Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 09/1809/1072. The contractual start date was in January 2010. The final report began editorial review in July 2014 and was accepted for publication in January 2015. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Steven Ariss was lead evaluator for one of the Collaborations for Leadership in Applied Health Research and Care (CLAHRCs) at the time of the evaluation. Richard Baker was the director of the National Institute for Health Research (NIHR) CLAHRC for Leicestershire, Northamptonshire and Rutland between 2008 and 2013. Ian Graham was a member of the advisory panel for one of the CLAHRCs at the time of the evaluation. Gill Harvey was employed by one of the CLAHRCs at the time of the evaluation. Jo Rycroft-Malone is a member of the Health Services and Delivery Research (HSDR) Board (commissioned research). Since completing this research she has been appointed as the editor-in-chief of the HSDR programme. Sophie Staniszewska is an associate member of the HSDR Board (researcher led). Carl Thompson was the CLAHRC Translating Research into Practice in Leeds and Bradford theme lead for the NIHR CLAHRC for Leeds, York and Bradford (2009–13).
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2015. This work was produced by Rycroft-Malone et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction
Policy context: the birth of Collaborations for Leadership in Applied Health Research and Care
The establishment of the Collaborations for Leadership in Applied Health Research and Care (CLAHRCs) in England was the culmination of a number of policy initiatives over several years to bridge the ‘knowing to doing’ gap,1 the gap between the acceptance of research and its adoption and routine use in practice. The time taken to incorporate research into routine practice can be ‘unacceptably long’ (p. 20). 1 Given this, there is now a widespread recognition of the need for an increase in resources to accomplish the translation and implementation of research to have an impact on patient outcomes. 2 As a consequence, governments in Europe, Canada, Australia and the USA have been making significant investments in translational research initiatives as a vehicle to bridge the metaphorical gap between bench and bedside.
Historically, the worlds of academia and practice have tended to be divided and disconnected; therefore, investments in translational initiatives have been focused on the potential of collaboration and in collaborative entities. When the users and producers of research are brought closer together, in theory, they can work collaboratively to find solutions to practical and relevant problems. Arguably, Canada led the way in such initiatives, with an early example being the Quebec Social Research Council’s grant programme that was set up in 1992 to encourage collaboration between decision-makers, researchers and practitioners. Since then, the USA has established the Quality Enhancement Research Initiative of the US Veterans Administration,3 the Netherlands has set up the Dutch Academic Collaborative Centres for Public Health4 and latterly in Australia Advanced Health Research Centres have been created. 5,6 The UK has followed this pattern with investment in a number of different entities designed to encourage collaboration, for example Academic Health Science Centres (AHSCs), Academic Health Science Networks, Biomedical Research Centres and Units, and, more recently, the CLAHRCs.
The landscape that led to the investment in and establishment of the variety of different collaborative entities in the UK was born from a number of policies. Shortly after the launch of a 5-year Research and Development Strategy for NHS England,7 which aimed to create a health system that supported leading-edge research based on patient need, the Cooksey Report8 drew attention to the undervaluing of applied health research (i.e. research that directly addresses questions and issues of practical importance) and highlighted two gaps in the translation of health research. Of relevance to this study, Cooksey highlighted the gap between the identification and evaluation of new effective interventions that are appropriate for everyday use, and their actual implementation in practice in the NHS [second gap in translation (T2)]. The report also focuses on the structures and cultures in the NHS that militated against the development and impact of applied health research, including a lack of strategy and cultural, institutional and financial barriers.
In 2007, the High Level Group on Clinical Effectiveness was tasked by the Chief Medical Officer to develop an action plan to enhance the effectiveness and efficiency of clinical care in England. 9,10 Its work led to a number of recommendations, including that there should be:
-
a more programmatic approach to the development and establishment of teams and investment in implementation
-
a gradual increase in investment through the National Institute for Health Research’s (NIHR’s) budget for this area
-
a long-term commitment to develop climates conducive to conducting implementation research and the activity of using research findings in practice
-
consideration of the establishment of a number of centres of excellence in implementation research. 10
These recommendations are directly relevant and related to the establishment of nine CLAHRCs in 2008. These entities were established to be collaborative partnerships between health-care organisations and higher education institutions (HEIs). Overall, the initiative received £100M funding by the NIHR for 5 years, with a similar amount of matched funding from participating partners. The CLAHRCs were funded to deliver on three interlinked functions:
-
conducting high-quality applied health research to generate knowledge to improve patient health and care
-
implementing findings from research in clinical practice for patient benefit
-
increasing the capacity of NHS organisations and the public, private and third sector organisations to engage with and apply research. 11
These functions were expanded on in the call for external evaluations of the initiative, in which the aims of the CLAHRC were described as follows (NIHR NCCSDO CLA258):
To secure a step change in the way that applied health research is done and applied health research evidence is implemented locally;
To increase capacity to conduct and implement applied health research through collaborative partnerships between universities and NHS organisations;
To link those who conduct applied health research with all those who use it in practice across the health community covered by the Collaboration;
To test and evaluate new initiatives to encourage implementation of applied health research findings into practice;
To create and embed approaches to conducting and implementing research that are specifically designed to take account of the way that health care is increasingly delivered across sectors and across a wide geographical area;
To focus on the needs of patients, and particularly on research targeted at chronic disease and public health interventions; and
To improve patient outcomes across the geographic area covered by the Collaboration.
There was no prescribed or single model for CLAHRCs; the expectation was that each would evolve to best reflect and serve local needs by being outward facing and community focused, which included active involvement of patients and the public and other relevant stakeholders. The CLAHRCs were designed to be pilots and a collaborative experiment in closing T2.
Framing the challenge: conceptual territory
The conceptualisation of the issue about what is known from evidence and what is practised is frequently framed as a metaphorical ‘know–do’ gap. Consequently, the way in which this gap is traversed, closed or bridged has been the challenge that has been taxing an ever-growing and interested community of researchers, practitioners and policy-makers. Many terms are used to describe the activity undertaken to solve the problem, including ‘diffusion’, ‘dissemination’, ‘implementation’, ‘knowledge transfer’, ‘knowledge mobilisation’, ‘linkage and exchange’ and ‘research into practice’. 12 On closer scrutiny, the terms are used to describe a multitude of overlapping concepts and practices, but also reflect the different perceptions and underpinning assumptions about the processes involved in knowledge and its action. Historically, the ‘know–do’ gap has been defined as a practice/service problem rather than a knowledge creation one, the conceptualisation of evidence has been relatively narrow and there has been a lack of attention to the situation of evidence use. 13
Over time there has been a shift (in the literature at least) from seeing knowledge and its mobilisation as an event to conceptualising it as a process. This has been in parallel to a greater recognition that such processes are not linear but that knowledge use is mediated by context, is complex and multifactorial and, therefore, is often unpredictable. Different conceptualisations reflect this shift in thinking, with, for example, the Pipeline Model14 representing action as following specific stages or phases and a linear trajectory, in contrast to others’ representations reflecting more complexity and a focus on action being situated within context. 15–20
Different terms also reflect underlying epistemologies and therefore assumptions. For example, ‘research into practice’ and ‘knowledge transfer’ tend to be used to reflect a more linear unidirectional conceptualisation of knowledge use, whereas the term ‘knowledge translation’ (KT), which has become particularly popular in Canada, embodies more complexity, for example:
Knowledge translation (KT) is defined as a dynamic and iterative process that includes synthesis, dissemination, exchange and ethically sound application of knowledge to improve the health of Canadians, provide more effective health services and products and strengthen the health care system. This process takes place within a complex system of interactions between researchers and knowledge users which may vary in intensity, complexity and level of engagement depending on the nature of the research and the findings as well as the needs of the particular knowledge user. 21
Similarly, the increasingly used terms (particularly in the UK and the USA) ‘knowledge mobilisation’ and ‘implementation’ (of research and practice) reflect multidirectional pathways for knowledge discovery, exchange and uptake, including the factors that might influence these processes. Therefore, within this report we use both terms (‘implementation’ and ‘knowledge mobilisation’) to refer to processes that concern being attentive to and acting on evidence, making changes to practice/service delivery that could be informed by propositional and non-propositional sources of knowledge, and taking account of action occurring within contexts that are complicated and complex, including with a variety of stakeholders. These conceptualisations are built on further as part of the development of the study’s evaluation framework reported in Chapter 3. The critical question about whether or not collaboration provides a condition for action was a central concern of this research study.
Reconceptualising the challenge
The conceptualisation of the challenge of using evidence in practice resulting from a gap between research and practice is perpetuated by the ‘two communities’ model of knowledge creation in which the producers and users of research occupy separate worlds. 22 It has been argued that, although there has been a huge investment in developing an infrastructure to fund and deliver high-quality health-related research in the UK, this has been achieved, in part, by splitting research production from the delivery of health-care services. 23 The impact of this has been an exacerbation of the boundary between research and practice, and a call for a change of paradigm.
Best and Holmes24 conceptualise three generations of thinking about how Knowledge to Action (K2A) has been conceived: linear models, relationship models and systems models.
The language incorporated within a linear model of framing the issue (e.g. ‘research uptake’, ‘research into practice’, ‘knowledge transfer’) suggests a one-way process, whereby researchers produce new knowledge, which is disseminated to end-users and then incorporated into policy and practice. Knowledge is seen as a product that is generalisable across contexts and its use is dependent upon effective packaging. 25 The exchange is seen as one-way, from research producer to research user, so effective dissemination is critical. The linear model is therefore the embodiment of the ‘two communities’ approach to knowledge creation and use.
Relationship models incorporate the linear model principles for dissemination and diffusion, and then focus on the interactions among people using the knowledge. The emphasis is on the sharing of knowledge, the development of partnerships and the fostering of networks of stakeholders with common interests (e.g. Graham et al. 17). Within this framing, knowledge is perceived to be derived from multiple sources, including research, theory, policy and practice, and its use is perceived to be dependent upon effective relationships and processes. Therefore, collaboration and shared learning are key features of knowledge creation and use through coproduction or engaged scholarship. 26
A systems model enhances linear and relationship conceptualisations by recognising that knowledge mobilisation processes are themselves organised and structured through structures and agents, that is systems. A systems thinking approach assumes that there is an interconnectedness and interdependency between components within a system and, therefore, knowledge mobilisation would be seen as only one aspect of a wider process of how organisations change and develop. Understanding knowledge mobilisation then needs to be understood in relation to how the system as a whole is operating.
As Best and Holmes’s24 conceptualisation highlights, there has been a growing emphasis over time on practice-based, collaborative and organisational approaches to knowledge and its use. They offer a contrast to an evidence-orientated understanding of knowledge use, which is predicated on an assumption that evidence is a product needing to be pushed out to its users over the academic–practice boundary. 27 Pushing out evidence in the form of, for example, guidelines has had some, but relatively limited, success (given the substantial investment in the development of such packages of evidence) in improving health outcomes. Therefore, reconceptualising the challenge by bringing together the creators and users of knowledge to cocreate solutions to real-world problems is appealing. In the context of this type of collaboration, in theory, the practice–academic boundary would be blurred, evidence would be created within communities of practice, it would be of relevance to that community and, therefore, the gap between practice and research would potentially be narrowed. 22 These sorts of partnerships are prevalent in industry, but less so in health care, particularly publicly funded health services.
Collaborations for Leadership in Applied Health Research and Care in a conceptual context
Collaborations for Leadership in Applied Health Research and Care were predicated on an assumption that providing a resource and the architecture to enable the research and practice community to work more closely together would facilitate the generation of more applied health research and accelerate its use in practice. Accordingly, the concept of CLAHRCs fits with interactional and relationship conceptualisations of knowledge mobilisation. We assume that that was the theory underpinning the creating and funding of CLAHRCs, which is tested in this study through a realist lens. Realist inquiry facilitates the building of context-rich, theory-led explanations of what is it about a programme that makes it work. The starting point for a realist inquiry is testing the ‘theory’ that was in the heads of the programme developers, namely that bringing HEIs and health-care organisations closer together accelerates knowledge mobilisation. We investigate this theory through some specific objectives:
-
to identify and track the implementation mechanisms and processes used by CLAHRCs and evaluate intended and unintended consequences (impacts) over time
-
to determine what influences whether or not and how research is used through CLAHRCs, paying particular attention to contextual factors
-
to investigate the role played by boundary objects in the success or failure of research implementation through CLAHRCs
-
to determine if and how CLAHRCs develop and sustain interactions and communities of practice
-
to identify indicators that could be used for further evaluations of the sustainability of CLAHRC-like approaches.
The report of this realist inquiry is structured as follows:
Chapter 1 sets the emergence of CLAHRCs within a policy context and in a conceptual territory.
Chapter 2 reports a rapid realist review that was conducted to identify and describe the existing evidence base underpinning the theory of whether or not and how bringing research producers and users together within a collaborative arrangement might accelerate knowledge mobilisation.
Chapter 3 describes the methodology and methods used in the study, including the conceptual platform developed and used to frame the evaluation.
Chapter 4 presents findings from each case framed around the conceptual platform used for the study.
Chapter 5 presents a cross-case and cross-framework narrative, which starts to build an explanation for what works, for whom, how and why knowledge mobilisation operated with CLAHRCs over time.
Chapter 6 presents a realist framed explanatory account of the findings through a set of context, mechanism and outcome configurations.
Chapter 7 outlines the key mechanisms and a programme theory, which provides an explanation for collective action in collaboration around implementation and is related to the wider literature. Finally in this chapter we draw some conclusions and implications about an area in which there is still much research and learning to be done.
Chapter 2 Collaboration between researchers and practitioners: how and why is it more likely to enable implementation? A rapid realist review
Introduction
As outlined in Chapter 1, closing the gap between research and practice has been a persistent and vexing challenge. It is widely acknowledged that, to date, relatively little attention has been paid to T2;28,29 however, CLAHRCs are one type of approach to closing this gap. As an example of a partnership model to knowledge mobilisation, the CLAHRC initiative has focused on translating high-quality research to meet the needs of patient groups through increasing capacity and capability by collaboration between academia and practice. 28 This approach embodies the view of KT as an ‘iterative, reciprocal exchange that takes place between researchers and research users’. 30
Although the benefits of collaboration provide a potentially attractive solution to the challenges of evidence use, the pathway from developing collaborative partnerships to the implementation of research or evidence in practice is far from straightforward, and yet to be established. In reality, ‘doing’ collaboration does not necessarily lead to the achievement of set goals, or to clarity about what outcomes may be achievable. 31 Moreover, the outcomes that are supposedly linked to collaboration are often described in abstract terms, for example related to the learning that occurs as a result of the collaboration,32 or to the development of new skills across partnerships. 33 However, whether or not and how collaboration promotes the implementation of knowledge by end-users is unclear. As this was the ‘theory’ in the heads of those who established and funded CLAHRCs, we undertook a rapid realist review to identify whether or not this theory is supported by evidence and, if so, why and how collaboration might prompt implementation. The review also provided some initial co-ordinates for the development of the study’s conceptual framework (described in Chapter 3).
Question
Why and how does organisational collaboration between researchers and practitioners enable implementation?
Rationale for realist review
Collaboration in health care is situated within complex social environments and described as a ‘nested phenomenon’. 34 Therefore, a realist approach seemed appropriate in that it focuses attention on seeking to understand what works, for whom, why, under which circumstances and how. 35 Realist review is a theory-driven method of synthesising knowledge, which is grounded in the realist philosophy of science. 36 It involves ‘an iterative process aimed at uncovering the theories that inform decisions and actions’. 37 For pragmatic reasons, we undertook a rapid realist review whereby the realist approach to knowledge synthesis is employed in resource-limited circumstances. 38 Rapid realist reviews use the principles of realist synthesis, within a restricted set of literature,25,35 with the aim of seeking out mechanisms that are specifically related to programme outcomes. 38 In addition, in contrast to a conventional realist review, the focus is not on the development of theory per se, so output may not (necessarily) include context–mechanism–outcome (CMO) configurations.
To safeguard against compromising the thinking behind the realist philosophy, the review used the principles of the traditional realist review and engaged with the evaluation research group, who became the ‘expert group’ and ensured that the parameters of the review question were observed throughout. 38 The question for the review was drawn from discussions with the research team (February 2012 and August 2013) and based on programme theory being developed by Rycroft-Malone et al. 39 Where subject content areas are sparse, reference groups and expert panels are drawn upon to describe ‘current best thinking’. 38
Background search
An initial background search of the literature was undertaken to understand how collaboration is represented, and to seek out examples of collaboration between organisations or researchers and practitioners. The search sought evidence about collaborations within health care and behavioural sciences (Table 1), as well as in the wider public services literature, for example education, environmental sustainability and youth programmes (see Appendix 1).
| Health care and behavioural sciences | Other types of literature |
|---|---|
|
|
Defining collaboration
The background search showed how collaboration is defined within and across disciplines, and how it is perceived as an integral component for the transformation of services. Collaboration is becoming recognised as a clearly defined area of scholarly research40 but is a contested territory. 40,41 It has been suggested that collaboration is a process ‘through which parties who see different aspects of a problem can constructively explore their differences and search for solutions that go beyond their own limited vision of what is possible’ (p. 5)42 that is rarely clearly defined. 43 In contrast, interorganisational collaboration has been defined as an entity: ‘a co-operative relationship among organisations that relies on neither market nor hierarchical mechanisms of control’. 44 Alternatively, collaboration has been perceived as a contingency: ‘a process that can emerge as organisations interact with one another to create new organisational and social structures’. 40 In non-profit organisations, collaboration is seen as the relationship required for application and sustainability of research in practice. 44 From the communities of practice literature, interprofessional collaboration relies on interaction between different actors and systems, and factors that determine success can relate to interpersonal factors or organisational structures. 45,46
The authors of conceptualisations, including frameworks and models, describe collaboration as a process or continuum42,47 involving dimensions of governance, administration, organisational autonomy, mutuality and norms. 40 For others, collaboration is considered to be a cyclical process involving negotiation, commitment and implementation. 48 Academic–practitioner (or cross-profession) collaborations are defined according to related professions and organisations,43 and estimations of their success are defined by considering the extent to which goals are met, as well as the perceived benefits for individuals and teams. 43
Academic and professional collaborations are discussed in terms of increasing research productivity and quality,49 improving learning32 and enhancing the development of new skills across partnerships. 33 Organisational collaboration is described as reaching outcomes or goals. 34 The literature reviewed in the background search describes outcomes or impacts of collaboration as, for example, the dissemination and implementation of guidelines;50 improving aspects of services and affecting health outcomes or public health;51–53 promoting successful change; and closing the gap between potential and actual performance. 51,54,55 Other authors refer to increasing the number of agencies working together and promoting users’ better engagement with intervention programmes;56 having an impact on macro-level outcomes related to enhancing innovation; and expediting the translation of science for patient-focused benefits. 57,58
In summary, the background search provided some understanding of how collaboration is defined in the literature, which led to the next step of the review, a purposive systematic search of the literature about whether or not collaboration provides the conditions for implementation.
Searching process
Consistent with realist principles, the search was progressive and iterative, and was receptive to different types of evidence, including ‘grey’ literature. 36,59 The main databases searched were limited to the health and behavioural sciences and included Applied Social Sciences Index and Abstracts, Cumulative Index to Nursing and Allied Health Literature, The Cochrane Library, PubMed, MEDLINE and JSTOR. A ‘snowball’ process was used to check and retrieve references cited in accessed articles if they were deemed to be relevant to the review. Links to relevant articles were also suggested by members of the research team. Initial search terms which referred to collaboration between researchers and practitioners were sought from the background search of the literature (see Appendix 2). It became evident as the review progressed that the wide range of potential search terms could lead to unmanageable amounts of retrieved literature; therefore, a decision was made to reduce the terms and focus the search on evidence that related to features to show if and how collaboration might enable implementation. The main search terms included ‘collaboration’, ‘coalition’, ‘co-operation’, ‘partnership’, ‘community partnership’, ‘inter-institutional relations’ and ‘joint working’. An additional search was conducted using more specific terms noted in the literature, for example ‘trans-disciplinary collaboration’ and ‘academic industry partnership’. The search was limited to documents written in English and published between 1994 and 2014, to capture the most relevant and recent evidence from the past 20 years. Methodological ‘filters’ were intentionally not used, to avoid missing any papers that could be relevant to the review. 36 The search was not confined to research studies, and included other evidence, for example case studies, column papers and reports.
Selection and appraisal of documents
Decisions about inclusion and exclusion of data from documents were based on judgements of relevance, as opposed to the overall quality of the document. The systematic search yielded an initial 6669 hits. Titles were screened for relevance, reducing the search to 87 papers. Papers were not saved if they related to implementing partnerships, developing and co-ordinating services, and service issues, or where reference to implementation was not apparent. Papers were not saved if they related to non-health-related disciplines, such as education. Screening of the abstracts reduced the papers to 18, which were then retrieved in full text. Further scrutiny of full text for relevance reduced the chosen papers to one, which was added to other relevant papers retrieved by chance, additional search and reference lists (nine).
The 10 papers retained were then subjected to a more rigorous review using the data extraction form designed for the review, as detailed below. The sequence of selection and appraisal is reported in Appendix 3.
The characteristics of the selected papers and their approach to describing implementation and knowledge mobilisation are reported in Table 2.
| Authors (year), title | Country | Paper type | Theme/main aims | Approach to describing implementation/knowledge mobilisation | Main findings/recommendations |
|---|---|---|---|---|---|
| Blevins et al. (2010),60 Collaborative research between clinicians and researchers: a multiple case study of implementation | USA | Original research report: evaluation study using mixed methods. Quantitative data consisted of survey and archival material, with qualitative data sourced from focus groups | Describes community-based participatory research in health, and reports an evaluation to establish the degree of collaboration across four funded projects in the Veterans Health Administration in the USA | Community-based participatory approaches conceptualised as acting on evidence-based interventions. Processes that have relevance (for the community), and sustainability or continuation of the intervention | Collaboration noted to contribute to better relationships and the production of research. Resources and support do not necessarily lead to sustainability of interventions. Collaboration not necessarily precursor to sustainability of interventions. Significance of clinicians’ prior research experience to the quality of the project |
| Kegler et al. (1998),61 Factors that contribute to effective community health promotion coalitions: a study of 10 Project ASSIST coalitions in North Carolina | USA | Original research report: survey conducted over 12-month period of 5-year intervention phase relating to local community health promotion coalitions | Paper relates to 7-year national project to reduce the numbers of smokers in US states (ASSIST). Aim of paper to seek factors that contribute to effective health promotion coalitions | Changes in health outcomes, community actions and community changes are perceived as ideal measures of coalition effectiveness. Processes of putting in place planned activities which are noted as measures of coalition effectiveness | Coalitions with higher levels of dedicated staff, with complex structures, and recognised as having better communication and cohesion than others are more likely to result in higher levels of implementation |
| Lasker et al. (2001),62 Partnership synergy: a practical framework for studying and strengthening the collaborative advantage | USA | Literature review and presentation of partnership synergy framework in health care | Partnership synergy postulated to influence partnership effectiveness and thus improve health and health-care issues. Determinants of partnership synergy identified in framework: resources, partner characteristics, relationships, external environment | Processes which lead to achievement of health and health system goals. Changes to programmes, policy and practice which affect health services | Partnership synergy conceptualised through framework which can be utilised to address policy issues relating to collaboration |
| Lesser and Oscos-Sanchez (2007),63 Community–academic research partnerships with vulnerable populations | USA and Canada | Review chapter | Reviews the state of community–academic research partnerships across the USA and Canada related to community health nursing | Processes which generate positive health outcomes and build capacity. Processes which result in communities and researchers becoming more empowered and knowledgeable. Impact influenced by how interventions appear specific to target population and culturally sensitive | Main findings relate to the importance of relationships to partnership success, allowing time to develop fruitful relationships, and how collaborations affect the conduct of research and improve processes |
| Olson et al. (2011),50 Factors contributing to successful inter-organisational collaboration: the case of CS2day | USA | Original research report. Online survey administered to 23 participants from nine organisations involved in CS2day health promotion collaboration to address tobacco smoking. Survey used adapted version of Wilder Collaboration Factors Inventory | Describes an interorganisational collaboration in continuing medical education (CS2day). Factors considered to contribute to success discussed | Actual and intended practice changes. Creation of best practices. More effective care | Findings highlight factors thought to contribute to collaboration success including choice of topic, environmental factors, structures and processes, shared vision, communication, having measurable targets and creating value |
| Ovretveit et al. (2002),51 Quality collaboratives: lessons from research | Sweden | Systematic evaluation report | Presents guidelines to support quality improvement collaboratives in health care to achieve their goals. Authors suggest that the guidelines can be useful for organising collaboratives and future research into collaboratives | How knowledge and innovation are spread. Processes which improve quality of services. Closing gaps between actual and potential performance. Successful change | Accentuates promise of new quality improvement methodology using a structured framework to make improvements through collaboratives. Collaboratives can be learning organisations which are motivating, and provide tools to help support quality problems. Findings accentuate importance of culture and leadership to collaborative success |
| Purcal et al. (2011),56 Does partnership funding improve coordination and collaboration among early childhood services? Experiences from the Communities for Children programme | Australia | Original research report. Mixed-methods study: service co-ordination study using qualitative and quantitative methods. Survey administered to 41 project sites, repeated once, elicited 744 responses. In-depth interviews (n = 222) | Evaluation of human service delivery partnerships operating under national Communities for Children programme in Australia. Authors allude to current lack of evidence to show partnership outcomes from national programmes. Collaboration perceived as mechanism of partnership working | Improvements in services and service experience. Improvements in health of service users. Cost-effective and holistic services for clients. Improvements in service efficiency | Partnership outcomes identified from project sites. Increase in collaboration for project agencies. Better working relationships noted. Highlighted significance of pre-existing networks. Negative impact related to time and investment required to establish partnership |
| Shortell et al. (2002),52 Evaluating partnerships for community health improvement: tracking the footprints | USA | Original research report. Midstream process evaluation of 25 community partnerships using qualitative and quantitative data | Focus of paper on community health partnerships and factors which can influence how they achieve objectives. Research questions focused on extent of partnership progression towards meeting objectives, and the factors considered to account for progress | Extent to which partnerships can positively influence outcomes. Improvements in quality outcomes. Improvements in community health | Six main characteristics identified in successful model partnerships which made most progress in implementation: managing size and diversity, three-component leadership, focus, how conflict managed, recognising life cycles, and partnership ability to ‘patch’ |
| Stokols et al. (2008),64 The ecology of team science: understanding contextual influences on transdisciplinary collaboration | USA | Report on empirical literature from team performance and collaboration | Main focus of paper on transdisciplinary team science | Translation of scientific knowledge into interventions and policies to improve public health (especially intermediate and long-term collaboration) | Typology of influences on transdisciplinary collaboration drawing on factors considered to enhance or hamper effective collaboration. Factors include leadership, establishing trust and respect, and collaboration readiness |
| Roussos and Fawcett (2000),65 A review of collaborative partnerships as a strategy for improving community health | USA | Literature review of published studies of collaborative partnerships in community health. Thirty-four studies included in review; most used experimental or quasi-experimental design | Lack of empirical data to show effectiveness of collaborative partnerships for community health improvement, and assumptions underlying collaborative working | Processes which relate to changes in population-level health outcomes. Improvements attributed to collaboration activities. Can be influenced by environment/behaviours | Review emerged with set of modifiable factors that can support partnerships to create the conditions required for improving health outcomes |
Data extraction
The review questions were used to determine the relevance of documents, or sections within the documents, to the review. Consistent with realist approaches, a bespoke data extraction form was developed to guide the review of the selected documents and for extracting or mining relevant information. The bespoke data extraction form incorporated areas of relevance to the review purpose. The data extraction form was developed around a number of different theory areas: the nature of collaboration, characteristics of research users and producers, and issues related to implementation (see Appendix 4). This form was used to extract information on each piece of evidence. Using the data extraction form ensured that the focus remained on eliciting any information to illuminate the review question66 and identify evidence which linked collaboration with implementation and knowledge mobilisation. The development of the form was guided by existing templates for realist reviews,67,68 and based on questions developed by the research team. 39
Analysis and synthesis processes
We used the test of relevance and rigour as the criteria for the selection of documents. 36 Relevance refers to how the data contribute to programme theory development: why, how and in which circumstances collaboration between researchers and practitioners enables implementation. Rigour refers to the reviewer’s judgement of the credibility of the data. 36 The analysis and synthesis of the data extracted from the search process were focused on answering the review question through an inductive and deliberative process.
Findings
The synthesis of evidence from the selected papers shows how collaboration has the potential to impact on implementation and knowledge mobilisation in different ways. The findings are reported based on how the evidence informed the questions used in the data extraction process, reflecting key features which emerged across the papers. The findings from the review are summarised in Table 3 to show what emerged under each of the data extraction areas.
| Nature/design/capacity/capability | Organisational factors | Roles/relationships/interplay |
|---|---|---|
| Infrastructure Size Complexity Communication Resources Setting measurable goals Time Planning Subject/topic |
Support Proximity |
Power sharing Shared vision Trust Reciprocal learning Leadership Membership History |
How the design of a collaboration can facilitate implementation
Collaboration infrastructures can promote a balance between partners, thus reducing pressures on them. 50 Technical assistance and the availability of resources within collaborations are key strengths for project completions. 60 The strategies employed by collaborations to communicate across partners are important, for example face-to-face meetings, regular teleconferences, use of e-mail and digital file sharing, uniform marketing templates and logos, and standard reporting forms. 50,64 In particular, Olson et al. 50 refer to the significance of early face-to-face meetings to foster transition from groups of individuals to functioning partnerships.
Setting measurable and achievable outcomes is proposed to contribute to collaboration success, facilitating monitoring and evaluation, and therefore enabling teams to learn from each other. 50,51 This leads to better co-ordination and success towards achieving deadlines. Additionally, where grant makers require reporting of evidence of intermediate outcomes, this has the potential to promote success in the longer term. 51,52,65 These findings are linked to what Shortell et al. 52 describe as ‘recognising life cycles’, suggesting that, where members are familiar with the stages of development of the collaborating partnerships, they are more able to address issues and seek solutions.
A collaboration is perceived as a ‘temporary learning organisation’ when it is allowed time to learn and consider how to sustain improvements. 51 Where time is protected to develop high-quality action plans which are commensurate with local needs, are clear, have measurable objectives and identify persons responsible for task completion, this facilitates implementation, either because taking action is facilitated, or because the ability to mobilise resources is greater. 61 Careful action planning is associated with increased rates of change; good-quality action plans are associated with synergistic partnerships that have potential for success,62 and better sustainability of events and adoption of interventions by other organisations not within the collaboration. 61,65
Olson et al. 50 suggest that the choice of topic is a significant factor for success of the collaboration. In their collaboration, tobacco smoking was a clinically focused topic of importance, with recognised evidence-based interventions but with identified gaps between desired and actual practice. 50 Olson et al. 50 found that the success of the collaboration is promoted where personal and emotional connections to the subject area are made by those involved and thereby provide the motivation to make changes and take action. Collaborations involving initiatives which are linked in such a way that they appear to be related to each other are more successful, according to Shortell et al. ,52 who suggest that this relates to the synergy between initiatives, allowing partnerships to achieve their intended objectives.
A link was postulated between coalition size and effectiveness, including implementation of activities. 61 Complexity was interpreted on the basis of the number of task forces and committee structures that are associated with the coalition. 61
Linking the structure/function of the collaborating organisation with implementation
Features that contributed to collaboration success also focused on the organisations responsible for hosting. The review suggests that how collaborations structure themselves and the nature of the policies and procedures that they have in place are important factors to support the collaboration without placing unnecessary pressure on resources. 50 Shortell et al. 52 found that most successful partnerships operate within organisations which provide stability and legitimacy across time, but maintain a low profile, allowing the partnership to flourish.
For Olson et al. ,50 factors around proximity contributed to the success of collaborations. These included the physical proximity of collaborating organisations, so that existing relationships between people in the organisations promote better communication and co-ordination. Another factor theorised to contribute to collaboration success through communication networks is the physical proximity of partnerships involved in the collaboration. 50
The role of individuals or teams, the nature of relationships, and the interplay between individuals and groups within collaborations
Sharing power can enable participation across all collaboration partners,50,63 and egalitarian collaboration is more likely to result in implementation of evidence-based practice because of the shift of power towards the clinician. 60 Through clarifying shared vision, prioritising goals, and setting strategies and outcomes, opinions become less divided, resulting in the formation of a broad guidance framework across collaborating partners. 50 Sharing power through collaboration suggests that partners (community and researchers) become more knowledgeable and empowered, according to Lesser and Oscos-Sanchez. 63 Shortell et al. 52 found that the ways in which successful partnerships are able to ‘nip problems in the bud’ are related to how conflict is forestalled through the development of trusting relationships.
Trust is essential to success in collaborative research, and can be reached more smoothly where there is previous experience of working with different organisations. 54,64 If collaborators are allowed time to develop mutual respect and trust, this leads to the development of meaningful relationships, a crucial factor for success according to Lesser and Oscos-Sanchez. 63 This links to the findings of Olson et al.,50 who theorised that starting the collaborative process with an underlying assumption of partners’ specific abilities and strengths promotes the creation of value, and collaborative benefits are distributed fairly and widely, through a productive process of developing resources and mutual learning. Additionally, a collaboration can improve the conduct of research through a reciprocal approach to partners’ engagement with refining research questions, developing theoretical frameworks, recruitment, and data interpretation and sharing. 63
Leadership is the most often reported factor for creating change,65 and elements relating to leadership are important factors for partnership success. In particular, having one consistent executive leader in a dedicated role and the ability to delegate leadership to people most closely involved with partnership projects, described as subsidiary leadership, appear to be important. 52 Furthermore, choosing and using leadership skills at different stages of the collaboration is important. For example, the leadership skills of facilitation and listening may be more effective at the start of the collaboration, whereas negotiation and advocacy skills may be required in the later stages to bring about changes which are true to the collaboration’s mission. 65
Opinion leaders who operate within or outside the collaboration can support the collaboration and contribute to its success. 50 In collaborations between researchers and clinicians, formal mentoring roles provide the encouragement required to complete projects, as long as mentors have the skills, not only in the conduct of research, but also in implementation and community engagement, so that they can facilitate both the programme and its sustainability. 60
Members who display certain traits (e.g. expertise, availability and certain social skills) within collaborations are more likely to contribute to success, especially where synergy is observed across individuals’ skills, resources and perspectives. 62 Successful partnerships are more likely to have members who clearly display readiness to collaborate, and are more able to manage conflict in ways that forestall problems. 52,64
Olson et al. 50 found that a relationship history between collaborators fostered better communication and co-ordination, and contributed to the collaboration’s success. Collaborations which draw on pre-existing networks, previous knowledge and experiences, and build on prior positive experiences and working relationships from earlier collaborations, are also more likely to succeed and contribute to strengthening future collaborations, especially where individuals are experienced in sharing risks, resources and responsibilities in seeking common goals. 56,64,65
Synthesis
Evidence about exactly how collaboration might affect implementation and knowledge mobilisation is sparse. Producing evidence to show the effect of collaborations on implementation can be a lengthy process, which takes much longer than the lifespan of the collaboration or partnership. Therefore, outcomes are difficult both to track and to evaluate. 52,56,65 We found little evidence to link collaboration directly to knowledge mobilisation. However, there are some implicit ideas and, in programme theory terms, some contingencies that might explain collaboration and implementation (Figure 1). These areas are presented below and by drawing on a wider body of literature where appropriate. This wider evidence base was scrutinised because it describes features of more or less successful collaboration; unfortunately, however, the evidence within it falls short of making the explicit link to how these have an impact on knowledge mobilisation.
FIGURE 1.
Theory areas: successful collaboration.
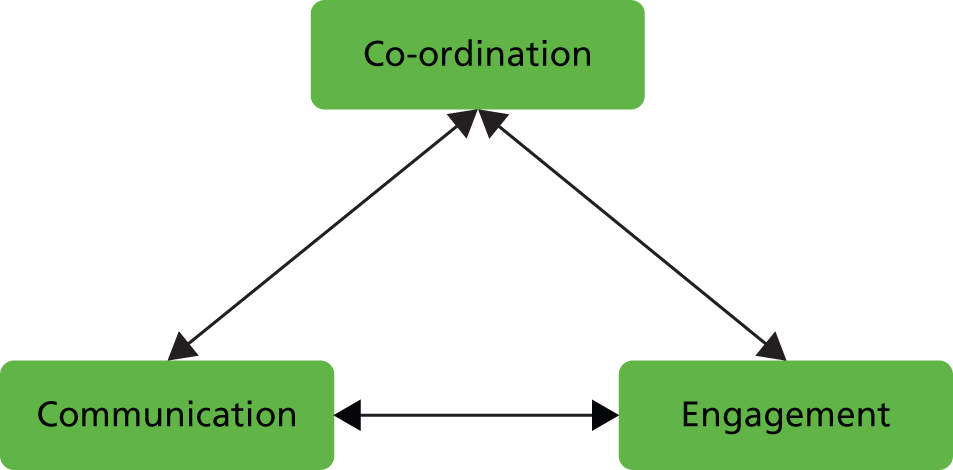
Co-ordination
Collaborations that pay attention to structures, infrastructures, processes and management50 are those that have the potential to facilitate the success of designated centres to work together, to design, implement and evaluate health-related interventions and programmes. 69 These features provide the potential conditions for co-ordinating activity, resources and people. Leadership has a key role to play in the co-ordination of the collaboration.
We found an association with infrastructure and size, and the potential of the collaboration to result in successful implementation. Collaborations are perceived to be moveable structures, which means that members and tasks shift from time to time,70 but evidence points to the importance of some common features about infrastructure. The wider literature supports the importance of governance frameworks, thus ensuring that effective processes are in place for decision-making, administration, management, regular communication, conflict resolution and addressing competition for priorities. 50,55 While small networks can be self-governed, there is some evidence to support the idea that larger collaborations are more effective where the lead organisation is the administrative host, or where collaborative partners represent the widest possible range of potential participants. 52,70
The wider literature supports the importance of setting clear parameters using contracts; defining clear roles and responsibilities; having active management and organisational understanding; ensuring the formation of steering groups to escalate issues and keep projects on track; and setting measurable and achievable targets for the progress of the collaboration. 50,51,58 Success is further promoted where there are clear, explicit statements about property rights. 70 Further, improving accountability through aligning academic and clinical institutions can be strengthened by ensuring common frameworks are in place to evaluate performance across the collaboration. 71
The ways in which outcomes are set and evaluated can have an impact on the success of the collaboration. Where evaluation is focused on intermediate (as opposed to final or long-term) outcomes, this can promote the function of the collaboration through focusing on intermediate success or failure, while at the same time enabling the celebration of small or large accomplishments; it helps the collaboration to redirect attention if required and identify potential barriers to success. 55,65 Furthermore, wider literature about collaboration points to operational planning and setting strategic initiatives as activities associated with successful collaborations. 65,72 Rigorous planning leads to more significant activities which link to programme outcomes. 73 Additionally, coalitions with action strategies that use task forces and action teams are reported to be more likely to impact on interorganisational partnership. 70
Collaboration partners require clear lines of accountability about the control of resources, and resources need to be directed towards network-level and organisational-level goals. Resources important to collaborative success include finance, space, equipment and goods. The wider literature also supports building on collaborative partners’ strengths and resources to promote the exchange of resources and enhance resource links between partners. 57,70,74
There is agreement in the literature that individuals in visible, senior, leadership positions contribute to the success of collaborative efforts in implementation and improvement. 51,53,75 Committed and active leaders encourage collaboration and commitment to projects; communicate the vision and mission of the collaboration to key stakeholders; support the engagement of other leaders to implement change; and possess skills that are facilitating and empowering, for example networking, diplomacy, listening, perseverance, dedication and adaptability. 32,52,55,65,69,70 They thus provide a co-ordinating function. The core characteristics of desirable leadership for collaborations include the ability to embrace the expertise of partners; the ability to demonstrate effective communication, facilitation, negotiation and networking skills; and previous experience in similar partnership work. 55,65,74
Evidence suggests that leaders who are reflective practitioners and who engage in formal collaboration evaluations70 are more likely to contribute to success in implementation, especially if facilitative characteristics such as being supportive, democratic and committed are identified. 64 The wider literature supports the view that leaders (or subsidiary leaders) who give direction and listen to others are likely to succeed. 52,65,76 It is reported that leaders with empowering styles are more likely to bring about successful implementation and achievement of collaboration outcomes,64 as are leaders orientated to action who demonstrate relationship-building skills. 77
Engagement
There is evidence to support the notion that relationships between partners are the foundational element of collaborative research. 78 The engagement and involvement of members and stakeholders in the collaboration is prompted through the quality of partner relationships, and a sense of trust, resonance and shared vision/mission in the collaboration. Continued efforts to build and rebuild trust and relationships are integral to success, but this is conditional upon both structured and unstructured interactions between partners. Setting the co-ordinates for the collaboration through defining a clear purpose seems to be important. Involving all partners, clear common aims should evolve as the collaboration grows, which involves setting a direction, taking action and building trust. 70,78 Conversely, where there is lack of clarity in the overall vision for the collaboration, this can have a negative impact on the success of the collaboration. 55 Furthermore, shared vision can be hindered by poor communication. 72
Trust in collaborations appears to be a key factor, perceived as a cyclical process which is built over time, and is often more strongly established on previous experiences and/or reputation than through formal agreements and contracts. 32,63,65,69,70,79 Given this, pre-formation has been shown to be important in creating strong foundations for the collaboration and linkage at the early stages. 16,73 Where examples are used to show how collaboration partners employ an element of pre-formative work (e.g. collecting data or analysing the system before commencing the collaboration), this appears to contribute to a better understanding of the issues. 54 Newly formed collaborations which work on the assumption that teams are not already formed and functioning, and provide time for team forming, are more likely to be successful. 51
Where there is equity among partners and commitment to ongoing self-reflection and self-critique, this could avoid power imbalances, and thereby enhance the collaboration’s chances of success. 63 Collaboration success is contingent on structures that allow shared power, whereby decision-making is by consensus; successful collaborations are built on trust, they can leverage support for the cause through agreement across partnerships so that they are fair and balanced, and they distribute work fairly among their members. 50,55 ‘Shared memory’ describes how consistent membership across collaborations can develop mutual respect and willingness to work together, and can promote learning from mistakes. 51,53,80
Within the communities of practice literature, successful collaborations are usually large, incorporating a full range of potential stakeholders who are engaged throughout the whole process of planning, implementation and evaluation of programmes. 57,70 Conversely, inadequate staffing for collaborative projects can have a negative effect on the chances of successful implementation. 55
The subject or topic area around which the collaboration is focused also seems to be important for its success. For example, quality- and community-based collaboratives appear to have more impact if subject areas are practice based and specific. 51,72 ‘Good’ subjects which are regarded as important and specific, with strong evidence of effective interventions and reflecting clear national research priorities, are linked with the success of the collaboration. 50,51,54,65 Wilson et al. 54 found that collaborations focused on broader topics are more likely to result in better implementation of innovations. However, Ovretveit et al. 51 question the effectiveness of collaborations which are associated with broad topic areas.
Communication
The success or failure of collaborative teams has been reported to be contingent on how partners communicate and consult with each other. 81 The evidence in this review indicates that communication between collaborators is a significant factor for collaboration success, supported by internal and external communication channels and multiple communication strategies. Physical proximity of team members and the level of technical communication strategies employed within the collaboration are also important for communication. 64 Furthermore, communication has the potential to facilitate sharing and therefore potentially to enable learning.
Findings from a study of interorganisational learning in health care showed that it is the learning activities, facilitated by the knowledge-sharing infrastructure provided within the collaboration to engage with learning, which ultimately lead to improvement, rather than the collaboration itself. 82 In community health and school health, evidence was found that indicates that the use of advisory boards and learning in teams can foster communication between partners and allow them to learn from each other. 52,74 Nembhard82 found that the likelihood of a collaboration’s being effective is increased where partners participate and use the infrastructure and the knowledge-sharing features within the collaboration. Tools and materials developed together in partnership can also foster opportunities for mutual learning, contributing to interorganisational collaboration success. 51 Furthermore, support for the collaboration in the form of technology platforms or technical assistance including training and support, described as virtual readiness, can enhance core competencies throughout the collaboration’s lifespan. 55,60,65,83
Structural links, agreements for working together, and the presence of specific and essential roles and resource mobilisation to support and nurture the collaboration are also important. 55,57,61,70 Committees and work groups which lead to a lack of cohesion and communication across partnerships are perceived to be a threat to the success of collaborations. 55 In contrast, promoting opinion leaders with high levels of technical competence, champions and stakeholders within and outside the collaboration can work effectively to secure change, and dispersed leadership prevents problems associated with sole leadership, such as manipulation. 54,64,65
Summary
This project begins with the theory in the heads of the creators and funders of CLAHRCs: that collaboration between organisations should have the potential to foster the application of research. However, the evidence to support this theory is largely absent. In this review we have attempted to find and summarise some of the emerging contingencies evident in the existing literature about collaboration related to knowledge mobilisation. This was challenging, as few studies make this explicit link. However, it appears that collaborations that offer opportunities to co-ordinate purpose, activities and people, that provide members and stakeholders with chances and resources to engage, that foster mutual trust, and that provide the ways and means for communication and interaction might be those that offer more conducive conditions. It is unclear, however, if and how these collaborative conditions and features have an impact on knowledge mobilisation itself.
Chapter 3 Design and methods
Design
This study was a longitudinal realist evaluation using multiple qualitative case studies. Overall, our purpose in this study was to develop explanatory theory about implementing research through CLAHRCs and answer the question ‘what works, for whom, why and in what circumstances?’ We did this by focusing on the following aims and objectives.
Aims
-
To inform the NIHR Health Services and Delivery Research programme about the impact of CLAHRCs in relation to one of their key functions: implementing the findings from research in clinical practice.
-
To make a significant contribution to the national and international evidence base concerning research use and impact, and mechanisms for successful partnerships between universities and health-care providers for facilitating research use.
-
To work in partnership so that the evaluation includes stakeholder perspectives and formative input into participating CLAHRCs.
-
To further develop theory-driven approaches to implementation research and evaluation.
Objectives
-
To identify and track the implementation mechanisms and processes used by CLAHRCs and evaluate intended and unintended consequences (impacts) over time.
-
To determine what influences whether or not and how research is used through CLAHRCs, paying particular attention to contextual factors.
-
To investigate the role played by boundary objects in the success or failure of research implementation through CLAHRCs.
-
To determine if and how CLAHRCs develop and sustain interactions and communities of practice.
-
To identify indicators that could be used for further evaluations of the sustainability of CLAHRC-like approaches.
Theoretical framework
The initial theoretical framework underpinning the study was a combination of two frameworks that focus on knowledge use in practice: Promoting Action on Research Implementation in Health Services (PARIHS)15,84 and K2A. 16
Promoting Action on Research Implementation in Health Services was conceived and developed as a means of understanding the complexities involved in the successful implementation of evidence into practice. As a framework that has been developing and refined over time through concept analysis and empirical validation and testing, it can serve as both a practical and a conceptual heuristic to guide and evaluate implementation. PARIHS maps out the elements that need attention before, during and after implementation efforts. Within PARIHS, successful implementation is represented as a function of the nature and type of evidence, the qualities of the context in which the evidence is being used and the process of facilitation. Each of these elements contains subelements:
-
evidence – research, clinical experience, patient experience and information from the local context
-
context – culture, leadership and evaluation
-
facilitation – the presence or absence of appropriate facilitation, including approaches ranging from task orientated to holistic.
These elements and subelements interact in different ways in different contexts to provide more or less conducive conditions for successful implementation.
The K2A framework was developed from a review of 31 planned action theories. The framework assumes a systems perspective and privileges social interaction and adaption of research evidence, taking local context and culture into account. The framework is a cycle of problem identification, local adaptation and assessment of barriers, implementation, monitoring and sustained use. Embedded within the cycle is attention to the knowledge creation process, knowledge synthesis and tools, and tailoring to local context. The authors state that adherence to each phase of the framework is not sufficient in itself for the successful application of knowledge; a key assumption underlying the framework is the importance of appropriate relationships between researchers and end-users, and between implementers and adopters.
These frameworks complement one another (e.g. they both consider the importance of context in implementation and that implementation is multifaceted), with PARIHS providing a conceptual map of the factors that have been demonstrated to lead to more successful implementation and K2A providing an action- or process-orientated representation of KT processes.
