Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 10/1010/06. The contractual start date was in July 2012. The final report began editorial review in February 2015 and was accepted for publication in August 2015. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Disclaimer
This report contains transcripts of interviews conducted in the course of the research and contains language that may offend some readers.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2016. This work was produced by Pinkney et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction, study objectives and literature review
Introduction
The demand for emergency medical care in the UK has escalated annually, leading to unparalleled pressures on emergency departments (EDs) and acute medical admissions units (MAUs). These pressures can adversely affect patient experience through overcrowding, long waiting times, delays in investigation and diagnosis, and potentially suboptimal decision-making. Negative consequences for acute hospitals include a persistent state of near-capacity bed occupancy, cancellation of elective work and pressures on the workforce. There has been a widely held view, supported by some evidence, that a significant proportion of acute admissions might be avoidable. The appropriateness of a hospital admission can be understood by examining the interactions, organisational culture and system contingencies that prevailed at the time that this decision was made. The Avoidable Acute Admissions (3A) project aimed to investigate the interplay of factors influencing decision-making about emergency admissions and to understand how the medical assessment process is experienced by patients, carers and practitioners. The study represented a collaboration involving the universities of Plymouth, Exeter and the West of England, and four acute hospital trusts in South West England, which are anonymised in this report. The research was led by the academic partners in partnership with clinicians and managers at these four hospitals. Patient and public involvement (PPI) throughout the research was supported by the Collaboration for Leadership in Applied Health Research and Care South West Peninsula (PenCLAHRC). The study received research ethics committee approval to commence on 1 July 2012 and was completed on 31 January 2015, following a 6-month no-cost extension agreed with the funder. The study’s final report has been elaborated using a combination of COREQ (consolidated criteria for reporting qualitative research) and STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) reporting guidelines. Prior to 3A, there had been little research on acute admissions from a perspective that attempted to understand patients’ and practitioners’ experiences and the processes involved in decision-making. The premise of the 3A study was that acquiring this understanding was a prerequisite for assessing the appropriateness of decision-making in patient journeys in particular. This research aimed to fill an evidence gap and inform policy-makers and NHS managers about the experiences of patients and practitioners in emergency medical departments. By investigating the care models used by different hospitals to organise their emergency service provision, the research aimed to identify service configurations and innovations that were associated with reduced likelihood of hospital admission, enhanced patient experience and best practice. Understanding the patient-centred perspective is likely to be of prime importance in planning improvements to emergency care in the NHS.
Overall aim
To investigate how clinician expertise and models of care in four contrasting hospitals contributed to appropriate decision-making regarding admissions in acute medical care; and to make recommendations about different admission avoidance models and their likely impact on workload management at the hospital front end.
Objectives
-
To investigate influences on decision-making about admissions in acute medical care.
-
To investigate how frontline experience and new models of care contribute to reducing avoidable acute admissions.
Research questions
-
What influences are operating in the acute admissions decision process?
-
This question was considered from the perspective of:
-
patients and relatives or carers
-
medical and other clinical staff responsible for decision-making (the role of early senior input in admission avoidance was specifically considered)
-
organisational factors that may influence decision-making.
-
-
How is the whole admissions process experienced by patients and practitioners?
-
How are the four models of care similar and different?
-
How does patient experience vary in each setting?
-
How are different ideas and policies and incentives adopted in each setting?
-
How often do the potentially critical components of care (e.g. early senior input) occur for potentially avoidable admissions? How does this vary by diagnostic group?
-
How is each model of care associated with demographically adjusted admission rates?
-
How does the cost of providing care during the unplanned admission process relate to different organisational models, and do such models have different impacts on workload management?
-
-
How can frontline expertise and new models safely reduce rates of admission?
Background
Literature relevant to the project was discussed in regular reading groups, where team members reviewed publications in specific areas (see Appendix 1). At the start of the project, researchers met to discuss key texts that had been identified in the initial study proposal. In subsequent meetings, the team developed a method for focusing reading groups on jointly reviewing collections of 6–11 texts relating to particular topics. The topics and texts were selected in response to emerging study findings, such as factors influencing decision-making, patient experience, safety and efficiency, senior input, and teaching and learning. The reading groups identified the themes in the sections that follow as particularly important for the study.
Growth of emergency admissions
The context for the 3A study was the 2010 Nuffield Trust report,1 describing the rapid growth of emergency admissions in the UK between 2004 and 2009, and local concerns in South West England. In this period, numbers of emergency admissions in England rose by 11.8%, resulting in 1.35 million extra admissions. There was a large rise in short-stay admissions, and one possible explanation was that this might reflect a decline in longer-stay admissions. Alternatively, it was possible that increasing numbers of less severe cases were being admitted, perhaps because the clinical threshold for admissions had been reduced. 1 More recently, the National Audit Office observed that there were 5.3 million emergency admissions to hospital in 2012–13, representing a 47% rise over 15 years. The annual cost to the NHS rose to around £12.5B. Overall, 26% of patients attending EDs were admitted. There was a 124% rise in short-stay admissions, and 850,000 acute bed-days were lost because of delayed discharges. Moreover, 50% of emergency medicine training posts were unfilled in 2011–12. 2
There was also significant variation between NHS trusts in England: in some, emergency admissions declined by a third, while in others they almost doubled. There was also variation between primary care trusts. These data suggested that admission rates are influenced by factors unrelated to medical need. Emergency admission rates were found to be twice as high in the most deprived areas as in the least deprived areas. 1 Research by O’Cathain et al. estimated that 22% of admissions were potentially avoidable, and that there was a threefold variation in potentially avoidable admissions. 3 This finding supported the results of an earlier meta-analysis. 4 However, O’Cathain et al. also linked high avoidable admission rates with unemployment. Furthermore, there was demographic variation in sociocultural expectations of emergency care, with evidence of significantly increased avoidable admission rates in urban compared with rural areas, and for younger compared with older patients. 3 Avoidable admission rates were also higher for hospitals with higher ED attendance rates, higher numbers of acute beds per 1000 population, and higher conversion rates from ED attendance to admission. 5
The Nuffield Trust report1 and the research by O’Cathain et al. 3,5 reinforce the idea that many acute hospital admissions are medically non-essential and therefore probably represent suboptimal use of resources, in addition to exposing people to potential iatrogenic harm. However, neither of these studies specifically sought the patient or ‘user’ perspective on ED attendance. The premise for the present study was that a significant proportion of emergency medical admissions are potentially avoidable for a range of different reasons, and that, if ED experience is better understood from the patient perspective, there may be opportunities to handle some acute admissions more appropriately, with resulting benefits for patients and the NHS.
Quality and efficiency
Since its introduction in 2000, the 4-hour standard has had a major influence on the way in which EDs have responded to rising demand. This target was introduced to improve patient experience and outcomes by ending lengthy ED waits, particularly for patients requiring admission. The target was also seen as an instrument to enhance patient safety, but it was not observed to promote safety and quality of care to the same extent as efficiency. NHS quality indicators were introduced in 2011 to address perverse effects of target compliance. 6 Although the target time for discharge or admission was designed to improve patient flow, co-operative working with other services and departments often presented a challenge. 7 Recent studies have found some indications of variation in the coding of admissions, with patients in some clinical areas coded as admissions while patients’ overnight stays in other clinical areas might not be coded as admissions or breaches. 8
The 4-hour target has been considered a blunt tool to drive quality improvement in emergency care systems. 9 The quality of hospital emergency care has come under new scrutiny, and the Royal College of Emergency Medicine has called for wholesale system redesign, better care integration, greater resourcing of clinical decision and ambulatory care units (ACUs), and improved governance, staffing and skill mixing. 10 Much existing literature focuses on systems and patient flow, in contrast to the lack of research on patient experience. 10
Crowding and waiting times
Crowding is a visible manifestation of high demand. While ED waiting times have attracted considerable attention, the phenomenon of crowding has been little addressed in the UK literature. 11 High demand that outstripped capacity was considered to increase risks of certain types of critical incident. 12 High demand appears not to be explained by frequent attenders; rather, this patient group generally has more urgent needs,13 and makes appropriate use of urgent care services. 14 Crowding and long waiting times may lead to poor user experience, and to safety being compromised: times of overcrowding in one ED were associated with an increased 10-day mortality rate. 15
Crowding occurs when demand outstrips capacity and may arise in the face of both appropriate and inappropriate demand. Higginson et al. suggested ways in which demand and capacity planning could address this problem. 16 Strategies to combat overcrowding were the focus of a report by the Royal College of Emergency Medicine,17 which recognised that a range of hospital and community initiatives were required to tackle the problem. Higginson et al. drew attention to the international recognition of crowding as a significant concern, raising the question of how to address this issue in the UK. 11 The 4-hour target alone has been an inadequate instrument to address complex issues responsible for crowding, long waiting times and quality issues. There has been concern that undue focus on flow may detract from patient-centred care. 9
Practitioner experience
High levels of demand for emergency medical assessment associated with ED crowding placed considerable expectations on staff. An ethnographic study from Australia described how the work of ED staff focused on management of patient flow,18 but the experiences of staff working in EDs have received little attention. Workplace pressures may significantly contribute to recruitment and retention problems in this specialty. 19
Several studies have investigated teamwork in EDs. Recent studies using social network analysis found wide variation in the frequency of communication between ED staff working on different shifts,20 which could influence quality of care. A systematic review found evidence that multidisciplinary teams in EDs probably reduce access block, and that physiotherapists could play a role in this. The need for ED teamwork and communication was also related to safety improvement and reduction of waiting times. 21 Communication at team handover was highlighted as an important factor influencing admit/discharge decisions and quality of care. Jeffcott et al. 22,23 introduced the concept of ‘resilience’ and, using clinical handover as the example, suggested that it could be beneficial to understand and adopt elements associated with good outcomes, rather than solely focusing on problems. Another recent study of clinical handover found that only 1.5–5% of handover conversation content related to patients’ social and psychological needs,24 when these were highly likely to influence outcomes.
Demand, capacity and safety
Significant variations in emergency attendances and admissions by day of the week and time of day are well known. 2 Although there are fewer attendances and admissions at weekends, a recent analysis of 4,317,866 episodes of emergency care in the UK observed 10% higher mortality at weekends. 25 Concern about fluctuations in the quality and safety of care across times and days of the week had led to recommendations for 24/7 staffing for acute service provision in hospitals. 10
Measures to reduce avoidable admissions
Decisions about hospital admission reflect the impact of policies generated both by financial and safety concerns. Influences on decision-making include medical need, social considerations, family and carer expectations, experience and seniority of decision-makers, system factors, policy directives and the availability of alternatives to admission. Efforts have been invested in exploring admission prevention and avoidance through the development of community-based chronic disease models. 26 However, there is more limited research to support the wide variety of initiatives currently being developed at the ‘front door’ of NHS hospitals and examined in this project. Early streaming of urgent and less urgent cases was first tested in the 1980s in order to reduce waiting times and reduce duration time in EDs27 and has since become widely adopted in many countries. However, few patient-centred data were found relating to the avoidability of acute admissions.
Early senior input and managing flow
Several studies supported the idea that early triage by more experienced staff might improve decision-making and patient flow. Early research showed that patients assessed by more experienced doctors were substantially less likely to be admitted or subsequently readmitted than those seen by less experienced doctors. 28 More recent research showed that early physician involvement reduced the time spent by patients in ED beds. 29 Physician screening of less urgent cases, and early initiation of care for more complex patients, were associated with reduced treatment and discharge times. 30
Compared with middle-grade and junior doctors, ED consultants admitted significantly fewer patients, referred fewer patients to clinics and had a faster patient turnaround time. 31 A variation of the ‘senior first’ model was a combined doctor–nurse early triage system that expedited medical assessment and discharge from an ED. 32 An observational study found that inpatient admissions were reduced by 12% and admissions to an acute medical assessment unit were reduced by 21% following early review by a senior clinician. 33
In December 2010, the Royal College of Emergency Medicine introduced a clinical standard relating to consultant review of high-risk patients. 34 This concept was adopted by the UK Department of Health as a key quality indicator for emergency care. 6 The Royal College of Emergency Medicine also highlighted the need for consultant expansion if capacity were to match demand for 24/7 access. 35 The Royal College of Emergency Medicine also argued against ‘gate-keeper’ functions and emphasised that early senior input was essential to control crowding. 17 However, most studies on the involvement of senior staff in emergency medicine have adopted a quantitative approach, have been based on relatively small samples and have not explored the experiences of patients and staff.
Reconfiguring hospital emergency care
The debate about how best to configure emergency medical care, and for which patients hospital admission is appropriate, is part of a wider dilemma between ‘senior/specialist first’ and ‘stepped care’ throughout the NHS. Several care configurations have been explored in attempts to reduce ED congestion. The presence in EDs of general practitioners (GPs) focusing on patients with primary care needs was found to reduce costs of emergency care. 36 A review by Carson et al. 37 found fewer referrals for admissions when GPs worked in EDs than with standard care. In another study, a hospital-based acute GP-led service, designed to provide support to community GPs, was found to modestly reduce numbers of GP admissions to the MAU, although the overall number of GP admissions to hospital wards was not necessarily reduced. 38
There was some evidence that specifically targeted measures might reduce inappropriate admissions of certain patient groups. A recent report highlighted the needs of elderly patients, emphasising better community-based services with rapid access, and improved recognition of problems such as confusion, falls, polypharmacy and safeguarding issues. It was suggested that greater use of care of the elderly liaison services in MAUs might increase the proportion of older people who could be managed in a community setting. The commissioning of evidence-based integrated health and social care was seen as essential. 39 A triage and early treatment system for elderly patients in London appeared to reduce avoidable acute hospital admissions. 40
There was much interest in reconfiguring the management of ambulatory care-sensitive conditions to reduce unnecessary admissions. A group of 19 common conditions, accounting for about one in six of all acute admissions, was considered suitable for medical management outside hospital,41 although it was acknowledged that concomitant social factors also had to be addressed. The related issue of avoiding unnecessary admission of people with chronic conditions was also recognised,42 together with evidence to support various interventions that could reduce unnecessary admissions. 43 Many acute hospitals have prioritised the identification and treatment of ambulatory care-sensitive conditions in order to avoid admission, as recently reported from Plymouth. 44
In summary, the literature pointed to potential advantages in reconfiguring various aspects of emergency care. There were possible disadvantages in terms of deployment costs and loss of training opportunities associated with having experienced practitioners at the front line. Given the lack of evidence in this area, there was a need to understand the benefits and disadvantages of different configurations.
Decision-making in acute medical admissions
Although decision-making is pivotal to admission and discharge planning, much remains to be understood about this process. The diversity of system and clinical practices that underpin decision-making during a patient’s journey through emergency care was noted by Lattimer et al. ,45 who studied this subject from the workforce perspective. The patient journey started with help-seeking in the community and initial contact with a professional either in the community or at the hospital ‘front door’. The scenarios and styles of decision-making were variable, ranging from entirely medical ‘paternalistic’ decision-making – particularly in medical emergency situations46 – through to more complex situations where there could be several options in which decision-making was shared between professionals, or between professionals and patients. Skill mixing involving other types of professionals might also enhance the speed and quality of decision-making in EDs, although Lattimer et al. 45 considered that further research was required on this subject. In support of this idea, however, non-medical emergency care practitioners (ECPs) were found to be able to deliver care to a similar standard to that offered by medical practitioners. 47
A priori, it was expected that decision-making would be broadly influenced by patient, practitioner and organisational factors, and that outcomes would be affected by individual beliefs, attitudes and expectations, personal resources and functioning, specific illnesses and comorbidity. 48 Domestic resources and the wishes and interventions of family members and carers could also be relevant. Research examining patients’ views of hospital admissions found that 70% of patients specified possible alternatives. 49 Professional factors included the experience, attitudes and beliefs of doctors. 50 Hensher et al. 51 examined decisions made about alternatives to hospital care, finding that consultants often chose hospital admission and were more likely than GPs to state that there was no alternative to this. A recent study considered why patients with primary care problems – often with long-term conditions – called for ambulances, and concluded that poor knowledge of alternatives, anxieties of carers and attitudes to risk were some of the factors that channelled people unnecessarily towards secondary care. 52
Organisational factors – including commissioning and monitoring arrangements, the model for admissions pathways and the governance and culture of organisations, as well as the wider health and social care system, including the availability of community-based care – could all contribute to the likelihood of hospital admission. Attention to these factors could also help to ensure provision of timely, appropriate and high-quality care. In summary, greater clarity is needed to understand the variations in, and influences on, decision-making in acute admission settings.
Contribution of the study
The aim of this study was to examine the patient journey, from initial help-seeking through to the consequences of the admission decision, in four hospital settings spanning novel and traditional approaches, focusing on research questions (RQs) informed by the above-mentioned evidence. The decision to admit or not to admit was the focal point of the 3A study. The study aimed not to test one approach against another, but rather to explore models developed in South-West England.
This literature review confirmed a paucity of evidence about the patient journey through the acute admission process, and about organisational and professional factors that contribute to individual decisions to admit or to discharge. A review by Nairn et al. 53 identified a range of patients’ concerns in emergency care including waiting times, communication, cultural aspects of care, treatment of pain and the care environment. However, that review did not examine how these concerns affected decision-making.
During the course of the study, new publications emerged in all the areas discussed above. Clinical practice has been influenced by a combination of ‘top-down’ and ‘bottom-up’ initiatives that aim to manage fluctuating demand in a capacity-limited system, maintain patient flow and ensure safety. As highlighted by the 2013 King’s Fund report on patient-centred leadership,54 in the wake of the 2013 Francis report55 there is a need for the NHS to embrace a primary focus on patient care and experience. The Royal College of Physicians’ report Future Hospital: Caring for Medical Patients56 emphasised many related themes including early specialist care when needed, multidisciplinary evaluation that meets the needs of all patients, including the elderly, and the need for improved communication at the community–hospital interface. However, the patient voice has been largely absent from this literature.
As is apparent from the literature review, the patient voice and the experience of patients and practitioners, have been largely absent from previous research on EDs. However, there is growing acknowledgement of the centrality of patient experience for the NHS, and of the need to consider practitioner experience and system design in planning and policy. We therefore undertook a mixed-methods study of patients’ journeys through emergency medicine departments at four acute hospitals with contrasting models of care. In 3A, journeys are captured from the perspectives of patients, carers and practitioners, and set in the context of the resources available in these emergency medical units. The study interprets decision-making in acute admissions by synthesising these streams of evidence and examining them through the lens of realist evaluation.
Chapter 2 Study design and methodology
Overall design
The project used a case study design, drawing on both qualitative and quantitative methods, for an analysis of service design and practitioner deployment on decision-making about admissions in four acute admission sites in South West England. The study was funded by the National Institute for Health Research (NIHR) Health Services and Delivery Research programme as part of a call for new research into the factors affecting emergency medical admissions to hospital (project reference number 10/1010/06) and ethical permission was obtained (Integrated Research Application System reference number 98931, Research Ethics Committee reference number 12/SW/0173).
The primary research comprised two main parts, with qualitative and quantitative phases of research on each site:
-
value stream mapping (VSM), to measure time spent on key events in patient pathways, with an embedded study of cost
-
ethnography with participant observation and semistructured interviews, incorporating observation of patient journeys, a selection of which were written up as ethnographic patient case studies.
We also gathered data and received support with interpretation through the involvement of patients and carers, and of managers and practitioners in clinical learning sets, clinical panels (see Appendix 2), and mid-project (see Appendix 3) and end-of-project workshops.
Members of the project’s PPI group, which had a total of 14 lay members, participated in four half-day workshops during the course of the project. In two of the workshops, participants analysed qualitative interview data and a selection of ethnographic patient case studies. Some PPI group members also participated in stakeholder discussions in the mid-term and end-of-project workshops, and in the two clinical panels that examined ethnographic and VSM patient case study material (see Appendix 12). PPI contributions to the project are further detailed in Appendices 4 and 5.
Managers and practitioners from the four research sites joined researchers in learning sets moderated by an experienced action-learning facilitator. The learning sets’ objectives were to channel professionals’ input to the project, enable the exchange of experiences, interpret some study data, validate emerging findings and identify actions that could address some of the problems encountered in the research. A total of 35 learning set members participated in one cross-site meeting, four site-specific meetings, and the mid-term and end-of-project stakeholder workshops. Learning set participants’ common themes, questions to the project and ‘burning issues’ are detailed in Appendix 6.
Hospital Episode Statistics (HES) data and documents from each site were used to describe the contexts in which decisions were made.
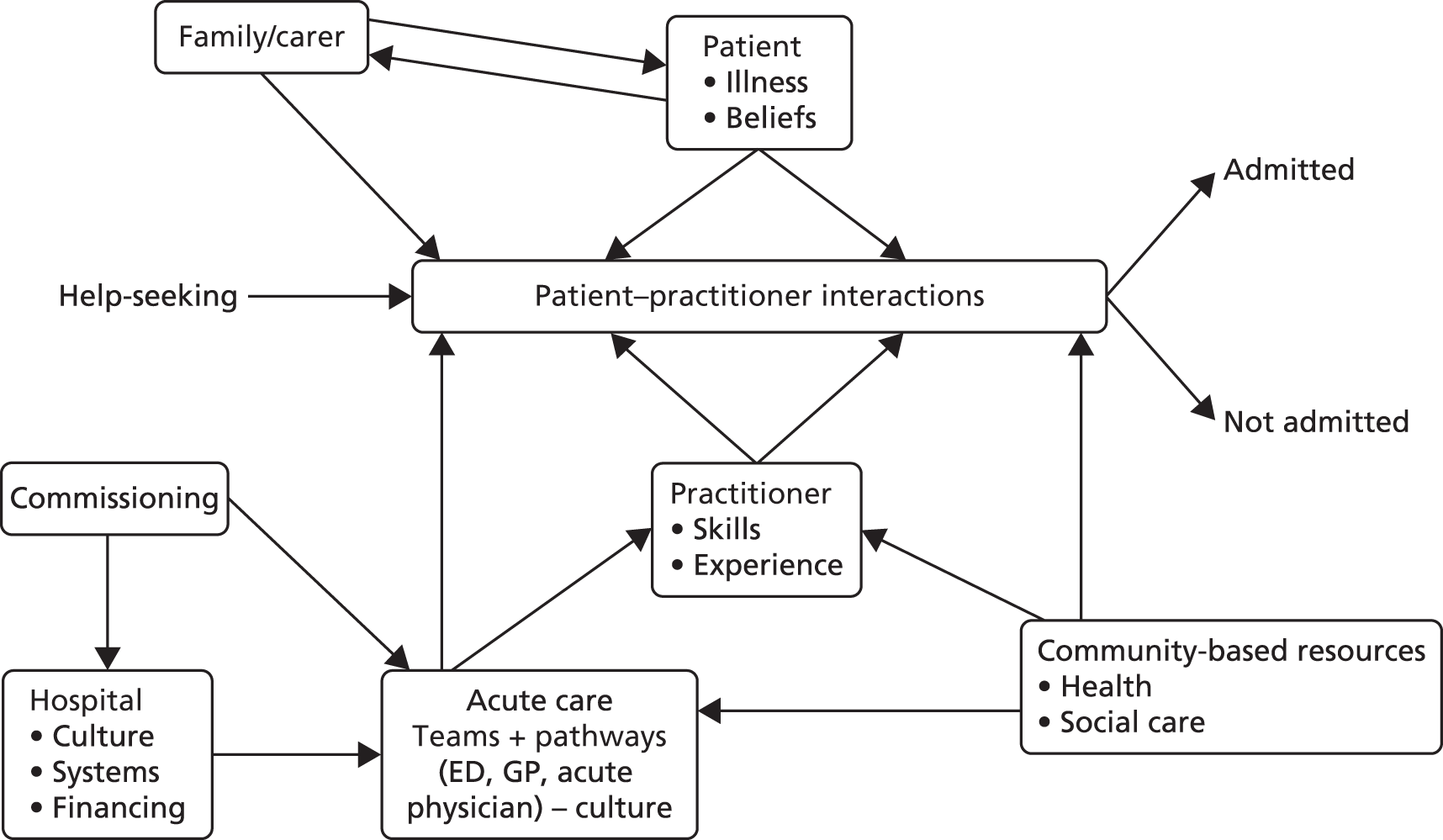
Critical realist evaluation57 was used as an overarching conceptual framework for the study and formed the basis of the method used to synthesise the different data streams and develop best-practice models. Figure 1 depicts the domains of influence on admission decisions that were brought together in the synthesis.
FIGURE 1.
A conceptual map of the influences on acute admission decisions.
Methodology and conceptual/theoretical framework
To achieve the project’s objectives, which were descriptive and exploratory in an area of care that has, to date, received little detailed attention, we selected a combination of qualitative and quantitative methods. We conceptualised each research site as a ‘case’, as set out in Stake’s typology,58 in which the collective case study aims to examine a number of cases in combination, to gain deeper understanding about a more general phenomenon. The idea of this type of study is to select varied cases (our four hospital sites) that are not necessarily representative of a wider pattern, but that show a certain balance and offer opportunities for comparison and learning.
In addition, in the VSM study and synthesis, we compared how components of the four services affected decision-making. Full individual case study analyses were not carried out and we did not aim to identify any one of the cases as having a superior model. The synthesis was concerned with understanding how best to achieve the key outcomes we identified: (1) appropriate admissions, (2) safe discharges and (3) improved patient experience. The synthesis generated a set of principles incorporating statements about how elements of a model of acute care can contribute to these outcomes. It did not aim to determine or quantify actual impact.
We conceived the decision-making process as occurring over some hours, involving practitioners from different teams and potentially a number of settings. While we sought to understand the influences on decision-making, we were aware that it would not be feasible to derive quantitative estimates for the effects of causal factors involving many individuals, teams and locations. We therefore selected methods that could enable in-depth analysis of decision-making alongside a broader investigation of the various influences.
We selected VSM, as a ‘Lean thinking’ method, which has been adapted for use in health services to study the timing and perceived value (or waste) incurred by different procedures and inputs throughout a pathway (see Appendix 7).
Ethnography has been used in many studies of health services. 59,60 It combines researcher observation and interviewing, and provides a flexible means of taking both a wide view on potential influences and a detailed picture of interactions between practitioners, patients and carers. In the qualitative phase of each hospital case study we used an ethnographic approach, incorporating fully participant observation and detailed fieldnotes, based on the epistemological understanding that:
-
the researcher is the primary instrument for generating (rather than ‘collecting’) data
-
the researcher’s identity and presence necessarily affect the process of generating data in interaction with study participants
-
participants’ awareness of the researchers’ presence and the study’s agenda can lead them to enact models of behaviour that exemplify values and practices they deem to be more publicly acceptable, but that nonetheless generate valuable study data.
In accordance with this interpretive approach, researchers pursued rigour from the outset of the study by doing preparatory work, individually and as a team, on our preconceived notions about the study theme and our expectations about fieldwork. We used reflexivity in team discussions throughout the study as a tool to minimise the effects of personal bias on selection of participants and ongoing analysis of data. Other aspects of rigour will be covered in Analysis of ethnographic data.
Ethnography is commonly associated with a constructivist stance but it has also been used in critical realist studies. 61 The critical realist framework allowed us to consider the admissions process as being influenced causally at two levels: that of the opportunities and resources available to practitioners within acute care settings, and that of interactions linking practitioners, patients and family members.
Mixed methods
We conducted the VSM and ethnography components separately, although each influenced the other, and both contributed to answering RQs 1–3 (see Chapter 1, Research questions). The ethnography was carried out during the first half of the project and informed the planning of the VSM study. Integration of VSM fieldwork and ethnographic analysis was promoted through regular meetings of both teams, and through researchers’ day-to-day input to an electronically shared file with notes on field observations. Findings from these and other project components were used to generate hypotheses about causation in acute admission decisions during the project and as part of the final synthesis. Initial analysis of the VSM data led to further analysis of the ethnographic data. To provide continuity following the site descriptions (see Chapter 3), the VSM study (see Chapter 4) precedes the ethnographic chapters (see Chapters 5 and 6), which are exploratory in nature. The synthesis of findings (see Chapter 7) makes some tentative hypotheses about how emergency care could best be provided, answering RQ 4 (see Chapter 1, Research questions).
Patients and carers
A PPI group (see Appendices 4 and 5), whose members had experience of acute admissions, worked with the team on the approach to obtaining informed consent, design of research instruments, interpretation of ethnographic data and patient case studies, and construction of value stream maps.
Managers and practitioners
On each study site, a lead practitioner or manager – who changed over time in two sites – was the main link with the project. A cross-site learning set was developed to enable practitioners, managers and researchers to discuss lessons learned about the acute admission process. Findings from both study phases were discussed for each site in the learning sets (see Appendix 6).
In the mid-project stakeholder workshop (January 2014), a total of 29 patients, carers, clinicians, managers and researchers (study team and external invitees) reflected on the initial analyses in relation to their experiences. In the final stakeholder workshop (November 2014), a similarly conformed group of 27 participants contributed to the synthesis by working together to identify mechanisms influencing acute admissions within and across sites.
Ethical and governance arrangements
Ethical permission was granted by National Research Ethics Service Committee South West – Cornwall & Plymouth, on 22 June 2012. The study steering group of nine members (see Appendix 8) was convened on five occasions. Changes to the protocol as agreed with NIHR are detailed in Appendix 9.
Study sites
Site selection was purposive. Three sites had already adopted innovative ways of providing input from experienced clinicians (including GPs, and emergency medicine and acute physicians) early in the patient pathway. The fourth site followed a more traditional model, but all four sites introduced changes during the course of the study. Quantitative considerations in sampling included numbers of new ED attendances, admissions via EDs and hospital acute beds, and percentages of bed occupancy (see Table 4 and Chapter 3, Hospital Episode Statistics). All the sites approached agreed to participate.
The four sites, for which we use pseudonyms in this report (anonymisation details below), represented different models of acute care. Porthaven and Churchtown offered an alternative acute route into the hospital in addition to their EDs: both had medical assessment units, and in Porthaven an acute GP service (AGPS) operated in peak hours. Underbridge accepted all patients through the ED, where the care model dictated that they should be assessed by ED staff before transfer to a medical team. Waterbury, with a more traditional model, accepted all arrivals through the ED but then used ED staff for medically unexpected patients, and medical team staff for medically expected patients.
Anonymisation and referencing of sites and participants
Study participants recruited at the sites were given unique identifiers for purposes of anonymity and referencing. Each participant included in the study was assigned a unique coded identifier. A simplified version of these identifiers was used to label study participants referred to or quoted in the report; the labels used the site pseudonym and consecutive numbering. Coded identifiers were kept in password-secured files and safe electronic and physical storage.
Clinical panel review used independent numbering systems for patient cases summarised from ethnographic data, in order to guard anonymity of patients and sites. To further protect anonymity, these numbering systems only differentiated between ethnographic patient cases, and did not reference particular sites.
Value stream mapping
Site maps
Site mapping was used to depict the acute access routes into each of the four sites. Preliminary site maps were constructed during the mid-project workshop, with input from participating clinicians.
Study participants
Value stream mapping patient inclusion criteria
To optimise generalisability, we focused on patients about whom there was known to be uncertainty regarding need for admission on initial assessment. Two groups, for which numbers were predicted to be sufficiently numerous, were defined for the study:
-
cardiorespiratory presentations (excluding those with protocolised admission decisions, such as suspected myocardial infarction)
-
presentations typical of older age, in patients aged 60 years or older (such as acute confusion, falls, incontinence and decreased mobility).
Patients were included from all acute unplanned admissions pathways for adult medical patients. These included EDs, acute medical units (AMUs) and AGPSs. Routes to the hospital (e.g. ambulance, self-presenting, GP referral) were recorded and did not affect the inclusion criteria. To understand the main pathways, we initially aimed for equal numbers of medically expected patients (seen by acute medical teams and acute GPs, as organised by the referring GP) and medically unexpected patients. In Porthaven and Churchtown this meant recruiting in the two separate areas of the hospital housing the EDs and AMUs. Towards the end of data collection there was some targeted sampling of patients to achieve a balanced sample by gender and type of presenting condition (conditions typical of older age vs. cardiorespiratory conditions).
