Notes
Article history
The research reported in this issue of the journal was joint funded by the HS&DR programme or one of its preceeding programmes and INVOLVE as project number 10/2001/36. The contractual start date was in September 2011. The final report began editorial review in March 2014 and was accepted for publication in January 2015. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2015. This work was produced by Wilson et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction
Since the late 1990s, a plethora of policies have emerged aimed at embedding public involvement within the NHS,1–4 and this impetus has been mirrored within health research within the UK. Researchers have increasingly been required through national governance frameworks5,6 to involve members of the public through working with them, rather than conducting research on them. This has been further encouraged through the integration of patient and public involvement (PPI) by most of the main UK funders of health research. 7 This drive towards public involvement in research is not limited to the UK; internationally there has been an increasing recognition of the importance of involving patients and the public in health-care governance and research. 8–11
The PPI in health has its roots in the increasing unease with and challenges to the medical institution. 12 The ethical argument for PPI grew and was taken up by policy-makers as characterised by the phrase ‘nothing about me without me’. 13 Politically, PPI is also seen as a way of addressing the democratic deficit by giving voice to the public in publicly funded health organisations and research. 14 In addition to the moral and political rationales for PPI, there are also a number of methodological claims regarding the positive impact of PPI in health research. These include increased relevance of the research through identifying research questions and prioritising research agendas, appropriate research conduct, addressing ethical tensions and matching research with policy objectives. 12,15–19
These three drivers have resulted in PPI being imperative for health research in the UK. However, despite this, PPI is poorly defined and conceptualised,20,21 with varied definitions and terms used to describe it. 22
Definition of patient and public involvement within the RAPPORT study
Within the ReseArch with Patient and Public invOlvement: a RealisT evaluation (RAPPORT) study, we define the process of PPI in research according to the definition offered by INVOLVE ‘as research being carried out “with” or “by” members of the public rather than “to”, “about” or “for” them’ (p. 6). 23 However, while the underpinning process of PPI is relatively clearly defined, albeit potentially not embraced or understood by the entire research community, the name is perhaps more contentious. INVOLVE and others24,25 use the term ‘public involvement’, as they argue this covers ‘patients, potential patients, carers and people who use health and social care services as well as people from organisations that represent people who use services’ (p. 6). 23 Conversely, others suggest that this fails to capture the ‘expert’ nature of the experiential knowledge brought specifically by patients or service users. 22 Equally, the connotation of passivity that the term ‘patient’ brings has also been criticised,26 as has the political dimension to the term ‘consumer’ involvement. 27 Jordan and Court22 suggest that controversy around the different labels used is unsurprising, as they are derived from a multitude of contexts and interests. They suggest that the term ‘lay’ is to be preferred, as it denotes a broader alternative perspective to that of the professional. What is clear is that no single label will be acceptable to everyone,28 and we took a pragmatic approach by agreeing with the RAPPORT PPI representatives what terms should be used within the report. We use two terms interchangeably: ‘PPI representatives’ to emphasise individuals undertaking diverse roles from patient representative through to a member of the general public, and ‘lay representatives’ to emphasise the overall perspective these individuals bring.
Rationale for the study
The relatively small amount of empirical evidence on the impact of PPI in research29 has been criticised as poorly reported21 and methodologically weak, often failing to fully explore the contextual factors surrounding PPI as a complex intervention. 30 Not only is there a notable lack of evidence on outcomes and impact of PPI,31 but what little there is tends to be observational evaluations which rarely consider the links between the context (when and where PPI happens), models of PPI (how it functions) and the outcomes of PPI (what difference it made). 32 As outlined in the next section, the RAPPORT study aimed to address these significant gaps in the evidence.
Aims and objectives of the RAPPORT study
The RAPPORT study sought to evaluate how different approaches to public involvement in research with different populations influence the identification of priorities, research conception, design, process, findings and knowledge transfer. Specifically, it aimed to identify what PPI approaches have applicability across all research domains, which are context specific and whether or not different types of public involvement achieve different outcomes for the research process, findings, dissemination and implementation of PPI. The RAPPORT study objectives are listed in Box 1.
The study objectives were to:
-
determine the variation in types and extent of public involvement in funded research in the areas of diabetes mellitus, arthritis, cystic fibrosis, dementia, public health, and intellectual and developmental disabilities
-
describe key processes and mechanisms of public involvement in research
-
critically analyse the contextual and temporal dynamics of public involvement in research
-
explore the experience of public involvement in research for the researchers and members of public involved
-
assess the mechanisms which contribute to public involvement being routinely incorporated in the research process
-
evaluate the impact of public involvement on research processes and outcomes
-
identify barriers and enablers to effective public involvement in research.
Structure of the report
The report presents the main findings from the RAPPORT study and discusses them within the context of the National Institute for Health Research (NIHR) Clinical Research Network portfolio. This portfolio consists of high-quality clinical research studies that are eligible for support from the NIHR Clinical Research Network in England. In Chapter 2 we provide scene setting through presenting the dominant arguments for PPI and an overview of the roots of PPI in health research, and summarise the existing available evidence of PPI impact. Chapter 3 sets out the underpinning methodology and methods used. We provide a discrete chapter to describe PPI within the RAPPORT study and evaluate the impact on the RAPPORT study itself. Chapter 5 presents findings from the national scoping and survey of PPI in research, and in Chapter 6 we provide the findings from our 22 case studies. Chapter 7 discusses our findings and in Chapter 8 we summarise the main conclusions of our research with particular regard to our key research questions. Drawing on our findings and discussion, we then identify implications for the research community and PPI representatives, and make recommendations for future research.
Chapter 2 Background
This chapter of the report sets the scene for PPI in health research. We set out the dominant arguments for PPI within the UK health system: the moral argument, founded on ethical and democratic principles, and the methodological argument. We briefly overview the roots of PPI within the NHS as a whole, then focus specifically on PPI in research and map out the policy frame for PPI in research. Although we have not undertaken a structured review of the literature, we provide an overview of a broad range of papers reporting PPI in research, and complete the chapter by presenting evidence from five structured reviews of the evidence on PPI in health research.
Search strategy
Literature was searched from 1995 to 2013 on the following electronic databases: MEDLINE, Cumulative Index to Nursing and Allied Health Literature (CINAHL), PsycINFO and The Cochrane Library. The InvoNet database was also searched for grey literature and published papers. Lateral searches were conducted from retrieved papers to provide historical background. Papers were restricted to those in English. Combinations of terms, one from each column in Table 1, were searched for.
| Population 1 | Population 2 | Intervention |
|---|---|---|
| Patient* Carer* Public* Citizen* User* Consumer* Lay Caregiver* Representative* |
Health Research* Health service Public health Primary health care Community |
Participate* Involve* Engage* Collaborate* Partnership Consult* Consumer panel Advisory group |
Links with experts in PPI also provided further papers and grey literature.
Patient and public involvement: historical roots
Patient and public involvement in health and social care is emblematic of the postmodern democracy. Challenges to the unquestioned authority of medicine from health service user groups can be traced back to the 1950s, with growing disillusionment over health-care decisions being made which failed to include the views and perspectives of the service user. 12 In the UK, health service users have evolved a collective voice and formed a number of groups which actively campaign for the right to have a voice in decisions directly affecting them. While such groups are often organised in relation to a specific health condition (such as diabetes mellitus) or a shared experience (such as domestic violence), the overall movement has questioned conventional assumptions of, for example, disability, and also provided the means for advocacy, political lobbying, provision of alternative forms of health and care services, and user-led research and training. 33,34 Further impetus for the challenge against biomedical authority was provided by a series of high-profile medical scandals including the retention of deceased children’s body parts for research without the knowledge or consent of parents35 and unexpectedly high mortality rates for children undergoing heart surgery. 36,37 This backdrop of a changing health service user response to established biomedical authority underpins one of the three main claims of PPI legitimacy: the moral argument. It has also actively shaped the second claim: the policy argument.
Patient and public involvement: the moral argument
A clear case for PPI is laid out as the right of citizens to have a voice in the public services for which they are paying through taxes and labour; this is particularly relevant to health and care services or publicly funded health research. This argument is founded on the notion of a previous democratic deficit38 and the concepts of rights and citizenship. 39 This right to be involved as a citizen has been further developed internationally,11 but it has also been criticised as often comprising too narrow a view of citizens, with the reality that the involved citizen is generally retired, white, middle-class and highly educated. 38 An alternative viewpoint is the ethical argument that the individual has a right to be fully involved about any health care or research intervention being done ‘to’ them as a person. As well as this ethical standpoint, there are also a range of emancipatory approaches40 that explicitly validate subjective knowledge and openly challenge the traditional medical model of knowledge. Characterised by user-led research, this approach attempts to give voice to knowledge that is seldom heard. 41 A key influence on this movement was the work of Paul Hunt, a resident of Leonard Cheshire Homes who was an early campaigner for residents’ rights in the 1970s and 1980s. The then Department of Health and Social Security commissioned research to explore the potential for residents’ participation in the running of care homes; the resulting report was heavily criticised by Hunt for failing to include the resident perspective. 42 That event was seen as a catalyst in the development of service user-led research. 43 However, while there is growing recognition of the importance of experiential knowledge being addressed alongside scientific understanding,44 there is also clearly often an intrinsic resistance to acknowledging lay knowledge, particularly in the sphere of biomedical research. 44,45
Patient and public involvement: the policy argument
Although some parts of the scientific community have contested what knowledge is credible,46 the public crisis in confidence in the way health and care services were being run contributed towards a policy shift through the 1990s whereby governance moved towards partnership and community involvement. 37 The consumerist movement in the 1980s provided a focus on customer satisfaction, and the involvement of patients and the public was perceived as a feedback system to ensure that the NHS was meeting the needs of service users. 47 However, with the advent of the 1990s and a procession of significant changes to the NHS48 there began a concerted effort to involve patients and the public in key decisions about the purchasing and delivery of health and care services. 49 The pace of policy change speeded up considerably with the new Labour government in the late 1990s. ‘Third way’ policy, with its emphasis on concurrent rights and responsibilities,50 produced a number of initiatives including developing patient expertise in self-management26 as a tool to increase an individual’s confidence and skills in involvement in their care. Public involvement became a statutory duty within the NHS and all organisations were required to involve patients and the public in planning and operational decisions about services. In the light of increasing political expectations of PPI, the NHS has had a succession of involvement bodies including community health councils (abolished in 2002), PPI forums (abolished in 2007), local involvement networks and, from 2013, Healthwatch. This frequent restructuring of mechanisms designed to enable the patient and public voice suggests that policy-makers are still seeking more effective ways of operationalising PPI. 47
While the policy argument has been presented in terms of PPI within the NHS as a whole, PPI within health research, although more recently established,46 has equally been shaped by policy-makers.
The policy approach to patient and public involvement in research
Since the 1990s, and mirroring the policy changes outlined above, there has been increasing mainstream acceptance of PPI in research. In 1996 the Department of Health set up an advisory group to support PPI in research. Originally known as Consumers in NHS Research (now INVOLVE), it commissioned a literature review on service user involvement51 which highlighted the need for flexibility, funding, shared values and the importance of the political philosophy. These key areas are reflected in the main policy papers, whereby PPI became a statutory part of the research governance framework,5 and which made the case for PPI to improve the relevance and more likely implementation of research findings. 6 The 2008 Health and Social Care Act consolidated legislation around PPI in the health service and health research, and in a relatively short time PPI has become embedded within the main UK health research funding streams, regulators and medical Royal Colleges. 52 Researchers applying to NIHR and most medical charity funding streams are now required to demonstrate how PPI has shaped the research proposal and how service users and the public will continue to be involved in the study.
Patient and public involvement: the methodological argument
In addition to the moral arguments, policy-makers have been receptive to the consequentialist case that PPI improves quality within the health service, particularly in terms of service delivery and patient outcomes. There is a growing body of evidence that involvement in care leads to improved health outcomes53,54 and patient experience,55,56 but less evidence on any impact of PPI on the planning and commissioning of health services. 57
Within the health research arena, the policy approach to PPI has been underpinned by various claims regarding the impact of PPI. It has been suggested that PPI in setting research priorities has had an impact on the amount of research conducted on rare conditions,28,29 and has shaped the research agenda for more common conditions, such as breast cancer. 58 Beyond priority setting, PPI is seen as having an important role in identifying specific research questions,59,60 with subsequent applications for funding being more successful. 61 Furthermore, PPI can ensure that the patient and carer perspectives are explicitly addressed within the research questions,62 and may result in research questions being further refined17,63 or even abandoning a research application if PPI suggests that the research questions are not meaningful for the target patient and service user population. 64
In addition to influencing researchers’ priorities, PPI has increasingly played a part in advising funding bodies on priority setting, for example in medical products,65 spinal cord injury66 and burns research. 67 Lay involvement in the review of research grant applications is seen to raise issues not previously identified and challenges scientist reviewers to think more about the service user perspective within their deliberations. 68,69 Overall, making PPI explicit within the research proposal development is seen as lending more credibility to the proposal and hence offering a greater chance of funding. 70,71 In particular, PPI is seen as being key to the development of plain English summaries as a requirement in many grant applications. 24,62
There are also claims that PPI improves the overall design in trials,72 particularly by ensuring the design is acceptable for potential participants. 73 Contributing to the design of interventions is reported as being an important aspect of PPI; examples include stroke research interventions74 and advising on the timing of interventions within Parkinson’s disease research. 75 PPI also has a role in ensuring that research tools are refined to more closely reflect the issues important for the target research population,76 ensuring tools are culturally sensitive and designing measures of patient expectations of treatment. 77 However, the most frequently cited claim for the value of PPI is in recruitment to studies,78 most commonly by ensuring that protocols and participant information are more relevant and accessible to participant groups. 70 PPI input is also seen as having importance in shaping the recruitment strategy by bringing local knowledge,79 or important links to the target population. 80 There are also examples where PPI has contributed to accessing marginalised and seldom heard populations81,82 and those with rare conditions,83 and played a role in promoting acceptance of researchers by previously sceptical communities. 84 More active involvement in mainly qualitative data analysis has been identified as improving interpretation of findings through the drawing out of relevant themes. 79,85–87 Moreover, qualitative data collection by service users as co-researchers has been claimed to improve validity and provide better-quality data. 88–90 Dissemination of research findings is also reported as gaining from PPI networks to increase access to peers81 and relevant sections of the community,15 and making information more broadly readable. 31,72 There are fewer published claims for PPI as playing a significant role in implementing findings, but, in a US public health research programme, Krieger et al. 86 report PPI-related implementation of changes by increasing their cultural relevance. Several researchers have identified that PPI has helped them address ethical dilemmas,17,71,78,85,91 for example ethically appropriate ways of contacting women with recently diagnosed breast cancer and the use of routine patient data. 92 There is also some suggestion that lay co-researchers have a role to play in helping safeguard potentially vulnerable participants. 82
The impact of PPI has a moral dimension in the reported outcomes for service users and the public involved in the study. This includes an increased sense of self-worth,87,93 peer support,94 improved quality of life95,96 and acting as a stepping stone to employment. 88 Being involved with a research team also provides service users and the public with a means of becoming more knowledgeable about health conditions, services and the research process. 58,93,95 Within community-based public health research, benefits of PPI are also reported in enhancing the capacity of community-based organisations to raise their value to their communities. 86
Finally, there are claims that PPI brings benefits to researchers beyond just the research study. Working with the public and service users is found to be a process whereby researchers learn to share control and develop facilitation skills. 88,97 PPI not only increases researchers’ confidence in their studies72 but perhaps most importantly fosters their greater understanding of the service user or patient perspective. 81,98
The evidence base for patient and public involvement in research
Despite the growing body of literature outlined in the previous section, there is relatively little evidence of PPI’s impact and outcomes. 99 Several factors contribute to the weak evidence base for PPI. First, previous evaluations have failed to use methodologies that take into account its complexity,100 arising from PPI being an interconnected, multifaceted social process, making it difficult to pinpoint specific impacts and contributions. 19 Second, there is little systematic appraisal and reporting of PPI impact and outcomes,101 further constrained by the conventions of academic publishing. 21 Nevertheless, there is a limited number of evidence reviews,19,29,99,101,102 here presented chronologically to illustrate the developing evidence base.
The systematic review by Oliver et al. 102 was the first to examine the evidence base on the impact of PPI on identifying and prioritising possible topics for research and development. They found detailed reports of 87 examples of PPI influencing the identification or prioritisation of research topics. While these reports highlighted the collective experience of research programmes in involving patients and the public, gaps were identified in training and preparing lay people. It also highlighted multiple barriers to service users’ ideas influencing research agendas, and a lack of collaborative working between the research programmes and lay people to address the way forward in collective decision-making. In addition, the majority of included reports were descriptive accounts written by researchers rather than service user representatives.
Staley’s 200919 review of the literature appraised papers published from 2007 within the INVOLVE collection of articles, systematically searched electronic databases and drew on grey literature obtained through networks via INVOLVE. A total of 89 articles (71 published papers and 18 from ‘grey’ informally published literature) were included in the review. While there was some evidence around the impact of PPI on influencing research questions, design, data collection, dissemination, implementation and research ethics, the most substantial body of evidence was on PPI’s impact on recruitment. However, particular gaps in evidence were found on PPI impact around grant-funding decisions, and on involvement in data analysis apart from qualitative methodology. There was some evidence of both positive and negative impacts of PPI on the public and researchers involved, and there were examples of positive impact for research participants in terms of PPI influencing a better research process, and impact on the wider community. However, as with Oliver et al. ’s review,102 because of the nature of the evidence available, inconsistent reporting and the context-dependent nature of PPI, it was not possible to carry out an in-depth analysis of different kinds of impact, or to judge the quality of the evidence and determine how generalisable the results were.
The Patient and Public Involvement in Research: Impact, Conceptualisation, Outcomes and Measurement (PIRICOM) systematic review29 aimed to examine the conceptualisation, measurement, impact and outcomes of PPI in health and social care research. Ninety papers published between 1995 and 2009 were included. Data were extracted from 83 papers (the remaining seven were not written in a format suitable for data extraction but were deemed sufficiently important to include within the conceptualisation of PPI). Of the 83 papers, 2 were randomised controlled trials (RCTs), 52 qualitative studies, 15 case study methodology, 4 cross-sectional studies and 10 structured reviews. As in Staley’s review,19 the papers provided more evidence around the processes of PPI rather than impact and outcomes, and found scant evidence of PPI impact on funding decisions. Hence, while there appears to be a reasonably robust level of evidence around the ‘architecture of PPI’, reporting of outcomes continues to be poor. Brett et al. 29 argue that most studies have attempted to conceptualise PPI mainly around context and process and have not sufficiently theoretically grasped the complexities of PPI. They did not find any evidence around systematic measurement of PPI outcomes, and furthermore found a lack of clarity on the differences between PPI impact and outcomes.
Jagosh et al. 103 addressed the complexity of PPI by utilising a realist review design. 104 Focusing on participatory research, which they define as the ‘co-construction of research between researchers and people affected by the issues under study . . . and/or decision-makers who apply research findings’, they reviewed published papers and grey literature on 23 studies or programmes of research where both service users and researchers either identified or set the research questions, selected the methodology, collected or analysed data and used or disseminated the research findings. In each example they attempted to map out the relationship between the context (any condition that triggers or modifies the behaviour of a mechanism), mechanism (a generative force that leads to outcomes) and outcomes (intended and unintended). As part of their realist review they generated three hypotheses to test within each example. Drawing on the concept of ‘partnership synergy’,105 their hypotheses were that partnerships are not always synergistic (e.g. because of previous history); that multiple stakeholder collaboration will enhance research outcomes beyond that which would be expected without the collaboration; and that partnerships may become more synergistic with time. They were unable to test the first hypothesis because of a lack of information about the history and previous context of each example. However, the other two hypotheses were supported in several examples. They conclude that partnership synergy often generates a virtuous circle, so that conflict and disagreement between the stakeholders is not necessarily a bad thing, as it may build more robust synergies through successful negotiation and resolution. However, as with the earlier reviews, Jagosh et al. 103 highlight the limited reporting of PPI and also suggest that negative outcomes are less likely to be reported.
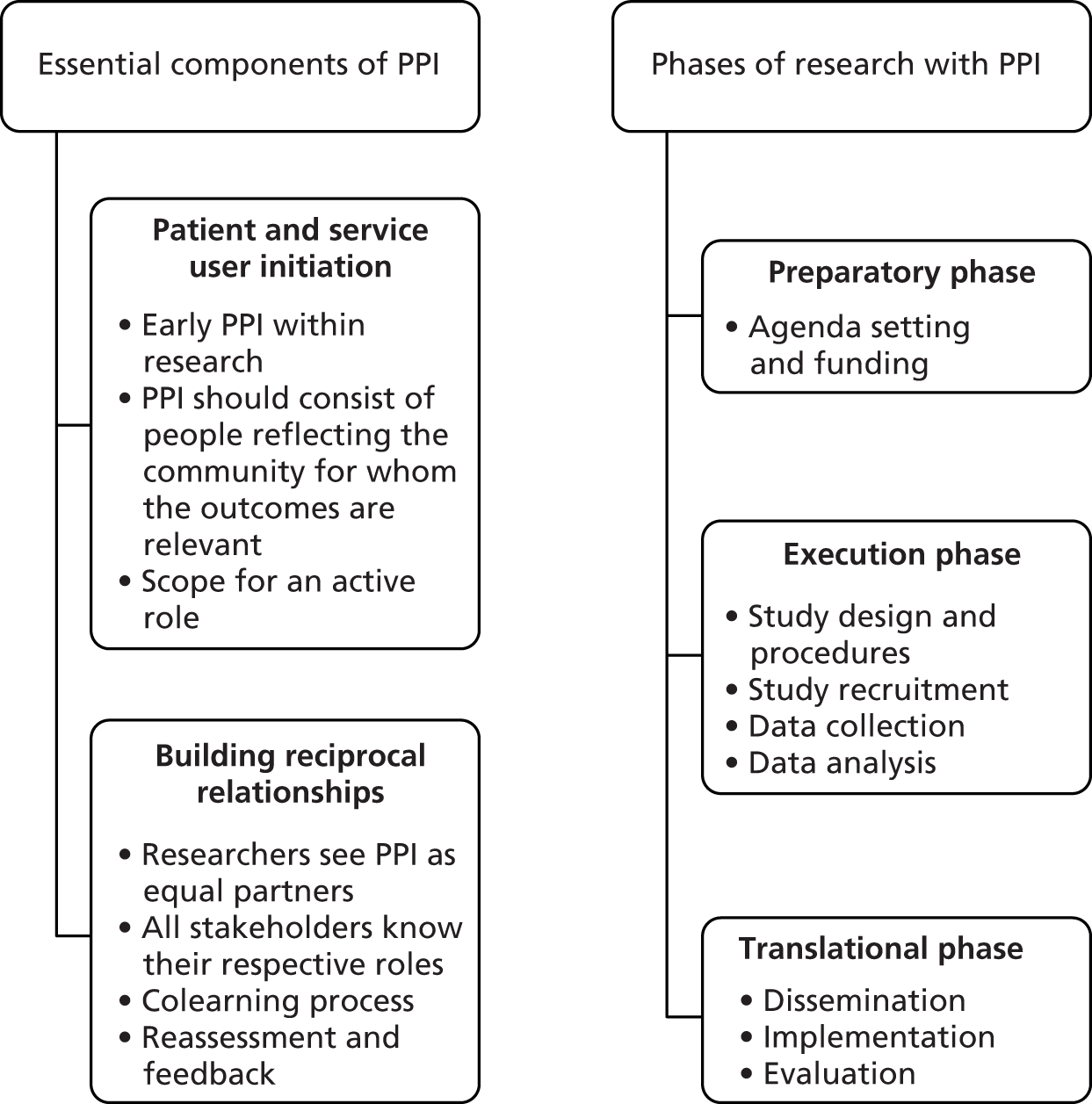
In a study published a year later, Shippee et al. 101 develop a conceptual framework (Figure 1) from their systematic review. They critique previous reviews as focusing on only one part of their proposed framework, suggesting that their approach is more comprehensive and recommending its use to guide future reporting of PPI. From an original 202 papers, the review included 41, with the findings mapped against the framework. They conclude that the evidence of PPI impact on funding decisions continues to be weak, with a notable lack of studies identifying the impact of PPI in data collection and analysis. In contrast, there is a growing body of evidence on the impact of PPI in addressing ethical issues and enhancing the validity of findings. The authors recommend that research be undertaken to compare and systematically report different methods of PPI, and that there be more robust indexing of such studies.
Conclusion
Embedding PPI in research continues within an overall policy framework which is built on specific contemporary moral and consequentialist arguments. However, while the body of literature describing PPI processes and the architecture required to enable PPI continues to grow, it still provides only comparatively weak evidence for impact and outcomes. One reason for this is the difficulty that confused terminology or poor reporting poses for finding evidence of PPI impact in the literature. What evidence there is tends to be descriptive, largely qualitative, often retrospective case studies,19,29,106 with only a few exceptional prospective longitudinal case studies,15 comparative multiproject evaluations107 or studies employing quantitative designs. 108 This reflects the significant methodological challenges in evaluating PPI as a complex intervention, and the length of time before impact may become visible. Key messages from the cumulative reviews of evidence on PPI in research suggest that an appropriate methodological approach must be sensitive to context and processes and their influence on outcomes, that PPI within a research study may shift and develop with time so that there is a need for a longitudinal approach, and that different models of PPI need to be evaluated and compared through a standardised design. In the next chapter we present our methodology designed with these conclusions in mind.
Chapter 3 Research design and methods
As outlined in the previous chapter, PPI in research is a complex social phenomenon, and can act as an ‘intervention’. 109 Providing a more robust evidence base for PPI policy requires moving beyond observational evaluations of PPI. 29,30 More conventional approaches to empirical evaluation would seek to examine whether or not programmes, interventions or innovations are effective using controlled trial designs to measure specified effects of each of a number of variables on outcomes. Although such designs are well suited to assess the effectiveness of clinical treatments, it has long been recognised110 that such research designs are less able to identify how exactly variables combine to create outcomes111 or to fully explain the processes through which programmes actually work. Furthermore, controlled trials are, by definition, able neither to examine the dynamic nature of those interventions which, will, of necessity, evolve over time nor to explore the effect and complexity of the wider social systems within which PPI takes place. For example, an experimental evaluation (RCT) which investigated the impact of PPI in developing participant information sheets (PISs) for a clinical trial108 concluded that PPI had little or no impact on participants’ understanding of the trial or on recruitment and retention, and the authors were able only to speculate that a wide range of contextual factors and limited understanding of the mechanism of gaining consent were responsible for this negative outcome. Yet, as Staley et al. argue:
If an experimental evaluation is not designed in a way that considers the contextual factors and aspects of the mechanism that have the potential to influence impact, then it may produce inaccurate or over-simplified conclusions about when and how involvement makes a difference.
p. 632
Realist evaluation (RE) is one of several theory-based approaches to evaluation developed within the social sciences, which seeks to address dynamism and context, rather than control for them, to explain more adequately how and, importantly, under what circumstances programmes, interventions or innovations will ‘work’ in real-world complex systems, such as those related to health care/research systems. 112 Such social science approaches highlight, specifically, how it can be the reasoning and actions of people (social actors), rather than inherent characteristics of the interventions themselves, that make them work. 113
In conclusion here, the evaluation of PPI in research necessitates a method of enquiry capable of capturing the interplay between outcomes and processes and the context in which PPI is conducted. As other authors have advocated in reviewing the evaluation evidence for PPI,32 a realist evaluation approach114,115 offered this research the capability of more fully investigating and understanding what type of PPI provided what kind of outcome in relation to different types of research and settings. We employed an overarching critical realist framework116,117 focused on the mechanisms embedded within PPI, to facilitate our understanding of outcomes present or absent depending on how they were triggered, blocked or modified. 118,119 RE,115 which draws upon this perspective, was used to inform the research design.
We continue this chapter with a brief introduction to RE and its application in this study. We then explain the three-stage research design and methods employed to test the links between context, mechanisms and outcomes of PPI. We also introduce Normalisation Process Theory (NPT) as the candidate programme theory to explain the ‘work’ required to embed PPI as normal practice. In particular, the focus of NPT on social action can help understand how and how far PPI may be ‘embedded’ within and across contemporary health-care research.
Method of enquiry: realist evaluation with Normalisation Process Theory
Both RE and NPT are theoretically informed approaches that can help researchers to further investigate, develop and refine middle-range theories (MRTs) to explain specific parts of programmes and interventions. Merton defines MRTs as ‘theories that lie between the minor but necessary working hypotheses and the all-inclusive systematic efforts to develop a unified theory that will explain all the observed uniformities of social behaviour, social organisation and social change’ (p. 39). 120 MRTs are thus sufficiently abstract to be applied to differing spheres of social behaviour and structure, but do not offer a set of general laws about these at societal level. Specifying the range of the theory is important here. The limited scope, conceptual range and claims of MRTs are what make them practically workable in analysing practice; both approaches (RE and NPT) can be applied across different types of social programmes at different scales.
The bodies of literature on empirical applications of both these approaches are relatively recent,112 especially NPT; its third and final development phase was reported only in 2009. 121
Realist evaluation is rooted in the philosophy of science situated between extremes of positivism and relativism, known as realism. 115,122 Realism understands the world as an open system, with structures and layers that interact to form mechanisms and contexts. RE research is concerned with the identification of underlying causal mechanisms, how they work, under what conditions and for whom. 115,123 The approach employs three key terms, for which definitions are provided in Box 2.
Context often pertains to the ‘backdrop’ of programmes (PPI in research): those conditions within which programmes are introduced that are relevant to operating the programme mechanisms (e.g. the research arena, previous working relationships or funding body). As these conditions change over time, the context may reflect aspects of those changes while the programme is implemented. Context can be broadly understood as any condition that triggers and/or modifies the mechanism.
MechanismMechanisms are the unit of analysis of RE. Mechanisms describe what it is about programmes and interventions (PPI in research) that bring about any effects (outcomes). Mechanisms are often hidden, as with a clock’s workings; they cannot be seen but drive the patterned movements of the clock’s hands. Mechanisms are linked to, but not synonymous with, the programme’s strategies (e.g. a strategy may be an intended plan of action for PPI in research, whereas a mechanism involves the researchers’ and PPI representatives’ reaction or response to the intentional offer of incentives or resources). Identifying the mechanisms (e.g. the design of PPI roles within research projects) advances the synthesis beyond describing what happened to theorising why it happened, for whom and under what circumstances.
OutcomesOutcomes are either intended or unintended consequences of programmes, resulting from the activation of different mechanisms in different contexts (e.g. if the research recruited more successfully because of PPI). Outcomes can be proximal, intermediate or final.
Because causal mechanisms are always embedded within particular contexts and social processes, their complex relationship with the effect of context on their operationalisation and outcome needs to be understood. Pawson and Tilley115 describe this as: context (C) + mechanism (M) = outcome (O). Rather than identifying simple cause-and-effect relationships, RE is concerned with finding out about what mechanisms work, in what conditions, why, to produce which outcomes and for whom. 124 RE does this through testing and refining configurations of context, mechanism and outcome (CMO) within analysis of data, as described in Box 3.
Context, mechanism and outcome configuring is a heuristic tool used to generate causative explanations pertaining to outcomes in the observed data. The process draws out and reflects on the relationship of CMO of interest in a particular programme. A CMO configuration may pertain either to the whole programme or only to certain aspects. One CMO may be embedded in another or configured in a series (in which the outcome of one CMO becomes the context for the next in the chain of implementation steps). Configuring CMOs is a basis for generating and/or refining the theory that becomes the final product of the evaluation. RE thus develops and tests CMOs conjectures empirically.
Although Pawson and Tilley did not provide a set of methodological rules for RE, and these are still much debated,112,125 they nonetheless suggest some principles for guiding evaluators. These include the identification of mechanisms and testing/refining of CMO configurations; stakeholder involvement and engagement; and a generative conception of causality (i.e. an explanation not of variables that are inter-related to one another but rather of how they are associated). 124
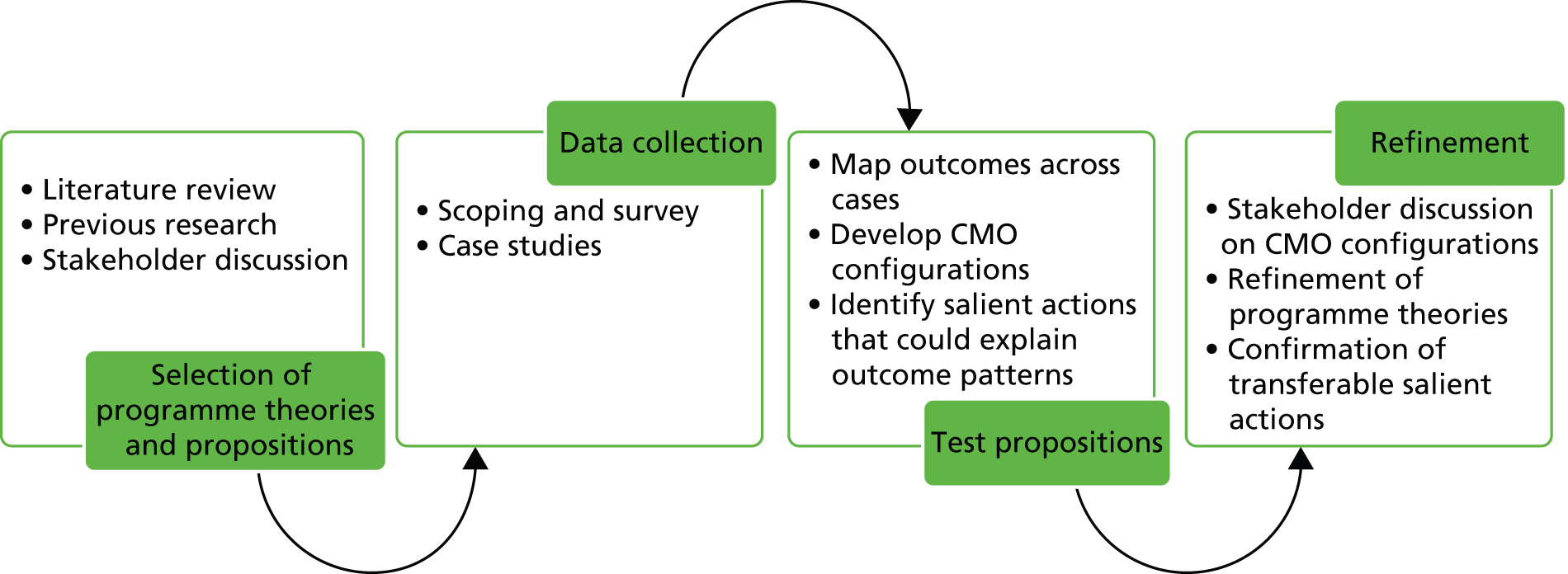
In practice, REs start with a MRT and end with a refined MRT, following four main stages as described by Pawson and Tilley. 114 The MRT can be formulated on the basis of existing theory, past experience and previous evaluations or research studies. The result is discussed with the stakeholders and finally results in the MRT that will be tested. The field study is then designed in relation to the MRT: the design, data collection tools and analysis tools are developed to enable testing the elements of the MRT. The outcomes of the fourth stage should lead to policy advice and recommendations. The application of these four stages in this research is shown in Figure 2.
Both a published literature review112 and critical discussions in the applied literature cite several methodological challenges associated with a RE approach, including deciding what constitutes a mechanism,127 and indeed differentiating between what is a mechanism and what is context. Barnes et al. ,128 for example, also caution against interpreting context as a purely external factor, arguing that context is shaped by actors as much as it constrains their activities.
Middle-range theories and hypotheses
Before the empirical work, we conducted a search of the literature to identify programme theories that would inform candidate CMOs. As described in Chapter 2, PPI can be defined through three different perspectives: moral, methodological and policy. We therefore sought explanatory theories that would underpin these approaches and predict outcomes. These are illustrated in Table 2.
| Dimension | Moral | Methodological | Policy |
|---|---|---|---|
| Purpose | To ensure citizens’ rights and the moral imperative | To improve research processes, outcomes and impact | To support and embed PPI in health research as normal practice |
| Expected outcomes of the programme (PPI) | Researchers ‘working with’ rather than ‘doing to’ patients and the public Patient and public satisfaction with levels of involvement Democratic deficit addressed |
Prioritisation of research questions with greatest relevance for patients and the public Improved overall research design leading to safer and more ethically robust research, participant-sensitive data collection tools, better recruitment rates, increased validity of interpretation of findings, wider dissemination, public engagement and longer-term impact Psychological benefit for patients and the public involved, and for researchers |
Democratic deficit addressed Researchers ‘working with’ rather than ‘doing to’ patients and the public Patient and public satisfaction with levels of involvement Lay people and researchers who are prepared for and supported in PPI Prioritisation of research questions with greatest relevance for patients and the public Improved overall research design leading to safer and more ethically robust research, participant-sensitive data collection tools, better recruitment rates, increased validity of interpretation of findings, wider dissemination, public engagement and longer-term impact |
| Expected developmental approaches to the programme (PPI) | Development of partnership approaches User-led research Emancipatory research |
Development of models of PPI and supportive infrastructure that optimises PPI impact on the research process | Governance frameworks Advisory organisations and guidance Public engagement |
| Programme theory | Critical theory (Habermas 1972129) Emancipatory concept of PPI (Gibson et al. 2012130) |
Architecture of involvement (Brett et al. 2010131) Multidimensional conceptual framework of PPI in health research (Oliver et al. 2008132) Partnership synergy (Lasker et al. 2001105) |
Normalisation Process Theory (May and Finch 2009121) |
We drew on the work of Habermas129 to predict the outcomes of PPI when operationalised through the moral perspective. Habermas proposes that critical theory challenges the traditional superiority of scientific knowledge and unmasks ideologies that seek to prevent the voice of marginalised groups from being heard. The case for emancipatory knowledge is put forward where personal knowledge is gained through self-reflection and leads to personal empowerment. This is amplified through communicative action where the interpersonal knowledge of groups comes together through mutual understanding. 129 Habermas’s work, alongside others, is used by Gibson et al. 130 to develop an emancipatory concept of PPI.
For the methodological perspective on PPI we used the multidimensional conceptual framework of PPI proposed by Oliver et al. ,132 the indicators of successful PPI developed by Boote et al. ,133 through consensus methodology, and the systematic review of Brett et al. ,29 which suggested the architecture required to enable effective PPI. As the methodological paradigm also depicts PPI in research as leading to improved outcomes for the research and for all those involved, we also drew on the partnership synergy model of Lasker et al. ,105 which proposes that synergistic partnerships (between PPI representatives and researchers) lead to high-quality (research) plans with more chance of a successful outcome.
A key MRT that informed our research approach was NPT. 121 Specifically, it is a candidate MRT to inform the policy perspective on PPI, but we found in practice that its constructs systematically inform all three viewpoints and therefore we used it explicitly to similarly inform our methodological approach (see Table 2).
Normalisation Process Theory
In attempts to help understand why it is that seemingly effective innovations often fail to flourish when rolled out in practice (context), NPT addresses two important problems that face service improvers as they try to get innovations into practice:
-
process problems – about the implementation of new ways of thinking, acting and organising
-
structural problems – about the integration of new systems of practice into existing organisational and professional settings.
Because PPI in research is not an entirely ‘new’ innovation, intervention, programme or phenomenon, but also is not yet fully normalised within contemporary research practice, it has been suggested15 that NPT offers unique potential for helping theorise how PPI is/is not routinely operationalised (embedded) and sustained (or not) in practice.
As an ‘action’ theory, NPT also sharpens our analytical focus on the actual work that people performing PPI do, or do not do, rather than people’s attitudes (how they feel about what they do) or their intentions (what they say they are going to do). 134 NPT distinguishes action according to a set of four constructs. Each of these represents a generative mechanism of social action. That is, each construct represents different kinds of work that people do in orienting themselves to a set of practices of PPI in research. These constructs and their components (domains) (Table 3) address the ways that people make sense of the work entailed in implementing and integrating PPI (coherence); how they engage with this work (cognitive participation); how they enact it (collective action); and how they appraise its effects and modify it (reflexive monitoring).
| NPT construct | Description | Components (domains) |
|---|---|---|
| Coherence | The sense-making work that people do individually and collectively when they are faced with the problem of operationalising some set of practices | Differentiation |
| Communal specification | ||
| Individual specification | ||
| Internalisation | ||
| Cognitive participation | The relational work that people do to build and sustain a community of practice around a new technology or complex intervention | Initiation |
| Enrolment | ||
| Legitimisation | ||
| Activation | ||
| Collective action | The operational work that people do to enact a set of practices, whether these represent a new technology or complex health-care interventions | Interactional workability |
| Relational integration | ||
| Skill set workability | ||
| Contextual integration | ||
| Reflective monitoring | The appraisal work that people do to assess and understand the ways that a new set of practices affect them and others around them | Systematisation |
| Collective appraisal | ||
| Individual appraisal | ||
| Reconfiguration |
Normalisation Process Theory has been developed for using in a flexible and dynamic way and can both direct and sensitise the practical and analytic trajectories of a research project. There is currently no published review of its empirical application, but it has been seen to have been applied to good effect in a number of social and health-care settings. 121,134,135 Of relevance in the RAPPORT study, and discussed in the following sections, is that case study methods have been seen to be more robust when theoretical propositions to guide data collection and analysis have been previously developed. 136 We have used NPT constructs and domains both to direct our data collection and to guide our analysis, particularly within our case study work. In effect, these domains map across to the RE, and are most significant in theorising PPI mechanisms and outcomes, and to some extent the context, but, as discussed below, were combined with additional questioning and coding to inductively explore other emerging significant themes.
We also drew on previous work focused on the architecture and infrastructure29,137 required for PPI to be operationalised.
Research design and methods
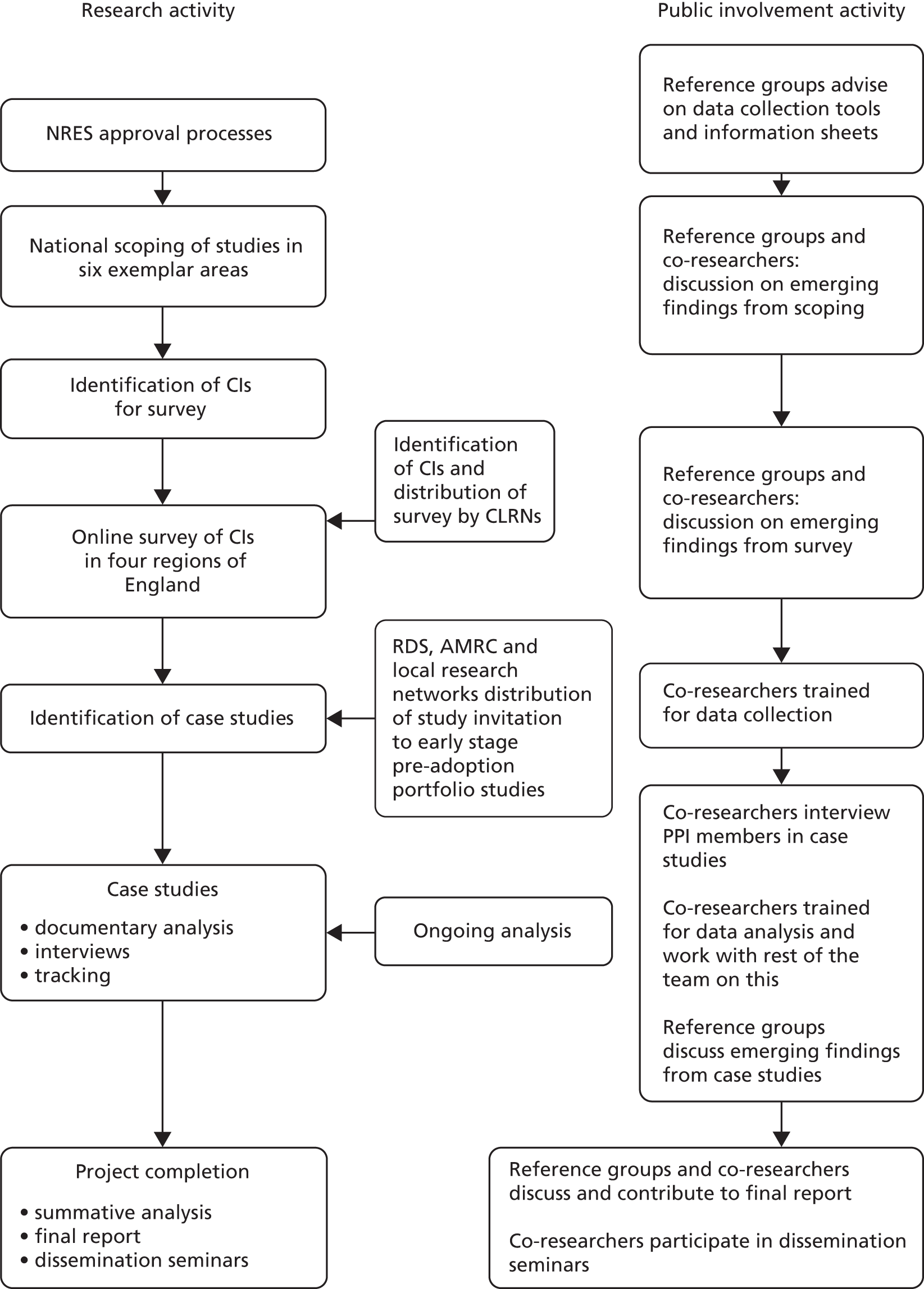
Both RE and NPT are method-neutral and often employ both qualitative and quantitative methods to collect sufficient information on the context (the setting and focus of the research), processes (type of involvement and formal support processes), structure and agency (organisational structures such as PPI frameworks and actions of stakeholders including researchers and lay representatives) within each case. Utilising a sequential, mixed-methods approach, the study was conducted in three stages, from May 2011 to February 2014. The project flow chart, shown in Figure 3, illustrates the phases of the research and methods employed and PPI.
FIGURE 3.
RAPPORT flow chart. AMRC, Association of Medical Research Charities; CI, chief investigator; CLRN, comprehensive local research network; NRES, National Research Ethics Service; RDS, Research Design Service.
The first two stages of the study comprised a scoping and survey which provided us with a contextual backdrop to PPI in current and recent research. These methods also informed us about what is recognised as PPI, and gave us an indication of the current level of PPI across six health research topic areas (see below). These findings informed the development of a sampling frame for the subsequent (third) phase, in-depth case studies.
To demonstrate which elements of PPI in research influence its outcomes, regardless of setting, those that are context specific, and what different approaches can and cannot achieve, we purposively selected six exemplar areas that by their focus and research tradition could capture the full continuum of PPI. These are:
-
Cystic fibrosis (CF). This life-limiting condition affects children and younger adults. Services are located within secondary care and specialist centres. There is a strong current laboratory-based research focus on gene therapy. Compared with the other topic areas, there is less of a history of PPI, with particular challenges in recruiting children and younger people.
-
Diabetes mellitus. This is characterised by a clear clinical diagnosis and its treatment emphasises self-management and lifestyle change. The disease affects people across the lifespan and services are predominantly delivered in primary care. PPI is well established particularly through powerful patient organisations.
-
Arthritis. This occurs through the lifespan but predominantly in older people. There are a range of treatments in a range of settings with an emphasis on preventing further deterioration. A strong patient organisation and recent history of involvement in research have informed the development of Expert Patients Programme.
-
Dementia. This is a condition of later life with a limited life expectancy. Characteristics that can shape PPI include the unclear trajectory of the disease, the stigmatising nature of the condition, reduced mental capacity and a population predominantly of older persons within a primary care setting. There is a well-established history of PPI in the identification of research priorities in the Alzheimer’s Society Quality Research in Dementia Network and an increasing recognition of the need to develop research to be inclusive for this population.
-
Intellectual and developmental disabilities (IDDs, also known as learning disabilities). Widely varying conditions mark out a marginalised group in terms of health-care delivery and health research. Despite the challenges of making research accessible for this group, there are a well-established history of PPI and well-developed theoretical and policy participative frameworks that inform policy, practice and research.
-
Public health. This includes participants across the lifespan who do not see themselves as service users. It may include community interventions and user-led projects in a variety of settings, but faces challenges in PPI, particularly in harder-to-reach groups.
These topic areas represented a diverse range of studies and associated models of PPI. They included studies with participants recruited across the lifespan (such as children and young people in CF studies, and older people in dementia studies), as well as different research designs (basic science to qualitative), settings (acute care, primary care) and traditions and history of PPI. For example, diabetes mellitus has a strong national patient organisation with a record of being involved in research and commissioning of health services. Both diabetes mellitus and dementia have a national research infrastructure that has well-established PPI mechanisms,78,138 and the IDD community at both policy and research levels has focused on inclusive practice. 139 Public health was incorporated to include community interventions and user-led projects and local populations who may not consider themselves as patients.
We built quality and rigour into the research process, from the method of sampling research studies for each stage, through data collection, to the ‘audit trail’ created during analytic phases.
Inclusion and exclusion criteria
We included researchers and service users and members of the public who:
-
were involved in a study eligible for adoption on the UK Clinical Research Network (UKCRN) portfolio in one of the six exemplar areas
-
were 13 years old and over
-
gave informed consent.
We excluded researchers and service users and members of the public who:
-
were not involved in a study eligible for adoption on the UKCRN portfolio in one of the six exemplar areas
-
were under the age of 13 years
-
did not give informed consent.
Ethical approval
This project had NHS approval (REC reference: 11/EM/0332), obtaining favourable approval by Nottingham Research Ethics Committee 1 Proportionate Review Sub-Committee on 13 August 2011 with no changes to the research protocol.
Ethical issues
It was not expected that any major ethical issues would emerge from this project. However, we were aware that we might be including younger people, people with IDDs and users of dementia services. The team was skilled in working in sensitive areas and with these groups, although few such participants were involved with or recruited to the case study phase of this research. We also foresaw that there might also be sensitivities in discussing experiences of a project with the potential to expose bad practice and misuse of PPI, so we were careful to remain neutral in our reactions to reports of practice, while also probing carefully in order to clarify understandings and gain fuller explanations. Informed consent was taken from all participants participating in interviews in stage 3.
Stage 1: national scoping of studies
To address objective 1, a national scoping of studies within the six exemplar areas was undertaken (October–December 2011).
Sample
Our sample here included current studies or those completed in the previous 2 years in the six exemplar areas and being undertaken in England. To ensure relevance to the NHS and scientific robustness, studies were limited to those registered with the UKCRN portfolio, excluding commercially funded studies. To ensure inclusion of studies most likely to have been designed since the embedding of PPI in the research governance framework,1 we excluded studies older than 2 years (end date of recruitment before 1 September 2009). We also excluded studies funded by commercial organisations because, despite current criticisms of the lack of transparency in drug trials,140,141 access to the study documents required was likely to be limited.
Data collection
Studies were identified using the using the search terms in Table 4.
| Topic area | Focus and key words/terms |
|---|---|
| CF | Key word ‘cystic fibrosis’ |
| Diabetes mellitus | Type 1 and type 2 and other |
| Arthritis | Musculoskeletal, inflammatory and immune, genetics, primary care |
| Dementia | Dementia and neurodegenerative diseases, Huntington’s disease, motor neurone disease, Parkinson’s disease, other |
| IDD | Searched on key words: ‘learning’, ‘attention’, ‘Downs’, intellectual’, ‘autism’, ‘Asperger’. Mental health: learning difficulties theme. Specific syndromes listed by Royal College of Psychiatry142 |
| Public health | Primary care, infection, key word ‘public health’ |
| All topics | Generic relevance and cross-cutting themes |
Details of each study were electronically searched via funding body databases. Relevant documentation such as reports, abstracts and protocols was reviewed for the type of research (e.g. laboratory based or qualitative) and any evidence of the nature and extent of PPI. Where information was not available electronically, the funding body was contacted and requested to provide further relevant details of the study. Indeed, one of our findings from this initial scoping exercise is that there is minimal direct open access to such study documentation. Significantly, even when the protocol was available on the funder’s or study’s website, there was little information about PPI. Therefore, we also contacted study teams directly or through collaboration with the Association of Medical Research Charities (AMRC) for PPI information.
Scoping response
In total, 1464 studies in the six broad topic/exemplar areas were downloaded from the UKCRN database. One hundred and two were excluded as not in the specific topic areas, 263 as more than 2 years old and 261 as commercially funded. A total of 838 studies were included (Table 5). These were then divided into the 478 included in the scoping, and 360 for the online survey. All of the latter group were within the four selected regions of England (Figure 4).
| Topic area | Number of studies identified on UKCRN portfolio | Number of studies for inclusion | % of total on UKCRN |
|---|---|---|---|
| CF | 23 | 8 | 35 |
| Diabetes mellitus | 512 | 277 | 54 |
| Arthritis | 399 | 188 | 46 |
| Dementia | 282 | 192 | 68 |
| IDD | 90 | 51 | 57 |
| Public health | 158 | 122 | 77 |
| Total | 1464 | 838 | 57 |
FIGURE 4.
Flow diagram of scoping and survey.