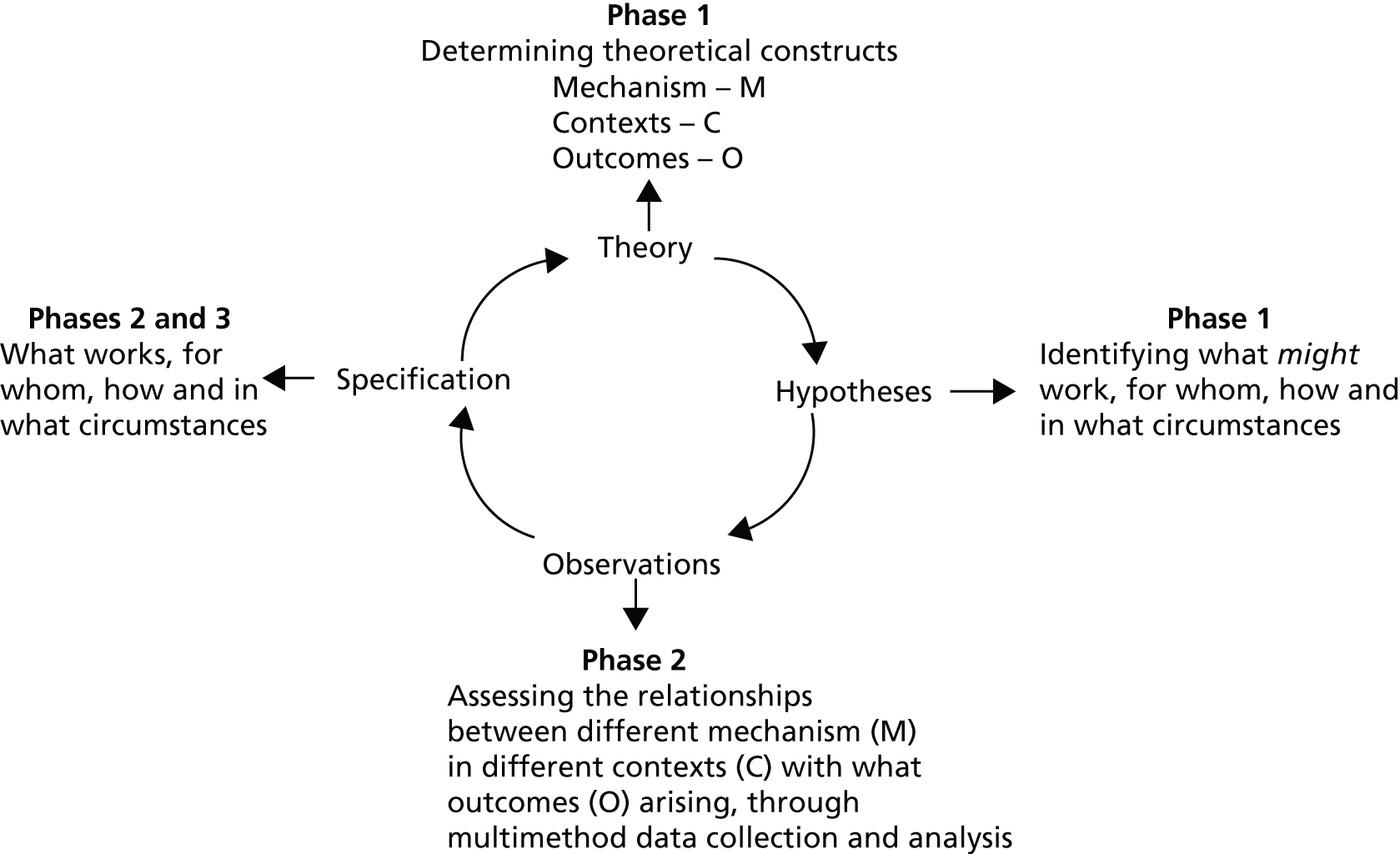
This framework provided an initial focus for the theory-building stage (phase 1) of the realist evaluation cycle (Figure 2). In practice this meant that, in the concept-mining phase of the development of the evaluation framework, concepts within the PARIHS and K2A frameworks were surfaced and combined with concepts from other sources of information and a subsequent mapping exercise was undertaken (see Development of conceptual framework and programme theories). Accordingly, PARIHS and K2A served as a starting point for the study, but through the theory-building process they became embedded in the evaluation framework and not visible in their original form.
FIGURE 2.
Study’s initial theoretical framework.

Realist evaluation
A fundamental assumption of realist evaluation is that ‘programmes are complex interventions introduced into complex social systems’ (p. 33). 85 Programmes are composed of theories, involve the actions of people, are rarely linear, and comprise a series of steps or processes that interact, are prone to modification and exist in open and dynamic systems that change as the result of learning. Realist evaluation is therefore an appropriate approach to exploring knowledge mobilisation within CLAHRCs, which, by their nature, are social systems, involve the actions of groups of people and have the potential to change over time. Observing CLAHRCs over time makes realist evaluation particularly appropriate because it is a cyclical and iterative approach.
Within realism, theories are framed as hypotheses about how mechanisms act in context to produce outcomes. We followed the realist approach promoted specifically by Pawson and Tilley. 86 Thus, programmes (in this study, CLAHRCs’ approaches to implementation) are interrogated to identify what it is about them (mechanisms) and the contextual conditions (context) that triggers these mechanisms to produce particular outcomes – commonly expressed as CMO (C + M → O) configurations. It is the CMOs that are the study hypotheses, which are refined and tested over time.
Contexts
The conditions that are necessary for a programme to trigger a mechanism to activate specific outcomes87 are critical for understanding how it works ‘for whom in what conditions’ (p. 72). 86 Context may be defined as space or place but can also be described as the ‘settings within which programmes are placed or factors outside the control of programme designers – people’s motivations, organisational context or structures’. 88 As such, context is not the backdrop to a site/study/case, as some have intimated,89 but is the condition that fires or triggers certain mechanisms.
Mechanisms
There is a paucity of literature relating to clarity of meaning of mechanisms; however, from the realist evaluator’s perspective, the underlying mechanisms that give rise to an event or outcome are the main focus of study. 90 Pawson and Tilley86 use the analogy of a clock to illustrate the meaning of a mechanism: it is only by examining the inside of the clock that it is possible to understand how it works, not by examining the clock face itself. Likewise with mechanisms, in realist evaluation the programme activity and processes are the mechanisms, which may be more or less hidden from view. Westhorp et al. 91 describe a mechanism in terms of how a programme changes people’s decision-making: what people do in response to the resources (of any kind) that a programme provides.
The other important aspect of mechanisms is that they lead to outcomes, but only when triggered by a particular context, or condition. 91,92 In realist evaluation the question is, therefore, not ‘does it work?’ but ‘how does it work and which mechanisms in which contexts give rise to particular outcomes?’.
Outcomes
In realist evaluation, outcomes ‘reflect, or represent, the responses to different mechanisms in particular contexts’ (p. 77). 93 Outcomes may include the learning from programmes or can be related to impact (e.g. a change in behaviour) or processes (whether or not an intervention worked). 94 In this study we captured a range of different types of impact CLAHRCs’ implementation activity might have, from those that are more direct to those that are more conceptual and processual.
Case studies
Case study was selected in order to undertake an in-depth exploration within three CLAHRCs. As Yin95 states, a case study is an empirical enquiry that investigates a contemporary phenomenon within its real-life context, especially when the boundaries between the phenomenon and the context are not clearly evident.
In this study, implementation was the phenomenon that we wanted to study in the real-life context of the CLAHRC. Case studies are appropriate where one does not need to (or wish to) control events, and when one is interested in answering ‘how’ and ‘why’ questions.
Realist evaluation and case studies are an appropriate ‘fit’ in that both aim to be explanatory in nature,86,95 are about understanding a phenomenon in context, and enable an approach that collects multiple sources of data. 96 For this study a ‘case’ is the implementation team/theme/programme within a CLAHRC.
Tracer issues
Tracer issues were chosen as a way to provide a common focus across CLAHRCs, which were heterogeneous, complicated and multifaceted entities. At the time of proposal writing (before the CLAHRCs had set their agendas and approaches), we had expected that these tracer issues might be clinical issues, for example diabetes or stroke; however, as the CLAHRCs began to establish themselves it was evident that there was huge variability and a lack of cross-cutting themes that could provide a common thread. Therefore, in collaboration with CLAHRC study collaborators it was decided to select tracer issues that reflected processes. These were viewed as a watermark in CLAHRC activities: something that could be seen when specifically looked for in projects and initiatives, but which was not in the foreground or the main point of their attention.
The tracer issues were discussed with the CLAHRCs at a stakeholder meeting (in January 2011) where members of all nine CLAHRCs were present, and a consensus was reached. This was then finalised through follow-up telephone calls with the CLAHRCs participating in this study, and included:
-
Change agency: the focus of this was on the people in change agent/boundary-spanning/facilitation roles (each CLAHRC had given these different job titles). Roles were a useful focus in the first instance, but the processes of change agency became an increasing focus in terms of facilitating implementation and the impact arising from this. It was what these people did that became the focus of the tracer issue.
-
Collaboration and partnership: one of the issues that came over strongly from stakeholders was the difficulty in identifying and separating the research and implementation functions of the CLAHRCs. As a tracer issue it provided scope to look into a variety of formal and informal collaborations and the processes of collaborating at different levels within the CLAHRCs. Again, it enabled the individual CLAHRCs to select the projects and initiatives that they felt would be able to focus on collaboration and partnership.
-
Sustainability, adaptability and spread: this tracer issue arose from the concern of the CLAHRCs that change and knowledge use needed to be sustainable beyond the end of individual projects, in a turbulent context and shared across the individual CLAHRCs and beyond where appropriate.
These issues mapped well onto the study’s evaluation framework (see Figure 4) and so were embedded in the questions asked at each round of data collection and in data analysis processes.
Sites
Given the collaborative nature of the CLAHRCs’ mission and realist evaluation’s emphasis on stakeholder engagement, we worked closely with those involved in CLAHRCs to develop the proposal and subsequently deliver the project. This included involving CLAHRC participants as coapplicants. We studied three CLAHRCs in depth (Ashgrove, Hazeldean and Oakdown) while providing opportunities for engagement with the wider CLAHRC community during stakeholder meetings and through an interpretive forum.
Patient and public involvement
As it was a stakeholder-driven project, patient and public involvement (PPI) was an important aspect of the study. Furthermore, we had been asked by the funder to ensure an explicit focus on PPI within implementation, as the other external evaluation projects were not funded to focus on this. Questions about how PPI happens within implementation are important and under-researched, and therefore warranted targeted attention in this project.
We also established a PPI group to help inform this aspect of the research and the work more generally. The group comprised five members: four from our case study CLAHRCs and one person from a non-CLAHRC area. Participants were nominated by the CLAHRCs themselves and as a group had experience of involvement as patients, as a lay member on a CLAHRC board and through participation in INVOLVE. An inaugural face-to-face meeting of the group was held on 12 December 2011. As part of agreeing ways of working, the preference was to engage with individual members of the group at points where their input would be most useful. Subsequently, they participated in the project by reading and commenting on, for example, draft reports, and through physical presence at research team meetings.
Data collection
The realist evaluation cycle represents the research process in three phases as hypothesis generation, refining and testing, and programme theory specification (over several rounds of data collection), as shown in Figure 3.
FIGURE 3.
Realist evaluation cycle.
Development of conceptual framework and programme theories
This relates to phase 1 (see Figure 3).
Realist evaluation is theory driven86 and theory guides us to know where to look and what to look for. It provides explanations and so directs us to vital explanatory components, their inter-relationships and the things that bring about those inter-relationships. 85 Interventions, for example CLAHRCs, begin as theories whereby there is always an expectation, hypothesis or ‘programme theory’ that if certain resources (social, cognitive, material) are made available this will lead to a change in action or behaviour. 97 As stated in Chapter 1, the establishment of CLAHRCs was a result of a theory in the creators’ and funders’ heads that collaboration would foster the conduct of applied research and the use of research in practice by providing an infrastructure, resources and a regional focus for building capability and capacity for implementation. There is no prescribed approach to the development of programme theories, or rules for working with implicit and explicit theory. Therefore, in this study a four-stage approach was used that was informed by Pawson and Tilley86 and Pawson85 to inductively identify the programme theories and a conceptual framework, while ensuring a focus on study objectives.
Development of the conceptual framework
The conceptual framework was developed through the following steps:
-
Concept mining: a number of sources of information such as the CLAHRC’s original commissioning brief, discussions with the participating CLAHRC’s directors, interviews with members of the commissioning panel and concepts from the explicit theory (K2A and PARIHS frameworks) underpinning the study were mined for key concepts. 17,84,98 The findings from the rapid realist review were also taken into consideration in that they provided an organising framework for exploring the implementation literature. This process resulted in a sizeable list of concepts relevant to the overarching research question and underlying intention of CLAHRCs to undertake research implementation.
-
Concept mapping: the list of concepts provided a focus for reviewing the implementation literature, which resulted in more detailed knowledge about the concepts and their potential meaning to the research question.
-
Mapping across concepts: a conceptual platform85 was developed by clustering the concepts including underpinning evidence into meaningful units or elements in the framework. The concepts underpinning the programme theory are context, knowledge and knowledge production, facilitation, PPI, knowledge sharing and exchange, geography, actors and agents, temporality, architecture and impact. These theory areas and the evidence underpinning them are described further by Rycroft-Malone et al. 39
-
Building the framework: considering the content in each dimension and revisiting the hypothesised purpose of the CLAHRCs implementation function, a framework that visually represents the potential interconnectedness between the dimensions was constructed.
This development process and the evidence underpinning the areas in the framework has been more fully described by Rycroft-Malone et al. 39
Consistent with the focus of realist evaluation on engaging with stakeholders, the framework was presented for comment at meetings with each of the three CLAHRC ‘cases’ and the wider evaluation research team. As a result a few minor modifications were made to the framework. The framework is shown in Figure 4.
FIGURE 4.
Conceptual framework. Source: Rycroft-Malone et al. 39 Reproduced with permission. CoP, Community of Practice.
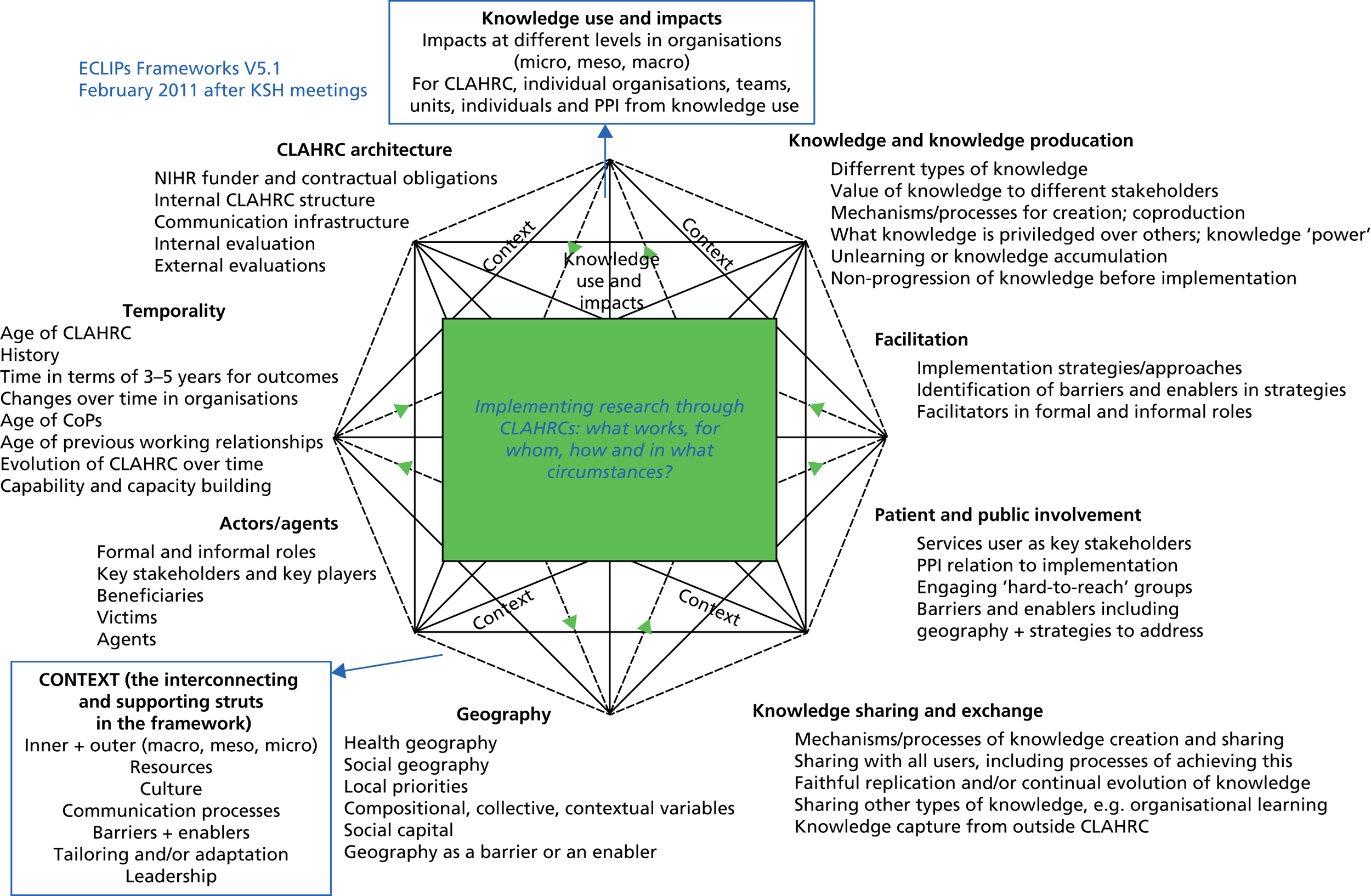
It was hypothesised that the elements in the framework would be more or less facilitative of a CLAHRC’s ability to deliver on its implementation function; however, at the outset we did not make any links or contingencies across them. Therefore, the framework provided a template upon which we focused data collection in round 1. Following round 1 data collection the realist task was to draw interferences and contingencies across the domains in the framework to provide explanations about CLAHRCs’ approach to implementation. These explanations or CMOs (see Chapter 6) were then refined and tested over the remaining three rounds of data collection.
What works, for whom, how and in what circumstances: data collection and analysis
This relates to phases 2 and 3 (see Figure 3).
Data were collected over four rounds between July 2011 and January 2014:
-
round 1, July 2011 to December 2011
-
round 2, July 2012 to December 2012
-
round 3, September 2012 to February 2013
-
round 4, September 2013 to January 2014.
As agreed when funded, and consistent with our collaborative approach to undertaking the research, at each stage discussions took place with CLAHRC directors about the focus of data collection activity. These discussions took into account the focus on tracer issues, topics of interest to the CLAHRCs themselves and the intent to build explanations about implementation within CLAHRCs over time.
Sampling
For each round of data analysis the sampling framework was based on a stakeholder analysis99 and used both theoretical and criterion sampling, which determined which stakeholders were essential, important and/or necessary to involve. 100 Details of potential participants were provided by CLAHRC directors or programme managers. Each potential participant was approached initially by e-mail invitation and then an information pack including participant information sheets and consent forms was sent by post. On receipt of consent to participate, interviews were arranged at a time to suit the participant. Snowball sampling was used to recruit other participants who met purposive sampling criteria and who were thought to have a perspective on implementation.
This resulted in an overall focus on implementation approach and roles, and the sample varied between CLAHRCs. Table 4 shows the focus of data collection across the four rounds. Tables 4 and 5 show the study participants and data collected.
| CLAHRC | Relationship to tracer issue | |||
|---|---|---|---|---|
| Round 1 (collaboration and partnership) | Round 2 (collaboration and partnership) | Round 3 (change agency) | Round 4 (change agency, collaboration and partnership, sustainability, adaptability and spread) | |
| Hazeldean | CLAHRC-designated roles, e.g. programme leads, directors, facilitators, theme leads | Mental and physical health project | Boundary spanning | Implementation roles and function |
| Oakdown | Health inequalities implementation theme | Bariatric surgery project | Boundary spanning | Implementation roles and function |
| Ashgrove | CLAHRC-designated roles, e.g. programme leads, directors, facilitators, theme leads | Cardiac rehabilitation project and COPD rehabilitation project | Boundary spanning | Implementation roles and function |
| Participants | Number |
|---|---|
| Members of seven CLAHRCs | 15 |
| Academics with an interest in knowledge mobilisation | 3 |
| Policy-makers | 3 |
| Members of the research team | 7 |
| Total | 28 |
Methods
Interviews
Semistructured, audio-recorded interviews were undertaken with individual participants by telephone and face to face (as convenient) and were guided by an interview guide. As we were developing explanations over time, the focus and schedule for interviews reflected this development, so we used four different interview schedules (see Appendix 5). The first round of data collection was exploratory and focused explicitly on the elements in the study’s evaluation framework. Following analysis of these data, data collection in rounds 2 and 3 focused on helping us refine the emerging explanations. Interviews in round 4 were focused on testing these explanations. Interviews were audio-recorded and lasted between 30 and 90 minutes. This type of interview process has been described as a realist interview or teacher–learner approach to interviewing. 85
Observation
Non-participant observation of some events and meetings (e.g. board meetings and stakeholder events) was conducted and recorded as field notes using Spradley’s101 nine dimensions of observation: space, actors, activities, objects, acts, events, time, goals and feelings. We asked site collaborators to alert us to observation opportunities. Given this study’s focus, we suggested that these could perhaps be strategic-level meetings about implementation plans, and/or more specific CLAHRC discussions about implementation-related activities. We followed up with CLAHRCs on a regular basis at each round of data collection to check if there were opportunities to which we could be invited.
Documentary data
Documents (see Appendix 6) were gathered from CLAHRCs to support the development of the programme theories and the contextualisation of data collected in the field (Table 6).
| Data sources | Hazeldean | Oakdown | Ashgrove | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Interviews | ||||||||||||
| Round of data collection | 1 | 2 | 3 | 4 | 1 | 2 | 3 | 4 | 1 | 2 | 3 | 4 |
| CLAHRC leadership role | 2 | – | – | 2 | 3 | – | – | 2 | 4 | 1 | 2 | 2 |
| Boundary-spanning/implementation role | 9 | 3 | 7 | 2 | 1 | 3 | 4 | – | 4 | 5 | 3 | 1 |
| Academic | 5 | – | 1 | 2 | 4 | 3 | – | 3 | – | 3 | 1 | 4 |
| Clinical academic | 2 | – | – | 1 | – | 1 | 1 | 1 | 2 | 1 | – | – |
| Clinician | 2 | 2 | – | 1 | – | 3 | 1 | – | – | 1 | – | – |
| NHS leadership role | – | 3 | – | – | – | 2 | – | 2 | – | – | – | – |
| PPI rolea | – | – | – | – | – | – | – | 1 | – | – | – | 1 |
| Subtotal for round | 20 | 8 | 8 | 8 | 8 | 12 | 6 | 9 | 10 | 11 | 6 | 8 |
| Subtotal for interviews | 44 | 35 | 35 | |||||||||
| Additional sources | ||||||||||||
| Observation of CLAHRC board meeting | One meeting (12 participants) | – | – | |||||||||
| Feedback from round 1 data collection to those in leadership roles in CLAHRCS | – | 3 | 2 | |||||||||
| Observation data from feedback sessions/workshops with mixed attendees | One session (24 participants) | – | One session (21 participants) | |||||||||
| Subtotal for additional sources | 36 | 3 | 23 | |||||||||
| Total evaluation reach b | 80 | 38 | 58 | |||||||||
Data analysis
Audio-recorded interviews were transcribed verbatim and contemporaneously with each round of data collection. Hand-written field notes were also transcribed into electronic text. The data analysis process was iterative and took place after each period of data collection in order to build explanations over time and enable us to focus subsequent data collection in areas of productive inquiry.
Drawing on the data analysis methods proposed by Miles and Huberman102 and the case study research methods of Yin95 we used a combined inductive and deductive approach to ensure that the process continually focused on the ‘propositional-building function of the CMO’ (p. 22). 85 Following each data collection period, the analysis process began with reading and rereading the transcripts and field notes before moving on to coding. We used interview data as our starting point and then moved on to observations and documents to help build explanations. In this sense they were purposively mined for information that would help us refine/challenge/develop CMOs. Each stage of analysis (summarised in Figure 5) became progressively focused on CMO configurations. In reality this process was not linear, but involved much iteration, discussion and deliberation between and across phases.
FIGURE 5.
Summary of analysis process.
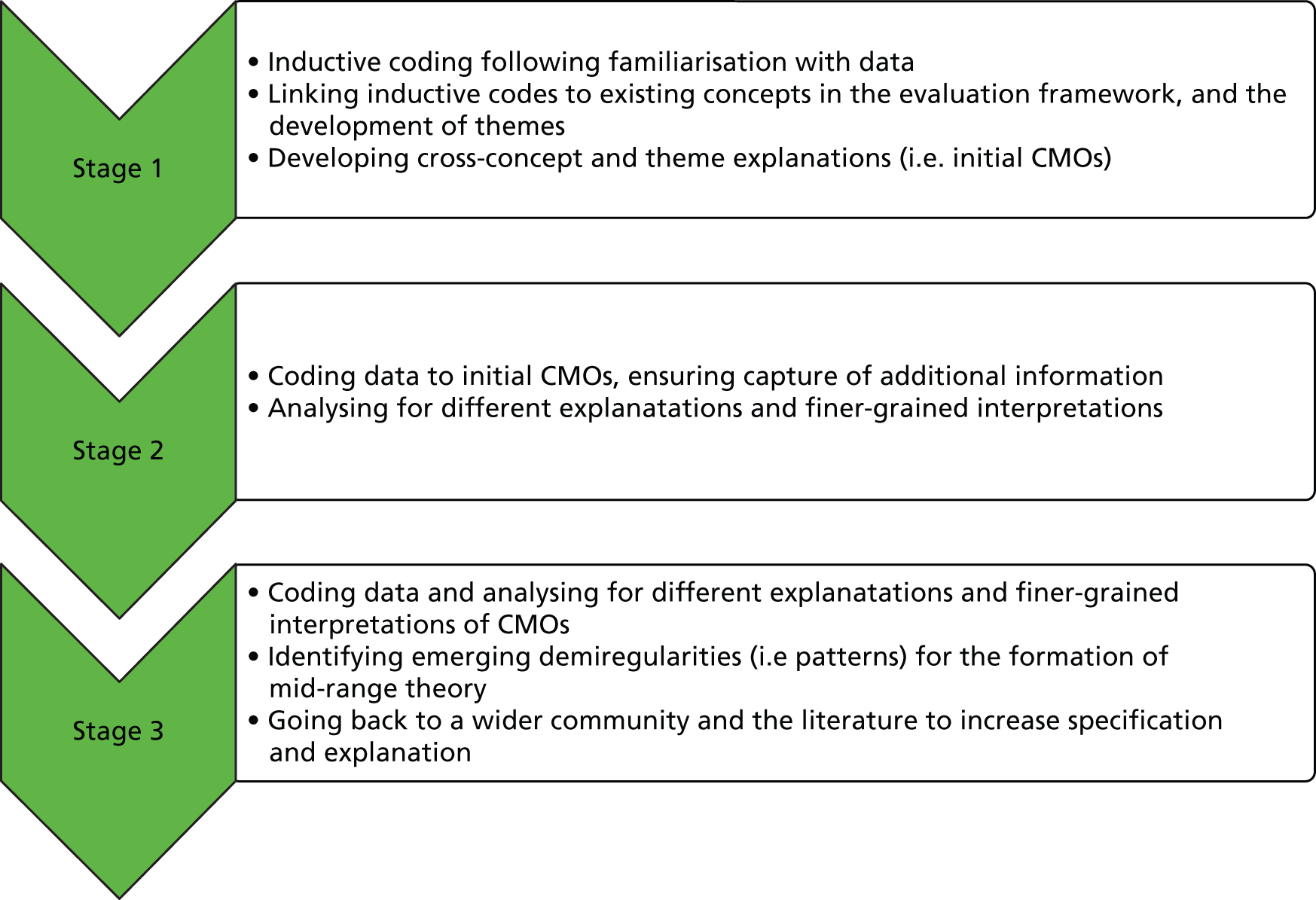
Consistent with the case study, data were analysed within data sources and cases, and then explanations were developed across cases, with attention to the realist task of uncovering contingencies and conditions, that is the relationships between factors that explain CLAHRCs’ approach to implementation, and the conditions in which they operate.
The analysis process was managed by three members of the core research team. However, members of the wider team (GH and BMc), including one from a participating CLAHRC, also engaged with this process. This engagement was useful for sense checking, building and refining explanations, and providing a further check on credibility.
Programme theory specification: interpretive forum
This relates to phase 3 (see Figure 3).
We closed the realist evaluation loop by ‘testing’ emerging findings with a wider community. The interpretive forum held in April 2014 was an opportunity to reflect on, interpret and surface viewpoints with a different group of stakeholders. Invitations to participate in this event were sent to participants in other CLAHRCs including members of CLAHRCs funded by the second wave of NIHR funding, and to other stakeholders who might have an interest and expertise in knowledge mobilisation, including policy-makers and our funder. Participants in the meeting are summarised in Table 5.
The workshop was externally facilitated and designed to give maximum opportunity for discussion and participation (see Appendix 7 for workshop description). Data were collected in field notes. This information was triangulated to facilitate further specification of CMOs.
Theory use and development thread
The use and development of theory is integral to realist evaluation. In this project we initially drew on explicit theory through reference to PARIHS and KTA in the early stages of our concept mapping processes. This provided an overall framework with which to interrogate the implementation research literature, which was then integrated with the findings of the rapid realist review. This process produced the conceptual framework illustrated in Figure 4. Figure 4, therefore, represents an amalgam of concepts that are embedded in existing theory (KTA and PARIHS) and in the literature about implementation and collaboration.
As a map, this conceptual framework informed the first round of data collection. Following analysis of these data an initial set of CMO configurations were developed (see Table 13) and then refined and then tested through a further three rounds of data collection, which resulted in a final set of CMO configurations (see Table 14). The contingencies between the elements in these CMOs are represented later in Figure 13. We then tested these configurations with a wider community and with reference to the wider literature and refined the programme theory, which is illustrated in later Figure 14. The whole theory development cycle of the project is summarised at the end of the report in Figure 15.
Ethical issues
Permission was sought and granted from a NHS Research Ethics Committee (study number YH0155) in June 2011. Once ethical approval had been granted it was necessary to obtain approval through the local [research and development (R&D)] governance processes. These procedures took some time, with the longest taking 7 months to grant access, as each CLAHRC covered more than one region. The procedures which were necessary for the study varied from one NHS organisation to another, with little consistency between them.
Burden
The main issue of concern was burden on individual participants through participating in a number of other evaluations, internal and external. Burden was minimised by negotiating access to potential participants with CLAHRC directors or programme managers prior to recruitment. Each participant was provided with an information pack about the study and was required to provide written consent prior to taking part. One potential participant (in Ashgrove) declined to be involved because of workload pressures; others were all given the opportunity to take part in interviews that were organised to be at their convenience. Participants who took part in more than one round of data collection were required to consent to each interview.
Confidentiality and anonymity
Each participant was assigned a unique numerical identifier for each round of data collection to protect anonymity. To ensure confidentiality each CLAHRC was given a pseudonym, and job titles, where used, were generalised to protect the anonymity of those in specialist roles or where job titles were specific to an individual CLAHRC. Protecting anonymity was, at times, troublesome, particularly over time when specific aspects of some of the CLAHRCs participating in this study became known about in the wider CLAHRC community or where CLAHRCs were collaborating together on projects.
Chapter 4 Findings from within each case
Introduction
The findings are presented in three chapters, which move progressively from description to explanation. From a realist perspective, this approach provided the opportunity to show the reader how we were able to develop and build an explanation about how, why and for whom knowledge mobilisation operates within the CLAHRC ‘programme’. These chapters are structured as follows:
-
Chapter 4: a high-level descriptive overview of the main issues evident from data collected in each case, organised around the theory areas in the conceptual framework (see Figure 4).
-
Chapter 5: an in-depth, narrative description of the main themes to emerge from data across cases and across the domains in the conceptual framework. As a cross-case and cross-framework narrative, this chapter also starts to highlight the factors, opportunities, choices and consequences that contribute to an explanation of implementation within CLAHRCs.
-
Chapter 6: a contingent explanation of implementation within CLAHRCs, structured as CMO configurations.
Within-case summaries
The following sections describe some of the main issues to emerge from the data collected that relate to the theory areas in the evaluation framework (Figure 6).
FIGURE 6.
Outline conceptual framework.
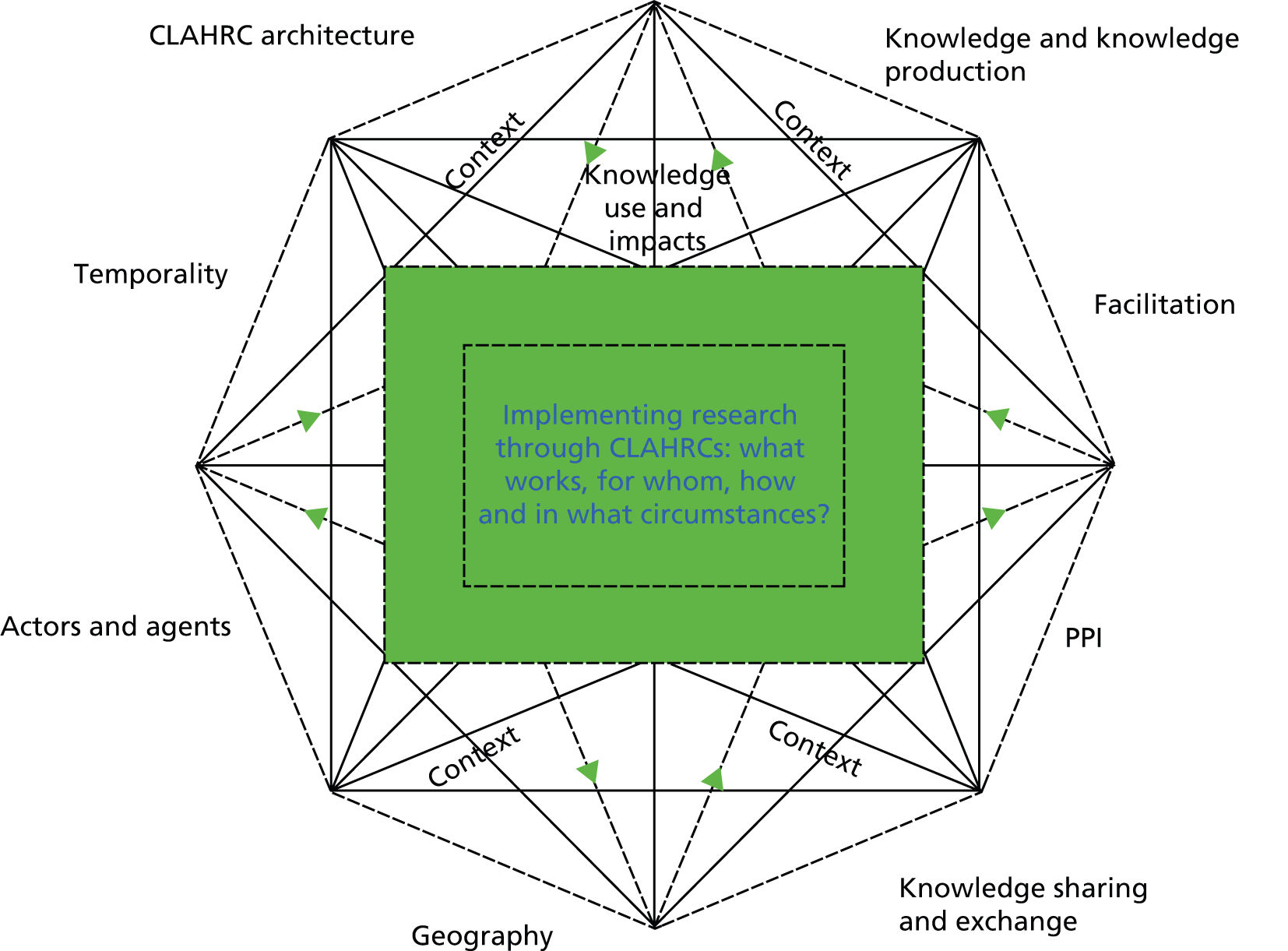
An overview of the structure and executive of each CLAHRC is outlined in Box 1.
One university and seven partners from the NHS, both acute and primary care trusts. These provided matched, in-kind funding for the CLAHRC.
StructureFour research themes: prevention, early detection, self-management and rehabilitation. In addition, it had five overarching themes for implementation: older people, health education, reducing emergency admissions, improving primary care services, and improving secondary care services. Each had a number of projects embedded within it.
ExecutiveLeadership was provided by a director, an associate director and a manager, and through a CLAHRC management board and executive committee with a team structure feeding into these. The executive committee comprised members from the partner organisations and the research and implementation theme leads.
Hazeldean Composition and fundingOne university and four NHS trusts (originally 10). Matched funding from participating NHS collaborators.
StructureFour research programmes (patients, practitioners, systems and services, later reduced to three: patients, systems and services) focused on people with long-term conditions; improving access to quality of care for people with depression in diabetes and coronary heart disease; and health information systems which developed systems for health-care planning for people with chronic vascular disease. It had one implementation programme focused on a range of cardiovascular conditions.
ExecutiveA director, a deputy director and a CLAHRC manager provided leadership.
The CLAHRC board consisted of two types of representatives: those with and without voting rights. Those with voting rights represented the NHS trusts that had provided direct or indirect (in-kind) funding to the CLAHRC. There were also representatives from a further seven organisations that did not provide CLAHRC funding and two lay members who did not have voting rights.
Oakdown Composition and fundingTwo universities, seven NHS trusts, five primary care trusts and five other organisations including a charity. It received matched funding from these organisations.
StructureTwo research arms – self-management and self-care of long-term conditions, and application of technologies – and an implementation/achieving translation arm, which had four themes with a number of embedded projects in each.
ExecutiveLeadership was provided by a core team through an executive board, which included a director, an associate director, a programme manager, an associate programme manager, a communications lead, administration staff, a lead for implementation, an evaluation lead, an evaluator, a PPI lead, a researcher and a research capacity lead. There was also a strategic board including senior members from universities, NIHR infrastructure partners and an intellectual property broker.
Ashgrove case summary
Geography
Ashgrove covered a substantial mixed urban and rural geographical area with a population of 1.34 million. 103 At the time of data collection, the background of the population was 50% white and 50% of other ethnicities. Deprivation indices showed a mixed picture of the area, with pockets of severe deprivation and related poor health and disability. Life expectancy was 9.4 years lower for men and 5 years lower for women in the most deprived areas than in the least deprived, and was lower than the average for England across the CLAHRC area. 104 Early deaths from heart disease and stroke were better than the average for England, and 16.2% of children in year 6 (aged about 10 years) were obese. Health priorities for the region, as identified by Public Health England,105 were ‘getting it right’ from childhood; early intervention and prevention; supporting the ageing population; and improving mental health and well-being.
In preparing the bid for CLAHRC funding, discussions with the directors of public health identified the following areas as priorities: cardiovascular disease; diabetes; stroke; and chronic obstructive pulmonary disease (COPD). The implementation projects were related to older people; health education; reducing emergency admissions; and improving services in primary and secondary care. However, the little time available to prepare the bid allowed limited interaction with NHS trusts:
We basically did what we could in the amount of time we got to put a proposal together; it really didn’t make it possible to have detailed discussions with the trusts. It was more a case of saying ‘This is what we want to do, what do you think?’
Joint appointment/leadership role, Ashgrove, R1
However, it was acknowledged that the context of health priorities was dynamic. For example, Ashgrove had some difficulty engaging the NHS in some projects, and vice versa:
The areas that were identified from the list of ideas tended to come from two specific areas within the trust, which were obstetrics and gynaecology and trauma and orthopaedics, which don’t really fit in with long-term conditions . . . and the head of CLAHRC said that they are not areas that particularly CLAHRC have a huge amount of expertise around, so it was kind of a mismatch really.
Implementation facilitator/boundary spanner, Ashgrove, R1
There was some suggestion that the shifts in activity within the implementation theme that emerged after an external evaluation reflected the priorities of NHS partners: ‘in terms of both service evaluation and also in terms of helping develop skills through the research capacity development need’ (leadership role, Ashgrove, R1).
The physical geography of the CLAHRC posed some challenges to aspects of implementation. For example, attempts to develop a CLAHRC-wide PPI group in the rehabilitation theme were not particularly successful, as patients were not physically well enough to travel the distances involved. Consequently, a number of groups were developed across the region, with some concern about duplication of effort and ‘silo working’:
and actually within our region, you’ve probably got three teams working on the same sort of projects, but if you work together you can pool resources and work together on their . . . yes it’s too silo’d.
Leadership role, Ashgrove, R3
Collaboration for Leadership in Applied Health Research and Care architecture
Ashgrove was organised around two strands, one for research, with four themes (prevention, early detection, self-management and rehabilitation), each with embedded projects, and one for implementation, with a number of projects embedded in it. These strands provided an organisational home for activity, encouraging ‘people to work within their themes [around] the research they wanted to do’ (implementation facilitator/boundary spanner, Ashgrove, R1).
Ashgrove created several roles, such as a communications manager, a knowledge manager and a research capacity development lead, which provided the main link between the NHS and the CLAHRC core team.
The majority of CLAHRC funding had been allocated by Ashgrove to its four research themes, with less resource to support implementation work and building capability and capacity. CLAHRC facilitators at times struggled to get funding for studies that they were trying to initiate in the NHS, and found it frustrating when, after they had generated interest, they had to turn people away because of a lack of resources.
Flexibility and sustainability funding was subsequently used to employ staff to undertake implementation in some themes. Thus, resources were not just financial, but also people and the expertise that they brought to the CLAHRC. This was thought to be particularly valuable in the implementation theme, where they were able to provide expertise to undertake service evaluations for the NHS:
We’ve not offered money, but we have provided staff resource and so we have provided advice, and we provided staff resources to actually conduct some of the evaluations or some aspects of the evaluations.
Leadership role, Ashgrove, R2
The CLAHRC was conducting an internal evaluation. Although this was not described in detail within our interview data, documents such as publications provide evidence of its focus and approach.
At the request of the CLAHRC board, Ashgrove had undergone an external advisory review in 2010, which was conducted by four experts in knowledge mobilisation. This review recommended a shift in focus away from the first of the CLAHRC aims (to conduct applied health research), towards implementation and building capability and capacity. The shift did not result in changes to CLAHRC structure, but prompted two changes in its activity:
-
The responsibility for implementing research was given to the applied research themes, resulting in an increasing amount of service evaluation activity being undertaken within the implementation theme: ‘we have made the decision to locate responsibility for implementation with the applied themes themselves and make sure that there is funding for that as well’ (academic/leadership role, Ashgrove, R4).
-
Each applied research theme was ‘developing its own implementation structure’ (theme manager, Ashgrove, R4).
The CLAHRC contributed to the external evaluations, with one participant commenting that the external evaluations drew attention to relevant issues and influenced the CLAHRC’s direction.
Knowledge and knowledge production
Ashgrove prioritised research-based policies and guidelines as a type of knowledge, and undertook the development of evidence summaries for use in partner NHS trusts. Knowledge creation seemed to have been focused on applied health research. By the end of 2013 Ashgrove had supported the publication of 230 academic papers, which was felt to be a significant achievement:
there is an element of credibility, and obviously with academic and especially with [CLAHRC university partner named], they’re looking at publications . . . because that’s what it’s all about, isn’t it?
Implementation facilitator/boundary spanner, R3
A key dimension of knowledge referred to in Ashgrove was the credibility of the knowledge bearer, usually associated with clinical seniority. There was less evidence of the cocreation of knowledge, although service user knowledge was used in the development of some products (patient manuals) and tools, and evaluation tools were modified after feedback from clinicians. Limited engagement of clinicians in the early stages of project design, for example around chronic kidney disease (CKD), was associated with implementation challenges:
There is some scepticism about the value of this type of CKD categorisation in primary care. For instance, general practitioners don’t believe in it really, they think it is all a waste of time and they don’t really think it is a disease. So there has been that sort of obstacle to come across, you know, and to get through.
Joint appointment/leadership role, Ashgrove, R1
There was a recognition that foreseeing the positioning of knowledge produced was important to ensuring its successful implementation. An example of this positioning was the need to undertake some unlearning in order to ‘make room’ for new practices ‘because the new stuff will not get in there, it is very difficult to shoehorn in’ (implementation facilitator/boundary spanner, Ashgrove, R2).
Knowledge sharing and exchange
Part of the knowledge-sharing strategy in Ashgrove was to push information and evidence out from the CLAHRC to users: ‘So I certainly see part of my role as being one of the pushers of communication, pushers of information and evidence out to people’ (leadership role, Ashgrove, R3). There was evidence of the use of marketing approaches to ‘sell’ their online cardiac rehabilitation tool, disseminating the tool via the internet. The CLAHRC also used press releases and social media to share important stories. Another key mechanism for sharing processual knowledge generated within Ashgrove was the development of tools for its evaluation and implementation work with NHS partners. Examples include an ‘online course on how to conduct evaluations . . . [and] a template for planning implementation’ (leadership role, Ashgrove, R2).
There was some evidence of sharing knowledge externally with other CLAHRCs. For example, collaboration between Ashgrove and Hazeldean around CKD saw Hazeldean providing knowledge and expertise in service improvement work, and Ashgrove providing an online audit tool to complement the Hazeldean contribution. There was some evidence of a lack of clarity in contributions: ‘I know that [Hazeldean] always talk about it as being their work, whereas whenever we talk about it we always talk about it being us and [Hazeldean]’ (leadership role, Ashgrove, R3).
Facilitation
To underpin the implementation approach within the CLAHRC, Ashgrove had opted to use the K2A model with principles of the dynamic knowledge transfer model106 (see Appendix 6, Ashgrove, document 5). However, there was a view that, by choosing that model, there was the possibility that organisational aspects of implementation might be neglected, and their later approach was augmented by an organisational excellence approach. 107 There was mixed evidence of shared understandings around implementation including among those with facilitation roles: ‘I’ve heard people define implementation in very different ways . . . there are different views about what constitutes implementation. And I guess perhaps even within our own group there are different views about what that means’ (leadership role, Ashgrove, R2).
The CLAHRC had employed seven boundary spanners (Box 2). Their role appears to have been more related to crossing boundaries and linkage of the NHS and the CLAHRC core team than supporting or facilitating implementation in the NHS, although their job description did include ‘to translate research findings into improved outcomes for patients within [CLAHRC named]; a highly complex task requiring understanding of the process of implementing research’ (see Appendix 6, Ashgrove, document 6).
-
Facilitators were employed in formal roles based in NHS R&D departments as boundary spanners between the trusts and the CLAHRC core team. Roles involved supporting trust staff in writing research proposals; providing training sessions on finding evidence; creating guidelines; and undertaking evaluations.
-
The majority of the facilitators had no NHS background and no experience of working in a similar role.
-
There were informal facilitation roles created for nurses to work on the CKD project.
-
One research theme had employed an implementation manager to lead the implementation of its rehabilitation projects.
-
One research theme had used lay people (not registered as health-care professionals) to implement its diabetes research and was evaluating the impact of this.
Success in these roles was felt to be dependent on a wide range of personal qualities and skills: ‘a good [boundary spanner] is someone who is basically a great people person, brings people together, communicates, organises, networks, speaks their minds, is great, says what’s what, someone with those qualities, that sort of skills, those interpersonal skills’ (joint appointment/leadership role, Ashgrove, R1). However, this needed to be complemented by credibility within the health-care setting: ‘We deliberately appointed someone who is Band 8 to make sure there was familiarity with the NHS and someone with decent punching power’ (joint appointment/leadership role, Ashgrove, R1).
The boundary spanner ‘model’ varied across partner NHS organisations, and each person had developed his or her own remit and role within the trust in which he or she was placed:
It was quite a woolly job description, it was sort of to help people do this, to help people do research, to help them implement the findings, that sort of level, so I thought ‘Right how do I do this?’ When I started I didn’t even know what the aims and objectives [of CLAHRC] were.
Implementation facilitator/boundary spanner, Ashgrove, R1
Actors and agents
The CLAHRC was led by a director and a deputy director, who both held clinical academic roles in addition to working within the CLAHRC. Complementing designated theme leads, there was strong medical leadership embedded throughout the themes. Leadership was variously described as distributed, embedded, developmental, sensitive and not ‘command and control’. One participant (NHS leadership role, Ashgrove, R4) felt that it had been more difficult to integrate NHS leadership into the CLAHRC leadership structure. One applied research theme (rehabilitation) had employed a formal implementation manager; other than this the CLAHRC employed no one in a formal role for supporting or undertaking implementation. Some CLAHRC staff were seen as being agents of the university and this made it difficult for them to integrate into the NHS:
I was the university person so yeah crossing the boundary into the NHS could be quite problematic. People, I think, a few were a bit wary of us in a way.
Leadership role, Ashgrove, R3
In the CKD project, where there was the use of an audit tool to increase case finding of patients with CKD, general practitioners (GPs) were thought to be beneficiaries thanks to the increase in Quality and Outcomes Framework (QOF) income as a result. The use of the Hazeldean CKD care improvement methods was also seen as a way in which GPs could increase QOF income through better management of patients with CKD.
An online cardiac rehabilitation project was seen by participants as a way in which the trusts could improve their income through Commissioning for Quality and Innovation (CQUIN) targets. Patients were thought to be beneficiaries through the provision and accessing of a cardiac rehabilitation programme that was flexible and accessible to suit patients’ lifestyles.
