Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 10/2002/23. The contractual start date was in April 2012. The final report began editorial review in August 2014 and was accepted for publication in December 2014. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2015. This work was produced by Pollock et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Background
Introduction
This report presents findings of a 2-year study (the Care and Communication study) funded by the National Institute for Health Research (NIHR) Health Services and Delivery Research programme. 1 The study investigates how seriously ill patients, their relatives and the health professionals caring for them understand and experience discussions about end of life care (EOLC) involving advance care planning (ACP) (Box 1).
. . . a voluntary process of discussion and review to help an individual who has capacity to anticipate how their condition may affect them in the future and, if they wish, set on record: choices about their care and treatment and/or an advance decision to refuse a treatment in specific circumstances, so that these can be referred to by those responsible for their care or treatment (whether professional staff or family carers) in the event that they lose capacity to decide once their illness progresses.
National End of Life Care Programme. Capacity, Care Planning and Advance Care Planning: A Guide for Health and Social Care Staff. Leicester: National End of Life Care Programme; 2011. 2 p. 6. Reproduced under Open Government licence. Crown Copyright 2011.
Advance care planning is a key component of current UK health policy to improve the experience of death and dying by enabling patients and their significant others to consider their options and preferences for future care. 3 It is considered important that patients have the opportunity to do this while they retain capacity to make and communicate decisions. ACP aims to enable family and professional carers to take account of, and where possible to implement, patients’ expressed wishes for care and treatment. ACP is considered an important means of protecting personal dignity and extending personal autonomy through the end of life. Evidence of the nature, frequency and outcomes of ACP discussions remains limited and frequently conflicting. 4 However, it is apparent that ACP remains uncommon in most areas of professional practice and that both professionals and patients tend to avoid discussions they find difficult. 5–14 Patient and family responses to ACP and its effect on EOLC outcomes remain poorly understood. This study contributes to the currently limited evidence relating to the nature and impact of ACP as well as a critical appraisal of its contribution within current EOLC policy. It employed qualitative methods to conduct an in depth investigation into how ACP is initiated and implemented in community health-care settings. It is based on two workstreams: a series of interviews with health professionals and a series of longitudinal patient case studies involving patients, family carers and nominated health professionals followed up over a period of approximately 6 months.
The rest of this chapter provides the background to the study, and considers the policy context in which it is set and the evidence available from earlier studies. Chapter 2 outlines the design and methods of the study before three findings chapters, which present demographic findings, the findings from the professional perspectives interviews and the findings from the patient case studies. Chapter 6 gives a discussion and critical appraisal of the findings in relation to the current literature, provides a summary of the study findings and their significance, and considers their implications for further research. Care of the dying is one of the most significant services to be provided within the NHS: it touches every person in the land and is a signal marker of the quality of national health care. EOLC has become a particular concern within modern industrial societies characterised by a changing demographic in which most deaths occur in great old age, after an extended period of increasing frailty and decline. These trends will continue, and even accelerate, far into the future. 15–17 They bring challenges to people’s experience and expectations of living as well as dying, and impose unprecedented social and economic demands in the organisation and resourcing of health and social care. 18,19 The difficulty of responding to these demands, and deep concern about the quality of care for dying patients, have been graphically documented in recent reports of gross shortcomings in institutional care for older people, including dying patients. 20 Care and treatment at the end of life are recognised to have often been inadequate and crisis driven. 15,21–23 In addition, there are ongoing concerns about the continuation of invasive and futile treatment for dying patients and the lack of recognition among professionals, as well as families, that patients are dying. 24,25 Although the Liverpool Care Pathway (LCP) for EOLC was introduced to implement a palliative approach towards the care of dying patients in hospital and community care settings,26 its widespread misapplication, and frequent reduction to a tick-box exercise rather than a holistic programme of care, has resulted in its withdrawal from service. Difficulties of communication between clinicians and patients and their families were identified as being a major contribution to the pathway’s demise. 27 In response, a coalition of 21 organisations, known as the Leadership Alliance for the Care of Dying People, has published a review prioritising the provision of compassionate care and emphasising the importance of early discussion and planning for death substantially in advance of the point at which an individual is recognised to have reached the end of life. 28
Concerns about the quality and equity of EOLC have arisen in the context of a well-established and progressive national End of Life Care Strategy (EOLCS), initially implemented in 2008 and subsequently supported by the National End of Life Care Programme (NEoLCP). 21,29 The EOLCS promoted the use of a six-stage EOLC pathway, beginning with, and hinging on, successful identification of patients who were in their last year of life. It also sought to promote patient involvement in decision-making about future care, and in particular, the fulfilment of patient choice of place of death, assumed in most cases to be home. 15,30,31 The NEoLCP incorporated a commitment to develop services to enable dying patients to be supported in the community. Reduction in unscheduled hospital admissions and their associated costs, and an increase in the proportion of patients dying at home have become key performance indicators within the Quality, Innovation, Productivity and Prevention workstream of the NEoLCP. Between 2008 and 2012 the number of home deaths (defined as usual place of residence, including care homes) had increased from 38% to 42%, with hospital deaths reducing to 51%. 29 The Quality, Innovation, Productivity and Prevention workstream has concentrated on the early part of the six-stage pathway: identifying people who are in their last year of life as a prerequisite for planning and co-ordinating care. ACP is one of the key initiatives involved in this programme of work.
Advance care planning
The current definition of ACP as a process of expressing and documenting preferences for future care to support autonomy refers to recent UK legislation regarding how decisions should be made in circumstances where individuals lose mental capacity. 32 However, the end of life care pathway (EOLCPW) and the very considerable body of resources and materials that have been developed to support it are oriented more broadly to ACP as a means of helping patients prepare for death and professionals to foresee, and make practical arrangements to meet, patient preferences for future care. Skilled communication, in broaching the topic of ACP and helping patients to explore their preferences and options, is essential to an ACP discussion. 21
Talking about death and dying: developing a public conversation
Discussion about ACP is the first step in implementing the pathway set out in the EOLCS, within which greater public openness and willingness to communicate about death and dying is seen as key to improving EOLC. However, public reluctance to talk about death and dying is widely assumed, and death is frequently regarded as a cultural taboo. 21,33 Consequently, the EOLCS set out a plan for an ‘information revolution’ to overcome this resistance, among professionals as well as patients and the public. This aimed to raise awareness and normalise the topic of death and dying as part of a process of encouraging people to consider and express their preferences for end of life well in advance of its occurrence. This campaign has been spearheaded by the Dying Matters Coalition, set up in 2009 and led by the National Council for Palliative Care. 34 There is expected to be a synergistic relationship between increased public awareness of death and dying and increased personal receptivity to the offer of an ACP discussion. Initiatives have also been directed towards health professionals, including a ‘Find your 1%’ campaign. This is led by the NEoLCP and aims to encourage general practitioners (GPs) to identify the expected 1% of patients within their practice lists who are in their last year of life, with a view to initiating a process of ACP and interdisciplinary planning and co-ordination of future care. 35
The origins and development of advance care planning
Advance care planning has developed within a movement to generalise the benefits of palliative care from hospice to wider hospital and community care settings. 36 It thus reflects the core components of a particular professional ideology and commitment to the nature and achievement for all patients of a particular construct of ‘the good death’. 37–40 This involves the excellent control of symptoms within a holistic approach to care, which acknowledges death as a natural, rather than a pathological, process. It incorporates a commitment to open awareness and communication about dying between all participants: patient, family and professionals. The good death occurs in a comfortable, non-medicalised environment: home is usually the preferred place, where dying can most easily be accompanied by the patient’s significant others. Open awareness of dying enables patients to engage actively with decisions about treatment, or their refusal, to foresee and plan for how they wish EOLC to be provided, to put their affairs in order and possibly also to realise personal goals and plans for living while these remain options available to them. Open awareness and communication about dying and patient involvement in planning for a future, however limited, satisfy a deeply held cultural commitment to preserving the dignity and autonomy of patients throughout their experience of greatest vulnerability and even to the end of life.
The protection of personal autonomy and patient determination of her or his own best interest was given a legal underpinning by the implementation of the Mental Capacity Act in 2005. 32,41 This set out the patient’s right to refuse particular forms of treatment, even when the outcome was life-threatening. It also supported the principle of precedent autonomy, whereby the expressed wishes of a competent individual were held applicable in the event that she or he subsequently lost capacity to make decisions, or the ability to communicate these, at some point in the future. Extending these principles to patients who are dying is a natural extension of the principled commitment to individual choice and self-determination.
Advance care planning does not need to be a formal process requiring documentation. It is recognised that some patients may be willing to discuss their preferences for future care, but may not be willing, or may not feel it necessary, to write these down. However, if patients’ wishes are not recorded and shared among the family members, health professionals and services involved in providing care, it is less likely that plans can be known and implemented, or that changes to previous plans may be acted on. Advance care plans carry no legal force [unless they involve the writing of a valid and applicable advance decision to refuse treatment (ADRT)], but should be taken into consideration by clinicians managing patient care in the process of determining best interests when the patient no longer has the ability to contribute to the discussion. Patients may record anything they like about their preferences for future care, and the environment and circumstances they would like to be in place during dying.
Advance decisions to refuse treatment and lasting power of attorney
Patients cannot command specific treatments or interventions, but they can refuse them. In the event that such refusal would have life-threatening consequences, it is necessary for a legally binding ADRT to be drawn up. In this case, if it is determined to be valid and applicable to the patient’s circumstances, clinicians must comply with the terms specified. In addition, patients may appoint persons to have a lasting power of attorney to make decisions on their behalf, in relation to property and financial affairs and/or health and well-being, in the event that they should lose capacity at some point in the future. Drawing up legally enforceable documents involves a level of bureaucratic complexity and, in the case of lasting power of attorney, a financial cost that act as a strong deterrent for many people. In practice, ADRTs have not been widely adopted or implemented. Even when clinicians have access to valid documents at the appropriate time, their content may be hard to interpret, or may fail to apply to the context in hand. 42–47 It is difficult for patients to foresee precisely what may happen, and yet accurate prediction and very precise specification are essential to the successful application of an ADRT. 48–50 In practice, and in consequence of these difficulties of application, ADRTs have been widely disregarded. The recent trend has been to shift the focus of anticipatory planning towards more informal processes of discussion and reflection about goals of care. 3,43,51–53
Cardiopulmonary resuscitation
A key decision in relation to patients who are extremely ill or frail relates to cardiopulmonary resuscitation (CPR) and how this is communicated to patients and their families. CPR is an emergency procedure to restart the heart and/or breathing following a cardiac or respiratory arrest. In the absence of an order not to attempt resuscitation (do not attempt cardiopulmonary resuscitation, DNACPR), it is a clinical decision whether or not to do so based on individual assessment of each patient’s case. 54 If there is doubt, the presumption must be towards preservation of life. Practice in relation to DNACPR decisions was re-emphasised in a court ruling after completion of data collection for this study. Unless such discussion is believed to cause the patient extreme psychological distress and harm, clinicians have an obligation to make sure decisions about resuscitation are clearly communicated to the patient (provided she or he has capacity) and her or his family and, ideally, their agreement obtained. 55 The decision that resuscitation should not be attempted on the grounds of futility remains a clinical responsibility and hence where the ‘expected benefit of attempting CRP may be outweighed by the burdens the patient’s informed views are of paramount importance’ (p. 3). 54 Thus, it is important that all patients with a significant chance of respiratory or cardiac failure should have the opportunity to understand the risks and benefits of CPR and state their preference about whether or not resuscitation should be attempted. Discussion of CPR and documentation of the patient’s wishes are a key component of ACP.
Preferred place of death
The focus of ‘choice’ in relation to EOLC has centred on supporting patients to die in their preferred place of death (PPOD). This is understood, in the great majority of cases, to be their home or usual place of residence. 16,56–61 It is widely stated that many people do not die in their preferred place, and that most of the 52% of patients who currently die in hospital would have preferred to die at home. 57,62,63 Hospital is regarded as an undesirable and expensive place of death and considerable efforts have been made to increase the resources available to community services to avoid ‘unnecessary’ hospital admissions at the end of life and enable patients to die at home. These include the introduction of specialist roles such as community matrons (CMs), practice liaisons and palliative care nurses (PCNs). 21,64
The proportion of home deaths is frequently taken to be a proxy indicator of quality of EOLC. 29 Indeed, a recent White Paper introduces the consideration that patients should be given the right to die at home. 29 Nevertheless, the evidence base underlying the axiom that home is most people’s PPOD is questionable. Much is derived from population surveys, often involving healthy adults representing a wide range of ages, and at a single point in time. 33,57,65 Responses to a question when it is purely hypothetical may be very different from those made in the light of hard experience. It is evident that preference for home as a place of death decreases as people get older and as the prospect becomes a more pressing reality. 51,59,66–69 Evidence from qualitative studies suggests that terminally ill patients may often feel uncertain about their preferences, which are likely to change throughout the course of illness. Such preferences are often not formulated clearly, especially in the face of uncertainty about what will happen throughout the experience of dying. Patients are pragmatic, also, about their options and how these depend on the circumstances that materialise. 6,22,43,50,51,67–73 Running like a leitmotif throughout the literature is that patients strongly desire not to impose a burden of care on their family members5,22,69,73–79 and it is evident that most people depend on the availability and willingness of informal carers to support their ability to die at home. 69,73,80 As the population ages, increasing numbers of the very old live alone and may not have carers available to help. However, dying alone is generally regarded as a very bad outcome, and for most patients it is not an acceptable option. 77,81,82
Death at home is frequently portrayed as a core component, perhaps even a prerequisite, for achieving a ‘good death’, in contrast to the impersonal, institutional and medicalised environment of the hospital. However, recent evidence suggests that control of pain and not being a burden are the important priorities for patients and the public. 33,79,83 Moreover, pain is reported to be best controlled in hospice, then hospital, and least well at home. 61
As people get older, they report an increased preference to die in hospice. 58 A recent survey of the English population indicated that 29% of respondents expressed a preference to die in hospice. This compares with 5% who actually do so. 57 Patients’ ability to die at home is limited by the availability of personal, family and service resources. Stated preferences for place of death are shaped by patient perceptions and awareness of the options practically open to them, and these may limit choice. Plans may be subject to rapid change as death draws closer. 22,43,51,67,69,70,72,84,85
The National Survey of Bereaved People (VOICES) of bereaved carers reported that, among the 44% of patients who had expressed a preference, 71% had wished to die at home. However, although the majority had died in hospital, most relatives (82%) subsequently felt that the patient had died in the most appropriate place. 61 Regardless of planning, circumstances may conspire to make hospital the only, and even the best, option. The findings of qualitative studies question the assumption that ‘home is best’ in relation to good-quality EOLC. 68,77,86 In the face of conflicting and uncertain evidence, it is important to establish a better understanding of how patients and caregivers develop their preferences, the role of health professionals in shaping these, the salience of choice and the importance patients attach to place of death. 69,74
The initiation of advance care planning
Advance care planning involves discussion of difficult issues that may be distressing to all participants. It is understandable that engaging in ACP discussions can be challenging for professionals as well as patients and their relatives. There is evidence that many professionals lack confidence in undertaking ACP and tend to avoid such discussions. 13,14,35,53,67,87,88 Several studies suggest that, as there is uncertainty about which professional should undertake discussion of ACP, there is a tendency, particularly among GPs, to defer responsibility to someone else. 9,12,53,64,67,89 Evidence also suggests that, although patients tend to expect professionals to take the initiative, there is a tendency for professionals to wait for patients to open the discussion. 5,43,87,90 As a result of this ‘bystander effect’ it is likely that the discussion never happens, or may occur too late, often in response to critical events, by which time options are restricted. 9,12,14 Reviews of patient preferences regarding discussion of end of life issues indicate they vary but tend towards an expressed desire for honesty and information. 91 However, there is also evidence of a discrepancy between stated and actual preferences for information, particularly about prognosis: people may want to know, but not too much. 92,93 It has been commonly reported that patients’ actual desire for information reduces as their illness progresses, and that this is often tempered by a preference for ambiguity and the ability to negotiate the degree of specificity involved. 25,81,91,93–98
Communication
Skilled communication is critical to ACP. 10,99 Poor communication about EOLC is a frequently cited source of patient and carer dissatisfaction and complaint, particularly in hospitals,100,101 and was identified as one of the key shortcomings which led to the withdrawal of the LCP. 27 Further research into improving communication has been identified as a research priority by patients. 102 Despite considerable promotion of ACP as a means of improving EOLC there is little evidence about how it is carried out, or the communication practices necessary to support successful discussion of patients’ future preferences and goals. 52,87,103 Evidence suggests that professional agendas tend to dominate discussions, which may include negative portrayals of life-sustaining treatments, and that patient goals and values are rarely explored in detail. 43,104 Professional influence on ACP discussions will have a very substantial impact on their outcome. Rather than reflecting established preferences, it is through the process of reflection and discussion involving coconstruction between patient and professional that choices for EOLC are established. 67 Preferences emerge and change through time. In this process, patients are likely to be strongly influenced by professional views and expectations, and to be directed towards what are seen to be ‘appropriate’ choices (dying at home, having a DNACPR order in place and, in some cases, opting to refuse further hospitalisation). Especially where patients are hesitant and uncertain, their ‘choices’ may be directed by professionals in line with prevailing assumptions about best interests. 63,67 Previous studies comment on patient apprehension about feeling coerced into formulating preferences for future care, or that statements made in advance might be abused, introducing euthanasia ‘by the back door’. 76,105 However, professional influence is not necessarily unwelcome or unwarranted. There is variation, and frequently uncertainty, in patient and public preferences to be involved in decisions about EOLC. 106 In a critical situation, many patients and their families may look to professionals for information, and also guidance. 49,67,81,101,107,108 Far from being ‘empowering’ for patients and their families, responsibility for decisions of great difficulty and significance may be experienced as burdensome and subsequently subject to uncertainty and regret. 101,109–111
Many studies describe the caution and circumspection that professionals employ when seeking cues about patient receptivity to ACP. 67,87,88 Open questions may be used as opportunities, or ‘offers’, which patients may elect to take up or ignore, and the use of ‘hypothetical’ questions and scenarios may soften the impact of confronting difficult issues directly. 104,112 Vague and indeterminate language, allusion and euphemism are employed by professionals as well as patients. 12,67,93,104,112,113 Reluctance to destroy hope is a common reason for professionals to avoid end of life discussions,12,88,92 and there is evidence that patients strive to balance understanding of their situation with the maintenance of hope. 95,114 Nevertheless, the outcome of interaction that is based on implicit communication and tacit understanding is likely to be misinterpretation and misunderstanding. 14,115 Several studies describe a process of collusion between patients and professionals in deflecting talk about a bad prognosis and limited life expectancy. 25,113,114 However, as Thé et al. 113 note, if patients remain unaware of their prognosis, they cannot plan. In this study, lung cancer patients who insisted on maintaining a ‘recovery story’ eventually confronted a difficult situation and found themselves unable to adjust or prepare for their impending death.
Barriers to advance care planning
Patient perceptions of professional communication skills strongly influence willingness to discuss EOLC. ACP can be undertaken by a range of professionals in hospital and community settings, so the generalisation of advanced communication skills to non-specialist practitioners is challenging. The complexity of modern health-care systems, the diversity of services involved in individual cases, and the number and turnover of professionals providing patient care militate against the achievement of continuity and sustained relationships that could support ACP as a process of ongoing discussion and review. While accepting the value of ACP in principle, professionals express uncertainty about how it should be implemented, and the feasibility of incorporating end of life discussions into routine practice. 53,89 Practical considerations such as lack of time, or a suitable and private location to hold discussions, which may be difficult and lengthy, are additional constraints. 11,67,87
The difficulty of prognostication emerges as one of the most important barriers to professional initiation of ACP, particularly in relation to patients with long-term conditions such as heart failure and chronic obstructive pulmonary disease (COPD) which are characterised by prolonged frailty and dwindling. 11,43,116–118 Professionals are cautious about predicting how long patients may live, from a reluctance to destroy hope or to be proved wrong. 119 This makes it difficult to identify the ‘right’ time to broach the topic. 52,114 Professionals report uncertainty about recognising appropriate opportunities to initiate ACP and are anxious not to cause distress. This leads to avoidance and procrastination. 11,53 In consequence, when it occurs at all, ACP is often undertaken very late, when the patient is already close to death. 8,96,120,121
Professionals are cautious also about raising discussion of ACP for fear of jeopardising relationships with patients who do not want, or are not ready, to consider this. It is evident that patients vary greatly in their receptiveness to ACP discussions and the point in time, if any, at which they are ready to engage with them. 5,12,67,78,88,92,106,122–124 Several studies report a preference among some patients to focus on living in the present, rather than thinking or talking about dying. This can be regarded as a positive means for maintaining a sense of personal integrity and engagement with life, rather than a negative strategy of ‘denial’. 5,2,70,72,107,125,126 There is evidence, also, that many patients simply do not see the relevance of considering issues of ACP while they are still relatively well. They prefer to leave, or only become receptive to, the invitation to consider the end of life much later, when they have become gravely ill and are clearly facing death. 6,12,24,43,51,96 Even when quite severely ill, patients may not realise, or wish to be aware, that they are dying. 12,61 The normative commitment to open awareness towards death and dying within palliative care and current EOLC policy is not borne out by research evidence of patient preferences. The concept of ‘the good death’ lacks public salience,70 as does the notion that dying may present an opportunity for personal fulfilment and growth. 81 It is evident that many patients do not want an open awareness of their impending death. 70,72,127
Professional caution in approaching the topic of ACP is understandable and frequently well founded and may well be sound in protecting the considerable minority of patients who do not wish, or are not yet ready, to engage in ACP. However, such circumspection deprives other patients, who would welcome such a discussion, of the opportunity to have one. The knowledge that patients are likely to change their preferences as their illness progresses may call in question the value of formulating plans in advance. There is wariness about raising expectations about future care that may prove impossible to meet. Whereas the policy rhetoric emphasises choice, in practice both professionals and patients know that options may be limited or illusory, and depend on the availability of resources to support a preferred death in hospice or at home, which may not be forthcoming. 53,121
Advocates of ACP view anticipatory planning as intrinsically beneficial. However, it is clear that patient and public responses to contemplating death and engaging in end of life discussions are complex and highly variable. Some studies have reported benefits and patient willingness to engage in ACP discussion. 128–132 However, as indicated above, an accumulating body of qualitative evidence suggests that a substantial minority of patients find the discussion of death and dying uncomfortable and distressing and do not wish to engage in ACP, or certainly not before their prognosis has become clearly limited. This applies particularly to older patients affected by chronic degenerative diseases such as COPD or heart failure, who tend to view their illness as a fact of life rather than a terminal condition, and do not see the relevance of discussing death and dying. 10,81 Patients may find it difficult to make decisions or anticipate their responses to a hypothetical future that is beyond imagination. Some patients may opt for denial as a positive coping strategy. Rather than plan for an uncertain future, some older patients confronted with their imminent mortality reportedly prefer to live in the present, and take each day as it comes. Acknowledgement of death and dying is resisted because it threatens to undermine the quality of remaining life lived in the present. 94,98,125 In a study of older UK patients with advanced heart failure, Gott et al. 81 found that patients did not want an open awareness of dying, or a precise prognosis. Nor did they value personal autonomy, choice or control over dying, preferring instead to delegate the burden of decision-making to trusted (professional and family) others. Far from its being dysfunctional, these authors acknowledge the value of denial as a positive coping strategy for patients in their management of chronic and debilitating illness. In another UK study of well older people’s views of ACP, Samsi et al. 98 found that, rather than engage in anticipatory planning, respondents preferred to confront future difficulties when they arose and to delegate decision-making to others. Similar findings are reported by Carrese et al. 94 in a study of chronically ill older patients in the USA. These findings suggest that a substantial number of older people, regardless of their current state of health, may not be receptive to the offer of an ACP discussion.
Advance care planning aims to enable patients to shape the experience of death and dying in accordance with their personal goals and preferences. The focus is on the patient as an autonomous agent. It is consistently reported that, rather than promoting personal preferences and autonomy, a key motivator for ACP is patients’ desire to relieve family members of the burden of care and responsibility for making difficult decisions. 65,76,81,82,133 ACP emerges largely as a professional construct framed as an intervention requiring professional mediation. Little is known about the extent or nature of discussions regarding end of life issues that may go on within families, though some studies report patients may look to relatives as well as, and possibly instead of, professionals for this purpose. 43,75,133,134 The availability and willingness of relatives to provide care is critical to enabling death to occur at home. 69,135 Relatives clearly have an important role to play in decisions about ACP and in providing hands-on care for patients dying at home. 133,136 However, carers’ entitlement to information about prognosis and their role in decision-making and future planning is frequently unclear, and carers assess professional communication about EOLC as inadequate. 100
Evidence for effectiveness of advance care planning
Despite the very considerable policy commitment to ACP in the UK as well as internationally, it remains uncommon in practice. Evidence of its effectiveness is limited and conflicting. 4,137 Some studies have reported benefits. 128,130–132,138,139 These tend to be based on surveys, and to focus on a comparative reduction in days and deaths in hospital and costs associated with care in the last year of life. Detering et al. 128 report the results of a randomised controlled trial in Australia in which patients receiving a structured ACP intervention were more likely to die in their preferred place. Carers expressed increased satisfaction with EOLC, and costs for health care were reduced. Abel et al. 132 conducted a retrospective cohort study of deaths among known hospice users and concluded that those who had an ACP in place spent fewer days in hospital and had lower costs of care than those without. However, a growing body of qualitative evidence gives an indication of the great complexity, ambivalence and variability of patients’ desire to engage in ACP, and their responses to professional invitations to do so. 12,25,67,69,81,88,94,98,122
Uptake and initiation of advance care planning
Despite the considerable efforts to change professional practice and public attitudes to death and dying, few people have made or recorded plans for future care. ACP remains uncommon. 9,65,105,140–143 National surveys report no strong resistance to or discomfort about talking about death among the public. 65,134 However, despite sustained campaigns to encourage public and professional engagement in ACP, only 5–6% of respondents have documented their preferences for EOLC. Fewer than half have discussed their own, or others’, future preferences. 33 Evidence suggests that on the one hand, there is a considerable divergence between current policy for ACP, and on the other, patient and public goals and values for making decisions about the end of life. However, little is known about lay and professional responses to the implementation of ACP, how patients and professionals initiate ACP discussions or how these affect the experience and outcomes of EOLC.
Context and justification for the Care and Communication study
For patients with capacity, discussion about ACP is the first step in implementing the EOLCPW (see Appendix 2) set out in the EOLCS. Poor documentation of ACP and lack of knowledge about patient and carer experiences and preferences, and how these may change and be communicated over time, make it impossible to assess the quality, range and frequency of ACP in the UK. However, the available evidence indicates that ACP remains undeveloped and that such discussions are not common. As part of the implementation programme of the EOLCS, each Strategic Health Authority was required to develop and support an EOLCPW to promote the regional uptake of ACP. The Nottinghamshire EOLCPW was established in 2009 as part of a national initiative to improve quality and increase access and equity of EOLC. 31 The Care and Communication study constitutes an instrumental case study144 of the development of ACP through the implementation of an integrated EOLCPW in the East Midlands. It constitutes an in-depth longitudinal investigation and triangulation of lay and professional perspectives of ACP, which will have local and national application in understanding and improving the patient experience of EOLC throughout the NHS. The study provides new knowledge about how patients and professionals initiate ACP in community care settings and how recorded preferences correspond with EOLC outcomes, and associated needs, for patients experiencing a range of terminal conditions as well as cancer (e.g. COPD, heart failure, stroke).
Chapter 2 Aim and methods
Aim
Within the context of a recently implemented EOLCPW in community care settings, the purpose of the study is to investigate how patients, carers and professionals negotiate the initiation of ACP and the outcomes of discussion and planning for EOLC in terms of how closely preferences for EOLC that have been expressed are realised.
Objectives
-
To investigate patient and professional perceptions and experiences of initiating, and subsequently reviewing, ACP discussions and decisions throughout the last 6 months of life.
-
To investigate patient and carer responses to the offer of an ACP discussion.
-
To identify barriers to the implementation of ACP.
-
To investigate outcomes for EOLC: how patient preferences for care, expressed and recorded during ACP, match care received in the last week of life.
-
To investigate how professionals, patients and carers assess the quality of EOLC.
-
To generate evidence for best practice in implementation of ACP.
-
To establish professional training and support needs for confident and skilful communication in ACP.
Methods
Study design
The study explores the applicability of a conceptual framework in which ACP is understood to involve a process of ongoing discussion, reflection and review, rather than constituting a ‘one-off’ recording of instructions for future medical treatment. This process may involve (1) input from several/diverse persons and perspectives (patient, family, professionals) and (2) change over time. A qualitative study design was employed to gather data in two workstreams:
-
workstream 1: professional perspectives interviews
-
workstream 2: patient case studies.
The research builds on methods and recruitment processes used successfully by the research team in earlier studies of patient choice and decision-making in palliative care145 and community nurses’ (DNs’) experiences of ACP. 53 Qualitative methods of data collection and analysis enable an in-depth exploration of participants’ views and perceptions of their experience. This is particularly valuable in discussion of little-known, complex and sensitive topics, especially where these are being studied over time. Semistructured interviews allow core topics to be raised for discussion, while leaving scope for the identification and exploration of unforeseen issues that may emerge as particularly significant or salient in respondents’ accounts, and to extend the discussion of these to establish clarity and depth of meaning. 146,147 Longitudinal case studies involving serial qualitative interviews have been used successfully to study patients’ evolving needs and experiences of palliative care. 90,148 Case studies are particularly suitable for exploring complex situations involving a variety of perspectives. 149 Detailed insights from well-constructed case studies also have an explanatory potential, in this instance in discerning how ACP practice is negotiated between participants and shaped by contextual factors at play in community care. 150,151
Setting/context
The study was based in generalist community health services providing supportive and EOLC to patients living with life-limiting and terminal conditions in their own or care homes and registered with GP practices in the East Midlands region of England.
Eligibility
Workstream 1: professional perspectives interviews
Health professionals: providing EOLC to patients in the community including GPs, DNs, CMs and clinical nurse specialists (CNSs) in palliative care and other specialities.
Workstream 2: patient case studies
Patients: living in their own or care homes; suffering from a progressive, terminal condition; assessed by health-care professional (HCP) to be within the last 6 months of life; with capacity to give informed consent; aged 18 years or older (there is no upper age limit); fluent English speakers.
Family carers: nominated by patient; in at least weekly contact with patient; with capacity to give informed consent; aged 18 years or older (there is no upper age limit); fluent English speakers.
Health professionals: nominated by patient; working in community health-care services providing palliative and EOLC to patients.
Recruitment
With support from the Primary Care Research Network, 10 GP practices were recruited from the study area. The network identified and contacted a range of GP practices. However, engaging practices willing to participate was a long and protracted process, and subsequently recruitment was extended to include a further practice.
Workstream 1: professional perspectives interviews
Health professionals providing EOLC to patients in the community were invited to take part. The initial plan was to recruit several professionals, including at least one GP and one DN, from each practice participating in the study. However, given the difficulty of recruiting professionals from participating practices, and consequently to ensure adequate representation from the different professional groups, the recruitment strategy was widened. Participants were recruited in a variety of different ways including via the participating GP practices, by accessing professional team meetings, by targeting training events and through direct invitation via a network of local contacts. Some participants were then asked to snowball this invitation to colleagues. In order to achieve inclusiveness and diversity and to gain a range of perspectives and experiences, care was taken to recruit GPs, DNs, PCNs and specialist nurses for a range of conditions such as heart failure, respiratory disease and neurological conditions. The aim had been to recruit 30 health professionals to this part of the study. However, in order to achieve the range of perspectives desired, a total of 37 health professionals were interviewed.
Workstream 2: patient case studies
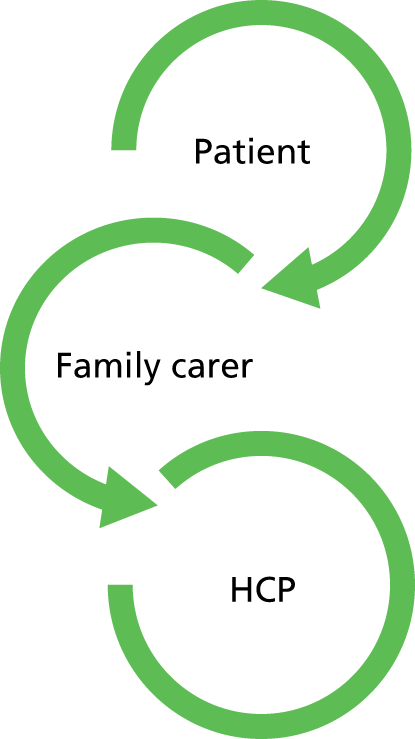
Case studies were prospective, longitudinal and multiperspective, with the patient as the centre of a network involving lay and professional carers148,152 (Figure 1). Initially, the participating GP practices were asked to identify patients considered likely to be within the last 6 months of life, and affected by a range of illnesses and comorbidity, such as cancer, stroke, respiratory disease and heart disease. These patients might be identified by their inclusion on the Gold Standards Framework (GSF) register or by GPs asking themselves the ‘surprise’ question, in this case specified as ‘would you be surprised if this patient were to die in the next six months?’148 What was relevant to the study was not the accuracy of prognosis, but the professional perception of the patient’s illness trajectory that was thought to be critical in initiating ACP.
FIGURE 1.
Make-up of cases.
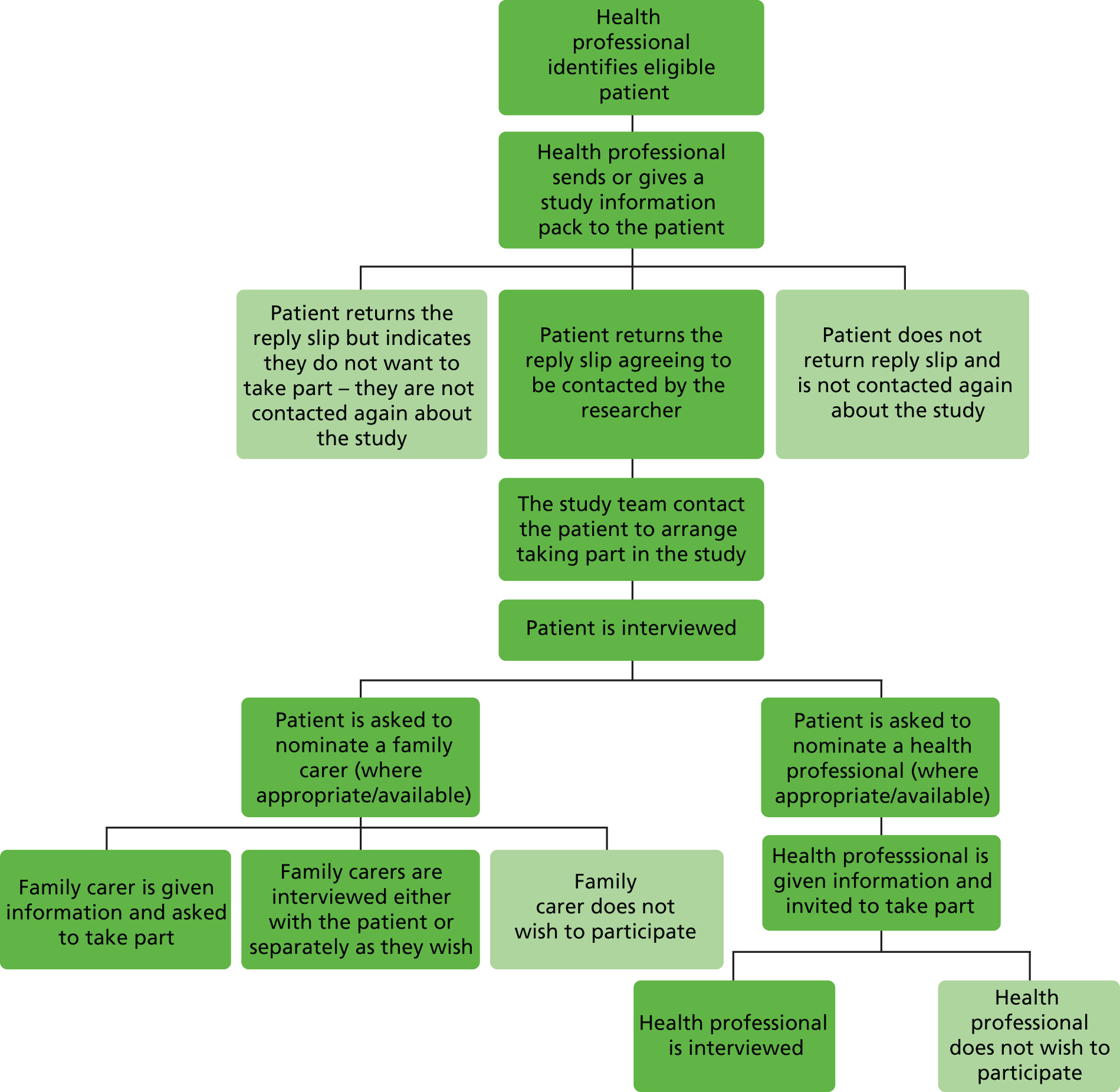
Once a suitable patient was identified, the health professional sent or gave them a pack with information about the study. The patient was then free to decide whether or not to participate by returning a reply form directly to the research team. When a reply slip indicating a wish to take part was received, the research team contacted the patient and arranged to visit for their initial interview. At this stage, written consent was taken and the patient was asked to nominate a family carer and a HCP to be included within the case study, if they wished to do so. Patients without informal carers or a key health professional were still included in the study. Hence the case studies are not uniform. Figure 2 shows the recruitment process.
FIGURE 2.
Recruitment process.
Recruitment of cases took place between August 2012 and November 2013, a total of 15 months, exceeding the initial 9-month target. By the end of the first 5 months of the recruitment period, 14 of the proposed 20 cases had been recruited. In order to boost recruitment, participating GP services were revisited, providing an additional four cases. In conjunction with this GP contact, specifically to widen the range of participants beyond those with cancer, recruitment packs were also distributed via CMs for patients with long-term conditions, and secondary care consultants of patients with respiratory and digestive diseases. This yielded three further cases, resulting in a total of 21.
Data collection
In response to a number of challenges, the recruitment period for the study was extended and, with allowance of a 6-month follow-up period for each of the case studies, data collection took place over a period of 22 months from July 2012 to April 2014. In line with the 6-month extension to the recruitment period, follow-up was also extended to allow all those recruited to be followed up for a period of at least 6 months. In addition to the difficulties of recruitment of GP practices, the project had been granted a 4-month no-cost extension to compensate for a period between the departure in May 2013 of Dimitris Vonofakos, who was originally appointed as the full-time research fellow on the project, and Eleanor Wilson’s being able to take up this post in September 2013.
Workstream 1: professional perspectives interviews
Semistructured interviews were used to gather data from a range of community-based health professionals. These interviews focused on respondents’ thoughts and experiences of delivering care towards the end of life, and the use or absence of ACP. Interviews were tailored to suit the time constraints of the participating health professionals. Consequently, one group interview was arranged to gather the thoughts of four CNSs for heart failure. This was initiated by the participants as the most expedient and appropriate approach to participation in the study given their pressures of time and availability. Professionals were also offered a telephone interview if they felt this would be more convenient; only one chose this option. Eight participants in the professional interviews were also nominated health professionals for case studies and took part in both workstreams of the study.
Workstream 2: patient case studies
The processes and outcomes of ACP, or its absence, were explored through (1) initial and follow-up interviews with each patient and each of their nominated family and professional carers and (2) analysis of medical records and documentation of ACP (accessed with permission).
-
Each patient recruited to the case study workstream was followed up for a period of approximately 6 months, or until their death if this occurred sooner. During this time, each member of the case study interview set (patient, family carer and HCP) was interviewed up to four times (Table 1 shows the number of interviews per case, broken down by participant type). The majority of patient and informal carer interviews were held jointly, according to preference. Follow-up contacts with patients and relatives were arranged to take account of relevant developments regarding treatment and care, including respondents’ wishes and state of health. Most follow-up contacts were carried out face to face, a few by telephone (two with patients, one with a family carer and seven with nominated health professionals). Follow-up interviews explored changes to participants’ health and experience of care, how these affected future preferences and plans, and whether or not there had been any changes or developments in discussion, documentation or implementation of planning for future care. Patient and family carer interviews took place in their own home and ranged from 12 minutes to 2 hours and 15 minutes in length.
-
Patients were asked to give permission for the researchers to review relevant parts of their medical records. This provided access to documentation of preferences for future care. Once the case study interviews had been completed, arrangements were made with the relevant GP practice and hospice (where applicable) to view the patients’ medical records. Information was extracted and notes made about recorded evidence of an ACP discussion; subsequent records relevant to ACP; DNACPR status; care in the last week of life; PPOD; and actual place of death. 145 This was possible for all but one case, in which clarity of consent could not be confirmed, without which it was felt inappropriate to access this patient’s medical records.
Patient and public involvement
Public involvement has been sought throughout all stages of this project in accordance with INVOLVE guidance for research. 153 An initial review of the ethical issues, patient recruitment documents and protocol was undertaken by a member of the Lancaster University patient and public involvement group. Further to this, a number of presentations were given to public groups including the Nottingham Older People’s Advisory Group, the Nottinghamshire Chinese Welfare Association, Medical Crises in Older People Patient and Public Advisory Group, Palliative Care Studies Patient and Public Group and the Newark & Sherwood Over 50s Forum. These presentations engaged the public in discussion of the topic and methods of data collection. These discussions raised the profile of the study and reinforced the significance and public salience of the topic and the relevance and value of the research. In preparation for data collection, a focused discussion was undertaken with a volunteer patient who had experience of cancer. This discussion reviewed the content of the patient interview schedule and the different reactions this might give rise to in potential participants. The session was particularly helpful in identifying ways in which interviews could be ended appropriately.
Throughout the recruitment and data collection phases, we engaged with the Nottingham and Sheffield Dementia, Frail Older People and Palliative Care Patient and Public Involvement Advisory Panel for advice, discussion and feedback on the progress of the study. The study findings were presented to the panel for discussion in June 2014. Seven members of the advisory panel reviewed a draft of the project report and their feedback has been incorporated into the final version, particularly concerning points and issues requiring clarification. The reviewer responses to the report were very positive. There was agreement that the study addressed an important topic and made a substantial contribution to the field, particularly in highlighting the gap between current policy and practice. The report was described as clearly written and easy to read. The aims and objectives were felt to be clearly stated and addressed by the study findings. The researchers were commended for the sensitivity and respectfulness with which they approached patients and carers during a very challenging period of their lives. The study findings were felt to have considerable value as a teaching tool for a wide range of professionals delivering EOLC. Panel members also reviewed the plain English summary and amendments were made in the light of their comments.
The Sue Ryder Care Research Group for the Study of Supportive, Palliative and End of Life care (SRCC) works with the panel on a regular basis and provides expenses for travel and time spent reviewing reports. Care is also taken to minimise burden, provide support, create a friendly environment and share research in a way suitable for non-professionals. The panel’s contribution to studies is valued highly, and additional funding is made available for training, education and attending wider meetings and conferences for members who wish to do so. The group meets five times a year and is made up of approximately 15 members, the majority of whom attend meetings on a regular basis.
Throughout the study the team has maintained and updated a web page, which is freely accessible and details the progress of the study. 154 The project has also been featured in a number of local, national, public and professional newsletters. These include national newsletters published by the National Council for Palliative Care, the Palliative Care Research Society and, locally, Nottinghamshire End of Life Care, the Nottingham Clinical Commissioning Group and the Nottinghamshire Chinese Welfare Association. These features have raised the profile of the study and contributed to the public debate around death and dying. All are accessible in the public domain in both hard copy and electronic formats.
Ethical approval
Approval for the study was sought through the National Research Ethics Service and approved by the Leicester NHS Research Ethics Committee on 21 March 2012. A substantial amendment to extend recruitment to a small number of secondary care settings was submitted and approved in September 2012. Research and development approvals and letters of access were issued by the NHS trusts participating in the study.
