitor costs Cater to patient demand Advertise the practice Look for new markets Portfolio careers |
Ownership responsibility logic
In medical practice, although there is less of an emphasis on the close-knit nature of the practice as a community of people (both staff and patients), there is still a deep sense of the importance of sustaining the medical practice as an entity for the sake of the staff employed by the enterprise and as a service to patients and the local community. Maintaining good working relationships among the team is key to the smooth running of the practice and to maintaining its functionality to provide effective care for patients.
Obviously the main thing is to look after the patients, provide decent care to the patients here and to maintain our function as a practice. Which is harder than it sounds. In that you have got a practice that is working together, people are working normally together with a good atmosphere and that’s harder than it sounds. It’s not just the job itself, it’s maintaining a good working atmosphere for everybody in the building so we have, we retain our good staff and we build on the clinical aspects of the practice rather than getting sidetracked by any other problems really . . . the practice will fall apart and people will start leaving.
DM2
You are responsible for running your premises, you’re responsible for employing your staff and of course most of all you are responsible for providing adequate care to your patients. So it’s threefold.
FM1
I mean obviously the essential one [practice goal] is providing the best possible medical care we can to our patients in line with current guidance and advice, whilst also striving to maintain a good atmosphere to work, adequate remuneration and quality of life . . . of working life for those working here.
CM2
I would say that they all [GMPs in the same way as GDPs] have that same level of you know, this is my . . . this is what I am supposed to be providing, this is my practice, this is what I do and I think they all kind of accept that responsibility.
2AC2
Keeping the business running is important and, to do this, importance is placed on monitoring income streams and maximising efficiency. The emphasis here is on maintaining a steady stable balance sheet, rather than on more commercial values associated with growth and profit. Running the business is geared towards survival, and commercial aspects are a ‘necessary evil’. This is a day-to-day activity and focus, since the balance between income and expenditure is tight. Because money is tight, efficiency and active management of resources are a necessity. The sense of responsibility experienced by partners is very real and not taken lightly.
We have to make sure that we are, you know, efficient and have a thorough system in place to make sure that we invoice for the work that we do, get recompense from the PCT so that, you know, all the staff can have their pay on time. So it has to run quite finely and the practice manager oversees all this.
FM1
On the other hand we have to check ourselves and our income which is important really and so we . . . we try to have a balance between all of these things so, keeping the practice running smoothly and on a daily basis given our income coming in and still to some extent, otherwise we wouldn’t be able to afford employing staff and running this practice and serving our community.
2FM3
Well we have always tried to keep our income stable but now we are more aware of the financial strains of the NHS more than anything.
2FM3
I would not like to describe it as such as making a profit. We just see it as earning a decent income and to keep our staff and the services running. In the interest of our patients really. We didn’t take business or medicine as a profession, I wasn’t there to make money as such, I am just here to have a decent living and on the other hand give a good service to our patients and keep our staff happy and giving them a good standard of living and good work environments really.
2FM3
You can’t become a partner simply because if you want to become a partner or . . . you have to function as a partner. Partnership comes with huge responsibility. It’s hard work and this is why I say people who talk about partnership they should not be underestimating partnership.
FM1A
We have to meet the QOF to continue as a practice.
2FM3
Every year the practice looks to make a profit. It has to to survive. So every year we decide what we can do, what we can afford and how much we’re looking to increase payments, even to the staff, and to the GPs themselves.
CM1
We are all just trying to keep a roof on our heads and keep our services going and patients happy. That’s the main reason why we are here really.
2FM3
Commissioners, too, often used the same language as GMPs to talk about the ownership role as involving maintaining a viable and stable business, rather than looking towards expanding profits in order to increase income.
That’s what it becomes about, what can they bring in to make their business more viable.
2AC2
Like dental practices, we found an importance placed on managerial autonomy. Discretion over how to spend income affords independence from commissioners. The managerial autonomy which comes from independent contractor status involves the ability to make decisions about how to run the practice efficiently in order to maintain a stable business. This has an impact on GMPs’ personal income but allows the organisation to reflect personal and practice goals. Decisions, for example how to reimburse staff using bonus systems to share rewards among the practice team when targets are reached, may mean that partners’ personal income is reduced.
You have the practice income from the PCT, and you choose to do with it what you want. That’s fine, that’s the way it should be. We’re an independent organisation that decides how best to . . .
CM2
I think it gives flexibility, you know, if I want some time off I ask and that’s my decision, a decision I take with my partners, without somebody else’s permission. If I want to be in Boston if I want to or reorganise my surgeries or provide this service in a different way because it’s better, I can just do that.
SKM1
In our practice we have invested heavily in senior management, our practice manager obviously gets a far bigger income than she would at another practice. We employ a practice pharmacist half time even though we’re not dispensing, to help us with our prescribing audits, advice, all those sort of things. We have a finance manager, who’s very efficient. We have an audit clerk who performs all our audits. All these people cost money and they have a net effect. We know that our income is as good, if not better, than any practice in town, but our personal . . . that’s the income from the PCT, but our personal income is less than most because we spend money internally.
CM2
We’re inordinately proud of the fact that we see it as a whole team effort to achieve the QOF targets, and every member of staff, whether they’re directly involved with QOF or not, will get a bonus.
CM2
Independent contractor status fosters a sense of responsibility for patients and the service. Hand in hand with greater managerial responsibility comes a greater sense of responsibility for the service for patients than is felt by, for example, a medical practitioner working on a salaried basis.
As a self-employed GP you are much more in control of what you do. It’s a small business and partners will determine who does what, how many patients you see in a morning, how many visits you do. And obviously it’s your business and if there is 10 visits, you do 10 visits. If you’re contracted as a salaried GP there will normally be a clear indication of what your day will entail. So you might expect to do two surgeries and two visits or maybe one extra if that’s how it works. And when I worked as a, latterly as a PCT-employed GP I continued to function like a self-employed GP and I worked with a guy who worked as a self-employed GP for many years and he did exactly the same. So we just did whatever came through the door. But thereafter, when we left, there have been several GPs who’ve just said ‘Actually I’m not doing that. That’s not my job.’
DM1
Duty to patients logic
The dominant logic of medical practice is a duty to patients. GMPs talked about ‘duty’ and being prepared to serve in a selfless way. This is a service to the individual patient who attends for care, and ‘doing your best’ for that patient is always the GMP’s prime concern.
For example, when a patient comes to see me I feel a sense of duty that John Smith has come in to see me and he has a need and I must satisfy that need. We end up helping people and guiding them about social issues, personal issues, domestic issues. And I do that out of a sense of duty. There is no other recompense for it.
FM1
General medical practitioners talked about their role as the patient’s advocate. In the same way as dentists, they frequently consciously acknowledge a professional responsibility to completely represent patients’ wishes and petition on their behalf. They are more likely to use the term ‘advocate’ when describing their role in acting as an agent on behalf of the patient, not altering what the patient is asking for in terms of care, but the professional principle is the same. Doctors talk about their role ‘speaking for the patient’, as a sense of responsibility which grows over several years of caring for the family. They are focused not purely on the ‘problem’ but on the ‘person’. When doctors use the term ‘patient advocate’, they mean that they set out to completely understand and appreciate the patient’s point of view. GMPs do not mean, however, that they necessarily accede to all patients’ demands, but instead that they set out to use their professional knowledge and skill to determine what care is best for the patient, albeit while still fully appreciating what the patient wants.
It goes back to what I said earlier about caring for the person, and that’s exactly what the advocacy refers to. I’m caring for the person, not just for that particular element . . . so, when I’m caring for the person, I have to bear in mind what will be the impact of any action I take relating to the patient on him or her as a person, not just on the problem. When the impact is likely to be so far-reaching then you have to bear the person’s best interest at heart all the time, and that’s what the advocacy comes before. It is feasible to strike a reasonable balance most of the time, because if you’re practising good medicine most of the time then you are automatically ensuring that the patient’s interest is at the forefront of the action that you process.
FM1A
I don’t know what any doctor is doing with their lives if they don’t think they are patient advocate. I’m surprised if you’ll find somebody who doesn’t believe they are. Well it’s just central to what you do. The minute you qualify it’s what you do. I struggle to envisage a scenario where that isn’t the case. The patient in front of you is always first, you should always listen to what they’re saying. Sometimes you’re not able to do what they would wish, you can’t do everything, but you should always try and understand what they are and be their advocate if appropriate.
CM2
I have known some patients for 20 years now and I have seen them grow up and seen them through quite a few things; you do feel very loyal to them and you just have an intrinsic feeling that you need to help them. They are completely trusting that you are going to help them as well so there is a very strong bond there. So you really are speaking for them.
DM2
I think so because the doctor basically has just got to learn the art of sitting there and listening and trying to act on what he hears.
FD1P3
Managerialism
The GMPs studied acknowledged that reaching targets set by commissioners was part and parcel of their work and a means by which income is allocated to the practice. This was recognised as part of the culture of the NHS and even recognised by patients. Counting patients as numbers is something which is necessary as part of a managerial focus concerned with effective and efficient management of resources at the practice level, geared towards maintaining practice stability.
Well if you’re a GP and in the NHS you know you’ve got targets to reach, you’ve got to see so many patients, you’ve got to make sure X number of your patients don’t die and all that to get your money.
AD2P4
The New Patient Check which allows us to slow down or keep a very close control of the numbers that come in. Otherwise we could get occasionally drowned by it.
CM1
Although doctors may be geared towards achieving targets mainly for financial ends, since these are tied to reimbursement arrangements, there is evidence that they derive more pride from achieving targets than do dentists, thus signifying that doctors consider targets to have some meaning in terms of the quality of service they provide. GMPs use and take note of benchmarking information. They adopt some management practices such as process mapping in order to improve practice efficiency. They place more value on some targets than others, recognising that some targets are derived on the basis of what represents good care and are a way of driving efficiency and progress towards worthwhile population health goals. Practices are strategic about deciding which targets they should work towards, and which they should ignore, depending on the benefits that are anticipated, both financially and clinically.
[Relations with nearby practices are] broadly friendly with a sort of slightly performance-based critical eye, you know, we don’t want any practice performing better than we do on anything. So there’s always that little competitive element to be the better performing, which I think is probably good for patient care. But I think we’re all pretty much like that, and all of us will be the best performing on some aspect and not on others. QOF targets, access targets, access ability, emergency admission rates, prescribing budgets, all sort of different things that you look at and clinically appropriate stuff.
CM2
So that’s the sort of target I think that they actually appreciate and understand and see it as a benefit because, if you don’t set a target on that, you know they’re not going to make sure that those numbers of patients are actually brought in or chased up to do the best they can to get those vaccinations delivered.
2AC2
So we get the graph and it has whatever, who the best, who the worst at a particular area. And I think one we came out we were high prescribers of non-steroidal drugs, Voltarol, ibuprofen, that type of thing. And there may be reasons for that or it may just be habit or it’s probably a mixture of all sorts of things. But you do think ‘Ohhh’.
FM2
I mean practically from a business point of view, you still have [to] sit down and you have to do your budgets and you basically admit you’re never going to get some and some operationally . . . you admit . . . you admit you’re never going get some . . . and some are entirely . . . we sit there and we say at the beginning . . . when we get the new targets we go ‘Well that one’s not worth the money and has got no clinical . . .’
BM1 director APMS
And recently as of Monday we did a process-mapping exercise with patient participation and I’ve never ever done that before and I was very very reluctant. It was looking specifically at heavy menstrual bleeding so we had two women, one of whom had waited something like 18 months before it was sorted. And the number of different referral routes they could have come through. And the number of times they had to go before they got what they wanted. So we are now looking at streamlining a pathway so it will takes all the variety out really.
DM1
I think it’s much more of a medical practice and hospital type things that have a target to achieve something.
2AC2
In our GMP sample, doctors recognised that the NHS budget is limited and finance is tight. GMPs therefore appeared not to resist attempts to restrain public spending. They accept rationing based on effectiveness criteria.
And we looked at the areas where the meds management team as it’s called would like GPs, primary care teams in general, to improve prescribing and most of it is aimed at reducing the costs. Now there is no point in people ducking and diving and I think it’s important that people do engage in low-cost prescribing wherever possible, as resources are limited.
FM1
General medical practitioners also recognise they are externally accountable to commissioners, and perceive a level of micro-management and supervision, which can be resented but is not overtly resisted.
But the PCTs and people in such echelons, they are given this feeling that their job is to supervise, which may be true to an extent, you need someone in supervision, we all need an element of supervision, that’s fine. I say the same thing to my children.
FM1
I think we are being so managed that goodwill fades on both sides really. You know you feel like because you are being watched and scrutinised and micro-managed in what you do you don’t want to necessarily go the extra mile but then you do. You go the extra mile for your patients . . .
FM2
Well I’ve got a line manager in the PCT for the safeguarding. And I suppose I have a manager for the sexual health service as well. Well, I do have (laughter). I have less – I feel less line-managed by her as I do by the other manager, who will call me in for one-to-ones on a regular basis and wants to know we are achieving all the things we are meant to achieve with CQC and things like that.
DM1
I would suggest they [GDPs] may not be treated in the same manner because they are seen as private contractors, whereas I don’t think we are. I think we are more rigorously controlled and one of the bugbears of most general practices that I know of anyway.
CM1
Public goods logic
General medical practitioners studied placed a value not just on providing high-quality services for individual patients, but on improving and developing services for the wider population. Working towards equality for patients is part of this duty, which GMPs carry out in addition to their work with individual patients. They understand that they have a responsibility as guardian of the public purse and understand that, by engaging with activities at a policy level outside the practice, they may bring benefits to their individual patients. They are used to dealing with managing competing priorities and arguing a case for investment and disinvestment at a service level.
On the other hand we try to all ourselves, doctors and CCG [Clinical Commissioning Group] board members trying to evolve services for patients and try to improve the standard and equality. I mean we are always trying to evolve and change and we try to provide services and things and get more involved with secondary care services and primary care services from outside.
2FM3
And there are some people who you meet and you say I believe this is a clinical priority and this is when you are coming back to the director and the performance manager at the locality. I said I believe this is a strong priority for this, this IT [information technology] system to enable people in the out of hours centre and A&E [accident and emergency] and on the acute medical unit to have more information, to make a better decision so to hopefully not admit as many people as we needed and they said, ‘Yes great idea let’s run with it as hard as we can and that’s fine.’
CM2
The most difficult relationship I’ve possibly got is with another GP and, because we disagree on priorities, it’s not with a manager . . . but we disagree on priorities, we both I’m sure are very committing to delivering effective health care in the best possible way but just different on priorities and then that just ends up with us trying to push our own particular way forward.
CM2
Obviously people need to be reasonable about what we can afford and what we can’t afford and maybe some services can be withdrawn. Directly we should focus on the big things and the important things that need care and daily care and disease management.
2FM3
In our GMP sample, doctors appeared to take on a role of guarding the public purse in their day-to-day work with patients. In their clinical decision-making they take account of what may be cost-effective care and what might not, knowing that, if they reduce waste, other patients within the practice will benefit.
We have got responsibility to look after patients and two-thirds of the NHS budget theoretically and we have to perform, otherwise our patients will suffer.
2FM3
The PCT has to rely on us to use NHS resources wisely.
FM1
[Our practice goals are] to provide cost-effective care to our patients. Because when you are being cost-effective, it does not mean you are losing your clinical perspective. Because the advocacy element as well as clinical efficiency. So if and only if you are practising good medicine will you be effective. And one cannot detract from the financial element because NHS resources are limited. So it has to be both.
FM1
So I do find myself in agreement with many government and quasi-government experts say, that there is a lot of waste in the NHS which if it was controlled and limited, we can’t do everything but if it was limited we would have more money for inward investment.
FM1
Entrepreneurial commercialism
While business aspects of the practice appear to be integral to work in medical practice, for many GMPs this is geared towards maintaining a viable practice in the long term, rather than to expand and generate profits in order to increase income. Business aspects are identified by many as a ‘necessary evil’ that comes with ownership responsibility. For some (a minority) of GMPs, though, more commercial aspects of running the practice are important, and they are geared towards growth. The way the GMS contract is constructed means that there are economic incentives for growth, embodied in a tailored set of targets, which are there to exploit. The possibility of taking on private work provides further opportunities for growth, which some commercially minded GMPs look to exploit.
The PCT will work out, based on the practice’s social demographics, what per cent of 15- to 24-year-olds are eligible for chlamydia screening and then it will say ‘OK, your target for screening this year of that number is this much per cent’, so if you have 100 patients who are eligible for screening and if we say to you we want you to achieve a target of say 30% and you will be paid £1 per patient that you screen so your total return would be £30. Of that £30 we will give you £15 upfront and the other £15 will be at the end of the year providing you screen 30 patients. If you don’t screen 15 patients then you only screen 10 so we take the five back from you. Yes, it’s what they call an aspirational payment. It appears that way on the face of it. But in actuality what is classed as more income is actually quality-predicated income. So it’s not a bonus: that is something for which you have to work extra to achieve it.
FM1
You have to to survive, actually. You have to; it’s imperative that one does that. It depends on how the world looks at it in terms of commercial. Commercial, that’s what we do all day long anyway. Everything is tied into some causality. For example QOF, LESs [local enhanced services] and DESs [direct enhanced services], it’s all commercial, you know, it’s all commercial and I do that. Yes, I have to do certain commercial things in order to stay afloat.
EM1
They are a business, independent business about running to make a profit, partly through the NHS and partly through private services. I don’t think they would view it in any different way than any other provider in that if there’s private work out there they will tap into it. As I say, the clinicians, again it depends on the individuals, some see these as . . . outside the contact areas as private things that they can make money doing, some of the clinicians probably think ‘Do you know what? I’ll just do it’ without even questioning it and they won’t charge, so it varies I think between each individual.
2AC2
Dealing with multiple income streams is a way in which GMPs can expand personal as well as practice profits. Some GMPs have ‘portfolio careers’ where they have several different roles and sources of income. This provides a means to expand personal income.
Perhaps I’ll get into trouble here if I start giving away how much partners earn in the practice. We have different ways of remuneration and methods and income streams and all the rest of it, so we all have separate income streams as well as that side, none of us do badly at all.
CM2
In our case studies, one of the most commercial and entrepreneurial-orientated GMP was a single-handed practitioner. While this GMP showed a sense that commerciality was integral to maintaining the viability of his practice, he was also more actively engaged in driving business aspects of the practice forward, rather than purely focusing on maintaining practice viability through a careful management of existing resources, as seen in most other practices. This GMP constantly looked for new opportunities and markets in order to expand his business, consciously using advertising to do this, and willing to cater to patient demand. In looking to develop initiatives he was willing to take calculable risks to move forward into new areas.
For example I take referral from the other GPs excise stuff for them. The PCT pays for them so for me that’s extra money, that’s extra income stream because not everyone does them, not every . . . I invest that money in the theatre upstairs to be able to do that so yes and if I had more time.
EM1
Because although there is the demand there [for private sector thread veining], but I feel they have more pitfalls than the other ones [areas of private work] I have been doing.
EM1
Quite a substantial number of them [patients] who are referred to me for operations or lumps and bumps, didn’t even know that there was a surgery here so they live nearby and they are ‘Oh I have been passing this road and I never knew there was a surgery here’ and when I took on this practice I had to invest in making my practice look different from the others because this is a terraced property so had it painted white so it looks a little bit different; there was never a sign so I’ve done a sign. We have a website, which is another way of finding us, so I see that as the first thing.
EM1
Entrepreneurship involves reaching forward and identifying new opportunities for growth. This commercially minded GMP was seen to actively seek and recognise new opportunities, using entrepreneurial language of ‘adventurism’ to express his goals. Entrepreneurial commercialism logic identifies less with maintaining the ‘venture’ but focuses on ‘ad-venture’. Private sector provision provides new markets, as do changes in the way services are commissioned.
I can see the opportunities, I’m already looking at the opportunities.
EM1
I do know that the whole plan is to move a lot of services from secondary care to primary care and I remember trying to get on the Any Qualified Providers [AQP]. Say for example increasing the basket of surgical procedure that I can carry out including, you know, things like carpel tunnel decompression operations. I see that as a big opportunity so I am seriously thinking about registering as a private company. I am seriously thinking about registering a health-care company so that when the time comes I’ll call CQC and ask them can I provide other services from here? And I’m seriously thinking about even the circumcision that I do.
EM1
I think that my sense of adventurism is above average if I should say!
EM1
The entrepreneurial minority are identified as being more ‘private sector’ orientated as opposed to having a public sector ethos. Some GMPs admit to being geared towards ‘making money’, but usually as secondary to their duty to patients. Having to make a profit is something which can get in the way of the main task of caring for patients.
I would position myself, we are within the public sector. The way, the way we’re paid . . . it is relevant and it does certainly impact on the way, on the decisions you make. There are a number, I don’t know, 10% of entrepreneurial people who might not agree with that and see themselves very clearly as business men and will have lots of things, lots of fingers in lots of pies.
SKM2
Well we want to provide the best patient care we can. And we want to make money; I know that sounds terrible.
FM2
I think, most GPs I know in this building, the majority are not, they are more interested in the day job than running a business.
SKM1
Commerciality involves having a strategic focus which looks at reducing costs at the same time as looking to expand into new markers.
You know all the vaccinations etc. that we do, those have to be invoiced for and claimed separately and then of course those payments are directly linked to the volume of work undertaken. But they are also linked to the purchasing of certain vaccines, you know like the flu vaccines from suppliers, so you have to make sure that your cost price of the raw material purchase is sensible, otherwise you end up doing a lot of work for very little return.
FM1
So . . . the great majority of GPs would I think, they’re not, we’re not businessmen, we’re not monitoring expenditure all the time, we’re not monitoring income all the time. The great majority of GPs at the end of the day will just accept what falls out. There are a small core [or small businessmen], but the great majority . . .
DM1
Interacting institutional logics in general medical practice
A pervading sense of duty to patients means that some GMPs are uncomfortable with commercial aspects of care. They may deny themselves NHS remuneration by charging for services on a private sector basis, or spend time undertaking tasks such as listening to patients for which they are not directly remunerated.
Public sector, without a doubt there are some limited services which we end up providing to our patients out of a sense of duty as much as anything else. You know they need insurance medicals and this and that that need doing and also forms that need filling, which are not part of our core general medical services contract, but if we are looking after those patients then we have a duty to assist them, you know.
FM1
Most of us are focused on delivering the best possible health care we can for our patients is the primary thing and accept that the way that remuneration is done means that, if we offer what we consider higher-quality, higher-class care, that will not be recognised in remuneration.
FM1A
While the dominant logic in medical practice is a duty to patients, alongside this, practitioners deal with what is best in terms of public goods logic: considerations about whether or not clinical decisions represent cost-effective care from the view of the ‘public purse’. While GMPs in the sample do not appear to consider financial implications when dealing with individual patients (their duty, first and foremost, is to consider these needs first), making sure that their clinical decisions represent good value for public money is a secondary consideration. Sometimes this means explaining what the patient can or cannot have in terms of care (e.g. in certain types of branded medicines), but this appears to be an easier task than sorting through the complexity of meeting the patients’ physical, psychological and social needs all at the same time.
I can honestly say that in my dealings face to face with patients, I never consider the financial implications of what the PCT is trying to do.
CM2
It’s not something I feel inwardly at all. It may be my role to explain to the patient with his bat ears why he can’t have the surgery, but that’s okay, I don’t mind that. I’m on the front line of many more things than rationing. I’m the interface between a patient and their health needs. I’m on the front line of a lot more things than rationing, it’s not a big deal.
CM2
While our findings indicate that GMPs find that duty to patients and public goods logics are not in conflict, the GMPs studied indicated that this can create conflicts in the view of patients. The conflict, therefore, is something which needs to be resolved in discussion with patients, making consultations in medical practice increasingly complex and time-consuming. Public goods logic and duty to patients logic may also conflict in terms of the time which practitioners have. Action to push forward a public goods logic often takes place outside the practice, in a struggle and argument with commissioners concerning the best use of resources, and reducing waste in public expenditure. This can be exhausting and reduce the time and energy that practitioners have to fulfil their primary role of serving their patients.
It does sometime, as I say, create problems . . . sometimes the patients . . . What can you say to them? ‘Well I can’t give you this drug or that drug because it costs more and the NHS can’t afford it’? We can’t, we try to be transparent with people and patients and you explain to them that if we don’t save money from this way then other patients or services will suffer.
2FM3
I say we want to make money, we want to make money for profit obviously for us but we are also trying all the time to save money on prescribing to save money for the NHS so it’s constant at the moment. It gets in the way.
FM2
It is making our daily consultation more complex really and more time-consuming really and sometimes it affects, with a few patients, our doctor–patient relationship. Because at the end of the day we are here to treat them and look after them and not to say to them ‘oh we are here to save money or score points’.
2FM3
But you can’t fight the system all the time. You can’t swim against the tide all the time because you will tire yourself out. So after some time I couldn’t help thinking, well, dash it, I’ve got to focus on my practice, my team and what I do for my patients.
FM3
Balancing ownership responsibility, duty to patients and public goods logics makes day-to-day work a conscious ‘juggling act’. Managerialism is experienced as both a tool to achieving these various goals, as well as a distraction.
Trying to balance the things the books and the policies and trying to please ourselves, please our patients, please the politicians and above all we have to do that in our budget and we can’t go above it really.
FM2
So they are trying to get on with the job and do things and keep up to the standards and create a budget and deal with services and do certain commissioning policies and run services and hit targets and all that stuff. So instead of having a stronger business [we’re] target juggling in the NHS in a way although nowadays they are veering off that.
FM2
Entrepreneurial commercialism can provide a means whereby GMPs are able to meet both duty to patients and public goods goals. Developing new income streams and working with commissioners to suggest creative solutions to developing better public services are ways in which they can deliver their sense of duty to patients and the public. Having flexibility within the medical practice allows new ventures to be developed to deliver better services for the community. We see this particularly in the APMS case, where there is a strong commercial awareness and strategic positioning of the business in the marketplace, but at the same time, an ethical focus which uses business expansion to deliver more and better services for the underserved.
The spec of the contract was kind of quite broad really in terms of . . . and by how you achieved those outcomes was up to you and how you modelled yourself was up to you and it was a great opportunity to be creative.
BM1
It’s about us bending mainstream services to serve our patients. I’m quite into bending mainstream to fit our patients. So then it’s things like co-ordinating the GP with the school. So simple things so it might be like . . . I mean we’ve had one case where we just deloused the kids of head lice and then amazingly school attendance goes up.
BM1
I want us to be deprivation specialists. I want us to know how to do health care in these really difficult areas and how to make it work. Then to be in a position where you pick work that suits that. I’ve got no desire to be big for big’s sake, but there’s always going to be deprived medicine.
BM1
Summary: contrasting dental and medical practice fields
While many of the same principles guiding everyday work were similar in dental and medical practices (ownership, professional values, population health managerialism, entrepreneurial commercialism), there were slight differences in how they were expressed, particularly in the extent that managerialism and public goods logics act in opposition to other logics. Commercialism appears less prominent in medical than in dental practice, and managerialism principles more readily accepted. In our study, medical practitioners recognised that, although they were independent contractors, they were relatively dependent on the NHS for their income. This brings a level of dependency and concurrence with NHS corporate values, including acceptance of scrutiny and supervision. Doctors see good clinical care as cost-effective care in ways that are rarely acknowledged by dentists.
General dental practitioners working with contract: micro-level chair-side behaviour
Institutional work theory recognises that, in the midst of larger-scale changes in the organisational field (e.g. concerned with increasing emphasises on commercialism, consumerism, managerialism, etc.), tensions are played out at a micro level – that is in the immediate daily task environment – as well as at the macro level, where arguments, negotiations, partnerships and struggles take place (both between GDPs and local commissioners and at a range of levels extending into the political and societal). Thus, since tensions are evident in the dental practice organisational field, we might expect this to shape behaviour which takes place in the dental surgery, as GDPs respond to and interpret contract rules. Hughes et al. 13 identify that providers adapt their practices according to contract rules – shaping their behaviour as intended by commissioners in some areas, but actively resisting the ‘spirit of the rules’ in some other areas (see Chapter 1, Grand theories of health-care contracting).
As soon as a new contract is established, existing areas of practice and behaviour are altered. Both GDPs and commissioners recognise the inevitability of grey areas of the contract, since the contract can never be completely specified. There is often a shared understanding of what the ‘spirit of the rules’ represents. GDPs, however, may work to the letter of the rules while recognising that this is against the spirit of the rules. Variation in practice exists at the boundaries of the letter of the rules. Decisions are rationalised and dentists constantly seek to justify their actions both to themselves and to others.
We’re now allowed to recall patients under NICE [National Institute for Health and Care Excellence]guidelines, so that means if I think it’s clinically necessary in my opinion to see a child every 3 months in accordance with legislation to apply fluoride, I will do. I get paid 1 UDA in return. Historically in the contract you could only claim for an examination once every 6 months. I still might have done it in the old contract, but I wouldn’t have got paid. I do have issues with dentists and the like who take that stance, and I can see where they are coming from, I can understand the reasoning.
CD1
I’ve read through [NICE guidelines] and, at the end of the day, many of my patients . . . I can find reasons, whether they smoke or whatever, whether it’s their gum health isn’t perfect, half the figures written down . . . I am writing so much more nowadays as every dentist is, . . . So, there’s enough to say if gums aren’t perfect, bring them back every 6 months . . . 3 months for the hygienist and I have a very good general standard of dental care amongst my little insular population.
ED1A
I think that the contract itself and people who understand the contract know where that line is. That’s not to say there aren’t people out there who abuse that line.
AC2
They introduced the scheme, just like the one with the doctors, and we sit down, we’re intelligent people, we think ‘How can we use this scheme to our advantage?’ Simple as that. Without breaking any rules. And they say there are no grey areas in this contract, which is an absolute myth . . . and basically you just use the scheme you have without breaking laws.
CD1
So you roll things out in a certain manner and there is a spirit to the thing isn’t there. You don’t expect to have to cover every eventuality when you set up a process but then it starts being abused.
APCR
He [the GDP] can, well certainly if he can rationalise it and therefore he can live with it but he will also justify it. I will justify a plastic plate to replace that because it looks **** good. The fact that you have got to take it out after every meal and clean it, so what, tough . . . that’s tough . . . but if you do that it looks good and it does the job. What’s your bitch, what are you complaining about? So you have got to clean it after each meal? You don’t like something on your palate? Tough. You want something . . . if you want your palate clear you pay me. Why should I charge the tax payer under public expenditure for something that you don’t really need? I will justify it.
SKDR2
The vast majority of dentists, all they have done is adapted the way they work to a system they work in and history shows that whenever there is a new contact, whether it’s 1948, 1990, 2006, the losers are the government because whenever you bring in a new system the dental profession is much quicker to adapt to the rules and new ways of the working than the department is.
SKDR1
While GDPs studied were aware of rules, for example, about not selecting particular types of patients as NHS patients, they were able work to the letter (e.g. demonstrate figures) but without complying with the spirit of the agreement.
I am not totally discriminatory because you’re not allowed to be. But there are ways of managing your patient practice and profile because I’ve worked that way from 1992; and I have . . . because they will show from the figures.
ED1A
General dental practitioners studied adjusted their behaviour in response to the contract in two ways. First, practice owners stepped back to make strategic decisions on how to operate. Strategies within the practice may be set by owners as a way to manage shortfalls in funding, for example limiting access to NHS crowns.
So if the junior colleague is doing that treatment provision, let’s say, and let’s just say hypothetically they are doing one crown, and this is all they’re doing, and it’s hypothetical, and one crown in the afternoon, let’s just round the £198 to £200. So effectively they’re doing £400 of patient charges in a day. So in a week it would be 5 × 400, which would be £2000, so if they were to do that for 50 weeks a year that’s £100,000. So the money that’s getting paid to train the junior colleague on the one hand is getting deducted and so through the contract system. So who is training the junior colleague? Who is paying their wages? Well, the money has been taken away and that’s a bizarre sort of scenario but that’s how it is. So of course we’re in a situation where I must say we don’t do crowns, we do.
AD1
Second, interpreting the contract rules appears as a daily activity which is undertaken at the chair side. There is a constant juggling of contract rules, decisions regarding timing, alternatives, charging and remuneration considerations according to different types of patients. Interpretation of contract rules (with consequences for remuneration) is intertwined with clinical decision-making, with many permutations.
It may be that given that my patients are exempt and they haven’t got the patient charges to pay, I might say ‘Right, OK, we’ll do immediate dentures in acrylic’ whereas having fee paid, yes, sometimes in the last 3 or 6 months, you can get it to 9 months at a push, I might say ‘That’s OK as we’ll replace it after 3 months’, which is perfectly clinically acceptable to do. And then suddenly whatever you think is appropriate. I might, you know, in some cases with my NHS patients I might say ‘OK, put a large filling in, you’ll benefit from a crown’ but I’ll wait for 3 months to make sure there is no repercussions of that filling being done. So immediately I’m going from what is a core providing a crown straight after I’m saying ‘OK, I get 3 UDAs for the filling, 3 months later I’ll get another 12’.
CD1
She actually works as [XXX’s] nurse in the surgery so that’s very useful and so obviously sort of regarding the UDAs and all that side of it, she knows a lot more.
AD11
The patients and their preferences are involved too, depending on the number of visits they are willing to make, all having an impact on patients’ charges and dentists’ reimbursement.
If a patient comes in . . . so I say to you ‘Right, well you’ve broken your tooth, I can either put you a dressing in it, leave it alone, or put you a new filling in it or change the filling altogether and put you a white one in – whichever.’ You’ll say to me ‘Well I’m too busy, I’ve got to pick up the kids, just put a dressing in it’. Okay, that’s £17 . . . 1.2 UDAs. If, however, you decide ‘well I tell you what, can you fix it properly’, I said ‘okay, fine, I’ll do that’, so in clinical terms I’ve put a new filling in it. It might take me a few minutes but . . . well that’s actually band 2 so that’s 3 UDAs. So instead of paying £17 you pay £47. You then say to me . . . You want a white filling doing, okay that’s fine. Well for argument’s sake we’re going to do that within the NHS, let’s say, so that’s going to cost you £65. So, if, however, we decide to do an inspection on your mouth there and then effectively I tell you what, we’ll just put your temporary [filling] there for now, get you back in a month, do the filling for you in amalgam, I then roll the course of treatment through as an examination, which then means you pay your £47. You haven’t had any emergency treatment. So it’s a 1 or 2 or 3. One visit or two visits.
AD11
Competing logics present themselves in micro-level decisions relating to deciding which UDA band to work within and consequently the level of patient copayment which comes with this. At the chair side there are strong pulls to provide a good deal for the patient, and consequently patients’ eligibility for charging can be under-represented, the GDP therefore acting as an ‘economic agent’ on behalf of the patient. 100 Out of a duty of fidelity, particularly where patients are felt to be vulnerable, dentists may promote patients’ interests above their own or above the state’s. In doing so, they move beyond being a silent partner in an arrangement which relies purely on the government and patient determining what should be funded.
There is a lot of conflict with that because, for example, erm, we’ve got a lot of elderly patients and frequently see them with a bit of tooth broken off or you know and then we know it’s difficult for them to come in, so we try to fix it there and then and really we ought to be charging a band 2. I think that’s the real conflict that we all have and I find that very difficult and we possibly do put quite a few of those down as 1.
