Notes
Article history
The research reported here is the product of an HS&DR Evidence Synthesis Centre, contracted to provide rapid evidence syntheses on issues of relevance to the health service, and to inform future HS&DR calls for new research around identified gaps in evidence. Other reviews by the Evidence Synthesis Centres are also available in the HS&DR journal.
The research reported in this issue of the journal was funded by the HS&DR programme as project number 13/05/12. The contractual start date was in October 2014. The final report began editorial review in April 2015 and was accepted for publication in June 2015. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2015. This work was produced by Turner et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Background
This rapid evidence synthesis has been written in response to a request by the National Institute for Health Research (NIHR) Health Services and Delivery Research (HSDR) programme to examine the evidence around the delivery of urgent care services. The purpose of the evidence synthesis is to assess the nature and quality of the existing evidence base, and identify gaps that require further primary research or evidence synthesis.
Demand for urgent care (including emergency care) has increased year on year over the last 40 years. This has been reflected in growth in emergency department (ED) attendances, calls to the 999 ambulance service and contacts with other urgent care services, including primary care and telephone-based services. 1 The reasons for this are only partly understood, but comprise a complex mix of changing demographic, health and social factors. Over the last 15 years there have been a number of reviews of urgent care, policy recommendations for service changes and service-level innovations, all of which were aimed at improving access to and delivery of urgent care. Figure 1 provides a summary of some of the key developments that have been widely adopted within the NHS and related policy initiatives. The timeline shows when developments were first introduced; however, these developments have not remained static but have grown and changed over ensuing years.
FIGURE 1.
Selected key developments and policy initiatives for the delivery of emergency and urgent care.

Despite these initiatives, the emergency and urgent care system has come under increasing strain and media attention,1 most commonly reported as failings in meeting government targets. Nationally, EDs have not met the target of treating and discharging or admitting 95% of attending patients within 4 hours for any year quarter from October 2012 to March 2015 (URL: www.england.nhs.uk/statistics/statistical-work-areas/ae-waiting-times-and-activity/weekly-ae-sitreps-2014-15/). Similarly, there has been a reduction in the ability of ambulance services to meet the national target of responding to 75% of life-threatening (Red 1) calls within 8 minutes. Performance nationally reduced from 76.2% in March 2014 to 73.4% in March 2015 (URL: www.england.nhs.uk/statistics/statistical-work-areas/ambulance-quality-indicators/), while at the same time the number of ambulance handover delays at EDs increased from 86,003 in November 2013–March 2014 to 139,970 for the same period in 2014/15 (URL: www.england.nhs.uk/statistics/statistical-work-areas/winter-daily-sitreps/winter-daily-sitrep-2013-14-data-2/).
In 2012/13, the intense public scrutiny culminated in a Health Select Committee inquiry,2 and this scrutiny has continued. The pressure of increasing demand has more recently been exacerbated by acute shortages of associated health-care professionals, particularly in emergency medicine,3 primary care4 and ambulance services. 5
It is increasingly recognised that provision of urgent care is a complex system of interrelated services and that this whole-system approach will be key to improvement and development in the future. In response to the clear pressure within the emergency and urgent care system, in 2012 NHS England embarked on a major review of urgent care services and in 2013 set out its strategy for development of a system that is more responsive to patients’ needs, improves outcomes and delivers clinically excellent and safe care. 6 The challenge now is to find ways to put this blueprint into practice.
Knowledge about the current evidence base on models for provision of safe and effective urgent care can support this process. The purpose of this rapid review is to examine what evidence there is on how efficient, effective and safe urgent and emergency care services can be delivered within the NHS in England, the quality of that evidence and the gaps in evidence which may need to be addressed.
Hypotheses tested in the review (research questions)
The NHS England review6 has set the agenda for urgent care, with recommendations on how the urgent care system and the services within it need to change. We have used the key themes identified in this review as the framework for this rapid evidence review to provide both focus and context for evidence appraisal and the identification of evidence gaps, which will be of direct relevance to future developments. The five key themes identified in the NHS England review are:
-
providing better support for people to self-care
-
helping people with urgent care needs to get the right advice in the right place, at the first contact
-
providing highly responsive urgent care services outside hospital so that people no longer choose to queue in accident and emergency (A&E) departments
-
ensuring that those people with more serious or life-threatening emergency care needs receive treatment in centres with the right facilities and expertise to maximise chances of survival and a good recovery
-
connecting all urgent and emergency care services, so the overall system becomes more than the sum of its parts.
The first theme, focused on providing better support for people to self-care, encompasses the much broader areas of health care related to reducing the need for urgent care. This theme warrants a separate review, as it involves complex issues such as management of long-term conditions, health promotion and injury prevention. As it targets an alternative health-care vision outside of urgent care; the potential scope was considered too broad and diffuse to be included within the constraints of this review. We have therefore excluded this theme and concentrated on the other four themes directly related to delivery of urgent care.
Within each of these four key themes the NHS England review sets out more specific proposals for service change and delivery, and these will form the focus of the primary scope for individual elements of this review. We have also added an additional underpinning theme, which was not identified as a separate issue by the NHS England review. In order to develop services that are responsive to the needs of the population using them, it is essential to understand the characteristics and drivers that underpin demand for services and the choices people make about how they use those services. Without this it is difficult to ensure alignment between service development and patient need. We have therefore included within our review a brief overview of a fifth theme focused on patterns and characteristics of the demand for urgent care (including change over time), and the factors that influence decisions about when and how to access urgent care.
Although these key themes provide focus, each one still potentially includes a range of issues. To keep the review process manageable within the time and resources available we have therefore restricted the research questions for some themes to a particular service area highlighted as of particular importance in the NHS England review.
Research questions
The research questions examine the evidence relating to the following:
-
To what extent does evidence on existing and proposed approaches to the delivery of urgent care support the development of four key themes in the NHS England review of urgent care?
-
Helping people to get the right advice in the right place, first time. This theme could potentially cover a range of services in terms of what care is eventually accessed. However, the process of providing advice and directing people to the right service when they first try to access care is firmly grounded in the NHS England review as the NHS 111 telephone service. This service is seen as the gateway to directing requests for emergency care to the right service. We have therefore focused on telephone-based access services in this review.
-
Providing highly responsive urgent care services outside hospital. This theme also potentially includes a range of community-based services; however, it was beyond the scope of this review to search and synthesise all of the potential literature about community-based urgent care. The 2013 NHS England review and related action plan make a clear statement that the ambulance service is considered a key provider in achieving this objective. We have therefore focused on the evidence for developing the ambulance service to manage more people in the community setting in this review.
-
Ensuring that people with serious or life-threatening emergency care needs receive treatment in appropriately staffed and resourced facilities. This theme is concerned with the provision of ED care, including both major regional facilities and local EDs. There is already a substantial evidence base about the impact of providing regionalised services (e.g. for stroke, heart attack), so there is no value in repeating this here. Furthermore, service pressure is greatest in general EDs (and major regional facilities also function as ‘local’ EDs). We have therefore focused this review on the evidence about different models and processes for delivering ED care to keep the review relevant to current NHS challenges.
-
Connecting urgent and emergency care services. The NHS England review sets out a clear view that the way to achieve this objective is through the development of urgent care networks to develop and manage local urgent care systems. We have focused this element of the review specifically on evidence about models of urgent care networks.
-
-
What evidence is there on characteristics of demand for urgent care, and why and how people access urgent care, that may help future service planning?
We have conducted and reported a rapid review for each of these five themes. For each review we have considered two additional questions:
-
What is the quality of that evidence?
-
What are the main/significant evidence gaps?
Chapter 2 Review methods
Overview of rapid review methods
This was a rapid framework-based evidence synthesis which needed to be completed within the relatively short time frame of 6 months to produce a review that met the HSDR programme’s needs. We have used rapid review methods to ensure the efficient identification and synthesis of the most relevant evidence. The multiple dimensions covered by the review questions posed a considerable challenge to the rapid review process. This challenge was further complicated by the fact that emergency and urgent care does not involve discrete populations or conditions, but encompasses whole populations and a heterogeneous mix of conditions and acuity, and care is delivered by a range of services. As a consequence there was a potentially huge pool of related literature.
Given the large scope and time and resource constraints we have not taken a standard approach to this review. Our aim was to provide a broad overview of the existing evidence base for each theme and any associated limitations. We have therefore applied the following criteria to structure the review process:
-
We have concentrated on identifying and synthesising the key evidence using a focused, policy-relevant framework to keep the task relevant and manageable. Framework-based synthesis has been identified as an efficient method for synthesising evidence to inform policy within relatively tight time constraints. 7
-
The review did not attempt to identify all relevant evidence or to search exhaustively for all evidence that meets the inclusion criteria; instead we have used a structured searching approach to identify the key evidence.
-
The data extraction and quality assessment have focused on the most critical information for evidence synthesis rather than aiming to exhaustively extract and critique all the available information in individual papers.
-
We have not appraised the evidence in terms of how future services should be provided, nor made recommendations about service configuration.
Framework
As the focus of this review is on models of care, that is service and system delivery, we have not searched for, or considered, evidence related to specific clinical interventions for specific conditions. We have also only included primarily evaluative research of actual interventions (although the definition of intervention can be broad and encompass changes to organisation, changing professional roles, new services, etc.) in order to provide an overview of what may or may not work in practice. For this reason we have purposely excluded the more theoretical literature, for example relating to organisational behaviour, professional development and clinical competence, work psychology, patient decision-making and behaviour. Where additional review in these related areas is of value, these have been highlighted in the individual review chapters as specific areas for further in-depth review and analysis.
For each of the four themes related to the NHS England review we have considered three main areas:
-
evidence on efficiency and clinical effectiveness and cost-effectiveness of service delivery for any identified operating models, including individual service and whole-system perspectives
-
evidence on associated workforce issues where this is primary research evaluating the effectiveness of changing or developing new professional roles in the delivery of urgent care and workforce planning
-
evidence on any related patient experience outcomes.
Urgent care provision in England is a rapidly changing environment. The NHS England review has prompted a range of work programmes8 and professional bodies, for example the Royal College of Emergency Medicine,9 to regularly publish recommendations about delivery of services. Where relevant, we have used key policy documents published before October 2014 specifically related to the implementation of the NHS England reform of urgent care to develop the review framework.
The additional fifth theme on understanding demand and use of services has focused on primary research that:
-
reports analysis of not only level of demand but also the characteristics of that demand (e.g. age profiles, condition profiles, whole-system demand for different types of service)
-
reports patient-derived explanatory research concerned with decisions to access urgent care.
This framework has provided a clear structure with which to guide the review while retaining the flexibility that has allowed the development of each individual theme in terms of defining the scope of the search strategies, defining inclusion and exclusion criteria to specify what types of studies will be included in each theme and evidence synthesis.
Search methods
A variety of search methods were undertaken in order to identify relevant evidence for each of the review questions and themes in a timely fashion. We have used a number of different search strategies for this review while using a general structure of combining relevant terms, such as:
-
Population
-
Users of the range of services within the emergency and urgent care system (ambulance services, ED, other urgent care facilities, telephone access services, primary care-based urgent care services).
-
-
Outcomes
-
Processes – ED attendances, emergency admissions, ambulance calls, dispatches or transports, demand, appropriateness of level of care, adverse events.
-
Patient outcomes – patient experience and satisfaction, decision-making, cost consequences and cost-effectiveness.
-
Searches were conducted in two stages:
-
Stage 1 – general search on MEDLINE.
-
Stage 2 – targeted database searches around telephone triage, ambulance, demand, organisation of EDs and networks. To increase efficiency, where appropriate, we have utilised existing search strategies from related research we have conducted within the School of Health and Related Research (ScHARR) or from existing related systematic reviews.
Database search strategies
General search
An initial broad-scoping search was conducted on MEDLINE. This broad search aimed to find studies that evaluated the impact of changes in organisation, policy, structure and systems on urgent care. Descriptive studies without an evaluative component were not considered relevant. Key issues for consideration were access to services, appropriate management of patients, service delivery, models of delivery and clinically appropriate management of patients. The general search strategy used a combination of free text and medical subject headings (MeSH), as well as appropriate subheadings. A detailed description of the search strategy is provided in Appendix 1. The search retrieved a large number of results and refinements were made to the search to reduce this number. One key modification was the removal of the term ‘ambulatory care’, as this term retrieved a large volume of results related to outpatient rather than urgent care. The final search retrieved 9488 results. After careful discussion it was decided that, because of time constraints, a sample of 20% would be considered for inclusion for this search and further targeted searches conducted relevant to each of the five themes. From the 20% sample of the general search, potential inclusions relevant to the five themes were identified using keywords and any additional references identified from this search, and not identified in the targeted search, were added to the list of potential inclusions for that theme.
Targeted searches
For the targeted searches the following databases were searched: MEDLINE (via Ovid SP), EMBASE (via Ovid), The Cochrane Library (via Wiley Online Library), Web of Science (via the Web of Knowledge) and the Cumulative Index to Nursing and Allied Health Literature (CINAHL; via EBSCOhost). Searches were limited to publication date from 1 January 1995 to current, in order to keep results relevant to current services, and publications were to be written in English. All searches were completed between October 2014 and January 2015. A detailed description of each of the targeted search strategies is provided in Appendix 1.
Targeted searches were conducted on the following areas: telephone triage, ambulance services, reorganisation of EDs, developing and building urgent care networks, and demand for emergency and urgent care services.
Telephone triage
Within ScHARR extensive previous work had already been completed on telephone triage and we were able to rerun an existing search strategy for this review with expansion of the dates from 1 January 1995 to 11 November 2014. After deduplication, there were 1127 unique references.
Ambulance services
The search on ambulance services focused on finding literature concerned with the impact of ambulance services treating people at home where appropriate and triaging them to more appropriate community or primary care services. Additionally, research was sought on developing the skills of ambulance personnel to enable them to perform extended roles. After deduplication, there were 4499 unique references.
Organisation of emergency departments
Targeted searches were also conducted on reorganisation of EDs. Targeted searches were conducted to find evaluative literature on service delivery following reorganisation of processes within the ED. After deduplication, there were 3539 unique references.
A recent report by the Royal College of Emergency Medicine9 recommended that all EDs should have a co-located primary care service. We identified an existing, relevant rapid evidence review conducted by the University of Warwick10 and updated the search strategy described in that review. After deduplication, there were 5724 unique references for this search.
Networks
Another targeted search focused on the development and use of networks within emergency and urgent care. After deduplication, there were 1301 unique references.
Demand for emergency and urgent care
The searches around demand for emergency and urgent care were based on searches previously completed for a project ScHARR conducted for the NHS Confederation, in 2013, and were expanded to encompass the full range of dates and databases. The search aimed to retrieve empirical research on urgent care demand, research on rising demand in the ageing population and empirical research on patient-derived reasons for accessing different emergency or urgent care services. After deduplication there were 1371 unique references.
The search results were downloaded into EndNote X7.2.1 (Thomson Reuters, CA, USA).
Given the scope of each search and the limited time available, we were not able to conduct extensive supplementary searching, for example citation searching. However, in addition to the database searches we also identified key evidence through:
-
scrutinising reference lists of included relevant systematic reviews
-
utilising our own extensive archives of related research, including a number of related evidence reviews
-
the evidence review that NHS England produced as part of its consultation
-
consultation with internal ScHARR topic experts and some external topic experts.
Review process
Inclusion and exclusion criteria
We have included both quantitative and qualitative empirical evidence in the review where relevant to one of the five themes. Both UK and international evidence have been included to ensure that alternative models of urgent care delivery designed to address the same objectives set out in the NHS England review (e.g. reducing ED attendances) are considered. We have only included published peer-reviewed evidence in order to ensure that we have synthesised evidence that has already undergone methodological and expert scrutiny. Emergency and urgent care changes rapidly in terms of demand, clinical care and service delivery, so we have limited the evidence included in the years from 1995 to 2014 to ensure that the evidence assessed has context and relevance to current policy and practice. Evidence for specific clinical interventions and conditions has been excluded as it is likely to be substantial for a large number of conditions; our focus is on whole services rather than narrow, condition-specific populations. However, we have included evidence for defined but broad (in terms of condition) populations, for example children or the frail elderly. To summarise, we have used a core set of inclusion and exclusion criteria for all five themes to ensure consistency in the review approach.
Inclusion criteria
-
Empirical data (all study designs).
-
Emergency/urgent care.
-
Report relevant outcomes.
-
Written in English.
-
Published between 1995 and 2014.
Exclusion criteria
-
Descriptive studies with no assessment of outcome.
-
Opinion pieces and editorials.
-
Non-English-language papers.
-
Conference abstracts.
Additional theme-specific inclusion and exclusion criteria were then applied to the core criteria. Theme-specific criteria are described in each review chapter.
Data extraction
Data extraction of included papers was undertaken for each theme. However, because of the number of themes and scope of each one, we could not complete detailed and exhaustive data extraction for all relevant inclusions. To make this task manageable, ensure consistency across the themes and enable comparisons to be made between themes we employed two strategies:
-
For each theme we used any existing, relevant systematic reviews identified from the searches as the starting point for decisions about which individual identified papers meeting the inclusion criteria we would extract data from. We did not extract data from individual papers already included in relevant systematic reviews, instead we extracted the data from the systematic reviews in to summary tables. Any additional papers not included in the systematic reviews had data extracted in to summary tables.
-
All data extraction was carried out directly in to summary tables rather than detailed data extraction forms, which would subsequently require summarising. Included research was highly heterogeneous, therefore we used a simple, broad template to summarise the key characteristics and findings from each included systematic review or individual paper. For each paper we summarised the study design used, population and setting, main purpose and objectives, including outcomes measured, and key findings and conclusions.
Quality assessment
Rather than using a standard checklist approach, we have focused on an assessment of the overall quality and relevance of the evidence included within each theme in the review. Relevance has been assessed based on various factors, including the number of relevant studies, particularly systematic reviews; study types and design; the country and health system in which the research was conducted; and whether the research is single centre or multicentre. Quality has been assessed based on study types, the strength of the evidence identified by related systematic reviews and other key factors. For each theme we have provided a narrative commentary on quality and relevance that will allow readers of the rapid evidence synthesis to make an assessment of the rigour and relevance of evidence included in the review.
We have effectively conducted five separate rapid reviews, one for each of the five themes set out in the research questions. We have therefore presented each review separately, describing any methods specific to that review, results, an appraisal and summary of the existing evidence and any evidence gaps identified which are likely to be critical to further development of the main urgent care delivery objectives related to a theme. This includes where additional, more detailed, topic-specific evidence reviews could be of value or where more primary research is needed, for example on a larger scale to provide definitive evidence of effectiveness.
The five reviews are presented in Chapters 3–7.
A summary of all the reviews, together with an appraisal of common evidence across themes to provide a more comprehensive overview that describes, compares and contrasts different approaches to the delivery of urgent care and a headline summary of key findings, is presented in Chapter 8. This review has been designed to identify evidence gaps and help inform future NIHR HSDR programme research priorities. As such, the analysis has been undertaken using a research-commissioning rather than service-commissioning perspective.
Chapter 3 Trends and characteristics in demand for emergency and urgent care
Introduction
The main focus of this rapid review is assessment of the evidence relevant to the NHS England review of urgent and emergency care. However, to provide context we have presented a short overview of the current state of knowledge of the characteristics and drivers that underpin demand for services. This may be of use in terms of future planning, the ability to develop services that are responsive to the needs of the population using them and ensuring alignment between service development and patient need, and so is of relevance to the later review about urgent care networks.
Increases in demand for ED care are well documented. In England, demand for ED care doubled from an estimated 6.8 million first attendances at type 1 (24-hour, consultant-led service) EDs to 13.6 million over the 40 years from 1966/7 to 2006/7 – equivalent to an increase from 138 to 267 first attendances per 1000 people per year. Since 2006/07 attendances at type 1 EDs have further increased to 14.3 million in 2012/13 and at the same time there has been a rapid increase in the use of minor urgent care services [type 3 – not 24 hours, may be run by nurses or general practitioners (GPs), limited facilities such as radiography], with attendances increasing by 46% from 4.7 million in 2006/7 to 6.9 million in 2012/13. 11 Similarly, demand for 999 ambulance services has also steadily increased from around 4 million calls per year in 1994/5 to 9 million in 2012/13 (an increase of 160%), with utilisation rising from 78 to 171 calls per 1000 people per year over the same time period. 1 People with health problems also access urgent care via NHS 111 and primary care, but NHS 111 is a relatively new service and there is a lack of national data on urgent care contacts with primary care, so it is difficult to assess whole-system demand for emergency and urgent care in England.
More detailed analysis of UK trends in demand is available in reports from the NHS Confederation1 and Nuffield Trust. 12 In this report we have examined the empirical evidence that may help explain why demand is changing.
Methods
The main inclusion and exclusion criteria, search strategies and review process have been described in Chapter 2. We have conducted previous reviews in this area and are aware of the relative scarcity of related evidence. In addition, this topic area is not concerned with interventions or service delivery and hence the effects on processes or patient outcomes. We have therefore included literature reviews that were not systematic reviews but which have described a structured search strategy. Search dates were from 1995 to 2014. For this review, specific additional inclusion and exclusion criteria were applied to studies investigating the following:
Inclusion criteria
-
Trends in demand for emergency and urgent care over time.
-
Analysis of characteristics of demand.
-
Empirical, patient-based studies examining reasons why people access emergency and urgent care and how they choose which service to access.
Exclusion criteria
-
Studies of demand that describe volumes of activity only at single points in time.
Review process
Studies were identified from updated and expanded database searching using a search strategy from one of our own previous reviews in this area1 and a review of the evidence on callers to the 999 service with primary care problems from an NIHR doctoral research fellowship currently awaiting publication in the NIHR Journals Library (Dr M Booker, University of Bristol, 2015, personal communication). As the aim of this part of the review was to describe an overview of current evidence to provide context for the more detailed rapid reviews on service delivery, we limited the studies included in three ways:
-
We previously conducted a scoping review of potential reasons for increases in ambulance demand and, as this is already in the public domain and available for reference, we have not considered papers included in this review. 13
-
We did not conduct a double 10% random sift of the results of the database searches. These were sifted by one reviewer (JT) and supplemented by potential inclusions identified in the 20% random sample from the general search, also sifted by the same reviewer.
-
Data extraction of individual papers meeting the inclusion criteria was only conducted for papers not included in relevant review papers identified in the searches.
The results of the review sifting process are given in Figure 2.
FIGURE 2.
A Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram for emergency and urgent care demand searches.

Results
We identified four relevant systematic or rapid reviews, and an additional 39 primary studies not included in the systematic reviews. Of these 39, eight related to demand and 31 were patient-based studies exploring reasons and choice in terms of accessing urgent care. The characteristics and findings of the included reviews and primary studies are summarised in Tables 1–3.
| Author, year | Study design | Population and setting | Purpose | Main findings |
|---|---|---|---|---|
| Lowthian, 201114 | Systematic review of published and unpublished reports generated between January 1995 and January 2010 | Attendances at ED in developed countries | To synthesise the evidence describing trends and drivers associated with increased ED attendances | A total of 56 peer-reviewed papers and additional (numbers not reported) related articles and reports included. Findings on trends and drivers were categorised under primary headings of ageing, which partly (but not wholly) explain growth in demand; loneliness and lack of social support; mainstreaming of psychiatric care and frequent attenders; organisation of services, access to primary care and co-payments; health promotion and health awareness; convenience and appropriateness of use; and risk aversion. Concluded factors associated with rising demand for ED services dependent on complex inter-related factors, including demographics, socioeconomic factors and community expectations |
| He, 201115 | Review article utilising multiple database searches and journal searching (Australian-based titles). Articles published between 1990 and 2011 | Attendances at ED, any setting. Paediatric attendances excluded | To identify factors affecting demand for ED care and describe the inter-relationships between these factors | A total of 100 papers and reports included. Utilised a conceptual framework to map the relationships between factors. Factors categorised as those describing patient health needs (chronic disease, acute illness, injury, drug/alcohol dependence); those predisposing patients to seek help (perceptions of severity, ability to self-manage, convenience, expected quality, population growth and ageing, seasonal influences); and policy factors (health insurance/payment, hospital number and size, availability of other services, geography – urban/rural). Review identified and mapped multiple inter-related factors affecting demand but no evidence on relative contribution of each factor |
| Lowthian, 201116 | Review article utilising Ovid MEDLINE and PubMed database searches supplemented by web-based Google and Google Scholar (Google Inc., Mountain View, CA, USA) searches and article reference list searches. Searches conducted for years 1996–2009 | Emergency ambulance calls in developed countries | To review the literature on trends in utilisation of emergency ambulances and identify the major potential drivers perceived to be contributing to increases in utilisation | A total of 45 papers and reports included. Descriptions of growth in the UK, USA, Canada, New Zealand and Australia that were in excess of population growth. Some association with ageing, with reported higher utilisation in > 65 years and incrementally increasing with age, and likely to be associated with increasing chronic illness and declining cognitive function. One Australian study showed age-related factor only accounted for 25% of increased demand. Other potential factors include decreased social support and increasing numbers living alone, insurance coverage, accessibility of primary care and increased patient expectations and health awareness. Most ambulance-based literature described ambulance activity and volumes with little examination of possible associations between rise in utilisation and patient, community or health-system factors |
| Gruneir, 201117 | Systematic review and narrative synthesis of published articles up to 2008 (start date not specified) Identified from electronic databases and searching reference lists | Older adults using ED, any setting. ‘Older’ not defined | Review of literature on trends, appropriateness and consequences of ED use by older adults. Looked at nursing home residents as a subpopulation | A total of 55 articles included. Consistent findings on greater and disproportionate use of EDs by older people, regardless of country or health-care system. Attendances spike at > 75 years and > 85 years. Reason for visits predominantly medical and injury from falls. Also associations with self-care problems, decreased functioning and lack of social support. Older adults have higher acuity of illness than younger ones, spend longer in EDs and have more diagnostic tests and more admissions. These increase with age, suggesting that visits are appropriate. Needs are complex; there is a lack of research on individual-level risk factors and a lack of population-based studies to support this research |
| Author, year, country | Study design | Population/setting | Purpose | Main findings |
|---|---|---|---|---|
| Leonard, 2014,18 Australia | Retrospective analysis of routine data | All ED presentations in Greater Sydney from January 2001 to December 2011 | To describe trends in population-based rates of ED presentation in the elderly. Measured age-specific rates for groups < 65 years, 65–79 years and ≥ 80 years | 11 million presentations included. 1.8% annual increase per 1000 population. Compared with the < 65 years group, adjusted incidence ratio was 1.6 times higher for the 65–79 years group (95% CI 1.4 to 1.8; p < 0.001) and 3.6 times higher for the ≥ 80 years group (95% CI 2.8 to 4.7; p < 0.001). For patients aged ≥ 80 years there were 40 patients per 1000 population more admissions compared with those aged < 65 years (β = 40, 95% CI 29 to 52; p < 0.001). The rate of increase in ED presentations in the group aged ≥ 80 years is disproportionate to population changes and higher admission rates |
| Pines, 2013,19 USA | Retrospective analysis of National Hospital Ambulatory Medical Care Survey | Patients 65 years or older attending EDs and recorded in survey, 2001–9 | To describe trends in use of ED by older adults, reasons for visits, resource use and care quality | Over an 8-year period, ED visits increased from 15.9 to 19.8 million (24% increase). Reasons for visits unchanged (main reasons chest pain, dyspnoea and abdominal pain). Resource use of investigations increased dramatically. The proportion seen in the ED, discharged and later admitted increased from 2% to 4.2%. If no changes to primary care, acute hospital facilities will need to plan for greater demand |
| FitzGerald, 2012,20 Australia | Time-trend analysis of ED presentations and population-utilisation rates over the 10-year period from 2000/1 to 2009/10 | Attendances at all public hospital EDs in all eight states and territories in Australia | To describe trends in ED use and population utilisation rates nationally and for individual states. Measured ED attendances ED utilisation rate per 1000 population |
Total growth in ED demand was 37% over the 10 years, with average growth of 3.6% per annum. Growth varied by state (range 14–73%). Some of this may be owing to reporting changes Trends varied, with a linear pattern in five areas, non-linear in two and no change in one. ED utilisation rates also varied between areas, from 38% lower in 2001 than in 2010 within one area to unchanged in three areas. Fluctuations in presentations during the 10 years Changes in ED presentations may be owing to population growth, but utilisation growth was greater than population growth. May be urban vs. rural differences, which cannot be detected from current data. Ageing population may have an effect, but this pattern was not consistent between areas |
| Lowthian, 2012,21 Australia | Retrospective analysis of routine public hospital data | All ED presentations in Metropolitan Melbourne from 1999/2000 to 2008/9 | To measure 10-year trends in volume and age-specific rates of ED presentations, population utilisation and ED LOS | Average annual 36% rise in rate of presentation after adjusting for population changes (95% CI 3.5 to 3.8). Almost 40% patients in ED for ≥ 4 hours in 2008/9 increasing for the acutely unwell. Patients aged ≥ 85 years were 3.9 times more likely to present than those aged 35–59 years (95% CI 3.8 to 4.0) and volume of older people doubled over a decade, more likely to arrive by ambulance more acutely unwell, 75% have ED stay ≥ 4 hours and 61% require admission vs. 35–59 years group. Presentation rates beyond those expected from demographic changes. Current models of emergency and community care do not meet needs for acute illness. The 4-hour targets were probably unachievable without whole-system redesign |
| Lowthian, 2011,22 Australia | Retrospective population-based analysis of routine ambulance data | All ambulance transports in Ambulance Victoria from 1994/5 to 2000/8 | To measure growth in ambulance use and the impact of population growth and ageing. Measured ambulance transportations and population utilisation rates for different age groups. Modelled future demand | Crude annual transports increased from 32 to 58 per 1000 people and by 75% (95% CI 62 to 89) over the 14 years. Represents average annual growth rate of 4.8% (95% CI 4.3% to 5.3%) beyond that explained by demographic changes. Patients aged ≥ 85 years were transported eight times more frequently than those aged 45–69 years. Forecast models suggest that the number of transports will increase by 46–69% from 2007/7 to 2014/15. Emergency ambulance use has risen dramatically beyond that expected by demographic changes. Increases were across all age groups, but more for older patients and likely to continue to increase |