Ethical issues
The principal ethical issues involved in the study relate to the involvement of patients and family carers confronting the challenge of life-limiting and terminal illness. The research involved a vulnerable patient population and investigation of a topic which participants may find challenging. Previous studies have found that respondents taking part in qualitative studies report this to be a positive experience, despite the discussion involving topics of a potentially difficult and distressing nature, and many welcome the opportunity to contribute to a research effort that may benefit others. 152,155–157 This applies also to patients with terminal conditions, or who knew that they were dying, and bereaved relatives of patients who had died. 156,158 Research has found that such patients may welcome the opportunity for their voice to be included and to make a contribution to research that will benefit others in future. 159–162 Consequently, it has been argued that excluding vulnerable patients from the opportunity to take part in research on the basis of assumptions made about their experiences and preferences is discriminatory and restrictive. 163–167 However, we were well aware of the need to approach contacts with patients and family carers with the utmost care and sensitivity, and to be suitably responsive to patient and family carer reactions and preferences throughout the research. This respect for emotional boundaries relied on the interviewers’ skills in recognising non-verbal cues in order to respond appropriately to each participant. As would be expected, some participants were more willing than others to talk about issues relating to EOLC, and interviewers took care to be guided by the participant on when and how much to discuss these issues. It was important to judge how to elicit relevant information about ACP without forcing people to confront issues or areas they were not comfortable talking about. Sometimes participants would give verbal indications by simply stating that they did not want to think about certain aspects of their care or illness, whereas others specifically introduced these topics themselves. In order to avoid causing distress to respondents who may not have been aware of, or did not wish to acknowledge, the terminal nature of their condition, the study was presented as research into the quality of care and communication about serious, chronic and life-limiting illness between patients, family carers and health professionals in community care settings. Initial discussion with patient and family carer participants was phrased in general terms and great care was taken to allow respondents to reveal their understanding of their condition and prognosis and to frame the interview discussion within the terms of their understanding, rather than assume that the individuals concerned had understood and accepted professional formulations of what these might be.
Care was taken during interviews to maintain clear boundaries between the role of researcher and professional. Researchers took no part in offering advice or support to patients and family carers, while always giving time for respondents to talk in detail about their perspectives on ACP and experience of care.
It is possible that involvement in the research may have altered the behaviour of respondents in such a way as to influence the nature of the data collected. For example, health professionals may have raised and pursued the issue of ACP with patients included in the study, when otherwise they would not have done so. The methodology of the study allowed for the flexibility to monitor and take account of such effects, and where appropriate explicitly address them as a topic of discussion in the interviews. Triangulation of data from workstreams 1 and 2 extended the scope to contextualise this phenomenon.
Written consent was obtained from participants before the first interviews commenced. Patients were also asked to identify whether or not they wished to be withdrawn from the study should they lose capacity either temporarily or permanently. They could also nominate someone to make this decision for them. However, loss of capacity did not materialise as an issue in any of the cases. For those professionals participating in both workstream 1 and workstream 2, a consent form was completed for each part of the study to indicate a clear understanding of the different aspects of the workstreams. Throughout the case studies the notion of process consent was used,168 allowing willingness to participate to be confirmed at each point of contact. This allowed participants to continue in the case studies as they wished. Patients and family carers were given the option of speaking on the phone or a home visit. Times for follow-up interviews were agreed with the participant based on their convenience, preferences and current health.
Confidentiality was a particular issue for the case studies in workstream 2, as most cases involved more than one participant. All participants were informed of the nature of the case studies and consented to participate. None of the participants raised concerns about issues of confidentiality at any point during the study, and they often encouraged the researchers to speak to other family members and health professionals. The majority of interviews with family members were undertaken as a joint interview with the patient, as they preferred.
Open discussion was maintained with all participants about the length of the study, and all patients and family members were happy to participate for the expected 6 months, where possible. In setting up the final interview date it was reiterated that this would be the last time contact would be made. The initial intention had been to conduct rounds of interviews with patients, family carers and professionals at approximately the same time. However, in practice it proved hard to synchronise professional and patient interviews in this way. We adopted a policy of working pragmatically with health professionals in terms of their willingness and availability to be interviewed (which varied) and in the context of what was happening with each case. In some instances where the patient was reasonably stable over part or all of the follow-up period, we judged that there was little to be gained by frequent follow-up with professionals involved,90 especially when they may have had little direct contact with the patient in the interim. In others, it was helpful to obtain an update on the case between patient and family carer follow-up interviews, rather than at the same time.
Analysis of multiple data sets
Most interviews were audio recorded with permission. However, there were three recording failures and four instances when only notes were taken, each when interviews were conducted over the phone. The study findings were derived from a number of data sets across the two workstreams:
-
workstream 1: professional perspectives interviews
-
workstream 2: patient case studies as sequential interviews over a 6-month period with patients, family carers and health professionals involved in their care, and documented records of patient care.
Each data set has been subject to both separate and integrated analysis. Data collected from serial follow-up interviews with case study participants go beyond cross-sectional and static accounts of specific stakeholders. This enables an understanding of communication about ACP and EOLC as a potentially ongoing process of communication between the multiple and changing perspectives of patients, family carers and professionals, by interrogating each case individually.
Coding and analysis was ongoing throughout the study and is an integral part of qualitative research. The qualitative software program NVivo 10 (QSR International, Warrington, UK) was used to facilitate organisation of a complex data set and support a thematic analysis of the data using the constant comparative method based on the principles of grounded theory. 146
Workstream 1: professional perspectives interviews
Once transcribed, checked and anonymised, interviews were imported into NVivo 10 along with written field notes. In addition to the freestanding professional interviews undertaken for this workstream, it became apparent that the nominated professional interviews that contributed to the patient case studies contained much relevant material relating to professional perspectives and experience of ACP. Consequently, relevant content from all professional interviews was incorporated into the professional interview coding frame. Use was made of both the ‘free’ and ‘tree’ node functions in the NVivo 10 software in order to sort and rank codes and to build hierarchical trees of related codes. Core categories and thematic inter-relations were established within and between each data set. 147 The evolving coding frame was discussed regularly by the researchers and within the project group meetings.
Workstream 2: patient case studies
Once data collection was completed for each of the case studies, all data from that case were reviewed and written up as an individual case profile including input from all case participants and data from medical records. This used a process of reconstruction and restorying of each case into an integrated narrative through detailed scrutiny of all relevant data sources. This analysis was extended with the documented evidence established by the review of medical records. Summaries of each case are provided (see Appendix 3). These outline key elements including participation in the study, involvement where applicable of nominated family carers and health professionals, changes over time, key incidents of care and any involvement in ACP. Building these individual narratives prevented cases from becoming swamped or disaggregated by cross-case analysis, enabling presentation of the particularity of each case within its own context. 144 Cross-case analysis was also undertaken to draw out common themes across the individual cases. The progression of each case was explored in relation to the occurrence or non-occurrence, and consequences, of ACP and the light this analysis shed on the salience and implementation of current EOLC policy for patient experience and professional practice.
Immersion in longitudinal studies and complex data collection can result in selective notions of what is important within the data. 169 The analysis was repeated over time and carried out by two researchers employing a systematic approach. Coding frames and data within codes were also presented to the advisory group in order to ascertain how much they resonated with practice. This multifaceted approach allowed a more robust and thorough analysis of the data.
Chapter 3 Findings: demographics
Workstream 1: professional perspectives interviews
Thirty-seven health professionals and allied health professionals (AHPs) were recruited to participate in this workstream of the study (Table 2). All interviews were undertaken on a one-to-one basis with the exception of one group interview, which included four heart failure nurse specialists. Most professional interviews were carried out face to face, with one being conducted by phone. They ranged in length from 12 to 59 minutes.
| Professional | Number interviewed |
|---|---|
| GPs | 12 |
| Community/district nurses | 5 |
| CMs | 6 |
| Heart failure specialist nurses | 6 |
| Specialist PCNs | 3 |
| Specialist nurses (other conditions) | 3 |
| AHPs | 2 |
| Total | 37 |
Eight of the professionals taking part in the professional perspectives interviews were interviewed in relation to one or more specific patient case and also feature in the case data. A further six professionals took part in the case studies as nominated professionals only. In addition to focusing on the individual patient, the case study interviews with professionals contained a considerable amount of more general material relating to respondents’ wider perspectives and experience of ACP. This material was coded in NVivo 10 and included in the analysis of findings relating to professional perspectives. Hence interviews from a total of 43 individual professionals were analysed and are reported in Chapter 4.
Data from the Public Health England website170 show a number of key demographics for all GP practices in England from 2011–13. Data were identified for 10 of the 11 practices included in this study. There were no data available for the remaining practice, which had recently merged with another and moved to new premises (practice L). Table 3 gives features of the different practices, including list size, the number of patients over the age of 65 years and the percentage with long-standing health conditions. These are presented alongside local demographics on deprivation scores, income deprivation for older people, number of Disability Living Allowance claims per 1000 patients, percentage of non-white ethic groups and unemployment status. All these statistics can be compared not only across the participant practices but also with the national average for England.
| Indicator | Practice | England average | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| A | B | C | D | E | F | G | H | J | M | ||
| Number of registered patients | 7094 | 2691 | 7918 | 12,048 | 11,360 | 6273 | 13,120 | 13,047 | 5323 | 9287 | 7041 |
| Number of GPs at the practicea | 5 | 3 | 2 | 10 | 7 | 5 | 7 | 7 | 3 | 8 | 6.8/10,000 populationb |
| Percentage (number) of patients on the GSF registerc | 0.35 (25) | 0.18 (5) | 0.48 (38) | 0.29 (35) | 0.18 (21) | 0.19 (12) | 0.14 (19) | 0.41 (54) | 0.3 (16) | 0.16 (15) | National target 1% |
| Percentage of patients over 65 years | 21.8 | 23.7 | 18.3 | 19.2 | 24 | 19.9 | 16.1 | 19.8 | 18.7 | 19 | 16.7 |
| Deprivation score (Index of Multiple Deprivation) | 21.5 | 16.3 | 42.2 | 26.9 | 19.3 | 12.5 | 10.5 | 30 | 31.6 | 23 | 21.5 |
| Income deprivation affecting older people (%) | 16 | 14 | 29 | 18 | 18 | 16 | 11 | 23 | 21 | 18 | 18.1 |
| Long-standing health conditions (%) | 58.9 | 55.9 | 64.3 | 55.4 | 59.5 | 52 | 52.1 | 65 | 66.4 | 48 | 53.5 |
| Disability Living Allowance claims per 1000 | 55.6 | 50.3 | 79.4 | 71.7 | 66.8 | 40.4 | 40 | 74.7 | 77.5 | 63.1 | 48.3 |
| Percentage non-white ethnic groups | 1.2 | 0.8 | 6.7 | 1.6 | 1.5 | 5.2 | 6.1 | 2.4 | 0.9 | 4.8 | Not cited |
| Unemployed (%) | 1.6 | 2.5 | 10 | 1.8 | 2.1 | 6.3 | 10.3 | 9.6 | 4.8 | 1.2 | 5.6 |
These data show that four (D, E, G and H) of the 10 practices have considerably higher than average numbers of patients registered and one (B) is well below the national average. Size of practice and number of GPs are reflected in the number of patients registered. However, these numbers can be considered only a guide, as practice websites did not specify the number of GPs working full- or part-time hours and calculations have been made between the number of GPs and their registered patient lists rather than the total population for the area.
All of the GP practices were registered on the GSF register or kept a register of palliative care patients. For clarity, the term ‘GSF register’ is used throughout the remainder of this document. When the size of practice list is combined with the number of patients registered on the GSF or palliative care register, all practices fell below the national target of 1%. Practices located in urban areas generally had higher deprivation scores. Rural practices in areas of less dense population, such as practice B, had smaller practice sizes and lower deprivation scores despite having a higher than average number of patients over the age of 65 years. All practices, apart from practice G, had higher than average levels of patients over the age of 65 years.
Comparisons between the GP practices used in the study and the national average show that the practices were broadly representative of GP practices in the UK. Marked differences relate to the location of the practices within either large cities or rural areas. Other practices present closer to the national average in terms of population distribution and demographic indicators, demonstrating a good spread of practice types within the study. All GP practices reported data on their GSF registers at one time point between March and April 2014.
Workstream 2: patient case studies
Recruitment
It was not possible to track the number of information packs that different practices and health professionals gave out to patients to invite participation in the case studies. However, from the number of reply slips returned, we are able to identify some characteristics of those who did not wish to take part as well as those who did participate (Table 4).
| Characteristic | Male | Female | Unknown | Total |
|---|---|---|---|---|
| Participated | 12 | 9 | – | 21 |
| Refused | 6 | 14 | 5 | 25 |
| Ineligible | 3 | 2 | – | 5 |
| Deceased prior to contact | 2 | – | – | 2 |
| Unable to arrange | 1 | – | – | 1 |
| Total | 24 | 25 | 5 | 54 |
Profile of cases
Twenty-one patients were recruited to the case studies. In addition, these cases included 13 family carers and 14 individual nominated professionals; four cases were made up of the patient alone. Eight had no family carer they wished to nominate, and seven did not nominate, or we were not able to contact, a HCP. The original intention had been to include only ‘complete’ cases in order to triangulate perspectives of patient, carer and key health professional. However, some patients did not wish to involve family or professional carers or could not identify a suitable individual to take part. It became apparent that a number of patients, particularly those who lived alone, lacked contact or significant relationships with local family members and/or health professionals. It was important to include the experience of such individuals, most likely representative of significant groups within the wider population, within the study. In addition, the sheer difficulty of recruitment called for a pragmatic strategy for inclusion. The demographics of the cases are collated in Table 5. Nominated family carers were predominantly spouses. Slightly more male than female patients took part in the study, resulting in a higher number of female family carers participating. Female patients were more likely to live alone, with the result that only three male family carers took part. Patients were most likely to nominate their PCN or CM. One PCN was nominated by two patients and another by three different patients. A further six nominated their GP or consultant in palliative medicine (CPM). In addition, three AHPs were nominated, demonstrating the range of professionals with whom patients and families built substantial relationships, and with whom they might discuss their end of life wishes. Patient ages ranged between 38 and 92 years. Sixteen were over the age of 65 years and eight of those were over the age of 80 years.
| Type | Characteristic | Number |
|---|---|---|
| Patients (n = 21) | Male (age range 62–91 years) | 12 |
| Female (age range 38–92 years) | 9 | |
| Family carers (n = 13) | Male | 3 |
| Female | 10 | |
| Spouse | 10 | |
| Son/daughter | 2 | |
| Sibling | 1 | |
| None | 8 | |
| Healthcare professionals (n = 14) | GP | 5 |
| PCN | 3 | |
| AHP | 3 | |
| CM | 2 | |
| CPM | 1 | |
| None | 7 |
Table 1 shows the number of interviews per case broken down by participant type. GP-held medical records were accessed for 20 of the 21 patients and, in a further four cases, hospice or care home notes were also reviewed. The names of all patients and family carers have been changed to provide anonymity and preserve confidentiality. Health professionals are referred to by grouped professional roles (see Appendix 1 for further information on these).
A total of 59 interviews were undertaken with patients as part of the case studies. Thirty-three were joint interviews with the patient and a family carer; 26 were with patients alone. In addition, seven interviews were with family carers alone, often after the death of the patient. The 14 individual nominated health professionals took part in a total of 31 interviews as part of the case studies. Apart from a few patients who died in the early stage of follow-up, all interviews took place over a period of approximately 6 months following recruitment to the study and were undertaken as and when was appropriate for each case. In total, 97 interviews were undertaken for the patient case studies. Nine (43%) patients died during the study follow-up period, some after only one interview.
Much previous research has focused on cancer patients. Our original aim had been to recruit patients with a wide range of conditions such as respiratory conditions, heart failure, neurological conditions and diabetes, as well as cancer, to reflect the most common causes of mortality and the type of case most frequently encountered in the community. However, this diversity proved hard to achieve. Patients recruited for the case studies had a range of conditions, and often more than one (Table 6). However, two-thirds (14 of 21) had been referred to the study because of a cancer diagnosis. Part of the struggle with recruitment resulted from the difficulty experienced by many professionals in identifying the end of life phase in patients, particularly those affected by conditions other than cancer, especially those with multiple crises and the frail elderly with multiple comorbidities. Most practices sought to identify eligible cases from their GSF registers, which, although reported to include a diversity of conditions, were predominantly made up of patients with a cancer diagnosis. The difficulty that health professionals evidently experienced in identifying suitable patients, particularly those who did not have cancer, is discussed further in Chapters 4–6.
| Condition | Number of cases | Notes |
|---|---|---|
| Cancer (including lung, oesophageal, pancreatic, stomach, brain, bladder and prostate) | 14 | Three had COPD in addition to cancer |
| COPD | 3 | One had renal disease in addition to COPD |
| Renal disease | 1 | |
| Liver disease | 1 | |
| Heart failure | 1 | Several had heart conditions in addition to their primary diagnosis |
| Spinal injury | 1 | |
| Total | 21 |
In addition to the challenges of identifying patients to refer to the study, some further difficulties with recruitment were identified. Several patients with liver failure were referred to the study through secondary care, of whom one was subsequently recruited to the study. These belong to a substantial group of hard-to-reach patients who have extensive contact with services but tend not to engage effectively with the system. The lifestyles of patients with substance abuse and/or mental health problems meant that they found it difficult to engage with the study despite their interest in taking part. Indeed the one patient from this group who was recruited was often difficult to contact and took part in only two interviews during the study period. No family or professionals were nominated for her case and consent could not be confirmed to access her medical records.
Recorded advance care planning
Medical records and data from the case study interviews were used to explore the incidence and prevalence of documented activity relating to ACP across 20 of the 21 cases (in one case we were unable to access medical records). We recognise that ACP is a nuanced process often involving discussion over time, much of which may not be documented. However, although medical records rarely capture the details of ACP discussion, they do often note when certain more tangible elements of ACP have been discussed and the elements of professional planning (e.g. fast track or anticipatory medicines) put in place for patients recognised to be in the last months of life. When recorded, these elements allowed data to be gathered on the types of anticipatory planning that were undertaken. These are summarised in Table 7.
| ACP element | Cases (%) (n = 20) |
|---|---|
| Any element documented | 17 (85) |
| GSF register | 15 (75) |
| DNACPR | 11 (55) |
| PPOC/PPOD | 11 (55) |
| Anticipatory medications | 7 (35) |
| Fast track | 5 (25) |
| DS1500 | 5 (25) |
| ADRT | 1 (5) |
The findings show that one or more element of anticipatory planning was documented in the medical notes of 17 (85%) cases. Excluding the patient whose records we did not gain access to, three patients had no documented, or reported, elements of any kind of ACP or anticipatory planning. Five had documented elements of professional planning such as placement on the GSF, but no evidence that this was discussed with them. Table 7 shows that 15 (75%) participants were included on their GP practice’s GSF register. Just over half (11 of 21) of the patients had a completed DNACPR form. Place of death had been recorded for the same number (although not necessarily the same cases). In two cases, the records stated both that home was the PPOD and that this had not been discussed with the patient. For a quarter of patients a fast track referral and a DS1500 had been recorded, although it is unclear if either was discussed with patients. Anticipatory medications were in place for just over a third of patients in this study (all of whom died during follow-up). Only one patient had an ADRT, completed at his instigation. An integrated pathway of care (IPOC) had been used in two of the nine cases in which the patient died during the course of the study. Figure 3 shows the recorded elements of anticipatory planning specifically in relation to those who died during the study period. Apart from registration on the GSF, elements of such planning were predominantly recorded for those who died during the study, indicating that ACP was generally undertaken near the end of life, rather than earlier.
FIGURE 3.
Elements of ACP documented per case, highlighting those who died. PPC, Preferred Priorities of Care.
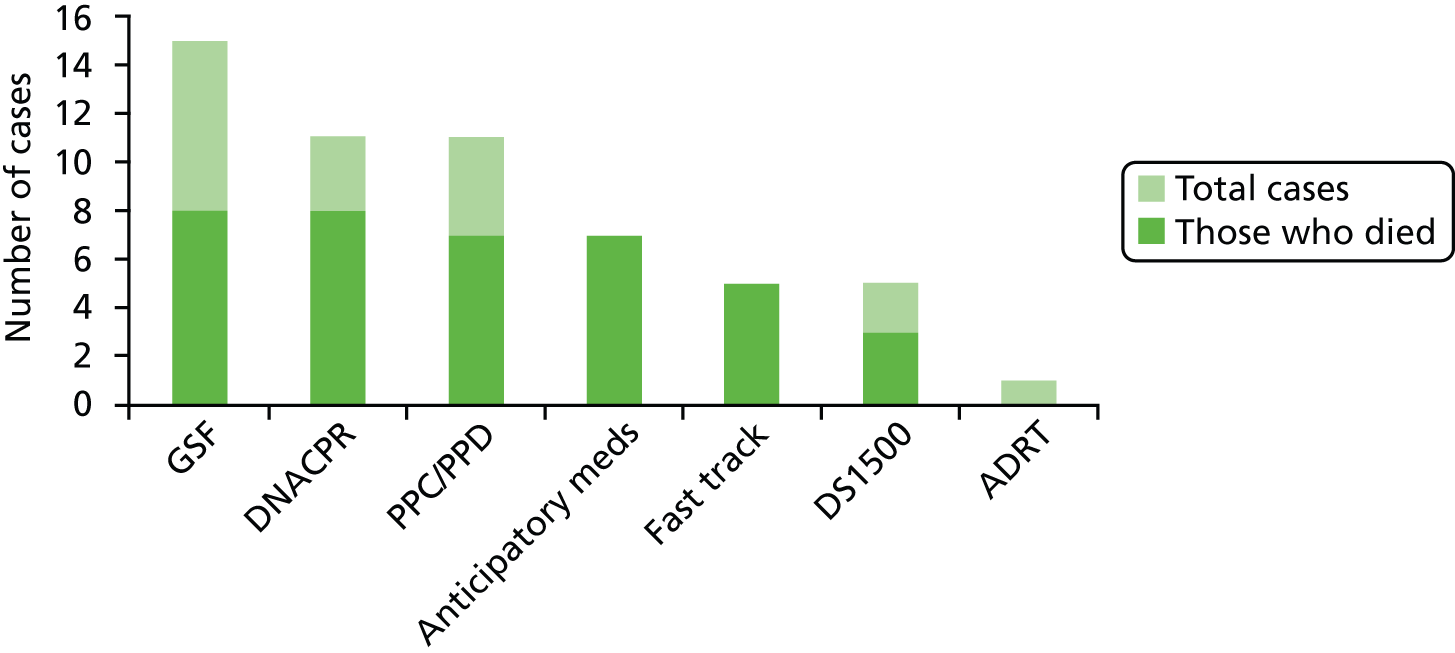
Fifteen patients participating in the case studies were identified as being on their GP practice GSF register (Table 8). It was not possible to identify an average length of time spent on the GSF register, as seven participants were still alive and remained on the register at the end of the data collection period (April 2014). However, of those who died during the study the average time on the register was 7.8 months, with a median of 4 months. One patient (Mr Patterson) who died during the study period was not recorded as being on the GSF register at his practice. These variations may be accounted for by the approach of each GP practice to the use of the GSF register. All seemed to differ in the types of patients they would consider eligible and at what point in the illness trajectory they would consider placing them on the register. However, as is discussed further in the following chapters, the difficulty and uncertainty of prognosis is an important factor accounting for the variable length of time that patients spent on the GSF register. As practices varied in size so too did the number of patients registered on the GSF, with a range of between five and 54 (see Table 2).
| Case | Case number | Time on GSF register |
|---|---|---|
| Mrs Tomlinson | 15 | 1 month until death |
| Mr Brown | 3 | 2 months until death |
| Mrs Jones | 5 | 2 months until death |
| Mrs Winters | 9 | 2 months until death |
| Mr Corley | 12 | 6 months until death |
| Mr Andrews | 13 | 10 months until death |
| Mr Farley | 19 | 14 months until death |
| Mr Williamson | 6 | 26 months until death |
| Mr Barlow | 4 | 6 months ongoing |
| Mrs Harrison | 21 | 12 months ongoing |
| Mr Roper | 17 | 14 months ongoing |
| Mr Arthur | 16 | 16 months ongoing |
| Mr Jenkins | 10 | 18 months ongoing |
| Mrs Elder | 11 | 22 months ongoing |
| Mrs Barker | 14 | 33 months ongoing |
Preferred and actual place of death
Using medical records in conjunction with interview data we were able to identify patients’ expressed PPOD, their recorded PPOD or preferred place of care (PPOC) and, for the nine patients who died, their actual place of death (Table 9).
| Case | Case number | Recorded PPOC/D | Expressed at interview | Actual place of death |
|---|---|---|---|---|
| Mrs Alderson | 1 | Not recorded | – | – |
| Mr Davis | 2 | Not recorded | – | – |
| Mr Brown | 3 | Home | Home/hospicea | Hospice |
| Mr Barlow | 4 | Home | – | – |
| Mrs Jones | 5 | Home | Home/hospicea | Home |
| Mr Williamson | 6 | Home/hospice | – | Home |
| Mrs Avery | 7 | Not recorded | Home/hospicea | – |
| Mr Patterson | 8 | No preference | Home | Hospice |
| Mrs Winters | 9 | Home | Hospice | Home |
| Mr Jenkins | 10 | Not recorded | – | – |
| Mrs Elder | 11 | Possibly home | Home | – |
| Mr Corley | 12 | Home | – | Home |
| Mr Andrews | 13 | Not recorded | – | Home |
| Mrs Barker | 14 | Not recorded | – | – |
| Mrs Tomlinson | 15 | Home | Home | Home |
| Mr Arthur | 16 | Not recorded | – | – |
| Mr Roper | 17 | Home | – | – |
| Mr Jacobs | 18 | Not recorded | Home | – |
| Mr Farley | 19 | Home/hospice | Hospice | Care home |
| Ms Lucas | 20 | Not recorded | – | – |
| Mrs Harrison | 21 | Home | Home | – |
Actual place of death generally reflected the recorded preferences for place of death. No deaths occurred in hospital and six of nine occurred at home. Of the six deaths occurring at home, three people remained at home to die as planned and three were admitted to hospital shortly prior to death. The fast track system was then utilised to facilitate discharge home to die. Health professionals’ accounts rarely differentiated explicitly between PPOC and PPOD, so it is not possible to identify which is recorded or intended. The charts in Figures 4 and 5 compare documented PPOD with actual place of death. For those in this study not achieving their PPOD, changes in circumstances and their health meant that home care was no longer a feasible option. This may not be reflected in the medical records when preferred and actual place of death are the only notations made. The complexities of this are discussed further in Chapter 5.
FIGURE 4.
Recorded preferred place of death.
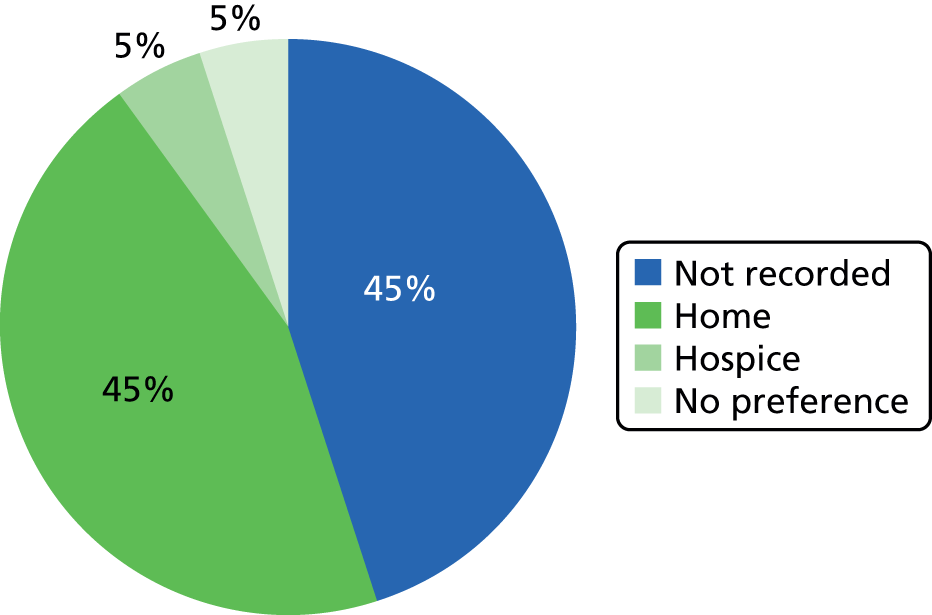
FIGURE 5.
Actual place of death.
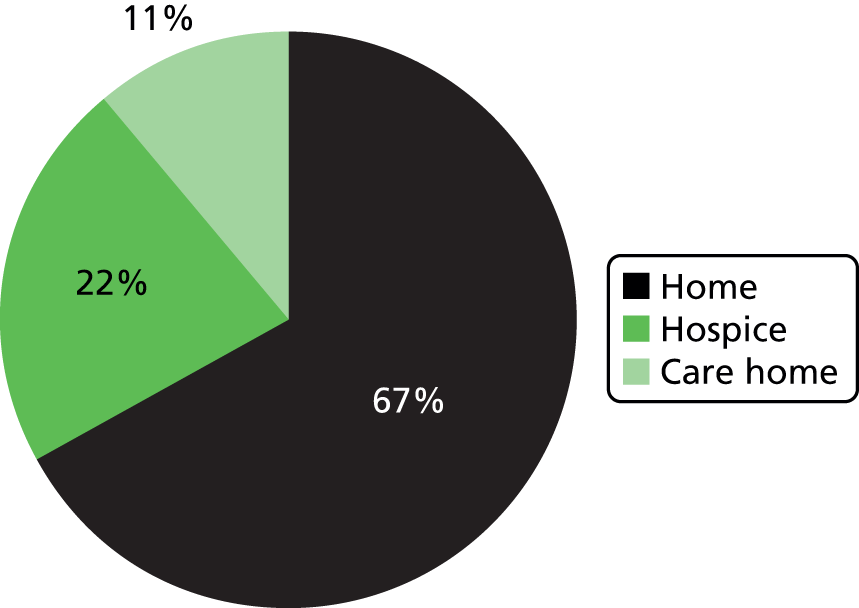
Throughout this report, the names of all patients and family carers have been changed to protect anonymity and confidentiality. Health professionals are referred to only by grouped professional roles.
Overview of findings
Types of planning
One of the aims of ACP is to involve patients, families and professionals in discussion and decisions about wishes for future care, particularly in the event that the patient loses capacity to make these decisions independently. However, this study has highlighted two additional levels of ‘professional’ and ‘personal’ anticipatory planning running in parallel, with varying points and degrees of intersection with the ‘formal’ process of ACP (Table 10). ‘Professional planning’ took place within the professional arena, such as during GSF meetings at GP practices, or through direct interprofessional communication and referral and a system of shared records. Its role was to anticipate a patient’s likely trajectory and plan the resources and arrangements that would be required to provide for their care needs. Areas of discussion might be identifying patients who were considered to be palliative and eligible for the GSF register or DNACPR status, completion of the DS1500 form, the timing and nature of referral to specialist services and the delegation of tasks within members of the multidisciplinary team (MDT). The nature of this level of planning was rarely communicated to patients and families. However, families themselves undertook their own ‘personal planning’ by preparing themselves practically and emotionally for death. This often took the form of practical arrangements for funeral planning, will writing and setting financial affairs in order, as well as personal reflection and discussion with significant others among friends and family. This personal planning was rarely shared with health professionals or embraced as part of ACP. The predominant focus of this report is on the process of ACP, and the components of this will be discussed in detail throughout the next chapters. However, approaches to both ‘professional’ and ‘personal’ planning informed the attitudes of patients, families and health professionals participating in this study and are apparent in their narratives of ACP.
| Type | Explanation |
|---|---|
| ACP | A process of discussion and reflection, which may involve health or other professionals, family and friends, regarding the patient’s wishes for future care, in the event that she or he loses capacity to make decisions at some point in the future. The outcome of ACP may be documented preferences for place of death, treatment and other interventions, including resuscitation. Verbal or written statements of preferences must be taken into account by professionals providing care. Patients may also complete ADRT forms in relation to specific treatments and interventions they do not wish to receive in specific circumstances. Valid ADRTs are legally binding documents. Patients may also delegate legal decision-making powers to a designated proxy, for health and welfare and/or financial affairs |
| Professional planning | Undertaken by professionals in order to plan resources for patient care, often without communication or consultation with the patient or family. Includes placing someone on the GSF register, arranging referrals to specialist services, discussing eligibility for the DS1500, flagging patients as palliative, implementing fast track scheme and arranging anticipatory medicines |
| Personal planning | Patients and families may undertake this for themselves, often without input from professionals, to prepare emotionally and physically for impending death. Includes making a will, funeral planning, getting financial affairs in order, arranging special holidays and events with family and friends and personal reflection |
Types of cases
During analysis of the data it became apparent that certain cases had specific qualities that affected the likelihood of ACP’s taking place. This finding allowed us to categorise patients into three broad groups or stages (Table 11). These were by no means discrete and some patients overlapped two groups or moved from one group to another in the course of the study. Sixteen of the 21 patients had lived with long-term conditions for many years, sometimes decades, and it seemed that it was only when cancer was diagnosed that ACP was instigated. Hence, these patients fell into both the long-term conditions and the rapid deterioration categories. Those spanning the elderly frail and long-term conditions categories were living with multiple comorbidities and advanced old age. When it occurred, ACP was likely to be prompted by a deterioration in one of their significant conditions. Those with cancer could fall into the long-term conditions group or the rapid deterioration group depending on the speed of their decline, but were more likely to be recognised as palliative on practice registers.
| Type | Explanation | Cases |
|---|---|---|
| Elderly frail | Those in advanced older age with multiple comorbidities but often no specific ‘terminal’ diagnosis. Prognosis was considered difficult but advanced age qualified them for the ‘surprise question’. EOLC was often not discussed and there was little indication of ACP or other planning | Mrs Alderson, Mr Davis, Mr Jenkins, Mrs Barker, Mrs Harrison, Mr Jacobs |
| Long-term conditions | Had a condition that they had been living with for a long period of time, which could be cancer. It was often not communicated or acknowledged in this group that their condition was terminal. Frequent exacerbations made prognosis or identification of dying difficult. Planning might be raised initially and then left until a clearer progression could be identified | Mr Barlow, Mr Williamson, Mrs Avery, Mr Patterson, Mrs Winters, Mr Jenkins, Mrs Barker, Mrs Tomlinson, Mr Arthur, Mr Roper, Mr Jacobs, Mr Farley, Ms Lucas |
| Rapid deterioration | Diagnosed with an advanced cancer or rapidly deteriorating condition that meant prognosis was more clearly expressed (usually less than a year); planning was more urgent, and had to be condensed into a shorter period | Mr Brown, Mrs Jones, Mr Patterson, Mrs Winters, Mrs Elder, Mr Corley, Mr Andrews, Mr Roper, Mr Farley |
Chapter 4 Findings: professional perspectives
Professional understanding of advance care planning
The professional respondents varied widely in their experience of supporting patients at the end of life and in their attitudes towards ACP. The term ‘ACP’ was rarely mentioned, while elements such as decisions about DNACPR or PPOD tended to be subsumed within the more general practice of EOLC. For this reason, we have differentiated the category of ‘professional planning’ as an activity distinct from ACP, although for convenience we refer to professional engagement with recording patient preferences for resuscitation and place of death as ‘ACP’. References to the wider aspects of ACP, specifically the element of planning for future incapacity, but also rejection of specific treatments, were very rare, except in the accounts of a few specialist nurses caring for patients with long-term trajectories such as multiple sclerosis or motor neuron disease. Some described discussion of these elements of ACP as an established part of their practice, a component of EOLC that they had undertaken over many years; others were less confident. Several respondents expressed an awareness of ACP as a recent phenomenon, a positive development that had been introduced to practice within the last few years. ACP was linked to a better experience of EOLC, particularly in supporting patients to die at home, made possible more often with the availability of more effective symptom control through interventions, such as anticipatory prescriptions and syringe drivers. In particular, ACP could give patients and families a sense of engagement and control over a process that was intrinsically frightening and uncertain.
Whereas if they’ve had time to discuss an advanced care plan, I’m not suggesting that they’re not fearful and that you haven’t got issues to deal with on the way, or things that might not have been addressed. But I think they have a greater control, I think they have taken a little bit of control about what’s happening to them.
CM4
Respondents who were supportive of ACP tended to emphasise the value of planning as a practical tool of management, a means of joining up care in an increasingly complex and fragmented system, rather than a vehicle for realising patient choice and self-determination. Nevertheless, it was evident that ACP was not common.
For long-term conditions, advanced care planning, it’s very, very difficult. It’ll happen but it’ll be rare. Yeah, could be one out of ten.
CM6
I think, for me, it just makes sure that everybody knows what’s happening. If you do it properly, you’ve communicated with the family and the patient and other people involved in that patient’s care . . . And, with the fragmentation of primary care, now we no longer have 24-hour responsibility and you’ve got out of hours services, you’ve got different providers for community service, I think it helps everybody to know what the pathway is and what the plan is, where different people are having different parts to play in that patient’s final journey.
GP7
Across the sample as a whole, there was a low level of expressed awareness of national policy developments or the extensive range of resources available locally to support ACP through the EOLCPW. Although broadly supportive, rather few respondents incorporated the vocabulary of ACP in their accounts or oriented to this as a discrete and specific aspect of their role. Several expressed their awareness of ACP as being linked to encouragement to achieve externally imposed goals, particularly regarding recorded place of death, completion of DNACPR orders and the avoidance of unscheduled and costly hospital admissions. These were linked to the introduction of new nursing roles, such as CM and practice liaison nurse. While the policy regarding ACP places emphasis on the role of forward planning in the event of lost capacity, the study respondents were oriented to eliciting and realising patients’ documented preferences regarding the key items of DNACPR decisions, PPOD and, less commonly, patients’ desire to avoid specific treatments (ADRT) and unscheduled hospital admissions. The emphasis was much more on helping patients to organise what happened in the future, and how they wished to manage dying, than on exercising precedent autonomy in the event that they lost capacity to make decisions for themselves in future.
A few respondents, mostly GPs, felt that ACP was inappropriate and potentially patronising, and could be harmful. These professionals felt that raising the topic could needlessly frighten patients, and was usually entirely unnecessary. Patients were assumed to understand their situation very clearly, and the current generation of frail elderly who had direct experience of the last world war knew more about death than the professionals providing care. There was, then, little to be gained in raising discussion of a topic which such patients would have considered blindingly obvious.
Professional division of labour
There was no formal division of labour directing responsibility for ACP: this could be undertaken by any health professional. There was also a wide variation in perceptions about the take-up of ACP within different professional roles. Perhaps because of their direct involvement and ongoing patient contact, especially in the home, nurses appeared to be more proactive than GPs in discussing ACP. Some specialist DNs, such as palliative care or neurology, became experienced in ACP by virtue of their role and caseload. However, the extent to which many professionals engaged in ACP seemed to be a consequence of individual preference and experience. Several respondents, especially GPs, did not engage in ACP, or did so only rarely, and were sceptical about its value. Where there was no specific allocation for the task, it was easy for individuals to assume, in line with the ‘bystander effect’, that someone else might have taken on responsibility, with the result that the topic of ACP was not broached at all, or not until very late. Initiation of ACP was often considered to be a difficult task, and some respondents expressed a preference to delegate to colleagues they considered to have more skill and confidence and, sometimes, also more time.
In some instances it’s the GPs, but they tend to be a bit briefer I think. They tend to go through the mechanical aspects, I would say, more. I try and be there for the initial discussion with them so that I know what’s been said, and then I remain there so I can explain it in a simple language really . . . So I think it can be either.
DN3
Some district nurses are really good, I’ll go in and it’s all been done. But, they’re not all, and they’re also under a lot of pressure.
PCN3
One reason for ACP being considered a job for nurses rather than GPs was because the discussion could be lengthy. It was also more appropriately done in the comfort and privacy of the patient’s home, rather than in the time-pressured and impersonal environment of a practice consultation room or clinic.
Gold Standards Framework registers and interdisciplinary working
Gold Standards Framework registers emerged as one of the most important resources for the implementation and coordination of EOLC, including ACP. These registers had clearly been highly instrumental in enabling practices to identify patients with palliative care needs, and to co-ordinate care and communication within the MDT. This was an important mechanism for supporting patients to die at home through timely referrals of appropriate community services including the setting up of anticipatory prescribing. The GSF registers constituted an important element of professional planning for EOLC. Good planning and accurate identification of palliative care needs are essential for identifying the point at which patients should be placed on the GSF register, and to enable them to receive the benefits this makes available. All the practices taking part in the study had GSF or palliative care registers, although they varied quite widely in the size and composition of the list and the frequency with which they held meetings: between 1- and 3-month intervals. All the registers were heavily oriented to patients with cancer, and some exclusively so. Some respondents reported that they did not tell patients that they were on the GSF register or, at least, the significance of this, saying merely that this meant that their case was subject to regular team discussion and improved co-ordination of care. Others felt that they could not place a patient on the register, or complete a DS1500 form, unless they had openly discussed the reasons for doing this, and its significance. However, the complexity of such a discussion, combined with the uncertainty of prognosis (which intensified the difficulty of discussion) could be a disincentive for placing patients on the register. The difficulty of prognosis was also a reason for the very variable length of time that patients could be on the GSF register (see Table 8).
Would you discuss with a patient that they were on the register?
Yeah I do but I, yeah no I do, but talk about it very much in terms of what that means so that it means that we talk about their care between the GPs and the nurses and that we’re communicating, rather than saying, ‘This means that you’ve got less than a year to live’.
In fact, I don’t think I’ve ever told anybody they’re on the register.
GP10
Recognition of which patients were eligible for the GSF and at what point they should be placed on the register was difficult and, apparently, tended to be serendipitous. Practices varied in their policies and processes, although these seemed to be generally ill defined. Several GPs expressed their awareness of recent drives to find more patients to put on the GSF register: the ‘1% campaign’ proposes that 1% of practice patients will be within the last year of life and, consequently, eligible for inclusion on the register and the initiation of ACP. At a practical level, however, there is a limit to how many patients can be actively managed within each practice GSF: it simply was not feasible to include anything near 1% of patients. Some practices were taking a relatively inclusive approach to putting patients on the register. Others tended to be more restrictive, including only patients who were clearly approaching death. However, respondents from practices operating with larger registers described systems of prioritising patients (sometimes through a ‘traffic light’ system) with active palliative care needs in GSF meeting discussions. Awareness of the difficulties of predicting the trajectory of long-term conditions such as COPD and heart failure made GPs reluctant to place them on the GSF; many respondents described patients, particularly those without cancer, who had remained on it for extended periods, even years.
I think that is one thing about the palliative care register, and has made me think more, when the sort of diagnosis made, the sort of terminal diagnosis is made, I’m very much more, I’ve got this tick box in my head of where do they want to die? What do they want to do? Shall we think about a DN[ACP]R?
GP10
Yes, in some ways I think it would be more useful to have a more focused register and make it back to a shorter length of time again and then be able to deal with a fewer number of patients. But the big push at the moment is . . . you know, we were told about a year ago ‘you haven’t got enough patients on your register’. Once it does get past a certain number of patients you can’t discuss that number of patients regularly anyway, and it becomes a bit pointless.
GP1
Practices varied in their arrangements for managing the GSF but GPs were responsible for placing patients on the register. Nursing respondents described how at meetings they might flag a patient as becoming appropriate for palliative care, and that their suggestions were often followed. GSF meetings were valued as a forum for sharing knowledge and experiential learning. Specialist nurses viewed the GSF meetings as an opportunity to inform and guide colleagues, including GPs, about aspects of EOLC. However, the introduction of financial incentives and quality appraisal targets for practices with GSF registers was evidently having some impact on their composition. Several respondents referred to patients being placed on the GSF to satisfy the requirement to hit targets, when in reality clinicians were not sure about the prognosis or suitability of patients for the register.
I think [the GPs] have to [have a register] because they get money for it, they get QOF [Quality and Outcomes Framework] points for it. So that’s the GP’s incentive, but it’s how you interpret.
DN2
The initiation of advance care planning
Regardless of experience, many respondents considered ACP to be a difficult area of practice. Expecting that many patients also found the subject difficult, professionals could be reluctant to broach the topic for fear of jeopardising the good relationship that they had established as the cornerstone of care.
I think, in the role that we’re doing, as matrons, it’s an extremely privileged role. We’re in patient’s own homes, you know, the power base is with them, it’s about us working with them and it’s a fragile relationship at times, so I wouldn’t want to do anything to jeopardise that.
CM3
I find it quite straightforward. It’s not easy, easy would be a wrong word but I find it quite straightforward with people who I know.
GP8
It was also apparent that, in some cases, professionals relied on their assumptions about what a patient would want in planning their EOLC, and took this knowledge to obviate the need for explicit discussion. Some expressed greater confidence, often linked to experience or sometimes the strength of their relationship with individual patients. Others – regardless of role and clinical seniority – described delegating this task to colleagues, not infrequently DNs. Another role for the GSF meetings was to confer authority on decisions and agreements arising from discussion among members of the MDT.
