Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 10/1010/05. The contractual start date was in January 2012. The final report began editorial review in September 2014 and was accepted for publication in December 2014. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2015. This work was produced by Wilson et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Background
This study was based on three premises: first, that a major challenge for health and social care is in reducing unplanned admissions is in those aged 85 years and over; second, that reducing unplanned admissions requires interventions at several inter-related points in a complex system; and, third, that an understanding of the practical challenges in implementing policies to reduce admission is necessary for successful adoption.
The challenge of unplanned admissions in those aged 85 years and over
The number of people aged 85 years and over in the UK is projected to more than double between 2009 and 2034, from 1.4 million to 3.5 million, compared with a 12% growth in the overall population. 1 Between 2001 and 2011, the number of people aged 85 years and over increased at three and a half times the rate of the rest of the population. 2 The proportion of emergency admissions contributed to by this age group rose between 2004/5 and 2008/9 from 9.5% to 11%,3 and will continue to increase as a result of these demographic trends.
Many, but not all, patients aged 85 years and over presenting to acute care have multiple comorbidities, polypharmacy, cognitive impairment and disability. Such patients are challenging to assess and manage, as the clinical presentation may be non-specific and difficult to interpret and relevant information may not be readily available. This leads to the high ‘conversion rates’ (the proportion of people attending acute care who are subsequently admitted to a bed). 4 Once admitted to hospital, older people have longer stays, are more prone to hospital-acquired complications, both physical and psychological (e.g. delirium), and may experience more difficulty returning home or to their usual place of residence due to disruption of previously established care packages. 5
Explanations for rising admission rates
Reasons for the rise of unplanned admissions in all age groups have been examined in detail in several reports. 2,3,6–10 A consistent finding was of unexplained variation in trends of admission rates, at hospital trust, primary care trust (PCT) and local authority levels, suggesting lessons can be learned from these different experiences.
In part, the increase in numbers of admissions is due to an ageing population; it has been estimated that demographic change accounted for 40% of the rise between 2004 and 2009. 3 There is no evidence of increased morbidity in the population, and so the consensus is that the majority of the increase is due to service factors, professional behaviour and public expectations.
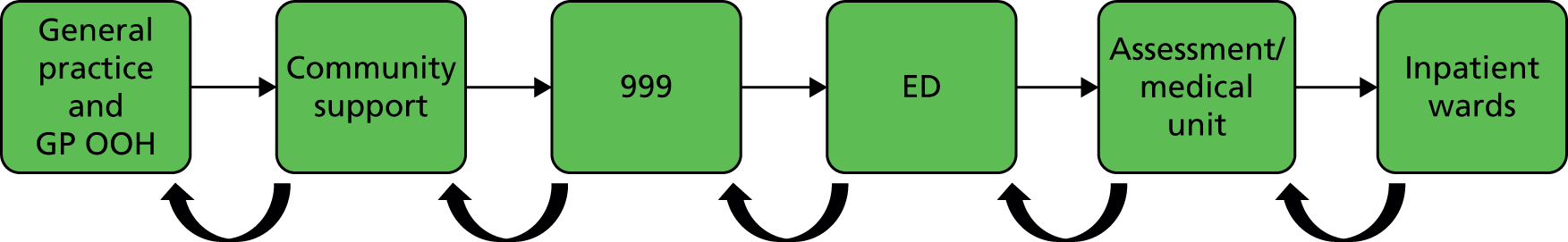
The patient journey from community to inpatient wards involves several steps, including all or some of the following: management in primary care, community support, emergency/ambulance services and emergency department (ED). The contribution of these to rises in admission is summarised below.
Primary care
Primary care can influence admission rates in two ways: first by optimal control of long-term conditions, such as blood pressure management to reduce risk of stroke, and second by early intervention in an acute condition to avoid the need for admission; for example, appropriate management of heart failure and exacerbations of chronic obstructive pulmonary disease (COPD) can prevent admissions. These have been referred to as ‘preventable’ and ‘avoidable’ admissions respectively,11 although the literature does not always use these terms consistently. Ambulatory care sensitive conditions (ACSCs) have been defined as those for which effective management in primary care should prevent admission to hospital, and include chronic and acute conditions as well as those that are vaccine preventable (e.g. influenza). Which conditions are included as ACSCs varies between reports. In 2009/10 in England, 19 ACSCs accounted for 16% of acute admissions overall, and 30% in those aged 75 years and older. 10 Using a broader definition of 27 ACSCs, Blunt reported that in England, between 2010 and 2013, rates of admission for these conditions rose by 26% after adjusting for an ageing population. 8 Within the older population, the biggest increases were for COPD, pneumonia and pyelonephritis, whereas in all age groups the rate of admission for chronic conditions declined. 8 This suggests that primary care (as well as public health measures, such as tobacco control) has been more effective in managing chronic conditions, but less effective in dealing with some acute conditions that could, in principle, be managed in the community.
There is some empirical evidence that lack of investment in primary care may contribute to increasing admissions. In a study of 16 acute trusts, it was found that, after adjusting for other factors such as age and deprivation, those serving communities with higher investment in primary care had lower ED attendance rates in those aged 65 years and above (admission data were not presented). 12 There is increasing evidence that access to and continuity in primary care affect ED attendance and admissions. 13 Evidence from the USA suggests that lower continuity of primary care (which includes family physicians, paediatricians and geriatricians) increases admission rates,14 a finding supported by recent work conducted by some of the authors. 15 Using the same data set from one English county, and adjusting for all known confounders, there was also a relationship between ED attendance rates and perceived access to general practice. 15 A similar study found the same relationship with emergency admissions. 16 National data, adjusting for age, also show that, where overall satisfaction with general practice and satisfaction with telephone access are lower, ED attendance rates are higher. 2 It has recently been estimated that, in England, over 5 million ED attendances (26.5%) were preceded by patients being unable to obtain an appointment with their general practitioner (GP). 17
The contribution of out-of-hours general practice, especially following the changes in 2004 which led to GPs being able to relinquish responsibility for this task, has been contested. Some authors have linked rising rates of ED attendance to these contractual changes,18 while others have noted that rates were already rising before they were introduced. 19 More certain is the fact that out-of-hours services vary in quality, including the proportion of patients they refer to hospital. 20 Although the introduction of the Quality and Outcomes Framework (QOF) in 2004 has improved management of individual long-term conditions, it has been suggested that this is at the expense of a more holistic approach, especially with older people. 21,22
Community support
One reason cited for rising admission rates of older people is the lack of community-based alternatives available to respond to the demographic changes outlined earlier. As far back as 2000, it was recognised that 50% of older people in hospital needed rehabilitation rather than acute care and that inappropriate use of in-patient bed-days by older people was greater than 20%. 23,24 This led to a commitment in the NHS plan25 to expand intermediate care provision, but evaluations have suggested that this has not been introduced on a sufficient scale and that, in many cases, these services have offered additional rather than substitute care. 26 Lack of community support has also been identified as a factor in the rising rates of readmission in the elderly. 27
Emergency departments and acute assessment units
By far the largest contributor to rises in emergency admission rates is the number of patients who come through EDs (accounting for 71% of admissions in 2012). Between 2003 and 2012, the number of attendances at major EDs increased by only 12.5%, but the percentage of attenders admitted (the conversion rate) increased from 19% to 26%. The National Audit Office estimated that this increase in the conversion rate accounted for 75% of the rise in emergency admissions through major EDs. 2 In 2010/11, people aged 80 years and over accounted for 6.5% and those aged over 90 years for 1.8% of first attenders to English EDs and, of those aged 85 years and over, 62% were admitted to hospital. Other factors identified in the report as explaining the rise in admissions include the 4-hour target (within which time ED attenders must be seen, treated, and admitted or discharged) and the introduction of acute assessment units, in which patients can be further assessed before a decision on management is made. Typically these units admit for a maximum of 72 hours. 28 Unfortunately, routine data do not distinguish between admission to such units and admission to an inpatient ward. It has recently been estimated that the increasing number of older people attending EDs between 2011/12 and 2012/13 accounted for 11% of the decline in reaching the 4-hour target. 29
In summary, the increase in the number of admissions from EDs has largely comprised short-stay admissions of less than 2 days (which increased by 124% in the 15 years to 20132) and has been driven more by a rise in conversion rates than by a rise in numbers attending. Clinical practice and government directives are likely to have contributed.
Initiatives to stem the rise of acute admissions
Several initiatives have been introduced to stem the increase in acute admissions, with many focused on the oldest old. The evidence base for these was summarised by Purdy in 2010. 6 They can be conceived as attempts to achieve the left-to-right shift illustrated in Figure 1, as proposed in the ‘Silver Book’. 30
Primary care
As outlined earlier, there is some evidence that improved access and continuity in general practice may reduce ED attendance. There have been several initiatives to improve access, particularly concerning targets for appointments to be offered within a defined time frame, but the effect of these on admission rates has not been evaluated. Risk profiling, to identify and support those at high risk of admission, was also introduced in 2005,31 but there is no firm evidence of effectiveness; for example, an evaluation of case management of those at high risk of admission showed no impact on admission rates,32 a finding supported by more recent evidence. 33
Additional services to improve access have been introduced in the last decade, including walk-in centres, minor injuries units, and telephone and web-based services such as NHS Direct. The first two of these are classified as accident and emergency (A&E) services in some data sets, and increased use of these services was reported by the Audit Commission as explaining the majority of the 32% increase in overall ED attendances between 2003/4 and 2012/13. In principle, these services could reduce emergency admissions by providing prompt management of acute conditions and by diverting people away from major EDs. Alternatively, they could increase admissions if their staff are less prepared to manage risk than standard primary care services. There are no empirical data to support either of these assertions and a recent systematic review found no evidence of effect, noting the lack of good-quality studies. 19
Community support
Community support to reduce acute admissions has focused on intermediate care, a term first used in the NHS Plan. 25 Intermediate care comprises services, primarily catering for older people, which seek to prevent unnecessary hospital admissions, facilitate earlier discharges and avoid premature admissions to long-term care. 34 Admissions avoidance schemes are services designed to provide an alternative to hospital admissions. Examples of such schemes include ‘rapid response’ (rapid assessment and access to short-term nursing/therapy support and personal care in the service user’s own home), ‘hospital at home’ (intensive support in the patient’s own home) and ‘residential rehabilitation’ (a short-term programme of therapy and enablement in a residential setting). There is good evidence from systematic reviews that, for selected patients, hospital at home can deliver similar or better outcomes than inpatient care, potentially at a lower cost;35,36 however, these schemes have not been implemented on a sufficient scale to show an effect on reducing admissions. The evidence base for early-discharge hospital at home schemes is less clear, although for some patient groups they may reduce long-term admissions to residential care. 37
A key driver of improving care for older people has been the promotion of ‘integrated care’. Although this concept includes ‘vertical’ integration (e.g. between primary and secondary care), in practice most activity has been improving ‘horizontal’ integration between general practice, community nursing and social services. Several such initiatives included the aim of reducing acute admissions. Surprisingly, a national evaluation of 16 schemes found that they resulted in a significant 2% increase in emergency admissions, but reduced planned admissions and outpatients attendances by 4% and 20% respectively. The authors suggest that increased availability of planned care in the community could explain these findings. 38
A specific area of activity aimed at reducing admissions has been work with care homes (nursing and residential). A number of different schemes have been introduced, including enhanced payments and different models for GP provision,39 specialist nursing and pharmacy teams, and input from geriatricians. A 2011 review included anecdotal reports that such initiatives could be effective in reducing admissions, but no one model of care was pre-eminent. 40
Ambulance and paramedic services
A recent trial of providing an emergency response by paramedics with enhanced skills found that this new service reduced ED attendances by 28% and admission rates by 13%. The mean age of participants was 82 years, and the most common conditions were falls, accounting for over 85% of cases. 41 A later systematic review supported this approach to falls,42 and there is evidence for the effectiveness of community management of these cases. 43 However, there is a lack of evidence for other conditions. 2
Emergency departments and acute assessment units
Several interventions have been introduced to reduce the proportion of ED attendances that result in admission. In 2007, the NHS published a list of conditions which could be managed in EDs without admission, for example pulmonary embolism. 44 Review by a senior clinician has been found to reduce admission rates to wards by 12% and to medical assessment units by 21%, compared with actions taken by a more junior clinician. 45 Similarly, the introduction of comprehensive geriatric assessment in an ED setting was found to reduce the ED conversion rate for people aged 85 years and over from 69.6% to 61.2%,46 a finding in line with other studies. 47–49
Although, as discussed earlier, admissions to acute admissions units are counted in the same way as those to traditional inpatient wards, there is good evidence that their introduction can increase the proportion of patients discharged within 72 hours, thereby reducing pressures on inpatient wards. 28
The need for a systems-level approach
The above sections demonstrate that, in experimental settings, individual initiatives can be shown to affect admission rates of older people. It is clear, however, that all elements of the system are inter-related; for example, the impact of senior medical assessment in EDs cannot be fully realised unless there is access to a range of services offering alternatives to acute admission. As The King’s Fund report notes:
in the real world, interventions will rarely be implemented in isolation. A combination of interventions intended to reduce admissions may be expected to have a ‘cumulative’ effect and, although each may have little effect individually, there may be greater benefit overall than the combined effects of single interventions.
p. 176
The need to understand how interventions inter-relate and contribute to the total system of care is particularly important in providing care for older people. 50 More recently, the National Audit Office concluded that ‘The effective management of the flow of patients through the health system is at the heart of reducing unnecessary emergency admissions and managing those patients who are admitted’. 2
Such a systems approach is attentive to the interconnections and configurations between various elements, transitions of care and handover, entities and processes that contribute to the performance, sustainability and capacity of an organisation or service. It suggests that complex social and organisational processes cannot easily be explained, or indeed changed, by focusing on single interventions, but rather that it is the relationships between these that contribute to both success and failure.
Systems theory therefore provides a holistic approach to understanding complex social and organisational processes, as exemplified by present-day health-care services that involve the co-ordination of multiple agencies, care processes and organisations. It is based on four underlying ideas: first, that ‘the whole is greater than the sum of the parts’ or that when different entities and processes interact there are emergent properties, including both intended and unintended consequences; second, that systems comprise entities or components with specialised functions and processes that often evolve in isolation and can be poorly aligned; third, that specialised elements are often grouped and over time brought together into subunits or organisations; and, fourth, that the challenge for systems thinking is the appropriate alignment and co-ordination of these elements and processes. This is because the components of the system have a tendency of organising themselves based on simple external rules. This self-organisation may not be aligned to the needs of the system as a whole. A systems approach offers a middle-range perspective to understanding complex organisations and processes, such as initiatives to reduce admissions of older people.
Implementing system change
The literature offers a range of models and approaches for understanding and implementing organisational change within organisations, including the health service. 51 This often centres on modifying the goals or mission of a unit, the culture and values of staff, the structures and operations within which people work, or looking for innovation or new technology. Much of this research, however, is focused at the organisational or unit level, with little attention given to the introduction of change at the system level, as outlined above. In other words, understanding the processes of change requires attention and the energy to change within the individual units or components that constitute the system together with the interconnections between them. This also means recognising that change management strategies that work within one unit, such as hospitals, might be very different from those needed in other units, such as commissioning groups. Utilising this ‘systems perspective’ therefore requires paying greater attention to the wider institutional conditions within which care services are organised and delivered. This includes the institutional pillars, such as regulatory systems, normative conditions and cognitive-cultural influences, that have been shown to shape health-care services and hinder strategic change. 52 Analysis of strategic change includes considering several ‘receptive conditions’ for change:
-
coherence of policy
-
leaders of change
-
environmental conditions and pressures
-
organisational cultures
-
managerial–clinical relations
-
co-operative interorganisational networks
-
clarity of goals and strategy
-
fit between the change ‘agenda’ and the local conditions.
System change, by its nature, is highly related to both the structure of an organisation and also its strategy. Strategy and structure are themselves tightly connected. Implementation will therefore always require a number of essential components that we can identify as being a strategy. Of strategy, Chandler53 identified three generic parts: it is the determination of long-term goals, followed by the adoption of courses of action, and finally the allocation of resources to meet the goals. Dealing with systems and, more accurately, ‘complex systems’ is difficult. In order to understand what a system is, we need to understand some of its key characteristics:
-
the interdependence of individual elements (objects, people, tools)
-
a holistic view (insight, obtained by observing the system as a whole, that observance of small elements would not provide)
-
entropy (accept there is a level of disorder in the system)
-
regulation (the complexity of feedback and controls within systems)
-
recursion (the manner in which the larger system is composed of smaller, similar systems, embedded within it, at lower hierarchical levels and aggregation)
-
differentiation (how smaller elements fulfil specific system tasks).
In summary, for a complex system to operate in an optimum manner, all subsystems must do so as well and in co-ordination with each other. Therefore, when systems elements are not working well, the ‘whole’ is compromised.
In the case of this change project, an effective way to identify that which we want to change was required. There are a number of different approaches or model structures that can help us to understand and analyse complex organisations. Among these are Porter’s Value Chain,54 McKinsey’s 7S framework,55 Beer’s Viable System Model,56 Galbraith’s Star Model57 and Mintzberg’s conceptual description of the organisation. 58
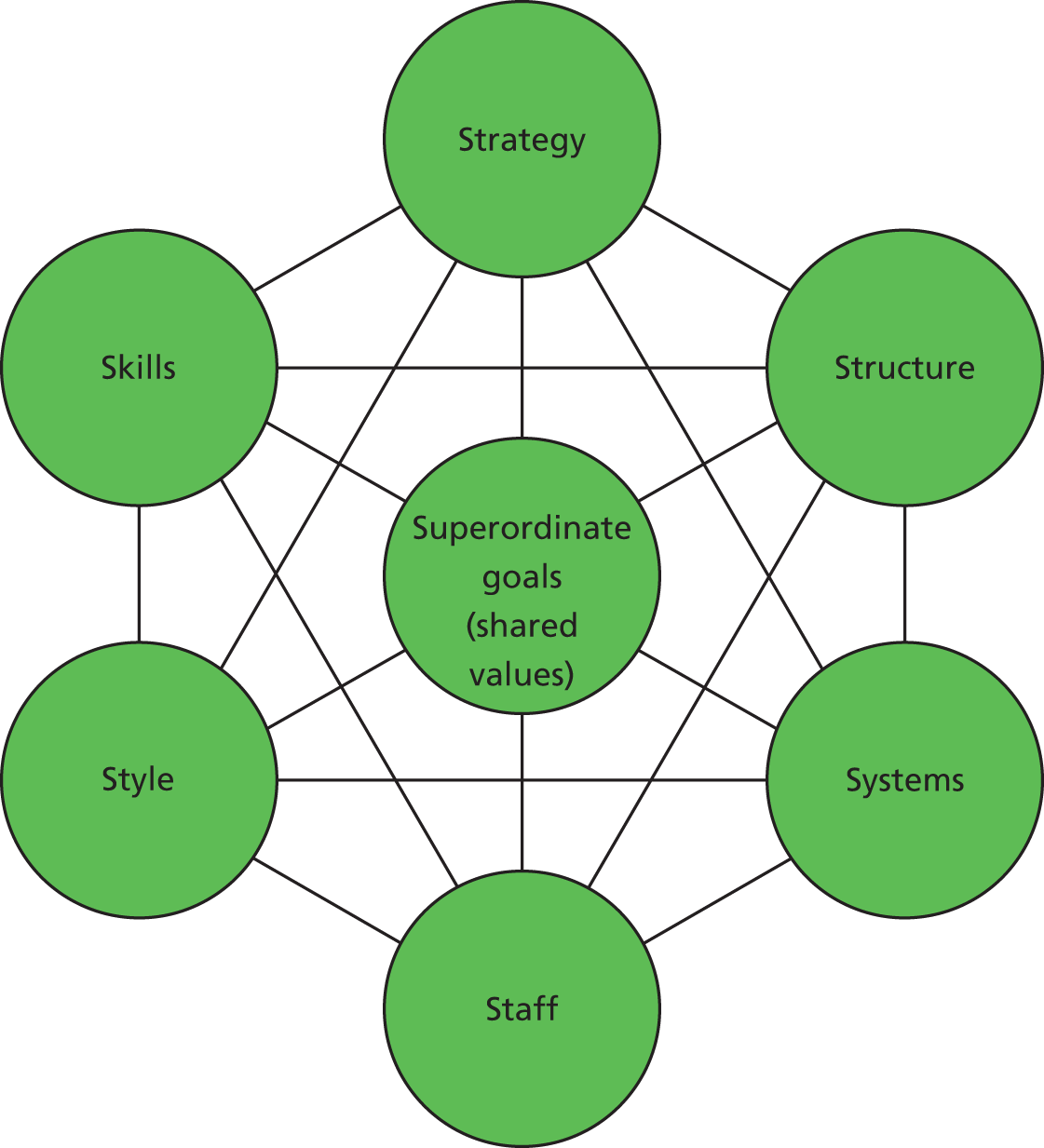
Of these models, the McKinsey 7S framework was seen as the most appropriate tool to capture and analyse the complex organisational structures we were to encounter. The 7S framework was originally designed to diagnose how the existing organisation operates and then to find ways to implement change. Moreover, the 7S framework has been proven in organisational study and design since its inception in the early 1980s. It has been widely adopted by researchers and managers in the NHS. 59 Its particular strength, relevant to this project, is in focusing on a systems-based approach, emphasising that, for change to be effective, changes in any one component must be accompanied by complementary changes in others. 51 It is often used in conjunction with PESTELI, a tool for analysing the environment in which an organisation operates (comprising Political factors, Economic influences, Sociological trends, Technological innovations, Ecological factors, Legislative requirements and Industry requirements). In this project our focus was more on the internal than the external environment, so PESTELI was not used. Although it might have contributed to contextual understanding, we considered this would be adequately covered by the 7S model.
The 7S framework segments different parts of the organisation (elements of the systems) so that they can be observed, studied, measured and understood at a meaningful level of aggregation. In addition, this tool crucially allows different organisational systems to be analysed by a common, simple yet effective framework (Figure 2).
The framework enables consideration of the key elements of the organisation/system as follows:
-
Structure: this is the way the organisation is structured, and specifically includes the reporting structure.
-
Strategy: this is the plan of activity for the system; importantly, it is also about how aligned the whole system is towards its objectives.
-
Systems: these are the processes and procedures of the system: the daily activities and routines.
-
Shared values: these are the norms and standards that guide the behaviour of the human elements within the system.
-
Style: this is essentially about the style of management used by the system leadership.
-
Staff: this element is concerned with the training, motivation and rewards of the staff.
-
Skills: this element is about the specific skills existing and required by staff in order to best execute their duties. It is also important during change management.
Chapter 2 Aims and objectives
Aims
To identify system characteristics associated with higher and lower increases in unplanned admission rates in those aged 85 years and over; to develop recommendations based on best practice to inform providers and commissioners; and to investigate the challenges of starting to implement these recommendations.
Research questions
-
What system characteristics (including commissioning arrangements and pathways of care) are associated with higher and lower than average changes in unplanned admission rates in those aged 85 years and over?
-
What are the antecedents, contextual and internal factors that influence these different characteristics of the management of care of those aged 85 years and over?
-
What are the lessons to be learned in terms of commissioning, system configuration and system change to reduce unplanned hospital admissions for those aged 85 years and over more widely across the NHS?
-
What are the practical challenges faced by providers and commissioners in starting to implement system change to reduce unplanned admissions in those aged 85 years and over?
Chapter 3 Methods
Overview
Our conceptual framework is the premise that emergency admissions are one outcome in a complex system which includes a range of inter-related services. Additionally, improvements will emerge not just from reconfiguration of services, but also from effective leadership and implementation. We define the system of interest as a healthy economy serving a defined population and comprising an acute hospital trust, commissioning groups, GPs, intermediate care services, care homes, ambulance service and social care. The principal method is a qualitative multiple explanatory case study. 61 This approach is designed not to be generalisable to a population but to develop and test theory. Multiple cases strengthen the results by replicating pattern matching, thus increasing confidence in the robustness of the theory. We examined three cases at each extreme of changes in admission rates, a sample large enough to develop and test theory while being small enough to be feasible. Other multiple case studies, including the national evaluation of intermediate care, to which several of this report’s authors contributed, included a similar number of sites. 62
Selection of study sites
A key consideration in multiple case study designs is the basis of case selection. This can be representative, purposive or guided by theoretical concerns, with the aim of providing a relevant basis for comparison. 63 For example, selection might include outliers or deviant cases with the express purpose of identifying and analysing factors potentially unique to the case and capable of generating novel conceptual insight. 61 For this study, the definition of case was the local health economy serving a defined population and comprising an acute hospital trust, commissioning groups, GPs, intermediate care services, care homes, ambulance service and social care. The basis of case selection was purposive and guided by prior statistical analysis; that is, cases were selected according to their distribution in relation to unplanned admission for people aged over 85 years, where case selection aimed to compare high- and low-performing cases as a means of understanding the factors (common and unique) that might account for unplanned admission.
We used PCTs as the basis of site selection, as these have a population base that can be used to derive admission rates. We chose changes in rates of admission for older people as the main criterion for selecting sites. This was chosen rather than absolute rates, as the latter are highly dependent on demographic factors such as age and deprivation. 6 By identifying and examining sites where rates had risen fastest and slowest we hoped to be able to understand how changes (or lack of changes) in systems of care influenced changes in admission rates.
A second criterion was a strong linkage between the PCT and an acute trust. This was applied because we wanted to explore areas in which there was at least a potential partnership between these organisations so that system change could occur. We defined this criterion as being achieved if more than 80% of acute admissions for people aged 85 years and over from a PCT were admitted to one acute trust. We excluded London PCTs, as their acute trusts have partnerships with several PCTs, even if the index PCT used one acute trust for a high proportion of its patients. Finally we excluded any site that was known to be experiencing significant reconfiguration as reflected in national publicity.
A third criterion in sample selection was to use a mix of urban and rural sites, and a range of deprivation. Finally, we excluded sites that were potential participants in the implementation phase of the project.
Admission rates for people aged 85 years and over were calculated for the latest 3 years for which Hospital Episode Statistics (HES) data were available (provided by the Nuffield Trust). These data are based on admissions, not individuals, and also provide information about the trust to which admissions were made. Data were not available for some PCTs because of mergers, etc. For the 143 PCTs for which we did have data, a regression coefficient was calculated for the change in admission rates over the 3-year period, adjusting for population size and age. The value of the slope indicates the annual change in admission rates, with a positive slope value indicating an increased admission rate.
Primary care trusts were ranked according to this statistic. The change in rates of admission of older people ranged from + 10% per annum at the bottom of the ranking to –6% per annum at the top. Of the 143 PCTs, 120 (84%) had increased admission rates. Sites at the top and the bottom of the ranking were considered as potential participants.
Table 1 shows a selection of sites at the top of our ranking. After we applied our criteria, sites ranked 4, 5 and 9 were selected. The selection at the bottom of the ranking is shown in Table 2. After applying our criteria, we selected sites ranked 132, 133 and 135.
| PCT rank for slope | 85 years and over admission rate (number of admissions/population) | Slope (per annum change) | % admissions to linked hospital trust | % aged 85 years and over | Reference in report | ||
|---|---|---|---|---|---|---|---|
| 2007 | 2008 | 2009 | |||||
| 1 | 0.61 | 0.53 | 0.49 | –0.06 | 66 | 1.5 | |
| 2 | 0.56 | 0.52 | 0.50 | –0.03 | 52 | 1.5 | |
| 3 | 0.71 | 0.69 | 0.67 | –0.02 | 43 | 1.5 | |
| 4 | 0.55 | 0.51 | 0.51 | –0.02 | 89 | 2.6 | I1 |
| 5 | 0.61 | 0.60 | 0.57 | –0.02 | 87 | 2.6 | I3 |
| 6 | 0.66 | 0.70 | 0.63 | –0.02 | 40 | 1.0 | |
| 7 | 0.53 | 0.54 | 0.50 | –0.02 | 40 | 2.5 | |
| 8 | 0.57 | 0.55 | 0.55 | –0.01 | 78 | 2.3 | |
| 9 | 0.41 | 0.41 | 0.39 | –0.01 | 83 | 2.2 | I2 |
| 10 | 0.40 | 0.41 | 0.38 | –0.01 | 66 | 2.2 | |
| PCT rank for slope | 85 years and over admission rate (number of admissions/population) | Slope (per annum change) | % admissions to linked hospital trust | % aged 85 years and over | Reference in report | ||
|---|---|---|---|---|---|---|---|
| 2007 | 2008 | 2009 | |||||
| 132 | 0.48 | 0.54 | 0.59 | 0.06 | 92 | 2.2 | D1 |
| 133 | 0.41 | 0.45 | 0.52 | 0.06 | 87 | 1.7 | D3 |
| 134 | 0.41 | 0.44 | 0.52 | 0.06 | 76 | 2.3 | |
| 135 | 0.49 | 0.59 | 0.61 | 0.06 | 83 | 1.8 | D2 |
| 136 | 0.51 | 0.58 | 0.64 | 0.06 | 90 | 2.1 | |
| 137 | 0.47 | 0.51 | 0.60 | 0.06 | 89 | 2.0 | |
| 138 | 0.46 | 0.54 | 0.60 | 0.07 | 75 | 1.6 | |
| 139 | 0.50 | 0.63 | 0.64 | 0.07 | 83 | 1.8 | |
| 140 | 0.41 | 0.56 | 0.56 | 0.07 | 80 | 2.2 | |
| 141 | 0.56 | 0.68 | 0.71 | 0.08 | 73 | 1.4 | |
| 142 | 0.33 | 0.51 | 0.50 | 0.09 | 50 | 1.8 | |
| 143 | 0.39 | 0.58 | 0.59 | 0.10 | 46 | 2.1 | |
Recruitment at sites
In the selected sites, invitations to participate were sent to the chief executives of the PCT and acute trust (see Appendix 1). In all cases, there was initial agreement from both parties. We then invited participation from the organisation responsible for community health services and social services. Table 3 shows final agreement of organisations by site. At site I1 there was a change of chief executive, and the incoming one withdrew the site from the study because of competing priorities. In site D3 the contract for delivering community health and adult social care was awarded to a social enterprise organisation. We were unable to obtain the confidentiality agreement from the university that this organisation required, so it did not participate.
| Site | Acute trust | PCT | Community health | Social services |
|---|---|---|---|---|
| I1 | No (withdrew support) | Yes | Yes | No |
| I2 | Yes | Yes | Yes (Care Trust Plus for both services) | Yes (Care Trust Plus for both services) |
| I3 | Yes | Yes | Yes | Yes |
| D1 | Yes | Yes | Yes | Yes |
| D2 | Yes | Yes | Yes | Yes |
| D3 | Yes | Yes | No (community enterprise) | Yes |
Quantitative methods
Improving and deteriorating sites were compared with national data using publicly available data and enhanced HES data. Publicly available data comprised the following:
-
HES online:64 admissions by PCT and hospital provider, aged 75 years and over (data on those aged 85 years and over were not available).
-
NHS Information Centre Indicator Portal:65 emergency admission rates (aged 85 years and over), changes in age structure of population, admissions for acute and chronic ACSCs, readmissions within 28 days of discharge (aged 75 years and over), deprivation.
-
NHS Better Care, Better Value Indicators:66 standardised emergency admissions rates for 19 ACSCs, financial and volume opportunities (i.e. potential financial and bed occupancy savings) rank.
-
GP Patient Survey:67 GP access, including out-of-hours services.
The enhanced HES data set enabled us to examine admissions in those aged 85 years and over up to the year 2011/12. These were used to calculate the following: admission rates, length of stay, seasonal variations and rank of admission rates, readmissions within 28 days, deprivation, ethnicity, health and disability index, breakdown of admissions by acute and chronic ACSCs, and admission from and discharges to care homes. Data are presented descriptively; given the small number of sites in each grouping and the purposive method of selection, it was not felt appropriate to apply statistical testing.
Qualitative methods
Following agreement to participate, two rounds of data collection were conducted at each site. In preparation for these interviews a profile was prepared for each site, using the quantitative data described earlier, and this was used to stimulate discussion during the interview.
In the first round, an understanding of the system’s history and drivers was sought in interviews with high-level key informants, including commissioners and managers of health and social care with responsibility for those aged 85 years and over, and clinicians and care providers with leadership roles in primary care, ED, social care, and intermediate and secondary care services. These interviews explored known system-level issues such as commissioning, interagency working, communication and knowledge sharing, culture, power relationships, incentives, boundaries, and successes and failures in implementation. We sought to understand what changes have been instigated in an attempt to reduce admissions in the 85 years and over bracket, the extent of their adoption, their outcome and reasons for success or failure. Respondents were also asked to allow the team access to any internal documents, audits, etc.
In the second round of data collection, we examined specific components of the system, using in-depth interviews and focus groups with those involved in delivering care, to explore issues involved in translating policy directives to changes in the actual provision of care. These included clinicians in ED and acute medical units, managers of intermediate and integrated care provision and clinicians in primary care. We had planned to conduct focus groups composed of individuals with similar roles, but in practice these were logistically difficult to arrange because of potential participants’ other commitments and so took place at only some sites.
In each site we aimed to convene a focus group, including representatives of carers and service users, to capture their perspectives on the impact of initiatives to reduce admissions in those aged 85 years and over. Participants were selected who were able to present a user perspective on service changes focused on admissions in those aged 85 years and over, and were drawn from local patient and public involvement (PPI) groups in primary and secondary care and charities such as Age UK.
Development of topic guide
The topic guide for interviews and focus groups with professionals was developed using the McKinsey 7S model as a starting point. The major themes were based around:
-
Strategy
-
Structure
-
Systems
-
Style
-
Staff
-
Skills
-
Shared values.
These areas for exploration were refined based on the topic of emergency admissions of older people. The project team discussed the areas which they believed would have an impact on emergency admissions in each of the seven major themes. The topic guide was further developed based on these discussions and was piloted on members of the project group. The topic guide was designed to be used in sections, whereby questions on the strategy and organisational structure were asked of senior staff and questions on service delivery and staff skills were given to frontline staff. The final topic guide can be found in Appendix 2.
Qualitative analysis
Interviews and focus groups were recorded and transcribed verbatim. Qualitative data analysis was undertaken in a stepwise approach following completion of data collection from the six case study sites. In the preliminary phases, all data from each case site were assigned to individual members of the project team for an initial phase of inductive, open coding. The aim of this initial stage was to develop a general descriptive account of each health system, paying particular attention to the management of care for people over 85 years old, and to determine the relevance and usefulness of systematically applying the 7S framework for subsequent data analysis. The initial case descriptions were shared and discussed among the wider project team with the aim of developing a common coding framework for the 7S model. Selection bias at the individual level was therefore minimised by group discussion and conferring.
The second and main stage of data analysis involved two independent researchers developing detailed case reports for each health system. This was informed by the 7S model and the preliminary phase of data analysis. Following a framework approach,68 all data items were systematically scrutinised, with extracts of data coded and sorted according to the 7S categories. This involved the close reading of all electronic data items, coding data extracts according to the 7S categories and copying these into the appropriate column of the framework spreadsheet. Guidance for coding was agreed by team members, including how items would be categorised according to the 7S framework (e.g. it was agreed that ‘Structure’ would be used to capture information about inter-relationships of services and ‘Systems’ for items related to individual component services). Where items of data did not easily fit within the 7S headings, a new open heading was produced. Throughout this phase, and in line with the principle of constant comparison, each category was systematically checked for its internal consistency and inter-relationships. 69,70 After this initial phase, data items within each category were further reanalysed to identify sub- and grouped themes. Through this process an initial narrative was produced to describe and characterise the findings within each category. The aggregated coding framework and initial descriptions were finally brought together to produce an initial case report for each site.
These case reports were then shared with the wider research teams for clarification and conceptual development, paying particular attention to the recommendations and learning points. At this time, one member of the study team used the data from each case report to produce a summary table for each case study site. For each of the 7S categories the table aimed to present the headline positive or negative features, for example those aspects of ‘Strategy’ that contributed either positively or negatively to the management of care for people aged over 85 years. For each of the identified features the table also sought to draw out from the case reports the possible reasons, source or influences that might explain these aspects, for example how local strategy was influenced by national policies, resource limitations or leadership structures. In this way, the table also starts to identify linkages between 7S categories, such as how Strategy and Skills are linked.
The final stage of data analysis involved members of the wider study team reviewing individual case reports and looking for overarching themes and accounts that might explain similar systems, features and processes. Comparison between case study sites provided the basis of conceptual and theoretical elaboration whereby tentative explanatory models were identified, developed and discussed among the study team with the aim of explaining similarities and differences among the study sites, especially between the improving and declining sites. These tentative propositions were then tested against the empirical data with the aim of producing recommendations for service improvement, before being validated through consultation with wider stakeholders and project advisors.
Ethics and governance
The project team applied for NHS ethics approval but was advised in September 2011 that the committee did not consider the project to be research. We therefore applied to the University of Leicester Ethics Committee, which granted approval in January 2012. Approval was also sought from the Research Group of the Association of Directors of Adult Social Services which in October 2012 agreed to recommend the project to social services departments. This study was included in the National Institute for Health Research Clinical Research Network Portfolio in August 2012, and sponsorship was agreed by University of Leicester.
Chapter 4 Results
Overview of quantitative data for improving and deteriorating sites
Emergency admission rates of people aged 85 years and over
Our selection of deteriorating and improving sites was based on their admission rates, expressed as number of hospital admissions in the age group of 85 years and over divided by the population of 85 years and over for each PCT, between 2007/8 and 2009/10. On average, the deteriorating sites experienced a rise in admission rates by about 5.5% annually during the period 2007/8–2009/10, higher than the average for England of 2% (Figure 3). In contrast, the improving sites experienced a fall in admission rates by 1% annually for the same period. At the start of the period, the deteriorating sites had, on average, rates below the English average, but at the end of the period these were higher than average. In contrast, improving sites started above the English average but were below at the end of the period. There was greater variation in absolute rates in improving sites than in deteriorating sites. As no sampling was used, error bars are not included.
FIGURE 3.
Eighty-five years and over admission rates for the period 2007/8–9/10 for study sites. Adapted from Ian Blunt, Nuffield Trust, 2011, personal communication.
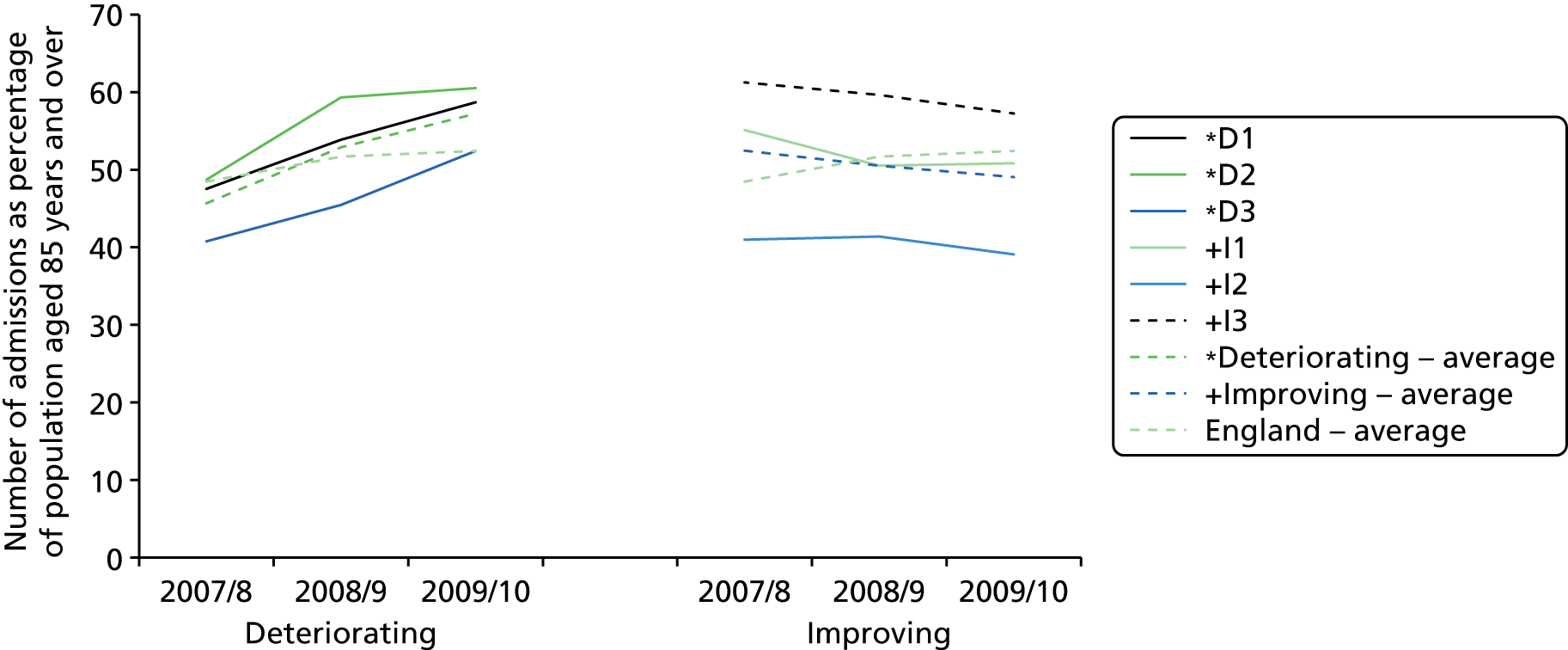
Data for later years show that in improving sites admission rates remained stable, whereas there was a small reduction in rates in deteriorating sites (Figure 4). Between using HES data for selection and this analysis, some corrections had been made to 2007/8 data, meaning the overall trends in reduced rates for improving sites were less pronounced.
FIGURE 4.
Eighty-five years and over admission rates for the period 2007/8–11/12 for study sites. Adapted from HES data set (Dean White, Health and Social Care Information Centre, 2012, personal communication).

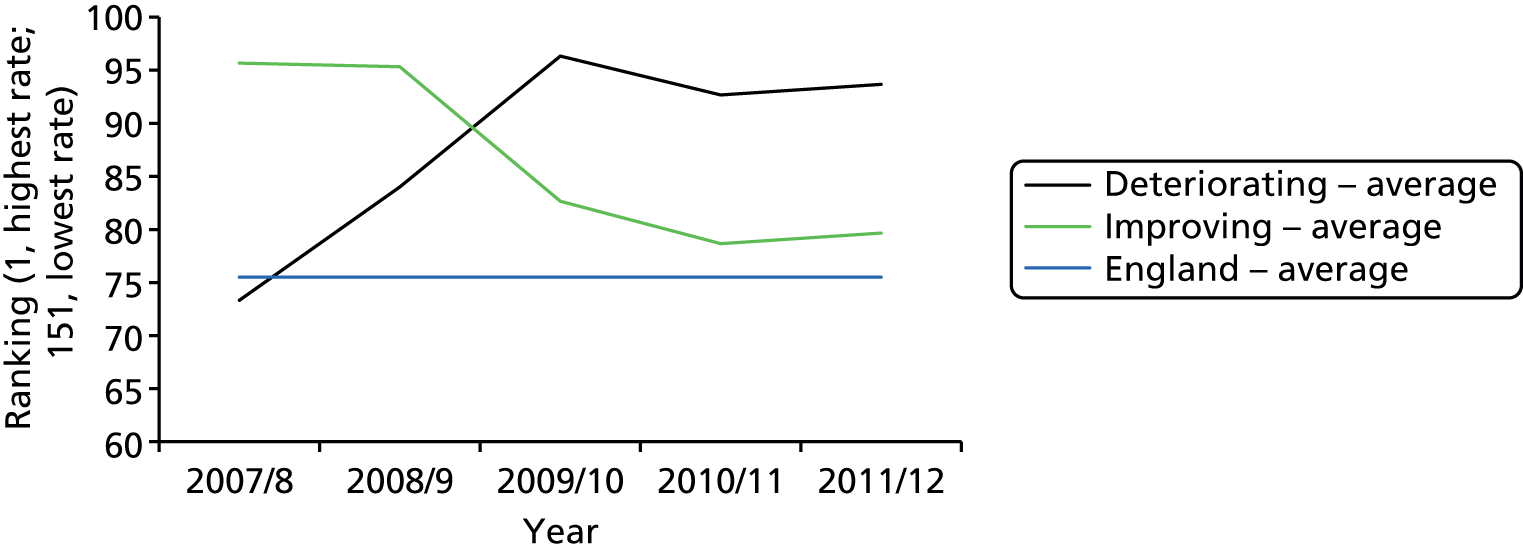
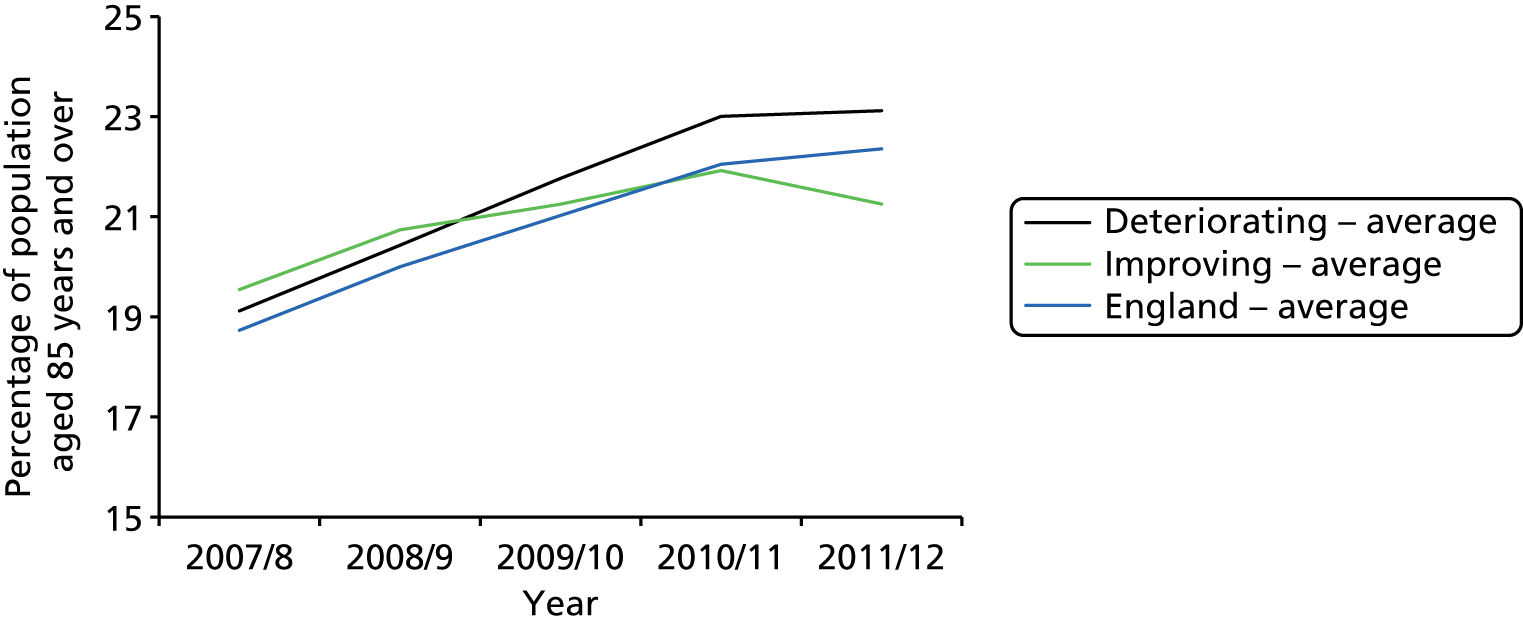
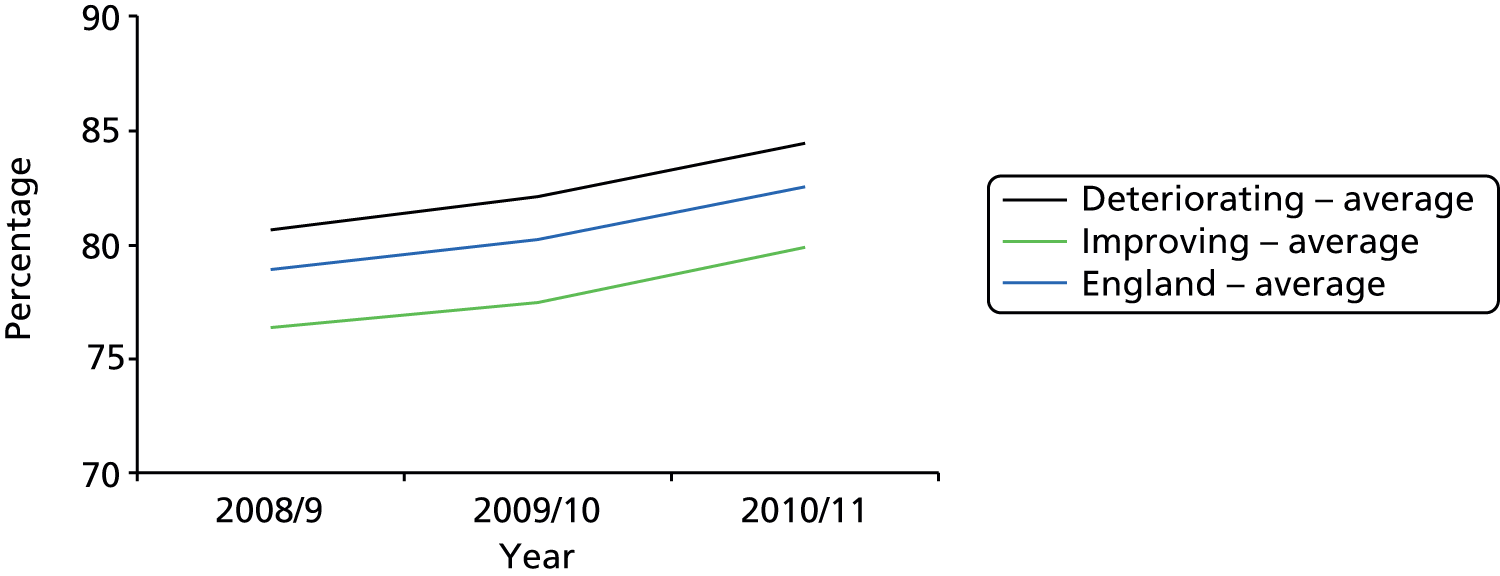
Differences in performance between improving and deteriorating sites were also explored by calculating their ranking in total admission rates compared with all 151 PCTs (Figure 5). In the first 3 years, the improving sites climbed the rankings and deteriorating sites fell back. Over the subsequent 2 years, the performance of both groups was stable.
FIGURE 5.
Rank fluctuations in total admission rates. Adapted from HES data set (Dean White, Health and Social Care Information Centre, 2012, personal communication).
We examined demographic changes as a possible explanation for differences between improving and deteriorating sites. During the period 2007–10 the population of 85 years and over residents in the deteriorating sites rose by 3.4%, which is above the England average of 2.8% for all 151 PCTs, while the population in the improving sites rose by only 1.3%. This pressure on services for older people may have increased more in deteriorating than improving sites.