| Chu, 2009,23 Australia | Retrospective ecological study of ED attendances from 2002 to 6 compared for two age groups: 14–65 years of age and > 65 years | All attenders at a major adult inner-city ED | To describe trends in ED use. Number of attendances Number in each category of the ATS Number of admissions Total ED time Access block (proportion of patients requiring admission, with total ED time ≥ 8 hours |
ED attendances increased by 7.7% over the 5 years. ED attendances in the age group > 65 years fell by 3.3%, whereas in the < 65 years group ED attendances increased by 9%. In both groups, ATS 5 (least serious) fell (–48.9%, > 65 years; –35.8%, < 65 years), ATS 1 and 2 decreased in the > 65 years group (–15.3%), but increased in the < 65 years group (16.1%), and ATS 3 and 4 increased in both groups. Percentage admitted fell in both groups, but higher rate in > 65 years group. Median ED time was higher in > 65 years group for admitted and discharged patients and increased overall for all patients. Access block increased from 7.7% to 33.3% over the 5 years Fall in attendances by the > 65 years group was unexpected. This reduction may be explained by population profile and change to aged care service. Increased demand by older people may not be uniform and local trends and population mix need to be considered for planning |
| Moll van Charante, 2007,24 the Netherlands | Prospective cross-sectional population study at two 4-month periods in 1997/8 and 2002/3 | All patient contacts with one GP co-operative and three EDs for a population of 62,000 | To assess OOH demand for GP and emergency care and referral patterns to ED by GP co-operatives and ambulance services | GPs managed 88% of OOH contacts and 12% of ED visits (275/1000 inhabitants vs. 38/1000 per year). A total of 43% of ED attendances were self-referrals, comprising 5% of all OOH contacts. ED self-referrals were predominantly young men with injuries. Patients taken to ED by ambulance or referred by GP were older and more likely to be admitted to hospital (p > 0.01). Most OOH urgent care needs were managed by GPs. GPs and ambulance services appropriately select patients who need ED care |
| Margolis, 2002,25 the United Arab Emirates | Retrospective cross-sectional survey of attendances abstracted from ED registers | Patients aged 65 years or older who visited ED in one hospital, 1989–9 | To describe change in ED use by the elderly in a major hospital ED | Visits increased from 321 to 1347 over 10 years. The mean age of patients aged 72.9 years did not change, but elderly attendances increased (3% to 5%; p < 0.001). The mean number of visits per person per year rose from 1.8 to 3.3 (p < 0.001). Acuity did not change, non-urgent attendances increased from 14% to 39% (p < 0.001), with a corresponding increase of dispositions to primary care |
| Author, year, country | Study design | Population/setting | Purpose | Main findings |
|---|---|---|---|---|
| Amiel, 2014,26 UK | Survey using self-completed patient questionnaires | Patients presenting to open-access urgent care centre attached to ED providing urgent care and normal GP services without appointment | To explore why patients with minor illness choose to attend an urban urgent care centre for their health-care needs | A total of 649 participants with a median age of 29 years. 72% were registered with a GP; more women (59%) attended than men. The majority of participants rated themselves as healthy (81%). Access to care (58%) and expectation of receiving prescription medication (69%) were main reasons for attending ED. GP dissatisfaction influenced 10% of participants decision to attend an urgent care centre. 68% did not contact their GP in the previous 24 hours before attending. Young adults mostly registered with a GP used urgent care centres because of convenience and ease of access rather than satisfaction levels with their GP |
| Booker, 2014,27 UK | Qualitative study using semistructured interviews and thematic analysis | Ambulance: patients and carers who had called an ambulance for a primary care-appropriate problem. Selected by research clinician in ambulance (n = 16) | To explore and understand patient and carer decision-making around calling an ambulance for primary care-appropriate health problems | The primary theme was patient and carer anxiety in urgent care decision-making, and four subthemes were: (1) perceptions of ambulance-based urgent care; (2) contrasting perceptions of community-based urgent care; (3) influence of previous urgent care experiences in decision-making; and (4) interpersonal factors in lay assessment, management of medical risk and subsequent decision-making Many calls are based on misconceptions about the types of treatment other urgent care avenues can provide |
| Lobachova, 2014,28 USA | Quantitative. Cross-sectional survey via questionnaire of patients and simultaneous web-based survey of PCPs | Patients presenting to all areas of ED (n = 1062). Survey of PCPs who were also responsible for care of patients who presented at ED (n = 275) | To measure the distribution and frequency of the stated reasons why patients choose the ED for care and why PCPs think their patients utilise the ED | The most common reason for which patients came to the ED was belief that their problem was serious (61%), followed by being referred (35%). In addition, 48% came at the advice of a provider, family member or friend. By self-report, 354 (33%) patients attempted to reach their primary care physicians and 306 (86%) of them were successful. PCP survey showed that PCPs believed the most common reasons patients attended ED was that the patient chose to go on their own (80%) and patients felt that they were too sick to be seen in the PCP’s office (80%) |
| Shaw, 2013,29 USA | Qualitative research through study using semistructured interviews conducted at discharge | Locally residing patients attending ED who were subsequently triaged to a ‘non-urgent area’ for treatment (n = 30) | To explore patients reasons for visit to ED, knowledge of other non-urgent options, patient satisfaction | A total of 7 out of 30 patients had no knowledge of alternative primary care options. A total of 23 out of 30 patients attended for the following six reasons: (1) instructed by a medical professional; (2) facing access barriers to their regular source of care; (3) perceiving racial issues with a primary care option; (4) defining their health-care need as an emergency that required ED services; (5) facing transportation barriers to other primary care options; and (6) factoring in costs to use other primary care options vs. the ED |
| Schumacher, 2013,30 USA | Observational, cross-sectional study design | Emergency department: adults ≥ 18 years of age presenting to an ED at an academic medical centre in an urban community | To examine the relationship between health literacy, access to primary care and reasons for ED use among adults presenting for emergency care | After adjusting for sociodemographic and health status, those with limited health literacy reported fewer doctor’s office visits (OR 0.6, 95% CI 0.4 to 1.0), greater ED use (OR 1.6, 95% CI 1.0 to 2.4) and had more potentially preventable hospital admissions (OR 1.7, 95% CI 1.0 to 2.7) than those with adequate health literacy. After further controlling for insurance and employment status, fewer doctor’s office visits remained significantly associated with patient health |
| Toloo, 2013,31 Australia | Quantitative, cross sectional survey by questionnaire while patients were waiting for or under treatment | Patients presenting at ED via ambulance or self-transport (n = 911; 223 by ambulance, 619 by own/public transport and 69 by police/other/not answered) | To describe patient views of perceived illness severity, attitudes towards ambulance, and reasons for using ambulance | Likelihood of using an ambulance increased by 26% for every unit increase in perceived seriousness. Patients who had not used an ambulance in the 6 months prior to the survey were 66% less likely to arrive by ambulance. Patients who had presented via ambulance stated that they considered the urgency (87%) or severity (84%) of their conditions as reasons for calling the ambulance. Other reasons included requiring special care (76%), getting higher priority at the ED (34%), not having a car (34%) and financial concerns (17%) |
| Agarwal, 2012,32 UK | Qualitative interviews with researcher | Purposeful sample of patients and their carers attending the ED and urgent care centre at a university hospital (n = 23) | To explore the reasons for attendance at the ED by patients who could have been managed in an alternative service and the rate of acute admissions to one acute hospital | Four main themes emerged from the interviews that are pertinent to patients’ decisions to attend the ED: (1) anxiety about their health and the reassurance arising from familiarity with knowledge of the emergency service; (2) issues surrounding access to general practice; (3) perceptions of the efficacy of the service; and (4) lack of alternative approaches to care. These factors are important predictors of ED attendance rates |
| Becker, 2012,33 South Africa | Qualitative questionnaire conducted by ED staff | Patients presenting to ED who were subsequently triaged as ‘green’ by the South African Triage Score (n = 277) | To determine the patient-specific reasons for accessing the hospital ED with primary health care problems | Of the cases, 88.2% were self-referred and 30.2% had complaints persisting for more than 1 month. Only 4.7% of self-referred green cases were appropriate for the ED. The three most common reasons for attending the ED were that the clinic medicine was not helping (27.5%), a perception that the treatment at the hospital is superior (23.7%) and that there was no primary health service after hours (22%). Strict referral guidelines are needed and better methods of channelling primary health-care patients to the appropriate level of care are needed |
| Fieldston, 2012,34 USA | Focus groups with 25 guardians and 42 health professionals participated | Emergency department: non-urgent, paediatric. Guardians of children, primary care practitioners and paediatric emergency medicine physicians | To determine and to describe guardians’ and health professionals opinions on reasons for non-urgent paediatric ED visits | Guardians focused on perceived illness severity of their child and the needs for diagnostic and other interventions, alongside accessibility and availability at times of day that worked for them Professionals focused on systems issues, concerning availability of appointments, as well as parents’ lack of knowledge of medical conditions and knowledge of when ED use is appropriate |
| Gomide, 2012,35 Brazil | Qualitative interviews | New patients presenting to the ED who were aged 18 years or over (n = 23) | To identify reasons why users turn to emergency care services in situations that are not characterised as urgent or emergencies | A total of 23 users were interviewed; 13 were female and the mean age was 40 years. Reasons why patients choose emergency care: difficult to get immediate care at other services; limited opening hours for primary care services and most patients work during primary care opening hours; and patients feel that EDs have greater amount of diagnostics |
| Marco, 2012,36 USA | Prospective study. Structured interview questions | Adult patients attending ED in an urban university hospital (n = 292) | To identify factors that influence patients’ decisions to seek care in ED and assess their access to primary care | Most participants had a PCP 73% (n = 4214) and a minority had called their PCP about their current problem. Most participants came to the ED because of convenience/location or preference for this institution. Participants came to the ED, rather than their regular doctor, because they had no PCP, an emergency condition or communication challenges. Convenience, location, institutional preference and access to other physicians were the most common factors influencing patients’ decisions to attend the ED |
| Müller, 2012,37 Switzerland | Self-administered, paper-based questionnaire | Walk-in patients presenting to the ED during the hours in which GPs were also open (n = 200) | To investigate why walk-in patients use a university ED during GP office hours | Most walk-in patients (82%) were registered with a GP. 39% of patients visited the ED because they had reported greater confidence in the hospital ED. Most patients stated that they preferred the hospital to their GP in any kind of emergency and the majority defined an emergency as either a condition requiring rapid attention or a life-threatening situation (53%) |
| Penson, 2012,38 UK | Patient questionnaire and subsequent notes review | Emergency department: patients aged 14 years and over presenting to the ED of an urban hospital (n = 285) | To estimate the potential of alternative providers of care for minor health problems to reduce demands on EDs | The notes review confirmed that more than two-thirds of the presenting conditions could have been managed in settings other than ED. Attendees’ reasons on the questionnaire indicated a strong belief that the only provider able to deal with their concerns at that time was the ED. For some users, ED was not the first contact with a health-care provider for the same health problem. Few believed that they would be seen quicker in the ED or that the ED was more convenient. The most frequent reason for presenting to the ED was ‘being advised to attend by someone else’. The ‘adviser’ was often a health professional (doctor or nurse or NHS Direct) rather than ‘friends or family’ |
| Wilkin, 2012,39 USA | Qualitative interviews in community forum groups moderated by researcher | Adults (aged ≥ 18 years) within a defined geographical area and previous 911 users (n = 52) | What factors influence residents’ decisions to use emergency vs. primary care? | Participants had a wide variety of health-care experiences The findings revealed unique barriers to primary care related to both medical literacy and class disparities. Residents were not always able to evaluate which health symptoms necessitated emergency care Barriers such as transportation, scheduling, ability to afford health-care costs, and patients’ attitudes towards available primary health-care options might prevent people from changing their health-care-seeking behaviours |
| Nelson, 2011,40 Scotland, UK | Qualitative telephone interviews using structured questionnaires | Emergency department: patients attending ED with ‘standard, non-urgent’ conditions (n = 27) | To understand patients’ perceptions of the urgency of their condition and how this influences their decision to attend EDs | A total of 85% of patients attended with injury and pain as main reason for attending. A total of 37% of patients felt they needed radiography (15% referred by GP, 7% advised by GP receptionist and 4% unable to obtain GP appointment). A total of 52% of patients attended because of health-care professionals and friends/family advising them to attend ED A total of 48% said condition was urgent, 52% said non-urgent. No patients rated their own condition as very urgent. A total of 37% of patients had made contact with a primary health-care provider before attending and 67% said they would attend again if problem was urgent (22% because it is open 24/7 and no appointment needed) |
| McGuigan, 2010,41 UK | Semistructured telephone interviews of a purposeful sample of patients | Self-referring patients aged over 16 years who presented to ED triaged as non-urgent (n = 196) | To discover factors influencing patients’ reasons for attending the ED for non-urgent treatment | Most patients in sample thought that their conditions required urgent attention The largest proportion of patients presented with soft tissue injuries or haematomas Females attended because of other people’s advice more than males. Family and friends rather than health-care professionals were most common source of advice |
| Oetjen, 2010,42 USA | Qualitative survey questionnaire | Emergency department: insured patients presenting to four ED departments within a single state (n = 438) | To understand why insured patients use EDs rather than more appropriate medical alternatives available to reduce the strain they are placing on this critical portal of entry | Patients can be grouped into proactive, reactive and reluctant ED users, the majority of patients being reactive Most patients (83%) had a PCP. There was no correlation between ED use and whether or not patients had a PCP. A total of 39% of patients did not contact a PCP before attending ED A variety of factors were identified as to why patients may choose to attend ED and choose a particular ED including: PCP being busy, PCP referral, OOH referral, patient perception of condition being serious, ED more convenient, friend’s recommendation, quality, location and staff |
| Adamson, 2009,43 UK | Mixed-method study (cross-sectional questionnaire survey and semistructured interviews) | Patients selected randomly from a single GP list (n = 911 survey; n = 22 interviews) | To quantify the prevalence of opinion on whether or not people use health services unnecessarily within primary care and A&E in order to examine the impact of these views on help-seeking behaviour | Survey data suggest that most people believe individuals use either GP or A&E services inappropriately (66%). Strong views relating to inappropriate health care use were not associated with reported seeking of immediate care. Responders tend to consider other people as time wasters, but not themselves. Individuals’ generally describe clear rationales for help seeking, even for seemingly trivial symptoms, and anxiety level was strongly predictive of health-seeking behaviour The findings suggest that people do not take the decision to consult health services lightly and rationalise why their behaviour is not time wasting |
| Scott, 2009,44 USA | Cross-sectional questionnaire survey of patients seeking care at an urgent care clinic within a large acute care safety net urban hospital | Urgent care clinic: patients presenting to an urgent care clinic (n = 1006) | To determine the motivation behind, and characteristics of, adult patients who choose to access health care in an urgent care clinic | A total of 54% of patients reported choosing the UCC because of not having to make an appointment, 51% because it was convenient, 44% because of same-day test results, 43% because of ability to get same-day medications and 15% because co-payment was not mandatory. A total of 68% of patients did not have a regular physician and 57% lacked a regular source of care. This study suggests that patients choose the urgent care setting based largely on convenience and more timely care |
| Benger, 2008,45 UK | Qualitative, semistructured questionnaire | Adult patients admitted to inner-city hospital after either ED or GP attendance (n = 200) | To determine the route by which patients with acute illness are admitted to hospital, the reasons and outcomes for the actions taken and the extent to which these may contribute to increased ED attendances and hospital admissions | Direct attendance at the ED was more common when help was sought by bystanders or persons known only slightly to the patient. Most patients who attended the ED directly did so as a result of the perceived severity or urgency of their condition and there was incomplete awareness of the OOH GP service. The majority of older patients who are admitted to hospital with an acute illness seek professional help from primary care in the first instance, whereas younger people contacted OOH or other services. OOH patients tended to attend ED more often than primary care patients |
| Jacob, 2008,46 USA | Survey. Convenience sample of ED patients | Emergency department: paediatric and adult patients presenting to the ED (n = 311) | To define the characteristics of ED patients who used ambulance transport compared with non-ambulance users and to determine reasons for ambulance use | Users (n = 71, 22.8%) were older than non-users, and were sicker according to self-rated illness severity, higher nurse triage score and higher admission rate. Patient decision regarding ambulance use was associated with both having someone who called an ambulance for them and self-estimation of illness severity (or lack thereof). Physicians agreed with transport method in 68% of users and 92% of non-users |
| Redstone, 2008,47 USA | A 31-item, cross-sectional, self-administered, anonymous survey | Patients over the age of 18 years with a primary care physician presenting to the ED who were subsequently triaged as non-urgent (n = 240) | To investigate why patients with minor problems and a PCP present to the ED. Results compared those attending in WDD and NWDD | There were high levels of self-perceived urgency for treatment; a strong majority felt they could not wait 1–2 days for treatment. More WDD patients felt their case was too difficult for the PCP to handle as opposed to NWDD patients. Around 24% of patients in both groups felt they needed to be admitted to hospital A total of 70% of WDD patients were willing to contact their PCP, despite 45% feeling their condition was too complex for their PCP; 45% did not contact PCP at all A total of 60% of patients across both groups felt the ED was more convenient than their PCP |
| Hodgins, 2007,48 Canada | Descriptive correlational study | Emergency department: low-urgency patients (n = 1612) | To what extent can patients’ responses to less urgent health problems be predicted using Andersen’s criteria (predisposing, enabling, need determinants) and do these characteristics differ based on the place (geographic location) in which health care is sought? | Differences were observed in the percentage of participants presenting at urban and rural EDs by type of health problem The two items with the highest mean scores reflected participants’ perceptions of need (severity of symptoms and concern problem will get worse), while the next two items dealt with characteristics of the context within which health care was sought (no other option and availability of family physician). The next three highest rankings were, convenience of service, needed service only available at ED and advice from family or friends |
| Norredam, 2007,49 Denmark | Quantitative, questionnaire survey of walk-in patients and care providers at four Copenhagen EDs | General ED (n = 4); migrant and national citizen usage of ED (n = 3426). Response rate 54% | To investigate the extent to which immigrants and patients of Danish origin have different motivations for seeking emergency room treatment, and differences in the relevance of their claims | Groups of foreign origin are more likely to consider contacting primary care providers before attending ED. A higher number of immigrants were unable to access primary care and immigrant ED attendance was often caused by not being able to access primary care. In contrast, more national patients claimed that the ED was more relevant for their needs. Patients from non-western or middle eastern origin were significantly more likely to attend ED because they did not live locally and could not access their normal primary care giver. Care providers reported that 21% of all ED attendances were not relevant to ED, a significantly higher proportion of non-western or middle eastern patients had irrelevant ED visits and irrelevant ED attendance was significantly related to not being able to access primary care |
| Campbell, 2006,50 Scotland, UK | Four focus groups and 51 in-depth interviews with 78 participants | Patients aged between 45 and 64 years in eight urban and rural general practices in north-east and south-west Scotland | To explore if, and how, patients’ consulting intentions take account of their perceptions of health-service provision | Anticipated waiting times for appointments affected consulting intentions, especially when the severity of symptoms was uncertain. Strategies were used to deal with this. In cities, these included booking early just in case, being assertive, demanding visits, or calling out of hours but in rural areas, participants used relationships with primary care staff, and believed that being perceived as undemanding was advantageous. OOH decisions to consult were influenced by opinions regarding OOH services. Some preferred to attend nearby EDs or call 999. In rural areas, participants tended to delay until their own doctor was available or might contact them even when not on call |
| Worth, 2006,51 Scotland, UK | Qualitative, community-based study using 36 in-depth interviews and eight focus groups with patients and/or their carers and 50 telephone interviews with patient’s GP and other key professionals | Urban, semi-urban and rural communities in three areas of Scotland. Patients with advanced cancer who had recently used OOH services | To explore the experiences and perceptions of OOH care of patients with advanced cancer, and with their informal and professional carers | Patients and carers had difficulty deciding whether or not to call OOH services because of anxiety about the legitimacy of need, reluctance to bother the doctor, and perceptions of triage as blocking access to care and OOH care as impersonal. Positive experiences related to effective planning, particularly transfer of information, and empathetic responses from staff. Professionals expressed concern about delivering good palliative care within the constraints of a generic acute service, and problems accessing other health- and social-care services |
| Palmer, 2005,52 UK | Semistructured telephone interviews of patients to discuss recent ED contact | Emergency department; patients presenting to ED triaged to 4 or 5 on the Manchester Triage Score (n = 321) | To investigate why and how patients decide to attend A&E departments, and to assess their satisfaction with the experience, in a predominantly rural west Wales population | Of the study sample, 78% attended with injury or illnesses of recent origin, and 50% with actual or presumed musculoskeletal injury, 73% of which were sustained within 10 miles of home. Travel to hospital was by private transport for 86%, average distance 7.4 miles. Most (90%) were registered with a local GP, but 32% felt A&E was the obvious choice, and a further 44% considered their GP inaccessible to their needs. Patient satisfaction was generally high. Among the 87 patients (27%) who reported a less satisfactory experience, 48 (55%) of these complained of dismissive attitudes of doctors |
| Foster, 2001,53 UK | Focus group methodology, with qualitative data analysis undertaken using a grounded theory (framework) approach | People aged between 65 and 81 years, from community groups based in south-east London (n = 30) | To explore older people’s experiences and perceptions of different models of general practice OOH services | Two related themes were identified: (1) attitudes to health and health-care professionals with reference to the use of health services prior to the establishment of the NHS, a stoical attitude towards health and not wanting to make excessive demands of health services; and (2) the experience of OOH care and perceived barriers to its use, including the use of the telephone and travelling at night. Participants preferred contact with a familiar doctor and were distrustful of telephone advice, particularly from nurses. Older people appear reluctant to make use of OOH services and are critical of the trend away from OOH care being delivered by a familiar GP |
| Coleman, 2001,54 UK | Questionnaire and review of notes | Adults presenting to ED triaged to the two lowest priority streams (n = 267) | To estimate the potential of general practice, minor injury units, walk-in centres and NHS Direct to reduce non-urgent demands on A&E departments taking into account the patient’s reasons for attending A&E | Using objective criteria, 55% of patients with non-urgent health problems who attend EDs should be treated in either general practice, a minor injury unit, a walk-in centre or by self-care after advice from NHS Direct. Nearly 25% of non-urgent patients who self-referred had previously accessed other health services for the same problem. Most patients attended, as they believed they required radiography. There are disparities between the professional view and the patient’s perceptions of the seriousness of the health problem, and expectations of care |
| Hoult, 1998,55 UK | Qualitative interviews with patients | OOH: patients calling OOH services within 2 days of a GP consultation (n = 20) | To determine the proportion of patients who call OOH within 2 days of a GP consultation and to explore the reasons for the OOH call | A total of 15% of patients who made OOH contact had had a GP appointment within the previous 2 days. Two out of three of the calls were related to the initial problem, but with no evidence of patient dissatisfaction. Less than one-quarter of calls were for ongoing medical conditions, and one-quarter were about medication prescribed at the first consultation. One-third of patients had mental health problems. Many patients were high users of other services, including A&E and private medicine. Some patients called with specific queries or to develop better understanding of illness |
| Shipman, 1997,56 UK | Quantitative data collection on demographics and nature of complaints. Telephone surveys with 82 people who attended ED | Patients presenting to OOH services in a large capital city. Data from GP (OOH) and ED (n = 2564) | To examine differential use of OOH general practice and ED use and to describe differences in service users | There are differences in age-related demand and presenting complaints for each service. Children constitute a great proportion of all OOHs contact and more families with children under 10 years presented to GP services More digestive, respiratory, viral/non-specific complaints presented to GP, whereas musculoskeletal problems accounted for the largest category of ED presenting problems. Usage relating to perceived and actual ability of services appeared interchangeable between sites. A collaborative method approach is required to respond to and influence demand |
Summary of findings
This review has been conducted to provide a brief overview and context for the subsequent more detailed reviews. We have therefore only identified key themes that have emerged from the available evidence.
Trends and characteristics of demand for emergency and urgent care
We identified four review articles and eight primary studies that explored trends in demand and associated characteristics. One review17 and two primary studies19,25 only considered older populations. Two studies16,22 investigated emergency ambulance utilisation, seven focused on ED attendances and one24 on ED and GP out-of-hours (OOH) attendances. The key common themes that emerged were:
-
The trend of increasing, year-on-year demand for emergency and urgent care is consistent across developed countries. Population utilisation rates are also increasing and this appears to be greater for ambulance services than EDs.
-
Population and demographic changes explain some, but not all, of the increases in demand. Elderly people do utilise emergency and urgent care more frequently, particularly those aged > 80 years and are more acutely unwell, but this group accounts for only about 25% of increased demand. The impact of ageing populations may also vary by locality and the relative health and socioeconomic status of the resident elderly population.
-
Demand is likely to be influenced by a range of other characteristics and factors, including health needs (chronic conditions, acute illness, drug and alcohol dependency), socioeconomic factors (isolation and loneliness, lack of social support, deprivation), patient factors (decision-making behaviours, awareness, expectations, convenience) and policy (insurance coverage, numbers of hospitals, access to primary care, geographical differences in provision), but there has been little research examining the association between the rise in demand and these factors.
-
There have been few attempts to identify and map the different influences on demand and the relative influences of each factor to create a comprehensive profile of the different health-care needs of populations accessing emergency and urgent care to inform health-service planning.
-
There is a lack of population-based studies, identification of independent risk factors associated with accessing urgent care and whole-system (rather than individual service) demand studies. This is particularly constrained by a lack of information about urgent care within the primary care setting and modelling studies that can forecast likely future changes in demand.
Patient-based studies examining reasons for accessing emergency and urgent care
We identified 38 relevant studies from the database searches, seven of which were included in the four systematic reviews and so are not included in the summary table. Of the 31 studies we have examined in more detail, 16 were qualitative interview or focus group studies,27,29,32–36,39–42,50–53,55 12 were surveys26,28,31,37,38,44–47,49,54,56 and three used mixed designs. 30,43,48 The majority (23/31) were conducted in the ED, predominantly involving patients who presented with urgent rather than emergency conditions; two considered ambulance patients and six were in other settings, such as GP surgeries and urgent care centres. A number of frequent and common themes emerged from these studies, which concern reasons why patients used emergency or urgent care and their choice of where to access care:
-
Access to and confidence in primary care were prominent concerns. Factors identified included lack of awareness of options (particularly OOH services), dissatisfaction with GPs, limited opening hours, anticipated waiting times for appointments, previous experience using OOH services and perceived barriers. The elderly, in particular, did not like or trust telephone-based OOH services. In many studies, a high proportion of patients attending the ED were registered with GPs but still chose to access the ED instead.
-
Perceived urgency, anxiety and the value of reassurance from emergency-based services.
-
Being advised to attend the ED by family, friends or health-care professionals.
-
A belief that their condition needed the resources offered by a hospital, including hospital doctors (rather than GPs), diagnostics (particularly radiography), and treatment.
-
In some health systems, costs and transport options affected decision-making.
-
Convenience, in terms of location, not having to make an appointment and opening hours, was a factor. Older people were more likely to contact a GP first, but younger patients contacted urgent care centres, ED or OOH services, as they found this more convenient.
Conclusions
Despite serious concerns about rising demand for emergency and urgent care and the impact this has on health services, there is remarkably little empirical evidence that can fully explain why this trend in behaviour has occurred. The evidence included here has highlighted a range of factors that may influence demand, but much of the research has focused on either individual services or populations, such as the elderly. Most of the evidence presented here has come from Australia and there were no UK-based studies. However, there is scope to replicate some of the Australian studies using UK data.
The four review articles helpfully brought together a broad literature of discrete studies on individual factors that may influence demand, and there is a substantial patient-focused literature that has examined the reasons why people choose to use emergency and urgent care and how they decide which service to access. The evidence gaps and challenges identified from the existing evidence concern the need to:
-
Examine demand from a whole-system rather than single-service perspective and gain better understanding of the relative proportions of demand for different parts of the system and the characteristics of patients within each sector. This more detailed understanding would allow more accurate assumptions to be made about changing care delivery, for example what is a realistic proportion of patients who could be managed out of hospital.
-
Build on the existing knowledge about the range of factors that may be influencing demand and develop more sophisticated research studies that can comprehensively map these issues into a coherent model. The conceptual model describe in the review by He et al. 15 is a useful starting point.
-
Explore the relationships and associations between individual influences and demand so that the relative contribution each one makes can be assigned to a map or model. This would then support the development of service design and planning to meet the needs of local populations19 and the development of predictive models that can be used to estimate likely changes in population needs for emergency and urgent health care. 22
-
All of these will require the development of robust, system-wide information systems to support these complex functions.
Chapter 4 Telephone triage and advice services
Introduction
A key principle of the NHS England urgent and emergency care review is provision of a telephone-based service that can act as a gatekeeper and direct people with urgent care needs so that they can get the right advice, in the right place, at the first point of contact. 6 NHS 111 is the cornerstone to this function and already provides a free, national, 24-hour, telephone-based service to triage, assess and signpost requests for urgent health care. However, the introduction and implementation of NHS 111 has not been without problems, and the NHS England review recognises the need to substantially enhance this service in order to deliver the intended benefits within the wider urgent and emergency care system. We have reviewed the broader evidence on use of telephone-based triage and advice services for access to and management of urgent care in order to summarise the current state of knowledge and identify evidence gaps that may need to be addressed to enable further development of this key service.
Methods
The main inclusion and exclusion criteria, search strategies and review process have been described in Chapter 2. Search dates were from 1 January 1995 to 11 November 2014. For this review specific additional inclusion and exclusion criteria were as follows.
Inclusion criteria
-
Requests for emergency/urgent care.
-
Telephone triage/advice/consultations.
-
Report relevant outcomes related to:
-
efficiency (triage accuracy; waiting times; adherence/compliance; other service impacts, e.g. reduction in ED visits)
-
effectiveness (safety; unplanned health service recontacts; patient outcomes; cost)
-
patient experience (satisfaction; acceptability; appropriateness; experience; access).
-
Exclusion criteria
-
Telephone services for single conditions.
-
Telephone services for non-urgent advice.
Review process
Studies were identified from database searching and through expert knowledge of the field of interest. In addition to the studies identified through database searching, the study team were aware of 10 further studies, which were assessed for inclusion in this review. The results of the review sifting process are given in Figure 3. A randomly generated 10% sample of studies from the database searches (n = 124) was double sifted by another member of the study team. The reviewers initially agreed on inclusion or exclusion for 88% of studies and agreed to exclude the remaining 10 studies after discussion. A total of 87 papers were included in the review, representing 83 individual studies.
FIGURE 3.
A PRISMA flow diagram for telephone triage and advice services searches.
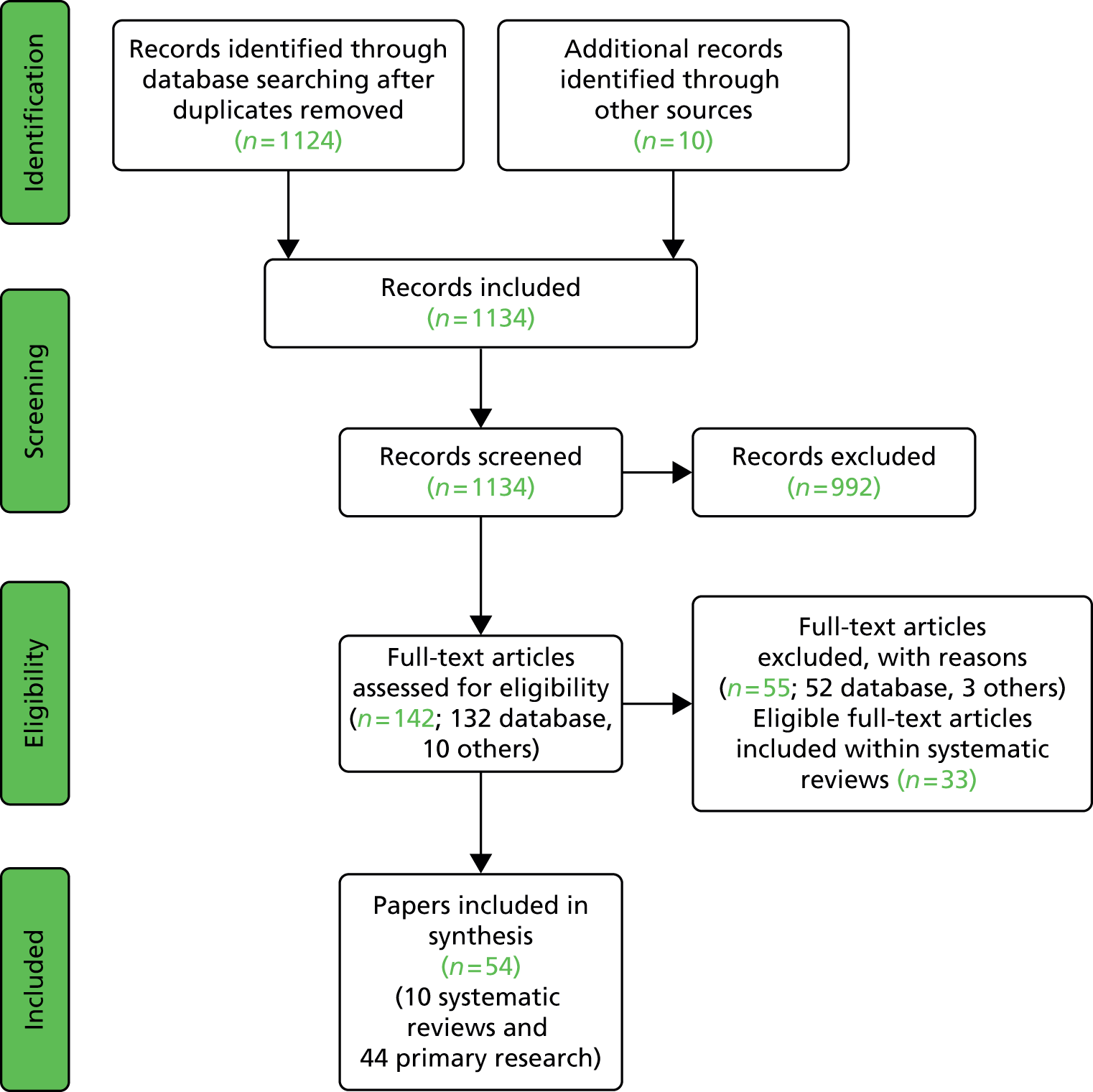
Systematic reviews included
Eighty-seven papers representing 83 studies were included in this review and of these eight57–65 were systematic reviews. The results from the eight reviews (10 papers57–65) are shown in Table 4. Many of the references included in the reviews overlapped. This overlap is shown in Table 5. Formal data extraction was not undertaken for the 33 papers66–98 meeting the inclusion criteria and included in systematic reviews, as this would have been conducted during the review process. Table 6 lists these 33 papers (32 studies66–98) and the systematic reviews in which they were included. A total of 43 studies (44 papers99–142) did not feature in any of the included systematic reviews and underwent full data extraction (Table 7).