We go to all the GSF meetings, so the Gold Standard Framework meetings, and I was only at one last week, the week before, and, it was brought up, and the doctor said, ‘I can’t do that, I can’t have that discussion, can you?’ And asked one of the district nurses if they could and she said, ‘No, I can’t’. But I have to say, as a community nurse, I often had those discussions with a patient, very often because I was best placed person.
Clinical nurse specialist – heart failure (CNS_HF) focus group
As indicated above, however, patients were not routinely informed that they had been placed on the register, so a degree of ‘professional planning’ and anticipation may have been conducted without their awareness or involvement. Regardless of whether or not patients were on the register, ACP discussions were not routine and tended to happen, if at all, at a late stage when it had become apparent that the patient was very close to death. This was particularly the case with patients suffering from chronic degenerative diseases such as heart failure or COPD, whose prognosis was particularly uncertain and characterised by an incremental decline.
I don’t think it’s easy. I’ve been a GP for 20 years so I suppose it gets easier. Some cases are relatively easy, I think when the patient knows and they’re ready for you to have that conversation, I often find it’s easier.
GP7
It’s a difficult subject to actually bring up. Especially, although it sounds paradoxical, the patients that I’ve been seeing over the years, they’ve been in and out of hospital, they’ve had their ups and downs, and you do start thinking, ‘Well, when, when, when do I introduce it? Is it too late to, to introduce it . . . ?’ So, or not too late but what point: yes, in a way, should I have brought this up months ago, or years ago, even? So you do kind of think, yeah, how are they going to feel if I suddenly start talking about it now when they’ve been acutely ill and, and survived it? And I do find that quite tricky.
AHP2
In principle, the initiation of ACP sets in motion an ongoing process of discussion, reflection and review. Patients are assured that plans are flexible, and that they can change their minds. In practice, where ACP happened at all, it was unlikely to be revisited, especially for routine review rather than in response to a rapid change in the patient’s circumstances close to death.
Professional strategies for initiating advance care planning
An important function of the GSF meetings was to allocate tasks and responsibilities for EOLC, including discussion of different components of ACP. In principle, any professional involved in providing patient care could raise the topic. In practice, such discussions tended to happen following a significant moment, after the patient had been referred to palliative care services. Conversations could be started while the patient was in hospital or hospice, but then tended to be taken up by professionals working in the community.
I find, in, it’s one of three people, either the hospice will do it if somebody’s in the hospice and gets discharged back home, often they’ll start that conversation. District nurses or ourselves and it’s really just knowing who’s doing what. . . . I think, ultimately, if somebody’s at home, it’s probably the GP’s responsibility to make sure that somebody’s had that conversation and it’s been documented.
GP7
So I certainly feel, even if a GP does initially have a conversation, the conversation is repeated and clarified and extended by a follow-up visit with a community nurse afterwards. Which I think is, is the right way to be because the patient’s gone away and has had time to mull it over and to think what’s been said and to think up new questions and then somebody’s going to see them so they can reiterate the conversation and they can clarify any questions or any concerns.
CNS_HF1
There were some accounts of professionals taking a very direct approach to the initiation of discussion of ACP and EOLC. However, most respondents found these discussions difficult. They described approaching ACP with great care and circumspection, searching for a window of opportunity to broach the topic. This was much easier when patients themselves openly took the initiative, or indicated their readiness to talk about their future care. Otherwise, professionals tended to move very gently, laying down cues and openings for the patient to respond to if she or he chose, and ready to back off rapidly at any suggestion of rebuff. A strong theme was that patients themselves will offer cues when they are ready to have an ACP discussion; this suggests that professionals are inclined to be responsive in their approach to broaching the topic. At the same time, it could be hard to interpret patients’ intentions: apparent cues as indicated, for example, by impulsive throwaway remarks might give a false, misleading impression that patients wished to initiate discussion of ACP and EOLC. Since professionals often felt that they needed patients’ ‘permission’ to raise the issue, if positive cues were not communicated, there was a tendency to avoid the topic altogether.
You can tell, when you’re talking to somebody, whether they’re going to be receptive or not or whether it’s the right time. And often, it’s the patient that will make a comment. You know, if they say,’ I don’t want to go back into hospital’, then you can say, ‘Well, where would you like us to look after you if you start to get more poorly?’ or [if] something happens, what would you want?
CNS_HF focus group
Sometimes I will sort of bring it into the conversation and say something like, ‘Have you thought about the future and, you know, how you’ll perhaps be in 6 months’ time? And you can often tell by the response whether it’s, ‘Don’t want to go there,’ or, you know, if they do want to talk about it.
CM1
From my perspective, it’s more about looking for those cues and what they’re saying. I think I’d try and get open conversation going on what they know . . . and I’ll say, ‘What have they said about your cancer and have they found it anywhere else and what have they said from the tests?’ And see where the patient takes it.
PCN4
Opinions varied about the importance of having an established and trusting relationship with the patient as a precursor to discussion of ACP. Some respondents felt that this was important, and that the patient’s ‘readiness’ to talk was calibrated on the degree of confidence and trust they felt in the professional. Where this was not in place, then ACP discussions were less likely to happen. On the other hand, by nature of their role, some specialist PCNs moved in to broach the topic immediately on referral. A few respondents referred to the existence of a close relationship with the patient as a barrier to ACP discussion. It could be more difficult to broach this topic with patients who had looked to them for support over an extended period of time: to start to talk about death and dying was construed as failure and betrayal. Respondents stressed the need to progress at the patient’s pace, and in a stepwise fashion, often as the significance of a further deterioration or critical event sank in. A particular strategy was the attempt to draw patients out so that the conversation used their words, and so it seems that ‘they end up saying it themselves’ (D103N).
Often, if you sow the seed and then go away. I’ve had people in the past that have rung up, said, ‘You know that thing we talked about, that form? I’ve been thinking’. It may be a week down the line, it might be a couple of months down the line.
CNS01
Some respondents expressed an awareness that patients often found it very difficult to raise the topic of dying, even when they wished to talk about it, and actually needed some directed help from professionals to enable this to happen. It could be necessary to take a more proactive stance when it was becoming clear that the patient was finally approaching death. For example, professionals might use the occurrence of a further exacerbation and hospitalisation, or the news that no further active treatment was possible, to raise the topic of how the patient felt about her or his progress and to reflect on the significance of this for future care. Respondents’ accounts conveyed a strong sense of discussions being much more about engendering a sense of realism rather than promoting ‘choice’. The task was to gradually move patients towards recognition of their situation and the limited options available.
We might talk about that things seem to be changing quite a lot each time I visit you, there’s things seem to be changing, and it may be tend to be talking about what their fears are with that. And then, suggesting that perhaps helping with those fears is to plan for their future and how they want their future care to work. And with that, often, that’s when you’ll get patients’ preferences.
CM4
A few respondents described an extended process of communication based on coded language or tacit understanding of the patient’s situation and the way it was developing: indicators of decline and mortality that were recognised by all, and did not require explicit discussion or acknowledgement. References to spirituality or the impact of a patient’s religious beliefs on their acceptance of ACP were notable by their rarity; several GPs said that they would not engage in such discussions because of their own non-religious perspective.
Patient responses to advance care planning
Respondents described patient responses to ACP as being very variable. A minority were reported to be quite up front about raising the topic, and quite explicit about their wishes for future care. More often patients might be uncertain, or even resistant to the prospect of the discussion, although professionals felt that they tended to be glad and relieved to have had the chance to think about ACP once the subject had been raised. Some patients had to arrive at a state of readiness to discuss the topic in their own terms and in their own time.
It was quite difficult with her [patient] because she does know that she’s not so good and things are probably going to get worse but she really doesn’t want to . . . Actually she said that ‘Yes, I do have worries and concerns but I really don’t want to talk about them at the moment’. And you sort of leave it at that. The sort of the first step has been made really and that may always be the case, she may never want to say anything else. But I think giving that opportunity and getting it out in the open seems to be the main thing.
GP2
And actually, the discussion is met with relief . . . That they know, at last, it’s out the box. We’ve all said, we know what we’re dealing with, and we can move on now. So often, it’s a very pleasing thing to discuss, it’s a very, very good consultation we have with them.
GP4
However, a significant number of patients – as many as 50%, in some estimations – were considered to be resistant to ACP and not to want to discuss the matter at any point in their illness.
Just thinking about it. I mean this is not scientific at all, but perhaps about 30% of people want to pursue, 30% don’t and 30% will partially engage. That’s just a feeling I’ve had thinking of the ones that I’ve been involved with over the last couple of years.
GP12
Some patients were characterised as being ‘in denial’, that is they did not recognise that they were near the end of life. Others were recognised to be aware of the situation, but preferred not to acknowledge or talk about it. These patients were understood to prefer taking ‘each day as it comes’, living their lives in an extended present which would be spoiled by direct confrontation with a limited future. A few respondents mentioned that religious beliefs might prevent an individual being receptive to ACP, because death was a matter for divine disposal. Another idea was that some patients refuse to countenance talk of ACP because to do so is regarded as ‘admitting defeat’ or ‘giving up’, when there is a strong cultural imperative towards ‘fighting’ for life.
When I said to him, ‘You know, we’ve got this diagnosis and you’re quite poorly, and you’re going to need some extra help and it, it’s probably likely that you won’t be, it won’t be that long’, he just said ‘I don’t want to hear any more’.
GP3
Some people can be in a certain amount of denial about their condition. And you try and sort of get in there and you realise that they don’t want to go there, they don’t want to talk about what’s going to happen. I guess that’s their way of dealing with it really. You have to leave it for now. And perhaps revisit it again at a later point when things have changed a bit, if that’s appropriate.
GP10
I think sometimes, they genuinely do know but they fight it. And they, they want to fight it, that’s their mentality, that’s how they’ve lived their life, and maybe it’s to protect their carer or their relative, or maybe it’s just the way that they want it to go.
CNS_HF6
Professionals described how, having raised a suggestion, or left a cue, they would ‘leave the door open’ to future discussion, or gradually work to encourage a change in a patient’s willingness and receptivity to return to the discussion. Even when patients were quite clear that they did not want to talk about ACP, some more proactive professionals felt that it was important to raise the topic explicitly, to give them the opportunity to talk. More commonly, respondents clearly found it more difficult to broach the topic in the face of manifest resistance.
The difficulty of prognosis and the limitations of planning
While some of the patient cases described asking directly about their prognosis at the time of first receiving their diagnosis, both the case study material and the professional accounts suggest that it is not common for patients to ask directly about prognosis, or return to the topic, throughout the progression of their illness. The difficulty of prognosis was a major barrier for professionals and patients undertaking ACP. This is a leitmotif running throughout the data. Even for cancer patients, assumed to have a relatively predictable trajectory, prognosis often proved to be uncertain and inaccurate. For those affected by a range of chronic degenerative diseases, such as COPD or heart failure, or extreme age and frailty, the difficulty of prognosis was immeasurably greater.
A difficulty I’ve had with patients in discussing these things and in patients accepting that they’re dying is the fact they’ve had so many ups and downs in their condition before. And they might have been told you’ve only got months to live but then they’ve pulled back and done quite well. So when it’s quite hard to call when it’s definitely the end but also getting the patients to understand that, because quite often, they’ve been there before, haven’t they, and they’ve got better again.
CNS_HF focus group
This reflects the professional orientation to ACP as a reactive, rather than a pre-emptive, measure. Health professionals reported that it could be hard, especially in the case of chronic degenerative diseases, for patients to be aware and accept that they are dying. This is partly because decline may be incremental, and partly because they are prone to acute episodes from which they recover, and they become accustomed to this pattern. In addition to the deterrent of intrinsic uncertainty, professionals were reluctant to discuss prognosis because of the credibility and trust that they would lose if subsequently proved wrong. In addition, inaccurate prognosis could be distressing and have very negative consequences for patients and their families. Professional accounts suggest that the purpose of broaching the topic of a limited prognosis was not so much to engineer an opening for ACP but rather to encourage the patient to understand and come to terms with her or his mortality. While such understanding may be a prerequisite for future planning, it seemed that the professional goal, operating largely independently of, or in parallel to, ACP, was more concretely and directly to support the patient through the experience of dying. Discussion at this point might focus on what could be expected in terms of symptoms and physical deterioration, and the range of resources and support services that could be made available in support.
We’ve always said, right from the release of the GSF, anybody with heart failure, no, you wouldn’t be [surprised], because the nature of heart failure is they could either deteriorate quickly or they could have a sudden death.
CNS_HF focus group
I could have given her a prognosis at the beginning and, you know, on the basis of my experience with metastatic lung cancer, people don’t live usually more than 3 months. So, she’s trumped that by living, I think, probably 18 months from, from when she got that point. And then we’ve got even the day before [the patient] died, if you’d asked me, I’d have said, ‘Well, I think she’s probably got about 3 or 4 weeks’ and she died the next day.
GP14
The difficulty of prognosis and reluctance to broach a speculative and uncertain future undermined the value of planning in advance, as did the knowledge that patients’ preferences and responses were liable to rapid and substantial change. In addition, professionals were well aware that, regardless of a patient’s initial preferences, their realisation depended on the availability of resources and the progression of the clinical condition. Hospice beds might not be available, circumstances might force a hospital admission, carers might find themselves unable to cope with the demands of caring for a dying relative at home, or patients themselves might change their minds. Consequently, professionals described being careful to manage expectations and to emphasise that patients were being asked to state their ‘preferences’ for care. While these were less likely to be realised if they remained unspoken and undocumented, there could be no guarantee that advance care plans could actually be implemented. In consequence, ACP discussions tended to be concentrated in the very last stage of life, when it was beyond doubt that death was imminent.
And if somebody’s saying to me that they want to die in the hospice, whilst acknowledging that is their preferred place, I would also say, given limitations, we can’t always guarantee, and try and put that across so they’re aware what other options would be. And as a second choice, some say, ‘Okay, well, I’d stay at home then’, if that was the choice, one or two have said hospital. But, I think, sometimes, it’s taken out of their hands if they go in with an acute episode of something and then don’t recover from it or deteriorate.
PCN4
Quite often it works, it works well, but, you don’t have that certainty that the services are always going to be there when you need them.
GP5
The unpredictability of long-term conditions might indicate that ACP could be taken to have a particular application. Nevertheless, there was no indication in the study findings that this circumstance prompted a more proactive stance to anticipatory planning in relation to this group of patients.
The components of advance care planning
Effectively, ACP was constrained and determined by the task-related documents associated with managing EOLC. These are often associated with policy goals and local targets, sometimes incentive driven, to complete DNACPR forms, record PPOD and keep patients out of hospital. The reduction of the wider project of ACP to a few key documented tasks reflects a professional orientation to planning as a management resource, rather than an existential goal. Many respondents referred to ACP’s being constituted, effectively, in the expression and documentation of a few key issues that were all contained on the DNACPR form and/or the patient’s medical record: whether or not the patient wished to be resuscitated, where she or he wished to die and whether or not she or he wished to remain at home rather than be admitted to hospital. Each of these outcomes could be documented, which, as some respondents acknowledged, was linked to practice audit and assessment. Throughout the study there was very little reference to respondents’ knowledge or use of available documents, resources or the EOLCPW, except for the DNACPR form, on which PPOD was also usually recorded. In addition, some services used versions of documents such as the LCP or an IPOC to document care in the last days of life, though most respondents made no reference to these, or occasionally observed that they did not use them.
The nature and extent of ACP was strongly defined by the nature and availability of the documents available for the purpose, and by respondents’ awareness of the local and national pressures to complete them. Several respondents described how they used ‘paperwork’ – and the need to complete this – as a way into the discussion of ACP, and also, effectively, to prompt patients to engage with the task. This could be either by explaining to the patient that there was some paperwork that the professional was required to fill in or by leaving the document with the patient to read and consider after the professional had departed, possibly to talk about during the next visit. There were very few accounts of any detailed and systematic use of wider resources to support ACP, and these tended to be from a few experienced specialist nurses. While completion of documents recording preferences could be used as a spur to further discussion through regular (perhaps annual) review and update, this was described as happening rarely. Generally, once the forms had been completed, or patient preferences documented, they were not revisited. Some professionals either disliked using the forms themselves or felt that patients tended to be unenthusiastic in their response to them. In particular, patients were felt to dislike and resist the formality of signed forms.
Capacity
The legal driver behind ACP relates to recent UK legislation protecting the rights of the individual to retain control of decisions about her or his future care in the event that she or he should lose capacity. 32 However, in this study, issues of capacity featured very little throughout the data. Only eight professionals made even brief or tangential references to this. The neurology specialist nurses were more confident and familiar with discussing ACP, but capacity did not seem to be an issue: one of these respondents could not think of a single patient who had lost the ability to make and convey her or his wishes for care.
Decisions about cardiopulmonary resuscitation
The completion of a DNACPR form was one of the most frequently encountered components of ACP, in both the professional perspectives interviews and the patient case studies. Eleven of the 21 patient cases in the study had completed DNACPR forms. For many professionals, this was clearly a key decision. DNACPR forms could be completed at varying points in the patient’s trajectory, though this tended to happen quite close to death. Acceptance of DNACPR was considered to be the best and most appropriate option for almost all frail and terminally ill patients, for whom attempted resuscitation was considered to be a futile and very distressing experience, emblematic of a ‘bad’ death. The availability of a DNACPR form was a factor strongly promoting its use. The procedure for completing DNACPR forms varied across the different services represented in the study. Any professional could instigate the discussion, and there was no clear hierarchy of responsibility for this. However, some respondents felt that this should be, and often was, the GP’s role, while acknowledging that nurses might be involved in follow-up discussions and support. However, a number of nurses expressed themselves to be confident and willing to undertake the process independently. Some described doing so. Usually, however, even when a nurse might take the lead or initiative in raising the topic, the form had to be signed by the patient’s GP. Several nurses complained of the difficulty they had in getting GPs to initiate discussion of DNACPR with patients and to complete the form; several GPs acknowledged the difficulty they experienced in carrying out discussion of DNACPR, and their relief when they could hand this task over to a nurse.
Trying to get a DNA[CP]R sometimes can be difficult. GPs don’t like to have that conversation, which happened, it was one weekend and obviously trying to pre-empt for a weekend situation getting a DNA[CP]R and anticipator[y medications] in, the GP said. ‘Oh, I’m not comfortable having that conversation at the moment with the patient’. Well somebody’s got to do it. They still didn’t do it, this GP still didn’t do the form.
DN5
I understand that it is a big conversation to have. I’m not saying that you should just hand it all over to us but I think if they’re empowering and training nurses to have those conversations, we should be able to validate the paperwork.
CM3
Professional opinions varied about the extent to which patients had a genuine choice regarding DNACPR decisions, or were involved in discussion as a largely nominal or bureaucratic task. Although policy asserts that resuscitation decisions should involve discussion with the patient and her or his family, DNACPR was a clinical decision which could be made without consultation with patients or family who sometimes do not want the burden of responsibility for deciding whether or not resuscitation should be attempted. However, recent changes to procedure had resulted in the DNACPR form being retained in the patient’s house. Its presence called for explanation. In broaching the topic, professionals (especially nurses) described reinforcing the idea that DNACPR decisions were the patient’s ‘choice’ and that documented decisions could be changed. However, it was clear that the preferred response was for patients to opt for not being resuscitated.
I try to introduce it as a treatment, ‘This is a treatment, [laughs] it’s not necessarily a choice, this is something, would we recommend it or not recommend it, just like chemotherapy, we wouldn’t recommend chemotherapy and we wouldn’t recommend resuscitation because it’s not going to work and we don’t want to cause more problems and more distress’. But some patients, even with that discussion, they would say, ‘Oh no’. And there’s no point in them having a DNA[CP]R form in the house, they might accept that if they go into hospital, that a form will be done without their permission.
PCN3
In describing how they handled DNACPR discussions, particularly when patients were resistant or reluctant to talk about it, several respondents described how they might feel it was appropriate to ‘force’ the issue a little – because of their awareness of the deterioration in the patient’s condition – and spell out the consequences of failure to make a decision: if they did not they risked a very unpleasant experience, and in any case their opportunity to make the decision would be over-ridden by professional judgement (not to resuscitate). This is so, even though it is clear from a number of accounts that patients quite commonly resist, or are upset by, DNACPR discussions.
I had one chap who, who we’d started the conversation about resuscitation, the cues were there, so we started the conversation but he got quite upset about it. And he decided he wanted resuscitating. That’s his choice. I mean, obviously, from a medical point of view, it would be completely futile. . . . So, we left it, and I said we would come back to it another time when he was ready to sort of think about it again. Unbeknown to me, the district nurses then went and had the same conversation and got the same response. So again, they sort of said, ‘That’s fine, you know, when you’re ready’. To which both of us fed back to the GP, so the GP rang the patient up and said, ‘I gather you want resuscitating, well, that’s completely inappropriate, medically, it would be futile and even if they attempted it, they’d break your ribs’.
PCN2
In addition to being distressed by discussion of the topic, patients could also be uncertain about their preferences. In many cases these were likely to be formulated in the course of discussion with the health professional rather than reflecting an established pre-formulated preference. It was clear from the professional accounts not only that respondents considered rejection of resuscitation to be the preferred and appropriate response, but also that a degree of more or less overt persuasion could be applied to achieve this end.
DS1500 forms
General practitioners expressed difficulties with getting the timing right for completion of the DS1500 form, which would enable patients to receive additional benefits during their last months of life. Here again, there were stories of people surviving well past their expected prognosis.
I remember doing a DS1500 on a patient once and 3 years later he was still alive and he kept coming back and seeing him . . . 3 years he lived after the DS1500.
GP1
Nursing staff described prompting GPs to think about completing DS1500 forms in GSF meetings when discussing ACP for patients. This was seen as part of the ACP process, although some considered completion of the DS1500 to come earlier than other aspects of ACP so it was not necessarily used as an opener for broader conversations about wishes for care.
I suppose it could be a way of discussing end of life care. It often isn’t, because it is often done really quite early on when that’s not necessarily appropriate or comfortable, to discuss it.
GP10
When the DS1500 was discussed with patients, it tended to be phrased in general terms of additional support. GPs steered away from highlighting that the patient’s prognosis was now approximately 6 months or less. One GP noted that she did not like to leave the form in the house, as the information it contained was too ‘direct’ to be read by patients and families.
I try and steer away from this idea of 6 months to live with it. And, you know, sometimes, I think people have, you know, people have questioned me on this or, then I say, ‘Well, we just don’t know, do we? Nobody knows.’ . . . And I have to say, that I do not give the relative a copy of that . . . because I just think it’s inappropriate in a sense, there’s a bit, you have to be fairly negative on the form.
GP11
Preferred place of care and death
Professional respondents expressed a strong commitment to support patients to die at home, which, in most cases, was assumed to be their preferred, and also the best, place. Supporting patients to die peacefully at home could be deeply satisfying. Notwithstanding some reservations, and uncertainty about their availability at a specific time, most respondents felt that they could access the resources they needed to enable most patients to die at home. However, lack of 24-hour sitting services or nursing support was felt to be a limiting factor. A few respondents commented on the imbalance in the resources available to support patients dying with cancer compared with those affected by other conditions. One respondent identified lack of availability and poor integration of social services with health care as the weakest link forcing some dying patients into hospital or institutional care unnecessarily. Although most professionals operated on the basis that most patients who wanted to die at home could be supported to do so, they were usually cautious not to provide an assurance that this would certainly happen, in case illness or lack of available resources presented an insuperable obstacle.
The vast majority of cases, people want to stay at home and they can stay at home if they provide the necessary support.
GP14
I do certainly find the majority of people I have those conversations with do tend to say they’d like to be at home, that then have had an awful lot of experience of patients wanting that but relatives not wanting that, in respect that that’s a big burden on a relative, to actually have that happen within their own home. But then I’ve had other scenarios where people have stayed at home, have had full care in that home and they’ve died at home and that’s been the best place and the relatives have been extremely grateful that that has happened.
CNS_HF1
Residential or nursing homes and hospices may be acceptable alternatives to home. Hospital was rarely seen as a good option, although in a minority of cases it may turn out to be a necessary one, and professionals considered that few patients set out with an initial preference to die there. There tended to be a response shift, throughout the interviews, depending on whether respondents were adopting a normative stance (home is best) or reflecting on direct experience of actual cases (families can find it difficult to cope with death at home). Thus, there were cases where hospital could turn out to be the best option in difficult circumstances, and even where patients and/or their families came to accept this. A critical factor in the ability of patients to stay at home was the availability and willingness of family carers to provide support. This, also, could change over the course of illness. The community and district nurses, in particular, expressed an understanding of the strain and difficulty that death at home could cause for families. Patients – and their families – could become frightened as death approached, and feel safer in the environment of a hospice or hospital. Some patients may retain a preference for death at home, but realise that this was outweighed by the demands of care, their own sense of vulnerability and/or their awareness of the burden home care was placing on their relatives. Any or a combination of these factors could tip the preference for place of death away from home.
I think the doctors [at the hospice] feel a duty to try and prevent admissions, almost, for people that want to die at home. But what happens then is you’ve got somebody that’s agreed to come in, but because it’s felt that they may be coming towards the end of their life, they don’t come in but then the symptom control, or the crisis that was looming at home, doesn’t get contained . . . when you’re working in the community and you’re seeing what they’re struggling with, you have to take the balance, I think, between what the patient’s wishes are, what the problems are and also how the family and the other health-care professionals are coping with it. And sometimes, the right decision is that they get admitted.
PCN3
I think, if you’re extremely proactive with this kind of conversation, surely all of us would say we want to be in our own bed in our own home to end our life but, then, when the time comes, a lot of my patients change their mind.
CM3
I think sometimes people make promises that then they feel they can’t break, if you know what I mean, and that family has made a promise that their loved one will not go into hospital or go into a [care] home and sometimes that’s unrealistic. And I suppose we’re there to support them in their decisions really.
DN2
A few respondents described giving patients the Preferred Priorities of Care (PPC) document as a prompt to discussion of PPOD. However, several others specifically commented on their dislike of this. The specialist neurology nurses were an exception, and described accessing tailored documents from the national charities, and also using these with their patients. One reason for the nurses’ antipathy towards the PCC document derived from a difference in perspective about the nature and purpose of planning. They did not appreciate the point or purpose of the PCC as a patient-focused document. Accustomed to very practical care planning, they felt the PCC lacked any scope for setting down the practical details and requirements of the patient’s future care as a professionally managed enterprise.
I don’t really quite see where [the PPC] sits . . . I don’t think that Preferred Priorities of Care document was launched in the right way. I think, actually, there should be some much simpler sheet. And I think it should be more health-care professional led. Because most patients and relatives, they wouldn’t know what to write down in a box and say, ‘What do you want?’ Even if they want to do an advanced decision, they often need quite a bit of guidance in terms of the wording.
PCN3
Well we’ve had that priorities of care plan, which we’ve not really got to grips with, because we don’t really like some of the questions on it. And actually when talking to GPs they didn’t know anything about it.
DN5
Advance decisions to refuse treatment
Validly formulated ADRT orders are legally binding documents that specify the nature and circumstances of interventions that the patient wishes to refuse, even in the event that doing so would shorten life. They are considered to be an important means for patients to exercise precedent autonomy, and are an optional component of ACP. Nevertheless, the limitations of ADRTs have been widely recognised, mainly because of the difficulty of applying them in practice. There are few references to ADRTs throughout the findings and, with the exception of one GP, all instances were given by nurses. All these respondents considered that ADRTs were rare in practice. Two nurses said they had never encountered ADRTs and several others were rather vague in describing their experience and indicated that they needed to know more. The exceptions were the specialist neurology nurses, who described being experienced and confident in using ADRT forms with their patients and took a very informed and proactive stance towards doing this, including the need for regular review. Respondents commented on the difficulty patients could experience with how to word their advance directives, and the professional help that was required, even to the point of influencing the content.
At the end of the form, there’s a box that you can put any other supporting information. And on that, I go right there, ‘Mrs X does not want wish to be readmitted into hospital under any circumstances, and her preferred place of care for end of life care, is at home. If this is not possible, then she might consider hospice, or hospital’. So I put it on there. I will then write a letter to the GP when I send the ADRT form out and say, their preferred place of care is at home.
CNSother1
When we sat down to do it, he decided to put, ‘I don’t want to go in hospital’ in the preference box. Which was, that, it was actually, it was my suggestion, ‘Why don’t you put it there?’ . . . it was a nice compromise for the family and they felt happier and he felt happier that it was on the form. . . . He never wanted to review it again.
CM4
Several respondents raised particular issues with ACP and ADRTs in relation to heart failure patients, not just because they fail to realise that their condition is terminal alongside a very difficult and uncertain prognosis, but because some people have implanted defibrillators, which necessitate a discussion of the need and timing for when they should be turned off. In addition, heart failure patients should be warned about the risk of sudden death to which they are all subject. In practice, respondents, including heart failure nurses, acknowledged that this advance discussion and awareness tends not to happen.
End of life care pathway
The EOLCPW seemed to mean different things to different people and was not clearly articulated by anyone. Some health professionals appeared to have limited knowledge of the pathway and its associated documents and supporting information. There was some apparent confusion between the EOLCPW and the LCP. There were variations, between individuals and services, in the documents used and information leaflets that were sometimes given to patients. Some respondents associated the pathway with cancer and felt that this did not work for conditions such as heart failure or COPD. Others valued the pathway and associated documents as a prompt to think through different aspects of palliative care and a reminder to consider all the elements with patients. However, there was a tension between the value of documentation and guidelines as a means of informing and standardising care, and the risk that they prompted a rigid, unreflective ‘tick-box’ exercise, which served to diminish and undermine the quality of care. Some respondents valued guidance; others felt that the recent drive to ACP did not add to their established expert practice, and saw little benefit in additional paperwork. However, several respondents, including GPs, referred to their awareness of being held accountable if they did not conform to policy guidelines for practice.
People often see all the procedures, along a pathway and actually they miss the end product that they’re looking for. So, you can tick all the boxes but actually, you’ve missed the spirit of the thing.
GP4
No, I think it is helpful and I think it certainly helps you, it helps you focus on what stages that you think the patient’s at and in theory, then what, what we should be thinking about at those different stages? I’m loath to call it a tick-box exercise because it’s not . . . I think it just reminds people.
PCN2
Yes, is that the Gold Standards Framework? Or is that different end of life, is that a different pathway? Is this where we’re looking at like all the little tick boxes whether everything’s been addressed, whether, discontinue inappropriate medication and all that kind of thing, is that the end of life [care pathway]?
DN2
Avoiding unscheduled hospital admissions
The remit to enable dying patients to avoid unscheduled hospital admissions and to support death at home was a strong theme throughout all the professional accounts, especially those of the specialist nurses and CMs. This was one reason for the importance of getting the patient to agree to put a DNACPR order in place. ACP could be a means of avoiding unscheduled hospital admissions through supporting patients and their relatives to feel confident about their ability to cope with dying at home, and thus enabling them to achieve a good and peaceful death. Another theme was that, despite well-laid plans, patients and, especially, their families were likely to panic when a crisis arose and summon the emergency services, who would tend to take the patient into hospital and, in the absence of a completed DNACPR form, would be obliged to attempt resuscitation. Some respondents considered such an outcome to constitute a failure in professional support and preparation. Others considered it understandable, if not inevitable, that families would react in such a manner when faced with the frightening reality of the patient’s deteriorating condition and impending death.
And I think relatives panic. . . . If you see your loved one struggling for breath, knowing everything that’s in place, you’ve been told, ‘Do not call 999’. What you going to do? Of course you’re going to, and that’s why we try and, you know, go on and on about it just because, we know it happens, reality is, who wouldn’t?
CNS_HF focus group
Several professionals linked their commitment to avoid hospitalisation to the need to keep costs down and/or meet local practice targets. Such statements tended to be qualified by an assurance that they would always act in the patients’ best interests. However, most professionals clearly felt that there was a convergence of interests given that, in most cases, the best course of action was for the patient to die at home. Although hospital was generally seen as a bad option, some respondents acknowledged that this was not always the case. Professionals recalled a few patients who stated hospital as their preference. For many others, admission proved to be unavoidable, either because of deterioration or because the family could no longer cope with care at home.
Documentation
Systems of documenting and sharing written information are critical elements of effective patient care especially in complex systems of delivery. The availability and content of forms defines the nature of tasks to be accomplished and directs professional attention towards certain topics rather than others. They also allow for audit and assessment of easily measurable aspects of professional practice and can be conveniently linked to targets as a means of evaluation of care and incentivising practice. In this sense, documentation functions as an important agent or mechanism of care. The study practices and associated services operated with a range of different systems and documents relating to ACP and EOLC. The GSF and its associated documentation was the principal means of identification and communication about patients needing palliative and EOLC. Nurses also communicated by written notes held in the patient’s house. These included completed DNACPR forms and documented preferences for place of death and any other written statements about EOLC that the patient may have made, which could be critical in communicating to professionals how future care should be managed. Transfer of patient information between services varied considerably in method and efficiency, and the extent to which all relevant records were available and could be shared electronically. Practices lacking integrated electronic records required nurses to make more use of the telephone and fax machine. Being in close proximity to colleagues, as was the case where practices were located in local health centres, facilitated verbal communication.
On [the shared computer system] it’s have they got the DS1500 done? It’s all documented. Is this done, is that bit done, has anybody spoken to the family, how are they coping with it all?
DN3
We have our own Macmillan notes. So, we don’t even have specialist palliative care notes. We have medical notes, we have inpatient notes, we have day care notes, we have our notes. If somebody’s come into [hospice] day care they will have the medical notes in the day care, that will all be together. Same on the ward. But for us, we need our own notes because we’re in a separate office. You’re having phone calls to and from all the time, you’re having quite a lot of contact, I document all of my stuff, I then ring the GP. We don’t use [the shared computer system].
PCN3
Documentation that an ACP discussion had taken place rarely gives an indication of the nature and depth of the discussion that might have accompanied this. Respondents rarely reported accounts of detailed or lengthy discussions, but tended to be oriented towards completion of tasks such as documenting DNACPR and PPOD. Several GPs felt that the pressure to conform to documented processes undermined their clinical autonomy and professional judgement. In this context, undertaking ACP was just another box that needed to be ticked for commissioning purposes and to demonstrate a task had been successfully completed. Regardless of its benefits, paperwork was felt to be burdensome and time-consuming, constantly replicating a multitude of forms which had little impact on care, and reduced the time that could be spend in direct contact with patients.
I do find all the forms and the DNA[CP]R stuff quite difficult actually. It’s just the time-consuming admin stuff, filling in forms; 15 years ago, people were allowed to die at home. [laughs] Now they can’t die at home unless you’ve filled in four or five forms.
GP11
General practitioners commented on their appreciation of being able to delegate this task to nurses. Some nurses reported that the formality of the ACP documents was off-putting to patients, who preferred a more informal approach to noting their preferences.
The paperwork is just paperwork to me, it’s very bland, it’s very clinical, very formal. And, unfortunately, when it comes to end of life care, patients don’t like formal. They like informal. They like you to feel like you’re really listening to them. So, producing a form, I don’t always think’s the best answer.
CNS_HF6
The completion of documentation was also clearly linked to practice targets and (financial) incentives, and quality appraisals. This introduced an additional level of constraint and compulsion. Respondents tended to qualify their accounts, saying that, regardless of external pressures, their first priority was to serve the best interests of the patient. However, the nature and extent of material relating to incentives and targets suggests some tension in relation to competing priorities.
There’s no pressure in that respect in the driver of keeping them out of hospital. I’ve not got the pressure, but obviously they wanted to reduce hospital admissions. But I know that they do – I don’t know what kind of point system it’s got, but if you’d filled an advanced care plan, or priorities of care, Preferred Priorities of Care in, it counted as one of their QOF points . . . So each one that you’d done, obviously, it looked better, and they did aim that everyone that was palliative had one of those in place.
DN4
Well we’ve had that priorities of care plan . . . Last year it just came out and I don’t know if it was a CQUIN [Commission for Quality and Innovation] target and one month we had to record how many people we’d given those out to. And whether they filled them in or not was irrelevant; it was just whether we’d offered that piece of paperwork. So we did it once, and then never really heard anything about that again . . . it was basically a quality marker of how well you’re doing . . . and there’s money attached to those. So it’s not really a target, but if you don’t meet that money gets taken from the organisation.
DN5
Language and communication
Respondents were aware of an increased focus on communication skills and how communication training and skills had improved substantially in recent years. Only a few of the nurses referred to having completed any specific continuing professional development or postgraduate courses in communication. However, this was not felt to be an issue for most respondents. Specialist nurses, in particular, expressed confidence in their skills in this area. Experience and learning through observation of skilled colleagues were considered to be more important than formal education. Training could help, but skills were considered to be intrinsic and largely developed by experience: some professionals were acknowledged to be naturally better than others at communicating skilfully. A few respondents acknowledged the lasting impact that positive or negative experiences of professional communication about significant events could have on patients and carers and the damage that could be done by bad or mistimed interventions.
As you become more experienced and more comfortable with your role and you’ve developed the communication skills, then, I think, those conversations are easier to manage. And when you’ve got somebody in bed and they say, ‘I’m dying, aren’t I?’ then what do you say? You know, you could say, ‘Oh no, don’t be silly’. Or you can say, ‘Well, I can see that you are struggling more and it may be, yes, that is happening’. But it’s how you communicate. And it comes down to experience.
AHP1
I think there is some inherent skills, they’re with you, you’ve got them or you haven’t. But you can definitely enhance them.
CM5
Vague language
Notwithstanding the varying degrees of confidence they had in their professional skills to communicate about ACP with patients, and also the guidance provided by associated documentation, it was clear that most respondents broached such discussions with great care and circumspection. Moreover, the language that was described for such conversations tended to be notably vague and euphemistic. ‘Soft’ words such as ‘if you become more unwell’, ‘very poorly’ or ‘for the time you have left’ were used instead of ‘hard words’ such as ‘death’ and ‘dying’. Nurses talked to patients about their hearts ‘getting tired’ or ‘having electrical problems’ and mentioned that their condition was one from which they would not get better, rather than being specific that their condition was terminal and inevitably progressing, albeit somewhat uncertainly, towards death.
I’m sure I used euphemisms rather than . . . We had a discussion that, you know, ‘If you were to become unconscious or slip or you’re slipping away, whether you’d want, if the ambulance came, to resuscitate you?’
GP14
Deliberate use of indeterminate language and gentle cues left interpretation open and so allowed patients to choose how they responded. They could take up the offer of an ACP discussion, or indicate by their lack of responsiveness that the professional should ‘back off’. However, adopting either of these options assumes that patients could accurately interpret the speaker’s underlying intent. There was a risk that the significance of the message, and also the opportunity to engage in ACP, might pass them by. A particular area of ambiguity concerns the critical distinction between where patients wish to be cared for and where they wish to die. These do not necessarily relate to the same place. However, since professionals describe rarely being explicit in making this distinction, it is not clear what may have been understood by patients asked a question such as ‘If you were to get more poorly, where would you like to be cared for?’
Not documentation. Not talked him through. Had the conversation and I’ve documented that home is where the preferred place of care will be . . .
And you’ve had the conversation about that, he’s actually said it?
For the event of death, no. For the event of care for your, how do I word it? I don’t use the word ‘death’. I find a different way of saying it. Something, I leave it an open end, ‘For all of the care that you will need, do you want it all to be here?’ Or something as open ended as that.
I think, yes, there are times when I’m, if they’ve come to me for initial [appointment] and I’m saying, ‘Yes, it looks like you’ve got COPD’. I tend, perhaps, . . . I say, you know, ‘It’s not something you’ll get better from’. But I do tend to shy away from saying, ‘Yes, you’re going to, have this for a long time and it’s going to get progressively worse and worse’.
If the professional intent was to ascertain the patient’s preference for place of death, it is likely that their response would be recorded as such. It is less clear what the patient may have understood from such discussion. Several respondents referred to the development of a tacit or implicit understanding with patients – a metacommunication – where both parties knew and understood the meaning of the other, but did not wish, or find it necessary, to be explicit about this. In the same vein, several respondents described knowing a patient’s preferences for place of death, and even having documented it on the notes, without having had an explicit discussion to that effect.
Persuasion
The goal of ACP is that, through a process of discussion and reflection, patients will be made aware of their options, and able to make an informed decision about their preferences for EOLC. However, patients – and their relatives – start from a position of great disadvantage in that in most cases they will have very limited experience of terminal illness and death and have to rely greatly on the guidance and advice provided by professionals. In most cases it can be expected that patient preferences are not pre-formed, to be uncovered and documented during discussion, but rather evolve during the process of talking and thinking about unfamiliar and difficult issues that may not have been previously considered. In this sense, ACP involves a process of coconstruction between the patient, the professional and any other involved and significant others. Many patients will undoubtedly be grateful for the advice and guidance of professionals, and may even prefer to leave decisions about their best interests to those they feel may be most competent to make them. However, there is also a possibility that the narrow boundary between advice/guidance and ‘persuasion’ may become blurred. In this case professional conviction about patients’ best interests being served by completion of DNACPR orders and dying at home may move inadvertently from guidance to influence, or even persuasion. There are a number of instances where this is suggested in the professional accounts.
So, I have a patient at the moment that’s, we’re just managing to turn him around to see that actually, no, he does want to be at home. Because [previously he thought] home couldn’t support his needs because there weren’t services in place. And there’s lots of reasons why that was, but I’ve now managed to manage that and get the services back again. It was all about communication, he now doesn’t want to go to hospital so we’re going to be able to keep him home successfully and save all that money, that unnecessary thousands and thousands of pounds.
CM5
Discussion of CPR tended to include graphic accounts of the traumatic and pointless nature of the procedure. While it may indeed be in the patient’s best interests to be made aware of this, it makes the ‘choice’ to refuse attempted resuscitation the obvious and default option. The same applies to home as place of death, where this is viewed by professionals as clearly the best and preferred option for most patients. At the very least, this position is reinforced by policy directives and incentives if not directly influenced by them. One consequence of this was the effort that some respondents describe to prevent patients and families calling an ambulance in response to a crisis after agreement had been reached that the patient would not undergo any further hospital admissions. Where professionals work more or less overtly to secure the family’s formal alignment with their point of view, it is likely that some patients who remain uncommitted to the suggestions made may subsequently change their minds. However, it is also likely that others may be directed towards accepting a ‘correct’ decision which, once formulated, carries its own force.
I think there’s the perception that the hospital can do something more for you that can’t be done at home. Now, when you actually talk to relatives, and you explain that, actually, you can do everything that the hospital can do, you can do at home, and once they meet the community nurses and they realise that you’re there providing support. . . . They’re always with you with that, as long as they can see that that support is there, and that they’re being kind of held.
GP11
Involving the family
Relatives play a crucial but variable role in discussion and implementation of ACP. Professionals acknowledged that without adequate family support the patient was unlikely to be able to stay at home to die. Relationships with families were important, though relatives could also cause difficulties in the event of conflict within families or disagreement with professionals about the best course of action. The boundaries of family involvement and entitlement were not always clear. Family members were frequently present during ACP discussions.
I think it’s always beneficial to involve the family when the patient is happy with that and often is easy because the first few meetings the family are there and there’s sort of implied consent or that you’ve given opportunity for the patient to speak on their own.
GP2
Occasionally professionals said that they preferred to have the initial discussion with the patient alone, in case there were things she or he wished to discuss in private. Another strategy was to indicate to the patient that the aim was to discuss difficult issues, and ask them if they preferred to have a family member present. However, difficult situations could arise when the patient or the relatives did not want the other party to know the patient was dying, or wished to withhold information from each other. Some patients indicated their clear preference not to be involved in discussion of ACP, in which case the locus of discussion and decision-making effectively passed to other members of the family. Regardless of issues of preference or confidentiality, there was a de facto progression to increasingly involve the family as the patient’s condition deteriorated, especially if capacity became impaired. In this case professionals might share information and make decisions with the family without direct involvement of the patient.
The hardest thing is you don’t always see one without the other . . . there may be things, sometimes you want to be able to prepare carers, even if the patient doesn’t want to talk about it, but then you don’t see the carers on their own, except on the doorstep.
PCN3
You know just thinking in particular about this lady with the head and neck cancer that, with the relatives I’ve obviously spoken to them about the risk of potential haemorrhages and things like that but I haven’t . . . discussed that with the patient. I think that would be quite distressing.
GP12
Facing death
Throughout the professional interviews there was rather little reference to issues about how people come to terms with death, reach a point of acceptance, or continue to resist or deny its imminent reality. There was no suggestion that discussion of existential issues is a topic that is frequently or explicitly discussed. It is not clear, however, to what extent patients look to professionals for this kind of exploration, or prefer to consult friends and family for such support. Professional accounts tended to focus on a task-oriented consideration of establishing preferences for resuscitation and place of death, and practical issues of managing resources. Several professionals indicated their awareness that patients and carers may be apprehensive about the experience of dying, and whether or not this will involve symptomatic distress, pain or problems with breathing. In that case, they were able to provide reassurance about the process of dying, which was described in quite benign terms: the patient would become sleepier, and drift off to sleep from which she or he would not awake. If pain or breathlessness was an issue then there were drugs to effectively deal with this.