Approach and consent
Study participants were selected opportunistically and consecutively from the time the researchers arrived in the department. Hospital staff were asked to identify patients for whom it was unclear whether they would be admitted or discharged, and who were likely to meet the inclusion criteria.
Staff then consulted the patients about the potential for their involvement in the study. If their cases appeared appropriate and they agreed, staff introduced each patient to the researcher, who explained the study and discussed the possibility of their involvement. In a few cases patients were approached directly by researchers because staff were unavailable for introductions. Patients were included if they were willing and able to give consent.
Participant characteristics
Data collection for phase II of the project, the VSM study, began in April 2014 with a team of four researchers including an academic GP. In total, 108 patient cases were collected, as described in Chapter 4.
Data on the patient journey
The direct observation of the process involved:
-
observation of what was happening (or not happening) to the patient at every step
-
assessment of the process from the perspective of the patients and practitioners involved.
The VSM method was adapted for this project to provide additional data for key liaison activities (e.g. nurses discussing patients with doctors or providing treatment, juniors gaining advice from seniors). These data were gained from direct observation of staff and debriefing with key staff.
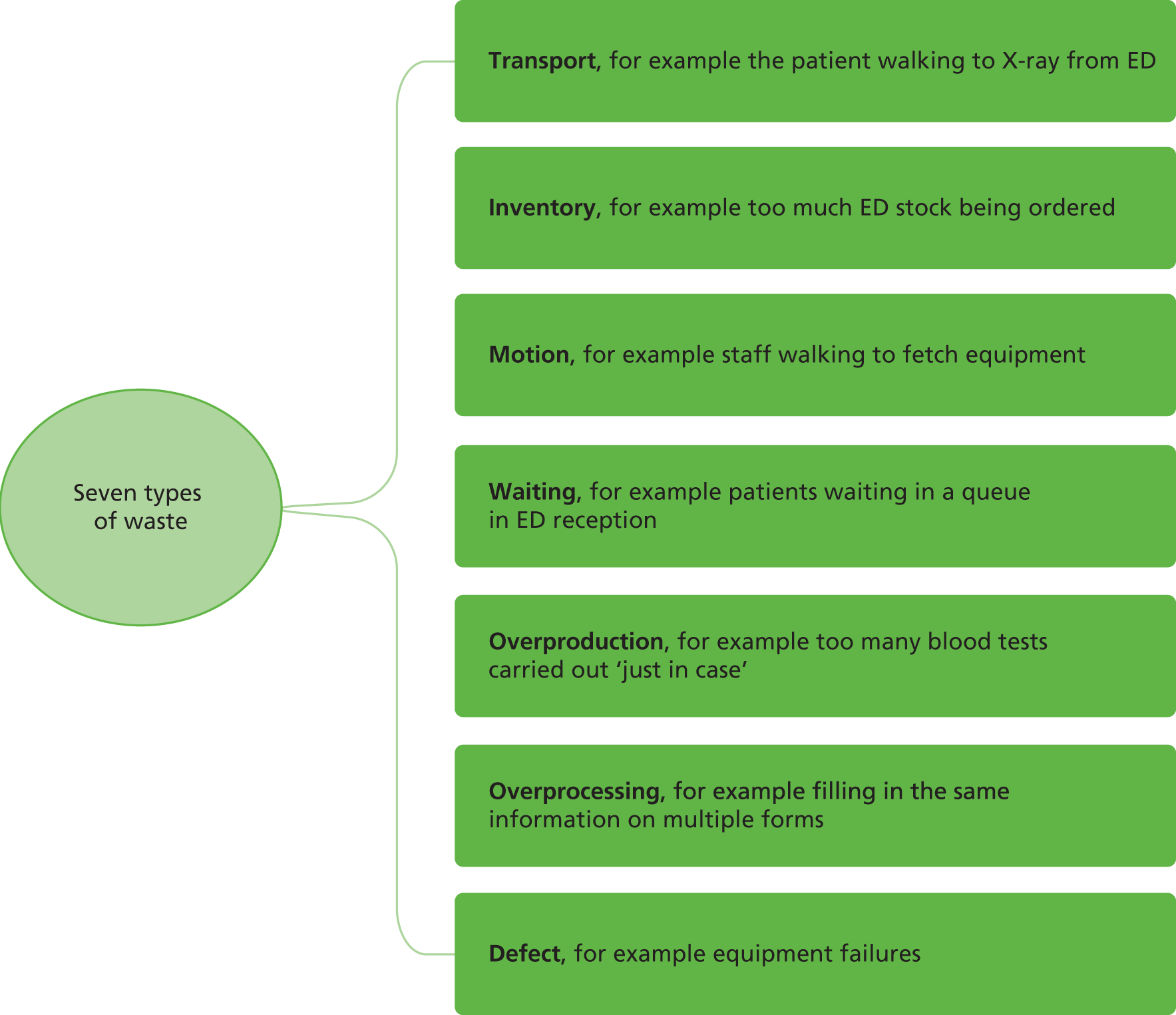
The details of each journey through acute care were recorded minute by minute, using the iPhone ‘HoursTracker’ application (Cribasoft LLC, Round Rock, TX, USA). The mapping process captured the seniority and number of medical staff involved in care, waiting times and diagnostic tests. The waste categories (such as transportation or looking for staff), and Lean values identified by Ohno,62 were applied by the researchers based on their interactions with patients and practitioners, in which they elicited views on the value of the care provided.
The ‘assessment of process’ was elicited from the principal clinical practitioner, who decided whether the patient would be admitted or discharged. These individuals were asked to consider, using a Likert scale, to what degree their decision had been affected by colleagues, the patient or his/her carer, availability of alternative care pathways, and additional factors.
This approach allowed us to apply the Lean principle of ‘thinking deeply’ about the problem to quantify and examine only those aspects of care processes that helped us to contrast the models of care at different sites.
The VSM study’s raw data therefore comprised detailed timings of stages of care throughout each patient’s journey, together with clinicians’ ratings of value, opinions on alternative care pathways and reflections upon their own decision-making.
Value stream mapping analysis
When conducting this analysis, we followed a methodological protocol to quantitatively describe and compare the acute care admissions pathways in the four NHS trusts (RQ 3), including:
-
patient pathway times overall
-
waste-to-value ratio
-
where in the ED process wastes were occurring
-
contrast among the proportions of patients who were admitted, were seen by different practitioners at different times and had investigations, including:
-
proportion of senior involvement
-
proportion of admitted patients
-
time first seen by a doctor
-
differences in patient hospital pathway
-
categorisation of known waits
-
patient pathway time for differing presenting conditions.
-
Economic analysis
We compared resource use and cost implications across the four sites for the core conditions and pathways, mainly through the value stream maps of the sampled patient pathways. Firstly, we compared economic data using data from each site relating to weekly staffing costs (grades and sessions/hours worked), to estimate the overall cost of care. Secondly, we used the data from the value stream maps to estimate how resources from the overall acute care system were reallocated to patients with potentially avoidable admissions. We then assessed the feasibility of estimating the opportunity cost of these resources.
The results of the two levels of cost analysis (hospital-level average costs; per-patient pathway VSM-based opportunity costs) are presented in the form of a ‘cost–consequence analysis’ alongside this provisional evidence of potential productivity differences (i.e. a simple balance sheet approach). Uncertainty and variability in cost estimates have been expressed quantitatively wherever possible (although, given the low number of, and non-randomly sampled, patient pathways for the VSM, these results are inevitably provisional and exploratory).
Ethnographic study
The ethnographic study was designed to generate understanding about influences on admission and discharge decisions, primarily through fully participant observation and semistructured interviews with patients and practitioners. During an initial period of orientation, researchers focused on understanding the ED’s geography, teams, systems and patient pathways; this included some in-depth interviews with managers and practitioners. Subsequently, the researchers collected data by following individual patient journeys.
Practitioners and organisation of services
Approach and consent of practitioners
We designed recruitment of practitioners on each site in conjunction with local collaborators. Flyers with general information about the study were handed out during researcher visits and posted on ward bulletin boards and in meeting rooms. Consent forms were distributed individually and at meetings so that staff had time to read them and decide if they wished to participate. In the case of 41 senior clinicians and managers who were purposively selected to be approached for in-depth interviews, information sheets and consent forms were delivered individually by e-mail or in person, together with a personalised letter. All these seniors gave their consent to be interviewed. The numbers of practitioners who consented to interview at each site is shown in Table 1.
| Site | Practitioners recruited through ethnography (number who gave senior in-depth interviews) | Practitioners recruited through VSM | Total practitioners recruited |
|---|---|---|---|
| A: Porthaven | 58 (11) | 26 | 84 |
| B: Churchtown | 69 (9) | 17 | 86 |
| C: Underbridge | 83 (10) | 39 | 122 |
| D: Waterbury | 72 (11) | 50 | 122 |
| Total | 282 (41) | 132 | 414 |
Semistructured interviews
On each site, 9–11 interviews were conducted with key informants: frontline clinicians (acute care consultants, acute GPs, lead nurses, ED consultants), senior managers and commissioners.
We used purposive sampling to identify individuals who were named by colleagues as experienced in decision-making and influential within the local model of care. Other health workers (including some seniors) were selected on pragmatic grounds to be approached for observation or brief interviews because of their roles in the care of patients who were the focus of ethnographic or VSM patient case studies. The overall strategy, combining purposive and pragmatic sampling, produced a broad sample of professionals that spanned varied staffing levels, types of contract and specialties.
During the set-up period, key informants were identified and topic guides for interviews developed and piloted (see Appendix 10). Interviews with clinicians combined semistructured questions about qualifications and experience of acute care settings, and open questions that explored perceptions about decision-making processes and factors influencing admission avoidance.
Participant observation of organisational processes, team composition and function (research questions 1, 3 and 4)
During set-up, we identified data-rich spaces where acute admission work could be observed. These included EDs, medical assessment and other units, and offices or clinical rooms used by patients and practitioners.
Patient journeys
Case study inclusion and exclusion criteria
Individual cases were selected on the basis of being ‘potentially avoidable’ admissions according to patient presentation. The selection of patients for ethnographic case studies was guided by the following criteria:
-
Cases were to be medical (not clearly surgical, although there was some overlap).
-
Cases were to be ‘uncertain’ enough for a decision to need to be made about whether or not they would be admitted (i.e. not a clear candidate for a predefined care pathway).
-
Patients were excluded if their condition, treatment or cognitive ability was not conducive to being approached by a researcher (e.g. in cases of severe illness, pain, reduced consciousness or states of dementia that did not allow sufficient recall for informed consent).
Sampling
Sampling of patients was both purposive (seeking patients with particular characteristics) and pragmatic (assessing which patients who were present could be suitable and available to participate in the study). We first checked patients who were suggested to us by staff against the inclusion and exclusion criteria listed above. We then enquired about the patient’s condition and treatment needs to avoid causing them any undue or unwanted disturbance. We purposively sought balance in sampling patients with particular types of presenting condition such as chest pain, ‘funny turn’ or collapse, shortness of breath, abdominal pain, and conditions typical of older age. We monitored our evolving sample in an ongoing way to achieve maximum variation in terms of gender, age and ethnicity. Notwithstanding South West England’s predominantly white UK demographic profile, a degree of ethnic diversity was purposively built into the sample on each site to maximise the potential for heterogeneity of patient experience. Pragmatic sampling was used to include relatives and carers who were present when patients were being observed or interviewed.
Approach and consent
Two strategies were used:
-
When researchers arrived for a fieldwork session, they asked co-ordinators and other staff to alert them about patients who might be suitable for case studies.
-
Researchers were guided by their own observations, which led them to identify certain patients as likely participants.
For both strategies, practitioners were asked to act as intermediaries, with the practitioner asking the patient if the researcher could make contact with them. If the patient accepted this initial contact, the researcher provided this patient with an information sheet (also available in large print) and gave further explanation as needed, using language that was comprehensible to that person. If any patients were unable to sign for themselves, relatives or carers could be asked to sign on their behalf.
Participant characteristics
As described in Table 2, 95 patients and carers gave their consent to participate in researcher observations, conversations and interviews. A further seven patients, and one carer, declined consent because they were too distressed or anxious or in too much discomfort to participate, or because they simply did not wish to participate in the study.
| Site | Patients | Gender | Age (years) range (median) | Ethnicity | Relatives and carers | Total participants | ||
|---|---|---|---|---|---|---|---|---|
| F | M | White British | Black and minority ethnic | |||||
| A: Porthaven | 13 | 9 | 4 | 26–92 (69) | 13 | 0 | 8 | 21 |
| B: Churchtown | 10 | 4 | 6 | 31–86 (68.5) | 8 | 2 | 6 | 16 |
| C: Underbridge | 14 | 7 | 7 | 23–89 (65) | 13 | 1 | 5 | 19 |
| D: Waterbury | 28 | 15 | 13 | 23–99 (73) | 24 | 4 | 11 | 39 |
| Total | 65 | 35 | 30 | 23–99 (70) | 58 | 7 | 30 | 95 |
Patient journeys
Ethnographic researchers documented patient journeys by making fieldnotes and holding recorded and non-recorded conversations and informal interviews with patients, carers and staff who had given consent before, during and after assessment and review of the case in question. Researchers made written fieldnotes during participant observation and/or as soon as possible after key events. Fieldnotes included descriptions of people, scenes, dialogues and decision-making processes, as well as personal experiences and reflections. Digital audio-recorders and smartpen recorders with Livescribe software were used to make recordings (Livescribe Echo Smartpen, Oakland, CA).
Transcription
All audio-recorded conversations and interviews were transcribed verbatim and uploaded to an NVivo (Version 10, QSR International Pty Ltd, Warrington, UK) ‘project’, or file used for data coding, which also incorporated researcher fieldnotes.
Analysis of ethnographic data
Coding
A framework approach63 was used to develop researchers’ understanding of key concepts in the study. The initial framework, expressed in the RQs, was based on the study proposal’s literature review. This was progressively adjusted in the light of findings that served to interrogate concepts that had formed part of the proposal, for example: How is an admission defined? Who is a senior? What meanings are given to patient waiting times?
We used two main elements from the framework approach:
-
The construction of a thematic tree that brought together categories from the project’s initial RQs, and categories that were inductively informed by coding of the initial field data. This is evidenced in Appendix 11, showing the final list of NVivo categories we used to code the ethnographic data.
-
Matrices that researchers constructed to tabulate data excerpts from specific NVivo nodes, ordered by research site, under headings referring to contexts, mechanisms and outcomes. We shared these in research team meetings and used them to elaborate context, mechanism and outcome configurations and analytical statements.
The body of data coded using NVivo 9 and included in the framework analysis consisted of ethnographic fieldnotes, interview transcripts and transcripts of audio-recorded conversations. This body of data came directly from fieldwork.
To maintain this coherence, the NVivo project did not include material that had undergone further processing by researchers, such as team meeting notes and the summaries of patient case studies, which were of two kinds: those compiled from ethnographic data, and those compiled from VSM data.
Researchers first coded their own data in separate NVivo projects, gradually adding more categories (‘nodes’) through an inductive process guided by grounded theory. The supervisors reviewed the data set and coded some data produced by each researcher. The four sets of codes were merged and, through a process of team discussion, the number of nodes was reduced to 49 (see Appendix 11); researchers then resumed coding using the agreed set. This instrument made the revised framework operational, and it enabled researchers to rapidly access and share ‘strings’ of data on particular themes. The process of opening up and redefining concepts was also informed by the reading group (see Appendix 1).
Integrated fieldwork, discussion and data analysis
Data analysis continued throughout fieldwork as an integrative part of the ethnographic method. Researchers discussed their insights and interpretations – gleaned from day-to-day field experiences, writing of fieldnotes, coding and revision of literature – in research team meetings (core team meetings, investigator meetings, fieldwork and analysis meetings, and one-to-one meetings with investigators who had specific expertise) and in activities such as the reading group, mid-project workshop, learning sets and PPI workshops. To stimulate input from the wider team, researchers presented emerging findings using visual maps incorporating illustrative quotations. Topics for analysis were chosen using the following criteria:
-
frequency and intensity of their appearance in the data, for example the ‘take-all’ way in which EDs were seen to operate
-
the singular impact of some occurrences, such as ‘stand-offs’ when practitioners expressed overt disagreement
-
conceptual clarification, for example unpicking differences between avoidability and appropriateness or inappropriateness, which aided definition of the clinical panel’s task
-
evidence of the use of divergent definitions, such as practitioners’ various different uses of the term ‘admission’, and the ‘bending’ of definitions and practices associated with breach avoidance
-
need for quantification through the VSM study, through analysis of HES data, or for follow-up in future research, for example number and proportion of acute admissions on each site that decision-makers considered to be ‘social admissions’
-
attention to silenced, taboo, minority-view or contentious issues, for example one stakeholder’s claim that hospitals were ‘hoovering up’ patients, especially the ‘frail elderly’, and seeking to swell their resource base with this justification.
Obvious differences and commonalities between sites were highlighted early on and these led to searches for further confirmatory or disconfirmatory data. We sought evidence of heterogeneity within sites, particularly regarding practitioners’ observed behaviour and reported beliefs and experiences.
In addition to the above procedures, the following methods were used to achieve rigour in the ethnographic data analysis:
-
The semistructured interviews with patients, carers and professionals were responsive to researchers’ ongoing field observations and conversations with participants. Alternation between these activities enabled us to explore, in interviews, some emerging questions and hypotheses.
-
Researchers refined their analytic statements by going from the NVivo node data excerpts ordered in framework analysis tables, back to the source transcripts, which gave greater indication of context.
-
Researchers tested and revised their emerging hypotheses in discussion with groups of research partners who had similar characteristics to the study participants: the PPI group; the learning sets of managers and clinicians on the four sites; the clinical panels; and the wider meetings of stakeholders comprising representation from all the above, and including the principal site collaborators.
-
In research team meetings, colleagues interrogated each other’s analytic statements and requested further examples of confirmatory and disconfirmatory evidence.
Data analysis
Researchers used the analytical method of printing and manually coding a relevant node (e.g. ‘Targets, time of day, time limits and avoiding breaches’), reading and rereading the data, highlighting phrases with particular impact and making notes on themes that became apparent. For example, a typology was developed of practitioners’ varying responses to pressure from busyness of the service and the 4-hour target. These ranged on a continuum from positive engagement to negative reaction, as staff members positioned themselves in different moments as doers and achievers, flexible team players, compliers and victims. These categorisations served to alert researchers about possible patterns to watch out for as they continued their fieldwork. When the ethnographic data set was completed, these provisional patterns were tested by seeking out tendencies within and across sites.
Ethnographic patient case studies
During the ethnographic study, researchers started to observe each patient journey with a view to creating an ethnographic patient case study. From these data, researchers selected the cases where they had been able to observe and conduct interviews during decision-making with involvement of practitioners, patients and sometimes carers. Six or seven of these patient case studies per site were collated and analysed as ethnographic case studies (see Appendix 12). The analysis involved comparing the views of the observer, patient, carer/family member and practitioners about their experience and the process of decision-making. The patient case studies were presented to two clinical panels (see Appendix 2) for discussion and for comments, which were incorporated into completed case studies for analysis within the main ethnography and within the synthesis. Two examples of case studies discussed by the clinical panels are provided in Appendix 2, which includes the clinical panel report.
Additional data sets and analysis
The following additional data were collected and analysed:
-
Documentary analysis (RQs 1, 3 and 4), including financial and business planning, governance, and implementation of process change, was used to identify key contextual features in each site.
-
Hospital Episode Statistics data were used to describe aggregated patient data for each site.
-
Data on costs of staff in each site (RQs 3 and 4), including typical staff mix, grades and sessions/hours worked at different times in each hospital, were used to estimate the cost of staffing EDs. It was not possible to quantify acute physician input owing to the complexity of shifts, rotas and job plans.
-
Analysis of the quality of decisions on admissions (RQ 4) by clinical panels of four or five clinicians (senior doctors and nurses in ED and acute medicine) and two local PPI representatives focused on the quality of the decisions made, based on collated ethnographic and VSM case studies. Two panels were assembled and chaired by a chief investigator. The northern panel reviewed cases from the two southern sites (Porthaven and Churchtown), and the southern panel reviewed cases from the two northern sites (Underbridge and Waterbury). First, members individually scored cases for likely appropriateness of decision-making. The research team then identified cases scored as potentially inappropriate or where there was panel disagreement. The panels then met to review these selected ethnographic patient case studies and individual patient VSM ‘charts’ and to agree a consensus score for whether or not the decision to admit or discharge appeared to be appropriate, and to comment in detail if care might have been improved. The panel process is described in detail in Appendix 2.
Synthesis
Approach to the synthesis across component studies
A critical realist approach64,65 provided the framework for integrating knowledge from each of the component studies, the stakeholder workshops, the clinical panels and the learning sets. We aimed to identify mechanisms that could explain how different outcomes arose in complex systems,66 with the goal of producing multifaceted explanations about how frontline expertise and new models can safely reduce admissions. We used the approach of Pawson and Tilley’s57 to identify potential mechanisms that result from the interaction of resource and opportunity with the reasoning of individuals and lead to behavioural change. In order to produce a more fine-grained analysis across the studies, we understood mechanisms as consisting of both reflexive and automatic responses.
Taking a realist perspective
Taking a realist perspective, the admission decision can be seen as a sequence, over time, of beliefs, knowledge and behaviours of the key actors: patients, carers and practitioners. The beliefs and actions of individual patients are affected by their immediate context, which can include both the cultural and structural context of their lives, family and home life, and their current state of physical and cognitive capacity. Patients and carers respond to the opportunities/resources provided (practitioners, acute care environment) with a variety of patterns of reasoning. It is the variety and detail of these patterns that we sought to understand.
Each of the practitioners involved in decision-making also has different beliefs and attitudes, based on previous training and experience that influence behaviours involved in the admission decision, such as further questioning, physical examinations, requesting tests or gathering opinions from other practitioners. Practitioner behaviour is also influenced by the organisational context in which the practitioners work: both structural – the teams, hierarchies, incentives, physical layout – and cultural – the norms and ideals of teamwork and professional conduct. Understanding how the immediate setting and wider hospital and health-care system beyond influence the individual practitioner’s reasoning is an important objective of the 3A study.
Individual practitioners also differ in their patterns of reasoning and capacity and respond differently to the same hospital and team environments, both in the immediate reasoning for the patient before them, and also over time in their acquisition of beliefs and cultural norms. This heterogeneity of practitioner responses may be one of the keys to understanding variations in acute admissions decision-making. In a contrastive way, we were also interested in seeing how practitioners as a group might respond to (1) the common and different resources and opportunities in existence at each of the four sites studied; (2) innovations that have been introduced, such as new types of teams, new diagnostic processes and pathways, or other innovations developed within the acute admissions system.
Integration of findings
We produced a set of analytic statements (see Appendix 13) from each study for presentation and discussion at researcher meetings and at the end-of-project stakeholder workshop. Wherever possible, we expressed these as causal ‘If . . . then’ statements that specified context, mechanism and outcome in relation to patient safety [i.e. appropriate (non-)admission decision]. For example, ‘If there is an acute bed shortage and pressure from management to decrease admissions (context) then clinicians may feel pressurised (mechanism) to discharge inappropriately (outcome)’.
However, in many instances it was necessary for the outcome stated to be a plausible stage on the decision-making route. For example, ‘If there is more than one team involved in the care of a patient (such as a specialist medical team) (context) then there can be confusion between practitioners (mechanism) about who is responsible for the care of the patient (outcome)’. Not all analyses or sources could support these types of causal statement. Where this was the case, we retained statements about context alone, for example, ‘Resource and time constraints may sway doctors towards admission as a safer option’. The statements were shared within and across teams so that an ongoing awareness of findings was cultivated. This also underpinned the development of collaborative working relationships, which in turn facilitated criticism and refinement of the synthesis.
We found that the common language of the ‘If . . . then’ statements helped us to group and look across project component studies. Our integration of findings focused on identifying how practitioners, patients and carers responded to each other, as well as how each responded to the resources and opportunities of the acute care setting.
In summary, the process was:
-
Based on the findings of each project component, ‘If . . . then’ statements (or other analytic statements or scenarios) were developed. A selection of these were further refined at the end-of-project workshop.
-
Refined statements were organised in tables by RQ and grouped by the participants in interactions (e.g. patient–carer–practitioner).
-
Through a process of reflection and discussion based on these refined statements (returning to the original data where necessary to clarify particular issues), we developed explanatory statements that incorporated all of the information in groups of refined statements (documents available on request from the authors). This typically involved the following tasks:
-
reading through to ‘sensitise’ ourselves to the issues
-
‘sense making’ – asking ‘How can we explain what has been observed here?’ and how we could account for context or rival explanations asking ‘What if?’ questions (i.e. looking for alternative explanations)
-
seeking disconfirming cases.
-
The statements were then brought together in narrative form within themes based around practice and service design in a narrative form referencing the analytic statement (see Appendix 13). Finally, we undertook an exercise of transforming negative statements into positive ones and setting these out as principles of practice that were likely to achieve particular objectives.
We focused on identifying mechanisms and the ways in which they could operate differently within varying contexts, as distinct from the pattern of events. 66 We endeavoured to recognise heterogeneity of responses as an inherent phenomenon within the system,67 acknowledging that, although social structures and culture have causal powers, people will interact with and respond differently to the same phenomena. 68
Chapter 3 Site descriptions, Hospital Episode Statistics and economic data
The four acute hospital sites
The 3A study was conducted at four major acute hospitals in South West England. These hospitals provide emergency medical care for much of the population of the south-west peninsula, and they serve varying catchments and populations with contrasting socioeconomic characteristics. The hospitals face similar pressures, demands on their workforces and resource constraints, and they are required to meet the same government targets. In response to these common challenges, however, the four sites also exhibited significant local innovations and therefore differences. In this chapter, the four hospitals are described using data collected by researchers during the study. HES data were used to describe activity and performance at each site, and to compare this data with national data. This chapter provides a detailed context for the ethnographic and VSM data that were subsequently collected, and for their interpretation.
Researchers examined the four hospitals, their structures and approaches to providing emergency medical care, and their innovations to improve performance and/or reduce admissions. Basic descriptive data – including location, catchment population, governance arrangements and some key aspects of infrastructure and staffing arrangements – are summarised in Table 3. While hospital size and overall numbers of emergency attendances and admissions were relatively similar, a range of local initiatives had evolved, some with similarities but others more unique, in order to expedite decision making and reduce admissions. The four hospitals were selected specifically because of these structural contrasts in their emergency medical admissions pathways, which existed at the start of the study (summarised diagrammatically in Appendix 14, Figure 20).
| Site features | A: Porthaven | B: Churchtown | C: Underbridge | D: Waterbury |
|---|---|---|---|---|
| Hospital location | 5 miles from city centre | 1.3 miles from city centre | In city centre | 1.5 miles from city centre |
| Population served | ≈450,000 | ≈350,000 | ≈612,000 | ≈500,000 |
| New ED attendances | 94,657 | 90,153 | 75,972 | 69,804 |
| Admissions via ED | 23,069 | 21,356 | 26,196 | 27,254 |
| Admissions to MAU | 3586 | 5332 | 0 | 0 |
| Particularities of trusts and CCGs | Covers a wide geographical area; managed by one CCG | Managed by one CCG; interacts with walk-in centre run by primary care; share site and reception | One trust that operates across two sites, served by one CCG | Covers a wide geographic area covering four counties and is served by four CCGs |
| ED configuration (see Appendix 14, Figure 21) | Minors, six cubicles; majors, 17 cubicles; resuscitation, four bays; CDU, 10 beds and a lounge area | Minors, nine cubicles; majors, nine cubicles; resuscitation, three cubicles; no CDU | Minors, eight cubicles; majors, nine cubicles, + majors 2, seven cubicles; resuscitation, four cubicles; no CDU | Minors, eight cubicles; majors, 18 cubicles; high care, six cubicles; resuscitation, four cubicles; observation ward, eight beds |
| ED senior cover | Consultant cover 09.00 to 20.30 weekdays and 09.00 to 17.00 weekends; 24-hour middle-grade cover | Consultant cover 08.00 to 22.00 weekdays and 09.00 to 22.00 weekends; 24-hour middle-grade cover | Consultant cover 08.00 to 22.00 every day of the week | Consultant cover 08.00 to 22.00 with on-call consultant cover between 22.00 and 08.00; 24-hour middle-grade cover |
| Medical assessment units/triage model | AMU, also called medical assessment unit: 52 beds in two single-sex areas; direct admission from GP referral or referral through ED AGPS 08.00 to 20.00 provides guidance for community GPs, sees ambulatory patients and refers to MAU |
AMU is a short-stay 44-bedded area with two high-care areas and two mixed-sex wards; medical triage unit, one with seven trolleys, one with seven seats, and three ‘see & treat’ rooms; receives patients from specialist clinics and through ED and GPs | Medical assessment unit (acute care unit A), a short-stay 25-bedded unit opposite ED, where admission is determined. Unscheduled treatment of patients in the acute sector: all patients come through ED and are seen by the ED clinicians | MAU with 34 beds located next to ED. All patients arrive through ED first for assessment by the acute medical team and are either discharged from ED or admitted to MAU |
| Ambulatory care model | Ambulatory care run jointly by the AMU and AGPS: eight treatment recliner chairs, four consultation rooms. Runs from 08.00 to 20.00. Consultant physician present 10.00 to 17.00 | Ambulatory area with six discharge seats. AMU consultant present from 08.00 to 22.00 | Ambulatory emergency care, new service being piloted, situated alongside medical day unit, some distance from the ED | Ambulatory care situated by MAU. Operates 08.00 to 22.00: three treatment rooms, two beds, five recliner chairs. Additional waiting area chairs |
Porthaven Hospital
Porthaven is a large university teaching hospital providing secondary and tertiary care services to a population of 450,000. Porthaven opened in 1981 and is situated 5 miles from the city centre. Porthaven serves both a large urban population and a widely dispersed rural population. There is wide socioeconomic variation, with particular pockets of urban deprivation. The hospital trains doctors, nurses and a range of other health-care professionals (HCPs).
Configuration of unscheduled care at Porthaven Hospital
Key initiatives to avoid admission/improve patient flow at Porthaven:
-
ED controller
-
clinical decision unit (CDU)
-
AGPS
-
ACU.
Porthaven receives approximately 95,000 emergency attendances per year. Unscheduled care is provided by two main units:
-
the ED and its associated CDU
-
an AMU/medical assessment unit, which includes an ACU.
The ED has six minors cubicles, 17 majors cubicles and four resuscitation bays. In addition, there is a 10-bed CDU, which incorporates a lounge area to accommodate low-risk patients for whom a quick turnaround may be possible, while they await test results and discharge. This short-stay area averts admission to a hospital ward and patients remain under the care of the ED team. The CDU lounge is an additional ambulatory area, with seats rather than beds, used for a variety of conditions where discharge home is expected.
The ED and the MAU are a 2- to 3-minute walk from each other. The MAU is a short-stay ward with 52 beds, divided into separate areas for female and male patients. The ACU is situated within the MAU and has four consultation rooms and eight treatment chairs. The ACU is run jointly by the acute medical team and an AGPS, and operates from 08.00 to 20.00. Originally, the ACU was set up as a joint venture between the ED and the MAU, but it is now run exclusively by the MAU.
