Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 10/1007/06. The contractual start date was in October 2011. The final report began editorial review in April 2014 and was accepted for publication in January 2015. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Disclaimer
This report contains transcripts of interviews conducted in the course of the research, or similar, and contains language that may offend some readers.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2015. This work was produced by Herepath et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction
Overview
This chapter introduces our study and is presented in three main parts. We begin by discussing the development of patient safety as the field of research that is concerned with one of the most significant social problems of our time: avoidable harm, waste and variation in health-care. Using the available literature, we outline the nature of this problem and present five factors which are thought to represent its foundations: (1) deficits in cultures of care, (2) leadership inadequacies, (3) ineffective team working, (4) problematic governance systems and (5) limited patient and public engagement. We then introduce the current agenda for patient safety improvement across the devolved NHS in the UK.
Second, we discuss the role of patient safety improvement programmes. We consider the design, implementation and evaluation of these complex social interventions and highlight the current lack of systematic analysis of relations between contextual (organisational and environmental) factors and the outcomes of patient safety interventions.
We then introduce the focal case of our study, the 1000 Lives+ national patient safety programme in Wales, and the three interventions selected for our detailed analysis: Improving Leadership for Quality Improvement (ILQI), Reducing Surgical Complications (RSC) and Reducing Health-care-Associated Infection (RHAI). We conclude this chapter by outlining the aim and objectives of our study, the structure of this report and the report’s intended audience.
Patient safety: a major social problem of our time
Since the publication in 2000 of To Err is Human: Building a Safer Health System,1 patient safety has become recognised as a major social problem of our time. It now sits at the centre of global debates about the quality, affordability and sustainability of health care. 2–6 Since 2000, understandings of the prevention, detection and mitigation of harm have improved. 4,7–13 Crucially, from an earlier concentration on individual factors, it is now recognised that the consistent delivery of high-quality, safe and effective health care is complex and multidimensional.
Considered at higher system levels of analysis, it has been shown that patient safety is shaped by government policy14–21 and demands a nuanced balance of health-care system design22,23 and resources to create high-reliability organisations. 24,25 At the organisational level of analysis, it has been demonstrated that patient safety is moulded by culture, capacity, processes and governance systems,26–28 and that each is enhanced by distributed (shared, see Glossary) leadership. 28–36 At the level of health-care practice, it is known that patient safety is informed by the beliefs and values of health-care professionals,37–41 and is ultimately underpinned by their personal commitment to care. 42,43
The extent and burden of the problem
Despite growing awareness of the challenges posed by patient safety,44–46 and concerted improvements efforts within some health-care systems,47,48 considerable hospital patient safety problems persist. Global estimates of the burden of harm vary. However, they are normally reported to be around 10% of all inpatient admissions with a range of 3.8–16.6%,49 though such results are influenced by the means of measurement employed. 50–53 In the UK, it is estimated that 1 in 10 NHS hospital patients is harmed during his or her care, and 1 in 300 dies as a result of adverse events such as acquired infection. 54,55 Along with these human costs, safety incidents are a drain on NHS resources, costing an estimated £3.5B per year in additional bed-days and negligence claims. 56
Avoidable harm takes various forms. Errors occurring during drug prescribing, supply and administration represent a significant and persistent burden. 57–62 So, too, do those that arise as a consequence of surgery. 63,64 A more hidden cause is, quite simply, incorrect diagnosis. 65–69 In addition, there is variation in the delivery of medical and nursing care. 70,71 Failure in the safety of care is a particular issue for high-risk patient groups,72,73 but all patients may be at risk of harm, for instance, from communication deficits at handover;74–77 from low staffing,78 especially at weekends; or because the delivery of care coincides with the influx of a new cohort of junior doctors in training. 79,80
Foundations of the problem
Rising concerns about patient safety have led, in recent years, to a number of public enquiries into highly publicised failures of the health-care system, such as patient safety failings at the Mid Staffordshire NHS Foundation Trust,81 events at the Bristol Royal Infirmary82 and the Royal Liverpool Children’s Hospital,83 and the actions of Dr Harold Shipman. 84 The major reports published following these enquiries have helped to identify reasons for the failures85 and have sought ways of improving the safety of patients. 86 Taken as a whole, the findings of successive UK inquiries have emphasised five issues that can be seen as foundations of the problem of patient safety: (1) deficits in cultures of care, (2) leadership inadequacies, (3) ineffective team working, (4) problematic regulatory oversight and governance systems and (5) limited patient and public engagement. We summarise these issues, and the recommendations made to address and eliminate them, in Table 1, as a way of introducing what was known (by us), prior to our study, about the context of patient safety.
| Deficits in culture(s) of care |
|---|
Recommended improvements
|
| Leadership inadequacies |
Recommended improvements
|
| Ineffective team working |
Recommended improvements
|
| Problematic regulatory oversight and governance systems |
Recommended improvements
|
| Limited patient and public engagement |
Recommended improvements
|
Culture(s) of care
Inquiries into the events at the Mid Staffordshire NHS Foundation Trust draw attention to ‘the culture of care in the NHS’. 5,87–89 Unfortunately, as noted by Professor Jon Glasby,81 ‘The trouble with culture is everyone blames it when things go wrong but no-one really knows what it is or how to change it’. This issue is compounded when viewing (as we do) health-care organisations as comprising multiple cultures/cultural frames, rather than as a single culture of care. These points notwithstanding, research indicates that five aspects of culture are of particular salience to patient safety: (1) the need for a culture of compassion in care;81 (2) the problematic intra- and interprofessional hierarchies, which privilege a perceived elite at the expense of the broader health-care team;41,90–92 (3) the culture of blame that retards the promotion of adverse incident reporting and disclosure of harm to patients;42,93–95 (4) the culture of bullying96–98 that, regrettably, appears to be widespread across the NHS;99–104 and (5) the culture of unrelenting pressure to attain government targets, which creates a range of unintended and dysfunctional consequences. 105–111
Leadership
It is well recognised that patient safety improvement requires ‘sustained investment in developing leadership skills at all levels in the NHS’ and its aligned regulatory organisations. 82 Failures in strategic leadership may arise across the public sector,112 with such failures attributed to, for instance, the detrimental impact of external pressures,113–115 structural change16 and the challenges posed by the global financial downturn. 116 Nevertheless, such contextual constraints do not obviate the need for distributed leadership in health care from board to ward. 30,36,117 The detrimental impact on patient safety of a weak board and senior management team, marred by professional disengagement, poor governance and a lack of focus on the standards of care, has been illustrated in the Francis Inquiry. 81 However, at the point of care, professional leadership, especially medical, remains paramount118–121 and may function as catalyst for, or barrier to, patient safety improvement. 28,90,122–125
Team work
Research shows that, given the complexity and multidisciplinary nature of modern health care, effective team working is an important element in patient safety,33,126,127 necessitating good communication and co-ordination,119,128 particularly in high-pressure environments such as the operating theatre. 74,75,129–133 It also requires a degree of consistency in the meanings, beliefs and values that frame different health-care professionals’ commitment to care. 39 Yet effective team working remains vulnerable to the adverse effects of hierarchy,134 poor staffing,81 enmity and conflict30 and the human factors that give rise to team fragility. 135 Greater understanding of such human factors, specifically with regard to (i) human error, (ii) the role of health-care worker performance and (iii) the design of health-care technology, is increasingly recognised as core to patient safety. 136–138 But to be successful, this, too, necessitates careful consideration of the local context and the informal culture of clinical practice. 139
Regulatory oversight and governance systems
Public inquiries into failures in patient safety have consistently sought to enhance regulatory oversight81,82 and heighten both professional and organisational systems of governance. 83,84,140 It has been argued that these pressures have eroded professional self-regulation,141 replacing this traditional mode of control with an increasingly legalised regulatory system. 142 As a consequence, organisational, professional and work group boundaries have shifted. 143 This has the potential to foster defensive activity,144 which, as evidenced in the Francis Inquiry,81 may prove detrimental to the safe provision of health care.
Patient and public engagement
A final foundation of the problem of patient safety that emerges from recent inquiries is the weak representation of patients, their families and carers at all levels of the health-care system. Lauded as a more bottom-up approach to service planning and provision,145 a robust patient-centred focus is increasingly considered a core dimension of health-care quality. 146 This involves providing opportunity for patient, and broader lay, involvement in professional oversight bodies84 and health-care organisations’ formal governance structures,147–150 as well as active patient engagement in decisions about their care and the ensuing evaluation of their experience. 151–156
The patient safety agenda
In 2013, the Francis Inquiry81 was accompanied by two major reports into hospital patient safety. The first was a review into the quality of care and treatment provided by 14 hospital trusts in England, led by Sir Bruce Keogh, National Medical Director for the NHS in England. 157 While this review acknowledged (as other commentators did158–160) the difficulties in adopting mortality measures as an indicator of hospital performance, it also set out core features of high-quality care for patients. The second, a report by the National Advisory Group on the Safety of Patients in England, led by Don Berwick, President Emeritus of the Institute for Healthcare Improvement (IHI),161 also endorsed these goals. Each addresses the foundations of the social problem of patient safety that are outlined in Table 1.
The improvement agenda proposed by these two recent reports is exacting. It demands changes in policies, the education of health-care professionals and wider NHS workforce and further research into the quality and safety of health care. 5
Patient safety improvement programmes
Recent reports and inquiries indicate that the global debate has progressed from the recognition and acknowledgement of the foundations of the problem of patient safety to the quest for systemic solutions to the challenges it poses. 88,162–167 In England, a special health authority of the NHS, the National Patient Safety Agency, was established in 2001 with the remit of monitoring patient safety. It identified the need to introduce patient safety improvement programmes to help foster local capacity and progress from a ‘blame’ culture to one that was perceived to be ‘just’ and capable of facilitating the open reporting of errors and near-misses. 168 Informed by the work of the US-based IHI,162 and advances in safety within other industries,22,169,170 NHS hospital patient safety programmes have typically sought to achieve improvements by implementing evidence-based clinical practices and enhancing performance monitoring systems. 171–173 Although the National Patient Safety Agency was dissolved in 2012, these policy goals continue to be pursued, in England, through the NHS Commissioning Board and the Safer Patients initiative sponsored by the Health Foundation, a charitable trust, and in Wales through the 1000 Lives campaign and its successor, the 1000 Lives+ national programme, the focus of this study.
1000 Lives+ national programme in NHS Wales
Patient safety interventions range from isolated interventions within a discrete health-care setting, such as the estimation of intraoperative blood loss174 or the validation of specific measures of harm,175 through to national programmes of the type we are investigating in this study. 176
In April 2008, the Welsh 1000 Lives+ campaign was launched by a collaborative involving the Welsh Assembly Government’s Clinical Governance Support and Development Unit, the Wales Centre for Health, the National Leadership and Innovation Agency for Healthcare, the National Public Health Service and the National Patient Safety Agency. It had two distinct goals: (1) to reduce by 1000 the number of deaths caused by suboptimal care and (2) to reduce by 50,000 the number of adverse incidents. All health-care organisations in NHS Wales volunteered to participate in the programme. In 2010, the campaign was superseded by the 1000 Lives+ national programme. This continued the ethos of high-quality person-centred care and offered a broader range of patient safety interventions, and aligned resources, for NHS Wales’ health boards to implement. This ambitious and complex intervention built on the momentum of its predecessor and now forms a core component of the Welsh Government’s delivery framework for the NHS in Wales. As illustrated in Figure 1, 1000 Lives+ comprises a complex array of 11 core programme improvement areas.
FIGURE 1.
1000 Lives+ national patient safety programme areas.
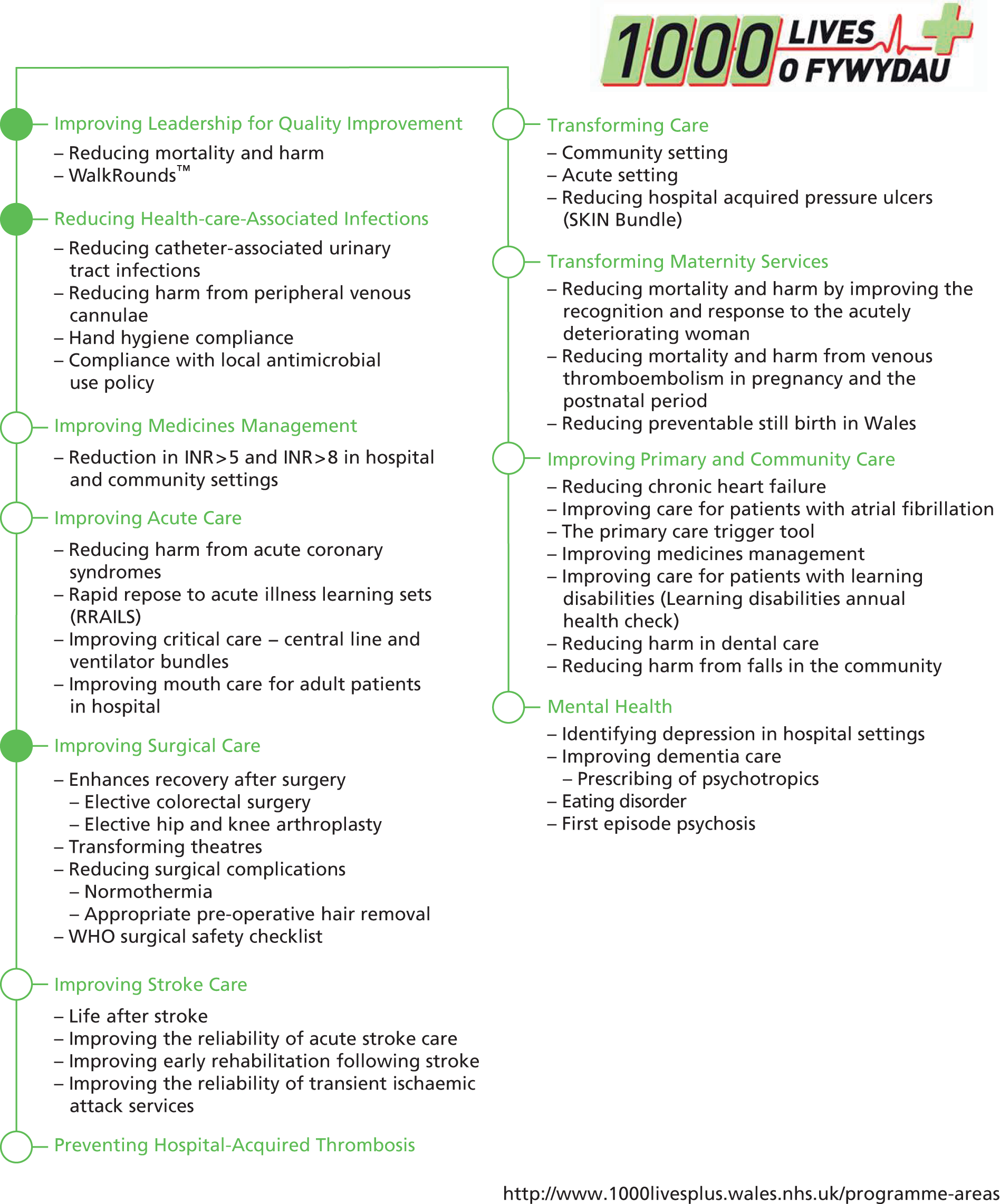
In this study, our attention is concentrated on three focal interventions: (1) ILQI, (2) RSC and (3) RHAI.
The 1000 Lives+ programme and its predecessor are adaptations of the IHI’s 100,000 Lives campaign. 162,177 Both are informed by the Model for Improvement (MI), developed by Langley et al. ,178 depicted in Figure 2. This model179,180 first directs attention to three questions: what are we trying to accomplish?; how will we know that a change is an improvement?; and what changes can we make that will result in improvement? It then prescribes the implementation of solutions through a Model for Improvement, Plan-Do-Study-Act (MI-PDSA) cycle.
FIGURE 2.
Model for improvement.
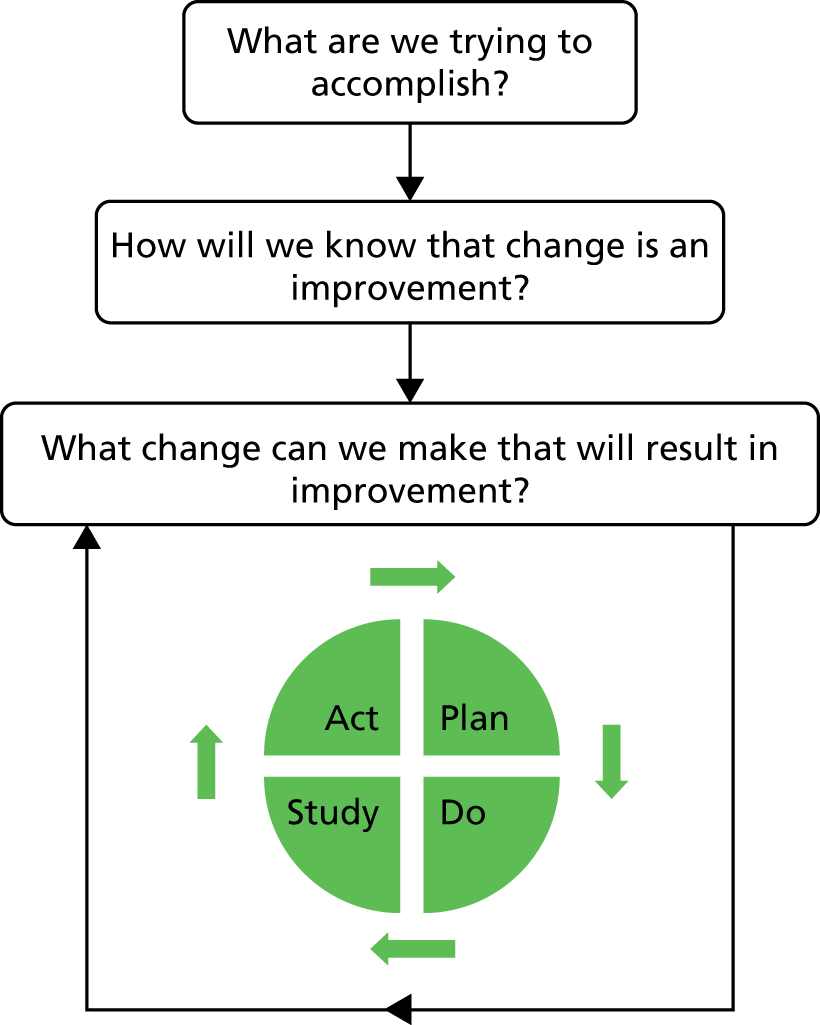
Centred on Deming’s system of profound knowledge,178 the MI-PDSA approach is an acknowledged cornerstone of the science of improvement,44,181 and is informed by a diverse array of theoretical perspectives.
The MI-PDSA cycle has been promoted by the IHI as the means to foster the transformation of patient safety. 172 The strength and success of this promotion is reflected in the way that the MI-PDSA approach has been applied across a range of contexts, and to a variety of issues. Many of these themes are of direct relevance to this study, including (i) the role of local champions in leading change;182–184 (ii) the education of health-care professionals in evidence-based practice change;185–188 (iii) the implementation of the World Health Organization Surgical Safety Checklist (WHOSSC);169,189–191 (iv) the development and implementation of anti-infective prescribing policies,192–194 including those for correct hand hygiene;195 and (v) the large-scale transformation of health-care services through a heightened emphasis on patient safety. 5,196
Design, implementation and evaluation
The 1000 Lives+ national programme incorporated a range of IHI-inspired patient safety interventions that have been utilised worldwide. 5 These include (i) the use of checklists; (ii) care bundles (checklists and associated directive guidelines) for high-risk drugs197 and invasive practices;192,198,199 (iii) multicomponent interventions, such as those advocated for the prevention and management of pressure ulcers, falls and hospital-acquired infections;200–203 and (iv) various other forms of intervention, including staff training,118,204–206 adverse event simulation,207,208 computer-assisted care management,62,209 national and/or local alert systems and trigger tools. 28,53,210,211
Hospital patient safety: a realist analysis
Context matters
Despite having a basic improvement approach in common, the differences in scale and scope of the patient safety programmes impact on both the complexity of their implementation and the evaluation of their outcomes5,168,212–215 and the reported outcomes of these interventions are marked by considerable variation. However, although public inquiries and research evidence now concur that patient safety is, in part, a matter of context,168 there has been very limited systematic and independent analysis of the relationship between organisational factors which shape the local context of health care and the outcomes of patient safety interventions. 124,216–223
Prior to this study, relationships between the recently advocated ‘four high-priority’ features of organisational context:5,223 (1) external factors such as regulatory requirements; (2) organisational structural characteristics; (3) leadership, team work and patient safety culture; and (4) management priorities – and the outcomes of safety programmes were both undertheorised and poorly understood in empirical terms. 224 As a result, the context of patient safety remained amorphous225 and ill defined. 226 In contrast, this study is designed to address the conceptual and empirical knowledge gaps involving the context of patient safety.
Aim and objectives
This study employs insights from institutional theory227 within a realist analysis framework228–235 to examine the impact of context on the implementation of the 1000 Lives+ national programme across the Welsh NHS. We present and explain our conceptual framework in Chapter 2.
Our approach arises from an appreciation that the influence of organisational features on hospital patient safety programmes cannot be readily understood from traditional evaluation methods. 236,274 Building on findings from previous studies of the design237 implementation,21,220,238,239 and outcomes146,240 of patient safety improvement programmes, we examine the implementation of three focal interventions in a multisite comparative-intensive case study of hospitals in NHS Wales. We seek to reveal the complex interplay of context and concerns,234,235 captured through the organisational factors and competing institutional logics – belief systems – which guide acceptance of, or resistance to, the local adoption and adaptation of patient safety programmes. 3,240
This realist analysis of patient safety aims to ascertain which contextual factors matter, and how, why and for whom they matter, in the hope that processes and outcomes of future improvement programmes may be improved. Hence the unit of analysis in this study is the process of local implementation of the 1000 Lives+ programme, centred on the three focal interventions (rather than an evaluation of the 1000 Lives+ programme per se). The study has five main objectives:
-
to identify and analyse the organisational factors (e.g. structure, culture and managerial priorities) pertinent to the health outcomes of hospital patient safety interventions
-
to identify and analyse the contextual mechanisms (logics or belief systems) that interact with organisational factors to generate the health outcomes of hospital patient safety interventions
-
to develop and test hypotheses concerning relationships between organisational factors, mechanisms and the health outcomes of hospital patient safety interventions
-
to produce a theoretically grounded and evidence-based model of which organisational factors matter, how they matter and why they matter
-
to establish and disseminate lessons for a broad range of stakeholders concerned with patient safety policy and management.
The achievement of these objectives should allow us to suggest how a particular configuration of organisational factors may influence the mechanisms that lead to more or less successful health outcomes of the three focal safety interventions considered. It is hoped that these findings will inform policy-makers, managers and practitioners, locally, nationally and internationally; will empower stakeholders to develop improvement interventions that are more likely to work in their local contingent circumstances; and may serve as a diagnostic tool to be used as a precursor to the design of more differentiated and context-sensitive interventions in future.
Report structure
The remainder of this report is presented in eight further chapters. Recognising the complexity of the subject matter and the novelty of our conceptual framework, we have produced an innovative set of explanatory schematics to accompany each chapter, in addition to our use of standard data tables and figures. Below, we outline the structure of this report and the way in which we combine text, explanatory schematics and other forms of data presentation to ensure the clarity of our reporting.
Chapter 2 presents the conceptual framework developed in this study – realist analysis – and defines our elaboration of established approaches to realist inquiry, centred on Archerian critical realism and augmented by sociological institutionalism and neo-institutional theory (see Figures 3–6).
Chapter 3 presents the research design – comparative case study – and multimethod approach to data collection and analysis (including our alignment to realist analysis) (see Figure 7 and Tables 2–5).
Chapters 4 and 5 present our analysis of the implementation and institutionalisation of the 1000 Lives+ programme in NHS Wales. Together, they form the foundation for our realist analysis of the three focal interventions selected from the programme. Chapter 4 presents our analysis of the bureaucratisation of 1000 Lives+ programme across NHS Wales, defining our preliminary understanding of the local implementation of the 1000 Lives+ programme (see Figures 8–11 and Tables 6–9). Chapter 5 explores interpersonal and individual engagement with 1000 Lives+ to offer an account of the normalisation of the programme at the level of the functional team within each health board (see Figures 12–15 and Table 10).
Chapters 6–8 present our realist analysis of the three focal interventions – ILQI, RSC and RHAI – and our understanding of the complex and dynamic relationships between organisational factors, generative mechanisms and the outcomes of hospital patient safety interventions: Chapter 6, Improving Leadership for Quality Improvement (see Figures 16 and 17, and Tables 11–21); Chapter 7, Reducing Surgical Complications (see Figures 18–20 and Tables 22–27); and Chapter 8, Reducing Health-care Associated Infection (see Figures 21 and 22, and Tables 28–33).
Chapter 9 presents the discussion and conclusion of our study, wherein we debate which contextual factors appear to impact on the implementation of patient safety improvement programmes, promoting or retarding their local success. In addition, we discuss the generalisability of our findings, the limitations of our study and potential for future work in this important area.
Intended audience
Throughout this report we have been concerned to ensure that our findings are accessible to the public, professionals, researchers and policy-makers wishing to (a) better understand existing improvement programmes and (b) design more effective ones in the future. We hope that our innovative use of neat description and summary graphics will assist in this objective, and the summaries presented in Chapters 1 and 9 are written for this extended audience in particular. In addition, we hope that much of the detailed narrative in the report will be of relevance to social scientists and others with an academic interest in the realist analysis of complex organisational phenomena.
Chapter 2 Conceptual framework
Overview
This chapter presents the realist analysis framework that was developed and then used in this study. It is presented in three main parts.
We begin by introducing the foundational realist philosophy of social science together with the approach to realist inquiry that underpins our framework. We then define the manner through which intervention, context, mechanism and outcome have traditionally been conceptualised and identify four challenges that have emerged.
The second section of this chapter, guided by Pawson’s241 belief that methods gain their spurs by thoughtful adaptation rather than mindless replication, introduces the conceptual resources from sociological institutionalism and Archerian critical realism that we have employed to address the challenges of applying realist inquiry.
In the final section, we draw from those resources and set out our innovative approach to the interplay of intervention, context and mechanisms in realist analysis. Briefly, our elaborations to realist inquiry are as follows. First, we include intervention as a separate analytical category in our realist analysis so that we may understand precisely ‘what’ is working, for whom, how and in what circumstances. Second, we forward a view of situated context as being stratified, conditioned, relational and temporally dynamic. Next, we distinguish the conceptual elements of mechanism from its ensuing outcomes and demonstrate the fundamental role of beliefs and values, institutional logics, on the propensity to act. Finally, in our realist analysis framework, outcome is not perceived as a simple, single aspect of change, such as a defined health outcome. Rather, we consider patterns of structural, political and ideational elaboration and maintenance.
Foundations of realist inquiry
Realist inquiry has emerged at the forefront of theory-informed policy evaluation methodology in health services and in other areas of social scientific enquiry. 228,241–243 Orthodox strategies for marshalling evidence in health-care research, epitomised by the Campbell and Cochrane Collaborations’ systematic reviews, seek to produce answers to the question ‘what works?’. In contrast, realist inquiry seeks to better bridge the gap between research, policy and practice244–246 by addressing the question ‘what works for whom, why and in what circumstances?’. 242,247 Within realist scholarship, two main approaches have gained prominence. Realist evaluation is the mode of inquiry for primary research, in which new data are collected from original sources. Its companion, realist review or synthesis, is the secondary research equivalent and involves analysis and interpretation of existing data. Both realist modes place emphasis on explanation of the interplay of contextual circumstances and mechanisms that foster the success or failure of an intervention. The principal aim is to refine understanding of how and why the intervention operates through the development of a more nuanced explication of what is termed programme theory, that is, the implicit or explicit hypotheses about anticipated outcomes on which a series of interventions (such as 1000 Lives+) are based. 247
Realist inquiry is rooted in the realist tradition in the philosophy of science. At base, realism steers a path between empiricist/positivist and constructivist accounts of scientific explanation243 and is regarded as the principal post-positivistic perspective. 242
The scholarship of Pawson and other realists is underpinned by a generative theory of causation. Hence the aim of realist research, such as ours, is not to identify variables that associate with one another as advocated by positivism. Instead, the research goal is to surface and explain how the association itself came about. 248 In this mode of inquiry, analysis is directed towards the identification and explanation of the underlying generative mechanisms which shape structure, agency, social relations and ensuing practices that are reproduced and/or transformed. 249,250 The realist approach to reviewing the evidence from complex interventions such as patient safety improvement programmes, therefore, assumes that deterministic theories cannot always explain or predict outcomes in every context. 251
The aim of realist inquiry is to further inform our understanding of the nuanced interplay between context, mechanism and outcome for particular interventions. 252–254 Its hallmark is, therefore, a quest to progress from a presumptive definition through to an evidence-informed refinement of a causal explanation. 247,255,256 Crucially, the conclusions of realist studies are recognised to be both provisional and fallible. 257
Realist inquiry
In realist inquiry, testable propositions of how an intervention is perceived to work are depicted through context–mechanism–outcome configurations (hereafter, CMO configurations). 228 In essence, a CMO configuration is a hypothesis that the programme outcome (O) emerges because of the action of some underlying mechanisms (M), which come into operation only in particular contexts (C). 256 Each CMO configuration, therefore, explicates and progressively refines the scope of the original programme theory. 258–260 In this manner, a virtuous circle is completed, fostering deeper understanding of the opportunities and challenges presented by an intervention, to inform future policy and practice.
Realist inquiry has gained increasing acceptance in health-care research, in part owing to its suitability for examining the implementation of complex interventions in heterogeneous, multiprofessional social systems. 261–266 However, a number of challenges have emerged concerning the operationalisation of each component of the CMO configuration. These challenges are discussed in the following four sections.
Intervention
Following Pawson, we recognise that while interventions designed to foster individual, organisational or system change (e.g. patient safety improvement programmes) are complex and diverse,260,267,268 they often depict consistent features. However, each intervention is dependent on collaborative human agency (motivated action) to achieve their effects. Consequently, the implementation chain of an intervention will be shaped by inconsistencies, as individuals and collectives, each differently enabled or constrained by the social system, engage with, adopt and adapt or ultimately reject the resources and reasoning provided by the programme. 251 The operationalisation of an intervention is, therefore, contextually dependent, influenced by the social system into which it is introduced and apt to mutate in situ. 251,269
There have been a number of realist approaches to analysing interventions in health-care organisations. For instance, an early application of realist inquiry into intervention in health care was research undertaken by Greenhalgh et al. into a major reorganisation of four inner-London health-care organisations176,261,270 They present an inclusive analysis of the interwoven components of an intervention, together with a postulated theory for each facet. 176,261,270,271 Similarly holistic approaches are illustrated in Byng et al. ’s evaluation of a complex health services intervention targeted towards people with long-term mental illness,264,272 Manzano-Santaella’s realist evaluation of financial incentives in English hospital discharge policy,273 and other causal explanations of interventions targeted at various stakeholder groups, including (i) patients;274–276 (ii) specific groups of health-care and aligned workers,277–284 and (iii) the standardisation of evidence-based practice through protocol-based care. 285–287
Alongside realist approaches that have been applied to consider ‘whole interventions’, more selective analyses of the discrete components of an intervention are depicted in studies such as Leone’s evaluation of an illicit drug deterrence programme. 288 This sanctions-based intervention is considered only with regard to the effects of its mandatory interview component. Similar approaches are demonstrated in other realist studies of health-care settings, such as (i) Blaise and Kegels’ evaluation of the development of the quality management movement in health-care systems in Europe and Africa;263 (ii) Ogrinc and Batalden’s evaluation of teaching about improvement of care in a clinical setting;289 and (iii) Pittam et al. ’s evaluation of employment advice provided to help people with mental health problems gain work. 290
Thus, it may be argued that previous applications of realist inquiry in health care have applied the concept of intervention inconsistently. Moreover, in our view, intervention is regularly underspecified and is too often conflated with context. As will be described later (see Intervention: a distinct analytical category), in this study we have tried to address these problems by treating intervention as a separate analytical category.
Context
In realist inquiry, four concentric layers of context are typically defined: (1) the broader infrastructural system, the outermost layer; (2) the institutional setting, encompassing the cultural aspects of a given contextual domain; (3) the interpersonal relationships which constitute the relational structure within which actors are embedded; and (4) the individual capacities of the key actors. 242 However, with rare exceptions (e.g. the work of Greenhalgh et al. 270 and of Byng et al. 264), realist studies in health care have, typically, been limited to a domain-specific notion of context. For example, focus may be directed towards the broader infrastructural system and associated aspects of the institutional setting as illustrated in Evans and Killoran’s realist evaluation of tackling health inequalities through partnership working291 or Pommier et al. ’s analysis of health promotion activities within the French education system. 292
Alternatively, realist inquiries have focused on discrete organisational sites293 as in Oroviogoicoechea et al. ’s evaluation of the impact of a computerised hospital information system on nurses’ clinical practice,294,295 Pittam et al. ’s evaluation of employment advice for those with mental health issues,290,296 and Tolson et al. ’s study of managed clinical networks in the care of individuals with cancer-related pain. 297
More recently, other aspects of context have been considered within realist studies in health care. These typically encompass the notion of organisational culture and influences emerging from wider interorganisational alignment. 3,298–300 Key contextual features include leadership, both by corporate management and by clinical health-care professionals,81,181,301 and governance systems, including performance monitoring, evaluation and feedback, which is increasingly patient informed. 28,146,302
Overall, as noted by Shekelle et al,223 many previous applications of realist inquiry have failed to agree on what elements of context are most influential and how context should be conceptualised. 27,303,304 We have tried to avoid this problem by using a multilevel approach to this issue (see Context: structural conditioning).
Mechanism
As originally described by Pawson, the mechanisms of a programme describe what it is about programmes and interventions that bring about any effects and are the processes by which subjects interpret and act on the intervention stratagem. 228,241,242 Thus, it is not programmes that work per se. Rather, it is the underlying reasons or resources that they offer subjects that generate change. 305 In this view, mechanisms explain causal relations by describing the powers, propensity or particular ways of acting inherent to a system and are linked to, but not synonymous with, the underlying programme theory. 306,307
Further insight into the nature of mechanisms is contributed by the work of Hedström and Ylikoski,308 who contend that a mechanism is a causal process that produces an effect or phenomenon. In addition, they posit that a mechanism has structure and operates in hierarchical sequence. This conceptualisation parallels that of Fleetwood,306 who sees mechanisms as consisting of a cluster of causal factors or components comprising social structures, practices, relations, rules and resources, with each cluster possessing the powers, capacities and potentials to do certain things. It is also important to appreciate that mechanisms produce contextually modulated effects according to their spatiotemporal relations with other objects, and have their own causal powers and liabilities, which may trigger, block or modify their action. 309,310
In realist inquiries, mechanisms are typically presented as part of a CMO configuration. 311,312 Indeed, some studies extend this explanatory analysis to expose the specific roles of different components of the intervention. This is exemplified in Mazzocato et al. ’s study,313 where candidate mechanisms, attributed to the operationalisation of service improvement methods, are used to define multiple CMO configurations. However, in studies where CMO configurations are not developed, merely disconnected mechanisms or outcomes, as opposed to a causal explanation, may be reported, as in Harris et al. ’s314 realist review of journal clubs and Gunawardena’s315 review of the effectiveness of geriatric day hospitals.
It is acknowledged in realist inquiry that one CMO configuration may be embedded in another or configured in a series (in which the outcome of one CMO becomes the context for the next in the chain of implementation steps). 307 This aspect of realist inquiry remains underdeveloped, as it demands a highly complex formulation of CMO configurations. 316–318
In addition, although it is acknowledged that mechanisms encompass the reasoning of its participants, this aspect of realist inquiry is also little explored,256 with few studies reporting participants’ thoughts about why they chose to change, or indeed adhere to, their established practice (for two exceptions, see Dieleman et al. 319 and Jackson et al. 320). The relative neglect of this aspect of mechanism may not be surprising as, as noted in Vassilev et al. ’s realist review of the role of social networks in the management of chronic illness,321 unpacking and conceptualising reasoning is fraught with difficulty as justifications for choices can operate within different, and often contradictory, stances.
Outcome
In realist inquiry, an outcome cannot be perceived as a simple, single aspect of change. The multifaceted nature of an intervention, particularly when implemented within different organisations, each shaped by their own contextual constraints and enablements, leads to different patterns of social transformation. 243,269
Many applications of realist inquiry in health care attempt to present the health outcomes of interventions. However, as noted by Floyd et al. ,322 the specification and measurement of outcomes poses challenges. For example, health outcomes may be obscured, merged with context and mechanism and depicted as factors,323 or simply framed in terms of the intervention’s effectiveness. 324 Outcomes supported by CMO configurations, and thus setting out a clear explanatory argument, such as Tilley’s325 realist evaluation of a British crime reduction programme, do something to tackle this problem. However, few studies explicitly address more subtle and aligned outcomes arising from the intervention.
To summarise, the above section has suggested that, despite the contributions made by realist inquiries in health care, four issues have consistently challenged researchers who have sought to apply existing models: (1) the tendency to conflate intervention with context; (2) the limited conceptualisation of context and mechanism, thereby inhibiting rigorous analysis of their boundaries; (3) the preoccupation with health outcomes, as opposed to wider organisational and systemic gains or losses; and (4) the limited capacity to frame the dynamic, temporal, interplay of intervention, context, mechanisms and outcomes. We now move on to explain how we sought to address these issues through an elaborated model of realist analysis.
Addressing the challenges of realist inquiry
In our realist analysis framework, we employ resources from sociological institutionalism and Archerian critical realism to help better specify context and mechanism and hence to address the challenges outlined above. In the next two sections we introduce the key concepts that inform the revised CMO model we present in Realist analysis: an elaborated intervention–context–mechanism–agency–outcome model.
Sociological institutionalism
Within organisation studies, there has been a ‘growing disenchantment’ with analytical perspectives that emphasise the influence of managerial rationality within organisational life. 326 Rejecting the tenets of strategic management and classical economic theory, sociological institutionalists examine the significance of institutions, the ‘regulative, normative and cognitive [see Glossary] structures that provide stability and meaning to social behaviour’. 327
Some of the main contributions to understanding institutional change and inertia in health care have emerged from analyses conducted at the level of organisational fields, defined as communities of organisations that ‘partake of a common meaning system and whose participants interact more frequently and fatefully with one another than with actors outside of the field’. 328 In a seminal example, DiMaggio and Powell329 suggest that within organisational fields, three forces – mimetic (copying those perceived to be successful), coercive (e.g. regulation) and normative (e.g. stemming from professional norms) – combine to produce powerful templates of what constitutes legitimate organisational structure and action, and we use these terms in our analyses of the data from our study.
In common with critical realism, sociological institutionalism depicts a world of virtual depth,330 stratified and organised through different levels of institutional structures, along with their logics, or commonly held sets of beliefs and values. There are higher, or macro-level, structures; these include societal systems such as the bureaucratic state, capitalist markets, democracy and religion. Then come meso-level structures characterised as organisation sectors or fields; these are composed of those organisations that are involved in a particular issue or policy community. The concept incorporates field-level structures, participating organisations and the people working within and between these organisations. For instance, the field of health-care organisations comprises distinctive actors, diverse institutional logics and distinct governance structures. Finally, there is the micro-level of the individual organisation, together with further intraorganisational levels or groups.
Typically, the multiplicity of logics in a given domain is represented as some combinations of (i) higher-order societal logics,331 (ii) field-level logics332 and (iii) institutional or ‘cultural’ logics. 333 At the societal level, heterogeneous higher-order logics sculpt the social world, conveying the core organising principles of different sectors. 331 Institutional logics orchestrate lower-level institutional strata and ensuing practices. They shape organisational interests, individual preferences, define actors’ expectations about each other’s behaviour and organise their enduring relations with each other. 330,334
Previous studies of UK health-care fields have concentrated on the role of, and dynamics among, three logics: professionalism, bureaucracy and market. Professional logic was dominant for much of the twentieth century and gave workers with specialised knowledge (e.g. doctors) cultural and material privileges, including the power to organise and control their own work and that of others. 335,336 The primary justification for these arrangements was that service delivery is optimised when it is under the control of experts acting with the altruism they are assumed to develop during prolonged training and socialisation. During the latter part of the twentieth century, successive governments promoted combinations of two alternative logics in health care: (1) bureaucratic logic, which holds that service delivery is improved under the administrative control of work using techniques of performance management, and (2) market logic, which holds that improved service delivery arises from conditions of competition among providers and choice among clients.
In our framework, multiple layers of logics constitute and provide the inherent structure to context. However, organisational actors (or agents) may go along with or actively resist these social prescriptions,337 thus inhibiting or supporting change. The process of institutional change is, therefore, both enabled and constrained by (i) the array of institutions, which compose and condition the substructure of the health-care field, and (ii) agential theorisation, reflexivity and ensuing modes of institutional work. 338–340 Accordingly, even though institutions provide meaning to social life, such conditioning is non-deterministic. 229,341
Realist social theory
To further elaborate realist inquiry, we turn to Margaret Archer’s seminal work on critical realism. 229–235 As in Herepath’s study,342 our approach employs Archer’s conceptual approach to structure,229 culture230 and agency,231 together with her later work on reflexivity. 232–235 Our reasons for incorporating Archer’s realist social theory are threefold.
First, Archer’s ontological stance holds structure (context) and agency (mechanism) as separate entities. Consequently, Archer offers help to researchers who struggle over this distinction when analysing the complex interplay of context and mechanism during the development of CMO configurations.
Second, an Archerian approach resonates with sociological institutionalism. 343,344 Hence by harnessing institutional theory within an Archerian approach, institutions are given their due recognition and temporal role as both symbolic constructions and a set of material practices which guide actors’ behaviours. 345 This helps to reveal the multiple logics which shape adherence to, or disregard for, the components of an improvement programme and its underlying ethos.
Third, an Archerian approach offers a robust methodological framework composed of three phases,229 which parallel the context, mechanism and outcome components of a CMO configuration. Therefore, methodologically, the researcher is guided by an aligned approach that helps to distinguish the boundaries between context and mechanism and to reveal possible causal links between them.
Realist analysis: an elaborated intervention–context–mechanism–agency–outcome model
This section explains how our model of realist analysis draws from the resources outlined above to address the challenges of realist inquiry.
Intervention: a distinct analytical category
Our first elaboration to realist inquiry is to include intervention as a separate analytical category in our realist analysis model. This stems from our recognition that although realist studies have adopted similar Pawsonian conceptions of intervention, the absence of intervention as an analytical component has encouraged its underspecification and conflation within context. 286
We therefore consider that there is an imperative within realist inquiry to (i) explicitly define the intervention ‘I’ and (ii) add this to Pawson’s original CMO formula to produce intervention–context–mechanism–agency–outcome (I-CMAO) configurations. This allows us to understand precisely ‘what’ is working in a situated context, for whom, how and in what broader circumstances. This refinement is depicted in Figures 3 and 4, and this method of representation forms the basis of all the translational schematics for the realist analysis presented in Chapters 6–8.
FIGURE 3.
Basic I-CMAO schematic.
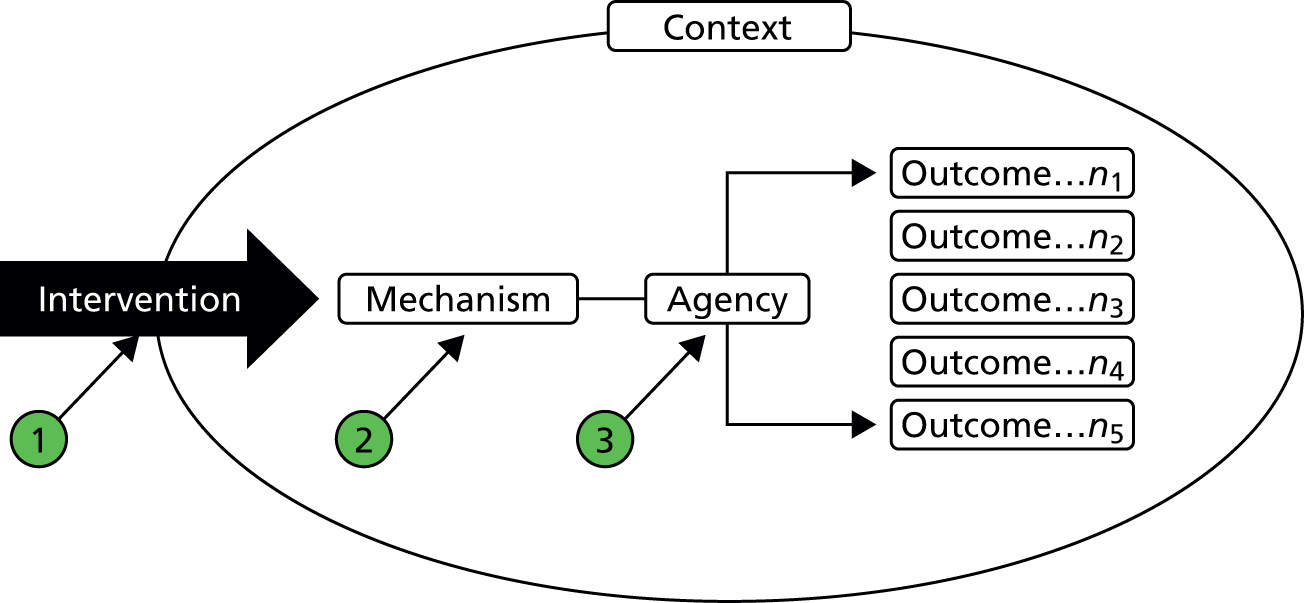
FIGURE 4.
Translation from a CMO configuration to an I-CMAO configuration.
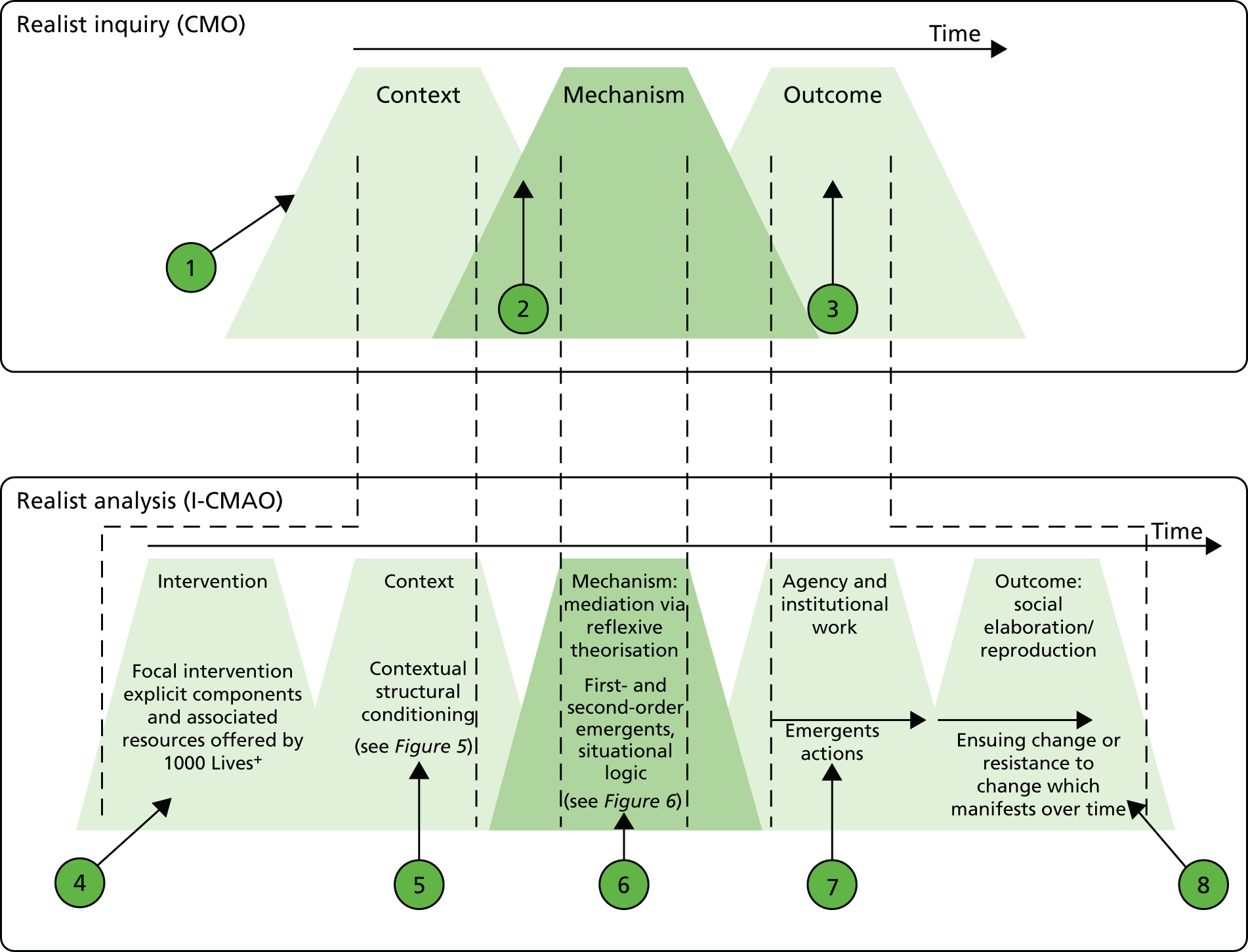
In the upper graphic of Figure 4 we depict a schematic representation of a CMO configuration. As asserted in Realist inquiry, a CMO configuration is a hypothesis that the programme outcome (O) emerges because of the action of some underlying mechanisms (M), which only come into operation in particular contexts (C).
Point 1 highlights the absence of intervention as a separate aspect of the analysis.
Point 2 highlights the difficulty that may arise in distinguishing context from mechanism in realist inquiry due, in part, to the lack of clarity and consistency with which context is conceptualised and operated.
Point 3 draws attention to outcome in realist inquiry. An outcome cannot be perceived as a simple, single aspect of change; however, few studies explicitly address more subtle and aligned outcomes, which arise consequential to the intervention, impacting social elaboration or reproduction.
To address these issues, in the lower graphic of Figure 4, we depict a schematic representation of our I-CMAO configuration and set out our four elaborations.
First, as indicated by point 4, we include intervention as a separate analytical category embedded with the context under consideration.
Second, at point 5 we forward a view of context as stratified, conditioned, relational and temporally dynamic, as expanded in Figure 5. In doing so, we seek to define the ‘situated context’, through the dominant structural and cultural emergent properties in play, their attendant mechanisms and, thus, the impact on lower contextual strata.
Third, at point 6 we apportion mediation and reflexive theorisation to mechanism. In this manner, we distinguish the conceptual elements of mechanism from its ensuing outcome (this is expanded in Figure 6).
Point 7 highlights our goal of examining the ensuing process of institutional change, as opposed to that which ultimately manifests as an outcome, thereby recognising that such change unfolds through time, may be contested and may be at different stages of maturation in different situational contexts.
Finally, as depicted in point 8, outcome is not perceived as a simple, single aspect of change. Rather, we seek to reveal structural and ideational differentiation.
Context: structural conditioning
As noted earlier, both realist inquiry and sociological institutionalism not only stress the importance of context228 but also warn that to enable meaningful explanatory analysis, context cannot be reduced to the spatial, geographical or institutional location into which a social programme is introduced and that a more nuanced understanding of the multiple layers that compose a given context must be established. 236,244,257
Guided by the approach to realist inquiry adopted by Pawson,228 we address the need to develop a more subtle analysis of context by specifying four main levels of contextual hierarchy (infrastructural system, institutional setting, interpersonal relations and individual) with all but the individual level divided into substrata (see Figure 5).
At the highest hierarchical level, we see the infrastructural system of the Welsh health-care state as comprising three strata: (1) the higher-order societal logics which mould this contextual arena; (2) the Welsh Government, as a devolved substate nation, and (3) the public sector partner agencies with regulatory oversight of health-care quality and patient safety, which operate in close liaison with, but distinct from, the Welsh Government and NHS Wales. The second highest hierarchical level of context, the institutional setting, is conceptualised through two strata: (4) NHS Wales, as a corporate whole, and (5) its seven constituent health boards as distinct multisite organisations. The third level, interpersonal relationships, which constitute the relational structure within which actors are embedded, is captured across two further strata: (6) a hospital site-based ward or multisite department and (7) the functional team (the group of people who carry out the tasks involved in running a ward or department). Our final stratum (8) describes the capacities of the individual actors.
However, a stratified model of context provides only the basic architecture of our argument, as it lacks the means to consider context as ‘situated’, meaning dynamic, conditioned, relational and temporally fluid. In essence, we see the dynamism of context as contoured by emergent structural, cultural and agential powers across time. Our recourse to Archerian critical realism, together with the work of Herepath,342 therefore offers a more complex yet nuanced means to develop I-CMAO configurations.
An underlying premise of realist theory and research is that context affects or mediates ensuing agential actions346 and hence the structural constraints and enablements of context are mediated to the agent as first-order emergents. First-order emergents encompass agents’ placement within their broader social context and roles, their vested interests, the opportunity costs associated with different courses of action and, thus, their perceived interpretive freedom. Such first-order emergents impact differently on each agent, enabling or frustrating the attainment of their desired goals depending on their social bargaining power, both as individuals and as members of groups. Consequently, our analysis of how context impinges on agents is stratified across three levels: social position, how their roles relate to others and the cultural logics of the institutional domain within which they are situated. In this way we expose the contextual constraints and enablements imposed on the agent.
The second stage by which the constraints and enablements of context are mediated addresses how agents, conditioned by their contexts, think about and influence the formulation of their desired projects, both individually and collectively. 232 These influences give rise to potential second-order emergents (i.e ‘the results of the results’ of the first-order emergent properties346), which in their turn affect the ways in which an intervention is implemented.
Accordingly, in our realist analysis, we separate context from its mediation (or the effects of the context on the intervention). As depicted in Figure 5, we first specify the explicit stratum concerned, so that hierarchical and heterarchical influences may be more readily appreciated within a situated context. Second, we identify dominant structural and cultural emergent properties within that context to define the structural conditioning in play. Third, we apportion its mediation to mechanism, as expanded in Mechanism: sociocultural interaction.
FIGURE 5.
Contextual strata: structural conditioning, hierarchical and heterarchical metamechanisms.
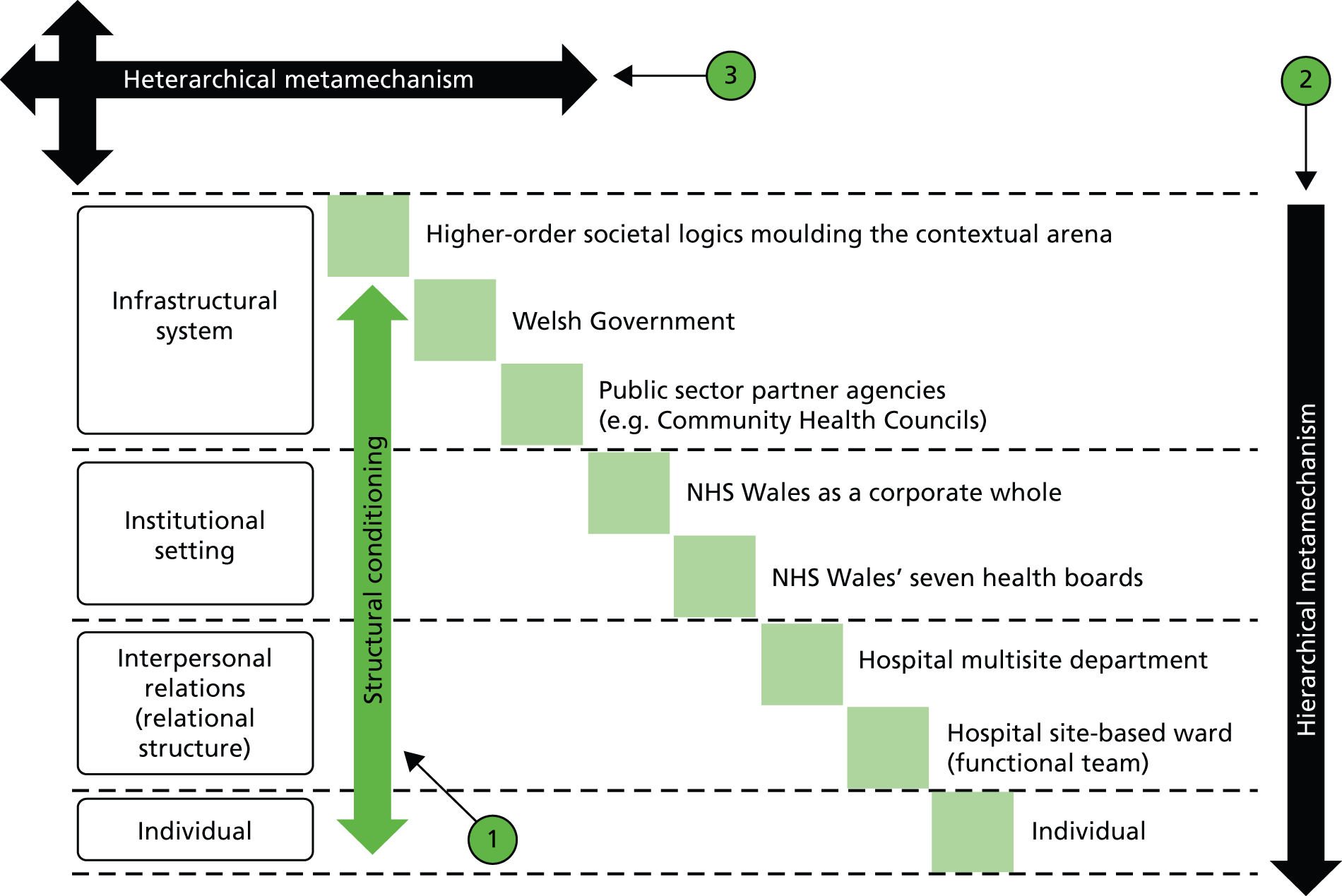
In Figure 5, we illustrate our view of context as stratified, conditioned, relational and temporally dynamic through the ‘steps’ of the contextual strata. This shows how the outcome of one I-CMAO becomes the context for the next in the chain of implementation steps.
In point 1, we depict the collective weight of structural conditioning impacting across contextual strata. This notion, as expanded in Context: structural conditioning, is an underlying premise of realist inquiry and Archerian realist social theory.
In addition, we highlight the notion of a ‘meta mechanism’ that functions as a ‘carrier’ for the 1000 Lives+ national programme across NHS Wales. Point 2, therefore, depicts a hierarchical meta mechanism emergent from the bureaucratisation of the programme across the policy/practice gap in NHS Wales.
Furthermore, point 3 depicts a heterarchical metamechanism inherent to normalisation of the programme at the level of the functional team across linked strata.
Mechanism: sociocultural interaction
In her later work, Archer has refined her conceptualisation of the mediation of contextual influences, which, she contends, is undertaken via two mechanisms: habituation, guiding routine action, and reflexivity, guiding those actions which demand a more creative response. 338 Critically, Archer asserts that such reflexive theorisation occurs through three stages: (1) discernment, the preliminary review stage of an issue of concern, where reflective retrospective and prospective thought informs practical action; (2) deliberation, involving the ranking of such concerns against others; and (3) dedication, entailing their prioritisation and alignment to foster a fallible yet correctable commitment to a chosen path. Reflexive theorisation thus represents the explicit interplay of social context and personal concerns that lies at the heart of Pawson’s notion of mechanism.
Following this approach, in our realist analysis we allocate contextual mediation to mechanism, and to this we add reflexive theorisation. Furthermore, as depicted in Figure 6, we distinguish the conceptual elements of mechanism from its ensuing outcome, illuminating the fundamental role of beliefs and values – institutional logics – on the propensity to act, and revealing the contested nature of institutional change and practice evolution.
FIGURE 6.
Mechanism: mediation via reflexive theorisation vs. habituation.
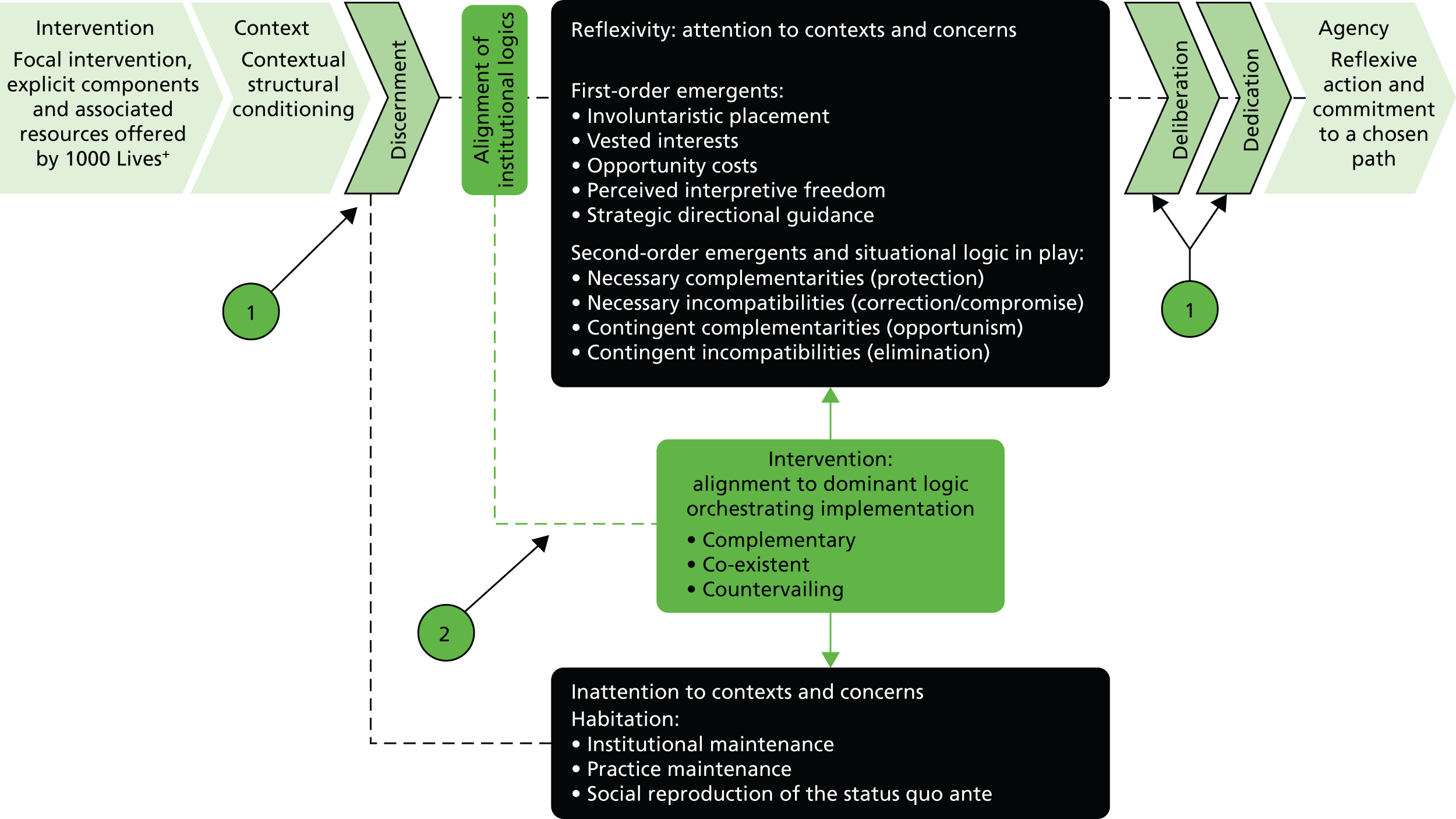
Figure 6 shows a preliminary outline of the key components of a mechanism. As noted in Figure 3, we apportion mediation and reflexive theorisation to mechanism. We thus distinguish the conceptual elements of mechanism from its ensuing outcome: the agential emergent properties, expressed through the unfolding strategic negotiation of change, and the mode of institutional work enacted, to deliver sustainable outcomes, be they elaborative or reproductive.
In point 1, we depict Archer’s refinement of her notion of contextual conditioning via the mediation of structure by agency. This, Archer contends, is undertaken via two mechanisms: habituation, guiding routine action, and reflexivity, guiding those actions that demand a more creative response. This manifests through three stages: discernment, the preliminary review stage of an issue of concern, where reflective retrospective and prospective thought informs practical action; deliberation, the ranking of such concerns against others; and dedication, their prioritisation and alignment to foster a ‘fallible yet corrigible’ commitment to a chosen path. Such reflexive agency thus represents the explicit interplay of social context and personal concerns.
In point 2 we assert that this three-stage process is modulated by the alignment of institutional logics. Complementarity, co-existence or contradistinction via a countervailing stance thus impact first- and second-order emergents to shape the individual’s situation logic and the ensuing stance that emerges from their deliberation and dedication to a chosen path.
In this study of the 1000 Lives+ programme, we examine the demarcation between context and mechanism, focusing on mediation, reflexive theorisation, ensuing agency via negotiation and the mode of institutional work enacted during two fundamental institutional processes: bureaucratisation and normalisation. These, we contend, operate as sociocultural and organisational meta mechanisms, the underpinning carriers347 of the processes of health-care change desired by 1000 Lives+. In essence, it is through successful embedding within these fundamental meta-mechanisms that the patient safety programme becomes institutionalised.
Bureaucratisation
Given that the logic of the bureaucratic state is predominantly that of command and control, we envisaged bureaucratisation as a vertical, top-down meta mechanism. In this manner, the Welsh Government has enacted state-centric control over NHS Wales. This is exemplified by the gradual bureaucratisation of the 1000 Lives+ national patient safety programme; specifically, the shift from optional engagement to mandatory engagement as defined in the Welsh Government’s tier 1 performance targets for NHS Wales. Such bureaucratisation now composes and conditions the substructure of the health-care field, creating a context of politicised force majeure. We therefore examine the consequences of adherence to the 1000 Lives+ programme and describe the mechanisms which foster institutional coupling to, and decoupling from, patient safety governance processes. 85,348,349
Drawing on the work of Greenwood et al. ,227 as well as terminology used by Lewin and Schein,350,351 we frame such institutional change through six stages – disconfirmation, deinstitutionalisation, preinstitutionalisation, theorisation, diffusion and reinstitutionalisation – and use these to develop our understanding of the local implementation of the 1000 Lives+ programme, as set out in Chapter 4.
Normalisation
We envisaged normalisation as a heterarchical metamechanism operating (i) horizontally across discrete functional teams, such as policy, health-care management or health-care clinical professionals; and (ii) hierarchically, bottom-up and top-down, across conceptual strata. Hence, to provide deeper insight into the implementation of the 1000 Lives+ programme, we use normalisation process theory, as developed by May et al. ,352–355 to refine our understanding of how agency embedded this patient safety improvement programme in a local context. The concept of normalisation acknowledges that those involved in the process of institutional change have to undertake institutional work – and thus theorise in a reflexive manner338,356– to reconfigure ensuing practices to meet local conditions. 357
This mid-range theory presented four possible generative mechanisms – coherence, cognitive participation, collective action and reflexive monitoring – which are viewed to be central to the embedding and integration of institutionally refined practices. As May and Finch353 point out, such mechanisms are subject to the power play of social actors. Therefore, by focusing on normalisation, our examination of the implementation of the 1000 Lives+ national programme was sensitised to the dynamic interplay of multiple logics.
Agency and ensuing outcomes: structural and cultural elaboration or reproduction
In our realist analysis framework, outcome is not perceived as a simple, single aspect of change such as a defined health outcome. Instead, it is recognised that the multifaceted nature of an intervention, particularly when implemented within different organisations, each shaped by their own contextual constraints and enablements, gives rise to discordant mechanisms which trigger different patterns of social transformation. 243,269 Moreover, such outcome patterns are contingent on all the tiny process and positioning issues that occur on the way to the goal. 244
Our framework is, therefore, concerned with the explication of these unfolding actions over time. Specifically, we seek to examine the means through which the health-care practice change advocated by the 1000 Lives+ programme, and the three focal interventions we consider in depth, are negotiated by the functional teams positioned within the contextual strata depicted in Figure 5. We thus seek to illuminate how health-care practice evolves (or not) over time, by considering the third-order emergents impacting within the contextual arena.
Third-order emergents arise from the effects of first- and second-order influences on the outcomes of the intervention. 229 This concept, therefore, captures structural and ideational differentiation, together with the regrouping inherent to the power play of a diverse array of agents.
Summary
We argue in this chapter that, as an established methodological complement to the critical realism of which Pawson is a key advocate, and as an innovative lens for realist inquiry, an Archerian approach provides both an explanatory framework for examining the interplay between structure (context) and agency (mechanism) and a viable means for developing and refining emergent I-CMAO configurations.
In seeking to demarcate context from mechanism and intervention, our stratified model of context depicts strata as hierarchical and interconnected. This purposely deviates from the notion of context bifurcated into external and internal domains,216,358 and echoes the broader realist literature in terms of a sociology divided into levels. 359,360 Moreover, by revealing the mechanisms that operate within and between these conceptual strata,316–318 as each action-level or arena is, simultaneously, a framework for action and a product of action,330 we carry forward these generative threads into our realist analysis to define the web of mechanisms operating within the focal context.
Chapter 3 Research design
Overview
This chapter sets out our research design and approach to data collection and analysis. First, acknowledging recent changes to research ethics and access permissions in NHS Wales, we provide a step-by-step account of our actions in the start-up stage to the study. Second, our comparative case study research design is presented, explaining our approach to realist analysis, case site selection and sampling strategy, and to data collection, coding and analysis. Finally, we reflect on the challenges encountered during our research across NHS Wales and discuss their impact on our realist analysis of hospital patient safety.
Research ethics and access permissions in NHS Wales
In February 2011, following notification of the award from the National Institute for Health Research Health Services and Delivery Research programme, an Integrated Research Application System project data set was developed prior to the formal start of the study in October 2011. Over the next 4 months, working in collaboration with the National Institute for Social Care and Health Research (NISCHR) Patient Safety and Healthcare Quality Registered Research Group, hosted by the School of Medicine, Cardiff University, and in close liaison with the Director General, Health and Social Services and NHS Wales Chief Executive, the ‘in principle’ engagement of all NHS Wales’ seven local health boards [Abertawe Bro Morgannwg University Health Board; Aneurin Bevan University Health Board; Betsi Cadwaladr University Health Board; Cardiff and Vale University Health Board; Cwm Taf University Health Board; Hywel Dda University Health Board; and Powys (Teaching) Health Board] was secured. In each health board, study contacts with delegated strategic oversight for patient safety were recruited at medical director or associate medical director level.
Having gained NHS Wales’ ‘in principle’ engagement, sponsorship of the study was secured from Cardiff University and the required documents were submitted to the Main Research Ethics Committee (MREC) for Wales. MREC approval was granted in August 2011 and site-specific NHS research and development forms were submitted to the newly established NISCHR Permissions Co-ordinating Unit. Following this, full ethical and research governance permissions were obtained from Cardiff Business School, Cardiff University, and research passports were obtained for Herepath and Kitchener. Research validation and global governance approval was obtained in September 2011. The research and development committees of the seven health boards granted site-specific research permission and researcher access by December 2011, and Herepath and Kitchener received either honorary research contracts or letters of access.
Anonymisation
All seven health boards in NHS Wales participated in the study. Summary data describing each organisation are presented in Appendix 1. To ensure anonymity from this stage of the report onwards, participant health boards are identified via a randomly assigned code letter from A to G. Numeric subscripts are then used to identify a constituent major hospital (X1), a constituent district general hospital (X2) or a constituent small local community hospital (X3).
Comparative case study approach
The study set out to examine which contextual factors matter and how they matter, and to explain why they matter in the hope that this may lead to improvement in the design, processes and outcomes of patient safety programmes. A comparative case study research design is appropriate for research of this nature361 and was therefore adopted and aligned to realist analysis as discussed below.
Comparative case studies in realist informed research are shaped by five methodological principles: (1) explication of structure and context; (2) explication of events; (3) abduction and retroduction362–364 (see Ontological andepistemological alignment to realist analysis, below); (4) empirical corroboration (ensuring that proposed mechanisms have causal power and better explanatory power than alternatives365); and (5) triangulation and multimethods (using multiple approaches to support causal analysis based on a variety of data types and sources, analytical methods, investigators and theories365). Each of these features are employed throughout Chapters 4–8.
Ontological and epistemological alignment to realist analysis
The basic premise, or ontology, of critical realist informed research is that the world may be viewed as stratified into three domains in which are apparent structures, mechanisms, powers and relations; events and actions; and experiences and perceptions. 362,363 Research in this tradition focuses on the identification and explanation of the underlying generative mechanisms that shape structure, agency and the social relations that are reproduced and/or transformed. 252
The nature of the approach taken by realist research does impose limitations on what may be revealed through a comparative case study research design. However, it is a viable means for discerning structures and mechanisms, conveyed through our understanding of the social world and, thus, subject to revision as our collective knowledge is refined. 363,365 Nevertheless, one cannot connect powers or causal mechanisms to events and perceptions easily or securely by simple inspection. 366 This is because, once set in motion, they continue to have an influence even if other countervailing powers and mechanisms prevent this influence manifesting itself. The act of drawing conclusions from a comparative case study is, therefore, a complex matter. It is informed by epistemology (what we think is known), the nature of the comparisons made between cases and the mode of inference employed.
Comparative case study research designs using a critical realist approach must, therefore, seek to define constraining and enabling social structures, encompassing organisations, groups and individuals, together with the rules, practices, technological artefacts, discourse and culture which they manifest. 365 In addition, social actors’ interpretations of such structures, and their beliefs, values and theories, require detailed consideration. The comparisons made between cases draw on abductive and retroductive modes of inference as opposed to inductive and deductive. 363,364 Abduction involves the production of an elementary account of a basic process or mechanism. 363 Retroduction builds on this analytical stage to reconstruct the basic conditions for such phenomena to be what they are, so fostering knowledge of the conditions, structures and mechanisms in play. 362,363 Abstraction forms the basis of both abduction and retroduction. As empirically demonstrated by Herepath,342 abstraction draws out the various components within the situated context so that the researcher may gain new insight into the way they combine and interact.