Yeah. And sometimes, people have quite specific fears or worries, and I always say to them, ‘If there are specific things worrying you, it’s better to talk about them’, because, actually, often, we can allay those anxieties and things, [are they] going to be in agony? Or not going to be able to breathe?
PCN3
And the amount of times somebody with motor neurone disease has said something like, I’m not frightened of dying but I’m frightened of how I’m going to die. And, it opens up that conversation . . . that reduces so much anxiety.
CNSother2
There were very few references to existential issues of emotional, psychological or spiritual distress. Several GPs indicated that they would not get involved in any discussion of spiritual issues because of their own lack of belief. Where they occur, existential issues were illustrated in professional accounts in descriptions of specific cases.
A range of perspectives was offered, but it was clear that not all respondents operate with a view that patients necessarily reach a point of acceptance or resignation about dying. Patient responses were variable and individual. Some patients viewed death as a relief or had reached a point of great age or prolonged suffering where they felt ‘ready to die’. Some never accepted death and might continue to adopt a stance of denial to the end.
I don’t think anybody ever accepts. I think you adapt, don’t think you necessarily accept.
CM6
Several references were made to the commitment to ‘fighting’ dying, as a personal disposition and also as a strongly engrained cultural stance. Several respondents referred to coping styles and resilience of patients as an individual thing. In a predominantly secular sample, there are very few references to the role and value of personal belief systems. A few commented on part of their role as being to offer help and support to patients in talking through their fears about death and dying and sometimes inviting them to do so, to try and help them come to terms with their situation. In some cases this discussion led on to an advance care plan in which patients were tremendously reassured to know that they had prevented an experience such as being resuscitated, or having a naso-gastric tube inserted, about which they had been very apprehensive. However, it seemed that professionals do not give this information routinely. It was also apparent that, in their discussion with patients, professionals tend to represent the experience of dying in notably benign terms.
There were very few explicit references to hope throughout the data. A few professionals talked about concerns that they do not destroy hope, and the desire not to damage hope was another reason to be cautious about initiating ACP. There was reference also to some patients being unrealistic in preserving false hope through committed denial as a means of coping with their situation. Patient denial of death, either temporary or continuing, was a recognised phenomenon and hard to shift. Some respondents accepted that this was some people’s preferred way of coping and should be respected, even if the consequences were very negative, in terms of a poorly managed death.
Summary
Most professional respondents in this study were positive about the improvement in patient care that had resulted from implementation of recent policy relating to ACP and EOLC. The GSF registers and associated activity were key to this process, as were recent developments in medical treatment and the recent introduction of specialist community nursing roles. These had enabled patients to remain at home when previously there would have been no option but to die in hospital. There was little reference to the EOLCPW or its resources, although some respondents were uncomfortably aware of practice incentives to meet local and national markers of quality appraisal. The introduction of GSF registers had improved identification of patients approaching the end of life and MDT discussion and co-ordination of their care. However, palliative care registers remained strongly oriented towards cancer patients, largely because these were easier to recognise as eligible for inclusion. The difficulty of prognostication, especially in long-term conditions, was a strong theme running through the data. It was a major barrier to initiating ACP discussions in an anticipatory, pre-emptive manner. ACP was described as relatively uncommon, and tended to occur when the patient was clearly close to death. Respondents approached discussion in a cautious, stepwise manner, searching for an opportune moment to raise the topic. They were wary of causing distress or damaging relationships with patients, and expected that a substantial number would not be receptive to ACP. Vague and indeterminate language allowed both parties to choose whether to evade or take up acknowledgement and discussion of ACP. However, this also risked misunderstanding and the formulation of unwarranted assumptions about what patients wanted. Professionals were strongly committed to the view that home is the best and usually PPOD. However, they also recognised that circumstances could sometimes conspire against this, and also that patients were prone to change their mind as death approached. These contingencies undermined the value of planning in advance. In practice, ACP tended to be task oriented and geared to completion of specific documents, particularly DNACPR and PPOD. Awareness of existential distress and physical suffering was mentioned infrequently. However, although it was not directly linked to ACP discussions, some respondents described the support they provided in reassuring patients who were apprehensive about the physical experience of dying.
Chapter 5 Findings from the case studies
Introduction
This chapter presents the overarching findings from the case study data, drawing on contributions from patients, family carers and nominated health professionals and review of medical records. The triangulation of different perspectives and data sources over a 6-month period of follow-up allowed a rare insight into the process – or absence – of ACP for patients with severe or chronic illness in the community. The longitudinal design and multiple sources of data offer an opportunity to explore the premise that ACP involves a process of ongoing discussion, reflection and review that may change over time. Each patient constitutes a unique and individual case. However, through our analysis it has been possible to identify several broad types of case and patterns of experience that, while not directly generalisable, may give rise to analytical insights that have widespread applicability through transferability to other settings and patient populations. The extent to which the insights from the patient case data are corroborated or challenged by the findings from the professional perspective interviews will be considered in the discussion.
Of the 21 case study patients, 14 had a form of cancer, sometimes alongside other conditions. The others suffered from a number of conditions including heart failure, renal disease and respiratory conditions. Nine of the 21 participants died during their involvement in the study follow-up. All had been referred because a health professional involved in their care had judged them likely to be within the last 6 months of life.
This chapter focuses on ACP but draws on highlighted elements of both ‘professional’ and ‘personal’ planning as illustrated by the descriptions of health professionals and patients. The next section of this chapter outlines some of the prevalent narratives evident in accounts of diagnosis and prognosis. In further sections, we discuss the barriers to ACP, the ways in which it was initiated and discussed by those participating in the case studies, and finally what impact these discussions and/or decisions might have had.
Responses to bad news: accounts of diagnosis and prognosis
This section explores patients’ narratives of receiving a diagnosis and prognosis that carried a critical intimation of mortality. This did not apply to everyone. Twelve patients had ongoing long-term conditions such as COPD, heart conditions and diabetes. Patients had become accustomed to living with these serious conditions, and did not always perceive themselves to be approaching death. Consequently, the topic of ACP and related issues did not arise during some case interviews. Multiple comorbidities were particularly characteristic of the eight participants who were over 80 years of age and made up a group of ‘elderly frail’. For a few (three) patients, their prognosis at the time of the study was relatively positive, maintaining their focus to continuing with life rather than planning for death. Most typically, for the patients in the study, it was the initial diagnosis of cancer, or the occurrence of a critical event such as suffering a stroke, that was immediately understood to signify that life expectancy was limited. The nature of the diagnosis contained an expectation of prognosis. Regardless of whether they asked for this or were directly told, and with whatever degree of specificity, awareness of an uncertain future initiated a process of some degree of preparation and planning. Some positioned themselves as information seekers (Mr Brown, Mrs Winters, Mrs Elder), wanting to find out more about their diagnosis and prognosis. Others resisted further knowledge and attempted to block out or deny the significance of the information they had been given.
Diagnosis
Respondents’ experiences of diagnosis varied widely. In two cases where patients were identified as having advanced cancer (Mr Brown and Mrs Jones) the diagnosis was made very quickly, allowing little time for the individual or her or his family to prepare for a drastically limited and uncertain future. Several patients described being shocked by the blunt nature of the disclosure, but were inclined, on reflection, to view this as a good thing: an indication of honesty and ‘straight talking’ in their clinician. In four cancer cases (Mrs Elder, Mr Corley, Mr Farley and Mr Roper) and one of renal disease (Mr Davis) delays in diagnosis were described, caused by a series of missed or misunderstood clinical signs and symptoms. Some clearly felt this delay had resulted in the unchecked spread or worsening of their disease and, consequently, a more unfavourable prognosis.
Looking back, I would rather have been told that I had a cancer than be told I’d got what I’d got, because I didn’t realise at the time that when they told me about it, I just didn’t realise the sort of utter complete change it would make of my life. . . . I’m just sitting round waiting for the wooden box. I can’t speed it up. I can’t make the getting there any easier.
Mr Barlow, interview 3
Yes, I think my present situation is I want to know where I am. I want to know where I am with my brain and I want to know where I am with the – when I’m given the information that you are there, I shall then have more of an idea of where I want to go to, but I can’t look ahead until I know where I am. I mean I’m not frightened of dying. I quite accept the fact I am going to die before too long. My only concern about dying is what I’ll leave [wife] with really.
Mr Farley, interview 2
Several respondents reported asking straight out, in response to hearing the diagnosis, what their prognosis was. For these patients, knowing allowed them an idea of how long they would have to prepare for death, both physically and emotionally. In knowing this, some, such as Mrs Jones and Mr Williamson, preferred to then get on with living and chose not to have further discussions about end of life; they had not asked and clearly did not want to know. Those affected by chronic degenerative diseases were less likely to have asked for, or been given, a prognosis of limited life expectancy at the time of diagnosis. It was often only when their condition had reached a very advanced stage that a prognosis was sought or offered. A notable feature of the elderly frail group of patients was that, despite being vulnerable through great age and poor health, they often had no specific condition pointing to clear or identifiable palliative care needs. These patients had evidently not engaged in discussion about prognosis and health professionals often did not consider it appropriate to initiate discussion about the end of life.
Personal planning
Some patients wanted to know their prognosis precisely so that they were able to engage in personal planning: setting their affairs in order, deciding how to spend the time left and, importantly, preparing themselves and their families for the prospect of death. For these patients, uncertainty in prognosis was upsetting because it made it difficult to plan ahead. In dealing with this uncertainty, Mr Barlow had tried to gain more insight into his prognosis so that he could make some plans for the future of his family. Consequently, being unable to obtain a precise prognosis could be a source of frustration. Mr Brown had discussed his prognosis with a number of health professionals, including his GP, in order to gather accurate information so that the family could plan to be together when the time came for his death. These discussions allowed Mr Brown to express his wishes and feel that he was able to make some plans about his future care that he had evidently thought about in some detail. However, in the event, despite fairly accurate prognostication, it did not prove possible to realise the plans he had intended. Mr Brown’s case is referred to again in the section Impact of and responses to advance care planning.
I’d asked [the respiratory nurse], hadn’t I, at one of those visits, if there is a time span on it, and she said, ‘You know, it’s not like cancer where they can say to you you’ve only got few weeks’ . . . Because I thought, at the time, you were going sort of downhill quite fast, weren’t you? And [the respiratory nurse] must have mentioned to [the consultant and he] just said, told us . . . I just basically really wanted to know what I’d got to [do], you know, if we were going to, well, you are, really, aren’t you?
Well, at the time, I needed to plan for the future, as it were. Not for my future but [my wife’s].
Mr and Mrs Barlow, interview 2
His main concern was, you know, having his family present when end of life does come for him. . . . I explained to him that even the consultants wouldn’t be able to sort of give him an exact day or time, they may give an estimation of weeks or months or years but nothing very, very specific. And we talked in depth about him knowing his own body and knowing what’s going on and he will notice maybe a change in his abilities and in his function and in, in how his body feels. He [seemed] to be quite reassured by that notion.
Mr Brown’s AHP, interview 1
Whereas most patients looked to health professionals as the main, and often the only, source of information about their illness, a few reported searching for information themselves, usually on the internet. At the time of her diagnosis, Mrs Winters was not given a prognosis and took it on herself to establish it. Internet research identified that she would probably have a prognosis of approximately 2 years, and she took this as her benchmark. Much of the focus of her narrative was about having time to prepare herself and, particularly, her adult family for her death. This was an ongoing project for her, made difficult by their continuing resistance and distress. She reported a stepwise approach to slowly get them to talk about her wishes. This left her with little support or space to discuss her own feelings within the family, and she expressed being glad of a good relationship with her GP.
Personal planning was usually undertaken independently of professionally brokered ACP discussions and focused on the more common elements of planning such as making a will or funeral arrangements, but also such things as planning holidays and family reunions (Mrs Tomlinson, Mrs Avery, Mrs Jones, Mrs Winters).
I’ve done my funeral, it’s all in place. It’s all done. Right down to the lining in the coffin, I’ve chose everything for my funeral. . . . I didn’t want my husband to think and worry ‘What would she have wanted? Would she have liked this, would she have wanted that?’ So, we have discussed it, we have talked about it and I chose a funeral directors . . . [my husband has] not got anything to worry about.
Mrs Jones, interview 1
In some cases this had been done prior to the patient’s diagnosis as part of people’s preparedness in life more generally (Mr Jacobs, Mrs Elder). It was clear that some participants were natural planners, accustomed to make arrangements in anticipation of changing circumstances. Often the focus of these plans was to alleviate the pressure on family members and reduce the burden of care and the disruption of death. An ongoing theme throughout Mrs Elder’s interviews was the desire to make things as easy as possible for her family during the process of EOLC and beyond, and not to be a burden. She had already planned and paid for her funeral, explaining this had been done prior to her diagnosis. She was also in the process of carrying out maintenance on her house and clearing away ‘clutter’ to make it more saleable when she was gone, reducing the work for her family when managing her estate.
In other cases, the diagnosis had clearly prompted patients’ thoughts about their future wishes and how best to live the life remaining. Some respondents described discussing these issues with family members. Others indicated that they had not spoken to anyone prior to the research interview. Following a stroke, Mr Barlow had quickly made changes to his financial arrangements to allow his wife access to his accounts and subsequently made the difficult decision to move from the family home to a bungalow to accommodate his increasing care needs. Mr Farley had insured the car in his wife’s name in case he was ‘not around when it next needed to be insured and dealt with’. Although personal planning tended to be undertaken independently of professional input, staff were sometimes involved. Mrs Tomlinson in particular talked at length about how staff at the hospice had helped her to create a living will and specify her wishes for her funeral (Box 2). Notably, however, she had asked for help to do this in response to a prompt from her daughter. This documented her wishes for after her death, including funeral plans such as selected music, readings and the clothes she wanted to wear, where she wanted her ashes to be scattered and that she wanted donations to the hospice instead of flowers.
‘You ought to do a bit of a will, mum’. So I says, ‘Well, I’ve got no money or nothing’, and I says, ‘The property’s not mine’. So she says ‘Just to put your mind at rest’. She says, ‘You know, what you want to happen to you when you die’. . . . So [I asked a member of the hospice team] ‘Wonder if you could help me write my living will out?’ . . . she were lovely, she done it for me, she put it all on the computer for me, sorted things out for me, . . . helped me with couple of things, a prayer, a lovely prayer.
Mrs Tomlinson, interview 2
She said something like ‘well I don’t want flowers, you must tell [my husband] I don’t want flowers!’ And I think I said to her, ‘Well, would you like to write down what you’d like and then [husband] won’t have to worry about it’. . . . I wrote it down faithfully how she said it, . . . because [husband] can then hear her say it almost . . . So we just wrote them on a piece of paper and I signed it and [so did] [the chaplain].
Mrs Tomlinson’s AHP, interview 1
Living with uncertainty
Health professionals were often challenged by the notion of providing an accurate prognosis. Some preferred not to offer this information, primarily because they were so often surprised by patients who either surpassed their expectations or who deteriorated more quickly than foreseen. Health professionals recognised that conditions other than cancer posed particular problems for prognostication. However, some cancers were also difficult to predict. Although patients with chronic degenerative diseases did not initially confront the shock of a terminal diagnosis, some were alerted to the reality of a constrained and limited future after the occurrence of a critical event. Three of the 21 cases (Mr Jacobs, Mrs Barker, Mr Arthur) had experienced complications from surgery or other coexisting conditions that had significantly worsened their prognosis. Mrs Barker had been left unable to walk and doubly incontinent after an operation for osteoporosis of the spine resulted in an infection and additional damage. Complications during an operation on his kidneys had left Mr Jacobs blind and with further renal problems in addition to his advanced COPD. Mr Arthur’s operation for oesophageal cancer had been considered curative. However, several postoperative chest infections combined with existing comorbidities complicated and limited his recovery.
Although there was a theme of approaching the certainty of a limited, if indeterminate, life expectancy with great focus and intent, another strand of responses took the stance of foreclosing the future: uncertainty in this case made planning difficult and unwelcome. These patients preferred not to look – or plan – too far ahead, opting to live as far as possible in the present, and deal with the future as it came. The slow rate of growth of Mrs Avery’s brain tumour since diagnosis in 2003 meant that both she and the health professionals involved in her care were particularly challenged in giving an accurate prognosis. She had been told that her tumour was inoperable but very slow growing. Living with such uncertainty, she found it difficult to think about her future.
I don’t think I think about the future. I think I just take it more or less a day at a time. . . . I can’t think long term because I know, like I said to you, I know I’m not going to get better. How long I’ve got? I don’t know. Because, how long is a piece of string? I mean, I don’t think they, doctors really know, do they?
Mrs Avery, interview 2
Mr Williamson had surprised health professionals several times. His GP noted during his interview in February 2013 that, when he had been diagnosed with spinal metastases 2 years previously, Mr Williamson’s prognosis had been approximately 6 months. Having seen this estimation greatly surpassed, the GP felt that again, his present prognosis would be for a further 6 months. It was clear throughout the study period that the emotional toll of such a protracted and debilitating illness had been extensive and Mr Williamson was often quite tearful during conversations.
I think we were surprised, I think, when we diagnosed him with spinal metastases, we didn’t expect him to live very long at all. You know, we were, I think, back in the late part of 2011, we were thinking probably 6 months . . . he’s surpassed all expectations. And even now, you know, towards the end of last year, he was quite poorly again with this confusion, and we thought . . . and he’s rallied and got better again. So the prognosis with [Mr Williamson] is really hard. But I would have thought, again, I think we’re looking probably at 6 months, but, he’s, he’s proved us wrong time and time again.
Mr Williamson’s GP, interview 1
Despite a diagnosis of cancer, both these patient cases seemed to fall within a category of long-term conditions leaving them living with extreme and even fluctuating uncertainty, which they found to be difficult and distressing.
Resisting information
In contrast to seeking information and taking a proactive stance to planning, some respondents explicitly did not want to know anything more than a vague prognosis. It would seem that patients and families used resisting information as a coping mechanism. This allowed them to distance themselves from the uncertainty of illness and likelihood of death. As Mrs Jones expressed it, she preferred things ‘just to happen’ as they would for anyone. Regardless of this approach, she wanted to continue to participate in life and had certain time periods and goals in mind which she aimed to reach. For these patients, confrontation, or even acknowledgement, of a poor prognosis threatened to spoil enjoyment of the life they had left. However, it seemed that health professionals often struggled to sanction this kind of blocking behaviour. In three successive letters to the GP, Mr Corley’s oncologist voiced concerns about his lack of understanding of his condition. The oncologist explained that he had been clear that the impending chemotherapy treatment was palliative and that their wishes to travel abroad were unlikely to be realised. Three months later he again expressed concern that Mr and Mrs Corley had not understood the significance of the spread of his cancer and the limited treatment options now available. Mr Corley’s PCN also expressed concerns and persisted to try to clarify the situation for the family, classifying this type of response as ‘difficult’. In her interview after her husband’s death, Mrs Corley reflected on this prognosis and suggested that, although they preferred to believe that the treatment would extend his life, she felt her husband was aware how serious his condition was. Perhaps this case illustrates that it was not that Mr Corley did not understand the information that he was being given about his prognosis, but rather that he chose to block that information as his preferred means of dealing with his impending death (Box 3).
I think he was quite difficult in a way, because he didn’t really, he wasn’t that, talking about things. So it was a bit challenging to do some of the advanced care planning. And when it was obvious he was starting to deteriorate, he was still not that comfortable with sort of raising the advanced care planning. So some things weren’t sort of quite in place . . . we’re thinking, ‘Oh, he’s not going to do well’. And I don’t think either of them really realised that, or they would sort of push it away a little bit. So, but once we needed to start talking about what, what the issues were and what the plans were and what were we doing keeping him at home and hospital bed and all those things, mostly that discussion was with [his wife].
Mr Corley’s PCN, interview 2
. . . he was diagnosed, so not very long really. And I thought longer, I just, well, he was doing so well, . . . I think both of us just believed the treatment would just allow him to carry on a little bit longer, I said, ‘Because, you know, people go on holiday in wheelchairs, we can still get about’, so that’s how we left it . . . it all happened sooner than . . . I think we just believed that we could go, have a bit longer.
So you weren’t prepared at all?
No. . . . No. No. But I, I, well, think perhaps [my husband] realised things weren’t good.
Mrs Corley, interview 2
Mr and Mrs Williamson focused on their day-to-day living throughout their interviews (Box 4). Their case shows how patients and families may consider engaging with ACP more appropriate at some times than others. Despite not wanting to discuss wishes for care on a regular basis, Mr Williamson had had some initial discussion with the palliative care team as his prognosis became more apparent. These conversations were revisited nearer to the time of his death. However, there was a considerable period of time in between when Mr Williamson did not want to engage with ACP. In a letter to his GP, the palliative care consultant identified that Mr Williamson was afraid of dying and managed this fear by not wishing to make choices about his care in advance but to ‘take each day as it comes’. Despite discussing some issues with Mr Williamson, the PCN did comment that DNACPR had not been raised with him. This was also noted by the GP. It was evident that this was completed during his final hospital stay 3 days before his death. When he deteriorated, although his preference was for the hospice there were no available beds and he was transferred to hospital and admitted via accident and emergency. Some days later he was fast tracked home to die.
We just take each day that comes.
We take days as, every day is a good day, if I’m all right.
You see, today is a good day. Another day you might come and he’s in bed all day.
Mr and Mrs Williamson, interview 1
Mr Williamson doesn’t really want to, wasn’t interested in discussing that, didn’t want to go there really. I think, as long as he’s, he’s at home and up and about, I think it, he represses the idea about prognosis and just doesn’t want to think about it really.
Mr Williamson’s GP, interview 1
We have talked about the future at various points when things aren’t looking so good and then that’s opened up conversation about the future and what might happen. He’s very aware that any treatment he’s having isn’t going to cure it. And that the disease is going to kill him but he prefers, well, when I’ve spoken to him, he’s preferred to take each day as it comes.
Mr Williamson’s PCN, interview 1
Mr Williamson’s case illustrates that health professionals seemed to feel that the process of ACP was hindered when patients did not want to discuss EOLC in advance. For health professionals this meant that they might not be able to accommodate patients’ wishes without due preparation, yet for some patients waiting until they are in or near the dying phase may just be seen as timely and appropriate. For patients and families, ‘appropriate’ timing for ACP discussion was prompted by deterioration in their condition. This point is explored further in the section Initiating advance care planning.
This section has focused on accounts of diagnosis and prognosis as experienced by patients and families. Once a diagnosis had been disclosed, we were able to identify themes around personal planning, living with uncertainty and blocking information. These differing approaches allowed patients to manage the information they were given and respond to the news of their diagnosis as best they could. Patients’ positions were not necessarily static within these approaches and could indeed fluctuate between wanting and seeking information and resisting further discussions. Such fluctuations often created challenges for health professionals in judging when to raise topics related to ACP, and patients’ responses did not always fit with their professional assumptions or agenda.
The next sections draw on smaller groups of cases that best illustrate the points discussed. A table at the beginning of each section summarises the cases relevant to the theme (Tables 12–15).
| Case | Diagnosis | Age (years) | Living situation |
|---|---|---|---|
| Mrs Alderson | Heart failure | 91 | At home alone |
| Mr Davis | Renal disease | 92 | At home alone |
| Mrs Avery | Brain cancer | 69 | At home alone |
| Mr Jenkins | Bladder and bowel cancer | 86 | At home alone |
| Mr Andrews | Stomach cancer | 85 | At home with his wife |
| Mrs Barker | Spinal injury | 86 | At home alone |
| Mr Arthur | Oesophageal cancer | 74 | At home with wife |
| Mr Roper | Bowel cancer | 76 | At home with wife |
| Ms Lucas | Liver disease | 38 | At home with mother |
| Case | Diagnosis | Age (years) | Living situation |
|---|---|---|---|
| Mr Barlow | COPD | 70 | At home with his wife |
| Mrs Avery | Brain cancer | 66 | At home alone |
| Mr Patterson | Lung cancer/COPD | 84 | At home with his wife |
| Mrs Winters | Lung cancer | 66 | At home with her partner |
| Mrs Elder | Lung cancer | 70 | At home alone |
| Mr Corley | Lung cancer | 64 | At home with his wife |
| Mr Jacobs | COPD/renal disease | 82 | At home with his wife |
| Mr Farley | Prostate cancer | 79 | At home with his wife |
| Case | Diagnosis | Age (years) | Living situation |
|---|---|---|---|
| Mr Brown | Lung cancer | 53 | At home with his wife and daughter |
| Mr Barlow | COPD | 70 | At home with his wife |
| Mrs Jones | Pancreatic cancer | 52 | At home with her husband |
| Mr Williamson | Oesophageal cancer | 68 | At home with his wife |
| Mr Patterson | Lung cancer/COPD | 84 | At home with his wife |
| Mrs Tomlinson | COPD | 62 | At home with her husband |
| Mr Corley | Lung cancer | 64 | At home with his wife |
| Mr Jacobs | COPD/renal disease | 82 | At home with his wife |
| Mr Farley | Prostate cancer | 79 | At home with his wife |
| Case | Diagnosis | Age (years) | Living situation |
|---|---|---|---|
| Mr Brown | Lung cancer | 63 | At home with his wife and daughter |
| Mr Patterson | Lung cancer/COPD | 84 | At home with his wife |
| Mrs Elder | Lung cancer | 71 | At home alone |
| Mr Corley | Lung cancer | 64 | At home with his wife |
| Mr Andrews | Stomach cancer | 84 | At home with his wife |
| Mr Jacobs | COPD/renal disease | 82 | At home with his wife |
| Mr Farley | Prostate cancer | 79 | At home with his wife |
Advance care planning
This section considers why ACP may not have been initiated, by highlighting the cases in which there was no evidence of ACP having been discussed between patients and health professionals. The process of professional planning is also illustrated. In nine of the 21 patient cases no involvement was reported, and no recorded evidence was found of discussions around EOLC or the patient’s wishes for ACP. Five of these participants had cancers and the other four had another long-term condition as a primary diagnosis. Almost all had other multiple comorbidities including COPD, diabetes, hypertension, kidney disease and degenerative conditions due to older age. Five of these nine participants lived at home alone. The majority were aged 70 years or over, with five being over the age of 85 years. Although not reporting any discussion of their wishes for future care with health professionals, several participants alluded to or directly expressed them in the interviews. They then reported a number of reasons why they had not discussed these issues with health professionals or, quite often, family members. For patients, these included lack of opportunity, communication issues and/or absence of a specific person with whom to raise these topics. For health professionals, barriers included lack of a clear prognosis, or continuation of active treatment, even if it was palliative. In some instances, advanced older age and multiple comorbidities seemed to be a barrier rather than a trigger for ACP. In others, even when there was no evidence of elements of ACP being communicated with patients and families, some areas of professional planning were nevertheless taking place.
The lack of a clear terminal diagnosis or prognosis seemed to prevent the initiation of ACP conversations, as did the continuation of ongoing active treatment, or if the patient was considered to be relatively well. Three male participants, Mr Davis, Mr Jenkins and Mr Roper, were all receiving ongoing active, but non-curative, treatment and seemed to be maintaining relatively good health. Each was being treated for bowel or bladder cancer or renal disease. Despite being considered to need palliative care, these conditions continued to be treatable. As Mr Jenkins described it, the treatments were ‘putting off’ death. These participants had consistent links with hospital outpatient departments but little if any contact with services or professionals within the community. Their consultations with health professionals seemed to focus specifically on the clinical aspects of care, giving little opportunity to discuss wider issues. These circumstances did not facilitate ACP being undertaken by primary or secondary care staff.
Five of the nine participants in this category had been placed on the GSF register by their GP practice (Mrs Barker, Mr Arthur, Mr Andrews, Mr Roper and Mr Jenkins), despite there being no recorded or reported discussion about their wishes for care. Mr Roper had been flagged as ‘amber’ on the GSF in his GP record, meaning that his prognosis was between 1 and 6 months, while Mr Jenkins was specifically flagged as ‘palliative’ on the GP system to allow him swift access to appointments. Mr Roper also had his PPOC recorded as home despite his PCN noting that it had been inappropriate to have this discussion with him. The fast track system and anticipatory medications were also instigated in Mr Andrews’s case. It would seem in these five cases that some anticipatory professional planning was taking place but without consultation or conversation with patients or families.
He realised it’s a matter of taking the results as they come and seeing how things go, but he didn’t want to enter into any other discussions at that point. He was more about the here and now, and I think I was a bit tentative because I didn’t want to distress him unnecessarily when he was a very anxious gentleman to start with . . . we have a section for, that’s a shared end of life care review that we normally fill in, I haven’t actually filled anything in for him, because potentially, it wasn’t at that point, an end of life situation. . . . If it was someone that had a palliative diagnosis, . . . yes, I will have anticipatory discussion, if that situation arose.
Mr Arthur’s PCN, interview 2
Long-term illness had resulted in Mrs Barker being nursed in bed for several years. Many health professionals were involved in her care, and professional carers attended four times a day to tend to her needs. Health professionals participating in this case seemed to regard discussion of plans for EOLC as inappropriate, even when Mrs Barker gave some initial cues that might have led health professionals to pursue a further discussion. Although Mrs Barker did not have a DNACPR in place, this was considered to be normal for someone with such ongoing care needs. When the topic of resuscitation was raised during a hospital admission, her family did not want a DNACPR order. The family consistently reported that they rarely discussed things directly with the professionals involved in Mrs Barker’s care and that they had very little contact with her GP, despite her poor health, recurring hospital admissions and constant monitoring via daily visits from the community nursing team. Nevertheless, her medical records note that Mrs Barker had been on the practice GSF register for over 33 months by the end of the study period (another instance of professional planning). Yet there appeared to be no one with the type of contact necessary to initiate or facilitate a discussion of ACP. Her family also displayed no inclination to discuss ACP; while aware of their mother’s age, they considered her to be reasonably well and in a steady state, making thoughts of ACP potentially unnecessary at this time. As in several other cases, it seemed the ongoing ‘normality’ of Mrs Barker’s poor health was a barrier rather than a facilitator to ACP.
Mrs Alderson was a 91-year-old woman with heart failure and multiple comorbidities including hypertension, diabetes, risk of stroke, falls, partial sight, partial deafness, dizziness and vertigo. Her GP did not consider her suitable for the GSF or ACP, but did feel she would fit the criteria for the ‘surprise’ question (if only by nature of her great age) and had referred her to the study on this basis. In interviews Mrs Alderson’s GP expressed a lack of support for ACP in general. In assuming that a knowledge that she might die was obvious to Mrs Alderson, he felt it would be inappropriate to talk about death with her. In her interviews Mrs Alderson did not express an explicit wish to engage with a discussion about ACP, and her son felt she would not wish to do so. However, Mrs Alderson felt that she had a generally poor relationship with health professionals. This was likely to inhibit any ACP discussions from taking place, even if she had wished to engage in them. In this case, being categorised as frail elderly with multiple comorbidities, but without a palliative care need, seemed to serve as a barrier rather than facilitator to ACP. Being considered not appropriate for the GSF register also meant that professional planning and discussion within the MDT was unlikely to occur.
I wouldn’t put her on [the GSF register]. . . . we’ve had no progressive disease where we can anticipate that she will gradually, irreversibly decline and die. . . . If I said to her, would you be surprised if you died in the next 6 months? I think she’d probably laugh. . . . And I think sometimes, so-called health professionals treat people like that as if they’ve never encountered death before. . . . That age, a lady with a history of heart disease, what else has she got? She’s atrial fibrillation and she’s on warfarin so she could have a stroke, she could have a serious bleed, she could have a major stroke and not recover from it. She could have a coronary, she’s had angina in the past. She’s got left ventricular failure, previous pulmonary embolism, she’s got lots of previous problems. . . . I’m never really surprised that any [one her age] . . . And I’m not sure what labouring the point to her that, or not labouring the point but saying it, that you might die in the next 6 months, I think she’d look at me as if I’d gone stupid, you know, as a fact, she couldn’t work that out for herself really.
Mrs Alderson’s GP, interview 1
This section has highlighted a number of barriers to ACP illustrated by participants in the study. Primarily, patients needed a strong enough relationship with a health professional for the topic to be raised. This was not the case for a number of patients and family carers, despite their experience of great age and frailty, combined with serious health conditions, and extensive contact with a wide range of health services and professionals. Communication was then illustrated as being central, both between health professionals and between professionals and patients and families. Within this theme there are a number of instances when health professionals felt that ACP would be inappropriate, particularly if a person was receiving ongoing or active treatment or when prognosis was uncertain. Health professionals would wait for a more appropriate time indicated by a specific ‘trigger’ such as deteriorating condition, or a ‘cue’ from the patient, as illustrated in the chapter outlining themes from the professional perspectives. However, these decisions were often based on assumptions, with little exploration of how much a patient may or may not wish to talk about the end of life.
Initiating advance care planning
Policy and guidance on ACP advocates a pre-emptive and stepwise approach that should start considerably in advance of predicted death, giving time for consideration, decision-making and review. For a few participants this was the case (see references to Mrs Elder, Mr Barlow and Mr Jacobs in particular). More commonly, any discussion and documentation of participants’ wishes for EOLC tended to be clustered towards the end of their illness trajectory. As indicated above, the difficulty of prognosis was a major barrier to professional initiation of ACP much in advance of the patient’s terminal decline. This section reports on the themes of timing and initiation of conversations and illustrates that both health professionals and patients prefer conversations to be prompted by a deterioration in the patient’s condition so that the timing of such conversations is considered to be ‘right’. There was agreement between patients and health professionals that not only was timing important but conversations were often initiated, and should be initiated, following deterioration in the patient’s condition. In several cases, the topic of ACP was broached, but not necessarily resolved, during a ‘window of opportunity’ following diagnosis or exacerbation, or when the patient was feeling very ill and emotionally at a very low ebb. When the immediate crisis passed, the topic might be ‘parked’ for an indefinite period while the patient remained relatively well, and adopted to a more hopeful, albeit ‘recovery orientation’. Professionals’ responses also seemed to correspond with this strategy, considering it necessary to confirm preferences for resuscitation and place of death late on in the illness trajectory, when the patient was close to death. Judging the right, or most appropriate, time to initiate discussion of ACP was difficult for patients as well as professionals. Mrs Winters, interview 2 (Box 5), talked about considering her future but had yet to broach this subject with health professionals, preferring to ‘just make the most of each day’.
Have you talked to anyone about that?
No, not yet because if I approach the subject, I get really scared. [laughs] Which, I don’t want to know the end result really.
Right, so you’d rather not?
Not at the minute, no. I mean, as time progresses, I don’t know. Or if the cancer progresses, I don’t know.
Mrs Winters, interview 2
I feel led by her really in terms of what issues she wants to bring up. But, if and when, well, when things get to the point where things start to deteriorate, then that will be the time then to have the discussion.
Mrs Winters’s GP, interview 1
It feels more appropriate when you really are seeing that someone’s in their, clearly in their final few months or weeks. Because at the moment, it sort of feels like, well, she could have a cardiac arrest, but actually, she’s reasonably well at the moment, so it wouldn’t feel unreasonable to try and resuscitate her from a cardiac arrest.
Mrs Winters’s GP, interview 2
However, getting this timing right was recognised to be difficult, as Mrs Winters went on to state she was able to think more clearly when she was feeling well: ‘I can do it better when I’m feeling all right. When I’m not very well I don’t want to know that part’. As Mrs Winters’s case demonstrates, it may be about getting the timing right not just for the patient but also for her or his family. Mrs Winters’s family were struggling to come to terms with her diagnosis and were resistant to discussing her prognosis or any plan she might have for the future. She attempted to raise the issue with her family on a number of occasions in order to give them time to adjust and cope with the devastation of the news.
If I bring it up, [the family will] say ‘No, no, no, we’re not there yet’. I keep saying, ‘You’ve got to face it, you’ve got to stand up and face this, I have to, you have to’. And then they see me, and say, ‘But mum, you’re all right’, and I don’t know whether they think that’s going to be forever, it is a hard subject to approach.
Mrs Winters, interview 2
Five months after Mrs Winters’s second interview she remained relatively well, which left her GP reluctant to discuss resuscitation with her, as he did not feel it was appropriate. Mrs Winters expressed some idea of when she would like the subject of end of life to be broached by the health professionals. She felt this should be once she had deteriorated but enough in advance that she would have time to plan what she wanted and where she would like to be. She had asked about her prognosis, and it was explained that it was not possible to predict this. However, this is did not lead to any further discussion of her wishes and Mrs Winters expected that this discussion might be prompted ‘when things get worse’. Mrs Winters’s GP also felt that these conversations would be prompted by changes in her health and that he would be led by her. Initiation of the discussion becomes a problem if each party is waiting for the other to broach the subject and hence a prompt such as change in condition might be the necessary catalyst.
Both Mrs Winters and Mrs Avery shared how they felt that a sign of further progression would prompt them to ask more about their prognosis and discuss their wishes. This was in line with the views of these patients’ GPs about the appropriate timing of these conversations. Mrs Avery’s GP was interviewed as her nominated health professional but struggled to recognise Mrs Avery as at the ‘end of life’. However, the GP reflected that any end of life conversations would be triggered by a change in Mrs Avery’s condition, such as if her scan showed growth of the cancer. Her GP felt that, prior to this decline, any discussion of ACP which was unprompted by the patient would be inappropriate. It was clear from Mrs Avery’s interviews that she agreed with this approach; she also stated that a change in the result from her scan would prompt her to ask more questions about her prognosis (Box 6).
Well, I mean, all I said was that I’d made this decision and would they sort of keep me comfortable and pain-free and they said yes, they would. And that’s as far as it’s gone at the moment. I suppose, perhaps, when I have the scan in October, November time, if it shows that the tumour’s grown a lot or something, they’d probably discuss things further.
Mrs Avery, interview 3
Well, I suppose we’ve not, we’ve (certainly not), we haven’t had a discussion about, you know, sort of where she wants to die or anything like that. . . . I suppose, she may, maybe it seems a little bit inappropriate to actually sort of have that discussion with her at this stage. If she raised it, I’d be happy to talk to her about it, if it was going through her mind but I think, to raise it with her, she’s going to think, ‘Oh, [my GP] thinks I’m going to be dying in the next few months’. . . . If there were sign[s] of progression on the scan, then I think I would maybe start to talk a bit more about the future and what her wishes were.
Mrs Avery’s GP, interview 1
As the cases of Mrs Winters and Mrs Avery illustrate, many patients and health professionals considered a change in condition to be a viable prompt to initiate ACP discussions. Health professionals’ accounts often identified an initial discussion and then plans to revisit these conversations as and when appropriate. Mrs Elder’s PCN described how Mrs Elder had initially raised the issue of DNACPR resulting in this being put in place. In three interviews with this health professional over a 10-month period, she demonstrated how some discussion of PPOC had been ‘touched on’ with Mrs Elder but would require reviewing at a more appropriate time (Box 7). Further discussion of ACP would be prompted by a change in her condition, which would motivate professional planning in terms of getting services and funding in place. The first interview also shows the PCN’s recognition that, although PPOC had been discussed in some way, this did not always equate to establishing PPOD. Hence, this element required further exploration. This was the only real display of recognition of this distinction from a health professional in the case study interviews.
She wants to stay at home but actually, that discussion, didn’t specifically say I want to die at home because that’s not always the same thing. And often, if you pin people down a bit more, they might say, ‘Well, I want to stay at home as long as possible’ or, ‘want to stay at home as long as I can cope’ or ‘as long as my carers are coping’ so there’s often a lot of, sort of provisos along with that really. And with her, I wouldn’t have pushed that for clarification necessarily because of how well she is. So with her, sure she would have been fine if I’d clarified, but actually, I didn’t feel it was necessary. And I’m still sort of testing the waters a little bit.
Mrs Elder’s PCN, interview 1
We sort of touched on where she would want to be, preferred place of care at, you know, right at that early point as well, and it will only be, I think, if she was, so I know, so I’d probably only revisit it with her when things actually were changing . . . if she was needing any extra – if she was needing support at home, from a practical point of view, at that point, I think we’d need to just clarify whether she’d had any more thoughts about preferred place of care.
Mrs Elder’s PCN, interview 2
In effect, this stepwise approach seemed to materialise as initially touching on the subject, potentially to establish the patient’s response to such conversations, and then leaving it until a trigger or prompt initiated a more essential group of discussions to establish the recordable elements of ACP and allow health professionals to fully undertake professional planning. As the prompt was often deterioration in the patient’s condition, these conversations then became clustered towards the end of life. It was really only in the case of the few proactive patients who initiated conversations for themselves that repeated discussion took place over an extended period of time. These individuals had strong views about certain elements of EOLC and it was their expression of these views that prompted further discussion with health professionals. The health professionals involved in Mr Jacobs’s and Mrs Harrison’s cases reported revisiting the issue a number of times as these patients regularly expressed their wishes and wanted to discuss their concerns. Mrs Harrison was anxious about dying alone and raised this a number of times in her interviews, reflecting the reports of her GP and annotations in her medical records. Her GP noted she wished to stay at home and had a DNACPR in her home-held notes (Box 8). Mrs Harrison’s medical records reflected a number of these conversations over a 1-year period and also showed that these took place with different health and AHPs, including other GPs. It was recognised that Mrs Harrison wanted to remain at home and her GP was keen to support that as far as possible. However, she noted that this would depend on her needs; if these changed dramatically then home might not be a feasible option. The GP revisited these issues a number of times in order to clarify and check for any changes.
Every so often, she sort of brings up about dying and her fears about it so, it is quite a sort of natural progression then to talk about these sorts of issues. So we have spoken about where she’d like to be cared for, which is home, and we’ve spoken about CPR as well. So she’s got a DNACPR decision in her house. They’re really the sort of main areas really.
Mrs Harrison’s GP, interview 1
I think it’s just a very sort of very gradual decline really I think. She’s still very highly anxious. We did talk about if she wasn’t able to tell us what she wanted, what sort of care she want, who would she want involved with her decisions, . . . And I think, yeah I mean we just covered a lot of things that she’s said a lot in the past again and again. . . . If that is her wish [to stay at home] we want to do what we can to try and support her with that . . . I think we just have to address these things as they arise really, and whether she agrees or doesn’t agree to things, just have to convince her at the time. . . . I don’t think there’s anything else that . . . it might just be that you know a crisis arises that means that the situation has dramatically changed, but at the moment we just carry on.
Mrs Harrison’s GP, interview 2
Mrs Elder had particular concerns about wanting a DNACPR order put in place and initiated several conversations with health professionals about this. After she raised the topic with her PCN, this information was conveyed to Mrs Elder’s GP, who visited her at home twice to discuss it further and to complete the form. However, there was little evidence of discussion or documentation of other elements of ACP, Mrs Elder’s preferences or the uncertainty she expressed about PPOD. Mr Jacobs had heard much of the negative media coverage of the LCP in 2013 and had experienced his mother dying slowly after a debilitating stroke. These factors informed his very strongly held view that he did not wish to go to hospital for any treatment. His GP and, primarily, CM had been able to support him in managing his illnesses in his own home. However, having discussed Mr Jacobs’s wishes on more than one occasion and helped him complete an ADRT, the CM felt there was currently little need to review the topic, as ‘his views about what he wanted . . . haven’t changed [and] there was nothing really in terms of this conditions that had suggested to me that we need to revisit the conversation’ (Mr Jacobs’s CM, interview 2).
Advance care planning could be initiated in various ways, by the patient or the health professional, although it was only proactive patients with a particular concern or wish who were likely to instigate the discussion. Indeed, it is likely that patients are not aware of issues such as resuscitation or place of death, and the possibility of considering them, until the topic is brought to their attention. Thus, either through patient preference or through lack of awareness, in most cases the topic of ACP is left for professionals to broach. Since health professionals often waited for clear cues and prompts from patients before raising ACP, consideration of the topic was likely to be avoided or delayed. However, patients and health professionals agreed that deterioration in the patient’s condition would be the most likely, and appropriate, prompt for any discussion. This meant that discussions of ACP tended to cluster towards the end of life. ACP could be raised by any health professional involved in the patient’s’ care. In this study, GPs primarily undertook the tasks of writing DNACPR orders and might initiate placing a patient on the GSF register, although some, such as Mrs Harrison’s doctor, did engage in ACP more fully. There was little evidence of ACP being carried out by DNs, although none was nominated for the study. It appeared that other elements of ACP were more likely to be addressed by specialist services such as PCNs, palliative care consultants and CMs. Hence, those without access or referral to these types of services often did not have the opportunity to discuss or implement ACP.