Patient and public involvement
In addition to representation on executive and management boards, Ashgrove’s work around PPI appeared to have crystallised in the appointment of a PPI champion and the construction of a PPI Forum. The strategic importance attached to PPI was evident in its external review:
there has been a lot of work to improve and increase the profile of PPI . . . one of the task groups that followed the external advisory review was about PPI specifically. And some of the money from [sustainability fund] . . . has been used to second someone from [research network] to lead on PPI.
Academic/leadership role, Ashgrove, R1
The dedicated investment of resources in PPI was not evident before the external review, and prompted significant attention to the processes, as distinct from the purposes, of PPI. These processes included communication strategies around implementation, such as consultation on the development of websites about self-management. There did not appear to be any substantial distinctions being made between PPI in research and PPI in implementation. Ashgrove was the only CLAHRC to report investment in a training programme, delivered by a university within its footprint, to support capability building around PPI.
Temporality
Prior to the development of the CLAHRC, while there were clinical academic posts in existence, with some of the research theme leads holding joint appointments, there did not appear to be a strong organisational link or relationship between the NHS and the university.
The key point in time for Ashgrove was the external review. This saw it reorganising responsibility for implementation and provided space for its boundary spanners to identify training and education needs, and to organise and deliver training and education sessions on doing and using research:
I think the external review did certainly help, particularly, and forced those of us who were arguing that we need to do more about helping people to use evidence and modify, you know, help to work with the NHS to change systems to incorporate views and evidence more.
Leadership role, Ashgrove, R1
The boundary spanners met regularly to discuss these issues and challenges. Inevitably, there was evidence that the shift around the organisation of implementation also played out at project level, where again there were reflections that the early focus on research had meant implementation issues were less developed:
What I am finding with [COPD rehabilitation manual] now in particular is that we are struggling a little bit because people hadn’t thought about the actual practicalities of delivering what they had designed, it hadn’t been considered at the outset.
Implementation facilitator/boundary spanner, Ashgrove, R2
At the end of the first round of funding Ashgrove merged with a neighbouring CLAHRC.
Hazeldean case summary
Geography
Hazeldean covered a large conurbation. At the 2011 census it had a population of 2.5 million with an ethnic mix broadly aligned with the population of England as a whole. Deprivation indices (2012) showed a mixed picture of poverty across the area, with pockets of severe deprivation around the main city and in some outlying boroughs. 105 Vascular conditions were seen by the CLAHRC as a priority and included diabetes, coronary heart disease, CKD and stroke.
The move to a vascular theme was consistent with regional public health strategy, with evidence of negotiation between Clinical Commissioning Groups (CCGs) [at that time primary care trusts (PCTs)] and NHS trusts in conjunction with the local AHSC. One of the challenges reported by participants was knowing at which level – system (health or social care system), CCGs (then PCTs) or GP practices – it was best to try to engage with stakeholders around health priorities, recognising also that different organisations had their own particular priorities:
Some of the trusts that we set out to work with . . . in the initial phase some of those trusts didn’t necessarily buy into the project as a whole, it wasn’t necessarily one of their priorities.
Implementation facilitator, Hazeldean, R1
It was reported to be easier for the CLAHRC to integrate and undertake implementation where the boroughs or PCTs already had knowledge of health geography and local priorities:
they had already established a hierarchy of clusters, those with high levels of poverty and deprivation in their areas or high ethnic, black and minority ethnic groups, so they had almost kind of stratified it, so it was much easier going into that organisation because they already had links to where we needed to put in place the programme.
Implementation facilitator, Hazeldean, R1
In terms of local priorities, there were a number of other initiatives working on improving patient care in the same geographical area as the CLAHRC. This created a challenge for making the CLAHRC’s contribution distinct from others:
we’re calling it a crowded landscape, but overcrowded is a better phrase. I am trying to carve out a distinct identity for [CLAHRC] in terms of what it does, which is to do research and put it into practice.
Academic/leadership role, Hazeldean, R4
The historical boundaries of services across the area served by the CLAHRC posed some challenges to implementation work across the CLAHRC as a whole. For example in a heart failure (HF) project, community HF specialist nurses were in post in some areas but not others:
it is like three different PCTs although they are supposed to be one, but they are like three separate PCTs that became one, but still operate very differently. It is like working with three separate organisations.
Implementation facilitator, Hazeldean, R1
In other projects, geography enabled implementation, such as a collaboration around CKD. Here, comparative clinical audits were fed back to GP practices as a means of motivating them to improve performance and share ideas:
The shared learning element is again something that we have had quite a lot of positive feedback on, practices don’t generally get the chance to share ideas even in a small geographical area . . . So it has helped give them some focus and really driven up their motivation to improve because they know other people are focusing on similar improvements in their area.
Improvement facilitator, Hazeldean, R1
Collaboration for Leadership in Applied Health Research and Care architecture
Hazeldean was initially structured around two main strands: a research strand with four research projects and an implementation strand with four main areas of work – CKD, diabetes, stroke and HF. Over time, the intention was to integrate implementation work into a single ‘vascular’ theme. In addition there were implementation projects relating to the self-monitoring of blood pressure and the physical health of people with severe and enduring mental health problems.
Implementation projects reported through programme managers to the CLAHRC assistant director and from there to the CLAHRC executive or CLAHRC board as appropriate. This flow of information was intended to ensure that ‘at the executive level they do have an understanding of what is going on in projects’ (management role, Hazeldean, R4).
Resources were more than financial, providing staff and ‘backfill’ for staff involved in CLAHRC projects, agreed on a project-by-project basis with the relevant NHS organisation. Hazeldean faced funding challenges early on; a reallocation of funds in primary care had a significant impact:
So once the NHS economy was under greater pressure for quite a lot of the PCTs in [CLAHRC area named] CLAHRC was a disposable expense really so in the initial setup we had 10 PCTs and where we are now we have four, so we lost a lot of the organisations we were working with.
Academic/leadership role, Hazeldean, R1
With most of the budget having been allocated to CLAHRC research projects, when the financial crisis struck it was implementation that saw a re-engineering in resource allocation. There was a reduction in the funding for the improvement collaborative approach in the CKD project and one research theme was halted.
Evaluation activity was built into each of the implementation projects and the reports of these were made available on the CLAHRC website. In addition, opportunities were taken to evaluate structural approaches to implementation, such as investment in implementation facilitator roles. Hazeldean participated fully in the external evaluations of which it was a part: ‘I have seen the results of the first round of data collection in this project but it wasn’t shared at all within the CLAHRC’ (academic/leadership role, Hazeldean, R4).
Knowledge and knowledge production
There were examples of different types of knowledge driving implementation work in Hazeldean, including research, national clinical guidelines, practitioner expertise, clinical consensus, local audit data and service user knowledge. Implementing the CLAHRC’s own research was not the focus of the implementation teams. Rather, other types of knowledge were used in service improvement projects focusing on HF, CKD, stroke and impaired glucose tolerance (pre-diabetes).
There did not appear to be a hierarchy of knowledge in use within the CLAHRC; different types were used where and when it was thought to be most appropriate. For example, in a stroke project, although national evidence from research was used to underpin poststroke assessment, decisions on the nature of assessment and content were taken after consultation and incorporated practitioners’ and service users’ experience.
Most of the implementation projects were focused on knowledge accumulation or new learning; however, implementation approaches had to be attenuated in line with financial constraints. For example, work on CKD became a ‘collaborative lite’ approach and this required some unlearning, for example to believe that undertaking webinars would have the same beneficial impact on the collaborative approach as undertaking face-to-face meetings.
Knowledge sharing and exchange
Hazeldean attended to knowledge sharing through a combination of artefacts and technologies. Sharing knowledge seemed to have been most readily achieved in the stroke project, where once the stroke assessment tool had been developed it was made openly available through the internet. Other projects also shared knowledge and information through websites and through the use of information technology; for example, the CKD project used webinars and learning events to connect people and processes. However, there was also a view that sharing knowledge was potentially limited:
We are sharing knowledge but it is kind of passive, if that is kind of a right way to say it. We are not doing it in a challenging way to further our understanding of knowledge of how to implement successfully in different contexts.
Management role, Hazeldean, R4
Sharing information also came in the form of the implementation project evaluations undertaken, which were valued by NHS partners:
I mean at project level we’ve done evaluation for all our projects and that has proved to be one of our successes in the sense that the partners really liked it.
Leadership role, Hazeldean, R4
The knowledge used in implementation activity, such as national and international guidelines, was sourced from outside the CLAHRC. In addition to this, there was some working across the CLAHRCs or with others who had similar projects, shared clinical topics or had particular improvement methodology expertise:
We are planning to do a stream of work with the AHSN [Academic Health Science Network] around kidney disease which will use the software package that developed as part of the implementation work with [Ashgrove].
Leadership role, Hazeldean, R4
Facilitation
Hazeldean used the Model for Improvement approach incorporating Plan, Do, Study, Act cycles, together with the PARIHS framework, to guide implementation activity. These were used to varying extents within the implementation projects, resulting in a perception that ‘across the four teams there are four completely different models of implementation that have been enacted in the first stage’ (clinical leadership role, Hazeldean, R1). However, some underlying principles, such as an assessment of context to determine barriers and enablers to implementation, appeared to have been undertaken in all projects, if only informally in some cases:
But perhaps we didn’t actually . . . wouldn’t do a formal context assessment of each practice or situation, it would be perhaps more ad hoc and more observational.
Implementation facilitator, Hazeldean, R1
Consistent with the adoption of the PARIHS framework, facilitator roles were created:
I think it started off that they employed like seven [facilitators] and our job was to facilitate the implementation of the evidence, whatever evidence into practice . . .
Implementation facilitator, Hazeldean, R1
The features of these roles are shown in Box 3.
-
Facilitators had varying backgrounds: some had clinical experience and others did not. This affected their credibility with clinicians. Their roles varied in different projects.
-
Education and training was provided for the implementation facilitators by one of the academics involved with implementation, who had expertise in facilitation.
-
As well as having a specific role in implementation, these roles were seen as providing a foot in either camp, undertaking boundary spanning between the academic and practice environments in CLAHRC.
-
During the second year of the CLAHRC, two of the implementation facilitators were promoted from Band 6 to Band 7 posts in more of a project management role and were working across, rather than within, implementation projects.
-
Changes were planned for the titles of both roles for CLAHRC 2, to reflect changes to the way the roles developed over time. There was also acknowledgement in the data that the work of the facilitators was very much a function of a team rather than of the individuals themselves.
There were some concerns expressed about facilitators’ lack of clinical credibility and knowledge of the context. There were reports that, with time, training and practical experience, facilitators had become more skilled in subsequent improvement projects. The CLAHRC also took on clinical staff with insider knowledge, expertise and perspective in seconded roles, to undertake similar work:
Some 23-year-old who has just finished their Masters, how are they supposed to go out and take on a GP who is being a bit bolshie when they have no facilitation background? This time round we had a secondment and we got quite an experienced nurse . . . and she did the first round of improvement work so she has got credibility, she’s walked the beat, she’s a natural facilitator, although she doesn’t have any formal training.
Clinical leadership role, Hazeldean, R1
There was a focus on using seconded staff from the NHS who had clinical expertise but lacked the project management skills or knowledge of the improvement methodologies, such as Hazeldean’s Plan, Do, Study, Act approach. This ‘imported’ clinical expertise to the projects had equipped the secondees with skills and experience that they could take back with them to their employing organisations:
Well, I think I will have learned huge amounts about managing projects and affecting change and working in different ways, and having confidence working with different organisations; and I think, or I hope, all of those things will stay with me.
Secondee to CLAHRC, Hazeldean, R2 (emphasis in the original)
Actors and agents
The CLAHRC was led by a director, who oversaw the research theme, and an assistant director, who oversaw the implementation theme. Their leadership styles were reported to be ‘very different’ (management role, Hazeldean, R4), with some ‘feeling there was no strong leadership’ (management role, Hazeldean, R4). However, there was also a sense from some participants that leadership had developed at different levels within teams:
I think the leadership was then really important in establishing relationships with the CCGs but that occurred up and down the whole hierarchy, certainly it wasn’t just up to the director or assistant director . . . and then we have had a lot of leadership within our teams which has developed.
Clinical leadership role, Hazeldean, R4
In addition to the facilitators and clinical secondees, there were two programme managers. The clinical and academic leads in each of the four main implementation projects were formal roles, but some of these posts were vacant for some time, and some were not replaced after people left. The extent to which individuals engaged in the role varied, as did their motivations for being involved:
I think for some of the clinical leads it was very much a chance to keep a toe in their own personal interests.
Academic/leadership role, Hazeldean, R4
Stakeholders had a key role in negotiating priorities or projects. For example, GPs and PCTs/CCGs were involved in negotiations about local priorities and projects:
I think the design of the project was mainly influenced by feedback from a range of stakeholders within primary care, GPs, leads, practice nurses, care co-ordinators, senior figures within the trust.
Implementation facilitator, Hazeldean, R2
The CKD project led to GP practices becoming clear beneficiaries, through increased QOF income from improved case finding and better CKD management. The impaired glucose tolerance project had patients as beneficiaries, with 52% (n = 26) of patients reverting to normal blood glucose levels (see Appendix 6, Hazeldean, document 3).
Patient and public involvement
Patient and public involvement was structured through lay involvement in the CLAHRC board, a specific research theme around PPI and involvement in individual implementation projects. The strategic importance attached to PPI was evident in two ways:
-
the regular, quarterly reporting of progress with PPI to the CLAHRC board
-
drawing on the external evaluation team to review learning around PPI in implementation and to support the development of action plans.
Data explaining involvement at a project level generally referred to representation, for example as ‘expert faculty’ (academic/leadership role, Hazeldean, R1) in a management group overseeing implementation work around CKD. Representation focused on the different type of knowledge that involvement could bring to bear on the work of the CLAHRC. This was particularly the case in work to integrate patient experience into cycles of improvement activity in primary care. However, other reports of PPI at project level included the involvement of participants in research studies, and advice on the development of practical strategies to engage with hard to reach or ‘marginalised groups’ (leadership role, Hazeldean, R1). Generally, approaches to PPI in research and in implementation were blurred, and described as a:
recursive [sic] relationship we have had between research and involving patients as research subjects and then feeding back into resources and how they are implemented . . .
Researcher, Hazeldean, R1
Temporality
Hazeldean built on existing collaborative working across organisations. For example, ‘good links between their PCTs and their GPs’ (implementation facilitator, Hazeldean, R1) were seen as an advantage. However, existing relationships were not seen to have been sufficiently established to facilitate implementation work; for example, ‘there was a large developmental time and . . . we found in implementation if you spend that time, if you don’t already have that engagement or credibility or relationships already built up, then it really helps’ (clinical academic/leadership role, Hazeldean, R1).
A key event in the history of Hazeldean was a funding crisis in year 2, which resulted in changes to the composition of the CLAHRC board. In addition, the implementation theme merged into one single vascular theme overarching the individual projects:
it was only as work progressed that some of the clinicians began to see that you could merge some of the work [into a single vascular theme], which in my mind was a good development. You would expect things to develop as time went on.
Academic/leadership role, Hazeldean, R1
There was a pressure of time, particularly in the early days of the CLAHRC, and participants felt the need to deliver: ‘we did choose to use a collaborative methodology I think from fairly early on . . . the good thing about it from our perspective was that you can kick things off quite quickly’ (clinical academic/leadership role, Hazeldean, R1). Much time in the early days was spent building relationships for implementation with NHS partners. Over time, this resulted in people approaching the CLAHRC to work with them, rather than the other way around:
what I find is the difference with other projects is the open doors that we’ve experienced. There was another project at the beginning of the CLAHRC that was very much kind of ‘please let us do our project with you, we can really do some good here’, whereas now we are being approached.
Implementation facilitator, Hazeldean, R2
Capability and capacity building to conduct and use research was addressed principally through two doctoral studentships attached to Hazeldean’s implementation theme. There was evidence of individuals developing knowledge and skills over time that would be of personal and organisational benefit, although some felt this could be strengthened.
As Hazeldean began to look forward and plan for renewal of funding, they reflected on CLAHRC 1, in terms of both how proposals should be constructed and the nature of implementation: ‘I think it is moving forward with what the CLAHRC has learned over the last three and a half years’ (implementation facilitator, Hazeldean, R2).
Oakdown case summary
Geography
Oakdown covered a large conurbation of metropolitan boroughs and in the 2011 census had a population of 1.34 million. 103 The ethnic background of the population is mostly white, with Asian or British Asian people being the largest other ethnic group. 103 The deprivation indices showed a mixed picture across the area, with pockets of severe deprivation and related poor health, disability and high unemployment. Life expectancy in the most deprived areas was 10.7 years lower for men and 7.7 years lower for women than in the least deprived. 105 Health priorities identified by Public Health England105 were reducing health inequalities, tobacco control and mental health. Early deaths from cancer and stroke were higher than the average for England, and 19.3% of children in year 6 (aged about 10 years) were classified as obese.
Oakdown agreed their priorities with NHS partners as COPD, depression, diabetes, stroke, obesity and genetics in the research themes, and tackling health inequalities in the implementation theme. Priorities for the K2A theme were set by the local NHS partners; they were nutrition, dysphagia and venous thromboembolism (VTE) in hospitalised patients. The identification of these priorities was seen by participants as crucial to the success of the implementation projects: ‘I think that what the CLAHRC did really well was pick up real service priorities’ (NHS senior leadership role, Oakdown, R4).
Collaboration for Leadership in Applied Health Research and Care architecture
Oakdown was organised in two strands: research and implementation. The implementation strand was organised thematically on health priorities (e.g. health inequalities) and implementation methods (e.g. K2A), with themes including a number of individual projects. They incorporated the potential to respond to NHS priorities for implementation:
of course the NHS had lots of priorities around implementation from day 1 so that is what we got on with.
Joint appointment/leadership role, Oakdown, R1
Organising themes around clinical topics was perceived to be appealing to NHS partners and for assisting with implementation, as it:
gave service providers a real solid point of contact, so if you were involved in diabetes care or stroke care . . . you had specific, very obvious, definite themes that you could link with that linked with your clinical area, and I think that really helped with implementation.
Academic/leadership role, Oakdown, R4
The CLAHRC had a number of management and leadership roles in each project that fed back directly through their role on the CLAHRC executive, and that linked the executive to the ‘front line’ or clinical staff in projects. In terms of linking to the NHS, one participant felt that there were good links between senior levels and the clinical front line, but that there were missing links to the middle management tier of the NHS. CLAHRC executive meetings were seen as a forum for sharing information:
I think it is undoubtedly one of the benefits, you would call it an additional benefit to having the CLAHRC’s structural processes. I think something similar happened at the CLAHRC executive meetings as well. I am keen to go to these meetings so I expect my colleagues feel similar and the reason I want to go is not just because I feel the need to be engaged with the CLAHRC business agenda, but because I know that at the meeting there will be a number of colleagues with whom I have a shared interest and I don’t think you can overestimate that slightly intangible benefit of CLAHRC.
NHS senior leadership role/theme lead, Oakdown, R1
Feedback within themes, and also back to the executive, incorporated brief summaries and newsletters, but the main method of communicating about projects was the theme meetings.
Oakdown was resourced through matched funding provided by NHS partners. There was a view of the CLAHRC being ‘overmatched’ and financially stable:
but certainly in terms of matched funding we are overmatched, that has been a great success, we are overmatched and that is because we are delivering.
Joint appointment/leadership role, Oakdown, R1
Oakdown had an internal evaluation programme, and there was evidence that evaluation outcomes were informing its ongoing development and, subsequently, preparations to respond to a second round of funding for the CLAHRC. In addition, there were evaluations undertaken within specific projects using audit and observations as a means of evaluating implementation. Oakdown participated fully in the external evaluations, although there was a view that outputs did not always fit the local context:
there was one particular external evaluation in that the information that was being fed back to us [we] felt it needed some knowledge translation work doing in it in that it was fairly inaccessible to the people that mattered.
Academic/leadership role, Oakdown. R4
Knowledge and knowledge production
Oakdown appeared to value a broad interpretation of evidence, encompassing research; national and international guidance; best practice knowledge; local and regional audit data; service user knowledge; service development knowledge; practitioner knowledge; policy knowledge; and organisational knowledge:
I think that should be an element for research, applied research and knowledge translation is actually if you don’t adopt all the different knowledges . . . you are on to a losing game really.
Leadership role, Oakdown, R1
Processes had been put in place to gather information from patients and the public: what the CLAHRC called coproduction events. These were based on Delphi techniques to whittle down the number of topics discussed and to decide on their importance. The bariatric surgery project in the obesity theme began in this way.
It was a really good workshop because service users, we thought of different ways of engaging them to make sure that people had a voice and we did things like having a market place as well as having a presentation to sell the ideas and to highlight the strength of the ideas.
Academic, Oakdown, R1
Health-care staff reported valuing research evidence, and other stakeholders (e.g. local councillors in a project spanning health and social care) contextualised decision-making within a wider context: ‘a decision might be evidence informed, but . . . there are a lot of other factors’ (academic, Oakdown, R1). The bearer of the evidence was more important than the strength of the evidence: if the person was credible and able to put forward a clear case then the evidence was accepted. This was particularly noted in the health inequalities theme, where participants reported ‘investments in things where the evidence was very thin but obviously the person who brought this to the table was convincing’ (academic, Oakdown, R1).
Knowledge sharing and exchange
Across Oakdown, attention was given to knowledge sharing through meetings; artefacts such as project summaries, newsletters and a K2A casebook; and project presentations, which were shared by theme leads, programme managers and the CLAHRC executive. These were also made available on the CLAHRC website as well as being distributed directly to interested parties. Oakdown’s emphasis on developing capability and building capacity for doing and using research was thought to be an important mechanism for sharing knowledge.
Creating a legacy through organisational learning and sustaining organisational memory was seen as important in the health inequalities implementation theme, particularly as PCTs were dissolved to make way for the CCGs. The CLAHRC had a role in preserving this:
I think it is a continual surprise to me how short organisational memory can be and how quickly we lose local evidence and I think we do that at our peril in a way because you run the risk of duplicating effort, not building on previous learning and wasting time and I think what the CLAHRC helps and has partly done is help preserve local memory but also share it across the patch.
Academic seconded to PCT, Oakdown, R1
In the health inequalities implementation theme, the CLAHRC architecture itself was seen as the mechanism by which knowledge was shared. Meetings that were arranged as part of the CLAHRC architecture, such as feedback meetings to the leadership, were seen by participants as providing a mechanism for two-way sharing of information.
At a project level, there was thought to be informal sharing through project steering groups, and through key appointments. For example, implementation activity on nutrition included a specialist nurse practitioner whose role was to work in the priority areas within the host NHS organisation, sharing learning from the individual projects.
Oakdown was working with other CLAHRCs around COPD, obesity and diabetes to develop ‘strategic knowledge exchange partnerships’ (joint appointment/leadership role, Oakdown, R1). Although these types of collaborations were seen to be a key potential benefit of the CLAHRC-wide network, for example by eliminating duplication of effort, there were some concerns about how this operated in a competitive context:
one of the areas of competition that was quite difficult to manage and I think potentially had a negative effect on the national programme as a whole regarding shared learning between the CLAHRCs. It wasn’t an environment which was very conducive to collaboration and sharing; it was more an environment which was very competitive.
Academic/leadership role, Oakdown, R4
Facilitation
Oakdown had adopted the K2A framework to underpin, guide and support implementation. Some staff also drew on the PARIHS framework to pay attention to key elements, such as the context of implementation, although not all themes adopted this approach. For example, there were no clear data about the approaches used to support implementation in the health inequalities theme. Not all participants felt that it was necessary to have a specific approach to implementation because of the nature of some of the more ‘improvement-oriented’ projects that were being undertaken:
I think I probably have a different view of how we get knowledge implemented in practice rather than just using a framework like that [K2A] . . . so a lot of the research projects we do are quite action orientated or have cycles of moving things on or have phases where we collect information . . . so directly influencing services and so I would suggest that is research being used in practice.
Leadership role, Oakdown, R1
In the third year, there was a change to the role of the implementation theme lead to oversee the whole of the CLAHRC’s implementation activity. This may have influenced the approach taken by the research teams:
initially I think it was the responsibility of the research themes to think about how they would be implementing their findings when they got them and then over the last year the [implementation lead] is taking over responsibility to support that.
Joint appointment/leadership role, Oakdown, R1
There were two different kinds of facilitators in formal roles within this CLAHRC: within the health inequalities implementation theme, two co-ordinator posts were created to be based in the PCTs’ R&D departments and to assist with implementation. In addition, in the K2A implementation theme there were a number of different formal and informal facilitation roles, the features of which are outlined in Box 4.
-
IFs were employed in formal roles to work across ward settings and to support information facilitators.
-
All the IFs had a health-care background and some experience of implementing change or of service improvement.
-
The IFs were seen as holding boundary-spanning roles and being able to bridge the academic and practice communities. They were seen as clinically credible.
-
Informal facilitator roles were created for clinical staff to support the work of the IFs on a day-to-day basis. They were known as ‘champions’ in some projects.
-
A specialist nurse practitioner had been employed to further the work of the IFs and champions by spreading learning across one NHS partner organisation.
-
Boundary-spanning roles in Oakdown were seen as part of a team or network of boundary spanners rather than one individual having to work at all levels within the trust.
IF, implementation facilitator.
Boundary-spanning roles were distributed across the CLAHRC, which was perceived to share out the responsibility for boundary crossing:
I think the key thing that we have worked on is developing boundary spanning roles within the team that operate on different levels so that it’s not for one individual to take account of all the boundary spanning.
Joint appointment/leadership role, Oakdown, R3
Actors and agents
Oakdown was led by a director, with an implementation lead responsible for overseeing all of the implementation work being undertaken within the CLAHRC. Both post holders held joint appointments with a local NHS foundation trust, and had done for a number of years before the CLAHRC came into being. The leadership style was described as distributed and supportive, with leadership embedded at all levels seen as important to the success of implementation projects:
I think that the other thing that has helped us or enabled us to be successful in some areas and less successful in others is what we know about the importance of clinical leadership. Where there is strong clinic leadership at the frontline level then change has been much easier to achieve.
Joint appointment/leadership role, Oakdown, R2
Stakeholders played a key role in projects or in deciding which projects should go ahead. Several coproduction events were held early on in the CLAHRC to decide research priorities; attendees included ‘providers, we had commissioners, we had voluntary organisations, we had some users, we had all sorts of people’ (CLAHRC project manager, Oakdown, R2). There were also a number of staff with joint appointments between the NHS foundation trust and the universities that were part of the CLAHRC, and there had been a move to give all the CLAHRC’s staff joint appointments.
Patient and public involvement
Alongside a dedicated leadership role for PPI, Oakdown’s approach was described as ‘devolved . . . completely embedded within the different teams and within the projects’ (PPI lead, Oakdown, R4). Embedding was reflected in plans for the allocation of central funding for PPI; themes were expected to allocate a percentage of their budget to engagement. The importance CLAHRC leaders attached to PPI was highlighted in the attention that was paid to raising its profile in their communication strategies, such as newsletters and project reports. Many projects described links with community groups, fulfilling both representation and opportunities for checking things out:
the patient group is extremely supportive and there are representatives who sit on the management group. Not only are they as individuals representing the patients’ perspective, but they also take things back to the group and get their views on things.
NHS senior leadership role, Oakdown, R1
Other strategies included priority setting and consultation activities, described as coproduction events to inform implementation plans.
In addition, the CLAHRC invested in a post to develop a research programme around PPI. This reflected a view that there was very little in the way of guidance about PPI in implementation. Oakdown also attempted to link its work around PPI with other NIHR bodies within the region, and develop a strategic PPI NIHR group.
Temporality
Oakdown was founded on established links with the local NHS trust through those staff who held joint appointments, and who had been applied health researchers prior to the formation of the CLAHRC. Within themes, previous working relationships were also important in providing a platform for activity and preventing duplication:
There was a huge amount of work already going on across the four PCT areas and therefore it was also very clear that what the CLAHRC should do was not, sort of, set up some separate inequalities-related project but find a way of supporting, facilitating, building on what was already going on across the region.
NHS senior leadership role, Oakdown, R1
As a CLAHRC, Oakdown appeared to have been fairly stable over the 5 years of its existence. As the majority of earlier implementation work was not based on the CLAHRC’s own research, there was a planned time schedule for implementation of home-grown research during the first period of funding:
I would be expecting quite serious delivery in year 4. I have no reason to suspect that isn’t going to happen but I wouldn’t have been anxious about it up to year 3, but you would expect delivery year 4, implementation year 5, you would be expecting.
Joint appointment/leadership role, Oakdown, R1
For some implementation projects based in primary care, the dissolution of the PCTs and their replacement with CCGs had an impact. The only changes that were noted over time were in the health inequalities theme, where they decided to adopt projects (or findings and implement them) that had begun before the CLAHRC. One such project was adopted by the CLAHRC to ensure that the findings of the research were not ‘lost’ in the dissolution of the PCTs.
The development of implementation capacity and capability accrued over the lifetime of the CLAHRC:
So I think we are really addressing some of the capacity issues and we have [person named] working with us now, and has for a year, running master classes and so on and I think our . . . capacity and capability around implementation is really growing as we have moved into year 4.
Joint appointment/leadership role, Oakdown, R1
The CLAHRC was increasingly described as a ‘pilot’, and this was illustrated by a change in the discourse over subsequent rounds of data collection, particularly as there was an expectation of further funding. There was a merger with a neighbouring CLAHRC in the second round of CLAHRCs.
Summary
In summary, there were both similarities and differences between Ashgrove, Hazeldean and Oakdown.
Geography
All three CLAHRC were in geographies with similar population profiles, and covered a mixture of urban and rural geography, although Hazeldean’s area was more metropolitan. The health challenges were similar and their areas of activity were cognisant of the local/regional challenges and national health priorities.
Architecture
Activity had been organised in themes within CLAHRCs, with the balance of activity on conducting applied health research rather than implementation. Oakdown had set up more mechanisms and therefore opportunities for communication within and across themes. Resource (roles, money, expertise) allocation was linked to how the CLAHRCs had prioritised their activity and, over time, how they had to respond to external events, such as the external review in Ashgrove and the changes to the NHS funding landscape in Hazeldean.
Knowledge and knowledge production
In contexts where research was more of a priority than implementation, research-based evidence was privileged. This was particularly evident in Ashgrove. In Hazeldean and Oakdown there was a more obvious appreciation of the value of other types of knowledge, particularly in the context of conducting service improvement projects.
Knowledge sharing and exchange
Different opportunities and mechanisms were used to share and exchange knowledge within and across the CLAHRCs, which were related to the way in which the CLAHRCs were organised (themes/strands) and their use of various tools and platforms. Formal mechanisms focused on pushing out information, for example newsletters and website presence. The CLAHRC’s architecture provided particular opportunities to share knowledge, for example through internal evaluations and through project activity. There appeared to be more opportunities for knowledge sharing and exchange in Oakdown than in either Hazeldean or Ashgrove.
Facilitation
All three CLAHRCs had established roles that were boundary spanning and/or concerned with facilitation (i.e. enabling the implementation of evidence in practice). In Ashgrove, individuals in these roles served as boundary spanners or linking agents between the NHS and CLAHRC activity; in Hazeldean and Oakdown, they were more focused on facilitation activity. These roles were variously linked to the particular theoretical/conceptual framework the CLAHRC had chosen to adopt, for example facilitators in relation to the use of the PARIHS framework in Hazeldean.
Actors and agents
The approach to leadership varied in all three CLAHRCs, with more or less centralisation versus distribution, and being more or less transformative versus command and control. Beneficiaries of CLAHRCs were similar across cases, with examples of being engaged in activity resulting in benefits such as increasing income through hitting QOF and CQUIN targets.
Patient and public involvement
All three CLAHRCs were aware of their challenges about how best to incorporate PPI within their implementation activity. Overall, they conflated PPI in research with PPI in implementation. Resource allocation for PPI varied and therefore so did their attention to it.
Temporality
All three CLAHRCs felt a pressure to deliver from the beginning of the funding period. Established links between higher education and health-care organisations were particularly obvious in Oakdown, where there had been a history of joint appointments. All three CLAHRCs at some point in the first 5-year funding period had to respond to different events, including changes to the funding environment and to external review. As they looked forward to renewed funding, all three CLAHRCs had reflected back and considered what they might do differently with the opportunity of continued funding.
Chapter 5 Cross-case and cross-framework narrative
In this chapter, findings are reported from an analysis of data across cases and across the theory areas in the evaluation framework. A number of inter-related themes emerged from our cross-case and framework analysis, which are summarised in Figure 7. Although this is a mainly descriptive account, as we began to draw together findings across the evaluation framework we inevitably began to identify some emerging interpretations and explanations about implementation within CLAHRCs. These explanations were fully developed through a process of proposition building and are described in Chapter 6.
FIGURE 7.
(a) Summary of inter-related themes from cross-site and cross-framework analysis and (b) antecedents.

Antecedents
There were a number of preceding conditions that appeared to influence the subsequent course and journey of the CLAHRCs, such that history and inheritance had an impact on establishing collaboration(s) and enacting their remit for implementation. These antecedents, which are not mutually exclusive, were starting point, interpretation of the CLAHRC brief and approach to priority setting.
Starting point
At the time of bid development, Ashgrove, Oakdown and Hazeldean each started at a different point in relation to the nature of the existing organisational relationships between the HEI(s) and local health services through which the collaborations needed to be established. This became an important issue in the context of the relatively short turn-around time between the call and the submission date for CLAHRC, and subsequently at the start of their funding and, therefore, action.
Within Oakdown it was reported that pre-existing relationships had been important at the time of bid development:
We had . . . a very sound framework for the CLAHRC before we started and those key folk contributed hugely to the writing of the application and we managed to put it together very swiftly and in terms of NHS partners because . . . key theme leads . . . were in the NHS and they were in academia so they weren’t full-time university professors . . . so this little group of people were very embedded in the NHS anyway.
Leadership role, CLAHRC core team, Oakdown, R1
Not only had these relationships facilitated the co-development of the bid but they had also created a starting point for the CLAHRC where individuals had not needed to ‘go out and create new relationships, there was already quite an intimate fabric there to build on and for people to engage with’ (leadership role, CLAHRC core team, Oakdown, R1).
In contrast, participants in both Hazeldean and Ashgrove reported a different sort of starting point, in which the relationships needed to be built on a project-by-project basis because these organisational connections had not been well established at bid development stage; for example:
I was told to go out and evaluate the service, first of all I had to find out about the service and this person [name] didn’t know anything about it. So suddenly to have this company called CLAHRC who was not heard of by anybody, because we were very new.
Implementation facilitator, Hazeldean, R1
Similarly, participants in Ashgrove reported that it had taken some time to develop relationships to be able to progress action on CLAHRC activities:
So it’s really taken 12 months, I think to build these clinical relationships with colleagues in primary care . . . get themselves known, to be accepted.
Clinical academic, Ashgrove, R1
The political landscape has changed and we didn’t have the links [with the NHS] there to begin with . . . there wasn’t time to develop the collaborations and although chief executives signed up that is not the same thing as collaboration.
Clinical academic, Ashgrove, R1
Interpretation of the Collaboration for Leadership in Applied Health Research and Care brief
The CLAHRC journey was also shaped by the way in which the call for proposals had been interpreted. The NIHR call set the establishment of the CLAHRC ‘pilots’ within the context of the ‘second gap in translation’ and of improving patient outcomes through the conduct and implementation of applied health research, including evaluating initiatives and strategies to increase the use of evidence in practice. 108 There was significant potential for flexible interpretation of the NIHR call and, therefore, inevitably those leading the bid writing for the CLAHRCs had interpreted the brief variously, particularly in relation to their role in the implementation and application of applied health research and the emphasis they placed on this in their plans.
There had been a trade-off in focus, and, therefore, resources, between conducting research and undertaking implementation-related activity. Overall, the balance tended to be weighted towards activity that focused on conducting, rather than implementing, research. Where the balance was weighted towards the generation of evidence, it was of course possible to conduct research in a more or less collaborative way, leading to the potential development of more or less implementable or implemented research. Oakdown, for example, explicitly set out to avoid the CLAHRC being perceived as ‘some sort of piglet [sic] research programme that has a limited life’ (NHS senior leadership role, Oakdown, R1). Given this, it espoused ‘coproduction’ as its preferred approach and ‘to provide a framework which will make it more systematic to think about how you scope evidence and apply it in practice when you are working on a particular issue’ (academic, Oakdown, R1).
There are also data to suggest that the interpretation of the CLAHRC’s remit may have been influenced by the background and knowledge of those involved in its development, including some political and philosophical tensions: ‘There are huge internal political divisions with the CLAHRC’ (clinical leadership role, Hazeldean, R1).
Some participants also acknowledged the need to learn more about implementation: ‘So this [implementation] is something we are trying to learn’ (clinical academic, Ashgrove, R1).
Once the teams had responded to the brief and received funding, it was perceived that there had been very little flexibility in their plans to make changes later on. One participant also reflected that there had been little dialogue with the funder about the funder’s expectations of the CLAHRC since the decision to fund was made:
The problem with that is that NIHR had done very little to clarify what they are looking for in a CLAHRC. So other than when we put in the original bid, the NIHR have been absolutely silent about what they expect from the CLAHRC.
Leadership role, CLAHRC core team, R1
Setting priorities
Although the broad parameters for CLAHRC activity were set within their proposals, the way in which CLAHRCs went about establishing and agreeing priorities differed. For example, participants in Hazeldean reported a level of pragmatism in their approach to trying to engage with local priorities in that a number of PCTs had funded the CLAHRC and therefore they had to have some work ‘done in them’ (academic, leadership role, Hazeldean, R1):
The minute we got the money and got started . . . you have partners paying, in our case NHS partners, and you have got to get on and do something. So it was much more – ‘we have got four clinical areas, who is interested in doing what?’
Leadership role, CLAHRC core team, R1
In contrast, a number of Ashgrove participants reported a potential disconnect between regional NHS priorities and CLAHRC activity (in the early stages mainly around research priorities):
the potential disconnect between the priorities of the NHS and the work that is being done, that is not to say our projects weren’t important, they were the priorities of some senior people in the NHS . . . but those things were defined possibly as much or even more by those people with their academic hat than the health priorities of the NHS they were serving.
Leadership role, CLAHRC core team, Ashgrove, R1
Over time, and in relation to their implementation remit, both these CLAHRCs shifted their approach to identifying priorities in a more service-orientated way, although still reliant on either party making an approach. It was reported that ‘alignment’ with a service’s priorities had made it easier to ‘implement things and achieve things’ (management role, Hazeldean, R1).
In contrast, participants in Oakdown reported that at bid development stage they had collaboratively identified priorities of relevance to the NHS. This, they stated, had facilitated continued engagement of the NHS ‘because of the implementation side that this wasn’t just about doing blue sky research, it was about embedding it in practice’ (leadership role, CLAHRC core team, Oakdown, R1). This CLAHRC had also developed a mechanism for identifying the ongoing prioritisation of projects through consensus development events/meetings.
However, participants in all three of these CLAHRCs reported the challenges of working to develop priorities with NHS partners in a continually changing landscape, including in their resources and boundaries.
Summary
At the conception of the CLAHRCs these antecedents established some of the conditions that played out in various ways in the subsequent life of the CLAHRCs we studied. The starting position for each CLARHC is mapped in Figure 8. For example, it was evident that the initial position of those developing the CLAHRC proposal on issues, such as the balance between implementation and research, determined the relative attention that was paid to these agendas in their plans. Additionally, a divide between higher education and service, and therefore the potential for different agendas and competing priorities, emerged early on in the life of the CLAHRC depending on the nature and quality of historical and existing organisational relationships. This set the tone for people’s motivation to engage with the CLAHRC and its activities. These starting points or positions set the direction of travel in an enduring way.
FIGURE 8.
Starting positions of CLAHRCs.
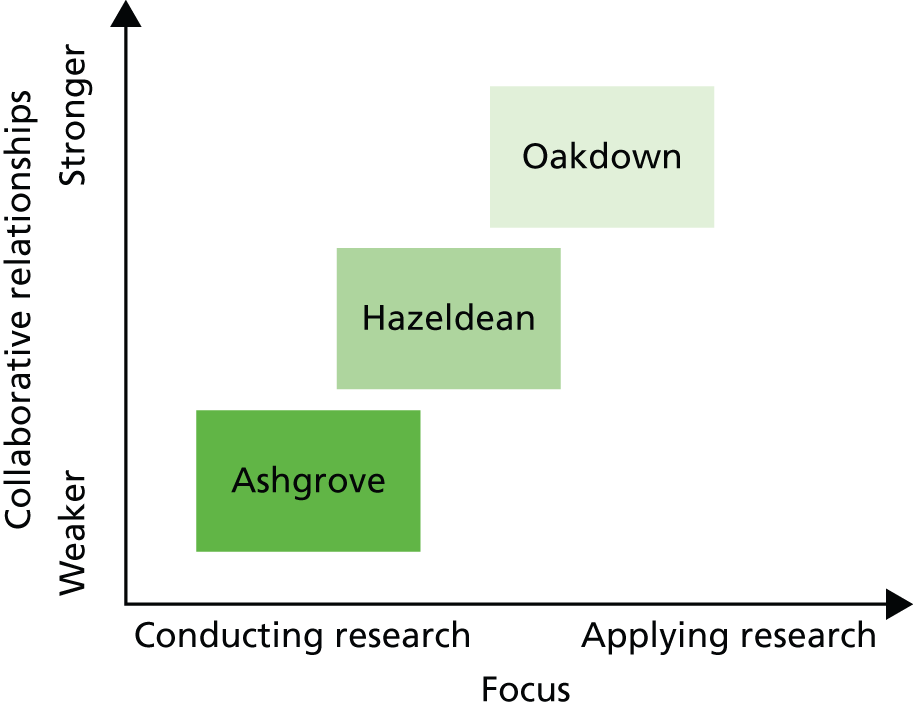
Architecture
The CLAHRCs’ architectures were constituted from multiple engineering, aesthetic and social factors (Figure 9). The architectures were made visible at micro, meso and macro levels within the CLAHRCs, from the accounts of those in leadership roles in CLAHRC central through to those at the coalface working at project level and at the interface between health-care organisations and higher education. These factors combined to create the environment and milieu in which any collective action around implementation was to be potentially catalysed and/or perpetuated.
FIGURE 9.
Collaboration for Leadership in Applied Health Research and Care architecture.

Engineered architecture: structure and space
As a distributed model for the conduct and application of applied health research across a health community and wide geographical area, the structures, roles and lines of accountability that were established within a CLAHRC provided a more or less supportive scaffold for communication, collaboration and implementation activity within and across its functions.
The activity within the CLAHRCs had been organised into themes. It was reported that this had been as a result of responding to the way the call had been constructed. The call for proposals had asked for detail about the specific research and implementation themes that would be pursued, including an overview of how they would relate to each other. The allocation of finances within the proposals was also distributed to themes and therefore, on balance, the majority of the financial allocation within CLAHRCs was to the generation of research, rather than its implementation.
Setting up the CLAHRCs as a collection of themes had resulted in the creation of boundaries between them as they operated in parallel and with limited connection between them and their functions:
it doesn’t work in parallel because the implementation teams started at the same time as the researchers and they had to get on implementing something and so they . . . went off and did their own thing . . . but it meant the strands went in different directions. I think that bridge [between research and implementation] has been difficult to properly bridge if people are honest with you.
Researcher, Hazeldean, R1
The consequences of the way in which the CLAHRCs had been engineered included challenges with communication, knowledge flow and sharing.
There were definitely problems with interaction, sometimes information did not flow easily.
Academic, Hazeldean, R1
There is not a shared understanding of what we are all working for because we do have these very separate applied themes who are lost in their research.
Implementation facilitator/boundary spanner, Ashgrove, R1
It was also reported that the issue of sharing across themes was compounded by an element of competition within the CLAHRC:
there was competition there so very often people were not keen to discuss things. They wouldn’t tell you what they were doing because there was some level of competition.
Academic, Hazeldean, R1
Participants suggested that the structural divides served to emphasise existing epistemic and professional differences:
I think the structures . . . have extenuated maybe ideological differences or philosophical differences in how research is done and how the research is gotten into practice. There has been a very big divide on that.
Clinical leadership role, Hazeldean, R1
Given the distributed nature of the CLAHRCs – ‘CLAHRC isn’t an organisation’, as one participant observed – and the challenges that had arisen from compartmentalised structures, their approach to governance became more important. There was evidence within Oakdown that, although the overall themed structure of the CLAHRC had created separation, its approach to governance, including reporting structures and processes, had facilitated some integration and knowledge sharing:
a lot of things around the governance and reporting structures actually helps to build that culture of what is expected and to consolidate that transfer . . . Individual projects without that organisation would be lost.
Leadership role, CLAHRC core team, Oakdown, R1
Although each CLAHRC had taken a similar approach to how it was engineered, there had been a recognition relatively early on that perhaps theme-type structures were not helpful; however, leaders in all three CLAHRCs perceived that there were limited possibilities to make changes partway through. The perception of inflexibility was particularly linked to the way that funding had been structured at the outset:
This CLAHRC as with most of the others, as it was putting itself together obviously came up with a budgetary split across the five themes . . . and that was allocated at that stage and pretty much committed . . . there was relatively little flexibility in the budget to make changes later on.
Leadership role, CLAHRC core team, Ashgrove, R1
Physical proximity between health services and higher education within the CLAHRC entity was a further feature of its engineered architecture. Relative closeness or distance to each other was determined by those setting the original course, related to existing relationships, position and view of a CLAHRC’s mission (e.g. the balance of research and implementation) and approach to doing business (e.g. more or less collaborative versus outreach/consultancy). Oakdown had deliberately decided at the outset to locate ‘CLAHRC central’ within a health service setting; the other two’s main centres remained in higher education settings, although NHS staff employed through CLAHRCs tended to be sited within NHS premises. The concept of colocation was important to Oakdown, as it was perceived to facilitate the development of productive partnerships:
[CLAHRC] brings a lot of likeminded people together in similar kind of areas and bridging that university and service provider divide. A lot of themes have got people from the universities working with service providers all working together and often colocated as well, which is quite important.
Leadership role, CLAHRC core team, Oakdown, R1
. . . so we had a kind of, if I can say, a very sound framework for the CLAHRC before we started and those key folk contributed hugely to the writing of the application . . . in terms of NHS partners because interestingly a lot of those key theme leads . . . they were in the NHS and academia so they weren’t whole-time university professors, so they were gynaecologists who ran clinics, a clinical psychologist who ran clinics, a speech and language therapist who was very involved with the trust speech and language department, myself, who always had a trust appointment as well as a university appointment, so it was this little group of people who were very embedded in the NHS anyway.
Leadership role, CLAHRC core team, Oakdown, R1
In Ashgrove and Hazeldean, those involved in project-level or boundary-spanning activity also recognised the value of sharing physical space as a way of providing opportunities for facilitating local buy-in to projects, building relationships, collaborative working, cross-fertilisation, sharing of ideas and an understanding about what a CLAHRC did; for example:
We are based in a hospital and some of the other themes are not . . . they are scattered and I think the fact that we are sitting together as a theme in one hospital with links with the clinicians and the managers . . . I think that is why actually we have got local enhanced knowledge of what CLAHRC does.
Management role, Ashgrove, R4
Aesthetic architecture: building an identity
Participants described CLAHRCs in various ways, including using the terms ‘consortium’, ‘network’, ‘movement’, ‘confederation’, ‘virtual’, ‘research organisation’, ‘consultancy’ and ‘umbrella organisation’. ‘CLAHRC’ was not a well-understood concept and the acronym itself was felt to be a barrier because it lacked meaning; this was particularly the case for service providers and those not closely aligned to a CLAHRC:
Ha ha, it is obscure . . . no one knows what CLAHRC stands for and those who are engaged with particular parts of CLAHRC do, they know about those parts of CLAHRC but I’m not sure anybody really, outside of the close CLAHRC community, knows what the purpose of a CLAHRC is.
Academic, Oakdown, R1
Both those in the CLAHRC executive and those working more locally in projects and/or in facilitation and boundary-spanning roles described ways in which they had either obscured or explained CLAHRC:
Well . . . number 1, you don’t really mention CLAHRC because nobody understands it.
Implementation facilitator/boundary spanner, Oakdown, R3
. . . also my job is about translation so . . . you know it’s important that our board and our executive team understand what CLAHRC is . . . it’s our job to translate that, make it meaningful to people who are at the bedside or in the clinic or in people’s homes . . . you might say it’s under this heading called CLAHRC but you can see people glaze over sometimes . . . if you use acronyms . . . we have a great role in translation, so they [practitioners] would know it was a project . . . they might not use the term ‘CLAHRC’.
NHS senior leadership role, Oakdown, R2
The challenges with the branding of CLAHRC were recognised as participants reflected on the need for a more active approach to marketing and publicity to raise their profile:
I don’t think a lot of people are aware . . . I think the CLAHRC themselves need to . . . advertise . . . some people have heard of it but they were very much in the minority.