Admission rates for ambulatory care sensitive conditions
As discussed in Chapter 1, the rising tide of admission for ACSCs is largely due to acute conditions, with an average annual increase of 2.7% from 2002/3 to 2009/10. Rates for chronic ACSCs remained fairly stable during this period. Acute conditions included in this group are H660–H664, suppurative otitis; I500, heart failure; J02–J06, acute upper respiratory infections; N159, renal tubulointerstitial disease; N300, acute cystitis; N39, urinary tract infection; I11, hypertensive heart disease; and J31, rhinitis, nasopharyngitis and pharyngitis. Chronic conditions included are J45–J46, asthma; and E10–E14, diabetes. 71
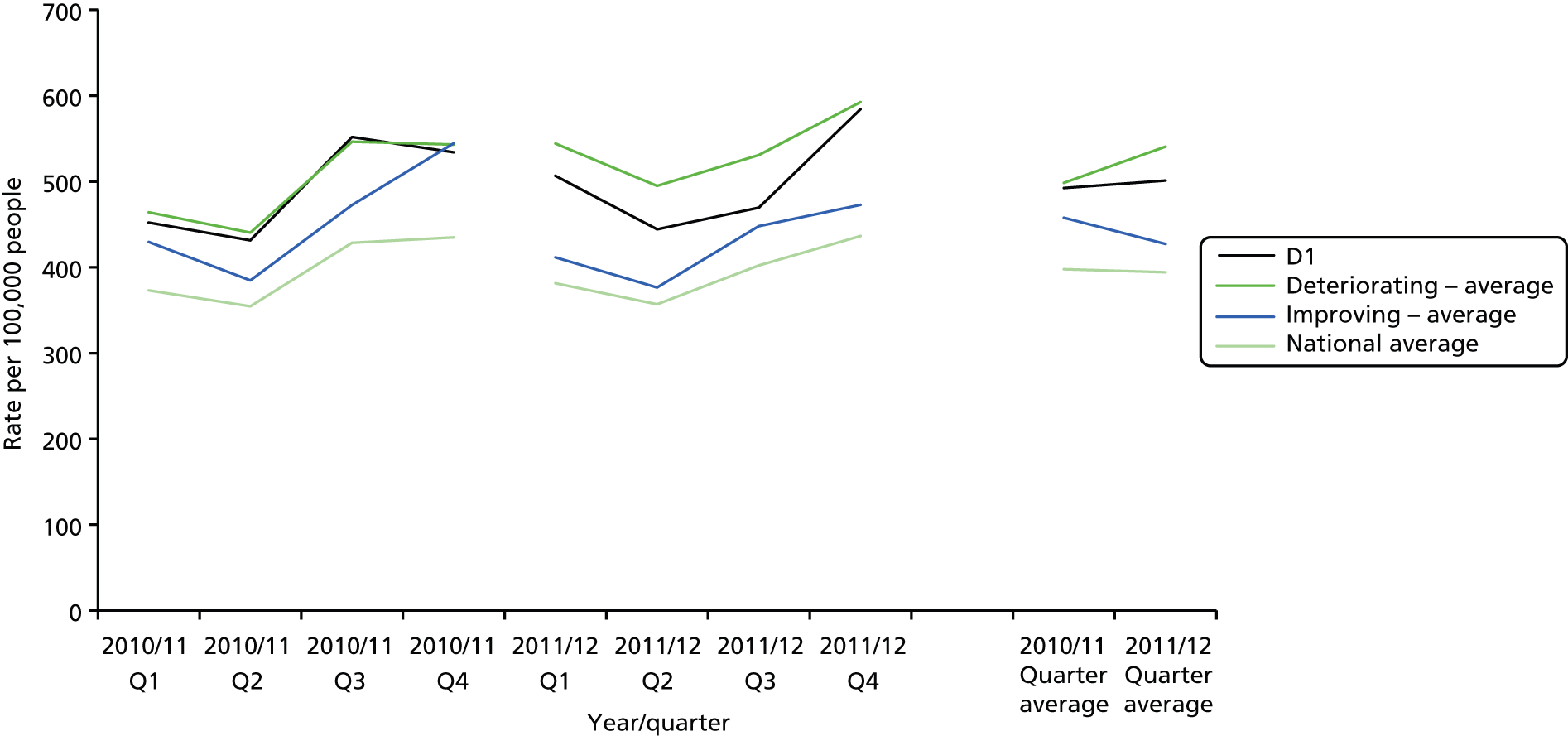
We examined admissions for ACSCs in study sites using the NHS information portal. The latest year for which data were available was 2009/10, and no data were available specifically for those aged 85 years and over. Emergency admissions for acute ACSCs exhibited a similar pattern to the overall admission rates for the age group of 85 years and over, which suggests that acute ACSCs may be a significant factor in explaining differences between improving and deteriorating sites. More specifically, the numbers of admissions in the deteriorating sites rose, while the numbers of admissions in the improving sites fell (Figure 6).
FIGURE 6.
Emergency hospital admissions: acute conditions usually managed in primary care. Indirectly age- and sex-standardised rate per 100,000, all ages. Adapted from https://indicators.ic.nhs.uk/. 65

Admissions for chronic ACSCs in the study sites were fairly stable during the period examined (Figure 7), although some variation is probably due to the low numbers of this type of admission (between 200 and 250 per 100,000 people).
FIGURE 7.
Emergency hospital admissions: chronic conditions usually managed in primary care. Indirectly age- and sex-standardised rate per 100,000, all ages. Adapted from https://indicators.ic.nhs.uk/. 65

Further information on ACSCs was obtained from the NHS Better Care, Better Value Indicators website. 66 It provides information on the emergency admissions for 19 ACSCs aggregated for patients from all ages. When accessed, this data set included admissions in 2010/11 and 2011/12 for the following conditions, standardised for age, sex and social deprivation: COPD, angina (without major procedure), ear, nose and throat infections, convulsions and epilepsy, congestive heart failure, asthma, flu and pneumonia (> 2 months old), dehydration and gastroenteritis, cellulitis (without major procedure), diabetes with complications, pyelonephritis, iron-deficiency anaemia, perforated/bleeding ulcer, dental conditions, hypertension, gangrene, pelvic inflammatory disease, vaccine-preventable conditions and nutritional deficiencies.
These data show that the changes in standardised average quarterly ACSC admission rate (per 100,000) between 2010/11 and 2011/12 were from 498 to 541 in deteriorating sites and from 458 to 427 in improving sites. Expressed as rankings of 151 PCTs, deteriorating sites moved from 90th to 96th, and improving sites from 87th to 85th.
This indicator also shows the financial opportunity per quarter of reducing the rate of emergency admissions per population head to those of the PCT at the 10th percentile. The estimate for national savings in quarter 4 of 2011/12 was £323M. From 2010/11 to 2011/12, this changed from £1.51M to £1.65M in deteriorating sites and from £1.30M to £1.38M in improving sites.
Length of stay
We examined whether or not differences in admission rates could be explained by differences in the length of stay of patients with acute admissions. Emergency admissions (all ages and 85 years and over) were divided into two categories: zero-day admissions (i.e. discharge on the same date as the admission) and multiday admissions (i.e. those discharged on a later date). For the latter category, average length of stay was calculated by dividing the sum of the bed-days by the number of admissions. Rates for zero-day admissions were calculated as a proportion of the population and as a proportion of the total number of admissions.
Multiday admissions
Across England and in both improving and deteriorating sites, there was a steady decrease in the length of stay (Figure 8). The average length of stay fell from 6.5 days in 2007/8 to 5.2 days in 2011/12, with no differences between types of site.
FIGURE 8.
Multiday admissions: average length of stay 2007/8–11/12, all ages. Adapted from HES data set (Dean White, Health and Social Care Information Centre, 2012, personal communication).

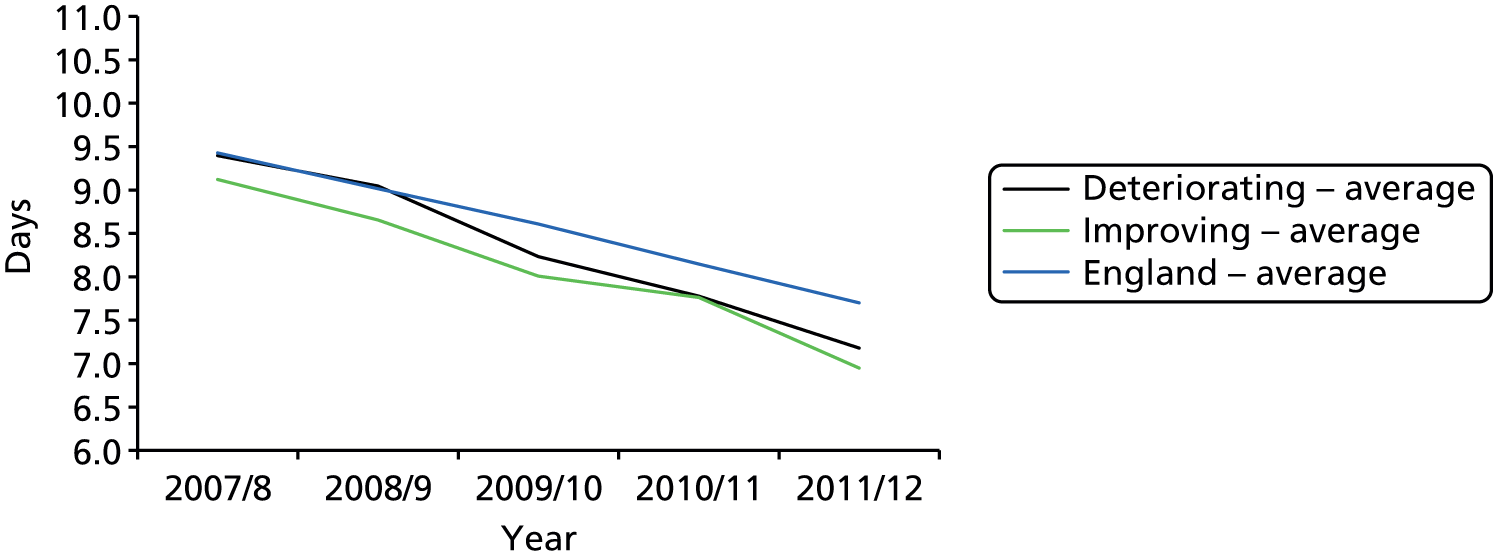
For those aged 85 years and over, stays were longer, but showed the same trend in reduction, from 9.3 days on average in 2007/8 to 7.2 days in 2011/12 (Figure 9). In the final year, both types of site had lengths of stay below the English average.
FIGURE 9.
Multiday admissions: average length of stay 2007/8–11/12, 85 years and over age group. Adapted from HES data set (Dean White, Health and Social Care Information Centre, 2012, personal communication).
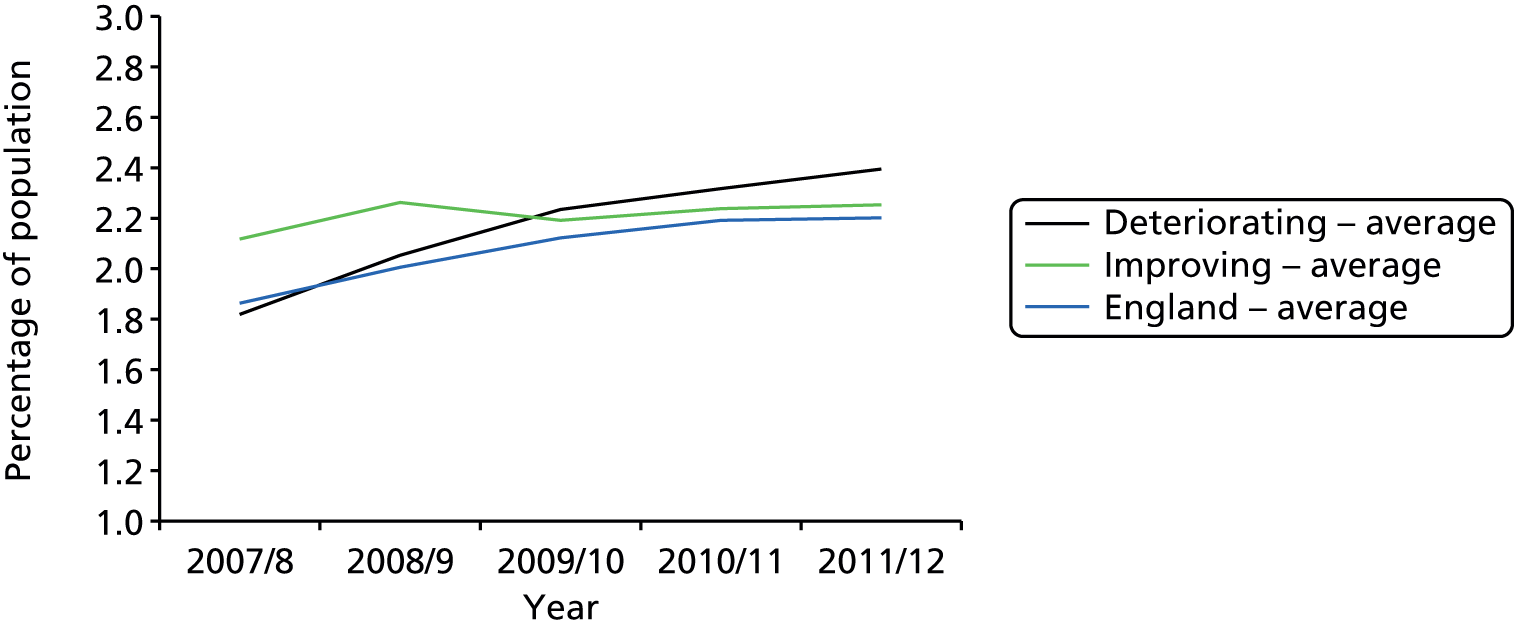
Zero-day admissions
Across England, same-day admissions constitute about one-third (28% to 30%) of all admissions. Their share was slightly rising from 2007/8 to 2010/11, when it seemed to peak (Figure 10). The two groups of sites differed markedly in trends for the proportion of 1-day admissions. The improving sites started out close to the England average in 2007/8 but the share declined until 2010/11. In contrast, the deteriorating sites started out well below the England average but increased the share of one-day admissions to that level by 2010/11. During the last year (2011/12) trends remained stable.
FIGURE 10.
Zero-day admission rate as a percentage of admissions, 2007/8–11/12, all ages. Adapted from HES data set (Dean White, Health and Social Care Information Centre, 2012, personal communication).
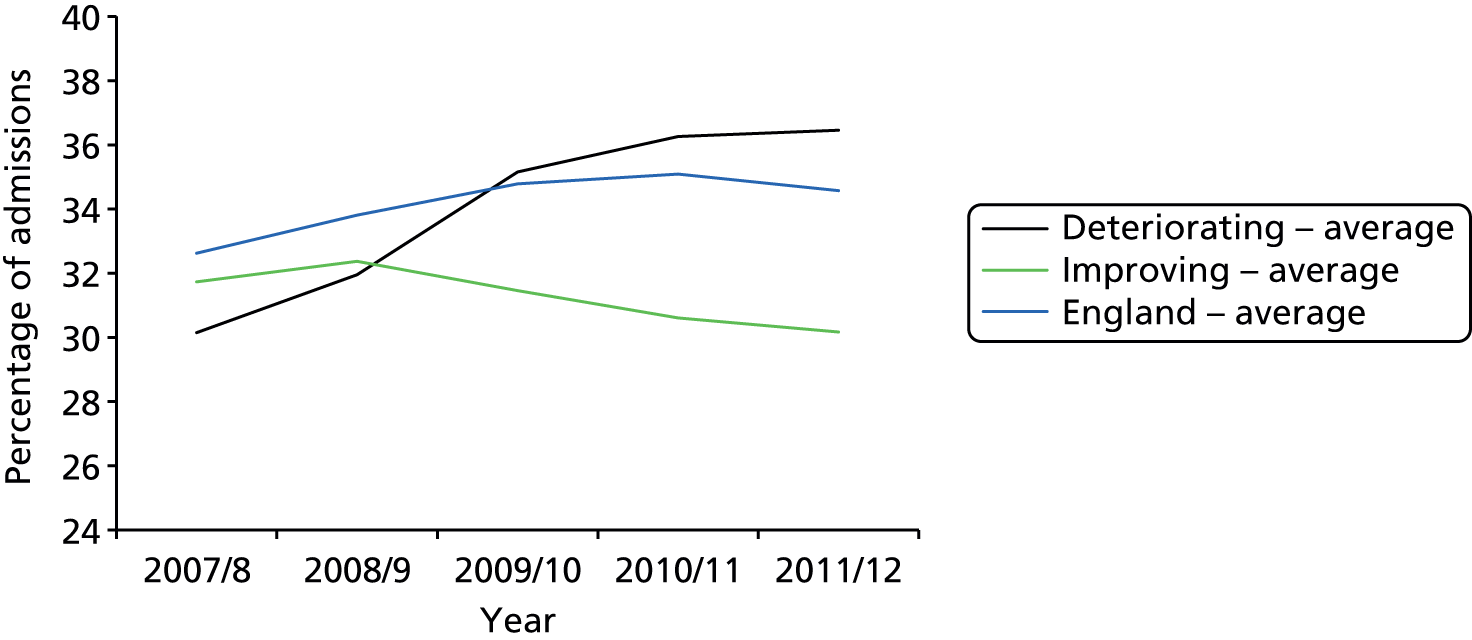
The zero-day admissions rate as a percentage of all admissions for the group aged 85 years and over followed the same trends as the rates for the whole population, with the exception that both the improving and deteriorating sites started out near the England average but then diverged (Figure 11). In 2010/11 the percentage of zero-day admissions in this age group was 30% in deteriorating sites, compared with 18% in improving sites.
FIGURE 11.
Zero-day admission rate as a percentage of admissions, 2007/8–11/12, 85 years and over age group. Adapted from HES data set (Dean White, Health and Social Care Information Centre, 2012, personal communication).
Rates of zero-day and multiday admissions were also examined for all age groups and those aged 85 years and over (Figures 12–15). In the latter group it can be seen that rates of zero-day admissions started close to the English average, but increased to 4.1% in deteriorating sites and fell to 3.0% in improving sites. Conversely, multiday admissions in those aged 85 years and over were stable in both types of site, and close to the national average. This trend was noted also by Blunt et al. ,3 who suggest that it is complex in nature, probably because of the interplay of several factors, and does not offer a causal explanation of the trend of increasing overall admission rates on its own.
FIGURE 12.
Zero-day admissions rate as a percentage of population, all ages. Adapted from HES data set (Dean White, Health and Social Care Information Centre, 2012, personal communication).

FIGURE 13.
Zero-day admissions rate as a percentage of population, 85 years and over age group. Adapted from HES data set (Dean White, Health and Social Care Information Centre, 2012, personal communication).
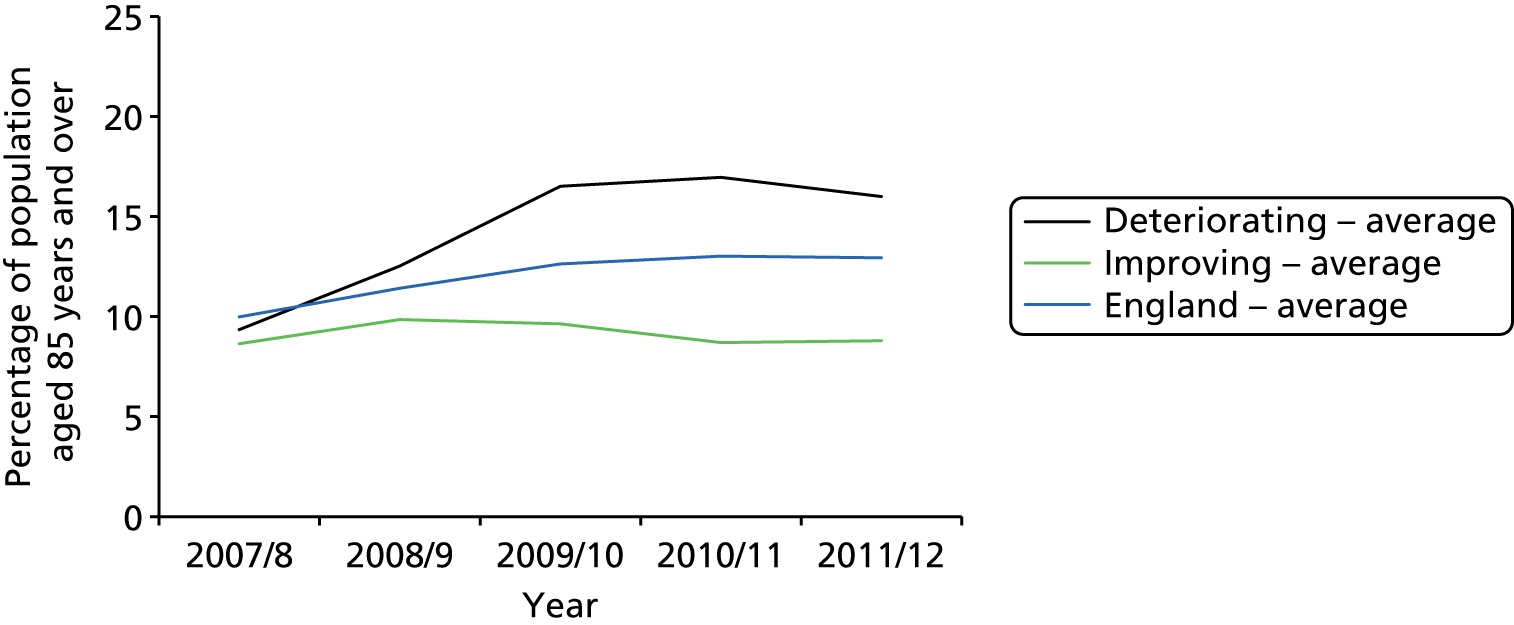
FIGURE 14.
Multiday admissions rate as a percentage of population, all ages. Adapted from HES data set (Dean White, Health and Social Care Information Centre, 2012, personal communication).
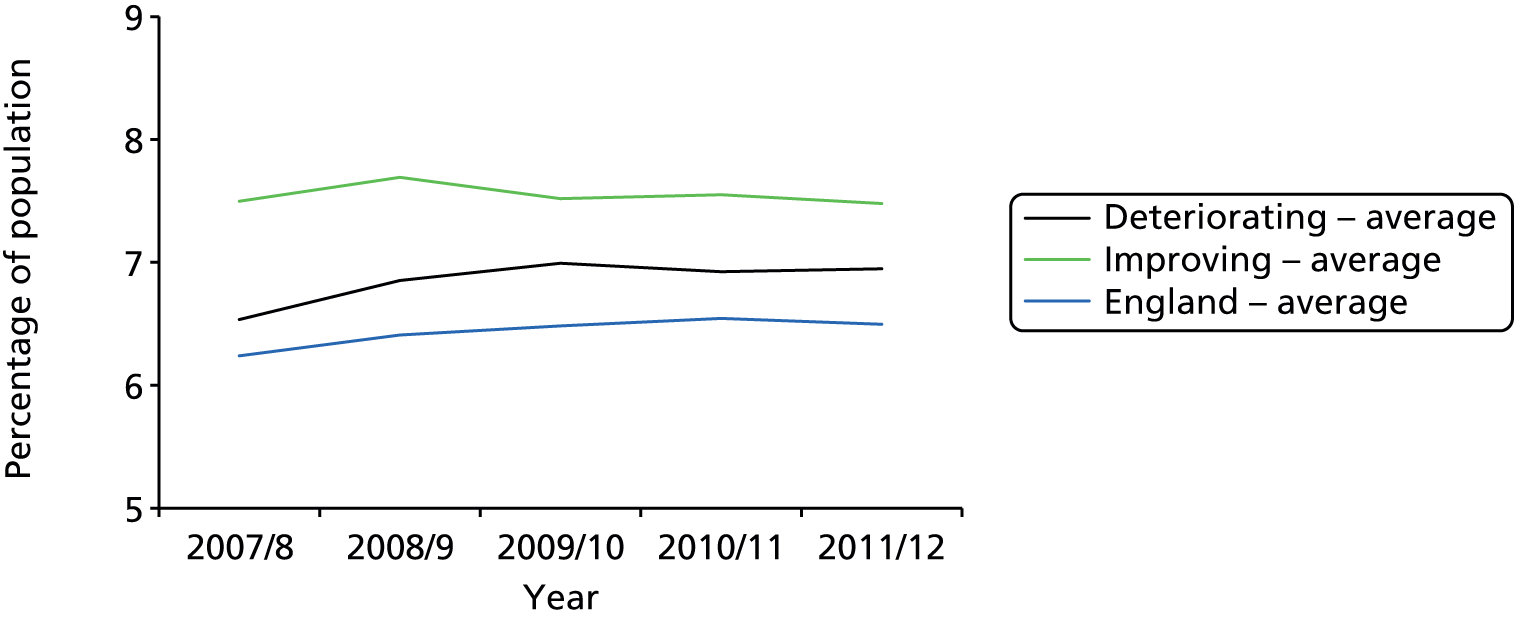
FIGURE 15.
Multiday admissions rate as a percentage of population, 85 years and over age group. Adapted from HES data set (Dean White, Health and Social Care Information Centre, 2012, personal communication).
Emergency readmissions within 28 days of discharge
The numbers of emergency readmissions within 28 days of a previous admission were calculated by populating an additional field in the HES database table with the date difference in days from the discharge date to the admission date. This was done regardless of the type of index admission, and so included planned admissions. This yielded the number of emergency admissions following an earlier discharge within 28 days. The number of readmissions for the first year was adjusted by half of 28/365 (= 0.038356) to account for lack of data on admissions in the preceding 28 days.
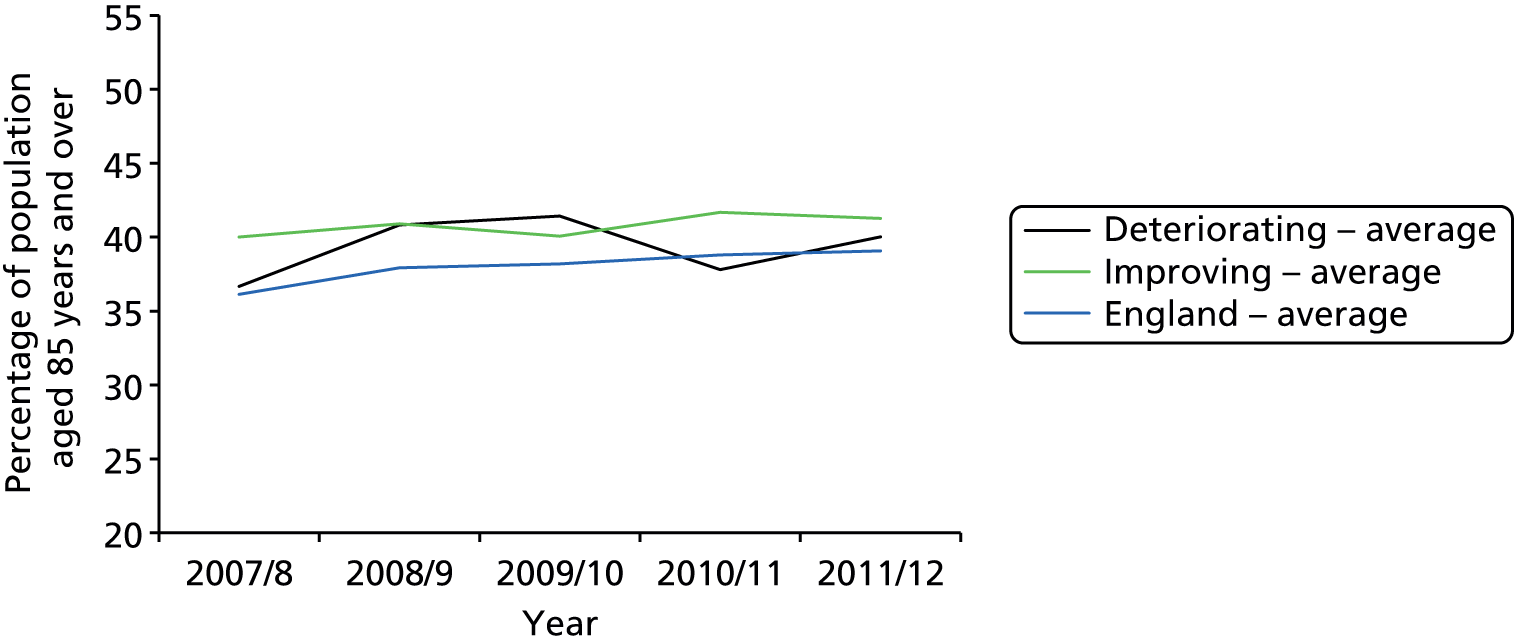
Emergency readmission rates as a percentage of the population
All ages
Across England, readmission rates increased from 2.0% to 2.2% of the total population between 2007/8 and 2011/12. Deteriorating sites started at close to this average, but showed a larger increase. In contrast, improving sites started above average but finished below (Figure 16).
FIGURE 16.
Emergency 28-day readmissions rate as a percentage of population, 2007/8–11/12, all ages. Adapted from HES data set (Dean White, Health and Social Care Information Centre, 2012, personal communication).
Age group 85 years and over
Readmission rates in this age group were higher but showed similar time trends. Both improving and deteriorating sites started close to the English average, but at the end of the period rates were 12.3% in the deteriorating group compared with 10.4 in the improving group (Figure 17).
FIGURE 17.
Emergency 28-day readmissions rate as a percentage of population, 2007/8–11/12, 85 years and over age group. Adapted from HES data set (Dean White, Health and Social Care Information Centre, 2012, personal communication).
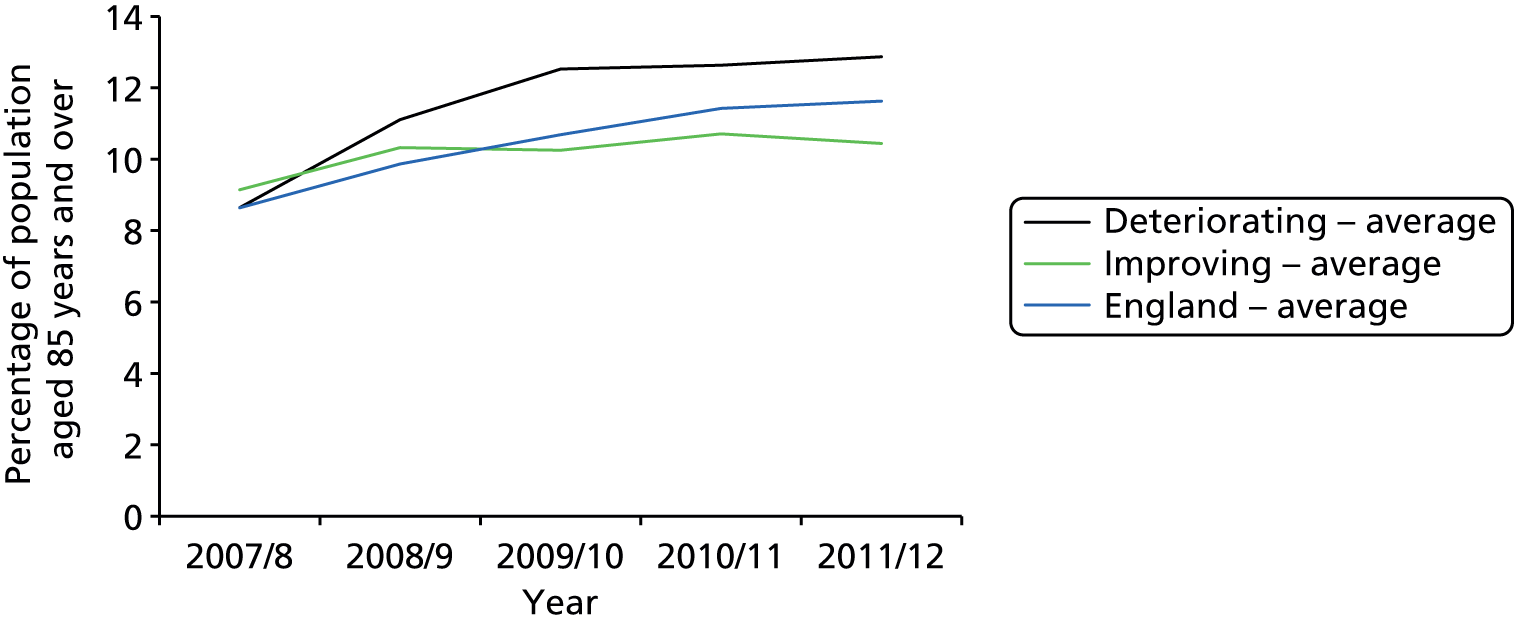
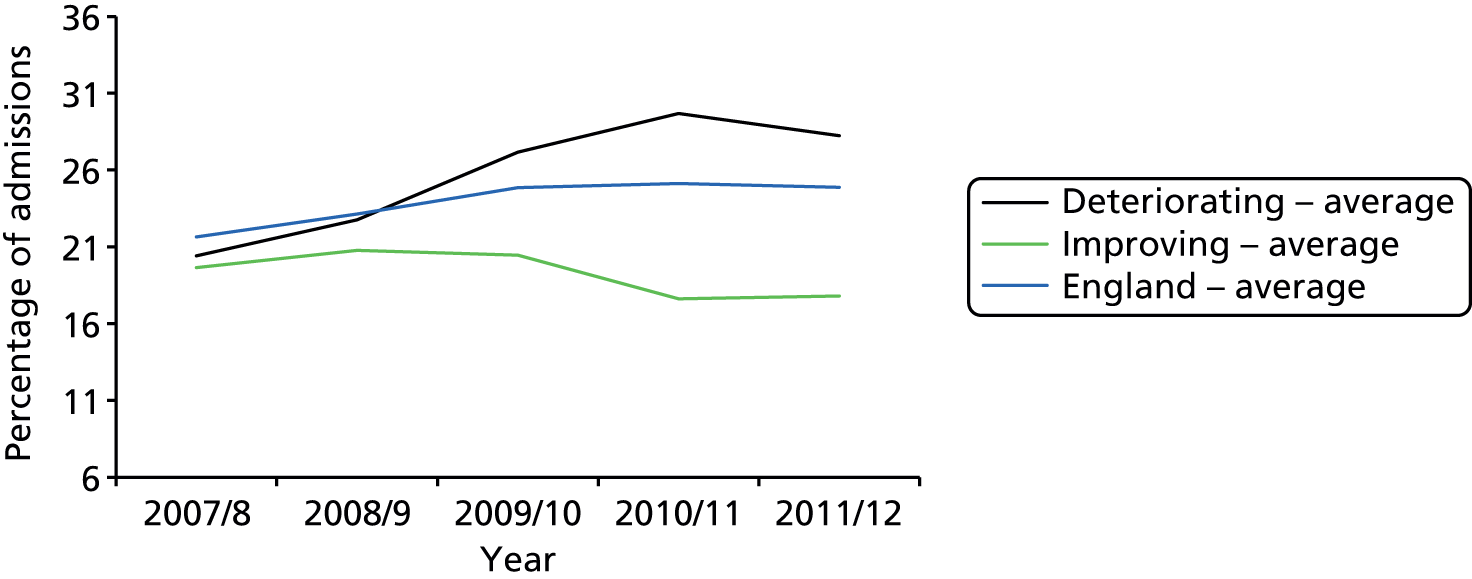
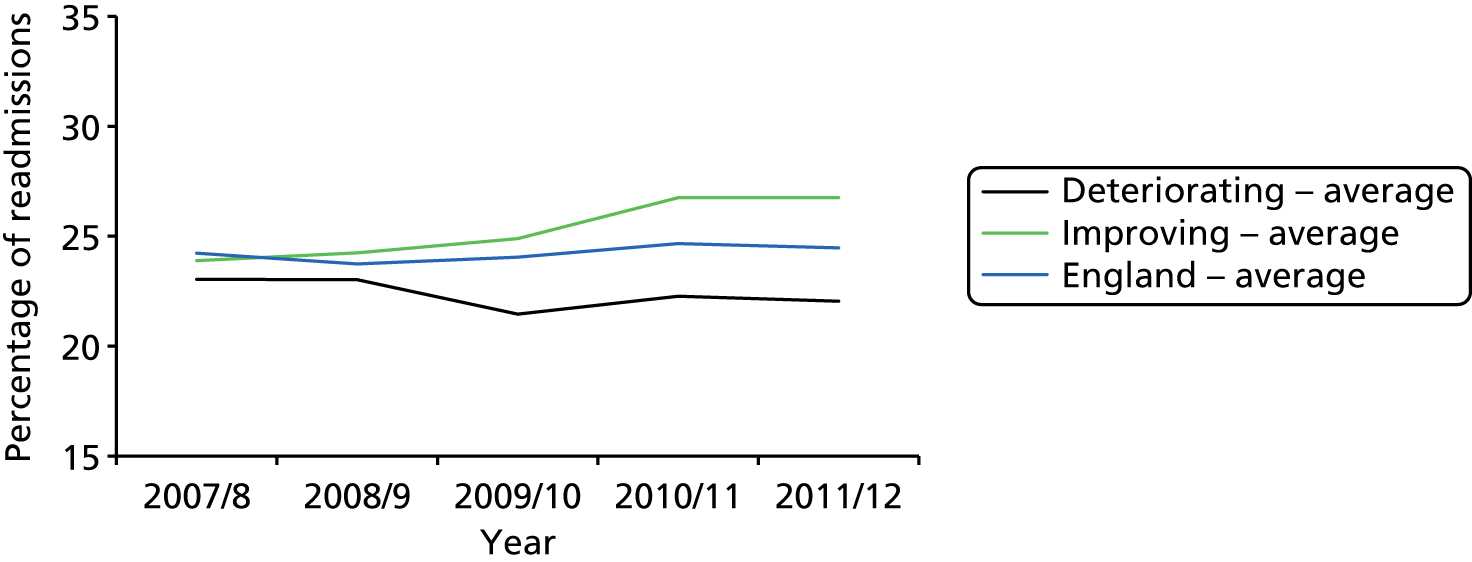
Emergency readmission rates as a percentage of admissions
Since admission rates and the readmission rates show similar trends, the ratio between them should be close to constant. This is what we observe in both graphs: for all ages (Figure 18) and for the age group 85 years and over (Figure 19). There is a slight trend of increase in the ratio, with the slope of the trendline for all ages in the deteriorating sites (= 0.61%) being higher than the slope of the trendline for the improving sites (= 0.35%) and closer to the England average (= 0.51%), which suggests that readmission rates are rising more than admission rates in the deteriorating sites. In 2011/12, for those aged 85 years and over, emergency readmissions comprised 23% of admissions, compared with 21% in improving sites.
FIGURE 18.
Emergency readmissions rate as a percentage of admissions, 2007/8–11/12, all ages. Adapted from HES data set (Dean White, Health and Social Care Information Centre, 2012, personal communication).
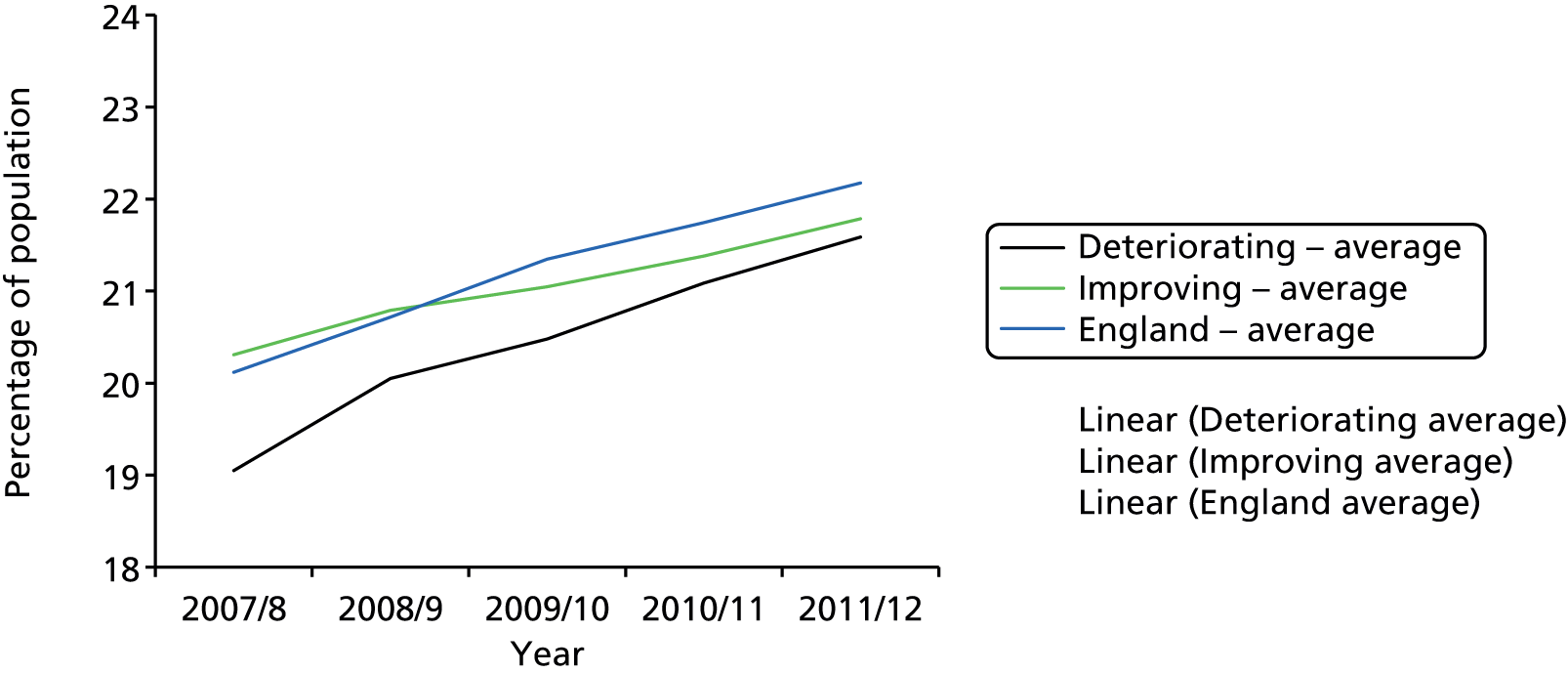
FIGURE 19.
Emergency readmissions rate as a percentage of admissions, 2007/8–11/12, 85 years and over age group. Adapted from HES data set (Dean White, Health and Social Care Information Centre, 2012, personal communication).
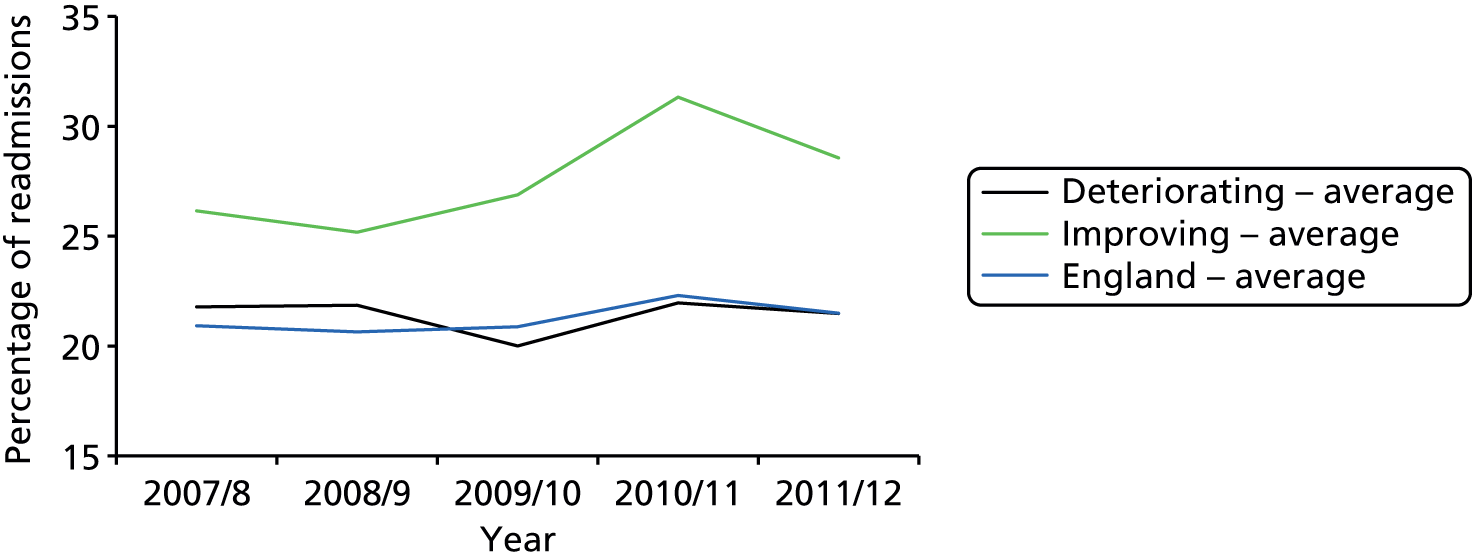
Emergency readmission rates following zero-day admissions
Emergency readmission rates following zero-day admissions were higher in improving sites, and this was more pronounced in those aged 85 years and over. There was an inverse relationship between zero-day admission rates and readmission rates following this type of admission. In the deteriorating sites, 1-day admission rates for all age groups rose from about 3% to about 4%, while the associated readmission rates fell from 23% to 22%. Conversely, the 1-day admission rates for all age groups in the improving sites fell slightly, from 3.2% to 3.0% of the population, while the associated readmission rates rose from 24% to 27% (Figure 20). This suggests that the absolute numbers of readmissions tend to remain stable, and the rates are affected mainly by the rising and falling admission numbers. It might also suggest that, in improving sites, people admitted for zero days are more ill and so more likely to be readmitted.
FIGURE 20.
Emergency readmissions rate following zero-day admissions, 2007/8–11/12, all ages. Adapted from HES data set (Dean White, Health and Social Care Information Centre, 2012, personal communication).
The pattern for the age group of 85 years and over (Figure 21) resembles the one for all ages. Deteriorating sites are very close to the English average, whereas readmission rates for improving sites are much higher.
FIGURE 21.
Emergency readmissions rate following zero-day admissions, 2007/8–11/12, 85 years and over age group. Adapted from HES data set (Dean White, Health and Social Care Information Centre, 2012, personal communication).
Admission to and from care homes
We aimed to examine differences in admissions from care homes, as the literature suggests initiatives based in these settings may be effective in reducing unplanned admissions. Unfortunately it was clear from examining HES data that, as shown in Table 4, these fields had not been reliably completed, so no conclusions are possible. Similarly, there were no reliable data for discharges to care homes.
| Site | 2007/8 | 2008/9 | 2009/10 | 2010/11 | 2011/12 |
|---|---|---|---|---|---|
| D1 | 91 | 54 | 17 | 13 | 6 |
| D2 | 57 | 59 | 21 | 32 | 24 |
| D3 | < 5 | < 5 | < 5 | < 5 | 8 |
| Deteriorating average | 50 | 38 | 13 | 15 | 13 |
| I1 | 9 | 5 | 5 | < 5 | < 5 |
| I2 | < 5 | < 5 | < 5 | < 5 | < 5 |
| I3 | 367 | 370 | 377 | 143 | 28 |
| Improving average | 126 | 125 | 128 | 49 | 10 |
General practitioner survey
Primary care trust-level results from the GP survey72 were examined for study sites. This survey is conducted regularly by Ipsos MORI. In 2014, 2.63 million patients were sent a questionnaire, which they could complete by post, by telephone or online. As in previous years, a response rate of around 34% was achieved and from 2009/10 onwards the results are adjusted for age, ethnicity, deprivation, etc.
Two questions about access which were included in 2008/9–2010/11 are shown in Figures 22 and 23. Similar questions were asked in 2007/8 and 2011/12, and these data are combined with the other 3 years. In all years, access scores were higher in improving than deteriorating sites, falling below and above the English average respectively. In all groups of sites, ease of access declined between 2007 and 2009 and then levelled off, and differences between improving and deteriorating sites persisted. Similar results were found in response to a question about ability to obtain an appointment (data are available only for 2008/9–2010/11).
FIGURE 22.
Able to see a doctor fairly quickly (question 7), percentage ‘yes’ answer. In 2007/8 and 2011/12 the question was defined differently. Adapted from GP Patient Survey. 72
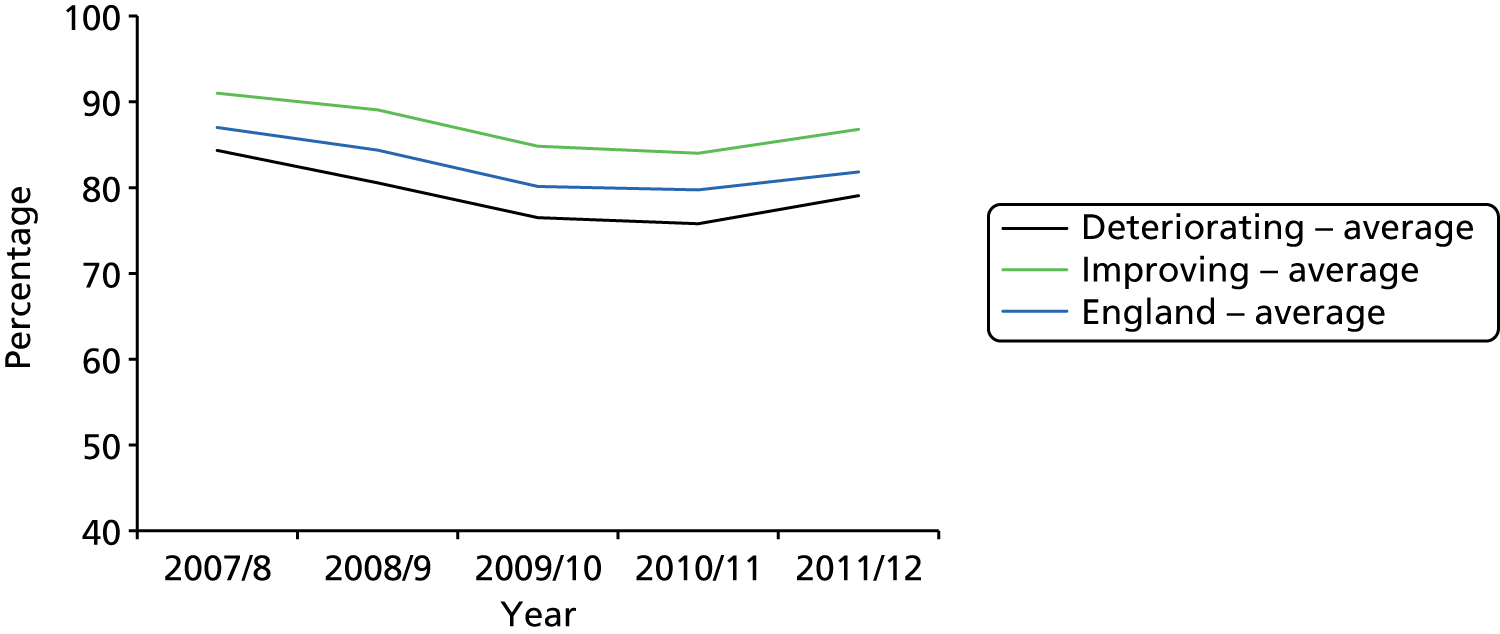
FIGURE 23.
Reasons for not being able to be seen fairly quickly (question 8), percentage ‘there weren’t any appointments’ answer. Adapted from GP Patient Survey. 72
The 2010/11 survey included a question about ease of contacting out-of-hours GP services by telephone. In deteriorating sites 23% reported it was ‘not very easy or not at all easy’, compared with 16% in improving sites.
Summary of quantitative findings
This analysis has revealed several factors that might explain differences in performance between improving and deteriorating sites, despite differences in admission rates for the 85 years and over being attenuated in the years after the period used to identify sites. The most important differences are the much lower proportion of zero-day admissions in improving sites, and lower overall readmission rates, suggesting that improving sites have been able to provide alternatives for these patients. The finding that readmission rates following 1-day admissions are higher in improving sites supports the suggestion that in these places admissions include a higher proportion of severely ill patients. Another reason for differences in performance is changes in admission rates for acute ACSCs, which rose sharply in deteriorating sites and declined in improving sites. This could reflect lower provision of community and GP services in these locations, as supported by evidence from the GP survey that access to GP services, including out-of-hours services, was poorer. Furthermore, problems with GP access are associated with increased use of EDs, which could itself increase admission rates, particularly for admissions for less than 1 day. The suggestion that both primary and secondary care services are under more strain in deteriorating sites is also supported by our finding that the oldest old population increased more rapidly in these locations.