CD3
Accountability to the patient
General dental practitioners find themselves accountable to patients as well as commissioners. Chair-side interactions with patients are shaped by wider societal views of the dental profession and the type of service it represents. We found patients had a greater level of cynicism regarding the profit motives of dental than medical practitioners. Patients also had a generally lower regard for dentists than for doctors. Dental practitioners are perceived as more overtly commercial than medical practitioners.
It is a profession that does inflict pain for a gain.
BD1
I don’t know what proportion of that money goes to the dentist and what goes to the NHS and stuff but I think it is seen as more of a money making. I can imagine people, but I could imagine some people would think of it that way, it’s like a business really isn’t it.
FD1P4
I think maybe people see doctors as being, what the word I am looking for . . . revered more than dentists.
FD1P4
Media stories, particularly about dental practitioners moving into the private sector, reinforce patients’ suspicions that GDPs are primarily self-interested and financially orientated. Prejudices can be hard to redress, sometimes spilling over into interactions between the dentist and patient at the chair side. While dental practitioners work daily to balance their professional clinical values and entrepreneurial commercialism, their behaviour and their balance between these two logics can be queried by patients. Conversations can be uncomfortable and difficult where dentists find their personal integrity called into question.
I trained to do clinical dentistry, that’s it. I know nothing about negotiating, I know nothing about politics, I’ve got no interest in politics and yet the patient can make huge judgements about you and your personality and whether you’ve got their best interests at heart. I actually got hate mail.
Did you?
Yes, hate mail, threat and what would happen to my car. My staff have had a few scenes when they’re going out shopping and it was awful, really awful. And you know, a practitioner down the road, he had police involved, threats of arson. I can’t describe it, I can’t describe it.
How long did that go on for?
Erm, gosh, about 12 months after [going private]. Even now you get patients who comment about dentists making loads of money and it’s absolutely never ending. It was purely based from the patient’s point of view, purely based on finance. Those people who did ask and when you explained to them were quite happy with the explanation given. But there is always a percentage of the population who just make up their own minds without any information at all.
An example that I can actually give, there was this gentleman who came and he needed quite a few things to be done and I gave him options, okay? NHS options and private options. The decision was going to be solely his, okay? He came back to me and said ‘I don’t quite like the provisions that you have given me under the NHS, I would like to go privately for those.’ I said, ‘By all means, there is no problem with that.’ I hit him with the estimate, he looked at me and said ‘This is fine.’ Then he goes home and his wife disagrees with him and he comes back and . . . he blatantly accused me of avarice, and I couldn’t take that! Because that is not where I come from. I was actually quite annoyed with him. I told him, look I did this and if you are not going to, if you don’t want me to see you I am more than happy to suggest that you see one of my colleagues here – I don’t want to be part of this, I don’t want my treatment to be from a polarised position, I don’t want that. And you know what, because I was straightforward with him and he could see . . . I had a catalogue of things that I had presented before him which justified my position and he had nothing to argue with me on that.
FD11
General dental practitioners have a gatekeeper role relating to the type and extent of NHS care which is available. Because dentistry is distinct from medicine in that copayment for routine care is involved, dental practitioners are put in a position of having to explain to patients why the state’s resources for dentistry are limited, a role that dentists can find difficult.
We, because we live in a society where there is a great feeling of entitlement, you know? People feel ‘I have paid my dues and if I want a situation like this should happen I don’t see why it should be denied me’. You know, as gatekeepers it is really difficult to defend a position like that, it clearly is difficult.
FD11
The NHS and private boundary
Under the 2006 UDA contract, whether care is provided under the NHS or privately is an area of ambiguity, and varies between dental practices, according to financial decisions made in terms of running the practice, as well as how choices can be justified at the chair side. The terms of the contract rely on language about ‘maintaining oral health’, which is inherently vague. Since a verbal concept is inadequate to capture the infinite variety of perceptions and experiences, decisions are often open to debate about whether or not a certain type of treatment is deemed necessary to maintain the oral health of the patient. Clinical decisions are involved in determining treatment options relevant to maintaining health and rehabilitating disease, and weighing the advantages and disadvantages of alternatives. Because patients have less information than dentists about alternatives and reasons for choices, this represents an area where commissioners feel that dentists have the freedom to go beyond the spirit if not the letter of the rules.
The crux of it is, if the clinician thinks the treatment provision is necessary to maintain the oral health of the patient, then in theory it’s available on the NHS. Yes, you could probably argue the toss, shall we say, but from a clinical standpoint I mean you have to try and be defined as where we’re going.
AD1
With the NHS obviously it’s about need rather than want. And securing oral health. Now for example I suppose the bridge is the best example of this – a bridge obviously looks better than a denture, works better for the patient than a denture would. However, the actual need to secure oral health is the denture, which is the cheaper option so sometimes where the patient needs the denture but wants a bridge and a bridge might be appropriate as an NHS patient, some practitioners are saying ‘No a bridge isn’t appropriate and you’ve got to pay privately’. There are other factors behind that and it’s difficult to get away from because then it’s clinical opinion and if the supporting teeth for the bridge, the surrounding teeth, aren’t strong enough to support the bridge then it’s not appropriate to put one in. The denture is the appropriate one and then the patient could choose to have the bridge but at the risk that it’s not going to work because of the surrounding teeth not being strong enough. But then that would be a private arrangement. However, it is that kind, there is that grey area where I think the practitioner knows what is and isn’t available and will play on the patient’s lack of knowledge of that.
AC2
There’s numbers being told they can’t have a white crown on the NHS for a back tooth. And that’s just not true.
CD1
Six grey areas of the contract
Because of the unavoidable vagueness of contract rules reliant on language, and the necessary flexibility needed to ensure the rules can be adapted to meet the complex and diverse needs of patients, it is no surprise that there are grey areas in the current dental contract. In our case studies and stakeholder interviews we identified six areas of common dental chair-side practice where GDP behaviour could be viewed as being against what was in the spirit of the 2006 dental contract rules. In two of these areas, GDPs’ behaviour could be interpreted as being more focused on the patients’ wishes than on those of commissioners (highlighted in Table 6); in the others, behaviour could be interpreted as self-interested behaviour on the part of the GDP. Table 6 describes these six grey areas, together with some indicative quotes.
| Grey area | Description | Indicative quotes |
|---|---|---|
| Not taking on a NHS patient because they represent financial loss | The dentist/practice discriminating against NHS patients who have poor oral health, requiring work that is not rewarded by a high number of UDAs. Dentists may steer patients towards private rather than NHS care or avoid accepting them for care | You just have a little suspicion that maybe, for their, you know, to avoid if you like . . . the sort of financial loss that they may be moving people from one scheme to another to suit their financial purposes.2KC1If you are in a contract you take the rough with the smooth and you do it and you don’t look at a child and think there’s 12 cavities there, you are not cost-effective, I am not going to do you.AD2 contract review |
| Restricting doing certain types of treatment such as root canal treatment | The dentist/practice avoiding treatments because they are time-consuming in relation to the amount of UDA value attached to them. They may also suggest that the treatment needs to be done privately because it is not covered by the NHS because the cost and price do not match | If you do think about it, if they’re chasing the UDA the easiest thing to do is to turn over the quickies and then get rid of anything else by referring into secondary care so you are, technically you haven’t got to sit down and do it properly with root canal.BC1 |
| Undertaking more band 3 treatments towards the end of the financial year | NHS dentists/practices in England that are behind in meeting their annual UDA targets attempting to address this shortfall by prioritising the treatments with the most UDA value at the end of the financial year, to avoid financial claw-back from the PCT | A normal amalgam would come under the £47 fee but if you go for an inlay and the inlay is the white ones, the white fillings and you do use them for clinical reasons but we have seen a significant use of inlays.BC1I think many people towards the end of a contract may start to do a lot more band 3s to try and catch up if they’re a bit behind. I can understand if you’re in a practice where it’s difficult to meet your UDAs (because you’ve got maybe a huge UDA contract value and a low UDA value, or you’ve got dentists who aren’t performing), then maybe you’ll try things like doing a lot more band 3s.BD31 |
| Stopping doing routine care for patients towards the end of the financial year (in the last 5 years) | NHS dentists/practices in England that are reaching the limit of their allocated UDAs for a financial year postponing certain treatments (check-ups, scale and polishes, fillings, etc.) until the next financial year, because they are aware that if they exceed their UDA quota by 4% they will not receive financial remuneration from the PCT for any additional work | Some practitioners . . . if they churn through their UDAs throughout the year and then they’re running out of UDAs and they think it’s a way of banging on the door and saying we want more money, then they are the ones that would routinely stop seeing patients in that period or reduced what they were offering and you tend to get the same practices doing that year on year.2AC2I’ve had a couple of practices that come towards year end [and] have said ‘I’ve done all my UDAs, I’ve done the 4% I can do over, I’m not now going to do it for free.’2GC1 |
| Undertaking some treatment as a band 1 rather than a band 2 (in the last 5 years)a | NHS dentists are concerned about the fairness of patient charges where, for example, a small filling needs to be made. This may be more commonplace in practices where the dentist has a long-standing relationship with the patient | You might get some doing that say if someone comes in for an urgent rather than a temporary filling, you know, the . . . the nicer dentists will say ‘well, I’ve got time to do the permanent filling now’. Depending obviously on how much drilling they’ve got to do . . . I just think someone who’s maybe had the relationship with their patients a little bit more and again it’s, it’s the practices that have got their regular patients . . . practices that have got your sort of stable patient list.2GC1 |
| Being more influenced by what the NHS patient wants, when setting a recall period, than in strictly following NICE guidelines (in the last 2 years)a | NHS dentists who are influenced by the patients regarding recall periods may be adhering to patient pressure in terms of what constitutes good (regular) service | I think occasionally . . . some practices will still have their kind of recalls, you know, every 6 months and . . . sometimes the patient does question that as to why and some patients want to [do that] because their children are coming back every six months and it’s easier . . .2GC1It’s one of the things that we do come across when we challenge things like reattendance rates and so on, is that, you know, some practitioners will say to us, well it’s difficult because the patients want to be seen that frequently . . . I think there’s still some people who sort of seem to think that it’s almost a right to have a 6-monthly check-up, and if they’re not then their dentist isn’t very good.2KC1 |
Summary: micro-level behaviour of dental practitioners
The immediate task environment, that is the dental chair side, is a place where tensions between competing logics are played out, and interpreting contract rules relating to the prescribing of care and accepting patients into the practice is integral to this. In our qualitative work we identified ways that dentists worked around the letter of the terms of the contract, acknowledging that their behaviour might be outside the spirit of the rules, but feeling still able to justify their actions morally. For many behaviours, however, interpretations of contract rules are not maximally rational, but a result of habits and heuristics against a backdrop of personal bias, knowledge of accepted practices, pressure from individual patients, etc., to reach satisfactory outcomes, most of the time. Actions are influenced by having to justify directly to the patient decisions involving payment, in an environment where the patients’ family, friends and wider society hold dentists in general in a relatively low regard. Interpreting contract rules, therefore, is a daily activity which involves constant juggling of competing priorities, sometimes supported by more strategy decisions made at the practice management level.
In the course of our qualitative work we identified six areas of micro-level practice to use in our quantitative work in order to test a hypothesis that behaviour is indeed shaped by the institutional logics of general dental practice which we outlined earlier, rather than solely by individually informed views of what is appropriate behaviour in these areas.
Commissioners working with contract: dealing with general dental practitioners
Hughes et al. 13 (see Chapter 1, Quasi-markets in health care) posit that purchasers as well as providers take contract rules issued centrally, and shape and interpret them in their dealings with providers. In our dental case studies we observed how commissioners did indeed work with areas of practice outlined by the contract, querying GDP practice, and through discussion and negotiations attempt to achieve some managerialist and public goods goals relating to increasing efficiency in the use of public funds and equity of access to NHS care. PCT commissioners stand between the centrally specified contract and targets set at higher levels of the NHS management structure, on the one hand, and GDPs, on the other. They use any flexibility around contract rules to enable them to negotiate delivery with GDPs in order to persuade providers to co-operate to deliver PCT goals and improve local services.
Flexibility around contract rules is used to take account of issues around practice delivery; it ‘greases the gears’ and forms the crux of the relationship between commissioners and providers. Commissioners use the same language as practitioners concerning being able to ‘justify’ their actions pertaining to certain areas of the contract which they have to ‘work around’.
We do, not break any rules but we do manipulate them to get the best for the PCT and the practice.
AC2
And what we have to do is try, as our Chief Exec used to say, ‘It’s easier to ask for forgiveness than ask for permission’, so we sometimes do what we know is best for [PCT A] . . . like the way we implemented the Darzi projects locally. We tailored within the rules just so that we could deliver what we knew was the best thing for [PCT A] but staying within the rules of the core criteria. And that’s the way we do it here.
AC1
And so it was bending the rules on what this money was meant to be used for . . .
AC2
We know exactly how many dentists they have got so, if they have underperformed by more than the 4% that they are allowed within the contract, rather than claw money back we may allow them to carry out, take 10% over because what will happen is as a PCT we can agree that and we are not breaking any rules.
APCR
What we always said to them was if patients are urgent see them because it’s only 1 UDA, all check-ups in March but any treatment, if you know it’s going to be a treatment then that can be held back as a routine appointment, just book them in the next month. But what we do and probably we’re quite lucky because the numbers are relatively low, relatively small so we do have quite a good relationship with the practices and understanding of all the practices.
AC2
Yes, you’ve got to. I mean it would be stupid not to but having said that I know other PCTs who’ve said ‘No’. For example we opened one practice in July of last year and we pro-rata-ed the number of UDAs to be delivered by, and took out the first quarter. And then what happened was he came back in towards the year end because of the 30% in the 6-month check point. If they are underdelivering by 30% then we have a chat with them and say ‘Well what’s going on?’ and they said ‘Well we’ve just not got the people coming in.’ ‘So go away, do this, this and this’ and at the year-end he was still short but what we said was ‘Well look, you’ve done what we asked you to do, you’ve taken mitigation against this and therefore it would be unreasonable for me to take this off you. What I’m saying is, if you can give me the assurance now, carry the lot forward.’ That was then, though.
BC1
We gave him the option. Because we are given a target from the SHA for access, we allow him to carry 4% so I think he had underachieved by maybe 6, 7%, so we said to him you’ve got an option, you can carry over your 4% and pay us back the remainder, or because of the exceptional circumstances and you’ve now got two brand new associates wanting to keep your patient base, keep the continuity in the [XXX] area and we have got problems with [XXX] for access for patients, so we didn’t want to block any access. So we said on this occasion we will allow you to carry over . . .
DPCR
So in order to pay for capital you have to convert it into capital. No, if there is ways around that by keeping it in, under a certain value and if you pay it to the practitioner through the payment system through the BSA [Business Services Authority] you can put them through as payments as I say for a small figure and it gets around it but it’s giving that then to the practitioner to assist with their capital.
AC2
We found however, that reinforcement and interpretation of contract rules by commissioners was becoming less flexible, usually as a result of pressure transmitted from higher levels of the NHS management hierarchy amid a steady tightening of finances. Reducing numbers of commissioners also meant that there was less scope for flexibility. Earlier agreements between commissioners and GDPs had been based on discussion rather than formal written agreements, but, as the environment and personnel changed, some of these verbal agreements had been rescinded.
And I think that it will probably become more formal and more . . . following the guidelines to the letter rather than having that flexibility.
AC2
But we had that flexibility and because we understand the practice we can work with them. I can see why another PCT, [XXX] for example, who have 70-odd dental contracts, they just, it wouldn’t, they need to be much more . . . stringent in speaking to the contract because you couldn’t possibly have a full understanding of each practice. Because their team isn’t that much bigger than ours so you know . . .
APCR
So, some of their predecessors may have said things, or promised things, and some of the people who have come in their place have not fulfilled those things. The problem is they were verbal agreements based on trust, or whatever, and they have now been not honoured, as you say. So I think the problem is (1) consistency of staff members in the institution, (2) to make clear-cut in writing what . . . any agreements that you make – you can’t then go back and then change it.
BD3
We found commissioners used various tactics in attempts to increase efficiency, and get more (service) for less (money). If persuasion and negotiation with GDPs was not effective they were prepared to try to revisit contract terms (e.g. UDA values) unilaterally. Struggles between commissioners and GDPs therefore concern implications for patients and the practice business on increasing productivity. The contract provides the legal front defining the extent of commissioners’ legitimate demands.
And he came down here and said ‘Discussion in this room is not going outside the room, do you all agree with that?’ and we said ‘Yes, OK.’ ‘We can combine the contract but we’re going to have to talk about either reducing the contract value or the revision of the UDAs.’ And I said ‘I didn’t come here to talk to a used car salesman. I think the meeting’s gone far enough.’
BD1
But I mean certainly we’re looking at that and I suppose what we’ve also said when we’ve had discussions with the LDC about waiting times and obviously people accepting new patients so the acceptance of new patients is an issue for us and we’re having those discussions with practices because what we’re saying to them is ‘Well unless you can actually get some of that productivity through we’re going to start looking at your UDA rates’ . . .
DC1
There is pressure to cut it down [20-minute appointments for patients] further because the PCT unofficially want to increase the targets by 10% now at 6 months’ review. And I am at the moment pulling together a letter to go to them today to illustrate that that is not possible and that things suffer in regards to that.
CD1A
I’m a bit cheeky at times, me. [XXX] and team [DH] said at every opportunity we should seek to maximise what we are getting for our buck. So said, hang on fellas, you’re all on £32 per UDA, if I agree to you going through and having one contract, I’m only going to offer you £31 per UDA actually and they said no . . .
BC1
They [senior PCT management] backed off and I knew I couldn’t do it. I checked with the legal team and everything else. Anyway 12 months later we carry on, blah blah blah, and then there was all this panic around dental QIPP [Quality, Innovation, Productivity and Prevention]. ‘We’re going to save money, we’re going to decommission.’ Errr, you can’t. Well what would be a neat trick is to get the overall UDA rate down because they seized on that one and we pointed out that’s illegal, you can’t do it, it has to be by mutual consent. And the paper that went into management was . . . And it said ‘Risk of legal challenge’ and that was it. So they were listening, they put it down.
BC1
Because they need to find £5000 because they’ve **** up the budget. They can’t actually do that. I know they can’t and I told them so. The contract says contract value and number of UDAs. It doesn’t mention UDA values anywhere in the contract. It doesn’t actually mention patients in the contract either, but that’s another thing. The . . . problem is that the contract value and all the UDAs cannot be changed without agreement on both sides, that’s in the contract. But the letter they sent didn’t mention that.
BD2
We found commissioners also attempt to use persuasion to limit what commissioners see as ‘gaming’ behaviour. Discussions are prompted where GDPs identified as outliers on the basis of statistical returns, and GDPs are put under pressure to justify their behaviour, with commissioners hoping that this will be instrumental in reshaping the practitioner’s behaviour more in line with group norms. Commissioners use persuasion with an escalation to more formal demands to try to shape behaviour while avoiding more costly legal action.
I hope we will arrive at an agreement. I am hoping it he will admit that he was claiming inappropriately and they will either pay things back or we will agree that they provide that work more appropriately. It’s the way it’s been claimed so I have not got concerns of him as a dentist, I just have the concerns about how he is running the practice and using the loopholes in the contract.
APCR
The guy . . . has quite an arrogant manner, has the dimension of being a European person working in Britain and plays the card of racial discrimination occasionally – so lots of underlying things, erm, to deal with it softly in the first instance. Okay. Lots of lots of visits, lots and lots of paperwork, lots and lots of letters, none of which produced a change in behaviour.
CC2
Summary: commissioners working with the contract
We found that it was not only practitioners who looked to ‘work around’ the contract rules; commissioners did too. They did this often strategically to try to reconcile competing imperatives: to adhere to bureaucratic rules passed down from the NHS hierarchy mandating that certain processes be followed, while trying to work towards a fair agreement with dental practitioners. We also observed commissioners willing to unilaterally revisit contract terms in order to achieve their managerialist and public goods goals where persuasion and negotiation with dental practitioners had failed. The terms of the contract becomes then the focus around which the struggle between commissioners and dental practitioners’ perspectives crystallise. With a contraction in the numbers of commissioners and a tightening of budgets, interpretation of dental contractual agreements was found to be becoming less flexible than previously.
Trust as an antonym for opportunism
In this section we move from the analysis of the behaviour of GDPs as agents and commissioners as principals, interpreting and working with the rules of the NHS dental contract, to explore the role of relationships in governing behaviour, as outlined in the theory review (see Chapter 1, Relational contracts). Proponents of this more sociological view of contracting argue that economic models concerned with opportunism place undue emphasis on unfavourable assumptions about the behaviour of agents. The sociological stance puts forward the relational theory view of contracting, presenting ‘trust’ as an antonym for opportunism, and thus a more favourable view of human nature.
In our qualitative data phase we explored the nature of relationships and trust in the dental and medical practice contracting context, to more fully understand what the concepts of ‘trust’ and ‘principal–agent relationships’ signify in these contexts. Their relationship to dental practice institutional logics, and to practitioner’s behaviour at both the micro level (dental chair side) and the macro level (approaches to commissioners), were then subsequently tested in our quantitative analysis.
Relationships and trust
Models of governance range from centralised command and control systems, as seen in the 1970s, to competitive market-based systems, as seen in the 1990s, which foster an adversarial approach between purchasers and providers. In the late 1990s, a ‘third way’ was proposed by the government, aimed at building on the strengths of each approach. The vision was to promote partnership and collaboration between clinicians and managers, focusing both parties’ energies on co-operation geared towards improving services. 28 This shift towards co-operation was intended as a cost-effective means of tackling the principal–agent problem. Central to this approach is the emphasis on developing mutual trust between purchasers and providers, with both parties appreciating that the contractual relationship is for the long term.
Trust is recognised as a multi-layered concept comprising a range of attributes. Although the term is freely used, it embraces at least three meanings: co-operation, confidence and predictability. 101 Synonyms for ‘trust’ often incorporate one or other of these meanings and the result is a verbal and conceptual morass. Previous study in this area is criticised as being surprisingly removed from context, even though relationships themselves are recognised as being embedded in social contexts. This is why, although we recognised from the theory review that trust and relationships would be important, we needed to define what they meant in the particular context we were studying.
We found that trust was most closely represented in the dental and medical practice context by the concept defined by Gambetta102 as ‘the probability that the Principal/Agent will perform an action that is beneficial or at least not detrimental to the other party, is high enough so that the principal/agent will consider engaging in some sort of co-operation with him’ (p. 217). We therefore conceptualised trust as ‘anticipated co-operation’. Trust is future orientated, and in the literature usually based on repeated previous interactions. 103 Lamothe and Lamothe104 use the same definition, and qualify ‘co-operation’ as including aspects of the contractual relationship which involve ‘fulfilling agreements and obligations, exhibiting fairness, sharing information and being flexible and responsive’.
Saunders and Thornhill105 identify that trust involves two elements: first having favourable expectations, and, second, a willingness to become vulnerable to the other party. Mistrust is conceptualised as the converse: having unfavourable expectations and an unwillingness to become vulnerable. 105 Others suggest that trust and mistrust are not two ends of a continuum, but represent different phenomena. 101 Our findings suggest that, in our context, trust and mistrust do represent different things. There is a further debate about whether mistrust is the same thing as distrust. However, since the terms ‘mistrust’ and ‘distrust’ are used interchangeably so often, there is a general agreement that they should be viewed as the same thing.
Summary: the role of trust
Trust is best conceived in the context of NHS dental contracting as ‘anticipated co-operation’. Our case studies indicate that, while trust (co-operation) is important, mistrust (or distrust) also has a role to play. Mistrust was best conceptualised in our study as having unfavourable expectations and being unwilling to be vulnerable.
Our findings also fit with the theory outlined by Atkinson and Butcher101 that, in certain contextual situations, sources of information from third parties (e.g. dental professional networks) influence relationships. Reputation is important. The theory indicates that stories from third parties invoke a process of amplification: they amplify mistrust in weak relationships more than trust in strong ones. This fits with the findings emerging from case studies, that shadows of the past, transmitted through political and professional networks, are influential in breeding mistrust. Moreover, while trust builds incrementally, mistrust has a more catastrophic quality.
The role of relationships
We found that relationships between commissioners and practitioners offered a means of changing mind-sets, enabling a working together to achieve public goods goals in partnership. The challenge for dental commissioners is greatest where GDPs logics are furthest from the managerialism and public goods logics of commissioners.
I want to understand why I can’t get dentists, some dentists, to change their bloody mind-set. The game of ‘I’m a dentist, end of story’ went years ago. You are a health-care professional with a specialisation in dentistry. You have premises and I want you to use that premises, I’d like to be able to turn around and say ‘Sarah comes in for a check-up, smoking cessation, I want you to deliver health checks, I want you to think outside of that bloody box for once and for all, but do not expect to get hundreds of millions of pounds cos I ain’t got it. Come in from the cold, don’t stay where you are’ and again, trust. They don’t trust us.
BC3
It’s difficult to establish a relationship how I’d explain it as better. I mean we’ve got one particular dentist who is single-handed; keeps himself very much to himself; doesn’t like any interference from the PCT, he’s never actually said that but . . . But that’s the feeling and whenever we’ve tried to move forward on anything it’s been very, very difficult to actually gain trust in each other and get that relationship going . . . but we’ve got him doing the clinical governance toolkit! Just about. But it’s certainly not easy to form a relationship with him because I don’t think he wants one.
BC2
Because it’s all about relationships and it’s about their understanding and sharing in terms of where you are . . .
2FC5
Building trust
Building relationships is time-consuming, but is a prelude to working co-operatively. Repeated positive and friendly interactions slowly and incrementally create an environment for mutual co-operation. It is also possible that mutual co-operation in itself creates a focus for the relationship to grow, giving rise to informality. Some commissioners have an active strategy to replace levels of mistrust with repeated, personal, more positive experiences. Moreover, when commissioners get to know practitioners and make positive assessments about their character, they also seem more open to move beyond suspicions of practitioner self-interest and engage in open discussion.
Getting to know the person is instrumental in building trust and overcoming mistrust. Conceptually therefore, we found it was personal trust (based on interpersonal interaction with a particular individual within a particular relationship) which was important in our context, as opposed to impersonal trust (based on roles, systems and reputation). 101 Building personal trust means that the parties are prepared to think the best of the other, when transactional interactions occur. Moreover, frequent and friendly interaction means that more adversarial conversations are avoided. It enables open conversations and honest exchange of views. Trust in this sense therefore breeds a sense of mutual reciprocation between parties rather than a general benevolence.
. . . what I’ve managed to achieve all these years has been largely through building good working relationships with individuals within the PCT on a one-to-one basis.
FM1
People get to know you and you develop mutual professional respect for them and they see you as someone decent, hard working and all those kinds of things, someone decent, honest, hard working, forthright, candid and all those things and you similarly find them as helpful sort of people who take their jobs seriously and are not just jobsworths who are there ticking boxes and you similarly develop respect for them. So when that direct interpersonal relationship is built up, you can get a lot of good work done.
FM1
What I liked about that was the fact that the practice that moved rang us and said ‘Can we have a chat’ and they pointed it out. They said ‘Look we are going to have to do this this and this and we are going to move over this particular weekend, we might not . . .’ so we are fully aware of it but thankfully we didn’t need to have a discussion. It’s when somebody does something and then they use it as an issue as to why they didn’t deliver.
BPCR
One of the things I introduced for the GPs was if a new practice manager came onto the patch into a practice I’d ring up and say ‘Hello, how are you? My name is [name deleted], how about coming in?’ ‘What for?’ ‘Well 10 minute conversation with the QOF Manager, 10-minute conversation with finance and blah blah blah, walk you round the building.’ Now any practice manager who joins this patch has a guided tour of the building and I introduce them to key players to bring down that level of mistrust.
AC1
I think once you’ve built up that rapport with them and they trust what you’re saying and they believe that if you say you’ll say something you do it, or if they, you know, if they’re assured that what you’re saying is either national policy or it’s something . . . you know the trust element is a massive part of the work with any of the professionals. Some of them it takes a little bit longer to build that up. So I think you build that with them and it really is a key element to anything. Even if it’s down to telling them that they can’t have something they understand that you’re not saying you can’t have it because I don’t like you, that you’re saying you can’t have it because it’s not available or you know it’s something that just can’t happen.
2AC2
He stands out because of the amount of the communications and respect that I think we have for each other . . .
BC1
Ironically dentists have rung me up about problems they’ve had with him [EC1] and things he’d said to them. Other dentists came by my way and phoned me up about it so I was disappointed because he’s always been proactive and a nice guy on the face of it who wouldn’t say bad things.
ED1
There are problems as well as benefits from the informality which gives rise to mutually co-operative relationships. Agreements based on ‘goodwill’ are often not committed to paper and, when circumstances change, verbal agreements prove to be worthless. Failure to honour the agreement can then give rise to a sense of violated justice. Informal relationships between some GDPs and commissioners give some practitioners access to soft information which can be commercially advantageous. For those without a close relationship, this can be interpreted as a lack of transparency and fairness.
And like I was in the area recently and just rang him on his mobile and said ‘I’m actually in another practice in [XXX], is it all right if I pop in’ so he said ‘Yes, make it 2 o’clock I’ve got a free . . . just pop in’. Because he is looking to move premises within the same locality because it’s not ideal where he is in a semi-detached house and you know he’s saying ‘What do you think of this, what do you think of this?’, you know looking at . . . and if I go for this is there any additional money?
DPCR
Had him [EC1] for about a year and he came and asked about more UDAs and I said ‘I’ll tell you what, [XX], don’t give me the money now. If I overperform then pay me. I don’t want you to pay me it all now because if you do and I underperform I don’t want to pay it back. If I have to then I’ll take the money and I’ll put it in an account and leave it’. It came to the stage where I’ve performed the UDAs, rang the PCT – ‘He’s left, someone else, [XX], lovely lady, all the time in the world for her’ – ‘Got no record of that, [XX], money’s gone’.
ED1
The trust environment: professional networks and distrust of the Department of Health
Mistrust diffuses through political and professional networks. The dyadic relationship between GDPs and commissioners is influenced by how GDPs feel about a third party: higher-level policy-makers. Memories, often about broken promises, go back to experiences from the 1990s, and from PDS pilots in the 2000s and since, and are influenced by professional networks. A ‘high trust environment’ was a policy phrase used at the time when relatively loosely specified early PDS contracts were created. Mistrust resides in networks of older generations of GDPs, but also permeates through dental networks. Online forums transmit reputational information from local to national networks and from national to local.
But there was also a bit of tension I think between [PCT C] and the dental fraternity. There was a bit of history of going back I think to the 1990s, before that even. Where they had not got the deal, perhaps again going back to this UDA value thing and financial deals at the time and the packages were not as good.
CC2
We are all very cautious. When we first went in the pilot scheme we were told by the Department of Health that you would have no financial implications upon your practice, we were guaranteed this. To be able to do the new pilot scheme we had, for example, to upgrade our software which was a financial cost to us and that wasn’t covered by the Department of Health and it wasn’t covered by the PCT.
BD31
My only experience of distrust has been from speaking to other dentists who have distrust with the Department of Health.
BD3
When we were in discussions with . . . and an LDC member they kept referring to ‘Well this is a high trusted environment’ and, basically, most dentists got their fingers burnt in some degree and that’s why we use it, it’s almost like a tongue in cheek . . . there is no trust, not any more. It is because it’s usually a subtle way of putting your point across to say that you know there is no high . . . the high-trust environment doesn’t really exist. It kept being used in LDCs, ‘It’s a high-trust environment, a high-trust environment’, and then all of a sudden, an awful lot of dentists were not so trusting shall we say? So when we say it’s because we’re saying we really don’t trust you any more.
CD1A
We have quite a lot of discussions anyway and we have a large network of dentists. So even though I am not directly involved with the LDC our network is big. So our conversations . . . it is just a different way of thinking. I think maybe, you know, without being ageist it is like the older-generation dentists, it is just more difficult to communicate with them. They are set in their ways, set in their mind-sets, you know, . . . they are too . . . stubborn in their own ways to be able to accept change, look for change or try and implement change, and they’ve had their fair share of distrust as well, so you can’t completely write off what they are saying because they have seen over the years how it’s gone and what mistrust they’ve had.
BD3
Equally we found evidence that mistrust of GDPs is transmitted through political and professional networks.
This is what we’re doing all the time because they do say that there’s a lot of money that’s being wasted through fraud.
BC Informal LDC
It’s more the, erm, you know I go to meetings and I went to Westminster Health Board, two of the industry ones, and it was talked about it a lot and it seems to be implied quite a lot that there are dentists who neglect patients.
CD3
Diplomatic means of managing competing logics
Discussions with commissioners are a means whereby commissioners hold GDPs accountable for their balance between competing logics: priorities concerned with their professional duty and other demands at the micro level (at the chair side). They are also a means to obtain a balance between similar conflicting logics at the macro level: achieving the most efficient use of public money while maintaining the viability of businesses. Relationships between practitioners and commissioners allow negotiation to reach mutually acceptable solutions increasing efficiency and equity while satisfying the goals of practitioners to maintain successful businesses and deliver high-quality care for individual patients. The work of commissioners therefore involves taking centrally defined policies and reconciling these with goals at the service delivery level. Being able to have a frank exchange of views represents a good working relationship, born out of a mutual respect for the other party. The nature of the relationship between contracting parties is one of diplomacy.
My relationship with the PCT as an individual has been on the whole, despite all my reservations about the PCT it has been a good professional relationship. So I’ve been quite fortunate in that sense to have a good working relationship.
FM1
They might ask my opinion on doing a specific function, and in the past they have. You know, ‘how did you find doing this piece of work’, just so that they can get an understanding of what they are asking, ‘is it difficult to do or is it easy to do, how much time has it taken you to provide this information?’ So I suppose if we didn’t have a good working relationship with them, they wouldn’t feel comfortable asking me and I wouldn’t feel as comfortable asking them.
FM21
I don’t mind having an open conversation and coming out with something that works for everybody, which is what we’re doing in [PCT B] now. What I can’t really deal with is the kind of the hiding and the letters to lawyers and the bullying.
BM1
I think the job of the PCT actually was to work to align its goals with that of its independent contractors and vice versa, and part of the ability for the PCT to be successful was how it was able to act as a filter almost for the information that was coming out of the SHA and the DH, and then work with the independent contractors to align what they were trying to deliver and build on their strengths that would then allow the PCT to deliver.
FC4
There were multiple ideas that got mooted and they actually went through each one. They [threatened to go private] you know they’ll move away, but if you do it with grown up wise everyone can say, you know I’ll take that, and they got the PCT access figures, they’ve hit their figures and we’ve got some more money and it’s actually worked as a team, rather than anything else, and I think that was the big plus.
ED3
I would give a balanced opinion with a common sense angle to it and certain things if they aren’t . . . if they’re not sensible, you just say so, it’s easier. People may not like that, particularly if they’ve spent a lot of time sitting down and drafting up various plans etc. I mean, it is public money and realistically, if certain ideas don’t work then you should really be aware of that. I mean it would be sensible to actually enhance, as I’ve said before, enhance effectively the practices that are already here . . . let them expand if they can.