| Identified studies | Number of studies | Number of papers |
|---|---|---|
| Systematic reviews | 8 | 10 |
| Included in systematic reviews | 32 | 33 |
| Not included in systematic reviews | 42 | 43 |
| Total | 83 | 87 |
| Author, year, country | Study design | Population/setting | Purpose | Main findings |
|---|---|---|---|---|
| Blank, 2012,57 UK | Systematic review and narrative synthesis using rapid evidence synthesis methods | In and OOH; primary and urgent; nurse (49/52 papers) | To synthesise evidence of the appropriateness of and compliance with different types of telephone triage advice | Triage decisions rated as appropriate varied between 44% and 98% and compliance ranged from 56% to 98%. Variation could not be explained by type of service or method of assessing appropriateness. Triage decisions to contact primary care may have lower compliance than decisions to contact emergency services or self-care |
| Purc-Stephenson, 2012,58 Canada | Meta-analytic review. Compares compliance rates by type of advice [attend ED; office care (GP); self-care] | In and OOH; primary and urgent; nurse | To investigate whether or not patients comply with triage advice from telenurses and to identify factors that may influence compliance | Thirteen studies were included. The overall compliance rate was 62%. Compliance by type of advice was:
|
| Carrasquiero, 2011,65 Portugal | Systematic review | In and OOH; primary and urgent care | To review telephone triage and advice service evaluation studies and compare results | A total of 55 papers were included. Key findings for each outcome:
|
| Huibers, 2011,62 the Netherlands | Systematic review of levels of urgency described in real and simulated patient studies | OOH primary and urgent; patients first request for help | To assess the research evidence on safety of telephone triage in OOH primary care | Thirteen observational studies showed that on average triage was safe in 97% (95% CI 96.5% to 97.4%) of all patients contacting OOH care and in 89% (95% CI 86.7% to 90.2%) of patients with high urgency. Ten studies that used high-risk simulated patients showed that, on average, 46% (95% CI 42.7% to 49.8%) were safe |
| Bunn, 2005,59 and Bunn, 200460 UK | Systematic review. Compares staff types and different services | In and OOH; primary and urgent; GP/nurse | To assess the effects of telephone consultation on safety, service usage and patient satisfaction | Nine studies included. Not all studies reported on each outcome. Three out of five studies reported decrease in GP visits but two out of five studies reported an increase in follow-up/return face-to-face GP appointments There was no increase in ED visits (6/7 studies), except for one study about a nurse-led telephone line |
| Chapman, 2004,63 UK | Systematic review. Compares across services and GP vs. nurse | In and OOH; primary and urgent care; GP/nurse | To review the evidence of seven recent innovations in service provision to improve access or equity in access to primary care | GP-led telephone services (five studies): decrease in demand for same-day appointments, but may increase subsequent contacts; patients view service as appropriate Nurse-led telephone services (four studies): nurses manage most OOH calls safely and effectively, with no increase in GP contact within 3 days; no difference between GP/nurse triage for 7-day mortality, hospital admissions or A&E attendances NHS Direct (one study): easily accessible, well used and high quality; high caller satisfaction rates; no less safe than other services; concern over delays in getting through/quality of self-care advice Telephone consultations (GP or nurse) can safely be substituted for face-to-face consultations, but it is not clear if this reduces face-to-face consultations over time |
| Leibowitz, 2003,61 UK | Systematic review. Compares different services and service provisions | OOH primary and urgent; nurses and physicians | To determine what evidence exists about the effect of different models of OOH primary medical care service on outcome | Results indicate that the introduction of a telephone triage and advice service for after-hours primary medical care may reduce immediate medical workload. Studies consistently showed patient dissatisfaction with telephone consultations. There was very little evidence about the advantages of one service model compared with another in relation to clinical outcome |
| Stacey, 2003,64 Canada | Systematic review. Compares across services and physician vs. nurse | In and OOH; primary and urgent care; nurse- and doctor-led services | To evaluate the effects of teletriage services on health service use, caller safety, satisfaction and health-related quality of life | Ten comparative studies met the inclusion criteria. Various delivery models were compared. Despite differences in interventions, the studies indicated that teletriage decreased immediate GP visits without increasing adverse outcomes (subsequent hospitalisations, ED visits or deaths). Half of the calls were fully managed by the teletriage service. Caller satisfaction ranged from 55% to 90% for registered nurse call centre programmes and was 70% for medical doctor teletriage. The effect of teletriage on immediate ED visits, subsequent contact with practitioners and health-related quality of life was less clear |
| Author, year | Systematic review | ||||||
|---|---|---|---|---|---|---|---|
| Blank, 201257 | Purc-Stephenson, 201258 | Leibowitz, 200361 | Bunn, 200559,60 | Huibers, 201162 | Chapman, 200463 | Stacey, 200364 | |
| Munro, 200066 | ✓ | ||||||
| Moore, 200267 | ✓ | ✓ | |||||
| Lattimer, 199868 | ✓ | ✓ | ✓ | ✓ | |||
| Gallagher, 199869 | ✓ | ||||||
| Christensen, 199870 | ✓ | ||||||
| Dale, 199771 | ✓ | ✓ | |||||
| Jackson, 199772 | ✓ | ||||||
| Giesen, 200773 | ✓ | ✓ | |||||
| Killip, 200774 | ✓ | ||||||
| Marklund, 200775 | ✓ | ✓ | |||||
| Stewart, 200676 | ✓ | ✓ | |||||
| Kempe, 200677 | ✓ | ✓ | ✓ | ||||
| St George, 200578 | ✓ | ||||||
| Bogdan, 200479 | ✓ | ✓ | |||||
| Richards, 200480 | ✓ | ||||||
| Sprivulis, 200481 | ✓ | ✓ | |||||
| Kempe, 200382 | ✓ | ✓ | |||||
| Foster, 200383 | ✓ | ||||||
| Belman, 200284 | ✓ | ||||||
| O’Connell, 200285 | ✓ | ✓ | |||||
| Jiwa, 200286 | ✓ | ✓ | |||||
| Kempe, 200187 | ✓ | ✓ | |||||
| Frisbee, 200188 | ✓ | ✓ | |||||
| Derkx, 200889 | ✓ | ||||||
| Hirsh, 200790 | ✓ | ✓ | |||||
| Labarère, 200391 | ✓ | ✓ | |||||
| Dale, 200492 | ✓ | ✓ | |||||
| Lee, 200393 and Lee, 200294 | ✓ | ✓ | ✓ | ||||
| McKinstry, 200295 | ✓ | ✓ | ✓ | ||||
| De Coster, 201096 | ✓ | ✓ | |||||
| Giesen, 200797 | ✓ | ||||||
| Thompson, 199998 | ✓ | ||||||
| Author, year, country | Study design | Population/setting | Purpose | Main findings |
|---|---|---|---|---|
| EMS-based studies | ||||
| Palma, 2014,104 Italy | Retrospective qualitative analysis of EMS telephone calls. Compares green-black calls with other calls | EMS; nurse | To analyse factors associated with registered nurse under-triage of EMS calls subsequently found to be associated with deaths (green-black code cases) | Characteristics associated with green-black calls: older patient (> 80 years); callers were individuals calling on behalf of patients, rather than patients themselves; callers reported non-life-threatening symptoms; nurse operators did not always ask about vital signs as required by the Medical Priority Dispatch System protocol; telephone conversations were shorter (54.26 seconds vs. 65 seconds) |
| Infinger, 2013,102 USA | Retrospective review of routine data and follow-up | Low-urgency ambulance | To analyse the impact of implementing transfer to an advice line nurse for low-acuity patients | A total of 329 (20%) patients were transferred to an advice line nurse and 204 (12%) received no ambulance response. A total of 118 of the patients who were not transported by ambulance (58%) completed telephone follow-up, 88% of whom reported that the non-transport option met their health-care needs. A total of 92% of the responders would accept the transfer again |
| Studnek, 2012,100 USA | Two-phased retrospective study with nurse telephone advice available in second phase. Compares telephone nurse vs. standard care | Low-urgency ambulance; nurse | To determine whether or not secondary telephone triage by a nurse was associated with subsequent hospital admission | In phase 2, 49% of eligible patients completed secondary triage by an advice line. Of these, 71% required immediate care and delayed care was appropriate for 29%. Those classified as requiring immediate care were more likely to be admitted to hospital than those classified as appropriate for delayed care (29% vs. 16%; p < 0.01). One patient classified for delayed care required an ICU admission. From the first phase (no telephone nurse), 25% of patients classified as requiring delayed care were admitted to hospital. In the second phase, a subset of patients was identified as requiring delayed care and these had a significantly lower frequency of hospital admission |
| Turner, 2006,101 UK | RCT and postal questionnaire. Compares telephone advice vs. standard care | Low-urgency ambulance | To assess the costs and benefits of transferring low-priority 999 calls to NHS Direct for further assessment and advice | The return rate to the ambulance service was 66.9% (range 36.1–75.5%). Of returned calls, 25% were returned for a 999 response and the remainder for transport or other non-clinical reasons. Callers were generally satisfied with the service |
| Dale, 2003,99 UK | Pragmatic controlled trial. Compares nurse telephone advice vs. standard response | 999 callers with urgent care problems; nurse/paramedic | To investigate the potential impact of providing telephone advice for low-urgency ambulance service callers | Nurses were more likely than paramedics to triage calls as not requiring an ambulance (OR 1.28, 95% CI 1.12 to 1.47). Of the 330 (52%) callers triaged as not requiring an emergency ambulance, 119 (37%) did not attend ED, whereas 55 (18%) of those triaged by a nurse/paramedic as requiring an ambulance did not attend ED (OR 2.62, 95% CI 1.78 to 3.85). A total of 9% of those triaged as not requiring an emergency ambulance were admitted to a hospital bed |
| Smith, 2001,103 USA | Two-phase prospective study. Compares nurse telephone advice vs. ambulance response | In- and OOH non-emergency 911; nurse | To examine the effects of transferring non-urgent 911 calls to a telephone consulting nurse | There were no adverse outcomes detected. Patients were satisfied with the outcome in 96% of the cases. Transferring 911 calls to a nurse line resulted in fewer basic life support responses |
| NHS 111-based studies | ||||
| Knowles, 2014,107 UK | Telephone survey (multiple sites) | In- and OOH urgent care; non-clinical | To identify any inequity in awareness or use of telephone-accessed health care | A total of 59% of respondents had heard of NHS 111 and 9% reported ever using NHS 111. Respondents were less likely to have used NHS 111 if they were older (p ≤ 0.001), male (p ≤ 0.001) and did not have a disability/limiting long-term illness (p ≤ 0.001) or own their home (p = 0.039) |
| O’Cathain, 2014,106 UK | Cross-sectional population survey | In- and OOH urgent care; non-clinical | To explore the user-acceptability of NHS 111 | A total of 41% of 4265 people responded. Over 90% said the advice was helpful or quite helpful. A total of 86% of people complied with the advice and 95% were satisfied. Users were less satisfied with the relevance of questions asked and the accuracy and appropriateness of advice given. Users who were auto-routed to NHS 111 from services such as GP OOH services were less satisfied than direct callers |
| Turner, 2013,105 UK | Controlled before-and-after study using routine data | In- and OOH urgent care; non-clinical | To measure the impact of the urgent care NHS 111 on the emergency and urgent care system | There was no change overall in emergency ambulance calls, ED attendances or urgent care use. Calls to NHS Direct reduced by 19.3% (95% CI −24.6% to −14%) and emergency ambulance incidents increased by 2.9% (95% CI 1.0% to 4.8%). Overall, emergency and urgent care system activity increased in each site, ranging from 4.7% to 12% per month; this remained when assuming that NHS 111 will eventually take all NHSD and GP OOH calls |
| Cost studies | ||||
| Navratil-Strawn, 2014,111 USA | Economic analysis. Compares compliance vs. non-compliance cost | 24-hour nurse telephone helpline | To identify whether or not compliance with nurse advice was associated with lower expenditure | Overall, 57% of callers were compliant with nurse recommendations. The average expenditures were US$328 lower among compliant callers |
| Lambert 2013,108 UK | Cost-minimisation study. Compares NHSD advice vs. patient-stated first alternative had NHSD not been available | In- and OOH emergency and urgent care; nurse; NHSD | To determine financial and quality-of-life impact of patients calling NHSD | An average per patient saving of £19.55 (36%) compared with patient-stated first alternatives, representing an annual cost saving of £97,756,013. Self-classified ‘urgent’ cases made significantly greater health gains than those who said they were ‘non-urgent’ (urgent by 21.5 points; non-urgent by 16.1 points) |
| Morimura, 2011,112 Japan | Before-and-after study using routine data. Compares ambulance use and cost before and after introduction of telephone line | Ambulance service callers; 24/7 nurse-run telephone advice line | To assess if a new telephone advice centre service reduced ambulance use in non-urgent cases and decreased ambulance costs | Compared with the previous year, the number of ambulance uses per 1 million people decreased (46,846 vs. 44,689; p < 0.0001). The emergency hospitalisation rate of ambulance cases increased significantly because of the decreased proportion of non-urgent cases (36.5%, vs. 37.8%; p < 0.0001). The total cost related to despatching ambulances was reduced by approximately £4,520,000 |
| Cariello, 2003,110 USA | Cost evaluative. Compares cost of original intentions with actions after the call | In- and OOH emergency and urgent care; nurse | This study evaluates service quality and cost of a nationally recognised nurse telephone helpline | Most callers rated the level of service quality very highly. The overall rating of service quality, measured by the total score on the SERVQUAL instrument, was a mean of 6.42/7. The action taken by the caller after the call resulted in cost savings (38.6% reduction in cost) |
| O’Connell, 2001,109 USA | Before-and-after cost analysis. Compares pre- and post-service introduction | In- and OOH urgent care; nurse | To assess patient satisfaction and a health plan’s return on investment associated with a telephone-based triage service | More than 90% of users were satisfied, and utilisation of hospital ED and physician office services decreased significantly after service implementation. Reductions in health-plan expenditures exceeded the costs of service provision. The plan’s estimated return for every dollar invested in the nurse triage service was approximately US$1.70 |
| All other studies | ||||
| Sakurai, 2014,113 Japan | Retrospective quality assessment. Compares telephone consultation advice with medical records | 24-hours nurse telephone helpline | To investigate the 7119 process by reviewing the outcome of triage in order to identify system problems | Problems identified with the telephone triage system were:
|
| Doctor, 2013,139 USA | Retrospective observational study. Expert review of telephone nurse ED referrals | OOH urgent; paediatric; nurse | To identify non-essential after hours referrals made by telephone nurses | A total of 73 out of 220 patients (33%) were classified non-essential and 67% as essential. Non-essential referrals were significantly younger (p < 0.05), had lower triage scores (p = 0.026) and shorter ED stays (p < 0.0001). The algorithms for ‘Fever – 3 months or Older’ (12.3%), ‘Vomiting without diarrhoea (8.2%) ‘Trauma – head’ (8.2%), ‘Headache’ (6.8%) and ‘Sore throat’ (5.5%) were determined most likely to result in a non-essential referral |
| Huibers, 2013,114 the Netherlands | Cross-sectional study of patients using a validated questionnaire. Compares age groups/experience | OOH nurse telephone helpline | To identify if patient/age experience of telephone consultations were associated with follow-up contact | Half of patients had a follow up contact. More probability of follow-up contacts in patients aged > 65 years (OR 2.39) or for co-operatives with high levels of telephone consultations (OR 1.02). Decreased probability for patients who had positive nurse–telephone experiences (OR 0.68) |
| Huibers, 2012,140 the Netherlands | Secondary analysis of telephone consultations by nurses at 29 centres. Compares quality of consultation vs. appropriateness of decisions | OOH nurse telephone helpline | To explore the impact of quality of consultation and estimated urgency on the appropriateness of decisions | A total of 90% of 6739 callers were non-urgent. Most decisions were appropriate (91% urgency, 96% follow-up advice, 95% timing). Higher-quality consultation was related to more appropriate estimates of urgency (OR 1.8, 95% CI 1.7 to 1.95), follow-up advice (OR 2.7, 95% CI 2.4 to 3.0) and timing (OR 2.4, 95% CI 2.2 to 2.6). High urgency was associated with suboptimal consultation quality |
| LaVela, 2012,127 USA | National cohort study (18 clinics) | In-hours primary care; staff type unknown | To understand patients’ experiences regarding telephone encounters for medically based purposes | Calling for an urgent medical issue was associated with dissatisfaction. Odds of call satisfaction were greater when patients thought staff were friendly (10 times), call answer was timely (five times) and needed medical information was provided (seven times) |
| Hansen, 2011,115 Norway | Assessment of medical scenarios compared with national guidelines | OOH nurse telephone helpline | To evaluate decisions about urgency made by nurses in OOH services in Norway | Among the acute, urgent and non-urgent scenarios, 82%, 74% and 81% were correctly classified according to national guidelines respectively |
| Ng, 2011,118 and Ng, 2012,119 Australia | Prospective observational study using chart review. Compares Health Direct referred vs. self-referred and GP referred | In- and OOH emergency and urgent care; nurse; Health Direct | To assess the appropriateness of Health Direct ED referrals | No differences in appropriateness between Health Direct-referred (72.9%) and self-referred (73.8%) patients (p = 0.72). GP-referred patients were significantly more appropriate (89.7%) than other groups (p < 0.01). Health Direct nurses used ambulance services appropriately in 97% of cases. Health Direct patients were often unwell; 25.7% required hospital admission, 37.9% required assessment by specialist inpatient teams and 67.5% required laboratory or radiological testing in the ED |
| Cook, 2010,116 UK | Expert review. Compares appropriateness of NHS 24 ED referrals reviewed by GPs and ED doctors | In- and OOH emergency and urgent care; nurse; NHS 24 | To compare different specialty doctors’ views on the appropriateness of NHS 24 referrals to ED | Agreement with ED disposal was 59.2% for ED doctors and 47% for GPs. ED doctors thought 20.8% of cases should have been referred to primary care; GPs, 35.7%. Results show GPs and ED consultants believe many NHS 24 ED referrals should be handled in primary care |
| Ernesäter, 2010,141 Sweden | Retrospective study of incident reports | In- and OOH urgent care; nurse | To conduct a retrospective study of incident reports from the national, nurse-led telephone triage system in Sweden | The 426 incident reports included 452 errors. Of the analysed incident reports, 41% concerned accessibility problems, 25% incorrect assessment, 15% routines/guidelines, 13% technical problems, 6% information and communication. Most frequent outgoing incident reports (i.e. sent from SHD to other health-care providers) concerned accessibility problems and most frequent incoming reports (i.e. sent to SHD from other providers) concerned incorrect assessment |
| Kinnersley, 2010,128 UK | Cross-survey using the validated OOH questionnaire. Compares across-service providers | OOH; GP; A&E; NHSD | To identify strengths and weaknesses of OOH service provision in Wales | Across providers and types of care, consistent strengths were the ‘manner of treatment by call operator’ and the ‘explanation of the next step by call operator’. Consistent weaknesses were the ‘speed of call back by the clinician’ and the ‘information provided by the GP’ |
| McKinstry, 2010,137 UK | Retrospective analysis of audio recordings. Compares telephone and face to face | Primary care/urgent; doctor | To investigate whether or not there are differences in quality and safety of family doctors’ telephone and face-to-face consultations | Telephone consultations were shorter (4.6 minutes vs. 9.7 minutes; p < 0.001), presented fewer problems (1.2 vs. 1.8; p < 0.001) and had less data-gathering, counselling/advice and rapport-building (all p < 0.001) than face-to-face consultations. Telephone consultations were less likely to include enough information to exclude serious illness. Patient involvement and satisfaction were similar for both groups |
| Al-Abdullah, 2009,117 Saudi Arabia | Prospective observational study. Compares appropriateness of different provider referrals | In- and OOH urgent care; ED; nurse telephone line; GP; self-referred | To determine the appropriateness of patient referrals by a telephone health service to a paediatric ED compared with self- and physician-referred patients | More physician-referred patients were rated appropriate than health-line (80% vs. 56%; p < 0.001) or self/parent-referred (63%; p = 0.002) (appropriateness assessed by the examining ED physician). Physician-referred patients were significantly more likely to have investigations/treatment, be admitted to hospital and have longer lengths of stay. Using explicit criteria that give equal weight to symptoms, diagnosis and parental concerns found no significant differences in visit appropriateness |
| Snooks, 2009,142 UK | Multimethod (postal questionnaire and expert review). Compares necessary vs. unnecessary and sufficient vs. insufficient advice | In- and OOH emergency and urgent care; nurse; NHSDW | To describe the appropriateness of advice and health-care contacts made following telephone calls | Over 80% of callers rated advice as appropriate. The clinical panel rated over 80% of callers as having taken necessary and sufficient actions following their calls. From two caller groups the clinical panel identified unnecessary advice was given to 17.1% and 11% of patients and insufficient advice was given to 1.4% and 3.3% respectively |
| Strom, 2009,129 Sweden | Qualitative method with a phenomenographic approach | Nurse | To describe patients’ perceptions of receiving advice via a medical care helpline | Patients perceived the helpline as professional, reliable and easily accessible; self-care promoted through personal advice and ‘back up’; satisfactory when the nurse is calm, friendly, confirming and shows respect; compliance and acceptance enhanced when patients feel involved in the decision-making process; and, perceived as simple and time-saving |
| Beaulieu, 2008,120 USA | Before-and-after study using a survey. Compares data for 12 months before and 12 months after service introduced | Primary care; paediatric; nurse | To examine the effect of a telephone advice nurse on parent/caregiver satisfaction and access to care | Post-implementation group said nurse–parent/caregiver-shared decision-making was important (100% vs. 75%; p < 0.05) No difference in satisfaction levels or views on the helpfulness of the nurse |
| Dunt, 2006,130 Australia | Pre- and post-trial telephone surveys of two random samples. Compares stand-alone call centre vs. GP co-operative | OOH; urgent | To study the impact of two stand-alone call centres and one GP co-operative in improving consumer access to services | Consumer acceptability and affordability increased in residents in the area served by the GP co-operative. Access, however measured, did not improve in either of the stand-alone call centre areas. Reduction in unmet need approached, but did not achieve statistical significance in most but not all trial areas |
| O’Cathain, 2005,121 UK | Qualitative interview study | In- and OOH emergency and urgent care; nurse; NHSD | To determine whether or not NHS Direct facilitates patient empowerment (helping people to be in control of their health, health interactions) | NHS Direct facilitates patient empowerment by:
|
| Hogenbirk, 2004,135 Canada | Retrospective analysis of call transcripts. Compares views on appropriateness by different staff (nurse, NP, GP) | In- and OOH urgent care; nurse | To assess the appropriateness of advice given by teletriage nurses | In 56% of the 73 calls, all three auditors judged the nurse’s advice as ‘appropriate.’ In 92% of the 73 calls, at least two of the three auditors judged the teletriage nurse’s advice as ‘appropriate.’ All calls were rated as ‘appropriate’ by at least one auditor. If not ‘appropriate,’ then auditors were three times more likely to rate the advice as ‘overly-cautious’ rather than ‘insufficient’ |
| O’Cathain, 2004,136 UK | Mixed-methods study. Semistructured interviews with 24 nurses. Multilevel analysis of 60,794 calls triaged by 296 nurses. Compares different types of nurses | In- and OOH urgent care; nurse; NHS Direct | To determine whether or not nurses with different clinical backgrounds make different triage decisions in NHS Direct | The proportion of calls triaged to self-care was 40%, varying by individual nurse from a 10th centile of 22% to a 90th centile of 60%, (adjusted for age, sex, time of the call). Variability was partly explained by length of clinical experience and type of software used: nurses with > 20 years’ clinical experience were more likely to triage callers to self-care than those with < 10 years’ experience (42% vs. 36% respectively; OR = 1.41, 95% CI 1.13 to 1.78). Proportions triaged to self-care differed by type of clinical decision support software used: 31% (Centramax), 37% (Access) and 44% (TAS) |
| Richards, 2004,126 UK | Cluster RCT. Compares NHSD vs. GP practice-based nurse triage for same-day appointments | In-hours primary and urgent care; nurse | To assess the effects on consultation workload and costs of off-site triage by NHS Direct for patients requesting same-day appointments | NHS Direct patients’ calls were less likely to be resolved by a nurse and more likely to have a GP appointment. NHS Direct calls took longer (mean 7.62 minutes longer) and costs were £2.88 more (95% CI £0.88 to £4.87) per patient triaged (difference between groups in proportions of patients at each final point contact after triage) |
| Leclerc, 2003,123 Canada | Secondary data analysis. Compares user recollection of advice vs. recorded advice | In- and OOH emergency and urgent care; nurse | To examine the telephone advice line users’ perception of the advice compared with recorded advice | Many callers appear to interpret advice to seek additional health care differently than intended. Advice to consult was recorded by the nurse in 42% of cases, whereas 39% of callers stated they had received a consultation. Overall disagreement between the two sources is 27% |
| Mark, 2003,122 UK | Mixed-method evaluation Compares call data before and after introduction of NHSD | In- and OOH emergency and urgent care; nurse; NHSD | To study the impact of introducing a telephone health line | Use of primary care centres declined following the arrival of NHS Direct; home visits initially increased then decreased; OOH doctor advice and A&E attendances showed a progressive increase; information calls increased during the study period |
| Monaghan, 2003,133 UK | Secondary analysis of routine data. Compares staff types | In- and OOH urgent care; children; nurse | To determine if there are differences in call length and outcomes of children presenting by telephone when triaged by different types of nurses | Mean call length of the registered sick children’s nurses was significantly shorter than registered nurses (p < 0001). Except for referrals for routine appointment with a GP, both types of nurse referred to other triage outcomes groups with equal frequency |
| O’Cathain, 2003,124 UK | Scenario-based comparisons. Compares agreement between nurses | In- and OOH emergency and urgent care; nurse; NHSD | To examine the consistency of triage outcomes by NHS Direct nurses | Overall agreement between the nurses using the four systems was ‘fair’ rather than ‘moderate’ or ‘good’ (κ = 0.375, 95% CI 0.34 to 0.41). For example, the proportion of calls triaged to EDs varied from 22% (26 of 119) to 44% (53 of 119) |
| Grant, 2002,134 UK | Observational study using standardised patients. Compares settings: walk-in centres, GPs and NHSD | In- and OOH primary and urgent care; nurse/face-to-face and telephone | To compare the quality of clinical care in walk-in centres with that provided in general practice and by NHS Direct | Walk-in centres had a significantly greater mean score for all scenarios combined than general practices (difference between groups 8.2, 95% CI 1.7 to 14.6) and NHS Direct (difference between groups 10.8, 95% CI 5.5 to 16.1). In contrast to general practices, walk-in centres and NHS Direct referred a higher proportion of patients (26% and 82% respectively) |
| Barber, 2000,138 USA | Blinded Delphi review of medical appropriateness. Compares telephone referral advice and other source referrals with physician view | Paediatric; hospital; nurse telephone advice | To examine the appropriateness of referrals to a paediatric ED by the PHIL, a hospital-based telephone service, vs. other referrals | Physicians reviewed 133 consecutive ED telephone referrals and 260 randomly selected control patients seen in ED for medical appropriateness. The telephone group had an appropriateness rate of 80.2%, compared with 60.5% for the control group (χ2 = 14.6369; odds ratio = 2.65, 95% CI 1.528 to 4.50). For the period studied, PHIL referrals to the ED had a 33% higher rate of appropriateness than controls |
| Crane, 2000,132 USA | Prospective observational study comparing recorded advice vs. parental actions | OOH primary and urgent care; paediatric residents | To determine parents’ compliance to after-hours telephone advice given by paediatric residents | A total of 83.6% of 493 caregivers followed the telephone advice. Of the 270 callers only given telephone advice, 90.4% followed the advice, 15 (5.6%) went to the ED, and 11 (4.1%) made an appointment for the next day. When a visit to the ED was recommended, 93.5% complied |
| Kempe, 2000,125 USA | Prospective evaluation. Compares nurse vs. doctor assessment of urgency | OOH emergency and urgent care; nurse | To examine the effect of second-level physician triage on the rate of AHR | From 955 eligible calls, 22% were initially given an urgent disposition by call centre nurses. Physician questionnaires were completed for 97%. Of patients triaged for AHR, 49% were given an AHR, 17% a next-day office referral, and 34% home care and advice. Second-level physician triage halved the number of AHRs |
| Kempe, 2000,131 USA | Prospective observational study. Compares nurse referral vs. physician view | OOH; urgent; paediatric; nurses; hospital | To evaluate the appropriateness of urgent AHR and parental compliance | Of the referred patients, 339 (82.9%) complied with the recommendation for AHR. A total of 90.7% of patient referrals were judged appropriate. Of evaluated patients, 37.0% had a diagnostic test, and in 43.5% of cases, the evaluating physician thought a therapeutic intervention was necessary that night. A total of 6.6% of patients were admitted to the hospital |
Summary of findings
A summary of the main characteristics of all included studies, excluding systematic reviews, is given in Table 8.
| Characteristics | Number of included studies, n (%) |
|---|---|
| Country | |
| USA | 25 (33) |
| UK | 28 (37) |
| Other Europe | 12 (16) |
| Other | 10 (13) |
| Study design | |
| RCT | 7 (9) |
| Observational | 12 (16) |
| Interviews | 3 (4) |
| Retrospective | 27 (36) |
| Controlled | 1 (1) |
| Before and after (uncontrolled) | 4 (5) |
| Before and after (controlled) | 1 (1) |
| Mixed-/multimethod | 6 (8) |
| Other | 14 (19) |
| Staff | |
| Doctor | 7 (9) |
| Nurse | 56 (74) |
| Non-clinical | 4 (5) |
| Multiple clinical | 5 (6) |
| Not stated | 3 (4) |
| Setting | |
| 24-hour urgent | 31 (43) (paediatric = 3) |
| OOH urgent | 25 (33) (paediatric = 10) |
| Primary care | 8 (11) (paediatric = 1) |
| EMS/ambulance | 8 (11) |
| ED | 1 (1) |
| Key themes | |
| Doctor vs. nurse | 7 (9) |
| Appropriateness/accuracy (advice/referrals) | 29 (39) |
| Compliance | 20 (27) |
| Safety | 18 (24) |
| Satisfaction | 22 (29) |
| Costs | 11 (15) |
| Service impacts (unplanned recontacts/workload) | 20 (26) |
| Access | 6 (8) |
Staff type comparisons
Seven studies (nine papers) reported on telephone triage performed by different staff types. 72,92–94,99,117–119,125 There was one randomised controlled trial (RCT),93 one controlled trial,92,99 three prospective observational studies117–119,125 and one retrospective study. 72
Two studies (three papers) compared the appropriateness of nurse telephone referrals with other referral sources. 117–119 Both studies found that GP or physician ED referrals were more appropriate than either nurse telephone-referred or self-referred patients when measuring appropriateness using clinical criteria.
Two studies directly compared nurse and doctor telephone triage. 72,93,94 One study reported that nurses were more likely to recommend higher-intensity advice than doctors, but that when the appropriateness of this advice was reviewed by experts the nurse advice was more likely to be appropriate. 72 The other study found that callers were significantly more likely to be satisfied and have higher compliance rates if their call was dealt with by a doctor rather than a nurse, whereas repeat calls for advice were significantly higher in the nurse group at both the 4- and 72-hour time intervals. 93,94 A different study looked at introducing second-level physician triage in a nurse telephone system. 125 Adopting this approach halved the number of OOH referrals.
One study looked at using telephone advice given by nurses and paramedics for low-urgency ambulance services. 99 They found that nurses were more likely to triage calls as not requiring an ambulance. The 330 cases triaged by a nurse or paramedic as not requiring an emergency ambulance were less likely to attend ED, but 9% of these patients were admitted to a hospital bed. The only included study of a service using non-clinical call handlers supported by clinicians was the evaluation of NHS 111 pilot sites,105 but no comparison was made of decision-making by non-clinical call handlers and clinicians.
Safety
Eighteen studies reported on safety of telephone triage. The related systematic review by Huibers et al. 62 included 10 of the papers identified in this review66,73,74,77,78,82,89–92 and reported that a high proportion (97%) of all OOH telephone triage contacts were safe but that the proportion of safe contacts decreased when looking at high-urgency patients. From 10 studies using high-risk simulated patients, the authors found that just 46% were safe, bringing into question whether telephone triage and advice is as safe for higher-urgency patients.
Of eight additional studies68,92,103,104,133,140–142 not included in the Huibers et al. review,62 one study also found that more safety issues were associated with higher-urgency calls140 and two studies, one set in primary care68 and one set in emergency medical service (EMS) care,103 both reported no adverse outcomes or differences in suboptimal outcomes for high-urgency calls.
One study looked at characteristics of calls coded as low-urgency that resulted in death. 104 The authors found that these calls related to older people who did not make the call themselves. The calls were short, did not always conform to the system protocol and non-life threatening symptoms were reported. This concurs with the findings from a primary care-based study,137 which found that telephone consultations were shorter and did not include sufficient information to exclude serious illness. However, a study by Snooks et al. 142 reported that the overall proportions of patients who receive insufficient advice were low (1.4–3.3%). Based on the information from a study that analysed the incident reports from errors, 25% of errors related to incorrect assessment. 141
Compliance
Twenty-one studies reported on compliance with telephone triage advice recommendations. There were also two systematic reviews (i.e. the review of Blank et al. 57 and Purc-Stephenson and Thrasher58) that reported on compliance, which contained 13 of the studies identified in this review. 67,76,77,79,81,83,85,87,88,91,93,94,96 Blank et al. 57 reported that compliance ranged from 56% to 98%, and Purc-Stephenson and Thrasher58 reported an overall compliance rate of 62% but that compliance rates differed by the type of advice received, with 63% complying with advice to attend A&E, 44% complying with a primary care referral and 78% complying with self-care advice. Of the studies not included in the systematic reviews, three studies reported compliance that was within the range identified by Blank et al. 66,111,132 One study143 identified a 20% refusal of telephone triage recommendations, whereas another123 reported that callers may interpret advice differently from how it is intended, resulting in unintentional non-compliance. Compliance with advice provided by callers to NHS 111 was 86%. 106 A qualitative study reported that compliance may be improved when callers feel involved in the decision-making. 129
Satisfaction
Twenty-two studies (23 papers) reported satisfaction data. 66,67,69–71,79,86,87,93–95,97,101–103,106,109,110,120,121,127,129,137 Satisfaction with telephone triage and advice services ranged from 55% to 97%. Dissatisfaction ranged from 2.3% to 18.3%. Dissatisfaction was higher for EMS-based studies where patients may have expected to receive an ambulance and instead received telephone advice. Qualitative research suggests that patients value feeling involved in the decision-making, that they appreciate the manner of the call handler being calm, friendly and respectful121,129 and that they feel it is a useful backup service where they can avoid being labelled as ‘time wasters’. 121
Where telephone advice provided by different staff types was compared, patients reported less satisfaction with nurse-led services than with doctor-led services. 93,94
Costs
Nine studies reported costs or cost savings. 75,79,86,101,108–112,126 The most common method of calculating and reporting costs was to report costs saved from callers’ change in subsequent health-care-seeking behaviour as a result of the call. 75,79,108,110 These were not consistently reported and were reported as average per patient savings, cost savings per call recommendation type, annual net savings and overall reduction, making comparison difficult. Two studies reported costs related to introducing a nurse telephone line for low-urgency ambulance patients. 101,112 One of these studies112 reported a cost reduction of £4,520,000 from reduced ambulance dispatch and one101 reported reductions in costs owing to reduced ambulance cycle times and fewer admissions to hospital. Only one study reported a cost increase and this related to the cost of the general practice telephone bill after the introduction of a telephone service. 86 A cost–consequence analysis conducted as part of the evaluation of NHS 111 pilot sites estimated that the service might potentially save the NHS £2.4M a month, although this was based on limited cost data and considerable assumptions. 144
Service impacts
Seventeen studies reported impacts on their own service or other services, either from increased or reduced service use and or increased or reduced staff workload68–70,86,95,98,99,101–103,105,109,112,114,122,126,134 One study found that NHS Direct referred a higher proportion of patients to other services when compared with general practice. 134
A RCT by Lattimer et al. 68 reported a 38% reduction in primary care appointments and a 23% reduction in home visits, whereas another study reported no change in primary care appointments but home visits reduced by 18%. 70
A number of studies reported that doctor workload fell after the introduction of a telephone service. One study reported a reduction in workload of 54% compared with the previous 3 months69 and that nurses were able to handle 26% of requests for GP appointments by telephone, whereas another study reported a 39% reduction in demand. 86 However, other studies have found that, while a telephone advice service may reduce demand for face-to-face appointments in the first instance, patients consult their GP more frequently in the subsequent weeks. 95 In particular, older patients were more likely to have follow-up contacts after receiving telephone advice. 114 The evaluation of NHS 111 pilot sites found no impact on attendances at EDs and contacts with urgent primary care services but a statistically significant increase in ambulance incidents. 105
Five studies found that the introduction of a telephone advice service for low-urgency ambulance service patients resulted in fewer ambulance responses being required. 99,101–103,112 However, some studies reported high call-return rates, where calls are passed back for an ambulance response, or that not as many calls as expected could be resolved by telephone. 101,102
Accuracy and appropriateness
Twenty-six studies reported data on the appropriateness or accuracy of telephone triage and advice services. 72,73,75–77,80–82,84,88–90,100,101,115–119,124,131,135,138–140 The systematic review by Blank et al. 57 also reported on appropriateness and 11 of the studies identified here were included in the review by Blank et al. 73,75–77,80–82,84,88,90 This review identified that triage decisions rated as appropriate varied between 44% and 98%. However, many different definitions of appropriateness were used, which leads to difficulty when trying to compare results.
Of the 15 other studies,72,89,100,101,115–119,124,131,135,138–140 four studies looked at the appropriateness of ED referrals. In terms of referral sources, no difference was found between telephone and self-referred patients,118 but doctor-referred patients were the most appropriate referrals. 117 One study identified 33% of ED referrals as non-essential139 and another identified that a high proportion of ED referrals should have been handled in primary care. 116
Most studies reported that a high proportion of referrals, often in excess of 90%, were appropriate. 131,140 Triage advice and referrals were more likely to be unnecessary than insufficient. 142 However, one study identified that acute and non-urgent scenarios were more likely to be classified correctly than urgent. 115
Where low-urgency ambulance calls were passed for telephone advice there was a high return rate for an ambulance response. 101
Quality
There is a large evidence base on telephone triage and advice, but studies are dominated by retrospective studies and observational designs, with only a small number of randomised trials. 8 This reflects the difficulties inherent in conducting randomised studies in this environment, particularly if the service being investigated is in a single site. Individual studies and systematic reviews assessed a range of different outcomes and only one systematic review conducted a meta-analysis for a single outcome, compliance. 58 Broad, relevant quality issues identified by the authors of systematic reviews and individual studies include:
-
different definitions of appropriateness and methods for measuring this outcome
-
different methods for measuring patient satisfaction
-
different clinical assessment systems used to triage calls
-
differences in operational design – 24-hour services versus those only available out of hours
-
differences in the wider health-care settings services have operated in with consequent variation in the availability of alternatives to ED care, such as primary care services.
The consequence is a wide variation in the range of reported outcome results, for example the systematic review by Blank et al. 57 found assessment of appropriateness ranged from 44% to 98%, which makes it difficult to make comparisons between studies and draw firm conclusions about the strength of evidence for some specific outcomes.
Conclusions
There is an existing, substantial evidence base about the operational and clinical effectiveness of telephone-based triage and advice services for management of requests for urgent health care. We have identified 87 relevant papers from 83 studies, including eight systematic reviews, reporting a range of outcomes. The most commonly reported outcomes were concerned with accuracy and appropriateness of decision-making, patient compliance with advice, safety of decision-making and patient satisfaction. Despite the limitations outlined above, some general conclusions can be made about these aspects of telephone triage and advice services:
-
Accuracy of decision-making is generally high with respect to minimising risk. Similarly, despite wide variation in reported assessments of appropriateness overall, the proportion assessed as appropriate was high in the majority of studies. Where calls were judged to have been inaccurately or inappropriately triaged, the tendency was to assign calls to a higher level of care than needed rather than a lower level. What is less clear is whether this is a function of the triage assessment systems, the individuals using the system or a combination of the two. With the exception of one early NHS Direct study, we have found no research that has compared the performance of different telephone triage clinical assessment systems.
-
A consequence of this apparent inherent risk-averseness is that, overall, telephone triage systems appear to be safe, although they may not be efficient. In the small number of studies where adverse patient events or outcomes have been measured, these were very low.
-
Reported compliance is also variable but overall tends towards a high level, although this varies depending on advice given, with self-care or ED visits appearing to have higher levels of compliance than advice to contact primary care. This may reflect patient perceptions and preferences and would align with the evidence described in Chapter 3 on patient perception of perceived difficulty in accessing primary care.
-
Patient satisfaction with telephone triage is generally high and the service well liked by users. Although only a small number of studies compared nurse-led services with doctor-led services, satisfaction appears to be higher in doctor-led services.
Other outcomes or aspects of service delivery have been less well investigated and warrant further study:
-
Only 17 of the included papers assessed the impact of telephone triage and advice services on other services associated with emergency or urgent care. The majority of these studies only assessed impact on a single other service (e.g. ambulance responses, ED attendances, primary care attendances). With the exception of one US study109 that assessed impact on both ED attendances and primary care activity, only the UK-based studies of NHS Direct66 and NHS 111105 have attempted to assess the impact of telephone services on multiple services within the emergency and urgent care system. Whole-system impact is a key outcome if one objective of telephone-based services is to contribute to improving system efficiency.
-
The included studies were predominantly concerned with nurse-led telephone services. Only nine papers from six studies explored the effects of different types of staff delivering these services. Most of these compared nurse- or doctor-led services, one compared nurses and paramedics and two papers from one study assessed lay operators in a GP OOH setting. The findings from these studies were mixed, with some reporting no differences in appropriateness of decisions between nurses and doctors while others found nurses more likely to refer to higher-level care than doctors. Acute problems and non-urgent problems appear to be more accurately identified than urgent problems, suggesting that the latter are more difficult to assess, and there is a suggestion that higher-level clinician assessment may improve accuracy of urgent problem identification. Only one study investigated two-level triage (nurse assessment followed by doctor assessment) for a subset of calls. The broad area of optimum skill levels and mix of clinicians and non-clinicians has not been addressed.
-
Few studies have examined the costs associated with telephone triage and advice services, and these have taken different approaches to estimating and reporting costs, which makes comparison difficult. The financial benefits of these services both at an individual-service and whole-system level remain unclear.
-
Given that a primary objective of telephone triage and advice services has been to improve and simplify access to urgent care, there is remarkably little evidence about the impact of these services on access. Only five included studies examined impact on access.
These four evidence gaps are of particular relevance to the continued development of the NHS 111 service within the NHS. Assuming that NHS 111 will continue to be a principal entry point for access to urgent care and that the existing clinical assessment system (NHS Pathways) will remain unchanged, the key challenges are based around improving the existing service so that it can fulfil the intended objectives. It is worth remembering that the scale and scope of the NHS 111 service is much greater than that of the services included in the existing evidence, including its predecessor NHS Direct. It is also the case that there have been significant technological advances over the 20+ years that the evidence spans, therefore evidence from early studies may lack relevance now. Previous services have mostly been small in scale and intended to provide advice and some direction about what service people should access.
The vision for NHS 111 is that it provides broader functions, including health information, signposting to other services to which patients can refer themselves, direct referral to other services on behalf of the patient (including ambulances, where needed, and appointments made in real time) and advice. Good decision-making at the time of the call is therefore key to an efficient and effective service. The most pressing research issue is therefore concerning staffing the NHS 111 service. NHS 111 is unique in that it is a national telephone urgent care-access service where non-clinical call handlers make the first assessment. The only evidence on impact of using non-clinical call handlers is the existing NHS 111 evaluation studies of pilot services. Qualitative research examining the role of non-clinical call handlers found the work had more in common with clinical work than other call centre work and that the requisite skills need to be carefully incorporated in to training. 145 These call handlers are supported by nurse or paramedic clinicians, and the NHS England review has stated that the addition of senior (doctor) clinicians to NHS 111 will be considered as part of the ongoing development of the service. Changes to the staffing profile of NHS 111 call handling services will provide a unique opportunity to address the questions around impact of different types of clinicians on accurate and appropriate call assessment and the proportions needed to provide an efficient service. Additional specialist clinical skills, such as mental health specialists and pharmacists, could also potentially be added to the mix. Adequate follow-up of callers would be needed in order to assess whether or not care pathways are shortened and care really is provided in the right place, at the right time, from the first call, as well as whether or not access improves. The early research on NHS 111 found it did not substantially change the way the population accesses urgent care; however, this may have changed since it became a national service. 107
Alongside this, the impact of different staffing models on whole-system activity can be measured. NHS 111 has been criticised for referring too many patients inappropriately to higher-level ambulance and ED care. The early evaluation of pilot sites did show an increase in ambulance incidents after the introduction of NHS 111 (the reasons for which remain unexplained), but not ED attendances. 105 More detailed evaluation of the accuracy and appropriateness of call assessment decisions would answer some of these questions and identify where there is scope to improve it, either through changing the staffing profile or modifying the clinical assessment system.
Changes to the staffing profile, particularly the addition of doctors and/or increasing the proportion of clinical advisors, and increased IT infrastructure to support real-time referrals will incur costs which will need to be offset by improving whole-system efficiency. Robust economic evaluation alongside other changes would provide evidence on the associated costs of providing this complex service, whether or not it provides value for money and the necessary cost shifting within the emergency and urgent care system needed to plan and support the service in the future.