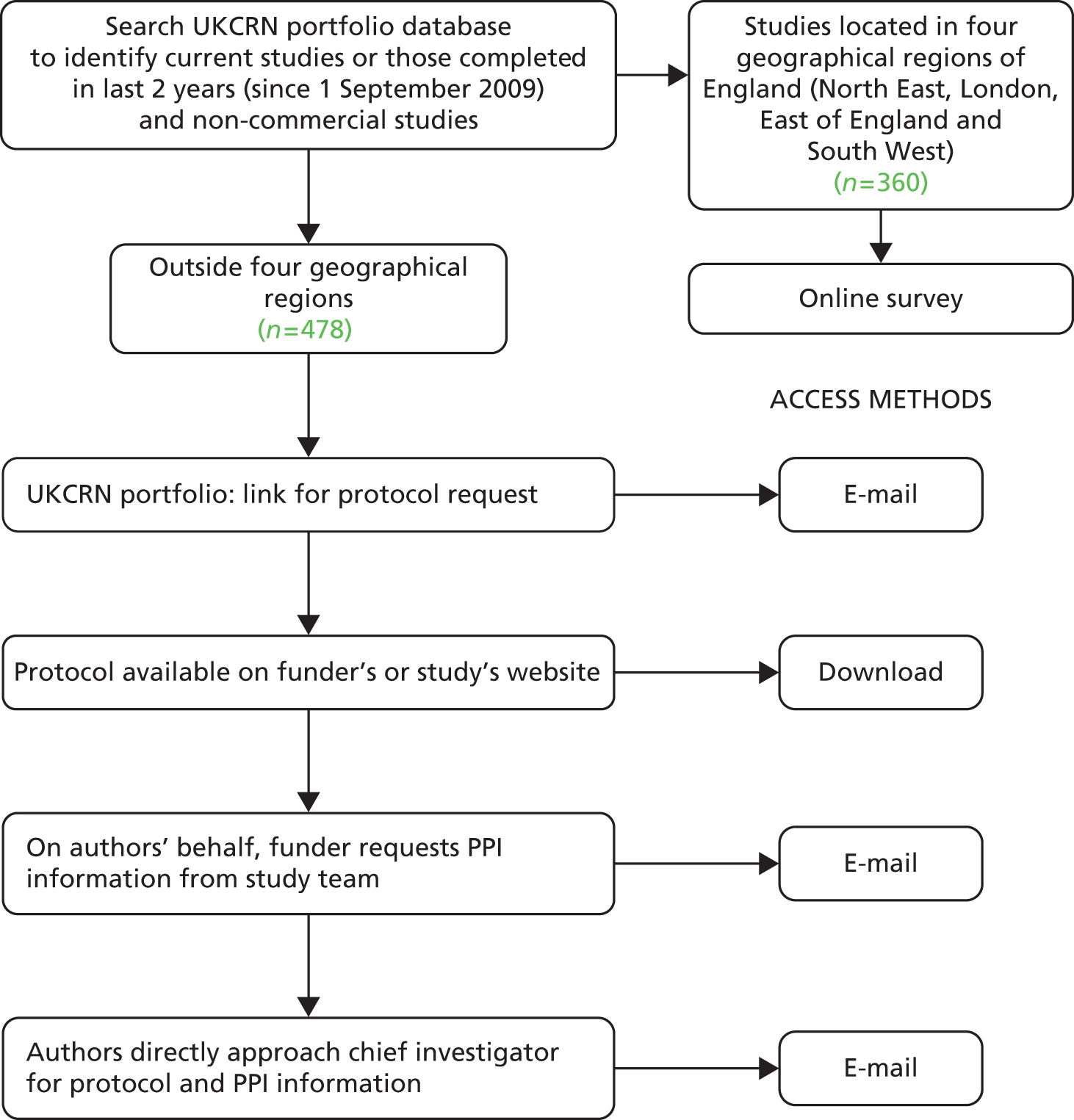
In the UK, clinical research networks have been established in each of the four UK nations funded by their health departments. These national networks form UKCRN. The UKCRN portfolio of studies was used as one single database to identify relevant research studies, and information including study title, sample size, end date of recruitment and contact details was downloaded into an Excel® (version 14, Microsoft Corporation, Redmond, WA, USA) spreadsheet.
For studies not covered by the online survey, that is running outside the four selected geographical regions, including studies in Scotland, Wales and Northern Ireland, direct requests were made. Documents or e-mail replies were then reviewed by two team members independently for background study information and any evidence of the nature, extent and activities of PPI. The scoping exercise obtained information about PPI from 182 studies out of a possible total of 478 (38%) (Table 6). Documents received in response to requests for PPI information included 93 protocols, 12 journal articles, 64 e-mail replies, 10 interim/final reports and 3 Integrated Research Application System (IRAS) forms. Other documents (such as grant applications, reports to funders and lay summaries) were also provided. Some studies provided more than one source of information. The studies in the scoping had sample sizes ranging from 12 to 250,000, with a median of 250. The two main funders were NIHR (29%) and charities (29%). The remaining funders were a mix of government departments, the European Union, research councils and others. Forty-two per cent of the scoping studies were clinical trials, 33% were mixed methods (qualitative and quantitative non-clinical trials), 10% were basic science and 15% were tissue bank/database.
| Topic | Scoping response rate (%) |
|---|---|
| CF | 40 (n = 2 of 5) |
| Diabetes mellitus | 34 (n = 46 of 137) |
| Arthritis | 42 (n = 55 of 132) |
| Dementia | 38 (n = 35 of 93) |
| IDD | 38 (n = 11 of 29) |
| Public health | 40 (n = 33 of 82) |
| Total | 38 (n = 182 of 478) |
Analysis
Variations in PPI were mapped against the type of research, topic area and funding body. Drawing on the conceptual framework of Oliver et al. 132 and the PIRICOM systematic review,29 a scoping framework was used to assess the stages of the research at which PPI took place, whether involvement was of lay groups or individuals and where it was located on the continuum of PPI from user-led to minimal PPI. We also assessed evidence of the ‘architecture of involvement’:29 those processes needed to enable PPI in research, which included a budget for PPI, defined roles for lay people, training and support, and means of communication between researchers and lay people. This was used to evidence the range of resources supporting PPI. The results from this analysis are presented in Chapter 5.
Stage 2: survey of lead researchers
Objectives 2, 3 and 6 were addressed by conducting an online survey (see Appendix 1) of lead investigators (January–February 2012). The design of the survey was drawn from indicators of successful PPI identified by Boote et al. ,133 including roles, resources, training and support, and recruitment. Informed by the findings of stage 1, the survey was conducted in four regions.
Sample
Four geographical regions in England were purposively selected for the survey to ensure maximum variation: the South West has a relatively large rural population and a long history of PPI;143 the East of England has established PPI networks144 with rural and urban areas; there is less evidence of any long-established PPI history in the North East, which has one major research hub and socioeconomic factors affected by a heavily industrialised past; and London is the most densely clustered in terms of research centres and has a relatively high population of people from black and minority ethnic (BME) groups.
Data collection
Drawing on the findings of the PIRICOM study,29 a validated online survey tool (Bristol Online Surveys, University of Bristol, Bristol, UK) was designed to collect data to assess how PPI is operationalised and its perceived impact on each study. Although the PIRICOM study found little evidence of PPI being theoretically conceptualised, there has been some work to develop a consensus on the principles and indicators of successful PPI,133 and this was used to underpin the survey design. The research team’s previous experience of using online survey tools suggested that good response rates are achieved when the survey remains focused, it takes no longer than 15 minutes to complete and rapid feedback is promised to participants. There was close working with the appropriate comprehensive local research network, specialty networks and local specialty groups to publicise and disseminate information about the study. The survey was electronically distributed to lead investigators across the four diverse regions and its findings also provided the test-bed for stage 3. Participants received a summary of findings.
Survey response and study characteristics
From the UKCRN portfolio 360 studies across the four regions were identified and an e-mailed invitation and link to complete the survey was sent out to all named chief investigators (CIs) or researchers. From the first e-mail there was a 17% response rate and following the reminder there was a total of 101 responses to the survey (28% response rate) (Table 7).
| Topic | Number replying | Total number sent |
|---|---|---|
| CF | 2 | 3 |
| Diabetes mellitus | 28 | 140 |
| Arthritis | 14 | 56 |
| Dementia | 31 | 99 |
| IDD | 5 | 22 |
| Public health | 21 | 40 |
| Total | 101 | 360 |
The 101 studies surveyed ranged in sample size from 5 to 300,000, and grants awarded ranged from less than £50,000 (8% of sample) to 30 over £1M (30% of sample). Funding was split evenly between NIHR (40%) and charities (40%). The survey included 40% clinical trials, 33% quantitative and qualitative, 12% basic science and 7% tissue/bank database and a further 7% were coded ‘other’ (as insufficient information to classify).
Analysis
The focus of the stage 2 survey was to describe researchers’ experiences and perceptions of positive and negative outcomes of PPI, and benefits and challenges of PPI for researchers. The focus of analysis in this stage was therefore the use of summary statistics alongside qualitative analysis of open-text responses. Using an electronic survey tool enabled rapid access to data that were readily transferred to SPSS (version 20, IBM SPSS Statistics, Armonk, NY, USA) for analysis. This analysis was mapped against the results of the scoping in stage 1 to identify any recurring patterns within and between types of research, stages in research process where PPI occurred and topic areas. The findings from these two phases were used to develop a sampling frame for the final case study phase. The survey findings were then used as one of the ways to identify research teams likely to be interested in taking part in stage 3.
Stage 3: case studies
Objectives 2–7 were addressed through in-depth case studies. Stages 1 and 2 provided a contextual backdrop, and findings from these stages informed what was recognised as PPI in current and recent research. Stage 3 delivered an in-depth RE of the CMO in specific research settings to increase understanding of at what points PPI has the most impact and effect on outcomes.
Case study methods are a recognised and well-established approach to conducting research in a variety of ‘real life’ settings including health care. 145 Yin146 defines case study research as ‘an empirical study that investigates contemporary phenomena within a real life context, when the boundaries between the phenomena and context are not clearly evident and which multiple sources of evidence are used’ (p. 18). This approach allowed us to employ a range of social science research techniques and designs, mainly qualitative, to gain in-depth understanding of the nature of engagement between service users, the public and local NHS organisations within their specific organisations. It also provided the methodological flexibility to generate some theoretical insights from our results. 147 We were thereby able to adopt an interactive approach to data collection and analysis, allowing theory development grounded in empirical evidence, which was the main strength of this design. 148
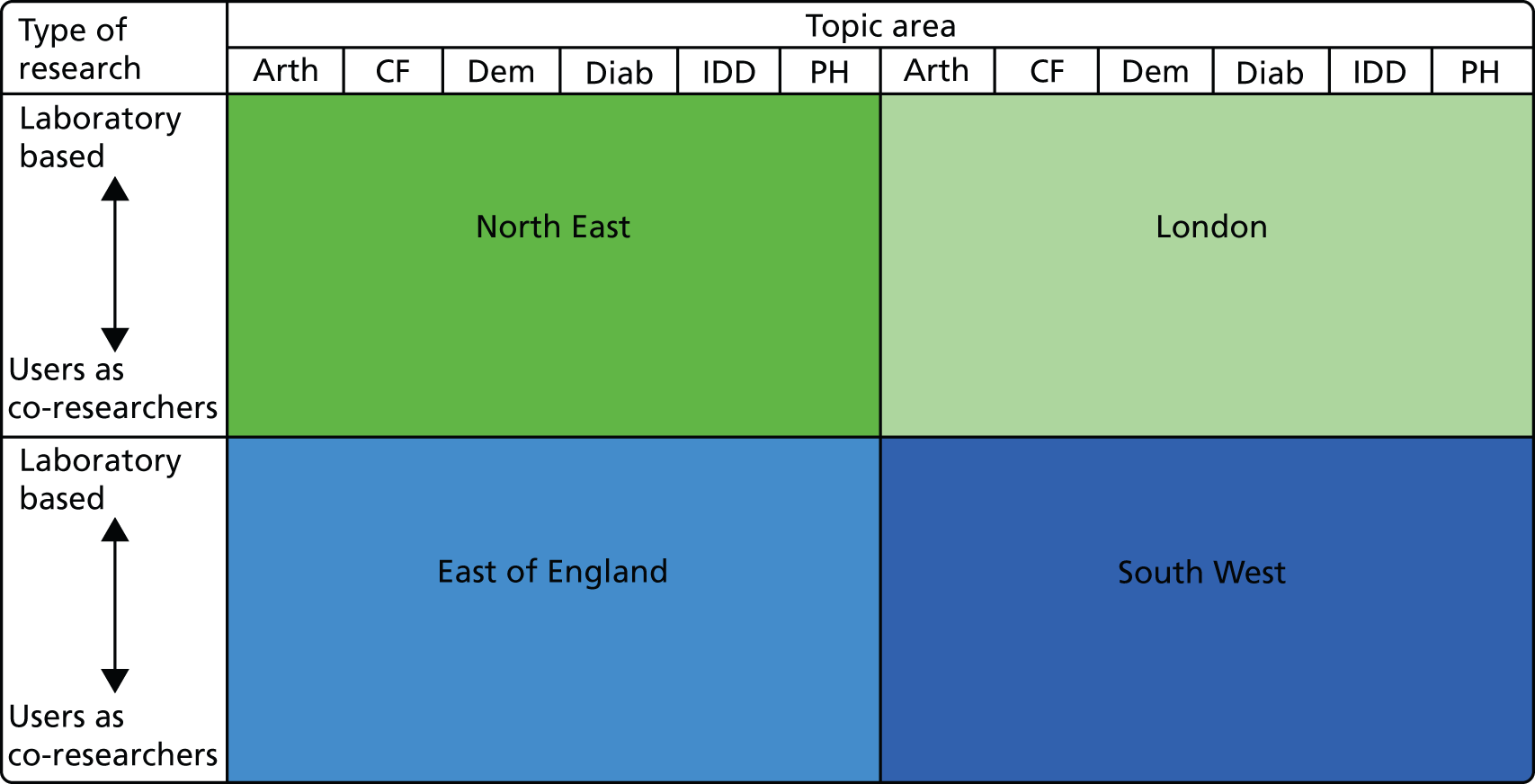
Sample
To ensure typicality and sufficient variation across topic areas, types of research and geographical regions, a sampling frame (Figure 5) developed from the previous stages was used to purposively select up to 20 case studies where the case is a single research study. This enabled maximum variation, but also allowed comparison within and between region, topic area and type of research.
FIGURE 5.
Sampling frame. Arth, arthritis; Dem, dementia; Diab, diabetes mellitus; PH, public health.
Data collection and recruitment
To ensure a range of studies that varied in their stage of research implementation, several recruitment strategies were employed:
-
Potential studies were identified from the survey.
-
Suitable early stage studies that had been awarded funding but had not yet been adopted on the UKCRN portfolio were identified by local Research Design Services (RDSs), by relevant charitable funding organisations from the AMRC, and by networks such as the Primary Care Research Network from their futures list. The RDSs, AMRC organisations and local research networks such as the Primary Care Research Network sent out information about the RAPPORT study and investigators interested in participating were asked to contact the RAPPORT study team.
Data were collected from each case study to inform the three stages of realist enquiry – context, generative mechanisms and outcomes119 – using the methods of documentary analysis, semistructured interviews with key informants from case studies, tracking and semistructured interviews with research funders and networks as follows:
Documentary analysis
Key documents from each project were requested and analysed149 to situate the project historically and capture the temporal dynamics of PPI at three levels of scale: micro (project), meso (host organisation) and macro (funding body). Documents requested included those pertaining to PPI policy, structures and support mechanisms (e.g. training) in the host [e.g. higher education institution (HEI)] and funding organisations. Project team and advisory/steering group meeting notes or minutes were also requested from participating case studies and (once anonymised) were added to the documentation collected in stage 1. Other relevant documents included, for example, PISs or publicity materials, which provided records or evidence of PPI impact/outcomes. Documents were requested and added to analysis throughout the data collection period of the RAPPORT study. A total of 278 documents were collated and analysed in the case study phase.
Semistructured interviews
Semistructured interviews were conducted with key informants in each case study. Depending on the study, this included the PPI members, lead/senior researcher, coapplicants, researchers, clinical partners and sometimes PPI co-ordinators within a host organisation. To maximise recruitment and participant convenience, interviews were conducted mainly by telephone and designed to take about half an hour to complete. The option of face-to-face interviews was also open to participants where preferred.
The interview guides developed (see Appendix 2) drew on, and were cross-referenced to, NPT,121 and focused on mechanisms and associated impact and outcomes of PPI. In the case of children and people with learning disabilities involved in studies, we had planned to review and modify data collection tools in collaboration with a reference group of people with learning disabilities, and a reference group of younger people with CF and their parents. However, all participants in this research were over the age of 18 years and, as seen below, a few participants with IDDs were recruited to the RAPPORT study. The only interviewee with a learning disability was high functioning and had experience of media interviews. Participants received an ethics committee-approved information sheet (see Appendix 3) and signed a consent form (see Appendix 4). All scheduled interviews were audio-recorded and professionally transcribed for analysis, and researchers checked them for accuracy and anonymised them upon receipt.
Tracking
Ongoing case studies were tracked over an 18-month period to identify public involvement processes. In negotiation with the study team this was expected to be a regular focused (telephone or occasionally face-to-face) interview with the lead investigator or other nominated member(s) of the research team but, as shown below, more often we were able to track PPI processes more fully by interviewing more than one researcher and/or a PPI member and supplement this data collection with e-mail exchanges/updates. The frequency of this contact depended on study characteristics and PPI milestones within the project, but occurred approximately every 12–16 weeks.
Semistructured interviews with research funders and research networks
To develop a fuller understanding of the dynamic and historical context of PPI, telephone interviews were also conducted with research funders and research networks. Key informants here included those professionals with responsibility for setting PPI policy and/or process for the funder/network and the studies funded within their research grant programmes. Other key informants here also included those with a PPI role within the funding body or network funding body – often as PPI representatives on research priority-setting panels or funding panels.
Interview guides here again drew on NPT (see Appendix 2), participants received an ethics committee-approved information sheet and signed a consent form (see Appendices 2 and 3) and interviews were audio-recorded and professionally transcribed for analysis and anonymised upon receipt.
Response and case study characteristics
In total we recruited 23 case studies in accordance with our sampling strategy as shown in Table 8.
| Topic | Region | Study design | Funder |
|---|---|---|---|
| Dementia | North East | Basic science involving humans | NIHR |
| East of England | CTIMP | NIHR | |
| Diabetes mellitus | North East | CTIMP | NIHR |
| London | Trial, cohort, qualitative | NIHR | |
| Mixed qualitative/quantitative | NIHR | ||
| Process of care, qualitative | Non-commercial | ||
| East of England | RCT to compare intervention | NIHR | |
| South West | Basic science involving humans | Charity | |
| Genetic epidemiology | Charity | ||
| Intervention (mixed quantitative/qualitative) | Charity | ||
| Arthritis | London | CTIMP | Charity |
| Research database | Research council/charity | ||
| East of England | Cohort | Charity | |
| South West | Qualitative methods | Research council | |
| Public health | London | RCT to compare intervention | NIHR |
| East of England | RCT to compare intervention | NIHR | |
| Survey admin questionnaires/interviews | Charity | ||
| South West | RCT | NIHR | |
| IDD | London | Questionnaire | NIHR |
| East of England | RCT to compare intervention | NIHR | |
| South West | Qualitative | NIHR | |
| Systematic review | NIHR | ||
| CF | London | CTIMP | NIHR/research council |
Considerable efforts were made to balance the recruitment of case studies according to region, topic area and research design. Other factors considered were the range of PPI models, PPI approaches, the stage the case study was at in its research process/cycle and the duration of the study. The cases we achieved appeared remarkably balanced, especially since the body of research in progress at any one time cannot be balanced according to our project’s specifications, but will be dictated by wider historical and political trends, biases and service needs.
Reflecting our emphasis on PPI processes and the tracking element of our research design, we over-recruited case studies in order to compensate for any potential dropout from the study. Standard consent to participation in research respects the right of individuals to withdraw from participation at any time, and for a variety of reasons research projects can be stopped before completion. Although we started with 23 case studies, after about 9 months into the RAPPORT study one withdrew from the study. There were two PPI representatives and two researchers in this study. These data were destroyed and removed from the analysis presented here.
Case studies were at various stages of progress during our RAPPORT data collection period and were tracked for between 8 and 18 months. Most case studies (17 of 22) had already begun before we started data collection, and approximately half (12 of 22) continued after RAPPORT data collection ended.
Initial and ongoing correspondence with case study CIs or a nominated research colleague identified potential documents and personnel (by role) to invite for interview for the RAPPORT study. In some cases it was acknowledged that some PPI representatives, more often those who had taken part in a larger one-off PPI event in the past, could no longer be identified or approached, as their contact details had been destroyed in line with the Data Protection Act (1998). 150 In addition, where studies in their development had been put to PPI panels that advise on a wider portfolio of research proposals [e.g. case study 01 (CS01)], it was deemed that they would have little to say regarding one of many studies they had reviewed in recent years.
Case studies were allocated to one of the three qualitative RAPPORT researchers at the University of Hertfordshire (PW and EM) and the University of East Anglia (JK). PPI co-researchers on the RAPPORT study (MC, DM and another PPI co-researcher) were affiliated to the University of Hertfordshire PPI group and thus were involved in case studies allocated there.
In total 129 participants [64 researchers, 48 PPI representatives, 7 PPI co-ordinators (attached to six of the case studies) and 10 funders/network representatives] were recruited for interview. The researchers and PPI representatives from the case studies were interviewed a number of times over the course of the study while the funders/network were interviewed only once; this gave a total of 206 interviews comprising 119 initial interviews with researchers and PPI representatives and 77 tracking interviews. The vast majority were conducted over the telephone. In accordance with participants’ preferences and geographical proximity/convenience, 17 of these interviews were conducted face to face (by JK).
The majority of researchers interviewed were female, although the sexes of the CIs were evenly split. Three-fifths of the CIs were over 50 years old whereas three-fifths of the other researchers were under 50 years. The majority (three-quarters) of PPI representatives were female and almost a quarter were over 65 years old.
In addition, approximately half (46%) of those PPI respondents who provided information had at least a degree and just under half of the PPI representatives interviewed were employed, full time or part time. Of those not employed, many were doing voluntary work.
The 22 case studies had a range of funders, including NIHR (Research for Patient Benefit, Health Technology Assessment, Efficacy and Mechanism Evaluation, Programme Grants for Applied Research), Collaboration for Leadership in Applied Health Research and Care (CLAHRC), charities and research councils. Eight representatives (both professional and lay) from various funding agencies were interviewed towards the end of the data collection period to explore the funding body’s perspective on PPI, including how this shaped the study context.
Overview of the analytic approach
Semistructured interview schedules for this study were informed by NPT, as was the initial coding frame, but, in line with guidance given regarding coding data using NPT, this did not preclude us from exploring other avenues in the data or limit our thinking.
If you are doing some form of coding via NPT constructs and components, you always need a code that is ‘other’, as in, issues and topics that do not clearly fit within the NPT. 151
Inductive codes were also developed.
Thematic content analysis was used first to identify key themes and common experiences as site specific and then to make cross-case comparisons. This established how different contexts (e.g. topic area, type of research and setting) affected processes (e.g. training and support), mechanisms (e.g. relationships and communication) and outcomes of PPI (e.g. evidence of changes, responsiveness to PPI input and impact on dissemination). Research team data analysis meetings provided a productive environment for generating themes, collective sense-making and enriched understanding through all stages of the study.
Utilising a similar approach to those of Schierhout et al. 152 and Rycroft-Malone et al. ,153 the analysis involved the following steps:
-
A subset sample of initial interview transcripts of interviews with both researchers and PPI representatives as conducted by various team members were coded independently (manually) by team members (PW, EM, JK, MC and DM). This was done both deductively, using an initial adapted version of the 16 NPT components, and inductively, capturing unforeseen themes which emerged within the data relating to our research questions. 154
-
A meeting was then held to discuss the coding of each sample interview, to address inconsistencies in the application of the coding categories and to refine collective understanding of them (increasing inter-rater reliability). We added several subcategories; for example, under the category ‘7. legitimation – participants do/do not buy in to the intervention (PPI)’ we added the subcodes ‘a) keen to do the research’ and ‘b) keen to do PPI’ to reflect distinctions within the accounts given by participants. We also further adapted the NPT coding frame to distinguish between where participants were discussing potential (hypothetical) and actual outcomes of PPI within case studies. In addition, given that NPT is an action theory, we ensured that coding categories captured where participants were reported not to have something as well as where they did have it, and that such instances were not labelled based on judgements or assumptions. Indeed, minor revisions were made throughout (e.g. the addition of inductive codes such as ‘background to project’).
-
All data relating to the identified categories were highlighted within the first round of interview transcripts and documents collated for each case study, using NVivo 9 (QSR International, Warrington, UK).
-
Data generated through interview were triangulated (including with study documents) to corroborate, elaborate, contradict or complement other data,155 in order to interpret PPI processes.
-
An initial summary of the NPT analysis and a RE were then written for each case study and shared within the team to check consistency in usage of the coding categories.
-
The Economic and Social Research Council-funded web-based NPT toolkit was then used151 to develop radar plots for each case study. These plots provided a temporal snapshot: a visual representation of the embeddedness of PPI within a case study within the four constructs and 16 domains. It must be noted that the expression of embeddedness is, of course, a function of the PPI design on different projects: the fuller the radar plots, the more fully embedded the PPI. Spikier plots illustrate internal variance in the degree of embeddedness (Figure 6).
FIGURE 6.
Levels of PPI embeddedness illustrated through NPT radar plots.
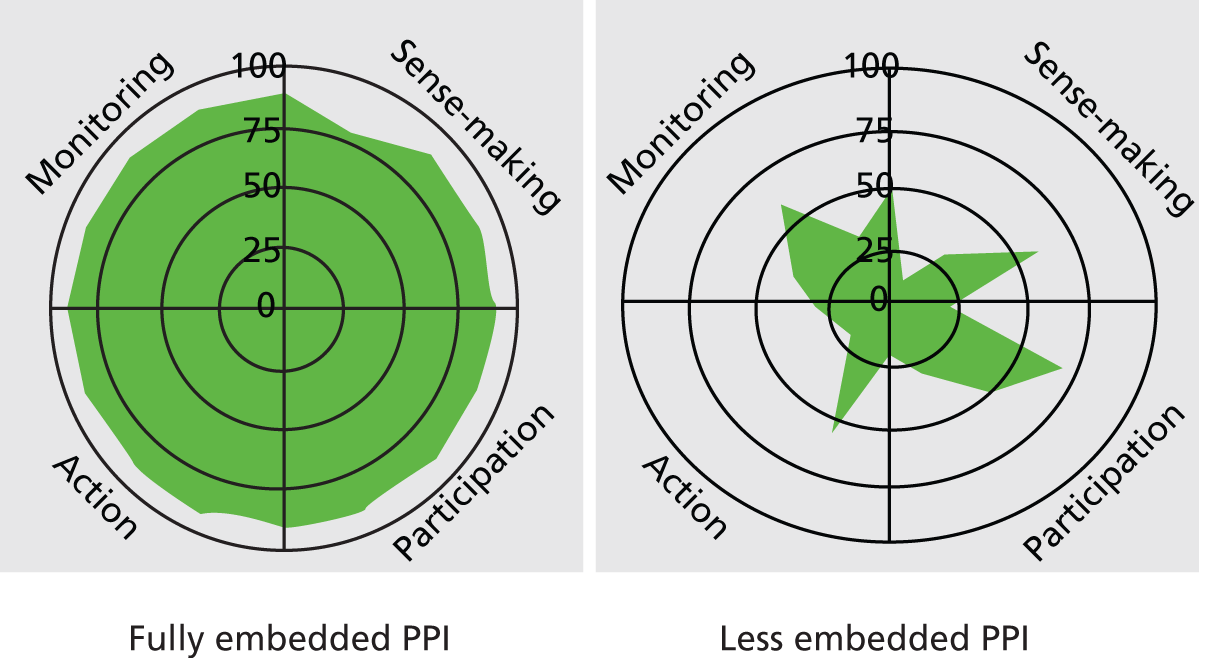
Radar plots supported our understanding of changes within case studies over time and ongoing comparison between them. Both the RE summaries and radar plots acted as aides-memoires for the research team throughout the research and also helped to maintain the specificity and wholeness of each case study. Summaries were updated and radar plots were re-evaluated at 18 months or the end of that study to capture/reflect any changes in PPI processes.
-
We repeatedly read, viewed and discussed and compared data from each case study at regular team meetings to develop our analysis and to identify emerging features of CMO across case studies.
-
We then tested CMO configurations across the data set as a whole, accepting, rejecting or refining CMO configurations through discussion.
-
Context, mechanism and outcome configurations were further refined through discussions with case study respondents, the reference groups and the RAPPORT advisory group, and four regional events conducted at the end of the study (see Appendix 5).
The steps above were initially undertaken in the order shown, although most were returned to repeatedly and iteratively.
A finalised NPT coding frame was devised and subcodes were added to the NPT constructs outlined earlier, and further inductive codes (such as PPI model description and personal narrative) were added. Analysis was informed by the research questions and RE, with methodological triangulation occurring during analysis and interpretation of results. 156
Quality assurance during the analytic phase
To make the analytic phase both transparent and rigorous, to increase the validity and reliability of our findings, transcripts were shared and coding was frequently and rigorously discussed and amended as analysis proceeded, maintaining reflexivity. This system of checking and critiquing the analysis was not merely to promote consensus but was a way of more deeply interrogating the data and exploring alternative explanations. 157 The co-researchers on the core research team were actively involved throughout the analysis and emerging findings/analysis discussed with an advisory group, which included PPI representatives, and with an IDDs reference group.
Research data management
Project-specific secure drives were set up at both the University of Hertfordshire and the University of East Anglia; only the research team had access to them. Both drives were backed up centrally each day. All interview data recorded on digital devices were uploaded onto university secure servers as soon as possible after interviews and deleted from devices. A file-labelling system was developed to ensure good housekeeping of data. Digital audio recordings for transcription were sent securely between the transcription agency and the research team. Upon receipt, transcripts were checked for accuracy and anonymised to protect the identities of the participating studies (personnel and place names, for example, were changed/removed).
Dissemination
Four regional dissemination events were held towards the end of the study. RAPPORT participants, local PPI and research groups attended (see Appendix 5). Our provisional findings were presented, and facilitated small group discussions were used as a means to confirm or refine CMO configurations.
Presentation of data in subsequent chapters
The findings chapters, Chapters 5 and 6, draw extensively upon statistics and illustrative examples from the data collected and analysed in order to describe six CMO configurations. In Chapter 7 we develop our analysis further to generate insights regarding the current embeddedness of PPI in health research in England. Excerpts from interview transcripts are included to bring findings alive and boxes are used to present case studies exemplifying each CMO configuration. Data from all 22 case studies are presented in the findings chapters. We have honoured our duty to respect confidentiality and protect research case studies by avoiding presenting too much data, which could be overly revealing. In Chapters 5 and 6, participants’ words are presented within embedded extracts or within speech marks within the text and speakers are broadly identified as funders or research network PPI co-ordinators, or by case study (CS) number and as being either paid academics on the research (Res) or PPI representatives (PPI). If there was more than one interview with a participant, interview number follows the participant code.
Chapter 4 Patient and public involvement in the RAPPORT study
As the RAPPORT study is a research project investigating PPI in contemporary health research in England, in this short chapter we begin by detailing the approach to PPI within the project itself, and then present an analysis of some of the reflections upon the experiences and processes of PPI.
This chapter was first drafted by one co-researcher and then expanded and elaborated with evidence by the research team, with comments from lay co-researchers and representatives.
Background to the project
The University of Hertfordshire had an existing PPI group: the University of Hertfordshire Public Involvement in Research Group (PIRG, established in 2005), with which the proposal to the Health Services and Delivery Research (HSDR) programme/INVOLVE was originally developed. The application included two coapplicants from PIRG, to be funded as co-researchers if successful. Additional expertise was added to the research team from coapplicants from the University of East Anglia. Lay representatives on the project advisory group were subsequently recruited from the Norfolk and Suffolk Patient and Public Involvement in Research (PPIRes) panel (established 2003), and the main support for this input linked with the University of East Anglia team. AH’s work with the Royal College of General Practitioners (RCGP) also allowed recruitment of a lay representative with a national overview of PPI in clinical settings (Chuter, then Chair of the RCGP Patient Partnership Group). The co-researchers, as members of the research team, attended the advisory group, but their roles were different: they were ‘embedded’ in the research project, where other lay contributors had episodic input. Finally, there were lay people linked with each research topic area as a reference point for the conditions under scrutiny. The study team aimed for a mixture of different PPI representatives: those who had worked together before (co-researchers from PIRG) and those who had not worked together before (PPIRes and the University of Hertfordshire); and experienced (> 10 years) PPI representatives and reference groups who had not worked with researchers before. It was one co-researcher’s first research project.
Patient and public involvement design
Coapplicants
Two members of the University of Hertfordshire PIRG were coapplicants on the RAPPORT study.
Co-researchers
There were three co-researchers: the two coapplicants plus a mother of a child with CF. These three were involved throughout the study, but were particularly involved in case study data collection (interviewing) and analysis. The two lay coapplicants were members of the research team (out of a total of 11 members), which met every 3–4 months. Team meetings were held face to face every 6 months, with a teleconference in between. The research team commented on all study documents, findings and publications.
Reference groups and representation
The project had reference links who were consulted during the progress of the study to add insight on PPI in each topic area. Some links were via the research team itself: one co-researcher had a child with CF, one had diabetes, one had arthritis, and two had cared for a family member with dementia and had been on other studies involved with dementia. Where links did not exist, reference groups were set up: an IDD group and a CF group of young people. The IDD reference group met face to face during the project to facilitate communication (including Easy Read materials); the CF reference group ran on a virtual basis.
Project advisory group
The project advisory group (a total of 22 members) met in person every 6 months and was well attended by the five lay representatives and the lay chair. The lay representatives consisted of two members from PPIRes, the two co-researchers from the University of Hertfordshire PIRG and one lay representative from the RCGP. In addition, the advisory panel included representatives linked to reference panels and lay groups: the Learning Disabilities Research and Development Manager (NHS North Essex) and the National Cancer Research Network Consumer Involvement Lead, who was later replaced by the Mental Health Research Network PPI Lead.
As for all advisory group members, PPI representatives reviewed all documentation concerning the research, and commented on emergent findings and study progress; meetings were minuted in detail so PPI contributions were included. The topic of PPI in the RAPPORT study was also an additional standing agenda item at each meeting, to ensure that feedback was welcomed and queries or concerns raised openly; this added to the reflective material utilised to assess impact within the study itself.
Patient and public involvement activities
Research design
Four members of the University of Hertfordshire PIRG submitted initial ideas for the research proposal; their contribution actively shaped and informed the proposal design. From the beginning, two research team/PIRG members actively contributed to the development of the full proposal, which was also discussed at regular PIRG meetings.
Data collection and data analysis
Three co-researchers were heavily involved in stage 3: case studies. The agreed main purpose of their input was to enable engagement with those playing PPI roles in some of the case studies: a peer-to-peer interview, as used in previous studies. 88–90 This was expected to add value to the study by allowing themes to emerge that were different from or additional to those captured by other means, even though the co-researchers were also involved in reflective analysis of the whole data set, not just their own interviews.
In recognition of the co-researchers’ needs, the whole research team developed a training session on interview techniques and the use of digital recorders, and co-researchers also helped develop the interview schedules. The peer interviews (with PPI representatives on case studies) were allocated according to interest, availability and background, sampling a total of eight case studies. Co-researchers were supported in carrying out the telephone interviews (the majority of interviews were by phone), either at the University of Hertfordshire or in the co-researchers’ homes, and carried out a total of 14 first interviews and three tracking interviews. The numbers of peer interviews were lower than originally planned because of difficulties in finding mutually convenient times for co-researchers and respondents. In reality, co-researchers had less availability and flexibility to accommodate interviews that other members of the research team.
Once the interviews were transcribed, 11 data analysis sessions (including training) were held with the researchers and the co-researchers (either individually or as a team). Only one further data analysis meeting was held without the co-researchers when they were unable to attend. The initial meetings were used to agree on coding structures and the use of NPT and to compare individually coded transcripts. Subsequently, data analysis meetings tested out the CMO configurations within and across the various case studies. PPI co-researchers also individually coded interview transcripts.
Dissemination
Conferences and meetings
The co-researchers copresented findings at four conferences and meetings while the project progressed. They were also fully involved in the RAPPORT national dissemination events, where the CI gave a formal presentation and the intention was to have a lay copresenter on each occasion. However, health needs of co-researchers prevented this from happening. One co-researcher attended two of the four dissemination events, and the two PPI representatives on the advisory group attended their local dissemination event. In addition to the roadshows, we have disseminated at key conferences including INVOLVE and the Higher Education Academy PPI seminar series, where both co-researchers presented and one made a podcast.
Papers
Two PPI coauthors contributed to a scoping and survey paper published in the International Journal of Consumer Studies (January 2014). 158 One co-researcher also submitted a piece on RAPPORT to Balance (Diabetes UK’s patient magazine) in August 2013; it was published in May/June 2014. Further publications with PPI input are expected. The overall general findings of the RAPPORT study will be available in Easy Read format once the report has been agreed.
Data sources for the analysis of patient and public involvement in the RAPPORT study
The following have been used to review the PPI input to the RAPPORT study:
-
documentation on the development of the original proposal (already submitted to INVOLVE as ‘Short report prepared for INVOLVE on public involvement in the development of a research proposal’, November 2010)
-
team minutes and field notes – these include audio recordings of discussions with the co-researchers, and researcher personal diaries (voluntary and self-held, but used for recall)
-
reference group discussions and notes of meetings
-
formal research team and advisory group minutes
-
all study documentation
-
records of interview schedule development, interviews, coding and analysis
-
formal ‘end of project’ reflective meetings, including individual notes from co-researchers, and two meetings held to reflect on the PPI process in the RAPPORT study, one with the research team and one with the advisory group.
Some quotes are shown here as evidence of different impacts in different phases.
Impacts of patient and public involvement in the RAPPORT study
Two co-researchers made some overall comments about the study:
None of this [PPI] has been tokenistic and lay contributors were treated as colleagues making contributions of equal value to that of the researchers throughout. Our comments and suggestions have been discussed and acted on where it was agreed they were appropriate. This has been made possible by ensuring we saw all relevant paperwork and were kept informed of issues as they arose and about progress as it took place.
Co-researcher01, 21 December 2014
I enjoyed everything about collaborating in the study but particularly participating in all the team and advisory meetings, the discussion on methodological issues and theoretical approaches. I appreciated being involved in all aspects and felt thoroughly involved and appreciated.
Co-researcher02, 15 January 2014
There were also reflections about specific stages of the research process.
Study development and protocol
Two quotes from the report of 2010 show that there was lay involvement as soon as the funding call came out and in developing the proposal:
Details of the call [for funding] were circulated to the PIRG for comment and initial ideas; four members responded. Responses were fed into the pool of initial ideas about the proposal. Ideas were fed back to the PIRG as they developed and after two weeks of on-line discussion PIRG members were asked what level of continuing activity they would like to undertake in the proposal development. Two members volunteered as co-applicants, the other two wished to contribute informally to the development. Additionally, the developing proposal was presented at the regular PIRG meetings to enable the whole group to have an input.
Early drafts of the outline proposal were circulated to the 2 PIRG members as part of the co-applicant team. They actively contributed to the development of the outline proposal by:
Data collection
Interviews carried out by PPI representatives (peer interviews) had some additional perceived benefits. PPI members often had more knowledge about a particular health condition than the researcher and could better relate to the interviewees:
I felt her [PPI’s] warm personality and humour shone through, and this made it very easy to build up a rapport with her quickly, and therefore make more effort to contribute. There was careful and gentle questioning, never intrusive, and she encouraged me carefully to think of other things I might have missed. Throughout the interviews I have had with her, I felt I was a real person and not an object of research.
RAPPORT PPI respondent CS17PPI01, e-mail exchange with respondent
[I had a] lot in common with her . . . think the connection we made was important, both had daughter with [health condition] . . . it felt more like you were having a chat as opposed to doing an interview.
Co-researcher03, 26 November 2012
The relationship between co-researcher and respondent also developed with time:
Yes, you know, it was like . . . she was asking about my daughter, I told her she might be going to hospital, she asked how was she and she said you have my number if you want to call me.
Co-researcher03, 26 November 2012
However, this benefit of peer interviewing was not considered to have the same impact across data collection. Not all experiences are shared: ‘I’m not sure user involvement made much difference in this interview as she was only [in her twenties] and not closely related to my experience’ (Co-researcher03, 18 October 2012).
One of the researchers commented that ‘re-designing the interview schedule so that it was more informal and chatty, involving people with real experience in talking to PPI reps in similar positions, helped make interviews more relaxed, open and reciprocal’ (reflections July 2014) (Box 4).
Original interview schedule first question: can you tell me how long you have been involved in research? How did your involvement come about?
Revised interview schedule first question: first we want to explore what do you understand by the term patient and public involvement in research? (sometimes called service user involvement/patient representation – other terms)
Before you were involved in xxx study what did PPI mean to you?
Data analysis
The RAPPORT team, including the co-researchers, used NPT as the candidate programme theory and also used it to shape the interview schedule and data analysis. One co-researcher found framing data analysis through NPT constructs ‘intellectually stimulating’ (Co-researcher02), while another found using interpretive approaches more generally (and NPT’s abstractions in particular) to be very challenging. This co-researcher devised her own set of inductive codes and analysed the transcripts using her own coding system. The use of this separate coding process added to the rigour and validity of data analysis as similar themes emerged:
I also think that having co-researchers independently coding transcripts added rigour to the process – I remember concerns from the 3 core researchers about whether there was data forcing into the NPT constructs. [X] went off, did free inductive coding and when we compared the same findings emerged – quite a relief!
Research team member reflections July 2014
Impact of patient and public involvement on representatives
As found within the RAPPORT study, the co-researchers gained personally from carrying out the research:
stimulating to get me back to using my brain a bit more and think about research.
Co-researcher03, 27 April 2012
However, this did not apply to the same extent to those who were not co-researchers:
I found this quite difficult to do, as I want to do more than you are asking me to do all the while.
Lay advisory group member, reflective meeting, 15 January 2014
Discussion of emergent findings
Patient and public involvement representatives on the research and advisory teams continually reminded the researchers of what is important, such as the current debate around PPI and professionalisation. The research team was able to test out the findings from the survey/scoping and case studies with PPI representatives as stakeholders who are aware of the current climate of PPI.
Enablers and challenges for patient and public involvement within the RAPPORT study
These were examined using the four NPT constructs:
Coherence
Roles and expectations of PPI representatives. The original project’s assumptions about the different roles, expectations and capacities of the various PPI representatives within the RAPPORT study needed revisiting over time: ‘Being on an advisory group I found quite limiting’. After a discussion at the end of a project meeting about whether or not being a PPI member of an advisory group was superfluous, it was then acknowledged that ‘they have a real role of accountability and PPI need to play a part in that’. There was also positive feedback about the improvements over time: ‘advisory groups have a bad reputation in PPI as having been tokenistic, this project did not feel like that’ (all three comments from the advisory group reflective meeting, 15 January 2014).
One co-researcher (Co-researcher02) was ‘disappointed’ that she was not able to do more interviews and had expectations of doing more than the research team were able to organise. However, she acknowledged this was also because of her own problems with availability of dates and different topic areas. She also felt she had ‘let the team down by not keeping to deadline’ (this was not seen as a problem by the research team). This co-researcher also reflected on the ‘difficulty of keeping sometimes, a lay role and not getting carried away with all the theoretical and methodological aspects . . . and a recognition of my own bias’. This comment resonates with the debate about ‘professionalisation’ of lay participants, and perhaps shows that there will not be one long-lasting ‘coherent’ view of PPI – rather a need for renegotiation and flexibility.
Participation
There was feedback that having support for personal and practical queries improved inclusiveness and contribution. Having a local person to co-ordinate PPI travel, expenses and other practical matters was found to be very important, as was accommodating preferences for written/hard copy materials rather than electronic communications:
paying attendance makes me feel valued, my time feel valued and respected, it is a big thing for me, not just paying me enough for the day, they are paying me, respecting me and my time.
Lay representative, advisory group reflective meeting, 15 January 2014
Collective action
Relationships. Replicating the findings from the RAPPORT study, the importance of relationships emerged as central in this study. Two of the co-researchers had a history of working with the CI and the team based at the University of Hertfordshire: there was prior shared understanding and trust, and this developed during the time of the project. The two PPIRes members on the advisory group already had relationships with coapplicants at the University of East Anglia but not with the University of Hertfordshire or other research team members, and new relationships across institutions developed over time. All advisory meetings started with lunch, allowing time to socialise. With hindsight, it was acknowledged that more time for the RAPPORT team to meet informally would have been beneficial, but lengthy journeys and budget constraints would have made this difficult. One co-researcher commented on:
the challenge of keeping everyone in PPI in ‘the loop’ being a task – with our other PPI colleagues being at a distance, but there was continued involvement and commitment to keeping all in touch and involved.
Co-researcher02,15 January 2014
Relationships had to develop with new members of the advisory group and with the reference groups, and these took time to establish. Explicit emphasis on this might have increased input and facilitated early project processes:
Usually I am approaching people to be on the advisory group that I have already have some relationship with or worked with before . . . it was quite different to have people recommended that I had not met in depth before, I think I had been quite naive before . . . if you haven’t got that relationship . . .
Team researcher reflections, 15 January 2014
Flexible provision for access. Respect for and accommodation of PPI representatives’ different skill mixes and requirements was an issue. For example, two of the co-researchers had different qualitative data analysis skills, two of the PPI representatives did not use computers and preferred to receive and annotate paper copies and one PPI representative on the advisory group asked for contact to be made by text.
Health/illness. Over a 2.5-year study, illness has meant that at times it was difficult for some PPI representatives to travel long distances or into London and be as involved in the RAPPORT study as they would have liked. Not all activities could be undertaken as expected, and the team worked around to find solutions. Every effort was made to be inclusive, by holding meetings locally wherever possible, organising convenient parking at the university, providing lifts, accompanying representatives on public transport, paying for taxis and so on.
Reflexive monitoring
Both lay advisory group representatives and research team members were encouraged to record formative reflections upon PPI and were provided with prompt questions and notebooks. However, as the study progressed, this proved difficult to maintain, with lay representatives reporting they did not do it immediately and then forgot to do it, so opportunities were instead created to prompt and audio-record reflections informally as conversations before or after certain meetings throughout the study. Two of the co-researchers, however, did provide the paper records of their formative thoughts at the end of the project.
A more formal summative reflective session on PPI in the RAPPORT study was conducted to capture the impact of PPI within the study. Two face-to-face meetings were held towards the end of the project: the first was with members of the research team (facilitated by two external facilitators) and a second for members of the advisory group. Each session was recorded and summary notes produced. An ‘ALPS’ [Amander’s Levels of Patient and Public Involvement Significance, a reflective tool developed by A. Wellings, a lay member of the advisory group, and reproduced with permission (Amander Wellings, PPIRes panel, 2014, personal communication)] was sent to all members before the reflective session and provided a stimulus for this discussion (see Appendix 6).
Summary
Overall, PPI has had a demonstrable impact on the RAPPORT study at all stages of the research cycle, particularly during the case study stage. As one PPI representative wrote, ‘there has been a large amount of public involvement across a range of roles within RAPPORT from its conception to its finish’ (Co-researcher01, 21 December 2014) – ‘Validating what themes are important, being there as a critical friend throughout the project’ (reflections on report July 2014). The key findings reflect those of the study itself: that both embedded PPI and periodic inputs can be valuable in different ways; and that relationships are key to making people feel included, getting their fullest contributions and solving practical problems. Clarity about different roles is important when there is more than one type of input from lay people into a project, and sufficient flexibility is needed for people whose other work or health may not allow predictable inputs. A strong emphasis on dialogue and feedback may assist both developing relationships and a sense of mutual respect and engagement, and allow concerns to be aired early. Previous experiences of PPI work may colour ongoing expectations, and may be worth exploring early on.
Chapter 5 Findings from scoping and survey
The scoping and survey had three main purposes. First, to provide some sense of the current landscape of PPI in terms of extent and types of models used. Second, to do some initial testing on enabling contexts for the embedding of PPI. We hypothesised that there were five important enabling contexts for PPI: funder requirements; topic area and design; resources; organisation of PPI; and the host organisation. Third, the results of the scoping and survey were used to further develop our sampling frame for the case studies, and to sharpen our questions and testing within them.
This chapter will present the main findings from the scoping and survey, drawing out implications for our hypotheses and the enablers and barriers for the candidate programme theory: NPT (see Chapter 3). The chapter commences with a summary of the key findings.
Summary of key findings
The scoping illustrated that there is a limited amount of publicly accessible information about PPI within research documentation and most of the information we obtained was through e-mailed requests to the study teams (see Chapter 3). Within the scoping we were unable to find evidence of any PPI in nearly half of the studies. Although within the normal parameters of an electronic survey,158 the disappointing response rate of 28% means that the results from the survey must be treated with caution (see Chapter 8, Reflections on and limitations of the research).
In both the scoping and survey it was clear that some respondents did not distinguish between involvement and study participation. There was also evidence of a dual role: study participants also acting as advisors either concurrently with being a participant, or sequentially.
There were differences in how PPI was approached by research topic; IDD had evidence of PPI in the highest percentage of studies. Basic science or tissue bank design studies appeared to have a limited role for PPI, although there were examples in the survey where these designs had PPI present.
From the survey we found that nearly half of PPI representatives were already known to the study team when it invited them to be lay advisers. Paradoxically, open-text responses in the survey emphasised the challenge of representativeness.
Survey respondents suggested that PPI impact is greatest in the early stages of research, although there were examples given of impact throughout the research process. With some noteworthy exceptions, there was sparse evidence of systematic evaluation of PPI within studies.
Studies without patient and public involvement
Within the scoping we were unable to find evidence of PPI in 49% of studies. This does not necessarily mean there was no PPI; rather, it may be indicative of the lack of accessible PPI-specific evidence. For example, protocols obtained directly from research teams confirmed that there was little space or official requirement to record PPI, with only one-third of protocols including any PPI information. Some respondents explained that other forms, such as funding applications and IRAS forms, had more detail of PPI:
We are happy to share our information on PPI. As the protocol does not reflect the level of PPI involvement in the design and conduct of the study I have highlighted fields from our original NIHR RfPB [Research for Patient Benefit] application form which reflect our level of PPI – see below.
Scoping: arthritis: clinical trial: identification code (ID) 49
Survey respondents were more likely than scoping respondents to report PPI within their study (79%), but 17% reported they did not have PPI, and for a further 4% (n = 4) it was unclear whether or not what was being described was PPI. In a short survey focused on gaining descriptive detail on the current extent of PPI, it was not possible to identify any specific rationale for not having PPI within a study (see Chapter 3). Although three out of seven tissue bank studies did not have PPI, studies with a basic science or tissue bank design did provide evidence of embedded PPI. Study design alone was not a predictor of engagement with PPI. However, there were some differences in how PPI was approached by research topic and study design.
Differences in the reported presence of patient and public involvement
Numbers of studies in some topic areas were very small (e.g. CF). In both the scoping and the survey, IDD studies, compared with the other topic areas, had the highest percentage of studies with evidence of the presence of PPI (scoping 91%; survey 100%) (Table 9). Second highest were arthritis (60%) in the scoping and dementia in the survey (87%). However, in the survey there was an overall trend for much higher levels of PPI across all topic areas than in the scoping.
| Design | Topic area (n) | Total | |||||
|---|---|---|---|---|---|---|---|
| CF | Diabetes mellitus | Arthritis | Dementia | IDD | Public health | ||
| Scoping studies | |||||||
| Clinical trial | 1 | 8 | 19 | 7 | 2 | 6 | 43 |
| Basic science | 0 | 0 | 2 | 1 | 1 | 0 | 4 |
| Qualitative and quantitative | 1 | 8 | 9 | 4 | 6 | 8 | 36 |
| Human tissue, data and tissue bank | 0 | 3 | 3 | 0 | 1 | 2 | 9 |
| Other | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Total | 2 | 19 | 33 | 12 | 10 | 16 | 92 |
| Survey studies | |||||||
| Clinical trial | 0 | 11 | 5 | 6 | 3 | 9 | 34 |
| Basic science | 0 | 4 | 1 | 3 | 0 | 0 | 8 |
| Qualitative and quantitative | 0 | 6 | 3 | 15 | 2 | 4 | 30 |
| Human tissue, data and tissue bank | 0 | 0 | 1 | 2 | 0 | 0 | 3 |
| Other | 0 | 1 | 1 | 1 | 0 | 2 | 5 |
| Total | 0 | 22 | 11 | 27 | 5 | 15 | 80 |
Using the IRAS definitions of study design (which were collapsed into four categories plus ‘other’), studies with mixed-methods designs (i.e. qualitative and quantitative) had the highest incidence of PPI (61% of scoping studies with this design had PPI; survey 91%), followed by clinical trials (scoping 56%; survey 81%). Both of them had higher levels of PPI than basic science (scoping 21%, survey 67%), tissue bank (scoping 33%, survey 43%) and other (observational studies and ‘cohort’) (scoping 0%, survey 71%). Basic science or tissue bank design studies appear to have a limited role for PPI.
However, the survey findings for the three topic areas of arthritis, dementia and public health showed examples of all four types of study design, and in these topic areas even basic science and tissue bank studies included some PPI elements. Written answers seemed to link this to the recognised need to build and sustain good relationships with patient groups in order to identify priorities and gain the research materials they needed:
all our work has been carried out in partnership with the families . . . often helps to focus what patients with a condition find most urgent to improve.
Survey: diabetes mellitus: basic science study: ID05
In this project probably all stages, from literature aimed at recruiting potential brain donors to lay people on the committee that gives ethical approval to researchers requesting tissue from the bank. We also invite a potential donor/carer to speak about brain donation from a personal perspective at our Ethics Training Days and this is always very highly rated by people contributing to brain donation, especially those without participant contact, such as mortuary services and neuropath lab staff.
Survey: dementia: tissue bank research: ID54
Relational work is a key element of the collective action construct within NPT and, as illustrated above, was perhaps even more important to focus on in research designs such as basic science, where there was an inevitable distance between researcher and end beneficiary of the study. This NPT construct proved important in our case studies (see Chapter 6). Furthermore, the survey showed that 50% of PPI representatives involved in research projects were patients or service users known to the researcher/clinician and that very few were recruited via their local NHS comprehensive local research network or RDS. PPI representatives were also recruited via voluntary organisations (40%) or from an established service user group (35%), and a quarter (25%) of survey respondents reported that their PPI representatives had replied to an open invitation (respondents could choose more than one option).
Organisation and resources for patient and public involvement
Survey results indicated that 29% of studies had 21 or more individual patient or public representatives involved. However, the PPI information in the scoping documents/e-mails was very limited and it was difficult to access who the PPI members were, how many there were and how they had been recruited. It was therefore not possible to make an accurate assessment about PPI models. Just over a one-third gave any information about PPI recruitment and only around one-quarter of the studies gave any information about the number of PPI representatives.