Case site selection and sampling strategy
Case site selection was based on a two-stage sampling strategy. In phase 1, four clear and readily operable criteria – corporate parent, complexity, function and geographical coverage – were employed to define the purposive sample of case-site hospitals within each health board (see Appendix 1), and three within-case comparators were selected from each health board: (1) a major hospital, (2) a district general hospital and (3) a small community hospital. This approach ensured theoretical variation in I-CMAO configurations by optimising the scope for description, interpretation and explanatory analysis, while reducing chance associations. 367–369 In contrast, in phase 2, the focus of the study was narrowed to four local health boards, and centred on deeper examination of the most promising I-CMAO configurations for the three focal interventions examined from the 1000 Lives+ programme.
Data collection, coding and analysis
In adopting an overarching approach that combined realist inquiry with regard to the explication of I-CMAO configurations, this study sought to examine the contextual conditioning which predated the launch of the 1000 Lives+ programme, together with the mechanisms which emerged from the social interaction of different groups of health-care workers engaged in its implementation, and the subsequent outcome on the embedded practices of day-to-day health-care practice. As illustrated by the schedule of data methods and sources illustrated in Figure 7, and expanded in the following four sections, a wide range of data collection methods were used. 256
FIGURE 7.
Schedule of data methods and sources.
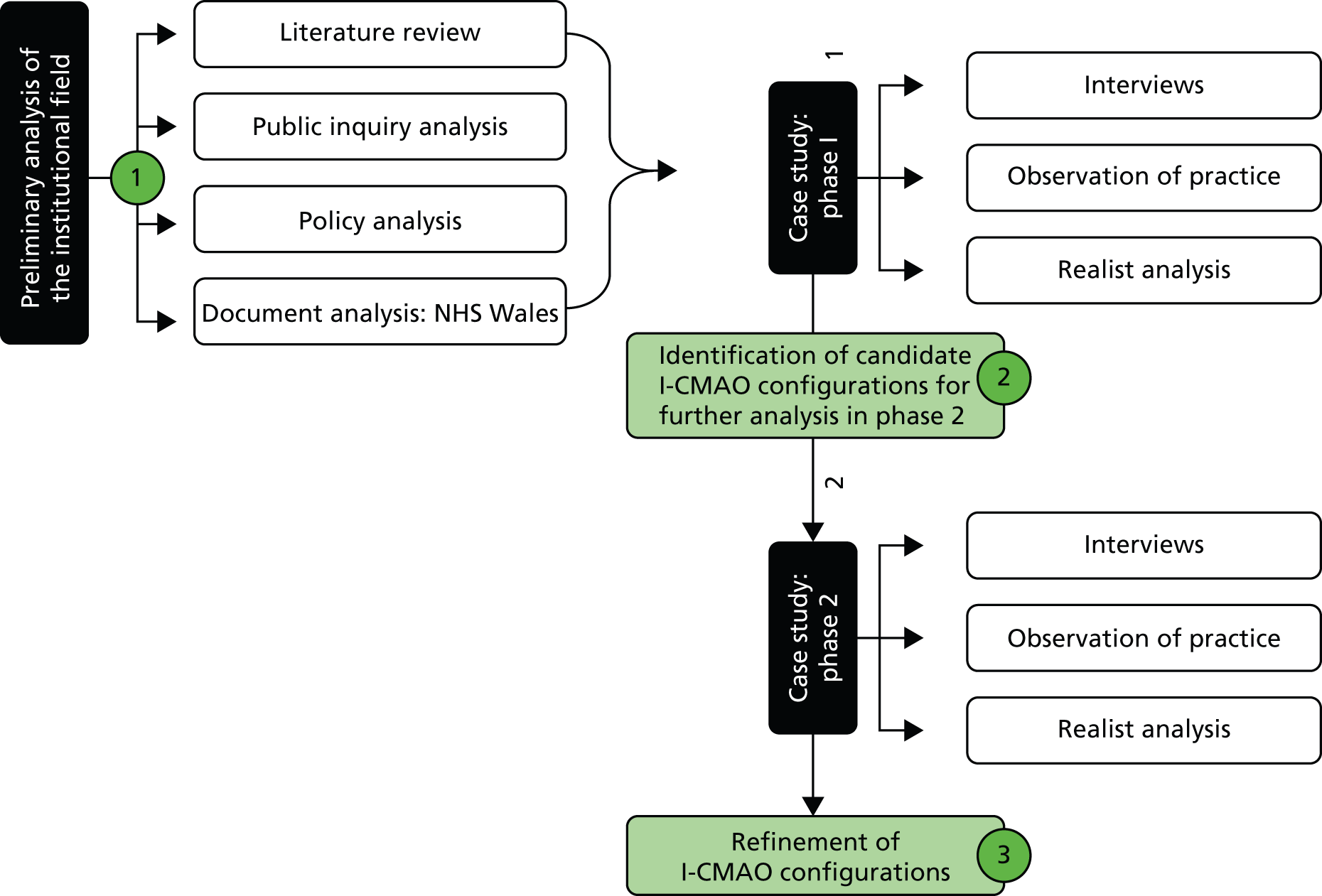
In Figure 7 we set out a schematic of data methods and sources, expanded below.
As set out in point 1, a series of data searches were undertaken. These included one that centred on public inquiries (see Table 5) as a means of gaining rapid awareness of significant systemic health-care delivery and patient safety failures. The literature review, policy and document analysis was maintained throughout the duration of the study. Points 2 and 3 depict the preliminary identification of candidate I-CMAO configurations and their progressive refinement throughout the study.
Welsh health-care policy context data
To build a coherent explanatory analysis of the context and events that led to the development and implementation of the 1000 Lives+ programme, our research commenced with an analysis of UK and devolved Welsh health-care policy spanning the period from 1997 to 2013. As indicated in Table 2, the UK coalition government’s White and Green Papers, together with other key legislative proposals, were accessed and downloaded from the Department of Health’s website. Those of the former UK New Labour government were sourced via the National Archives. Relevant Welsh Government documents, together with those from the National Assembly for Wales, were accessed from site-specific policy archives. In addition, Welsh health circulars and ministerial letters spanning the period 1997–2012 were accessed via the Health of Wales Information Service (HOWIS) intranet. A repository in excess of 1700 documents was established and archived in an electronic database to facilitate the exploration of the structural conditioning of the Welsh health-care system.
| UK government policy |
|---|
|
| Welsh Government policy |
|
Three analytical frameworks informed the coding of these data: (1) Friedland and Alford’s depiction of higher-order societal logics;331 (2) Barber’s three paradigms of public sector reform;370 and (3) Hood’s doctrinal components of new public management. 371,372 Collectively, these focused our approach to contextual conditioning and set out the requisite ‘vocabulary’373 through which the infrastructural system – specifically, the organisational and professional governance processes structuring health-care quality and patient safety – could be abstracted from the policy archive. As illustrated in Chapter 4, this centred on the interplay of the higher-order societal logic of the bureaucratic state with the field-level logics of the market, professionalism and democracy in health policy.
Analysis of these data revealed the systemic, paradigmatic, dominant and subordinate institutional logics, which condition NHS Wales structurally and culturally, and impact on infrastructural systems underpinning hospital patient safety. In addition, our consideration of bureaucratisation and normalisation sensitised us to the generative mechanisms which foster institutional coupling to and decoupling from patient safety governance processes, as well as the complex web of constraints and enablements which impact on differently positioned social actors and condition their response to the development and implementation of the 1000 Lives+ programme.
Semistructured realist interviews
To refine our explanatory analysis of the context and events that led to the development and implementation of the 1000 Lives+ programme, we sought empirical corroboration from participants in the seven Welsh health boards. In each health board, an initial section of potential research participants was identified in close liaison with the study’s local contact. As summarised in Table 3, individuals were purposively drawn from a wide range of organisational roles. These encompassed the corporate management structure, clinical professionals and those occupying hybrid positions such as health-care clinical professionals in managerial roles.
Following confirmation of individuals’ consent to participate in the study, realist interviews were undertaken,228 guided by the questionnaire defined in Appendix 2. In addition, during each interview, respondents were asked to suggest further potential research participants. This ‘snowball’ approach helped to secure access to staff across NHS Wales with relevant knowledge and expertise in the three focal patient safety interventions examined. It also provided the opportunity to gain permission to observe meetings and the established practices of health-care delivery.
Additional research participants for the study were drawn from the research team’s extensive network of contacts across the Welsh public service, comprising (i) the Welsh Government’s Department of Health and Social Services; (ii) external organisations tasked with the strategic oversight of patient safety in NHS Wales; and (iii) health-care professional bodies.
Finally, to help refine the study’s emergent findings, world-leading academics with research interests in health-care quality and patient safety were also interviewed. Therefore, as summarised in Table 3, a total of 160 interviews, face to face or by telephone, digitally recorded and professionally transcribed, were undertaken across phases 1 and 2 of the study. Interviews ranged in duration from 30 minutes to 90 minutes, with a mean time of 40 minutes.
| Exampler roles | Number |
|---|---|
| Welch Government | 10 |
|
|
| NHS Wales, board-level executive directors | 20 |
|
|
| NHS Wales, sub-board-level associate directors | 20 |
|
|
| NHS Wales, medical and surgical staff | 20 |
|
|
| NHS Wales, nursing staff | 40 |
|
|
| NHS Wales, pharmacy staff | 20 |
|
|
| 1000 Lives+ national programme | 10 |
|
|
| External stakeholders | 20 |
|
|
| Total | 160 |
The transcript of each interview was validated by (i) correcting errors, predominantly typographical, that arose most typically from the use of complex medical terminology; and (ii) correcting queries, annotated and time-marked by the transcriber, that arose from the use of medical and health policy acronyms (e.g. ‘VTE’ meaning venous thromboembolism; ‘AQF’ meaning ‘annual quality framework’). These data were then coded in a two-stage process.
First, a central registry data file was created on an external hard drive, including (i) the interviewee’s assigned anonymisation code; (ii) their name; (iii) their gender; (iv) their profession; (v) their role; (vi) their hybrid status; (vii) the anonymisation codes for their employing health board (or other organisation) and, if relevant, (viii) the anonymisation codes for their base site hospital. Access to this data file was password protected and restricted to Herepath and Kitchener. Second, transcripts were coded in accordance with the framework defined in Table 4, and records linked to the central registry data file.
| Theme | Subtheme | |
|---|---|---|
| Preliminary coding framework: NHS inquiries recommendations impacting health-care quality | ||
| Regulation |
|
|
| Corporate governance |
|
|
| Clinical governance |
|
|
| Patient engagement |
|
|
| Supplementary coding framework: infrastructural system – Welsh Government | ||
| Health-care policy and patient safety |
|
|
| Developing an ethos of patient safety |
|
|
| Internal oversight of patient safety |
|
|
| External oversight of patient safety |
|
|
| Supplementary coding framework: institutional setting – NHS Wales as a corporate whole/NHS Wales’ health boards | ||
| 1000 Lives+ national programme |
|
|
| Developing an ethos of patient safety |
|
|
| External oversight of patient safety |
|
|
| Internal oversight of patient safety |
|
|
| Impact of reconfiguration of patient safety |
|
|
| Supplementary coding framework: institutional setting and interpersonal relations – hospital multisite department/hospital site-based ward (functional team) | ||
| 1000 Lives+ national programme |
|
|
| Context of health-care delivery |
|
|
| Supplementary coding framework: mechanism | ||
| Institutionalisation |
|
|
| Normalisation |
|
|
| Reflexive theorisation |
|
|
| Supplementary coding framework: agency | ||
| Institutional work mode and disposition to act |
|
|
| Supplementary coding framework: outcome | ||
| Perception of outcome |
|
|
Initially, as described in Chapter 2, our data were analysed to examine the bureaucratisation of 1000 Lives+ programme (see Chapter 4), and its ensuing normalisation at the level of the functional team within each health board (see Chapter 5). This stage of our analysis drew on two institutional theories. First, as noted in Chapter 2, we utilised the work of Greenwood et al. 227 and their six linked institutional mechanisms: disconfirmation, deinstitutionalisation, preinstitutionalisation, theorisation, diffusion and reinstitutionalisation. Second, guided by the work of May et al. ,352,353 the process of local implementation was framed through the mechanisms that foster the normalisation of complex interventions in daily health-care practice. These stages shaped our deliberation and explication of the 1000 Lives+ programme’s I-CMAO configuration spanning the Welsh health-care institutional field.
These data were further interrogated through our innovative approach to realist analysis, as illustrated in Chapters 6–8. Drawing on the work of Herepath,342 interview transcripts were analysed to identify first-, second- and third-order emergents. In this manner, interviewees’ perceptions of their situated context were ascertained, together with the power play inherent to strategic negotiation of change, and ensuing outcome. These latter stages involved abstraction to draw out various components of the focal intervention and so facilitate the conceptualisation of their interplay, through combination and interaction, in the situated context. This was then supplemented by retroduction. Therefore, the generative mechanisms that operated through an emergent causal configuration were surfaced through a combination of theory and experimental observation. 228
Given the number of interview data collected, the selection of excerpts for inclusion in the report had to be constrained. To respond to this requirement we adopted the following format for references to transcription data in Chapters 4–8. First, succinct statements, which captured interviewees’ perceptions of context and their beliefs, values and reflections – and, thus, the reflexive theorisation inherent to mechanisms – together with ensuing actions, and outcomes, were prioritised. Throughout Chapters 4–8, such data excerpts are identified by a chapter code and number. For example, ‘transcription 4:01, below’, indicates the first transcription excerpt included in Chapter 4. Where data from interviews are used to make a point but excerpts are not included in the text, this is indicated in a similar way, but without ‘below’. Full transcripts of all interview data, including those discussed but not illustrated in the report owing to editorial word constraints, are archived in a supplementary data file. These may be obtained for personal research use only from the corresponding author of this report.
In contrast to the wealth of interview data included, limited observational data are alluded to in this report. This deliberate restriction is a result of the marked disparity between overt observation of practice undertaken during the study and inherently opportunistic covert observation of practice that arose across multiple case sites.
Supplementary organisational data
Six supplementary forms of case site-specific data were also collected. These encompassed (i) Executive Board papers; (ii) health board mortality data; (iii) Welsh health-care-associated infection programme data; (iv) external inspection reports from Healthcare Inspectorate Wales (HIW), Community Health Councils (CHCs) across Wales, the Wales Audit Office and the Public Services Ombudsman for Wales (PSOW); (v) 50 hours’ observation of established day-to-day health-care practice undertaken to discern embedded leadership, theatre and infection prevention and control (IPAC) practices; and (vi) feedback sessions to NHS Wales and the 1000 Lives+ team, during which our posited I-CMAO configurations were tested and refined.
Supplementary secondary data
To gain an in-depth appreciation of the contextual issues impacting on hospital patient safety, and sensitise our subsequent analysis, the reports generated by six public inquiries into safety failures in the NHS, listed in Table 5, were collected.
|
For the purposes of this study, data in the form of 954 reported recommendations – the espoused lessons to be learned for the future – to improve the design, delivery and sustainability of safe health-care services were collected and archived in an electronic database. This provided further rich insight into the infrastructural system underpinning hospital patient safety, its complex nature and embedded institutions.
Acknowledging that the notion of comparing the reports and recommendations from different public inquiries is somewhat ‘contestable’,378 we therefore coded the abstracted recommendations descriptively, across (i) regulatory oversight, (ii) corporate governance, (iii) clinical governance and (iv) patient engagement. These data were then coded once more in accordance with the nature of the ‘problems/issues’ identified, as depicted in Table 4.
The analysis of these data with respect to extant NHS governance processes helped to identify institutional decoupling – the creation and maintenance of gaps between symbolically adopted formal policies and actual organisational practices379 – which foster institutionalisation of aberrant practice. 346 In this manner, we identified the common vulnerabilities which impact adversely on patient safety, and their advocated remedies. This analysis informed both the development of our interview tool and the selection of our preliminary I-CMAO configurations.
Patient and public involvement
Current hospital patients were not involved in the design, development or operationalisation of this study. However, a broader lay (and patient) perspective was actively sought. Working in close liaison with the NISCHR Clinical Research Centre’s Involving People Programme, two lay representatives were appointed to the study’s advisory board. Each provided insight into the patient experience of health care. Moreover, this was augmented by their collective insight into (i) patient advocacy, (ii) participation in health-board-level stakeholder reference groups and (iii) prior experience of advisory board roles in other health-care studies implemented in NHS Wales.
Challenges encountered in the operationalisation of the study
Two issues arose during the operation of our study that required deviation from the original research protocol.
Access to patient stories and organisational culture survey data
During the design and development of the grant application for this study, the research team was assured of access to an archive of patient stories and organisational culture survey data held by the 1000 Lives+ programme team. Following the commencement of the study, working in close liaison with the 1000 Lives+ programme team, three critical issues emerged on review of these data. First, and most importantly, these data lacked ethical approval and informed patient consent for use for research purposes. Second, the patient stories data had been collected via inconsistent means and lacked the requisite information to verify or contact data sources. Given such issues, these data were, therefore, used in a restricted manner to inform the phase 1 interview guide. Third, with respect to the organisational culture survey data, that archive reflected the organisational boundaries prior to the reconfiguration of NHS Wales. The research teams therefore considered that such historical data provide limited insight into NHS Wales’ evolving cultural composition post reconfiguration. These data were, therefore, used only to inform the research team’s understanding of organisational context, and the organisational legacy effect that it imparts, within each reconfigured health board.
Supplementary quantitative data quality
During phases 1 and 2 of the study, data from interviews and documentary analysis indicated that, with respect to the focal interventions ILQI and RSC, the desired supplementary quantitative data were of inconsistent quality. This issue did not impact RHAI because mandatory surveillance data were available via the Welsh Healthcare Associated Infection Programme (WHAIP) led by Public Health Wales. The research team discussed this issue at length with the study’s advisory board and commissioners, who advocated the continued investigation of the three focal interventions adjusted to reflect the broader organisational outcomes of the 1000 Lives+ programme and focal interventions.
Chapter 4 Institutionalisation of the 1000 Lives+ national programme in NHS Wales: bureaucratisation, health-care policy and patient safety
Overview
Chapters 4 and 5 present our analysis of the implementation and institutionalisation of the 1000 Lives+ programme in NHS Wales. Together, they form the foundation for our analyses of the three focal interventions – ILQI, RSC and RHAI – that are presented in Chapters 6, 7 and 8, respectively. This chapter presents our analysis of the bureaucratisation of the 1000 Lives+ programme at the higher, infrastructural system level of the Welsh health-care field. In contrast, Chapter 5 is focused at lower contextual levels and explores interpersonal and individual engagement with 1000 Lives+ to offer an account of the normalisation of the programme at the level of the functional team.
In this chapter, we first explore the institutional logics moulding the Welsh health-care field and explain how these conditioning influences have framed the implementation and ensuing bureaucratisation of the 1000 Lives+ programme. Second, to penetrate beyond the rhetoric of policy and espoused best practice, we examine actors’ perceptions of the manner in which the 1000 Lives+ programme has become an integral part of Welsh health-care policy. Specifically, we consider its integration with organisational and professional patient safety governance processes operating across the Welsh health-care field. In doing so, we gain further insight into the bureaucratisation of 1000 Lives+ and set out our understanding of the pragmatic issues which foster institutional coupling to, or decoupling from, these governance processes. This chapter, therefore, serves to sensitise our subsequent analyses to the development of patient safety practices in NHS Wales. Finally, we set out our understanding of the local implementation of the 1000 Lives+ programme, anchored to the underpinning MI-PDSA approach.
Institutional logics framing the bureaucratisation of 1000 Lives+
At a systemic level, the post-devolution Welsh health-care field parallels that of the UK – English – NHS and is characterised by the central role of government in overseeing the collective production, provision and consumption of health care. 380 The underlying principles and values underpinning the NHS in Wales remain grounded in the traditional social democratic communitarian ethos apparent at the inception of the NHS in the 1940s381 and access to its operational service infrastructure remains based on the principle of citizenship. 382
When considering the provision of public services at the infrastructural level, Barber370 suggests three paradigms – bureaucratic command and control, quasi-markets, and devolution and transparency370,383 – which may be deployed within a government system if it is to balance equity and diversity with support for high quality.
The classical notion of bureaucratic command and control is forwarded as the means of pursuing change to address public service failure, policy or program priorities, and to demonstrate this response to a wider public and political audience. The alternative formation of a quasi-market logic is supported by governments that wish to introduce market forces within a public service system to provide the individual with choice across a range of providers to improve performance. Finally, the devolution of responsibility to frontline units, augmented by the overt communication of performance measures to patients and staff to enable informed comparisons to be made (transparency), stems from a logic of choice. This is deemed necessary to reform a service where the conditions for the success of quasi-markets are not present.
In practice, according to Barber,370 all of these paradigms are likely to co-exist within large-scale systems, such as health care, although the precise balance of paradigmatic institutional logics within a given health-care field positions one into dominance while the remainder function in a subordinate capacity. Hence we would argue that, while the UK remains emblematic of new public management,384 our data suggest that NHS Wales is far more representative of a new public service logic with the paradigmatic logic of bureaucratic command and control occupying a dominant position, tempering the logics of the market, professionalism and democracy in health policy. Patient safety and associated governance processes appear, therefore, to be primarily structured and directed by the regulatory agency of the Welsh Government.
Bureaucratic state logic
As illustrated in Figure 8, the logic of the bureaucratic state is expressed through an array of structural features that inculcate a pervasive performance measurement and management ethos across the Welsh health-care field. 385,386 Much of this was introduced under the UK New Labour government, such as new systems for clinical governance, a statutory duty of quality and evidence-based national service frameworks. That government also laid the foundations for an array of arm’s-length bodies that retain the scope for direct intervention in the NHS in England and Wales. 387 Some have even seen this as a precursor to the legitimisation of the role of the state as the guarantor of social provision, rather than as the sole provider,388 a stance which resonated with the policy approach of the 2010 UK Conservative–Liberal Democrat coalition government. However, while the logic of the bureaucratic state imposes a sense of control, the efficient use of resources resides largely within the control of discrete professionals. 389 This logic is, therefore, tempered by the wielding of professional power at the individual and group level,390 as illustrated in Figures 8 and 9.
In Figure 8 we depict a schematic representation of the Welsh health-care institutional field. As indicated in Chapter 2 (see Sociological institutionalism), the multiplicity of logics in this domain are represented as some combinations of (i) higher-order societal logics; (ii) field-level logics; and (iii) institutions or ‘cultural logics’, each composed of regulative, normative and cultural-cognitive pillars.
Point 1 illustrates the heterogeneous higher-order logics (the bureaucratic state, capitalist market, democracy, nuclear family and religion) that sculpt the social world, conveying the core organising principles of these different sectors. In both connection and contention with each other, they are held in dynamic tension due to their inherent complementarities and contradictions. Such institutional logics, therefore, orchestrate lower-level institutional strata and ensuing practices: shaping organisational interests; individual preferences; and the ensuing repertoire of anticipated behaviours which define actors’ expectations about each other’s behaviour and organise their enduring relations with each other.
Point 2 depicts the expression of this interplay at the level of the Welsh health-care field. Here, the higher-order societal logic of the bureaucratic state is dominant. Accordingly, the paradigmatic logic of bureaucratic command and control predominates.
Point 3 of our explanatory schematic illustrates the field-level expression of the dominant logic of the bureaucratic state, expressed through an array of structural features that inculcate a pervasive performance measurement and management ethos across the Welsh health-care field.
Point 4 depicts the field-level expression of the subordinate logics of collaboration, professionalism and democracy.
In Figure 9, informed by the findings of our realist analysis in Overview, we illustrate how the dominance of one logic vs. another is influenced by contextual strata.
Point 1 depicts the logic of the bureaucratic state as dominant across the infrastructural and institutional setting of our study.
However, as indicated at point 2, the logic of democracy is dominant for public sector partner agencies with strategic oversight of patient safety.
In addition, as indicated at point 3, at lower contextual strata – specifically, a hospital multisite department or site-based ward – the functional team is orchestrated by a dominant professional logic.
As indicated in point 4, this therefore draws different professional logics into contention and potential conflict with that of the bureaucratic state.
FIGURE 8.
Institutional logics in the Welsh health-care institutional field.
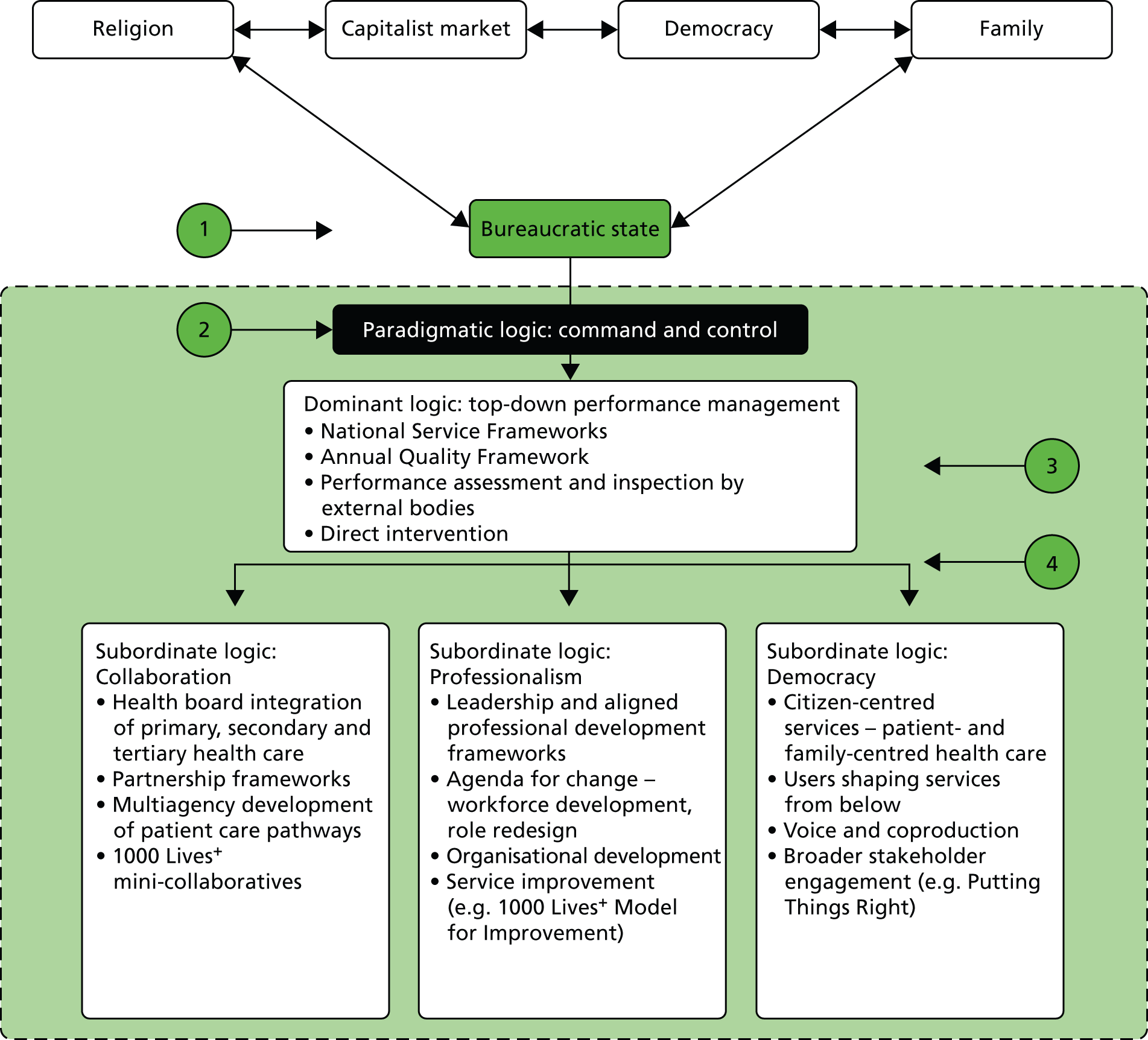
FIGURE 9.
Institutional logics in the Welsh health-care institutional field: dominant and subordinate logics in a complementary, co-existent or countervailing alignment.
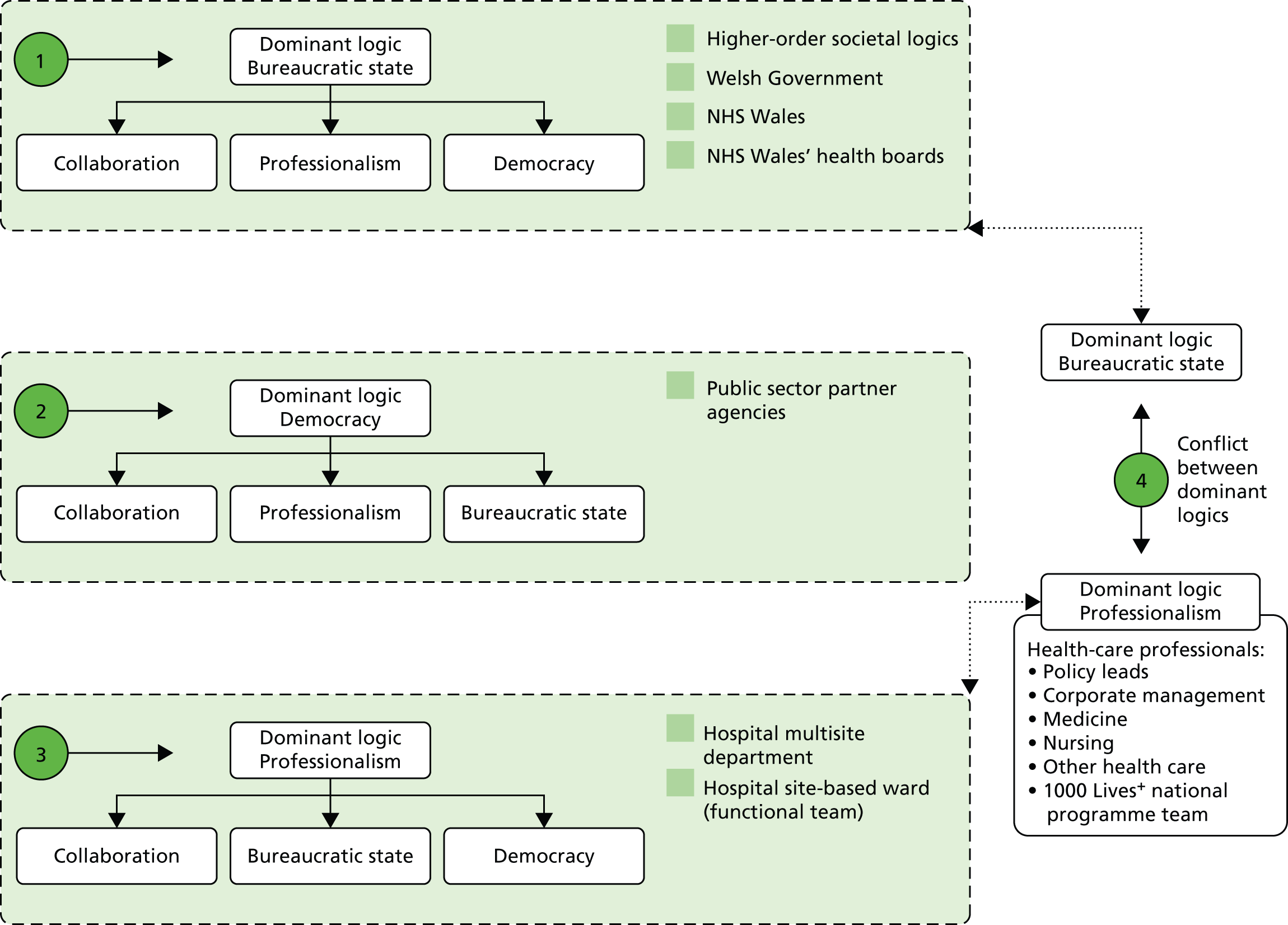
In Wales, the bureaucratic state logic of the Welsh Government orchestrates the top-down performance measurement and management of the 1000 Lives campaign and the successor 1000 Lives+ programme. For example, under the mantle of 1000 Lives+, NHS Wales’ constituent organisations are tasked to (i) set appropriate local targets for the reduction of harm and hospital mortality, initially by employing the Trigger Tool for hospitals; (ii) demonstrate participation in 1000 Lives+ through the appointment of executive leads; and (iii) collect robust data so that local variation in service provision may be identified, analysed and understood, resulting in the development of intelligent targets for service improvement and patient safety. 391 Strategic oversight of such actions rests with the National Quality and Safety Forum instituted in 2012.
Capitalist market logic replaced by collaboration
The UK New Labour government followed the Conservative adherence to new public management, aiming to increase the efficiency and quality of service provision through the logic of the capitalist market. For the UK health-care field this approach could be seen in the encouragement of aspects of competition, contestability and practice-based commissioning, and the same stance lingered on in the 2010 UK Conservative–Liberal Democrat coalition government’s health-care policy. However, in the post-devolution Welsh health-care field, this logic has been opposed and replaced by collaboration. 392 Importantly, the Government of Wales Act (2006) requires the Welsh Government to work in formal partnership with the voluntary sector, local government and businesses. This constitutes a set of operational requirements not paralleled elsewhere in the UK. 393
The NHS reforms in Wales have, therefore, sought to inculcate a new set of behaviours – replacing competition with collaboration, joint working and whole-systems thinking – to foster a greater emphasis on quality and patient safety outcomes. This collaborative logic is interwoven throughout the 1000 Lives+ programme, as evidenced by its integral mini-collaboratives, and national learning and networking events, which foster co-operation, knowledge sharing and peer challenge. Furthermore, strategic oversight of health-care standards and patient safety performance in Wales requires collaboration across the National Quality and Safety Forum, Welsh Government, HIW, PSOW, CHCs and health-care providers, including those in the independent sector.
Professional logic
Despite Wales’ adoption of a collaborative approach, the ideological approach to public management reform adopted by the UK government still impacts on Wales through its reserved powers. Thus, at the field level, professional logic – be that corporate management or the array of hierarchically positioned health-care professionals394 – remains constrained. Indeed, what can be seen is an explicit focus on workforce development (and, thus, organisational development) through a managerialist variant of transformational leadership,395 role redesign and adherence to prescriptive standards that seek to build staff capacity and capability while reducing service variation. 396 This logic is inescapably interwoven with performance management. As asserted in the current quality delivery plan for NHS Wales,391 the operationalisation of the 1000 Lives+ programme is central to the building of staff capacity and capability across NHS Wales:
1000 Lives+ will continue to be the core NHS improvement programme, ensuring a common and consistent language and approach to improvement.
Health Boards and Trusts will agree a plan to train 25 per cent of their directly employed and contractor workforce in quality improvement methodology (at basic, expert or leadership level) by the end of March 2014, supported by 1000 Lives+.
Achieving Excellence: The Quality Delivery Plan for the NHS in Wales 2012–2016 (2012)391
Democratic logic
Although the logic of democracy, expressed in policy through the desire for heightened user participation, engagement and control over public services, appeared in the Conservative Party’s general election manifesto of 1979, it reached new heights during the first term of the New Labour government. Beginning with the promotion of openness and public involvement in the NHS,397 it progressed to the heightened legitimacy and authority of lay voices398 and the later adoption of a Scandinavian model of explicit patient choice which evolved into individualisation and coproduction. However, it is uncertain if this approach can or will be fully realised, as its implementation is dependent on many factors, not least that appropriate program design is essential if engagement with the citizen-consumer is to be effective. 399,400
In the Welsh health-care field, given the overt rejection of market logic, the policy levers for provider pluralism and ensuing choice were not available. Wales has, therefore, embraced a citizen-centred model,392 adhering to notions of collectivism and standardisation as in the traditional socialist values of equality, social justice and social inclusion in policy. 401 The 1000 Lives+ programme explicitly seeks to actively engage patients in the coproduction of their health care. Indeed, as expanded in Chapter 6, patient stories represent an important means of gaining feedback. In addition, an aligned programme, Putting Things Right, launched in April 2011 (www.wales.nhs.uk/sites3/home.cfm?orgid=932), facilitates the communication of what are collectively termed ‘concerns’ (complaints, claims and incidents reports) into the standards of health-care delivery and patient safety in NHS Wales. This operates in parallel with NHS Wales’ governance framework.
1000 Lives+, health policy and patient safety
The 1000 Lives+ programme is a complex, multicomponent patient safety intervention and is an integral part of the Welsh Government’s policy framework for NHS Wales. 391,402 All health boards and trusts are involved in its operation. The Welsh Government and Public Health Wales host its codirectors and core team of improvement facilitators. Strategic oversight is provided by a dedicated programme board. 1000 Lives+ is supported by a faculty comprising a small group of senior clinical and managerial leaders who are tasked to ensure the rigour and clinical credibility of the evidence-based interventions promoted. In addition, the faculty builds capacity and capability at local and national levels by providing mentorship within clinical arenas, and through its contribution to the design and delivery of resources and training materials. The 1000 Lives+ core team and faculty are augmented by an active network of students and academics committed to quality improvement and patient safety in NHS Wales.
As outlined in Chapter 1, the 1000 Lives+ programme seeks to support organisations and individuals to deliver health care of the highest quality for the people of Wales. Composed of an array of aligned improvement programmes, summarised in Figure 1, it adheres to an internationally recognised MI-PDSA178 approach. This supports the use of small tests of change to establish new ways of working that can be replicated and adapted across NHS Wales. The broader infrastructure of 1000 Lives+ includes a website (www.1000livesplus.wales.nhs.uk) that enables access to publications and resources. These provide tailored support for each improvement area, together with notification of national events, opportunities for networking, knowledge mobilisation and collective learning. These resources are aligned to a web-based national learning programme for all NHS Wales staff and contractors (Improving Quality Together: www.iqt.wales.nhs.uk/home) together with the resources offered by Patient Safety Wales (www.patientsafetywales.org.uk).
Our discussions with policy leads, drawn from the upper echelons of the Welsh Government, highlighted the manner in which the 1000 Lives+ programme has become established in the Welsh health-care field and a core policy lever for health-care transformation in NHS Wales, as expressed in the excerpt from transcription 4:01, below (N.B. the full text of all transcriptions can be found in a supplementary data file; see Chapter 3, Data collection, coding and analysis, Semistructured realist interviews).
1000 Lives+ has become institutionalised – it’s become part of the fabric – it’s part of the way in which policy is being delivered and therefore all of the mechanisms that report progress on policy are by proxy reporting 1000 Lives+ progress; albeit I don’t think it’s quite that explicit. But I think the bureaucracy that sits behind the politics of policy have become enmeshed with 1000 Lives+.
Policy lead, Welsh Government (146); transcription 4:01
The 1000 Lives+ programme was widely viewed to have been built around the Welsh Government’s tier 1 performance targets for NHS Wales (transcriptions 4:02 and 4:03). Indeed, the relative success of 1000 Lives+ had enabled other policy programmes to be associated with and linked to this complex intervention (transcription 4:04, below).
1000 Lives+ is something that people are using in order to be able to engage NHS staff in improvement work – it’s a badge, a brand – and, what has happened here is that things have ended up being tagged onto 1000 Lives+. Through its own relative success 1000 Lives+ has become a magnet for lots of other things that people want to get in on the back of; it’s almost become a Trojan horse way of getting something in the policy system! But it’s mandated now, it’s how we do change.
Policy lead, Welsh Government (150); transcription 4:04
Respondents also saw ministerial advocacy as important to the institutionalisation of the 1000 Lives+ programme (transcription 4:05, below).
[T]hey stuck their head out, well above the political parapet by coming out and publically endorsing, or at least acknowledging that, in health care, things can go wrong – we can cause harm, be it through variation, misjudgement, error or malpractice: we damage patients.
Policy lead, Welsh Government (081); transcription 4:05
Such advocacy was augmented by elite engagement across NHS Wales (transcription 4:06). Isomorphic institutionalism (increased similarity over time), vectored through the work of the IHI, was also perceived to have played a central role in brokering ministerial and wider elite engagement (transcriptions 4:07 and 4:08, below).
There was an awareness, back in 2006 and 2007, that we should be doing better in terms of patient safety. I think that awareness was raised by the work of the Institute for Healthcare Improvement to some extent – some of the key protagonists in the original campaign were closely involved with the IHI – but it was a bold commitment by the minister, the decision to actually launch the 1000 Lives Campaign. The label – 1000 Lives – that label, it implied that there were 1000 avoidable deaths, which is quite a brave thing to say. I’m not sure that we’re still that brave.
Policy lead, Welsh Government (145); transcription 4:08
However, such elite engagement had also given rise to a context marred by coercive isomorphism329 (enforced similarity), one in which it was difficult to criticise the 1000 Lives+ national programme for fear of jeopardising relationships with future leaders of the Welsh NHS (transcription 4:09, below).
Wearing my naive yet political hat, the one thing you do not do is tell 1000 Lives+ it’s failing – that is like insulting their firstborn and saying it’s ugly – too many people high up the food chain – politicians, chief executive, medical directors – have signed up to this, and to publicly say it’s not working is dangerous, not just for getting the process done but dangerous for individuals. So you need to be a bit more savvy about that!
Wales is a very small community – everyone knows everyone – so I am very mindful that if I pissed off someone here: you piss off today’s medical director, you are enemies with tomorrow’s chief exec of NHS Wales!
Policy lead, Welsh Government (144); transcription 4:09
Indeed, the human factors inherent to policy development – the barriers created through personal enmity and petty jealousies – compounded this note of discord (transcription 4:10, below).
The 1000 Lives+ national programme is a source of hostility. [Why do you think it is a source of hostility?] There’re a number of elements in play but, to be frank, it comes down to personalities and personal jealousies. It’s about how, and with whom, it all started. In the beginning, we had [Name 1] and [Name 2] – both strong, charismatic personality types, who have their advocates and detractors, and who were, especially [Name 1], closely tied to the minister [Minister for Health and Social Services]. Now, these were the key figures, and some people across the service are advocates of them – not the 1000 Lives+ national programme – whilst others are not: but that’s just the way it is, in all walks of life, some people reject what you’re saying, not because they’ve thought about it, or hold a contrary view but just because you’re saying it: so it’s personal enmity. There’re a number of ****ed-up relationships out there! God, you know how bloody parochial it can be. So, these personal tensions and jealousies – because that’s what they are, jealousies about who’s standing in the ministerial limelight; who is flavour of the month – these cause significant barriers to programme uptake, buy-in, and implementation.
Policy lead, Welsh Government (081); transcription 4:10
Patient safety governance processes in NHS Wales
The 1000 Lives+ programme has now become integrated within organisational and professional patient safety governance processes operating across the Welsh health-care field and this complex patient safety intervention was perceived to symbolise and be part of the language of working together (transcription 4:11, below).
I think 1000 Lives+, certainly, because by its very nature it’s a collaborative approach, it gives you a way of getting people in a room. Also, because it’s badged 1000 Lives+ it probably doesn’t feel as threatening to some board-level stakeholders – it’s a convenient badge that’s become a metaphor for working together – the terminology, it’s become part of the patient safety language of NHS Wales.
Policy lead, Welsh Government (146); transcription 4:11
Strategic oversight of patient safety
The 1000 Lives+ programme functions under the auspices of the statutory Quality and Safety Committee in each health board. The programme was typically supported by a local steering group at hospital level (transcription 4:12, below, and transcriptions 4:13 and 4:14).
We have a structure that, I think, is pretty much standard for health boards in Wales. Our main committee is the Quality and Safety Committee – every organisation has statutory duty to have a Quality and Safety Committee or something termed along those lines – but we also have a subgroup of the Quality and Safety Committee called the Clinical Effectiveness Committee, which is a group led by the Medical Director, and, as the name implies, that receives the reports of the 1000 Lives+ work as well as internal, external audits, research and development, and stuff like that.
Associate Director, case site G1 (011); transcription 4:12
Within this organisational structure, delegated strategic oversight routinely rested with three core board-level roles (transcription 4:15, below).
We have a 1000 Lives+ implementation group that’s chaired by the medical director, the director of nursing and the director of therapies and health sciences – the three with the clinical portfolio – but it’s also supported and attended by the director of public health.
Associate Director, case site D1 (049); transcription 4:15
The strategic oversight of patient safety was supported by other board-level and non-executive positions, and this had impacted the culture of the organisations (transcription 4:16, below, and transcription 4:17).
My view is that everything that’s in the portfolio of the Workforce and Organisation Development Director is about safety. It’s about quality and safety because that is the ultimate aim. The quality and the safety of the services provided are as high as they can be achieved within the resources available. So, that’s at the heart of everything that’s in the portfolio – from recruitment, job design, right away through to performance management and ongoing development, CPD [continuous professional development] and leadership development – I think that all of those elements, which are central to human resource management, are around systems and processes that build or undermine the culture of patient safety. They are all core planks of my role, I think, and the role of my team.
Executive Director, Workforce and Organisation Development, case site G1 (012); transcription 4:16
Sub-board-level managers also played a role in supporting the operation of 1000 Lives+. This was typically centred on data collation and reporting to the Quality and Safety Committee (transcriptions 4:18 and 4:19).
Patient safety practices and the burden of proof
The 1000 Lives+ programme was perceived to have improved front-line practitioners’ awareness of the safety of their patients. However, this was dependent on the successful embedding of the underpinning MI-PDSA methodology178 (transcriptions 4:20 and 4:21). The programme was also associated with increased paperwork and audit processes (transcriptions 4:22 and 4:26, below).
1000 Lives+ generates a lot of paperwork but it’s not just 1000 Lives+ that generates paperwork. I think, with nursing, it’s just that, you know, we have to keep records – it’s proof, proof, proof all the time; prove that you’ve done it, prove that you’ve done it – and now there is just so much documentation just to admit a patient takes an awfully long time. But the government want proof, they want us to know that yes we’ve got 1000 Lives+ in place. But there’s so much paperwork and some of it doesn’t always follow the patient because we share notes now, sometimes, and that almost muddies the water in some respect. It’s a huge amount on notes and things! Plus there’s the amount of audits we do – we get audited to death – [What do you get audited on?] We get audited on use of sharps bins; we get audited on the environment and whether we’re using the correct bins; we get audited on infection control; documentation audits, you know, it just seems that there’s so much auditing. Mattresses get audited: there’s just heaps of audits that go on.
Ward manager, case site G3 (086); transcription 4:24
There’s an awful lot of paperwork involved in patient care today. With 1000 Lives+ for every bundle that is developed you think: ‘oh boy, here we go!’ The delivery of care has got to be the paramount importance to us, it’s no good thinking: ‘yes, I can tick all the boxes but not actually doing the care’. So, you give the care, and then you have to find the time to do the assessments, the evaluations, and tick the boxes and everything. Also, you have to have the care plans that go with the bundle or care pathway, and they have to be linked and cross-referenced. Those have to be updated every week, sometimes more than that, depending on the stability of the patient because obviously that can vary. It would be nice if the documentation could be streamlined in such a way that, instead of having so many new documents, perhaps we could have one document that encompasses many things.
Ward manager, case site B2 (056); transcription 4:26
The burden of data collection in order to document adherence to prescribed care practices, together with the growth of nursing metrics (transcription 4:27, below), may pose a fundamental risk to 1000 Lives+, as it may foster disengagement from the purpose of the programme and threaten reducing adherence to a tick-box exercise. One respondent commented that it could become simply ‘a massive bureaucracy to feed the minister’ (transcription 4:28).
[What performance indicators and nursing metrics are collected at ward level to monitor patient safety?] Bloody hell, what are the performance indicators? Everything! There’s a whole set – they go through to the Welsh Government – there’s a whole section on patient safety, infection control, workload, sickness absence, 1000 Lives+! It’s just measures: it’s a way of auditing us at a ward level. It’s split into different sections but the one section you’d be interested in with 1000 Lives+ is the one with patient safety. [What issues do they monitor?] They look at things like, well there’s quite a few parts which would relate to it, like you audit how many patients have had their armbands on. So you say, choose 12 patients, go round the 12, how many of the 12 have got armbands on, and it gives you a percentage figure. Once you’ve clicked that button and it’s gone in, you can’t change anything. So it does help, at the ward level, it gives me an indication, it gives me an indication if things are lacking.
Ward manager, case site B1 (060); transcription 4:27
In addition, decoupling of practice from the intent of policy was fostered through the failure to validate data and to enforce adherence to guidelines (transcriptions 4:29 and 4:30).
External oversight of health-care quality and patient safety
In Wales, HIW, CHCs and the PSOW provide external oversight of health-care quality and patient safety. Such audit processes were seen as helping to validate the delivery of appropriate health-care standards, promoting change through identifying service failings (transcription 4:31, below).
Healthcare Inspectorate Wales did a spot audit here, last October I think it was, and on the particular morning they came in – I wasn’t here, I wasn’t on duty, and the sister wasn’t here and there were a couple of staff off – it was absolutely bedlam! There were two patients dying, so two lots of family in and there were doctors everywhere, because it was after 9 o’clock and a load of medical students came to the ward. The linen trolley with the fresh linen for the day had been thrown in. People were doing breakfast; they were still doing breakfast! It looked like an absolute bombsite apparently. And in the audit they completely floored us . . . but, since then, I think it did us a favour because there were some things that we’d been fighting to get done because, as you know, this is an old ward. So there are things that we’ve managed to get changed on the back of this audit. So it’s done us little favours.
Ward manager, case site B1 (060); transcription 4:31
Furthermore, audits provided an important external source of data, countering parochialism and strengthening democratic challenge across NHS Wales (transcription 4:32, below).
[Do you report back to the Welsh Government?] For Welsh Government – well, there’s a firewall between them and us [a CHC in Wales] – but we are an agent of government. However, having said that, we are a pain in their side – we say things they don’t want to hear – the political view is obviously very different. But it’s my duty to tell the truth to government, to tell them: ‘actually you’re not providing sufficient care, or your health boards with sufficient money to provide that care, and patients are struggling. Ultimately, you’re to blame guys – don’t blame the health boards – you’re to blame’. Basically, we’re seeing the NHS being removed by stealth. The government are going to be very cross with me, but I have a duty to speak on behalf of patients, so there you go!
[Does the politicisation of health care make it difficult for you to expose problems?] Yes, if it lands in the minister’s lap and the minister doesn’t like it! There’ll be a level of ‘ball bouncing’ between government civil servants and the CHCs simply because they don’t want that to land on the Minister’s desk. I can’t say I blame them. But it is my job to speak honestly on behalf of patients. Patients are David to the NHS’ Goliath and how on earth can they possibly fight that giant?
Chief Executive, CHC in Wales (073); transcription 4:32
The role of ‘critical friend’, working in creative tension with a partner health board, is central to the scrutiny of local health services and advocacy support to complainants (transcription 4:33). However, for some health boards, these vital relationships may be fraught (transcription 4:34). Moreover, in discussions with such external organisations, though awareness of the 1000 Lives+ programme was evident, monitoring of adherence to its practices was overshadowed by the use of competing performance measures. Health boards were also concerned with this issue (transcription 4:35, below).
The Healthcare Standard we’ve just got used to, well, for me, it’s now much more of a narrative – you tell your story – it’s like we’ve gone from a series of MOTs and driving tests and garage inspections to a sticker on the back of the car saying: ‘How’s my driving?’. It’s a bit like: ‘here’s the standards for health care, how do you think you are doing?’. Not one of them is a genuine standard, which really confuses staff; they’re basically a list of aspirational statements and we’re left essentially to our own devices about how we decide whether we meet them or not. My joke was that they could have saved a lot of time and money by just printing a lot of mouse-mats with the standards on because it’s an aide memoire – it’s basically a wish list. So that’s a different approach to quality improvement. We’re now encouraged to be more self-reflective and self-reliant but it is difficult because people always get things wrong and screw up and how do you legislate for that?
Executive Director, case site G1 (011); transcription 4:35
Patient safety and competing contextual challenges
The 1000 Lives+ programme, and the predecessor 1000 Lives campaign, have been implemented during a major structural reconfiguration of NHS Wales. This has created a contextual challenge, specifically for the leadership and communication of the patient safety agenda (transcription 4:36, below) adding to the potential for distraction (transcriptions 4:37 and 4:38).
Post reconfiguration, I suppose, the size of the organisation brings its own challenges – it’s a huge challenge – how do you communicate things effectively when you’re that big? For 1000 Lives+ and other health board strategies, my biggest challenge is keeping in touch with what the organisation’s priorities are – what is [name] chief priority as chief executive, how is he driving that forward – if we’re going to make things change in line with his strategy, you’ve got to know what it is. If you don’t know what it is, how on earth are we going to do that? There’re so many tiers to go through now. I don’t want to harp back all the time but it’s a valid comparison because before I could talk directly to the chief executive because I’d see him in the corridor, and the medical director; those relationships were direct then, weren’t they? Before you had the key people in your organisation – that physical proximity, almost a direct route on a formal and informal basis – you would be kept up to speed when things were going on. But now, it’s lost.
Associate Director, case site B2 (009); transcription 4:36
However, the greatest challenge arises, unsurprisingly, from unstinting financial pressures. All areas of NHS Wales are expected to do more with less and this confronts the 1000 Lives+ programme with a stark challenge (transcriptions 4:39 and 4:40, below).
If we are to keep up the momentum on 1000 Lives+ the area that we need to keep pushing is the business case for quality – to have the evidence from all of the 1000 Lives+ improvement programmes to show where the cost savings are – to build that bank of evidence for cost savings through quality improvement; that’s where we need to get to.
Policy lead, Welsh Government (065); transcription 4:40
1000 Lives+ institutionalisation: preliminary understanding of local implementation
Our study focused on the complex interplay of the 1000 Lives+ national programme in the context of the Welsh health-care institutional field. The unit of analysis in this study was the process of local implementation of 1000 Lives+ and the three focal interventions selected for detailed consideration: ILQI, RSC and RHAI.
The first stage of our analysis sought to examine the process of institutional change as it emerged during the progressive bureaucratisation of 1000 Lives+ programme, in order to understand the manner in which the programme has become part of the context of the Welsh health-care institutional field. Drawing on the work of Greenwood et al. ,227 as well as terminology used by Lewin350 and Schein,351 we framed such institutional change through six linked stages: disconfirmation (Greenwood et al. 227 see this stage as triggered by ‘precipitating jolts’, in this instance recognition that patient safety is a continuing problem), deinstitutionalisation, preinstitutionalisation, theorisation, diffusion and reinstitutionalisation. We also reflect on the impact and interplay of institutional logics in the Welsh health-care field and, as illustrated in Figures 8 and 9, consider the relationships between dominant and subordinate logics, be they complementary, co-existent or countervailing.
Disconfirmation
The overarching goals of 1000 Lives+ signal the need for institutional change through an admission that patients are not being cared for as well as they should be: what Schein, building on Lewin’s theories of planned change, calls an act of disconfirmation350,351 (Figures 10 and 11 and Tables 6–9). Thus, the process of institutional change in the Welsh health-care field begins with the transmission of the IHI’s influential MI-PDSA approach via elite institutional carriers,403,404 such as ministers and government officials, who, by conveying their political advocacy for such change – ‘sticking their heads above the political parapet’, as one respondent put it – promote the concept, encouraging others to introduce its ethos and practices by processes of imitation (mimetic institutional isomorphism329) and/or official directive (coercive institutional isomorphism329). In this context, the logic of the bureaucratic state is dominant, rendering the logics of collaboration, profession and democracy into a complementary stance under the influence of ministerial authorisation. However, it should be noted that implementation may be undermined when actors find it difficult to meet the organisational goals by using the explicit policies and procedures, and proceed to modify them, a process known as ‘gaming’405 (see Figure 11, point 2, and Chapter 7, Realist analysis and comparative case study, Sociocultural interaction: agency and strategic negotiation).
FIGURE 10.
Bureaucratisation of 1000 Lives+: hierarchical metamechanism operating across the contextual strata of the infrastructural system and institutional setting.
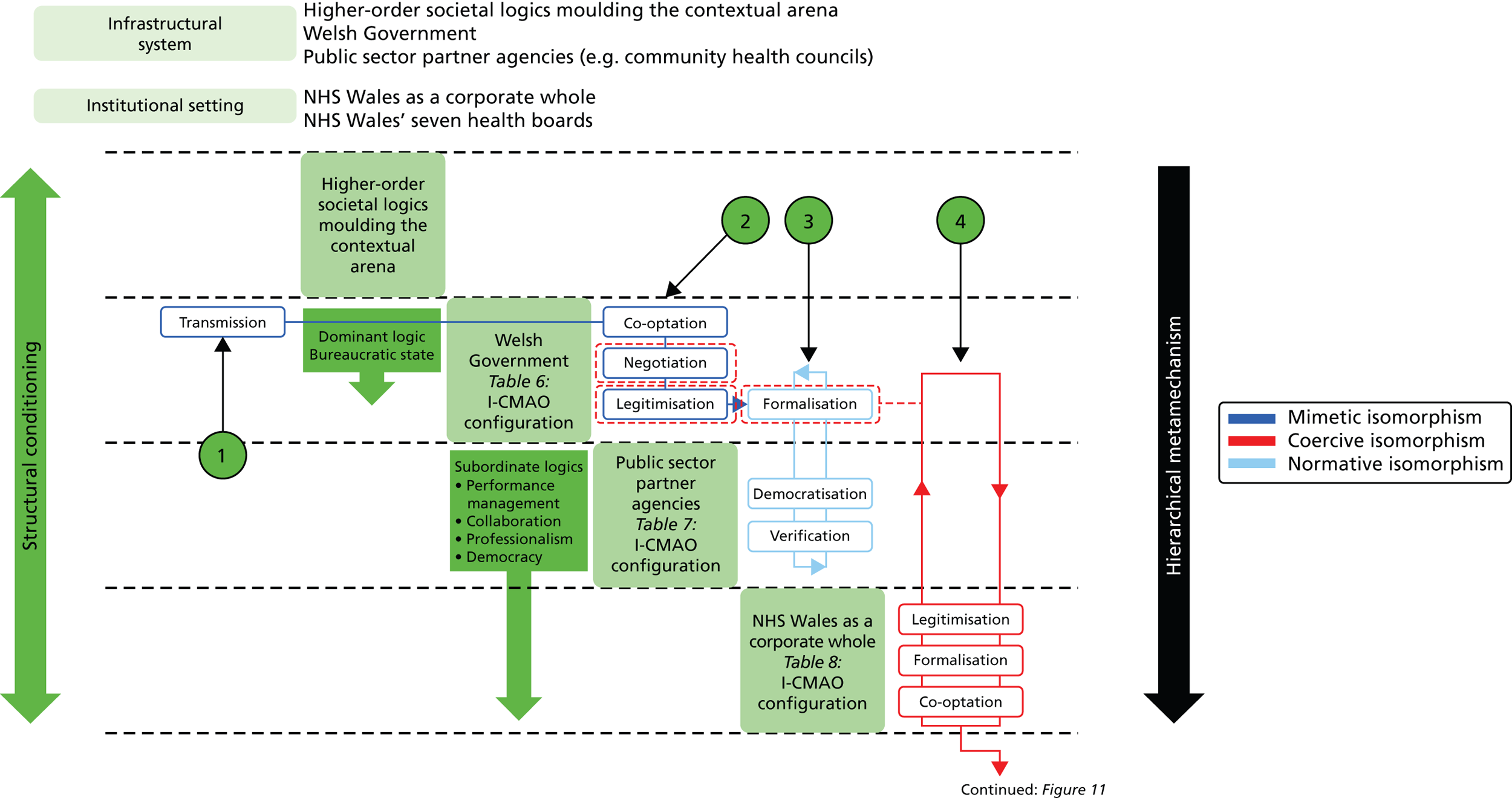
In Figure 10 we depict the bureaucratisation of the 1000 Lives+ national programme across the infrastructural system and institutional setting of the Welsh health-care field.
In point 1 the process of institutional change begins with the transmission of the IHI’s hegemonic MI-PDSA approach via elite institutional carriers, who enact mimetic institutional isomorphism to introduce its practices within the Welsh health-care field.
In point 2 elite institutional agents, through acts of co-optation and negotiation, spread and legitimise the MI-PDSA approach, gradually co-opt others through mimetic and coercive institutional isomorphism. The legitimisation of the IHI’s MI-PDSA approach is signalled by the aligned names – 1000 Lives+ campaign and 1000 Lives+ national programme.
In point 3 the formalisation of the 1000 Lives+ national programme is marked by the embedding of its patient safety interventions in Welsh health-care policy – notably tier 1 performance targets – and associated internal and external governance systems. In this manner, the context is conditioned for NHS Wales, its constituent health boards and their employees at the departmental level or that of the ward-based functional team.
In point 4 following the legitimisation of the 1000 Lives+ programme’s mandate, adverse events are reframed as a social problem to be addressed through the collaborative engagement and the ensuing agency of health-care professionals in NHS Wales’ constituent health boards. Localised formalisation is seen, catalysing multiprofessional and multisite co-ordination of patient safety via the statutory Quality and Safety Committee and aligned governance structures, augmented by distributed leadership of the patient safety agenda across the managerial strata.
FIGURE 11.
Bureaucratisation of 1000 Lives+: hierarchical metamechanism operating across the contextual strata of the interpersonal system within NHS Wales’ health boards.
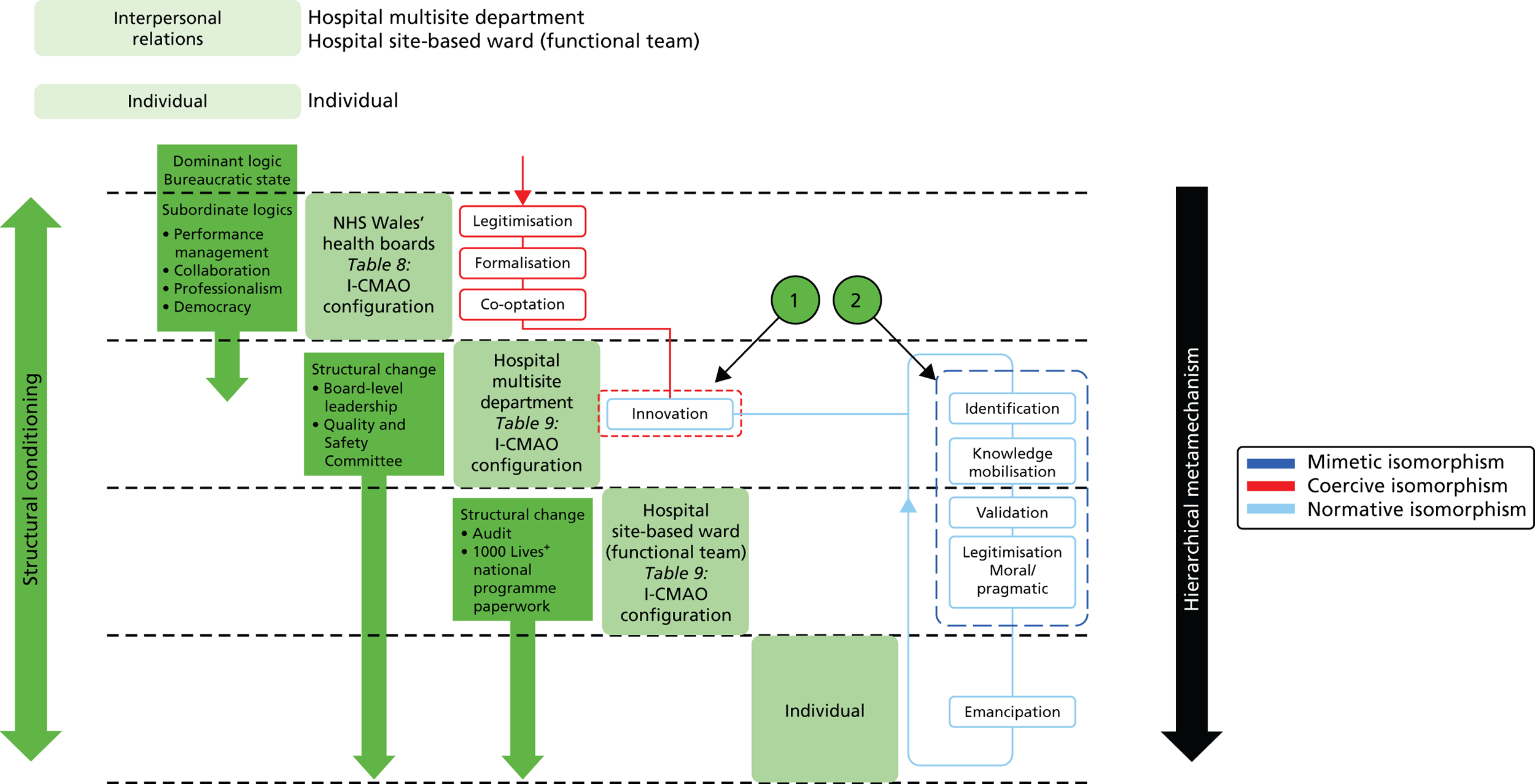
In Figure 11 we extend our depiction of the bureaucratisation of the 1000 Lives+ national programme to consider the interpersonal level.
In point 1 innovation is seen to be brokered through the pragmatic evidence-based learning of the 1000 Lives+ embedded MI-PDSA approach. This is driven by coercive, mimetic and normative institutional isomorphism. Importantly, at this juncture, as illustrated in Figure 9, professional logic asserts dominance, thereby generating the potential for discord.
In point 2 identification and awareness of systemic patient safety failings, fostered through the testing of a rapid cycle of change with the MI-PDSA approach, heightens collaboration and communication across the multidisciplinary team, giving rise to knowledge mobilisation and greater understanding of variation in health-care service delivery. Yet the burden of data collection and demands of validation may retard meaningful engagement and give rise to the situated practice of gaming. This increased knowledge and understanding of the unfolding change reveals common areas of failing – systemic and human – so that the conceptualisation of the desired institutional change is further refined. In this manner, the moral and pragmatic legitimisation of 1000 Lives+ arises, helping to overcome reluctance and resistance to engage and its institutionalisation across NHS Wales.
| Intervention | 1000 Lives+ national programme | ||
|---|---|---|---|
| Context | Welsh Government | ||
| Mechanism | Institutional isomorphism: mimetic, coercive and normative | ||
| Agency and institutional work |
|
Exemplar transcriptions:
|
|
|
Exemplar transcriptions:
|
||
|
Exemplar transcriptions:
|
||
|
Exemplar transcriptions:
|
||
|
Exemplar transcriptions:
|
||
| Outcome | 1000 Lives+ national programme institutionalised into policy processes | ||
| Intervention | 1000 Lives+ national programme | |
|---|---|---|
| Context | Public sector partner agencies | |
| Mechanism | Institutional isomorphism: predominantly normative | |
| Agency and institutional work |
|
|
|
Exemplar transcriptions:
|
|
|
Exemplar transcriptions:
|
|
| Outcome | 1000 Lives+ national programme institutionalised within existing processes supporting the external oversight of patient safety | |
| Intervention | 1000 Lives+ national programme | ||
|---|---|---|---|
| Context | NHS Wales as a corporate whole/NHS Wales’ health boards | ||
| Mechanism | Institutional isomorphism: coercive | ||
| Agency and institutional work |
|
Exemplar transcriptions:
|
|
|
Exemplar transcriptions:
|
||
|
Exemplar transcriptions:
|
||
| Outcome | 1000 Lives+ national programme institutionalised within existing processes supporting the internal oversight of patient safety | ||
| Intervention | 1000 Lives+ national programme | |
|---|---|---|
| Context | Hospital multisite department/hospital site-based ward (functional team) | |
| Mechanism | Institutional isomorphism: coercive, mimetic, progressing to normative | |
| Agency and institutional work |
|
Exemplar transcriptions:
|
|
Exemplar transcriptions:
|
|
|
Exemplar transcriptions:
|
|
|
Exemplar transcriptions:
|
|
|
Exemplar transcriptions:
|
|
|
Exemplar transcriptions:
|
|
| Outcome | 1000 Lives+ national programme institutionalised in daily health-care practice | |
At the level of the infrastructural system (see Table 6), the systemic legitimisation of the IHI’s MI-PDSA approach is signalled by the aligned names: 1000 Lives campaign and 1000 Lives+ national programme. Meanwhile, its formalisation is marked through the embedding of these patient safety interventions in Welsh health-care policy and governance systems.
As expanded in Table 7, both added democracy and authentication come from public sector partner agencies tasked with the external oversight of health-care quality and patient safety, with their inspection regimens encouraging adherence to 1000 Lives+ standards, beliefs and norms. Indeed, during the transition from the campaign to the national programme, the use of the 1000 Lives+ and associated MI-PDSA approach became embedded in the Welsh Government’s health-care policy, notably in its tier 1 targets and aligned performance metrics.
Deinstitutionalisation
At the level of NHS Wales and its constituent health boards, deinstitutionalisation, the second facet of the 1000 Lives+ local implementation, can be seen as the 1000 Lives+ programme’s mandate is legitimised via the Welsh Government’s Department of Health and Social Care (see Table 8). Formalisation then ensues as the programme is placed under the statutory oversight of local Quality and Safety Committees (see Figure 11). Through local acts of co-optation in each health board, leaders are assigned to each focal intervention. They are tasked to identify potential systemic failures, anticipate adverse events and reframe such issues as a social problem to be addressed through collaboration with health-care professionals across NHS Wales’ constituent health boards.
A wider range of health-care actors are gradually co-opted into 1000 Lives+ contributing to the multiprofessional and multisite co-ordination of patient safety. This generates internal challenge through which previously accepted standards of quality and safety – for example, the nature and frequency of adverse outcomes in theatre169,191,406 or for central venous catheter-related bloodstream infections407 – are viewed in a pejorative light. Practitioners, acting as institutional entrepreneurs,41 now collectively adopt a new normative standard leading to practice-based change181 and the rejection of old habits. This leads to institutional change and strengthens the collective will to create an organisational culture attuned to quality improvement. 408
Preinstitutionalisation
This constitutes the third facet of the local implementation of the 1000 Lives+ programme and is demonstrated at the interpersonal level, impacting functional teams, be they the executive board or ward-based clinicians. Importantly, as illustrated in Figure 9, in the context of the hospital department or ward-based functional team, professional logic (re)gains dominance. This creates the potential for discord between the different professional logics of health-care management, medicine, nursing and other allied professional groups, although Table 9 depicts this in a benign manner.
As illustrated in Figure 11, innovation can emerge from the evidence-based learning of the MI-PDSA approach. 172,409,410 The use of data to inform practice heightens the identification and awareness of systemic patient safety failings. 24,181,411 Furthermore, collaboration and communication across the multidisciplinary team is increased through testing of a rapid cycle of change. 172,180,187,412 This gives rise to knowledge mobilisation and greater understanding of variation in health-care service delivery. 187 However, the burden of data collection and demands of validation may retard meaningful engagement and give rise to the practice of gaming. 405 In addition, because performance measurement and monitoring systems are mandatory, the logic of the bureaucratic state again asserts dominance. This again creates the potential for discord among logics as illustrated by the decoupling expressed in the exemplar transcriptions.
Theorisation
This is central to the conceptual framework employed in our study. Greenwood et al. 227 contend that this manifests through the (i) specification of general organisational failings; (ii) justification of abstract possible solutions; and (iii) assertions of moral and pragmatic legitimacy. Hence, in refining perceptions of cause and effect, reflexive theorisation represents a key stage in individual and collective social actors’ adaptive response to institutional change. 413 It underpins the notion of mechanism, set out in Chapter 2, as the embodiment of an agent’s reasoning and their selective attention to the disparate resources offered through the 1000 Lives+ national programme.
As depicted in Figure 11, the implementation and bureaucratisation of 1000 Lives+ increases knowledge and understanding of the unfolding change, revealing common areas of failing and enabling refinements to be made. Such legitimisation helps to overcome reluctance and resistance to engage,127,414,415 and so aids its institutionalisation across NHS Wales. This end may be achieved through multidisciplinary team-based discussion,169,189,219 including focus groups with patients151,416 and health-care professionals,417 together with dedicated support for interorganisational learning. 261,418 Such processes aid emancipation of staff, giving them the authority, whatever their rank, to insist on correct safety procedures being followed. However, should this theorisation stage fail to change people’s values and attitudes appropriately, this may precipitate institutional decoupling,348,349 giving rise to the emergence of a legitimacy façade85 and the failure of the intervention.
Diffusion
Diffusion through wider adoption constitutes the fifth facet of the local implementation of the 1000 Lives+ programme. However, as noted by Berwick,419 continuous effort is required to maintain and spread the gain associated with such practice change. As illustrated in Table 7, at this interface the logic of democracy assumes dominance, fostering the external oversight of patient safety via public sector partner agencies’ inspection regimens to support this goal.
Reinstitutionalisation
This is the final facet of the 1000 Lives+ local implementation, reflecting widespread organisational acceptance of and adherence to the new programme. However, this, too, in acknowledging an ongoing commitment to the embedded MI-PDSA approach, must evolve with the shifting dynamic of the evidence-base3–5 and progressive rehabitualisation. 222
Summary
In Chapter 4, we analyse the structural change inherent to bureaucratisation of the 1000 Lives+ programme at the higher, infrastructural system level of the Welsh health-care field. This analysis defines our preliminary understanding of the programme’s local implementation and how the 1000 Lives+ programme becomes part of the context of the Welsh health-care institutional field.
Chapter 5 Institutionalisation of the 1000 Lives+ programme in NHS Wales: normalisation, health-care practices and patient safety
Overview
This chapter continues our examination of the institutionalisation of the 1000 Lives+ patient safety programme in NHS Wales. Presented in three main parts, it is focused at contextual levels below the field level and explores interpersonal and individual engagement with 1000 Lives+ to gain a deeper understanding of its progressive normalisation across NHS Wales.