Implementation facilitator/boundary spanner, Oakdown, R3
There was also evidence of an effort to sell CLAHRC to get buy-in and involvement through promoting its potential benefits including those for individuals and for services. The individual benefits of accessing education and training opportunities were made evident by, for example, ensuring certification for professional development portfolios and producing practical tools for practitioners to use. For services, useful ‘carrots that you can dangle in front of them’ (boundary spanner, Ashgrove, R3) had proved to be the potential benefits and incentives of engaging with projects and initiatives that would help them meet targets and gain points in the QOF and/or CQUIN Framework. It was also recognised that the benefits of being involved in CLAHRC activity needed to be realised quickly and obviously by both individuals and organisations.
The perception of ‘CLAHRC as other’ was exacerbated by a view that the partnership was aligned with academia rather than service. Within Ashgrove and Hazeldean, CLAHRC was perceived as academic input or an ‘organisation’ that was based in the universities, with the service side being described separately. There was also a pervasive theme in the data about CLAHRCs being a research funding body, a large programme grant. Given that there was more resource (finance) and attention (themes) on research, and NIHR reporting requirements focused on academic-related metrics, this is perhaps an unsurprising perception and is reflected in the data through scepticism, particularly from service providers, about what a CLAHRC was and what it was there to do:
There was a lengthy discussion about CLAHRC 2 and it was felt that it was going to be important to demonstrate strong partnerships and that ‘money won’t be forthcoming just to do interesting projects, like in CLAHRC 1’. The discussion continued with various academics suggesting that they didn’t do enough as researchers to find out what the priorities of the NHS were, with others feeling that they need to be talking to the NHS now [2011] to find out what their priorities are. This brought a mixed response from others, with the opinion expressed that the NHS changes its priorities so it was pointless asking them. There was concern expressed that by involving the NHS, that they would be seen by others, such as the local AHSC as doing ‘dustbin category’ research rather than pure academic research.
Hazeldean fieldnotes, board meeting 2 December 2011
The perception of CLAHRC as an ‘academic machine’ was perpetuated in cases where there was a higher proportion of ‘pure academics’, who, it was reported, were:
pretty much untouched by the implementation agenda and not that interested and didn’t want to have a dialogue with that half of the CLAHRC.
Clinical leadership role, Hazeldean, R1
The separateness or isolation of the CLAHRC from service providers was also evident in the discourse of participants describing both the design and the execution of project work:
I think we [CLAHRC name] have just been completely in the driving seat as project managers and I guess in an ideal world we would have liked to have someone in the trust . . . on the project management side.
Management role, Hazeldean, R2
Given this, in this example the CLAHRC had taken on more of a consultancy or supplier of services role in supporting trusts to deliver on their priorities. The cofunding arrangements set up an expectation that NHS bodies were going to get a free service. Although that term was used to describe their approach, it was also acknowledged that this approach needed to be balanced by joint working:
it is different with this kind of consultancy with the CLAHRC and it is certainly a balancing act to make sure that you not only have the buy-in but you have people commit to you and work jointly together.
Implementation facilitator, Hazeldean, R1
The identity, role and visibility of CLAHRCs remained a challenge, and participants continued to make observations about this across rounds of data collection, particularly in the context of other, related, policy initiatives such as Academic Health Science Networks. However, as one participant stated and as our data show, the perception of the CLAHRC brand or identity is completely context dependent and therefore patchy. For an academic and/or senior person in the organisation it was more likely that the CLAHRC was visible and that one could have been a beneficiary (e.g. in receipt of financial resources to undertake a project). In contrast ‘in the clinical front line it depends on if the experience was good and the relationships were good and sometimes they weren’t’ (clinical leadership role, Hazeldean, R4). Thus, some people felt part of something called CLAHRC, while others were on the periphery or not involved. These findings probably reflect the distributed nature of a CLAHRC and that it was separate from existing structures in the NHS landscape:
The fact is that although we are a co-operative, a collaborative, in many ways we are not . . . I think it is likely that CLAHRC will be seen as an external organisation in which the trust and CCG deal. It won’t be ‘this is an organisation we are part of’, it won’t be ‘this is a club I am part of’, it will be ‘this is an organisation I am aware of who does things for us because we give them money’.
Leadership role, CLAHRC core team, Ashgrove, R4
In contrast to some of the more negatively framed challenges of ‘CLAHRC’ described above, the CLAHRC label/brand also had the potential to be a boundary object. Organically and over time, which included opportunities for sense making and increasing familiarity, CLAHRCs’ capability in bringing people together to work on common goals developed: ‘well I think it’s the name of the CLAHRC that has enabled this to happen’ (facilitator, Oakdown, R2).
Social architecture: leadership, collaboration and boundaries
Although there were mixed views about what a CLAHRC was, and describing it as an ‘organisation’ in a traditional sense is potentially misleading given its distributed nature, CLAHRCs did directly employ people to deliver work and created environments and spaces for activity and action. Each CLAHRC was strategically and operationally led by some form of executive team, who by virtue of their role and function were the social architects of their CLAHRC, in that they were responsible for creating the milieu to encourage desired action and behaviour. There were a number of features of the social environment that created the conditions in which CLAHRCs approached collaboration and therefore the context through which any implementation activity was mediated.
Leaders as the social architects
In general terms, the backgrounds and therefore positions of the leaders and leadership teams differed across the CLAHRCs participating in this study. Some were grounded in clinical research and practice, some in allied health research and practice, and others in management and health services research, and there were differences in gender balance of the executive teams. These characteristics appear to have played out in a number of ways, for example in a CLAHRC’s focus, such as more or less attention being paid to implementation versus conducting research, and in its way of working:
I wouldn’t say [one of the leaders] had a very progressive view of implementation of research. [Leader] used to see it very much as a one-way type of process from academia, following out to clinical areas, the service or organisations . . . rather than a dialogue.
Clinical leadership role, Hazeldean, R4
Across the CLAHRCs, leadership was perceived to be more or less centralised and distributed. More distributed leadership capability resulted in greater CLAHRC visibility and enhanced opportunities for feedback from, and integration of activities across, networks. Centralised versus distributed leadership also appeared to be related to descriptions about leadership style: where leadership was described as more distributed (Oakdown), this corresponded to descriptions of these people being ‘open’, ‘collaborative’, ‘shared’ and ‘democratic’; for example:
I think the director has provided clear leadership for the CLAHRC but has done this in a collaborative and participative way so that . . . the leadership style . . . has been participatory and more transformative in bringing a range of ideas to bear.
Leadership role, core team, Oakdown, R4
In contrast, some participants had felt that a more centralised and controlling leadership approach had been detrimental to potentially more productive ways of working, including sharing information:
it was quite a traditional leadership style . . . sort of divide and rule . . . so it was much easier to keep people in their clearly defined boxes and manage those in a conventional vertical way rather than risk putting people together in much more informal cross-projects, cross-functional groups and my sense would be that is probably where some of the barriers developed . . . there was relatively little horizontal movement of people or information or knowledge because the systems weren’t set up in that way really.
Leadership role, Hazeldean, R4
There were also mixed perceptions from participants about whether or not there had been clear and shared visions both within and across the organisations involved in the CLAHRC. This variation may also have resulted from different leadership styles, approaches and engineered architectures:
I found the whole thing to be challenging, because . . . there was no kind of vision of what we were trying to achieve as a CLAHRC.
Management role, Hazeldean, R1
Collaboration and competition
Despite the call for collaboration embodied by the CLAHRC concept, in practice, participants’ reflections often represented different points along a continuum between co-operation and collaboration. Furthermore, it was evident that the nature of collaboration varied at different levels: at an organisational level between the academic institutions and health services involved in the CLAHRCs, at the level of CLAHRC projects and in relation to cross-CLAHRC collaboration. Perhaps unsurprisingly, given the distributed nature of the CLAHRCs, overall there were varying perceptions about the nature and the quality of collaborations within and across these levels. Within the different levels of the CLAHRCs there were perceptions that, where collaboration through positive relationships worked at the level of projects, this might not necessarily be reflected at CLAHRC organisational level:
I suppose relationship building comes at all levels, I don’t think we have done it very well, generally on the whole when we are working down at a practice level we have built good relationships with individual practices . . . I think what we haven’t done very well is that relationship at a more senior level.
Leadership role, Hazeldean, R4
It was also noted that the development of the relationships and understanding required to develop productive and meaningful collaborations takes time:
I’m not sure whether collaboration works . . . straight away . . . there is a bedding-down phase, I think.
Implementation facilitator/boundary spanner, Oakdown, R3
A number of different factors seemed to contribute to facilitating and mediating collaboration, including where the CLAHRCs started from in their relationships with partners, and the resources, structures and infrastructures they created to operationalise their plans. As outlined earlier, the quality and nature of the relationship between the academic institutions and health services at the foundational stage of the CLAHRCs varied. As a consequence, the development of collaborations also varied after the funding decision: more established relationships catalysed collaborative contexts in a shorter time scale.
Other factors that played a role in driving or forging collaboration included the nature of funding: ‘we’ve got to collaborate with our NHS and academic partners because they’re providing matched funding’ (leadership role, core team, Ashgrove, R3). However, there was also evidence that funding from organisations does not necessarily lead to commitment: ‘it was almost like a three-line whip where it was just top-sliced basically from 10 PCTs . . . but, as we learned, that doesn’t actually mean commitment’ (leadership role, core team, Hazeldean, R4).
The desire of people on the service side to meet targets in frameworks such as CQUIN and QOF, and their priorities to improve services, led them to engage with the CLAHRC:
Because obviously we were implementing guidance that was linked to CQUIN’s targets . . . so of course they were very supportive.
Implementation facilitator/boundary spanner, Oakdown, R3
There were other infrastructures that helped with building the potential for collaboration, including the roles that were invested in within each CLAHRC. While labelling them differently, each CLAHRC had made an investment in some form of boundary-spanning role: individuals who worked under the auspices of the CLAHRC (i.e. CLAHRC ‘employees’) but straddled academic and service boundaries (see Boxes 1–3 for more detail about these roles and their function). They played a critical role as links and linchpins for collaboration because they were responsible for building relationships through their activities; this role was helped by greater physical proximity to end-users:
Our [facilitators] have become competent, knowledgeable and experts in their field who have been able to credibly build relationships at that level.
Leadership role, Hazeldean, R4
Something like just being on a different floor can make things a little bit more difficult and it’s easier when they’re based next to you and you can just lean over and have a conversation or have a chat in the kitchen.
Implementation facilitator/boundary spanner, Ashgrove, R3
However, in contexts where collaboration at an organisational level was less established, individuals in these roles may have had less impact:
We could have done with finding a way to formalise the work at the level of the individual trusts . . . whereas what they’ve done is really manage the research teams for the academics whereas my view is they should have been much more integrated into a collaborative function. The CLAHRC [boundary spanners] were a bit too junior to do that effectively.
NHS partner, Ashgrove, R4
Joint appointments were another example of how CLAHRCs managed their resource to enhance collaboration between academia and services. This model was evident in Oakdown, which had set out to establish this as a preferred way of working, commented on by this NHS chief executive:
One of the features I’d pick out was we exploited to the max and had more joint appointments . . . so it felt like the joint appointments were integrated . . . it almost demonstrated the relationship between academics and practice as part of people’s role or demonstrated the synergy between the organisations where people had joint appointments . . . so I think the structure that we put in place and that developed over time helped with implementation.
NHS senior leadership role, Oakdown, R4
This participant had experienced a ‘really strongly collaborative’ CLAHRC, which had ‘brought together academics and people from clinical practice’. Therefore, these roles, alongside the boundary-spanner or facilitation-type roles, had the potential to create integration and connectivity between academia and the NHS, particularly in CLAHRC contexts where the research and implementation themes were running separately and/or in parallel to each other.
The CLAHRCs’ approach to collaboration was also manifest in the way they set the agenda and in their approach to implementation. For example, there was evidence of collaboration within the service improvement collaborative model, in contrast to a more ‘doing for’ consultancy-type approach to working with services, which may be less conducive to building genuinely collaborative relationships. However, over time, while there seemed to be a shift to more collaborative ways of working, there was an underlying tension regarding the balance between support, ownership and delivery:
there is actually buy-in from the trust executive . . . but at the same time it is almost easy for us, or difficult for us not to fall back into a consultancy role that we will deliver for them and I think that is often a fine line . . . we are driving the project, we are delivering it with them but the ownership lies with us.
Implementation facilitator, Hazeldean, R2
Greater evidence of collaboration (in addition to flexible matched funding arrangements) may have also provided some protection or resilience in the context of significant changes to the NHS landscape partway through the funding period. Having closer relationships between partners gave the potential to be quickly aware of what was going on and to be engaged in the discussions about its impact on roles and activity, including the sustainability of the CLAHRC programme.
There were a number of examples of CLAHRCs collaborating with each other around the use of tools and approaches, and two CLAHRCs had also set up a ‘Strategic Knowledge Exchange Partnership’. Oakdown had developed a ‘Strategic Knowledge Exchange Partnership’ with another CLAHRC around the use of Oakdown’s COPD discharge bundle, through which the two CLAHRCs exchanged information and expertise on telehealth. Hazeldean and Ashgrove worked together on CKD using resources developed by each of the CLAHRCs. These were used to more effectively find patients with CKD in general practice registers, using the audit tool developed by Ashgrove, and to support staff and patients by using the patient and staff information developed by Hazeldean.
At the interpretive forum, the development of a shared (across CLAHRCs) repository of tools and resources was discussed among participants. Some felt that this would be a worthwhile and potentially useful endeavour because it would enable sharing in a more systematic way, but others expressed concerns about there being issues around, for example, intellectual property, which might prohibit some from entering into this type of joint venture.
However, over the rounds of data collection, although there was evidence of collaboration within and between CLAHRCs, evidence emerged about rivalry and competition. Within CLAHRCs this was seen in competing for resources between the organisations aligned with the CLAHRC for projects, such that there was a feeling of losing out to the bigger institutions within the network. Across the nine CLAHRCs there was evidence of competition or rivalry because each was being scrutinised for success and potentially benchmarked against the others. Participants in all three of the CLAHRCs in this study made reference to a competitive element:
success was going to be evaluated between other institutions and I think with coming up to funding for CLAHRC 2 the focus has sharpened a little bit. However, we were continually being told by [X] and [Y] that [Z] CLAHRC was doing very, very well by whatever internal benchmark NIHR applied . . . but we were told that we were doing really rather well.
Clinical leadership role, Hazeldean, R4
. . . we’ve enjoyed being in the top two [CLAHRCs] and we’ve wanted to keep that position.
NHS senior leadership role, Oakdown, R4
We all have to do annual reports to NIHR . . . and when they are collated we will be saying, ‘look, we have collected three times as many patients as them, we have got twice as many research papers and publications as x, y, z CLAHRC’ . . . I don’t think that is unhealthy at all because there has also been a great deal of co-operation.
Leadership role, Ashgrove, R4
Competition became more visible in a lack of sharing as speculation mounted about the potential of funding being made available for ‘CLAHRC 2’. The competition intensified when the call was released and it became clear that the CLAHRCs would be competing with each other. This resulted in a number of reactions and responses including a reluctance to share, guarded communication and reduced attendance at meetings (e.g. directors’ meetings), which it was acknowledged may not have been helpful for CLAHRC as a national initiative.
Boundaries
Multiple types of boundaries were evident in our data (Table 7). The way in which CLAHRCs had engineered their architectures resulted in the construction of boundaries between research and practice, between higher education and health services and between communities. The different perspectives individuals and groups brought to the issue were a function of, and perpetuated, professional and epistemic boundaries. These professional and epistemic boundaries resulted in semantic ones. The geographic delineation of the CLAHRC resulted in physical and spatial boundaries.
| Type | Description | Example |
|---|---|---|
| Organisational | Boundaries that are created or exist between different organisations or between different departments/divisions in organisations and CLAHRCs | . . . so primary care, secondary care, university, PCT all sorts really so having different ways of communicating I thinkAshgrove, leadership role, core team, R3. . . it did have these distinct research and implementation strands . . . there was a massive gap between themHazeldean, leadership role, R1 |
| Epistemic | Boundaries created from differences in where individuals/teams/CLAHRCs ‘come from’ (philosophically) in relation to knowledge and its implementation | . . . a lot of people who are doing applied research . . . actually think they’re doing implementation as part of their applied health research because they’re working with NHS users or NHS staff but they come with a very different sort of epistemological understanding of what implementation is. And I think that has probably been reinforced over the 4 years of the CLAHRC rather than being broken down in any wayHazeldean, leadership role, R3 |
| Semantic | Boundaries arising from different understandings about meaning and language | . . . using a language . . . into ways that people at different levels of an NHS organisation . . . away from research language . . . developing a shared language that takes the project forwardOakdown, leadership role, core team, R3 |
| Professional | Boundaries between different professional groups in different contexts | I think one of the barriers to crossing boundaries was that introduction of ‘I’m a dietitian’, well you’re a dietitian, you’re not a nurse, sometimes can be a barrierOakdown, implementation facilitator/boundary spanner, R3I mean academia and the NHS are two quite distinct sort of cultures . . . and they’ve got their own sort of characteristics and sort of nuances . . . and what they see as a priorityAshgrove, implementation facilitator/boundary spanner, R3. . . there is warfare between various disciplines of implementation . . . I’m the social scientist, the psychologists, the management scientists and they’re all badgering each other and got different views and you get them together and they’re sort of polite but then you get them separately and you get different viewsAshgrove, leadership role, core team, R1 |
| Geographical | Boundaries created by the physical and NHS geography of a CLAHRC | . . . that is all completely scrambled because of the new NHS landscape . . . CCG leads . . . probably feel no obligation to support the CLAHRC because they weren’t in existence when the CLAHRC was initiatedAshgrove, leadership role, core team, R1Between primary care practice . . . there’s no sharing of best practice . . . within a locality . . . just each for their own . . . our huge challenge is spreadHazeldean, leadership role, R3 |
From an implementation perspective, boundaries could be conceptualised as barriers because they have to be overcome, permeated, spanned or eliminated for some form of productive action to take place. Therefore, the resilience of boundaries to be crossed and the effort required to find some shared space resulted in challenges with engagement and getting implementation work done. In this context, credible individuals in boundary-spanning roles were a key resource in facilitating the CLAHRC and its implementation agenda (described further in Boxes 1–3):
And so establishing and doing these sort of teaching sessions at first, we did quite a lot of study days where staff came from the trust. And [name of facilitator] was the biggest help in getting over any sort of barriers and boundaries because she was there, she knew the trust, she could sort of go and . . . work with the staff at a ward level . . . and constantly reinforce the message.
Implementation facilitator/boundary spanner, Oakdown, R3
There was also evidence that CLAHRCs had had a role in breaking down boundaries, in resourcing and creating a shared space for different groups of people, primarily academics and practitioners, to meet and network:
certainly strengthened by CLAHRC, it’s almost provided a hub for us to get to know each other a lot better. It has created links between people who mainly work in academia and people who work mainly in the health service so I think it’s made things perhaps slightly more relevant to people who are purely academically focused.
Implementation facilitator, Ashgrove, R2
Summary
The CLAHRCs’ engineered, aesthetic and social architectures shaped the conditions and space for collective action around implementation whereby their governance arrangements prompted varying opportunities for connectivity and engagement. Furthermore, organising activities in themes, which all CLAHRCs had done, emphasised the epistemic and professional differences within and between higher education and practice. The architectures were a consequence of the interpretation of the CLAHRC call, in particular the positioning of implementation and associated resources relative to other functions such as research. Leaders and executives were the social architects of CLAHRCs in that they set the course and the tone for their particular CLAHRC and for delivering the plan. More distributed leadership within a CLAHRC was associated with the social architects being ‘open’ and ‘collaborative’. There were dominant perceptions across all three CLAHRCs, particularly earlier on in their life cycle, that they were academic entities; as a consequence the nature and quality of interaction varied along a co-operation–collaboration continuum. The CLAHRC identity was constructed over time through activities (e.g. project meetings, training sessions) and roles that brought researchers and practitioners together, and thus started to become a known ‘brand’. As each CLAHRC was a distributed and mainly virtual entity, and as a result of the way it had been engineered, multiple types of boundaries were evident. These boundaries then hindered the potential for productive interaction and engagement, and required extra work to overcome them. The negotiation of these boundaries was entrusted to those in boundary-spanning roles, which, as described below, were a CLAHRC’s main investment in knowledge mobilisation.
Knowledge and its mobilisation
Our ability to focus on the CLAHRC’s purpose of the ‘application of applied health research’ was mediated by how much attention was paid to this aspect of their remit (Figure 10). As indicated in Antecedents above, in general, their main investment was in the generation of applied health research, which was perpetuated by the reporting metrics (e.g. numbers of outputs, grant income) of the NIHR. However, the conduct of applied health research can be achieved in more or less collaborative ways and thereby catalyse the potential of mobilising and applying knowledge through the research process.
FIGURE 10.
Knowledge and its mobilisation.

A number of overarching themes emerged about knowledge and its mobilisation within the context of the three CLAHRCs in this study. They include motivation to engage with implementation, theory and its application, different types of implementation incorporating how different types of knowledge become privileged, facilitation roles and approaches, the role of boundary objects, and PPI in CLAHRC’s implementation agenda.
Motivation to engage with implementation
Motivations to engage emerged over time in the narrative of participants. The motivation or incentive to engage with the implementation function of CLAHRCs was dependent on constituency – the ‘what’s in it for me’ factor. Those that did engage were incentivised by seeing something in it for them. For health services this was expressed in terms of some form of pay-back on their financial investment:
NHS side that we have invested a good deal of money and we want to see ourselves getting something out of it . . . something that will benefit patients and so we should really try very hard to make sure that we hold the CLAHRC to that.
Leadership role, core team, Ashgrove, R4
Services also saw CLAHRCs as an opportunity for support with service priorities and in the improvement of patient care, with the benefit of doing that based on an academic evidence base:
I think the project management support elements of it . . . the academic input side of things, so thinking that they are actually going to get some academic input in how to manage change in their organisation or change a particular culture or context or whatever it might be so that was a big motivator.
Leadership role, Hazeldean, R4
What the CLAHRC did really well was pick up on real service priorities. So it wasn’t a piece of research that was sort of sitting on its own in glorious isolation, it was picking up on real priorities . . . and to have an evidence-based approach to addressing them and getting them into practice was a real motivation for clinical staff . . . we could use CLAHRC as a vehicle to carry out work that enabled us to address those real tricky, wicked problems.
NHS senior leadership role, Oakdown, R4
As described earlier, and reinforced throughout the rounds of data collection, responding and improving on service priorities also had a knock-on effect of meeting targets such as QOF and CQUIN:
The nutrition project and the VTE project were identified by the organisation because they were CQUINs targets and if they didn’t meet the CQUINs targets they would lose a percentage of their income.
Leadership role, Oakdown, R2
For academics, the motivation and incentive to engage presented opposing stances. On the one hand the idea of having the opportunity to be more closely aligned with services and other providers was viewed positively:
From a university’s point of view what we do is public service and public health research . . . so the CLAHRC is just a vehicle for doing the sort of research that we do with the added bonus of close engagement with other providers, the NHS and indeed some industry groups as well so it enabled a much clearer model of coproduction.
Academic, Oakdown, R4
However, for some, the applied research and implementation focus of CLAHRCs did not meet the perceived academic standards that the Research Excellence Framework (REF) demands.
The differences of opinion between the communities explained why there were differences in whether or not they engaged in collective action. This serves to highlight the importance of mutual benefit. It was observed that that benefit tends to arise from the quality of relationships, which, as described earlier, were in varying stages of development even later on in the life cycle of CLAHRC 1:
I think that getting people engaged in it is about them seeing there’s some mutual benefit and where there wasn’t seen as any mutual benefit it doesn’t happen. But seeing there’s mutual benefit has come from relationship building, and there are plenty of times, and I know other CLAHRC directors feel a bit the same, that you feel like you’re a salesperson going round trying to sell things.
Leadership role, core team, Hazeldean, R4
Theory and its application
Both Oakdown and Hazeldean had articulated the use of a particular framework to guide their implementation activity. Hazeldean had framed its bid around the use of the PARIHS framework, and Oakdown had based its on the K2A framework. At the outset, Ashgrove had not articulated a particular theoretical position or starting point, but later ‘talked about our approach, which is the K2A cycle’ (leadership role, core team, Ashgrove, R1). How the use of these frameworks played out in practice varied, particularly at the level of the CLAHRC as a whole; however, their use was more easily described at project level.
In Hazeldean the use of PARIHS alongside a Plan, Do, Study, Act approach was mentioned, although more than one participant agreed that their knowledge, experience and application of both had been limited:
looking at the PARIHS framework was something I think we all adhered to but I don’t think it was something which we made an effort towards working with . . . so all the elements regarding evidence, context and facilitation, we knew they were key parts . . . But perhaps we didn’t actually do a formal context assessment of each practice or situation, it would perhaps be more ad hoc and more observational.
Implementation facilitator, Hazeldean, R1
However, in one of the improvement projects conducted within this CLAHRC, an assessment based on the context element of PARIHS had been undertaken. This discrepancy serves to highlight a disconnect between the expectations of the CLAHRC as a whole and what was happening at project level. That is, there was not a consistency of expectation about the use of PARIHS as the framework of choice for implementation activity. This became more visible in the reporting from a different participant, who was using normalisation process theory in her project activity (although it was not clear how this theory was being used either):
We have used the normalisation process model a lot in our interventions and working with clinicians to change their practice as they go along and I suppose it is a bit arrogant but I thought that that model worked and wasn’t prepared really to engage with a different model.
Researcher, Hazeldean, R1
A lack of consistency in expectation about the use of the PARIHS framework meant that:
across the four teams there are four completely different models of implementation that have been enacted.
Implementation facilitator, Hazeldean, R1
Within Oakdown, it was reported that it used the K2A framework to guide its implementation efforts. Although it was not always articulated how the framework was being used at either CLAHRC or project level, it seemed that different stages/phases within this planned action theory were being operationalised. For example, there was evidence that baseline audits had been conducted within projects, and there were reports that action arising from them had been undertaken. This activity corresponds with stages of the cyclical approach of K2A. For example:
We go through exercises based on literature reviews we did around the evidence of what influences the effectiveness of teams . . . then from that day we have actions that we take forward and we have half a day kind of action learning sets . . . there’s quite a lot of evidence gathering that goes on around it as well . . . all make sure we are not doing any harm but also see areas that we might improve as a result of the changes we are making and we can start to feed that back as well to various patients and staff and indicators.
Leadership role, core team, Oakdown, R1
Clear and explicit links between theory and action, that is theoretical fidelity, were difficult to find in Oakdown and Hazeldean and were absent from the data we collected from Ashgrove.
Type of knowledge mobilisation
The different views, values, interpretations and visions come together to result in a mixed picture, with varying amounts of implementation taking place within each of the CLAHRCs in this study. Over time we identified six types of activity that capture how knowledge was, or had the potential to be, mobilised and actively used, each with the possibility of being approached in interactive and coproductive ways:
-
Service improvement – the implementation of quality improvement methods within and across sites to improve specific service and/or clinical issues, for example in CKD, helping GP practices to diagnose patients with CKD earlier and helping to raise awareness on how to manage the condition more effectively.
-
Making evidence accessible – taking National Institute for Health and Care Excellence guidance and translating it into easily digestible, practical and potentially useable resources/packages, for example taking blood pressure targets and developing aides-memoire for clinical staff to use in practice.
-
Taking national evidence and getting it into practice – typically evident through a focus on prioritising the implementation of guidance (local or national) in local services, for example in improving care for people with VTE based on national guidance and quality standards through helping local implementation of a VTE assessment tool.
-
Mobilising local evidence – examples of intelligence gathering around implementation projects and potential sharing of local evidence about effective practice within and across CLAHRCs, for example using knowledge from one service improvement project to inform a different initiative, and as a result tinkering with the model/approach.
-
Using home-grown research – there was an aspiration, linked to funder expectations, that CLAHRCs should be implementing the research they generate within the 3- to 5-year period of funding. This aspiration was achieved in Ashgrove, which implemented its own research from CKD and COPD projects and an online cardiac rehabilitation tool.
-
Paying attention to implementation in the conduct of research – breaking down the divide between research and its use by considering implementation at the beginning of the research process, and/or adopting an approach to conducting research that could be described as coproductive.
In reality we observed a mixture of these different types of implementation within and across CLAHRCs. However, each CLAHRC tended to coalesce around certain types; for example, Hazeldean’s approach focused on service improvement and Oakdown’s on implementing guidance. Across the three CLAHRCs there was a greater balance towards knowledge transfer approaches than towards those that were more coproduced.
Additionally, each CLAHRC came from a different starting point with respect to both its view and its experience of knowledge mobilisation, and all were going through some form of journey in figuring it out. For example, participants from Oakdown were very clear that at the outset their approach would be one of ‘coproduction’. This then played out in their approach to working with partners in the way they conducted their research, and their implementation work was led by a practitioner-researcher experienced in evidence-based practice. Individuals in Ashgrove gave a very honest account of their contrasting starting point with respect to their implementation remit:
I think where I have found it difficult is understanding this second part of the CLAHRC, this implementation translation, and I think it has come across, we just don’t know how to do this.
Leadership role, core team, Ashgrove, R1
In this case, it was recognised that this issue was not helped by the fact that ‘the lines of communication between academics and the health trust are not well formed and so there isn’t an obvious route for implementation’ (leadership role, Ashgrove, core team, R1), and that implementation had not been clearly articulated in early plans because ‘a lot of us . . . weren’t up to speed with this agenda and how that would work’ (leadership role, core team, Ashgrove, R1).
Privileging of evidence
Different types of implementation privileged different types of evidence from different sources of knowledge. Perhaps unsurprisingly, in contexts where the research function of a CLAHRC was more prominent, research and academic knowledge tended to be privileged. In contexts where there was a broader appreciation of the CLAHRC remit, and evidence of implementation, such as service improvement activity, the value of incorporating different sources of knowledge was recognised; for example:
I think in our CLAHRC there is quite a lot of service improvement going on and service evaluation where different knowledge is used to inform and measure it over time . . . there is a move towards knowledge as practice or research as practice . . . if you don’t adopt all the different knowledges including research knowledge . . . practitioner knowledge, policy knowledge, user knowledge, if you don’t use those to interpret it [research] and put it into practice you are into a losing game really.
Leadership role, Oakdown, R1
Patient and public involvement in knowledge mobilisation
Although there was considerable variation in PPI across implementation projects within CLAHRCs, Hazeldean’s focus on service improvement claimed a mixed use of patient perspectives in different improvement activities, with some coproduction of project outputs. Oakdown’s claimed aspirations around coproduction saw mixed progress with PPI, but with a determined intention to enhance their activity through investing in research into PPI approaches. Ashgrove’s approach to implementation emphasised the potential of the patient experience as a means of unlocking barriers to implementation, for example through the production of patient education resources. External evaluation produced a renewed emphasis on PPI, although this focused on the research process as a whole. Generally participants conflated PPI in research and PPI in implementation, regardless of the predominant approach to implementation in each of the three CLAHRCs. A key distinguishing feature, however, was the issue of funding:
[PPI in research] costs money, but you can put that into the preplanned research budget, and obviously when the research ends, so does the consultation or the joint work with patients and the public.
Leadership role, core team, Hazeldean, R1
Types of patient and public involvement
Even where research themes within CLAHRCs had a history of PPI, and some infrastructure to support it, they found it difficult to augment the focus of PPI in research to include implementation. The data demonstrate a lack of conceptual clarity about PPI, with cited examples including:
-
patients as research study participants
-
consultation activity across all CLAHRCs, but including qualitative research into the patient experience in Ashgrove
-
using PPI as a focus for learning at improvement events, either directly or through patient stories
-
using PPI as a source of knowledge/expertise to be represented in improvement work
-
collaborating in product and service development
-
dissemination, including the design and content of websites.
Hazeldean’s work on the development of a framework for assessment at 6 months after stroke was held up as an example of coproduction, and specifically its focus groups with patients ‘looking at what they considered to be the problems they had after their stroke’ (implementation facilitator, Hazeldean, R1). Indeed, in other CLAHRCs, although coproduction was usually couched in terms of ‘events’, there was a desire for future CLAHRCs to pay more attention to coproduction as an approach to meaningful PPI. Although participants across all CLAHRCs felt that progress had been made in embedding PPI in implementation projects, and clear instances of impact on activity and products were evident, PPI was viewed as a work in progress requiring sustained and strategic action in subsequent CLAHRC-type initiatives.
Influences and mediators of patient and public involvement
How the CLAHRCs had organised their research and implementation functions inevitably influenced how PPI was conceptualised. For example, where an initial approach to implementation focused predominantly on the (future) use of home-grown evidence in Ashgrove, then participants reported difficulty in contemplating the interplay between evidence from research and the patient voice: ‘asking patients what they want from services isn’t the same as injecting research evidence into those services’ (leadership role, core team, Ashgrove, R1). Further on, the development of ‘project groups’, with PPI representatives adopting an advisory role, was reported by both Hazeldean and Oakdown as helpful in providing a structure for melding different types of information for implementation.
In a context where there was a lack of early strategic intent around PPI, projects relied on efforts to engage patients in feedback on ‘redesign rather than design’ (secondee to CLAHRC, Hazeldean, R1) implementation initiatives. This led to a perception that PPI efforts were mostly around ‘catch-up’ (implementation facilitator, Hazeldean, R1), even in the context of a strong push from leadership around PPI. This was particularly evident in Ashgrove, where, after an external review, the appointment of a PPI champion led to the development of a PPI forum to cover both research and implementation CLAHRC functions. This led to input into all applied research projects. Attention to leadership was also mirrored by investment of resources in the training PPI. These changes led to the construction of a framework for PPI across the knowledge production and utilisation cycle, which aimed to enhance the implementability of research: ‘if everybody is being consulted at the right points throughout the process, you’re not going to have those barriers to implementation’ (implementation facilitator/boundary spanner, Ashgrove, R3).
Within the context of a programme of work to improve CKD services, there was a disconnect between research and implementation which meant that PPI fed into implementation/service improvement activity rather than the research upon which products were produced.
The data demonstrate that participants were persuaded of the importance of PPI: ‘everyone knows they should be doing it and most of them do it, and some of them do it outstandingly well. Others need to be monitored and encouraged’ (leadership role, core team, Hazeldean, R1). This view was mirrored in Ashgrove, where gaps between intention and action were crystallised: ‘no one seems to be very sure about how to set it up’ and there was ‘a problem in understanding what it is and what it consists of’ (implementation facilitator/boundary spanner, Ashgrove, R1). Intentions to engage patients in service improvement activities were sometimes thwarted through limited capacity for patient engagement within the service side: ‘most practices have underdeveloped systems for consulting their patients’ (leadership role, core team, Hazeldean, R1). However, there was a contrary perspective around positive intention in the data, where PPI was not always seen as essential, for example where ‘you are spreading proven innovation’ (leadership role, core team, Hazeldean, R1). PPI was often perceived as a NHS responsibility, although there was a recognition that capacity and capability were limited (leadership role, core team, Hazeldean, R1). Where the focus of implementation activities was principally conceived as generating a change in clinician behaviour, there also appeared to be little interest in PPI, other than in the production of patient information resources as in the case of HF work in Hazeldean. However, a sense of a moral dimension to PPI emerged in the narratives, specifically about PPI being the ‘right thing to do’. This was echoed by leaders, who reported that staff should ‘feel at least guilty for not doing it’ (leadership role, core team, Hazeldean, R1).
Patient and public involvement seemed to work well where there was a clear clinical focus around which patients and professionals could collaborate, as in the case of Oakdown’s work on diabetes research, as this provided a ‘shared interest’ to motivate engagement (NHS senior leadership role, Oakdown, R1). However, where there was a lack of agreement on the feasibility or appropriateness of the implementation activity, as appears to be the case for Hazeldean’s work around CKD management in primary care, there was little appetite for early patient engagement. The absence of a clear PPI strategy in the early stages of CLAHRC development probably reflects a predominant narrative in the data around PPI being something to be done when projects were up and running. There was no evidence in our data of PPI informing the selection of implementation projects to be conducted at CLAHRC level.
There was a general reliance on tapping into patient groups and networks that were already in existence, and serendipity about whether or not there was the right mix of resources. In Hazeldean, projects tended to ‘work with whoever just happens to be there and not if they aren’t’ (leadership role, core team, Hazeldean, R1). This appeared to reflect concerns about the significant costs associated with the development of infrastructure to support PPI. Oakdown also reported that its PPI activity was mostly through voluntary organisations and advocacy groups. However, Hazeldean’s work around HF, and the associated networking of professional groups and stakeholders, was successful in creating access to a ‘lot of patient of patient groups that existed, but nobody actually knew where they were’ (implementation facilitator, Hazeldean, R1). Data show that the further formation of service user groups or networks in this CLAHRC had been useful in informing the design of aspects of implementation projects, for example in establishing ‘what success would look like’ (management role, Hazeldean, R2), and was considered a key PPI success for the CLAHRC. Sustaining these was highlighted by both Hazeldean and Oakdown as a strategic challenge for the next round of CLAHRCs, given the considerable amounts of time and resources associated with group or network development. Continuing investment in PPI leadership was seen as key to the future in Ashgrove.
The strongest perspective in the data that emerged around PPI was the view of patients as holding a knowledge resource which could be tapped. The use of this resource appeared to be the most significant early impact of PPI, specifically in the capture and use of this knowledge to design patient information materials. Within Ashgrove, for example, concerns about the uptake of cardiac rehabilitation services, which were described as ‘really poor’ (implementation facilitator, Ashgrove, R2), were addressed through the coconstruction of a web-based support programme. Other more obvious impacts reported were around increasing access to hard-to-reach or ‘marginalised’ (leadership role, core team, Hazeldean, R1) groups such as ‘men with coronary heart disease in isolated circumstances’ (researcher, Hazeldean, R1).
Reflecting on their approaches to patient and public involvement
Strategic uncertainty about PPI within the CLAHRC appeared to be associated with reported challenges about scaling up, or learning about PPI, which both Hazeldean and Ashgrove recognised as requiring improvement, although progress with this appeared slow. This was also reinforced during the interpretive forum in which participants reiterated their challenges with operationalising PPI, particularly in the absence of an evidence base for PPI within implementation. Despite a learning event to reflect on PPI, Hazeldean had not developed any guidance on PPI. This left feelings of tokenism, with ‘little visibility’ (leadership role, Hazeldean, R4) of any achievement of PPI, and a concern that future efforts might not be ‘progressive and meaningful’ (clinical leadership role, Hazeldean, R4). In this CLAHRC, and despite processes for reporting progress with PPI, the board was reported to lack any ‘systematic view of how integral PPI is across the research theme or implementation theme. They get snapshots . . . they don’t get any real feeling of actual engagement’ (leadership role, Hazeldean, core team, R1). It appears that, in this case, board lay members were particularly exercised about this.
As time went on, there was evidence of a recognition that there was a lack of guidance around PPI. As a result, Ashgrove undertook a review of the literature on PPI in implementation, and engaged in other networking activity across CLAHRCs to further this aspect of their mission.
Although most CLAHRCs had made progress in the establishment or consolidation of PPI networks around projects, concerns emerged in later data collection rounds around the democratic nature of representation. Specifically, concerns were addressed around what agenda PPI representatives were bringing to programmes, and that the ‘same people were popping up all the time’ (management role, Hazeldean, R4). Despite these concerns, the development of more infrastructure for PPI was associated with a ‘less reactive’ (management role, Hazeldean, R4) approach, reflecting greater knowledge and confidence of PPI issues.
Perspectives from a different Collaboration for Leadership in Applied Health Research and Care
The configuration and range of experiences were checked out in one additional CLAHRC, which had adopted a more embedded approach to PPI from the outset. As with Ashgrove, leadership was key to driving PPI forward, although in this CLAHRC the leadership was part of a long-standing programme of public engagement around health issues within the CLAHRC footprint, including a ’10-year programme of doing user-led research’ (leadership role, PPI CLAHRC, R4). Additionally, leadership was sustained through dedicated funding for PPI staffing and related activities such as patient costs. The embedded approach to PPI was made explicit with a clear strategy for PPI at the inception of the CLAHRC, defined as ‘Engagement by Design’, and covered research priority setting and design issues such as the selection of outcome domains and measures. This reflected a recognition of the need to attend to implementation issues in the earliest phases of the knowledge production cycle. There was an assumption that, in this way, ‘the knowledge we’ve produced is actually much more likely to be taken up into practice’ (leadership role, PPI CLAHRC, R4). Whereas in our partner CLAHRCs PPI had been associated with surfacing patients’ experiential knowledge as a resource for improvement, and was ‘the right thing to do’, the ambitions of PPI in this CLAHRC were broader. Here there was an emphasis on changing the discourse of health through involvement at a regional level, increasing collaborative and collective capacity for implementation as ‘patients and professionals are learning about the evidence base together’ (PPI lead). Extending PPI beyond CLAHRC projects in this way appeared to reflect a regional tradition of activism around health, which provided the foundation for this CLAHRC’s approach to PPI. While other CLAHRCs worried about the professionalisation of PPI through the ‘usual suspects’ (PPI lead), this CLAHRC paid less attention to representation and more to the ‘authenticity of the experiences round the table’ (leadership role, PPI CLAHRC, R4) being brought to bear through PPI.
Facilitation and boundary-spanning roles
Implementation was enacted through the establishment of roles to fulfil facilitation and boundary-spanning functions (see Boxes 1–3 for a more detailed description). The rationale for the type of roles that were established within each CLAHRC was not clearly articulated; however, there did appear to be links to the frameworks they had selected to guide their implementation activity. Specifically, in Hazeldean the facilitator role was developed around the concept of knowledge transfer and was informed by the PARIHS framework’s facilitation element.
Oakdown had created a number of different facilitator roles, with a focus at different organisational levels. In the PCTs, two R&D facilitator posts were developed and, although these were ultimately not seen by participants as successful because of changes to the health service landscape, they were created to act as agents of the CLAHRC within the PCT:
The original conception was to have R&D facilitators who would be absolutely embedded in local PCT public health teams, which is where we saw the focus as being, but of course when the coalition came in and announced that they were getting rid of PCTs and that responsibility for inequalities in public health was all moving to local government, kind of . . . essentially ever since the White Paper we have had to rethink how we actually do things.
NHS senior leadership role, Oakdown, R1
These posts fell into abeyance when post holders left and were not replaced. The posts were funded by the CLAHRC but the holders ‘were perceived as somebody extra rather than a core member of the team’ (NHS senior leadership role, Oakdown, R1). However, within the implementation theme a number of facilitator roles were developed to link with the theoretical model that this CLAHRC had adopted to underpin implementation.
Within Ashgrove, individuals were appointed to co-ordinate and deliver training sessions. They were based in the R&D departments of health-care trusts, which did not appear to be linked to a particular approach or model/framework: ‘the implementation objectives have started to evolve as we have gone on, it is a bit more iterative and I don’t think it was entirely clear in our initial plans’ (clinical academic, Ashgrove, R1). As one participant noted, these were new posts and as a result would take time to embed:
these are very new roles where there really is no template for action and there is no clear guidance as to what they should or shouldn’t be doing. So I think it has taken all of the time to bed in and work out for themselves how best they might support their organisations and support the CLAHRC.
Leadership role, Ashgrove, R1
Although the Hazeldean implementation facilitators’ roles were linked to the implementation framework (PARIHS), there was still a lack of clarity about what the role would/should entail, which caused some uncertainty for the post holders:
For me personally [it was difficult that it was an undefined role] . . . I think some other people struggled more than myself. I think because of the way I am and the way I am used to working, I am quite a good self-motivator . . . The downside of that is that perhaps I wasted energy and time in areas that were not applicable, but I think at that time and regarding the role, I don’t think it was actually known what was needed in certain areas.
Facilitator, Hazeldean, R1
Role in knowledge mobilisation
Individuals in these roles generally said that they had vague job descriptions, particularly at the outset. However, in all three CLAHRCs those appointed to these roles were expected to engage in activity that ranged from training in research and evaluation to being focused on facilitating knowledge mobilisation. In contrast to the training and education function of individuals in Ashgrove, the implementation facilitators in Oakdown were more focused on knowledge mobilisation. Here, they were involved in the development of tools and procedures in three projects to support the use of knowledge in practice. This involved providing e-learning resources, training staff and working with steering groups to develop tools and procedures for implementing evidence. In addition, they had a supporting role for the ward-based champions, who had been identified as another means of knowledge mobilisation. In this sense there was the enactment of an external–internal facilitator-type approach:
One [approach] was to introduce ward-based nutritional champions so members of the ward team would help facilitate that change in practice with support of what we would call [implementation facilitators], who come from CLAHRC.
Leadership role, core team, Oakdown, R2
Oakdown facilitators were also expected to spread evidence-based improvements across the hospitals in which they were working:
there’s been spread through our [implementation facilitators] that we appointed to work across the wards and help disseminate so there’s been, I suppose, formal approaches like the workshops and the newsletter and there have been less formal ones where there’s been spread through people meeting informally.
Leadership role, core team, Oakdown, R3
There was also some clarity about the role of the facilitators in Hazeldean, where they were expected to implement evidence into practice:
I think it started off that they employed like seven [implementation facilitators] and our job was to facilitate the implementation of evidence, whatever evidence into practice.
Implementation facilitator, Hazeldean, R1
Boundary spanning
In all three CLAHRCs these individuals also served as boundary spanners; this was most obvious in Oakdown, where, in descriptions of the implementation facilitators and their role, ‘boundary spanning’ or ‘boundary spanners’ was the dominant discourse. Here, there was a recognition that it was necessary to have boundary spanners functioning at different levels within the health-care organisation:
I think what has become evident for us is the importance of boundary spanning at different levels . . . it is about the importance of boundary spanning at executive and board level going down to middle managers and steering committee members, key clinicians in the trust as well as middle managers and then importantly boundary spanning with frontline staff, the people whose practice we are trying to change.
Leadership role, core team, Oakdown, R2
Likewise in Ashgrove, the skills and qualities of the boundary spanner were identified in outlining their role:
we needed somebody in the trust to bring the organisations and the researchers together . . . a good [boundary spanner] is someone who is basically a great people person, brings people together, communicates, organises, networks, you know, speaks their minds . . . It’s not necessarily about the evidence, but it is about the people skills . . . we see them as sort of boundary spanners really, getting people across the boundaries and letting things happen that way.
Leadership role, core team, Ashgrove, R1
The critical feature of success for people in these roles was their credibility. Therefore, over time, Hazeldean augmented the work of its boundary spanners by employing clinical staff on secondment, because the people they had employed lacked clinical credibility, which had been a problem. In clinically embedded projects (CKD and HF), these roles were seen as important because the people had knowledge of the health-care context, including clinical knowledge:
So across the CLAHRC as a whole now we’ve got as least as many seconded people in knowledge transfer-type roles as we have people we originally recruited because that does bring that much more informal knowledge of people, networks and the clinical knowledge you know, and although there’s a few of those who we recruited who are good facilitators, in view of credibility and particularly the confidence that goes with those abilities are very important I think.
Leadership role, Hazeldean, R3
In contrast, Oakdown had employed only staff with a clinical background in its implementation facilitator roles, so they brought with them the clinical and contextual knowledge (i.e. local knowledge) that was seen as important for implementation success. In Ashgrove, boundary spanners were based in PCT R&D departments. In addition to the implementation facilitators in the PCTs, one of the research themes in Ashgrove had employed a full-time senior nurse as an implementation manager. This was seen as bringing clinical credibility to the role along with a sound knowledge of the health-care context, including barriers and enablers to implementation.
Overall, it was perceived that individuals in these roles were pivotal to knowledge mobilisation within CLAHRCs through facilitation and boundary spanning. They were also the most visible presence of the CLAHRC within health services. The focus of their function was allied to the particular position the CLAHRC had taken around research versus implementation, and in relation to the use of particular frameworks/models to underpin its activities. These individuals were perceived to be credible messengers – credible in the sense that they could interface with individuals at various levels of organisations and in that they brought clinical and contextual savvy to the implementation situation. The investment in them also provided the potential to build capability and capacity for implementation and research within health services.
Boundary objects
Boundary objects are described as vague concepts with strong cohesive properties, flexible to local needs but remaining recognisable across contexts to enable the translation of knowledge from one group to another. 109 Allen110 argues that it is because of their vagueness that they have the potential to facilitate communication between individuals and/or groups. However, historically, there has been a tendency to apply the concept of boundary objects to concrete shared objects, with less attention given to the conceptual. Within this study we identified the potential role of boundary objects in translating knowledge into action on a continuum from concrete to conceptual. Additionally, we have gained an understanding about how boundary objects move from boundary objects in theory into boundary objects in use.