An important innovation at Porthaven is the hospital-based AGPS, established in 2006. The service replaced a previous system wherein AMU nurses received calls from GPs seeking advice on patient treatment. Currently, the AGPS is delivered by GPs who take calls from community GPs from 08.00 to 20.00 on weekdays and provide advice, guidance and signposting for community treatment. Additionally, for ambulatory patients who require investigations or assessment but not admission, the AGPS will accept and see patients in the ACU. Finally, they will refer patients who require admission to the MAU. All referrals from community GPs to the medical team come through the AGPS during these hours. The AGPS also has the ability to directly book patients to a number of outpatient clinics.
Model of care
Patients self-present to the ED, come by ambulance or are referred to unscheduled care by their GP. The GP-referred patients will be seen either by the AGPS or by the acute physicians in the MAU. These patients have direct access to the ACU/MAU without the need to pass through the ED, unless they need emergency medical treatment, in which case they will be sent to the ED. Alternatively, patients who self-present to the ED and require medical admission can also be referred to the MAU. Early senior clinician input is also a key aspect of the staffing model adopted by Porthaven.
Space and working environment
Porthaven ED has a spacious ‘majors’ area surrounding two central desks (see Appendix 14, Figure 21). This allows practitioners to maintain most patients clearly in view. The department includes three cubicles with doors, rather than curtains, for patients with more sensitive issues or for infection-control purposes. A significant innovation at this site is the ‘controller’ – typically a consultant – who assumes the central position in the unit, responds directly to requests from junior staff and other colleagues, and oversees the whole department, focusing on the resuscitation (‘resus’) and majors area. Managerially, this operates as a hub and spoke system with the controller at the centre. Opposite the controller sit the senior emergency nurse and the patient flow co-ordinator (PFC), also in central positions within easy conversational distance. The PFC supports the medical and nurse co-ordinators. A public address system facilitates communication throughout the ED and the adjoining offices and staff rooms.
Churchtown Hospital
Churchtown is a university teaching hospital with foundation trust status. It serves a population of roughly 350,000 people, including urban and rural areas, and has many summer visitors. The site is 1.3 miles from the city centre and operates a park-and-ride scheme for patients. The site has been occupied for 250 years although the current building was completed during the 1990s.
Configuration of unscheduled care at Churchtown Hospital
Key initiatives to avoid admission/improve patient flow at Churchtown:
-
rapid assessment and triage team
-
acute care of the elderly (ACE) team
-
rapid outpatient review
-
onward care team
-
ambulatory care area.
Churchtown receives approximately 90,000 ED attendances per year. The ED shares the same site and reception area as the primary care walk-in centre and GP out-of-hours service. Although these services are colocated, they are separate entities. Triage staff can reallocate patients between these entities.
Patients self-present to ED, are brought by ambulance or are directly referred by a GP. On arrival in ED, patients are triaged, usually by experienced nurses who assign patients to the appropriate area. There are six ‘see and treat’ rooms in ED reception for patients who can be treated by senior nurses and discharged. Some patients are referred to the walk-in centre directly from triage. Patients with more serious conditions are sent directly to ED majors.
General practitioner referrals go directly to the medical triage unit (MTU) for assessment by the on-call medical team under the care of the medical consultant. These patients are assessed, treated and admitted or discharged within the 4-hour time limit. Those admitted are moved to the adjacent AMU for ongoing care before moving on to specialty wards as appropriate.
For patients arriving into ED majors, a rapid assessment and triage model was introduced whereby patients are seen by a consultant on arrival for a brief assessment to instigate investigations and early management and co-ordinate ongoing care, including admission or discharge planning. Patients are then seen and managed by ED doctors until onward referral or discharge. There are some exceptions, such as patients suspected of having a stroke, who are immediately referred to the acute stroke team.
The ACE team is a recent innovation. Eligible patients arriving in ED are seen by a multidisciplinary specialist team, under the supervision of a geriatrician, aiming to ensure that they are immediately guided towards the most suitable patient pathway and that hospital admission is avoided where appropriate. This team supports appropriate discharge by liaising with community and primary care resources.
Rapid outpatient review: rapid pre-arranged clinic appointments are available for patients who need follow-up after being treated in the ED. Examples include some burns, bites and replacement plaster casts. This is a consultant-led service running 7 days a week; senior nurses are also involved in treating such patients.
The onward care team is a team of physiotherapists and occupational therapists who can assess patients’ mobility and ability to be safely discharged. The team has a comprehensive knowledge of local initiatives and resources for care in the community.
Model of care
Patients self-present to the ED, arrive by ambulance or occasionally are directly referred by a GP. Patients who are referred by their GP to the medical team go directly to the MTU for assessment by the on-call medical team under the care of the medical consultant. The care model at Churchtown also promotes early experienced clinician input.
Space and working environment
There is a spacious triage area with side rooms (see Appendix 14, Figure 21). The children’s ED is colocated within the unit and incorporates a small play area and dedicated children’s ward. Majors and minors areas are located on either side of the main corridor linking the ambulance bay with the rest of the hospital.
Churchtown ED has a relatively compact majors area so that most beds are clearly visible from the central desk, and the bays have externally visible observation monitors. There is more limited desk space for staff.
One flow controller sits centrally in the majors area and another in the minors area. Both use whiteboards to track patient location and investigations. These individuals also manage patient records. There are four side rooms used as majors beds, but they can also be used to admit patients for observation outside the 4-hour target.
The AMU is a 5-minute walk away, near the opposite end of the hospital. The AMU consists of a MTU where new patients are assessed and either offered ambulatory care or moved to a small bedded ward. From here, further assessment and diagnosis are undertaken. If necessary, patients may be admitted directly to the adjacent AMU ward. While diagnostics (X-ray) are very close to ED, they are much further away from the AMU. Finally, the MTU ambulatory area co-ordinates several specific treatment pathways such as deep-vein thrombosis and cellulitis treatment, aimed at reducing the need to admit such patients.
Underbridge Hospital
Underbridge is a district general hospital close to the city centre. This modern hospital was developed in the 1960s. It is one of two acute hospitals, each with its own ED, run by the same foundation trust. However, 24-hour emergency care is provided only by Underbridge, whereas the partner ED accepts only walk-in patients at night-time, who are treated by ECPs. Underbridge provides care for a large urban and rural area, including districts of both high deprivation and relative affluence.
Configuration of unscheduled care at Underbridge Hospital
Key initiatives to avoid admission/improve patient flow at Underbridge:
-
ambulatory emergency care (AEC) (nurse led)
-
integrated discharge team (IDT)
-
older person’s assessment and liaison (OPAL) team
-
rapid access (hot) clinics.
Underbridge ED receives approximately 76,000 attendances per year. Unscheduled care consists of care within the ED, acute care unit A (ACUA) and medical day unit (MDU) and, more recently, AEC. The ED has recently been extended and consists of an eight-cubicle minors area and a 16-cubicle majors area, divided into two sections, and with a four-cubicle resuscitation bay. There is no CDU or observation unit at Underbridge; instead, patients requiring observation are admitted to ACUA.
Acute care unit A is positioned opposite the ED in a 25-bed ward designed for short-stay assessment. This has five four-bedded bays and five side rooms. Although a senior review is performed when the consultant arrives at 08.00, at the time of this study there was no formal structure to the review process. While it appeared to differ somewhat by consultant, reviews were usually undertaken to ensure that patients were seen and treated efficiently.
The MDU at Underbridge is an area for patients who require acute medical care but not admission. Patients are directed here by the medical team by prior arrangement. Therefore, the MDU is not a destination for patients admitted through the ED.
Since September 2013, a new initiative – AEC – has been operational. AEC is a unit led by nurse practitioners with medical support. They identify patients who either self-present or are referred by GPs to the ED and who, while not requiring admission, may require assessment or investigations that take longer than 4 hours. Once a potentially suitable patient is identified by nurse practitioners, ED staff will refer him/her to AEC.
A local innovation is the IDT: a team of physiotherapists, nurses and occupational therapists with extended competencies. They are employed by community services and operate from 08.00 to 20.00 Monday–Friday and from 09.00 to 17.00 at weekends and on bank holidays. This team assesses the functional needs of elderly patients in order to secure safe discharges, and, if necessary, arrange packages of care or transfer to community beds.
Another innovation is the OPAL team: a team of two consultant geriatricians who assess the special needs of elderly patients at the request of the ED or MAU, and who work closely with the IDT.
A recent pilot initiative in ED involved a collaboration with a number of local GP surgeries that provided access to primary care medical records in order to facilitate emergency decision-making.
Finally, there is a series of rapid access (hot) clinics available for patients in need of urgent review but not necessarily admission. There are several routes into these clinics, including referral by the ED or by GPs.
Model of care
A distinctive aspect of care at Underbridge is that all emergency attendance and referrals are assessed by ED staff. Patients attending the ED self-present, arrive by ambulance or are sometimes referred by another professional, generally their GP. All patients are assessed by ED nurses and reviewed by ED clinicians, who then decide whether or not the patient needs admission and, if so, to which specialty. In contrast to this route of entry, the majority of GP referrals are received by a service known as the ‘single point of clinical access’, which is based within the Clinical Commissioning Group (CCG) but historically was managed by the ED. Anecdotal accounts from the ED staff suggest that, since the service has moved, the threshold for accepting GP referrals has lowered, resulting in greater numbers arriving in the ED.
Underbridge was included in this study because it had initiated a new model for ED care. The unscheduled treatment of patients in the acute sector (UTOPIA) model was designed to address increasing problems of crowding and was introduced in August 2009. In this model, all patients come through the ED and are seen by ED clinicians regardless of whether or not they have already been assessed by another health-care provider such as their GP.
The relationship between the ED and ACUA was reputed to work well for patients requiring medical admission. In addition, clinicians from the acute medical team monitor the ED, and if they identify a patient with a significant medical need they will assess him/her in the ED and expedite the decision to admit or discharge. The success of this relationship has been attributed to both departments being under the same management division. This is not the same for all other specialties, where some practitioners still prefer to make their own decisions. This can result in patients waiting for review in the ED. The main observation made locally about UTOPIA is that the model would require large numbers of senior decision-makers, for whom insufficient funding was available.
Space and the working environment
The physical space in the ED is designed with patient cubicles positioned around a central working desk, so that patients and staff are within easy sight of each other (see Appendix 14, Figure 21). The proximity of minors and majors areas allows close working and overlap. The co-ordinator has a dedicated space in which to work, but otherwise the nursing and clinical staff work in the same space; this appears to result in a degree of integration between the teams.
Although the flow of patients through the department is primarily the responsibility of the co-ordinator (senior nurse), this is undertaken in partnership with the ED consultants. To aid monitoring of patient flow, a computer screen on the wall displays numbers and situations of all patients.
Acute care unit A is similar to the ED in staffing arrangements, although numbers per shift are smaller. ACUA is a new purpose-built ward that is bright and airy. A co-ordinator oversees the whole ward. The doctors’ and nurses’ offices are situated next to each other and there is a high level of interaction between team members. AEC has a smaller staff quota, with one nurse practitioner and either a staff nurse or an experienced health-care assistant (HCA). The unit does not always have a member of medical staff present but there is immediate access to both the ED and ACUA doctors as necessary.
It was understood that recruitment and retention of both nursing and medical staff had been a recent challenge and, during this project, it was observed that a significant number of locum staff were employed.
Waterbury Hospital
Waterbury is a large district general hospital providing care for a large, predominantly rural, population covering four counties with relatively low levels of deprivation and some areas of high affluence. The hospital is located 1.5 miles from the city centre.
Configuration of unscheduled care at Waterbury Hospital
Key initiatives to avoid admission/improve patient flow at Waterbury:
-
Senior With A Team (SWAT)
-
discharge assessment team
-
rapid access (hot) clinics
-
access to GP records.
Unscheduled care in Waterbury is given in an ED. It includes an observation unit, an MAU and an ACU, all of which are classed within the same managerial structure.
The ED occupies a large physical space and includes an eight-cubicle minor area, a 24-cubicle major area with six cubicles classed as ‘high care’, and a resuscitation area with four further cubicles. There is also an eight-bed observation ward for patients who may require assessments that take longer than 4 hours but who do not require admission (see Appendix 14, Figure 21).
The MAU provides short-stay admission for patients who require further assessment and investigation for up to 48 hours. The MAU is located next to the ED and has 34 beds in three bays. There are three main daily rounds for senior review: the ‘post-take’ rounds at 08.00 and 18.00, when all recently admitted patients are reviewed by a consultant physician (not a MAU consultant); a geriatric round at 08.00, when patients identified on the basis of age and complexities of medical and social needs are reviewed by a consultant geriatrician; and a ‘post-post-take round’, when patients who have been on the unit for over 24 hours receive consultant review. In addition, the MAU consultants review all patients who are being clerked/admitted at 11.00, 14.00 and 17.00. Clerking of patients is undertaken by nurse practitioners and junior doctors.
An ACU is attached to the MAU and provides an alternative to admission for ambulant patients who have referred by their GP or the ED to the medical team, but require assessment or investigations that can be completed within 8 hours between 08.00 and 20.00.
There have been several recent initiatives at this site:
‘Senior With A Team’ (SWAT) is a new initiative implemented in early 2014. A consultant, aided by a senior nurse and either a junior nurse or a HCA, can have the use of two to four cubicles to expedite decisions and reduce delays in patient assessments.
Discharge assessment team is a recent initiative comprising a team of discharge therapists (physiotherapists or occupational therapists) with extended competencies who assess the functional needs of elderly patients prior to discharge and the provision of care packages, and are also able to arrange community beds. The service operates from 08.00 to 19.00 Monday to Friday and from 08.00 to 12.00 at weekends and on bank holidays.
A range of rapid access (hot) clinics are also available for patients requiring prompt medical treatment but not necessarily admission. ED clinicians can refer patients electronically to these clinics.
Direct access to GP records is a recent initiative to improve information sharing from a selection of local surgeries that are taking part in the pilot project.
Model of care
Patients self-present to the ED, come by ambulance or are referred by a health professional, usually a GP. At Waterbury, all patients present first to the ED and are identified as ‘ED patients’ or ‘expected patients’ (those referred from elsewhere to a particular specialist team). All patients are assessed by ED nurses and, depending on their needs, are then assessed by a physician from either the ED or another medical specialty, and a decision to admit or discharge is often made in the ED. Patients who require further investigations or observation before the decision are admitted to the observation unit (ED patients expected to be discharged within 12–24 hours) or the MAU (medically expected patients). Patients who self-present to the ED and are identified as requiring medical admission will also be referred to the medical team in the MAU. Although patients referred to the medical team would ideally be assessed initially in the ED and then be referred direct to the MAU, in reality patients regularly wait in the ED for a MAU bed to become available.
Space and working environment
The ED is a large physical space where cubicles are not clearly visible from the central desk (see Appendix 14, Figure 21). Staff may not be in visual contact and a public address system is used. Significant movement is required by both patients and staff. Similarly, movement is required to perform functions such as computer data entry, record writing, and accessing equipment and drugs. In addition, there are separate dedicated spaces for medical and nursing staff. The co-ordinator also has an allotted space where patients can be assessed and the department overseen.
The flow of patients through the ED is managed primarily by the co-ordinator (a senior nurse), who oversees patients on arrival and the general movement of patients in and out of the hospital. The co-ordinator records patients’ names, times of arrival and named nurses on a whiteboard. There is co-ordination with the consultant and the site manager, who has oversight of the hospital’s bed occupancy. In addition, the departmental manager may be involved at times of high workload and if patients are at risk of breaching the 4-hour target.
The ACU is staffed by a small permanent team including a medical nurse practitioner (MNP), a staff nurse, a HCA and a receptionist. Patients are referred to the ACU by their GP or occasionally by the ED. A MAU consultant attends for morning and afternoon rounds to see patients who require a clinical decision, but much of the workload is handled, and some of the decisions are made, by the MNP. The unit is managed by a co-ordinator (MNP), who is able to undertake a number of clinical procedures that patients may require, and make autonomous decisions to admit or discharge. There is also a staff nurse with a dual role, to provide nursing care within the ACU and take calls from the GP referral service.
The MAU is similar to the ED in staffing arrangements, although staff numbers are smaller. Nursing staff are based in bays overseen by a co-ordinator. Medical staff move between bays and the ED, where they spend much of their time. The doctors have a separate office off the corridor.
Most of the calls referring patients to the medical team come via an access team who take GP calls. The access team may also identify community beds. An additional facility is the ‘consultant hotline’, which GPs are able to ring to discuss patients.
Hospital Episode Statistics
Hospital Episode Statistics were used to investigate the activity and pressures at the four sites, along with several key performance indicators for 2009–13. Formal statistical analysis was beyond the scope of this project, and the data are presented here for descriptive purposes.
Sources of emergency admissions at the four sites
The sources of referrals and admissions at the four sites closely reflected national data, with about 70% of emergency admissions referred through EDs (Figure 2), about 15% by GPs and 15% from other sources. The statistics for Waterbury and Underbridge were similar to national patterns, although Porthaven and Churchtown exhibited relatively higher numbers of GP referrals in relation to admissions through EDs.
FIGURE 2.
Sources of all emergency admissions at the four study sites compared with national data. Data are from HES, 2009–13. Hospital Episode Statistics data were accessed through the Health and Social Care Information Centre (www.hscic.gov.uk/hes) using the Lightfoot signalsfromnoise (SFN) tool (Lightfoot, Bracknell, UK).

Demand and activity at the four sites
The times of arrival of patients in the four EDs of the studied sites were similar and in line with national data (Figure 3). Arrivals reached a nadir at 05.00–06.00 and then rose rapidly to a significant peak around 11.00, before reaching a plateau throughout the afternoon. A small peak was observed around 18.00 followed by a gradual decline throughout the night.
FIGURE 3.
Diurnal variation in patient arrival times at the four sites compared with national statistics. Data are from HES, 2009–13. Hospital Episode Statistics data were accessed through the Health and Social Care Information Centre (www.hscic.gov.uk/hes) using the Lightfoot signalsfromnoise (SFN) tool (Lightfoot, Bracknell, UK).

At these four sites, numbers of ED attendances peaked on Mondays, in line with national data. Numbers were lower from Tuesday to Saturday before a small increase on Sunday. Waterbury and Underbridge exhibited very similar patterns to the national profile, whereas Porthaven and Churchtown also exhibited peaks in attendance on Sundays that equalled the Monday attendances.
Emergency admissions tended to reflect the attendance rate, with a corresponding peak on Mondays, declining somewhat from Tuesday to Friday, followed by a 20–25% reduction on Saturdays and Sundays. Nationally, the decline in emergency admissions is associated with a fall in GP referrals. Waterbury and Underbridge reflected the national pattern, whereas Porthaven and Churchtown also showed some decline in admissions through the EDs at weekends.
Similarly, all sites showed typical daily fluctuations in the number of beds occupied with emergency admissions. Bed occupancy peaked on Mondays and declined through the week to a nadir on Fridays, before climbing over the course of the weekend. The emergency patient bed occupancy varied by 5–6% on average throughout the week. Length of stay was a little lower at the four sites than the national average, and was around 5.0 days at the time this study was conducted.
Annual attendance, admission and performance data at the four sites
National data show that attendances at EDs increased each year from 2009 to 2013. However, this increase was lower at all four study sites than the national average, and Porthaven experienced an absolute fall in attendances (Table 4). On the other hand, compared with the national average, all four sites exhibited somewhat higher conversion rates from attendance to admission. The admission rates were generally in line with national data, with the exception of Porthaven, which again showed a decline. The proportion of attendances and admissions that breached the 4-hour target did not differ significantly from national statistics.
| Site characteristic | National data | Porthaven | Churchtown | Underbridge | Waterbury |
|---|---|---|---|---|---|
| Attendance and admission (%) | |||||
| Growth rate of A&E attendances | 5 | –1.8 | 2.6 | 3.8 | 1.3 |
| Conversion rate of A&E attendance to admission (range) | 20–24 | 26–34 | 22–28 | 30–36 | 30–40 |
| Growth rate of emergency admissions | 0.4 | –2.6 | 1.9 | 0.4 | 1.5 |
| Breach of 4-hour target (%) | |||||
| Proportion of A&E attendances that breach 4 hours (range) | 4–9 | 2–8 | 2–10 | 2–12 | 3–8 |
| Proportion of admissions that breach 4 hours in A&E (range) | 10–26 | 5–20 | 10–25 | 5–30 | 5–20 |
| Older population and case complexity | |||||
| Proportion of A&E attendees aged ≥ 70 years (%) | 15.5 | 17.6 | 19.5 | 20.9 | 24.6 |
| Proportion of A&E attendees admitted aged ≥ 70 years (%) | 36.9 | 37.9 | 42.7 | 43.7 | 46.7 |
| Number of diagnoses per emergency spell | 7.5 | 9.1 | 7.9 | 6.6 | 7.6 |
| Readmission rates (%) | |||||
| Emergency readmission rate (48 hours) | 2.0 | 1.5 | 1.4 | 1.4 | 1.8 |
| Emergency readmission rate (7 days) | 6.6 | 5.8 | 5.3 | 5.3 | 6.0 |
| Emergency readmission rate (30 days) | 14.0 | 12.8 | 11.7 | 11.9 | 12.6 |
| Emergency readmission rate (30 days, same specialty) | 6.9 | 5.6 | 6.6 | 4.8 | 5.5 |
The proportion of older people attending and admitted through the EDs was greater than the national average, with the highest percentage in Waterbury. Numbers of diagnoses linked to a case – a possible surrogate measure of diagnostic complexity – were similar in each site. Numbers of diagnoses appeared higher than average for Porthaven.
All four sites had emergency readmission rates a little lower than the national average. Readmissions within 48 hours (‘failed discharges’) were noticeably lower (by 10–25%) than the national average.
Summary
The provision of emergency care posed similar challenges for each of these hospitals. However, differences were apparent between the models of care that had evolved. The four sites contrasted in many ways including their locations and catchment areas and the sociodemographic characteristics of their population, and several also had marked seasonal fluctuations in workload. There were differences in the availability and configuration of local community services, the ease of access to other medical specialties and ambulatory care, the physical size and layout of their EDs and the associated units, and the attendant impact of these factors on local working practices. There were some contrasts in staffing levels, recruitment and retention, use of locum staff, medical–nursing interaction and staff hierarchies, and use of modes of communication such as whiteboards, public address systems and radios. These differences were associated with contrasts in models of care and working environments.
A wide variety of initiatives was evident in these departments, including efforts to promote early triage and ‘senior first’ decision-making, ambulatory care, GP involvement, colocation of ED and GP services, areas to keep selected patients under necessary observation without breaching the 4-hour target, ‘hot’ outpatient clinic reviews and teams to support safe discharge of elderly patients with complex care needs. Some initiatives were widely adopted in one form or another, whereas others were unique to one site.
There were significant strategic differences between the four sites in terms of physical structure and space; the number of CCGs influencing service configuration; the hospital management and divisional structures; the relative emphasis on escalation policies; differences in patient data software; communication channels between EDs and the rest of the hospital; presence of local policies and adherence to national guidelines; and the influence of other associated organisations such as universities.
Hospital Episode Statistics data confirmed similarities between the sites in the temporal patterns of workload, although the patients overall were slightly older than the national average. One hospital had observed a reduction in ED attendance and admissions. There was a suggestion that flow of unscheduled attendance through ED might be inversely associated with entry by GP referral. Breach rates for the 4-hour target and emergency readmissions were similar across the sites.
We acknowledge the limitations of these site descriptions, in terms of both the researchers’ impressions, based on observation and interviews, and the inherent limitations of the HES data. Infrastructure and pathways were in a constant state of evolution at all four sites – with new initiatives being tested while others were being discarded – as each hospital sought to meet the challenge of high demand for emergency care. Therefore, the components and structures of care at each hospital were subject to a degree of change during the project.
In conclusion, the emergency care provided by these four hospitals has evolved to meet the challenges of rising local demands for 24-hour services. All four sites balanced the adoption of measures that helped to meet performance targets, such as ‘senior first’ policies, against the training needs of doctors, nurses and other HCPs. Team spirit was in evidence at all four sites and each hospital was engaged with its own new initiatives to reduce avoidable acute admissions.
Chapter 4 Value stream mapping of patient journeys in hospital emergency medical care
Introduction
The hospital emergency medical care systems, and patient experience of these systems, were examined from the perspective of ‘Lean theory’, and using the quantitative methodological approach of VSM. This chapter explains how VSM was applied to our research and presents the quantitative findings. We describe care processes and waiting times between process steps, investigating the impacts of different care models on patient experience. Our data, recorded through direct observation of patient journeys at the four sites, provide evidence from which hypotheses can be generated and potential solutions to problems identified. They also establish the context for the ethnographic chapters which follow. Differences in site configuration (described in Chapter 3 and Appendix 14), especially in the availability of ambulatory care, AGPSs and observation units, may have an important impact on patient journey times and waits.
The origins and theoretical background of Lean theory and VSM are included in Appendix 7, and the VSM method is described in Chapter 2. As part of this analysis, the ED staff costs for this group of patients were also estimated. The interpretation of VSM data was aided by transcripts of the clinical panels of senior clinicians and patient representatives who undertook recorded case discussions of a selection of case studies. The methodology for the clinical panel is described in Chapter 2 with additional material in Appendix 2.
Results
Uptake rates
Of the 124 patients identified as meeting the inclusion criteria and then approached, 108 consented to the study, giving an uptake rate of 87% (Figure 4). Ten per cent of patients declined to participate, mainly because they were in pain or they were fearful of the emergency situation. Another 3% were excluded by the researchers either because they could not ensure that informed consent had been obtained or because the patient became too unwell to continue with the consent process.
FIGURE 4.
Patient recruitment flow chart for the VSM study.

Overall, of the participants recruited, 48% were discharged and 52% were admitted to hospital. This approximately even split indicated that the criteria of admission ‘uncertainty’ had been applied effectively during the patient selection process.
Participants
The characteristics of the VSM study participants are summarised in Table 5.
| Site | Number of patients | Gender | Age group (years) | Age (years) summary (range, median) | Ethnicity | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| F | M | 18–44 | 45–64 | 65–74 | 75–84 | ≥ 85 | White | Black and minority ethnic | |||
| Porthaven | 30 | 15 | 15 | 5 | 8 | 5 | 8 | 4 | 26–94, 65 | 29 | 1 |
| Churchtown | 30 | 16 | 14 | 2 | 6 | 4 | 10 | 8 | 18–93, 78 | 30 | 0 |
| Underbridge | 24 | 12 | 12 | 4 | 7 | 2 | 6 | 5 | 23–94, 70 | 24 | 0 |
| Waterbury | 24 | 12 | 12 | 0 | 4 | 3 | 9 | 8 | 47–99, 82 | 24 | 0 |
| Total | 108 | 55 | 53 | 11 | 25 | 14 | 33 | 25 | 18–99, 76 | 107 | 1 |
There was a broad age range of participants and a balance of male and female participants and of presenting conditions. There was limited ethnic variation, reflecting regional demographics.
Participants were recruited from all acute access routes and from both groups of presenting conditions at each site (Table 6).
| Site | ED | Presentation | Medically expected (MAU, MTU, AGPS) | Presentation | ||
|---|---|---|---|---|---|---|
| Cardiorespiratory | Older age | Cardiorespiratory | Older age | |||
| Porthaven | 19 | 10 | 9 | 11 | 9 | 2 |
| Churchtown | 23 | 9 | 14 | 7 | 6 | 1 |
| Underbridge | 13 | 6 | 7 | 11 | 10 | 1 |
| Waterbury | 17 | 9 | 8 | 7 | 5 | 2 |
| Total | 72 | 34 | 38 | 36 | 30 | 6 |
Although it was expected that elderly people might make more use of non-emergency acute routes into the hospital, a somewhat greater proportion of this patient group was found to have come through the ED route.
All non-ED patients arrived at hospital following referral from their GP or an outpatient clinic. In contrast, many participants arrived in ED either in response to first seeking advice through another health professional, such as a GP or the 111 service, or following a 999 ambulance call. Table 7 summarises the routes followed before patients arrived in the ED.
| Site | ED attendees | Prompt to attend a hospital ED | |||||
|---|---|---|---|---|---|---|---|
| Rang 999 | GP advice | Rang 111 | Carer or nurse | MIU/outpatient clinic | Own initiative | ||
| Porthaven | 19 | 7 | 6 | 1 | 3 | 2 | 0 |
| Churchtown | 23 | 11 | 5 | 0 | 1 | 2 | 4 |
| Underbridge | 13 | 6 | 2 | 1 | 2 | 1 | 1 |
| Waterbury | 17 | 7 | 1 | 0 | 7 | 2 | 0 |
| Total | 72 | 31 | 14 | 2 | 13 | 7 | 5 |
Porthaven had the lowest proportion of ED attenders using the 999 service. It also had the highest proportion arriving as a result of GP advice (31%). Churchtown had the highest proportion of patients attending the ED on their own initiative (17%), while Waterbury had a particularly high proportion attending the ED on the advice of a carer or nurse (41%).
Analysis
This study aimed to describe what happens to patients as they traverse acute medical pathways that may result in hospital admission. To do this, admission decision pathways were mapped for each site. Visual representations of these pathways (or ‘value stream maps’) are shown in Appendix 7. It soon transpired that these value stream maps represented an ideal, in which certain process tasks happened in sequence. The observed reality was that multiple factors affected the pathway, so that processes could happen in a different order from that presented by the value stream map, and additional processes were sometimes added and others removed, depending on the needs of the patient and the context in which the patient arrived. Consequently, the patient pathways were analysed by examining the overall picture rather than by abstracting the timings for a specific patient in relation to a generic value stream map.
To understand the patient journeys at each hospital, timing data was used to analyse journey time (known in Lean terminology as ‘lead time’), at what points in the patient pathway waits occurred, and time attributed to either value-adding activity (predominantly contact time with patient) or non-value-adding activity from a patient’s perspective (how long the patient was waiting). The VSM timing data were then used to address three RQs relating to the quantification of patient pathways:
-
How do medical staff and other practitioners contribute to decision-making?
-
How do organisational factors affect decision-making?
-
How are the four models of care similar and different?
Firstly, the VSM analysis examined patient journey time by site. The box-and-whisker plot in Figure 5 shows median journey times, which ranged from 195 to 243 minutes, with a mean of 223 minutes.
FIGURE 5.
Median patient journey time by site. max., maximum; min., minimum.