Participants in qualitative interviews
We were able to gain participation from all key organisations in four of the six study sites. As outlined in Chapter 3, in site I1 the acute trust withdrew following a change of chief executive and the social services department declined to participate. In site D3, we were not able to secure an agreement with the social enterprise organisation with responsibility for community services. As shown in Table 5, we interviewed over 140 individuals in total, including some focus groups, with the number of participants at each site ranging from 15 to 43. Table 6 shows the background of those we interviewed. Across the sites we were able to capture the views of a range of professionals, including senior managers involved in commissioning and delivery, operational staff and clinicians from medicine, nursing and rehabilitation.
| Site | Acute trust | PCT/Clinical Commissioning Group | Community services | Social services | PPI | Total |
|---|---|---|---|---|---|---|
| I1 | Declined | 2 | 13: 7 individual, 2 focus groups (n = 2 and 4) | Declined | 0 | 15 |
| I2 | 6 | 6 | 16: 7 individual, 2 focus groups (n = 9)a | Focus group (n = 5) | 33 | |
| I3 | 5 | 3 | 24: 4 individual, 3 focus groups (n = 6, 6 and 8) | 2 | Focus group (n = 9) | 43 |
| D1 | 7 | 3 | 3 | 2 | Focus group (n = 5) | 20 |
| D2 | 10 | 3 | 2 | 4 | Focus group (n = 5) | 24 |
| D3 | 2 | 3 | Declined | 1 | 1 | 7 |
| Total | 30 | 20 | 58 | 9 | 25 | 142 |
| Site | PCT/CCG | Community services | Acute trust | Social services | Patient participation group |
|---|---|---|---|---|---|
| I1 | Locality transformation manager Commissioning manager, urgent care |
Manager, rehab Head, reablement Manager, end of life care Head of adult services Demand, capacity and resilience team leader Deputy head, community services Advanced nurse practitioners Head occupational therapist Head nurse Team manager, integrated care Team manager, falls (physio) GP and lead for roving GP services |
|||
| I2 | Service lead, unplanned care Clinical lead, unplanned care Nurse commissioner Strategic advisor, adult social care Director of commissioning Commissioning chairperson (GP) |
Chief executive (nurse) Head of service, intermediate tier Team manager, intermediate care Discharge team manager (nurse) Advanced nurse practitioner, rapid response Manager, older people Head of service, demand management and commissioning |
Clinical director, ED Assistant director of operations Director of operations Manager, medicine group Operations centre manager Clinical director for medicine (geriatrician) |
Manager, adult social services Manager, access and assessment |
Chairperson of Engage Voluntary worker Care home manager Lay member, CCG |
| I3 | Commissioning manager planned care (nurse) Commissioning manager urgent care Chief operating officer Chief operating officer (nurse) |
Medical director (GP) Manager, community nursing Service lead, therapies Clinical director (GP) Discharge co-ordinator (nurse) Team leaders, intermediate care (3) Alternatives to hospital nurses (2), administrators (2) Nurse practitioner, older people Community matrons (4) Community nurses (3) |
Older People’s Parliament: chairperson and five members Age UK project manager |
||
| D1 | GP member, CCG Head of development Service redesign manager |
Director of operations Deputy director of operations General manager |
Co-ordinator, services for older people Clinical director, acute and elderly medicine Consultant in acute medicine Associate director, non-elective care Nurse specialist, older people Practice facilitator (matron) |
Assistant director, adult social care Assistant director |
Older people’s partnership Age UK |
| D2 | CCG chairperson (GP) Urgent care lead (GP) Director of commissioning |
Clinical lead reablement (nurse) Mental health and dementia lead (nurse) |
Clinical director, unscheduled care Divisional nurse manager Manager, unscheduled care (2) Matron Manager, clinical assessment unit Clinical lead, clinical assessment unit Manager, medical assessment unit (nurse) Manager, acute nursing |
Head, adult care services Commissioning manager Hospital social worker Manager, community rehab |
Chairperson, user carer forum Members, user carer forum (4) |
| D3 | CCG board member (GP) CCG lead, unscheduled care (GP) Locality commissioning director |
Chief executive (medical) Geriatrician |
Head of policy, adult social care | Head of Healthwatch |
Site reports
A detailed qualitative case report can be found for each in-depth study in Appendix 3. These reports provide more detailed analysis of each site in terms of broader system configuration in line with the 7S framework and include illustrative extracts of data from study participants and other empirical sources. These case reports also provide summary tables that draw out the main findings from each site, which were subsequently used to inform and develop recommendations for system improvement (see Chapter 5). In this chapter, we draw on both quantitative and qualitative data to provide a brief descriptive overview of each study site and present an account of their main learning points. After reviewing each site, the chapter provides a cross-case comparison to draw out the main learning points from both the deteriorating and improving groups with the aim of elaborating recommendations. It is worth noting that the primary focus of these short case summaries is on the organisation and delivery of unplanned care for patients aged 85 years and over between 2007 and 2010, but many other aspects of service configuration were described to the research team through comparison with current practices. For example, participants often talked of more recent initiatives as a way of highlighting previous shortcomings. Given this, there is an inevitable hindsight bias to some of the accounts provided by participants and possibly a desire to present an improving picture. Readers are also encouraged to examine the more detailed case reports found in Appendix 3, where primary data support the summary account provided below.
Deteriorating sites
Site D1
The PCT of D1 has a large urban population base, classified as a ‘centre with industry’ by the Office for National Statistics (ONS). 73 For total population it ranked 56th out of 151 PCTs, and had higher than average population growth, including in those aged 85 years and over. Its deprivation rank is 43rd of 151, meaning it is in the most deprived third of PCTs. Its admissions rate for the age group of 85 years and over ranked 37th out of 143 PCTs, which is the second highest of the sites included in this report. As many as 92% of acute admissions from the PCT are to the linked acute trust. As shown in Tables 7 and 8, admission rates for people aged 85 years and over and readmission rates for those aged 75 and over rose more rapidly than the average for our deteriorating sites. Between 2010 and 2011, emergency admission rates for ACSCs rose slightly, but less than the average for deteriorating sites (Figure 24). Results from the GP survey for access to GP services and out-of-hours services were similar to the average for deteriorating sites.
| Site | 2007/8 | 2008/9 | 2009/10 |
|---|---|---|---|
| D1 | 48 | 54 | 59 |
| Deteriorating sites – average | 46 | 53 | 57 |
| England – average | 48 | 52 | 52 |
| Site | 2007/8 | 2008/9 | 2009/10 |
|---|---|---|---|
| D1 | 15.5 | 16.0 | 18.0 |
| Deteriorating sites – average | 15.3 | 15.9 | 16.7 |
| England – average | 14.4 | 14.9 | 15.4 |
FIGURE 24.
Emergency admissions for ACSCs 2010/11–11/12 (per 100,000 people, all ages, sum of 19 conditions), site D1.
Site D1 comprised a large acute teaching hospital (NHS trust) formed in 2006, consisting of over 1200 beds and providing an extensive range of acute and specialist services. The hospital was located in the main administrative city of the county and provided acute services to city and county, and specialist services to bordering counties. Two smaller NHS trusts provided a selective range of acute and non-acute services to the wider county area and surrounding catchment populations. A community health-care NHS trust was formed in 2006 and provided a range of community services and rehabilitation to the city and county. This trust provided inpatient, community and day clinics as well as specialist services to a population of over 850,000. The organisation provided services from more than 80 locations and employed more than 4000 dedicated staff. Over 60 GP practices served the principal administrative city, with many being operated by single-handed GPs or in small practices. An urgent care walk-in centre was also provided in a city-centre location.
The over-riding finding from D1 was the absence of any coherent or system-wide strategy for managing urgent, unplanned care, particularly for those aged 85 years and over. Specifically, the strategy developed over the preceding 5 years had largely been in relation to the formation and development of specialist acute services within the NHS acute trust provider, rather than primary or community services. Linked to this, participants described an operational strategy driven by prevailing national targets, especially for 4-hour ED attendance, which could admit patients with more complex needs as inpatients. Where innovations and changes had been adopted across the wider health system, they often lacked strategic leadership or alignment between acute and community care, focusing instead on expanding acute care. In addition, many innovations were based around rapid improvement projects, many of which failed to complete or were overtaken by new initiatives before being completed and evaluated.
Reflecting the above strategy, the structure of the health system at site D1 was largely centred around the main acute NHS trust, with the emphasis on building up the expertise and resources of this trust to meet the growing needs of older people. Accordingly, a number of systems had been put in place in and around the ED to improve the flow of patients into and through the acute hospital and avoid breaches of the 4-hour target. This also seemed to drive a set of values around the importance of meeting targets.
The organisation and delivery of community care had recently undergone change, with care being provided by multidisciplinary care teams, but with limited evidence of integration with either acute or primary care services. However, with increased admissions to the acute trust and evidence that certain patient groups were receiving restricted packages of care, there had been a move to develop alternative forms of community provision based upon care at home. The involvement of GPs in the management of longer-term and acute care for those aged over 85 years was uneven and widely seen as a problem, especially for smaller practices, which struggled to respond to urgent patient needs. In particular, urgent access to GPs was commonly identified as a problem, although where access was available it was believed that medical expertise was usually adequate to manage patient care needs. Some areas of primary care witnessed increased specialisation in the care of older people, including specialist nurses and geriatricians working in the community, but this recent development was not necessarily meeting demand throughout the entire city and county. Additional concerns were also raised about the management, resources and inspection of nursing homes. As well as difficulties with recruitment and training for complex care needs, it was reported that nursing home staff were poorly supported by primary or community health-care specialists, making it difficult to manage urgent care needs without referring the patient to the ED. It was also felt that patients aged 85 years and over struggled to navigate the care system and that there was a growing reliance on families and other carers to service the needs of these groups.
In sum, site D1 illustrated a system highly centred on acute care, with some degree of fragmentation of other primary and community services. The problems of urgent care attendance at the ED for those aged 85 years and over was, accordingly, managed by streamlining the acute care system to avoid breaches of targets over and above the better management of complex care needs in the community. The lack of integration and planning at a wider system level was further evidenced by widespread concerns about the lack of communication between care providers, and a lack of shared vision or strategy about the management of care for older patients.
Site D1 offers possible lessons for the management of urgent care for patients aged 85 years and over. These include:
-
Strategy
-
Define a specific strategy for the care of patients aged 85 years and over.
-
Align this strategy with existing local and regional service strategies.
-
National pressures and targets need to take into account the impact they have on older people.
-
Learn from pilots and implement good practice.
-
-
Structures
-
Better integrate acute, community and primary care.
-
Restrengthen relationships between GPs and community nursing where these are no longer colocated.
-
-
Systems
-
Provide greater transparency of service availability and provision.
-
Longer-term packages of care need to be provided.
-
Systems to access GPs may need to improve.
-
-
Shared values
-
Service providers should unite around the quality of care and communicate with each other.
-
Alignment of staff and public values regarding care and funding of care for older people.
-
-
Style
-
Overcome cultural differences between care providers.
-
Improve communication and manage expectations between different professional members/roles, between staff and family, and between practitioners and patients.
-
-
Staff
-
Consider specialised roles such as community geriatricians and specialist nurses.
-
-
Skills
-
Champion recognised ways to overcome existing practical problems, in terms of both health-care provision and organisational make-up.
-
Site D2
The PCT of D2 is in a mixed urban and rural area, classified as a ‘centre with industry’ by the ONS. 73 It has a relatively small population, ranked 120th out of 151 PCTs. Its deprivation rank is 22nd out of 151, meaning it is in the most deprived fifth of PCTs. Its admission rate for the age group of 85 years and over ranked 30th out of 143 PCTs, which is the highest of the sites included in this report. Some 83% of acute admissions from the PCT are to the linked acute trust. As shown in Tables 9 and 10, admission and readmission rates for people aged 85 years and over rose more rapidly than the average for our deteriorating sites, with most of the increase occurring between 2007/8 and 2008/9. Between 2010 and 2011, emergency admission rates for ACSCs rose sharply, more than the average for deteriorating sites. This pattern is also reflected in admissions for ACSCs (Figure 25). Results from the GP survey for access to GP services and out of hours were similar to the average for deteriorating sites.
| Site | 2007/8 | 2008/9 | 2009/10 |
|---|---|---|---|
| D2 | 49 | 59 | 61 |
| Deteriorating sites – average | 46 | 53 | 57 |
| England – average | 48 | 52 | 52 |
| Site | 2007/8 | 2008/9 | 2009/10 |
|---|---|---|---|
| D2 | 16.5 | 17.7 | 16.8 |
| Deteriorating sites – average | 15.3 | 15.9 | 16.7 |
| England – average | 14.4 | 14.9 | 15.4 |
FIGURE 25.
Emergency admissions for ACSCs 2010/11–11/12 (per 100,000 people, all ages, sum of 19 conditions), site D2.
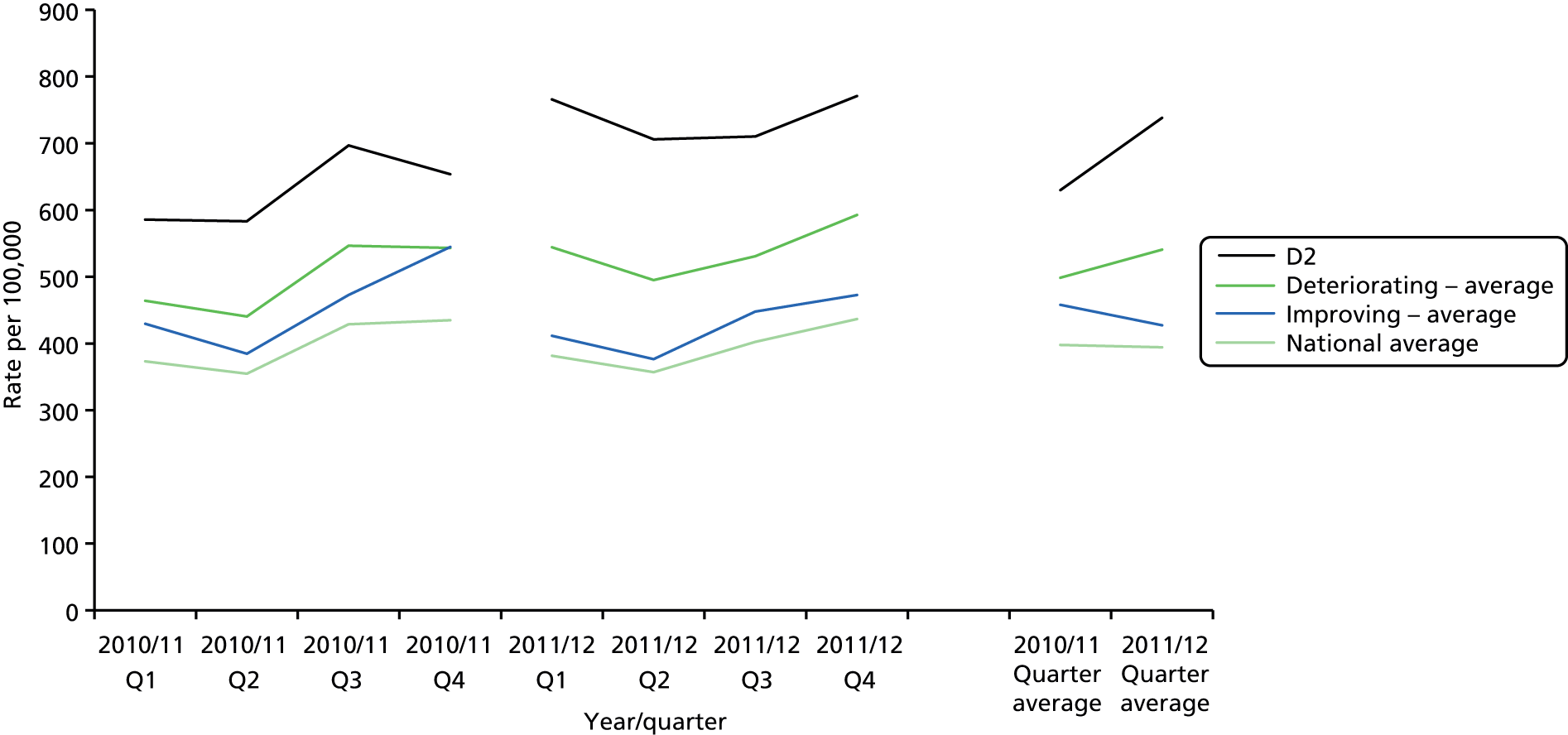
Site D2 involved a highly complex system of health- and social care provision arranged over three small to medium-sized towns located within the same metropolitan borough of a large county. Acute hospital services were provided by a NHS trust that managed four acute district general hospitals and some community and specialist services. This included the hospital and urgent care services provided within the D2 catchment area, as well as those provided in adjoining areas, which broadly reflected prevailing PCT borders. In the years preceding and included within the analysis, the acute care system had witnessed significant transformation in the organisation and provision of acute and emergency care. This included the downgrading of D2’s acute hospital’s ED to an urgent care centre, with the transfer of emergency cases to an acute hospital managed by the NHS trust but located outside the D2 catchment area. This also reflected a general diminution of acute care provision with the D2 area, with the main hospital providing limited inpatient treatment and more day-based outpatient clinics and community care services. GP services in the surrounding area were characterised by a mix of small and medium-sized group practices and a range of private nursing and care homes operated across the area. The study found that service leaders placed strategic priority on managing and supporting discharge from hospital and reducing readmissions, as reflected in the support for a Short Term Assessment and Reablement Service (STARS) which provided a 6-week package of care for patients after they left hospital. The changes in service configuration and urgent care provision across the area were described by some as creating additional pressures on the local ambulance service.
Alongside, and possibly reflecting, the major structural changes that the study found, site D2 had little in the way of an overarching or shared strategy or vision for managing the care of older people or reducing unplanned admissions for patients aged 85 years and over. Rather, the over-riding strategy was aimed at reducing the length of acute hospital stays improving hospital discharge and reducing readmission, as illustrated by the STARS and the widespread need for investment in community services to reduce delays in discharge. In broad terms, there was little recognition or priority given to reducing unplanned urgent care; rather, the emphasis was on establishing appropriate systems that ensured patients were either seen with the urgent care centre within the D2 area, or transported to the ED outside the area. In short, the wider reconfiguration of urgent and emergency care appeared to overshadow efforts to better manage the need for urgent or unplanned care within the community setting. In line with this, the study found that local improvement and transformation projects aimed to ensure appropriate and timely access to and discharge from hospital care. This strategy was further evidenced by changes introduced in 2010 whereby additional investment was made by the NHS trust in community services and hospital prevention schemes that aimed to offer more proactive management of complex patient needs before escalating care.
The reconfiguration of service might also have led to, or exacerbated, fragmentation among the wider health- and social care system. It was widely reported that there was a lack of partnership working or collaboration between individual service providers, especially between primary and secondary care. It appeared that GP practices had little by way of strategy or systems for managing chronic or complex care needs in the community, and there were significant concerns about out-of-hours GP provision, which might further add to the demand for unplanned care. Instead there was a reliance on community health-care services, such as community matrons, and local authority reablement services. However, these were also aligned to the management of postdischarge care rather than avoiding unplanned admission.
In sum, site D2 highlighted a preoccupation with, and the longer-term repercussions of, making large-scale system change, whereby the emphasis was on improving access to and discharge from hospital rather than reducing demand for hospital care. This shaped the organisation and delivery of services for a significant period during data capture and only recently have services started to respond with a different approach. Site D2 offers possible lessons for the management of urgent care for patients aged 85 years and over. These include:
-
Strategy
-
Aim for better integration between care providers, especially community and acute care trusts and health- and social care providers.
-
Minimise disruption due to reorganisations.
-
Reduce the tension between localism versus regionalism.
-
-
Structures
-
Develop clearer pathways across the region.
-
When focusing on reconfiguring (hospital) urgent and acute care, consider primary care and urgent care in the community.
-
-
Systems
-
Increase engagement between acute care services and ambulance trusts.
-
Tackle variations in GP provision and coverage.
-
-
Style
-
Primary and secondary care need to adopt a collaborative approach.
-
-
Staff
-
Address staffing problems across the region.
-
Site D3
The PCT of D3 is in a mixed urban and rural area, classified as a ‘new and growing town’ by the ONS. 73 It has a relatively small population, ranked 118th out of 151 PCTs. Its deprivation rank is 119th out of 151, meaning it is in the least deprived quartile of PCTs. Its admission rate for the age group of 85 years and over ranked 67th out of 143 PCTs. A total of 87% of acute admissions from the PCT are to the linked acute trust. As shown in Tables 11 and 12, admission and readmission rates for people aged 85 years and over were below the English average in 2007/8, but increased rapidly over the subsequent 2 years to reach the average. This pattern is also reflected in admissions for ACSCs (Figure 26). Results from the GP survey for access to GP services and out of hours were similar to the average for deteriorating sites.
| Site | 2007/8 | 2008/9 | 2009/10 |
|---|---|---|---|
| D3 | 41 | 45 | 52 |
| Deteriorating sites – average | 46 | 53 | 57 |
| England – average | 48 | 52 | 52 |
| Site | 2007/8 | 2008/9 | 2009/10 |
|---|---|---|---|
| D3 | 13.9 | 14.2 | 15.3 |
| Deteriorating sites – average | 15.3 | 15.9 | 16.7 |
| England – average | 14.4 | 14.9 | 15.4 |
FIGURE 26.
Emergency admissions for ACSCs 2010/11–11/12 (per 100,000 people, all ages, sum of 19 conditions), site D3.

Health-care services within site D3 were predominantly organised around a large acute and community health-care NHS trust. The trust was formed in 2003 and provides a full range of acute services at a single hospital site located in the main administrative city for the area, together with a range of community rehabilitation, nursing and care services provided across the wider county, but not for the city area. Community care in the city area is currently provided by a social enterprise organisation established in 2011, which formed after the dissolution of PCT care provision. In line with previous NHS provision, the social enterprise provides integrated communication and social care through a single point of access (SPA), including a crisis service, community matrons, out-of-hours GP services and urgent care facilities, based within the acute hospital. Despite the perceived benefits of community matrons in managing urgent care demand, it was widely believed that these services were being overstretched by growing demand. A walk-in service was also provided within the city centre area, which was considered by many to be successfully diverting patients from EDs. Traditionally, there had been close working between the former PCT and the social service department, which might explain the range of services now offered through the social enterprise, but notable changes included the reduction in consultant-led services in favour of more nurse-led services.
The findings suggest that, despite the extensive coverage of acute and community care within the area, there remained significant problems in primary care. In particular, primary care services were described as highly fragmented and not well integrated with other community and acute services. For some this was expressed in terms of the problems of accessing primary care, as demonstrated by patient surveys, but for GPs there was a sense of being disconnected from other services. This had recently been addressed with, for example, enhanced information sharing between acute and primary care in terms of numbers of ED attendances. There were also new initiatives to support GPs in risk-profiling patients in order to intervene early in care management and avoid unplanned admission.
The problems of developing a coherent strategy for unplanned care, especially for patients aged 85 years and over, were widely seen as stemming from frequent reorganisations at both national and local levels: first, in terms of community health-care provision; second, in terms of the role of national targets and commissioning frameworks; and, third, in terms of wider health system restructuring. For example, the changes in city and country community care provision were widely viewed as beneficial but also as creating considerable flux in local strategy, with attention focused on establishing new services rather than managing care needs. Substantial restructuring since 2007, for example, saw many old facilities closed and a new intermediate care centre (ICC) being built. At the same time, commissioning decisions were greatly influenced by national targets and financial incentives which exacerbated competition between care providers rather than enhancing collaboration and integration. However, the development of these services did not always appear to fully consider the staffing and resource implications, with questions raised about the level of specialist geriatric input, the location of services and integration with other community providers.
Site D3 revealed no significant or stand-out issues that prevented the management of unplanned care for older people, but rather a preoccupation with structural change and working within changing commissioning and service frameworks. The range of acute, community and primary care services generally appeared to reflect the diverse needs of both city and county patients, but little strategic thought had been given to how these services should align or integrate within each other. Site D3 therefore offers a number of learning points:
-
Strategy
-
Minimise disruptions due to reorganisations and staff changes.
-
Avoid transient pilots with no follow-through.
-
Admission reduction strategies need to include investment in primary care.
-
-
Structures
-
Develop a SPA for community and intermediate care services.
-
Integrate information systems for walk-in centres, urgent care centres and ambulatory care services.
-
-
Systems
-
Assess the need for geriatrician input to intermediate care.
-
-
Shared values
-
Develop a vision of high-quality care for older people, including medical, functional and managerial perspectives.
-
Avoid perverse incentives [e.g. payment by results (PbR) to manage demand].
-
-
Style
-
Recognise the importance of clinical leadership.
-
Synthesis of deteriorating sites
The three deteriorating sites reveal a picture of uncertain and complex health system change, where service leaders did not always display a shared vision, clear understanding of or foresight about how different system elements should interact with each other. However, it would be misleading to suggest these three sites exhibited only negative qualities; rather the case reports show how each area was characterised by an array of positive features relating to existing organisational resources and strengths. However, in the changing context of older patients’ requirements, as well as regional and national shifts in resources and policy, a number of over-riding features appeared to outweigh these positive elements and tip the balance in favour of poor system performance. Looking across the three sites, a number of common features might explain the described findings.
First, all three sites revealed no evidence of overall ‘system strategy’. Although individual system components might have quite developed strategies for aspects of unplanned care, such as the ED, there was little appreciation of how the components of the wider health system should fit and work together. In short, service leaders need more a strategic and system-wide understanding of shared problems.
Second, strategies tended to be dominated by acute care provision and system changes to support the reconfiguration of acute care. This could be seen in all three sites, to the detriment of policies to expand or improve primary and community care. This might suggest some form of capture or dominance by large acute trusts when working with commissioners.
Third, strategies were driven by prevailing national targets, which also reinforced the importance of acute care and potentially fragmented community care. This was exemplified by the preoccupation with delayed hospital admission and discharge over and above preventing hospital attendance, and changes in commissioning arrangements that transformed the provision of primary and community services.
Fourth, where improvement projects were identified, these tended to be highly reactive and short-lived, with little follow-through, strategic alignment or consideration of the resource implications, such as developing specialist geriatric services within the community. This might reflect constantly changing local and national priorities and an overarching sense of strategic planning in each area.
Fifth, there was widespread underinvestment in and planning for primary care. GP practices were generally seen to be managing chronic care and needing to direct urgent care demand to appropriate service providers. There was little understanding of the potential role of primary care providers in providing holistic case management.
Sixth, there was little evidence of integration between acute, primary and community services. Each was characterised by distinct governance and funding arrangements, divergent cultures and values, and different ways of working. These occupational and organisational boundaries hinder the potential for integration.
Seventh, there was little understanding of or planning for whole-pathway care; that is, understanding the complex journeys that patients travel through the health- and social care systems. As above, there was often emphasis on key care stages, such as admission and discharge, but not on the wider constellation of agencies, handovers and transitions that patients face across the system.
Eighth, there was excessive demand on limited services, especially community-based services, because of the failure to align or integrate other services. This meant that many specialist community teams were routinely overstretched and struggled to provide comprehensive packages of care.
These factors are summarised in Table 13, which classifies them according to the McKinsey 7S model and examines their interconnections and their positive or negative impact.
| Dimension | Strong/positive type | Stems from | Influences | Weak/negative type | Stems from | Influences |
|---|---|---|---|---|---|---|
| Strategy | New recognition of strategic deficit by CCGs Increased provision of reablement funding and service innovation around care of older people Close working between PCT and social services New projects that have a strong social element to them |
Restructuring Recognised need to address health- and social care problems New funding opportunities for integrated working More investment in community services (2010) |
Commissioning | Unaware of overall strategy on unplanned admissions for those aged 85 years and over Strategies are influenced by changes in leadership roles too often Targets and incentives, such as the 4-hour target, may increase admissions Elective care dominated service planning ahead of urgent admission Piloting of initiatives but often no sustained change Reducing length of stay instead of admissions Frequent restructuring at different organisational levels |
Higher-status professional specialisation challenged by complexity of treatment requirements for very old people Lack of consistent leadership Poor communication across regions National strategies Commissioning strategy Emphasis on quick fixes rather than sustained improvements Lack of strategic communication at regional level |
Higher-status professions more narrowly driven by progression of natural science research instead of social science Shortage of investment and planning for care for old people Constant change and uncertainty |
| Structure (of care system) | New forms of health provision in community, e.g. virtual wards being supported Consultant-led services can positively influence structural organisation Some regions developing SPA and integrated care teams for community health and social care Some new community providers with embedded practices for rapid patient support outside hospital Access to GPs in many areas very good |
Increased funding Changes in local care planning Service innovations and pilots that work |
Community care provision is hampered when multidisciplinary teams cannot function Structure of GP practices: many are single-handed, which relates to trouble in managing service hours Hospital amenities for older people are limited Constant change in system structure and team configurations, including change in hospital sites, new intermediate facilities, and a shift towards more nursing care Lots of pilot change Poor integration between primary care and secondary care Lack of partnership working |
Changes in how packages of care are delivered. This can involve new organisations funded by existing trusts Existing style of work is less flexible to modern challenges Lack of strategic planning Reactive strategy Wider system change Organisational barriers between system actors Lack of strategic planning |
Limited forward planning Reduction in family support and out-of-hours care Integration and co-ordination of services Staff and skill mix Patient planning and care pathway Reduced communication between staff at executive levels |
|
| System (processes) | New services being piloted using new technologies Reduced bureaucracy and streamlined information systems (recent) Integrated processes for SPA and associated services Some restructuring has provided new assessment and re-ablement services |
Recognising opportunities for change Improved integration Recognising opportunities for change |
Structural change in primary and social care | Overcomplexity of community care. Patients are confused by the ever-changing numbers and names of services Systems to support and work with family carers could be improved Lack of resources to prevent patients bouncing back into A&E GP waiting and opening times Quality of care in nursing homes reduced Concept of ‘safe discharge’ inadequate for very old patients Inadequate technology systems Lack of integration between care processes, especially primary, community and secondary Difficulty of access to primary care (patient survey) Incentive systems encourage excessive medication and polypharmacy Lack of integration between ambulance and acute trust interface New projects are sporadic – lack of system consistency Varied out-of-hours services |
Design and communication of community services not as well supported Lack of funding Existing work style and culture Diminished care home inspections Existing style of work with very old people Technology incompatible, knowledge sharing challenged and lack of training Structural change Persistent organisational and occupational boundaries Lack of primary engagement in service planning Troubled design of processing structural change |
Recognition of service user perspective lacking Government policy not implemented to define standards Shared values Teamwork Role of primary care teams in SPA and other services |
| Shared values (for system working) | There was an implicit agreement that avoiding hospital admissions of old people was valuable Emphasis on patient function rather than age |
Poor communication about community provision between trusts and providers Age of GP can be found to influence motivation for change Cultural and normative differences between primary and secondary care Conflict between the medical model and therapist nurse model Frail older people are disadvantaged by the care system Tension between clinical and managerial values in the care system Culture was not team focused Blame culture too apparent |
Established culture of work Sustained organisational and occupational boundaries Prioritisation of elective and non-elderly care |
Scope for integrated working | ||
| Skills | Gerontologists have a very good skill set for dealing with very old people Skills of geriatricians and community matrons are very well utilised |
|||||
| Style | 2010 NHS reforms on clinical leadership is associated with positive change Clinical leadership associated with positive change |
Challenging to engage the right staff earlier before admission Change of culture of service user families around the expectation of provision In connection with this culture is reactive culture of admission by practitioners Lack of stability and high turnover in senior management Lack of integrated working Emphasis on quick fixes rather than sustained improvements Pressure to discharge was not matched with effective team linkages Pressures have been seen to increase the divide between primary and secondary care |
Contact between services is poor, patients are described as being ‘offloaded’ Societal shift in family composition and geographical location Constant change Lack of strategy Emphasis on quick wins |
Too much of a workload to cater for the demand Setting issues around wealth and family values Culture and values Service integration Strategy development |
||
| Staff | Community matrons have a central role in care provision for frail older adults and supporting GPs to identify repeated hospital activity. They provide a key mechanism for reducing unplanned admissions Increase of consultant involvement, for example in ambulatory care units or A&E, can display improved service function |
Care home staff claimed to be underskilled Care home staff not supported by other professionals working in the community Overmedication by some staff can lead to falls and medically it is unclear what the correct policy is on this Access to GPs is increasingly difficult Recruitment of good staff in deprived areas Turnover of senior managers and leaders Lack of geriatric health-care professionals in community Primary care teams had become fragmented and disjointed There are not enough staff Poor skill mix of staff – reduction in A&E consultants Defining role boundaries is a constant issue |
Lack of investment in community staff | Specialist input into strategy and process | ||
| Setting | Existing political issues can cause problems, for example concerning where services are geographically located A poor relationship between primary and secondary care may be historically established Ease of access to services in some locations might push up admissions |
Improving sites
Site I1
The PCT of I1 is in an urban centre, classified as a ‘regional centre’ by the ONS. 73 It has an average population base, ranked 85th out of 151 PCTs. Its deprivation rank is 56th out of 151. Its admissions rate for the age group of 85 years and over ranked 79th out of 143 PCTs, which is the second lowest of our selected sites. Eighty-nine per cent of acute admissions from the PCT are to the linked acute trust. As shown in Tables 14 and 15, admission and readmission rates for people aged 85 years and over were above the English average in 2007/8, but declined over the subsequent years to end below the average. Readmission rates increased slightly, in line with other improving sites. Admissions for ACSCs declined to a similar extent to that seen in the other improving sites (Figure 27). Results from the GP survey for access to GP services and out-of-hours services were similar to the average for improving sites.
| Site | 2007/8 | 2008/9 | 2009/10 |
|---|---|---|---|
| I1 | 55 | 51 | 51 |
| Improving sites – average | 52 | 51 | 49 |
| England – average | 48 | 52 | 52 |
| Site | 2007/8 | 2008/9 | 2009/10 |
|---|---|---|---|
| I1 | 15.3 | 15.7 | 16.3 |
| Improving sites – average | 14.1 | 15.0 | 15.1 |
| England – average | 14.4 | 14.9 | 15.4 |
FIGURE 27.
Emergency admissions for ACSCs 2010/11–11/12 (per 100,000 people, all ages, sum of 19 conditions), site I1.

A large university NHS trust managed and provided acute and specialist services for site I1. This included one teaching hospital, one specialist children’s hospital, one general hospital and a walk-in centre within the I1 catchment area, together with other specialist hospitals in adjacent counties. Urgent and emergency services were provided through the large teaching hospital located in the centre of the county’s principal city. A community NHS trust provided locality rehabilitation, therapies and nursing care across the county through a number of community hospitals, outpatient clinics and home care services. A range of private providers offer additional home, residential and nursing care, including intermediate care and out-of-hours nursing care. There are over 45 GP practices in the area, ranging from small to large practices.
A prominent finding from site I1 was a longstanding strategic commitment to community care, including the integration of acute, primary and community care (although, as reported earlier, the acute trust did not participate in the research). There was no specific strategy for the care of people aged 85 years or over, but there was a strategic recognition of the need to better manage care needs in the community before patients sought urgent or unplanned care. This view was widely supported and shared by different strategic actors, including GPs, acute specialists, community care providers and commissioners, revealing a strong set of shared priorities around the management of patient need. A significant feature of site I1 was the existence of a single unitary community health-care provider that covered the range of services for both city and county. This was seen as not only producing efficiencies and cost savings but also supporting integration across the range of services rather than different services being provided by a range of agencies.
This strategy was further exemplified by a number of significant interventions and approaches found within the I1 site. This included sustained financial investment in community care services, such as new clinics, outreach services and community hospitals. It was also described how change had been backed and driven by both strong service leadership and widespread engagement with clinical and patient groups, to garner and secure support for change initiatives. The importance of this was further reported in relation to recent leadership changes and the belief that transformation was now more difficult. It was also suggested that change agents had persevered in the face of adversity to realise a shared strategic vision for enhanced community care. In addition, service transformation programmes were described as being clearly aligned to overall strategic objectives, well led and resourced, and supported with workforce development and education.
A further feature of site I1, which might stem from the unitary community care provider, was the strategic and operational emphasis of integrated care, between both health- and social care agencies, and between acute and community care providers. This was supported by the cofunding of improvement projects and the joint commissioning of services. Where changes might have run counter to this integrated approach, such as with the introduction of a private provider for out-of-hours primary care, it was reported that services still operated on the basis of integration and collaboration, rather than competition. Integration within the area was described as being supported by targeted technologies. Although these were also described as inhibiting integration in some circumstances, in most cases they were described as enabling timely and effective communication and knowledge exchange across occupational and organisational boundaries. This was described as enabling frontline care providers to direct patients to more appropriate services rather than to the ED.
In sum, site I1 revealed an overarching strategic commitment to supporting patient care in the community and where specialist or urgent care was a necessary last resort. This was matched by giving strategic leadership to community agencies and working to integrate acute and community services through a variety of financial, structural and technological activities. It was also found that the close integration of services supported learning both within and across organisational boundaries, revealing a form of system resilience and dynamism. In addition to these headline findings, site I1 offered a number of associated learning points:
-
Strategy
-
Create and maintain a shared vision and agree a strategy across health- and social care services.
-
Allow time for relationships to develop so that it is possible for this vision to succeed and survive.
-
Work hard to keep the vision alive over time through reorganisations and changes in key decision makers.
-
-
Structures
-
Vehicles such as system-wide urgent care boards can play a key role in overseeing service change and service integration.
-
Clustering services under the same provider can be a constructive strategy through which to foster integration.
-
Address the challenge of creating integrated primary care teams inclusive of general practice and out-of-hours care.
-
-
Systems
-
Develop information technology (IT) systems that are integrated across acute, community and primary care.
-
Support and involve families, carers and care homes in the management of vulnerable patients.
-
-
Shared values
-
Work towards seeing people as based in the community and help them to continue to support themselves there.
-
-
Style
-
Retain and support leaders who can champion the right culture.
-
-
Staff
-
Make all staff accountable for their contribution in achieving the organisational goals.
-
-
Skills
-
Assess need to improve IT systems training.
-
Site I2
The PCT of I2 is in a rural area with several towns, classified as a ‘manufacturing town’ by the ONS. 73 It has a relatively small population base, ranked 139th out of 151 PCTs. Its deprivation rank is 40th out of 151, meaning it is in the most deprived third. Its admissions rate for the age group of 85 years and over ranked 137th out of 143 PCTs, by far the lowest of our selected sites. Eighty-three per cent of acute admissions from the PCT are to the linked acute trust. As shown in Tables 16 and 17, admission rates for people aged 85 years and over were well below the English average in 2007/8, and fell further over the subsequent 2 years. Readmission rates were below the average for England and improving sites, but increased slightly, in line with other improving sites. Admissions for ACSCs declined to a similar extent to that seen in the other improving sites (Figure 28). Results from the GP survey for access to GP services and out-of-hours services were similar to the average for improving sites.
| Site | 2007/8 | 2008/9 | 2009/10 |
|---|---|---|---|
| I2 | 41 | 41 | 39 |
| Improving sites – average | 52 | 51 | 49 |
| England – average | 48 | 52 | 52 |
| Site | 2007/8 | 2008/9 | 2009/10 |
|---|---|---|---|
| I2 | 10.6 | 12.3 | 11.9 |
| Improving sites – average | 14.1 | 15.0 | 15.1 |
| England – average | 14.4 | 14.9 | 15.4 |
FIGURE 28.
Emergency admissions for ACSCs 2010/11–11/12 (per 100,000 people, all ages, sum of 19 conditions), site I2.
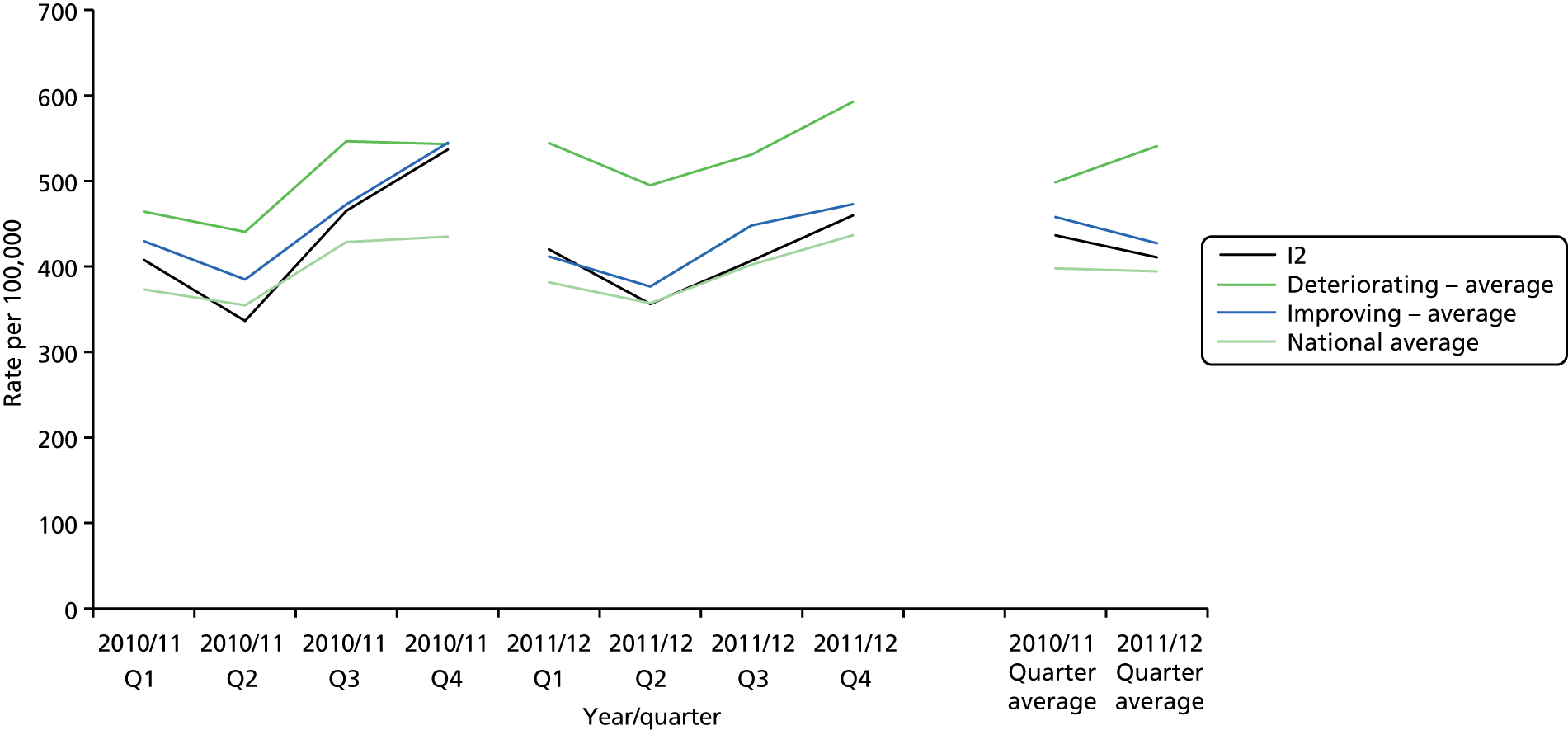
Site I2 is a largely rural and in some places remote geographical area comprising three small to medium-sized towns. The area is served by a single NHS acute trust which manages three district general hospitals, one in each town, which together provide a wide range of acute services. Although some specialist services are provided by the trust, many patients travel out of the area to a regional teaching hospital for specialist care. Emergency services are provided by two of the larger hospitals, while the smaller hospital offers an urgent care centre. The trust is also the primary community health-care provider and manages a number of community-based clinics. In 2007 a new Care Trust Plus was established, which involved the transfer of adult social care from the local authority to the NHS trust, which was premised on the idea that the NHS should focus on disease management and older people. In addition, a community care agency, which is a nationally funded initiative, operates across the region alongside existing health- and social care providers. A range of social enterprise and private care providers also operate within the area, including a local authority volunteer scheme which includes over 250 volunteers helping with a range of community and social care services. The local PCT also provides a walk-in centre at the largest town. There are over 40 GP practices in the area, of which about 54% are single-handed GPs.
The findings suggest site I2 was characterised by a high degree of integration and coordination between acute, community, primary and social care services. This was exemplified by the fact that the main NHS trust managed and provided both acute and community adult care services, involving a transfer of some community and social care services from other agencies. This therefore enabled closer integration of services across the patient pathways and a strong sense of organisational cohesion. For example, there was evidence of services being provided by one organisation, which could reduce the need for discussion about resource allocation. More generally, it was felt that services shared a sense of purpose and there was generally a good working relationship between different component parts of the health- and social care system.
The sense of integration between sectors was further evidenced by the use of explicit and transparent care pathways and relatively simple system designs that could help commissioners, referrers and patients navigate the care system, as well as clearly defining the roles and responsibilities of different systems actors. In particular, there was evidence of close strategic working between the NHS trust and the local authority, as illustrated by the transfer of adult services, as well as co-ordinated working with the wider range of private and voluntary care providers. This sense of collaboration and co-ordination made it easier to share information between service providers and deliver more patient-centred holistic care, and also enabled the targeting of interventions to better manage patient care needs. For example, GPs operated a personal medical service that helped to proactively assess and manage the needs of patients to avert unplanned admissions. GPs also remained active in managing the local out-of-hours services, rather than relying on external contractors, therefore providing continuity of care in terms of available information and clinical resources. In particular, a rapid response service was introduced to explicitly manage unplanned admissions through addressing the needs of deteriorating patients at home or in the community rather than referring to the ED. Also of significance was the large team of voluntary workers who helped to manage patient needs in the home. The range of support included meals, personal care, mobility and home help among many other initiatives. This also involved specific community-based campaigns to support older patients, such as during winter. In parallel, efforts had been made across the region to improve and monitor the standard of care homes through the local authority.
At a strategic level, it was reported that there had been clear and relatively stable leadership at senior levels across the health- and social care system. This had enabled services to respond effectively and quickly to funding cuts and work in more co-ordinated ways to help share financial shortcomings and potential risks to service delivery. In frontline services it was also reported that relative stability and continuity of staff had enabled strong and open working relationships to develop and to ensure that any uncertainties brought about by changes in wider system structure, for example commissioning, were mitigated by continuity of leaders and staff.
In sum, site I2 highlights the scope for integrated working between health- and social care providers across public, private and third sectors, in particular for strategic actors to align and co-ordinate their activities in ways to support more integrated and co-ordinated frontline services. Further learning points from across this site include:
-
Strategy
-
Allow time for integration between new local partners, encouraging the spread of common goals.
-
Vertical integration enables services across the patient pathways to work more closely and provides a strong sense of organisational cohesion.
-
-
Structures
-
Integration can be facilitated if leaders in each service stream (primary care, community care, social care) are matched to partner leads in the other services.
-
Colocation, when practical, helps improve interactions between services.
-
-
Systems
-
Rapid response services on a sufficient scale are a key means of reducing unplanned admissions.
-
Integrate social work and nursing teams that cross the boundary between community and hospital.
-
Keep patient pathways simple and transparent.
-
Integrate clinical information systems.
-
-
Shared values
-
Share values across the leadership of all involved organisations.
-
Promote and share the value of enabling older people to stay at home.
-
-
Staff
-
Consider incentives for staff to encourage them to stay within the region.
-
Champion strong leadership.
-
-
Style
-
Foster mutual respect to improve quality of working relationships.
-
Site I3
The PCT of I1 is in a mixed urban and rural area, classified as ‘industrial hinterlands’ by the ONS. 73 It has an average population base, ranked 42nd out of 151 PCTs. Its deprivation rank is 50th out of 151, with pockets of affluence and severe deprivation. Its admissions rate for the age group of 85 years and over are higher than average, ranked 42nd out of 143 PCTs. Eighty-seven per cent of acute admissions from the PCT are to the linked acute trust. As shown in Tables 18 and 19, admission rates for people aged 85 years and over were well above the English average in 2007/8, but fell over the subsequent 2 years. Readmission rates were also above the average for England and improving sites, and increased slightly, but by less than the national trend. Admissions for ACSCs declined to a similar extent to that seen in the other improving sites (Figure 29). Results from the GP survey for access to GP services and out-of-hours services were similar to the average for improving sites.
| Site | 2007/8 | 2008/9 | 2009/10 |
|---|---|---|---|
| I3 | 61 | 60 | 57 |
| Improving sites – average | 52 | 51 | 49 |
| England – average | 48 | 52 | 52 |
| Site | 2007/8 | 2008/9 | 2009/10 |
|---|---|---|---|
| I3 | 16.4 | 16.8 | 16.9 |
| Improving sites – average | 14.1 | 15.0 | 15.1 |
| England – average | 14.4 | 14.9 | 15.4 |
FIGURE 29.
Emergency admissions for ACSCs 2010/11–11/12 (per 100,000 people, all ages, sum of 19 conditions), site I3.
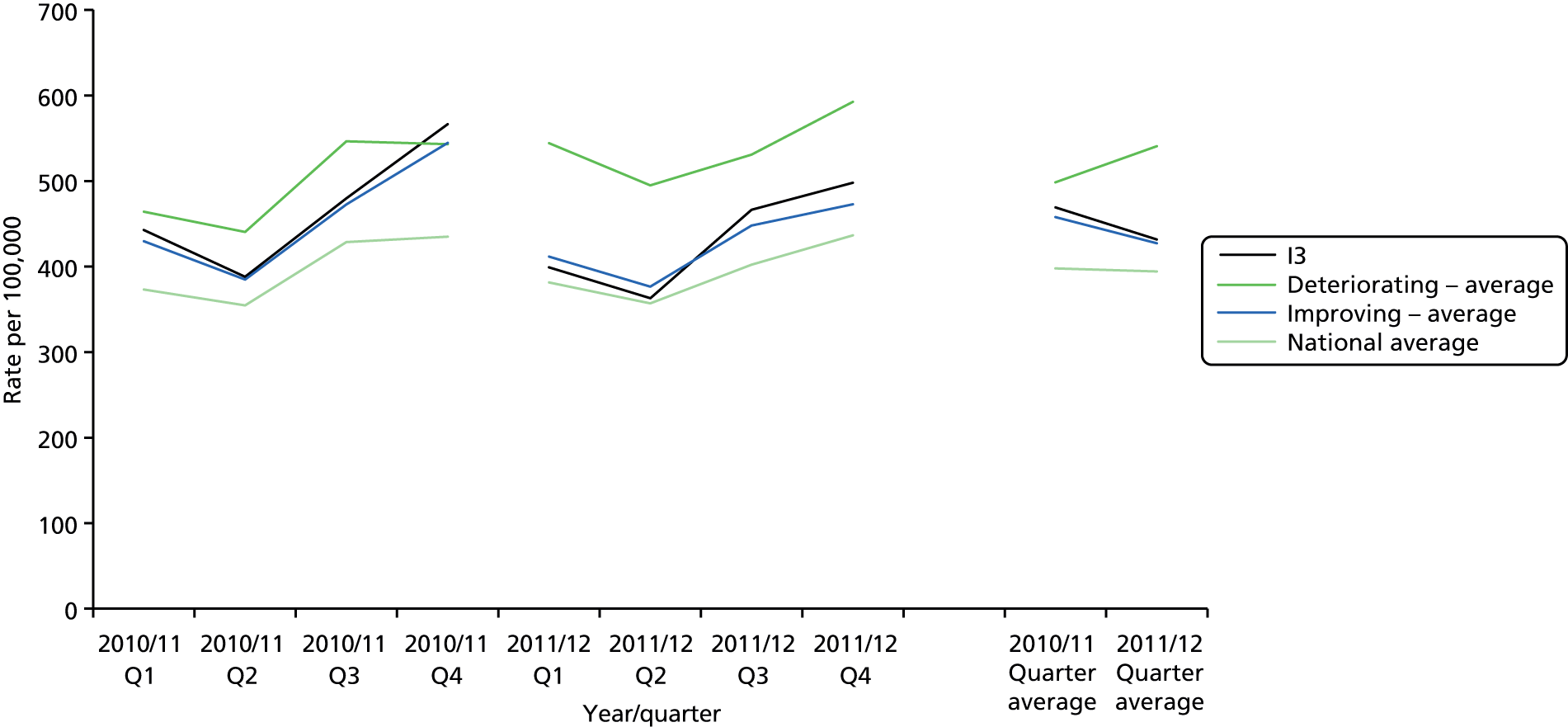
Site I3 is a semirural and urban conurbation in close proximity to a large metropolitan area. Although the majority of acute and community health-care services are organised and managed within this catchment area, local authority services are managed by a larger authority that extends outside the catchment area. Within site I3 a single NHS foundation trust provides a wide range of acute and emergency services, across two hospital sites, each located in a small commuter town. Although some specialist services are provided by the trust, other specialist services are provided at hospitals located in adjacent metropolitan areas. Alongside the two distinct general hospitals, the trust also operates one community hospital and a health centre providing outpatient services. Community health-care services are provided by a single NHS trust, including community nursing, out-of-hours GP services and dedicated services for unplanned care, including SPA service. These services are provided through community hospitals, three walk-in centres and an urgent care centre colocated with the acute trust. The region relies heavily on care homes, in which a rapid-access (intermediate care) scheme has been introduced that provides urgent beds for patients. This both facilitates discharge and avoids unplanned admission, and is funded collaboratively by the local authority and the health-care commissioners’ fund.