Documentary analysis of a range of CLAHRC documents uncovered a number of different objects, which had the potential to have the properties of boundary objects in use (i.e. enabling shared meaning). These are summarised in Table 8, in which Star and Griesemer’s109 taxonomy is used with the addition of a further column, ‘Catalysts?’
| Object | Repository | Standardised methods and forms | Objects, models and maps | Symbolic object | Catalysts? (intended) |
|---|---|---|---|---|---|
| Web-based cardiac rehabilitation programme | ✓ | ✓ | ✓ | ||
| Annual and other reports | ✓ | ✓ | ✓ | ||
| Assessment tools | ✓ | ✓ | ✓ | ||
| Audit tools | ✓ | ✓ | ✓ | ||
| Blog | ✓ | ✓ | ✓ | ||
| Space COPD manual | ✓ | ✓ | ✓ | ||
| Care pathway | ✓ | ✓ | ✓ | ||
| CRD questionnaire | ✓ | ✓ | ✓ | ||
| Chronic condition audit tool (CKD) | ✓ | ✓ | ✓ | ||
| Diabetes UK booklet on diabetes and depression | ✓ | ✓ | ✓ | ||
| Lesser diabetes score | ✓ | ✓ | |||
| Chronic disease registers (CKD/HF) | ✓ | ✓ | |||
| ✓ | ✓ | ✓ | |||
| Guideline | ✓ | ✓ | ✓ | ||
| K2A framework | ✓ | ✓ | |||
| KT casebook | ✓ | ✓ | ✓ | ||
| Ashgrove self-assessment risk score | ✓ | ✓ | |||
| Malnutrition Universal Screening Tool + | ✓ | ✓ | |||
| PARIHS framework | ✓ | ✓ | |||
| Implementation protocols | ✓ | ✓ | ✓ | ||
| Self-management manual | ✓ | ✓ | |||
| CLAHRC website | ✓ | ✓ | |||
| Implementation worksheets | ✓ | ✓ | |||
| Evidence-based practice concept | ✓ | ||||
| Implementation concept | ✓ | ||||
| CLAHRC vision | ✓ |
General overview of the types of things that can be classified as boundary objects in theory
Those objects listed in the columns labelled ‘Standardised methods and forms’ and ‘Objects, models and maps’ suggest a considerable overlap between classes (many of these listed items can occupy both classes). However, multiple classification is a feature of many boundary objects, and a single boundary object may reside in several classes simultaneously.
During interviews with participants who were operating as boundary spanners, conceptual (e.g. CLAHRC concept) entities also emerged that appeared to operate as boundary objects, and it became evident that whether or not the boundary objects in theory operated as boundary objects, in practice was a function of the way in which they evolved and the meaning that was attached to them. Interviews with participants verified if and how boundary objects in theory (i.e. those that were evident in documents; Table 9) played out in practice as boundary objects in use.
| Repositories | Standardised methods and forms | Objects, models and maps (representations) | Symbolic objects | Boundary spanners |
|---|---|---|---|---|
| Disease registers | Care pathways Formal implementation methods Assessment tools Best practice guidelines Standards of care Quality improvement methods and tools, i.e. PDSA, audit tools Change packages |
Models and frameworks of implementation, e.g. K2A, PARIHS, CFIR Concrete models Diagrams and visual representations Published output Annual reports Newsletters Multimedia Electronic communications |
CLAHRC concept and vision Evidence-based practice Implementation/knowledge mobilisation |
Knowledge brokers Knowledge transfer associates Nutritional champions Health trainers and educators CLAHRC co-ordinators Other formal/informal roles |
Concrete to conceptual boundary objects
A range of what could be described as concrete boundary objects was evident in the discourse of the boundary-spanner interviewees. The nature and properties of some of these are outlined in Table 10. These objects had the potential to share meaning and knowledge and to catalyse action among those who coalesced around them.
| Boundary object | Properties |
|---|---|
| Nutrition action plan (Oakdown) | Prompted open communication between ward staff and CLAHRC implementation facilitators in order to develop a boundary object that is meaningful at an individual-ward scale, and within the scope of the ward team |
| VTE assessment form (Oakdown) | VTE assessment tool relocated to span the boundary between knowing and doing more effectively, increasing its potential as a boundary object in use |
| Disease register (Hazeldean) | Generates a repository of standardised information which can be accessed by different parties across different contexts. However, the disrepair and inaccuracy of the repositories meant that implementation work is co-ordinated around their interrogation and validation |
| CKD improvement guide (Hazeldean) | An object to be shared across PCTs, spanning the boundaries between GP practices as individual businesses around which a common approach to improvement is developed |
| Evaluation toolkits (Ashgrove) | Each toolkit provides a reference point prompting and guiding dialogue and sharing information between different groups of stakeholders |
| Data and targets, e.g. QOF (all CLAHRCs) | Communication opened up at levels of commissioners and PCTs. Identification of shortfall, potential to improve service delivery, assistance in reaching targets. QOF data represent a compelling case for participating in implementation work – a powerful and persuasive message |
In addition to the tangible objects that were identified as potential boundary objects, less tangible entities, conceptual or symbolic, emerged that could also have boundary object properties attached. CLAHRCs as a concept served as a boundary object, in that they possessed some cohesive property (which varied across them) in catalysing the potential to cultivate collaboration. There were varying perceptions about what a CLAHRC is, which were related to the type of stakeholder expressing the opinion: those in CLAHRC leadership roles were clearer about it than those in the front line of the health service. Over time, and through a process of collective sense making, CLAHRCs as a concept became clearer for some:
we really sort of got our heads together about what CLAHRC was, and actually what we should be doing . . . yeah, we kind of just worked something out ourselves and just created a job and created work for ourselves, based on our interpretations of . . . of what it is . . . it’s a programme of work to promote collaborative . . . collaborative work between academia and health care to . . . ensure research evidence is used quickly, and it is . . . is . . . worthwhile, it’s wanted, and it’s used.
Implementation facilitator/boundary spanner, Ashgrove, R3
However, CLAHRCs’ catalytic potential to bring about collaboration was hindered by their architectures.
There were also examples of language being used to create a shared meaning around issues and topics, and thereby acting as a symbolic boundary object. In this example a facilitator had been using what she described as a slogan to engage practitioners’ attention:
I’m tending to use a slogan that I suppose is about patient safety . . . Everybody’s business. So those are sort of catchphrases that capture people’s interest.
Implementation facilitator/boundary spanner, Oakdown, R3
Clinical issues also had the potential to have cohesive properties. For example, in Oakdown shared clinical topics such as nutrition and dysphagia were boundary-spanning concepts, which were meaningful to a range of stakeholders including practitioners and patients.
I think the thing with nutrition is it’s not a hard sell . . . I really don’t think anybody thinks it’s not important . . . everybody thinks it is important . . . And most people, and I can’t think . . . as I say, most people believe nutrition is important . . . So it’s not a hard sell. What’s the hard sell is how to do it.
Implementation facilitator/boundary spanner, R3
In this example, nutrition was a useful symbolic boundary object that resonated across contexts and was perceived to be universally important, providing a focus around which to catalyse engagement and potential action for improvement.
The evolution of boundary objects: collective action
The potential of boundary objects to have cohesive properties appeared to be partly a function of the way in which they evolved. Those objects that transformed from objects in theory to object in use had similarities in terms of their collective generation. Collective generation occurred through discussion and collaborative activity in developing, amending and tailoring objects for use. There are a number of examples in the data where particular tools had emerged from collective endeavours, which had involved the engagement of relevant stakeholders and resulted in their use in practice [e.g. CKD audit tool at Ashgrove and Hazeldean, Malnutrition Universal Screening Tool (MUST)+ and VTE assessment tools at Oakdown and HF alert card at Hazeldean]. In this way they mobilised knowledge between communities because the process involved the integrating of local evidence and experience with external evidence from guidance and thereby became meaningful to stakeholders.
Box 5 provides an example of how collective action around a shared symbolic object was transformed into a concrete boundary object, something that was relevant and had resonance with its end-users, which was then used in practice.
Through a mapping exercise of HF services undertaken by members of Hazeldean’s implementation theme, poor communication between primary and secondary care was identified as a problem:
The problem came from them and then we just tried to find a solution for it.
Implementation facilitator, Hazeldean, R1
Specifically, community HF specialist nurses were not being notified when patients on their caseload were admitted to hospital and discharged home. Through discussion with HF practitioners and service users during stakeholder meetings facilitated by Hazeldean CLAHRC, the idea of an emergency card emerged as a way of conveying information regarding a patient’s HF status across primary and secondary care settings. One of the facilitators took this idea and developed it through discussions with stakeholders into a credit card-sized HF alert card to be shown by patients at secondary care appointments:
So we came up with a heart failure alert card . . . you know, the patient has this card . . . and it’s got the contact details . . . it’s got kind of . . . patient . . . a few details about the patient, but it’s also got the contact details of the heart failure nurses, and also states . . . please contact my heart failure nurse, you know, on admission or whatever.
Implementation facilitator, Hazeldean, R1
Feedback gathered 12 months later confirmed that the implementation of the card had been evaluated as a success by primary care professionals:
it was quite successful. And from that there’s . . . quite a few heart failure services, you know, across Hazeldean, are using it now . . . And one practice nurse is going to trial it for me . . . and actually, you know, making sure that patients are receiving the treatment that they . . . that’s best suited to them.
Implementation facilitator, Hazeldean, R1
According to the HF alert card report there are now recommendations to spread the card to different services, for example community matrons, active case managers, secondary care HF specialist nurses and GPs. The format of the alert card would remain the same but the information on the card would be revised to reflect the service.
Within Oakdown there were also reports of collective tailoring of standardised generic objects that had originated externally from the CLAHRC organisations, including the MUST and VTE assessment tools. These tools underwent a process of tailoring and contextualisation, including the incorporation of local knowledge:
things like the MUST screening tool or the Department of Health VTE assessment form and the idea that those are then adapted to the local context so MUST was developed to what we called MUST+ because it had an extra question that we felt was appropriate.
Clinical academic, core team, Oakdown, R3
. . . without us . . . without doing enough tailoring . . . I think what we learnt was you have to do a lot more tailoring than you think.
Implementation facilitator/boundary spanner, Oakdown, R3
If there was not enough collective action involving relevant stakeholders in either development or tailoring, the result was that a concrete boundary object in theory potentially operated in an inhibitory rather than catalytic way in practice; for example:
they decided, because . . . South Asian communities have a higher incidence of diabetes at a lower BMI [body mass index] . . . this was a real . . . it was important, and obviously Ashgrove has a very high South Asian population; it was really important that this tool worked for that group . . . They’d done a literal translation, which was in places quite offensive . . . and the . . . the . . . as a visual aid, it’s like a traffic light . . . you know, red, two ambers and a green, and they couldn’t get why you would have two ambers. It really . . . you know, it stopped the purpose of the tool, it . . . you know, they were saying ‘Oh why . . .’ you know, ‘How do I know which amber I am?’ and things like this. So those discussions, if they hadn’t have taken place that tool would have gone out, I mean it is out, Diabetes UK host it, it is a really valuable tool . . . But it would not have worked for that group if they hadn’t had that conversation.
Leadership role, Ashgrove, R3
Our data show that meaningful collaboration provided a condition in which the potential of boundary objects may be released, because this provided a receptive context and opportunity for attaching meaning, resonance and value, which enabled knowledge mobilisation. Therefore it could be predicted that, in environments in which there is more and good-quality collaboration, the power and potential of boundary objects might be greater.
Summary: knowledge and its mobilisation
Different levels of attention were focused on CLAHRCs’ implementation function. These levels linked back to how the CLAHRC initially interpreted the brief (i.e. its position about what CLAHRC was for), and the positioning of resources to enact its plans. However, we identified a number of different types of activity that mobilised knowledge or had the potential to mobilise it, and around which each CLAHRC tended to coalesce. On balance these approaches were concerned more with knowledge transfer than with coproduction; that reflected an emphasis on CLARHCs as producers rather than users of applied health research. CLAHRCs were figuring out PPI within knowledge mobilisation and articulated their challenges with this remit. Generally, they had conflated PPI in research and PPI in implementation, which demonstrated a lack of conceptual clarity around this issue and their challenge in operationalising it in a CLAHRC context. Engaging with the CLAHRC agenda and around knowledge mobilisation was an enactment of ‘what’s in it for me’; different stakeholder motivations provided a loop of reinforcement for engagement. Motivations to engage also differed between health services and academia; those in practice perceived CLAHRCs to be dominated by an academic agenda.
The CLAHRCs positioned financial investment in implementation through the creation of boundary-spanning roles. Individuals who were credible and visible in these roles played a significant role in mobilising knowledge (and in making a CLAHRC real). They developed and had at their disposal a number of ‘things’ that were, or became, boundary objects. Potentially meaningful collaboration (e.g. in the creation of objects) provided the conditions in which the potential of boundary objects was released.
Impacts
The data contain many examples of both perceived and actual impacts that were attributed to the existence of the CLAHRCs. CLAHRCs certainly appeared to have catalysed action through the provision of resources, opportunities and the ‘space’ for collective action. The impacts from CLAHRC activity have been made visible in reports, publications, websites and the verbal accounts of those participating in this study. We captured a variety of impacts that ranged from those that were more direct (e.g. actual impact on practice and/or patient outcomes) to those that were more conceptual and processual (Figure 11). We also discovered that involvement in CLAHRCs had led to impacts that could be described as personal.
FIGURE 11.
Impacts.
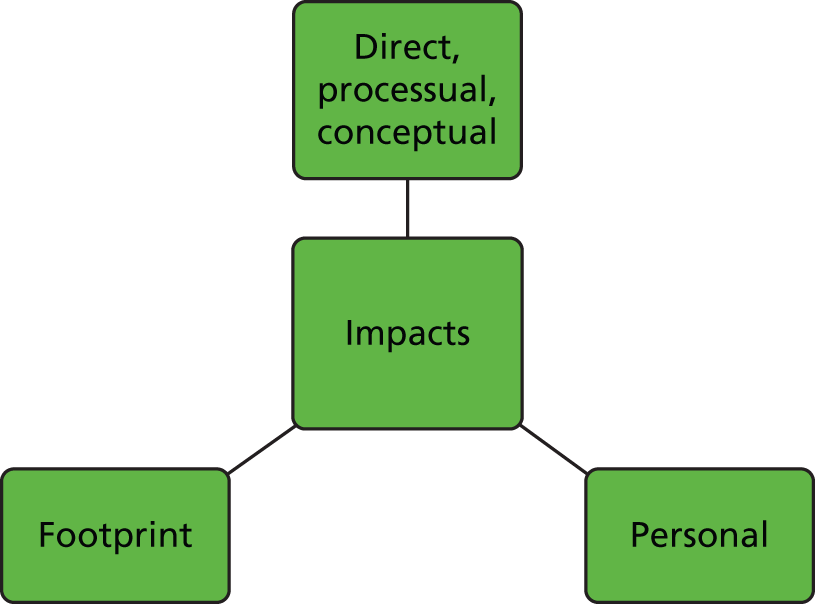
Direct, processual and conceptual impacts
Throughout the rounds of data collection there was a consistent narrative about needing to demonstrate impact. This was particularly acute in the early stages of the life cycle of the CLAHRCS: ‘high expectations from the trust and the funding, there is a lot we need to achieve in a quite short space of time and I think that is quite difficult or I personally found quite difficult, quite a lot of pressure in a sense to achieve results quickly’ (implementation facilitator, Hazeldean, R2). Given the time that it takes to generate impact, particularly in relation to changes in practice, service delivery and patient outcomes, it was perhaps unsurprising that evidence of more direct impacts accumulated over time and was, therefore, more obvious at the point of transition between CLAHRC 1 and CLAHRC 2, when data collection in this project was finishing. Appendix 8 provides a list of evidence extracted from a variety of documents about the direct impacts that CLAHRC’s had generated and reported. Some of these impacts are illustrated in Table 11. The most prominent source of these more direct types of impacts from implementation activity appears to be service/quality improvement-type projects. Discussions between CLAHRC participants at the interpretive forum acknowledged that the (regional) public health impacts expected in the original CLAHRC bid had not been realised as intended, and that perhaps this was partly a result of the types of metrics they were being asked to deliver and report on.
| CLAHRC | Document | Impact |
|---|---|---|
| Hazeldean | Document 5: local evaluation | Stroke assessment tool pilot: 464 unmet needs were identified in 137 post-stroke reviews |
| Document 9: website screen shot | CKD second-wave projects: 539 additional patients on the CKD register of the 11 practices involved. This was 154% of the target that was set for the practices. The percentage of patients with proteinuria recorded improved from 92% to 95%. The recording and management of blood pressure (in line with NICE-recommended targets) increased from 60% to 83%. This represents 972 patients who now achieve recommended blood pressure targets or have blood pressure readings better recorded | |
| Oakdown | Document 2: CLAHRC newsletter, autumn 2013 | VTE project: by regular monitoring, the project was able to demonstrate that up to 90% of patients were risk-assessed for VTE and prescribed appropriate preventative treatment. As a result the trust exceeded the national CQUIN target for VTE quality indicators |
| Document 5: progress report for funder, 2013 | Implementation of COPD care bundles: since they began, the percentage of patients to whom the care bundle was applied increased from 15% in June 2013 to 93% in January 2014. Care bundle compliance for all components increased from 0% in June 2013 to 93% and above in September 2013. From patient surveys returned (n = 72) 90% of patients felt confident to cope at home; 97% felt that they were informed about COPD and ready for discharge; 94% felt confident about how and when to take medication; and 87% felt confident about recognising signs of their condition worsening | |
| Ashgrove | Document 7: progress report to funder, 2013 | COPD care bundle: since April 2012 and the introduction of the COPD care bundle more than 2000 patients have benefited from the new service. Since the implementation of the care bundle there have been substantial increases in referrals to pulmonary rehabilitation and smoking cessation services, and fewer home visits as well as increased satisfaction ratings for both staff and patients |
| Document 7: progress report to funder, 2013 | CKD identification tool which can identify GP practice patients at risk of CKD: it has been implemented in more than 19 PCT areas and an additional 250 GP practices, where it has identified more than 21,500 people at risk from CKD |
In addition to an increasing accumulation of direct impacts, we also heard about different sorts of impacts arising from the implementation of specific projects and from being involved in a CLAHRC. For example, respondents reported impacts on the processes of care through the implementation of particular tools, which, in the case of the illustration below, if assessment led to appropriate action, had the potential to impact on outcomes:
So it was huge . . . when we got that in [VTE assessment into documentation] I mean I did an audit when it had been in about 2 or 3 months and the . . . compliance you could see had just gone up. It’s not by any means perfectly completed, but they are risk-assessing and, you know, it’s much better.
Implementation facilitator/boundary spanner, Oakdown, R3
There were also other processual impacts on service delivery processes. For example, a care pathway to co-ordinate the physical health of people with enduring mental health problems between primary, community and inpatient services was implemented, and that had impacts on communication:
Communication had improved between GPs and the trust . . . but also communication within the trust had improved with greater numbers of referrals of patients to lifestyle services who were able to offer advice about smoking cessation and weight loss for service users.
NHS partner, Hazeldean, R2
Further, partly as a function of the closeness of relationships between a CLAHRC’s constituent services and HEIs, including joint appointment, there was also evidence that learning through a CLAHRC had an impact on curriculum development: ‘we can influence the curriculum and how the curriculum can respond more quickly to the learning from CLAHRC’ (implementation facilitator/boundary spanner, Oakdown, R3).
Additionally, there were numerous reports of changes to thinking, knowledge, skills and attitudes as a result of project-related activity. However, the gap between conceptual and direct impacts was also noted:
We did get some nice changes in attitude and knowledge using the questionnaire but . . . it was much more difficult to see what had actually changed . . . so it was more of a conceptual use of knowledge rather than the instrumental use of knowledge.
Implementation facilitator/boundary spanner, Oakdown, R2
The challenge of spreading impacts beyond the projects from which they originated and beyond the boundaries of the CLAHRC was an issue that was articulated consistently by those in leadership positions within CLAHRCs:
It has got to be about the impact and the scale of it and the spread of it so you know it is something that not just a handful of people are benefiting from because there is so many pockets of good practice and things being done well but then if you are the unfortunate person who doesn’t fit into that pocket then you don’t get the benefit and I think it has got to be the scale of it.
Management role, Hazeldean, R4
However, there were examples of particular tools developed through CLAHRCs (e.g. an online cardiac rehabilitation programme) that had proved to be popular (i.e. useful and relevant) and spread across the UK, and their translation/extension into other disease groups had been initiated. Tools such as these had been developed collaboratively and had been driven by a service-identified need.
Personal impacts
Data show that different sort of impacts were important for different stakeholders. Academics valued publications and the provision of opportunities to increase grant capture. CLAHRCs had concentrated or focused expertise and academic talent within England, which has resulted in increased activity around grant applications and awards. However, the applied nature of the CLAHRC work has caused a tension for some, particularly in relation to career framework expectations and REF 2014:
I think some of it [CLAHRC activity] is considered subscience and I think they like the fact that it is going on and I wonder if people are glad that it is happening but not them doing it . . . the so-called hard core scientists actually like to leave it to others and now I understand why, because these things, however good, and PPI and all that sort of stuff, it doesn’t impact on REF or is more difficult to impact on REF-type activities . . . I am not sure it is of hard core value in the world of academia, certainly not yet.
Academic, Ashgrove, R4
Although it was noted by participants at the interpretive forum that, in the context of the (then) forthcoming outcome of REF 2014, impact stories, for which CLAHRC activity provides a natural pipeline, may contribute to the survival of the CLAHRC concept and a shift in thinking by academics to value engagement with more applied research and its implementation as a rewarding activity.
It is clear that CLAHRCs have provided opportunities for capability building and for individuals to develop personally and professionally. Involvement in activities and projects has provided job satisfaction to those who have felt that they have contributed to making a difference, and it has given others the chance to develop their curriculum vitae, while in parallel developing implementation capability within the system:
I think importantly what it has also done for a lot of people is develop their own knowledge and skills around implementation, so my core team had varying knowledge about implementation when they started but through projects that we have done, the reading that we have done through their engagement in KU [knowledge utilisation] events . . . people have been exposed to a different environment . . . in the NHS . . . working in partnership with academics in universities that often they don’t do that, so I think they have learnt more about the process of research of the process of rigorous evaluation through that process . . . they have developed their CV [curriculum vitae] so we had people promoted through readership to personal chairs . . . through the NHS from Band 6s to Band 7s and taking on more leadership responsibility.
Leadership role, core team, Oakdown, R4
Development and personal growth impacts were very particular to those individuals who took on boundary-spanning and facilitator-type roles. However, there was also evidence from others that being involved in a CLAHRC had provided a platform for career development and an opportunity for personal profiling:
I am the director of [NHS organisation] – how did that happen?! That was a direct result of [CLAHRC]; there is absolutely no way that I would have the kind of experience I needed . . . I wouldn’t have had that experience to go to the trust board if it hadn’t have been for [CLAHRC] . . . it would have taken me another 10 years to get where I am if it hadn’t been for [CLAHRC].
NHS partner, Oakdown, R4
You know they’ve [facilitators] all . . . you know, become experts in their fields over the years, and some of them did that very quickly and were then able to transfer knowledge very quickly. I think the lady who runs the . . . post-stroke assessment . . . dare I say probably . . . at a national level known quite well as an expert in stroke . . . she would be seen probably as an opinion leader in her own right.
Academic leadership role, Hazeldean, R3
Collaboration for Leadership in Applied Health Research and Care ‘footprint’
As the above examples begin to illustrate, there were many and varying types of impacts that could be attributed to the existence of a CLAHRC. However, one issue that was discussed within the interpretive forum and was thought to be either missing or not yet articulated was the ‘footprint’ left by CLAHRC. This means the impact that CLAHRC had had on an area and the NHS as a whole, and cultural change: the ‘way we do research’ or the ‘way we do implementation’. The ability to see the footprint was potentially impeded by changes to the NHS landscape, including frequent changes in relationships and health service boundaries. However, the ability to identify the footprint might also be linked to the absence or presence of mechanisms and processes for meta-learning within and across CLAHRCs.
Summary: impacts
We observed many different types of impact from CLAHRC activity. These could be considered to be positioned on a continuum, in that direct impacts (on practice and service delivery) took time to realise and were preceded by other types of impacts, which were less instrumental, including those that were more personal to individuals engaged in CLAHRC roles. Participants stressed their desire and need to make an impact, and the funder’s monitoring focused attention on particular metrics, for example number of publications and amount of research funding. External reporting requirements fuelled an emphasis on particular types of metrics and on a need to demonstrate volume of activity. Locally generated reports also included case studies and stories of impact. The impact of the CLAHRC was an accumulation of project-level impacts rather than a demonstration of cultural change in a region or in the NHS, and therefore the imprint left by the CLAHRC footprint as a whole was still faint when we stopped collecting data.
Evaluation and learning
There was attention to both internal and external evaluation of CLAHRCs and their activity (Figure 12). Internally, there were varying levels of attention paid to evaluation through a dedicated theme of work (in two of the CLAHRCs) and to some extent (but this was patchy) embedded within individual projects. The other CLAHRC, which had not included explicit attention to evaluation (as a theme) within its original bid, reflected in early rounds of data collection that this had been an oversight and had looked to other ways of building in evaluation.
FIGURE 12.
Evaluation and learning.
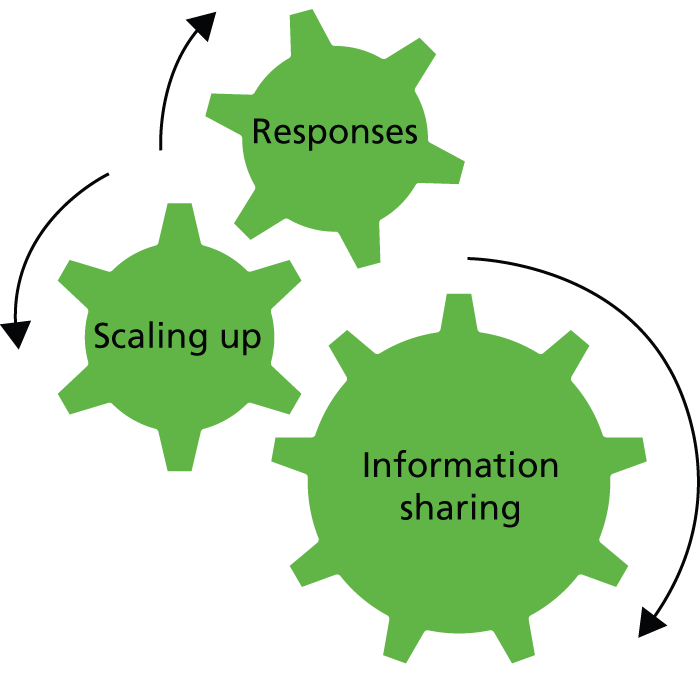
I don’t think had a good enough internal evaluation strategy . . . so I don’t feel that we have pulled all the learning we have done in a systematic a way as possible. I think looking at the individual CKD project in the CLAHRC programme, the communication across the projects could have been much, much better; it has ended up almost feeling like they are in competition to each other rather than one big implementation effort.
Leadership role, Hazeldean, R1
Information sharing
When asked to reflect on the processes and mechanisms for learning within CLAHRCs, most participants talked about sharing information between projects and themes through, for example, reports, meetings and knowledge-sharing events. However, a common perception that emerged from participants across all three CLAHRCs was that sharing of information tended to be focused on metrics, at the level of individual projects, and for the purpose of feeding into 6-monthly returns for the NIHR:
There was a process, there was some really dysfunctional research and implementation meetings but nothing got done. They tended to be focused around things like the 6-monthly NIHR reports and the annual report.
Leadership role, Hazeldean, R4
Information sharing within a CLAHRC was hindered by the structures that had been established (engineered architecture), the leadership approach and style (more or less transparent and open to critique and learning) and the communication mechanisms that had been developed and sustained. In contrast, where there were strong relationships and connections between individuals, teams and services, this created openness, which facilitated information sharing. However, most participants felt that sharing for learning within and across CLAHRCs could have been better. The prevalent reason for sharing was, as one participant put it, provision of information rather than sharing for learning by bringing challenges to the table and learning from each other. It was noted, however, that the potential to learn would require a different sort of forum from that which currently existed:
There is a difference between going to a meeting where there is an agenda, one to six different projects, and a meeting where we are beginning to think . . . about what is the same, what is different, what have we learned, is any of it generalisable, can it be used in theory. Those are different kinds of meetings. Most of the meetings have been A rather than B.
NHS partner, Ashgrove, R4
Scaling up
Given this, although there were information sharing and feedback mechanisms in place within CLAHRCs, it was unclear how this information was being used to learn or scale up from individual projects. This finding was corroborated at the interpretive forum, at which participants reflected that not formally evaluating the question ‘what have we learnt?’ was a missed opportunity. However, it was reported by CLAHRC directors that there had been some ‘organisational’ learning in CLAHRC 1 that was being taken forward in revisions to structures (fewer divisions between structures) and some processes (considering more opportunities for learning) for CLAHRC 2. Furthermore, it was felt that the externally funded evaluations were not universally helpful because in reality it had been a challenge for them to provide timely formative information, and because some of the projects had not been designed in an interactive way. These problems were not perceived positively by some CLAHRC directors.
Responses
The CLAHRCs within this study responded in different ways to different (mainly externally located) stimuli prompting changes to the way things were being done. There were considerable changes to the NHS landscape during the life cycle of CLAHRC 1; these significantly affected Hazeldean, which had set up a funding structure that was reliant on actual (rather than in-kind) resource from primary care partners. During this time, health service partners left the collaboration, withdrawing their money, which necessitated the CLAHRC’s cutting its cloth accordingly: prioritising activities with the resources they were left with and doing less. In the first 2 years of its existence, the board of Ashgrove (the body the CLAHRC was accountable to) instigated a formal external review, which in itself signalled a need and openness to receive feedback. The review team critiqued its approach, specifically the balance of activity, which was felt to be too weighted towards research and not enough towards its application, and building capacity and capability. The external review resulted in a course correction for this CLAHRC, through which it began to pay more attention to implementation:
Yes definitely, that it [implementation] had to be incorporated and I think it was a difficult concept really because we were doing clinical trials and we thought, actually you are doing this trial because you don’t know the answer, so it is difficult to think about implementation . . . but now [after the evaluation] if you are embarking on a clinical trial then we do appreciate that you have to talk to patients, you have to talk to commissioners and you have to think about implementation . . . so I think gradually you know the penny had dropped and so it has changed, will change our view over the longer term.
Management role, Ashgrove, R4
In contrast, Oakdown took an ongoing approach to reviewing its activity and approach through reflection and negotiation with internal and external stakeholders. This seemed to have insulated the CLAHRC from changes in the primary care landscape and enabled it to be responsive to partners without compromising its ongoing activity and future plans.
Summary: evaluation and learning
Learning within and across Ashgrove, Oakdown and Hazeldean was patchy, with varying levels of receptiveness and therefore varying levels of attention being given to evaluation and to structures and processes that could mediate feedback and sharing. Learning at a project level was more evident than learning from the CLAHRC as a whole; however, from our data it was not clear how project learning was being incorporated into doing things differently in the future. Equally, their potential to learn from the externally funded evaluations had been varied, with issues raised about the timing and format of the feedback provided. However, there had been different externally driven prompts in Ashgrove and Hazeldean that had necessitated review and resulted in adaption. Oakdown took a more ongoing approach to reflection and subsequent refinement. It was also evident that learning from CLAHRC 1, or the ‘pilot’, had been taken forward into proposals for CLAHRC 2.
Emerging explanation
These findings have shown how there are a number of interconnected issues that begin to explain how the CLAHRC programme might have provided the conditions and released the resources for action around knowledge mobilisation. At the outset, the vision of what a CLAHRC was, and particularly the interpretation of the funder’s brief, were fundamental to the way in which the CLAHRC as an entity was operationalised. This vision and interpretation were influenced by a number of factors including views about collaboration, implementation, knowledge and its mobilisation, and by the different approaches to leadership. Any subsequent action such as resource allocation, focusing activity and establishment of structures and processes was determined and remained set early on in the CLAHRCs’ life cycle. These provided the conditions for different stakeholders to have different motivations and potentials to engage, including opportunities for exchange, sharing and learning. Brokering, linking and bridging were facilitated by investment in individuals who took on these roles and their work was supported by the development of tools and other resources, which had the capacity to create shared meaning through collective development processes. These issues combine to result in varying levels of commitment and engagement to CLAHRCs over time, in determining their approach and progress in implementation, and in their impacts. These contingencies are unravelled in more detail in the following chapter.
Chapter 6 Context–mechanism–outcome configurations
The realist task was to draw out inferences and identify contingencies that provide theoretical explanations about CLAHRCs’ approach to implementation. This required moving from a description of the findings as provided thus far, through to explanation by identifying context (C), mechanism (M) and outcome (O) threads, which connect the domains in the evaluative framework. In this way it was possible to uncover the relationships between factors that explain CLAHRCs’ approach to implementation, and the conditions in which they operate.
This did not involve allocating themes into separate context, mechanism and outcome elements, which were then assembled into CMO configurations; rather, the analytical process in this study involved an ongoing and deliberative approach to uncover linked CMO patterns: the vital explanatory components85 that might theoretically explain how, why, for whom and with what impact(s) CLAHRCs implement research.
The first phase of analysis resulted in the emergence of an initial six conjectured hypotheses or CMO configurations (Box 6; see Rycroft-Malone et al. 39 for more detail about these CMOs including the evidence from round 1 data from which they emerged).
-
Stakeholders’ physical, cognitive and conceptual positioning at micro, meso and macro levels in a CLAHRC led to individual and group interpretations of collaborative action that resulted in variable types of implementation.
-
CLAHRCs’ governance arrangements, including both structures and processes, at micro, meso and macro levels prompt different opportunities and approaches to build relationships, including communication methods and styles, which resulted in varying types and quality of collaboration(s), and levels of engagement and commitment to CLAHRC over time.
-
The availability of dedicated resources, including additional funding for implementation, such as roles, people and opportunities, increased the potential for engagement across service and academic boundaries, which resulted in varying levels of commitment and ownership in the implementation activities and functions of a CLAHRC.
-
The CLAHRC ‘brand’ triggered opportunities for knowledge exchange, which led to the managing and sharing of knowledge to greater or lesser extents within and across CLAHRCs.
-
Different professional agendas and competing drivers prompt different motivations for engagement by stakeholders, which results in a variation of understanding and opinion about CLAHRC outcomes and goals.
-
A CLAHRC’s degree of openness to internal and external evaluation, critique and feedback prompts the potential for learning, which results in adaptation of varying types, and of varying degrees.
Over subsequent rounds of data collection and analyses these conjectured CMOs were refined and finally tested in round 4, including through the interpretive forum. In practice this involved moving backwards and forwards across the concepts and themes described in Chapters 4 and 5 as they emerged over the course of the study. The resultant CMO configurations, which have undergone varying degrees of transformation, are described below, including the underpinning rationale that explains their development and how the differences and similarities between CLAHRCs injected some explanatory power into our interpretation.
Context–mechanism–outcome configurations
Positioning and interpretation
Conceptual, cognitive and physical positioning of stakeholders at micro, meso and macro levels led to individual, group and CLAHRC interpretations of collaborative action, which resulted in setting and sustaining a particular direction of travel or path dependency, including approach to implementation.
The figuring out, mainly organically, of their specific purpose and approach to implementation was set within a broader context of the way in which the CLAHRCs had interpreted their purpose, related activity and way of working. This varied interpretation appeared to be a function of a mixture of conditions including:
-
how they had made sense of the brief, that is where they started from and their ‘cognitive positioning’
-
what they individually and collectively brought to the issue, that is their ‘conceptual positioning’
-
how constituencies and stakeholders positioned themselves geographically, that is their ‘physical positioning’.
The course or direction of the CLAHRCs appeared to be fairly fixed at the time of bid development and subsequent award of funding because their proposals became part of the contract on which they were held to account. Therefore, their starting point and where they came from on a number of issues played out in a pervasive and persistent way. That is, the contingent relationship between the context or condition of positioning and the mechanism of interpretation was one of reinforcement during CLAHRC 1.
Interpretation of the ‘brief’ created a path dependency. Given this, fulfilling a role and function around what the NIHR call described as the application of research findings (i.e. implementation) was contextualised within a broader view or position about a CLAHRC’s overall remit. Specifically, their resultant approaches to implementation were a function of:
-
how much attention was paid to implementation by CLAHRCs per se
-
their existing knowledge about implementation
-
how they had interpreted collaboration between services and academia, and whether implementation was perceived to be a more or less collaborative act.
Data show that views about collaboration varied from viewing it as a challenge and something that was not well understood – ‘the nature of the call is collaboration, that is the key word, and the nature of collaboration with the NHS is not terribly well founded in my view’ (Clinical academic, Ashgrove, R1) – to a perception that ‘the CLAHRC as a whole is a very collaborative approach and joint appointments were integrated and demonstrated . . . the synergy between the organisations’ (NHS partner, Oakdown, R4).
A CLAHRC’s decisions about the balance between research and implementation were critical to the allocation of resources (financial and human) and consequently the relative attention afforded to each area of activity. Each of the CLAHRCs in this study had traded research activity and implementation activity in a similar way and our findings show that, in response to the perceived terms of the call, greater emphasis was placed on the generation of research than its mobilisation in practice:
We have, I suppose 80% more or less for applied health research themes and one implementation theme, broadly the money’s been distributed 20% each . . . I think if I were bidding again we could certainly change that distribution.
Leadership role, CLAHRC core team, Ashgrove, R1
However, within Oakdown there was a commonly expressed aspiration that both the creation and use of knowledge in practice could be achieved through coproductive and integrated ways of working: ‘but again see it more as a shared endeavour to get more research embedded in what they are doing’ (leadership role, Oakdown, R1). Accordingly, the purpose of the CLAHRC, which incorporated its role and function for knowledge mobilisation, was conceived differently across the CLAHRCs involved in this study. There were also some honest accounts from some participants that they were being challenged by the concept of implementation and were on a journey of ‘figuring out’ the implementation function and role of their CLAHRCs’ remit: ‘we just don’t know how to do it . . . a lot of us aren’t up to speed with this [implementation] agenda’ (leadership role, Ashgrove, R1). However, fundamentally, their interpretation seemed to be dependent upon how they had interpreted the first ‘C’ of CLAHRC in combination with their experience and expertise in knowledge mobilisation.
Physical proximity was both a condition for, and a function of, their view of implementation as a collaborative act/process, for example whether the CLAHRC leadership team was situated within health services or HEI(s). Oakdown had purposively positioned its senior/core team within the health service, and the other two were based within universities, although they posted secondees and boundary spanners out to the service setting. Being physically embedded within the service setting was symbolic in the context of the raison d’être of a CLAHRC, but was also a function of a history of closer working relationships between services and higher education. Where this history did not exist, collaborative and trusting working relationships took time to establish, particularly ‘that getting to know time . . . as to how people work’ (implementation facilitator, Oakdown, R3). Building up the collaborations was further compounded by the issue of time early in the life cycle, when there was a pressure to do something: ‘The minute we got the money and got started . . . you have partners paying, in our case NHS partners, and you have got to get on and do something’ (leadership role, CLAHRC core team, Hazeldean, R1). Therefore, more established relationships catalysed collaborative contexts in a shorter time.
The different views, values, interpretations and visions came together to result in a mixed picture, with more or less implementation (i.e. explicit activity concerned with the actual use of evidence, in its broadest sense, in practice and service delivery) taking place. During the course of this study, we distilled the approaches to mobilising knowledge into the following categories:
-
service improvement, that is implementation of quality improvement methods
-
making evidence accessible, that is converting evidence/guidance into more practical products
-
implementing national and/or local guidance into practice
-
mobilising local evidence, that is sharing intelligence about local evidence of effective practice
-
implementing home grown evidence – a stated, but minimally realised, aspiration
-
paying attention to aspects of implementation in the conduct of research, from paying attention to intervention implementation in a trial to conducting research that could be described as coproduced.
As this categorisation makes evident, the different types of knowledge mobilisation could be placed on a continuum from knowledge transfer to coproduction, with the overall balance weighted towards knowledge transfer-type approaches. In Oakdown, there was evidence of historic collaboration and an aspiration for coproduction; in contrast, these conditions were less obvious in the other two CLAHRCs. However, within specific projects in Hazeldean and Ashgrove there was evidence of engagement in the absence of established partnerships. Furthermore, there were different approaches embedded and evident within these knowledge mobilisation categories, such as taking on a consultancy or supplier of services type role to the partnered health care organisations. This makes more visible the particular conceptual, cognitive and physical positioning of a CLAHRC: in this example, as something slightly removed or separate from the service, which reinforced a ‘potential disconnect between the priorities of the NHS and the work that is being done [in the CLAHRC]’ (leadership role, Ashgrove, R1).
Furthermore, conceptual positioning and theoretical fidelity should in theory be conditional upon and aligned with each other. Other than providing a focus for talking about implementation, it was difficult to uncover exactly how the theories and frameworks that CLAHRCs had signed up to were being operationalised in implementation practice and research. However, in Hazeldean and Oakdown, where they had articulated the use of particular frameworks, it was possible to see traces of their use, such that they provided a heuristic for project, group and individual activity and thinking:
Normally often within the NHS people launch straight into a project and they don’t necessarily look at barriers and enablers . . . they don’t necessarily think about evaluation or feedback loops and mechanisms. They don’t always think about the KT strategy the facilitation approach that they’re going to be using. So we’ve used the K2A cycle to help people to understand that as we’ve gone through . . . The facilitators at times have occasionally referred to PARIHS framework . . . At a very superficial level on the basis of the concepts of evidence facilitation and context to help people understand the different dimensions that we’re bringing the evidence, that we need to take account of the change of context at different levels.
Leadership role, Oakdown, R3
The interpretation of implementation within these two CLAHRCs, including their use of theory, came from greater attention to implementation within their plans, and the existence of implementation research and practice expertise within their senior teams (i.e. their cognitive and conceptual positioning).
There also appeared to be a link between a CLAHRC’s interpretation of the brief and its attention to different types of evidence. A cognitive position where there was more attention to the production of research (e.g. Ashgrove) led to (perhaps unsurprisingly) the privileging of research and less attention to other sources of evidence. In contrast, within the service improvement efforts in both Hazeldean and Oakdown and in the facilitation of guidance into practice projects in Oakdown, there were accounts of seeking and incorporating evidence from propositional and non-propositional sources of knowledge into practice and research.
The reinforcing contingency between positioning and interpretation had determined CLAHRCs’ approach to implementation, which was evident early in their life cycle. Over time it became more apparent that the CLAHRCs’ starting point in relation to their mission more generally (i.e. their view about the purpose of CLAHRC and how collaboration should operate) provided an additional explanation of why they did what they did, and why they then persisted with that direction of travel. The CMO about learning and review provides evidence of how a direction of travel could be disrupted, if not completely redirected.
Governance and connectivity
The CLAHRCs’ governance arrangements, including both structures and processes between people, places, ideology and activity, prompted different opportunities for connectivity, which affected the potential to have productive relationships and interactions for collaborative action around implementation.
The engineered, aesthetic and social architectures, including leadership approaches in CLAHRCs, provided a physical and aesthetic scaffold with which individuals, teams and organisations could potentially connect. In reality there were varying levels of connectivity within and to CLAHRCs that affected the type and quality of collaboration, and therefore how productive relationships for collaborative action around implementation were.
As a distributed model across a large geography containing many individuals, teams and health-care organisations, the way in which the CLAHRCs organised themselves became critical to their potential for collaboration and action. Their architectures provided a more or less supportive scaffold for communication, collaboration and therefore any implementation activity that was to result. The degree of fit and integration across different activities and constituencies varied, with some being more integrated and networked than others. Organising the work of the CLAHRCs within themes or strands appeared to be counterproductive to working in an integrated way because ‘it meant strands went in different directions’ (academic, Hazeldean, R1). In all three CLAHRCs the structures were not obviously connected. Organising themselves in themes also inhibited sharing information, enacting the vision for the CLAHRC and embedding PPI. However, in Oakdown, for example, where there appeared to be supplementary mechanisms for integration, accountability (i.e. reporting structure) and communication, in combination with an internal evaluation, connections between projects, activities and people were facilitated. Additionally, in Oakdown, Hazeldean and Ashgrove, the decision to resource roles such as boundary spanners and facilitators had provided opportunities for connectivity, and therefore the potential for more action around implementation.
In these contexts, boundaries of varying types were created and/or emphasised rather than bridged. Such boundaries mediated the potential for connections to be made, requiring greater effort to overcome them. Of particular note is that the structure of CLAHRCs had in some cases emphasised the professional and epistemic differences between higher education and practice because they had reinforced both the metaphorical and the physical distance between them:
There was quite a lot of siloed behaviour of that being research and that being implementation and I think that a lot of those people didn’t really budge position at the end of 5 years, so from that sense it wasn’t a roaring success.
Clinical leadership role, Hazeldean, R4
This also played out in behaviour through tribalism between groups, such that ‘if you helicoptered over this room . . . it had all the implementation theme down one end of the room in a big circle . . . and then there was one research team up one end, another two wandered in and another two somewhere else’ (leadership role, Hazeldean, R4). This feature links to the path dependency described above, in that the conceptualisation of CLAHRC had played out in features of its engineered architecture; relative closeness or distance was a feature of the operationalisation of collaboration.
Less integrated structures were overcome by creating opportunities, and therefore resources, for connections to be catalysed and for connectivity to be enacted through specific activities and project work. Opportunities that created ‘space’ for connections between services and higher education to be made, for ideas and knowledge to be shared among different communities and for cross-fertilisation and learning had resulted in some productive relationship building around specific CLAHRC activities. This led to collective action around research and/or implementation. Over time all three CLAHRCs had managed successfully to create these spaces. The added value of these activities was that they also made the CLAHRC itself visible and increased the likelihood that individuals would feel connected to it as a concept.
In contrast to CLAHRC creating or reinforcing a distance between services and academia, the CLAHRC ‘brand’ had also provided a potential catalyst for many different opportunities, including as a vehicle to stimulate exchange. The resources of the CLAHRC had prompted activities, from formal events to creating the space to enable projects and ideas to happen serendipitously. It had also provided opportunities that might otherwise not have occurred, including providing a space for testing out ideas and new ways of working before rolling them out. In this sense the CLAHRCs were perceived to be a legitimate test bed, such that, if ideas failed, the cost was accepted as part of the natural CLAHRC experiment. Furthermore, over time, the CLAHRC itself began to act as a boundary object: as something that encouraged and facilitated communication across different individuals, groups and organisations. Additionally, for some, the brand became trusted and had established a reputation and some kudos:
I think universities align themselves with the brand because it is prestigious and it gives them access to money . . . it allows universities to do their jobs.
Academic, Oakdown, R4
I think we have got a good one [CLAHRC brand] . . . When you first start out and nobody knows you and you are not quite sure what you are doing it was much more difficult . . . But once you have done things and some group has worked with you, we found it much easier to recruit practices and in fact with the CCGs we had a very good reputation.
Clinical leadership role, Hazeldean, R4
. . . it was heavily dominated by the University of [place] and that was where the kudos was going to sit.
Clinical leadership role, Hazeldean, R4
Connectivity was a response that operated variously across the layers or levels of CLAHRCs. Projects, for example, provided another potential for engagement, which may not have been mirrored at the organisational level of a CLAHRC. There were a number of examples, for example within Hazeldean, of service improvement projects having provided an opportunity to successfully engage relevant stakeholders from both health-care organisations and academia to work on relevant issues to positive effect. These effects were realised in terms of bringing about positive health benefits (e.g. in the assessment and detection of CKD) through the use of evidence, and doing so in a way that facilitated the sharing of expertise among stakeholders, and in building capacity and capability in improvement approaches. In this sense, the CLAHRC programme had catalysed collective action around particular implementation challenges by providing the space, conditions and resources for these projects to happen. The question remains how CLAHRCs then become greater than their constituent activities and projects, particularly in conditions where the CLAHRC network is less integrated and established.
The social architects of CLAHRCs were their leaders. Social architects shaped the environment that encouraged certain types of behaviour towards particular goals, which made them powerful agents within their CLAHRCs: ‘the leads very much feel they have influenced the thinking behind the CLAHRC and how that CLAHRC has evolved over time’ (leadership role, core team, Oakdown, R4). Given this, the leadership approaches and styles of CLAHRCs’ leaders were critical to creating a more or less facilitative milieu and in providing the conditions for internal and external stakeholders to engage and connect with a CLAHRC and its activity. A more centralised leadership approach, which was obvious in one CLAHRC participating in our study, led to closer and tighter networks that were more difficult for people to penetrate. This contrasted with more distributed leadership, which provided opportunities for engagement at various levels and intersections. Further, more centralised versus distributed leadership approaches were linked to descriptions of leadership style; those who were more centralised were described as command and control, or divide and rule, in contrast to those encouraging a more distributed approach, which were described as open and facilitative. These different styles provoked responses that were both practical (‘keep people in their clearly defined boxes and manage in a vertical way’) and emotional (‘I found the whole thing to be challenging’) (leadership role, core team, Hazeldean, R4). This led to variable feelings of connectivity with and within a CLAHRC, and therefore potential opportunities for collective action.