The advance care planning discussion
In a number of the case study narratives there was evidence about how ACP was discussed with patients and relatives. This emerged as an important theme and was recounted by both health professionals and patients and families. However, there was little direct reference to patient’s or carers thoughts about being offered an ACP discussion. In this section, data are presented about how discussions were implemented, aspects of care and the types of language used. It seemed that resuscitation compelled a much more definitive and clear explanation and discussion than other aspects of ACP.
In a couple of instances there was evidence that ACP and professional planning had taken place but the patient’s death prevented further exploration of these issues. It was clear that Mrs Jones had some discussion about her wishes for care, and her medical notes recorded a DNACPR, a DS1500 in place and, latterly, anticipatory medications in the home. In addition, Mrs Jones had also discussed her PPOC and stated she would like to be cared for at home unless there was a medical need for her to be moved to the hospice. She stated this was ‘all planned out’, but as this was a single interview it is not possible to know the extent of this or who the plans had been shared with. The medical records indicated that a ‘long conversation’ had taken place between Mrs Jones and her GP during a home visit. However, no further details were given about the nature and extent of the discussion.
The language used by health professionals in discussing ACP was often described as being ‘soft’ or indirect. However, this was specifically not the case for conversations about resuscitation. Together with PPOD, DNACPR seemed to be the most commonly reported and recorded aspect of ACP. Completed DNACPR forms were held in the patient’s notes in her or his home, although the patient was not required to sign it. As it remained with the patient, professionals tended to feel under some pressure to discuss its contents. DNACPR discussion could be initiated by hospital staff during an admission and then taken on for completion by community staff after discharge so that the DNACPR form could be placed in the home with the patient. Mrs Tomlinson’s case provides an example of how this DNACPR discussion took place in the hospital and was then taken up by her GP.
We were talking at the [hospital] and that and when I found out [how] I was, I was in the fourth stage of it, and that ‘There’s nothing we can do now, we can just keep you comfortable’ . . . And then he says, ‘I don’t like asking you, [Mrs Tomlinson]’, but he says, ‘It’s a new law, we’ve got to ask people now’, he says, ‘If anything happened, would you want resuscitating?’ and I said ‘No’. I’d made my mind up then, because I don’t think it were fair on my family. And, they says, ‘Well, not only that, it’s not fair on you, because, where you are at the moment, with your illness, it’s just going to put more pressure on to you, perhaps bring you round for a couple of minutes and you could be gone again’. It’s not fair to keep doing it and I made my mind up.
Mrs Tomlinson, interview 1
Mr Barlow was a 70-year-old man with COPD and a history of stroke. After his stroke he had asked for his prognosis, and been told by his consultant that it was 2 years. His GP had told the CM referred to his case that he was considered to be in need of palliative care. Mr Barlow’s CM described how discussions about DNACPR had taken place (Box 9). Mr Barlow and his wife referred to the DNACPR document when asked about how well informed they felt about the future. They noted that the CM had initiated this with them by giving them a leaflet and leaving them to decide what they wanted. In her second interview, at the end of the study period, the CM talked about potentially revisiting the DNACPR decision with Mr Barlow, but did not feel this was necessary.
It was about [saying] ‘with a chest infection and eventually your heart can get tired, if it did stop beating and then therefore you would maybe stop breathing, would you want an ambulance crew to physically try to resuscitate you? Or would you want them to come and be with you and help, but without actually the physical chest compressions?’ . . . And, ‘you don’t have to answer me now, you and [your wife] can talk about this’. And, so it took, took a couple or three more visits before we got an answer to that.
Mr Barlow’s CM, interview 1
We’ve got a letter in the bedroom, haven’t we, which is already sorted, if he, well, don’t know what word it is, what do you call it? If any, if ambulance man has to come, if he has to be resuscitated.
I don’t want to.
He doesn’t want to. So that’s all sorted.
Mr and Mrs Barlow, interview 2
We’ve done the Do Not Attempt Resuscitation form and it’s at the front of the notes so every time I open it, there’s this big, red form, and he sees that, I see that. . . . So, no, I haven’t discussed it again and because, that’s probably my fault, if there is a fault to be had because I don’t see why I need to remind him of something that’s so abundantly obvious. . . . I feel like we all know.
Mr Barlow’s CM, interview 2
This decision about DNACPR appears to have been discussed and documented with a shared understanding of what it means between the health professional, Mr Barlow and his wife. However, issues around PPOC and PPOD are much more complex and ambiguous. From discussions with Mr Barlow about his time in hospital, the CM identified that she felt he would want to die at home because he had expressed a clear wish not to go into hospital. She had specified his PPOD as ‘home’, despite not having this direct conversation with him. In interviews, Mr and Mrs Barlow expressed complex views about going to hospital. He stated that he did not want to go to hospital, but recognised that he would do so if the consultant felt it was necessary. Mr Barlow felt that not only was the hospital very busy and without his home comforts but it was hard for his wife and family to visit him. Reducing the burden of care for his wife was an important consideration. However, when a crisis occurred, Mr Barlow became very scared and distressed by breathing difficulties and was willing to be admitted. Given his ongoing resilience and recovery from exacerbations, it could not be confidently predicted that any admission was likely to be his last. The CM also had some concerns that the couple perhaps did not agree about whether or not to go to hospital in the future. Overall, Mr Barlow seemed less averse to going to hospital than his wife, but the CM wondered if she would remain so resistant if she felt her husband was actually dying. It was interesting to note that she did not feel the need to openly discuss these issues with this couple so that a clear plan could be made in preparation for this eventuality.
He wants to be at home, yes, in a roundabout way, not a direct way, as ‘Where do you want to spend the last days of your life?’ I haven’t asked that direct question. What I have said is, ‘Your time in hospital, you never enjoy that time. Everything we’re trying to do is about trying to be at home, is that what you want to happen?’ . . . He really, really does not want to go to hospital. Even for IV [intravenous antibiotics] where he knows he’ll respond because he’s had the experience and comes home again. And so, I, so from that, I’ve elicited that he really desperately doesn’t want to be in hospital, for any reason, least of all to die.
Mr Barlow’s CM, interview 1
I mean, if he’s got capacity, that’s where that all comes in, then he will always have that ultimate choice. If not, it’ll be [his wife]. So I think [his wife] would think an acute admission was suitable and [Mr Barlow] wouldn’t so I think that they’re the two that are going to have the difficulties there . . . So I’m not sure how that’s going to play out, [his wife] wouldn’t want him, she wouldn’t want him to go without a fight, she’ll want all, I think, all treatment, therapies offered and delivered if at all possible. Whereas I think [Mr Barlow] is more like, ‘Oh, just let me be peaceful here at home’.
Mr Barlow’s CM, interview 2
The CM’s assumptions about Mr Barlow’s PPOD are based on his expressed views about not wanting to go to hospital, yet not wanting to go to hospital is not the same thing as wanting to die at home or indeed not wanting to die in hospital. The lack of expressed conversation on this topic and clear language about PPOC as distinguished from PPOD leads to an unclear picture of what might happen or who would make these decisions when Mr Barlow was finally considered to be dying. Although she recognised Mr Barlow as getting ‘more frail’, and despite the extended period of time he had been designated as requiring palliative care, Mr Barlow’s resilience to continued exacerbations made it difficult for the CM to identify when he should be considered to be at the end of life and therefore when to initiate more focused conversation about his wishes.
Professional use of vague language appeared to be a source of frustration for some patients and families, who wanted explicit information so that they could be clear about the situation. Mr Patterson was an 83-year-old man who had lived with COPD for 8 years and had more recently been diagnosed with lung cancer. When Mr Patterson was admitted to the hospice for respite, his wife reported receiving vague messages about his prognosis. It was only when her daughter asked staff for a direct answer to her question about what was happening that they were able to make decisions about Mr Patterson’s care in light of his sudden deterioration.
I think he knew, basically, he wasn’t coming home. From his attitude. And on the Monday afternoon, we had a long conversation with the whole team. And they were very nice and skirting the issues, we, both myself and my daughters wanted to be in there, saying, ‘Look, just tell me what’s the bottom line?’ [laughs] And in the end, my eldest daughter who’s a bit impetuous, she said, ‘Well, you’ve been very helpful but I just want a straight answer. What are the chances of me taking my dad home?’ And he looked and said, ‘Very slim, he’s very poorly at the moment’. So I made the decision there and then, having discussed it with [my husband] over the years and I said, ‘Well, if that’s the case, then, I want him to be kept comfortable and pain free’. So, they said ‘Fine’.
Mrs Patterson, interview 2
Mr Jacobs, an 82-year-old man with COPD and renal disease, was the only participant to have an ADRT in place. It appeared, however, that the ADRT was not as comprehensive as Mr Jacobs and his wife thought. Throughout his interviews he was consistent in his narrative about his wish not to go to hospital and how this had been documented. However, this is not explicitly stated in his ADRT, his electronic medical records or his home-held notes. The ADRT document merely stated ‘Even if my life is at risk as a result I do not want intravenous or artificial feeding or fluid’ in the circumstances that he was unable to ‘carry out independently all activities of daily living’. These rudimentary and ambiguous statements did not meet Mr Jacobs’s expressed needs. In this case, and despite regular discussions, a lack of clear communication and documentation had resulted in a disparity in understanding between Mr Jacobs and his wife, on the one hand, and his CM, on the other (Box 10). In all his interviews Mr Jacobs was clear that he did not want to go to hospital and wished to die at home. It seemed that both his CM and his GP recognised this but it was not documented in his records. In addition, Mr Jacobs and his wife were both clear that he did not want to be resuscitated and that he had ‘a form’ in place to this effect. However, again, this was not documented in his records and the CM stated in both her interviews that she had not completed the DNACPR form and indeed was of the belief that Mr Jacobs did want resuscitating. Mr Jacobs held his CM in very high regard and often stated that it was her management of his conditions that allowed him to remain at home and avoid hospital admissions. He was also very clear about his wishes and expressed them frequently, so it is unclear in this case why these wishes were not documented more explicitly.
I suppose we never quite got round the DNACPR . . . it was something he didn’t want to be in place, even though there is almost a kind of contradiction in terms of what he has put in his advance directive. But again, but [Mr Jacobs] is very much somebody that wants to be in control and gets frustrated. I know his wife would say how difficult he finds it that he has to be dependent on other people and therefore it is very important that he has what he wants in that advance directive. And whether there are discrepancies or anomalies or, that doesn’t really matter, it’s about his own peace of mind I think.
Mr Jacobs’s CM, interview 2
Oh no, no, I don’t want to go back in [to hospital].
So, have you talked that through with the community matron? . . .
Yes. Yes. Yes. She knows. She knows the position.
And he signed, he’s signed papers and everything . . . Even if I have to call an ambulance . . . they know that it’s on the records that he does not want to be resuscitated.
You’ve got a form for not being resuscitated in place then?
Yes. Everything’s in place, because the matron explained it all to me, how that works. And she explained everything to me. And, she said that with my problems that I’ve got, my bag and everything, you know, she said, ‘It’s entirely up to you’, she said, but, she said, ‘How you are, I don’t think they would resuscitate you anyway’. I said, ‘Well, I don’t really want to, because’, I said, ‘I never want to finish up like my mother’.
Mr and Mrs Jacobs, interview 1
Oh, I’m not going to hospital. No way. No way. No way. . . . Matron has got everything written down and I’ve signed a sheet, you know, and . . . signed the form and everything. When I die, I want to die here.
Mr Jacobs, interview 2
Like Mr Jacobs, Mr Brown and Mr Farley were considered by health professionals to have an ‘open’ attitude to conversations about death and dying. Such ‘openness’ was considered to help when health professionals had to have difficult conversations. Patients were likely to be more receptive following the occurrence of critical developments such as diagnosis or exacerbation of their illness, or at a time when they were feeling particularly ill. Having raised the topic, Mr Farley’s PCN left him leaflets to read about ‘Planning your future care’ and resuscitation, with the option to discuss these further at a later meeting. Having received the leaflets, Mr Farley reported that this prompted him to think about the issues. The conversation was returned to on a number of occasions, both by the PCN and latterly by the DN on his transfer to the care home.
He was quite easy in terms of assessment and things because he was just really open, so, right from the beginning, he was just sort of quite straight[forward] . . . he was quite clear at the beginning that he wanted to try and stay and home.
Mr Brown’s PCN, interview 1
At that time, he knew it was advanced disease, he knew it was palliative and he knew, at some point, it potentially could get worse. . . . And I think, because he was quite open with that conversation, I gave it, we’ve got a Do Not Attempt Resuscitation booklet, information booklet, and gave him that as well, . . . I’d been a couple of times before that cropped up, and he said he’d keep it on one side. . . . He sort of took the option of, ‘Well, yes, I might have to consider that at some point but, as we are now, this is what I want to focus on’.
Mr Farley’s PCN, interview 1
Impact of and responses to advance care planning
This section looks at how people responded to making plans for end of life in advance and the kinds of impact experienced by patients and their families when ACP was or was not put in place. None of the nine patients who died during follow-up did so in hospital; six died at home, which was their stated PPOD. In the cases of Mrs Jones, Mrs Winters and Mr Corley, ACP seemed to be instrumental in things turning out as planned and facilitating their deaths at home as they wished. Certainly, Mr Corley’s case provided an example of the impact of having a DNACPR in place when paramedics were called and required this document in order to allow a natural death to occur without any attempt at resuscitation.
The only thing that [my husband] wrote down was that he didn’t want to be resuscitated if ever anything happened. . . . [On the morning he died] I rang the district nurse team and they said, ‘Do you want paramedics or police?’, I said, ‘Well, I don’t know . . .’. And they sent the paramedics, thankfully, they were lovely. They were lovely. Even though I knew he didn’t want to be resuscitated, but you’re just in a, you’re in a panic, you don’t know what you’re saying, I didn’t know who I needed to come, I just needed somebody here, they just, they just took control then and, [the paramedic] kept saying, ‘I need proof that he doesn’t want resuscitating’, but then, the district nurse file was there.
Mrs Corley, interview 2
Preferred place of death was also achieved for Mr Williamson, Mr Andrews and Mrs Tomlinson by making use of the fast track system and transferring them home from hospital to die. A small number of patients such as Mr Farley and Mr Jacobs expressed being reassured by having an ACP in place.
I’ve signed the form here to say that I don’t want resuscitation . . . if I get to a situation where that is the only way to prolong my life, . . . I felt it was appropriate . . .
Yes. You were pleased, weren’t you?
I thought that my condition was such that it was one of the things I ought to be aware of.
Mr and Mrs Farley, interview 1
However, unless health professionals, patients and families all agreed to the same plan its existence became somewhat superfluous. Mr Jacobs expressed being pleased that his wishes had been taken into account by his CM and GP and that these had been recorded in his notes. However, as identified in the previous section, Mr Jacobs’s understanding of what was documented differed from what was recorded in his medical records and expressed by his CM in interviews. Hence, he may have been falsely reassured. In an astute observation Mrs Elder recognised that ACP in itself may offer a false reassurance, as circumstances may dictate the actual outcome. Patients and families seemed to recognise the limitations of plans, which were likely to be overtaken by events.
I said I would prefer if possible, at home. But I think they’ve stopped one of the services that the Macmillan nurses used to provide, where they come and stay with you. So I don’t know whether that would still be allowed, but I don’t want to go into hospital, I’d rather go to the hospice, if I, well, I won’t have a choice, will I, really?
Mrs Elder, interview 2
This tendency constitutes a clear limitation of ACP. In three cases the initial PPOD was not achieved because of changes in the circumstances of the patient’s health and the availability of resources at the time.
Mr Farley was a 79-year-old man with advanced prostate cancer. His wife had been caring for him at home. However, suspected brain metastases caused Mr Farley to behave in a confused manner. Mrs Farley had the support of home carers but ultimately their house was not suitable for the level of care required. Mr Farley had initially expressed a preference to die at home, but from the outset was aware that this might not be possible, and considered hospital to be the likely and acceptable alternative. His preferences were largely determined by his desire not to burden his wife. As his condition deteriorated, he began attending hospice as a day patient, and, having become aware of this as an option, specified this as his PPOD. However, when he needed to be admitted for terminal care, the hospice did not have any available beds and Mr Farley was moved to a local care home. Mrs Farley subsequently reported being very happy with the care her husband received, and recognised that, in the circumstances, his move to a care home had been the most appropriate action. Yet she noted that not being able to achieve her husband’s PPOD left her with some feelings of guilt.
The one thing that we didn’t get right was that he decided he wanted to go to the hospice. . . . One or two people knew that he would have liked to go to the hospice but then, you see, as it turned out, because he was ill at the bank holiday time, it was a case of, they’d get him a bed anywhere they could. . . . And so, he didn’t, he never went to the hospice. And I always, I still felt a bit guilty after that.
Mrs Farley, interview 5
Mr Brown, a 63-year-old man with a diagnosis of advanced lung cancer, had expressed his wish to die at home. During an admission to the local hospice for respite care and symptom control, he had become increasingly confused, and his pain remained uncontrolled. Hospice staff assessed his capacity as fluctuating and 2 days before his death reported that he was likely to have suffered a stroke. In addition, it was clear that his wife was very anxious about the prospect of her husband returning home to die, and felt that she would not be able to cope. In these circumstances, the hospice staff felt that Mr Brown was not able to return home, despite his clearly expressed wish to do so (Box 11).
He wanted to go home but it was evident that his wife was completely terrified about the idea of him going home. . . . But I think, at the end of the day, doesn’t matter how much a patient wants to die at home, if the family aren’t going to cope, . . . you’re setting them up to fail and then everyone feels worse. . . . He did want to get back home and he was deteriorating, because of the confusion, I just think that his wife just, she was so relieved in the end, when the decision was to keep him here.
Mr Brown’s PCN, interview 1
There was every intention with that admission of admitting him and getting him home because that was well recorded as his preference to the end . . . His clinical condition changed . . . his choices were fluctuating almost hour by hour. . . . his wife, his partner, became progressively more, more frightened by the fact that he was deteriorating but also, these changes in his confusion. . . . Because if we took his best interests and ignored everything else that was going on around him that might actually not be in his best interests to ignore all those other things.
Mr Brown’s CPM, interview 1
Changing plans were a pragmatic and acknowledged element of ACP and could be precipitated by a change in the patient’s wishes as well as a change in circumstances. Mr Patterson had stated home as his PPOD. However, Mrs Patterson, also in her eighties, was struggling to care for her husband at home. She was especially concerned about caring for him at night and the impact interrupted sleep was having on her own health and ability to continue his support. After some discussion between health professionals and the family, Mr Patterson felt he did not want to go to a nursing home but would be happy to be placed on the waiting list for the hospice. After a short wait, Mr Patterson was admitted to the hospice for what was expected to be respite care. His wife related that ultimately he had been relieved to be admitted to the hospice and was happy and comfortable to die there. He died 3 days after his admission.
Mr Brown’s and Mr Patterson’s cases also illustrate the importance of family carers to the outcome of any plan, through their availability, willingness and capacity to support the patient to die at home. Indeed, many patients identified this as a caveat in their planning, most citing that they would like to stay at home ‘as long as’ it was feasible or ‘until’ it was no longer feasible because of the burden of care for their families. For family carers, managing this burden of care could mean that they had little time for anything else. Mrs Corley and Mrs Farley both talked of how the tasks of ‘doing’ took over, giving them little time to think about future plans. Like Mrs Brown, Mrs Farley was quite clear, in a subsequent interview, that she had not wanted her husband to die at home.
The lack of ACP and clear communication about foreseen care needs and wishes could have negative impacts for carers into bereavement. Mr Andrews was an 85-year-old man with stomach cancer. Once metastases were identified, Mr Andrews had been considered suitable for palliative care by health professionals. However, this did not seem to have been communicated adequately to either himself or his wife, with both reporting that the cancer had not returned. The community nursing team were involved but the couple reported that the nurses had little time to talk to them about their concerns or feelings, prioritising physical care. Although clearly concerned about Mr Andrews’s health and the prospect of recurrence or spread of cancer, the couple had not raised or discussed these issues with any of the professionals providing care. Although they described feeling left in the dark, it appeared also that they were highly ambivalent about exploring Mr Andrews’s prognosis further. Clearly emotional, during interviews, about the recognition that their time together might be limited, and apprehensive about the future, they also seemed inclined to temporise, trying to push the prospect of death out of the near future. Mr Andrews died 1 month after his second interview, shortly after a further admission to hospital with back and hip pain. Despite visiting her husband every day in hospital, Mrs Andrews reported that she had remained unaware that he was dying. In response to his wish to go home, Mr Andrews had been discharged from hospital with an extensive care package involving nurses/carers visiting four times a day. However, Mrs Andrews reported that there was still no reference to the reality of what was happening, and even up to the moment of death she did not appreciate that her husband was dying. Overall, despite a number of nurses being involved in Mr Andrews’s care, especially towards the end of life, it was clear no effective relationships had developed with these or any other of the health professionals involved in his care. The case medical records indicated a number of elements of professional planning. Mr Andrews had been placed on the GSF register with his GP practice several months before his death, and his eligibility for the DS1500 had been discussed at the MDT. He had been fast tracked home from his final hospital admission with anticipatory medications in place and been upgraded to ‘amber’ on the GSF register. These elements of professional planning appear to have taken place without effective communication with Mr Andrews or his wife. There was some indication that Mr Andrews knew he was dying during his final stay in hospital but it seemed that his wife distanced herself from this knowledge as a way of coping. In a later interview she recognised that she had possibly missed cues or ignored signs (Box 12). Although a lack of open discussion and planning in Mr Andrew’s case seems to have left his wife ill prepared for his death, she reflected that denial had been her coping strategy.
The district nurses, when they come, just writ[e] things and, and the folder’s in there, and the reports, they don’t ask me any questions really.
And how about your GP [. . .]?
Oh, she asks a lot of questions but never once mentioned cancer until [my wife] did.
Mr Andrews, interview 2
On the day he died he had not wanted to eat or drink. . . . In the afternoon Mr Andrews had become agitated and at this point she [Mrs Andrews] had phoned the nurse and asked her to come down – and two of them did. But she still did not realise what was happening. . . . But again, she thinks, she should have realised the significance of the nurses’ action – the first thing they did was put a waterproof sheet under her husband. The nurses were there for about half an hour – when one of them said that ‘she didn’t think it would be long now’, and the other said immediately ‘I think he’s gone now’.
Notes from telephone interview with Mrs Andrews, interview 3
Some patients and family carers commented on what having planning in place meant to them. Some considered it to be reassuring to have their wishes documented so that they were more likely to be carried out. However, others recognised the fluidity of plans and their susceptibility to changes in response to circumstances. Among the nine patients who died, it was clear that, although ACPs could have a positive influence on outcomes such as a avoiding resuscitation, plans for preferred place of care and death were dependent, predominantly, on family carers and also the availability of community services. Three cases in this study also showed the importance of the fast track system in allowing transfers from hospital to home once the dying phase was recognised. This system can work well, but can also mean that efforts to achieve death at home result in very late transfers, made when the patient is very close to death. In Mrs Tomlinson’s case, although her family were happy she had died at home, as they felt this complied with her wishes, she was comatose by the time she was transferred home and died only a few hours later, which potentially queries the emphasis placed on where death occurs.
Chapter summary
In this chapter we have used examples of individual cases to illustrate prevalent themes from the data. These include responses to bad news in patients’ accounts of diagnosis and prognosis, in which we address areas of information seeking for personal planning, the impact of living with uncertainty and the role information blocking might play in coping with facing mortality. We then explored themes of barriers to ACP, initiating ACP, the discussion of ACP and the impact of ACP in shaping the circumstances of death and dying.
Patients’ accounts show the diversity of responses to ACP. Some were proactive in their engagement and information seeking, whereas others resisted discussion of ACP, or engaged with this only in response to prompting. These approaches seemed to reflect patient attitudes to planning more widely. Proactive patients incorporated aspects of ACP as an extension of their personal planning and preference to achieve control in managing their lives. The majority expressed wishes to remain at home until that was no longer possible, and many placed their own caveats on what service provision or level of care need would constitute a limit for home care. Patients were pragmatic about the uncertainty of planning and prioritised not burdening their family over place of death. A prime consideration was to be comfortable and pain free. Patients and health professionals generally agreed that it was not necessary or appropriate to hold ACP discussions while the patient remained relatively well. The timing of such discussions was often prompted by a deterioration in the patient’s condition which heralded the approach of death. Plans documented in advance were likely to be subject to revision later. Contrary to the aims of current policy, ACP tended to be reactive rather than anticipatory and pre-emptive.
The themes derived from these data clearly illustrate the importance of family carers in achieving plans for the patient to remain at home throughout death and dying. Personal planning was often undertaken with, and perhaps prompted by, family members rather than health professionals. Some family carers expressed the need for prognostic information in order to prepare themselves to support the patient and for their impending loss. In approaching and undertaking ACP conversations, health professionals often focused on making sure a DNACPR was in place and recording a preference for place of death. Other areas of ACP tended to be more vaguely executed and not always directly discussed. Predicting the right time to have conversations, especially in relation to the uncertainties of prognosis, was reported to be challenging for health professionals. Most suggested they would be led by the patient’s indication that they were receptive, or prompted by a change in the patient’s condition. Professional planning incorporated those elements of ACP which influenced the allocation of resources and provision of care for patients and were in line with practice incentives and performance targets. However, professional planning extended far beyond these limited aspects of ACP and went on largely beyond patients’ awareness.
Medical records provided a valuable element of data for exploring ACP in practice. In some cases there was no evidence of ACP in either interview accounts or medical records. Some records showed evidence of professional planning by noting when patients had been discussed at the MDT or GSF meeting, when the issue of the DS1500 form might have been raised, and referrals made to specialist services. However, even carefully maintained records with special sections for palliative care did not capture the extent to which interviews reported EOLC conversations to have taken place. In the majority of cases, elements of ACP were reduced to tick boxes and brief annotations. These issues are discussed further in Chapter 6.
Chapter 6 Discussion and conclusions
Introduction
Advance care planning has become an important component of the EOLCS to improve the quality of care for dying patients and their families. In its wider formulation, ACP involves a process of reflection and discussion about the individual’s wishes for future care, not only regarding the end of life, and particularly in the event she or he loses capacity to make decisions independently. 172–174 Ideally, ACP should be undertaken when people are relatively well, or at least when their condition is stable, with regular review and revision of documented or verbal plans. 4,43 The EOLCS aims for ACP to be initiated when patients are identified as likely to be within the last year of their life. ACP has developed within a cultural and professional ideology combining commitment to the value of individual autonomy and choice and a practice of palliative care promoting a particular vision of ‘the good death’. 38,39 The good death is a professionally brokered experience and focuses on the patient being comfortable, free from pain, in her or his preferred place and accompanied by family and significant others. An open awareness of dying enables communication and transparency about the circumstances of death. ACP is reported to increase the chances of patients dying in their preferred place, assumed usually to be home, and experiencing less invasive (and less costly) treatment. 128,130–132,138,139 Nevertheless, evidence regarding the effectiveness of ACP is limited and conflicting. 4 The policy is not based on evidence about patients’ and the public’s understanding and experience of ACP, their preferences for how and when this should be discussed, or their attitudes to death and dying. 175
This study supports findings from previous research that ACP remains uncommon, is often limited to documentation of a few key decisions about CPR and place of death, is reported to be challenging by many health professionals, is not welcomed by a substantial number of patients and tends to be postponed until death is clearly imminent. 5–14 The current model of ACP presupposes a high degree of prognostic accuracy in identifying patients entering the last year of life that is not achievable in practice. This applies particularly to patients with comorbidities and long-term conditions,43,117,118,120 but also to those with cancer, which has often been assumed to display a more predicable trajectory. 116
Professional respondents expressed a low awareness of current policy and guidelines relating to ACP. 53 Very few made any reference to the EOLCPW or use of the many text and web-based resources available to support patients and professionals in discussion of ACP. Professionals undertook specific aspects of ACP, such as completion of DNACPR forms and documenting patients’ PPOD, within the wider framework of organising and coordinating EOLC. Practice GSF meetings provided an important forum for prompting recognition and discussion of palliative cases and allocation of tasks among the MDT, including, sometimes, those related to ACP. Although most UK practices have GSF registers,23 the majority (75%) of patients are not on these when they die, and only a quarter of those who are have conditions other than cancer. 120,176 GPs have been encouraged to find the 1% of patients in each practice who are expected to be eligible for inclusion on the register. None of the study practices had approached this figure, and the target was judged to be unrealistic, making registers unmanageable.
The correspondence between current guidelines and implementation of ACP as evidenced in the study data was poor. Respondents rarely referred to ‘advance care planning’ explicitly, and there was a confusion of terminology and intent between ACP and usual care. 176 ACP tended to be operationalised in terms of a few specific, discrete and easily measurable tasks, rather than viewed as a means of exploring patient goals and values for future care, particularly in the event of lost capacity. This raises a question about exactly how ACP should be defined: what has to happen in order to be able to say that ACP has been undertaken? Is it enough for a patient to record her or his preferences for resuscitation or place of death, or is more than this required? Is consideration of capacity essential? Uncertainty about how this question should be answered makes it difficult to recognise when ACP has been accomplished: within the study data the phenomenon remained elusive. Nevertheless, for the purposes of this discussion, we refer to ACP having taken place when there was evidence that any of its discrete elements had been discussed or documented.
How established is advance care planning in community care?
The study findings support reports from other studies that ACP is not well established in community care settings11,35,80,88 and that it tends to be limited and perfunctory in extent. 43 Most professionals found ACP difficult, and such discussions were not common. In nine of 21 patient cases there was no indication of any element of ACP. Although 15 of 21 patients’ cases had been placed on the practice GSF register, not all were aware of this, or its significance. The reasons for some patients’ inclusion remained unclear. By the end of follow-up, just over half (11 of 21) of patient cases had a DNACPR order and the same number had a documented preference for place of death. One patient had a (poorly worded) ADRT, completed at his instigation.
An important finding of the study was identification of a category of frail elderly patients, often living alone with debilitating comorbid conditions, who slipped through the net in terms of ACP. Despite great age, complex health problems and substantial input from a range of health services, these individuals had not developed needs that were recognised as requiring palliative care, or established significant relationships with any professionals providing care. Lack of connection with a GP was a notable feature of these cases, especially if their care was mainly provided through the secondary sector. Nevertheless, these patients, characterised by great vulnerability and lack of social support, were walking on very thin ice in terms of imminent mortality, and lacked supportive structures or anticipatory care as they approached the end of life.
Who initiates advance care planning?
Professional accounts indicated that discussion of ACP was much easier when the patient took responsibility for initiating the conversation. This was described as being relatively unusual. Generally, however, it was considered appropriate for professionals to start the discussion, and patients are often thought to wait for this to happen. 5,43,87 Anyone from a wide range of professional services could initiate ACP, which meant that it was not always clear who should or did. This is consistent with the aim of generalising EOLC skills across professional roles throughout community care. In relation to the study data, initiation of the topic was most commonly undertaken by specialist nurses. Occasionally it was apparent that several different professionals might be involved at different times, including secondary care clinicians. Consideration of matters relevant to ACP could be distributed over time and place. However, some GPs and senior nurses expressed reluctance to broach the topic, and preferred to delegate this task to colleagues. Specialist nurses with a specific EOLC remit, or who were involved in supporting patients with an extended illness trajectory, such as multiple sclerosis or motor neuron disease, described greater confidence and experience in undertaking ACP as an ongoing aspect of their practice. Otherwise, the occurrence of ACP seemed to be determined largely by the personal inclination, confidence, judgement and communication skills of individual practitioners. Indeed, professionals justified the lack of allocated roles for ACP discussion to allow for the flexible application of variable skills and motivation among individual practitioners. There were also practical reasons underlying professional engagement with ACP: GPs lacked knowledge or regular contact with some patients with whom a good relationship had not been established. Practice appointments were acknowledged to be a difficult and time-constrained environment for undertaking ACP. Some specialist services, such as Macmillan nurses, incorporate a specific remit to support dying patients, and these staff may be more accustomed to raising issues around ACP as a reason for referral. Ideally, however, respondents felt that ACP was best approached from within an established relationship. The lack of such a connection was one reason for the lack of ACP among the group of frail elderly patients. However, an established relationship could also pose a barrier to ACP discussion. Some professionals described the difficulty they would have in raising issues of death and dying with patients they had worked to support and help positively cope with life for an extended period of time: this transition was felt to signify failure and betrayal.
When is advance care planning initiated?
The data support findings from previous studies that professionally brokered ACP discussions tend to occur reactively, rather than pre-emptively, and late in the day, when it has become clear that the patient is approaching death. 8,96 The GSF register was a key mechanism for co-ordination of palliative care, including the initiation of ACP. However, registers were dominated by cancer patients. Patients tended to be placed on the register only when they were judged to be in the last months or weeks of life. Professionals were sceptical about the feasibility or benefits of more accurate prognostication, especially among those affected by long-term conditions.
Patients were also reluctant to commit to decisions about an uncertain future, and tended to take a cautious, pragmatic approach to their options for future care. As in previous studies, ACP was often not considered relevant until illness had become advanced. 6,12,43,123 This congruence between patient and professional preferences for the timing of ACP is notable. ACP was thus often triggered by events rather than being carried out pre-emptively. GP respondents, in particular, expressed the view that decision-making for EOLC would be driven by the progression of the patient’s illness. This tended to negate the perceived need or value of planning in advance, particularly as everyone recognised the provisional nature of plans liable to change. Recognition of the purpose of ACP as a means of preserving autonomy in the event of future lost capacity was virtually absent from the data.
Documenting advance care planning
Systems of documenting and sharing written information are critical elements of effective patient care, especially in complex systems of delivery. The content and availability of forms and templates defines the nature of the tasks to be completed and directs attention towards certain topics rather than others. They also allow audit and assessment of easily measurable aspects of professional practice and can be conveniently linked to targets as a means of evaluating care and incentivising practice. In this sense, documentation functions as an important agent or mechanism of care. ACP is promoted as a voluntary activity directed by patient preferences that need not result in formal documentation of decisions about end of life. Nevertheless, without effective methods of recording and, crucially, sharing information between services, it is difficult to see how ACP could be implemented effectively. Somewhat paradoxically, as the focus of anticipatory planning moves from the formality of ADRTs to the informality of ACP, a plethora of templates, documents and resources has developed to encourage the recording of patients’ EOLC preferences and to support professional and patient discussion. The documented records relating to ACP discussions were usually brief and uninformative. Practices participating in the study varied in the arrangements in place for transferring information between professionals and the extent to which electronic transmission was enabled. Regardless of this, it is interesting that in a complex and sometimes fragmented system of health care it was the face-to-face GSF meetings that brought the MDT together and that continued to be a key mechanism in arranging and co-ordinating EOLC for practice patients.
When they had been completed, DNACPR and PPOD forms remained in the patient’s home to enable immediate professional access. The presence of these forms prompts discussion of their purpose and content and is, consequently, an important spur to initiation of talk about resuscitation and place of death. However, the forms focus on these very limited issues, and do not in themselves prompt discussion of wider concerns and aspirations which patients may wish to express in relation to death and dying, including treatments and interventions they may wish to refuse. Some professional respondents described the value of documentation, including EOLC pathways, in providing checklists and prompting discussion. Documents may enable and structure, but also inhibit and constrain, the content of conversations. Consequently, there was also ambivalence, particularly among GPs, towards the reduction of ACP to a simplistic ‘tick box’ exercise underpinning the need to meet quality appraisal and financial incentive targets. ‘Paperwork’ was described as time-consuming and burdensome and also as deflecting attention from the essential focus on communicating with the patient. The task of ‘having to fill in forms’ could also detract from professional authority, although some respondents found it helpful to use the need to complete these documents as a way into initiating discussion of ACP.
Barriers to the implementation of advance care planning
Prognostication
The uncertainty of prognosis presents a major barrier to professional identification of patients as needing palliative care, their inclusion on GSF registers and the initiation of ACP, and to patients’ understanding of their prognosis and receptivity to discuss plans and options for EOLC. This was a prominent theme throughout the study findings, and well established in the wider literature. 12,43,88,96,117,118,120 One reason for professional caution was the knowledge of the harm and distress occasioned by an inaccurate prognosis. In particular, if this turned out to overestimate the patient’s survival, the consequences for the doctor’s relationship with the family, not to mention her or his professional credibility, could be very damaging.
Professional responses
Professionals varied greatly in their confidence, experience, and personal inclination to engage in discussion of ACP, but many described this as challenging and infrequent. 35,88 Respondents tended to shift perspective in different contexts, acknowledging that ACP was a good idea in principle, but moving to describe its limitations in practice. 53,89 Professionals were aware of organisational and financial incentives to meet quality appraisal targets relating to avoidance of hospitalisation, maintaining the GSF register and documenting PPOD. There were also some concerns, especially among GPs, about the imposition of ACP as a bureaucratic ‘tick box’ task, which undermined clinical judgement and autonomy. 53,85 An important disincentive was the expectation that a substantial number of patients would not be receptive to discussion and might be harmed by inappropriate timing of ACP discussions and the distress and destruction of hope these might entail. 12,88,92 Professionals were understandably wary of causing distress and harming relationships that were the cornerstone of care. Unless patients themselves directly broached the topic, it was difficult to judge their readiness to engage in ACP. Deconstructed parts of ACP, such as decisions about PPOD and DNACPR, tended to get subsumed within the more general management of EOLC, and it is this that respondents talked about, rather than ACP. The term was never used by patients.
Vague language and professional persuasion
Effective ACP depends on skilled and sensitive communication, including transparency and mutual understanding. Nevertheless, as widely reported in other studies, professional approaches tended to be cautious as they sought to identify cues from patients, or offer cues for patients to identify, if and when they were willing to pursue the topic. 11,88,122 Such offers, on both sides, were characterised by ambiguity and suggestion. This has the advantage of allowing either party to back off, and to avoid patients feeling under pressure to discuss difficult topics unless they want to do so. Professionals expected that a substantial number of patients would not be receptive to discussion or decision-making about ACP. 12,70,88,92,106,123,126 Patient denial, and failure to realise that they were dying, was cited as an important barrier to ACP discussion. 88 Discussion tended to be hedged by vague and euphemistic language. 12,67 Although some professionals maintained that tacit understanding was sufficient, this strategy risked misunderstanding and uncertainty about what had actually been established. This was particularly pertinent in relation to the distinction between patients’ preferences for place of care and place of death; vague language elides the distinction between these. 69,84 It is evident that there may be a considerable discrepancy between patient and professional recall and understanding of what was said and what was meant in ACP discussions. 14,115 Misplaced confidence in tacit understanding also inclined professionals to make, and sometimes document, assumptions about patient preferences, which may not correspond with what was actually intended or preferred. 67,115
Patient and carer responses to the offer of an advance care planning discussion
The study data support established findings that take-up of ACP in community care practice remains limited. 80 Nearly half of patient cases (9 of 21) had no reported or documented discussion of ACP. We cannot know if the topic had been broached, or indeed if cues to open a discussion may have been offered but disregarded or unreported. However, in the context of the wider study findings, this seems unlikely. The remaining cases illustrate the diversity of responses to ACP and willingness and motivation to discuss EOLC. Only three of the patients had initiated the topic for discussion. The careful, stepwise approach to introducing ACP described by most professionals fitted well with patients’ preferences to consider this late on, and in response to a significant deterioration in their condition. It was important to find the time when patients indicated they were ‘ready’ to consider ACP, and this tended to be when they were close to dying. 14,177 Patients could also shift in their receptiveness to consider ACP at different stages in their illness. This intensified the difficulty for professionals wishing to raise, or pursue, the topic for discussion. A few patients maintained a clear awareness and explicit focus on the approach of death. More commonly, accounts indicated a preference to park the prospect of a limited future until the imminence of death could no longer be denied. Some initial consideration of anticipatory planning might be undertaken at or around the point of diagnosis, to be replaced by a limited positive recovery orientation in which the focus is on living in, and enjoying, the present rather than look too closely into an uncertain future. A clear theme running through the data and the wider literature concerns the variability of patient preferences and responses to ACP discussions and their timing, and the tendency for such preferences to change. 5,12,70,78,84,88,92,123,126,178
Preferred place of death
Home has become established as the best and, most usually, PPOD. This underpins its status as a proxy indication of the success of ACP and quality of EOLC. However, much evidence about patient and public attitudes to place of death derives from population surveys16,60 and quantitative methods of inquiry. 128,132,139 These do not capture the complexity of choices patients make when confronted with the experience of frailty and comorbidity in great old age. 179 There is (largely qualitative) evidence that the desire for a home death decreases with age and severity of illness. 67–69,179 The current orthodoxy that home is the best, and usually preferred, place of death is coming under challenge. Evidence accumulates about the complex situational factors underlying decisions and the varied preferences which may subsequently be expressed. 22,59,66,69,142,180 The focus on place has deflected attention from how death is experienced in different settings. 69,72,73,77,179 Patients tend to adopt a pragmatic stance to place of death. Home might be preferred in principle, but that preference over-ridden by contextual factors,67,69 and hospital is not necessarily dispreferred. 69,72–74,77,86 Some carers may not want their relative to die at home. 73 There is consistent evidence that the key priority for patients is control of pain, followed by not imposing a burden on family members. 5,65,69,74,76,78,81,82,107,125,133,181 Indeed, the desire to makes things easier for family members is stated to be one of the principal reasons for patients to engage in ACP.
The study findings support this revision of the current orthodoxy that home is, by default, the best and PPOD. Six of the nine patients who died did so at home, which was their preferred place. However, respondents expressed uncertainty about what would happen to them during dying, and how they might respond to it. Consequently, they rarely articulated a strong desire or commitment regarding place of death. Their preference was mostly to remain at home for as long as they could, while acknowledging that circumstances might force a relocation. Professionals were strongly committed to the idea that home was the PPOD, and to support patients to die at home. However, they also acknowledged that this was not always possible. Nurses, in particular, expressed awareness of the struggle and difficulties that could be experienced by families in the effort to keep a dying patient at home. Several reflected that home was not necessarily the best option, and might even result in a ‘bad’ death. Thus, the fact that patients do not die in what has been documented as their PPOD does not necessarily mean that they died in the ‘wrong’ place. Conversely, correspondence between documented wishes and place of death does not necessarily signify that patients died well, or in the ‘right’ place. Three patients did not achieve their documented preference for place of death, when circumstances forced a change of plan. Two of their nominated carers had not wanted the patient to die at home. However, they experienced guilt that the patients’ stated preference for place of death was not achieved.
Parallel planning
In analysing the case studies we identified three distinct levels or strands of ‘anticipatory planning’. These levels ran in parallel with various degrees and points of intersection within individual cases; in an ideal (policy) world, all three would be intertwined. ACP, ideally, involves patients, families and health professionals engaging in a process of ongoing discussion about preferences for EOLC, particularly in the event of lost capacity. In practice, however, these aspects were often broken down by health professionals into documentable elements such as DNACPR, PPOD and decisions to avoid further admissions to hospital. In addition, it was clear that a process of ‘professional planning’ also took place, which was not directly oriented to ACP as a patient-centred activity and did not necessarily involve or engage with patients. This kind of planning was undertaken by professionals in the course of managing the case, and in anticipation of the arrangements and resources that would have to be mustered as the patient’s condition deteriorated. Although timing was uncertain, professionals had a clear understanding and anticipation of the likely trajectory of decline as the patient approached the end of life. This knowledge was largely beyond the understanding of patients and their carers. However, regardless of whether or not decisions and anticipations were openly shared with patients and their families, professional planning went on ahead of future need. The principal forum for such professional discussion and decision-making was the regular practice GSF meetings. Here patients were identified as suitable for palliative care and eligible to be placed on the register, and with varying degrees of urgency. Decisions were made about DNACPR status, completion of DS1500 forms, the timing and nature of referral to specialist services, and the delegation of tasks among the members of the MDT.
The third element has been termed ‘personal planning’ and refers to the practical and emotional anticipatory work that patients and families undertake in preparation for death. This encompasses purely pragmatic and practical matters, for example making a will, paying for and planning funerals, and setting financial and other affairs in order. It also involves the existential work of preparing self and others for the experience of death and dying. ACP is a professional construct and tends to be framed as an intervention requiring professional mediation. Little is known about the extent or nature of discussions about end of life issues that may go on within families, though some studies report that patients may look to relatives as well as, and possibly instead of, professionals for this purpose. 133 Within the cases, personal planning seemed largely to occur outside professional engagement or awareness. This was more directly focused on the clinical tasks of resource management and control of symptoms.