AD1A
I suppose it depends upon the relationship that you have with the person from the PCT. We have a very good working relationship with the lady that has been coming to the meetings, and at times we might say ‘Sorry, if you feel like we are criticising, but this our point of view’ and then you will get her point of view. And then you can see the middle ground then. It is always good to get another opinion.
FM21
Some of the PCTs have tried to just to whip the rug out from underneath the dentist’s feet and it’s been a very uncommunicative way, whereas our PCT have the dentists involved with it, we came in with a solution with them . . .
ED3
Obviously our role is to challenge just as much as they were challenging us.
2AC2
They will always try and throw that in, I think, that you know . . . I’m, you know, I’m a clinician and I feel I’ve got ethical duties and I’ve got these duties to my patients. And I’m making the decisions based on what I think’s best for the patient. Rather than I’m just doing it to, you know, count activity or count access numbers or count whatever. So usually that is one of the main, I would have said the main argument.
2IC1
I mean to be honest you’re going to have conflicts with people who don’t believe your priorities are the right priorities or have different priorities and it’s then trying to persuade them that . . . you know come to a mutually agreed thing.
CM2
So you do try and be a diplomat in between certainly [name of DBC] and my bosses and the PCT. Because you still have to maintain that good relationship no matter what the pressure is from above [corporate managers].
CD2
While the ‘chemistry’ of personal commissioner–practitioner relationships is important, it is not all-important, for both practitioner and commissioners may adopt an active strategy that they will work co-operatively together, overlook any personality clashes and set aside disagreements.
I mean there’s people you don’t agree with but that happens in every walk of like. You just have to say this is a professional thing and just get on with it.
CM2
I have always said to [our practice manager] ‘Please try and get on well with these people, it’s really really important that we are not falling out with anybody. We will toe the line’. I want them to think we are good practice. So I am always, I am sure [our practice manager] does that and she is on good terms with them all and we don’t try and stand out as being obstructive in any way.
DM2
Not all PCTs, though, were equally receptive to working with GDPs; some practitioners attempting to suggest solutions found themselves ignored. A perceived lack of openness in the contractual relationship makes it difficult to work together.
I wrote a fairly boring three-page letter explaining to the PCT how we could fund it and how we could do this and how we could do that and what the benefits of it all where. But that was ignored, they didn’t even reply to it. That’s an example of the PCT, they didn’t even reply to the letter.
BD2
. . . having meetings with the PCT, we give them information but it doesn’t come back. It’s not a relationship, it’s more dictatorial.
BD1
You are open with what you are delivering, they are open with what they are giving out and what they are looking at – it can work really well. But if you are dealing with people who are very closed behind doors, not very flexible, lack of contact, then it gets very difficult.
BD3
There are mutual benefits where practitioner–commissioner relationships are co-operative. Where commissioners have a working relationship with practitioners with opportunities to work up solutions together and shape commissioning decisions, practitioners more fully appreciate what commissioners are trying to achieve (and vice versa). This type of relationship is seen more often between GMPs and commissioners than with GDPs. Practitioners working with commissioners may see benefits in terms of expanding their businesses because of new developments.
If something’s fully engaged and I said aligned, twin pillars, something like a double helix, that they are so intertwined, so that when you’re setting out what you want to deliver with the service you’ve got clinicians engaged, shaping your thinking and that they’re fully linked in to each part of the cycle, each part of the commissioning cycle, so that they are aware of what you’re setting out to do, what’s your problem, have you assessed your need, have you communicated that need to clinicians, and then what services need to respond to that need, how much, where should they be, what should they look like, again, clinicians need to be engaged.
SKP4
I’m just taking patients on anyway, we took 300 new patients on last month and it’s really worked. We’ve worked with the PCT rather than against each other and actually just talking.
ED3
He piloted when we first did this clinical governance toolkit, he piloted that with his staff. We provided some funding for him to expand, but it was all part of those discussions and having a good relationship that he felt he could come . . . and he felt that there was a very good relationship there and he still today will ring me up ‘I’ve got this bit of problem and I don’t know . . . what do you think?’
BC2
It’s worked symbiotically, it’s got the NHS PCT sorry, out of their hole because they’ve had to provide a service, fraction of the cost for them and it’s . . . compared to normal NHS work, relatively lucrative.
ED12
Without a relationship between commissioners and practitioners which is based on mutual respect and co-operative working, the relationship becomes adversarial, with reduced willingness to engage in benevolent behaviour. The terms and form of the contract determine the balance of power between the parties. Instead of a virtuous cycle of mutual co-operation, the contract can be used increasingly as a means for exerting control over practitioners, and as a way for practitioners to defend their position.
[PCT A], with all due respect, aren’t very interactive with the practitioner. It could even be, as I see quite a few of the practitioners in the locality, one could even sense that the practitioners would consider that there is possibly even an element of bullying that does occur. Well, I think the thing is that practitioners are vulnerable and obviously the contract that the primary care trust holds, you have to comply with and it’s a very powerful weapon. And the primary care trust can abuse their power and indeed choose almost what they want to do.
AD1
Sometimes clinicians feel that things are done to them, they don’t always understand the terms of the contracts or for that matter they see measures within contracts that don’t capture what they’re delivering to their patients and what they value, which might be quality, which might be taking time with someone who’s got very high needs and that perhaps the contract terms and the contract as a tool isn’t capturing what they’ve delivered and they don’t feel valued and therefore they’re disengaged and they feel disempowered.
SKP4
I think there is always room for negotiation. And I’m not sure people retain what’s in that contract in their head. And if you’re somebody who knows your contract by heart then you’re probably less flexible than is ideal in this kind of work.
DM1
If they try and make the contract more rigid, these are the elements of good practice which are not contractually binding, will just fall by the wayside, because the more people are put under pressure the less room there is for them to, you know, to be, sort of, you know, going beyond their call of duty.
FM1A
We need to sit down with four of them and say ‘Right, what’s going on?’ Cos I know what they have done, I mean the contract variation they are quoting chapter and verse on, that’s fine, but I don’t get a pink and fluffy feeling about this.
BPCR
I’ve got contracts at home I dare not leave in the practice just in case the practice burns down because it’s the only thing I’ve got, my rights in this contract. And it’s got the Chief Executive’s signature on it and that’s fine.
BD1
Perceived injustice in a fragmented professional network
Contractual justice has three elements: (1) a fair exchange; (2) honest dealing; and (3) keeping one’s promises. 100 While some PCTs use a flexible approach in negotiating with practitioners, outside the dyadic commissioner–provider relationship, this can give rise to problems. Relational contracting by its very nature is informal and does not lend itself to transparency and consistency. Since GDP networks are fragmented and because dental practices are commercially orientated, there is a suspicion of some practitioners being given more favourable deals than others. Fairness in terms of one immediate relationship between commissioner and GDP can be viewed as unfair by other practitioners looking on. Without open channels of communication, conspiracy theories arise. Dental practitioners are characterised as more individualistic than medical practitioners, and more isolated from their peers, which fosters a spirit of suspicion. Information is transmitted through networks as rumour, and allegations of dishonest dealings arise. GDPs can accuse commissioners of exploiting the fragmented professional network to exert power, even attempting to ‘divide and rule’ between partners in a practice.
I think part of the problem is compared to the medics we’re a bunch of individuals.
BD2
Dentists are left on their own, dentists are isolated people, we are isolated and we’re all in our own little practices, we don’t get an awful lot of communication, we have meetings with the PCT, dentists, etc. But you’re all sort of in your own practices, you’re a little bit isolated . . . I think you’re really left to your own devices a lot and that’s the way it always has been.
AD2
They wouldn’t tell us what our UDA value was going to be. They kept telling us we would work things out in this way or that way but it was not in the slightest bit transparent. They started to get individual practitioners and do deals with them, which was pretty obvious to me and all the dentists round here. It was to my mind a bit divide and conquer.
DD1
We should all go and tell . . . tell the CQC where to get off because if none of us register then they can’t deregister all of us. But, you know, even Arthur Scargill couldn’t keep it together. Oh, herding cats. Yeah, they’re very, it’s a very selfish profession. I don’t mean selfish greedy, I mean selfish cut off and I’m the best dentist in [PCT B] – if you ask [BD1] when I’m not in the room, he’s the best dentist in [PCT B].
BD2
And there is sort of this attitude of divide and conquer, and obviously a couple of practices have been expanded, we don’t resent that. But we’re not quite sure why those practices expanded and we weren’t approached. We thought, it seemed to be grace and favour . . . and they were giving different deals to different people for different reasons. And we thought ‘No, not interested really’.
BD1
Now we did find quite a lot of conflict in our . . . but we had to manage that in terms of, you know, leaving their LDC hat at the door, their contractual hat and concerns about their individual contracts and just think of the wider population and the patient base and it was very difficult.
2AC2
They just get on with things in their own little isolation, they don’t know what’s going on nationally, they don’t know what’s going on with the PCT.
APCR
There are some dentists who they [PCT E] don’t like and some that they do like and he’s in the ‘do like’ category. I mean there’s another couple of dentists you know who do all right with them.
ED2A
They approached one of our partners independently, individually, and said ‘Would you like to stay in the NHS?’ for example.
DD1
Co-operation alongside mistrust
Stories from other GDPs as well as their own experiences with commissioners, where verbal promises were made by a particular commissioner and then not honoured, have meant GDPs are guarded about becoming vulnerable. This does not mean that these practitioners will not adopt a strategy of co-operation with commissioners; rather, where they decide to co-operate, they will protect their own interests, knowing that the agreement and the relationship may change. While practitioners who trust are likely to co-operate with commissioners, practitioners may still co-operate even if they mistrust. This suggests, as put forward by Saunders and Thornhill,105 that trust (anticipated co-operation) and mistrust (unfavourable expectations and unwillingness to be vulnerable) are not mutually exclusive, because it is possible to both trust and mistrust at the same time, sometimes concerning different issues. Lamothe and Lamothe104 talk about ‘the shadow of the past’, but suggest that some providers may view this as merely as a ‘sunk cost’ because the past relationship is not part of calculating the benefits of future co-operation – the ‘shadow of the future’ is more pertinent. Thus practitioners, while being guarded, may decide to co-operate.
I was agreeing to something that I didn’t know. It was a leap of faith and there was no . . . that trust relationship had well and truly gone.
CD1
Oh yes, you can’t do all of this work without the trust. There has to be an element of trust and notwithstanding all my reservations I do trust them. I don’t necessarily trust them 100% largely because I don’t trust them to look after my interests. I’ve . . . I trust them because they have a job to do.
FM1
Do I raise a fuss and scream and shout because there are records of the meetings somewhere, he came here and who is going to turn away money? Practice manager could have screamed and shouted and raised issues with the PCT, but I have my contract value and I don’t want to get ‘What’s the point in crying over spilt milk, what’s the point of saying that you promised me’ . . . there is nothing going to happen, one. Two, you’ll get their backs up, ruin personal relationships.
ED1
General dental practitioners expressed mistrust in terms of expectations that they might be treated unfavourably, with consequent passive or hesitant behaviour when relating to commissioners. Our data also confirm that, while trust takes a long time to build, mistrust occurs more easily, with the ‘leap of faith’ often taking place at an earlier stage.
I was told that we’d still listen but yes the decision had been made. I just felt it would have been . . . for someone who has been down for the first time it may have been fair to say okay you can have 50% claw back or you know . . . like I mentioned I thought it would have been fair to have the 4% over because we were so close to it and maybe claw back that 0.8% or something, but there was no . . . and from that day then it also put in my head that the days of being flexible are gone. Because in the past, not that we were ever down, but I know previous people have been down and they’ve been much more down than us and not had the reasons we had and they have been allowed to carry over. I mean obviously if they’re down again that’s different. So I just felt from that . . . for all of us it was a bit of a shock, a bit of a surprise and we thought we need to be on our guard.
BD3
What trust has been built up for those dentists has totally gone and other dentists who . . . I’ve had a great working relationship with [PCT B], it makes me super wary, anything I get in the letter, any letter, any post, any formal meetings, any informal meetings, makes me very, very wary.
BD3
The balance of power: general dental practitioners, general medical practitioners and commissioners
The dental contract is more specific than the one governing medical practice. Greater specificity of the dental contract provides more levers for performance management, but at the same time affords more protection for the providers to defend what is legitimate. The extent of information gathered about practice activity allows questions to be raised about the way the contract is delivered.
With a GMS contract you’ve got essentially additional services and a very loose – about eight statements are loose . . . ‘to provide family planning services’, ‘to provide minor surgery’ . . . and the definitions are very very poor and then the rest of the contract is about definitions and terms, what this might include and what that might include. And then that’s backed up with standard financial instructions so they’ve got a series of entitlements they can claim. The dental contract is fantastic because it says ‘BC1, if this dentist doesn’t deliver within 4% tolerance, have a word’. It says in black and white, it’s brilliant.
BC1
What I’m saying is the contract is a damn sight easier to manage than the GP one. Where the power balance is not necessarily in my, sorry, our favour. I think it’s more biased because dentists can turn around and say ‘Go away, stop playing silly beggars’ and that’s fine, I don’t mind that because I think some PCTs would abuse that if they had the chance. But equally it makes it simple if it says in the paragraph ‘Let’s just do it’. So I think the balance of power is a lot more shared and a lot better than the GMS and the GPs because the GPs certainly have the balance of power with that contract. We can’t, it’s difficult.
BC1
I’ve been in the trenches now for 6 years where I’ve worked with doctors, dentists, pharmacists and opticians and the easiest or the hardest one to work with is the GPs because even in the contract it says ‘You must provide reasonable services between 8 a.m. and 6 p.m. for patients blah blah blah’. OK guys, so that tells me your doors have got to be open between 8 a.m. to 6.30 p.m. No it doesn’t. It says provide reasonable services, well, what do you mean by that? Well, we put our phones through and take them back at 8.30, 9 a.m., and that time the patient can ring up but the patient can’t get access to you can they? No. Can they make an appointment? No. Can they pick up a repeat prescription? No. That’s not reasonable. Define reasonable. And that’s the type of semantics you get into. But with the dentist it’s open at 9 a.m., closed at 5 p.m., if you’re closed on a Thursday afternoon then make sure somebody else has got that written in the contract. It is and at least it removes the ambiguity and the dentist has very little room for their own interpretation, clinically obviously. But it makes it because the relationship can be so much more civilised.
BC1
Dependency
Some dental cases showed GDPs trusting commissioners that they would be treated favourably, most notably in a relatively new practice set up in premises owned by the PCT (case AD3). This case was characterised by a high degree of dependency and hope rather than expectations of being treated favourably based on prior experience, because of a co-ownership of assets between the PCT and GDP, and mutual contract goals. PCT investment in the practice as a PDS+ practice was geared towards meeting PCT access targets. This meant that commissioners had an interest in the new practice succeeding as a business in order to deliver public goods goals. The GDP, recognising the mutual interest and dependency in the relationship, held (perhaps naively) favourable expectations of future PCT actions despite his professional network colleagues pointing to the PCT’s reputation, which indicated otherwise. The relationship here though looks more akin to an employee–employer relationship than a market-based governance model. There were other examples, too, where the PCT had invested heavily in terms of both financial risk and risk of delivery of access targets, with commissioners again becoming closely involved in delivery issues as if they were directly managing the service.
Again there might be some leeway in September and they might give a couple of thousand UDAs extra if you are continuously over. There is definitely a way you can speak to them; you can tell them you are way beyond the targets on a regular basis.
AD3
I had words from my solicitors saying the PCT doesn’t have a good . . . things like that but trust me I have nothing bad to say about the PCT at the moment.
AD3
He feels like we’re micromanaging him. But we’ve got to. We’re anxious about the service, we’re anxious about the financial risk to the PCT, so there’s lots of issues. So it has been a hard slog and we are constantly, because its literally down the road, we are constantly . . . and he does feel like we’re big brother monitoring him, but it’s a new start-up, we’ve given him lots . . . , we’ve got to.
DPCR
The relationship of GMPs with commissioners is also characterised by a mutual dependency. They have greater ties to the NHS in terms of transaction-specific assets (premises, computers, etc.), and the relationship is geared more towards hierarchical than market-based governance.
Although we are self-employed a lot of GPs do act as almost on an employed basis.
SKM1
The NHS supports GP practice in a much greater way than it supports dentists because obviously GPs get their rent reimbursed, they get, you know, all their computers provided, so it’s a ‘business’ in a very loose sense of the word, whereas a dental practice, the only thing that they get from us apart from the contract is we reimburse business rates, which is, in the great scheme of things, is minimal you know and that’s the only real reimbursement they get.
2AC2
They [GMPs] need to make sure that their relationship with anyone who’s in control of their NHS income . . . are appropriate. The relationships are there. They assume that they are going to receive the money when they wish to have it. If they’re wishing to develop any of their premises on behalf of their patients, again, they are assuming there is going to be the funding to support them in that. So they, their future and the development of their practices is all tied in with them being NHS.
2HC1
Summary: the role of relationships
Repeated positive and friendly interactions slowly and incrementally create an environment for mutual co-operation between practitioners and commissioners. Trust breeds a sense of mutual reciprocation between parties rather than just a general benevolence. Relationships therefore give a forum for a diplomatic resolution of differing practitioner and commissioner perspectives. The downside of building relationships between practitioners and commissioners is that informality opens the door to a lack of transparency and perceptions of unfairness by those not involved in the relationship. With commissioning structures and personnel in flux, verbal agreements can be over-ridden, with resultant perceptions of unjust dealings. While trust takes a long time to build, mistrust occurs more easily, with the ‘leap of faith’ often taking place at an earlier stage. Mistrust diffuses through political and professional networks and online forums transmit reputational information from local to national networks and from national to local.
General dental practitioners working with the contract: macro-level behaviour
Strategies which GDPs adopt in how they communicate or resist commissioners can be pictured as macro-level behaviour (see Chapter 1, Quasi-markets in health care).
Insights from institutional theory suggest that resistance to institutional change can take many forms. Oliver87 suggests a range of strategic behaviours are employed by actors, ranging from passive conformity to proactive manipulation. Our case studies indeed showed a range of strategic approaches employed by GDPs in relation to PCT commissioners, although the typology is not an ‘either–or’ arrangement, because practitioners may move through a range of approaches as events unfold. We describe below the types of GDP approaches observed in relationships with commissioners.
Active co-operation
Some GDPs set out to develop open lines of communication with commissioners in order to foster a spirit of co-operation. Whether or not this is a form of ‘proactive manipulation’ described by Oliver87 is hard to judge because motives are not always clear. The proactive co-operation strategy does appear (sometimes) to bring business benefits where GDPs set out to understand the commissioner’s agenda and ‘way of doing things’, and some GDPs will actively champion the PCT reputation among the dental network.
But I think it is important to establish a good relationship with the PCT and if you have that relationship there then you can get the help there as well.
BD3
You just try and build a relationship with them which says ‘Commission with what you know’. But it doesn’t work (laughter). It just doesn’t work.
CD1
But since then we’ve worked closely, we’ve actually increased contract values through a bidding process, his contract values increased and his . . . he actually writes professional bids and he listens to what we’re saying and what we’re looking for. He sits on our Dental Health Steering Group and again listens to what’s going on, gives us his feedback.
AC2
I have a very good relationship with the PCT and I’m actually going to do something totally about that and I’ve even written something on the internet on a blog site . . .
ED1A
Acquiescence
We found some practitioners neither actively co-operating nor openly defiant and resistant to commissioners. They complied with PCT procedures by obeying rules and accepting new norms in a resigned acceptance, or imitated them by mimicking new practices while continuing old ones – merely giving an appearance of compliance. The latter here suggests a pacifying tactic and represents only partial compliance. Oliver87 characterises pacifiers as typically mounting a minor level of resistance to institutional pressures but devoting most of their energies to appeasing or placating the source of pressure. Compliance may also take the form of compromise and balance, where practitioners attempt to accommodate conflicting demands. They take the rules, and then go away and work out a way to make them work for their practice.
So three of us went, confronted him with this, he basically said ‘Hands up I’ve been doing it wrong’, but pleaded ignorance.
CC2
No, there is nothing I can do to influence it. Well, you can work longer hours but you can’t work long hours because you already work long enough. But having said that if you are over, which it was last year, I think I had a couple of days off in March.
DD2
So if you had, little white lies, and you went through and ticked all the boxes and then if you actually did get past that you could then go back and do it all. That’s the way.
BD1 LDC Debrief
So I said ‘All right if that’s what you’re giving everybody’, I took him at his word, and I said ‘I’ll have that’. Yes, we had no idea, you know. I mean I could have played hardball, it would have been very interesting to see if I could have got any more; you don’t know how desperate they were at the time. At the moment it’s working. It’s not too bad. You know on the average I’d like to be on £25, same as everyone else. But it’s working reasonably well.
FD2
No, what they did, it’s dead sneaky. You’ve got a contract, you make a partner on your contract – ta dah. So you retain your £32 per UDA but I’m on there to provide UDA so if you carry off on holiday I can do work on your behalf.
BC1
Defiance
Oliver87 suggests that defiance as an active form of resistance to institutional pressures can be expressed as three tactics in order of increasing resistance: dismissal, challenge and attack. In case studies we observed all of these approaches.
I thought it was an outrage and I wanted to send a nasty letter back but the solicitor stopped me so no letter went back to him. He did demand a response but he never got one.
ED2A
He can just challenge everything you do. Like if you wanted to come he would . . . ‘Why? What?’ . . . He likes to challenge!
BC2
He was always maligning the PCT, he never had a good word for the PCT. He had written in umpteen letters . . . in fact we only ever sent letters via the lawyers to him to stop writing these letters, it was alleging that I was, you know . . . it was my fault that the emergency dental out of hours service was poor and that it was my fault that I never listened to him when he was on the LDC and he was very . . . his letters were aggressive and vindictive and without foundation and, at one point the PCT was going to involve that clause . . . what’s the clause when someone is . . .
DC3
Challenging because we’re constantly on the phone to inform him of what’s happening but we’ll always be trying, I feel is always trying to catch me out or trying to, if we’ve got changes we’re trying to implement he’ll always try to throw a spanner in the works with it. So there is . . . it challenges my knowledge of how things work.
AC2
When the infection control team had to go in, we had two infection control senior nurses who were on the Look Back exercise. I needed one of these nurses to come to one of the practice manager’s meetings a month later. It must have been about 6 months later after this incident had all been sorted and forgotten and he did a presentation on the infection control and the HDMO105 and she was firing questions. She must have questioned him on about six occasions, whereas other practice managers may have asked one question and he came out of that meeting and he said ‘I am totally drained. She’s purposely done that to try’. To try to make him fall down in front of everybody.
DC2
[GDP] you’ve caught me out. I’ve no idea. I didn’t realise there was an alert . . . I will have a chat with [BC2] first thing in the morning and come back to you.
Yes, it’s not an ambush. I only got the e-mail myself this morning.
BC and GDP B Informal LDC
By the time you’re hammered, you know not only will I destroy you but I’ll sue your arse off you as well and I’m happy to have that sort of ‘fight’ shall we say, but it’s not going to be consistently comfortable for whoever wanted to try and do that.
AD11
Sometimes the battle takes the form of attrition with each party trying to wear the others’ resistance down.
To cut a long story short he decided to take me to the NHS Litigation Authority. So that went on for months and months and months and months and ultimately thankfully they’ve come down in our favour and upheld. And at one point it was getting quite nasty because he was throwing so many information requests which kept us busy for weeks and I think he was hoping I was going to go away but I don’t. I never go away, I never do.
BC1
When he’s worn us all down he’ll probably retire!
BC2
He’s one of these people who compulsively comes back and back and back and asks us again. I am sure he asked me when I took over from somebody else, I am fairly certain he will be asking [XXX]. [XXX] and I work closely together, so he won’t get a different answer.
CC2
Case studies revealed many examples of defiance in the form of legal challenges, some of which arose during the course of the study. Resolution through a legal route though was potentially costly in time and money and had to be carefully considered, for both GDPs and commissioners.
But we haven’t got the time to go off and get people up in court. We can take it to the NHS LA [Litigation Authority] if we wish to.
BD1
And it went so far with solicitors and the PCT decided to back down and reinstate the contract on a smaller scale.
DPCR
Yes, judicial review, everything, and he refused, we ended up offering to settle out of court and he refused and was very very nasty. And I felt really really sorry for [AC1] during the whole thing. We spent days in court together and it wasn’t pleasant.
AC2
To cut a long story short he decided to take me to the NHS Litigation Authority. So that went on for months and months and months and months and ultimately thankfully they’ve come down in our favour and upheld.
BC1
Summary: macro-level behaviour of dental practitioners
A range of strategic approaches are employed by GDPs in relation to their dealings with PCT commissioners. Practitioners may proactively co-operate, have a resigned acceptance (acquiescence) or be defiant (either openly or subversively). The typology, however, is not an ‘either–or’ arrangement, because practitioners may move through a range of approaches as events unfold.
Quantitative findings
In this section we report the findings of our quantitative work, the methods of which we have outlined earlier (see Chapter 3, Questionnaire to general dental practitioners). We have included the description of the sample and response rate in the methods section. Here we focus on predicting GDPs’ behaviour relating to six grey areas of the NHS dental contract (their micro-level, i.e. dental chair-side, behaviour) and their more strategic (macro-level) behaviour towards commissioners. In our quantitative work we particularly investigated whether or not the institutional logics we had identified earlier in our qualitative work could be substantiated and confirmed by the quantitative work, and whether or not these have a role in predicting how GDPs behave in relation to the contract.
Reported behaviour in relation to six grey areas of the contract, descriptive and injunctive norms
All six types of behaviour were reported by at least some of the GDPs respondents, with around 20–70% reporting having behaved in that way in the previous 2 years. Descriptive and injunctive norms were higher (Table 7). Over a quarter of GDPs thought that almost all GDPs would approve of either not taking on NHS patients or restricting types of NHS treatment because it represented a financial loss to the practice. Alongside this we present the views of commissioners gathered from phase 3 telephone interviews (Table 8). Although the sample of commissioners is small because of the qualitative method used, commissioners saw these six types of behaviours as mainly undertaken exceptionally or occasionally, while recognising that over 50% of GDPs would approve of behaving in that way.
| Grey area | Behaviour | % GDPs estimating what proportion of GDPs would approve of the behaviour | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Never | Rarely | Once | Often | Routinely | None | < 10 | 10–50 | 50–75 | Almost all | ||
| Avoiding high-cost patients (NHS dentists/practices in England not taking on a NHS patient because that patient represents financial loss) | Past | 65.8 | 16.3 | 11.8 | 3.8 | 2.2 | 1.3 | 12.9 | 36.0 | 24.6 | 24.9 |
| Intended | 45.3 | 20.1 | 16.8 | 10.4 | 7.4 | ||||||
| Other dentists | 3.4 | 5.3 | 27.6 | 43.6 | 19.7 | ||||||
| Restricting high-cost treatment (NHS dentists/practices in England restricting doing certain types of treatment such as root canal treatment) | Past | 53.4 | 21.4 | 14.7 | 7.3 | 3.2 | 0.9 | 9.4 | 30.7 | 30.4 | 28.2 |
| Intended | 41.3 | 23.4 | 19.7 | 11.0 | 4.8 | ||||||
| Other dentists | 1.3 | 2.8 | 27.3 | 46.7 | 21.6 | ||||||
| Over-representing patients’ diagnoses (NHS dentists/practices in England undertaking more band 3 treatments towards the end of the financial year) | Past | 43.5 | 23.3 | 22.7 | 8.6 | 1.6 | 2.2 | 23.0 | 37.1 | 24.0 | 12.8 |
| Intended | 35.8 | 26.1 | 25.2 | 10.6 | 3.3 | ||||||
| Other dentists | 2.2 | 11.1 | 40.0 | 34.0 | 11.7 | ||||||
| Inequitable care (NHS dentists/practices in England stopping doing routine care for patients towards the end of the financial year) | Past | 74.0 | 11.5 | 8.7 | 4.5 | 1.0 | 4.1 | 28.0 | 36.0 | 18.8 | 12.4 |
| Intended | 63.1 | 19.4 | 10.7 | 4.9 | 1.6 | ||||||
| Other dentists | 3.2 | 14.9 | 48.1 | 27.5 | 5.7 | ||||||
| Under-representing patients’ copayment [NHS dentists/practices in England undertaking some treatment as a band 1 rather than a band 2 (filling) where the filling is small and they are concerned about fairness of patient charges] | Past | 34.4 | 13.8 | 23.8 | 17.4 | 9.6 | 8.3 | 37.1 | 34.5 | 11.2 | 8.0 |
| Intended | 34.1 | 17.4 | 24.4 | 15.1 | 8.0 | ||||||
| Other dentists | 8.2 | 33.9 | 40.8 | 12.3 | 4.1 | ||||||
| Overallocation of treatment resources because of patients’ demands (NHS dentists in England being more influenced by what the NHS patient wants when setting a recall period than in strictly following NICE guidelines) | Past | 8.1 | 23.9 | 32.0 | 27.5 | 8.1 | 0.6 | 18.7 | 40.6 | 28.9 | 10.5 |
| Intended | 8.7 | 22.7 | 34.3 | 26.2 | 7.8 | ||||||
| Other dentists | 0.3 | 16.5 | 38.9 | 36.4 | 7.6 | ||||||
| Grey area | n (%) GDP past behaviour | n (%) GDPs who would approve | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Never | Exceptionally | Occasionally | Routinely | Don’t know | None | < 10% | 20–50% | 50–75% | Almost all | |
| Avoiding high-cost patients (NHS dentists/practices in England not taking on a NHS patient because that patient represents financial loss) | 1 (11.1) | 3 (33.3) | 5 (55.6) | 0 (0) | 0 (0) | 1 (11.1) | 1 (11.1) | 1 (11.1) | 3 (33.3) | 3 (33.3) |
| Restricting high-cost treatment (NHS dentists/practices in England restricting doing certain types of treatment such as root canal treatment) | 0 (0) | 3 (33.3) | 4 (44.4) | 2 (22.2) | 0 (0) | 0 (0) | 1 (11.1) | 2 (22.2) | 3 (33.3) | 3 (33.3) |
| Over-representing patients’ diagnosis (NHS dentists/practices in England undertaking more band 3 treatments towards the end of the financial year) | 0 (0) | 5 (55.6) | 3 (33.3) | 0 (0) | 1 (11.1) | 0 (0) | 1 (11.1) | 2 (22.2) | 3 (33.3) | 3 (33.3) |
| Inequitable care [NHS dentists/practices in England stopping doing routine care for patients towards the end of the financial year (in the last 5 years)] | 0 (0) | 5 (55.6) | 3 (33.3) | 1 (11.1) | 0 (0) | 0 (0) | 1 (11.1) | 3 (33.3) | 3 (33.3) | 2 (22.2) |
| Under-representing patients’ copayment [NHS dentists/practices in England undertaking some treatment as a band 1 rather than a band 2 (filling) where the filling is small and they are concerned about fairness of patient charges (in the last 5 years)] | 3 (33.3) | 6 (66.7) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 5 (55.6) | 0 (0) | 2 (22.2) | 2 (22.2) |
| Overallocation of treatment resources because of patients’ demands [NHS dentists in England being more influenced by what the NHS patient wants when setting a recall period than in strictly following NICE guidelines (in the last 2 years)] | 0 (0) | 2 (22.2) | 5 (55.6) | 2 (22.2) | 0 (0) | 1 (11.1) | 5 (55.6) | 1 (11.1) | 2 (22.2) | 0 (0) |
Table 7 shows the distributions of responses relating to various behaviours, intentions to engage in behaviours over the next 2 years, and descriptive and injunctive norms. Higher levels of past and intended behaviour were observed for patient-interested behaviours (under-representing need for patients’ co-payment and over-riding NICE recall guidelines to accommodate patient wishes). These two items also showed greater correspondences between prior and intended behaviour. Intentions to engage in the first four behaviours were considerably higher than previous behaviour, but not the final two. This may be an artefact of the methodology, but one interpretation for this is that dentists were intending to change their behaviour to engage in more behaviour against the interests of commissioners than in the past (possibly as a consequence of completing the questionnaire).
Factor analysis of institutional logics
Following on from our qualitative work in which we identified four interacting institutional logics reflecting the ‘common meanings’ of dental practitioners, we used factor analysis to examine the structure of these logics, hypothesising that the 47 items put into the analysis would form identifiable factors that were analogous to the four logics uncovered. The items did indeed emerge from the analysis around four factors, although the four factors gave a slightly different, and more nuanced, conceptualisation of institutional logics than had been drawn from the qualitative work. Table 9 shows the final analysis with eigenvalues and the percentage of variance accounted for by each factor, loadings of individual items of greater than 0.30 on the pattern matrix and interfactoral correlations.
| Factor 1: entrepreneurial commercialism | Factor 2: duty to staff and patients | Factor 3: managerialism | Factor 4: public goods | |
|---|---|---|---|---|
| Eigenvalue | 8.30 | 4.39 | 2.44 | 1.50 |
| Variance (%) | 21.84 | 11.56 | 6.41 | 3.96 |
| Pattern matrix loading | ||||
| 2 Supporting staff through personal difficulties | 0.587 | |||
| 3 Having a practice business plan | 0.435 | |||
| 4 Having harmonious relations in the practice | 0.630 | |||
| 5 My responsibility for the care provided | 0.489 | |||
| 6 Happy atmosphere amongst staff | 0.655 | |||
| 7 Opportunities to sell to the patient | 0.548 | |||
| 8 Reputation of the practice in the local community | 0.374 | |||
| 9 Maintaining business to secure staff employment | 0.517 | |||
| 11 Staff should share same work related values | 0.578 | |||
| 12 Identifying new business opportunities | 0.764 | |||
| 13 Practice endures for longstanding patients | 0.648 | |||
| 14 Retaining staff in the practice | 0.725 | |||
| 15 Receiving support from staff | 0.643 | |||
| 16 Equal care standards whether NHS or private | 0.359 | 0.348 | ||
| 18 Discuss treatment options with patients | 0.408 | |||
| 19 Dentists professionally responsible for patients | 0.421 | |||
| 20 Financial implications of advising patients | 0.316 | |||
| 23 Patient satisfaction with care provided | 0.456 | |||
| 24 Accountable to commissioners for care | –0.379 | 0.384 | ||
| 25 Review of practice policies and procedures | –0.726 | |||
| 27 Care as part of a publicly funded system | 0.656 | |||
| 28 Expanding the practice as a business | 0.859 | |||
| 29 Building goodwill to enhance value of practice | 0.548 | |||
| 30 Paper trail of practice procedures | –0.655 | |||
| 31 Payment schedule statistics for performance information | 0.403 | |||
| 32 Supporting staff through professional difficulties | 0.640 | |||
| 33 Using public money in cost-efficient way | 0.585 | |||
| 34 Feeling part of the NHS | 0.592 | |||
| 35 Expanding the practice as a business | 0.863 | |||
| 36 The branding of the practice | 0.741 | |||
| 39 Business aspects of the practice | 0.667 | |||
| 40 Positioning the practice in the market place | 0.772 | |||
| 42 Reducing population inequalities in oral health | 0.567 | |||
| 43 Adapting the business in a changing environment | 0.563 | |||
| 44 Remuneration in line with years of training/skills | 0.341 | |||
| 45 Identifying new business opportunities | 0.867 | |||
| 46 Regular review of practice policies and procedures | –0.785 | |||
| 47 Being highly regarded by other local dentists | 0.404 | |||
| Factor intercorrelations | ||||
| Factor 1 Entrepreneurial commercialism | 0.19 | –0.19 | 0.10 | |
| Factor 2 Duty to staff and patients | –0.29 | 0.18 | ||
| Factor 3 Managerialism | –0.15 | |||
Factor 1 closely resembled the entrepreneurial commercialism logic which was described in the qualitative work: characterised by higher loadings on the importance of seeking commercial opportunity; particularly geared towards expansion and marketing of the business.