First, guided by the model proposed by May et al. ,352,353 we analyse the patient safety literature to consider mechanisms that may foster the normalisation of complex interventions in daily health-care practice. Second, we enrich this explanatory analysis through consideration of in-depth discussions held with a wide range of health-care practitioners concerning their perceptions of the normalisation of 1000 Lives+ and the development of patient safety practices in NHS Wales. Specifically, we examine the 1000 Lives+ MI-PDSA approach, the distributed leadership and the teamwork inherent to its operationalisation. We then illustrate the nuanced impact of pride and shame in building the ethos of patient safety and examine the pragmatic issues that foster institutional coupling to, or decoupling from, such activities. Finally, we elaborate our understanding of the local implementation of the 1000 Lives+ programme. This forms the foundation for our analyses of the three focal interventions presented in Chapters 6–8.
Possible mechanisms fostering the normalisation of 1000 Lives+
As discussed in Chapter 2, we draw on institutional theory to inform our understanding of the generative mechanisms, specifically the roles of contextual constraints and enablements, and ensuing reflexive theorisation; and May’s352,353 modulating roles of coherence, cognitive participation, collective action and reflexive monitoring, thought to foster the normalisation of 1000 Lives+ in NHS Wales.
Coherence
As expressed in May’s normalisation process theory,352,353 coherence means that a practice – an ensemble of beliefs, behaviours and acts that manipulate or organise objects and others – is made possible by a set of ideas about its meaning, uses and utility and by socially defined and organised competencies. 353 In this regard, the 1000 Lives+ programme may be seen as a material object which facilitates the improvement of the patient safety in NHS Wales through the way in which the health-care team, both individually and collectively, think about and understand its meaning and carry out the practices involved.
As evident from patient safety studies undertaken in NHS Wales,210 the coherence and foundational competence of the 1000 Lives+ programme is clearly linked to the underpinning MI-PDSA approach. 178,219 This method of service improvement has been advocated in health care for many years420–423 and its widespread adoption in developed health-care systems promotes health-care actors’ awareness of the MI-PDSA approach as accepted practice,353 so aiding its embedding into day-to-day working. 186
Cognitive participation
The 1000 Lives+ programme is normalised through ongoing cognitive participation, defined by May and Finch353 as ‘the symbolic and real enrolments and engagements of human actors that position them for the interactional and material work of collective action’.
Although cognitive participation in the 1000 Lives+ programme is underpinned by the MI-PDSA approach, specifically with regard to the promotion of a consistent approach across its multicomponent improvement programmes,424 other resources make valuable contributions. For example, the 1000 Lives+ programme team, improvement guides and local and national learning events each facilitate cognitive participation through education and practice-based skill development. Such learning, whether at an individual,187,421,425–427 an organisational12,411 or a system-wide level,24,428 is fundamental to health-care practice change, as is the need for senior organisational leaders to develop a comparable level of awareness of 1000 Lives+, the MI-PDSA approach and associated drivers. 429 Cognitive participation thus helps to ensure that systemic and organisational factors giving rise to patient neglect are addressed,430 while knowledge sharing and trust are enhanced. 431
Collective action
The cognitive participation of social actors gives rise to collective purposive action aimed at some goal. However, with respect to the 1000 Lives+ programme, such goal-orientation may include resistance, subversion or reinvention, as well as affirmation and compliance with the core features of this patient safety programme. The normalisation of 1000 Lives+ is, therefore, dependent on institutional and professional work that defines and operationalises the desired features of 1000 Lives+, aligned factors which promote or inhibit social actors’ enacting of 1000 Lives+ and social actors’ collective investment of effort in such practices. 353
For the 1000 Lives+ programme, two processes which facilitate collective action are interactional workability and relational integration. 352 These involve cross-team co-operation,432 notably via enhanced communication;433,434 the development of shared goals, meanings and expectations;435 and accountability and confidence in the internal and external credibility fostered by mandated local and national monitoring of 1000 Lives+. Furthermore, given the explicit steps defined in each discrete patient safety intervention, 1000 Lives+ represents a valid and recognised practical aide memoire. In this way, the programme helps to increase awareness of patient-related issues, procedures and anticipated risks across functional health-care teams,436 including both public and population health care. 437
Other processes which facilitate collective action are skill-set workability and contextual integration. 352 Skill-set workability describes how work is divided up among practitioners with different but complementary skills. 353 For example, empirical investigation of the WHOSSC, the focal intervention discussed in Chapter 7, supports the view that defined allocation of work, where the assessment of intraoperative blood loss is apportioned to surgeons, patient-specific airways management to the anaesthesia team and sterility and equipment issues to nurses,438 enhances the performance of the operating theatre team. However, such task definition does remain susceptible to entrenched role boundaries and perceived surgical autonomy, which may impact adversely on safety culture. 439 Contextual integration, as the term suggests, refers to the integration of 1000 Lives+ within a social context and its interplay with extant structures and organisational procedures. As May and Finch353 point out, integration may not be easy to achieve in some contexts and will require collective effort from those involved.
Reflexive monitoring
Practices, even when established, demand reflexive monitoring to ensure appropriate performance. 338,353,440 Patterns of collective action, and their outcomes, are therefore continuously evaluated by participants in implementation processes, both formally and informally, and with a greater or lesser degree of intensity depending on their interest and involvement. 353 The normalisation of the 1000 Lives+ programme in day-to-day practice is, therefore, dependent on institutional and professional work that defines and organises the everyday understanding of 1000 Lives+, aligned factors which promote or inhibit social actors’ appraisal of 1000 Lives+ and social actors’ collective investment in its ongoing theorisation and refined understanding. 353
Individual and collective reflection of actual practice against explicit and more tacit norms, while central to the embedding of a practice,356,441–444 may differ markedly from formal governance procedures and standards, in some cases giving rise to a façade of legitimacy. 85 Empirical studies of patient safety have also highlighted the human barriers to incident reporting, despite its central role in organisational learning and the establishment of a stronger safety culture. 412 In the following section, we seek to examine the views and experiences of individuals and groups during the institutionalisation of the 1000 Lives+ programme, and so to understand the processes involved in the operationalisation, subversion or reconstruction of its associated practices.
1000 Lives+, health-care practice and patient safety
During in-depth discussions with a wide range of health-care practitioners across NHS Wales, we asked each participant to reflect on the notion of context. As set out below, transcription 5:01 succinctly expresses the sense of context as situated, demarcated by relational ties and distinct from that of the wider organisation.
I think what is key, when you consider the way in which 1000 Lives+ is implemented, is consideration of context. [What do mean by context?] The immediate area of its implementation and the people involved. Look, you can work with one ward to implement it. They do it there, and you can then spread it; but when you do spread it you have to customise it to make it work for the people who are there – in that new context. You can’t just pick up something developed in one area of your organisation and assume it will fit into another without you, at least, considering where they’re coming from! So, you can’t really define organisational context – to implement, context has to be kept really small – you work within that area, have a testing period, and then spread and renew. That’s how it’s done. I think that is key to a lot of what we can manage.
Associate Director, case site C2 (014); transcription 5:01
This perception is replicated throughout our discussions and subsequent analysis of the implementation and operationalisation of 1000 Lives+. As one respondent described, 1000 Lives+ has normalised in discrete pockets. This has created disparity between adjacent wards within a given hospital case site (transcription 5:02, below).
What I see is pockets of interests in 1000 Lives+. It’s led by individuals who have cultivated a team around them and given them work to do, so it’s being led by people who are enthusiastic or buy into certain areas where their interests lie. But it’s not systemic: there are good pockets in the organisation and areas that aren’t reached – you can have wards on opposite sides of a corridor where one’s engaged and the other isn’t. As a consequence, it’s relying on enthusiasm rather than a systematic approach. Sustainability at an organisational, corporate level is needed, so that everything is aligned toward patient safety.
Executive Director, Workforce and Organisation Development, case site G1 (012); transcription 5:02
Normalisation is, thus, restricted to those who perceive meaning in 1000 Lives+ owing to alignment with their beliefs, and whose cognitive participation and commitment builds and co-ordinates the engagement of others. This finding offers explanatory insight into the perceived failure of such complex patient safety interventions168 and underscores Pawson’s iron law of evaluation: the expected value of any net impact assessment of any large scale social program is zero. 241
Acknowledgement of the fragmented nature of its normalisation does not, however, detract from the undeniable focus that 1000 Lives+ offers health-care practitioners in NHS Wales. Those who value the initiative consider it as something real and visible that they can use to help them to forward the cause of patient safety (transcription 5.03, below).
Before 1000 Lives and 1000 Lives+ – before SPI [Safer Patients Initiative] – people were saying: ‘we want to keep patients safe, we don’t want to do them harm’. Well, of course, that’s what we want to do, I mean, that’s a given. But with patient safety now, we have the 1000 Lives+ logo, we have information at the front of the hospital; there’s something you can hang your hat on! It has real organisation! It’s not just some nebulous patient safety concept. There’s somebody leading it, there were newsletters, there are graphs so that you can see, you can see the improvements that have been made. 1000 Lives+ is making it real, I would say – not that it wasn’t real before – but, you know, now it has something; it’s tangible, it’s all coordinated, it’s centralised. So, say if somebody had a good idea for improving patient safety, rather than saying: ‘shall I go to my line manager? Well, they’re never any good, they’ll nod but they won’t do anything, who else can I go to?’. They’ve got someone you can go to! You’ve got the 1000 Lives+ patient safety group, and you just go on the intranet and find out the relevant person, and you know they will take it seriously. They may or may not be managing it but you know they will take it seriously because that’s what they do – that’s the hat that they wear – so they’re not trying to juggle between clinical effectiveness, patient safety, and saving money. Patient safety isn’t just something competing for their time, their skills and resources. That is what 1000 Lives+ is: it starts and finishes with patient safety.
Pharmacist, Antibiotics Medicines Management, case site D2 (020); transcription 5:03
Such coherence appears to resonate equally with patients and with the public (transcription 5:04).
On the other hand, there is a sense that bureaucratic impatience may be hampering the successful implementation of 1000 Lives+ across NHS Wales, leaving some staff in its wake (transcription 5:05, below).
I think with 1000 Lives+ we have been pushed on to get on to the next ones [improvement programmes] before it’s sort of embedded. For example, the NEWS Score [National Early Warning Score] is not embedded, it’s embedding.
Ward manager, case site C3 (T080); transcription 5:05
For instance, although aware of the 1000 Lives+ programme, some key medical staff remain disengaged (transcriptions 5:06 and 5:07, below).
I’ve had doctors telling me that it’s, you know, not nonsense but it’s one of those fads. So they’ve obviously made up their mind they’re not going to pay any attention to 1000 Lives+ and it’s of no relevance to them. I think, as with anything, you have people just being bloody minded for whatever reason!
Associate Director, case site F1 (026); transcription 5:06
I think some consultants aren’t aware of 1000 Lives+. They have it in their peripheral field. They are aware that it exists but it doesn’t impact on their lives, and some think it’s probably a good thing but it still doesn’t impact on their lives.
Consultant gastroenterologist, case site F1 (027); transcription 5:07
The policy pacing and positioning of the 1000 Lives+ programme across NHS Wales is, therefore, contributing to the fragmentation of its normalisation. Unequal engagement with the resources offered by this patient safety intervention further stymies progress, as its main adherents are those who are involved in, and already agree with, the aspirations of the programme (transcription 5:09, below).
I think with 1000 Lives+ they’re selling it to those who’ve bought in – you know, the people who are designing the programmes and delivering them – I think it’s important to them. But whether staff in the NHS are really engaged, I don’t know. I mean, here, and this is a small hospital, we don’t get all doctors following the sticker initiative [antibiotic prescribing guidelines]. Some do, some don’t: there’s always an excuse not to do it, whether it’s too much work, too time-consuming, whatever, they always have excuses. Another aspect to this, though, is the rate of turnover. FP1–2s [junior doctors undertaking foundation training] rotate so quickly, and they may not be within the same health board, let alone hospital, so there’s little time for them to learn the system before they’re off again. On the whole, it’s the staff that don’t rotate that maintain the system against, or despite, those who are just passing through.
Pharmacist, Antibiotics Medicines Management, case site B2 (001); transcription 5:09
The meaningful engagement of wider NHS staff is undeniably key to the normalisation and sustainability 1000 Lives+. Specifically, non-rotating staff are central, as they provide the contextual and relational continuity necessary for coherence. This is the foundation the programme must return to, and reinforce, to prevent the dissipation of its goals (transcription 5:10).
Model for Improvement, Plan-Do-Study-Act approach
The central role of the MI-PDSA approach, asserted in Putative mechanisms fostering the normalisation of 1000 Lives+, is clearly evident in the study’s participant health boards. This approach provides a recognised framework for health-care practice change and feedback that, through the Improving Quality Together website, benefits from institutional work via the ongoing support of the 1000 Lives+ national programme (transcription 5:11, below, and transcription 5:12).
The PDSA approach provides a framework for improvement but you still need leadership, you need ideas and execution, so you’ve still got to generate the will in the people that you’re working with first. Then you’ve got to have change ideas that are based on evidence and not just plucked out of the air – you actually have things that have to be tested – and then you test them; you don’t just assume they’ll work in practice. But the approach gives people the freedom to test them, measure and learn from the process. So, I think, if I was to say anything, it’s a framework, and its helped teams to focus on a name, on a measure, that will tell them whether or not they’re getting towards their aim, and on a change that will hopefully help them to achieve that aim.
Welsh Government, policy lead (033); transcription 5:11
Transcription 5:13, below, describes the role of PDSA in building coherence, cognitive participation and collective action to enable health-care staff to design and deliver practice change.
The model for improvement [MI-PDSA], well it’s, it’s a tried and tested approach, part of improvement science. Look, traditionally we’ve gone: ‘here’s a problem; here’s the solution’, and we’ve tried to fit the problem to the solution even if it involves putting a square peg in a round hole just get on and do it! And, for all sorts of reasons, people don’t just get on and do it because, because things aren’t fit for purpose. So the issue of using the model for improvement is you enable people. You start from the very beginning, you know – you expose the need – you properly measure and identify the problem and enable people to understand that the problem lies with them and that they can do something about it, which is quite empowering. And then, obviously, you guide a solution, and some of those solutions are their own, though most of the time we take an evidence-based practice approach. We introduce them to the evidence-based practice and the methodology – the improvement methodology – so that they can go out and they can get started straight away by having an idea, testing it on one patient one time, one nurse, one doctor! It’s quick and easy, it doesn’t require whole engagement of masses of staff, they can just go out and gradually, gradually build and learn from those very small tests of change and they can adapt existing material to make it fit for purpose. We’ve got the methodology – it’s simple, it’s safe – it requires little or no investment at the beginning in terms of staff resource. There is strong leadership over supporting all of these programmes, so that there is an accountability route, so you can’t just go away and do nothing, there are lines of accountability through local working, through direct and divisional quality and safety meetings, and then through to the steering – the 1000 Lives+ steering group – and the quality and safety committee. But it’s simple, the methodology is simple, it’s intuitive, logical, and it’s really enabling people to develop and make the system do what is right to do, easy to do.
Associate Director, case site D1 (049); transcription 5:13
The inherent simplicity of the approach is viewed to aid its adoption and the sense of local ownership and engagement that underpin its normalisation across NHS Wales (transcriptions 5:14, 5:15 and 5:16). Moreover, as illustrated in transcription 5:17, below, the MI-PDSA approach helps in surfacing the need for improvement, and confidence in the efficacy of its structured processes gives a sense of security that facilitates positive small steps towards change.
Well, I think, fundamentally, it provides us with a focal point to get around the table – to actually acknowledge there’s a problem in the first place – and that we’ve got a structure to follow that’s going to take us in the direction towards solving it. That we might not necessarily solve it in the first place – it might take a couple of times of going through the process to resolve it – but it gives us that format to be able to: it’s a building block to start to look at what the problem is, within a structured way. And I think it’s something, it’s almost like a baby’s dummy, I think it’s something that we just, it’s almost a comfort blanket for us.
Ward manager, case site G3 (084); transcription 5:17
This markedly positive stance places emphasis on the MI-PDSA’s incremental approach to service development and the empowerment of staff (transcription 5:18). However, two issues countervail: the potential for misuse as an instrument of control (transcription 5:19), and disagreement over the validity of the evidence base for the efficacy of the 1000 Lives+ programme (transcription 5:20, below).
1000 Lives+ programme team are, in the main, focused on achieving practical, pragmatic activities across NHS Wales which seek to generate service improvements and change. But in NHS Wales, on the other side, you’ve got medical and other professionals – and academics – who work to a completely different standard of evidence in terms of rigorous knowledge-based scientific work: you know how explicit medical or epidemiological statistical modelling is! So, for them, the introduction of 1000 Lives+ is, well, it’s completely counter-cultural. The reports that the 1000 Lives programme team were stating were the outcomes of the initial programme, in terms of mortality statistics, well some view it all as some political conspiracy that’s being sold to the NHS, and the public – it’s spin, fluff, crap – it’s not valid data, it’s not collected in a robust manner, it’s flawed. Oh God: please save me from the tyranny of evidence! [What do you mean by the tyranny of evidence?] It’s a killer phrase, isn’t it, in fact it’s the killer phrase. [What do you mean?] It’s used by professionals in health care to stop action, to destroy the potential for change: ‘Oh, we can’t do that, the evidence-base is too weak; their argument is flawed, the data’s mismanaged’. [Anything to maintain the status quo?] Status quo ante! The evidence-based for the 1000 Lives+ national programme has been systematically attacked by the other factions – for one side, it’s evidence and truth; for the other, it’s spin and fluff – and reality is caught in the middle.
Policy lead, Welsh Government (081); transcription 5:20
Board leadership, followership and change
Executive-level leadership of patient safety augments the normalisation of the 1000 Lives+ programme in NHS Wales (transcription 5:21, below).
If the job of the Executive Team is not about patient safety – organisational fitness, systems, processes, governance structures – then I don’t understand the job!
Executive Director, Workforce and Organisation Development, case site G1 (012); transcription 5:21
Beyond the board, there is acknowledgement of the need for leaders with expertise in quality improvement methodology to support staff and maintain their commitment to patient safety (transcription 5:22, below). Such roles are, therefore, pivotal for the successful transition of the ownership of the patient safety agenda from the 1000 Lives+ programme team to the health board.
My reflection on the PDSA process and instruction is, as a methodology, it’s a very good one. The problem with regards to its application is that you need somebody who is a PDSA expert within the organisation – a leader and change management mentor who can support the various mini-collaboratives with quality improvement methodology – to harness what people are doing.
Associate Director, case site F1 (026); transcription 5:22
However, some respondents indicated a degree of resentment about the obligatory nature of the 1000 Lives+ programme and suggested that such commands to engage may be left unheeded (transcriptions 5:23, and 5:24 below).
The 1000 Lives+ national programme and the campaign – it’s command and control rather than a grass-roots culture change – it hasn’t been created by the people. It’s not of the people. It’s an imposition. It’s control. It’s from Cardiff. It’s very much a Cardiff thing that is being pushed to everyone else because: ‘we know better’. Outside Cardiff, it feels remote and distant and not part of us, it’s something that we all recognise as important, clearly, but we don’t necessarily own it.
Consultant gastroenterologist, case site F1 (T027); transcription 5:24
There was a widespread belief that effective board leadership of patient safety is paramount (transcriptions 5:25 and 5:26) but the importance of clinical leadership of patient safety throughout the organisation, so directing teamwork, communication and collaboration to deliver the desired practice change, was also emphasised (transcription 5:27, below).
Clinical leadership is key – credible clinical leadership – and that’s all about empowerment of band 7 nurses. When we’re in escalation, when beds are crazy, that’s when it’s hard. It’s then you need your band 7 nurses to turn around and tell you what isn’t safe. That’s something we’re working really hard at but that’s a whole culture change. But the 1000 Lives+ PDSA cycles did give them a feeling of empowerment that they could make and own changes, they could take chances in the way that suited their ward or theatre or wherever they were doing it: it wasn’t that we were telling them how to do it, it was about them trying it and seeing how it worked, and changing it until it did work in their area. So, I think that they, the areas that did feel empowered through 1000 Lives+, combined with the data that they were collecting, well they knew whether they were doing something good or not, and those two things would motivate change.
Associate Director, case site A2 (T069); transcription 5:27
Teamwork, collaboration and emancipation
For health-care practitioners who have invested meaning in the 1000 Lives+ programme, and who adhere to its practices, the programme functions as a rallying point, building collective action and ensuing teamwork. This aids collaboration and communication across different areas of the employing health board and represents an important aspect of the institutional maintenance work that helps to reproduce the norms and beliefs inherent to 1000 Lives+ (transcription 5:28, below, and transcription 5:29).
There are other nurse managers and practice development nurses within the organisation that I tend to work with quite closely. For example, with my colleague in surgery, we delivery similar sort of teaching about 1000 Lives+, so we link up and deliver sessions together. That way we could pull staff from both of our Directorates, increase numbers, and it’s easier when you’ve got someone else there. We also meet as a group four times a year, so any development and training needs, and that kind of thing, can be discussed and we can agree how things may be taken forward. I know certain of my colleagues were very heavily involved with the SPI [Safer Patients Initiative] work and the first phase of 1000 Lives – they delivered all the corporate training around the PDSA methodology and that type of thing. They’re good contacts to have!
Ward manager, case site D1 (T010); transcription 5:28
In teamwork situations, the 1000 Lives+ programme is perceived to empower health-care staff in roles traditionally subordinate to the profession of medicine. The emancipation of these staff helps to break down the entrenched barriers that prohibit challenge and scope for change (transcription 5:30, below).
1000 Lives+ gives them [nursing staff] the freedom to question, which they might not previously have had the confidence to do, as it gives them a format to do it and it’s standardised. Also, you get less challenge back when you are questioning something because everybody here’s been exposed to 1000 Lives+.
Theatre manager, case site A1 (T008); transcription 5:30
Empowerment and engagement with others similarly motivated by 1000 Lives+ is seen to have led to patient safety improvements (transcription 5:31). However, there is a view that the latent potential of staff is yet to be realised in NHS Wales (transcription 5:32, below).
I think the key to the next step is, if you like, taking the stabilisers off the bike. 1000 Lives+ has supported staff to do specific projects and that has enabled them to have the confidence to say: ‘this is why, and this is how we’re going to do it’. The next step is: ‘this is my idea, and this is what I want to do’. But how is that picked up and supported by the organisation when it’s not an external prompt is the question. I think the NHS is quite bad at thinking about change normally because we’re reeling from it being imposed.
Associate Director, case site G1 (T011); transcription 5:32
Building the ethos of patient safety: pride and shame in health-care practice
During discussions with the wide range of health-care practitioners interviewed across NHS Wales, the 1000 Lives+ programme appeared to be aligned with feelings of both pride and shame in health-care practice.
On the one hand, a strong sense of achievement is depicted in transcriptions 5:33 and 5:34 (below) and highlights the reinforcing role of individual reflexive monitoring – and objective success – in fostering meaningful engagement.
Our last pressure ulcer was approximately – we’ve had two in the last three and a half years – we’ve got a very good record. I’m so proud of our record on pressure ulcer prevention. We have nurses, now, who’ve never seen pressure ulcers. I’m really proud of it. I have this massive thing about pressure ulcers; I have a zero tolerance of them!
Nurse manager, case site A2 (T058); transcription 5:33
If you’ve had 300 days free of MRSA [meticillin-resistant Staphylococcus aureus], C. diff. [Clostridium difficile] or pressure ulcers in this organisation, it is celebrated with cake! I think, maybe a few years ago, I might have been: ‘that’s a bit gimmicky’ but, actually, the feedback from staff and patients is really positive, and we make sure that patients are involved in that celebration. So, we’ll do media, some publicity around it as well, there’s always features in our local press about a team, ward or department that’s working particularly well. I think that’s positive for our organisation but actually it’s positive from a public perspective because it gives some confidence in the service. Too often bad news is good news, isn’t it?
Associate Director, case site A1 (T025); transcription 5:34
Indeed, receiving praise for their efforts is seen as central to staff’s continued motivation and commitment to 1000 Lives+ (transcription 5:35).
This positive stance is, however, balanced by the use of blame and shame, prompted via the reporting mechanisms inherent to its governance structures across NHS Wales (transcription 5:36).
Another respondent spoke of the ‘desensitising’ effect of being perceived to fail, suggesting that this led to an exaggerated determination not to go beyond the strict parameters of their current task (transcription 5:37, below).
Rather than bad practice being done, there are less opportunities for good practice. People are becoming desensitised by public perceptions of failure. It is normal, now, to sit next to a phone and not answer it because it isn’t going to be for you, and you’re going to be interrupted from your job. The nurse is in a tabard saying do not disturb me on my drug round; that’s wonderful, but you’ve got three consultants doing their ward round too! In the good old days, a sister or staff nurse would come round with me. Now, I’ve got to try and find a nurse and all you get is: ‘it’s not my bay, I’m sorry, I’m on Bay B’, so they don’t know the patient – how many nurses does it take to change a light bulb? Oh sorry, that light bulb isn’t in my bay – it’s that compartmentalised. The sisters have got an awful time; they’ve got, they’re getting kind of beaten at all ends. The number of staff you have on the wards – the ratio of nurses to patients has gone down – apparently, there’s some paper which says that’s safe but then there’s all the other things as well. I think that’s, you know, that’s the concern.
Consultant, palliative medicine, case site A1 (T052); transcription 5:37
In addition, for those who welcome the new emphasis on patient safety and take a pride in adhering to the precepts of 1000 Lives+, there may be a deep sense of shame when failures in patient safety do occur (transcription 5:38, below).
So, with 1000 Lives+ we thought we’ve cracked it, it’s done! But I was walking out of the ward one evening at about 9 o’clock at night, and we have, always on our ward, we have a policy of putting our safety crosses in the public area. So, I was walking out of the ward and I saw this red square on the pressure ulcer monitoring, and I said to myself: ‘some idiot’s made a mistake on the safety cross’. I went back into the ward and they said: ‘no, actually, we’ve had a pressure ulcer’, and we all wanted to cut our wrists, really, it was a very depressing moment.
Consultant surgeon, case site B1 (T062); transcription 5:38
The ethos of care stimulated by the 1000 Lives+ programme is, therefore, constrained by the fragmented nature of its normalisation. As expressed in transcription 5:39, and more so in transcription 5:40 below, there is a profound disjuncture. For some, 1000 Lives+ and its associated MI-PDSA approach have been actively embraced, resulting in its progressive normalisation: 1000 Lives+ is, therefore, absorbed into daily practice. Yet for others, although its mandated nature enforces engagement, this has been resisted: 1000 Lives+ is, therefore, only adsorbed onto (i.e. there is token commitment only and it is not properly integrated) daily practice – and, in this transitional state, it may fail to institutionalise across NHS Wales.
Sometimes it can feel we’re doing 1000 Lives+ for the sake of 1000 Lives+! Well because, you know, people don’t necessarily see their mini-collaborative within the context of the overall quality improvement, patient safety improvement – reducing waste, variation, and harm from the policy perspective – and I don’t think as an organisation we’ve been very good at placing those mini-collaboratives within the context of the overall quality improvement and patient safety improvement agenda. I think that’s why – it just sometimes feels like one of those stand alone things that people do – and, I think, we’ve lost a trick.
Associate Director, case site F1 (T026); transcription 5:40
1000 Lives+ institutionalisation: elaborated understanding of local implementation
Previously, in Chapter 4, we set out our analysis of the bureaucratisation of 1000 Lives+ programme across the higher levels of context, thereby defining our preliminary understanding of the local implementation of 1000 Lives+. Building on the findings presented in this chapter, we now seek to integrate the role of the mechanisms that appear to be involved in the normalisation of the 1000 Lives+ programme at lower levels of context.
Figure 12 demonstrates three ways in which existing institutional logics, or the collective beliefs and value systems of those involved, may affect the outcomes of an intervention. First, where logics are not aligned, the intervention may be opposed, with people deliberately seeking to maintain existing and habitual practices, and actively challenging attempts to impose new ways of working. Second, where institutional logics co-exist, while they may not actively reject, people may nonetheless ignore or give little thought or attention to the imposed changes. While this may lead to apparent revision of practice, because people’s values and belief systems have not been changed it is likely that if the coercive element is removed practice will revert to the status quo ante. Hence implementation of an intervention can be effective only when beliefs and value systems are aligned within a particular context, as shown in the third element of Figure 12. In these circumstances, coherence, cognitive participation and reflexive monitoring of the desired institutional change are fostered and new procedures are absorbed into daily practice and become routinised over time.
FIGURE 12.
Normalisation of 1000 Lives+: heterarchical meta-mechanism operating across contextual strata.
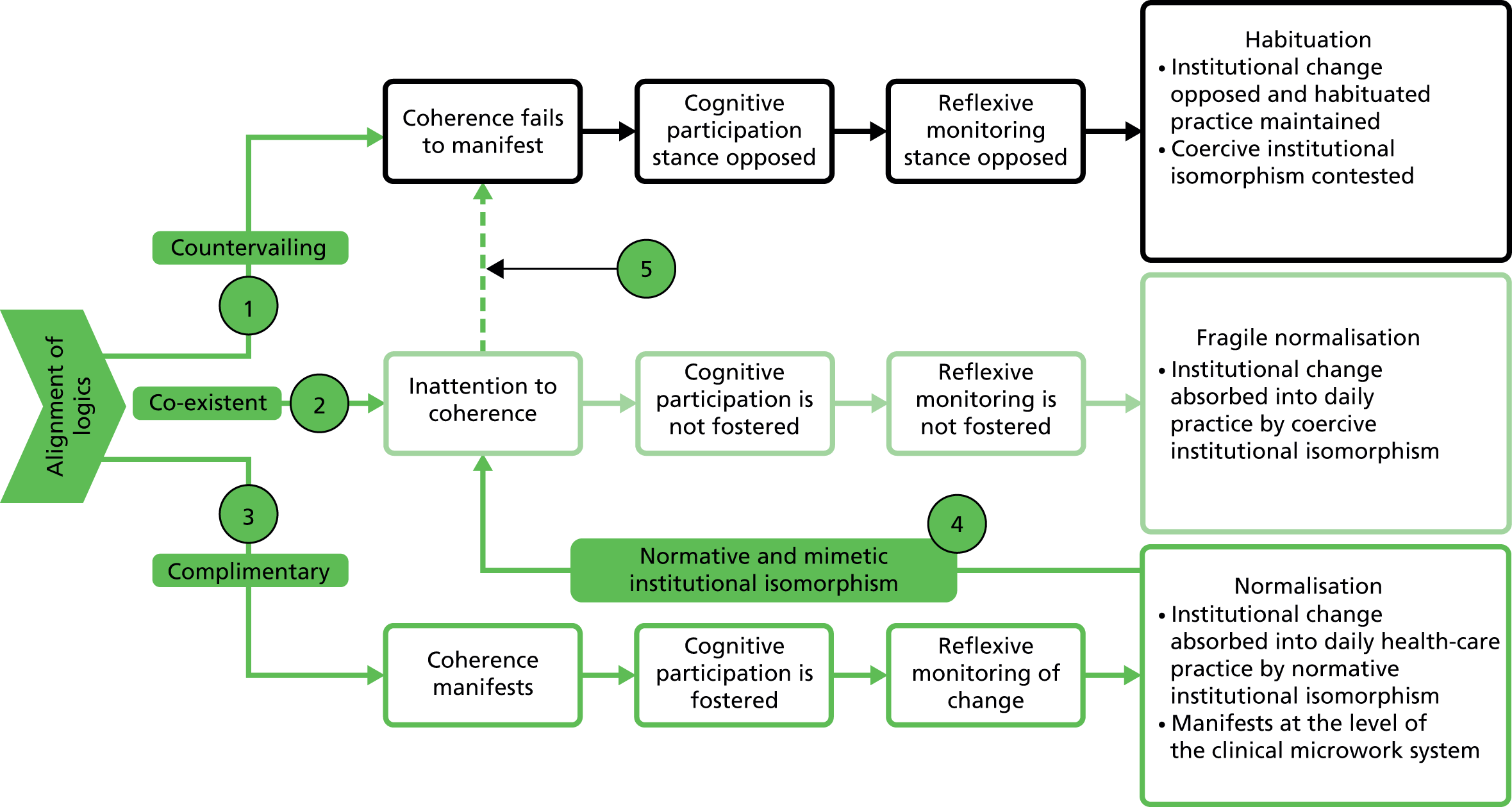
In Figure 12 we depict the mechanisms that foster normalisation – coherence, cognitive participation and reflexive monitoring – and set out the impact on the alignment of institutional logics, as expanded below.
In point 1, institutional logics are not aligned, limiting the potential for coherence. In such a scenario the desired institutional change is resisted, habituated practices continue and attempts to impose change are challenged.
-
Under these situated contextual conditions, mechanisms to generate change, although operational, are ineffectual.
In point 2, institutional logics co-exist without fostering contradistinction and conflict. However, in this scenario, the potential for coherence to manifest is limited owing to inattention. Accordingly, cognitive participation and reflexive monitoring do not occur and people’s beliefs and values are not revised. A fragile normalisation occurs, through which the mandated institutional change is compulsorily imposed onto, but not into, daily practice. However, if such forces are removed, the desired institutional change may revert to the status quo ante.
-
Under these situated contextual conditions, such generative mechanisms, though operational, are limited.
In contrast, in point 3, the alignment of institutional logics is complementary. This, we assert, fosters coherence, cognitive participation and reflexive monitoring of the desired institutional change, and new practices are absorbed into daily practice.
-
Under these situated contextual conditions such generative mechanisms catalyse the desired institutional change and facilitate the evolution of health-care practice. Furthermore, such sites act as foci for change through normative and mimetic isomorphic institutionalism (processes of imitation and normalisation) and will gradually influence change in initially less receptive areas (see points 4 and 5).
Importantly, as explored in later figures, such generative mechanisms are modulated by the relational structures within the situated context, specifically by the interplay of local leadership, team working and encultured values.
It is from such environments, which function as foci for change, that areas initially less receptive to the proposed changes may be gradually recruited through processes of imitation and normalisation.
Table 10 sets out aligned transcription dyads showing divergent stances to normalisation. These reveal the impact of coherence, cognitive participation, collective action and reflexive monitoring in a situated health-care context.
| Intervention | 1000 Lives+ national programme | |
|---|---|---|
| Component | MI-PDSA | |
| Context | Hospital multisite department/hospital site-based ward (functional team) | |
| Mechanisms |
|
|
| Agency and institutional work | Normalisation: coupling to 1000 Lives+ and MI-PDSA approach | Habituation: decoupling from 1000 Lives+ and MI-PDSA approach |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Outcome |
|
|
| Exemplar transcriptions | ||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Figures 13–15 portray the institutional change driven by the bureaucratisation of 1000 Lives+. Our discussion considers three examples of processes involved in the normalisation of the 1000 Lives+ programme: (1) legitimisation, (2) formalisation and (3) innovation.
FIGURE 13.
Normalisation of the 1000 Lives+ heterarchical metamechanism operating across contextual strata: legitimisation.

In Figure 13 we depict the legitimisation of the 1000 Lives+ national programme across the Welsh health-care institutional field, centred on lower contextual strata at health board, hospital multisite department, hospital site-based ward and individual levels.
In point 1, in situated contexts where logics are in alignment:
-
Agency – legitimisation – elite institutional actors and co-opted others embrace 1000 Lives+ and MI-PDSA approach and embed in health-care policy and performance frameworks.
-
Institutional work – creation – elite institutional actors enact political work to reconstruct rules, rights and access to resources, thereby linking 1000 Lives+ national programme to tier 1 performance targets.
In point 2, in situated contexts where logics are in alignment:
-
Agency – legitimisation – 1000 Lives+ becomes part of the language and positioned-practices of patient safety in NHS Wales, fostering collaboration and systemic challenge among institutional entrepreneurs who reassert a new normative standard to precipitate practice-based change.
-
Institutional work – creation – elite board-level institutional actors enact political work to reconstruct rules, rights and access to resources, thereby linking 1000 Lives+ national programme to the attainment of the Welsh Government’s tier 1 performance targets.
In point 3, in situated contexts where logics are in alignment:
-
Agency – legitimisation (moral/pragmatic) – 1000 Lives+ moral and pragmatic legitimacy fosters mainstreaming of the intervention across NHS Wales.
-
Institutional work – creation – functional team’s belief and meaning systems reconfigured.
In point 4, the impact of co-existent or countervailing institutional logics is depicted as corrosive feedback that challenges legitimisation and, therefore, normalisation.
FIGURE 14.
Normalisation of the 1000 Lives+ heterarchical metamechanism operating across contextual strata: formalisation.
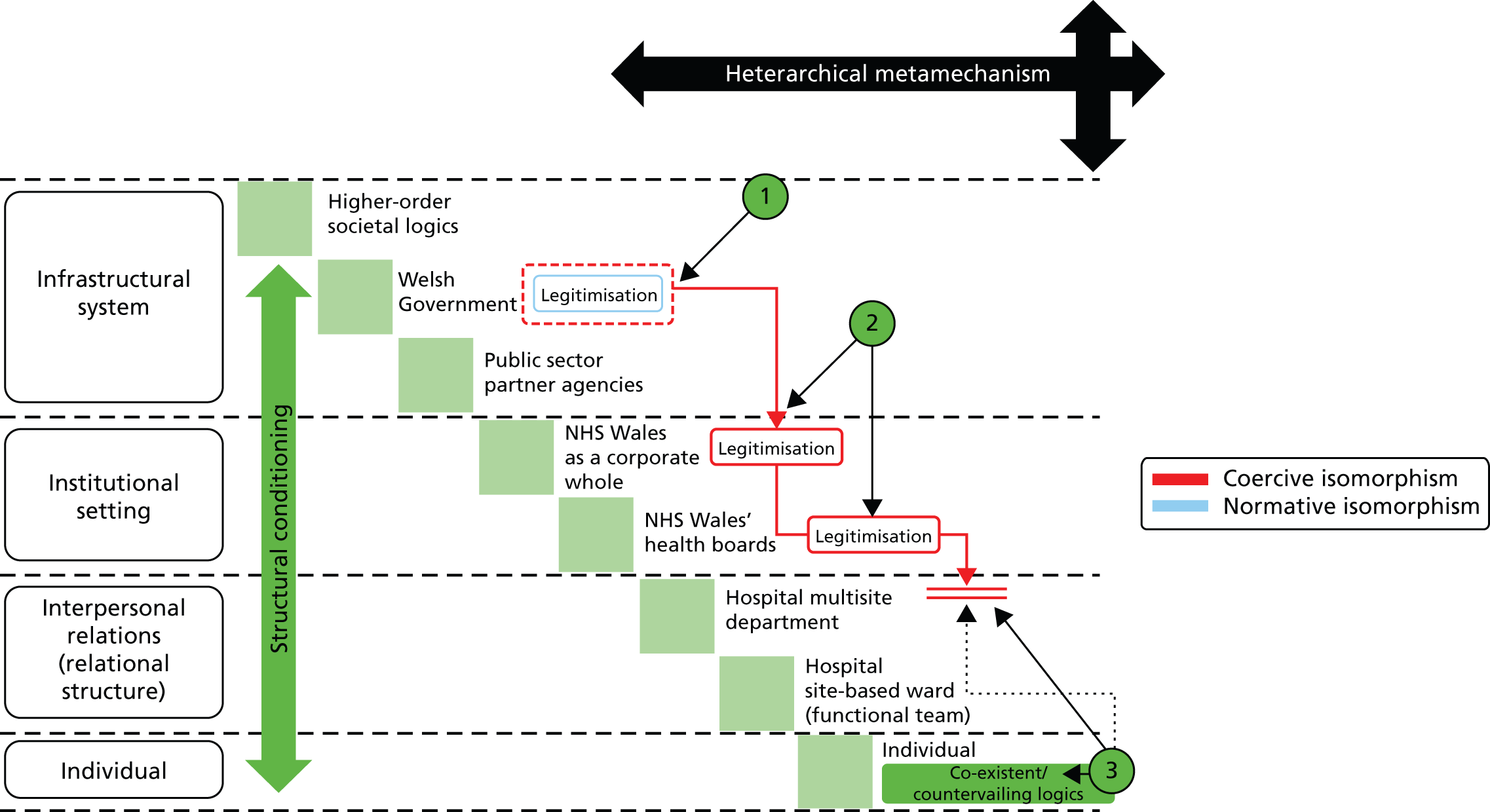
In Figure 14 we depict the formalisation of the 1000 Lives+ national programme across the Welsh health-care institutional field, centred on lower contextual strata at health board, hospital multisite department, hospital site-based ward and individual levels.
In point 1, in situated contexts where logics are in alignment:
-
Agency – formalisation – mandated engagement with 1000 Lives+ and the MI-PDSA approach to address NHS Wales’ organisational failings and attain national health-care standards.
-
Institutional work – creation – elite institutional carriers enact political work to reconstruct rules, rights and access to resources, thereby linking 1000 Lives+ national programme to tier 1 performance targets.
In point 2, in situated contexts where logics are in alignment:
-
Agency – formalisation – multiprofessional and multisite co-ordination of patient safety via the statutory Quality and Safety Committee and aligned governance structures.
-
Institutional work – creation – elite board-level institutional actors enact political work to reconstruct rules, rights and access to resources, thereby linking 1000 Lives+ national programme to the attainment of the Welsh Government’s tier 1 performance targets.
In point 3, the impact of co-existent or countervailing institutional logics is depicted as corrosive feedback. However, this is insufficient to over-ride mandated performance management and governance processes.
FIGURE 15.
Normalisation of the 1000 Lives+ heterarchical metamechanism operating across contextual strata: innovation.

In Figure 15 we depict innovation catalysed by the 1000 Lives+ national programme across the Welsh health-care institutional field, centred on lower contextual strata at health board, hospital multisite department, hospital site-based ward and individual levels.
In point 1, in situated contexts where logics are in alignment:
-
Agency – innovation – individual and organisational pragmatic evidence-based learning manifests through adherence to the MI-PDSA approach.
-
Institutional work – creation – functional team’s belief and meaning systems reconfigured.
In point 2, the impact of complementary institutional logics is depicted as positive feedback that supports the formalisation of evidence-based innovation across NHS Wales.
In point 3, the impact of co-existent or countervailing institutional logics is depicted as corrosive feedback.
1. Legitimisation: Table 10, transcriptions 5:02 and 5:24 and Figure 13 show how legitimisation is modulated. In transcription 5:02 (see 1000 Lives+, health-care practice and patient safety), complementarity between bureaucratic state, professional and collaborative logics results in perceptions of coherence with 1000 Lives+. However, the ensuing cognitive participation of those who ‘buy into certain areas where their interests lie’ promotes contained collective action, directed to deliver the aligned vested interests of those who occupy the orchestrating leadership position in this situated context.
In contrast, transcription 5:24 (see Building the ethos of patient safety: pride and shame in health-care practice) depicts the overt rejection of the dominant logic of the bureaucratic state. Professional logic is, therefore, shifted from its subordinate role into an ascendant position. Given the contradiction between these co-existent logics, theorisation prevents coherence from developing. This inhibits cognitive participation and collective action. As a result, 1000 Lives+ is viewed as ‘not part of us’. In this context, decoupling from the national programme arises.
2. Formalisation: Table 10, Figure 14 and transcription 5:29 (see reference in Teamwork, collaboration and emancipation) suggest that formalisation is modulated by complementarity between bureaucratic state, professional and collaborative logics. This promotes adherence to the governance structures which support the 1000 Lives+ national programme. However, the subtleties of individuals’ reasoning and use of the resources provided by 1000 Lives+ are exposed in transcription 5:36 (see reference in Building the ethos of patient safety: pride and shame in health-care practice). Although no overt rejection of the dominant logic of the bureaucratic state is expressed, professional logic and collaborative logic are not held in a complementary stance. Instead, they occupy a co-existent stance that fosters professional protection and a lack of collaboration. In this context, coupling to the governance structures that support 1000 Lives+ is fragile.
3. Innovation: Table 10, Figure 15 and transcriptions 5:13 and 5:20 demonstrate how innovation is modulated, while transcription 5:13 (see Model for improvement and PDSA approach) illustrates the nuances of normalisation. Once again, the logic of the bureaucratic state is embraced and held in close alignment with professional and collaborative logics. This promotes strong coherence with the 1000 Lives+ national programme – ’The model for improvement [MI-PDSA], well it’s, it’s a tried and tested approach, part of improvement science’ – resulting in the cognitive participation, collective action and reflexive monitoring of health-care staff who ‘can go out and they can get started straight away by having an idea, testing it on one patient one time, one nurse, one doctor!’. In contrast, transcription 5:20 (see Model for improvement and PDSA approach) highlights a profound disjuncture between the logic of the bureaucratic state and one facet of medical professional logic – the contestation between care and science373 – that stymies engagement with 1000 Lives+ owing to disagreement over the validity of the evidence base: what the respondent in this transcription calls the ‘tyranny of evidence’. This fundamental discord impacts on theorisation. It limits coherence and erodes the means for meaningful engagement with 1000 Lives+. As a result, normalisation and, thus, institutionalisation are hampered.
We suggest that the mechanisms that appear to foster normalisation modulate the processes of bureaucratisation through amplification of the complementarity or contradiction between logics in the institutional field. However, of those considered – coherence, cognitive participation, collective action and reflexive monitoring – only three are seen as generative mechanisms (coherence, cognitive participation and reflexive monitoring), while collective action is simply an outcome of such reflexive theorisation and, thus, an expression of agency.
In the next chapter we examine and develop I-CMAO configurations for three focal interventions from the 1000 Lives+ programme using theories of structure, agency and social change.
Summary
In Chapter 5, we analysed the cultural change inherent to normalisation of the 1000 Lives+ programme at the level of the functional team. We explored the role of contextual constraints and enablements, and ensuing reflexive theorisation, across the dynamic interplay of multiple logics, and considered the modulating roles of coherence, cognitive participation and reflexive monitoring.
Chapter 6 Improving leadership for quality improvement
Overview
Chapters 6–8 set out our realist analyses of the three focal interventions selected from the 1000 Lives+ programme in NHS Wales: ILQI, RSC and RHAI. To aid the explanation of our argument, each is structured in the same manner, as set out below.
In this chapter we examine ILQI, a programme aimed at helping organisational leaders to take a systematic approach to the implementation of practical interventions. We first consider three leadership activities designed to build the will to make measurable systemic improvement, specifically (i) setting aims and monitoring progress through local mortality reviews; (ii) demonstrating visible leadership via WalkRounds™; and (iii) the use of patient stories at board level. We review such practices to highlight their acknowledged benefits and the barriers that impede their normalisation into daily practice.
Second, we undertake a realist analysis of the progressive institutionalisation of ILQI, thereby setting out our comparative case study of sites A, B, C and D. In doing so, we explain the structural conditioning, sociocultural interaction and structural elaboration or reproduction fostered through the actions of three groups of key actors – directors of medicine, nursing, and therapies and health science – together with their colleagues in respective associate roles. We concentrate on these actors because they are formally tasked with the implementation of the ILQI under the 1000 Lives+ programme. In addition, to aid our understanding of context and mechanism, we examine the perspectives of policy leads, health board chairs, chief executive officers and other managerial staff aligned to these professional groups. Finally, informed by the findings of our realist analysis, we set out our understanding of the ILQI I-CMAO configuration.
Focal intervention, aim and drivers
Improving Leadership for Quality Improvement is the first of the three focal interventions considered in this study. This improvement programme aims to support board members and other organisational leaders to take a systematic approach to the implementation of practical leadership interventions to promote transformational quality improvement. ILQI has gradually become embedded in NHS Wales’ annual operating frameworks,445 quality frameworks446 and associated delivery plans. 391,402 Furthermore, ILQI is supported by an aligned organisational and workforce development strategy,447 a web-based national learning programme for all NHS Wales staff and contractors – Improving Quality Together (www.iqt.wales.nhs.uk/home) – and associated online resources offered by Patient Safety Wales (www.patientsafetywales.org.uk).
Improving Leadership for Quality Improvement is centred on the appointment of executive level leads for the different interventions within the 1000 Lives+ programme. It calls for the application of the underpinning MI-PDSA approach to inform the development of intelligent targets for priority clinical services. As illustrated in Figure 16, ILQI advocates three drivers for change. The first aims to build the will to make measurable improvement as quickly as possible. This directs senior leaders to cultivate staff engagement, enthusiasm and commitment at all levels of the organisation. The second aims to encourage and spread ideas about alternatives to the status quo, which are robust enough to form the basis of new working systems. This challenges senior leaders to support staff to implement such change. The third aims to oversee the implementation of a range of improvement initiatives within the organisation. This tasks senior leaders to develop a culture of health-care quality and patient safety. ILQI, as a core part of a Welsh health-service-wide governance agenda, therefore assists health boards to set local targets to reduce harm and mortality.
FIGURE 16.
Driver diagram: ILQI.
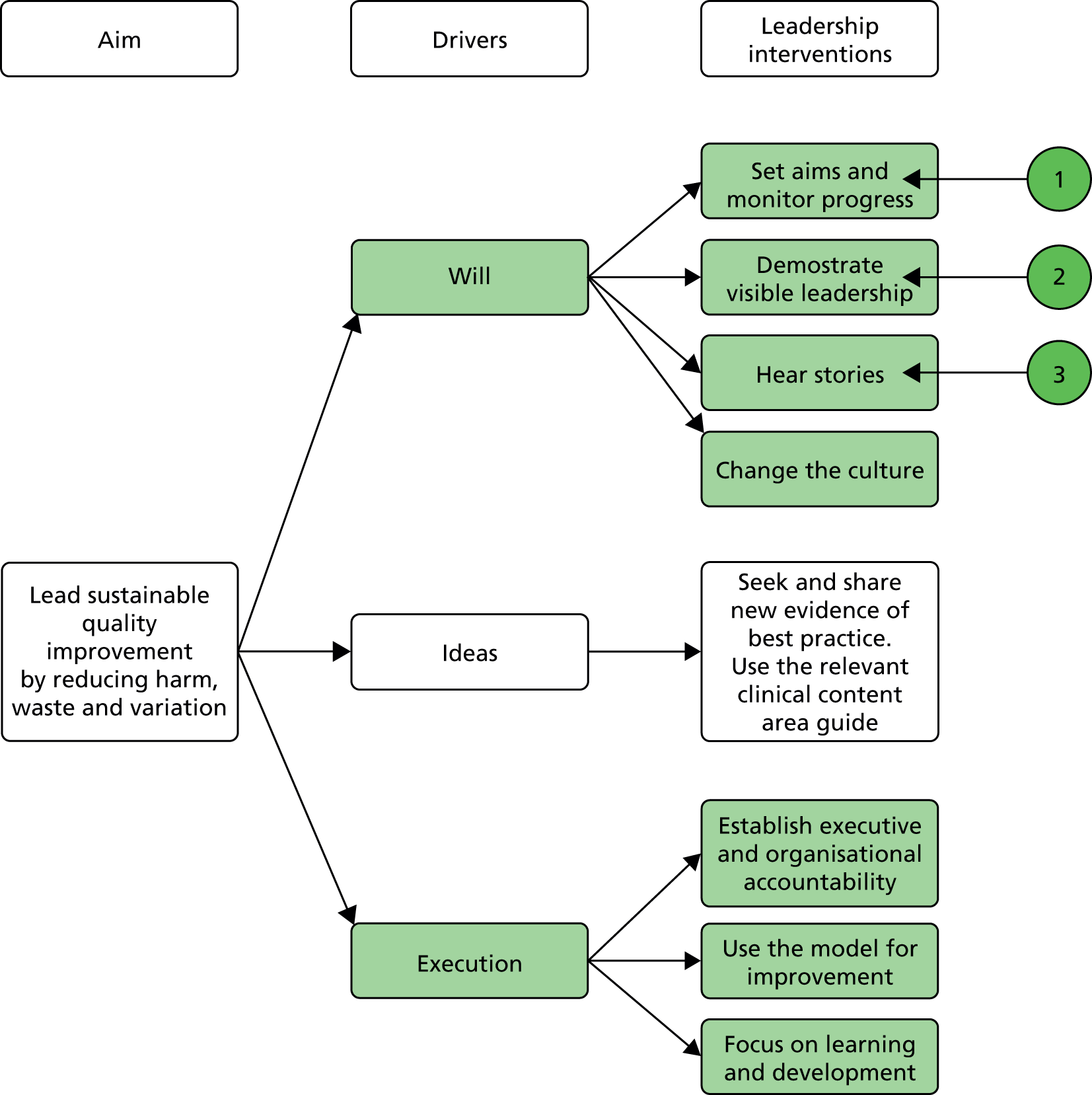
Figure 16 depicts the driver diagram for the focal intervention, ILQI. Attention is directed to three leadership activities designed to build the will to make measurable systemic improvement, as defined below:
-
point 1, setting aims and monitoring progress through local mortality reviews
-
point 2, demonstrating visible leadership via WalkRounds and
-
point 3, the use of patient stories at board level.
To aid our understanding of the interplay of context and mechanism in the operationalisation of this focal intervention, the perspectives of policy leads, health board chairpersons, chief executive officers and other managerial staff aligned to these professional groups enrich our analysis.
Acknowledging the interconnected features of this intervention, our attention focused on three leadership activities designed to build the will to make measurable systemic improvement to patient safety, specifically (i) setting aims and monitoring progress through local mortality reviews; (ii) demonstrating visible leadership via WalkRounds; and (iii) the use of patient stories at board level.
Mortality reviews, WalkRounds and patient stories
As outlined in Chapter 1, health-care quality and patient safety demand effective and co-ordinated leadership from politicians,448,449 executive-level managers81,450 and their subordinate staff – whether corporate or clinical professionals451 – who interact with patients, directly or indirectly,4,88,204,452,453 in the coproduction of their care. 146,155,454 Health-care leadership is, therefore, inherently distributed30,36,455,456 and complex,457 and necessitates active followership. 458 Furthermore, it is modulated by a range of other factors which impact patient safety and the culture of care,459–461 most notably (i) organisational governance processes, audit and monitoring systems;462–465 (ii) management processes and their reception by staff;29,466–469 (iii) team-centred learning and local commitment to education;11,207,470–474 (iv) an individual and collective focus on practice innovation;43,475 and (v) the development of an organisational culture of care, wherein transparency, communication and mutual respect are valued. 22,476–478
Mortality reviews
In the aftermath of the public inquiry into failings at the Mid Staffordshire NHS Foundation Trust,81 excess mortality has been openly debated as a means to flag concerns with hospital patient care. 479–482 Beyond the NHS, this approach has been used in other developed health-care systems to monitor organisational performance and to compare such performance between hospitals. 483,484 However, the validity and reliability of the Hospital Standardised Mortality Ratio (HSMR) and other means of measurement, such as the risk-adjusted mortality index (RAMI), is dependent on comprehensive, accurate and consistently applied clinical coding. Consequently, the use of such measures as HSMR as a screening tool for distinguishing low-quality hospitals from high-quality hospitals remains in doubt158–160,485 because the link between HSMR and organisational factors is ambiguous. 160 In addition, it has not yet been proved that HSMR reporting necessarily leads to worthwhile improvement in quality of care and patient outcomes. 483
Given this unresolved debate, and wide variation in hospital mortality, the impact of leadership on mortality, whether or not adjusted for case-based severity and cross-linked with resource measures,486,487 appears somewhat unclear. However, hospital-based monitoring of all-cause mortality through review meetings constitutes an important board-level and medical governance resource and may provide deeper insight into emergent patterns, thereby helping to identify trends to guide local improvement efforts488 and to reveal their impact on the provision of care over time. 489,490 In addition, they may provide assurance that patients are not dying as a consequence of unsafe clinical practices. 491
Other markers or proxy measures of leadership are associated with mortality. For example, a significant and positive association has been found between a higher percentage of clinicians on boards, the quality ratings of service providers and lower morbidity rates;32 Mortality rates have also been linked to greater use of high-performance human resource practices;492 nursing staffing ratios and skill mix78,493 and hospital pay for performance. 494 Wright et al. 495 also found that good leadership, organisational management practices and information systems, supported by a quality improvement strategy based on robust local evidence, training and a community-wide approach, may be effective in reducing hospital mortality. The evidence suggests, therefore, that mortality measurement may assist boards in thinking strategically about what it takes, from a systems perspective, to achieve patient safety. 496
WalkRounds
Board engagement in the patient safety agenda can also be increased by enhancing their collective literacy in health-care quality, governance processes and aligned service improvement methods. 497 One means to achieve this is WalkRounds. 498–500 Perceived as a key leadership practice in health care, WalkRounds foster situational awareness and help management to periodically assess new or unresolved vulnerabilities that may affect safety and care quality. WalkRounds, therefore, potentially provide (i) a forum for front-line staff to report and discuss patient safety problems with local leaders, so that the voice of the caregiver influences the ongoing board-level debate;501 (ii) an opportunity to improve teamwork and communication within and across units; and (iii) a supportive environment in which staff and leaders help to develop potential solutions for patient safety and service delivery issues502–505– all refined through the underpinning MI-PDSA approach. 506
Improvements in patient safety have been linked to the frequency of exposure to WalkRounds507 but their sustained operation demands significant organisational will, project management and commitment from board-level leaders. 499 Research is now beginning to penetrate the complex social processes that underpin WalkRounds so that their potential to foster executive-level learning is enhanced. 508,509 However, the development and maintenance of appropriate organisational feedback mechanisms is known to be a significant challenge. 510,511
Patient stories
These are a means for the patient and their family, advocate or carer to forward their personal narrative of harm in order to actively contribute to the coproduction of safe care. 512,513 Considering the notion of harm from the perspective of the patient offers insight into alternative health-care priorities,514 including (i) the psychological and emotional aspects of harm515 and (ii) the harm and distrust caused by delays in communicating patient safety incidents to patients,516 compounded by (iii) that which arises owing to their exclusion from the critical conversations which shape the provision of their individual care. 132,153
By providing rich insight into the reality of health-care provision through description and dialogue, patient stories can inform organisational governance processes517–519 and service redevelopment through experience-based design. 520 However, although patient stories may inform, equip and challenge organisational leaders to improve the delivery of health care, they also expose them to the fear of reputational and financial risk generated by the broader dissemination of harrowing narratives of harm. 521 This presents a barrier to the development of a safety culture. Tasking board-level leaders to hear patient stories as the first agenda item at every board meeting may reveal the human face of harm. 522 However, if rendered down to just another performance measure, amid an array of others, such narratives will do little to foster appropriate remedial action. 105 Indeed, dysfunctional consequences may arise owing to entrenched historical and cultural precedents, specifically beliefs anchored to health-care performance and autonomy. 523–527 Cognitive psychological explanations of the way such individuals process patient feedback of this type, together with the corresponding social rules which frame their ensuing action or inaction,303,527–529 therefore constitute an important arena of patient safety research for social scientists. 530
Realist analysis and comparative case study
To examine the dynamic interaction of the focal intervention and context, ascertaining emergent mechanisms and ensuing outcomes, we now undertake a critical realist analysis of the progressive institutionalisation of the 1000 Lives+ programme’s ILQI. Our case study considers sites A, B, C and D, which, owing to high levels of access and wide-ranging staff engagement, offered rich insights into the unfolding implementation of the ILQI. Our analysis focuses primarily on three groups of key actors – directors of medicine, nursing, and therapies and health science, together with their colleagues in respective associate roles – tasked with the implementation of the ILQI under the auspices of the 1000 Lives+ programme. However, we also use data from policy leads, health board chairpersons, chief executive officers and other managerial staff aligned to these professional groups.
First, we consider the focal intervention in context and explore the dominant structural and cultural emergent properties impacting board-level actors. Next, to reveal the generative mechanisms in play, we examine mediation via first- and second-order emergents and the resultant situational logic. Then, to examine the initiation of change, we explore the unfolding strategic negotiation of change and the mode of institutional work enacted. Finally, we reflect on the nature of any sustained outcome, be that elaborative or reproductive. This analysis forms the foundation of our refinement of the I-CMAO configuration spanning the Welsh health-care field in 1000 Lives+ institutionalisation: ILQI – local implementation of the focal intervention and contribution to the I-CMAD configuration spanning the Welsh health-care field.
Structural conditioning: structural and cultural emergent properties in the Welsh health-care field
Initially, we discussed the dominant structural and cultural influences impacting health board-level actors during the institutionalisation of the 1000 Lives+ programme and ILQI with policy leads in the Welsh Government. As commented in transcriptions 6:01 and 6:02 (below) – and as previously reflected in transcription 4:01 – the 1000 Lives+ programme was deeply integrated with health-care policy development in Wales.
The 1000 Lives+ national programme has been a vehicle to do lots and lots of things; it’s been very useful. Now, for pretty much all projects – when we get to the stage where there’s some policy that we need to do in Welsh Government and, I think, even more so following Francis – the implementation is designed with the methodology that sits behind 1000 Lives+ in mind because it’s there, and people can understand it, and so they can use it in order to be able to move stuff forward.
Policy lead, Welsh Government (145); transcription 6:01
What we’ve started to introduce this year – this new financial year just started – is we’ve tweaked the tier 1 targets and we’ve created basically five domains of quality. So we’ve tried to reflect much more broadly what boards are doing. We’ve piloted alongside it the principle of what I would call a bit of improvement methodology. We’ve sort of laid out a series of matrixes or grids of competencies that we expect boards to be able to display on a scale of 1 to 5 – a scale of maturity – so what we’re trying to do is to move it away, a bit, from just target driven to being more about development. As I’m trying to make it more developmental, it is starting to get closer to the 1000 Lives+ type approach.
Policy lead, Welsh Government (146); transcription 6:02
Such policy actors held robust views on the dominant structural emergent properties impacting health boards: ‘it’s finance, reconfiguration, staffing, and health-care quality performance’ (transcription 6:03, below).
What are the structural constraints on the 1000 Lives+ national programme? That’s an interesting question, we could probably spend the next hour just discussing that; but I’ll do my best to be succinct. The first structural constraint is, obviously, the financial difficulties that all public services now face in light of the global economic downturn. Second, for NHS Wales, it’s the major reconfiguration, and that’s still ongoing, as we have to address the configuration of services and their provision across Wales, so there’s a ripple effect across all health boards as they reconfigure. All that will create heated political and public debate because, in Wales, as elsewhere, people are fiercely protective of their health-care services – they still criticise them – but they don’t want services shifted to other sites away from their locality. That creates staffing constraints for all health boards, especially those further off the M4 corridor. As I’m sure you are aware, there are major difficulties in some areas of Wales, in terms of the recruitment and retention of general practitioners, some acute specialisms, accident and emergency, and others. And then, of course, we have the Francis Report, which, I believe, will heighten governance and performance management systems, as we saw after the Kennedy Report into Bristol Royal Infirmary. So, it’s finance, reconfiguration, staffing, and health-care quality performance, they’re the main ones, at least!
Policy lead, Welsh Government (143); transcription 6:03
Financial constraints were also seen to have a specific adverse effect on patient safety (transcription 6:04).
Beyond the goals of 1000 Lives+ and ILQI, these acknowledged structural constraints shaped the strategic context to the delivery of the Welsh Governments’ tier 1 targets, and their active management and mitigation was central to the bureaucratic control exerted over each health board (transcription 6:05, below).
[How do you hold NHS Wales’ health boards to account for their performance?] We have an escalation framework – basically four levels of escalation, five if you include zero – we monitor health boards, as they have to perform against the targets that they’re supposed to achieve, and if they’re performing against all of the standards then they wouldn’t be escalated. Basically, they’re allowed to get on with it and, to a degree, we actually pull away from the level of assurance that we seek. So we could get to the stage where you might only, you know, touch them quarterly or half-yearly. But we’re not at that point with anybody at the moment. Once things start to go wrong – somebody’s missing their targets – we then escalate to level 1, 2, 3 and up to 4. At each of those levels there’s a slightly higher level of intervention. Each of these would be just a bit more forceful: ‘you need to have got to a recovery plan by this’; ‘we need you to be showing you’re doing a recovery plan’, if they don’t do that they go up another level and that carries on and the frequency increases. Basically, by the time we’ve got to level 4, the chair will probably be having conversations with the minister, and the chief executive will be probably having conversations with the chief executive of NHS Wales. Throughout this process what we’re looking at is, essentially, what have we got to do with this board; is there something that’s needed in way of turning around behaviour, turning around attitude, turning around performance? Does that mean we have to bring something or someone in? We can bring to bear quite a lot of sanctions, in terms of alterations to their allocation of money. Now, we don’t normally get to that stage but we’re very close with a few boards at the minute – we do have to recognise, as is happening in NHS England, that performance is very difficult in the current financial environment – so the whole system is just basically not quite as slick as it would have been even a year ago.
Policy lead, Welsh Government (146); transcription 6:05
Another respondent viewed the Francis Report to have been the main cultural impact on health boards during the institutionalisation of the 1000 Lives+ programme and ILQI (transcription 6:06).
Other structural and cultural constraints arose from the institutionalised delegation of strategic oversight of patient safety – and, thus, 1000 Lives+ and ILQI – to the leadership of directors and associate directors of medicine, nursing, and therapies and health science (transcriptions 6:07 and 6:08, below, and transcription 6:09).
Post Francis, I think that the cultural constraints which will impact on NHS Wales’ health boards and 1000 Lives+ national programme stem from driving forward a transparent culture of compassionate care – we’ve set out our views on that – so, that is all about the professions, their traditional practices, turfs and turf wars, recognising that errors do happen, and that we can make change to mitigate some of them, though it will take real leadership and time to change the culture.
Policy lead, Welsh Government (145); transcription 6:07
The quality of our services and patient safety issues, though they fall within my remit as accountable officer, are delegated to other board members. You’ll find this across NHS Wales. Certainly, for 1000 Lives+ it’ll be the medical director, nursing director, and the one for therapies and health sciences – or whatever title is applied for this type of board-level role – that hold the strategic focus for the patient safety agenda. Typically, it’ll be their associate directors who will be more involved, operationally, in the roll-out of 1000 Lives+. This isn’t an abdication or abrogation of responsibility, it’s delegation through to the clinical professionals who ultimately deliver care to patients and whose practices 1000 Lives+ is attempting to transform. [What about your engagement in mortality measurement, WalkRounds, and use of patient stories at board level?] Yes, we do those. But that is only part of what we do, there’s more to managing this health board than addressing 1000 Lives+.
Chief Executive, case site A1 (078); transcription 6:08
First-order emergents for board-level actors central to the institutionalisation of ILQI
The dominant structure and culture described in the previous section shaped the context and conditioned the actions of the board-level directors and associate directors central to the institutionalisation of the ILQI. Below, we set out how actors in such professional role-positions reflected on first-order emergents such as their delegated leadership of the ILQI, their vested interests and perceived opportunity costs associated with various courses of action, and seek to discern how this shaped their interpretive freedom and scope for purposive action to support patient safety.
Director of medicine and associates
The vested interests of directors of medicine and their associates, tasked with the strategic oversight of the 1000 Lives+ programme and ILQI, lay primarily in the successful development of a systematic locally agreed approach to undertaking the mortality review in the aftermath of the structural reconfiguration of NHS Wales (transcriptions 6:10 and 6:11, below, and transcriptions 6:12 and 6:13).
In terms of 1000 Lives+, my main focus is the mortality reviews, and reporting through the system that has been established with the Welsh Government. We’ve done a board paper, two board papers in a row, which address how do we measure harm, how do we measure our morbidity, our mortality. So it’s a key role. With 1000 Lives+, the mortality reviews have been around a programme of work looking at how we, how do we actually understand where the harm is occurring. It’s a systematic process – one of the main things that [name, NHS Wales Chief Executive and Director General, Welsh Government] asked the medical directors to do, probably in 2010, was to do systematic case notes reviews – so we have a system whereby I was probably looking at 25% of the deaths, not all the deaths, because we have 50 deaths a week! So we embarked upon learning through reviewing about 15 sets of notes a week with the senior governance adviser and with also one of the associate directors of medicine. We tried various different ways, in terms of pro formas, and we did all the PDSA-type work but in the end we’ve settled on a detailed notes review using the global trigger tool. I have to say that we continued that right up until January when there was the debate about publishing RAMI. Although we didn’t feel that we learnt in excess, we did learn above and beyond what we knew about the organisation through that process.
Medical Director, case site D1 (117); transcription 6:10
[Prior to 1000 Lives+ was there any systematic process for reviewing mortality across the health board’s hospital sites?] Well the kick-off, actually, was, you know, when this organisation came into being; there had been chaos! There was the organisation, and predecessor organisation or organisations – as you know, we’ve had to endure a lot of change – we had the interim trust with a completely different executive team, and a completely different interim medical leadership and management structure, that was just basically trying to keep the thing ticking over really. Then we were presented as a new edition, [health board name], and more systematic scrutiny of our statistics started, and one them was that our RAMI which was worrying. So, that was the situation when the health board came into being and, obviously, as medical director, I was tasked to do something about it.
Certain parts of the organisation may well have been looking at quality initiatives before that but really I think getting a grip on the mortality review and embracing 1000 Lives+, which we did as organisation at that point, added coherence to the whole thing. So, when you asked me specifically what had been done before, I would say that it was very hit and miss. Now, with 1000 Lives+, I have a clear focus on mortality. I don’t want to harp on about it, but you’re asking about leadership and what we do as an organisation, I think that’s a very good example how it’s been successful. I mean, at the moment we’re into year 3, something like week 12 or 13, where every single week, every single death in the organisation is looked at by a senior medical – a senior doctor – every single one, and a report goes to the chief executive. The information from that review – which, of course, when we get concerns highlighted, concerns are investigated more deeply and reported back, hopefully through auspices of medical director – the lessons learned, the themes, and so forth are communicated back, right the way across the whole of the organisation, primary care and everything.
Medical Director, case site F1 (042); transcription 6:11
Moreover, such vested interests were closely aligned to those of policy leads with the Welsh Government. Therefore, through the 1000 Lives+ programme and ILQI, the systematisation of mortality reviews brought bureaucratic state logic, professional (medical) logic and a collaborative logic into a complementary stance (transcription 6:14, below).
I think, in Wales, because we had a well-developed sort of collaborative approach, we were able to engage clinicians in the audit of their local mortality levels, and what was going on. But we’re using the national indicator in a very, very simplistic way, which I think is good, to just say: ‘hey look, this will tell us if there is a problem’. But we then go into that audit work – that real work on the ground, to say – well actually, are they doing all the things they should be doing to really understand and make sure that this is right. [Long pause]
In a way, what we’ve avoided, so far, is getting dragged into this idea that’s going on in England where you keep hauling out the top five and sort of having a public process about their mortality levels. What we’ve tended to go for is: ‘well let’s get them working on it’. Now having done that, and it being, at least so far, quite a successful approach, we’re now looking at how that set of principles could be carried into other areas. So when we start looking at developing unscheduled care markers, or planned care, or whatever it might be, we’re looking at whether we could underpin it with an audit type approach, which says: these are all the good things you should be doing, how are you doing against all of these; if you’re doing all these things, how are you monitoring your outcomes.
Actually, some of these higher-level measures are underpinned now with something that’s a bit more substantial than just making sure you’re getting everybody through. So we’re trying to adopt almost a two-tier approach – a set of national standard type measures – which we’ll try and keep as simple as we can, but underpin it with a different approach around a more detailed understanding and audit.
Policy lead, Welsh Government (146); transcription 6:14
Director of nursing and associates
In contrast to the directors of medicine, the vested interests of directors of nursing and their associates were aligned with the successful local co-ordination of the various patient safety interventions emergent from 1000 Lives and 1000 Lives+. Though the formal remit of their roles was to be professionally accountable for nursing practice, such roles typically absorbed a wide range of other ‘stuff’ (transcription 6:15, below).
As Director of Nursing, I’m professionally accountable for nurses and midwives across the health board – about 5500 registrants and 3000 health-care support workers – so I advise the board on the professional agenda. I’ve also hold joint executive responsibility with the medical director and director of therapies and health scientist for clinical governance. In respect of 1000 Lives+ I’ve got some key executive lead roles, for example infection prevent and control; but I also have executive lead roles for the Transforming Care programme. Directors of nursing often label ourselves directors of nursing and stuff because we tend to pick up a lot!
Director of Nursing, case site B1 (030); transcription 6:15
Work associated with the 1000 Lives+ programme and ILQI was frequently co-ordinated with medical leads, highlighting the complementary alignment of professional (nursing) and professional (medical) logics (transcription 6:16, below).
I am one of the assistant directors of nursing – we’re each site based in a district general hospital – and I work very closely with the site-based assistant medical director. We work together to ensure that we undertake safety WalkRounds, and other features of the 1000 Lives+ national programme to build leadership capacity, and to ensure that we provide that support and visibility for front-line staff. So it’s very important that, between ourselves, that we undertake them jointly, preferably.
Assistant Director of nursing, case site C1 (093); transcription 6:16
Executive nurse leadership was viewed as pivotal for the successful institutionalisation of the 1000 Lives+ intervention ‘bundles’ apportioned to nursing for their implementation (transcription 6:17, below).
The 1000 Lives+ skin bundle has got an executive lead – our assistant director of nursing – who’s very active. They have study days are coordinated by her secretary, and they have three sessions that they run for each area. In contrast, my experience with the catheter bundle has been difficult. I couldn’t facilitate that for my area because I haven’t had an active executive lead. But the skin bundle, certainly with their executive lead, has worked really well, and spread to areas from across the health board, including private nursing homes and things! We’d love to do that with the catheters, but we just haven’t been able to break down the barriers to get across and to access people who can make those links for us.
Senior nurse, IPAC, case site D1 (034); transcription 6:17
Director of therapies and health science and associates
Directors of therapies and health science were newly established board-level roles (transcription 6:18). Consequently, their vested interests centred on ‘coming up to speed’ with the demands of the role as well as their executive leadership of 1000 Lives+ interventions associated with ILQI. In this regard, the professional logic enacted was firmly aligned to professional (medical), professional (nursing) and professional (management) logics in a complementary stance (transcription 6:18, below, and transcription 6:19).
My learning curve with the original 1000 Lives campaign and now the 1000 Lives+ national programme, you know, it’s been particularly steep over the last 3 or 4 years! Just coming into the director role for therapies and health sciences – we didn’t have these director roles previously, so we’re all new to boards in the first place – and so the medical and nursing directors’ portfolios have shifted around.
But this definitely felt like quite a daunting prospect, I felt it needed a level of expertise; I’d need to have an enormous amount of expertise. I have obviously been learning and asking questions, just the same with any board role, we all need to have teams, support around us, people who can give you expert advice. So I’ve had to ask questions and get into some of the detail, just to get my head around it, and I’ve come back out again. Do you see what I mean?