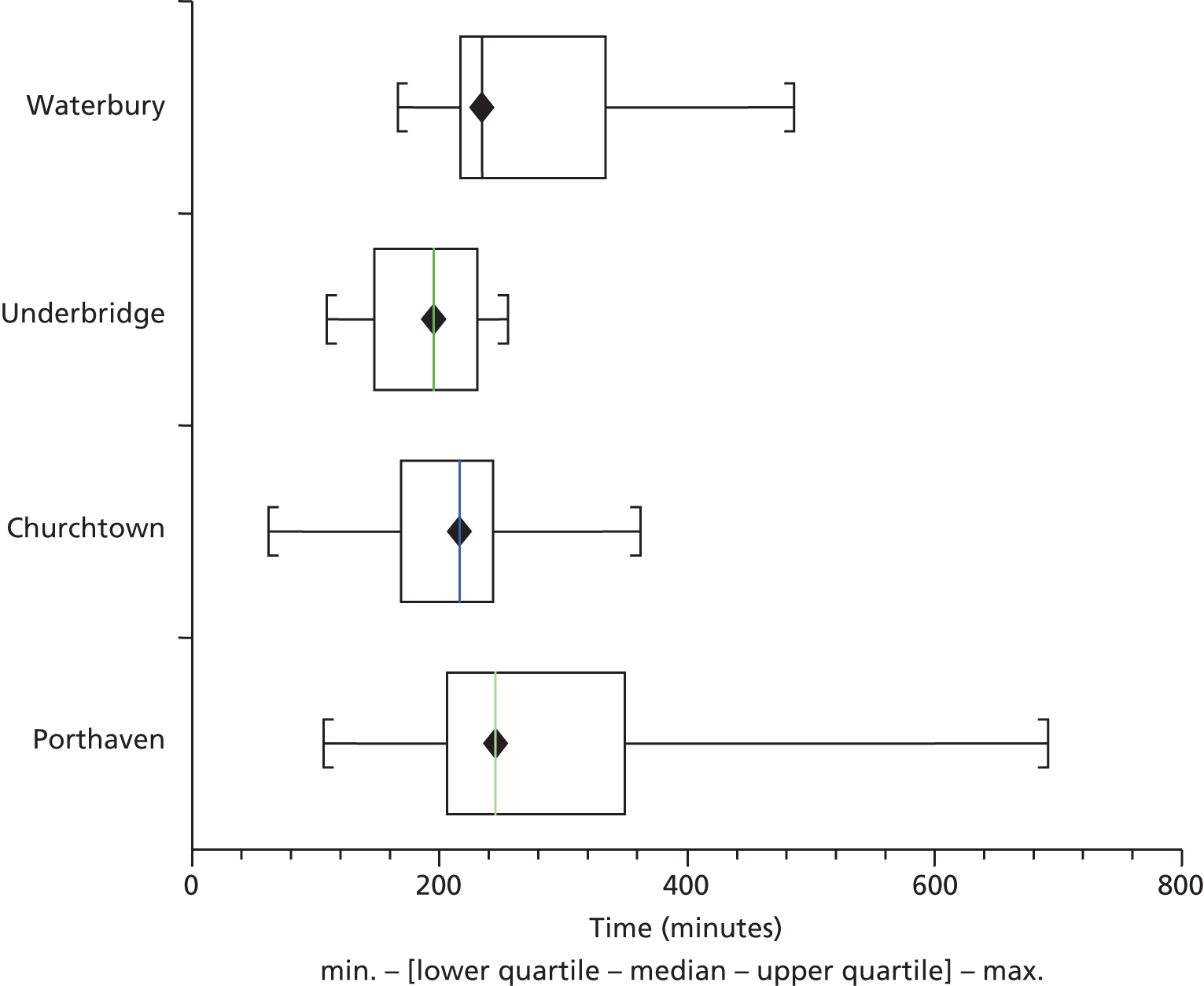
A wider range in overall patient journey times is clearly evident at the Porthaven site. In contrast, Underbridge, with the smallest range of journey times, also has the lowest median time.
During these journeys, the ratio of value (contact) to waste (predominantly non-contact time and waiting) ranged from 39% to 52%, with an average of 45.5% at each site (Figure 6).
FIGURE 6.
Value-to-waste ratio for each site.
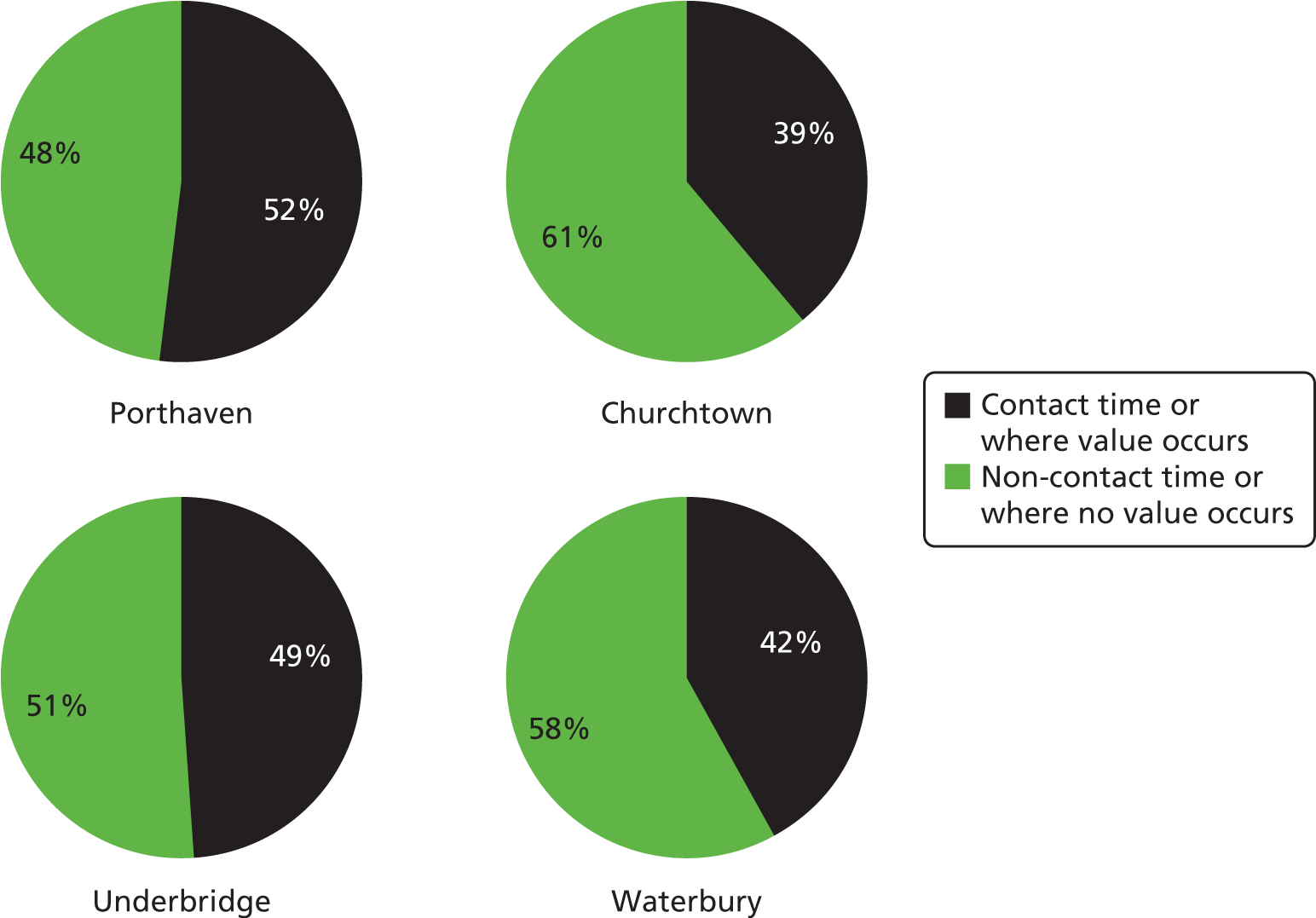
There was no significant difference between the ratios of percentage waste and value times at the four sites. However, total waste time at the four sites differed significantly [one-way analysis of variance (ANOVA); p = 0.007]. Thus, the mean waste time in Underbridge (95 minutes) was significantly less than in Churchtown (128 minutes), Porthaven (138 minutes) and Waterbury (151 minutes). The total value time also differed significantly between the four sites (one-way ANOVA; p = 0.01). Value time was significantly higher at Porthaven (150 minutes) than at Churchtown (82 minutes), Underbridge (93 minutes) and Waterbury (111 minutes).
To understand where wastes (non-value activity when patients were mainly waiting) were occurring, wastes were attributed to key time frames in the patient pathway. The key time points chosen were:
-
waits after the patient arrived but before being assessed by a doctor
-
waits after assessment by a doctor but before a final admission decision
-
waits after a final admission decision but before the patient left the department or was admitted to a ward.
A breakdown of waste stage, by site, is shown in Figure 7. The pie charts indicate a clear variation between sites in the stage at which the greatest proportion of waste occurred. At Underbridge, almost half of the time the patient spent waiting was before the patient was assessed by a clinician. Waste time after assessment but before final decision was in the range of 30–39% for three sites, but lower at Waterbury (20%). This time interval typically represented the wait for diagnostic test results. The wait after the final decision was shortest at Underbridge (23%), and similarly lengthy at both Churchtown and Waterbury (51–54%).
FIGURE 7.
Stage of patient care where waste occurred.

These process points – arrival, assessment, decision and leaving – were used, as they were carried out for every patient and occurred in a specific order, whereas other process points, as shown in Appendix 15, occurred less consistently (in both occurrence and order). Although these process points were chosen because they occurred routinely, there were a few occasions when a final decision had been made at the point when an assessment occurred, and this could influence the results. However, in general, a working decision was made at the point of assessment, and the final decision was made after the diagnostic tests.
Research question 1: how do medical staff and other practitioners contribute to decision-making?
The first RQ addressed by the VSM study related to the role of different medical staff in the decision-making process. The data captured the grade of medical staff who conducted the assessment and who made the final decision. It also captured whether there had been direct senior medical staff involvement in either the assessment or the decision-making, or indirect involvement through liaison with junior medical staff. Figure 8 shows the proportion of patients who were observed to have direct consultant involvement. In comparing consultant involvement and admission rates, it appeared that sites with greater consultant involvement had higher discharge rates. Overall, this fell short of significance (p = 0.06; Fisher’s exact test).
FIGURE 8.
Proportion of consultant involvement and admission rate by site.
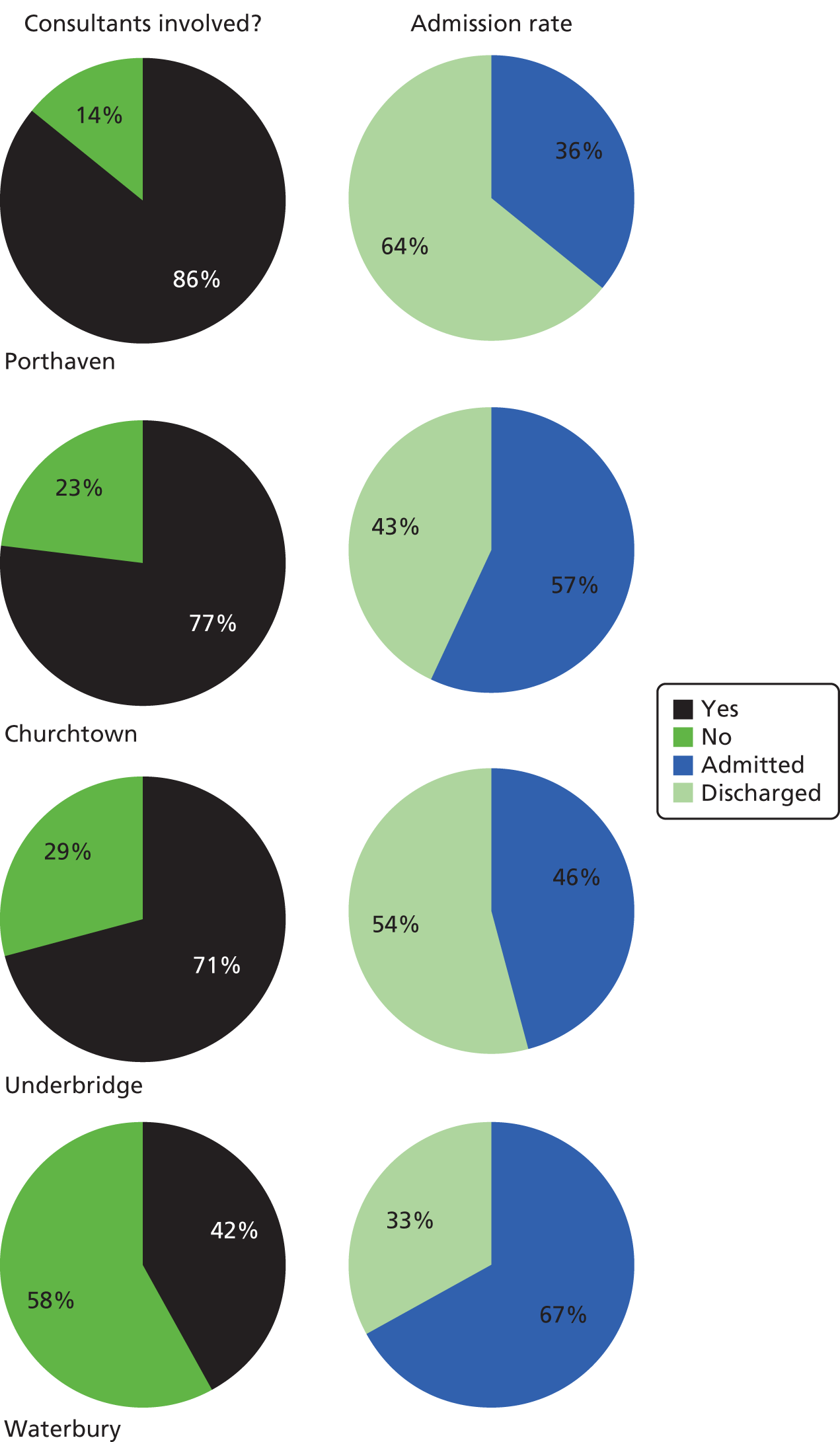
In comparing patients who had consultant involvement, we also plotted their overall journey time against patients without direct consultant involvement. The bar chart in Figure 9 suggests that patient journey time on average (median) was little affected by senior involvement.
FIGURE 9.
Median patient journey time and consultant involvement.
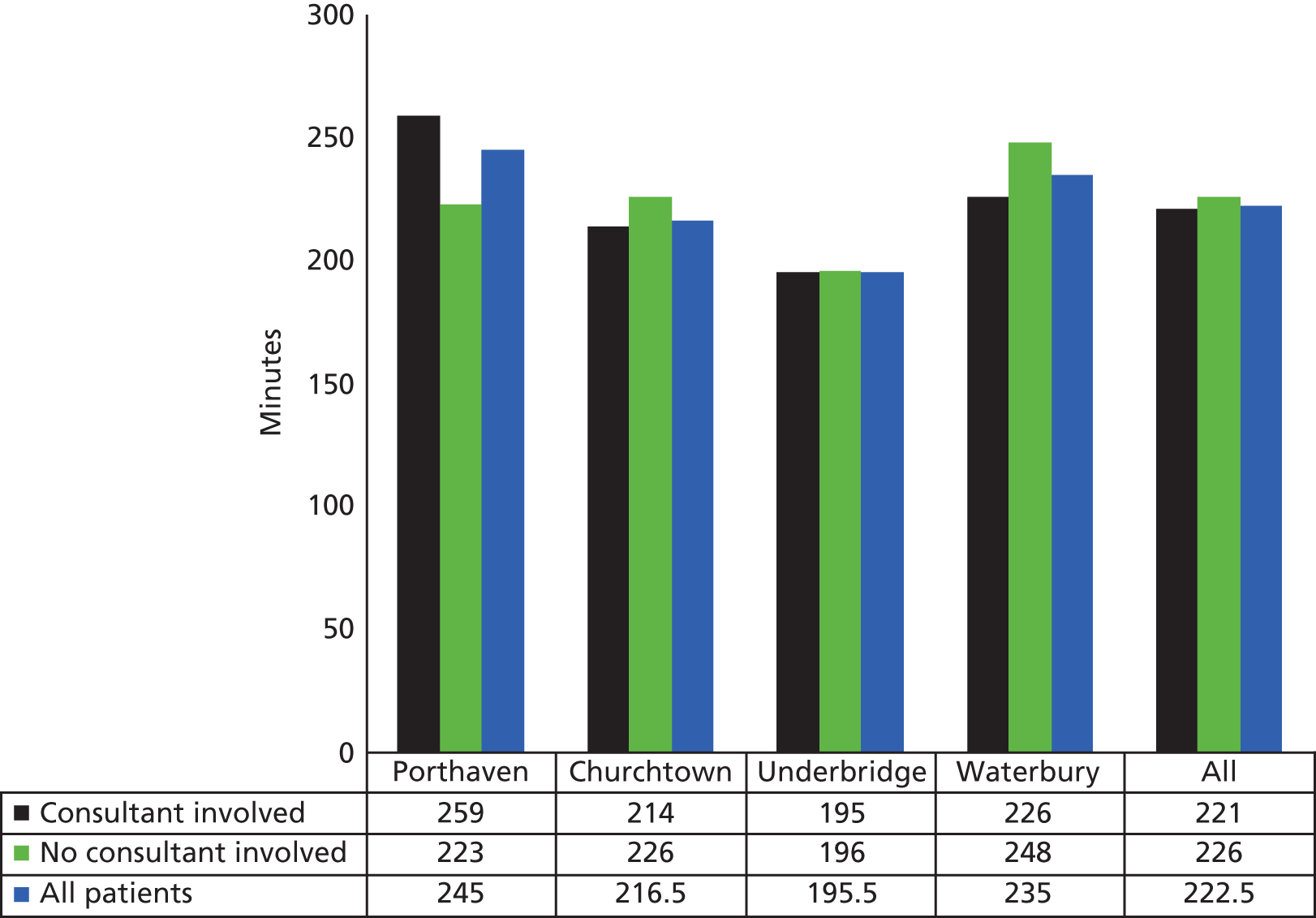
The shortest patient journey time, of 195 minutes, occurred at Underbridge. The data show that consultant involvement for that site accounted for only a 1-minute difference, on average, in journey time. In contrast, the longest patient journey time was observed at Porthaven, lasting 259 minutes, where a consultant was involved. This site experienced longer journey times with consultant involvement, but it also regularly used an observation unit for patients who required time-consuming diagnostic tests. During the observation unit stay, the patient remained under the responsibility of the ED staff.
To further investigate the involvement of medical staff in decision–making, we examined the time point when a doctor first saw the patient. Across the four sites, the median times to first review by a doctor ranged from 32 to 66 minutes, but averaged 55 minutes. We observed no significant association between time to first assessment and overall journey time [r = 0.13; p = 0.17 (Table 8)].
| Relationship between variables | Correlation coefficient (Pearson’s r) | Significance (p) |
|---|---|---|
| All patients: time of initial assessment to overall journey time | 0.13 | 0.17 |
| ED patients: time to initial assessment to overall journey time | 0.20 | 0.09 |
| Time of senior involvement to overall journey time | 0.25 | 0.03 |
We found that time to senior involvement was correlated significantly with overall journey time (r = 0.25; p = 0.03), represented by the scatter plot in Figure 10. This association suggested that earlier senior involvement could expedite decision-making. The connection observed tended to be more marked in cases seen in an ED (and it did not include alternative acute medical decision-making routes), but it did not reach statistical significance in this subgroup (r = 0.20; p = 0.09).
FIGURE 10.
Time to consultant involvement against journey time.
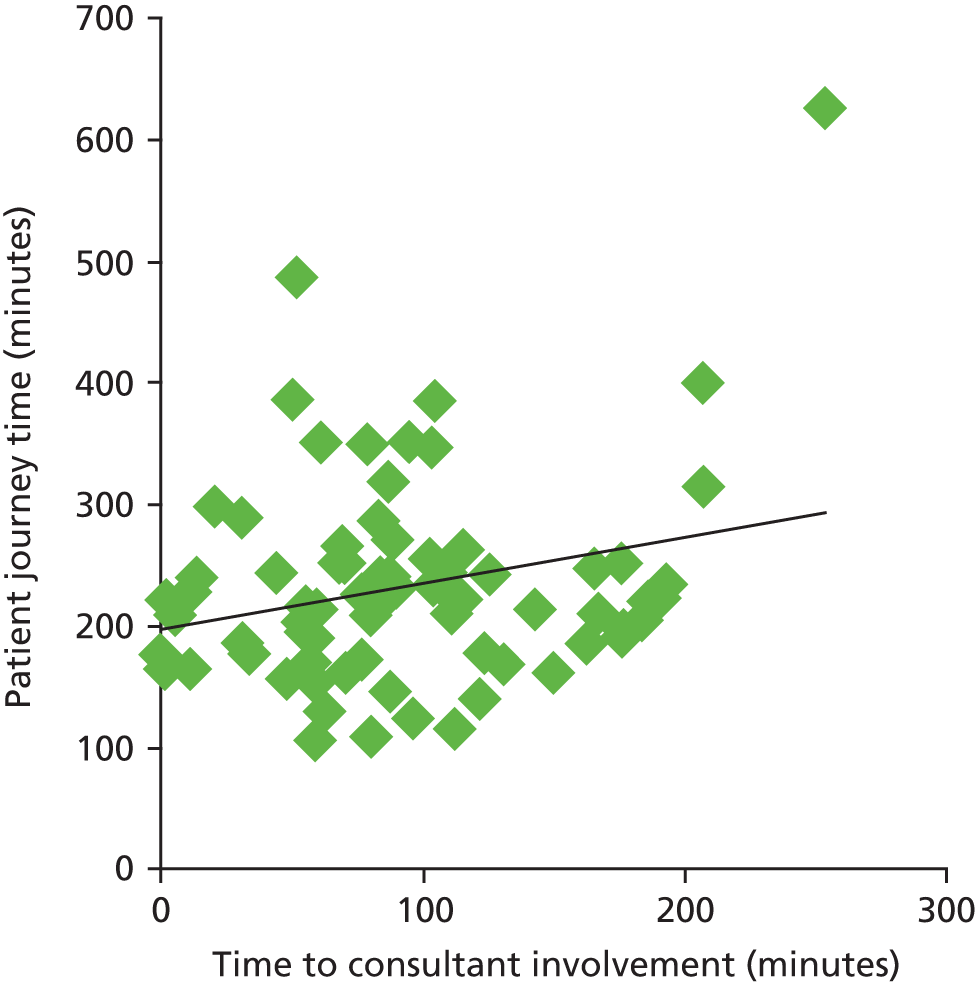
Research question 2: how do organisational factors affect decision-making?
The main organisational factor affecting the time to admission and discharge decisions was the 4-hour target, the impact of which can be seen in Figure 11.
FIGURE 11.
Admission and discharge decisions by time from arrival.

Few, if any, decisions were reached in the first hour, but the number of decisions rose rapidly and peaked at 223 minutes, close to the 4-hour target. A small tail of longer waits was also evident.
In considering the second RQ we also compared the acute care pathways at each site. The box-and-whisker plot in Figure 12 shows the journey time of patients divided by hospital pathway. In general, median journey times through both the ED and alternative pathways at each of the four sites appeared relatively similar.
FIGURE 12.
Patient journey time by hospital pathway for each site. max., maximum; min., minimum.
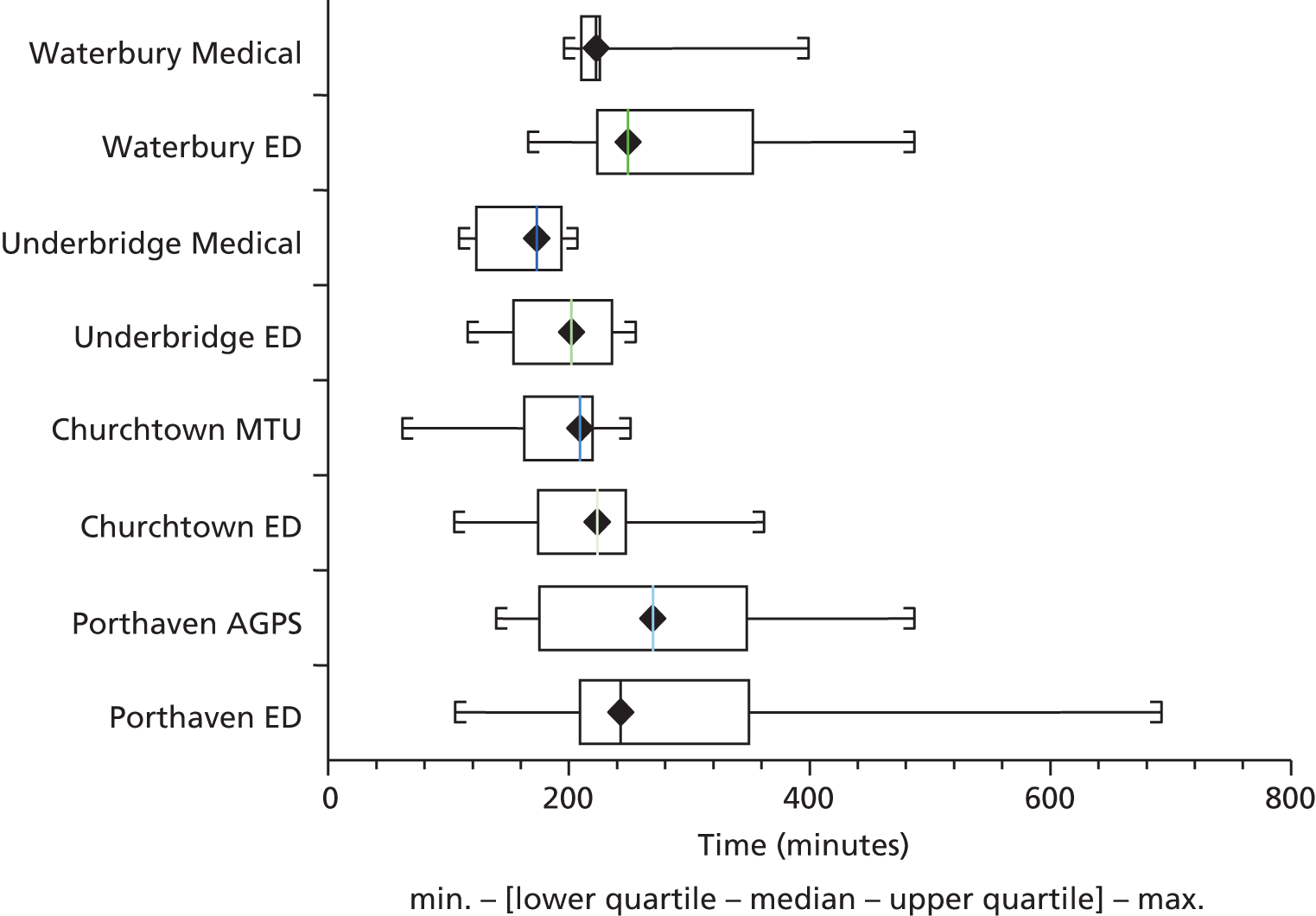
There may be several reasons for any time differences between medical pathways. Patients entering through the medical referral route had already had GP assessments; senior staff interviews and the clinical panel discussions suggested that these prior assessments were important in expediting decision-making. This factor could have offset the tendency towards slower assessment through the medical route, with consultant review often being based on periodic ‘board rounds’ between formal ward rounds, whereas consultant work patterns in EDs were more geared to continuous availability. However, beyond the ED/medical pathway dichotomy there were other organisational factors that were linked to the different models of care at the four sites, and these were considered separately.
Research question 3: how are the four models of care similar and different?
The third question addressed through the VSM data was that of the similarities and differences between the four sites. The overall patient journey times were similar for all four sites (see Figure 5). Although value-to-waste ratios were also similar at each site (see Figure 6), the stages in the pathways with lengthier waits differed (see Figure 7). Waiting prior to assessment varied significantly across the four sites (one-way ANOVA; p = 0.002). In general, significantly longer waits prior to assessment were observed at Underbridge (mean 45 minutes) and Waterbury (33 minutes) than at Porthaven (27 minutes) and Churchtown (17 minutes). It is possible that the shorter waits were at sites that made more frequent use of alternative entry points for GP-referred patients (i.e. direct to AMU and/or AGPS/ACU at Porthaven, and MTU at Churchtown), whereas sites where single-entry points predominated (Underbridge and Waterbury) appeared to have somewhat longer pre-treatment waits. However, Waterbury differed from Underbridge in accepting GP-referred patients through the ED because of lack of capacity in the medical assessment unit.
Safer and speedier decision-making was facilitated at Porthaven, a site with faster time to assessment, involving a central decision-maker within the ED, where the senior consultant had a designated advisory role, did not see patients directly and was clearly visible to juniors. However, Churchtown was the site with the shortest times to assessment. Churchtown also had a consultant in charge but did not use a controller in exactly the same way as Porthaven. At the sites without a controller, consultants moved around the departments or saw patients in addition. Possibly as a result, junior staff appeared to spend time locating the decision-maker, and this could have been a factor that slowed down decision-making.
Although waiting times after assessment, but prior to final decision, did not differ significantly across the sites (one-way ANOVA; p = 0.13), waiting times tended to be longer at Porthaven (mean 58 minutes). These times did not differ significantly from Churchtown (46 minutes) or Waterbury (30 minutes), but appeared slightly longer than at Underbridge [mean 28 minutes; p = 0.06 (t-test, unequal variance)]. There are several possible explanations for this, including the availability and use of observation units such as the CDU at Porthaven, where patients were ‘off the clock’ (see Chapter 5). Although the underlying explanation cannot be clearly identified, it may be speculated that there was a trade-off between longer waiting times for a decision and management plan that resulted in discharge – and thus less overall time in hospital – and an early decision to admit for observation and to await investigations and results, which resulted in a lengthier hospital stay.
Waits after the final decision also differed significantly between the sites (one-way ANOVA; p = 0.02). There was nearly a fourfold variation in mean wait at this stage. Waits were significantly shorter at Underbridge (mean 22 minutes), compared with 57 minutes at Porthaven (p = 0.02), 65 minutes at Churchtown (p = 0.01) and the longest waits, of 82 minutes, at Waterbury (p < 0.001). The time from the final decision to the time the patient left the assessment area, either admitted or discharged, is shown in Figure 13.
FIGURE 13.
Time from final decision to leaving department. max., maximum; min., minimum.
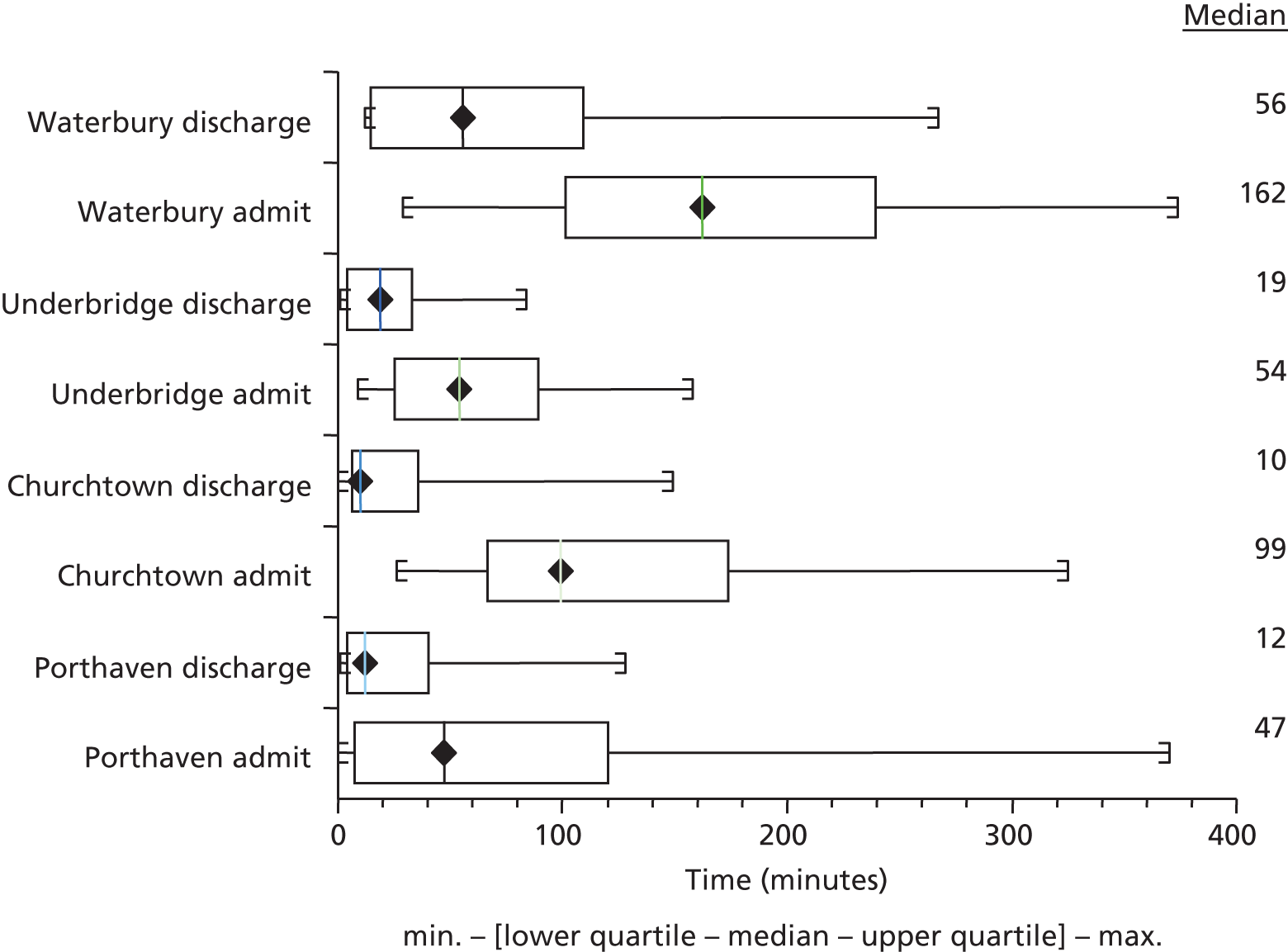
At all sites, discharged patients left the departments more quickly than those admitted. At Waterbury, the median time to discharge was nearly an hour after the decision, which appeared longer than at the other sites. All sites took nearly 1 hour or more to admit patients to a ward. It seems probable that differences in population dispersal and transportation could influence time to discharge, while in-hospital factors such as bed availability influenced time to admission.