To elicit any embedded PPI organisation, the survey respondents with PPI in their studies were asked if working with regional/local public involvement groups had altered their practice when writing proposals. Seventy-nine per cent of researcher respondents said they knew of a local or regional and public group that had supported research. Sixty-three per cent had used such a group and 36% said that this group had altered their practice when writing the proposal. The main way in which the researchers said they had altered their practice had been by consulting PPI at proposal writing stage to ‘define research questions’ and making objectives ‘more realistic’ and ‘patient-orientated’.
The survey provided information on what roles and activities lay representatives were undertaking. The most frequently represented PPI activities were being on an advisory/steering committee (65% in the scoping study) and patient information leaflet development (73% in the survey). Low levels of involvement were reported in data analysis, data collection and report writing in either the scoping study or the survey (Table 10).
| PPI activities | Scoping (%) | Survey (%) |
|---|---|---|
| Advisory/steering committee | 65 | 71 |
| Development of participant information materials | 35 | 73 |
| Dissemination materials | 16 | 49 |
| Review of reports/lay summaries | 8 | 48 |
| Design of research methodology | 62 | 45 |
| Identification of research topic | 17 | 21 |
| Report writing | 3 | 9 |
| Data analysis | 12 | 8 |
| Data collection | 3 | 6 |
| Other | 10 | 10 |
The possible activities were then totalled into a score and the survey revealed that IDD had the highest median level of activities, followed by arthritis and dementia (4.0 for IDD and 3.0 for arthritis and dementia). However, Figure 7 shows that there is little difference in the overall range of activities between each topic area.
FIGURE 7.
Survey: box plot of number of activities for those studies with PPI by topic (showing range of the number of activities, 75th percentile, median and 25th percentile). a, maximum value; b, 75th percentile; c, median; d, 25th percentile; e, minimum value. Note: the number of activities was calculated only for those studies with PPI.

Topic area was therefore not predictive of the range of PPI roles within a study. However, simply knowing ranges of roles does not provide an in-depth analysis of whether or not the roles were appropriately allocated and supported. We found only 9% of studies from the scoping with any evidence of training, whereas over one-quarter (28%) of studies with PPI in the survey had provided training for their PPI members, and 43% had directly costed for training of PPI members in the grant application.
Funder requirements
The influence of funders could also be seen in that higher levels of PPI were found in NIHR-funded studies (scoping 75%; survey 89%) and charity-funded studies (scoping 58%; survey 78%). Researchers acknowledged that PPI is a relatively recent expectation from funders, and for some studies the external expectation was key to the development of PPI:
We have had no structured PPI for this study. There are a number of reasons for this: The study was developed a while ago and there was less of an expectation for PPI.
Scoping: diabetes: mixed qualitative/quantitative: ID24
Alzheimer’s Society uses a PPI [representative] for peer review of grants and so these proposals are written with this in mind.
Survey: dementia: basic science: ID73
Neither scoping nor survey found any relationship between sample size or geographical area and levels of PPI. There were similar proportions of studies having PPI in the older studies (as measured by being ‘closed’ on the UKCRN portfolio) and in the open studies. However, evidence of PPI was further blurred because of inconsistencies in how PPI was defined.
Defining patient and public involvement
Our analysis showed that various interpretations of PPI were apparent among researchers. As a reminder to recipients, the scoping requests for information and survey highlighted the INVOLVE definition23 of PPI. However, the survey results suggested that a minority of respondents were equating PPI with participation in research:
Survey Question: in your opinion at what stage of the research does service user/public involvement have the most impact?
patient completes questionnaires. Results help to understand/control disease in specific population
Survey: public health: case control study: ID81
We also found evidence in the survey and case studies that a dual role of being both participant and lay representative was being undertaken. The four studies reporting this in the survey suggested the benefit of this was the provision of direct feedback which could be used to improve research processes and outcomes:
we are continually listening to the comments of our participants in relation to study material and where possible modify accordingly. At the end of the sessions they are asked to complete a feedback form with their comments.
Survey: public health:mixed qualitative/quantitative: ID93
Collective understanding is a distinct NPT construct and the survey highlighted this as an area to be tested in the case studies, particularly how PPI was understood by respondents, and the extent to which the dual role was present. A lack of coherence in understanding the purpose and positive impact of PPI could potentially create a number of tensions.
The challenges of patient and public involvement
Free-text responses in the survey identified challenges as recruitment, communicating the research to lay people, extra resources needed, the potential for tokenism, bureaucracy, confidence of individuals to participate, managing expectations of the PPI individuals and threats to long-term commitment (such as illness). The most common theme that emerged was recruitment and how to gain access to ‘representative’ service users, mentioned by about one-third of respondents:
trying to get a representative sample and not just the usual suspects.
Survey: dementia: qualitative studies: ID50
The only challenge is in finding appropriate representatives, they need to be able to understand the basics of the type of research that you’re doing but if they are all former academics and/or health professionals it kind of defeats the purpose, we were fortunate to get a mixture.
Survey: dementia: mixed qualitative/quantitative: ID57
Finding suitable people to take part that are able to see the broader picture and aren’t solely focused on their own personal issues. Cost.
Survey: arthritis: other clinical trial: ID83
These comments may suggest that some researchers feel that the PPI representatives currently volunteering for research studies are not necessarily those they feel should be involved, are not authentically representing the views of others or do not offer enough diversity. There was also some evidence of concern about PPI representatives losing the service user perspective through a process of socialisation into the research world:
in some contexts, we are engaging with a cadre of service users/public that become ‘professionalised’, that they are being repeatedly asked to speak for others.
Survey: arthritis: qualitative: ID37
In addition to recruitment issues, the next most common challenge highlighted by researchers was being able to communicate their research (i.e. complex design) to lay people and the time (to comment and build relationships) and resources required to make the research accessible and supportive of PPI. Researchers were also aware of the challenge of involving the public in a meaningful and real way. The management of expectations about what the study could deliver was mentioned by some researchers, as was reconciling the sometimes competing priorities of researchers and PPI representatives. This is a particular issue in research which might not bring benefits in the lifetime of the PPI representatives.
Mainly the wish of families to believe that the genetic, clinical or cell studies will provide rapid answers and treatments.
Survey: diabetes: basic science: ID05
The research approach did appear to influence what particular aspects of PPI were highlighted by respondents as challenging. Topic-specific issues were mentioned, with dementia studies identifying the extra time needed for PPI and diabetes mellitus studies the need to clearly explain information about the research. In terms of NPT, this highlights the construct of collective action where the necessary tasks for PPI are performed; as per our hypothesis, the survey findings suggested that certain topic areas and study designs have different influences on researchers when working with PPI representatives.
Impact of patient and public involvement
More recently there has been a growing emphasis on making attempts to assess the impact of PPI. 19,29,31,32,159 While fairly limited in the amount of evidence this would elicit about the benefits of PPI in research, the survey included an open question where respondents could write about at which stage they felt PPI had the most impact. The most frequent type of answer given was ‘the design stage/at the beginning/as early as possible’. Studies which were clinical trials had the highest proportion of respondents naming PPI as having the most impact at the design stage. The next most frequent was ‘at every stage’, and mixed methods had a higher proportion of respondents naming PPI as having the most impact at all stages:
Think there is an impact at many different stages of the process, all of which have equal rating in terms of importance: Design – improves the potential uptake to a trial as the impact has been evaluated prior to recruitment commencing and what would be an acceptable level of intervention/participation. Review of supporting documents improves clarity for patients and reduces the requirement to alter the documents when they are reviewed by ethics committees – these aspects improve the timescales of studies being given ethical approval and reduce the time delay before study recruitment begins. On-going evaluation – this can be a very useful component if there is difficulty recruiting to a study. Dissemination – this can be very useful to ensure that the correct members of the public are informed of the results of the study to ensure that the results are getting back to the relevant patient population.
Survey: dementia: other clinical trial: ID75
Beyond describing where PPI potentially has the most impact in research, we also found some limited evidence of a systematic approach to evaluating PPI impact within research.
Systematic evaluation of patient and public involvement
Although we were provided with very few examples, documents submitted as part of the scoping exercise did provide some evidence of thinking around systematically evaluating PPI:
The proposed trial provides an opportunity to develop user research capacity for future trials and the opportunity for user voices to develop recommendations and tools to support clinical practice. It is imperative to evaluate involvement in this trial from a multi-stakeholder (members of the project team and the user advisory group) perspective. This will inform the design of future studies with significant user involvement. A focus group consisting of all the stakeholders will be conducted at the end of the project. An independent user researcher will facilitate this, as well as undertaking the analysis. Lessons learned and future recommendations will be disseminated widely.
Scoping: public health: clinical trial: ID151
Reflexive monitoring in order to evaluate PPI systematically and, in the light of this appraisal, reconfigure work in the future is the fourth major construct within NPT:
Another change we would make would be to encourage three user group members (rather than two) to join the project management group. This would help to promote better continuity, as well as provide additional support for users, for example on the occasions when one person was unable to attend.
Scoping: public health: mixed qualitative/quantitative: ID160
However, there was relatively sparse evidence of systematic evaluation happening overall. This finding was replicated in the case studies (see Chapter 6).
Conclusion
An unexpected finding was the invisibility of publicly accessible information on PPI in research studies. This lack of information has implications for transparency, evaluability and accountability (see Chapter 7). We had hypothesised that topic area, study design and funder requirements would be significant influences on the embedding of NPT. The findings from the scoping and survey suggest that funder requirements and study design appear to be the biggest influences on the extent of PPI within a study. We also expected that resources would also be an enabler of PPI and yet fewer than half of the survey studies had actually costed for PPI in their proposals.
The scoping and survey did not provide enough information to give a clear sense of the organisation or models of PPI, or what part the host organisation was playing in embedding PPI. However, in applying the NPT framework to the findings there were indications of barriers to embedding PPI.
Coherence
A surprising finding was the existence of a dual role. It was not clear whether this role was deliberately created or was due to a lack of understanding in the difference between participation and involvement.
Cognitive participation
Enthusiasm or buy-in to PPI was often evident in the free-text responses; however, the extent of this buy-in must be questioned when 17% of studies from the survey reported having no PPI.
Collective action
It was also surprising that the relational work to embed PPI was so prominent. For basic science and tissue banks reporting PPI, this work appeared particularly important in an area of research where PPI was less commonly found. The necessary tasks for PPI did appear to have some slight differences in topic areas, but the scoping and survey were unable to capture these nuances in detail.
Reflexive monitoring
Free-text responses clearly highlighted some positive appraisal of PPI. While there was some evidence of systematic evaluation, overall evidence for this was sparse.
Chapter 6 Findings from the case studies
In this chapter we present the findings from the 22 case studies. We provide a rationale for why NPT was found to be the most comprehensive and predictive programme theory for PPI and present the 16 NPT informed mechanisms that were tested within the case studies. We then summarise the key findings and list the contexts that enabled mechanisms. CMO tables are provided, illustrating salient actions within the case studies, potential contexts, plausible mechanisms and potential outcomes. Organised under the major case study actions, data are presented to illustrate how the CMO tables were arrived at. We draw on specific case studies, including their NPT radar plots, to provide illustrative exemplars. The chapter concludes with evidence of PPI impact and outcomes.
Normalisation Process Theory as the candidate programme theory being tested
Our testing within case studies was framed by the 16 NPT mechanisms grouped under the four headings (see Chapter 3) and presented in Table 11. When applied to the 22 case studies, NPT121,134 had sufficient explanatory power to predict which case studies had PPI embedded as normal practice; therefore, it predicted both policy outcomes and the processes and infrastructure required for effective PPI that had positive outcomes both methodologically and morally. Using NPT as a MRT developed out of health service research, we directly interpreted PPI as the complex intervention, which then shaped our data collection tools and analytical framework (see Chapter 3).
| Number | Mechanism |
|---|---|
| Coherence (sense-making) | |
| M1 | Understanding PPI as a different way of working in research |
| M2 | Collective agreement about the purpose of PPI |
| M3 | Individuals understand what PPI requires of them |
| M4 | Individuals construct the potential value of PPI for their work |
| Cognitive participation | |
| M5 | There is a key individual driving PPI forward |
| M6 | There is individual agreement that PPI should be part of their work |
| M7 | Researchers and lay people ‘buy in’ to PPI |
| M8 | There is continued support for PPI |
| Collective action | |
| M9 | The necessary tasks for PPI are performed |
| M10 | Trust in each other’s PPI work and expertise is maintained |
| M11 | Allocation of PPI work to individuals is appropriate |
| M12 | Appropriate support for PPI is provided by the host organisation |
| Reflexive monitoring | |
| M13 | Information about the impact and outcomes of PPI is systematically assessed |
| M14 | PPI is collectively appraised as being worthwhile |
| M15 | PPI is individually appraised as being worthwhile |
| M16 | PPI approaches and work are changed in response to the appraisal |
Summary of key findings
This is one of the first studies to contribute significantly to our understanding of PPI as a concept, through the analysis of a large number of case studies, selected to capture varying levels of PPI embeddedness, in order to understand how it may change over time during the research process.
In testing whether or not topic area had an influence on the embedding of PPI, we found similarity between the nature of the clinician–patient relationship and the way PPI was enacted. This was further influenced by the topic area’s history of PPI and the tacit models that had evolved. For example, we found PPI in IDD studies to be framed by an empowerment model and resonant of the long history of partnership working between practitioners and service users. Well-established PPI structures in some topic areas such as dementia provided a pragmatic source for the lay perspective, but we found unintended outcomes for this model, including the outsourcing of PPI to external parties with little researcher engagement. It also exemplified a ‘one-off’ model whereby PPI was limited to a single task.
Researcher perceptions of what lay representatives could be expected to understand or be interested in, coupled with a lack of effort to communicate in an accessible way, sometimes led to limiting lay involvement in parts of the research process, potentially limiting impact. However, we also found in areas such as basic science and tissue banks, where PPI has traditionally been seen as having a limited role, that research teams were enabling PPI, leading to improved relevance of research priorities and questions.
While still challenging for a number of studies and funders, recruiting a diverse range of lay people was enhanced when the study setting interfaced with a diverse population. Particular PPI structures helped, including an outreach model with either a specific lay person or a co-ordinator acting as a bridge to a broader community. The quality of such connections was important to create the context for involvement. The resulting impact was culturally sensitive, participant-focused research designs.
In contrast, researchers’ descriptions of ‘usual suspects’ as lay representatives reflected a perception of concerns about the professionalisation of PPI. However, our findings suggested this was at odds with reality and with the advantages of the experienced lay representative being able to develop a number of skills that helped their role, and enabling a career trajectory for the lay person within PPI.
An important finding in both the survey and the case studies was the dual role, whereby the lay advisor was also a study participant. Although this had the benefit of real-time feedback about the impact of the research design and enhanced a sense of ownership of the study for lay respondents, there was also evidence of conflicts of interest and a blurring of roles. In some case studies the dual role was a deliberate PPI design; however, in others it clearly demonstrated that involvement was not understood as being different from participation, and highlighted the level of PPI drift away from INVOLVE definitions. It was also indicative of a lack of training or experience in PPI, particularly in novice researchers. Training or on-the-job experience not only helped researchers to differentiate between involvement and participation, but also enhanced an understanding of what both parties bought to the table. Development of positive relationships underpinned by trust was the minimal requirement for any form of PPI; this led to improved self-worth for lay people, and increased researchers’ confidence in their work. Breakdown in this relationship had a profound effect on levels of PPI embeddedness over time.
It was clear from the case studies that PPI was most likely to be embedded when hosted in well-resourced research centres with a dedicated budget and PPI co-ordinator. PPI groups and panels had continued engagement with the research host organisation, were reimbursed equitably and had social interaction with the research teams; these are crucial to the sustaining of positive relationships. Resourcing PPI in such a way also enabled a fully entwined model of PPI, in which lay people and researchers worked seamlessly together, with research priorities and research questions created by the lay people involved. This generated some research programmes that would not have been run without lay involvement. However, embedding PPI to this level required not only resources but also time to develop.
We found that funder requirements played a key role in influencing levels of reimbursement. In addition, how PPI was operationalised in individual studies could be traced back to the funder’s ethos of PPI. Within funding organisations there was a growing interest in evaluating processes and outcomes of PPI within studies. However, even with funder expectations, only a limited number of case studies were reflecting on and evaluating PPI in an ongoing way to improve the quality of PPI processes and outcomes.
Enabling contexts
The findings suggested there were eight enabling contexts for the mechanisms (Box 5). Five of these (funder, topic area and design, resources, organisation of PPI and research host) were expected, based on the literature, and shaped our sampling framework to ensure a range of case studies as a test-bed. The other three (training, positive relationships and positive experience) became visible during data collection and analysis.
C1 Funder requirements for PPI in research.
C2 Training of lay people or researchers.
C3 Topic area and study design.
C4 Resources supporting PPI.
C5 Positive relationships between researchers and lay people.
C6 Organisational structures that support PPI.
C7 Research host support for PPI.
C8 Positive experience of PPI, both researchers and lay people.
Context–mechanism–outcome configurations
As described in Chapter 3, through an iterative process we tested candidate CMO configurations within each case study and discussed our findings with case study respondents in the tracking interviews, with our reference groups and finally at the four regional events. We identified six CMO configurations that explained salient case study actions, potential contexts, plausible mechanisms and potential outcomes, both intended and unintended. CMO configurations focus on immediate outcomes within a study. It was not possible to include longer-term outcomes of a study, as these evolve over a longer period of time. Tables of each CMO are presented and then illustrated by data and case study exemplars. Within exemplars, NPT radar plots will be shown, and any change in PPI embeddedness over time will be illustrated through tracking radar plots.
Purpose, structure and role of patient and public involvement
Table 12 illustrates the CMO configuration for this action. Funder requirements were a significant enabling context, and had resulted in a more structured approach to PPI. It was also facilitated by host organisations with an established PPI infrastructure, such as an established group or panel, and access to training. At the time of data collection, this enabling context was provided by some topic areas (dementia and diabetes mellitus) with network support for PPI. Having adequate resources to maintain this group in terms of administration and reimbursement was vital for sustained engagement with PPI in research.
| Salient CS action | Potential contexts | Plausible mechanisms | Potential outcomes | Case study exemplars |
|---|---|---|---|---|
| A clear purpose, role and structure for PPI are ensured within the study | This action was enabled if grant applications required detailed proposed PPI structure (C1). It was also enabled by host organisations (C7) with an established PPI structure (C6) such as a group or panel, designated colocated lead and access to PPI training (C2). Involvement in a number of research projects enabled continued engagement with PPI for members. Having adequate resources (C4) to maintain this group in terms of administration and reimbursement was fundamental. Topic area had some influence; for example, in diabetes mellitus and dementia studies there was often access to well-established PPI structures (C3) | PPI was seen as a different way of working (M1) and therefore required a clear structure which was agreed by all (M2). The structure specification helped everyone to understand their role (M3). It was further enabled by having an identified person leading the PPI strategy (M5), but also there was buy-in (M7) that PPI was part of everyone’s research work (M6). The purpose and structure of PPI also required continued support (M8) and trust in each other’s expertise (M10). Within the PPI structure, work needed to be allocated appropriately (M11) and supported by the host organisation (M12), and people needed to have the necessary skills to carry out their respective roles (M9) | Moral:
|
CS02 (see Box 11) |
| CS03 (see Box 10) | ||||
| CS07 (see Box 17) | ||||
| CS11 (see Box 15) | ||||
| CS13 (see Box 16) | ||||
| CS18 (see Box 9) | ||||
| CS21 (see Box 6) | ||||
| CS05 (see Box 14) | ||||
| CS08 (see Box 13) | ||||
| CS14 (see Box 26) | ||||
| CS16 (see Box 20) | ||||
| CS17 (see Box 23) |
For some case studies, the purpose, structure and role for PPI were an inherent part of the research design. For example, CS03 (see Box 10) and CS23 (see Box 21) were funded to coproduce an intervention (self-management website and mobile phone applications for young people with diabetes mellitus). Other case studies sometimes had to craft a PPI structure from new because of the funder’s requirements.
Funder requirements
Researchers were particularly aware that when applying for specific grants there were even stronger imperatives to have PPI as a funding requirement. PPI was recognised as a part of the contemporary research landscape, and some reflected that having formalised PPI as a requirement was beneficial, as experience of good PPI usually leads to more in the future:
more researchers are willing to engage, whether that’s because they want to or whether because they have to because of the grant application, I think there’s a bit of both there, but then again, that’s fine because those that . . . engage because they have to kind of start to begin to see the worth of it anyway.
CS07Res01-01
Overall, the funder respondents clearly asserted that PPI both in research and at funder and system level had developed significantly over the previous 5 years, describing a journey along a continuum of learning and understanding of PPI, despite noting that there was still some way to go until it was fully embedded as normal practice:
I think organisationally that’s been a sea-change . . . Externally with researchers I sense there has broadly been a change but there’s still a lot to do, but certainly the quality of the PPI anecdotally that we’re getting in our applications is on the up, possibly to do with . . . everything being reviewed by a public contributor.
Funder01
Structures and processes for PPI within funder organisations themselves inevitably varied and strongly reflected the influence of their core funding source, mission, scale and length of service. PPI structures had developed either quite systematically or more recently and organically as part of the overall PPI movement.
Working closely with INVOLVE, two overarching programme management organisations and two research programmes that are funded by central government had, over a number of years, developed similar, embedded structures for PPI within their organisations. However, the sheer volume of applications to process could potentially result in the PPI representatives having to work with a conveyor belt approach. The industrial scale of PPI as metaphor was also picked up by one of the lay representatives:
I think, having started from a low base, it’s [PPI] now in danger I think of almost becoming an industry; that is that everybody concerned with health care has to have some public involvement, and that goes for GP practices, hospitals, and very much in research, all areas of research . . . It sometimes strikes me that it’s a kind of bandwagon. Don’t get me wrong, I think it’s one of the most useful things in the health economy, but it seems to have made jobs for an awful lot of people, let’s put it that way.
Funder07(lay rep.)
The other funding bodies taking part in the RAPPORT study had only recently started to implement PPI strategies in their organisations. A government-funded research council had endorsed its PPI strategy only a year before and there was now a strategic vision around PPI. The structure of this funding organisation was less complex and was led by a member of staff responsible for both public involvement and engagement. This organisation had a PPI panel of around 20 members who were offered the opportunity to be involved in particular funded projects; alternatively, the organisation would ask specific medical charities to nominate lay representatives for particular condition-specific projects. Another large national funder, financed through endowments, had a different stance on PPI, focusing more on public engagement:
patient and public involvement doesn’t just have to be people in a focus group or a patient representative on a steering committee, it can, you can use kind of more engagement approaches that can still inform and can kind of be part of the research process . . . sometimes when I talk to people in the patient and public involvement sphere there’s quite a narrow definition of how they see patient and public involvement, and so yeah, I can see it a bit wider than that.
Funder08
Public engagement was seen as a key policy driver within this organisation, and strategically it focused on facilitating research teams to improve its public engagement, with PPI being seen as operationalised at research team level.
We also interviewed two representatives from condition-specific medical research charities. Their PPI strategies had gradually developed over recent years:
we’re currently looking at expanding it, so it is something that’s definitely on the radar of people within the charity, it’s just the technicalities. I think, you know, everyone’s definitely willing to do it and I know that our Medical Director is very keen on PPI, and I think it is almost evolving organically . . .
Funder01(CharityA)
A major finding from the interviews with funder representatives was that their stances or values (and thus PPI structures and processes) were actively shaped by the origin of their funding and their histories. The funding organisations that received government public funding as part of a national research agenda clearly articulated the reasons for PPI in methodological terms:
It [PPI], you know, is likely to improve recruitment. It makes sure that it meets patient needs so that when it gets out the other end if you like into the implementation phase that it can actually have a possibility of having impact on an individual with a said condition.
Funder04
In contrast, the medical charities reliant on fundraising spoke of PPI in terms of an ethical rationale:
we get our money from the public, from people with the condition, so it’s really important that we include viewpoints of people with the condition in our decision.
Funder02(CharityB)
Hence, funders influenced PPI in subtly different ways depending on their organisational values. Case studies funded by NIHR funding streams were required to have PPI as a different way of working within the actual research process because of the emphasis on the methodological importance of PPI. In contrast, those funded by charities tended to have less focus on a requirement for PPI in the actual research process, with structures in their organisation concentrated more on ensuring PPI in funding decisions.
Structures for patient and public involvement
Host organisations, and in particular CLAHRCs, were instrumental in providing a PPI infrastructure. This often involved having a designated lead for PPI. Six of the case studies had a dedicated PPI co-ordinator who was separate from the research team, and a further case study had a research team member who took on the role of the PPI co-ordinator as part of their duties. Case study 21 (Box 6) had a colocated co-ordinator who, as a non-researcher, was seen to bridge the gap between researchers and the public:
The research centre hosts a large PPI group made up of parents.
A project-specific ‘expert reference group’ was established, made up of the PPI representatives, and reviewed the data collected.
Normalisation Process TheoryCoherence: roles and expectations of PPI clearly defined by all. Coherence in describing the approach and philosophy of PPI in the organisation and research team.
Participation: key person drives it forward. Model adapted from elsewhere and now underpins the entire centre’s work.
Collective action: roles clearly described and training given. Relationships seen as key; trust and making it fun.
Reflexive monitoring: no formal evaluative tool used but it is actively piloting tools developed within the CLAHRC. All describe how they appraise PPI and modify their actions subsequently.
Radar plots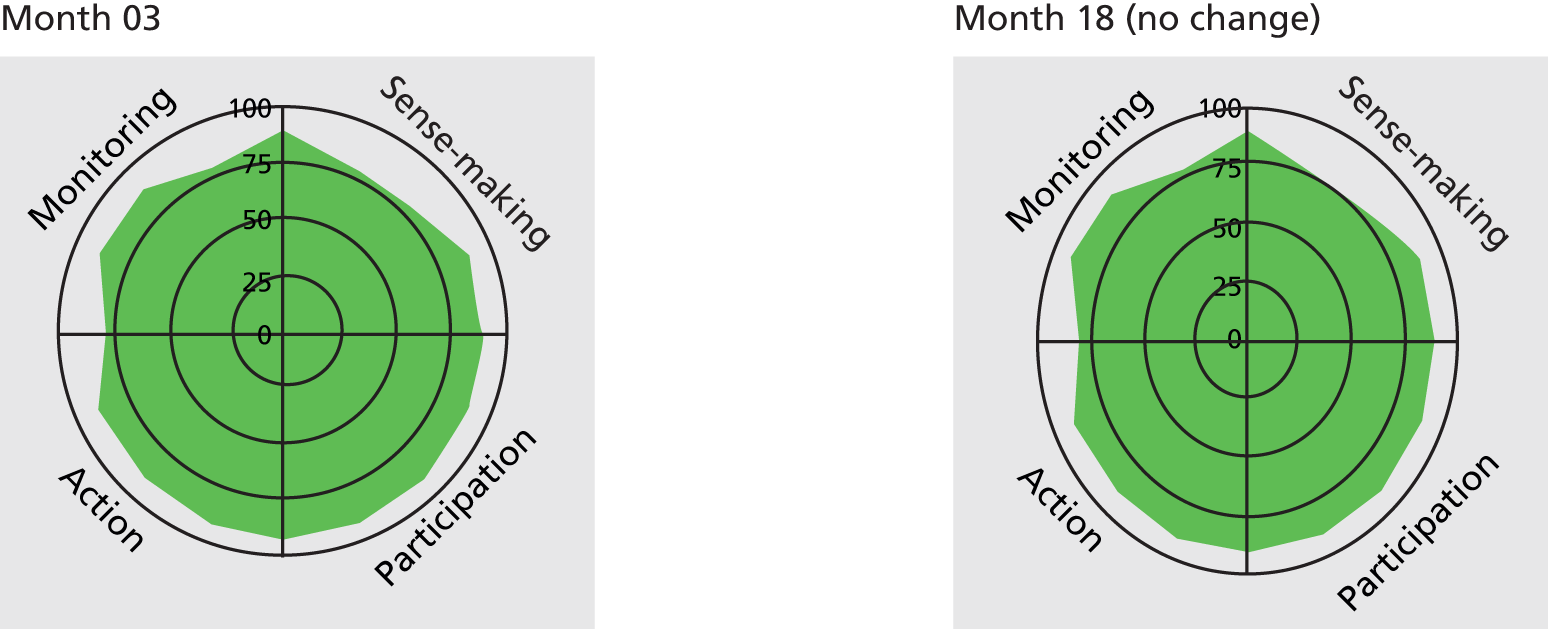
Research question setting: the group are encouraged to put forward research questions and this idea originated from one of the parents.
Design of the study: sensitivity of statements on questionnaires.
Recruitment: recruitment improved through postcard-size reminders.
Outcome measures: increased relevance of outcome measures; parents set the inclusion criteria for the systematic review.
Dissemination: conference presentations by lay reps and lay summary.
Impact for PPI representatives: increased knowledge of health services (parents), increased self-worth (parents), respite from caring (parents).
she’s become a great interface between us and the families because she helps, she’s . . . she knows enough about research to be able to explain what we do, but equally doesn’t know enough that she can challenge me or others in the team to explain more clearly what we’re asking of families. And I think that’s probably the greatest reason for our success has been the sort of creation of that role and the development of it.
CS21Res01-01
Case study 21 exemplified fully embedded PPI which was enabled by all eight identified contexts. It also demonstrated an ‘entwined’ model of PPI in which research and PPI were wrapped together much like a double helix. It was hosted within a research centre primarily funded by a charity (C1) with a topic area (children with severe cognitive disabilities) (C3) where active involvement of parents was seen as a prerequisite of meaningful research. The study design (systematic review) (C3), compared with the ongoing qualitative research being undertaken in the programme of work, required more effort from the research team to ensure that parents were involved and the review was rigorous. The research centre (C7) had an established PPI system (C6) including a funded co-ordinator who supported parents and undertook extensive outreach work. The centre was also part of a CLAHRC with a vibrant PPI community and resources for PPI (C4), and parents were reimbursed for their time and received training (C2) for their role. Resources also included the time researchers needed to work with parents on the systematic review. This level of resources was necessary for an entwined model of PPI (see Chapter 7). There was a strong focus on positive relationships (C5) that were developed over time and enhanced by social activities. This led to a positive experience of PPI (C8) for all involved and the sustaining of a virtuous cycle whereby PPI became increasingly embedded. At the start of data collection PPI was already embedded in CS21, so there was no change in the tracking radar plots over time.
The need for time to develop a PPI infrastructure that could support embedded PPI was also clear in CS22 (Box 7). The topic area of CF had little history of established PPI structures, and the study designs are more commonly towards basic science. This case study captured the early days of study set-up and developing PPI, so radar plots were less full. After a year and despite focused work by a PPI champion, the radar plots remained unchanged, suggesting that embedding PPI requires a significant amount of time: at least 5 years. The limited impact of PPI may reflect the very early stages of a research study; however, as other case studies show significant impact in the early stages of the research cycle, it may also be indicative of a neophyte PPI structure which is not enabling a fuller impact.
Parents of children with CF (one member of charity). Experience of committees.
Stages: steering committee, four afternoons a year. One PPI representative also gives up about 3 days a month, as they sit on a monthly committee.
Recruitment of PPI: known to researchers (through clinic or other committees).
Normalisation Process TheoryCoherence: PPI has recently become a new way of working for PPI reps, researchers and PPI co-ordinators. Those interviewed have similar ideas about PPI but report some of the scientists/researchers in the hospital are not so supportive or understanding of PPI.
Participation: PPI should be part of work, but not all clinicians see it that way. PPI representative wants to find a cure in their child’s lifetime. Disagreement between researchers that PPI could understand all the science (this is reported evidence). PPI representative was unsure about research progress over time.
Collective action: training has been provided on research and governance, more recent training provided by charity – researchers and PPI representatives trained together. There has been a PPI co-ordinator for 3 years. There is a formal procedure to include PPI in research proposals.
Reflexive monitoring: PPI representatives get feedback that proposals have been successful, how their views were taken on board and how their suggestions on the protocol have been taken up.
Radar plots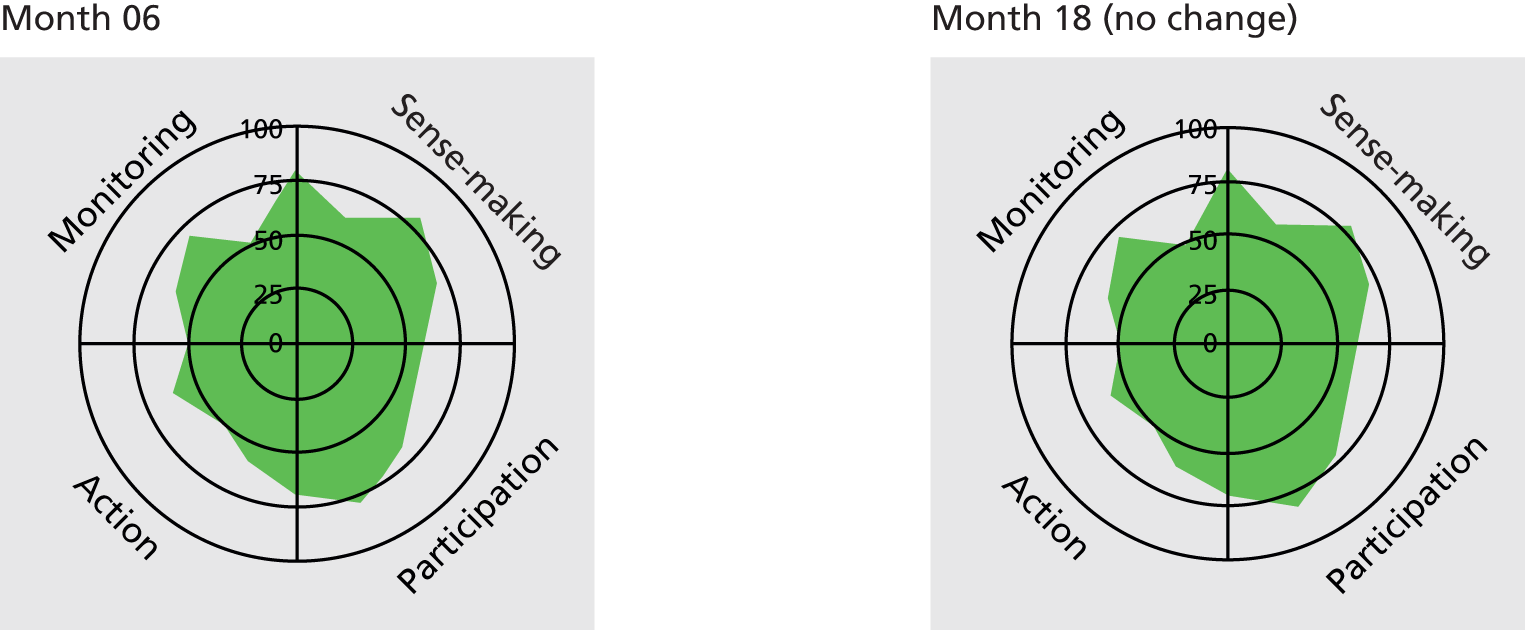
Recruitment: improved patient leaflets.
Outsourcing patient and public involvement
For case studies not hosted by organisations with existing PPI structures, an alternative was to recruit an ad hoc, project-specific group of people or individuals to support the study as PPI. However, another possibility was for research teams to access external PPI groups or panels. Topic area (C3) was an enabling factor and respondents from two national networks covering dementia and diabetes mellitus both held a list of names of interested PPI representatives. One network had a formal registration process on its website (which was updated annually and had around 3000 names) and the other spoke of a more informal, dynamic list based on personal relationships. Both networks had ready access to around 150–250 regularly involved and engaged PPI representatives; had been approached by researchers (in this topic area and beyond) for PPI in protocol development, funding before the application stage, help with PPI budgets and recruitment; and often organised local focus groups to gather PPI views.
Panels were preferred by some because they were more focused on a specific question and were hoped to consult with a wider population:
I think that the PPI, you get from a reference panel is potentially more focused on specific important questions . . . for example a Trial Steering Committee which might only meet twice a year or, and if the layperson can’t attend.
ResearchNetwork02
Panels were felt to be a very effective way of using PPI time and skills, and easy access to existing groups made PPI feasible within the time line of a project. However, although convenient, recruiting solely through local PPI networks with trained and prepared members of the public was seen as not always appropriate for effective PPI. Researchers within some of our case studies expressed concern about the difficulty of recruiting more than just the ‘usual suspects’:
one of the problems is ensuring that you actually are getting real and representative user involvement and not just the people who happen to be around who always get signed up to these user involvement things . . . actually it’s quite easy I think to get the usual suspects.
CS23Res04-01
There was also evidence that relying on an external group had led to a ‘one-off’ model of PPI in which researchers had requested help for just one task and there was an absence of PPI throughout the rest of the research process. This limited the potential impact of PPI and was characterised by a more ambivalent view towards the value or impact of PPI. In a few case studies, the CI appeared unconvinced of the value of PPI:
but where’s the evidence that it [PPI] does work, maybe there’s scientific management for a programme that should just be done by scientists, internal, external and managers and maybe there are other elements that really need a PPI input, I don’t think that’s terribly well worked out at the moment.
CS01Res02-01
Case study 01 (Box 8) provides an example of this model.
Panel: an established local research network panel with a paid co-ordinator, who has worked with CI before. Panel asked for views on access to patient notes.
Normalisation Process TheoryCoherence: PPI co-ordinator feels PPI is about recruitment, researcher feels it is about better research and CI feels it is good for PIS and ethics committees but not necessarily design of studies. Both CI and researcher see dissemination to participants as PPI. A journal letter on patient involvement is focused on providing feedback to participants.
Participation: low legitimisation/enrolment. CI reservations that PPI can delay research, good for ethics but not for research design.
Collective action: CI prefers to deal with panel rather than having one or two potentially idiosyncratic views on a committee. Newer studies now have more contact with research network and PPI co-ordinator. Little support for PPI from researchers; this is provided through the research network.
Reflexive monitoring: CI’s view ‘maybe PPI does work, maybe it doesn’t, we are not really sure’. No systemic appraisal at research network, although a spreadsheet is maintained of PPI reps’ activity but not impact. PPI reps are becoming more involved, but it is not clear if researchers are using more PPI in further studies.
Radar plots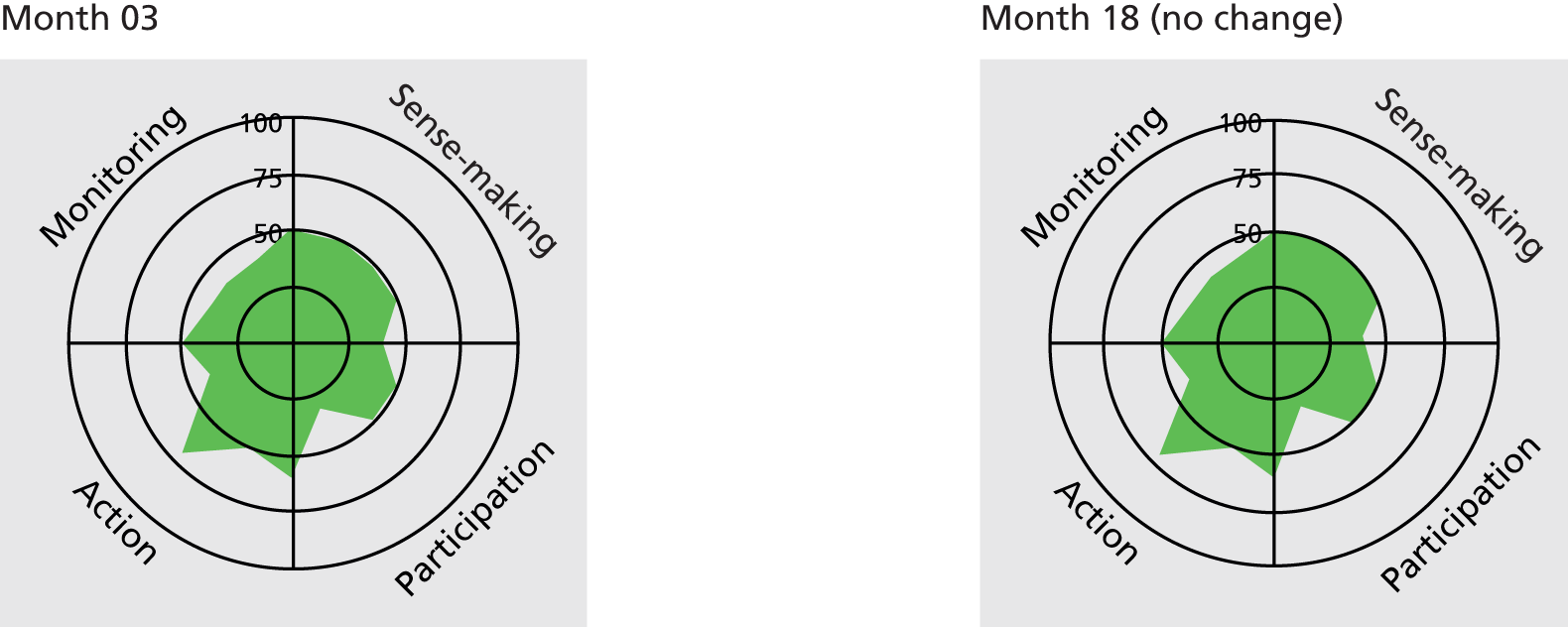
Study design: research design is acceptable to patients.
Recruitment: increase recruitment to studies (PPI co-ordinator’s priority to increase recruitment to studies).
Training
The evidence suggested that training around PPI for researchers was likely to be an enabling context, but there were mixed and even polarised views on training for lay representatives. Nevertheless, even in case studies with embedded PPI, researchers had not received formal training on PPI. Rather, they had learned through experience within an environment supportive of PPI.
Understanding PPI as different from study participation was a prerequisite for the development of appropriate structures, purposes and roles for PPI. Most researchers could articulate the difference; however, it was significant that many junior researchers could not. This lack of understanding was attributed by some to a lack of formal training:
there was no formal training, I just, you know, from what my colleagues and supervisors have just briefly mentioned but nothing formal on it and I think it would be an important part early on for trainees interested in research.
CS14Res02-01
Of those lay respondents in the case studies who had received training, the majority had been provided by CLAHRCs, public involvement groups or research networks. However, the need for training for lay representatives did not emerge so strongly from the data as for early-career researchers. Indeed, various arguments were put forward against training, such as potentially compromising the lay perspective, or skills already existing because of extensive PPI experience or transferable skills from work life:
I don’t think there was any necessity for training at all. There’s certainly obviously one or two people have got good committee experience who are sitting round the table, on the lay side, so no, I don’t think there was any necessity at all.
CS13PPI05-01
In stark contrast a minority of lay representatives suggested it was impossible to contribute meaningfully without some understanding of research:
I don’t think that you can just so easily shove inexperienced patients in to a PPI role without them being, having some training and having some support because there’s no question that, you know, the whole research agenda is incredibly complicated and they talk in a language which is, you know, if you’re not a researcher you sometimes have no idea what they are talking about when they’re talking about face validity and constructs and confidence intervals and so on and so on.
CS14PPI02-01
However, the above quote suggests that this lay representative felt it was essential for the PPI representative to be able to cope with the research world, rather than the research community needing to make the effort to include the lay world in an accessible way. Making the effort also included working towards recruiting lay representatives who reflected the diversity of a study population.
Recruiting lay representatives reflecting the diversity of a study population
Table 13 illustrates the CMO configuration for this action. Formal training for researchers played a part in helping them to identify the need for this action, but experience on the job of recruiting diverse lay representatives was a more common enabling factor. It was easier to achieve this action when the research setting interfaced with and had access to a diverse population. Particular topic areas such as IDD had developed links with less-heard groups, and in a number of case studies these links were provided by a PPI co-ordinator or a lay person within an outreach model. In a few case studies, recruiting lay members as representative of the study population was actually operationalised through recruiting study participants to also have advisory input: a dual role.
| Salient CS action | Potential contexts | Plausible mechanisms | Potential outcomes | Case study exemplars |
|---|---|---|---|---|
| The research team actively recruit lay representatives who are likely to have an understanding of the diverse viewpoints of the study’s target population | This action was potentially enabled by PPI training for researchers (C2), or at least some experience of recruiting diverse lay representatives. Training or experience of PPI was in turn enabled by resources (C4), a host organisation such as a CLAHRC with an established PPI structure (C7). It was also enabled by a study setting that interfaced with a diverse population (C7). Certain topic areas (such as IDD) had an established history of reaching out to enable diverse representation (C3), and for other case studies PPI was organised (C6) in such a way that this recruitment was done through either a co-ordinator or an outreach model of PPI | The research team ‘buy in’ to the concept of PPI (M7) | Moral:
|
CS02 (see Box 11) |
| CS03 (see Box 10) | ||||
| CS07 (see Box 17) | ||||
| CS11 (see Box 15) | ||||
| CS13 (see Box 16) | ||||
| CS18 (see Box 9) | ||||
| CS21 (see Box 6) | ||||
| Some research teams also recruited lay representatives to undertake a dual role of both study participant and advisory lay representative. It was enabled by a positive relationship where there was confidence that these roles would be treated as distinct (C5) | The potential value of this dual role was seen by researchers and lay representatives (M4). The necessary tasks for this dual role were performed (M9) and the work associated with this role was appropriately allocated to the lay representative (M11) | Moral:
|
CS05 (see Box 14) | |
| CS08 (see Box 13) | ||||
| CS14 (see Box 26) | ||||
| CS16 (see Box 20) | ||||
| CS17 (see Box 23) |
Strategies for recruiting lay representatives
Being able to understand the research through the viewpoint of a target population was seen as key:
I was sat on a table with speech and language therapist, physiotherapists, paediatricians, and a handful of parents, all as equals, you know? . . . and I was just thinking ‘What does that mean to me as a parent’, thinking of my child’s capabilities and all the other children that I knew.
CS21PPI01-01
However, finding lay representatives who they felt could present the viewpoint of the research study’s target population was often challenging for research teams. This was more frequently cited for BME groups. We attempted to include case studies that were likely to have a target population from the BME community. One case study specifically focused on the experiences of a particular ethnic group living with arthritis (CS18). One of the study sites was located in an area with a high percentage of people from this ethnic background, and the lay representative was recruited through that site:
I was going to the clinic, attending the clinic and the nurse actually asked me if it’s okay because I speak different, three or four different languages.
CS18PPI02-01
This opportunistic recruitment meant that CS18 benefited from the input of a lay representative who demonstrably understood the enablers of recruitment in far more depth than the research team:
what we had was an audio CD because a lot of people do not read the script, [specific language], so some of our interviewees did not speak English so we got the information sheet translated and put onto CD and she [PPI01] listened to that and gave feedback on that because there are different dialects of [specific language], apparently some are deemed posher than others and there’s all sorts of things that I was not aware of initially.
CS18Res01-01
While there was trust in this lay representative’s expertise demonstrated by the peak in the collective action segment of the radar plot (bold outline) (Box 9), the construct as a whole was affected by one major challenge: that the CI (who was effectively the PPI lead within this study) and the PPI representative were located at a significant distance from each other.
Patient and public involvement representatives normally recruited to each study via an established PPI group based at the university. Only one took part in CS18. Expert by experience (has condition). This PPI representative was recruited through second university user group.
Normalisation Process TheoryCoherence: PPI representative slightly hesitant about role and impact. Researcher clear that PPI helped and provided reassurance. Another, more experienced, PPI withdrew through ill health. Both feel it important to give patient view and experience.
Participation: arthritis – outcome measures about pain were introduced because a patient spoke up.
Collective action: paid PPI co-ordinator. Training is provided once a year and group meet together. Sometimes difficult to commit, because of illness (flares).
Reflexive monitoring: PPI representative found it worthwhile for herself. CI found PPI input very valuable. In the future would involve two representatives. If the CI moved to another institution they would definitely set up a similar organisational PPI approach.
Radar plots
Data analysis: ensured it was culturally sensitive.
Dissemination: published paper with PPI representative in acknowledgements.
Cultural reassurance for CI (from other researcher and PPI representative).
Outcomes for PPI: hearing and reading about other people’s situations helped PPI representative personally.
Enabling contextsFunder requirements: NIHR (C1). Study design: qualitative (C3). Research host (C7): CI located in an organisation with embedded ‘established system’; each research project is automatically assigned two patient representatives. However, this context was significantly counteracted by the research site being at a distance.
We also included four case studies focused on type 2 diabetes mellitus with the expectation that these would include a relatively high percentage of research participants from BME groups susceptible to this condition. One of these case studies (CS03) (Box 10) had used strategies (advertising and interviewing applicants) to recruit a diverse range of lay representatives:
Experts by experience, different levels:
-
Focus groups involving diabetic and health professionals.
-
Eight to ten people with diabetes mellitus were selected through interview. The PPI recruited mostly through Diabetes UK magazine. Newly established group or panel meets once a month for a year.
-
Two patient representatives on steering committee (one PPI representative volunteers for local diabetes support group and Diabetes UK network, is involved in another charity and was involved in a project at the research centre before; second PPI representative not available for interview).
Coherence: high. PPI representatives and researchers use the same language (everyday life, real-world knowledge), pooling experiences, diversity of views. Value for PPI individuals: confidence, mental stimulation. They value the importance of the research and website.
Participation: key person (one of the researchers) approachable, supportive, interested; trust is strong, all voices heard, researcher says ‘you have to take a back seat’ and that PPI have ownership.
Collective action: PPI representatives are a selected subgroup from a larger group. They know exactly what they have to do, they are given clear instructions and they are set appropriate tasks as homework, which is made clear at the beginning of each meeting. They are supported in terms of parking and venue. PPI embedded within department but not whole university. Some underestimation about what PPI representatives can do (by researchers).
Reflexive monitoring: PPI representatives know that their ideas have been used. Homework set each month and representatives given feedback on why their ideas have been incorporated into the website or why not. Comments clearly written up. Collectively think it is worthwhile, users shaping the intervention, broader measure will be if website gets used.
Radar plots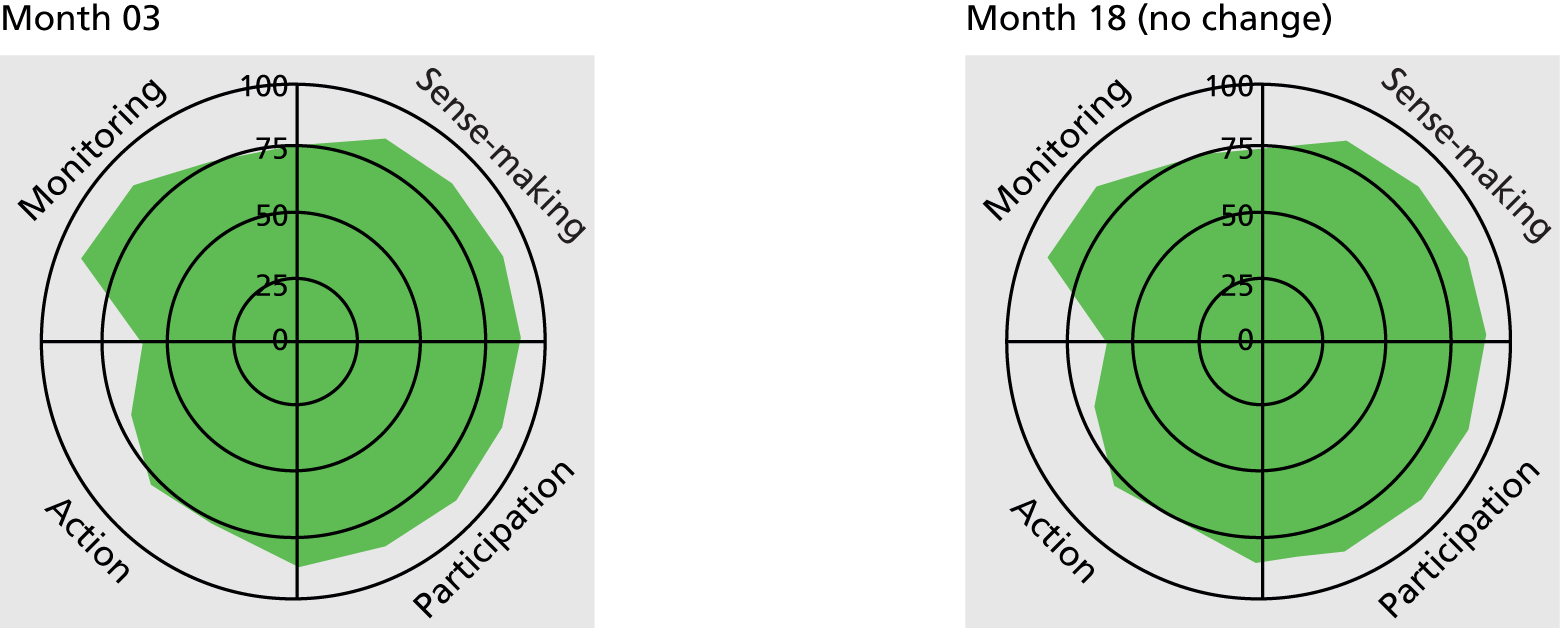
Recruitment: two PPI representatives on steering group involved in suggesting changes to documents.
Design of intervention: self-management tool.
Outcomes for PPI: PPI representatives feel valued, sense of worth, benefits for society.
we wanted a really representative mix of people with diabetes . . . we wanted to be quite diverse in sort of the sociodemographic, those variables so we got a really nice ethnicity mix and age mix and gender and so that’s what formed our regular groups . . . Because sort of in the population, diabetes is more prevalent in sort of the Afro-Caribbean, South East Asian population, . . . it was one of the things that sort of influenced our decision as well.
CS03Res03-01
Strategies used when recruiting individual PPI representatives reflected researchers’ attempts to involve people who could bring both specific and broader perspectives. Recruitment of individual lay representatives was from five main groups: general public; expert by experience; carer/parent; patient representative; study participant. Individuals could take on multiple roles and represent their views at different levels. However, relying on just one or two individuals also raised the issue of representativeness:
it’s impossible, you can’t expect one person to speak on behalf of everyone so I guess the question would be what would be useful, or truly influential patient involvement? Is it enough to have just one person or two people who will be very, very good and who will be enthusiastic, but the question is, how representative are their opinions into their input?