A significant finding from site I3 was the absence of boundary complexity or disputes between different health- and social care agencies. In part, this might reflect the particular geography of the area, but there was close alignment between primary, acute and community care boundaries, while borough (not county) authorities also aligned with these boundaries. This was seen as making it easier to design and enact co-ordinated services and streamlined issues of accountability and communication. Reflecting this, it was reported that services were well integrated, despite some discrepancies and tensions between acute and community care where, for example, both provided similar or linked services. Similarly, the provision of out-of-hours GP service by the community NHS trust was seen as supporting integration with primary care.
Urgent and emergency care was widely recognised as a common strategic priority across site I3. This was evidenced through aligned policies, common care pathways and a range of specific service interventions aimed at reducing unplanned admission and supporting care management in the community. Of particular note is that these strategies were explicitly targeted at older patient groups. This included, for instance, an admission prevention service, which provided rapid response to patients in need, a SPA and multidisciplinary clinics for managing older people’s care needs. These clinics were described as being well suited to understanding and managing the complex care needs typically associated with older patients.
Alongside enhanced NHS services, additional co-investment was made by local authority and NHS services in intermediate care to help avoid admissions or support care transition. This included the provision of additional bed capacity in private or statutory care homes through the introduction of a rapid-access service. Linked to this, additional activities, including community nursing and geriatric care, were introduced within the care home sector to better manage patient care and reduce admissions.
Site I3 shows how the alignment of organisational boundaries can help to align potentially divergent modes of working and encourage a more combined strategy. It also highlights a sustained commitment to reducing unplanned admission across organisational sector boundaries by better and more proactive management of complex patient needs through alternative community pathways. Further evidence and detail from site I3 are presented in the case report in Appendix 3 and additional learning points are summarised below:
-
Strategy
-
Create and maintain a shared vision across health and social care.
-
Minimise disruptions due to reorganisations and staff changes.
-
Avoid multiple initiatives which are inadequately marketed.
-
-
Structures
-
Maintain a clear organisational structure.
-
Consider using the social fund to purchase admission avoidance/supported discharge schemes.
-
-
Systems
-
Intermediate care provision should be integrated with 24/7 availability and a SPA.
-
Offer home-based intermediate care to reduce the risk of institutionalisation.
-
Support care home staff training by more skilled NHS nursing staff.
-
Develop IT systems that are integrated across acute, community and primary care and all work roles.
-
-
Shared values
-
Create a more patient-centred approach to overcome service delivery disagreements.
-
-
Skills
-
Improve IT systems and training.
-
Allow community and hospital staff to learn each other’s skills for dealing with the very old.
-
-
Staff
-
Push and champion high standards of staff in care homes.
-
Establish strong and reliable leaders.
-
-
Style
-
Recognise that staff need to perform different roles and help them bridge the gap between health and corporate performance.
-
Synthesis of improving sites
The three improving sites provide a picture of a health system which, in contrast with the deteriorating sites, involved greater stability and continuity among a range of well-co-ordinated health- and social care service providers. Each case identifies key areas and issues relevant to the challenge of dealing with unplanned admissions (please also refer to the individual case reports) and, collectively, these build up a picture of the common attributes that might explain how these systems managed better and had reduced levels of unplanned admissions of patients aged 85 years or over. Looking across these three sites, and in comparison with the first three sites, a number of headline features can be identified.
First, all three improving sites exhibited a shared and comprehensive strategy for managing unplanned care, including specific policies and procedures for older patient groups. These were linked to a range of interventions to better manage patient care in the community, which includes rapid-access service, intermediate care service, out-of-hours care and support from voluntary sectors. Significantly, these strategies and policies were not isolated to individual care providers. Instead, they were shared across the wider health- and social care setting, suggesting an underlying basis of collaboration and co-ordination between care providers, reducing the risk of dominance by one provider that was noted in deteriorating sites.
Second, and possibly influencing the first feature, each site was characterised by stable and clear strategic leadership, whether by individual change agents or by co-ordinated agencies that provided continuity of purpose, fostered collaborative working and maintained commitment to improvement. Significantly, there was less evidence of knee-jerk change or projects not being brought to completion.
Third, and supporting the above, improvement projects were generally well resourced, often through cofunding or matched funding arrangements between local agencies and national bodies. Moreover, change projects were usually given time to develop and embed into practice rather than being subject to changing fashions or emerging policies.
Fourth, these sites typically provided integrated community health (and in some cases social) care provision through a single or main NHS organisation. This could either be a typical community health-care provider or a unified community and acute care provider. Significantly, the integration of community care within one provider not only enabled efficiency savings but, more importantly, enhanced integration between specialist teams of care providers. It also meant that the introduction of service innovations could be more easily aligned with and integrated into existing services, rather than seen as operating in competition.
Fifth, there was also closer alignment of out-of-hours GP services with either community or acute NHS providers. As above, this facilitated closer integration of primary, acute and community services, especially for information sharing, continuity of care and joined-up working more generally.
Sixth, these services also seemed to make more explicit and strategic use of voluntary care agencies. These often provided service in more responsive and dynamic ways that eluded traditional health-care providers.
Finally, and as a final point of clarification, it is worth noting that all three improving sites were relatively small and geographically bounded and composed of smaller cities or towns with surrounding rural areas. Only one had a large city and none had large metropolitan areas. In two sites, acute services were predominantly provided through traditional district general hospitals with limited teaching and specialist services, and specialist services were managed out of the area. Given this, it might be that these acute trusts could easily focus on organising and prioritising reductions in acute care and working in collaboration with local health- and social care partners; that is, these acute hospitals did not act as large centres of excellence and dominate the regional health economy. That being said, one of the improving sites did have a large specialist teaching hospital and continued to work collaboratively with regional care providers.
These factors are summarised in Table 20, which classifies them according to the McKinsey 7S model and examines their interconnections and their positive or negative impact.
| Dimension | Strong/positive type | Stems from | Influences | Weak/negative type | Stems from | Influences |
|---|---|---|---|---|---|---|
| Strategy | Good investment in community care Early engagement of all practitioners in key strategic decisions Strategic decisions made in a care trust, which allowed integrated decision-making from acute to social care in the community Strategy to focus on needs assessment for very old people helped reduce unplanned admissions Smart ways of dealing with the funding cuts Urgent care was a top strategic priority Recognised importance of community care |
Structuring Integration of acute, primary and community services Good understanding of patients’ needs and management Forward thinking and collaboration Executive decision-making |
Commissioning Design of trusts |
More recent lack of clarity in strategy for urgent care Increased professional barriers Targets and incentives, such as the 4-hour target, may increase admissions Lack of strategy for patients aged 85 years and over More recent changes with the shift to CCGs mean organisational goals are still up in the air – unsettled and difficult to plan |
National strategic funding cuts National strategies Lack of recognition of rising importance Significant organisational change |
Government policy Government policy and cuts |
| Structure (of care system) | Good governance structure, integration of all service providers at top level Good level of autonomy to design and deliver services Placement of staff whose knowledge complements new structural implementation Accountability of GP services through Personal Medical Services service design Interdisciplinary teams set up Out-of-hours services previously run by GPs as a co-operative Rapid response seen as an essential structure in the organisation in reducing unplanned admissions Lack of boundary issues helps to keep a clear structure Investment in interdisciplinary clinics with specialist services for old people Out-of-hours services run through the community trust successfully |
One of the few places in the country with a dedicated community trust Regional layout and planning Commissioning |
Out-of-hours services are not clearly structured and reliable Recent changes in out-of-hours services threaten existing reliability An increasing number of providers threatens to complicate the existing strengths of the organisational structure Gradual reduction in intermediate care in care homes, but not much has been done to replace the deficit in bed numbers Reduction in nursing and care home support |
GPs expressing interest only when it suits them Recognised damage of institutionalisation Costs and workload |
||
| System (processes) | Evidence of innovative technology systems being employed Pilots trialled new methods of work that were often successful GP out-of-hours services works well at the point of access, as well as rapid response 24/7 phone triage service through GPs and nurses allowing further access to rapid response if required – recognition of family need for advice Simple system design makes it clear for patients and families whom they can call – one acute trust Good support and training for care home patients and staff Good community initiatives and volunteering, especially in winter A focus on key programmes for urgent, stroke and end of life care puts systems in place to reduce unplanned admissions Good integration with care and nursing homes to allow staff engagement and development Attention to the importance of polypharmacy and initiatives to reduce falls |
Recognised need for the sharing of information Good strategic decisions around innovation Resources in the right places, upstream defence Collaborative delivery and good relationships |
Leaders focused on patient-centred care Commissioning |
Interface between teams weakening and struggling to provide services Care homes are not always visited by more qualified staff Some technology systems are not good enough, dangerous for patients Pilots being used but lack of education around them Lack of IT systems that allow the sharing of information between all providers is highly troublesome. A&E often going in blind, which is incredibly dangerous A&E targets can sidetrack professionals’ judgement |
Lack of strong leadership/short-term contracts/staff turnover/high level of demand Workload pressures and overlap of professional boundaries Existing professional boundaries stifling innovation Systems for evaluating pilots are not in place Professional boundaries/lack of investment/poor choice of computer systems |
Government policy |
| Shared values (for system working) | Clear direction and strategies fostered shared value in reaching goals Professionals willing to work together and bend hierarchies in order to put the patient first Strong organisational cohesion Health over politics Families tuned in to help the care of their older relatives Good communication and energy for providing good-quality care for old people |
Good governance and leadership/good communication Build up systems fostering long-term relationships |
Shared values of families towards the care of old people being challenged by the requirement for work and travel Recognition that government cuts stifle cohesion Patient-centred care is sometimes lost because of boundary issues |
Increased workload and costs | ||
| Skills | Perseverance of staff to see projects through and get people on board Very good at overcoming disagreements. Staff/organisations have developed interpersonal skills that enable effective working relationships Nursing staff are highly skilled and effective |
Strong values and goals Longstanding teams |
Variance in skill set of GPs Hospital staff very risk-averse High readmission rates suggest problems with community care |
Lack of GP governance Risk-averse culture Care pathways back into the community not available |
||
| Style | Regular contact and meetings between hospital and community professionals is arranged A lot of pride in providing services that keep older people out of hospital Effective working relationships, especially between GPs and other services Systems to integrate and educate the community on health-care issues for old people |
Willingness to come together and deal with the negative aspects of acute/community barriers Built upon over time |
Culture of patient-centred care | Risk of complacency; knowing that some services work well can lead to excessive dependency Some blame culture when services are pressured Lack of contact with frontline care can create problems when commissioners wish to understand patient experiences |
Leadership weakening | |
| Staff | Multidisciplinary teams in intermediate care are particularly beneficial for treating very old people Recognised need to involve pharmacists to reduce excessive medication Loyalty and effort of staff at a high level – long-standing and close relationships Previously had very strong leadership |
Close working relationships and simple structure | Communication challenges with ambulance services General trouble with attracting and keeping high-quality staff within the region (GPs, nursing and care home staff included) Staff at the very top of the organisation tend to be quite academically and research-orientated Staff boundaries and competencies are not always used effectively – especially regarding specialist staff Skills required for the best-quality community care are not always understood or appreciated by hospital staff Care home staff can make a huge difference to unplanned admissions and the well-being of old patients A lot of leadership change |
Systems for experiential learning are not in place Lack of regulation of staff and care home inspections |
||
| Setting | Rapid response and intermediate care being geographically integrated improves patient pathways Dense population used to advantage, but all areas are recognised as having specific problems Increased unemployment in the region has led to more volunteering (the value of community help has been recognised) Recognised the challenges for people with less money, and tailored services and provided information as well as possible |
Inequalities in wealth greatly affect the health-care challenge Risk of hospital losing teaching status, affecting staff numbers, skill sets and attraction to the region Ease of getting to hospital can discourage patients and their families from using other services |
Comparison between improving and deteriorating sites and concluding observations
It is first worth reiterating that further empirical and analytical detail can be found in Appendix 3 for each case study site and that the account given above aims to capture the main findings and learning points. It is also important to highlight the enormous challenge of describing and understanding local health- and social care systems, because they are inherently complex and characterised by relatively distinct configurations and characteristics. That being said, comparison both within and between the deteriorating and improving sites makes it possible to identify system features that might explain the observed variations in unplanned admission of people aged 85 years and over. A detailed list of possible recommendations was developed through cross-case comparison and subsequently verified and clarified through respondent validation (see Chapter 5), from which recommendations for change were developed with the implementation sites (ISs) (see Chapter 6). However, a number of significant issues have been identified here.
An overall strategy for unplanned care, in particular, and system integration, more broadly, appears to be essential. This needs to encompass more than the main health-care providers, such as acute hospitals, and be inclusive of primary, community and social care. Moreover, the strategy should be focused on the collective system, not isolated components or subsystems. For example, focusing strategy on acute care at the expense of community care might lead to unintentional bias in service development. Extending this line of analysis, strategy should be developed at the level of the local or regional system rather than component organisations. This might be challenging given the diversification and pluralisation of care provision and the extension of more competitive market mechanisms to drive performance.
Second, strategies need to reflect national policy priorities and targets, but these should not be addressed at the expense of local patient and community needs. As powerfully illustrated by the Francis Report,74 care providers can easily become trapped in a culture of doing the system’s business where what is measured gets managed (see also Bevan and Hood75). In addition, local strategies need to have continuity of purpose and direction, while recognising that wider structural change is an inevitable and cyclical feature of health policy. In this regard, consistency of service leadership which includes leaders who not only represent the interests of their individual organisation but understand the interdependencies between service organisations and the need for integrated working, seems important.
Third, and reflecting the above issue, strategies should place at their heart a commitment to integration and co-ordination between the entire health- and social care systems, recognising that all service providers, commissioners and other stakeholders have an active role to play. This also encompasses full inclusion of the voluntary and social enterprise sectors as key actors in meeting and managing patient demand. Significant in this regard is the need for investment and support for primary care to play an active and full role in system performance. This might involve transforming the image of the GP as a gatekeeper to acute or specialist services, and instead regarding him or her as a champion of managing patient need and co-ordinating the wider health systems around the patient.
Fourth, improvement and innovation projects are common across both deteriorating and improving sites, but what characterised the latter was a focus on aligning change projects to the overall systems strategy, establishing continuity of change and seeing change through, and providing sufficient resources, time and skills to enable change to become embedded in practice. In contrast, the former were associated with a plethora of short-lived, sectional improvement projects that were not given the opportunity to become embedded because they did not provide quick wins. This suggests, therefore, that a change in culture away from short-term strategy and improvement towards a greater number of longer-term and shared goals should be recommended.
Chapter 5 Development of recommendations
Transcripts of interviews from all sites were analysed by members of the research team to identify lessons that could inform recommendations. Draft recommendations from each site were compiled separately and then combined. Appendix 4 shows the first draft, with items colour coded to indicate from which site they were derived.
This version was revised following comments by all members of the research team. Evidence (for and against) each recommendation was sought from the literature, and references were added to alert readers to the evidence base to support them. This did not aim to be a comprehensive review of the literature; evidence was included only for topics related to the recommendations.
Using SurveyMonkey (www.surveymonkey.com; Survey Monkey Inc, Palo Alto, CA, USA), this version was then sent to all site respondents and external members of the project steering group, of whom 21 and 3, respectively, responded after two reminders. Table 21 shows details of site respondents.
| Characteristic | Category | n |
|---|---|---|
| Organisation | CCG | 3 |
| Acute trust | 6 | |
| Community trust | 4 | |
| Social services | 2 | |
| Other | 6 | |
| Role | Senior manager | 10 |
| Service manager | 5 | |
| Service provider | 3 | |
| Other | 3 | |
| Professional background | Medical | 3 |
| Nursing | 5 | |
| AHP | 3 | |
| Management | 6 | |
| Other | 4 |
Respondents were asked to indicate their agreement or disagreement with each recommendation on a 5-point Likert scale: 5, strongly agree; 4, agree; 3, neutral; 2, disagree; 1, strongly disagree. Results and average scores are presented in Table 22, with averages from all respondents and steering group members presented in separate columns. An agreement and disagreement score was also calculated by counting strongly agree/disagree as 2 and agree/disagree as 1. Items with the low levels of agreement are highlighted in blue and green, with blue indicating strongest disagreement. Respondents were also invited to add free-text comments. In some cases, the number of responses to individual questions was less than 24 because of missing data. It can be seen that, for several items, scores allocated by the steering group members differed from those of all respondents, although it should be remembered that numbers are small.
| Recommendation number | Recommendation | Average: all respondents | Strongly disagree (1) | Disagree (2) | Neutral (3) | Agree (4) | Strongly agree (5) | Disagree score | Agree score | Net score | Steering group average |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Strategy | |||||||||||
| Long term | |||||||||||
| R1 | Create and maintain a shared vision across health and social care: be aware that ‘big ideas’ and ‘national must dos’ and reorganisations come and go | 4.25 | 1 | 0 | 2 | 10 | 11 | 2 | 32 | 30 | 4.50 |
| R2 | Aim to maximise integration between care providers: community and acute care trusts and health and social care | 4.50 | 1 | 0 | 2 | 4 | 17 | 2 | 38 | 36 | 4.75 |
| R3 | Work at relationships with the local authority and acknowledge that this is a political organisation | 4.33 | 0 | 0 | 2 | 12 | 10 | 0 | 32 | 32 | 3.75 |
| R4 | Allow time for relationships to develop between the local partners, involving the emergence of common goals | 3.88 | 1 | 1 | 5 | 10 | 7 | 3 | 24 | 21 | 4.25 |
| R5 | Avoid tension between localism versus regionalism | 3.92 | 1 | 0 | 5 | 12 | 6 | 2 | 24 | 22 | 3.50 |
| R6 | Try to reconcile tensions between competition and collaboration | 4.04 | 1 | 1 | 1 | 14 | 7 | 3 | 28 | 25 | 4.00 |
| Medium term | |||||||||||
| R7 | Focus on reconfiguring according to the needs of the whole system, not isolated pockets | 4.30 | 1 | 0 | 1 | 10 | 11 | 2 | 32 | 30 | 4.50 |
| R8 | Minimise disruptions due to reorganisations and staff changes: these need to be risk managed | 4.13 | 1 | 0 | 2 | 12 | 8 | 2 | 28 | 26 | 4.50 |
| R9 | Admission reduction strategy needs to address underinvestment in primary care | 4.17 | 0 | 1 | 5 | 6 | 11 | 1 | 28 | 27 | 4.25 |
| R10 | Integration of funding and plans should include collectively shared and mutually dependent performance management | 4.13 | 1 | 0 | 1 | 14 | 7 | 2 | 28 | 26 | 4.25 |
| Short term | |||||||||||
| R11 | Avoid transient pilots with no follow-through and multiple initiatives which are inadequately promoted/marketed | 4.43 | 0 | 1 | 1 | 8 | 13 | 1 | 34 | 33 | 3.75 |
| R12 | Assess measures directed towards productivity and savings carefully and so avoid downside impact on quality and/or capacity | 4.30 | 1 | 0 | 0 | 12 | 10 | 2 | 32 | 30 | 4.50 |
| R13 | There are perverse incentives in the system; CCG should challenge trusts through active performance management of admissions and length of stay | 3.74 | 1 | 3 | 2 | 12 | 5 | 5 | 22 | 17 | 4.50 |
| R14 | Consider direct-to-public marketing to influence health utilisation behaviours | 3.48 | 2 | 1 | 6 | 12 | 2 | 5 | 16 | 11 | 3.25 |
| R15 | Invest in the full range of evidence-based intermediate care services (e.g. early supported discharge for orthopaedic patients) | 4.30 | 1 | 0 | 1 | 10 | 11 | 2 | 32 | 30 | 3.75 |
| R16 | Be prepared to take risks by investing in new models of care that as yet have a poor evidence base | 3.52 | 1 | 1 | 9 | 9 | 3 | 3 | 15 | 12 | 3.00 |
| R17 | CCGs could consider using social fund to purchase admission avoidance/supported discharge schemes | 3.78 | 1 | 0 | 6 | 12 | 4 | 2 | 20 | 18 | 3.75 |
| R18 | Acknowledge that some services will be decommissioned in the process of service redesign | 3.83 | 1 | 0 | 3 | 17 | 2 | 2 | 21 | 19 | 4.50 |
| R19 | Providers prefer broad specifications for service change that are outcome focused, as this enables them to make best use of their resources | 3.91 | 0 | 2 | 5 | 9 | 7 | 2 | 23 | 21 | 3.75 |
| R20 | Commissioners are purchasing services for their own patients while providers serve more than one commissioner; mechanisms need to be in place to enable tailoring of services to populations served | 3.74 | 1 | 3 | 2 | 12 | 5 | 5 | 22 | 17 | 3.50 |
| Structure (between services) | |||||||||||
| R21 | Forums such as system-wide urgent care boards should play a key role in overseeing service change and service integration | 3.82 | 0 | 1 | 6 | 11 | 4 | 1 | 19 | 18 | 3.00 |
| R22 | Integration can be facilitated by leaders in each service stream (primary care, community care, social care) being matched to partner leads in the other services | 4.00 | 0 | 0 | 5 | 12 | 5 | 0 | 22 | 22 | 3.33 |
| R23 | Clustering services under the same provider can be a constructive strategy through which to foster integration | 3.73 | 0 | 2 | 5 | 12 | 3 | 2 | 18 | 16 | 2.67 |
| R24 | Integrate social work and nursing teams that cross the boundary between community and hospital | 4.18 | 1 | 0 | 2 | 10 | 9 | 2 | 28 | 26 | 4.00 |
| R25 | Effort is needed to integrate mental health trusts in system change, especially when community staff sit in other organisations | 4.00 | 1 | 0 | 3 | 12 | 6 | 2 | 24 | 22 | 4.67 |
| R26 | Consider how palliative care teams are integrated as part of the overall system of care | 4.32 | 1 | 0 | 1 | 9 | 11 | 2 | 31 | 29 | 4.00 |
| R27 | Where district nursing teams are no longer based in GP surgeries, relationships should be restrengthened with more formal links | 4.00 | 0 | 1 | 3 | 13 | 5 | 1 | 23 | 22 | 2.67 |
| R28 | Maximise opportunities for colocation of services | 4.14 | 1 | 0 | 3 | 9 | 9 | 2 | 27 | 25 | 4.67 |
| R29 | Integrate clinical information systems for primary care, walk-in centres, urgent care centres, ambulatory care and social care | 4.36 | 1 | 0 | 1 | 8 | 12 | 2 | 32 | 30 | 5.00 |
| R30 | Understand and address the impact that early-discharge policies can have on admissions unless additional and compensatory changes are made to the system to accommodate these patients | 4.32 | 1 | 0 | 1 | 9 | 11 | 2 | 31 | 29 | 3.67 |
| Systems (individual services) | |||||||||||
| Emergency care | |||||||||||
| R31 | Review skill mix in EDs, consider specialist geriatric cover (24/7), GPs, community matrons, occupational therapists and social workers | 4.18 | 0 | 0 | 4 | 10 | 8 | 0 | 26 | 26 | 4.33 |
| R32 | Review skill mix (including GP and geriatrician input) in assessment units (and consider integrating with primary care assessment unit) | 4.32 | 0 | 0 | 0 | 15 | 7 | 0 | 29 | 29 | 4.33 |
| R33 | Implement a system for assessment and management of people who fall with ambulance trusts and extend this to reduce the conveyance of patients with other conditions | 3.95 | 0 | 0 | 6 | 11 | 5 | 0 | 21 | 21 | 4.67 |
| R34 | Consider ambulatory care centres (which allow patients who would normally be treated as inpatients to be seen as day cases) to take referrals from GP and divert from ED | 4.05 | 0 | 0 | 4 | 13 | 5 | 0 | 23 | 23 | 4.33 |
| Intermediate care | |||||||||||
| R35 | Intermediate care provision should be integrated, with 24/7 availability and a SPA | 4.19 | 1 | 0 | 2 | 9 | 9 | 2 | 27 | 25 | 4.67 |
| R36 | Acknowledge that community ‘beds’ is an old and discredited model for care in the community | 3.10 | 0 | 7 | 7 | 5 | 2 | 7 | 9 | 2 | 2.67 |
| R37 | Assess the need for geriatrician input to intermediate care | 4.29 | 1 | 0 | 0 | 11 | 9 | 2 | 29 | 27 | 4.33 |
| R38 | A roving GP supported by a consultant geriatrician may oversee use of a limited number of ‘step up’ and ‘step down’ beds | 3.81 | 1 | 1 | 4 | 10 | 5 | 3 | 20 | 17 | 3.33 |
| R39 | Consider telehealth as an addition to community matron provision for COPD and heart failure | 3.38 | 3 | 1 | 5 | 9 | 3 | 7 | 15 | 8 | 2.00 |
| R40 | Provide a specialist community-based 24/7 response service for people with urgent mental health needs | 4.33 | 1 | 0 | 1 | 8 | 11 | 2 | 30 | 28 | 4.33 |
| Geriatric services | |||||||||||
| R41 | Provide GPs with access to urgent geriatric advice (telephone) and urgent clinic appointments | 3.95 | 1 | 0 | 3 | 12 | 5 | 2 | 22 | 20 | 4.33 |
| GP and extended hours services | |||||||||||
| R42 | Monitor the performance of GPs in urgent care provision | 4.33 | 1 | 0 | 1 | 8 | 11 | 2 | 30 | 28 | 3.67 |
| Care homes | |||||||||||
| R43 | Work closely with nursing homes hosting beds to assure the quality of care in this setting | 4.43 | 1 | 0 | 1 | 6 | 13 | 2 | 32 | 30 | 4.67 |
| R44 | Be flexible about community nurses supporting residents of nursing homes | 4.33 | 0 | 0 | 2 | 10 | 9 | 0 | 28 | 28 | 4.33 |
| Shared values | |||||||||||
| Vision | |||||||||||
| R45 | Develop and communicate a shared vision on quality of care for older people, accommodating medical, functional and managerial perspectives | 4.24 | 0 | 0 | 2 | 12 | 7 | 0 | 26 | 26 | 2.67 |
| R46 | Be proactive in creating the kind of future that is needed; do not wait to be pushed | 4.29 | 1 | 1 | 1 | 6 | 12 | 3 | 30 | 27 | 3.67 |
| Culture and change | |||||||||||
| R47 | Accept and accommodate role changes, including the cultural shift needed for hospital-trained staff to work in the community | 4.19 | 1 | 0 | 1 | 11 | 8 | 2 | 27 | 25 | 4.33 |
| R48 | Community nurses and GPs need to better understand each other’s worlds, priorities and ways of working | 4.24 | 1 | 0 | 0 | 12 | 8 | 2 | 28 | 26 | 4.00 |
| R49 | Accept that a key role for NHS managers is to manage uncertainty | 4.43 | 0 | 0 | 2 | 8 | 11 | 0 | 30 | 30 | 5.00 |
| R50 | Acknowledge that new organisations (CCGs) need to find their feet and build relationships | 3.95 | 0 | 1 | 5 | 9 | 6 | 1 | 21 | 20 | 3.00 |
| Relationships | |||||||||||
| R51 | Consider trust-building initiatives to improve relationships between commissioners and providers | 3.71 | 1 | 1 | 6 | 8 | 5 | 3 | 18 | 15 | 3.33 |
| R52 | Avoid blaming other organisations or groups for things that are not going well; collaborative solutions are more likely to work | 4.10 | 1 | 0 | 2 | 11 | 7 | 2 | 25 | 23 | 3.67 |
| R53 | Focus on the needs of the patient; there is no room for ego | 4.52 | 1 | 0 | 0 | 6 | 14 | 2 | 34 | 32 | 3.67 |
| R54 | Focus on building relationships and supporting staff through redesign | 4.33 | 1 | 0 | 0 | 10 | 10 | 2 | 30 | 28 | 3.67 |
| R55 | Break down role boundaries wherever they get in the way of effective care | 4.38 | 1 | 0 | 0 | 9 | 11 | 2 | 31 | 29 | 2.33 |
| Skills | |||||||||||
| R56 | Integrate long-term condition nurses into primary care teams, blending specialist knowledge and generic skills | 4.10 | 0 | 0 | 3 | 13 | 5 | 0 | 23 | 23 | 3.33 |
| R57 | Assure all relevant disciplines are given the opportunity to contribute to MDTs | 4.38 | 0 | 0 | 1 | 11 | 9 | 0 | 29 | 29 | 3.00 |
| R58 | Look to role extension as an alternative to increasing complexity of MDTs | 3.81 | 0 | 1 | 6 | 10 | 4 | 1 | 18 | 17 | 3.67 |
| R59 | Assess the need to improve IT systems training | 4.19 | 1 | 0 | 2 | 9 | 9 | 2 | 27 | 25 | 3.67 |
| R60 | Invest effort in developing skills of key groups, e.g. staff in care homes | 4.57 | 0 | 0 | 0 | 9 | 12 | 0 | 33 | 33 | 4.33 |
| Staff | |||||||||||
| R61 | Manage pressures at work; stretched or stressed staff resort to silo mentality, which will ultimately work counter to integration | 4.38 | 1 | 0 | 1 | 7 | 12 | 2 | 31 | 29 | 4.33 |
| Style | |||||||||||
| R62 | Leadership by key individuals makes a difference especially when working across organisations; take advantage of these people | 4.48 | 0 | 0 | 1 | 9 | 11 | 0 | 31 | 31 | 4.33 |
| R63 | Recognise the importance of clinical leadership: clinician managers can offer particular perspectives | 4.48 | 0 | 0 | 2 | 7 | 12 | 0 | 31 | 31 | 3.67 |
| R64 | Recognise that different leadership styles are appropriate to different problems and situations. Aggressive/tenacious leaders can get things done; liberal, inclusive, charismatic leaders have their strengths; all can be relevant | 4.29 | 0 | 1 | 1 | 10 | 9 | 1 | 28 | 27 | 2.67 |
Results from this consultation exercise were considered at a meeting of the project management group and a revised and shortened list was produced. Changes were made based on results from the consensus exercise, consideration of the evidence base and the views of the research team. Some items were dropped completely and others were rephrased or consolidated. Details of the changes are listed below.
Strategy Item 5 was dropped, as it scored below 4 with both groups and was felt to reflect a particular problem at one site. Item 16 scored low and so was rephrased and combined with items 15 and 18, emphasising that non-evidence-based services should be introduced only as part of an evaluation. Items 14 and 20 scored low and so were dropped.
Structure All items had high levels of agreement by site respondents and were retained, although some were rephrased for clarity.
Systems In general, levels of agreement were high, apart from items 36 (about community beds) and 39 (about telehealth). These items were dropped, and it was also noted that recent reviews do not support the extension of telehealth. Item 42 was also dropped, as it was felt to be too general to be useful, and items 43 and 44 (about care homes) were combined.
Shared values Although all items scored highly, there was felt to be some duplication, and so the number of recommendations in this section was consolidated from 11 to 6.
Skills Items 57 and 58 (about multidisciplinary teams) were combined.
Staff and Style All items scored highly and so were retained, although some were rephrased for clarity.
This resulted in a reduction in the number of recommendations from 64 to 47. The final list, with the accompanying evidence, is shown in Box 1.
Letters in brackets refer to the evidence base at the end of the document.
Strategy Long term-
Create and maintain a shared vision across health- and social care, despite the fact that ‘big ideas’, ‘national must dos’ and reorganisations come and go (A).
-
Aim to maximise integration between care providers (primary care, community and acute care trusts, health- and social care), acknowledging the major cultural shift needed to make this happen (B)(C).
-
Work at relationships with the local authority and acknowledge that this is a politically led organisation. Recognise the role of Health and Wellbeing Boards.
-
Allow time for relationships to develop between the local partners, involving the emergence of common goals and consensus that will last (D).
-
Try to reconcile tensions between competition and collaboration by putting the needs of patients first.
-
Focus on reconfiguring according to the needs of the whole system, not isolated pockets (E).
-
Minimise disruptions due to reorganisations and staff changes: these need to be risk managed through wide involvement and engagement of staff.
-
Admission reduction strategy needs to address underinvestment in primary care, including out-of-hours care (F).
-
Integration of funding and plans should include collectively shared and mutually dependent performance management (G).
-
Avoid transient pilots with no forward planning and multiple initiatives which are inadequately promoted (E).
-
There are perverse incentives in the system; the CCG should challenge trusts through active performance management of admissions and length of stay (H).
-
Assess measures directed towards productivity and savings carefully and thereby avoid downside impact on quality and/or capacity.
-
Invest in evidence-based intermediate care services (I) and be prepared to invest in new models of care that lack an evidence base if part of a robust evaluation. Acknowledge that some services will be decommissioned.
-
Commissioners could consider using flexible funding (e.g. Social Fund) to purchase admission avoidance/supported discharge schemes.
-
Commission services on well-defined outcomes rather than process, as this enables providers to make best use of their resources.
-
Forums such as system-wide urgent care boards should play a transparent role in overseeing service change and service integration (J).
-
Consider facilitating integration by matching leaders in each service stream (primary care, community care, social care) to partner leads in the other services (K).
-
Clustering services under the same provider can be an effective strategy through which to foster integration (L).
-
Integrate social work and nursing teams that cross the boundary between community and hospital.
-
Effort is needed to integrate mental health trusts in system change, especially when community staff sit in other organisations.
-
Maximise the integration of palliative care teams with the overall system of care.
-
Where district nursing teams are no longer based in GP surgeries, relationships should be restrengthened with more formal links.
-
Maximise opportunities for colocation of services and, where this is not possible, use technology to bridge the gap.
-
Integrate clinical information systems for primary and secondary care, walk-in centres, urgent care centres, ambulatory care and social care (N).
-
Understand and address the impact that early discharge policies can have on admissions unless additional and compensatory changes are made to the system to accommodate these patients.
-
Review skill mix in emergency departments and acute assessment units, consider specialist geriatric teams/frailty units (24/7), GPs, community matrons, OTs and social workers (M).
-
Implement a system for community assessment and management of people who call emergency ambulance services. This could start with those who fall and be extended to patients with other conditions (P).
-
Consider equipping ambulatory care centres (which allow patients who would normally be treated as inpatients to be managed as day cases) on hospital sites to take referrals from GPs and divert from emergency departments (Q).
-
Intermediate care provision should offer a SPA, with 24/7 availability (L).
-
Assess the need for geriatrician input, from GP with geriatrician support to multidisciplinary intermediate care services (R).
-
Provide a specialist community-based 24/7 response service for people with urgent mental health needs.
-
Provide GPs with access to urgent geriatric advice (telephone) and urgent clinic appointments.
-
Be flexible about community nurses supporting residents of nursing homes and assure quality of care where homes provide intermediate care.
-
Develop and communicate a shared vision on quality care for older people, accommodating medical, functional and managerial perspectives (A).
-
Accept and accommodate role changes, including the cultural shift needed for hospital-trained staff to work in the community and vice versa.
-
Break down role boundaries wherever they get in the way of effective care.
-
Professionals across the system need to better understand each other’s roles, priorities and ways of working, including recognising that a key role for managers is to manage uncertainty; consider rotating staff through services to enhance this knowledge transfer.
-
Avoid blaming other organisations or groups for things that are not going well; collaborative solutions are more likely to work.
-
Focus on the needs of the patient, building relationships and supporting staff through redesign.
-
Integrate long-term condition nurses into primary care teams, blending specialist knowledge and generic skills.
-
Ensure all relevant disciplines are given the opportunity to contribute their skills to multidisciplinary teams and look to role extension as an alternative to increasing their complexity.
-
Assess the need to improve staff training in IT skills.
-
Invest effort in developing the skills of key groups, for example staff in care homes.
-
Manage pressures at work; stretched or stressed staff may resort to silo mentality.
-
Leadership by committed and charismatic individuals makes a difference, especially when working across organisations; take advantage of these people but build in succession planning.
-
Recognise the importance of clinical leadership: clinician managers can offer particular perspectives.
-
Recognise that different leadership styles are appropriate for different problems and situations. Aggressive/tenacious leaders can get things done; liberal, inclusive leaders can increase cohesion; aim to achieve a balance.

-
The national evaluation of integrated care pilots38 concluded that strong leadership and shared vision were facilitators for success, and that ‘national policies, processes and legislation’ and ‘the bureaucratic nature of NHS and local government processes’ were barriers (p. 20).
-
The national evaluation of integrated care pilots38 showed an increase in emergency admissions but a decrease in planned admissions and outpatient visits.
-
The King’s Fund9 concluded that ‘areas that have well developed integrated services for older people have lower rates of hospital bed use’ and that ‘any local strategy should look across the system and align ways of working between primary, community and acute care to reduce avoidable admission and length of stay’ (p. 1).
-
The national evaluation of integrated care pilots38 found ‘pre-existing relationships at a personal level across organisations’ facilitated success. The King’s Fund9 found commissioners buying a high proportion of activity from one provider had lower rates of bed use among those aged 65 years and over.
-
The King’s Fund report9 concluded that ‘the key to improvement lies in changing a system rather than piecemeal initiatives. A set of unaligned projects will not produce system-wide results’ (p. 19).
-
The FTN briefing12 found a negative association between primary care spending and ED attendances in those aged 65 years and over (admissions not presented).
-
The national evaluation of integrated care pilots38 recommended ‘developing a monitoring framework to demonstrate the continuing benefits of integrating activities’ (p. 93). The National Audit Office2 identified a number of barriers to closer integration, including differences in funding, performance management and culture between the organisations.
-
The national evaluation of integrated care pilots38 recommended ‘developing a monitoring framework to demonstrate the continuing benefits of integrating activities’ (p. 93).
-
The King’s Fund6 concluded that Hospital at Home was an effective intervention to reduce admissions. This draws on evidence from two Cochrane reviews suggesting that Hospital at Home delivers similar clinical outcomes to inpatient care, that it is preferred by older people and that admission avoidance schemes may be cost saving.
-
The National Audit Office2 noted (p. 41):
These groups bring together health and social care partners to build consensus, learn from best practice and identify how urgent care services can best be delivered locally. However, decisions about the use of resources will be the responsibility of the individual budget holding organisations.
-
In its report on integrated care, The King’s Fund76 emphasised the importance of shared leadership at all levels, not just at the top of organisations.
-
The King’s Fund76 reports that ‘experience indicates the importance of a single point of access, a single assessment process and close alignment between the work of the team and other providers’ (p. 4).
-
There is observational evidence that senior review in EDs can reduce admissions by 12%. 45 FTN12 reported that trusts that provide early specialist geriatric assessment of older patients in EDs and short-stay medical units achieve significantly fewer admissions and shorter lengths of stay in hospital.
-
The National Audit Office2 noted that (p. 44):
Patient information is key to better joint working and integration. Patient information is not commonly available across all parts of primary care, social care, community care and secondary care. Patient information is often fragmented and hard to access out of hours.
-
Enhanced paramedic training can reduce the conveyance rate (relative risk 0.72, 95% confidence interval 0.68 to 0.75) to hospital in older people, including those with cognitive impairment. 41 Falls prevention for those assessed by the ambulance crew but not conveyed to hospital is clinically effective and cost-effective. 43,77
-
There is systematic review evidence that assessment/admission units reduce unnecessary admissions. 78
-
The FTN briefing12 also concluded that ‘ensuring the expert geriatric workforce is available at times of peak demand from older patients will improve operational efficiency’ (p. 1).
Prioritised recommendations
Finally, a list of ‘top 20’ recommendations was produced, selecting those with the highest scores in the poll of participants, for each component of the 7S model, combining the sections on Skills, Staff and Style. The numbers in parentheses refer to the number of the recommendation in the full list. Our findings support the view that recommendations addressing strategic issues should be given the highest priority as they will facilitate the adoption of more operational objectives and ensure their integration both with each other and with the wider system.
Strategy
-
Aim to maximise integration between care providers: community and acute care trusts and health and social care (R2).
-
Work at relationships with the local authority and acknowledge that it is a political organisation (R3).
-
Focus on reconfiguring according to the needs of the whole system, not isolated pockets (R7).
-
Avoid transient pilots with no follow-through, and multiple initiatives which are inadequately promoted/marketed (R11).
Structure
-
Consider how palliative care teams are integrated as part of the overall system of care (R21).
-
Integrate social work and nursing teams that cross the boundary between community and hospital (R19).
-
Integrate clinical information systems for primary care, walk-in centres, urgent care centres, ambulatory care units and social care (R24).
-
Understand and address the impact that early-discharge policies can have on admissions unless additional and compensatory changes are made to the system to accommodate these patients (R25).
Systems
-
Review skill mix in EDs and acute assessment units; consider specialist geriatric teams/frailty units (24/7), GPs, community matrons, occupational therapists (OTs) and social workers (R26).
-
Assess the need for geriatrician input to intermediate care (R30).
-
Provide a specialist, community-based, 24/7 response service for people with urgent mental health needs (R31).
-
Be flexible about community nurses supporting residents of nursing homes and assure quality of care where homes provide intermediate care (R33).
Shared values
-
Develop and communicate a shared vision on high-quality care for older people, accommodating medical, functional and managerial perspectives (R34).
-
Break down role boundaries wherever they get in the way of effective care (R36).
-
Enable professionals across the system to better understand each other’s roles, priorities and ways of working, including recognising that a key role for managers is to manage uncertainty; consider rotating staff through services to enhance this knowledge transfer (R37).
-
Focus on the needs of the patient, building relationships and supporting staff through redesign (R39).
Skills, staff and style
-
Ensure all relevant disciplines are given the opportunity to contribute their skills to multidisciplinary teams and look to role extension as an alternative to increasing the teams’ complexity (R41).
-
Invest effort in developing the skills of key groups, for example staff in care homes (R43).
-
Acknowledge that leadership by committed and charismatic individuals makes a difference, especially when working across organisations; take advantage of these people but build in succession planning (R45).
-
Recognise the importance of clinical leadership: clinician managers can offer particular perspectives (R46).
Chapter 6 Implementation
Aim
The aim of this phase of the project was to identify the practical challenges faced by providers and commissioners in starting to implement system change to reduce unplanned admissions of very old people. More specifically, we wanted to establish the necessary conditions and contribute to drivers for initiating change and better practice for improved system performance for people aged 85 years and over with urgent care needs. This is not easy in a complex and dynamic environment. The King’s Fund report notes:
in the real world, interventions will rarely be implemented in isolation. A combination of interventions intended to reduce admissions may be expected to have a ‘cumulative’ effect and, although each may have little effect individually, there may be greater benefit overall than the combined effects of single interventions.
p. 176
Identification of sites
In the original proposal, we planned to identify two ISs in the East Midlands: one large teaching acute trust and one district general hospital. Despite approaching several district general hospitals at the start of the project, we were unable to find a volunteer, but gained expressions of interest from two university-linked trusts. A primary factor in their selection was that these two agreed to engage with the implementation phase of the project. Equally important was the fact that these sites were local and already had links with the research team. Unfortunately, after initial engagement and several meetings, one of these sites was unable to continue with the project because of staff sickness, so, with permission from Health Services and Delivery Research (HSDR), we focused implementation activity on one site.
Methodological approach
The original plan for implementation was to have one research associate lead implementation within the two identified sites. However, following discussions at the two selected sites, the project team decided that a better way to effect change within the complex system would be to enlist ‘champions’ within each site. Research by Soo et al. 79 strongly recommends this as a demonstrably effective method of effecting change within health-care systems. This change in direction envisaged identifying and enlisting an individual within the system who would be able to engage at all the necessary levels, from patients, commissioners, ED clinicians, GPs and social care managers, throughout the management structures to chief executive level. Key capabilities of such a person included the ability to network, a root and branch understanding of the health-care system and a willingness to promote the recommendations and assist in dissemination of the work. This approach was modelled on previous work on knowledge diffusion. 80
Implementation focused on the dissemination and engagement of people on a system-wide level. This type of engagement understandably takes time to establish. Key factors included being aware of the timing of strategic planning and reviews, and being able to take advantage of this. In addition to this, an understanding of current and future strategic priorities was also very helpful, particularly with regard to advising about the ‘fit’ of some of the recommendations with the specific strategic initiative.
Profile of the implementation site
The IS was profiled in the same manner as previously done for improving and deteriorating sites in the earlier part of the research.
The health economy of the IS has a catchment population of 1.08 million and includes a single large teaching hospital with one ED, three Clinical Commissioning Groups (CCGs) covering 154 GP practices and one large provider of community health services.
Population demographics are diverse, with 13% of the population in the city (total population 380,000) and 23% of the population in the county (total population 628,000) being over the age of 65 years. There is one CCG for the city and two for the county, covering the east and west sides respectively. There is also a budding ‘Better Care Together’ (BCT) programme and fund in place, with an identified frail older persons’ workstream.
Many projects related to older people have been ongoing for several years, including work on end of life care and on acute care in the ED and acute medical assessment units.
Key contextual messages from the research that informed our approach to implementation were:
-
Population seemed from the study sites to be an important factor underlying increasing or decreasing admissions rates, as it grew more rapidly in the deteriorating sites than in the improving sites. It may be the case that more rapid population growth puts more stress on primary care and emergency systems, resulting in patients being admitted to hospitals more readily. IS has an above average population base and a rapidly increasing number of admissions in the age group of 85 years and over, growing much faster than the population numbers.
-
Admissions for ACSCs also suggest that deteriorating sites are less able to cope with increased demand for primary care and emergency services. The evidence for this comes from the seasonal variations in admissions and their effect on the ranking of the PCTs. The deteriorating PCTs slip down in the rankings during the cold season, while the improving PCTs go up in the rankings. The IS had much higher admission rates for ACSCs than average, but in the last few years has been improving on this measure and now conforms to the seasonal trends.
-
The out-of-hours GP service and the ease of access to GP services seem to be worse in the deteriorating sites, which may be a reason for higher rates of transfers to hospital care. The IS’s results are very close to the deteriorating PCTs’ averages, except in the lack of appointments category, for which the IS’s results were below this average.
-
The chronic versus acute admission rates comparison, as well as the readmission rates and the deprivation profile, offers complementary evidence of pressures on the primary care system. The IS is one of the most deprived of our selection of PCTs and does relatively poorly on those measures.
Dissemination activity
The dissemination fellow is an ED consultant and the acute trust’s Associate Medical Director for Clinical Quality and Improvement. He has also been a member of the BCT programme clinical reference group and the BCT fund’s frailty task group since March 2014.
The dissemination of the recommendations, although a partially promotional activity, is essentially planning and searching for means to present and describe the recommendations to both system-wide and decision-making stakeholders.
The draft recommendations were initially presented to the Board of the West [county] CCG in September 2013. It was well received with an initial desire to tackle some aspects of the findings, especially those that affected community services. The East [county] CCG had an annual local GP forum, also in September 2013, where some of the draft recommendations were also presented but with no response. Several unsuccessful attempts were made through e-mails and verbally to have the recommendations from the project presented at the IS’s urgent care board. This was more a reflection of the current crisis faced by the local emergency care system, which constantly failed to achieve the 4-hour emergency access target, and its effect on prioritisation rather than anything against the project.
Another opportunity arose in February 2014, when Pfizer invited the dissemination fellow to help organise a NHS–Pfizer collaboration lab in London, where the theme proposed on behalf of IS was reducing admissions in older people. Despite representation from the three CCGs and the acute trust, nothing has happened as follow-up. The stated intention was to work together towards developing more joint programmes on reducing admissions.
However, the fact that inability to reduce admissions in older people may be a vital contributor to the system’s inefficiencies may not have been acknowledged to the necessary extent. Further avenues are being pursued towards a dissemination that would result in change packages.
In May 2014, the IS appointed a transformation advisor. This advisor is a senior geriatrician with knowledge of improvement methodology. He was given access to the draft recommendations to attempt to integrate some of the principles within the urgent care transformation workstream.
In June 2014, the IS set up an older person’s strategy group to improve care of frail older people within the hospital and in line with the recommendations from the ‘Silver Book’. 30 Currently a summit is also being planned to present the recommendations of the project to the directors of strategy in the IS to assist with transformation programmes aligned to the outcomes from the BCT projects.
Feedback on recommendations or gauging system-wide response is being planned to include the members of the frailty task group as primary responders. CCGs and other project boards are to be included at a later date.
Understanding the challenges of implementation
For providers and commissioners to begin implementing system change, there are significant barriers to overcome. These include elements such as resources, funding, infrastructure, skills, culture and a dynamic economy. Parkin81 notes how policy-makers have struggled with understanding and managing the NHS (as a national system) and view it as a ‘1940s system in a 21st century world’ (p. 4).
Practitioners and commissioners will have to approach implementation from a systems perspective. This is an approach which is well recognised and established within the health-care environment, but difficulties in achieving it have been described in the literature. Plsek and Greenhalgh82 highlight the key aspects of complexity in health care and state that: ‘In complex systems, unpredictability and paradox are ever present, and some things will remain unknowable’ (p. 625). In addition: ‘Clinical practice, organisation, information management, research, education, and professional development are interdependent and built around multiple self-adjusting and interacting systems’ (p. 625).
These different elements are essentially the same as those we have tried to capture in this research by use of the McKinsey 7S framework. The framework attempted to capture and classify the whole system into the seven categories of Structure, Strategy, Systems, Shared values, Style, Staff and Skills.
On implementing change, Parkin81 states that: ‘Implementing change in healthcare is difficult, challenging and often results are short-lived’ (p. 7). This should be understood by commissioners, and implementation seeks to clearly avoid such short-termism of outcome. This is a very important point and informed the project team’s rationale for deciding to engage a dissemination fellow to interact with the system components.
The tasks of the dissemination fellow are ongoing and include:
-
encouraging adoption of better practice among system stakeholders
-
guiding an approach that seeks alignment with existing projects
-
advising on ‘fit’ of recommendations within the IS
-
assisting in the dissemination of the project findings.
Management of change and overcoming resistance
As noted above, a major barrier to change for stakeholders to negotiate is culture. Scott et al. 83 identify a number of different factors that can impede change, with which some our own findings resonate and which are highlighted below. Bate84 points to structure, process and context as three core dimensions through which to understand and frame change. In this project, the McKinsey 7S framework can be readily mapped onto these core dimensions and provides a more detailed understanding of the environment under study. Campbell85 emphasises the point that context (situation) as well as psychology is key in change these core dimensions management practice. Further, in terms of Parkin81 levels of analysing change models (macro, meso and micro), our concern here is meso (organisations, institutions, health trusts) and micro (individuals, groups, interactions).
Moving on from understanding and analysis, Kotter and Cohen86 proposed a change management model that was effectively followed in this project. Kotter and Cohen86 identified three phases of change implementation that were referred to as creating a climate for change, engaging and enabling the whole organisation and, finally, implementing and sustaining the change. The greatest concern for this project, and where most effort was expended, was the first two of Kotter’s phases: preparation and engagement. Much of this ongoing activity is reported above in Dissemination activity.
In overcoming resistance to implementing change, stakeholders are advised of the following pitfalls developed from Scott et al. (pp. 114–17),83 which are also captured by our research and implicitly incorporated into our recommendations (numbers relate to Chapter 5).
The lack of ownership by individuals and groups can create loss and confusion. People have to ‘buy in’ to proposed changes.
Example from our recommendations:
-
No. 34: Develop and communicate a shared vision on quality care for older people, accommodating medical, functional and managerial perspectives.
Complexity and the multifarious influences on culture within the system should be acknowledged.
Examples from our recommendations:
-
No. 17: Consider facilitating integration by matching leaders in each service stream (primary care, community care, social care) to partner leads in the other services.
-
No. 3: Work at relationships with the local authority and acknowledge that this is a politically led organisation. Recognise the role of Health and Wellbeing Boards.
External influences such as policy, will occasionally cast a shadow over internal directions and initiatives. These must be managed.
Examples from our recommendations:
-
No. 1: Create and maintain a shared vision across health and social care, despite the fact that ‘big ideas’, ‘national must dos’ and reorganisations come and go.
-
No. 2: Aim to maximise integration between care providers (primary care, community and acute care trusts, health and social care), acknowledging the major cultural shift needed to make this happen.