With the 1000 Lives+ national programme, I think, possibly, it’s been even more challenging for my nurse director colleague. From an organisational perspective across Wales, 1000 Lives+, a great deal does come down to the director of nursing. It is very much a nursing domain.
Director of Therapies, case site C1 (118); transcription 6:18
Second-order emergents and situational logic
In case sites A to D, the interplay of structural, cultural and agential emergent properties impacted on the three groups of actors central to the institutionalisation of the 1000 Lives+ programme and ILQI. Structurally, the presence of necessary and internal linkages of a complementary nature between structures such as the mandated bureaucratic performance management systems and associated 1000 Lives+ and ILQI goals, notably the RAMI, which was integrated into local mortality measurement practices, rendered these performance management and governance institutions mutually reinforcing. Similarly, structural resilience emerged from the co-ordinated action of directors of medicine, nursing, and therapies and health sciences, as collective champions of 1000 Lives+ and the broader patient safety agenda.
Second, at board level, the institutionalisation of 1000 Lives+ and ILQI draws professional logic into alignment with that of the bureaucratic state. Moreover, there is coalescence and cohesion across medical, nursing, allied professional and health-care management logics. This places each into a complementary stance, fosters the cross-cultural systematisation of facets of 1000 Lives+ and ILQI across NHS Wales and promotes the reproduction of such practices across each health board. Consequently, at board level, the ILQI operated under a situational logic of protection that moulded sociocultural interaction, agency, strategic negotiation and the ensuing mode of institutional work.
Sociocultural interaction: agency and strategic negotiation
A situational logic of protection emerged from a context of necessary and internal linkages of a complementary nature between systemic structures and harmonising logics. However, given the status of the people involved, the inherent change agenda overarching the 1000 Lives+ programme and, thus, the ILQI were executed from a position of high negotiating strength. Below, we highlight this complex interplay in both a discrete case site and across multiple case sites, drawing out different degrees of bureaucratisation and normalisation to help understand the interplay of the focal intervention, context and mechanism.
Power-induced compliance and political sanction
To examine the adoption of power-induced compliance under a board-level situational logic of protection and to trace its impact across management tiers, we reflect on some of our discussions with respondents in case site B. At this site the chief executive had visibly responded to the bureaucratic demand for engagement with 1000 Lives+ and ILQI, and WalkRounds had also become successfully integrated and thus normalised as an expected professional role-position practice (transcription 6:20, below).
Our approach to 1000 Lives+ is reflected by the leadership of the health board. WalkRounds are a central aspect of 1000 Lives+ but [name, chief executive officer] is out and about to each of the main hospital sites to deliver our monthly team brief, and that team brief is expected to be cascaded out to other managers – then they speak to their leads, their teams, on a one to one, that’s the expectation – so that leadership and visibility is there in addition to the WalkRounds. That’s about four a month, or eight a month with the team briefings and the open forums, on top of which the director of nursing also does theirs – about four a year – and goes out and about and meet the nurses and midwives across the organisation. So they try their best to communicate and be visible, but they can’t be as visible as they used to be because of the size of the organisation.
Associate Director, case site B2 (009); transcription 6:20
Thus, under a situational logic of protection, the chief executive enacted the practices mandated for his role, building them into an ambassadorial display that promoted similar enactment by other board-level and sub-board managerial actors. Furthermore, such activity was appreciated for its ‘very hands-on’ and ‘approachable’ manner (transcription 6:21).
Transcription 6:22 (below) reveals the impact of the Francis Report81 as a parallel driver for change across NHS Wales, one that was used in an overt act of professional role-positional power to deliver higher standards of care.
One of the things that I did, to address patient safety, was to remove a ward sister from the ward – and we changed the team – because there was a deep-rooted culture in that ward, that went back years and years and years. So I removed the ward sister and put two registered nurses through a disciplinary. It was like a volcano going up.
I don’t want to turn this into a blame culture but where there are failings and poor standards of practice or poor leadership – they either want to be a ward sister and all that entails or they don’t – so we’re making some quite hard moves at the moment and I think that, given Francis, I think it’s the right time to do that now.
Director of Nursing, case site B1 (030); transcription 6:22
Such power was also used to enable those involved to drive forward their evolving patient safety agenda by the display of visible leadership (‘walk the wards’); the engagement and co-option of medical staff to act as clinical champions for 1000 Lives+ (‘we must have the medical champions out there’); and building the will for change across the functional health-care team (‘strong clinical leadership to give teams the confidence to challenge’) (transcriptions 6:23 to 6:25).
Reciprocal exchange and the harmonisation of desires
A more subtle deployment of power arose through reciprocal exchange and the harmonisation of desires with other key professional actors. At case site A, board-level actors exerted their managerial control and co-opted their associates who demonstrated interest and relevant clinical expertise to lead the implementation. Thus, the implementation of 1000 Lives+ gained further visible professional leadership closer to the point of care (transcription 6:26, below).
Given my professional background, and experience of service delivery, I’ve always been really interested in quality and safety, so as associate director, I was tasked with patient safety and patient experience. I’m responsible for sorting out the patient experience agenda – working out how we can capture the patient experience – and making sure that we close the loop. So if we discover something about patient experience through patient satisfaction, patient stories, complaints or anything like that, I aim to ensure that we close the loop in terms of the organisational learning. And for good practice as well because, obviously, as part of that feedback, I get to find out what’s really good about our service. It’s not always about what’s really bad about our services. . .!
I also work with clinicians and managers to put in any action plans, in terms of any work, if things aren’t up to standard, or if there’s some developmental work that needs to be put in place. So, if my early warning system is telling me that I’ve got signs of a problem in an area then, obviously, I’ll work with the area and the managers to see what needs to be done to improve quality and service. And I work with clinicians to make sure our policies and procedures are up to date and fit for purpose.
Associate Director, case site A1 (048); transcription 6:26
Such leadership, in itself, fostered the engagement of consultant medical staff with aligned clinical interests. This promoted further medical engagement with 1000 Lives+, [‘. . . if you’ve got somebody at that level that drives it, it’s so much easier. Medical leadership makes it work a lot quicker than management’ (transcription 6:28)] and, ultimately, the local leadership of discrete interventions [’it’s local leadership because they understand the pressure within the organisation, and what makes a difference within that particular area’ (transcription 6:29)]. Creative institutional work, targeted at those who were believers in the aims of 1000 Lives+ programme and, therefore, motivated to engage by a strong sense of coherence, aided its normalisation in practice (transcription 6:27, below).
The thing that enabled it to happen [1000 Lives+ national programme], the places where it happened, it was due to the individuals who were committed to it. [Was that limited to consultant-level clinical leadership or were others involved?] Both. In our health board, here, there’s myself and there’s a consultant, and we’re both who committed to it. You need – rightly or wrongly people listen to consultants, people listen to doctors – you can have the best nurse in the world, who’s an expert in something, but they’re still a nurse. It’s a hierarchical culture in the NHS. Doctors don’t learn – doctors are not prepared to learn from nurses – they’ll learn from doctors: it’s completely wrong. Some of the universities are now doing a lot more multiprofessional learning, the Peninsular Medical School, you know, they’re fantastic at this sort of stuff. So, because there’s this hierarchical thing, you do need consultant leadership but that can’t work on its own. [You need nurse leadership and broader followership to embedded 1000 Lives+ into practice?] Yes.
Consultant, palliative medicine, case site A1 (052); transcription 6:27
In case sites B, C and D, the deployment of power through reciprocal exchange and the harmonisation of desires led to similar patterns of expert co-optation to promote resource control of the 1000 Lives+ programme at the point of care. However, discussions at each case site exposed different features. For example, in case site B, reciprocal exchange, manifested through knowledge, flows from board to ward and to the 1000 Lives+ programme team (transcriptions 6:30 to 6:33). At case site C, reciprocal exchange was deployed to build intraprofessional coherence and commitment to 1000 Lives+ for medical and nursing professionals (transcriptions 6:34 and 6:35). Finally, at case site D, reciprocal exchange manifested, once again, through knowledge flows from board to ward (transcriptions 6:36 and 6:37). This was also marked by a subtle shift in expertise to lower management tiers, illustrating the normalisation of 1000 Lives+, and, thus, the inherent successful implementation of ILQI.
Structural elaboration or reproduction in the Welsh health-care field
We also sought to gauge key actors’ perceptions of the structural elaboration or reproduction that had emerged under a situational logic of protection. A national programme team member described how, through the formalisation of ILQI, a network of patient safety leaders, health-care professionals from managerial, medical, nursing and other allied groups, had evolved (transcription 6:38, below).
Well, throughout the 1000 Lives campaign and 1000 Lives+, there were some specific interventions that were focused on board-level leaders. But we quickly recognised that, actually, the people that we needed to get at were often senior leaders who didn’t have a formal board-level role. Another thing was that, because of the level of disruption with the NHS in Wales – due to the reconfiguration – there weren’t people in all the formally appointed board roles, so you had a much more, a looser coalition of senior leaders that we needed to engage with. But one of the things that we have recognised, increasingly, is that to achieve a connection between the clinical teams working on programmes and an organisation level focus involves much more than board-level leaders and front line leaders. It involves a network of people throughout the organisation.
1000 Lives+ national programme team member (089); transcription 6:38
This notable structural change, in indoctrinating others, promoted the distributed leadership of patient safety and the local integration of the 1000 Lives+ programme at each case site. Furthermore, the structural change associated with the integration of mortality reviews into the Welsh Government’s performance management framework was viewed to have added an important ‘critical lens’ through which to view patient safety, providing a valued means of organisational learning (transcriptions 6:39 to 6:41).
In contrast, cultural change was viewed as far more fragmented. This was viewed as owing partly to the pejorative perception of 1000 Lives+ as a nurse-dominated agenda and partly to the time demanded for such cultural evolution, if not revolution (transcriptions 6:42 to 6:44, below).
One success is that it’s certainly been embraced by the nursing profession but I’d like to see it embraced by the multidisciplinary teams in a broader context. Some of the other professions are quite dismissive: ‘it’s a nursey-nursey thing’.
Policy lead, Welsh Government (140); transcription 6:42
I do think we have driven structural change through 1000 Lives+ but, I think, cultural change is slower. It’s happening, no doubt, and the new website will, I hope, help NHS Wales to build a workforce that has a detailed understanding of service improvement – the skills and knowledge, the capabilities to sustain patient safety – and the sense of empowerment to act.
Policy lead, Welsh Government (145); transcription 6:43
That notion, that simple acknowledgement that, in the Welsh NHS, we do harm. It’s politically difficult to stand-up and say that but I believe it’s the start of real culture change: a revolution in care.
Policy lead, Welsh Government (081); transcription 6:44
Importantly, the cultural change that was in play included some notes of discord. For instance, the means of guiding care could become an end in itself, much to the detriment of the patient (transcription 6:45, below).
The nurses have become conditioned, in some respects to, if they’re having a problem with a patient, they reach for a piece of paper to document behaviours. So I’ll give you an example of one of the recent wards that I’ve been working on – it’s a very, very busy trauma ward – and we have a big problem with older people becoming delayed transfers of care because it’s difficult for us to discharge older people, with high intensity needs, out into a more appropriate setting once their orthopaedic and the trauma care is finished.
One of our patients on this particular ward has, is completely dependent, unable to verbalise her needs or her wants, bed bound, reliant on us for everything, from feeding, to turning, to toileting, to trying to interpret communication. And in that, clearly, she becomes very frustrated. So she’s taken to grabbing out or grabbing nurses as they’re turning her. Instead of the nurses stopping and thinking how can we better interact with her, and how can we reassure her more, they’ve reached for a behaviour chart. So now her behaviours are being documented – instead of actually stopping and thinking about what can we do differently – let’s document the bad behaviour is their response. I think, as a nurse leader, that’s what we’re conditioning our nurses to do.
Associate Director, case site C1 (119); transcription 6:45
In addition, some aspects of WalkRounds and the use of patient stories were found wanting. For some respondents, WalkRounds were centred on ‘good news stories’ that lacked feedback and action at ward level rather than providing a means for transparent and open discussions (transcriptions 6:46 to 6:49), and ownership of the voice behind the patient story was a source of concern for others. However, overall the 1000 Lives+ programme’s ILQI was considered to be a catalyst for change (transcription 6:50).
In Wales, the NHS is characterised by a management style which is probably best described as pace setting, so it tends to have a pace setting management style. And 1000 Lives+ and collaborative working and engagement with the public and all of those sorts of things, is more about a coaching style. So for me, it’s getting that right balance between targets setting a pace and underpinning it with something, which then coaches people at the best way of how they can do those maturely, so it’s how we go about bringing that together, which for me is the absolute challenge that we’ve got. And it seems very easy to say that but when you think of the characteristics that you’re changing to do that, it’s immense.
Policy lead, Welsh Government (146); transcription 6:50
1000 Lives+ institutionalisation: ILQI – local implementation of the focal intervention and contribution to the I-CMAO configuration spanning the Welsh health-care field
In this section, we seek to further our understanding of the local implementation of ILQI and define its contribution to the 1000 Lives+ programmes’ I-CMAO configuration spanning the Welsh health-care field.
In case sites A–D, ILQI was targeted primarily at executive board-level actors. Hence this focal intervention connected the infrastructural system of the Welsh Government and the Department of Health and Social Care to NHS Wales’ health boards. Viewed at a high level of abstraction, as illustrated in Figure 17, the institutional change inherent to formalisation, therefore, shaped the context of action for such actors.
FIGURE 17.
Improving Leadership for Quality Improvement: heterarchical metamechanism operating across contextual strata.
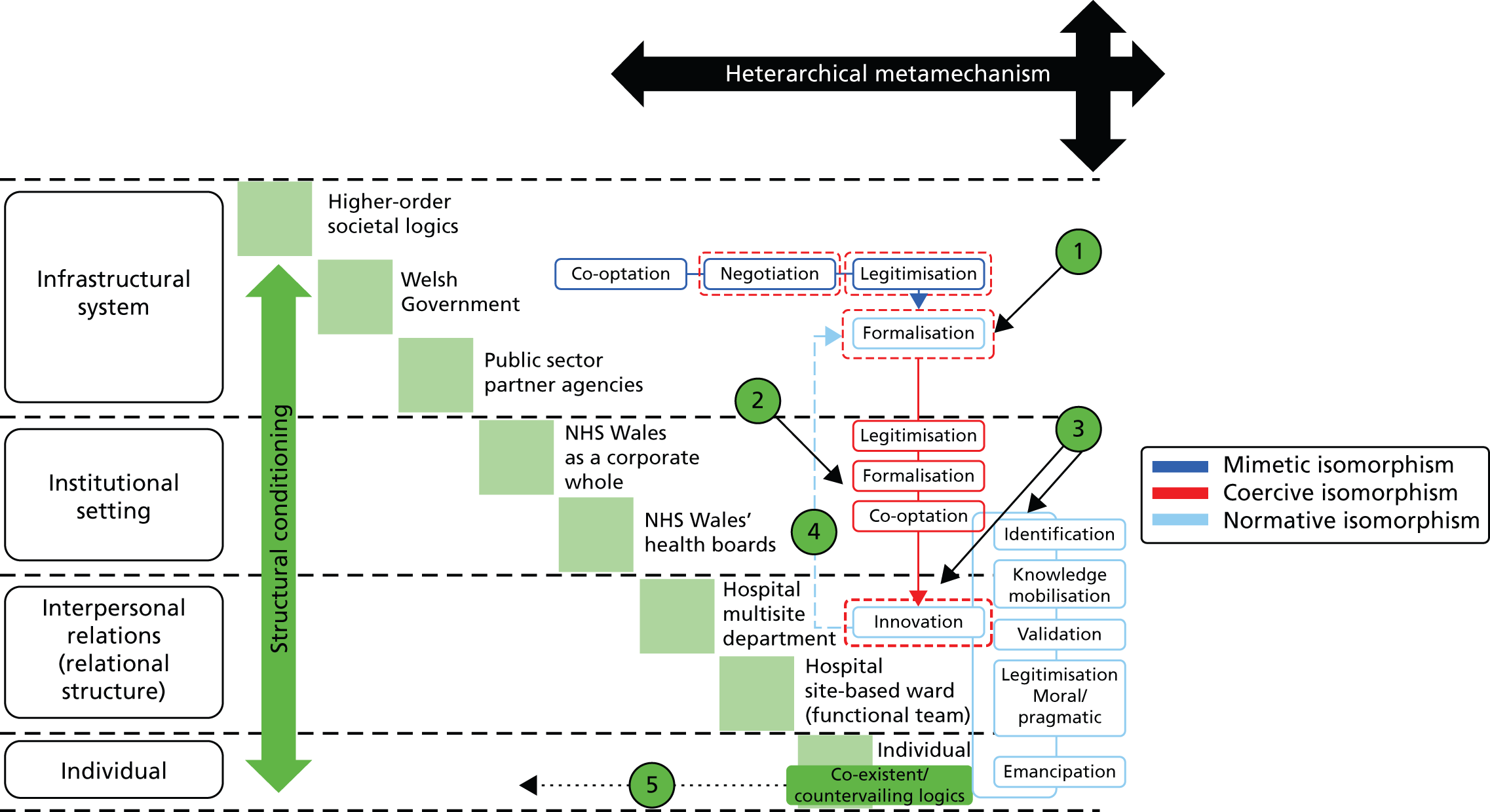
In Figure 17 we depict the implementation of the mortality review component of the ILQI focal intervention.
In point 2 structural constraint impacts at the level of the executive team, fostering the co-optation of other medical leads and clinical coding staff, who are to operationalise the mortality review across the health board together with its associated audit practices.
In point 3 mandated engagement drives the innovation cycle in the situated context, so that new practices for measuring harm, morbidity and mortality emerge. This, therefore, functions as a fundamental stage in organisational learning with respect to health-care quality and patient safety.
In point 4 we depict feedback to Welsh Government and public sector partner agencies as the implementation and operationalisation of the mortality review component of the ILQI focal intervention gradually systematises across NHS Wales.
In point 5 co-existent and countervailing logics are muted by structural constraint.
The 1000 Lives+ and the MI-PDSA approach were embedded in Welsh Government tier 1 targets and associated escalation framework. The ILQI, therefore, served to define expected performance across the Welsh health-care field. Such bureaucratisation, through command and control of board-level actors, signalled the legitimisation of the ILQI’s mandate. Board-level negotiation, formalisation and co-optation of others promoted the deinstitutionalisation of redundant board practices and fostered the preinstitutionalisation of mortality reviews, associated RAMI (see Tables 17–23), WalkRounds and the use of patient stories at board level. Hence across each case site, with respect to the 1000 Lives+ programme and ILQI, the mandated context for all was comparable and overtly coercive.
In each health board, innovation emerged from the evidence-based learning arising from the MI-PDSA approach. As clearly illustrated with respect to mortality reviews in transcriptions 6:10 and 6:11 (see Director of medicine and associates), identification of problems and systematic failings, catalysed knowledge mobilisation and the validation of extant clinical coding practices, thus promoting the broader moral and pragmatic legitimisation of the newly normalised practice. In this manner, the actors involved drew on the resources of the 1000 Lives+ programme, notably RAMI monitoring guidelines.
Tables 11–13 show, respectively, I-CMAO configurations illustrating the infrastructural system of the Welsh Government, the institutional setting of NHS Wales and its constituent health boards and interpersonal relationships within the institutional settings.
| Intervention | 1000 Lives+ national programme | |
|---|---|---|
| Component | ILQI (centred on mortality review as an exemplar) | |
| Context | Welsh Government | |
| Mechanisms |
|
|
| Agency and institutional work | Normalisation: coupling to 1000 Lives+, ILQI and mortality review | Habituation: decoupling to 1000 Lives+, ILQI and mortality review |
|
|
|
| Outcome | 1000 Lives+ national programme, ILQI and mortality review institutionalised into policy processes | |
| Exemplar transcriptions | ||
|
|
|
| Intervention | 1000 Lives+ national programme | |
|---|---|---|
| Component | ILQI (centred on mortality review as an exemplar) | |
| Context | NHS Wales/NHS Wales’ health boards | |
| Mechanisms |
|
|
| Agency and institutional work | Normalisation: coupling to 1000 Lives+, ILQI and mortality review | Habituation: decoupling to 1000 Lives+, ILQI and mortality review |
|
|
|
|
|
|
|
|
|
|
|
|
| Outcome |
|
|
| Exemplar transcriptions | ||
|
|
|
|
|
|
|
|
|
|
|
|
| Intervention | 1000 Lives+ national programme | |
|---|---|---|
| Component | ILQI (centred on mortality review as an exemplar) | |
| Context | Hospital multisite department/hospital site-based ward (functional team) | |
| Mechanisms |
|
|
| Agency and institutional work | Normalisation: coupling to 1000 Lives+, ILQI and mortality review | Habituation: decoupling to 1000 Lives+, ILQI and mortality review |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Outcome |
|
|
| Exemplar transcriptions | ||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Tables 14–20 illustrate the type of information about mortality rates in hospitals made publicly available as part of the new emphasis on transparency in relation to patient safety.
| Reporting period | Health board | Morriston | Singleton | Neath Port Talbot | Princess of Wales |
|---|---|---|---|---|---|
| January 2011 to December 2011 | 122 | 115 | 122 | 123 | 125 |
| February 2011 to January 2012 | 119 | 112 | 121 | 118 | 120 |
| March 2011 to February 2012 | 115 | 109 | 117 | 119 | 115 |
| April 2011 to March 2012 | 114 | 109 | 117 | 117 | 112 |
| May 2011 to April 2012 | 113 | 107 | 112 | 120 | 112 |
| June 2011 to May 2012 | 110 | 103 | 109 | 117 | 111 |
| July 2011 to June 2012 | 109 | 102 | 107 | 113 | 111 |
| August 2011 to July 2012 | 109 | 101 | 106 | 113 | 112 |
| September 2011 to August 2012 | 107 | 100 | 106 | 112 | 114 |
| October 2011 to September 2012 | 108 | 102 | 101 | 109 | 112 |
| November 2011 to October 2012 | 105 | 100 | 100 | 107 | 112 |
| December 2011 to November 2012 | 105 | 99 | 100 | 106 | 111 |
| January 2012 to December 2012 | 104 | 98 | 102 | 109 | 109 |
| Reporting period | Health board | Royal Gwent | Neville Hall | Ystrad Fawr |
|---|---|---|---|---|
| January 2011 to December 2011 | 107 | 111 | 97 | 83 |
| February 2011 to January 2012 | 107 | 111 | 97 | 105 |
| March 2011 to February 2012 | 107 | 113 | 93 | 116 |
| April 2011 to March 2012 | 107 | 115 | 91 | 101 |
| May 2011 to April 2012 | 108 | 119 | 89 | 98 |
| June 2011 to May 2012 | 107 | 118 | 87 | 99 |
| July 2011 to June 2012 | 106 | 116 | 88 | 100 |
| August 2011 to July 2012 | 106 | 117 | 87 | 96 |
| September 2011 to August 2012 | 107 | 118 | 86 | 96 |
| October 2011 to September 2012 | 106 | 117 | 86 | 92 |
| November 2011 to October 2012 | 106 | 117 | 86 | 90 |
| December 2011 to November 2012 | 106 | 118 | 87 | 93 |
| January 2012 to December 2012 | 108 | 120 | 88 | 99 |
| Reporting period | Health board | Gwynedd | Glan Glwyd | Wrexham |
|---|---|---|---|---|
| January 2011 to December 2011 | 114 | 103 | 101 | 126 |
| February 2011 to January 2012 | 112 | 101 | 99 | 124 |
| March 2011 to February 2012 | 111 | 97 | 98 | 123 |
| April 2011 to March 2012 | 109 | 95 | 98 | 124 |
| May 2011 to April 2012 | 108 | 95 | 98 | 122 |
| June 2011 to May 2012 | 107 | 94 | 97 | 119 |
| July 2011 to June 2012 | 108 | 96 | 97 | 119 |
| August 2011 to July 2012 | 107 | 95 | 98 | 118 |
| September 2011 to August 2012 | 107 | 97 | 98 | 116 |
| October 2011 to September 2012 | 108 | 97 | 99 | 115 |
| November 2011 to October 2012 | 107 | 98 | 99 | 115 |
| December 2011 to November 2012 | 107 | 100 | 99 | 115 |
| January 2012 to December 2012 | 107 | 101 | 99 | 113 |
| Reporting period | Health board | Wales | LLandough |
|---|---|---|---|
| January 2011 to December 2011 | 99 | 104 | 85 |
| February 2011 to January 2012 | 99 | 105 | 85 |
| March 2011 to February 2012 | 100 | 106 | 86 |
| April 2011 to March 2012 | 100 | 107 | 84 |
| May 2011 to April 2012 | 101 | 108 | 83 |
| June 2011 to May 2012 | 99 | 107 | 81 |
| July 2011 to June 2012 | 99 | 105 | 81 |
| August 2011 to July 2012 | 99 | 105 | 81 |
| September 2011 to August 2012 | 97 | 103 | 81 |
| October 2011 to September 2012 | 98 | 102 | 84 |
| November 2011 to October 2012 | 98 | 102 | 83 |
| December 2011 to November 2012 | 97 | 101 | 83 |
| January 2012 to December 2012 | 97 | 99 | 85 |
| Reporting period | Health board | Royal Glamorgan | Prince Charles |
|---|---|---|---|
| January 2011 to December 2011 | 115 | 123 | 99 |
| February 2011 to January 2012 | 114 | 121 | 98 |
| March 2011 to February 2012 | 113 | 119 | 97 |
| April 2011 to March 2012 | 113 | 120 | 97 |
| May 2011 to April 2012 | 111 | 116 | 95 |
| June 2011 to May 2012 | 111 | 115 | 94 |
| July 2011 to June 2012 | 111 | 114 | 95 |
| August 2011 to July 2012 | 117 | 113 | 98 |
| September 2011 to August 2012 | 112 | 111 | 100 |
| October 2011 to September 2012 | 113 | 112 | 100 |
| November 2011 to October 2012 | 113 | 112 | 100 |
| December 2011 to November 2012 | 114 | 114 | 99 |
| January 2012 to December 2012 | 112 | 114 | 96 |
| Reporting period | Health board | Bronglais | Glangwili | Prince Philip | Withybush |
|---|---|---|---|---|---|
| January 2011 to December 2011 | 100 | 101 | 100 | 97 | 103 |
| February 2011 to January 2012 | 99 | 97 | 98 | 95 | 104 |
| March 2011 to February 2012 | 97 | 98 | 96 | 94 | 101 |
| April 2011 to March 2012 | 96 | 97 | 94 | 92 | 100 |
| May 2011 to April 2012 | 97 | 100 | 96 | 91 | 101 |
| June 2011 to May 2012 | 96 | 98 | 95 | 92 | 99 |
| July 2011 to June 2012 | 96 | 99 | 94 | 92 | 98 |
| August 2011 to July 2012 | 95 | 99 | 94 | 91 | 98 |
| September 2011 to August 2012 | 94 | 98 | 93 | 90 | 97 |
| October 2011 to September 2012 | 94 | 95 | 95 | 89 | 97 |
| November 2011 to October 2012 | 92 | 92 | 94 | 87 | 95 |
| December 2011 to November 2012 | 91 | 90 | 94 | 84 | 93 |
| January 2012 to December 2012 | 92 | 90 | 97 | 85 | 91 |
| Hospital site | Discharges, n | Deaths, n | Mortality, % |
|---|---|---|---|
| Brecon | 460 | 35 | 7.61 |
| Bronllys | 337 | 36 | 10.68 |
| Ystradgynlais | 242 | 23 | 9.50 |
| Knighton | 200 | 17 | 8.50 |
| Llandrindod Wells | 396 | 40 | 10.10 |
| Machynlleth | 153 | 19 | 12.42 |
| Llanidloes | 230 | 32 | 13.91 |
| Newtown | 230 | 10 | 4.35 |
| Welshpool | 264 | 30 | 11.36 |
We now turn to the findings of our realist analysis. For illustration, we focus only on the mortality review component of the ILQI, and thus primarily on the generative mechanisms and ensuing agency attributed to directors of medicine. Figure 17 and Table 21 support our discussion.
| Intervention | Leading the Ways to Safety and Quality Improvement (ILQI) | |
|---|---|---|
| Component | Mortality review | |
| Context | Structural conditioning of the institutional setting: NHS Wales health boards’ executive-level implementation of 1000 Lives+ national programme | |
| Structural emergent properties |
|
|
| Cultural emergent properties |
|
|
| Social actors |
|
|
| Social position |
|
|
| Role-position practices |
|
|
| Mechanism | Mediation of structural conditioning to core actors and their reflexive theorisation | |
| Institutional logics and nature of alignment between core actors | The institutionalisation of 1000 Lives+ and ILQI draws professional logic into alignment with that of the bureaucratic state. Moreover, there is coalescence and cohesion across medical, nursing, allied professional and health-care management logics, thereby placing each into a complementary stance. This fosters the systematisation of 1000 Lives+ and ILQI across the cultural system level of NHS Wales, and promotes the reproduction of such practices across each health board | |
| First-order emergents | The vested interests of directors of medicine and their associates, tasked with the strategic oversight of the 1000 Lives+ programme and ILQI, lay primarily in the successful development of a systematic locally agreed approach to undertaking the mortality review in the aftermath of the structural reconfiguration of NHS Wales | |
| Second-order emergents | Necessary complementarities | |
| Situational logic | Protection | |
| Reflexive theorisation | Complementarity between the dominant logic of the bureaucratic state, professional (medical) logic and collaborative logic fosters coherence, cognitive participation and reflexive monitoring. This results in the discernment of issues, deliberation of their importance and dedication of ensuing agency in alignment to the goals of the ILQI | |
| Agency and institutional work | Agency, the unfolding strategic negotiation of change, and the mode of institutional work enacted | |
| Agential emergent properties | Given the high status of such actors, the inherent change agenda overarching the 1000 Lives+ programme, and thus the ILQI, was executed from a position of considerable negotiating strength | |
| Strategic negotiation |
|
|
|
|
|
| Institutional work | Primarily creative and augmented by actions which maintain relevant associated practices | |
| Outcome | Social elaboration, reproduction or invariance | |
| Structural | Integration of mortality reviews into the Welsh Government’s performance management framework was viewed to have added an important ‘critical lens’ through which to view patient safety and the maturation of the health-care quality agenda in NHS wales amid organisational reconfiguration | |
| Cultural | Cultural change was viewed to be far more fragmented | |
| Agential | A network of patient safety leaders, health-care professionals from managerial, medical, nursing and other allied groups, evolved | |
As signposted in Table 21, the bureaucratic sense of force majeure that drove engagement with ILQI gave rise to aligned first-order emergents in board-level actors. This included compliance with task allocation and appropriate action to ensure delivery in accordance with the dominant logic of the bureaucratic state. Given the complementary linkages between systemic structural and cultural logics, this fostered a situational logic of protection. 229 In part, this was self-referential: board-level actors had to engage, visibly, in the leadership of patient safety, so aiding the normalisation of such practices within the board.
The sociocultural interaction encouraged by board-level activity centred on strategic negotiation across management tiers and professional networks. Driven by the board and honed through the 1000 Lives+ MI-PDSA approach, legitimisation, formalisation and co-optation ensued. This drove the innovation cycle, as illustrated in Figure 17.
An objective outcome of ILQI was the normalisation of the three practices – mortality reviews, WalkRounds and patient stories – examined in this chapter. The relational structure at each site had also evolved, encouraging the diffusion of the ILQI, and thus the 1000 Lives+ programme, and promoting a culture of organisational learning. However, cultural change was restricted by medical disengagement, notably via challenge to the moral and pragmatic legitimacy of some components of the 1000 Lives+ programme, the burden of documentation and weak feedback from boards to wards. We return to these issues in Chapter 7, where we examine the implementation of our second focal intervention under far more challenging constraints.
Summary
In Chapter 6, we examined the local implementation of the focal intervention ILQI and discussed its contribution to the 1000 Lives+ programmes’ I-CMAO configuration across the Welsh health-care field.
Chapter 7 Reducing Surgical Complications
Overview
In this chapter we examine RSC, the second focal intervention drawn from the 1000 Lives+ national programme. Our focus is explicitly directed to one strand of this complex intervention: the WHOSSC. To begin, we set out a brief overview of RSC, defining its multicomponent structure, aim and drivers. This we augment with a review of the WHOSSC, highlighting its emergence, acknowledged benefits and the perceived barriers that impede its normalisation into daily practice.
Second, we undertake a realist analysis of the institutionalisation of RSC and the WHOSSC, through a comparative case study of sites A, B, C and D. In doing so, we explain the structural conditioning, sociocultural interaction and structural elaboration or reproduction fostered through the actions of three groups of key actors: theatre managers, consultant surgeons and anaesthetists, and theatre nurses. We concentrate on these groups as they were formally tasked with the implementation of the RSC within the 1000 Lives+ programme. Again, to aid our understanding of context and mechanism, we also consider the perspectives of policy leads and other senior health-care management staff. Finally, informed by the findings of our realist analysis we set out our understanding of the RSC-WHOSSC I-CMAO configuration.
Focal intervention, aim and drivers
Reducing Surgical Complications aims to support theatre department staff to deliver high-quality, safe and effective care for adult patients undergoing surgical procedures in a hospital setting. As illustrated in Figure 18, RSC is composed of four interventions to reduce the number of infections after surgery, two interventions to improve teamwork and three to facilitate patient involvement in their care. In this study, attention focused on the WHOSSC,531 a tool for clinical teams to improve the safety of surgery by reducing deaths and complications.
FIGURE 18.
Driver diagram: RSC.
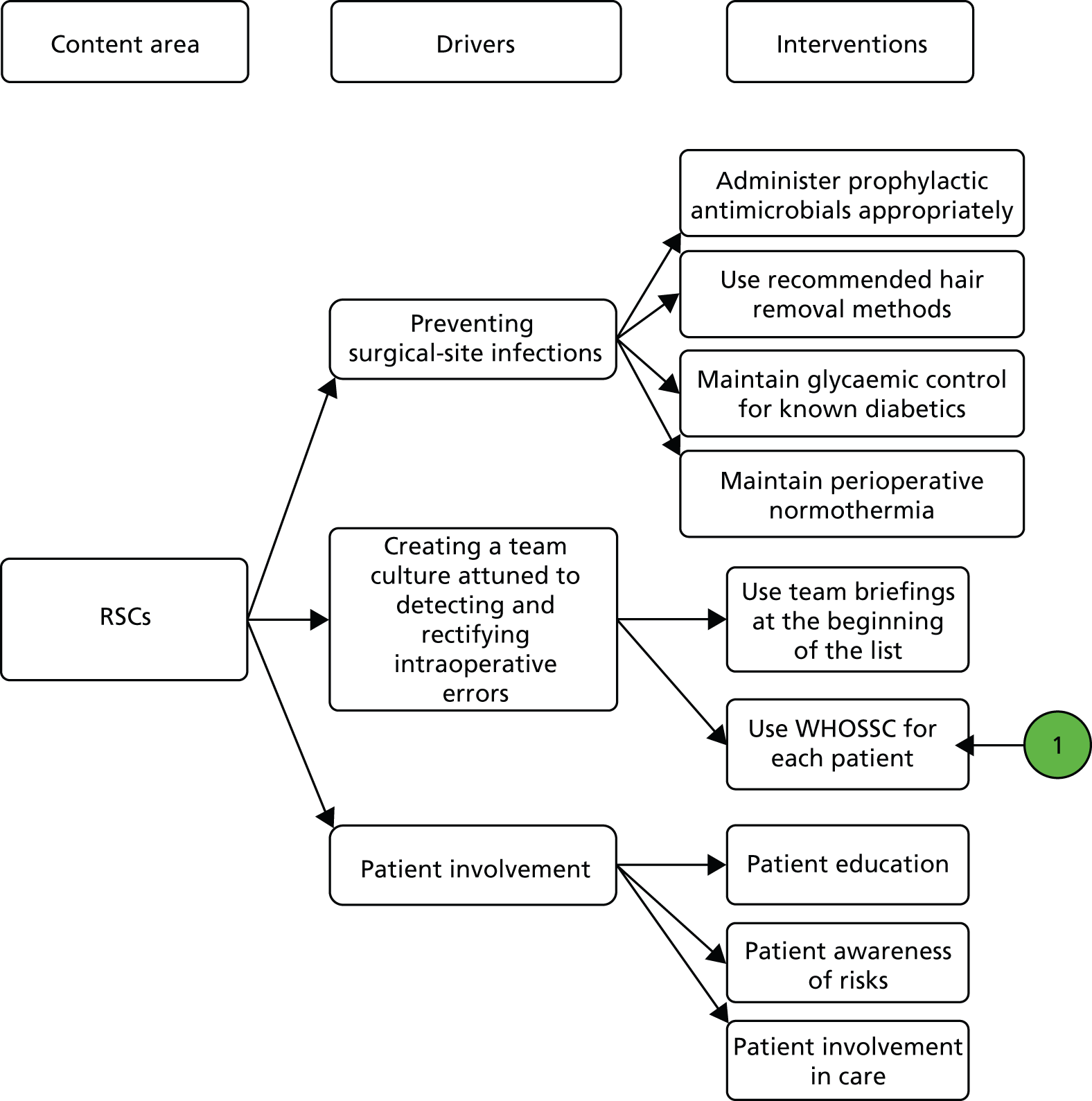
Figure 18 depicts the driver diagram for the focal intervention, RSC, focusing specifically on one strand of this multicomponent intervention, the WHOSSC. To aid our understanding of the interplay of context and mechanism in the operationalisation of this intervention, we sought the perspectives of theatre managers, consultant surgeons and anaesthetists, and theatre nurses, each tasked with the implementation of the RSC and WHOSSC under the auspices of the 1000 Lives+ national programme.
World Health Organization Surgical Safety Checklist
The WHOSSC evolved from the Safe Surgery Saves Lives initiative, established by the World Alliance for Patient Safety as part of the World Health Organization’s (WHO) efforts to reduce the number of surgical deaths across the world. This initiative sought to harness political commitment and clinical will to address important safety issues. The principal concerns were poor communication among team members; inadequate surgical and anaesthetic safety practices; and avoidable surgical infection. 531
As illustrated in Figure 19, the WHOSSC is characterised by simplicity and brevity, and is composed of a series of questions to guide the co-ordinated actions of the theatre team. Notably, many of the individual steps advocated are accepted as routine practice. But, as expanded below, such acceptance does not reduce the barriers to its collective adoption. 531 It is, therefore, acknowledged that to foster engagement and enhance compliance,532 each theatre team must adapt the WHOSSC to their needs and routine operative workflow and to address many different types of surgery. 533–545
FIGURE 19.
The WHOSSC. Source: http://whqlibdoc.who.int/publications/2009/9789241598590_eng_Checklist.pdf. Reproduced with permission.
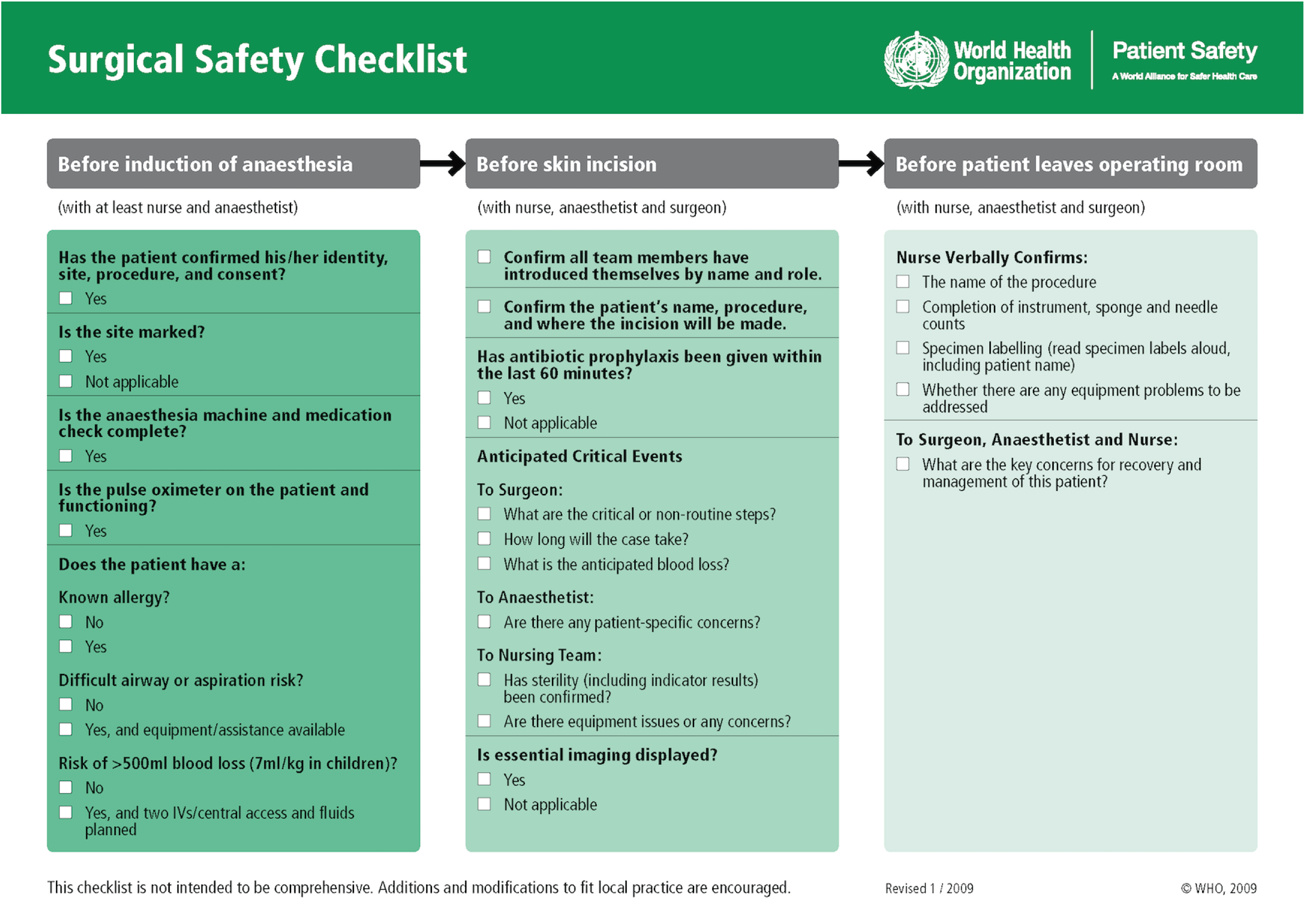
With increasing acceptance of the WHOSSC,546 aligned approaches have been adapted to address broader surgical issues and hazards. 547–550 There have also been more subtle changes such as the adjustment of the timing of questions likely to cause anxiety to patients. 173
Since its inception, the WHOSSC has proved to be a robust means of reducing perioperative complications. 70,406,551,552 Empirical research supports assertions that the WHOSSC (i) saves lives;553–557 (ii) improves communication across the surgical team;558 (iii) reduces the occurrence of wrong-site surgery;63 (iv) promotes adherence to defined antibiotic protocols, thereby reducing the incidence of surgical-site infection;559–561 and (v) fosters more efficient use of theatre time and resources,556 while supporting appropriate staffing levels. 439
Despite such obvious benefits, operationalisation of the WHOSSC may be poor. 70,190,562–564 Failures to follow the checklist include not identifying the patient; undertaking a wrong-site surgery or procedure;565 and failing to identify staff members. 123,566 In addition, pressure of time may lead to surgical procedures being started before the checklist is completed. 567–569 Failure to complete sign out is another common deviation. 122 Poor engagement by anaesthetists,71 surgeons570 and nursing staff due to resistance and gaps in knowledge has also been reported. 435,543,571
Realist analysis and comparative case study
We now undertake a critical realist analysis of the institutionalisation of the 1000 Lives+ national programme’s RSC and WHOSSC. Again, our case study considered sites A, B, C and D. Our analysis focuses on three groups of key actors, theatre managers, consultant surgeons and anaesthetists, and theatre nurses, tasked with the implementation of the RSC under the auspices of the 1000 Lives+ national programme.
First, we consider the focal intervention in context and explore the dominant structural and cultural emergent properties impacting key personnel in the theatre departments at each case site. Next, to reveal the generative mechanisms in play, we examine mediation via first- and second-order emergents and the resultant situational logic. Then, to examine the initiation of change, we explore the unfolding strategic negotiation of change and the mode of institutional work enacted. Finally, we reflect on the nature of any sustained outcome, be that elaborative or reproductive, that occurred following the implementation of the RSC and WHOSSC. This analysis forms the foundation of our refinement of the I-CMAO configuration spanning the Welsh health-care field in 1000 Lives+ institutionalisation: RSC – local implementation of the focal intervention and contribution to the I-CMAO configuration spanning the Welsh health-care field.
Structural conditioning: structural and cultural emergent properties in the Welsh health-care field
Completing the WHOSSC surgical checklist was a compulsory element of the overarching policy mandate of the 1000 Lives+ national programme (transcription 7:01, below).
1000 Lives+– well, it’s not rocket science by any stretch of the imagination – it’s an incredibly simple approach and that is one of the reasons why it works. The PDSA cycles and all of that stuff it’s created a language that they like: it’s language that they all understand. The WHO checklist just adds another element to it, which is recognised world-wide. It’s mandated as a practice – in policy and professionally – so they’ve just got to do it. After all it saves lives, we know it saves lives.
Policy lead, Welsh Government (146); transcription 7:01
In addition, the WHOSSC was strongly advocated by the WHO, the IHI and the array of associated medical professional Royal Colleges, placing the dominant logic of the bureaucratic state into close alignment with that of professional medical logic within the theatre environment (transcription 7:02, below).
The WHO checklist – it’s compulsory – so it was a little bit more straightforward because, at the end of the day, if people didn’t comply then they were in breach of contract with their controlling body. So that was it, essentially.
Consultant surgeon, case site D1 (083); transcription 7:02
Such structural constraint was amplified by a parallel programme, Transforming Theatres, representing a Welsh adaptation of the NHS Institute for Innovation and Improvement’s Productive Series, The Productive Ward and The Productive Operating Theatre (transcription 7:03).
The dominant cultural emergent properties, which moulded the institutionalisation of the 1000 Lives+ RSC and WHOSSC, arose from the institutional system of the theatre departments in case sites A–D. First, such theatre departments were perceived to function in relative isolation within the base hospital and parent health board (transcription 7:04, below).
Theatre attracts extroverts – you wouldn’t work here if you didn’t have thick skin and couldn’t deal with some of the issues that we have to deal with – but they feel quite isolated from the organisational agenda in a way. Theatre is its own little world. There isn’t that link between the theatre and the rest of the wards, and the larger organisation. But there is a link across the different operating theatres in the health board even though they are all different.
Theatre manager, case site A1 (008); transcription 7:04
The perception of a distinctive functional and professional culture underscored this sense of separation (transcription 7:05) and this second cultural emergent property fostered the potential for conflict. Across each case site, the traditional view that the surgeon was in charge still lingered. This created a schism: a managerial logic aligned to the nursing profession versus a counterpoised stance aligned to surgeons and their medical colleagues. This tension was not a key issue at all case sites. However, such institutionalised professional role-positions arose as a perceptible fault-line throughout many discussions (transcription 7:06, below).
In theatre, traditionally, the surgeon was the captain of their ship – they ran the show and all the rest of it – and people just did their bidding. But today that’s completely the wrong way round! That’s completely not what modern surgery’s about because you’re only as good as your parts. Now a lot of people won’t believe that still! So if you’re trying to get people to implement the WHO checklist and yet they believe that everything depends on them performing correctly and that they don’t make errors [laughs] then it’s a very difficult task! You’re far more likely to engage with people that actually are slightly less self-assured because they understand there may be a better way to improve the care of the patients. So my gambit with some of my colleagues was to say: ‘I’m not as perfect as you – but do you know your error rate? Are you perfect? Are you one in a million perfect? And if it is that one in a million then what are you going to do to improve’– but people have to accept there’s a problem before they’ll look for a solution. I think they have to see that it’s a problem before they’ll change their practice.
Consultant surgeon, case site A1 (063); transcription 7:06
Such cultural constraints highlight the critical role of agential emergent properties. Most notably these include leadership and orchestrated collective action within the multidisciplinary theatre team to address perceived problems (transcription 7:07, below).
There was a surgeon I worked with – an orthopaedic surgeon – who I really respected. One day, because I’d just been on a course and knew the proper way of doing the procedure he was going to do, I realised he was going to use the wrong approach. Basically, he was going to go in from the other side of the leg. I knew he was wrong, so I told his registrar, because I couldn’t tell him. The registrar knew he was wrong, and he couldn’t tell him. That’s the example I always use with theatre clinicians: ‘if the most senior consultant was just about to stick a knife into someone, and the most junior member of the department walked in and said – excuse me, stop – what would be the response?’ Would the response be: ‘OK, what have you got to say?’ or would it be ‘get the hell out of my theatre’ with somebody throwing something at him? That usually raises a smile, and once you start talking about it, they realise that the teams that they think were good teams are actually not. Getting back to my example, I said to him in the end: ‘Mr [Name], so you’re using the medial approach today, are you?’, and it was as if somebody switched a switch on in his brain. You could see him almost like come awake and go: ‘no, I think I will go in laterally’. But he couldn’t say to me, you know: ‘thanks for that, I was going to make a mistake’ – we both had to play the game – this whole thing about hierarchies!
1000 Lives+ national programme team member (041); transcription 7:07
Consideration of the underlying contextual strata at the interpersonal and individual levels further reveals the impact of this cultural fault-line and exposes the deeply held belief systems anchored to such discordant professional logics. Different cultural stances could lead some individuals to pay little attention to the RSC and WHOSSC. For instance, it was reported that some consultant surgeons did not believe the WHOSSC to be necessary and, thus, viewed it as little more than a management weapon to exert control (transcriptions 7:08 and 7:09). As succinctly expressed in an excerpt from transcription 7:10, below, the institutionalisation of the WHOSSC was dependent on flattening the professional role-based hierarchy in the theatre department.
Our theory on it is if people get the briefings right – where they develop a real team by flattening the hierarchy – and there’s respect for everyone in the theatre, the whole checklist sails through! People start to understand – they’re not worried about challenging a surgeon – they see the value of it!
1000 Lives+ national programme team member (041); transcription 7:10
First-order emergents for key actors central to the institutionalisation of the World Health Organization Surgical Safety Checklist
A distinctive set of structural and cultural emergent properties shaped the context in which individuals who were central to the institutionalisation of the WHOSSC found themselves and conditioned their ensuing actions. Deeply entrenched professional role-positions orchestrated the operation of the theatre departments, and we asked theatre managers, consultant surgeons and anaesthetists, and theatre nurses to reflect on their placement, their vested interests and the perceived opportunity costs associated with various courses of action to determine how this shaped their activities.
Theatre managers
In case sites A–D, theatre managers’ placement shaped their vested interests towards ensuring the successful implementation of the 1000 Lives+ national programme’s RSC and WHOSSC initiatives. They operated under a professional logic aligned to health-care management and, for hybrid professional staff, the nursing profession. Given the need to succeed, their activity centred on the brokerage of support resource to leverage the RSC and WHOSSC via the emotions of pride and shame. To achieve this they drew on the core resources of the 1000 Lives+ programme’s team, the MI-PDSA approach and the aligned Transforming Theatre team (transcriptions 7:11 and 7:12, below, and transcription 7:14).
We did have problems with the WHO checklist but they were picked up by 1000 Lives+ team, and they were followed through via the Transforming Theatre Team. They did their own audits and glitch lists. They’d go to each and every health and safety briefing and they would name and shame – which theatre was doing well, which ones weren’t; which surgeons were turning up, which ones weren’t – that caused huge amounts of conversation! But I think you can say it was nothing but positive because, even when they were arguing, they did start improving because they did not like seeing their poor results. That really helped get our WHO checklist and safety briefings on track. So we used both 1000 Lives+ and Transforming Theatre.
Theatre manager, case site A1 (008); transcription 7:11
To begin with we had difficulty with the PDSA approach. Yes, we had difficulty with that! We had difficulty in getting our heads around it – we thought we’d mastered it but we hadn’t – but we did eventually get through it! We worked with the 1000 Lives+ team and the Transforming Theatre team and looked at what we could improve. With the PDSA, well, we didn’t understand it very well: we couldn’t get our heads around it! At times we thought we’d mastered it but then they’d say: ‘no, that’s not right’, and we thought: ‘oh God, you know, somebody please give us a simple explanation so we can just get it right’. We’d sort of grasped it but we were trying to do it in sort of one hit and not doing small things – small rapid cycles of change – and then sort of escalating it gradually.
Theatre manager, case site B1 (005); transcription 7:12
Consultant surgeons and anaesthetists
The behaviour of the consultant surgeons and anaesthetists interviewed during our study was markedly influenced by the nature of their engagement with the 1000 Lives+ national programme. For those who were simply participants, lacking the burden of professional and managerial accountability for the programme’s implementation, the RSC and WHOSSC were viewed with a degree of disdain. In case site A, surgeons were perceived to be in a position of security, given NHS Wales’ assumed reluctance to ‘play heavy handed’. In response, surgeons tended to ignore the medical director’s efforts at control (transcription 7:15, below).
If you want to play heavy handed then what you need to do is – which is what they’ve done in many trusts in England – is they sack people. It happens, that’s what NHS England does. But we don’t do that in Wales. Surgeons are in a position where we have security and the stick that the medical director can wield is just not big enough.
Consultant surgeon, case site A1 (063); transcription 7:15
Such disengagement rendered the implementation of the RSC and WHOSSC into ‘quite an interesting shambles’, with senior medical professionals deciding to ignore the initiative (transcription 7:16, below). Thus actors’ vested interests lay in maintaining their professional role-positional power, as there appeared to be no sanctions associated with their disengagement. The dominant logic of the bureaucratic state and aligned professional health-care management logic were, therefore, countervailed by professional medical logic.
One surgeon didn’t want to play, he thought: ‘why should I introduce myself to the anaesthetist? I’m busy writing up my previous case, so I’m not going to. . .’ Also, the WHO checklist was all done, sort of, at the wrong time – you know, the end of the case bit, well it was done sort of retrospectively rather than live! [Laughs] It was all quite an interesting shambles actually. The senior people decided that they were above it all basically.
Consultant anaesthetist, case site A1 (064); transcription 7:16
In contrast, in case site B, the theatre manager was able to broker wider medical participation through effective leadership of the implementation (transcription 7:17, below).
We have a really proactive Theatre manager, who is really good at working with the doctors and surgeons, so I think the WHO checklist was a breeze! I am assured that it is fully implemented because I have spot-checked them. I spoke to [Name, Theatre manager] when I first came into the organisation and I saw that we were 100% compliant. So, yeah, we seem to be rocking with the WHO checklist!
Consultant surgeon, case site B1 (062); transcription 7:17
However, this overtly positive perspective was diluted by a respondent who pointed out that, despite apparent use of WHOSSC, mistakes had not been entirely eliminated, and suggested that not everyone at site B was enthusiastic about the initiative (transcription 7:18, below).
I gather, here, it’s got its enthusiasts and it’s got its detractors. But across NHS Wales we’ve had disasters even with the checklist being used: wrong site surgery, instruments left in, etcetera. [Even though the WHO Surgical Safety Checklist is being used?] Yes! In other words it’s not being used properly. It will never cure all problems but you do wonder whether it’s being used properly or whether people just pretend it’s being used.
Consultant anaesthetist, case site B1 (059); transcription 7:18
In contrast, for those chosen and tasked with the implementation of the 1000 Lives+ national programme, the RSC and the WHOSSC met with approval. In case sites C and D, such actors’ vested interests lay in brokering participation with the WHOSSC with their professional colleagues to ensure that the checklist did not merely function as a ‘tick-box exercise’. Their agency was directed to managing the tension promoted by the countervailing stance of professional medical logic (transcriptions 7:19 and 7:20, below).
When I first started in the health board, I got asked to assist with the implementation of the WHO checklist. I think – I’m not quite sure if I had an official title as such – but I was responsible for some of the surgical aspects. [Did you encounter any resistance towards the WHO checklist?] Ah yes . . . [Long pause] . . . that was an old chestnut, we had to deal with it at the time. I think with a lot of these projects where people are looking to try and implement change the difficulty is the people who volunteer to do them, of course, they’re the believers! And the people who don’t volunteer are not the believers. So, there’s always a sort of a clash of culture, I guess, between the two. But clinicians like to see themselves as being very independent. Surgeons probably more than most! They have a certain arrogance and belief in themselves that they need in order to survive their day-to-day job. So, yes, you’re right, there were a lot of, I don’t know, issues. There were lots of little teething problems. One of which was how you actually record that you’ve done it!
Consultant surgeon, case site D1 (083); transcription 7:20
This contested terrain is expressed in transcription 7:21, below. It reveals that other facets of the RSC, essentially the easy, less controversial ones that did not impugn surgical ability, were adopted first as readily achievable ‘quick wins’.
When you think about the WHO checklist . . . [long pause] . . . Well you can understand why theatre nurses are going to choose to do normothermia! [Another component of the 1000 Lives+ RSC intervention] It’s simple! You take a temperature, you make sure they’re kept warm – the intervention is easy and there’s no controversy – everyone knows normothermia is good; everyone knows good glycaemic control matters. Safe hair removal, it’s fine, we just ban razors and go to clippers! We just stop procuring them, problem sorted. Done! So in some of the RSC interventions, all of those people are able to go: ‘look, we are a success, and we’ve done it quickly’. So they’ve had the quick win. But the message is people choose the path of least resistance. The WHO checklist is more complex and so it’s harder to achieve.
Medical Director, case site D1 (117); transcription 7:21
Theatre nurses
Theatre nurses in case sites A–D, though their vested interests were aligned to the implementation of the RSC and the WHOSSC, varied in their perception of the degree to which their roles allowed them freedom to act according to its precepts. In case site A, engagement of all staff was promoted by a surgical consultant who, from personal experience of a surgical ‘never event’, was committed to the WHOSSC. However, others who showed only ambivalent adherence diluted such clear strategic surgical leadership (transcription 7:22, below).
We have one surgeon who was doing the WHO checklist before it was even implemented here – they had their own sort of version of it – and that because . . . [long pause] . . . they had had an incident happen, I think it was here, a wrong site surgery. From that moment on, they now make sure that everybody stops, everybody agrees, so that they get it right. They’re the biggest convert! But most of them are ambivalent about it and just realise that they’ve got to do it.
Theatre nurse, case site A1 (024); transcription 7:22
Theatre nurses in case site B, however, perceived that their role in the implementation of the RSC and especially of the WHOSSC was facilitated by the professional role-position of scrub nurse. The expertise and knowledge enacted through this role-position helped to level the entrenched professional hierarchy of the theatre department, particularly for surgeons in training, ensuring that they ‘learn to listen’ (transcription 7:23). This empowered and emancipated stance set the strategic direction for other theatre nurses to follow, aiding the normalisation of the WHOSSC in daily practice.
In case site C, rudimentary contextual constraints, such as a surgeon’s family commitments preventing his attendance at the eight o’clock briefing, posed formidable barriers to engagement which nurses lacked the role-positional means to counter (transcription 7:24), while in case site D, the placement of one theatre nurse tasked with the implementation of the RSC and WHOSSC was devoid of resource support and expertise. This rendered the nurse ill equipped and isolated, limiting the extent to which she was able to promote the implementation (transcription 7:25, below).
I was seconded, part-time, to theatres. From my perspective, I was brought in late. It [1000 Lives+ RSC focal intervention] had already started, and the staff, which were heading it up for [name, health board], had already gone and had their briefing session. So I felt I was brought in blind. I didn’t really understand it at the start to be honest. But we were given drivers of things that we needed to address – improvements that we needed to achieve; change in practice and audit really – and told to gather data to see if we were meeting the drivers and the standards. It was my job to tell the staff about what the standards and the drivers were, and how we were going to identify how we were going to change practice in line with what they were saying we needed to do. I had to gather all the data, put it into a graph, and then present that on a monthly basis. But I was isolated. I did the PDSA cycles – I tried to involve people, I tried my hardest, I even had champions – but I was doing the PDSA cycles, writing them up, because they wanted written evidence that they were being done. It’s embarrassing when you’re presenting data that you haven’t got – so I was doing it to make sure I had data to present – so that I wasn’t going to be standing there saying: ‘well sorry, I haven’t got anything’. When theatre staff are working clinically they’ve got the pressure of patients coming through – and they come first – this is [WHO checklist] just a bit of paper that doesn’t do anything.
Theatre nurse, case site D1 (028); transcription 7:25
Second-order emergents and situational logic
In case sites A–D, the interplay of structural, cultural and agential emergent properties impacted on the three groups of actors central to the institutionalisation of the 1000 Lives+ national programme, the RSC and the WHOSSC, enabling or frustrating the position they adopted and their role in implementation.
Where structure was concerned, the RSC and WHOSSC emerged into a context moulded by internal and necessary linkages that reflected both complementarities and contradictions. However, as illustrated in the transcriptions above, culturally there was deep discord as the key actors were confronted by the constraining contradictions (necessary incompatibilities) between the dominant logic of the bureaucratic state with its aligned professional health-care management logic versus that of professional medical logic. This led to development of a situational logic of correction/compromise, where those tasked with the implementation of the WHOSSC confronted a context fraught with the power play of different professional groups and had to act in a manner that sought to ameliorate this sociocultural constraint.
Sociocultural interaction: agency and strategic negotiation
At each case site, the situational logic of correction/compromise motivated an essentially concessionary negotiating stance among the key actors. Below, we elaborate two features in depth to highlight this complex interplay across multiple case sites.
Power-induced compliance and political sanction
To examine the adoption of power-induced compliance and political sanction under a situational logic of correction/compromise, we considered individual actors’ strategic negotiating stances across each case site. In transcription 7:26, below, the medical director admitted using reference to the Mid Staffordshire scandal and threats of losing their jobs to coerce colleagues into compliance with new practices.
With 1000 Lives+, the WHO checklist, whatever, resistance to that sort of change has to be managed in an open and transparent way, and it has to be managed in terms of saying a number of things – different drivers – if you like.
I haven’t yet used the F word, but we’ll use it now – Francis [Report of the public inquiry into Mid Staffordshire NHS Foundation Trust] – Francis will act as an important driver. Francis is ground breaking. So, I will use Francis, as a lever, to say: ‘If you are not. . .’. But revalidation is another important lever; so we’ve got two levers. The third is: ‘Well, the Welsh Government expects this of you. . .’, and I don’t like using that as a lever but why not chuck it in! [It causes more resistance. . .] Yes, it does.
But where I need to get to as a medical director is to have a culture where I go to a consultant and say: ‘Oh dear, I hear your complication rates are a bit high’, to which I get an open answer in which they say: ‘Yes they are, and do you know what, I’m doing an audit to check whether . . .’, as opposed to ‘No, I’m fine’. So, I think, that we want to develop is that candour culture that Francis wants.
With revalidation everybody has to reflect now – I’ve just revalidated all the medical directors, so I’m reflected out! – but now you have to reflect on everything! This is good; but they’re going to have to do that. So, now, if they say to me: ‘No, everything’s fine’, then they won’t revalidate.
So that is how I will be moving forward, in terms of driving openness and transparency, and saying: ‘You have no choice but to engage in this because otherwise those mechanisms will see to it that you are removed’.
Medical director, case site D1 (117); transcription 7:26
However, some argued that such compliance was only token, with checklists being completed casually and inaccurately (transcriptions 7:27 and 7:28, below).
The WHO checklist should be 100% compliant: end of story! But drilling down through our data for that in more detail revealed problems. We do the safety briefings but what we were finding was it was a tick-box exercise – they were being done – but they were being done without the presence of the key members of the team, such as the consultant; they were being done a little bit flippantly, not necessarily with the real information that we needed for patients on the list; there were assumptions. They were very much nurse-led. . . [Long pause]. Look, I’m not confident that the data is accurate. I couldn’t actually find evidence as to who was not doing it but whether or not it’s 100% reliable I’m not sure. But the trend that we’re setting is that we’re 98–100% compliant.
Theatre manager, case site A1 (008); transcription 7:27
I get the monthly reports from the computer system on the checklist compliance and it’s always about 99 something per cent! I don’t suppose that’s true for a moment because people are just ticking the box on the computer. [You don’t think that’s a representative value?] No, I don’t believe it: 99% every month, no way! My problem with all this is it’s quantitative data being collected about a qualitative process. Take the incident that happened back last year. Somebody sat there in front of me, after it had all happened, and said: ‘well, I did do the checklist’, and I said: ‘well, how do you account for the fact that they nearly did the wrong operation?’, ‘I don’t know, perhaps the surgeon didn’t hear me’. So they ticked the boxes on the checklist but they didn’t do the checklist if you know what I mean.
Theatre nurse, case site D1 (029); transcription 7:28
Observation of practice revealed computer-based systems that recorded completion of the WHOSSC via a simple yes-or-no option with progress through subsequent screens being prohibited by a no response, thus completely negating the purpose of the checklist and decoupling it from the physical enactment of the WHOSSC. Thus, under a situational logic of correction/compromise, the contested institutionalisation of the WHOSSC corrupted and was decoupled from meaningful governance processes. However, such subversions of the purpose of the checklist were felt likely to be exposed by growing public awareness of the WHOSSC, and the possibility of subsequent legal challenge in the face of surgical adverse or never event was perceived to be a latent generative mechanism for change and one that would be a ‘very, very quick way to get it up to speed’ (transcription 7:29).
Reciprocal exchange and harmonisation of desires
In case site B, the actions of the nurse theatre manager in ensuring that the WHOSCC was completed facilitated detailed examination of the use of strategic negotiation via reciprocal exchange and resource control. In this context, the manner of negotiation that held sway bordered on the coercive and the bureaucratic policy mandate for the RSC and the WHOSSC was employed to manifest effect. The role of nurse empowerment, in aiding normalisation, was also evident, with the manager and other nursing staff having sufficient confidence to insist that the checklist was completed. This illustrated both coherence of purpose and commitment to the WHOSSC as a practice (transcription 7:30, below).
[How did you get surgeons to participate in the WHO checklist?] Well, they didn’t have a choice! [Laughs] Don’t tape that! We said to them: ‘you know, we’ve got to do the WHO checklist’ – it is a mandatory patient safety check – ’so we haven’t got a choice, you’ve got to be part of it, and we’ll do it with the patient, and you, in here [Theatre], so you’re going to have to listen’. Basically, we came to an agreement with the surgeons. We agreed that the scrub nurse would not start helping the surgeon until the WHO checklist was completed. So they had to be part of it! In the end, I think, they came to the conclusion that they hadn’t a choice really. It was a bit of a battle at the very beginning because they started arguing with us, and we just said: ‘no, we don’t want to argue about this, we haven’t got a choice, we’ve got to do it’. We took the same approach with visiting consultants. [How did you manage them?] Well, actually, that was the easy bit. What I said was: ‘if you’re doing it in the [name, alternative hospital theatre site in health board], well then it doesn’t bother you to do it here, does it?’
Theatre manager, case site B1 (005); transcription 7:30
Such processes were enabled by the dominance of the professional role-position of theatre manager, manifesting through their long-honed expertise and social capital within the relational structure of the theatre department. Under such orchestration the situational logic of correction/compromise resulted in the progressive institutionalisation of the RSC and the WHOSSC.
In case site D, the situational logic of correction/compromise that held sway was attributable to five key individuals: an associate director with strategic oversight for the theatre department; the theatre manager tasked with the strategic oversight of its implementation; the consultant surgeon leading the clinical implementation of the WHOSSC; and two theatre nurses (transcriptions 7:31 to 7:35).
As illustrated in the excerpt from transcription 7:31, below, difficulties in brokering change, due to the entrenched schism between the managerial logic aligned to the nursing profession and the counterpoised stance aligned to surgeons and their medical colleagues, were acknowledged with the setting up of a multiprofessional team to support the implementation of the RSC and the WHOSSC.
Before the WHO checklist came out we were trying to introduce safety briefings in theatres. That was generally, sort of, well we tried, tried to be led by a nurse – a nurse-led approach – but there was a lot of challenge and resistance because the general thinking was that: ‘we already do this, it’s a waste of time, and how dare other people come in and try to tell us what to do!’ But then there was a great team set up with one of our senior anaesthetists who worked with a nurse practice educator in operating theatres and we had even had a consultant surgeon! So, really, the three of them worked together and put their own house in order to set the example.
Associate Director, case site D1 (049); transcription 7:31
Despite this apparently successful implementation, it was clear that the normalisation of the RSC and the WHOSSC remained contested, with some staff treating the WHOSSC in a cavalier manner, undermining it as a meaningful practice and eroding its value to that of a joke. Such disruptive institutional work diminished the legitimacy and moral foundation of the practice. It also served to limit the requisite remoulding of underlying belief systems to aid cognitive participation, collective action and reflexive monitoring during the implementation of the RSC and the WHOSSC (transcription 7:32, below).
I’ve had students come and tell me: ‘Oh, the surgeon introduced themselves, they did the checklist’ – so the tick on the box said: ‘yes, we did it’ – but then they tell me: ‘they introduced themselves as Mickey Mouse’, so they weren’t taking it seriously. When you question them on that, they will say, quite rightly: ‘we’ve worked together for 5 years, we all know each other’. We have even had: ‘I am Spartacus, no I’m Spartacus!’ when they go round introducing themselves. About 99% of our audit data is saying they’re doing it, and yes, they might. But they’re probably not doing it that often and, even when they are doing it, it might not be as fully comprehensive as it should be.
Theatre manager, case site D1 (068); transcription 7:32
In the excerpt from transcription 7:33, below, the strategic negotiation led by the consultant surgeon exposes the reasons given by some surgical colleagues for their reluctance to adopt the WHOSSC.
. . . When we started we also went to people, individually, and spoke with them and gauged their resistance to it – you have to negotiate that with the individuals – a lot of it was, you know, a lot of people were fairly positive; but as I said they were the believers in the first place. Some people said: ‘well OK, well it won’t do any harm, so I might as well just do it just to please you’, which isn’t particularly positive but they did it.
Now, there are always going to be a group of people that will simply refuse and we basically ignored them – that was too big a fish to fry – because they were worried about other issues of their job of which the WHO checklist was a very small part. I mean colleagues would say, in as many words: ‘why would I worry about doing the WHO checklist at the beginning of the list when I can’t even guarantee that all of my patients get into hospital!’, which is understandable and real problem and it’s something we all grapple with. So it’s very difficult to say to them: ‘OK, well this is only a small change that you’re going to make and I can’t help you with your patients’ access’ as some will just say: ‘well, OK, I’ll help you out’ but others will say: ‘sort out my issues first, then I’ll help you!’. One way or the other, they’re sort of trying to get leverage.
Consultant surgeon, case site D1 (083); transcription 7:33
Transcription 7:34, and transcription 7:35, below, illustrate the nuanced negotiation that is demanded under a situational logic of correction/compromise and the creative institutional work involved in reconstructing the social rules impacting on each operating theatre team, despite the lingering barriers of professional power and legitimacy.
We can only persuade people that it’s what they need to do. I can do very little – I have no authority over any of the medical staff – I have some power to tell staff what to do. But I think all along we’ve taken the approach that we’re trying to get people on our side, to understand the importance of the WHO checklist because what I’m asking people to do is – before you hand the knife over to the surgeon, after you’ve prepped and draped the patient, and it’s all ready to go, the anaesthetist is ready to go – is that you stop and get everybody’s attention and there is a point where you have that opportunity. But they have that power because they’ve got the knife. If they don’t hand it over and say: ‘right, we’re going to do the time out, we don’t start operating’ because if you give them the knife then they’re away, and they’re doing it. But it’s the constant sort of having to nag – it needs quite a strident person to be able to stand there, an empowered person – to stand there and say: ‘you’re not starting until you’ve done this’.
Theatre nurse, case site D1 (029); transcription 7:35
Structural elaboration or reproduction in the Welsh health-care field
In examining the contested institutionalisation of the WHOSSC under a situational logic of correction/compromise we sought to gauge key actors’ perceptions of emergent outcomes. Structural change, wrought through the introduction of the WHOSSC and its integration into governance processes, was viewed to have been achieved. However, some interviewees openly acknowledged decoupling from governance processes and the diminishing of the RSC and WHOSSC to a ‘tick-box exercise’ (transcriptions 7:36 and 7:37, below).
As far as the WHO checklist [long pause]. I think it’s disappointing that the figures that are sent in to the centre about compliance bear no resemblance to what’s actually going on out in the service. I just worry that people at the top may be comfortable in the fact that everyone’s having a WHO checklist done and that’s not – that’s not – the case.
Theatre manager, case site C1 (006); transcription 7:36
I think they saw the benefit but the time constraints get in the way – it became a tick-box exercise – and they weren’t being filled in properly. I remember going round to pick up the form, and seeing someone quickly take it off the stand and tick it, so that data was not really true. The worth wasn’t seen immediately.
Theatre nurse, case site D1 (113); transcription 7:37
Yet other interviewees, who viewed the institutionalisation of the RSC and WHOSSC pragmatically, perceived structural progress, albeit blended with residual gaps due to professional cultural contradictions. Transcription 7:38, below, captured a cautionary viewpoint that acknowledged that discrete aspects of the WHOSSC had indeed failed to fully embed into daily practice. This reveals an important issue to be addressed when seeking to attain such cultural change: the act of brokering alignment between discordant professional logics demands ongoing creative institutional work to promote the desired alignment and unification at the cultural-system level.
The WHO checklist does work now, generally, but there are gaps. The things that didn’t really take off were things like the theatre briefings before the meetings – they keep being revisited but they keep failing – and they’re trying to relaunch those in [name, different health board] too! They talk about these ‘champion theatres’ of course but nobody knows what champion theatres are! If you ask anyone who’s not in the know – who isn’t a believer – then they won’t have a clue! It’s then very difficult to say: ‘look, the guys in Theatre 3 are doing really good work, can you do the same?’ And they say: ‘well I don’t know anything about it, why should I do that? What’s in it for me?’ It’s compulsory! But even then it won’t be taken care of.