CS03Res02-01
Nevertheless, one model of using a single lay representative as a conduit to a broader constituency appeared to work well. The outreach model, as exemplified by CS02 (Box 11), involved one representative from a charity who then linked with 20 members of the support group in an iterative way to inform the study design and recruitment materials. An unforeseen impact from this PPI was to raise concerns over the safety of the study, resulting in extra study visits and a questionnaire (see Impact and outcomes of patient and public involvement).
Steering committee: national representative. One PPI representative (senior position in charity) sits on trial steering committee. PPI representative then consults the (20) panel members, invites feedback, collates answers and then sends it back to research study team. Provided study with letter of support from charity. Involved at a number of stages during the research study. At second interview PPI was in a lull while trial up and running. PPI representative wanted to write something for charity newsletter. PPI representative leads and initiates involvement when appropriate.
Recruitment of PPI: PPI representative known to CI; charity recruits to panel.
Normalisation Process TheoryCoherence: high. CI and one researcher new to PPI, other researcher 2–3 years’ experience. Recognition that funding agencies now require PPI. Agreed PPI was about patient views, perspective, real life, everyday life. Overall, in agreement that PPI does bring value for research.
Participation: medium. PPI representative now gets approached by lots of people for PPI. One researcher had had negative experience of PPI, unsure about benefits and CI feels PPI might not be involved in research applications (PPI might not agree with what clinicians feel is an important research question). ‘Involvement might not be in the best interests of a partnership’ (CI).
Collective action: skills of PPI representative are put to good use, collating views, information more patient-friendly. Communication appears to be good. PPI representative is supported by her charity, not really by the research institution.
Reflexive monitoring: PPI representative believes PPI should be from the beginning and early involvement should be assessed by funding bodies. However, recognition that PPI does take more time. CI thinks PPI representatives not so useful at commenting on research design but great at commenting on how patients might feel to take part, adding questionnaire about safety and reassuring patients with an extra visit. PPI representative can see their ideas have been taken on board.
Radar plots
Design of study: protocol changed to include extra visit.
Safety of study: PPI suggested adding in a 3-month visit for patient reassurance. Patient concerns about safety so a safety questionnaire was added.
Recruitment: changed language of documents (more readable/PIS altered); designed a small card (with hospital telephone number, emergency number and information on); suggested avoiding the word ‘mortality’.
Some case studies also bought together project-specific panels. Case study 12 (Box 12) was particularly enabled by being located in a teaching hospital with relatively good resources for research (C4), which were sufficient for PPI honoraria.
Newly formed panel: experts by experience, participants on the trial, mentors on the trial. Less PPI at the early stages of the research, became involved with study documents. One lay representative had already worked with the CI, others were new.
Normalisation Process TheoryCoherence: researcher and PPI representative agree an outsider’s view is needed especially when testing a service which will be eventually used by pre-diabetics. Value of the psychological support for coming to terms with having diabetes mellitus (PPI). Good for ethics.
Participation: PPI representatives and researchers agree it should be part of their work. Wider than just the research project.
Collective action: PPI representatives do perform activities asked of them; relationships not a strong focus, but PPI representatives do not articulate this as a need, being very experienced working on committees (feel they do not need the support); skill set seems appropriate.
Reflexive monitoring: do not formally evaluate PPI, although meetings minuted; all feel PPI is worthwhile.
Radar plots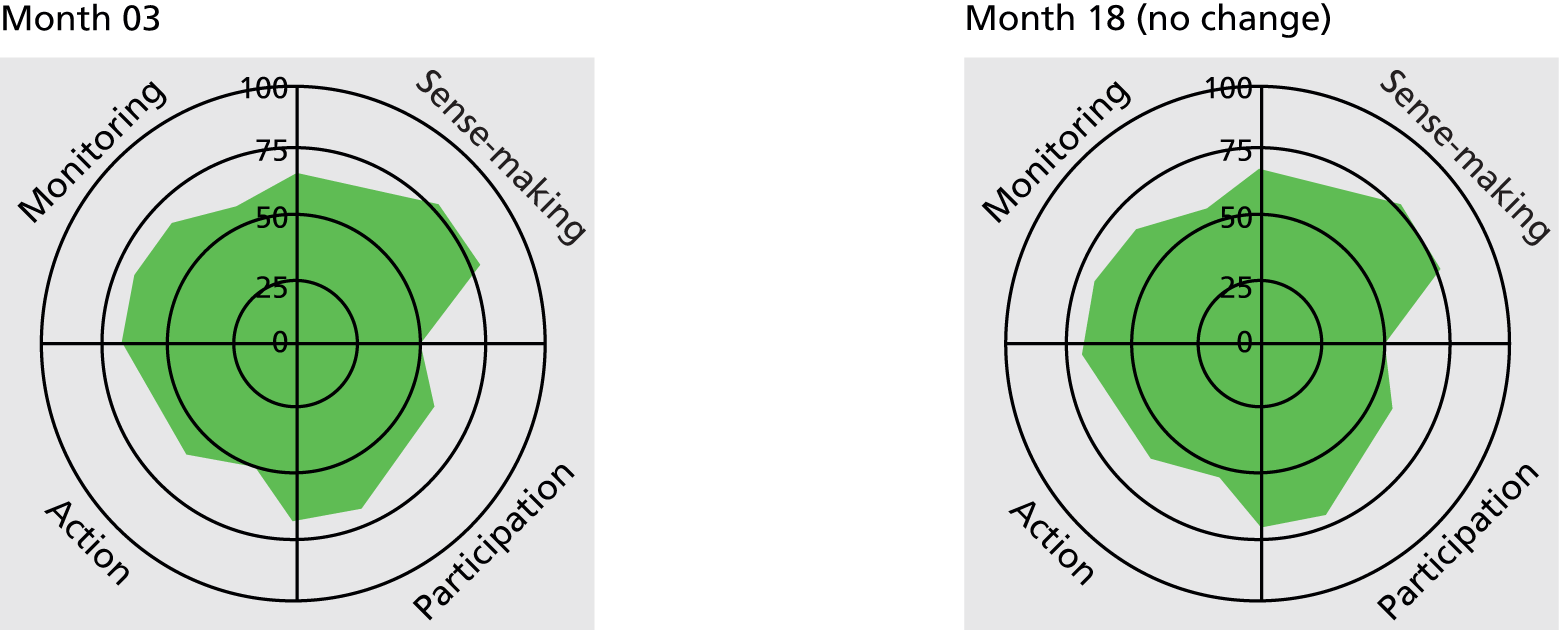
Ethics: enhanced approvals process as materials reviewed by PPI representatives before submission.
Recruitment: increase recruitment to study by clarifying paperwork. PPI looking at reasons for withdrawals from study.
Challenges in ensuring diversity
Researchers acknowledged there was much work to be done to ensure diversity in PPI. The fact that only a very few of our PPI respondents were not from a white British background exemplifies the common problem as described by one of the funders:
we have as much of a problem as anyone about, you know, diversity and all those issues are still issues which we need to explore further. I think often public, people who get involved with PPI are a self-selecting group and it’s really difficult to bring in groups wider and that’s a usual excuse and I hate it, and I hate it when researchers say it. But I, it, you know, for example if somebody couldn’t read and write how would we include them in this process? If someone wasn’t, we do manage to include people who are not computer literate but then these days how are they going to even find out about us if they don’t have a computer? How are they going to know who to ring?
Funder01
Difficulties in accessing ‘representative’ PPI were particularly marked for public health studies when the focus was on healthy or ‘at-risk’ populations with particular lifestyles. The difficulties for public health studies was also linked to the setting (e.g. broad communities) in which they took place. Those studies taking place in settings with ready access to patients obviously had greater potential for recruiting both participants and PPI representatives onto their studies:
the problem at the university is that those researchers that aren’t clinical or don’t have good links into the clinical setting, it becomes very difficult to identify service users to sit on a panel like that so we’re in quite a privileged position because we’re right next to the outpatients clinic and that makes our life a lot easier for maintaining that model.
CS18Res01-01
The dual role
Clinicians who were also researchers had the added advantage of having ready access to patients as potential PPI representatives. For example, one case study (CS14) (see Box 26) hosted by a district general hospital with few embedded PPI structures was able to involve patients through an active condition-specific support group facilitated by clinical department staff. However, the distinction between being involved and being a research participant was often blurred in this case study, with PPI being understood by many of the respondents as a dual role. This dual role was overt in another arthritis-related study (CS08) (Box 13), where the PPI respondent was also a study participant. While there are potential ethical conflicts here, this lay representative actively recruited participants through her own network and had a strong sense of purpose. This action-orientated approach to PPI resulted in a fuller quadrant in the radar plot denoting a positive appraisal of the PPI within CS08 (see bold outline in box figure).
Dual role: PPI representative already known to CI through being on funding committee but also has joint issues so is participating in the research as well as acting as an advisor.
Normalisation Process TheoryCoherence: there is a general understanding of what PPI means but also some confusion and acknowledgement that this is not a typical example of PPI. PPI representative has particularly strong views on the limitations of PPI whereas the CI appears to be increasingly converted to its possibilities.
Participation: the CI is fully enrolled, but the other two respondents have some doubts over whether or not the value of PPI outweighs the effort required. There is no key leader for PPI.
Collective action: the roles of involvement and participation are blurred. However, the relationship between CI and PPI representative is key and characterised by continuity and reciprocity. Both CI and PPI representative agree that there is the ‘right sort of person’ for PPI. There is mixed acknowledgement of reimbursement for time and travel, as some members of the research team see PPI as a voluntary role not requiring reimbursement for time.
Reflexive monitoring: CI can identify the impact of PPI in the study and to a lesser extent so can the PPI representative. However, the CI is concerned about the difficulties in evaluating PPI formally and talks of needing numbers for an evaluation. CI has clearly learned from this study and would have earlier and fuller PPI; all seem to think dual role is useful, particularly in terms of ongoing feedback during a study.
Radar plots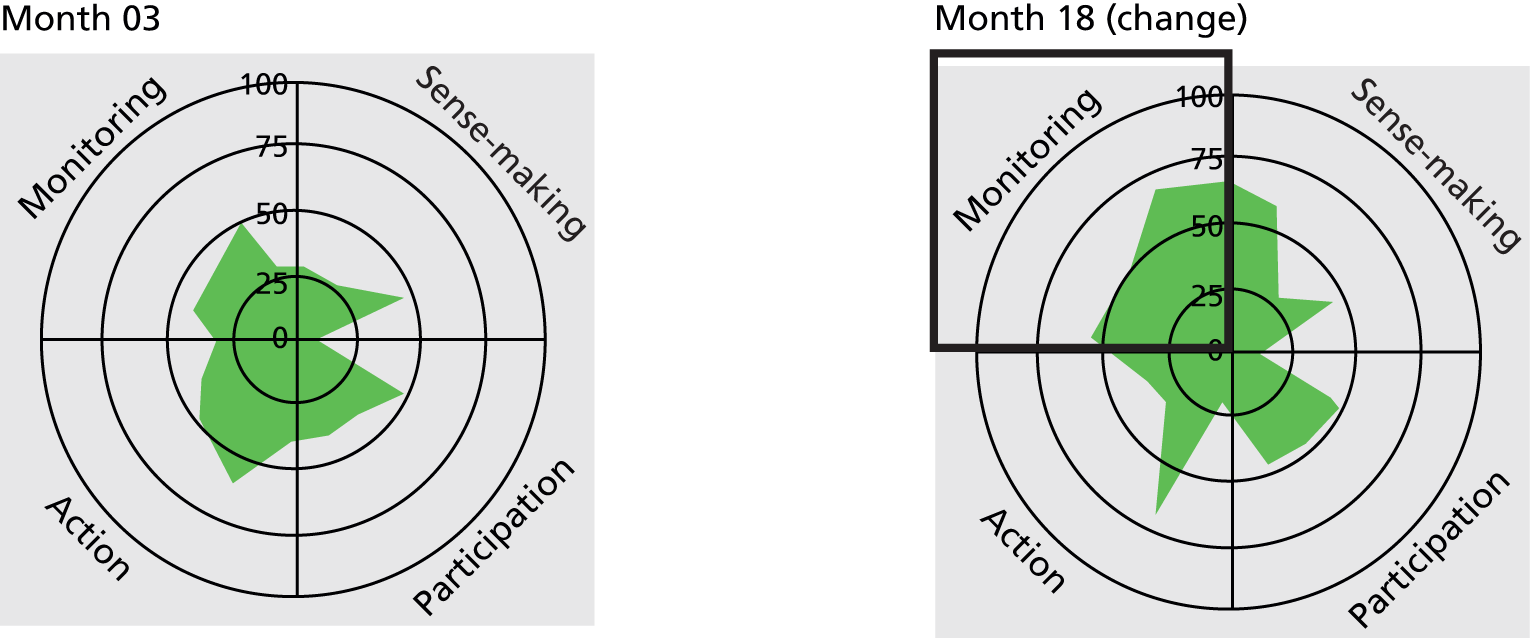
Design of study: changes in the way the study was run (subtle touches such as introducing staff, cups of tea).
Recruitment: actual recruitment by PPI representative to study, changes to PIS.
Enabling contextsStudy design: low-risk observational study so lay rep. comfortable recruiting others (C3). Research host (C7): study being conducted in labs with little interface with the public; CI relying on existing contacts for lay representation but this established relationship also enabled trust (C5).
Although respondents in CS08 were comfortable with this dual role, it was operationalised in an ad hoc manner that was unlikely to lead to any embedding of PPI. In contrast, this dual role was carefully constructed and managed in a longitudinal cohort study (CS13, see Box 16). A rolling PPI panel was drawn from study participants and the role was clearly defined and separated. The impact of this role included both increased public engagement with the study and improved participant retention. This model of PPI was enabled by topic area (public health with healthy participants) and the longitudinal design, which allowed relationships to be developed and sustained over time. This was a well-resourced study with dedicated PPI staff and good organisation, and was run from community hospitals at the heart of local populations. For the public undertaking this dual role, there was a sense of ownership of the study, with subsequent sustained engagement. Two tissue bank studies also had lay representatives who advised but also had donated samples. In CS17 (see Box 23), engagement was sustained, but for the other (CS16, see Box 20) the sense of ownership became a cause of conflict, which is presented in Enablers and barriers to trust.
If this dual role was to have a positive impact, then the purpose, structure and clear role boundaries needed to be defined.
Whole research team is engaged with patient and public involvement
A distinct action of case studies where PPI was embedded was engagement of the whole team with PPI, and having the skill set to do this. Funder requirements (C1) for plain English summaries were bringing into sharp focus the need to be able to explain technical aspects of the research in an accessible way, and the most effective way of doing this was to work in partnership with lay representatives (C5). This needed time to achieve (C4) and could also be helped through specific training (C2). It was particularly evident as an action in the IDD topic area (C3). The CMO configuration for this action is shown in Table 14.
| Salient CS action | Potential contexts | Plausible mechanisms | Potential outcomes | Case study exemplars |
|---|---|---|---|---|
| All researchers in the team engage with PPI, acknowledge the need to explain technical aspects of the research and have the skills to do so | Whole team engagement with PPI was particularly evident in IDD as a topic area (C3). Funder requirements (C1) for plain English summaries were triggering an acknowledgement that this was a required skill for researchers, best achieved when working in partnership with lay reps through a positive relationship (C5). Training (C2) for researchers could further enable this. In complex research, or where lay reps had little experience of research, this was a time-consuming activity that required adequate resources (C4) (e.g. Easy Read documents, time) | Researchers needed to understand that this was an essential component of PPI (M3), was part of their role (M6) and was not left to the lay rep. to do all the work in making sense of the research (M11). There is collective appraisal of PPI as worthwhile (M14) | Moral:
|
CS11 (see Box 15) |
| CS13 (see Box 16) | ||||
| CS16 (see Box 20) | ||||
| CS17 (see Box 23) | ||||
| CS21 (see Box 6) |
Relying on one person to lead patient and public involvement
As described in Purpose, structure and role of patient and public involvement, having someone to lead and co-ordinate was important in embedding PPI. If there was not a designated co-ordinator, this role was often carried out in addition to a junior researcher role and was not part of the original job description. Different levels of commitment to this role were found and PPI representatives spoke of often not having one ‘designated person’. Continuity of personnel with responsibility for PPI was an issue. For example, one PPI representative reported seeing someone different at each meeting (CS05) (Box 14) and another said the enthusiastic support ‘gradually dwindled’ (CS14). If the whole team was not engaged with PPI, the loss of the PPI champion had a detrimental impact.
Steering committee: one expert by experience, recruited through national arthritis body, who was a patient of the CI. Was asked to change consultants. Nursing background and interested in research. Understands some of the medical terminology.
Stages: PPI representative on steering committee throughout the project. Steering committee meets every 6 months.
Normalisation Process TheoryCoherence: PPI representative is ‘patient voice’. Mixed views from the research team about PPI processes within the study. PPI representative believes PPI can be bridge between clinical decision and actual opinion. CI thinks PPI is ‘neutral’ in terms of recruitment.
Participation: PPI seen by some as just another change in the research landscape. Qualitative researcher within department (not involved with this research) very keen on PPI. PPI representative keen to take part.
Collective action: steering committee every 6 months and few e-mails in between. Not much work for PPI representative to do in between times. Lack of continuity with change of study managers (hard for PPI to maintain a relationship), PPI representative accepts she will not understand everything, she communicates the patient perspective. Researcher agrees that PPI representative might not be able to be involved in clinical practice. CI says PPI support needs to be tackled centrally, not at individual study level.
Appraisal: no feedback to PPI representative. PPI representative has some doubt about how much impact PPI has. PPI representative made comments on protocol, concern regarding radiography and reducing medication. PPI rep. feels views taken on board, but less evidence that research team evaluate these as changes.
Radar plots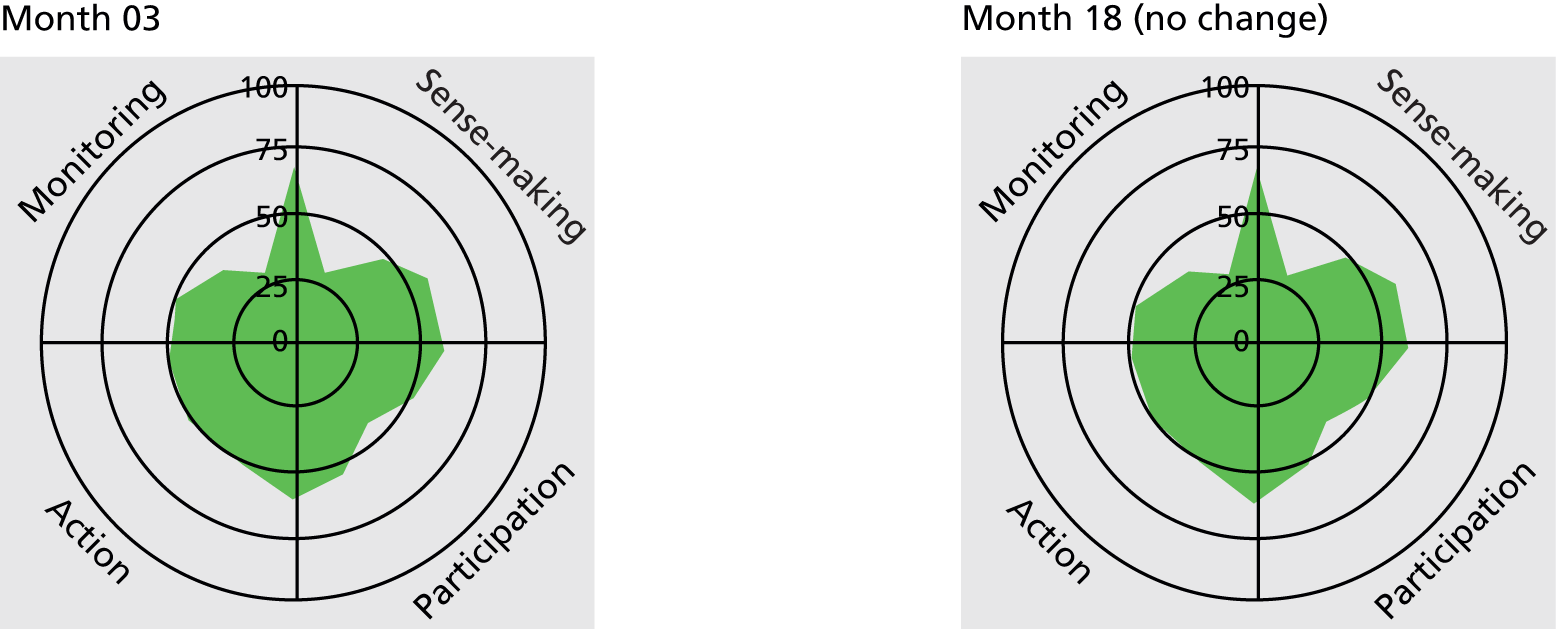
Protocol: PPI suggested changes to protocol; concern regarding radiography and impact of reducing medication.
Patient and public involvement as a collective action
Case studies demonstrating agreement of all individuals in the team that PPI should be part of their work were particularly strong within the IDD topic area, where there is an acknowledged history and strong investment in PPI. The CI from CS11 (Box 15) clearly articulated this:
Two PPI representatives are new to PPI in research (one voluntary worker, one carer) and one more experienced (expert patient). Preference for PPI recruitment from established condition-specific networks (built on previous relationships and personal recommendations) rather than local (generalised) PPI networks.
Normalisation Process TheoryCoherence: CI (clinician) has much more of an overview of PPI in the project (and its genesis) and deeper understanding of politics/history of PPI in this area than other (less experienced) researchers interviewed. PPI representatives have a good understanding of role/purpose of PPI in this study.
Cognitive participation: strong investment in PPI in this research topic, and on this project. CI drives participation. PPI members see participation as (1) part of their job, (2) their only job, (3) a voluntary role with potential benefits for those affected, including family members.
Collective action: PPI members feel valued and identify importance of being assertive. One PPI representative feels that research team could use that representative’s skills more. Interpersonal aspects of PPI: a few examples of issues which have arisen and been managed well are given, which stem from health condition and professional boundary issues. The word ‘mindful’ is used a couple of times in respect of this. Effective chairing of meetings very important.
Reflexive monitoring: nothing systematic in place, but some clear contributions outlined in minutes and interviews and lots of important small changes made, in line with PPI recommendations.
Radar plots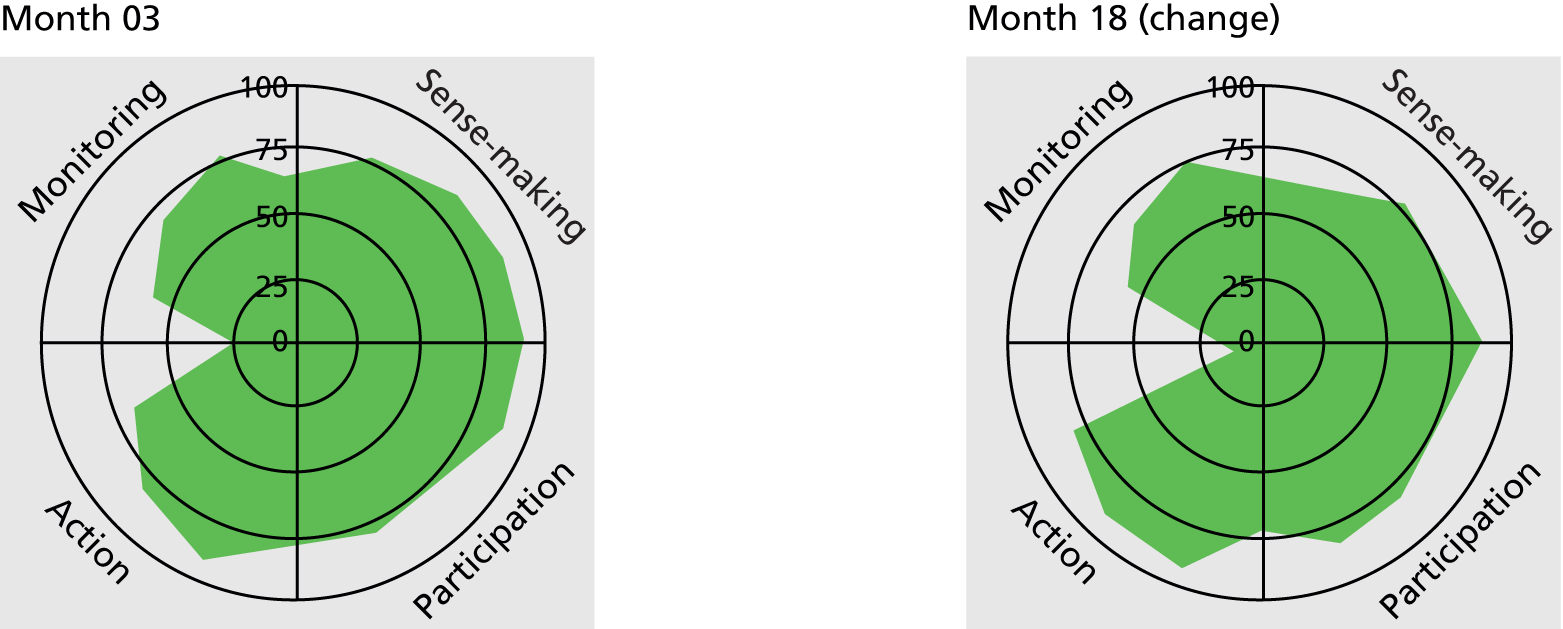
Intervention: refining intervention and testing acceptability of intervention.
Recruitment: better recruitment/retention of participants to trial.
Outcome measures: more meaningful.
PPI outcomes: taking part improves curriculum vitae to get more work of this nature, including consultant/trainer work.
in order to understand and develop theory effectively, you need to really have a conversation with service users and probably somebody who has the problem with the condition, and that is how psychological theory develops. You know, it is that, ‘Are you doing something to people or are you doing it with people?’ and doing it to people, you know, there’s such a power imbalance, and given the backdrop and the history associated with people with disabilities internationally, that’s not politically palatable to me personally and to, you know, society, I suppose.
CS11Res01
Although the NIHR funding (C1) was used to pay out-of-pocket expenses, this case study was hosted by a medical school, with the CI reporting limited engagement with PPI. However, it is the topic area (C3) that is the strongest enabling feature, suggesting a culture where ‘nothing about me without me’ shaped research practice. This CI also framed the challenge to explain technicalities more clearly to lay audiences positively, as good practice for communicating ideas to the public:
saying things like, ‘Oh, this is a stepped wedge design,’ and ‘We’re randomising,’ . . . you can use that language, but people aren’t going to understand it. So, you’re going to spend all your time explaining what you mean, so you might as well just use simpler language to start with, and perhaps really as a researcher or scientist, that’s a good thing because it helps improve your communication skills with lay people and the general public.
CS11Res01-01
This whole team engagement was not unique to IDD as a topic area. For example, in CS13 (public health) (Box 16) although a project-specific PPI panel was facilitated by a lead person, all senior researchers took it in turns to attend panel meetings. The embedding of PPI in this study was enabled through access to resources from grant monies (C4) and a longitudinal design (C3) that enabled relationships to be sustained (C5).
‘Consultation’ panel hybrid model, built upon earlier, less formalised (mass consultation, participant feedback) PPI panel drawn from large cohort study (now mostly retirement age). Panel meet quarterly with an annual general meeting with a rolling membership of 15.
Patient and public involvement in all research stages apart from data collection and analysis.
Normalisation Process TheoryCoherence: PPI approach (roles and purpose) of consultation type panel clearly understood across team with strong leadership; other historical PPI mechanisms have been utilised in cohort study, for example to identify study priorities.
Cognitive participation: run by dedicated and respected member of team. Strong buy-in communicated from outset/CIs: verified from researchers and PPI panel members interviewed. Lots of thought put into planning: how to set up the panel, following best-practice principles.
Collective action: All very satisfied with the way the PPI is run and managed. Shared decision-making regarding panel name, frequency of meetings, level of commitment, when/where meeting and level of input required. Light touch, structured but engaging, elements of fun. Panel only more recently being asked to help set the agenda of meetings, but do feel comfortable to challenge any points put to them for consideration.
Reflexive monitoring: panel are given clear, itemised feedback on why all suggestions are/are not taken on board. All queries are reported back on. They can clearly see their impact in before/after versions of documents. They enjoy taking part and feel highly valued. Annual general meeting reviews PPI contribution and model.
Radar plots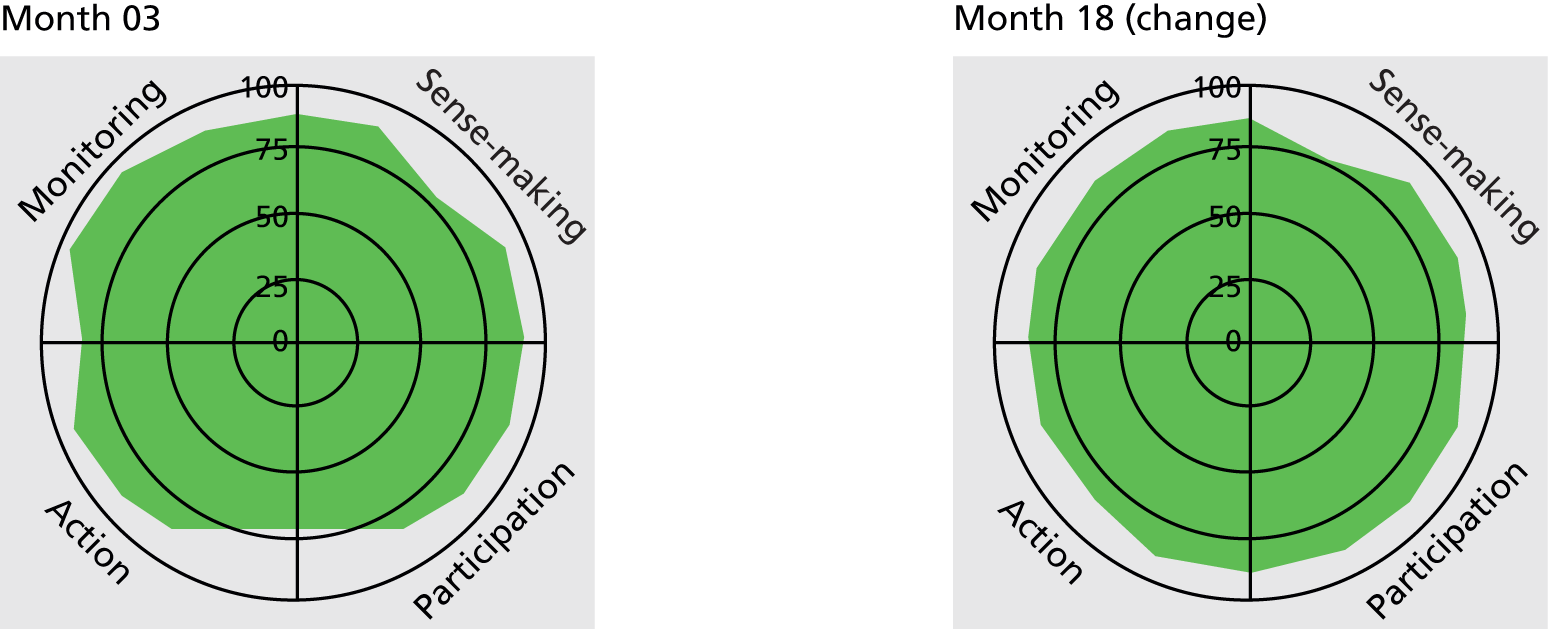
Research priority setting: helping identify research questions.
Design of the study: testing acceptability (refining) of data collection tools of proposed phases.
Recruitment: redesigning website to be more user friendly.
Design of intervention: testing acceptability of future intervention studies.
Standardise outcome measures: patient-focused outcome measures.
Dissemination: presentation to an audience of researchers on PPI and being a panel member. PPI representatives involved in public engagement work. Newsletters.
Other: improved participant retention.
Mutual understanding and trust
While formal training (C2) had a part to play in helping both researchers and the public to understand each other’s roles in research, positive relationships (C5) sustained over time led to PPI as a positive experience (C8) and the development of trust, which was key for this action. Reimbursement of out-of-pocket expenses and time contributed to maintaining trust. If clearly articulated, funders’ expectations (C1) of reimbursement were an enabling context, as was the topic area (C3) if reimbursement was normal practice. Host organisations (C7) had a key role in providing resources (C4) for reimbursement and ensuring payment was smooth. The CMO configuration for this action is shown in Table 15.
| Salient CS action | Potential contexts | Plausible mechanisms | Potential outcomes | Case study exemplars |
|---|---|---|---|---|
| Researchers and lay reps acknowledge, understand and trust each other’s contributions | Training (C2) or significant experience of PPI was an enabling context for the acknowledgement and an understanding of what both parties bought to the research table. This was further enabled through positive experiences of PPI in research (C8), and the development of positive relationships (C5) with time. For many respondents, acknowledgement of each other’s roles was formalised through reimbursement of out-of-pocket expenses and time. Available resources (C4) were clearly an enabling context. These were provided either by the host organisation (C7), which also had a pivotal role in ensuring that payment was seamless and easy, or by the grant awarded. Funder requirements (C1) were also enabling when clearly articulated as an expectation of PPI reimbursement. Topic areas (C3) also had a role to play, as reimbursement is firmly established in some areas such as IDD. Resources were also required to enable social activities that were important in sustaining positive relationships (C5) | Researchers and lay reps needed to understand that PPI was a different way of working from traditional research (M1), and have a belief in the potential value of PPI (M4). Maintaining trust in each other’s work (M10) was key, and needed to be evaluated positively by both researchers and lay reps (M14, M15). Reimbursement was also important in maintaining trust. Understanding that contemporary PPI was different from the traditional notion of ‘volunteer’ (M1), and agreeing together that the role is different (M2), were important mechanisms. Ways of managing continued support of PPI (M8) needed to be developed once grant funds came to an end and in some case the host organisation played an important part in this (M12) | Moral:
|
CS02 (see Box 11) |
| CS03 (see Box 10) | ||||
| CS04 (see Box 22) | ||||
| CS06 (see Box 24) | ||||
| CS07 (see Box 17) | ||||
| CS09 (see Box 27) | ||||
| CS10 (see Box 25) | ||||
| CS11 (see Box 15) | ||||
| CS12 (see Box 12) | ||||
| CS13 (see Box 16) | ||||
| CS15 (see Box 21) | ||||
| CS17 (see Box 23) | ||||
| CS18 (see Box 9) | ||||
| CS21 (see Box 6) | ||||
| CS23 (see Box 21) |
Coherence in understanding the contribution of patient and public involvement
As the bedrock for trust, lay representatives and researchers needed to have a shared understanding of the purpose of PPI. Novice researchers were more likely to be unable to fully distinguish PPI as separate from research participation. For example, a registrar in CS14 defined PPI as:
patients contributing to research and enrolling into research studies, whether they had portfolio status or not.
CS14Res02-01
While this impeded an understanding of what PPI could offer to the research process, other researchers and PPI representatives provided a variety of reasons for carrying out PPI including gaining insight into the lived experience of a particular health condition, and to provide reassurance for researchers that their research question resonates with the patient community. This was exemplified in CS07 (Box 17).
Experts by experience panel (≥ 10 patients who have lived with diabetes mellitus for over 5 years). Recruited from diabetes research network panel. Members of the CS07 panel are on their own Diabetes UK voluntary group (access to another level of PPI). There is also an online panel. Involved in different stages (involved at beginning and in recruitment and CI hopes they will be involved in dissemination).
Normalisation Process TheoryCoherence: CI says ‘patients are the experts’, ‘find it incomprehensible that you wouldn’t ask patients first’. Researcher had been involved with PPI in service redesign before – ‘it’s the way forward’. Involve people from the concept and design through to dissemination. ‘PPI runs throughout the study’. Ethics committee had been very positive. PPI representative believes PPI to ‘humanise research’, ‘white coat jargon – words of one syllable’.
Participation: researchers buy into PPI as does the PPI representative.
Collective action: meetings set up only when needed. Training through research network, not sure PPI representative wants any more technical training as providing lay perspective. PPI representatives distributed questionnaires to their own Diabetes UK groups, so got lots of feedback. PPI representative accepts limitations of specialist knowledge and terminology. CI feels PPI is embedded within her organisation. Taxi organised for PPI representative as has mobility problems.
Reflexive monitoring: involved in protocol (randomisation), PIS, design of questionnaire, video used when recruiting practices to the trial. PPI representative intends to be involved in dissemination (not analysis). Researchers listen, PPI representative feels contribution is valued. Researchers recognise importance of feedback (it is an agenda item). PPI representative says feedback very complimentary on the video. Dissemination so far: PPI poster designed for UK annual conference, newsletters.
Radar plots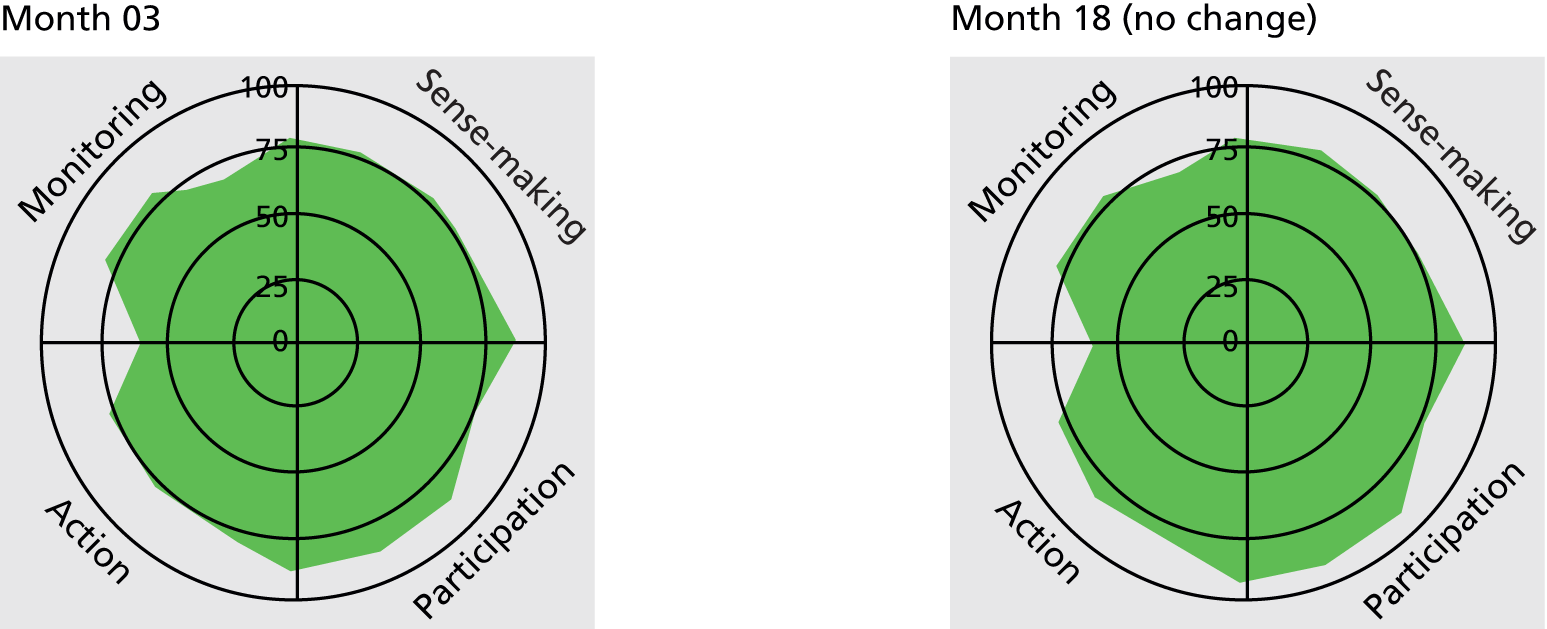
Design of study: psychological element (scale has been shortened), whether to do partial or full RCT. Panel commented on proposal of this study at the beginning. Introduction, how to phrase the study.
Design of intervention: refined – changed the questionnaire six times, eight pages to three. Validated the questionnaire (panel sent out to their user groups and through diabetes database).
Recruitment: through video – PPI representatives took part.
Case study 07 was enabled through an established diabetes (C3) network group (C6) housed in the host organisation (C7). The study focus on processes of care (C3) also enabled coherence. PPI members met regularly and were involved in a number of projects which helped promote sustained engagement (C5). However, lay representatives were not reimbursed for their time because of bureaucratic difficulties; rather, they were taken out for a social meal.
Whereas the experience of established panels was seen by many researchers as a bonus, others spoke of the tension between wanting someone who was ‘outside’ the research environment and wanting someone who was also able to engage with research studies (possessing some research skills) and thus perceived as being able to perform the necessary PPI tasks. This notion of wanting the right person with a short distance between direct experience and its interpretation but who also can feel comfortable in a research environment is maybe a contradiction in itself. There was evidence of an ongoing debate about whether or not the experience of a condition (direct or indirect) was seen as less legitimate because of that person’s professional background, experience or training in research or health care:
we’re all patients . . . yeah, and some of us have PhDs and some of us don’t, so it’s quite difficult to kind of define what is a lay representative . . . they’re really just people who, actually, through their qualifications, they should be research assistants but don’t happen to have a job in research but are on a lay panel. And I kind of think ‘what . . . are you really a lay person? You’re just an unpaid researcher’, but I’m not entirely sure whether that’s right . . .
CS17Res01-01
Our findings suggested that defining PPI as a discrete and commonly understood component of research was difficult but the range of PPI representatives can be summarised through a fourfold typology based on an insider/outsider perspective (on one axis) and a range of research skills (on the other) (Figure 8). Research studies can be placed along these axes; however, within one research study there may be a mixture of individuals with varying skills and perspectives.
FIGURE 8.
Insider/outsider perspective.

While the insider/outsider debate was articulated in a number of case studies, those that had embedded PPI were likely to have sustained engagement with the same group of PPI representatives over a long time.
Building relationships over time
We found that the relationship between the researchers and PPI representatives was a key factor for successful PPI. Relationships took time to establish, which was particularly difficult at the beginning of research (or even before the proposal is written). One finding from the case studies was that the majority of PPI representatives had a previous working relationship with the research team. Of the 51 PPI representatives, 33 (64.7%) had some prior working relationship with either the CI or members of the research team (three were patients of the CI and also members of a service user group, so had worked together before), nine (17.6%) had a more distant acquaintance (but described themselves as being within the same loose network) and nine (17.6%) PPI representatives were completely new to the research team (recruited from outside existing structures). The obvious advantage of having a previous relationship meant that PPI could start as soon as possible within the research project, whereas more time was needed to establish relationships through informal small meetings if the lay representatives and researchers had not previously met.
Research teams spoke of initial meetings where everyone got to know each other and having these times of informality before starting on the ‘academic’ business. The benefits of PPI representatives having the opportunity to get to know each other also provided support later in the project. Social elements were important in encouraging and maintaining continual engagement in the research study and should not be underestimated by researchers. Some of the case studies also ran social events outside the research, which again helped to build and maintain relationships:
We do these family fun days as well, which we get together once a year, just to get together at the zoo or something. [PPI co-ordinator] works phenomenally hard to build relationships with the families that . . . So, it’s a partnership really.
CS21Res01-01
In more formal advisory or steering committee meetings, PPI representatives spoke of being specifically welcomed into the meeting (sometimes being met beforehand). Most importantly, during the meeting, successful PPI was being ‘genuinely’ listened to and their comments taken on board. The relationship between the researchers and the PPI representatives was key to fully embedding PPI within the research study. The researchers needed certain social skills, which included being approachable, good listening skills and group work skills:
initially facilitating and always presented a positive, welcoming, friendly, supportive space to you.
CS17PPI01-02
Patient and public involvement representatives reported that meetings needed to have a ‘flat structure’ where PPI representatives felt free and at ease to speak.
Relationships could change over time, either through loss of trust or as trust developed, as illustrated in CS19 (Box 18). Although only subtly different, the radar plots show a change in all quadrants but particularly in collective action (bold box), where M10 (trust in each other’s PPI work and expertise is maintained) is included as a mechanism. This reflects clarification of roles and the improving relationship and trust in the PPI work:
Committees: two representatives (one a coapplicant) on trial steering committee (meet twice a year). Two PPI representatives on trial management group (meet once/twice a year).
PPI in all but data collection and analysis stages of research.
Recruitment of PPI representatives: two research-related professionals already known to CI who had had experience of the intervention.
Normalisation Process TheoryCoherence: mixed understandings and tensions about the purpose and role of PPI in general and specifically on this project. CI sees PPI as normalised and indistinct from other research partnerships.
Cognitive participation: CI drives the PPI. Qualitative researchers unsure how PPI will impact. PPI coapplicant bought in from the start. Agreement on commitment to PPI but mixed views on how it needs developing further in the study.
Collective action: PPI coapplicant very effective to begin with but has had to step down. Other PPI representative feels that team need to think about patient experience and is unsure whether or not the team is responding to the PPI representative’s message. PPI representative feels both she and the other PPI representatives could be more involved.
Reflexive monitoring: no systematic process for appraising PPI in place, but clear, if weak, examples given of contributions of PPI to the study after initial protocol development; some reflections on how PPI could be strengthened.
Radar plots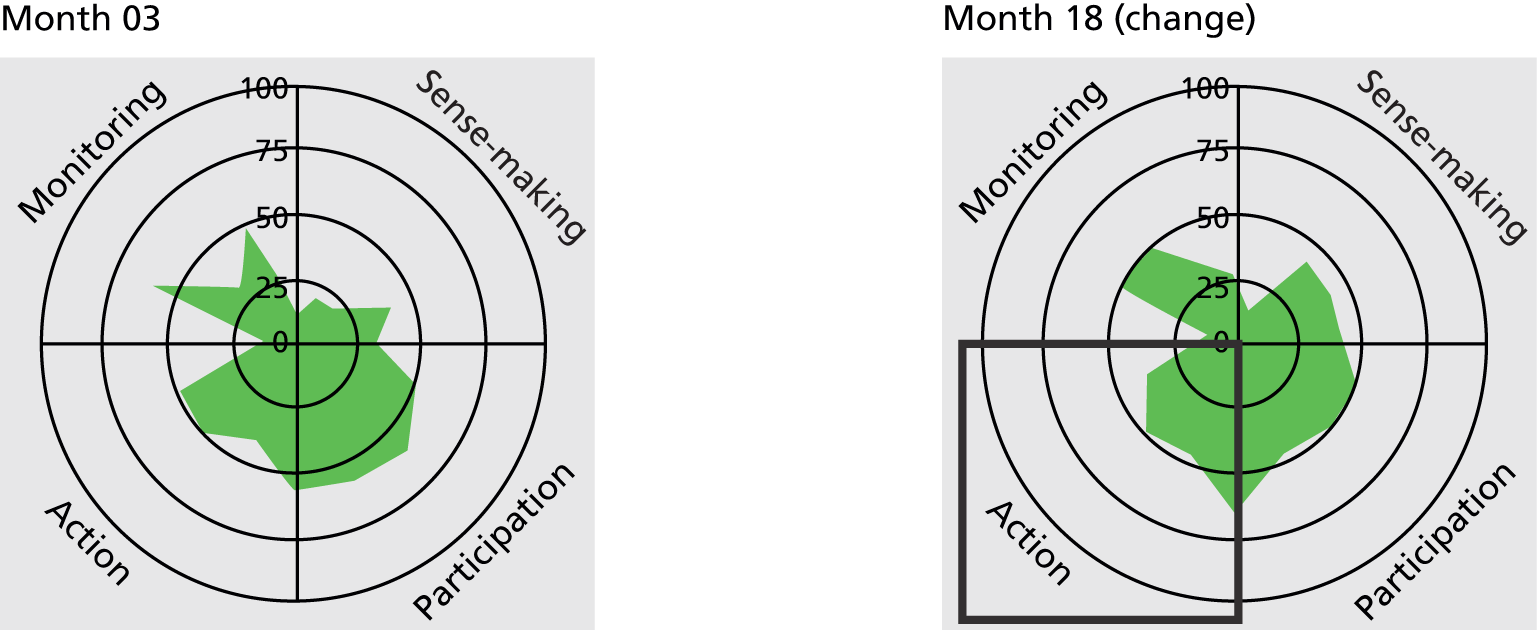
Marketing of study: awareness that study logo might be inappropriate/insensitive.
Design of study: timing of nutrition questionnaire; PPI representative felt this is too invasive.
Design of intervention: testing acceptability of intervention; asking too much of patients in each visit.
Recruitment: recruitment pack, information.
Dissemination: PPI representative invited to coauthor a paper.
I don’t know what they want me to prepare for, I don’t know what they want me to do, and I don’t know if the confusion is because of my professional role [. . .] and I don’t know if they’re waiting for me to take the lead, and I’m waiting for them to treat me as a patient. . . . I’m a little bit disappointed. It feels almost tokenistic.
CS19PPI02-01
Conflict between roles resolved . . . CS19PPI02 feels happier now that they are no longer post-surgery, less vulnerable. They had a long chat with a rheumatology person in department who had done a lot of PPI work who reassured CS19PPI02 that one PPI voice is better than none, more confidence to feel you don’t have to represent all patients, can just give your own experience. Different way of looking at the value of their contribution.
CS19PPI02, notes of tracking interview 6 months later
Trust as the foundation for patient and public involvement
A relationship framed by trust was the minimum requirement for PPI to have a positive impact. Although PPI was not embedded within CS14 (see Box 26), the relationship between lay representatives and the clinician was based on trust built up from a clinician–patient relationship with continuity over time:
there’s a trust there, I trust them that they wouldn’t ask me to do something that wouldn’t be, you know, it would be difficult or wouldn’t necessarily be appropriate or whatever.
CS14PPI01-01
Some researchers also trusted their lay representatives to undertake the work in a way that was workable for the researcher:
It’s always good, you know, on research it’s you need good people you can work with and that’s what I would be looking for, to set up some relationship of trust and mutual respect . . . Without thinking of them as a hindrance.
CS15Res03-01
Case study 15 (Box 19) exemplified how, even when resources were minimal for PPI, the very existence of mutual trust resulted in positive PPI impact. This study was housed in an organisation with no PPI infrastructure and with minimal resources for PPI despite the study being funded by the NIHR. The research setting [intensive care unit (ICU)] provided particular challenges: consent and recruitment difficulties in a high-stress environment; difficulty in recruiting lay representatives, as they were often traumatised by their time in ICU; and lack of resources, as there was no large charitable funder. The lay representative in CS15 had an impact on recruitment processes for the study and provided a valid argument to present to the ethics committee for this approach:
One national representative. PPI role confined to trial steering group.
Activities include review of PIS before ethical approval, project management. Involvement in dissemination expected.
A topic area with particular challenges in recruiting lay representatives.
Normalisation Process TheoryCoherence: lay representative very experienced in different PPI roles (although first clinical trial of an investigational medicinal product) but all research team very new to PPI and some find it hard to differentiate from obtaining feedback from participants. Despite some difficulties in clearly defining PPI and describing their own role in PPI, all the research team articulated potential value of PPI including bringing patient perspective, advising on consent process, improving recruitment and dissemination and raising awareness of the research.
Participation: CI sees role to drive PPI forward as a requirement of funders, whereas the research nurse feels this is something that could be developed in her role. There is no resistance to the idea of PPI and there is evidence that the team are likely to continue supporting PPI.
Collective action: some acknowledgement by the team that regular communication is a requirement for PPI. Trust is a key feature but unlike many of the other case studies it is trust in the PPI representative that is more articulated. Research team trust the PPI representative. This will make dealing with PPI representative easier, and representative will feed back appropriately and not mind if they do not take up PPI suggestions. The PPI representative sees the relationship with the CI as key.
Reflexive monitoring: minimal – had not thought of systematically evaluating PPI impact. CI evaluates PPI input as useful to date, but no evidence of any reconfiguration.
Radar plots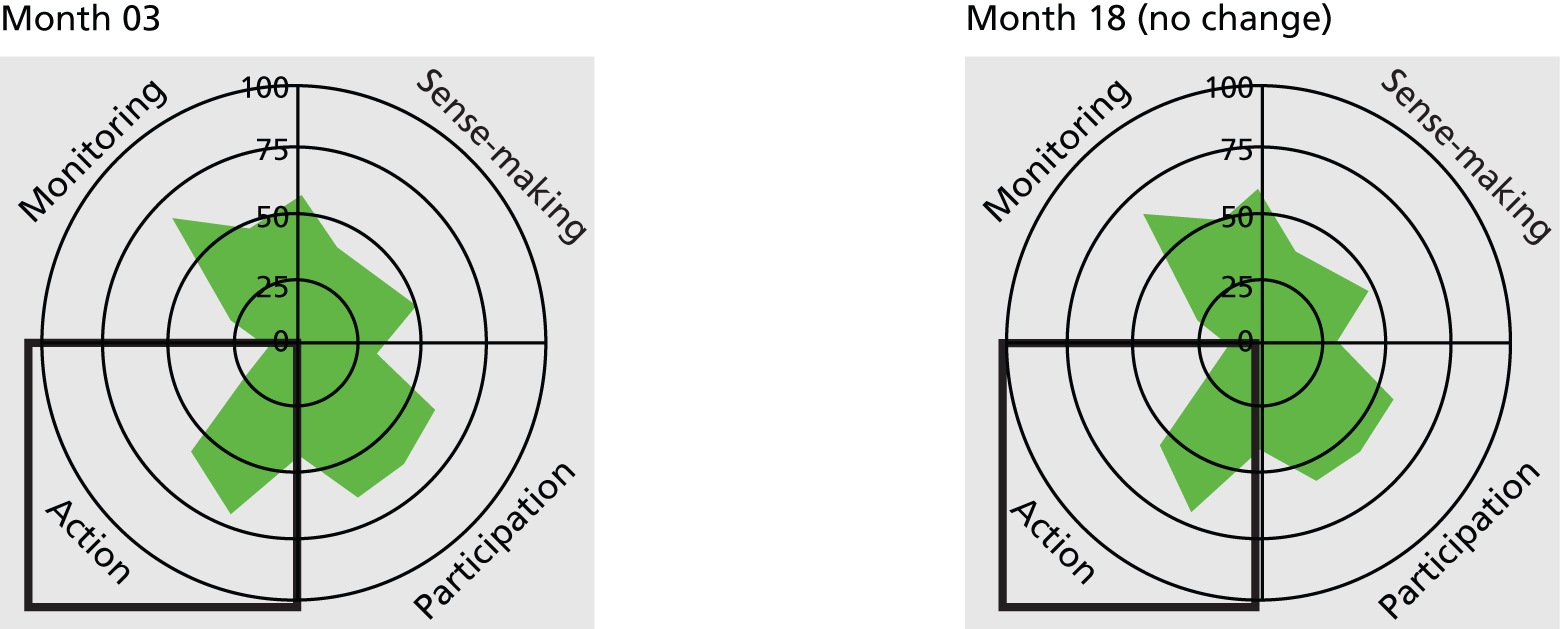
Recruitment: too early to tell but is seen mainly in terms of improving recruitment because of refinement of PIS, in particular making the wording more sensitive to relatives who will be consenting.
we put a thing here saying in the consent ‘to continue information now you’ve regained consciousness, we would like your permission to continue in the research’, now [PPI01 has] written ‘I realise this might not be possible but in my own experience of delirium I was regarded as having capacity long before I was in my right mind or capable of rational decision making. I appreciate this may be beyond the scope of the study but if there were any way to change the emphasis for the patient remaining in the study unless they chose to opt out, I think that would be much better’.