Factor 2 was characterised by higher loadings of items concerning a ‘duty to staff and patients’ and was therefore labelled as such. Items most highly correlated within this factor concerned reciprocal relationships with staff within the practice, although also correlated were items related to a responsibility to patients and the importance of professional reputation. All the items which fell within factor 2 were derived from what we had pictured as expressions of either ownership responsibility logic or professional clinical values logic from our case study work. There were also a few other items originally composed in relation to expressions of ownership responsibility (‘being able to determine the “ethos” of the practice’) and professional clinical values (‘doing the best for the patient’, ‘putting the patients’ interests higher than business interests’, ‘making treatment decisions dispassionately’), but these were not correlated sufficiently to load onto factor 2, nor did they feature in a separate factor.
Factor 2 prompts us to query our previous conceptualism of professionalism logic. In the qualitative work we identified ‘professional clinical values’ logic as embracing various aspects of professionalism, which includes the focus on high standards of clinical excellence alongside self-governance of the profession and altruistic motivations to work in the best interests of the patient – a concept previously articulated in the wider literature on professionalism. 106 Our quantitative analysis, however, showed a strong relational form, where caring was seen as an extended process that radiates from high-quality relationships within the practice to encompass patients and the community. This incorporates characteristics of ownership logic, whereby practitioners try to cultivate practice cultures of solidarity around key service values. We emphasise that this means not that dentists regard more traditional elements of professional practice as unimportant, but merely that these elements are not integrated into a unitary schema of professional practice. We tentatively interpret this as a response to specific pressures on dentists to ensure the survival of the practice, whereby the altruistic components of professionalism become functionally redefined in terms of high-quality relationships within and outside the practice that hold survival value. We also note that factor 2 was statistically related to a commercialism factor (factor 1), whereby clinicians view their practice as an active competitor in an opportunistic marketplace. We speculate that both logics may be compatible responses to the problems of practice survival.
Factor 3 and 4 both contained elements of what we previously described as ‘population health managerialism’; however, the factor analysis made a distinction between importance being placed on ‘procedural diligence’ and public goods. Factor 3 was consequently labelled as managerialism, being characterised by negative loadings of the importance of practice review, preparing a paper trail and accountability to commissioners. Factor 4 on the other hand was characterised by high loadings on the importance of publicly funded health care, reducing health inequalities and accountability for public money. We consequently labelled this ‘public goods’. Public goods are defined as goods and services from whose benefits no one can be excluded and where consumption by one person does not diminish consumption by another. 107 The term carries a sense that one person’s contribution confers a benefit on a group of people. Moreover, there is no presumption that the service is delivered by a public sector provider. 108 It could equally be delivered by a provider within the private sector, albeit on a not-for-profit basis. This is why we labelled factor 4 ‘public goods’ rather than ‘public sector’ logic.
The analysis indicated that those who score highly on ‘duty to staff and patients’ are more likely to score highly on ‘public goods’ but score lower for ‘entrepreneurial commercialism’ and ‘managerialism’. Entrepreneurial commercial practitioners are more likely to also score highly on public goods and may also be more anti-managerialism. The small correlations show a statistical independence between the logics, meaning that any one dentist’s score on any logic will provide a poor prediction of that dentist’s score on the other logics. This independence of logics is in line with institutional theory literature, which suggests that multiple logics can coexist,109 and these can play out both competitively as well as in tandem in everyday work.
Summary: factor analysis of institutional logics
Undertaking a factor analysis of 47 items relating to institutional logics allowed us to test the hypothesis which we had developed in the course of our qualitative work, that several distinct logics exist in general dental practice, and these are formed around ownership, commercialism, professionalism and managerialism issues. The results confirmed that a logics structure of several strands did indeed exist, with a coherence shown around items concerned with entrepreneurial commercialism in the same way as had been identified in the qualitative work. Items relating to professional clinical values and ownership responsibility, however, emerged as not distinct in themselves, but having a coherence which indicated these logics are closely entwined. Thus we refined our notion of these logics as a ‘duty to staff and patients’, which caused us to query how professionalism is currently expressed in dental practice. Finally, our factor analysis enabled us to elaborate on our conception of population health managerialism formed from the qualitative work. We identified that two separate logics – managerialism and public goods – exist, and these two aspects, which are sometimes complementary, may also be competing.
Do institutional logics and norms predict micro-level chair-side behaviour in relation to the contract?
In our quantitative analysis we hypothesised that the four institutional logics would predict behaviour in the six grey areas of the contract. We were unclear about the directions in which specific logics might influence decision-making, and made two-tailed predictions that logics would be associated with both self-reports of previous engagement in grey areas of practice and intentions to engage in practices within the next 2 years. The regression analysis also examined the unique prediction of behaviour by descriptive and injunctive norms, as well as correlations between behaviour and demographic, practice type and practice finance variables.
Correlations between predictor variables and behaviour in relation to six grey areas
Table 10 shows correlations for a range of predictor variables (demographic, practice type, practice finance, descriptive and injunctive norms, institutional logics) and behaviour in relation to the six grey areas of the NHS contract. Pearson and point-biserial correlations show that female GDPs were less likely to engage in grey area behaviours relating to treatment resulting in a financial loss to the practice. Practices having a higher proportion of NHS patients in their practice were also found to have fewer intentions to refuse patients who might represent a financial loss to the practice, and more intentions to under-represent patients’ copayments for the sake of the patient.
| Variable | Refuse NHS patient who represents financial loss | Restrict treatments that represent a financial loss | Band 3 treatments towards end of financial year | Stopped routine care towards end of financial year | Chosen band 1 rather than 2: fairness of charge | Patient wishes on recall period over-ride NICE guidelines |
|---|---|---|---|---|---|---|
| Gender | –0.23** | –0.17** | 0.02 | –0.10 | –0.02 | –0.05 |
| Years in practice | 0.06 | 0.05 | –0.09 | –0.01 | 0.02 | 0.03 |
| Number of dentists per practice | –0.10 | 0.07 | 0.00 | 0.06 | 0.04 | –0.03 |
| Percentage NHS patient mix | –0.16** | –0.04 | –0.04 | 0.00 | 0.38** | 0.01 |
| Past behaviour | 0.59 | 0.75 | 0.84 | 0.83 | 0.94 | 0.92 |
| UDA price | –0.05 | –0.07 | 0.05 | 0.18** | 0.22** | –0.03 |
| Profit trend | 0.18** | 0.07 | 0.00 | 0.11 | 0.13 | –0.04 |
| Turnover trend | –0.01 | 0.00 | 0.03 | 0.01 | 0.02 | 0.02 |
| Descriptive norm | 0.36** | 0.32** | 0.42** | 0.23** | 0.51** | 0.70** |
| Injunctive norms | 0.42** | 0.41** | 0.41** | 0.26** | 0.37** | 0.61** |
| Entrepreneurial commercialism logic | 0.08 | 0.23** | 0.06 | 0.12* | –0.26** | –0.02 |
| Duty to staff and patients logic | –0.11* | –0.11* | –0.12* | –0.09 | –0.09 | –0.02 |
| Managerialism logic | 0.04 | 0.14* | 0.07 | 0.03 | 0.02 | 0.27** |
| Public Goods logic | –0.17** | –0.12** | –0.04 | –0.05 | 0.24** | –0.07 |
Transfer of dentists from a FFI remuneration system to a UDA system was made using calculations based on historical levels of activity of each practice, to generate a contract value. This created an anomaly whereby some dentists were remunerated at a higher price per UDA earned than others (these practices generally representing patterns of previous care with high levels of complex types of treatments). In our analysis, unexpectedly, dentists having higher UDA values in their contract were more likely to reduce routine care towards the end of the financial year, although they were also more inclined to under-represent the level of patient copayment by allocating treatment to band 1 for band 2 work, to reduce patients’ charges.
Both descriptive and injunctive norms were positively related to all six behaviours. The first four behaviours, which reflect practitioner’s self-interested responses to the contract, were generally predicted by the practitioner placing a higher importance on entrepreneurial commercialism (factor 1) and a lower importance on ‘duty to staff and patients’ (factor 2) and public goods values (factor 4). Under-representing patients’ copayment was related to having a lower sense of entrepreneurial commercialism logic and a higher score for public goods logic. Overriding NICE guidelines related to recall periods was associated with placing a low importance on managerialism logic (factor 3).
Regression analysis predicting intentions to engage in chair-side behaviour relating to six grey areas of the contract
Regression analyses are presented in Table 11. Past behaviour was used as the only covariate because it subsumed variance explained by demographic and practice variables. In the full sample, higher descriptive or injunctive norms scores were associated with the first three behaviour intentions. Higher entrepreneurial commercialism logic scores were associated with intentions to restrict treatments that represent a financial loss and reduce routine care near the end of the financial year but also a lower intention to adjust bands in favour of patients to reduce their copayment level. ‘Duty to staff and patients’ logic scores were associated with a lower intention to refuse NHS patients who might represent a financial loss to the practice and over-ride NICE guidelines relating to dental recall periods. Neither managerialism logic nor public goods logic uniquely predicted any behavioural intentions to interpret contract rules in favour of the practice and/or patients (Table 11).
| Avoiding high cost patients (refuse NHS patients who represent financial loss) | Restricting high-cost treatment (restrict treatments that represent a financial loss) | Over-representing patients’ diagnosis (band 3 treatments towards end of financial year) | Inequitable care (stopped routine care towards end of financial year) | Under-representing patients’ co-payment (chosen band 1 rather than 2: fairness of charge) | Overallocation of treatment resources because of patients’ demands (patient wishes on recall period over-ride NICE guidelines) | |
|---|---|---|---|---|---|---|
| Full sample | ||||||
| R2 (adjusted) | 0.41** | 0.63** | 0.73** | 0.70** | 0.88** | 0.84** |
| Past behaviour | 0.47** | 0.76** | 0.77** | 0.80** | 0.87** | 0.82** |
| Descriptive norm | 0.12* | 0.04 | 0.10* | 0.04 | 0.04 | 0.08 |
| Injunctive norm | 0.19** | 0.13** | 0.05 | 0.04 | 0.04 | 0.05 |
| Entrepreneurial commercialism logic | 0.07 | 0.10* | 0.01 | 0.08* | –0.05* | –0.03 |
| Duty to staff and patients logic | –0.11* | –0.06 | –0.01 | –0.04 | –0.03 | –0.06* |
| Managerialism logic | –0.05 | 0.06 | 0.01 | 0.02 | 0.03 | 0.02 |
| Public goods logic | –0.04 | 0.06 | 0.05 | 0.00 | 0.06 | –0.02 |
| Negotiation subsample | ||||||
| R2 (adjusted) | 0.42** | 0.61** | 0.71** | 0.67** | 0.86** | 0.85** |
| Negative commissioning experience (Neg) | 0.12* | 0.04 | 0.05 | 0.05 | –0.06 | –0.02 |
| Neg × entrepreneurial commercialism logic | 0.13* | 0.05 | –0.02 | 0.05 | 0.00 | –0.05 |
| Neg × duty to staff and patients logic | –0.06 | 0.01 | –0.04 | –0.03 | –0.01 | –0.02 |
| Neg × managerialism logic | 0.14* | 0.07 | 0.00 | 0.03 | 0.01 | 0.01 |
| Neg × public goods logic | 0.14* | 0.02 | –0.04 | 0.03 | –0.03 | 0.03 |
Summary: institutional logics and norms and micro-level behaviour
General dental practitioner descriptive and injunctive norms predicted micro-level behavioural intentions related to the six grey areas of the contract. Institutional logics were also predictive, but only entrepreneurial commercialism and duty to staff and patients logics, and these only in relation to certain behaviours, depending, for example, on whether the behaviour was orientated towards the patients’ wishes or to the benefit of practice finances.
Do dentists’ negative experiences with commissioners predict chair-side behaviour?
In our analysis we also hypothesised that, among dentists who had experience in dealing with commissioners over the previous 2 years, negative experiences would be directly associated with interpretation of contract rules to the advantage of practitioners and/or patients, but at the expense of the commissioners’ wishes; and also that negative experiences with commissioners would moderate the effects of logics. Moderated regression analyses presented in Table 11 show that the interaction terms predicted behaviour in only one of the six grey areas of the contract: avoiding high-cost patients. Following procedures of Aiken and West,110 we graphically modelled the three interaction terms. These figures (Figures 2–4) show that in three of the four logics (entrepreneurial commercialism, managerialism and public goods logics), these orientations were associated with increased intentions to behave in a self-interested way (i.e. refuse to accept NHS patients who represent a financial loss to the practice), but only if these dentists reported having had negative experiences in their dealings with commissioners.
FIGURE 2.
Interaction between GDPs’ negative experiences with commissioners and entrepreneurial commercialism in relation to refusing to take NHS patients representing a financial loss to the practice.
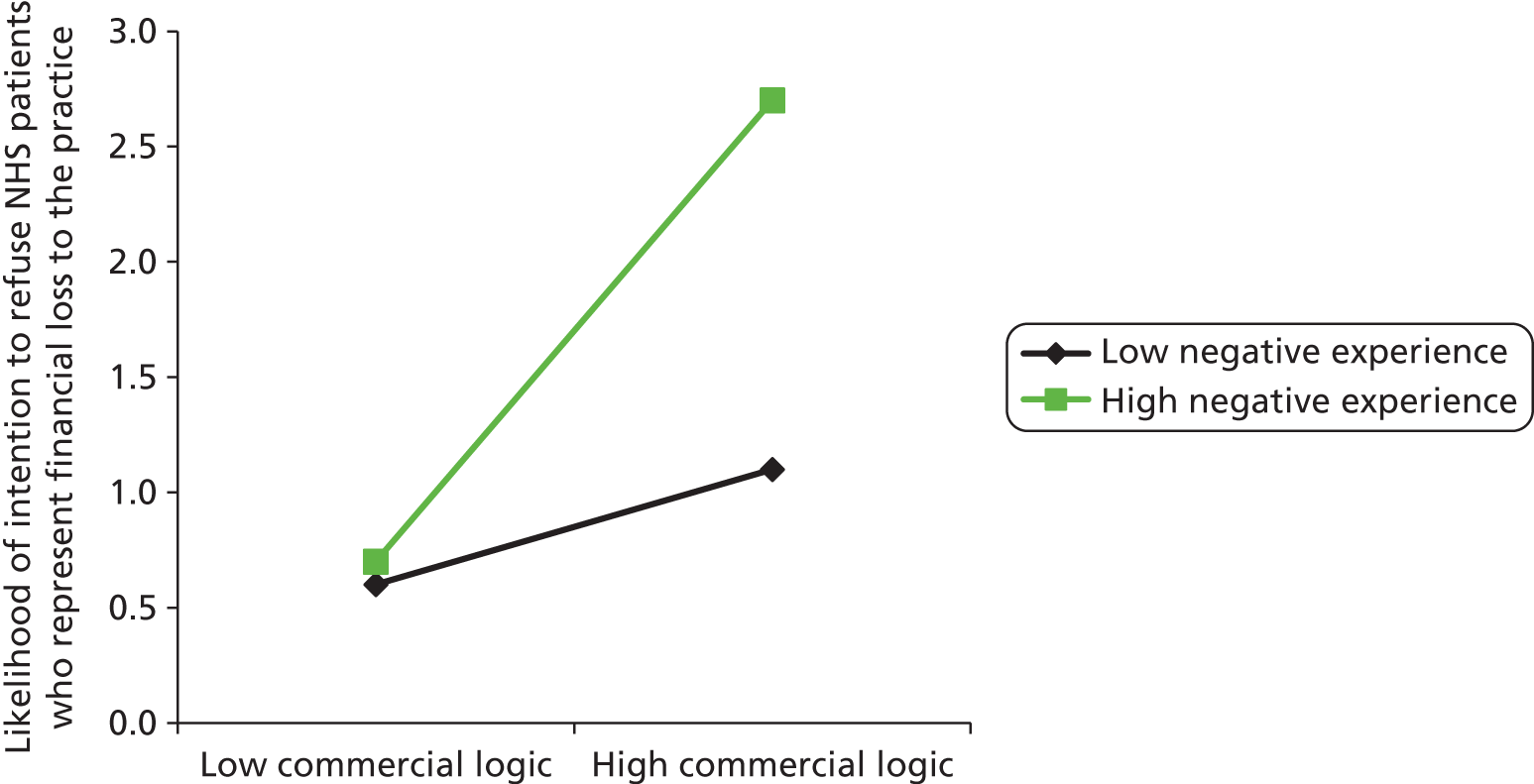
FIGURE 3.
Interaction between GDPs’ negative experiences with commissioners and managerialism logic in relation to refusing to take NHS patients representing a financial loss to the practice.
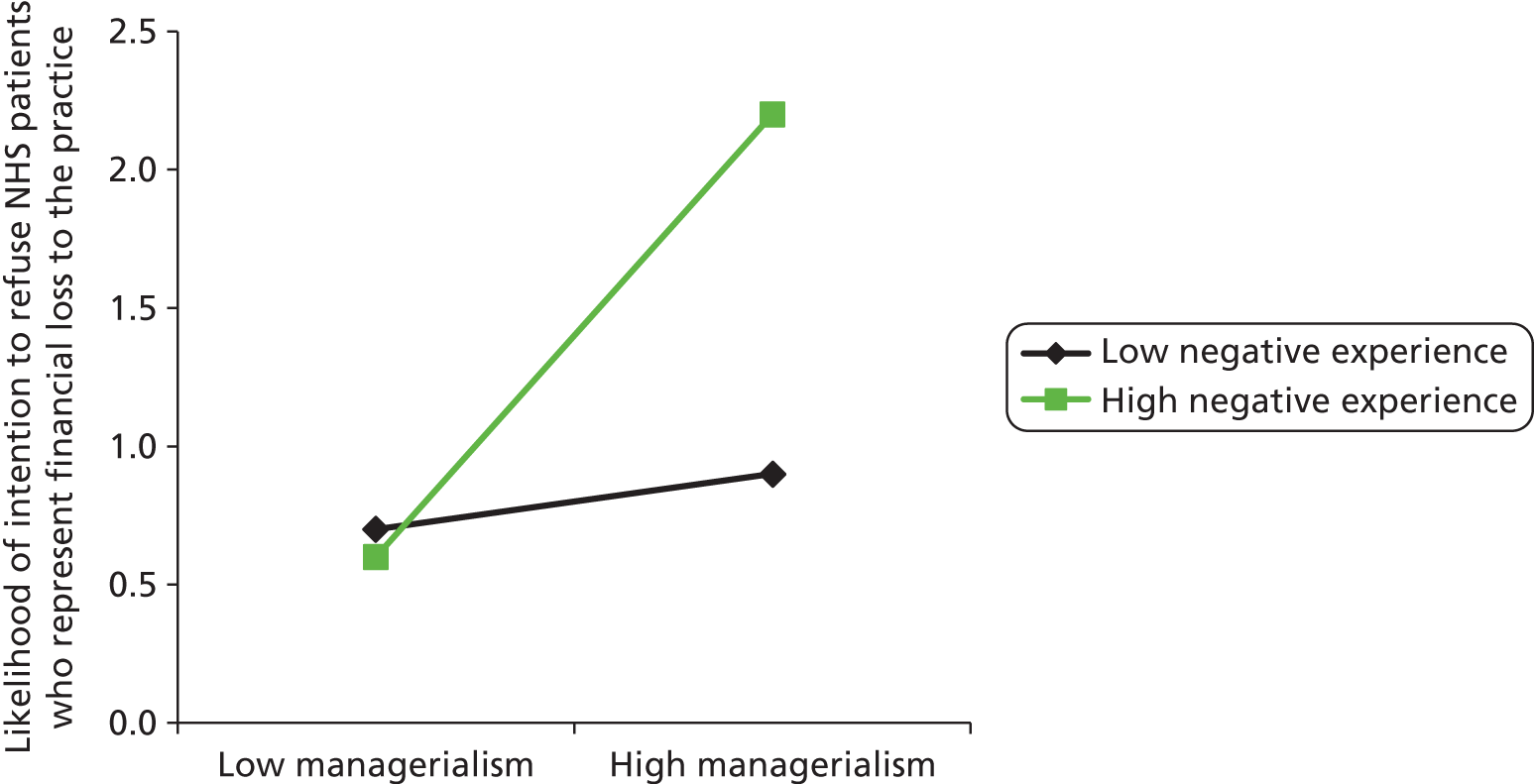
FIGURE 4.
Interaction between GDPs’ negative experiences with commissioners and public goods logic in relation to refusing to take NHS patients representing a financial loss to the practice.
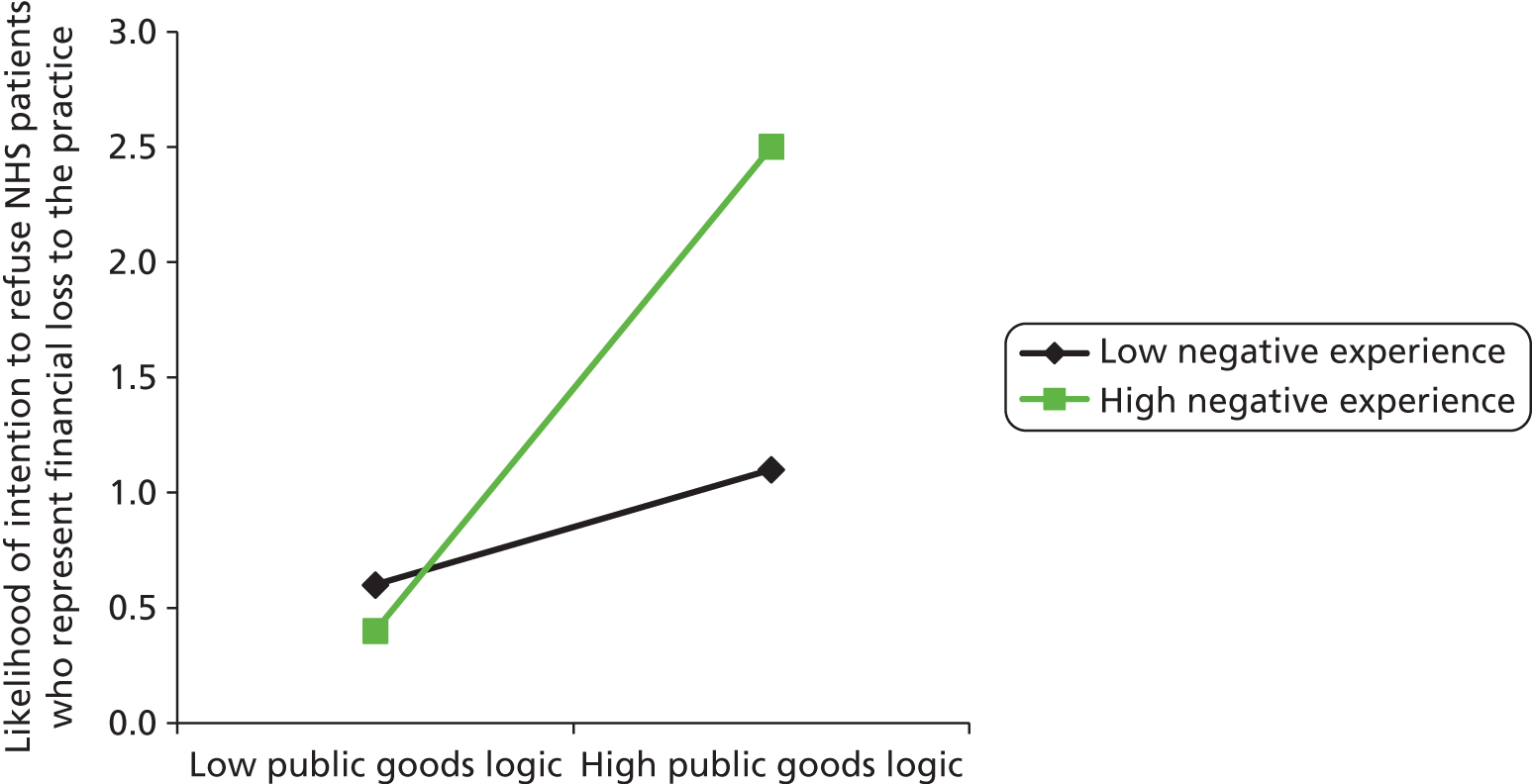
Where dentists reported negative experiences with commissioners, they were more likely to avoid high-cost NHS patients, where their outlook reflected entrepreneurial commercialism, managerialism or public goods logic. We therefore conclude that, in an area where practitioners appear to act in a self-interested way (refusing to take on NHS patients who represent a financial loss), this behaviour is motivated not purely by self-interest but also by the breakdown of trust in relationships with commissioners.
Do institutional logics predict macro-level behaviour?
Factor analysis of macro-level behaviour
We undertook a factor analysis of items related to the macro-level behaviour of dental practitioners in order to test our analysis of qualitative data: that dentists respond to commissioners in a number of ways, by strategically co-operating, acquiescing or being defiant. The factor analysis was undertaken on data from 268 dentists who completed the 15 items pertaining to macro-level behaviour – items which had been developed from our qualitative work. An initial factor analysis of intended macro-level behaviour showed three factors with eigenvalues greater than 1.0 with the scree plot showing a cut-off after the third factor. The item ‘To write to the dental press or online forums in support of commissioners’ was removed from the final analysis because of a low communality (< 0.30). The principal components analysis showed three clear factors explaining a total variance of 56%. Table 12 shows the final analysis with means for all macro-level behaviours, eigenvalues and the percentage of variance accounted for by each factor, loadings of individual items of greater than 0.30 on the pattern matrix and interfactoral correlations (partial correlations between factors while statistically controlling the third are presented on the lower diagonal).
| Mean (SD) | Argumentative behaviour | Co-operative behaviour | Acceptance behaviour | |
|---|---|---|---|---|
| Eigenvalue | 3.98 | 2.18 | 1.68 | |
| Percentage variance | 28.42 | 15.47 | 11.96 | |
| To do a favour for commissioners | 1.08 (0.38) | 0.784 | ||
| Challenge legitimacy or threaten legal action | 1.81 (0.89) | 0.624 | ||
| Speak out in public to challenge policy | 1.91 (0.95) | 0.463 | 0.319 | |
| Work together with commissioners to solve problems | 2.47 (1.02) | 0.901 | ||
| Work closely with the commissioners | 2.34 (1.01) | 0.919 | ||
| To query competency of commissioners | 1.87 (0.86) | 0.814 | ||
| To be unhappy with deal but use adaptive strategies at practice level | 2.36 (1.00) | 0.328 | 0.633 | |
| Accuse of unfairness or incompetence | 1.58 (0.80) | 0.748 | ||
| Take action to protect practice against consequences of unfavourable deals | 2.20 (1.08) | 0.306 | 0.444 | |
| Present mitigating circumstances to the PCT during negotiations | 2.07 (0.94) | 0.402 | 0.472 | |
| Persist in arguing with PCT to wear them down | 1.49 (0.81) | 0.779 | ||
| Accept commissioners ‘decision without questioning and bear consequences | 2.04 (0.99) | 0.861 | ||
| Work closely with commissioners to obtain benefits for yourself or practice | 2.12 (0.99) | 0.486 | ||
| Not raise issues for the sake of long-term relationship | 2.25 (0.96) | 0.777 | ||
| Interfactor correlations (partial correlations on lower diagonal) | ||||
| Argumentative behaviour | – | 0.26** | 0.13* | |
| Co-operative behaviour | 0.24** | – | 0.15* | |
| Acceptance behaviour | 0.10 | 0.12* | – | |
Interpretation of the three factors appears to be clear. Factor 1 refers to an argumentative behaviour whereby the dentist engages in some level of confrontation. Factor 2 seems to involve a co-operative behaviour of working closely with the PCT. The item ‘Worked closely with PCT to obtain benefits for yourself or practice’ implies that this may be done manipulatively, but this item shows a lower loading than others and it would be unwise to conclude that high scores on this factor involve manipulativeness. Factor 3 seems to represent decisions that are passively accepted while suppressing objections so as not to endanger relationships. The interfactor correlations were all positive and significant. Partial correlations between argumentative and relational, and between relational and acceptance were significant, suggesting that dentists use these behaviours together or interchangeably, possibly intending to choose the strategy that maximises prospects of success.
The intended negotiation strategies factors were saved as variables using the regression method, producing standardised scores. Negotiation tactics used during the previous 5 years were entered into a similar analysis, showing almost identical results. The three factor scores were saved as standardised scores and used as predictor variables representing past behaviour in the inferential analyses.
Predicting macro-level behaviour from trust, professional networks and institutional logics
Table 13 shows correlations between all predictor variables and intentions to use each macro-level tactic. No demographic variables predicted macro-level tactics, and none were used as control variables in the inferential analyses. Higher UDAs were associated with higher intentions to use argumentative and co-operative strategies, while bigger practices (defined by a greater number of practices and dentists) were more likely to intend to use co-operative strategies. Other correlations were largely as expected: intentions to use an argumentative tactic were associated with more dental network contacts, lower trust and an entrepreneurial commercialism logic; intentions to use a co-operative strategy were associated with more dental network contacts, greater trust and entrepreneurial commercialism, managerialism and public goods logics. An acceptance strategy was predicted by only negative experiences.
| Variable | Mean (SD) | Argumentative strategy | Co-operative strategy | Acceptance strategy |
|---|---|---|---|---|
| Age (years) | 49.20 (8.78) | 0.13 | 0.02 | –0.01 |
| Time since qualification | 26.69 (9.71) | 0.09 | 0.02 | –0.03 |
| Gender | 0.06 | –0.04 | –0.04 | |
| Percentage NHS practice work | 63.19 (34.95) | 0.16* | 0.30** | 0.03 |
| UDA | 24.39 (6.16) | 0.23** | 0.19* | 0.02 |
| Number of surgeries at the practice | Median = 3, IQR 2–4 | 0.06 | 0.22* | 0.03 |
| Number of dentists at the practice | Median = 3, IQR 2–4 | 0.06 | 0.25** | 0.06 |
| Past strategy use | 0.00 (1.00) | 0.58** | 0.57** | 0.55** |
| Dental network memberships | 2.64 (1.79) | 0.20** | 0.13* | 0.04 |
| GDP discuss difficulties with dental network | 3.21 (0.80) | 0.33* | 0.10 | 0.08 |
| Dental network contact outside the practice | 2.03 (1.06) | 0.17* | 0.13* | 0.01 |
| Negative experience | 3.01 (0.92) | 0.32** | –0.18* | 0.17* |
| Trust | 2.96 (0.91) | –0.36** | 0.20* | –0.10 |
| Entrepreneurial commercialism logic | 0.00 (1.00) | 0.17* | 0.19** | 0.06 |
| Duty to staff and patients logic | 0.00 (1.00) | –0.06 | 0.07 | 0.09 |
| Managerialism | 0.00 (1.00) | –0.02 | –0.22** | 0.04 |
| Public goods logic | 0.00 (1.00) | 0.08 | 0.30** | 0.07 |
Regression analyses predicting macro-level behaviour
Regression analyses were conducted by regressing past behaviour, trust, the three dental network items and the four logics items onto the three macro-level behaviour factors. We did not use practice-related items (e.g. UDA value) because initial analyses showed that they did not add to prediction afforded by macro-level behaviour used in the previous 5 years. We also did not use the negative experiences variable because it was strongly associated with trust (r = –0.79) and did not add to the prediction of outcome variables.
Table 14 shows findings from the regression analyses. After statistical control of macro-level behaviour used in the previous 5 years, the use of an argumentative strategy was associated with lower trust scores, a greater perceived likelihood that dentists would discuss difficulties with others and higher scores on the entrepreneurial commercialism logic. Unlike the argumentative strategy, intentions to use a co-operative strategy were associated with higher scores on trust and public goods logic, but, similar to the argumentative strategy, higher scores on the entrepreneurial commercialism logic.
| Argumentative behaviour | Co-operative behaviour | Acceptance behaviour | |
|---|---|---|---|
| Full sample R2 (adjusted) | 0.42** | 0.39** | 0.29** |
| Strategy use previous 5 years | 0.48** | 0.55** | 0.58** |
| Trust | –0.10* | 0.12* | 0.10 |
| Dental network memberships | 0.09 | –0.08 | –0.03 |
| Dental network discussions | 0.25** | 0.10 | 0.06 |
| Dental network contacts | –0.04 | –0.03 | –0.05 |
| Entrepreneurial commercialism logic | 0.12* | 0.14** | 0.00 |
| Duty to staff and patients logic | –0.08 | –0.07 | 0.05 |
| Managerialism logic | –0.02 | –0.10 | 0.07 |
| Public goods logic | 0.05 | 0.13* | 0.02 |
The role of trust and relationships in mediating micro- and macro-level behaviours
A study focus was the concept of trust between dentists and commissioners and its relationships to micro- and macro-level behaviours. One feasible model is that trust or mistrust emerges from an agent’s perceptions of how he or she is treated in negotiations, which influences both approaches to new negotiations and honouring the contract. In statistical terms, this should mean that trust would mediate the relationship between negative experiences with commissioners and micro- and macro-level behaviour. Mediational analyses, controlling past behaviour, were conducted to ascertain whether or not this occurs. Table 15 shows these. The mediation estimate estimates the extent of the mediation relationship, where trust mediates any influence of negative experience of negative experiences on intentions to engage in an argumentative stance in negotiation. No other mediating relationships were observed.
| Variable | Mediation estimate | Lower 95% CI | Upper 95% CI |
|---|---|---|---|
| Chair-side decisions to benefit practice (behaviours 1–4) | 0.0099 | –0.0933 | 0.1107 |
| Chair-side decisions to benefit patients (behaviours 5–6) | 0.0505 | –0.0137 | 0.1197 |
| Argumentative behaviour intention | 0.1479* | 0.0190 | 0.2886 |
| Co-operative behaviour intention | –0.0991 | –0.2852 | 0.0690 |
| Acceptance behaviour intention | –0.0646 | –0.2477 | 0.0733 |
This shows that trust mediates the relationship between negative experiences and only the intention to adopt argumentative (and not co-operative or acceptance) behaviour (Figure 5). This fits with findings from our qualitative work, that, while practitioners might mistrust, they may still adopt co-operative behaviour. Exploring the qualitative data set again, having seen the results from this area of quantitative analysis, we further observed that, in some cases where an argumentative stance had been adopted, practitioners involved were from minority ethnic/religious groups. So practitioner ‘trust’ may be shaped by other influences, for example by their experience of belonging to a marginalised group. We need to point out that these findings relate only to a very small data set. However, they may still be useful in indicating a possible area for future research.