Finally, evaluation of improvements in the NHS 111 service itself, together with measurement of whole-system changes in volumes of activity in different associated services and some specific population-based research, would also begin to address issues about access and whether or not the service produces real changes and improvements in the way people access urgent care.
Chapter 5 Management of patients with urgent care problems by ambulance clinicians outside hospital
Introduction
Another key principle of the NHS England review is to provide more urgent care services away from hospitals and so encourage people not to choose A&E services. Enhancing urgent care outside hospital involves a range of services, including GPs, primary care and community services, community pharmacists and ambulance paramedics. There was not scope to consider all of these services within the time frame for this review. Particular emphasis has been placed in the NHS England review on development of the ambulance service by extending paramedic training and skills so they can manage more people on-scene and avoid unnecessary journeys to hospital. We have therefore focused our rapid review for this principle on identifying and summarising the existing evidence around initiatives implemented by the ambulance service to support this objective.
Methods
The main inclusion and exclusion criteria, search strategies and review process have been described in Chapter 2. Searches were conducted for the years 1 January 1995–26 November 2014. For this review, specific additional inclusion and exclusion criteria were used to identify studies investigating the areas detailed below.
Inclusion criteria
-
Extended care paramedics (community paramedics, advanced paramedics, paramedic practitioners, emergency care practitioners).
-
‘Treat and refer’ (to community setting).
-
‘Treat and leave’.
-
ED avoidance.
-
Conditions which could be managed at home/in the community.
Exclusion criteria
-
Acute conditions requiring hospital care.
Review process
Studies were identified from database searching and through expert knowledge of the field of interest. In addition to the studies identified through database searching, the study team identified 10 additional studies and these were assessed for inclusion in this review. A randomly generated 10% sample of studies from the database searches (n = 462) was double sifted by another member of the study team. The reviewers initially agreed on inclusion or exclusion for 97% of studies. The remaining 12 studies were discussed with a third reviewer; of these, six were included and six excluded. The results of the review sifting process are given in Figure 4.
FIGURE 4.
A PRISMA flow diagram for ambulance management in the community searches.
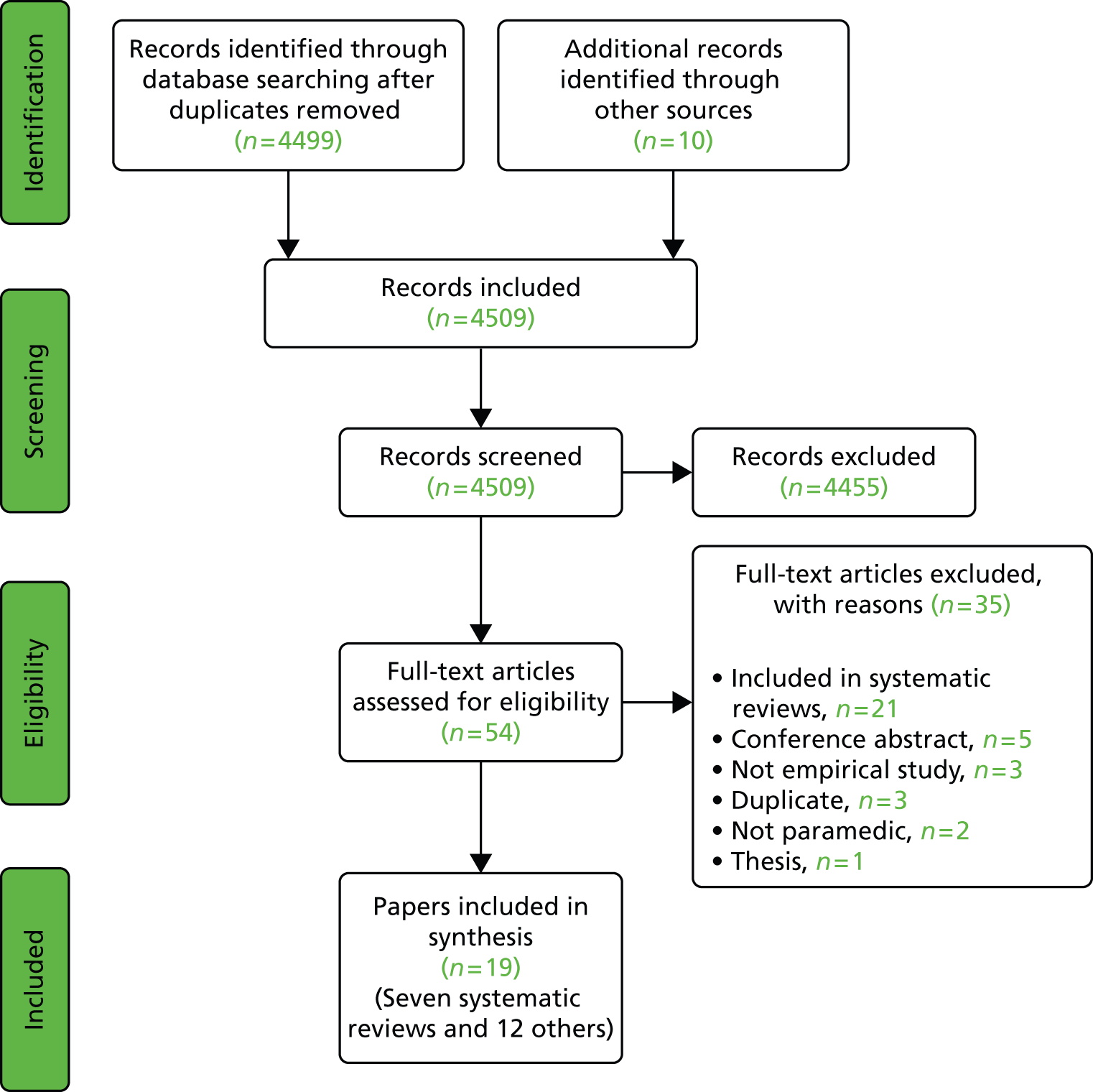
Results
We identified seven relevant systematic reviews and, within these, 64 papers from 57 studies were included, although only 21 of these papers met the inclusion criteria for this review. We also identified an additional 12 primary studies not included in the systematic reviews. Formal data extraction was not undertaken for the 21 papers meeting the inclusion criteria and included in systematic reviews, as this would have been conducted during the review process. Table 9 lists these 21 studies and the systematic reviews in which they were included.
| Primary study | Systematic review | |||||
|---|---|---|---|---|---|---|
| Bigham, 2013146 | Cooper and Grant, 2009147 | Evans, 2014148 | Hill, 2014149 | Mikolaizak, 2013150 | Tohira, 2014151 | |
| Adams, 2005152 | ✓ | ✓ | ||||
| Coates, 2012153 | ✓ | ✓ | ||||
| Cooper, 2004154 | ✓ | ✓ | ✓ | ✓ | ||
| Cooper, 2007155,156 | ✓ | ✓ | ||||
| Cooper, 2008157 | ✓ | ✓ | ✓ | ✓ | ||
| Department of Health, 2004158 | ✓ | ✓ | ||||
| Dixon, 2009159 | ✓ | ✓ | ✓ | |||
| Gray and Walker, 2008160 | ✓ | ✓ | ✓ | |||
| Halter, 2006161 | ✓ | ✓ | ✓ | |||
| Halter and Ellison, 2008162 | ✓ | ✓ | ||||
| Knowles, 2011163 | ✓ | ✓ | ||||
| Mason, 2006164 | ✓ | ✓ | ||||
| Mason, 2007165 | ✓ | ✓ | ✓ | ✓ | ✓ | |
| Mason, 2008166 | ✓ | ✓ | ||||
| Mason, 2007167 | ✓ | ✓ | ✓ | |||
| Mason, 2012168 | ✓ | ✓ | ||||
| O’Hara, 2012169 | ✓ | ✓ | ||||
| O’Keeffe, 2011170 | ✓ | ✓ | ||||
| Shah, 2010171 | ✓ | ✓ | ||||
| Stirling, 2007172 | ✓ | ✓ | ||||
Studies fall in to two broad groups: those concerned with a focus on investigating expanded professional roles for pre-hospital care providers (predominantly ambulance paramedics) and those focused on investigating alternatives to transport to ED, which encompasses broader professional groups rather than just those with enhanced skills.
We have summarised the characteristics and findings of the seven systematic reviews146–151,173 (Tables 10 and 11). Data on the 12 papers174–185 not included in the systematic reviews were extracted in to summary tables (Tables 12–14).
| Author, year | Study design | Population/setting | Purpose | Main findings |
|---|---|---|---|---|
| Bigham, 2013146 | Systematic review of research articles (any design). Search of three databases from January 2000 to 30 September 2011 | Extended scope paramedics working in any type of community paramedic programme | Impact of extended scope paramedics on any patient- or system-related outcome. Reported outcomes included clinical indicators (ED attendance and length of stay); operational outcomes (time on task and transport rates); patient satisfaction; economic impact; safety; and attitudes and satisfaction of paramedics with training | Eleven articles were included (one RCT). Community paramedic programmes in the UK, Australia and Canada appeared promising. The UK RCT showed benefits for paramedic practitioners over standard care paramedics. Role of CPs is currently unclear and desired outcomes need to be established by consensus Areas for research included safety of CP programmes, dispatch algorithms to identify patients needing CP services and deployment models for CP units |
| Cooper, 2009147 | Systematic review. Three databases, plus Google, Google Scholar and Journal of Emergency Primary Health Care were searched to July 2008 | Ambulance, nursing or medical staff with extended roles in out-of-hospital emergency care | Appraisal of evidence on impact of new and emerging out-of-hospital clinician roles on conveyance rates, immediacy of treatment and referral, patient satisfaction, cost savings and inter-professional working | Thirty-four articles were included, with 14 empirical studies analysed in detail. Authors concluded that ECP and PP roles significantly improve conveyance rates, treatment and referral rates and patient satisfaction, with some evidence of financial savings Areas for research included safety, barriers to implementation and cost–benefit trade-offs of investment in education and training vs. efficiencies within the health economy |
| Evans, 2014148 | Systematic review. Six bibliographic databases and various grey literature sources were searched from 1990 to March 2012 | Paramedics with extended skills; UK ECPs were excluded | Identify evidence of paramedics trained with extra skills and the impact of this on patient care and related services. Skills defined by the British Paramedic Association’s core paramedic competences and associated outcomes | Nineteen articles were included. Authors concluded that there is evidence on paramedics assessing and managing patients autonomously to reduce ED conveyance and that this is acceptable to patients and carers Areas for research included paramedics working with GPs, paramedic referral to hospital departments other than the ED and paramedics assessing and managing minor acute conditions in elderly patients |
| Hill, 2014149 | Systematic review. Five bibliographic databases plus Google, Google Scholar and the Department of Health website were searched from 2003 to August 2012 | ECPs in any UK setting | Summarise evidence on impact of ECPs on health-care delivery effectiveness of practise and resource use. Outcomes included staff or patient perceptions of the acceptability or performance of the ECP role, health-care costs and clinical working practices of ECPs | Fifteen peer-reviewed articles and six project reports were included. There was support from patients and staff for ECP services. A number of high-quality studies reported care processes provided by ECPs as being equivalent to or better than those provided by staff with traditional roles. Prehospital ECPs reduced unnecessary referrals to EDs Further research is needed to establish whether or not apparent cost savings associated with ECPs apply across all operational settings and patient groups |
| Author, year | Study design | Population/setting | Purpose | Main findings |
|---|---|---|---|---|
| Brown, 2009173 | Systematic review and meta-analysis. Search of three databases from inception to February 2008 | US paramedics; patients for whom 911 or similar emergency call was activated and ambulance transport requested | Comparison of paramedic determinations of need for transport with a reference standard. Primary outcome was NPV of paramedic determinations; other diagnostic accuracy outcomes were also reported | Five articles were included, of which only two reported full accuracy data. Pooled NPV was 0.91 (95% CI 0.71 to 0.98). Authors concluded that there is insufficient evidence to support paramedics determining whether patients need ambulance transport No explicit research recommendations provided |
| Mikolaizak, 2013150 | Systematic review. Six bibliographic databases plus reference lists of included studies were searched from inception to December 2011 | Emergency ambulance services; older people (60 years and older) who have fallen | Summarise evidence on non-conveyance, outcomes following non-conveyance and outcomes from alternative care pathways for older people following a fall | Twelve studies included. Non-transportation rates ranged from 11% to 56%. Non-transported people were likely to access health care following the incident fall: up to 49% had unplanned health-care contact within 28 days of the initial fall. One study reported that ECPs reduced subsequent hospital admission compared with standard ambulance crews Authors recommended research to explore non-ED pathways that can support ambulance services’ decision-making around transportation |
| Tohira, 2014151 | Systematic review and meta-analysis of comparative studies. Four bibliographic databases were searched from 2002 to early 2013. Supplementary search of Emergency Medicine Journal contents and article reference lists | Extended role NPPs, including ECPs, PPs and extended care paramedics; patients who sought an ambulance service | Assessment of impact of NPP roles on number of patients discharged at the scene; number transported to the ED; subsequent ED attendance; and appropriateness of care provided/decisions made | Thirteen studies (20 articles) were included. Meta-analysis showed that NPPs were less likely to take patients to the ED and more likely to discharge them at the scene than standard ambulance crews Pooled ORs: 0.09 (95% CI 0.04 to 0.18) for transport to ED and 10.5 (95% CI 5.8 to 19) for discharge at the scene. Most studies did not control for important confounders. Evidence for subsequent ED attendance and appropriateness of care was unclear Areas for research included safety of patients attended by NPPs and impact (if any) of NPPs in alleviating ED crowding |
| Author, year, country | Study design | Population/setting | Purpose | Main findings |
|---|---|---|---|---|
| Burrell, 2013,174 UK | Qualitative interview study | Ambulance staff working in south London | To assess the decision-making process by ambulance staff managing patients with epilepsy | Interviewees (n = 15) stated that complex seizures that self-resolve are difficult to triage. They reported insufficient training and guidance and relied on experience to guide their decisions. Transport to hospital was encouraged by fear of possible litigation, patient expectation and lack of access to patient information or alternative care pathways. Authors concluded that improved guidance should be developed |
| Halter, 2011,175 UK | Qualitative interview study | Ambulance staff in London | To understand the decision-making process of emergency ambulance staff with older people who have fallen | Twelve staff participated in semistructured interviews. Thematic analysis revealed a similar assessment and decision-making process among participants. This was complex and involved predominantly informal decision-making processes. Need for further support was highlighted. Authors recommended research into how new care pathways offering alternatives to the ED may influence decision-making |
| O’Hara, 2014,176 UK | Qualitative study using multiple methods | Ambulance service staff working in three different NHS ambulance trusts | To examine influences on safe decision-making by ambulance staff to identify areas for intervention and for further research | The NHS system was characterised as fragmented and inconsistent. Pressure to reduce transport to EDs intensifies the need for appropriate training, but operational demands were seen as conflicting with this. Perception of the ambulance service as primarily a transport service was seen as a barrier to working across professional and service boundaries |
| Author, year, country | Study design | Population/setting | Purpose | Main findings |
|---|---|---|---|---|
| Clesham, 2008,177 UK | Prospective ‘diagnostic accuracy’ study | Ambulance staff serving a major urban teaching hospital | To assess the ability of ambulance staff to predict which patients will require hospital admission | Questionnaires completed on arrival at ED (n = 396 cases). Staff predicted 182 (46%) would be admitted and 214 (54%) discharged. Actual dispositions were 187 (47.2%) and 209 (52.8%) respectively. Sensitivity of predicting admission was 71.7% (95% CI 65% to 78%) and specificity 77% (95% CI 71% to 81%). Ambulance staff showed reasonable accuracy in predicting admission and correctly identifying patients who able to leave |
| Cornwall, 2012,178 USA | Prospective ‘diagnostic accuracy’ study | EMTs in an urban fire department | To assess EMTs’ ability to identify intoxicated people not requiring transport to an ED | Questionnaires completed on arrival at ED (n = 197 cases). Overall sensitivity and specificity of identifying those requiring admission were 93% (95% CI 66.1% to 99.8%) and 40% (95% CI 33.3% to 47.9%). Potential for intermediate level EMTs to play an important role in triage of intoxicated patients to ED or alternative sobering facilities |
| Newton, 2014,179 UK | Service evaluation (diagnostic accuracy study) | Ambulance staff working in North West Ambulance Service NHS Trust | To evaluate the clinical utility and safety of triage support tools (Paramedic Pathfinder tools for medical and trauma patients to assess need for ED care) | Paramedic Pathfinder tool applied to 367 medical and 114 trauma patients. Agreement between ambulance staff and ‘gold standard’ was 80.5%. Sensitivity of the tools was 94.8% and specificity 57.9%. A total of 20.9% of medical patients and 30.7% of trauma patients transported to the ED could have been safely treated elsewhere. Demonstrated acceptable sensitivity in identifying patients who require ED care |
| Schmidt, 2000,180 USA | Prospective ‘diagnostic accuracy’ study | Ambulance EMTs | To determine whether or not EMTs can safely apply protocols to assign transport options | EMTs categorised 1300 patients. Overall sensitivity and specificity for identifying patients needing ambulance transport were 94.5% and 32.8% respectively. Between 3% and 11% of patients determined at the scene not to need an ambulance had a critical event. EMS systems need to determine an acceptable rate of under-triage |
| Snooks, 2014,181 UK | Cluster RCT | Ambulance staff attending older patients for a reported fall | To assess the clinical effectiveness, cost-effectiveness and safety of CCDS for ambulance staff attending older people who have fallen. Outcomes included referral rates, quality of life, job cycle times, contacts, non-conveyance rates and costs | Paramedics using CCDS referred 42 (9.6%) patients to falls services, compared with 17 (5.0%) seen by control paramedics (OR 2.04, 95% CI 1.12 to 3.72). No adverse events related to the intervention and no significant differences between groups in subsequent emergency contacts; quality of life and non-conveyance. Average cost £208 per patient with CCDS and £308 without. Ambulance paramedics using CCDS referred twice as many patients to a falls service with no difference in safety. CCDS is potentially cost-effective, especially in settings with existing electronic data capture |
| Author, year, country | Study design | Population/setting | Purpose | Main findings |
|---|---|---|---|---|
| Jensen, 2014,182 Canada | Qualitative focus group study | Residents in LTC facilities | To identify lessons from implementation and operation of a novel paramedic programme to provide on-site emergency assessment and care to LTC residents suffering acute illness or injury | Twenty-one stakeholders took part in four focus groups. The programme was positive for relationships between EMS and LTC, required additional paramedic training and could positively affect LTC patient experience of acute medical events. Paramedics found involvement with end-of-life care rewarding |
| Logan, 2007,183 UK | Service evaluation | Older people not taken to hospital after a fall and attended by an emergency ambulance | Assessment of impact of referral to intermediate care services by ambulance clinicians for older people after a fall. Outcomes measured: referrals to intermediate care service, admissions and deaths of referred patients within 6 months | Fifty-four patients were referred to intermediate care between July 2004 and June 2006. Of these, 21 were accepted by the service. Twelve patients were admitted and four died over 6 months. Intermediate care appeared to be acting as a single point of referral and referred people to other services after assessment. Service evaluation with no control group for comparison |
| Sach, 2012,184 UK | Economic evaluation alongside a RCT | People aged over 60 years who had fallen and called an emergency ambulance but were not taken to hospital | To estimate cost-effectiveness of referral to a community falls prevention service for older people not taken to hospital after a fall | Mean difference in health and personal social services costs was –£1551 per patient over 1 year (95% CI –£5932 to £2829), favouring the intervention group. The intervention group experienced, on average, 5.34 fewer falls (95% CI –7.06 to –3.62). The mean difference in QALYs was 0.07 (95% CI 0.01 to 0.15) in favour of the intervention group. The community falls prevention service was likely to be cost-effective in this high-risk group |
| Walker, 2006,185 UK | Service evaluation | People with diabetes mellitus who had called an ambulance for acute hypoglycaemia | To evaluate the effectiveness of ambulance crew referral to a diabetes mellitus specialist nurse team on patient satisfaction | Thirty-eight patients were referred and reviewed by telephone; 30 also required a clinic review. A total of 26 patients returned a satisfaction questionnaire, 88% agreed that their understanding of hypoglycaemia had improved and 73% felt more able to treat a hypoglycaemic episode in future. Referral was associated with high patient satisfaction and improved confidence in dealing with hypoglycaemia |
Summary of findings
The main characteristics of the 33 primary papers (21 papers included in systematic reviews and 12 additional papers) are summarised in Table 15.
| Characteristics | Number of primary studies, n (%) |
|---|---|
| Country | |
| UK | 28 (85) |
| USA | 3 (9) |
| Canada | 1 (3) |
| Australia | 1 (3) |
| Study design | |
| ‘Diagnostic accuracy’ study | 4 (12) |
| Interviews | 4 (12) |
| Survey/questionnaire | 5 (15) |
| Service evaluation (uncontrolled) | 3 (9) |
| Cluster RCT | 3 (9) |
| Economic evaluation alongside RCT | 2 (6) |
| Focus groups | 1 (3) |
| Quasi-experimental | 3 (9) |
| Mixed/multimethod | 7 (21) |
| Audit | 1 (3) |
| Principal outcomes | |
| Insight into decision-making processes | 7 (21) |
| Accuracy of decision-making | 4 (12) |
| Referrals/admissions | 9 (27) |
| Transport to ED | 3 (9) |
| Cost-effectiveness | 3 (9) |
| Patient/carer satisfaction | 5 (15) |
| Other | 2 (6) |
| Populations covered | |
| General population or not applicable | 19 (58) |
| Older people including those who have fallen | 9 (27) |
| Long-term care | 1 (3) |
| Epilepsy | 1 (3) |
| Intoxication | 1 (3) |
| Diabetes | 1 (3) |
| Children | 1 (3) |
The majority of related research has been conducted in the UK and eight of the included papers were outputs from two large studies by Mason et al. (i.e. Mason et al. 2007165 and Mason et al. 2012168). There were only two randomised studies165,181 and one relevant economic evaluation associated with a larger trial of a community falls service. 186 The main outcomes studied were rates of transportation to EDs, accuracy and safety of decision-making and patient satisfaction. Over 50% of studies included the broad emergency ambulance population, with specific populations dominated by older people who have fallen. The small number of studies that have considered costs were also associated with the three randomised trials highlighted above.
Effectiveness
Six of the systematic reviews146–148,150,151,187 found evidence that prehospital professionals can successfully reduce the number of patients transported to EDs and provide autonomous care and appropriate referral in the community setting. The evidence is predominated by schemes to provide ambulance paramedics with extended and enhanced clinical skills. Two studies160,165 showed that hospital admissions were also reduced in patients managed at home by paramedic practitioners and that patients managed at home had no more subsequent health contacts. 167
Four of the UK studies154,157,161,168 involved emergency care practitioners (ECPs), a role open to other health-care professionals such as nurses, although in reality dominated by ambulance paramedics, and practised in settings other than ambulance services. The review by Evans et al. ,148 which was concerned only with paramedics with extended skills, excluded studies of ECPs. The title ‘ECP’ has created problems as the generic ‘practitioner’ part of the title proved confusing. It conflicts with the regulators’ ability to ensure patients know who is treating them and was opposed by paramedic professional bodies. 188 The title ECP has been replaced (for paramedics) with titles listed in the paramedic career framework, such as specialist and advanced paramedic. 189
A smaller number of studies have investigated whether or not ambulance clinicians other than those with advanced skills can manage patients out of hospital and reduce transports to EDs. Snooks et al. 190 evaluated ‘treat and refer’ protocols for paramedics and found these did not increase the number of patients left at home. More recently, a trial of computer decision support software to aid paramedic on scene decision-making about referral to a falls service has shown some promise in terms of increasing the number of patients referred and left at home, although the numbers included in the study were small. 181
Where measured, the evidence on patient satisfaction and acceptability of initiatives to manage patients out of hospital and closer to home is positive. The UK studies on paramedic practitioners and ECPs165,168 found that patient satisfaction was higher in the groups receiving care from the advanced practitioners than those receiving usual care, and other studies of ECPs also found high levels of patient satisfaction191 and that patients found advice and explanations were clearer. 161,191 A positive effect for carers has also been reported. 192 Another study found that patients left at home following an episode of diabetic hypoglycaemia and referred to a specialist nurse reported high patient satisfaction and increased confidence in managing future episodes. 185
Only a small number of studies have examined costs but, where an economic evaluation has been done, management of patients by ambulance clinicians out of hospital has been reported as having lower costs and as being likely to be cost-effective when compared with conventional hospital care. 167,181,186,193
Safety and decision-making
Reducing transports to hospital is linked to safe and appropriate decision-making. Studies of advanced practitioners have shown that decision-making is generally safe and appropriate. 161,166,169 A number of studies have also examined the accuracy of ambulance clinician decision-making around whether or not to transport to hospital for the wider workforce and not just paramedics with advanced skills. The systematic review by Brown et al. 173 assessed the evidence on paramedic decision-making about need for transport and concluded that there was insufficient evidence to establish whether or not paramedics can accurately determine who needs transport. However, only five papers were included in this review.
More recently, one UK study has assessed the ability of ambulance staff to predict which patients need hospital admission and found that they showed reasonable accuracy in determining who needed admission and could correctly identify patients who did not. 177 A US study assessed emergency medical technicians’ ability to identify intoxicated people who did not need transporting to hospital and found there was potential for emergency medical technicians to accurately triage patients to alternatives to ED. 178 Another recent UK study evaluated the utility and safety of a triage support tools (Paramedic Pathfinder) for deciding which medical and trauma patients needed transporting or could be left at the scene. 179 Sensitivity was high, with reasonable specificity; however, the tools were used in shadow form (all patients were still transported) and there is currently no published evaluation of the tool in real practice.
A small number of more recent qualitative studies have provided some valuable insight into the difficulties associated with the decision-making processes faced by paramedics and advanced paramedic practitioners when deciding whether or not to transport patients. A detailed study on safety and decision-making by ambulance staff highlighted that, as the need to reduce transports to hospital increases, the requirement for appropriate training and education to equip ambulance clinicians for this role also increases. 176 Two studies on decision-making by ambulance staff for patients with epilepsy174 and elderly fallers175 both identified a need for additional training and support to aid safe decision-making, as did one Canadian study that focused on out-of-hospital management of patients with long-term conditions. 182
Implementation of initiatives
Some studies have highlighted the challenges, facilitators and barriers to implementation of initiatives to enable ambulance clinicians to manage more patients out of hospital, although these aspects of service provision are less well reported. The systematic review by Bigham et al. 146 highlighted issues associated with identifying patients suitable for advanced paramedic practitioner intervention and appropriate dispatching at the time of the emergency call as a potential barrier to using these practitioners effectively. As discussed above, training to support decision-making has been identified as a facilitator, but also, where it is felt to be insufficient, as a barrier. Issues about effects of integration with the wider urgent and emergency care system on successful implementation and, in particular, the need to have clear information about patients and about access to alternative care pathways for patients have also been raised. 150,174,176 Other relevant issues identified which impede patient management out of hospital include the conflicting demands of maintaining operational performance and meeting response-time targets (which reduces opportunities for training), barriers between professional groups, a continuing perception that the ambulance service is still primarily a transport service and fear of litigation which is associated with complex decision-making. 174,176
Quality
Although there is a substantial evidence base associated with the development of the ambulance service as a provider of out-of-hospital care, as evidenced by the seven systematic reviews included in this rapid review, there is a lack of robust, high-quality RCTs. Much of the relevant evidence included in the systematic reviews is derived from the two UK studies comprising a cluster randomised trial of paramedic practitioners165 and a community intervention trial of ECPs. 168 There is also a single randomised trial of use of computerised clinical decision support (CCDS) software for management of fallers. 181 The rest of the evidence is based in a range of study designs that introduce a number of limitations identified by study authors, including:
-
use of small convenience samples in some studies, which introduce potential bias from self-selection of participants and may not be representative of the intended clinician group
-
use of service evaluation approaches with no control group and, therefore, reported results do not account for any potential bias or confounding effects
-
studies of decision-making where clinicians have recorded intended rather than actual decisions (i.e. patients have still been transported to hospital), which limits applicability to actual clinical practice. Compliance rate in completing questionnaires is often low
-
important outcomes such as adverse events and subsequent health-care utilisation are, with a small number of exceptions, not recorded or reported.
More generally, most studies have been small scale, in single sites and usually involved a subpopulation of patients and clinicians, thus limiting generalisability to wider clinical practice.
Conclusions
Extended paramedic roles have been implemented in various health systems and settings and, based on a small number of high-quality studies, appear to be successful at reducing transports to hospital, making safe decisions about the need for transport and delivering acceptable care out of hospital, as well as being potentially cost-effective. The evidence on safety of decision-making about need for transport to hospital in the broader paramedic workforce without advanced skills is less clear and questions remain about safety. Studies concerned only with decisions about whether or not to transport to hospital also tend to ignore the important issue: that a decision not to transport requires good clinical care to be provided at the scene as an alternative. Good-quality care out of hospital is about more than just the decision to transport.
The authors of the seven systematic reviews and 12 individual papers included in this rapid review have made a range of recommendations for further research, including:
-
further work on the safety of decision-making and development of better guidelines, decision support systems (including CCDS) and training to support decision-making
-
further assessment of the risk of under-triage associated with decision support tools
-
barriers to implementation
-
cost-effectiveness of investment in training and potential cost savings across different settings and patient groups
-
further development and exploration of out of hospital care pathways for a range of conditions to support decision-making as effectiveness of initiatives to reduce transport to ED will depend on availability of alternative pathways and services
-
assessment of the impact of prehospital interventions on ED crowding.
These areas warranting further research have direct application to the NHS England review and the review’s expectations of an enhanced role for the ambulance service in managing more patients with urgent health problems in the community setting. It could be argued that at least some of these areas, for example resolving issues around safety, cost-effectiveness and wider system impact, are precursors to any widespread adoption of increased out-of-hospital management of patients by ambulance clinicians. However, pragmatically, it is the case that ambulance services in England have been progressively reducing the proportion of patients it transports to EDs over a number of years, both through managing more patients at the time of their call (‘hear and treat’, discussed more fully in Chapter 4, Costs and Service impacts) and outside hospital (‘see and treat’). Currently, the mean non-conveyance rate to ED is 37%, although this varies from 22% to 55% between individual ambulance trusts (www.england.nhs.uk/statistics/statistical-work-areas/ambulance-quality-indicators/ambulance-quality-indicators-data-2014-15/).
The reasons for this variation are unclear and the HSDR programme has already funded research to explore this. 194 However, this does illustrate that the ambulance service already manages a substantial number of its calls outside hospital. Given this and the clear important strategic role of the ambulance service in the NHS England review implementation plans,8 the future questions relevant to the continued development of the ambulance service as an out-of-hospital care provider are not about if it should be providing this service but how it can continue to expand and improve this aspect of service delivery. There are four key evidence gaps that could be addressed to support this process:
-
Clearly a key component to achievement of the NHS England plans is development of the paramedic workforce. The available evidence has shown the potential of advanced paramedic practitioners, but these have been relatively small scale and are likely to have involved highly motivated individuals willing to advance their practice. There is no evidence about the implications of developing the paramedic workforce at scale to achieve national objectives. One of the issues highlighted in the existing evidence is the possible ‘gap’ in decision-making skills between paramedics and paramedics with advanced skills. The paramedic workforce is changing, with a much clearer professional framework,189 and is rapidly moving towards a graduate-based profession;195 however, at present it is unknown to what extent this change may reduce the gap. There is a pressing need to begin to investigate the necessary skill mix of the paramedic workforce and the proportions of paramedics and paramedics with advanced and specialist skills needed to provide a safe and high-quality, community-based service for patients. The implications for the educational and training needs of the paramedic workforce that will be needed to fulfil this enhanced role, at scale, will need to be considered at the same time.
-
More broadly, and to support paramedic workforce planning, some clarity is needed about volume of activity and, specifically, the proportion of patients who could be managed outside hospital. Although the NHS England review has a clear view that ambulance services can manage more patients out of hospital, it stops short of stating how many patients this might encompass. As stated earlier, we already know that there is substantial variation in the non-conveyance rate to hospital across ambulance trusts in England, and it is reasonable to assume that there is scope for services with low non-conveyance rates to move towards performance of services comparable with higher rates of non-conveyance. What is uncertain is whether or not there is a threshold for non-conveyance beyond which the risks of leaving people at home begin to outweigh the benefits.
-
The qualitative research studies that have explored in more depth the barriers and facilitators to developing management of patients in the community have highlighted the need to develop robust clinical care and referral pathways for a range of different conditions as alternatives to transport to hospital. Without these pathways and confidence that onward referrals will be actioned,176 efforts to manage more people at home will be thwarted. Development of pathways is linked to development of robust guidelines and tools to support clinical decision-making at-scene. This will require wider system collaboration rather than small-scale, individual, local initiatives. It may be the case that not all patients who can be left at home need an advanced practitioner if they can be referred to an appropriate alternative provider. The existing evidence suggests that there is potential for CCDS software and triage tools (such as Paramedic Pathfinder) to improve and support decision-making; further research in this area is needed, but this will need to be aligned to workforce development, as graduate paramedics with higher-level skills may circumvent the need for this type of triage tool. However, it is likely that, as the range of alternatives increases, so the need for decision support tools increases.
-
The existing research evidence is based in small studies which, although showing local effects on reducing transports to ED, have not been at sufficient scale to assess system impacts across a range of services, both in terms of activity and associated costs. Expanded care by ambulance services in community settings may reduce ED attendances and hospital admissions but increase contacts with primary care, community and social services. Ambulance services themselves may need additional resources (staff, vehicles and equipment) and have increased training costs to support this expansion of their service. Future evaluation of initiatives to develop paramedic practice and increase the number of patients managed in community settings needs to assess the impact of these initiatives at scale and at a whole-system rather than individual-service level.
Chapter 6 Delivery of emergency department services
Introduction
The NHS England review6 has a focus on managing more urgent conditions outside acute hospitals, including, for example, urgent care centres. It also recognises the need to provide higher-level care for some health-care problems and sets out a strategy for emergency care that can deliver treatment in the right type of facilities and maximise patient outcomes. The model envisaged includes two types of facility: (1) major emergency centres, with highly specialised services; and (2) emergency centres, which can treat most emergency conditions and, where appropriate, refer on to a major emergency centre. A core principle for both centres is the presence of senior clinicians 7 days a week. This ‘model’ has been interpreted to some extent as creating a two-tier service but, in reality, reflects current provision, and NHS England states it expects the number of centres to remain broadly the same as the current number of EDs.
Reviewing the evidence on delivery of ED services poses significant challenges. Unlike the two preceding reviews, which had a focused, well-defined method (telephone triage) or aspect (paramedic management of patients out of hospital) of service delivery, provision of ED care encompasses the much broader set of issues associated with whole-service delivery. These include organisation and operations, service dynamics (flow), clinical roles of different professional groups, demand, clinical complexity of a heterogeneous population of users and relationships with other parts of the health service. Consequently, there is also a vast evidence base of related research.
The commissioning brief for these reviews has a focus on models of delivery. We have not reviewed the evidence on highly specialised and regionalised care (acute cardiac care, stroke, major trauma) as these have been extensively reviewed elsewhere. 196 Instead, we have focused this review on the evidence on the organisation and operations associated with delivery of general ED services (which are also provided in major centres). The Royal College of Emergency Medicine produced a report in 2014, which identified 13 recommendations for changes needed to build a sustainable and resilient emergency and urgent care system. 9 We used some of these recommendations, specifically regarding delivery of ED care (rather than whole-system issues) to further refine the focus. We have therefore conducted two linked but separate rapid reviews:
-
A key recommendation is that every ED should have a co-located primary care OOH facility. We have updated an existing related rapid evidence review published in 2010 to assess the current evidence for this model of care.
-
We have also reviewed the broader evidence on ED organisation and operation and, on advice from a senior clinician, have kept the emphasis on ED flow (including front-door assessment and back-door discharge), the related area of clinician role and the key growing area of managing the complex elderly patients in EDs.
Co-location of primary care and emergency departments
Methods
For this review we replicated and updated the search strategy used in a previous rapid review,10 which is described in detail in Chapter 2, Database search strategies. Searches were conducted from 1 January 2009 to 20 January 2015. We also applied the same inclusion criteria used in this review:
Inclusion criteria
-
Studies reporting primary data on interventions for managing patients with primary care-type conditions, however defined.
-
Included objective measures attributable to a defined intervention, either within or allied to the ED.
Review process
Studies were identified from the updated database search and were supplemented using the reference list of studies identified and included in a related systematic review recently conducted and in preparation for publication by authors within ScHARR (Dr Shammi Ramlakhan, Sheffield University Teaching Hospitals NHS Trust, 2015, personal communication). This paper identified four additional studies, which were assessed for inclusion in this review. A randomly generated 10% sample of studies from the database searches (n = 572) was double sifted by another member of the study team. The reviewers initially agreed on inclusion or exclusion for 96.4% of studies and, after discussion, agreed to exclude the remaining 26 studies.