Helping patients to prepare for death
Advance care planning aims to enable patients to have a sense of control over future care. In the context of the EOLCS, ACP is considered to be the first stage in the EOLCPW. Consequently, the focus of ACP within current policy implementation is very clearly on approaching death. Anticipatory planning is regarded as a key component in the achievement of a ‘good death’, with the positive and reassuring connotations this conveys. Dying in a chosen place, without the threat of aggressive interventions such as CPR, is a hallmark of ‘dying well’. Professional representations of death in the Care and Communication study were predominantly benign. Respondents talked in terms of supporting patients to have the death they ‘wanted’. Acknowledgement of suffering, or the experience of physical and emotional distress, was rare throughout the data. In contrast, the hard work of dying is depicted graphically in patients’ own accounts and the review of medical records: the relentless rounds of medical tests and appointments, home visits, unremitting pain, constant and debilitating symptoms. A signal issue in EOLC is the extent to which professionals support patients through the acknowledgement of fears about what happens during dying. 182–185 Some respondents were willing to take on board a discussion of patients’ concerns about the physical and existential experience of dying. Such discussions were described as focusing on the present and immediate future, concerned with moving in a stepwise progression to help patients foresee and understand what was likely to happen next, and the kinds of support that could be provided, to help them deal with worsening symptoms and distress, extending gradually to the point of death. This kind of supportive and advocacy role could also be undertaken by professionals in relation to a range of ‘in the moment’ decisions50 about whether or not to have further treatment such as chemotherapy.
‘Choice’ and autonomy
Professionals often talked of presenting ACP decisions to patients in terms of ‘choice’. In relation to the end of life, forward planning is taken to be ‘empowering’, preserving the autonomy and dignity of patients throughout a state of greatest vulnerability and peril. However, as indicated in the findings from this study, while strong efforts may be made to realise patient choices, these are not guaranteed. Some patient trajectories offer greater scope for realising preferences through anticipatory planning, for example neurological conditions and some cancers. For many patients, however, the uncertainty of prognosis makes planning very difficult. Patients themselves were often pragmatic in their appraisal of uncertainty. Patients may wish to ‘choose’ the option that is least difficult for their family, keenly aware that one person’s choice may become another’s burden. It is clear that family support is usually critical to a patient’s ability to remain at home to die. 69,76,186 However, relatives may feel that they have failed in their obligation to support the patient in dying at home if this turns out to be impossible, and they find themselves unable to cope. Alongside an in-principle commitment to home as the PPOD, professional respondents, especially nurses, recognised the difficulty and struggle that could ensue from patient choices, and families’ commitment to support their relative to die at home.
Patient preferences for ACP rarely spring ready formed into discussion, but will be shaped or ‘coconstructed’ through dialogue with others. 67 A strong theme throughout the data is that professionals perceived their role as to guide patients to make the choices that they genuinely believed to be in their best interests. The ideal is to achieve a convergence between (professionally defined) ‘needs’ and patient ‘wants’. In practice, this often involves professionals guiding patients to ‘choose well’. ‘Choices’ are framed by professional knowledge and the availability of restricted options. 48,187 Some people are unaccustomed to making plans, and not disposed to choose, especially when faced with decisions about matters of great significance of which they have no prior knowledge or experience. Indeed, the obligation to choose may be experienced as burdensome. 110 Patients can rarely gain the knowledge required to make decisions on the basis of ‘full’ information. 50,188,189 In a critical situation, they may look to professionals for guidance.
The discourse of choice in relation to the circumstances and options for future care presumes an unrealistic ability to control the future circumstances of death and dying. Resistance to open awareness of prognosis highlights the discrepancy between patient preferences and the current discourse of autonomy and empowerment. The language of ‘choice’ and autonomy – precedent or otherwise – does not sit easily, nor does it appear to carry salience, for many patients and families confronting death and dying. 25,69,81,190 ‘Choice’ in EOLC turns out to be largely illusory, and may be troubling for many patients. However, it has a tremendous symbolic significance as a means of maintaining agency in the face of death.
Professional training and communication skills
Professionals acknowledged that ACP discussions called for skilled and sensitive communication, but they varied in the extent to which they felt they had the requisite confidence and experience to engage with patients about this topic. This was not necessarily related to seniority or specialist roles but was strongly linked to experience and confidence. One theme was that communication skills were felt to be largely innate. They could improve through training and experience, but remained fundamentally an individual attribute. A few respondents mentioned having undertaken specialist communication training. More commonly, however, professionals valued experiential learning. The GSF meetings provided a valuable forum for sharing skills between staff from different disciplines and varying experience.
Several respondents had either completed some continuing professional development or postgraduate training, or acquired specialist knowledge of ACP in the course of working with patients facing incapacity at the end of a long illness trajectory. Others referred to having opportunities for in-house training about a range of topics relating generally to EOLC. The need for additional training in ACP was rarely stated, even though professionals’ expressed awareness of ACP policy and guidelines, including recent legislation relating to decision-making and mental capacity, was overall rather low. 53
Assessing the impact of advance care planning
The elusive nature of ACP revealed in this study makes it hard to assess when or how well it has been implemented and consequently, also, how to assess its outcome. Professionals usually worked with a limited operationalisation of ACP as concerning decisions about resuscitation and place of care. This is in contrast to the model of ACP as a means of enabling patients to make a range of decisions about future care in the event of lost capacity. However, as evidenced in the literature cited in this report, it has become customary for research and professional practice relating to ACP to be concerned with a narrower, task-based view of planning as a tool for co-ordinating EOLC. It is evident, also, that concerns about capacity, autonomy and future planning were not salient to the majority of patients. Professional respondents perceived the impact of ACP to be broadly positive, specifically to the extent that it enabled resources to be put in place to support patients to die at home, and avoid the trauma of futile resuscitation. An unplanned death was likely to be less well managed, from the practical perspective of having services and care packages in place. However, respondents were keenly aware that events might force a change of plan, and also that patient and family preferences might change.
As indicated above, studies reporting the success of ACP have focused on discrete and easily measurable components, such as an increased proportion of patients dying at home, and reduction in hospital deaths and health-care costs, as evidence of effectiveness. 137 Qualitative work, including the findings of the present study, indicates a more complex and ambiguous picture. Preferences for place of death may be uncertain and equivocal, even when documented. It is possible, also, that rapid change in preferences and plans close to death may go undocumented, or even unexpressed, and, consequently, unrealised. The distinction between patient preferences for place of care and place of death merits close attention. Many patients may wish to remain at home for as long as possible, but accept that this may be not the best, or even preferred, place in which to die. Professional assumptions about patient preferences and best interests, combined with the use of vague and ambiguous language, may result in a documented preference for home that is not entirely warranted.
The variability of patient and professional responses to ACP, and the difficulty its implementation posed in practice, raise questions about its future application. The aim in UK policy has been to support professionals in a range of roles to undertake ACP. However, the evidence suggests that uptake is patchy, and implementation variable. In the present study, ACP rarely amounted to more than discussion of decisions about place of death and resuscitation, which tended to occur in response to clear clinical deterioration. Professionals described practical difficulties in undertaking ACP, particularly related to the uncertainty of prognostication, and also expressed reluctance to initiate discussions. Professional strategies of caution and late initiation of ACP seemed to chime with many patients’ preferences for approaching death. However, current practice means that patients who would be receptive to ACP, but do not themselves raise the topic, may experience difficulty in engaging in discussion of their concerns and preferences for future care. There is scope, as at present, for fitting discussion of PPOD or DNACPR decisions into routine practice of EOLC. Some experienced and confident professionals will engage in a deeper exploration of patient concerns and plans. However, it is difficult to see how a more substantial exploration of goals and preferences for ACP, especially as this relates to future incapacity, could easily be incorporated within existing constraints of time, resources and professional engagement in generalist community care settings. 89 An alternative would be to develop ACP as a discrete and specialist referral, in line with the Respecting Choices programme originating in Wisconsin and widely implemented in areas of Canada and Australia. 44,137,191 This allows patients to decide if they wish to take part in one or more discussions of ACP with a trained facilitator, involving detailed exploration of goals and preferences for future care, not just at the end of life. This will include consideration of treatments and interventions that may be expected in specific conditions, and the individual’s preferences in relation to lost capacity. The Respecting Choices programme is currently being trialled in six European countries, including the UK. 192–194 It is likely that the appeal of the Respecting Choices intervention may be quite specific, to individuals who are predisposed to maintain control over their affairs and those who confront an extended illness trajectory with an expected outcome. It is possible that a few of the study patients would have been interested in the opportunity for such a discussion. Overall, however, the data did not convey a sense of need for, or receptivity to, a more extended consideration of ACP among either patient or professional participants. As is reported in the wider literature, many patients do not perceive a need to plan for future care. Concern with precedent autonomy, capacity and open awareness of death and dying contrasts with the clearly and consistently articulated patient priorities: to be free from pain, to live in an extended present and to avoid imposing a burden on their family members. We conclude that current policy regarding ACP has not translated easily to health-care practice in community settings.
Strengths and limitations of the study
The Care and Communication study generated a substantial body of qualitative data, enabling triangulation of professional and patient experiences of, and perspectives on, the initiation and implementation of ACP in community care settings and the documented records relating to this. The patient case studies enabled follow-up over a 6-month period and the comparison of respondents’ perspectives at different points in time, as well as between different members of each case. Cross-case analysis revealed the diversity of individual responses as well as the occurrence of recurring themes and patterns. The triangulation of different data sources and perspectives and the longitudinal follow-up of cases are particular strengths of the study. The findings cannot be directly generalised to other settings, but they are strengthened by their congruence with reports from previous research and the high degree of thematic correspondence between the data from the professional perspectives and case study interviews. We believe that the findings of the Care and Communication study make a substantial contribution to the currently limited evidence relating to the implementation of ACP in community care settings, how patients and professionals communicate about EOLC, and how patients and their families wish to anticipate, and prepare for, the experience of death and dying. One of the strengths of qualitative research is flexibility to respond to issues of significance as they arise in the course of data collection, and to pick up on concerns and experiences that are particularly salient to participants. Such research has to deal with the world as it is, rather than how it was predicted. Some objectives turn out to be not relevant, perhaps not possible to realise, while new and unexpected issues establish salience. This applies to certain aspects of the Care and Communication study, with some consequences for the objectives as these were originally formulated. Overall, the study findings relate more comprehensively to the first three objectives as stated in the protocol than to the rest.
The initial aim had been to recruit patients expected to be within the last 6 months of life and follow the process of ACP through to the outcomes of EOLC. A key finding of the study was the extent to which the uncertainty of prognostication posed a barrier to the identification of patients requiring palliative care, and also for the initiation of ACP. In fact, 12 of 21 patient cases outlived the 6-month follow up, so the outcomes of ACP could be established in only nine cases and family assessments of care in even fewer. This limited what we could say about outcomes in relation to expressed preferences for care or how patients and carers assess the quality of EOLC. A further deviation from the study protocol was the inclusion of cases in which it was not possible to recruit the full triad of participants: four cases consisted of the patient alone. This was a pragmatic response to the difficulties of recruitment. However, it was also a telling reflection of the circumstances of a substantial number of patients, particularly those who are frail and elderly and live alone, and who lacked significant relationships with health professionals and/or locally residing family carers whom they considered it would have been appropriate to invite to take part in the study. While it inevitably reduced the data relating to each case, specifically the carer and professional perspectives, widening the case composition extended the diversity of respondents who participated in the study, and picked up on the experience of important groups of patients which would not otherwise have been included.
We had aimed to follow up each case participant at approximately 6- to 8-week intervals over a period of 6 months: up to four times in all. This was inevitably going to be a theoretical maximum. As we expected, a degree of attrition was inevitable when some patients died within the 6-month follow-up period. In addition, as indicated above, four cases consisted of patients alone. Some cases lacked either a carer or professional participant, and some carer and professional respondents took part in fewer than four interviews. However, we had always proposed to work flexibly with study participants, accepting the degree of involvement with which they felt comfortable and found convenient. Sometimes we had to work around the exigencies of fluctuations in the patient’s health, and the wider commitments of both patients and carers. It sometimes proved difficult to fit interviews into the busy schedules of health professionals, and these could take some time to arrange. In a number of cases, where the patient’s condition was clearly relatively stable, we judged that it was not necessary or appropriate to conduct the full set of interviews, especially with health professionals when there was little new to report, and little contact had been made with the patient in the interim. Consequently, the interval between contacts was extended. We adopted a pragmatic approach to follow-up according to what was possible and appropriate in the context and unfolding circumstances of each case.
It is important to note that the data represent retrospective accounts of participants’ engagement with ACP, and how this was documented in medical records. This provides valuable insight into participants’ recall, understanding, recording and attitudes towards ACP, but does not reveal the content of discussions, or how closely they correspond to respondents’ accounts. EOLC in patients with long-term conditions has been relatively neglected, yet these account for the majority of deaths. The study aim was that the majority of patient cases would be affected by conditions such as heart and renal failure or COPD, rather than cancer. However, the process of recruitment to the study was difficult and protracted and, in the end, only seven of the 21 patient case studies did not have cancer. This reflects the composition of the GSF registers that professionals used to identify eligible potential cases. It is also an expression of the difficulty professionals found in judging prognosis for non-cancer patients. The difficulty of prognostication is also illustrated by the survival of over half (12 of 21) of the patient cases beyond the 6-month follow-up period. Professionals were asked to identify patients using the surprise question: ‘would you be surprised if this patient were to die in the next 6 months?’ However, as it emerged during the course of the study, the difficulty of prognostication was such that, if the question asked had been ‘would you be surprised if this patient were to remain alive for the next 6 months?’, in most cases the (negative) response would have been the same. Qualitative research involves detailed exploration of a relatively small number of cases. Consequently, the scope for diversity is limited. The study did not include any representatives from the substantial and important categories of care home residents and black and ethnic minority groups.
We had originally set out to generate evidence for best practice in implementation of ACP as a core component of the EOLCPW. As things turned out, however, the concept and relevance of ACP came under scrutiny and the notion of ‘best practice’ became remote. In consequence, we ended up with little to say about establishing professional training and support needs for effective communication in ACP. Instead, the findings shed light on the very limited extent to which ACP is implemented, in large part because, as currently undertaken, it proved to be of little relevance to patients or professionals. However, the tendency to reduce ACP to a rather perfunctory task-based exercise, particularly when staff felt under pressure to respond to financial incentives linked to quality assurance measures and appraisal, raised some further issues of concern. In particular, the study findings challenge the firmly held assumption that home is always or necessarily the best and PPOD or that patients welcome, and benefit from, an open awareness of death and dying. They raise the risk of patients coming under subtle pressure to conform to normative expectations about the best and appropriate way to die, and of professional assumptions about patient preferences being translated into actual care. The findings highlight the difficulties and uncertain relevance of ACP, as currently formulated, in many health-care settings. They raise the potential of developing ACP as a more substantial intervention delivered by specialist facilitators, and targeted at specific groups of patients rather than the wider population. At the very least, the study findings indicate that much greater conceptual clarification and debate regarding the nature and purpose of ACP is required before issues of quality, training and best practice can be addressed.
Implications for research
-
The study findings support those of previous research in highlighting the gap between policy and practice regarding ACP. They demonstrate the value of longitudinal studies incorporating a case study design. Topics for future research include:
-
investigation, especially qualitative, of public attitudes to death and dying, the value of anticipatory planning and attitudes to place of death
-
an exploration of experiences and assessment of death in different settings (home, hospital, hospice, care home) and the nature and contribution of ACP to such assessment, from the perspective of health professionals and bereaved relatives
-
longitudinal investigation of the importance of place of death for patients affected by different diseases, and at different stages of the illness trajectory
-
longitudinal investigation of the impact of different conditions on patients’ receptiveness to ACP, particularly those confronting an extended trajectory (such as multiple sclerosis, motor neuron disease or dementia) which is bound to result in physical and/or mental incapacity
-
investigation of ACP in conditions which carry a strong need for awareness and future planning, such as patients with implantable cardiac defibrillators
-
investigation of the views and experience of ACP in minority and ethnically diverse groups and how these currently engage with EOLC
-
ACP among those who live alone and/or lack family support.
-
-
In addition to patients with cancer and long-term conditions, the research identified two categories of patients whose EOLC needs are currently neglected, and which call for further recognition and investigation:
-
the frail elderly who manage complex comorbid conditions with substantial input from health and social services, but without establishing a relevant profile as vulnerable cases or significant relationships with individual health professionals providing community care
-
patients with a wide range of health problems, including hard-to-reach groups and those affected by stigmatised conditions such as serious mental illness or substance abuse, who fail to engage constructively with a wide range of services and are not recognised as suitable referrals for palliative and EOLC.
-
Conclusion
The study findings raise the question ‘How does ACP as envisaged in government policy and practice guidelines add to the quality of patient care, preparation for, and experience of death and dying?’ Studies reporting benefits from, and patient willingness to engage in, ACP discussions tend to involve trials or surveys. These focus on limited and easily documented and measurable aspects of ACP, such as preferences for resuscitation and place of death, or impact on health-care costs. In contrast, there is now a reasonably substantial literature, mainly qualitative, and including the present study, which explores the complexity, diversity and uncertainty involved in patient and professional responses to, and engagement with, ACP and EOLC. Nearly half the patients in the study had no evidence of any kind of ACP. For the rest, planning was largely confined to completion of DNACPR forms and documenting PPOD. Understanding of ACP as a means of establishing patients’ precedent autonomy was unusual. The difficulty of prognostication presented a major barrier to initiating ACP in a timely fashion. Professionals describe engaging patients in discussion of EOLC as difficult. They expect that many patients will not want to do this and may be distressed by ill-timed initiation of ACP. Professionals approach the topic with great caution, searching for cues that patients are willing to discuss the future. The focus of care is on control and anticipation of symptoms, supporting patients through a stepwise progression towards death. Patient responses to ACP are diverse, shifting and not infrequently ambivalent and resistant. Some patients wish to be, and remain, informed about their prognosis and to make plans for future care. Others are less certain: wanting to know, but not too much, preferring to set aside the future for as long as possible. The current strategy of professional caution in initiating discussion of ACP corresponds with the preferences of many patients, who do not see the relevance of ACP, and do not wish to deal with death and dying before they have to. In consequence, however, those who wish for, or would be receptive to, open awareness regarding their prognosis may find it difficult to engage in ACP. The findings point to the potential value of ACP as a structured intervention delivered by specialist facilitators, rather than a task to be incorporated by professionals delivering EOLC in community settings.
The study findings build on previous evidence that current policy relating to ACP does not translate easily to practice because it does not resonate with the aspirations of many patients or the real world constraints of health-care practice. ACP has developed in the absence of strong evidence or consultation about public preferences and perspectives about death and dying. However, a growing body of evidence indicates that patient and public goals regarding the ‘good death’ and what is most important to the experience of dying may differ from those incorporated within ACP. This particularly applies among patients from different cultures and minority ethnic groups, whose experience and preferences in relation to death and dying remain largely unexplored. Many patients who undertake ACP do so because they are strongly motivated to avoid burdening their families with the responsibility for difficult decisions about their care. Far from opting to preserve autonomy, patients frequently wish to protect their families. Decisions are formulated through networks of interpersonal relationships and obligation rather than by patients acting as self-directed and independent agents. Evidence suggests that the importance of home as a place of death (as opposed to care) has been overstated, and the diverse and dynamic nature of patient preferences for EOLC has not been recognised sufficiently. Many patients do not want, or value, the open awareness of dying that is a fundamental premise of the palliative care ideology on which ACP is based. The really important issue emerging from the study findings does not relate to achievement of precedent autonomy or the maximisation of patience ‘choice’ and decision-making in advance of an uncertain and hypothetical future. Rather, what matters most is the capacity of health professionals in a wide variety of roles to engage in effectively supporting patients and their families through the present and unfolding experience of death and dying.
The study findings revealed a considerable distance between the abstract formulation of ACP as a means of achieving precedent autonomy, its policy application in the EOLCPW and its pragmatic implementation in community care settings. Indeed, the construct of ‘advance care planning’ has become disaggregated: it is at once a policy to support the exercise of patient choice and precedent autonomy, a strategy to improve the patient and family experience of death and dying, a policy to reduce the number of hospital admissions and associated costs of EOLC, a means of facilitating professional management and planning, an aid to help patients and families foresee and come to terms with the reality of death and dying, a policy to encourage public awareness of death and greater responsibility for managing care of dying patients, a bureaucratic process of documentation and audit, and an incentivised strategy for changing professional practice. In particular, there are tensions between the goals of ACP as a means of extending patient autonomy, as reducing health-care costs and as a consumerist promotion of ‘patient choice’. We conclude that much greater critical scrutiny of the concept of ‘advance care planning’ as well as greater understanding of its public salience and acceptability is required before recommendations about future implementation and professional training can confidently be made.
Acknowledgements
This project was funded by the NIHR Health Services and Delivery Research programme (project number 10/2002/23). Further information is available at www.nets.nihr.ac.uk/projects/hsdr/10200223
This report presents independent research commissioned by the NIHR. The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NIHR Evaluation, Trials and Studies Coordinating Centre, the Health Services and Delivery Research programme or the Department of Health. The views and opinions expressed by the interviewees in this publication are those of the interviewees and do not necessarily reflect those of the authors, the NHS, the NIHR, NIHR Evaluation, Trials and Studies Coordinating Centre, the Health Services and Delivery Research programme or the Department of Health.
The University of Nottingham acknowledges the support of the NIHR, through the Primary Care Research Network, in carrying out this study.
We thank the patients and families for their generosity in taking part in the study during a very difficult period in their lives when their time was so valuable. Without their contributions, this study would not have been possible. We also acknowledge the input of the health professionals who took part in this study as interviewees and also in recruiting patients to the case studies. Thanks also to the practice managers who made reviewing patients’ records possible.
We thank Irene McGill, from the Lancaster University Patient and Public Involvement Group, for undertaking a review of the study protocol, ethical issues and patient recruitment documents in the early stages of the study. We have very much appreciated the support given to the study by the Nottingham University Dementia, Frail Older People and Palliative Care Patient and Public Involvement Advisory Panel. In particular, we would like to thank the following members of the panel for reviewing and commenting on a draft of the final report: Maureen Godfrey, Heather Redshaw, Michael Osborne, Brian Hodges, Caryl Kelly, Janet Norris and Elizabeth Thraves.
Contributions of authors
Kristian Pollock (Principal Research Fellow, School of Health Sciences, University of Nottingham) was the principal investigator and conducted study design and delivery including data collection and analysis and the writing of final report.
Eleanor Wilson (Research Fellow, School of Health Sciences, University of Nottingham) was involved in day-to-day management of the project, data collection, analysis and writing of the final report from September 2013 to August 2014.
Contributions of the research team
Dimitris Vonofakis (Research Fellow, School of Health Sciences, University of Nottingham) was involved in day-to-day management of project, data collection and analysis, and review of the final report from April 2012 to April 2013.
Jane Seymour (Sue Ryder Care Professor in Palliative and End of Life Studies, School of Health Sciences, University of Nottingham) was involved in study design and development, project overview, review of findings and the final report.
Karen Cox (Professor of Cancer and Palliative Care, School of Health Sciences, University of Nottingham) was involved in study design and development, project overview and advisory support, review of findings and the final report.
Greg Finn (Consultant in Palliative Medicine, John Eastwood Hospice, Nottinghamshire) was involved in study design and development, project overview and advisory support, facilitation of recruitment and liaison with health professionals and services, review of findings and the final report.
Vincent Crosby (Consultant in Palliative Medicine, Nottingham University Hospitals NHS Trust) was involved in study design and development, project overview and advisory support, facilitation of recruitment and liaison with health professionals and services, review of findings and the final report.
Helen Scott (Senior Public Health Manager, NHS Nottinghamshire County) was involved in study design and development, project overview and advisory support, facilitation of recruitment and liaison with health professionals and services, review of findings and the final report.
Tony Avery (Professor of Primary Health Care, Faculty of Medicine and Health Sciences, University of Nottingham) was involved in project overview and advisory support, facilitation of recruitment and liaison with health professionals and services, review of findings and the final report.
Data sharing statement
This is a qualitative study and therefore data generated are not suitable for sharing (beyond that contained in the report). Further information can be obtained from the corresponding author.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
References
- National Institute for Health Research . Health Services and Delivery Research (HS&Amp;DR) Programme n.d. www.nets.nihr.ac.uk/programmes/hsdr (accessed 22 May 2015).
- Capacity, Care Planning and Advance Care Planning: A Guide for Health and Social Care Staff. Leicester: National End of Life Care Programme; 2011.
- Thomas K, Lobo B. Advance Care Planning in End of Life Care. Oxford: Oxford University Press; 2011.
- Mullick A, Martin J, Sallnow L. An introduction to advance care planning in practice. BMJ 2013;347. http://dx.doi.org/10.1136/bmj.f6064.
- Barnes K, Barlow C, Harrington J, Ornadel K, Tookman A, King M, et al. Advance care planning discussions in advanced cancer: analysis of dialogues between patients and care planning mediators. Palliat Med 2011;9:73-9. http://dx.doi.org/10.1017/s1478951510000568.
- Knauft E, Nielsen E, Engelberg R, Patrick D, Curtis J. Barriers and facilitators to end-of-life care communication for patients with COPD. Chest 2005;127:2188-96. http://dx.doi.org/10.1378/chest.127.6.2188.
- Schickendanz AD, Schillinger D, Landefeld CS, Knight SJ, Williams BA, Sundore MD. A clinical framework for improving the advance care planning process: start with patients’ self-identified barriers. J Am Geriatr Soc 2009;57:31-9. http://dx.doi.org/10.1111/j.1532-5415.2008.02093.x.
- Leung J, Udris EM, Uman J, Au DH. The effect of end-of-life discussions on perceived quality of care and health status among patients with COPD. Chest 2012;142:128-33. http://dx.doi.org/10.1378/chest.11-2222.
- Gott M, Gardiner C, Small N, Payne S, Seamark D, Barnes S. Barriers to advance care planning in chronic obstructive pulmonary disease. Palliat Med 2009;23:642-8. http://dx.doi.org/10.1177/0269216309106790.
- Janssen D, Engelberg R, Wouters E, Curtis J. Advance care planning for patients with COPD: past, present and future. Patient Educ Couns 2012;86:19-24. http://dx.doi.org/10.1016/j.pec.2011.01.007.
- Momen N, Barclay S. Addressing ‘the elephant on the table’: barriers to end of life care conversations in heart failure – a literature review and narrative synthesis. Curr Opin Support Palliat Care 2011;5:312-16. http://dx.doi.org/10.1097/SPC.0b013e32834b8c4d.
- Momen N, Hadfield P, Kuhn I, Smith E, Barclay S. Discussing an uncertain future: end-of-life care conversations in chronic obstructive pulmonary disease. A systematic literature review and narrative synthesis. Thorax 2012;67:777-80. http://dx.doi.org/10.1136/thoraxjnl-2012-201835.
- Hancock K, Clayton J, Parker S, der Wal S, Butow P, Carrick S, et al. Truth-telling in discussing prognosis in advanced life-limiting illnesses: a systematic review. Palliat Med 2007;21:507-17. http://dx.doi.org/10.1177/0269216307080823.
- Wright A, Zhang B, Ray A, Mack J, Trice E, Balboni T, et al. Associations between end-of-life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment. JAMA 2008;300:1665-73. http://dx.doi.org/10.1001/jama.300.14.1665.
- NHS Confederation . Improving end-of-life care. Leading Edge 2005;3:1-8.
- Leadbetter C, Garber J. Dying for Change. London: Demos; 2010.
- OECD Factbook 2009: Economic, Environmental and Social Statistics. Paris: OECD Publishing; 2009.
- Barnett K, Mercer S, Norbury M, Watt G, Wyke S, Guthrie B. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet 2012;380:37-43. http://dx.doi.org/10.1016/S0140-6736(12)60240-2.
- Bardsley M, Georghiou T, Dixon J. Social Care and Hospital Use at the End of Life. London: Nuffield Trust for Research and Policy Studies in Health Services; 2012.
- Francis R. Independent Inquiry into Care Provided by Mid Staffordshire NHS Foundation Trust January 2005–March 2009, Volume I. London: The Stationery Office; 2010.
- End of Life Care Strategy: Promoting High Quality Care for All Adults at the End of Life. London: Department of Health; 2008.
- Patient and Carer Experiences Regarding End of Life Care in England. Leeds: National Audit Office; 2008.
- End of Life Care: Results of Census of Primary Care Trusts. London: National Audit Office; 2008.
- Death and Dying: Understanding the Data. London: Marie Curie Cancer Care; 2013.
- Richards N, Ingleton C, Gardiner C, Gott M. Awareness contexts revisited: indeterminacy in initiating discussions at the end-of-life. J Adv Nurs 2013;69:2654-64. http://dx.doi.org/10.1111/jan.12151.
- Ellershaw J, Murphy D. The Liverpool Care Pathway for the Dying Patient (LCP). Liverpool: Marie Curie Research Institute, Liverpool; 2011.
- More Care, Less Pathway: A Review of the Liverpool Care Pathway. London: Department of Health; 2013.
- One Chance to Get It Right: Improving People’s Experience of Care in the Last Few Days and Hours of Life. London: Leadership Alliance for the Care of Dying People; 2014.
- End of Life Care Strategy: Fourth Annual Report. London: Department of Health; 2012.
- Liberating the NHS: No Decision about Me without Me. Further Consultation on Proposals to Secure Shared Decision-Making. London: Department of Health; 2012.
- Nottinghamshire End of Life Care Pathway for All Diagnoses. Nottingham: NHS Nottinghamshire County, NHS Nottingham City, Bassetlaw PCT and Local Authorities; 2009.
- Mental Capacity Act 2005, Code of Practice. London: The Stationery Office; 2005.
- Death and Dying Survey. 2011.
- National Council for Palliative Care . Dying Matters n.d. http://dyingmatters.org/ (accessed 22 May 2015).
- Dying Matters Coalition . The Dying Matters GP Pilot Project 2011 Evaluation 2011. http://dyingmatters.org/sites/default/files/user/FINAL%20EVALUATION%20EXEC%20SUMMARY%20+%20SUMMARY%202010_11%20-%2013-1-12.pdf (accessed 22 May 2015).
- Seymour J. Looking back, looking forward: the evolution of palliative and end-of-life care in England. Mortality 2010;17:1-17. http://dx.doi.org/10.1080/13576275.2012.651843.
- Hart B, Sainsbury P, Short S. Whose dying? A sociological critique of the ‘good death’. Mortality 1998;3:65-77. http://dx.doi.org/10.1080/713685884.
- McNamara B. Good enough death: autonomy and choice in Australian palliative care. Soc Sci Med 2004;58:929-38. http://dx.doi.org/10.1016/j.socscimed.2003.10.042.
- Payne S, Langley-Evans A. Perceptions of a ‘good’ death: a comparative study of the views of hospice staff and patients. Palliat Med 1996;10:307-12. http://dx.doi.org/10.1177/026921639601000406.
- Seale C. Good and bad death: introduction. Soc Sci Med 2004;58:883-5. http://dx.doi.org/10.1016/j.socscimed.2003.10.034.
- Chapman S, Makin A, Thomas K, Lobo B. Advance Care Planning in End of Life Care. Oxford: Oxford University Press; 2011.
- Evans N, Bausewein C, Meñaca A, Andrew E, Higginson I, Harding R, et al. A critical review of advance directives in Germany: attitudes, use and healthcare professionals’ compliance. Patient Educ Couns 2012;87:277-88. http://dx.doi.org/10.1016/j.pec.2011.10.004.
- Davison SN, Holley JL, Seymour J, Chambers EJ, Brown E, Germain M. Supportive Care for the Renal Patient. Oxford: Oxford University Press; 2010.
- Lee M-J, Heland M, Romios P, Naksook C, Silvester W. Respecting patient choices: advance care planning to improve patient care at Austin Health. Health Issues 2003;77:23-6.
- Thompson T, Barbour RS, Schwartz LJ. Adherence to advance directives in critical care decision making: vignette study. BMJ 2003;327:1-7. http://dx.doi.org/10.1136/bmj.327.7422.1011.
- Wilkinson A, Wenger N, Shugarman LR. Literature Review on Advance Directives. Rand Corporation: Santa Monica, CA; 2007.
- Widdershoven GAM, Berghmans RLP. Advance directives in dementia care: from instructions to instruments. Patient Educ Couns 2001;44:179-86. http://dx.doi.org/10.1016/S0738-3991(00)00190-7.
- Tonelli MR. Pulling the plug on living wills a critical analysis of advance directives. Chest 1996;110:816-22. http://dx.doi.org/10.1378/chest.110.3.816.
- Perkins HS. Controlling death: the false promise of advance directives. Ann Intern Med 2007;147:51-7. http://dx.doi.org/10.7326/0003-4819-147-1-200707030-00008.
- Sudore RL, Fried TR. Redefining the ‘planning’ in advance care planning: preparing for end-of-life decision making. Ann Intern Med 2010;153:256-61. http://dx.doi.org/10.7326/0003-4819-153-4-201008170-00008.
- Fried TR, O’Leary JR. Using the experiences of bereaved caregivers to inform patient- and caregiver-centered advance care planning. J Gen Intern Med 2008;23:1602-7. http://dx.doi.org/10.1007/s11606-008-0748-0.
- Horne G, Seymour J, Payne S. Advance care planning: evidence and implications for practice. End of Life Care 2009;3:58-64. http://dx.doi.org/10.1016/j.ijnurstu.2011.12.003.
- Seymour J, Almack K, Kennedy S. Implementing advance care planning: a qualitative study of community nurses’ views and experiences. BMC Palliat Care 2010;9. http://dx.doi.org/10.1186/1472-684X-9-4.
- Decisions Relating to Cardiopulmonary Resuscitation. London: British Medical Association; 2007.
- Tracey v. Cambridge University Hospitals NHS Foundation Trust, Secretary of State for Health, Equality and Human Rights Commission and Resuscitation Council (UK) 2014.
- What Do We Know Now That We Didn’t Know a Year Ago? New Intelligence on End of Life Care in England. London: National End of Life Care Intelligence Network; 2012.
- Gomes B, Calanzani N, Higginson IJ. Local Preferences and Place of Death in Regions within England. London: Cicely Saunders International; 2011.
- Higginson I, Sen-Gupta G. Place of care in advanced cancer: a qualitative systematic literature review of patient preferences. J Palliat Med 2000;3:287-300. http://dx.doi.org/10.1089/jpm.2000.3.287.
- Gomes B, Calanzani N, Gysels M, Hall S, Higginson I. Heterogeneity and changes in preferences for dying at home: a systematic review. BMC Palliat Care 2013;12:1-28. http://dx.doi.org/10.1186/1472-684x-12-7.
- Gomes B, Higginson I, Calanzani N, Cohen J, Deliens L, Daveson B, et al. Preferences for place of death if faced with advanced cancer: a population survey in England, Flanders, Germany, Italy, the Netherlands, Portugal and Spain. Ann Oncol 2012;23:2006-15. http://dx.doi.org/10.1093/annonc/mdr602.
- First National VOICES Survey of Bereaved People: Key Findings Report. London: Department of Health; 2012.
- Time to Choose: Making Choice at the End of Life a Reality. London: Macmillan Cancer Support; 2013.
- Thomas C. The place of death of cancer patients: can qualitative data add to known factors?. Soc Sci Med 2005;60:2597-607. http://dx.doi.org/10.1016/j.socscimed.2004.10.020.
- Burt J, Shipman C, Addington-Hall J, White P. Palliative Care: Perspectives on Caring for Dying People in London. London: The King’s Fund; 2005.
- Shucksmith J, Carlebach S, Whittaker V. Dying: British Social Attitudes. London: NatCen Social Research; 2012.
- Reyniers T, Houttekier D, Cohen J, Pasman RH, Deliens L. What justifies a hospital admission at the end of life? A focus group study on perspectives of family physicians and nurses. Palliat Med 2014;28:941-8. http://dx.doi.org/10.1177/0269216314522317.
- Munday D, Petrova M, Dale J. Exploring preferences for place of death with terminally ill patients: qualitative study of experiences of general practitioners and community nurses in England. BMJ 2009;338:1-9. http://dx.doi.org/10.1136/bmj.b2391.
- Thomas C, Morris SM, Clark D. Place of death: preferences among cancer patients and their carers. Soc Sci Med 2004;58:2431-44. http://dx.doi.org/10.1016/j.socscimed.2003.09.005.
- Murtagh F, Bausewein C, Petkova H, Sleeman K, Dodd R, Gysels M, et al. Understanding Place of Death for Patients with Non-malignant Conditions: A Systematic Review. London: NIHR SDO programme; 2012.
- Difficult Conversations with Dying Patients and Their Families. London: Marie Curie Cancer Care; 2014.
- Kass-Bartelmes BL, Hughes R. Advance Care Planning: Preferences for Care at the End of Life. Agency for Healthcare Research and Quality: Rockville, MD; 2003.
- Small N, Rhodes P. Too Ill to Talk? User Involvement and Palliative Care. London: Routledge; 2000.
- McCall K, Rice AM. What influences decisions around the place of care for terminally ill cancer patients?. Int J Palliat Nurs 2005;11:541-7. http://dx.doi.org/10.12968/ijpn.2005.11.10.19983.
- Chapple A, Evans J, McPherson A, Payne S. Patients with pancreatic cancer and relatives talk about preferred place of death and what influenced their preferences: a qualitative study. BMJ Support Palliat Care 2011;1:291-5. http://dx.doi.org/10.1136/bmjspcare-2011-000091.
- Singer P, Martin D, Kelner M. Quality end-of-life care: patients’ perspectives. JAMA 1999;281:163-8. http://dx.doi.org/10.1001/jama.281.2.163.
- Seymour J, Gott M, Bellamy G, Ahmedzai SH, Clark D. Planning for the end of life: the views of older people about advance care statements. Soc Sci Med 2004;59:57-68. http://dx.doi.org/10.1016/j.socscimed.2003.10.005.
- Gott M, Seymour J, Bellamy G, Clark D, Ahmedzai SH. Older people’s views about home as a place of care at the end of life. Palliat Med 2004;18:460-7. http://dx.doi.org/10.1191/0269216304pm889oa.
- O’Sullivan EM, Higginson IJ. ‘I’ll continue as long as I can, and die when I can’t help it’: a qualitative exploration of the views of end-of-life care by those affected by head and neck cancer (HNC) [published online ahead of print 13 May 2014]. BMJ Support Palliat Care 2014. http://dx.doi.org/10.1136/bmjspcare-2014-000664.
- Bausewein C, Calanzani N, Daveson B, Simon S, Ferreira P, Higginson I, et al. ‘Burden to others’ as a public concern in advanced cancer: a comparative survey in seven European countries. BMC Cancer 2013;13. http://dx.doi.org/10.1186/1471-2407-13-105.
- What We Know Now 2013: New Information Collated by the National End of Life Care Intelligence Network. London: Public Health England; 2013.
- Gott M, Small N, Barnes S, Payne S, Seamark D. Older people’s views of a good death in heart failure: implications for palliative care provision. Soc Sci Med 2008;67:1113-21. http://dx.doi.org/10.1016/j.socscimed.2008.05.024.
- Clarke A, Seymour J. ‘At the foot of a very long ladder’: discussing the end of life with older poeple and informal caregivers. J Pain Symptom Manage 2010;40:857-69. http://dx.doi.org/10.1016/j.jpainsymman.2010.02.027.
- Higginson I, Gomes B, Calanzani N, Gao W, Bausewein C, Daveson B, et al. Priorities for treatment, care and information if faced with serious illness: a comparative population-based survey in seven European countries. Palliat Med 2013;28:101-10. http://dx.doi.org/10.1177/0269216313488989.
- Agar M, Currow D, Shelby-Jones T, Plummer J, Sanderson C, Abernethey A. Preference for place of care and place of death in palliative care: are these different?. Palliat Med 2008;22:787-95. http://dx.doi.org/10.1177/0269216308092287.
- Cox K, Moghaddam N, Almack K, Pollock K, Seymour J. Is it recorded in the notes? Documentation of end-of-life care and preferred place to die discussions in the final weeks of life. BMC Palliat Care 2011;10. http://dx.doi.org/10.1186/1472-684X-10-18.
- Seymour J, Payne S, Chapman A, Holloway M. Hospice or home? Expectations of end-of-life care among white and Chinese older people in the UK. Sociol Health Illn 2007;29:872-90. http://dx.doi.org/10.1111/j.1467-9566.2007.01045.x.
- Almack K, Cox K, Moghaddam N, Pollock K, Seymour J. After you: conversations between patients and healthcare professionals in planning for end of life care. BMC Palliat Care 2012;11. http://dx.doi.org/10.1186/1472-684X-11-15.
- Barclay S, Momen N, Case-Upton S, Kuhn I, Smith E. End-of-life care conversations with heart failure patients: a systematic literature review and narrative synthesis. Br J Gen Pract 2011;61:e49-62. http://dx.doi.org/10.3399/bjgp11X549018.
- Robinson L, Dickinson C, Bamford C, Clark A, Hughes J, Exley C. A qualitative study: professionals’ experiences of advance care planning in dementia and palliative care, ‘a good idea in theory but . . .’. Palliat Med 2013;27:401-8. http://dx.doi.org/10.1177/0269216312465651.
- Murray S, Kendall M, Carduff E, Worth A, Harris F, Lloyd A, et al. Use of serial qualitative interviews to understand patients’ evolving experiences and needs. BMJ 2009;339. http://dx.doi.org/10.1136/bmj.b3702.
- Parker S, Clayton JM, Hancock KM, Walder S, Butow PN, Carrick S, et al. A systematic review of prognostic/end-of-life communication with adults in the advanced stages of a life-limiting illness: patient/caregiver preferences for the content, style, and timing of information. J Pain Symptom Manage 2007;34:81-93. http://dx.doi.org/10.1016/j.jpainsymman.2006.09.035.
- Curtis J, Engelberg R, Young J, Vig L, Reinke L, Wenrich M, et al. An approach to understanding the interaction of hope and desire for explicit prognostic information among individuals with severe chronic obstructive pulmonary disease or advanced cancer. J Palliat Med 2008;11:610-20. http://dx.doi.org/10.1089/jpm.2007.0209.
- Barnes S, Gott M, Payne S, Seamark D, Parker C, Gariballa S, et al. Communication in heart failure: perspectives from older people and primary care professionals. Health Soc Care Commun 2006;14:482-90. http://dx.doi.org/10.1111/j.1365-2524.2006.00636.x.
- Carrese JA, Mullaney JL, Faden RR, Finucane TE. Planning for death but not serious future illness: qualitative study of housebound elderly patients. BMJ 2002;325. http://dx.doi.org/10.1136/bmj.325.7356.125.
- Davison S, Simpson C. Hope and advance care planning in patients with end stage renal disease. BMJ 2006;333:886-90. http://dx.doi.org/10.1136/bmj.38965.626250.55.
- Fried TR, Drickamer M. Garnering support for Advance Care Planning. JAMA 2010;303:269-70. http://dx.doi.org/10.1001/jama.2009.1956.
- Innes S, Payne S. Advanced cancer patients’ prognostic information preferences: a review. Palliat Med 2009;23:29-3. http://dx.doi.org/10.1177/0269216308098799.
- Samsi K, Manthorpe J. ‘I live for today’: a qualitative study investigating older people’s attitudes to advance planning. Health Soc Care Commun 2011;19:52-9. http://dx.doi.org/10.1111/j.1365-2524.2010.00948.x.
- Janssen D, Curtis J, Au D, Spruit M, Downey L, Schols J, et al. Patient–clinician communication about end-of-life care for Dutch and US patients with COPD. Eur Respir J 2011;38:268-75. http://dx.doi.org/10.1183/09031936.00157710.
- Spotlight on Complaints: A Report on Second Stage Complaints about the NHS in England. London: Commission for Healthcare Audit and Inspection; 2008.
- Russ AJ, Kaufman SR. Family perceptions of prognosis, silence and the ‘suddenness’ of death. Cult Med Psychiatry 2005;29:102-23. http://dx.doi.org/10.1007/s11013-005-4625-6.
- Perkins P, Booth S, Vowler S, Barclay S. What are patients’ priorities for palliative care research? A questionnaire study. Palliat Med 2008;22:7-12. http://dx.doi.org/10.1177/0269216307085180.
- McDonagh J, Elliott T, Engelberg R, Treece P, Shannon S, Rubenfeld G, et al. Family satisfaction with family conferences about end-of-life care in the intensive care unit: increased proportion of family speech is associated with increased satisfaction. Crit Care Med 2004;32:1484-8. http://dx.doi.org/10.1097/01.CCM.0000127262.16690.65.
- Tulsky J, Fischer GS, Rose MR, Arnold RM. Opening the Black Box: how do physicians communicate about Advance Directives?. Ann Intern Med 1998;129:441-9. http://dx.doi.org/10.7326/0003-4819-129-6-199809150-00003.