Consultant surgeon, case site D1 (083); transcription 7:38
In contrast, no pejorative stance muted the perceived success reported in transcriptions 7:39 and 7:40; although the respondent in transcription 7:40, below, was concerned about disparity in theatre department practice, this was mitigated by the belief that auditing such engagement would accommodate, though not reconcile, such variation.
The WHO checklist has been rolled-out across the organisation for some time now and it’s used in each of our theatre suites. But how it’s used is different, it’s different: some of them will do their team debrief on the same day, others will do the WHO meetings all in the meeting, and then it’s managed differently. But whatever they’re doing it’s audited. The activity around the WHO checklist is audited every month.
Associate Director, case site C1 (119); transcription 7:40
Such varied responses underline the need for leadership and skilled strategic negotiation to broker compromise, contain discord and disregard among the disbelievers and deliver successful change to promote local patient safety practices.
1000 Lives+ institutionalisation: RSC – local implementation of the focal intervention and contribution to the I–CMAO configuration spanning the Welsh health-care field
We now seek to further our understanding of the local implementation of RSC-WHOSSC in theatre departments, and to define its contribution to the 1000 Lives+ programmes’ I-CMAO configuration spanning the Welsh health-care field.
As illustrated in Figure 20 and Tables 22–26, the RSC and WHOSSC were a mandatory part of the 1000 Lives+ programme, signalling systemic legitimisation and promoting negotiation across those staff tasked with the implementation of the intervention. This ensured that formalisation and the co-optation of others occurred. It also promoted the deinstitutionalisation of redundant theatre practices and fostered the preinstitutionalisation of the WHOSSC, together with other less controversial practices.
FIGURE 20.
Reducing Surgical Complications: heterarchical metamechanism operating across contextual strata.
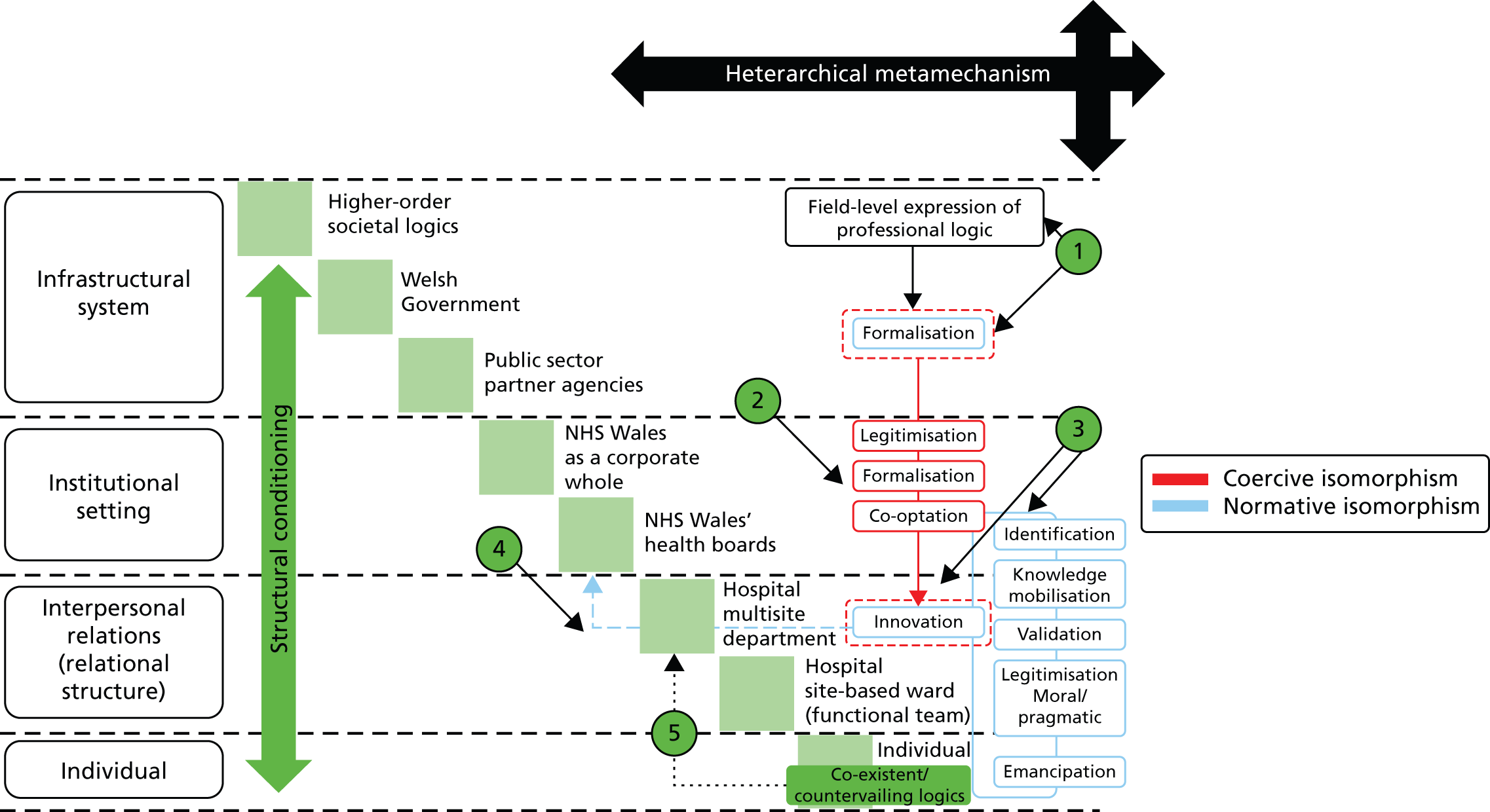
In Figure 20 we depict the implementation of the WHOSSC component of the RSC focal intervention.
In point 1 we draw attention to the formalisation of this process via professional guidelines and Welsh Government policy, thereby mandating engagement by all health boards and relevant theatre department staff.
In point 2, such structural constraint impacts at the level of the theatre department, fostering the co-optation of others, primarily surgical, anaesthetic, nursing and operation department practitioner staff, to support the implementation of the WHOSSC.
In point 3 such mandated engagement drives the innovation cycle in the situated context, so that new practices associated with the WHOSSC are enacted.
In point 4 we depict feedback through the multisite department to the health board as the operationalisation of the WHOSSC component of the RSC focal intervention gradually systematises across NHS Wales.
In point 5 we depict co-existent and countervailing logics, which, though muted by structural constraint, nonetheless impact at the level of the multisite department.
| Intervention | 1000 Lives+ national programme | |
|---|---|---|
| Component | RSC and WHOSSC | |
| Context | Welsh Government | |
| Mechanisms |
|
|
| Agency and institutional work | Normalisation: coupling to 1000 Lives+ and WHOSSC | Habituation: decoupling to 1000 Lives+ and WHOSSC |
|
|
|
| Outcome | 1000 Lives+ national programme, RSC and WHOSSC institutionalised into policy processes | |
| Exemplar transcriptions | ||
|
|
|
| Intervention | 1000 Lives+ national programme | |
|---|---|---|
| Component | RSC and WHOSSC | |
| Context | NHS Wales as a corporate whole/NHS Wales’ health boards | |
| Mechanisms |
|
|
| Agency and institutional work | Normalisation: coupling to 1000 Lives+ and WHOSSC | Habituation: decoupling to 1000 Lives+ and WHOSSC |
|
|
|
|
|
|
|
|
|
|
|
|
| Outcome |
|
|
| Exemplar transcriptions | ||
|
|
|
|
|
|
|
|
|
|
|
|
| Intervention | 1000 Lives+ national programme | |
|---|---|---|
| Component | RSC and WHOSSC | |
| Context | Hospital multisite department/hospital site-based ward (functional team) | |
| Mechanisms |
|
|
| Agency and institutional work | Normalisation: coupling to 1000 Lives+ and WHOSSC | Habituation: decoupling to 1000 Lives+ and WHOSSC |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Outcome |
|
|
| Exemplar transcriptions | ||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Health board | Type of surgical ‘never events’ | Details |
|---|---|---|
| Abertawe Bro Morgannwg University Health Board |
|
|
| Aneurin Bevan University Health Board |
|
|
| Betsi Cadwaladr University Health Board |
|
|
| Cardiff and Vale University Health Board |
|
|
|
|
|
| Cwm Taf Health Board | None recorded | None recorded |
| Hywel Dda Health Board |
|
|
| Powys (Teaching) Health Board | None recorded | None recorded |
| Health board | Type of surgical ‘never events’ | Details |
|---|---|---|
| Abertawe Bro Morgannwg University Health Board |
|
|
| Aneurin Bevan University Health Board |
|
|
| Betsi Cadwaladr University Health Board |
|
|
| Cardiff and Vale University Health Board |
|
|
| Cwm Taf Health Board |
|
|
| Hywel Dda Health Board |
|
|
| Powys (Teaching) Health Board | None recorded | None recorded |
Tables 25 and 26 illustrate the type of information made publicly available as part of the new emphasis on transparency in relation to patient safety. They relate to the incidence of so-called ‘never events’ in surgery that the WHOSSC was designed to prevent.
Across each case site, the situated context was essentially comparable and overtly coercive; however, relational structures – the ties that bind social actors – were different. In each health board, innovation emerged from the MI-PDSA approach. Though this led to the identification of problems and systematic failings, thereby catalysing knowledge mobilisation and the validation of practices, the broader moral and pragmatic legitimisation of the WHOSSC remained contested.
To forward our I-CMAO configuration we turn to the findings of our realist analysis. First, in Figure 20, we consider the overall scheme of the intervention across the different structural contexts. Following this, in Tables 25–27, respectively, we show I-CMAO configurations illustrating the infrastructural system of the Welsh Government, the institutional setting of NHS Wales and its constituent health boards, and interpersonal relationships within the institutional settings.
| Intervention | RSC | |
|---|---|---|
| Component | WHOSSC | |
| Context | Structural conditioning of the institutional setting: NHS Wales health boards’ implementation of 1000 Lives+ national programme’s RSC | |
| Structural emergent properties |
|
|
| Cultural emergent properties |
|
|
| Social actors |
|
|
| Social position |
|
|
| Role-position practices |
|
|
| Mechanism | Mediation of structural conditioning to core actors and their reflexive theorisation | |
| Institutional logics and type of alignment between core actors | Consultant surgeons tasked with the implementation of the WHOSSC operated under a professional logic that was aligned to the dominant logic of the bureaucratic state and professional health-care management logic. However, their actions were directed to managing the tension promoted by the countervailing stance adopted by other surgeons | |
| First-order emergents | The vested interests of consultant surgeons, tasked with the implementation of the RSC and WHOSSC, lay primarily in the successful brokerage of theatre staff engagement with the WHOSSC | |
| Second-order emergents | Constraining contradictions (necessary incompatibilities) between the dominant logic of the bureaucratic state and aligned professional health-care management logic vs. that of professional medical logic held by surgeons opposed to the introduction of the WHOSSC | |
| Situational logic | Correction/compromise | |
| Reflexive theorisation | For consultant surgeons tasked with the implementation of the WHOSSC, their logic is shaped by alignment between the dominant logic of the bureaucratic state, aligned professional health-care management logic, and that of their professional medical logic. This therefore fosters coherence, cognitive participation and reflexive monitoring focused towards addressing the constraining contradictions, which arise as a result of the countervailing professional medical logic held by surgeons opposed to the introduction of the WHOSSC, and who remain disengaged The reflexive theorisation of consultant surgeons tasked with the implementation of the WHOSSC is, therefore, directed towards the discernment of issues impairing such logical alignment, the deliberation of their importance, and dedication of ensuing agency to broker compromise to correct and counteract the opposing stance thereby normalising the WHOSSC into daily practice |
|
| Agency and institutional work | Agency, the unfolding strategic negotiation of change, and the mode of institutional work enacted | |
| Agential emergent properties | Agency was directed to managing the tension promoted by the countervailing stance of professional medical logic | |
| Strategic negotiation |
|
|
|
|
|
| Institutional work | Multimodal | |
| Agency and institutional work | Agency, the unfolding strategic negotiation of change, and the mode of institutional work enacted | |
| Outcome | Social elaboration, reproduction or invariance | |
| Structural | Structural change, wrought through the introduction of the WHOSSC and its integration into governance processes, was achieved. However, the openly acknowledged decoupling from governance processes distorted coherence and commitment to the RSC and WHOSSC by diminishing it to a tick-box exercise | |
| Cultural | Cultural change limited as harmonising discordant professional logics demands prolonged creative institutional work to promote the desired coalescence and unification at the cultural system level | |
| Agential | Invariant | |
Finally, in Table 27, and focusing, for expediency, primarily on the generative mechanisms and ensuing agency attributed to consultant staff tasked with the implementation of the RSC and WHOSSC, we present our realist analysis linking the empirical data to I-CMAO.
As alluded to above, a sense of structural force majeure was evident, but its influence was reduced by theatre departments’ feeling of relative separation from the parent health board and wider health-care institutional field. Consultant staff, tasked with the implementation of the RSC and the WHOSSC, were confronted by the contradictions between the dominant logic of the bureaucratic state and aligned professional health-care management logic and that of professional medical logic. In such circumstances a situational logic of correction/compromise arose that was open to the power play of different professional groups, each seeking to turn such sociocultural constraint to their advantage.
As set out in Table 27, the reflexive theorisation of consultant staff tasked with the implementation of the RSC and the WHOSSC focused on addressing the concerns of surgeons opposed to the introduction of the WHOSSC. Their thinking and actions were, therefore, directed towards seeking the reasons for such opposition and seeking ways of finding compromise positions and/or solutions which would be acceptable to the dissidents and enable the WHOSSC to be normalised into daily practice.
The structural elaboration evident across each case site was shaped by the integration of the WHOSSC into governance processes. However, the openly acknowledged decoupling of the insulated surgical theatre world from such governance processes distorted coherence and commitment to the RSC and the WHOSSC by diminishing it to a tick-box exercise. Indeed, the large number of ‘never events’ (serious patient safety violations) which occurred in NHS Wales’ health boards during the period 1 April 2012 to 30 September 2013 (see Tables 28 and 29), while unable to necessarily be directly attributed in part or in whole to failure to implement the WHOSSC, serve only to underscore such decoupling.
This contested institutional change highlights the time required to negotiate alignment between discordant professional logics and stresses the complexity of the creative institutional work required.
Summary
In Chapter 7, we furthered our understanding of the local implementation of the focal intervention, RSC, centred on the WHOSSC, and defined its contribution to the 1000 Lives+ programmes’ I-CMAO configuration spanning the Welsh health-care field.
Chapter 8 Reducing Health-care-Associated Infection
Overview
In this chapter we examine RHAI, the final focal intervention drawn from the 1000 Lives+ programme. Our attention was directed to two aspects of this patient safety intervention: (1) hand hygiene and (2) the appropriate use of antimicrobial drugs. Importantly, in contrast to the other focal interventions selected from the 1000 Lives+ national programme, set out in Chapters 6 and 7, such interventions do not represent practice innovations. Instead, they represent the consolidation of established best practice. We begin with a brief overview of the RHAI, defining its multicomponent structure, aim and drivers. This we augment with a review of health-care-associated IPAC, highlighting key issues and the challenges that confront developed health-care systems.
Second, we undertake a realist analysis of the institutionalisation of RHAI in Wales, as illustrated by our comparative case study of sites A, B, C and D. We explain the structural conditioning, sociocultural interaction and structural elaboration or reproduction fostered through the actions of three groups of key actors: consultant microbiologists, IPAC nurses and pharmacists specialising in antibiotics medicines management. We concentrate on these three groups because they are directly involved in the operation of RHAI under the 1000 Lives+ programme, but we also include in our analysis the perceptions of a wide range of health-care professionals. Finally, informed by the findings of our realist analysis, we set out our understanding of the RHAI I-CMAO configuration.
Focal intervention, aim and drivers
Reducing Health-care-Associated Infection, the last of the three focal interventions considered in this study, aims to support health-care staff to reduce the overall burden of nosocomial (hospital-acquired) infection in NHS Wales. As illustrated in Figure 21, RHAI comprises four interventions to prevent the transmission of infection, two of which are aligned to promote the effective treatment of infection, and a further three interventions to facilitate patient involvement in their care. During the period of this study RHAI was augmented with further advice on the appropriate and timely use of invasive devices, specifically guidance aimed to reduce peripheral venous cannula (PVC) and catheter-associated urinary tract infections (CAUTI). This extension was beyond the scope of our research protocol and ethics submissions, and so our research focused on standard precautions for hand hygiene to prevent the transmission of infection and the appropriate use of antimicrobial drugs to ensure the effective prevention and treatment of infection. Nonetheless, the publicity surrounding the launch and implementation of the PVC and CAUTI interventions impacted on the context of care.
FIGURE 21.
Driver diagram: RHAI.

Figure 21 depicts the driver diagram for the focal intervention: RHAI. Attention is directed to two of the four aspects of this patient safety intervention which are focused at clinical and other staff, as defined below:
-
point 1, standard precautions for hand hygiene to prevent the transmission of infection and
-
point 2, appropriate use of antimicrobial drugs to ensure the effective prevention and treatment of infection.
To aid our understanding of the interplay of context and mechanism in the operationalisation of this focal intervention, the perspectives of consultant microbiologists, IPAC nurses and pharmacists specialising in antibiotics medicines management, each directly involved in the operationalisation of the RHAI under the auspices of the 1000 Lives+ national programme, enrich our analysis.
In contrast to the other focal interventions selected from the 1000 Lives+ national programme, standard precautions for hand hygiene and the appropriate use of antimicrobial drugs do not represent practice innovations but are merely the consolidation of established best practice.
Health-care-associated infection, prevention and control
Health-care-associated infection (HCAI), prevention and control is an issue that impacts on developed and developing health-care systems. 572–574 It is a source of concern for politicians, health-care professionals, patients and the public alike. 575,576 Addressing the human costs in terms of morbidity and mortality is paramount,577,578 but there is also a need to minimise the cost burden incurred through protracted treatment and extended lengths of stay. 577,579–582 A range of patient safety interventions have been designed to improve this problem. 181,583–590 Such interventions typically encompass (i) mandatory reporting and surveillance programmes;591–594 (ii) ensuing targets, standards and performance indicators for IPAC,595–620 especially for high-risk clinical practices600–602 and vulnerable patient groups;603–606 and (iii) heightened control over the use of antimicrobial drugs in the face of the changing epidemiology of HCAIs,589,607–610 exemplified by the rise of MRSA and extended-spectrum beta-lactamase (ESBL)-producing strains of Escherichia coli and Klebsiella pneumonia. 609,611–619
In the NHS, following major outbreaks of hospital-acquired (nosocomial) infection,620 national targets for the reduction of MRSA bacteremias (blood infections) and C. difficile (gastrointestinal) infection are supported by enhanced mandatory surveillance. Oversight rests with the Health Protection Agency in England and Scotland,592,597,621 and, in Wales, the WHAIP led by Public Health Wales. In this manner, IPAC is placed at the centre of clinical and corporate governance. 622 Indeed, the Health Act 2006 Code of Practice mandates adherence to national and local policies and protocols. 623 Zero tolerance of HCAIs624,625 is a primary policy goal.
Core to success is the enactment of good hand hygiene across health-care practitioners, support workers626–630 and patients. 631–635 This standard precaution, perceived to be fundamental to safe health-care practice,636 is captured through the WHO’s ‘five moments of hand hygiene’. 637 These guidelines harness a substantial evidence base in support of hand antisepsis to limit the incidence of HCAIs. 587 However, such education requires regular updating638–640 to promote the adoption of, and continued adherence to, evidence-based improvements,641,642 and monitoring systems are necessary to audit compliance. 595,596,643–645
Although existing studies highlight success in limiting HCAIs48,181 through hand hygiene195,639,646–648 and wider reaching educational programmes,649–653 a high level of non-compliance with basic infection control measures persists among health-care professionals. 654 Indeed, junior medical and nursing staff copy the aberrant behaviour of their superiors,655–657 which results in the entrenchment of non-compliance across successive generations. 655–660 IPAC teams, therefore, have a central role to play in active staff engagement,661 support for peer-to-peer education,662 and the monitoring of HCAIs to reduce the burden of avoidable harm to patients and its associated untoward costs. 581,663–689
The changing epidemiology of HCAIs607,608,611,612,617,666–694 also places demands on medical microbiologists and clinical pharmacists specialising in antibiotic medicines management. 57,671 Collectively, their active stewardship of antibiotic prescribing is acknowledged to limit overprescribing672 and improve adherence to guidelines. 673–676 However, their oversight of surgical prophylaxis is constrained by the charting and timing of the administration of such drugs within the theatre environment. 677–679
There are many other ways in which patients may acquire infections while in hospital. These include the use of invasive medical devices such as ventilators,48,680–710 intravenous and arterial cannulae605,687–690 and various sorts of catheter691–695 However, these sources of infection and the precautions taken to avoid them are not considered in this study.
Realist analysis and comparative case study
We now undertake a critical realist analysis of the institutionalisation of the 1000 Lives+ programme’s RHAI. Again, our case study considers sites A, B, C and D. Our analysis focuses on three groups of key actors: consultant microbiologists, IPAC nurses and pharmacists specialising in antibiotics medicines management. Each is directly involved in the operation of RHAI under the auspices of the 1000 Lives+ national programme. However, as HCAIs are an issue for all to address, we include the perceptions of a wide range of health-care professionals in our analysis.
As in the two previous chapters, we consider the focal intervention in context and explore the dominant structural and cultural emergent properties impacting key actors involved in the operation of the RHAI. Next, to reveal the generative mechanisms in play, we examine mediation via first- and second-order emergents and the resultant situational logic. Then, to examine the initiation of change, we explore the unfolding strategic negotiation of change and the mode of institutional work enacted. Finally, we reflect on the nature of any sustained outcome, be that elaborative or reproductive, that occurred following the implementation of RHAI. This analysis forms the foundation of our refinement of the I-CMAO configuration spanning the Welsh health-care field in 1000 Lives+ institutionalisation: RHAI – local implementation of the focal intervention and contribution to I–CMAO configuration spanning the Welsh health-care field.
Structural conditioning: structural and cultural emergent properties in the Welsh health-care field
In contrast to the other focal interventions selected from the 1000 Lives+ programme and analysed in Chapters 6 and 7, the discrete interventions selected from RHAI – standard precautions for hand hygiene to prevent the transmission of infection and the use of antimicrobial drugs to ensure the effective prevention and treatment of infection – did not represent practice innovations. The dominant structural emergent properties impacting the RHAI were, therefore, the complex array of established alternative frameworks and the ongoing surveillance of their effectiveness via the WHAIP (transcription 8:01, below).
The question for me is, how do we untangle 1000 Lives+ from all of the other elements in play – it’s complicated, confounded – because what’s happening is happening between 1000 Lives+, all of the other frameworks and antimicrobial guidelines that are out there, and mandatory surveillance reporting and feedback via WHAIP.
So, it’s through one or a combination of all of those things that the higher echelons, if you like, of hospital management are now faced with infection control, and its importance, much more so than they were 10 years or so ago, or even less than that. So I think, whether it’s due to 1000 Lives+, other frameworks, or the surveillance processes in place, I think it’s achieving something – because they have to be aware and address HCAI due to WHAIP reporting to the Welsh Government – my impression is that they are aware of it and they feel accountability.
Now when you have accountability in the higher levels of management, the way that they effect that accountability, quite rightly, is through delegation and spreading the message in terms of what needs doing. The previous medical director here, who was spectacularly engaged, even before 1000 Lives+, with the idea of infection control provided a real sense of leadership, and had an awful lot of insight. I don’t know why that was, perhaps he just saw it as part of his role, I don’t know, but he did it very well. But now, now that we’re a lot bigger, and we have a wider range of – I don’t want to use that term ‘lower’ – some of the next tier down levels of management, like director level and their associates or assistants, that message is dissipated.
Consultant microbiologist, case site C1 (034); transcription 8:01
Other structural issues also surfaced during discussions with respondents, notably the compounding impact of the reconfiguration of NHS Wales on framework alignment, and the need for the co-ordination and consolidation of different guidelines under a health-board-wide and emergent all-Wales remit (transcriptions 8:02 and 8:03, below).
The reconfiguration of NHS Wales, the formation of health boards that’s occurred during the roll-out of the original 1000 Lives campaign and 1000 Lives+, I think this has created issues which are problematic. I think that the creation of much larger health boards has created barriers to the roll-out of 1000 Lives and 1000 Lives+. So, for example, something that’s seen to be an incredibly high priority within this health board, quite rightly, is the fact that before we were [number] Trusts, and we all had, I imagine, a pretty good spread of infection control policies that were broadly in line, and in their own way ticked the boxes for national recommendations. But they were not the same. Now a priority, here, is that we have harmonised consistent policies. So, you know, we all have workable policies that we could just leave alone to would work on each site; but no, we are required to have single harmonised policies that we all agree to. Now the differences that existed were there for a reason. But now we’ve got to try and overcome those differences, agree amongst ourselves, and then get wider agreement across the consultants. And the point being that that’s a job of work that takes time and is outside the time requirements that might be put into 1000 Lives+.
Consultant microbiologist, case site A1 (035); transcription 8:02
Working with consultant microbiologists, we produce and review the antibiotic policies used across the health board. There’re planning to have all Wales antibiotic policy guidelines. [Have they been produced and published?] No, no way: it’s still at a very early stage of discussion, about 6 months in, and I think it will take years to agree: there’s so much disagreement about what to use, when, and some doctors simply refuse to follow any guidelines, no matter who produces them: ‘where’s the evidence; the evidence is disputed; it’s not that clear cut; it’s my freedom to prescribe how I see fit for my patient’. We get that same old argument, from some of them, all the time.
So, we produce the health board’s antibiotic guidelines and monitor them through audit cycles across each ward or base hospital; we do the education associated with antibiotic usage for the junior doctors, nurses, and other staff, including other pharmacists; and we do antibiotic ward rounds with consultant microbiologists – this is a small hospital, so consultant microbiologists don’t have junior doctors attached to them, so, in a way, we act like their juniors – this involves antibiotic prescribing and follow-up, checking that the drug and indication are appropriate, that the dose, route, are all correct, that sort of stuff. I don’t think of the context outside so much, I suppose; for me, it’s about the people I talk to and work with each day.
Pharmacist, Antibiotics Medicines Management, case site B2 (001); transcription 8:03
In addition to the structural constraints arising from various existing guidelines, a previous patient safety improvement programme, the Safer Patients Initiative, had a legacy effect which resonated strongly with some IPAC nurses interviewed as part of this study (transcription 8:04, below, and transcription 8:05).
If I’m honest with you, when it [1000 Lives] came out originally, it was a bit of a spin-off from the SPI [Safer Patients Initiative], you know, the IHI approach, wasn’t it?
It came out at the time when we were reorganising the health service in Wales. So, I think, a lot of the correspondence went to people whose positions have changed and so on and so forth. They started off at a very high level but there was a lot going on in the organisations and it didn’t really filter down – the leadership was a little bit fragmented at that time – I think in the last 2 years we’ve sort of taken hold of it.
We were a little bit at odds with the priorities of the RHAI programme initially because we had done our own prevalence survey, internally, and we hadn’t identified problems with catheter-associated UTIs [urinary tract infections]. We did an incident survey over a period of 1 month in wards in the organisation and there were no issues with catheter-associated infections at that point in time. However, we identified problems with peripheral venous cannulas during our point prevalence survey. But the campaign was mandating a focus on short-term urinary catheters, whereas our priority at that time was more to do with peripheral lines. So it was a little bit of, it was a little bit, you know, sort of didactic I guess: ‘this is a priority, and this is what you must do’, and I was thinking, well, in our organisation, this is our priority and we will do that, at the moment we need to focus on that.
Senior nurse, IPAC, case site A2 (076); transcription 8:04
Such structural constraints were interwoven with the current financial challenge; as one respondent commented, ‘the biscuits are gone!’ (transcriptions 8:06 and 8:07).
The cultural emergent properties impacting staff involved with infection control arose from their different but interlocking roles. It was clear that there was close liaison between each professional group (transcriptions 8:08 and 8:09, below).
I’m aware that there are different models, if you like, with the consultant leading, consultant microbiologist, the infection control doctor leading the service. Here it’s a flat model – a flat model between the lead infection control nurse and the lead infection control doctor – and it is something that I feel not only works well but is appropriate because we bring different skills to the mix, and I’m not sure that any set of skills is more important than the other.
Consultant microbiologist, case site C1 (T034); transcription 8:08
Well, predominantly, in infection control, our role is for support and advice to staff. That’s our role. But we’re also involved in conducting audits – particularly things like hand hygiene audits, commode audits, environmental audits, and those kind of things – and those are fed back to ward staff, the results and an required action. But we also carry out things like surveillance, so we’ll monitor our alert organisms [for WHAIP]. If there’s any kind of change – an indication that there’s an increase in health-care-associated infections, or an increase in any of our WHAIP alert organism, such as MRSA, MSSA [meticillin-sensitive S. aureus], C. diff, Group A strep [Group A Streptococcus], E. coli, any of the alert organisms, we’ll go and find out, and liaise with the consultant microbiologist.
Senior nurse, IPAC, case site D2 (017); transcription 8:09
Such liaison also gave rise to professional networks which enabled processes of interprofessional knowledge mobilisation that were perceived to be operating at a more challenging level than those of 1000 Lives+ (transcription 8:10, below).
If I’m facing something that new, a bit different to what I’ve handled before, I would first contact other antibiotic specialist pharmacists – there’s a network across Wales – so that would be one source of information and advice. The others, naturally, are the consultant microbiologists and IPAC nurses. Also, there’s a formal meeting twice a year of the Antibiotic Stewardship Forum, which consists of medical microbiologists, pharmacists, and some specialist nurses. They don’t meet that often but they’re a great source of information, and an opportunity to share learning and development.
[Are there any other groups that you would contact for advice or support?] Yes, the UK CPA [UK Clinical Pharmacy Association] is another source of information. They have an infection management group – they’re more advanced in England – there’s a good web site, support materials, that sort of stuff which is very helpful. In England, they have developed the consultant pharmacists role – we don’t have those in Wales yet; but I think one is due to be developed in Renal Pharmacy, which is an incredibly complex field. So that sort of recognition, legitimacy almost, is absent in Wales. Another group is the British Society for Antimicrobial Chemotherapy. They’ve got a useful website, and they run all Wales study days, which, in terms of the evidence and focus, are pitched at a far higher level than 1000 Lives+. I feel like I’m learning something new when I attend these, not just being told to wash my hands before I go onto a ward, or to make sure that a course of antibiotics has a defined stop date! Another is the Welsh Microbiological Association and again, they run study days, really focused on education, and this is linked into Public Health Wales. So this is all at a level above 1000 Lives+.
Pharmacist, Antibiotics Medicines Management, case site B2 (001); transcription 8:10
First-order emergents for key actors central to the institutionalisation of Reducing Health-care Associated Infection
Such structural and cultural emergent properties shaped the context in which key actors, central to the institutionalisation of the RHAI now found themselves and conditioned their ensuing actions. We therefore asked consultant microbiologists, nurses specialising in IPAC and pharmacists specialising in the management of antibiotic medicines to reflect on their placement, their vested interests and the perceived opportunity costs associated with various courses of action, to determine how this shaped their activities.
Consultant microbiologists
The vested interests of consultant microbiologists lay in the day-to-day operational management of IPAC, centred on the provision of their expert advice, and the ongoing demands which arose from WHAIP surveillance (transcriptions 8:11 to 8:13). The 1000 Lives+ national programme and RHAI, though aligned to such tasks, were a secondary consideration (transcription 8:12, below).
Well, of course, a lot of the mandatory reporting used to be done manually by microbiologists – that used to take up our time, particularly statistics for bacteraemia – but that’s all done centrally now. So all that information is sucked out of the data store in Wales.
In terms of mandatory requirements, there’s, in theory, there’s less for us to do. But I strongly suspect that – I’m not alone here, in fact I guarantee you that all microbiologists who used to do it, still do it – because there is an expectation that, a requirement for us, when reports are generated centrally through WHAIP before those reports come out as you know the raw data is circulated back to us to check if we think it’s correct but we would only know that if we were doing the same data collection that we ever did!
But we would want to do it anyway – not just to check the accuracy of WHAIP reports, bearing in mind that some of those reports are somewhat retrospective – because if we relied on them to find out if we were having an out of the ordinary rise in numbers of C. diffs in a given area or MRSA bacteraemia associated with line use in a certain area, we’d miss the boat and problems would have deteriorated. So we have, we need to do these things, relatively, real time. So that’s one form of reporting pressure if you like. I mean we see it as part of our work – as our normal role – and that’s why I’m fairly confident that it doesn’t matter who you ask in Wales they’ll probably give you that exact same answer. But nonetheless it’s a time pressure that needs, a role that needs to be fulfilled.
On top of that you’ve then got two other pressures. So, one is the one I’ve just mentioned, whereby you’re noticing your own local priorities with these figures that you’re generating for WHAIP, so that we can focus our attention and look at the interventions that should be being made, and audit whether they are being made, and how well they’re being done and that kind of thing. But at the same time we might be receiving instructions that we should be looking at other areas – and it’s not that those areas aren’t important – but then our time is split because there’s the thing that we see, that we feel we have an immediate need, and then there’s the requirement to fit in with 1000 Lives+ I suppose.
Consultant microbiologist, case site B1 (036); transcription 8:12
In focusing on the broader remit of IPAC, as opposed to the progressive institutionalisation of RHAI, consultant microbiologists operated under a professional (medical) logic co-existent with and complementary to professional (health-care management) and bureaucratic state logics. Thus, the RHAI was absorbed and integrated into existing and culturally entrenched monitoring processes. This aided its adoption and reproduction across NHS Wales’ health boards.
Infection prevention and control nurses
The vested interests of IPAC nurses at each case site, captured in transcriptions 8:14 to 8:21, again reflected the impact of their traditional role jurisdictions. These overshadowed and pre-dated the 1000 Lives+ national programme and RHAI (transcriptions 8:14 and 8:15, below).
We do all the audits – environmental audits, hand hygiene audits – ward-based teaching, like the session that you’re going to see this afternoon, and just general support for the wards, and where we find a problem, we like to go back and offer a solution and support the staff to eradicate hospital-acquired infections.
Nurse, IPAC, case site A2 (003); transcription 8:14
We were doing all this before 1000 Lives and 1000 Lives+ – including looking at urinary catheter-associated infections and peripheral and central line infections – so the interventions 1000 Lives+ promotes are already integrated into our monitoring systems, and it would be the same for all health boards.
Senior nurse, IPAC, case site A2 (002); transcription 8:15
In addition, some aspects of infection control lay far beyond the scope of RHAI (transcription 8:17, below).
It is unacceptable to have a case of Clostridium difficile, and if you have two within a 28-day period, a formal meeting is called. [What do you do if you have a persistent problem with Clostridium difficle?] If there was a continuing problem, then we’d look to Bioquel the ward – bio-bomb it with hydrogen peroxide – they go in, in their decontamination suits, and close the doors. They do it one section at a time, they vapour blast it with hydrogen peroxide, they leave all the equipment in there, all the beds, everything stays in there, so there’s no risk of us missing something really. After that the domestic staff will go in and just clean – soap and water, detergent – and then we put the patients back in the ward. So far, that seems to be very effective. But we’ll only do that if we have real hotspots.
Nurse, IPAC, case site B1 (131); transcription 8:17
The newer 1000 Lives+ interventions associated with RHAI, though beyond the scope of this study, were an extension of established practice. However, owing to medical resistance, some specified changes were a source of concern (transcription 8:18, below).
The new 1000 Lives+ intervention was launched nationally last year, and we’ve been rolling out the PVC bundle but we have the catheter bundle in place for about 4 years now. The PVC bundle has proved a little more difficult to implement really, in that there’s been a change to practice, there’s also been a lot of medical opposition. [Why?] Because they’ve got to do stuff! What they’re saying is: ‘where’s the evidence to say that they’re not doing things properly, and that we’ve got a high rate of infection? Why should I change my practice without the evidence that there’s a problem in the first place?’ [They don’t perceive a problem in their current practice or the rates of infection?] Because they don’t believe they’ve got a problem. They don’t believe that by changing practice, or being forced to evidence that they’re doing what they should be doing, that that will make any difference. And, in one respect, you could sort of see their point, in that there is a low rate of peripheral venous infections. But we do get catheter-related bloodstream infections and the incidence of MSSAs [meticillin-sensitive S. aureus] within the health board has been increasing. But what we asking them to do, due to 1000 Lives+, well, for them, it just takes too long.
Nurse, IPAC, case site C1 (132); transcription 8:18
In regards to 1000 Lives+, I’d say the introduction of the bundles and the STOP campaign is probably all the infection control team have been involved with and some of that just involved minor changes to our practice.
Nurse, IPAC, case site D2 (019); transcription 8:21
In focusing their agential activity on the broader remit of IPAC, in addition to the institutionalisation of the RHAI, specialist nurses operated under a professional (nursing) logic that was complementary to professional (health-care management) and bureaucratic state logics.
Antibiotic medicines management pharmacists
Transcriptions 8:22 to 8:29 suggest that the vested interests of pharmacists with expertise in antibiotic medicines management were poorly aligned to RHAI, which they saw as irrelevant given their level of expertise (transcriptions 8:24 and 8:25, below).
[When you think about the knowledge and information that you use within you role, do you draw on the 1000 Lives+ resources?] No, I don’t use them. There’s little information in them that relevant to me; I mean, it’s just so basic – really bottom-end stuff, basic, mundane – if you don’t know it, you shouldn’t be working as a clinical pharmacist.
1000 Lives+ is, it’s too basic, directed at lower-level nurses. For me, it offers little. [Do you use the driver diagrams?] No, they’re not relevant: they’re basic. I do a ward round with a consultant microbiologist each day and there’s more to that than hand washing! The diagrams aren’t education. I mean, we are using the key points in our stickers, developed as part of the antibiotic care bundle, but it’s our system. [Do you use the PDSA cycle?] No, we have ongoing audit cycles, which, I guess, serve the same function but they’re part of the health board’s audit regimen and not informed by the 1000 Lives+ programme.
Pharmacist, Antibiotics Medicines Management, case site B2 (001); transcription 8:24
[When you think of 1000 Lives+, what does it mean to you?] That’s a good question. What does it mean to me? I’d say it’s pretty much invisible. I guess it’s one of a number of elements that we take into account on a day-to-day basis. It’s tricky because you’re undertaking CPD [continuous professional development] all the time. It’s probably not recorded as CPD but every article you read in the PJ [Pharmaceutical Journal] is all CPD. For example, I’m going to have a lunchtime teaching session, and there could be two or three things in that that I will take away, and then use in my day-to-day practice. But as a consequence there are things that I will probably drop out by day-to-day practice because they’re become superseded by something else more important. 1000 Lives+ is just one element. There are lots of other things you’re taking in and trying to maintain as current all the time.
Pharmacy manager, case site B2 (016); transcription 8:25
Such disregard was augmented by the notion that, for pharmacists, aspects of 1000 Lives+ have not been ‘translated to pharmacy-speak’ (transcription 8.26). Hence, for this professional group, the resources offered by RHAI were not considered to be a worthwhile innovation in practice (transcription 8:28, below).
If you look the 1000 Lives+, although I think this might have existed with 1000 Lives as well, but I mean, with 1000 Lives+ – I forget what the terminology is but the project theme or something for health-care-associated infection – you have the key intervention areas, if I remember correctly, you’ve got things like standard precautions, hand hygiene and decontamination; isolation precautions, that would be another, and antimicrobial stewardship and so on and so on. But all of these are in the strategies we’ve had in Wales for years! So they, they’re not new and they’re not separate are they?
Pharmacist, Antibiotics Medicines Management, case site D2 (020); transcription 8:28
Second-order emergents and situational logic
In case sites A–D, the interplay of structural, cultural and agential emergent properties impacted on the three groups of actors directly involved in the operationalisation of RHAI. First, in structural terms, RHAI was integrated into the social system-level but was overshadowed by existing systems. Second, in cultural terms, though internal and necessary complementarities could be seen between the RHAI and the array of professional logics in play, this was not considered to add much to already existing principles and procedures and was largely disregarded. RHAI, therefore, operated under a situational logic of protection that was primarily directed towards the pre-existing structural and cultural system-level, and thus to sociocultural interaction aligned with long-established practices.
Sociocultural interaction: agency and strategic negotiation
As discussed in Chapter 6, a situational logic of protection is typically associated with a defensive negotiating stance. However, for RHAI, prior systems of HCAI surveillance and developed IPAC practices overshadowed the intervention. The progressive institutionalisation of the 1000 Lives+ national programme and RHAI, therefore, unfolded in a terrain marred by a degree of disdain. We highlight this complex interplay in both a discrete case site and across multiple case sites, again drawing out different degrees of bureaucratisation and normalisation to help enrich our understanding of the institutional work complementary to the interplay of the focal intervention, context and mechanism.
Power-induced compliance and political sanction
To examine the issues of power-induced compliance and political sanction, we considered individual actors’ strategic negotiating stances across different case sites and professional roles.
It was clear that the IPAC team, in the broader sense, were connected to the managerial core (transcription 8:30). However, they were also intermittently connected to ward-based functional health-care teams, though IPAC nurses and pharmacists undertook regular ward visits as part of their practice. This created a context in which such roles, while offering advice and expertise, also functioned as part of the ward-based governance of IPAC.
However, this oversight role was compromised. Poor practice was adapted in the presence of IPAC nurses, changing so that it demonstrated, while observed, close adherence to the hand washing guidelines of RHAI (transcriptions 8:31 and 8:32, below). This finding was corroborated by our observation of practice at each case site.
There’s some wards you go to and, you know, 1000 Lives+ is just an aside, an extra element of work. For example, you ask them about commode cleaning and they say: ‘well, we don’t have to clean it after every patient’, and then we say: ‘but you’ve got to, that is part of the task, it’s part of the commode bundle’, and they roll their eyes and argue: ‘well, we haven’t got the time’.
I think, wow, if you haven’t got time to just clean a commode, what else have you not got time for? It’s almost as if everything on some wards is seen as on top of what they’re trying to do, you know, because they’re so run ragged, which is understandable, but that’s when it’s harder, then, to implement something new: when they can’t even be doing the things that they should be, you know?
[Can you mandate adherence to these guidelines?] Yes, we tell them, and we audit them, but because we are all known to staff, the minute we walk onto a ward their practice changes. [So they adopt the expected behaviour when you are present?] Yes.
Nurse, IPAC, case site D2 (019); transcription 8:31
About 90% of the staff in ITU [intensive therapy unit] are familiar with me. So, they all know me, and they all know what my job is. When I walk in twice a year, even if they don’t know my name, they know who I am – that sounds really self-important, and that not the issue, but they know me and it’s a problem – and people often will come up, and they’ll stand and chat to me and wash their hands, and I know perfectly well that they’ve done absolutely nothing – they haven’t been near a patient – it’s just that conscious effort to demonstrate hand washing. They’ll walk into ITU, they’ll have a squirt of alcohol gel, and they’ll be watching me, looking at me, to check I’m watching them. So now I sent up [namea] and [nameb], both IPAC as most of the staff don’t know them. So, they went up, on the pretext of looking through patients’ notes, and the hand hygiene practice was not acceptable. But, as soon as they realised that they were being audited, their practice changed immediately. They were like washing their hands, alcohol gel, everything changed.
Nurse, IPAC, case site B1 (137); transcription 8:32
The IPAC staff demonstrated the professional role-positional power to challenge poor practice within extant bureaucratic governance processes. However, confronted by normalised malpractice and decoupling from pre-existing and repacked RHAI standards, their institutional work was predominantly corrective.
Similar corrective institutional work was also demonstrated in the ward-based actions of pharmacists with expertise in antibiotic medicines management (transcriptions 8:34 and 8:35, below).
We don’t get all doctors following the antibiotic prescribing guidelines. Some do, some don’t. So it’s a core part of the role for pharmacists to challenge and change that when they do their ward rounds.
Pharmacy manager, case site D1 (021); transcription 8:34
[What happens if a doctor prescribes off guidelines within the health board?] We challenge them. I had one, a few days ago, who I challenged because he had prescribed two drugs, and only one was needed for the patient’s indication; but all he said was: ‘so what’s the problem, it’s not illegal is it?’ But it’s a waste of money, medicine, and more of a risk and inconvenience for the patient. I think that a lot of my role is really about education and changing the culture in the health board. [But is that refusal to follow the guidelines reported to anyone?] Yes, all the audits go to the medical director. But it’s anonymised data: ward level, not prescriber level. One of my colleagues in [name, health board] has done this per consultant team, and they’ve had good results in changing prescribing because the data is ranked. Everyone knows who’s playing ball, and more importantly, who’s not, so to speak.
Pharmacist, Antibiotics Medicines Management, case site B2 (001); transcription 8:35
In this example, though such staff demonstrated the professional role-positional power to challenge poor practice and enacted corrective institutional work, the lack of transparency and feedback at this site, compared with the respondent’s example of another site, where ’everyone knows who’s playing ball, and more importantly, who’s not, so to speak’, only served to erode the goals of RHAI.
Reciprocal exchange and harmonisation of desires
Gaining widespread support and agreement for a harmonised approach to IPAC, and thus RHAI, proved difficult due, in part, to individual prescribing preferences and ensuing practices. Indeed, this issue was a consistent theme at each case site and across professional groups (transcriptions 8:36 and 8:37, below).
Getting agreement between the all of the consultant microbiologists in the health board is quite demanding but that pales into insignificance when we have to start telling other medical consultants or surgeons what they are supposed to prescribed for a given indication. You know this as much as me! They’re all got their preferred drugs, ones that they have used for years, new ones that offer more, and cost more, it’s that debate that difficult, and it’s one we are having to address due to the formation of the health board.
Consultant microbiologist, case site B1 (036); transcription 8:36
I don’t know if they’ll all agree to a health board-wide antibiotic policy. I mean, we’ll get agreement on the overarching health-care-associated issues – say C. diff management because that’s changing, and it’s our area per se: they don’t want to claim that for themselves – but it’s harder to negotiate with respiratory physicians, orthopaedics, all the rest, as they’ve got their preferred drugs. So changing their prescribing practice is difficult. Our policy is monitored by pharmacists, and IPAC nurses, as they work at ward level, so they are at the sharp end.
Consultant microbiologist, case site C1 (034); transcription 8:37
The comment from a respondent that ‘To change something – whether you’re talking about the 1000 Lives+ work, adherence to current policy guidelines, or the development of new guidelines across the health board, you’ve got to know the people involved in the system’ (transcription 8:38) highlights the critical role of contextual relational structure and social interaction in the brokerage of such contested change. Leadership and the use of co-opted medical power were also seen as central to the negotiating stance employed (transcriptions 8:39 and 8:40, below).
On the wards, well, you’ve got issues, other things, you know, if you’ve got high sickness rates on a ward as well, motivation is often low, so when you’re trying to introduce 1000 Lives+ guided change that’s going to impact more on their workload, often that’s seen as a negative. The key issues then is, how do you really sell that to them because it’s no good us saying: ‘this is all the new paperwork, go on, use this’, the wards have got to see the benefits of that, and own it, and want it, for it to work. I think that’s where good leadership comes in because it’s sort of, you know, if they sell it, if the ward manager sells it as this is a positive thing: ‘if we do this we can reduce our rates’, the staff will be on board.
Lead nurse, IPAC, case site A1 (037); transcription 8:39
We’re having problems with the PVC insertion bundles because we went on the sticker route for the insertion bundles, whereby you put the sticker on the prescription chart, on the PRN [as required medication] side of the prescription chart. Well, every time they went to change a cannula they would just need to sign the prescription chart to say that they’d changed it, and the sticker will have things like hand hygiene, personal protective equipment, and the right dressing on it, you know. But doctors insert venflons and doctors don’t like to document that they’ve inserted something! So when we spoke with the associate medical director at the time, he suggested that we approached clinical champions to try and embed that a little bit further. So with the audit work and the regular feedback, and identifying clinical champions, we’ll begin to see an improvement in compliance, you know, if we don’t, we’ll feed it back to them.
Nurse, IPAC, case site B1 (131); transcription 8:40
Although these IPAC nursing staff demonstrated the professional role-positional power to challenge poor practice, their corrective institutional work, buttressed by the power of others, was directed towards the maintenance of best practice and its evolution through RHAI.
Structural elaboration or reproduction in the Welsh health-care field
In examining the progressive institutionalisation of the 1000 Lives+ national programme’s RHAI we sought to gauge key actors’ perceptions of the structural elaboration or reproduction that had manifested under a situational logic of protection. For consultant microbiologists, attributing improved outcomes in HCAIs to 1000 Lives+ or RHAIs was considered to be very challenging, owing to the interplay and collective impact of multiple IPAC policies on WHAIP’s robust epidemiological modelling (transcription 8:41, below).
If you’re looking at say, catheter care policy, now, looking for it to reduce catheter-associated UTIs [urinary tract infections] then that’s going to be a small subset. So, it’s very, very difficult to be able to draw and demonstrate a reduction. It’s technically possible, if you have a big enough study population. However, practices in hospital are not static, things change, for the better, for the worse, for a whole host of reasons, and controlling any one aspect through 1000 Lives+ policy, or something of that nature, that may have one impact but there may be contrary aspects that the main path is working on. So, it can be, I think, very challenging, and very difficult to really show a reduction and improvement in outcomes.
Consultant microbiologist, case site A1 (035); transcription 8:41
Structural change was apportioned to the ward-based functional health-care team. In enacting RHAI and other IPAC guidelines, such staff not only delivered change (transcription 8:42, below), but were continually motivated to do so through fear of exposure of failings (transcriptions 8:43 and 8:44).
Our C. difficile rates have actually gone down, a reduction again on last year. So it’s good. But, you know, that’s where our support and advice has come in. But at the end of the day, in infection control, we’re not there on the coalface, if you like, it’s the staff who put that into practice, into place, you know, they carry on with what we advise. So, you know, a lot of the hard work is down to them.
Nurse, IPAC, case site D2 (019); transcription 8:42
Cultural change, by contrast, was perceived to be far more marked, with a professional logic of zero tolerance of HCAIs emerging across NHS Wales, although it remained far removed from the reality of day-to-day health-care practice (transcription 8:45, below).
I think the culture is changing, I mean, I’ve seen it in the short time I’ve been in infection control, the ownership at ward level for infection control has shifted. Whereas, you know, if there was a problem on the ward, often the wards wouldn’t call us, so we would find out by our surveillance!
But now wards are contacting us to say: ‘I think we’ve got a problem’, so there’s the acceptance of their role in infection prevention and control. Before, for Clostridium difficile, it was accepted that it’s just a consequence of being in hospital – the attitude was: ‘what do you expect, you’re going to have antibiotics, you’re elderly, you’re bound to get it’ – but that is changing now. Now people are saying: ‘no, they shouldn’t be getting a health-care-associated infection, it’s just not good enough’. There should be zero tolerance on infection, health-care-associated infection. [But they still happen, don’t they? And patients still die as a consequence, don’t they?] Yes. [Long pause] But I think at ward level staff now are not accepting that patients should acquire an infection as a result of being in hospital.
Nurse, IPAC, case site B1 (131); transcription 8:45
In addition, though tangential to RHAI, the normalisation of the 1000 Lives+ MI-PDSA approach was evident (transcriptions 8:46 and 8:47). However, the crux of such cultural change lay in the education of staff (transcription 8:48, below, and transcriptions 8:49 and 8:50).
Education is key, too, not just education for the sake of antibiotic education but to change the culture. But, again, we face a huge problem here as the attitude is: ‘well, what’s the problem; why do we need to change how we do things; the evidence is weak’, it’s always the same.
I don’t want to sound cynical, I don’t. I love my job. But getting people to change is difficult, especially doctors, though they do know that I know what I’m on about. But we go through the same issues with each junior doctor rotation – I feel that I have to re-prove myself to them because they prescribe, wrongly – I know what they should be prescribing better than they do. So, a large part of what I do is education, and not just about drugs.
[Do you think that the junior doctors respect the work you do?] If they’re arrogant, and think they know it all, probably not; but they’re the most dangerous. Once you’re stopped them from killing a patient, once or twice; once they’ve realised how fallible they’re, and how, within the NHS, you’re lucky if you got a good team around you, who all know their own profession and offer different expertise, they start to listen. They’re not all like it, thankfully. Some are really good, and with more joint training early on in health-care professional careers, I think the issue of professional respect is getting better. But the best doctors are those that listen, and, more importantly, they ask for information and advice, they’re keen to learn, and you know they’re going to be good because they work constructively within the team. But with some with doctors, we often just get point blank refusal to co-operate.
[What are the consequences of this? How does the audit cycle, and associated governance processes intervene to feedback in such circumstances?] Well, the pharmacy audit will be sent to the medical director but, with the lack of prescriber identification, and data aggregation, it gets blunted.
Pharmacist, Antibiotics Medicines Management, case site C1 (013); transcription 8:48
1000 Lives+ institutionalisation: RHAI – local implementation of the focal intervention and contribution to the I–CMAO configuration spanning the Welsh health-care field
Our efforts to understand the local implementation of RHAI, and define its contribution to the 1000 Lives+ programmes’ I-CMAO configuration spanning the Welsh health-care field, were limited, as there was a profound sense of it being overshadowed by the complex array of established alternative frameworks and the ongoing surveillance of their effectiveness via the WHAIP. Indeed, RHAI was found to be, in some respects, a leftover theme from the predecessor 1000 Lives campaign. Furthermore, for some staff, the legacy effect of the Safer Patients Initiative was more pertinent. Consequently, though the institutional change inherent to formalisation shaped the situated context of action for all, the impetus of RHAI, nonetheless, dissipated.
Turning now to the findings of our realist analysis, we first consider, in Figure 22, the overall scheme of the intervention across the different structural contexts, focusing, for simplicity, on only one of the two processes researched in this part of the study, namely the appropriate use of antimicrobial drugs to ensure the effective prevention and treatment of infection.
FIGURE 22.
Reducing health-care-associated infection: heterarchical metamechanism operating across contextual strata – management of antibiotic drugs.
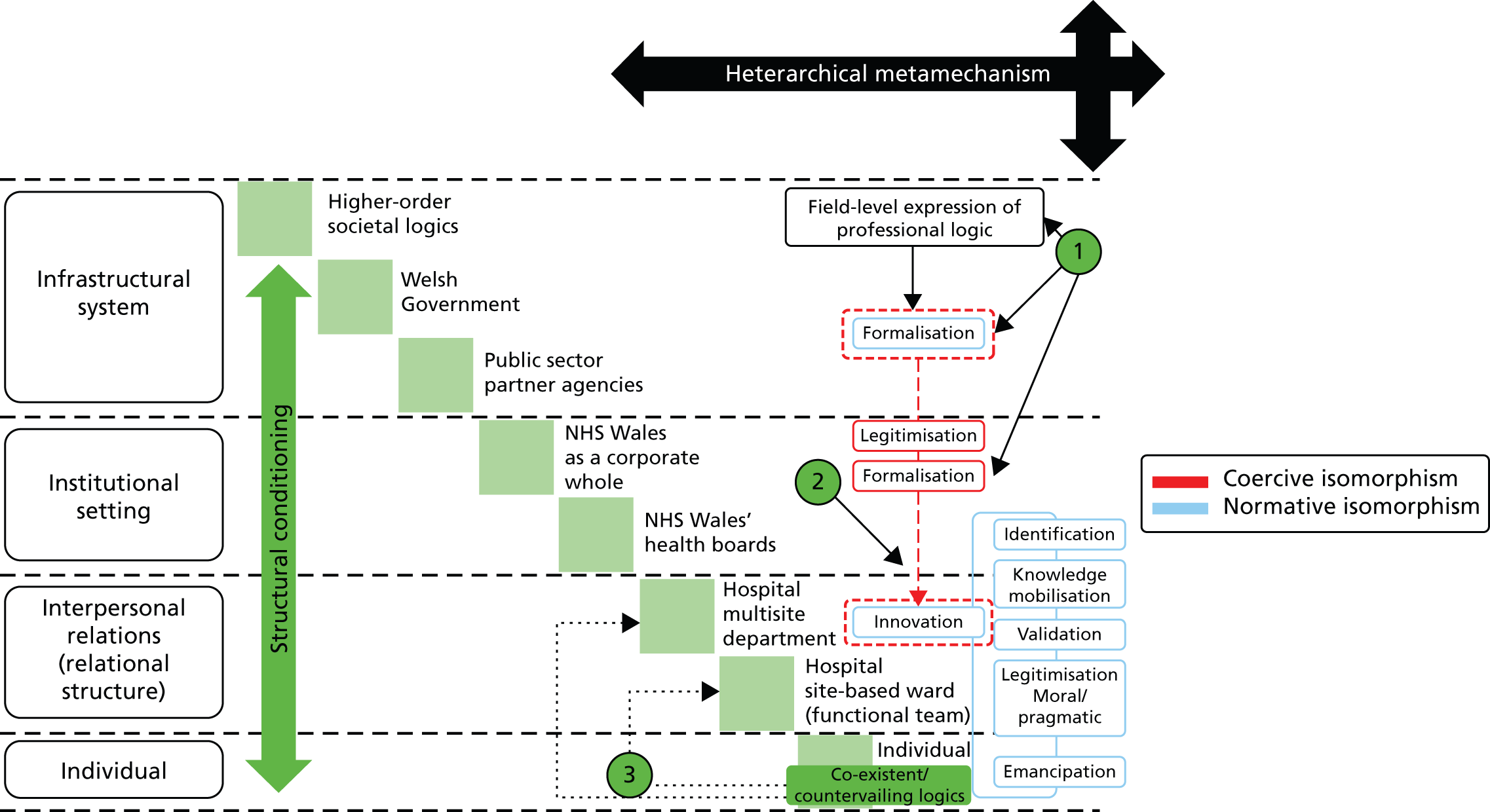
In Figure 22 we depict the implementation of local antibiotic guidelines in association with the RHAI focal intervention.
At point 1 we draw attention to the formalisation of this process via professional guidelines and Welsh Government policy, thereby mandating engagement by all health boards, health-care staff with prescribing privileges and pharmacists with expertise in antibiotics medicines management.
In point 2 we highlight that, although such practices are legitimate and formalised, under the 1000 Lives+ national programme they represent established practices which do not represent or drive innovation.
Point 3 highlights illustrates that such mandated engagement may be opposed across the micro-work system.
In Tables 28–30 we show, respectively, I-CMAO configurations for the implementation of RHAI, illustrating the infrastructural system of the Welsh Government, the institutional setting of NHS Wales and its constituent health boards, and interpersonal relationships within the institutional settings.
| Intervention | 1000 Lives+ national programme | |
|---|---|---|
| Component | RHAI | |
| Context | Welsh Government | |
| Mechanisms |
|
|
| Agency and institutional work | Normalisation: coupling to 1000 Lives+ and RHAI | Habituation: decoupling to 1000 Lives+ and RHAI |
|
|
|
| Outcome | 1000 Lives+ national programme and RHAI institutionalised into policy processes via WHAIP | |
| Exemplar transcriptions | ||
|
|
|
| Intervention | 1000 Lives+ national programme | |
|---|---|---|
| Component | RHAI | |
| Context | NHS Wales/NHS Wales’ health boards | |
| Mechanisms |
|
|
| Agency and institutional work | Normalisation: coupling to 1000 Lives+ and RHAI | Habituation: decoupling to 1000 Lives+ and RHAI |
|
|
|
|
|
|
|
|
|
|
|
|
| Outcome |
|
|
| Exemplar transcriptions | ||
|
|
|
|
|
|
|
|
|
|
|
|
| Intervention | 1000 Lives+ national programme | |
|---|---|---|
| Component | RHAI | |
| Context | Hospital multisite department/hospital site-based ward (functional team) | |
| Mechanisms |
|
|
| Agency and institutional work | Normalisation: coupling to 1000 Lives+ and RHAI | Habituation: decoupling to 1000 Lives+ and RHAI |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Outcome |
|
|
| Exemplar transcriptions | ||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Tables 31 and 32 report data relating to the incidence of two types of hospital-acquired infection made publicly available as part of the new emphasis on transparency in relation to patient safety.
| Health board | Monitoring period | ||||
|---|---|---|---|---|---|
| 1 April 2012 to 31 March 2013 | 1 April 2011 to 31 March 2012 | 1 April 2010 to 31 March 2011 | 1 April 2009 to 31 March 2010 | 1 April 2008 to 31 March 2009 | |
| Abertawe Bro Morgannwg University | 4 | 4 | 6 | 5 | 8 |
| Aneurin Bevan University | 4 | 5 | 4 | 5 | 8 |
| Betsi Cadwaladr University | 7 | 8 | 8 | 7 | No comparable WHAIP data |
| Cardiff and Vale University | 4 | 6 | 7 | 10 | 12 |
| Cwm Taf University | 5 | 4 | 4 | 9 | 8 |
| Hywel Dda | 4 | 6 | 5 | 7 | 8 |
| Powys (Teaching) | 0 | 0 | No comparable WHAIP data | No comparable WHAIP data | No comparable WHAIP data |
| Health board | Monitoring period | ||||
|---|---|---|---|---|---|
| 1 April 2012 to 31 March 2013 | 1 April 2011 to 31 March 2012 | 1 April 2010 to 31 March 2011 | 1 April 2009 to 31 March 2010 | 1 April 2008 to 31 March 2009 | |
| Abertawe Bro Morgannwg University | 26 | 24 | 21 | 24 | 22 |
| Aneurin Bevan University | 23 | 23 | 23 | 25 | 26 |
| Betsi Cadwaladr University | 23 | 26 | 26 | 25 | No comparable WHAIP data |
| Cardiff and Vale University | 27 | 26 | 30 | 29 | 32 |
| Cwm Taf University | 20 | 15 | 15 | 24 | 23 |
| Hywel Dda | 30 | 25 | 26 | 28 | 26 |
| Powys (Teaching) | 1 | 1 | No comparable WHAIP data | No comparable WHAIP data | No comparable WHAIP data |
Finally, in Table 33, we present our realist analysis linking the empirical data to I-CMAO.
| Intervention | RHAI | |
|---|---|---|
| Component | Antibiotics medicines management | |
| Context | Structural conditioning of the institutional setting: NHS Wales health boards’ implementation of 1000 Lives+ national programme’s RHAI | |
| Structural emergent properties |
|
|
| Cultural emergent properties |
|
|
| Social actors |
|
|
| Social position |
|
|
| Role-position practices |
|
|
| Mechanism | Mediation of structural conditioning to core actors and their reflexive theorisation | |
| Institutional logics and nature of alignment between core actors | For this professional group, their agential activity therefore manifested under a professional (pharmacy) logic that, though co-existent to others in the field, express disregard for the RHAI | |
| First-order emergents | The vested interests of pharmacists with expertise in antibiotic medicines management was poorly aligned to the RHAI as it was perceived to lack relevance | |
| Second-order emergents | The RHAI emerged into a context moulded by internal and necessary linkages of a complementary nature to extant structures. The RHAI was integrated into the social system-level but, in so doing, it was overshadowed. Though internal and necessary complementarities manifested between the RHAI and the array of professional logics in play, this was tainted by disregard | |
| Situational logic | Protection (of status quo ante) | |
| Reflexive theorisation | Although the RHAI emerged into a context moulded by internal and necessary linkages of a complementary nature to extant structures – thereby in alignment to the dominant logic of the bureaucratic state, and collaborative logic, and professional (pharmacy) logic – the reflexive theorisation that manifested was, as indicated above, not considered to add much to already existing principles and procedures and largely disregarded. Coherence, cognitive participation and reflexive monitoring were, therefore, anchored to the past, such that the discernment of issues, deliberation of their importance, and dedication of ensuing agency in alignment to the goals of the RHAI were superficial as, for these actors, little had changed | |
| Agency and institutional work | Agency, the unfolding strategic negotiation of change, and the mode of institutional work enacted | |
| Agential emergent properties | Agency was directed to the maintenance of practice | |
| Strategic negotiation |
|
|
|
|
|
| Institutional work | Primarily maintenance | |
| Outcome | Social elaboration or reproduction | |
| Structural | Reproduction | |
| Cultural | Reproduction | |
| Agential | Invariant | |
In this context, deinstitutionalisation did not occur. After all, no appreciable change to practice was required. As illustrated in Tables 31–33, RHAI placed emphasis on well-established health-care practices, each supported by a wealth of tacit knowledge and a burgeoning evidence base, which were institutionalised in NHS Wales. Hence the information offered by the discrete components of this intervention was neither new nor challenging to extant practice. Instead, these components were merely the continuation of standard precautions for hand hygiene, together with the ongoing debate on appropriate antimicrobial prescribing and the merger of guidelines that was required following the reconfiguration of NHS Wales.
In addition, the transcriptions set out in in Tables 28–30 depict high levels of decoupling. This finding is supported by the wider literature. For example, it is known that hand hygiene benefits from entrenched ideas about its meaning and broader social utility. 352 This most basic of practices, therefore, constitutes a cognitive and behavioural ensemble that demands little by way of organised competencies. 595,626 However, in order to be effective, hand hygiene must be enacted as a conscious activity. 630 But its broader social utility positions this practice as routine and somewhat mindless696 and habitual,697 which limits the individual’s reflexive monitoring and appraisal of the practice.
Moreover, as RHAI did not demand change, theorisation was not triggered, so that established factors inhibiting actors’ meaningful participation629,645,658 persisted. Compounded by environmental contamination,698 these factors encouraged the spread of nosocomial infection.
As illustrated in Table 33, and supported by the explanatory schematic Figure 22, our realist analysis adds insight. Centred on pharmacists with expertise in antibiotic medicines management, sociocultural interaction through the wide range of activities depicted in this study, though undertaken in logical alignment to the RHAI, were marred by the lack of appreciable change demanded. Indeed, only the new interventions, focused on the appropriate and timely use of invasive devices – specifically guidance aimed to reduce PVC and CAUTI – prompted cognitive participation and collective action to deliver change. Accordingly, little structural elaboration was displayed across each case site, compounded by the view expressed by some pharmacists that RHAI did not offer any substantive enhancement of their practice.
Summary
In Chapter 8, we furthered our understanding of the local implementation of the focal intervention RHAI and defined its contribution to the 1000 Lives+ programmes’ I-CMAO configuration spanning the Welsh health-care field.
Chapter 9 Discussion and conclusion
Overview
In this chapter we present the discussion and conclusion of our study. Here, the explicit intention is to move beyond simple iteration. We therefore present our closing argument in four main parts.
First, we return to the original research questions posed in the aim and objectives of this study and address them guided by our empirical findings. In this manner, we forward our conceptualisation of context, mechanism, agency and ensuing outcome, and develop insights from the local implementation of the three focal interventions selected from the 1000 Lives+ national programme: ILQI, RSC and RHAI. Second, we acknowledge the limitations of our study and set out our stance regarding the generalisability of our findings. Next, we consider the contribution of this study to the study of patient safety, outline the future outputs from this project and suggest areas for future research. Finally, we consider the implications of the research for health-care practice and patient safety.
Which contextual factors matter: how, why and for whom?
In this study, we sought to ascertain which contextual factors matter, how, why and for whom, in order that processes and outcomes of future patient safety programmes may be improved. Our study therefore deviated, quite markedly, from the traditional focus of realist inquiry, and the newly established RAMESES publication standards for realist syntheses (www.ramesesproject.org). Most significantly, our unit of analysis was the process of local implementation of the 1000 Lives+ programme, as opposed to the evaluation of the 1000 Lives+ programme per se.
Before we could begin to address this issue, the notion of context demanded clarification. As Bate699 has recently commented, context is everything. However, there has been very limited systematic and independent analysis of the relationship between organisational factors, which shape the local context of health care, and the outcomes of patient safety interventions. 124,216–223 In this study, guided by the established approach to realist inquiry,228,241,242,247 we specified four main levels of contextual hierarchy: infrastructural system, institutional setting, interpersonal relations and individual. All levels except the individual are divided into substrata (see Figure 5). Through this depiction we sought to capture and convey the accumulated sense of contextual constraints and enablements, structural and cultural, which impact differently positioned actors within the Welsh health-care field to shape their scope and perceived discretion to act. Context was, therefore, conceptualised as ‘situated’. By this we mean that context is stratified, conditioned, relational and temporally dynamic.
Importantly, our view of context was reflected in our findings. At the level of the functional team, context was perceived to be distinct from that of the wider organisation. Indeed, it resonated with that of a bounded health-care managerial or clinical micro-work system. 163,164,166,700–704 Accordingly, we suggest that this finding challenges the use of the health-care organisation as a unit of analysis for patient safety programmes, as adopted in this study and as advocated in the ‘four high-priority’ features of organisational context. 5,223,705 Indeed, our use of a comparative case-study design across major, district general and small community hospital sites within each participant health board was somewhat confounded.
In phase 1 of our analysis, despite the bureaucratic mandate to engage with the 1000 Lives+ programme that was evident at the field level of analysis (see Chapter 4), our examination of the normalisation of 1000 Lives+ at the suborganisational level (see Chapter 5) surfaced a complex pattern. At this level, discrete pockets of high adherence sat alongside areas of enforced but somewhat disengaged adoption. As such, even within case sites, it was not uncommon to find disparity between adjacent wards. In essence, two polarised types of situated context emerged. In the first type, 1000 Lives+ was normalised and absorbed into daily practice, becoming integral to care. In the second type of situated context, engagement with 1000 Lives+ was merely adsorbed (attached to but not fully integrated with) onto daily practice. It was then perceived to be an additional burden above and beyond the routine demands of health-care provision. The local implementation of the 1000 Lives+ programme was, therefore, positioned across a spectrum between these polarised stances. This highlights the transitional and fragile state of its progressive institutionalisation across NHS Wales. We therefore contend that focus directed at the level of the ‘micro-work system’163–170,706–711 may offer greater insight into the impact of patient safety improvement programmes at the point of patient-centred care. Indeed, this may even help to challenge Pawson’s iron law of evaluation: the expected value of any net impact assessment of any large-scale social program is zero. 241
Contextual organisational factors pertinent to the health outcomes of hospital patient safety interventions
In this section we build on our conceptualisation of a situated context. Informed by our realist analysis of the local implementation of the 1000 Lives+ programme’s three focal interventions – ILQI, RSC and RHAI – we identify and analyse the supraorganisational and organisational factors in the Welsh health-care field which are pertinent to the health outcomes of these hospital patient safety interventions.
What supraorganisational factors matter: how, why and for whom?
In this study, we have drawn on the long-held view that multiple institutional logics co-exist. 331 As illustrated in Figures 8 and 9, at the higher-order societal level, the balance between these logics shapes what is expected and accepted behaviour for broader society. Moreover, at the level of the Welsh health-care institutional field, their expression orchestrates the rituals, routines and practices constituting day-to-day professional work. 38 The interplay between logics and their inherent tensions give rise to the institutional complexity that all health-care practitioners confront. 712 Consequently, each individual – whether positioned as a policy lead in the Welsh Government, a health board chief executive or board-level director, or a hospital doctor, nurse or other aligned professional group – has to negotiate individually, and as part of a functional team, the consequences of countervailing, co-existent and complementary logics. Existence within such a system demands nuanced institutional work. This is typically executed through role and professional position-based power to attain a state of force majeure, or to broker a workable sense of reconciliation and compromise. 713
Our findings indicate that the precise balance of the institutional logics moulding the Welsh health-care institutional field impacts patient safety in a particular way. First, the paradigmatic logic of bureaucratic command and control, which fosters mandated engagement with 1000 Lives+ via coercive institutional isomorphism, structures the health-care policy context for elite individuals such as policy leads, members of public sector partner agencies tasked with the strategic oversight of patient safety and board-level personnel in NHS Wales’ seven health boards.
Although this logic was dominant at the level of the infrastructural system, as illustrated in Figures 8 and 9, professional logic was found to dominate contextual strata at sub-board organisational levels across each health board. This gave rise to conflict between logics. In the example of the mandated completion of the WHO checklist, cited in Chapter 7, while the moral and pragmatic legitimacy of the 1000 Lives+ programme was promoted by the logic of policy leads and health-care managers, it was challenged by the logic of some groups of health-care clinical professionals. Importantly, it was not the central issue of patient care that promoted such contestation, but the means through which it was imposed. Mandated engagement was perceived in a pejorative light as a means of management control that eroded professional autonomy: a core component of professional logic. 335,336 This created tensions that provoked decoupling from the goals and practices advocated by the 1000 Lives+ programme.
What organisational factors matter: how, why and for whom?
Our findings set out in Chapter 4 illustrated that the paradigmatic logic of bureaucratic command and control inculcated a pervasive performance measurement and management ethos across the Welsh health-care field. Mandated engagement with 1000 Lives+ was, therefore, legitimised as a core policy lever for health-care transformation. This clearly impacted on board-level actors in NHS Wales’ seven health boards. Specifically, it caused their actions to be directed to the (i) co-optation, negotiation and legitimisation of the distributed leadership of change across the relational structure of their personal managerial and professional networks; and (ii) the formalisation of patient safety governance processes, specifically the statutory Quality and Safety Committee, aligned to the Welsh National Quality and Safety Forum.
Such mandated engagement was, however, hindered by the challenges posed by the structural reconfiguration of NHS Wales. Indeed, our findings highlight that the emergence of health boards has (i) added management tiers, which now distort communication channels formerly shaped by proximity and close relational ties for health-care managers and health-care clinical professionals alike; and (ii) disrupted the relational structures of clinical micro-work systems due to clinical service reconfiguration across formerly distinct organisations. Furthermore, the profound challenges posed by the economic downturn impact patient safety and NHS Wales’ organisations engaged with 1000 Lives+ have to do ‘more with less’.
Reflecting on such issues at the level of the functional team added further insight into the nature of situated context. For example, the organisational factors impacting the focal intervention ILQI, set out in Chapter 6, were found to be closely integrated with the 1000 Lives+ programme’s position as a legitimised core policy lever for health-care transformation across NHS Wales. Formalised through the Welsh Government’s tier 1 targets, this structural constraint drove board-level engagement and severely limited the scope for decoupling. Moreover, it was compounded by demands for heightened transparency with respect to the publication of health board and discrete hospital site RAMI data (see Tables 14–20) and board papers conveying the use of patient stories.