Results
Nine papers were included in the review:10,143,197–203 two systematic reviews,10,197 which included 28 individual papers, and seven additional papers. 143,198–203
The results of the review sifting process are given in Figure 5.
FIGURE 5.
A PRISMA flow diagram for management of primary care in ED searches.
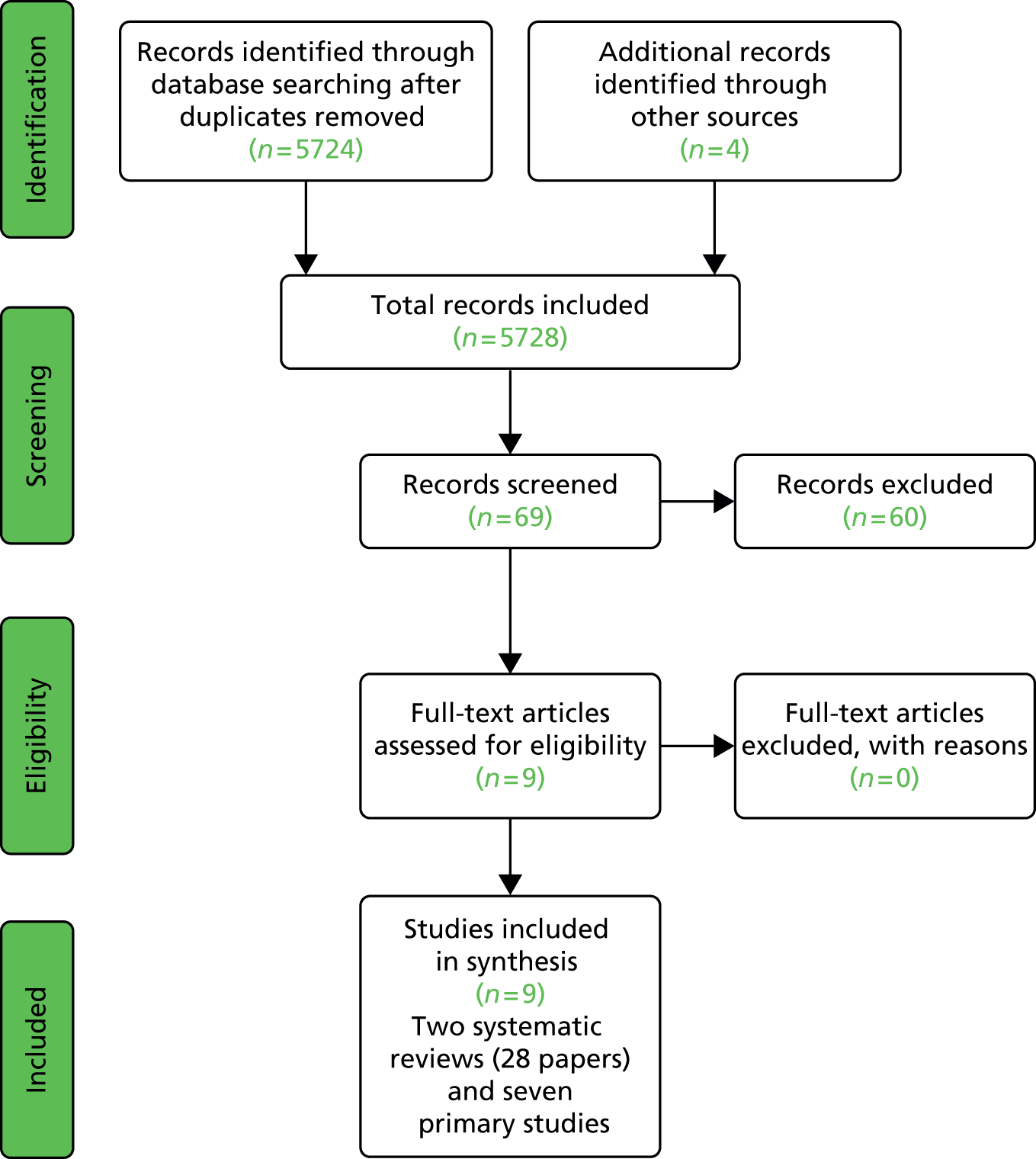
A summary of the characteristics and findings of the included papers are given in Tables 16 and 17.
| Author, year | Study design | Population/setting | Purpose | Main findings |
|---|---|---|---|---|
| Fisher, 201010 | Rapid review of the literature and narrative analysis | Patients of all ages seeking primary care attending a service:
|
Assessment of evidence on interventions for managing patients with primary care-type conditions, either within or allied to the ED Outcomes included: attendance at primary care, attendance and/or reattendance at ED, adverse events, patient satisfaction, investigations and referrals requested and prescriptions issued |
Twenty-eight studies included. A GP working in the ED may result in fewer referrals for admission and fewer tests being undertaken. Cost benefits may exist but the evidence is weak Redirect away from ED has variable results in terms of predicting future attendances. Assessments of safety of this intervention have variable results. Primary care appointments made for patients redirected from the ED may not be kept Educational interventions do not show a change in attendance patterns There is a paucity of evidence available to support the current system |
| Khangura, 2012197 | Systematic literature review | Patients who present to hospital EDs with illness or injury suitable for primary care | Effect of primary care professionals working in hospital EDs (including GPs, NP, optometrists and dentists) on admissions, length of stay, resource use, costs, follow-up care and health-care utilisation and adverse events | Three studies included. Two studies reported that GPs used significantly fewer health-care resources than EPs, with fewer blood tests, radiography, admissions to hospital and referrals to specialists. One study reported no difference in number of prescriptions made by GPs compared with EPs, and one that GPs prescribed significantly more than EPs. These two studies showed marginal cost savings from introducing GPs in hospital EDs The third study failed to identify a significant difference in the number of investigations or admissions to hospital, but identified a significantly greater number of referrals to specialists and prescriptions made by GPs compared with EPs. There is insufficient evidence to draw conclusions about the effectiveness and safety of GPs vs. EPs for non-urgent patients in the ED |
| Author, year, country | Study design | Population/setting | Purpose | Main findings |
|---|---|---|---|---|
| Boeke, 2010,198 the Netherlands | Before-and-after comparative study of a new care method in the ED of an Amsterdam university medical centre | Adult patients who self-presented to ED on weekdays during the day (10.00–17.00 hours) | Evaluation of impact of introducing GP services into ED to manage primary care conditions on patient satisfaction, time from arrival to departure, time from start of consultation to departure and referrals for aftercare | Patient satisfaction with the treatment increased significantly The mean process time decreased from 93 to 69 minutes (p < 0.001). The mean treatment time decreased from 60 to 35 minutes (p < 0.001) |
| Bosmans, 2012,199 the Netherlands | Before-and-after design | Self-referrers who attended the ED on weekdays during the day (10.00–17.00 hours) | Evaluation of impact of adding a GP to the ED to manage primary care problems on patient satisfaction, process time and costs | Significantly reduced process time, significantly higher patient satisfaction and no statistically significant difference in the number of correct diagnoses after intervention introduced. Total costs per patient were €217 in the new service compared with €288 before (mean difference –€71, 95% CI –€121 to –€23) |
| Enard and Ganelin, 2013,200 USA | A non-equivalent comparison group, quasi-experimental study design | Patients older than 18 months and younger than 65 years who frequently use the ED for primary care and are publicly insured | Impact of a primary care patient-navigation referral programme on PCR-ED attendance and cost per person of a PCR-ED visit | Patient navigation intervention was associated with decreased odds of returning to the ED in less-frequent PCR-ED users. For patients who returned to the ED for PCR reasons, the pre-/post-mean visits declined significantly over 12 months but not 24 months. Savings associated with reduced PCR-ED visits were greater than the cost of implementing the navigation programme |
| Salisbury, 2007,201 UK | A controlled before-and-after study | Patients consulted, admitted or discharged monthly from 6 months before the opening of walk-in centres to 6 months after | Evaluation of the impact of opening walk-in centres located alongside EDs on attendance rates, duration of visits, costs and outcome of care | At most sites, the walk-in centres did not have a distinct identity and there were few differences in the way services were provided compared with control sites. Overall, there was no evidence of an increase in attendance at sites with walk-in centres, but considerable variability across sites. Proportion of patients managed within the 4-hour target improved at intervention and control sites. No evidence of any difference in reconsultation rates, costs of care or patient outcomes at sites with or without walk-in centres |
| Sharma and Inder, 2011,143 Australia | Observational study of ED waiting times over 1 year in the state of Victoria | Emergency (category 2) and non-urgent (category 5) patients in 38 hospital EDs | Analysis of differences in patient waiting times (difference between arrival time and time first seen by treating doctor) at EDs with and without co-located GP services | The degree of choice for non-urgent patients has a non-linear effect: more choice for non-urgent patients is associated with longer waits for emergency patients at lower values and shorter waits at higher values of degree of choice. Increasing choice of ED for non-urgent patients related to longer wait for emergency patients in EDs. Waiting time for emergency patients in hospitals with co-located GP clinics was 19% (mean 1.5 minutes) less than in hospitals without co-located GP clinics |
| Thijssen, 2013,202 the Netherlands | Longitudinal observational study 3 years before and 3 years after the start of an ECAP | All attendances at ED and GP co-operatives over the 6-year period of 2006 to 2012 | Evaluation of the impact of introducing an integrated after-hours care model on ED and GP co-operative self-referrals, non-self-referrals and follow-up contact | ED attendances decreased by 13% after the start of the ECAP (59,182 before vs. 51,513 after). Self-referred ED patients decreased by 99.5% (OR 0.003, 95% CI 0.002 to 0.004) Referred patients increased by 213.4% and ED hospital admissions increased by 20.2%. Planned outpatient follow-up increased by 5.8% (OR 1.968, 95% CI 1.870 to 2.071). Regional general practitioner co-operative consultations increased by 26.0% (183,782 vs. 232,246) |
| Wang, 2014,203 USA | Before-and-after study | Consecutive patients attending ED with ambulatory care conditions from 1 October 2007 to 12 November 2007 before intervention (n = 451) and routed to HGP from 6 April 2010 to 14 May 2010 post intervention (n = 342) | Evaluation of the effects of implementing of a new HGP service on time from admission to discharge and time intervals between different stages of care | Median time from admission to discharge was 120 minutes in the ED (IQR 80–165 minutes) vs. 60 minutes in the HGP (IQR 40–90 minutes) (p < 0.001) The adjusted OR of receiving any additional diagnostics was 1.86 (95% CI 1.06 to 3.27; p = 0.032) for ED doctors vs. GPs controlled for age, sex and injury-related medical problems |
The characteristics of primary studies included in the two systematic reviews and the seven additional studies are described in Table 18.
| Characteristics | Number of studies, n (%) |
|---|---|
| Country | |
| USA | 14 (40) |
| UK | 6 (17) |
| Other Europe | 14 (40) |
| Other | 1 (3) |
| Study design | |
| Before-and-after study | 21 (60) |
| Randomised control trial | 5 (14) |
| Prospective | 3 (9) |
| Observational study | 4 (11) |
| Systematic review | 1 (3) |
| Retrospective audit | 1 (3) |
| Patients | |
| Adults and children | 11 (31) |
| Children | 7 (20) |
| All | 12 (34) |
| Adults | 5 (14) |
| Setting | |
| Co-located | 10 (29) |
| Not co-located | 25 (71) |
Summary of findings
Two systematic reviews10,197 examining the evidence on the clinical effectiveness and cost-effectiveness of primary care services associated with EDs included findings from 28 studies. Both concluded that, although there was some evidence that locating primary care services within or close to EDs could reduce ED attendances may save resources by using fewer diagnostics and referrals for admission and potentially could reduce costs, the evidence base to support development of this model of care was weak and based on poor-quality studies. Our search identified a further seven more recent studies which, overall, presented more positive findings on the potential benefits of integrating GPs within EDs. Two studies in the Netherlands, where GPs were located within the ED,198,199 found process and treatment times were reduced and patient satisfaction increased after the introduction of this service, and that there were cost savings. However, these were both uncontrolled before-and-after studies, so the influence of other potential confounding factors is unknown. A study of a primary care patient navigation service significantly reduced the likelihood of ED readmission for less-frequent primary care-related ED users200 and produced cost savings, while a hospital-integrated general practice service was shown to have potential to significantly reduce the time from admission to discharge and resource use as primary care doctors used fewer diagnostics than ED physicians. 203 A broader study examined longitudinal trends in ED attendances over 3 years after introducing integrated OOH GP co-operatives. 202 The findings were that, overall, ED attendances, and in particular self-referrals, decreased but referrals from GPs to EDs increased, as did ED admissions. Unsurprisingly, GP co-operative consultations increased and what is unclear is the net effect of patient movement between these services. Again, all of these studies were uncontrolled. The only comparative trial was conducted in the UK and investigated the impact of introducing walk-in centres in the vicinity of EDs. 201 This study found that, while ED attendances decreased in some centres, in others there was no change. Overall, there was no evidence of impact on reconsultations, patient outcomes or costs. The lack of success may have been owing in part to the walk-in centres not having any clear identity and hence not being visible to the public as an alternative to EDs. Of the available evidence, the most convincing seems to be from models where GPs or primary care professionals are located within the ED itself rather than alongside it or as stand-alone units. Intuitively, this makes sense, as it creates a single ‘front door’ which may reduce confusion for the public and allow more efficient streaming between ED and primary care, with a single entry and assessment point. It is also possible that this intervention may be most suitable for simple single episodes and that complex conditions and frequent users need more specialist and sophisticated care. 200 Boerke et al. 198 make an important point about the influence of general societal and cultural factors on health-care-seeking behaviour, and suggest that interventions to reduce the amount of ‘inappropriate’ use are likely to fail and that strategy might be better focused on enhancing adequacy of care than on trying to match health-care-seeking behaviour to the services.
Quality
The quality of the available evidence is generally poor. Of the 35 included studies, there were only five RCTs and a high preponderance of uncontrolled before-and-after studies, which cannot control for other system effects. For example, the study by Thijssen et al. 202 acknowledges that closure of hospitals during the study period may have had some influence on the findings. The authors of the two systematic reviews identified a range of limitations to the studies included in their reviews, including small sample sizes in the form of low response rates, lack of data on patient waiting times, length of hospital stay, adverse effects or mortality and a lack of consideration of patient safety issues. 197 The review by Fisher et al. 10 also identified the poor research design and reporting of studies, including variability in study design and length, sample size, period of follow-up and definitions of primary care/non-urgent type condition. Individual authors of included studies have acknowledged the difficulties of conducting randomised trials in this difficult environment. 199 The majority of studies were set in single centres, which limits generalisability. This is exacerbated if the focus is a particular group, such as the uninsured, the elderly or children, and may also be limited by the health-care system in which an intervention operates. 200 The trial by Salisbury et al. 201 identified some additional limitations and important considerations, particularly the low quality of available routine data, the need to allow new services time to mature (and hence to design studies of sufficient length to detect real effects) and the need to conduct studies at scale and assess true impact across a whole system rather than single sites.
Emergency department organisation and operation
Methods
The main general inclusion and exclusion criteria, search strategies and review process described in Chapter 2, Review process, have been applied to this review. Searches were conducted from 1 January 1995 to 17 December 2014. Specific inclusion and exclusion criteria used in this review were as follows.
Inclusion criteria
-
Empirical studies that had evaluated changes to ED service delivery.
-
Associated with the key areas of ED flow management, workforce or management of frail elderly.
-
Applied to the broad ED population (not specific conditions).
Exclusion criteria
-
Descriptive studies of only a service intervention, with no assessment of impact.
Review process
Studies were identified from the database search and were supplemented using our internal topic expertise. The searches identified 3539 records. Early in the search sifting process it became clear that, with such a broad range of processes present within ED, the volume of potential inclusions was prohibitive in terms of including and synthesising individual papers or studies. The initial sifting identified a large number of existing, related systematic reviews, and so a decision was made that we would only include these systematic reviews in our synthesis.
Results
Twenty-two systematic reviews were included. 204–225 The results of the review sifting process are given in Figure 6.
FIGURE 6.
A PRISMA flow diagram for delivery of ED services search.
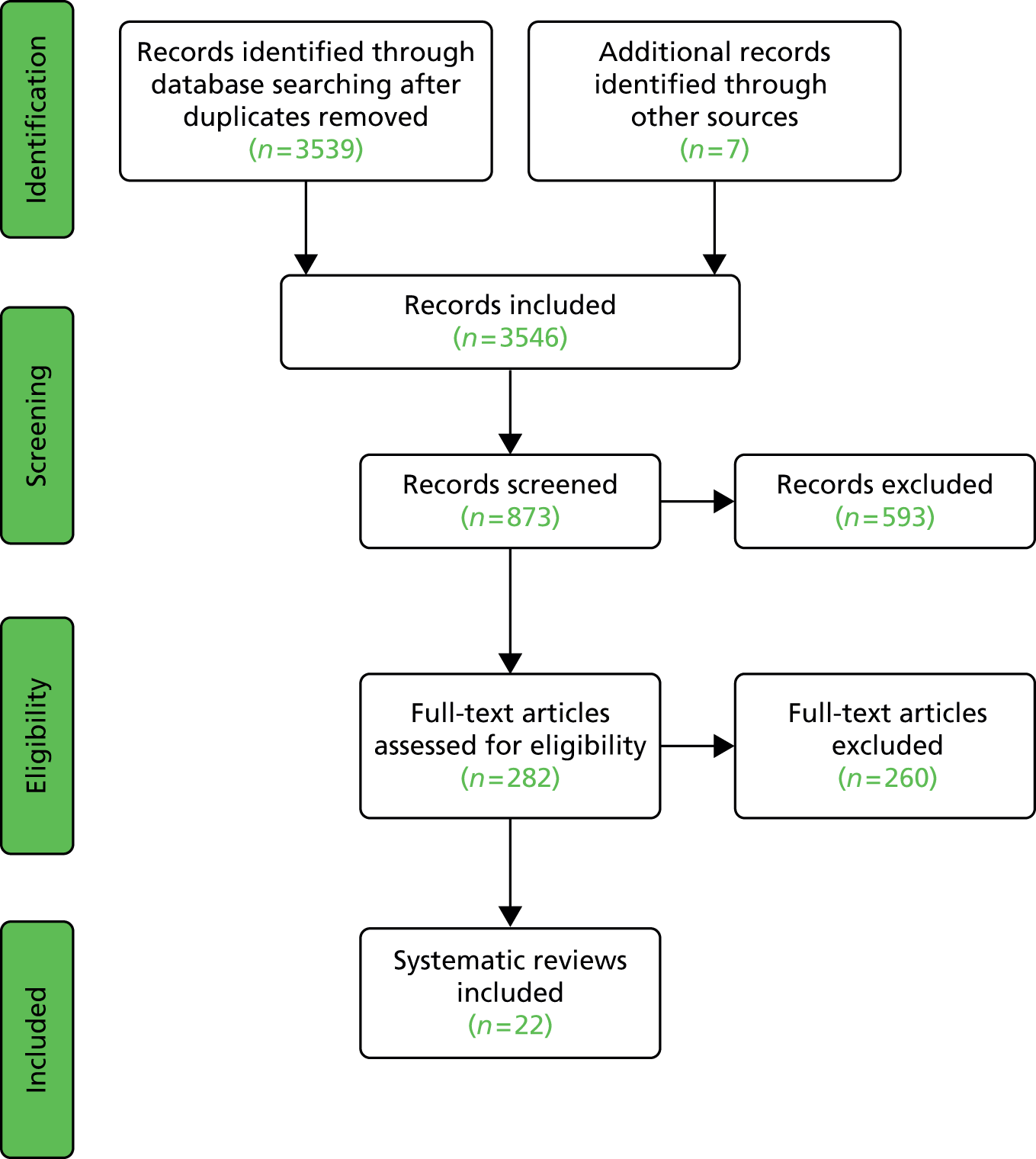
A summary of the characteristics and findings of the included systematic reviews are given in Tables 19–21.
| Author, year | Study design | Population/setting | Purpose | Main findings |
|---|---|---|---|---|
| Abdulwahid, 2015204 | Systematic literature search with assessment of relevance and bias using the Effective Public Health Practice Project bias tool | ED, senior doctor triage | To review and synthesise studies with the primary aim of investigating the effect of senior doctor triage on ED quality indicators: waiting time, LOS, LWBS, left without treatment complete | A total of 25 studies with a control group were included. Most studies showed that using senior doctor triage improved ED performance measure results. Pooled results from two out of four RCTs showed a significant reduction in LOS for medium acuity patients (WMD –26.26 minutes, 95% CI –38.50 to –14.01 minutes). Two other RCTs showed waiting times significantly reduced when using senior doctor triage (WMD –26 minutes, 95% CI –31.68 to –20.65 minutes). LWBS was reduced in two RCTs (RR 0.79, 95% CI 0.66 to 0.94). This was similar to most pre–post study designs. Senior doctor triage had no effect on adverse events or clear benefits for patient satisfaction or cost-effectiveness. Nine studies were of moderate quality, four were of strong quality and 12 were of weak quality |
| Bullard, 2012205 | Narrative synthesis, grouped by outcome | ED, rapid assessment zones/pods | To synthesise evidence on the use of rapid assessment zones/pods to reduce overcrowding in adult EDs | There were four included studies (one RCT, one controlled trial and two before-and-after studies), with sample sizes between 200 and 12,305, representing 23,189 participants. Study quality was assessed as weak for three of the studies The review reported that rapid assessment zones/pods have the following benefits:
|
| Cooke, 2003206 | Qualitative systematic review | ED, assessment/admission wards | To review the advantages and disadvantages of the use of assessment/admission wards | A total of 17 studies included. Most suggest assessment or admission wards are beneficial; they improve patient satisfaction, are safe, reduce length of stay, provide earlier senior involvement and reduce unnecessary/inappropriate admissions. May be particularly useful for certain diagnostic groups, but have little effect if care is already good. Observation wards may reduce ED workload and improve patient flow. Reduced pressure on hospital staff allows more time for important decision-making such as diagnosis, ensuring appropriate admissions that may reduce costs. Some studies advise that patients should be transferred out within 24 hours to prevent inappropriate use |
| Daly, 2003207 | Systematic review (comparative studies) | ED, SOUs | To conduct a systematic review of how SOUs affect the efficiency of health-care delivery and the quality of services provided | Reported potential benefits of SOUs are reduced length of stay, improved ED efficiency and reduced cost, but there was variation between studies regarding reported benefits
|
| Flores-Mateo, 2012208 | Systematic review (n = 48) | ED | To systematically review the effectiveness of organisational interventions designed to reduce ED utilisation | Most studies were of poor methodological quality. Results were reported in the following categories:
|
| Georgiou, 2013209 | Systematic review of quantitative studies | ED, CPOE systems. ED settings or ED outcomes | A systematic review of the quantitative literature related to the effect of computerised provider order entry systems in the ED | Twenty-two studies met the inclusion criteria. CPOE was associated with an increase in time spent on computers (up to 16.2% for nurses and 11.3% for physicians), but with no significant change in time spent on patient care. CPOE with decision support systems showed significant decreases in prescribing errors (ranging from 17 to 201 errors per 100 orders), potential adverse drug events (0.9 per 100 orders) and prescribing of excessive dosages (31% decrease for a targeted set of renal disease medications). There was a high possibility of publication bias towards studies with positive results reported |
| Harding, 2011210 | Systematic review, no study design restrictions. Data were analysed using descriptive synthesis | ED, triage systems | What effect do different triage systems have on patient flow? | The authors identified that triage systems may improve quality of patient care across multiple settings through reduced waiting time, shorter waiting lists and reduced LOS. Some evidence that services providing triage and initial treatment have a positive effect on patient flow, but conflicting evidence on patient flow for systems providing triage without initial treatment Eight studies conducted in hospital EDs with a doctor at the triage desk in conjunction with standard nurse triage found some evidence of benefit for reducing LOS, number of patients who left without being seen and ED waiting time Three studies evaluated use of a multidisciplinary triage clinic and found over 20% of patients were discharged at triage and waiting times were reduced Half of the included studies were considered poor quality |
| Holden, 2011211 | Critical review | EDs introducing Lean methods of working | To critically review 18 articles describing the implementation of Lean in 15 EDs within the USA, Australia and Canada | Lean is a process improvement approach designed to eliminate waste. Within ED this relates to patient flow and over-triage/unnecessary investigations. Patient care usually improved after implementation of Lean, with many EDs reporting decreases in LOS, waiting times, and proportion of patients leaving the ED without being seen. Few null or negative patient care effects were reported, and studies typically did not report patient quality or safety outcomes beyond patient satisfaction. The effects of Lean on employees were rarely discussed or measured systematically, but there were some indications of positive effects on employees and organisational culture. Success factors included employee involvement, management support and preparedness for change |
| Hoot and Aronsky, 2003212 | PubMed search and synthesis | General ED | To identify and report on articles that study causes, effects or solutions of ED overcrowding | Causes of crowding were: non-urgent visits, frequent attenders, influenza season, inadequate staffing, inpatient boarding and hospital bed shortages Effects of crowding included: increased patient mortality, transport delays, treatment delays, ambulance diversion, patient elopement and financial effect Solutions of crowding included: additional personnel, observation units, hospital bed access, non-urgent referrals, ambulance diversion, destination control, crowding measures and queuing theory |
| Katz, 2012213 | Systematic review | ED and post-ED treatment plans; urban, rural, multicentre, single centre | A systematic review on the clinical effectiveness of ED-based care co-ordination interventions | Of 23 included articles, 14 were RCTs and nine were quasi-experimental studies. The many different types and settings of EDs made it difficult to compare results. Most care co-ordination interventions have been implemented in single-centre EDs, with good results. Two-thirds of studies described interventions that were clinically effective in improving their primary outcome. A total of 19 studies developed post-ED plans and 12 were clinically effective in improving follow-up rates or reducing repeated ED visits. However, four studies found higher ED visit rates Of the four studies that used educational services for continuing care, two were effective. Of the two studies evaluating information transfer, one was effective |
| Lee, 2008214 | Systematic review; acute ED presentations | ED | This review systematically evaluated the literature on ED consultations with other specialities | Twelve studies included, with little new research published since the mid-1990s. Eleven out of 12 studies were from the USA or Canada, so may not reflect EDs in other countries. Overall, four studies examined ED consultation proportions, six identified the rate of consultation for special populations of ED presentations and two examined interventions to improve consultations. Only two published studies on interventions to reduce or control ED consultations. Consultation rates varied from 20% to 40% for all patients, usually reported for patient subgroups and varied by setting. Limited research on how to improve the ED consultation process and the relationship with overcrowding |
| Paul, 2010215 | Systematic review | ED, overcrowding | The aim of this systematic review was to highlight the contributions of simulation studies to our understanding of ED overcrowding and to explore how simulation can be better used as a tool to address crowding | Most studies aimed to identify potential improvements in costs and competition, efficiency, re-engineering and quality of service Studies examined resource-, process- and environment-related scenario
|
| Porter, 2014216 | Systematic review. Evaluation of innovation without comparator, or comparison of innovation with usual care | ED, adult patients; clinician-led rapid assessment teams to streamline patient handover and flow in the ED | The systematic review was undertaken to identify rapid assessment models used to expedite patient care and treatment in EDs and evidence about their effects | Studies reported that rapid assessment models reduced waiting time, length of stay and numbers of patients who left without being seen. Interventions tended to benefit all patients in the ED, not just target conditions, as reducing time in ED for low-acuity patients freed resources for patients with more urgent needs. Staff and patients reported positive reactions. Methodological and reporting quality of papers was mostly moderate or weak, so evidence about the effect of these interventions should be treated with caution |
| Roberts and Mays, 1998217 | Systematic review | ED, patients with minor illness or injury | To assess the extent to which primary–secondary substitution is possible in emergency care | A total of 34 studies of a range of interventions were included. Variable methodological quality. Demand for ED may be reduced by increasing access to primary care or introducing barriers to ED care (e.g. charges), but cost-effectiveness of these approaches is unknown. An alternative, more cost-effective approach is to use primary care professionals within ED to treat patients with non-urgent needs. At the time of the review there was little evidence on impact and cost-effectiveness of telephone triage, minor injuries units and GP OOH co-operatives The results showed no evidence of any significant differences in patient satisfaction or health outcomes between GP and hospital doctor management of patients, and suggests that restricted hospital access carries low levels of risk and was acceptable to patients |
| Egleston, 1998218 | Systematic review | ED, patients with minor illness or injury | A systematic review of the literature on the cost-effectiveness of alternative models of A&E care for the primary care attender | A total of 17 papers were included, 12 of which were from the USA. There was variation in study inclusion criteria, sample size, study length and the definition of a primary care patient. The studies considered different interventions so no conclusions could be drawn on the most cost-effective model of service provision. Summary of the evidence:
|
| Rowe, 2011219 | Systematic review | ED, adult only (> 17 years) or mixed (i.e. child and adult) populations | A systematic review to examine the effectiveness of TLPs on mitigating the effects of ED overcrowding | Twenty-eight studies were included: 13 journal publications, 12 abstracts and three web-based articles. Most studies employed before-and-after designs; 23 of the 28 studies were considered to be of weak quality. Pooling of data from two RCTs found TLPs resulted in shorter ED LOS compared with nurse-led triage (WMD –36.85 minutes, 95% CI –51.11 to –22.58 minutes). One RCT showed a significant reduction in the time to physician assessment associated to TLP presence (WMD –30.00 minutes, 95% CI –56.91 to –3.09 minutes); the other RCT showed no change in LWBS rates (RR 0.82, 95% CI 0.67 to 1.00) |
| Rowe, 2011220 | Systematic review | ED, adult only (> 17 years) or mixed (i.e. child and adult) populations | A systematic review to examine the effectiveness of TNO on ED overcrowding, ED LOS and time to physician initial assessment | Fourteen, mostly single-centre ED, studies included. Most studies had methodological issues. The evidence showed TNO appeared effective at reducing ED LOS, particularly for cases of injury or possible fractures. For injured patients with suspected fracture, three RCTs indicated TNO interventions produced a significant reduction in ED LOS (pooled mean difference –19.7 minutes, 95% CI –37.5 to –1.9 minutes), but result has high heterogeneity (I2 = 92%) TNO interventions comparing emergency physician and emergency NP ordering radiography found a significant reduction in ED LOS (mean difference –37.2 minutes, 95% CI –44.1 to –30.3 minutes) |
| Author, year | Study design | Population/setting | Purpose | Main findings |
|---|---|---|---|---|
| Carter and Chochinov, 2007221 | Systematic review (MEDLINE and CINAHL) | ED; NP | To assess the use of NPs in the ED setting in relation to waiting times; patient satisfaction; quality of care and cost-effectiveness | Quality of care: doctors and NPs were equally competent and accuracy was associated with experience regardless of profession Patient satisfaction: consistently high for both NPs and physicians, but often higher for NPs. NPs explained procedures better than physicians (14.3% for NPs and 6.1% for residents) Waiting times: introducing a NP in a minor injury unit, ED or free-standing unit associated with reduced waiting times Cost-effectiveness: costs of NPs are higher when compared with resident physician costs, but there are no data comparing the cost of NPs with hiring additional medical professionals |
| Wilson, 2009222 | Systematic review | ED; patients aged > 16 years with minor injuries | A systematic review to determine the clinical effectiveness of ED NPs in assessment, treatment and management of minor injuries | Nine studies included in the review: five experimental studies and four descriptive surveys No significant differences in terms of significant errors in care or number of patients followed up for emergency NPs compared with junior doctors or standard care (two RCTs, n = 1652). There was no evidence of statistical heterogeneity for these analyses. The review findings support the use of NPs for management and treatment of minor injuries in adults, but more high-quality studies are needed |
| Doan, 2011223 | Systematic review | EDs employing physician assistants | To describe the role and impact of PAs in the ED | A total of 66 studies, mainly of limited methodological quality, were included. More academic medical centres report using PAs in the ED (65–68% vs. 13–18%). Most of the evidence shows that PAs are able to assess some medical complaints and perform procedures, and are accepted by both ED staff and patients. Evidence is limited as to whether PAs improve ED flow or are cost-effective |
| Author, year | Study design | Population/setting | Purpose | Main findings |
|---|---|---|---|---|
| Conroy, 2011224 | Systematic review of RCTs | Acute hospital setting, discharge of frail older (> 65 years of age) patients, rapid discharge (< 72 hours) | To review the evidence on the impact of CGA on outcomes for frail older patients attending ED | There were only five trials of sufficient quality to include. There was no clear evidence of benefit for CGA interventions for mortality (RR 0.92, 95% CI 0.55 to 1.52), readmissions (RR 0.95, 95% CI 0.83 to 1.08) or for subsequent institutionalisation, functional ability, quality of life or cognition. Study quality was poor and more research is recommended |
| Graf, 2011225 | Systematic review (MEDLINE) | ED, geriatric | To review the literature on the use and value of CGA in ED for evaluation of older patients and its influence on adverse outcomes | Eight controlled or matched studies using CGA efficiency and 14 on screening tools. Use of CGA in ED decreases functional decline, ED readmission and potentially nursing home admission in high-risk patients. Validated screening tools can be applied to detect high-risk patients who will benefit most from CGA There is no evidence that undertaking CGA in ED had any effect on mortality. It is more efficient than age-based screening and, if it is followed by appropriate interventions, will lead to improvements in patient outcomes |
Summary of findings
Reviews of the evidence associated with managing emergency department flow
The interventions included in this theme were most commonly concerned with early patient management processes, such as triage, initiatives to manage flow within the department, such as assessment/observation units and short-stay wards, and initiatives to reduce ED attendances. The most commonly reported outcome measures were reductions in length of ED stay, the proportion of patients leaving without being seen and ED waiting time. Harding et al. 210 found reductions in all three when they examined triage with management options against triage with prioritisation only. Katz et al. 213 found that interventions that developed post-ED plans were generally effective in improving follow-up rates or reducing repeat visits to ED. Porter216 found the same effect when examining rapid assessment models. Triage liaison physicians were reported to have had an impact in reducing ED lengths of stay, compared with nurse-led triage,219 and senior doctor triage could reduce both waiting times and length of stay in the ED. 204
Three reviews assessed the evidence on use of observation or assessment units and short-stay wards. One concluded that assessment or observation units had potential to produce benefits, including facilitating early senior clinician involvement and reducing length of stay and inappropriate admissions, but that this may only apply to specific diagnostic groups. 206 This review did highlight that these process benefits reduced workload, which in itself could then impact on better decision-making. Similarly, a review of short-stay wards for chest pain and asthma patients found potential to reduce length of stay and produce cost savings, but the number of included studies was small and the results not consistent. 207 Another review focused on rapid assessment zone/pod initiatives to reduce ED overcrowding and found that, although the results appeared to suggest a positive effect, the available evidence to support its implementation was limited and weak. 205 A much broader review by Hoot and Aronsky212 identified a number of solutions that may potentially mitigate ED crowding, including use of observation units, increasing staff, referring low-acuity patients out and using queuing theory to manage processes.
Flores-Mateo et al. 208 found that interventions that aim to increase access to primary care and ED cost-sharing are effective in reducing ED use. Both this review and that by Egleston et al. 218 reported that patient education programmes did not have a significant impact on patients with primary care conditions using EDs.
A review assessing the evidence on using Lean processes within ED found that, although there was some indication that they may reduce waiting time, length of ED stay and the proportion of patients leaving without being seen, the evidence was weak and no studies had examined impact on quality of care or patient outcomes. 211
Workforce
We have included a small number of systematic reviews that have focused on assessing the evidence on different professional roles in the ED and particularly changing or expanding roles. A systematic review by Carter and Chochinov221 examined the potential impact of nurse practitioners (NPs) and found that NPs could function as competently as doctors, with consistently high rates of patient satisfaction reported. They concluded that supplementing existing ED staff with NPs can help to manage demand more effectively, especially in high-volume EDs and may also have an important role to play in treating lower-acuity patients in minor injury units. Another review of management of minor injuries by emergency NPs came to broadly the same conclusion that this was a safe and effective way of managing this patient group. 222
The evidence on the clinical effectiveness and cost-effectiveness of physician assistants was less clear. While they were found to be more reliable in assessing particular medical complaints, were more trusted with performing procedures and were approved of by ED staff and patients, there is limited evidence on whether they can improve patient flow or are a cost-effective response. 223 The physician assistant role is well embedded in the US health system, but not in the NHS, so may be of limited relevance. Workforce issues were raised in several other reviews. The review of evidence on use of Lean methods in EDs considered impact on employees and found that Lean thinking may have encouraged frontline staff to take control of their own work and contribute to creating an environment committed to continuous improvement. The increasing ability of staff to take control of their own work was also one of the key findings in the review of rapid assessment models. 216 In addition, the authors also found that rapid assessment models encouraged team working and collective responsibility and helped to improve communication, but also had potential for negative consequences creating longer shifts and more demanding working conditions.