Figure 14 shows a detailed breakdown of the known, observed reasons for waste time (with unknown reasons for waste excluded). Using the Lean definition, the largest source of waste from the patient perspective was in ‘waiting’. We therefore grouped the other categories of Lean waste into one, labelled ‘system wastes’, and explored the known reasons behind the waiting categories more fully. It can be seen from these figures that there appeared to be significant variation. For instance, in both Churchtown and Waterbury about 40% of wait time was attributable to waiting for a bed, compared with 9% at Porthaven and 3% at Underbridge. In Porthaven, 50% of observed wait times were associated with waiting for investigations or results, compared with 22–28% at the other three sites. At Underbridge, 28% of waits were for staff availability, compared with 21% at Porthaven, 12% at Waterbury and 8% at Churchtown.
FIGURE 14.
Types of waste from the patient’s perspective.
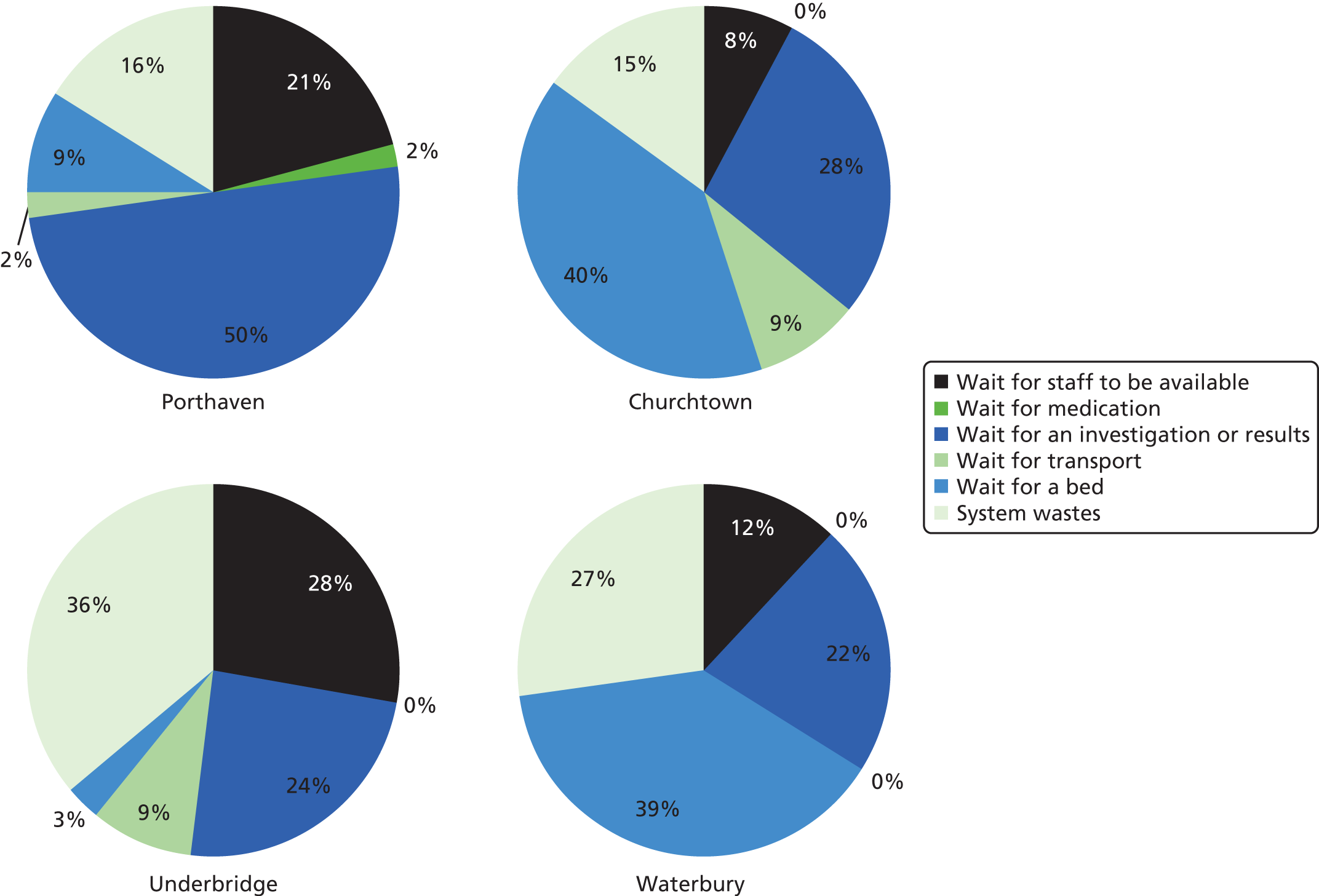
However, these figures should be treated with caution because they relate only to known waste. Some sites may have lent themselves more than others to the identification of reasons for waste, be they related to the observer’s location and the physical layout, ease of access to certain staff, or differences in information technology systems. In view of these considerations, no formal statistical comparison was undertaken on the data in Figure 14. Long waits for beds could have reflected high bed occupancy, slower turnaround or poor communication. Waits for tests or their results could have reflected differences in staffing, ability to move patients between different areas, proximity of X-ray departments, laboratory staffing and speed of diagnostic tests, or the information technology systems used to communicate results. The prominence of staff availability as a factor at one site suggests that waste time may have increased with workload, indicating reduced efficiency.
At the time of this study, it was reported that there were significant numbers of locum and agency staff at Underbridge. That may have been associated with decision-making by practitioners who were less well informed about local care pathways, and it also suggested staffing shortfalls.
Overall patient journey times were compared at each site for discharged and admitted patients, and in relation to presenting medical conditions. Figure 15 shows that median journey times were relatively similar for both admitted and discharged patients.
FIGURE 15.
Patient journey time and decisions to admit or discharge. max., maximum; min., minimum.
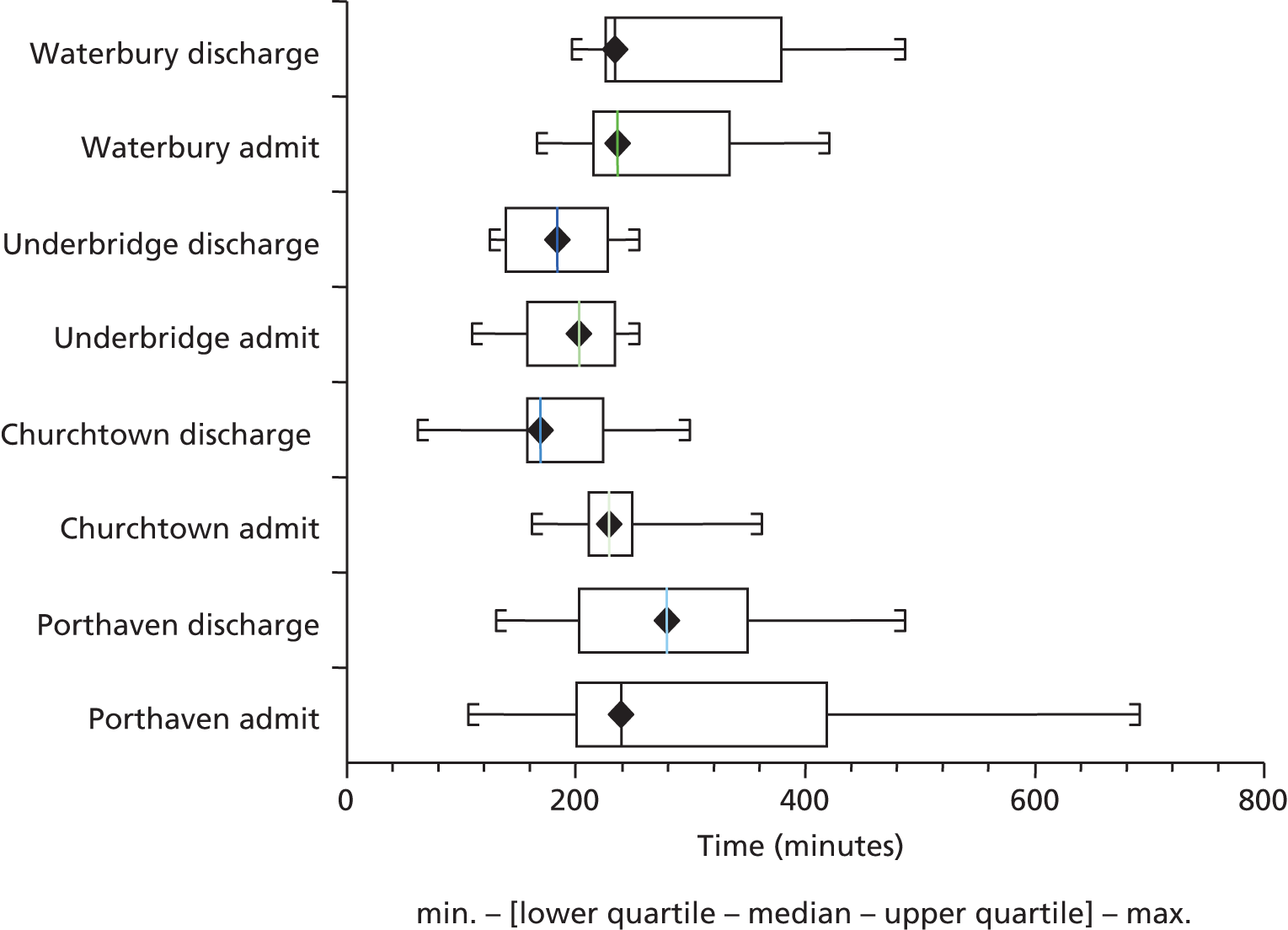
Similarly, there appeared to be relatively little difference between the journey times of cardiorespiratory and elderly patients at each site, although elderly patients tended to have longer journey times than cardiorespiratory patients at Waterbury. It is possible that this might have reflected differences in services for elderly patients with more complex conditions. Porthaven also included some considerably longer journey times for both patient categories (Figure 16).
FIGURE 16.
Overall patient journey times by category of presenting condition. max., maximum; min., minimum.
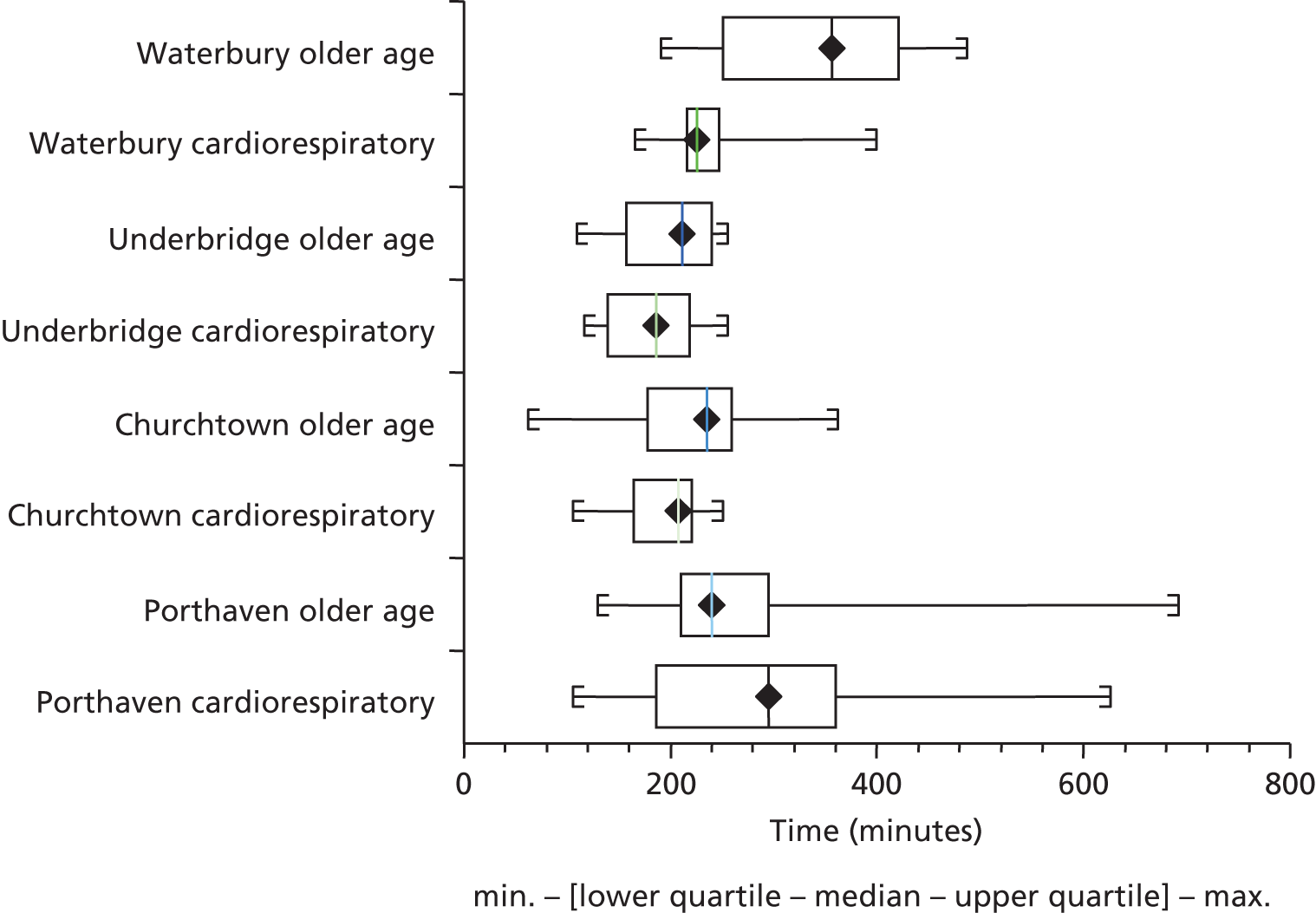
Estimates of staff costs at the four sites
We used routine NHS data to estimate the cost of NHS staff time spent on face-to-face interaction with VSM patients and on other observed patient-related activities (see Chapter 2 for method). Table 9 shows that there was an approximately twofold variation in the number of different staff seen by each VSM patient between Porthaven (median 4 staff seen) and Waterbury (median 8.5 staff seen).
| ED (number of patients) | Number of staff encountered per patient | |||||
|---|---|---|---|---|---|---|
| Mean | Median | Maximum | Minimum | 25th percentile | 75th percentile | |
| Porthaven (30) | 4.5 | 4.0 | 10 | 2 | 3.0 | 5.0 |
| Churchtown (30) | 6.7 | 5.0 | 21 | 2 | 3.3 | 8.8 |
| Underbridge (24) | 7.1 | 7.5 | 12 | 3 | 5.0 | 8.0 |
| Waterbury (24) | 8.4 | 8.5 | 13 | 6 | 6.75 | 9.25 |
There appeared to be differences between two pairs of sites: Porthaven and Churchtown on the one hand, and Underbridge and Waterbury on the other. More than three-quarters of patients in the latter two EDs saw over five different members of staff, compared with three-quarters of patients in Porthaven and Churchtown EDs seeing over three different members of staff. The maximum recorded number of staff was seen in Churchtown (21), illustrating the high number of practitioners that a patient might encounter during the journey through acute care.
The difference across sites in staff cost per patient was rather less marked (Table 10), suggesting that, in those EDs where patients saw more staff, the additional encounters were shorter and/or mainly with lower-grade (less highly paid) staff. Once again, Churchtown stood out from the other sites by having the widest range of staff costs, from £15 minimum to £253 maximum. It is not possible to ascertain the reasons for such variation in cost but it may imply significant variation in the complexity of individual patient journeys.
| ED (number of patients) | Cost of staff encounters per patient (£) | |||||
|---|---|---|---|---|---|---|
| Mean | Median | Maximum | Minimum | 25th percentile | 75th percentile | |
| Porthaven (30) | 64 | 61 | 128 | 18 | 34 | 85 |
| Churchtown (30) | 77 | 64 | 253 | 15 | 48 | 99 |
| Underbridge (24) | 77 | 73 | 181 | 17 | 55 | 85 |
| Waterbury (24) | 92 | 75 | 205 | 37 | 68 | 105 |
Table 11 shows a comparison of staff cost between admitted and discharged patients. Porthaven and Churchtown ED patients who were ultimately admitted to hospital had lower staff costs than those discharged. In contrast, the opposite was observed for Underbridge and Waterbury, where discharged patients had higher average staff costs than those admitted.
| Site | Number of patients admitted | Cost per admitted patient (£) | Number of patients discharged | Cost per discharged patient (£) | ||
|---|---|---|---|---|---|---|
| Median | Range | Median | Range | |||
| Porthaven | 13 | 61 | 18–99 | 17 | 66 | 22–128 |
| Churchtown | 17 | 65 | 15–128 | 13 | 60 | 16–253 |
| Underbridge | 11 | 85 | 36–181 | 13 | 57 | 17–87 |
| Waterbury | 18 | 87 | 37–205 | 7 | 73 | 37–177 |
Although analysis of their data was based on smaller subsamples of patients, Underbridge and Waterbury had higher staff costs for older patients than for those with cardiorespiratory problems, whereas average staff costs for older and cardiorespiratory patients in Porthaven were similar (Table 12).
| Site | Number of cardiovascular patients | Cost per cardiovascular patient (£) | Number of older patients | Cost per older patient (£) | ||
|---|---|---|---|---|---|---|
| Median | Range | Median | Range | |||
| Porthaven | 14 | 58 | 22–128 | 16 | 63 | 18–106 |
| Churchtown | 18 | 60 | 34–104 | 12 | 76 | 15–253 |
| Underbridge | 19 | 57 | 17–181 | 5 | 128 | 77–148 |
| Waterbury | 17 | 74 | 37–158 | 7 | 100 | 61–205 |
Although these results should be viewed cautiously because of the low numbers and limited sampling approach, they indicate some interesting differences in staffing arrangements and variation in models of care across sites.
Review of value stream mapping data by clinical panels
The review of selected VSM patient case studies by the clinical panels (see Appendix 2) resulted in rich discussions that also aided the interpretation of the VSM data.
The clinical panels commented on a patient whose VSM data identified a very rapid decision to admit in the face of an element of diagnostic uncertainty, followed by a long wait in the ED for a bed. The panel considered that the admission was probably inappropriate and might well have been avoidable, had the decision by the clinician been delayed, and had more time been spent on identifying a suitable alternative. Alternative options suggested were a dedicated rapid assessment team – had this been available – or placement in a community bed, which was apparently not explored. It was speculated that this was an example of the 4-hour target influencing a clinician to make an early, but ultimately suboptimal, decision. The availability and use of a CDU/observation ward in this case might have allowed more time to make a more appropriate decision for both patient and hospital (case VAP103).
The VSM data of another patient, who the panel considered was probably appropriately admitted, prompted the comment that admissions for observation can occur to avoid breaching the 4-hour target (case VAP121).
A further patient, whose admission was considered understandable but probably avoidable, had a long VSM time, being transferred to a ward 12 hours later. The clinical panel considered that this was a good example of a complex patient, perhaps inappropriately referred to the ED, when he could have received more appropriate and timely care by the relevant specialist team, probably without hospital admission (case VAP101). This case again highlighted the importance of accessible alternatives to admission for some patients; yet there was often difficulty in accessing these alternatives once a patient reached the ED and decision-making was subject to the 4-hour target.
Another patient’s VSM data revealed very rapid assessment and discharge, which was considered entirely appropriate (case VCP108), although the panel considered that such quick turnaround was relatively unusual, and in some contrast to the medical and social complexity of many of the patients commonly seen in EDs and AMUs.
The importance of patient safety and the risk of a wrong decision also arose in the case of another patient (case VDP101), whose admission was considered inevitable on the grounds of potential diagnosis and risk, and therefore it was not appropriate to consider alternatives.
In summary, the clinical panel discussions highlighted some key influences on decision-making in this selection of VSM cases. Whether an admission was avoidable or not depended ultimately on practitioners’, patients’ and carers’ perceptions of the medical and social risk of discharge; but also on practitioners having access to relevant background medical details, information about social circumstances and the availability of alternatives including community options, observation wards and appropriately resourced ambulatory care pathways. The availability of sufficient time appeared to be an overriding requirement in order to make the best decisions in more complex cases.
Discussion
Research question 1: how do medical staff and other practitioners contribute to decision-making?
Overall, senior clinician input was not significantly associated with admission rates, although there was a weak but significant correlation between early senior involvement and journey time. The site with most consultant involvement also appeared to have the lowest admission rate, while the site with the least consultant involvement had the highest admission rate, suggesting that there might be some relationship between the two.
All four sites had prioritised the ‘senior first’ approach, although this manifested in contrasting ways. While ethnographic analysis can help us to understand how senior clinicians (medical and/or nursing) became involved in patient care and what factors influenced this, it cannot necessarily ascertain how senior clinicians chose to distribute their time between direct involvement in decision-making for medically complex patients, and supervising and advising more junior staff. The VSM findings may question the claim that the ‘senior first’ policy – at least ‘consultant-led senior first’ – is essential for expeditious care and admission avoidance in all cases. Indirect senior input via juniors and nurses or via a ‘controller’, as at Porthaven, could provide alternative or complementary models and could have several advantages in terms of costs of staffing and training. The organisational ethnography (see Chapter 5) suggests that there may also have been differences among sites in the extent of skill-mixing, and the involvement and autonomy of nurse practitioners in decision-making.
Senior clinician input also appeared to exert relatively little influence on the duration of the patient journey. However, this could have been because all sites prioritised senior input (see Chapter 5), making differences less apparent. This finding could also be explained by the patient groups studied: for many of these patients, medical or social uncertainty was high at the outset; alternatively, other undetermined, factors were more influential than senior input. The 4-hour target was clearly a driving force that affected journey times, and senior input may have been a factor in adherence to this target.
It is possible to speculate that senior input may have been a significant factor in deciding whether patients were to be kept in admissions areas for longer or transferred to observation areas (e.g. a CDU such as Porthaven) where they were not subject to the 4-hour target, for observation (including ‘watchful waiting’), treatment and discharge planning. This flexibility could have had the added benefit of reducing peaks in patient movement as the 4-hour benchmark approached, thereby promoting a more even and predictable distribution of resources.
Research question 2: how do organisational factors affect decision-making?
The acute care pathway that patients followed was determined by their route of entry into the system. Patients’ experiences of care included overall journey times to admission or discharge, of which VSM gave a detailed breakdown. There was some suggestion that organisational factors could influence decision-making processes. For example, the AGPS in Porthaven – a feature not present at other sites – had lower admission rates than units for similar patients elsewhere.
However, journey times at other sites were also shorter for patients seen by medical teams than for those seen in the ED (p = 0.04). To access these faster pathways, patients usually had to be referred by their GP. Patients and GPs may have perceived attending the ED as resulting in quicker tests and diagnosis, but this was not necessarily the case. It may be suggested that a better understanding of these systems could favourably influence the way in which patients access health care and GPs make referrals. In turn, this could help to manage demand and influence future service planning. The Royal College of Emergency Medicine has proposed that ‘best practice’ is for all medical patients with GP assessments to be taken directly to the MAU (p. 2, recommendation 2N). 10 Our findings support the view that patients can receive treatment as promptly from medical teams as from the ED.
There was evidence that organisations’ responses to the 4-hour target influenced overall patient journey time, and therefore decision-making. All four sites had similar patient journey times, and admissions and discharges peaked around the 4-hour point. This suggested that the 4-hour target was driving the time point at which a decision was made and the patient was moved from the ED (or department associated with the 4-hour target).
Research question 3: how are the four models of care similar and different?
In addition to similar overall journey times, the amount of time spent waiting at each of the four sites was similar: a little less than half of the total time was spent waiting. This high proportion of waiting time is consistent with previous Lean work conducted in EDs. 69 The wait time may have reflected intrinsic elements of the clinical assessment process, such as the need for time to run tests and obtain results, or attend to personal care (e.g. eating, drinking, toileting), or may have been part of a more complex system of queuing in acute health care. However, the reasons for waiting, and the points in the journey where the longest waits occurred, differed significantly between sites.
One possible reason for differences in waiting times across sites might have been differences in the location and capacity of ACUs, as described in Chapter 3. Moreover, the ways in which these resources were used could also vary. At Porthaven, ED consultants had the option of both a CDU and ACU and referred to both of these, while the ACU was also used by the AGPS and medical assessment unit. At Churchtown, where there was no ED observation unit, the ACU was within the triage area of the medical assessment unit (remote from the ED) and patients were taken mostly via GP referrals. At Underbridge, appropriate patients were directed to the ambulatory emergency unit directly from the ED. At Waterbury, there was an eight-bedded observation unit (situated in the ED) as well as ambulatory care, used by ED and medical staff. Although 3A was not designed to compare the performance of individual pathways formally, it is clearly plausible that greater use of ACUs may reduce waits for assessment, investigation and discharge, while transfer of significant numbers of patients into CDUs may also shorten measured waiting times.
It is also possible that differences in waiting times may result from deliberate planned decisions about resource allocation. One explanation is that this could indicate a lack of sharing of best practice and innovations that could reduce waits. Sharing insights and best practice could reduce waits in different areas for all patients, thereby reducing waiting times and journey times overall, in all hospitals. For example, hospitals with longer waits for assessment or for discharge might benefit from adopting specific practices associated with shorter waits. Sharing of ideas and practice, promoting a best-practice model of care, could reduce waiting and journey times and enhance patient experience.
There were no substantial differences between the sites in the ratio of waste to value, and patients were waiting in the ED for nearly half of the time. Although value-adding activities could have been occurring behind the scenes, during waiting periods, this value ratio may give some indication of patient experience. However, there were significant differences in types of waits at the four sites. The project’s PPI group felt that some waits were more acceptable than others: waiting for triage and assessment could be experienced as less acceptable than subsequent waiting for test results. Waiting for first assessments was more adverse because the patient was not yet in the system and treatment could not commence. In contrast, waiting for test results could be more understandable, and patients were more amenable to waiting at this stage.
Therefore, the points in the patient journey where significant waits occurred could have a significant impact upon patient experience. Figure 7 shows that the waits occurred at different places in the patient journey at the four sites. Presumably, a relatively large proportion of waiting before being seen by an assessing doctor could have a detrimental effect on the patient’s overall experience. Assuming also that journey times and the ratio of waste to value remained similar across the sites (which we found), the model of care for each site could have a significant impact on different waits and therefore patient experience.
The finding of longer patient journey times for admitted than discharged patients was not overly surprising. The decision to admit triggered the quest for a bed in hospitals with uniformly high rates of bed occupancy. However, identifying the exact reasons for this waste time might identify organisational factors that can be improved. Porthaven was an exception to this trend, suggesting that this particular site may have some characteristic that expedites admissions. Similarly, Porthaven did not fit the pattern seen in Figure 16 of journey times in relation to category of presenting medical condition (i.e. older age group or cardiorespiratory). Three of the four sites had somewhat longer journey times for older patients than for cardiorespiratory patients, whereas Porthaven showed little or no difference.
Although the four sites exhibited similar value-to-waste ratios, the economic data suggested that there might be differences in cost per patient between the sites. These data must be treated with caution, in view of the assumptions upon which they are based, the limited sample sizes, and the fact that different models of care are being compared. Waterbury, the site with most staff per patient case, appeared to have the least consultant input and perhaps the highest admission rate. Porthaven and Churchtown, the sites with lower pre-assessment waste, had lower costs for admitted patients than for those discharged. At Underbridge and Waterbury, where costs for discharged patients appeared greater, there was greater post-assessment waste. At Waterbury, the ED staff costs for elderly patients appeared greater than those for cardiorespiratory patients.
In conclusion, the present study has generated some of the first VSM data for acute medical admissions in the UK, and it has used this method to evaluate and compare four sites with contrasting models of care. While this approach provided several unique insights, it also has limitations, which are discussed in Chapter 8. Several potentially significant differences in system performance were found, and these have possible implications for patient experience, organisational of care and running costs. The findings may be used to generate new hypotheses on the relative merits of different approaches to care, and to suggest solutions to challenges currently faced by the NHS.
Summary
-
Overall patient journey times were similar at all four sites, for both cardiorespiratory and elderly patient groups and for both the ED and medical admissions pathways.
-
The majority of patient admissions or discharges occurred close to the 4-hour target, suggesting that this target strongly influenced decision-making at all four sites. However, the 4-hour target may also have hastened some admissions that were avoidable.
-
Earlier senior involvement in decision-making had a weak but significant association with reduced patient journey time (a correlation that was stronger in ED cases).
-
The lowest admission rate was at the site with the highest level of senior involvement, and this site had also adopted several specific initiatives including a ‘controller’ to oversee ED activity, a dedicated CDU within the ED for observation, an ambulatory care pathway and an AGPS. The highest admission rate appeared to occur at the site with least senior involvement, although this site also differed in its care model.
-
Avoiding unnecessary acute admissions required time to establish alternatives, and this was sometimes not available within 4 hours. Initiatives aiming to reduce admission rates may do so by providing more time and information so that more appropriate decisions can be reached.
-
The CDUs/observation wards were a way to take potentially dischargeable patients with medical and/or social complexity ‘off the clock’, to allow time for tests, periods of observation or discharge arrangements, but their use varied significantly between the four sites.
-
The AGPS and ACU models could provide useful alternative pathways, mainly for pre-selected, GP-identified ambulatory patients who required hospital diagnostics but not a bed.
-
Waste and value were very similar at each site, but the sites contrasted in the stages where waste occurred. Sites where single-entry points predominated tended to have longer pre-assessment waits. Time spent awaiting test results or hospital beds also signified important sources of waste at some sites. Patients who were admitted had greater waste time than those discharged. Time waiting to leave the department after a decision to discharge also varied considerably between the four sites. These differences may also be associated with significant differences in staffing costs. The VSM study insights indicate several areas where performance could potentially be improved and ways to improve patient experience at these sites.
Chapter 5 Practitioner experience and organisational ethnography
This chapter explores decision-making about admission and discharge from the perspectives of clinicians and managers. The ethnographic data convey experiences of working in the highly charged environment of unscheduled care where practitioners sought to balance patient safety, resources (such as available staff, beds and transport) and 4-hour target compliance. Some particularities were associated with the site configurations and models described in Chapter 3: Porthaven with its spacious ED, acute GP unit and ‘controller’ departmental oversight; Churchtown with its restricted ED space, rapid senior assessment, medical triage and ambulatory care model, and pressure on nursing time; Underbridge with its single point of entry for all patients, and emergency services spread across two hospitals; and Waterbury with its senior nurse co-ordination of the all-through-the-front-door model, and emphasis on teaching and training. Staff on all sites had frequent discussions about appropriateness of attendance and avoidability of admissions with reference to primary and community health services and patients’ home care situations.