In addition, in the aftermath of the Francis Report,714 cultural constraints and enablements centred on heightening awareness of systemic failings and the need to foster a culture of high-quality compassionate care. This gave rise to the institutionalised division of delegated strategic oversight of patient safety – and thus 1000 Lives+ and ILQI – to the directors of medicine, nursing, and therapies and health science. Given the board-level status and professional role-positions of such actors, the inherent change agenda overarching the 1000 Lives+ programme and, thus, the ILQI were executed from a position of high negotiating strength.
Structural elaboration was, therefore, displayed across each case site. Indeed, an objective outcome of the ILQI was the normalisation of the three practices examined in Chapter 6. In addition, the relational structure at each site had evolved, promoting the diffusion of the ILQI, and thus the 1000 Lives+ programme, while engendering a culture of organisational learning. However, cultural change was restricted by medical disengagement – notably via challenge to the moral and pragmatic legitimacy of some components of the 1000 Lives+ programme. The two key issues we identified were the burden of documentation and weak feedback from boards to wards.
The organisational factors impacting at the level of the functional team for the focal intervention RSC and the associated WHOSSC, set out in Chapter 7, were, once again, shaped by the bureaucratic processes of formalisation emergent from the infrastructural system of the Welsh Government’s Department of Health and Social Care. However, in this regard, the overarching policy mandate of the 1000 Lives+ programme was augmented by the compulsion to undertake the WHOSSC forwarded by professional Royal Colleges.
Cultural constraints and enablements centred on the institutional system emblematic of the theatre departments. Two critical features surfaced in this study were a sense of separation from the broader health board that was compounded by distinctive functional and dominant professional cultures.
In essence, the local implementation of the RSC and the WHOSSC demanded skilful brokerage of institutional change across two groups of theatre department staff. The first group were consultant surgeons who lacked the burden of managerial accountability for the implementation of the RSC and WHOSSC, and who, therefore, were, quite simply, participants in its local operationalisation. This group of actors viewed the change with a degree of disdain: ’It was all quite an interesting shambles actually. The senior people decided that they were above it all basically’. The second group were consultant surgeons, supported by theatre managers, who were explicitly tasked with the strategic oversight of the local implementation of the RSC and the WHOSSC. Given the professional role-positions of such theatre department actors and the inherent change agenda overarching the 1000 Lives+ programme, the RSC and the WHOSSC were executed through negotiated compromise through multimodal institutional work.
Once again, as set out in Chapter 7, structural elaboration was evident across each case site. This was illustrated by the integration of the WHOSSC into governance processes. However, the openly acknowledged decoupling from such governance processes distorted coherence and commitment to the RSC and the WHOSSC by diminishing it to a tick-box exercise. Such a contested change highlights the time demanded to bring discordant professional logics into alignment. It also underscores the complexity of the prolonged period of creative institutional work required to promote the desired coalescence and unification at the cultural system level.
In contrast, the organisational factors impacting the focal intervention RHAI centred on the complex array of established alternative frameworks and ongoing surveillance of their effectiveness via the WHAIP. This was compounded by different but interlocking professional roles across the local IPAC team. Accordingly, in such a situated context, no appreciable change to practice was required and deinstitutionalisation did not occur. The 1000 Lives+ programme and RHAI were, therefore, blunted through adherence to alternative frameworks of perceived heightened professional legitimacy via institutional maintenance work.
Mechanisms that interact with contextual organisational factors to generate the health outcomes of hospital patient safety interventions
In this section, first, we reflect on the notion of a mechanism. Then we set out how our findings have identified critical mechanism substructures which impact the local implementation of the 1000 Lives+ programme.
From mechanism to causal configuration
In realist inquiry, mechanisms are considered to be the engines of explanation embodied in an agent’s reasoning and their selective attention to the disparate resources offered through a social programme. 228,241,242 However, consideration of social actors’ contextually situated reflexive reasoning remains underdeveloped. 256 One reason for this arises from the inherent problems associated with unpacking and conceptualising reasoning, specifically as justifications for choices may operate within different, and often contradictory, stances. 321
The notion of ‘a mechanism’, in the sense of a unitary phenomenon, obscures its inherent structure and operation within a broader causal configuration. Hence, in this study, mechanism, while centred on agents’ reasoning, is theorised as part of a causal configuration emergent from a cluster of contextual factors and organisational components. These typically encompass a complex array of social structures, practices, relations, rules and resources. Yet, collectively, it is these factors which possess the powers, capacities and potentials to do certain things when operating in a spatio-temporal relationship with other objects. 306,309,310 Conceptualised in this manner, mechanisms, and their attendant causal I-CMAO (CMO) configurations, may be embedded in another or configured in a series, so that the outcome of one configuration becomes the context for the next in the chain of implementation steps. 307 This aspect of realist inquiry remains underdeveloped, as it demands the formulation of I-CMAO configurations, which pervade and connect contextual strata, in the form of bidirectional (top-down and bottom-up) nested causal cascades or metamechanisms. 316–318
In this study, our aim was to contribute to these conceptual challenges by examining the nuanced demarcation between context and mechanism across defined yet linked contextual strata, each involved in the operationalisation of the 1000 Lives+ programme within the Welsh health-care field. Hence, to examine the process of the local implementation of this complex and ambitious patient safety programme, we drew on two fundamental institutional processes – bureaucratisation and normalisation – which, we argue, operate as sociocultural and organisational metamechanisms. Bureaucratisation and normalisation, therefore, act as the underpinning carriers347 of the processes of health-care institutional change and ensuing practice-based change advocated by 1000 Lives+. In essence, it is through successful embedding within these fundamental metamechanisms that the patient safety programme becomes institutionalised.
Our findings from Chapters 4–8 illustrated three mechanism substructures, which collectively compose core components of the causal configuration for the local implementation of the 1000 Lives+ programme and further enrich our appreciation of the complex interplay of context and mechanism.
Mechanism substructure I: institutional isomorphism – mimetic, coercive and normative – coupling and decoupling
Institutional theory has arguably become the dominant approach for the study of macro-organisational phenomena. 715 Indeed, in institutionally informed health-care research it is acknowledged that institutions are primary and mould the context in which the varied health-care actors’ interests operate. 716 Dominant institutional logics are, therefore, a critical field-level mechanism717 that focus attention on the manner through which the attendant ‘culture’718 influences lower-level organisational change. 719
As set out in Chapter 4, our findings indicated that, within the Welsh health-care field, institutionally prescribed values were orchestrated at field level and echoed at the organisational level of the Welsh Government and NHS Wales, though they manifested in a distinctive manner in functional subgroups. This stance has been identified in other complex, institutionally dense organisations. 720 However, it was the discrete professions embedded within this institutional field that operated as the ‘pre-eminent institutional agents’, enacting isomorphic institutionalism through mimetic, coercive or normative means. 404,721 Furthermore, our findings highlight that such institutional work engendered legitimacy which impacted strategy and culture as well as associated structures and processes, in part, due to the statutory accountabilities and governance structures enmeshed with patient safety practices across NHS Wales.
Voronov et al. 722 have identified the important role of ‘glocalisation’ – fidelity to global norms with aligned adaptation to local conditions – in institutional maturation and change. In our study, this effect was apparent in the transmission of the IHI patient safety practices via mimetic isomorphic forces, driven by the dominance of the IHI’s position and their acceptance by elite institutional actors with close professional ties to policy leads within the Welsh Government. Indeed, our data highlighted that for social actors embedded within the policy domain of the Welsh Government, mimetic isomorphic forces drove acts of imitative entrepreneurship even for those who expressed questions over the legitimacy of the 1000 Lives+ programme. Mimetic isomorphism also arose through the institutional work of ‘believers’ in the 1000 Lives+ programme’s ethos and values, thereby catalysing co-optation and engagement of others. Yet despite the salience and assumed core values enshrined in the notion of patient safety, this institutional mechanism, as previously illustrated by Van Wijk et al. ,723 was marred by the disruptive distributed brokerage of change.
Coercive institutionalism was apparent throughout our study. It emerged from dominating organisational structures tied to health-care policy, health board performance and the ‘legitimating rhetoric’724 of governance – external and internal – of patient safety. Yet this, too, was challenged by professional, predominantly medical, power-based structures of membership and specialism identity. 725
In addition, isomorphic institutionalism through normative means was apparent in some long-established interventions, which had previously operated under the banner of the 1000 Lives campaign and, indeed, the Safer Patients Initiative, together with others associated with the 1000 Lives+ programme. However, as illustrated in Chapter 5, such normalisation was fragmented and isolated in discrete pockets.
Normalisation of the 1000 Lives+ programme was also associated with clear leadership of change, internal health-care practice maturation emergent from the MI-PDSA approach, and complex ‘boundary brokerage’34,91,726 to signal an identity for the programme, its adherents and associated health-care practices. The creative institutional work required to change beliefs, values and, through time, associated norms of practice was frequently displayed by actors occupying hybrid professional roles, including nurse-managers, associate directors with dual management and clinical portfolios, and board-level clinical practitioners. This finding parallels that of Reay et al. 222,408
Our findings illustrated that, while the local implementation of the 1000 Lives+ programme fostered strong institutional coupling that was moulded by the institutional isomorphism inherent to its bureaucratisation and normalisation, the operationalisation of 1000 Lives+ in everyday practice was distorted by adaptive and maladaptive decoupling.
Adaptive decoupling arose in the focal intervention RHAI, as already established alternative IPAC guidelines and the ongoing surveillance of their effectiveness via the WHAIP were perceived to offer more rigor and, thus, heightened legitimacy across the core professional groups examined in our study. Hence given the embedded nature of such alternatives, and their aligned clinical practices, the 1000 Lives+ programme was simply circumvented.
In contrast, maladaptive decoupling was apparent in the local implementation of the focal intervention RSC, centred on the WHOSSC. Given the Welsh health-care policy commitment to this practice, as well as its world-wide professional advocacy,439,565,727 it is worth considering the means through which such maladaptive decoupling manifested, that is, the simple and common failure to identify the members of the theatre team in the checklist. This practice reduced the possibility of individuals being blamed for any failures, undermining belief in the WHOSSC as a meaningful practice. Indeed, such disruptive institutional work diminished the legitimacy and moral foundation of the practice and hindered the remoulding of underlying belief systems. Perceived as a threat to the entrenched professional dominance of surgeons, the resistance rendered the WHOSSC down to a tick-box exercise which was interpreted by respondents to demonstrate that it was having little effect on reducing error ’. . .across NHS Wales we’ve had disasters even with the checklist being used: wrong site surgery, instruments left in, etcetera . . . In other words it’s not being used properly’.
Mechanism substructure II: alignment of institutional logics – countervailing, co-existent and complementary – and ensuing coherence, cognitive participation and reflexive monitoring
At the level of the Welsh health-care institutional field, the nature of the alignment of institutional logics - be they complementary, co-existent or countervailing – impact patient safety. As discussed in Contextual organisational factors pertinent to the health outcomes of hospital patient safety interventions, What supra-organisational factors matter: how, why and for whom?, and as illustrated in Figures 8 and 9, this centred on the interplay of the logic of the bureaucratic state and professional logic. However, previous studies have illustrated that, within health care, professional logic does not manifest in unitary manner. 37,38,222,373,728 Rather, different interprofessional logics and attendant institutions are displayed, each connected by some semblance of an overarching ‘logic of care’. 373
Our findings illustrated the dynamic and complex nature of this relationship. When a complementary alignment of professional logics arose, as in the case of the focal intervention ILQI, coherence, cognitive participation and reflexive monitoring of the health-care practices advocated by the 1000 Lives+ programme was fostered, thereby aiding its normalisation in daily practice. In contrast, a countervailing alignment of logics, or their mere co-existence, was found to have stymied normalisation. Such varied permutations may be found both between different health-care professional groups, and within a discrete health-care professional group, and are typically dependent on two factors. The first is variation in individual practitioners’ reflexive theorisation, encompassing their discernment of the patient safety practice in question, deliberation over the issues and dedication to a chosen action guided by their situational logic. The second factor is variation in the situational logic apparent at the level of the functional team.
Normalisation, a pivotal stage of institutionalisation, was therefore found to be dependent on the actions of those who were the ‘believers’: perceiving meaning in 1000 Lives+ due to alignment with the beliefs and values of their professional logics. When such coherence manifested, it promoted cognitive participation and reflexive theorisation in the individual and, importantly, at the level of the functional team, building commitment and co-ordinated engagement with the programme across the bounded clinical micro-work systems. Underscoring the fundamental role of leadership and effective teamwork to orchestrate the actions of the functional team, such processes were central to local innovation and adaptation of the health-care practices advocated by 1000 Lives+ and appeared to be a viable means of developing micro-competences across the functional team.
Mechanism substructure III: relational structure – role position-practices and profession – and the power to change health-care practice
Across Chapters 4–8, our findings highlight the role of the relational structure of the functional team in the local implementation of the 1000 Lives+ programme. This mechanism substructure places attention on the human relationships. By this we mean the ties that bind the functional team, its orchestrating situational logic, ethos and values, and the presence of hierarchical or distributed leadership. 729,730 These factors collectively impact team-level performance and, in turn, patient safety. Hence relational structure is moulded by the interplay of role position-practices and profession within the multidisciplinary team, and the power to change health-care practices is aligned to leadership functions across managerial and clinical micro-work systems.
In Chapters 4–8, those in professional role-position practices shaped by high levels of social capital – typically board-level managers and consultant medical or surgical health-care practitioners – were found to have had a valued role to play in reconfiguring other actors’ belief systems to support the local implementation of 1000 Lives+. Our findings therefore echo those that recognise the role of managerial, medical and nurse leadership in patient safety, especially in the brokerage of change across different functional teams. 34,731,732 Despite this, there were some such actors who, as the following comment illustrates, overtly rejected the 1000 Lives+ programme: ’The 1000 Lives+ national programme and the campaign – it’s command and control rather than a grass roots culture change – it hasn’t been created by the people. It’s not of the people. It’s an imposition. It’s control. It’s from Cardiff. It’s very much a Cardiff thing that is being pushed to everyone else because: “we know better”. Outside Cardiff, it feels remote and distant and not part of us, it’s something that we all recognise as important, clearly, but we don’t necessarily own it’.
However, such demonstrable leadership was not the exclusive jurisdiction of high-status actors. Social actors across an array of managerial and clinical roles, who expressed their belief in the 1000 Lives+ programme and actively engaged in creative institutional work to imbue a similar sense of meaning in others, were undeniably central to the local implementation of 1000 Lives+ and the ongoing discourse of patient safety across NHS Wales. This was expressed in the view that ’Clinical leadership is key – credible clinical leadership – and that’s all about empowerment of Band 7 nurses’, underscoring the empowerment and emancipation of those in roles traditionally subordinate to the profession of medicine. Therefore, in supporting staff at all levels, an important outcome of the 1000 Lives+ programme was the progressive erosion of entrenched professional barriers that prohibit challenge and scope for health-care practice change.
Mediation and reflexive theorisation
In defining such mechanism substructures, our findings help to reveal how the structural constraints and enablements of context are mediated to social actors engaged in the local implementation of the 1000 Lives+ programme. As expanded in Chapter 2, these influences give rise to four potential second-order emergents, which foster the accompanying situational logics of protection, correction/compromise, opportunism and elimination, thereby guiding the generative mechanisms in play.
Our findings illustrated that the focal intervention ILQI drew professional logic into alignment with that of the bureaucratic state. This fostered the systematisation of 1000 Lives+ and ILQI across the cultural system level of NHS Wales and promoted the reproduction of such practices across each health board. Consequently, at board level, ILQI operated under a situational logic of protection that guided sociocultural interaction, agency, strategic negotiation and ensuing modes of institutional work.
The focal intervention RSC, centred on the local implementation of the WHOSSC, confronted a more contested terrain, with the coalescence and cohesion manifest between the views of theatre managers, consultant surgeons tasked with the implementation of the WHOSSC, and theatre nurses, stymied by the countervailing stance adopted by some surgeons. These constraining contradictions (necessary incompatibilities) between the dominant logic of the bureaucratic state and aligned professional health-care management logic versus that of professional medical logic held by surgeons opposed to the introduction of the WHOSSC therefore created a situational logic of correction/compromise. This logic guided sociocultural interaction, agency, strategic negotiation and ensuing modes of institutional work along its disrupted path.
The focal intervention RHAI emerged into a context moulded by internal and necessary linkages of a complementary nature to existing structures. Nonetheless, a situational logic of protection of the status quo ante manifested. Reflexive monitoring was found to be anchored to the past, to preferred and more highly rated organisational and professional processes currently in use. Under these conditions, there was only superficial interest in and action to engage with RHAI.
Development and hypothesis testing of relationships between contextual organisational factors, mechanisms and the health outcomes of hospital patient safety interventions
In this study, we sought to develop and test hypothesis regarding the nature of the relationships between contextual organisational factors, mechanisms and the health outcomes of hospital patient safety interventions. Yet given the ontological commitment to critical realism, set out in Chapter 2 (see Addressing the challenges of realist enquiry, Realist social theory) and Chapter 3 (see Comparative case study approach, Ontological and epistemological alignment to realist analysis), such hypothesis testing was markedly different from that commonly adopted in positivistic studies. In essence, our approach centred on the progressive explanation and refinement of our understanding of the local implementation of the 1000 Lives+ programme, and the three focal interventions considered in more depth, all framed through our I-CMAO configurations.
Across Chapters 4–8, this approach revealed the nuanced relationships associated with the bureaucratisation and normalisation of the 1000 Lives+ programme, as illustrated in the explanatory schematics and accompanying data tables. What emerged from our data was the role of structural and cultural conditioning on the individual, embedded at the level of the functional team – managerial and clinical – and their ensuing disposition and scope to act to effect institutional change in support of patient safety. Such social structure, understood as the internal and necessary relations between social positions and positioned-practices, gave rise to emergent causal powers as the material cause of social activity. 733–735 Perceived through our non-reductionist critical realist ontological stance, patient safety is, therefore, an emergent property of the micro-level organisation of health care.
In examining the bureaucratisation and normalisation of the 1000 Lives+ programme, together with the local implementation of the three focal interventions selected, the underpinning role of the MI-PDSA approach, depicted in Figures 2–11, was revealed. 1000 Lives+, together with this core resource, were found to have become ’part of the patient safety language of NHS Wales’ . . . ’PDSA cycles and all of that stuff it’s created a language that they like: it’s language that they all understand’. That, supported by the 1000 Lives+ dedicated website, and aligned resources from Improving Quality Together and Patient Safety Wales, now provide the means to spread such practices across NHS Wales.
However, although innovation through identifying failings and honing local knowledge and skills to change health-care practice was evident throughout our study, there were those who challenged the evidence that the programme was working: ‘The evidence-base for the 1000 Lives+ national programme has been systematically attacked by the other factions – for one side, it’s evidence and truth; for the other, it’s spin and fluff – and reality is caught in the middle’.
Limitations of the study
Although we contend that our realist analysis framework presents an innovative and suitable means to address the research questions posed, we must acknowledge inherent limitations. There are three main sets of limitations to this work: (1) those posed by the processs of realist analysis itself, (2) those consequent on any qualitative social science research, and (3) those posed by a lack of the type of quantitative data which would have added further validity to our findings.
The most significant limitation in producing a narrative which is true to the tenets of critical realism is in the abstraction, abduction and retroduction inherent to the data analysis. Abstraction draws out the various components within the situated context, facilitating the conceptualisation of their interplay, through combination and interaction, so that the researcher may gain new insight. 310 Abduction involves the production of an elementary account of a basis process or mechanism. 363 Retroduction builds on this analytical stage. The aim is to reconstruct the basic conditions for such phenomena to be what they are, so fostering knowledge of the transfactual conditions, structures and mechanisms in play. 363 In this study, this process was aided by the hierarchical bureaucratisation of the Welsh health-care institutional field, which facilitated the explication of the internal and necessary relationships underpinning structural and cultural emergent properties.
To be adequate, as noted by Herepath,342 this approach must abstract from particular conditions, excluding those which are believed to have no significant effect, in order to focus on those which do and identify relations of different types: ‘substantial’, ‘formal’, ‘external or contingent’ and ‘internal or necessary’. 310 Only once this step has been achieved may it be possible to combine or synthesise the various separate understandings into a unity that reconstitutes, or provides a better understanding of, the concrete. 736 Thus, an explanatory structure is devised through a combination of theory and experimental observation. 228
Inevitably, such analysis is open to the criticism that, as it must be influenced by the investigator’s perspective, beliefs and experience, the data represent only individual interpretation. To counter such criticism we made considerable efforts to ensure the data collected were as robust as possible. We achieved this triangulation of data collection by accessing documentary evidence and conducting on-site observation, as well as interviewing a large and varied number of individuals.
A further limitation of our study is our inability to derive detailed linkage of quantitative data to the qualitative data relating to each specific intervention studied. Paradoxically, given the engagement in the study of all seven of the health boards in NHS Wales, detailed linkage of quantitative data was prohibited as it would have proved impossible to ensure anonymisation at organisational, hospital case site and individual level. The best we were able to do was to accommodate for this deficit by giving illustrative public source data for each health board, as set out in Tables 14–20 (RAMI data), Tables 25 and 26 (‘never events’ across NHS Wales’ health boards) and Tables 31 and 32 (MRSA per 100,000 bed-days and S. aureus per 100,000 bed-days).
Possible applications
As this study centred on the local implementation of the 1000 Lives+ national patient safety programme across NHS Wales, a substate nation with devolved oversight of health-care policy, it is pertinent to consider to what extent our findings may be applicable to other developed or developing health-care systems.
There is, of course, a global debate on patient safety, and patient safety programmes have been widely integrated into developed health-care systems on a world-wide scale. In that sense, some of the processes and practices seen in our study of the implementation of 1000 Lives+ in NHS Wales may well be identified in other settings and, therefore, offer insights into other similar processes and practices elsewhere. Nevertheless, the extent to which our findings may be directly transferable to other health-care systems implementing major programmatic changes is limited by a number of factors.
First, as presented in Chapter 4, NHS Wales is shaped by a distinctive health-care policy trajectory in which engagement with the 1000 Lives+ programme is mandated and monitored. This created a health-care institutional field moulded by coercive isomorphism in addition to the normative and mimetic modes more typical to studies of the diffusion of patient safety practices. 358
Furthermore, the study period overlapped the period of transition following the reconfiguration of health services in Wales. As such, health boards, through the merger of other former NHS Wales’ hospital trusts with primary care organisations, were newly established. Each organisation, therefore, confronted a strategic agenda burdened by the managerial demands of reconfiguration, including change to management cadres and clinical director roles, together with the politicised and public constraints fostered through the ongoing reconfiguration of hospital service provision across each territory. Though such circumstances are far from unique in developed health-care systems, they were distinctively shaped by the particular context of health care in Wales, and these factors do limit the degree to which the lessons learned from this study may be transferable to other settings.
Another limitation of applicability is that, although in our research protocol our case site selection criteria encompassed a major hospital, an intermediate hospital and a small local community hospital within each health board, to offer a desirable mix of different organisational features the strategic oversight of the 1000 Lives+ programme and its leadership was predominantly centred within the major hospital sites. Indeed, the 1000 Lives+ programme was, ostensibly, acute in its focus, with fewer interventions applicable to small case hospitals. This limited our scope to explore the implementation of each focal intervention across the range of organisations. Our findings are, therefore, more broadly applicable to large and intermediate hospital settings.
Case study participants were initially selected by the research team’s local contact at each case site and, thus, a degree of bias must be acknowledged. However, we sought to mitigate this issue through our use of a snowball sampling strategy, as discussed in Chapter 3. As evidenced by the candid and occasionally very blunt comments embedded in Chapters 4–8, the research team is confident that the data collected accurately represented the views of those interviewed, although, as a degree of self-selection was involved, we cannot discount the possibility that others who were not interviewed might have held different views.
Despite these caveats, however, we would argue that, at the micro-level of functional teams in wards and departments, the processes and practices of implementation identified in this study may well mirror those to be found in similar circumstances in other health-care systems, and that our findings may thus have relevance and offer lessons to be learned elsewhere.
Contribution of the study to patient safety research
This study offers conceptual, methodological and empirical contributions to patient safety research. In conceptual terms, we developed a theoretically grounded and evidence-based realist model of which organisational factors matter, how they matter and why they matter. To do this, we introduced conceptual resources from sociological institutionalism and Archerian critical realism to address challenges associated with applying realist inquiry. Our model incorporates four elaborations of the established approach to realist inquiry.
First, so that we may understand precisely ‘what’ is working, for whom, how and in what circumstances, we include intervention as a separate analytical category in our realist analysis. Second, we forward a view of ‘situated context’ as stratified, conditioned, relational and temporally dynamic. This involves identifying the dominant structural and cultural emergent properties in play and separating context from its mediation. Third, we apportion mediation and reflexive theorisation to mechanism. In this manner, we distinguish the conceptual elements of mechanism from its ensuing outcomes, which include the agential emergent properties, expressed through the unfolding strategic negotiation of change, and the mode of institutional work enacted, to deliver sustainable outcomes, be they elaborative or reproductive. This fine-grained realist analysis therefore explicates the fundamental role of beliefs and values – institutional logics – on the propensity to act, to reveal the contested nature of institutional change, health-care practice evolution, and thus social elaboration or, indeed, reproduction. Finally, in our realist analysis framework, outcome is not perceived as a simple, single aspect of change, such as a defined health outcome. Rather, we reveal structural and ideational differentiation, together with the regrouping inherent to the power play of the diverse array of agents embroiled in the institutionalisation of a complex patient safety improvement programme.
In methodological terms, this is one of the first studies of patient safety to apply realist philosophy of social science across inception, design, fieldwork, analysis and writing. This has generated a number of features that may inform and challenge the field of patient safety research.
First, in contrast to the majority of health services research studies, this study has taken seriously, and explicated, realist epistemology and ontology. These foundations of our research conditioned its design, conduct and reporting. They helped shape our concern for ontological depth and contextual strata, and they directed us towards the identification and explanation of the underlying generative mechanisms which shape structure, agency, social relations and the ensuing practices that are reproduced and/or transformed. In terms of analysis, this is one of the first health services research studies to conduct abstraction, abduction and retroduction363 to devise an explanatory structure through a combination of theory and experimental observation. While we have earlier noted the challenges posed by this approach, we believe that this study has demonstrated the value of the analytical approach in helping to reconstruct the basic conditions for focal phenomena to be what they are, so fostering knowledge of the conditions, structures and mechanisms in play. In addition, the conclusions of our realist analysis are recognised to be both provisional and fallible.
In terms of empirical contribution, for each of the three focal interventions of 1000 Lives+ programme, this study offers a nuanced explanation of how local conditions relating to each level of our stratified model of context differentially combine with mechanisms (the engines of explanation embodied in people’s reasoning) to derive outcomes in terms of structural and cultural reproduction or change. Reflecting social reality, these causal configurations are complex and nested. To aid our elucidation of these configurations we augment our textual description with a series of graphics. This approach to presentation of our findings allows us to clearly specify how particular configurations of factors across multiple layers of context (e.g. logics, power relations) combine with two metamechanisms (bureaucratisation and normalisation) and three submechanisms (isomorphism, logic alignment and relational structure) to generate outcomes that are variously viewed as more or less successful by multiple stakeholders.
We believe these findings will provide a valuable resource for policy-makers, managers and practitioners, locally, nationally and internationally, and will enable stakeholders to develop improvement interventions that are more likely to ‘work’ (for specified stakeholders) in their local contingent circumstances. They may also serve as a diagnostic tool to be used as a precursor to the design of more differentiated and context-sensitive interventions in future.
Future project outputs
This report addresses gaps in conceptual, methodological and empirical knowledge about the influence of context on the local implementation of patient safety programmes so that we may discern which contextual factors matter – how, why and for whom – in order that processes and outcomes of future improvement programmes may be improved. Future research outputs will seek to contribute to a broad range of academic and professional literatures.
Active dissemination of emergent findings to academic audiences has commenced via participation in relevant national and international conferences [Academy of Management (US); British Academy of Management; European Group for Organizational Studies; Health Services Research Network; International Organisational Behaviour in Healthcare; International Research Society for Public Management]. Dissemination will now continue through the submission of papers to leading academic journals. The first of such papers is currently under review.
As well as disseminating our findings to academic audiences, we intend to work with case site organisations in NHS Wales and, potentially, to reach out to a wider audience in NHS England, through a series of interactive seminars for health-care policy and professional audiences. These discussions will be disseminated through publications targeted specifically at NHS professional audiences including, for example, the Health Service Journal.
Future research
While the work conducted in this study could be developed in a number of ways, we believe that three options are most promising.
First, although this study adopted the organisation as the primary unit of analysis, we now consider that the micro-work system – managerial and clinical – could be a more fruitful unit of analysis from which to develop further insight into the implementation of patient safety programmes. Indeed, this offers the potential to examine the complexity inherent to the delivery of patient-centred care across discrete care pathways, thereby spanning organisational boundaries between primary, secondary and, potentially, tertiary-based functional teams. Such an approach, we believe, will help to explicate the true demands of leadership, followership, and empowered and emancipated team working, which underpin health-care practice innovation and commitment to the delivery of health care of the highest quality for all.
Second, this study has placed great significance on the role of, and interplay between, logics operating across the multiple strata of our model of context. In our case based in Wales, a critical dynamic occurs between the field level, where the paradigmatic logic of bureaucratic command and control shapes the activity of elite actors, while actors at sub-board organisational levels are influenced primarily by professional logics. It will, therefore, be important to compare the processes and outcomes from that context with (i) settings with similar institutional arrangements (possibly Scotland), and (ii) arenas with alterative arrays of dominant logics across contextual strata (possibly England, where the dominant paradigmatic logic is competition augmented by devolution and transparency).
Furthermore, given the mandated nature of engagement with the 1000 Lives+ programme in our study, and the tensions thereby fostered for some health-care clinical professionals, it will also be important to compare future patient safety interventions which emerge at the level of the functional team so that their insights may be effectively harnessed and their diffusion aided within, and across, health-care organisations.
Finally, this study has illustrated the complex interplay that lies behind the 1000 Lives+ programme’s summary I-CMAO configuration. Indeed, it has exposed that distinctive ‘cultures of care’ emerged and operated throughout the local implementation of the 1000 Lives+ programme. These ranged from ‘discrete pockets of high adherence’ to situated contexts of ‘enforced but somewhat disengaged adoption’. This finding demonstrates the time and institutional work needed to achieve change amid competing priorities, contested professional values and notions of control. Future research should address the relational dynamics of the functional team within a situated context to refine our understanding of high-performing micro-work systems and thus penetrate beyond the illusory notion of a cohesive culture of care.
Priorities for practice
Below, we set out the implications of our findings for realist informed research and the design and operationalisation of complex patient safety interventions.
Realist analysis
The realist analysis undertaken in this study is different from established approaches to realist inquiry. It is neither a realist evaluation of the success or failure of the 1000 Lives+ patient safety programme, nor a realist synthesis of extant data to inform the future redesign of the 1000 Lives+ patient safety programme and associated policy in NHS Wales. Rather, as set out in in the introduction to this report, our approach to realist analysis defines an alternative means to analyse the complex interplay of this patient safety intervention within a specified ‘situated’ context. This creates challenges and opportunities for the field.
The challenges posed are primarily conceptual and methodological, and arise from the need to integrate distinct research traditions – realist inquiry, critical realism and institutional theory – with the information to be assimilated from aligned medical, health-care policy and health-care organisational and professional fields. However, we would argue that the opportunities offered by the adoption of our approach, and the generation of I-CMAO configurations within other studies, arise from the more nuanced understanding to be gained of the organisation and operation of developed health-care safety practices at the level of the functional team. This, we consider, possesses the potential to enrich our understanding of the emergence of patient safety as a dynamic capability within high-performing health-care teams, thereby informing the design of patient safety interventions.
Realist analysis: refinement of the concepts of context and mechanism
Our conceptual refinement of the situated context of care suggests that future patient safety research will need to consider context as more than a mere amorphous residual. While it may not be practicable for all research designs to actively embrace our stratified, conditioned, relational and temporally dynamic approach, a heightened awareness and account of context will foster cumulative insight and contribute to appreciation of the locus of change within complex health-care systems or discrete organisations.
Similarly, in future realist informed research, apportioning both the mediation of contextual forces and reflexive theorisation to mechanism will help to refine our understanding of what drives social agents – be they organisations, professions or individuals – to actively embrace and normalise a new patient safety practice or reject and retard such change. This will help to clarify the role of that such mechanisms play within larger and more complex causal configurations.
Realist analysis: refinement of agency and outcome
This study suggests that the combination of Archerian critical realism and institutional theory offers a robust means to examine mechanism across aligned or conflicted institutional logics in different organisational and professional jurisdictions. This feature of an I-CMAO configuration, therefore, helps to further inform our understanding of the operationalisation of patient safety practices, specifically by offering insight into the actions that unfold within and across functional teams. Accordingly, both patient safety research and the implementation of such interventions will benefit from an enhanced understanding of practice, centred on the unfolding strategic negotiation of change and mode of institutional work enacted to deliver sustainable outcomes.
Design of patient safety improvement programmes
This study demonstrates that complex patient safety interventions, though targeted at whole-systems or multisite health-care organisations, do not embed and normalise into practice in such a totalising manner. Rather, acceptance and adherence is piecemeal and fragmented. This suggests that their design may be more logically framed at the level of the functional team and associated discrete high-risk health-care practice. This has marked implications for the leadership of localised change and support provided, and the emancipation of front-line health-care professionals may further the development of innovative patient safety practices at the point of care.
Oversight of the implementation and operationalisation of patient safety improvement programmes
This study has demonstrated a significant cause for concern by capturing the ready acceptance of gaming,405 under a legitimacy façade, that obscures the failure to adhere to recommended patient safety practices. Such actions are diverse – ranging from hollow engagement with WalkRounds and disconnected recording of the WHOSSC in computer-based systems to the overt ‘performance’ of observed hand-washing – but they suggest the need for (i) clearly visible and meaningful leadership of patient safety and (ii) integration of the oversight of patient safety programmes into corporate governance and organisational development programmes, with ensuing accountability for performance and staff development. To this end, as outlined in Chapter 5 (specifically in the sections Putative mechanisms fostering and normalisation of 1000+ Lives, Cognitive participation and Collective action), cognitive participation is an essential component of collective action to ensure that systemic and organisational factors giving rise to patient neglect are addressed, while knowledge sharing and trust are enhanced.
Acknowledgements
We acknowledge the valuable advice received from members of our advisory group, namely Professor Graeme Currie, Warwick Business School; Mrs Janet Davies, policy lead, Welsh Government, and codirector of the 1000 Lives+ national programme in NHS Wales; Dr Andrew Goodhall, chief executive officer (CEO) of Aneurin Bevan University Health Board; Mr Bob Hudson, CEO of Public Health Wales; Mr Alwyn Rowlands, lay representative (NISCHR Involving People Programme); and Dr Neil McKenzie, lay representative (NISCHR Involving People Programme).
We are also grateful for the support of all the anonymous participants in the study. We benefited greatly from discussions with colleagues working on other NIHR research projects, notably at the events that brought teams together. We thank academic and administrative staff at NIHR for their expert support, especially Ruth Saw.
In addition, we wish to acknowledge the generous support and encouragement provided by Dr Andy Bailey, Director of the Sir Roland Smith Centre for Strategic Management, and designate Head of the Department of Entrepreneurship, Strategy and Innovation, Lancaster University Management School, who very sadly died on 28 June 2015. Requiescat in pace Andy.
The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the HSDR programme, NIHR, the NHS or the Department of Health.
Contributions of authors
Dr Andrea Herepath PhD MBA PhD, coprincipal investigator, Lecturer, Sir Roland Smith Centre for Strategic Management, Department of Entrepreneurship, Strategy and Innovation, Lancaster University Management School, Lancaster University, Lancaster, UK, and formerly Senior Research Fellow, Cardiff Business School, Cardiff University: participated in the design of the study, managed the study, conducted the fieldwork and analysis, and drafted the report.
Professor Martin Kitchener BSc (Econ) MBA PhD, principal investigator, Dean and Head of School, Cardiff Business School, Cardiff University: designed and led the study, oversaw the fieldwork and analysis, and contributed to the drafting of the report.
Professor Justin Waring BA MSc PhD, coprincipal investigator, Professor of Organisational Sociology, Nottingham University Business School, University of Nottingham: participated in the advisory board, contributed to the academic development of the project and commented on the draft report.
Data sharing statement
Owing to the nature of the study and condition of ethics approvals, we are unable to share data related to this study.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
References
- Kohn LT, Corrigan JM, Donaldson MS. To Err Is Human: Building a Safer Health System. Washington, DC: Committee on Quality of Health Care in America, Institute of Medicine; 2000.
- Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press; 2001.
- Wachter RM, Pronovost PJ, Shekelle PG. Strategies to improve patient safety: the evidence base matures. Ann Intern Med 2013;158:350-2. http://dx.doi.org/10.7326/0003-4819-158-5-201303050-00010.
- Vincent C. Science and patient safety. CMAJ 2013;185:110-11. http://dx.doi.org/10.1503/cmaj.120792.
- Shekelle PG, Pronovost PJ, Wachter RM, McDonald KM, Schoelles K, Dy SM, et al. The top patient safety strategies that can be encouraged for adoption now. Ann Intern Med 2013;158:365-8. http://dx.doi.org/10.7326/0003-4819-158-5-201303051-00001.
- Leape LL, Berwick DM. Five years after to err is human: what have we learned?. JAMA 2005;293:2384-90. http://dx.doi.org/10.1001/jama.293.19.2384.
- Øvretveit J. Contemporary quality improvement. Cad Saúde Pública 2013;29:424-6. http://dx.doi.org/10.1590/S0102-311X2013000300002.
- Marshall M, Pronovost P, Dixon-Woods M. Promotion of improvement as a science. Lancet 2013;381:419-21. http://dx.doi.org/10.1016/S0140-6736(12)61850-9.
- Luoto J, Maglione MA, Johnsen B, Chang C, Higgs ES, Perry T, et al. A comparison of frameworks evaluating evidence for global health interventions. PLOS Med 2013;10. http://dx.doi.org/10.1371/journal.pmed.1001469.
- Shekelle PG, Pronovost PJ, Wachter RM, Taylor SL, Dy SM, Foy R, et al. Advancing the science of patient safety. Ann Intern Med 2011;154:693-6. http://dx.doi.org/10.7326/0003-4819-154-10-201105170-00011.
- Vincent C, Batalden P, Davidoff F. Multidisciplinary centres for safety and quality improvement: learning from climate change science. BMJ Qual Saf 2011;20:i73-8. http://dx.doi.org/10.1136/bmjqs.2010.047985.
- Harvey G, Fitzgerald L, Fielden S, McBride A, Waterman H, Bamford D, et al. The NIHR collaboration for leadership in applied health research and care (CLAHRC) for Greater Manchester: combining empirical, theoretical and experiential evidence to design and evaluate a large-scale implementation strategy. Implement Sci 2011;6. http://dx.doi.org/10.1186/1748-5908-6-96.
- Rycroft-Malone J, Wilkinson JE, Burton CR, Andrews G, Ariss S, Baker R, et al. Implementing health research through academic and clinical partnerships: a realistic evaluation of the Collaborations for Leadership in Applied Health Research and Care (CLAHRC). Implement Sci 2011;6. http://dx.doi.org/10.1186/1748-5908-6-74.
- Martin GP, Finn R. Patients as team members: opportunities, challenges and paradoxes of including patients in multi-professional healthcare teams. Sociol Health Illn 2011;33:1050-65. http://dx.doi.org/10.1111/j.1467-9566.2011.01356.x.
- Boyne GA, Meier KJ. Burdened by bureaucracy? Determinants of administrative intensity in public organisations. Int Public Manag J 2013;16:307-27. http://dx.doi.org/10.1080/10967494.2013.817261.
- Andrews R, Boyne G. Structural change and public service performance: the impact of the reorganization process in English local government. Public Adm 2012;90:297-312. http://dx.doi.org/10.1111/j.1467-9299.2011.01956.x.
- Nutley S, Levitt R, Solesbury W, Martin S. Scrutinizing performance: how assessors reach judgements about public services. Public Adm 2012;90:869-85. http://dx.doi.org/10.1111/j.1467-9299.2011.02022.x.
- Martin S, Webb A. ‘Citizen-centred’ public services: contestability without consumer-driven competition?. Public Money Manage 2009;29:123-30. http://dx.doi.org/10.1080/09540960902768038.
- Ferlie E, Fitzgerald L, McGivern G, Dopson S, Bennett C. Public policy networks and ‘wicked problems’: a nascent solution?. Public Adm 2011;89:307-24. http://dx.doi.org/10.1111/j.1467-9299.2010.01896.x.
- Jonesa L, Exworthy M, Frosini F. Implementing market-based reforms in the English NHS: bureaucratic coping strategies and social embeddedness. Health Policy 2013;111:52-9. http://dx.doi.org/10.1016/j.healthpol.2013.03.010.
- Anand P, Exworthy M, Frosini F, Jones L. Autonomy and improved performance: lessons from an NHS policy reform. Public Money Manage 2012;32:209-16. http://dx.doi.org/10.1080/09540962.2012.676279.
- Walshe K, Shortell SM. When things go wrong: how health care organizations deal with major failures – important opportunities for improvement will be missed if we fail to investigate and learn from the ‘airplane crashes’ of health care. Health Aff 2004;23:103-11. http://dx.doi.org/10.1377/hlthaff.23.3.103.
- Berwick DM. Launching accountable care organizations – the proposed rule for the Medicare shared savings program. New Engl J Med 2011;364. http://dx.doi.org/10.1056/NEJMp1103602.
- Pronovost PJ, Berenholtz SM, Goeschel CA, Needham DM, Sexton JB, Thompson DA, et al. Creating high reliability in health care organizations. Health Serv Res 2006;41:1599-617. http://dx.doi.org/10.1111/j.1475-6773.2006.00567.x.
- Pronovost P, Sexton B. Assessing safety culture: guidelines and recommendations. Qual Saf Health Care 2005;14:231-3. http://dx.doi.org/10.1136/qshc.2005.015180.
- Exworthy M, Frosini F, Jones L. Are NHS foundation trusts able and willing to exercise autonomy? ‘You can take a horse to water . . .’. J Health Serv Res Policy 2011;16:232-7. http://dx.doi.org/10.1258/jhsrp.2011.010077.
- Fitzgerald L, Ferlie E, Addicott R, Baeza J, Buchanan D, McGivern G. Service improvement in healthcare: understanding change capacity and change context. Clin Manag 2007;15:61-74.
- Turner S, Ramsay A, Fulop N. The role of professional communities in governing patient safety. J Health Organ Manag 2013;27:527-43. http://dx.doi.org/10.1108/JHOM-07-2012-0138.
- Parand A, Dopson S, Vincent C. The role of chief executive officers in a quality improvement initiative: a qualitative study. BMJ Open 2013;3. http://dx.doi.org/10.1136/bmjopen-2012-001731.
- Fitzgerald L, Ferlie E, McGivern G, Buchanan D. Distributed leadership patterns and service improvement: evidence and argument from English healthcare. Leadership Q 2013;24:227-39. http://dx.doi.org/10.1016/j.leaqua.2012.10.012.
- Ferlie E, Crilly T, Jashapara A, Peckham A. Knowledge mobilisation in healthcare: a critical review of health sector and generic management literature. Soc Sci Med 2012;74:1297-304. http://dx.doi.org/10.1016/j.socscimed.2011.11.042.
- Veronesi G, Kirkpatrick I, Vallascas F. Clinicians on the board: what difference does it make?. Soc Sci Med 2013;77:147-55. http://dx.doi.org/10.1016/j.socscimed.2012.11.019.
- Chreim S, Langley A, Comeau-Vallée M, Huq JL, Reay T. Leadership as boundary work in healthcare teams. Leadership 2013;9:201-28. http://dx.doi.org/10.1177/1742715012468781.
- Long JC, Cunningham FC, Braithwaite J. Bridges, brokers and boundary spanners in collaborative networks: a systematic review. BMC Health Serv Res 2013;13. http://dx.doi.org/10.1186/1472-6963-13-158.
- Burgess N, Currie G. The knowledge brokering role of the hybrid middle level manager: the case of healthcare. Br J Manag 2013;24:132-42. http://dx.doi.org/10.1111/1467-8551.12028.
- Currie G, Lockett A. Distributing leadership in health and social care: concertive, conjoint or collective?. Int J Manag Rev 2011;13:286-300. http://dx.doi.org/10.1111/j.1468-2370.2011.00308.x.
- Reay T, Hinings CR. Managing the rivalry of competing institutional logics. Organ Stud 2009;30:629-52. http://dx.doi.org/10.1177/0170840609104803.
- Goodrick E, Reay T. Constellations of institutional logics: changes in the professional work of pharmacists. Work Occupat 2011;38:372-416. http://dx.doi.org/10.1177/0730888411406824.
- Travaglia JF, Nugus PI, Greenfield D, Westbrook JI, Braithwaite J. Visualising differences in professionals perspectives on quality and safety. BMJ Qual Saf 2012;21:778-83. http://dx.doi.org/10.1136/bmjqs-2011-051755.
- Parand A, Burnett S, Benn J, Pinto A, Iskander S, Vincent C. The disparity of frontline clinical staff and managers’ perceptions of a quality and patient safety initiative. J Eval Clin Pract 2011;17:1184-90. http://dx.doi.org/10.1111/j.1365-2753.2010.01506.x.
- Lockett A, Currie G, Waring J, Finn R, Martin G. The role of institutional entrepreneurs in reforming healthcare. Soc Sci Med 2012;74:356-63. http://dx.doi.org/10.1016/j.socscimed.2011.02.031.
- Wachter RM. Personal accountability in healthcare: searching for the right balance. BMJ Qual Saf 2013;22:176-80. http://dx.doi.org/10.1136/bmjqs-2012-001227.
- Corbett A, Travaglia J, Braithwaite J. The role of individual diligence in improving safety. J Health Organ Manag 2011;25:247-60. http://dx.doi.org/10.1108/14777261111143518.
- Batalden P, Davidoff F, Marshall M, Bibby J, Pink C. So what? Now what? Exploring, understanding and using the epistemologies that inform the improvement of healthcare. BMJ Qual Saf 2011;20:99-105. http://dx.doi.org/10.1136/bmjqs.2011.051698.
- Shojania KG, Dixon-Woods M. Bad apples: time to redefine as a type of systems problem?. BMJ Qual Saf 2013;22:528-31. http://dx.doi.org/10.1136/bmjqs-2013-002138.
- Vincent C, Davy C, Esmail A, Neale G, Elstein M, Cozens JF, et al. Learning from litigation. The role of claims analysis in patient safety. J Eval Clin Pract 2006;12:665-74. http://dx.doi.org/10.1111/j.1365-2753.2006.00634.x.
- Jeong HJ, Pham JC, Kim M, Engineer C, Pronovost PJ. Major cultural – compatibility complex: considerations on cross-cultural dissemination of patient safety programmes. BMJ Qual Saf 2012;21:612-15. http://dx.doi.org/10.1136/bmjqs-2011-000283.
- Dixon-Woods M, Leslie M, Tarrant C, Bion J. Explaining Matching Michigan: an ethnographic study of a patient safety program. Implement Sci 2013;8. http://dx.doi.org/10.1186/1748-5908-8-70.
- Sari A, Sheldon T, Cracknell A, Turnbull A, Dobson Y, Grant C, et al. Extent, nature and consequences of adverse events: results of a retrospective case note review in a large NHS hospital. Qual Saf Health Care 2007;16:434-9. http://dx.doi.org/10.1136/qshc.2006.021154.
- Hoonhout LHF, De Bruijne MC, Wagner C, Asscheman H, Der Wal GV, Van Tulder MW. Nature, occurrence and consequences of medication-related adverse events during hospitalization: a retrospective chart review in the Netherlands. Drug Safety 2010;33:853-64. http://dx.doi.org/10.2165/11536800-000000000-00000.
- Vincent C, Saunders A. Patients and doctors experiences of iatrogenic injury. Z Arztl Fortbild Qualitatssich 2004;98:593-9.
- Dolores Menéndez M, Rancaño I, García V, Vallina C, Herranz V, Vázquez F. Use of different patient safety reporting systems: much ado about nothing?. Rev Calid Asist 2010;25:232-6. http://dx.doi.org/10.1016/j.cali.2010.02.001.
- Asavaroengchai S, Sriratanaban J, Hiransuthikul N, Supachutikul A. Identifying adverse events in hospitalized patients using Global Trigger Tool in Thailand. Asian Biomed 2009;3:545-50.
- Donaldson L. Keynote Speech to NHS Confederation Annual Conference 2007. www.health.org.uk/nhs_managers.html (accessed 22 May 2008).
- Thomas AN, Taylor RJ. Review of patient safety incidents reported from critical care units in North-West England in 2009 and 2010. Anaesthesia 2012;67:706-13. http://dx.doi.org/10.1111/j.1365-2044.2012.07141.x.
- Patient Safety. London: The Stationery Office; 2008.
- Takata GS, Taketomo CK, Waite S. Characteristics of medication errors and adverse drug events in hospitals participating in the California Pediatric Patient Safety Initiative. Am J Health Syst Pharm 2008;65:2036-44. http://dx.doi.org/10.2146/ajhp070557.
- Dean B, Schachter M, Vincent C, Barber N. Causes of prescribing errors in hospital inpatients: a prospective study. Lancet 2002;359:1373-8. http://dx.doi.org/10.1016/S0140-6736(02)08350-2.
- McLeod MC, Barber N, Dean Franklin B. Methodological variations and their effects on reported medication administration error rates. BMJ Qual Saf 2013;22:278-89. http://dx.doi.org/10.1136/bmjqs-2012-001330.
- Avery AJ, Ghaleb M, Barber N, Dean Franklin B, Armstrong SJ, Serumaga B, et al. The prevalence and nature of prescribing and monitoring errors in English general practice: a retrospective case note review. Br J Gen Pract 2013;63:e543-53. http://dx.doi.org/10.3399/bjgp13X670679.
- Franklin BD, McLeod M, Barber N. Comment on ‘prevalence, incidence and nature of prescribing errors in hospital inpatients: a systematic review’. Drug Safety 2010;33:163-5. http://dx.doi.org/10.2165/11319080-000000000-00000.
- Baysari MT, Westbrook J, Braithwaite J, Day RO. The role of computerized decision support in reducing errors in selecting medicines for prescription: narrative review. Drug Safety 2011;34:289-98. http://dx.doi.org/10.2165/11588200-000000000-00000.
- Panesar SS, Noble DJ, Mirza SB, Patel B, Mann B, Emerton M, et al. Can the surgical checklist reduce the risk of wrong site surgery in orthopaedics? – can the checklist help? Supporting evidence from analysis of a national patient incident reporting system. J Orthop Surg Res 2011;6. http://dx.doi.org/10.1186/1749-799X-6-18.
- Martinez EA, Thompson DA, Errett NA, Kim GR, Bauer L, Lubomski LH, et al. High stakes and high risk: a focused qualitative review of hazards during cardiac surgery. Anesth Analg 2011;112:1061-74. http://dx.doi.org/10.1213/ANE.0b013e31820bfe8e.
- McDonald KM, Matesic B, Contopoulos-Ioannidis DG, Lonhart J, Schmidt E, Pineda N, et al. Patient safety strategies targeted at diagnostic errors: a systematic review. Ann Intern Med 2013;158:381-9. http://dx.doi.org/10.7326/0003-4819-158-5-201303051-00004.
- Schwartz A, Weiner SJ, Weaver F, Yudkowsky R, Sharma G, Binns-Calvey A, et al. Uncharted territory: measuring costs of diagnostic errors outside the medical record. BMJ Qual Saf 2012;21:918-24. http://dx.doi.org/10.1136/bmjqs-2012-000832.
- Chang J, Ronco C, Rosner MH. Computerized decision support systems: improving patient safety in nephrology. Nat Rev Nephrol 2011;7:348-55. http://dx.doi.org/10.1038/nrneph.2011.50.
- Caldwell G. What is the main cause of avoidable harm to patients?. BMJ 2010;341. http://dx.doi.org/10.1136/bmj.c4593.
- Graber ML, Wachter RM, Cassel CK. Bringing diagnosis into the quality and safety equations. JAMA 2012;308:1211-12. http://dx.doi.org/10.1001/2012.jama.11913.
- Sparks EA, Wehbe-Janek H, Johnson RL, Smythe WR, Papaconstantinou HT. Surgical safety checklist compliance: a job done poorly!. J Am Coll Surg 2013;217:867-73. http://dx.doi.org/10.1016/j.jamcollsurg.2013.07.393.
- O’Connor P, Reddin C, O’Sullivan M, O’Duffy F, Keogh I. Surgical checklists: the human factor. Patient Saf Surg 2013;7. http://dx.doi.org/10.1186/1754-9493-7-14.
- Shake JG, Pronovost PJ, Whitman GJR. Cardiac surgical ICU care: eliminating ‘preventable’ complications. J Cardiac Surg 2013;28:406-13. http://dx.doi.org/10.1111/jocs.12124.
- Tropello SP, Ravitz AD, Romig M, Pronovost PJ, Sapirstein A. Enhancing the quality of care in the intensive care unit. A systems engineering approach. Crit Care Clin 2013;29:113-24. http://dx.doi.org/10.1016/j.ccc.2012.10.009.
- Hannaford N, Mandel C, Crock C, Buckley K, Magrabi F, Ong M, et al. Learning from incident reports in the Australian medical imaging setting: handover and communication errors. Br J Radiol 2013;86. http://dx.doi.org/10.1259/bjr.20120336.
- Nagpal K, Arora S, Vats A, Wong H, Sevdalis N, Vincent C, et al. Failures in communication and information transfer across the surgical care pathway: interview study. BMJ Qual Saf 2012;21:843-9. http://dx.doi.org/10.1136/bmjqs-2012-000886.
- Farhan M, Brown R, Woloshynowych M, Vincent C. The ABC of handover: a qualitative study to develop a new tool for handover in the emergency department. Emerg Med J 2012;29:941-6. http://dx.doi.org/10.1136/emermed-2011-200199.
- Farhan M, Brown R, Vincent C, Woloshynowych M. The ABC of handover: impact on shift handover in the emergency department. Emerg Med J 2012;29:947-53. http://dx.doi.org/10.1136/emermed-2011-200201.
- Shekelle PG. Nurse–patient ratios as a patient safety strategy: a systematic review. Ann Intern Med 2013;158:404-9. http://dx.doi.org/10.7326/0003-4819-158-5-201303051-00007.
- Palmer WL, Bottle A, Davie C, Vincent CA, Aylin P. Dying for the weekend: a retrospective cohort study on the association between day of hospital presentation and the quality and safety of stroke care. Arch Neurol 2012;69:1296-302. http://dx.doi.org/10.1001/archneurol.2012.1030.
- Young JQ, Ranji SR, Wachter RM, Lee CM, Niehaus B, Auerbach AD. ‘July effect’: impact of the academic year-end changeover on patient outcomes. Ann Intern Med 2011;155:309-15. http://dx.doi.org/10.7326/0003-4819-155-5-201109060-00354.
- Francis R. Report of the Mid Staffordshire NHS Foundation Trust Public Inquiry (Volumes 1–3). London: The Stationery Office; 2013.
- Kennedy I. Learning From Bristol: The Report of the Public Inquiry into Children’s Heart Surgery at the Bristol Royal Infirmary 1984–1995. London: The Stationery Office; 2001.
- Redfern M. The Royal Liverpool Children’s Inquiry. London: The House of Commons; 2001.
- Smith J. The Shipman Inquiry: Independent Public Inquiry into the Issues arising from the Case of Harold Frederick Shipman (First Report: Death Disguised, 2002; Second Report: The Police Investigation of 1998, 2003; Third Report: Death Certification and the Investigation of Deaths by Coroners, 2003; Fourth Report: The Regulation of Controlled Drugs in the Community, 2004; Fifth Report: Safeguarding Patients: Lessons from the Past – Proposals for the Future, 2004; Sixth Report: Shipman: The Final Report, 2005). London: The Stationery Office; 2001.
- MacLean TL, Behnam M. The dangers of decoupling: the relationship between compliance programs, legitimacy perceptions, and institutionalized misconduct. Acad Manag J 2010;53:1499-520. http://dx.doi.org/10.5465/AMJ.2010.57319198.
- Alaszewski A. The impact of the Bristol Royal Infirmary disaster and inquiry on public services in the UK. J Interprof Care 2002;16:371-8. http://dx.doi.org/10.1080/1356182021000008319.
- Dixon-Woods M, Baker R, Charles K, Dawson J, Jerzenbek G, Martin G, et al. Culture and behaviour in the English National Health Service: overview of lessons from a large multimethod study. BMJ Qual Saf 2014;2:106-15. http://dx.doi.org/10.1136/bmjqs-2013-001947.
- Dixon-Woods M, McNicol S, Martin G. Ten challenges in improving quality in healthcare: lessons from the Health Foundation’s programme evaluations and relevant literature. BMJ Qual Saf 2012;21:876-84. http://dx.doi.org/10.1136/bmjqs-2011-000760.
- Davies HTO, Mannion R. Will prescriptions for cultural change improve the NHS?. BMJ 2013;346. http://dx.doi.org/10.1136/bmj.f1305.
- Currie G, Lockett A, Finn R, Martin G, Waring J. Institutional work to maintain professional power: recreating the model of medical professionalism. Organ Stud 2012;33:937-62. http://dx.doi.org/10.1177/0170840612445116.
- Battilana J, Casciaro T. Change agents, networks, and institutions: a contingency theory of organizational change. Acad Manag J 2012;55:381-98. http://dx.doi.org/10.5465/amj.2009.0891.
- Battilana J, Casciaro T. Overcoming resistance to organizational change: strong ties and affective cooptation. Manag Sci 2013;59:819-36. http://dx.doi.org/10.1287/mnsc.1120.1583.
- Waring JJ. Beyond blame: cultural barriers to medical incident reporting. Soc Sci Med 2005;60:1927-35. http://dx.doi.org/10.1016/j.socscimed.2004.08.055.
- Wachter RM. Patient safety at ten: unmistakable progress, troubling gaps. Health Aff 2010;29:165-73. http://dx.doi.org/10.1377/hlthaff.2009.0785.
- Exworthy M, Smith G, Gabe J, Jones IR. Disclosing clinical performance: the case of cardiac surgery. J Health Organ Manag 2010;24:571-83. http://dx.doi.org/10.1108/14777261011088665.
- Patrick K. Barriers to whistleblowing in the NHS. BMJ 2012;345. http://dx.doi.org/10.1136/bmj.e6840.
- Burnes B, Pope R. Negative behaviours in the workplace: a study of two primary care trusts in the NHS. Int J Public Sect Manag 2007;20:285-303. http://dx.doi.org/10.1108/09513550710750011.
- Stewart K, Wyatt R, Conway J. Unprofessional behaviour and patient safety. Int J Clin Leadersh 2011;17:93-101.
- Crump H, Moore A. Investigation. DH will probe how row over targets led to bullying claims. Health Serv J 2009;119:4-5.
- Gillen S, Duffin C. Mid Staffs ward sisters refute bullying and misconduct charges. Nurs Stand 2013;27. http://dx.doi.org/10.7748/ns2013.03.27.28.8.p10760.
- Hands DM. We need aggregated data on bullying in the NHS. BMJ 2012;345. http://dx.doi.org/10.1136/bmj.f209.
- Kmietowicz Z. Bullying and harassment rife in Manchester unit, report says. BMJ 2003;327. http://dx.doi.org/10.1136/bmj.327.7417.697.
- O’Dowd A. Manager who took settlement after being ‘exhausted’ fighting his dismissal describes ‘bullying’ NHS culture. BMJ 2013;346. http://dx.doi.org/10.1136/bmj.f1896.
- Reid J. The NHS must support staff to speak out against poor practice. Nurs Times 2010;106.
- Mannion R, Braithwaite J. Unintended consequences of performance measurement in healthcare: 20 salutary lessons from the English National Health Service. Intern Med J 2012;42:569-74. http://dx.doi.org/10.1111/j.1445-5994.2012.02766.x.
- Gabe J, Exworthy M, Jones IR, Smith G. Towards a sociology of disclosure: the case of surgical performance. Sociol Compass 2012;6:908-22. http://dx.doi.org/10.1111/j.1751-9020.2012.00490.x.
- Walker RM, Brewer GA, Boyne GA, Avellaneda CN. Market orientation and public service performance: new public management gone mad?. Public Adm Rev 2011;71:707-17. http://dx.doi.org/10.1111/j.1540-6210.2011.02410.x.
- Lamb RM, Studdert DM, Bohmer RMJ, Berwick DM, Brennan TA. Hospital disclosure practices: results of a national survey. Health Aff 2003;22:73-8. http://dx.doi.org/10.1377/hlthaff.22.2.73.
- Jacobs R, Mannion R, Davies HTO, Harrison S, Konteh F, Walshe K. The relationship between organizational culture and performance in acute hospitals. Soc Sci Med 2013;76:115-25. http://dx.doi.org/10.1016/j.socscimed.2012.10.014.
- Greener I. Unpacking the evidence on competition and outcomes in the NHS in England. J Health Serv Res Policy 2012;17:193-4. http://dx.doi.org/10.1258/jhsrp.2012.012032.
- Tickle M, McDonald R, Franklin J, Aggarwal VR, Milsom K, Reeves D. Paying for the wrong kind of performance? Financial incentives and behaviour changes in National Health Service dentistry 1992–2009. Community Dent Oral Epidemiol 2011;39:465-73. http://dx.doi.org/10.1111/j.1600-0528.2011.00622.x.
- O’Reilly D, Reed M. ‘Leaderism’: an evolution of managerialism in UK public service reform. Public Adm 2010;88:960-78. http://dx.doi.org/10.1111/j.1467-9299.2010.01864.x.
- Andrews R, Boyne GA. Organizational environments and public-service failure: an empirical analysis. Environ Plann C 2008;26:788-807. http://dx.doi.org/10.1068/c69m.
- Andrews R, Boyne GA, Enticott G. Performance failure in the public sector: misfortune or mismanagement?. Public Manag Rev 2006;8:273-96. http://dx.doi.org/10.1080/14719030600587612.
- Andrews R, Boyne GA, Law J, Walker RM. External constraints on local service standards: the case of comprehensive performance assessment in English local government. Public Adm 2005;83:639-56. http://dx.doi.org/10.1111/j.0033-3298.2005.00466.x.
- Andrews R, Boyne GA, Walker RM. Overspending in public organizations: does strategic management matter?. Int Public Manag J 2012;15:39-61. http://dx.doi.org/10.1080/10967494.2012.684017.
- Denis JL, Langley A, Sergi V. Leadership in the plural. Acad Manag Ann 2012;6:211-83. http://dx.doi.org/10.1080/19416520.2012.667612.
- Detsky AS, Berwick DM. Teaching physicians to care amid chaos. JAMA 2013;309:987-8. http://dx.doi.org/10.1001/jama.2013.620.
- Baker GR, Denis JL. Medical leadership in health care systems: from professional authority to organizational leadership. Public Money Manage 2011;31:355-62. http://dx.doi.org/10.1080/09540962.2011.598349.
- Ham C. Doctors in leadership: learning from international experience. Int J Clin Leadersh 2008;16:11-6.
- Øvretveit J. Leading improvement. J Health Organ Manag 2005;19:413-30. http://dx.doi.org/10.1108/14777260510629661.
- Vogts N, Hannam JA, Merry AF, Mitchell SJ. Compliance and quality in administration of a surgical safety checklist in a tertiary New Zealand hospital. NZ Med J 2011;124:48-5.
- Rydenfält C, Johansson G, Odenrick P, Åkerman K, Larsson PA. Compliance with the WHO surgical safety checklist: Deviations and possible improvements. Int J Qual Health Care 2013;25:182-7. http://dx.doi.org/10.1093/intqhc/mzt004.
- Walrath JM, Dang D, Nyberg D. An organizational assessment of disruptive clinician behavior: findings and implications. J Nurs Care Qual 2013;28:110-21. http://dx.doi.org/10.1097/NCQ.0b013e318270d2ba.
- Locock L, Dopson S, Chambers D, Gabbay J. Understanding the role of opinion leaders in improving clinical effectiveness. Soc Sci Med 2001;53:745-57. http://dx.doi.org/10.1016/S0277-9536(00)00387-7.
- Lamb BW, Taylor C, Lamb JN, Strickland SL, Vincent C, Green JSA, et al. Facilitators and barriers to teamworking and patient centeredness in multidisciplinary cancer teams: findings of a national study. Ann Surg Oncol 2013;20:1408-16. http://dx.doi.org/10.1245/s10434-012-2676-9.
- Aveling EL, Martin G, Armstrong N, Banerjee J, Dixon-Woods M. Quality improvement through clinical communities: eight lessons for practice. J Health Organ Manag 2012;26:158-74. http://dx.doi.org/10.1108/14777261211230754.
- Auerbach AD, Sehgal NL, Blegen MA, Maselli J, Alldredge BK, Vittinghoff E, et al. Effects of a multicentre teamwork and communication programme on patient outcomes: results from the Triad for Optimal Patient Safety (TOPS) project. BMJ Qual Saf 2012;21:118-26. http://dx.doi.org/10.1136/bmjqs-2011-000311.
- Sevdalis N, Wong HWL, Arora S, Nagpal K, Healey A, Hanna GB, et al. Quantitative analysis of intraoperative communication in open and laparoscopic surgery. Surg Endosc 2012;26:2931-8. http://dx.doi.org/10.1007/s00464-012-2287-3.
- Hull L, Arora S, Aggarwal R, Darzi A, Vincent C, Sevdalis N. The impact of nontechnical skills on technical performance in surgery: a systematic review. J Am Coll Surg 2012;214:214-30. http://dx.doi.org/10.1016/j.jamcollsurg.2011.10.016.
- Wong HWL, Forrest D, Healey A, Shirafkan H, Hanna GB, Vincent CA, et al. Information needs in operating room teams: what is right, what is wrong, and what is needed?. Surg Endosc 2011;25:1913-20. http://dx.doi.org/10.1007/s00464-010-1486-z.
- Sehgal NL, Fox M, Sharpe BA, Vidyarthi AR, Blegen M, Wachter RM. Critical conversations: a call for a nonprocedural ‘time out’. J Hosp Med 2011;6:225-30. http://dx.doi.org/10.1002/jhm.853.
- Finn R. The language of teamwork: reproducing professional divisions in the operating theatre. Hum Relat 2008;61:103-30. http://dx.doi.org/10.1177/0018726707085947.
- Finn R, Currie G, Martin G. Team work in context: institutional mediation in the public-service professional bureaucracy. Organ Stud 2010;31:1069-97. http://dx.doi.org/10.1177/0170840610376142.
- Gurses AP, Ozok AA, Pronovost PJ. Time to accelerate integration of human factors and ergonomics in patient safety. BMJ Qual Saf 2012;21:347-51. http://dx.doi.org/10.1136/bmjqs-2011-000421.
- Carayon P, Xie A, Kianfar S. Human factors and ergonomics as a patient safety practice. BMJ Qual Saf 2014;23:196-205. http://dx.doi.org/10.1136/bmjqs-2013-001812.
- Fawcett TN, Rhynas SJ. Re-finding the ‘human side’ of human factors in nursing: helping student nurses to combine person-centred care with the rigours of patient safety. Nurse Educ Today 2014;34:1238-41. http://dx.doi.org/10.1016/j.nedt.2014.01.008.
- Vincent CJ, Li Y, Blandford A. Integration of human factors and ergonomics during medical device design and development: it’s all about communication. Appl Ergon 2014;45:413-19. http://dx.doi.org/10.1016/j.apergo.2013.05.009.
- Timmons S, Baxendale B, Buttery A, Miles G, Roe B, Browes S. Implementing human factors in clinical practice. Emerg Med J n.d.;32:368-72. http://dx.doi.org/10.1136/emermed-2013-203203.
- Walshe KMJ. New structures of governance are needed. BMJ 2003;326. http://dx.doi.org/10.1136/bmj.326.7392.764.
- Sheaff R, Marshall M, Rogers A, Roland M, Sibbald B, Pickard S. Governmentality by network in English primary healthcare. Social Policy Adm 2004;38:89-103. http://dx.doi.org/10.1111/j.1467-9515.2004.00378.x.
- McGivern G, Fischer M. Medical regulation, spectacular transparency and the blame business. J Health Organ Manag 2010;24:597-610. http://dx.doi.org/10.1108/14777261011088683.
- Waring J, Dixon-Woods M, Yeung K. Modernising medical regulation: where are we now?. J Health Organ Manag 2010;24:540-55. http://dx.doi.org/10.1108/14777261011088647.
- Hyde P. Managing across boundaries: identity, differentiation and interaction. Int J Innov Learn 2006;3:349-62. http://dx.doi.org/10.1504/IJIL.2006.009560.
- Hirschman A. Exit, Voice and Loyalty. Cambridge, MA: Harvard University Press; 1970.
- Wiig S, Storm M, Aase K, Gjestsen MT, Solheim M, Harthug S, et al. Investigating the use of patient involvement and patient experience in quality improvement in Norway: rhetoric or reality?. BMC Health Serv Res 2013;13. http://dx.doi.org/10.1186/1472-6963-13-206.
- Ocloo J, O’Shea A, Fulop N. Empowerment or rhetoric? Investigating the role of NHS foundation trust governors in the governance of patient safety. Health Policy 2013;111:301-10. http://dx.doi.org/10.1016/j.healthpol.2013.05.005.
- Ocloo JE, Fulop NJ. Developing a ‘critical’ approach to patient and public involvement in patient safety in the NHS: learning lessons from other parts of the public sector?. Health Expect 2012;15:424-32. http://dx.doi.org/10.1111/j.1369-7625.2011.00695.x.
- Greenfield D, Hinchcliff R, Moldovan M, Mumford V, Pawsey M, Westbrook JI, et al. A multimethod research investigation of consumer involvement in Australian health service accreditation programmes: the ACCREDIT-SCI study protocol. BMJ Open 2012;2. http://dx.doi.org/10.1136/bmjopen-2012-002024.
- Braithwaite J, Travaglia JF. An overview of clinical governance policies practices and initiatives. Aust Health Rev 2008;32:10-22. http://dx.doi.org/10.1071/AH080010.
- Kazimierczak KA, Skea ZC, Dixon-Woods M, Entwistle VA, Feldman-Stewart D, N’Dow JMO, et al. Provision of cancer information as a ‘support for navigating the knowledge landscape’: findings from a critical interpretive literature synthesis. Eur J Oncol Nurs 2013;17:360-9. http://dx.doi.org/10.1016/j.ejon.2012.10.002.
- Lloyd A, Joseph-Williams N, Edwards A, Rix A, Elwyn G. Patchy ‘coherence’: using normalization process theory to evaluate a multi-faceted shared decision making implementation program (MAGIC). Implement Sci 2013;8. http://dx.doi.org/10.1186/1748-5908-8-102.
- Elwyn G, Tsulukidze M, Edwards A, Légaré F, Newcombe R. Using a ‘talk’ model of shared decision making to propose an observation-based measure: observer option 5 item. Patient Educ Couns 2013;93:265-71. http://dx.doi.org/10.1016/j.pec.2013.08.005.
- Edwards AG, Naik G, Ahmed H, Elwyn GJ, Pickles T, Hood K, et al. Personalised risk communication for informed decision making about taking screening tests. Cochrane Database Syst Rev 2013;2. http://dx.doi.org/10.1002/14651858.cd001865.pub3.
- Couët N, Desroches S, Robitaille H, Vaillancourt H, Leblanc A, Turcotte S, et al. Assessments of the extent to which health-care providers involve patients in decision making: a systematic review of studies using the OPTION instrument [published online ahead of print 4 March 2013]. Health Expect 2013.
- Russell J, Greenhalgh T, Burnett A, Montgomery J. ‘No decisions about us without us’? Individual healthcare rationing in a fiscal ice age. BMJ 2011;342. http://dx.doi.org/10.1136/bmj.d3279.
- Keogh B. Review into the Quality of Care and Treatment Provided by 14 Hospital Trusts in England: Overview Report. London: Department of Health; 2013.
- Lilford R, Pronovost P. Using hospital mortality rates to judge hospital performance: a bad idea that just won’t go away. BMJ 2010;340:955-7. http://dx.doi.org/10.1136/bmj.c2016.
- Girling AJ, Hofer TP, Wu J, Chilton PJ, Nicholl JP, Mohammed MA, et al. Case-mix adjusted hospital mortality is a poor proxy for preventable mortality: a modelling study. BMJ Qual Saf 2012;21:1052-6. http://dx.doi.org/10.1136/bmjqs-2012-001202.
- Mohammed MA, Lilford RJ. Two incorrect assertions about study of hospital standardised mortality ratios in the West Midlands. BMJ 2013;346. http://dx.doi.org/10.1136/bmj.f1088.
- A Promise to Learn – A Commitment to Act: Improving the Safety of Patients in England. London: National Advisory Group on the Safety of Patients in England; 2013.
- Berwick DM, Calkins DR, Joseph McCannon C, Hackbarth AD. The 100,000 lives campaign: setting a goal and a deadline for improving health care quality. JAMA 2006;295:324-7. http://dx.doi.org/10.1001/jama.295.3.324.
- Nelson EC, Godfrey MM, Batalden PB, Berry SA, Bothe AE, McKinley KE, et al. Clinical microsystems, part 1. The building blocks of health systems. Jt Comm J Qual Patient Saf 2008;34:367-78.
- Wasson JH, Anders SG, Moore LG, Ho L, Nelson EC, Godfrey MM, et al. Clinical microsystems, part 2. Learning from micro practices about providing patients the care they want and need. Jt Comm J Qual Patient Saf 2008;34:445-52.
- Godfrey MM, Melin CN, Muething SE, Batalden PB, Nelson EC. Clinical microsystems, part 3. Transformation of two hospitals using microsystem, mesosystem, and macrosystem strategies. Jt Comm J Qual Patient Saf 2008;34:591-603.