-
No. 12: Assess measures directed towards productivity and savings carefully and so avoid downside impact on quality and/or capacity.
Lack of appropriate leadership will smother any efforts at implementing change. In our research we noted clear issues where leaders had remained in post for relatively short lengths of time. This somewhat led to discontinuity in organisational direction.
Examples from our recommendations:
-
No. 45: Leadership by committed and charismatic individuals makes a difference, especially when working across organisations; take advantage of these people but build in succession planning.
-
No. 47: Recognise that different leadership styles are appropriate to different problems and situations. Aggressive/tenacious leaders can get things done; liberal, inclusive leaders can increase cohesion; aim to achieve a balance.
Cultural diversity can establish barriers to change. For example, subgroup cultures generally differ between nurses, doctors, managers and patient groups. Ideally there should exist a balance between power and effectiveness between these subgroups.
Examples from our recommendations:
-
No. 34: Develop and communicate a shared vision on quality care for older people, accommodating medical, functional and managerial perspectives.
-
No. 37: Professionals across the system need to better understand each other’s roles, priorities and ways of working, including recognising that a key role for managers is to manage uncertainty; consider rotating staff through services to enhance this knowledge transfer.
-
No. 38: Avoid blaming other organisations or groups for things that are not going well; collaborative solutions are more likely to work.
Dysfunctional consequences are usually the unwanted outcomes of some initiatives. An example of this can be seen as the recent policy drive for targets and performance measures. Although it is a useful device for process improvement, the side effects have been detrimental to the service received by patients.
-
No. 12: Assess measures directed towards productivity and savings carefully and so avoid downside impact on quality and/or capacity.
-
No. 11: There are perverse incentives in the system; CCG should challenge trusts through active performance management of admissions and length of stay.
-
No. 9: Integration of funding and plans should include collectively shared and mutually dependent performance management.
Chapter 7 Discussion
Summary of findings
Using a mix of methods we were able to identify important differences between sites in which admission rates for people aged 85 years and over had increased most rapidly between 2007/8 and 2009/10 and sites in which these rates had stabilised or declined. Our selection was based on rates of change, not absolute rates, so it should be remembered that some improving sites had higher admission rates than deteriorating sites. On average, in improving sites these rates per 100 of the population at risk fell from 51% to 49%, and in deteriorating sites they increased from 53% to 57%. For acute ambulatory care conditions (all ages, as data on those aged 85 years and over are not available), differences in rates were greater, decreasing from 0.49% to 0.45% in improving sites and increasing from 0.46% to 0.55% in deteriorating sites.
The main contributor to these differences in rates of admission for those aged 85 years and over was changes in the proportion of zero-day admissions (i.e. people who were admitted and discharged on the same day). In improving sites these fell as a proportion of total admissions and were stable (at 9%) when expressed as a rate of the population at risk. Conversely, in deteriorating sites, zero-day admissions increased both as a proportion of total admissions and from 10% to 15% of the population at risk. Another contributor to differences between sites was emergency readmission rates for those aged 85 years and over, which were fairly stable in improving sites but rose from 9% to 13% in deteriorating sites. However, readmission rates following a 1-day admission were higher in improving sites. There are several possible reasons for this, including case mix (i.e. fewer patients with lower levels of need were admitted) and that patients were discharged at an earlier stage of their recovery.
Higher rates of zero-day admissions could reflect a lack of alternatives, such as provision (or co-ordination) of intermediate care, ambulatory care centres and other community services; there was evidence from qualitative interviews that this was the case in deteriorating sites. These services appeared to work best when fully integrated with each other, offering round-the-clock availability with a SPA, shared information systems and specialist nursing and geriatric support. There were examples of improving sites where all such services were provided by a single organisation, including, in one case, vertical integration through provision by an acute trust. These conclusions are in line with those of a recent national audit of intermediate care, which found that these services were still fragmented, particularly in relation to mental health. 87
We also found that, in deteriorating sites, GP access, including out-of-hours services, was worse. Poor access is associated with increased use of emergency departments, which could itself increase admission rates, particularly for less than 1 day. Interview data suggested that, in all three deteriorating sites, there had been less focus on developing GP and community services when tackling emergency care. Again, integrated organisational structures, for example a community trust taking responsibility for out-of-hours provision, appeared to be important.
Within EDs, difficulties in reaching the 4-hour target were reported as increasing the risk of admission because there may have been insufficient time to offer alternatives. We found evidence of effective strategies for reducing the proportion of older people attending EDs who were subsequently admitted. These included review of skill mix, provision of specialist geriatric teams, and GPs and community matrons who could facilitate support in the community after ED attendance. The suggestion that both primary and emergency care services were under more strain in deteriorating sites is supported by our interview findings, which included excessive demand for community-based services, which were themselves poorly aligned with each other and with other services. A contributory factor for services being under strain is likely to be our finding that the oldest old population increased more rapidly in these locations.
However, our interviews showed that the most striking differences between improving and deteriorating sites were not the presence or absence of specific services, but overwhelming differences in leadership, culture and strategic development at the system level; that is, not just confined to individual organisations or providers. All three improving sites had strong, stable strategic leadership, enabling the development of a comprehensive system-wide strategy for managing unplanned care, including specific policies and procedures for older people, which were shared across an integrated health- and social care setting. This encouraged longer-term, consistent development, often in the face of changing national imperatives; this in turn avoided the risk of short-term, isolated projects. Conversely, in deteriorating sites, strategies were piecemeal, confined to individual organisations and disjointed, and there was less appreciation of how the components of the wider health system should fit and work together. Care was less well integrated, with divergent cultures, values and ways of working.
Development of recommendations
As outlined in earlier sections, transcripts were reviewed to derive a list of recommendations from each study site, drawing on negative and positive findings. Despite clear differences between improving and deteriorating sites, all were able to provide examples of what appeared to work well and less well, and several findings were common to more than one site. The 7S framework proved useful in encouraging consideration of all elements of organisational performance when deriving recommendations, especially broader issues, such as shared values, which might have been under-recognised using a more service-oriented approach. We tried to draw a clear distinction between ‘structures’, which lie above individual services, and ‘systems’, which are the services themselves. Inevitably some recommendations could be classified under more than one category; for example, lack of community-based geriatricians could be considered under ‘systems’, ‘skills’ or ‘staff’. However, we felt these distinctions were less important than the holistic approach that the 7S model encouraged. By compiling recommendations in this way, we inevitably constructed a long list that could be seen as unwieldy. Although participation in the consensus exercise was lower than we had hoped, it did allow us to eliminate some items where there was a low level of agreement and to consolidate others. Although the unique feature of our recommendations is that they are derived from empirical findings, we felt it was important to identify how far they are supported by external evidence and expert opinion. The original list of 64 recommendations was shortened to 47, based on results from the consensus exercise, consideration of the evidence base and the views of the research team. Some items were dropped completely and others were rephrased or consolidated. Of the list of 47 recommendations, 16 were supported by external evidence, ranging in strength from Cochrane reviews to observational studies and reports by organisations including The King’s Fund and the Nuffield Trust. In no case did the evidence contradict a recommendation (the only case in which it could have happened was regarding telehealth, which scored very low in the consensus exercise and so was removed). Although the final list of recommendations remains long, it will be used by organisations such as commissioning groups and urgent care boards, which are likely to have considered several of the issues; therefore, it will be most useful for encouraging a strategic and system-wide approach and as a checklist for specific issues. Finally, a list of ‘top 20’ recommendations was produced, selecting those with the highest scores in the poll of participants, for each component of the 7S model, combining the sections on Skills, Staff and Style.
Implementation
The implementation phase of the project evolved with the project team’s developing insights, as well as resources available for use at that time. The original plan of enlisting a research associate to work with and promote our recommendations was amended following discussions at intended ISs. The conclusion was that real change within the system could be accomplished effectively only by a person in a very particular type of role, and from within the organisation in question. This person would be required to operate at every level within the system, and outside if needed, and would need a root-and-branch understanding of the system. To this end, two dissemination fellows were enlisted, one to operate at each of the two intended ISs. This followed the model of ‘diffusion fellows’, which have been described as ‘champions for change, translating and disseminating knowledge from practice into the research studies and vice versa, taking the knowledge developed by academics back into their own practice environments’ (p. 1). 80 Unfortunately, as reported earlier, because the dissemination fellow at one site had to take long-term sick leave, work at this site was not pursued, and the project team decided to commit resources to only one site.
There have already been a number of successful interventions at the IS, including presentations to relevant CCG boards and a high-profile national event, organised by the NHS and Pfizer, at which the dissemination fellow was invited to describe the site’s approach to reducing admissions in older people. Recommendations have also been presented to the site’s recently appointed transformation advisor, a senior geriatrician charged with developing a whole-systems approach to urgent care. Presentation of the recommendations to directors of strategy is planned and a feedback survey is currently being developed in order to gauge opinion of recommendations on a system-wide scale.
Implementation will be ongoing, however, as it is recognised that management of change can take time. The important points for the project implementation phase are that our findings are carefully and appropriately enfolded within the ongoing needs and priorities of the IS. Lessons learned that can be applied to more widespread dissemination of our recommendations include the need for a champion with credibility and understanding of the whole system, an appreciation that all sites will have a significant programme of ongoing work with which recommendations have to fit, and the importance of identifying when, where and by whom key strategic decisions are made. Further work will be needed to test the impact of the project’s recommendations in other settings.
Strengths and limitations
The study design enabled an in-depth examination of the study sites at the extremes of rankings for rates of change in the admission of people aged 85 years and over in recent years. The mixed-methods approach allowed quantitative and qualitative approaches to complement each other in several ways. Routinely available HES data enabled us to calculate rates of change within sites and to calculate rates of admission, while effectively controlling for factors such as age and deprivation, which are the major drivers of admission rates. More detailed HES and other NHS data allowed us to profile each site in detail to inform the content of interviews with participants and trigger discussion. Interviewers felt that providing as well as seeking information in this way contributed to interviewees’ engagement with the project. By using both qualitative and quantitative data in the analysis we were able to build a complete picture for each site by both measuring changes and identifying reasons to explain them.
A multiple case study design that takes into account the local and wider context is seen as offering strong internal validity through in-depth analysis within each case, and as providing a basis for external validity and theoretical generalisation through structured comparison between cases. 61 By following a multiple case study design, this study aimed to describe similarities in and differences between the chosen cases and, through comparison of in-depth cases, identify and develop theoretical generalisations that explain differences among cases, especially in regard to levels of unplanned admission for people aged 85 years and over.
Notwithstanding the increased scope for both internal and external validity from multiple case study research, considerations of validity and reliability in qualitative research are often superseded by those of confidence and trustworthiness given the integral role of the researcher in the research process. According to Lincoln and Guba,88 trustworthiness can be assessed in terms of a study’s credibility (the extent to which the reader can have confidence in the findings), transferability (the extent to which the findings are applicable beyond the given context or case), dependability (the extent to which the findings are consistent) and confirmability (the extent to which research bias is addressed and considered). In line with Lincoln and Guba’s suggestions, the design and conduct of this study reflects a number of features directed at enhancing trustworthiness. In terms of establishing credibility, case selection included analytically distinct (negative) cases, such as high- and low-performing systems; data collection was in depth and over time; case analysis combined multiple data sources, including statistical, documentary and interview data; and findings were sense-checked with relevant stakeholders and experts. In terms of establishing transferability, the study involved multiple cases with common methods of enquiry, with the express aim of establishing more transferable and generalisable lessons based upon structured case comparison. In terms of dependability, the case study approach was designed with a common method of data collection and all instances of individual data collection and analysis were subject to open scrutiny by the wider research team and advisors. Finally, in terms of confirmability, the researchers were all supported in being reflexive about their own role in the data collection process, including through regular review meetings with the wider research team to discuss data collection, while multiple data sources were used to systematically question emerging assumptions and to look for alternative interpretations. Furthermore, the emerging findings and analysis were regularly reviewed by external advisors and specialists to sense-check emerging lines of interpretation.
However, the study did have several limitations, some inherent to the methods used and some due to the climate in which the research was conducted. Our selection criteria were based on change in recent years and so would not have identified sites which had achieved and maintained optimally low admission rates for older people, or those in which rates were consistently higher than expected. Both of these categories of sites could have provided insights relevant to our aims. Although we used the most recent routine data available to us to select sites, inevitably these were historical by the time fieldwork commenced, and they represented a fairly short time frame. The strongest interview data came from informants who had been in post, or at least in the locality, for the period of interest and so had an institutional memory, but inevitably many respondents were relatively new in post and were more able and inclined to describe the current situation than historical events. However, it is notable that, in all study sites, trends for admission rates remained fairly stable when recalculated using more recent data. Lack of good-quality routine data also hampered our ability to understand parts of the whole system in detail. For example, although HES data aim to capture information on admission from and discharge to care homes, this was not adequately recorded. Another part of the system for which routine data are not available is intermediate care, so it was not possible to objectively examine the opinion of several participants that increased provision had an impact on admission rates, particularly for older people.
The McKinsey 7S framework was used as a method to capture key elements of highly complex health-care systems. 55 Although the 7S framework was very effective in enabling the systematic investigation of these structures, it did not and indeed does not allow the context or external climate to be examined. The context was captured by detailed and extended interviews as part of the mixed-methods approach. A further limitation of the 7S framework is that there is a limit to the level of granularity that can be rendered effectively by this technique. Again this was captured to some extent by the rounds of face-to-face interviews. The study findings suggest the 7S model might be better suited to examining individual organisations or groups of organisations, rather than complex systems of interdependent heterogeneous system actors. Furthermore, the empirical findings reveal aspects of the local health- and social care system that were not well addressed or covered by the 7S model. These included, for example, the wider social and demographic ‘setting’ and the influence of wider ‘stakeholders’, especially patient and public representative groups and dispersed communities.
The feature of the external climate that most affected the study was the fact that the NHS was undergoing a major reorganisation during the course of the study; for example, PCTs, which were used as the sampling frame, ceased to exist and were replaced by CCGs, which in some cases were not coterminous and in most cases involved change in personnel, meaning that a historical perspective was more difficult to obtain. This reorganisation, and the associated uncertainty about their future that it imposed on staff, meant it was very difficult in some cases to engage potential participants, despite organisational support, and interviews and focus groups were much more time-consuming to arrange than would have been the case in more stable periods. Furthermore, reorganisation led one acute trust to withdraw from the study before fieldwork could begin, and at another site we were unable to recruit a social enterprise organisation because it raised issues about confidentiality and research governance that had not yet been resolved. Thus, although our sample remained large for a qualitative study, further interview data would have provided opportunities for more recommendations to be developed across rather than within study sites. Finally, obtaining NHS permissions at a time of organisational change led to severe delays, as new organisations did not have fully established procedures.
Need for further research
This project has emphasised that research on individual components of care for older people needs to take account of their impact on the system as a whole, and this is our main recommendation for future research. Parts of the system that appear important in managing admission rates in older people include primary care, especially access in and out of hours, capacity of intermediate care and management of older people in EDs.
In primary care there is a need for intervention studies to demonstrate whether or not improving services for older people, particularly in terms of access and continuity, will result in reduced admissions. A number of initiatives are currently taking place, in part as a result of the implementation of the Better Care Fund, a ‘£3.8 billion single pooled budget for health- and social care services to work more closely together in local areas, based on a plan agreed between the NHS and local authorities’ (p. 1). 89 These include a named doctor for older people, longer appointments and the provision of a care plan for people at high risk of admission. This provides an opportunity to gather much-needed evidence on the impact of initiatives in primary care.
The Better Care Fund is also likely also to lead to an expansion of intermediate care services. Key issues for research include methods to determine the optimal capacity of these services, their skill mix and how they can best be integrated with other parts of the system. As noted earlier, a major limitation in researching these services is the lack of consistent routine data.
Finally, there is a lack of evidence about how frail older people can best be managed in EDs, including the need for specialist geriatric teams and acute frailty units.
Conclusions and recommendations
Both quantitative and qualitative data supported the conclusion that rising admission rates for older people were seen in places where several parts of the system were under strain. Pressure points in the system that contributed to this outcome included worse access to GPs both in and out of hours, excessive demand on EDs and lack of provision of intermediate care. Places which had stemmed the rising tide of admissions had done so through strong, stable leadership and shared vision, strategy and values across the system, and our findings suggest these are the most important points to address. The following is a summary of our main recommendations (with some clarification of wording following peer review).
Strategy
-
Aim to maximise integration between care providers: community and acute care trusts and health and social care.
-
Work at relationships with the local authority and acknowledge that it is a political organisation.
-
Focus on reconfiguring according to the needs of the whole system, not isolated pockets.
-
Avoid transient pilots with no follow-through, and multiple initiatives which are inadequately promoted/marketed.
Structure
-
Consider how palliative care teams are integrated as part of the overall system of care.
-
Integrate social work and nursing teams that cross the boundary between community and hospital.
-
Integrate clinical information systems for primary care, walk-in centres, urgent care centres, ambulatory care units and social care.
-
Understand and address the impact that early-discharge policies can have on readmissions unless additional and compensatory changes are made to the system to accommodate these patients.
Systems
-
Review skill mix in EDs and acute assessment units; consider specialist geriatric teams/frailty units (24/7), GPs, community matrons, OTs and social workers.
-
Assess the need for geriatrician input to intermediate care.
-
Provide a specialist community-based 24/7 response service for people with urgent mental health needs.
-
Be flexible about community nurses supporting residents of nursing homes and assure quality of care where homes provide intermediate care.
Shared values
-
Develop and communicate a shared vision on high-quality care for older people, accommodating medical, functional and managerial perspectives.
-
Break down role boundaries wherever they get in the way of effective care.
-
Enable professionals across the system to better understand each other’s roles, priorities and ways of working, including recognising that a key role for managers is to manage uncertainty; consider rotating staff through services to enhance this knowledge transfer.
-
Focus on the needs of the patient, building relationships and supporting staff through redesign.
Skills, staff and style
-
Ensure all relevant disciplines are given the opportunity to contribute their skills to multidisciplinary teams and look to role extension as an alternative to increasing the teams’ complexity.
-
Invest effort in developing the skills of key groups, for example staff in care homes.
-
Acknowledge that leadership by committed and charismatic individuals makes a difference, especially when working across organisations; take advantage of these people but build in succession planning.
-
Recognise the importance of clinical leadership: clinician managers can offer particular perspectives.
Acknowledgements
We are grateful for the support of members of the steering group throughout the project, and for advice from the Leicestershire, Northamptonshire and Rutland Older People’s Research Patient and Public Involvement Forum. Many thanks also to Lorraine Pollard and Lewis Hyland, who contributed to the qualitative analysis, Munira Arkate, who provided administrative support during fieldwork, and Robert Weinmeister, who helped to compile the final report. Most of all we would like to acknowledge participants at all study sites for their time and the candid insights they provided.
Contribution of authors
Andrew Wilson (Professor of Primary Care Research) Co-ordinated the project, led on development of recommendations, drafted the final report.
Richard Baker (Professor of Quality in Healthcare) Contributed to analysis and development of recommendations, advised on quality improvement and primary care issues.
John Bankart (Senior Lecturer in Medical Statistics) Led on-site selection, including quantitative data analysis.
Jay Banerjee (Consultant in Emergency Medicine) Contributed to analysis and development of recommendations and implementation, advised on emergency care issues.
Ran Bhamra (Senior Lecturer in Engineering Management) Led on implementation, advised on systems theories.
Simon Conroy (Consultant Geriatrician) Contributed to analysis and development of recommendations, advised on emergency care and geriatric issues.
Stoyan Kurtev (Data Officer) Led on acquisition and analysis of quantitative data.
Kay Phelps (Research Fellow) Developed topic guides, liaised with study sites, conducted fieldwork.
Emma Regen (Research Fellow) Developed topic guides, liaised with study sites, conducted fieldwork.
Stephen Rogers (Consultant in Public Health) Contributed to analysis and development of recommendations, advised on quality improvement and commissioning issues.
Justin Waring (Professor of Organisational Sociology) Led on qualitative analysis, contributed to analysis and development of recommendations.
All authors contributed to the final report, and none have conflicts of interest to declare.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
References
- Mid-year Population Estimates. London: ONS; 2010.
- Emergency Admissions to Hospital: Managing the Demand. London: HMSO; 2013.
- Blunt I, Bardsley M, Dixon J. Trends in Emergency Admissions in England 2004–2009. London: Nuffield Trust; 2010.
- Ferguson C, Woodard J, Banerjee J, Conroy S. Operationalising frailty definitions in the emergency department: a mapping exercise. Age Ageing 2010;39.
- Sager MA, Franke T, Inouye SK, Landefeld CS, Morgan TM, Rudberg MA, et al. Functional outcomes of acute medical illness and hospitalization in older persons. Arch Intern Med 1996;156:645-52. http://dx.doi.org/10.1001/archinte.1996.00440060067008.
- Purdy S. Avoiding Hospital Admissions: What Does the Research Evidence Say?. London: The King’s Fund; 2010.
- Reducing Unplanned Hospital Admissions: What Does the Literature Tell Us?. Birmingham: HSMC; 2006.
- Blunt I. Focus on Preventable Admissions. London: Health Foundation and Nuffield Trust; 2013.
- Imison K, Poteliakhoff E, Thompson J. Older People and Emergency Bed Use: Exploring Variation. London: The King’s Fund; 2012.
- Tian Y, Dixon A, Gao H. Emergency Hospital Admissions for Ambulatory Care Sensitive Conditions: Identifying the Potential for Reductions. London: The King’s Fund; 2012.
- O’Cathain A, Knowles E, Maheswaran R, Pearson T, Turner J, Hirst E, et al. A system-wide approach to explaining variation in potentially avoidable emergency admissions: national ecological study. BMJ Qual Saf 2014;23:47-55. http://dx.doi.org/10.1136/bmjqs-2013-002003.
- Foundation Trust Network . FTN Benchmarking: Driving Improvements in Elderly Care Services 2012. www.foundationtrustnetwork.org/resource-library/ftn-benchmarking-elderly-care-services-briefing-2012/ (accessed 15 June 2015).
- Huntley A, Lasserson D, Wye L, Morris R, Checkland K, England H, et al. Which features of primary care affect unscheduled secondary care use? A systematic review. BMJ Open 2014;4. http://dx.doi.org/10.1136/bmjopen-2013-004746.
- Gill JM, Mainous AG. The role of provider continuity in preventing hospitalizations. Arch Fam Med 1998;7:352-7. http://dx.doi.org/10.1001/archfami.7.4.352.
- Bankart MJ, Baker R, Rashid A, Habiba M, Banerjee J, Hsu R, et al. Characteristics of general practices associated with emergency admission rates to hospital: a cross-sectional study. Emerg Med J 2011;28:558-63. http://dx.doi.org/10.1136/emj.2010.108548.
- Gunther S, Taub N, Rogers S, Baker R. What aspects of primary care predict emergency admission rates? A cross sectional study. BMC Health Serv Res 2013;13. http://dx.doi.org/10.1186/1472-6963-13-11.
- Cowling TE, Harris MJ, Watt HC, Gibbons DC, Majeed A. Access to general practice and visits to accident and emergency departments in England: cross-sectional analysis of a national patient survey. Br J Gen Pract 2014;64:e434-9. http://dx.doi.org/10.3399/bjgp14X680533.
- Thompson C, Hayhurst C, Boyle A. How have changes to out-of-hours primary care services since 2004 affected emergency department attendances at a UK District General Hospital? A longitudinal study. Emerg Med J 2010;27:22-5. http://dx.doi.org/10.1136/emj.2008.068817.
- Ismail SA, Gibbons DC, Gnani S. Reducing inappropriate accident and emergency department attendances: a systematic review of primary care service interventions. Br J Gen Pract 2013;63:e813-20. http://dx.doi.org/10.3399/bjgp13X675395.
- Improving Out of Hours Care: What Lessons Can Be Learned from a National Benchmark of Services?. Lewes: Primary Care Foundation; 2010.
- Oliver D. QOF and public health priorities don’t improve care in ageing. BMJ 2008;337. http://dx.doi.org/10.1136/bmj.a1403.
- Lester HE, Hannon KL, Campbell SM. Identifying unintended consequences of quality indicators: a qualitative study. BMJ Qual Saf 2011;20:1057-61. http://dx.doi.org/10.1136/bmjqs.2010.048371.
- Henderson C, Sheaff R, Dickinson A, Beech R, Wistow G, Windle K, et al. Unplanned admissions of older people: exploring the issues. Serv Deliv Organ 2011;20.
- McDonagh MS, Smith DH, Goddard M. Measuring appropriate use of acute beds: a systematic review of methods and results. Health Policy 2000;53:157-84. http://dx.doi.org/10.1016/S0168-8510(00)00092-0.
- NHS Plan: A Plan for Investment, a Plan for Reform. London: The Stationery Office; 2000.
- Martin GP, Peet SM, Hewitt GJ, Parker H. Diversity in intermediate care. Health Soc Care Community 2004;12:150-4. http://dx.doi.org/10.1111/j.0966-0410.2004.00481.x.
- Glynn N, Bennett K, Silke B. Emergency medical readmission: long-term trends and impact on mortality. Clin Med 2011;11:114-18. http://dx.doi.org/10.7861/clinmedicine.11-2-114.
- Scott I, Vaughan L, Bell D. Effectiveness of acute medical units in hospitals: a systematic review. Int J Qual Health Care 2009;21:397-40. http://dx.doi.org/10.1093/intqhc/mzp045.
- Blunt I. Focus on: A and E Attendances. Why Are Patients Waiting Longer?. London: Health Foundation, Nuffield Trust; 2014.
- Banerjee J, Conroy S. Quality Care for Older People with Urgent & Emergency Care Needs: ‘Silver Book’. London: British Geriatric Society; 2012.
- Billings J, Dixon J, Mijanovich T, Wennberg D. Case finding for patients at risk of readmission to hospital: development of algorithm to identify high risk patients. BMJ 2006;333. http://dx.doi.org/10.1136/bmj.38870.657917.AE.
- Gravelle H, Dusheiko M, Sheaff R, Sargent P, Boaden R, Pickard S, et al. Impact of case management (Evercare) on frail elderly patients: controlled before and after analysis of quantitative outcome data. BMJ 2007;334:31-4. http://dx.doi.org/10.1136/bmj.39020.413310.55.
- D’Souza S, Guptha S. Preventing admission of older people to hospital. BMJ 2013;346. http://dx.doi.org/10.1136/bmj.f3186.
- Woodford HJ, George J. Intermediate care for older people in the UK. Clin Med 2010;10:119-23. http://dx.doi.org/10.7861/clinmedicine.10-2-119.
- Shepperd S, Doll H, Angus RM, Clarke MJ, Iliffe S, Kalra L, et al. Admission avoidance hospital at home. Cochrane Database Syst Rev 2008;4. http://dx.doi.org/10.1002/14651858.cd007491.
- Shepperd S, Doll H, Angus RM, Clarke MJ, Iliffe S, Kalra L, et al. Avoiding hospital admission through provision of hospital care at home: a systematic review and meta-analysis of individual patient data. CMAJ 2009;180:175-82. http://dx.doi.org/10.1503/cmaj.081491.
- Shepperd S, Doll H, Broad J, Gladman J, Iliffe S, Langhorne P, et al. Early discharge hospital at home. Cochrane Database Syst Rev 2009;1. http://dx.doi.org/10.1002/14651858.cd000356.pub3.
- National Evaluation of Department of Health’s Integrated Care Pilots. Cambridge: RAND Europe; 2012.
- Briggs D, Bright L. Reducing hospital admissions from care homes: considering the role of a local enhanced service from GPs. WWOP 2011;15:4-12. http://dx.doi.org/10.5042/wwop.2011.0114.
- Quest for Quality. London: British Geriatrics Society; 2011.
- Mason S, Knowles E, Colwell B, Dixon S, Wardrope J, Gorringe R, et al. Effectiveness of paramedic practitioners in attending 999 calls from elderly people in the community: cluster randomised controlled trial. BMJ 2007;335:919-22. http://dx.doi.org/10.1136/bmj.39343.649097.55.
- Mikolaizak AS, Simpson PM, Tiedemann A, Lord SR, Close JCT. Systematic review of non-transportation rates and outcomes for older people who have fallen after ambulance service call-out. Australas J Ageing 2013;32:147-57. http://dx.doi.org/10.1111/ajag.12023.
- Logan PA, Coupland CAC, Gladman JRF, Sahota O, Stoner-Hobbs V, Robertson K, et al. Community falls prevention for people who call an emergency ambulance after a fall: randomised controlled trial. BMJ 2010;340. http://dx.doi.org/10.1136/bmj.c2102.
- Purdy S, Griffin T. Reducing hospital admissions. BMJ 2008;336. http://dx.doi.org/10.1136/bmj.39394.402465.BE.
- White AL, Armstrong PAR, Thakore S. Impact of senior clinical review on patient disposition from the emergency department. Emerg Med J 2010;27:262-5. http://dx.doi.org/10.1136/emj.2009.077842.
- Conroy SP, Ansari K, Williams M, Laithwaite E, Teasdale B, Dawson J, et al. A controlled evaluation of comprehensive geriatric assessment in the emergency department: the ‘Emergency Frailty Unit’. Age Ageing 2014;43:109-14. http://dx.doi.org/10.1093/ageing/aft087.
- Pareja-Sierra T, Hornillos-Calvo M, Solís JR, Sepúlveda-Moya DL, Bassy-Iza N, Martínez-Peromingo FJ, et al. Implementation of an emergency department observation unit for elderly adults in a university-affiliated hospital in Spain: a 6-year analysis of data. J Am Geriatr Soc 2013;61:1621-2. http://dx.doi.org/10.1111/jgs.12433.
- Wright PN, Tan G, Iliffe S, Lee D. The impact of a new emergency admission avoidance system for older people on length of stay and same-day discharges. Age Ageing n.d.;43:116-21. http://dx.doi.org/10.1093/ageing/aft086.
- Salvi F, Morichi V, Grilli A, Giorgi R, Spazzafumo L, Polonara S, et al. A geriatric emergency service for acutely ill elderly patients: pattern of use and comparison with a conventional emergency department in Italy. J Am Geriatr Soc 2008;56:2131-8. http://dx.doi.org/10.1111/j.1532-5415.2008.01991.x.
- Kodner DL. Whole-system approaches to health and social care partnerships for the frail elderly: an exploration of North American models and lessons. Health Soc Care Community 2006;14:384-90. http://dx.doi.org/10.1111/j.1365-2524.2006.00655.x.
- Iles V, Sutherland K. Organisational Change: A Review for Health Care Managers, Professionals and Researchers. London: National Institute for Health Research; 2001.
- Pettigrew A, Ferlie E, McKee L. Shaping Strategic Change: Making Change in Large Organizations. The Case of the National Health Service. London: Sage Publications; 1992.
- Chandler A. Strategy and Structure: Chapters in the History of American Enterprise. Cambridge, MA: MIT Press; 1962.
- Porter M. Competitive Advantage: Creating and Sustaining Superior Performance. New York, NY: Simon and Schuster; 1985.
- Peters TJ, Waterman RH. In Search of Excellence: Lessons from America’s Best-Run Companies. New York, NY: Harper & Row; 1982.
- Gabayan GZ. VSM Guide 2014. www.esrad.org.uk/resources/vsmg_3/screen.php?page=preface (accessed 29 May 2014).
- Star Model 2014. www.jaygalbraith.com/services/star-model (accessed 16 July 2015).
- Mintzberg H, Lampel JB, Quinn J, Ghoshal S. The Strategy Process: Concepts, Contexts, Cases. Harlow: Pearson; 2014.
- Jackson S. Organisational effectiveness within National Health Service (NHS) trusts. Int J Health Care Qual Assur 1998;11:216-21. http://dx.doi.org/10.1108/09526869810243926.
- Pkor43 . File:McKinsey 7S framework.Svg 2007. http://commons.wikimedia.org/wiki/File:McKinsey_7S_framework.svg (accessed 29 May 2014).
- Yin RK. Case Study Research: Design and Methods. Thousand Oaks, CA: Sage Publications; 2009.
- Regen E, Martin G, Glasby J, Hewitt G, Nancarrow S, Parker H. Challenges, benefits and weaknesses of intermediate care: results from five UK case study sites. Health Soc Care Community 2008;16:629-37. http://dx.doi.org/10.1111/j.1365-2524.2008.00788.x.
- Swanborn P. Case Study Research. London: Sage; 2010.
- Health and Social Care Information Centre . Hospital Episode Statistics, Admitted Patient Care, England: 2013–14 2015. www.hscic.gov.uk/searchcatalogue?productid=17192&q=title%3a%22Hospital+Episode+Statistics%3a+Admitted+patient+care%22&sort=Relevance&size=10&page=1#top (accessed 29 May 2015).
- Health & Social Care Information Centre . Indicator Portal n.d. www.hscic.gov.uk/indicatorportal (accessed 29 May 2015).
- NHS Improving Quality . NHS Better Care, Better Value Indicators n.d. www.productivity.nhs.uk/ (accessed 15 June 2015).
- GP Patient Survey . Surveys and Reports n.d. https://gp-patient.co.uk/surveys-and-reports (accessed 3 September 2014).
- Gale N, Heath G, Cameron E, Rashid S, Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol 2013;13. http://dx.doi.org/10.1186/1471-2288-13-117.
- Spencer J, Ritchie L, Bryman A, Burgess R. Analysing Qualitative Data. London: Routledge; 1993.
- Strauss A, Corbin JM. Basics of Qualitative Research: Grounded Theory Procedures and Techniques. Thousand Oaks, CA: Sage Publications; 2008.
- Purdy S, Griffin T, Salisbury C, Sharp D. Ambulatory care sensitive conditions: terminology and disease coding need to be more specific to aid policy makers and clinicians. Public Health 2009;123:169-73. http://dx.doi.org/10.1016/j.puhe.2008.11.001.
- Ipsos MORI. GP Patient Survey n.d. www.gp-patient.co.uk/results/ (accessed 15 June 2015).
- Office for National Statistics . 2011 Area Classifications n.d. www.ons.gov.uk/ons/guide-method/geography/products/area-classifications/ns-area-classifications/ns-2011-area-classifications/index.html (accessed 29 May 2014).
- Francis R. Report of the Mid Staffordshire NHS Foundation Trust Public Inquiry: Executive Summary. London: The Stationery Office; 2013.
- Bevan G, Hood C. What’s measured is what matters: targets and gaming in the English public health care system. Public Adm 2006;84:517-38. http://dx.doi.org/10.1111/j.1467-9299.2006.00600.x.
- Ham C, Walsh N. Making Integrated Care Happen at Scale and Pace: Lessons from Experience. London: The King’s Fund; 2013.
- Sach TH, Logan PA, Coupland CAC, Gladman JRF, Sahota O, Stoner-Hobbs V, et al. Community falls prevention for people who call an emergency ambulance after a fall: an economic evaluation alongside a randomised controlled trial. Age Ageing 2012;41:635-41. http://dx.doi.org/10.1093/ageing/afs071.
- Cooke MW, Higgins J, Kidd P. Use of emergency observation and assessment wards: a systematic literature review. Emerg Med J 2003;20:138-42. http://dx.doi.org/10.1136/emj.20.2.138.
- Soo S, Berta W, Baker GR. Role of champions in the implementation of patient safety practice change. Healthc Q 2009;12:123-8. http://dx.doi.org/10.12927/hcq.2009.20979.
- Rowley E. Protocol for a qualitative study exploring the roles of ‘Diffusion Fellows’ in bridging the research to practice gap in the Nottinghamshire, Derbyshire and Lincolnshire Collaboration for Leadership in Applied Health Research and Care (CLAHRC-NDL). BMJ Open 2012;2. http://dx.doi.org/10.1136/bmjopen-2011-000604.
- Parkin P. Managing Change in Healthcare: Using Action Research. London: Sage Publications; 2009.
- Plsek PE, Greenhalgh T. The challenge of complexity in health care. BMJ 2001;323:625-8. http://dx.doi.org/10.1136/bmj.323.7313.625.
- Scott T, Mannion R, Davies HT, Marshall MN. Implementing culture change in health care: theory and practice. Int J Qual Health Care 2003;15:111-18. http://dx.doi.org/10.1093/intqhc/mzg021.
- Bate SP. Strategies for Cultural Change. Oxford: Butterworth-Heinemann; 2010.
- Campbell RJ. Change management in health care. Health Care Manag 2008;27:23-39. http://dx.doi.org/10.1097/01.hcm.0000285028.79762.a1.
- Kotter JP, Cohen DS. The Heart of Change: Real-Life Stories of How People Change Their Organizations. Boston, MA: Harvard Business Press; 2002.
- National Audit of Intermediate Care. Manchester: NHS Benchmarking Network; 2013.
- Lincoln YS, Guba EG. Naturalistic Inquiry. London: Sage; 1985.
- Bennett L, Humphries R. Making Best Use of the Better Care Fund: Spending to Save?. London: The King’s Fund; 2014.
Appendix 1 Information for case study sites
Appendix 2 Full topic guide for interviews
Establishing System Change for Admissions of People 85+ (ESCAPE 85+)
Topic guide for interviews: full topic guide.
Code:
Date of interview:
Interviewer:
Permission to tape record: (transcript required?) yes/no.
Introduction.
Interviewer to introduce themselves and thank interviewees for taking part.
Interviewer to check the interviewees have a copy of the information sheet.
Interviewer to give an indication of how long the interview will last.
Interviewer to explain the use of the recorder, confidentiality and data protection and ascertain whether the interviewees would like a copy of the interview transcript.
Interviewer to ensure the consent forms are signed.
Interviewer to confirm arrangements and timescale for feedback/access to final report.
Interviewer to answer any questions the interviewees may have.
Interviewer to mention that support mechanisms are available if required.
Introduction to the project
-
The research is looking at unplanned/emergency admission to hospital of people aged 85+. We are therefore focussing on the very old and the policies and services which affect them.
-
Sites have been chosen as to whether their rates of admissions for 85+ were increasing or decreasing during the time period 2005–9. We are therefore interested in a historical perspective.
-
Present site data to be discussed in the interview.
-
Request further data which may be collected/collated locally which will inform the study.
Structure of the interview schedule
-
General views on unplanned admissions.
-
General views on system characteristics.
-
Specific questions on system characteristics.
-
Changes and recommendations.
-
PPI involvement.
-
Outcomes.
Unplanned admissions in the area: priorities, levels and changes
Ask interviewee to give a reaction to the data presented to them giving the rates of unplanned admissions of people 85+ in their area during 2005–9.
Historical perspective from 2005 onwards.
Possible questions and prompts:
-
Were you aware of the rate of unplanned admissions to hospital of people 85+ in your area?
-
Did you know if your rates were increasing decreasing or staying the same?
-
– What would you say were the reasons for that?
-
-
Are the rates of unplanned admissions to acute hospital of people 85+ an issue in your organisation?
-
– Do they need to be reduced?
-
-
Do you collect/collate any local data on unplanned admissions and if so can we see the reports/have access to the data?
Whole system characteristics, configuration, monitoring and changes over time
What are the important elements/components which you believe have the most effect on the rates of unplanned admissions of people 85+ in your area?
Possible prompts (could use star model to illustrate):
-
Policies.
-
– Procedures, service delivery, working practices.
-
-
People, staffing, leadership, behaviour.
-
Finance and budgets.
-
Infrastructure, geography, buildings, IT.
-
Partner organisations.
-
Shared vision.
Possible questions:
-
What characteristics are associated with changes in unplanned admissions of people 85+?
-
What changes have you made as a result of the increasing number of people over 85?
-
What changes do you think you need to make to reduce unplanned admissions of people 85+?
-
What changes are planned to reduce unplanned admissions of people 85+?
-
What have been the historical drivers of change?
-
– Leadership.
-
– Finance.
-
– Targets.
-
-
When making changes what have been the main challenges?
-
What have been the main outcomes of change?
-
– Did it achieve what was hoped for?
-
-
Reasons for success or failure of changes.
Policy on unplanned admissions
-
How have/do policies in your organisation affect unplanned admissions of people aged 85+?
-
– Historical perspective as well as current.
-
– E.g. A&E, ED, Primary Care, out-of-hours services, Ambulance, Staffing.
-
-
What have been/are your organisation’s policies around unplanned admissions?
-
– Historical perspective as well as current.
-
-
Have policies around unplanned admissions been linked/coherent with the policies of other organisations in your area?
-
– Historical perspective as well as current.
-
-
What policy changes have you made as a result of the increasing number of people over 85?
-
Have there been/are there clear strategies/goals within your organisation around unplanned admissions of people 85+?
-
Please can you supply policy documentation on unplanned admissions of people 85+ from 2005 to the present?
Budgets/finance/commissioning of emergency care
-
Is there a specific budget for unplanned/emergency care for people aged 85+/older people?
-
– Historically and currently.
-
-
How much is spent on emergency care for people aged 85+?
-
– Historically and currently.
-
-
How much is spent on older people compared with other areas?
-
– Historically and currently.
-
-
What are the commissioning arrangements for unplanned admissions (of people 85+) in your area?
-
– CCGs.
-
– PCTs.
-
– Involvement of secondary care.
-
-
How have these arrangements changed since 2005?
-
What part have financial imperatives (cost/resources) played in commissioning services for unplanned admissions?
-
What are the incentives in commissioning which affect unplanned admissions?
Partnership working between acute and community health and social care
-
How have acute and community health and social care worked together in the area to tackle unplanned admissions and care of older people?
-
Has there been a whole systems approach to planning care or do all the organisations commission, plan and deliver service separately? E.g.
-
– Cooperative interorganisational networks.
-
– Sharing information and communication.
-
– Shared protocols and procedures.
-
– Shared policy on unplanned admissions – linked/coherent?
-
-
Have there been any integrated services or is this planned?
-
What have been the incentives to a whole systems approach?
-
What have been the challenges to a whole systems approach and how does cooperation/competition pose challenges?
-
Do the health- and social care organisations in your area have clearly defined boundaries?
-
– What are the boundaries?
-
– Are boundaries a problem?
-
– Different measurement criteria for success?
-
– Different organisational cultures?
-
– Different regulation?
-
-
Outcomes of partnership/integrated planning/services?
-
– Successes and challenges.
-
– Reasons for success or failure.
-
– Obtain copies of any partnership agreements.
-
People, leadership, managerial and clinical relationships, staffing
-
Who has led policy and/or changes affecting unplanned admissions of people over 85 in this area?
-
– Organisational leadership.
-
-
Have there been any professional tensions, allegiances and hierarchies which affect unplanned admissions in this area?
-
Have there been any staff satisfaction surveys carried out in your organisation?
-
– Can we have report?
-
-
Have job planning and staffing changes had an impact on unplanned admissions?
-
What impact has training had on unplanned admissions?
Infrastructure and contextual factors influencing unplanned admissions of 85+
-
Have there been any local infrastructure or contextual factors or pressures influencing unplanned admissions of 85+ in this area?
Possible prompts:
-
– Geography.
-
– Buildings/facilities.
-
– Technology/IT systems.
-
– Transport – ambulance services.
-
– Environmental conditions.
-
– Local pressures.
-
Procedures/service delivery
-
Are there any issues around service delivery in your area which have affected unplanned admissions of people 85+?
Possible prompts:
-
–Who delivers urgent care services in the acute sector?
-
–Who delivers urgent care services in the community sector?
-
–Commissioning arrangements.
-
–Pathways of care.
-
–Access points for urgent and emergency care.
-
–Admission pathways.
-
–Management of acute care.
-
–ED configuration.
-
–Integrated care.
-
–Access to and responsiveness of social care.
-
–Management of chronic conditions.
-
–Out-of-hours provision in the community.
-
–Ambulance service.
-
–Discharge procedures.
-
–IT systems (Dashboard, NHS Pathways, discharge monitoring systems, etc.).
-
–Governance systems (emergency care networks, joint governance frameworks).
-
Interventions, outcomes and evaluation
-
What interventions in the whole system have affected or changed the levels of unplanned admissions?
-
– Intermediate care.
-
– Integrated care.
-
– Reablement
-
– End of life care.
-
– Residential/nursing home care.
-
– Community matrons.
-
– Alternatives to acute admission.
-
– Discharge initiatives.
-
– Social care initiatives.
-
– Chronic conditions management.
-
– Geriatrician assessment/outreach.
-
– Hospital outreach.
-
– Hospice care/outreach.
-
-
Who delivers these services?
-
What has been the effect of these interventions on the whole system of care?
-
What is the relationship between interventions?
-
How available and accessible are alternatives to unplanned admission?
-
– E.g. primary and social care services.
-
-
Have the outcomes of the interventions been measured or evaluated?
-
What are the reasons for the success of these interventions?
-
What are the reasons for the failure of these interventions?
-
Can I have copies of any internal evaluations?
Recommendations for reducing emergency admissions
-
What changes have been made/need to be made to reduce unplanned admissions?
-
– Strategy.
-
– Organisational.
-
– Partnership.
-
– Commissioning.
-
– Policy.
-
– Service delivery.
-
– Leadership/staffing.
-
-
What lessons have you learnt in trying to reduce unplanned admissions for those 85+?
-
– What are the challenges?
-
– What have been the successes?
-
PPI involvement
-
What PPI involvement do you have in your organisation in this area?
-
What PPI involvement do you have in policy making in this area?
-
What PPI involvement do you have in commissioning in this area?
-
What PPI involvement do you have in strategy development in this area?
-
What PPI involvement do you have in system development in this area?
-
What PPI involvement do you have in leadership and decision making in this area?
-
What PPI involvement do you have in service delivery in this area?
-
What changes have resulted from PPI involvement?
Outcomes and impact for older people and carers
-
How do you measure outcomes for older people and carers?
-
What service changes have most affected older people and carers in this area?
-
– What has been the impact?
-
-
What has been the impact of particular initiatives to reduce unplanned admissions?
-
– Refer to initiatives already mentioned above.
-
– What is the patient experience of these services?
-
-
Have outcomes for older people and carers changed over the last 5 years?
-
– For the better?
-
– For the worse?
-
-
What changes are needed to improve emergency services and outcomes for older people 85+ and carers?
-
What are the benefits to older people and their carers of reducing unplanned admissions?
-
What are the disadvantages to older people and their carers of reducing unplanned admissions?
-
Have you carried out any patient satisfaction surveys in emergency/unplanned/urgent care in the last 5 years?
-
– Can we have the report?
-
-
Have you carried out any service evaluation looking at urgent care services for people over 85?
Suggestions of interviewees/focus groups
Can you suggest other people in the area who you feel we need to talk to?
Name:
Role:
Organisation:
E-mail:
Phone:
Base:
Other info:
Name:
Role:
Organisation:
E-mail:
Phone:
Base:
Other info:
Name:
Role:
Organisation:
E-mail:
Phone:
Base:
Other info:
Documentation
-
Do you have any policy documents concerned with unplanned admissions?
-
– Emergency/urgent/unplanned care.
-
– A&E.
-
– Acute admissions.
-
– Emergency primary care.
-
– Out of hours primary care.
-
– Ambulance service.
-
– Staffing of emergency services.
-
– Staffing of out-of-hours care.
– Can I have copies – who from?
-
-
Do you have any operational documents concerned with unplanned admissions?
-
– Emergency/urgent/unplanned care.
-
– A&E.
-
– Acute admissions.
-
– Emergency primary care.
-
– Out of hours primary care.
-
– Ambulance service.
-
– Staffing of emergency services.
-
– Staffing of out-of-hours care.
– Can I have copies – who from?
-
-
Copies of any internal evaluations.
Data
Do you have any local data on:
-
Numbers of unplanned admissions from own homes?
-
Numbers of unplanned admissions from care homes?
-
Unplanned admissions by district?
-
Unplanned admissions by living circumstances?
-
(live alone/with spouse in care home etc.)
-
-
Unplanned admissions resulting in death?
-
Acute condition?
-
Chronic condition?
-
Terminal condition?
-
Readmission rates?
Notes/post-interview comments.
Appendix 3 Site reports
Aims
To identify system characteristics associated with higher and lower increases in unplanned admission rates in those aged 85 years and over. To develop recommendations based on best practice to inform providers and commissioners, and to investigate the challenges of starting to implement these recommendations.
Methods
Interview transcripts and field notes were reviewed by members of the research team, and learning points from each site were categorised using McKinsey’s 7S model. Informants from PCTs or CCGs are coded A, those from community services are coded B and those from acute trusts are coded C.
McKinsey’s 7S model
The 7S model focuses on the seven internal aspects of an organisation that need to work well together if it is to be successful. The seven Ss are strategy, structure, systems, shared values, skills, style and staff (see Figure 2).
All the elements depend on each other and a change in one can affect all the others.
The seven Ss of the model are divided into hard and soft elements. Strategy, structure and systems are considered to be the hard elements of the model, whereas the soft elements consist of shared values, skills, style and staff. Senior management has direct influence and control over the hard elements of the model, whereas the soft elements are usually influenced by the organisation’s culture, and they are therefore more difficult to control.
Use
The 7S model can be used in two ways:
-
Strengths and weaknesses of an organisation can be identified by considering the links between each of the Ss. No S is a strength or a weakness in its own right; it is only its degree of support, or lack of support, for the other Ss which is relevant. Any Ss which harmonise with all the other Ss can be thought of as strengths, any dissonances as weaknesses.
-
The model highlights how a change made in any one of the Ss will have an impact on all of the others. Thus, if a planned change is to be effective, then changes in one S must be accompanied by complementary changes in the others.
Site report for I1
Setting
The main hospitals are both university hospitals. There is also a health centre, which has a walk-in facility. Community care is mainly provided by a NHS Trust. There are 46 GP practices in the region and some other private services provide out-of-hours nursing service from 08.00 until 20.00.
Data analysis
The transcribed data from the nine interviews, one focus group, field notes and reports were analysed by the research team. The key themes were identified, agreed on and coded against the McKinsey 7S model.
Hard elements
Strategy
Definition: what is the purpose or goal of the system/organisation?
What we found:
Investment
The reason for this region doing better than average on unplanned admissions may have been increased investment in community care (2005).
Yeah, I mean I think if it’s going back that far we had, we made a conscious decision to kind of really buy in to the whole shifting care in the community close to home. So, and that kind of fitted with kind of bigger strategic objectives across kind of health authority areas. There were lots of initiatives around reconfiguring acutes at the time like best care, best place and things like that. So I think we as a PCT, I’m not kind of sure where it came from really. I think we just kind of, I don’t think there was one particular driver. We had quite a visionary GP, head of commissioning at the time.
A-01a
I think that money – the NHS was funded a lot better during that period, and so there were opportunities for people like myself with the vision and whatever to bid – you know, we had winter pressure monies and – so anything that came along . . . and because I made contacts in the hospital, you know, with the discharge co-ordinators and everything, we wrote loads of bids. And also the PCTs had just developed so, you know, things like the falls services were all being developed and I just – I jumped up on any bandwagon, really, that I could to expand the community, I think.
B-02
Engagement
Trust in the strategy by many in senior positions enabled it to work effectively, and this was achieved by the early engagement of many practitioners. Interestingly there was not a particular strategy for patients aged 85 years and over, but rather an overall recognition of the importance of community services.
No, I suppose nothing that we’ve implemented is for the over-eighty-fives specifically, is it? So maybe they were having more of an impact on the younger older people, sort of 70–85 rather than the over 85.
A-01b
We got them on board after we’d kind of written the strategy the first time and I think there was just, there was a willingness within kind of senior managers within the organisation to kind of take a bit of a leap of faith and invest actually quite a lot of money in community services.
A-01a
But I think that’s kind of partly some of our successes that we got the GPs on board so early, so we were on board in 2005/6 and that’s just been the way we’ve done things. Obviously we could have done it even better in terms of clinical engagement. Hopefully the CCG will provide us with opportunities to do that even more.
A-01a
Leadership
More recently there has been a lack of strategy which could be connected to leadership issues, with a corollary increase in unplanned admissions.
I think also been lacking for me is a clear strategic direction around certain areas. So for example when the acute trust decided to do commissioner GPs in the urgent centre, we didn’t have a view as an organisation of what we thought of that or what our response would be. So that, we just kind of let it happen.
A-01a
I think there’s no clear strategic plan around urgent care at the moment which everybody has signed up to. There are lots of people and services dabbling in it. They’ve all got different views or they change their views or they listen to the acute trust about something and then decide that that’s the way to go and I think we need to be much clearer about what we as an organisation are going to deliver, because when we had that clear strategic route before, we got on really well and delivered.