FIGURE 5.
Path diagram showing mediation of intentions to adopt an argumentative stance.
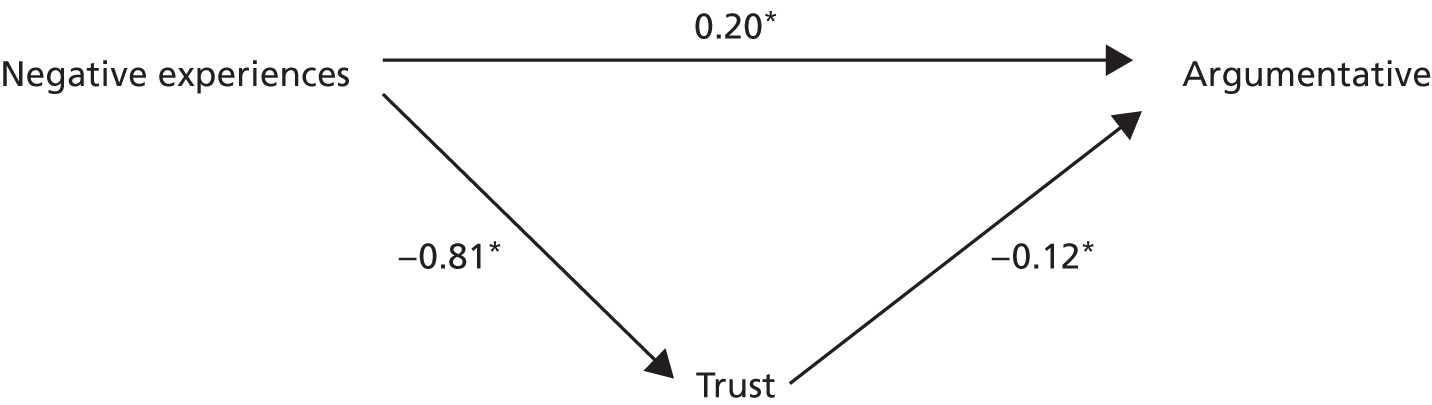
Summary: predicting macro-level behaviour of dental practitioners and the role of trust
Neither age nor gender predicted the type of macro-level behaviour which practitioners said they would adopt. We focused our regression analysis, which takes account of confounding variables, on the type of macro-level behaviour that practitioners said they would adopt in the future; this gives a stronger analysis as a basis for making judgements of cause and effect relationships (the ‘cause’ needs to precede the ‘effect’). We found that institutional logics predicted the type of macro-level behaviour said they would adopt; in particular, a logic of entrepreneurial commercialism predicted adopting both an argumentative and a co-operative strategy. This entirely fits with the concept of entrepreneurialism, usually characterised as having an adaptive ability to seize opportunities and act strategically. Having a high degree of trust in commissioners was found to be predictive of practitioners intending to adopt a co-operative stance, and low trust predictive of an argumentative approach. Having more discussions with dental professional colleagues was also predictive of taking an argumentative approach, demonstrating, as found in our qualitative work, how resistance to contracting is influenced by more distal ingredients than the perceptions of individual practitioners relating to their dyadic relationship with commissioners. Our meditational analysis suggests that trust is particularly pertinent in determining which practitioners decide to adopt an argumentative form of resistance to commissioners. This substantiates our qualitative findings that, while practitioners may mistrust, they may still decide to co-operate strategically with commissioners.
Are macro- and micro-level approaches correlated?
It is feasible that micro- and macro-level approaches to contracts are correlated. For example, dentists who accept contracts that they believe favour commissioners may be more prone to try to ‘rebalance’ any perceived inequity by making chair-side decisions that benefit the practice. Table 16 shows the Pearson’s values between the six grey areas of micro-level (chair-side) behaviour and macro-level behaviour concerned with approaches to dealing with commissioners. It should be noted that all correlations in this table represent small effect sizes. The analysis suggests a tendency whereby dentists adopting a tactic of ‘acceptance’ attempt to use the resources available to them at a micro level, possibly in order to make up for deficiencies at the macro level. 100 This is shown in two areas of behaviour concerned with the financial interests of the practice.
| Six grey areas micro-level (chair-side) behaviour | Argumentative behaviour | Co-operative behaviour | Acceptance behaviour |
|---|---|---|---|
| Avoiding high-cost patients (refuse NHS patients who represent financial loss) | 0.05 | –0.04 | 0.07 |
| Restricting high-cost treatment (restrict treatments that represent a financial loss) | 0.11 | –0.11 | 0.13* |
| Over-representing patients’ diagnosis (band 3 treatments towards end of financial year) | –0.07 | –0.06 | 0.14* |
| Inequitable care (stopped routine care towards end of financial year) | 0.14* | 0.06 | 0.12 |
| Under-representing patients’ copayment (chosen band 1 rather than 2: fairness of charge) | 0.07 | 0.15* | 0.11 |
| Overallocation of treatment resources because of patients’ demands (patient wishes on recall period override NICE guidelines) | 0.03 | 0.02 | 0.08 |
Moreover, dentists adopting co-operative behaviour were more likely to be orientated towards the patients’ interests (micro-level behaviour 4). Dentists adopting argumentative behaviour were also more inclined to stop undertaking care towards the end of the financial year (once targets had been reached), with this behaviour being a means of expressing this type of defiant behaviour.
Integration of qualitative and quantitative work streams
Our empirical work involved two methodologies: qualitative and quantitative work. As outlined in Chapter 3, Research design, this is a strength, for it allows us to overcome some of the deficiencies inherent in either method. We undertook the qualitative work first, and identified different sets of institutional logics, conceptualisations of the role of trust and wider determinants of responses to contracts such as professional network links. Arising from this analysis we were able to test these ideas in a less select and wider group of practitioners. The preceding qualitative work allowed us to identify six grey areas of the current NHS dental contract around which we could analyse the behavioural intentions of dental practitioners at the micro level. It also allowed us to generate items for our quantitative work which we subsequently subjected to factor analysis to explore our conceptualisation of institutional logics and macro-level behaviour.
In particular, our quantitative work allowed us, first, to test and refine our conceptualisation of institutional logics. Our earlier conceptualisation involved four logics (ownership responsibility, professional clinical values, population health managerialism and entrepreneurialism). Our quantitative work allowed us to refine this and see that ownership responsibility and professional clinical values are particularly intertwined in dental practice, together representing a ‘duty to staff and patients’ which is felt as an ethical obligation. We also identified that there are two strands to population health managerialism (managerialism and public goods), which, while sometimes acting synergistically, may also on occasion be competing. While practitioners may be resistant of managerialism in principle, they may be less resistant of public goods goals, if resources are sufficient to allow satisfaction of the other possibly competing imperatives relating to ownership, professionalism and commercial values. Second, the quantitative work allowed us to test the hypotheses formed in our qualitative work, that institutional logics are predictive of both micro-level and macro-level behaviours of dental practitioners. Third, it enabled us to explore how relationships between practitioners and commissioners shaped responses to contracting, given all the other determinants concerned. Our quantitative findings did indeed confirm our suggestion that the context as well as the ‘self’ is predictive of responses to contracting. Institutional logics were found to be predictive of some aspects of responses to contracts at both the micro and macro levels, with practitioners’ wider view of commissioning relationships shaping the extent of practitioners’ responses.
Chapter 5 Discussion and implications
Introduction
Both the qualitative and quantitative analyses explored the perspectives of practitioners and commissioners, and their responses to contracts governing their relationship. In the literature review we identified a wide range of factors which shape practitioners’ responses to contracts, from those pertaining to their immediate contractual relationship with commissioners, to wider influences such as the extent of competition and political and professional networks. In our qualitative work we undertook a detailed exploration of dental practice and were able to describe the prevailing logics which characterise the dental practitioner’s self and context. We also described medical practitioners’ and commissioners’ logics. In the quantitative work we were able to substantiate and further refine our dental practice logics, as well as relate them to their responses to the current NHS dental contract, at both the micro level (chair side) and macro level (responses to commissioners). In this chapter we start by summarising study limitations and then return to our original research questions and discuss some of the insights we have gained from our study. We then end with a discussion of implications for commissioning and further research.
Study limitations
Readers will need to consider some study limitations before interpreting our findings. First, an element of bias in the recruitment of dental practice cases exists: practices willing to be involved in this study may have held particularly strongly to the public goods logic, for example, or had particular views from their previous dealings with commissioners. The inclusion of a subsequent quantitative phase involving a wider, less select group of practitioners was designed partly to address this issue. Second, social desirability will have influenced the honesty of participants’ responses in both our qualitative and quantitative work. Our case-study approach, however, which included observations and triangulation of responses by interviewing several members of staff in the practice, on different occasions, and exploring inconsistencies in subsequent interviews, enabled us to address this issue to some extent. The influence of social desirability on responses to some parts of the questionnaire is, however, indicated by the finding that fewer dentists report engaging in opportunism than their reported estimates of descriptive norms and injunctive norms (perceived acceptability of the behaviour) among fellow dentists, and this has to be borne in mind when interpreting results. Currently our results indicate that the proportion of dentists who engage in opportunism is relatively low. Most report that they are engaged in ‘business as usual’, with little or no thought given to opportunism, most of the time.
While the quantitative phase of the work allowed us to widen participation to a wider sample of dental practices, the response rate of 43% needs to be considered when thinking about the generalisability of results. A response rate of less than 50%, however, is not unusual for postal questionnaires of this type, particularly for questionnaires involving sensitive questions (such as opportunistic behaviour and difficult relationships with commissioners). Comparing the profile of respondents (mix of NHS/private work, gender of practice owners, see Chapter 3, Phase 3: questionnaire and commissioner interviews), though, reassures us that questionnaire respondents are fairly representative of English dental practitioners as a whole. Unfortunately we had insufficient data on the individual characteristics of all those in the sampling frame to make a direct comparison between respondents and non-respondents, and thus we were unable to explore the impact of response bias further.
Limited numbers of questionnaire responses also meant that we had to rely on exploratory techniques rather than confirmatory factor analytic techniques in the analysis of institutional logics. Since most items used in the questionnaire were developed directly from our qualitative work, while this had the advantage of improving their relevance to dentists’ expressed concerns, it also had a disadvantage in that there was no evidence of instrument reliability or validity, save for the face validity of the items, that was independent of the current data set.
The study took place at a time of turbulence in the NHS. In April 2013 the dental commissioning role, previously the responsibility of PCTs, was transferred to newly formed organisations: NHS Area Teams, which have a slightly wider footprint than PCTs. It was intended that, in phase 3, telephone interviews with commissioners in 14 PCTs would be carried out, but because of a merging of areas, and a flux in the commissioning workforce, very few of the dental commissioners from the six PCTs involved in the case study work remained in post (see Chapter 3, Telephone interviews with commissioners). Some who did remain declined further involvement in the study on the basis that restructuring (reduced numbers of commissioners, wider areas) had placed new and greater work pressures on them. Moreover, the commissioners who were interviewed in phase 3 were generally less concerned to discuss issues relating to the ‘day-to-day’ aspects of commissioning, and instead were keener to discuss their concerns relating to organisational uncertainty and the impact of the recent restructuring on their workload and roles. Thus the organisational environment of NHS dental commissioners has clearly changed from that present during the collection of earlier qualitative data in phase 2, and may even change again as the new organisational structures settle down and relationships and roles evolve and emerge. Nevertheless, the emphasis in our study on identifying underlying tensions between different values and elements of the commissioning role means that these may still hold once this period of turbulence in NHS commissioning has passed. Since institutional theory suggests that logics are dynamic83 (see Chapter 3, Institutional logics and general dental practice as an organisational field) and shaped by agents reacting to their environment, as well as by agents acting on their environment, we cannot assume that commissioners’ practices, norms and values still remain the same today.
Finally, our study was influenced to only a limited degree by patient and public involvement. Although our advisory group included a patient and public involvement member who was involved in the design of data collection and the interpretation of results, the scope for patient and public involvement could have been greater. While the study focused on contractual aspects of dental practice work, which is mainly the preserve of the dental practice owner, and commissioners with whom they deal, the impact is often felt by patients and public in terms of access to services, fairness, etc. While we included interviews with patients of some of the practices within our case study data collection, some practices were unwilling to be involved to this extent or lacked the facilities to interview patients in private areas. Interviewing patients at home or members of the public was outside the scope of the study, but would have strengthened the validity of this aspect of the research.
The next three sections are structured according to our three study objectives stated at the outset (see Chapter 2, Aims and objectives).
What is contract ‘success’ for general dental practitioners and commissioners?
Within our overarching study aim, to identify the factors which facilitate and hinder the use of contractual processes to manage and strategically develop general dental services, we set out to identify what ‘success’ in contractual agreements represents from the different perspectives of dental practitioners and commissioners (objective 1; see Chapter 2, Aims and objectives). Following our extensive literature review and deeper understanding of the factors influencing NHS dental practice contracts, arising particularly from our qualitative work, we now see ‘contractual success’ as something which must be of mutual benefit to each party.
From our literature review and empirical work, we recognise that in any contractual situation which involves a complex product (such as providing care) there is an inevitability of adverse selection and moral hazard (see Chapter 1, Grand theories of health-care contracting). Each party in the contract will always seek to act in its own self-interest, within the bounds of its rationality. Behaviour (either practitioners responding to the contract or even commissioners also implementing the contract) is influenced by the fact that people occupy perspectives which are shaped by rational responses from a range of what is understood to be appropriate (determined by loyalty groups, e.g. professional networks, and authority, e.g. hierarchies and law).
Decisions are taken pragmatically as a result of habit and heuristics rather than being maximally rational, and it is these habits, framed by personal bias and historical preferences, that give rise to behaviour which is aimed at the satisfactory as opposed to the ideal. The ‘ideal’ here is the maximally efficient outcome which features in classical economic models of contracting. In other words, practitioners, in their behaviour, aim for what is satisfactory in meeting their goals of everyday practice; and this is based on what has proved successful before, rather than ideal. Heuristics are rules of thumb and habit which become embedded into practice in a way that is so dispositional that it becomes the ‘divine law’ by which the dentist practices. Regular 6-monthly recall of regular patients, for example, is one such habit that we can see arising from a context where the organisational structure involves practitioner ownership of assets, with patient satisfaction and local reputation important to practice viability in a competitive market. This is called into question by commissioners and policy-makers geared towards managerialism and public goods goals concerned with rationing of resources according to effectiveness and equity criteria. We therefore observe institutional work at play where new forms of contract and regulation cause heuristics and habit to surface. Existing practices (such as routine 6-monthly recall of regular patients) are queried, forcing practitioners to acquiesce, defy or co-operate with the shifting environment.
Principal–agent models of contracting recognise that self-interest is inevitable. It may be helpful to rephrase this as ‘self-centredness’, which (being less commonly used in this context) may feel less pejorative, and captures the tension which was particularly evident in our context: that perspectives from GDPs and commissioners (and higher-level policy-makers) differ substantially. A ‘successful’ contract therefore is one where neither party involved in the contract promotes its own self-interest above the other’s. The focus should be on obtaining a ‘satisfactory’ rather than a ‘utilitarian’ (i.e. good versus bad) agreement between the contracting parties.
Factors which influence contractual ‘success’
Following our deeper understanding of the role of contracts in NHS dental practice, we bring together here revised versions of the various research questions posed at the start of the study (see Chapter 2, Institutional work theory rather than activity theory):
-
What are the institutional logics which prevail in general dental practice?
-
How do these differ from commissioners’ institutional logics?
-
What does variation in micro-level (chair-side) behaviour of dental practitioners tell us about how GDPs pursue their ‘self-centred’ interests?
-
What role do relationships and trust have in influencing the responses of GDPs?
-
What other factors influence the responses of GDPs?
-
What does the difference between GDPs and GMPs tell us about the challenges and solutions to contracting with NHS independent contractors?
General dental practitioners’ and commissioners’ institutional logics
In our qualitative work we mapped the ‘common meaning system’ of GDPs, GMPs and commissioners. We identified several different institutional logics interwoven and running through the work of GDPs and commissioners. We found a dominant logic in dental practice concerned with ownership responsibility, as well as a strong sense of an ethical responsibility to serve the patients’ best interests, the whole field being marbled with commerciality. Population health managerialism was found to be emergent in dental practice, and less in sympathy with other logics. Balancing coexisting and competing logics was a tension carried by GDPs in their everyday work. In our quantitative work we were able to further explore these logics and to refine the notion of population health managerialism logic into separate managerialism and public goods logics.
Our qualitative work with commissioners also enabled us to more fully understand that even managerialism and public goods logics may not always be in sympathy. Moreover, we identified a bureaucratic logic as evident among PCT commissioners and this further constrained some of the flexibility and innovation necessary to realise goals driven by public goods logics. Managing competing interacting institutional logics is not purely confined to the work of dental practitioners. It affects the work of commissioners too.
Micro-level (chair-side) behaviour and pursuing self-interest
Institutional rules act as constraints (or a lack of constraint) to action because they express people’s fundamental understanding of the nature of the social exchange between dentists and patients (see Chapter 3, Case studies as a methodological approach in the study of institutions).
While our qualitative study identified various areas of practice which could be interpreted as provider opportunistic behaviour, which were further substantiated by our quantitative work, what is worth noting first is that the proportions of GDPs engaging in this type of behaviour were relatively low. While a degree of response bias and reporting bias may account for this, fewer GDPs reported engaging in opportunistic behaviour themselves than they reported perceiving descriptive and injunctive norms (perceived acceptability of that type of behaviour) among fellow practitioners (see Chapter 4, Do institutional logics and norms predict micro-level chair-side behaviour in relation to the contract?). We should therefore recognise that, as argued by Williamson,111 most agents (GDPs) are engaged in ‘business-as-usual, with little or no thought to opportunism, most of the time’.
In our quantitative work we were able to identify the way the institutional logics of GDPs shaped their responses and interpretation of some grey areas present in the current NHS dental contract (see Chapter 4, Do institutional logics and norms predict micro-level chair-side behaviour in relation to the contract?). While the six areas we identified are specific to the current UDA contract, they may be generalised too (e.g. indicating how GDPs might react in terms of limiting high-cost treatment, selecting low-risk treatments, overinflating complexity, etc.). We can therefore use the findings to predict how different types of practitioners may react to new forms of dental contract, and other new areas of ‘gaming’ which become identified as soon as the new contract rules are set.
The role of relationships and trust
Relationships between dental practitioners and commissioners were observed to provide a diplomatic means of resolving and working out competing institutional logics in order to reach mutually beneficial goals. In our qualitative work we were able to conceptualise ‘trust’ in the context of the dental contractual relationship as being geared to working towards working co-operatively with commissioners. Mistrust, on the other hand, concerned an unwillingness to become vulnerable to commissioners. We found that, while trust built relatively slowly over time, particularly through getting to know the people involved, mistrust had a more catastrophic quality and was transmitted through personal, political and professional networks. Having mistrust of commissioners, however, did not preclude a willingness to work co-operatively. Our quantitative work confirmed the importance of trust and mistrust, finding that, even if GDPs mistrust, they may choose to co-operate strategically. This does not preclude, however, the fact that mistrust can also influence others who have bad experiences of commissioning, in deciding to take an argumentative approach.
The role of personal, political and professional networks and the media
Our study recognises that practitioner motivation, which lies at the heart of opportunism, is set in a much broader network of relationships and influences (see Figure 1). Personal, political and professional relationships influence motivation, as does the indirect relationship between the state and professional bodies. The media have a role to play, influencing the role of the state as well as wider levels of trust between the dental profession and society. These higher-level factors shape what happens in the more immediate dental practice environment, and provide indirect mechanisms to influence behaviour. There is a wider societal mistrust of dental practitioners than of doctors. This places a greater onus on GDPs to justify their actions to the patients: we see clinical interactions involving dental practitioners having to justify their moral stance directly to patients (see Chapter 4, Commissioners working with contract: dealing with general dental practitioners). Their role as gatekeeper to the NHS is therefore made all the more difficult. Thus the patient themselves and the attitude of wider society towards dentistry contribute to the institutional constraints which give rise to the institutional rules structuring interactions in the dental practice environment (see Chapter 1, Synthesis of theory and a logic model of the theory of health-care contracting), and are forces which should not be ignored.
The nature of the dental profession itself is also an important factor. In our qualitative work, dental professional networks emerged as less cohesive than in medical practice. An ethos of partnership was apparent in several aspects of medical practice approaches, whereas, in dentistry, approaches tend towards the individualistic. A greater degree of commercial competition between practices may account for dental practitioners being generally more geared towards working as individuals within a practice, and as individual practices, than medical practitioners are. We also found that the nature of dental practice work and the contractual arrangements in place had a tendency to make dental practitioners more isolated. Many GMPs have time away from practice, and we even observed a move towards portfolio careers. Portfolio careers entail a mixture of jobs and working arrangements which give individual doctors a freedom to move between contractual arrangements and organisations (see Chapter 4, Institutional logics in general medical practice, Entrepreneurial commercialism). In contrast, many GDPs tend more to completely focus exclusively on their own practice environment. This inevitably leads to a narrower focus on the practice, rather than the wider population and the collegiality concerned with being a member of the wider dental profession.
Differences between general dental practitioners and general medical practitioners
We started our work by identifying that GDPs and GMPs have a common status as independent contractors to the NHS, and that policy shifts since the 1990s have curtailed professional autonomy in both groups in favour of greater levels of accountability within a managerialist system. As our work progressed however, it became apparent, as outlined in the introduction (see Chapter 1, General dental practitioners and general medical practitioners as independent contractors to the NHS: ownership of assets and modes of governance), that although independent contractor status might initially appear to represent a type of market-based system of governance as opposed to a hierarchical (employer–employee) model, in practice the contractual relationship between the contractor/client still has the scope to operate more as a hierarchy than as a market.
The different ways dental and medical practice contracts are structured and supported mean that modes of governance and the relationships between commissioners and practitioners are very different. For example, the scope for alternative sources of income outside the NHS for medical practice has (until relatively recently) been tied to shared asset ownership (rent reimbursement). Although our medical case-studies showed GMPs geared towards tightly managing income and expenditure in their practices in order to ensure long-term viability of the business; sources of income were mainly from the NHS and dependable. The medical practice contract too was limited in the extent to which the main NHS sources of income to medical practice could be curtailed through performance management. Rather, the medical system is geared towards stretching towards incentives and attaining targets for bonuses. Although medical practice emerged as less overtly commercial than dental practice, there did appear the scope for entrepreneurialism to realise expansion of profits, which were often then reinvested to improve the range and quality of services for patients.
We found the medical practice contract and the relationship between GMPs and commissioners characteristic of a contract build around mutual dependency (see Chapter 1, Grand theories of health-care contracting, Relational contracts and Chapter 4, General dental practitioners working with the contract: macro-level behaviour, Dependency). Both principal and agent have few alternatives other than to maintain their current contractual relationship. Moreover, we found the balance of power between GMPs and commissioners very different from that between GDPs and commissioners (see Chapter 4, General dental practitioners working with the contract: macro-level behaviour, Balance of power). Finally, and perhaps most importantly of all, we found institutional logics prevailing in medical practice less in conflict with each other, and with commissioning logics. Perhaps because less conflict in institutional logics exists, working towards shared goals occurs more easily. The level of co-operation between some medical practitioners and commissioners working together to achieve public goods goals can therefore be likened more to a joint venture organisation (see Chapter 1, Grand theories of health-care contracting, Relational contracts) as opposed to a rather more oppositional market-based system. While examples of codependency and working closely towards common goals did occur within the dental cases studies, these were less common than in the medical practice setting.
Implications for commissioning
Our study comes at a time when significant policy decisions are being made concerning contracts in NHS general dental practice. As outlined in Chapter 1, Different dental contract models: Personal Dental Service, Personal Dental Service Plus, nGDS, nPDS, new contract pilots, plans for reform of the NHS dental contract are being made, with national implementation likely in the next few years. At the same time, the commissioning structure within NHS dentistry is undergoing significant reformulation. Following the 2010 White Paper Equity and Excellence: Liberating the NHS,112 the previous structure, involving local relationships between dental commissioners and GDPs, was replaced by a national dental commissioning structure under NHS England. A much smaller number of dental commissioners means reduced emphasis on the relational aspects of dental contracting under this new model. Thus dentistry has departed from having the same commissioning structure as medical practice. Commissioning structures in medical practice are still locally based, around Clinical Commissioning Groups, with doctors leading the management of commissioning (see Appendix 2). The professional representation in dental commissioning, on the other hand, is now by local dental networks, with new roles, responsibilities and ways of working still being worked out. Our study points to the possible consequences and challenges of this new dental commissioning model as well as the prospect of successfully implementing a new form of NHS dental contract:
-
Our study separates out the drivers operating at the dental practice level. In doing so, we remove the focus from the behaviour of individual GDPs or commissioners, and the tendency to blame different actors for behaving in self-interested ways. We have identified different strands of dental practice and NHS commissioning which coexist and interact with each other (ownership responsibility; duty to staff and patients; managerialism; public goods; bureaucracy; entrepreneurial commercialism). This enables policy-makers to recognise that these logics exist and work towards creating an environment where any one of these might be shaped in order to better realise mutually beneficial goals. For example, policy-makers might seek to provide an environment which recognises and enhances the scope for entrepreneurial commercialism to deliver public goods – an environment which appears more readily seen in the general medical practice context than in the dental practice context at present. Recognising, for example, that NHS dental practices need to make a profit, and making this explicit, open and unashamed, would be important in fostering this approach. Securing Excellence in Commissioning NHS Dental Services113 identifies a need to align current levers and enablers in order to successfully discharge the NHS commissioning board’s function (p. 9). Our work directly addresses this requirement, making clearer what is often taken for granted but rarely made explicit in the complex environment of dental practice.
-
Although the commissioning structure has changed since the outset of our study, the institutional logics we described and the wider influences which shape contractual behaviour in NHS dental contracting are not fixed in a single policy context. In exposing the underlying motivations and tensions which exist within the system, we provide clarity which is easily transferred as organisational structures change.
-
The new commissioning structure affords less opportunity for the conflicting self-interests of GDPs and commissioners to be recognised, discussed and resolved, ultimately reaching for a mutually beneficial solution at the level of individual dental providers. A diminution in the numbers of local commissioners means there will be less exchange at this one-to-one level, which in turn means that the role of relationships in ‘building trust’ through ‘knowing the person’ (see Chapter 4, General dental practitioners working with the contract: macro-level behaviour) will be largely lost. Commissioners will have less opportunity to communicate managerialism and public goods logics to individual practitioners. Moreover, the new structure is also likely to afford less flexibility to adapt contractual agreements at a local level to make them fair and take account of practice delivery issues. Unfair contractual arrangements can offend distributive injustice: the basic fairness of outcomes and allocations. Our study shows this as an element of ‘negative experiences’ of commissioning, which lead GDPs to look towards preserving their own self-interest.
-
On the other hand, the new commissioning structure will give more transparency and consistency in the negotiations which take place between commissioners and local GDPs. In Securing Excellence in Commissioning NHS Dental Services,113 the vision for a greater consistency in commissioning runs throughout; the word ‘consistency’ features seven times in the two-page executive summary alone. Greater consistency between local areas in approaches to commissioning is trumpeted as one of the key benefits of a new commissioning structure reliant on a central NHS commissioning board to determine strategic direction, set characteristics of high-quality services and carry oversight for securing and monitoring all dental services, as well as developing clinical information and intelligence systems to underpin this monitoring role and to challenge existing practice through benchmarking. The shift is clearly to be away from the relational and towards a transactional view of contracting. The bywords of ‘flexibility’ and ‘trust’ expressed as key features of successful contracting models in our study, where commissioners and practitioners work together to achieve mutually beneficial solutions, would seem to have little place in this new era of dental commissioning.
-
That is not to say that addressing a lack of consistency in commissioning is not needed. The lack of consistency experienced in dealings between dental practitioners and commissioners, combined with the rumour-mill method of communication of information arising from the relatively fragmented professional network which exists in NHS dental practice, was in our study revealed to contribute to perceptions of distributive injustice. A greater consistency in commissioning, particularly at a local level, is predicted by our study to yield benefits in perceptions of contractual justice (see Chapter 1, Quasi-markets in health care), and, through that, how practitioners will respond to contractual arrangements. One of the interesting findings in our quantitative work is that perceived ‘negative experiences’ of commissioning shape GDPs’ responses to resisting and/or working with the dental contract, at the micro level (chair side) and macro level (co-operating or challenging approaches to commissioning). Furthermore, we found an interaction between dental practitioner logics, their perceived experiences with commissioning and how they responded in one dental chair-side behaviour studied: taking on NHS patients where they represented financial loss to the practice. In other words, where practitioners perceive contractual injustice, they either steer patients from NHS towards private care or avoid accepting certain high-need patients for NHS care, and this significantly exacerbates the stance they would have taken given the institutional logics which guide their everyday practice. Thus, if there is perceived contractual injustice as new models of commissioning and contracting are implemented, there may be access and equity consequences as practitioners seek to protect their self-interest.
-
Alongside moves towards a greater centralisation of commissioning decisions comes a move towards a greater national consistency in the form of the NHS dental contract itself. Development and piloting of a new national dental contract is ongoing. Our study shows contracting to be a dynamic process, where rules are set and negotiated centrally, but then interpreted, resisted and adapted in a process of local implementation which results in further adjustments at a central level (see Chapter 1, Quasi-markets in health care). The extended period of piloting and shaping of the new contractual arrangements entirely fits with this view. While contract design decisions may be made centrally, translation takes place at the micro-level. Whatever form the new contract arrangements may take, there will still be a necessity to resolve competing tensions between ownership, professional values, population health managerialism and commercial demands.
-
The reforms to NHS dental commissioning acknowledge the need for a greater involvement of clinicians in shaping local strategy. 113 With the restructuring of dental commissioning arrangements, the task of negotiating competing perspectives and values held by commissioners and dental practitioners will pass from one-to-one relationships between commissioners and GDPs (through knowing the person and building trust) to relationships and negotiations at the local dental network level. The new arrangements expect that centrally developed and held information intelligence on local practice will be passed to area teams who will be charged with ‘addressing unwarranted variation’ and ‘enabling clinically led decisions’. 113 Much will depend on the balance of power and responsibility among clinicians and commissioners at the local level. There is a danger, though, which is indicated in our study findings, that clinical leaders who move themselves into positions of the professional elite become somewhat removed from grass-roots levels and viewed with a degree of suspicion by the wider network of dental practitioners. The fragmented nature of the dental practitioner network where competition exists for contracts may need to be addressed if wider clinical engagement is to be achieved. For example, doctors, in contrast with dentists, often have more time away from their surgeries (increasingly adopting portfolio careers, for example), which facilitates a wider diffusion of new ideals into everyday practice. Achieving wider clinical engagement is an area which will demand resource if the strategy of ‘socialising the commissioning direction of the NHS commissioning board’ and forming ‘productive relationships’113 is to be achieved in dentistry. Different models of local dental networks are emerging, but it is interesting that some have identified a need for several tiers of clinical representation. 114 Work done by the Greater Manchester local dental network, focused around a public health campaign to increase numbers of young children visiting dental practices in the area, involved not just practitioner membership on the local dental network itself, but diffusion of practice ideas and goals through a network of ‘clinical champions’ as well as a number of wider engagement meetings involving several hundred grass-roots practitioners. 114
-
The study allows us to recognise more fully the significance of the shift from a FFI system of dental remuneration to a model based around contractual governance. In the FFI system the set of choices (400 or so items of treatment) were clear and transparent. In a traditional piece-rate, factory production line system, there is relatively little need for accountability and management in the form of organisational structure; terms are clear. This relies, however, on being able to specify the product in terms of both quantity and quality. Dental care as a product is less easily specified than some other commodities (treatment quality and diagnoses are often debated), but on the other hand we can also argue that dental care is more easily quantified than many other aspects of health care (we can count fillings, look at radiographs, etc.) – hence the feasibility and relative success over many years of the FFI system.
-
Once the wider nature of the production of dental services, however, is recognised, seeking to more fully capture elusive aspects of quality such as patient satisfaction, the need for organisation and contractual governance escalates. Organisational form and management structures are needed to make sense of the complex nature of the work going on. The paradox, though, is that the more organisational structures are needed to manage the transaction, the greater the transaction costs. An ever-increasing focus on stipulating and monitoring quality standards is set to fail on account of the inevitability of opportunism. As each quality standard is identified and monitored, it creates the same amount of new opportunities to act against the spirit of the rules. As we invent rules, we also invent the boundaries of the rules (see Chapter 4, Commissioners working with contract: dealing with general dental practitioners). The alternative path to the escalation of regulation and transaction costs is to foster and place greater emphasis on the role of professional values in shaping behaviour and suppressing opportunism – recognising too that local practice reputation is important in the maintaining of business viability.
-
While our report mainly generalises about the interpretation of contract rules by dental practitioners at the dental chair side and focuses on frictions which arise when approaches vary from what is seen by commissioners as appropriate behaviour, our analysis also informs us about how tensions between various clinicians relating to differences in interpretation of contract rules. The relationship between the practice owner and contract holder who also provides care (the provider) and any dentists they subcontract care to (performers) is shaped by the logics of ownership, professional values, population health managerialism and entrepreneurial commercialism. Central to the logic of ownership is a responsibility for practice leadership, which involves setting practice goals and ways of doing things (see Chapter 4, Institutional logics in general dental practice). This is also informed by professional clinical values as well as commercial values. This makes subcontracting to performers a risky thing to do. Providers feel the need to employ people with the same values in order to avoid conflict within the practice and may be hesitant to expand the practice because of this (seen clearly, for example, in the actions of AD3 and ED1 in our case studies). Some dentists thus prefer to rely on family members as colleagues, to maintain a close-knit and relatively friction-free community. Avoiding the principle of ‘outsourcing’ though goes against one of the elements espoused by NPM approaches embodied in population health managerialism as advocated by commissioners. Our study thus shows how managing within-practice tensions is bound up in wider responses to institutional change.
-
Our study portrays responses to contracts as something which happens at several levels. Although there are reactions to the rules at the dental chair side, our study reveals these to be shaped at least to some extent by how tensions are resolved relating to the contractual agreement at a higher level. For example, we found correlation of behaviour such as restricting high-cost treatment (e.g. root canal treatment) and over-representing the patients’ diagnosis (e.g. more band 3 towards the end of the financial year) with ‘acceptance behaviour’ in response to commissioners – and not with practitioners who were inclined to either co-operate or argue. In other words, such acceptance behaviour represents a form of compromise and balance, which pushes the practitioner back to the practice level to try to resolve the resource issue (see Chapter 4, General dental practitioners working with the contract: macro-level behaviour). As described by Morreim,100 we see here the dentist as an economic agent forced to use his or her ability to still control resources at the micro level by exploiting the ambiguity and flexibility of contract rules, because of his or her loss of control of resources at a higher level. Opportunism is sorely tempting because it offers escape from a seeming impossible situation, allowing the practitioner to still secure indirectly what he or she can no longer control directly. There are several reasons why opportunism is undesirable, such as that by definition it represents a degree of duplicity which offends honesty, which is a basic tenet of moral integrity. It also offends distributive justice. Thus it is necessary not to foster an environment where the practitioner tends to over-ride, undermine and otherwise ‘correct’ the contract because he or she has personally judged it to be inadequate; rather, as Morreim100 suggests:p. 454
Contractual justice is better served when bad contracts are openly challenged than when they are covertly under-mined.