- McKinley KE, Berry SA, Laam LA, Doll MC, Brin KP, Bothe A, et al. Clinical microsystems, Part 4. Building innovative population-specific mesosystems. Jt Comm J Qual Patient Saf 2008;34:655-63.
- Waring J, Rowley E, Dingwall R, Palmer C, Murcott T. Narrative review of the UK Patient Safety Research Portfolio. J Health Serv Res Policy 2010;15:26-32. http://dx.doi.org/10.1258/jhsrp.2009.009042.
- Safer Patients Initiative Evidence: Phase One and Two. London: Health Foundation; 2011.
- Low DK, Reed MA, Geiduschek JM, Martin LD. Striving for a zero-error patient surgical journey through adoption of aviation-style challenge and response flow checklists: a quality improvement project. Paediatr Anaesth 2013;23:571-8. http://dx.doi.org/10.1111/pan.12121.
- Travaglia JF, Hughes C, Braithwaite J. Learning from disasters to improve patient safety: applying the generic disaster pathway to health system errors. BMJ Qual Saf 2011;20:1-8. http://dx.doi.org/10.1136/bmjqs.2009.038885.
- Sutcliffe K, Weick K. Managing the Unexpected: Assuring High Performance in an Age of Complexity. San Francisco, CA: Jossey-Bass; 2001.
- Gillam S, Siriwardena AN. Frameworks for improvement: clinical audit, the plan-do-study-act cycle and significant event audit. Qual Prim Care 2013;21:123-30.
- Doshi J, Badran K, Minhas S. A completed audit cycle – what do patients think of the World Health Organisation (WHO) Surgical Checklist?. Otorhinolaryngologist 2012;5:39-42.
- Solon JG, Egan C, McNamara DA. Safe surgery: how accurate are we at predicting intra-operative blood loss?. J Eval Clin Pract 2013;19:100-5. http://dx.doi.org/10.1111/j.1365-2753.2011.01779.x.
- Douglas A, Letts L, Eva K, Richardson J. Measurement of harm outcomes in older adults after hospital discharge: reliability and validity. J Aging Res 2012;2012. http://dx.doi.org/10.1155/2012/150473.
- Greenhalgh T, MacFarlane F, Barton-Sweeney C, Woodard F. ‘If we build it, will it stay?’ A case study of the sustainability of whole-system change in London. Milbank Q 2012;90:516-47. http://dx.doi.org/10.1111/j.1468-0009.2012.00673.x.
- Berwick DM, Hackbarth AD, McCannon CJ. IHI replies to ‘The 100,000 lives campaign: a scientific and policy review’. Jt Comm J Qual Patient Saf 2006;32:628-30.
- Langley GJ, Moen RD, Nolan KM, Nolan TW, Norman CL, Provost LP. The Improvement Guide: A Practical Approach to Enhancing Organizational Performance. San Francisco, CA: Jossey Bass; 2009.
- Courtlandt CD, Noonan L, Feld LG. Model for Improvement – Part 1: a framework for health care quality. Pediatr Clin North Am 2009;56:757-78. http://dx.doi.org/10.1016/j.pcl.2009.06.002.
- Schriefer J, Leonard MS. Patient safety and quality improvement: an overview of QI. Pediatr Rev 2012;33:353-60. http://dx.doi.org/10.1542/pir.33-8-353.
- Dixon-Woods M, Bosk CL, Aveling EL, Goeschel CA, Pronovost PJ. Explaining Michigan: developing an ex post theory of a quality improvement program. Milbank Q 2011;89:167-205. http://dx.doi.org/10.1111/j.1468-0009.2011.00625.x.
- Damschroder LJ, Banaszak-Holl J, Kowalski CP, Forman J, Saint S, Krein SL. The role of the ‘champion’ in infection prevention: results from a multisite qualitative study. Qual Saf Health Care 2009;18:434-40. http://dx.doi.org/10.1136/qshc.2009.034199.
- Holland R, Meyers D, Hildebrand C, Bridges AJ, Roach MA, Vogelman B. Creating champions for health care quality and safety. Am J Med Qual 2010;25:102-8. http://dx.doi.org/10.1177/1062860609352108.
- Campbell J. The effect of nurse champions on compliance with keystone intensive care unit sepsis-screening protocol. Crit Care Nurs Q 2008;31:251-69. http://dx.doi.org/10.1097/01.CNQ.0000325050.91473.0b.
- Weingart C, Herstich T, Baker P, Garrett ML, Bird M, Billock J, et al. Making good better: implementing a standardized handoff in pediatric transport. Air Med J 2013;32:40-6. http://dx.doi.org/10.1016/j.amj.2012.06.005.
- Singh K, Sanderson J, Galarneau D, Keister T, Hickman D. Quality improvement on the acute inpatient psychiatry unit using the model for improvement. Ochsner J 2013;13:380-4.
- Marcellus L, Harrison A, MacKinnon K. Quality improvement for neonatal nurses, part II: using a PDSA quality improvement cycle approach to implement an oral feeding progression guideline for premature infants. Neonatal Netw 2012;31:215-22.
- Curran ET, Bunyan D. Using a PDSA cycle of improvement to increase preparedness for, and management of, norovirus in NHS Scotland. J Hosp Infect 2012;82:108-13. http://dx.doi.org/10.1016/j.jhin.2012.07.007.
- Low D, Walker I, Heitmiller ES. Implementing checklists in the operating room. Paediatr Anaesth 2012;22:1025-31. http://dx.doi.org/10.1111/pan.12018.
- Lal N, Lewington E, Nepogodiev D, Bhangu A, Pathak R. A prospective audit cycle with an intervention of active feedback improves completion rates of the World Health Organisation Surgical Safety Checklist. Chirurgia (Turin) 2012;25:179-83.
- Styer KA, Ashley SW, Schmidt I, Zive EM, Eappen S. Implementing the World Health Organization Surgical Safety Checklist: a model for future perioperative initiatives. AORN J 2011;94:590-8. http://dx.doi.org/10.1016/j.aorn.2011.03.012.
- McPeake J, Cantwell S, Malcolm G B, Malcolm D. Central line insertion bundle: experiences and challenges in an adult ICU. Nurs Crit Care 2012;17:123-9. http://dx.doi.org/10.1111/j.1478-5153.2012.00491.x.
- van Tiel FH, Elenbaas TWO, Voskuilen BMAM, Herczeg J, Verheggen FW, Mochtar B, et al. Plan-do-study-act cycles as an instrument for improvement of compliance with infection control measures in care of patients after cardiothoracic surgery. J Hosp Infect 2006;62:64-70. http://dx.doi.org/10.1016/j.jhin.2005.05.016.
- Pulcini C, Crofts S, Campbell D, Davey P. Design, measurement, and evaluation of an education strategy in the hospital setting to combat antimicrobial resistance: theoretical considerations and a practical example. Dis Manag Health Outcome 2007;15:151-63. http://dx.doi.org/10.2165/00115677-200715030-00004.
- White CM, Statile AM, Conway PH, Schoettker PJ, Solan LG, Unaka NI, et al. Utilizing improvement science methods to improve physician compliance with proper hand hygiene. Pediatrics 2012;129:e1042-50. http://dx.doi.org/10.1542/peds.2011-1864.
- Leape LL, Berwick D, Clancy C, Conway J, Gluck P, Guest J, et al. Transforming healthcare: a safety imperative. Qual Saf Health Care 2009;18:424-8. http://dx.doi.org/10.1136/qshc.2009.036954.
- Franklin BD, Taxis K, Barber N. Parenteral drug errors: reported error rates are likely to be underestimation. BMJ 2009;338. http://dx.doi.org/10.1136/bmj.b1814.
- Pronovost PJ, Marsteller JA, Goeschel CA. Preventing bloodstream infections: a measurable national success story in quality improvement. Health Aff 2011;30:628-34. http://dx.doi.org/10.1377/hlthaff.2011.0047.
- Goeschel CA, Holzmueller CG, Pronovost PJ. Hospital board checklist to improve culture and reduce central line – associated bloodstream infections. Jt Comm J Qual Patient Saf 2010;36:525-8.
- Mathiesen ASM, Norgaard K, Andersen MFB, Moller KM, Ehlers LH. Are labour-intensive efforts to prevent pressure ulcers cost-effective?. J Med Econ 2013;16:1238-45. http://dx.doi.org/10.3111/13696998.2013.832256.
- Spears GV, Roth CP, Miake-Lye IM, Saliba D, Shekelle PG, Ganz DA. Redesign of an electronic clinical reminder to prevent falls in older adults. Med Care 2013;51:37-43. http://dx.doi.org/10.1097/MLR.0b013e31827807f8.
- Miake-Lye IM, Hempel S, Ganz DA, Shekelle PG. Inpatient fall prevention programs as a patient safety strategy: a systematic review. Ann Intern Med 2013;158:390-6. http://dx.doi.org/10.7326/0003-4819-158-5-201303051-00005.
- Denham CR, Angood P, Berwick D, Binder L, Clancy CM, Corrigan JM, et al. Chasing zero: can reality meet the rhetoric?. J Patient Saf 2009;5:216-22. http://dx.doi.org/10.1097/PTS.0b013e3181c1b470.
- Berwick DM. Preparing nurses for participation in and leadership of continual improvement. J Nurs Educ 2011;50:322-7. http://dx.doi.org/10.3928/01484834-20110519-05.
- Clay-Williams R, McIntosh CA, Kerridge R, Braithwaite J. Classroom and simulation team training: a randomized controlled trial. Int J Qual Health Care 2013;25:314-21. http://dx.doi.org/10.1093/intqhc/mzt027.
- Spigelman AD, Debono DS, Oates K, Dunn AG, Braithwaite J. Patient safety teaching in Australian medical schools: a national survey. Clin Risk 2012;18:46-51. http://dx.doi.org/10.1258/cr.2012.012004.
- Walker ST, Sevdalis N, McKay A, Lambden S, Gautama S, Aggarwal R, et al. Unannounced in situ simulations: integrating training and clinical practice. BMJ Qual Saf 2013;22:453-8. http://dx.doi.org/10.1136/bmjqs-2012-000986.
- Sandahl C, Gustafsson H, Wallin CJ, Meurling L, Øvretveit J, Brommels M, et al. Simulation team training for improved teamwork in an intensive care unit. Int J Health Care Qual Assur 2013;26:174-88. http://dx.doi.org/10.1108/09526861311297361.
- Coleman JJ, Hemming K, Nightingale PG, Clark IR, Dixon-Woods M, Ferner RE, et al. Can an electronic prescribing system detect doctors who are more likely to make a serious prescribing error?. J R Soc Med 2011;105:208-18. http://dx.doi.org/10.1258/jrsm.2011.110061.
- Wolfenden J, Dunn A, Holmes A, Davies C, Buchan J. Track and trigger system for use in community hospitals. Nurs Stand 2010;24:35-9. http://dx.doi.org/10.7748/ns2010.07.24.45.35.c7905.
- Nicolini D, Waring J, Mengis J. The challenges of undertaking root cause analysis in health care: a qualitative study. J Health Serv Res Policy 2011;16:34-41. http://dx.doi.org/10.1258/jhsrp.2010.010092.
- Waring J. Patient safety: learning the lessons in primary care. London J Prim Care 2010;3:88-92.
- Waring JJ. Constructing and re-constructing narratives of patient safety. Soc Sci Med 2009;69:1722-31. http://dx.doi.org/10.1016/j.socscimed.2009.09.052.
- Burnett S, Renz A, Wiig S, Fernandes A, Weggelaar AM, Calltorp J, et al. Prospects for comparing european hospitals in terms of quality and safety: lessons from a comparative study in five countries. Int J Qual Health Care 2013;25:1-7. http://dx.doi.org/10.1093/intqhc/mzs079.
- Benn J, Burnett S, Parand A, Pinto A, Vincent C. Factors predicting change in hospital safety climate and capability in a multi-site patient safety collaborative: a longitudinal survey study. BMJ Qual Saf 2012;21:559-68. http://dx.doi.org/10.1136/bmjqs-2011-000286.
- Bate P, Mendel P, Robert G. Organising for Quality: The Improvement Journey of Leading Hospitals in Europe and the United States. Oxford: RAND Health Research; 2008.
- Nosrati H, Clay-Williams R, Cunningham F, Hillman K, Braithwaite J. The role of organisational and cultural factors in the implementation of systemwide interventions in acute hospitals to improve patient outcomes: protocol for a systematic literature review. BMJ Open 2013;3. http://dx.doi.org/10.1136/bmjopen-2012-002268.
- Øvretveit JC, Shekelle PG, Dy SM, McDonald KM, Hempel S, Pronovost P, et al. How does context affect interventions to improve patient safety? An assessment of evidence from studies of five patient safety practices and proposals for research. BMJ Qual Saf 2011;20:604-10. http://dx.doi.org/10.1136/bmjqs.2010.047035.
- Nadeem E, Olin SS, Hill LC, Hoagwood KE, Horwitz SM. Understanding the components of quality improvement collaboratives: a systematic literature review. Milbank Q 2013;91:354-94. http://dx.doi.org/10.1111/milq.12016.
- Krein SL, Damschroder LJ, Kowalski CP, Forman J, Hofer TP, Saint S. The influence of organizational context on quality improvement and patient safety efforts in infection prevention: a multi-center qualitative study. Soc Sci Med 2010;71:1692-701. http://dx.doi.org/10.1016/j.socscimed.2010.07.041.
- Kitson AL, Rycroft-Malone J, Harvey G, McCormack B, Seers K, Titchen A. Evaluating the successful implementation of evidence into practice using the PARiHS framework: theoretical and practical challenges. Implement Sci 2008;3. http://dx.doi.org/10.1186/1748-5908-3-1.
- Reay T, Goodrick E, Casebeer A, Hinings CR. Legitimizing new practices in primary health care. Health Care Manage Rev 2013;38:9-19. http://dx.doi.org/10.1097/HMR.0b013e31824501b6.
- Shekelle PG, Pronovost PJ, Wachter RM, Taylor SL, Dy S, Foy R, et al. Assessing the Evidence for Context-Sensitive Effectiveness and Safety of Patient Safety Practices: Developing Criteria. Rockville, MD: Agency for Healthcare Research and Quality; 2010.
- Shortell S, Rundall T, Hsu J. Improving patient care by linking evidence-based medicine and evidence-based management. JAMA 2007;298:673-6. http://dx.doi.org/10.1001/jama.298.6.673.
- Bamberger P. Beyond contextualization: using context theories to narrow the micro–macro gap in management research. Acad Manag J 2008;51:839-46. http://dx.doi.org/10.5465/AMJ.2008.34789630.
- Kaplan HC, Brady PW, Dritz MC, Hooper DK, Linam WM, Froehle CM, et al. The influence of context on quality improvement success in health care: a systematic review of the literature. Milbank Q 2010;88:500-59. http://dx.doi.org/10.1111/j.1468-0009.2010.00611.x.
- Greenwood R, Suddaby R, Hinings CR. Theorizing change: the role of professional associations in the transformation of institutionalized fields. Acad Manag J 2002;45:58-80. http://dx.doi.org/10.2307/3069285.
- Pawson R, Tilley N. Realistic Evaluation. London: Sage; 1997.
- Archer MS. Realist Social Theory: The Morphogenetic Approach. Cambridge: Cambridge University Press; 1995.
- Archer MS. Culture and Agency: The Place of Culture in Social Theory. Cambridge: Cambridge University Press; 1996.
- Archer MS. Being Human: The Problem of Agency. Cambridge: Cambridge University Press; 2000.
- Archer MS. Structure, Agency and the Internal Conversation. Cambridge: Cambridge University Press; 2003.
- Archer MS. Making our Way in Through the World. Cambridge: Cambridge University Press; 2007.
- Archer MSE. Conversations about Reflexivity. London: Routledge; 2010.
- Archer MS. The Reflexive Imperative in Late Modernity. Cambridge: Cambridge University Press; 2012.
- Boaz A, Ashby D, Denyer D, Egan M, Harden A, Jones DR, et al. A multitude of syntheses: a comparison of five approaches from diverse policy fields. Evid Policy 2006;2:479-502. http://dx.doi.org/10.1332/174426406778881755.
- Gustafson DH, Sainfort F, Eichler M, Adams L, Bisognano M, Steude H. Developing and testing a model to predict outcomes of organizational change. Health Serv Res 2003;38:751-76. http://dx.doi.org/10.1111/1475-6773.00143.
- Damschroder L, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci 2009;4. http://dx.doi.org/10.1186/1748-5908-4-50.
- Helfrich CD, Li Y-F, Sharp N, Sales AE. Organizational readiness to change assessment (ORCA): development of an instrument based on the Promoting Action on Research in Health Services (PARIHS) framework. Implement Sci 2009;4. http://dx.doi.org/10.1186/1748-5908-4-38.
- Grol R, Berwick DM, Wensing M. On the trail of quality and safety in health care. BMJ 2008;336:74-6. http://dx.doi.org/10.1136/bmj.39413.486944.AD.
- Pawson R. The Science of Evaluation: A Realist Manifesto. London: Sage; 2013.
- Pawson R. Evidence-Based Policy: A Realist Perspective. London: Sage; 2006.
- Wong G, Greenhalgh T, Westhorp G, Buckingham J, Pawson R. RAMESES publication standards: realist syntheses. BMC Med 2013;11. http://dx.doi.org/10.1186/1741-7015-11-21.
- Boaz A, Pawson R. The perilous road from evidence to policy: five journeys compared. J Soc Policy 2005;34:175-94. http://dx.doi.org/10.1017/S0047279404008530.
- Pawson R, Owen L, Wong G. Legislating for health: locating the evidence. J Public Health Policy 2010;31:164-77. http://dx.doi.org/10.1057/jphp.2010.5.
- Cruickshank J. Positioning positivism, critical realism and social constructionism in the health sciences: a philosophical orientation. Nurs Inq 2012;19:71-82. http://dx.doi.org/10.1111/j.1440-1800.2011.00558.x.
- Pawson R, Greenhalgh T, Harvey G, Walshe K. Realist review – a new method of systematic review designed for complex policy interventions. J Health Serv Res Policy 2005;10:21-34. http://dx.doi.org/10.1258/1355819054308530.
- Noyes JP, Williams A, Allen D, Brocklehurst P, Carter C, Gregory JW, et al. Evidence into practice: evaluating a child-centred intervention for diabetes medicine management – the EPIC project. BMC Pediatr 2010;10. http://dx.doi.org/10.1186/1471-2431-10-70.
- Ekstrom M, Danermark B. The study of power mechanisms – an interactive and generative approach to a case study of Swedish urban renewal. Scand Hous Plan Res 1991;8:153-70. http://dx.doi.org/10.1080/02815739108730269.
- Reed MI. Organization, trust and control: a realist analysis. Organ Stud 2001;22:201-28. http://dx.doi.org/10.1177/0170840601222002.
- Wong G, Greenhalgh T, Pawson R. Internet-based medical education: a realist review of what works, for whom and in what circumstances. BMC Med Educ 2010;10. http://dx.doi.org/10.1186/1472-6920-10-12.
- Reed M. Reflections on the ‘realist turn’ in organization and management studies. J Manag Stud 2005;42:1621-44. http://dx.doi.org/10.1111/j.1467-6486.2005.00559.x.
- Newton T, Deetz S, Reed M. Responses to social constructionism and critical realism in organization studies. Organ Stud 2011;32:7-26. http://dx.doi.org/10.1177/0170840610394289.
- Greener I. Path dependence, realism and the NHS. Br Polit 2006;1:319-43. http://dx.doi.org/10.1057/palgrave.bp.4200021.
- Pawson R. Middle-range realism. Arch Eur Soc 2000;41:283-325. http://dx.doi.org/10.1017/S0003975600007050.
- Pawson R, Manzano-Santaella A. A realist diagnostic workshop. Evaluation 2012;18:176-91. http://dx.doi.org/10.1177/1356389012440912.
- Pawson R, Tilley N. Realistic evaluation bloodlines. Am J Eval 2001;22:317-24. http://dx.doi.org/10.1177/109821400102200305.
- Pawson R. Digging for nuggets: how ‘bad’ research can yield ‘good’ evidence. Int J Soc Res Methodol 2006;9:127-42. http://dx.doi.org/10.1080/13645570600595314.
- Pawson R. Protocols, policy making and scientific progress. J Epidemiol Community Health 2012;66:386-7. http://dx.doi.org/10.1136/jech-2012-201061.
- Pawson R, Wong G, Owen L. Known knowns, known unknowns, unknown unknowns: the predicament of evidence-based policy. Am J Eval 2011;32:518-46. http://dx.doi.org/10.1177/1098214011403831.
- Best A, Greenhalgh T, Lewis S, Saul JE, Carroll S, Bitz J. Large-system transformation in health care: a realist review. Milbank Q 2012;90:421-56. http://dx.doi.org/10.1111/j.1468-0009.2012.00670.x.
- Black J. Transforming the patient care environment with Lean Six Sigma and realistic evaluation. J Healthc Qual 2009;31:29-35. http://dx.doi.org/10.1111/j.1945-1474.2009.00028.x.
- Blaise P, Kegels G. A realistic approach to the evaluation of the quality management movement in health care systems: a comparison between European and African contexts based on Mintzberg’s organizational models. Int J Health Plann Manag 2004;19:337-64. http://dx.doi.org/10.1002/hpm.769.
- Byng R, Norman I, Redfern S. Using Realistic Evaluation to evaluate a practice-level intervention to improve primary healthcare for patients with long-term mental illness. Evaluation 2005;11:69-93. http://dx.doi.org/10.1177/1356389005053198.
- Cheyne H, Abhyankar P, McCourt C. Empowering change: realist evaluation of a Scottish Government programme to support normal birth. Midwifery 2013;29:1110-21. http://dx.doi.org/10.1016/j.midw.2013.07.018.
- Williams L, Burton C, Rycroft-Malone J. What works: a realist evaluation case study of intermediaries in infection control practice. J Adv Nurs 2013;69:915-26. http://dx.doi.org/10.1111/j.1365-2648.2012.06084.x.
- Pawson R, Wong G, Owen L. Myths, facts and conditional truths: what is the evidence on the risks associated with smoking in cars carrying children?. CMAJ 2011;183:E680-4. http://dx.doi.org/10.1503/cmaj.100903.
- Wong G, Pawson R, Owen L. Policy guidance on threats to legislative interventions in public health: a realist synthesis. BMC Public Health 2011;11. http://dx.doi.org/10.1186/1471-2458-11-222.
- Wong G, Greenhalgh T, Westhorp G, Pawson R. Realist methods in medical education research: what are they and what can they contribute?. Med Educ 2012;46:89-96. http://dx.doi.org/10.1111/j.1365-2923.2011.04045.x.
- Greenhalgh T, Humphrey C, Hughes J, MacFarlane F, Butler C, Pawson R. How do you modernize a health service? A realist evaluation of whole-scale transformation in London. Milbank Q 2009;87:391-416. http://dx.doi.org/10.1111/j.1468-0009.2009.00562.x.
- Macfarlane F, Barton-Sweeney C, Woodard F, Greenhalgh T. Achieving and sustaining profound institutional change in healthcare: case study using neo-institutional theory. Soc Sci Med 2013;80:10-8. http://dx.doi.org/10.1016/j.socscimed.2013.01.005.
- Byng R, Norman I, Redfern S, Jones R. Exposing the key functions of a complex intervention for shared care in mental health: case study of a process evaluation. BMC Health Serv Res 2008;8. http://dx.doi.org/10.1186/1472-6963-8-274.
- Manzano-Santaella A. A realistic evaluation of fines for hospital discharges: incorporating the history of programme evaluations in the analysis. Evaluation 2011;17:21-36. http://dx.doi.org/10.1177/1356389010389913.
- Allen D, Cohen D, Hood K, Robling M, Atwell C, Lane C, et al. Continuity of care in the transition from child to adult diabetes services: a realistic evaluation study. J Health Serv Res Policy 2012;17:140-8. http://dx.doi.org/10.1258/jhsrp.2011.011044.
- Douglas FC, Gray DA, Van Teijlingen ER. Using a realist approach to evaluate smoking cessation interventions targeting pregnant women and young people. BMC Health Serv Res 2010;10. http://dx.doi.org/10.1186/1472-6963-10-49.
- Goicolea I, Coe AB, Hurtig AK, San Sebastian M. Mechanisms for achieving adolescent-friendly services in Ecuador: a realist evaluation approach. Glob Health Action 2012;5. http://dx.doi.org/10.3402/gha.v5i0.18748.
- Kazi MAF. Realist evaluation of social services: what works and in what circumstances. Int J Interdiscipl Soc Sci 2010;4:75-84.
- Kazi MAF, Pagkos B, Milch HA. Realist evaluation in Wraparound: a new approach in social work evidence-based practice. Res Soc Work Pract 2011;21:57-64. http://dx.doi.org/10.1177/1049731510371345.
- Goicolea I, Vives-Cases C, Sebastian MS, Marchal B, Kegels G, Hurtig AK. How do primary health care teams learn to integrate intimate partner violence (IPV) management? A realist evaluation protocol. Implement Sci 2013;8. http://dx.doi.org/10.1186/1748-5908-8-36.
- Ranmuthugala G, Cunningham FC, Plumb JJ, Long J, Georgiou A, Westbrook JI, et al. A realist evaluation of the role of communities of practice in changing healthcare practice. Implement Sci 2011;6. http://dx.doi.org/10.1186/1748-5908-6-49.
- Wand T, White K, Patching J. Refining the model for an emergency department-based mental health nurse practitioner outpatient service. Nurs Inq 2008;15:231-41. http://dx.doi.org/10.1111/j.1440-1800.2008.00407.x.
- Wand T, White K, Patching J. Applying a realist(ic) framework to the evaluation of a new model of emergency department based mental health nursing practice. Nurs Inq 2010;17:231-9. http://dx.doi.org/10.1111/j.1440-1800.2010.00488.x.
- Wand T, White K, Patching J, Dixon J, Green T. An emergency department-based mental health nurse practitioner outpatient service: part 1, participant evaluation. Int J Ment Health Nurs 2011;20:392-400. http://dx.doi.org/10.1111/j.1447-0349.2011.00744.x.
- Wand T, White K, Patching J, Dixon J, Green T. Outcomes from the evaluation of an emergency department-based mental health nurse practitioner outpatient service in Australia. J Am Acad Nurs Pract 2012;24:149-59. http://dx.doi.org/10.1111/j.1745-7599.2011.00709.x.
- Rycroft-Malone J, Fontenla M, Bick D, Seers K. Protocol-based care: impact on roles and service delivery. J Eval Clin Pract 2008;14:867-73. http://dx.doi.org/10.1111/j.1365-2753.2008.01015.x.
- Rycroft-Malone J, Fontenla M, Bick D, Seers K. A realistic evaluation: the case of protocol-based care. Implement Sci 2010;5. http://dx.doi.org/10.1186/1748-5908-5-38.
- Rycroft-Malone J, Fontenla M, Seers K, Bick D. Protocol-based care: the standardisation of decision-making?. J Clin Nurs 2009;18:1490-500. http://dx.doi.org/10.1111/j.1365-2702.2008.02605.x.
- Leone L. Realistic evaluation of an illicit drug deterrence programme: analysis of a case study. Evaluation 2008;14:9-28. http://dx.doi.org/10.1177/1356389007084673.
- Ogrinc G, Batalden P. Realist evaluation as a framework for the assessment of teaching about the improvement of care. J Nurs Educ 2009;48:661-7. http://dx.doi.org/10.3928/01484834-20091113-08.
- Pittam G, Boyce M, Secker J, Lockett H, Samele C. Employment advice in primary care: a realistic evaluation. Health Soc Care Community 2010;18:598-606. http://dx.doi.org/10.1111/j.1365-2524.2010.00929.x.
- Evans D, Killoran A. Tackling health inequalities through partnership working: learning from a realistic evaluation. Crit Public Health 2000;10:139-40. http://dx.doi.org/10.1080/09581590050075899.
- Pommier J, Guével MR, Jourdan D. Evaluation of health promotion in schools: a realistic evaluation approach using mixed methods. BMC Public Health 2010;10. http://dx.doi.org/10.1186/1471-2458-10-43.
- Schatzki TR. The sites of organization. Organ Stud 2005;26:465-84. http://dx.doi.org/10.1177/0170840605050876.
- Oroviogoicoechea C, Elliott B, Watson R. Review: evaluating information systems in nursing. J Clin Nurs 2008;17:567-75. http://dx.doi.org/10.1111/j.1365-2702.2007.01985.x.
- Oroviogoicoechea C, Watson R. A quantitative analysis of the impact of a computerised information system on nurses’ clinical practice using a realistic evaluation framework. Int J Med Inf 2009;78:839-49. http://dx.doi.org/10.1016/j.ijmedinf.2009.08.008.
- Pittam G, Secker J, Ford F. The role of interprofessional working in the pathways to work condition management programmes. J Interprofess Care 2010;24:699-70. http://dx.doi.org/10.3109/13561821003590831.
- Tolson D, McIntosh J, Loftus L, Cormie P. Developing a managed clinical network in palliative care: a realistic evaluation. Int J Nurs Stud 2007;44:183-95. http://dx.doi.org/10.1016/j.ijnurstu.2005.11.027.
- Fulop N, Protopsaltis G, King A, Allen P, Hutchings A, Normand C. Changing organisations: a study of the context and processes of mergers of health care providers in England. Soc Sci Med 2005;60:119-30. http://dx.doi.org/10.1016/j.socscimed.2004.04.017.
- Xue D, Zhou P, Bundorf MK, Huang JX, Chang JL. The association of strategic group and organizational culture with hospital performance in China. Health Care Manag Rev 2013;38. http://dx.doi.org/10.1097/HMR.0b013e3182678f9a.
- Stetler CB, Ritchie JA, Rycroft-Malone J, Schultz AA, Charns MP. Institutionalizing evidence-based practice: an organizational case study using a model of strategic change. Implement Sci 2009;4. http://dx.doi.org/10.1186/1748-5908-4-78.
- Ferlie EB, Shortell SM. Improving the quality of health care in the United Kingdom and the United States: a framework for change. Milbank Q 2001;79:281-315. http://dx.doi.org/10.1111/1468-0009.00206.
- Braithwaite J, Westbrook MT, Robinson M, Michael S, Pirone C, Robinson P. Improving patient safety: the comparative views of patient-safety specialists, workforce staff and managers. BMJ Qual Saf 2011;20:424-31. http://dx.doi.org/10.1136/bmjqs.2010.047605.
- Dixon-Woods M, Tarrant C, Willars J, Suokas A. How will it work? A qualitative study of strategic stakeholders’ accounts of a patient safety initiative. Qual Saf Health Care 2010;19:74-8. http://dx.doi.org/10.1136/qshc.2008.029504.
- Löfgren S, Hansson J, Øvretveit J, Brommels M. Context challenges the champion: improving hip fracture care in a Swedish university hospital. Int J Health Care Qual Assur 2012;25:118-33. http://dx.doi.org/10.1108/09526861211198281.
- Pawson R. Evidence-based policy: the promise of ‘realist synthesis’. Evaluation 2002;8:340-58. http://dx.doi.org/10.1177/135638902401462448.
- Fleetwood S. Ontology in organization and management studies: a critical realist perspective. Organization 2005;12:197-222. http://dx.doi.org/10.1177/1350508405051188.
- Jagosh J, MacAulay AC, Pluye P, Salsberg J, Bush PL, Henderson J, et al. Uncovering the benefits of participatory research: implications of a realist review for health research and practice. Milbank Q 2012;90:311-46. http://dx.doi.org/10.1111/j.1468-0009.2012.00665.x.
- Hedström PY, Ylikoski P. Causal mechanisms in the social sciences. Ann Rev Soc 2010;36:49-67. http://dx.doi.org/10.1146/annurev.soc.012809.102632.
- Sayer A. Method in Social Science: A Realist Approach. London: Hutchinson; 1984.
- Sayer A. Realism and Social Science. London: Sage; 1999.
- Maluka S, Kamuzora P, SanSebastián M, Byskov J, Ndawi B, Olsen ØE, et al. Implementing accountability for reasonableness framework at district level in Tanzania: a realist evaluation. Implement Sci 2011;6. http://dx.doi.org/10.1186/1748-5908-6-11.
- Timmins PM, Miller C. Making evaluations realistic: the challenge of complexity. Support Learn 2007;22:9-16. http://dx.doi.org/10.1111/j.1467-9604.2007.00439.x.
- Mazzocato P, Savage C, Brommels M, Aronsson H, Thor J. Lean thinking in healthcare: a realist review of the literature. Qual Saf Health Care 2010;19:376-82. http://dx.doi.org/10.1136/qshc.2009.037986.
- Harris J, Kearley K, Heneghan C, Meats E, Roberts N, Perera R, et al. Are journal clubs effective in supporting evidence-based decision making? A systematic review. Med Teach 2011;33:9-23. http://dx.doi.org/10.3109/0142159X.2011.530321.
- Gunawardena I. Effectiveness of the geriatric day hospital – a realist review. Rev Clin Gerontol 2011;21:267-9. http://dx.doi.org/10.1017/S0959259811000050.
- Bunge M. Mechanism and explanation. Philos Sol Sci 1997;27:410-46. http://dx.doi.org/10.1177/004839319702700402.
- Bunge M. How does it work? The search for explanatory mechanisms. Philos Soc Sci 2004;34:182-210. http://dx.doi.org/10.1177/0048393103262550.
- Mayntz R. Mechanisms in the analysis of social macro-phenomena. Philos Soc Sci 2004;34:237-59. http://dx.doi.org/10.1177/0048393103262552.
- Dieleman M, Gerretsen B, van der Wilt GJ. Human resource management interventions to improve health workers’ performance in low and middle income countries: a realist review. Health Res Policy Syst 2009;7. http://dx.doi.org/10.1186/1478-4505-7-7.
- Jackson L, Langille L, Lyons R, Hughes J, Martin D, Winstanley V. Does moving from a high-poverty to lower-poverty neighborhood improve mental health? A realist review of ‘Moving to Opportunity’. Health Place 2009;15:961-70. http://dx.doi.org/10.1016/j.healthplace.2009.03.003.
- Vassilev I, Rogers A, Sanders C, Kennedy A, Blickem C, Protheroe J, et al. Social networks, social capital and chronic illness self-management: a realist review. Chronic Illn 2011;7:60-86. http://dx.doi.org/10.1177/1742395310383338.
- Floyd M, Pilling D, Garner K, Barrett P. Vocational rehabilitation: what works and in what circumstances. Int J Rehabil Res 2004;27:99-103. http://dx.doi.org/10.1097/01.mrr.0000127638.09376.cd.
- Morgan G. Evidence-based health policy: a preliminary systematic review. Health Educ J 2010;69:43-7. http://dx.doi.org/10.1177/0017896910363328.
- Connelly JB, Duaso MJ, Butler G. A systematic review of controlled trials of interventions to prevent childhood obesity and overweight: a realistic synthesis of the evidence. Public Health 2007;121:510-7. http://dx.doi.org/10.1016/j.puhe.2006.11.015.
- Tilley N. Applying theory-driven evaluation to the British Crime Reduction Programme: the theories of the programme and of its evaluations. Crim Just 2004;4:255-76. http://dx.doi.org/10.1177/1466802504048465.
- Barley S, Tolbert P. Institutionalization and structuration: studying the links between action and institution. Organ Stud 1997;18:93-117. http://dx.doi.org/10.1177/017084069701800106.
- Scott WR. Institutions and Organizations. London: Sage; 1995.
- Scott WR, Hans-Ulrich Derlien M, Uta Gerhadt M, Scharpf FW. Systemrationalitat und Partialintereresse. Baden-Baden: Nomos Verglagsgesellschaft; 1994.
- DiMaggio P, Powell W. The Iron Cage revisited: institutional isomorphism and collective rationality in organizational fields. Am Sociol Rev 1983;48:147-60. http://dx.doi.org/10.2307/2095101.
- Holm P. The dynamics of institutionalization: transformation processes in Norwegian fisheries. Adm Sci Q 1995;40:398-422. http://dx.doi.org/10.2307/2393791.
- Friedland R, Alford RR, Powell WW, DiMaggio PJ. The New Institutionalism in Organizational Analysis. Chicago, IL: University of Chicago Press; 1991.
- Freidson E. Professionalism: The Third Logic. Chicago, IL: University of Chicago Press; 2001.
- Mutch A, Meyer RE, Sahlin K, Ventresca MJ, Walgenbach P. Institutions and Ideology (Research in the Sociology of Organizations, Volume 27). 2009.
- Thornton PH, Ocasio W, Greenwood R, Oliver C, Sahlin-Anderson K, Suddaby R. The Sage Handbook of Organisational Institutionalism. London: Sage; 2008.
- Kitchener M. Mobilizing the logic of managerialism in professional fields: the case of academic health centre mergers. Organ Stud 2002;23:391-420. http://dx.doi.org/10.1177/0170840602233004.
- Kitchener M, Exworthy M, McKee L, Ferlie E, Hyde P. Organizing and Reorganizing: Power and Change in Health Care Organizations. Hampshire: Palgrave MacMillan; 2008.
- Sillince JAA, Barker JR. A tropological theory of institutionalization. Organ Stud 2012;33:7-38. http://dx.doi.org/10.1177/0170840611425735.
- Archer MS. Routine, reflexivity, and realism. Sociol Theory 2010;28:272-303. http://dx.doi.org/10.1111/j.1467-9558.2010.01375.x.
- Hoffman AJ, Ventresca MJ. The institutional framing of policy debates: economics versus the environment. Am Behav Sci 1999;42:1368-92. http://dx.doi.org/10.1177/00027649921954903.
- Lawrence TB, Suddaby R, Clegg S, Hardy C, Lawrence TB. Handbook of Organization Studies. London: Sage; 2006.
- Seo M-G, Creed WED. Institutional contradictions, praxis, and institutional change: a dialectical perspective. Acad Manag Rev 2002;27:222-47.
- Herepath A. In the loop: a realist approach to structure and agency in the practice of strategy. Organ Stud 2014;35:857-79. http://dx.doi.org/10.1177/0170840613509918.
- Hesketh A, Fleetwood S. Beyond measuring the human resources management-organizational performance link: applying critical realist meta-theory. Organization 2006;13:677-99. http://dx.doi.org/10.1177/1350508406067009.
- Mutch A, Delbridge R, Ventresca M. Situating organizational action: the relational sociology of organizations. Organization 2006;13:607-25. http://dx.doi.org/10.1177/1350508406067006.
- Greenwood R, Díaz AM, Li SX, Lorente JC. The multiplicity of institutional logics and the heterogeneity of organizational responses. Organ Sci 2010;21:521-39. http://dx.doi.org/10.1287/orsc.1090.0453.
- Archer MS. For structure: its reality, properties and powers: a reply to Anthony King. Sociol Rev 2000;48:464-72. http://dx.doi.org/10.1111/1467-954X.00226.
- Scott WR. Institutional carriers: reviewing modes of transporting ideas over time and space and considering their consequences. Ind Corp Change 2003;12:879-94. http://dx.doi.org/10.1093/icc/12.4.879.
- Pache AC, Santos F. Inside the hybrid organization: selective coupling as a response to competing institutional logics. Acad Manag J 2013;56:972-1001. http://dx.doi.org/10.5465/amj.2011.0405.
- Tilcsik A. From ritual to reality: demography, ideology, and decoupling in a post-communist government agency. Acad Manag J 2010;53:1474-98. http://dx.doi.org/10.5465/AMJ.2010.57318905.
- Lewin K. Resolving Social Conflicts and Field Theory in Social Science. American Psychological Association; 2010.
- Schein EH. Kurt Lewin’s change theory in the field and in the classroom: notes towards a model of management learning. Syst Pract 1996;9:27-4. http://dx.doi.org/10.1007/BF02173417.
- May C. A rational model for assessing and evaluating complex interventions in health care. BMC Health Serv Res 2006;6. http://dx.doi.org/10.1186/1472-6963-6-86.
- May C, Finch T. Implementing, embedding, and integrating practices: an outline of normalization process theory. Sociology 2009;43:535-54. http://dx.doi.org/10.1177/0038038509103208.
- May C. Towards a general theory of implementation. Implement Sci 2013;8. http://dx.doi.org/10.1186/1748-5908-8-18.
- May C. Agency and implementation: understanding the embedding of healthcare innovations in practice. Soc Sci Med 2013;78:26-33. http://dx.doi.org/10.1016/j.socscimed.2012.11.021.
- May CR, Finch T, Ballini L, MacFarlane A, Mair F, Murray E, et al. Evaluating complex interventions and health technologies using normalization process theory: development of a simplified approach and web-enabled toolkit. BMC Health Serv Res 2011;11. http://dx.doi.org/10.1186/1472-6963-11-245.
- Murray E, Treweek S, Pope C, MacFarlane A, Ballini L, Dowrick C, et al. Normalisation process theory: a framework for developing, evaluating and implementing complex interventions. BMC Med 2010;8. http://dx.doi.org/10.1186/1741-7015-8-63.
- Greenhalgh T, Robert G, Macfarlane F, Bate P, Kyriakidou O. Diffusion of innovations in service organizations: systematic review and recommendations. Milbank Q 2004;82:581-629. http://dx.doi.org/10.1111/j.0887-378X.2004.00325.x.
- Mouzelis NP. Modern and Postmodern Social Theorizing: Bridging the Divide. Cambridge: Cambridge University Press; 2008.
- Layder D. Understanding Social Theory. London: Sage; 2006.
- Yin RK. Case Study Research: Design and Methods. London: Sage; 2009.
- Bhaskar R. A Realist Theory of Science. Brighton: Harvester; 1978.
- Danermark B, Ekström M, Jakobsen L, Karlsson J. Explaining Society: An Introduction to Critical Realism in the Social Sciences. London and New York, NY: Routledge; 2002.
- Bergene AC. Towards a critical realist comparative methodology: context sensitive theoretical comparison. J Crit Realism 2007;6:5-27. http://dx.doi.org/10.1558/jocr.v6i1.5.
- Wynn D, Williams CK. Principles for conducting critical realist case study research in information systems. MIS Q 2012;36:787-810.
- Ackroyd S, Fleetwood S. Realist Perspectives on Management and Organisation. London: Routledge; 2000.
- Eisenhardt KM. Building theories from case study research. Acad Manag Rev 1989;14:532-50.
- Eisenhardt KM, Graebner ME. Theory building from cases: opportunities and challenges. Acad Manag J 2007;50:25-32. http://dx.doi.org/10.5465/AMJ.2007.24160888.
- Dopson S. The potential for case study method for organisational analysis. Policy Polit 2003;31:217-26. http://dx.doi.org/10.1332/030557303765371708.
- Barber M. Three Paradigms of Public-Sector Reform. London: McKinsey and Company; 2007.
- Hood C. A public management for all seasons?. Public Adm 1991;69:3-19. http://dx.doi.org/10.1111/j.1467-9299.1991.tb00779.x.
- Hood C. Contemporary public management: a new global paradigm?. Public Policy Adm 1994;10:104-17.
- Dunn MB, Jones C. Institutional logics and institutional pluralism: the contestation of care and science logics in medical education, 1967–2005. Adm Sci Q 2010;55:114-49. http://dx.doi.org/10.2189/asqu.2010.55.1.114.
- Ritchie J. An Inquiry into Quality and Practice within the National Health Service arising from the actions of Rodney Ledward. London: The Stationery Office; 2000.
- The Kerr/Haslam Inquiry: Full Report. London: The Stationery Office; 2005.
- Redfern M, Keeling JW, Powell E. The Royal Liverpool Children’s Inquiry Report. London: The Stationery Office; 2001.
- Midstaffsinquiry . Mid Staffordshire NHS Foundation Trust Inquiry n.d. www.midstaffsinquiry.com/ (accessed March 2012).
- Burgess A. The changing character of public inquiries in the (risk) regulatory state. Br Polit 2011;6:3-29. http://dx.doi.org/10.1057/bp.2010.15.
- Meyer JW, Rowan B. Institutional organizations: formal structure as myth and ceremony. Am J Sociol 1977;83:340-63. http://dx.doi.org/10.1086/226550.
- Financing and Delivering Health Care: A Comparative Analysis of OECD Countries. Paris: OECD; 1987.
- Cole A, Jones JB, Storer A. Inside the National Assembly for Wales: the Welsh civil service under devolution. Polit Q 2003;74:223-32. http://dx.doi.org/10.1111/1467-923X.00532.
- Burau V, Blank RH. Comparing health policy: an assessment of typologies of health systems. J Comp Policy Anal Res Pract 2006;8:63-76. http://dx.doi.org/10.1080/13876980500513558.
- Piatt W. The UK Government’s Approach to Public Service Reform. London: Prime Minister’s Strategy Unit, Cabinet Office; 2006.
- Ferlie E, Pettigrew A, Ashburner L, Fitzgerald L. The New Public Management in Action. Oxford: Oxford University Press; 1996.
- Boyne G, Martin S, Walker R. Explicit reforms, implicit theories and public service improvement. Public Manag Rev 2004;6:189-210. http://dx.doi.org/10.1080/1471903042000189092.
- Fernandez S, Pitts DW. Under what conditions do public managers favor and pursue organizational change. Am Rev Public Adm 2007;37:324-41. http://dx.doi.org/10.1177/0275074006293467.
- Reconfiguring the Department of Health’s Arm’s Length Bodies. London: Department of Health; 2004.
- Sullivan M. Wales, devolution and health policy: policy experimentation and differentiation to improve health. Contemp Wales 2005;17:44-65.
- Le Grand J. The Labour Government and the National Health Service. Oxf Rev Econ Policy 2002;18:137-53. http://dx.doi.org/10.1093/oxrep/18.2.137.
- Fiol CM, O’Connor EJ, Aguinis H. All for one and one for all? The development and transfer of power across organizational levels. Acad Manag Rev 2001;26:224-42. http://dx.doi.org/10.2307/259120.
- Achieving Excellence: The Quality Delivery Plan for the NHS in Wales 2012–2016. Cardiff: Welsh Government; 2012.
- Making the Connections: Delivering Better Services for Wales – The Welsh Assembly Government Vision for Public Services. Cardiff: Welsh Assembly Government; 2004.
- Quinn M. Evidence based or people based policy making? A view from Wales. Public Policy Adm 2002;17:29-42. http://dx.doi.org/10.1177/095207670201700303.
- Currie G, Finn R, Martin G. Accounting for the ‘dark side’ of new organizational forms: the case of healthcare professionals. Hum Relat 2008;61:539-64. http://dx.doi.org/10.1177/0018726708091018.
- Currie G, Lockett A. A critique of transformational leadership: moral, professional and contingent dimensions of leadership within public services organizations. Human Relat 2007;60:341-70. http://dx.doi.org/10.1177/0018726707075884.
- Trust, Assurance and Safety – The Regulation of Health Professionals in the 21st Century. London: The Stationery Office; 2007.
- The New NHS: Modern, Dependable. London: Department of Health; 1997.
- Delivering the NHS Plan: Next Steps on Investment, Next Steps on Reform. London: Department of Health; 2002.
- Dixon A, Le Grand J, Henderson J, Murray R, Poteliakhoff E. Is the British National Health Service equitable? The evidence on socioeconomic differences in utilization. J Health Serv Res Policy 2007;12:104-9. http://dx.doi.org/10.1258/135581907780279549.
- Thomson S, Dixon A. Choices in health care: the European experience. J Health Serv Res Policy 2006;11:167-71. http://dx.doi.org/10.1258/135581906777641703.
- Cole GDH. A History of the Labour Party from 1914. London: Routledge and Kegan Paul; 1948.
- NHS Wales Delivery Framework: 2013–2014 and Future Plans. Cardiff: Welsh Government; 2013.
- Whittington R. Completing the practice turn in strategy research. Organ Stud 2006;27:613-34. http://dx.doi.org/10.1177/0170840606064101.
- Scott WR. Lords of the dance: professionals as institutional agents. Organ Stud 2008;29:219-38. http://dx.doi.org/10.1177/0170840607088151.
- Rieley J. Gaming the System: How to Stop Playing the Organizational Game and Start Playing the Competetive Game. London: Pearson Education; 2001.
- Walker IA, Reshamwalla S, Wilson IH. Surgical safety checklists: do they improve outcomes?. Br J Anaest 2012;109:47-54. http://dx.doi.org/10.1093/bja/aes175.
- Dixon-Woods M, Leslie M, Bion J, Tarrant C. What counts? An ethnographic study of infection data reported to a patient safety program. Milbank Q 2012;90:548-91. http://dx.doi.org/10.1111/j.1468-0009.2012.00674.x.
- Reay T, Chreim S, Golden-Biddle K, Goodrick E, Williams BEBW, Casebeer A, et al. Transforming new ideas into practice: an activity based perspective on the institutionalization of practices. J Manag Stud 2013;50:963-90. http://dx.doi.org/10.1111/joms.12039.
- Gapp R, Fisher R. Developing an intrapreneur-led three-phase model of innovation. Int J Entrepreneur Behav Res 2007;13:330-48. http://dx.doi.org/10.1108/13552550710829151.
- Pronovost PJ, Berenholtz SM, Goeschel C, Thom I, Watson SR, Holzmueller CG, et al. Improving patient safety in intensive care units in Michigan. J Crit Care 2008;23:207-21. http://dx.doi.org/10.1016/j.jcrc.2007.09.002.
- Koetsier A, van der Veer SN, Jager KJ, Peek N, Keizer NF. Control charts in healthcare quality improvement: a systematic review on adherence to methodological criteria. Method Inf Med 2012;51:189-98. http://dx.doi.org/10.3414/ME11-01-0055.
- Sujan MA. A novel tool for organisational learning and its impact on safety culture in a hospital dispensary. Reliabil Engineer Syst Saf 2012;101:21-34. http://dx.doi.org/10.1016/j.ress.2011.12.021.
- Strang D, Meyer JW. Institutional conditions for diffusion. Theory Soc 1993;22:487-511. http://dx.doi.org/10.1007/BF00993595.
- Goodrick E, Reay T. Florence nightingale endures: legitimizing a new professional role identity. J Manag Stud 2010;47:55-84. http://dx.doi.org/10.1111/j.1467-6486.2009.00860.x.
- Benning A, Ghaleb M, Suokas A, Dixon-Woods M, Dawson J, Barber N, et al. Large scale organisational intervention to improve patient safety in four UK hospitals: mixed method evaluation. BMJ 2011;342. http://dx.doi.org/10.1136/bmj.d195.
- Varkey P, Sathananthan A, Scheifer A, Bhagra S, Fujiyoshi A, Tom A, et al. Using quality-improvement techniques to enhance patient education and counselling of diagnosis and management. Qual Prim Care 2009;17:205-13.
- Brodie A, Kinross J, Bailey M, Aggarwal R, Vincent C. Using failure mode and effects analysis to identify hazards within resuscitation. Int J Risk Saf Med 2009;21:201-15.
- Currie G, Finn R, Martin G. Spanning boundaries in pursuit of effective knowledge sharing within networks in the NHS. J Health Organ Manag 2007;21:406-17. http://dx.doi.org/10.1108/14777260710778934.
- Berwick D. Spreading innovation. Qual Connect 1997;6:1-3.
- Berwick DM. Developing and testing changes in delivery of care. Ann Intern Med 1998;128:651-6. http://dx.doi.org/10.7326/0003-4819-128-8-199804150-00009.
- Cleghorn GD, Headrick LA. The PDSA cycle at the core of learning in health professions education. Jt Comm J Qual Improv 1996;22:206-12.
- Lovitt MR. The new pragmatism: going beyond Shewhart and Deming. Qual Prog 1997;30:99-105.
- Dooley K. Use PDSA for crying out loud. Qual Prog 1997;30:60-3.
- Brilli RJ, McClead RE, Crandall WV, Stoverock L, Berry JC, Wheeler TA, et al. A comprehensive patient safety program can significantly reduce preventable harm, associated costs, and hospital mortality. J Pediatr 2013;63:1638-45. http://dx.doi.org/10.1016/j.jpeds.2013.06.031.
- Coleman MT, Headrick LA, Langley AE, Thomas JX. Teaching medical faculty how to apply continuous quality improvement to medical education. Jt Comm J Qual Improv 1998;24:640-52.
- Seary JA, Chui C, Fu R, Lo J, Min E. Learning by doing: experiences of an interdisciplinary student quality improvement team. U Toronto Med J 2011;88:156-9.
- Oyler J, Vinci L, Johnson JK, Arora VM. Teaching internal medicine residents to sustain their improvement through the quality assessment and improvement curriculum. J Gen Intern Med 2011;26:221-5. http://dx.doi.org/10.1007/s11606-010-1547-y.
- Farbstein K, Clough J. Improving medication safety across a multihospital system. Jt Comm J Qual Improv 2001;27:123-37.
- Walley P, Gowland B. Completing the circle: from PD to PDSA. Int J Health Care Qual Assur 2004;17:349-58. http://dx.doi.org/10.1108/09526860410557606.
- Reader TW, Gillespie A. Patient neglect in healthcare institutions: a systematic review and conceptual model. BMC Health Serv Res 2013;13. http://dx.doi.org/10.1186/1472-6963-13-156.
- Chang CW, Huang HC, Chiang CY, Hsu CP, Chang CC. Social capital and knowledge sharing: effects on patient safety. J Adv Nurs 2012;68:1793-803. http://dx.doi.org/10.1111/j.1365-2648.2011.05871.x.
- Norton EK, Rangel SJ. Implementing a pediatric surgical safety checklist in the OR and beyond. AORN J 2010;92:61-7. http://dx.doi.org/10.1016/j.aorn.2009.11.069.
- Carney BT, West P, Neily J, Mills PD, Bagian JP. Differences in nurse and surgeon perceptions of teamwork: implications for use of a briefing checklist in the OR. AORN J 2010;91:722-9. http://dx.doi.org/10.1016/j.aorn.2009.11.066.
- Takala RSK, Pauniaho SL, Kotkansalo A, Helmiö P, Blomgren K, Helminen M, et al. A pilot study of the implementation of WHO Surgical Checklist in Finland: improvements in activities and communication. Acta Anaest Scand 2011;55:1206-14. http://dx.doi.org/10.1111/j.1399-6576.2011.02525.x.
- Hurtado JJD, Jiménez X, Pẽalonzo MA, Villatoro C, De Izquierdo S, Cifuentes M. Acceptance of the WHO Surgical Safety Checklist among surgical personnel in hospitals in Guatemala city. BMC Health Serv Res 2012;12. http://dx.doi.org/10.1186/1472-6963-12-169.
- Pronovost PJ, Morlock L, Davis RO, Cunningham T, Paine L, Scheulen J. Using online and offline change models to improve ICU access and revenues. Jt Comm J Qual Improv 2000;26:5-17.
- Livingood WC, Sabbagh R, Spitzfaden S, Hicks A, Wells L, Puigdomenech S, et al. A quality improvement evaluation case study: impact on public health outcomes and agency culture. Am J Prev Med 2013;44:445-52. http://dx.doi.org/10.1016/j.amepre.2013.01.011.
- Böhmer AB, Wappler F, Tinschmann T, Kindermann P, Rixen D, Bellendir M, et al. The implementation of a perioperative checklist increases patients’ perioperative safety and staff satisfaction. Acta Anaest Scand 2012;56:332-8. http://dx.doi.org/10.1111/j.1399-6576.2011.02590.x.
- Haugen AS, Søfteland E, Eide GE, Sevdalis N, Vincent CA, Nortvedt MW, et al. Impact of the World Health Organization’s Surgical Safety Checklist on safety culture in the operating theatre: a controlled intervention study. Br J Anaest 2013;110:807-15. http://dx.doi.org/10.1093/bja/aet005.
- Gherardi S. Practice-based theorizing on learning and knowledge in organizations. Organization 2000;7:211-23. http://dx.doi.org/10.1177/135050840072001.
- May C, Finch T, Mair F, Ballini L, Dowrick C, Eccles M, et al. Understanding the implementation of complex interventions in health care: the normalisation process model. BMC Health Serv Res 2007;7. http://dx.doi.org/10.1186/1472-6963-7-148.
- May CR, Finch TL, Cornford J, Exley C, Gately C, Kirk S, et al. Integrating telecare for chronic disease management in the community: what needs to be done?. BMC Health Serv Res 2011;11. http://dx.doi.org/10.1186/1472-6963-11-131.
- Finch TL, Mair FS, Odonnell C, Murray E, May CR. From theory to ‘measurement’ in complex interventions: methodological lessons from the development of an e-health normalisation instrument. BMC Med Res Methodol 2012;12. http://dx.doi.org/10.1186/1471-2288-12-69.
- Finch TL, Rapley T, Girling M, Mair FS, Murray E, Treweek S, et al. Improving the normalization of complex interventions: measure development based on normalization process theory (NoMAD): study protocol. Implement Sci 2013;8. http://dx.doi.org/10.1186/1748-5908-8-43.
- NHS Wales Annual Operating Framework: 2010–2011. Cardiff: Welsh Assembly Government; 2010.
- NHS Wales Annual Quality Framework: 2011–2012. Cardiff: Welsh Assembly Government; 2011.
- Working Differently – Working Together: A Workforce and Organisational Development Framework. Cardiff: Welsh Government; 2012.
- Fulop N, Walters R, Perri, Spurgeon P. Implementing changes to hospital services: factors influencing the process and ‘results’ of reconfiguration. Health Policy 2012;104:128-35. http://dx.doi.org/10.1016/j.healthpol.2011.05.015.
- Miller EA, Banaszak-Holl J. Cognitive and normative determinants of state policymaking behavior: lessons from the sociological institutionalism. Publius 2005;35:191-216. http://dx.doi.org/10.1093/publius/pji008.
- Morello RT, Lowthian JA, Barker AL, McGinnes R, Dunt D, Brand C. Strategies for improving patient safety culture in hospitals: a systematic review. BMJ Qual Saf 2013;22:11-8. http://dx.doi.org/10.1136/bmjqs-2011-000582.
- Sheaff R. Medicine and management in english primary care: a shifting balance of power?. J Soc Policy 2009;38:627-47. http://dx.doi.org/10.1017/S0047279409990183.
- Braithwaite J, Westbrook M, Nugus P, Greenfield D, Travaglia J, Runciman W, et al. A four-year, systems-wide intervention promoting interprofessional collaboration. BMC Health Serv Res 2012;12. http://dx.doi.org/10.1186/1472-6963-12-99.
- McCaughey D, Halbesleben JRB, Savage GT, Simons T, McGhan GE. Safety leadership: extending workplace safety climate best practices across health care workforces. Adv Health Care Manag 2013;14:189-217. http://dx.doi.org/10.1108/S1474-8231(2013)00000140013.
- McGuckin M, Govednik J. Patient empowerment and hand hygiene, 1997–2012. J Hosp Infect 2013;84:191-9. http://dx.doi.org/10.1016/j.jhin.2013.01.014.
- Ruchlin HS, Dubbs NL, Callahan MA. The role of leadership in instilling a culture of safety: lessons from the literature. J Healthc Manag 2004;49:47-58.
- Best A, Saul J, Willis C. Doing the dance of culture change: complexity, evidence and leadership. Healthc Pap 2013;13:64-8. http://dx.doi.org/10.12927/hcpap.2013.23346.
- Lindstrom RR. Leadership needs to shift in the health system: three emerging perspectives to inform our way forward. Healthc Pap 2013;13:48-54. http://dx.doi.org/10.12927/hcpap.2013.23343.
- Whitlock J. The value of active followership. Nurs Manag 2013;20:20-3. http://dx.doi.org/10.7748/nm2013.05.20.2.20.e677.
- Deilkås ET, Hofoss D. Psychometric properties of the Norwegian version of the Safety Attitudes Questionnaire (SAQ), Generic version (Short Form 2006). BMC Health Serv Res 2008;8. http://dx.doi.org/10.1186/1472-6963-8-191.
- Alahmadi HA. Assessment of patient safety culture in Saudi Arabian hospitals. Qual Saf Health Care 2010;19. http://dx.doi.org/10.1136/qshc.2009.033258.
- Singer SJ, Vogus TJ. Reducing hospital errors: interventions that build safety culture. Annu Rev Public Health 2013;34:373-96. http://dx.doi.org/10.1146/annurev-publhealth-031912-114439.
- Sullivan N, Schoelles KM. Preventing in-facility pressure ulcers as a patient safety strategy: a systematic review. Ann Intern Med 2013;158:410-16. http://dx.doi.org/10.7326/0003-4819-158-5-201303051-00008.
- Chassin MR, Loeb JM. High-reliability health care: getting there from here. Milbank Q 2013;91:459-90. http://dx.doi.org/10.1111/1468-0009.12023.
- Heenan M, Khan H, Binkley D. From boardroom to bedside: how to define and measure hospital quality. Healthc Q 2010;13:55-60. http://dx.doi.org/10.12927/hcq.2013.21615.
- Reid J. Respect, compassion and dignity: the foundations of ethical and professional caring. J Periop Pract 2012;22:216-19.
- Yoon SH, Kim B, Kim SY. Development and validation of the Korean patient safety culture scale for nursing homes. J Korean Acad Nurs 2013;43:379-88. http://dx.doi.org/10.4040/jkan.2013.43.3.379.
- Brunoro-Kadash C, Kadash N. Time to care: a patient-centered quality improvement strategy. Leadersh Health Serv 2013;26:220-31. http://dx.doi.org/10.1108/LHS-02-2013-0011.
- Scott C, Gerardi D. A strategic approach for managing conflict in hospitals: responding to the joint commission leadership standard, part 1. Jt Comm J Qual Patient Saf 2011;37:59-6.
- Yule S, Flin R, Davies JM, McKee L. Healthcare CEOs’ leadership style and patient safety. Hum Fac Erg Soc P 2008;52:820-4. http://dx.doi.org/10.1177/154193120805201212.
- Stott DL. Whole team training. J Periop Practice 2013;23.
- Siassakos D, Fox R, Bristowe K, Angouri J, Hambly H, Robson L, et al. What makes maternity teams effective and safe? Lessons from a series of research on teamwork, leadership and team training. Acta Obstet Gynecol Scand 2013;92:1239-43. http://dx.doi.org/10.1111/aogs.12248.
- Miskelly P, Duncan L. ‘I’m actually being the grown-up now’: leadership, maturity and professional identity development [published online ahead of print 28 February 2013]. J Nurs Manag 2013.
- Kaufman G, McCaughan D. The effect of organisational culture on patient safety. Nurs Stand 2013;27:50-6. http://dx.doi.org/10.7748/ns2013.06.27.43.50.e7280.
- Duff B. Creating a culture of safety by coaching clinicians to competence. Nurs Educ Today 2013;33:1108-11. http://dx.doi.org/10.1016/j.nedt.2012.05.025.
- Weng RH, Huang CY, Chen LM, Chang LY. Exploring the impact of transformational leadership on nurse innovation behaviour: a cross-sectional study. J Nurs Manag 2015;23:427-39. http://dx.doi.org/10.1111/jonm.12149.
- Gluck PA. Physician leadership: essential in creating a culture of safety. Clin Obstet Gynecol 2010;53:473-81. http://dx.doi.org/10.1097/GRF.0b013e3181ec1476.
- Weaver SJ, Lubomksi LH, Wilson RF, Pfoh ER, Martinez KA, Dy SM. Promoting a culture of safety as a patient safety strategy: a systematic review. Ann Intern Med 2013;158:369-74. http://dx.doi.org/10.7326/0003-4819-158-5-201303051-00002.
- Thomas L, Galla C. Building a culture of safety through team training and engagement. BMJ Qual Saf 2013;22:425-34. http://dx.doi.org/10.1136/bmjqs-2012-001011.
- Valabhji J. Excess inpatient mortality for those with diabetes in England. Diabet Med 2013;30:1391-2. http://dx.doi.org/10.1111/dme.12311.
- Spiegelhalter D. Are you 45% more likely to die in a UK hospital rather than a US hospital?. BMJ 2013;34. http://dx.doi.org/10.1136/bmj.f5775.
- Jarman B. Quality of care and patient safety in the UK: the way forward after Mid Staffordshire. Lancet 2013;382:573-5. http://dx.doi.org/10.1016/S0140-6736(13)61726-2.
- Jarman B. In defence of the hospital standardized mortality ratio. Healthc Pap 2008;8:37-42. http://dx.doi.org/10.12927/hcpap.2008.19974.
- Scott IA, Brand CA, Phelps GE, Barker AL, Cameron PA. Using hospital standardised mortality ratios to assess quality of care – proceed with extreme caution. Med J Aust 2011;194:645-8.
- den Ouden AL, van der Wal G. The usefulness of the hospital standardized mortality ratio as an indicator of hospital mortality. Ned Tijdschr Geneeskd 2008;152:1191-2.
- Penfold RB, Dean S, Flemons W, Moffatt M. Do hospital standardized mortality ratios measure patient safety? HSMRs in the Winnipeg Regional Health Authority. Healthc Pap 2008;8:8-24. http://dx.doi.org/10.12927/hcpap.2008.19972.
- Teres D. The value and limits of severity adjusted mortality for ICU patients. J Crit Care 2004;19:257-63. http://dx.doi.org/10.1016/j.jcrc.2004.08.007.
- Mitchell PH, Shannon SE, Cain KC, Hegyvary ST. Critical care outcomes: linking structures, processes, and organizational and clinical outcomes. Am J Crit Care 1996;5:353-63.
- Lau H, Litman KC. Saving lives by studying deaths: using standardized mortality reviews to improve inpatient safety. Jt Comm J Qual Patient Saf 2011;37:400-8.
- Wen E, Sandoval C, Zelmer J, Webster G. Understanding and using the hospital standardized mortality ratio in Canada: challenges and opportunities. Healthc Pap 2008;8:26-3. http://dx.doi.org/10.12927/hcpap.2008.19973.
- McKinley J, Gibson D, Ardal S. Hospital standardized mortality ratio: the way forward in Ontario. Healthc Pap 2008;8:43-9. http://dx.doi.org/10.12927/hcpap.2008.19975.
- Higginson J, Walters R, Fulop N. Mortality and morbidity meetings: an untapped resource for improving the governance of patient safety?. BMJ Qual Saf 2012;21:576-85. http://dx.doi.org/10.1136/bmjqs-2011-000603.
- West MA, Guthrie JP, Dawson JF, Borrill CS, Carter M. Reducing patient mortality in hospitals: the role of human resource management. J Organ Behav 2006;27:983-1002. http://dx.doi.org/10.1002/job.396.
- Nicklin W, Graves E. Nursing and patient outcomes: it’s time for healthcare leadership to respond. Healthc Manage Forum 2005;18:9-13. http://dx.doi.org/10.1016/S0840-4704(10)60298-0.
- Sutton M, Nikolova S, Boaden R, Lester H, McDonald R, Roland M. Reduced mortality with hospital pay for performance in England. Obstet Gynecol Surv 2013;68:187-9. http://dx.doi.org/10.1097/01.ogx.0000428158.81933.54.
- Wright J, Dugdale B, Hammond I, Jarman B, Neary M, Newton D, et al. Learning from death: a hospital mortality reduction programme. J R Soc Med 2006;99:303-8. http://dx.doi.org/10.1258/jrsm.99.6.303.
- Sheps SB. Measure for measure? The challenge of new thinking about patient safety. Healthc Pap 2008;8:62-7. http://dx.doi.org/10.12927/hcpap.2008.19979.
- Joshi MS, Hines SC. Getting the board on board: engaging hospital boards in quality and patient safety. Jt Comm J Qual Patient Saf 2006;32:179-87.
- Rubin MS, Stone RK. Adapting the ‘managing by walking around’ methodology as a leadership strategy to communicate a hospital-wide strategic plan. J Public Health Manag Pract 2010;16:162-6. http://dx.doi.org/10.1097/PHH.0b013e3181c6b68a.
- Frankel A, Grillo SP, Pittman M, Thomas EJ, Horowitz L, Page M, et al. Revealing and resolving patient safety defects: the impact of leadership walkrounds on frontline caregiver assessments of patient safety. Health Serv Res 2008;43:2050-66. http://dx.doi.org/10.1111/j.1475-6773.2008.00878.x.
- Frankel AS, Leonard MW, Denham CR. Fair and just culture, team behavior, and leadership engagement: the tools to achieve high reliability. Health Serv Res 2006;41:1690-709. http://dx.doi.org/10.1111/j.1475-6773.2006.00572.x.
- Saladino L, Pickett LC, Frush K, Mall A, Champagne MT. Evaluation of a nurse-led safety program in a critical care unit. J Nurs Care Qual 2013;28:139-46. http://dx.doi.org/10.1097/NCQ.0b013e31827464c3.
- Menéndez MD, Martínez AB, Fernandez M, Ortega N, Díaz JM, Vazquez F. Walkrounds and briefings in the improvement of the patient safety. Rev Calid Asist 2010;25:153-60. http://dx.doi.org/10.1016/j.cali.2009.12.008.
- Jensen EB. Single-patient rooms. Enestuer 2009;171:1772-5.
- Frankel A, Graydon-Baker E, Neppl C, Simmonds T, Gustafson M, Gandhi TK. Patient safety leadership walkrounds. Jt Comm J Qual Improv 2003;29:16-2.
- Frankel A, Gandhi TK, Bates DW. Improving patient safety across a large integrated health care delivery system. Int J Qual Health Care 2003;15:i31-40. http://dx.doi.org/10.1093/intqhc/mzg075.
- Taylor AM, Chuo J, Figueroa-Altmann A, Di Taranto S, Shaw KN. Using four-phased unit-based patient safety walkrounds to uncover correctable system flaws. Jt Comm J Qual Patient Saf 2013;39:396-403.
- Schwendimann R, Milne J, Frush K, Ausserhofer D, Frankel A, Sexton JB. A closer look at associations between hospital leadership walkrounds and patient safety climate and risk reduction: a cross-sectional study. Am J Med Qual 2013;28:414-21. http://dx.doi.org/10.1177/1062860612473635.
- Burnett S, Parand A, Benn J, Pinto A, Iskander S, Vincent C. Learning about leadership from patient safety WalkRounds™. Int J Clin Leadersh 2008;16:185-92.
- Verschoor KN, Taylor A, Northway TL, Hudson DG, Van Stolk DE, Shearer KJ, et al. Creating a safety culture at the Children’s and Women’s Health Centre of British Columbia. J Pediatr Nurs 2007;22:81-6. http://dx.doi.org/10.1016/j.pedn.2006.08.012.
- Gandhi TK, Graydon-Baker E, Huber CN, Whittemore AD, Gustafson M. Closing the loop: follow-up and feedback in a patient safety program. Jt Comm J Qual Patient Saf 2005;31:614-21.
- Frankel A, Grillo SP, Baker EG, Huber CN, Abookire S, Grenham M, et al. Patient safety leadership WalkRounds at Partners Healthcare: learning from implementation. Jt Comm J Qual Patient Saf 2005;31:423-37.
- Hill S. The Knowledgeable Patient: Communication and Participation in Health. Oxford: Wiley-Blackwell; 2011.
- Greenhalgh T, Wengraf T. Collecting stories: is it research? Is it good research? Preliminary guidance based on a Delphi study. Med Educ 2008;42:242-7. http://dx.doi.org/10.1111/j.1365-2923.2007.02956.x.
- Berwick DM. The stories beneath. Med Care 2007;45:1123-5. http://dx.doi.org/10.1097/MLR.0b013e31815d18e6.
- Kuzel AJ, Woolf SH, Gilchrist VJ, Engel JD, LaVeist TA, Vincent C, et al. Patient reports of preventable problems and harms in primary health care. Ann Fam Med 2004;2:333-40. http://dx.doi.org/10.1370/afm.220.
- Pinto A, Faiz O, Vincent C. Managing the after effects of serious patient safety incidents in the NHS: an online survey study. BMJ Qual Saf 2012;21:1001-8. http://dx.doi.org/10.1136/bmjqs-2012-000826.
- Kerfoot K, Sarosi GM. Hero making through storytelling: the nurse manager’s challenge. Nurs Econ 1993;11.
- Morath J, Leary M. Creating safe spaces in organizations to talk about safety. Nurs Econ 2004;22:344-51, 354.
- Kitson A. Nursing leadership: bringing caring back to the future. Qual Health Care 2001;10:ii79-84. http://dx.doi.org/10.1136/qhc.0100079.
- Pickles JP, Hide EH, Maher LM. Experience based design: a practical method of working with patients to redesign services. Clin Govern 2008;13:51-8. http://dx.doi.org/10.1108/14777270810850634.
- Quaid D, Thao J, Denham CR. Story power: the secret weapon. J Patient Saf 2010;6:5-14. http://dx.doi.org/10.1097/PTS.0b013e3181d23231.
- Conway J. Getting boards on board: engaging governing boards in quality and safety. Jt Comm J Qual Patient Saf 2008;34:214-20.
- Amalberti R, Auroy Y, Berwick D, Barach P. Five system barriers to achieving ultrasafe health care. Ann Intern Med 2005;142:756-64. http://dx.doi.org/10.7326/0003-4819-142-9-200505030-00012.
- Travaglia JF, Westbrook MT, Braithwaite J. Implementation of a patient safety incident management system as viewed by doctors, nurses and allied health professionals. Health 2009;13:277-96. http://dx.doi.org/10.1177/1363459308101804.
- Westbrook MT, Braithwaite J, Travaglia JF, Jorm C, Iedema RA. Promoting safety: longer-term responses of three health professional groups to a safety improvement programme. Int J Health Care Qual Assur 2007;20:555-71. http://dx.doi.org/10.1108/09526860710822707.
- McDonald R, Waring J, Harrison S, Walshe K, Boaden R. Rules and guidelines in clinical practice: a qualitative study in operating theatres of doctors’ and nurses’ views. Qual Saf Health Care 2005;14:290-4. http://dx.doi.org/10.1136/qshc.2005.013912.
- McDonald R, Waring J, Harrison S. Rules, safety and the narrativisation of identity: a hospital operating theatre case study. Sociol Health Illn 2006;28:178-202. http://dx.doi.org/10.1111/j.1467-9566.2006.00487.x.