CS15Res03-01
It can be clearly seen how M10 appears as a peak in the collective action section of the radar plot (bold square).
Enablers and barriers to trust
Sustained feedback to PPI representatives was a clear enabler of trust and continued engagement:
and they’re always thanking us for our participation. All the time. Always saying, you know, I get it in e-mail messages, we get it at the meetings and they always say how valuable our input is, you know, they make us feel worthwhile and that is good.
CS13PPI03-04
This feedback was recognised by many researchers as being important:
I think it’s important, what I’ve learnt is that if you are going to ask them things you need to feed back to them so that it’s terrible to actually ask their opinion and they never hear again, so I’m quite good now, it’s an agenda item that you know, I feed back what I’ve heard from different people, because they’re left wondering . . .
CS07Res01-01
The forum in which researchers and lay representatives came together was also an important enabling context for trust. The majority of our case studies had PPI representatives as members of steering committees (one or more lay representatives per study) which met every 3 or 6 months to advise the research team but did not necessarily have a ‘hands-on’ role with the research. However, different research teams made different uses of their steering committee members, with some members making comments only during the meeting and others who were asked to comment on documents throughout the study. As shown in CS04 (see Box 22), there was a varying sense of equality within the committee:
it wasn’t run by the Professor from the top down in sort of military fashion, it was a round table discussion where anybody could contribute . . . whilst it could have been intimidating actually it was very welcoming, and the person who chaired the meeting was very sensitive to that.
CS04PPI02-01
However, the formal term ‘steering committee’ put some PPI representatives off: ‘if they said someone to be on the Steering Group I mean I would never, I would have just thought well that wouldn’t be . . . that sounds too high powered for me’ (CS04PPI01-01).
Despite it often being seen as good practice, there was little evidence that this relational integration was being formalised through job descriptions or contracts for the PPI representatives. However, at the start of the study researchers often clarified expected commitments to attending meetings; other PPI input was often less formalised. Those case studies which had high levels of PPI activity could achieve this through flexibility and allowing PPI representatives to ‘dip in and out’ as their other commitments also varied:
parents will stick with the programme because they know that they can step in and out if needs be, and the team also think about how they can include people that might not be able to travel, so whether it’s joining in a meeting by phoning in to it and participating over the phone or sending responses or comments and feedback in an e-mail, so it’s made it available and it’s made accessible.
CS21PPI02-01
However, trust in CS16 (Box 20) was lost because of a lack of formal agreements about access and ownership of a database. This issue appeared midway through data collection and the impact can be quite clearly seen on the radar plots tracked over time. The impact can also be seen in the way the PPI was appraised (hatched box); because of this experience the charity would get legal documents drawn up before working with researchers again.
National expert network: charity. Dual role (participants and representatives).
Patients meet once a year but charity has ongoing contact.
Recruitment of PPI: through charity.
Normalisation Process TheoryCoherence: CI has worked with patients with a particular rare condition (which is related to diabetes mellitus) since the 1980s. CI received money to fund a clinic (but not the research). With parents of children with the condition, PPI and charity reps, the CI developed a grant application which was awarded by the charity. CI very committed to PPI. PPI representatives believe in patient voice. All three PPI reps work for charity, very involved. PPI representatives feel clinicians/researchers do not fully understand the condition as a whole. Come together for conference once a year.
Participation: PPI seen as essential, as patients/parents are in unique position to understand experience of condition.
Collective action: CI believes PPI not appropriate for all areas and sometimes realistically there is no time to involve patients – depends on the study. Scientists having an open mind to be challenged and be able to explain things simply. CI thinks funders should make PPI compulsory but the sponsor also needs to be signed up to PPI. The charity owns the database and wants to access it but there are research governance issues.
Reflexive monitoring: PPI representative keeps an events log of conferences, events. As study progressed, ownership of database became contested. PPI work will be reconfigured in future studies to include a formal contract.
Radar plots
Study design: sensitive research tools, how to undertake procedures and examinations.
Recruitment: changing the wording of PIS. Language: employ people at the charity who speak Urdu or Punjabi so not just relying on interpreter from the hospital – so can have open discussion.
Dissemination: will be from the charity, which is hoped will be more effective coming from patients.
Virtual patient and public involvement
There has been a recent move towards the increasing use of technology and teleconferences being used as a means to include lay representatives who might otherwise not be able to attend meetings. However, this move towards ‘virtual’ contact as opposed to ‘face to face’ has implications for the establishment of relationships. One lay representative said that they always wanted an initial face-to-face meeting to make any following (virtual) meetings easier. As presented in Strategies for recruiting lay representatives, being unable to meet in person also caused problems in CS18, where the CI and lay representative were in different regions. The challenges of building and sustaining relationships through virtual contact were also raised by a funder. Maintaining arm’s length relationships was acknowledged to be difficult for the army of remote lay reviewers, and they found it difficult to sustain any more active involvement. Case study 23 (Box 21) provided an example of virtual PPI with young adults, and also demonstrated how this medium provided an outreach model (see Discussion).
Four YPD as advisory group.
One local community volunteer (experienced in PPI) also a coapplicant.
Another PPI coapplicant was meant to be a co-researcher but dropped out. A third coapplicant was an expert by experience.
Involved in developing initial idea, bid writing, design of study, giving feedback on mobile phone applications (apps), contribution to e-mail discussions.
Recruitment of PPI: coapplicant PPI through previous research contact, and local voluntary representative.
Normalisation Process TheoryCoherence: divergent understanding within the team regarding the PPI model, as research is user led. Concerns that the YPD on PPI advisory panel may not fully represent the (hard to reach) service users. Strong belief in value of PPI for more effective, relevant research/service development.
Cognitive participation: PPI in study has assigned co-ordinator from HEI cluster who runs YPD advisory group with research assistant. Strong buy-in across research team – allied to study being user-led research, but YPD have to be prompted to do their PPI tasks. Continued PPI has been a challenge to maintain here because of other demands on time and geographical remoteness. Coapplicant also dropped out.
Collective action: ‘virtual PPI’; never had a full team meeting – lots of e-mail discussion. YPD advisory group run separately (at their request) but mechanisms for feeding their input back to researchers unclear. Payment for PPI well handled – some flexible use of the project’s PPI budget to support participation. PPI on steering group believes they have challenged the team.
Reflexive monitoring: strong interest in evaluating PPI within the HEI cluster, but very little in evidence on this project. No minutes of meetings; mechanisms by which PPI informs study clear at bid development phase, but not always so in running of the project. Mixed assessments of the value of impact of PPI YPD advisory group.
Radar plots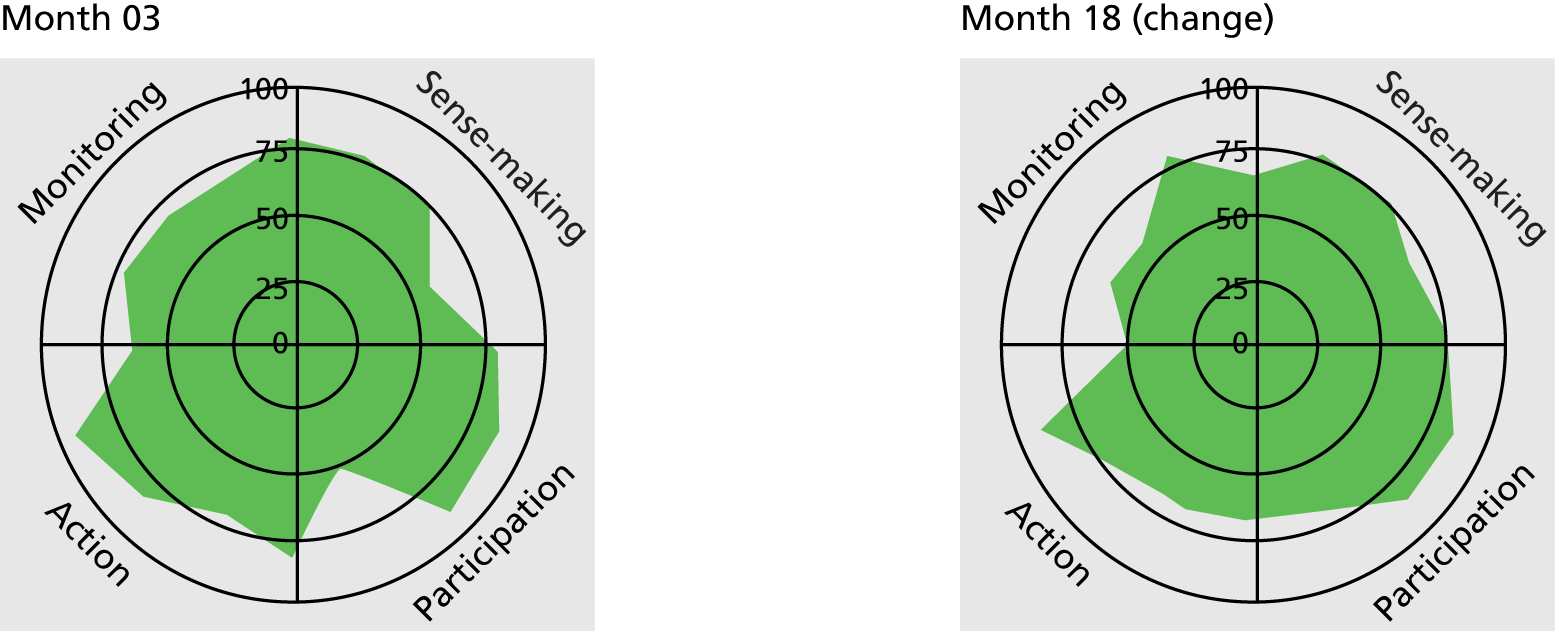
Research priority setting: original research idea builds on PPI coapplicant’s website.
Study design: research question and design confirmed as relevant but more clearly defined by diabetes service users ‘expert patients’ panel; split original proposal into two target populations and approaches.
Recruitment: research web pages more younger person-friendly and language less clinical in style. Young person with diabetes mellitus helped to recruit participants to test apps via social media.
Dissemination: researcher and a main participant/informant on Twitter coauthored an invited journal paper.
The benefit of this virtual form of PPI was obvious:
I’ve got a main informant on Twitter . . . asked her if she could work with me on developing a paper and she’s a young person . . . and so she basically threw some question out to Twitter to her one and a half thousand followers . . . and we sort of put some questions to them and we’d written a paper within 3 weeks.
CS23Res04-01
Case study 23 also had an advisory PPI group made up of four young people with the condition. At their request, this group was hosted separately from the research team meetings and deliberately had an ‘informal feel’. These separate meetings were envisaged to be a series of evening, face-to-face meetings with monies allocated to cover travel expenses. However, in reality, as a result of competing demands placed on the attention of this age group, the group did PPI ‘virtually’. Co-ordinating such involvement was a significant workload, which was difficult to predict and cost for. However, as this was adapted to over time, the tracking radar plot became fuller.
Reimbursement
Reimbursing lay representatives for their time is intuitively an enabler of trust and seen as normal good practice, yet payment for time was surprisingly rare in the case studies, although all were paid for out-of-pocket expenses. This was not only because of financial restraints but also reflected a continuing debate from a minority of respondents on how payment fitted with the notion of volunteerism. For example, in CS08 (see Box 13) PPI was felt to be more of a voluntary role, which payment would then ‘professionalise’:
No, I think it should be voluntary . . . because you’ll be paying for services for like, I guess, advice or public feedback, if you’re paying them then it’s, I don’t think, it’s more official, I guess . . .
CS08Res02-01
This was rejected by many lay representatives:
It is and part of the problem is that people just kind of make an assumption, oh they’re patients, we won’t need to pay them. And you know our time in our life is just as . . . important as a researcher’s or a doctor’s.
CS14PPI02-01
Among the five case studies reimbursing for time, the amounts ranged from £25 per meeting to £75. This was often enabled by the host organisation, such as a CLAHRC or research centre. However, even within well-funded host organisations such as HEIs, researchers related institutional barriers to paying lay representatives within institutional systems reliant upon inappropriate standardised status classifications (such as lay people having to be classed as visiting lecturers), electronic forms and difficulties dealing with cash refunds, as well as payments affecting lay volunteers’ benefit payments and tax arrangements. Hence, the host organisations that managed reimbursement and arrangements seamlessly made lay representatives feel a collegial partner with the organisation.
National charity representatives reported that they were being asked to be involved with an increasing number of research studies, which is not necessarily the main part of their work. One PPI representative called for there to be some recognition of cost to the organisation and the consequences:
there must be other charities like me in other therapeutic areas who are getting the same issues . . . So I would have thought that we should be looking at this at a national level to say if patients are going to be involved in research in a way that they have not been previously then they need support to do that and it should not, all of the cost of doing that, should not fall solely on the third sector. We should be getting some kind of NHS/government DH [Department of Health] support for this.
CS14PPI02-01
One paid charity representative said her workload was such that she did PPI work in her own time. Perhaps in acknowledgement of this, another charity representative in a PPI role was contracted (part time) by the research project – yet further blurring the lines between PPI and researcher. It could also be argued that paid employment also introduces different obligations and commitments to involvement, although it has the potential to clarify an otherwise open-ended commitment.
Opportunities for patient and public involvement throughout the research process
A characteristic of studies with fully embedded PPI was that opportunities for PPI in all parts of the research process were fully exploited. The CMO configuration for this action is shown in Table 16. As an enabling context for embeddedness, it was not necessarily how the PPI was organised but how much PPI representatives were encouraged to be involved and were exposed to different areas of the study throughout its stages where they could have an impact. There were reservations from some researchers on the potential for PPI in the early work of basic science designs (C3). However, we found that, with appropriate training (C2) and experience, lay representatives were effectively contributing to funding decisions for basic science studies, and prioritisation for tissue bank studies. This was further enabled by having a pool of lay representatives (C6) with sufficient interest and expertise to contribute effectively at all stages of the research.
| Salient CS action | Potential contexts | Plausible mechanisms | Potential outcomes | Case study exemplars |
|---|---|---|---|---|
| Opportunities for PPI in all parts of the research process are fully exploited | Study design (C3) had an influence on how many stages of the research had active PPI, with reservations from some researchers about the potential for PPI in the early work of basic science designs. However, training and experience (C2) of both lay reps and researchers could enable more extensive PPI in all research designs. If this was further facilitated by the organisation of PPI (C6) such as having a pool of lay reps with sufficient interest and expertise to contribute effectively at all stages, then PPI was evident in the early stages of, for example, a systematic review. Positive experiences (C8) of more extensive PPI led to a virtuous cycle | This required all mechanisms associated with coherence: understanding PPI as a different approach (M1), individual and collective agreement about the purpose (M2, M3) and constructing the potential value (M4). It also required agreement that PPI should be part of the work at that particular stage of research (M6), and that lay reps were supported to do the tasks required (M9). Finally, the worth of PPI in more parts of the research process needed positive appraisal (M14, M15), with adjustments made if necessary (M16) | Moral:
|
CS02 (see Box 11) |
| CS03 (see Box 10) | ||||
| CS04 (see Box 22) | ||||
| CS06 (see Box 24) | ||||
| CS07 (see Box 17) | ||||
| CS09 (see Box 27) | ||||
| CS10 (see Box 25) | ||||
| CS11 (see Box 15) | ||||
| CS13 (see Box 16) | ||||
| CS16 (see Box 20) | ||||
| CS17 (see Box 9) | ||||
| CS18 (see Box 22) | ||||
| CS21 (see Box 19) | ||||
| CS23 (see Box 21) |
Patient and public involvement and the research cycle
Performing the necessary tasks for PPI appeared limited to certain stages of the research cycle. Some researchers recognised the importance of having PPI before studies were funded but acknowledged the difficulty of finding appropriate PPI representatives in a short time frame. Many researchers felt comfortable involving PPI representatives in the general review of study documents but not so certain about involvement in other parts of the research process. In most case studies there was significant PPI during study set-up, but this often decreased as the research progressed, for example when patient recruitment or data collection started. Researchers often reported that the pressure to recruit research participants (during data collection) resulted in less capacity to enable involvement of PPI representatives. This impacted most on relational aspects, with changes evident in this sector of the NPT radar plots.
The distinctive characteristic of case studies that enabled involvement at all stages of the research process was the presence of a dedicated individual facilitating PPI (e.g. CS21, see Box 6). A complementary or alternative approach was having a lay coapplicant who was fully involved from the inception of the design, and sometimes undertook an outreach role, or worked as an integral part of the research team. Case study 04 (Box 22) had one experienced lay member as coapplicant; this was enabled by the research topic being focused on a patient evaluation tool, and by having an established PPI group with experienced lay members.
Experts by experience.
Number of levels: focus group, consensus event (10 people) (not consented so counted as public involvement); two lay representatives on steering committee (one of the lay representatives is also on the research team and is particularly experienced; has been on diabetes user group for 3–4 years and been involved in other research projects).
Stages: involved throughout, as one PPI representative is on research team.
Recruitment of PPI: diabetes user group and known to CI.
Normalisation Process TheoryCoherence: both researchers new to PPI, but both felt PPI essential to research: ‘seems ridiculous . . . without’. Consensus event considered to be PPI. Researchers and PPI representatives agree on purpose of PPI; real situations, bigger picture, quality of life, well-being and sense of worth.
Participation: CI is approachable, in contact a lot; ‘invaluable to have someone with the condition involved’. PPI representatives view ‘amazing piece of research’.
Collective action: CI felt PPI not embedded within institution. PPI rep. talks of flat structure (relationship), managing expectations, welcomed, included, round table discussion, not intimidating. Other PPI rep. had thought she would not be sort of person for steering committee, as sounds too high powered, but persuaded through personal contact. Travel, support organised.
Reflexive monitoring: comments given on questionnaire are recorded. Second PPI representative does not consider self to have contributed very much. The end result is that questionnaire is unrecognisable from original form (so can see impact of PPI input). Felt to increase validity of research, more balanced. PPI representative suggested changing area of country when researching the education courses (national coverage). Questions were ambiguous and section on pumps changed.
Radar plots
Protocol: input into proposal (keep the patient in mind).
Design of intervention: questionnaire, issues added not thought of by researcher.
Dissemination: two papers written, one submitted to journal with PPI representative’s name as coauthor.
Outcomes of PPI: rewarding for PPI reps.
Patient and public involvement in different research designs
Funders and some researchers espoused stereotypical assumptions about the limitations of PPI in certain research designs, such as basic science, which has traditionally been an area with little PPI. A PPI co-ordinator working in a medical setting and talking about CTIMP (clinical trial of an investigational medicinal product) research observed that, because some researchers believed patients have difficulty in understanding the science and bench side of research, they find it hard to engage and have meaningful PPI. Similarly, one funder suggested PPI was more compatible with applied science:
I think it comes down to the complexity of science and the type of research that you’re talking about, some studies: when it’s very kind of lab based and it’s very molecular, doesn’t really lend itself to being able to involve the public or patient, you know, at a very kind of technical level. But there are a lot of opportunities in medical research where it is viable and it is possible to do it.
Funder03
Other researchers also felt that involving PPI representatives in ‘technical’ discussions about certain research designs was tokenistic, as they were able to contribute very little:
I mean we’re doing a review of reviews . . . so it’s methodologically very challenging, it’s conceptually quite challenging, half the academics feel out of their depth, intellectually and conceptually. The PPI feel . . . that’s not to denigrate them or to put them down in any way at all, it’s not what PPI is about, . . . No, they come to the steering group and then they feel a bit left out and I think it’s a shame, I think it’s, you know I think it’s disrespectful in a way that not having, I mean I think, for that project it would be more respectful not to have PPI, does that make sense?
CS03Res04-01
There was also some evidence that researchers felt concerned that some PPI representatives who lacked scientific understanding could jeopardise a study at the design stage. However, another funder challenged assumptions about the ability of experienced PPI to review less applied, more basic science applications:
when we set up these committees, there was a fear or a worry that they would have trouble reviewing basic science applications and therefore they would be more drawn towards the clinical ones, but actually what happens is, it’s quite funny really, it’s almost the other way round. I think they can see the pipedream or the hope at the end, and almost they’re more critical about clinical studies, I think maybe because it’s closer to the patient benefit.
Funder01
Indeed CS17 (Box 23) successfully involved PPI in approving bench research proposals in genetic epidemiology through a panel model whereby the PPI representatives are presented with lay protocols written specifically for the panel.
Established panel for over 10 years; about 30 on panel and two attend each monthly meeting (usually invite four). Meeting and reviewing papers. PPI mixture of research-naive and ‘professional lay people’. PPI work more widely than just the panel – work with primary care research network. Some of the PPI representatives do have samples in the biobank (therefore participants as well).
Stages: involved at the beginning at proposal stage, sometimes PIS.
Recruitment of PPI: diabetes mellitus research network, county shows, shop staff, researchers go out to recruit.
Members decide which researchers should have access to database. Some members also from diabetes mellitus research network.
Normalisation Process TheoryCoherence: new way of working for CI (was a tick box previously). Panel running some time (PPI now formal), previously PPI more ad hoc. PPI representatives had not realised how powerful PPI could be before being involved (changing the way studies go, outcomes relevant to patients). Researcher and PPI representatives seem to be in agreement about the purpose of PPI and the value of it. PPI to help other people, intellectual stimulation.
Participation: PPI representatives have sense of ownership. PPI representatives write articles for newsletters and magazines encouraging people to take part in the research. CI committed to PPI and is the main contact. All feel it should be part of their work. The CI uses the database budget to fund PPI.
Collective action: workload is manageable. PPI representatives know what they have to do, including commenting on proposals, PIS and consent forms; ensuring more accessibility to lay people. Direct feedback in the meetings, for example intervention is too onerous for people, information from own experience and own health background. The panel votes on whether or not they think proposed research is a good use of the database and samples. PPI representatives feel welcomed, communication is good. CI says group has to be managed well. CI would like to offer the panel some training in the future (governance processes and ethics). PPI representatives feel supported.
Reflexive monitoring: PPI representatives feel valued. PPI representatives suggested a toolkit for when you start on a project (time commitment, travel expenses for different research networks). Feedback all the time – PPI representatives know what happens after the meeting – whether proposals are approved or not.
Radar plots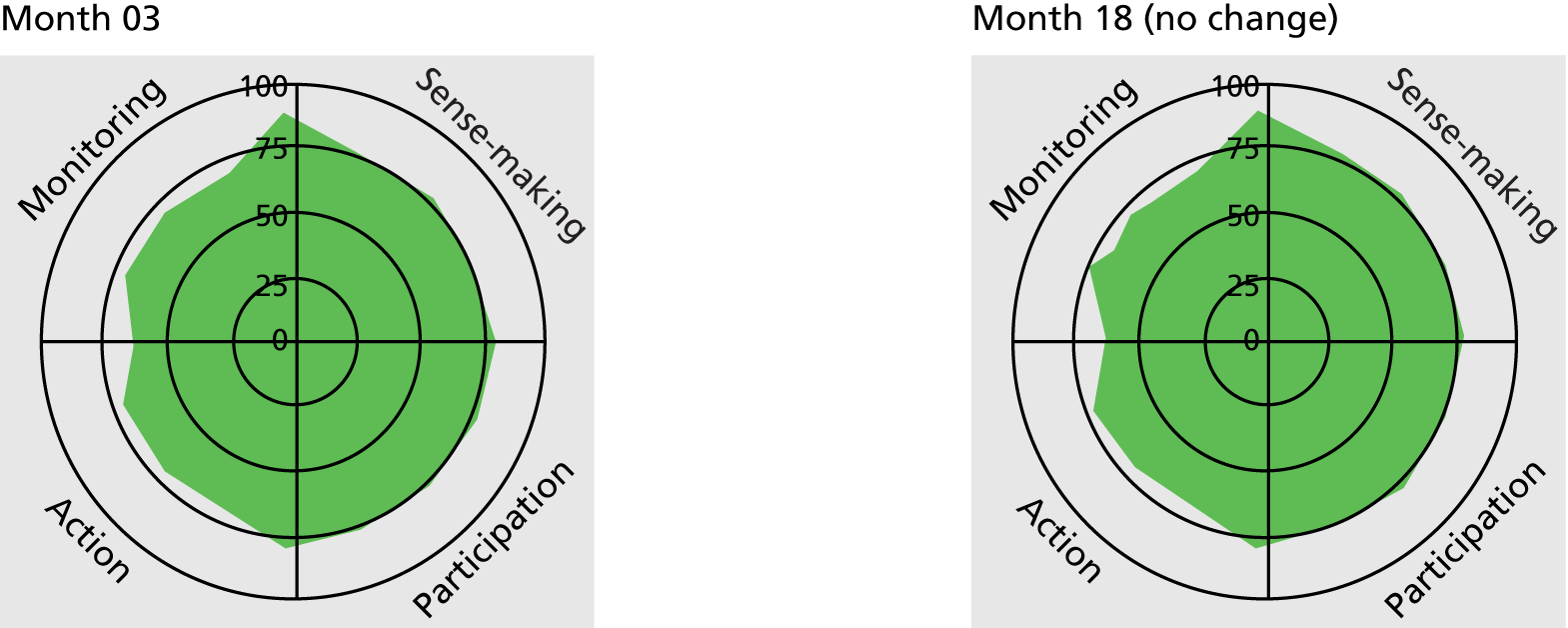
Research priority setting: PPI representatives decide on which researchers have access to database/biobank.
Ethics: PPI adds strength to ethics committee submissions.
Recruitment: PPI representatives involved in writing articles to involve patients. PPI representatives tell friends about a new study. Research more patient friendly (PIS).
Outcomes for PPI: PPI provides intellectual stimulation; socially, meet like-minded people.
Levels of involvement
Beyond stages of research, respondents identified themselves as working at different ‘levels’ or degrees of consultation and collaboration. Rather than being polarised, these approaches could be used interchangeably throughout the project:
I mean research is knocking a billiard ball gently down a table to the other end and the role of the public bit is to just have to influence and push it to the left, push it to the right, give the researchers, oh it’s difficult to describe, isn’t it? Because it’s not, I understand entirely it’s not complete consultation and on some occasions it’s taken seriously. I think, put it this way, to keep the researchers in touch.
CS03PPI02-01
To me, I mean, I think there are different levels at which you can involve people through the standard three levels. I mean, to me, we like to work with people as collaboratively as possible. I realise there is a role for consultative involvement in research but, for me, it’s being able to work in partnership really with members of the public to help design and to have ideas for research really.
CS21Res02-01
Although none of our case studies was user-led, as described in the previous section some did have lay representatives as coapplicants or co-researchers (CS04, CS19, CS21 and CS23), although levels of involvement also varied. Although CS17 (see previous section) did involve lay representatives at all stages, researchers also raised as an issue the move towards lay representatives as coapplicants. There were concerns that this was becoming the ‘gold-standard’ of PPI and people questioned if all study designs are suited to having PPI representatives as coapplicants:
it is difficult to have coapplicants on the kind of research we do, because of the nature of it, you know, if a member of the public came up and said I think you should compare the level of HbA1C [glycated haemoglobin] compared to glucose, they wouldn’t be a member of the public, they would be a scientist, to even know what the question was . . . because I think there is the idea that being coapplicants, and making videos is a measure of doing good PPI.
CS17Res01-04
Nevertheless, some felt that funding was more likely with a PPI representative as coapplicant; but this was not confirmed by any of our funder respondents. However, there was clearly a lack of reflection on whether or not having lay coapplicants made any particular impact on the research process and outcomes.
Reflection, appraisal and evaluation
Only two of the case studies provided any evidence of systematically appraising the PPI contribution to their study. However, funders’ requirements (C1) for an evaluation of PPI in the final report were beginning to have an influence, but any evaluative work was less commonly a collaborative endeavour for a research team. In contrast, host organisations (C7) that had embedded PPI infrastructures were more likely to evaluate and fine-tune PPI processes in a collaborative way. Having developed over time, embedded PPI infrastructures also enabled positive relationships (C5) in which researchers and lay members could reflect honestly on what and what had not worked well. Table 17 illustrates the CMO configuration for this action.
| Salient CS action | Potential contexts | Plausible mechanisms | Potential outcomes | Case study exemplars |
|---|---|---|---|---|
| Researchers and lay reps participate in ongoing reflections and evaluate PPI in order to improve quality of PPI processes and outcomes | Funder requirements (C1) for an evaluation of PPI within a study’s ongoing and final report had some influence, but were rarely articulated as a collaborative activity. A more enabling context was the host organisation (C7), with some case studies benefiting from a PPI infrastructure that sought collaborative evaluation and fine-tuning of PPI processes. The organisation of PPI (C6) also had an influence: long-established panels were more likely to be involved in evaluative processes. Collaborative evaluation also required positive relationships (C5), in which people felt able to share honestly what had and what had not worked so well | The mechanisms associated with reflexive monitoring were central here: systematically assessing information about PPI (M13), individual and collective appraisal of PPI (M14, M15) and fine-tuning of PPI work (M16). In addition, there needed to be trust (M10) between all parties for honest evaluation | Moral:
|
CS03 (see Box 10) |
| CS13 (see Box 16) | ||||
| CS17 (see Box 23) | ||||
| CS21 (see Box 6) |
Systematic appraisal of patient and public involvement
Of the two case studies with systematic appraisal, CS13 (see Box 16) had an annual evaluation, with a review of the PPI contribution and model at the panel annual general meeting. The researcher co-ordinating PPI ‘measures’ the extent of PPI against published best practice guides to assess if PPI can be of use in further phases of the research:
The NIHR, five or six points in the research cycle in which people should be involved, I’ve always bought into that notion, so we try and use that as a template for judging how we’re doing internally.
CS13Res05-01
Case study 21 provided the RAPPORT study with numerous documents which recorded PPI activities and impact but currently did not formally evaluate PPI. However, the case study site was actively involved in piloting an evaluative framework for PPI with clear intentions to change its PPI practices in future to include systematic appraisal.
However, researchers often did not have the time or resources to record PPI activities and reflect on PPI input, and some did not see it as something they should be doing. Respondents from CS06 (Box 24) saw PPI as an implicit part of the research process and hence not requiring discrete evaluation:
Hybrid model consisting of one-off events for less experienced PPI, and an advisory group including a more experienced PPI with more commitment/ongoing responsibility required. Member of the general public. Three development focus groups (approximately 60 people) held with participants from earlier pilot.
One PPI focus group (nine people) to look at project participant paperwork, before ethics committee approval.
One PPI member on advisory group from local community voluntary service.
Chief investigator also got feedback on dissemination materials from three older people: one trial participant and relatives of researcher.
Stages: in all stages, apart from data collection/analysis.
Recruitment of PPI: participants in pilot study and local (recommended) voluntary representative.
Normalisation Process TheoryCoherence: CI less experienced at using PPI, so takes steer from highly experienced coapplicant (has a deep working knowledge of PPI in this field and at HEI, where PPI is strongly embedded). Other research team members see PPI as closely linked to trial participation. PPI representative on advisory group sees PPI in wider context of community voluntary service participation in service/policy consultation.
Cognitive participation: all research team very keen, PPI members in focus groups strongly perceived to have been very keen too – there was a waiting list.
Collective action: coapplicant is highly attuned to power dynamics of PPI. Research team employ their different professional skills/relationships with PPI to good effect. Previous/ongoing relationship of research nurse with PPI (part of GP practice) highly significant. Providing food/refreshments significant in light of no payment. PPI representative on advisory group has a lot of trust in team and their professionalism. Pacing of implementation focus group was perhaps too intense according to CI. No training offered or requested.
Reflexive monitoring: clear contributions systematically recorded, with implications, but changes not necessarily fed back to those involved in focus groups. PPI representative on advisory group sees the endeavour of PPI as intrinsic to research.
Radar plots
Marketing the study: changed project logo and images used on PISs.
Design of study: participants on previous (pilot) study ‘came up with’ study design for this RCT.
Design of intervention: refined participant intervention – time taken to complete, better tailored to older ‘healthy volunteers’.
Recruitment: changed language used to identify participants, not ‘seniors’ or ‘elderly’ but age range. Clarity of invitation letters, PIS, trial handbook improved. Include images of older people from different ethnic groups and both single and couples, and specify exactly what the intervention group and control group did in the trial.
I wouldn’t say it has added value, I think it’s actually fundamental to, to the research inquiry . . . it’s not just added value, it’s intrinsic to the inquiry.
CS06PPI01-01
However, as the NPT radar plots illustrate (bold box), although there was no systematic evaluation of PPI, respondents did individually appraise PPI as worthwhile in the study.
Other researchers struggled to evaluate PPI because there was little guidance or knowledge on how to carry out this task and recognised: ‘it’s quite hard to evaluate I would have thought’ (CS08Res01-02). Despite the lack of systematic evaluation, some research projects did record PPI activities, providing a baseline to document PPI input.
For some researchers a lack of robust evidence on the value of PPI was a problem. In CS10 (Box 25) it was explicitly recognised that what was seen as ‘worthwhile’ by the general public might not be seen in the same way by researchers:
Experts by experience, using a ‘consultation’ approach.
Two PPI representatives on trial steering committee (one could not attend meetings and did not comment on materials).
One PPI representative (ex-smoker) gave one-off feedback on intervention booklets.
Local PPI patient involvement group provided (one-off) feedback on PIS, for further linked qualitative study. PPI co-ordinator attached to this patient involvement group, little input.
New PPI representatives 2013: one person to take on the trial steering committee role (replacement) and another interested in the qualitative study (both have academic backgrounds).
Stages: development and developing study materials, refining intervention and on committee.
Recruitment of PPI: local PPI group and CI recruited other ‘lay’ representative. Mixture of smokers and ex-smokers.
Normalisation Process TheoryCoherence: research team less clear on purpose of PPI in this project, or its potential further application. PPI contribution as mostly collaborating to redesign booklets and giving feedback on additional qualitative study bid. PPI representative recruited by CI was not aware of PPI as a broader ‘movement’.
Cognitive participation: CI less experienced in using PPI and not clear on validity of PPI, especially when recruited via PPI networks. Researchers: normal practice to them; see the PPI in this study as relatively straightforward, unproblematic. PPI representatives have mixed views on the value of PPI in this study.
Collective action: researchers understand the importance of PPI in tailoring process to suit volunteers, although they question costs associated with local PPI group model. Secretarial aspects of checking project materials for clarity suited PPI representative but less confident about commenting on research design (although has had training). Lay PPI representative happy to help, would have done it for free (convenient, interesting, local).
Reflexive monitoring: CI and lay PPI question the contribution PPI actually has to project. Very little supporting documentary evidence, not clear what specific changes PPI made to intervention booklets or PIS for qualitative study. No PPI in minutes from first two committee meetings (did not attend or send comments), in final committee no comments attributed to new PPI person. PPI rep. feels they made a minor contribution.
Radar plots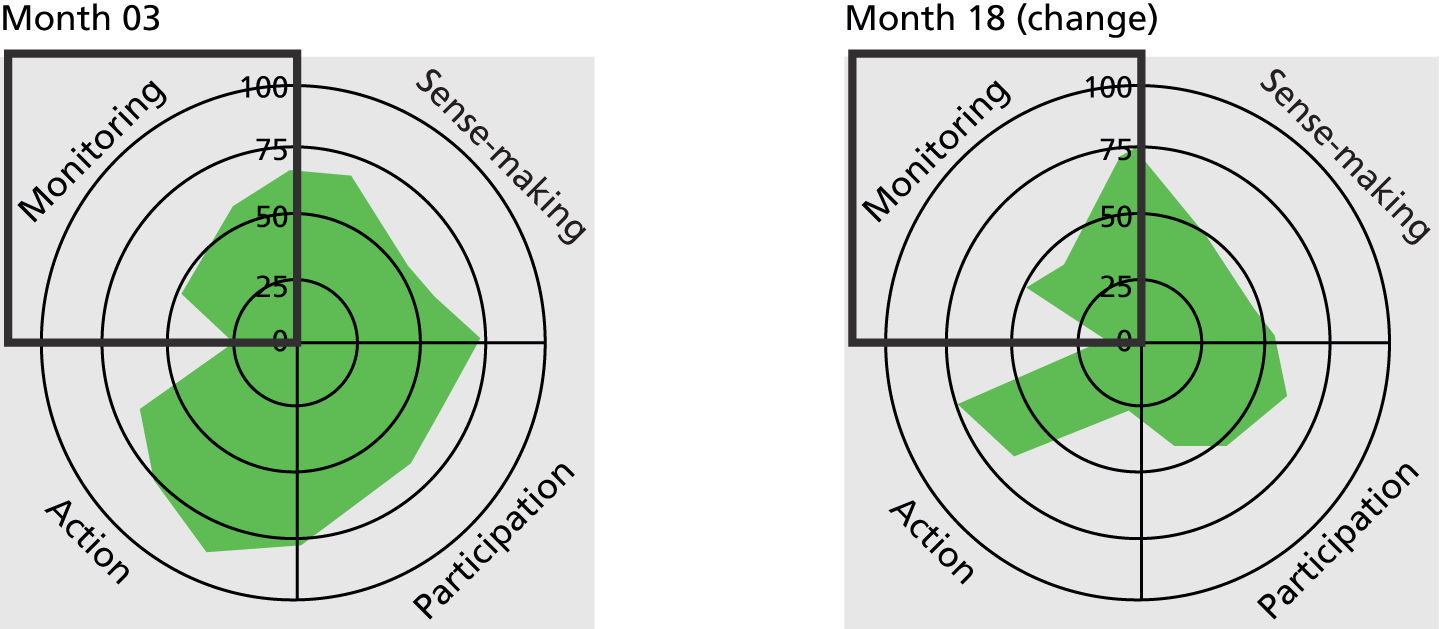
Design of study: PPI representative on trial steering committee (along with other local panel members) provided timely feedback on lay summary for additional qualitative bid. Two new PPI members have input into the interview topic guide.
Intervention: refine self-help booklets – better tailored to population targeted. Clarity of PIS improved.
especially not to researchers. To people outside the world of research, I can reason very happily [on the value of PPI]. But researchers want evidence and that’s the holy grail, and I haven’t seen it yet.
CS10Res04-01
The rather mixed view on the value of PPI within CS10 can be seen in the radar plot in the case study summary. Within the tracking radar plot, the impact of questioning the value of the PPI in this study is marked.
Enabling contexts for evaluating patient and public involvement
Funders’ requirements (C1) were a strong enabling context for evaluation. For example, the requirement to report on PPI when NIHR-funded projects were completed was a major incentive for researchers to review processes and benefits of PPI in the project. Indeed, some case studies agreed to be part of the RAPPORT study as an aid to meet this requirement. However, approaches to evaluating the outcomes and impact of PPI were shaped by the funding organisation’s stance towards PPI. The data from the programme management organisations strongly resonated with the methodological argument for PPI; hence, the organisations were actively seeking ways of evaluating the impact of PPI on research outcomes. Approaches cited, however systematic, seemed descriptive and biased towards ‘good news’: the collection of illustrative case studies and the specific identification of PPI in the final research report, as described below.
I ask that all the monitoring programme managers, if they spot something really interesting or good or unusual or positive, that they just let me know. And then I keep a spreadsheet of all of those for posterity, for, you know, when I start doing, we’re doing a lot of work on impact here . . . we’ll have more ability to really get in and look at good examples of PPI.
Funder04
There was evidence that this focus on evaluation, although not fully assessing and comparing impact, was resulting in some modification to the funder’s PPI work, for example developing advice to support lay representatives on trial steering committees.
For the funding organisations framing PPI more in the engagement paradigm, evaluation was focused on the impact of public engagement activities, and a web-based tool was used for researchers to record their public engagement activities and outcomes. For the condition-specific medical charities, again perhaps shaped by their moral stance on PPI, there was anecdotal evidence of where PPI has had an observable impact: ‘I think that they [grant applicants] have an increased awareness of the fact that they have to write a good lay summary’ (Funder01). However, there was no systematic appraisal of this.
For lay representatives, a positive appraisal of PPI was shaped not only by a positive experience (C8), but also by personal outcomes. Described further later, these outcomes included increased understanding of their health condition:
I read some of the interviews from other patients . . . it really helped me because personally . . . reading about how people are suffering from it and I’m not the only one, other people are also going through the same sort of problems, yeah. So some people do get better, people still live a happy life.
CS18PPI02-01
For others it was a sense of giving something back to the health-care system:
I then felt well if I can do anything, you know for the greater good, I was happy to do it and so I get out of it the feeling I’m making a contribution towards the research and the further development of treatment for patients with rheumatoid.
CS14PPI01-01
A number of researchers also felt PPI was worthwhile to them personally beyond impact just on the research process and outcomes. Researchers spoke of PPI bringing them closer to patients or service users, and reminding the researcher about the real aim of the research:
remind you a bit why you’re doing it because sitting in front of a load of numbers you sort of think, you know you’re doing it for those people. Because that’s the population you’re working with.
CS13Res01-01
A positive experience of PPI was often the start of the process to establish PPI as normal practice:
she’s really been the one that’s been my epiphany for understanding patient involvement more than anyone.
CS08Res01-01
Equally, a negative experience of PPI could hold up this process for some time:
I did an informal questionnaire amongst patients who we saw in the secondary care clinic, research patients, asking them to identify, you know, suitable research topics. However, I didn’t find it was very useful, patients mainly said that research should be concentrating on identifying a cure for diabetes, and that’s not completely helpful as that’s like a very long-term goal in research . . . then that sort of coloured my views of PPI for a little while afterwards thinking, hmm, I’m not sure really what patients want to get out of it or whether they have enough knowledge about the research process and personnel involved to be able to contribute effectively.
CS02Res02-01
Modifying future work
The majority of the case studies reflected on their PPI approaches only informally towards the end of the study, so there was minimal evidence of any changes within actual case studies. However, in a longitudinal cohort study (CS14) there was also evidence that being a case study within the RAPPORT study provided the opportunity for participants to reflect on PPI and plan things differently for the future:
you’re making me think [interviewer], maybe I should do a little leaflet to send out to show them all what we are doing with their information. So as I’ve been talking to you that’s something I will be doing differently and I’ll bring it up at the meeting that we should be sending them an update or feedback.
CS14Res03-03
This case study (Box 26) was supported by minimal PPI infrastructure but the impact of reflection can be seen in the tracking radar plots (bold box).
Hybrid: national representative, local service user group and expert by experience. However, these components did not come together and hence there was no cross-fertilisation. The national representative has advised nationally (multicentre) but the other lay representatives are just asked to be involved when needed, for example in the training of research nurses.
Recruitment of PPI: the national representative was formally recruited but the service user reps and expert patient were invited as CI’s patients. Service users also undertook dual role as study participants.
Age of study: started well before PPI in research movement, so rather ad hoc.
Normalisation Process TheoryCoherence: Less evidence of a shared understanding of the purpose and definition of PPI.
Participation: different levels of buy-in and some hesitation over recruiting PPI representatives who do not just talk to a personal agenda.
Collective action: relationship key and is underpinned by a long-term clinician–patient relationship. The national representative is finding the workload of being involved in a number of studies challenging. The lack of reimbursement of their time is a problem and has consequences for the national charity. Limited PPI infrastructure means ad hoc approaches. Blurring of PPI in service delivery and PPI in research.
Reflexive monitoring: more how it has impacted on research process rather than outcome. Lots of personal benefit for PPI representatives. Using a service user group was seen as having benefits but may require a different way of working in the future.
Radar plots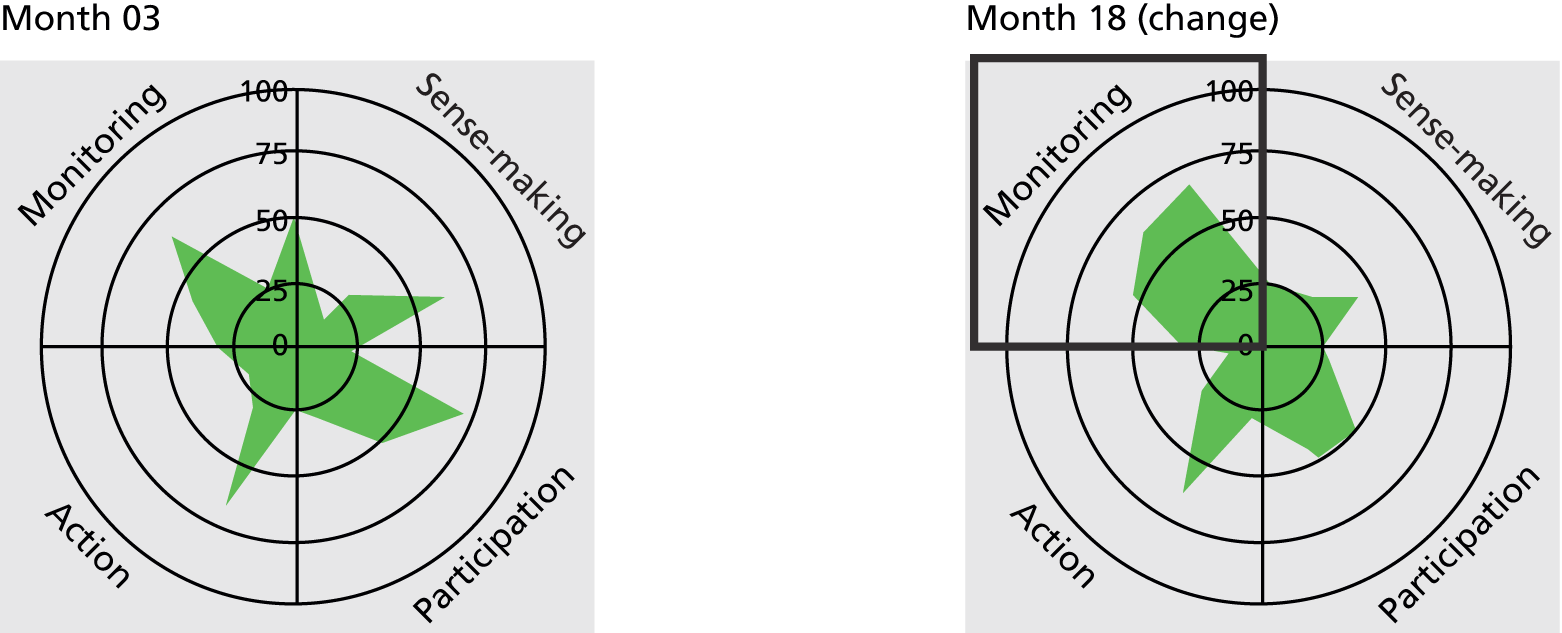
Design of study: PPI representative on trial steering committee (along with other local panel members) provided timely feedback on lay summary for additional qualitative bid. Two new PPI members have input into the interview topic guide.
Intervention: refine self-help booklets – better tailored to population targeted. Clarity of PIS improved.
For the majority of case studies, either modifications to PPI approaches would be operationalised in future studies, or the influence of that particular case study was affecting PPI approaches within other studies:
What is great now, lots and lots of studies are coming through . . . other departments who weren’t doing any PPI or patients, it is forcing them, I have access to a group of volunteers, pre-screened; you need to do PPI to get them! . . . we are getting sport scientists, oncologist, all sorts of people; the meetings are becoming more and more interesting . . . now the meeting [panel] has such a wide diversity of studies that are being discussed.
CS17Res01-03
Hence, while the CS17 (see Box 23) tracking radar plot showed minimal change in the reflexive monitoring segment, if expanded to the research environment in which it was hosted then a far more significant change could be noted.
Nevertheless, extensive future changes to PPI approaches could be inhibited by a lack of understanding of what is possible, as exemplified by CS09 (Box 27):
Two national representatives of two different support groups. Both PPI representatives sit on project advisory group; one of them carries out much of the qualitative analysis.
Normalisation Process TheoryCoherence: PPI representatives have seen an increase in PPI activity over the years. PPI rep. believes formal structures for PPI are a good thing. PPI believed to be important, valuable and worthwhile. Agreement among PPI representatives and researchers. PPI representatives feel listened to and not just because they have to have PPI.
Participation: can make medical ideas understandable for users; PPI is extra work but not a negative. Researchers will definitely use PPI in future (and one PPI representative is now a coapplicant on next grant).
Collective action: PPI representatives are confident to put views across, PPI representative doing qualitative analysis (skills), other PPI representative commenting on main themes (sees her lack of research skills as advantage), reassurance for researcher in a sensitive topic. One PPI representative and researcher know each other personally.
Reflexive monitoring: talk of track changes to documents but back copies not routinely collated. PPI representative has led on documents and views taken on board. Suggests a PPI mentor for less experienced PPI representatives. Research paper changed because of comments made by PPI representative. Researcher would like to work with individual women also but not sure how to go about it, unless through the charity.
Radar plots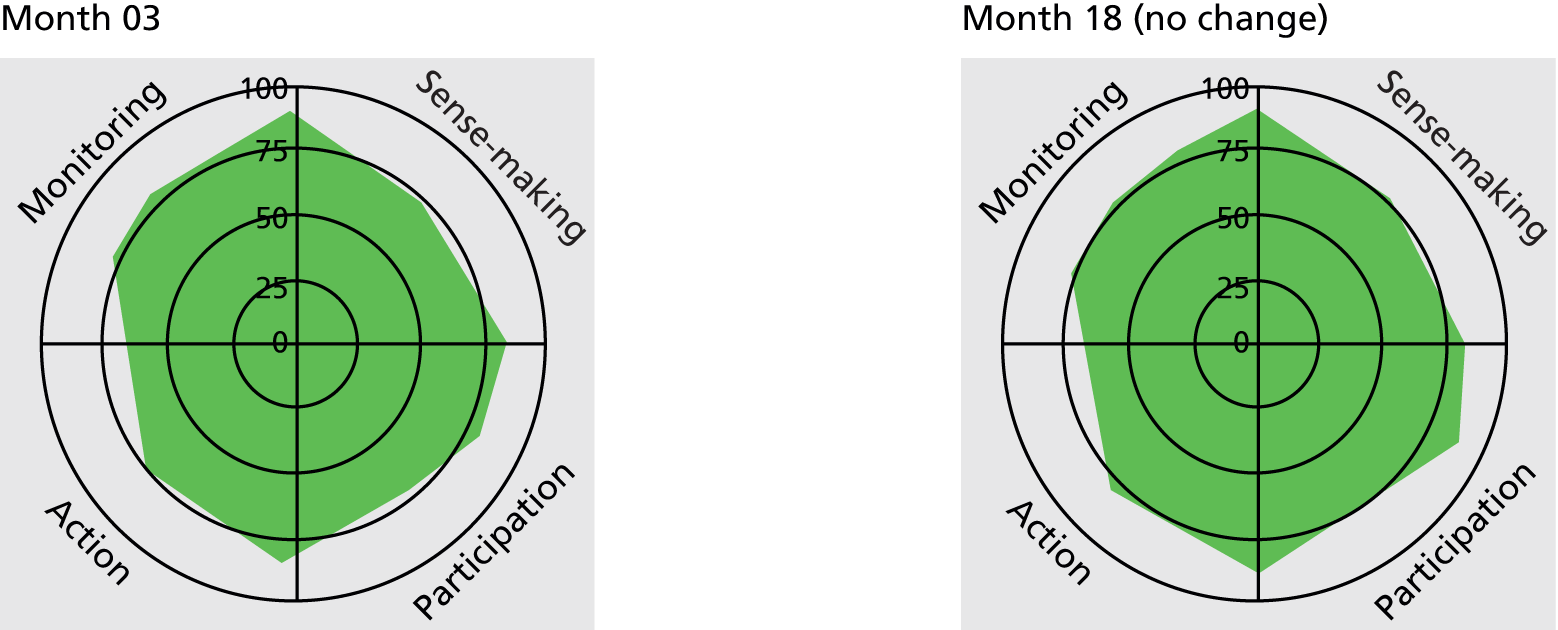
Design of study: PPI representative on trial steering committee (along with other local panel members) provided timely feedback on lay summary for additional qualitative bid. Two new PPI members have input into the interview topic guide.
Intervention: refine self-help booklets – better tailored to population targeted. Clarity of PIS improved.
I don’t know how you go about involving patient and public in planning research, that maybe sounds a bit silly; in my mind I have a big question mark about how it works: before you recruit anyone to the study you need ethical approval, and to me asking patients potentially what they want research to entail, is in a way recruiting them to a mini study before the main study.
CS09Res02-01
While the radar plots indicate a comparatively embedded level of PPI, future potential impact of PPI is constrained by researchers’ beliefs. This reinforces findings presented earlier where potential PPI impact was inhibited by boundaries set by the research team.