Managing the frail elderly in emergency departments
We identified just two systematic reviews that had appraised the evidence on specific management of the frail elderly patient in the ED and both focused on comprehensive geriatric assessment (CGA), which is a dimensional and usually interdisciplinary diagnostic process to assess a frail older person’s condition. Neither study provided conclusive evidence as to the effectiveness of CGA. Conroy et al. 224 did not find clear evidence for the benefit of CGA on mortality, readmissions, institutionalisation, functional ability, quality of life or cognition. They were also unable to identify any models of care that realise the benefits of CGA in acute, short-term inpatient care. In addition, nor were they able to find any evaluations for interventions for frail older people who are discharged from acute medical units, which are increasingly used in the UK.
Graf et al. 225 suggested that CGA can have a significant impact across many domains, including reducing functional decline and ED readmission. Some of their studies showed that CGA did not have a significant impact on outcomes nor mortality, while others suggested that such an intervention could reduce functional decline. There was mixed evidence over institutionalisation. Applying CGA in the ED was considered to be time-consuming, with the authors presenting the case for shorter and more routinely applicable alternatives.
The literature on CGA suffers from being limited in nature and of variable quality. Some areas, such as adverse outcomes, are under-researched and limited patient outcome data were reported, while the small number of studies examined made it difficult to draw meaningful conclusions.
Quality
Quality issues were generally the same as those discussed in the section on quality in the earlier section in this chapter on GP services in ED. Overall, the quality of the available evidence is generally poor, with a paucity of RCTs. Only one of the 22 systematic reviews we have included utilised solely RCTs in the review;224 another included 14 RCTs in a review of post discharge interventions, but there was a broad range of interventions and settings so general conclusions were difficult to form. 212 Variable metrics used to assess performance precluded meta-analysis in most of these reviews. As previously, there was a high reliance on before-and-after studies and the authors of the reviews included here identified a similar range of limitations as previously discussed, such as poor study design and small sample sizes. Very few studies considered the cost consequences and cost-effectiveness of interventions, and inclusions were dominated by single-centre studies with consequent implications for generalisability; none considered whole-system effects and the impact they may have on the success or failure of particular interventions. Four of the systematic reviews we have included are now quite old (two published in 1998217,218 and two in 2003206,207). Delivery of emergency and urgent care continues to develop and operates in a rapidly changing environment so, although not without some value, at least some of the studies included in these reviews and the inferences drawn from the results may have limited relevance to current service provision.
We have also conducted a simple quality assessment of the 22 systematic reviews included in this section,204–225 using four basic methodological criteria: adequate search, assessment of risk of bias in included studies, use of an appropriate method to synthesise the studies (e.g. meta-analysis or narrative synthesis) and whether or not the authors’ conclusions reflected the evidence presented. Critical appraisals from the Database of Abstracts of Reviews of Effects (DARE) were used, if available. For other reviews, quality was assessed by one researcher, using the full text of the review. The results are given in Table 22.
| Author, year | Adequate search | Risk of bias assessed | Appropriate method of synthesis | Conclusions justified by evidence presented |
|---|---|---|---|---|
| Reviews on managing ED flow | ||||
| Abdulwahid, 2015204 | Yes | Yes | Yes | Yes |
| Bullard, 2012205 | Yes | Yes | Yes | Yes |
| Cooke, 2003206 | Yes | No | Unclear | Unclear |
| Daly, 2003207 | Yes | Unclear | Yes | Unclear |
| Flores-Mateo, 2012208 | Yes | Yes | Yes | Yes |
| Georgiou, 2013209 | Yes | No | Yes | Yes |
| Harding, 2011210 | Yes | Yes | Yes | Unclear |
| Holden, 2011211 | Yes | No | Yes | Yes |
| Hoot and Aronsky, 2008212 | No | No | Yes | Unclear |
| Katz, 2012213 | Yes | Yes | Yes | Unclear |
| Lee, 2008214 | Yes | Yes | Unclear | Yes |
| Paul, 2010215 | Yes | No | Yes | Unclear |
| Porter, 2014216 | Yes | Yes | Yes | Yes |
| Roberts and Mays, 1998217 | Yes | Yes | Yes | Yes |
| Egleston, 1998218 | Yes | No | Yes | Yes |
| Rowe, 2011219 | Yes | Yes | Yes | Yes |
| Rowe, 2011220 | Yes | Yes | Yes | Yes |
| Reviews on ED workforce | ||||
| Carter and Chochinov, 2007221 | Yes | No | Unclear | Yes |
| Wilson, 2009222 | Yes | Yes | Yes | Unclear |
| Doan, 2011223 | Yes | Yes | Unclear | Yes |
| Reviews on management of frail elderly | ||||
| Conroy, 2011224 | Yes | Yes | Yes | Yes |
| Graf, 2011225 | No | No | Unclear | Unclear |
Overall, the reviews performed reasonably well against the four criteria. All except two of the reviews212,225 had an adequate search scope (covering at least two databases and/or other sources). These two reviews only searched MEDLINE or PubMed, therefore they may not have located all relevant studies.
Risk of bias of included studies was assessed using recognised checklists or scales in 13204,205,208,210,213,214,216,217,219,220,222,224 out of 22 reviews. 204–225 In the remainder, risk of bias was either not assessed or no results were reported. In the absence of a risk of bias assessment, it is more difficult to assess the strength of the evidence underlying the review’s conclusions.
Seventeen reviews204,205,207–213,215–220,222,224 were judged to have used an appropriate method to synthesise the studies. In most cases a narrative approach was used because the included studies were too heterogeneous for meta-analysis. Reviews that provided a narrative discussion of the included studies without any description of methods of synthesis have been classified as ‘unclear’.
In most reviews (14204,205,208,209,211,214,216–221,223,224 out of 22204–225), the evidence presented was judged to support the authors’ conclusions. Reviews where the DARE appraisal considered that the authors’ conclusions were potentially unreliable or should be treated with caution have been scored as ‘unclear’.
Conclusions
This rapid review attempting to assess the evidence on different models of delivering ED services has been particularly challenging. The broad focus on a whole service means there are a whole range of potential areas to assess that are of pressing concern, including operational processes at different stages as patients progress through an ED and the issues associated with that (front-door assessment, flow through the department, exit block); workforce issues (who does what, when, how many); and the associations with the wider emergency care or hospital system that impact on performance. The more focused review on co-location of primary care within the ED did identify a relevant and manageable set of existing systematic reviews and primary research studies to allow some synthesis of evidence. Practical constraints meant that for the second part we have only been able to conduct a ‘review of reviews’ but, given the extensive evidence available, we have probably not done this topic area justice and there will be many relevant aspects that we have not considered at all. In addition, given the complexity, it has been difficult to identify clear and unambiguous evidence gaps. However, the review has highlighted some areas that are worth further consideration and can guide future research in this area:
-
In the process of conducting these rapid reviews we have conducted extensive searches and have created a substantial library of relevant research articles. Given the complexity of the topic area, more focused reviews could be carried out utilising the work already done here with, where necessary, targeted focused additional searches. Because of the complexity and because of the rapidly changing environment and pressure on services to implement change, there are already policy and guidance documents from a range of sources, such as the Royal College of Emergency Medicine, setting out interventions that should be implemented,226 many of which may not have a solid evidence base. Before further, more focused reviews are carried out, it may be prudent to consult with the Royal College of Emergency Medicine and identify which specific topic areas would benefit from a more detailed analysis.
-
Although management of the frail elderly is seen as a key area for development9 there is remarkably little research on interventions to improve care for this population. There is scope to identify more recent primary studies from our existing search library to supplement the two existing systematic reviews, as both were published in 2011, and to further review this important area.
-
One clear evidence gap identified from the research we have appraised here is lack of studies that take a broader system approach to identifying, implementing and evaluating interventions to try to improve emergency and urgent care. This has important implications for future service design and planning. Future ED-focused studies could be broadened out to encompass these wider system issues. If this is ignored there is always a risk that some specific interventions may appear to be inefficient or not deliver intended benefits at an individual service level and be abandoned when in fact the benefits may be being achieved elsewhere or some external system issue may be inhibiting an intervention from working optimally.
Chapter 7 Emergency and urgent care networks
Introduction
The final element of the NHS England review6 is focused on the development of broad emergency and urgent care networks with the aim of connecting services together as a system. The vision for these networks is that they will reduce boundaries between hospital- and community-based services and support information flow and expertise across sectors so that patient care can be delivered in the most appropriate and convenient setting. The review initially envisaged that major emergency centres would take the lead in this development, but NHS England has subsequently outlined a wider model based on a combination of strategic and operational functions with no specification on lead (www.england.nhs.uk/2014/05/30/jonathan-benger-2/).
The emphasis on providing emergency and urgent care has seen a shift towards a consensus that a whole-system approach is needed, and emergency and urgent care networks are seen as being central to the achievement of system-wide objectives. In this review, we have attempted to identify whether or not there is any empirical evidence on the organisation, function and effectiveness of emergency and urgent care networks in improving the delivery of emergency and urgent care.
Methods
The methods and search strategy have been described in detail in Chapter 2. Searches were conducted from 1 January 1995 to 21 January 2015. For this review the specific inclusion and exclusion criteria were as follows.
Inclusion criteria
-
Focused on whole-system emergency and urgent care.
-
Network operating models used in practice.
-
Empirical assessment of network performance or effectiveness.
Exclusion criteria
-
Descriptive studies with no assessment of effect.
The results of the searches are given in Figure 7.
FIGURE 7.
A PRISMA flow diagram for emergency and urgent care networks searches.
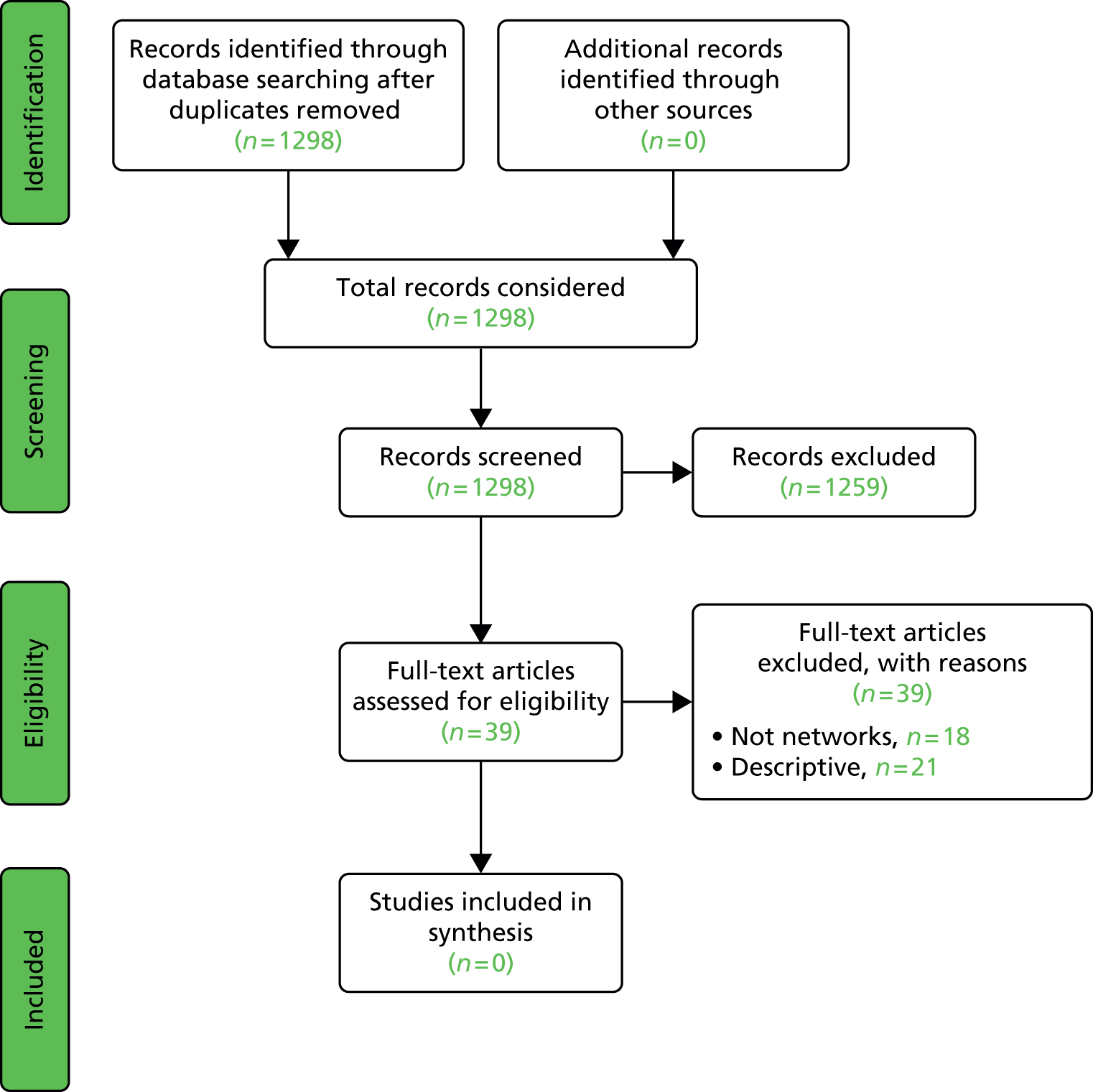
Results
We found no relevant papers that fulfilled the inclusion criteria; that is, that provided a description of an operating emergency and urgent care network model with some empirical evidence of how it performed and produced an impact on health-care delivery. There were 21 papers that were related to networks and the delivery of health care, but these were predominantly related to the following study types:
-
Descriptive studies of clinical networks for specific conditions or patient groups, but with no assessment of effect. For example, a clinical network to provide care pathways for aboriginal and Torres Straights populations with acute coronary syndromes,227 a model of a trauma network in the USA228 and, perhaps more relevant, a network for integrating ambulance services and acute hospitals in the Netherlands. 229 The description for this network included a statement that government policy had been put in place to monitor development, but no outputs have been identified.
-
Studies reporting data on activity within clinical networks for specific conditions such as stroke,230,231 trauma,232,233 primary or community care234,235 and ST elevation myocardial infarction. 236 Most of these studies claimed that clinical networks had improved care by, for example, increasing numbers of patients admitted to specialist facilities,230,232 receiving thrombolysis for stroke231 and improving mortality from trauma,233 but all of them reported current activity and had not made any assessment of differences in care compared with before the network became operational or, therefore, whether the network had improved care.
Perhaps more useful in terms of providing insights into factors that aid or inhibit network function, and so provide lessons for emergency and urgent care network development, are the small number of qualitative studies that have examined this area in more detail. One study of health-care professionals’ perceptions about the functioning of a gerontological network highlighted three key characteristics: (1) the central role of GPs in co-ordinating care, (2) geriatrician’s intervention in assessment of older patients’ needs and (3) the interface between hospitals, GPs and homecare. Lack of collaboration hindered network function. 237 A UK study of the network governance lessons from a programme aimed at improving care for older people and reducing emergency bed-days identified some helpful lessons. 238 The study found features associated with effective network governance included the selection of a small number of evidence-based services, co-ordination by a network-based strategic group with clear responsibility for implementation at operational level and a ‘joined at the top’ implementation group.
There were a small number of papers that did have an emergency and urgent care network focus but were of limited value in terms of providing evidence on successful and effective network models. One UK paper describes attempts to develop an early emergency care system in Surrey,239 although this is now old, the NHS environment has changed substantially since then and there appear to be no subsequent outputs demonstrating success or further development. Two papers emerged from a US consensus conference on integrated networks of emergency care. One sets out a conceptual framework for how categorise, designate and regionalise services within a network and identifies a range of research opportunities needed to support this process, including contributing to design, processes, utility and impact on patient outcomes. 240 The other sets out a research strategy for developing methods for defining and measuring success in emergency care networks and the infrastructure needed to support it, including identifying key metrics, scaling, network data systems and data linkage. 241 These two papers set out an ‘aspirational’ view of future emergency care networks and there may be some value in considering the conceptual approaches they have described when thinking about network development; however, they do not provide any information on how these aspirations might be operationalised into a functioning network.
Conclusions
We have found no evidence base on how to best organise and operate an emergency and urgent care network with associated empirical evidence to demonstrate the effectiveness of a network model in managing and improving delivery of care. There is some related evidence from other types of clinical networks but these are very focused in their remit. While they may provide some useful insight for network development, strategies that work in improving care for specific conditions or groups of patients with clear and well-developed care pathways may not be transferable to the complex, broad population-based, whole-system-based focus of emergency and urgent care networks. Literature on networks within the specific topic area of emergency and urgent care is scant and confined to descriptive articles or ‘think pieces’ about the conceptual and aspirational frameworks for network-based models rather than examples of functioning network models. We conducted some descriptive research on this topic for the Department of Health in 2007, which described a small number of embryonic emergency and urgent care networks in existence at the time,242 but which subsequently disbanded or changed with multiple reorganisations. This report did suggest some principles for network development based on the experiences of the early study sites, which have been translated into the NHS England suggested model, but we did not measure network effectiveness.
Given that emergency and urgent care networks are a key component of the delivery of the NHS England review, there is remarkably little evidence and information available to inform this development. Anecdotally, health economies are building networks, but there is no information available at a national level about the structure and operating models of existing networks, nor indeed about how many there are. It is likely that networks are developing in isolation, which limits opportunities for sharing experiences about network model design, development and implementation.
There are some key and pressing research activities that could support emergency and urgent care-network development:
-
A more detailed and targeted rapid review could be undertaken to further explore the more theoretical literature about network model development and implementation to supplement the small descriptive evidence we have identified. More detailed synthesis could provide evidence on central components and strategies for successful network development that could be used to underpin network development now taking place.
-
Of course, it may be the case that this additional evidence review would come too late and that nationally network development is already under way, although there may still be some value in modifying existing models. There is a paucity of information about activity in an area viewed as being of such strategic importance in terms of delivering a whole-system approach to emergency and urgent care. Some rapid scoping research to identify and map current emergency and urgent network development nationally could provide useful information about numbers, size, models, state of maturity, etc. This could be supplemented by more qualitative work to identify the more detailed issues associated with developing and implementing a network model, including challenges, barriers and facilitators, which can then be shared.
-
A programme of research to evaluate emergency and urgent care progress using case study sites identified from the work suggested above. This would need to be a long-term strategy involving comparing different models of networks to assess processes, operation and management and, ultimately, to measure effectiveness and the extent to which different models change and improve the delivery of urgent care and achieve the objectives set out in the NHS England review plan.
-
Information will be a central component of network function. Chapter 3 set out the importance of whole-system information systems that will allow better understanding of demand and inform planning of services needed to meet that demand. Chapters 4, 5 and 6 have highlighted the need to evaluate service developments in terms of whole-system as well as individual service impact. Development of robust and linked patient-based data systems will be needed to support these activities. Research to better understand the information needs of emergency and urgent care systems and networks and map this onto existing information-system development by other parts of the NHS, for example the Academic Health Science Networks, the Health & Social Care Information Service, NHS England and local initiatives, could inform the development of a coherent national plan for network information-system development.
Chapter 8 Discussion and conclusions
Summary of main findings
We have conducted five separate rapid reviews spanning a range of themes relevant to the NHS England review of emergency and urgent care. 6 A comprehensive discussion and conclusions are provided at the end of each review chapter. The main findings from each review are briefly summarised here.
Demand for emergency and urgent care
Despite serious concerns about rising demand and the impact this has on health services, there is remarkably little empirical evidence that can fully explain why this has occurred. Much of the evidence has focused on individual services or populations, such as the elderly. Although there is a substantial evidence base that has explored patient reasons for accessing urgent care, there is a lack of any sophisticated understanding about what is driving demand for individual emergency and urgent care services and no published literature on whole-system demand. In the UK, the only recent evidence about whole-system demand is that available in the evaluation examining the impact of NHS 111 pilot sites,105 and a lack of any data within this on in-hours GP urgent care means the whole picture remains unclear. There is a broad literature of discrete studies on individual factors that may influence demand. The key evidence gaps and challenges identified from the existing evidence relate to:
-
a need to examine demand from a whole-system perspective and to gain better understanding of the relative proportions of demand for different parts of the system and the characteristics of patients within each sector
-
development of research studies that build on existing knowledge about factors which may be influencing demand and the contribution each one makes and map these in to a coherent system model. This would then support the development of service design and planning to meet current and future needs of local populations.
Telephone triage and advice
There is an existing, substantial evidence base about the operational and clinical effectiveness of telephone-based triage and advice services for management of requests for urgent health care. Overall, these services provide accurate, appropriate and safe decision-making and patient compliance with advice is generally high, as is patient satisfaction. Where calls have been judged to have been inaccurately or inappropriately triaged, the tendency is to assign calls to a higher level of care than needed rather than a lower level so although services appear to be safe, they may not be efficient. Evidence gaps and aspects of service delivery that warrant further study include:
-
Further assessment of the whole-system impact of telephone access services for emergency and urgent care, including the associated costs, to establish how it contributes to improving system efficiency.
-
More focused research on the broad area of the optimum requirements for different skill levels needed in the NHS 111 service, which provides a unique mix of non-clinical, clinical and senior/specialist clinical professionals.
-
More detailed evaluation of the accuracy and appropriateness of call assessment decisions would help answer some of the questions about the appropriateness of referrals made by the NHS 111 service and identify where there is scope to improve it, either through changing the staffing profile, modifying the clinical assessment system or developing better referral pathways.
Management of patients with urgent care needs by the ambulance service in community settings
Extended paramedic roles have been implemented in various health systems and settings and, based on a small number of high quality studies, appear to be successful at reducing transports to hospital, making safe decisions about the need for transport, delivering acceptable care out of hospital and potentially cost-effective. The key evidence gaps and areas for further research we have identified include:
-
Further work on the development of methods to support paramedic decision-making in the community, together with development and assessment of out of hospital care pathways for a range of conditions that mediate safe management in the community.
-
More detailed study on the necessary skill mix of the paramedic workforce, optimum proportions of paramedics and paramedics with advanced and specialist skills needed to provide a safe and high-quality, community-based service for patients and the educational and training needs to support this enhanced role at scale. The potential impact of increasing paramedic prescribing rights will also need to be considered.
-
More accurate estimations of the likely proportion of patients who could be safely managed out of hospital to support paramedic workforce planning.
-
Further evaluation of the impact of initiatives to develop paramedic practice and increase the number of patients managed in the community is needed to assess the impact of these initiatives at scale and at a whole-system level and the cost consequences.
Models of service delivery in the emergency department
Attempting to assess the evidence on different models of delivering ED services has been particularly challenging, as there is a substantial range of potential areas to assess. The more focused review on co-location of primary care and EDs identified potential for this initiative. Practical constraints meant that, for the second part, we have only been able to conduct a ‘review of reviews’ and, given the extensive evidence available and complexity of the subject area, it has been difficult to identify clear and unambiguous evidence gaps. The review has highlighted some areas worth further consideration:
-
More focused reviews could be carried out utilising the work already done here with, where necessary, targeted and focused additional searches. Because of the complexity and the rapidly changing environment, some consultation with the Royal College of Emergency Medicine would help to identify which specific topic areas would benefit from a more detailed analysis.
-
Management of the frail elderly is considered a key area for development, but there is little evidence on interventions to improve care for this population. There is scope to identify more recent primary studies from our existing search library to supplement the analysis of two related systematic reviews.
-
One clear evidence gap is the lack of studies conducted at scale and that have considered wider system effects and impact. Given the emphasis on developing co-located primary care services within EDs, this is one area where there is a clear opportunity to begin to undertake these broader studies.
Emergency and urgent care networks
We have found no evidence base on how to best organise and operate an emergency and urgent care network, nor any empirical evidence on effectiveness of a network model in managing and improving delivery of care. There is some related evidence from other types of clinical networks, but these are very focused in their remit. Although they may provide some useful insight for network development, strategies that work in improving care for specific conditions may not be transferable to the complex, broad population, multiple service-based focus of emergency and urgent care networks. Literature on networks within the specific topic area of emergency and urgent care is scant and confined to descriptive articles. Given that emergency and urgent care networks are a key component of the delivery of the NHS England review, there is a significant evidence gap and hence some key and pressing research activities that could support emergency and urgent care network development:
-
A more detailed and targeted rapid review could be undertaken to further explore the more theoretical literature on network model development and provide evidence around central components and strategies for successful network development.
-
Network development is already under way, so some rapid scoping research to identify and map current emergency and urgent network development nationally could provide useful information on numbers, size, models, state of maturity and issues associated with developing and implementing a network model.
-
A programme of research to evaluate emergency and urgent care network progress using case study sites to compare different models of networks and assess processes, operation and management. In the longer term, studies are needed to measure effectiveness and the extent to which different models change and improve the delivery of urgent care and achieve intended objectives.
Evidence sources
For some themes a substantial proportion of the existing evidence came from the UK. A total of 85% of the included studies on expanded roles for paramedics were conducted in the UK, as were 37% of the studies on telephone triage. A relatively small proportion of studies on providing primary care in EDs (17%) were conducted in the UK. No studies on trends in demand came from the UK, but almost half of the studies examining patient reasons for accessing urgent care (48%) came from the UK.
Common themes across subject areas
We have conducted five separate reviews focused on specific areas of service delivery, and the synthesis of evidence for each individual review revealed a number of common themes that spanned one or more topic areas. This fits with the view that delivery of emergency and urgent care needs to be viewed from a whole-system perspective and highlights the clear interdependencies between the different system components that contribute to efficiency and effectiveness.
Although the theme on understanding demand for urgent and emergency care is not a key theme in the NHS England review, we included it in this rapid review to provide context for the underlying issues that are contributing to pressure in the emergency and urgent care system and hence the need for service change. The issues and evidence gaps identified from the analysis of evidence on trends in and characteristics of demand were relevant to several subject areas. The most highly relevant was emergency and urgent care networks. The envisaged primary function of a network is to design and plan an emergency and urgent care system that can meet the needs of a heterogeneous and changing population with a range of complex health problems ranging from acute and life-threatening to minor and chronic illness and injury. To do this, a detailed understanding of the profile of the population accessing care, the different types of care they will need and the relative proportion of people requiring different types of service within the system is needed. The identified need to develop more sophisticated models that map demand and the needs of local populations and can begin to estimate how this will change as population characteristics change has direct relevance to the potential successful functioning of an emergency and urgent care network.
At an individual service level this also has implications for the success of the expected changes in delivery of care. For example, clear estimates and thresholds for the likely proportion of patients who could be safely managed in the community by the ambulance service would inform ambulance service resource and workforce planning. Similarly, initiatives in the ED to better manage specific patient groups require information on the likely volumes of patients who, for example, will be suitable for GP care in a co-located primary care unit or a specialist major trauma or frail elderly care service.
System design and developed care and referral pathways
The need for system wide, integrated care and referral pathways was highlighted in the chapters on Telephone triage and advice and Management of patients with urgent care needs by the ambulance service in community settings. In both cases this was seen as critical to further development of these services if they are to operate efficiently and fulfil their potential. The development of these pathways and testing their effectiveness links to the functioning of networks.
Whole-service and -system impact
A common theme across all three service delivery-related reviews was the lack of evidence about the impact of initiatives and interventions at scale. The available evidence is based almost exclusively on evaluations of single initiatives in single centres. This means that, for example, the impact of NHS 111 on delivering system benefits by directing people to appropriate care nationally or at a single-service level, now that services are much bigger than the pilot services, is unknown. Likewise, although there is good evidence that paramedics can safely manage people in the community, the implications for scaling up interventions for ambulance services and associated primary and community care services (particularly as the desired proportion of patients managed in this way increases) and the impact on, for example, ED crowding, are unknown. The impact of scaling-up initiatives on both individual and whole-system activity, effectiveness and costs is a clear research gap. A final and related theme is that future evaluations of initiatives should be of sufficient length to allow the intervention to mature and function as intended. The risk of not doing this, and of only evaluating the impact on the ‘host’ service rather than the system, is that promising and potentially effective interventions are abandoned, owing not to lack of evidence but lack of the right sort of evidence. 104,201 Well functioning networks with robust information systems will be essential for enabling measurement of whole-system impacts and costs.
Limitations
The scope of this rapid review and the volume of evidence included mean we have not been able to conduct a detailed analysis of the quality of the evidence base; however, we have provided a broad assessment and commentary of relevant issues in each of the separate review chapters. We have included a substantial number of systematic reviews within this review and have drawn on the findings of these studies to identify significant methodological issues. In addition to the limitations regarding lack of scale and measurement of system impact already discussed, some key themes have been identified that are common across the reviews:
-
Overall, the evidence base on clinical effectiveness and cost-effectiveness of different models of care for delivering emergency and urgent care is weak. Only a small number of interventions have been evaluated using RCT designs. It is acknowledged, however, that this is a difficult environment in which to conduct this type of study.
-
There is a high reliance on uncontrolled before-and-after studies within the overall evidence base, with consequent serious limitations on interpretation of findings. The majority of studies were single-site and small in scale, with small sample sizes. This makes generalisability difficult, particularly in terms of relevance to different health systems. There is a lack of population-based studies to inform development of emergency and urgent care systems and services.
-
The majority of studies have measured processes, such as times, attendance or contact rates, re-admission and recontact rates, to assess effectiveness. With a few exceptions, patient outcome measures have been confined to patient satisfaction, and there has been little consideration of important patient outcome measures concerned with safety, such as adverse events. The reviews on telephone triage and management of patients by paramedics in the community did identify studies that included patient safety.
-
Little attention has been paid to the costs and cost-effectiveness associated with interventions.
There are some limitations to the rapid review method we have used. First, we have not been able to exhaustively search for and synthesise all the relevant literature for each of the five themes. We have drawn extensively on existing systematic reviews and only extracted detailed information on primary studies not included in these reviews. This has allowed us to provide a comprehensive overview of the existing evidence base for each theme. However, this was a particular limitation for the review of models of care for delivering ED services. For this theme we only included systematic reviews and therefore have not been able to confidently identify the related evidence gaps. This theme warrants additional, more focused reviews.
Second, emergency and urgent care encompasses a broad patient population, range of services and related factors. Given the potential scope and scale, we have used a framework to guide the reviews, based on the key policy objectives for emergency and urgent care set out in the related NHS England review,6 in order to provide focus and relevance. This framework also guided the systematic search strategies tailored to each individual review but, given the scope, we have further restricted the focus of two themes (helping people get the right advice and managing more urgent care outside hospital) to the specific areas of telephone-based triage and advice and management of patients by paramedics in the community, respectively. This does mean that the broader literature on community-based urgent care services has not been addressed.
Third, although using the framework provided structure that enabled us to synthesise a large body of evidence in a short time frame, it does mean that there are related themes and subject areas that have been excluded from this review. The most obvious gap is a separate review of models of urgent care within primary care. There is significant overlap within the existing reviews, for example, telephone triage, management of patients by paramedics within the community setting and provision of primary care services within the ED. However, there may be more specific evidence we have not considered. There is scope to conduct an additional review within this area utilising the search libraries we have generated for this review. We have also not considered the specific but important issues related to the emergency and urgent care workforce, such as education, training, skills, recruitment and retention. This may also warrant an additional review, although it would be large in scope as there is a wide range of professional groups to consider.
Finally, the short time frame and volume of included material meant we were not able to include any patient and public involvement input in this review. However, this perspective will be important when considering future research commissioning. We have identified a substantial number of evidence gaps which will need to be prioritised, and patient and public involvement assessment of those gaps and questions will be of value in understanding which ones are most important to patients and the public and which need most urgently addressing.
Conclusions
We have conducted five separate rapid evidence reviews on themes related to the delivery of emergency and urgent care in the NHS. These themes were (1) trends in and characteristics of demand; (2) telephone triage and advice; (3) management of patients in the community by ambulance clinicians; (4) models of service delivery in the ED; and (5) emergency and urgent care networks.
We have found there is a paucity of evidence to explain the complex reasons that have driven the increases in demand for emergency and urgent care and the detailed characteristics and consequent service needs of the population. There exists a considerable evidence base on the effectiveness of some interventions for improving service delivery, but overall the evidence base is weak and based in small single-site studies, with no assessment of impact at scale or on the wider emergency and urgent care system. A small number of interventions have been robustly evaluated. The delivery of ED care is complex and multidimensional and it was beyond the scope of this review to identify clear evidence gaps. Furthermore, more focused evidence reviews are needed in this area. There is no evidence to support the development of emergency and urgent care networks.
We have identified a number of evidence gaps across the reviews. The gaps that appear to be in most immediate need of addressing are detailed below:
-
Research to characterise and map demand at a population level and link this to service need so that emergency and urgent care systems can be designed that can effectively, efficiently and safely respond to patient needs.
-
An assessment of the current state of play in the development of emergency and urgent care networks and longer-term evaluation of the effectiveness of different network models to identify how best networks can deliver NHS England objectives.
-
Expanding the current evidence base on existing interventions that are viewed as central to delivery of the NHS England plan, such as increasing the number of patients managed by paramedics in the community, by developing integrated care pathways and assessing the implications of increasing the intervention at scale. Measurement of the costs and system impact will be critical to the assessment of effectiveness and resource requirements needed to support expansion.
Although not an evidence gap, a clear theme that emerged across the reviews was the need for robust, high-quality and linked patient data to support service planning, measure whole-system benefits and costs and support research. This may need to be addressed alongside any newly commissioned research studies.
There is also a need to plan and design better-quality research studies. Some of the problems associated with existing research studies have been highlighted above. Future research will need to address these problems. The broad range of questions evident from the research gaps means a range of designs will be needed to adequately answer these questions. It is not possible to be prescriptive, as each question will need a different approach, but there is a clear need to move away from uncontrolled studies toward better use of quasi-experimental observational studies that do allow comparison against current practice. Evidence gaps concerned with scaling-up interventions would benefit from mixed-methods approaches that can consider a range of associated issues. Clinical effectiveness may have been demonstrated, but translating this into common practice needs consideration of both the population (quantitative) effects across multiple sites or whole systems and, as importantly, the ‘real-world’ processes that effect change and mediate successful adoption of new ways of delivering services. Valuable knowledge can be gained from more qualitative studies that can identify the factors and processes that contribute to success or failure of service change. This is linked to the clear lack of consideration of workforce implications apparent in the existing evidence. Future studies, particularly those concerned with scaling up, cannot ignore this component, and specific studies providing a primary assessment of workforce and skill mix requirements may need to be a precursor to any large scale expansion of interventions. Existing studies have also been limited by only measuring short-term process and outcome changes and future studies could make better use of, for example, interrupted time series designs to provide a more robust assessment of the impact of service changes in the longer term. Robust economic evaluations should also be conducted alongside any changes to assess cost-effectiveness, as well as the broader cost shifting that occurs around an emergency care system when large-scale service delivery changes are implemented.
There are significant problems within the emergency and urgent care system in the NHS. In consequence, there is pressure to instigate change and services are operating in a rapidly changing environment. Specific programmes, such as the NHS England review delivery plan,8 refer to a number of existing pilot schemes and interventions under development. There are also broader programmes across the NHS that may also have an impact on emergency and urgent care, such as the move to 7-day working, the Prime Ministers Challenge Fund to improve access to primary care (URL: www.england.nhs.uk/ourwork/qual-clin-lead/calltoaction/pm-ext-access/) and vanguard sites for new models of care deliver (URL: www.england.nhs.uk/ourwork/futurenhs/5yfv-ch3/new-care-models/ and local initiatives). These programmes mean that there are already potentially large numbers of relevant initiatives already under way or in development, but it is difficult to identify the range and scope of existing projects. Before new research to address evidence gaps is commissioned, it may be worth considering commissioning a preliminary project to identify and map existing plans and initiatives to distinguish if any evaluation research is already under way, whether or not the planned evaluation is robust and whether or not there are potentially suitable initiatives that are at development stage but have no evaluation plan in place. This could reduce duplication of effort and help ensure new models of care are rigorously assessed before they are adopted on a large scale.
Acknowledgements
The authors of this report have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HSDR editors have tried to ensure the accuracy of the authors’ work and would like to thank the reviewers for their constructive comments; however, they do not accept liability for damages or losses arising from material published in this web report.
The National Institute for Health Research Health Services and Delivery Research team
Professor Suzanne Mason (University of Sheffield) provided assistance with identifying key components of ED processes and accessing related papers currently in press and in preparation.
Dr Matthew Booker (University of Bristol) provided access to references included in a recently completed related review undertaken as part of an NIHR postdoctoral research fellowship.
Professor Andy Newton (Chair of the College of Paramedics) advised on current developments in paramedic education.
Contribution of authors
Ms Janette Turner (Senior Research Fellow) undertook reference sifting and evidence synthesis for the review on demand for urgent care; undertook reference sifting, data extraction into summary tables and evidence synthesis for the review on emergency and urgent care networks; contributed to writing the report, including the discussion and conclusions; and managed the project.
Mrs Joanne Coster (Research Fellow) undertook reference sifting, data extraction into summary tables, evidence synthesis and contributed to writing the report for the review on telephone triage.