- Currie G, Humpreys M, Waring J, Rowley E. Narratives of professional regulation and patient safety: the case of medical devices in anaesthetics. Health Risk Soc 2009;11:117-35. http://dx.doi.org/10.1080/13698570902784257.
- Addicott R, Ferlie E. Understanding power relationships in health care networks. J Health Organ Manag 2007;21:393-405. http://dx.doi.org/10.1108/14777260710778925.
- Vincent C. Social scientists and patient safety: critics or contributors?. Soc Sci Med 2009;69:1777-9. http://dx.doi.org/10.1016/j.socscimed.2009.09.046.
- Implementation Manual: Surgical Safety Checklist. Geneva: World Alliance for Patient Safety, World Health Organization; 2008.
- Alnaib M, Al Samaraee A, Bhattacharya V. The WHO surgical safety checklist. J Periop Pract 2012;22:289-92.
- Munigangaiah S, Sayana MK, Lenehan B. Relevance of World Health Organization surgical safety checklist to trauma and orthopaedic surgery. Acta Orthop Belg 2012;78:574-81.
- Clark SC, Dunning J, Alfieri OR, Elia S, Hamilton LR, Kappetein PA, et al. EACTS guidelines for the use of patient safety checklists. Eur J Cardiothorac Surg 2012;41:993-1004. http://dx.doi.org/10.1093/ejcts/ezs009.
- Knepil GJ, Harvey CT, Beech AN. Marking the skin for oral surgical procedures: improving the WHO checklist. Br J Oral Maxillofac Surg 2013;51:413-15. http://dx.doi.org/10.1016/j.bjoms.2012.09.010.
- Da Silva-Freitas R, Martín-Laez R, Madrazo-Leal CB, Villena-Martin M, Valduvieco-Juaristi I, Martínez-Agüerosa JÁ, et al. Establishment of a modified surgical safety checklist for the neurosurgical patient: initial experience in 400 cases. Neurocirugia (Astur) 2012;23:60-9. http://dx.doi.org/10.1016/j.neucir.2012.04.006.
- Burbos N, Morris E. Applying the World Health Organization Surgical Safety Checklist to obstetrics and gynaecology. Obstet Gynaecol Reprod Med 2011;21:24-6. http://dx.doi.org/10.1016/j.ogrm.2010.09.009.
- Leff DR, Vincent C, Al-Mufti R, Cunningham D, Darzi A, Hadjiminas DJ. A clinical ‘near miss’ highlights risk management issues surrounding ultrasound-guided and wire-localised breast resections. Patient Saf Surg 2012;6. http://dx.doi.org/10.1186/1754-9493-6-15.
- Kelly SP, Steeples LR, Smith R, Azuara-Blanco A. Surgical checklist for cataract surgery: progress with the initiative by the Royal College of Ophthalmologists to improve patient safety. Eye (Lond) 2013;27:878-82. http://dx.doi.org/10.1038/eye.2013.101.
- Cavallini GM, Campi L, De Maria M, Forlini M. Clinical risk management in eye outpatient surgery: a new surgical safety checklist for cataract surgery and intravitreal anti-VEGF injection. Graefes Arch Clin Exp Ophthalmol 2013;251:889-94. http://dx.doi.org/10.1007/s00417-012-2206-2.
- Helmiö P, Takala A, Aaltonen LM, Blomgren K. WHO Surgical Safety Checklist in otorhinolaryngology-head and neck surgery: specialty-related aspects of check items. Acta Otolaryngol 2012;132:1334-41. http://dx.doi.org/10.3109/00016489.2012.700121.
- Helmiö P, Blomgren K, Takala A, Pauniaho SL, Takala RSK, Ikonen TS. Towards better patient safety: WHO Surgical Safety Checklist in otorhinolaryngology. Clin Otolaryngol 2011;36:242-7. http://dx.doi.org/10.1111/j.1749-4486.2011.02315.x.
- Avansino JR, Javid P, Katz C, Drugas G, Goldin A. Implementation of a standardized procedural checklist in a children’s hospital. Am J Surg 2011;201:655-60. http://dx.doi.org/10.1016/j.amjsurg.2011.01.014.
- Morgan PJ, Cunningham L, Mitra S, Wong N, Wu W, Noguera V, et al. Surgical safety checklist: implementation in an ambulatory surgical facility. Can J Anest 2013;60:528-38. http://dx.doi.org/10.1007/s12630-013-9916-8.
- Perea-Pérez B, Santiago-Sáez A, García-Marín F, Labajo González E. Proposal for a ‘surgical checklist’ for ambulatory oral surgery. Int J Oral Maxillofac Surg 2011;40:949-54. http://dx.doi.org/10.1016/j.ijom.2011.04.004.
- Lee MJ, Fanelli F, Haage P, Hausegger K, Van Lienden KP. Patient safety in Interventional radiology: a CIRSE IR Checklist. Cardiovasc Interv Radiol 2012;35:244-6. http://dx.doi.org/10.1007/s00270-011-0289-5.
- Truran P, Critchley RJ, Gilliam A. Does using the WHO surgical checklist improve compliance to venous thromboembolism prophylaxis guidelines?. Surgeon 2011;9:309-11. http://dx.doi.org/10.1016/j.surge.2010.11.024.
- Halikar VG, Galitzine S, Popat MT. Wrong side peripheral nerve blocks. Le Praticien En Anesthésie Réanimation 2012;16:373-7. http://dx.doi.org/10.1016/j.pratan.2012.04.009.
- Economides CP, Christodoulou L, Kyriakides T, Soteriades ES. An unusual case of suprascapular nerve neuropathy: a case report. J Med Case Rep 2011;5. http://dx.doi.org/10.1186/1752-1947-5-419.
- Rocos B, Donaldson LJ. Alcohol skin preparation causes surgical fires. Ann R Coll Surg Engl 2012;94:87-9. http://dx.doi.org/10.1308/003588412X13171221501221.
- Enright A. Review article: safety aspects of anesthesia in under-resourced locations. Can J Anest 2013;60:152-8. http://dx.doi.org/10.1007/s12630-012-9856-8.
- Kasatpibal N, Senaratana W, Chitreecheur J, Chotirosniramit N, Pakvipas P, Junthasopeepun P. Implementation of the world health organization surgical safety checklist at a university hospital in Thailand. Surg Infect 2012;13:50-6. http://dx.doi.org/10.1089/sur.2011.043.
- Weiser TG, Haynes AB, Lashoher A, Dziekan G, Boorman DJ, Berry WR, et al. Perspectives in quality: designing the WHO surgical safety checklist. Int J Qual Health Care 2010;22:365-70. http://dx.doi.org/10.1093/intqhc/mzq039.
- Weiser TG, Haynes AB, Dziekan G, Berry WR, Lipsitz SR, Gawande AA. Effect of a 19-item surgical safety checklist during urgent operations in a global patient population. Ann Surg 2010;251:976-80. http://dx.doi.org/10.1097/SLA.0b013e3181d970e3.
- Sparkes D, Rylah B. The World Health Organization surgical safety checklist. Br J Hosp Med 2010;71:276-80. http://dx.doi.org/10.12968/hmed.2010.71.5.47908.
- Seme ME, Resch S, Haynes AB, Funk LM, Bader A, Berry WR, et al. Adopting a surgical safety checklist could save money and improve the quality of care in U.S. hospitals. Health Aff 2010;29:1593-9. http://dx.doi.org/10.1377/hlthaff.2009.0709.
- Haynes AB, Weiser TG, Berry WR, Lipsitz SR, Breizat AHS, Dellinger EP, et al. A surgical safety checklist to reduce morbidity and mortality in a global population. New Engl J Med 2009;360:491-9. http://dx.doi.org/10.1056/NEJMsa0810119.
- Mohammed A, Wu J, Biggs T, Ofili-Yebovi D, Cox M, Pacquette S, et al. Does use of a World Health Organization obstetric safe surgery checklist improve communication between obstetricians and anaesthetists? A retrospective study of 389 caesarean sections. BJOG 2013;120:644-8. http://dx.doi.org/10.1111/1471-0528.12041.
- Tillman M, Wehbe-Janek H, Hodges B, Smythe WR, Papaconstantinou HT. Surgical care improvement project and surgical site infections: can integration in the surgical safety checklist improve quality performance and clinical outcomes?. J Surg Res 2013;84:150-6. http://dx.doi.org/10.1016/j.jss.2013.03.048.
- Kwok AC, Funk LM, Baltaga R, Lipsitz SR, Merry AF, Dziekan G, et al. Implementation of the World Health Organization Surgical Safety Checklist, including introduction of pulse oximetry, in a resource-limited setting. Ann Surg 2013;257:633-9. http://dx.doi.org/10.1097/SLA.0b013e3182777fa4.
- Moriyama K. Preoperative evaluation and perioperative prevention of infectious diseases. Jpn J Anesthsiol 2010;59:1146-8.
- Van Klei WA, Hoff RG, Van Aarnhem EEHL, Simmermacher RKJ, Regli LPE, Kappen TH, et al. Effects of the introduction of the WHO ‘surgical safety checklist’ on in-hospital mortality: a cohort study. Ann Surg 2012;255:44-9. http://dx.doi.org/10.1097/SLA.0b013e31823779ae.
- Levy SM, Senter CE, Hawkins RB, Zhao JY, Doody K, Kao LS, et al. Implementing a surgical checklist: more than checking a box. Surgery 2012;152:331-6. http://dx.doi.org/10.1016/j.surg.2012.05.034.
- Fourcade A, Minvielle E, Blache JL, Bourgain JL. Assessment of the French surgical checklist: the experience of 17 French cancer centres. Ann Fr Anesth Reanim 2011;30:495-500. http://dx.doi.org/10.1016/j.annfar.2011.04.001.
- Toor AA, Nigh-e-Mumtaz S, Syed R, Yousuf M, Syeda A. Surgical safety practices in Pakistan. J Pak Med Assoc 2013;63:76-80.
- Collazos C, Bermudez L, Quintero A, Quintero LE, Díaz MM. Checklist verification for surgery safety from the patient’s perspective. Rev Colomb Anestesiol 2013;41:109-13. http://dx.doi.org/10.1016/j.rca.2013.01.001.
- Sheena Y, Fishman JM, Nortcliff C, Mawby T, Jefferis AF, Bleach NR. Achieving flying colours in surgical safety: audit of World Health Organization ‘Surgical Safety Checklist’ compliance. J Laryngol Otol 2012;126:1049-55. http://dx.doi.org/10.1017/S002221511200165X.
- Nugent E, Hseino H, Ryan K, Traynor O, Neary P, Keane FBV. The surgical safety checklist survey: a national perspective on patient safety. Ir J Med Sci 2013;182:171-6. http://dx.doi.org/10.1007/s11845-012-0851-4.
- García DR, González AN, Bates MLP, Villarreal GC. Level of compliance and factors that influence in the application of safe surgery checklist. Rev Mex Enf Cardiol 2012;20:47-53.
- Reinelt P, Härting H, Lübke B, Jirak P, Schönherr U. Clinical risk management in high-volume cataract surgery. Spektrum Augenheilkd 2011;25:372-6. http://dx.doi.org/10.1007/s00717-011-0057-6.
- Sewell M, Adebibe M, Jayakumar P, Jowett C, Kong K, Vemulapalli K, et al. Use of the WHO Surgical Safety Checklist in trauma and orthopaedic patients. Int Orthop 2011;35:897-901. http://dx.doi.org/10.1007/s00264-010-1112-7.
- Jarvis WR. What can Canada learn from the USA’s experience in reducing healthcare-associated infections?. Clin Govern 2012;17:149-54. http://dx.doi.org/10.1108/14777271211220862.
- Pittet D, Allegranzi B, Storr J, Nejad SB, Dziekan G, Leotsakos A, et al. Infection control as a major World health Organization priority for developing countries. J Hosp Infect 2008;68:285-92. http://dx.doi.org/10.1016/j.jhin.2007.12.013.
- Krein SL, Kowalski CP, Hofer TP, Saint S. Preventing hospital-acquired infections: a national survey of practices reported by U.S. Hospitals in 2005 and 2009. J Gen Intern Med 2012;27:773-9. http://dx.doi.org/10.1007/s11606-011-1935-y.
- Gould D, Drey N, Millar M. Patients and the public: knowledge, sources of information and perceptions about healthcare-associated infection. J Hosp Infect 2009;72:1-8. http://dx.doi.org/10.1016/j.jhin.2009.01.024.
- Lomas C. Why infection control is everybody’s business. Nurs Times 2008;104:14-5.
- Vandijck D, Cleemput I, Hellings J, Vogelaers D. Infection prevention and control strategies in the era of limited resources and quality improvement: a perspective paper. Aust Crit Care 2013;26:154-7. http://dx.doi.org/10.1016/j.aucc.2013.07.005.
- Kavanagh KT. Financial incentives to promote health care quality: the hospital acquired conditions nonpayment policy. Soc Work Public Health 2011;26:524-41. http://dx.doi.org/10.1080/19371918.2011.533554.
- Graves N, Halton K, Doldge S. Who bears the cost of healthcare-acquired surgical site infection?. J Hosp Infect 2008;69:274-82. http://dx.doi.org/10.1016/j.jhin.2008.04.022.
- Nosrati M, Boroumand M, Tahmasebi S, Sotoudeh M, Sheikhfathollahi M, Goodarzynejad H. Excess costs associated with common healthcare-associated infections in an Iranian cardiac surgical unit. J Hosp Infect 2010;76:304-7. http://dx.doi.org/10.1016/j.jhin.2010.07.003.
- Raschka S, Dempster L, Bryce E. Health economic evaluation of an infection prevention and control program: are quality and patient safety programs worth the investment?. Am J Infect Control 2013;41:773-7. http://dx.doi.org/10.1016/j.ajic.2012.10.026.
- Waters HR, Korn R, Colantuoni E, Berenholtz SM, Goeschel CA, Needham DM, et al. The business case for quality: economic analysis of the Michigan keystone patient safety program in ICUs. Am J Med Qual 2011;26:333-9. http://dx.doi.org/10.1177/1062860611410685.
- Clarke J. Patient Safety First: supporting improvements in infection prevention. J Infect Prev 2010;11:2-5. http://dx.doi.org/10.1177/1757177409358217.
- Gould DJ, Hewitt-Taylor J, Drey NS, Gammon J, Chudleigh J, Weinberger JR. The Clean Your Hands Campaign: critiquing policy and evidence base. J Hosp Infect 2007;65:95-101. http://dx.doi.org/10.1016/j.jhin.2006.09.028.
- Kiernan M. High impact intervention tools for acute care. Nurs Times 2007;103:4-5.
- Mears A, White A, Cookson B. Healthcare-associated infection in acute hospitals: which interventions are effective?. J Hosp Infect 2009;71:307-13. http://dx.doi.org/10.1016/j.jhin.2008.12.004.
- Pittet D, Allegranzi B, Storr J, Donaldson L. ‘Clean care is safer care’: the global patient safety challenge 2005–2006. Int J Infect Dis 2006;10:419-24. http://dx.doi.org/10.1016/j.ijid.2006.06.001.
- Reichardt C, Eberlein-Gonska M, Schrappe M, Gastmeier P. Clean Hands Campaign: no chance for hospital infections!. Unfallchirurg 2009;112:679-82. http://dx.doi.org/10.1007/s00113-009-1631-0.
- Mielke M. Prevention and control of nosocomial infections and resistance to antibiotics in Europe – primum non-nocere: elements of successful prevention and control of healthcare-associated infections. Int J Med Microbiol 2010;300:346-50. http://dx.doi.org/10.1016/j.ijmm.2010.04.004.
- Pratt RJ, Pellowe CM, Wilson JA, Loveday HP, Harper PJ, Jones SR, et al. epic2: National evidence-based guidelines for preventing healthcare-associated infections in NHS hospitals in England. J Hosp Infect 2007;65:1-59. http://dx.doi.org/10.1016/S0195-6701(07)60002-4.
- Durlach R, Mcllvenny G, Newcombe RG, Reid G, Doherty L, Freuler C, et al. Prevalence survey of healthcare-associated infections in Argentina: comparison with England, Wales, Northern Ireland and South Africa. J Hosp Infect 2012;80:217-23. http://dx.doi.org/10.1016/j.jhin.2011.12.001.
- Humphreys H, Newcombe R, Enstone J. Four country healthcare associated infection prevalence survey 2006: risk factor analysis. J Hosp Infect 2008;69:249-57. http://dx.doi.org/10.1016/j.jhin.2008.04.021.
- Sheps SS, Birnbaum D. Mandatory reporting of healthcare associated infections: can US experience inform Canadian policy?. Clin Govern 2012;17:96-100. http://dx.doi.org/10.1108/14777271211220871.
- Worth LJ, Bull AL, Thorpe SM, Richards MJ. Meeting national recommendations for surgical site infection surveillance: examples and lessons from the Victorian Healthcare-Associated Infection Surveillance System. Healthc Infect 2009;14:119-22. http://dx.doi.org/10.1071/HI09106.
- Cookson B, Mathai E, Allegranzi B, Pessoa-Silva CL, Bagheri NS, Schneider A, et al. Comparison of national and subnational guidelines for hand hygiene. J Hosp Infect 2009;72:202-10. http://dx.doi.org/10.1016/j.jhin.2009.03.022.
- Cookson B, Mackenzie D, Coutinho AP, Russell I, Fabry J. Consensus standards and performance indicatiors for prevention and control of healthcare–associated infection in Europe. J Hosp Infect 2011;79:260-4. http://dx.doi.org/10.1016/j.jhin.2011.07.008.
- Kanerva M, Ollgren J, Lyytikäinen O. Inter-hospital differences and case-mix in a nationwide prevalence survey. J Hosp Infect 2010;76:135-8. http://dx.doi.org/10.1016/j.jhin.2010.05.017.
- Millar M. Are national targets the right way to improve infection control practice?. J Hosp Infect 2009;73:408-13. http://dx.doi.org/10.1016/j.jhin.2009.02.022.
- O’Neill E, Humphreys H. Use of surveillance data for the prevention of healthcare-associated infection: risk adjustment and reporting dilemmas. Curr Opin Infect Dis 2009;22:359-63. http://dx.doi.org/10.1097/QCO.0b013e32832d04c0.
- Conway LJ, Larson EL. Guidelines to prevent catheter-associated urinary tract infection: 1980 to 2010. Heart Lung 2012;41:271-83. http://dx.doi.org/10.1016/j.hrtlng.2011.08.001.
- Coello R, Brannigan E, Lawson W, Wickens H, Holmes A. Prevalence of healthcare device-associated infection using point prevalence surveys of antimicrobial prescribing and existing electronic data. J Hosp Infect 2011;78:264-8. http://dx.doi.org/10.1016/j.jhin.2011.01.028.
- Pronovost PJ, Cardo DM, Goeschel CA, Berenholtz SM, Saint S, Jernigan JA. A research framework for reducing preventable patient harm. Clin Infect Dis 2011;52:507-13. http://dx.doi.org/10.1093/cid/ciq172.
- Cairns S, Reilly J, Booth M. Prevalence of healthcare-associated infection in Scottish intensive care units. J Hosp Infect 2010;76:308-10. http://dx.doi.org/10.1016/j.jhin.2010.05.010.
- Cairns S, Reilly J, Stewart S, Tolson D, Godwin J, Knight P. The prevalence of healthcare-associated infection in older people in acute care hospitals. Infect Control Hosp Epidemiol 2011;32:763-7. http://dx.doi.org/10.1086/660871.
- Rosenthal VD, Jarvis WR, Jamulitrat S, Silva CP, Ramachandran B, Dueñas L, et al. Socioeconomic impact on device-associated infections in pediatric intensive care units of 16 limited-resource countries: International Nosocomial Infection Consortium findings. Pediatr Crit Care Med 2012;13:399-406. http://dx.doi.org/10.1097/PCC.0b013e318238b260.
- Apostolopolou E, Raftopoulos V, Terzzis K. Infection Probability Score, Apache II and Karnofsky scoring system as predictors of infection onset in haematiology-oncology patients. J Clin Nurs 2010;19:1560-8. http://dx.doi.org/10.1111/j.1365-2702.2009.03011.x.
- Durante-Mangoni E, Zarrilli R. Global spread of drug-resistant Acinetobacter baumannii: molecular epidemiology and management of antimicrobial resistance. Future Microbiol 2011;6:407-22. http://dx.doi.org/10.2217/fmb.11.23.
- Fierobe L, Lucet JC, Decré D, Muller-Serieys C, Deleuze A, Joly-Guillou ML, et al. An outbreak of imipenem-resistant Acinetobacter baumannii in critically ill surgical patients. Infect Control Hosp Epidemiol 2001;22:35-40. http://dx.doi.org/10.1086/501822.
- Lin MY, Hayden MK. Methicillin-resistant Staphylococcus aureus and vancomycin-resistant enterococcus: recognition and prevention in intensive care units. Crit Care Med 2010;38:335-44. http://dx.doi.org/10.1097/CCM.0b013e3181e6ab12.
- Mastoraki A, Douka E, Kriaras I, Stravopodis G, Manoli H, Geroulanos S. Pseudomonas aeruginosa susceptible only to colistin in intensive care unit patients. Surg Infect 2008;9:153-60. http://dx.doi.org/10.1089/sur.2007.004.
- Apisarnthanarak A, Kiratisin P, Mundy LM. Clinical and molecular epidemiology of healthcare-associated infections due to extended-spectrum beta-lactamase (ESBL)-producing strains of Escherichia coli and Klebsiella pneumonia that harbour multiple ESBL genes. Infect Control Hosp Epidemiol 2008;29:1026-34. http://dx.doi.org/10.1086/591864.
- Burke L, Humphreys H, Fitzgerald-Hughes D. The revolving door between hospital and community: extended spectrum beta-lactamase-producing Escherichia coli in Dublin. J Hosp Infect 2012;81:192-8. http://dx.doi.org/10.1016/j.jhin.2012.04.021.
- Pearson A. Historical and changing epidemiology of healthcare-associated infections. J Hosp Infect 2009;73:296-304. http://dx.doi.org/10.1016/j.jhin.2009.08.016.
- Tong SY, Chen LF, Fowler VG. Colonization, pathogenicity, host susceptibility, and therapeutics for Staphylococcus aureus: what is the clinical relevance?. Sem Immunopathol 2012;34:185-200. http://dx.doi.org/10.1007/s00281-011-0300-x.
- Thole S, Daniels-Haardt I. A seal of quality for hospitals and nursing homes – background, concept and experiences. Hygiene Medizin 2012;37:202-8.
- Gould D. MRSA: implications for hospitals and nursing homes. Nurs Stand 2011;25:47-56. http://dx.doi.org/10.7748/ns2011.01.25.18.47.c8234.
- Carey AJ, Long SS. Staphylococcus aureus: a continuously evolving and formidable pathogen in the neonatal intensive care unit. Clin Perinatol 2010;37:535-46. http://dx.doi.org/10.1016/j.clp.2010.05.002.
- Duerden BI. MRSA: why have we got it and can we do anything about it. Eye 2012;26:218-21. http://dx.doi.org/10.1038/eye.2011.314.
- Sánchez A, Gattarello S, Rello J. New treatment options for infections caused by multiresistant strains of Pseudomonas aeruginosa and other nonfermenting gram-negative bacilli. Sem Respir Crit Care Med 2011;32:151-8. http://dx.doi.org/10.1055/s-0031-1275527.
- Pellatt G. Progress made, but more to be done for infection control. Br J Neurosci Nurs 2007;3. http://dx.doi.org/10.12968/bjnn.2007.3.12.27893.
- Kilpatrick C. What is Health Protection Scotland up to?. Br J Infect Control 2008;9:4-5. http://dx.doi.org/10.1177/1469044608089700.
- Brannigan ET, Murray E, Holmes A. Where does infection control fit into a hospital management structure?. J Hosp Infect 2009;73:392-6. http://dx.doi.org/10.1016/j.jhin.2009.03.031.
- Duerden B. Controlling healthcare-associated infections in the NHS. Clin Med 2008;8:140-3. http://dx.doi.org/10.7861/clinmedicine.8-2-140.
- Zingg W, Walder B, Pittet D. Prevention of catheter-related infection: toward zero risk?. Curr Opin Infect Dis 2011;24:377-84. http://dx.doi.org/10.1097/QCO.0b013e32834811ed.
- Shabot MM, Monroe D, Inurria J, Garbade D, France AC. Memorial Hermann: high reliability from board to bedside. Jt Comm J Qual Patient Saf 2013;39:253-7.
- Jenkins K. Back to basics: practice guidelines for correct hand hygiene. J Ren Nurs 2011;3:226-9. http://dx.doi.org/10.12968/jorn.2011.3.5.226.
- Kelcikova S, Skodova Z, Straka S. Effectiveness of hand hygiene education in a basic nursing school curricula. Public Health Nurs 2012;29:152-9. http://dx.doi.org/10.1111/j.1525-1446.2011.00985.x.
- West KH, Cohen ML. Standard precautions – a new approach to reducing infection transmission in the hospital setting. J Intrav Nurs 1997;20:7-10.
- Didiodato G. Just clean your hands: measuring the effect of a patient safety initiative on driving transformational change in a health care system. Am J Infect Control 2013;41:1109-11. http://dx.doi.org/10.1016/j.ajic.2013.01.039.
- Ryan K, Russo PL, Heard K, Havers S, Bellis K, Lindsay Grayson M. Development of a standardised approach to observing hand hygiene compliance in Australia. Healthc Infect 2012;17:115-21. http://dx.doi.org/10.1071/HI12022.
- Banfield KR, Kerr KG. Could hospital patients’ hands constitute a missing link?. J Hosp Infect 2005;61:183-8. http://dx.doi.org/10.1016/j.jhin.2005.03.016.
- Burnett E, Lee K, Rushmer R, Ellis M, Noble M, Davey P. Healthcare-associated infection and the patient experience: a qualitative study using patient interviews. J Hosp Infect 2010;74:42-7. http://dx.doi.org/10.1016/j.jhin.2009.07.027.
- DeLa Cruz RF, Caillouet B, Guerrero SS. Strategic patient education program to prevent catheter-related bloodstream infection. Clin J Oncol Nurs 2012;16:E12-17. http://dx.doi.org/10.1188/12.CJON.E12-E17.
- Davis RE, Pinto A, Sevdalis N, Vincent C, Massey R, Darzi A. Patients’ and health care professionals’ attitudes towards the PINK patient safety video. J Eval Clin Pract 2012;18:848-53. http://dx.doi.org/10.1111/j.1365-2753.2011.01688.x.
- Martin M, Zingg W, Hansen S, Gastmeier P, Wu AW, Pittet D, et al. Public reporting of healthcare-associated infection data in Europe. What are the views of infection prevention opinion leaders?. J Hosp Infect 2013;83:94-8. http://dx.doi.org/10.1016/j.jhin.2012.10.010.
- Reichardt C, Gastmeier P, Eberlein-Gonska M, Schrappe M. ‘Action clean hands’ – don’t give hospital infections a chance!. Krh Hyg Inf Verh 2008;30:82-5.
- WHO Guidelines on Hand Hygiene in Health Care: First Global Patient Safety Challenge Clean Care is Safer Care. Geneva: World Health Organization World Alliance for Patient Safety; 2009.
- Allegranzi B, Pittet D. Role of hand hygiene in healthcare-associated infection prevention. J Hosp Infect 2009;73:305-15. http://dx.doi.org/10.1016/j.jhin.2009.04.019.
- Jamal A, O’Grady G, Dalton A, Andresen D. Improving hand hygiene in a paediatric hospital: a multimodal quality improvement approach. Br Med J Qual Saf 2012;21:171-6. http://dx.doi.org/10.1136/bmjqs-2011-000056.
- Cassidy I. Student nurses’ experiences of caring for infectious patients in source isolation. a hermeneutic phenomenological study. J Clin Nurs 2006;15:1247-56. http://dx.doi.org/10.1111/j.1365-2702.2006.01404.x.
- Wyeth J. Hand hygiene and the use of personal protective equipment. Br J Nurs 2013;22:920-5. http://dx.doi.org/10.12968/bjon.2013.22.16.920.
- Storr J, Kilpatrick C. Hand hygiene improvement in the community: a systems approach. Br J Community Nurs 2012;17:S24-9. http://dx.doi.org/10.12968/bjcn.2012.17.Sup3.S24.
- Gould D. Auditing hand hygiene practice. Nurs Stand 2010;25:50-6. http://dx.doi.org/10.7748/ns2010.09.25.2.50.c7988.
- Scheithauer S, Oberröhrmann A, Haefner H, Kopp R, Schürholtz T, Schwanz T, et al. Compliance with hand hygiene in patients with methicillin-resistant Staphylococcus aureus and extended spectrum beta-lactamase-producing enterobacteria. J Hosp Infect 2010;76:320-3. http://dx.doi.org/10.1016/j.jhin.2010.07.012.
- Boscart VM, Levchenko AI, Fernie GR. Defining the configuration of a hand hygiene monitoring system. Am J Infect Control 2010;38:518-22. http://dx.doi.org/10.1016/j.ajic.2010.02.007.
- Macbeth D, Murphy C. Auditing hand hygiene rates for quality and improvement. Healthc Infect 2012;17:13-7. http://dx.doi.org/10.1071/HI11030.
- Dixit D, Hagtvedt R, Reay T, Ballermann M, Forgie S. Attitudes and beliefs about hand hygiene among paediatric residents: a qualitative study. BMJ Open 2012;2. http://dx.doi.org/10.1136/bmjopen-2012-002188.
- Doron SI, Kifuji K, Hynes BT, Dunlop D, Lemon T, Hansjosten K, et al. A multifaceted approach to education, observation, and feedback in a successful hand hygiene campaign. Jt Comm J Qual Patient Saf 2011;37:3-10.
- Moureau N. Safe patient care when using vascular access devices. Br J Nurs 2013;22:14-21. http://dx.doi.org/10.12968/bjon.2013.22.Sup1.S14.
- Peterson TH, Teman SF, Connors RH. A safety culture transformation: its effects at a children’s hospital. J Patient Saf 2012;8:125-30. http://dx.doi.org/10.1097/PTS.0b013e31824bd744.
- Uneke CJ, Ogbonna A, Oyibo PG, Onu CM. Bacterial contamination of stethoscopes used by health workers: public health implications. J Infect Dev Ctries 2010;4:436-41. http://dx.doi.org/10.3855/jidc.701.
- Matlow A, Stevens P, Urmson L, Wray R. Improving patient safety through a multi-faceted internal surveillance program. Healthc Q 2008;11:101-8. http://dx.doi.org/10.12927/hcq.2008.19659.
- Gurses A, Seidl K, Valdya V. Systems ambiguity and guidelines compliance: a qualitative study of how intensive care units follow evidence-based guidelines to reduce healthcare-associated infections. Qual Saf Health Care 2008;17:351-9. http://dx.doi.org/10.1136/qshc.2006.021709.
- Rosenweg PN, Langan-Fox J. Culture and Compliance with Hospital Infection Protocols. Melbourne, VIC: Faculty of Business and Enterprise, Swinburne University; 2009.
- Brady RRW, McDermott C, Gibb AP, Paterson-Brown S. Factor infection: do surgical trainees known enough about infection control?. Ann R Coll Surg Engl 2008;90:647-50. http://dx.doi.org/10.1308/003588408X321756.
- McHugh SM, Hill ADK, Humphreys H. Preventing healthcare-associated infection through education: have surgeons been overlooked?. Surgeon 2010;8:96-100. http://dx.doi.org/10.1016/j.surge.2009.11.009.
- Mittal MK, Morris JB, Kelz RR. Germ simulation: a novel approach for raising medical students awareness toward asepsis. Simul Healthc 2011;6:65-70. http://dx.doi.org/10.1097/SIH.0b013e318206953a.
- Erasmus V, Brouwer W, Van Beeck EF, Oenema A, Daha TJ, Richardus JH, et al. A qualitative exploration of reasons for poor hand hygiene among hospital workers: lack of positive role models and of convincing evidence that hand hygiene prevents cross-infection. Infect Control Hosp Epidemiol 2009;30:415-19. http://dx.doi.org/10.1086/596773.
- Ward DJ. Attitudes towards infection prevention and control: an interview study with nursing students and nurse mentors. BMJ Qual Saf 2012;21:301-6. http://dx.doi.org/10.1136/bmjqs-2011-000360.
- Cole M. Patient safety and healthcare associated infection. Br J Nurs 2011;20:1122-6. http://dx.doi.org/10.12968/bjon.2011.20.17.1122.
- Nichols A, Badger B. An investigation of the divisions between espoused and actual practice in infection control and of the knowledge sources that may underpin this division. Br J Infect Control 2008;9:11-5. http://dx.doi.org/10.1177/1469044608088621.
- McHugh SM, Corrigan MA, Dimitrov BD, Cowman S, Tierney S, Hill AD, et al. Preventing infection in general surgery: improvements through education of surgeons by surgeons. J Hosp Infect 2011;78:312-16. http://dx.doi.org/10.1016/j.jhin.2011.03.023.
- Cook E, Marchaim D, Kaye KS. Building a successful infection prevention program: key components, processes, and economics. Infect Dis Clin North Am 2011;25:1-19. http://dx.doi.org/10.1016/j.idc.2010.11.007.
- Rothe C, Schlaich C, Thompson S. Healthcare-associated infections in sub-Saharan Africa. J Hosp Infect 2013;85:257-67. http://dx.doi.org/10.1016/j.jhin.2013.09.008.
- McKinley L, Auel C, Bahr M, Hutchings A, Leary M, Moskal N, et al. Building global partnerships in infection prevention: a report from APIC Badger and the Nairobi Infection Control Nurses Chapter. Am J Infect Control 2013;41:281-2. http://dx.doi.org/10.1016/j.ajic.2012.03.024.
- Joo EJ, Chung DR, Ha YE, Park SY, Kang SJ, Kim SH, et al. Community-associated Panton–Valentine leukocidin-negative methicillin-resistant Staphylococcus aureus clone (ST72-MRSA-IV) causing healthcare-associated pneumonia and surgical site infection in Korea. J Hosp Infect 2012;81:149-55. http://dx.doi.org/10.1016/j.jhin.2012.04.018.
- Milianai K, L’Hériteau F, Lacavé L, Carbonne A, Astagneau P. Imipenem and ciprofloxacin consumption as factors associated with high incidence rates of resistant Pseudomonas aeruginosa in hospitals in northern France. J Hosp Infect 2011;77:343-7. http://dx.doi.org/10.1016/j.jhin.2010.11.024.
- Casapao AM, Kullar R, Davis SL, Levine DP, Zhao JJ, Potoski BA, et al. Multicenter study of high-dose daptomycin for treatment of enterococcal infections. Antimicrob Agents Chemother 2013;57:4190-6. http://dx.doi.org/10.1128/AAC.00526-13.
- Cooke FJ, Holmes AH. The missing care bundle: antibiotic prescribing in hospitals. Int J Antimicrob Agents 2007;30:25-9. http://dx.doi.org/10.1016/j.ijantimicag.2007.03.003.
- Lode H, Raffenberg M, Erbes R, Geerdes-Fenge H, Mauch H. Nosocomial pneumonia: epidemiology, pathogenesis, diagnosis, treatment and prevention. Curr Opin Infect Dis 2000;13:377-84. http://dx.doi.org/10.1097/00001432-200008000-00009.
- Tauman AV, Robicsek A, Roberson J, Boyce JM. Health care-associated infection prevention and control: pharmacists’ role in meeting national patient safety goal 7. Hosp Pharm 2009;44:401-11. http://dx.doi.org/10.1310/hpj4405-401.
- Sharvill J. Antibiotic overprescribing: who are the bad guys?. Br J Gen Pract 2013;63. http://dx.doi.org/10.3399/bjgp13X671515.
- Ostrowsky B, Sharma S, Defino M, Guo Y, Shah P, McAllen S, et al. Antimicrobial stewardship and automated pharmacy technology improve antibiotic appropriateness for community-acquired pneumonia. Infect Control Hosp Epidemiol 2013;34:566-72. http://dx.doi.org/10.1086/670623.
- Tea CK, Baysari MT, Day RO. Compliance with antibiotic prescribing policy: perspectives of policymakers and prescribers. Aust J Pharm 2013;94:74-7. http://dx.doi.org/10.1002/j.2055-2335.2013.tb00212.x.
- Wickens HJ, Farrell S, Ashiru-Oredope DAI, Jacklin A, Holmes A. The increasing role of pharmacists in antimicrobial stewardship in English hospitals. J Antimicrob Chemother 2013;68:2675-81. http://dx.doi.org/10.1093/jac/dkt241.
- Vettese N, Hendershot J, Irvine M, Wimer S, Chamberlain D, Massoud N. Outcomes associated with a thrice-weekly antimicrobial stewardship programme in a 253-bed community hospital. J Clin Pharm Ther 2013;38:401-4. http://dx.doi.org/10.1111/jcpt.12079.
- Andersson AE, Bergh I, Karlsson J, Eriksson BI, Nilsson K. The application of evidence-based measures to reduce surgical site infections during orthopedic surgery – report of a single-center experience in Sweden. Patient Saf Surg 2012;6. http://dx.doi.org/10.1186/1754-9493-6-11.
- W-Dahl A, Robertsson O, Stefánsdóttir A, Gustafson P, Lidgren L. Timing of preoperative antibiotics for knee arthroplasties: improving the routines in Sweden. Patient Saf Surg 2011;5. http://dx.doi.org/10.1186/1754-9493-5-22.
- Thouverez M, Lallemand S, Bailly P, Bertrand X, Talon D. Determination of indicators for non-compliance with guidelines for surgical antimicrobial prophylaxis. Pathol Biol (Paris) 2002;50:547-51. http://dx.doi.org/10.1016/S0369-8114(02)00352-8.
- Al-Dorzi HM, El-Saed A, Rishu AH, Balkhy HH, Memish ZA, Arabi YM. The results of a 6-year epidemiologic surveillance for ventilator-associated pneumonia at a tertiary care intensive care unit in Saudi Arabia. Am J Infect Control 2012;40:794-9. http://dx.doi.org/10.1016/j.ajic.2011.10.004.
- Arora SC, Mudaliar YM, Lee C, Mitchell D, Iredell J, Lazarus R. Non-bronchoscopic bronchoalveolar lavage in the microbiological diagnosis of pneumonia in mechanically ventilated patients. Anaest Intens Care 2002;30:11-20.
- Flanders SA, Collard HR, Saint S. Nosocomial pneumonia: state of the science. Am J Infect Cont 2006;34:84-93. http://dx.doi.org/10.1016/j.ajic.2005.07.003.
- Klompas M. Advancing the science of ventilator-associated pneumonia surveillance. Crit Care 2012;16. http://dx.doi.org/10.1186/cc11656.
- Kollef MH, Kollef KE. Antibiotic utilization and outcomes for patients with clinically suspected ventilator-associated pneumonia and negative quantitative BAL culture results. Chest 2005;128:2706-13. http://dx.doi.org/10.1378/chest.128.4.2706.
- Leblebicioglu H, Yalcin AN, Rosenthal VD, Koksal I, Sirmatel F, Unal S, et al. Effectiveness of a multidimensional approach for prevention of ventilator-associated pneumonia in 11 adult intensive care units from 10 cities of Turkey: findings of the International Nosocomial Infection Control Consortium (INICC). Infection 2013;41:447-56. http://dx.doi.org/10.1007/s15010-013-0407-1.
- Patterson JE, Malani PN, Maragakis LL. Infection control in the intensive care unit: progress and challenges in systems and accountability. Crit Care Med 2010;38:265-8. http://dx.doi.org/10.1097/CCM.0b013e3181e69d48.
- O’Connor I, Wilks M, Hennessy E, Millar M. Control of vascular access device associated blood stream infection in a large London teaching hospital. J Infect Prev 2012;13:79-83. http://dx.doi.org/10.1177/1757177412443169.
- Easterlow D, Hoddinott P, Harrison S. Implementing and standardising the use of peripheral vascular access devices. J Clin Nurs 2010;19:721-7. http://dx.doi.org/10.1111/j.1365-2702.2009.03098.x.
- Cherry RA, West CE, Hamilton MC, Rafferty CM, Hollenbeak CS, Caputo GM. Reduction of central venous catheter associated blood stream infections following implementation of a resident oversight and credentialing policy. Patient Saf Surg 2011;5. http://dx.doi.org/10.1186/1754-9493-5-15.
- Choi SW, Chang L, Hanauer DA, Shaffer-Hartman J, Teitelbaum D, Lewis I, et al. Rapid reduction of central line infections in hospitalized pediatric oncology patients through simple quality improvement methods. Pediatr Blood Cancer 2013;60:262-9. http://dx.doi.org/10.1002/pbc.24187.
- Curran E, Murdoch H. Aiming to reduce catheter associated urinary tract infections (CAUTI) by adopting a checklist and bundle to achieve sustained system improvements. J Infect Prev 2009;10:57-61. http://dx.doi.org/10.1177/1757177408097755.
- Nazarko L. Reducing the risk of catheter-related urinary tract infection. Br J Nurs 2008;17:1002-10.
- Pellowe CM. Using evidence-based guidelines to reduce catheter related urinary tract infections in England. J Infect Prev 2009;10:44-8. http://dx.doi.org/10.1177/1757177408096889.
- Clarke K, Tong D, Pan Y, Easley KA, Norrick B, Ko C, et al. Reduction in catheter-associated urinary tract infections by bundling interventions. Int J Qual Health Care 2013;25:43-9. http://dx.doi.org/10.1093/intqhc/mzs077.
- Saint S, Kowalski CP, Forman J, Damschroder L, Hofer TP, Kaufman SR, et al. A multicenter qualitative study on preventing hospital-acquired urinary tract infection. Infect Control Hosp Epidemiol 2008;29:333-41. http://dx.doi.org/10.1086/529589.
- Bourdieu P. The Logic of Practice. Cambridge: Polity Press; 1990.
- Heidegger M. What is Called Thinking?. New York, NY: Harper Perennial; 2004.
- Biddle C. Semmelweis revisited: hand hygiene and nosocomial disease transmission in the anesthesia workstation. AANA J 2009;77:229-37.
- Perspectives on Context: A Selection of Essays Considering the Role of Context in Successful Quality Improvement. London: Health Foundation; 2014.
- Godfrey MM, Nelson EC, Wasson JH, Mohr JJ, Batalden PB. Microsystems in health care: part 3. Planning patient-centered services. Jt Comm J Qual Saf 2003;29:159-70.
- Batalden PB, Nelson EC, Mohr JJ, Godfrey MM, Huber TP, Kosnik L, et al. Microsystems in health care: part 5. How leaders are leading. Jt Comm J Qual Saf 2003;29:297-308.
- Mohr JJ, Barach P, Cravero JP, Blike GT, Godfrey MM, Batalden PB, et al. Microsystems in health care: part 6. Designing patient safety into the microsystem. Jt Comm J Qual Saf 2003;29:401-8.
- Huber TP, Godfrey MM, Nelson EC, Mohr JJ, Campbell C, Batalden PB. Microsystems in health care: part 8. Developing people and improving work life: what front-line staff told us. Jt Comm J Qual Saf 2003;29:512-22.
- Batalden PB, Nelson EC, Edwards WH, Godfrey MM, Mohr JJ. Microsystems in health care: part 9. Developing small clinical units to attain peak performance. Jt Comm J Qual Saf 2003;29:575-85.
- Taylor SL, Dy S, Foy R, Hempel S, McDonald KM, Øvretveit J, et al. What context features might be important determinants of the effectiveness of patient safety practice interventions?. BMJ Qual Saf 2011;20:611-17. http://dx.doi.org/10.1136/bmjqs.2010.049379.
- Etchegaray JM, Thomas EJ. Engaging employees: the importance of high-performance work systems for patient safety [published online ahead of print 11 February 2014]. J Patient Saf 2014. http://dx.doi.org/10.1097/PTS.0000000000000076.
- Weinberg DB, Avgar AC, Sugrue NM, Cooney-Miner D. The importance of a high-performance work environment in hospitals. Health Serv Res 2013;48:319-32. http://dx.doi.org/10.1111/j.1475-6773.2012.01438.x.
- Leggat SG, Balding C. Achieving organisational competence for clinical leadership: the role of high performance work systems. J Health Organ Manag 2013;27:312-29. http://dx.doi.org/10.1108/JHOM-Jul-2012-0132.
- Robbins J, Garman AN, Song PH, McAlearney AS. How high-performance work systems drive health care value: an examination of leading process improvement strategies. Qual Manag Health Care 2012;21:188-202. http://dx.doi.org/10.1097/QMH.0b013e31825e88f6.
- Leggat SG, Bartram T, Stanton P. High performance work systems: the gap between policy and practice in health care reform. J Health Organ Manag 2011;25:281-97. http://dx.doi.org/10.1108/14777261111143536.
- Etchegaray JM, St. John C, Thomas EJ. Measures and measurement of high-performance work systems in health care settings: propositions for improvement. Health Care Manage Rev 2011;36:38-46. http://dx.doi.org/10.1097/HMR.0b013e3181f685a4.
- Greenwood R, Raynard M, Kodeih F, Micelotta ER, Lounsbury M. Institutional complexity and organizational responses. Acad Manag Ann 2011;5. http://dx.doi.org/10.1080/19416520.2011.590299.
- Lê JK. When contradictory logics coexist: how work practices and institutional accounts reconfigure instituational logics. Acad Manage Proc 2011;1:1-5. http://dx.doi.org/10.5465/AMBPP.2011.65869706.
- Delivering Safe Care, Compassionate Care: Learning for Wales from the Report of the Mid Staffordshire NHS Foundation Trust Public Inquiry. Cardiff: Welsh Government; 2013.
- Suddaby R. Challenges for institutional theory. J Manag Inq 2010;19:14-20. http://dx.doi.org/10.1177/1056492609347564.
- Goodrick E, Salancik GR. Organizational discretion in responding to institutional practices: hospitals and cesarean births. Adm Sci Q 1996;41:1-28. http://dx.doi.org/10.2307/2393984.
- Washington M, Ventresca MJ. How organizations change: the role of institutional support mechanisms in the incorporation of higher education visibility strategies, 1874–1995. Organ Sci 2004;15:82-97. http://dx.doi.org/10.1287/orsc.1030.0057.
- Hinings B. Connections between institutional logics and organizational culture. J Manag Inq 2012;21:98-101. http://dx.doi.org/10.1177/1056492611419798.
- Thornton PH, Jones C, Kury K, Jones C, Thornton PH. Transformation in Cultural Industries (Research in the Sociology of Organizations, Volume 23). Emerald Group Publishing Limited; 2005.
- Danisman A, Hinings CR, Slack T. Integration and differentiation in institutional values: an empirical investigation in the field of Canadian national sport organizations. Can J Adm Sci 2006;23:301-17. http://dx.doi.org/10.1111/j.1936-4490.2006.tb00609.x.
- Muzio D, Brock DM, Suddaby R. Professions and institutional change: towards an institutionalist sociology of the professions. J Manag Stud 2013;50:699-721. http://dx.doi.org/10.1111/joms.12030.
- Voronov M, De Clercq D, Hinings CR. Conformity and distinctiveness in a global institutional framework: the legitimation of Ontario fine wine. J Manag Stud 2013;50:607-45. http://dx.doi.org/10.1111/joms.12012.
- Van Wijk J, Stam W, Elfring T, Zietsma C, Den Hond F. Activists and incumbents structuring change: the interplay of agency, culture, and networks in field evolution. Acad Manag J 2013;56:358-86. http://dx.doi.org/10.5465/amj.2008.0355.
- Greenwood R. Focusing the asteroid belt of organizations. J Manag Inq 2008;17:152-6. http://dx.doi.org/10.1177/1056492608316917.
- Flood AB, Scott WR. Professional power and professional effectiveness: the power of the surgical staff and the quality of surgical care in hospitals. J Health Soc Behav 1978;19:240-54. http://dx.doi.org/10.2307/2136557.
- Balogun J, Gleadle P, Hailey VH, Willmott H. Managing change across boundaries: boundary-shaking practices. Br J Manag 2005;16:261-78. http://dx.doi.org/10.1111/j.1467-8551.2005.00463.x.
- Editorial . WHO’s patient-safety checklist for surgery. Lancet 2008;372. http://dx.doi.org/10.1016/S0140-6736(08)60964-2.
- Scott WR, Ruef M, Mendel PJ, Caronna CA. Institutional Change and Healthcare Organizations: From Professional Dominance to Managed Care. Chicago, IL, and London: University of Chicago Press; 2000.
- Sayer A. Dignity at work. Deut Z Philos 2012;60:557-72. http://dx.doi.org/10.1524/dzph.2012.0042.
- Elder-Vass D. Integrating institutional, relational and embodied structure: an emergentist perspective. Br J Sociol 2008;59:281-99. http://dx.doi.org/10.1111/j.1468-4446.2008.00194.x.
- Goeschel CA, Wachter RM, Pronovost PJ. Responsibility for quality improvement and patient safety: hospital board and medical staff leadership challenges. Chest 2010;138:171-8. http://dx.doi.org/10.1378/chest.09-2051.
- Pronovost PJ, Miller MR, Wachter RM, Meyer GS. Perspective: physician leadership in quality. Acad Med 2009;84:1651-6. http://dx.doi.org/10.1097/ACM.0b013e3181bce0ee.
- Bhaskar R. The Possibility of Naturalism. Hemel Hempstead: Harvester Wheatsheaf; 1979.
- Kaidesoja T. Exploring the concept of causal power in a critical realist tradition. J Theory Soc Behav 2007;37:63-87. http://dx.doi.org/10.1111/j.1468-5914.2007.00324.x.
- Lewis PJ. Realism, causality and the problem of social structure. J Theory Soc Behav 2000;30:249-68. http://dx.doi.org/10.1111/1468-5914.00129.
- Archer MS, Bhaskar R, Collier A, Lawson T, Norrie A. Critical Realism: Essential Readings. London: Routledge; 1998.
Appendix 1 Summary of case study organisations
| Corporate parent | Abertawe Bro Morgannwg University Health Board | Aneurin Bevan University Health Board | Betsi Cadwaladr UHB University Health Board | Cardiff and Vale University Health Board | Cwm Taf University Health Board | Hywel Dda University Health Board | Powys (Teaching) Health Board |
|---|---|---|---|---|---|---|---|
| Geographical area | South | South | North | South | South | Mid | Mid |
| Population (000) (URL: www.wales.nhs.uk/sitesplus/922/home) | 518 | 577 | 688 | 472 | 293 | 382 | 133 |
| Major hospital with accident and emergency services | 2 | 2 | 3 | 1 | 2 | 3 | 0 |
| District general hospital with minor injuries unit | 2 | 2 | 9 | 1 | 2 | 1 | 4 |
| Small hospital/clinic without accident and emergency/minor injuries unit | 11 | 10 | 37 | 7 | 3 | 13 | 6 |
Appendix 2 Semistructured interview questionnaire
Part 1
Information about the interviewee
This opening section of the interview aims to discuss the interviewee’s role, professional background and management reporting relationships within the hospital case site.
-
What is your current role within the organisation?
-
How long have you worked in that role?
-
What did you do before you took up your current role?
-
-
What is your professional background? [Asked if not explicit from comments above.]
-
Please will you tell me a little more about what your role involves on a day-to-day basis?
-
Who do you report to?
-
Who reports to you?
-
Part 2
Awareness, understanding, and personal involvement in the 1000 Lives+ national programme and predecessor 1000 Lives campaign.
-
When and how did you first become aware of the 1000 Lives campaign or 1000 Lives+ national programme?
-
What does the 1000 Lives+ national programme mean to you?
-
How is the 1000 Lives+ national programme managed in your organisation?
-
Who is involved in the local leadership of the 1000 Lives+ national programme?
-
How would you describe your involvement in the 1000 Lives+ national programme?
-
Part 3
Discussion of I-CMAO configurations for 1000 Lives+ national programme and relevant focal interventions.
Intervention
-
What patient safety interventions have been adopted?
-
Do you use any of the resources supported by the 1000 Lives+ national programme? [Ascertain awareness web site and support materials.]
-
Do you use the Model for Improvement, Plan-Do-Study-Act Cycle in your functional team?
Context
-
What do you consider to be the context in which you work: how would you describe it?
-
Awareness of Welsh health-care policy commitment to the 1000 Lives+ national programme.
-
How is an ethos of patient safety advocated and developed?
-
What organisational- or team-level governance processes are in place to measure and monitor the internal oversight of patient safety? [Assess visits via WalkRounds.]
-
What external governance processes are in place to measure and monitor patient safety? [Assess inspection visits by Healthcare Inspectorate Wales, Community Health Councils, etc.]
-
What happens if you have a patient safety incident?
-
Can you explain your complaints procedure?
-
-
How has the reconfiguration of NHS Wales/the health board impacted patient safety?
Mechanism
-
Do you think the 1000 Lives+ national programme improves patient safety?
-
Why/how do you believe it works?
-
What has helped or hindered the local implementation and ongoing operationalisation of the 1000 Lives+ national programme?
Outcome
-
How do you measure and monitor the impact of the 1000 Lives+ national programme on patient safety?
-
Awareness of monitoring processes for local targets, data collection, ownership, analysis and reporting.
-
How is such data reported, to whom, formality and frequency?
-
What changes in health-care practice have been encouraged by the 1000 Lives+ national programme?
-
-
If you could change the 1000 Lives+ national programme in any way, what would you do?
Appendix 3 Data search strategy
| Databases | Research domain | ||||
|---|---|---|---|---|---|
| Social science | Business | Health-care studies | Medicine | Nursing | |
| ABI/INFORM Global (ProQuest) | ✓ | ||||
| AMED (Allied and Complementary Medicine) (via Ovid) | ✓ | ✓ | |||
| ASSIA (Applied Social Sciences Index and Abstracts) | ✓ | ✓ | |||
| Biomed Central | ✓ | ||||
| British Humanities Index (via CSA) | ✓ | ||||
| British Nursing Index (via Ovid) | ✓ | ✓ | |||
| CINAHL (Cumulative Index to Nursing and Allied Health Literature) | ✓ | ✓ | |||
| COPAC | ✓ | ✓ | |||
| EBSCOhost Business Source Premier | ✓ | ||||
| EMBASE (Excerpta Medica) (via Ovid) | ✓ | ✓ | ✓ | ||
| Emerald Library (via Emerald) | ✓ | ||||
| Ingenta Connect | ✓ | ✓ | |||
| JSTOR | ✓ | ||||
| MEDLINE (via Ovid) | ✓ | ✓ | |||
| MEDLINE In-Process & Other Non-Indexed Citations | ✓ | ✓ | |||
| PsycINFO (via Ovid) | ✓ | ✓ | ✓ | ✓ | |
| PubMed | ✓ | ✓ | ✓ | ||
| ScienceDirect – all subscribed content – V4 (Elsevier) | ✓ | ✓ | |||
| SCOPUS – V4 (Elsevier) | ✓ | ✓ | ✓ | ||
| SwetsWise | ✓ | ✓ | |||
| Web of Knowledge | ✓ | ✓ | |||
| Zetoc | ✓ | ✓ | ✓ | ||
Research themes and key author-based searches
-
Harm.
-
Health-care-associated infection.
-
Health-care management.
-
Health-care leadership and followership.
-
MI-PDSA cycle.
-
Mortality review and organisational performance
-
Patient safety culture.
-
Patient stories.
-
Public inquiries.
-
Shared decision-making.
-
WalkRounds™.
-
WHO Surgical Safety Checklist.
-
Allen D.
-
Andrews R.
-
Banaszak-Holl J.
-
Barber N.
-
Batalden P.
-
Berwick D.
-
Boyne G.
-
Braithwaite J.
-
Currie G.
-
Dixon-Woods M.
-
Dixon A.
-
Dopson S.
-
Exworthy M.
-
Ferlie E.
-
Finn R.
-
Fitzgerald L.
-
Franklin B.
-
Fulop N.
-
Greener I.
-
Greenhalgh T.
-
Ham C.
-
Hyde P.
-
Kirkpatrick I.
-
Kitchener M.
-
Le Grand J.
-
Lilford R.
-
Lockett A.
-
Mannion R.
-
Marshall M.
-
McDonald R.
-
McGivern G.
-
McKee L.
-
Ovretveit J.
-
Pronovost P.
-
Rycroft-Malone J.
-
Schofield J.
-
Shekelle P.
-
Vincent C.
-
Wachter R.
-
Walshe K.
-
Waring J.
-
Critical realism.
-
RAMESES publication standards (realist syntheses).
-
Realist analysis.
-
Realist evaluation.
-
Realist review.
-
Realist synthesis.
-
Ackroyd S.
-
Archer M.
-
Bhaskar R.
-
Cruickshank J.
-
Danermark B.
-
Edwards P.
-
Elder-Vass D.
-
Fleetwood S.
-
Hartwig M.
-
Mutch A.
-
Outhwaite W.
-
Pawson R.
-
Potter G.
-
Sayer A.
-
Searle J.
-
Smith C.
-
Vincent S.
-
Bureaucratisation.
-
Institutional change.
-
Institutional creation.
-
Institutional disruption.
-
Institutional entrepreneurship.
-
Institutional isomorphism (coercive, mimetic, normative).
-
Institutional logics.
-
Institutional maintenance.
-
Institutional structure.
-
Institutional work.
-
Normalisation.
-
Battilana J.
-
Boxenbaum E.
-
Dacin T.
-
Dcoupling.
-
Dorado S.
-
Goodrick E.
-
Greenwood R.
-
Hardy C.
-
Hinings B.
-
Lawrence T.
-
Leca B.
-
Lounsbury M.
-
Meyer R.
-
Ocasio W.
-
Phillips N.
-
Reay T.
-
Scott W.
-
Suddaby R.
-
Thornton P.
-
Tracey P.
-
Ventresca M.
-
Vermeulen P.
-
Voronov M.
-
Washington M.
-
Zietsma C.
-
Zilber T.
Appendix 4 Study invitation letter, information sheet and consent to be interviewed form
Glossary
- Abduction
- Abduction is a hypothesis or inference that explains an observation. It differs from deduction or induction because it infers a prior condition that gives rise to what is observed, rather than making assumptions about what will be true as a consequence of the observation. Abduction is a ‘logic of discovery’ used in realist research to set out an explanatory account of a mechanism acting in a given context.
- Abstraction
- In realist research, abstraction is a step in the analytical process that is used to identify and isolate in thought discrete aspects of an object. The point of abstraction is, therefore, to select one or more aspects, components or attributes and their relationships in order to understand how they impact social reality.
- Actor
- An individual who performs specific acts (see Agent).
- Agency
- The purposive action of individuals (and organisations) that is the foundation of changing practice.
- Agent; agentic
- An agent is similar to an actor, but is one who acts within a social structure, although there is debate about the degree to which the structure may or may not affect the action. In agentic transactions, people are seen as producers as well as products of social systems.
- Agentic emergent properties
- See Emergent properties.
- The Campbell Collaboration
- The Campbell Collaboration is an international research network that produces systematic reviews of the effects of social interventions (see Systematic review).
- Causality; causal configuration
- See Mechanism.
- Cochrane
- Cochrane is an international research network that produces systematic reviews of the effects of health-care interventions (mainly randomised controlled trials) to assist the decision-making of policy-makers, health-care professionals and others (see Systematic review).
- Coercive force
- In terms of organisational change, a coercive force is one that imposes a change (e.g. by regulation).
- Cognitive
- Cognitive processes are the mental processes of perception, memory, judgement and reasoning. They may be used consciously or happen unconsciously. Cognitive processes use existing knowledge and generate new knowledge.
- Comparative case study
- A research design that facilitates the longitudinal intensive analysis and comparison of different ‘cases’, typically an organisation or a discrete function within an organisation.
- Constraints
- In Archerian critical realism, constraints are causal powers that are internal to structural and cultural emergent properties. For anything to exert the power of a constraint it has to obstruct the achievement of a specific enterprise.
- Context–mechanism–outcome configuration
- A configuration, used in realist inquiry, to explain what aspects of an intervention work, for whom, why and in what circumstances.
- Coupling–decoupling
- With regard to patient safety interventions, coupling refers to the deliberate connection to – and decoupling to the deliberate disconnection from – organisational structures and associated practices that enhance the legitimacy and effectiveness of such interventions.
- Critical realism
- Critical realism is a complex body of ideas: a movement in philosophy, the human sciences and similar practices that describes an interface between the natural and social world. It is most closely associated with the work of Roy Bhaskar, Margaret Archer and Andrew Sayer, among others.
- Cultural emergent properties
- See Emergent properties.
- Distributed leadership
- Distributed leadership is leadership which, rather than being performed solely by one person, is shared between several people. It refers to purposive, concertive action, rather than aggregated, individual acts. Important forms of concertive action are collaboration, intuitive understandings that emerge from close working relationships and a variety of structural relations and institutionalised arrangements. Under distributed leadership some functions may be shared by several members of a group, some may be allocated to individual members and a particular function may be performed by different people at different times.
- Ear, nose and throat surgery
- Otolaryngologists (or otorhinolaryngologists) are commonly referred to as ENT (ear, nose and throat) surgeons and deal with the diagnosis, evaluation and management of diseases of the head and neck and, principally, the ears, nose and throat.
- Emergents; emergent properties
- Emergents or emergent properties are new features or transformations that differ qualitatively from the elements from which they came and, therefore, cannot be returned to their previous forms (e.g. the NHS, once formed, could not be returned to the private institutions which predated it). Agential emergent properties are transformations that come about as a result of deliberate action at the level of the individual, group or organisation (e.g. the NHS was created by Aneurin Bevan and the Labour government of the day). Cultural emergent properties are transformations that are influenced by the cultural situation (the prevailing climate shaped by people’s collective beliefs, values or ideologies) in which they occur (e.g. the NHS was influenced by both egalitarian principles and a belief that free health care would profit the nation by improving the health of the workforce). Structural emergent properties are transformations that are influenced by the circumstances in which they occur, be they physical or social (e.g. the structure of the NHS was influenced by existing health-care structures and the perceived needs of the post-war population).
- Enablements
- In Archerian critical realism enablements are causal powers that are internal to structural and cultural emergent properties. For anything to exert the power of an enablement it has to aid the achievement of a specific enterprise.
- Epistemology
- The nature and scope of knowledge – what we think can be known about the world. Additionally, the study of knowledge, and justified belief, centred on the creation and dissemination of knowledge in particular areas of inquiry.
- Escherichia coli
- Escherichia coli are a group of bacteria that are an important part of the normal intestinal flora of humans. Most strains of E. coli are harmless. However, some strains of E. coli can cause illness, typically diarrhoea or urinary tract, respiratory or blood infections.
- Extended-spectrum beta-lactamase
- Some strains of E. coli and Klebsiella pneumonia produce an enzyme called extended-spectrum beta-lactamase. This enzyme can break down antibiotics and make them ineffective. Infections caused by extended-spectrum beta-lactamase-producing strains of these bacteria are, therefore, difficult to treat.
- First-order emergents (see Emergents)
- First-order emergents are the results of social interaction. In Archerian critical realism, first-order emergents manifest as the agent’s involuntaristic placement within the broader social context and role array; their vested interests; the opportunity costs associated with different courses of action; and their perceived interpretive freedom and scope for strategic directional guidance.
- Functional team
- The group of people who carry out the tasks involved in running a ward or department.
- Generative mechanism
- See Mechanism.
- Health-care-associated infection
- Health-care-associated infection refers to infections that occur as a result of contact with the health-care system.
- Heterarchy
- A non-hierarchical system of organisation characterised by horizontal positioning of power and authority, with individuals sharing the same status.
- Hierarchy
- A system of organisation characterised by vertical ranking relative to status or authority.
- Higher-order societal logics
- See Institutions and Institutional logics.
- Hospital-acquired infection
- Hospital-acquired infection – also known as nosocomial infection – refers to an infection that develops in a patient ≥ 48 hours after admission to a hospital. Infections that occur within the first 48 hours are referred to as community-acquired.
- Hospital standardised mortality ratio
- Hospital standardised mortality ratio is the ratio of the actual number of acute in-hospital deaths to the expected number of in-hospital deaths.
- Institutional logics
- Institutional logics focus on how broader belief systems shape organisational interests and individual preferences, define actors’ expectations about each other’s behaviour and organise their enduring relations with each other. In institutional theory, higher-order societal logics refer to the central institutions of contemporary societies – for example the family, the capitalist market, organised religion, the state and democracy – which inform the core organising principles of these different sectors of society. Institutional logics also operate at the level of professions.
- Institutional pillars: regulative, normative and cultural-cognitive
- Institutions are conceptualised as composed of three pillars: the regulative pillar, which stresses rule setting, monitoring and sanctioning activities, both formal and informal; the normative pillar, which sets out what is considered to be appropriate behaviour given the demands of the situated context; and the cultural-cognitive pillar, which emphasises the centrality of common schemas that guide behaviour.
- Institutional theory
- Institutional theory is one of the dominant perspectives within organisation and management theory.
- Institutional work
- The purposive action of individuals and organisations aimed at creating, maintaining, enhancing and disrupting institutions.
- Institutions
- Institutions are the taken-for-granted social prescriptions that guide the behaviour of actors in different societal, organisational and professional contexts.
- Intervention–context–mechanism–agency–outcome configuration
- A configuration used in realist analysis to explain what aspects of an intervention work, for whom, why and in what circumstances.
- Intransitive dimension (see Ontology)
- The intransitive dimension is synonymous with ontology and refers to the objects in the domain of the real of any human inquiry, theoretical or practical.
- Isomorphic institutionalism
- Increased similarity between institutions over time.
- Klebsiella species
- Klebsiella species are a group of bacteria that are an important part of the normal intestinal flora of man. Usually, healthy people do not get Klebsiella infections. However, in health-care settings, patients who are receiving long courses of certain antibiotics and those whose care requires invasive medical devices such as ventilators (breathing machines) or intravenous (vein) catheters are at risk of Klebsiella infections.
- Legitimacy façade
- In respect to patient safety interventions, a legitimacy façade is the outward appearance of adhering to guidelines while, in reality, deviation from such guidelines is seen in day-to-day practice.
- Mechanism
- The power to bring about change: the characteristic way(s) of acting possessed by things by virtue of their intrinsic structures. In realist enquiry, mechanisms refer to the engines of explanation embodied in an agent’s reasoning and their selective attention to the disparate resources offered through a social programme. Mechanisms are also part of a causal configuration emergent from a cluster of contextual factors and organisational components.
- Mediation of structure by agency
- In Archerian critical realism, the mediation of structure by agency refers to the conditioning influence of context on the actions of individuals.
- Metamechanism
- A metamechanism is a complex ‘bundle’ of mechanisms.
- Metaphysics
- The branch of philosophy that deals with the first principles of things, including abstract concepts such as being, knowing, identity, time and space.
- Methodology
- Methodology is the systematic, theoretical analysis of the methods used in research.
- Meticillin-resistant Staphylococcus aureus
- Staphylococcus aureus is a type of bacteria commonly found on human skin. Most of the time, S. aureus does not cause any harm. Meticillin-resistant S. aureus is a bacterium that is resistant to many antibiotics. In the community most meticillin-resistant S. aureus infections are skin infections. However, in health-care settings, such as hospitals and nursing homes, meticillin-resistant S. aureus may cause life-threatening bloodstream infections, pneumonia, endocarditis (infection of the heart valves), osteomyelitis (bone infection) and surgical site infections.
- Mimetic force
- In terms of organisational change, a mimetic force is one which copies a change perceived to be successful elsewhere.
- Morphogenesis
- The process of social transformation.
- Morphogenetic-morphostatic cycle
- The morphogenetic-morphostatic cycle is a method of analysing the complex interplay of structure, culture and agency across three temporal phases: structural conditioning, sociocultural interaction and structural reproduction or elaboration.
- Morphostasis
- The process of social reproduction.
- ‘Never events’
- Serious, largely preventable patient safety incidents that should not occur if the available preventative measures have been implemented. They include incidents such as wrong site surgery and a retained instrument after operation.
- Normative force
- In terms of organisational change, a normative force is one in which change is aligned with what is perceived to be an existing norm, or standard.
- Nosocomial infection
- See Hospital-acquired infection.
- Ontology
- The branch of metaphysics that deals with the nature of being or the way we think the world is.
- Peripheral venous cannula
- A peripheral venous cannula is a very thin tube inserted into a small peripheral vein for therapeutic purposes such as the administration of medications, fluids or blood products.
- Point prevalence survey
- A point prevalence survey is a count of the number of patients with a particular condition or treatment (in this report either a health-care-associated infection or an antimicrobial agent) at a particular time (a specified day), as a proportion of the total number of patients who are hospitalised at that particular time. A point prevalence survey counts the condition or treatment only if it is present on the specified day of the survey, and does not count it if it is present at other times during the patient stay in the hospital.
- Reflexive agency
- In Archerian critical realism, reflexive agency originates within the internal conversation of the individual’s domain of mental privacy.
- Reflexive theorisation
- Reflexive theorisation, the final stage of the mediation of structure by agency, occurs through three stages: discernment, the preliminary review stage of an issue of concern, where reflective retrospective and prospective thought informs practical action; deliberation, involving the ranking of such concerns against others; and dedication, entailing their prioritisation and alignment to foster a fallible yet corrigible commitment to a chosen path.
- Relational structure
- Relational structure refers to social relations, or the ties that bind social actors, specifically the pattern of causal interconnections and interdependencies among agents occupying defined roles, and their subsequent actions. Relational structure is, therefore, the nexus of connections among actors causally affecting their actions and, in turn, causally affected by them.
- Reproduction
- In realist research, reproduction refers to a lack of change, persistence of the status quo ante.
- Retroduction
- In realist research, retroduction is a step in the analytical process that is used to refine understanding of a distinctive process or mechanism when the basic conditions for its existence have been elaborated.
- Risk-adjusted mortality index
- Risk-adjusted mortality index is a statistical tool by which an estimate is made of probability of death for all admitted patients. Taking into account factors such as age, sex, diagnoses, procedure, clinical grouping and admission type, it allows a calculation of risk of death. From this prediction it calculates the number in a population expected to die. In publishing such data, comparisons are made between the numbers of patients who actually die and those predicted. Where the numbers are the same, the risk-adjusted mortality index will be reported as 100.
- Second-order emergents
- Second-order emergents are the results of necessary and internal relations among first-order emergents. In Archerian critical realism, the second stage of the mediation of structure to agency addresses how an individual or group, confronted by contextual conditioning, exercise their subjective and reflexive mental powers to formulate their strategic goals, individually or collectively. This array of influences gives rise to four potential second-order emergents –’necessary complementarities, necessary incompatibilities, contingent complementarities and contingent incompatibilities’ – which foster the accompanying situational logics of protection, correction/compromise, opportunism and elimination. The situational logic ultimately brought to pass through strategic negotiation – be that via power-induced compliance, reciprocal exchange or the harmonisation of desires – represents the mechanism of morphogenesis or morphostasis.
- Situated context
- Situated context refers to one of the many contexts in which groups and individuals live and work, and which influence their actions in a particular environment.
- Situational logic: contingent complementarities
- A prevailing situational logic of contingent compatibilities entails a situational logic of pure opportunism that generates fundamental change.
- Situational logic: contingent incompatibilities
- A prevailing situational logic of contingent incompatibilities gives rise to the tensions in the strategic arena and fosters morphogenesis. Here, opposing factions become party to the situational logic of elimination, where the greatest gain coincides with inflicting maximum injuries on the other side.
- Situational logic: necessary complementarities
- A prevailing situational logic of necessary complementarities depicts a strategic arena in which transformation threatens the loss of vested interest all round. Necessary complementarities, therefore, generate a situational logic of protection that is conducive to morphostasis.
- Situational logic: necessary incompatibilities
- A prevailing situational logic of necessary incompatibilities depicts a strategic arena that is marked by incompatibilities between institutions, which are nonetheless internally and necessarily related. Accordingly, a situational logic of compromise arises because necessary incompatibilities means that the promotion of vested interests has to be a cautious balancing act – a weighing of gains against losses – where to accrue bonuses is also to invite or incur penalties. The fragility of this structural conditioning, therefore, offers a subtle potential for change.
- Situational logic of protection
- See Situational logic: necessary complementarities.
- Structural emergent properties
- See Emergent properties.
- Systematic review
- A systematic review is a literature review that aims to identify, critically appraise, select and synthesise published research studies that address a particular research issue. A systematic review typically includes a description of the findings of the collection of research studies. The systematic review may also include a quantitative pooling of data called a meta-analysis.
- Third-order emergents
- In Archerian critical realism, third-order emergents arise from the effects of first- and second-order influences on the outcomes of the intervention. This concept, therefore, captures structural and ideational differentiation, together with the regrouping inherent to the power play of a diverse array of agents.
- Transitive dimension
- The transitive dimension is synonymous with epistemology and refers to human understanding of the objects in the domain of the real.
- Venous thromboembolism
- Venous thromboembolism is a condition that includes both deep-vein thrombosis and pulmonary embolism. Deep-vein thrombosis is the formation of a blood clot in a deep vein, usually in the leg or pelvic veins. Pulmonary embolism is a sudden blockage in a lung artery, usually caused by a blood clot that travels to the lung from a vein in the leg.
List of abbreviations
- CAUTI
- catheter-associated urinary tract infection
- CHC
- Community Health Council
- CMO
- context–mechanism–outcome
- HIW
- Healthcare Inspectorate Wales
- HOWIS
- Health of Wales Information Service
- HSMR
- Hospital Standardised Mortality Ratio
- I-CMAO
- intervention–context–mechanism–agency–outcome
- IHI
- Institute for Healthcare Improvement
- ILQI
- Improving Leadership for Quality Improvement
- IPAC
- infection prevention and control
- MI-PDSA
- Model for Improvement, Plan-Do-Study-Act
- MRSA
- meticillin-resistant Staphylococcus aureus
- NISCHR
- National Institute for Social Care and Health Research
- PSOW
- Public Services Ombudsman for Wales
- PVC
- peripheral venous cannula
- RAMI
- risk-adjusted mortality index
- RHAI
- Reducing Health-care-Associated Infection
- RSC
- Reducing Surgical Complications
- WHAIP
- Welsh Healthcare Associated Infection Programme
- WHO
- World Health Organization
- WHOSSC
- World Health Organization Surgical Safety Checklist