A-01b
Political environment
Some respondents revealed that more recently the cuts in funding have resulted in a reduction in professional integration. This in turn would be a problem for the care of patients aged 85 years and over because many rely on integrated teams for care.
I think as funding starts to dry up, barriers start to go up as well and, you know, obviously we’re in a different political environment since 2008 and so budgets are very tight. I don’t think that helps at all.
B-02
Structures (interactions between components of system)
Definition: How is the system organised? The way an organisation’s teams or services work with each other.
What we found:
Integration
Structural factors that contributed to keeping this region under the national average for unplanned admissions of those aged 85 years and over included good integration.
Yeah, so, and we did have, you know, we’ve had a whole governance structure around that and another local iteration of a kind of urgent care group as well, which is, you know, when it was kind of working really well it was actually really good. Had everybody round the table, had some good ideas around the stuff. Got things, things got delivered.
A-01a
Yeah, we’ve always worked quite closely with the local authority and our community provider. You know we’ve got a lot of history with joint commissioning with the local authority.
A-01a
Unitary community trust and autonomy
This region was only one of two in the country that had a dedicated community trust. This meant it had more autonomy to design and deliver community services.
Going back to, kind of, commissioning relationships is that one thing I would say is that the commissioners, the PCT was one of only two PCTs in the country that didn’t actually run any community services.
B-01
So [name of organisation] was one of the few dedicated community trusts in the country. And so the PCT couldn’t really control us either and they certainly couldn’t control [X].
B-01
It was quite an exciting time, actually, developing services like the falls service, community neuro service, community services was developing, OTs were going into MDT [multidisciplinary team] teams . . .
B-02
Then in 2006/7, probably around about 2007, I think, sort of in line with the Darzi report, when we started to see specialist services coming out into the community.
B-03
We were all starting to move into efficiency savings, cost-efficiency savings and moving towards that commissioner-based/provider relationship. And I think what made us perhaps a bit ahead of the game on that one was the view that [I1] were one of the only unitary trusts in the country. We were employed by the PCT and therefore, you know, quite early on we had to develop those relationships with the commissioners.
B-03
Out of hours
A particular structural change that has affected services is that out-of-hours services became privately run in this region. Striving towards trauma centre status also resulted in some changes; however, it is suggested that more focus on community services is the answer to improving care for older people.
Our vision was originally, many years ago, was that we had a fully integrated urgent care centre with out-of-hours care located with a GP skill mix. That’s changed . . . they wanted major trauma centre status. So they needed 24/7 consultant cover. So we got rid of GPs and replaced them with A&E consultants . . . And then they basically pushed the out-of-hours service out so they’re on the acute side, but they’re not in A&E any more.
A-01
I think there needs, particularly round older people, there needs to be a step change in thinking about care of the elderly consultants, because they really don’t accept that about 40% of people being admitted could actually be managed in the community.
A-01a
Out-of-hours services are generally private but it was suggested that there are ‘lots of GPs with their fingers in the pie around there. You know, there’s always some kind of interest’ (B-01). However, the main issue was with reliability of the out-of-hours services in this region. Other structural issues concern the understanding of accessibility and risk of community services, and the funding that is required to support them.
I’ve often heard, especially the clinicians, the medics sort of say ‘We can’t close our doors at A&E’ and you think well actually you can because you divert quite a lot whereas actually in the community we don’t have doors and we’re managing risk in the community, which I don’t think they are appreciative of. I also think community trusts in general, not just us, I think the push has been for the care to come into the community much earlier than it used to, so you’re managing a higher acuity but the money hasn’t followed it, the resources haven’t come with it.
B-05
Systems
Definition: the procedures and processes that characterise how work is to be done.
What we found:
System integration
Some respondents mentioned that it was difficult to keep up good communication between teams.
And some of the things we found with the [intermediate care] services that are provided within . . . there’s a lot of the problems are between teams. So for example we know the interface between the community rapid response team and the integrated primary care team, which are both services provided by [community trust], that interface doesn’t always work. And that we found that very frustrating, because that should be something that an organisation, you know, strong leadership within an organisation should be able to sort out.
A-01b
Contributing factors to this are the turnover of staff and workload.
Yeah and we’ve also been stymied a bit by things like contracts coming to an end and having to do procurements possibly not in a time, you know, at a time when it doesn’t suit us and, you know, like in an ideal world we’d take a year to consider what we wanted to do and then start procuring. Whereas we had to do procuring.
A-01b
And the idea is that they, you know, they work – the stratification tools to, so they used the stratification tools to identify, you know, where they can intervene with individuals and work with them to support them in the community, but they also have, kind of, have existing caseloads that they work with as well. It’s worked well in some areas and less so in others. I think in certain areas they’ve struggled with the level of demand.
A-01a
Systems to manage caseloads may result in targeting certain services over others. Care homes, for example, may not always be visited if staff are under pressure.
We kind of wanted to get away from this, we had lots of services with lots of criteria like [inaudible], but the district nursing service, I mean they didn’t go in to the nursing homes because they have their own nurses, you know, and we just wanted it to be different and actually just do what needs to be done and it is like that, isn’t it? But as you say, sometimes leads to being abused.
A-01b
Technology systems
Technology was found to be a great enabler and barrier to the effective provision of care. The benefits of technology are that it enables effective systems for communicating knowledge and professional understanding of a particular patient. This knowledge exchange is then taken up in the formation of action that can result in the patient being treated by other means in the community, rather than being admitted to a hospital.
Hermes facilitates three-way conversations; sorry, that’s a key bit of information. So the GP will be on the line, the nurse from Hermes would be on the line and the acute physician from AMU [the acute medical unit] would be on the line and having a conference about whether or not it’s appropriate that person ought to go to hospital.
A-01a
We’ve got a service, something like the ambulance service has got, is a web-based tool that crews have access to on which you can upload the patients’ care plans. So when they’re, when they attend to a patient they should be able to access the care plan and follow that care plan. It will say what to do with the patient and what their normal stats are, things like that. So I mean we don’t get to see very much evidence of that making much of a difference but I think it’s got potential to make a difference once we’ve got more people on it. So you know for mental health patients it might just say, oh, this person just needs a cup of tea and a chat or have you asked them if they’ve spoken to [name] today and they might just be after some sympathy.
A-01b
We’ve enhanced the, we’ve got this thing called e-BURS, which basically is a 24/7 response service for people who are in crisis . . . It didn’t use to be 24/7 so we’ve improved that. It’s telephone access, there’s a rapid – over a 24-hour period people can access the service via the phone or they can go to a rapid access clinic.
A-01a
Overall, many respondents thought that technology could be much better and that professional integration would be easier if it were. People were hopeful for the future and there was hope that the affordances of sharing systems would be utilised to bring down unplanned admissions.
I think IT systems could be so much better. If we’re all on the same system . . . if patients held records and all this were ever to really take off, I think it would draw all the professions together and all the organisations together, but I might be banging on about that, you know, for the next 20 years. I hope not but I’ve always thought that – that I should have my own records and, you know, professionals should be having to communicate with each other. And I think a lot of GPs are now on System One and we’re going – [name of trust] are going – you know, some of the services are already on System One. So that might be a way forward to share.
B-02
I think telehealth and the internet. I know for my generation it’s going to make a huge difference to us. You know, I’m sure we will find ways and means of helping us with our own mobility.
B-02
Commissioned services and education systems
There was quite a lot of discussion around new projects that develop services and education systems. These were thought to provide ways to reduce unplanned admissions, but they were not found to become more firmly established; this also connects to ways of educating staff about new ideas.
We’ve got a, commissioned a really good service from Age UK, a crisis service, and don’t know whether it really prevents admissions, but maybe the odd one or two.
A-01b
No, we communicate an awful lot with GPs about all these different things, I think, I think that there is a gap at the moment. There’s nowhere for us to educate GPs about new things other than we communicate mostly through a newsletter, don’t we, but there is no sort of education for them or . . .
A-01b
So the falls service was based at [name of hospital]. It was multidisciplinary and the idea was to sort of give someone an MOT [Ministry of Transport test]. So anybody who had fallen in the past or the geriatrician just felt was likely to fall, they’d come into the falls service and we used to do sort of balance classes and educational classes and there was an osteoporosis nurse within the team . . . so to sort of enable people to stay at home a lot longer because – what I felt was, as well, is sometimes – once you’ve fallen and broken your hip, it’s too late, really, because you’re in the system.
B-02
I think for the very elderly it probably depends what time they might need to call an ambulance or something like that at the weekend if you can’t get hold of a GP. You need to call an ambulance and then the ambulance might convey you, when actually if they were more aware of the services out there they could stop that conveyance. One of my team has just done a pilot in A&E and that was exactly working with the elderly frail, working at the front door of A&E, working with the elderly frail as they were brought in by the ambulance, assessing them at the front door and then, with her knowledge around what community services were out there, trying to turn them back round again and stopping their admission. And in 3 weeks 47 people were diverted away from the A&E department, back to community services.
B-06
Family and carers
Family and carers were said to play an important role in the successful functioning of services. Their ability and willingness to communicate with staff had an impact on the services’ abilities to act quickly and prevent unplanned admissions.
The issue with the matrons and, certainly I remember this when I was managing them, we tried all sorts of things to try and get the patient or the family or the hospital to let them know that somebody had been admitted, because quite often what was happening was they’d go in and the matron wouldn’t even know about it.
B-03
When it did work, when they, when a family member rang the matron or the hospital, you know, did phone the matron for whatever, through the assessment process, they realised that actually there was a matron involved and the individual in the hospital took it upon themselves to contact them. Then when that did happen then it worked really well. They would be able to go in and work indirectly with them and actually facilitate early discharge. Make sure, you know, that everything was ready for when they came home.
B-03
Soft elements
Shared values
Definition: what the organisation stands for and what it believes in. The characteristics that guide practices and systems.
What we found:
Organisational goals and aims
The data revealed that having clear direction provided shared values for people to abide by organisation-wide. Further, this fostered enthusiasm and flexibility to work as and with teams, as there was a source of gratification and a sense of reward.
We had the audacious goal programme this year, which was all about reducing emergency admissions, and we had quite a lot of buy-in at the beginning of that process to a whole-system approach to reducing emergency admissions. So we had the ambulance service and the council, the community trust and a private provider that we use very engaged, but that for a variety of reasons has, the enthusiasm I think for that has waned and people have, the system has been under quite a lot of pressure for the past 6 months and that’s taken people’s eye off the ball.
A-01b
I think admission avoidance, expediting discharge – all those things are sort of in health professionals’ DNA now. As is multidisciplinary working. I think that’s grown up over the last 20 years and, you know, like, some community teams don’t mind as much being managed by a physio or an OT, whereas in the past that was thought of as absolutely dreadful.
B-02
Shared values in society
Some respondents felt that a lack of intergenerational cohesion in society resulted in increased pressures on the health services. Further, this highlights the fact that, regardless of the quality of patient care services can provide, treatment of patients in the community or hospital will increase because of cultural shifts in the social and geographical mobility of patients and family members.
I think obviously I’m going to sound really intermediate here, a lot of it’s culture, where we’re paying the price of a kind of a secular culture or a culture that is just here, there and everywhere, you know, families, you know, I think are key to being close to the older generations and because we’re more mobile and because of the way economics are and demographics and culture development is that the price of all these kind of changes and advances is later on in life you might be a little bit more lonely because your daughter or son is not there by you.
B-01
Style
Definition: the cultural style of the organisation and how managers behave in achieving the organisation’s goals.
What we found:
Relationships
The respondents revealed that good relations between professional groups fostered a positive organisational culture. Organising meetings to maintain collaboration fostered a good cultural style.
We had a, and it happened frequently, we used to do it sort of every month. The discharge meeting . . . with the discharge co-ordinators. And we used to go over incidents that had happened, because I think again I don’t think it’s unusual in this trust, but if you had incident reporting in the community that involved the hospital and you followed the flow chart and it seemed to disappear in to a big, black hole and you never hear about it. And the same thing would happen again and again. So I think off the back of that, we did actually set up those meetings to review incidents, see, you know, where they’d gone wrong . . . I think having those meetings was quite useful, was very useful, because the discharge matrons obviously have a greater understanding of that sort of crossover team – hospital and community – and were able to go back directly to their own staff and say, you know, can I just talk you through the consequences of this and, you know, I think there’s learnings from that as well.
B-03
We have a systems board that always met on a Wednesday so [I1-B-04] and I were there and the acutes and adult social care and the commissioners met every Wednesday so you could debunk some of that sort of anecdotal rubbish . . . We’ve turned it into the urgent care board now but, yes, it still goes on [all year].
B-05
And so I think there was an awful lot of pride around that kind of working, so that you had the intermediate carers in the community, they’re in effect preventing people from going into hospital and you had the integrated section 31 intermediate care beds that we had as well. We had a number of community matrons established as well.
B-01
However, some respondents voiced concern about the ability of local management to attend to specific services, given its large agenda.
We’ve got good relations with the local management. I do have concerns about their executive involvement, because they’re a bigger trust distracted by other areas and other issues and I’m not sure we get the same level of kind of executive oversight that we probably needed. Because we’ve had two big change areas with them. One was our integrated primary care, which was kind of like our long-term conditions, community nursing teams.
A-01a
And services and the community rapid response has got a reputation for being able to fix things and sort things out quickly. So consequently it picks up work from other teams that it probably shouldn’t do, but because it’s got a ‘can do’ attitude people, and everyone knows it will get things sorted. They go to the [community rapid response] and it gets abused. But I would expect somebody within [commissioning team] at a senior level to be picking that up as a problem and dealing with it, but that doesn’t happen.
A-01a
Changing role demands and performance
Some respondents mentioned that part of the learning curve was shaping behaviour to different styles of organisational management that they encountered. Principally, the management of care and the management of projected care are balanced. It was also suggested that shaping care around the patient is an important factor in organisational style.
And I think it’s the commissioners are the same, they, you know, they share what they need to share at those commissioner meetings at a corporate level. I think it’s those, it’s remembering to be corporate when you’re in those kinds of meetings. And it was all sort of a learning curve for everybody, but I suppose in the long run what that did was help relationships at that time, because it helped to develop trust I think.
B-03
Setting
Definition: the context in which the organisation operates.
What we found:
Regional specifications
There were a few attributing factors that were specific to the culture of this region of the UK that influenced service provision and patient flow.
We’ve got a real parochial mentality. In many ways, that’s good because you kind of, it’s kind of evolves around the needs of each area, the cultural needs of each area, but it’s very difficult to –, well some people will want to see things strategically, but you’ll realise that [name of area] is different to [name of area] is different to [I1] and within [I1] it’s fantastic, a complete mix of the lowest deprivation in the country with alongside, you know, high salubrious areas.
B-01
But there’s a lot more social deprivation, a lot more poverty. There’s a lot of elderly poverties, which is quite hidden poverty, so you’ve got people in big, fat houses living in just one tiny little room that can’t pay for their gas, electric or heating, but live in a massive house in a nice, posh area.
B-07
Amenity layouts
Detailed geographic location of patient organisation in the hospital was also found to be of significance when wishing to understand admission rates.
Well I think it’s a physical issue I think because you’ve got everybody, intermediate care are on this floor and then rapid response two floors up. So we have them all in the same building, well we’ve got them in the same building but need them on the same floor and we are looking at changing some of the estate’s plans to accommodate that. If they were on the same floor it would be amazing and it would work far better. But they’re not at the moment. And even we’ve got an access point, we’ve got two access points. We’ve got one up at rapid response and one here at intermediate care where they screen calls through as well. They all come through one number but they get kind of finalled off, but we are looking at the access point joining, once we can get the building plans through.
B-06
Staff
Definition: the numbers and types of staff within the organisation.
What we found:
Multidisciplinary teams
Staff types have often been mixed to provide the best care for patients. When this works, services are very efficient; however, there are issues around the right composition and numbers of staff, and difficulties also arise when staff are not willing to be as flexible as required.
The multidisciplinary teams in intermediate care, really, have made a difference. I’m such a believer in multidisciplinary teams rather than uniprofessional teams because you – when I first qualified, I was a community OT out in [name of county] and I was so lonely. You know, it sort of – much better to be within a multiprofessional environment where you can share expertise, you reduce duplication – you know, sometimes, one person’s seeing a physio, an OT and a nurse, and they just need to see one member of the team.
B-02
So there’s a lot of, with our elderly here in [I1] a lot of the reasons why an elderly person might go into a crisis is polypharmacy, they’re taking the wrong drugs and not the right drugs and we’re just trying to get an agreement with the PCT to fund pharmacy or a pharmacist as part of the multidisciplinary team.
B-06
I can only speak generally for the country, if you had more nurses on wards and more therapists, then they would be able to implement discharge planning when a patient arrived on the ward.
B-01
The only thing I would say was at that time there was a bit of protectionism already, you could see that they were starting to think ‘oh, actually we don’t mind some of this going out in to the community, but we want to hold on to our outpatients’ appointments’.
B-03
Communication and accountability
Some respondents highlighted issues regarding certain staff not being easily contactable and also not being held to account.
Yeah, I mean a good example would be we’ve tried to encourage our, we’ve developed this new pathway whereby ambulance crews can ring the roving GP when they attend to a patient who’s short of breath and doesn’t need to be taken to hospital and could be managed if their own GP turned up. We can’t have promoted the service any more than we have done, yet the pathway is barely being taken up, but even, but we know from looking at the data there’s still, that the ambulance crews are still taking people to hospital who could have been managed on that pathway. And we can, we just there is no way we could communicate any more with [name of organisation]. They just seem like an impossible bunch to, you know, to get them to change the way they do things, it’s really difficult.
A-01b
And what it, you know, we had quite challenging expectations placed on our ambulance service this year in terms of reducing conveyances etc., which they haven’t delivered and that was the mechanism for holding them to account and they haven’t really been held to account have they?
A-01b
Skills
Definition: the distinctive capabilities of personnel or of the organisation as a whole.
What we found:
Skill variance
In some parts of the region the skill set of staff is not quite up to the same standard as in others, which causes disparities in the service.
I think there are some practices that are very good and there are some that you wouldn’t want to go to if you didn’t have to. So I mean we do often say that some of the reason we have such high numbers of people going to A&E is because access in some of our practices isn’t great.
A-01b
Perseverance
Perseverance of personnel was found to be a particular asset to the organisation as a whole. This particular skill set also relates to managers who can see where things will work down the line and where things will not.
Yeah, I think so, I mean we’ve had, you know we’ve had lots of iterations of urgent care over the past and the things we’ve done that have worked have worked because we’ve had that kind of multiagency engagement. It’s pulling teeth sometimes, isn’t it? Like trying to get CRS [Community Response Service] out, it’s a nightmare, but once we got it set up it’s been brilliant, hasn’t it?
A-01a
I can remember going round with these specialist services, supporting them in, you know, going to GP practices and saying ‘this is a brand new service for you’ and them raising their eyes as if to say ‘oh not another one’. And yet, you know, as it went on and they could see that these were worthwhile services, they then started to engage a lot more.
B-03
I1 summary
| Dimension | Strong/positive type | Stems from | Influences | Weak/negative type | Stems from | Influences |
|---|---|---|---|---|---|---|
| Strategy | Good investment in community care Early engagement of all practitioners a key strategic decision |
Structuring | Commissioning | More recent lack of clarity in strategy for urgent care Increased professional barriers Targets and incentives, such as 4-hour target, may increase admissions |
National strategic funding cuts National strategies |
Government policy |
| Structure (of care system) | Good governance structure, integration of all service providers at top level Good level of autonomy to design and deliver services |
One of the few places in the country with a dedicated community trust | Out-of-hours services not clearly structured and reliable | GPs expressing interest only when it suits them | ||
| System (processes) | Evidence of innovative technology systems being employed Pilots trialled new methods of work that were often successful |
Recognised need for the sharing of information Good strategic decisions around innovation |
Leaders focused on patient-centred care | Interface between teams weakening and struggling to provide services Care homes not always visited by more qualified staff Some technology systems not good enough, dangerous for patients Pilots being used but lack of education around them |
Lack of strong leadership/short-term contracts/staff turnover/high level of demand Workload pressures and overlap of professional boundaries Existing professional boundaries stifling innovation Systems for evaluating pilots not in place |
|
| Shared values (for system working) | Clear direction and strategies fostered shared value in reaching goals Professionals willing to work together and bend hierarchies in order to put the patient first |
Good governance and leadership/good communication Build up systems fostering long-term relationships |
Shared values of families towards the care of older people being challenged by the requirement for work and travel | |||
| Skills | Perseverance of staff to see through projects and get people on board | Strong values and goals | Variance in skill set of GPs | Lack of GP governance | ||
| Style | Regular contact and meetings between hospital and community professionals arranged A lot of pride in providing services that keep older people out of hospital |
Willingness to come together and dealing with the negative aspects of acute/community barriers | Risk of complacency; knowing that some services work well can lead to excessive dependency | |||
| Staff | Multidisciplinary teams in intermediate care particularly beneficial for treating very old people Recognised need to involve pharmacists to reduce excessive medication |
Communication challenges with ambulance services | ||||
| Setting | Rapid response and intermediate care being geographically integrated improves patient pathways | Social deprivation |
Site report for I2
Setting
One of the main hospitals in the region is part of a NHS foundation trust.
In 2007 the care trust arrangement was set up; it transferred adult social care to the local NHS, and children’s commissioning and public health to the local authority. The rationale was that the NHS should focus on disease management and care support, particularly for older people.
There are roughly 45 GP practices, 54% of which are said to be single-handed. There is a walk-in centre, and there are 42 care homes in the region. In this region the workforce are very well supported by volunteers. The council was found to have at least 270 volunteers helping run community services such as meals on wheels and a falls collaborative.
Data analysis
The transcribed data from the 19 interviews, two focus groups, field notes and reports were analysed by the research team. The key themes were identified, agreed on and coded against the McKinsey 7S model.
Hard elements
Strategy
Definition: what is the purpose or goal of the system/organisation?
What we found:
Integrated services under the trust
This factor may have contributed to a low rate of unplanned admissions, from 2007 to 2010, in those aged 85 years and over. This region was one of a few in the country that had a care trust, which improved the provision and integration of services.
The care trust, which must have been 5 years ago now, was obviously – well, in the country I believe in terms of what it was an integrated – the health organisation held the social care budget on behalf of the council and still does as we go into an integrated CCG. But that alone meant that the approach to commissioning was truly integrated at the budget and organisational level. So that I think is fundamental.
A-01–2
When we became integrated much more in 2007 we became a Care Trust Plus. I think that further supported the work on unplanned care. So we were – because for us the responsibility doesn’t just stop when they no longer need health care; it goes right into social care. So we have constantly focused on putting in lower-level support to help maintain people’s independence for longer and to help keep them out of hospital . . . the stability of the people in the area, i.e. the teams working to help manage some of this, and that’s not only within the PCT, CTP [Care Trust Plus], CCG, whatever we are now. I think that relates to the hospital as well. Our relationships with adult social care etc. and just in general all the people that are working to strive to achieve the objective because we’re [inaudible] of those different things it helps in terms of building those relationships and building trust really and allowing us to perhaps take more risks in our patch than would perhaps be allowable in other patches where they don’t have that trust and relationship.
A-02
I would argue in terms of the low rates of admissions it’s about the chronic disease management, it’s about needs assessment, risk assessment, putting in actions to address those needs, putting in actions to mitigate the risks that you anticipate happening and responding if those risks come to fruition in a timely and comprehensive and integrated way and then picking up when you look at the readmissions when people coming out actually doing the same thing in terms of doing that when they come out as well.
A-05
Managing funding cuts
There has been robust strategic thinking on how to manage the cuts, which has also been a key reason that the region has prevented a rise in unplanned admissions.
We’ve been very smart over the last . . . taken 13 million out so far without – I think without harming the delivery model by being much smarter around price, much more efficient about process, getting skills mixed differently, managing demand very differently and integrating money across health and social care to produce the intermediate tier.
A-03
It’s been OK because we’ve been smart, we’ve gone really lean, we’ve changed skills mix, we’ve managed demand differently, we’ve put rehab/re-enablement together in an intermediate tier with extended functionality of that and the level of interventions, but to have to take another great chunk of money out will test the relationship, I think.
A-03
Structures (interactions between components of system)
Definition: how is the system organised? The way an organisation’s teams or services work with each other.
What we found:
Consistency in people maintains structure
While there have been numerous changes across the organisation, there has also been a reshuffling of the same people, which has produced a sense of continuity. Further, the changes in overall structure were not sudden; rather, the relationship progressed, which made the transition more manageable.
We have seen a change of people at the local authority, we’ve seen a change of people at the hospital but I think our organisation has remained fairly consistent. We’ve had one or two changes but I think it still has been fairly consistent. The other thing is, I think, it is about the relationship. I often equate our relationship with the local authority because as I said we were on a journey from 2000 as a PCT to get to that integration. So I kind of – from 2000 to 2007 we were sort of – if you put it in courtship terms we were engaged but then got married in September 2007 because we had a legally binding piece of paper.
A-02
General practitioner services
Many of the GP practices in this area are Personal Medical Services (PMS) practices. This form of contract may have translated into the practices being more proactive for individual patients.
Round here I think GPs are more proactive in managing their patients. I don’t know whether that’s because of the PMS leaders. For example, if you’re a GMS [General Medical Services] practice there’s no incentive for you keeping your admission – I know there is now because of the new QOF changes – but before the new QOF changes we had our PBC [practice-based commissioning] budgets and if we were within our budget there’d be some financial reward for that. That’s the wrong word for that – but so you’d a vested interest to making sure your patients were managed appropriately and not in hospital unnecessarily. When I started here in 2006 as a GP we used to have regular MDT [multidisciplinary team] meetings where you look at the patients who’d been into hospital and you’d have a community matron there, you’d have a GP, your practice nurse, receptionist, and you work out ways of trying to avoid admissions the next time. So you’d go and actively manage this patient who went into hospital. There’s been a big drive for COPD locally as well – this has been going on for the last 6 or 7 years, the community matrons with a background in managing COPD, so they pick up patients who went into hospital, work out why they went into hospital and try and avoid them going back into hospital as part of the MDT that the GP practices would have.
A-01-1
General practitioners also used to be responsible for out-of-hours services. That was found to be successful, but more recently the structure of the service has changed.
GP out of hours has been run as a co-operative since 1997. Now that’s located in the hospital and historically all GP practices would give up a GP as a co-operative to work in the GP unit. So you had local doctors also working there as well and we’ve – GP out of hours has now become a private provider, it’s not longer a co-operative – but we still have local GPs working in the GP out-of-hours service who also are in the hospital.
A-01-1
Rapid response is a key service in reducing unplanned admissions
Rapid response services were found to be an instrumental part of the service structure. This is because patients aged 85 years and over were often found to deteriorate in a hospital environment if admitted.
And our rapid response service was tasked and set up to avoid A&E attendances and admissions.
A-01-2
They go out as a social care crisis response team – it does tend to be health driven but the link into what somebody might need to keep in the home – obviously which you sort of have the social care there.
A-01-2
Well, we have a single point of access for rapid, community health and adult social care, 24/7. We have no hospital social work team because it adds 30% to expenditure costs in adult social care, in my view. Most hospital social work teams are unqualified social workers under huge pressure [inaudible]. It adds – when we looked at it locally, about 30% of your budget is being taken up by hospital discharge . . . So we took the view that we’d manage both hospital admissions and long-term care placements and crisis health referrals and all adult social care new referrals and even some from past history differently, so we have a single point of access manned by advice officers, behind which there are three levels of triage which are all about, really – at every level of triage it’s an integrated triage between health and social care. And behind those three levels of triage lies the intermediate tier on the one hand, and on the other hand lies, where it’s just absolutely adult social care, a whole range of third-party providers, mainly voluntary and community.
A-03
Integrated community and social care
In this region it was found that the increasing number of providers may lead to a less efficient system.
Two years ago, it would be two organisations dealing with that, the PCT plus [name of area] Hospital; now if the lady was confused there would still be two organisations, now you have got in [name of area], Care Plus Group, the CCG, [name of social enterprise], and you’ve also starting up a social work . . . social enterprise. You’ve got all these organisations so it’s very fragmented, where before it was two organisations and it worked very closely together. I come from social services, my colleague from the cancer collaborative came from health. I believe we was working really, really closely together; however, I feel that because we’ve fragmented these organisations and we’ve put in the competition side to it, I think there’s everybody fighting for their corner.
B-06
The acute trust provides some community element and Care Plus also provides some community element, like they provide the intermediate care and intermediate care services and things like the intermediate tier. So there is a – yeah, it’s not a standard – you can’t say all community therapy services are provided by Care Plus or we provide all the acute. That isn’t . . . we provide the mix from the acute but the Care Plus don’t provide any acute.
C-02
Systems
Definition: the procedures and processes that characterise how work is to be done.
What we found:
Out of hours and fast response
Some respondents suggested that mechanisms put in place to prevent patients being admitted to A&E were very effective.
By – mostly out of hours to begin with, short-term health interventions and stabilisation that didn’t involve a GP because you may not have got a GP there overnight and that intervention was meant to last 1 day, 2 days at the most in terms of being in that service. But the point is it was fast response to something that traditionally something might have just gone to A&E with.
A-01-2
You know, people would go up to A&E and may end up – actually end up in GP out of hours instead and that’s right, you know, because they’re there, you can do that. They’re there hooked into the same call-handling core services as the rapid are, so there might be some passing around of appropriate patients at that point and avoiding admissions and attendances and ending up in GP out of hours. So I agree – that’s definitely what’s there.
A-01-2
We have a 24-hour triage service. It was set up to run GP out of hours – to take the calls for the GP out of hours, but we leave the phone line open 24 hours. If anything comes in through the GP out-of-hours line that we think may need a home visit, we’ll ask rapid to go rather than the GP, so the GP home visit rate has gone down to . . . a lot.
B-02
And they provide that support 24/7. We then link that to our GP out-of-hours service and the calls to that. So out of hours the calls go through A&E but there are nurses sitting there as well to provide that advice and support. So I think all those sort of things help to stop people ending up in hospital because they have access to rapid response teams who can go out and assess people and that is day and night to provide support and into people’s homes. Because often people – in terms of the things we’ve looked at and questioned the population about and people who use the services, a lot of families just want advice and support and reassurance.
A-02
Transparent care providers and pathways
This region benefits from a simpler system through which patients can be navigated. A corollary benefit is that it means that any issues which arise can be sorted out quickly because relationships between services are better.
There’s not several different providers. Patients can’t get moved around the system because there’s only basically GP practices, intermediate tier and one acute trust.
A-01-1
And that’s actually really important because from a management point of view we try to get all people in the system in a room, blame free, and try and sort the issues out. I mean as a commissioner I personally meet the general manager responsible for A&E every week. I go – on a Friday I’m at the hospital.
A-01-2
So you know that’s just a – so the relationship is very, very close. I can’t imagine in a [name of city]-type environment where you’ve got multiple PCTs and multiple general hospitals.
A-01-2
Information technology systems
Some respondents recognised the dangers of not having a shared medical record, especially when patients enter A&E. This may also lead to overcautious behaviour when patients are admitted, because practitioners in A&E do not know what might be unusual about a patient’s circumstances.
IT systems. I mean the government have – I was going to swear the right word – have messed around with this one care for everything for years and they’ve spent loads of money on it and it’s just very simple. But the fact is you can go into an A&E department and they know nothing about you and that’s kind of dangerous I think. Because at least if my patients phone me up I’ve got the whole record in front of me and it’s one of the issues of [inaudible] as well, you know with my commissioning hat, with regards to risk of 111 [NHS non-emergency call line]. GP out of hours use the same records as GP in hours – so when I work in the GP out-of-hours unit, when a patient comes in I’ve got a full record of what they’re on, if they’ve had this problem before, if they fainted last week then it’s probably the same thing. But these A&E doctors, they’ve got one hand tied behind their back because they’re going in blind.
A-01-1
This was found to be an issue related to disparity in commissioning across the health-care system, where practitioners were not found to communicate which systems they were using.
As commissioners we can’t force all practices to use the system and we haven’t yet. Because the government had GP systems of choice, they gave them the choice of what systems to use.
A-01-2
When you try and get competing manufacturing systems to get their systems to talk to each other . . . They don’t unless it’s going in their favour and what the history tells us that what they’ll do is they’ll say ‘well, actually we’re not going to do that because over time we’ll be the prevailing system, so we’re not going – no interest in it’ – so it’s incredibly complicated and unbelievably frustrating because the notion of information sharing is fundamental.
A-01-2
Accident and emergency
The 4-hour target was found to increase admissions. Many people were admitted to avoid not reaching the target.
I mean I don’t know if there’s any hard evidence but when I worked in A&E one day in this GP pilot, I read through the previous admissions and what time they were admitted and they were all around the 3-hour-30 mark.
A-01-1
General practitioners have been involved in A&E for a long period and this has had positive benefits.
GPs in A&E – well, GPs have been in the hospital ever since I’ve been here, so they’ve either been colocated, so very close to A&E, or in A&E.
A-02
Care homes
Some respondents revealed that there are systems in place to keep the standards high in care homes, in terms of both care home staff and organisations that can support care home staff.
There’s quality standards for the care homes and incentives for them to develop, for example, training, staff development and the like but also incentives for Care Plus to support care homes in terms of helping them. . . . So, if you say ‘why would you put time and effort into supporting the development of staff in a provider you’ve got no direct interest in?’, it’s about aligning incentives. That’s the sort of commissioning approach, how do we align the incentives between providers so that’s mutual benefit?
A-05
So we have 14 specialist nurses and three of those are specifically to support care homes . . . but all of them will support care homes. So we have staff who will go in – so we do infection control in our care homes; don’t charge. We’ve got diabetic specialists who will go in and support care homes. We have a tissue viability [service] that supports care homes. We have a system for managing pressure sores that is specific to care homes that we invented here, that our care homes have all adopted. We support them to get onto the Liverpool Care Pathway before it got out of fashion – for end of life care. We support them with Gold Standard. So we will do that. All their training – their staff training here, currently, is free.
B-01
Community systems
There were a number of clever systems put in place by staff to avoid older people having to venture out when it is snowing, which often results in their falling over and being admitted to A&E. There are a number of effective winter campaigns that taught them to prepare for the snow, but staff recognised patterns in their behaviour. For example, on pension day:
So they waited and waited and waited and waited and then thought, ‘I’m going to have to go. I’m going to have to go. I’ll go on pension day.’ So they all set off on the same day, they all got to the bottom of the gate, they all fell over and they all lay next to one another in A&E. So, October 20th, 2009, [name of falls co-ordinator] rang me and said, ‘What are we going to do to stop a ninth of January this winter?’ And she’s just based over there. So I went over and had a chat and she said, ‘We need to make sure they never run out of bread and milk.’ . . . I rang Meals on Wheels and I said, ‘I need you to go and collect all this gear from [shop] every Wednesday and create these food parcels.’ And my Meals on Wheels staff, I’m ashamed to say, are the least-paid of my staff. And they all came in on annual leave, days off, sick, that morning at 7 o’clock in the morning, went to [shop], collected all that gear, banged it all up and then delivered 1000 food parcels. And we did that every week for 6 weeks.
B-01
Soft elements
Shared values
Definition: what the organisation stands for and what it believes in. The characteristics that guide practices and systems.
What we found:
Organisational cohesion
The structure of the organisation was found to foster closer working relationships. The way that these relationships played out in one organisation meant that workers could elide the discussion of money, and instead focus on the tasks.
So we’ve – effectively because we’re all – well, at that time we were all in the same organisation, you worked together to find the best solution rather than focusing around the money all the time and worrying about the cost. We just focused on the solutions rather than the money.
A-02
The public have a shared value in looking after each other, but in more affluent areas the family support is not there because people are more often away or have permanently flown the nest.
Because [I2] has got quite a lot of deprivation in it, in the areas of deprivation you’ve got more chronic disease and ME [myalgic encephalomyelitis]. And in those areas of deprivation what you’ve got is often quite large families and in [I2] specifically you find that families haven’t left, they haven’t gone away anywhere else, they’re still here. So in the areas where there is the most chronic disease such as the most risk of people being admitted, there’s a higher proportion of family members or the community, although it’s poor, looks after its own.
B-05
Style
Definition: the cultural style of the organisation and how managers behave in achieving the organisation’s goals.
What we found:
Good working relationships
The cultural style of the service provider relationships is very good. There are close links between GPs and the service providers that play a key role in the organisation of patients.
We have a good relationship with our primary care practitioners – GPs and primary care services – because we have local contracts with them for PMS contracts. So that helps to build up a good relationship because we have regular dialogue and contact with the primary care.
A-02
We have a GP sat in telephone triage on a Saturday morning, here, physically with the staff, and he also gives advice to rapid or to the district nurses that are out in the community. And we’re also looking at a mentor programme for rapid to sit with that GP when they’re in out of hours. So we are forging quite good links.
B-02
The number of small systems in place amount to a sense of organisational style that is integrated into the community. The solutions are well designed around indigenously understood problems. The complexity of this is recognised as difficult to define in terms of systems, as it goes beyond the formalisation of health-care provision.
What they actually did, they went round with campaign materials and asked people in the area about what sort of phrase would resonate with them regarding winter and keeping warm, they tried all sorts of different promotional logos but they came back for [I2] was ‘keeping snug as a bug’ so they designed some campaign materials around that and about the need to keep your living room at least 21 [°C] and your bedroom 18 [°C] and some thermometers, they tried varying freebies to give out and you’ve got a list of them here, so we run those each year, I can pass you the figures what we had last year, I think we did 64 events last year.
B-06
The other side of the card is talking about winter planning buddies, so what we did last . . . the first year, it’s the third year now, we asked people to volunteer to be called a buddy, so if, like, I live in village called [name of village], I’m a co-ordinator in [name of village] and a buddy so if it’s really bad weather I can’t get out to work and A&E have a . . . somebody rings up, ‘I live in [name of village]’, and says ‘I’ve got a Mrs Jones, she needs a loaf of bread getting in’.
B-06
It was the human element, jus the humanism of somebody that’s on the phone that does come regularly and is interested in you and they had confidence . . . So I think it’s that and I know we’re proposing, aren’t we, all this computerised checking tools and a lot of things like that, whereas I really think that that human element is what made a difference.
B-05
Setting
Definition: the context in which the organisation operates.
What we found:
Inequalities in wealth detrimental to health
The region’s wealth inequalities were found to pertain to the quality of people’s health, which challenged the health organisations’ and services’ ability to improve health in the community. This has an impact on unplanned admissions of those aged 85 years and over, but there is a good level of social cohesion that brings people together for support.
We’ve got significant inequalities. I mean one of our super output areas is the second worst in the country, which for somewhere like [I2] you wouldn’t think that’s the second most deprived super output area in the whole country when you think of places like [names of cities] and places. So yeah, we have significant pockets of deprivation and 9 years’ life expectancy difference when people can be living less than 2 miles apart and you can live one side of the hospital compared to the other side of the hospital and have a 9-year variation in terms of life expectancy. That’s one of the things that we’re trying to, with the development of the CCGs, is what’s the role of general practice in terms of community leadership. So some of the wider determinants of health are actually stepping up and owning some of these disadvantaged communities, whether geographical communities or communities of common interest, you know, dementia patients or patients with Parkinson’s, whatever it is, but trying to take on more of a wider community leadership role.
A-05
This region has a very dense population; although that is partly what characterises it as deprived in terms of living standards, it also provides benefits for the organisation of health care.
We have the densest population in the UK, including east London before they bulldozed it for the Olympics. We have 8.3 people per hectare; national average is 2.7; [I2] is 0.3. And if I took you 300 yards from here, to where all the fishing things are, it’s tight. So we have a really dense population. And everything’s compact, so it’s easy for us to do what you’ve just seen, because we know we can cover everything quite quickly. It also means your relationships are key because we don’t have cross- – we have cross-boundary issues, but not in that kind of way. You know, it’s not like being in – I don’t know – [name of city], where you’ve got [name of city] on one side and [name of city] on one side and [name of area] and [name of city].
B-01
However, while there are others in the region who are financially better off, this may not translate into being in a better position to receive care, so they have also been recognised as vulnerable.
We started off in high-density populations of older people in poor areas of [I2] but since then because of the success of the programme we’ve expanded and we’ve now got . . . we’ve got representatives, we’re working 15 areas of [I2], we’ve got 15 social clubs running. The reason being we originally started off in poor areas but if you look at the social isolation issues some of them can be, I wouldn’t say financially well off, but better off older people but isolated because [I2] is a bit of a . . . we’ve got a very small town but we’ve got lots of villages in the outlying areas and the issue is a lot of people come to [I2] to retire and if their partner dies and they don’t drive or if their partner dies and they do drive and they’ve got no family and they’ve got no connections that means they’re very socially isolated so that’s why a lot of our areas we started . . . we’ve moved that into leafy suburbs.
B-06
The increase in unemployment levels during the recession has meant that there are more people volunteering to hold the community together.
I think we got a huge third-sector hub here within [I2]. I think because of where we are on the map, they don’t actually come through us to get to somewhere else, people actually come here for a specific reason and, obviously, tourism is the bigger attraction. I think people, kind of, find a sense of . . . that feeling of home, whether you’re from here or not, it’s a sense of feeling at home, and I think that gets people generated, but I think, because we’ve got quite a big population of unemployment now, lots more people are volunteering. So I think that big society element fits into a lot of our model of what we do.
B-10
Hospital locations, size and amenities
There are concerns over the hospitals’ ability to cope with existing demand because of changes in junior doctor rotations. This reveals that the junior staff has been a valuable resource over the 2007–10 period.
But that’s – you know we’re not a teaching hospital town or city. The rotations don’t tend to come through [I2] and the acute trust is at risk of shrinking so they could lose their status as a teaching hospital – they could lose their rotational status for the young junior doctors.
A-01-1
I think the hospital feels vulnerable in this sort of day and age where they can see increasing activity coming into the hospital, because that’s the traditional model – everything goes to the hospital and what I’m trying to do is take things forward and say ‘well, actually some of the hospital could come out into the community’.
A-02
Staff
Definition: the numbers and types of staff within the organisation.
What we found:
Staff interest in the region
The region is relatively isolated, meaning that many staff are attracted to other places. This is particularly the case for newly trained staff, who may prefer to live in a city, and this may have an impact upon the quality of services.
Yeah, but the people here – because [I2] is a – not a backwater, but it’s very isolated, so if you are here you tend to stay here don’t you? So the managers – OK, they might move around the system and they might be in different parts of the acute trust and they might move into primary care – but generally they’re the same people. For example the people that [I2-A-01] referred to have been in that hospital for the last 15 years in one form or another.
A1-01-1
Yeah, the people who are here came from here but even though that is the case people who do get educated here tend to – majority of people leave and not come back. It’s hard to get people to come into the area, I think, so you have to home grow them and get them to stay.
A-01-1
Like with GPs as well, it’s hard to get GPs. I mean I’m a GP at this surgery but you can’t get anyone with anything about them because there’s no medical school here – well, there is, there’s [name of place].
A-01-1
If you had choices most people would either go . . . they either want to go to a centre of excellence with research opportunities and a lot of staff working for you or you choose to go and work in a nice leafy suburb with comfortable lifestyle and probably a degree of private practice. [I2] doesn’t offer either of those.
A-05
A lot of the nursing services, they’re struggling to recruit because they’ve run out of local recruits, you know, how do you advertise nationally and say ‘come to [I2]’?
A-01-2
Leadership and the prioritisation of health
With regard to leadership at the very top of the organisation, it was suggested by some respondents that the more academic, research-orientated leaders are less focused on the functioning of day-to-day care. This results in confusion about the nature of what is most important to the health in the region.
No, there’s nobody clinical, there’s nobody caring, there’s nobody who actually does the business of looking after people, particularly the frail elderly, who are messy and don’t fit into a clear protocol, because a lot of this is around, you know, you talk about is medicine a science or an art, well I would say it’s the art of applying the science but particularly when you get to the frail elderly it’s much more art than science and it’s about how you actually come up with solutions that makes sense of that individual because they won’t fit into a nice clean care pathway.
A-05
The ethos of a past chief executive was championed.
Going back to the PCT days – so we were a – by all parameters of the DH [Department of Health], we were a top-performing PCT. We were in the top five, top 10. We were third best world-class commissioner in the assessments. But we knew that we had 1000 people, who we could name, who would not/could not/did not receive care. And our chief exec at the time, [name of person], said, ‘As long as we are failing the 1000 people who need us most, we’re crap. Don’t care what the DH says.’
B-01
Close relationships and time in post
Some respondents stressed the benefits of long-term working relationships, since this enabled them to learn each other’s behaviours. A key benefit to this is that they can learn how to get the best out of each other.
The relationships help. Most of us have been here a long time, so most of us have grown old together, fallen out together . . . we know each other really, really well; we can be straight with one another. We can fall out without falling out, so you can have your say. So, hence, I’m not that bothered about confidentiality ’cause there’s nothing I’m going to say to you that I ain’t said to their faces and, like, vice versa. So we all know each other. Our staff, therefore, are really, really connected to this community.
B-01
Multidisciplinary approaches using a variety of staff were found to be very effective in this region.
We find a multidisciplinary approach works, ’cause you . . . these patients, they might have health needs, but sometimes they fall over because of their social needs, and vice versa, so by having a combined approach, we can put the best professional in for that patient. And sometimes we do a multiple assessment, so you’ll send a nurse and a social worker or a nurse and a physio to assess the patient. Whatever looks appropriate at the time. We also have, within Care Plus Group, two mental health nurses. Because a lot of these patients are depressed or undiagnosed dementias – you know, they fall over because they’re confused, we treat for a chest infection or a UTI [urinary tract infection], which are usually the reasons the elderly get confused; if they’re not improving on their antibiotics and there is some mental health impairment, we’ll get our two mental health nurses to go and do an assessment and they will refer into mental health services or the memory clinic if they need to, or pick up undiagnosed depressions, etc. So they add an extra element to the team, as well.
B-02
Skills
Definition: the distinctive capabilities of personnel or of the organisation as a whole.
What we found:
Overcoming disagreements
Many of the staff in this region displayed a high propensity for getting over differences of opinion by focusing on what is best for patients.
We do have disagreements, of course we do, like any big family, but we can put them aside to focus on what is best for the people in [I2] and we are good at making compromises. Now one thing I will say is going to probably sound a bit sexist but the senior team in [I2] is predominantly female and has been for some time and that’s what I mean in terms of negotiation and compromise because I think negotiation and compromise are more a strength of women than men. So I don’t mean it to sound sexist, I’m just trying to attribute some skills that I think have worked well in [I2].
A-01
I2 summary
| Dimension | Strong/positive type | Stems from | Influences | Weak/negative type | Stems from | Influences |
|---|---|---|---|---|---|---|
| Strategy | Strategic decisions made in a care trust, which allowed for integrated decision-making from acute to social care in the community Strategy to focus on needs assessment for very old people helped reduce unplanned admissions Smart ways of dealing with the funding cuts |
Integration of acute, primary and community Good understanding of patients’ needs and management Forward thinking and collaboration |
Design of trusts | |||
| Structure (of care system) | Placement of staff whose knowledge complements new structural implementation Accountability of GP services through PMS service design Interdisciplinary teams set up Out-of-hours services previously run by GPs as a co-operative Rapid response seen an essential structure in the organisation in reducing unplanned admissions |
Recent changes in out-of-hours services threaten existing reliability An increasing number of providers threatens to complicate the existing strengths of the organisational structure |
||||
| System (processes) | GP out-of-hours service works well at the point of access, as well as rapid response 24/7 phone triage service through GPs and nurses allowing further access to rapid response if required – recognition of family need for advice Simple system design makes it clear for patients and families whom they can call – one acute trust Good support and training for care home patients and staff Good community initiatives and volunteering, especially in winter |
Resources in the right places, upstream defence Collaborative delivery and good relationships |
Commissioning | Lack of IT systems that allow the sharing of information between all providers highly troublesome. A&E often going in blind, which is incredibly dangerous A&E targets can sidetrack professionals’ judgement |
Professional boundaries/lack of investment/poor choice of computer systems/computer systems chosen | Government policy |
| Shared values (for system working) | Strong organisational cohesion Health over politics Families tuned in to help the care of their older relatives |
|||||
| Skills | Very good at overcoming disagreements. Staff/organisations have developed interpersonal skills that enable effective working relationships | |||||
| Style | Effective working relationships, especially between GPs and other services Systems to integrate and educate the community on health-care issues for older people |
Built upon over time | Culture of patient-centred care | |||
| Staff | Loyalty and effort of staff at a high level – long and close working relationships Previously had very strong leadership |
General trouble with attracting and keeping high-quality staff within the region (GPs, nursing and care home staff included) Staff at the very top of the organisation tend to be a bit academic and research-orientated |
||||
| Setting | Dense population used to advantage, but all areas recognised as having specific problems Increased unemployment in the region has led to more volunteering (the value of community help has been recognised) |
Inequalities in wealth greatly affect the health-care challenge Risk of hospital losing teaching status, affecting staff numbers, skill sets and attraction to the region |
Site report for I3
Setting
There are four main hospitals and four walk-in centres across the region. During some of the period between 2007 and 2010 there was a walk-in centre in one town at a hospital (and also a minor injuries unit with X-ray facilities). There was also a walk-in centre at another hospital site and at a third location. A Darzi centre was colocated with the walk-in centre on a fourth site.
Rapid access was set up in 2010. Previously this type of service was collaboratively managed by certain care homes; the beds are now situated in different care homes. This is not a home-visit service in any capacity, just a bed service which was funded by social services. Therapy for those patients, however, is funded by the CCG/health fund.
Data analysis
The transcribed data from the 14 interviews, three focus groups, field notes and reports were analysed by the research team. The key themes were identified, agreed on and coded against the McKinsey 7S model.
Hard elements
Strategy
Definition: what is the purpose or goal of the system/organisation?
What we found:
Emergency/urgent care has been a top priority
Urgent care has been a priority in this region, with the result that care pathways for patients, including those aged 85 years and over, are well supported. This strategy has had an impact on unplanned admissions because some services prevent admissions.
[Urgent care] has been one of the top priorities in both organisations. For the whole time I’ve been here it’s been a top priority. And the main reason for that is that, one, you know, we want the urgent care pathways to be as high quality as possible for our patients, we’ve got a huge number of patients going through urgent care services every year, and secondly – and this is important – it’s a very large proportion of our expenditure as a commissioning organisation.
A-02
Some of the initiatives that have put in by the commissioners with regards to a rapid access . . . that was initiated a couple of years ago. They put money in where they’ve purchased packages of care and they’ve purchased care home beds . . . To support either preventing hospital admission or being able to facilitate discharge from hospital.
B-01
Specific strategies for those aged 85 years and over unknown
Some respondents recognised the particular problems for patients aged 85 years and over, but also expressed a difficulty in knowing how to solve them. While there is a good volunteer workforce, beyond this it is difficult to help very old people in social ways that may reduce unplanned admissions.
We’ve got a very good volunteer workforce. But the voluntary service can only do what they can do within the constraints of finance and what they can provide. I think, particularly in [I3], especially West [I3], a lot of the elderly patients, because of the loss of the extended family, people are more mobile, go away, they tend to be left. They spend a lot of time on their own or their families have grown up and gone off. But I do feel that we probably don’t do as much as we probably could for the over-eighty-fives. I don’t know what the answer is.
B-01
More recent organisational change
The more recent organisational changes have meant that overall strategy is more confused. In particular, the speed of change and lack of consistency in decision-making result in an inability to plan ahead.
The whole health system has been chaotic. Our acute trust has had a complete change of board and there was a new chief exec who arrived, I think he’s a year in post now, and there’s only one existing director in post from the original regime so there’s a complete change of board within the acute trust. Within the local authority they’ve had a huge deficit to manage as well and so their cost improvement plans are coming in at the moment and that’s got a huge impact on health. We’ve changed from a PCT and we’ve gone into lots of different directions, which is Public Health England, NHS England, CCG, community trusts, so there’s an absolute huge disarray and chaos within the system and at the same time patients still come in, come out, come in, and still expect to be treated as well while you’re trying to settle all this down really.