The concomitant contingency between governance and connectivity in CLAHRCs had provided opportunities for joining up people, teams and organisations working across different boundaries, disciplines and mind-sets, and in different places and spaces. More integrated structures and processes of governance provided greater resources for connectivity. Opportunities for meeting, communicating and interacting provided occasions for catalysing collaborative action on knowledge mobilisation.
Given the critical role that leadership styles, roles and approaches appeared to play in practice and in the minds of participants, leaders (at all levels in a model of distributed leadership), in their capacity as social architects, could be considered the oil that lubricated the CLAHRC system.
Resources and facilitation
Positioning and availability of resources, including funding for implementation, roles, opportunities and tools, prompted facilitation, resulting in a range of impacts including engagement, capability and capacity building, improved care processes and patient outcomes, and personal benefits.
Facilitative capacity and capability was released in the context of CLAHRCs’ position and approach to implementation, and the associated resources that were made available for this function, thus reinforcing the path dependency described in Positioning and interpretation. There was a catalytic contingency between resources and facilitation in that their interaction stimulated the potential for action and thus different types of impacts, including, in the later stages of our study, direct impacts on outcomes. In this context, the mechanism of facilitation encompassed enabling, freeing up, helping and making things easier, and had potential impact on individuals, teams and services.
Investment in formal roles was an obvious and visible investment in knowledge mobilisation in the CLAHRCs. Individuals in these jointly appointed roles served a boundary-spanning and/or facilitation-type function. Their functions related to a CLAHRC’s stance on knowledge mobilisation, including what they perceived it to be and where it was on the continuum between collaborative action around implementation and knowledge transfer. These roles were also loosely linked or aligned to the frameworks CLAHRCs had chosen to adopt and/or adapt, for example an investment in roles called ‘facilitators’ in the context of using the PARIHS framework in Hazeldean. Those in boundary-spanning roles (linking service and academia) were most evident in contexts where the balance was weighted towards research production and knowledge transfer was the dominant model of knowledge mobilisation:
I’ve been involved in an introductory training package . . . which was all around trying to develop a sort of an introduction to research and evaluation techniques for NHS staff. But also to have it led and taught by NHS staff so the idea was for it to be a sustainable thing to sort of increase research . . . to sort of build up research capacity.
Implementation facilitator/boundary spanner, Ashgrove, R3
In contrast, facilitators (those enabling implementation processes) were visible within contexts where there was more of a focus on projects and activities ‘to help facilitate that change in practice’ (leadership role, Oakdown, R2), for example in guideline/guidance implementation and service improvement projects. Clearly, these functions were not mutually exclusive – that is, those in facilitator-type roles could also act as boundary spanners. However, it was less likely that those in boundary-spanning roles were undertaking facilitation because of their defined remit in training and education in, for example, research skills and awareness.
Individuals in these roles were important ambassadors of the CLAHRCs. Through enacting the CLAHRC’s position on knowledge production and knowledge mobilisation they were the visible face of the CLAHRC and made it more tangible. This was an important function, particularly in the early days of the CLAHRCs, when there was a lack of clarity in participating communities and constituencies about what the CLAHRC was. Their ability to communicate, make connections and network across the various service and academic boundaries was critical in establishing engagement with the CLAHRC generally and in its activities (e.g. training events and projects) specifically. They did this in a variety of ways, including through ‘informal’ techniques such as coining and using appropriate language and phrases to encourage ward staff to become involved in the quality improvement initiatives, for example seeing patients’ safety as ‘everyone’s business’ (boundary spanner, Oakdown, R3).
Therefore, the personal qualities and skills were an important condition of the success of individuals in these roles being both the credible messengers and the public face of a CLAHRC. The clinical credibility of these individuals was particularly important. This had not been foreseen when the CLAHRCs were first set up, which was part of what Hazeldean and Ashgrove in particular learned. This is a further illustration of how the starting position of the clinical–academic partnerships supported by CLAHRC funding affected on the success of their plans. In contexts where the relationships were not established and required time to be developed, creating credible links to a CLAHRC, which at this point was perceived by some to be an ‘academic machine’ (NHS clinician, Ashgrove, R4), was partly dependent on people in these linking roles being able to influence others about the value of CLAHRC. For those in health-care organisations, their response to the presence and work of these individuals was enhanced by perceptions of clinical credibility, which resulted in bridging to those in health-care organisations: ‘I think the [facilitators] have done a really good job of bridging the boundaries between the university and the NHS, not perfectly, but at a relationship level, they have, I think’ (leadership role, Hazeldean, R3).
The availability and targeting of resources in, for example, implementation and improvement projects and the development of tools released facilitative potential in that they created opportunities for engagement and collaboration. The collective generation of, for example, clinically relevant tools (e.g. VTE assessment form or CKD improvement guide) resulted in the mobilisation of knowledge, which had an impact on care processes and outcomes. These tools acted as boundary objects; that is, they had the potential to facilitate communication and common understanding between individuals and/or groups.
These tools and resources developed as boundary objects because of the way in which they evolved. The transition from boundary objects in theory to boundary objects in use was a function of their collective generation, amendment and tailoring for contexts and practical use through collaborative activity. This established their catalytic properties. Collective generation provided opportunities for end-users to attach meaning and resonance to these tools, which increased the likelihood of their being valued and used. Those that did not go through such processes operated in an inhibitory rather than catalytic way. In Hazeldean and Oakdown, where there had been greater attention and commitment of resources to implementation tools, activities and facilitator roles, there was more evidence of these types of generative processes resulting in tools with catalytic properties.
Over time, positioning and availability of resources and facilitative capacity and capability led to an accumulation of impacts. This was the foundation upon which further impacts were catalysed and accrued. Accruing impacts was a function of the time needed to establish relationships, priorities and work plans and then to commence activity. There was evidence of a shift from evidence of what could be described as conceptual and processual impacts, including building capability and capacity in the system for ‘doing’ implementation, to those were more direct or instrumental: actual changes to practice and service outcomes. Actual changes to practice were particularly evident in relation to the conduct of improvement projects. Both Hazeldean and Oakdown had used this approach as part of their implementation activity, and they accumulated a number of direct impacts within the funding period. Across all three CLAHRCs, their investment in boundary-spanning type roles had resulted in personal impacts, such as career development and opportunities for building individuals’ personal profiles.
Agendas and competing drivers: motivations to engage
Stakeholder agendas and competing drivers prompted different motivations to engage, resulting in a variety of understandings about CLAHRC goals and outcomes.
The CLAHRC was an amalgam of many different individual, group and organisational stakeholders, agendas and therefore potentially competing drivers. This context triggered different motivations to engage with the CLAHRC in the first place, and on a more sustained basis. This was evident across all three CLAHRCs and in the different motivations between stakeholder groups (e.g. practitioners and academics). These motivations were made visible through the views and opinions of stakeholders about the purpose of CLAHRCs, whom they were serving and what their expected outcomes would be. One manifestation of the mechanism of motivation was how ‘what’s in it for me’ was enacted through the incentives and rewards that were perceived to be available through engagement in a CLAHRC’s activities. Sustaining a CLAHRC may therefore be a function of how successfully they worked with different agendas, drivers and motivations while realising planned goals, in parallel to being responsive to issues that arose through continued interaction.
The service–academic divide had played out in a number of ways in the CLAHRCs that we studied and was foundational at the stage of bid development. This division was evident in the different reasoning of people and their motivations to engage, particularly where the CLAHRC was perceived as something separate. This separateness had created different degrees of belonging or buy-in to it as a concept and therefore as something people should or would want to engage with. The sceptics were mainly those working within health-care organisations, because they perceived the CLAHRC to be dominated by an academic agenda:
It was clear from the trusts that they were . . . a bit frustrated in what CLAHRC was doing in that it just seemed to have a pre-set agenda, a research agenda that it was pursuing . . . they had been expecting something significantly different from the CLAHRC . . . so they were a bit frustrated . . . they didn’t have a great deal of enthusiasm.
Leadership role, CLAHRC core team, Ashgrove, R1
This view was perpetuated by those researchers within CLAHRCs who, because they perceived they would be unable to conduct research that would be of an appropriate academic standard, did not show an interest in the implementation or more service-orientated agenda:
I don’t think it worked from a REF perspective . . . I would be interested to know how many people who have been involved in CLAHRC have been producing international-style papers with T2-style research.
Academic, Ashgrove, R4
These different agendas were evident in the discourse and behaviour of stakeholders because there was a lack of a shared value base, language and understanding. Where they (CLAHRCs and individuals within CLAHRCs) positioned themselves (conceptually and cognitively) fundamentally affected their level of engagement and therefore what they expected to get out of it:
it will be seen as an external organisation . . . It won’t be ‘this is an organisation we are part of’, it won’t be ‘this is a club I am part of’, it will be ‘this is an organisation I am aware of who does things for us because we give them money’.
Leadership role, Ashgrove, R4
Therefore, there were questions about what the CLAHRC is, and who ‘belongs’ to it, which did provoke some strong feelings and reactions. These issues also related to the conception of CLAHRC as a distributed model for the conduct and application of health research across a health community, and how its architecture and branding was managed to facilitate connectivity and potential engagement. In contexts where there was no history of collaboration, where there had been less activity around jointly setting priorities either at the bid development stage (e.g. Ashgrove) or through ongoing prioritisation mechanisms (e.g. Ashgrove and Hazeldean), the need to sell the benefits of CLAHRC to encourage or incentivise engagement was evident.
Tapping into the different motivations of stakeholders was a particularly useful mechanism; for example, selling the message to health-care organisations that ‘this is what we [the CLAHRC] can do for you to help you meet your CQUINs targets or your service improvement challenges’ (leadership role, CLAHRC core team, Oakdown, R4) did incentivise engagement. However, motivations were different between constituencies. For example, some academics did not engage because they believed there would be no benefits to them in terms of the requirements for the REF. However, others valued the opportunity to engage more closely with practice and practitioners, and take advantage of the roles and opportunities that were afforded by the additional resource of the CLAHRCs.
These findings provide further explanation of what we observed to be involvement along a co-operation to collaboration continuum, highlighting that stakeholders will have different agendas and therefore different motivations (‘what’s in it for me’), which need to be accessed if engagement is going to be both meaningful and sustained. This included the motivation to work across CLAHRCs, which was eroded by the call for CLAHRC 2, which set up an agenda of competition and resulted in a gradual withdrawal from each other:
Going into the second round of funding applications there was an organisational decision that we wouldn’t share very much about what we had learned and what we were doing and what we were planning . . . we were in a competitive environment . . . I think it potentially had a negative effect on the national programme as a whole . . . it wasn’t an environment that was very conducive to collaboration and sharing, it was more an environment which was very competitive.
Leadership role, Oakdown, R4
Fundamentally, these findings show that any exchange, including engagement, needs to result in mutual benefit because this acts as a reinforcing loop.
The mainly professional (whether that be related to academia or practice) agenda as a context for motivating engagement was particularly evident in CLAHRCs’ approach to PPI, which had been poorly conceptualised and therefore challenging to operationalise within the three CLAHRCs in this study. PPI in research and PPI in implementation had been conflated. Honest accounts were provided of the challenges in knowing how to engage patients and the public in their implementation activity: ‘we were a bit off the mark, I would say . . . we are stronger in research than implementation in PPI’ (academic, Oakdown, R4). These accounts showed that PPI tended to be conceived as an add-on rather than an embedded activity, and therefore it was operationalised on a project-by-project basis rather than by the CLAHRC as a whole. As a result, and despite representation of service users at a strategic level, PPI remained a mainly professionally led agenda. This was evident, for example, in academics making choices about what sort of projects would be appropriate to engage patients and the public in, the sort of aspects within projects that would benefit from their input and how that input would be made. In this context, PPI appeared to focus on surfacing the patient experience, focusing particularly on information resources for patients and the public, and was seen as the ‘right thing to do’.
Although this was not represented within our partner CLAHRCs, testing out our findings with a CLAHRC that had an early strategic intent around PPI, including dedicated funding, showed more activism and potential success around PPI. Where there was a history of leadership and progress with public engagement around health, it was possible to adopt a more bottom-up approach that linked PPI across knowledge production cycles and aimed to increase capacity and capability for engagement in implementation. While there was a consensus about the importance of PPI and a view that it was ‘work in progress’, the approach that had been taken related back to the positioning of PPI in the original plans (e.g. strategic intent and resource allocation) and therefore to the interpretation of the brief, which links naturally to how stakeholders’ agendas also played out.
Receptiveness to evaluation and learning: review and reflection
A CLAHRC’s receptiveness to evaluation and learning led to review and reflection, which resulted in adaption and refinement.
The openness of a CLAHRC’s mind-set and engineered structures (how connected its structures and processes were) to internal and external evaluation and learning prompted the potential for review and reflection, which over time resulted in thinking about and doing things differently. There had been a number of opportunities, occasions and events that had required (e.g. external evaluation), and in some cases forced (e.g. change to funding environment), CLAHRCs to make a response, in contrast to taking an ongoing approach to review, reflection and negotiation. Across all CLAHRCs there was a sense of learning over time and learning by doing, particularly as the funding for CLAHRC 2 was announced and they reflected on what they might learn from, and do differently in a new funding proposal for a refreshed entity.
Their capacity for learning and evaluation was mediated by the importance they attached to it and therefore the attention they gave it. The relative focus on evaluation and learning was a function of:
-
the leadership approach (i.e. openness to critique and learning)
-
the way that they had organised themselves (i.e. themes without communication mechanisms impeded connections and information sharing)
-
the type of evaluation and review information that was valued and therefore collected (i.e. the data that could incentivise review and reflection).
Relationships and connections, which were facilitated or impeded through a CLAHRC’s social and engineered architectures, created the potential for information sharing, but not necessarily learning from information collected and/or shared. While all CLAHRCs had to collect metrics about their progress and achievements for the funder (e.g. grant income, papers published, examples of impact), this had been potentially restrictive and resulted in less attention to process and other types of impact:
but NIHR are one of the stakeholders . . . who put a particular performance management framework on what you do . . . you have to make a decision . . . whether you allow that to drive the design of your CLAHRC, which is what we did . . . I don’t really think, if CLAHRCs are going to achieve what they need to achieve with their partners, you can do that.
Leadership role, Hazeldean, R4
The original direction of travel of two CLAHRCs had been disrupted by events and had prompted a response. For example, the course correction taken by one CLAHRC following an external review demonstrated that openness to evaluation could result in adaptation by reallocation of both resources and attention to (implementation) functions. Another CLAHRC had to cut its cloth through having to review its programme of activities in the context of a reduction in resources, which resulted in radically adapting its original plans. However, there were also examples of CLAHRCs reflecting internally on how they might do things better or differently, particularly the way that they had structured and organised their activities.
There was also some reflection on, and acknowledgement of, their challenges with PPI (as findings show, PPI in research was conflated with PPI in implementation), with some additional activity to figure out how this might be approached differently. However, these efforts did not result in changes that were progressive and meaningful. Additionally, any fundamental changes to their activities and structures seemed to be thwarted by a lack of receptiveness to revising plans partway through the funding cycle within the performance framework that had already been set.
Structures and processes to facilitate review and learning within the various layers and components of CLAHRC were absent: ‘I don’t know that we’ve done enough on evaluating the whole approach’ (leadership role, Hazeldean, R4). This impeded the potential for demonstrating how a CLAHRC was something greater than the sum of its parts, that is a set of activities, projects and roles. The potential for meta-learning by scaling up within and across CLAHRCs was not realised and therefore the footprint left by them was not yet clearly visible.
Structures, positions and resource alignment: release of potential for collective action
Where structures, positions and resources are aligned, this releases the potential for, and unlocks barriers to, purposeful collective action for implementation, the successful delivery of projects and positive impacts on processes and outcomes.
In contexts where there was greater alignment between structures, including the way that the CLAHRC had organised its implementation activity, allocation of appropriate resources including people and expertise in implementation, and their positioning about knowledge mobilisation, greater potential for collective action was released and cognitive and practical barriers were more likely to be overcome. This resulted in positive impacts on processes and outcomes through the successful delivery of projects.
This CMO configuration relates to the need for things to come together to provide the conditions for a more successful outcome to be achieved. Successful outcomes – particularly direct impacts on patient outcomes – were a result of the accrued benefits of things coming together or lining up in a way that increased the effect. This particular explanation for successful project outcomes emerged over time, which highlights how temporality (once again) influences the development of collective action around implementation within collaborative entities, and therefore the realisation of any potential impacts.
The broader context of CLAHRCs determined the specific or more local conditions of the projects nested in them. It is clear from our findings that a number of factors, both tangible and less concrete, came together to create the environment and milieu which catalysed and fuelled the delivery of projects. Specifically, the alignment of vision, values, goals and purpose around both the nature of collaboration and knowledge mobilisation led to more impactful project work because this synergy released opportunities and resources, including social, financial and intellectual capital. Any synergy realised was as a result of a CLAHRC’s starting point (its positioning and therefore interpretation of the brief), its leadership, and its structures and processes, including potential for ongoing reflection and learning. Leadership structures and approaches were particularly critical to enabling alignment: ‘distributed so that is not only directive but shaped by principles . . . You know, there is some co-ordination, cohesion but it’s usually around the way we do things’ (academic lead, Oakdown, R4). Structures and processes which were more integrated between health-care organisations and HEIs, and less centralised within a CLAHRC, together with facilitative leadership, including the development and articulation of a shared vision, added to a facilitative context. Aligning understanding and expertise in implementation with the allocation of appropriate resources had an additive effect, enabling things to happen.
Potential was released in various ways including unblocking channels of communication, overcoming boundaries, providing space (cognitive and physical) and opportunities, adding legitimacy and enabling connectivity. Evidence of this release in potential was observed at project level through implementation projects and improvement initiatives, for example in Oakdown and Hazeldean, which had led successfully to an impact on patient outcomes and care processes. The greater the alignment between features and factors, the greater potential these projects had for successful outcomes. However, we also observed that some projects succeeded in the absence of alignment at a higher level within a CLAHRC, for example where the structure of a CLAHRC was perceived to inhibit collaboration and where leadership was centralised. Therefore, the success of projects at a local level was not always and consistently reliant on complete alignment. Successful outcomes from collective action reinforced synergy.
Summary
The final set of CMO configurations, which were developed, refined and tested over the four rounds of data collection, are summarised in Box 7.
Conceptual, cognitive and physical positioning of stakeholders at micro, meso and macro levels led to individual, group and CLAHRC interpretations of collaborative action, which resulted in setting and sustaining a particular direction of travel or path dependency, including approach to implementation.
CLAHRCs’ governance arrangements, including both structures and processes between people, places, ideology and activity, prompted different opportunities for connectivity, which affected the potential for productive relationships and interactions for collaborative action around implementation.
Positioning and availability of resources, including funding for implementation, roles, opportunities and tools, prompted facilitation, resulting in a range of impacts including engagement, capability and capacity building, improved care processes and patient outcomes, and personal benefits.
Stakeholder agendas and competing drivers prompted different motivations to engage, resulting in a variety of understandings about CLAHRC goals and outcomes.
A CLAHRC’s receptiveness to evaluation and learning led to review and reflection, which resulted in adaption and refinement.
Where structures, positions and resources are aligned, this releases the potential for, and unlocks barriers to, purposeful collective action for implementation, the successful delivery of projects and positive impacts on processes and outcomes.
The relationship these CMOs have to each other and in creating the potential for collective action on knowledge mobilisation is represented in Figure 13. This figure also demonstrates development and movement from the conceptual map or framework that we presented at the start of the project (see Figure 4) in that it begins to highlight some contingencies between the elements of the CMOs. This figure shows a path dependency, which starts with the position of stakeholders on key issues on collaboration, knowledge and implementation. These positions influence how knowledge mobilisation within the context of collaboration is both organised and operationalised. The degree of alignment between these positions and features determine outcomes. It is hypothesised that greater alignment leads to impacts that are more relevant and timely for stakeholders and services. The development and progress of implementation through collective action will be influenced by the collaboration’s approach to evaluation and learning and their response to any signals or events.
FIGURE 13.
Representation of contingencies between CMO configurations. –ve, negative; +ve, positive.
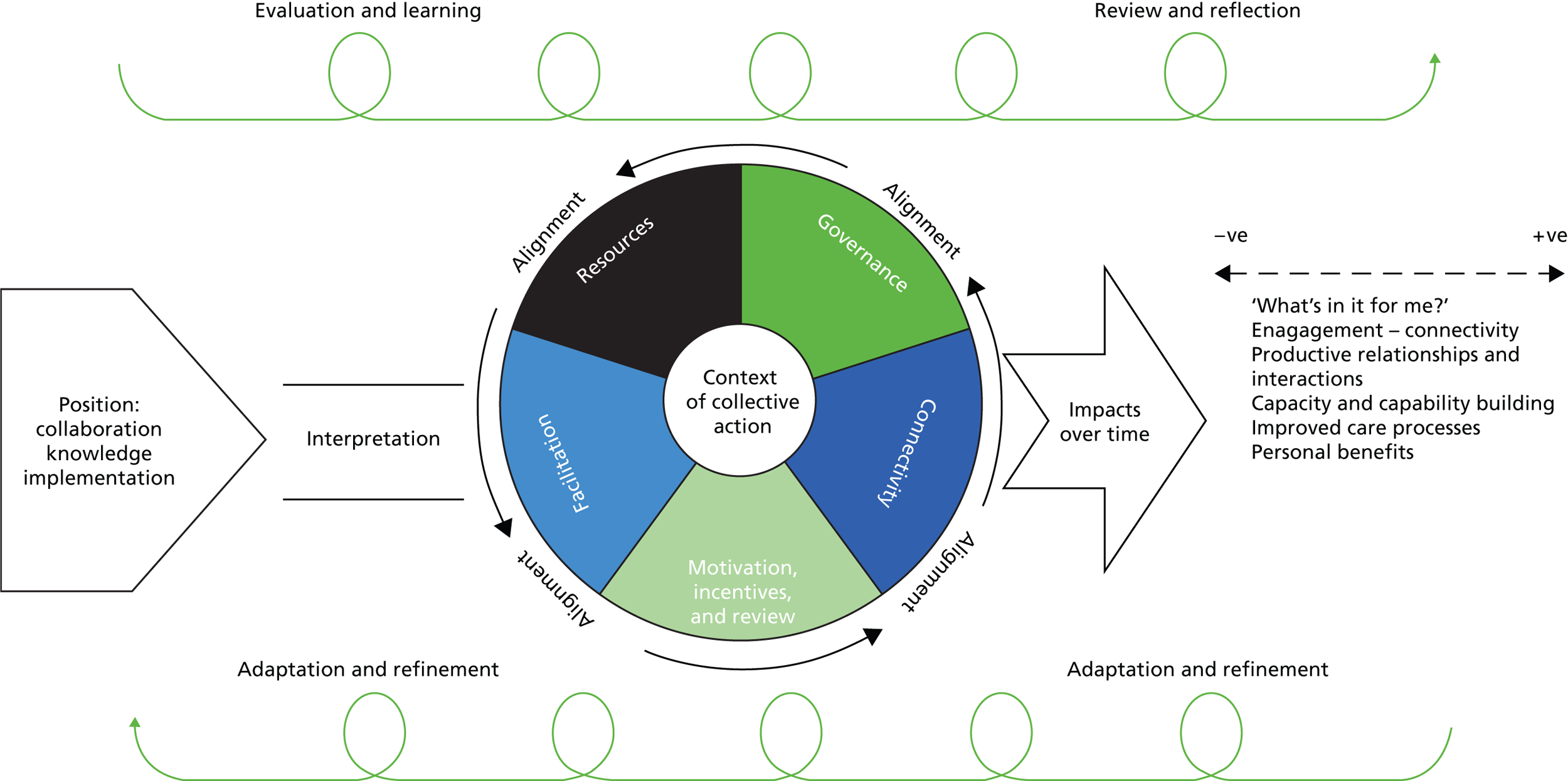
Chapter 7 Discussion, conclusions and implications
Introduction
In this chapter we summarise some key issues that are fundamentally important to the processes and outcomes for promoting implementation within collaboration. Our findings reinforce a growing body of evidence that draws attention to the complexities surrounding the mobilisation and use of knowledge in practice. To date, however, the majority of research conducted within a health-care context that comes to this conclusion has been as a result of studying implementation within one-off projects, such as the implementation of a guideline into practice. Although there are some exceptions to this (e.g. Dopson and Fitzgerald,111 Crammer et al. ,112 Stetler et al. 113), we know little about how and/or why implementation might take place within more sustained interactions such as organisational partnerships and collaborations like CLAHRCs. While reinforcing some aspects of the existing evidence base, such as that implementation is multifaceted and context is important, our findings also provide a more detailed narrative about the nature and pattern of interactions. We also provide a more nuanced understanding about context and a temporal account of how patterns of action and interaction can be formed and influenced, including an explanation of the potential for CLAHRCs and CLAHRC-like models to close the metaphorical gap between research and practice. We summarise how our findings address the objectives we sought to address at the start of the evaluation in the context of some wider literature and before a further specification of the emerging programme theory. We end the chapter with some implications for implementation practice and research.
Revisiting the research objectives
In the following sections we summarise how our findings meet the objectives we set out to address.
To identify and track the implementation mechanisms and processes used by Collaborations for Leadership in Applied Health Research and Care and evaluate intended and unintended consequences (impacts) over time
Undertaking a longitudinal study meant we were able to successfully track the journey of three CLAHRCs over time, including identifying their strategies and approaches to implementation. Being able to study CLAHRCs over time led us to identify the potential of a life cycle or ecology of implementation as they evolved and developed. The temporal thread was evident in their evolution, and in one site more of a revolution, around the implementation agenda. The life cycle of the CLAHRC, and more fundamentally the stage of development of the collaboration itself, provided the conditions for collective action around knowledge mobilisation. Individuals, groups and therefore the CLAHRCs went through a process of sense making. Over time, through engagement and reflection on events, meaning and understandings about CLAHRCs were constructed. In contrast to previous conceptualisations, this sense making did not necessarily result in a consensus about a shared identity or cohesiveness114,115 CLAHRCs were not born within a vacuum, and our findings indicate that CLAHRC-like entities need time to learn and develop,51 particularly in the absence of history50,116 or any pre-formative work. 16,54,73
Their ongoing formation and development, rather than reflecting the stages and phases that others have proposed (e.g. Centers for Disease Control and Prevention117), was more iterative and dynamic. Furthermore, their evolution was influenced by factors that were sometimes not in their sphere of control (e.g. changes to NHS structures and funding arrangements). Their response to such events was a function of their perspective on, and approach to, evaluation and learning, and their perceived capacity to adapt and adjust. More reflection and potential learning could result in greater potential to evolve within a shorter time frame. The 5-year funding period was both enabling (need to get on and do something) and constraining (direct impacts were difficult to realise).
The ebb and flow of the CLAHRC’s life cycle points to the notion of an ecology of implementation. Collaborations as well as implementation projects have lifespans in that they are conceived, live and potentially degenerate and/or transform in response to their particular conditions of existence. The complex relationships and interactions between actors (‘organisms’ in ecological terms) and their environments (including territories) create the dynamic in which both collaboration and implementation evolve.
As reported, a CLAHRC’s specific attention to implementation was in some part shrouded by its focus on fulfilling the remit around the conduct of applied health research. However, as described, we identified a number of different types of knowledge mobilisation operating within CLAHRCs. Overall, however, implementing home-grown research within the initial 5-year funding period remained an unattained aspiration. The predominant focus and most common mechanism for mobilising knowledge were through the use of boundary spanners. These individuals had varied functions, from training, sharing knowledge and linking people and groups together, to engaging in the facilitation of ‘evidence into practice’ activities and projects.
Perhaps unsurprisingly, given what is already known about the gap between implementation activity and direct impact on practice and policy, the direct impacts from CLAHRCs’ activity were slow to be realised. Service improvement activities appeared to be having an impact on service delivery, which was translating into patient outcomes (e.g. early detection). Additionally, we observed a number of different types of other effects of project-related activity, including perceived changes to thinking, knowledge, skills, attitudes and practice, and impacts on the personal and professional development of those involved in CLAHRCs, particularly those in boundary-spanning functions. Scaling up project-related impacts into an effect that was demonstrative of a CLAHRC’s ‘footprint’ was difficult for us to detect and for those in CLAHRCs to articulate. An unexpected consequence we observed was the tension and rivalry within a CLAHRC (e.g. internal competition for resources) and across the interface between CLAHRCs, which was made visible as speculation mounted about the potential of funding for CLAHRC 2. This element of competition resulted in reluctance to share and reduced communication: features that are the antithesis of collaboration.
To determine what influences whether or not and how research is used through Collaborations for Leadership in Applied Health Research and Care, paying particular attention to contextual factors
Our investigation was focused on how context influenced whether or not research was used in CLAHRCs. Specifically, realist inquiry focuses the investigator’s attention on context as a condition rather than a backdrop for action. In this way we were able to gain a detailed understanding and develop an explanation of how particular conditions in the contexts of CLAHRCs affected fulfilling the programme’s remit around the application of research.
Collaboration was expected to provide both the structure and the opportunity for developing a shared space or spaces in and around which knowledge mobilisation could occur. Sharing of both physical space(s) and cognitive space(s) was realised by the three CLAHRCs in this study to varying extents. Approaches to coproduction118 and engaged scholarship26 emphasise a positive link between stakeholder engagement and the production and implementation of knowledge. However, achieving genuinely shared space requires the blurring of epistemological, role and practical boundaries and therefore the relinquishing of power and influence held by individuals, teams and organisations, which is notoriously challenging. 119 As Orr and Bennett point out, politics and other ‘tricky issues’ arise from ‘co-producing research involving cooperative interactions between members of two communities that have distinct interests, expectations and priorities’. 120
Preceding conditions influenced the subsequent course and journey of the CLAHRCs. This included where they started from in their relationships with partners, including the presence or absence of a history of working together. These conditions determined how long it took to engage in meaningful collective action around implementation. Their interpretation of the brief in relation to the specific expectations about knowledge mobilisation in the context of conducting more applied research and building capacity and capability (the vision) played out in the way they engineered their structures and processes and in how resources were allocated.
The context of action was critical in that there was an interconnection and interaction of enabling and restraining forces that interlocked and had an impact on how each CLAHRC delivered on its implementation function. These interactions not only included actors but extended to interactions between the actors and context. Negotiation and renegotiation of a shared space in the development of genuine and collaborative action was explained by multiple contexts including:
-
temporal (historical, longitudinal and living history of relationships and working together)
-
cognitive (collective and individual differences and similarities about notions of collaboration, evidence, knowledge and implementation)
-
emotional (thoughts and feelings of individuals and the collective – what people thought about the CLAHRC, how they enacted ‘what’s in it for me’)
-
professional (epistemic, professional)
-
physical (structures and processes, geography).
These contexts then acted and reacted so that they became more than a backdrop to action but coalesced to create the conditions and contingencies that explain relationships, activity and subsequent outcomes.
Governance arrangements were a condition or context that linked to different opportunities for connectivity and engagement. Collaborations that pay attention to structures, infrastructures and management are those that have the potential to facilitate the success of centres and people working together. 50,69,70 Additionally we found that distribution and use of resources, including financial as well as social and intellectual capital, was a precursor to a CLAHRC’s attention to implementation. A collaboration’s engineered social and aesthetic architectures provided both a tangible (e.g. organisation of activity/projects, resource management) and a less tangible (e.g. clarity around decision-making, buy-in and belonging) collaborative scaffold for aligning strategy, people and activity.
Given that CLAHRCs are networks of stakeholders, governance arrangements that facilitate connectedness and connectivity, particularly through face-to-face interaction, provided greater scope for creativity and for sustainable activity around implementation. This includes a network of actors who are systematically arranged and managed to pursue a set of activities under a collective goal around implementation. Therefore the flexibility of these arrangements and how they operate across all levels of the collaboration – from the project(s) to the ‘organisation’ or network as a whole – will help explain a collaboration’s ability to ensure appropriately resourced activity and the capacity to respond to wider issues and pressures as they arise. It has been suggested that an organisation’s ambidexterity, that is its ability to be aligned and adapt to demands, has been found to be a prerequisite of organisational survival and success,121 and arguably for its resilience too. The way in which concepts such as these might transfer to a ‘constellation of interconnected practices’122 such as CLAHRCs, is in their potential to explain how these networks evolve and then sustain themselves (or not). Walter et al. 123 observed that sustainable partnerships provide the conditions that allow researchers to better support users to test and implement research findings and encourage collaborative reflection beyond the knowledge production process and on to research use processes.
Leadership (designated and distributed style and approach) were a critical part of a CLAHRC’s governance arrangements and therefore vital to establishing the collaboration, and to determining and then enacting a vision around implementation. Research shows that a blend and alignment of designated leadership with distributed leadership has been shown to provide a necessary condition and mechanism for collective action around implementation. 16,113 It has been suggested that leadership within collaboration is concerned with making things happen – specifically, the formulation of the collaboration’s plan/policy and activity agenda. 76 The importance of leadership for successful change, innovation and implementation is reflected in existing theory and frameworks (e.g. Pettigrew and Whipp,124 Greenhalgh et al. ,16 Rycroft-Malone et al. 15) and was reinforced in this study.
As we observed, leaders contributed to shaping the context of collaboration through structure and agency. 125 A number of principles have been identified that include facilitating interorganisational collaboration demands of leaders, including inspiring commitment and action, leading as a peer problem solver, building broad-based involvement, and sustaining hope and participation. 126 Additionally, leaders need to attend to their personal style and approach, as the practice of leadership for collaboration demands power-sharing, practice-based leadership, systems thinking and being ‘managers of meaning’. 125 This resonates with our findings. In a context where there was more aligning of vision, structures, processes, people and resources through credible, authentic and embedded leadership, the collaboration seemed to be more robust, and there was a greater focus on collective action around implementation. Leadership roles, style and approach are the ‘oil’ that lubricates the system. Furthermore, a life-cycle view of collaboration, including the idea of ecology of implementation, suggests the need for regular renegotiation (e.g. arrangements, relationships, agreements) requiring a flexible approach that is tactical and strategic, and contextually situated.
The potential success of collective action in implementation appears to be at least in part a function of an alignment in organisational structures, processes and the reasoning of those in the collaboration. As Jagosh et al. 127 remind us, collaborations are not de facto synergistic but their success is predicated on some effort to align values, goals and purpose. More successful and impactful attempts at collective action in implementation were determined by the alignment of a number of features, including foundational relationships, vision, values, structures and processes (including the potential for greater learning and meta-learning), purpose and thoughts about the nature of the collaboration and knowledge mobilisation (including theory and approaches). Strategically and structurally the potential for alignment was vested in the leaders of the collaborations, and within projects and activities this was entrusted to individuals in boundary-spanning roles. Therefore the presence of both designated and distributed leadership at all levels appears to be important for alignment. Furthermore, Best et al. 25 suggest that large-system transformation in health care is enabled through alignment between top leadership and distributed leadership because this can reduce cognitive dissonance and facilitate integration between intraorganisational boundaries. Given this, it could be hypothesised that knowledge mobilisation within a collaborative context could be enhanced by creating opportunities for alignment across all the levels and corners of the collaboration in ways that facilitate synergy between structure and agency.
Within an ecological view of implementation, synergy has the potential to develop and build over time where successful outcomes from collaborative knowledge mobilisation activity provide reinforcement. Additionally, alignment has the potential to develop over time where there is attention to learning and evaluation with appropriate adaptation. 127 However, it is unclear if some degree of misalignment or tension within the implementation ‘system’ could potentially act as a form of catalyst for action, which could minimise the potential for entrenchment, habitual thinking and behaviour. 128 It is conceivable, for example, that alignment may stop being a catalytic mechanism if consensus and groupthink develop. Creating opportunities for renewal and refreshment through reflection, evaluation and learning may militate against potential stability versus stagnation.
To investigate the role played by boundary objects in the success or failure of research implementation through Collaborations for Leadership in Applied Health Research and Care
The CLAHRC model was predicated on an assumption that providing resources and an architecture would enable the research and practice community to work more closely together – to close the metaphorical ‘know–do’ gap. Within this networked model of collaboration we observed both the creation and blurring of boundaries. The CLAHRCs’ architectures and different perspectives and positions resulted in the construction of a number of different types of boundaries, including:
-
organisational, between different organisations and divisions/departments within institutions
-
epistemic, between the different philosophical perspectives about knowledge and its mobilisation
-
semantic, between people and groups because of different understandings about meaning and language
-
professional, between different groups in different contexts
-
geographical, as a result of the physical geography of the CLAHRC, the CLAHRC network and NHS geography.
Collaborations for Leadership in Applied Health Research and Care have been described as an example of an institutionalised ‘constellation of interconnected practices’. 129 They comprise numerous boundaries and therefore territories that need to be negotiated and/or bridged if meaningful action is to take place. Furthermore, demarcated boundaries between the ‘worlds’ of researchers and practitioners, each with their different epistemic cultures, can result in communication challenges and tensions. Co-ordinating and sharing knowledge across boundaries have converged around three primary perspectives,130,131 which also resonate with our findings: information processing – knowledge is viewed as objective and therefore needs to be codified, stored and retrieved across people and contexts; cultural – knowledge is embedded within members of the community and therefore shared through creating a shared language and negotiated through the use of boundary objects and/or through boundary spanners; and political – knowledge is rooted in the accumulated know-how of the community and shared through the use of different types of shared communicative devices. Where boundaries were blurred and knowledge sharing and/or implementation occurred this was as a result of the creation of boundary objects and through the agency of those in boundary-spanning roles, including facilitators.
Van de Ven and Johnson132 describe ‘Arbitrage, dialectical inquiry and constructive conflict management among researchers and practitioners’ as central to engaged scholarship. These processes require active management and skilled facilitation, and therefore investment in a network of actors across the collaboration as linking and bridging agents. If people in boundary-spanning and facilitator roles share an understanding of both collaboration and implementation, they have the potential to manage activity, enable interactions, develop shared spaces and negotiate tensions and conflict. Tools to include in their armoury include their skills, credibility and opportunities to collectively develop ‘artefacts’ that have the potential to become boundary objects, to which people in different territories and across various boundaries can attach meaning, resonance and value. We found that what activated boundary objects in theory to be realised as a boundary objects in use was related to how they evolved. Those objects that transformed from objects in theory to objects in use are similar in terms of their collective generation. The creation of, for example, different practice tools through meaningful collaboration provided an opportunity for different stakeholders to come together and engage in a process that involved integrating local evidence and experience with external evidence from guidance. The process of collective design made the artefacts meaningful to different stakeholders in different groups and increased their potential to be used in practice. Therefore, it could be predicted that the potential of boundary objects to mobilise knowledge would be enhanced if developed in contexts in which there is good-quality collaboration, with planned opportunities for joint creation and design among stakeholders.
To determine if and how Collaborations for Leadership in Applied Health Research and Care develop and sustain interactions and communities of practice
The potential of the CLAHRC context to create opportunities to develop and sustain interactions and communities of practice was fulfilled to varying extents. Communities of practice can analyse practice and solve practice-related problems and encourage mutual learning and the sharing of knowledge. Given this, CLAHRCs had created opportunities for groups and teams to come together for sharing knowledge and expertise, but to a lesser extent for learning. Interactions were facilitated through opportunities to engage in specific projects and by those in boundary-spanning roles who were perceived to be credible and helpful. However, their potential was mediated by some role confusion and by the context in which they were operating. In this way, project communities were created and sustained for the life of the project. We do not know whether or not these interactions will be sustained beyond the life of projects and the initial CLAHRC funding period.
Engagement of stakeholders was contingent upon incentives, benefits and/or rewards individuals and organisations perceived they would reap from CLAHRCs. Therefore, the levers or motivations for engagement varied over time so the success of implementation activity within a shared space was also mixed. Different theoretical perspectives from organisational theory help explain potential motivations, which include, for example, learning and communities of practice. 133
The notion that communities of practice would work together on ‘something’ is a central element of much of the literature. 134,135 However, developing a shared understanding of what that ‘something’ is not a one-off event or exercise; it takes time to develop and involves ongoing negotiation and renegotiation with participating organisations and individuals. 70,76 Working on a shared endeavour helps to build group identity and integrate individuals while still allowing them to retain their identity and links with their organisation of origin. 136 It is the interaction of individuals and active collaboration137 that creates group identity as individuals create meaning through sense making. 138 Within the current study we observed this happening to some extent through specific projects, such as those that employed more interactive methods, for example improvement projects. This supports the idea that the topic or subject area around which a collaboration is focused is also important for its success. 51,72
However, the mediating issues of power and, particularly, competition are neglected in the communities-of-practice literature. The motivation to engage in these shared endeavours may build over time as trust is developed through the development of relationships and ties, which may turn into reciprocity. The need to navigate different types of boundaries, including the geographical boundaries that precluded colocation and close proximity between individuals and groups, limited the potential for interaction and therefore the development of communities of practice. Equally, fundamental epistemic differences between groups were difficult to resolve and were challenged by different motivations to engage in joint enterprise and by differentials in power and authority.
Many of the discussions about interaction and engagement make the assumption that members are getting (or perceive they will get) something from being involved in a community of practice. Further, individuals and organisations may be motivated to engage in collaborative activities that minimise transaction and maximise opportunity costs. Therefore, if researchers and practitioners are going to work together productively over time there needs to be recognition of scope for bidirectionality in benefits and rewards, which need to be made visible for individuals as well as organisations.
Sustaining interactions and communities of practice is, at least in part, likely to be related to the capacity of a collaboration to pay attention to evaluation and learning in an ongoing way. Our findings show that there was evidence of within-project evaluation (and potential learning), but structures and processes that paid attention to systematic evaluation and learning at a higher level and between CLAHRCs was absent. Organisational learning theories suggest that the ability of an organisation to learn is a characteristic of an adaptive organisation, that is one that picks up signals from its internal and external environment and adapts accordingly. 139 The ability to pick up signals requires deliberate attention to the establishment of feedback loops in which evaluation that blends hard and soft metrics at different levels of the system could both incentivise and reward engagement and activity.
Collaborations for Leadership in Applied Health Research and Care were created to catalyse a step change in the conduct and application of high-quality research in the English NHS within regional contexts and health priorities. Their ability to engineer this could be enhanced by greater attention to systems and processes that accumulate and use (reflect on and adapt appropriately) the knowledge from the experience of individuals, teams and organisations that are part of their distributed network. While there was some evidence of this, their own reflections provided an honest account of how they could have ‘done this better’ (leadership role, CLAHRC core team, Oakdown, interpretive forum), particularly in relation to how CLAHRCs could have combined and learned from a collective intelligence. At this stage, therefore, it is difficult to describe how CLAHRCs were greater than the sum of their parts (i.e. projects, activities and people).
It could be hypothesised that implementation within collaboration may be enhanced if a continuous improvement approach to the collaboration and its component activities is adopted. Paying greater attention to both the structures and mechanisms for ongoing reflection and learning would also increase the potential for meta-learning.
To identify indicators that could be used for further evaluations of the sustainability of Collaboration for Leadership in Applied Health Research and Care-like approaches
Our findings provide a reference point for future evaluations of CLAHRC-like approaches to the mobilisation of knowledge.
These contribute to a potential ‘re-usable conceptual platform’ (p. 86)85 about how implementation within collaborations might work. As a middle-range theory it provides a starting point, some co-ordinates and the conceptual ground for any future evaluation and learning that is cumulative. We also provide a starting point for those at the beginning of the journey in creating the conditions for collection action for knowledge mobilisation, including paying attention to:
-
surfacing and articulating the different perspectives of all stakeholders around collaboration, knowledge and implementation, including engaging in pre-formative activity and continued dialogue
-
the organisation and operationalisation of the collaboration, particularly around the structures and processes that will be needed to bring people together, and how activity will be resourced and managed
-
setting up opportunities and mechanisms to facilitate the bridging and brokering of boundaries, the employment of people in facilitator-type roles
-
purposefully creating spaces (physical and cognitive) for sharing and learning
-
tapping into the motivations that different groups, individuals and organisations will have for engaging, and using these to both incentivise and reward them
-
resourcing and mobilising formal and distributed leadership in a way that galvanises and motivates both the collaboration and its activities for knowledge mobilisation.
Life cycle of collective action for knowledge mobilisation
At the end of Chapter 6 we presented a final set of CMO configurations and a representation of how their elements fitted together in a path-dependent and contingent way in Figure 12. Further reflection on our findings, including the opportunity to present findings to a wider group via the interpretive forum and contextualising the reflection and discussion in the interpretive forum within a wider literature, added a further layer of explanation, which is shown in Figure 14. This process closes the theory development loop, which is illustrated in Figure 15.
FIGURE 14.
Life cycle of collective action for knowledge mobilisation.
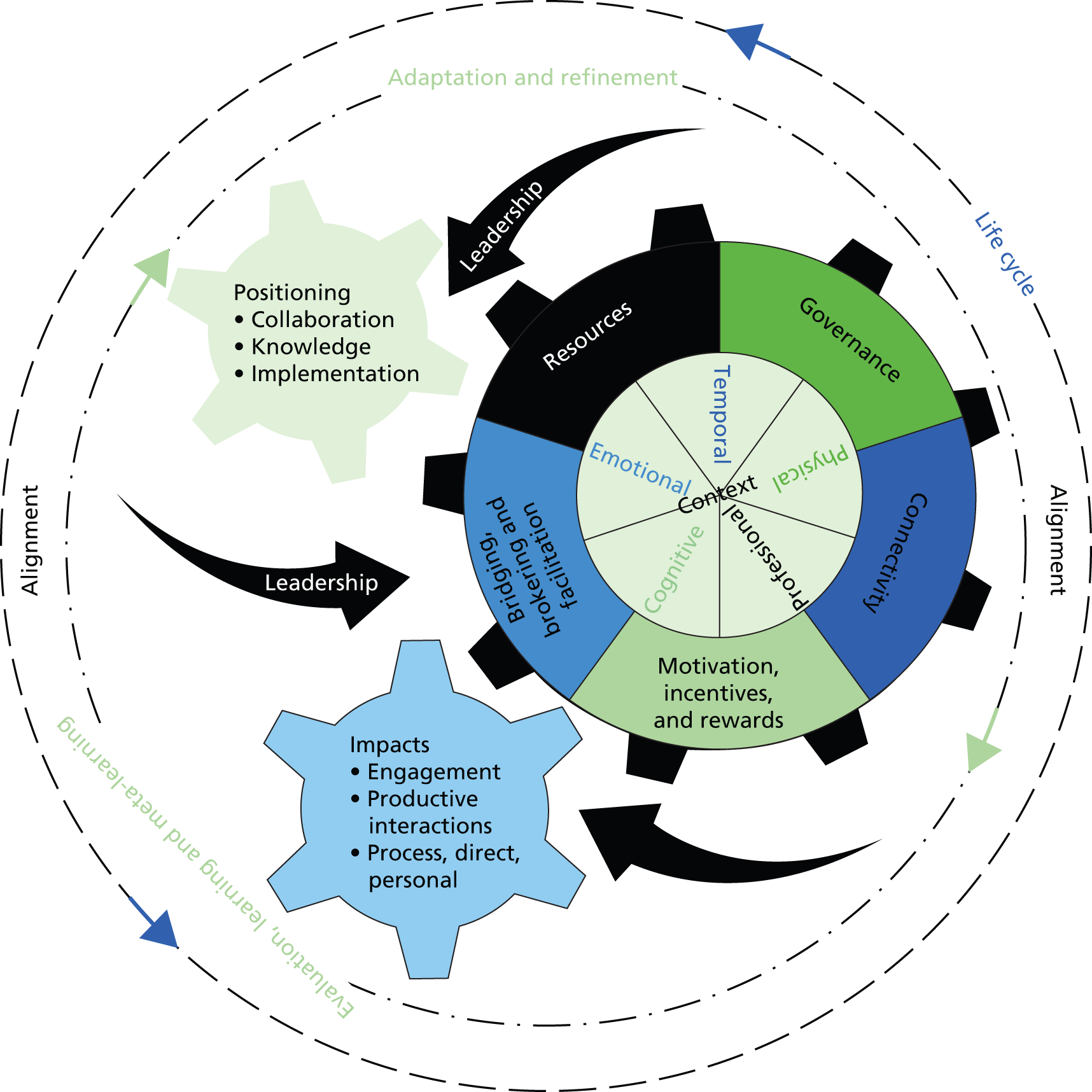
FIGURE 15.
The theory development loop. –,ve, negative; +ve, positive.