Dr Duncan Chambers (Research Fellow) undertook reference sifting, data extraction into summary tables, evidence synthesis and contributed to writing the report for the review on management of patients by ambulance clinicians in the community.
Mrs Anna Cantrell (Information Specialist) contributed to the proposal writing, designed and ran the literature searches, and contributed to writing the report.
Mr Viet-Hai Phung (Research Assistant) undertook reference sifting, data extraction into summary tables and evidence synthesis, and contributed to writing the report for the review on models of care in the ED.
Dr Emma Knowles (Research Fellow) undertook reference sifting for the review on management of patients by ambulance clinicians in the community.
Mr Daniel Bradbury (Medical Student) undertook data extraction into summary tables for the review on demand for urgent care.
Professor Elizabeth Goyder (Professor of Public Health) contributed to the proposal writing.
Data sharing statement
No new data have been created.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
References
- Emergency Care Forum. Ripping Off the Sticking Plaster: Whole System Solutions for Urgent and Emergency Care. London: NHS Confederation; 2014.
- Urgent and Emergency Services. London: The Stationery Office; 2013.
- Stretched to the Limit: A Survey of Emergency Medicine Consultants in the UK. London: College of Emergency Medicine; 2013.
- Securing the Future GP Workforce: Delivering the Mandate on GP Expansion. GP Taskforce Final Report. London: Health Education England; 2014.
- Partial Review of the Shortage Occupation Lists for England and Scotland. London: Migration Advisory Committee; 2015.
- High Quality Care for All, Now and for Future Generations: Transforming Urgent and Emergency Care Services in England – Urgent and Emergency Care Review End of Phase 1 Report. Leeds: NHS England; 2013.
- Dixon-Woods M. Using framework-based synthesis for conducting reviews of qualitative studies. BMC Med 2011;9. http://dx.doi.org/10.1186/1741-7015-9-39.
- Urgent and Emergency Care Update. August 2014. Leeds: NHS England; 2014.
- Acute and Emergency Care – Prescribing the Remedy. London: College of Emergency Medicine; 2014.
- Fisher J, Salman B, Cooke M, Carson D, Clay H, Stern R. Primary Care and Emergency Departments. London: Primary Care Foundation; 2010.
- Nicholl J, Mason S. Return of the “corridors of shame?”. BMJ 2013;346. http://dx.doi.org/10.1136/bmj.f4343.
- Blunt I, Edwards N, Merry L. What’s Behind the A&E ‘Crisis’? Policy Briefing No.3. London: Nuffield Trust; 2015.
- Turner J. Building the Evidence Base in Pre-hospital Emergency and Urgent Care: A Review of Research Evidence and Priorities for Future Research. London: Department of Health; 2010.
- Lowthian JA, Curtis AJ, Cameron PA, Stoelwinder JU, Cooke MW, McNeil JJ. Systematic review of trends in emergency department attendances: an Australian perspective. Emerg Med J 2011;28:373-7. http://dx.doi.org/10.1136/emj.2010.099226.
- He J, Hou XY, Toloo S, Patrick JR, Fitz Gerald G. Demand for hospital emergency departments: a conceptual understanding. World J Emerg Med 2011;2:253-61. http://dx.doi.org/10.5847/wjem.j.1920-8642.2011.04.002.
- Lowthian JA, Cameron PA, Stoelwinder JU, Curtis A, Currell A, Cooke MW, et al. Increasing utilisation of emergency ambulances. Aust Health Rev 2011;35:63-9. http://dx.doi.org/10.1071/AH09866.
- Gruneir A, Silver MJ, Rochon PA. Emergency department use by older adults: a literature review on trends, appropriateness, and consequences of unmet health care needs. Med Care Res Rev 2011;68:131-55. http://dx.doi.org/10.1177/1077558710379422.
- Leonard C, Bein KJ, Latt M, Muscatello D, Veillard AS, Dinh MM. Demand for emergency department services in the elderly: An 11 year analysis of the Greater Sydney Area. Emerg Med Australas 2014;26:356-60. http://dx.doi.org/10.1111/1742-6723.12250.
- Pines JM, Mullins PM, Cooper JK, Feng LB, Roth KE. National trends in emergency department use, care patterns, and quality of care of older adults in the United States. J Am Geriatr Soc 2013;61:12-7. http://dx.doi.org/10.1111/jgs.12072.
- FitzGerald G, Toloo S, Rego J, Ting J, Aitken P, Tippett V. Demand for public hospital emergency department services in Australia: 2000–2001 to 2009–2010. Emerg Med Australas 2012;24:72-8. http://dx.doi.org/10.1111/j.1742-6723.2011.01492.x.
- Lowthian JA, Curtis AJ, Jolley DJ, Stoelwinder JU, McNeil JJ, Cameron PA. Demand at the emergency department front door: 10-year trends in presentations. Med J Aust 2012;196:128-32. http://dx.doi.org/10.5694/mja11.10955.
- Lowthian JA, Jolley DJ, Curtis AJ, Currell A, Cameron PA, Stoelwinder JU, et al. The challenges of population ageing: accelerating demand for emergency ambulance services by older patients, 1995–2015. Med J Aust 2011;194:574-8.
- Chu K, William AB, Lukin W. Local trends in emergency department attendances by older patients in an ageing national population. Aust Health Rev 2009;33:117-23. http://dx.doi.org/10.1071/AH090117.
- Moll van Charante EP, van Steenwijk-Opdam PC, Bindels PJ. Out-of-hours demand for GP care and emergency services: patients’ choices and referrals by general practitioners and ambulance services. BMC Fam Pract 2007;8. http://dx.doi.org/10.1186/1471-2296-8-46.
- Margolis SA, Reed RL. Changing use of the emergency department by the elderly in the United Arab Emirates, 1989 and 1999. East Mediterr Health J 2002;8:409-15.
- Amiel C, Williams B, Ramzan F, Islam S, Ladbrooke T, Majeed A, et al. Reasons for attending an urban urgent care centre with minor illness: a questionnaire study. Emerg Med J 2014;31:E71-5. http://dx.doi.org/10.1136/emermed-2012-202016.
- Booker MJ, Simmonds RL, Purdy S. Patients who call emergency ambulances for primary care problems: a qualitative study of the decision-making process. Emerg Med J 2014;31:448-52. http://dx.doi.org/10.1136/emermed-2012-202124.
- Lobachova L, Brown DFM, Sinclair J, Chang YC, Thielker KZ, Nagurney JT. Patient and provider perceptions of why patients seek care in emergency departments. J Emerg Med 2014;46:104-12. http://dx.doi.org/10.1016/j.jemermed.2013.04.063.
- Shaw EK, Howard J, Clark EC, Etz RS, Arya R, Tallia AF. Decision-making processes of patients who use the emergency department for primary care needs. J Health Care Poor Underserved 2013;24:1288-305. http://dx.doi.org/10.1353/hpu.2013.0140.
- Schumacher JR, Hall AG, Davis TC, Arnold CL, Bennett RD, Wolf MS, et al. Potentially preventable use of emergency services: the role of low health literacy. Med Care 2013;51:654-8. http://dx.doi.org/10.1097/MLR.0b013e3182992c5a.
- Toloo G, FitzGerald GJ, Aitken PJ, Ting JYS, McKenzie K, Rego J, et al. Ambulance use is associated with higher self-rated illness seriousness: user attitudes and perceptions. Acad Emerg Med 2013;20:576-83. http://dx.doi.org/10.1111/acem.12149.
- Agarwal S, Banerjee J, Baker R, Conroy S, Hsu R, Rashid A, et al. Potentially avoidable emergency department attendance: interview study of patients’ reasons for attendance. Emerg Med J 2012;29. http://dx.doi.org/10.1136/emermed-2011-200585.
- Becker J, Dell A, Jenkins L, Sayed R. Reasons why patients with primary health care problems access a secondary hospital emergency centre. S Afr Med J 2012;102:800-1. http://dx.doi.org/10.7196/samj.6059.
- Fieldston ES, Alpern ER, Nadel FM, Shea JA, Alessandrini EA. A qualitative assessment of reasons for nonurgent visits to the emergency department: parent and health professional opinions. Pediatr Emerg Care 2012;28:220-5. http://dx.doi.org/10.1097/PEC.0b013e318248b431.
- Gomide MFS, Pinto IC, de Figueiredo LA. Accessibility and demand at an Emergency Care Unit: the user’s perspective. Acta Paul Enferm 2012;25:19-25. http://dx.doi.org/10.1590/S0103-21002012000900004.
- Marco CA, Weiner M, Ream SL, Lumbrezer D, Karanovic D. Access to care among emergency department patients. Emerg Med J 2012;29:28-31. http://dx.doi.org/10.1136/emj.2010.103077.
- Müller U, Winterhalder R, Businger A, Zimmermann H, Exadaktylos AK. Why do walk-in patients prefer a busy urban emergency department during office hours? A pilot survey of 200 consecutive patients from Switzerland. Swiss Med Wkly 2012;142. http://dx.doi.org/10.4414/smw.2012.13565.
- Penson R, Coleman P, Mason S, Nicholl J. Why do patients with minor or moderate conditions that could be managed in other settings attend the emergency department?. Emerg Med J 2012;29:487-91. http://dx.doi.org/10.1136/emj.2010.107276.
- Wilkin HA, Cohen EL, Tannebaum MA. How low-income residents decide between emergency and primary health care for non-urgent treatment. Howard J Commun 2012;23:157-74. http://dx.doi.org/10.1080/10646175.2012.667725.
- Nelson J. Why patients visit emergency units rather than use primary care services. Emerg Nurse 2011;19:32-6. http://dx.doi.org/10.7748/en2011.04.19.1.32.c8448.
- McGuigan T, Watson P. Non-urgent attendance at emergency departments. Emerg Nurse 2010;18:34-8.
- Oetjen RM, Oetjen DM, Rotarius T, Liberman A. Emergency department utilization by insured users: a study of motivating factors. Health Care Manag 2010;29:199-212. http://dx.doi.org/10.1097/hcm.0b013e3181e8e077.
- Adamson J, Ben-Shlomo Y, Chaturvedi N, Donovan J. Exploring the impact of patient views on ‘appropriate’ use of services and help seeking: a mixed method study. Br J Gen Pract 2009;59:e226-33. http://dx.doi.org/10.3399/bjgp09X453530.
- Scott DR, Batal HA, Majeres S, Adams JC, Dale R, Mehler PS. Access and care issues in urban urgent care clinic patients. BMC Health Serv Res 2009;9. http://dx.doi.org/10.1186/1472-6963-9-222.
- Benger JR, Jones V. Why are we here? A study of patient actions prior to emergency hospital admission. Emerg Med J 2008;25:424-7. http://dx.doi.org/10.1136/emj.2007.050856.
- Jacob SL, Jacoby J, Heller M, Stoltzfus J. Patient and physician perspectives on ambulance utilisation. Prehosp Emerg Care 2008;12:176-81. http://dx.doi.org/10.1080/10903120701710058.
- Redstone P, Vancura JL, Barry D, Kutner JS. Nonurgent use of the emergency department. J Ambul Care Manage 2008;31:370-6. http://dx.doi.org/10.1097/01.JAC.0000336555.54460.fe.
- Hodgins MJ, Wuest J. Uncovering factors affecting use of the emergency department for less urgent health problems in urban and rural areas. Can J Nurs Res 2007;39:78-102.
- Norredam M, Mygind A, Nielsen AS, Bagger J, Krasnik A. Motivation and relevance of emergency room visits among immigrants and patients of Danish origin. Eur J Public Health 2007;17:497-502. http://dx.doi.org/10.1093/eurpub/ckl268.
- Campbell NC, Iversen L, Farmer J, Guest C, MacDonald J. A qualitative study in rural and urban areas on whether – and how – to consult during routine and out of hours. BMC Fam Pract 2006;7. http://dx.doi.org/10.1186/1471-2296-7-26.
- Worth A, Boyd K, Kendall M, Heaney D, Macleod U, Cormie P, et al. Out-of-hours palliative care: a qualitative study of cancer patients, carers and professionals. Br J Gen Pract 2006;56:6-13.
- Palmer CD, Jones KH, Jones PA, Polacarz SV, Evans GWL. Urban legend versus rural reality: patients’ experience of attendance at accident and emergency departments in west Wales. Emerg Med J 2005;22:165-70. http://dx.doi.org/10.1136/emj.2003.007674.
- Foster J, Dale J, Jessopp L. A qualitative study of older people’s views of out-of-hours services. Br J Gen Pract 2001;51:719-23.
- Coleman P, Irons R, Nicholl J. Will alternative immediate care services reduce demands for non-urgent treatment at accident and emergency?. Emerg Med J 2001;18:482-7. http://dx.doi.org/10.1136/emj.18.6.482.
- Hoult L. Why do patients call out-of-hours following a recent consultation with their GP? A qualitative study in one general practice. Fam Pract 1998;15:S30-5.
- Shipman C, Longhurst S, Hollenbach F, Dale J. Using out-of-hours services: general practice or A&E?. Fam Pract 1997;14:503-9. http://dx.doi.org/10.1093/fampra/14.6.503.
- Blank L, Coster J, O’Cathain A, Knowles E, Tosh J, Turner J, et al. The appropriateness of, and compliance with, telephone triage decisions: a systematic review and narrative synthesis. J Adv Nurs 2012;68:2610-21. http://dx.doi.org/10.1111/j.1365-2648.2012.06052.x.
- Purc-Stephenson RJ, Thrasher C. Patient compliance with telephone triage recommendations: a meta-analytic review. Patient Educ Couns 2012;87:135-42. http://dx.doi.org/10.1016/j.pec.2011.08.019.
- Bunn F, Byrne G, Kendall S. The effects of telephone consultation and triage on healthcare use and patient satisfaction: a systematic review. Br J Gen Pract 2005;55:956-61.
- Bunn F, Byrne G, Kendall S. Telephone consultation and triage: effects on health care use and patient satisfaction. Cochrane Database Syst Rev 2004;3. http://dx.doi.org/10.1002/14651858.cd004180.pub2.
- Leibowitz R, Day S, Dunt D. A systematic review of the effect of different models of after-hours primary medical care services on clinical outcome, medical workload, and patient and GP satisfaction. Fam Pract 2003;20:311-7. http://dx.doi.org/10.1093/fampra/cmg313.
- Huibers L, Smits M, Renaud V, Giesen P, Wensing M. Safety of telephone triage in out-of-hours care: a systematic review. Scand J Prim Health Care 2011;29:198-209. http://dx.doi.org/10.3109/02813432.2011.629150.
- Chapman JL, Zechel A, Carter YH, Abbott S. Systematic review of recent innovations in service provision to improve access to primary care. Br J Gen Pract 2004;54:374-81.
- Stacey D, Noorani HZ, Fisher A, Robinson D, Joyce J, Pong RW. Telephone Triage Services: Systematic Review and a Survey of Canadian Call Centre Programs. Ottawa, ON: Canadian Coordinating Office for Health Technology Assessment; 2003.
- Carrasqueiro S, Oliveira M, Encarnacao P. Evaluation of telephone triage and advice services: a systematic review on methods, metrics and results. Stud Health Technol Inform 2011;169:407-11.
- Munro J, Nicholl J, O’Cathain A, Knowles E. Impact of NHS direct on demand for immediate care: observational study. BMJ 2000;321:150-3. http://dx.doi.org/10.1136/bmj.321.7254.150.
- Moore JD, Saywell RM, Thakker N, Jones TA. An analysis of patient compliance with nurse recommendations from an after-hours call center. Am J Manag Care 2002;8:343-51.
- Lattimer V, George S, Thompson F, Thomas E, Mullee M, Turnbull J, et al. Safety and effectiveness of nurse telephone consultation in out of hours primary care: randomised controlled trial. The South Wiltshire Out of Hours Project (SWOOP) Group. BMJ 1998;317:1054-9. http://dx.doi.org/10.1136/bmj.317.7165.1054.
- Gallagher M, Huddart T, Henderson B. Telephone triage of acute illness by a practice nurse in general practice: outcomes of care. Br J Gen Pract 1998;48:1141-5.
- Christensen MB, Olesen F. Out of hours service in Denmark: evaluation five years after reform. BMJ 1998;316:1502-5. http://dx.doi.org/10.1136/bmj.316.7143.1502.
- Dale J, Crouch R, Patel A, Williams S. Patients telephoning A&E for advice: a comparison of expectations and outcomes. J Accid Emerg Med 1997;14:21-3. http://dx.doi.org/10.1136/emj.14.1.21.
- Jackson DAS, Wall TC, Fargason CA, Byars TL, King WD, Steiger C. Pediatric telephone management, a comparison of pediatric residents and a nurse triage system. Ambulatory Child Health 1997;2:311-7.
- Giesen P, Ferwerda R, Tijssen R, Mokkink H, Drijver R, van den Bosch W, et al. Safety of telephone triage in general practitioner cooperatives: do triage nurses correctly estimate urgency?. Qual Saf Health Care 2007;16:181-4. http://dx.doi.org/10.1136/qshc.2006.018846.
- Killip S, Ireson CL, Love MM, Fleming ST, Katirai W, Sandford K. Patient safety in after-hours telephone medicine. Fam Med 2007;39:404-9.
- Marklund B, Strom M, Mansson J, Borgquist L, Baigi A, Fridlund B. Computer-supported telephone nurse triage: an evaluation of medical quality and costs. J Nurs Manag 2007;15:180-7. http://dx.doi.org/10.1111/j.1365-2834.2007.00659.x.
- Stewart B, Fairhurst R, Markland J, Marzouk O. Review of calls to NHS Direct related to attendance in the paediatric emergency department. Emerg Med J 2006;23:911-4. http://dx.doi.org/10.1136/emj.2006.039339.
- Kempe A, Bunik M, Ellis J, Magid D, Hegarty T, Dickinson LM, et al. How safe is triage by an after-hours telephone call center?. Pediatrics 2006;118:457-63. http://dx.doi.org/10.1542/peds.2005-3073.
- St George I, Cullen M, Branney M. Healthline: do primary care doctors agree with the advice?. N Z Med J 2005;118.
- Bogdan GM, Green JL, Swanson D, Gabow P, Dart RC. Evaluating patient compliance with nurse advice line recommendations and the impact on healthcare costs. Am J Manag Care 2004;10:534-42.
- Richards DA, Meakins J, Tawfik J, Godfrey L, Dutton E, Heywood P. Quality monitoring of nurse telephone triage: pilot study. J Adv Nurs 2004;47:551-60. http://dx.doi.org/10.1111/j.1365-2648.2004.03132.x.
- Sprivulis P, Carey M, Rouse I. Compliance with advice and appropriateness of emergency presentation following contact with the HealthDirect telephone triage service. Emerg Med Australas 2004;16:35-40. http://dx.doi.org/10.1111/j.1742-6723.2004.00538.x.
- Kempe A, Luberti A, Belman S, Hertz A, Sherman H, Amin D, et al. Outcomes associated with pediatric after-hours care by call centers: a multicenter study. Ambul Pediatr 2003;3:211-7. http://dx.doi.org/10.1367/1539-4409(2003)003<0211:OAWPAC>2.0.CO;2.
- Foster J, Jessopp L, Chakraborti S. Do callers to NHS Direct follow the advice to attend an accident and emergency department?. Emerg Med J 2003;20:285-8. http://dx.doi.org/10.1136/emj.20.3.285.
- Belman S, Murphy J, Steiner JF, Kempe A. Consistency of triage decisions by call center nurses. Ambul Pediatr 2002;2:396-400. http://dx.doi.org/10.1367/1539-4409(2002)002<0396:COTDBC>2.0.CO;2.
- O’Connell JM, Towles W, Yin M, Malakar CL. Patient decision-making: use of and adherence to telephone-based nurse triage recommendations. Med Decis Making 2002;22:309-17. http://dx.doi.org/10.1177/0272989X0202200409.
- Jiwa M, Mathers N, Campbell M. The effect of GP telephone triage on numbers seeking same-day appointments. Br J Gen Pract 2002;52:390-1.
- Kempe A, Luberti AA, Hertz AR, Sherman HB, Amin D, Dempsey C, et al. Delivery of pediatric after-hours care by call centers: a multicenter study of parental perceptions and compliance. Pediatrics 2001;108. http://dx.doi.org/10.1542/peds.108.6.e111.
- Frisbee SJ, Malloy M, Meurer JR, Kuhagen KA, Kini NM. Urban Wisconsin pediatric patients using an after-hours telephone triage service: outcomes and compliance. WMJ 2001;100:55-8.
- Derkx HP, Rethans JJE, Muijtjens AM, Maiburg BH, Winkens R, Van Rooij HG, et al. Quality of clinical aspects of call handling at Dutch out of hours centres: Cross sectional national study. BMJ 2008;337:676-9. http://dx.doi.org/10.1136/bmj.a1264.
- Hirsh DA, Simon HK, Masseyd R, Thornton L, Simon JE. The host hospital 24-hour underreferral rate: An automated measure of call-center safety. Pediatrics 2007;119:1139-44. http://dx.doi.org/10.1542/peds.2006-1986.
- Labarère J, Torres J, Francois P, Fourny M, Argento P, Gensburger X, et al. Patient compliance with medical advice given by telephone. Am J Emerg Med 2003;21:288-92. http://dx.doi.org/10.1016/S0735-6757(03)00087-1.
- Dale J, Williams S, Foster T, Higgins J, Snooks H, Crouch R, et al. Safety of telephone consultation for “non-serious” emergency ambulance service patients. Qual Saf Health Care 2004;13:363-73. http://dx.doi.org/10.1136/qshc.2003.008003.
- Lee TJ, Baraff LJ, Wall SP, Guzy J, Johnson D, Woo H. Parental compliance with after hours telephone triage advice: nurse advice service versus on-call pediatricians. Clin Pediatr 2003;42:613-9. http://dx.doi.org/10.1177/000992280304200707.
- Lee TJ, Guzy J, Johnson D, Woo H, Baraff LJ. Caller satisfaction with after-hours telephone advice: nurse advice service versus on-call pediatricians. Pediatrics 2002;110:865-72. http://dx.doi.org/10.1542/peds.110.5.865.
- McKinstry B, Walker J, Campbell C, Heaney D, Wyke S. Telephone consultations to manage requests for same-day appointments: a randomised controlled trial in two practices. Br J Gen Pract 2002;52:306-10.
- De Coster C, Quan HD, Elford R, Li B, Mazzei L, Zimmer S. Follow-through after calling a nurse telephone advice line: a population-based study. Fam Pract 2010;27:271-8. http://dx.doi.org/10.1093/fampra/cmq003.
- Giesen P, van Charante EM, Mokkink H, Bindels P, van den Bosch W, Grol R. Patients evaluate accessibility and nurse telephone consultations in out-of-hours GP care: Determinants of a negative evaluation. Patient Educ Couns 2007;65:131-6. http://dx.doi.org/10.1016/j.pec.2006.06.021.
- Thompson F, George S, Lattimer V, Smith H, Moore M, Turnbull J, et al. Overnight calls in primary care: randomised controlled trial of management using nurse telephone consultation. BMJ 1999;319. http://dx.doi.org/10.1136/bmj.319.7222.1408.
- Dale J, Higgins J, Williams S, Foster T, Snooks H, Crouch R, et al. Computer assisted assessment and advice for “non-serious” 999 ambulance service callers: the potential impact on ambulance despatch [sic]. Emerg Med J 2003;20:178-83. http://dx.doi.org/10.1136/emj.20.2.178.
- Studnek JR, Thestrup L, Blackwell T, Bagwell B. Utilization of prehospital dispatch protocols to identify low-acuity patients. Prehosp Emerg Care 2012;16:204-9. http://dx.doi.org/10.3109/10903127.2011.640415.
- Turner J, Snooks H, Youren A, Dixon S, Fall D, Gaze S, et al. The Costs and Benefits of Managing Some Low-Priority 999 Ambulance Calls by NHS Direct Nurse Advisers. Southampton: National Co-ordinating Centre for NHS Service Delivery and Organisation R&D (NCCSDO); 2006.
- Infinger A, Studnek JR, Hawkins E, Bagwell B, Swanson D. Implementation of prehospital dispatch protocols that triage low-acuity patients to advice-line nurses. Prehosp Emerg Care 2013;17:481-5. http://dx.doi.org/10.3109/10903127.2013.811563.
- Smith WR, Culley L, Plorde M, Murray JA, Hearne T, Goldberg P, et al. Emergency medical services telephone referral program: an alternative approach to nonurgent 911 calls. Prehosp Emerg Care 2001;5:174-80. http://dx.doi.org/10.1080/10903120190940092.
- Palma E, Antonaci D, Coli A, Cicolini G. Analysis of emergency medical services triage and dispatch errors by registered nurses in Italy. J Emerg Nurs 2014;40:476-83. http://dx.doi.org/10.1016/j.jen.2014.02.009.
- Turner J, O’Cathain A, Knowles E, Nicholl J. Impact of the urgent care telephone service NHS 111 pilot sites: a controlled before and after study. BMJ Open 2013;3. http://dx.doi.org/10.1136/bmjopen-2013-003451.
- O’Cathain A, Knowles E, Turner J, Nicholl J. Acceptability of NHS 111 the telephone service for urgent health care: cross sectional postal survey of users’ views. Fam Pract 2014;31:193-200. http://dx.doi.org/10.1093/fampra/cmt078.
- Knowles E, O’Cathain A, Turner J, Nicholl J. Awareness and use of a new urgent care telephone service, NHS 111: cross-sectional population survey. J Health Serv Res Policy 2014;19:224-30. http://dx.doi.org/10.1177/1355819614535571.
- Lambert R, Fordham R, Large S, Gaffney B. A cost-minimisation study of 1,001 NHS Direct users. BMC Health Serv Res 2013;13. http://dx.doi.org/10.1186/1472-6963-13-300.
- O’Connell JM, Johnson DA, Stallmeyer J, Cokingtin D. A satisfaction and return-on-investment study of a nurse triage service. Am J Manag Care 2001;7:159-69.
- Cariello FP. Computerized telephone nurse triage. An evaluation of service quality and cost. J Ambul Care Manage 2003;26:124-37. http://dx.doi.org/10.1097/00004479-200304000-00005.
- Navratil-Strawn JL, Ozminkowski RJ, Hartley SK. An economic analysis of a nurse-led telephone triage service. J Telemed Telecare 2014;20:330-8. http://dx.doi.org/10.1177/1357633X14545430.
- Morimura N, Aruga T, Sakamoto T, Aoki N, Ohta S, Ishihara T, et al. The impact of an emergency telephone consultation service on the use of ambulances in Tokyo. Emerg Med J 2011;28:64-70. http://dx.doi.org/10.1136/emj.2009.073494.
- Sakurai A, Morimura N, Takeda M, Miura K, Kiyotake N, Ishihara T, et al. A retrospective quality assessment of the 7119 call triage system in Tokyo – telephone triage for non-ambulance cases. J Telemed Telecare 2014;20:233-8. http://dx.doi.org/10.1177/1357633X14536347.
- Huibers L, Koetsenruijter J, Grol R, Giesen P, Wensing M. Follow-up after telephone consultations at out-of-hours primary care. J Am Board Fam Med 2013;26:373-9. http://dx.doi.org/10.3122/jabfm.2013.04.120185.
- Hansen EH, Hunskaar S. Telephone triage by nurses in primary care out-of-hours services in Norway: an evaluation study based on written case scenarios. BMJ Qual Safe 2011;20:390-6. http://dx.doi.org/10.1136/bmjqs.2010.040824.
- Cook R, Thakore S, Morrison W, Meikle J. To ED or not to ED: NHS 24 referrals to the emergency department. Emerg Med J 2010;27:213-5. http://dx.doi.org/10.1136/emj.2008.064261.
- Al-Abdullah T, Plint AC, Shaw A, Correll R, Gaboury I, Pitters C, et al. The appropriateness of referrals to a pediatric emergency department via a telephone health line. CJEM 2009;11:139-48.
- Ng J, Fatovich D, Turner V, Wurmel J, Skevington S, Phillips M. Does contact with healthdirect lead to appropriate use of the emergency department and ambulance services? A prospective, observational study comparing healthdirect, general practitioner and self-referred patients. Emerg Med Australas 2011;23:28-9.
- Ng JY, Fatovich DM, Turner VF, Wurmel JA, Skevington SA, Phillips MR. Appropriateness of healthdirect referrals to the emergency department compared with self-referrals and GP referrals. Med J Aust 2012;197:498-502. http://dx.doi.org/10.5694/mja12.10689.
- Beaulieu R, Humphreys J. Evaluation of a telephone advice nurse in a nursing faculty managed pediatric community clinic. J Pediatr Health Care 2008;22:175-81. http://dx.doi.org/10.1016/j.pedhc.2007.05.006.
- O’Cathain A, Goode J, Luff D, Strangleman T, Hanlon G, Greatbatch D. Does NHS Direct empower patients?. Soc Sci Med 2005;61:1761-71. http://dx.doi.org/10.1016/j.socscimed.2005.03.028.
- Mark AL, Shepherd ID. How has NHS Direct changed primary care provision?. J Telemed Telecare 2003;9:S57-9. http://dx.doi.org/10.1258/135763303322196367.
- Leclerc BS, Dunnigan L, Cote H, Zunzunegui MV, Hagan L, Morin D. Callers’ ability to understand advice received from a telephone health-line service: comparison of self-reported and registered data. Health Serv Res 2003;38:697-710. http://dx.doi.org/10.1111/1475-6773.00140.
- O’Cathain A, Webber E, Nicholl J, Munro J, Knowles E. NHS Direct: consistency of triage outcomes. Emerg Med J 2003;20:289-92. http://dx.doi.org/10.1136/emj.20.3.289.
- Kempe A, Dempsey C, Hegarty T, Frei N, Chandramouli V, Poole SR. Reducing after-hours referrals by an after-hours call center with second-level physician triage. Pediatrics 2000;106:226-30.
- Richards DA, Godfrey L, Tawfik J, Ryan M, Meakins J, Dutton E, et al. NHS Direct versus general practice based triage for same day appointments in primary care: cluster randomised controlled trial. BMJ 2004;329:774-7. http://dx.doi.org/10.1136/bmj.38226.605995.55.
- LaVela SL, Gering J, Schectman G, Weaver FM. Optimizing primary care telephone access and patient satisfaction. Eval Health Prof 2012;35:77-86. http://dx.doi.org/10.1177/0163278711411479.
- Kinnersley P, Egbunike JN, Kelly M, Hood K, Owen-Jones E, Button LA, et al. The need to improve the interface between in-hours and out-of-hours GP care, and between out-of-hours care and self-care. Fam Pract 2010;27:664-72. http://dx.doi.org/10.1093/fampra/cmq056.
- Strom M, Marklund B, Hildingh C. Callers’ perceptions of receiving advice via a medical care help line. Scand J Caring Sci 2009;23:682-90. http://dx.doi.org/10.1111/j.1471-6712.2008.00661.x.
- Dunt D, Day SE, Kelaher M, Montalto M. The impact of standalone call centres and GP cooperatives on access to after hours GP care: a before and after study adjusted for secular trend. Fam Pract 2006;23:453-60. http://dx.doi.org/10.1093/fampra/cml020.
- Kempe A, Dempsey C, Whitefield J, Bothner J, MacKenzie T, Poole S. Appropriateness of urgent referrals by nurses at a hospital-based pediatric call center. Arch Pediatr Adolesc Med 2000;154:355-60. http://dx.doi.org/10.1001/archpedi.154.4.355.
- Crane JD, Benjamin JT. Pediatric residents’ telephone triage experience – Do parents really follow telephone advice?. Arch Pediatr Adolesc Med 2000;154:71-4.
- Monaghan R, Clifford C, McDonald P. Seeking advice from NHS direct on common childhood complaints: does it matter who answers the phone?. J Adv Nurs 2003;42:209-16. http://dx.doi.org/10.1046/j.1365-2648.2003.02602.x.
- Grant C, Nicholas R, Moore L, Salisbury C. An observational study comparing quality of care in walk-in centres with general practice and NHS Direct using standardised patients. BMJ 2002;324. http://dx.doi.org/10.1136/bmj.324.7353.1556.
- Hogenbirk JC, Pong RW. An audit of the appropriateness of teletriage nursing advice. Telemed J E Health 2004;10:53-60. http://dx.doi.org/10.1089/153056204773644580.
- O’Cathain A, Nicholl J, Sampson F, Walters S, McDonnell A, Munro J. Do different types of nurses give different triage decisions in NHS Direct? A mixed methods study. J Health Serv Res Policy 2004;9:226-33. http://dx.doi.org/10.1258/1355819042250221.
- McKinstry B, Hammersley V, Burton C, Pinnock H, Elton R, Dowell J, et al. The quality, safety and content of telephone and face-to-face consultations: a comparative study. Qual Saf Health Care 2010;19:298-303. http://dx.doi.org/10.1136/qshc.2008.027763.
- Barber JW, King WD, Monroe KW, Nichols MH. Evaluation of emergency department referrals by telephone triage. Pediatrics 2000;105:819-21. http://dx.doi.org/10.1542/peds.105.4.819.
- Doctor K, Correa K, Olympia RP. Evaluation of an after-hours call center: are pediatric patients appropriately referred to the Emergency Department?. Pediatr Emerg Care 2014;30:798-804. http://dx.doi.org/10.1097/PEC.0000000000000262.
- Huibers L, Keizer E, Giesen P, Grol R, Wensing M. Nurse telephone triage: good quality associated with appropriate decisions. Fam Pract 2012;29:547-52. http://dx.doi.org/10.1093/fampra/cms005.
- Ernesäter A, Engström M, Holmström I, Winblad U. Incident reporting in nurse-led national telephone triage in Sweden: the reported errors reveal a pattern that needs to be broken. J Telemed Telecare 2010;16:243-7. http://dx.doi.org/10.1258/jtt.2009.090813.
- Snooks H, Peconi J, Munro J, Cheung WY, Rance J, Williams A. An evaluation of the appropriateness of advice and healthcare contacts made following calls to NHS Direct Wales. BMC Health Serv Res 2009;9. http://dx.doi.org/10.1186/1472-6963-9-178.
- Sharma A, Inder B. Impact of co-located general practitioner (GP) clinics and patient choice on duration of wait in the emergency department. Emerg Med J 2011;28:658-61. http://dx.doi.org/10.1136/emj.2009.086512.
- Turner J, O’Cathain A, Knowles E, Nicholl J, Tosh J, Sampson F, et al. Evaluation of NHS 111 Pilot sites. Final Report to the Department of Health. Sheffield: Medical Care Research Unit, University of Sheffield; 2012.
- Turnbull J, Prichard J, Halford S, Pope C, Salisbury C. Reconfiguring the emergency and urgent care workforce: mixed methods study of skills and the everyday work of non-clinical call-handlers in the NHS. J Health Serv Res Policy 2012;17:233-40. http://dx.doi.org/10.1258/jhsrp.2012.011141.
- Bigham BL, Kennedy SM, Drennan I, Morrison LJ. Expanding paramedic scope of practice in the community: a systematic review of the literature. Prehosp Emerg Care 2013;17:361-72. http://dx.doi.org/10.3109/10903127.2013.792890.
- Cooper S, Grant J. New and emerging roles in out of hospital emergency care: a review of the international literature. Int Emerg Nurs 2009;17:90-8. http://dx.doi.org/10.1016/j.ienj.2008.11.004.
- Evans R, McGovern R, Birch J, Newbury-Birch D. Which extended paramedic skills are making an impact in emergency care and can be related to the UK paramedic system? A systematic review of the literature. Emerg Med J 2014;31:594-603. http://dx.doi.org/10.1136/emermed-2012-202129.
- Hill H, McMeekin P, Price C. A systematic review of the activity and impact of emergency care practitioners in the NHS. Emerg Med J 2014;31:853-60. http://dx.doi.org/10.1136/emermed-2013-202660.
- Mikolaizak AS, Simpson PM, Tiedemann A, Lord SR, Close JC. Systematic review of non-transportation rates and outcomes for older people who have fallen after ambulance service call-out. Australas J Ageing 2013;32:147-57. http://dx.doi.org/10.1111/ajag.12023.
- Tohira H, Williams TA, Jacobs I, Bremner AP, Finn J. The impact of new prehospital practitioners on ambulance transportation to the emergency department: a systematic review and meta-analysis. Emerg Med J 2014. http://dx.doi.org/10.1136/emermed-2013-202976.
- Adams A, Wright K, Cooke M. Evaluation of the NHS Changing Workforce Programme’s Emergency Care Practitioners Pilot Study in Warwickshire. Coventry: Division of Health in the Community, Medical School, University of Warwick; 2005.
- Coates D, Rawstorne S, Benger J. Can emergency care practitioners differentiate between an avoided emergency department attendance and an avoided admission?. Emerg Med J 2012;29:838-41. http://dx.doi.org/10.1136/emermed-2011-200484.