The emergency department ‘take-all’ model
Across the four sites, managers, consultants, and medical and nursing staff often spoke about the ‘take-all’ way in which EDs functioned, the only department that operated 24/7 and acted as a filter for other units. This was especially true of Waterbury, where, because of high occupancy of medical assessment beds, the ED also routinely housed GP-referred patients as they awaited medical review: ‘When a ward is full, it’s full. We never stop taking patients’ (Waterbury manager 1). Staff described the ED as the place where the doors were always open: ‘Patients will still keep continuing to come here because it’s the place with the lights on’ (Underbridge practitioner 1). Practitioners also represented it negatively as the place where ‘everybody gets dumped’ through inappropriate referrals (Waterbury practitioner 1) and in positive terms as the department known for giving a quick turnaround:
we’re the default position . . . for when every other system of health in this country fails, . . . so we’re sort of victims really of success. . . . I can see why people come here with GP stuff, because they know that we see them within 4 hours so they don’t have to wait 2 weeks for an appointment.
Porthaven practitioner 1
Effects of the 4-hour target
A parameter of reference for staff with longer experience in the system was the state of EDs before 2000, when the NHS introduced the 4-hour target: ‘Patients were waiting 8–12 hours routinely on hospital trolleys’ (Churchtown practitioner 1). Several practitioners said that they would not wish to return to that situation and, in that sense, the target had been a boon to them and to patients: ‘it isn’t good to have people in trolleys in the emergency department for a long time’ (Waterbury manager 2).
Emergency departments were designed as a route towards other places where a patient’s medical care and social needs could be more fully met: back at home with adequate support, in a community facility or on a hospital ward. There were other units where patients could ‘stop over’ if a diagnosis sufficient to guide further care could not be completed within 4 hours, if lack of beds or community resources impeded transfer or referral, or if there were transport delays. These could be observation, medical assessment, clinical decision or ACUs, or ‘holding bays’ for patients awaiting beds. Trolley waits in corridors still occurred, although these were said to be less frequent than in pre-target times.
There was widespread recognition by staff of the achievements of acute care in reducing waiting times, despite the increase in demand coupled with a diminishing bed base and closure of many community services: ‘It does work well, like even on busy days, I mean I think we try and see everybody promptly’ (Waterbury practitioner 2). Nevertheless, staff found it challenging to keep up with some of the accident and emergency (A&E) clinical quality indicators. 6 They described tensions in their efforts to ensure safety, avert breaches and provide patient-centred care, knowing that failure on any of these counts could generate financial penalties, patient harm and complaints:
I was aware of the time going by. Um, but I was quite late in deciding whether the patient was going to come into hospital or go home. . . . when the vascular surgeon came and had finished him and he said that he was happy for him to go home, then it was quite close to the 4-hour deadline, so then I was able to get his medication sorted . . . , to get him home before, before the 4 hours.
Waterbury practitioner 3
There was little slack in the system to accommodate peaks in demand, and practitioners described ‘constantly battling away against the crisis’ (Churchtown practitioner 2) as a routine state in medical assessment units as well as in EDs.
Practitioner views about factors influencing inappropriate attendance and admission
Practitioners across all sites believed there were high levels of what they regarded as ‘inappropriate attendances’ at EDs and MAUs, which affected admission levels. The designation of ‘inappropriate attendance’ triggered the expectation that admission could be avoided.
in our new protocol . . . [t]here’s ‘attendance avoidance’ so by a contact and advice over the phone, stopping people coming. ‘Admission avoidance’, which means you attend but we sort you out rapidly and we get you home.
Churchtown manager 1
Study respondents mentioned factors operating on the levels of the wider hospital system, external agents such as primary and community health-care services, and attitudes to risk of the individual practitioner and the patient or carer that contributed to inappropriate attendances and avoidable admissions:
you’ve got people . . . who don’t need hospital care but they can’t go home because they live on their own and you can’t sort out a social package out of hours, so they come into a hospital bed, which is not appropriate. So if there were more community beds there’d be less people in hospital.
Churchtown practitioner 3
[One consultant] says that he over-admits. . . . He says that . . . it is easier to admit than to turn them around. He’s risk averse . . . [and says that] the risk is also about not meeting the target and not just patient safety.
Porthaven fieldnotes 2
The role and responsibility of GPs and community nurses to reduce attendances and admissions was frequently mentioned, with some exceptional cases of acute staff expressing a collegiate approach to GPs, believing that they, too, brought skills to the cause of admission avoidance:
we’re quite good at risk-stratifying people and risk managing. So I think that’s something shared by us and GPs . . . they’re very good at managing risk without admitting to hospital, whereas the easy option is to admit.
Waterbury practitioner 4
Practitioners also mentioned the capacity of the ED and levels of staffing needed for rapid decision-making as being critical factors in admission avoidance. This was a particular concern in Churchtown, where the ED had the lowest capacity of the four sites:
if they are on a day when it’s full, when there’s more people coming in and there’s no outflow, then we haven’t got that capacity to [deal with it]. . . . It sort of backs up and then . . . the whole system gets in admission. . . . our rapid assessment . . . is stuff that we’ve been trying to do, but . . . I mean that works when it works well. And the problem with that again is staffing, is that if we’re tied up in Resus [the resuscitation unit] we can’t rapid-assess.
Churchtown practitioner 4
Working with time pressure
The ED environment could prove stimulating to staff who enjoyed high levels of activity:
I like . . . the challenges and the fact you don’t know what each day’s going to bring, . . . and the type of people you get through. . . . I don’t get bored in A&E whereas I did on the wards a little bit.
Waterbury practitioner 5
A valued feature of some EDs was the culture of teamwork: ‘We’ve always got each other and . . . you never have to make a decision all by yourself if you don’t want to’ (Waterbury practitioner 1). However, relations could become strained with professional groups and units outside EDs and MAUs that had different time frames and priorities.
Tension between emergency departments and medical specialty wards
The drive to avoid admissions was more visible in EDs than in other parts of the system, because of the pressure of continuous arrivals. MAUs also depended on possibilities for onward referral:
Acute medical units are . . . reliant on the wider medical wards. . . . we do everything we can do to speed up our processes . . . , but if beyond the back door [the unit] isn’t working, then we’re not going to work . . . and then that builds up to . . . a pile-up in ED, for want of a better phrase.
Underbridge manager 1
Target breaches officially belonged to trusts, but ED co-ordinators often carried prime responsibility for averting them. Practitioners from within and outside EDs could feel that they were being made individually responsible for delays affecting throughput:
[A specialty consultant] arrives at this point and takes the [patient’s] notes. The [ED manager] points out the time on the clock forcefully to him and reminds him of the breach target. He rather irritatedly says ‘Yes I know’.
Churchtown fieldnotes 4
Emergency department practitioners on all sites made efforts to reduce patients’ duration of hospital stay, even if this meant keeping them in the department for longer periods of observation and testing. Staff expressed concern about patients, especially the elderly, getting lost in the system. When people left the ED, the sense of urgency could be lost on the wards, paperwork became burdensome, and patients could ‘languish in the system’ (Churchtown fieldnotes 4), resulting in iatrogenic illnesses:
if you let people progress beyond [the ED] . . . they get unnecessarily trapped in a diagnostic and therapeutics spiral which takes days, costs hundreds of thousands of pounds, and doesn’t benefit the patient anyway. So I try and sort them out definitively in [the ED] if possible.
Porthaven practitioner 3
Underbridge staff identified their single-point-of-entry model as a system that attempted to avoid the above-mentioned loss of momentum, by enabling management of all patients – both those needing emergency care and those referred for medical assessment – to be initiated in the ED within the 4-hour limit.
Tipping points
Staff spoke of ‘tipping points’ that took them from a calm situation to one that felt unsafe. A nurse described these as regular rather than exceptional, feeling there were ‘just too many’ patients: ‘they overrun us and we couldn’t cope with it’ (Churchtown practitioner 6). Objective situations of bed occupancy blended with subjective limits when they started to feel out of control:
the department goes from a state of kind of normal business where it is flowing, we are meeting the targets, . . . we’ve got our noses above the water, and then suddenly, whether it be a surge in patient numbers or acuity or whatever it is and we tip over to, . . . we need to make people safe now, and the targets are largely irrelevant. But I find the most stressful bit of my work is . . . trying to hold onto the reins while we are tipping into crisis management.
Consultant in learning set 1
Moving patients through the system
Several nurses and some clinicians commented that the managerial drive for efficiency tended towards packaging and moving patients through the system like objects on a production line:
I think as nurses, um, if you forget that you’re dealing with human beings and you start thinking you’re dealing with boxes, which is sometimes how you get made to feel you should do.
Churchtown practitioner 7
Practitioners sometimes gave positive connotations to commodification of flow, which they explained in terms of not only achieving targets but also reducing delays:
we’ve tried to explain that I have 10 expecteds to come in and I’m moving them because it’s the right thing to do, because we shouldn’t have people awaiting beds, we shouldn’t have people awaiting treatment.
Underbridge manager 2
However, staff’s attention to flow meant that time for basic nursing care was reduced:
the human element to me is why I do my job, and it’s vital that we have the time to do that. . . . we get site management phone us and say, ‘This patient is on . . . 3 hours 55, why haven’t they gone to the ward?’ And it’s like, ‘Because they’ve just been incontinent and actually I want to wash them and put them on a clean bed, because I wouldn’t want to be wheeled down the corridor on a bed covered in urine, would you?’ . . . and I understand that that’s their job, to do the boxes: move that box from there within 4 hours, and it just doesn’t always work like that.
Churchtown practitioner 7
Time for patient care and communication
Flow management under pressure left little time for dialogue with patients and relatives, and staff acknowledged that this generated problems:
there’s lots of complaints that are made against the hospital and against the emergency department, most of which are to do with communication.
Porthaven practitioner 2
Senior clinicians tended to focus on ‘hard’ safety outcomes rather than ‘softer’ aspects of quality of care. Some associated spending time on practitioner–patient interaction with other staff roles, levels or ‘styles’ of delivery:
I get around very quickly, I discharge. . . . I don’t get any more complaints. My readmission rate’s no higher than anybody else, my mortality – so it’s not like I’m discharging people willy-nilly without any sort of safety checks in place. . . . some of the others will have some of the softer stuff that’s a bit more educational with the trainees. . . . they may spend a bit more time with the patients than I would. . . . it’s just a style thing really.
Underbridge practitioner 2
Practitioners made decisions by ‘ruling out’ risk factors rather than ‘ruling in’ to acute care (Underbridge practitioner 3), giving an expulsive movement to the service. A clinician in a stakeholder workshop said that the ‘ED is designed to frontload diagnostics, not “care”’. A learning set participant, however, expressed concern about communication with patients:
a quick way that would make a difference to the patient experience is how we manage to improve our communication of what’s happening with the patient, so that we have a policy where the patient knows what’s going on, . . . why they are waiting at all times.
Learning set 2
When staff did not feel pressured, they could show sensitivity in persuading patients to agree to a move that they considered appropriate. This was apparent in the case of a Churchtown specialist geriatrician who took time to visit the ED with the care of the elderly team, in search of patients they might help to discharge:
What do you think about that? Would you be happy with that?
You’re the doctor, you tell me what to do [laughing]. . . .
What do you think? Does that sound okay? [laughing]
Yeah. If Mum’s happy – if you’re happy for her to go home and you’ve obviously done a lot of tests and whatever and that’s fine.
Churchtown practitioner 8
Some practitioners linked being ‘busy and manic’ (Underbridge manager 2) with a default to admit patients. This state could generate a hyper-efficient, but confusing, mode of delivery, observed in MAUs as well as EDs, that unwittingly obstructed two-way communication:
Sorry about that. . . . such efficiency. . . . If you’re in in the morning, the doctors do a ward round. They usually finish by about 12 o’clock but you’re more than welcome to ring and see how she’s got on, but they might say, ‘We can’t give you any new information until the consultant has seen you’. All right? Any other questions that I can answer for you?
No that’s –
Are you going to go home and put your feet up and have a sleep? Are you going to be all right to drive home? As long as you – do you want to call a taxi? Do you want to use our phone here? Do you know a taxi number that you’d like to use?
No.
Guys, does anybody know a taxi number?
Churchtown practitioner 9
In observation and ambulatory facilities at Churchtown and other sites, the less pressured model of care gave opportunities for more relaxed and frequent communication with patients:
[The nursing assistant] takes it as part of her responsibility to check with patients while they are in the ambulatory area . . . if they have had fluids and foods.
[The staff nurse] comes in to ask [a patient] about her drugs and discusses the dosage . . . before she goes. . . .
Doctors are not based in ambulatory care but keep up with [patients’] progress via Patient First, and go in to see them as needed.
A junior doctor comes to speak to a patient who is waiting to go home. . . .
The junior doctor [says to another patient], ‘You can go home now. [We] will send the letter to the GP in the post. You can take ibuprofen. [I] suspect things will settle down in time. If it doesn’t, you can see your doctor’.
The nursing assistant says to a patient: ‘Sorry for the wait’ [for transport].
Churchtown fieldnotes 5
Effects of pressure on staff
Staff experienced strain between delivering patient-centred care and guarding acute beds:
family members think we’re holding our opinions more important and we’re thinking about resources. . . . an acute bed is a very special thing nowadays . . . so therefore we have to ring-fence them even more . . . everyone should be happy to try and not have you in one, as opposed to the other side that’s always been that a hospital is always there, it’s always safe, it’s always open, it’s always got beds, and that now just doesn’t exist any more.
Waterbury practitioner 6
A staff member described the effects of pressure on a cohort of senior nurses who left one ED:
we were getting more pressure to hit targets, and as senior nurses they were just saying . . . I don’t need this. . . . Roughly at the time . . . we all kind of went, hmm . . . we’ll just take a side-step. . . . [The ED has] lost a lot of nurses, . . . and the new nurses that we’ve recruited have had to be taught the skills to work in A&E, . . . we had to frantically put a lot of them through the triage training. . . . there’s 10 nurse posts out to advert at the moment for A&E here.
Churchtown practitioner 7
Decision-making about admission and discharge
One ED consultant explained that, whereas other specialties ‘throw their net very wide’ and ‘try to find out everything that might be seen to be going on’ with a patient, emergency practitioners focused ‘right down on the problem that’s brought them in’ and quickly tried to decide whether they required admission or not (Waterbury practitioner 7). Across all sites, decisions were rarely taken by just one practitioner in either the ED or the MAU; decision-making was frequently an evolving process combining the viewpoints of different grades of emergency or medical doctors and, where appropriate, professionals from other specialties and discharge teams:
it’s really a decision that’s made by everybody . . . if she’s been seen by another specialist and they have an opinion and they’re experienced in that, then I’m going to . . . go with what they say. I will state my case and say, ‘. . . the GP thought this and the community nurse thought this and, you know, clinically she’s well to go home, but . . . if you have genuine concerns then I’m not going to undermine those’.
Churchtown practitioner 10
Balancing risk and ensuring safety
Across the four sites decision-making was a dynamic process of evaluating the consequences of practitioner decision-making for three principal actors: for the patient, in terms of their safety and well-being; for the practitioner in terms of their reputation and feelings of self-worth; and for the hospital system in terms of resource implications and liabilities. Practitioners sometimes described decision-making as a rational process based on clinical judgement and knowledge of ‘statistics and success rates’ (Porthaven fieldnotes 4). At other moments they said that ‘You have to go with your gut feeling . . . within a reasonably safe parameter’ (Waterbury practitioner 8):
it’s like a sixth sense, it’s like a feeling of . . . failing the end-of-bed-o-gram, . . . and I think even consultants will still admit that feeling that there’s something that they’re not happy with but there’s no physiological complete signs for it, but if something’s not quite right the safest thing to do is . . . to admit them.
Porthaven practitioner 4
Although the attraction of working in ED was partly linked to making rapid decisions, this could also be experienced as the most stressful aspect of the job. Practitioners were acutely aware of the consequences of an inappropriate discharge decision:
I know colleagues who have been harmed by [the fact that] they missed a subarachnoid haemorrhage [or] they missed an aortic dissection and a young person went home and died, . . . and they suffer from that bias from the patient they’ve seen last. I think it’s then difficult to step back and actually go, ‘Just because I had a bad experience it’s not fair to inflict the negatives of over-testing on all the other patients I’ve seen’.
Porthaven practitioner 3
Practitioners often said that concern for patient safety outweighed all other factors (including targets) as an indicator for admission. This concept included the patient’s ability to live independently with or without support, to have their pain adequately managed, and to care for their emotional state or mental health. In responding to this spectrum of needs, acute care often acted as a substitute for social care:
we would obviously never discharge anyone that’s unsafe medically . . . ; and then there’s socially safe. Can somebody look after themselves? Are they going to be all right waiting for their carers that we can’t set up until the next day? . . . and the anxiety-related safe. Are they going to get home and become so anxious they phone an ambulance, in which case that’s not ideal either.
Waterbury practitioner 9
Practitioners characterised patient cases as ‘complex’ according to the combination of medical conditions present together with disability or social care needs. To manage such cases (see Appendix 12), acute care staff gathered information and criteria from various sources including other clinical specialties and, where available, specialist discharge teams. In other cases – typically of younger patients – there was less medical and social complexity, but commonly a level of anxiety that influenced their decision to seek acute care, sometimes out of general practice opening hours. Such patients were sometimes referred to by practitioners as the ‘worried well’ (Porthaven practitioner 4). Nevertheless, researchers observed several instances in which patients who had been described as anxious were assessed case by case to exclude serious conditions.
System contingencies and out of hours
Clinical need was not always the primary consideration in decision-making. Resource constraints, and system contingencies could sway practitioners towards admission. These factors were particularly compounded by the timing of the patient’s presentation at hospital. Practitioners stressed that their decision-making out of hours was influenced by lack of availability of diagnostics and specialist teams within the hospital and a perceived difficulty in setting up community-based support:
if we know that the family situation is breaking down, that the frail little old lady care package isn’t adequate and it can’t be changed, there isn’t a community system that’s responsible enough, um, to make that happen quickly, then I usually find I admit patients – and that’s frequently out of hours, so weekends, evenings – um, because you’re just going to make a difficult situation worse, on the whole, even though the patient may not necessarily be acutely unwell enough to require admission.
Underbridge practitioner 4
Although [the patient] looks clinically well and I think this could potentially be managed in the community hospital . . . I discussed it with [the medical consultant] and she sort of agreed that . . . now [the patient] is here she could come in under us.
Underbridge practitioner 4
Decision-making with limited time and information carried risks including readmission:
I think to myself: ‘What if I missed something? How would it look? But if we keep readmitting . . . it’s not helpful. If at any time anything happens, [the patient] can come back to A&E.
Waterbury practitioner 9
Emergency consultants described their hallmarks as having the confidence to bear risk and an eye for probability:
Admitting people is the easy option actually. Taking the risk and the responsibility to send somebody home is [a] more difficult decision sometimes.
Porthaven practitioner 4
I think it’s the confidence to be able to let them go home with the proviso that they can always come back as well.
Underbridge practitioner 2
Some senior clinicians, especially when occupying the central decision-maker or ‘controller’ role in Porthaven, concentrated on departmental management and reviewed cases by liaising with other practitioners without necessarily seeing patients. Other clinicians emphasised the importance of ‘eyeballing’ the patient (Underbridge practitioner 5) and basing their judgement on the patient’s appearance and a first-hand conversation.
Target compliance
Target compliance was a basic factor influencing the moment at which ED decisions were made:
I would say 9 times out of 10 that decision-making is done because the pressure that’s felt to move those patients out of the emergency department, either ’cos, you know, the general feeling that it’s unsafe or simply because, you know, the clock is ticking and we’re getting to that 4 hours.
Waterbury manager 2
Admissions were observed to occur where there was uncertainty about admission or discharge and a breach time approached, in order to ‘buy time’ for making assessments of an evolving condition:
a lot of the time we admit patients that don’t need to be admitted, they just need a bit longer, so either they need a blood test to be taken for example, 6 hours after a bit of chest pain, and . . . if we want that we potentially have to admit them to wait for that blood test.
Porthaven practitioner 5
The decisions of ED practitioners were often tempered by the threat of sanctions governed by audits. Tension was created between risk aversion and a culture of admission avoidance within a strict time frame:
I think a lot of the junior doctors who haven’t chosen the specialty find that taking risk is very stressful . . . because we do get blamed if we’re . . . I’m not convinced that we’re adequately supported in that and I think if there was better support for backing up risk, as it were, then people would be more willing to take the chance of sending a patient home.
Waterbury practitioner 1
Pressure from patients’ relatives
Practitioners reported that the need to ‘give the relatives the option’ about admission for elderly patients (Churchtown practitioner 7) acted as a pressure in the course of decision-making:
Sometimes [relatives] can really have an impact if they say, ‘Actually, you know, we can’t manage at home, you know, we’ve tried to do this, we’ve tried to do that and actually we want somebody to sort this out’ . . . the wards will say, ‘Well actually [relatives] said can [the patient] stay in another night because they have got to do something and then they’ll come and collect them tomorrow?’ and you think, ‘Really?’ . . . but just by the same token some people will say, ‘No they’re not staying, and I’m taking them home.’
Churchtown manager 2
Defensive practice
Practitioners balanced the risk that might be posed to a patient by admission or discharge, or by investigations that might be requested. They were also influenced by what was safest for the hospital, other patients, the community at large, and practitioners themselves: ‘you could potentially be putting them at risk and subsequently yourself at risk from a defensive perspective’ (Waterbury practitioner 10). Practitioners were concerned that their professional reputation was often at stake in the rapid decisions required of them:
staff are not going to put their jobs on the line by reducing the threshold to discharge patients when it’s not their issue. If you’re left to look after a patient and to medically look after the patient and that’s what you’re there for they’re not going to worry that patients are not getting in through the door, because that’s people’s reputation on the line isn’t it and that patient’s experience of sending them home – all that’ll happen is they’ll just go home and come back in again.
Waterbury practitioner 12
Practitioners said that admission was more likely if a time-consuming process was needed for discharge, where there were staff shortages, and if there were a high number of acutely ill patients:
if you’ve gone down from 9, 10, 11 doctors, to 4 doctors, and the acuity of the patients has gone up – the numbers of new attendances [is] slightly lower at two in the morning than two in the afternoon, but the acuity will be worse – . . . [then] the doctors will be very pressurised in terms of decision-making and much more likely . . . to opt for the path of least resistance and get a patient admitted, rather than try and initiate a whole series of things that are going to be very hard to try and undertake at two o’clock in the morning.
Underbridge practitioner 4
Access to general practitioner notes
Background information about patients was considered important for safe decision-making. This could come from the patient or carer, from referral letters or from GP notes if available. However, it was emphasised that access to primary care information was impossible if patients attended out of hours:
If you’ve got a complex patient who is not the best of historians . . . then trying to piece together . . . enough of the picture to make the decision can be very challenging. . . . if you go out of hours and the GP is no longer open . . . you’re working with far less information and then you have to veer on the side of safety . . . and because you’re going to be more cautious, . . . then you will admit more.
Underbridge practitioner 5
Access to GP notes varied across sites. The AGPS at Porthaven had direct electronic access, and Waterbury ED was piloting a system of electronic access to notes from selected GP practices:
we have access to [notes from] a significant number . . . , probably about half of GP systems at the moment, and that’s going to increase, which has been dramatically helpful in deciding.
Waterbury practitioner 4
However, for one patient in Waterbury ED, access was attempted but was observed to be unsuccessful:
[The consultant] suggested that they utilise a new system whereby they are able to access GP notes, with the patient’s permission. Unfortunately this proved unsuccessful, although the consultant [said] that the new initiative had made decision-making easier when they were able to view GP assessments of patients.
Waterbury fieldnotes 5
On sites without access to GP notes, clinicians could decide to call the GP, although this was rarely observed in our patient case studies. Instead, ED practitioners generally preferred to rely on the accounts of patients and relatives.
The role of senior input
Services had evolved on all four study sites to ensure that senior practitioners – including nurse co-ordinators, advanced nurse practitioners (ANPs), experienced middle-grade doctors, managers and consultants – were available to make early decisions about admission and discharge. Admission avoidance initiatives included input from seniors at the hospital ‘front door’, pathways such as ‘ratting’ (rapid assessment and treatment) or Emergency Physicians Integrated Care (EPIC) at Churchtown and Underbridge, and AGPSs such as those offered at Porthaven.
Senior status was attributed to practitioners on different grounds: formal position and institutional authority; clinical and technical knowledge; and breadth of local experience, which locums did not necessarily have. The role of emergency consultants was said to be different from that of any other specialty. Practitioners recognised their broad clinical experience and knowledge of alternatives to acute admission. Critical to the ability to discharge was the consultant’s relative certainty that the patient could safely leave the hospital, over and above considerations about institutional capacity:
it’s just seeing thousands and thousands of cases and seeing how they’ve panned out. And it helps you to spot the slightly unusual as well, and that can help you prevent something going wrong.
Churchtown practitioner 1
Dealing with multiple roles
Drawing on their authority, knowledge and local experience, consultants integrated what they called ‘predictive and proactive management’ into their multiple activities:
trying to maintain an awareness of . . . the whole department and managing . . . the clinical resource, so both nursing and medical . . . but also managing the clinical risk and safety for each patient . . . so within that I might have um, influences in terms of, you know, how busy is the department . . . how busy is the rest of the hospital, how busy are my specialty colleagues, . . . what’s happening outside in the pre-hospital environment, . . . what’s the likely scenario that’s going to happen over the next hour?
Waterbury practitioner 11
Multitasking was a visible feature of the work dynamic of senior managers and clinicians: ‘I remember one patient looked at me and said, “Do you know you’ve had 30 conversations in 15 minutes?”’ (Underbridge practitioner 6). ED seniors generally had limited opportunities to plan their workload, since they responded to all in the department. Consultants’ decision-making expertise was acknowledged, but less recognition was given to their ability to oversee the department, support juniors and maintain flow, and simultaneously attend to their own caseload: ‘that’s often one of the biggest challenges, is trying to do both of those roles at the same time’ (Underbridge practitioner 11). Porthaven used a different model whereby consultants took turns acting as managerial lead without seeing patients, reportedly with several benefits:
when we started to put in lots of consultants on the shop floor, the problem we discovered very rapidly was there were lots of chiefs. . . . so we have what’s called a Fat Controller . . . whose job is not to see patients but . . . to sit and run the department. So they liaise with the senior nurse, they liaise with the specialties, . . . with people like radiology, and they . . . make sure that patients are all seen appropriately, [that] flow is maintained . . . Fat Controller should know a bit about every patient in the department. . . . you’re the focal point for junior doctors to discuss patients with. So it means the other consultants . . . can get on with seeing patients . . . we think it works very well.
Porthaven practitioner 2
Cherry-picking
Some seniors selected cases where they felt they could give most value by diagnosing or discharging them in less time than junior doctors could do:
Sometimes I’ll cherry-pick things that I think I might sort out more quickly or be more likely to send home than other people. So if I see someone that I think is potentially dischargeable then I might see them myself.
Waterbury practitioner 1
An alternative version of ‘cherry-picking’ was choosing to see frequently attending patients, nicknamed ‘frequent flyers’, to avoid junior doctors getting drawn into unnecessary admissions:
if I see someone who is, let’s say, er, a well-known patient, say, who has a problem so like alcoholic, so someone who keeps coming in and complaining of a problem which has been ruled out repeatedly in the past, . . . I’ll go see them because I’ll be able to make the decision much faster than a junior doctor.
Porthaven practitioner 2
Fixing, not delegating
Emergency department consultants described how, if they wanted something done, they just did it, whether that was taking a blood test, arranging for an admission or securing a clinic appointment, particularly when their knowledge of the system allowed them to take shortcuts:
maybe apart from anaesthesia you would struggle to find a consultant doing blood tests, yet here, if I see a patient and they need bloods done I’ll do them.
Porthaven practitioner 2
. . . before going to see [the patient] I was expecting I was going to try and do things for this afternoon . . . a CT [computerised tomography] scan, making sure I’d seen his ECG [electrocardiogram], and have blood tests done. . . . I wanted to [get the patient seen by a] TIA [transient ischaemic attack] clinic which runs Monday to Friday . . . but not at weekends. . . . knowing the system and the seniority allowed me to do those things more quickly.
Underbridge practitioner 7
Seniors could have the confidence to reverse a decision on the basis of further observation and test results, also considering pressure on beds:
if he was pain free and we’d had a CT and it’s normal, and he still hasn’t . . . got a bed on the ward, then we could potentially review things at that point, couldn’t we? . . . reverse the decisions.
Churchtown practitioner 4
Staff acknowledged the speed with which seniors could operate and their ability to take responsibility for discharge:
a consultant was brought in on the weekend and he discharged 16 patients. Now if you’ve got a junior, they won’t do that . . . there is this thing about having a senior person around to say, actually, you can go home, you don’t need to come here.
Underbridge manager 3
In combining multitasking with a hands-on approach, consultants tended to ‘make it happen’ rather than delegate tasks, although they were sometimes observed to delegate to senior nurse co-ordinators. Some ED consultants spoke more of doctors and nurses working ‘together as a team’ in a different way from ward culture, which was said to be ‘more them and us’ (Porthaven practitioner 1). The culture of joint working between doctors and nurses was not however, shared across all sites, and in some departments tensions were reported.
Seniors could facilitate consultations across departments and requests for speedy testing, in ways that were not generally accessible to juniors:
if one of the acute physicians was in the department and I see them, . . . with their specialist interest in a particular area, I might run something by them. Radiologists I’ll phone up if I’m uncertain about a scan or an X-ray. . . . I feel completely comfortable to phone anybody in the hospital if I wanted advice from them and generally they’re very happy to give it. . . . also consultant status means everyone’s nice to you. [Laughs] The junior doctors may not have such an easy time asking for advice or favours or ‘Could you just fit this one in?’ or ‘Could I just have that scanned?’
Waterbury practitioner 1
Training junior doctors and other staff
While making increasing demands for rapid decision-making, the hospital emergency system allowed little time for seniors to train staff in this skill, in triage and in the network of services for referral. Pressure on consultants’ time meant that they sometimes ‘fixed’ issues rather than talking juniors through the process: ‘I’ll just make the decision’ (Underbridge practitioner 3). A Waterbury co-ordinator pointed out one potential disadvantage of the ‘senior first’ model:
if someone senior has already seen [the patient] and said [to a junior doctor], ‘You need to do this, this and this, and this is what the outcome’s likely to be’, then it takes away that kind of decision-making process . . . and [juniors] become a more admin type.
Waterbury practitioner 4
One ED consultant considered that it was characteristic of emergency medicine to have a ‘very high hit rate’ of juniors requesting decision-making support from seniors: ‘It’s hard for you to have your own clinical workload’ (Waterbury practitioner 11). Some consultants acknowledged that taking time to teach was an intrinsic part of their work and beneficial to all. Modes of support varied across sites: Porthaven seniors slotting in micro teaching sessions; Churchtown consultants discussing reasoning processes in decision-making with juniors; Underbridge seniors, from both emergency and medical departments, balancing teaching with safe cover in the department; and Waterbury being known as a site where seniors felt themselves to be particularly accessible. Despite this advantage, new intakes of junior doctors took time to develop their own decision-making skills:
we’re very visible in our department, there’s always somebody [juniors] can ask 24 hours a day and most people are very approachable . . . sometimes you find you’ve got a queue of three people constantly, you know, for 8 hours at a time waiting to ask you to make their decisions for them.
Waterbury practitioner 1
In their early training stages, juniors were said to compound busyness. They underwent rapid training, acquired experience on the job, and moved on:
when we’re quieter the junior doctors will get more support . . . you get your new doctors, you get a really busy department, you just go, well, we’ve just got to survive, we’ve just got to get through this period.