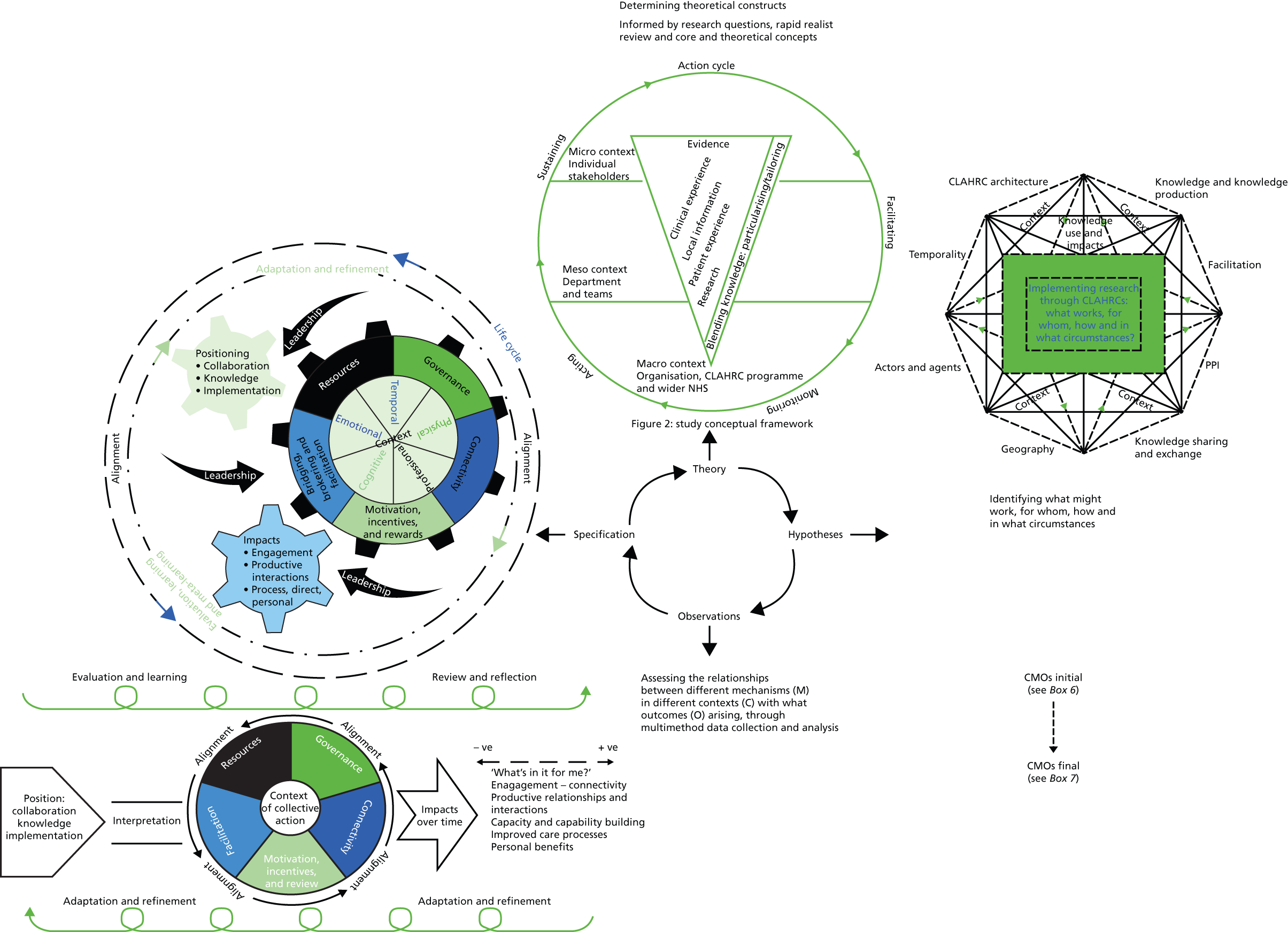
The key ways in which this representation builds on Figure 13 are as follows:
-
The contingencies and path dependency, which starts with the position of stakeholders on the key issues of collaboration, knowledge and implementation, determine how knowledge mobilisation within a CLAHRC-like context is organised, governed and resourced, including investment in bridging, brokering and facilitation activities and roles, and whether or not this sets the condition for people to be motivated to engage. There are multiple contexts of action that can both enable and restrain. All of this is set within a life cycle of organisational collaboration for knowledge mobilisation.
-
The life cycle observed in our partner CLAHRCs was influenced by responses to evaluation and learning activities over time. We expect that different approaches to evaluation and learning about knowledge mobilisation will be more effective when they correspond to how mature the collaboration is. We also acknowledge that the interplay between starting position, organisation and operationalisation and resultant impacts is mediated by the distributed nature and visibility of leadership, including leaders’ characteristics and style.
Study limitations
Our findings should be read in the context of their potential limitations. First, we focused on three CLAHRCs as in-depth case studies and cannot make claims about the extent to which our findings are representative of all nine CLAHRCs. We gave other CLAHRCs the opportunity to contribute to the study on more than one occasion, including via the interpretive forum in April 2014 and by interviewing an additional stakeholder in a different CLAHRC about PPI. These provided a means through which others could express an opinion on the resonance of our approach and emerging findings. We have provided a rich and detailed description of cases and of the findings, from which readers can make judgements about theoretical transferability to different contexts. We also encourage others to read our findings in the context of the reports and outputs of the other external evaluations, to enable judgements about transferability to be made.
We used a purposive sampling strategy based on a stakeholder analysis to identify potential participants. The stakeholder analysis enabled us to identify those who were perceived to be essential to interview in relation to the focus of interest during particular rounds of data collection. An initial approach was made through CLAHRC directors or their deputies/nominees (as agreed by the NIHR at the stage of funding) to direct us towards the respondents that would be most likely to be able to answer our questions (‘essential’ stakeholders). On interviewing key stakeholders we also then used snowball sampling, asking initial respondents to suggest others who might have knowledge about the focus of data collection during particular data collection rounds. This approach may have introduced some bias. We attempted to minimise the bias of self-report in interviews by triangulating data sources. Where possible we established the trustworthiness of emerging findings by means of observations, documents and feedback sessions with participants.
Opportunities to engage in observation were more limited than we had originally expected or hoped. Reasons for this included that the meetings we were invited to were few (e.g. because there were issues regarding sensitivity about finances, refunding, etc.), the focuses of meetings were not highly relevant (i.e. more or less focused on implementation and related issues) and the timing of meetings/events meant for practical reasons a physical presence was not possible. There was also an over-riding concern from the CLAHRCs throughout this project that the external evaluations were potentially burdensome. We do not know if this influenced decisions about inviting us or not to meetings/events. Not having as many opportunities for observations as we had originally hoped may have affected the interpretation of our findings. As is typical of case study research and realist evaluation, analysis starts with the most prominent source of data, in this case interviews, and then seeks confirming or disconfirming evidence from other sources. It is therefore possible we missed some nuances by being unable to draw on a volume of field notes from observations.
We were also mindful of the balance that needed to be struck between pursuing data collection opportunities to full advantage and burden on potential participants. We were particularly aware of the involvement of the CLAHRCs in more than one of the external evaluations as well as their own internal evaluations. We therefore made two approaches to each potential participant and did not pursue them further if they did not respond.
We fed back findings to the CLAHRCs through meetings/workshops and conference calls. In addition, the interpretive forum included participants from all nine CLAHRCs, and others with an interest in knowledge mobilisation and CLAHRC-like approaches. We used this as an opportunity to present findings from all four rounds of data collection and to check out the resonance of these with participants. Overall, it appeared that participants felt the findings resonated with their experiences and their own theories about implementation within CLAHRCs.
In the interests of transparency it is worth reflecting on the fact that the theoretical starting point for this study was the PARIHS and K2A frameworks and that authors related to both those frameworks are authors of this report. As previously described, these frameworks provided a theoretical starting point for the development of the evaluation framework of the study. As such, they were not retained in their entirety, but their concepts became embedded in the evaluation framework, therefore minimising the risk of the slavish application of our own theories.
Implications
Our findings and conclusions highlight a number of implications for both implementation practice and implementation research.
Implications for implementation practice
Collaboration does not appear out of a vacuum; therefore, attention needs to be given to pre-formative work in which stakeholders have the opportunity to develop relationships and established shared goals. In the absence of pre-formative work, implementation strategies that rely on organisational collaboration should allow time, space and other resources for the creation of partnerships between individuals and teams. Activity around developing relationships and collaboration should be balanced with building in opportunities to achieve some ‘quick wins’ early on in the collaboration’s life cycle. These should be relevant and meaningful to stakeholders, and could therefore be linked to relevant incentives and policy/practice priorities for maximal impact.
Over time, partnerships should use, or allow the creation of, a variety of boundary objects that provide a focus for collective effort around the different interfaces within implementation, for example:
-
professional boundaries – patient stories, clinical guidelines
-
organisational boundaries – governance and reporting frameworks, learning events and artefacts
-
epistemological boundaries – mid-range theories that provide sufficient specification and abstraction for action, and learning across implementation programmes.
Our findings show that the potency and catalytic action of boundary objects is born out of the collective and deliberative processes of their development, which includes involving the right stakeholders.
Reflecting the multiple approaches to implementation observed within our data, organisations contributing to CLAHRC-like programmes/initiatives should provide opportunities for the collaborations to develop a shared vision and common language about implementation. Our findings show that this is best achieved through opportunities for face-to-face interaction between relevant stakeholders, including patients and the public. Implementation models and frameworks may be effective boundary objects in this respect by, for example, providing a useful heuristic around which to begin conversations.
In addition, engaging with multiple stakeholders in the systematic identification of priorities for action on implementation can help enhance the relevance of this vision, and increase organisational buy-in to the collaboration. Ensuring synergy between the vision and the governance arrangements will provide the foundation on which participating organisations’ expectations and commitments, including funding arrangements, can be managed.
Organising implementation activity in cognate themes or programmes provides a focus that has currency with clinicians, managers and other stakeholders. Organising activity within clinical topics was a typical approach used by the CLAHRCs in this study. However, with this approach there is also a danger of working in silos, so a theme-based approach should be balanced with the adoption of strategies that allow cross-theme or cross-programme communication and working to increase access to implementation expertise, and to share learning. The potential for cross-theme working should also be built in to governance, including reporting arrangements. Where this was working well in one of the CLAHRCs, we observed greater opportunities for ongoing review and learning.
Leadership has been identified within the implementation literature as critical for creating the conditions for success. Our findings show that a more distributed approach to leadership within CLAHRC-like programmes appears to be most effective in making strategy around implementation visible. Investing in individuals not in designated leadership roles (such as boundary spanners) can also create some synergy between the different levels and corners of the collaboration.
In this study, implementation was achieved through resource allocation and therefore investment in the establishment of roles to fulfil facilitation and boundary-spanning functions. Generally, people in these roles were successful, although attention needs to be paid to their skills, experience and credibility. We found that credibility was not necessarily related to seniority, but was more about their currency within the context in which they were working. Our findings indicate that, when boundary spanners do not have experience of, and credibility within, a health service setting, their impacts can be dampened. Secondment of clinical staff from service delivery to boundary-spanning roles appears to generate buy-in to the collaboration, and has the potential to increase capability within the system for implementation. Furthermore, clarity about role descriptions, ongoing development and succession planning needs to be built into any organisational investment in facilitation/boundary-spanner programmes.
There is a very limited evidence base for how to involve patients and other lay stakeholders in implementation. Findings from data collected in a CLAHRC that was not one of the three forming the main focus of this evaluation showed that its success in involvement was a result of building on a long history of user-led research. This implies that, where possible, implementation and involvement activity should draw on existing lay involvement initiatives and networks. Furthermore, patient experience should be viewed as a credible form of evidence for implementation.
Individuals and organisations are motivated by different incentives and our findings show that the ‘what’s in it for me’ factor was strongly linked to engagement in CLARHC activities, particularly implementation. Therefore, ensuring that clinicians and academics who are expected to engage in CLAHRC-like initiatives can transparently map their engagement onto relevant professional and career development frameworks will generate buy-in, and ensure that expectations and experiences can be more effectively managed. Engagement in this context should include both project-based activities and more formal capability-building approaches such as embedded doctoral programmes. Similarly, aligning implementation activity where possible around policy and organisational incentives (e.g. QOF) will also increase the relevance and impact of drivers for engagement in implementation.
Minimising any unintended consequences of competition for external funding may be achieved through the sharing of learning about what works in implementation. Virtual repositories of products that could be developed within a CLAHRC as well as ones that are shared across the CLARHC network, such as implementation reports and other artefacts, may provide a platform to facilitate sharing and learning.
A combination of internal and external review has provided some opportunity for learning and a re-evaluation of implementation activity. However, there is still uncertainty about the CLAHRC footprint. Therefore, there are implications about balancing different types of performance metrics, which focus on process as well as outcomes. Learning and research should focus on the core underlying mechanisms of change that are associated with implementation activity. The mechanisms and their contingencies embedded within our programme theory could provide some direction. It would also be important to ensure there is capacity and capability within the system to ensure the potential to scale up from individual project-level metrics to the collaboration, and to the network of collaborations as a whole. Furthermore, our findings imply that it would be useful to identify the different pathways to impact early on in the collaboration’s life cycle. This would provide the platform upon which to develop a prospective evaluation strategy and for tracking impacts as they occur.
In summary, creating the conditions for collection action for implementation requires paying attention to:
-
surfacing and articulating the different perspectives of all stakeholders around collaboration, knowledge and implementation, including engaging in pre-formative activity and continued dialogue
-
the organisation and operationalisation of the collaboration, particularly around the structures and processes that will be needed to bring people together, and how activity will be resourced and managed
-
setting up opportunities and mechanisms to facilitate the bridging and brokering of boundaries, the employment of people in facilitator-type roles
-
purposefully creating spaces (physical and cognitive) for sharing and learning
-
tapping into the motivations that different groups, individuals and organisations will have for engaging, and using these to both incentivise and reward them
-
resourcing and mobilising formal and distributed leadership in a way that galvanises and motivates both the collaboration and its activities for knowledge mobilisation.
Implications for implementation research
Organisational commitment to implementation should be structured to exploit opportunities to advance implementation research by paying attention to two key areas:
-
identifying opportunities for capability building by, for example, embedding doctoral training programmes
-
paying attention to the advancement of theory in the development and evaluation of implementation programmes.
As a relatively young field, implementation science provides space for a number of different epistemological positions, and their associated methodologies and methods. Explanatory, mid-range theory of what works in implementation can provide a potential middle ground around which these different contributions can meld. Paying attention to the role of theory and how this plays out in implementation efforts (theoretical fidelity) could provide some useful insights into how to achieve a balance between practical relevance and rigour.
Our data indicate a variety of drivers for implementation operating in different personal, project, team, programme, professional and organisational contexts. Research that further investigates the importance of alignment between these, such as the balance of collaboration, rivalry and competition, is warranted, including a focus on the expected and unforeseen consequences.
Findings demonstrate that there was limited attention to particularising implementation strategies to circumstances. There is still much to learn about how implementation interventions and approaches are tailored to and in different contexts, including how context is assessed and judgements made about selecting and then implementing different strategies.
Although we found that a distributed approach to leadership for implementation was important, further investigation of the influence of different types of leadership and power in implementation over time, how they are constructed and manifested, and their influence in different implementation contexts would be valuable.
Theory comes in many guises, and this study has shown the potential of combining explicit theory with the inductive development of a middle-range theory in studies about implementation processes and outcomes. We advocate the need to pay greater attention to theory use and development within future implementation research efforts.
Although it is a longitudinal study, we had limited opportunity to observe medium-term consequences of implementation activity within CLAHRCs. Further research could usefully investigate a more extended life cycle of implementation, focusing on the cues for both the creation and the refreshment of organisational collaboration on implementation over a longer time. The second wave of funding for CLAHRC might present some opportunities to do this research.
The research team and CLAHRC participants observed that there had been a lack of attention to scaling up of successful implementation approaches/projects. There is the potential, therefore, to study how best to scale up from individual projects/initiatives, and the facilitators and barriers to this in the context of a distributed network structure.
Acknowledgements
First, we would like to acknowledge the contribution and support of all the participants in our three cases, ‘Hazeldean’, ‘Oakdown’ and ‘Ashgrove’, for their willingness to give their time to be interviewed, particularly those who were willing to participate in more than one round of data collection. We would like to thank the CLAHRC directors and the NIHR Health Services and Delivery Research programme for their ongoing engagement and support in this project.
We are very grateful to the five members of our evaluation PPI group, Maureen Daley, Gavin Eyres, John Hughes, Enid Hurst and Tony Sargeant, who contributed a very specific and valuable perspective to the evaluation.
Thanks to Professor Graham Martin, who contributed to project meetings and provided comments on a draft of the final report.
Our thanks go to Dr Cheryl Stetler, Professor Brian Williams and Professor Sandra Nutley, who have acted as advisors to the research team and have provided insight at critical points in the study.
We are also very grateful to Nyree Hulme, Lois Wilkinson and Heledd Owen-Griffiths for their work as transcribers. We also thank Nyree Hulme for her help with research administration and for her work on compiling and formatting this report.
Contributions of authors
Professor Jo Rycroft-Malone was the principal investigator, led the design of the study, was involved in data collection and analysis, and is lead author of this report.
Dr Christopher Burton was coapplicant and was involved in study design, data collection and analysis, and the writing and general preparation of this report.
Dr Joyce Wilkinson took day-to-day responsibility for data collection and project management, and was involved in analysis and in the preparation of this report.
Professor Gill Harvey was coapplicant and was involved in study design, data analysis (particularly in relation to realist evaluation and implementation) and the preparation of this report. She also brought a CLAHRC perspective to the project.
Professor Brendan McCormack was coapplicant and was involved in study design, data analysis (particularly in relation to realist evaluation and implementation) and the preparation of this report.
Professor Richard Baker was coapplicant, was involved in study design, brought a CLAHRC view to the project and was involved in the preparation of this report.
Professor Sue Dopson was coapplicant and was involved in study design (particularly around organisational perspectives on implementation) and the preparation of this report.
Professor Ian Graham was coapplicant, was involved in study design, participated in research team meetings, contributed a K2A perspective and was involved in the final preparation of this report.
Dr Sophie Staniszewska was coapplicant, was involved in study design, participated in research team meetings (particularly in relation to PPI in implementation) and was involved in the final preparation of this report.
Professor Carl Thompson was coapplicant, was involved in study design, participated in research team meetings, contributed a CLAHRC view to the project and was involved in the final preparation of this report.
Dr Steven Ariss participated in research team meetings, contributed a CLAHRC view to the project and was involved in the final preparation of this report.
Ms Lucy Melville-Richards led on data collection for round 3 around the role of boundary objects in CLAHRCs’ implementation work and was involved in the analysis process and the preparation of the report.
Dr Lynne Williams led the conduct and write-up of the realist rapid review (see Chapter 2).
Publications
Rycroft-Malone J, Wilkinson J, Burton C, Andrews G, Ariss S, Baker R, et al. Implementing health research through academic and clinical partnerships: a realistic evaluation of the Collaborations for Leadership in Applied Health Research and Care (CLAHRC). Implement Sci 2011;6:74.
Rycroft-Malone J, Wilkinson J, Burton C, Harvey G, McCormack B, Graham I, et al. Collaborative action around implementation in Collaborations for Leadership in Applied Health Research and Care: towards a programme theory. J Health Serv Res Policy 2013;18:13–26.
Data sharing statement
All available data can be obtained from the corresponding author.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
References
- Graham ID, Tetroe J. How to translate health research knowledge into effective healthcare action. Healthc Q 2007;10:20-2. http://dx.doi.org/10.12927/hcq. 18919.
- Rosenberg RN. Translating biomedical research to the bedside, a national crisis and call to action. JAMA 2003;289:1305-6. http://dx.doi.org/10.1001/jama.289.10.1305.
- US Department of Veterans Affairs . QUERI: Quality Enhancement Research Initiative n.d. www.queri.research.va.gov/ (accessed 2 October 2015).
- ZonMw . Programme: Academic Collaborative Centres Public Health n.d. www.zonmw.nl/en/programmes/academic-collaborative-centres-public-health/links/ (accessed 2 October 2015).
- Brooks P. Explainer: Why Australia Needs Advanced Health Research Centres 2011. www.theconversation.com/explainer-why-australia-needs-advanced-health-research-centres-1139 (accessed 2 October 2015).
- Fisk NM, Wesslingh SL, Beilby JJ, Glasgow NJ, Puddey IB, Robinson BG, et al. Academic health science centres in Australia: let’s get competitive. Med J Aust 2011;194:59-60.
- Best Research for Best Health: A New National Health Research Strategy. The NHS Contribution to Health Research in England. London: Department of Health; 2006.
- Cooksey D. A Review of UK Health Research Funding. London: HM Treasury; 2006.
- Clinical Effectiveness Research Agenda Group . Implementation Research Agenda Report 2008. http://preview.implementationscience.com/content/supplementary/1748-5908-4–18-s1.pdf (accessed 2 October 2015).
- Eccles M, Armstrong D, Baker R, Clearly K, Davies H, Davies S, et al. An implementation research agenda. Implement Sci 2009;4. http://dx.doi.org/10.1186/1748-5908-4-18.
- NHS Confederation . Integrating Research into Practice: The CLAHRC Experience 2012.
- Wilson PM, Petticrew M, Calnan MW, Nazareth I. Disseminating research findings: what should researchers do? A systematic scoping review of conceptual frameworks. Implement Sci 2010;5. http://dx.doi.org/10.1186/1748-5908-5-91.
- Harvey G, Loftus-Hills A, Rycroft-Malone J, Titchen A, Kitson A, McCormack B, et al. The many meanings of evidence: implications for the translational science agenda in healthcare. Int J Health Policy Manag 2013;1:1-2. http://dx.doi.org/10.15171/ijhpm.2013.34.
- Glasziou P. The paths from research to improved health outcomes. ACP J Club 2005;142:A8-10.
- Rycroft-Malone J, Kitson AL, Harvey G, McCormack B, Seers K, Titchen A, et al. Ingredients for change: revisiting a conceptual framework. Qual Safe Health Care 2002;11:174-80. http://dx.doi.org/10.1136/qhc.11.2.174.
- Greenhalgh T, Robert G, MacFarlane F, Bate P, Kyriakidou O. Diffusion of innovations in service organisations: systematic review and recommendations. Milbank Q 2004;82:581-629. http://dx.doi.org/10.1111/j.0887-378X.2004.00325.x.
- Graham ID, Logan J, Harrison MB, Straus SE, Tetroe J, Caswell W, et al. Lost in translation: time for a map?. J Contin Educ Health Prof 2006;26:13-24. http://dx.doi.org/10.1002/chp.47.
- Nutley SM, Walter I, Davies HTO. Using Evidence. London: Policy Press; 2007.
- Kitson Al, Harvey G, McCormack B. Enabling the implementation of evidence-based practice: a conceptual framework. Qual Health Care 1998;7:149-58. http://dx.doi.org/10.1136/qshc.7.3.149.
- Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci 2009;7. http://dx.doi.org/10.1186/1748-5908-4-50.
- Canadian Institutes of Health Research (CIHR) . More about Knowledge Translation at CIHR 2014. www.cihr-irsc.gc.ca/e/39033.html#Definition (accessed 26 March 2014).
- Rycroft-Malone J. From knowing to doing: from the academy to practice. Comment on ‘The many meanings of evidence: implications for the translational science agenda in healthcare’. Int J Health Policy Manag 2014;2:1-2. http://dx.doi.org/10.15171/ijhpm.2014.08.
- Walshe K, Davies HTO. Health research, development and innovation in England from 1988 to 2013: from research productions to knowledge mobilisation. J Health Serv Res Policy 2013;18:1-12. http://dx.doi.org/10.1177/1355819613502011.
- Best A, Holmes B. Systems thinking, knowledge and action: towards better models and methods. Evid Policy 2010;6:145-59. http://dx.doi.org/10.1332/174426410X502284.
- Best A, Greenhalgh T, Lewis S, Saul J, Carroll S, Bitz J. Large-system transformation in health care: a realist review. Milbank Q 2012;90:421-56. http://dx.doi.org/10.1111/j.1468-0009.2012.00670.x.
- Van de Ven AH. Engaged Scholarship: A Guide for Organisational and Social Research. Oxford: Oxford University Press; 2007.
- Dopson S, Bennett C, Fitzgerald L, Ferlie E, Fischer M, Ledger J, et al. Health Care Managers’ Access and Use of Management Research: Final Report. Southampton: NIHR Service Delivery and Organisation Programme; 2012.
- Rycroft-Malone J, Wilkinson J, Burton C, Andrews G, Ariss S, Baker R, et al. Implementing health research through academic and clinical partnerships: a realistic evaluation of the Collaborations for Leadership in Applied Health Research and Care (CLAHRC). Implement Sci 2011;6. http://dx.doi.org/10.1186/1748-5908-6-74.
- Grimshaw JM, Eccles MP, Lavis JN, Hill SJ, Squires J. Knowledge translation of research findings. Implement Sci 2012;7. http://dx.doi.org/10.1186/1748-5908-7-50.
- Jansson SM, Benoit C, Casey L, Phillips R, Burns D. In for the long haul: knowledge translation between academic and nonprofit organizations. Qual Health Res 2010;20:131-43. http://dx.doi.org/10.1177/1049732309349808.
- Van Raak A, Paulus A, Mur-Veeman I. Why do health and social care providers co-operate?. Health Policy 2005;74:13-2. http://dx.doi.org/10.1016/j.healthpol.2004.12.006.
- Denis J-L, Lomas J. Convergent evolution: the academic and policy roots of collaborative research. J Health Serv Res Policy 2003;8:1-6. http://dx.doi.org/10.1258/135581903322405108.
- Denis J-L, Lehoux P, Hivon M, Champagne F. Creating a new articulation between research and practice through policy? The views and experiences of researchers and practitioners. J Health Serv Res Policy 2003;8:44-50. http://dx.doi.org/10.1258/135581903322405162.
- Woodland R, Hutton M. Evaluating organisational collaborations: suggested entry points and strategies. Am J Eval 2012;33:366-83. http://dx.doi.org/10.1177/1098214012440028.
- Wong G, Greenhalgh T, Westhorp G, Pawson R. Realist methods in medical education research: what are they and what can they contribute?. Med Educ 2012;46:89-96. http://dx.doi.org/10.1111/j.1365-2923.2011.04045.x.
- Wong G, Greenhalgh T, Westhorp G, Buckingham J, Pawson R. RAMESES publication standards: realist synthesis. BMC Med 2013;11. http://dx.doi.org/10.1186/1741-7015-11-21.
- McCormack B, Rycroft-Malone J, DeCorby K, Hutchinson A, Bucknall T, Kent B, et al. A realist review of interventions and strategies to promote evidence-informed healthcare: a focus on change agency. Implement Sci 2013;8. http://dx.doi.org/10.1186/1748-5908-8-107.
- Saul JE, Willis CD, Bitz J, Best A. A time-responsive tool for informing policy making: rapid realist review. Implement Sci 2013;8. http://dx.doi.org/10.1186/1748-5908-8-103.
- Rycroft-Malone J, Wilkinson J, Burton C, Harvey G, McCormack B, Graham I, et al. Collaborative action around implementation in collaborations for leadership in applied health research and care: towards a programme theory. J Health Serv Res Policy 2013;18:13-26. http://dx.doi.org/10.1177/1355819613498859.
- Thomson A, Perry J, Miller T. Conceptualising and measuring collaboration. J Public Adm Res Theory 2007;19:23-56. http://dx.doi.org/10.1093/jopart/mum036.
- Williams P, Sullivan H. Working in Collaboration: Learning from Theory and Practice. Cardiff: National Leadership and Innovation Agency for Healthcare; 2007.
- Gray B. Collaborating: Finding Common Ground for Multiparty Problems. San Francisco, CA: Jossey-Bass Publishers; 1989.
- Amabile T, Patterson C, Mueller J, Wojcik T, Odomirok P, Marsch M, et al. Academic–practitioner collaboration in management research: a case of cross-profession collaboration. Acad Manag J 2001;44:418-31. http://dx.doi.org/10.2307/3069464.
- Phillips N, Lawrence B, Hardy C. Interorganizational collaboration and the dynamics of institutional fields. J Manag Stud 2000;37:23-4.
- Sibbald S. A Focused Literature Review on Integrated Knowledge Translation Partnerships (IKTP). Ottawa, ON: Canadian Institutes of Health Research; 2010.
- Pfaff K, Baxter P, Jack S, Ploeg J. An integrative review of the factors influencing new graduate nurse engagement in interprofessional collaboration. J Adv Nurs 2013;70:4-20. http://dx.doi.org/10.1111/jan.12195.
- Himmelman AT, Huxham C. Creating Collaborative Advantage. Thousand Oaks, CA: Sage Publications; 1996.
- Ring PS, van de Ven AH. Developmental processes of cooperative interorganisational relationships. Acad Manage Rev 1994;19:90-118.
- Rynes SL, Bartunek J, Daft R. Across the great divide: knowledge creation and transfer between practitioners and academics. Acad Manage J 2001;44:340-55. http://dx.doi.org/10.2307/3069460.
- Olson CA, Balmer JT, Mejicano GC. Factors contributing to successful inter-organisational collaboration: the case of CS2day. J Contin Educ Health Prof 2011;31:S3-12. http://dx.doi.org/10.1002/chp.20143.
- Ovretveit J, Bate P, Cleary P, Cretin S, Gustafson D, McInnes K, et al. Quality collaboratives: lessons from research. Qual Safe Health Care 2002;11:345-51. http://dx.doi.org/10.1136/qhc.11.4.345.
- Shortell SM, Zukosli AP, Alexander JA, Bazzoli GJ, Conrad DA, Hasnin-Wynia R, et al. Evaluating partnerships for community health improvement: tracking the footprints. J Health Polit Policy Law 2002;27:49-91. http://dx.doi.org/10.1215/03616878-27-1-49.
- Hall KL, Stokols D, Moder RP, Taylor BK, Thornquist MD, Nebeling LC, et al. Findings from the National Cancer Institute’s TREC year-one evaluation study. Am J Prev Med 2008;35:S161-71. http://dx.doi.org/10.1016/j.amepre.2008.03.035.
- Wilson T, Berwick DM, Cleary PD. What do collaborative improvement projects do? Experience form seven countries. Jt Comm J Qual Saf 2003;29:85-93.
- Baker EA, Wilkerson R, Brennan LK. Identifying the role of community partnerships in creating change to support active living. Am J Prev Med 2012;43:S290-9. http://dx.doi.org/10.1016/j.amepre.2012.07.003.
- Purcal C, Muir K, Patulny R, Thomson C, Flaxman S. Does partnership funding improve coordination and collaboration among early childhood services? Experiences from the Communities for Children programme. Child Fam Soc Work 2011;16:474-84. http://dx.doi.org/10.1111/j.1365-2206.2011.00766.x.
- Goes JB, Ho Park S. Inter-organisational links and innovation: the case of hospital services. Acad Manag J 1997;40:673-96. http://dx.doi.org/10.2307/257058.
- Academic–NHS–Industry Collaboration in Experimental Medicine. London: Department of Health; 2011.
- Pawson R. Evidence-Based Policy: A Realist Perspective. London: Sage Publications; 2006.
- Blevins D, Farmer MS, Edlund C, Sullivan G, Kirchner JE. Collaborative research between clinicians and researchers: a multiple case study of implementation. Implement Sci 2010;5. http://dx.doi.org/10.1186/1748-5908-5-76.
- Kegler MC, Steckler A, McIerou K, Malek SH. Factors that contribute to effective community health promotion coalitions: a study of 10 Project ASSIST coalitions in North Carolina. Health Educ Behav 1998;25:338-53. http://dx.doi.org/10.1177/109019819802500308.
- Lasker RD, Weiss ES, Miller R. Partnership synergy: a practical framework for studying and strengthening the collaborative advantage. Milbank Q 2001;79:179-205. http://dx.doi.org/10.1111/1468-0009.00203.
- Lesser J, Oscos-Sanchez MA. Community–academic research partnerships with vulnerable populations. Annu Rev Nurs Res 2007;25:317-57.
- Stokols D, Misra S, Moder RP, Hall KL, Taylor BK. The ecology of team science: understanding contextual influences on transdisciplinary collaboration. Am J Prev Med 2008;35:S96-114. http://dx.doi.org/10.1016/j.amepre.2008.05.003.
- Roussos ST, Fawcett SB. A review of collaborative partnerships as a strategy for improving community health. Annu Rev Public Health 2000;21:369-402. http://dx.doi.org/10.1146/annurev.publhealth.21.1.369.
- Jackson L, Langille L, Lyons R, Hughes J, Martin D, Winstanley V. Does moving from a high-poverty to lower-poverty neighborhood improve mental health? A realist review of ‘Moving to Opportunity’. Health Place 2009;15:961-70. http://dx.doi.org/10.1016/j.healthplace.2009.03.003.
- Dieleman M, Kane S, Zwanikken P, Gerretsen B. Realist Review and Synthesis of Retention Studies for Health Workers in Rural and Remote Areas. Geneva: World Health Organisation; 2011.
- Rycroft-Malone J, McCormack B, Hutchinson AM, DeCorby K, Bucknall TK, Kent B, et al. Realist synthesis: illustrating the method for implementation research. Implement Sci 2012;7. http://dx.doi.org/10.1186/1748-5908-7-33.
- Lantz PM, Viruell-Fuentes E, Israel BA, Softley D, Guzman R. Can communities and academia work together on public health research? Evaluation results from a community-based participatory research partnership in Detroit. J Urban Health 2001;78:495-507. http://dx.doi.org/10.1093/jurban/78.3.495.
- Best A, Hall N. Rapid Review on Inter-organizational Partnerships. Vancouver, BC: Healthshares; 2006.
- Ovseiko PV, Heitmueller A, Allen P, Davies SM, Wells G, Ford GA, et al. Improving accountability through alignment: the role of academic health science centres and networks in England. BMC Health Serv Res 2014;14. http://dx.doi.org/10.1186/1472-6963-14-24.
- Kilbourne A, Neumann M, Waxmonsky J, Bauer M, Kim H, Pincus H, et al. Public–academic partnerships: evidence-based implementation: the role of sustained community-based practice and research partnerships. Psychiatr Serv 2012;63:205-7. http://dx.doi.org/10.1176/appi.ps.201200032.
- Kreuter MW, Lezin NA, Young LA. Evaluating community-based collaborative mechanisms: implications for practitioners. Health Promot Pract 2000;1:49-62. http://dx.doi.org/10.1177/152483990000100109.
- Butler J, Fryer CS, Reed EA, Thomas SB. Utilising the School Health Index to build collaboration between a university and an urban school district. J Sch Health 2011;81:774-82. http://dx.doi.org/10.1111/j.1746-1561.2011.00657.x.
- Provan KG, Nakama L, Veazie MA, Teufel-Shone NI, Huddleston C. Building community capacity around chronic disease services through a collaborative inter-organisational network. Health Educ Behav 2003;30:646-61. http://dx.doi.org/10.1177/1090198103255366.
- Huxham C. Theorizing collaboration practice. Public Manag Rev 2003;5:401-23. http://dx.doi.org/10.1080/1471903032000146964.
- Bazzoli G, Casey E, Alexander J, Conrad D, Shortell S, Sofaer S, et al. Collaborative initiatives: where the rubber meets the road in community partnerships. Med Care Res Rev 2003;60:63S-94S. http://dx.doi.org/10.1177/1077558703259082.
- Pinto RM. Community perspectives on factors that influence collaboration in public health research. Health Educ Behav 2009;36:930-47. http://dx.doi.org/10.1177/1090198108328328.
- Vangen S, Huxham C. Nurturing collaborative relations: building trust in interorganizational collaborations. J Appl Behav Sci 2003;39:5-31. http://dx.doi.org/10.1177/0021886303039001001.
- Clark MA, Rogers ML, Boergers J, Kahler CW, Ramsey S, Saadeh FM, et al. A transdisciplinary approach to protocol development for tobacco control research: a case study. Transl Behav Med 2012;2:431-40. http://dx.doi.org/10.1007/s13142-012-0164-1.
- Ross S, Lavis J, Rodriguez C, Woodside J, Denis J-L. Partnership experiences: involving decision-makers in the research process. J Health Serv Res Policy 2003;8:S26-34. http://dx.doi.org/10.1258/135581903322405144.
- Nembhard LM. When Do Organisations Learn from Each Other? Inter-Organisational Learning in Health Care n.d. www.web.mit.edu/is08/pdf/Nembhard.pdf (accessed 26 November 2015).
- Puga F, Stevens KR, Patel DI. Adopting best practices from team science in a healthcare improvement research network: the impact on dissemination and implementation. Nurs Res Pract 2013;2013. http://dx.doi.org/10.1155/2013/814360.
- Kitson AL, Rycroft-Malone J, Harvey G, McCormack B, Seers K, Titchen A. Evaluating the successful implementation of evidence into practice using the PARIHS framework: theoretical and practical challenges. Implement Sci 2008;3. http://dx.doi.org/10.1186/1748-5908-3-1.
- Pawson R. The Science of Evaluation: A Realist Manifesto. London: Sage Publications; 2013.
- Pawson R, Tilley N. Realistic Evaluation. London: Sage Publications; 1997.
- Tilley N. Realistic Evaluation: An Overview 2000. http://evidence-basedmanagement.com/wp-content/uploads/2011/11/nick_tilley.pdf (accessed 2 October 2015).
- Timmins P, Miller C. Making evaluations realistic: the challenge of complexity. Support Learn 2007;22:9-16. http://dx.doi.org/10.1111/j.1467-9604.2007.00439.x.
- Dixon-Woods M. Perspectives on Context: A Series of Short Essays Considering the Role of Context in Successful Quality Improvement. London: The Health Foundation; 2014.
- Wilson V, McCormack B. Critical realism as emancipatory action: the case for realistic evaluation in practice development. Nurs Philos 2006;7:45-57. http://dx.doi.org/10.1111/j.1466-769X.2006.00248.x.
- Westhorp G, Prins E, Kusters C, Hultink M, Guijt I, Brouwers J. Realist Evaluation: An Overview. Report from an Expert Seminar. Wageningen: Wageningen UR Centre for Development Innovation; 2011.
- Astbury B, Leeuw FL. Unpacking black boxes: mechanisms and theory building in evaluation. Am J Eval 2010;31:363-81. http://dx.doi.org/10.1177/1098214010371972.
- Williams L. What Works? A Realist Evaluation of the Role of Intermediaries in Promoting Best Practice in Infection Prevention and Control. Bangor: Bangor University; 2013.
- Kazi M. Realist Evaluation in Practice: Health and Social Work. London: Sage Publications; 2003.
- Yin RK. Case Study Research: Design and Methods. London: Sage Publications; 1994.
- Yin RK. Case Study Research: Design and Methods. London: Sage Publications; 2003.
- Pawson R, Sridharan S, Killoran A, Kelly MP. Evidence-Based Public Health Effectiveness and Efficiency. Oxford: Oxford University Press; 2010.
- Rycroft-Malone J, Harvey G, Seers K, Kitson A, McCormack B, Titchen A. An exploration of the factors that influence the implementation of evidence into practice. J Clin Nurs 2004;13:913-24. http://dx.doi.org/10.1111/j.1365-2702.2004.01007.x.
- Patton MQ. Utilization Focused Evaluation. Thousand Oaks, CA: Sage Publications; 2008.
- Guba EG, Lincoln YS. Fourth Generation Evaluation. Thousand Oaks, CA: Sage Publications; 1989.
- Spradley JP. Participant Observation. Belmont, CA: Holt, Rinehart, & Winston; 1980.
- Miles MB, Huberman AM. Qualitative Data Analysis: An Expanded Sourcebook. Thousand Oaks, CA: Sage Publications; 1994.
- Office for National Statistics . Census: Aggregate Data (England and Wales) 2011. http://infuse.mimas.ac.uk (accessed 2 October 2015).
- Office for National Statistics . Region and Country Profiles: Key Statistics and Profiles 2012. http://census.ukdataservice.ac.uk/use-data/citing-data (accessed 2 October 2015).
- Public Health England . English Indices of Deprivation 2012. www.apho.org.uk/resource/view.aspx?RID=125886 (accessed 2 October 2015).
- Parent R, Roy M, St-Jacques D. A systems-based dynamic knowledge transfer capacity model. J Knowl Manag 2007;11:81-93. http://dx.doi.org/10.1108/13673270710832181.
- Walter I, Nutley S, Percy-Smith J, McNeish D, Frost S. Knowledge Review 7: Improving the Use of Research in Social Care Practice. London: Social Care Institute for Excellence; 2004.
- National Institute for Health Research . CLAHRC – Call for Proposals for Pilots n.d. www.nihr.ac.uk/files/pdfs/CLAHRC%20-%20Call%20for%20Proposals%20for%20Pilots.pdf (accessed 7 July 2014).
- Star SL, Griesemer JR. Institutional ecology, ‘translations’ and boundary objects: amateurs and professionals in Berkeley’s Museum of Vertebrate Zoology. Soc Stud Sci 1989;19:387-420. http://dx.doi.org/10.1177/030631289019003001.
- Allen D. From boundary concept to boundary object: the practice and politics of care pathway development. Soc Sci Med 2009;69:354-61. http://dx.doi.org/10.1016/j.socscimed.2009.05.002.
- Dopson S, Fitzgerald L. Knowledge to Action? Evidence-Based Health Care in Context. Oxford: Oxford University Press; 2005.
- Crammer A, Morgan D, Stewart N, McGilton K, Rycroft-Malone J, Dopson S, et al. The hidden/complexity of long-term care: how context mediates knowledge translation and use of best practices. Gerontologist 2014;54:1013-23. http://dx.doi.org/10.1093/geront/gnt068.
- Stetler CB, Ritchie JA, Rycroft-Malone J, Shultz AA, Charns MP. Institutionalising evidence-based practice: an organizational case study using a model of strategic change. Implement Sci 2009;4. http://dx.doi.org/10.1186/1748-5908-4-78.
- Taylor JR, Van Every EJ. The Emergent Organization: Communication as its Site and Surface. Mahwah, NJ: Erlbaum; 2000.
- Weick KE, Sutcliffe KM, Obstfeld D. Organizing and the process of sensemaking. Organ Sci 2005;16:409-21. http://dx.doi.org/10.1287/orsc.1050.0133.
- Greenhalgh T, Humphrey T, Hughes J, MacFarlane F, Butler C, Pawson R. How do you modernize a health service? A realist evaluation of whole-scale transformation in London. Milbank Q 2009;87:391-416. http://dx.doi.org/10.1111/j.1468-0009.2009.00562.x.
- Drug Resistant Streptococcus pneumonia Surveillance Manual. Atlanta, GA: CDC; 2003.
- Nowotny H, Scott P, Gibbons M. Rethinking Science: Knowledge in an Age of Uncertainty. Cambridge: Polity Press; 2001.
- Dickinson H, Glasby J. Why partnership working doesn’t work: pitfalls, problems and possibilities in English health and social care. Public Manag Rev 2010;12:811-28. http://dx.doi.org/10.1080/14719037.2010.488861.
- Orr K, Bennett M. Public administration scholarship and the politics of co-producing academic–practitioner research. Publ Admin Rev 2012;22:487-95. http://dx.doi.org/10.1111/j.1540-6210.2011.02522.x.
- Raisch S, Birkinshaw J. Organizational ambidexterity: antecedents, outcomes, and moderators. J Manag 2008;34:375-409. http://dx.doi.org/10.1177/0149206308316058.
- Gherardi S, Nicolini D. Learning in a constellation of interconnected practices: canon or dissonance. J Manag Stud 2002;39:419-36. http://dx.doi.org/10.1111/1467-6486.t01-1-00298.
- Walter I, Davies H, Nutley S. Increasing research impact through partnerships: evidence from outside health care. J Health Serv Res Policy 2003;8:S58-61. http://dx.doi.org/10.1258/135581903322405180.
- Pettigrew A, Whipp R. Managing Change for Competitive Success. Oxford: Blackwell; 1991.
- Sullivan H, Williams P, Jeffares S. Leadership for collaboration. Public Manag Rev 2012;14:41-66. http://dx.doi.org/10.1080/14719037.2011.589617.
- Grint K. Problems, problems, problems: the social construction of ‘leadership’. Hum Relat 2005;58:1467-94. http://dx.doi.org/10.1177/0018726705061314.
- Jagosh J, Macaulay AC, Greenhalgh T. Uncovering the benefits of participatory research: implications of a realist review for health research and practice. Milbank Q 2012;90:311-48. http://dx.doi.org/10.1111/j.1468-0009.2012.00665.x.
- Nilsen P, Roback K, Brostrom A, Ellstrom P-E. Creatures of habit: accounting for the role of habit in implementation research on clinical behaviour change. Implement Sci 2012;7. http://dx.doi.org/10.1186/1748-5908-7-53.
- Kislov R. Boundary discontinuity in a constellation of interconnected practices. Public Admin 2014;92:307-23. http://dx.doi.org/10.1111/padm.12065.
- Kellog KC, Orlikowski WJ, Yates J. Life in the trading zone: structuring co-ordination across boundaries in postbureaucratic organisations. Organ Sci 2006;17:22-4. http://dx.doi.org/10.1287/orsc.1050.0157.
- Carlile PR. Transferring, translating, and transforming: an integrative framework for managing knowledge across boundaries. Organ Sci 2004;15:555-68. http://dx.doi.org/10.1287/orsc.1040.0094.
- Van de Ven AH, Johnson PE. Knowledge for theory and practice. Acad Manage Rev 2006;31:802-21. http://dx.doi.org/10.5465/AMR.2006.22527385.
- Wenger E, McDermott R, Snyder WM. Cultivating Communities of Practice. Boston, MA: Harvard Business School Press; 2002.
- Lave J, Wenger E. Situated Learning: Legitimate Peripheral Participation. New York, NY: Cambridge University Press; 1991.
- Le May A. Communities of Practice in Health and Social Care. Oxford: Wiley; 2009.
- Agterberg M, van den Hooff B, Huysman M, Soekijad M. Keeping the wheels turning: the dynamics of managing networks of practice. J Manag Stud 2010;47:85-108. http://dx.doi.org/10.1111/j.1467-6486.2009.00867.x.
- Probst G, Borzillo S. Why communities of practice succeed and why they fail. Eur Manage J 2008;26:335-47. http://dx.doi.org/10.1016/j.emj.2008.05.003.
- Veenswijk MC, Chisalita CM. The importance of power and ideology in communities of practice. Info Technol People 2007;20:32-5. http://dx.doi.org/10.1108/09593840710730545.
- Senge PM. The Fifth Discipline: The Art and Practice of the Learning Organization. London: Random House; 1990.
- Chauhan M, Bankart MJ, Labeit A, Baker R. Characteristics of general practices with numbers of elective admissions. J Public Health n.d.;34:584-90. http://dx.doi.org/10.1093/pubmed/fds024.
Appendix 1 References for rapid realist review
Appendix 2 Initial concepts and search terms
| Collaboration OR |
Academia OR |
Health Services OR |
Implementation OR |
|---|---|---|---|
| Co-operation Co-operative enquiry Interaction Networks Negotiation Interdependency Co-ordination Partnerships Joint working Trials Co-production Integration Interdisciplinary Teamwork Joined-up working Service integration Inter-institutional relations Coalitions Partnership Community partnership |
HEIs Academics Academy (Engaged) Scholarship Research partnerships University Scientists Joint research project Theory |
Practitioners Practice Multi-agency working Hospital Community Healthcare professionals |
Building capacity Impact Research Sustainability |
Appendix 3 Search strategy
Search strategy. ASSIA, Applied Social Sciences Index and Abstracts; CINAHL, Cumulative Index to Nursing and Allied Health Literature.

Appendix 4 Data extraction form
-
How is the collaboration initiated and how established – does this have impact on implementation success?
-
How does the nature of the collaboration (e.g. funding/lifecycle/focus; e.g. regional/national) have an impact on implementation?
-
How does the nature of the organisation(s) (structure/function) contribute (or not) to the impact of the collaboration on implementation?
-
How does collaboration enhance capacity and capability?
-
How do individuals/teams within the collaboration impact on implementation?
-
What is the nature of relationships between collaborators (e.g. symbolic/asymmetric/egalitarian) and how do relationships impact on the extent of implementation?
-
What is the nature of the intervention/knowledge?
-
What are (if any) reported impacts?
-
What is the source/origin of knowledge?
Appendix 5 Interview schedules
High-level research questions for interviews
Each of these maps across to the evaluation framework and addresses an element from the framework and covers the 3 tracer issues. These would form the topic areas for semi-structured interviews. The specific areas covered will depend on the role and responsibilities of the individual participant (not all will be relevant to every participant) and will be augmented by observational and documentary data.
Data collection round 1: interview schedule
Element in evaluation framework
Knowledge and knowledge production
-
Different types of knowledge used.
-
Value of knowledge to different stakeholders.
-
Types of knowledge privileged over others.
-
Processes for knowledge creation and co-production.
-
Processes of unlearning or accumulation (link to capacity building).
-
Non-progression of knowledge implementation processes before utilisation.
Facilitation
-
Strategies and rationale for implementation and approaches used.
-
Identification of barriers and strategies to address.
-
Maximising enablers to implementation and utilisation processes.
-
Facilitators (factors not individuals) of co-production of knowledge and utilisation.
-
Formal and informal roles for facilitating implementation and utilisation processes.
Patient and public involvement
-
Involvement of service users as key stakeholders in co-production of knowledge – how and what is the nature of this.
-
Engagement of hard to reach groups – how has this been approached and what has worked.
-
Identification of barriers and enablers to PPI in knowledge generation and utilisation and strategies to address these or maximise.
Knowledge sharing and exchange
-
Processes of knowledge sharing additional to co-production.
-
Sharing with all potential users – how is this achieved.