Implications for further research
Previous work on dental contracting has concentrated on describing dentists’ behavioural responses to changes in incentives mainly by way of reporting natural experiments associated with contract change,115,116 focusing the debate on the relative efficiency of different types of dental remuneration system and designing monitoring systems to close loopholes. Unfortunately, in these types of studies the strategic behaviour of dental practitioners remains unexplored, since the stance still tends towards a neoclassical assumption of hyper-rationality where the dental practitioner is seen as making optimal choices from a sharply defined set of possibilities. 15 These previous approaches are weakening by focusing too narrowly on dental practices as production functions with technological outputs, and ignoring the wider context, which also shapes behaviour.
Our study, while recognising the inevitability of moral hazard, adds to studies of health-care contracting by demonstrating that practitioners’ behaviour is not entirely explained by a classical economic approach based on assumptions of self-interest. Rather, behaviour is interpreted as acting in the mutual interest of ‘self’ and ‘context’. In our qualitative work we showed, in a more explicit description than previously, what it means to experience moral hazard in the dental practice context (and even the commissioning context too), as a constant interchange between self and context. The finding in our quantitative work that institutional logics are predictive of behaviour in areas of the contract open to opportunism substantiated this view. This leads us to new areas of research where the context is seen as having a role in shaping behavioural responses to contracts. We demonstrated clearly, for example, how practitioners’ perception of their dealings with commissioners shaped their behaviour. In a context which is clearly changing very rapidly in this area of health care, it will be important to explore the impact of this on how practitioners (and commissioners acting at the local level) respond to NHS contracts.
Our perspective throws open new and under-researched areas which are relevant to investigating behavioural responses to NHS contracts. Our logic model (see Figure 1) identifies several pathways, besides contract design and monitoring mechanisms and dyadic relationships between practitioners, which influence opportunism; practitioners and commissioners are influenced by wider forces such as how dentists and the NHS are portrayed in the media, relationships between the government and professional bodies, etc., all of which inform and motivate behaviour. Indeed, social and professional networks in particular may be a powerful way in which opportunism is constrained, a mechanism which is currently relatively unexplored. In reality it is likely that multiple mechanisms are relevant in restraining opportunism and there is a need for more research to understand how different mechanisms are used concurrently, and supplement and reinforce each other in combination. 117
New commissioning strategies indicate an increased emphasis on involving clinicians (local dental networks) and wider public engagement in shaping dental commissioning at a local level to shape policy. 113 This changing context, as well as changes such as the rise in DBCs and private sector provision are responses to shifts in the interplay between institutional logics. Thus, logics change structures and practice, and are changed by them in a constant interplay between agents (practitioners, patients, policy-makers, commissioners) and their environment. Study of these wider changes (e.g. the growing importance of DBCs in the dental market) is needed to more fully understand practitioners’ responses to contracts at the micro level.
Our study showed the logic of population health managerialism as emergent but often resisted in dental practice. This was less apparent in medical practice, although our data set there was relatively limited. More work exploring interacting logics in medical practice is needed, particularly looking more closely to see how doctors manage the tensions between ownership, professionalism, commercialism and logics driving a public health approach. It would also be interesting to follow up our initial work on medical practice with some quantitative work. In our dental quantitative work we were able to move on from our view of population health managerialism, which we developed in the qualitative phase of the study, to identify managerialism and pubic goods as separate logics. Many dentists fundamentally want to carry out a duty to wider society and see managerial approaches (particularly bureaucracy) as hindering rather than supporting this goal. The real struggle seems to be between managerial and professional jurisdictions, but not in the way that it is often portrayed. 117 Our study, particularly through the quantitative work, reveals professionalism in dentistry in a new light: less concerned with medical dominance and self-governance than with the relational aspects of engaging with patients who also contribute to the cost of their care. Practitioners feel an obligation to maintain the viability of the practice for the sake of staff, patients and the wider community. We see these as particular responses to pressures on dental practices to ensure financial survival in a structure where there is no co-ownership of assets and little shared contractual risk. The social contract traditionally described in medical professionalism, involving ethical obligations to society, appears redefined as one between the dentist, dental staff, patients and the local community. It is this which tends to resist to managerial efforts to reduce inequalities (e.g. allocating patients to practices from waiting lists), rather than an underlying unwillingness to serve the wider public interest.
In the doctors’ data we saw how entrepreneurial commercialism sometimes enabled investment in the practice which could be used to loosen constraints and allow expansion to improve services for their patients and the wider community. Certainly, we saw in dental practice, undertaking private work allowed dentists to do work for NHS patients at a standard that satisfied their professional and practice ownership responsibilities. Thus the lines between ‘public’ and ‘private’ sectors start to become blurred. It will be important to explore further whether or not entrepreneurial commercialism can provide a cost-effective means to achieve public goods goals while satisfying these professional and ownership sensitivities. This brings us back to NPM approaches whereby conversion of non-public goods from the public to the private sector is a key doctrine. 2 The same challenges, though, will need to be explored, with regard to what mechanisms can be used to ensure that outcomes still satisfy public values such as social and cultural equity, homogeneity and universality of service. 3
Acknowledgements
We are grateful to the National Institute for Health Research Health Services and Delivery Research programme for funding the research and for all the participants who generously contributed to the study. We are also grateful to members of the Project Advisory Group, who met periodically during the project and gave advice on design, recruitment, interpretation of results and dissemination of findings.
-
Carolyn Temple: GDP and practice owner.
-
Edwin Morgan: currently Chair of Liverpool Healthwatch. An experienced lay patient representative, having previously served as a Patient Liaison Group member at the Royal College of Surgeons (RCS) of England until January 2013, he has also served as a Health & Social Care Ambassador for Liverpool LINk in University Hospital Aintree NHS Foundation Trust and Liverpool Clinical Commissioning Group.
-
Kirk Beyon: formerly Primary Care Development Manager at Knowsley PCT, now Commissioning Officer, Merseyside Area Team, NHS England.
-
Amanda Longsdale: formerly Primary Care Contracting and Performance Manager (West Cheshire PCT), now Joint Commissioning Lead For Adults at NHS West Cheshire Clinical Commissioning Group and Programme Lead – Ageing Well at NHS West Cheshire Clinical Commissioning Group.
-
Mark Gabbay: Professor of General Practice and Head of Department of Health Services Research, Institute of Psychology, Health and Society, University of Liverpool.
-
Jenny Gallagher: Professor/Honorary Consultant in Dental Public Health, University of London.
Contributions of authors
Rebecca Harris (Professor/Honorary Consultant, Oral Health Services Research) was responsible for the original concept and project design, led the project, did paper screening and extraction, wrote the literature review, conducted most of the stakeholder interviews and some case study interviews, undertook data analysis of qualitative data, led questionnaire design and wrote the report. Professor Harris is a member of the Department of Health Evidence and Learning group advising on the evaluation of pilots of NHS dental practice contract reform.
Elizabeth Perkins (Professor, Community Nursing) contributed to the project design, literature review, data analysis of case study data, design of the questionnaire and the report revision.
Robin Holt (Professor, Organisation and Management) contributed to the project design and qualitative data analysis.
Steve Brown (Senior Lecturer, Clinical Psychology) contributed to the project design and design of the questionnaire, undertook the quantitative analysis and contributed to the report.
Jayne Garner (Research Associate) did title and abstract screening, recruited phase 2 participants, collected phase 2 data and administered the questionnaire.
Sarah Mosedale (Research Fellow) did the electronic literature search, title and abstract screening, recruited phase 2 participants, collected phase 2 data and did some stakeholder interviews.
Phil Moss (Research Assistant) collected phase 2 data relating to medical practice and was involved in this aspect of the qualitative analysis, wrote Appendix 2 and formatted the report.
Alan Farrier (Research Assistant) collected phase 3 commissioner interview data and did one medical practice interview.
Publications
Harris R, Holt R. Interacting institutional logics in general dental practice. Soc Sci Med 2013;94:63–70.
Harris R, Mosedale S, Garner J, Perkins E. What factors influence the use of contracts in the context of NHS dental practice? A systematic review of theory and logic model. Soc Sci Med 2014;108:54–9.
Harris R, Garner J, Perkins E. A discourse of disconnection: challenges to clinical engagement and collaborative dental commissioning. Br Dent J 2015;218:393–7.
Harris R, Brown S, Holt R, Perkins E. Do institutional logics predict interpretation of contract rules at the dental chair-side? Soc Sci Med 2014;122:81–9.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
References
- Bennet C, Ferlie E. Contracting in theory and practice: some evidence from the NHS. Public Adm 1996;74:49-66. http://dx.doi.org/10.1111/j.1467-9299.1996.tb00857.x.
- Simonet D. The new public management theory in the British health care system: a critical review. Adm Soc 2013;20:1-25. 10.1177/0095399713485001.
- Ferlie E, Pettigrew A, Ashburner L, Fitzgerald L. The New Public Management in Action. Oxford, UK: Oxford University Press; 1996.
- Working for Patients. London: HMSO; 1989.
- Butler J, Robinson R, Le Grand J. Evaluating the NHS Reforms. London: The King’s Fund; 1993.
- Palmer N. The use of private-sector contracts for primary health care: theory, evidence and lessons for low-income and middle-income countries. Bull World Health Organ 2000;78:821-9.
- Enthoven A. Reflections on the Management of the National Health Service. London: Nuffield Provincial Hospitals Trust; 1985.
- Asthana S. Liberating the NHS? A commentary on the Lansley White Paper. Equity and Excellence. Soc Sci Med 2011;72:815-20. http://dx.doi.org/10.1016/j.socscimed.2010.10.020.
- Boyett I, Finlay D. The quasi-market, the entrepreneur and the effectiveness of the NHS business manager. Public Adm 1995;73:393-411. http://dx.doi.org/10.1111/j.1467-9299.1995.tb00835.x.
- Jensen M, Meckling W. The nature of man. J Appl Corporate Finance 1994;7:4-19. http://dx.doi.org/10.1111/j.1745-6622.1994.tb00401.x.
- Howden-Chapman P. Doing the splits: contracting issues in the New Zealand Health Service. Health Policy 1993;24:273-86. http://dx.doi.org/10.1016/0168-8510(93)90046-R.
- Roberts JA. Managing markets. J Public Health Med 1993;15:305-10.
- Hughes D, Griffiths L, McHale JV. Do quasi-markets evolve? Institutional analysis and the NHS. Camb J Econ 1997;21:259-76. http://dx.doi.org/10.1093/oxfordjournals.cje.a013669.
- Light DW. Managed competition, governmentalility and institutional response in the United Kingdom. Soc Sci Med 2001;52:1167-81. http://dx.doi.org/10.1016/S0277-9536(00)00237-9.
- Ferlie E. The creation and evolution of quasi markets in the public sector: a problem for strategic management. Strateg Manag J 1992;13:79-97. http://dx.doi.org/10.1002/smj.4250130907.
- Hall CS, Gardener L. Theories of Personality. New York, NY: John Wiley and Sons; 1957.
- Kerlinger FM. Behavioural Research: A Conceptual Approach. Philadelphia, PA: Rinehart and Winston Holt; 1979.
- Doty DH, Glick WH. Typologies as a unique form of theory building: toward improved understanding and modelling. Acad Manag Rev 1994;19:230-51. http://dx.doi.org/10.2307/258704.
- Ratcliffe J. Extra-market incentives in the new NHS. Health Policy 1993;25:169-83. http://dx.doi.org/10.1016/0168-8510(93)90110-B.
- Levaggi R. Regulating internal markets for hospital care. J Regul Econ 2007;32:173-93. http://dx.doi.org/10.1007/s11149-007-9035-y.
- Williamson OE. Markets and Hierarchies: Analysis and Anti-trust Implications. New York, NY: Free Press; 1975.
- Williamson OE. Transaction cost economics: the governance of contractual relations. J Law Econ 1979;22:233-61. http://dx.doi.org/10.1086/466942.
- Ferlie E, McGivern G. Relationships between Health Care Organisations: A Critical Overview of the Literature and the Research Agenda. London: Imperial College; 2003.
- Dawson D, Goddard M. Long-term contracts in the NHS: a solution in search of a problem?. Health Econ 2011;8:709-20. http://dx.doi.org/10.1002/(SICI)1099-1050(199912)8:8<709::AID-HEC482>3.0.CO;2-0.
- Granovetter M. Economic action and social structure: the problem of embeddedness. AJS 1985;91:481-510. http://dx.doi.org/10.1086/228311.
- MacNeil I. The New Social Contract. London: Yale University Press; n.d.
- Ferguson B, Posnett J. Pricing in the NHS internal market. Health Econ 1994;3:133-6. http://dx.doi.org/10.1002/hec.4730030302.
- Goddard M, Mannion R. From competition to co-operation: new economic relationships in the National Health Service. Health Econ 1998;7:105-9. http://dx.doi.org/10.1002/(SICI)1099-1050(199803)7:2<105::AID-HEC333>3.0.CO;2-K.
- Taylor-Gooby P. Trust and welfare state reform: the example of the NHS. Soc Policy Adm 2008;42:288-306. http://dx.doi.org/10.1111/j.1467-9515.2007.00592.x.
- Donato R. Extending transaction cost economics: towards a synthesised approach for analysing contracting in health care markets with experience from the Australian private sector. Soc Sci Med 2010;71:1989-96. http://dx.doi.org/10.1016/j.socscimed.2010.09.016.
- Ferlie E. The creation and evolution of quasi-markets in the public sector: early indications from the National Health Service. Policy Polit 1994;22:105-12. http://dx.doi.org/10.1332/030557394782453744.
- Smith SR. Transforming public services: contracting for social and health services in the US. Public Adm 1996;74:113-27. http://dx.doi.org/10.1111/j.1467-9299.1996.tb00860.x.
- Baxter S, Killoran A, Kelly MP, Goyder E. Synthesizing diverse evidence: the use of primary qualitative data analysis methods and logic models in public health reviews. Public Health 2010;124:99-106. http://dx.doi.org/10.1016/j.puhe.2010.01.002.
- Whynes DK, Baines DL. Income-based incentives in UK general practice. Health Policy 1998;43:15-31. http://dx.doi.org/10.1016/S0168-8510(97)00078-X.
- Greenwood R, Hining C, Brown J. ‘P2 form’ strategic management: corporate practices in professional partnerships. Acad Manag J 1990;33:725-55. http://dx.doi.org/10.2307/256288.
- Kravitz AS, Treasure ET. Manual of Dental Practice Version 4.1. Cardiff: The Council of European Dentists; 2009.
- Department of Health . Standard GDS Model Contract: November 2012 Update 2012. www.gov.uk/government/publications/dental-services-contracts-updated-for-2012 (accessed 3 June 2014).
- Primary Care Contracting . Briefing Paper: Termination of Dental Contracts and Sale of Goodwill 2006 2006. www.pcc-cic.org.uk/sites/default/files/articles/attachments/goodwill_briefing_paper.pdf (accessed 27 May 2015).
- The Future of GP Practice Premises. London: BMA; 2010.
- Webster C, Loudon I, Horder J, Webster C. General Practice under the National Health Service 1948–1997. Oxford: Clarendon Press; 1998.
- O’Donnell CA, Ring A, McLean G, Grant S, Guthrie B, Gabbay M, et al. The New GMS Contract in Primary Care: The Impact of Governance and Incentives on Care 2011.
- Harris RV, Sun N. Translation of remuneration arrangements into incentives to delegate to English dental therapists. Health Policy 2012;104:253-9. http://dx.doi.org/10.1016/j.healthpol.2011.11.013.
- Howden-Chapman P, Ashton T. Shopping for health: purchasing health services through contracts. Health Policy 1994;29:61-83. http://dx.doi.org/10.1016/0168-8510(94)90007-8.
- Internal Revenue Service . Independent Contractor Defined 2013 2015. www.irs.gov/Businesses/Small-Businesses-%26-Self-Employed/Independent-Contractor-Defined (accessed 27 May 2015).
- Walsh K, Deakin N, Smith P, Spurgeon P, Thomas N. Contracting for Change: Contracts in Health, Social Care and Other Local Government Services. Oxford: Oxford University Press; 1997.
- Stinchcombe A, Heimer C. Organisation Theory and Project Management: Administering Uncertainty in Norwegian Offshore Oil. Oslo: Norwegian University Press; 1985.
- McDonald R. Market reforms in English primary medical care: medicine, habitus and the public sphere. Sociol Health Illn 2009;31:659-72. http://dx.doi.org/10.1111/j.1467-9566.2009.01165.x.
- Buck D, Newton JT. Dental access: The privatisation of NHS dentistry? A national snapshot of general dental practitioners. Br Dent J 2001;190:115-18. http://dx.doi.org/10.1038/sj.bdj.4800900.
- Calnan M, Silvester S, Manley G, Taylor-Gooby P. Doing business in the NHS: exploring dentists’ decisions to practise in the public and private sectors. Sociol Health Illn 2000;22:742-64. http://dx.doi.org/10.1111/1467-9566.00229.
- BBC News . Dentists’ ‘Private Work Tops NHS’ 2006 2006. http://news.bbc.co.uk/1/hi/health/5366490.stm (accessed 27 May 2015).
- Understanding Public and Patient Attitudes to the NHS. London: Healthcare Commission; 2006.
- British Medical Association . Guidance: Focus on Private Practice 2010 2004. http://bma.org.uk/-/media/Files/PDFs/Practical%20advice%20at%20work/Private%20practice/Focus%20on%20private%20practice%20July%202010.pdf (accessed 27 May 2015).
- Pulse . Premises Rule Change May Allow GPs Freedom to Ramp Up Private Work 2013 2013. www.pulsetoday.co.uk/your-practice/practice-topics/premises/premises-rule-change-may-allow-gps-freedom-to-ramp-up-private-work/20002582.article (accessed 27 May 2015).
- King RS. The dash for dentures: the turbulent introduction of NHS dentistry. Br Dent J 1988;185:14-8. http://dx.doi.org/10.1038/sj.bdj.4809715.
- Reay T, Hinings CR. The recomposition of an organizational field: health care in Alberta. Organ Stud 2005;26:351-84. http://dx.doi.org/10.1177/0170840605050872.
- Promoting Better Health. London: HMSO; 1987.
- Report of the Committee of Enquiry into Unnecessary Dental Treatment. London: HMSO; 1986.
- Lynch M, Calnan M. The changing public/private mix in dentistry in the UK: a supply side perspective. Health Econ 2003;12:309-21. http://dx.doi.org/10.1002/hec.728.
- Bloomfield K. Fundamental Review of Dental Remuneration: Report of Sir Kenneth Bloomfield KCB. HMSO; 1992.
- Health Committee. Fourth Report of Session 1992–93, Dental Services, HC 264–I n.d.
- Improving NHS Dentistry 1994.
- Choice and Opportunity – Primary Care: The Future. London: HMSO; 1996.
- Health and Social Care (Community Health and Standards) Act 2003. n.d.
- The National Health Service (Primary Care) Act 1997 (Commencement No. 2) Order 1997. n.d.
- Goodwin N, Morris AJM, Hill KB, McLeod HS, Burke FJT, Hall AC, et al. National evaluation of personal dental services (PDS) pilots: main findings and policy implications. Br Dent J 2003;195:640-3. http://dx.doi.org/10.1038/sj.bdj.4810781.
- NHS Dental Services in England: An Independent Review Led by Professor Jimmy Steele. London: Department of Health; 2009.
- Ward P, Mehra A. The Big Decision: The NGDS Contract; NHS or Private; Which Way Should I Go?. London: Samera; 2006.
- British Dental Association. GDPC Responses to LDC Conference Motions 2010 n.d. www.ldcuk.org/documents/doc_view/117-2010-conference-motions-gdpc-response (accessed 27 May 2015).
- NHS Dental Contract: Proposals for Pilots. London: Department of Health; 2010.
- Engeström Y. Expansive learning at work: toward an activity theoretical reconceptualization. J Educ Work 2001;14:133-56. http://dx.doi.org/10.1080/13639080020028747.
- Denzin NK. The Research Act: A Theoretical Introduction to Sociological Methods. New York, NY: Praeger; 1978.
- Bouchard TJ. Unobtrusive measures: an inventory of uses. Sociol Methods Res 1976;4:267-300. http://dx.doi.org/10.1177/004912417600400301.
- Boring EG. The rôle of theory in experimental psychology. Am J Psychol 1953;66:169-84. http://dx.doi.org/10.2307/1418724.
- Johnson RB, Onwuegbuzie AJ, Turner LA. Toward a definition of mixed methods research. J Mixed Methods Res 2007;1:112-33. http://dx.doi.org/10.1177/1558689806298224.
- Hartley J, Cassell C, Symon G. Essential Guide to Qualitative Methods in Organisational Research. London: SAGE Publications; 2004.
- Eisenhardt KM. Building theories from case study research. Acad Manag Rev 1989;14:532-50. http://dx.doi.org/10.2307/258557.
- Yin R. Case Study Research: Design and Methods. London: SAGE; 2009.
- Bergen A, While A. A case for case studies: exploring the use of case study design in community nursing research. J Adv Nurs 2000;31:926-34. http://dx.doi.org/10.1046/j.1365-2648.2000.01356.x.
- Barley S, Tolbert P. Institutionalisation and structuration: studying the links between action and institution. Organ Stud 1997;18:93-117. http://dx.doi.org/10.1177/017084069701800106.
- Lawrence T, Suddaby R, Leca B. Institutional Work: Actors and Agency in Institutional Studies of Organisations. Cambridge: Cambridge University Press; 2011.
- Berger P, Luckmann T. The Social Construction of Reality: A Treatise in the Sociology of Knowledge. New York, NY: Anchor Books; 1967.
- Selznick P. Leadership in Administration: A Sociological Interpretation. Berkeley, CA: University of California Press; 1984.
- DiMaggio PJ, Powell WW. The iron cage revisited: institutional isomorphism and collective rationality in organisational fields. Am Sociol Rev 1983;48:147-60. http://dx.doi.org/10.2307/2095101.
- Lawrence TB, Suddaby R, Clegg S, Hardy C, Lawrence TB, Nord W. Handbook of Organisation Studies. London: Sage; 2006.
- Friedland R, Alford RR, Powell WW, DiMaggio PJ. The New Institutionalism in Organisational Analysis. Chicago: University of Chicago Press; 1991.
- Thornton PH, Ocasio W. Institutional logics and the historical contingency of power in organizations: executive succession in the higher education publishing industry, 1958–1990. Am J Sociol 1999;105:801-43. http://dx.doi.org/10.1086/210361.
- Oliver C. Strategic responses to institutional pressures. Acad Manag Rev 1991;16:145-79.
- Scott WR. Institutions and Organisations. Thousand Oaks, CA: Sage; 2001.
- Wells AS, Hirshberg D, Lipton M, Oakes J. Bounding the case within its context: a constructivist approach to studying detracking reform. Educ Res 1995;24:18-24. http://dx.doi.org/10.3102/0013189X024005018.
- Shepherd J. A Classification of Primary Care Trusts in England Based upon the New Definitions of Rural Areas. London: Rural Evidence Research Centre at Birkbeck College, University of London; 2005.
- Health and Social Care Information Centre . NHS Dental Statistics for England, Quarter 3, 31 December 2008 2009. www.hscic.gov.uk/searchcatalogue?productid=549&topics=1%2fPrimary+care+services%2fDental+services&sort=Most+recent&size=100&page=1#top (accessed 28 May 2015).
- Numagami T. The infeasibility of invariant laws in management studies: a reflective dialogue in defense of case studies. Organ Sci 1998;9:2-15. http://dx.doi.org/10.1287/orsc.9.1.1.
- Fernandez S. Understanding contracting performance: an empirical analysis. Adm Soc 2009;41:67-100. http://dx.doi.org/10.1177/0095399708330257.
- Dental Earnings and Expenses, England and Wales, 2010/2011. 2013.
- Trafimow D. Problems with change in R2 as applied to theory of reasoned action research. Br J Soc Psychol 2004;43:515-30. http://dx.doi.org/10.1348/0144666042565344.
- Deem R, Brehony KJ. Management as ideology: the case of ‘new managerialism’ in higher education. Oxf Rev Educ 2005;31:217-35. http://dx.doi.org/10.1080/03054980500117827.
- Milewa T, Valentine J, Calnan M. Managerialism and active citizenship in Britain’s reform health service: power and community in an era of decentralisation. Soc Sci Med 1998;47:507-17. http://dx.doi.org/10.1016/S0277-9536(98)00150-6.
- Checkland K, Harrison S, Snow S, McDermott I, Coleman A. Commissioning in the English National Health Service: what’s the problem?. J Soc Policy 2012;41:533-50. http://dx.doi.org/10.1017/S0047279412000232.
- Walton E. The persistence of bureaucracy: a meta-analysis of Weber’s model of bureaucratic control. Organ Stud 2005;26:569-600. http://dx.doi.org/10.1177/0170840605051481.
- Morreim EH. Gaming the system: dodging rules, ruling the dodgers. Arch Intern Med 1991;151:443-7. http://dx.doi.org/10.1001/archinte.1991.00400030013003.
- Atkinson S, Butcher D. Trust in managerial relationships. J Manag Psychol 2003;18:282-304. http://dx.doi.org/10.1108/02683940310473064.
- Gambetta D. Trust: Making and Breaking Cooperative Relations. Oxford: Blackwell; 1998.
- Chan M. Some theoretical propositions pertaining to the context of trust. Int J Organ Anal 1997;5:227-48. http://dx.doi.org/10.1108/eb028868.
- Lamothe M, Lamothe S. To trust or not to trust? What matters in local government–vendor relationships?. J Public Adm Res Theory 2011;22:867-92. http://dx.doi.org/10.1093/jopart/mur063.
- Saunders M, Thornhill A. Trust and mistrust in organizations: an exploration using an organizational justice framework. Eur J Work Organ Psychol 2004;13:493-515. http://dx.doi.org/10.1080/13594320444000182.
- Hanlon G. Professionalism as enterprise: service class politics and the redefinition of professionalism. Sociology 1998;32:43-6. http://dx.doi.org/10.1177/0038038598032001004.
- World Health Organisation . Trade, Foreign Policy, Diplomacy and Health 2013 n.d. www.who.int/trade/glossary/story041/en/index.html (accessed 28 May 2015).
- Sugden R. Reciprocity: the supply of public goods through voluntary contributions. Econ J 1984;94:772-87. http://dx.doi.org/10.2307/2232294.
- Reay T, Hinings C. Managing the rivalry of competing institutional logics. Organ Stud 2009;30:629-52. http://dx.doi.org/10.1177/0170840609104803.
- Aiken L, West S. Multiple Regression: Testing and Interpreting Interactions. Newbury Park, CA: SAGE; 1991.
- Williamson O. Opportunism and its critics. Manag Decis Econ 1993;14:97-107. http://dx.doi.org/10.1002/mde.4090140203.
- Equity and Excellence: Liberating the NHS. 2010.
- Securing Excellence in Commissioning NHS Dental Services. London: NHS; 2013.
- Brocklehurst P, Bridgman C, Davies G. A qualitative evaluation of a Local Professional Network programme ‘Baby teeth DO matter’. Community Dent Health 2013;30:241-8.
- Chalkley M, Tilley C, Young L, Bonetti D, Clarkson J. Incentives for dentists in public service: evidence from a natural experiment. J Public Adm Res Theory 2010;20:1207-23. http://dx.doi.org/10.1093/jopart/muq025.
- Tickle M, McDonald R, Franklin J, Aggarwal VR, Milsom K, Reeves D. Paying for the wrong kind of performance? Financial incentives and behaviour changes in National Health Service dentistry 1992–2009. Community Dent Oral Epidemiol 2011;39:465-73. http://dx.doi.org/10.1111/j.1600-0528.2011.00622.x.
- Thorne M. Colonizing the new world of NHS management: the shifting power of professionals. Health Serv Manag Res 2002;15:14-26. http://dx.doi.org/10.1258/0951484021912798.
- Light DW. From Managed Competition to Managed Cooperation: Theory and Lessons from the British Experience 1997;75:297-341. http://dx.doi.org/10.1111/1468-0009.00058.
- Ranade W. The theory and practice of managed competition in the National Health Service. Public Adm 1995;73:241-62. http://dx.doi.org/10.1111/j.1467-9299.1995.tb00826.x.
- Allen P. Plus ça change, plus c’est la meme chose: to the internal market and back in the British National Health Service?. Appl Health Econ Health Policy 2002;1:171-8.
- Broomberg J. Managing the health care market in developing countries: prospects and problems. Health Policy Plann 1994;9:237-51. http://dx.doi.org/10.1093/heapol/9.3.237.
- Segall M. From cooperation to competition in national health systems – and back? Impact on professional ethics and quality of care. Int J Health Plann Manag 2000;15:61-79. http://dx.doi.org/10.1002/(SICI)1099-1751(200001/03)15:1<61::AID-HPM573>3.0.CO;2-4.
- Vining AR, Globerman S. Contracting-out health care services: a conceptual framework. Health Policy 1999;46:77-96. http://dx.doi.org/10.1016/S0168-8510(98)00056-6.
- Enthoven AC. On the ideal market-structure for 3rd-party purchasing of health-care. Soc Sci Med 1994;39:1413-24. http://dx.doi.org/10.1016/0277-9536(94)90236-4.
- Palmer N, Mills A. Classical versus relational approaches to understanding controls on a contract with independent GPs in South Africa. Health Econ 2003;12:1005-20. http://dx.doi.org/10.1002/hec.792.
- Propper C, Burgess S, Gossage D. Competition and quality: evidence from the NHS internal market 1991–9. Econ J 2008;118:138-70. http://dx.doi.org/10.1111/j.1468-0297.2007.02107.x.
- Woolhandler S, Himmelstein DU. Competition in a publicly funded healthcare system. BMJ 2007;335:1126-9. http://dx.doi.org/10.1136/bmj.39400.549502.94.
- Randall GE, Williams AP. Exploring limits to market-based reform: managed competition and rehabilitation home care services in Ontario. Soc Sci Med 2006;62:1594-604. http://dx.doi.org/10.1016/j.socscimed.2005.08.042.
- Propper C. Market structure and prices: the responses of hospitals in the UK National Health Service to competition. J Public Econ 1996;61:307-35. http://dx.doi.org/10.1016/0047-2727(95)01561-2.
- Propper C. Regulatory reform of the NHS internal market. Health Econ 1995;4:77-83. http://dx.doi.org/10.1002/hec.4730040201.
- Libby AM, Wallace NT. Effects of contracting and local markets on costs of public mental health services in California. Psychiatr Serv 1998;49:1067-71. http://dx.doi.org/10.1176/ps.49.8.1067.
- Propper C, Soderlund N. Competition in the NHS internal market: an overview of its effects on hospital prices and costs. Health Econ 1998;7:187-97. http://dx.doi.org/10.1002/(SICI)1099-1050(199805)7:3<187::AID-HEC349>3.0.CO;2-F.
- Propper C, Wilson D, Soderlund N. The effects of regulation and competition in the NHS internal market: the case of general practice fundholder prices. J Health Econ 1998;17:645-73. http://dx.doi.org/10.1016/S0167-6296(98)00029-0.
- Levaggi L, Levaggi R. Strategic costs and preferences revelation in the allocation of resources for health care. Int J Health Care Finance Econ 2010;10:239-56. http://dx.doi.org/10.1007/s10754-010-9079-x.
- Chalkley M, Malcolmson JM. Competition in NHS quasi-markets. Oxf Rev Econ Policy 1996;12:89-9. http://dx.doi.org/10.1093/oxrep/12.4.89.
- Whynes DK. The NHS internal market: economic aspects of its medium term development. Int J Health Plann Manag 1993;8:107-22. http://dx.doi.org/10.1002/hpm.4740080204.
- Propper C, Burgess S, Green K. Does competition between hospitals improve the quality of care? Hospital death rates and the NHS internal market. J Public Econ 2004;88:1247-72. http://dx.doi.org/10.1016/S0047-2727(02)00216-5.
- Brekke KR, Cellini R, Siciliani L, Straume OR. Competition and quality in health care markets: a differential-game approach. J Health Econ 2010;29:508-23. http://dx.doi.org/10.1016/j.jhealeco.2010.05.004.
- Allen P. A socio-legal and economic analysis of contracting in the NHS internal market using a case study of contracting for district nursing. Soc Sci Med 2002;54:255-66. http://dx.doi.org/10.1016/S0277-9536(01)00025-9.
- Allen P, Croxson B, Roberts JA, Archibald K, Crawshaw S, Taylor L. The use of contracts in the management of infectious disease related risk in the NHS internal market. Health Policy 2002;59:257-81. http://dx.doi.org/10.1016/S0168-8510(01)00183-X.
- Levaggi R. NHS contracts: an agency approach. Health Econ 1996;5:341-52. http://dx.doi.org/10.1002/(SICI)1099-1050(199607)5:4<341::AID-HEC196>3.0.CO;2-7.
- Rosenthal MB, Minden S, Manderscheid R, Henderson M. Typology of organizational and contractual arrangements for purchasing and delivery of behavioral health care. Adm Policy Ment Health 2006;33:461-9. http://dx.doi.org/10.1007/s10488-005-0025-z.
- Burgoyne JG, Brown DH, Hindle A, Mumford MJ. A multi-disciplinary identification of issues associated with ‘contracting’ in market-oriented health service reforms. Br J Manag 1997;8:39-4. http://dx.doi.org/10.1111/1467-8551.00038.
- McGuire TG, Riordan MH. Contracting for community-based public mental health services. Adv Health Econ Health Serv Res 1993;14:55-69.
- Chalkley M, Malcolmson JM. Contracting for health care with unmonitored quality. Econ J 1998;108:1093-100. http://dx.doi.org/10.1111/1468-0297.00331.
- Chalkley M, Malcolmson JM. Contracts for the National Health Service. Econ J 1996;106:1691-701. http://dx.doi.org/10.2307/2235210.
- Kuhn M, Siciliani L. Performance indicators for quality with costly falsification. J Econ Manag Strategy 2009;18:1137-54. http://dx.doi.org/10.1111/j.1530-9134.2009.00240.x.
- Chalkley M, McVicar D. Choice of contracts in the British National Health Service: an empirical study. J Health Econ 2008;27:1155-67. http://dx.doi.org/10.1016/j.jhealeco.2008.05.005.
- Csaba I, Fenn P. Contractual choice in the managed health care market: an empirical analysis. J Health Econ 1997;16:579-88. http://dx.doi.org/10.1016/S0167-6296(96)00533-4.
- Fenn P, Rickman N, McGuire A. Contracts and supply assurance in the UK health market. J Health Econ 1994;13:125-44. http://dx.doi.org/10.1016/0167-6296(94)90020-5.
- Chalkley M, Khalil F. Third party purchasing of health services: patient choice and agency. J Health Econ 2005;24:1132-53. http://dx.doi.org/10.1016/j.jhealeco.2005.04.002.
- Mukamel DB, Weimer DL, Mushlin AI. Interpreting market share changes as evidence for effectiveness of quality report cards. Med Care 2007;45:1227-32. http://dx.doi.org/10.1097/MLR.0b013e31812f56bb.