Churchtown practitioner 7
Senior nurse managers as well as consultants monitored and supported junior doctors: ‘Some juniors can be very good, it’s an individual thing . . . they’re sort of safety-netted by our senior team so [as] to reduce risk of bad management’ (Porthaven practitioner 1).
Emergency department pressures were said to leave insufficient time for training staff in decision-making:
undertrained staff . . . are not confident to make a decision and therefore defer this decision to others, which often [means] admitting until someone can review the decision. It is not these individuals who are at fault . . . they do not receive adequate training and support.
Underbridge practitioner 8
On some sites, the decision-making role of ANPs was said to be inadequately supported:
they’re actually very nervous of making those sort of decisions without getting another senior review . . . I think generally it’s about having senior people within the department. If you’ve got emergency nurse practitioners . . . who will . . . look at the X-ray and say, ‘You can go home’ – it’s about training, skill, competence, seniority, I suppose, as opposed to more formal systems.
Underbridge manager 3
This was reflected in one ANP’s comments regarding her limited role in decision-making, which she linked with a deficit in authority, and possibly also in clinical knowledge:
none of us are able to . . . we don’t have that, the authority to say this patient’s going home . . . when you’ve seen the patient . . . we’re not clinical decision-makers in that I couldn’t discharge someone solely off my own back.
Waterbury practitioner 9
Middle-grade doctors who had developed skills and knowledge of the local system over years were observed to bring considerable benefits to teams. Some staff commented that waiting for senior review could cause greater delays to patients than decision-making by capable middle-grades. It was important for safety that they could judge whether or not it was necessary to seek the opinion of a senior:
if I’m fairly happy with what I’m doing then I don’t need to discuss everything with somebody senior. . . . I’ve kind of gone with my . . . gut instinct and I manage him. . . . I know that he’s going to [medical assessment] . . . so I think he’ll be relatively safe.
Porthaven practitioner 5
Trainees’ skill in decision-making was said to be favoured not only by their expanding knowledge and local experience, but also by having a temperament that was neither overly risk averse nor excessively bold:
it’s down to the individual, there are certain docs you are – have got on your radar, . . . the ones that tend to be just a little bit too reckless and also the ones that tend to be too cautious.
Underbridge practitioner 3
Admission avoidance initiatives
Early senior input was taken to be pivotal for acute care improvements on all sites. This element in admission avoidance was not necessarily protocolised, but, to be successful, it was said to require sufficient availability of diagnostic tests, community beds, access to GP notes and collaboration from medical specialists:
we are throwing money at the problem by doing consultant triage . . . I mentioned EPIC to you where you come in and you’ll be seen by a consultant immediately and test ordered immediately and plans made immediately, so that should help things. Erm, but [it’s] the most expensive way of doing it, is the only problem with that. . . . I think ultimately . . . it’s the back-up services; you need the tests to be able to be done quickly and to be interpreted quickly. And the resource available if there’s an issue to be able to make that decision.
Porthaven practitioner 2
Acute medical specialists
Some practitioners considered that input from medical specialists early in decision-making could reduce admissions to acute wards, particularly for the type of patients with uncertain medical diagnoses on which this study focused:
a lot of our doctors are GP trainees, and they’re not necessarily A&E or they’re not necessarily medical . . . they’re not specialised in medicine or . . . surgery, so therefore they’ll admit most people. Whereas if we had a specialty doctor in the department – so if we had a medical doctor specifically – they could say, actually, you don’t need to be admitted. Like we’ve got one of our consultants from medicine down here, at the moment, having a look at one of our patients to decide whether they actually need to go to the ward or not.
Churchtown practitioner 11
Medical physicians sometimes came to assess ‘medical and uncertain’ patients and attempted to achieve their discharge, where appropriate, directly from the ED, thus preventing potential waits for beds to become available in MAUs. This was routine practice in Underbridge, because of the single-point-of-access model in which medical and emergency physicians worked together in the ED. It was also the default practice in Waterbury, where the high occupancy rates of MAU beds rendered it expedient for on-call medical physicians to make admission or discharge decisions directly from the ED. On both sites, the transfer of patients was facilitated by the close proximity of the ED and the MAU.
Even where the geographical distance between units was greater, the working relationship between emergency and medical physicians was emphasised as productive for admission avoidance. A Churchtown medical consultant made occasional, unplanned visits to ED:
had we [the medical team] got to the gentleman in time who has since gone to the ward, we’d have thrown him straight out. . . . this lady here is going to go straight home . . . because we don’t think she needs the blood test that ED want to do. . . . we have a greater confidence because we have greater experience of medical patients.
Churchtown practitioner 2
Initiatives from the ground up
Given manifestations of overload on the front line, EDs were observed and reported to run with remarkable efficiency for much of the time. System improvements operated partly in response to policy mandates, but organisational resilience was fundamentally achieved through a strategy of teams pulling together in EDs and other acute care units in multiple efforts to avoid inappropriate admissions. Practitioners on each site mentioned at least 15 concurrent initiatives that they associated with admission avoidance, including acute GP units, ambulatory care, attendance-avoidance phone advice, care of the elderly teams, CDUs, discharge teams, ‘hot’ clinics, nurse practitioner roles, observation units, physiotherapy within 24 hours of admission, rapid assessment on arrival, short-stay units and urgent care groups. Additionally, clinical protocols to reduce the likelihood of admission had been established for conditions such as cellulitis and pulmonary embolism (PE), and for chest pain investigation (Triple Marker system). Informal initiatives included interpersonal strategies such as ‘begging and chatting people up’ for extra CT-scan slots (Waterbury practitioner 12).
Some initiatives were short-lived pilots, such as an eight-bedded trolley area run by nurse practitioners within a medical assessment unit: ‘We trialled it twice but . . . it lasted about 24 hours before it was filled with inpatients and therefore we sort of adapted our role to now go to the patient wherever they arrive in the hospital’ (Waterbury practitioner 9). Initiatives were constantly adapted in response to changes in site configuration, staff availability, seasonal demand and policy mandates. An AGPS was disbanded at Churchtown shortly before our data collection commenced, and during the course of this study an ACU was opened at Underbridge.
The plethora of initiatives did not depend on formal oversight and seemed to have a motivating effect on teams working towards a common goal:
we’ve launched [AEC] . . . and we’ve got . . . the Go In team, who . . . look at people at the front door rather than admit them straight away. . . . we have got mental health support . . . We have a paediatric assessment unit, . . . It’s kind of like a [CDU] . . . we do have a couple of emergency clinics . . . that we’re able to admit directly into.
Underbridge manager 9
Varying concepts of admission and admission avoidance
Far from being subject to a unitary definition, the term ‘admission’ was used in various ways associated with the ground-up initiatives employed across sites. There were formal trust and commissioner definitions of what constituted an ‘admission’, some associated with tariffs:
Admission for me is when we get the paid money for an admission . . . so [as CDU] we get a tariff for that . . . it’s several hundreds of pounds, I don’t know what the locally negotiated rate is, but it’s normally sort of like £400 to £600.
Porthaven practitioner 3
At the moment, [in ambulatory care], if we pull a patient from the emergency department and we then admit that patient, we don’t get paid for that presentation, which is a risk.
Underbridge practitioner 10
There were corresponding local and informal ideas of what constituted an admission for practitioners:
what we’ve got to understand is [getting] away from admitting patients long-term. . . . At some point we still have to treat our patient. . . . are we saying avoidable admission? No, people still need to be admitted for treatment. . . . That can’t change. What we’re looking at is avoidable length of stay – is probably more correct.
Underbridge practitioner 6
Differences also occurred within sites and across departments in what counted as an admission. Practitioners variously referred to patients breaching the 4-hour target, on a bed in a ward base, in hospital overnight and referred to a specialist team as constituting admissions, while expedient moves to another (bedded) department once a target had been reached, and with the knowledge that the patient would probably leave the hospital on the same day, were not consistently seen as admissions:
technically speaking, the fact that [the patient] moved from ED to [MAU], I’m sure she would count in some measurement as an admission when actually she wasn’t, she was moved here because the ED had their 4-hour wait. . . . once we’ve had all our tests back we’ll see if she can go. And she’s not truly an admission really.
Waterbury practitioner 13
Observation areas ‘off the clock’
In the context of financial penalties for breaches, target workaround allowed patients who required longer periods of observation to be taken ‘off the clock’ and moved from trolleys to beds or into holding bays, observation or short-stay units. Porthaven and Waterbury had observation or decision-making units where patients were under ED care but no longer ‘on the clock’. In Waterbury’s bedded observation ward these patients were regarded as ‘admitted’, although most were awaiting investigation results and formal decisions. On the other sites, where this facility did not exist, or where such areas were for seated patients only, some practitioners believed that a bedded short-term observation area would provide a solution to the problem of patients holding space in the ED, and an alternative to longer-term admission to a ward: ‘We could observe them and send them home from there without them touching the surgeons’ (Churchtown practitioner 4):
we don’t have a CDU where they can wait for things like ultrasounds or CT scans, but all of those types of things cause huge delays, . . . because we can’t get these patients out and there’s no beds. . . . We’ll look at some and we’ll say, ‘Actually, you don’t need to be seen here,’ and we’ll put them directly into [a ward] somewhere so they can be seen by the specialty. . . . They are just a GP admission that has gone to a ward to avoid queuing in a corridor.
Underbridge manager 4
At Churchtown, ED patients were kept within the department for observation:
there’s three cubicles that we call ‘AFO’, Admit For Observation. . . . We don’t AFO them so they don’t breach, because we’re not allowed to do that, you know, we AFO them for genuine reasons. . . . they come off the [clock] . . . so they’re in a cubicle and they go onto a bed. . . . as long as they stay in that cubicle that’s fine . . . it’s like being an inpatient because you’re not on a trolley.
Churchtown manager 3
Patients marked as AFO on the ED whiteboard were counted by managers as a type of admission prior to ‘actual’ admission to a ward:
they’re not on the 4-hour clock any more, but there are very, very strict criteria that we’re allowed to admit for observation . . . people that are awaiting bloods, for example . . . so we can monitor them for the 6 hours and then decide either that they’re OK and they can go home or actually that they need admitting.
Churchtown manager 2
However, some ED consultants had a more nuanced understanding of the term ‘admitted’:
I suppose . . . technically, they’re put on a hospital bed, they’re in an area where they can be kept overnight, so I guess that, you know, that’s an admission . . . I don’t personally see it as an admission really, . . . mainly because . . . it’s within our nine major cubicles as it were, and because those are used flexibly, . . . I wouldn’t see it so much as an admission. Particularly as often it’s used as a period of observation with an expectation that the patient’s going to be discharged home. . . . It’s a way to carry on managing those patients outside the 4-hour target, essentially.
Churchtown practitioner 1
Practitioners across all sites tended to favour the introduction of short-stay units where patients could be monitored without being subject to the 4-hour target. They appreciated observation time as providing a third option in decision-making, beyond the binary concept of admit to a ward/discharge:
it would be better for patients though as well . . . if we could just park them somewhere for a short while. I know that happens on [the acute care unit] but we almost need another area where we can do that. . . . and you haven’t got that pressure then of the 4-hour target, ‘cos you’ve . . . just moved them sideways for an hour or so.
Underbridge manager 3
However, researchers observed that the use of such units sometimes led to a loss of momentum in decision-making and, particularly on bedded units, to patients’ expectation that they would subsequently be admitted.
Ambulatory care and avoiding admission expectations
Ambulatory care was used on all sites, with reported benefits in reducing admissions by allowing patients to be seen, treated and observed, generally by small teams and in seated areas, without the expectation that they would stay overnight. Ambulatory areas across sites showed variations in staffing, consultant input, processes of referral to these units and whether or not patient pathways were subject to the 4-hour target. Porthaven, Waterbury and Churchtown ambulatory units were under MAU management, and they typically received medically expected patients from medical triage, although Porthaven also worked closely with the AGPS. At Porthaven and Churchtown, patients from pathways allowing next-day outpatient appointments were not on a 4-hour target time, as it was expected that they would be investigated and treated, and then return home. Other patients referred by GPs, or occasionally by the ED, were seen on the same day and within a 4-hour limit, as investigation could indicate the need for admission, although the patients were not sufficiently unwell to be in a bed:
our aim is to avoid admissions . . . that’s what we have our ambulatory area for, it’s kind of like the walking wounded . . . so anybody that doesn’t actually need to be within this area on a trolley, or somebody who we feel could come back potentially the next day, or is suitable. . . . so we’ve got the cellulitis pathway, we’ve got the PE pathway and a couple of others as well.
Churchtown practitioner 12
Policy mandates and financial incentives supported the setting up of such units:
we were given an incentive so the tariff was increased to make sure we had more zero-length-stay patients. . . . patients are less at risk of acquiring hospital-acquired infections, patient experience is supposed to be better. . . . and obviously reducing beds as well . . . you get very frustrated about seeing a patient who possibly didn’t need to come in . . . and once they get into the system of the hospital it’s an extended length of stay. That’s why we’re trying to set up the short-stay ward as well.
Porthaven manager 1
The recently established ambulatory area at Underbridge was led by the ED and acted as an alternative pathway for patients who required an assessment that might exceed 4 hours, but who were likely to be discharged. The difficulty for practitioners lay in defining what was ‘ambulatory’:
Obviously, your classic, you know, ‘20-something’ that walks in is clearly ambulatory. . . . But what about your, um, little old lady that mobilises two steps at home with her Zimmer frame because that’s her normal – is that ambulatory or not? I’d say yes, it is . . . They’re not walking but they are ambulatory.
Underbridge practitioner 10
Irregular use of admission avoidance initiatives
Where ambulatory care was effectively signposted and used, it could result in admission avoidance. However, there were indications that ambulatory care and other alternative pathways were not used consistently. This was partly because of confusion about the patient types that could be referred to these units, and partly because the units did not always come to mind when practitioners weighed up alternatives to admission:
If at all possible, I’d like to get you out today.
To where she should have been in the first place: to ambulatory care.
A completely avoidable admission. She is not that unwell. We have an ambulatory care set-up where she should have been.
Porthaven practitioner 7
. . . there is no reason why a patient like her couldn’t have come to ambulatory care, sat, and had everything done for her in there. But because she came in with chest pain, which is what we get hyped up about . . . – so the only reason she’s in MAU is because of the ED 4-hour wait thing, so I guess with that in mind she’s probably more an avoided admission, rather than somebody who’s actually admitted and discharged the same day.
Waterbury practitioner 13
Where ambulatory units were led by the medical team, they were not generally accessed directly from the ED, even though ED practitioners believed this could be beneficial:
I think having well-established . . . pathways for investigating some things that could be done on an outpatient basis is important, and we’ve already got things like that, like . . . ambulatory care pathways . . . They’re helping – having well-established links with those. Sometimes they’d perhaps be better co-ordinated and more available directly from the emergency department.
Churchtown practitioner 1
The somewhat haphazard ensemble of initiatives gave rise to some duplication and irregular use of both formally established and newly created pathways:
I think the ADU [sic] – I’m still confused as to whether I should be calling it MDU, ADU, AEC [laugh] and I have to admit I haven’t quite got my head round what the different acronyms do in terms of which patients I can send where – . . . the service has been in one location and then it’s in a different location and now it’s called this and then it’s called that, I don’t think the department has worked out when to use it and when not to use it.
Underbridge practitioner 5
New intakes of junior doctors were often unaware of the pathways available:
Hi [name], [ACE] team. Anything for the [name of team] geriatricians?
Oh maybe, yes, that might be good. Dunno . . .
70-year-old collapse?
Yeah, that sounds right up your street.
Churchtown practitioners 8 and 13
This junior doctor’s inclination to admit was reversed when the care-of-the-elderly consultant secured agreement for discharge from the patient and her daughter, and arranged an outpatient appointment for the next day. The junior’s reflection illustrated how initiatives involving specialist teams could work in a serendipitous way, even though they had not been integrated by all practitioners as regular pathways:
what happened with that lady is how the system should work, but I think certainly it’s quite a variable . . . [the care of the elderly team] happened to be here and therefore it worked really well, and that’s great.
Churchtown practitioner 13
Summary
The ability to rapidly assess and safely discharge a heterogeneous mix of patients was regarded as critical to the effectiveness of EDs. Where community resources were limited and time was needed to make plans for safe discharge, hospital admission could be the line of least resistance. Insufficient collaboration from medical specialties was noted as a barrier to patient flow. Admission avoidance was a goal pursued by all staff through multiple initiatives, partly for patient benefit and alleviation of departmental pressure, and partly to aid 4-hour target compliance. The target, while benefiting patients by reducing time in the acute care department, could also lead staff to admit by restricting time for observation and driving them to avoid breach penalties. In response to this dilemma, the study sites introduced ambulatory care, and observation and short-stay units, some situated in the ED and others in MAUs. These initiatives allowed practitioners to buy time ‘off the clock’ for observing a patient’s evolving condition and assessing how best to meet that patient’s needs.
Chapter 6 Ethnography of patient experience and decision-making
Following on from the organisational ethnography and analysis of practitioner experience (see Chapter 5), in this chapter we examine how service users – 65 patients and 30 carers (see Chapter 2) – weighed up risk and responsibility in their use of emergency services, how they contributed to decision-making and how they described their experiences. Across the four sites, patients, carers and practitioners collaborated to guard patient safety within a resource-constrained system by using self-help, staff time, the acute bed as a scarce commodity, and teams and units within and outside the hospital. This collaboration allowed overburdened EDs to be sustained as the repository for a broad spectrum of health-care and social care needs. Patients’ willingness to use alternatives to the ED was concordant with admission avoidance policy, and with practitioners’ efforts to keep patients out of hospital. However, this approach could be thwarted by what was reported to be the slow or ineffective response of community services, long waits for outpatient appointments or shortfalls in home care arrangements.
Patients’ considerations in deciding to seek acute care
Patients’ decision-making began at the onset of worrying symptoms or a critical event or episode, when they had to assess the need for a hospital visit. Patients’ decisions were influenced by a series of considerations: a generalised reluctance to attend hospital, especially on the part of the elderly; concern for the emergency system and appropriate use of NHS resources; lack of confidence in community alternatives for urgent care; a desire for quick resolution of their problem, sometimes linked to the ‘pull’ factor of the ED’s reputation for efficient turnaround; self-assessment of the seriousness of their condition, aided by advice from companions and carers; patients’ ranking of need, comparing their own situation with that of others attending the service; a sense of fairness regarding the delivery and use of emergency care; a commonly expressed wish to avoid admission; and the perceived importance of patients’ own interests, pragmatically weighed against any of the above-mentioned factors.
Reluctance to go to hospital
Rather than a drive to overuse emergency services, our data indicated a clear preference among patients on all sites for using community-based services and avoiding hospital visits:
the pain started again today, and I ignored it around 12 o’clock, because I’ve got two children I don’t want to stress myself. . . . it kept on and I took co-codamol. But it just could not go, then she [GP] said to come here [to the ED].
Waterbury patient 1
A 51-year-old woman from Waterbury had attempted to consult her GP about chest pain. The practice was closed, so she called 111, whereupon she was advised to attend the ED by ambulance:
I just kept saying to people on the phone this morning that I was quite happy to – I just thought they’d send me down to [X community hospital], [X] would give me some painkillers or something and sort of ship me off home again. And I was quite happy to do that. I even said ‘I’m going to see the [GP]’, didn’t I?
Waterbury patient 2
The wish to avoid hospital was especially common among members of the older generation, who tended to associate emergency services with dire situations and also felt the need to justify their use of such services to others. A 69-year-old woman with a pre-existing heart condition attended Porthaven ED after a ‘funny turn’. She was admitted to the medical assessment ward for cardiac and neurological investigations:
Perhaps it’s the way you’re brought up. . . . that you just get on with things. . . . I daren’t tell a couple [of] people that I’ve come in, God. . . . I just feel so embarrassed about it. . . . it’s as though you’re going in for something trivial just because you’re not feeling well.
Porthaven patient 1
Concern for the system
Patients on all sites expressed concern about the appropriate use of emergency services in the context of generalised public support for the NHS and awareness of pressures on its staff and resources. The patient cited above had learned as a carer that ambulance services were not to be overused:
I looked after my husband a lot when he was ill so I know . . . when you should and when you shouldn’t call [an ambulance].
Porthaven patient 1
Some people come in and want to be seen like that [snaps fingers]. Not me. I wouldn’t even call an ambulance. I’d get myself here. I don’t want to waste their time.
Porthaven carer 1
A man accompanying his 82-year-old mother to the ED in an ambulance after a fall echoed practitioners’ comments about the department’s ‘take-all’ model, inappropriate use, and alternative pathways for accessing urgent care:
A&E . . . pick up everything don’t they? There would be a lot of people who don’t need to come here. . . . who could go to the GP or . . . they’ve got a . . . drop-in GP service here.
Porthaven carer 2
Lack of confidence in community services
Despite many patients’ preference for using primary care, past experiences could undermine their confidence in using the community system for urgent care. There were several references to long waits for outpatient appointments and a shortfall in out-of-hours services. Some patients reported delays in receiving test results, and these delays could generate complaints:
We know that the NHS is stretched. We know it’s tremendously stretched. But he had an echocardiogram and we’ve never had the results. And this was months ago, wasn’t it? . . . you’ve written a –
Got the letter there somewhere.
Porthaven patient 2
Some patients expressed doubts about the speed and effectiveness of GP response to their concerns:
I think they [GPs] would have referred me in a few days hence. . . . and I was very concerned . . . this is the first time that the pain had become really violent. . . . I’ve always felt pressure with the heart thing before. So I was rather alarmed and more felt that I needed to see someone . . . as quickly as possible.
Porthaven patient 2
Desire for quick resolution
The VSM study (see Chapter 4) found that only 5 of the 72 patients attending EDs across the four sites had done so on their own initiative. The ethnography, too, found relatively few reports of ED attendance that had been decided by individual patients. Some of these patients had chronic conditions and knowledge of associated risks, such as a 73-year-old Waterbury woman with a recent heart attack and triple bypass who called an ambulance herself:
I’d been in extreme pain for 3 days. . . . because I’ve had operations, and because I’ve had known blockages in my arteries, I wonder whether I had another blockage in my left side. . . .
. . . what made you decide to come here rather than seek some other place for your care?
Well, I wanted a resolution fairly quickly.
Waterbury patient 3
A 24-year-old woman attended Underbridge ED on her own initiative with a recurrence of symptoms that she described as a TIA:
when I first had anything like this happen and I went to the doctor’s, they didn’t do anything . . . when I had a TIA . . . again my GP wouldn’t look into it. . . . last week when I phoned the 111 number . . . thinking, well maybe I should go to the emergency doctors or something, but they said, no, you need to go to A&E. . . . so this week rather than phoning [111] first, we just thought, right, let’s just come [to the ED].
Underbridge patient 1
This account indicates possible communication problems between the patient, who may have self-diagnosed a TIA, and the GP, who may have disagreed but did not make this clear to the patient.
Assessing the seriousness of symptoms
Deciding whether or not symptoms were serious could be confusing, and some patients found it hard to accept that their condition could warrant a hospital visit. A 66-year-old woman with cancer was suffering from chest pain and her GP advised her to attend Waterbury ED:
That surprised me, I must say, that he [GP] did take it more seriously than I did. I just wanted the painkillers or something, you know. So it was just an annoyance, actually, rather than a concern.
Waterbury patient 4
Two patients interviewed in Churchtown’s ambulatory care area had attended GP appointments and, to their surprise, been advised to make their own way to hospital for assessment. One of these patients was a 67-year-old man experiencing breathlessness following recent heart surgery. He was pleased to be discharged after being diagnosed with a routine postsurgical complication that would self-resolve (Churchtown patient 1). The second patient was a 31-year-old man who sought GP advice about a headache and was referred for medical assessment, a move he felt was unfounded:
It’s just a headache really as far as I’m concerned. . . . [the GP] said that my blood pressure was a bit low and she couldn’t get a clear view of my eye or something. . . . I came here and there’s . . . nothing wrong with my blood pressure and they can see clearly in my eye, so it makes you wonder. . . . it was a locum GP so I’m not sure.
Churchtown patient 2
This patient’s mistrust of the GP’s advice may have been exacerbated by poor communication. However, the acute medicine doctor explained to the patient that she wished to exclude life-threatening conditions (subarachnoid haemorrhage, meningitis or raised intracranial pressure). Following negative results from a CT scan and lumbar puncture, the patient was discharged with pain relief.
Once patients had acknowledged that their condition might be serious, they were keen to seek hospital care and ‘get to the bottom’ of the problem (Underbridge patient 2):
We expect that someone will say to us if all is all right, if it is something serious or not, what’s going on, basically.
Waterbury patient 5
A 55-year-old woman with cancer was advised by her oncologist to attend Waterbury ED, and she too considered that her symptoms required urgent attention:
I had lots of shivers, and sweats as well, last night. And I’ve had quite a lot of other symptoms as well, but it’s mainly achy and flu-ey, which is a strong indicator, with a temperature, that you’ve got an infection beginning.
Waterbury patient 6
Patients’ ranking of need
Patients’ desires not to be in the category of serious cases could lead them to compare their situation with that of others, who might be more in need of emergency care. A 60-year-old woman living in a rural area, who had a recurrence of TIA symptoms after a recent suspected mini-stroke, felt ‘shaken up’ when her GP fast-tracked her to the ED by ambulance: ‘I don’t need an ambulance, you know? I thought it’s taking it from somebody who probably needed one’ (Porthaven patient 4). Older patients tended to combine such arguments with their preference for care at home:
Well, I would rather be at home than in a nursing home actually . . .
Or in hospital.
Well, certainly not in hospital.
Why not?
Well . . . I just think I’m clogging a hospital bed, aren’t I, really, when I don’t need to . . . possibly.
Porthaven patient 3 and carer 2
Patients’ concepts of ranking need also included more straightforward doubts about the legitimacy of their place in the system. A 69-year-old woman from Porthaven felt as though she was ‘making a fuss’ or that she was in the ED ‘under false pretences’ when she arrived in an ambulance after a ‘funny turn’ that could have been due to her heart condition or a mini-stroke (Porthaven patient 4). A 65-year-old woman from Underbridge who had collapsed at home said she ‘felt a bit of a . . . a con, ’cos, you know, I don’t feel ill but I’m not right’ (Underbridge patient 3).
Patients sometimes felt caught between nervousness about attending the ED unnecessarily – ‘you just don’t want to bother them’ (Waterbury patient 6) – and fear of being at fault if they failed to attend and ultimately caused more trouble for themselves and the system. A 74-year-old man who had experienced a fainting episode was given a choice by an Underbridge ambulance crew whether or not to attend hospital: ‘I didn’t want to come, but I was going to look like a fool if I had gone home and collapsed there’ (Underbridge patient 4). A Porthaven patient blamed herself for not attending in time to prevent the worsening of a chest infection that led to her admission in the medical assessment unit: ‘I didn’t feel well enough to go out . . . so I stayed put, which was silly . . . and of course I ended up in here’ (Porthaven patient 5).
A sense of fairness regarding service delivery and use
Patients could find it confusing that some who were waiting might be seen before others. In Waterbury and Underbridge, all patients, whether referred by a GP or self-referring, were assessed in the ED under the ‘single point of entry’ system. They were generally unaware of the difference between their status as either medical or emergency patients. Patients in Waterbury, especially, did not necessarily know that patients referred by GPs to the medical team could wait longer for doctors to come and see them in the ED. Patients were often unaware of the 4-hour target that applied to all patients seen in the ED.
Patients commonly acknowledged that other cases could be more urgent than theirs. However, if they perceived that resources were being allocated to ‘undeserving’ cases, they could feel justified in seeking attention for their own needs:
I rang up NHS Direct and they were harping on about chest pain and because I’ve got a little bit of an upper respiratory tract infection . . . I have got a little bit of pain up here. . . . It was like, ‘I’m not worried about that’. . . . I was thinking ‘Oh my God, [the hospital is] wasting resources’ and stuff like that, but then on the other hand I think, well, the amount of people that I’ve seen in hospital that really don’t need to be in here.
Underbridge patient 3
A 40-year-old man attending the ED with pain from a kidney stone, who was frustrated about lack of communication from staff, expressed his view about the right to access urgent care when needed:
Well I pay my taxes don’t I? [laughs] I live in this country that affords us these privileges, and we pay for the right to fitness as well? I see no reason why I shouldn’t be here if the need arises.
Churchtown patient 3
Desire to avoid admission
Other patients alluded to their right not to be admitted and to the inconvenience of unnecessary admissions when their voices were not heard. An 86-year-old man with diabetes, who lived independently with his wife, suffered symptoms that were taken to be suggestive of a heart attack. He felt that there was nothing wrong and that he was being admitted unnecessarily because his knowledge about his condition was not being listened to: ‘I can’t get it through to people, that always happens if I get hungry. . . . because I have got a bad hernia there’ (Waterbury patient 7).
One ethnographic case study concerned a 66-year-old woman presenting with chest pain who resisted admission because she and her husband disliked hospital and had experienced lengthy delays in the past. The patient, who was receiving treatment for bowel cancer, had called the chemotherapy nurse, who advised a GP visit. The GP referred her to the AMU with a possible PE. The patient was seen by a senior house officer (SHO), who wanted to admit her to help ‘speed things up’ (Waterbury fieldnotes 1). Her case was reviewed by a consultant, who discussed it with an oncologist and offered a compromise: she could return the next day for a scan and ambulatory care review. In this case the patient’s wish to avoid admission was taken on board and she effectively influenced decision-making.
Patients putting their interests first
Consideration for the emergency system was often emphasised in patients’ narratives, unless they were in severe pain or in a state of anxiety, when they put their own needs first. A few patients declared the influence of their own pragmatic interests in the way they used the emergency system:
[The patient] had been advised to attend on Friday but had waited until [Monday] as it was more convenient to her.
Underbridge fieldnotes 1
I’m going to New Zealand . . . in a few weeks’ time and I didn’t want none of this, that’s why I didn’t want to come in, . . . I thought, ‘Oh God, we’re going on holiday, I don’t want a blip!’ you know because I suppose I will have to ring up my travel insurance to tell them that I’ve been in A&E now won’t I?
Porthaven patient 6
The relative speed of emergency investigations could act as a ‘pull’ factor for patients:
I feel well cared for, you know, and investigated and they haven’t said, ‘Well, you’ve got to wait until Wednesday week before we can tell you all that’, you know.
Porthaven patient 7
One ethnographic case study focused on a 23-year-old woman who had made 21 visits to Porthaven hospital with various complaints since the age of 7 years. This visit was prompted by a call to her GP:
I told him about the symptoms and said I had a pain in my chest. He said, ‘Go to hospital, we can’t take any chances’.
Waterbury patient 8
Certain elements in the patient’s narrative suggested that she had made pragmatic use of the service, starting with her self-awareness about her definition of the presenting symptom – severe chest pain – which prompted a series of tests, and her estimate of the time needed for results, which would allow her to return home by the evening:
How was the patient journey for you?
A lot quicker this time. It was the symptom, they prioritise that.
How long do you expect to be here?
An hour and a half . . . a rough estimate. ’Cos obviously, they want to get you in and out as quickly as possible. . . . By seven? It gives them an adequate amount of time.
Why seven?
I’d give them an hour [for the tests] and add a bit.
Waterbury patient 8
The tests showed negative results and the doctor gave indications for discharge. In expressing satisfaction with the care received, the patient acknowledged the worry that had led to her seeking urgent care: ‘Two relatives have had atrial fibrillation, a heart condition. My uncle had it when he was my age. He never went to the doctor – and it was too late’ (Waterbury patient 8). She also mentioned travel plans that she felt free to undertake having been reassured that her heart function was good (Waterbury fieldnotes 2).