- Cooper S, Barrett B, Black S, Evans C, Real C, Williams S, et al. The emerging role of the emergency care practitioner. Emerg Med J 2004;21:614-8. http://dx.doi.org/10.1136/emj.2003.011247.
- Cooper S, O’Carroll J, Jenkin A, Badger B. Collaborative practices in unscheduled emergency care: role and impact of the emergency care practitioner–quantitative findings. Emerg Med J 2007;24:630-3. http://dx.doi.org/10.1136/emj.2007.048058.
- Cooper S, O’Carroll J, Jenkin A, Badger B. Collaborative practices in unscheduled emergency care: role and impact of the emergency care practitioner–qualitative and summative findings. Emerg Med J 2007;24:625-9. http://dx.doi.org/10.1136/emj.2006.043943.
- Cooper S, O’Carroll J, Jenkin A, Badger B. Emergency care practitioners (ECP): practice and performance in the UK West country--a case study. Int Emerg Nurs 2008;16:180-4. http://dx.doi.org/10.1016/j.ienj.2008.04.004.
- Right Skill, Right Time, Right Place. The ECP report. London: Department of Health; 2004.
- Dixon S, Mason S, Knowles E, Colwell B, Wardrope J, Snooks H, et al. Is it cost effective to introduce paramedic practitioners for older people to the ambulance service? Results of a cluster randomised controlled trial. Emerg Med J 2009;26:446-51. http://dx.doi.org/10.1136/emj.2008.061424.
- Gray JT, Walker A. Avoiding admissions from the ambulance service: a review of elderly patients with falls and patients with breathing difficulties seen by emergency care practitioners in South Yorkshire. Emerg Med J 2008;25:168-71. http://dx.doi.org/10.1136/emj.2007.050732.
- Halter M, Marlow T, Tye C, Ellison GTH. Patients’ experiences of care provided by emergency care practitioners and traditional ambulance practitioners: a survey from the London Ambulance Service. Emerg Med J 2006;23:865-6. http://dx.doi.org/10.1136/emj.2005.032912.
- Halter M, Ellison G. A Study of the Processes and Outcomes of Clinical Decision-Making (Project Report). London: Faculty of Health and Social Care Sciences, Kingston University and St George’s, University of London; 2008.
- Knowles E, Mason S, Colwell B. An initiative to provide emergency healthcare for older people in the community: the impact on carers. Emerg Med J 2011;28:316-9. http://dx.doi.org/10.1136/emj.2009.084616.
- Mason S, Coleman P, O’Keeffe C, Ratcliffe J, Nicholl J. The evolution of the emergency care practitioner role in England: experiences and impact. Emerg Med J 2006;23:435-9. http://dx.doi.org/10.1136/emj.2005.027300.
- Mason S, Knowles E, Colwell B, Dixon S, Wardrope J, Gorringe R, et al. Effectiveness of paramedic practitioners in attending 999 calls from elderly people in the community: cluster randomised controlled trial. BMJ 2007;335. http://dx.doi.org/10.1136/bmj.39343.649097.55.
- Mason S, Knowles E, Freeman J, Snooks H. Safety of paramedics with extended skills. Acad Emerg Med 2008;15:607-12. http://dx.doi.org/10.1111/j.1553-2712.2008.00156.x.
- Mason S, O’Keeffe C, Coleman P, Edlin R, Nicholl J. Effectiveness of emergency care practitioners working within existing emergency service models of care. Emerg Med J 2007;24:239-43. http://dx.doi.org/10.1136/emj.2006.035782.
- Mason S, O’Keeffe C, Knowles E, Bradburn M, Campbell M, Coleman P, et al. A pragmatic quasi-experimental multi-site community intervention trial evaluating the impact of Emergency Care Practitioners in different UK health settings on patient pathways (NEECaP Trial). Emerg Med J 2012;29:47-53. http://dx.doi.org/10.1136/emj.2010.103572.
- O’Hara R, O’Keeffe C, Mason S, Coster JE, Hutchinson A. Quality and safety of care provided by emergency care practitioners. Emerg Med J 2012;29:327-32. http://dx.doi.org/10.1136/emj.2010.104190.
- O’Keeffe C, Mason S, Bradburn M, Iheozor-Ejiofor Z. A community intervention trial to evaluate emergency care practitioners in the management of children. Arch Dis Child 2011;96:658-63. http://dx.doi.org/10.1136/adc.2010.201889.
- Shah MN, Caprio TV, Swanson P, Rajasekaran K, Ellison JH, Smith K, et al. A novel emergency medical services-based program to identify and assist older adults in a rural community. J Am Geriatr Soc 2010;58:2205-11. http://dx.doi.org/10.1111/j.1532-5415.2010.03137.x.
- Stirling CM, O’Meara P, Pedler D, Tourle V, Walker J. Engaging rural communities in health care through a paramedic expanded scope of practice. Rural Remote Health 2007;7.
- Brown LH, Hubble MW, Cone DC, Millin MG, Schwartz B, Patterson PD, et al. Paramedic determinations of medical necessity: a meta-analysis. Prehosp Emerg Care 2009;13:516-27. http://dx.doi.org/10.1080/10903120903144809.
- Burrell L, Noble A, Ridsdale L. Decision-making by ambulance clinicians in London when managing patients with epilepsy: a qualitative study. Emerg Med J 2013;30:236-40. http://dx.doi.org/10.1136/emermed-2011-200388.
- Halter M, Vernon S, Snooks H, Porter A, Close J, Moore F, et al. Complexity of the decision-making process of ambulance staff for assessment and referral of older people who have fallen: a qualitative study. Emerg Med J 2011;28:44-50. http://dx.doi.org/10.1136/emj.2009.079566.
- O’Hara R, Johnson M, Hirst E, Weyman A, Shaw D, Mortimer P, et al. A qualitative study of decision-making and safety in ambulance service transitions. Health Serv Deliv Res 2014;2.
- Clesham K, Mason S, Gray J, Walters S, Cooke V. Can emergency medical service staff predict the disposition of patients they are transporting?. Emerg Med J 2008;25:691-4. http://dx.doi.org/10.1136/emj.2007.054924.
- Cornwall AH, Zaller N, Warren O, Williams K, Karlsen-Ayala N, Zink B. A pilot study of emergency medical technicians’ field assessment of intoxicated patients’ need for ED care. Am J Emerg Med 2012;30:1224-8. http://dx.doi.org/10.1016/j.ajem.2011.06.004.
- Newton M, Tunn E, Moses I, Ratcliffe D, Mackway-Jones K. Clinical navigation for beginners: the clinical utility and safety of the Paramedic Pathfinder. Emerg Med J 2014;31:e29-34. http://dx.doi.org/10.1136/emermed-2012-202033.
- Schmidt T, Atcheson R, Federiuk C, Mann NC, Pinney T, Fuller D, et al. Evaluation of protocols allowing emergency medical technicians to determine need for treatment and transport. Acad Emerg Med 2000;7:663-9. http://dx.doi.org/10.1111/j.1553-2712.2000.tb02041.x.
- Snooks HA, Carter B, Dale J, Foster T, Humphreys I, Logan PA, et al. Support and Assessment for Fall Emergency Referrals (SAFER 1): cluster randomised trial of computerised clinical decision support for paramedics. PLOS ONE 2014;9. http://dx.doi.org/10.1371/journal.pone.0106436.
- Jensen JL, Travers AH, Marshall EG, Cain E, Leadlay S, Carter AJ. Insights into the implementation and operation of a novel paramedic long-term care program. Prehosp Emerg Care 2014;18:86-91. http://dx.doi.org/10.3109/10903127.2013.831506.
- Logan P, Stoner-Hobbs V, McCloughry H, Foster C, Fitzsimmons D, Williams J, et al. Intermediate care for older people. Nurs Older People 2007;19:25-8. http://dx.doi.org/10.7748/nop2007.06.19.5.25.c4644.
- Sach TH, Logan PA, Coupland CA, Gladman JR, Sahota O, Stoner-Hobbs V, et al. Community falls prevention for people who call an emergency ambulance after a fall: an economic evaluation alongside a randomised controlled trial. Age Ageing 2012;41:635-41. http://dx.doi.org/10.1093/ageing/afs071.
- Walker A, James C, Bannister M, Jobes E. Evaluation of a diabetes referral pathway for the management of hypoglycaemia following emergency contact with the ambulance service to a diabetes specialist nurse team. Emerg Med J 2006;23:449-51. http://dx.doi.org/10.1136/emj.2005.028548.
- Sach TH, Logan PA, Coupland CA, Gladman JR, Sahota O, Stoner-Hobbs V, et al. Community falls prevention for people who call an emergency ambulance after a fall: an economic evaluation alongside a randomised controlled trial. Age Ageing 2012;41:635-41. http://dx.doi.org/10.1093/ageing/afs071.
- Hill H, McMeekin P, Price C. A systematic review of the activity and impact of emergency care practitioners in the NHS. Emerg Med J 2014;31:853-60. http://dx.doi.org/10.1136/emermed-2013-202660.
- Newton A. Specialist practice for paramedics: a bright future?. Journal of Paramedic Practice 2011;3:58-61. http://dx.doi.org/10.12968/jpar.2011.3.2.58.
- Paramedic Curriculum Guidance and Career framework. Bridgwater: College of Paramedics; 2014.
- Snooks H, Kearsley N, Dale J, Halter M, Redhead J, Cheung WY. Towards primary care for non-serious 999 callers: Results of a controlled study of “Treat and Refer” for ambulance crews. Qual Saf Health Care 2004;13:435-43. http://dx.doi.org/10.1136/qshc.2003.007658.
- Halter M, Marlow T, Mohammed D, Ellison GTH. A patient survey of out-of-hours care provided by Emergency Care Practitioners. BMC Emerg Med 2007;7. http://dx.doi.org/10.1186/1471-227x-7-4.
- Knowles E, Mason S, Colwell B. An initiative to provide emergency healthcare for older people in the community: the impact on carers. Emerg Med J 2011;28:316-9. http://dx.doi.org/10.1136/emj.2009.084616.
- Dixon S, Mason S, Knowles E, Colwell B, Wardrope J, Snooks H, et al. Is it cost effective to introduce paramedic practitioners for older people to the ambulance service? Results of a cluster randomised controlled trial. Emerg Med J 2009;26:446-51. http://dx.doi.org/10.1136/emj.2008.061424.
- O’Cathain A, Siriwardena A, Jacques R, O’Hara R, Turner J, Williams J. Project Portfolio Number 13 54 75: Understanding Variation in Rates of Ambulance Service Non-Conveyance of Patients to an Emergency Department n.d. www.nets.nihr.ac.uk/projects/hsdr/135475.
- Lovegrove M, Davis J. Paramedic Evidence Based Education Project (PEEP): End of Study Report. High Wycombe: Allied Health Solutions and Buckinghamshire New University; 2013.
- Pickering A, Cooper K, Harnan S, Holmes M, Sutton A, Mason S, et al. Comparison of Direct Transfer to Specialist Care Centres with Delivery to the Nearest Hospital: A Systematic Review and Economic Evaluation. Final Report. Southampton: NIHR Service Delivery and Organisation programme; 2014.
- Khangura JK, Flodgren G, Perera R, Rowe BH, Shepperd S. Primary care professionals providing non-urgent care in hospital emergency departments. Cochrane Database Syst Rev 2012;11. http://dx.doi.org/10.1002/14651858.cd002097.pub3.
- Boeke AJP, Van Randwijck-Jacobze ME, De Lange-Klerk EMS, Grol SM, Kramer MHH, Van Der Horst HE. Effectiveness of GPs in accident and emergency departments. Br J Gen Pract 2010;60:e378-e87. http://dx.doi.org/10.3399/bjgp10X532369.
- Bosmans JE, Boeke AJ, Randwijck-Jacobze ME, Grol SM, Kramer MH, Horst HE, et al. Addition of a general practitioner to the accident and emergency department: a cost-effective innovation in emergency care. Emerg Med J 2012;29:192-6. http://dx.doi.org/10.1136/emj.2010.101949.
- Enard KR, Ganelin DM. Reducing preventable emergency department utilization and costs by using community health workers as patient navigators. J Healthc Manag 2013;58:412-27.
- Salisbury C, Hollinghurst S, Montgomery A, Cooke M, Munro J, Sharp D, et al. The impact of co-located NHS walk-in centres on emergency departments. Emerg Med J 2007;24:265-9. http://dx.doi.org/10.1136/emj.2006.042507.
- Thijssen WA, Wijnen-van Houts M, Koetsenruijter J, Giesen P, Wensing M. The impact on emergency department utilization and patient flows after integrating with a general practitioner cooperative: an observational study. Emerg Med Int 2013;2013. http://dx.doi.org/10.1155/2013/364659.
- Wang M, Wild S, Hilfiker G, Chmiel C, Sidler P, Eichler K, et al. Hospital-integrated general practice: a promising way to manage walk-in patients in emergency departments. J Eval Clin Pract 2014;20:20-6. http://dx.doi.org/10.1111/jep.12074.
- Abdulwahid MA, Booth A, Kuczawski M, Mason S. The impact of senior doctor assessment and triage on emergency department performance measures: systematic review and meta-analysis of comparative studies [published online ahead of print, 16 July 2015]. Emerg Med 2015. http://dx.doi.org/10.1136/emermed-2014-204388.
- Bullard MJ, Villa-Roel C, Guo X, Holroyd BR, Innes G, Schull MJ, et al. The role of a rapid assessment zone/pod on reducing overcrowding in emergency departments: a systematic review. Emerg Med J 2012;29:372-8. http://dx.doi.org/10.1136/emj.2010.103598.
- Cooke MW, Higgins J, Kidd P. Use of emergency observation and assessment wards: a systematic literature review. Emerg Med J 2003;20:138-42. http://dx.doi.org/10.1136/emj.20.2.138.
- Daly S, Campbell DA, Cameron PA. Short-stay units and observation medicine: a systematic review. Med J Aust 2003;178:559-63.
- Flores-Mateo G, Violan-Fors C, Carrillo-Santisteve P, Peiro S, Argimon JM. Effectiveness of organizational interventions to reduce emergency department utilization: a systematic review. PLOS ONE 2012;7. http://dx.doi.org/10.1371/journal.pone.0035903.
- Georgiou A, Prgomet M, Paoloni R, Creswick N, Hordern A, Walter S, et al. The effect of computerized provider order entry systems on clinical care and work processes in emergency departments: a systematic review of the quantitative literature. Ann Emerg Med 2013;61:644-53. http://dx.doi.org/10.1016/j.annemergmed.2013.01.028.
- Harding KE, Taylor NF, Leggat SG. Do triage systems in healthcare improve patient flow? A systematic review of the literature. Aust Health Rev 2011;35:371-83. http://dx.doi.org/10.1071/AH10927.
- Holden RJ. Lean Thinking in emergency departments: a critical review. Ann Emerg Med 2011;57:265-78. http://dx.doi.org/10.1016/j.annemergmed.2010.08.001.
- Hoot NR, Aronsky D. Systematic review of emergency department crowding: causes, effects, and solutions. Ann Emerg Med 2008;52:126-36. http://dx.doi.org/10.1016/j.annemergmed.2008.03.014.
- Katz EB, Carrier ER, Umscheid CA, Pines JM. Comparative effectiveness of care coordination interventions in the emergency department: a systematic review. Ann Emerg Med 2012;60:12-23. http://dx.doi.org/10.1016/j.annemergmed.2012.02.025.
- Lee RS, Woods R, Bullard M, Holroyd BR, Rowe BH. Consultations in the emergency department: a systematic review of the literature. Emerg Med J 2008;25:4-9. http://dx.doi.org/10.1136/emj.2007.051631.
- Paul SA, Reddy MC, DeFlitch CJ. A systematic review of simulation studies investigating emergency department overcrowding. Simul Trans Soc Model Simul Intl 2010;86:559-71.
- Porter A, Evans B, Gammon B, Harris R, Poulden M, Rees N. Streamlining Patient Handovers from Ambulances to the Emergency Department. Swansea: Swansea University; 2014.
- Roberts E, Mays N. Can primary care and community-based models of emergency care substitute for the hospital accident and emergency (A & E) department?. Health Policy 1998;44:191-214. http://dx.doi.org/10.1016/S0168-8510(98)00021-9.
- Egleston CV, Leydon GN, Lawrenson R, Meakin R, Freeman G. Cost of alternative models of care for primary care patients attending accident and emergency departments. J Accid Emerg Med 1998;15:77-83. http://dx.doi.org/10.1136/emj.15.6.435-b.
- Rowe BH, Guo X, Villa-Roel C, Schull M, Holroyd B, Bullard M, et al. The role of triage liaison physicians on mitigating overcrowding in emergency departments: a systematic review. Acad Emerg Med 2011;18:111-20. http://dx.doi.org/10.1111/j.1553-2712.2010.00984.x.
- Rowe BH, Villa-Roel C, Guo X, Bullard MJ, Ospina M, Vandermeer B, et al. The role of triage nurse ordering on mitigating overcrowding in emergency departments: a systematic review. Acad Emerg Med 2011;18:1349-57. http://dx.doi.org/10.1111/j.1553-2712.2011.01081.x.
- Carter AJ, Chochinov AH. A systematic review of the impact of nurse practitioners on cost, quality of care, satisfaction and wait times in the emergency department. CJEM 2007;9:286-95.
- Wilson A, Zwart E, Everett I, Kernick J. The clinical effectiveness of nurse practitioners’ management of minor injuries in an adult emergency department: a systematic review. Int J of Evid Based Healthc 2009;7:3-14. http://dx.doi.org/10.1111/j.1744-1609.2009.00121.x.
- Doan Q, Sabhaney V, Kissoon N, Sheps S, Singer J. A systematic review: The role and impact of the physician assistant in the emergency department. Emerg Med Australas 2011;23:7-15. http://dx.doi.org/10.1111/j.1742-6723.2010.01368.x.
- Conroy SP, Stevens T, Parker SG, Gladman JR. A systematic review of comprehensive geriatric assessment to improve outcomes for frail older people being rapidly discharged from acute hospital: ‘interface geriatrics’. Ageing 2011;40:436-43. http://dx.doi.org/10.1093/ageing/afr060.
- Graf CE, Zekry D, Giannelli S, Michel JP, Chevalley T. Efficiency and applicability of comprehensive geriatric assessment in the emergency department: a systematic review. Aging Clin Exp Res 2011;23:244-54. http://dx.doi.org/10.1007/BF03337751.
- Crowding in Emergency Departments. London: Royal College of Emergency Medicine; 2014.
- Spetz J, Parente ST, Town RJ, Bazarko D. Scope-of-practice laws for nurse practitioners limit cost savings that can be achieved in retail clinics. Health Aff 2013;32:1977-84. http://dx.doi.org/10.1377/hlthaff.2013.0544.
- Sox CM, Swartz K, Burstin HR, Brennan TA. Insurance or a regular physician: which is the most powerful predictor of health care?. Am J Public Health 1998;88:364-70. http://dx.doi.org/10.2105/AJPH.88.3.364.
- Boom PS. Emergency medical care in the Netherlands. Eur J Emerg Med 1999;6:263-6. http://dx.doi.org/10.1097/00063110-199909000-00017.
- Derex L, Philippeau F, Blanc-Lasserre K, Cakmak S, Vallet AE, Flocard E, et al. A regional emergency stroke network yields a high rate of thrombolysis. The resuval (Rhone Valley, France) thrombolysis registry. Cerebrovasc Dis 2013;35. http://dx.doi.org/10.1159/000381866.
- Kiechl S, Tuer A, Geley T, Kreuzer H, Schoech H, Jaeger N, et al. Comprehensive stroke care pathway and network in Tyrol. Cerebrovasc Dis 2013;35.
- Ang D, Norwood S, Barquist E, McKenney M, Kurek S, Kimbrell B, et al. Geriatric outcomes for trauma patients in the state of Florida after the advent of a large trauma network. J Trauma Acute Care Surg 2014;77:155-60. http://dx.doi.org/10.1097/TA.0000000000000272.
- Ruchholtz S, Lefering R, Lewan U, Debus F, Mand C, Siebert H, et al. Implementation of a nationwide trauma network for the care of severely injured patients. J Trauma Acute Care Surg 2014;76:1456-61. http://dx.doi.org/10.1097/TA.0000000000000245.
- Wierdsma AI, Poodt HD, Mulder CL. Effects of community-care networks on psychiatric emergency contacts, hospitalisation and involuntary admission. J Epidemiol Community Health 2007;61:613-8. http://dx.doi.org/10.1136/jech.2005.044974.
- Manns BJ, Tonelli M, Zhang J, Campbell DJ, Sargious P, Ayyalasomayajula B, et al. Enrolment in primary care networks: impact on outcomes and processes of care for patients with diabetes. CMAJ 2012;184:E144-52. http://dx.doi.org/10.1503/cmaj.110755.
- Solla DJ, Paiva Filho Ide M, Delisle JE, Braga AA, Moura JB, Moraes Xd, et al. Integrated regional networks for ST-segment-elevation myocardial infarction care in developing countries: the experience of Salvador, Bahia, Brazil. Circ Cardiovasc Qual Outcomes 2013;6:9-17. http://dx.doi.org/10.1161/CIRCOUTCOMES.112.967505.
- Ghadi V, Vedel I, Routelous C, de Stampa M, Ankri J, Cassou B, et al. A gerontological network as an interface between health-care professionals and homecare professionals. Sante Publique 2011;23:317-28.
- Sheaff R, Windle K, Wistow G, Ashby S, Beech R, Dickinson A, et al. Reducing emergency bed-days for older people? Network governance lessons from the ‘Improving the Future for Older People’ programme. Soc Sci Med 2014;106:59-66. http://dx.doi.org/10.1016/j.socscimed.2014.01.033.
- Navein J, McNeil I. The Surrey Emergency Care System: a countywide initiative for change. Emerg Med J 2003;20:192-5. http://dx.doi.org/10.1136/emj.20.2.192.
- Martinez R. Academic Emergency Medicine Consensus Conference BRINoC. Keynote address – redefining regionalization: merging systems to create networks. Acad Emerg Med 2010;17:1346-8. http://dx.doi.org/10.1111/j.1553-2712.2010.00945.x.
- Glickman SW, Kit Delgado M, Hirshon JM, Hollander JE, Iwashyna TJ, Jacobs AK, et al. Defining and measuring successful emergency care networks: a research agenda. Acad Emerg Med 2010;17:1297-305.
- Turner J, Nicholl J, O’Cathain A. A Preliminary Study of Emergency and Urgent Care Networks. Report to Department of Health Urgent Care Strategy Team. Sheffield: Medical Care Research Unit, University of Sheffield; 2007.
Appendix 1 Search strategies
General search strategy
MEDLINE (via Ovid SP)
Date range searched: 1 January 1995 to 5 November 2014.
Date of searched: 5 November 2014.
Search strategy
-
Ambulances/
-
“ambulance*”.ab,ti.
-
exp Emergency Medical Services/
-
(pre-hospital or pre hospital or prehospital).ab,ti.
-
Emergency Service, Hospital/
-
“emergency department*”.ab,ti.
-
“emergency service*”.ab,ti.
-
“accident and emergency”.ab,ti.
-
(urgent adj3 care).ab,ti.
-
After-Hours Care/
-
‘out of hours care’.ab,ti.
-
after hours care.ab,ti.
-
‘out of hours medical care’.ab,ti.
-
‘after hours medical care’.ab,ti.
-
‘out of hours service$’.ab,ti.
-
after hours service$.ab,ti.
-
‘out of hours medical’.ab,ti.
-
‘out of hours clinic$’.ab,ti.
-
after hours medical.ab,ti.
-
after hours clinic$.ab,ti.
-
or/1-20
-
“Delivery of Health Care”/
-
(classification or economics or legislation jurisprudence or manpower or organization administration or standards or statistics numerical data or supply distribution or trends or utilization).fs.
-
(service adj1 (deliver$ or reform$ or reorganis$ or reorganiz$ or restructur$ or chang$ or innovat$)).ab,ti.
-
22 or 23 or 24
-
21 and 25
-
limit 26 to (english language and yr=“1995 -Current”)
-
(efficien$ or effectiv$).ab,ti.
-
(reduc$ or shorten$ or cut$).ab,ti.
-
(demand or ‘waiting time$’).ab,ti.
-
29 and 30
-
right care.ab,ti.
-
appropriate care.ab,ti.
-
right place.ab,ti.
-
right time.ab,ti.
-
Patient Satisfaction/
-
Patient Readmission/
-
readmi$.ab,ti.
-
reattend$.ab,ti.
-
re-attend$.ab,ti.
-
re-admi$.ab,ti.
-
revisit.ab,ti.
-
re-visit.ab,ti.
-
Crowding/
-
crowd$.ab,ti.
-
reduc$.ab,ti.
-
44 or 45
-
46 and 47
-
Health Services Accessibility/
-
28 or 31 or 32 or 33 or 34 or 35 or 36 or 37 or 38 or 39 or 40 or 41 or 42 or 43 or 48 or 49
-
26 and 50
-
limit 51 to (english language and yr=“1995 -Current”)
-
Comment/
-
Letter/
-
Editorial/
-
(comment or letter or editorial).pt.
-
53 or 54 or 55 or 56
-
52 not 57
Targeted search strategies
Telephone triage search strategy
MEDLINE (via Ovid SP)
Date range searched: 1 January 1995 to 28 December 2014.
Date searched: 28 December 2014.
Search strategy
-
*Telephone/ or *Hotlines/
-
(triage or consultation).mp. [mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier]
-
(“nhs direct” or “nhs 24”).mp. [mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier]
-
telephone triage.mp. [mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier]
-
call centre triage.mp. [mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier]
-
advanced nursing.mp. [mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier]
-
appropriate*.mp. [mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier]
-
quality framework*.mp. [mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier]
-
under?referral.mp. [mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier]
-
inappropriate.mp. [mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier]
-
safe*.mp. [mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier]
-
danger*.mp. [mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier]
-
satisf*.mp. [mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier]
-
consistency.mp. [mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier]
-
consequence*.mp. [mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier]
-
(adherance or compliance).mp. [mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier]
-
decision-making.mp. or Decision-making/
-
Decision Support Systems, Clinical/
-
Needs Assessment/
-
Technology Transfer/
-
experience.mp. [mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier]
-
recommend*.mp. [mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier]
-
6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22
-
1 and (2 or 3)
-
4 or 5 or 24
-
23 and 25
-
limit 26 to (english language and yr=“1995 -Current”)
Ambulance search strategy
MEDLINE (via Ovid SP)
Date range searched: 1 January 1995 to 7 December 2014.
Date searched: 7 December 2014.
Search strategy
-
Ambulances/
-
ambulance$.ab,ti.
-
Emergency Medical Services/
-
(pre-hospital or pre hospital or prehospital).ab,ti.
-
allied health personnel/ or emergency medical technicians/
-
paramedic$.ab,ti.
-
emergency care assistant$.ab,ti.
-
emergency medical technician$.ab,ti.
-
emergency care practitioner$.ab,ti.
-
or/1-6,8-9
-
extend$ role$.ab,ti.
-
extend$ skill$.ab,ti.
-
great$ role$.ab,ti.
-
avoid$.ab,ti.
-
alternative care.ab,ti.
-
(treat$ or manag$ or care).ab,ti.
-
Primary Health Care/
-
(primary adj3 care).ab,ti.
-
Community Mental Health Services/ or Community Health Services/
-
(community adj4 service$).ab,ti.
-
(community adj4 care).ab,ti.
-
intermediate care.ab,ti.
-
17 or 18 or 19 or 20 or 21 or 22
-
16 and 23
-
community management.ab,ti.
-
pathway$.ab,ti.
-
service referral$.ab,ti.
-
Staff Development/
-
(workforce adj3 (develop$ or skill$ or competenc$)).ab,ti.
-
or/11-15,24-29
-
10 and 30
-
(service adj2 (deliver$ or reform$ or reorganis$ or reorganiz$ or restructur$ or chang$ or innovat$)).ab,ti.
-
(efficien$ or effectiv$).ab,ti.
-
(reduc$ or shorten$ or cut$).ab,ti.
-
(demand or ‘waiting time$’).ab,ti.
-
34 and 35
-
right care.ab,ti.
-
appropriate care.ab,ti.
-
right place.ab,ti.
-
right time.ab,ti.
-
patient satisfaction.ab,ti.
-
patient experience$.ab,ti.
-
Patient Satisfaction/
-
patient view$.ab,ti.
-
Health Services Accessibility/
-
safety/ or patient safety/
-
safe$.ab,ti.
-
or/32-33,36-47
-
31 and 48
-
limit 49 to yr=“1995 -Current”
Emergency department demand search strategy
MEDLINE (via Ovid SP)
Date range searched: 1 January 1995 to 21 December 2014.
Date searched: 21 December 2014.
Search strategy
-
*Emergency Medical Services/
-
emergency care.ti,ab.
-
urgent care.ti,ab.
-
*Ambulances/
-
ambulance*.ti,ab.
-
(emergency adj2 service*).ti,ab.
-
EMS.ti,ab.
-
*Emergency Service, Hospital/
-
emergency department*.ti,ab.
-
ED.ti,ab.
-
“accident and emergency”.ti,ab.
-
A&E.ti,ab.
-
emergency unit*.ti,ab.
-
or/1-13
-
trend*.ti,ab.
-
*“Health Services Needs and Demand”/
-
demand*.ti,ab.
-
Crowding/
-
crowding.ti,ab.
-
or/15-19
-
14 and 20
-
*Empirical Research/
-
empirical.ti,ab.
-
cause*.ti,ab.
-
*“Aged, 80 and over”/ or *Aged/ or *Population Dynamics/
-
ageing population.ti,ab.
-
reason*.ti,ab.
-
factor*.ti,ab.
-
22 or 23 or 24 or 25 or 26 or 27 or 28
-
21 and 29
-
22 or 23
-
21 and 31
-
Empirical Research/
-
23 or 33
-
21 and 34
-
limit 35 to yr=“2003 -Current”
-
from 36 keep 1,3,5,7,9-10,12,14,17,20-21,24,28
-
((rise or rising or increas*) adj3 (demand* or use* or using or utili* or access*)).ti,ab.
-
14 and 38
-
“rising demand”.ti,ab.
-
16 or 40
-
14 and 41
-
14 and 40
-
((rise or rising or increas*) adj3 demand*).ti,ab.
-
14 and 44
-
limit 45 to yr=“2003 -Current”
-
from 37 keep 1-13
-
from 46 keep 2,7-8,15,17,19-20,22-29,31-34,36,41-42,48-52,54-58,60-61,64-67,69-70,72-74,76,79-85,87,89,91-92,96,98-100
-
from 46 keep 101-102,104-107,109,111,117,122,125-127,129-130,133,135-138,140-141,143-145,147-151,153,156,159-160,162,168-169,171-177,181,184-185,188-192,194
-
48 or 49
-
from 50 keep 1-112
-
25 or 26
-
14 and 52
-
limit 53 to yr=“2003 -Current”
-
54 not 46
-
from 55 keep 1,3,7-8,12,14,16-19,22,24,27-28,30-34,36-37,39-54,56-57,59-60,64,66-67,70-71,73-75
-
from 56 keep 1-49
-
18 or 19
-
14 and 58
-
limit 59 to yr=“2003 -Current”
-
36 or 46 or 54
-
60 not 61
-
crowding.ti.
-
*Crowding/
-
63 or 64
-
14 and 65
-
66 not 61
-
emergenc*.ti.
-
63 and 68
-
69 not 61
-
limit 70 to yr=“2003 -Current”
-
limit 69 to (english language and yr=“1995 -Current”)
-
limit 53 to (english language and yr=“1995 -Current”)
-
limit 45 to (english language and yr=“1995 -Current”)
-
limit 35 to (english language and yr=“1995 -Current”)
-
72 or 73 or 74 or 75
-
or/15-17
-
14 and 77
-
34 and 78
-
limit 79 to (english language and yr=“1995 -Current”)
-
73 or 74 or 80
Emergency department reorganisation search strategy
MEDLINE (via Ovid SP)
Date range searched: 1 January 1995 to 17 December 2014.
Date searched: 17 December 2014.
Search strategy
-
*Emergency Service, Hospital/
-
*Emergency Medical Services/
-
*Emergency Medicine/
-
(emergency adj2 service$).ab,ti.
-
emergency care.ab,ti.
-
urgent care.ab,ti.
-
emergency department$.ab,ti.
-
or/1-7
-
*Efficiency, Organizational/
-
patient outcome$.ab,ti.
-
*“Quality of Health Care”/
-
*Models, Organizational/
-
organi?ation$.ab,ti.
-
*Cost-Benefit Analysis/
-
cost$.ab,ti.
-
effectiveness.ab,ti.
-
efficacy.ab,ti.
-
efficiency.ab,ti.
-
utilization.ab,ti.
-
*Health Services Accessibility/
-
(service adj1 (deliver$ or reform$ or reorganis$ or reorganiz$ or restructur$ or chang$ or innovat$)).ab,ti.
-
or/9-21
-
“out of hours”.ab,ti.
-
“walk in centres”.ab,ti.
-
“fast track areas”.ab,ti.
-
“fast track unit”.ab,ti.
-
*Nurse Practitioners/
-
*Nurse Administrators/
-
*Triage/
-
copayment.ab,ti.
-
“cost sharing”.ab,ti.
-
“incentive based”.ab,ti.
-
“coinsurance”.ab,ti.
-
“tiered benefit”.ab,ti.
-
“patient charge”.ab,ti.
-
gatekeeping.ab,ti.
-
*Gatekeeping/
-
*Primary Health Care/
-
“urgent care centre$”.ab,ti.
-
“patient flow$”.ab,ti.
-
emergency care access point$.ab,ti.
-
stream$.ab,ti.
-
or/23-42
-
8 and 22 and 43
-
Editorial/
-
Letter/
-
Comment/
-
(editorial or comment or letter).ab,ti.
-
or/45-48
-
44 not 49
-
limit 50 to (english language and yr=“1995 -Current”)
Warwick review update search
MEDLINE (via Ovid SP)
Date range searched: 1 January 2009 to 20 January 2015.
Date searched: 20 January 2015.
Search strategy
-
primary care.mp. or exp Primary Health Care/
-
exp Physicians, Family/
-
general practitioner$.mp.
-
exp After-Hours Care/
-
(out-of-hours or OOH).mp. [mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier]
-
1 or 2 or 3 or 4 or 5
-
7. exp Emergency Medical Services/ or exp Emergency Service, Hospital/
-
((accident and emergency department) or emergency department or casualty).mp. [mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier]
-
7 or 8
-
16 and 9
-
1limit 10 to (humans and yr=“2009 -Current”)
Networks search strategy
MEDLINE (via Ovid SP )
Date range searched: 1 January 1995 to 21 January 2015.
Date searched: 21 January 2015.
Search strategy
-
Ambulances/
-
“ambulance*”.ab,ti.
-
exp Emergency Medical Services/
-
(pre-hospital or pre hospital or prehospital).ab,ti.
-
Emergency Service, Hospital/
-
“emergency department*”.ab,ti.
-
“emergency service*”.ab,ti.
-
“accident and emergency”.ab,ti.
-
(urgent adj3 care).ab,ti.
-
After-Hours Care/
-
‘out of hours care’.ab,ti.
-
after hours care.ab,ti.
-
‘out of hours medical care’.ab,ti.
-
‘after hours medical care’.ab,ti.
-
‘out of hours service$’.ab,ti.
-
after hours service$.ab,ti.
-
‘out of hours medical’.ab,ti.
-
‘out of hours clinic$’.ab,ti.
-
after hours medical.ab,ti.
-
after hours clinic$.ab,ti.
-
or/1-20
-
inter-professional collaboration.ab,ti.
-
interagency relation$.ab,ti.
-
inter-organisational relationship$.ab,ti.
-
interprofessional relation$.ab,ti.
-
interinstitutional relation$.ab,ti.
-
Community Networks/
-
(care adj3 network$).ab,ti.
-
(clinical adj3 network$).ab,ti.
-
(hospital adj3 network$).ab,ti.
-
(health adj3 network$).ab,ti.
-
(research adj3 network$).ab,ti.
-
(practice adj3 network$).ab,ti.
-
(emergency adj3 network$).ab,ti.
-
(trauma adj3 network$).ab,ti.
-
or/22-35
-
21 and 36
-
limit 36 to (english language and yr=“1995 -Current”)
List of abbreviations
- A&E
- accident and emergency
- CCDS
- Computerised Clinical Decision Support
- CGA
- comprehensive geriatric assessment
- CINAHL
- Cumulative Index to Nursing and Allied Health Literature
- DARE
- Database of Abstracts of Reviews of Effects
- ECP
- emergency care practitioner
- ED
- emergency department
- EMS
- emergency medical service
- GP
- general practitioner
- HSDR
- Health Services and Delivery Research
- NIHR
- National Institute for Health Research
- NP
- nurse practitioner
- OOH
- out of hours
- PRISMA
- Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- RCT
- randomised controlled trial
- ScHARR
- School of Health and Related Research