A-03
From a provider services organisation they can’t plan because the commissioners change what they want by the minute and they do try and respond to that but the commissioners say ‘jump’ and we jump; half doesn’t make the grade and the other half fall down, don’t they? You know, it’s sort of that’s what it’s like, you know, it’s what the commissioners say goes and they change their minds like pussy cats.
B-05
It’s quite hard to deliver a service when you’re only given 3 months and there doesn’t seem to be any overall strategy. I think they’re looking at it and they will develop a strategy but for us on the ground doing the work it doesn’t feel as though there’s any joined-up strategy, I would say.
B03
Structures (interactions between components of system)
Definition: how is the system organised? The way an organisation’s teams or services work with each other.
What we found:
Lack of cross-boundary problems in the region
The region benefits from a simple system design and, while there are still some communication difficulties, a transparent and ordered structure of the health service organisations helps reduce complications.
We always say we should be able to do it on [I3] because we hardly have any cross-boundary issues, as you say, at all. You know, it’s just one social services department, one acute trust, one community trust, one mental health trust and one health commissioner – that’s it.
A-02
Multidisciplinary clinics for old people and increasing consultant numbers
A very useful organisational structure has been the use of multidisciplinary clinics, with services specifically for old people. Their often more complex symptoms can be managed by a number of specialists in one location.
About a year to 18 months ago, we introduced our Opera clinic, an older persons’ representative. It runs 5 days a week, GPs refer it to . . . they can refer it today, and patients can be seen tomorrow. So yes, geriatrician, who has access to an OT, a physio, a social worker, who then has access to a range of alternatives to admission. So we started off that, that’s had fantastic reviews from the GPs; they love it. And we’ve developed that further now, that they’ve actually got a phone line they are calling from, faxing in a referral, if they’ve got an elderly patient with them in the surgery, they’re just not sure what to do, they just pick up this phone line, and there’s a geriatrician who will advise them. So there’s that.
C-04
There has also been an increase in consultant numbers and specialist services elsewhere in the region.
The last three to five [years] really. We’ve almost doubled our consultant numbers. So we run an all-singing, all-dancing 24/7 stroke unit, which takes all ages but obviously it’s predominantly elderly. We’ve got two orthogeriatricians. So we do a lot of in-reach into the surgical wards. We’ve got a specialist that does predominantly cardiology and heart failure for our older population. We’ve got a movement disorders consultant that has been with us for the last two and a half years and we have appointed . . . we’ve got two community geriatricians as well and that was work that we did with, well it was the PCT, now CCG, and they’ve actually funded those posts. It’s quite a tight service specification but it was quite evident.
C-05
Out of hours
Out-of-hours services are run through the community trust quite successfully.
It’s run by our community trust so they have the contract for the GP out of hours and then yes it’s run . . . as I say, it’s run and managed by them and then there’s loads of GPs on it and that might be some of our GPs may decide to be employed or do a locum or whatever, so some of them will be local GPs, some of them will be locums and some of them will be GPs from out of the area; it just depends, really.
A-03
Structural changes and reductions in intermediate care
Intermediate care has gone through a significant amount of reshuffling, with services being provided by a number of different care homes and in varying capacity. More recently, an element of intermediate care has been termed ‘rapid access’, but that is not to be confused with ‘rapid response’, which does not exist in this region. The service has basically become the same existing intermediate care, and the structure of services has been designed to meet the needs of very old people. However, the numbers of beds have decreased.
I’ve got intermediate care service, OK? It used to be on three sites actually and there were 52 beds . . . Probably about up until about 18 months ago I’d say, and then there were so many of those beds, residential beds, and I think there were 16 of those beds, nursing care beds, and I think they were struggling to manage the more complex patients because they were identifying nursing needs within the intermediate care . . . So then they opened these rapid access beds, which was 20 beds across five nursing homes. Now in intermediate care they’re saying that they should be in those beds for about 6 weeks. We do well if they’re only in for that long. They’re so complex, the patients. Rapid access, the target is those patients should only stay in those beds for 6 weeks and, as I say, 85 year old, it’s very rare you can turn, 85. I mean the average age is nearer 90 that we see in those beds . . . It’s rare that you can turn a patient round that quick who is that frail, to be honest. So they opened the rapid access beds and soon realised, ‘Well actually we need therapists to get patients home out of these beds.’ So they commissioned us to provide a rapid access therapy service to these 20 beds with a KPI [key performance indicator] that patients should be seen and assessed within 3 days of them being admitted to that bed.
B-03
We used to have intermediate care beds in [I3] and over the last few years the CCG have closed most of them down. So we have very, very little, based on any area I’ve ever worked in, community-based beds. I don’t remember the exact numbers now, because they seem to change every time you ask, but we used to have about 60–80 intermediate care beds. Now it’s down to about 30–40, if that. There is very little provision in the community for patients with cognitive impairment. So, for example, there’s no intermediate care or nursing home base for patients to have dementia and they can’t access those facilities.
C-05
Reduction in rapid response, nursing and care home support
One of the services that helped keep unplanned admissions low was the [name of place: X] admission prevention service (XAPS). This was recognised as a very good service; however, more recently the commissioning groups disbanded it, and there is less support for services that enter the home. Further to this there has been some structural change around nursing home assessment.
[XAPS] was a really, really good service, they were very skilled nurses that had a lot of care and experience round COPD, for example, so I think that’s been a bit of a backward step for us . . . We do have a nursing service, but we are very restricted and we don’t have the resource to pull in, to support keeping people at home.
B-01
There’s not been a lot of buy-in from GPs around nursing home assessment. So there’s no service, you know, locally enhanced scheme for GPs [in I3] to assess their nursing home population, despite multiple attempts. So we’ve got quite a large nursing home population that doesn’t get a lot of regular review by primary care. So in terms of admission avoidance there’s just not the regular review happening. We’ve also got our out-of-hours service that provides all of the outside usual working hours working for GPs. We’ve got very few practices that actually do their own out of hours. It’s all been centralised in [I3].
C-05
Systems
Definition: the procedures and processes that characterise how work is to be done.
What we found:
Key programmes and systems
Systems connected to the regional focus on urgent care enabled them to see to patients quickly and efficiently, which is particularly important for those aged 85 years and over who are very fragile and at risk of quick deterioration. This was coupled with other big programmes run by the PCT at the time.
The other thing we had on there was a single front door service, because in our urgent care services we have several different services on our key hospital site and like three or four front doors to our urgent care service on the [name of hospital] site. And I think the network wanted to try and get to a point where we had one point of streaming.
A-02
There are a number of other initiatives which will have impacted on the demands as well, it wasn’t just the urgent care programme, I mean we have a stroke programme, you know, we had a huge programme around cancer and end of life care, mental health programme . . . I’m just trying to think of the main ones. Those are the main ones. So it wasn’t just the urgent care programme, there were other initiatives that were part of this development that allowed the PCT to do things.
A-02
Accident and emergency
Similarly to many other sites, the A&E targets are met when time is running out.
Now when you throw in the 4-hour target and the pressures that people are under, it’s exactly as you say, so you’re working with risk-averse because I don’t know these people and I’ve also got a manager or somebody going, you know, it’s 3 hours 58 minutes, 3 hours 58, 3 hours 59 . . . what are you going to do? You’re going to admit.
A-03
Admittance to homes
Some respondents highlighted the problems around patients not being admitted to the right homes, and also around the mixture of services in homes being too broad. This could cause deterioration in healthier older patients.
There was patients coming through that might have needed nursing and some didn’t need nursing, they decided that, if we just commission beds in nursing homes, they’ll have the nursing element there and then if they’re lower-level need then the nurses just don’t need to so much, but the difficulty is then that you’ve got patients coming in that they’re not even really needing residential care and they’re put in an environment that’s scary for them really, they’re seeing patients that need hoisting or can’t communicate or dementia and a lot of them will take to their room instead of us trying to promote let’s get out here, and let’s remobilising, they’re staying in their room and refusing to come out.
B-05
Reducing unplanned admissions from nursing homes
The respondents reported on a number of initiatives that helped to reduce unplanned admissions from care homes, of which there are a particularly high number in the region.
There’s been a number of initiatives that we’ve tried to do to keep it where it is, I think there’s work that’s gone on with nursing homes so there’s been things like we’ve commissioned education into nursing homes so we’ve educated nursing home staff, we’ve implemented the Care of the Dying Pathway, we’ve implemented things like the Anticipatory Care Pathway, so it’s things like preferred place to die and things like that. We’ve also introduced, in some nursing homes doctors or some GPs actually go in and do ward rounds so we have like a GP going in, a nursing home GP, because what we were finding with some of our nursing homes was that they would just dial 999 at the drop of a hat because their perception was, ‘well, it’s difficult to get our GP and it’s difficult to do this and it’s difficult to do that’, so what we’ve tried to do is find out what triggers an emergency admission from a nursing home to do that and then by putting in the education, by putting in different tools, decision-making things, we’ve been able to . . . I think that’s certainly had an input.
A-03
A key component of this has been reducing the number of drugs old people are receiving, because polypharmacy can make them drowsy and likely to fall.
The other thing that we have done as well is we’ve put in pharmacy and medicines management support as well because we also found that polypharmacy was quite a problem as well because it was then giving two issues really; I think one of them was it was actually making some patients worse and knocking people off and there was also something about the reviews weren’t happening properly either so it’s given people the opportunity to have a good medicines management review, it’s helped them then to reduce the amount of polypharmacy that they’re having, which then can reduce the amount of falls and drowsiness and all things associated with taking tons and tons of drugs so I think from a nursing home point of view I think that’s certainly helped. We’ve also done work around a falls pickup service as well and that’s around . . . there’s been some upstream things so we’ve got our falls service, so there’s things like the sloppy slippers campaign and things like that.
A-03
Some innovative ideas have supported this work, with staff in the region recognising and changing some of the smaller idiosyncratic features that cause falls.
What we actually did is we went out and we did like slipper exchanges so we made elderly people give their slippers and we fitted them with proper slippers . . . and things like that but again it’s just trying to reduce the incidents of falls, so it’s simple things like that that we’ve done. The other things that we’ve done around falls is we do have a falls team so again it’s a multidisciplinary team with OT and physios and things like that, so again people who might attend with a fall or have a history of falls, our teams go out and look at their home, look at putting in aids, adaptations, whether it’s a grab rail here, whether it’s the slippers, whatever it is, to try and prevent some falls from occurring. We also have a falls pickup service, so again working with the ambulance service and saying because people fall doesn’t necessarily mean it’s an attendance to hospital, so the ambulance service will fill in and look at doing an assessment and if they’re pretty certain that there’s no break, there’s no damage, da de da de da, or there’s no underlying medical condition that caused them to fall, they will pick the patient up and they’ll stay in their same home again and then the falls service will come in the next day or the district nurse and so it will trigger another referral but it doesn’t trigger an automatic attendance to accident and emergency.
A-03
Technology
Technology systems are regarded as a particular problem in this region; outdated systems and systems which do not communicate add further complexity to tasks and increase workload.
The biggest bit we’re waiting for is our IT, ’cause that will make a massive difference ’cause we’re drowning in paperwork. Everything’s done manually, the work allocation. It’s huge, massive . . . I mean on a daily basis it takes 2–3 hours for two staff to do that, write all the list of all the patients to be seen the following day and then allocate them to the nurses. I mean it’s massive. So if it was all electronic you’d be able to have all your case load and you’d be able to allocate them across to the nurses.
B-01
We’re all paper based, so there’s a massive, massive piece of work going on about getting an electronic community nursing system. . . . We’ve got another, like the integrated care at home one, team around the person, they’re looking at an IT system. I thought ‘why are you looking for an IT system for that when we’re building an IT system for that?’ The hospital’s got another IT system and we’re going to have our own and social services are going to . . . how does it all tie together? And all the GPs in [I3] don’t use the same system.
B-01
But even the GPs because they’ve got ENDS [electronic nursing documentation system] and we’ve got ENDS and you can talk to each other and you can’t because one’s got the GP version and one has got a community version and there’s no integrating software.
B-05
Communication issue is that systems often, GPs will all have their own IT system, different one for different GPs, the hospitals will all have, social care have their own, the nurses have their own and so on, so what we are looking for, and we don’t think we will ever solve that, but what we are looking for is a kind of bolt-on system that can kind of interrogate data from the different systems and bring the relevant information to the relevant agencies and what we are looking for is a local integrated team that would be able to have that information and be able to plan from there basically.
D-01
Soft elements
Shared values
Definition: what the organisation stands for and what it believes in. The characteristics that guide practices and systems.
What we found:
Political and health misalignment
Some respondents recognised that the coalition government cuts had made things far more difficult, and this displays a lack of shared value in the health requirements that are felt by health practitioners. The practitioners have to align and make sense of the cuts in an organisational sense.
I think it’s fair to say that there has been some political moves, you know things like the Conservatives, for example, wanting to demonstrate that they’ve cut budgets and been able to meet the financial targets and as a result making some quite draconian decisions about social services, and they have done, but I mean that’s almost a moot point now because the cuts to the council are so big that any administration is having to make quite draconian decisions. And I do think we are trying to show as much understanding as we possibly can of the financial pressure that our social services department is under, because a lot of this now is not about them being funny with us, it’s about them being under the most extraordinary financial pressure that we’ve ever seen. And we have to show a level of understanding of that as a health community and I think we are, you know, through this SLA [Service Level Agreement] process, trying to show some understanding of it whilst also getting the outcomes that we need for the investment of our health money. It’s a difficult conversation, I’m not going to flower over that, it’s a really, really difficult conversation – massively difficult.
A-02
Ownership of patient responsibility
The data revealed that there were some issues over who should treat a particular patient. The merging of care provision by different practitioners might be in contradiction with how they each manage their cohort, resulting in some patients slipping through the net. The focus on the patient is lost here and there is no shared value found in the opportunity to treat them.
I think as well some of the patients that get put into the social care fund beds or the rapid access beds, because they’re trying to prevent admissions, they are people who often do actually need an admission and they’re in the beds and then we’re fighting the GPs because it’s not their local . . . it’s not their permanent GP who covers them, it’s a temporary GP, so then they won’t look at necessarily even medications reviews or they won’t come and see the patient and we’re saying they need X-ray and you’re trying to ring the permanent GP who’s saying ‘well, I haven’t seen them for this length of time’ . . . I do wonder what GPs do these days, they don’t seem to care for their patients, some of them are very good and we shouldn’t put them all in the same basket, but why, if you know somebody’s poorly, why don’t you say I’ll see you next week, but they don’t, they wait for the patients to come back with the next crisis.
B-05
Style
Definition: the cultural style of the organisation and how managers behave in achieving the organisation’s goals.
What we found:
Relationships and boundaries
In the region there was some cultural behaviour of blame, especially between primary, acute and community, where the demarcations could explain why something was not working.
I think there’s an element at times where it’s easier to sort of blame . . . I don’t know if that’s a bit of a strong word . . . but it’s easier to sort of think ‘right, OK, patient goes into hospital, that now becomes the hospital’s problem and I can hands-off here’, whereas actually what I think we need to be doing is being quite mature about it and having a really strong working relationship to actually say this is a shared responsibility here.
A-03
The issue of communication technologies exacerbates interprofessional relationships, in that communication should also provide the opportunity for collaborative working; failure to achieve this is treated negatively.
Communication and sharing information is a big, big factor because we don’t share communication and information well. We all don’t get what we need with regards to the transfer of patients and patient information and what’s happened. Sometimes you’re lucky if you get anything. The district nursing teams are lucky if they get anything at all.
B-01
Lack of contact with the front line
A number of issues have arisen with the commissioners, who lack an understanding of patients’ needs that could be provided by other staff.
The commissioners have just produced a questionnaire that they want us to send out to patients and it’s just so inappropriate . . . it’s awful, and they want it to go pre-assessment, at discharge, 6 months and 9 months; is a 95-year-old going to remember who saw them 6 months ago and whether it was a nurse or physio? . . . plus it’s not only our services that are producing these leaflets and giving them to the patients, it’s the podiatrists, dieticians, and they could have three different, the same things, and get that form three times, it’s just not fully feasible is it?
B-05
My impression is that the commissioners really don’t, themselves don’t have a good understanding of the services that are being provided or what they want.
B-05
I think the things that work really well on the [I3] are the relationships at an operational, and to a degree going into strategic work, and I think those individual relationships, and people knowing each other and having a level of trust ’cause that’s very, very difficult. I think there is a huge potential for a massive distrust between all the organisations and I think commissioning generally at the moment is in quite a uncomfortable place.
C-02
Setting
Definition: the context in which the organisation operates.
What we found:
Regional specifications
Within the region there are areas of significant deprivation that have resulted in big disparities in health.
We do have, in some places in [I3] a large ageing population as well and again it does bring its problems with it, so within [I3], if you look at us, . . . you’ve got the [name of motorway] that runs in between it and we’ve got the west side and the east side of [I3] and the east side of [I3] is a largely deprived area and we have a number of young people and we have teenage pregnancies, drugs, alcohol-related issues and when you look on the west side we have an ageing population . . . you’ve got this huge divide between the west and the east and so you’ve got an ageing population and actually that brings a lot of demands as well, having an ageing population, and when you look at life expectancy between the west and the east, there’s a 15-year age difference.
A-03
Say breast screening services, if we use that as an example, the breast screening uptake is very good on the west side of [I3] but on the east side it’s poorer, so what do you need to do in order to encourage that? Well, do you need to get some sort of mobile breast screening? How do you get people? Because again that’s what brings up the life expectancy, your health and quality things, people don’t attend for cervical screening, breast screening, and yet on the other side yes they do, there’s also things around access to public transport, car ownership and things like that, so when we’re thinking about commissioning services sometimes just putting them into one place isn’t always the answer; you might need to have locality-based things because it’s easier for people to get to, so we look at, say . . . we’ve got some smaller sort of community hubs that it’s easier for local people to get to rather than sort of get two buses to get up to the main hospital or to get somewhere else, so it does affect our commissioning in some ways.
A-03
The rate of unplanned admissions to A&E may be influenced by the ease of getting to the hospital.
Do you know what, just coming at the point, it’s just something that having looked at other areas, what you have to remember is the geography of [I3] is so limited because we’re a [geographic term] and anywhere on [I3] you’re 10 minutes from this hospital. Therefore hospital is also a very easy option.
C-03
Staff
Definition: the numbers and types of staff within the organisation.
What we found:
Staff responsibilities not always properly defined and met
Within the region, staff with expertise may not be utilised to full effect.
We do a lot of end of life care in relation to syringe drivers because they haven’t got competent staff on duty. So we manage the syringe driver element, supporting the care home staff around symptom management etc. . . . we’ve got the specialist palliative care team . . . Who are part of specialist nursing, which is part of community nursing. But they don’t do any hands-on at all.
B-01
And the reason we’ve got quite large community nursing teams, they’re skill-mixed teams, is around economies of scale. And it’s covering the service ’cause we’ve got to cover the service 24/7.
B-01
Specialist training for community work is not always provided.
I think . . . or sometimes when you . . . if you bring hospital staff out into the community I think there’s some training needed to understand that living in the community there is a risk and sometimes we have to manage those risks, we don’t always automatically send up. Now whether that’s new GPs coming straight out of hospital they don’t always know, I don’t know, but I find that hospital staff, their knowledge finishes at the front gate and it’s a different skill set out in the community and sometimes it’s recognition of that.
B-03
The quality of staff in care homes can make a huge difference to unplanned admissions.
And also I think it’s the care agencies because of the people . . . some of the care agencies on [I3], some companies will pay their staff travelling between houses and I think they’ll be costing their hours. Other agencies don’t and some of them will pay them the bottom of the minimum wage, so they’ll get very young people, but it’s about dealing with the older person, or they’ll send a male to a Miss, you know to administer personal care – well, that’s not appropriate. You just think those little things, subtleties make a huge difference to a patient and what they feel is acceptable to them, but I think the other issue for us is that because [I3] Council has got £3 million to save, you know, everything is pared down to the minimum. But in the long term that’s not going to be effective because our patients then are prone to urinary tract infections, if they’ve got a catheter they need to drink at least 2 litres of fluid a day, so somebody’s got to push fluids, because if they don’t they’re going to get a blocked catheter, urinary tract infections – it’s a no-brainer.
B-04
Leadership change
Change in leadership is seen as an important factor in developing relationships between services.
I think we’ve in the last 5 years probably had three chief executive social services, we’ve had three chief execs, and it must be very difficult to form relationships at a very senior level and they set the tone. You know, your chief exec sets the tone for all of these services, and in CCGs the very senior GPs who have history and people know them. So I think it’s been quite difficult ’cause I think leadership changes on a very regular basis, and this should be about systems, not about people, and sometimes I think it becomes about people, not systems.
C-02
Skills
Definition: the distinctive capabilities of personnel or of the organisation as a whole.
What we found:
Difference between community and hospital staff
The hospital staff is found to be more risk-averse, which is not necessarily best for some very old patients.
What I’m saying is the hospital staff are more risk-averse, so they won’t take the risk of sending somebody home, they will admit, whereas in the community we probably manage them. So it’s sharing those skills really, but I do wonder if in the past there’s been a lot of junior doctors in A&E and I’m just wondering if they’ve got the skill to be able to identify where a risk can be managed, because a doctor will say admit and then you’ll get these admission prevention nurses that have been part of this pull team to pull people out and they’ll go in and say, ‘Oh no, come on, we can manage you at home.’ So whether you need that joint approach at the front door at hospital I don’t know.
B-03
Skill variance
Within the region some of the hospitals have high rates of readmission, which suggests there are a number of problems with care pathways back out in the community. However, the nursing team is regarded as doing a good job.
Our hospital do not discharge particularly well at the moment . . . They don’t plan well and they just discharge them, sometimes without any support. So we get a element of revolving door . . . well, they’re just told ‘get them out’ and they just get them . . . they discharge them at 8 o’clock, 9 o’clock, 10 o’clock at night . . . With no services, sometimes no equipment.
B-01
We provide an excellent community nursing service. I think the quality that we provide, and I think that’s borne out by our exceptional results: our healing rates for leg ulcers, our end of life care we provide. That’s not to say there is room for improvement, but there’s always room for improvement. But I think we’ve always met our targets, we’ve always met what’s been expected of us and I think we provide an excellent community nursing service, it’s truly 24/7. And I don’t think there’s a lot of areas that can actually say that they provide that. We’ve no gaps in service and we’ve got a very dedicated committed workforce.
B01
I3 summary
| Dimension | Strong/positive type | Stems from | Influences | Weak/negative type | Stems from | Influences |
|---|---|---|---|---|---|---|
| Strategy | Urgent care a top strategic priority Recognised importance of community care |
Executive decision-making | Lack of strategy for patients aged 85 years and over More recent changes with the shift to CCGs means organisational goals still up in the air – unsettled and difficult to plan |
Lack of recognition of rising importance Significant organisational change |
Government policy and cuts | |
| Structure (of care system) | Lack of boundary issues helps keep a clear structure Investment in interdisciplinary clinics with specialist services for old people Out-of-hours services run through the community trust successfully |
Regional layout and planning Commissioning |
Gradual reduction in intermediate care in care homes, but not much has been done to replace deficit in bed numbers Reduction in nursing and care home support |
Recognised damage of institutionalisation Costs and workload |
||
| System (processes) | A focus on key programmes on urgent, stroke and end of life care puts systems in place to reduce unplanned admissions Good integration with care and nursing homes to allow staff engagement and development Attention to the importance of polypharmacy and initiatives to reduce falls |
Strategic decision-making at board level Regional reliance on care homes very high so blanket policy |
Lack of IT systems that allow the sharing of information between all providers Care home patient variance can lead to early deterioration A&E targets sidetrack professionals’ judgement |
Professional boundaries/lack of investment/poor choice of computer systems Cost saving National targets |
Government policy | |
| Shared values (for system working) | Good communication and energy for providing good-quality care for old people | Recognition that government cuts stifle cohesion Patient-centred care sometimes lost because of boundary issues |
Increased workload and costs | |||
| Skills | Nursing staff highly skilled and effective | Longstanding teams | Hospital staff very risk-averse High readmission rates suggest problems with community care |
Risk-averse culture Care pathways back into the community not available |
||
| Style | Some blame culture when services are pressured Lack of contact with frontline care can create problems when commissioners wish to understand patient experiences |
Leadership weakening | ||||
| Staff | Overall a good level of cohesion between staff Good levels of support and integration |
Close working relationships and simple structure | Staff boundaries and competencies not always used effectively – especially regarding specialist staff Skills required for the best-quality community care not always understood or appreciated by hospital staff Care home staff can make a huge difference to unplanned admissions and the well-being of older patients A lot of leadership change |
Systems for experiential learning not in place Lack of regulation of staff and care home inspections |
||
| Setting | Recognised the challenges for people with less money, and tailored services and provided information as well as possible | Inequalities in wealth greatly affect the health-care challenge Ease of getting to hospital can prevent patients and their families from using other services |
Site report for D1
Setting
A new hospital opened in 2006 and provides community services in conjunction with acute services. The older hospital is a separate hospital people can visit if registered with a GP in site D1. It is run by the new hospital and the local NHS trusts. One trust provides a range of hospital- and community-based services to 300,000 people in three districts.
A NHS trust formed in 2006 and integrated with community services from NHS site D1 in April 2011 to provide a range of community services for people in D1. They also provide inpatient, community and day clinics as well as specialist services to a population of about 850,000 living within D1 and the county. The organisation provides services from more than 80 locations with an income of about £200 million, and employs more than 4000 dedicated staff.
There are 63 GP practices in D1; many are run on a small scale, being operated by single-handed GP’s or partners. In 2013, CCGs replaced the PCT and Strategic Health Authority, but this report focuses on the period between 2007 and 2012. All but two care homes in D1 are contracted, and there are a number of providers of social care across the region.
Data analysis
The transcribed data from the 14 interviews, one focus group, field notes and reports were analysed by the research team and the key themes were identified, agreed on and coded against the McKinsey 7S model.
Hard elements
Strategy
Definition: what is the purpose or goal of the system/organisation?
What we found:
A lack of strategy and understanding about specific care for people aged 85 years and over
This factor may have contributed to an increase in unplanned admissions from 2007 to 2010 in those aged 85 years and over. Some respondents did not know the extent to which unplanned admissions are a problem for people aged 85 years and over, or the specific care required:
I wasn’t aware personally that that was a particular problem but then obviously I haven’t actually seen the most up-to-date figures, so I don’t quite know which direction we’re going.
D1-A-01
I’m not sure there’s enough evidence to really clearly say which is the key magic bullet to solving care home admissions and that does include thoughts of residential homes and maybe even houses with care, houses with support, houses with wardens, ’cause there’s quite a lot of admissions from those areas.
D1-A-03
The evidence base for treating most conditions in somebody over 85 is distinctly lacking.
D1-A-01
This lack of strategy has been recognised by the more recent CCG formations, and this presents an opportunity for change.
I’m sure that I’m not the only person in a CCG where the people at the top, and this unfortunately includes some of the managers, have still not got programme management heads and strategy heads. The system plans are great, links into public health, needs analysis, all those things, but it’ll have bullets like we’ll support care close to home but we’ll support financial sustainability of the acute hospitals. Unless you have some sort of integration, those two things are mutually exclusive in the long term. But there is no strategy to say ‘our strategy is that means integration but converts some hospital beds to step down or mental health’, you know, to replace out-of-area replacements and all those things. We are just lacking in that meaningful strategy.
D1-A-03
I think what we probably need now is clinically led provider organisations, ’cause you’ve still got managerial-led provider organisations and I think if we can get the doctors talking to each other it will work better. The doctors do talk to each other but then they don’t talk to the managers and the managers talk about a different thing, so it’s not necessarily connected.
D1-A-02
Changes in leadership roles and health service strategy across the region
The data set revealed concerns around changes in key leadership roles in the past:
So what I would say is, given the level of pressure they’re under, the partnership working has been reasonable and I think it’s getting better and, again, I think that’s because of the leadership capacity, I think, in the system has improved in the last year or so. We’ve got better people in the system, now, who are prepared to work together . . . whilst we’ve had some difficulties with the different personnel bobbing in and out in the past.
D1-B-02
A few respondents raised the issue of changes to the regional strategy, which may have affected admission rates over this time period in D1:
The other thing I don’t know if anyone else has mentioned, just in case I forget, but one reason why, well part of the reason why our figures might have gone up in old admissions is because two things started over the last sort of 5 or 6 years, which is primary PCI [percutaneous coronary intervention] for heart attacks and thrombolysis for strokes. So we’re getting a lot of patients being admitted, and a lot of them to tend to be older, that wouldn’t have come to this hospital 10 years ago, because it’s a regional centre now for thrombolysis for stroke and for primary stenting for MIs [myocardial infarctions]. So we get patients from [name of city], [name of city], you know, who 10 years ago would have gone to [name of hospital] etc. We’re getting those in.
C-03
The opening of the new university hospital is also suggested to have lured patients in:
I think or it would have been in line with the averages and in 2006/7 they opened a whopping, beautiful new hospital.
D-02
Targets and incentives
The strategy of using 4-hour targets has also been shown to increase admissions of very old people because they often present as more complex cases that take longer to understand.
Again I don’t know how that impacted on [D1-C]’s 4-hour targets. You know, somebody turns up in A&E and because it’s probably quite difficult to get things sorted out quickly, especially with the very elderly they just said ‘oh, we’d better admit them’ or they’re actually not very well but there hasn’t been a huge change and therefore they didn’t feel it safe enough to just send them back.
D1-A-01
It’s a target that overtakes anything else that seems to happen in this hospital. Rightly or wrongly, that’s the way it is and as such we’ve had everybody in reviewing it; . . . we’ve had a company called [name of company] doing some work with us on the front door to see if they can improve our performance. To date hasn’t shown much so far.
D1-C-04
Service innovation and pilots
Many of the respondents agreed with the information they were presented with on the increasingly ageing population and how this presents new challenges for the organisation of health care. As a reaction to this, many recognised that an increase in the integration of services and teams in the community would help deal with this. In D1 the ‘hub system’ was recognised as not effective, so the strategy changed to an integrated system through different funding arrangements:
We’ve certainly tried to sort it through reablement funding over a year or so back, we put well over half a million pounds or so into reablement services with a view to them working closer together.
D1-A-02
Funding for pilots has also been used to seek out more effective ways of preventing the admittance of very old people into hospital.
Pilot for urgent visits to residential care homes where if a request for a visit comes into a practice and it is deemed relatively urgent – so can’t wait till the next day or end of surgery – it’s passed onto another GP visiting service, who will go in within half an hour or so, and the idea behind that was to actually reduce the temptation for a doctor or practice to actually say ‘well, I’m sorry I can’t get there for 2 or 3 hours; phone 999’ and they’d get admitted that way.
D1-A-01
However, such pilots are not always implemented following their completion, and this is often because of uncertainties around the best strategy to use regarding staff:
Because the way it was set up, having fulfilled its aims – because one of the aims was also for the GPs to be able to educate the staff and so on but they found that for various reasons that didn’t work out and in fact the practice that’s been supervising it all has said probably using GPs is not the best way to provide that kind of a service.
D1-A-01
The overall consensus is that a main strategy is for staff to work together more as well as to provide specialist services for old people. However, there are concerns with the extra costs of having this service improvement.
So we have the gerontology strategy, which has a number of strands but, basically, one is rehabilitation including autogeriatrics, which we’ve gone some way to developing. The other is subspecialty rotas and rapid access clinics. Again, we’re not there yet. And then there’s the community strand – the care home support and that side of things. . . . But what we need to do is develop a geriatric subspecialty rota. So that there’s daily geriatric review, we need a daily rapid access clinic to pick up patients that could be seen via that route and we also want to convert some of the beds on the short-stay ward into short-stay geriatric assessment beds.
D1-C-02
We’re back to building individual relationships with the team leaders, the community matrons, the district nursing sisters and the GP practice. The downside for us, if it was a downside, is that – well, it’s been an upside and downside – it’s more expensive.
D1-B-01
Structures
Definition: how is the system organised? The way an organisation’s teams or services work with each other.
What we found:
Changes in community care provision
Changes in community care provision have led to reports of restricted access to certain packages of care for old people. Services are found to rely on multidisciplinary teams (MDTs) working together, and the lack of integration between organisations can prove troublesome:
Social care is fairly peripheral, I would say. I mean, most of it goes down the [name of organisation] route. I mean all care packages used to be provided by social services so you knew, if you needed a care package, it was social services. But now we’ve got this system whereby, if it’s a new package of care, it has to go through [name of organisation], which is funded by social services but is separate from them somehow. And [name of organisation] don’t seem to be able to provide the same packages of care that we used to get through social services. So, for example, if we need two carers four times a day, it’s virtually impossible to get that from [name of organisation].
C-02
Structure of GP practices and services
Within the community, GP practices were seen as an integral part of the structure of services that affected the quality and capacity of care for old people. If this was not felt to be reliable, patients were liable to go to the hospital. Key issues were around the number of single-handedly run GP practices, which may not be able to deal with fluctuations in patient demand, and this is also connected to restricted service hours.
We still have significant numbers of single-handeds.
D1-B-02
General practice [in D1] still closes on a Thursday afternoon.
D1-A-02
Out-of-hours services were also found to lack reliability, and once people have trouble accessing these services a deeper reliance on hospitals can be established because they know that someone will be there to help them.
People have learned that the hospital doors are always open. Out of hours also I think need to be quite strongly looked at because it’s got used to using the hospital as a resource rather than it being seen as a resource.
D1-A-02
Hospital size and amenities
The size and amenities of the hospital is also seen as an important structure, and since hospital services have been used more by old people there are processes that stem from its current ability to deal with demand.
One of the things that struck me when I first worked here was (a) how few geriatric beds and consultants there seemed to be for the size of the hospital and the catchment area. I mean I think when I did all my training in [name of city] and [name of city] had, you know, the catchment area was similar sort of inner city, similar sort of daily admission numbers and they had about six or seven elderly care wards and about 20 elderly care consultants. And here you’ve got like one plus one elderly care ward plus another sort of outlying elderly care ward and about five or six consultants and it just seems like woefully inadequate for the population and the catchment size and I think, you know, that has a big impact as well, because if patients aren’t, the frail older group that we’re talking about, if they’re not getting the sort of, because it’s as specialist as a cardiologist doing like a stent for an MI, is assessing a frail, older, confused, delirious patient. And if those patients aren’t getting the sort of specialist input that they need before they’re discharged then it’s sort of easy to see why they keep bouncing back again time after time. So I think readmissions are a big problem.
C-03
New forms of health provision in the community
As a reaction to the increase of admissions and the knowledge that the condition of patients aged 85 years and over will often get worse from just being in a hospital, some restructuring of health-care provision in the community has been implemented. The delivery of care in the patient’s home is seen as a suitable way to prevent the deterioration of health and a perfectly viable option given the skills of certain staff.
To try and maintain them in the home. It’s seen like a virtual ward. It’s an intensive input into those patients who would normally come into hospital. So we’ve got those in place. We’ve appointed senior nurses into the care homes to support – to do training with nursing staff to assess patients and to reduce admission to hospital. There are now three GPs who are salaried purely to look after the care homes in [D1]. So that’s been some good pieces of work around there.
D1-C-04
There’s a lack of understanding in acute hospitals that, actually, lots of things go out and the majority of care is actually given in the community. And it’s some very complex stuff. And that’s partly, I guess, our fault as well for not blowing the trumpet loud enough, but if you saw the complexity, particularly in children but in the elderly as well – the things that community nurses now deal with – it’s all acute, really complex stuff.
D1-B-01
Systems
Definition: the procedures and processes that characterise how work is to be done.
What we found:
Community systems
Patients are presented with a vast array of services to get in touch with, many of which change frequently. Given this complexity, patients aged 85 years and over may not be able to understand how to access them and may be deterred from trying to.
You know, the services are so complex that we as health professionals find it difficult and I think . . . for then, for somebody who is over 85 or not necessarily – for anybody I think it’s really difficult for them to understand where to go for help and, I think, so by default people know that this [A&E] is open 24 hours a day, you can literally just walk in and you’ll be helped.
D1-C-01
The other dynamic with that age group is, I don’t want to trouble a doctor. So they’re waiting until they’re actually quite poorly. So that’s the other dynamic.
D1-A-02
Family support in the community is also becoming more difficult to rely upon. These are important systems of care that in many cases work alongside professional care.
I mean we’d like more people with dementia to be able to go home, but there’s not the supportive service for them at home. You know and some families are saying I can’t look after them and that’s fair enough, I think that’s, we shouldn’t be pressurising them, you know, to say you’ve got to look after them if they’re coming home. There should be services available to look after people in their own home.
D1-C-06
In addition to this, some of the professional services do not have the resources to cater for all patients, and long-term packages of care often cannot be implemented.
What is borne out in the data is that if – we’ve got, at the moment – and it goes back to resources, sadly – we’ve got a palliative care team in the community that basically, because of resource issues, runs 5 days a week.
D1-B-02
If somebody who’s had a short-term package for up to 6 weeks for the reablement period, if they then need a long-term package of care – I know in the past that’s been very difficult. So I think there’s blocks both ends, so it’s not necessarily that they haven’t – they’re not trying to respond, I think it’s their capacity which has been so difficult and whether that just – I don’t know whether it’s processes, if you see what I mean, rather than the actual capacity that they’ve got.
D1-C-01
General practitioner service systems can have an impact on patient-centred care, especially if time is limited to 10 minutes per session and if there are long waiting times in the walk-in centres.
And the other thing again is the staffing of these situations, is one GP enough to be looking at the X amount of people and all that. He has 10 minutes when you sit down, you know, and is that enough to look at someone? Could there be an alternative situation where you have, in the old days when you were a doc, you knew your clientele and Mr O’Donnell called you, ‘oh he’s got such and such, I’ll go up and see him.’
D1-PPI
That’s why the A&E is getting so much because you can’t get near a doctor. You’ve got the walk-in centre, which we were there at the opening of that years ago. We always recommended people go there. I’ve since heard now you can wait 8 hours down there.
D1-PPI
The extension of access to services in the community has entailed more complex systems because of professional disintegration.
What we call it now is the community services pathway. So what happens is that there are really – there should only be one way in but, again, GPs wanted their own dedicated line – so there are two ways into the service: one is for GPs and one is for everybody else. So what we’ve got is, if a GP wants to make an urgent referral – I mean, they’ll use the usual referral mechanisms within their team, but if they want to make an urgent referral, something’s cropped up, what we’ve done is we’ve given them dedicated lines for their geographical or their cluster area, which is always manned. So they can ring up and a district nursing sister will take the referral and they’ll action it and they’ll sort out what needs to be done. And that’s immediate, on a daily basis.
D1-B-01
Systems in place to keep high standards of care in residential and nursing homes have not been supported, which may have resulted in higher admissions to EDs.
Well, maybe this particular problem goes back into the fact that the inspections of homes have been diminished, diminished by government policy, by not adding to, firming up on the inspection. If you inspect a home properly you would then look at staffing levels, training levels and feeding and whatever, medication, particularly the application of medication. That’s extremely important. But the culture that’s being encouraged in this country at the moment is that you get away with what you can so that you don’t have to cost so much so you’re making the profits.
D1-PPI
Accident and emergency in practice and discharge from hospital
There are a number of systems in place in A&E to make sure patients go to the right place quickly. Many older patients are admitted because of the fragility and complexity of their condition. The acute medical service takes up to 60% of people from EDs, many old, because of this.
I think most of us would want to accept them, because we end up inheriting most of them anyway, it’s just 3 days down the line and they’re sicker or, you know, you thought ‘if I’d have known about this patient earlier I could have stopped that drug, I could have done this, I could have referred on to this or whatever’ and it’s just a bit too late often, yeah. So I’m, you know, the more I think about it, the more I think that system is in part responsible for our increase in lengths of stay and complication rates and readmissions and things.
D1-C-03
We are, it’s been a bit of a Cinderella service and we’ve not really, you know, like in ED you’ve got people who look at stroke. You’ve got cardiac practitioners. You know, and then obviously you’ve got a response for stroke, but those kind of things people see straight away and it’s like a big thing, we’ve got to get this done, but older people, they’ve just been seen as like ‘well, we’ll pass them through the system’, but having somebody who understands that would be better and there is a lack of that definitely.
C-06
There are issues around the discharge of patients aged 85 years and over because they are often in a very fragile condition. This challenges the professional understanding of what a ‘safe discharge’ is, and there are also issues around professional disintegration making safe discharge more difficult.
You know – I don’t think a safe discharge is something that exists for older people. Because these people are frail, elderly, they risk a fall . . . You know, you could keep them in for 6 months; send them home; 5 minutes later they fall over. You know, you cannot sort of stop some things happening.
C-02
Once they get in hospital, it’s very hard to turn some of them round because the care homes say they need to come and assess them, the packages of care stop and so all the relatives say, ‘Oh, you can’t possibly send them home; they’ve been struggling for months.’
C-02
. . . and you’ll have someone on a ward, say even cardiology, say, cardiology is the place to be if you’ve had a heart attack, but it’s not the place to be if you want your discharge plan sorted out, is it? Because they just, they look after the heart but don’t see the rest of the person.
C-05-A
Technology systems to support integrated work practice
Technology is seen as an important tool for facilitating collaborative work, integrating teams and providing the delivery of services and care for patients of all ages. When it was brought up in interview, respondents recognised both this and the challenge of harnessing opportunity for things such as the single patient record; for example:
We put IT systems in in the health service, and have done for years, and never train anybody, and then wonder why they don’t use them.
B-01
And we’ve not got a very good system ’cause they can’t look at our system so they don’t know whether they’re known or not, ’cause we’re separately entities so the NHS IG [information governance] doesn’t allow you to look at other people’s computers, which is completely potty. So unless they actually talk to the matron and say, ‘Is this patient known to you?’ . . . and often, obviously, their pressure of work means that they’ve just got on with the daily what’s in front of them rather than thinking ahead.
B-01
Not going to happen before I die. We haven’t even got a single record in our organisation, let alone across organisations.
B-01
And you’ve only to look at what the health service has done over the last 15 years: billions of pounds spent on IT systems that don’t [. . .] work, because everybody has an opinion and they’ll listen to every opinion. And there needs to be some benign autocracy around some of this. But, of course, no government will take on the medical body – even Margaret Thatcher didn’t take on the doctors ’cause she’d have lost.
B-01
However, there are some initiatives that present opportunities to overcome these boundaries, including the use of telehealth, which might be a catalyst to ingrate service and care for the over-85s in particular:
Developing the computer systems with something called ‘Script Switch’ so people were alerted to something that might be better value and things like that. Repeat prescription systems – so there’s all sorts of things. Not prescribing things that were ‘black listed’ or should we say of low clinical value.
D1-A-01
I think you could probably provide just as much with somebody in their own home if you’ve actually got the monitoring and whether telehealth will do any of that I don’t know – I think the jury is out on telehealth with regards – but that’s more for chronic conditions rather than an acute situation.
D1-A-01
We’ve still got a rapid response, single point of access call centre that we’ve introduced in the last 3 months from a previous setup where the ambulance service took the calls and did the triage. We do all that now in house, so we’ve now got a much, much more seamless service, ’cause it’s directly triaged by people who know the business. They can put a care package in within 4 hours. If it’s mainstream, that can be referred straight through with a single phone call and it’s on a workload management system as well – so it’s computerised so we can track it to the team that that patient relates to and to the GP that that patient relates to.
B-01
Shared values
Definition: what the organisation stands for and what it believes in. The characteristics that guide practices and systems.
What we found:
Community, primary and acute
Many respondents revealed that there has been a lack of communication between care providers. Certain roles were identified as key mediators between services.
I think from the community provision things did not go well because we’ve had a lot of problems – and actually probably still do have some problems with the partnership trust, you know, that runs the community services and they’re not – and it’s very difficult to get information from them. What has now changed is that we’ve got – literally in the last couple of weeks – have got integrated teams for our district nurses.
D1-A-01
The motivation for change is difficult to manufacture in some cases where providers have established norms. This challenges the shared values of the organisation in terms of dealing with higher rates of admission to EDs.
We’ve got a high proportion of GPs in [D1], I wouldn’t hazard to give you the proportion but it’s I think over 50% who have retired, taken their pension and come back. So there is no motivation for them to change at all. Some of them are quite old, and I mean in their seventies plus, they’ve been in [D1] for years, their patients love them but there is no motivation for them to change.
D1-A-02
Funding health
Some respondents commented on the issue of funding the increased demand for care, which raises interesting questions around what family-/friend-based care is worth to society in monetary terms. Shared values on the quality and style of care may be challenged, which brings to the surface the plethora of competing views on the treatment of older people and how much money they have to support themselves.
I think to some extent we’re coming across our own culture here and we’ve either got to agree to a much higher rate of taxation so that we can support people or begin to think, well actually whose responsibility is it? ’Cause I think personally we all see it necessarily that it’s the state’s problem rather than our problem and it’s not the state’s problem, we can’t afford it as a state. And I think we try to duck and dive and come up with all kinds of ways of meeting the demand that actually isn’t manageable because people are getting older.
D1-A-02
So there’s more people – I guess maybe linked with the age possibly or just that there are people with multiple comorbidities, complex home situations, lack of kind of family support I suppose, very sort of on their own – quite a lot of sort of vulnerable adult sort of cases or sort of possible safeguarding from the community and there are people – well, safeguarding and vulnerable is different, but the vulnerable sort of aspect of it you know when people are living in kind of poverty situations or you know especially this time of year and it’s to do with heating, water, all those sorts of things, well.
D1-C-01
Style
Definition: the cultural style of the organisation and how managers behave in achieving the organisation’s goals.
What we found:
Communication between services
A lack of communication is at the root of many problems, but may also be symptomatic of bigger strategic, structural and systematic issues that have been outlined. Nevertheless, the respondents recounted how these broader decisions affect the provision of care at the service delivery level.
Some of our biggest problems or challenges that we’ve got with the health economy is getting the communications right. ’Cause quite often people end up in A&E whereas if the GP, if the other professional had known these individuals were already known to a community matron or to a district nurse team, that sometimes could be avoided, and then you stop all the deterioration and the disorientation that happens particularly with the elderly.
B-01
Because of the funding issues, you’ll have very strict criteria from health saying ‘this person doesn’t merit having money from us’, they’ll go back to social services, social services are then having to pick up a bill, but they’ll go for the least expensive option because that’s their thing to do and they’re not saving money for health, because if they come back in again, it’s health that are going to bear the cost. So it’s not joined up and it’s everybody trying to, sort of, offload.
C-05-A
Communication with family
Some of those interviewed felt that it occasionally it was difficult to ask families to help because of cultural changes in how the nature of the service was understood and the expectations of it.
And people are frightened to ask family, you see, because we’re so turning to this service industry where they’re customers and I suppose they’re, you know, but actually why shouldn’t families take some responsibility if they’re able to? Because you get some families that are working so hard and never ask for help and others who, you know, won’t do anything, so there’s got to be some sort of joint working again, hasn’t there, in partnership in caring for the person.
C-05-A
People don’t want to wait for a GP appointment any more and they won’t tolerate certain things and whilst this is an elderly age group we’re talking about, which probably are more tolerant, their children and their carers possibly aren’t.
B-02
In the hospital
Following on from the shift in how patients and families wish to use health-care services, practitioners were found to fear the consequences of failing to meet those expectations.
I think there’s been a societal shift about what people’s expectations are. I think there’s been – I think some of this will be around the fear of litigation. . . . I think there’s a lot of junior doctors who are not supported in the way that junior doctors used to be. I think there’s lots of – so I think there’s a bit more absentee consultism. You’ve got lots more consultants around but, are they there? No. The Working Time Directive – I think all that, coming together, has conspired to underpin some of this stuff about ‘Crikey, we’d better admit them, just in case.’
D1-B-01
Well, there is a culture of admission in this hospital – again, it’s not unique to here, probably, but there is a culture of, someone comes to the front door, they see a junior doctor, admit them. They get admitted onto the ward; what’s the first thing a nurse does? Admits them. So, I mean, you know, if I go on a post-take ward round and see a patient that’s been admitted to one of these wards on the same day – you know – and say they can be discharged, the nurse looks at me as though I’m some sort of idiot – you know: ‘What are you talking about discharge? I haven’t finished admitting them yet.’
D1-C-02
Setting
Definition: the context in which the organisation operates.
What we found:
Site
Debates on the site of the hospital still reverberate through the organisation; differing views on where it should be located affect the cohesion of service provision.
There’s a lot of politics which goes right back to when this new hospital was built. Public and the PCT wanted it in the city centre; the chief exec at the time didn’t; it got built here. I think there’s a historical issue there. You know, there always has seemed to be a lot of politics around this place, particularly.
D1-C-02
So the relationship between primary care and secondary care or acute care has not historically been that good – is that what you’re saying to me?
I think that’s a bit euphemistic. [Laughter]
D1-A-01
Ease of access
The geographical location of hospitals, catchment area and expectation of service provision may influence the increase in patient numbers.
But again there’s a lot of other factors that come in to play for that, because I’ve heard like ambulance crews talking about like I’ll say to them ‘why have you brought this patient here, they normally go to X, Y, Z hospital’ and they’re like ‘well, you always have the shortest queues.’
C-03
I think at the end of the day some of it is just patient choice. They choose where they go, so maybe if they live this side of the city it’s easier to get here than it would be to get to the walk-in centre in town.
C-01
Staff
Definition: the numbers and types of staff within the organisation.
What we found:
Care home staff
There were a number of issues reported around the training, medical experience and expertise of care and residential home staff:
I think some of it might well be to do with the way that the local authority and the care home and residential home contracts run because I’m not so sure that they’ve been monitored through kind of good and clear performance management. I’m not sure that they’ve ever necessarily been set KPIs. So we know that what happens is that the nursing care residential homes are very often staffed by either part-timers or people who really don’t want the hassle. So if somebody gets quite ill their immediate reaction is to send them to hospital.
A-02
I think one of the problems that we’ve got is that a lot of people – a lot of these very elderly probably are being overtreated with medication, so that causes problems. A lot of them perhaps should have end of life care pathways, which are not in place, but I think one of the big problems though is actually the – when we’re talking about residential homes is they – they just don’t have staff that are trained and so, you know, if something happens their knee-jerk reaction is to pick up the phone and dial 999, which actually should be the last thing that they should be doing.
D1-A-01
The people that work in care homes often are untrained or unregistered nurses and, you know, some of them have not had that much caring experience and pay is not always great.
C-06
But the incentive, you’re right, there is an incentive for organisations to keep hold of people, right, but if that person gets to the end of their 6 weeks with an agency, we don’t – they don’t necessarily stay with that agency, but we’d review them, we’d put them back out to the market for like another provider, so there’s no guarantee of continuity . . . if I was running a provider I wouldn’t invest in staff training on the back of your annual contract, just wouldn’t do it.
D-01
Other comments regarding care home staff revealed that they were not supported very well by the other health-care service and practitioners, even when they knew that the staff are paid relatively low wages and have less medical expertise.
The care home staff don’t feel that they’re being supported by the local GPs to keep these patients out of hospital. So they’ll ring up and they’ll get through to a locum GP who’s like covering that patch and they’ll say ‘oh, I don’t know, just admit them to hospital’ sort of thing ‘I can’t be bothered to come in to the home.’ So they’re, I know that our region has one of the worst access to GP problems.
D1-C-03
General practitioner provision and specialisation
It was clear from the corpus of data that some barriers to GPs exist within the community. This may begin from the inception, when the telephone call is made, through to disparities in quality across the region, opening times, out-of-hours services and home visits.
It is not always the GP that takes the call, it’s the receptionist, and the receptionist hearing urgent will say ‘take them to the hospital’. So care homes over time have learned: don’t bother to ring the GP; it’s urgent; take them straight to the hospital.
A-02
And we also have – you know – inner city area, and some of the areas are extremely deprived, we do struggle to attract, I would imagine, the better-quality GPs in some of those areas. But we’ve got some very good GPs, as well. So I’d say it’s variable.
B-02
As a primary care system. Well, it’s increasingly difficult to get GP appointments; they very rarely go out to people’s houses.
C-02
So – you know – they spend quite a lot of time in education; their contract – they don’t do out of hours, da de da . . . You know, so I think the GP contract nationally has had an impact. So there’s less out-of-hours care, primary care. So of course they all pitch up the front door here . . . there’s a tendency to default to phoning for an ambulance, particularly if the GP doesn’t know the patient. You know, it’s easier for them to just say ‘phone an ambulance, come up here’. So we’re dealing with a lot of primary care in ED.