Impact and outcomes of patient and public involvement
As presented in each CMO configuration, case study actions led to a number of methodological and moral impacts and outcomes. This section draws on the interview and documentary data to provide evidence of the methodological impacts and outcomes of PPI within the case studies. Here we define impact as the immediate effects of PPI, which may be intended as part of the objective for PPI within each study, or unintended. Outcomes are longer-term effects of PPI in relation to the overall goal for PPI in each study. 160 Eight of the 22 case studies concluded during the RAPPORT data collection period, so participants could provide summative assessments of the impact and also possible longer-term outcomes of PPI. However, it should be recognised that there are likely to be longer-term outcomes of studies that were not possible to capture within the time scale of the RAPPORT study.
Impact and/or outcomes were described within 13 stages of the research cycle/process and there were a range of topic areas with evidence of impact and outcomes (Table 18). The following section provides evidence of PPI methodological impact and outcomes with specific examples from the 22 case studies. Impact and outcomes are applicable only to certain research designs and, of course, are a function of the original PPI objectives and overall goal.
| Stage of involvement | Number of studies reporting impact/outcomes by topic area | ||||||
|---|---|---|---|---|---|---|---|
| Ar | De | Di | IDD | PH | CF | Total | |
| Research priority setting | 1 | 0 | 3 | 0 | 1 | 0 | 5 |
| Identifying research questions | 1 | 0 | 0 | 1 | 0 | 0 | 2 |
| Linking to the wider community | 1 | 0 | 2 | 1 | 0 | 0 | 4 |
| Recruitment of research staff | 0 | 0 | 0 | 1 | 0 | 0 | 1 |
| Marketing the study | 0 | 0 | 0 | 0 | 2 | 0 | 2 |
| Study design | 1 | 1 | 6 | 1 | 4 | 0 | 13 |
| Study safety | 0 | 0 | 1 | 0 | 0 | 0 | 1 |
| Intervention design | 0 | 0 | 2 | 1 | 4 | 0 | 7 |
| Ethics submission | 0 | 0 | 2 | 0 | 0 | 0 | 2 |
| Recruitment (documents and direct recruitment) | 2 | 2 | 8 | 2 | 3 | 1 | 18 |
| Standardising outcome measures | 1 | 0 | 1 | 1 | 1 | 0 | 4 |
| Data collection/analysis | 1 | 0 | 1 | 1 | 0 | 0 | 3 |
| Dissemination | 1 | 0 | 4 | 1 | 1 | 0 | 7 |
Research priority and question setting
Five of the case studies reported that PPI representatives had been involved in research priority setting. For example, the panel in CS17 had input into deciding which research should be funded, although we received no documentary evidence to show the impact on decision-making. We were provided evidence of PPI impact in identifying research questions. For example, the research centre hosting CS21 has a large PPI group who are encouraged to put forward research questions, and this particular case study originated from one of the parents. The structure of the research centre and the priority that this organisation gives to PPI ensure that the ideas relevant to service users are carried out:
Because the very idea of the whole thing came from a parent, it’s been a very natural process to have families involved in it all of the time, and I think that’s the beauty of getting the idea from the family. You don’t have to then try and shoehorn PPI in, it’s already there. So, it’s just been from the word go.
CS21Res01-01
Linking to the wider community
Four case studies utilised PPI to provide links to the wider community. Case study 02 exemplified this approach, with the single lay representative on the steering committee consulting with wider range of people from the study target population. A newsletter to this group provides evidence of the impact of this approach (Box 28).
[Patient organisation] members recommended changes to the draft proposal and these were incorporated into the final version and into the current protocol. The suggestions included:
-
the type of quality of life questionnaires given to patients to complete;
-
the option that follow-up visits can also be conducted at the patient’s home;
-
the assurance that as far as possible the same researcher will carry out all assessments for home visits to ensure continuity of care;
-
and the request for additional laboratory safety tests midway during the study.
In CS23, this PPI bridging role to the wider population (in this case younger people) was done via social media and was an effective way of getting one-off input from an often less-heard group. This input was used as a basis for a practice-focused article and also informed the development of the study (Box 29).
. . . what apps and websites are YPD [young people with diabetes] using? In order to review the use of apps and other online resources by YPDs, one of the authors (PPI rep.) discussed the use of apps with her followers on Twitter and friends on Facebook, asking three questions. 1. What apps/sites do you use in relation to your diabetes? 2. What do you like about apps/sites and what don’t you like? 3. If your DSN [diabetes specialist nurse] needs to know one thing about diabetes apps/sites what is it? At least 30 respondents posted responses.
Lay representatives were also used as a link to recruit study participants. Examples included writing articles for newsletters to encourage participants to take part, being filmed as part of the recruitment video, using social media or approaching people directly through their networks (support groups).
Such connections with other groups of members of the public or service users proved to be valuable in recruitment, and in harnessing a wider range of (less accessible) PPI representatives/experiences, reassuring researchers who were concerned about the PPI representatives not being a ‘typical’ lay person.
Marketing the study
Two of the studies had PPI input regarding study logos, and in the first study the logo was changed (Box 30).
There was a lot of discussion about the photographs used. They preferred the picture of the couple walking in the wood, as this looked active and upbeat. However, they felt that there was also value in the older woman with a walking stick, as there would be patients recruited who used walking sticks and this might appeal to them. They suggested having the picture of the couple on the front and the older woman with a walking stick and possibly a similar one of an older man walking on his own, on the back of the leaflet.
Action taken: We will stick to the idea of giving out the leaflet when participants come to see the research assistant. We will use the picture of the couple on the front of the leaflet and the older woman with the stick and a picture of an older man on the back of the leaflet.
However, in CS19 PPI advice was not taken on board, as the logo had been already commissioned and developed by the team (and PPI coapplicant), but it was later criticised as being potentially insensitive by steering group PPI representatives:
it was about their logo [. . .] I just hated it on sight, and their response to that was, ‘But we paid someone to do it and . . . maybe . . . [other] people wouldn’t feel like that.’
CS19PPI02
Design of study
Patient and public involvement representatives made comments on the protocol and design of the study in 13 of the case studies, particularly regarding lay summaries, data collection instruments and study information (Box 31). In other case studies PPI representatives were consulted over study design; for example, they were asked whether a RCT or partial randomised control design should be used, and PPI representatives’ suggestion of a RCT design (CS07) was accepted. In another case study the PPI representatives were asked if they approved of particular methods of accessing patients’ notes (CS01). Data collection tools such as questionnaires were ‘softened’ by PPI representatives in terms of language and sensitivity (CS09, CS21).
It was suggested at the last meeting that the third health-check webpage is too heavy on text and if the big paragraphs could be reduced with the option to expand if someone is interested in reading more information. The ‘read more’ function is tricky technically. [XX] has adjusted image and text so it fits better.
Safety of study
Involving patients’ groups in the governance of a study had evidence of potentially improving patient safety. In the original proposal of CS02, the researcher conceded that the research study was presented in a very clinical fashion and, because it was asking people to reduce the amount of a particular drug that they were taking, the safety element (from the patient’s point of view) had not been considered. PPI views (through a national charity panel) changed the application to include a safety questionnaire:
when I put together the original application, it didn’t really have much in terms of the safety element because I had taken it for granted that people are already on [x drug], reducing the dose wouldn’t make a big difference and I would have seen it in a clinical fashion, but as soon as we got the patients on board and had their comments coming through, one of the things that seemed to be coming through was a concern, or a potential concern from the patients that would it make them feel unwell or would it do anything to them? So therefore we then added an extra element asking patients about how they felt, safety questionnaires.
CS02Res01-01
The outcome of PPI here was reassurance for patients in terms of safety and also improved recruitment rates, and a 3-month visit (for reassurance) was added to the study design for participants.
Design of intervention
In those studies which contained an intervention as part of their study design, PPI representatives helped to design or make suggestions to existing interventions to make them more acceptable/feasible. In CS03 one PPI representative suggested there should be more content on pre-pregnancy and diabetes mellitus, and the documentation confirmed that more was added into the resource intervention (Box 32).
I fully understand that you don’t want to go into the complexities of pregnancy with diabetes but I feel more is needed to inform women of the importance of pre-pregnancy planning and quick action once they suspect they are pregnant. Asian and Afro-Caribbean women are developing Type 2 at younger ages than the general population and also the increase in obesity is likely to see an increase in younger women with type 2 . . . [She goes on to explain about her personal experience of pregnancy and diabetes].
Action: to include more information pre-pregnancy.
When the intervention was a questionnaire (CS04, CS07) the questionnaire was altered to include items not previously considered by the researcher:
I’m sort of embarrassed to admit it, but I went to that meeting thinking, ‘I know everything that should go in this questionnaire’, but I so didn’t, and loads of stuff came out in that meeting that I just never would have thought of.
CS04Res01-01
In another case study (CS07) PPI representatives were involved in the validation of 260 pre- and post-questionnaires (which were used as part of the intervention). The PPI representatives took the questionnaire back to their local user groups and asked them to complete the questionnaire as a pilot. However, there was also evidence that researchers perceived an unintended outcome of PPI. In CS23 the CI (who was also a clinician) felt that the PPI representatives had steered the project off course, and that the interventions developed were neither innovative nor adequately focused on the research question.
Research ethics submission
Two of the case studies felt that having PPI helped their ethics submission by saying that materials had been viewed and approved by PPI representatives:
they [research ethics committee] take note it, of course the committees have their own lay people and I mean the one thing about lay people is they’re individuals like all of us, it’s a bit like a peer review and you might get lay members of the panel who don’t really agree but they take note of it and I think it carries quite a bit of weight, doesn’t always carry the day though.
CS01Res02-01
Recruitment
One of the most frequently stated outcomes for PPI in our case studies was a perceived increase in recruitment rates to the research study (18 of the 22 case studies). Researchers commonly attributed recruitment success to the PPI input to materials (suggestions on layout, size, language, colour, length, readability, clarity and design; evidenced by tracked changes/before and after versions of documents) used for recruitment (PIS, invitation letters, consent forms). Suggested changes were made either directly by the PPI representatives themselves or by taking materials back to wider reference groups for further comments; for example parents showing the PIS to their children. PPI representatives made changes to language such as taking out the word ‘mortality’ or explaining technical words such as ‘lung function’. They introduced a summary section at the start of the PIS and produced information in a small, credit card-sized, format for people to carry in their wallets. Changes also included images of actual people wearing equipment or lying on scanners, and extra information about the length of procedure and the weight and size of any equipment was added (CS13 PIS).
One researcher felt able to quantify the increase in recruitment because of such PPI changes. A number of different versions of the PIS and invitation letter had been submitted to ethics committees:
we changed a few things but we did [a] stage [at a] time so we could see what had an impact, and that certainly did increase recruitment by, only you know, 1 or 2%, but 1 or 2% when you’re sending out thousands a month . . .
CS12Res02-01
Outcome measures
Research teams advocated the use of PPI for outcome measures that were relevant to patients; this was particularly relevant to one arthritis study:
it was appreciated that there were certain things that we were measuring that we thought were really important, these patients actually weren’t interested in at all and didn’t deem relevant, whereas other issues we didn’t think were . . . well, we thought they were important, obviously, otherwise we wouldn’t measure them, but we didn’t realise how important they were to patients.
CS14Res01-01
There was qualifying evidence here that the outcome measures had been changed or added to in the research design. Respondents also reported that this change of emphasis was fed into clinical guidelines, which may have an impact on patient experience.
Data analysis and collection
Two studies had PPI representatives involved directly in data collection. The PPI representative in CS18 was involved in data analysis; she was asked because of her cultural knowledge and to reassure the researchers that the analysis resonated with her experience of the ethnic ‘community’:
I want to check with the community that I’m not sort of completely going way off track here so I guess in some ways that was her main role, more than in this situation the experience of living with the illness really, it was actually her cultural knowledge that was most helpful.
CS18Res01-01
In one case study where this PPI role could have been applicable but was not utilised (CS21), this was a deliberate restriction because of ethical considerations; many of the study participants would have been known to the PPI representatives.
Patient and public involvement representatives also made a contribution to data analysis (Box 33).
As you say, the difference in preference is interesting. What I could really do with – if you ever have five minutes – is for you just to talk me through one or two of the tables as I am rubbish at interpreting graphic info. And then you could also help me with understanding things like ‘conditional logit model’.
Was there any difference in responses from the [xxx] sample? I was just wondering whether they would value accuracy fairly highly as they were painfully aware . . .
The impact of this was clearly described by the researcher:
When I initially did a straight comparison women’s views versus health professional’s views, [PPI02] suggested I break down the women, into those that had experience with [xxx] or [xxxx], compared them to women who haven’t had any problem [xxxx] and we found quite big differences between the two groups.
CS09Res01-02
Dissemination
Two of the case studies (CS17 and CS21) mentioned that the PPI representatives had presented the study findings at conferences, and six examples of academic papers with PPI representatives as coauthors were submitted to the RAPPORT study. One of the PPI representatives, who was working as an academic researcher 3 days a week on the project, was first author of a paper (and her organisation was the charity mentioned in the paper). Other representatives were mentioned in the acknowledgements at the end of the paper. Some case studies in the RAPPORT study had not yet reached dissemination phases; however, our tracking interviews suggested that, in a number of cases where it had been planned that PPI representatives would be involved in dissemination, this had not happened.
Moral impact and outcomes
In addition to the outcomes which were identified in terms of the research project, the researchers and PPI representatives also identified personal outcomes associated with their PPI role. The personal benefits of PPI have been well documented, and those reported here echo previous studies. These included increased self-confidence and mental challenge. The PPI role helped people to keep mentally active in retirement or unemployment and provided the possibility of leading to other roles or responsibilities:
. . . enriches our research but also enriches their lives.
CS21Res01
. . . it just opens up a world of opportunities.
CS21PPI01
Interestingly, some PPI representatives spoke of the benefits of their involvement to the wider society: ‘maybe it’ll change the world a little bit’ (CS11PPI02-01). In CS03, the PPI representatives felt that they could pass back information to their wider network and again be ‘boundary spanners’ (which Williams161 describes as ‘individuals who have a dedicated job role or responsibility to work in collaborative environments’) between the academic world and the patient community:
I have met since my diagnosis other people who’ve had [condition] for many many years who haven’t necessarily had access to much information or they haven’t, or they have had access to information and services but it’s been a bit sporadic and I always wanted to kind of pass that information along or back to people that I’d met, so . . . I’ve kind of been a lay tutor.
CS03PPI04-01
Longer-term outcomes
The RAPPORT study was designed to include studies that concluded during our data collection period, with the expectation that outcomes of PPI could be summatively assessed. Among the eight that were completed, we found no evidence of any immediate outcomes of PPI for the research findings. However, out of these eight studies, five had demonstrated clear embedding of PPI and interestingly it was these studies that clearly identified the outcome as developing further grant applications, as more research was required. These five case studies were continuing to work with their lay representatives to generate further research questions. Out of the remaining three, one was in follow-up, we could find no evidence from the other two case studies of any particular outcome, and from a dissemination perspective there was nothing publicly accessible providing results or outcomes of the studies. It is clear that, as in all evaluation of research impact, longer-term outcomes influenced by PPI need an extensive time to detect.
Conclusion
Collective understanding about the purpose and role of PPI was an important mechanism leading to positive outcomes, and was enabled by training and certain topics and study designs. Values quite clearly shaped this understanding, and there was some questioning of whether or not PPI was appropriate in all study designs. Three main models of PPI were identified: a bounded, one-off model, an outreach model and a fully intertwined model. Even in research settings with minimal PPI infrastructure, there was clear evidence that establishing and maintaining relationships was crucial and required time. PPI as a dynamic process was significantly compromised when relationships broke down. It was also clear that a dual role (participant/involvee) was relatively common, and that an unintended consequence of the evolving national and regional PPI structure was an outsourcing of PPI, with associated researcher disengagement. These key areas will now be explored further in the discussion.
Chapter 7 Discussion
Within the scoping, survey and case studies we tested what contexts were required to enable the mechanisms informed by NPT to embed PPI in UK health research as normal practice. We have presented six CMO configurations detailing the NPT mechanisms, enabling contexts and outcomes of salient actions for PPI. These actions were focused on:
-
the purpose, role and structure of PPI
-
recruiting lay representatives likely to have an understanding of the diverse viewpoints of the target study population
-
engagement of the whole research team with PPI
-
mutual understanding and trust between researchers and lay representatives
-
opportunities for PPI in all parts of the research process
-
reflection, appraisal and evaluation of PPI.
This chapter discusses the implications of the findings, and explores in more depth those results which were unexpected. These include:
-
lack of transparency, publicly accessible information and ongoing evaluation of PPI
-
a lack of coherence in understanding and defining PPI
-
within the national research infrastructure, the nuanced shaping of PPI through values
-
frameworks and models of PPI
-
enabling contexts for PPI, in particular the importance of relationships
-
the impact of PPI.
How embedded is patient and public involvement within a national research infrastructure?
Despite the limitations of the survey, it did provide some evidence that the proportion of studies which included PPI has increased over recent years. Two surveys conducted in 2000162 and 2003163 attempted to quantitatively capture the extent of PPI in English health research. The survey by Telford et al. 162 of 66 NHS research and development leads had a 73% response rate but fewer than 25% reported any PPI in research activity within their respective NHS organisations. The survey by Barber et al. ,163 conducted 2 years later, comprised a randomly selected sample of 900 researchers from the National Research Register and had a response rate of 58%. This indicated even less PPI activity in research, with only 17% reporting PPI in their research studies. In comparison, our survey findings, with 79% of respondents reporting PPI in their research study, show a notable increase in the extent of PPI activity. This is unsurprising in the light of the flow of successive national policies aimed at increasing and embedding PPI in research. 1,5,6,164 Major research funders now expect to see details of PPI in their grant application and this was reflected in our results, where NIHR-funded studies (which require PPI details) were more likely to confirm the presence of PPI.
Despite these encouraging findings indicating that PPI in research is becoming more widespread in England, a number of limitations persist. A major finding from the scoping was the limited amount of publicly accessible information about PPI contained in research documents, despite PPI having become a requirement of many funding agencies. While the expectations of the funder were identified as a key influence on PPI within grant applications and study designs, not only was there a lack of transparency within documentation about how PPI would be operationalised, but there was equally a lack of follow-through. This reflected the overall low quality of reporting PPI in studies. 21 Paradoxically, while PPI processes may be articulated within grant applications, there is no corresponding documentation providing evidence of monitoring or how the PPI strategy within a study may have changed as the research developed. This contrasts starkly with the usual reporting of other amendments in study protocols, which routinely undergo rigorous and transparent external monitoring and research governance auditing.
Furthermore, some responses received in the scoping, survey and case studies indicated that, although the UK has one of the most extensive PPI research infrastructures in the world,165 there was evidence of a persisting lack of coherence in understanding and defining PPI.
Coherence: how was patient and public involvement understood?
Echoing the earlier survey of Barber et al. ,163 the RAPPORT survey findings suggested that some researchers still have difficulty in distinguishing between research participation and PPI activities. There was some evidence of this, albeit minimal, in the case studies. As described in the first two CMO tables, understanding PPI as a different way of working was needed particularly to enable a clear role, purpose and structure for PPI, and to ensure lay representatives were recruited who would have an understanding of the diverse viewpoints of the study population.
The respondents most likely to confuse these terms were those less involved in submitting grant applications, such as research assistants or research nurses. In the case of the latter, this may be caused by less uptake of research training. 166 Many of our senior researcher respondents were also unlikely to have received any formal preparation for PPI, but the actual process of submitting bids (particularly for NIHR funding applications) requires increasingly detailed descriptions of proposed PPI, potentially encouraging more clarity in defining PPI.
Engagement, feedback or involvement?
While confusion between participation and involvement still persists among some junior and indeed some senior staff, the boundaries between ‘engagement’ and ‘involvement’ were sometimes even less firmly defined. In differentiating between engagement and involvement, we draw on definitions offered by INVOLVE167 and National Voices168 which view involvement as a deliberative activity characterised in various two-way processes such as collaboration or partnership. Our findings suggested that, in a minority of case studies, simply providing feedback on, for example, the study results, despite being one-way information giving, was seen by some participants as active involvement.
A recent study exploring PPI in commissioning services for long-term conditions57 suggested a model of involvement as the product of engagement plus experience. Peckham et al. 57 defined engagement as a commitment to respond or interact. In terms of PPI in research this could mean the public attending dissemination sessions, reading research summaries or going to engagement events. One of our respondents from a funding organisation very clearly defined PPI in terms of this kind of engagement, discussed in more depth later in this chapter. Our PPI respondents’ experiences were varied and included public service, experience of a health condition as patient or carer and being a research participant.
If PPI is limited to engagement, this precludes the full potential of involvement. The model of partnership synergy proposed by Lasker et al. 105 illustrates the full potential of involvement where the sum of the whole (PPI and researcher working together) is greater than the sum of its parts. Synergistic collaboration leads to thinking that is comprehensive and holistic, creative, practical and transforming.
In one RAPPORT case study (CS10), a PPI representative was identified as such because he had the appropriate experience of the public health issue being researched, but not of prior engagement with the research process. His involvement in this study was limited to a one-off event and the data suggested he was unlikely to actively seek to be involved in any future studies.
The study of Peckham et al. 57 also identified the impact of failing to maintain a two-way interactive process, which leads to disengagement. Some of our PPI respondents reported feeling disengaged from projects because of long periods of silence, and, if results of studies were not fed back, disenchanted with research overall.
The dual role
While some researchers appear not to understand the differences between involvement, engagement and participation in research,167 there is also developmental evidence of some explicit merging of research participant and PPI roles, in which patients undertake a dual role as participants and also as lay representatives. With the current focus on increasing patient participation in research trials169,170 and given that involvement and participation are listed alongside each other in the NIHR’s aims for patient and public awareness of research, the time may now be appropriate to examine the potential advantages and implications of this dual role further. In particular, the ethical implications and the robustness of knowledge gained in this way need to be explored further.
We found little evidence within the literature of the dual role, and discussions at our dissemination events also suggested that this was seen as very unusual, if not ‘bad’ practice. However, Goodman et al. 171 describe the benefits of involving young people in a study on transport and health as advisors, co-researchers and study participants. While they acknowledge it is more in the research team’s interests to recruit study participants, there were notable outcomes for the same young people in acting as advisors: increasing self-worth and understanding of research, and having enjoyable work experiences. While aware of potential ethical issues, the authors describe a reciprocal win–win situation for the young people, schools and research team. Where managed carefully, such experience for both research teams and lay representatives was also evidenced in the RAPPORT study.
Patient and public involvement: is it always needed?
While the majority of our survey respondents and case studies did report having some form of PPI, they varied considerably in how many research stages and which levels of PPI activity this involved, with a few case studies showing PPI as entailing only minimal, one-off activity. Not everyone believed that PPI was essential to each stage of a study or was persuaded that benefits far outweighed potential risks, particularly for studies nearer the laboratory end of the ‘bench to bedside continuum’. 172 Arguments for seeing PPI as less essential or more risky included there being a lack of evidence of PPI effectiveness in this type of research. However, our analysis suggested that underpinning this assertion were several researcher beliefs, including that lay representatives would not be comfortable with the more basic science and that they lack the knowledge to understand it. A small number of researchers appeared to minimise the general ability and skills of PPI representatives to contribute to research. Some respondents, including a funder, had changed their view on this, and after initial surprise reported now seeing their lay representatives as being able to understand and offer more than originally envisaged. 27
Narratives also included researchers’ stories of lay representatives being seen as overstepping boundaries and dabbling in science. A few researchers perceived a threat of the lay person taking over, an anxiety reported in other studies. 28 The supposed menace of experiential, subjective knowledge overturning scientific notions of neutrality, objectivity and distance173 has been described in terms of a clash of two worlds. 130 However, McKevitt et al. ,16 in reflecting on PPI in a stroke research study, argue that the moral status of PPI balances out any asymmetry between these two worlds. Some of our case studies at the basic science end of the research continuum did bear out the sustainability of such a viewpoint, with researchers making great efforts to ensure active involvement.
In terms of amount of activities, PPI was most likely to be limited in basic science studies, where lay knowledge was generally seen by researchers as less useful in this kind of research. 39 Callard et al. 172 argue that failing to have PPI in the early stages of translational research may result in failing to capitalise on the potential contributions lay representatives could make, including ensuring that the end product of bench research must be appropriately designed for the end-user, and that ethical issues arising between any academic and commercial interests are challenged. The basic science studies in the RAPPORT study that did have a firm PPI underpinning adopted a partnership approach,105 even though at times this partnership came under strain, particularly over issues of who had more say in decisions about the use of data. Conflict or tension, while posing difficulties to resolve, is not necessarily undesirable and, indeed, is evidence of engagement,105,174 so much so that where it was managed well, through, for example, clear guidelines, dialogue and consensus, it was seen to add to the strength of the case study in terms of how embedded PPI was.
Values shaping patient and public involvement approaches
Two main stances, methodological and moral, appeared to shape the ways in which our respondents viewed and operationalised PPI. A third stance (policy) described in Chapter 2, was the initial trigger for many of the researchers and the centrally funded funders to engage with PPI. Analysis of the data from these respondents suggested three pathways (see Figures 9 and 10).
A frequently found narrative, illustrated in Figure 9, was of researchers ‘having to do’ PPI because of revised governance requirements. 5 However, this often shifted to a subsequent ‘conversion’ to PPI when they appraised outcomes of PPI as having had a benefit on the research outcomes. Policy was then no longer required as the main trigger, so PPI activity became a self-sustaining virtuous cycle. A variation found in this pathway, also demonstrated in our analysis, identified not only a ‘conversion’ in terms of the methodological benefits of PPI, but also a move towards the moral value set whereby PPI became a process that one should do because it is ‘right’. Of course, some respondents were embedded in this moral paradigm and their pathways can be depicted in Figure 10. In particular, the funder representatives from condition-specific charities articulated PPI as a moral imperative and, perhaps paradoxically, had given little to no thought to if and how their PPI strategies should be evaluated as appropriate or successful. In contrast, some case studies from the IDD topic area clearly presented a strongly coherent moral stance on PPI. However, as well as seeing PPI as a given, the approach taken by researchers from these case studies was an open one, actively seeking to explore ways of capturing the impact of PPI on their research outcomes.
FIGURE 9.
‘Virtuous cycle’ of PPI triggered by policy.
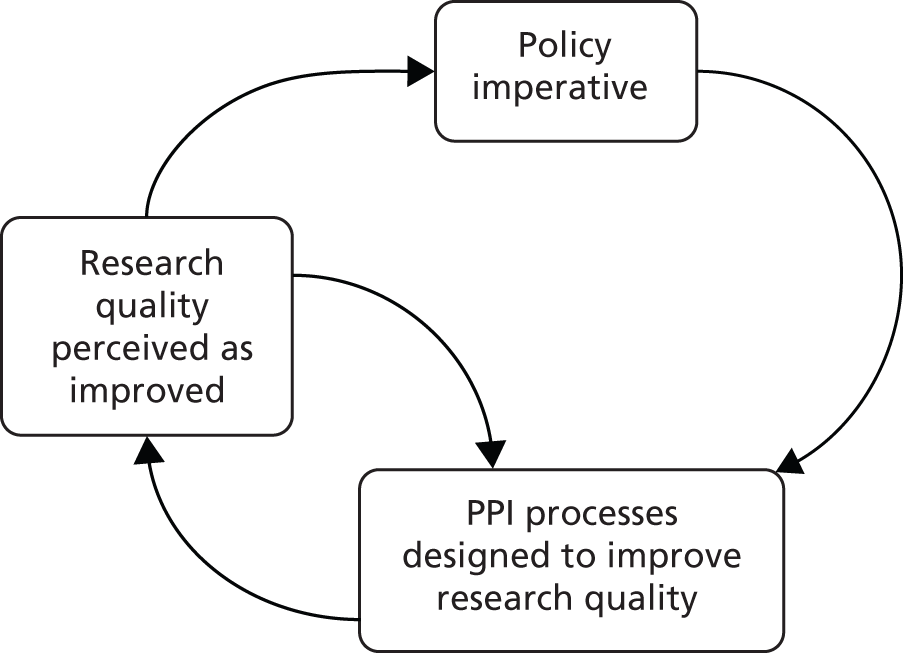
FIGURE 10.
Pathways triggered by moral value set.
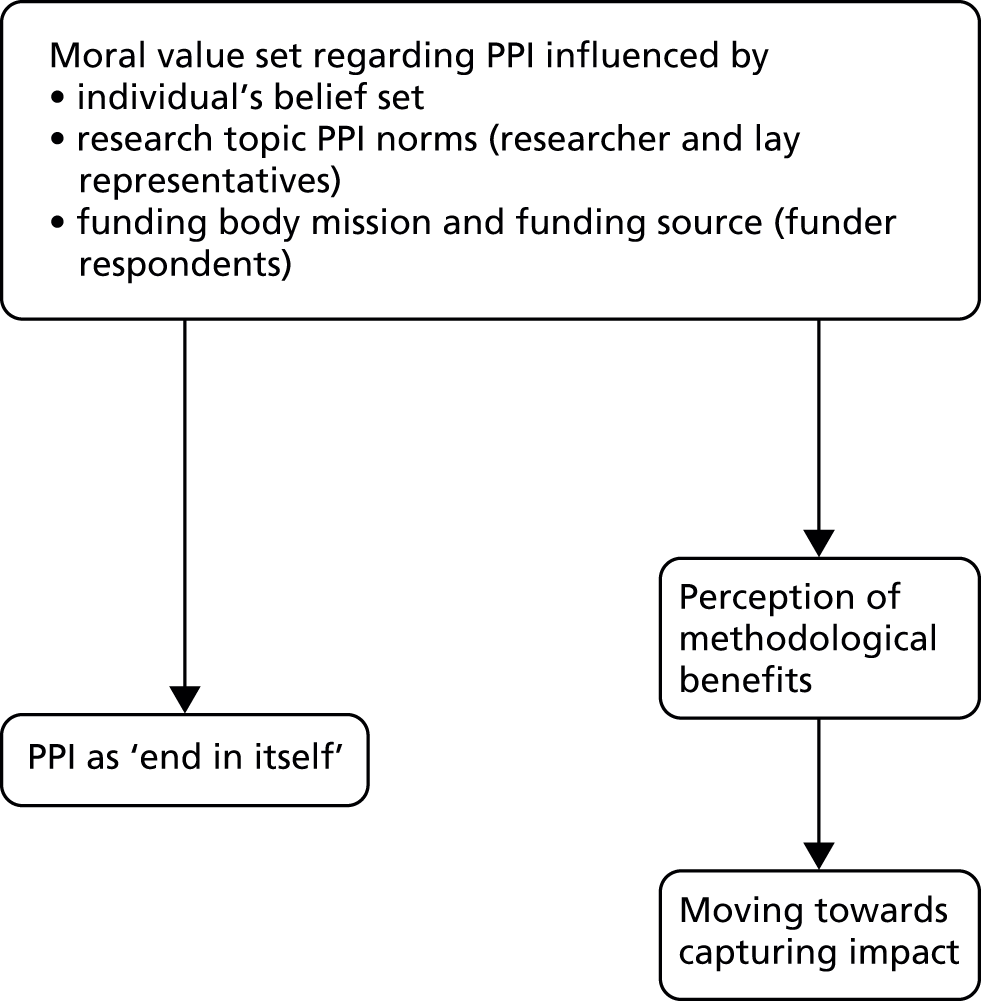
That values should have such a profound impact on shaping PPI processes is unsurprising and will be discussed further in other sections. A project running at the same time as the RAPPORT study explored values in more depth and suggested three value sets: normative (which we have termed ‘moral’), substantive (which we have termed ‘methodological’) and process. 25,175 Its process value set included concepts such as partnership and equality, respect, trust and honesty, which we have mostly subsumed under our ‘moral’, ‘methodological’ and ‘policy’ value sets. However, whichever labels are used to define value sets, it is clear that different value sets are seen to lead to diverse constructions of PPI,28,174 and can affect whether or not and how PPI is evaluated. 52
It was specifically notable that values could be seen to shape the way PPI was organised within funding bodies, with impact on how they evaluated PPI within their funded projects. The centrally funded programme management organisations placed a clear focus on developing ways of capturing the methodological impact of PPI, in contrast to the condition-specific charities, which followed a clear moral imperative to involve the people who put coins into the tin. The influence of values on funders was further highlighted by the approach of the large national funding body funded through endowments, for which the obligation was one of engagement rather than any moral imperative to involve. An earlier study on funders also suggested that charities and centrally funded organisations adopted different approaches and rationales for PPI. 176 It should also be noted that O’Donnell and Entwistle176 and van Bekkum and Hilton177 suggest that funders had many anxieties about PPI such as its ‘distorting’ the research agenda. This was not reflected in the RAPPORT findings on current views of funder organisations; the main concern from our data was the potential to overload lay representatives with reviews.
The metaphor of an ‘industrialised’ scale of research suggested by our data echoes the similar argument of Ward et al. 39 that the trend towards consumerism has shaped the commodification of research. Although we had no evidence of any of our lay respondents ‘shopping around’ for research projects to be involved in, it could also be seen that one of the condition-specific charities had framed the end-user of the research as being the consumer, and consequently including both patient and clinician as their ‘user representatives’. Kreindler27 also argues that the consumer paradigm is predicated on consumer satisfaction, so that methods for implementing PPI will centre on feedback. Our case studies offered examples of PPI approaches adopting such methods, such as focus groups.
Models and commitment to patient and public involvement
While values were seen to have a major influential role in all our data, narratives also offered evidence that values can and do change over time. One influence on such shifts was from the model of PPI used, which, as seen earlier, is often triggered by one value set and then either the model is reinforced over time or a subsequent shift in values leads to a new model being adopted.
Dynamic framework for patient and public involvement
The RAPPORT data supported a typology of PPI in research based on:
-
who the PPI representatives were
-
what the forums for the PPI representative–researcher interface were
-
the approaches used.
This typology is not dissimilar to the conceptual framework suggested by Oliver et al. 132 However, the RAPPORT data suggested a far more dynamic framework (Figure 11) than that of Oliver et al. ,132 recognising subtle changes over time. Within this more dynamic framework, the PPI approaches, forums and PPI representatives may be seen to change during the research process, or several approaches and forums may run throughout the life of a study. In contrast to previous observations18 that PPI conceptualisations have not addressed the dynamic nature of PPI within research, our analysis, and the framework that it underpins, is able to take into account a dynamic concept of PPI within a research study.
FIGURE 11.
Dynamic framework of PPI.

Value sets greatly influence PPI processes within a study; and relatedly, in turn, the model of PPI in each study was seen to be influenced by the CI’s desired outcomes from the PPI input. 18 For example, one case study (CS01) recorded only a one-off narrowly defined PPI input, which reflected the CI’s reservations about any benefits of PPI.
Patient and public involvement within a study was also partially shaped by the lay recruitment method. Varying the methods of PPI recruitment was one means by which researchers tried to address the issue of PPI representativeness, an often-questioned issue. The quest to find a person (or a group) with characteristics as close as possible to a target study population173 was particularly challenging for research teams in public health studies, where the target population would not necessarily see themselves as having a health condition or need. Interestingly, those of our case studies which involved marginalised groups, such as those with learning disabilities and IDDs, did not have particular problems in recruiting PPI representatives thanks to the existing infrastructure for PPI developed in these areas. As argued by Barnes et al. ,178 representativeness in providing perspectives was achieved by merit of the lay representative’s personal experience, particular characteristics (e.g. being an older person) or links with other networks (e.g. representatives from local or national charities). However, what particularly vexed some researchers was the perceived repeated recruitment of the same group of lay people, rather than of those able to bring a fresh outsider perspective (discussed in Impact of involvement on patient and public representatives).
Our data also suggested that existing groups or panels were a pragmatic source of recruitment for many researchers, and had benefits such as PPI members having some basic knowledge about the research process, providing more than one voice and having support mechanisms in place. Many of these groups were also able to reimburse lay members for work in developing grant applications, a particularly challenging issue raised by many17 that could then be addressed. However, the PPI costs required in a grant application proved a surprise to a minority of researchers, suggesting that further work needs to be done in helping researchers understand the resource implications of supporting PPI. How often PPI representatives were involved in successive research stages in our case studies could be presented as a decreasing double bell shape, with activity focused on project set-up and to a lesser extent the dissemination phase.
The forums in which PPI representatives and researchers came together provided similarly contrasting data. The most common forum in our case studies was some form of study management committee. In many of these committees lay representatives felt well supported and that their voice was heard, often primarily enabled by relational work (discussed in Contextual enablers for patient and public involvement: relationships). However, in some committees, other PPI representatives reported feeling lost by language, procedures and lack of support, and unable to contribute effectively to these committees.
Scott179 suggests a number of rules and norms that govern such forums:
-
regulative – the system of rules that shape and monitor actions
-
normative – the rules for appropriate behaviour in that particular forum
-
cultural-cognitive – the shared meanings that lead to unwritten agendas of ‘how we do things here’.
Regulative rules may be written and formalised, for example in research governance frameworks, but may not be understandable to lay representatives even if documents are provided. However, it is the other two sets of norms that can cause most problems, as they may be unwritten and therefore not visible to a PPI representative who is working with a research team for the first time, or is new to the work of study management committees. Barnes et al. 178 argue that these rules and norms have specific effects on such forums. First, proscribing groups with which studies engage may affect access to such committees. So, for example, certain lay representatives such as those with poor literacy or lacking access to a computer may not be invited to be part of the committee. Second, rules and norms can define agenda setting, including which items are included and who can take part in the discussion. Some of our data suggested that some lay representatives felt unable to contribute to any item on the agenda, and certainly had no say in adding any agenda item. Finally, the normative and cultural-cognitive rules and norms guide the way the deliberation proceeds and is conducted. So, for example, some lay representatives sitting on committees alongside eminent scientists followed unspoken rules that the scientists be allowed more talk-time than other members of the committee. Effective chairing could often ameliorate this, and several PPI respondents articulated the role of the chair in moving key PPI contributions beyond only tokenistic membership of a committee.
Models of patient and public involvement
While we found different forums, approaches and people involved in a dynamic framework of PPI, and traditional models of PPI with two or more representatives fully involved as part of a steering committee, our findings also suggested three specific models of PPI which resulted in different levels of PPI impact.
The one-off model of patient and public involvement
We found evidence of a model with one-off, limited PPI input into the study with boundaries set by the CI (Figure 12). While such involvement did achieve its purpose from the CI’s perspective, it also precluded any further potential positive impact of PPI.
FIGURE 12.
Model 1: the ‘one-off’ PPI.

As this model was indicative of a CI who had reservations about PPI, it was unsurprising that we had few case studies that exemplified this model, as we would expect that those agreeing to take part in the RAPPORT study would be more engaged with PPI. Therefore, it is likely that this model may be rather more common in the wider research community and so merits further exploration. It is also an interesting model, as our analysis suggests that an unintended outcome was commodification, whereby PPI was ‘bought’ by the CI for a specific task.
We can draw on Habermas’s theory of communicative action180,181 to illuminate this further. Habermas suggests that the modern capitalist society comprises a ‘lifeworld’ where public and private experiences and values are culturally and socially integrated, sustained and reproduced. Here, for example, we could see how people living with dementia exist in a ‘lifeworld’ where experiences can be shaped by stigmatising processes182 that are sustained and reproduced. One rationale for PPI in dementia research is therefore to be able to gain understandings of these experiences from the perspective of service user and carer, and how these experiences inform research priorities and design.
Alongside the ‘lifeworld’, Habermas argues, is the ‘system’ made up of bureaucracies, markets and policies;129 for example, this would include the bureaucratic and policy processes, and economic drivers of health research. A key mechanism within the ‘lifeworld’ is communicative action, a consensual process whereby people understand and share experiences. Within the RAPPORT study we can see communicative action within one particular case study with families of children with disabilities (CS21), where they shared experiences which were translated into research priorities. In contrast to the ‘lifeworld’, the ‘system’ is sustained by strategic action, which may be conscious or unconscious. Therefore, the requirement for PPI as a condition for research funding could be seen as a conscious strategic action. However, the tacit shaping of PPI through a process of commodification would, through the Habermas perspective, be seen as the colonisation of the ‘lifeworld’ by the bureaucratic and market interests of the scientific-technical system,183,184 which will then influence and rationalise the ‘lifeworld’. In the case study with more limited PPI, PPI was bought in by the CI as a commodity to demonstrate that those representing the target population would find the accessing of medical notes acceptable. Because there was no sustained engagement with the PPI representatives, we were unable to interview any of them, but our interviews with other PPI representatives suggested it would be unlikely that this one-off activity could lead to engagement with the research study, or therefore any connection with PPI representatives’ ‘lifeworld’.
The fully intertwined model of patient and public involvement
Seven of our case studies (CS03, CS04, CS07, CS09, CS13, CS17 and CS21) demonstrated a fully entwined model (Figure 13), in which PPI was integral and ongoing within the research study. This model demanded more resourcing, including a discrete co-ordination role, reimbursement of larger numbers of PPI representatives, ongoing and proactive communication and building and sustaining relationships between the research team, centre or host organisation and lay representatives. However, this model produced greater impact than the one-off model and, without exception, had the fullest NPT radar plots, indicating that PPI was embedded as normal practice.
FIGURE 13.
Model 2: fully intertwined PPI.
This model was particularly exemplified in two case studies (CS13 and CS21), which had the most embedded PPI as shown in the radar plots (see Chapter 6). The context for both was research being conducted in a well-resourced research centre, jointly or totally hosted by a university. However, they differed in research design, topic area (IDD and public health) and, hence, their tradition and history of PPI. They also differed in PPI approaches, with CS21 tending more to user-led research in that the research question had been identified by service users, but the actual research itself was conducted in partnership with researchers. In CS13, the approach was characterised by a collaborative approach, with the panel an integral part of the research process but as collaborators, not co-researchers. The key enablers for this model appeared to be the ‘work’ described in all four NPT constructs and, in particular, values, PPI co-ordination role and relationships. Both studies also had time, core funding and stability to develop a fully entwined model of involvement, where PPI was integral to the research process. Therefore, this model was not possible for all our case studies even when actively sought, because of limited resources.
The outreach model of patient and public involvement
A third model was identified, which we termed the outreach model. This still entailed entwinement but was looser and generally involved fewer PPI representatives: just one in some cases. The key feature of this model was that this small number of PPI representatives provided a conduit to and from a wider population from which they would bring back perspectives and views (Figure 14).
FIGURE 14.
Model 3: outreach PPI.
Recent literature has also promoted this model if the PPI representative is well connected to and has credibility with the target population. 185 Although this appeared to be an effective model which required fewer resources, the resource implications are from the research team’s perspective and we had evidence that this model increasingly relied on charities to perform the outreach function. This escalation of demand on charities without associated funding to support this work has significant implications for sustainability, and is discussed further later. Van Bekkum and Hilton’s study on funding bodies177 also suggests that this model is being adopted by some funders, seeking representatives who could act as a ‘middle-man’ between the worlds of research and the public. While CS02 demonstrated a collaborative approach, it also showed the potential for tokenism in this model if the individual is operating just to provide endorsement of the study by the target population.
Contextual enablers: organisation of patient and public involvement
We wished to test out in our case studies and survey whether or not the principles identified for successful PPI,137 or architecture for PPI in research,29 would be found to be prerequisites for effective and embedded PPI. The PIRICOM study architecture for PPI included the principles gained through consensus by Telford et al. ,133,137 grouped here under three headings: processes (PPI activities/research interface), resources and relationships (see Figure 15).
As reported in Chapter 6, having a clear purpose, role and structure for PPI was a salient action undertaken by case studies with embedded PPI. As illustrated in Figure 15, we found that adequate resources and the development of relationships over time were important enabling contexts, and these will be discussed in Contextual enablers for patient and public involvement: resources and Contextual enablers for patient and public involvement: relationships. However, what is not so explicit within the Brett et al. 29 architecture is the need for someone to lead, and in particular co-ordinate PPI.
The co-ordinator role
A major feature of the case studies where PPI was strongly embedded was the presence of a person with designated responsibility for co-ordinating and facilitating PPI within the research study. In some case studies this was undertaken by a paid co-ordinator with general responsibility for a research centre’s programme of work, for a UKCRN network or for a public involvement group serving a geographical area. In other case studies this role was undertaken by the CI or assigned to another researcher in the team. For the paid co-ordinators and assigned researchers, the role comprised various components (Figure 16). Some of these components were also evident in the work of the CIs and the funding bodies’ PPI leads, and all could be described as providing a bridge between two worlds: research and lay. This idea of bridging fits well with the social network theory-derived definition of ‘boundary spanner’161 (see Chapter 6). Further exploration of the specific features of this bridging role helps tease out the different approaches of these co-ordinators.
FIGURE 16.
Components of PPI co-ordination work.
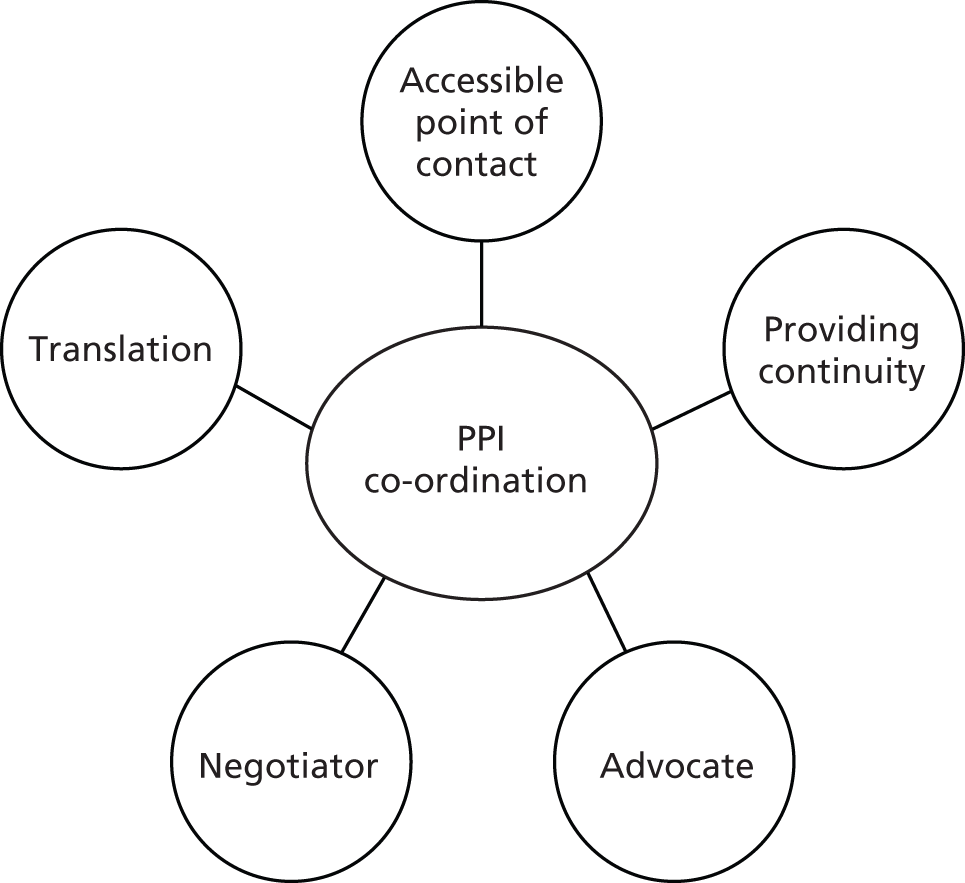
Clavier et al. 186 propose three aspects of bridging: cognitive translation, strategic translation and logistic practices (Table 19).
| Aspect | Actions | RAPPORT findings |
|---|---|---|
| Cognitive translation | Bringing insights in from the public and translating them into research questions | Case studies 21 and 23 had forums specifically designed to do this, with members of the public facilitated in turning needs into research questions |
| Strategic translation | Circulating and translating information derived from research and public perspectives. Establishing committees and procedures. Clarification of expectations | Case study 17 PPI co-ordination was facilitated by the CI. Panels and structures plus effective lines of communication were a feature (see also CS13) |
| Logistic practices | The practical work and time required to enable both translations | Well-resourced case studies had discrete administrative support for PPI, or researchers would take the time and make the effort to carry out these tasks |
One of our case studies (CS21) exemplified cognitive translation by bringing the public and service users into the research centre and helping them translate their perceived needs into research questions. Strategic translation was often undertaken by CIs who facilitated PPI within their study. They emphasised ensuring good communication and feedback, and setting up structures for PPI within their study. For both aspects of translation to work well, various logistical practices were required to ensure that PPI ran smoothly, usually in the administrative tasks such as payment of expenses. In some case studies the dedicated co-ordinator also carried out these tasks; in others this work had to be absorbed by the research team.
Our interviews evidenced respondents carrying out the PPI co-ordination role as displaying certain traits reflecting Williams’s boundary spanners’ skills requirements187 (Figure 17), focused on managing complexities through negotiation and building sustainable relationships. The nature, development and facilitation of such relationships will be discussed more in Contextual enablers for patient and public involvement: relationships, but our findings made clear that effective PPI co-ordination, whether within research teams or funding bodies, depended heavily on the ability to build and sustain relations.
However, to see PPI co-ordination simply as a bridge between two worlds disguises its complexity. As illustrated in Figure 11, within each case study, PPI was not static and boundaries between the research and lay world were dynamic, constantly shifting. For example, over time, PPI representatives may become less research naive and the nature of relationships and the boundary dividing the research and lay worlds may subtly shift. Equally, researchers’ assumptions regarding PPI may change with time and again affect the nature and permeability of the boundary. The evaluation of knowledge translation processes within CLAHRCs by Evans and Scarborough188 suggested that the bridging model described above may keep the two worlds apart. They argue that a ‘blurring’ approach is more effective in creating transformation. Rather than rely on a single PPI co-ordinator to perform the boundary-spanning role, the blurring approach requires both researchers and PPI representatives to adapt the skills they have to accommodate new ways of working. This theory may partly explain why in the case studies with minimal PPI co-ordination there could still be positive outcomes from PPI, and why in one case study with formal PPI co-ordination there was minimal PPI impact: the worlds of research and lay had remained separated by a boundary that only the co-ordinator could cross.
Overall, the co-ordination role facilitated effective PPI, including work to clarify PPI role descriptions and expectations.
Patient and public involvement role descriptions and expectations
A pertinent finding in the RAPPORT study was the lack of formalised PPI role descriptions and expectations in the majority of case studies. Indeed, in some case studies, it was seen as an explicit requirement that roles and expectations were left as open as possible. The logic given was that, if a research team wanted PPI representatives because of their personal experience of complex needs, then the role needed to be flexible enough to accommodate these complex needs. Indeed, as CMO Table 12 illustrated, tightly bound work specification for PPI representatives could limit their potential impact.
However, there was also evidence that a lack of clarity around role expectations could lead to a breakdown of trust, with a negative impact on relationships and outcomes for PPI. Hence, it would seem that some careful balancing between flexibility and clarity around expectations was required to enable sustained embedding of PPI within a research study.
Contextual enablers for patient and public involvement: resources
As seen in the findings, some of our case studies did include PPI during the grant development phase, but most exhibited an intense ‘PPI phase’, usually when developing ethics applications, and to a lesser extent when findings including the development of a lay summary were disseminated. Surprisingly, and in contrast to best practice,189 whereas all case studies reimbursed PPI representatives for their out-of-pocket expenses, only around a quarter of case studies reimbursed for time. As discussed earlier, there was evidence that this was becoming a very contentious issue, particularly for PPI representatives from relatively small charities. There were five such representatives. One was a representative from the charity partially funding the study so did not expect any remuneration. The second was being paid as a part-time researcher, and a third took an altruistic stance, giving time free in the interests of those she represented. However, two respondents who ran national organisations expressed doubts that it was sustainable for them to undertake this PPI work with no recompense, as their absence had implications for the work of the charity. They also called into question the idea that it was morally defensible to expect them to undertake an increasing workload of PPI requests without some significant financial reimbursement. There was evidence that both these charities were putting in place consultancy procedures and costs that would need to be met in future grant applications.
Interestingly, PPI respondents also rarely mentioned the need for training. Although some had received appropriate training, many lay representatives did not feel they required any particular training. However, there was some evidence that researchers (particularly those relatively new to research) did want more training and preparation for PPI.
The strongest theme to emerge from our data was the centrality of relationships to PPI. Whereas previous work has highlighted the importance of the researcher–lay relationship, the RAPPORT findings illuminate this further by teasing out the components that result in relationships being one of the most important enabling contexts in leading to positive PPI outcomes.
Contextual enablers for patient and public involvement: relationships
Truman and Raine190 suggested that ‘the creation of evidence in health research is shaped by the social relations of the research process as well as by the methodologies used’ (p. 215). This was very evident in the RAPPORT case studies, with several clearly recognising the importance of emotional as well as rational deliberation (cf. Martin 2011191). There were four components in enabling relationships: time, reciprocity, arenas and skills.
Time for relationships to develop
Our data showed that meaningful relationships took time to develop, and this need had been reduced within the great majority of case studies by having PPI representatives already known to the research team; only 6% of lay representatives were completely new to the team. This may be a reflection of our sampling, as CIs with UKCRN portfolio studies tend to be more experienced. Generally, PPI representatives were known to the researchers through being involved in previous studies, being part of an established PPI group attached to the research centre or being a patient or acquaintance. The temporal aspect of relationship building supported the development of trust. 192 For researchers this could mean trusting the PPI representative to not derail the project, behave according to the rules and norms of that context179 and/or make a positive contribution to the study. For PPI representatives, trust was a sense of security at meetings that they would not be made to look foolish and their comments would be listened to; this was always enhanced when research teams provided feedback on their response to lay comments. For PPI representatives in a governance role, there was also a sense of trust that the research team would alert them if there were any safety issues with the study. Time also allowed PPI representatives to develop their skills192 to enable them to contribute to the study; many saw this ‘learning on the job’ as equally effective as formalised training, if not more effective.