-
Faithful replication of knowledge or attenuation over time through the sharing processes.
-
Sharing of other types of knowledge such as organisational learning approaches.
-
Knowledge capture from outwith CLAHRCs and exchange between CLAHRCs.
Geography
-
Links to health geography, social geography, human geography for determining local priorities (as a source of knowledge and how utilised).
-
Knowledge as social capital.
-
Geography as a barrier or enabler to co-production, implementation or utilisation.
Actors/agents
-
Formal and informal roles of individuals in CLAHRCs.
-
Key stakeholders and key players in knowledge utilisation processes.
-
Beneficiaries, victims and agents in relation to knowledge co-production and utilisation.
Temporality
-
Historical aspects of the pre-CLAHRC organisations and working relationships.
-
Knowledge production, implementation and utilisation processes over time.
-
Communities of practice over the time-span of the CLAHRC.
-
Aspects of capability and capacity building developing over time for increasing scope for knowledge generation, receptivity and utilisation.
Collaboration for Leadership in Applied Health Research and Care architecture
-
The impact of contractual obligations to NIHR.
-
Internal structures of CLAHRC including communication processes.
-
Internal and external evaluations and their impact on knowledge utilisation activities and processes.
Context
Observational and documentary data will be the main ways in which data about context is gathered but will be augmented by specific questions in interviews if there is a need for clarity or more information about any aspect or any level of context: resources; culture; leadership; communication processes; barriers and enablers to knowledge production and utilisation; tailoring of strategies to address contextual aspects or adaptation of context to ameliorate these.
Data collection round 2: interview schedule
Within this project, what are the gaps between knowledge and practice that you are trying to close?
-
How were these identified?
-
Had anything been tried before – tell me about the history of the project?
-
How was it prioritised (who decided) or what made it a priority? Was it influenced by particular organisations and people’s agendas? Was there any PPI involvement in this?
-
How does this fit with the CLAHRC implementation strategy?
-
How does it link to other initiatives within or outwith CLAHRC?
What activities are planned or undertaken to close the gaps?
-
What has influenced the design of the project?
-
What has worked and why and has there been any learning from the project? How is this fed back to the CLAHRC? Are there any impacts/outputs that have led to things being done differently?
Who will be/is included in the project and why (who are key stakeholders and why?)
-
In what ways have people worked together?
-
What has helped/hindered?
How has the Collaboration for Leadership in Applied Health Research and Care contributed to/influenced initiation or progress of the project or activities within it?
-
Access to resources (people/money/others).
-
Use of different types of knowledge/expertise/evidence – who, what and why privileged and how are they integrated/used?
What from the Collaboration for Leadership in Applied Health Research and Care contribution has worked and why – how do you know/how will you know? What will ‘success’ look like? (Contribution and consequences)
-
Has this changed over time and if so in what ways?
-
Has there been any shift in barriers and enablers?
On the basis of this project how has/will capacity and capability for implementation changed or how do you anticipate it will change?
-
What opportunities has the CLAHRC provided?
-
Who has benefited and in what ways?
-
What levels of impact have you observed/captured and how do you/will you know? Levels – individual, organisational, public, etc.
Anything else about the project setup that you want to mention?
Data collection round 3: interview schedule
The aim is to explore experiences of implementation and the sorts of things and ideas that have been helpful in facilitating collaboration and working together towards service improvement and knowledge use. In this case implementation refers to the process and methods of translating evidence – in its broadest sense, into practice. Other terms that are often used include improving patient safety, quality improvement and so on.
Your role in Collaboration for Leadership in Applied Health Research and Care
-
Can you describe your role, what sorts of things you do or are involved in?
-
Tell me about some of the implementation projects that you’ve been involved in . . .
-
Can you tell me a little bit more about communication and what sorts of things were helpful in opening up a dialogue?
-
-
Shared understanding
-
Can you tell me about an implementation project that you’ve been involved in when it became clear that people did not understand each other?
-
And one when everyone understood each other?
-
Was there anything that this understanding hinged on? For example was there a specific moment when it became clear that everyone understood each other, or was it a gradual process?
-
How was this understanding reached?
-
-
Knowledge exchange
-
Can you describe an instance when it became clear that knowledge had not been shared been those involved in implementation work (for example a knowledge gap between different stakeholders that had not been identified or met)?
-
Can you tell me about a time when you’ve shared knowledge with other people during implementation work?
-
What was the outcome?
-
How did this help or hinder?
-
-
Collaboration – working together
-
Can you describe an example of when you worked in partnership with other people and groups involved in implementation work?
-
Can you think of any factors that led to the success of this collaboration?
-
There are different levels of collaboration across different projects, for example the role of patients and the public varies in some projects compared to others. Is there a ‘bottom line’ for working together, for example what degree of collaboration is good enough in terms of implementation?
-
-
Boundaries and crossing
-
We are interested in finding out how boundaries are crossed when different groups work together to get evidence into practice through CLAHRCS, such as those between healthcare services and higher education. Can you tell me about some of the boundaries that you have encountered?
-
What sorts of things have been useful in crossing boundaries? Are there any things, ideas, approaches or strategies you’ve found helpful and why?
-
How would you describe their role when boundaries are crossed?
-
-
Cross-boundary relationships
-
Part of boundary crossing is about being able to establish rapport and develop relationships across different boundaries. How have you gone about establishing rapport across the different boundaries you work across?
-
How have you maintained these relationships?
-
Recap and summarise.
Anything else participant would like to add that hasn’t been covered in relation to implementation?
Thanks.
END.
Data collection round 4: interview schedule
Focus on implementation not research – focus on obtaining explanation rather than description
-
How would you describe your CLAHRC’s approach to implementation? (prompt re four types we have identified so far)
-
Is there any other approach that they have been using?
-
What has influenced this CLAHRC’s approach to implementation
-
-
What are the motivations, incentives or disincentives for different people/groups to engage with your CLAHRC’s implementation agenda?
-
What did organisations expect to get out of the collaboration for implementation?
-
What helped in closing the implementation gap?
-
Has there been any competitive element to the CLAHRC (such as reputational competition or university competition)?
-
-
In what way has this CLAHRC prompted health services to do implementation differently? (think added value and what would have happened anyway?)
-
Has the CLAHRC shifted the responsibility for implementation away from the health services?
-
Examples?
-
-
Leadership at all levels seems to have been an important factor in how CLAHRCs have gone about their business, including implementation. How would you describe the leadership style within this CLAHRC?
-
What sort of impact has this had?
-
Does this fit with your approach to leadership, how (or not)?
-
-
How has the structure of this CLAHRC facilitated or impeded engagement/relationship building needed to conduct its implementation activity? (Bear in mind the three types of trust: companion trust; competence trust and commitment trust)
-
What improvements do you think could have been made?
-
How would you describe the link between what happens on the ground (i.e. in projects) and what happens at the CLAHRC executive level?
-
-
How would you describe the CLAHRC ‘brand’ (identity)?
-
Why do people align themselves with the brand (or why not) and what do they bring to implementation?
-
Why do you think people might feel like ‘insiders or outsiders’?
-
-
What formal mechanisms/process are in place for this CLAHRC to learn from its implementation activity/projects/programmes and how does this feed into future planning?
-
How do they feed into the management of the CLAHRC?
-
How do projects share feedback with one another?
-
How could these processes/approaches be improved?
-
Have they learned anything from the external evaluations of CLAHRCs, if so, what? (ask for examples)
-
-
Over time, in what ways has the CLAHRC adapted and changed in relation to its implementation activity?
-
Why/what prompted this?
-
And to what effect? (ask for examples)
-
-
What has the CLAHRC learned about PPI in implementation?
-
What has been taken forward?
-
Anything left out or won’t be taken forward?
-
-
We have identified a number of different kinds of impacts from CLAHRC, one of these is the potential for unexpected personal, professional opportunities from being involved with a CLAHRC. Have you experienced anything like this, or have others that you know of?
-
CLAHRC director level, what have they learned, how would they do things differently and what did they keep in the new CLAHRC proposals, what did they change?
END.
Observational data collection schedule
Spradley’s nine dimensions of observation will be the basis for data collection. Field notes will be analysed according to these nine dimensions.
-
SPACE: for example where the observations are taking place, in a meeting or workshop and where this is in relation to the CLAHRC.
-
ACTORS: for example who is involved, what are their roles in the CLAHRC?
-
ACTIVITIES: for example what a specific meeting is about and what are the main activities of the participants – listening, contributing, leading, presenting and so on.
-
OBJECTS: for example in a CLAHRC Board meeting, the objects might be specific presentations or documents.
-
ACTS: providing fuller explanation about specific involvement in a CLAHRC Board meeting such as leading on an agenda item, providing feedback or facilitating a discussion.
-
TIME: for example when a meeting takes place, how long it lasts and if any of the other dimensions change over time (such as additional people joining or leaving a meeting which might change the dynamic of the meeting).
-
EVENTS: for example specific events that take place during a meeting such as presentations by an external speaker or a conference call that takes place for a short time in the meeting. Also covers aspects of the meeting that become ‘eventful’ such as a hotly debated agenda item.
-
GOALS: what the purpose of the meeting was, what goals are achieved during the meeting and what are the goals of those involved.
-
FEELINGS: for example feelings expressed by an individual in a meeting; the ‘mood of the meeting’ or issues that relate to wider contextual issues such as NHS funding and the impact on CLAHRCs.
Appendix 6 Documents used in documentary analysis
Hazeldean
| Document no. | Anonymised title | Date |
|---|---|---|
| 1 | CKD paper published in BMJ Quality & Safety | 2012 |
| 2 | Report on phase 1 of the CKD collaborative | 2010 |
| 3 | IGT project evaluation report | 2011 |
| 4 | Evaluation of the stroke assessment tool | 2013 |
| 5 | Post-stroke review pilot project report | 2010 |
| 6 | CLAHRC HF alert cards evaluation report | 2012 |
| 7 | Physical and mental health project evaluation report | 2013 |
| 8 | Primary care HF project evaluation report | 2012 |
| 9 | Website page on CKD project evaluation second wave | 2013 |
| 10 | Final report of Hazeldean CLAHRC to the funder | 2014 |
| 11 | Added value examples from the CLAHRC report to funder | 2014 |
| 12 | CKD paper submitted to International Journal of Quality in Health Care | 2014 |
| 13 | Paper on communities of practice published in Journal of Management Inquiry | 2013 |
| 14 | Paper on HF alert cards published in European Journal of Cardiovascular Nursing | 2013 |
| 15 | Paper on communities of practice published in Implementation Science | 2012 |
| 16 | Paper on stroke assessment tool published in Clinical Rehabilitation | 2012 |
| 17 | Website page on the use of the stroke assessment tool | 2013 |
Oakdown
| Document no. | Anonymised title | Date |
|---|---|---|
| 1 | Executive summary of evaluation of the dysphagia e-learning package | 2012 |
| 2 | Oakdown CLAHRC autumn newsletter ‘Impacts and Sustainability’ | 2013 |
| 3 | Oakdown CLAHRC KT casebook | 2011 |
| 4 | Internal evaluation report executive summary | 2011 |
| 5 | Final report of Oakdown CLAHRC to the funder | 2014 |
| 6 | Added value examples from the CLAHRC report to the funder | 2014 |
Ashgrove
| Document no. | Anonymised title | Date |
|---|---|---|
| 1 | Executive summary of report on CLAHRC co-ordinators | 2012 |
| 2 | Spanning boundaries: an interim review of the CLAHRC coordinator role | 2012 |
| 3 | Elective admissions paper published in Journal of Public Health | 2012 |
| 4 | Summary of recommendations from the external advisory review of Ashgrove CLAHRC | 2010 |
| 5 | Approach to KT for Ashgrove CLAHRC | 2011 |
| 6 | Job description of CLAHRC co-ordinators | No date |
| 7 | Final report of Ashgrove CLAHRC to the funder | 2014 |
| 8 | Ashgrove publications for 2013 | 2014 |
Appendix 7 Interpretive forum
Collaboration to enhance the use of knowledge in practice: a workshop for sharing and learning
We held a 1-day interpretive forum on 2 April 2014. The day was open to all CLAHRCs and specific invitations went out to those who had been part of our case study sites and to others with an interest or expertise in knowledge mobilisation or collaborative ways of working across sectors. We had a total of 28 participants from seven CLAHRCs and associated HEIs. The programme was as follows:
Collaboration to enhance the use of knowledge in practice: a workshop for sharing and learning
Facilitated by Professor Huw Davies and the ECLIPS team.
Held in Radisson Blu Edwardian, Free Trade Hall, Peter Street, Manchester M2 5GP.
| 10:30 | Tea/coffee available |
| 11:00 | Welcome & introduction; purpose of workshop |
| 11:10 | Overview of the project, including emerging findings [please read Journal of Health Services Research & Policy paper (18 {suppl 3}, 3–26) before the meeting] |
| 11:30 | Group discussion 1: reflection on how emerging findings resonate with participants’ experiences and plans (small group and plenary discussion) |
| 12:30 | Lunch |
| 13:15 | Drawing together themes/issues from the morning’s discussions |
| 13:30 | Group discussion 2: looking forward and taking action – reflecting on the most and least important ingredients in developing a collaboration to enhance and facilitate knowledge use (small group and plenary discussion) |
| 14:45 | Summary remarks and what next |
| 15:00 | Close |
This workshop is part of an NIHR funded project (HS&DR 09/1809/1072).
Project details: www.nets.nihr.ac.uk/projects/hsdr/0918091072.
As can be seen, the day took the form of an interactive workshop with a short presentation (below) of the high-level emerging findings (participants had been asked to read a published paper prior to the meeting) and then small-group work to check out the resonance of these with participants. This ended with a plenary session, with small-group feedback to the whole group.
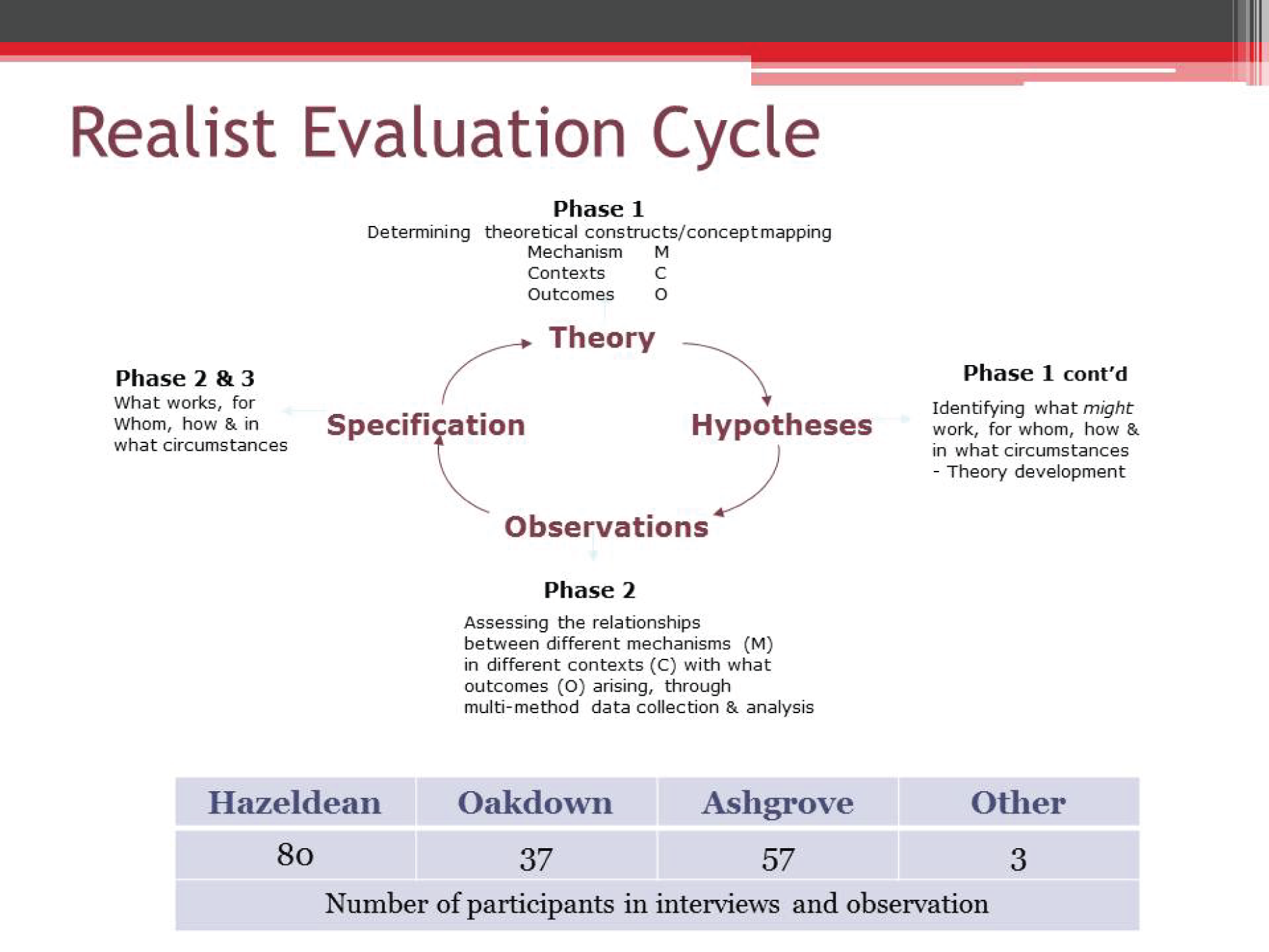
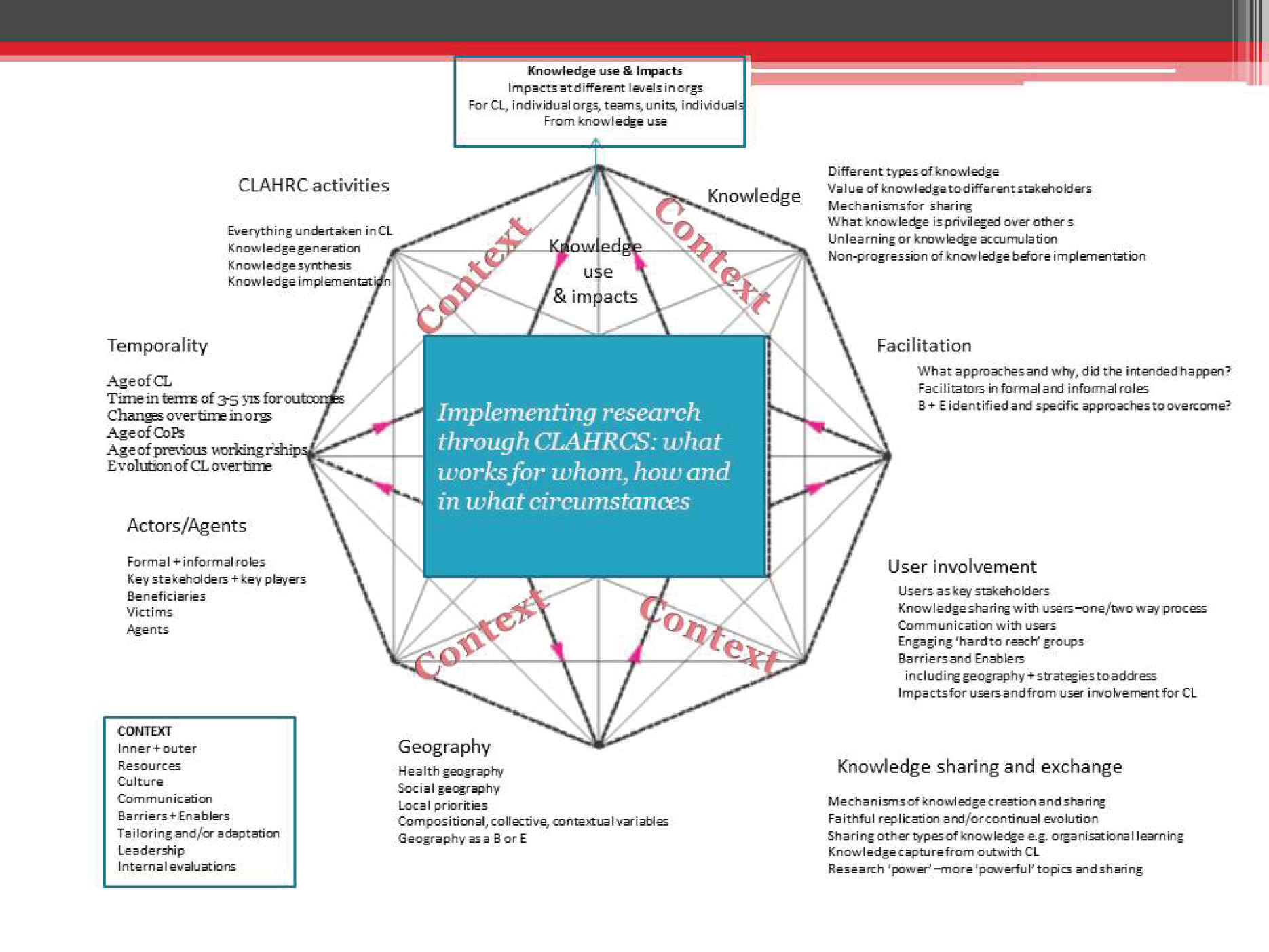
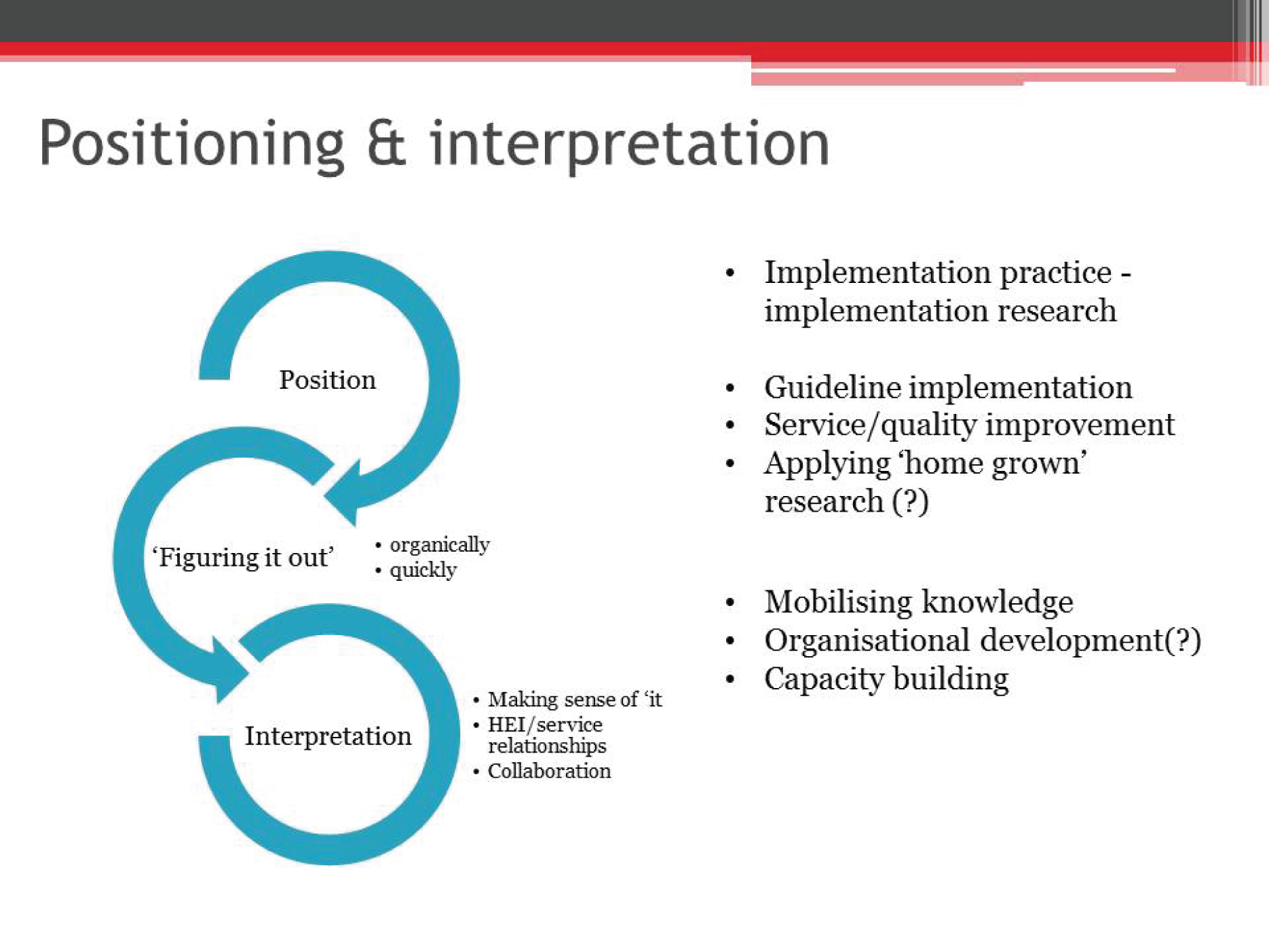

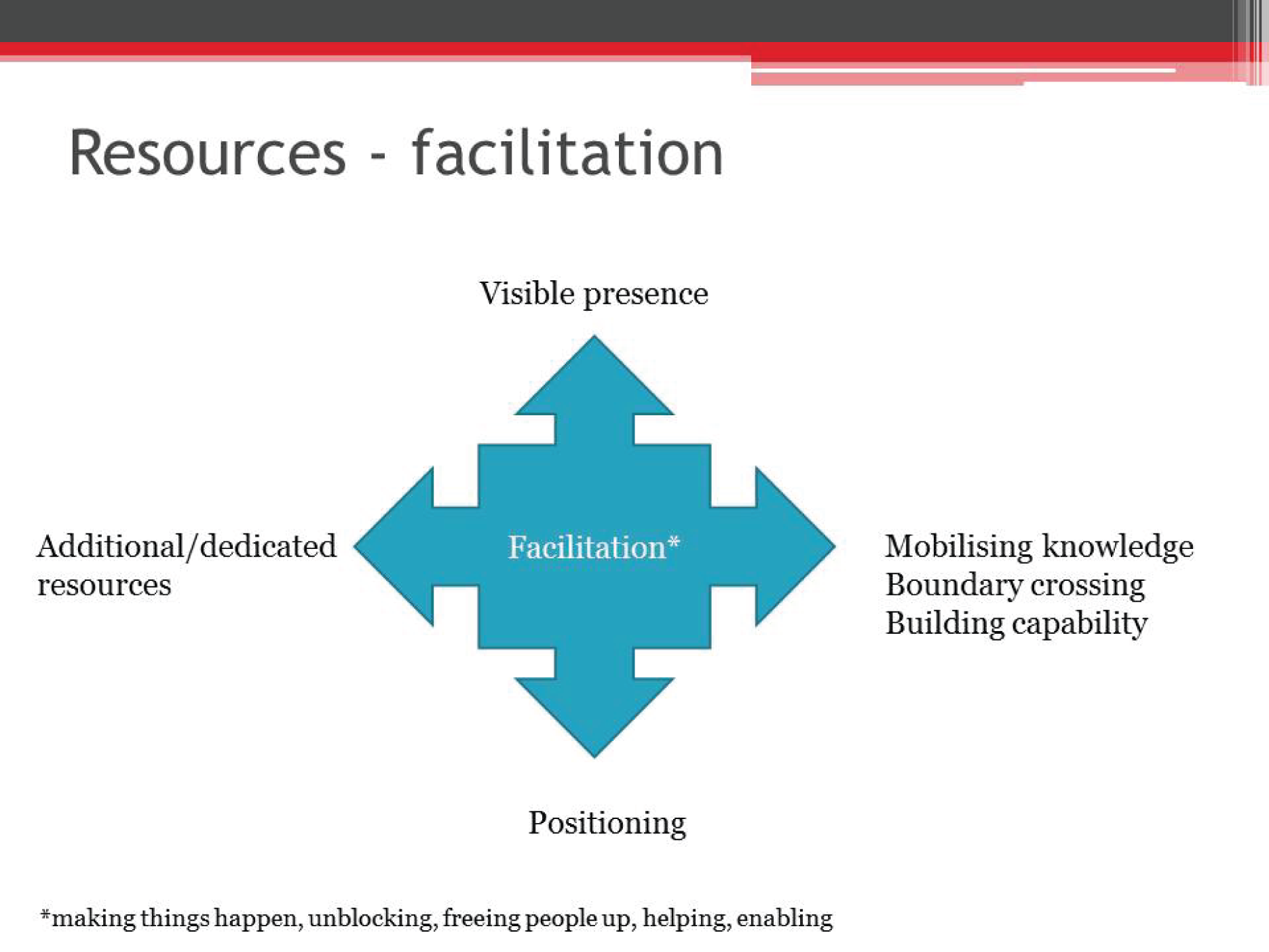
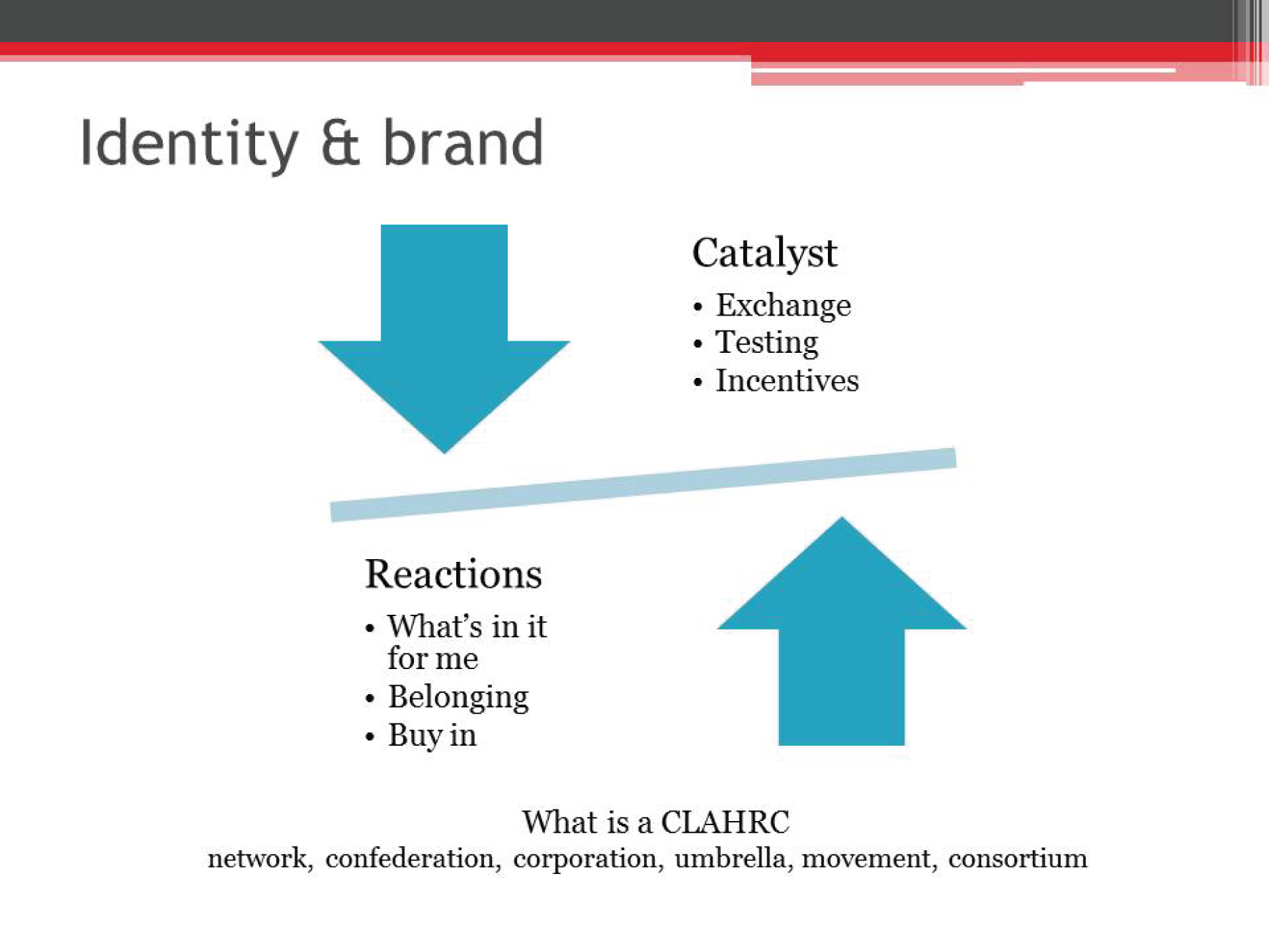
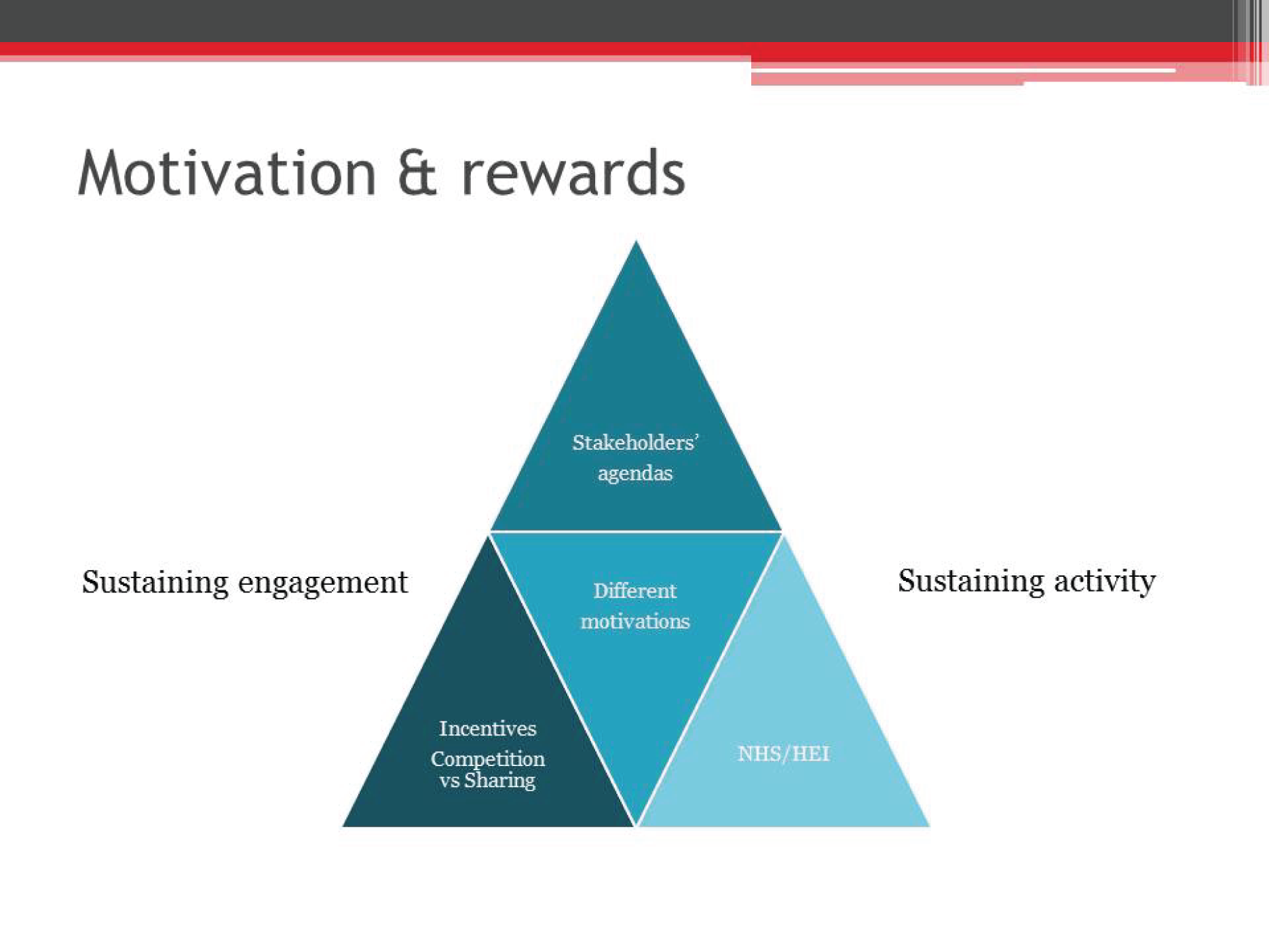
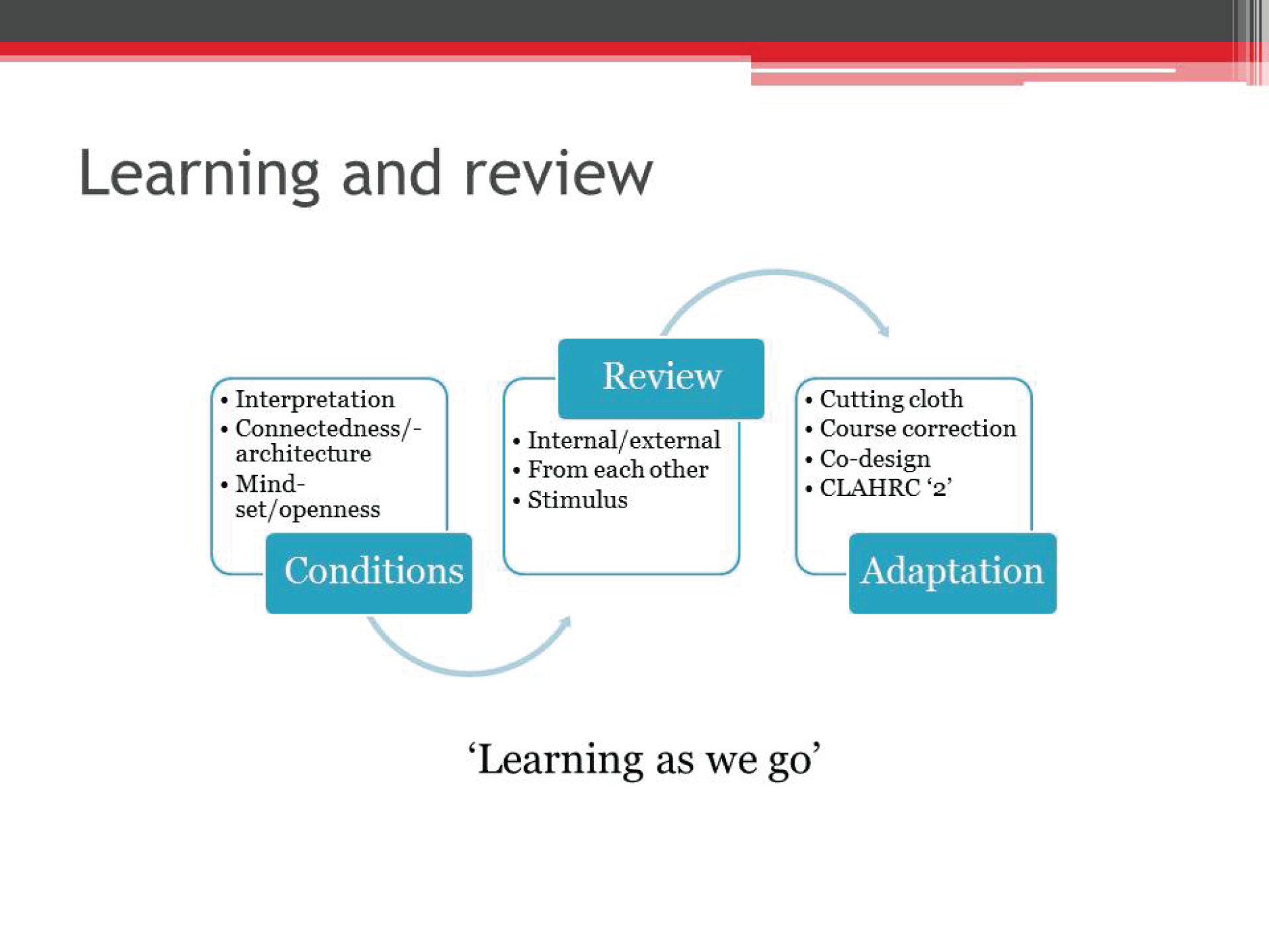
The afternoon session provided participants with a list of potential factors to take into consideration when developing collaborations and asked them to consider in small groups which were the most and least important ingredients in developing a collaboration to enhance and facilitate knowledge use.
Group discussion 2
Here are some of the characteristics of CLAHRCs’ approach and ways of working in facilitating implementation. If you were to start again in building organisational collaborations to facilitate the implementation if evidence, which of these would you give most attention to and why?
-
Approach to implementation (e.g. links with research, responsiveness vs. fidelity).
-
Vision (e.g. commonly understood, shared, bought into).
-
Impacts (what was expected to be important/any shift?).
-
Resource flow (e.g. targeted, flexible).
-
Leadership (e.g. centralised, distributed).
-
Brokering and bridging processes and people (including roles and skills).
-
Incentives and incentivisation.
-
Learning, evaluation and meta-learning (including capability and capacity building).
-
Engagement (e.g. quality and nature of relationships, over time).
-
Organisations.
-
Teams and people.
-
Patient and public involvement (e.g. starting point, purpose and integration).
-
Flexible structures/architectures (including governance).
This also ended with a plenary session, with small groups feeding back to the whole group.
Feedback from both sessions was positive and attendees related that the findings presented resonated strongly with their own experience of collaborative working to enhance knowledge use.
Appendix 8 Table of impacts from documents
| CLAHRC | Document no. | Impact |
|---|---|---|
| Hazeldean | 1 | CKD collaborative: practices identified 1324 patients with CKD over 12 months, equating to 92% of target set |
| CKD collaborative: 40% improvement of patients on CKD registers being managed within NICE blood pressure targets, the equivalent of up to 1800 patients getting better BP management | ||
| CKD collaborative: 55% improvement in patients registered with CKD having urine tested for protein | ||
| CKD collaborative: in one PCT the participating practices showed a reduction of 43% of referrals to secondary care | ||
| 3 | IGT care call project: 77% of patients achieved their overall goal of lifestyle change | |
| IGT care call project: 74% (n = 35) of patients achieved a significant weight loss through the time of the care call | ||
| IGT care call project: 69% (n = 20) of patients reduced their Finnish Diabetes Risk Score (FINDRISC), with eight patients reducing their score enough to drop to a lower classification | ||
| IGT care call project: 63% (n = 26) of patients reduced their BMI score by an average of 3.02 points per person | ||
| IGT care call project: at the start of the project 35% (n = 18) of patients reported having no daily fruit or vegetable intake. Of these 83% (n = 15) increased their fruit and vegetable intake to daily following their participation in the project | ||
| IGT care call project: 38% (n = 20) initially reported not taking any regular exercise activity at the start of the programme. On completion of the programme 75% (n = 15) reported participation in regular exercise activity | ||
| IGT care call project: of 41 patients who had an OGTT performed at the end of the care call programme, 75% (n = 31) showed a reduction in their 2-hour OGTT | ||
| IGT care call project: on completion of the programme 51% (n = 21) had a fasting blood glucose and OGTT result within the normal range and were no longer classified as having IGT | ||
| 4 | Stroke assessment tool: the stroke assessment tool is being used in 24 services across England | |
| Stoke assessment tool: over 4000 patients have already been reviewed using the tool | ||
| 5 | Stroke assessment tool pilot: 464 unmet needs were identified in 137 post-stroke reviews | |
| 6 | HF alert cards: over the 12-month period of the pilot, 74% (n = 119) of patients on the HF specialist nurses (HFSN) caseloads were issued with HF alert cards | |
| HF alert cards: in 80% (n = 49) of cases the HFSNs were informed that a patient on their caseload had been admitted to hospital | ||
| HF alert cards: of the above 49 cases, 37% of notifications came from secondary care, which was a 100% increase from the previous 12 months | ||
| HF alert card: in two of the 49 cases (above) the HFSNs were contacted by a hospital outwith their catchment area and once by a rehabilitation unit as a direct result of the alert card, which had never happened before | ||
| 7 | Mental and physical health project: the consensus (100%, n = 10) from the post-project interviews with GPs, practice nurses, care co-ordinators and community physical health checks (CPHCs) is that physical health care is becoming more co-ordinated between primary care and the community mental health team | |
| Mental and physical health project: 69% (n = 9) of care co-ordinators stated that the MDT meetings had a positive impact on patient care, with 92% of them having carried out actions generated from MDT meetings | ||
| Mental and physical health project: in 24 MDT meetings (September 2012 to March 2013) 101 service users were discussed and 163 actions relating to their physical health were agreed | ||
| Mental and physical health project: an audit of the GP clinical practice systems relating to the information recorded about service users’ physical health showed that there was a marked improvement of 25.7% in the amount of information recorded. During the exploratory stage there were missing data for 62% (n = 115) of service users; after the project this had improved, with data missing for only 42% (n = 79) of service users | ||
| 8 | HF investigation tool (HFIT): at reaudit of GP practice registers 78.96% (n = 259) were appropriately on the HF register, an increase of 32.19%. The proportion of patients requiring investigation was 18.29% (n = 60), a decrease of 16.02% | |
| HFIT: there was an improvement in the prescribing patterns for ACE inhibitors and beta blockers for patients with left ventricular systolic dysfunction. Reaudit showed that there was an increase in the prescribing of recommended ACE inhibitors of 30.53% and an increase in recommended beta blocker prescribing of 35.08% | ||
| HFIT: reaudit showed that the percentages of patients documented as contraindicated and where ACE inhibitor therapy was being up-titrated increased by 27.91 percentage points and 11.74 percentage points respectively | ||
| HFIT: reaudit showed that the percentages of patients documented as contraindicated and where beta blocker therapy was being up-titrated increased by 97.95 percentage points and 8.61 percentage points respectively | ||
| HFIT: the number of HF reviews performed in primary care increased by 216.72% and the number of patients attending specialist services decreased by 25.82% | ||
| HFIT: in the 10 practices reaudited, the overall prevalence of HF increased from 0.56% to 0.67% | ||
| HFIT: as a direct result of participating in the HF project, one GP practice decided to implement long-term condition reviews that incorporated HF, rather than conducting individual disease reviews | ||
| 9 | CKD: second wave projects:
|
|
| Oakdown | 1 | Dysphagia e-learning programme: all participants reported gaining new knowledge about dysphagia. The majority also said that they acquired new knowledge and skills about thickening fluids. The most important learning points related to practical strategies, reducing risks and educating patients and their families |
| Dysphagia e-learning programme: all health-care assistants (n = 10) demonstrated improved practical knowledge on the post-programme and follow-up questionnaires. Their increasing scores indicate the acquisition, retention and further development of ‘know-how’ in the weeks after the training | ||
| Dysphagia e-learning programme: most staff reported putting their action plan into practice, giving specific examples, especially about medicines management, thickening fluids, oral hygiene and educating others | ||
| Dysphagia e-learning programme: there was discussion and actions about dysphagia-related topics such as oral hygiene, refeeding syndrome, the administration of medicines via enteral tubes and first aid/using the Heimlich manoeuvre with patients in bed or a wheelchair | ||
| 2 | Implementation of COPD care bundles: bundle implementation in one named place has facilitated the achievement of a specific bundle CQUIN target within the trust | |
Implementation of home oxygen pathway resulted in:
|
||
As a result of the EQONS (Enhancing the Quality of Oral Nutrition Support) project:
|
||
VTE project:
|
||
Dysphagia project:
|
||
Findings from the Keeping Warm in Later Life (KWILLT) project have been incorporated into, for example:
|
||
| 3 | Comfort Club – supporting women with post-natal depression through community empowerment. A number of impacts from attending the clubs were noted:
|
|
A proactive tissue viability service: preventing pressure ulcers: as a result of this initiative there has been:
|
||
| Ashgrove | 1 | Role of CLAHRC co-ordinators:
|
| 2 | Role of CLAHRC co-ordinators:
|
|
| 3 | Creation of evidence: results of a research study into elective hospital admissions found:140
|
Appendix 9 Participant information sheet
Appendix 10 Participant consent form
Glossary
- Plan, Do, Study, Act
- An improvement approach based on achieving small, incremental changes.
- Research Excellence Framework
- A national exercise carried out to judge the quality of research output in the UK.
- Second gap in translation
- The gap between the development of an effective intervention and its routine use in practice.
List of abbreviations
- AHSC
- Academic Health Science Centre
- CCG
- Clinical Commissioning Group
- CKD
- chronic kidney disease
- CLAHRC
- Collaboration for Leadership in Applied Health Research and Care
- CMO
- context–mechanism–outcome
- COPD
- chronic obstructive pulmonary disease
- CQUIN
- Commissioning for Quality and Innovation
- GP
- general practitioner
- HEI
- higher education institution
- HF
- heart failure
- K2A
- Knowledge to Action
- KT
- knowledge translation
- MUST
- Malnutrition Universal Screening Tool
- NIHR
- National Institute for Health Research
- PARIHS
- Promoting Action on Research Implementation in Health Services
- PCT
- primary care trust
- PPI
- patient and public involvement
- QOF
- Quality and Outcomes Framework
- R&D
- research and development
- REF
- Research Excellence Framework
- T2
- second gap in translation
- VTE
- venous thromboembolism