- Chalkley M, Malcolmson JM. Contracting for health services when patient demand does not reflect quality. J Health Econ 1998;17:1-19. http://dx.doi.org/10.1016/S0167-6296(97)00019-2.
- Jelovac Z. Physicians’ payment contracts, treatment decisions and diagnosis accuracy. Health Econ 2001;10:9-25. http://dx.doi.org/10.1002/1099-1050(200101)10:1<9::AID-HEC560>3.0.CO;2-Y.
- Shmueli A, Glazer J. Addressing the inequity of capitation by variable soft contracts. Health Econ 1999;8:335-43. http://dx.doi.org/10.1002/(SICI)1099-1050(199906)8:4<335::AID-HEC433>3.0.CO;2-O.
- Siciliani L. Optimal contracts for health services in the presence of waiting times and asymmetric information. B E J Econ Anal Policy 2007;7. http://dx.doi.org/10.2202/1935-1682.1661.
- Ashton T. Contracting for health services in New Zealand: a transaction cost analysis. Soc Sci Med 1998;46:357-67. http://dx.doi.org/10.1016/S0277-9536(97)00164-0.
- Ashton T, Cumming J, McLean J. Contracting for health services in a public health system: the New Zealand experience. Health Policy 2004;69:21-3. http://dx.doi.org/10.1016/j.healthpol.2003.11.004.
- Flynn R, Pickard S, Williams G. Contracts and the quasi-market in community health services. J Soc Policy 1995;24:529-50. http://dx.doi.org/10.1017/S0047279400025423.
- Burke C, Goddard A. Internal markets: the road to inefficiency. Public Adm 1990;68:389-96. http://dx.doi.org/10.1111/j.1467-9299.1990.tb00767.x.
- Guinness L. What can transaction costs tell us about governance in the delivery of large scale HIV prevention programmes in southern India?. Soc Sci Med 2011;72:1939-47. http://dx.doi.org/10.1016/j.socscimed.2011.01.019.
- Petsoulas C, Allen P, Hughes D, Vincent-Jones P, Roberts J. The use of standard contracts in the English National Health Service: a case study analysis. Soc Sci Med 2011;73:185-92. http://dx.doi.org/10.1016/j.socscimed.2011.05.021.
- Ham C. Managed markets in health care: the UK experiment. Health Policy 1996;35:279-92. http://dx.doi.org/10.1016/0168-8510(95)00789-X.
- Preker AS, Harding A, Travis P. ‘Make or buy’ decisions in the production of health care goods and services: new insights from institutional economics and organizational theory. Bull World Health Organ 2000;78:779-90.
- Joslyn E. Contracting in the National Health Service (NHS): recognizing the need for co-operation. J Nurs Manag 1997;5:151-6. http://dx.doi.org/10.1046/j.1365-2834.1997.00112.x.
- Raftery J, Robinson R, Mulligan J, Forrest S. Contracting in the NHS quasi-market. Econ Health Care Syst 1996;5:353-62. http://dx.doi.org/10.1002/(SICI)1099-1050(199607)5:4<353::AID-HEC215>3.0.CO;2-8.
- Exworthy M, Powell M, Mohan J. The NHS: quasi-market, quasi-hierarchy and quasi-network?. Public Money Manag 1999;19:15-22. http://dx.doi.org/10.1111/1467-9302.00184.
- Gustafsson RA. Open the black box: paradoxes and lacunas in Swedish health care reforms. Int J Health Serv 1995;25:243-58. http://dx.doi.org/10.2190/F81H-W0PL-PMWA-1J0R.
- McHale JV, Hughes D, Griffiths L. Disputes in the NHS internal market: regulation and relationships. Med Law Int 2011;2:215-27. http://dx.doi.org/10.1177/096853329600200302.
- Exworthy M. Localism in the NHS quasi-market. Environ Plann C: Government Policy 1998;16:449-62. http://dx.doi.org/10.1068/c160449.
- Fredriksson S, Olli H, Mattila M, Wass H. The politics of competitive tendering: political orientation and attitudes towards contracting out among Finnish local politicians. Local Government Stud 2010;36:637-54. http://dx.doi.org/10.1080/03003930.2010.506977.
- Abbott S, Proctor S, Iacovou N. NHS purchaser–provider relationships in England and Wales: the view from primary care. Soc Policy Adm 2009;43:1-14. http://dx.doi.org/10.1111/j.1467-9515.2008.00642.x.
- Mannion R. General practitioner commissioning in the English National Health Service: continuity, change, and future challenges. Int J Health Serv 2008;38:717-30. http://dx.doi.org/10.2190/HS.38.4.h.
- Liu XZ, Hotchkiss DR, Bose S. The impact of contracting-out on health system performance: a conceptual framework. Health Policy 2007;82:200-11. http://dx.doi.org/10.1016/j.healthpol.2006.09.012.
- Fry J. General Practice and Primary Health Care 1940s–1980s n.d. www.nuffieldtrust.org.uk/sites/files/nuffield/publication/General_Practice.pdf.
- Glendinning C. GPs and contracts: bringing general practice into primary care. Soc Policy Adm 1999;33:115-31. http://dx.doi.org/10.1111/1467-9515.00138.
- Goodwin N, Dixon A, Poole T, Raleigh V. Improving the Quality of Care in General Practice: Report of an Independent Inquiry Commissioned by The King’s Fund n.d. www.kingsfund.org.uk/sites/files/kf/improving-quality-of-care-general-practice-independent-inquiry-report-kings-fund-march-2011_0.pdf.
- Levitt R, Wall A. The Reorganised National Health Service. London: Croom Helm; 1984.
- Wyke S, Mays N, Street A, Bevan G, McLeod H, Goodwin N. Should general practitioners purchase health care for their patients? The total purchasing experiment in Britain. Health Policy 2003;65:243-59. http://dx.doi.org/10.1016/S0168-8510(03)00040-X.
- Robinson J. From contracts to service agreements: what can be learned from total purchasing?. J Manag Med 1998;12:370-7. http://dx.doi.org/10.1108/02689239810243896.
- British Medical Association . Personal Medical Service (Agreements): Guidance for GPs n.d. http://bma.org.uk/-/media/Files/PDFs/Practical%20advice%20at%20work/Contracts/gppmsagreements0904.pdf.
- Maisey S, Steel N, Marsh R, Gillam S, Fleetcroft R, Howe A. Effects of payment for performance in primary care: qualitative interview study. J Health Serv Res Policy 2008;13:133-9. http://dx.doi.org/10.1258/jhsrp.2008.007118.
- Curry N, Goodwin N, Naylor C, Robinson R. Practice-Based Commissioning: Reinvigorate, Replace or Abandon? n.d. www.kingsfund.org.uk/sites/files/kf/Practice-based-Commissioning-Reinvigorate-replace-abandon-Curry-Goodwin-Naylor-Robertson-Kings-Fund-November-2008.PDF.
- Ellins J, Ham C, Parker H. Choice and Competition in Primary Care: Much Ado about Nothing? n.d. http://epapers.bham.ac.uk/745/1/choice_competition_primary_care.pdf.
- Smith J, Holder H, Edwards N, Maybin J, Parker H, Rosen R, et al. Securing the Future of General Practice: New Models of Primary Care 2013. www.nuffieldtrust.org.uk/sites/files/nuffield/130718_securing_the_future_of_general_practice-_full_report_0.pdf.
- Heins E, Pollock AM, Price D. The commercialisation of GP services: a survey of APMS contracts and new GP ownership. Br J Gen Pract 2009;59:e339-43. http://dx.doi.org/10.3399/bjgp09X472638.
- Ellins J, Ham C, Parker H. Opening up the primary care market. BMJ 2009;338:798-800. http://dx.doi.org/10.1136/bmj.b1127.
- Davidson S, Evans P. NHS Unlimited? Who Runs Our GP Services (ND) n.d. www.nhscampaign.org/uploads/documents/NHS.
- NHS Employers Federation . Investing in General Practice: The New GMS Contract n.d. www.nhsemployers.org/SiteCollectionDocuments/gms_contract_cd_130209.pdf.
- Naylor C, Curry N, Holder H, Ross S, Marshall L, Tait E. Clinical Commissioning Groups: Supporting Improvement in General Practice? 2013. www.kingsfund.org.uk/sites/files/kf/field/field_publication_file/clinical-commissioning-groups-report-ings-fund-nuffield-jul13.pdf.
- Bostock N. GP Contract 2014 15: Third of QOF Cut As GPs Take On Wider Elderly Role 2013. www.gponline.com/News/article/1221068/GP-contract-2014-15-Third-QOF-cut-GPs-24-7-elderly-role/.
Appendix 1 Systematic review tables of health-care contracting theory with references
| Theory | Constructs (in bold) and relationships | Citations |
|---|---|---|
| Grand theory (1) | ||
| Benefits of a quasi-market | Competition enhances efficiency because this addresses root causes of efficiency, which are embedded in professional and organisational culture and institutional rules | Light (1997),118 Light (2001),14 Ranade (1995)119 |
| By using public agencies to act as purchasers on behalf of consumers, asymmetry of information can be minimised | Levaggi (2007),20 Allen (2002)120 | |
| Competition requires extensive regulation and strong management to guard against provider profit-making compromising equity | Broomberg (1994),121 Segall (2000)122 | |
| Market incentive mechanisms | To secure a reasonable share of the market, providers must offer the goods/service at an attractive selling price. To maximise profits, production costs must be kept low. There is an incentive to demonstrate high quality of care to acquire and maintain long-term contracts | Ratcliffe (1993)19 |
| Mid-level theory (1) | ||
| Quasi-market conditions to achieve improvements in efficiency, equity and patient responsiveness | Five conditions must be present: (1) the market must be contestable, with barriers to entry and exit not too high; (2) both purchaser and provider should have access to cheap and accurate information on cost and quality; (3) transaction costs should not exceed efficiency gains; (4) suppliers must be motivated at least in part by financial self-interest to respond to price signals in the market place and purchasers should be motivated by the needs and wishes of patients; (5) there must be no incentives for providers to select low-risk patients | Ranade (1995),119 Levaggi (2007),20 Broomberg (1994)121 |
| Imperfect markets in health care | Characteristics of highly competitive markets are unlikely to be found in health-care systems but the benefits of high competition can be achieved if the market is contestable (threat of new entrants) | Roberts (1993),12 Allen (2002),120 Ferlie (1992)15 |
| Purchasers’ interests in protecting in-house production or co-ordinating decisions with other providers may contribute to contestability problems | Vining and Globerman (1999),123 Enthoven (1994)124 | |
| Where competition does not exist, purchaser/provider dependency results in ‘lock-in’ to relationships | Palmer and Mills (2003)125 | |
| Because of high levels of uncertainty in health care, consumers and their proxies will be willing to pay more to reduce the perceived risk of poor-quality services | Ferlie (1992)15 | |
| Competition and localism | Competition in health-care markets is not possible in some areas because of geography | Propper et al. (2008)126 |
| Downsides of health-care markets | The pursuit of provider profits/survival may have the following adverse effects: (1) selection of low-risk patients; (2) segmentation of the market; (3) differentiating the product; (4) biasing of information. Purchasers need to continually structure and adjust the market to overcome tendency towards inequity and failure Where there are structural barriers to market entry and few providers exist, introducing managed competition can lead to higher costs and reduced access to services |
Roberts (1993),12 Woolhandler and Himmelstein (2007)127 Randall and Williams (2006)128 Broomberg (1994)121 |
| Effect of competition on prices and cost | Market concentration leading to competition can lower prices and therefore cost savings, but not in all circumstances. Because neither purchaser nor provider has an interest in disclosing real price information in a negotiation process which has long-term collaborative objectives, this can mean that competition does not lower costs | Propper (1996),129 Propper (1995),130 Libby and Wallace (1998),131 Propper and Soderlund (1998)132 |
| Competition may lead to higher prices where there are non-binding budget restraints. If parties pass on costs, competition may be on quality | Propper et al. (1998)133 | |
| The degree of bargaining power of purchasers where there is more than one purchaser can influence price | Propper (1995)130 | |
| The NHS regulatory framework does not mean that competition has no impact on prices | Propper and Soderlund (1998)132 | |
| Competition is associated with lower prices but where purchasers do not have good information this can be diluted | Propper et al. (1998)133 | |
| Providers may have an incentive to reveal their prices or private information but only if it can make a substantial change in the allocation of resources | Allen (2002)120 | |
| If purchaser and providers are equally well informed on costs, a ‘take-it-or-leave-it’ offer may be made to specify the services wanted at a price which exactly reflects costs, even if there are no competitors. Where purchasers are less well informed, competition may be a way to increase efficiency | Levaggi and Levaggi (2010)134 | |
| Price elasticity may be determined by market concentration. Given a non-profit constraint, cost plus pricing contracts, in the absence of competition, give weak incentives for providers to minimise costs | Chalkley and Malcolmson (1996),135 Ferguson and Posnett (1994)27 | |
| Effect of competition on quality | Quality for any given price will be increased if competition exists | Chalkley and Malcolmson (1996),135 Whynes (1993)136 |
| The effect on quality depends on the effect of competition on price e.g. if competition increases the elasticity of the quality signal more than the price signal then the effect will be to increase quality | Propper et al. (2004)137 | |
| If quality signals are weak or noisy the impact of competition on price may dominate. Quality may fall rather than rise as a result of competition | Propper et al. (2004)137 | |
| In competitive markets unmeasured and unobserved quality may be reduced to improve measured and observed quality | Propper et al. (2008),126 Chalkley and Malcolmson (1996)135 | |
| Where investment in quality is costly, marginal cost is increasing and providers can observe and take into account current conditions, then competition’s beneficial effects on quality will be less than that predicted by static models | Brekke et al. (2010)138 | |
| Theory | Constructs (in bold) and relationships | Citations |
|---|---|---|
| Grand theory (2) | ||
| Principal–agent problem | Both principals (P) and agents (A) tend to act in a self-interested way. In the face of uncertainty (e.g. stochastic patient demand), where incentives/objectives are compatible, even though information asymmetry exists, an optimal solution is possible. If incentives/objectives differ but there is no information asymmetry, an optimal solution is possible. Information asymmetry and incompatible objectives lead to opportunism and moral hazard (misrepresenting effort ex post) and/or adverse selection (misrepresenting competence ex ante). Principals therefore need to induce agents to act in their interests where there is poor information about the behaviour and circumstances of the agent | Goddard and Mannion (1998),28 Allen (2002),139 Allen (2002)120 Allen et al. (2002),140 Roberts (1993),12 Levaggi (1996)141 Rosenthal et al. (2006),142 Burgoyne et al. (1997),143 McGuire and Riordan (1993)144 |
| Mid-level theory (2) | ||
| Contract choice and risk allocation | In a world of asymmetric information and uncertainty, the choice between a block contract, cost + volume and cost per case depends on risk aversion and contractual experiences. The block contract allows the purchaser to shift risk to the provider and avoids problems of asymmetric information. In the long run this may have perverse effects especially if uncertainty is stable over time (a purchaser’s role in a block contract is reactive) | Levaggi (1996)141 |
| For short-term prospective payment contracts (cost + volume) can be improved by adding an element of cost reimbursement where purchaser information is poor. Cost sharing allows providers to share risks | Chalkley and Malcolmson (1998),145 Chalkley and Malcolmson (1996)146 | |
| Contract choice and quality | Inclusion of payments based on numbers of patients demanding treatment rather than on numbers of patients treated for each diagnostic group can induce providers to maintain quality even if not all aspects of quality are monitored | Chalkley and Malcolmson (1998a),145 Chalkley and Malcolmson (1996b)146 |
| Within an adverse selection model, manipulation reduces the optimal level of quality effort but generally increases the optimal level of reported quality | Kuhn and Siciliani (2009)147 | |
| Contract choice and characteristics of the service being purchased | The nature of the service (amount of variation in demand and uncertainty over costs), purchaser and provider concentration influence choice of contract: whether or not any account is taken for ex post adjustment of payment | Chalkley and McVicar (2008)148 |
| Purchasers prefer block or cost and volume contracts to transfer risk to providers where patient demand is stochastic, budgets are fixed and there is limited local capacity | Csaba and Fenn (1997),149 Fenn et al. (1994)150 | |
| Contract choice and patient demand response | Outcome-based payment is more effective than treatment-based payment in utilising patients’ demand response (deciding when and where to be treated) as an incentive instrument in mitigating the effects of moral hazards Patient demand response is more important for elective and less severe conditions than acute and life-threatening illnesses |
Chalkley and Khalil (2005)151 |
| Contract choice, patient demand response and quality | Providing new information on quality can influence demand. Where patient demand reflects quality, this can be used to reduce costs at the same time as maintaining quality. Where patient demand does not reflect quality, choice of contract depends on how benevolent the providers are: with fully benevolent providers there are roles for block and cost + volume contracts; for partly benevolent, some degree of cost reimbursement is recommended; if fully self-interested, a cost per case contract is indicated | Mukamel et al. (2007),152 Chalkley and Malcolmson (1998)153 |
| Contract choice and moral hazard | Compared with fixed-price contracts (FFI), supply-side cost-sharing contracts (e.g. capitation) incentivise the provider to reduce the cost of treatment and do not lead to moral hazard in under-representing the patient’s condition. The downside is that quality can be lower and high-cost patients avoided (adverse selection) – but where there is a long-term provider–patient relationship this may be minimised | Jelovac (2001)154 |
| Contract choice and equity | Although capitation contracts have ex ante equity (before the arrival of the first patient, all have access to equal care), because physicians prefer the present patient to future ones and budgets may be exhausted, future patients may receive lower quality and quantity of care A mixture of capitation contract and a retrospective FFI contract may be more equitable over time |
Shmueli and Glazer (1999)155 |
| Contracting for higher activity and longer waiting times | Providers can influence demand by altering waiting times. Where there is asymmetric information, purchasers should contract for higher activity and longer waiting times for hospitals with high potential demand | Siciliani (2007)156 |
| Theory | Constructs (in bold) and relationships | Citations |
|---|---|---|
| Grand theory (3) | ||
| TCE | It may be more economic to internalise transactions into organisations such as hierarchies than to proceed through a market where transaction costs are high. Behavioural (bounded rationality, opportunism) and informational factors (uncertainty, information asymmetry) as well as the characteristics of the product (complexity of the product and its environment, asset specificity, measurability, frequent exchange) influence transaction costs. Transaction costs are higher if there is less competition: supplier opportunistic behaviour is curtailed by the threat of losing a contract. Asset specificity may increase the ‘lock-in’ and produce problems with small numbers bargaining | Allen (2002),139 Allen (2002),120 Allen et al. (2002),140 Ashton (1998),157 Ashton et al. (2004),158 Ferlie (1992),15 Flynn et al. (1995),159 Goddard and Mannion (1998)28 Howden-Chapman and Ashton (1994),43 Palmer (2000)6 Roberts (1993),12 Vining and Globerman (1999),123 Burke and Goddard (1990),160 Guinness (2011),161 Petsoulas et al. (2011)162 |
| Mid-level theory (3) | ||
| Governance by hierarchies | Organisations economise on transaction costs by altering governance arrangements to mitigate risk that accompanies arm’s-length transactions, e.g. formally internalising the contract or informally entering into networks | Ham (1996),163 Guinness (2011)161 |
| Elements of informality in contracts can be understood as informal elements of a hierarchical system rather than a relational contract. In centralised political cultures, hierarchies may be a more efficient mode of governance to improve quality than the use of internal markets | Allen (2002),139 Allen (2002)120 | |
| The more contestable and measurable are goods, the more appropriate is the use of the market rather than vertically integrated hierarchies | Preker et al. (2000)164 | |
| Purchaser–provider splits can lead to a failure in continuity in management, which is essential in securing effective outcomes | Joslyn (1997)165 | |
| Long-term contracts improve efficiency | Two types of asset specificity are important in health care: site specificity (buyer and seller located near to each other reduces transport costs) and dedicated assets (investments by the supplier that if the contract were terminated would result in spare capacity). A long-term contract increases the likelihood that the least-cost ‘transaction-specific’ investment will be made rather than the lower-risk, more generalised investment | Dawson and Goddard (2011)24 |
| The more important asset specificity is in the transaction, the longer a duration of the contract is required, until vertical integration is the most efficient arrangement | Goddard and Mannion (1998)28 | |
| Purchaser investment in assets | Where asset specificity is high, opportunistic hold-up may be reduced and efficiency enhanced by the purchaser investing and leasing the asset to the provider | Vining and Globerman (1999)123 |
| Impact of transaction costs on competition | The transaction costs associated with the contracting bidding process may deter smaller providers and result in less competition than expected | Randall and Williams (2006)128 |
| Theory | Constructs (in bold) and relationships | Citations |
|---|---|---|
| Grand theory (4) | ||
| Classical and neoclassical theory of contracts | The classical model of the contract focuses on a single exchange between two parties who are free to choose whether or not to contract and with whom. Contracts are complete (all eventualities covered) and there is full advance allocation of risk. Disputes are resolved through law. The neoclassical model recognises that the contract is not a one-off event and the contract therefore allows some flexibility. A third party may judge whether or not performance is satisfactory | Allen (2002),139 Bennet and Ferlie (1996)1 Ferlie (1992)15 |
| Relational contracts | The contract is embedded in a social relation with its own history and norms such as reciprocity, solidarity and a sense of duty. Relational contracts involve an ongoing relationship between the parties involved and are driven by the need to maintain the relationship. Since future events cannot be foreseen, the parties will need to revisit the agreement and jointly deal with problems | Allen (2002),139 Allen et al. (2002),140 Bennet and Ferlie (1996)1 Ferlie (1992),15 Ashton (1998),156 Flynn et al. (1995),159 Goddard and Mannion (1998),28 Palmer (2000),6 Raftery et al. (1996)166 Palmer and Mills (2003),125 Petsoulas et al. (2011)162 |
| Mid-level theory (4) | ||
| Relationships as a means of governance | Diffuse norms may be more important in regulating behaviour than purpose-designed governance systems. Macro-level norms such as obligation, co-operation and solidarity are mechanisms for control and generating trust. The process norm of reciprocity may also be important. These norms are developed and embedded in micro-level personal networks Economic action is achieved through actors operating in networks, not as atomised individuals. It is through networks of intersecting interests (purchasers, providers) that information is transmitted regarding quality, thereby conveying trust and reputation effect. Networks can constrain opportunism |
Ferlie (1992)15 Allen et al. (2002)140 Exworthy (1999)167 |
| Dense ties have mutual dependency, pooling of resources and reciprocity but, where there is performance ambiguity and little agreement on goals, hierarchies are more efficient | Flynn et al. (1995)159 | |
| New organisational forms | Faced with the need to negotiate new forms of contract, innovators arise who devise new organisational forms which are more efficient, e.g. stable networks rather than markets or hierarchies | Ferlie (1992),15 Donato (2010)30 |
| Wage rationality and care rationality | Care is contextually bounded and embedded in local customs and habits. Behaviour is therefore bound by general rules of conduct as well as self-interest. When wage rationality ‘rules of conduct’ are set up, this may be an obstacle to care rationality | Gustafsson (1995)168 |
| Incomplete contracts and ex post allocation of power | Since contracts are never complete, ex post allocation of power or control is important to reduce hold-up behaviour (haggling). Some sort of integration or long-term relationship may lead to more efficient outcomes | Palmer (2000)6 |
| Consequences of relational contract | Subsequent rounds of contracting deteriorate into pair-like bondings. A fundamental transformation arises where a specialised language develops, personal and institutional loyalties evolve and ex post management becomes lax | Roberts (1993),12 Smith (1996)32 |
| Role of personnel in the contractual relationship | Purchaser–provider relationships depend more on the personnel involved in the negotiation process than on the nature of the service Relationships change when there is a difference of opinion, especially with respect to the degree of trust, e.g. where poor information leads to a loss of trust |
Ashton (1998)157 |
| Loyalty to providers | Personal knowledge and contacts may facilitate a conciliatory approach. Purchasers without these links may be prepared to be more pugilistic. Loyalty to existing providers conditions subsequent dispute processes | McHale et al. (2011)169 |
| Discrete (e.g. consent and choice) and relational norms (flexibility and reciprocity) | Conflicted and adversarial relationships are predicted when discrete norms are unduly accentuated at the expense of relational norms | Petsoulas et al. (2011)162 |
| Factors affecting localism | Localism varies according to (1) spatial factors (urban/rural, level of competition, capital stock and capacity of local providers, role of private sector in local provision, transaction costs, social values, norms and meaning placed on space) and (2) temporal factors (personnel changes, technology changes) | Exworthy (1998)170 |
| Trust, incentives and co-operation | The greater the degree to which economic relationships are based on trust, the lower the costs of the incentives (or threat) required to encourage a given degree of co-operation, enforcing and monitoring | Goddard and Mannion (1998),28 Allen (2002)139 |
| Trust may be less likely to develop when the institution is distant and interaction is limited | Palmer and Mills (2003)125 | |
| Role of law in contractual relationship | The role of law in contractual relations is inversely related to the need for and the presence of co-operation | Goddard and Mannion (1998),28 McHale et al. (2011)169 |
| Theory | Constructs (in bold) and relationships | Citations |
|---|---|---|
| Grand theory (5) | ||
| Social relations both personal and institutional | Networks of personal and political relations shape institutions (the state and the professions) and these influences shape trading in markets | Ferlie (1994),31 Exworthy (1998),170 Flynn et al. (1995),159 Ferlie (1992),15 Ranade (1995),119 Palmer and Mills (2003)125 |
| Purchasing ‘regimes’ | The relationship between purchaser and provider is akin to long-term relationships between nation states. The contracting regime is rarely balanced between purchasers and providers. Both purchaser and provider have multiple constituents. The relationship is governed by norms and rules | Smith (1996)32 |
| Mid-level theory (5) | ||
| Political orientation | Political orientation is influential in the perception of likely benefits in increasing competitive tendering | Fredriksson et al. (2010)171 |
| Role of central government | Central government is the single most important factor in contract resolution. The influence of purchasers on provider behaviour is weak because of the disparity of power, the nature of the contract, centrally determined policies and the need to ensure that providers do not succumb to financial risk | Abbott et al. (2009),172 Allen (2002),139 Allen (2002)120 |
| Path dependency | Policy-makers may be ‘hemmed in’ by existing structures that channel them along established policy paths. Relative merit of current policy increases compared with alternatives because the cost of switching to an alternative rises over time | Mannion (2008)173 |
| Role of the media | The media are an arena for struggles over the meaning of competing discourses from different parties. It is usually the provider that uses the media as a lever in contract negotiations to strengthen its position | Liu et al. (2007)174 |
| Development of social trust in institutions | In market-led systems, non-rational trust in the health-care institution is developed | Taylor-Gooby (2008)29 |
Appendix 2 Summary of medical practice contracts
The origins of the General Medical Services contract date back to the National Health Insurance (NHI) Act of 1911. The Act established principles and conditions of service which were largely unchanged with the creation of the NHS in 1948. The contract was to be provided on a self-employed independent contractor basis, with the contract between the GMP and a local insurance committee. The contract provided an agreed range and standard of medical services with remuneration to the GMP by capitation fee for each registered patient. 175
The Second World War provided an opportunity to develop a system of regional organisation and administration for the nation’s health provision. The state effectively nationalised all local authority and voluntary hospitals through the establishment of the Emergency Medical Service. During this period of war a joint report by the British Medical Association and the Royal Colleges, which pre-dated the 1942 Beveridge Report, called for the extension of private medical insurance to 90% of the population. Remuneration for GMPs was to remain by capitation plus extra fees for the provision of a small range of ‘special’ services. In addition, the report urged the introduction of group practices with a range of staff supporting the work of the GMP. 175
When the NHS was established in 1948, GMPs were one of three groups of health-care providers, alongside GDPs and opticians, who remained independent contractors. General practice became both responsible for all personal medical care, with a reduced role in hospital and public health care, and the portal for patient access to hospital and specialist care. Remuneration was through a capitation-based system, which encouraged competition for patients between local practices. 176,177 Administration of the first NHS GMP contracts was the responsibility of local Executive Committees and, later, Family Practitioner Committees, both of which were directly responsible to the then Department of Health and Social Security. Neither committee, however, was responsible for the quality, coverage or development of GMP services. 176 In these early years there was a lack of defined standards for general medical practice. 176,177
Given this context, therefore, the quality of care offered by the medical contract at that time varied widely. The 1950 Collings Report, the first major review of quality in general practice, found poor standards of care and working conditions. 177 It reported that there was no planning surrounding general practice and the system provided few incentives for good practice. The review advocated group practice from state-owned health centres. 175
By the 1960s, there was widespread low morale in general practice, with dissatisfaction over working conditions and low levels of pay compared with other countries. Medical migration to the USA and Australasia resulted in a temporary shortage of GMPs. The threat of mass resignation by GMPs from the NHS resulted in the first major contractual change in 1966. 175 The new contract resulted in significant increases in GMP income. Loans and grants for building or refurbishing premises were made available and financial support was established for employing support staff and allowances for GMP training and collaboration. 177 A three-part payment system was introduced which comprised a basic practice allowance, alongside capitation fees, and with additional payments for out-of-hours provision and specified items of service such as contraception and immunisation. In addition, financial support was made available for group practices of three or more doctors and for undertaking work in underdoctored areas. 41,175 These measures resulted in improvements in relation to GMP retention and recruitment and an increase in group practices with support staff. 177
Despite the incentives, however, the new contract continued to fail to address the continued variability in general practice service delivery. Indeed, the contract itself ensured that the profession was protected from explicit state intrusion into members’ work as professional practitioners under their independent contractor status. There were few levers available to influence the distribution of GMPs, or the quality and range of services they provided. 176
In 1974 there was a complete administrative reorganisation of the NHS which resulted in the management and organisation of all health services falling under the responsibility of regional and area health authorities. 178 The 1970s and 1980s saw the continued trend in general practice away from single-handed practices towards partnership working and multiprofessional team working, led by GMPs and including in-house practice nurses, and district nurses and health visitors attached to practices. This period also saw the increasing use of practice managers by GMPs. 176 Moreover, the 1980s saw a major policy change in the government’s approach to managing the NHS. The adoption of the recommendations of the 1983 Griffiths Report introduced private sector management principles into the NHS. In essence this meant a drive towards efficiency and accountability with a consequent reduction in professional autonomy. The result was the replacement of demand-led provision with cash-limited budgets. 176
This new era of control and accountability, alongside the ongoing concern about variability in the quality of primary medical care, was the backdrop to the 1990 medical contract. The 1990 GMS contract, imposed by the Conservative administration despite significant opposition by the profession, aimed to specify in greater detail the terms of service of GMPs. It introduced new minimum service standards; for example, the requirement to offer health checks to newly registered patients, to those patients who had not seen their GMP for 3 years or more and to all patients over 75 years. It also tied elements of GMP remuneration more closely to the provision of specific services; for example, immunisation, cervical screening and health promotion clinics. The contract introduced financial incentives and penalties geared towards to managing medical practitioners’ performance, and altering the overall balance of GMP remuneration. 177 A smaller proportion of GMP income was derived from basic allowances; a greater proportion came from capitation payments and income from incentives to provide specific services such as immunisation and screening programmes. These specific services were often provided by practice nursing staff. 176
In April 1991 the Conservative government introduced an internal market for health provision which organisationally split health care between purchasers and providers. At the same time it introduced GMP fundholding. The main purchasing role for health services was undertaken by the health authority, which also had responsibility for assessing the health-care needs of its local population. Under the reforms, GMPs were allowed to volunteer to be allocated an annual budget by their health authority to purchase some hospital and community health services on behalf of and for their patients. 173,179 The range of services included elective surgery, diagnostic tests and investigations, outpatient referrals, district nurse and health visiting services, and prescribing. GMP fundholders were self-selectors into the scheme in seven waves up until 1997/8. As a result, around half of all general medical practitioners eventually become fundholders. 173
A piloted extension to GMP fundholding, ‘total purchasing’ was also introduced under the 1991 reforms. Its aim was also to further improve efficiency and the quality of care in hospitals and widen patient choice. Under these arrangements, a medical practice or group of practices was delegated a budget by its local health authority to purchase unplanned or emergency hospital and community health services for their patients, which would otherwise be purchased by the health authority and were excluded from the standard fundholding scheme. The total purchasing pilots began with four ‘pioneer’ sites in 1994. A further 53 pilots were then established in a first wave which went live in 1996, and 35 in a second wave a year later. 180
Towards the end of the decade, and immediately prior to the general election of the same year, the 1997 NHS (Primary Care) Act gained royal assent. This introduced (initially intended to be for only 3 years) three forms of contracts that were to become known collectively as Personal Medical Services (PMS) pilots: (1) the employment of individual GMPs on a salaried basis by the local health authority with contracts to provide a specific range of services – these were later to become known as PCT medical services (PCTMS), the main purpose of which was to recruit GMPs to poorly supported areas of care, such as deprived areas where few GMPs had set up in practice; (2) the PMS contract itself (which was a contract with the practice rather than an individual GMP, financed by a cash-limited budget) – these types of pilots were the ‘practice’ equivalent of the GMS contract, with the objective to improve the range and/or quality of services in the locality they served; and finally (3) PMS+, which was similar to PMS-only projects but also offered an extended range of medical services beyond the standard PMS/GMS contract. 176
The defining feature of these three types of PMS contracts was their local nature. Unlike GMS contracts, which were negotiated nationally between the profession and the government, the PMS contracts were negotiated locally and not initially subject to national directives. They remained as ‘pilot’ agreements until the 2004 GMP contract. Since then they have attained an equal status to the GMS contract as a contractual option, and as of 2004 almost half of medical practices were PMS. 181 Since 2004, the differences between GMS and PMS contracts have narrowed to the point where they are effectively indistinct. 177
General practitioner fundholding, however, was relatively short-lived. The election of a Labour administration in 1997 saw its abolition in April 1999. It was replaced with primary care groups (PCGs), later evolving into PCTs. Initially PCGs were subcommittees of their local health authorities, but by April 2002 all PCGs had become PCTs. PCTs had responsibility for developing, organising and commissioning virtually all health care for their localities, retaining the purchaser/provider split. Their defined area of influence was based on the patient populations of their constituent GMP practices, which was typically 20 to 25 practices. 173
These measures were followed by a new medical practice contract in April 2004. One of the perceived main issues with the previous contract was the apparent lack of financial incentives to improve quality of care within general practice. The introduction of the QOF was used to address this issue. Originally comprising 146 indicators across seven areas of practice, QOF provided doctors with the opportunity to earn points related to each indicator, with the points translating into extra income for the practice. Around half of the indicators were associated with clinical activity, defined as indicators of good-quality care, and the remainder related to practice organisation and patient experience. The clinical domains with the most indicators associated with them included coronary heart disease, hypertension and diabetes. In 2006, care indicators for renal disease and depression were included within QOF. 182
A year after the 2004 contract, practice-based commissioning (PBC) was introduced, reinvigorating the idea of practice-led commissioning associated with GMP fundholding. Once again GMPs could volunteer to be become involved in the commissioning of primary care services, as well as being providers. It was believed that engaging practitioners in this way would lead to improvements in the quality of services, by stimulating local service provision and shifting care from the hospital sector, therefore allowing the better management of patient demand. 183
Under the system, medical practices would make use of an additional indicative commissioning budget allocated by their PCT to commission and provide services for their locality. The proposals suggested that, in order to improve efficiency and obtain economies of scale, GMPs should organise themselves into PBC groups or networks, so that they could work together on areas of service redesign. Various terms have been used to describe such joint working: clusters; consortiums; localities and neighbourhoods. The scheme provided a range of financial incentives to encourage participation by GMPs. First, a direct enhanced payment for their involvement in PBC began in 2005 and was available until 2007/8. Second, any PBC income not spent or ‘saved’ at the end of the financial year could be retained by the practice, although it had to be spent on ‘approved’ projects related to PBC activity, such as practice capital development, investment in administrative capacity and training in commissioning skills. 183
The 2004 GMP contract also attempted to deal with issues surrounding equitable access for patients to primary care. The introduction of APMS contracts was developed to encourage new types of providers to enter the market place of primary medical care to compete for patients and deliver innovative services. 184 APMS contracts may contain GMS-type services, but can also include a range of other services not normally associated with traditional medical practices. For example, they can provide unscheduled care for non-registered patients through ‘walk-in centres’, or improved access for patients through extended opening hours, or set additional quality standards for selected areas of care over and above those associated with QOF indicators. 185
Alternative provider medical services contracts usually involve one of three types of ownership: public companies with shares traded on the stock exchange; private companies; social enterprise businesses or community interest companies. The first two are ‘for-profit’ businesses while social enterprise organisations are typically ‘not-for-profit’. 186–188 Social enterprise organisations are often referred to as a ‘third way’, combining the innovation, entrepreneurship and flexibility associated with private companies with the public ethos of the NHS. They can have a number of different governance structures: from companies limited by guarantee to more co-operative/mutual models. They may be owned by their users, customers, employees, the wider community, trustees, public bodies or a combination of different stakeholder groups, including GMPs, and may employ salaried GMPs. 188
Like the PMS contract, the 2004 GMS contract was now with the practice rather than individual medical practitioners. On the other hand, however, the PMS contract had taken on many of the component parts of the GMS contract, such as QOF, enhanced services, information technology investment and pension improvements. 181 Alongside the 2004 contract, there have been other moves to introduce stronger regulation and governance mechanisms within general practice. Annual appraisals for GMPs were introduced in 2002. From 2011 all medical practices are required to register with the CQC, and mandatory revalidation of doctors’ fitness to practice will become a requirement. 177
The 2004 contract was the last incarnation of the medical contract prior to the NHS reforms of 2013. The core of the contract comprises ‘essential’ and ‘additional’ services. Essential services are mandatory and very broadly defined to include the management of ill patients for the duration of the illness who are normally expected to recover; or have a chronic, long-term disease; or are terminally ill. Additional services are nominally optional, but, if practitioners decide to opt out, money is deducted and used by the PCT to commission the services from other providers. Additional services include provision such as immunisation, child health surveillance, maternity services and standard contraceptives. Payment for both types of service is based on capitation (weighted for deprivation, etc.). 189
These core services are supplemented with ‘enhanced’ services, comprising three forms. The PCT must commission ‘direct enhanced services’ for everyone and may not alter them; GMPs are the preferred providers. The PCT must commission ‘national enhanced services’ only if needed by the local population and may not alter them; the PCT is free to use providers other than GMPs. Payment for these two sets of services is typically by lump sum with the capitation per patient included. The third form is ‘local enhanced services’, which are designed in collaboration between the PCT and local GMPs according to the needs of the local population. Payment may be capitation-based, target-based or procedure-based. 189
The creation of the coalition government in 2010 brought with it significant reform for the NHS and social care system. From 2013, PCTs and SHAs were abolished and GMPs are at the centre of clinically led commissioning of health care for their local populations through the legal requirement for GMP practices to be members of Clinical Commissioning Groups (CCGs), controlling around two-thirds of the NHS budget. The aim of the reforms is to ensure clinicians play a much more significant role in deciding how funds are spent when shaping services to meet local needs. The new commissioning groups have two distinct roles. On the one hand they will be responsible for commissioning hospital and community care services for their local populations. Primary care itself is commissioned through the new national commissioning agency, NHS England, and its 27 area teams.