Reciprocity
To enable PPI, reciprocal trust and relationships needed to be built. 101,193 Reciprocity is often defined as a co-operative or mutual exchange of gifts or privileges. 194 Criticisms of PPI include tokenism and power asymmetries between researcher and lay representative. 27,52,173 However, Ben-Ari and Enosh194 suggest that focusing on such exchanges is too simplistic and that, within health research, reciprocity between researcher and the lay representative occurs less through the exchange of gifts and privileges, but more through sharing an issue of common concern or interest, reflecting the notion of mutual gain. 195 This was certainly evident in some of our case studies: PPI representatives willingly gave up their time to contribute to a project for which they could see longer-term benefits. However, our data suggested that there was another form of reciprocity, although not necessarily exclusive to the shared and vested interest in the research topic. PPI respondents often reported an increased sense of self-worth and confidence as an outcome of their PPI activity. 196 Others stated that, if they gained knowledge of a specific condition or services available for it, this was of personal benefit to them. There were others for whom the reciprocal favour was either access to services or perceived maintenance of good services. For example, patients of clinical researchers would often agree to undertake PPI as something to ‘give back’ for the quality care they had received. Finally, for a minority, the reciprocal gift was monetary.
Arenas for relationships
Those case studies with embedded PPI, or that were particularly strong in relational integration, both used arenas outside the formal research structures, where relationships could develop and flourish. Examples ranged from entire days devoted to an exclusively social activity to, more commonly, the provision of food and meals outside a research meeting. Although our research was not designed to observe such arenas ethnographically, the interview data did suggest that the arenas were explicitly being used to nurture relationships. This included sharing personal narratives, which Barnes197 argues is important in ensuring mutual recognition, and allows the researcher to understand where the PPI representative is ‘coming from’. 193 In the theoretical conceptualisation of PPI by Gibson et al. ,130 there is a call for a ‘plurality of arenas’ where the different voices (lay and professional/researcher) can be heard. Many of the RAPPORT case studies suggested that different arenas were created to enable the emotive and rational voices to be heard and to contribute to the research study. Conversely, this may also imply that the formal arenas such as trial steering committees were unlikely to provide much space for personal narratives. Rather, our data suggest that prevailing norms and rationalistic discourse continued to dominate these arenas.
Our findings pinpoint specific issues if PPI is to be conducted solely through virtual media. Having an arena where relationships could flourish was a shared characteristic of the case studies with strongly embedded PPI. As relationships are created through, for example, social networking, blogs, followers and tweets, there is no reason why virtual PPI could not work within plural arenas. This area merits further research.
Skills for enabling relationships
Whatever arena within which relationships developed, there were discrete skills and traits needed by those facilitating relationships. Others have highlighted the challenge of encouraging and maintaining relationships in PPI,193 and the need for training to do this. 29,101
As discussed earlier, knowledge about boundary spanners helps illuminate the skills and traits that enable this work. Williams187 describes four aspects to building sustainable relationships (Figure 18), and these skills and traits were described within our data. Some of these aspects are amenable to development through training; others may be seen as personality traits. The RAPPORT data gave a sense of the PPI co-ordinator or person leading on PPI being that kind of person: approachable, sensitive, tolerant and open.
Impact and outcomes of patient and public involvement
The findings from the RAPPORT case studies identified the impact and outcomes of PPI, which were overwhelmingly articulated by our respondents as positive, although some negative experiences were also described. The case for evaluating PPI impact draws upon the methodological case for the need to know what is working and what does not work well in PPI,198 and the economic case, as PPI is relatively resource-intensive. 30 However, our survey and scoping, and previous systematic and structured reviews of PPI in research, showed that there is little recording of PPI activity and costs in publicly accessible research study information, and in published papers. 19,29 Our analysis of the case studies clearly showed that outcomes of PPI were far easier to identify than the mechanisms and context that led to them. The majority of PPI-related outcomes were those expected and desired by the research team.
Impact of patient and public involvement
There is a drive towards public involvement and engagement in a number of sectors beyond health research. Impact of public or community engagement in these sectors may shed light on the PPI impact we may expect in health research.
Community engagement in housing through, for example, tenant management organisations has been cited as an approach leading to improved processes and outcomes in social housing. 199 A systematic review200 on the impact of community engagement on health and social outcomes found that community engagement helped with planning and management of housing services, enabled partnership working and better communication between stakeholders and provided a conduit to a broader community. Although there was evidence of impact on members of the public, such as development of skills, conclusive evidence of the impact of community engagement on service delivery could not be found. The authors suggest this is because of the difficulty in attributing improvements to PPI, as so many factors are involved.
There is also a broad body of work on public participation and involvement in ecological and conservation work. 201 Desired longer-term outcomes for PPI in this arena include sustained conservation202 and empowerment for the public involved. 203 However, as in social housing, longer-term impacts of PPI are rarely measured and noticeable long-term outcomes may occur only 10 years or more after the project has been set up. 201 Nevertheless, evaluation of PPI within social housing and conservation suggests that PPI enables positive outcomes in:
-
processes including management and governance
-
accessing knowledge that would otherwise be unavailable
-
improved partnership working, communication and broader links with the community.
Impact and outcomes of patient and public involvement in the RAPPORT study
The most commonly reported outcome of PPI was in improving recruitment rates, particularly through refining participant information literature, and also through providing links with participant populations. However, there was no evidence on how this affected research outcomes. This effect of PPI on study recruitment has been reported widely elsewhere,70,78–86,88 but the range of case studies within the RAPPORT study allows the specific components to be teased out (Figure 19).
FIGURE 19.
Patient and public involvement processes and outcomes in study recruitment.
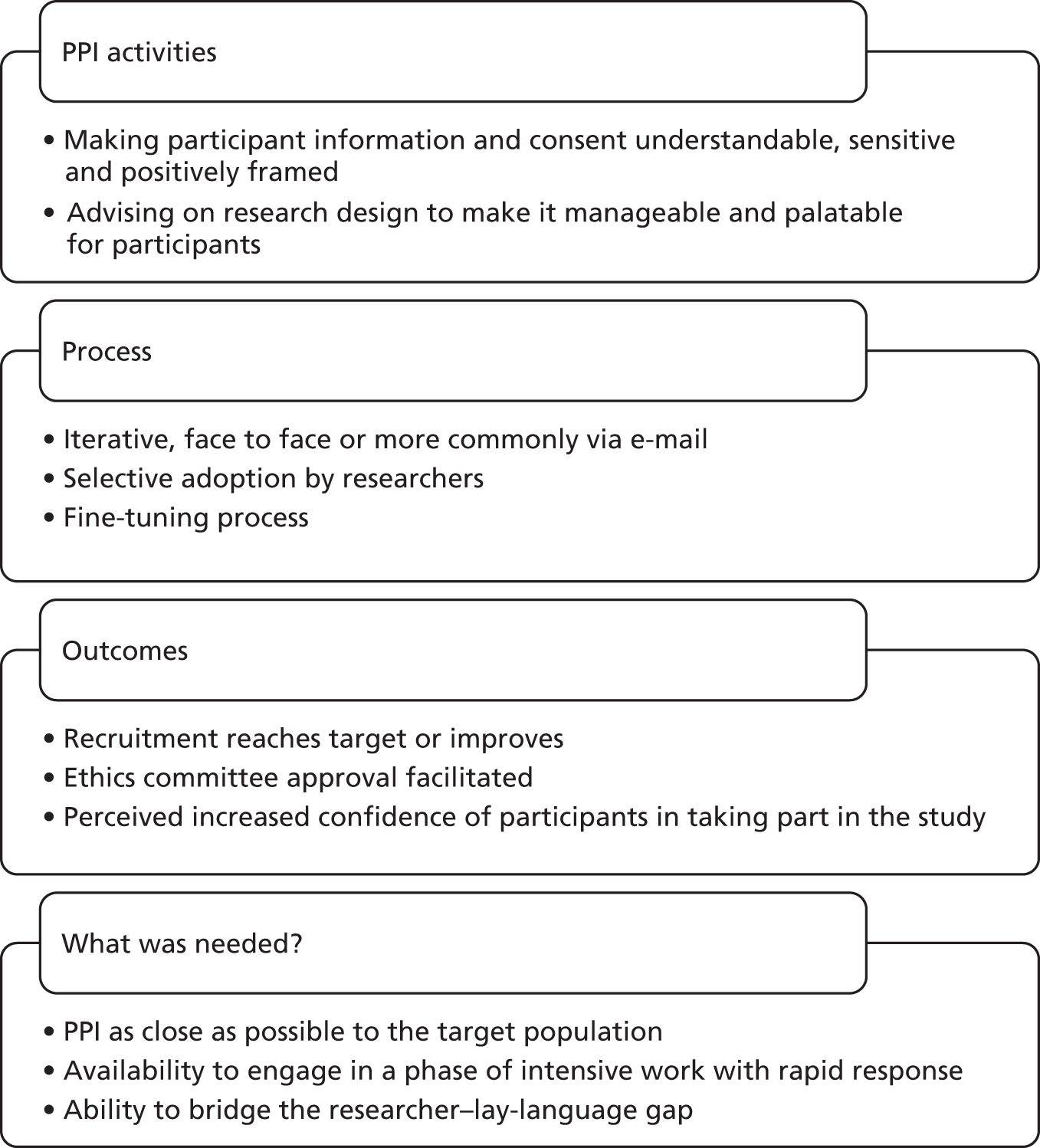
Five out of the 22 case studies had PPI representatives involved in setting research priorities, and again this has been previously demonstrated (see Chapter 2). Impact of PPI on this outcome was particularly facilitated by formal structures which ensured that lay representatives were part of the decision-making process and could influence the final decision.
Whereas the majority of outcomes from PPI for the research studies are reported previously, one notable exception was an unexpected outcome in one case study where both researchers and PPI respondent reported an impact on participant safety. Although this could be subsumed under PPI impact on the overall research design, it is particularly interesting that the lay representative, by being able to put herself in the shoes of the participants, could identify potential safety issues not seen by the research team. It is also significant that this outcome was unexpected by the research team, and carried implications for research teams who set strict boundaries on what outcomes PPI representatives may affect. It also raises some questions about current developments in building evaluative frameworks for PPI, which will be discussed in Evaluating patient and public involvement in research studies.
It should be noted that, while the RAPPORT studies did provide evidence of PPI impact on research design, the research stakeholder (including PPI) consensus study by Barber et al. 159 concluded that it was not possible to evaluate PPI impact in this area. The positive impact of the fully intertwined model on the research process was clearly observable, and ranged from identifying research questions to disseminating research findings; however, this was not exclusive to this model. Some of the case studies typifying a more traditional approach to PPI, such as two or more representatives involved in a project steering committee, also demonstrated a positive impact on research processes. Rather than a specific model being the enabler, it was the six salient actions as described in the CMO tables (see Chapter 6) that were key. However, it is significant that all the case studies demonstrating an intertwined model achieved the salient actions and exemplified fully embedded PPI.
Nevertheless, as with other sectors it was difficult to tease out the impact of PPI on the research results. This is unsurprising given the difficulties in distinguishing the impact of PPI from other factors, but, as recognised in the Higher Education Funding Council for England Research Excellence Framework, impact is often not immediate and can take 15 years to become visible. 204 We are therefore not able to determine whether or not the resources required for the fully intertwined model are merited in terms of long-term impact on research findings. However, our findings suggest that the fully intertwined model is likely to lead to increased relevance of research questions, and hence may have greater long-term outcomes in terms of research orientated towards patient priorities.
This issue also illuminates the ongoing debate on what constitutes PPI success. 205 Attaining seemingly small PPI impacts on research processes may mark important steps in achieving greater change within the complex system of health research. 205 However, there is consensus that the impact of involvement on PPI representatives themselves is easier to evaluate. 159
Impact of involvement on patient and public representatives
As reported widely elsewhere (see Chapter 2), involvement had a significant impact on many of our PPI respondents in terms of psychological outcomes and knowledge (see Chapter 6). It was also clear that, for some, involvement in a single study had been the start of a PPI trajectory that moved as the individual’s knowledge, confidence and interest grew. Some of the PPI co-ordinators had been patient representatives, and the PPI respondents we interviewed from funding programmes also described a journey from involvement at study level moving towards a more strategic level.
This PPI career trajectory is a hotly debated subject. Many of our researcher respondents expressed concerns about the same PPI representatives being repeatedly involved and the need to ‘refresh’, a euphemism generally denoting removing PPI incumbents and recruiting new ones. As raised by others,206 for the PPI representatives, the challenge was to remain authentically credible after having developed enough research knowledge to reduce some demands on the research team’s time. The ‘ideal’ PPI representative from many researchers’ perspectives would be at the stage indicated by the star in Figure 20.
FIGURE 20.
Credibility versus understanding research.
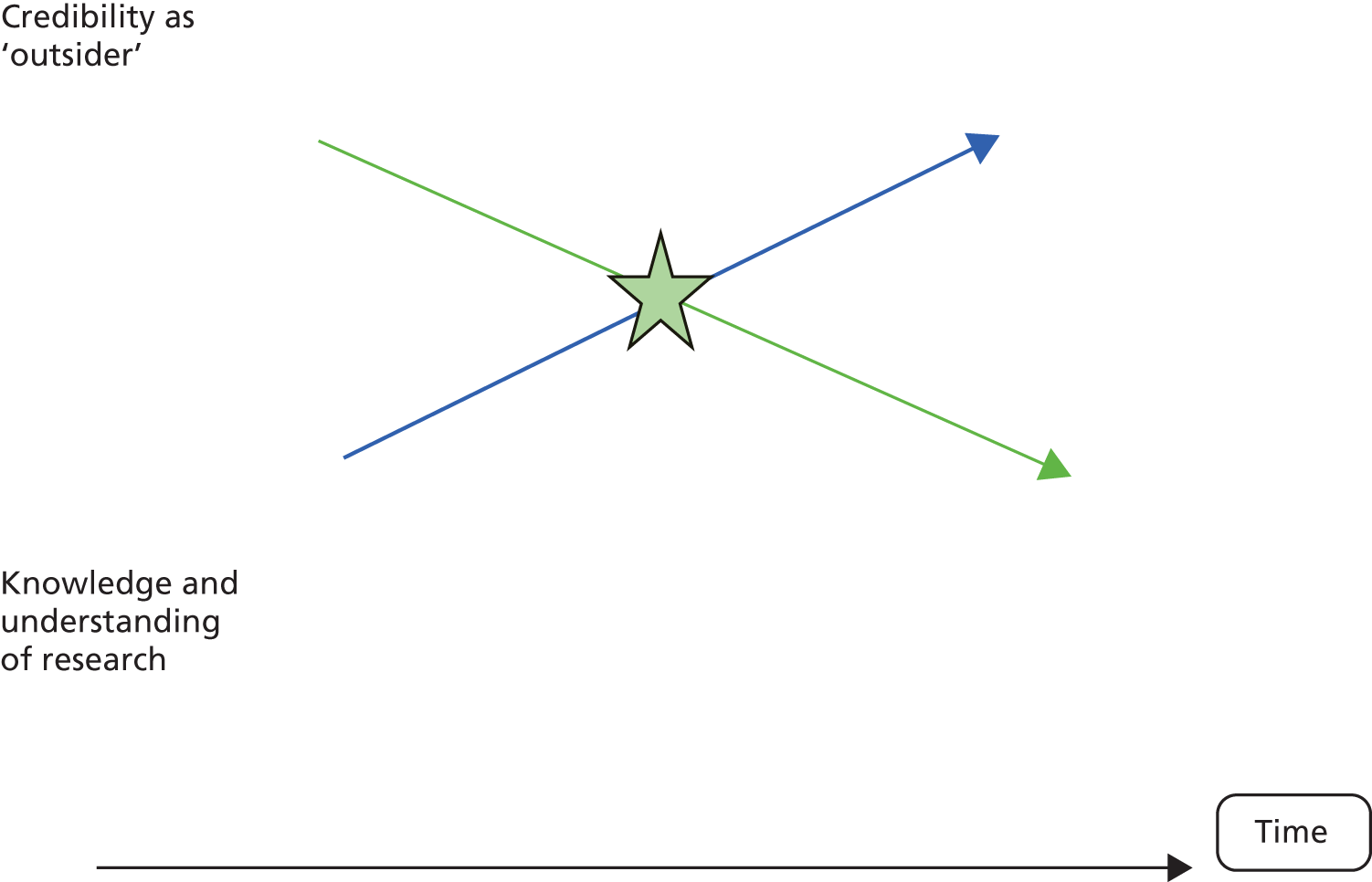
Making judgements about which lay representatives were credible and competent involved shaping processes and practice for PPI207 to exclude those moving beyond the star. So the argument ricochets between training and ‘professionalisation’ of PPI resulting in the loss of the lay perspective22,208 and also to counter the moral argument for PPI,208 and the need for some training209,210 to carry out certain tasks required in the PPI role. Although this was not articulated by any of our PPI respondents, in the ethnographic study conducted by Thompson et al. 46 they describe the balancing act carried out by the PPI respondents to have enough knowledge to be able to contribute within a trial steering committee, but also to remain credible.
It was clear in those RAPPORT case studies with strongly embedded PPI that developing knowledge and skills in research was not seen as detracting from credibility as an authentic PPI representative. Indeed, in many of these case studies the involvement trajectory was enabled and PPI representatives were encouraged to take on more strategic roles or act as co-researchers or coapplicants. This fits well with notions of equality, for it is unlikely that any researcher would in such cases be ‘refreshed’ because they had become too skilled.
Evaluating patient and public involvement in research studies
As indicated in the findings chapter, the weakest NPT construct in our analysis of case studies was appraisal, in which the PPI is evaluated and work is reconfigured in the light of this evaluation. There were few case studies which provided any evidence of systematic evaluation (see CMO Table 17) and these demonstrated very different approaches influenced by their research design. One RCT was able to demonstrate that rises in recruitment rates could be linked to participant information amended by PPI representatives. This was possible because of the duration of recruitment. However, in another case study, which was a systematic review, linking PPI to recruitment rates would not be relevant. In this study all PPI activities, input and outcomes were carefully recorded to provide a ‘storyline’ of impact.
The findings suggested that, in the case studies where PPI was strongly embedded, the research teams were already intuitively following evaluative processes suggested by the Public Involvement Impact Assessment Framework (PiiAF) project with values identification and impact theory. 175 Their value sets and understanding of PPI were coherent, and they were evaluating PPI impact appropriate for their study design. However, for many other case studies such systematic evaluation would be difficult because coherence levels were lower. In addition, many of these studies were working to short, intensive time scales, so would be unlikely to enter into the group thinking that the PiiAF project suggests lays the foundation for impact evaluation. However, outside the research study, it is likely that the value clarification exercises suggested by PiiAF would contribute much to the training and preparation for PPI requested by many of the less experienced researcher respondents. A point of note is that any evaluative framework must be flexible enough to capture any unforeseen outcomes; simply measuring whether or not expected outcomes had been met would not provide a full evaluation.
A key challenge for some of our researcher respondents (mainly clinical) was that their research approaches were clearly placed within the positivist paradigm, so they found it very difficult to articulate how they would evaluate PPI by preserving their focus on measurable and observable changes.
It should be noted here that some case studies were recruited to the RAPPORT study because they wanted an external evaluation of their PPI. Having regular tracking interviews revealed the complex temporal dynamics of PPI in some case studies; the challenge for these researchers is now to provide published evidence of the impact of PPI in as robust a form as in reporting their RCT findings. 21
Summary
A widespread lack of transparency in how PPI is operationalised, and with what impact, impedes any clear summative assessment of the extent of PPI embeddedness within the research infrastructure. Our case studies clearly indicated a widespread lack of any systematic evaluation of PPI. This is compounded by the inherent difficulties in assessing PPI impact on research outcomes due to the time required for impact to become visible and the difficulties in teasing out individual contributions. However, the widespread and diverse impact on all those involved and the research process was marked and should not be underestimated within the context of a complex system such as health research.
One clear constraint on PPI becoming embedded is the drifting of definitions between involvement and participation. While this sometimes illustrated a lack of common coherence, there was also evidence of a deliberate dual role. This poses the potential of ethical concerns, but there also appeared to be a positive impact when taking on such a dual role was well-managed through clear boundaries, transparency and informed choice. Within a dynamic framework of PPI we found evidence of traditional models of PPI with two or more representatives fully involved as part of a steering committee, and three specific models of PPI which resulted in different levels of PPI impact.
The one-off model at one end of a continuum of involvement was characterised by tokenistic and limited PPI where full impact could not be realised. At the opposite end of this continuum, the fully intertwined model displayed PPI as integral to the research impact, which resulted in a range of positive outcomes. However, for the host organisations and research teams this model proved also to be resource-intensive. The outreach model provided a way of linking with a broader target population through a credible and well-connected lay representative. To avoid tokenism required a collaborative and iterative process between research team, PPI representative and the broader community. While more resource-efficient for the research team and host organisation, this entailed resource and workload implications for the lay representative taking on this role.
Such a ‘bridging’ role with a broader community was also undertaken by some PPI co-ordinators, who appeared to be central in leading and enabling PPI. Part of this role was to develop and sustain relationships, which we found to be the fundamental enabler for PPI. However, it was important that the co-ordinator role was not being used by other researchers within the team to abdicate engagement with PPI.
Chapter 8 Conclusions
The RAPPORT study looked at studies started more than 6 years after PPI became a statutory part of the health research governance framework. 5 This policy was reflected in many of the case studies where there was evidence of well-established structures to support and resource PPI. However, the complex nature of PPI means it is challenging to pinpoint its impact and distinct contributions to research studies. 19,100 The varied nature of PPI in terms of structures, roles and relationships required a methodology capable of exploring and evaluating context-specific mechanisms. 32 It was also important to evaluate how far PPI had become embedded as normal practice within research adopted by the UKCRN portfolio.
This chapter revisits the research objectives and provides a summary of the key findings under each objective. We then present the main conclusions and reflect on the RAPPORT study research process and limitations. We discuss the implications for PPI practice derived from our findings and highlight the responses to these from our stakeholder dissemination events (Appendix 5). Finally we present recommendations for future research.
The RAPPORT study research objectives were to:
-
determine the variation in types and extent of public involvement in funded research in the areas of diabetes mellitus, arthritis, CF, dementia, public health and IDDs
-
describe key processes and mechanisms of public involvement in research
-
critically analyse the contextual and temporal dynamics of public involvement in research
-
explore the experience of public involvement in research for the researchers and for members of the public involved
-
assess the mechanisms which contribute to public involvement being routinely incorporated in the research process
-
evaluate the impact of public involvement on research processes and outcomes
-
identify barriers and enablers to effective public involvement in research.
What was the variation in types and extent of patient and public involvement across the topic areas?
The six research topic areas were purposively selected to ensure a diverse range of study design, study participants and different histories of engagement with PPI, traditions and associated models of PPI. Within the scoping and survey phase it was clear that our assumptions about some of the topic areas were supported. In particular, IDD, with its long history and focus on service user involvement and inclusion,139 had the largest proportion of studies which included PPI. We had expected that, with its well-established PPI networks and a clear drive towards inclusive practices for people with reduced capacity,78 dementia studies would have a large proportion of studies with PPI. However, although this proved to be the case in our survey findings, significantly fewer dementia studies with PPI were found through the scoping study. This pattern of a larger proportion of topic-specific studies with PPI in the survey than in the scoping was also found for diabetes mellitus studies, perhaps reflecting the fact that researchers who used PPI were more likely to respond to the survey. The topic area of CF was particularly interesting as an example of where PPI has developed from minimal engagement to a strategic commitment to patient and family involvement in research. CF was selected not only because it would include younger research participants, but also because it is a research area orientated towards biomedical, laboratory-based research. There were few CF studies on the UKCRN portfolio so our sample was very small. Within the CF area it proved very difficult to identify PPI leads, and many research centres we contacted (with the exception of the centre where the one CF case study was hosted) suggested that, that for them, PPI was not a top priority, as very close relationships already existed between research participants and research teams. As the RAPPORT study progressed there were clear signs of involvement beginning to develop in this area. These indicators were present both in the case study and in the latest research strategy of the CF Trust, which states its aims as ‘to ensure people with cystic fibrosis are more fully involved in the design, commissioning and management of clinical research, and we will be exploring ways to ensure the voice of patients and their families are better heard in this area’ (p. 23). 211
It was study design rather than topic area that was more predictive of the extent of PPI. Unsurprisingly, PPI was likely to be limited in basic science or tissue bank designs, although we found noteworthy exceptions to this in our case studies.
What were the key processes and mechanisms of patient and public involvement in research?
Values were a key mechanism in shaping PPI within a research project and, at funder level, a finding consistent with a previous study. 174 Funding organisations often drew a focus on either the moral or the methodological rationale for PPI, and this shaped requirements for PPI within research projects. Funders primarily articulating the methodological perspective expected greater detail about PPI processes and placed increasing emphasis on capturing the impact of PPI.
Key processes and mechanisms were also distinctively shaped by the model of PPI adopted. Three models were identified within the RAPPORT study. The least common was that entailing a one-off PPI activity; while addressing needs for PPI from the researcher’s perspective, this also limited the impact PPI could have on research processes and outcomes. In contrast, there were seven studies with a fully intertwined model where PPI was closely entwined with the research process. This model produced the greatest range and extent of PPI-related outcomes but was also the most resource-intensive and so could only be sustained by research centres with a well-developed infrastructure for PPI. The third model entailed an outreach component whereby relatively few PPI representatives would engage with the study at regular points, but would also act as a bridge to a wider constituency and so provided a two-way conduit to a broader population. This model required lay representatives who could perform this function, but for the research community it was less resource-intensive and demonstrated a range of PPI-influenced outcomes for the study. However, charities undertaking this function expressed concerns about how sustainable this model was without realistic funding. Case studies demonstrating a more traditional model of PPI, with two or more lay representatives being members of a study steering committee, could also produce a range of PPI-related impact. Rather than a specific model, achievement of six salient actions was central to the effectiveness of PPI. These actions were having a clear purpose, role and structure for PPI; ensuring diversity; whole research team engagement with PPI; mutual understanding and trust between the researchers and lay representatives; ensuring opportunities for PPI throughout the research process; and reflecting on, appraising and evaluating PPI within a research study.
The inherent pragmatism of PPI recruitment found in the case studies ran counter to the expectations of INVOLVE and the list of potential sources of PPI. 23 The process of finding lay representatives generally meant recruiting those previously known to the research team or using an established PPI group or panel. Only a few of our case studies actually recruited new representatives independently via other sources such as the media. Ease of access and established support systems made pragmatic sense in time-constrained projects. However, unless the researcher had worked with members of the group before, the relationship between the PPI representatives and research team would be less developed, and the team would be more likely to see PPI as a commodity to be bought in.
How PPI representatives and researchers came together was also an important mechanism, and for the majority of studies the forum for this was a formal meeting. Some of our case studies took care that meetings were arranged on neutral ground, but most were conducted in the researcher’s organisation. The chairing of these meetings was an important process,23 and many of the lay respondents cited the difference a facilitative chair could make.
Meetings were also settings where relationships were often established and developed. However, it was important that meetings allowed time for a social element to enable more informal engagement. On a practical level, this has implications for hospitality costs. However, the creation and sustenance of meaningful relationships between PPI representatives, specific researchers and the research team as a whole proved to be a far more important mechanism than previously reported in the literature. This was a key finding in the RAPPORT study. PPI underpinned by a lay/researcher relationship characterised by trust and reciprocity determined positive processes and outcomes of PPI in research.
What are the contextual and temporal dynamics of patient and public involvement in research?
Activities that provided a clear structure, and allowed enough time for trust to develop within a framework where roles are defined and understood, supported relationships characterised by trust. 23 This was important even when lay representatives and researchers were familiar with each other. For PPI activity, this tended to be most intense in the pre-funding and project set-up stages, and clearly PPI representatives need to be aware of the timing of these concentrated periods of work.
The RAPPORT study evidenced the dynamic nature of PPI in research studies as recognised by INVOLVE. 23 Hence, although clear structures and expectations are helpful, they may nonetheless need to be revised as the circumstances of the research, and of all those involved, change. Some of these changes can be foreseen and planned for, whereas others cannot. For example, the loss of a PPI lead had the potential for negative impact on relationships; that could, however, be mitigated if other members of the research team had been fully engaged with PPI.
How did researchers and lay representatives experience involvement?
For lay respondents, PPI was overwhelmingly a positive experience. While for some it improved understanding about their condition or services they could access, for most the increased sense of self-worth and confidence was most frequently reported. This echoes other studies87,93,212,213 and was particularly marked in people who because of retirement, unemployment or family caring roles were grateful for the mental stimulation provided through the PPI role. Moreover, this role opened up further opportunities for them, with many describing a career trajectory of PPI.
Less positive experiences for lay representatives arose from role ambiguity, from whether or not PPI knowledge was valued and from how much they felt part of the research team. The dual role we described in Chapters 5 and 6 could be a problem for some when clear boundaries were not identified. This dual role also encompassed being a consultant’s patient one day and then the PPI representative on that consultant’s study the following day. Although many respondents welcomed the reciprocal nature of this relationship, others felt their needs as a patient were not being fully met when the clinician continued the lay–researcher relationship within the clinical environment. Other less positive experiences included frustration or intimidation when the lay representative felt unable to contribute at meetings, when the generalisability of their experience was questioned and when they lacked or lost contact with studies. Lack of communication was one of the main triggers for a lay representative becoming disengaged with the study, sometimes leading to longer-term disengagement with PPI.
Some of our researcher respondents also articulated some negative experiences of PPI, although more often framed within previous studies rather than any of the case studies in the RAPPORT study. A small minority felt that PPI could be tokenistic and an imposed add-on which had not been thought through well. Others expressed frustration if they perceived lay representatives bringing only a personal agenda rather than seeing the broader picture. However – and unsurprisingly, as researchers had agreed to participate in the RAPPORT study – the vast majority spoke of their experience of PPI only in positive terms. On a practical level, PPI helped develop the skills of researchers, such as being able to communicate with the public in an accessible way. Moreover, the depth of this positive experience was illustrated by the often-used religious metaphors of PPI as being like an ‘epiphany’ or a ‘Damascene moment’. PPI had made them look at their research in a completely new way and, further, a way to which they were fully converted and which they would be unwilling to relinquish. The transformative effect of PPI is often represented as an aspiration linked to what is morally the right thing to do; these findings provide evidence of PPI as a mechanism for change and for redefining research questions and interpretation of findings.
What mechanisms were needed to routinely incorporate patient and public involvement into research?
Normalisation Process Theory134 was used to guide our data collection and analysis to understand which mechanisms were needed to routinely incorporate PPI into research. In the case studies with the most embedded PPI, researchers and lay representatives clearly had a shared understanding of PPI. However, our tracking of studies also showed that understandings could change with time, generally towards more coherence but occasionally away from it. For the newer researchers and the majority of lay representatives, PPI was not a new concept. However, newer researchers found it more challenging to distinguish between research participation and involvement, which may reflect their inexperience in developing grant applications requiring a detailed PPI strategy. This was further compounded by a lack of training on PPI for researchers.
Patient and public involvement was significantly helped by having a defined lead for PPI. 23 If this person was a member of the research team, it was important that they had enough time to fully carry out this role, and often the demands of the role were hidden, particularly when providing a ‘lay representative centred approach’ by going the extra mile. Dedicated PPI co-ordinators appeared to be most effective if they were colocated with research teams.
The operational work required to incorporate PPI routinely was considerable. This included ways of managing payments in good time, having a central point of contact, regular communication and engagement. Having a developed infrastructure to support this operational work reaped benefits in terms of embedding PPI. Although clear in INVOLVE guidance,189 for some of our respondents the principle of reimbursement for time was a contentious issue. A minority of researchers felt that payment for time was in danger of professionalising PPI,208 which should be undertaken as volunteer activity. This view was not articulated in case studies with embedded PPI. However, some lay representatives who led patient organisations felt strongly that lack of reimbursement for time was devaluing PPI and those undertaking this role. This was confirmed by other PPI respondents, who saw symbolic value in the payment. Interestingly, few of our case studies had formal job descriptions for their PPI representatives, which contrasts with INVOLVE guidance. 23 The emphasis was more on enabling a flexible approach that could be hindered by any prescriptive roles; nevertheless, there remained a need to clarify expectations at the beginning of a study. Equally, few lay respondents reported any particular need for training, or highlighted previous training as essential. Instead they described learning on the job and the need for a supportive relationship with the research team. This contrasted with several of the newer researchers we interviewed, who highlighted their lack of preparation for PPI and voiced this as a need. However, as discussed earlier, the most important operational work was the building and sustaining of relationships. This was enhanced when people had confidence in each other and a relationship based on trust was established. If this relationship between lay representatives and researchers was present and maintained, then PPI was enabled to have positive impact even in studies with minimal infrastructure.
There was very little systematic evaluation of discussion of the processes and impact of PPI within a study. There was some evidence of informal evaluations, with respondents describing how they might refine processes in the future. There were a number of reasons for this. First, some researchers had not thought of evaluating PPI, as they just saw it as part of the whole research process and so as not requiring particular evaluation. Second, there was no time built into the study to do this. Third, because of the dynamic and flexible nature of PPI it was difficult for researchers to know which parts to ‘capture’. Finally, and reflecting previous commentaries on evaluating PPI,19 researchers felt that PPI was too complex to evaluate in any objective way.
What was the impact of patient and public involvement on research processes and outcomes?
The majority of researcher respondents readily offered their perceptions of PPI impact on processes and outcomes of their study, but most PPI respondents found it more difficult to articulate what difference they had made. However, this proved markedly different in the case studies with embedded PPI, probably reflecting the robust feedback mechanisms to assess lay participation employed in these case studies.
One case study linked improvement in recruitment rates to PPI. Apart from this example, the impact of PPI was rarely quantified. Recruitment was the most frequently mentioned area in which PPI was seen as having a ‘visible’ impact, and is a recurring focus in the literature. 70,78–86 Recruitment processes were part of the overall research design and provided a natural entry for PPI. Case studies had evidence of PPI impact on other elements of the design such as choice of outcome measures, ensuring tools were participant-sensitive or involvement in developing the intervention.
The impact of PPI on research priority and question setting was most evident in the case studies categorised as exemplifying the fully intertwined model. The potential safety of participants was a particularly interesting PPI impact. There has been a growing interest in PPI and its potential impact on improving patient safety in health care. 214–218 Arguments for PPI in patient safety include providing a final ‘buffer’ to prevent errors214 and reinforcing the moral argument that patients should be included in processes regarding their own care and treatment. 216 However, what is surprising is the lack of consideration of PPI in health-care research acting as the final check for participants. The RAPPORT study did not include the perspective of those participating in the research of each case study (unless in a dual role). However, a recent consultation exercise conducted by Ipsos MORI and the NHS Health Research Authority identified that potential participants feel reassured if they know that there has been PPI during the design of the study. 219 Teasing out the impact of PPI on research participant safety and lessons to be drawn from broader health-care delivery merits further exploration.
What are the barriers and enablers to effective patient and public involvement in research?
A lack of a shared understanding of what PPI was, and of its purpose, was seen to be the main barrier to effective PPI. The discourse of the RAPPORT respondents tended to be framed within either a methodological or a moral perspective, but these viewpoints were not mutually exclusive, and did not appear to have a negative impact on each other. For example, researchers may articulate PPI more from the methodological perspective (to improve research quality), whereas lay representatives within the case study may frame their involvement more from the moral viewpoint (a right to be involved or an altruistic motive). As suggested by others,25,174 as long as both of these perspectives were acknowledged then PPI was enabled. However, there were a few examples when conflict arose because, rather than being synergistic values, they worked in tension, for example PPI role in management and governance of study versus PPI right to have joint ownership of data because of charitable funding of the study.
Other barriers to PPI impact derived from how far lay involvement was limited and constrained by the researchers as indicative of the one-off model of PPI. Although we acknowledge that modest levels of PPI activity may be appropriate in certain studies, our concerns are that adopting such modest levels should be justified. For example, the impact of PPI on potential safety issues for participants had an unexpected outcome and might not have happened if the lay representative had not been so fully involved. On a practical level, lack of time was a significant barrier to PPI. Short, intense projects with relatively small research teams found it more difficult to operationalise PPI in their study.
Access to established PPI groups or panels was seen as an efficient and time-saving approach to PPI. However, this also ran the risk of being a tick box exercise and worked against the relationship building so necessary for effective PPI within a study. Equally, while we endorse the guidance from INVOLVE on identifying a lead for PPI,23 we found that the PPI co-ordinator role also had potential for research team members to abdicate responsibilities for engaging with PPI. However, a co-ordinator working alongside fully engaged research teams was a significant enabler. This is linked to the establishing and sustaining of relationships based on mutual trust and respect as being the over-riding principal enabler. This endorses current guidance on organisational responsibilities. 23 The RAPPORT study findings suggest that case studies with fully embedded PPI treated lay representatives in the same way as other valued members of the team, including considering their long-term future beyond the current study.
Key conclusions
Relational work appears to be the foundation stone for effective PPI and, while relationships are acknowledged to be part of the architecture of PPI,29,101,137 their central importance above other processes and resources has not been previously highlighted. These relationships are framed by trust, mutual respect and responses between researchers and lay representatives being framed by synergistic team membership. 105
A dedicated PPI co-ordinator either within or outside the team is a significant enabler of PPI. However, there can also be unintended consequences of this role in that acting as a bridge188 between the research team and lay representatives could result in research teams abdicating any responsibilities for PPI engagement. Equally, PPI panels such as those established in the NIHR78 or regional15,144 research infrastructure could also have the unintended consequence of PPI becoming a commodity and, in a few examples, reinforce the separation between lay and research worlds.
Finally, concerns raised elsewhere that there is little systematic evaluation of PPI by researchers in their studies21,30 were also highlighted in the RAPPORT study findings. Research teams that are already fully engaged with PPI and well resourced in terms of PPI staff and time are likely to work towards systematic evaluation of impact, for example as suggested by the PiiAF project. 175 However, for research teams with fewer resources it is unlikely that without further incentives they will undertake any evaluative work which diverts them from the intense nature of running a study with limited staff and time. There is still an argument for developing instruments to measure impact in the future,21 and also a more formalised accountability framework to increase transparency of PPI reporting and monitoring.
Reflections on and limitations of the research
The RAPPORT study sample was limited to six topic areas; while these were purposively selected to provide a broad range in terms of designs, settings and target participant populations, we acknowledge that this does not include areas where, for example, there is a growing body of user-led research, such as in mental health. 173,220 Basing data collection on the UKCRN portfolio will have also excluded smaller charity-funded projects; however, the portfolio does represent mainstream health-care research. In addition, some numbers within a topic area are very small, making analysis/significant differences difficult to calculate in the scoping and survey. Because publicly accessible documents were rarely available within the scoping we had to request documents from research teams. Therefore, in all three phases of the research our respondents were more likely to be positive towards PPI than those who did not accept the invitation to participate.
We identified case studies through the survey, and our sampling frame ensured a range of study designs and topic areas. However, we did not include in the frame the range of possible PPI activities and roles, and it was not possible to explore the increasing use of codesign methods and co-researcher roles that define the study approach.
We had case studies at the early stages of the research process. Whereas we were able to capture PPI-specific issues relating to project start-up and recruitment, this meant that PPI outcomes and impact were more challenging to assess within the study time frame.
The RAPPORT study is one of the most extensive in-depth empirical studies of PPI in research with international relevance. To the best of our knowledge it is also one of the first studies to combine the use of NPT and a RE framework. We found NPT to be particularly useful in teasing out why PPI appeared to work better in some case studies, and it fitted well within the RE framework.
Implications for patient and public involvement practice
There already exists a great volume of guidance for PPI in health research, for example from INVOLVE,23 the Mental Health Research Network,221 RDS,222 British Paediatric Surveillance Unit,223 Dementias and Neurodegenerative Diseases Research Network224 and CLAHRCs. 225 Rather than produce another set of guidance, this section presents the key learning from the RAPPORT study as practical points that further illuminate existing guidelines. These are based on our key findings presented in the six CMO configuration tables (see Chapters 5 and 6):
-
the purpose, role and structure of PPI
-
recruiting lay representatives likely to have an understanding of the diverse viewpoints of the target study population
-
whole research team engagement with PPI
-
mutual understanding and trust between researchers and lay representatives
-
opportunities for PPI in all parts of the research process.
Reflection, appraisal and evaluation
Purpose, role and structure of patient and public involvement
-
Shared understanding of the purpose of PPI can be enabled if time is set aside as early as possible to discuss both researcher and lay perspectives and understanding.
-
Training on PPI, particularly for early-career researchers, could address some of the misconceptions. The dissemination events confirmed this as a priority area, suggesting that this training would be best undertaken jointly with lay representatives. Incorporating input on PPI within good clinical practice training was also identified as a way of enhancing understanding.
-
Clarity of roles with terms of reference should be developed early on, but these must be flexible to ensure that roles can adapt to the individual lay representative’s needs and the needs of the research study.
Recruiting lay representatives likely to have an understanding of the diverse viewpoints of the target study population
-
Specific models of PPI are more likely to enable links with a more diverse population. The fully intertwined model involved drawing in a broad range of PPI representatives who were fully involved in the research process. Typically, a large number of lay representatives are involved in this model who need support from a dedicated co-ordinator, training and supplementary social events outside the research study core business. This model requires adequate resources in terms of reimbursement (financial or other, such as accredited training) for PPI, research organisation staffing, time and costs for support.
-
The outreach model involves smaller numbers of PPI representatives whose role is to link out with a diverse population. However, to succeed they must have the links and credibility with the wider community and networking skills. As with all models, there should be appropriate reimbursement which is realistic and sustainable, including adequate funding for any charity or voluntary group involved.
-
The dual role whereby study participants are also invited to advise or be involved in the study is one way of ensuring the perspective of the target population is captured. Our dissemination stakeholders voiced concerns over potential ethical issues, but also acknowledged its potential advantages. As in all models, no individual can represent a whole population, so careful thought is required about specifically which and how many participants are playing this dual role. Most importantly, the potential ethical issues must be thought through. For example, how roles should be separated, at times when an individual is a participant and also involved, what terms of reference are necessary and how participants may be approached to avoid any sense of obligation.
-
Some case studies used advertising as a successful way of recruiting more diverse PPI representatives. Our dissemination stakeholders suggested that spreading the message more widely about PPI needed to be undertaken at a more strategic level.
Whole research team engagement with patient and public involvement
-
Having a PPI co-ordinator and ease of access to existing PPI groups is an enabler of PPI. However, all those involved need to reflect on whether or not reliance on a single individual to lead PPI and pragmatically using existing groups are hindering whole team engagement with PPI.
-
To engage researchers with PPI, the added value to them needs to be made clearer. For example, engaging the public with science is increasingly a remit for researchers, and PPI can help develop and hone the skills required for this.
Opportunities for patient and public involvement in all parts of the research process
-
Researchers and lay representatives need to work together to ensure that the potential impact of PPI is fully realised. This may require research teams to try out new approaches in partnership with lay representatives, and learn from other research teams’ experiences.
Mutual understanding and trust between researchers and lay representatives
-
If PPI representatives and research team are not already known to each other, time must be built in early on for social engagement; hospitality costs should also be covered.
-
Building early relationships with representatives in virtual PPI must be carefully planned.
-
Lack of feedback is a major cause of disengagement. Feedback should always be given to PPI representatives on responses to their suggestions, and studies’ results.
-
Maintain links with PPI representatives even after the project has completed; regular communication (e.g. biannual emails/newsletters) maintains engagement. Enable or signpost further PPI opportunities for representatives when a study completes.
Reflection, appraisal and evaluation
-
Build in the evaluation strategy early on so that information on PPI impact and outcomes can be collected and reflected upon as the study progresses. This strategy should be kept simple and manageable. Evaluative frameworks should be utilised that can also capture unforeseen PPI outcomes.
-
Information should routinely be collected on the level and extent of PPI, methods of recruiting PPI, impact on research processes and, where possible, impact on research outcomes.
Implications for lay representatives
Our dissemination events confirmed that the RAPPORT study had several implications for lay representatives. These are summarised as key messages in Box 34.
-
As a minimum, you and the research team need to clarify your PPI role and responsibilities and maintain a good working relationship with you to support you to undertake tasks.
-
There should be a named link person on the research team with whom you feel comfortable liaising with in the first instance.
-
Be prepared to challenge the research team if there are things that need to be changed for you to undertake these tasks, or to renegotiate them. You may feel that you need support to do this, so have some options.
-
Be aware of existing support structures locally and nationally that can offer advice, support and opportunities for further involvement or training.
-
Keep researchers informed of any changes in circumstances that may affect your ability to undertake specific tasks, what to put in place to support you or how tasks could be reallocated or changed.
-
Wherever possible, work with the research team to record both your input and associated outcomes.
Recommendations for future development and research
It was clear from the RAPPORT study that research host organisations with core funding and stability for PPI were able to embed PPI as routine practice, which has implications for the national research infrastructure. However, it was also evident that PPI could be enabled if the relational work was appropriately achieved. A focus on this area of work needs to be incorporated into training for researchers, particularly those less experienced in PPI and research. Seven clear areas have been identified from the RAPPORT study:
-
Virtual PPI needs further evaluation. The move towards virtual PPI can be mapped within health-care commissioning and delivery,226 and is a common model for general practice patient participation groups. 57 It is also becoming increasingly common in health research. However, as the RAPPORT study has highlighted the importance of relationships in PPI, further research is required to evaluate how this can be best managed within the virtual world. The requirement of access to e-mail and its impact on including seldom-heard groups should also be included in this evaluation.
-
Virtual PPI is potentially an effective way of involving younger people. Only one case study had lay representatives primarily from this age group, and there were challenges in maintaining engagement. Further research is therefore recommended into the particular issues of engaging young people in PPI.
-
The PPI training needs of researchers need to be explored, using the findings of the study and the NPT process as a framework for the curriculum. So does understanding the balance between supportive infrastructure and the potential for research teams to abdicate engagement with PPI and externally source it for a one-off activity.
-
Further evaluation is required of the impact of PPI on issues of participant safety in clinical trials.
-
A future costs analysis and economic evaluation of the different models of PPI is recommended that could consider relative impact on key outcomes such as recruitment, study milestones and dissemination and uptake of study findings by patient groups.
-
Little is known about the extent, experience, outcomes and implications of the dual role in PPI. More research is required to explore this further, and specific guidance should be developed.
-
Outcomes of PPI on research findings and impact on services and clinical practice requires a longer-term follow-up study. The RAPPORT study has collected rich data from 18 months of a research study. Tracking the longer-term impact of these studies and how PPI has influenced this would be a unique opportunity to determine longer-term PPI outcomes.
Acknowledgements
The research team would like to thank members of the RAPPORT advisory group for all their support during the study:
Ruth Sawtell (lay chair)
Antony Chuter (lay member)
Penny Vicary (lay member)
Amander Wellings (lay member)
Fiona Brooks (professor and head of adolescent and child health research)
Katherine Froggatt (senior lecturer in health research)
Thomas Kabir (Mental Health Research Network service users in research co-ordinator)
Mike Kelly (professor and director of the Centre for Public Health – National Institute for Health and Care Excellence)
Carl May (professor of health-care innovation)
Jackie Ord (learning disabilities research and development manager)
Gurch Randhawa (professor of diversity in public health).
We would also like to thank our lay co-researcher, Sue Miller, and all the members of the CF and IDD reference groups.
All members of the University of Hertfordshire Public Involvement in Research Group contributed to the original idea and design of the RAPPORT study, and we acknowledge with thanks their contribution and ongoing support.
Contributions of authors
Professor Patricia Wilson (Professor in Primary and Community Care). Chief investigator, designed the study, provided overall direction, led on four case studies, analysed data and drafted sections of the report.
Dr Elspeth Mathie (research fellow, patient and public involvement). Managed the project, led on 12 case studies, analysed data and drafted sections of the report.
Dr Julia Keenan (senior research associate, patient and public involvement). Led on six case studies, analysed data and drafted sections of the report.
Mrs Elaine McNeilly (research assistant, patient and public involvement). Conducted data collection, analysed data and drafted sections of the report.
Professor Claire Goodman (Professor of Health Services Research). Coapplicant, advised on the study and reviewed the report.
Professor Amanda Howe (Professor of Primary Care). Coapplicant, advised on the study, including approaches to analysis, and reviewed the report.
Professor Fiona Poland (Professor of Social Research Methodology). Coapplicant, advised on the study and reviewed the report.
Dr Sophie Staniszewska (senior research fellow, patient and public involvement and patient experiences). Coapplicant, advised on the study and reviewed the report.
Professor Sally Kendall (Professor of Nursing and Director of Centre for Research in Primary and Community Care). Coapplicant, advised on the study and reviewed the report.
Ms Diane Munday (member of the University of Hertfordshire Public Involvement in Research Group). Coapplicant, performed data collection and analysis and drafted sections of the report.
Ms Marion Cowe (member of the University of Hertfordshire Public Involvement in Research Group). Coapplicant, performed data collection and analysis and reviewed the report.
Professor Stephen Peckham (Professor of Health Policy). Coapplicant, advised on the study and reviewed the report.
Publications
Mathie E, Wilson P, Poland F, Mcneilly E, Howe A, Staniszewska S, et al. Consumer Involvement in health research: a UK scoping and survey. Int J Consum Stud 2014;38:35–44.
Data sharing statement
All available data can be obtained from the corresponding author subject to safeguarding confidentiality and anonymity of participants.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
References
- Patient and Public Involvement in the New NHS. London: Department of Health; 1999.
- Patient and Public Involvement in Health: The Evidence for Policy Implementation. London: Department of Health; 2004.
- Stronger Voice, Better Care. London: Department of Health; 2008.
- Liberating the NHS: No Decision about Me without Me. Government Response to the Consultation. London: Department of Health; 2012.
- Research Governance Framework for Health and Social Care. London: Department of Health; 2005.
- Best Research for Best Health. London: Department of Health; 2006.
- Staniszewska S, Denegri S. Patient and public involvement in research: future challenges. Evidence Based Nurs 2013;16. http://dx.doi.org/10.1136/eb-2013-101406.
- Boivin A, Currie K, Fervers B, Gracia J, James M, Marshall C, et al. Patient and public involvement in clinical guidelines: international experiences and future perspectives. Qual Saf Health Care 2010;19:1-4. http://dx.doi.org/10.1136/qshc.2009.034835.
- National Institutes of Health . Director’s Council of Public Representatives n.d. www.nih.gov/about/copr/index.htm (accessed March 2014).
- Consumers Health Forum of Australia . What We Do n.d. www.chf.org.au/who-we-are.php (accessed March 2014).
- World Health Organization . Ninth Futures Forum on Health Systems Governance and Public Participation n.d. www.euro.who.int/document/e89766.pdf (accessed March 2014).
- Entwistle VA, Renfrew MJ, Yearley S, Forrester J, Lamont T. Lay perspectives: advantages for health research. BMJ 1998;316:463-6. http://dx.doi.org/10.1136/bmj.316.7129.463.
- Delbanco T, Berwick DM, Boufford JI, Edgman-Levitan S, Ollenschlager G, Plamping D, et al. Healthcare in a land called PeoplePower: nothing about me without me. Health Expect 2001;4:144-50. http://dx.doi.org/10.1046/j.1369-6513.2001.00145.x.
- Baggott R. Health and Health Care in Britain. Basingstoke: Palgrave Macmillan; 2004.
- Howe A, Delaney S, Romero J, Tinsley A, Vicary P. Public involvement in health research: a case study of one NHS project over 5 years. Prim Health Care Res Dev 2010;11:17-28. http://dx.doi.org/10.1017/S1463423609990405.
- McKevitt C, Fudge N, Wolfe C. What is involvement in research and what does it achieve? Reflections on a pilot study of the personal costs of stroke. Health Expect 2009;13:86-94. http://dx.doi.org/10.1111/j.1369-7625.2009.00573.x.
- Staniszewska SH, Jones N, Newburn M, Marshall S. User involvement in the development of a research bid: barriers, enablers and impacts. Health Expect 2007;10:173-83. http://dx.doi.org/10.1111/j.1369-7625.2007.00436.x.
- Smith E, Ross F, Donovan S, Manthorpe J, Brearley S, Sitzia J, et al. Service user involvement in nursing, midwifery and health visiting research: a review of evidence and practice. Int J Nurs Stud 2008;45:298-315. http://dx.doi.org/10.1016/j.ijnurstu.2006.09.010.
- Staley K. Exploring Impact: Public Involvement in NHS, Public Health and Social Care Research n.d. www.invo.org.uk/pdfs/Involve_Exploring_Impactfinal28.10.09.pdf (accessed March 2014).
- Forbat L, Hubbard G, Kearney N. Patient and public involvement: models and muddles. J Clin Nurs 2009;18:2547-54. http://dx.doi.org/10.1111/j.1365-2702.2008.02519.x.
- Staniszewska S, Brett J, Mockford C, Barber R. The GRIPP checklist: strengthening the quality of patient and public involvement reporting in research. Int J Technol Assess Health Care 2011;27:391-9. http://dx.doi.org/10.1017/S0266462311000481.
- Jordan Z, Court A. Reconstructing consumer participation in evidence-based health care: a polemic. Int J Consum Stud 2010;34:558-61. http://dx.doi.org/10.1111/j.1470-6431.2010.00906.x.
- Hayes H, Buckland S, Tarpey M. Briefing Notes for Researchers: Public Involvement in NHS, Public Health and Social Care Research. Eastleigh: INVOLVE; 2012.
- Boote JD, Twiddy M, Baird W, Birks Y, Clarke C, Beever D. Supporting public involvement in research design and grant development: a case study of a public involvement award scheme managed by a National Institute for Health Research (NIHR) Research Design Service (RDS) [published online ahead of print October 1 2013]. Health Expect n.d.
- Gradinger F, Britten N, Wyatt K, Froggatt K, Gibson A, Jacoby A, et al. Values associated with public involvement in health and social care research: a narrative review [published online ahead of print December 10 2013]. Health Expect n.d.
- Wilson PM. A policy analysis of the Expert Patient in the United Kingdom: self-care as an expression of pastoral power?. Health Soc Care Commun 2001;9:134-42. http://dx.doi.org/10.1046/j.1365-2524.2001.00289.x.
- Kreindler SA. Patient involvement and the politics of methodology. Can Public Admin 2009;52:113-24. http://dx.doi.org/10.1111/j.1754-7121.2009.00062.x.
- Thompson J, Barber R, Ward PR, Boote JD, Cooper CL, Armitage CJ, et al. Health researchers’ attitudes towards public involvement in health research. Health Expect 2009;12:209-20. http://dx.doi.org/10.1111/j.1369-7625.2009.00532.x.