C-02
While it was clear that access to GP services was a problem, some respondents suggested that their medical expertise was good enough to deal with many problems, and that specialisation could increase costs and make health care more difficult to manage for older people.
You know, I don’t think you necessarily need to be expert in a subspecialty to be able to look after 99% of somebody’s condition.
D1-A-01
Increasing specialisation, subspecialisation is one of the difficulties that we’ve got.
D1-A-01
Interestingly, the specialisation of care around older people was not seen as a negative trend. Rather, the increase in numbers of specialist nurses and geriatricians in the community was seen as remedial to the problem of overadmittance of older people to EDs.
It would be much better to actually have specialist nurses involved in geriatric care to actually do that work instead.
D1-A-01
The geriatricians should be really should be almost based in the community.
D1-A-01
Community nurses and matrons
Similarly to the suggested increase in geriatricians, community matrons were seen by many to be useful because they could prevent admissions of older people, having a more detailed knowledge of patients’ conditions.
Our community matrons basically work with long-term conditions, predominantly the elderly and the more complex end. She will see somebody that she says ‘great, we can, you know, this patient will be better off at home; it’s in this patient’s best interest. Yes, I know this patient has COPD and the stats are low but this is normal for that patient.’
B-03
However, the relationship between community matrons was unclear, and this created some tensions:
We put three-quarters of a million pounds into district nursing, some of it was to do with the fact that GPs had become very focused on community matrons and we kind of moved away from district nurses to community matrons. Everything became community matron. And the community matrons weren’t necessarily getting into all the practices, didn’t have the capacity. And district nurses began to feel a bit disenfranchised.
A-02
General staff sourcing, training and integration
While there have been particular staffing problems and opportunities defined by role category, there were broader staffing issues that related to variance in character, work ethic, ability to source and cohesion of roles across the health economy.
You know, what I have found across the whole health economy is staff don’t grow on trees. It’s all very well, I mean let’s take the GP initiative. So at the moment I’m starting an out-of-hours GP service. Voluntary. These are GPs that some of them, most of them are on bank. I’ve only got a couple that are actually work within the trust that actually are trust contract. So I’m reliant on these GPs wanting to work in the out-of-hours service. I then need to now start looking at providing a service at [D1-C] which I haven’t been able to do for 2 weeks ’cause I haven’t got the GPs so I’ve just sourced them. Now if I’m asked to do GP drivers, paramedics, there comes a point where I haven’t got the resources. The same with nurses, you know. I mean not just nurses, AHPs [allied health professionals] as well. They don’t grow on trees and I think that is something that needs to be, so it’s all very well as a commissioner to say ‘here we are, I’m giving you some more money, go out and get two more move on co-ordinators’. Well, I can’t find them. They’re not out there. So then, social care, can you provide somebody? Yes we will. Three months down the line they haven’t. Then it’s ‘well, we’ll provide somebody but can they run it as a clinic. Can I come and sit there as a clinic?’ No, I need you out there in your car visiting patients and moving them on, supporting them, making sure the goals are reached, working with the physios, working with the carers, working with the family. And then again we’re back to cultures.
B-03
The disjointed service provision, while useful for organising to one standard, has implications for patients who challenge existing professional paradigms.
What we’ve realised, I think, is that as a nurse on a hospital ward – and certainly this would be my experience when I worked in hospitals – you have very little understanding of what district nursing colleagues can manage in terms of the complexity of a patient. So what we found was, looking at a piece of work, actually, that was done at [name of hospital], is that you would say to – if you had a patient in front of you with all the details, etc., a district nurse would say, ‘We can manage that’, and a hospital nurse would never have thought in a million years that they could manage that patient.
B-02
Skills
Definition: the distinctive capabilities of personnel or of the organisation as a whole.
What we found:
Holistic aprroach and communication
It was recognised by many respondents that the care of older people is complex and requires a great deal of specialist knowledge and skill, especially when it comes to patients suffering from dementia.
It’s very complex and you’ve got to have a very good knowledge of physical as well as mental and psychological and I think a lot of the problems we’ve had here is due to not being holistic, people seeing delirium very much as a mental health problem, because most of the patients we see are physically unwell and I think a lot of the problems can be reduced if they really understood the person, the patient, so I’m really, that’s where my interest is, is trying to be therapeutic, isn’t it?
C-05-A
There are certain skills that can be practised effectively with older people if the right opportunities are provided within a role. Excessive medication and treatment was one key aspect of this shift in care for older people.
The gerontologists are very, very good and they know to talk to people, communicate with people and to find out how much people want. Not everybody at 86 wants to be, you know, have everything done to them. But I find in other areas it’s not so measured and it’s not so, it’s almost ‘this is our pathway for this process, so that’s what they’re on’.
C-05-A
D1 summary
| Dimension | Strong/positive type | Stems from | Influences | Weak/negative type | Stems from | Influences |
|---|---|---|---|---|---|---|
| Strategy | New recognition of strategic deficit by CCGs Increased provision of reablement funding and service innovation around care for older people |
Restructuring | Commissioning | Unaware of overall strategy for unplanned admissions of those aged 85 years and over Changes in leadership roles and regional strategies occurred too often Targets and incentives, such as 4-hour target, may increase admissions |
Lack of consistent leadership Communication across region poor National strategies |
|
| Structure (of care system) | New forms of health provision in community, e.g. virtual wards being supported | Increased funding | Community care provision is hampered when multidisciplinary teams cannot function Structure of GP practices: many singledhanded, which relates to trouble in managing service hours Hospital amenities for older people limited |
Changes in how packages of care are delivered. This can involve new organisations funded by existing trusts Existing style of work is less flexible to modern challenges |
Limited forward planning on the detail of new work connections Reduction in family support and out-of-hours care |
|
| System (processes) | New services being piloted using new technologies | Recognising opportunities for change | Overcomplexity of community care. Patients are confused by the ever-changing numbers and names of services Systems to support and work with family carers could be improved Lack of resources to prevent patients bouncing back into A&E GP waiting and opening times Quality of care in nursing homes reduced Concept of ‘safe discharge’ inadequate for very old patients Inadequate technology systems |
Design and communication of community services not as well supported Lack of funding Existing work style and culture Diminished care home inspections Existing style of work with very old people Technology incompatible, knowledge sharing challenged and lack of training |
Recognition of service user perspective lacking Government policy not implemented to define standards |
|
| Shared values (for system working) | Poor communication about community provision between trusts and providers Age of GP can be found to influence motivation for change |
Established culture of work | ||||
| Skills | Gerontologists have a very good skill set for dealing with very old people | |||||
| Style | 2010 NHS reforms on clinical leadership associated with positive change | Challenging to engage the right staff earlier before admission Change of culture of service user families around the expectation of provision In connection with this culture is reactive culture of admission by practitioners |
Contact between services is poor, patient described as being ‘offloaded’ Societal shift in family composition and geographical location |
Too much of a workload to cater for the demand Setting issues around wealth and family values |
||
| Staff | Community matrons instrumental in preventing admissions | Care home staff claimed to be underskilled Care home staff not supported by other professionals working in the community Overmedication by some staff can lead to falls and medically it is unclear what the correct policy is on this Access to GPs increasingly difficult Recruitment of good staff in deprived areas |
||||
| Setting | Existing political issues around the location of the hospital still cause problems Historically the relationship between primary and secondary care has not been good Ease of access might push up admissions |
Site report for D2
Setting
In D2 the rate of unplanned admissions for those aged 85 years and over increased between 2007/8 and 2009/10. Subsequently there has been a decrease in the rate.
Data analysis
The transcribed data from the 17 interviews, three focus groups, field notes and reports were analysed by the research team and the key themes were identified, agreed on and coded against the McKinsey 7S model.
Hard elements
Strategy
Definition: what is the purpose or goal of the system/organisation?
What we found:
Focus of strategy
In the strategy for 2005–9, it seems that the focus was on reducing length of stay rather than reducing admissions to hospital.
Bringing down length of stay is a definite strategy . . . the direction of travel for hospitals is exactly what we are doing, which is shortening the length of stay and having more zero length of stay and far fewer long-stay beds.
Participant 5
Other respondents were unaware of any policy on unplanned admissions, and felt that the focus had been on delivering the trust’s Healthy Futures strategy.
The focus from an organisational point of view around strategy has been based on Healthy Futures. That has been the trust strategy.
Participant 6
Development hampered by restructuring and regional projects
Reference is made to the frequent reorganisation and restructuring. These may have distracted attention from core business, as this quote illustrates:
Everything was restructured about that time.
Participant 3
Respondents felt that regional projects were hampering the development of a local strategic plan and reducing the focus on local issues.
But the downgrading of [a previous A&E facility] to an urgent care centre was on the back of two massive [name of city] projects – Healthy Futures and Making It Better. Obviously Making It Better was the paediatric . . . review and Healthy Futures was medical surgical, etc. So really it wasn’t led by us as an acute trust, it was these two massive regional projects.
Participant 6
Joint working
Interviewees felt that the rate of unplanned admissions was attributable to lack of partnership between organisations and called for greater unification and integration.
I don’t think it is managed very well really in this area [unplanned admissions], which is one of the reasons why you see relatively high admission rates. And I think part of the reason for that is because there are separate organisations each with their own agendas and each with their own pressures, OK. I think if those organisations, you know, particular health and social care, were to be unified or have much more, sort of, closer working, then that would remove some of the barriers which are occurring. Now, you know, over the years, we’ve always had fairly good relations with social care, to be quite honest anyway, but what we have to acknowledge is that they are under even greater pressures than we are and, to be quite honest here, I mean, I said it before and I’ll say it again, I think money is inappropriately tied up in health care which should be going into social care which would, you know, fund a lot more care in the community than, you know, persons stuck in hospital and we need to – and we also know that there’s double the number of hospitals in this region than there should be.
Participant 5
Response
In 2010 there was a change of direction resulting in more investment in community services and hospital prevention initiatives which have a strong social element to them; for example, the Partnerships for Older People project was launched, aiming to reduce social isolation and prompt independence. More recently there has been joint working on the dementia strategy and pathways.
I know strategically the service directors and director are working on that relationship and bringing that together better.
Participant 2
Structures (interactions between components of system)
Definition: how is the system organised? The way an organisation’s teams or services work with each other.
What we found:
Lack of partnership working
This was the main contributory factor that had a significant role in the increased unplanned admissions from 2007 to 2010 in those aged 85 years and over. Respondents expressed their frustrations about the lack of collaboration between the NHS trusts in the region, as this quote demonstrates:
I think we have worked as three separate organisations, there is absolutely no doubt about that. I don’t necessarily think that we’ve worked together as we should . . . we are massive and so complicated, it’s difficult for us. If we had one trust and one PCT and one local authority it might be slightly easier but we’re not in that position.
Participant 6
Systems
Definition: the procedures and processes that characterise how work is to be done.
What we found:
Ambulance trust
Throughout the transcripts it is apparent that more engagement is needed at the ambulance and acute trust interface, as this quote illustrates:
I think the other thing that we need to do is change massively [name of ambulance service]’s approach to how they deliver our patients to us [name of trust] because we’ve got the wrong people going to the wrong place.
Participant 6
Community services and intermediate care
These had been substantially restructured since a new provider took over community services. It seems that initiatives have been launched, such as STARS, which has 80 care staff and provides up to 6 weeks of care. It is an urgent community-based service and accepts referrals from the hospital discharge team. The service is available for people over the age of 18 years. However, some initiatives have been described as ‘a bit piecemeal – only happen on one site’ (Participant 6).
There have been some changes at the intermediate care level:
We had 20 intermediate care beds across two of the local residential homes. And health staff put the therapy in. We also had a hospital avoidance service which was rapid response and we had nurses and therapists working in that service and we took all referrals from GPs of people who they were trying to avoid admission to hospital. So they were sick and we did the hospital avoidance. We linked into the A&E department, did all the assessments on A&E, medical admissions units and those type of patients. I also had attached to my services the hospital discharge co-ordinators. They were part of my service; I was responsible for hospital discharge processes. And also, in my early stage, when I went into intermediate care, I developed the care – the community matron role in [name removed] and [name removed].
Participant 1
It seems that more investment in community services is needed in order to reduce delays in discharging patients:
they didn’t have any capacity to step down any of the patients.
Participant 13
Out-of-hours general practitioner services
The variation in GP cover and provision was highlighted as a contributing factor to unplanned admissions.
I think it’s locality based because we’ve got a different rapid response from [D2B] and I think north will be different as well.
Participant 13
Soft elements
The soft elements of the 7S model are less tangible and more influenced by culture. These soft elements are as important as the hard elements if the organisation is to be successful.
Shared values
Definition: what the organisation stands for and what it believes in. The characteristics that guide practices and systems.
What we found:
Culture change
It was expressed that the culture within NHS Trust needs to change, to become more team focused.
I think the culture needs to change, we need to get a different culture, certainly in the trust where they’re more open to listen to issues and try and work together to resolve the issues, rather than a blame culture. We need to tackle things as adults with each other, so if there’s five [D2-CR] patients block, why don’t they just contact them and see what we can do about it, what together can we do about it?
Participant 1
Style
Definition: the cultural style of the organisation and how managers behave in achieving the organisation’s goals.
What we found:
Discharge and community link
There was a pressure to discharge patients, but the linkage between the hospital and community needed to be enhanced, which happened through the re-ablement team.
It’s more about getting out of hospital, I mean, we don’t have any reason, I suppose, to be monitoring hospital admission in a way, I mean, we know that we obviously get pressure from hospital discharge team, you know, well, we have hospital discharge teams who are linked to the hospitals and they will be under pressure if people are in hospital when they shouldn’t be, you know, so it’s about that getting them out appropriately and with the right services so they’re not representing, you know, we’ve got responsibilities there and that’s what, you know, again that’s why, sort of, the reablement-type services assist us.
Participant 2
Clinical leadership
The 2010 NHS reforms changed management styles in the NHS commissioning organisations from being managerial/business-led to being clinical-led. This change has been welcomed and has led to greater collaboration between the acute trust and CCG management:
the senior management of the hospital had met the CCG management and they got the impression that there was a much more co-operative feeling, much more possibility of negotiation and so on.
Participant 20
Primary and secondary care
Respondents felt that pressures on primary and secondary care had caused a division and that perhaps adopting a collaborative approach might be a way forward in terms of improving services for patients.
Primary/secondary care divide I think the collaborative view of clinicians working together, the patient’s best interests has been sequentially lost and I think that the current set of reforms will do nothing to make those any better . . . When I arrived in ’95 there were regular meetings between primary and secondary care, where there were educational meetings, or whatever meetings, where you could meet and talk to GPs and GPs could talk to hospital consultants, specialists and services. What has happened since then is that each group has had a huge pressure built upon them.
Participant 7
Staff
Definition: the numbers and types of staff within the organisation.
What we found:
Level of staffing
Concerns about staff levels were highlighted in the interviews
And all we get told all the time is, ‘Oh, well, we’ve no staff’.
Participant 8
Medics
The role and the numbers of A&E consultants are pivotal to admission rates and to ensuring that the skill mixture keeps staff from being put under too much pressure, as this quote demonstrates:
Think workforce issues are a constant pressure and they’re actually often why services don’t deliver, right. So, you know, for instance, our A&E department, we’ve lost a couple of A&E consultants, right, which means that there’s fewer around and that puts pressure on the department and, you know, that can affect your outcome data and stuff like that . . . when you’ve got workforce pressures, it means that things aren’t done as slickly as possible so length of stay goes up and when that goes up then it just incurs, sort of, problems, you know, and that can back up to the, sort of, A&E and you then trigger long waits in the A&E.
Participant 5
Response
Since 2009, consultant cover and hours have increased, and there has been discussion of widening their remit to include an outreach service.
So we’ve been allocated more consultants and the medical division have seen that as having a senior position at the front door 7 days a week. You know – they work till 9 o’clock at night now, where they all finished at 5 before, so there’s senior cover on the shop floor, so they’re there for advice and – you know. And the same on the MAUs [medical assessment units], as well, that we’ve got – you know – a more senior consultant where we’d have one or two and you’d have a middle grade doing a – we have consultant ward rounds all the time so you’ve got a senior person seeing the – making the management plan and making decisions.
Participant 8
[Name of town] PCT are looking at an outreach service now, so we’ve got [X] consultants at [name removed] looking at doing it now.
Participant 7
Community matrons
Generally community matrons seemed to have a central role in care provision for the frail older adults, as they provide a community step-up service:
So it might be that when the doctors see somebody at home and think ‘hang on a minute, they’re not stable’ they might refer to the community matrons themselves.
Participant 3
Social workers
Social workers have faced a number of challenges and their role and remit has changed considerably:
The proposal is they’re making redundant (xx) social workers across the borough, so the proposal is they’re going to go from [xx] posts to [xx] but they are going to recruit unqualified workers into the gap. So it’s not losing any numbers, it’s changing the skill mix.
Participant 3
Geriatricians’ remit
There were calls to have specialist mental health geriatricians with a remit to cover acute and community care. This would help to reduce admissions.
I mean, I don’t know whether we have it or not, but do we have like a geriatrician who would, who specialises in like mental health, you know, that type of role because we get an awful lot of confused people, they’re not confused because they’ve got a UTI, they’re just confused generally. So, I mean, but I don’t know whether that’s a psychogeriatrician in the community, that kind of service, that would be helpful.
Participant 7
Skills
Definition: the distinctive capabilities of personnel or of the organisation as a whole.
What we found:
Community matron and geriatrician numbers
It is evident that there has been investment in geriatricians and community matrons. The respondents expressed the view that both professional groups have an important role in the future care model for older adults (65 years and over).
We’ve appointed acute physicians with a background in geriatrics and they, sort of, give, sort of, community sessions as their sort of specialist interest. So what we’ve done is tried to create a model which we think will probably be the future model for a lot of areas because long-stay beds will decrease, so you won’t want your traditional geriatrician any longer, 60% of hospital admissions are in the over, you know, 65 age group so, you know, actually you want more geriatricians on the acute medical unit.
Participant 5
. . . like the medical division have invested in the matrons who are clinically free to be able to go and support the ward managers in issues that they’re struggling with.
Participant 8
Other factors
Some emerging important themes are relevant characteristics that interviewees felt influence admissions rates and are beyond the 7S framework.
Social
Social aspects, such as where people live, level of deprivation, access to transport, support links to family and friends, played an important role in people’s health and well-being.
I think the key challenge in this area is, one: the deprivation. The deprivation is significant; it is very significant and I think part of what goes with that is that there is reasonable community support for the elderly people in that their families live close by but the families as well are deprived; they don’t own cars and things like that; so when problems start to happen I think quite a lot of the families don’t have the ability to get the information that they need; I don’t think they have the ability to access support and the services as well as the worried well; they don’t have that, so crises happen, I think, more than they do in other areas; I mean that’s my thought on it.
Participant 10
D2 summary
| Dimension | Strong/positive type | Stems from | Influences | Weak/negative type | Stems from | Influences |
|---|---|---|---|---|---|---|
| Strategy | New projects that have a strong social element to them | More investment in community services (2010) | Governance | Reducing length of stay instead of admissions Unaware of clear strategy on unplanned admissions Frequent restructuring at different organisational levels |
Emphasis on quick fixes rather than sustained improvements Lack of strategic communication at regional level |
Lack of investment and planning Constant change and uncertainty in funding |
| Structure (of care system) | Lack of partnership working Poor integration between primary care and secondary care |
Lack of strategic planning Organisational barriers between system actors |
Reduced communication between staff at executive levels | |||
| System (processes) | Some restructuring has provided new assessment and reablement services | Recognising opportunities for change | Structural change in primary and social care | Lack of integration between ambulance and acute trust interface New projects are sporadic – lack of system consistency Varied out-of-hours services |
Troubled design of processing structural change | Shared values |
| Shared values (for system working) | Culture was not team focused Blame culture too apparent |
|||||
| Skills | Skills of geriatricians and community matrons very well utilised | |||||
| Style | 2010 NHS reforms on clinical leadership associated with positive change | Pressure to discharge was matched with effective team linkages Pressures have been seen to increase the divide between primary and secondary care |
Not enough team meetings Not enough meetings between primary and secondary care providers |
Increase in workload | ||
| Staff | In 2009 there was an increase in consultant allocation to A&E Community matrons provide a key mechanism for reducing unplanned admissions |
Funding reallocation GPs allowing certain professionals to have patient contact and care provision |
There are not enough staff Poor skill mix of staff – reduction in A&E consultants Defining role boundaries is a constant issue |
Lack of investment in community staff | ||
| Social | Evidence that areas of deprivation in the region make it very difficult to combat health problems |
Site report for D3
Setting
In site D3, the rate of unplanned admissions in those aged 85 years and over rose from 2007 to 2010 and then stabilised over the next 2 years (2010–12). Rates for ACSCs rose in 2010–11 but are below the national average. The proportion of 1-day admissions has consistently been above the national average. GP access survey results are worse than the national average. This led to the PCT commissioning a report from the Primary Care Foundation.
A hospital was opened in 2002 and provides community health services for the county but not D3. The hospital includes a consultant-led ambulatory care unit (10.00–18.00), opened in 2011.
In the past there was close working between the PCT and social services, with a range of intermediate care provision, but this was reconfigured in 2007–8, moving from a consultant-led to a nurse-led service.
A social enterprise organisation was set up in 2011, incorporating many former staff from the PCT provider arm and adult social care. It provides community health and social care with a SPA, including the community intermediate care (crisis team), community matrons, the out-of-hours GP service and an intermediate care unit (urgent care centre) based on the hospital campus. Another social enterprise provides a walk-in centre based in the town centre.
Comparing the organisations’ functioning in the first 3 years with that in the subsequent 2 years will identify the key changes that produced the beneficial outcomes.
Data analysis
The transcribed data from the eight interviews, field notes and reports were analysed by the research team and the key themes were identified, agreed on and coded against the McKinsey 7S model.
Hard elements
Strategy
Definition: what is the purpose or goal of the system/organisation?
What we found:
Lack of strategy and investment in primary care
This factor may have contributed to an increase in unplanned admissions from 2007 to 2010 in those aged 85 years and over. This was reported by the Primary Care Foundation and echoed in the narratives:
There’s been underinvestment in primary care, there hasn’t been a clear primary care strategy . . . there is a view that there’s been underinvestment in primary care local enhanced services compared to other places. So the other thing coming out from the Primary Care Foundation was actually our GPs seem to work a lot harder than others; now that begs the question: was that effective?
Participant 3
The amounts of funding [for primary care] have not shifted over the last few years and our ability to develop those things is constrained by some of the other changes. You know, it’s a perfect storm.
Participant 1
The respondents were unaware of any organisation’s policies for unplanned admissions for people aged 85 years and over.
I don’t know that we’ve had a specific policy. Are we expected to have had specific policies for the over-eighty-fives? I mean, I’m showing my ignorance here.
Participant 5
Change in population
Interviewees felt that the increase in acute admissions (2007–10) was in response to an ‘increasing population (including the elderly) . . . so, overall, there has been just an increase in numbers. So, I mean, I suspect the increasing admission rate has as much to do with that’ (Participant 1). However, the specific health need of those aged over 85 years was recognised by the NHS organisations and social care, which reacted to the increased demand by prioritising it as a concern and undertaking work to address the need.
Response
In 2008, the [D3] Strategic Partnership, in which NHS [D3] plays a full and active role, agreed a partnership agenda with the council and produced a joint strategic plan. This outlined the partnership’s ambitions, areas of priority and plans in order to improve health and care for the population of D3. In this strategy document there is a section dedicated to people who are older, placing an emphasis on preventative care, where GPs, Age Concern and telecare have a role. This change of direction may have contributed to the decrease in unplanned admissions rates in those aged 85 years and over in 2010–12.
Strategic development hampered by frequent reorganisation and staff changes
Throughout the transcripts reference is made to frequent reorganisation and restructuring. This may have distracted attention from core business, as this quote illustrates:
I think the change we’ve had in the system in the 2 years as anything, you know, the eye goes off the ball and you start to internalise – And I think you know we haven’t been as engaging, as coherent as we could have been with all our . . . That’s just the way it is.
Participant 2
The reorganisations and restructuring have led to ‘constant change . . . the frontline, commissioners, GPs and community nurses are actually probably the most long-lasting members. Actually, the senior management have turned over repeatedly’ (Participant 1). Some interviewees felt that this change was disruptive: ‘the last thing you needed was yet another navel-gazing, internal reorganisation following the last navel-gazing, internal reorganisation following the previous one’ (Participant 1). Some also felt unsupported at a managerial/business level: ‘I’m amazed anybody in commissioning land are still – I’m surprised it hasn’t fallen over yet ’cause I don’t really know who the hell to talk to’ (Participant 4).
Targets and incentives
Commissioning decisions are influenced by nationally set targets and financial incentive schemes intended to enhance performance in certain areas. Some interviewees felt that this may have been an influence in decision-making about services.
So the elective issues held sway and older people’s services were part of the spectrum of service provision that was felt could be sacrificed because it didn’t meet a short-term or elective admission target.
Participant 6
Others felt that:
the criteria forces admission into an acute hospital, actually I can understand that because all the funding at the moment, because of the way the funding streams work ends up in the acute hospitals because of PbR and actually that’s part of the problem. The whole incentivisation strategies around admission work in the wrong way.
Participant 4
Commitment to innovation
Although there is evidence of innovation, it seems that a lack of investment and commitment may have been barriers to new initiatives being fully implemented:
we’ve piloted lots of good things, but it’s been the usual story of just doing pilots and not doing them at sufficient scale, we’ve dabbled in things and haven’t really followed them sufficiently through.
Participant 3
Structures (interactions between components of system)
Definition: how is the system organised? The way an organisation’s teams or services work with each other.
What we found:
Community services provider
Community services were now being provided by a social enterprise (which won a Cabinet Office award). The provider has worked to make the system easier for GPs and others to navigate, and to integrate community services with primary care. Having a SPA was welcomed.
New community provider . . . they’ve embedded ways of working, roles of community matrons, crisis teams, step-up beds . . . elderly patient with multiple problems and that traditionally might have been an emergency admission, we would ring the . . . the crisis team, and you then get an experienced nurse team – sort of SWAT team of nurses and social care and they’d put a crisis pack in place to support the person either in the home or even with placement in a care home or – you know – for a crisis assessment . . . And it’s a lot clearer to GPs about how we access it now, as well . . . there’s a single telephone number.
Participant 1
Disconnection
Regret was expressed about the loss of practice-based teams, as this has left GPs feeling disconnected from other community teams. Having practice-based teams enhanced the sharing of information more readily with the MDT without going through the referral process.
We’ve now got all these different teams and people doing bits and they’re not based around practices . . . and being able to talk quickly to appropriate people that don’t involve 15 form fillings and referral processes and referral criteria. They just involve being able to speak to someone, hopefully colocated, that allows us to actually deal with the complexities.
Participant 1
Competition
It was stated that the PbR system is leading to competition between the community provider and the acute trust, whereas collaboration between the two would lead to a smoother transition of care for those aged 85 years and over.
There’s the conflict that [acute trust] wants the income through payment by results by bringing patients in, but then also it’s got to have a bit of an interest in seeing [name of community provider] fail because it could be potentially a competitor.
Participant 3
Alignment of processes
However, problems remain with integrating health and social care, leading to what one respondent described as organisational abuse, as highlighted below. This indicates that the two organisations need further alignment.
There is a game when it comes to the patients with dementia to say ‘ah, is this a mental health issue or is it a social services issue?’ And both sides will then procrastinate or draw their heels in or wait for due process before they will work in the patient’s best interest. And for me this is a form of organisational abuse.
Participant 6
Admissions prevention initiatives
New technologies and care homes
The new community service provides support to care homes and the use of new technologies, both of which are welcomed by the interviewees.
They’ve got community matrons and nurses that go into the care homes to training and support, the crisis team will even support people in a care home.
Participant 1
[Name of community provider] have been really quite successful in terms of managing using telehealth as an enabler with their community matrons. And we know that this period of time also is that we started to get the sort of very high, intensive user list out fortnightly.
Participant 1
Risk profiling
Recently GP practices have been receiving information on their patients’ activity at the hospital, such as A&E attendances. This has helped GPs to identify patients who might be at an increased risk of attending A&E in the future. This information enables GPs to develop various interventions aimed at reducing hospital activity. It was felt that the innovation was successful but more work was needed on walk-in-centre data.
We’ve been doing a lot with primary care, which hasn’t been happening before, that is starting to change behaviours, we are starting them – they now get daily information on their patients’ activity with the hospital, so they get to know who’s been admitted the day before, they get to know who’s been discharged the day before, they get to know who’s been an A&E attendance, we’re hoping that they will get data on who’s been to the walk-in centre, but the walk-in centre doesn’t collect the information in the same way as the rest of the health system does it, but we’re trying to get that data. We are getting the data from our community provider in terms of the patients who are now on the virtual ward.
Participant 3
Intermediate care centre
In addition, the community matrons have been admitting patients to the ICC, as they have access to five beds. The matrons are admitting patients who do not necessarily need acute care but need monitoring for a short period of time, and they are leading on virtual wards.
Relationship between primary and secondary care
There were obviously problems in the interface and relationship between primary and secondary care. Addressing these could facilitate further reduction in unplanned admissions.
So you’ve got a big divide: primary care good, hospital bad. Actually you’ve got the skills between the two that actually could solve the problem. And it’s breaking that kind of, some of those kind of cultural barriers really that we’ve got. So you mention certain GPs’ names in the hospital and they groan, you know. And this is a really . . . a bit fortress, [place name], so they see everything as needing hospitalisation.
Participant 4
Systems
Definition: the procedures and processes that characterise how work is to be done.
What we found:
Ambulatory care centre
The ambulatory care centre was established in 2011 (and won a national award). Situated next to the ED and taking GP referrals, the centre offers an alternative to an inpatient admission. There is a consensus that the ambulatory care centre has been a success in terms of reducing unplanned admissions.
. . . we’ve set up is an ambulatory care service. We’re only admitting 30% and we’re turning around 70% . . . and there’s very much an admission avoidance in that department, so admission is failure. That’s how they see it. We’ve been able to take out nearly 70 beds. The other way they can come in is through a GP phoning a consultant. The consultant can either give advice over the phone, therefore the GP doesn’t need to admit, or they bring them in to ambulatory care, do diagnostics and send them away again and come away with a management plan. And I think that’s what you see in there. I genuinely do. I think it’s having a big impact on us because they’re not hitting the hospital wards.
Participant 4
However, an interviewee, although agreeing that the ambulatory centre was successful at reducing admissions, questioned how relevant it was for very old people: ‘not terribly useful for the 85-plus group’ (Participant 1).
Community provider services
Intermediate care centre
This had witnessed substantial restructuring since 2007, with the old facilities, which were based on three sites, being closed, and a new ICC being built on the hospital campus. There have also been changes within the intermediate care service, from being medical-led to now being more nurse-led. Some interviewees felt that this major restructuring led to the increase in unplanned admissions:
When intermediate care services became required [name] was well ahead of the game. So that had a big impact. And these are all geriatrician run and supported with some nurses . . . somewhere around 2007–8 they systematically closed them. They served three different functions. One function was for respite for very frail elderly people. It was felt to be a luxury provision and closed. The consequence of that was that some of these patients died. Some of these patients went into long-stay nursing homes because the carers felt unable to look after them any more without the support they were giving them, and a proportion then started to bounce in and out of hospital. If the service that we had had been in place then, I think a significant proportion of those people would still be at home being supported as the families’ primary choice. And that was a mixed unit with physio, OT, social workers involvement, run jointly both by primary and secondary care. We had general practitioners with special interests working in that unit. And that again was a well-respected and a high-occupancy unit. The bottom line is that as the PCTs ran short of money these units were sequentially closed . . . which is why I’m not terribly surprised that when you look at the figures there has been a serial rise in hospital admissions.
Participant 6
And as the new hospital was being built it became clear that there was a bed shortfall and at relatively short notice the intermediate care centre was built, which was a 60-bedded unit built on the same campus. So I think that your admission rate, 2010–11, would tie in with the admission avoidance with frail elderly people not being admitted and going into the intermediate care centre.
Participant 6
Although the new ICC is on the main hospital campus, it is a separate building, and it was highlighted that there is a need for integration with the main hospital.
Last year with the intermediate care they decided, sort of slightly overnight, that it would be a step up – but of course they haven’t got junior doctors and, well, they stopped wanting to use ours and so they ended up having quite a few inappropriately too sick patients – And although they’re on site, you have to call an ambulance, although they’re only 20 yards away.
Participant 5
Assessment, investigation and triage needs to be in a facility where they have access to all the relevant up-to-date, investigative facilities. Patients going into ICC don’t have access to that. It’s a physically separated building. If you want an X-ray you have to book an ambulance to go across to get it.
Participant 6
The ICC also seems to have been hampered by changes in the referral process which were not communicated by commissioners sufficiently quickly.
They [commissioners] changed the criteria halfway through the year ’cause they were all step down at one point. Now they’re half step up, half step down. Didn’t communicate that with us. Their commissioners now have to come over to this hospital. Whereas before we could directly admit, they now have to come over and see whether or not they meet the criteria so we put yet another step in the process.
Participant 4
Concern was raised that care was time-limited by being focused on length of stay rather than patients’ needs.
I have a great problem if they’re saying ‘well, we’re going to have a rehab service of 16 days and once you get to 16 days you’re out’, which means that the moment you go in you’re planning their exit and you’re not actually planning what’s the matter with them and how you’re going to achieve your rehab smart goal. And that’s been one of the fundamental problems I have had with the way [name] have run. They run it according to the length of stay not according to patient need. I do not think that age discrimination is appropriate in this day and age. But if the PCT are the ones that are promoting it for their financial benefit there is a conflict of interest.
Participant 6
The walk-in centre
This is also considered to be successful at diverting patients from A&E and reducing unplanned admissions. However, there is concern about its location and its integration in the care pathway.
The walk-in centre seems to be incredibly successful and the activity in the walk-in centre is just growing and we’ve helped that by rediverting patients, which doesn’t necessarily help patient satisfaction because they turn up in [name] and then get pushed down to the town centre, so that’s not ideal. So I think we have go to think about how we use the walk-in centre and where it fits in our pathways in terms of the bigger picture.
Participant 3
Primary care
Access to primary care is a recognised problem, as reported by the Primary Care Foundation and demonstrated in the patient survey report.
[We are] doing some work about how we can improve access to primary care services, so that hopefully that will reduce inappropriate attendances at A&E and potentially some admissions into hospital . . . the Primary Care Foundation thought in terms of the patient satisfaction survey we were actually one of the worst that they’d ever come across.
Participant 3
Some felt that primary care in town was of lower quality than in the county, resulting in higher admissions, including at the end of life. There were also concerns about out-of-hours care, linked to underinvestment.
I think we see a great deal of admission here for things that actually probably could be managed better in primary care. And so you’ve got a different culture amongst the general practice there and you haven’t got such good out-of-hours cover so, you know, you compare [name] with [name] and you see quite different things in primary care, much higher quality in [name], much higher resources actually.
Participant 4
End of life care
Developing systems to enable people to make the choice to die in their own home was recognised as an area to advance.
. . . is that 70% of all people that die in [name] die in this hospital and that used to be the number, I’m sure [name] was the same, but they’ve now got it down to 40%.
Participant 5
I think the model that we’ve got at the moment doesn’t really help some of that end of life.
Participant 4
Inpatient bed management
One respondent felt the acute trust’s management of bed crises exacerbated the problem by producing a vicious circle of inefficiency.
When we get to bed crisis, and we’ve had bed crisis for all bar the last 2 weeks, patients go everywhere. And the moment they go everywhere your rates of flow go down and your levels of risk go up and your failures go up, so we then start to work in a very inefficient manner, which means that our rates of flow go down even further and, you know, how do we get, we should have our maximum efficiency when we’re under greatest pressure, which is not what happens. We’re at our minimum efficiency when we’re under greatest pressure and then people are surprised we’ve got a bed crisis. So what we need to do is to look at the processes in the hospital and channel them so that they are condition and age specific.
Participant 6
Soft elements
The soft elements of the 7S model are less tangible and more influenced by culture. These soft elements are as important as the hard elements if the organisation is going to be successful.
Shared values
Definition: what the organisation stands for and what it believes in. The characteristics that guide practices and systems.
What we found:
Avoiding unnecessary hospital admissions
There was an implicit agreement that avoiding hospital admissions in very old people was valuable and that community-based care is more suitable.
Acute hospitals are fundamentally not the right place for over-eighty-fives, they really are not because you’re packing – to put it bluntly you are, you’re body’s packing up at 85-plus, you’re aged, and therefore you’re going to have things . . . you’re far better in your home environment or in a supported environment that’s not hospital ’cause acute wards, they’re busy and actually they’re not the best places to get better. And I don’t feel we’re having that debate in a really imaginative way. But I’m just seen as a big bad [removed] of a hospital and actually I don’t believe in bedded models so I really think beds are the wrong places for a lot of the population actually but particularly the over-eighty-fives.
Participant 4
Focus on functional not chronological age
How a patient is functioning and their ability are just as important as their biological age.
So I think age alone is not a very useful marker of this. It’s about people’s ability and comorbidities and the complexity around their social situation that have much more effect.
Participant 1
Medical model and therapist nurse model
There seems to be a conflict between the medical model and the therapist nurse model.
Now what we did with those five [intermediate care] beds is that we almost wanted to distance the medical input, because what we, and this isn’t a criticism, but what both the nurses and the therapists were saying is, is that they felt that it was overmedicalised . . . what they did was that they did it from a therapist nurse model, because what the medics were doing, they wanted to investigate more.
Participant 2
A minority felt that frail older people were not given the same level of service, and that this was decided on the basis of the patients’ age.
I think that if you have two processes – no, let me phrase this the correct way. I strongly believe that frail older people should not be expected to go through a process that gives them a second-class service. So, whether you’re 30 or 90, if you’re ill you need to have appropriate assessment, investigation and treatment that is right for you. If that’s in a district general hospital, that’s fine. If it’s, you have your investigation treatment to go home, that’s fine. If it’s actually, you can be managed in an intermediate care centre, that’s fine as well. But that primary issue about assessment, investigation and triage needs to be in a facility where they have access to all the relevant up-to-date investigative facilities. Patients going into [name] ICC don’t have access to that. It’s a physically separated building. If you want an X-ray you have to book an ambulance to go across to get it.
Participant 6
Prescribing behaviour
There were concerns that the QOF system is leading to overmedication and to polypharmacy:
a lot of these people that are – this group have got cognitive impairment or dementia, limited social resource and ability to cope, and it’s not actually a medical response that’s needed, often; it’s actually the most important response is actually stopping half the tablets, ’cause that’s usually what’s causing them to be ill in the first place.
Participant 1
Conflict of values
Throughout the interviews it was highlighted that there was tension between clinical and managerial values within the acute trust and between commissioners and providers, as these quotes demonstrate:
I think we’ve got a dichotomy at the minute in the NHS around a business customer focus model around competition versus vocational public sector provision.
Participant 2
. . . the tension our providers have with us as commissioners and our clinical colleagues, we will have consultants sat in the room with us and they will say . . . ‘all you’re interested in is money’ and I’m going ‘listen, all I’m interested in is that you are creating an overdraft for us in effect and that overdraft over and above the activity I need as money to invest in the right places. You are sucking people in.’
Participant 2
I desperately look at them [name] and I’m hearing what I hear and I want to go to them ‘you’re going to have to pull your socks up. You’re going to have to really get a grip of this’ . . . we’ve now got a real, real problem in the system. I asked for all the escalation plans. I get a telephone message from [name] saying ‘well, it’s business as normal’. And I’ve gone back to them and said ‘it isn’t business as normal. Where’s your increased capacity? Where’s your extra social workers? Where’s your extra staff?’
Participant 2
The conflict between managerial and clinical values is echoed throughout the transcripts. Some interviewees felt that the financial incentives, such as PbR, are diverting the focus away from the quality of care that patients receive and their experiences.
PbR and the tariff has meant there’s very clear transactional costs, but actually it’s measuring the wrong thing. It’s measuring footfall across doorways rather than quality and passage of care. The system is more fragmented now than it was . . . going through McKinsey-style competency frameworks without actually addressing the real issues about patient care, experience, relational transactions, relational care that patients get and the feeling they have about their care and the empowerment about making choices about their care . . . get pushed to the side because of the transactional nature of the incentives in the system.
Participant 1
Monitoring regulation and innovation
Interviewees acknowledged the need for regulation; however, they felt that innovation also has an important role and too much regulation could stifle that.
The problem is we’re being overly regulated now so we’ve got a really tight framework and they have a view about how that should be done, they’re like ‘monitor a lot now’, they’re accountants by and large, so they’ve never run hospitals in their lives and so the whole framework at the moment isn’t helping. And that’s what The King’s Fund are saying, so The King’s Fund are saying they’re stifling innovation.
Participant 4
Style
Definition: the cultural style of the organisation and how managers behave in achieving the organisation’s goals.
What we found:
Clinical leadership
The 2010 NHS reforms changed management styles in the NHS commissioning organisations, from being managerial/business-led to being clinically led. This change has been welcomed and several interviewees were hopeful that it would lead to a greater engagement with primary care.
. . . certainly with the clinical leaders that I, the GPs that I have most contact with, they are incredibly optimistic, positive and enthusiastic about the changes and thinking that yes they can really add clinical value and make a difference and that’s really good news . . . what we’ve been doing is obviously getting the CCG leadership on board because it’s their vision, their mission, etc. and they are definitely coming on and we’ve got some good strong clinical leaders around that, so that is definitely good news.
Participant 3
In addition, the change in management has led to a greater collaboration between the acute trust and CCG management.
The senior management of the hospital had met the CCG management and they got the impression that there was a much more co-operative feeling, much more possibility of negotiation and so on.
Participant 8
However, not everyone agrees, as there is some evidence of tension in the relationship between CCG commissioners and the acute trust. It might have been caused by confusion about role boundaries and CCG expectations of the acute trust. This has been attributed to the CCG feeling disconnected from the hospital. Perhaps a way forward could be adopting flexible leadership in order to engage with the different CCGs, as they are very different organisations.
[Name] is the head of the CCG there; he sort of sees the world as how he’s got to improve the hospital and he feels a bit of a disconnect and generally we’ll get a lot of stroppy letters from the [name] GPs telling us how we’re not measuring up to their high standards, whereas in [name] we’re more likely to have a dialogue. So . . . but I don’t – you know – they’re much harder to deal with, [name]. But maybe that’s the nature of the practices. Maybe people are different.
Participant 5
Clinical leadership of the ambulatory care services has been considered to be a contributing factor to the reduction of acute admission rates between 2010 and 2012:
it’s the clinical leadership in ambulatory care seems to have made that work.
Participant 4
The welcome change of management seems to offer inspiration in comparison with the previous managerial/business-orientated management style, which some interviewees considered to be ‘personality driven’ and hierarchical:
Which is really great so he’s providing a lot of leadership to our GPs, so in our vision and our strategy and our mission statement, etc., those are all being revamped under [name]’s championship, which is brilliant. Chief execs can talk a good talk but will it get down to the senior managers, down to the operational managers or whatever and that’s just, so that’s all down to personalities and managing how people behave in what’s not seen as their territory by others . . . it’s all tribalism and stuff, isn’t it?
Participant 3
Staff
Definition: the numbers and types of staff within the organisation.
What we found:
Community matrons
Generally, community matrons seemed to have a central role in care provision for the frail older adults, as their remit is wide. Their work seems to range from working with care homes – ‘community matrons and nurses that go into the care homes to training and support’ (Participant 1) – to supporting GPs to identify repeated hospital activity.
And at the minute that’s the only data that we’ve got to see any evidence of repeated activity with people. And that goes out to the community matrons and they will go through it based on the practices that they cover. They will then go armed with that information and they meet with the GPs and they’re saying, you know, look, did you realise this person and it interestingly was in 2000, sort of 10, 11, when we started to really focus on that information, there was one particular individual that not only got admitted something like 24, 30 times, he also attended ED 40 times. And it was around catheter care.
Participant 2
The matrons also have been advising and
. . . challenging ED, particularly the consultants. So the community matrons, we’ve got quite a lot of clinical management notes available to ED to say if this person turns up because the ambulance have brought them, because their saturation rate has reduced or something, read the notes, because their sats are always in their eighties and this is how we manage them.
Participant 2
However, concern was raised that community matrons’ capacity was being outstripped by the demand for their services, which could have an impact on their effectiveness.
The role of the community matrons came in, but they’re too few and they’re not based in practices directly. They’re based through [name] in an office. I know who our community matron – very able, very nice lady, but, actually – you know – you have to track her down. She’s dashing round like a blur, dealing with the cases, and actually not . . .
Participant 1
Geriatricians’ remit
Several participants felt that increased input from geriatricians would help to reduce admissions, but organisational barriers appear to inhibit their role in the community.
Geriatricians used to do domiciliary visits; you’d feel to speak to a geriatrician – they’d come in, you’d have a big conversation with them, they’d come in, maybe see someone at home and they’d say, ‘Well, I agree with you; it’s absolutely barking mad to do anything else; why don’t we do this, that and the other and don’t worry about it?’ Whereas, now, the only way you can do that is either by taking that risk yourself, or by admitting them.
Participant 1
We have offered to the PCT whilst they’re in their pomp as much geriatric cover as they wanted with community geriatricians and at one level, to be fair, they thought that was a good model, but it hasn’t really come to fruition. So we’re here, keen to offer geriatric in the community if that’s the way they want to go, but as of yet, they don’t have it in [name], they’ve got a geriatrician from [place] who they really love and want us to mirror that in the community, but [name] don’t do that.
Participant 5
Some respondents suggested that geriatricians could provide an outreach service to care homes, as this has been previously identified as an area needing support.
There’s an argument for getting more outreach from here in geriatric care out into care homes.
Participant 1
Fragmentation of primary care teams
There was an indication that primary care teams had become fragmented and disjointed:
We’ve now got all these different teams and people doing bits so that – and they’re not based around practices . . . bizarre fragmenting of continuing health care and social care. Well, what came in was the role of the community matrons came in, but they’re too few and they’re not based in practices directly.
Participant 1
Stability at senior management level
There are calls for stability at senior management level: ‘no one’s in place long enough’ (Participant 1); ‘I’ve seen out the acute sector, six chief executives. That’s in 18 years, our sixth one now. So the life cycle of a chief executive is necessarily relatively short’ (Participant 6). In addition to wanting stability, the interviewees expressed a desire for senior management to be committed to the organisation ‘because they [chief executives] have, come in, they’re like politicians, have to make a high impact in a short space of time and are looking to say “well this is what we can do to get a quick win” ’ (Participant 6).
Skills
Definition: the distinctive capabilities of personnel or of the organisation as a whole.
What we found:
Numbers of community matrons and geriatricians
It has been acknowledged that the demographic of the population is changing as people are living longer; consequently the skills mix of the NHS workforce needs to reflect this.
As a consultant base we currently have three whole time in what’s geriatrics, we have a vacancy which we have been unable to recruit to but there is a recognition that we are undermanned in terms of workforce for the geriatric population and we have funding in place for a further four geriatricians. So with a view to expand geriatrics from four to eight but we have been unable to recruit as yet and that’s a big issue.
Participant 6
We also recognise that we need to significantly increase the capacity of [name of community provider] as our current community provider to be able to provide more community matrons, to be able to provide more district nurses, to get the virtual wards working properly, etc. I don’t think [name] they’ve got the capacity to do all of the things we ask of them and they haven’t currently really got the information system to effectively manage themselves, let alone for us to use as commissioners to improve, so that, and they are getting a new information system. I think if we’re going to put the risk stratification tool in, it’s all very well putting a tool in, but you actually need something behind it to support it, so I think we will want some sort of case managers.
Participant 3
Summary
During the 5-year period from 2007 to 2012, NHS organisations underwent massive restructuring and change. Introducing change can be hampered by a lack of trust and shared values, and facilitated by strong clinical leadership. During this time there was a change in direction at strategic level, resulting in the launch of a new strategy produced by [D3] Strategic Partnership in 2008. This provided a strategic vision, with a focus on people who are older, which is system-wide. Previously there seemed to be a lack of organisational polices for unplanned admissions for those aged 85 years and older, and an underinvestment in primary care may have contributed to the increase in unplanned admissions. There may be an association between ICC provision and unplanned admissions: when the centres closed, rates increased, and then, following the opening of a new centre, rates decreased. When developing intermediate care, thought needs to be given to specialist geriatric input, location and organisational boundaries. The interviews refer to observational data that the ambulatory care centre has reduced admissions, but not all interviewees agreed.
D3 summary
| Dimension | Strong/positive type | Stems from | Influences | Weak/negative type | Stems from | Influences |
|---|---|---|---|---|---|---|
| Setting (context) | Increasing population of older people Health system reform and uncertainty Constant change in commissioning and service configuration |
Regional and national policy-makers ‘Wicked problems’ |
Strategy, resourcing, structure, systems | |||
| Strategy | Close working between PCT and social services | Recognised need to address health- and social care problems New funding opportunities for integrated working |
More recent changes | Elective care dominated service planning ahead of urgent admission Lack of explicit policy or strategy for over-85s Piloting of initiatives but no sustained change |
Commissioning strategy Acute care strategy Emphasis on quick fixes rather than sustained improvements |
Shortage of investment and planning for care for older people Constant change and uncertainty |
| Structure (of care system) | Consultant-led ambulatory care unit (10.00–18.00), opened in 2011 SPA and integrated care teams for community health and social care (recent) New community provider with embedded practices for rapid patient support outside hospital (recent) Better access to GP (recent) |
Changes in local care planning (recent) Service innovations and pilots that work |
Constant change in system structure and team configurations, including change in hospital sites, new intermediate facilities, shift towards more nursing care Lots of pilot change Poor integration between primary care and secondary care |
Lack of strategic planning Reactive strategy Wider system change Organisational barriers between system actors |
Integration and co-ordination of services Staff and skill mix Patient planning and care pathway |
|
| System (processes) | Reduced bureaucracy and streamlined information systems (recent) Integrated processes for SPA and associated services |
Improve integration | Structural change in primary and social care | Lack of integration between care processes, especially primary, community and secondary Difficult access to primary care (patient survey) Incentive systems encourage excessive medication and polypharmacy |
Structural change Persistent organisational and occupational boundaries Lack of primary engagement in service planning |
Shared values Teamwork Role of primary care teams in SPA and other services |
| Shared values (for system working) | There was an implicit agreement that avoiding hospital admissions of older people was valuable Emphasis on patient function rather than age |
Cultural and normative differences between primary and secondary care Conflict between the medical model and therapist nurse model Frail older people disadvantaged by care system Tension between clinical and managerial values for care system |
Sustained organisational and occupational boundaries Prioritisation of elective and non-elderly care |
Scope for integrated working | ||
| Skills | ||||||
| Style | Clinical leadership associated with positive change | Lack of stability and high turnover in senior management Lack of integrated working Emphasis on quick fixes rather than sustained improvements |
Constant change Lack of strategy Emphasis on quick wins |
Culture and values Service integration Strategy development |
||
| Staff | Community matrons have a central role in care provision for frail older adults, and supporting GPs to identify repeated hospital activity Consultant-led ambulatory care unit (10.00–18.00), opened in 2011 |
Turnover of senior managers and leaders Lack of geriatric health-care professionals in community Primary care teams had become fragmented and disjointed |
Lack of investment in community staff | Specialist input into strategy and process |
Appendix 4 First draft of recommendations
List of abbreviations
- A&E
- accident and emergency
- ACSC
- ambulatory care sensitive condition
- BCT
- Better Care Together
- CCG
- Clinical Commissioning Group
- COPD
- chronic obstructive pulmonary disease
- ED
- emergency department
- GP
- general practitioner
- HES
- Hospital Episode Statistics
- ICC
- intermediate care centre
- IS
- implementation site
- IT
- information technology
- MDT
- multidisciplinary team
- ONS
- Office for National Statistics
- PbR
- payment by results
- PCT
- primary care trust
- PMS
- Personal Medical Services
- PPI
- patient and public involvement
- QOF
- Quality and Outcomes Framework
- SPA
- single point of access
- STARS
- Short Term Assessment and Reablement Service