The area teams of NHS England will have a remit to hold CCGs to account as well as providing the groups with developmental support. CCGs have a relationship with the newly created Health and Wellbeing boards of local authorities. These boards are intended to act as local forums for strategic co-ordination of local health economies and as a means to enhance the accountability of the local health economy to the local population. CCGs are required to take account of the local Health and Wellbeing board strategies when they are considering commissioning services for the local community. 190
Clinical Commissioning Groups were established in shadow form in 2010, originally called GMP commissioning consortia. Before they were able to take on their full responsibilities in April 2013, they had to go through a strict authorisation process to establish that they had the core competencies necessary to undertake their duties and responsibilities. The groups will be subject to an ongoing assurance process overseen by NHS England area teams. Proposals for this assurance process include quarterly checkpoint meetings and an annual ‘health check’, assessing organisational capabilities, delivery and support needs. 190
Given the scale of the changes introduced as a result of these reforms, continual amendments to the medical contract have been made to take account of the organisational and relational developments. Fundamentally, however, the key elements of the contract – essential, additional and enhanced services – have remained largely unaltered. Two significant changes under the 2013/14 contract, however, have recently been agreed. First, patients over 75 years will now have a named GMP at their practice to be accountable for the care they receive; second, there will be a ‘substantial’ reduction in the size of the QOF. Over a third of the QOF will be abandoned, with the funding associated with it moved into core payments for GMPs. 191
Appendix 3 Timeline of key events in dental practice organisational field
| Date | Event |
|---|---|
| 1948 | NHS is established following passage of the National Health Service Act 1946, and general dental practice care is made available to everyone, free at the point of delivery, provided they can find a dentist |
| 1951 | Legislation introducing patient charges for dentures |
| 1981 | Government Dental Strategy Review Group reports |
| 1985 | Patient charges for dental examinations introduced |
| General Dental Council amends regulation on advertising | |
| 1986 | Schanschieff Committee of Enquiry into Unnecessary Dental Treatment |
| 1987 | Government White Paper Promoting Better Health |
| 1990 | New dental contract introduces registration, written treatment plans, practice leaflets |
| 1992 | Fee cut and Bloomfield Report |
| 1993 | House of Commons Health Select Committee on Dental Services |
| 1996 | Government White Paper Choice and Opportunity: Primary Care – The Future |
| 1998 | Personal Dental Services (PDS) schemes established |
| 2001 | House of Commons Health Select Committee on Access to NHS Dentistry |
| 2002 | NHS Dentistry: Options for Change vision for NHS dentistry |
| 2003 | Health and Social Care Act 2003: PCTs to be responsible (from April 2005) for contracting locally with dentists as part of their commissioning role |
| 2006 | New dental contract based on bands: courses of treatment with new banded system of patient charges |
| Removal of restrictions on number of Dental Bodies Corporate | |
| 2008 | General Dental Council, previously composed of members elected by the profession, replaced by independently appointed professionals and lay members |
| House of Commons Health Select Committee | |
| 2009 | Steele independent review of NHS Dental services |
| 2012 | New dental contract piloted |
| 2013 | PCTs abolished and commissioning role taken by NHS Commissioning Board |
Appendix 4 Important features of previous NHS dental contract and the new contract model currently being piloted
| Contract type | General Dental Service (GDS) | Personal Dental Service (PDS) | Personal Dental Service Plus (PDS+) | 2006 dental contract (nGDS or nPDS) | New dental contract pilot |
|---|---|---|---|---|---|
| Date | 1948–2006 | 1998–2006 | 2009 to present | 2006 to present | 2011 to present |
| Summary | Centrally managed FFI |
Locally designed and commissioned Few if any activity targets Different models include capitation and sessional payments |
Locally commissioned Compliance with KPIs, plus measures of access and service |
Locally commissioned UDAs Attainment of targets and compliance with standards monitored locally |
Overseen and evaluated nationally Care pathways and weighted capitation |
| Contract design | Not specified | Loosely specified | Highly specified | Specification on what must be provided | Care pathways specified |
| Relational contracts | GDPs are autonomous No relationship |
Room for negotiation with commissioners | Little room for negotiation | Little room for negotiation | Would provide a national framework with little negotiation |
| Goal difference purchaser and provider | No purchasers | Agreement of shared goals Voluntary scheme |
General new tenders and therefore agreement of goals | Focus on activity differs from individualised high-quality patient care | Preventative care pathways represent a shared goal |
| Patients select services on quality | Market forces but little information for patients or incentives to inform/involve patients Value on ‘goodwill’ |
Room for GDPs to provide high-quality care (or not) Value on ‘goodwill’ |
KPIs include measures of quality as perceived by patients No value on ‘goodwill’ |
Focus on activity may limit capacity to deliver high-quality care for individual patients Monitoring of patient satisfaction by purchasers No value on ‘goodwill’ |
Information for patients on their oral health risk and disease involves them in care Blended contract would include KPIs on quality as perceived by patients No value on ‘goodwill’ |
| Information asymmetry | GDP has all the information on need, cost, performance and effort | Little information gathered GDPs have most of information on need, cost, performance and effort |
Purchasers gather more information from GDPs | Purchasers gather information from GDPs and are able to compare different practices to raise questions | Computer-based algorithms generate a lot of information for purchasers, e.g. on need, cost, performance |
| Transaction costs (monitoring and negotiating) | Low | Medium | High | High | Unknown |
| Allocation of risk to purchaser/GDP | All the risk with the purchaser | Shared risk | Risk transferred to the GDP | Risk transferred to the GDP | Unknown |
Appendix 5 Qualitative data: detail of stakeholder participants
| Type of stakeholder | Code | Number of interviews |
|---|---|---|
| Commissioning stakeholder | SKC | 2 |
| Dental practice service delivery level | SKD | 5 |
| Macro-level dental professional representative | SKDR | 5 |
| Dental corporate above service delivery level | SKDC | 6 |
| Legal stakeholders | SKL | 3 |
| Medical practice, macro-level medical representative or medical corporate | SKM | 3 |
| Policy-level and public health stakeholder | SKP | 4 |
Appendix 6 Coding scheme anonymising participant quotes
-
If the extract starts with the number 2, this represents a phase 3 interview with a commissioner.
-
If the first two letters are SK, this was a stakeholder interview. SKD denotes a dental practice stakeholder; SKDR denotes a macro-level (professional representative) stakeholder; SKDC denotes a dental corporate stakeholder above service delivery level; SKP represents a policy (DH) or public health stakeholder; SKC is a commissioning stakeholder; SKM is a medical stakeholder with a mixture of practice-level professional (e.g. Local Medical Committee)/medical corporate representatives; SKL is a legal representative. All are then numbered sequentially in each group (see Appendix 5).
-
First letter: A, B, C, D, E and F denote PCTs all involved in case studies (phase 2); G, H, I, J, K, L, M and N denote PCTs involved in phase 3 interviews with commissioners.
-
The next character represents interview or observation data from D, a dental practice, M, a medical practice, or C, a commissioner.
-
The next character is a number. This represents which dental practice was studied within that PCT. For example, AD1 is dental practice 1 in PCT A and AD2 is dental practice 2 in PCT A.
-
If the next character is a P, this is a patient interview, and these are numbered sequentially for interviews undertaken in the same practice. For example, AD1P3 represents the third patient interview in dental practice 1, PCT A.
-
If the interview was with a member of staff and not a patient, the numbering after the first three characters denotes whom the interview was with (principal, associate, area manager, practice manager, etc.).
Appendix 7 Qualitative data: detail of dental practice case-study participants
| Dental practice characteristics | Interviewee characteristics | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Code | Contract | Structure | Surgeries | % NHS | Code | Role | Gender | Date qualified | Interviews |
| AD1 | nPDS | Partnership plus associates | 4 | > 90 | AD1 | Partner dentist | M | 1979 | 4 |
| AD11 | Practice manager | F | n/a | 1 | |||||
| AD1P1–4 | Patients | 1M 3F | 4 | ||||||
| AD1 observation | 1 | ||||||||
| AD2 | GDS child only | Principal plus associate | 2 | ≈ 10 | AD2 | Principal dentist | F | 1982 | 1 |
| AD2P1–4 | Patients | 3M 1F | 4 | ||||||
| AD2 contract review | 1 | ||||||||
| AD2 contract debrief | 1 | ||||||||
| AD3 | PDS+ | Principal plus associates | 3 | > 90 | AD3 | Principal dentist | M | 1996 | 2 |
| AD31 | Receptionist | M | n/a | 1 | |||||
| AD32 | Practice manager | F | n/a | 1 | |||||
| AD3P1–4 | Patients | 3M 1F | 4 | ||||||
| AD3 contract review | 1 | ||||||||
| BD1 | nPDS | Partnership | 6 | > 90 | BD1 | Partner dentist | M | 1974 | 1 |
| BD12 | Partner dentist | M | 1978 | 1 | |||||
| BD1A LDC debrief | 1 | ||||||||
| BD2 | N/A | LLC, directors plus associates | 5 | 0 | BD2 | Director dentist | M | 2001 | 1 |
| BD3 | NCP | Partnership plus associates | 2 | > 90 | BD3 | Partner dentist | M | 2002 | 1 |
| BD31 | Partner dentist | M | 1999 | 1 | |||||
| CD1 | nGDS child and exempt | LLC, directors plus associates | 4 | < 50 | CD1 | Director dentist | F | 1995 | 2 |
| CD11 | Associate dentist | M | 2005 | 1 | |||||
| CD1P1–5 | Patients | 5F | 5 | ||||||
| CD2 | PDS+ | Multisite corporate | 6 | > 90 | CD2 | Area manager | F | n/a | 2 |
| Patients | 3F 2M | 5 | |||||||
| CD3 | NCP | Principal plus associates | 4 | > 90 | CD3 | Principal dentist | F | 1986 | 1 |
| DD1 | N/A | Partnership plus associates | 4 | 0 | DD1 | Partner dentist | M | 1977 | 2 |
| DD2 | nGDS | Principal | 1 | > 90 | DD2 | Principal dentist | M | 1979 | 2 |
| DD21 | Practice manager | F | n/a | 1 | |||||
| ED1 | nGDS child and exempt | Principal | 2 | < 50 | ED1 | Principal dentist | M | 1982 | 3 |
| ED12 | Practice manager | F | n/a | 1 | |||||
| ED1P1–4 | Patients | 2M 2F | 4 | ||||||
| ED2 | nGDS | Principal | 1 | > 90% | ED2 | Principal dentist | M | 1974 | 2 |
| ED21 | Practice manager | F | n/a | 2 | |||||
| ED22 | Practice nurse | F | n/a | 1 | |||||
| ED2P1–9 | Patients | 6F 3M | 9 | ||||||
| ED3 | NCP | Principal plus associates | 4 | > 90% | ED3 | Principal dentist | M | 1998 | 2 |
| FD1 | nGDS | Multisite corporate | 5 | > 90% | FD1 | Practice manager | F | 1988 | 2 |
| FD11 | Associate dentist | M | n/a | 1 | |||||
| FD1P1–4 | Patients | 3M 1F | 4 | ||||||
| FD2 | nGDS | Principal plus associates | 2 | 50–90% | FD2 | Practice manager | M | n/a | 1 |
Appendix 8 Qualitative data: detail of medical practice case-study participants
| Practice characteristics | Interviewee characteristics | ||||||
|---|---|---|---|---|---|---|---|
| Code | Contract | Structure | Code | Job | Gender | Date qualified | Interviews |
| BM1 | APMS | Community Interest Company | BM1 | Director | F | n/a | 1 |
| BM2 | Finance director | M | n/a | 1 | |||
| CM1 | PMS | Partnership | CM1 | Practice manager | F | n/a | 1 |
| CM2 | Partner doctor | M | 1985 | 1 | |||
| DM1 | PMS | Partnership plus associates | DM1 | Associate doctor | F | 1988 | 1 |
| DM2 | Partner doctor | F | 1989 | 1 | |||
| EM1 | PMS | Principal | EM1 | Principal doctor | M | 1992 | 2 |
| FM1 | GMS | Principal plus associates | FM1 | Principal doctor | M | 1996 | 2 |
| FM12 | Practice manager | F | n/a | 1 | |||
| FM2 | GMS | Partnership plus associate | FM2 | Partner doctor | F | 2000 | 1 |
| FM21 | Practice manager | F | n/a | 1 | |||
| 2FM2 | Partner doctor | M | 1998 | 1 | |||
Appendix 9 Qualitative data: detail of commissioner participants
| PCT | Code | Title | Gender | Interviews |
|---|---|---|---|---|
| A | AC1 | Head of Primary Care Commissioning | F | 1 |
| AC2 | Dental Commissioning Lead | M | 2 | |
| B | BC1 | Head of Primary Care Commissioning | M | 2 |
| BC2 | Dental Commissioning Lead | F | 2 | |
| C | CC1 | Head of Primary Care Commissioning | F | 1 |
| CC2 | Dental Commissioning Lead (retired) | M | 1 | |
| CC3 | Dental Commissioning Lead | F | 2 | |
| D | DC1 | Head of Primary Care Commissioning | F | 1 |
| DC2 | Dental Commissioning Lead | F | 2 | |
| DC3 | Dental Practice Advisor | M | 1 | |
| E | EC1 | Head of Primary Care Commissioning | F | 2 |
| F | FC1 | Dental Commissioning Lead | F | 2 |
| FC2 | Medical Commissioning Lead | F | 1 | |
| FC3 | Chair, GP Commissioning Consortium | M | 1 |
| Code | Title | Gender | Interviews |
|---|---|---|---|
| 2AC2 | Contract Officer | M | 1 |
| 2CC4 | Primary Care Commissioning Manager – Dental | F | Declined |
| 2EC1 | Head of Primary Care Commissioning | F | Declined |
| 2FC4 | Contracts Manager | F | 1 |
| 2GC1 | Assistant Contract Manager – Dental Lead | F | 1 |
| 2HC1 | Contracts Manager | F | 1 |
| 2IC1 | Assistant Contract Manager – Primary Care | M | 1 |
| 2JC1 | Contracts Manager Dental and Optometry | F | 1 |
| 2LC1 | Dental Commissioning Lead | F | 1 |
| 2KC1 | Dental Commissioning Lead | M | 1 |
| 2MC1 | Contracts Manager (Dental) | M | 1 |
Appendix 10 Interview guides
The guides provided in this appendix were those used in the initial data collection of each type. As data collection and analysis progressed, we refined the topic guides to take account of and explore emergent themes in more depth.
Stakeholder interview topic guide
-
Who are the main stakeholders in the system?
-
What are the main issues regarding setting up a dental contract?
-
What would you say would be success in terms of a dental contract?
-
Is the contract a one-off thing where two parties come and agree a contract, or more of an on-going process that you’re working on something together?
-
What does failure look like then?
-
What is clinical engagement?
-
Who should bear the financial risk in dental contracts?
-
Is the role of the contract to try to regulate against poor performance like that or do you think regulation should be done in a different way?
-
Do you think GDPs generally have public or private sector type values?
-
Comparing dentistry with medicine, what makes dental practice distinct, is it just the history or is it something about dental practice?
-
What role has the media played in contractual relationships?
Dental practice case studies: interview guide
The practice and the contract
Some of this section could be gathered from the practice manager to shorten the interview
-
Tell me about the practice and how it’s set up
-
How long been here as a practice
-
Is this a branch practice – are there others you are involved with?
-
How many surgeries
-
Is it computerised?
-
Rough % NHS vs. private
-
Is the Practice contract or do performers have separate contracts with the PCT?
-
Do you have a partnership? With who? Is this a Limited Liability Partnership/Corporation?
-
No. in patient list
-
I’d like to map out what the FTE [full-time equivalent] staffing (dentists and staff) is, can I do this with the practice manager to save your time?
-
-
Tell me about your PCT contract
-
What type of contract do you have?
-
Is the contract for everyone or child only/exempt contract?
-
Is it PDS or GDS and have you changed from one to another?
-
PDS plus or new contract pilot – what type of contract have you had previously?
-
Current UDA value
-
Current target no. UDAs/contract value
-
-
What risks do you take in accepting an NHS contract? What risks do you think the PCT takes?
-
Success
-
What are your practice goals?
-
Do you identify with being part of the public or private sector?
-
Do you feel part of the NHS?
-
What do you think the PCT goals are?
-
What is success in terms of the contract?
-
What is failure?
Competition
-
Who is your customer?
-
Do patients come from the local area or wider afield?
-
What is the competition like?
-
Is access to NHS care an issue in the area?
-
Do you advertise?
-
What do you think of corporates?
-
Have you ever tendered for a new contract?
Business
-
To what extent do you analyse income and expenditure?
-
Who helps to run the business?
-
Do you have an accountant? How often do you meet? What does he do?
-
What does the practice manager do?
-
How do you manage the contract – in order to make sure you hit targets but don’t go over?
-
What would you do if you went over the target?
-
Have you ever had clawback? How was this handled?
-
To what extent do patient charges influence your work?
PCT relationship
-
Tell me about your relationship with the PCT?
-
Describe examples
-
If bad relationships was this retrievable and how?
-
To what extent was this to do with personality clashes or clashes in views?
-
-
Do you trust them? Explain what constitutes trust
-
Are they ‘open’ with you?
-
How do they communicate with you?
-
How often do you meet – how are contract reviews undertaken?
-
Do you have one person you contact at the PCT or is it a set of people?
-
How involved do you feel with the whole NHS?
-
Have you ever submitted applications for grant monies from the PCT etc.
-
Do you think they treat dentists differently to doctors, why?
External influences
-
What do you think of the role of the BDA in representing the profession?
-
Do you trust the Dept of Health?
-
Some people have talked about the ‘dental community’; who is in it?
-
How do you find out information about what is happening in the dental world?
-
Web based forums
-
Free dentists’ magazines
-
Do you read the BDJ [British Dental Journal]?
-
From company reps?
-
A group of local dentists?
-
People I was at dental school with
-
The newspaper
-
-
Do you go to the LDC? What is their role?
Norms
-
Are you aware of how other practitioners behave for example in relation to how they work within the UDA system to achieve their targets? There are stories of people say splitting courses of treatment to get more rewards. What do you think of this? Is it just a few people?
-
Do you ever try and work out how other practices and dentists handle things like this?
-
There is a lot of talk of dentists (and doctors) doing things like cherry picking patients (selecting patients who will give the greatest reward). Is this acceptable?
-
How do you avoid things like this happening?
Medical practice case studies: interview guide
The practice and the contract
Some of this could be gathered from practice manager
Tell me about the practice and how it’s set up
-
How long been here as a practice
-
Is this a branch practice – are there others you are involved with?
-
Is it computerised?
-
Who owns the practice/shares the profit? Is it a partnership – who is involved?
-
No. in patient list
Tell me about your PCT contract
-
What type of contract do you have?
-
What risks do you take in accepting an NHS contract? What risks do you think the PCT takes?
Success
-
What are your practice goals?
-
Do you identify with being part of the public or private sector?
-
Do you feel part of the NHS?
-
Do you think dentists are part of the NHS in the same way?
-
What do you think the PCT goals are?
-
What is success in terms of the contract?
-
What is failure?
Competition
-
Who is your customer?
-
Do patients come from the local area or wider afield?
-
How likely would patients be to move to another doctor in the area?
-
Would you want to expand and how would you do that?
Business
-
To what extent do you analyse income and expenditure?
-
Who helps to run the business?
-
Do you have an accountant? How often do you meet? What does he do?
-
What does the practice manager do?
-
What sort of targets do you have? And how do they affect your remuneration?
-
How do you manage the contract – in order to make sure you hit targets but don’t go over?
-
What would you do if you went over target?
PCT relationship
-
Tell me about your relationship with the PCT?
-
Describe examples
-
If bad relationships was this retrievable and how?
-
To what extent was this to do with personality clashes or clashes in views?
-
-
Do you trust them? Explain what constitutes trust
-
Are they ‘open’ with you?
-
How do they communicate with you?
-
How often do you meet – how are contract reviews undertaken?
-
Do you have one person you contact at the PCT or is it a set of people?
-
How involved do you feel with the whole NHS?
-
Have you ever submitted applications for grant monies from the PCT etc.
-
Do you think they treat dentists differently to doctors? Why?
External influences
-
What do you think of the role of the BMA in representing the profession?
-
Do you trust the Dept of Health?
-
Is there such a thing as a ‘medical community’ – we hear talk about a ‘dental community’ – who is in it?
-
How do you find out information about what is happening in the medical world?
-
Web based forums
-
Free doctors’ magazines
-
Do you read the BMJ [British Medical Journal]?
-
From company reps?
-
A group of local doctors?
-
People I was at medical school with
-
The newspaper
-
-
Do you go to the LMC? What is their role?
Norms
-
Are you aware of how other practitioners behave for example manipulating the contract to get more profit? What do you think of this? Is it just a few people?
-
Do you ever try and work out how other practices and doctors handle things like this?
-
There is a lot of talk of dentists (and doctors) doing things like cherry picking patients (selecting patients who will give the greatest reward). Is this acceptable?
-
How do you avoid things like this happening?
Differences between doctors and dentists
-
What are the differences between doctors and dentists in terms of their work and relationship in contracts with the PCTs?
Dental patients interview topic guide
-
Why do you come to this dentist rather than another one?
-
Have you ever thought of ‘shopping around’ for a new dentist?
-
Have you ever made a complaint about a dentist?
-
Do you think people see doctors and dentists differently?
Phase 2 commissioners interview topic guide
The structure in the PCT
-
Tell me about who is involved in dental commissioning in the PCT.
-
Has there been much turnover of staff?
-
Who do they answer to in terms of performance? i.e. the dental commissioner answers to primary care directorate answers to Chief Exec? etc.
-
Who else is involved in dental commissioning in the PCT? Consultant in Dental Public Health? Dental Practice Advisor?
-
How is their input gathered? What do they do? How do you feel about this?
-
Does the LDC have any input into the commissioning process?
Performance management and PCT culture
-
How is performance of the PCT monitored? – by SHA and DH?
-
Is dental performance different to performance say of GMPs?
-
How is performance of staff monitored in the PCT? Is it informal or formal?
-
What happens if the PCT doesn’t meet the targets say for delivering the number of UDAs to be commissioned?
-
Does this have any consequences for you as a member of staff?
Dental contracts
-
What type of contracts have you got across the patch?
-
How did you decide this?
-
How did you decide on the UDA value? Are all practices on the same UDA value or different?
-
Explain the contract review process. Do you go out to the practices or do they come to the PCT? How often? Or is it done by letter – get an example
-
Did many GDPs go private in 2006?
-
Have you ever been flexible with contracts not being met? Introducing new variations? Stepped contracts for new practices?
-
How is risk handled?
-
How is dental commissioning/contracting different to medical commissioning?
-
Do dental contracts tend to be shorter-term than doctors’ contracts?
-
Can anything be done to avoid the insecurity of short-term contracts?
-
How much do you identify dentists as being part of the NHS?
-
Do dentists have the same opportunities to go for say growth money as doctors in the PCT?
-
Do you ever feel you’re limiting the clinical freedom of dentists/doctors?
-
Are GDPs/GMPs more regulated?
-
Is the regulation handled differently?
-
How do you minimise monitoring costs?
Relationships
-
Do GDPs tend to contact one person in the PCT or several?
-
Is it usually formal or informal contact?
-
Do you visit the practices?
-
What other communication do you have? e.g. newsletters – gather example
-
Would you say that you have good relationships with GDPs? Give an example of a good or bad relationship
-
For bad relationships – was it about a clash of personalities or issues?
-
Are there examples of a bad relationship becoming good or a good relationship going bad? How did this happen?
-
Do you trust GDPs?
-
Do you think they trust you?
-
To what extent are you ‘open’ with GDPs?
-
What about GMPs – are the relationships there any easier to handle?
-
Do you think there is a greater degree of mutual trust with GMPs?
Success
-
What is success to you in the use of contracts?
-
What is failure?
-
Do you ever worry about a dental practice not being able to run a viable business or being stressed delivering the contract?
Competition
-
To what extent is there competition in the dental market locally?
External influences
-
How do you get your information about forthcoming changes in dentistry?
-
How much do you swap information with other commissioners?
-
Do you read any of the dental magazines or the British Dental Journal?
-
Do you go to the LDC meetings? What input, if any, do you have?
-
What about the LMC for doctors?
Norms
-
Outline a day. What is your main activity and object of activity?
-
Who do you have most frequent contact with in your daily work?
-
How are things ‘normally done’?
Triangulation
Before the interview identify the anecdotes from case studies about negotiations over corporation, difficult relationships – either insert them into the interview schedule at the appropriate place or raise them at the end.
Phase 3 commissioners interview topic guide
Background (brief)
-
What is your role now? What did you do previously? Do you only commission GDPs or do you have experience of commissioning other primary care (e.g. medical)?
Ownership
-
Do GDPs have a strong sense of being responsible for ‘their’ practice?
-
What is this sense of ‘ownership’ rooted in?
-
Is there a different sense of this in medical practice?
Professionalism
-
What do you think about how ready GDPs are to criticise fellow practitioners’ work, both in the same practice and in different practices?
-
Is this any different in medical practice?
-
Have you encountered any dental practitioners who are more ‘old school’ in their approach? How would you characterise this?
-
What about medical practitioners?
Population health managerialism
-
Do some practitioners ‘get’ the population perspective?
-
Is there a ‘clash’ between this and the culture in most dental practices?
-
How do you think GDPs feel about the resource constraints on the NHS and the PCT’s ways of managing this?
-
What do GMPs think of this?
-
How do you think GDPs feel about the NHS brand?
-
What do GMPs think of this?
Commercialism
-
We are interested in the extent to which practitioners are orientated towards a commercial outlook. Do you recognise the description?
-
Do you see a variation in how dentists approach the commercial side of their businesses?
-
Are those who are less commercial any less likely to be able to meet PCT targets?
-
Do different practices approach the role of practice managers differently?
-
Is it generally a business planning role or is it mainly administration?
Relationships
-
To what extent are the relationships between commissioners and practitioners based on trust?
-
Is it necessary to have a relationship with trust because of contractual issues?
Appendix 11 Questionnaire (phase 3)
Appendix 12 Links to project outputs
Papers
Harris R, Holt R. Interacting institutional logics in general dental practice. Soc Sci Med 2013;94:63–70. URL: www.sciencedirect.com/science/article/pii/S0277953613003766
Harris R, Mosedale S, Garner J, Perkins E. What factors influence the use of contracts in the context of NHS dental practice? A systematic review of theory and logic model. Soc Sci Med 2014;108:54–9. URL: www.sciencedirect.com/science/article/pii/S0277953614000598
Conference abstracts
Harris R, Mosedale S, Garner J, Perkins E. A systematic review and logic model of health care contracting theory. 18th Annual Congress of the European Association of Dental Public Health in a Joint Meeting with the Council of European Chief Dental Officers, St Julians, Malta, 14–16 November 2013. URL: www.eadph.org/downloads/2013_abstracts.pdf
Harris R, Brown S, Holt R, Perkins E. Do institutional logics predict macro-level behaviour of dental practitioners? International Association for Dental Research, Capetown, South Africa, June 2014. URL: https://iadr.confex.com/iadr/14iags/webprogram/Paper190349.html
Appendix 13 Participant information sheets
Appendix 14 National Research Ethics Service letter of approval
Glossary
- Alternative Provider Medical Services
- Type of medical practice contract.
- British Dental Association
- National professional association and registered trade union for dentists.
- British Medical Association
- National professional association and registered trade union for doctors.
- Clinical Commissioning Group
- Commissioner of most services funded by the NHS in England, replacing primary care trusts in April 2013.
- Dental Bodies Corporate
- A unique class of corporations which are registered with the General Dental Council and entitled to carry out the business of dentistry in the UK.
- Department of Health
- Department of the UK government responsible for health matters.
- Direct Enhanced Services
- Optional services commissioned in all areas from primary care providers and linked to national priorities.
- General dental practitioner
- Dentist working as an independent contractor.
- General Dental Service
- NHS dentistry provided under General Dental Service contract terms and conditions.
- General medical practitioner
- Doctor working as an independent contractor.
- General Medical Service
- Service governed by a nationally negotiated NHS general medical practice contract.
- Local Dental Committee
- Local representative committee of NHS dentists to represent their interests in their locality.
- Local Dental Network
- Network of local NHS dental clinicians informing local commissioning.
- Local Enhanced Services
- Services commissioned from primary care providers agreed locally between primary care commissioners and providers.
- Local Medical Committee
- Local representative committee of NHS medical practitioners to represent their interests in their locality.
- National Enhanced Services
- Additional services commissioned using national specifications and benchmark prices, from primary care providers, if identified as being needed by the local population.
- New contract pilot
- Practices involved in piloting elements of a new NHS dental contract.
- New public management
- Management ideology underpinning public sector reform emphasising competition as a means of maximising resource efficiency.
- nGDS
- Type of General Dental Service contract after the 2006 reform involving Units of Dental Activity.
- nPDS
- Type of Personal Dental Service contract after the 2006 reform involving Units of Dental Activity.
- Personal Dental Service
- Pilot from 1998 to 2006 involving locally negotiated contracts with a range of contract currencies.
- Personal Dental Service Plus
- Contract based on Personal Dental Service arrangements but including measures related to service, access, performance.
- Personal Medical Service
- Type of medical practice contract.
- Practice-based commissioning
- General medical practice-led commissioning introduced after the 2004 general medical practice contract.
- Primary care organisation
- Local organisation responsible for commissioning, for example primary care trust.
- Primary Care Trust
- Up until April 2013, the NHS organisation responsible for commissioning health care locally.
- Quality and Outcomes Framework
- System for the performance management and payment of general practitioner services in the NHS.
- Strategic Health Authority
- NHS organisation responsible for leading the strategic development of local health services and managing primary care trusts and NHS trusts; abolished in 2013.
- Unit of Dental Activity
- 2006 contract currency.
List of abbreviations
- APMS
- Alternative Provider Medical Services
- BDA
- British Dental Association
- CQC
- Care Quality Commission
- DBC
- Dental Body Corporate
- DH
- Department of Health
- dmft
- number of decayed, missing and filled primary teeth per child
- FFI
- fee-for-item
- GDP
- general dental practitioner
- GDS
- General Dental Service
- GMP
- general medical practitioner
- GMS
- General Medical Service
- GP
- general practitioner
- IQR
- interquartile range
- KPI
- key performance indicator
- LDC
- Local Dental Committee
- MeSH
- medical subject heading
- NCP
- new contract pilot
- nGDS
- type of GDS contract after 2006 reform involving UDAs
- NICE
- National Institute for Health and Care Excellence
- nPDS
- type of PDS contract after 2006 reform involving UDAs
- NPM
- new public management
- PCO
- primary care organisation
- PCT
- Primary Care Trust
- PDS
- Personal Dental Service
- PDS+
- Personal Dental Service Plus
- QOF
- Quality and Outcomes Framework
- SD
- standard deviation
- SHA
- Strategic Health Authority
- TCE
- transaction cost economic theory
- UDA
- Unit of Dental Activity