- Sahm S, Will R, Hommel G. Attitudes towards and barriers to writing advance directives amongst cancer patients, healthy controls, and medical staff. J Med Ethics 2005;31:437-40. http://dx.doi.org/10.1136/jme.2004.009605.
- Daveson BA, Bausewein C, Murtagh FE, Calanzani N, Higginson IJ, Harding R, et al. To be involved or not to be involved: a survey of public preferences for self-involvement in decision-making involving mental capacity (competency) within Europe. Palliat Med 2013;13:418-27. http://dx.doi.org/10.1177/0269216312471883.
- Waterworth S, Jorgensen D. It’s not just about heart failure: voices of older people in transition to dependence and death. Health Soc Care Commun 2010;18:199-207. http://dx.doi.org/10.1111/j.1365-2524.2009.00892.x.
- Ekdahl AW, Andersson L, Friedrichsen M. ‘They do what they think is the best for me’: frail elderly patients’ preferences for participation in their care during hospitalization. Patient Educ Couns 2010;80:233-40. http://dx.doi.org/10.1016/j.pec.2009.10.026.
- Hickman R, Daly B, Eunsuk L. Decisional conflict and regret: consequences of surrogate decision making for the chronically critically ill. Appl Nurs Res 2012;25:271-5. http://dx.doi.org/10.1016/j.apnr.2011.03.003.
- Botti S, Orfali K, Iyengar SS. Tragic choices: autonomy and emotional responses to medical decisions. J Consum Res 2009;36:337-52. http://dx.doi.org/10.1086/598969.
- Botti S, McGill AL. When choosing is not deciding: the effect of perceived responsibility on satisfaction. J Consum Res 2006;33:211-19. http://dx.doi.org/10.1086/506302.
- Lutfey K, Maynard DW. Bad news in oncology: how physician and patient talk about death and dying without using those words. Soc Psychol Q 1998;61:321-41. http://dx.doi.org/10.2307/2787033.
- Thé B, Hak A, Koeter G, van der Wal G. Collusion in doctor–patient communication about imminent death: an ethnographic study. West J Med 2001;174:247-53. http://dx.doi.org/10.1136/ewjm.174.4.247.
- Broom A, Kirby E, Good P, Wootton J, Adams J. The troubles of telling: managing communication about the end of life. Qual Health Res 2014;24:151-62. http://dx.doi.org/10.1177/1049732313519709.
- Hancock K, Clayton J, Parker S, Walder S, Butow P, Carrick S, et al. Discrepant perceptions about end-of-life communication: a systematic review. J Pain Symptom Manage 2007;34:190-20. http://dx.doi.org/10.1016/j.jpainsymman.2006.11.009.
- Murray SA, Kendall M, Boyd K, Sheikh A. Illness trajectories and palliative care. BMJ 2005;330:1007-11. http://dx.doi.org/10.1136/bmj.330.7498.1007.
- Finucane TE. How gravely ill becomes dying: a key to end-of-life care. JAMA 1999;282:1670-2. http://dx.doi.org/10.1001/jama.282.17.1670.
- Coventry P, Grande G, Richards D, Todd C. Prediction of appropriate timing of paliative care for older adults with non-malignant life-threatening disease: a systematic review. Age Ageing 2005;34:218-27. http://dx.doi.org/10.1093/ageing/afi054.
- Christakis NA. Death Foretold: Prophecy and Prognosis in Medical Care. Chicago, IL: University of Chicago Press; 1999.
- Zheng L, Finucane A, Oxenham D, McLoughlin P, McCutcheon H, Murray S. How good are we at identifying patients who need palliative care? A mixed methods study. Eur J Palliat Care 2013;20:216-22.
- Munday D, Dale J, Murray S. Choice and place of death: individual preferences, uncertainty, and the availablity of care. J R Soc Med 2007;100:211-17. http://dx.doi.org/10.1258/jrsm.100.5.211.
- Horne G, Seymour J, Shepherd K. Advance care planning for patients with inoperable lung cancer. Int J Palliat Nurs 2006;12:172-9. http://dx.doi.org/10.12968/ijpn.2006.12.4.21014.
- Barnes K, Jones L, Tookman A, King M. Acceptability of an advance care planning interview schedule: a focus group study. Palliat Med 2007;21:23-8. http://dx.doi.org/10.1177/0269216306073638.
- Fried TR, Bullock K, Iannone L, O’Leary JR. Understanding advance care planning as a process of health behavior change. J Am Geriatr Soc 2009;57:1547-55. http://dx.doi.org/10.1111/j.1532-5415.2009.02396.x.
- Horne G, Seymour J, Payne S. Maintaining integrity in the face of death: a grounded theory to explain the perspectives of people affected by lung cancer about the expression of wishes for end of life care. Int J Nurs Stud 2012;49:718-26. http://dx.doi.org/10.1016/j.ijnurstu.2011.12.003.
- Willems DL, Hak A, Visser F, Van der Wal G. Thoughts of patients with advanced heart failure on dying. Palliat Med 2004;18:564-72. http://dx.doi.org/10.1191/0269216304pm919oa.
- My Life until the End: Dying Well with Dementia. London: Alzheimer’s Society; 2012.
- Detering K, Hancock A, Reade M, Silvester W. The impact of advance care planning on end of life care in elderly patients: randomised controlled trial. BMJ 2010;340. http://dx.doi.org/10.1136/bmj.c1345.
- Steinhauser KE, Christakis NA, Clipp E, McNeilly M, Grambow S, Parker J, et al. Preparing for the end of life: preferences of patients, families, physicians, and other care providers. J Pain Symptom Manage 2001;22:727-37. http://dx.doi.org/10.1016/S0885-3924(01)00334-7.
- Ratner E, Norlander L, McSteen K. Death at home following a targeted advance care planning process at home: the kitchen table discussion. J Am Geriatr Soc 2001;49:778-81. http://dx.doi.org/10.1046/j.1532-5415.2001.49155.x.
- Teno J, Gruneir A, Schwartz Z, Nanda A, Wetle T. Association between advance directives and quality of end-of-life care: a national study. J Am Geriatr Soc 2007;55:189-94. http://dx.doi.org/10.1111/j.1532-5415.2007.01045.x.
- Abel J, Pring A, Rich A, Malik T, Verne J. The impact of advance care planning of place of death: a hospice retrospective cohort study [published online ahead of print 14 March 2013]. BMJ Support Palliat Care 2013. http://dx.doi.org/10.1136/bmjspcare-2012-000327.
- Singer P, D M, Lavery J, Theil E, Kelner M, Mendelssohn D. Reconceptualizing advance care planning from the patient’s perspective. Arch Intern Med 1998;158:879-84. http://dx.doi.org/10.1001/archinte.158.8.879.
- A Good Death Consultation: Full Research Findings. Newcastle upon Tyne: NHS Public Health North East; 2010.
- Gomes B, Higginson IJ. Factors influencing death at home in terminally ill patients with cancer: systematic review. BMJ 2006;332:515-21. http://dx.doi.org/10.1136/bmj.38740.614954.55.
- Davison S. Facilitating Advance Care Planning for patients with end-stage renal disease: the patient perspective. Clin J Am Soc Nephrol 2006;1:1023-8. http://dx.doi.org/10.2215/CJN.01050306.
- Brinkman-Stoppelenburg A, Reitjens J, Van der Heide A. The effects of advance care planning on end-of-life care: a systematic review. Palliat Med 2014;28:1000-25. http://dx.doi.org/10.1177/0269216314526272.
- Zhang B, Wright A, Huskamp H, Nilsson M, Maciejewski M, Earle C, et al. Health care costs in the last week of life: associations with end of life conversations. Arch Intern Med 2009;169:480-8. http://dx.doi.org/10.1001/archinternmed.2008.587.
- Houben CH, Spruit MA, Groenen MT, Wouters EFM, Janssen DJA. Efficacy of advance care planning: a systematic review and meta-analysis. J Am Dir Assoc 2014;15:477-89. http://dx.doi.org/10.1016/j.jamda.2014.01.008.
- Caplan G, Meller A, Squires B, Chan S, Willett W. Advance care planning and hospital in the nursing home. Age Ageing 2006;35:581-5. http://dx.doi.org/10.1093/ageing/afl063.
- Exley C, Bamford C, Hughes J, Robinson L. Advance Care Planning: an opportunity for person-centred care for people living with dementia. Dementia 2009;8:419-24. http://dx.doi.org/10.1177/14713012090080030702.
- Formiga F, Chivite D, Ortega S, Casas S, Ramon J, Pujol R. End-of-life preferences in elderly patients admitted for heart failure. Q J Med 2004;97:803-8. http://dx.doi.org/10.1093/qjmed/hch135.
- Robinson L, Bamford C, Beyer F, Clark A, Dickinson C, Emmet C, et al. Patient preferences for future care: how can Advance Care Planning become embedded into dementia care – a study protocol. BMC Geriatrics 2010;10. http://dx.doi.org/10.1186/1471-2318-10-2.
- Stake RE. Multiple Case Study Analysis. London: Guildford Press; 2006.
- Cox K, Seymour J, Moghaddam N, Almack K, Porock D, Pollock K. Choice and Decision-Making in Palliative Care: A Study of Patients’, Carers’ and Health Professionals’ Experiences. Nottingham: University of Nottingham; 2008.
- Charmaz K. Constructing Grounded Theory: A Practical Guide through Qualitative Analysis. London: Sage; 2006.
- Strauss A, Corbin J. Basics of Qualitative Research, Techniques and Procedures for Developing Grounded Theory. Thousand Oaks, CA: Sage Publications; 1998.
- Pinnock H, Kendall M, Murray S, Worth A, Levack P, Porter M, et al. Living and dying with severe chronic obstructive pulmonary disease: multi-perspective longitudinal qualitative study. BMJ 2011;342. http://dx.doi.org/10.1136/bmj.d142.
- Yin R. Case Study Research, Design and Method. London: Sage; 2008.
- Payne S, Field D, Rolls L, Hawker S, Kerr C. Case study research methods in end-of-life care: reflections on three studies. J Adv Nurs 2007;58:236-45. http://dx.doi.org/10.1111/j.1365-2648.2007.04215.x.
- Ingleton C, Addington-Hall J, Bruera E, Higginson I, Payne S. Research Methods in Palliative Care. Oxford: Oxford University Press; 2007.
- Cook A. Ethical issues in berevement research: an overview. Death Studies 2001;19:103-22. http://dx.doi.org/10.1080/07481189508252719.
- National Institute for Health Research . INVOLVE n.d. www.invo.org.uk/ (accessed 22 May 2015).
- Sue Ryder Care Centre of the Study of Supportive Palliative and End of Life Care . Care and Communication Between Health Professionals and Patients Affected by Severe or Chronic Illness in Community Care Settings n.d. www.nottingham.ac.uk/research/groups/srcc/projects/care-communication.aspx (accessed 22 May 2015).
- Lowes L, Gill P. Participants’ experiences of being interviewed about an emotive topic. J Adv Nurs 2006;55:587-95. http://dx.doi.org/10.1111/j.1365-2648.2006.03950.x.
- Rosenblatt P. Ethics of qualitative interviewing with grieving families. Death Studies 1995;19:139-55. http://dx.doi.org/10.1080/07481189508252721.
- Carter S, Jordens C, McGrath C, Little M. You have to make something of all that rubbish do you? An empirical investigation of the social process of qualitative research. Qual Health Res 2008;18:1264-76. http://dx.doi.org/10.1177/1049732308321753.
- Cook A, Bosley G. The experience of participating in bereavement research: stressful or therapeutic?. Death Studies 1995;19:157-70. http://dx.doi.org/10.1080/07481189508252722.
- Pesson H, Galieta M, Nelson C, Brescia R, Rosenfeld B, Breitbart W. Burden and benefit of psychosocial research at the end of life. J Palliat Med 2008;11:627-32. http://dx.doi.org/10.1089/jpm.2007.9923.
- AlQurainy R, Collis E, Feuer D. Dying in acute hospital setting: the challenges and solutions. Int J Clin Pract 2009;63:508-15. http://dx.doi.org/10.1111/j.1742-1241.2008.01991.x.
- Casarett D, Ferrell B, Kirschling J, Levetown M, Merriman M, Ramey M, et al. NHPCO Task Force Statement on the ethics of hospice participation in research. J Palliat Med 2001;4:441-9. http://dx.doi.org/10.1089/109662101753381566.
- Lawton J. Gaining and maintaining consent: ethical concerns raised in a study of dying patients. Qual Health Res 2001;11:693-705. http://dx.doi.org/10.1177/104973201129119389.
- Cowdell F. Engaging older people with dementia in research: myth or possibility. Int J Older People Nurs 2008;3:29-34. http://dx.doi.org/10.1111/j.1748-3743.2007.00096.x.
- Moore T, Hollett J. Giving voice to persons living with dementia: the researcher’s opportunities and challenges. Nurs Sci Q 2003;16:163-7. http://dx.doi.org/10.1177/0894318403251793251793.
- Lloyd V, Gatherer A, Kalsy S. Conducting qualitative interviews research with people with expressive language difficulties. Qual Health Res 2006;16:1386-404. http://dx.doi.org/10.1177/1049732306293846.
- Addington-Hall J. Research sensitivities to palliative care patients. Eur J Cancer Care 2002;11:220-4. http://dx.doi.org/10.1046/j.1365-2354.2002.00343.x.
- Adshead G. Studying the mind: ethical issues and guidance in mental health research. Clin Ethics 2008;3:141-4. http://dx.doi.org/10.1258/ce.2008.008026.
- Dewing J. Participatory research: a method fro process consent with persons who have dementia. Dementia 2007;6:11-25. http://dx.doi.org/10.1177/1471301207075625.
- Rubin H, Rubin I. Qualitative Interviewing: The Art of Hearing Data. London: Sage; 2005.
- Public Health England . National General Practice Profiles n.d. http://fingertips.phe.org.uk/profile/general-practice (accessed 22 May 2015).
- Nuffield Trust . GP Numbers Relative to UK Populations n.d. www.nuffieldtrust.org.uk/data-and-charts/gp-numbers-relative-uk-populations (accessed 22 May 2015).
- Henry C, Seymour J. Advance Care Planning: A Guide for Health and Social Care Staff. Department of Health, End of Life Care Programme: Leicester; 2008.
- Planning for Your Future Care. London: National Council for Palliative Care; 2009.
- Advance Care Planning, National Guidelines. London: Royal College of Physicians; 2009.
- Cox K, Bird L, Arthur A, Kennedy S, Pollock K, Kumar A, et al. Public attitudes to death and dying in the UK: a review of published literature. BMJ Support Palliat Care 2013;3:37-45. http://dx.doi.org/10.1136/bmjspcare-2012-000203.
- Thomas KJ, Corner H, Stobbart-Rowlands M. National primary care audit in end of life care and ACP and recommendations for improvement. BMJ Support Palliat Care 2012;2. http://dx.doi.org/10.1136/bmjspcare-2012-000250.83.
- Mack JW, Cronin A, Taback N, Huskamp HA, Keating NL, Malin JL, et al. End-of-life care discussions among patients with advanced cancer: a cohort study. Ann Intern Med 2012;156:204-10. http://dx.doi.org/10.7326/0003-4819-156-3-201202070-00008.
- Clayton J, Hancock K, Butow P, Tatersall M, Currow D. Clinical Practice Guidelines for communicating prognosis and end-of-life issues with adults in the advanced stage of a life-limiting illness and their carers. Med J Aust 2007;186:77-108.
- Wood C, Salter J. A Time and a Place. London: Sue Ryder; 2013.
- Morris ZS, Fyfe M, Momen N, Hoare S, Barclay S. Understanding hospital Admissions Close to the End of life (ACE) study. BMC Health Serv Res 2013;13. http://dx.doi.org/10.1186/1472-6963-13-89.
- Vig EK, Pearlman RA. Good and bad dying from the perspective of terminally ill men. Arch Intern Med 2004;164:977-81. http://dx.doi.org/10.1001/archinte.164.9.977.
- Kleinman A. The Illness Narratives, Suffering, Healing and the Human Condition. United States: Basic Books; 1988.
- Macdonald E. Dying in Distress: The Limitations of Good Palliative Care. London: Commission on Assisted Dying; 2013.
- Mason B, Nanton V, Epiphaniou E, Murray SA, Donaldson A, Shipman C, et al. ‘My body’s falling apart’: understanding the experiences of patients with advanced multimorbidity to improve care – serial interviews with patients and carers [published online ahead of print May 28 2014]. BMJ Support Palliat Care n.d. http://dx.doi.org/10.1136/bmjspcare-2013-000639.
- Horne G, Payne S. Removing the boundaries: palliative care for patients with heart failure. Palliat Med 2004;18:291-6. http://dx.doi.org/10.1191/0269216304pm893oa.
- Payne S, Brearley S, Milligan C, Seamark D, Thomas C, Wang X, et al. The perspectives of bereaved family carers on dying at home: the study protocol of ‘unpacking the home – family carers’ reflections on dying at home. BMC Palliative Care 2012;11. http://dx.doi.org/10.1186/1472-684X-11-23.
- Agledahl K, Førde R, Wifstad Å. Choice is not the issue: the misrepresentation of healthcare in bioethical discourse. J Med Ethics 2011;37:212-15. http://dx.doi.org/10.1136/jme.2010.039172.
- O’Neill D. Present, rather than, advance directives. Lancet 2001;358:1921-2. http://dx.doi.org/10.1016/S0140-6736(01)06973-2.
- Drought TS, Koenig BA. ‘Choice’ in end-of-life decision making: researching fact or fiction?. Gerontologist 2002;42:114-28. http://dx.doi.org/10.1093/geront/42.suppl_3.114.
- Seymour J, Witherspoon R, Gott M, Ross H, Payne S, Owen T. End-of-Life Care: Promoting Comfort and Well-Being for Older People. Bristol: Policy Press; 2005.
- Hammes B, Rooney B. Death and end-of-life planning in one Midwestern community. Arch Intern Med 1998;158:383-90. http://dx.doi.org/10.1001/archinte.158.4.383.
- Hammes BJ, Rooney BL, Gundrum JD. A comparative, retrospective, observational study of the prevalence, availability, and specificity of advance care plans in a county that implemented an advance care planning microsystem. J Am Geriatr Soc 2010;58:1249-55. http://dx.doi.org/10.1111/j.1532-5415.2010.02956.x.
- ACTION . ACTION: Advance Care Planning n.d. www.action-acp.eu/ (accessed 22 May 2015).
- Gundersen Health System . Respecting Choices® Advance Care Planning n.d. www.gundersenhealth.org/respecting-choices (accessed 22 May 2015).
Appendix 1 Definitions of professional roles
General practitioner
A GP is considered to be the main point of contact for general health care for UK residents. GPs are highly skilled doctors who support patients throughout their lives. They help to manage health and prevent illness and are trained in all aspects of general medicine. GPs will assess, diagnose and treat illness and issue prescriptions. They will also make referrals to community specialists and hospital teams as and when appropriate. GPs work directly with a team of other health professionals including DNs, midwives, pharmacists and health advisors as well as with practice staff such as practice nurses, health-care assistants, practice managers and administrative staff.
District/community nurse
Central to community nursing, DNs provide 24-hour nursing care services to patients in their own homes. They work in teams, linked to a number of GP practices and covering a wide geographical area, especially out of hours. Teams usually comprise a number of DNs of differing levels of experience led by a more senior DN with additional qualifications.
District nurse teams work with large and varied caseloads. EOLC is only one aspect of their role. This is considered fundamental in enabling patients to remain at home at the end of life, as they provide the most hands-on care at this time, including the setup and management of syringe drivers and anticipatory medications. DNs can engage with ACP.
A new role of practice liaison nurse was introduced during the study period. These nurses with community nursing qualifications were tasked to identify patients at risk of hospital admission and to help reduce admissions. It was not clear how this differed from the CM role other than being more generic in its remit. These posts had been funded for 1 year initially. For the purposes of this study these nurses have been collated under the umbrella of DN.
Allied Health Professional
This is a generic term for a wide range of professionals working to support the needs of patients. For the purposes of this report these include roles such as occupational therapists, physiotherapists, home carers, practice nurses, sitters and hospice staff. Qualifications varied depending on the profession but all carried their own caseloads and worked as part of a MDT to provide care.
Community matron
The role of CM was introduced in 2004 with the aim of managing people with long-term conditions and multiple health-care needs in the community. CMs are experienced senior nurses who provide hands-on care and work as case managers, acting as a single point of contact for help and advice. CMs saw their role as managing complex cases in the community, with a view to reducing the incidence of inappropriate or unnecessary hospital admissions, supporting other professionals involved in their patients’ care, providing a link between hospital and the community, and co-ordinating care with a case management approach.
Clinical nurse specialist
The CNS role is undertaken by advanced practice-registered nurses with expertise in a certain area, such as palliative care. The role involves a system-wide approach to patient care. This role incorporates responsibility for diagnosis and treatment, disease management, health promotion and the prevention of ill health and risky behaviours by patients, families and communities.
In this study we have separated CNS roles into those with specialist palliative care training (see PCN role below) and those who specialised in specific conditions such as heart failure or neurological conditions (referred to as CNS_HF or CNSother). These nurses varied in their engagement with ACP with patients. The CNSs specialising in neurology were more proactive in their approach, while those concerned with heart failure recognised that they rarely instigated or discussed ACP with their patients.
Palliative care nurse
Palliative care nurses are CNSs in palliative care. For the purposes of this report they include Macmillan nurses, who worked mainly with cancer patients, and those who specialised in care of patients with respiratory and cardiac conditions. The Macmillan nurse role is to support patients with complex and difficult symptoms or psychological issues that could not be managed by generalists. The Macmillan nurses participating in this study had a caseload that meant they were able to take only cancer patients. PCNs saw people in their own homes as well as at the hospice or GP surgery. They also maintained a system of telephone contact with those they perceived to have less need of direct contact. These nurses took on a specialist role and co-ordinated with other members of the MDT by attending GSF meetings and using shared notes, as well telephone and fax contact. They sometimes engaged in ACP, initiating conversations and supporting others in doing so.
Consultant in palliative medicine
A consultant is a senior physician or surgeon who has completed specialist training in a chosen area such as palliative care. CPMs work within multiprofessional teams and services. In hospitals and the community, the role of these teams is advisory; the overall responsibility for medical care remains with the hospital consultant or the GP. In specialist palliative care units, CPMs have overall medical responsibility for the patients.
In this study CPMs reported working as part of the palliative care team providing advice to clinical colleagues and working closely with PCNs. They were based at a local hospice or hospital where they saw patients in outpatient clinics and inpatient units, rather than in their own homes.
Appendix 2 The end of life care pathway
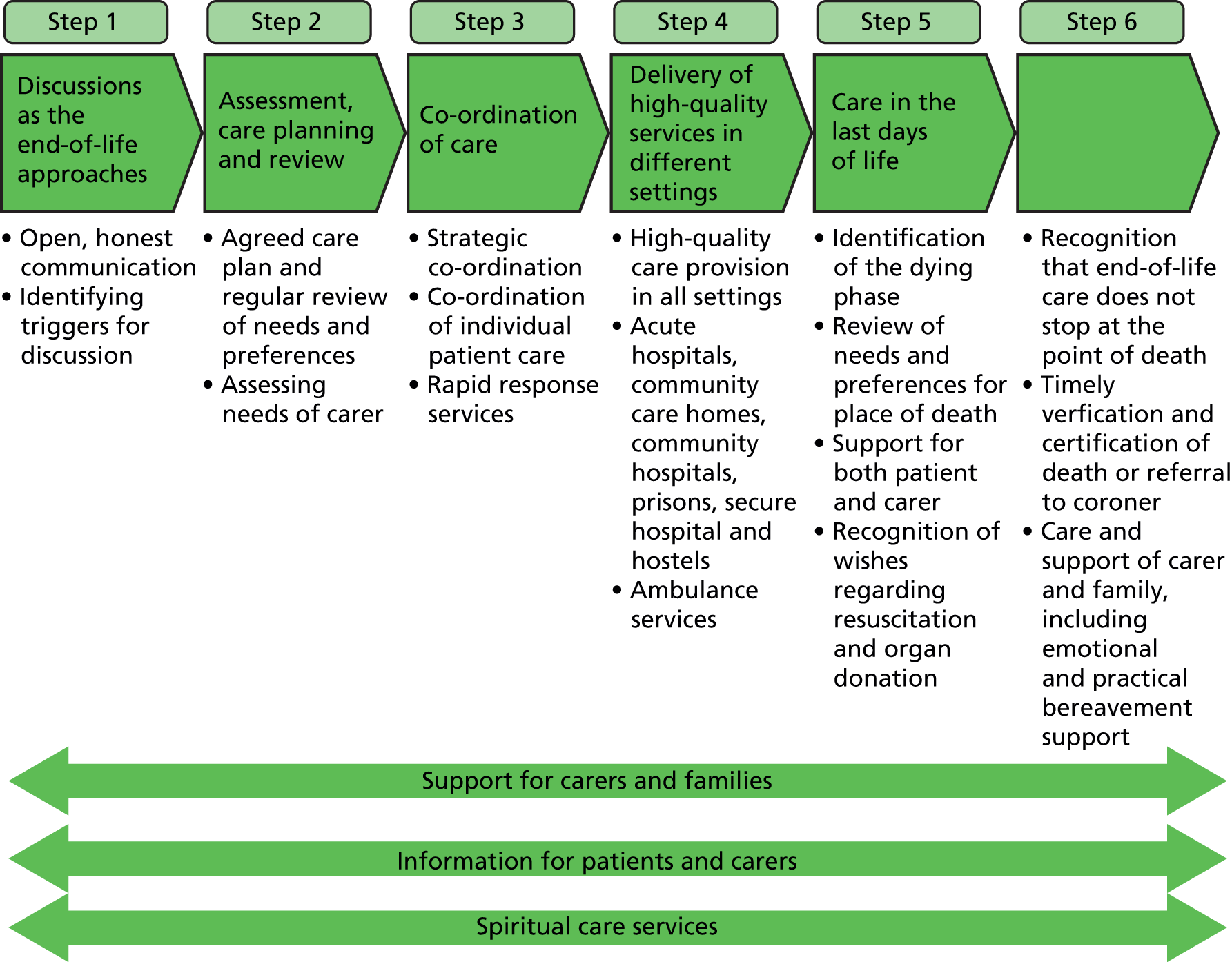
Source: Department of Health. End of Life Care Strategy: Promoting High Quality Care for All Adults at the End of Life. London: Department of Health; 2008. 21 Reproduced under Open Government licence. Crown Copyright 2008.
Appendix 3 Patient case profiles
Mrs Alderson
| Age | 91 years |
| Sex | Female |
| Medical history | Heart failure (pacemaker fitted), multiple comorbidities including hypertension, diabetes, risk of stroke, falls, partial sight, partial deafness, dizziness and vertigo. Several emergency hospital admissions due to falls and hypertension in past 2 years |
| Living situation | Home alone |
| Family carer | Son (two interviews) |
| HCP | GP (two interviews) |
| Participation in study | Four interviews over 8 months |
| Patient group | Elderly frail |
| ACP: no evidence throughout | |
|---|---|
| GSF register | No |
| DNACPR | None |
| PPOC/D | None recorded |
| Anticipatory medications | No |
| DS1500 | No |
| Fast track | No |
| Personal planning | None expressed |
| Place of death | n/a |
Mrs Alderson was a 91-year-old widow who lived alone and fairly independently, with support from family nearby. Mrs Alderson felt she would prefer not to have regular input from the DN or other community services to avoid being ‘made an invalid’ or be tied to set times for nurses to visit. She had been referred to the rapid response physiotherapy team, but was resistant to the equipment offered. She often felt health professionals did not listen to her and did not explain what was going on sufficiently. These communication issues were often a source of discussion and concern for her during interviews.
We found no evidence of documented or verbal wishes for ACP or EOLC from any of the data sources included in the study. Despite having several unplanned hospital admissions within the previous 2 years, Mrs Alderson stated several times that she did not want to go into hospital. Mrs Alderson’s GP considered her not to be suitable for the GSF register or discussion of ACP despite feeling she would fit the ‘surprise question’ because of her age. This was based on knowledge of the patient and the fact that she did not have a definite diagnosis and prognosis requiring palliative care.
In her final interview Mrs Alderson revealed some fears and concerns about dying suddenly. These fears seemed to be preventing her from undertaking some activities she would have liked to engage in. She said that she had not expressed these fears to her family or others, but they appeared to stem from a lack of understanding of her condition and what might or might not happen because of it. It seemed that Mrs Alderson had had very little discussion with any one about her wishes for care or any future plans. Her son reported that they had not discussed the future, as his mother had simply ‘brushed it off’.
Mrs Alderson fell into a category of elderly frail patients who were clearly vulnerable as a result of great age and complex health problems. However, because these problems were long-standing, and no critical event had occurred signalling the need for palliative care, these patients slipped under the radar for ACP. Despite manifest health problems and the experience of several emergency hospital admissions, Mrs Alderson’s continuing ability to remain relatively distant from regular health service input served as a concrete indication of her continuing independence and ability to manage. However, as a consequence she had not developed any close relationships with individual professionals who might have taken on the task of ACP. Mrs Alderson was not receptive to discussion of death or EOLC throughout the interviews, though latterly she made a few brief references to this as a topic of some concern.
Mr Andrews
| Age | 86 years |
| Sex | Male |
| Medical history | Metastatic stomach cancer, history of asthma/COPD and gastric problems |
| Living situation | At home with wife |
| Family carer | Wife (three interviews) |
| HCP | None nominated |
| Participation in study | Two interviews over 4 months |
| Patient group | Rapid deterioration |
| ACP: none discussed with patient | |
|---|---|
| GSF register | Yes (10 months) |
| DNACPR | No |
| PPOC/D | None recorded, PPOC document in notes; not known if completed |
| Anticipatory medications | Yes |
| DS1500 | Discussed eligibility, not clear if put in place |
| Fast track | Yes |
| Personal planning | None expressed |
| Place of death | Home |
Mr Andrews lived at home with his wife. He was initially diagnosed with operable stomach cancer. However, during the operation, metastases were identified and he was then considered to need palliative care. A second interview with Mr Andrews and his wife revealed a number of concerns. With no family or friends close by, the couple felt they needed additional support from health professionals. The community nursing team was involved at this time but it seemed they were not clear about Mr Andrews’s history and focused on physical tasks rather than offering the couple an opportunity to talk about their feelings or concerns about Mr Andrews’s illness and prognosis.
Mr Andrews was in the rapid deterioration group and died 1 month after his second interview. Unusually for a patient in this grouping, it seemed that no ACP was undertaken. However, his records show professional planning taking place, which included placing him on the GSF register, prescribing anticipatory medications and the use of the fast track system. A follow-up phone call to his wife reported that he had been admitted to hospital with back and hip pain. It seems by this point Mr Andrews was aware of his poor prognosis but did not raise this with his wife. Hence, despite visiting him every day in hospital she remained unaware that he was dying. In retrospect she recognised she had missed several ‘hints’ and failed to read the signs and later reflected that she had adopted denial as a means of coping. After he indicated he wished to go home, an extensive care package was put in place to allow nurses/carers to attend to him at home four times a day. However, Mrs Andrews reported that there was still no reference to what was happening and, literally up to the moment of the event, she did not realise he was dying.
Mr Arthur
| Age | 74 years |
| Sex | Male |
| Medical history | Cancer of the oesophagus, long-standing COPD, atrial fibrillation, stage 4 kidney disease and hypotension |
| Living situation | At home with his wife |
| Family carer | Wife (three interviews) |
| HCP | PCN (two interviews) |
| Participation in study | Four interviews over 8 months |
| Patient group | Long-term conditions |
| ACP: none discussed with patient | |
|---|---|
| GSF register | Yes (16 months) |
| DNACPR | No |
| PPOC/D | No |
| Anticipatory medications | No |
| DS1500 | No |
| Fast track | No |
| Personal planning | None expressed |
| Place of death | n/a |
Mr Arthur had lived with COPD, a heart condition and kidney disease for some years and had recently been diagnosed with cancer of the oesophagus. Surgery was considered curative, but his protracted and complicated recovery left him with a number of problems. Although generally satisfied with his care at the hospital, Mr Arthur and his wife reported that they did not always have enough information about what was happening. He was referred to the Macmillan service for support after the community nursing team had noticed signs of depression. The GP prescribed antidepressants, and regular contact with the PCN was maintained to discuss his worries and concerns. Her early assessment noted that it was not appropriate to discuss PPOC or resuscitation at this time and placed his GSF status as ‘green’, indicating a prognosis of at least 6–12 months.
As his health improved, the PCN slowly withdrew, focusing more on phone follow-up than on home visits. As Mr Arthur’s operation had been potentially curative, the PCN reported that she had not initiated any end of life discussion with him. Although his case was discussed at GSF meetings he was not officially considered to be receiving palliative care. She felt that the focus needed to be on improving his mental health and anxiety and such a conversation would neither have been welcomed by Mr Arthur nor done him any good.
Throughout the interviews, Mr and Mrs Arthur voiced concerns about the possibility that his cancer might spread. These fears were intensified when, shortly before his last interview, Mr Arthur attended a routine check with a different hospital consultant and learnt that his cancer was considered to be at stage 3 and ‘could return’. He was clearly anxious about the significance of this information, which seemed at odds, as did his long-term placement on the GSF register, with his own and his PCN’s assessment of his surgery as ‘curative’. It was on this basis that the PCN judged that it was not helpful or appropriate to raise the issue of ACP. However, there appears to have been some uncertainty and confusion between professionals about the circumstances of this case.
Mrs Avery
| Age | 68 years |
| Sex | Female |
| Diagnosis | Brain cancer diagnosed over 10 years previously, partial epilepsy, anxiety and depression |
| Living situation | At home alone |
| Family carer | None nominated |
| HCP | GP (one interview) |
| Participation in study | Three interviews over 7 months |
| Patient group | Long-term conditions |
| ACP: expressed wish to be comfortable and pain free – not recorded | |
|---|---|
| GSF register | No |
| DNACPR | No |
| PPOC/D | Not recorded |
| Anticipatory medications | No |
| DS1500 | No |
| Personal planning | Will written and funeral planned |
| Place of death | n/a |
Mrs Avery’s brain tumour was identified as very slow growing and after some initial palliative chemotherapy she requested no further treatment. A few years before the study Mrs Avery’s husband had died unexpectedly and since that time she had suffered with anxiety and depression. She found the support from her local hospice counselling service to be helpful in expressing her distress since her husband’s death.
Mrs Avery had adult children who provided support and visited regularly. Since being referred to the hospice Mrs Avery reported seeing little of her GP. She felt all her needs were met by the oncology department at the hospital and MDT at the hospice. Her condition meant that prognostication was challenging, making it difficult for health professionals and Mrs Avery herself to think about the future. Her GP struggled to recognise Mrs Avery as at the ‘end of life’, and there was no documented discussion about her wishes for care. She was not on the practice GSF register and, although Mrs Avery reported expressing a wish to die at the hospice if her needs could not be met at home, this seemed to be an informal discussion and was not recorded in her notes. Her GP felt that any end of life conversations would be triggered by change in her condition such as if her scan showed growth, and felt any discussion unprompted by the patient would be inappropriate at this time. It was clear that Mrs Avery agreed with this approach and she also stated that a change in her scan would prompt her to ask more questions about her prognosis.
Mrs Avery is considered to be within the long-term conditions category of patients. She had knowledge that she would die from her illness but had no clear prognosis at the time of the study. Routine outpatient appointments and links to her local hospice meant that Mrs Avery had limited engagement with community services. She was referred to the Macmillan team but after assessment it was felt her needs would be best met by the counsellor at the hospice. Mrs Avery had undertaken some personal planning and had spent some time with her daughter-in-law talking about her wishes for her funeral. She also reported having made a will. There appeared to be agreement between Mrs Avery and her health professionals which combined open awareness of her diagnosis, the ongoing stability of her condition and her uncertain prognosis with a sense that further discussion of this or future planning for EOLC was unnecessary and inappropriate. All were waiting for a clear indication of clinical deterioration to signify that the time had come for this to be addressed.
Mrs Barker
| Age | 86 years |
| Sex | Female |
| Medical history | Musculoskeletal degenerative condition, type 1 diabetes, poor eyesight |
| Living situation | At home alone |
| Family carer | Daughter (four interviews) |
| HCP | AHP (two interviews) |
| Participation in study | Four interviews over 11 months |
| Patient grouping | Long-term conditions and elderly frail |
| ACP: none discussed with patient | |
|---|---|
| GSF register | Yes (31 months) |
| DNACPR | No; issue raised with family, who wished for resuscitation |
| PPOC/D | Not recorded |
| Anticipatory medications | No |
| DS1500 | No |
| Fast track | No |
| Personal planning | None expressed |
| Place of death | n/a |
Mrs Barker had become unable to walk following orthopaedic surgery. An extensive package of care was provided by DNs and paid home care assistants who visited daily. In addition, Mrs Barker received substantial support from her adult children, who were keen for their mother to continue living at home. The complexity of care resulted in some communication difficulties between the family and the care teams. Medical records show that in July 2011 Mrs Barker was put on the practice GSF register, although it is not clear what prompted this and there was no indication that this had been discussed with Mrs Barker or her family. Other than this, there appears to have been very little engagement with planning from the health professional perspective or instigated by the family. During hospital admission for acute infection, staff had raised the issue of resuscitation with the family, who were clear that they did not want a DNACPR order to be put in place. It is not clear if this was ever discussed directly with Mrs Barker herself. Despite Mrs Barker’s long-term care needs and advanced age no prognosis had been discussed, nor had ACP been considered. She seemed to span the elderly frail and long-term conditions categories, as she remained in a relatively stable state with no specific triggers for ACP.
Mr Barlow
| Age | 70 years |
| Sex | Male |
| Medical history | COPD, recognised as severe for a number of years, with frequent acute exacerbations, stroke several years previously |
| Living situation | At home with his wife |
| Family carer | Wife (four joint interviews) |
| HCP | CM (two interviews) |
| Participation in study | Four interviews over 8 months |
| Patient group | Long-term condition |
| ACP: discussion about wishes and prognosis | |
|---|---|
| GSF register | Yes |
| DNACPR | Yes |
| PPOC/D | Recorded as home but not discussed with patient |
| Anticipatory medications | No |
| DS1500 | Yes |
| Fast track | No |
| Personal planning | Organ donation form completed, moved to bungalow, made financial arrangements, anticipating death |
| Place of death | n/a |
Mr Barlow was a 70-year-old man living at home with his wife, with support from two adult children living nearby. He had suffered from COPD for nearly a decade and his condition had gradually worsened. Mr Barlow now had very little energy and spent much of his day resting on the bed. He often had exacerbations of his condition and multiple courses of antibiotics to fight infections. He had regular contact with a CM and regular outpatient follow-up at a respiratory clinic at the hospital. He cited his consultant, the respiratory nurses and his CM as his main sources of professional health input and support. He was on good terms with his GP, but described seeing him rarely.
Over the course of his illness it was clear that Mr Barlow had had a number of discussions about his future with different health professionals and made some arrangements regarding his affairs in consequence. Much of this personal planning seemed to be prompted by his stroke. Mr Barlow had asked his consultant directly for a prognosis at this time, and been told it was likely to be 2 years. He seemed to derive some satisfaction from having already exceeded this forecast at the time of his involvement in the study. Mrs Barlow had also asked the specialist nurse about her husband’s prognosis around the time he had had a stroke. Continued exacerbations meant that Mr Barlow became increasingly unwell, but showed great resilience in overcoming a number of acute infections. Several discussions took place in order to plan for Mr Barlow’s care. A DNACPR form had been completed, which recorded ‘home’ as PPOD. However, despite having recorded his PPOD as ‘home’, his CM described not having discussed this matter with him explicitly.
Mr Barlow falls into the long-term conditions category. He had suffered with worsening COPD for a number of years, although it was the occurrence of a stroke 2 years previously that prompted concerns about his future life expectancy and awareness of a limited prognosis. While everyone was clearly aware of the gravity of his illness, his wife and CM maintained a positive orientation to the future. During interviews Mr Barlow indicated his awareness of his limited life expectancy, though he also seemed inclined to temporalise, in expecting death to be a more medium- than short-term prospect. However, he also expressed the frustration and despair the limitations of his illness caused him.
Mr Brown
| Age | 63 years |
| Sex | Male |
| Medical history | Lung cancer |
| Living situation | Lived at home with his wife and daughter |
| Family carer | None nominated |
| HCP | AHP (one interview), PCN (one interview), palliative care consultant (one interview), informal discussion with GP |
| Participation in study | One extended interview and phone contact over 2 months |
| Patient group | Rapid deterioration |
| ACP: wanted accurate prognosis to plan for death | |
|---|---|
| GSF register | Yes (2 months) |
| DNACPR | Yes |
| PPOC/D | Home |
| Anticipatory medications | Discussed but not issued |
| DS1500 | No |
| Fast track | No |
| Personal planning | Preparing for death, planning to bring family together |
| Place of death | Hospice; LCP used in last days of life |
Mr Brown was faced with an unexpected diagnosis of cancer and a short prognosis. He had been diagnosed with lung cancer after reporting some pain in his neck. The cancer had already metastasised to his spine, lymph nodes and bones. Mr Brown reported asking his consultant directly about his prognosis, which was given as 9 months. This proved to be an accurate forecast. Mr Brown immediately engaged in a considerable amount of personal planning, to prepare himself emotionally and practically for death. He was also unusually open about his situation and willing to discuss this with a number of different professionals, as well as during the research interview. He wanted to know this as accurately as possible, and also to plan for his family to be together at his death. PPOD had been discussed and documented. Despite wanting to remain at home, Mr Brown recognised that this would be determined by the course of his illness and the level of dependency this caused. He felt it would not be acceptable for him to remain at home in the event that he became incontinent or unable to manage his personal hygiene independently. Mr Brown’s preferred places of care and death were discussed in various ways with a number of health professionals, allowing him to express his concerns and help him prepare for his death. However, it appeared that he was not easily able to discuss his prognosis or impending death with his wife or children.
Towards the end of his life Mr Brown experienced intransigent symptoms, including uncontrolled pain, and was admitted to the hospice to try to control these. However, it became apparent that his condition was deteriorating rapidly and his mental capacity was beginning to fluctuate. His wife felt that she could not cope with his symptoms or manage his care at home. In his final days Mr Brown was also thought to have suffered a stroke. His care needs at this point meant that it was no longer feasible for Mr Brown go home, despite that being his wish.
The key issue for Mr Brown was that he was a cancer patient with rapidly advancing disease and symptoms that meant that, although he had an extensive and well worked out ACP in place, deterioration in his condition meant that plans needed to change. His case demonstrates the importance of family carers, the additional resources needed to facilitate home deaths for those with complex symptoms and that plans need to remain flexible to accommodate change. It also highlights the limitations of planning and provision of choice in terms of place of death and wishes for care.
Mr Corley
| Age | 63 years |
| Sex | Male |
| Medical history | Lung cancer with bone metastases, previous skin cancer, deep vein thrombosis |
| Living situation | At home with wife |
| Family carer | Wife (two interviews) |
| HCP | PCN (two interviews) |
| Participation in study | One interview |
| Patient group | Rapid deterioration |
| ACP | |
|---|---|
| GSF register | Yes (6 months) |
| DNACPR | Yes |
| PPOC/D | Yes |
| Anticipatory medications | Yes |
| DS1500 | Yes |
| Fast track | No |
| Personal planning | None stated |
| Place of death | Home |
Mr Corley lived at home with his wife. After presenting to various GPs a number of times with hip and leg pain, he was finally diagnosed with lung cancer with secondary bone metastases. During his radiotherapy, a discussion with the PCN clarified that his cancer could not be cured, leading to a discussion of Mr Corley’s prognosis. However, both the PCN and Mr Corley’s oncologist had concerns that the couple were not clear about the extent of Mr Corley’s cancer and his limited prognosis. Mr Corley’s deterioration was fairly rapid and the PCN acknowledged that she had not had a discussion about ACP with him, as he had resisted these conversations. She completed the DNACPR form a couple of days later in discussion primarily with Mrs Corley. She also requested anticipatory medications and recorded that she had discussed PPOC and PPOD with Mr Corley and his wife, although it was not noted what these preferences were. Four days later Mr Corley was visited at home by the GP, who suspected deep vein thrombosis. He died at home 3 days later. The paramedics were called and requested to see the DNACPR form to confirm that no attempts at resuscitation should be made. In her bereavement interview Mr Corley’s wife acknowledged that she had not been ready to hear the seriousness of her husband’s condition and focused on the tasks that needed ‘doing’ during his final days. Mr Corley’s rapid deterioration and resistance to ACP meant that this was hastily condensed into the final few days of his life and discussions primarily took place with his wife.