- Brett J, Staniszewska S, Mockford C, Herron-Marx S, Hughes J, Tysall C, et al. Mapping the impact of patient and public involvement on health and social care research: a systematic review. Health Expect 2014;17:637-50. http://dx.doi.org/10.1111/j.1369-7625.2012.00795.x.
- Staniszewska S, Adebajo A, Barber R, Beresford P, Brady L-M, Brett J, et al. Developing the evidence base of patient and public involvement in health and social care research: the case for measuring impact. Int J Consum Stud 2011;35:628-32. http://dx.doi.org/10.1111/j.1470-6431.2011.01020.x.
- Barber R, Beresford P, Boote J, Cooper C, Faulkner A. Evaluating the impact of service user involvement on research: a prospective case study. Int J Consum Stud 2011;35:609-15. http://dx.doi.org/10.1111/j.1470-6431.2011.01017.x.
- Staley K, Buckland SA, Hayes H, Tarpey M. ‘The missing links’: understanding how context and mechanism influence the impact of public involvement in research. Health Expect 2014;17:755-64. http://dx.doi.org/10.1111/hex.12017.
- Baggott R, Allsop J, Jones K. Speaking for Patients and Carers: The Role of Health Consumer Groups in the Policy Process. Basingstoke: Palgrave; 2005.
- Barnes M, Simmons R, Powell M, Greener I. The Consumer in Public Services. Bristol: Policy Press; 2009.
- The Royal Liverpool Children’s Inquiry: Summary and Recommendations. London: The Stationery Office; 2001.
- The Report of the Public Inquiry into Children’s Heart Surgery at the Bristol Royal Infirmary 1984–1995: Learning from Bristol. London: The Stationery Office; 2001.
- Morrow E, Boaz A, Brearley S, Ross F. Handbook of Service User Involvement in Nursing and Healthcare Research. Chichester: Wiley-Blackwell; 2012.
- Martin GP. ‘Ordinary people only’: knowledge, representativeness and the publics of public participation in healthcare. Sociol Health Illn 2008;30:35-54. http://dx.doi.org/10.1111/j.1467-9566.2007.01027.x.
- Ward PR, Thompson J, Barber R, Armitage CJ, Boote JD, Cooper CL, et al. Critical perspectives on ‘consumer involvement’ in health research: epistemological dissonance and the know–do gap. J Sociol 2010;46:63-82. http://dx.doi.org/10.1177/1440783309351771.
- Oliver M. Changing the social relations of research production?. Disability Handicap Soc 1992;7:101-14. http://dx.doi.org/10.1080/02674649266780141.
- Cotterell P, Morris C, Barnes M, Cotterell P. Critical Perspectives on User Involvement. Bristol: Policy Press; 2012.
- Hunt P. Settling accounts with the parasite people: a critique of ‘A Life Apart’ by E.J. Miller and G.V. Gwynne. Disability Challenge 1981;1:37-50.
- Barnes M, Cotterell P, Barnes M, Cotterell P. Critical Perspectives on User Involvement. Bristol: Policy Press; 2012.
- Caron-Flinterman JF, Broerse JEW, Bunders JFG. The experiential knowledge of patients: a new resource for biomedical research?. Soc Sci Med 2005;60:2575-84. http://dx.doi.org/10.1016/j.socscimed.2004.11.023.
- Prior L. Belief, knowledge and expertise: the emergence of the lay expert in medical sociology. Sociol Health Illn 2003;25:41-7. http://dx.doi.org/10.1111/1467-9566.00339.
- Thompson J, Bissell P, Cooper C, Armitage CJ, Barber R. Credibility and the ‘professionalized’ lay expert: reflections on the dilemmas and opportunities of public involvement in health research. Health 2012;16:602-18. http://dx.doi.org/10.1177/1363459312441008.
- Barnes M, Cotterell P, Barnes M, Cotterell P. Critical Perspectives on User Involvement. Bristol: Policy Press; 2012.
- The NHS and Community Care Act. London: HMSO; 1990.
- Lupton C, Peckham S, Taylor P. Managing Public Involvement in Healthcare Purchasing. Milton Keynes: Open University Press; 1998.
- Connelly J. Public health policy: between victim blaming and the nanny state – will the third way work?. Policy Stud 1999;20:51-67. http://dx.doi.org/10.1080/01442879908423766.
- Baxter L, Thorne L, Mitchell A. Small Voices Big Noises: Lay Involvement in Health Research. Lessons from Other Fields. Eastleigh: INVOLVE; 2001.
- McKevitt C. Experience, knowledge and evidence: a comparison of research relations in health and anthropology. Evid Policy 2013;9:113-30. http://dx.doi.org/10.1332/174426413X663751.
- Greene J, Hibbard JH. Why does patient activation matter? An examination of the relationships between patient activation and health-related outcomes. J Gen Intern Med 2012;27:520-6. http://dx.doi.org/10.1007/s11606-011-1931-2.
- Self-Care Reduces Costs and Improves Health: The Evidence. London: EPP; 2010.
- Wilson PM, Goodman C. Evaluation of a modified chronic disease self-management programme for people with intellectual disabilities. J Nurs Healthc Chronic Illn 2011;3:310-18. http://dx.doi.org/10.1111/j.1752-9824.2011.01105.x.
- Wilson PM, Kendall S, Brooks F. The Expert Patients Programme: a paradox of patient empowerment and medical dominance. Health Soc Care Commun 2007;15:426-38. http://dx.doi.org/10.1111/j.1365-2524.2007.00701.x.
- Peckham S, Wilson PM, Williams L, Smiddy J, Reay J, Bloomfield L, et al. Commissioning for long-term conditions: hearing the voice of and engaging users. Health Serv Deliv Res 2014;2.
- McCormick S, Brody J, Brown P, Polk R. Public involvement in breast cancer research: an analysis and model for future research. Int J Health Serv 2004;34:625-46. http://dx.doi.org/10.2190/HPXB-9RK8-ETVM-RVEA.
- Stevens T, Wilde D, Hunt J, Ahmedzai S. Overcoming the challenges to consumer involvement in cancer research. Health Expect 2003;6:81-8. http://dx.doi.org/10.1046/j.1369-6513.2003.00214.x.
- Wright D, Corner J, Hopkinson J, Foster C. Listening to the views of people affected by cancer about cancer research: an example of participatory research in setting the cancer research agenda. Health Expect 2006;9:3-12. http://dx.doi.org/10.1111/j.1369-7625.2006.00353.x.
- Staley K. A Series of Case Studies Illustrating the Impact of Service User and Carer Involvement on Research. London: Mental Health Research Network; 2013.
- Oliver S, Armes D, Gyte G. Public involvement in setting a national research agenda. Patient Centered Outcomes Res 2009;2:179-90. http://dx.doi.org/10.2165/11314860-000000000-00000.
- Walker D-M, Pandya-Wood R. Can research development bursaries for patient and public involvement have a positive impact on grant applications? A UK-based, small-scale service evaluation [published online ahead of print September 19 2013]. Health Expect n.d.
- Boote JD, Dalgleish M, Freeman J, Jones Z, Miles M, Rodgers H. ‘But is it a question worth asking?’ A reflective case study describing how public involvement can lead to researchers’ ideas being abandoned. Health Expect 2012;17:440-51. http://dx.doi.org/10.1111/j.1369-7625.2012.00771.x.
- Elberse JE, Pittens CACM, de Cock Buning T, Broerse JEW. Patient involvement in a scientific advisory process: setting the research agenda for medical products. Health Policy 2012;107:231-42. http://dx.doi.org/10.1016/j.healthpol.2012.05.014.
- Abma TA. Patient participation in health research: research with and for people with spinal cord injuries. Qual Health Res 2005;15:1310-28. http://dx.doi.org/10.1177/1049732305282382.
- Broerse JEW, Zweekhorst MBM, van Rensen AJML, de Haan MJM. Involving burn survivors in agenda setting on burn research: an added value?. Burns 2010;36:217-31. http://dx.doi.org/10.1016/j.burns.2009.04.004.
- Andejeski Y, Bisceglio IT, Dickersin K, Johnson JE, Robinson SI, Smith HS, et al. Quantitative impact of including consumers in the scientific review of breast cancer research proposals. J Womens Health Gend Based Med 2002;11:379-88. http://dx.doi.org/10.1089/152460902317586010.
- Royle J, Oliver S. Consumers are helping to prioritise research. BMJ 2001;323:48-9.
- Lindenmeyer A, Hearnshaw H, Sturt J, Ormerod R, Aitchison G. Assessment of the benefits of user involvement in health research from the Warwick Diabetes Care Research User Group: a qualitative case study. Health Expect 2007;10:268-77. http://dx.doi.org/10.1111/j.1369-7625.2007.00451.x.
- Carter P, Beech R, Cox D, Thomas MJ, Jinks C. Mobilising the experiential knowledge of clinicians, patients and carers for applied health-care research. Contemp Soc Sci 2013;8:307-20. http://dx.doi.org/10.1080/21582041.2013.767468.
- Vale C, Thompson L, Murphy C, Forcat S, Hanley B. Involvement of consumers in studies run by the Medical Research Council Clinical Trials Unit: results of a survey. Trials 2012;13. http://dx.doi.org/10.1186/1745-6215-13-9.
- Edwards V, Wyatt K, Logan S, Britten N. Consulting parents about the design of a randomized controlled trial of osteopathy for children with cerebral palsy. Health Expect 2011;14:429-38. http://dx.doi.org/10.1111/j.1369-7625.2010.00652.x.
- Fairbrother P, McCloughan L, Adam G, Brand R, Brown C, Watson M, et al. Involving patients in clinical research: the Telescot Patient Panel [published online ahead of print September 30 2013]. Health Expect 2013. http://dx.doi.org/10.1111/hex.12132.
- Paterson C, Allen JA, Browning M, Barlow G, Ewings P. A pilot study of therapeutic massage for people with Parkinson’s disease: the added value of user involvement. Complement Ther Clin Pract 2005;11:161-71. http://dx.doi.org/10.1016/j.ctcp.2004.12.008.
- Miller E, Cook A, Alexander H, Cooper S, Hubbard G, Morrison J, et al. Challenges and strategies in collaborative working with service user researchers: reflections from the academic researcher. Res Policy Plann 2006;24:197-208.
- Hofmann D, Ibrahim F, Rose D, Scott DL, Cope A, Wykes T, et al. Expectations of new treatment in rheumatoid arthritis: developing a patient-generated questionnaire [published online ahead of print April 25 2013]. Health Expect n.d.
- Iliffe S, McGrath T, Mitchell D. The impact of patient and public involvement in the work of the Dementias & Neurodegenerative Diseases Research Network (DeNDRoN): case studies. Health Expect 2013;16:351-61. http://dx.doi.org/10.1111/j.1369-7625.2011.00728.x.
- Savage CL, Xu Y, Lee R, Rose BL, Kappesser M, Anthony JS. A case study in the use of community-based participatory research in public health nursing. Public Health Nurs 2006;23:472-8. http://dx.doi.org/10.1111/j.1525-1446.2006.00585.x.
- Langston AL, McCallum M, Campbell MK, Robertson C, Ralston SH. An integrated approach to consumer representation and involvement in a multicentre randomized controlled trial. Clin Trials 2005;2:80-7. http://dx.doi.org/10.1191/1740774505cn065oa.
- Dewar BJ. Beyond tokenistic involvement of older people in research: a framework for future development and understanding. J Clin Nurs 2005;14:48-53. http://dx.doi.org/10.1111/j.1365-2702.2005.01162.x.
- Goodman CM, Mathie EJ, Cowe M, Mendoza A, Westwood D, Munday D, et al. Talking about living and dying with the oldest old: public involvement in a study on end of life care in care homes. BMC Palliat Care 2011;10. http://dx.doi.org/10.1186/1472-684x-10-20.
- Terry SF, Terry PF, Rauen KA, Uitto J, Bercovitch LG. Advocacy groups as research organizations: the PXE International example. Nat Rev Genet 2007;8:157-64. http://dx.doi.org/10.1038/nrg1991.
- Burrus BB, Liburd LC, Burroughs A. Maximizing participation by black Americans in population-based diabetes research: the Project DIRECT pilot experience. J Community Health 1998;23:15-27. http://dx.doi.org/10.1023/A:1018718803890.
- Caldon LJM, Marshall-Cork H, Speed G, Reed MWR, Collins KA. Consumers as researchers: innovative experiences in UK National Health Service Research. Int J Consum Stud 2010;34:547-50. http://dx.doi.org/10.1111/j.1470-6431.2010.00907.x.
- Krieger J, Allen C, Cheadle A, Ciske S, Schier JK, Senturia K, et al. Using community-based participatory research to address social determinants of health: lessons learned from Seattle Partners for Healthy Communities. Health Educ Behav 2002;29:361-82. http://dx.doi.org/10.1177/109019810202900307.
- Williamson T, Brogden J, Jones E, Ryan J. Impact of public involvement in research on quality of life and society: a case study of research career trajectories. Int J Consum Stud 2010;34:551-7. http://dx.doi.org/10.1111/j.1470-6431.2010.00909.x.
- Faulkner A. Beyond Our Expectations: A Report of the Experiences of Involving Service Users in Forensic Mental Health Research. London: National Programme for Forensic Mental Health R&D; 2007.
- Clark CC, Scott EA, Boydell KM, Goering P. Effects of client interviewers on client-reported satisfaction with mental health services. Psychiatr Serv 1999;5:961-3. http://dx.doi.org/10.1176/ps.50.7.961.
- Philpot M, Collins C, Trivedi P, Treloar A, Gallacher S, Rose D. Eliciting users’ views of ECT in two mental health trusts with a user-designed questionnaire. J Mental Health 2004;13:403-13. http://dx.doi.org/10.1080/09638230410001729843.
- Koops L, Lindley RI. Thrombolysis for acute ischaemic stroke: consumer involvement in design of new randomised controlled trial. BMJ 2002;325. http://dx.doi.org/10.1136/bmj.325.7361.415.
- Forbes LJ, Nicholls CM, Linsell L, Graham J, Tompkins C, Ramirez AJ. Involving users in the design of a randomised controlled trial of an intervention to promote early presentation in breast cancer: qualitative study. BMC Med Res Methodol 2010;10:1471-2288. http://dx.doi.org/10.1186/1471-2288-10-110.
- Rhodes P, Nocon A, Booth M, Chowdrey MY, Fabian A, Lambert N, et al. A service users’ research advisory group from the perspectives of both service users and researchers. Health Soc Care Commun 2002;10:402-9. http://dx.doi.org/10.1046/j.1365-2524.2002.00376.x.
- Palmer R, Paterson G. To what extent can people with communication difficulties contribute to health research?. Nurse Res 2013;20:12-6. http://dx.doi.org/10.7748/nr2013.01.20.3.12.c9491.
- Cotterell P, Clarke P, Cowdrey D, Kapp J, Paine M, Wynn R, et al. Creative Engagement in Palliative Care. Oxford: Radcliffe Publishing; 2007.
- Schneider B, Scissons H, Arney L, Benson G, Derry J, Lucas K, et al. Communication between people with schizophrenia and their medical professionals: a participatory research project. Qual Health Res 2004;14:562-77. http://dx.doi.org/10.1177/1049732303262423.
- Sutton J, Weiss M. Involving patients as advisors in pharmacy practice research: what are the benefits?. Int J Pharm Pract 2008;16:231-8. http://dx.doi.org/10.1211/ijpp.16.4.0005.
- Hewlett S, de Wit M, Richards P, Quest E, Hughes R, Heiberg T, et al. Patients and professionals as research partners: challenges, practicalities, and benefits. Arthritis Care Res 2006;55:676-80. http://dx.doi.org/10.1002/art.22091.
- Jagosh J, Pluye P, Wong G, Cargo M, Salsberg J, Bush PL, et al. Critical reflections on realist review: insights from customizing the methodology to the needs of participatory research assessment. Res Synthesis Methods 2014;5:131-41. http://dx.doi.org/10.1002/jrsm.1099.
- Macaulay AC, Jagosh J, Seller R, Henderson J, Cargo M, Greenhalgh T, et al. Assessing the benefits of participatory research: a rationale for a realist review. Global Health Promot 2011;18:45-8. http://dx.doi.org/10.1177/1757975910383936.
- Shippee ND, Domecq Garces JP, Prutsky Lopez GJ, Wang Z, Elraiyah TA, Nabhan M, et al. Patient and service user engagement in research: a systematic review and synthesized framework [published online ahead of print June 3 2013]. Health Expect n.d.
- Oliver S, Clarke-Jones L, Rees R, Milne R, Buchanan P, Gabbay J, et al. Involving consumers in research and development agenda setting for the NHS: developing an evidence-based approach. Health Technol Assess 2004;8. http://dx.doi.org/10.3310/hta8150.
- Jagosh J, Macaulay AC, Pluye P, Salsberg J, Bush PL, Henderson J, et al. Uncovering the benefits of participatory research: implications of a realist review for health research and practice. Milbank Q 2012;90:311-46. http://dx.doi.org/10.1111/j.1468-0009.2012.00665.x.
- Pawson R, Greenhalgh T, Harvey G, Walshe K. Realist review: a new method of systematic review designed for complex policy interventions. J Health Serv Res Policy 2005;10:21-34. http://dx.doi.org/10.1258/1355819054308530.
- Lasker RD, Weiss ES, Miller R. Partnership synergy: a practical framework for studying and strengthening the collaborative advantage. Milbank Q 2001;79:179-205. http://dx.doi.org/10.1111/1468-0009.00203.
- Boote J, Wong R, Booth A. ‘Talking the talk or walking the walk?’ A bibliometric review of the literature on public involvement in health research published between 1995 and 2009. Health Expect 2012;4:44-57.
- Kreis J, Puhan MA, Schunemann HJ, Dickersin K. Consumer involvement in systematic reviews of comparative effectiveness research. Health Expect 2013;16:323-37. http://dx.doi.org/10.1111/j.1369-7625.2011.00722.x.
- Guarino P, Elbourne D, Carpenter J, Peduzzi P. Consumer involvement in consent document development: a multicenter cluster randomized trial to assess study participants’ understanding. Clin Trials 2006;3:19-30. http://dx.doi.org/10.1191/1740774506cn133oa.
- Medical Research Council . Developing and Evaluating Complex Interventions: New Guidance 2008. www.mrc.ac.uk/complexinterventionsguidance (accessed March 2014).
- Fulop N, Allen P, Clarke A, Black N. Studying the Organisation and Delivery of Health Services. Research Methods. London: Routledge; 2001.
- Fiss P. A set-theoretic approach to organizational configurations. Acad Manag Rev 2007;32:1180-98. http://dx.doi.org/10.5465/AMR.2007.26586092.
- Marchal B, van Belle S, van Olmen J, Hoerée T, Kegels G. Is realist evaluation keeping its promise? A review of published empirical studies in the field of health systems research. Evaluation 2012;18:192-21. http://dx.doi.org/10.1177/1356389012442444.
- Wand T, White K, Patching J. Applying a realist(ic) framework to the evaluation of a new model of emergency department based mental health nursing practice. Nurs Inq 2010;17:231-9. http://dx.doi.org/10.1111/j.1440-1800.2010.00488.x.
- Pawson R, Tilley N. Realistic Evaluation. London: Sage Publications; 2001.
- Pawson R, Tilley N. Realist Evaluation 2004. www.communitymatters.com.au/RE_chapter.pdf (accessed March 2014).
- Collier A. Critical Realism: An Introduction to Roy Bhaskar’s Philosophy. London: Verso; 1994.
- Bhaskar R. Scientific Realism and Human Emancipation. London: Verso; 1986.
- Kontos PC, Poland BD. Mapping new theoretical and methodological terrain for knowledge translation: contributions from critical realism and the arts. Implement Sci 2009;4. http://dx.doi.org/10.1186/1748-5908-4-1.
- Connelly JB. Evaluating complex public health interventions: theory, methods and scope of realist enquiry. J Eval Clin Pract 2007;13:935-41. http://dx.doi.org/10.1111/j.1365-2753.2006.00790.x.
- Merton RK. Social Theory and Social Structure. New York, NY: Free Press; 1968.
- May C, Finch T. Implementing, embedding, and integrating practices: an outline of normalization process theory. Sociology 2009;43:535-54. http://dx.doi.org/10.1177/0038038509103208.
- Delanty G. Beyond Constructivism and Realism. Buckingham: Open University Press; 1997.
- Wilson V, McCormack B. Critical Realism as emancipatory action: the case for realistic evaluation in practice development. Nurs Philos 2006;7:45-57. http://dx.doi.org/10.1111/j.1466-769X.2006.00248.x.
- Rycroft-Malone J, Fontenla M, Bick D, Seers K. A realistic evaluation: the case of protocol-based care. Implement Sci 2010;5. http://dx.doi.org/10.1186/1748-5908-5-38.
- Tolson D, McIntosh J, Loftus L, Cormie P. Developing a managed clinical network in palliative care: a realistic evaluation. Int J Nurs Stud 2007;44:183-95. http://dx.doi.org/10.1016/j.ijnurstu.2005.11.027.
- Hewitt G, Sims S, Harris R. The realist approach to evaluation research: an introduction. Int J Ther Rehabil 2012;19:250-9. http://dx.doi.org/10.12968/ijtr.2012.19.5.250.
- Astbury B, Leeuw F. Unpacking black boxes: mechanisms and theory building in evaluation. Am J Eval 2010;31:363-81. http://dx.doi.org/10.1177/1098214010371972.
- Barnes M, Matka E, Sullivan H. Evidence, understanding and complexity: evaluation in non-linear systems. Evaluation 2003;9:265-84. http://dx.doi.org/10.1177/13563890030093003.
- Habermas J. Knowledge and Human Interests. Boston, MA: Beacon Press; 1972.
- Gibson A, Britten N, Lynch J. Theoretical directions for an emancipatory concept of patient and public involvement. Health 2012;16:531-47. http://dx.doi.org/10.1177/1363459312438563.
- Brett J, Staniszewska S, Mockford C, Seers K, Herron Marx S, Bayliss H. The PIRICOM Study: Systematic Review of the Conceptualization, Measurement, Impact and Outcomes of Patient and Public Involvement in Health and Social Care Research. London: UKCRC; 2010.
- Oliver SR, Rees RW, Clarke-Jones L, Milne R, Oakley AR, Gabbay J, et al. A multidimensional conceptual framework for analysing public involvement in health services research. Health Expect 2008;11:72-84. http://dx.doi.org/10.1111/j.1369-7625.2007.00476.x.
- Boote J, Barber R, Cooper C. Principles and indicators of successful consumer involvement in NHS research: results of a Delphi study and subgroup analysis. Health Policy 2006;75:280-97. http://dx.doi.org/10.1016/j.healthpol.2005.03.012.
- May C, Finch T, Ballini L, MacFarlane A, Mair F, Murray E, et al. Evaluating complex interventions and health technologies using normalization process theory: development of a simplified approach and web-enabled toolkit. BMC Health Serv Res 2011;11. http://dx.doi.org/10.1186/1472-6963-11-245.
- May C, Mair F, Finch T, MacFarlane A, Dowrick C, Treweek S, et al. Development of a theory of implementation and integration: Normalization Process Theory. Implement Sci 2009;4. http://dx.doi.org/10.1186/1748-5908-4-29.
- McDonnell A, Lloyd JM, Read S. Practical considerations in case study research: the relationship between methodology and process. J Adv Nurs 2000;32:383-90. http://dx.doi.org/10.1046/j.1365-2648.2000.01487.x.
- Telford R, Boote JD, Cooper C. What does it mean to involve consumers successfully in NHS research? A consensus study. Health Expect 2004;7:209-20. http://dx.doi.org/10.1111/j.1369-7625.2004.00278.x.
- Matthews DR, Kennedy ED, Darbyshire JH, Johnston DG. The UK Diabetes Research Network: an opportunity and a challenge. Diabet Med 2007;24:7-9. http://dx.doi.org/10.1111/j.1464-5491.2007.02005.x.
- Department of Health . Valuing People Now: A New Three-Year Strategy for Learning Disabilities n.d. http://webarchive.nationalarchives.gov.uk/20130107105354/http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/documents/digitalasset/dh_093375.pdf (accessed March 2014).
- Thompson M, Heneghan C. We need to move the debate on open clinical trial data forward. BMJ 2012;345. http://dx.doi.org/10.1136/bmj.e8351.
- Chalmers I, Glasziou P, Godlee F. All trials must be registered and the results published. BMJ 2013;346. http://dx.doi.org/10.1136/bmj.f105.
- Royal College of Psychiatry . Clinical Syndromes Associated With Learning Disability n.d. www.rcpsych.ac.uk/pdf/CLINICAL%20SYNDROMES%20ASSOCIATED%20WITH%20LEARNING%20DISABILITY.pdf (accessed June 2015).
- Purttell R, Gibson A, Lloyd CE, Heller T. Long-Term Conditions: Challenges in Health and Social Care. London: Sage; 2012.
- Howe A, MacDonald H, Barrett B, Little B. Ensuring public and patient participation in research: a case study in infrastructure development in one UK Research and Development consortium. Prim Health Care Res Dev 2006;7:60-7. http://dx.doi.org/10.1191/1463423606pc269oa.
- Exworthy M, Peckham S, Powell M, Hann A. Shaping Health Policy: Case Study Methods and Analysis. Bristol: Policy Press; 2012.
- Yin RK. Case Study Research Design and Methods. London: Sage Publications; 2009.
- Marinetto M. Studies of the Policy Process: A Case Analysis. London: Prentice Hall Europe; 1998.
- Hartley J, Cassell C, Symon G. Essential Guide to Qualitative Methods in Organizational Research. London: Sage; 2004.
- Abbott S, Shaw S, Elston J. Comparative analysis of health policy implementation: the use of documentary analysis. Policy Stud 2004;25:259-66. http://dx.doi.org/10.1080/0144287042000288451.
- Data Protection Act. London: The Stationery Office; 1998.
- May C, Murray E, Finch T, Mair F, Treweek S, Ballini L, et al. Normalization Process Theory On-Line Users’ Manual and Toolkit 2010. www.normalizationprocess.org (accessed March 2014).
- Schierhout G, Hains J, Si D, Kennedy C, Cox R, Kwedza R, et al. Evaluating the effectiveness of a multifaceted, multilevel continuous quality improvement program in primary health care: developing a realist theory of change. Implement Sci 2013;8. http://dx.doi.org/10.1186/1748-5908-8-119.
- Rycroft-Malone J, Wilkinson J, Burton CR, Harvey G, McCormack B, Graham I, et al. Collaborative action around implementation in Collaborations for Leadership in Applied Health Research and Care: towards a programme theory. J Health Serv Res Policy 2013;18:13-26. http://dx.doi.org/10.1177/1355819613498859.
- Strauss A, Corbin J. Basics of Qualitative Research: Grounded Theory Procedures and Techniques. Newbury Park, CA: Sage Publications; 1990.
- Brannen J. Mixing methods: the entry of qualitative and quantitative approaches into the research process. Int J Soc Res Methodol 2005;8:173-84. http://dx.doi.org/10.1080/13645570500154642.
- O’Cathain A, Murphy E, Nicholl J. Three techniques for integrating data in mixed methods studies. BMJ 2010;341. http://dx.doi.org/10.1136/bmj.c4587.
- Barbour R. Checklists for improving rigour in qualitative research: a case of the tail wagging the dog?. BMJ 2001;332:1115-17. http://dx.doi.org/10.1136/bmj.322.7294.1115.
- Mathie E, Wilson P, Poland F, McNeilly E, Howe A, Staniszewska S, et al. Consumer involvement in health research: a UK scoping and survey. Int J Consum Stud 2014;38:35-44. http://dx.doi.org/10.1111/ijcs.12072.
- Barber R, Boote JD, Parry GD, Cooper CL, Yeeles P, Cook S. Can the impact of public involvement on research be evaluated? A mixed methods study. Health Expect 2012;15:229-41. http://dx.doi.org/10.1111/j.1369-7625.2010.00660.x.
- Hawe P, Degeling D, Hall J. Evaluating Health Promotion: A Health Worker’s Guide. Sydney, NSW: MacLennan and Petty; 1990.
- Williams P. We are all boundary spanners now?. Int J Public Sector Manag 2013;26:17-32. http://dx.doi.org/10.1108/09513551311293417.
- Telford R, Beverley CA, Cooper CL, Boote JD. Consumer involvement in health research: fact or fiction?. Br J Clin Governance 2002;7:92-103. http://dx.doi.org/10.1108/14664100210427606.
- Barber R, Boote JD, Cooper CL. Involving consumers successfully in NHS research: a national survey. Health Expect 2007;10:380-91. http://dx.doi.org/10.1111/j.1369-7625.2007.00457.x.
- National Institute of Health Research . Making the Difference 2011. www.crncc.nihr.ac.uk/Resources/NIHR%20CRN%20CC/PPI/Documents/Making%20the%20difference%20May%202011.pdf (accessed 29 July 2013).
- Patient Empowerment: For Better Quality, More Sustainable Health Services Globally. London: APPG on Patient and Public Involvement in Health and Social Care; 2014.
- Badger FJ, Daly W, Clifford C. Educating tomorrow’s clinical researchers: a review of research preparation in undergraduate education. Nurse Educ Today 2012;32:737-43. http://dx.doi.org/10.1016/j.nedt.2012.04.010.
- INVOLVE . What Is Public Involvement in Research? 2012. www.invo.org.uk/find-out-more/what-is-public-involvement-in-research-2/ (accessed March 2014).
- National Voices . Patient Involvement n.d. www.nationalvoices.org.uk/patient-involvement (accessed February 2014).
- Department of Health . Innovation Health and Wealth, Accelerating Adoption and Diffusion in the NHS 2011. www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/documents/digitalasset/dh_131784.pdf (accessed 12 November 2012).
- National Cancer Research Institute . Action on Access: Widening Patient Participation in Clinical Trials 2012. www.ncri.org.uk/includes/Publications/reports/action_on_access_report_final.pdf (accessed 12 November 2012).
- Goodman A, Roberts H, Green J. Reciprocity: Combining Youth Involvement, Engagement and Participation in Health Research 2013. http://researchonline.lshtm.ac.uk/1410529/ (accessed March 2014).
- Callard F, Rose D, Wykes T. Close to the bench as well as at the bedside: involving service users in all phases of translational research. Health Expect 2012;15:389-400. http://dx.doi.org/10.1111/j.1369-7625.2011.00681.x.
- Beresford P. Developing the theoretical basis for service user/survivor-led research and equal involvement in research. Epidemiologia E Psychiatria Sociale 2005;14:4-9. http://dx.doi.org/10.1017/S1121189X0000186X.
- Snape D, Kirkham J, Preston J, Popay J, Britten N, Collins M, et al. Exploring areas of consensus and conflict around values underpinning public involvement in health and social care research: a modified Delphi study. BMJ Open 2014;4. http://dx.doi.org/10.1136/bmjopen-2013-004217.
- PiiAF Study Group . Public Involvement Assessment Framework (PiiAF) n.d. http://piiaf.org.uk/index.php (accessed June 2015).
- O’Donnell M, Entwistle V. Consumer involvement in decisions about what health-related research is funded. Health Policy 2004;70:281-90. http://dx.doi.org/10.1016/j.healthpol.2004.04.004.
- van Bekkum JE, Hilton S. UK research funding bodies’ views towards public participation in health-related research decisions: an exploratory study. Health Serv Res 2014;14. http://dx.doi.org/10.1186/1472-6963-14-318.
- Barnes M, Newman J, Sullivan H. Power, participation, and political renewal: theoretical perspectives on public participation under New Labour in Britain. Social Politics 2004;11:267-79. http://dx.doi.org/10.1093/sp/jxh034.
- Scott WR. Institutions and Organizations. Thousand Oaks, CA: Sage; 2001.
- Habermas J. Theory of Communicative Action Volume One: Reason and the Rationalization of Society. Boston, MA: Beacon Press; 1984.
- Habermas J. Theory of Communicative Action Volume Two: Lifeworld and System. A Critique of Functionalist Reason. Boston, MA: Beacon Press; 1987.
- Batsch NL, Mittelman MS. World Alzheimer Report 2012: Overcoming the Stigma of Dementia. London: Alzheimer’s Disease International; 2012.
- Held D, Thompson JB, Held D. Habermas Critical Debates. London: Macmillan; 1982.
- Roderick R. Habermas and the Foundations of Critical Theory. London: Macmillan; 1986.
- McNichol E, Grimshaw P. An innovative toolkit: increasing the role and value of patient and public involvement in the dissemination of research findings. Int Pract Dev J 2014;4.
- Clavier C, Sénéchal Y, Vibert S, Potvin L. A theory-based model of translation practices in public health participatory research. Sociol Health Illn 2012;34:791-805. http://dx.doi.org/10.1111/j.1467-9566.2011.01408.x.
- Williams P. The competent boundary spanner. Public Admin 2002;80:103-24. http://dx.doi.org/10.1111/1467-9299.00296.
- Evans S, Scarborough H. Supporting knowledge translation through collaborative translational research initiatives: ‘bridging’ versus ‘blurring’ boundary-spanning approaches in the UK CLAHRC initiative. Soc Sci Med 2014;106:119-27. http://dx.doi.org/10.1016/j.socscimed.2014.01.025.
- INVOLVE . Cost Calculator Tool n.d. www.invo.org.uk/resource-centre/involvement-cost-calculator/ (accessed October 2014).
- Truman C, Raine P. Involving users in evaluation: the social relations of user participation in health research. Crit Pub Health 2001;11:215-29. http://dx.doi.org/10.1080/09581590110066667.
- Martin GP. The third sector, user involvement and public service reform: a case study in the co-governance of health service provision. Public Admin 2011;89:909-32. http://dx.doi.org/10.1111/j.1467-9299.2011.01910.x.
- Tritter JQ, McCallum A. The snakes and ladders of user involvement: moving beyond Arnstein. Health Policy 2006;76:156-68. http://dx.doi.org/10.1016/j.healthpol.2005.05.008.
- Barnes M. Passionate participation: emotional experiences and expressions in deliberative forums. Crit Soc Policy 2008;28:461-81. http://dx.doi.org/10.1177/0261018308095280.
- Ben-Ari A, Enosh G. Power relations and reciprocity: dialectics of knowledge construction. Qual Health Res 2013;23:422-9. http://dx.doi.org/10.1177/1049732312470030.
- Titmuss R. The Gift Relationship. London: Allen and Unwin; 1970.
- Brett J, Staniszewska S, Mockford C, Herron-Marx S, Hughes J, Tysall C, et al. A systematic review of the impact of patient and public involvement on service users, researchers and communities. Patient 2014;7:387-95. http://dx.doi.org/10.1007/s40271-014-0065-0.
- Barnes M. The same old process? Older people, participation and deliberation. Ageing Soc 2005;25:245-59. http://dx.doi.org/10.1017/S0144686X04002508.
- Staniszewska S, Herron-Marx S, Mockford C. Measuring the impact of patient and public involvement: the need for an evidence base. Int J Qual Health Care 2008;20:373-4. http://dx.doi.org/10.1093/intqhc/mzn044.
- Cairncross L, Morrell C, Darke J. Tenants Managing: An Evaluation of Tenant Management Organisations in England. London: ODPM; 2001.
- Milton B, Attree P, French B, Povall S, Whitehead M, Popay J. The impact of community engagement on health and social outcomes: a systematic review. Commun Dev J 2011;47:316-34. http://dx.doi.org/10.1093/cdj/bsr043.
- Shirk JL, Ballard HL, Wilderman CC, Phillips T, Wiggins A, Jordan R, et al. Public participation in scientific research: a framework for deliberate design. Ecol Soc 2012;17. http://dx.doi.org/10.5751/es-04705-170229.
- Pattengill-Semmens CV, Semmens BX. Conservation and management applications of the REEF volunteer fish monitoring program. Environ Monit Assess 2003;81:43-50. http://dx.doi.org/10.1023/A:1021300302208.
- Middleton JV. The Stream Doctor project: community-driven stream restoration. BioScience 2001;51:293-6. http://dx.doi.org/10.1641/0006-3568(2001)051[0293:TSDPCD]2.0.CO;2.
- Decisions on Assessing Research Impact. Bristol: Higher Education Funding Council for England; 2011.
- Nathan S, Stephenson N, Braithwaite J. Sidestepping questions of legitimacy: how community representatives manoeuvre to effect change in a health service. Health 2014;18. http://dx.doi.org/10.1177/1363459312473617.
- Renedo A, Marston C. Healthcare professionals’ representations of ‘patient and public involvement’ and creation of ‘public participant’ identities: implications for the development of inclusive and bottom-up community participation initiatives. J Commun Appl Soc Psychol 2011;21:268-80. http://dx.doi.org/10.1002/casp.1092.
- Barnes M, Newman J, Knops A, Sullivan H. Constituting ‘the public’ in public participation. Public Admin 2003;81:379-99. http://dx.doi.org/10.1111/1467-9299.00352.
- Ives J, Damery S, Redwod S. PPI, paradoxes and Plato: who’s sailing the ship?. J Med Ethics 2013;39:181-5. http://dx.doi.org/10.1136/medethics-2011-100150.
- Staley K. There is no paradox with PPI in research. J Med Ethics 2013;39:186-7. http://dx.doi.org/10.1136/medethics-2012-100512.
- Parkes JH, Pyer M, Wray P, Taylor J. Partners in projects: preparing for public involvement in health and social care research. Health Policy 2014;117:399-408. http://dx.doi.org/10.1016/j.healthpol.2014.04.014.
- Cystic Fibrosis Trust . Cystic Fibrosis: Investing in Research to Change Lives n.d. www.cysticfibrosis.org.uk/media/175431/Cystic%20Fibrosis%20Trust%20Research%20Strategy%202013-2018-Low-res.pdf (accessed March 2014).
- Meyer MC, Torres S, Cermeno N, MacLean L, Monzon R. Immigrant women implementing participatory research in health promotion. West J Nurs Res 2003;25:815-34. http://dx.doi.org/10.1177/0193945903256707.
- Minogue V, Boness J, Brown A, Girdlestone J. The impact of service user involvement in research. Int J Health Care Qual Assur Inc Leadersh Health Serv 2005;18:103-12. http://dx.doi.org/10.1108/09526860510588133.
- Davis RE, Jacklin R, Sevdalis N, Vincent C. Patient involvement in patient safety: what factors influence patient participation and engagement?. Health Expect 2007;10:259-67. http://dx.doi.org/10.1111/j.1369-7625.2007.00450.x.
- Davis RE, Sevdalis N, Jacklin R, Vincent CA. An examination of opportunities for the active patient in improving patient safety. J Patient Saf 2012;8:36-43. http://dx.doi.org/10.1097/PTS.0b013e31823cba94.
- Entwistle VA. Differing perspectives on patient involvement in patient safety. Qual Saf Health Care 2007;16:82-3. http://dx.doi.org/10.1136/qshc.2006.020362.
- Ocloo JE, Fulop NJ. Developing a ‘critical’ approach to patient and public involvement in patient safety in the NHS: learning lessons from other parts of the public sector?. Health Expect 2012;15:424-32. http://dx.doi.org/10.1111/j.1369-7625.2011.00695.x.
- Schwappach DLB. Review: engaging patients as vigilant partners in safety – a systematic review. Med Care Res Rev 2010;67:119-48. http://dx.doi.org/10.1177/1077558709342254.
- Hunn A. Patient and Public Engagement Project: Patient and Public Dialogue Workshops 2013. www.hra.nhs.uk/documents/2013/08/patient-and-public-workshops-dialogue-report.pdf (accessed March 2014).
- Pitt L, Kilbride M, Nothard S, Welford M, Morrison AP. Researching recovery from psychosis: a user-led project. Psychiatr Bull 2007;31:55-60. http://dx.doi.org/10.1192/pb.bp.105.008532.
- Armes D, Barrett J, Hindle D, Lemonsky F, Trite J. Mental Health Researchers’ TOOLKIT for Involving Service Users in the Research Process 2011. www.mhrn.info/pages/mental-health-researchers-toolkit-for-involving-service-users-in-the-research-process.html (accessed March 2014).
- Research Design Service London . Patient and Public Involvement in Health and Social Care Research: A Handbook for Researchers by Research Design Service London 2010. www.rdslondon.co.uk/RDSLondon/media/RDSContent/copy/RDS_PPI-Handbook_web.pdf (accessed March 2014).
- British Paediatric Surveillance Unit . Patient and Public Involvement: Guidance for Researchers Supported by the BPSU 2013. www.rcpch.ac.uk/system/files/protected/page/BPSU_PPI_Guidance4.pdf (accessed March 2014).
- McGrath T. Patient and Public Involvement Guidance Document for ESRC n.d. www.dendron.nihr.ac.uk/wp-content/uploads/Guidance-DTC-Individual-representation-or-advice-FOR-ESRC.pdf (accessed March 2014).
- Collaboration for Leadership in Applied Health Research and Care . Patient and Public Involvement (PPI) Guidance n.d. www.clahrc-northwestlondon.nihr.ac.uk/inc/files/documents/ppi-resources/clahrc_ppi_guidance_v1_0.pdf (accessed March 2014).
- Patient and Public Involvement Solutions . Patient Participation: Community Voices Project to Support Practice Based Commissioning 2010. www.patientpublicinvolvement.com/wp-content/uploads/2013/01/Community-Voices-resource.pdf (accessed March 2014).
Appendix 1 Online survey
Appendix 2 RAPPORT interview schedule
Researchers and funders
| NPT statement | |
|---|---|
| 1 | Has patient and public involvement been a feature of your research/the research you fund for some time – or is it a fairly new way of working for you/your organisation? Can you tell me a little bit about how this way of working has developed? |
| 2, 3 | In your opinion, what is the purpose & role of PPI in research? |
| 4, 14, 15 | In your opinion, how does PPI bring added value? Do you find your colleagues share this view? |
| 5, 11 | Is there someone in particular who is responsible for PPI in your research team/organisation? |
| 6, 9 | What do you think are the best ways to enable PPI to work well? What needs to be in place? |
| 7, 8, 10 | What do you think are the downsides to PPI? |
| 12 | Do you feel that PPI is embedded within your organisation? If so, how? Prompts: Is there a local or regional PPI group? Is this group always used as the first resource in PPI? |
| 13, 15 | How do you judge whether PPI has made a difference to your study(ies)? |
| 16 | Can you give me any examples of how you have changed your study/the way you fund studies because of PPI? |
Normalisation Process Theory statements
-
Participants distinguish the intervention from current ways of working.
-
Participants collectively agree about the purpose of the intervention.
-
Participants individually understand what the intervention requires of them.
-
Participants construct potential value of the intervention for their work.
-
Key individuals drive the intervention forward.
-
Participants agree that the intervention should be part of their work.
-
Participants buy in to the intervention.
-
Participants continue to support the intervention.
-
Participants perform the tasks required by the intervention.
-
Participants maintain their trust in each other’s work and expertise through the intervention.
-
The work of the intervention is appropriately allocated to participants.
-
The intervention is adequately supported by its host organisation.
-
Participants access information about the effects of the intervention.
-
Participants collectively assess the intervention as worthwhile.
-
Participants individually assess the intervention as worthwhile.
-
Participants modify their work in response to their appraisal of the intervention.
Service user/public interview schedule
| 1 | Can you tell me how long you have been involved in research? How did your involvement come about? |
| 2, 3 | In your opinion, what is the purpose & role of PPI in research? |
| 4, 14, 15 | In your opinion, how does PPI bring added value? Do you think that members of the research team share this view? |
| 5, 11 | Who do you deal with most in the research team? What kind of things do they do for you? |
| 6, 9 | What do you think are the best ways to enable PPI to work well? What needs to be in place? |
| 7, 8, 10 | What do you think are the downsides to PPI? |
| 12 | In your experience do you feel that PPI is really believed in or more of a tick box exercise? |
| 13, 15 | How do you judge whether PPI has made a difference to the study you are involved in? |
| 16 | Can you give me any examples of how the study has been changed because of PPI? |
Normalisation Process Theory statements
-
Participants distinguish the intervention from current ways of working.
-
Participants collectively agree about the purpose of the intervention.
-
Participants individually understand what the intervention requires of them.
-
Participants construct potential value of the intervention for their work.
-
Key individuals drive the intervention forward.
-
Participants agree that the intervention should be part of their work.
-
Participants buy in to the intervention.
-
Participants continue to support the intervention.
-
Participants perform the tasks required by the intervention.
-
Participants maintain their trust in each other’s work and expertise through the intervention.
-
The work of the intervention is appropriately allocated to participants.
-
The intervention is adequately supported by its host organisation.
-
Participants access information about the effects of the intervention.
-
Participants collectively assess the intervention as worthwhile.
-
Participants individually assess the intervention as worthwhile.
-
Participants modify their work in response to their appraisal of the intervention.
Easy speak interview schedule
| 1 | Tell me about how you started helping the researchers with this study Prompts: How did they know about you? Who asked you to help? What happened? |
| 2, 3 | Why do you think the researchers ask people like you to help them with their study/work? |
| 3, 4, 14, 15 | How do you help the researchers? |
| 5, 11 | Who do you talk to most in the research team? How do they help you? |
| 6, 9 | What kind of things helps people like you to be involved in research? |
| 4, 7, 8, 10, 14, 15 | What do you like best about being involved in the research? What do you find difficult when helping the researchers/being involved? |
| 12 | Have you been involved/helped out with other research studies? What was that like? |
| 13, 15, 16 | Do the researchers tell you if they have changed anything in their study because of what you have said? Tell me a bit more about this |
Normalisation Process Theory statements
-
Participants distinguish the intervention from current ways of working.
-
Participants collectively agree about the purpose of the intervention.
-
Participants individually understand what the intervention requires of them.
-
Participants construct potential value of the intervention for their work.
-
Key individuals drive the intervention forward.
-
Participants agree that the intervention should be part of their work.
-
Participants buy in to the intervention.
-
Participants continue to support the intervention.
-
Participants perform the tasks required by the intervention.
-
Participants maintain their trust in each other’s work and expertise through the intervention.
-
The work of the intervention is appropriately allocated to participants.
-
The intervention is adequately supported by its host organisation.
-
Participants access information about the effects of the intervention.
-
Participants collectively assess the intervention as worthwhile.
-
Participants individually assess the intervention as worthwhile.
-
Participants modify their work in response to their appraisal of the intervention .
Appendix 3 Participant information sheet
Appendix 4 Consent form
Appendix 5 Dissemination events
Dissemination
| Area | Date | Local partners |
|---|---|---|
| London | 19 March 2014 | London Diabetes Research Network PPI panel |
| North East | 27 March 2014 | Dendron, Voice North |
| South West | 1 April 2014 | Researchers at University of the West of England, CLAHRC South West Peninsula |
| East of England | 28 April 2014 | CLAHRC East of England, RDS |
In total 221 people attended the events and the mixture was roughly twice as many researchers/health professionals (n = 147) as PPI representatives (n = 74). The gender balance was roughly twice as many females as males.
| Area | ‘Professionals’ | Lay members | Total |
|---|---|---|---|
| London | 28 | 19 | 47 |
| North East | 20 | 24 | 44 |
| South West | 40 | 14 | 54 |
| East of England | 59 | 17 | 76 |
| Total | 147 | 74 | 221 |
Feedback from the small group work
There was a variety of feedback to the RAPPORT study findings from the small group work; training for researchers came out as a clear top priority at the London event. There was a general feeling the NIHR needs to ‘self-publicise’ and help the public understand what patient and public is and how to get involved. The need to widen participation and representativeness of PPI representatives were repeated at each event. The feedback from the four events is given below.
London dissemination event
Top priorities
Table 1: representativeness, population, age, gender.
Table 2: spread the news, catchy, government funding, positive outcomes, NIHR to advertise in the media.
Table 3: training, resources (caps on funding), providing feedback to participants, PPI involved throughout.
Table 4: NIHR training requirement for research (like GCP training), qualify, evaluating impacts of PPI, NIHR to take a role in this.
Table 5: training for researchers.
North East dissemination event
Top priorities
Table 1: publicity – widening participation, general public, NIHR.
Table 2: defining PPI – umbrella term, one definition, branches and categories, evaluation PPI, where is the evidence?
Table 3: PPI co-ordinator – identified, ease/help research, ‘tick box’ exercise, a set point of contact.
Table 4: researcher training – PPI training – ALL. Not tokenistic, genuine, PPI before ethics.
Table 5: training – who needs it? Overall, capacity, more people, the right people, funding and time, evaluation, impact, research base.
Table 6: ageing, extended to all research, contacts with existing groups, training for researchers.
Table 7: NIHR – what does it stand for? Need for clarity, how can people get involved?
Raising awareness, do general public know what PPI is? Does the public and research community know it is more than just engagement?
South West dissemination event
Top priorities
Table 1: raising awareness of the general public, meaningful PPI, feedback (specific feedback at all stages of research).
Table 2: engagement; NIHR role, ability of general public working in partnership whichever part of the NIHR it is, throughout NIHR.
Table 3: amount of time. Training (joined up), clinicians, researchers, PPI in same room, same training. Partnership working, skills for high-quality research, modular, different stages to dip in and out, accredited training (university accredited).
Table 4: NIHR – funding issue, what is the quality of PPI in bids that get funded? Whether the research gets funded or not. Culture change.
Table 5: do you want patients to be involved or evidence of better care and outcomes?
Table 6: joined-up thinking, ethics and NIHR. PPI should be traceable throughout. Do what you said you would do in the protocol. Standalone report for PPI, lay summary/plain English.
Table 7: CLAHRCs – evidenced, make a difference, making PPI inescapable and making PPI part of medical curriculum (student level).
Table 8: communicate – NIHR plain English, benefits of research to public, PPI Healthwatch, how fitted together, how relevant.
Table 9: NIHR self-publicise, man on the street, more aware of what NIHR is doing and how they can get involved.
East of England dissemination event
Table 1: Top Priority: Ownership of PPI – it always happens under the radar and someone should take ownership – should this be Healthwatch?
Finance – lead up to grants (no resources), visible hubs (e.g. PPI groups to spread message), pathways for involvement and engagement.
Table 2: Top Priority: Making PPI standard across all research topic areas and healthcare areas – standardisation but at a local level.
Health research authority needs to make IRAS form more robust to make CI think about PPI throughout the research cycle.
Table 3: Top Priority: Educating researchers – researchers to listen to understand patient representatives – get them young when at university – get them to understand PPI right from the start. For more established researchers help them to understand barriers and enables of effective PPI.
Involving younger people more and understanding what incentivises young people.
Table 4: Top Priority: Overall marketing strategy needed, very difficult to get an understanding of who and what are involved, normalising PPI.
Who is mentoring lay representatives etc. succession planning etc.
Make sure we get the views of younger people and the older person.
Campaigns like the Australian one for sun protection to increase research participation.
Employment status of people in PPI – and their performance management.
Table 5: Top Priority: Feedback to 1. lay representatives and 2. general public re: possibilities of PPI. Start at school level and people must feel comfortable in challenging.
Involve lay people right from the beginning – need a balance of new and experienced lay people.
NIHR should have more of a monitoring role in PPI.
Publicity re: research at primary care level especially in GP surgeries.
Table 6: Education – start in schools e.g. health literacy and introduce partnership working.
Joint training, service users and researchers.
Training on innovative approaches for researchers.
Continue to build evidence base on PPI.
Co-ordination of different organisations involved in PPI, reduce confusion.
PPI has become an industry and is at risk of becoming introverted.
Increase diversity; Increase embedding of PPI.
Table 7: Evaluation of impact (e.g. Til Wykes) and qualitative research approaches.
Cost-effectiveness – public investment so need to be at least cost neutral.
Don’t lose good practice through transition to new structures.
One-stop shop to hear of local innovations and get out nationally.
Raising awareness – can’t do anything if people aren’t aware.
Table 8: Involvement should be at different levels so public, carers, service users, etc. should be able to be involved at what level they’re comfortable at.
Skill mix – new PPI reps and experienced PPI group meetings.
Grant allocation should be available and reflect the model of PPI; training for researchers.
Table 9: Top Priority: Annual audit (as per MRC [Medical Research Council]) of PPI, this will need costing. Data analysis @ NIHR.
Strategic level – people having PPI activities audited and include lay representatives.
More realistic costings of PPI.
Appendix 6 Amander’s Levels of Patient and Public Involvement Significance (ALPS), reproduced with permission [Amander Wellings, Norfolk and Suffolk Patient and Public Involvement in Research (PPIRes) panel, 2014, personal communication]
-
Please score your gut feeling experience of this expedition (meeting/event) on the mountain graph below.
-
Please use the space below to reflect on any ‘mountain tools’ gained, for example new knowledge or good practices you experienced at the Group meeting.
-
Please use the space below to reflect on any ‘avalanches’ or negative experiences you experienced at the group meeting.
-
Are there any places during the expedition where you can now see that help from your fellow climbers would have eased your ascent?
-
Please think of any’ base camps’ you could build, so as you need not start from the bottom each time (use the answers from 2, 3 and 4 to help inform this).
Reproduced with kind permission from Amander Wellings, RAPPORT advisory group member.
List of abbreviations
- AMRC
- Association of Medical Research Charities
- BME
- black and minority ethnic
- CF
- cystic fibrosis
- CI
- chief investigator
- CLAHRC
- Collaboration for Leadership in Applied Health Research and Care
- CMO
- context, mechanism and outcome
- CS
- case study
- HEI
- higher education institution
- HSDR
- Health Services and Delivery Research
- IDD
- intellectual and developmental disability
- IRAS
- Integrated Research Application System
- MRT
- middle-range theory
- NIHR
- National Institute for Health Research
- NPT
- Normalisation Process Theory
- PIRG
- Public Involvement in Research Group
- PIRICOM
- Patient and Public Involvement in Research: Impact, Conceptualisation, Outcomes and Measurement
- PIS
- participant information sheet
- PPI
- patient and public involvement
- PPIRes
- Norfolk and Suffolk Patient and Public Involvement in Research
- RAPPORT
- ReseArch with Patient and Public invOlvement: a RealisT evaluation
- RCT
- randomised controlled trial
- RDS
- Research Design Service
- RE
- realist evaluation
- rep.
- representative (also service user, lay representative)
- UKCRN
- UK Clinical Research Network
- YPD
- young people with diabetes mellitus