Mr Davis
| Age | 92 years |
| Sex | Male |
| Medical history | End-stage renal failure and multiple comorbidities including very limited vision and ongoing cardiac problems, which resulted in shortness of breath and limited walking distance |
| Living situation | Home alone |
| Family carer | None nominated |
| HCP | None nominated |
| Participation in study | Four interviews over 8 months |
| Patient group | Elderly frail |
| ACP: no evidence throughout | |
|---|---|
| GSF | No |
| DNACPR | None |
| PPOC/D | None recorded |
| Anticipatory medications | No |
| DS1500 | No |
| Fast track | No |
| Personal planning | None expressed |
| Place of death | n/a |
Mr Davis lived alone and did not nominate any HCPs to participate in the study. He reported good support from his family, although none of them lived locally, so they were not nominated to take part in the case study. He attended dialysis three times a week. He was clearly aware of his diagnosis and recognised that he would need dialysis for the rest of his life. His main professional contacts were with the nurses and a nephrologist at the hospital. Mr Davis felt there was little his GP could add to his overall care.
Mr Davis’s GP records show no discussions about wishes for care or ACP. Mr Davis also reported that he had not discussed his future care with the nephrologists, as consultations generally focused on clinical aspects of care. Like other elderly patients, Mr Davis had a number of monitored comorbidities which caused him problems intermittently. Being connected to the dialysis unit also gave Mr Davis access to other services such as dietetics and social services.
Mr Davis belongs to the category of elderly frail patients without ACP and, despite extensive ongoing contact with, and input from, health professionals, no significant relationships with any. This was evident in his inability to nominate a key professional for the study, not because he was unwilling: he simply could not think of anyone he felt he knew well enough. As a patient with ongoing chronic health problems, he was managed routinely in secondary care, largely bypassing his GP and primary care services. It was evident that Mr Davis looked to his nephrologist for support and referral for a number of other health issues. Nevertheless, though he had most contact with a range of hospital staff, it seemed none of them had taken on board the task of initiating discussion of ACP. Although Mr Davis was evidently not disposed to discuss death and dying during the interviews, he made a number of brief references to his limited life expectancy.
Mrs Elder
| Age | 71 years |
| Sex | Female |
| Medical history | Lung cancer, history of asthma |
| Living situation | At home alone |
| Family carer | Daughter lives nearby (two interviews) |
| HCP | PCN (two interviews) |
| Participation in study | Four interviews over 10 months |
| Patient group | Long-term conditions |
| ACP | |
|---|---|
| GSF register | Yes (22 months) |
| DNACPR | Yes |
| PPOC/D | Possibly home |
| Anticipatory medications | No |
| DS1500 | Yes |
| Fast track | No |
| Personal planning | Funeral planned and paid for, getting house in order, actively working to arrange affairs to reduce burden of her death for her family |
| Place of death | n/a |
Mrs Elder lived alone in a bungalow. She had a daughter who visited regularly and the support of her wider family. After a number of years of chest infections and treatment for asthma and bronchial conditions, she was diagnosed with inoperable lung cancer. Since diagnosis she had had regular and sustained input from the Macmillan team, the community nursing team and consultants at the hospital and hospice. She reported not having confidence in her GP practice and avoided contact.
Mrs Elder had been clear from the outset that she did not wish to be resuscitated. She initiated this discussion with her PCN. An ongoing theme throughout her interviews was the desire to make things as easy as possible for her family. She had planned and paid for her funeral, was in the process of carrying out maintenance on her house and had, as far as possible, arranged her affairs to make things as easy as possible for her family after her death. The relationship she had with the hospice suggested implicitly that there was an option to go there if/when she needed to do so. However, she had expressed a wish to remain at home if services could be put in place to lessen the trouble for her family. PPOC had been discussed but the PCN recognised that this did not always equate to PPOD and that as things developed this would need to be revisited.
During the study Mrs Elder’s health manifested a gradual deterioration. Her PCN considered that this trajectory could continue for some time, although the onset of a rapid deterioration was also a possibility. Mrs Elder was well aware of her situation and future prospects and had discussed these, especially her wish not to be resuscitated, with her family and several professionals. She was proceeding through a worked-out sequence of personal planning. Despite this awareness, and as with other cases, Mrs Elder indicated a preference for bracketing the reality of her limited prognosis, to focus on the possibility of an ongoing future.
Mr Farley
| Age | 79 years |
| Sex | Male |
| Medical history | Cancer of the prostate with widespread metastases, longstanding heart disease |
| Living situation | At home with his wife until moving to a care home |
| Family carer | Wife (4 interviews) |
| HCP | PCN (2 interviews) |
| Participation in study | 3 interviews over 6 months |
| Patient group | Long-term conditions leading to rapid deterioration |
| ACP | |
|---|---|
| GSF register | Yes (14 months) |
| DNACPR | Yes |
| PPOC/D | Home/hospice (changed over time) |
| Anticipatory medications | Yes |
| DS1500 | No |
| Fast track | Yes |
| Personal planning | Finances, administrative and home affairs in order |
| Place of death | Care home; IPOC used in care home |
Mr Farley lived at home with his wife until towards the end of the study period, when he moved to a care home, where he later died. He had lived with heart conditions for a number of years. When diagnosed, his cancer was already quite advanced. He had community nursing at home and Macmillan services. The PCN gave him leaflets on ‘Planning your future care’ and resuscitation to prompt discussion of ACP.
The couple had also made some of their own plans in terms of sorting out their finances and other affairs. They felt that ACP being raised by the nurse was part of this process and were reassured that this had been discussed, as they would not have known to raise it themselves. Initially the PCN had noted that Mr Farley wanted to stay at home as long as possible but she had not felt it was appropriate to discuss place of death at this time. As he deteriorated, regular contact was maintained with a number of services, and a number of items of equipment were put into the home. Latterly, PPOC was discussed and recorded as home. However, as his condition worsened and after Mr Farley visited the hospice for day care, he stated that he might like to die there. This was documented as his second choice for place of death, if home was no longer an option.
As Mr Farley became increasingly confused because of brain metastases, discussions were held with his family about how best to support his care. As the hospice had no available beds, it was agreed that fast track funding would be used to facilitate a move to a local care home. At the care home an IPOC document was started and a DNACPR form completed. It was also noted that a decision had been made that non-essential medication had been discontinued and pre-emptive medications written up.
After he had lived with a long-term condition for over 20 years, Mr Farley’s diagnosis of metastatic cancer and subsequent rapid deterioration prompted several elements of ACP to be initiated. Mr and Mrs Farley were aware of the likelihood that Mr Farley’s life expectancy was limited, and adopted a systematic approach to preparing for his death. Following experience as a day patient, his preference shifted from home to hospice as a place of death. However, Mr Farley was clear that location was subordinate to the desire not to impose a burden of care on his wife. In the event, a hospice bed was not available, and Mr Farley was moved to a care home for the last month of his life. By this time he had lost capacity to be involved in decisions about care. Although Mrs Farley was happy with the care received, she expressed feeling guilty that it had not been possible for her husband to die in hospice. She was quite clear, also, that she had not wanted him to die at home.
Mrs Harrison
| Age | 92 years |
| Sex | Female |
| Medical history | Cancer of the breast, depression, severe osteoporosis |
| Living situation | At home alone |
| Family carer | None |
| HCP | GP (two interviews) |
| Participation in study | Three interviews over 5 months |
| Patient group | Elderly frail and long-term conditions |
| ACP | |
|---|---|
| GSF register | Yes (12 months) |
| DNACPR | Yes |
| PPOC/D | Home |
| Anticipatory medications | No |
| DS1500 | No |
| Fast track | No |
| Personal planning | None expressed |
| Place of death | n/a |
Mrs Harrison lived at home on her own. She had daily input from a care agency to help her with personal care. Her son visited twice a week but had no input in her physical care. She had a history of complicated and estranged relationships with other family members. She was diagnosed with a recurrence of breast cancer, although she admitted putting off getting a diagnosis for some time and did not want any treatment. A number of comorbidities restricted her mobility. Mrs Harrison had a long history of mental health problems and her GP reported trying a number of avenues to support her needs and concerns over the years. She had accessed local hospices, but felt she did not want to go back despite the level of social interaction this would have afforded.
Mrs Harrison expressed her wish to remain at home for as long as possible but asserted that she was afraid of dying alone and was often anxious when on her own, particularly at weekends. She reported having a good relationship with her GP and some of her home carers, but no particular relationship with the visiting community nursing team. She had discussed her fear of dying to a counsellor provided by the hospice, the GP and the DNs who visited. Her notes record a number of discussions about PPOC, whom she would like to be consulted should she lose capacity to speak for herself, and that a DNACPR had been put in place.
Along with her advanced age, Mrs Harrison lived with several serious conditions resulting in a slow deterioration and limited prognosis. A number of community professionals were engaged in her care, and efforts were being made to provide for her wishes regarding EOLC. As she lived alone and would often reject options to support her needs, health professionals recognised that achieving her wish to die at home might not be possible.
Mr Jacobs
| Age | 82 years |
| Sex | Male |
| Medical history | COPD, kidney and liver disease, blindness, asthma, recurrent infections |
| Living situation | At home with his wife |
| Family carer | Wife (three interviews) |
| HCP | CM (two interviews) |
| Participation in study | Four interviews over 7 months |
| Patient group | Long-term conditions |
| ACP: frequently discussed but little accurate record of decisions | |
|---|---|
| GSF register | No |
| DNACPR | Discussed but not in place |
| PPOC/D | Discussed but not recorded |
| Anticipatory medications | No |
| DS1500 | No |
| Fast track | No |
| Personal planning | Requested an ADRT, made will, arranged burial plot |
| Place of death | n/a |
Mr Jacobs lived at home with his wife. He had a long-term diagnosis of COPD and renal failure. In addition, failing eyesight left him almost completely blind. Despite this, he was able to get around his house and still undertook most of his own activities of daily living. One daughter who lived nearby provided support in the form of shopping, getting medication and driving the couple to appointments when necessary.
During the study period Mr Jacobs was supported at home by a CM. He had a fairly good relationship with his GP but relied on his CM as a first port of call. He had raised end of life issues with her as a stable figure in his health care. This seemed to be prompted by a television programme, recent media coverage of the LCP and past experience of watching his mother die slowly after a debilitating stroke. Mr Jacobs and the CM had a number of discussions that he initially did not want documenting officially. After further discussions over some months, his wishes were formalised in an ADRT written with the support of the CM, and witnessed by his wife. The ADRT stated that he did not wish to be artificially hydrated or fed. However, it did not record his frequently expressed wish to avoid future hospitalisation. Mr Jacobs did not have a DNACPR order in place. His CM reported that when she had raised this issue Mr Jacobs had stated that he did wish to be resuscitated. However, this conflicted with the couple’s reports, both of them stating that he had a DNACPR in place.
Mr Jacobs’s case is interesting in illustrating an open desire to discuss and document ACP, alongside apparent misunderstanding between him and key health professionals, who apparently had not clearly documented the wishes he had expressed.
Mr Jenkins
| Age | 84 years |
| Sex | Male |
| Medical history | Bladder and bowel cancer, multiple operations for both, angina |
| Living situation | At home alone |
| Family carer | None |
| HCP | None |
| Participation in study | Three interviews over 8 months |
| Patient group | Long-term conditions and elderly frail |
| ACP: none discussed with him | |
|---|---|
| GSF register | Yes (18 months) |
| DNACPR | No |
| PPOC/D | Not recorded |
| Anticipatory medications | No |
| DS1500 | No |
| Fast track | No |
| Personal planning | Made a will |
| Place of death | n/a |
Mr Jenkins had lived alone since the death of his wife, without any locally resident family. He considered himself to have a number of good friends and neighbours whom he was involved with socially. Mr Jenkins had a kidney removed because of cancer approximately 6 years before and he now managed bowel and bladder cancers with medications and was monitored via teleclinic with the hospital and through blood tests taken at his surgery. Small recurrences of cancer in his bladder had been managed with surgery. Mr Jenkins was aware that such recurrences would continue. He saw his treatments as ‘putting off’ death. He also recognised that death was a common occurrence in his age group. However, all recent scans had been clear and his follow-up had been reduced to yearly.
Mr Jenkins remained very well throughout the study. He was generally very happy with the care he received. He had strong links forged over a number of years visiting the hospital outpatient clinic and felt he required little from his GP. He had no home care services and did not feel he required this kind of support.
Mr Jenkins spans the elderly frail and long-term conditions groups. This case illustrates a group of patients who are not involved with their GP, who have serious health-care problems but no palliative care referrals, and whose illness is being largely managed in secondary care. Mr Jenkins had little contact with services in the community and his conditions were managed through outpatient appointments. Despite his age he was considered to be quite well and was managing well at home. It seemed there had been no discussion with Mr Jenkins about ACP or EOLC wishes.
Mrs Jones
| Age | 63 years |
| Sex | Female |
| Medical history | Pancreatic cancer, some palliative chemotherapy, syringe driver set up for optimum management of symptoms |
| Living situation | Home with husband |
| Family carer | None nominated |
| HCP | None nominated |
| Participation in study | One interview |
| Patient group | Rapid deterioration |
| ACP | |
|---|---|
| GSF register | Discussed at palliative care MDT |
| DNACPR | Yes |
| PPOC/D | Home |
| Anticipatory medications | Yes |
| DS1500 | Yes |
| Fast track | No |
| Personal planning | Son’s wedding brought forward, funeral planned, trip with family |
| Place of death | Home |
Mrs Jones lived at home with her husband, in frequent contact with an extended family living close by. After some months of unidentified back pain, a tumour of the pancreas was found. Mrs Jones was told her cancer was inoperable and care was palliative from diagnosis. Despite knowing her time was likely to be short, Mrs Jones stated that she did not want an accurate prognosis and preferred for things to ‘just happen’ as they would for anyone. With the help of her husband she had planned her funeral.
Mrs Jones had been referred to the Macmillan team and had regular contact with her GP and a DN team that visited daily to manage her syringe driver and additional injections. She had also discussed her PPOC and stated she would like to be cared for at home unless she had a medical need to be moved to the hospice. Shortly after the research interview her condition deteriorated and she was admitted to hospice for a week for symptom management. She then returned home with anticipatory medications in place alongside her syringe driver. Medical records note that she remained at home for 12 days before she died.
Mrs Jones falls in the rapid deterioration category. She had two short admissions, one to the hospital and one to the hospice for symptom control, but otherwise the syringe driver and additional anticipatory medications allowed her to remain at home with input from community services. Such a rapid deterioration in this case meant that we were able to conduct only one interview with Mrs Jones and were not able to gain input from family or health professionals in this case. It seems that her death did go to plan. However, although quite aware of her situation, and having set up some plans for the future, Mrs Jones was explicit that she was not interested in knowing too much about her prognosis.
Ms Lucas
| Age | 38 years |
| Sex | Female |
| Medical history | Liver disease |
| Living situation | Between home with mother and brother and living with a partner |
| Family carer | None nominated |
| HCP | None nominated |
| Participation in study | Two interviews over 3 months |
| Patient group | Long-term conditions |
| ACP: none reported, not able to gain access to medical records | |
|---|---|
| GSF register | Unknown |
| DNACPR | Unknown |
| PPOC/D | Unknown |
| Anticipatory medications | Unknown |
| DS1500 | Unknown |
| Fast track | Unknown |
| Personal planning | None expressed |
| Place of death | n/a |
Ms Lucas lived between her mother’s house and that of her partner. She had several school-age children, all of whom lived with other family members or their fathers. It seemed that an operation during which she suffered a massive bleed due to her liver disease was the start of her mortal illness. She had since been admitted to hospital several times with ongoing liver problems. Ms Lucas was aware that her condition was due to excessive drinking of alcohol. When asked what she had been told about her condition she stated that she knew it was ‘severe’ but it was not clear what this meant for her.
Ms Lucas reported having no contact with any community health professional and seeing different health professionals each time she was in hospital, despite being on the same wards. She reported feeling that they ‘did a good job’ at the hospital and were supportive of her, although she seemed to lose confidence when at home because of a lack of support.
After losing contact with Ms Lucas, we felt it was not appropriate to access her medical records without checking her initial consent. That limited the information available for this case but it appeared that Ms Lucas fell into the long-term conditions category and had support only through secondary care because of exacerbations of her condition. Indeed contact with Ms Lucas was erratic and difficult to organise despite her desire to take part in the study. Although a singular case, Ms Lucas represents a wider group of patients with stigmatised conditions and complex and disorderly lifestyles who do not engage with services effectively. A further patient from this group was also referred to the study and agreed to participate but, because of poor health, an appropriate time to do so could not be established. Ms Lucas belongs to a discrete group of patients with long-term conditions that are unrepresented in palliative care research.
Mr Patterson
| Age | 84 years |
| Sex | Male |
| Medical history | Lung cancer and COPD, a number of comorbidities including heart failure and eye problems, requiring a number of hospital admissions via accident and emergency |
| Living situation | At home with his wife |
| Family carer | Wife (two interviews) |
| HCP | None |
| Participation in study | One interview |
| Patient grouping | Long-term conditions to rapid deterioration |
| ACP | |
|---|---|
| GSF register | No |
| DNACPR | Yes |
| PPOC/D | None recorded |
| Anticipatory medications | No |
| Fast track | Yes |
| Personal planning | Spoken to solicitor; wanted doctors to decide the best course of action in his care, so as not to burden his family |
| Place of death | Hospice |
Mr Patterson was diagnosed with COPD and lung cancer. He initially had some radiotherapy treatment for his lung cancer but his COPD made him increasingly unwell. Approximately 16 months before his death, it was recorded in his notes that the oncology department could not offer him ‘any further active treatment’. Mr Patterson had regular monitoring of his blood and frequent home visits and phone contacts with his GP. Some months later Mr Patterson was admitted to hospital with pneumonia following an emergency call-out by the GP. A DNACPR was completed on the ward. Following discharge home, the DN team contacted the GP to arrange fast track funding for home care. A week after Mr Patterson returned home, his GP visited and it is recorded in his notes that EOLC was discussed. A DNACPR form to hold at home and the local Emergency Medical Services form were completed by the GP.
It became increasingly difficult for Mr Patterson’s wife to cope with his care at home. The couple were aware that the GP had referred them to continuing care funding through fast track and that this enabled them to have carers in twice a day to help Mr Patterson get up and dressed, and washed in the evenings. After some discussion with his family and health professionals Mr Patterson stated he would prefer the hospice to a care home if his wife could not manage his care at home. He was admitted to the hospice for respite care and died somewhat unexpectedly 3 days after his admission.
Mr Patterson spanned all the patient groupings in various ways but his long-term diagnosis of COPD and heart disease place him in the long-term conditions group. Once his cancer was diagnosed he experienced a more rapid deterioration. Some discussion related to ACP seems to have taken place at a very advanced stage of Mr Patterson’s illness. Although there is evidence of active professional planning and management of this case, Mr Patterson had not been included on his practice GSF register.
Mr Roper
| Age | 76 years |
| Sex | Male |
| Medical history | Bowel cancer with liver metastases, long-standing history of COPD, asthma and diabetes |
| Living situation | At home with his wife |
| Family carer | Wife (three interviews) |
| HCP | None |
| Participation in study | Three interviews over 7 months |
| Patient group | Long-term conditions |
| ACP: none discussed with patient | |
|---|---|
| GSF register | Yes (14 months) |
| DNACPR | No |
| PPOC/D | Home |
| Anticipatory medications | No |
| DS1500 | No |
| Fast track | No |
| Personal planning | None expressed |
| Place of death | n/a |
Mr Roper had been living with COPD and diabetes for a number of years but had more recently been diagnosed with bowel cancer. Eight months after he was diagnosed he had an operation to remove the cancer from his bowel but felt the delay in diagnosis had resulted in secondaries in his liver which could not be surgically removed. He and his wife both struggled to communicate with their oncologist and often requested feedback from their GP after a consultation. Having found his first round of chemotherapy to be very difficult, Mr Roper did not feel he wanted further treatment at this time. He was aware that his cancer was not curable and that any treatment was just to keep it at bay. However, he remained unclear about the stage his cancer had reached and why he had been told by the hospital team that they could not operate.
Mr Roper’s medical records indicate that his GP had classified him as for palliative care. The record of an initial visit from the PCN noted that Mr Roper was on the GSF as ‘amber’. Despite recording it as inappropriate to have a discussion about PPOC, she notes this to be ‘home’. After a couple of initial home visits by the PCN it had been arranged that the couple would contact the nurse if needed.
Generally Mr Roper’s bowel cancer caused few symptoms that affected his daily life. He reported being more restricted by his COPD. However, this remained under control throughout the study period and he experienced no serious exacerbations of his condition. He seemed to fall into the long-term conditions category, as he had been given no prognosis and, although some professional planning had taken place, his cancer diagnosis and progression had not yet prompted discussion of ACP.
Mrs Tomlinson
| Age | 62 years |
| Sex | Female |
| Medical history | Long-standing COPD, with a number of recent exacerbations |
| Living situation | At home with her husband |
| Family carer | Husband (three interviews) |
| HCP | AHP (one interview) |
| Participation in study | Two interviews over 6 months |
| Patient group | Long-term conditions |
| ACP | |
|---|---|
| GSF register | Yes (1 month) |
| DNACPR | Yes |
| PPOC/D | Home |
| Anticipatory medications | Yes |
| DS1500 | No |
| Fast track | Yes |
| Personal planning | Made living will including funeral plans |
| Place of death | Home |
Mrs Tomlinson lived at home with her husband. She had experienced a series of exacerbations and hospital admission for COPD over a number of years. During an extended hospital admission it became apparent that she was in the advanced stages of her illness and considered suitable for palliative care by the consultant. She was referred to the hospital Macmillan team and local hospice. The issue of resuscitation was initially raised by the consultant and a form completed for the hospital. On discharge, the DNACPR form was completed by the GP, to be held in her home. He also completed forms for the ambulance service for out-of-hours calls. Another DNACPR was then completed to be held at the hospice. The GP had also prescribed anticipatory medications at this time. However, he did not explain what these were for and Mrs Tomlinson had to ask her DN to explain why they had been prescribed. While at the hospice she was supported to create a ‘living will’ that documented her wishes for after her death, including funeral plans and where she wanted her ashes to be scattered.
During a further hospital admission caused by a chest infection, it became clear that Mrs Tomlinson was dying. Her husband reported that she was sleeping most of the time and not conscious at all for the last couple of days. At this stage, the family was asked if she wanted to die at home and all agreed they wanted her to be at home. The fast track system was used to get her home, where she died only a few hours later.
Mrs Tomlinson’s case illustrates the recognition of the tipping point to rapid deterioration of a long-term condition as the trigger to discussion of ACP as well as professional and personal planning. Open awareness of her limited prognosis allowed Mrs Tomlinson to undertake some personal planning and health professionals to co-ordinate care. This case is striking, also, in illustrating the strength of commitment among professionals and family to realise patients’ expressed preferences for death at home. This involved the transfer of a comatose and dying woman from hospital to home, where she died a few hours later. It is unlikely that Mrs Tomlinson could have had much, if any, awareness of her situation at this stage. Nevertheless, her family expressed great appreciation that they had been able to honour her wishes to die at home.
Mr Williamson
| Age | 68 years |
| Sex | Male |
| Medical history | Oesophageal cancer; spinal metastases; increasing bony metastases |
| Living situation | At home with his wife |
| Family carer | Wife (three joint interviews) |
| HCP | GP (two interviews), PCN (one interview) |
| Participation in study | Three interviews over 7 months |
| Patient group | Long-term conditions to rapid deterioration |
| ACP: ‘plan of care’ discussed with family | |
|---|---|
| GSF register | Yes (26 months) |
| DNACPR | Yes |
| PPOC/D | Home/hospice |
| Anticipatory medications | Yes |
| Fast track | Yes (3 days) |
| DS1500 | No |
| Personal planning | None expressed |
| Place of death | Home |
Mr Williamson had been very ill for a number of years since a diagnosis of oesophageal cancer during a routine medical check required for his work. Following surgery, severe back pain was diagnosed as a tumour on his spine, which rendered him bedridden. Since that time he had been identified as needing palliative care and had attended the local hospice for outpatient appointments with the palliative care team and the PCNs as and when needed. He had several times exceeded clinical expectations about his life expectancy and his GP found it difficult to give a prognosis.
Despite not wanting to discuss his wishes for care on a regular basis, Mr Williamson had had some initial discussion when he was referred to the palliative care team. Subsequent discussions were led by a change in his condition, with the focus often on the physical process of dying rather than what his wishes for future care might be. However, issues of ACP were revisited nearer to the time of his death. During his final stay in hospital a ‘plan of care’ was discussed with Mr Williamson and his family and it was recorded that he wanted to go home with a care package but would consider the hospice as a PPOD if his family could not support him at home. The DNACPR was also completed and the fast track referral system was used to transfer him home, where he died 3 days later. Mr Williamson’s package of care included night sitters to support his wife at home.
Despite having a cancer diagnosis, Mr Williamson falls in the long-term conditions category, as his cancer was slow to progress and he suffered several exacerbations that shifted expectations and made it difficult to determine his prognosis. However, the cancer diagnosis made it apparent that Mr Williamson would die from his condition at some point and could be seen as the catalyst for ACP following his referral to the palliative care team. Some professional planning was undertaken, as Mr Williamson had been placed on the GSF register to alert the MDT to his foreseen needs. However, his placement on the GSF register for over 2 years indicates the challenge of prognosis in this case. A DNACPR was put in place by the hospital team only when he was being discharged home to die.
Mrs Winters
| Age | 65 years |
| Sex | Female |
| Medical history | Lung cancer, chronic stage 3 kidney disease, fibromyalgia, depression and a previous cancer diagnosis |
| Living situation | Living at home with her husband |
| Family carer | Husband (one joint interview) |
| HCP | GP (three interviews) |
| Participation in study | Three interviews over 6 months |
| Patient group | Long-term conditions, rapid deterioration |
| ACP | |
|---|---|
| GSF register | Yes (2 months) |
| DNACPR | Yes |
| PPOC/D | Home |
| Anticipatory medications | Yes |
| DS1500 | Yes |
| Fast track | Assessment made on the day of death |
| Personal planning | Took own initiative in determining prognosis and subsequently invested considerable emotional work in preparing her family for her death. Declined further treatment. Planned funeral and insurance |
| Place of death | Home |
Mrs Winters was living in a warden-aided flat with her husband. At the time of diagnosis she was not given a prognosis by doctors but did some research for herself on the internet and found that it was likely to be approximately 2 years. After suffering severe side effects from chemotherapy, she subsequently declined further treatment. Mrs Winters expressed a desire to know what was happening so that she could prepare for death, and also to make the most of the time she had remaining. In particular, she was concerned about supporting her family to come to terms with the fact that she was dying. Despite her awareness and willingness to talk about her death, Mrs Winters continued to place this somewhere in an indeterminate future. Shortly before her death she rejected an initial invitation to consider resuscitation on the grounds that this would not be appropriate until she was much closer to dying; evidently she did not realise that this was, indeed, imminent. As her condition deteriorated, discussion about her wishes did take place, although this was prompted by the DNs, who requested a DNACPR and anticipatory medications. A DNACPR was eventually completed the day before she died. With significant input from her family and the community nursing team, she was able to die at home as she wished. She had maintained regular contact with her GP, who provided considerable support throughout her illness.
Mrs Winters had a number of long-term conditions but it was when her cancer caused her to deteriorate rapidly that ACP was instigated, predominantly through professional planning.
Appendix 4 Interview topic guides
Patient interview topic guide
NB: Question wording and follow up will be tailored to patient circumstances and phrased sensitively and appropriately according to context.
-
Introduction.
-
To researcher and study.
-
Nomination of lay and professional carers for study.
-
Issues of future consent and capacity.
-
Completion of advance statement of preferences.
-
-
Completion of consent to interview.
-
-
Background and current circumstances.
-
Current health: what’s been happening?
-
Main issues re illness and treatment
-
Who is providing care and support?
-
Informal.
-
Professional.
-
-
Current problems/concerns/coping?
-
-
Knowledge and understanding of illness and prognosis.
-
Nature and goals of current treatment.
-
Future options: proposals, preferences for care and treatment.
-
Preferences for information: verbal, written, full, partial.
-
Adequacy and sources of information.
-
-
Making decisions and involvement in care.
-
Preferences re involvement/responsibility for decisions about treatment.
-
Specific/general options and issues.
-
Carer involvement/influence in decisions (who).
-
Issues/concerns?
-
-
-
Thinking about the future.
-
How does Patient see the future, at this point in time?
-
Discussed with others (who: family, friends, HCPs)?
-
Recorded preferences for future care? (As appropriate).
-
Issues/concerns?
-
-
Communication.
-
Review and reflection: how does patient feel about ease and quality of communication:
-
with informal carer(s)
-
with Health Professionals
-
issues/concerns?
-
-
-
Conclusion
-
Anything else, not discussed?
-
Confirm personal details (if not known/as appropriate).
-
Age; former employment; illness history and duration; network of informal and professional support, family circumstances.
-
-
-
Debriefing.
-
How does Patient feel after the interview?
-
Explore concerns, offer contacts for support, bring discussion to a neutral plane.
-
Arrangement for follow up.
-
Thanks!
-
-
Carer/relative interview topic guide
NB: Question wording and follow up will be tailored to respondent/patient circumstances and phrased sensitively and appropriately according to context.
-
Introduction.
-
To researcher and study.
-
Issues of patient’s future capacity and consent.
-
Completion of consultee form if R [Respondent] is nominated carer.
-
Completion of consent to interview form.
-
-
-
Background and current circumstances.
-
Relationship with Patient; involvement with care and support.
-
What has been happening: Patient’s current health and main issues re illness and treatment.
-
Professional support and care for patient.
-
How Respondent is coping, care and support available, all sources.
-
Issues/concerns regarding Patient’s current care.
-
-
Knowledge and understanding of illness and prognosis.
-
Understanding of nature and goals of current treatment.
-
Awareness of proposals/options/preferences for future care and treatment.
-
Preferences for information (written, verbal, full, partial).
-
-
Making decisions and involvement in care.
-
Discussion and involvement: Patient, Relative, HCPs
-
Responsibility for decisions.
-
-
Thinking about the future
-
Knowledge and anticipation.
-
Discussion with: Patient, HCPs and others?
-
Recording of preferences?
-
Current concerns.
-
-
Communication and discussion.
-
Review and reflection: how does Respondent feel about ease and quality of communication:
-
With patient.
-
With HCPs providing care for patient
-
With others, e.g. family and friends?
-
-
-
Conclusion
-
Anything else, not discussed?
-
Confirm personal details, e.g.
-
Age, employment, health, family circumstances, etc.
-
-
-
Debriefing
-
How does Respondent feel after interview?
-
Explore concerns, offer contacts for support.
-
-
Arrangement for follow-up.
-
Thanks!
-
Nominated health professional interview topic guide
-
Introduction.
-
Introduction to researcher and study.
-
Issues of patient’s future capacity and consent.
-
Completion of consultee form if Respondent has been nominated for this role.
-
Completion of consent to interview.
-
-
Background and history of care.
-
Relationship with patient; involvement in care and support.
-
What has been happening: Patient’s current health and main issues re illness and treatment.
-
Other services/HCPs respondent liaises with in providing care.
-
Communication/exchange of information.
-
Patient and family coping.
-
Issues/concerns regarding current care.
-
-
Knowledge and understanding of illness and prognosis.
-
Process of recognising patient approaching end of life.
-
instigating palliative/end of life care
-
GSF?
-
-
Patient/family awareness of prognosis.
-
Understanding of treatment.
-
-
-
Thinking about the future.
-
What will happen to patient over the next 6–8 weeks?
-
Anticipation of care management during this period.
-
Issues/concerns about Patient’s present or future care.
-
-
Making decisions and management of care.
-
Discussion of future care and options.
-
With patient, family and other HCPs
-
-
Responsibility for care/decisions across professional network
-
Communication/information exchange between HCPs/services
-
Recording of preferences for care?
-
-
Communication.
-
Review and reflection: how does Respondent feel about ease and quality of communication.
-
With patient, family, other HCPs involved in case.
-
-
Conclusion.
-
Anything else, missed, not discussed?
-
Confirm personal details as required: age, professional role and position, length in current post, experience, specialist training in palliative and EOLC, ACP.
-
-
Debriefing.
-
How does respondent feel after interview?
-
Explore concerns, suggest contacts for support.
-
Arrangement for follow-up.
-
Thanks!
-
Professional perspective interview guide
Professional interview topic guide
-
Introduction.
-
To researcher and study.
-
Completion of consent to interview.
-
-
Background information
-
Age; position (how long); training and experience: palliative/EOLC.
-
-
Case account
-
Discussion of recent patient case involving palliative and EOLC.
-
Circumstances, diagnosis, trajectory, recognition of dying/terminal illness, process of referral and professional/service engagement; coordination of care; involvement with patient and family, decision making, communication about end of life, ACP; documentation of discussion; transfer of information.
-
-
Was this case typical, unusual: in what way?
-
Main issues in providing EOLC for this patient?
-
ACP in place/not; relevance
-
-
Generalise discussion.
-
To other patients/diagnostic conditions.
-
Recognising dying; decision making and discussion within MDT.
-
Communication with patient/carers.
-
Transition from active to comfort care/LCP.
-
Consideration of ‘futility’.
-
Initiation of ACP: documentation and sharing of information.
-
Follow up and review.
-
Realising patient preferences for EOLC:
-
place of death
-
DNR orders.
-
-
Patient/family acceptance/rejection of specific treatments.
-
Patient/family attitudes re information and discussion.
-
Hospital admission
-
Most challenging/rewarding aspect of work with dying patients and their families?
-
-
EOLC pathway
-
Familiarity with EOLC pathway: training, knowledge and use of resources
-
Assessment of EOLC pathway: resources and tools (PPC, GSF, LCP; website)
-
Use of pathway resources with patients/carers
-
Specific tools: PPC, GSF, ADRT, LCP?
-
-
Impact of EOLC Pathway on practice
-
Communication with patients and carers
-
Initiation and follow up of ACP
-
Documentation
-
Need for additional resources, training support to improve confidence and skills?
-
-
Conclusion
-
Any other issues to add/not already discussed?
-
Query how R is feeling following interview
-
Thanks for taking part: details and preferences for feedback of findings
-
Appendix 5 Patient information sheet
Participant information sheet
Patient case study
Patients
Title of study: Care and communication between health professionals and patients affected by severe or chronic illness in community care settings.
Name of researcher(s):
-
Kristian Pollock
-
Eleanor Wilson
We would like to invite you to take part in our research study. Before you decide we would like you to understand why the research is being done and what it would involve for you. One of our team will go through the information sheet with you and answer any questions you have. Talk to others about the study if you wish. Ask us if there is anything that is not clear.
What is the purpose of the study?
The purpose of the study is to find out about the care provided by a range of community services to patients who are affected by severe, chronic or life-limiting illness. We are interested in how patients, family carers and health professionals communicate with each other and exchange information and how this impacts on patients’ treatment and experience of care. Good information about illness and treatment, and the chance to discuss this, is considered essential for patients and their carers to understand what is wrong, what can be done about it, and to enable them to play an active part in making decisions about treatment options and their future care if they wish to do this.
Why have I been invited?
You have been invited to take part in this study because you are a patient affected by severe, chronic or life-limiting illness and you are on the list of one of the GP practices which is participating in the research. A health professional currently providing care for you has identified you as someone who might be interested in taking part in the study. We are inviting 20 participants like you to take part.
Do I have to take part?
No. It is up to you to decide whether or not to take part. If you do decide to take part you will be given this information sheet to keep and be asked to sign a consent form to say that you have agreed to take part in the study, and understand what this involves. If you decide to take part you are still free to withdraw at any time and without giving a reason. This would not affect your medical care or legal rights. You may indicate your decision to withdraw from the study either directly to the researchers, or through your nominated health professional, either verbally or in writing/by email.
What will happen to me if I take part?
The research is a two-year study which is based on a series of detailed patient case studies. Each case will include a patient, a carer and a health professional. If you decide to get involved in the study you will be invited to take part in an initial interview and then follow up contacts at six- to eight-week intervals over the following six months. This will involve between four to six contacts in all. The first will be an interview and will last for about an hour. Interviews may take place in your home, at a clinic, or another location of your choice. Follow-up contacts are likely to be shorter (probably between 20–40 minutes) and may involve a combination of interview, phone, email or Skype, depending on your preference and convenience. Interviews and follow-up contacts will be arranged entirely at your convenience, and will be cancelled or rearranged if you are not feeling well on a particular day.
The interviews will be about your experience of care, the information you have received about your illness and its treatment, and the extent to which you wish to be involved in making decisions about your present and future care. With your permission we would like to record the interviews. We will also ask if you are willing to let us access your medical records to find out how different services are recording and sharing information about your care. However, you can still take part in the study even if you do not want us to do this.
We are also interested in the experiences of your close family members or friends who might help to support you. You will be invited to nominate someone close to you, for example a relative or a friend (aged 18 and over), who might be willing to take part in the study. Finally, we will ask you to nominate a health professional who you feel is most involved in providing care for you just now. We would like to ask them about their role in providing care for you, how they engage with other services involved in providing care for you, and how information about your treatment and preferences for care is communicated between relevant staff and services. If you prefer, you may choose to involve an additional health professional to be part of your case, rather than a relative or informal carer.
Nominating a consultee
It is possible that serious illness can cause people to become unable to make decisions for themselves. This can be for a short time, or may last for a longer period. If you decide to take part you will be asked to say whether or not you wish to remain in the study in the event that you should become unable to make this decision for yourself. You may prefer to leave this decision to your relative or another person chosen by you. The Mental Capacity Act (section 32) allows you to nominate a person who is willing to be consulted about whether it is in your best interests to remain in the study if this circumstance should arise. We will discuss this decision with you before you take part in the study, and you may wish to consult others also.
Expenses and payments
Participants will not be paid to participate in the study. Travel expenses will be offered for any visits incurred as a result of participation.
What are the possible disadvantages and risks of taking part?
Serious illness naturally causes anxiety and distress for patients and their families. We ask you to consider very carefully how you would feel about sharing this experience with the researcher, and over an extended period of time. It is important that you understand what is involved and discuss this fully with the researchers before you decide to take part. It is possible that you may feel distressed at some times during the interviews. However, you will never be under any pressure to answer questions or talk about topics that you prefer not to discuss. The interviews will focus on your experience of your care and treatment and what is important to you. You can stop an interview, or withdraw from the study at any time.
What are the possible benefits of taking part?
We cannot promise the study will help you but the information we get from this study may help health professionals to understand patients’ experience of serious illness and preferences for care. This should help to improve the care and support provided by community health services to patients and their families in future. We hope participants will find involvement in the study to be an interesting experience. Some people find it helpful to have the opportunity to reflect on, and share, difficult experiences such as illness and disability with someone who is not directly involved in providing care.
What if there is a problem?
If you have a concern about any aspect of this study, you should ask to speak to the researchers who will do their best to answer your questions. The researchers’ contact details are given at the end of this information sheet.
If you would like to discuss your concerns with a senior member of University staff who is independent of the research study, you are welcome to contact Professor Patrick Callaghan, Director of Research/Head of School Elect, School of Nursing, Midwifery and Physiotherapy, Tel. xxxx xxxxxxx or email xxxxxxxxxxx.
If you remain unhappy and wish to complain formally, you can do this by contacting NHS Complaints through NHS Direct on 0845 464, or at: http://www.nhsdirect.nhs.uk/members/membersmagazinearchive/togethersummer10/thenewnhscomplaintsprocedure
Will my taking part in the study be kept confidential?
Yes. We will follow ethical and legal practice and all information about you will be handled in confidence, in accordance with the Data Protection Act, 1998.
If you join the study, some parts of your medical records (if you have given permission for these to be accessed) and the data collected for the study will be looked at by authorised persons from the University of Nottingham who are organising the research. They may also be looked at by authorised people to check that the study is being carried out correctly. All will have a duty of confidentiality to you as a research participant and we will do our best to meet this duty.
All information which is collected about you during the course of the research will be kept strictly confidential, stored in a secure and locked office, and on a password protected database. Any information about you which leaves the university will have your name and address removed (anonymised) and a unique code will be used so that you cannot be recognised from it.
Your personal data (address, telephone number) will be kept for 3–6 months after the end of the study so that we are able to contact you about the findings of the study if you have told us that you would like to receive these. All other data (research data) will be kept securely for 7 years. After this time your data will be disposed of securely. During this time all precautions will be taken by all those involved to maintain your confidentiality; only members of the research team will have access to your personal data.
The only circumstances under which confidentiality would be broken would arise if the researchers were made aware of actions or situations resulting in serious risk of harm to yourself or others. The researchers would discuss this with you and consider the need to raise the matter with senior clinical managers of the services involved.
What will happen if I don’t want to carry on with the study?
Your participation is voluntary and you are free to withdraw at any time, without giving any reason, and without your legal rights being affected. If you withdraw then the information collected so far cannot be erased and this information may still be used in the project analysis.
Involvement of the General Practitioner/Family doctor (GP)
The researchers will not inform your GP that you are taking part in the study. It is up to you if you would like to let your doctor or other health professionals know that you are doing this. You may wish to discuss your taking part in the study with them.
What will happen to the results of the research study?
The results of the study will be used to help health care staff improve the care and support they provide to patients affected by serious and chronic illness and the carers who support them. The researchers will prepare a report for the National Institute for Health Research (NIHR) Health Services and Delivery Research Programme, which has funded the study. The results of the research will be made more widely available through professional and academic journal publications and conference presentations. You (and your relative, if they take part) will not be identified in any report or publications resulting from the research. All participants will be sent a summary of the findings and recommendations at the end of the study if they would like to receive this.
Who is organising and funding the research?
This research is being organised by the University of Nottingham and is being funded by the National Institute for Health Research Health Services and Delivery Research programme (NIHR HSDR).
Who has reviewed the study?
All research in the NHS is looked at by an independent group of people, called a Research Ethics Committee, to protect your interests. This study has been reviewed and given favourable opinion by the Leicester Research Ethics Committee.
What do I have to do?
Please use the reply form and prepaid envelope included with this information sheet to let the researchers know if you are interested in taking part, or would like to find out more about the study. They will contact you directly to discuss this. You do not have to respond if you do not want to take part. However, it would be very helpful if you could indicate this by signing and returning the reply slip: you do not need to include any additional contact details. Returning the reply slip will prevent a reminder letter being sent to you. You may also contact the researchers directly by phone or email using the contact details given in this information sheet (please see over page).
Further information and contact details
Dr Kristian Pollock
Senior Research Fellow
School of Nursing, Midwifery and Physiotherapy
University of Nottingham
Queen’s Medical Centre
Nottingham NG7 2HA
Tel: 0115 8230810
Email: kristian.pollock@nottingham.ac.uk
Dr Eleanor Wilson
Research Fellow
School of Nursing, Midwifery and Physiotherapy
University of Nottingham
Queen’s Medical Centre
Nottingham NG7 2HA
0115 8231201
eleanor.wilson@nottingham.ac.uk
Glossary
- DS1500
- A short report written by a clinician to certify a patient has a terminal diagnosis to allow them to claim certain benefits in the last months of life.
- Fast track
- Referral system allowing rapid access to funding and services for those with palliative care needs.
- Integrated pathway of care
- A documented plan of care to guide health professionals caring for patients recognised to be dying.
- Quality and Outcomes Framework
- Incentive programme to resource and reward general practices achieving results in certain areas of care.
See also Appendix 1 for definitions of professional roles.
List of abbreviations
- ACP
- advance care planning
- ADRT
- advance decision to refuse treatment
- AHP
- Allied Health Professional
- CM
- community matron
- CNS
- clinical nurse specialist
- CNS_HF
- clinical nurse specialist – heart failure
- COPD
- chronic obstructive pulmonary disease
- CPM
- consultant in palliative medicine
- CPR
- cardiopulmonary resuscitation
- DN
- district/community nurse
- DNACPR
- do not attempt cardiopulmonary resuscitation
- EOLC
- end of life care
- EOLCPW
- end of life care pathway
- EOLCS
- End of Life Care Strategy
- GP
- general practitioner
- GSF
- Gold Standards Framework
- HCP
- health-care professional
- Int
- interview
- IPOC
- integrated pathway of care
- LCP
- Liverpool Care Pathway
- MDT
- multidisciplinary team
- NEoLCP
- National End of Life Care Programme
- NIHR
- National Institute for Health Research
- PCN
- palliative care nurse
- PPC
- Preferred Priorities for Care
- PPOC
- preferred place of care
- PPOD
- preferred place of death
- QOF
- Quality and Outcomes Framework