The 3A PPI group reflected that this patient’s self-interest, as well as concern about her family medical history, might have motivated her use of the emergency system on this occasion to obtain rapid tests and diagnosis. They queried the GP’s role in referring her, and the junior doctor’s role in running tests without consulting a senior. At the same time, they acknowledged that the patient had been assessed on a case-by-case basis without prejudice about her being a ‘serial’ ED attender.
Roles of carers and relatives
The category of carers, as well as those formally employed for this purpose, included partners, relatives, companions, and friends or neighbours who supported or acted on behalf of the patient. As well as advising patients about using the system, prompting them to attend the ED and accompanying them to hospital, carers could play other roles: observing and giving information about a patient’s condition or treatment; making efforts to avoid unnecessary admissions; and seeking hospital stays for elderly relatives, a role that sometimes led to conflict with the wishes of patients themselves.
Observing and informing about a patient’s condition and treatment
Carers had a primary role in alerting staff to symptoms that might be indicative of a serious condition:
Because I was actually sitting next to his mother when she had her stroke so . . . as soon as I saw him having trouble speaking I basically started to engage him and ask him questions . . .
So something clearly wasn’t right.
Yeah. You still are struggling with your ‘R’s.
Yeah a little bit, yeah.
Yeah, I can see the way you’re talking there.
Underbridge carer 1
When accompanying their relatives during hospital visits, carers often contributed to filling gaps in a patient’s medical history, especially when they arrived without referral letters and when GP notes were not available. Some could have detailed conversations with clinicians about symptoms, tests and results:
So have they checked the urine? Was there anything?
Yeah, the urines came back clear, didn’t they, ’cos they sent some off? [checking with patient’s wife] I mean, it has been an ongoing problem with Dad that unfortunately he has high infection markers . . .
OK. Right.
And he was tried on a number of antibiotics. They started testing spinal fluid and everything because nothing appeared to work. And then suddenly after a while he gets better [laughs].
That’s the thing with inflammatory markers, . . . they can’t show us urine infection. They don’t really tell us where . . .
No, I mean, he’s also [had] problems with gout in the past.
Churchtown carer 1
Carers could aspire to being partners in decision-making, especially when they had background clinical knowledge or when they had researched treatment options. Some were aware of their importance as information-givers, but they described being valued in this capacity as an exceptional experience:
. . . what’s been good is that the doctors have actually listened to what we’ve said . . . with his previous brain injuries they would have thought he would have needed . . . scans . . . but we, from our previous experience as a family, think it’s more related to some sort of infection. . . .
. . . it was a positive thing that they were prepared to listen and take that on board because we were giving him some history on [patient] that he wasn’t aware of.
Churchtown carers 1 and 2
. . . she [GP] was marvellous! Because right from the beginning when I asked, with [patient]’s permission, could I go in with him, he needed me to help him, and she treated me with every bit of respect, and that was amazing! I can’t tell you, through [patient]’s years of being ill, often I have not even been looked at, let alone acknowledged.
Waterbury carer 1
Some practitioners’ apparent disregard for relatives’ contributions may have been linked to their wish to keep the patient as an active participant in the centre of the discussion:
I remember a case recently where a young man had come in with his wife and his wife was telling me all about his abdominal pain and I was like, I want to hear it from him, not the wife. Erm, but in elderly patients who do suffer with cognitive impairment I think carers can often be very useful at telling us . . . what they are like at baseline.
Underbridge practitioner 1
Avoiding unnecessary admissions
Carers who were knowledgeable about emergency services could make efforts to prevent their relatives from being admitted unnecessarily, but they did not always feel supported by the existing system:
There’s no form that can be filled in for the family to say, ‘Look, he’s a frequent faller, . . . don’t bring him in!’ . . . Last week [the carer’s father] fell in the garden and bumped his head . . . the ambulance crew really wanted to bring him in and I said, ‘He’s absolutely fine. It’s just a little graze. Pick him up and put him in his chair.’ I said, ‘I’ll stay with him’. . . . but if I had been at work, they would have brought him in.
Porthaven carer 3
A participant in a PPI workshop was the carer for his wife, who had complex care needs following a subarachnoid haemorrhage and a diagnosis of dementia. After efforts that lasted for several months, he obtained a GP letter that the family could show to emergency services, if the need arose, to avoid unwanted admissions:
Mr [X] would prefer to avoid acute admissions in the future. We suggest that if [patient’s] mobility deteriorates . . . when the surgery is closed, she should be assessed by [out-of-hours doctors] and, if no acute medical problem is diagnosed necessitating admission, then a short-term increased package of care should be organised. . . . rapid response is another route to go down if the former proves unsuccessful.
GP letter shared by carer in PPI workshop
This carer and others in the PPI workshop reflected that their knowledge was often discounted and that there was a cost to the system of not listening to relatives who wished to avoid acute admissions.
Seeking hospital stays for elderly relatives
Whereas some carers made efforts to avoid unnecessary admissions, others tried to persuade staff of the need to admit patients, fundamentally because of difficulties with home care. Practitioners gathered information about the availability of family support for transport and other needs, but sometimes they made inferences that were rectified by patients:
And then you’ll get, ‘You can’t phone my daughter to pick me up, you know, she’s busy, she’s got a busy life! Can’t I have an ambulance?’
Porthaven practitioner 1
It was frequently reported and observed that relatives sought hospital stays on behalf of elderly patients whom they had difficulty caring for at home – known by staff as ‘boarding’ – whether or not the clinical need was evident. A Porthaven carer was concerned about his mother’s deteriorating condition and the prognosis for her degenerative spinal disease, which did not allow her to adequately care for herself in her sheltered accommodation:
is she going to need to stay in hospital . . . that would be a good idea, as she needs to rest and a bit of TLC [tender loving care], which is very difficult for us to give her. . . . My wife and I both work, you know . . . I’d just like to keep her in overnight and just, you know, just keep an eye on her. . . . at the moment it’s safer in hospital, especially if she’s got to take more morphine and stuff like that. . . . And er, being quite frail anyway, I think it’s not a bad thing.
Porthaven carer 2
. . . she’s a bit wobbly and stuff, so it’s probably best that . . . she stays here. . . . both myself and my brother . . . we haven’t room to sort of have her staying with us and we both work full time and got young families, so that’s quite difficult.
Porthaven carer 4
Carers’ requests for boarding could feel somewhat taboo to voice to staff, since they implicitly breached two moral codes: families’ duty of mutual support and citizens’ responsibility to use hospital services appropriately:
Can you not keep her in for a week?
Pardon?
Can you not keep her in for a week?
Not in this hospital but it depends – because this is an acute hospital, if your partner couldn’t manage at home following this assessment we’d look at what options there are –
That was supposed to be a joke!
Oh was it? [Laughs] I took it very seriously. That’s fine. Well some people do – you know want to stay in the hospital but it’s not always the best place for their care so –
But it’s going to be difficult for her to move about at home.
Well, that’s what we’re going to assess now, so . . . are you at home all the time together?
Yeah.
. . . if your mobility is good enough for you to go home [Mrs X], would you accept having some carers in on a short-term basis? . . .
Carers in? Well I think . . . oh . . . [makes a negative face].
Churchtown carer 3 and patient 4
Conflict was sometimes observed between the desire for admission avoidance, which elderly patients shared with practitioners, and relatives’ wish for hospital stays:
I was saying, Mum, that, if need be, it would be a good idea for you to have a couple of days in, to be looked after, get a bit of TLC –
Mmmm. [Laughter from those present] I would still like to get home, I really would, but if I – if I agree to more help, I should think I should go home actually.
It depends what you’ve done, doesn’t it?
Yes, oh of course it does, because what I’ve done –
It’s very, very difficult for me to get her to agree to more help.
Porthaven patient 8 and carer 2
Factors influencing patients’ experience of care
Patients’ experience of emergency care was influenced by a series of factors: the layout and geography of the service, and features of design that affected self-care and recovery; practitioners’ consideration of the individual needs of patients and carers; patients’ self-rationing and reduced expectations regarding what could reasonably be expected from a service under pressure; arrangements for safe discharge and forward care; involvement in decision-making; service efficiency combined with care for patients’ basic needs; timely communication; the offer of fluids and food; and, last but not least in patients’ ranking, being under the care of a named nurse.
Use of chairs, beds and trolleys
On some sites there were both seated and bedded areas for patients waiting for investigations and decisions or, after a decision, awaiting discharge and transport. Ambulatory units across sites were largely seated, or with reclining chairs, sometimes with one or two beds for patients who were considered to be less mobile. The use of chairs, beds and trolleys was observed to influence patients’ expectations of admission or discharge. In seated areas, patients tended to move around, they often voiced their desire to go home and they accepted a wait, as they felt comfortable:
[The patient] is not concerned that he has had to wait to see a doctor for initial assessment, as he finds the seated waiting area quiet and comfortable and he has access to drinks and food. He also values the fact that he is kept informed about why he is waiting.
Churchtown fieldnotes 1
Some practitioners believed that putting a patient into a bed increased their expectation of an admission:
if ED feel that that patient [is going to need] admission, . . . then they’ll say this patient is for admission so they automatically go into a bed, which, one, raises patient expectation; two, the relatives go home because they think the patient’s in a bed so they’re staying in hospital; and [it] also builds in a huge delay. So if they were to come to ambulatory care, they’d be seen first-hand by a consultant, . . . they’d still have their clothes on, . . . so there’s not the expectation, not the sheets . . . and the thing. Relatives [are] still there because they’re waiting to see what’s going to happen. . . . the consultant sees the patient and makes an immediate decision, you’re fine, you’re not going to need to come in, we’re going to do this, this, this and this. . . . to avoid admission from here is so much easier than . . . from a bed. Once you get into a bed you go through another junior doctor clerking, another layer, which builds in on average about 4 to 8 hours’ delay.
Porthaven practitioner 2
Where there were only bedded areas for investigations and waiting, patients who did not feel unwell could be frustrated by being put into a bed:
the patient . . . had been referred to the ambulatory care unit by her GP for a scan but they had no space so she was sent to ED. The lady was not impressed at having to go through the ED system, and after being asked to undress she then sat in the chair. . . . the nurse then asked the patient to get onto to the trolley, which the patient did reluctantly for an ECG. . . . when the nurse had finished, the patient got off the trolley and sat back in the chair, as she told [the researcher] this was more comfortable. Later the patient was sent for an X-ray, and again she was instructed to get back onto the trolley so that the porter could push her round. After a review by the medical team, the decision was made that she did not require admission and she was discharged.
Waterbury fieldnotes 3
In another example from the same site, a 99-year-old woman was put into the bedded observation ward awaiting discharge and transport. The patient was surprised to have the sides of the bed raised, and she found it distressing when she wished to use the toilet, attempting to climb out of the bed around the cot sides. When she returned from the toilet, the nurse again put her into bed, although she was destined to go home (Waterbury fieldnotes 4).
Consideration for individual needs
Patients and relatives sometimes alluded to the diminished status of individuals in a crowded system:
We never anticipated all this; we thought we would be in and out in half an hour.
Did you? [To partner] Ah, what did you think?
No. Well you don’t just go in and out of hospital, you know, because there are hundreds of other people before you always.
Churchtown patient 4 and carer 3
Patients’ and carers’ sensitivity about competing with the needs of others was reinforced by practitioners’ allusions to the volume of demand:
I wish they would just come and say, I am sorry there is [sic] delays, and I had to ask the young nurse there, excuse me what is happening? And she said there is [sic] an awful lot of sick people here, so . . . I don’t expect to jump the queue, I don’t.
Waterbury patient 9
When practitioners’ time was short, they could sometimes miss attention to communication and other needs of patients or carers with disabilities that were not immediately apparent:
[The patient] had been identified as suitable [for inclusion in the study] by one of the nursing staff although she warned me that the husband did not seem very happy at all. I [researcher] went to speak to the patient and she was very keen to participate and although I could see her husband was less keen I then realised that this was due to his inability to understand fully what was happening as he was deaf. Once I had approached him with this in mind, he was very happy to participate.
Waterbury fieldnotes 1
Even in cases of ‘social admissions’ that some staff might have considered inappropriate, patients frequently acknowledged that their needs had been taken into account, and many expressed appreciation for the care received:
. . . did you want to stay in hospital or – ?
Well, I had no choice, love, did I really? I had no choice. They just said, ‘We would like to keep you’. . . . I was grateful to be kept. . . . You see if I had somebody at home, I could have . . . but it was really offered to stay. And I was grateful.
And why did you want to stay? . . .
Because I have no one to go home to. That’s why.
Porthaven patient 9
Patients who were known to staff as ‘frequent flyers’ because of their recurrent attendance also reported positive experiences of care, with safe as well as satisfactory outcomes when their levels of risk were considered case by case:
I have always had very happy . . . I mean I have had several trips in here and it has been brilliant. . . . it has always been for my stomach, and they have been absolutely fantastic. Well enough that I have been recognised and they are all saying hello!
Porthaven patient 10
I’m happy! They’ve done a lot of tests today. I’m happy, but with a precaution, to see the GP.
Waterbury patient 8
Self-rationing and system expediency
There were exceptions to these positive accounts. A 41-year-old woman attended the Waterbury ED as a result of a 111 ambulance call for an acute episode of chronic neck pain, apparently associated with a spinal lesion. She had attended the ED on three previous occasions for this problem, and on her last visit, 2 days earlier, she had been admitted to the observation ward for pain relief. Her condition improved and she was discharged soon afterwards in the middle of the night:
they sort of morphined me, given me diazepam, and then dismissed me at two o’clock in the morning, which was a bit dramatic . . . they sent me home in a taxi, and like, high as a kite on drugs. I was crawling up my stairs to get to bed. I don’t think really that should have happened. They did know I was on my own as well. . . . But anyway, I know they’ve got limits to . . . who they can keep in and stuff like that. . . . I said, ‘That’s fine,’ you know. ‘Give me the tablets and let’s go,’ sort of thing. . . . I knew it wouldn’t take the problem away. But I thought, ‘Oh, it might bring it back down to a level where I can cope at home, until I was due to see the pain clinic . . . and hopefully this [neurological] appointment. But obviously I ended up back here, which is just a bit frustrating.’
Waterbury patient 10
In this example of self-rationing, the patient demonstrated a reduced expectation of consideration for her needs. She showed willingness to make allowances for the system under pressure, even though she reported an unpleasant experience and a subsequent need to return to the ED.
As unsatisfactory discharge also occurred in the case of the 60-year-old rural woman who was ‘fast-tracked’ by her GP to Porthaven ED in an ambulance after she consulted about stroke-like symptoms. This patient experienced her whole process of care as troublesome. Having been informed that it had been a mistake to send her in via the ED, she expressed confusion about what was happening:
the doctor told me they’re doing four different things, and I don’t know what they are. One’s taking blood, doing an ECG, that might have been two, I don’t know, and to bring an overnight bag in case I had to stay overnight.
Porthaven patient 3
The patient experienced delay with long waits for a CT scan, and she was eventually discharged with an outpatient appointment for the next day. Since she was considered ‘not unwell’, she was not provided with transport. She was unhappy about travelling home alone on two buses late in the evening and having to return in the morning, and the instruction to bring an overnight bag had added to her expectation that she might stay in hospital. In this case too, discharge and travel arrangements were expedient for the system but were not felt by the patient to be in her best interests. Her experience was negatively affected by miscommunication and lack of consideration for her travel difficulties. The junior doctor was unaware of transport issues and considered this to be part of the nurses’ role (Porthaven patient 3).
Arrangements for safe discharge
Specialist teams could assist with decision-making, provide outpatient alternatives and enable community support to be included in the package of care. Patients were not always aware that this was happening or which staff were members of these specialist teams. At Churchtown, a 70-year-old woman who attended after a fainting episode was hoping not to be admitted, although her daughters were concerned about the possibility of her injuring herself at home. Although a junior doctor had planned to admit the patient for further testing, a senior geriatrician from the ACE team showed tact and skill in giving her the option of going home with a prompt outpatient appointment, to the satisfaction of both patient and family (Churchtown patient 5).
Patients’ safe referral into the community could be facilitated by discharge teams, which had different acronyms across the four sites. However, community resource constraints could limit the impact of such teams. An elderly Churchtown patient with dementia had been considered suitable for a community bed, but lack of availability meant that she stayed for over 3 weeks in an acute ward. The hospital was some distance from her home and her partner had difficulty visiting, which added to her distress (Churchtown fieldnotes 2).
Involvement in decision-making
Whereas practitioners tended to refer to the ‘influence’ or ‘impact’ of patients and carers on decision-making, patients themselves often demonstrated their capacity for active involvement in decisions about treatment and admission or discharge. One case where this was observed concerned an 82-year-old woman who had been admitted to Porthaven medical assessment unit following a fall some days earlier. She had a history of two strokes, and she lived at home alone with no carers. Her relatives, who visited her daily, were worried about her breathing, although the doctor examining her had found no problem there. The patient had pain on her right side, but she reported feeling quite well in herself. An X-ray showed no fractures. A MAU consultant on a ward round with a junior doctor visited the patient, who described her fall and symptoms in detail. Although her relatives had noted problems with her speech, perhaps fearing a stroke, the patient was lucid and communicative. The consultant took time to converse with her, involved her in treatment decisions, and gave instructions to facilitate her discharge:
What was the problem yesterday? Why did they [family] call the ambulance?
I don’t know.
[The junior doctor and consultant both laugh.]
They said, ‘Mum, you’re talking funny.’ I said, ‘I’m not talking funny, I’m talking natural!’
[Everyone laughs. The consultant examines her.]
Well done. The ambulance crew were a bit bothered because the oxygen levels were a bit lower than we would like.
They’ve been taking my temperature all night.
[Consultant asks about medication the patient is supposed to have been taking.]
I can’t get to the toilet in time. Not being personal . . . [I have] accidents. So [I’m only taking] it once every 2 or 3 days.
Take it every day but in a slightly lesser dose: 20 mg instead of 40 mg. Each day. A little bit of benefit without the problems.
If you like, I’ll take a whole tablet every day.
We’ll try and get you a bit more mobile. [To junior doctor] Get the rapid response team. [To patient] If the physio thinks you’ll be OK, I’d be happy to get you home.
When I’m at home, I’ve got a walking frame. I’m OK.
I’ll try and get you home this afternoon. If you behave! [To junior doctor] Medications. GP to keep an eye on.
Porthaven fieldnotes 5
There could be intrinsic constraints to patient involvement when patients had significant cognitive impairment. In such situations, carers could supplant the role of patients in communicating with practitioners, and patients could be vulnerable to a failure to detect their needs in a timely way:
He’s a very good patient.
Yeah, and very, I know. Very nice.
He doesn’t, he doesn’t complain about anything, he, he doesn’t tell you anything. He doesn’t ring the bell.
Yeah.
He’s the best and worst patient, isn’t he?
[Laughter]
He’s quiet but before you know it, he’s on the floor.
Yeah, yeah. That’s not always, not a great thing.
[Laughter]
Churchtown carers 1 and 2 and practitioner 14
Efficiency and care
Just as practitioners gave positive value to the speedy movement of patient flow, patients too expressed appreciation for efficiency as well as ‘customer-aware’ care in a system that was acknowledged to be chronically busy:
Can you tell me something about now when you went to X-ray, what it was like? . . .
Very efficient, very fast. Um . . . about a 2-minute wait, if that. Wheeled straight in. The, um, the staff was [sic] very, she was very polite, very friendly, eye contact, all the things that you would expect a professional to do.
Waterbury patient 3
When staff did make time for the ‘softer’ aspects of care, patients regarded such an approach as exceptional, given the pressures on their time:
They’re very efficient. You can tell everyone’s very busy but they make time for you. And certainly the paramedic was just – couldn’t do enough, you know. . . . Made you feel at ease, which was helpful.
Porthaven patient 11
So what’s your impression so far of the care that you’ve had here?
Oh it’s fantastic. I really appreciate it, from the time I entered until now, the nurses are just running everywhere, they’re helping. And I actually saw the doctor as well.
Waterbury patient 1
The patient’s use of ‘actually’ here could imply that time with doctors was valued as a scarcer resource, or one for which longer waits were expected. Patients could be confused about how decisions were made, as the process was not always visible to them. They could be happy to wait for test results or decisions if they were kept informed of the reason for delays:
I expect it, that I’ll wait at a hospital. Everyone’s been polite and courteous and told me they’re just waiting for a doctor to look at my case, so. It would have been different if I’d just been sat here and no one had said anything to me. I would have been a bit annoyed.
Churchtown patient 2
Sometimes ED practitioners’ focus on speedy throughput could detract from their attention to the symptom that had brought the patient into the department. One patient who disliked hospitals was pleased to be going home but felt that her reason for presenting had not been resolved:
So what are you hoping and expecting?
Well, I’m hoping . . . you know, I wanted someone to take the pain away, and, um, I’ve had a couple of paracetamols and the pain’s, okay, it comes and goes, but nobody’s actually dealt with the pain.
Waterbury patient 4
Timely communication
Just as practitioners reached ‘tipping points’ when they felt a loss of control over the dynamic of maintaining patient flow and providing safe care, patients and carers too experienced moments that took them over the limit of tolerance within the overstretched system, and made them feel dissatisfied with the level of care they were receiving. This feeling could be exacerbated when patients believed that cases less deserving than their own were being given priority or when they were experiencing high levels of pain. The most frequently expressed reason for patient dissatisfaction was the lack of information and updates on their status within the system. This was particularly noted when patients were waiting for test results and admission or discharge decisions. All sites formally emphasised the need for patients to be able to identify a lead or named nurse in charge of their care. However, there was significant variation in how far the lead nurse was involved with a patient’s treatment, and whether or not the patient knew who this individual was.
The VSM study (see Chapter 4) found variation across sites in the stages of patient journeys at which the longest waits occurred. At Churchtown, a large proportion of waits occurred after the final admission or discharge decision. This was reflected in the experience of a 40-year-old patient: the decision had been made to admit him to a ward 1 hour after his arrival in the ED, but he then waited 5 more hours for a bed. During this time, he was not sure what he was waiting for. Whereas at Porthaven there was clear identification of the main decision-maker in charge of a patient’s care, at Churchtown patients were sometimes uncertain about whom they could ask for updates:
. . . it wasn’t until after the CT scan that I started getting worried. So up till then . . .
And what do you mean by worried?
Just no communication.
Yeah. And how could that have been improved, do you think?
Someone just to say, ‘Hi, I’m in charge of you at the moment, umm, while you’re in this ward if there’s anything you need to know talk to me and I’ll tell you everything you need to know.’ I’d just like some formal, like, ‘I’m in charge of your case. There will be 15 other people you’ll see and that’s normal but if you have anything come to me.’
Churchtown patient 3
Patients could understand that staff were busy, and they could also accept that they might be discharged without a clear diagnosis of their presenting condition: ‘I would rather go . . . if there’s nothing wrong, if there’s nothing they can do, “Fine, let’s go home”’ (Waterbury patient 2). However, patients could express annoyance when information about their status was not forthcoming:
I want to see somebody now, to say that I’d be going home. . . . usually they’re very quick at sending you home. . . .
And can you just take me through what happened?
I, um . . . got woken by a doctor and then I got moved to the ward, got me tablet, then woken again for the [inaudible], then woken again to go down for an X-ray at half past three in the morning.
Porthaven patient 12
This patient was aware of pressure on beds, and she hoped to receive a prompt decision with a view to discharge. Her admission experience was negatively affected by the repeated disturbance of moves and procedures during the night, and, it appears, by the sense that she was passively undergoing an instrumental form of processing through the system with insufficient regard for her felt needs:
Have you had any updates at all?
No. I don’t know when, it’s as and when I think, you can’t get one, but I don’t want to stop in here another night, that’s why I’m [annoyed at myself] for coming in . . . I’m getting right frustrated now.
I guess it’s just not knowing um, what’s going to happen in the next 6 hours.
Well, I think they should be able to contact somebody, you know, bleep them or something, and just say I need discharging . . . I think that’s what they could do, I mean if they were short of a bed they would.
Porthaven patient 12
This patient’s initially supportive attitude to the service changed to discontent when she perceived that staff actions such as moving her to a ward, dispensing treatment, organising tests and facilitating discharge were dispensed ‘as and when’ convenient for the hospital rather than primarily with her personal well-being in mind. She experienced not only frustration at the lack of information, but also disillusionment on sensing that her being left ‘in limbo’ was because system needs were prioritised over patients.
Patients approaching breach time could generate concern among staff, and this was often observed to be focused on target compliance, or on investigations that were key to an admission decision, rather than the patient’s comfort or communication needs:
[The patient] seemed irritated by the doctor’s questioning and remarked that he kept having tests on his heart but that no one was telling him why or if there was a problem. . . . [The patient] was frustrated by having to wait for the results of his tests as he was hoping to go home. . . . the co-ordinator and [the consultant] were concerned about the slow progress of [the patient], who had now been in the department for 3.38 hours. . . . [The consultant] went to speak to the patient, who, at this point, looked very uncomfortable, as he had slipped down the bed, resulting in him hanging off the end and having to look up in order to speak . . . but no-one addressed this.
Underbridge fieldnotes 2
In such situations, it was also observed that patients and carers self-rationed their communication with staff about basic care needs when they perceived that practitioners were busy:
For the past half-hour [the patient] has been mentioning that the back of the bed is uncomfortable – not a good neck position. . . . I suggest [the daughter] might ask the nurse in charge of her mother. She looks out for him in the nursing area and we see him moving quickly about between patients. She says ‘He looks a bit busy’ and does not pursue this. The patient remains with an arm behind her head, trying to prop herself up.
Churchtown fieldnotes 2
Offer of fluids and food
The cultures within different acute care units (anonymised in this section) significantly affected patient experience. Where food and drink were provided, or clinicians encouraged access to them, patients appeared to feel less anxious about waiting. One site introduced a ‘discharge lounge’ from the single point of entry ED where patients awaiting final medication, paperwork and transport could wait and also help themselves to food and drink. Another site designated a similar area, available to MAU, triage and ambulatory patients, where ward routines of meal times and the offer of fluids were built into practice.
In EDs, these routines were less evident, and some patients were observed to go for long periods without being offered food and drink. A senior nurse in an observation area suggested: ‘I don’t know that [ED staff] are as good as us at asking the patients, because they’ve got so many, and they’ve got lots of other things to do’ (site X practitioner 8). In one ED, relatives were observed to seek advice from staff when they or the patient were hungry or thirsty, but they were unclear about whom to ask and expressed concern about disrupting practitioners whom they perceived to be busy. Patients’ requests in this area were sometimes not attended to in a timely way:
The patient says ‘Can I have a drink now?’ [Support staff] tell the [PFC] that the patient would like a drink. [The PFC] mentions this to nurse [X]. The nurse is carrying out a procedure with another patient and does not respond to this request at the time I am observing.
Site X fieldnotes 1
So aren’t I supposed to be on fluids and stuff like that?
Well, fluids aren’t critical if you are managing to drink.
Well, I’m not.
Because they haven’t brought you anything or because you’re not thirsty?
Because they haven’t brought me anything. . . .
Right. Do you want something to eat and drink now?
Am I allowed to eat?
Yes!
Oh thank God! Yes please!
Let’s see what we can find.
Site X patient 1
Doctors at this site voiced their concern that staff retention difficulties and pressure on nurses to complete administrative tasks meant that their attention to patient care could be compromised:
the other thing is the nursing staff, . . . having enough nurses to kind of deal with the jobs, the procedures . . . how do you prioritise the . . . jobs for those patients, because then that delays getting a patient ready for the ward and all the rest of it.
Site X practitioner 1
This issue was observed to be a particular problem where patients were elderly, had disabilities, had impaired cognitive functioning or were in too much pain to express their needs, including their capacity to report on their intake of fluids and foods as they were moved between hospital departments. On the same site, an 86-year-old woman with dementia had fallen in the night and had not eaten or drunk for many hours by the time she was transferred to the MAU. The patient herself only asked for a cup of tea after what was reported by her carer to be some 20 hours without food (site X fieldnotes 2).
Summary
Patients frequently alluded to self-rationing and self-regulation to avoid admission, decrease the burden on staff and reduce the duration of hospital stays for their own benefit and that of the system. The desire of patients and practitioners to avoid ED attendance or admission was shared to a lesser extent by carers. Families caring for elderly relatives often felt the strain on their time and resources and could pressure staff for lengthier hospital stays in the absence of clinical need. Patients and relatives made allowances for the overstretched system, but their tolerance diminished if they felt resource allocation to be unfair, or if they were not kept informed about reasons for delays and barriers to discharge. Late-night transfers, bed moves and discharges were sometimes carried out in ways that were expedient for the system but had negative effects on patients. Despite expressing generally high levels of satisfaction, patients could at times feel that they were giving too much, in terms of understanding the system, empathising with staff, making allowance for their busyness, rationing their expectations of care and avoiding demands on resources. Some dissatisfaction was associated with a lack of clear communication from community and hospital practitioners about risk exclusion and the rationale for hospital visits and tests. Patient care could be seen to be less than optimal in ED environments where attention to ‘softer’ needs and the offer of food and drink were not always observed. Even more than reduced waiting times per se, patients’ most commonly expressed requests and complaints concerned availability of staff to provide basic nursing care, information about reasons for delays and updates on their status in the system.
Chapter 7 Synthesis of findings and implications
Introduction
This chapter synthesises the findings from the component studies to provide insights from the study as a whole. Based on the synthesis, we propose elements for a model of care and service organisation aimed at improving patient experience and admissions decisions. We aim not to evaluate the impact of each element but rather to show how each might have an effect.
The synthesis covers three areas that relate to the design and delivery of models for care: practitioners’ interactions, the internal acute care system and the wider urgent care system. Analytic statements developed from the component studies and team/stakeholder discussions are referred to by number in this synthesis (e.g. no. 21) and listed in Appendix 13.
Challenges for patients, practitioners and the system
Risk and decision-making
The decision to access acute care
Determining whether or not symptoms warranted their access to acute care could be confusing for patients and carers. The decision was frequently driven by anxiety, but was often mediated by patients’ and carers’ levels of knowledge and understanding about symptoms, underlying conditions, individual medical history (no. 97), alternatives to acute care (no. 93) and the advice given – by a GP, another professional or the 111 service (no. 109) – about attending acute care. People could be reluctant to access acute care if previous experiences had been considered ‘difficult’ (no. 76).
Tolerance of risk within a resource-constrained system
While patient safety was the primary consideration declared by practitioners, decision-making incorporated considerations of what was safest for clinicians, the hospital, other patients and/or the community as a whole (no. 19). Where doubt existed, the limit to which practitioners would tolerate risk about missing potentially important diagnoses, or keeping patients in unstable social circumstances, could lead to a default decision to refer to acute physicians (no. 81) or to admit (no. 18; no. 19). This may also have reflected an experiential understanding that it could cost less in practitioner time to admit than to discharge a patient (no. 108), and the decision could be further compounded by staffing pressures and a high number of acutely ill patients (no. 41). Tolerance of risk, and willingness to share risk, could be higher among doctors in both primary and acute care than among other health professionals (no. 83) but also varied within a group of HCPs of the same grade, with some being seen as more risk averse than others. Practitioners could feel that their professional reputation was at stake and that an unsafe decision would impact negatively on their sense of self-worth (no. 113). Practitioners were also more comfortable in making a decision if the patient or carer bore some of the risk him-/herself (no. 114).
Practitioners’ interactions
Acute care was ‘pressurised’ in terms of workload, patient acuity and targets, and this could lead to suboptimal interaction between patients, carers and practitioners.
Communication between practitioners, patients and carers
Patients experienced anxiety when they were not kept informed about diagnostic wait times, decision-making processes and plans for their treatment (no. 38). This could be intensified when mobility was limited, sometimes leading to frustration and regret about the decision to access acute care (no. 77). However, waiting could provide a time interval that enabled more fully informed decision-making and a shorter overall time spent in hospital (no. 107).
Carers had similar expectations to patients about accessing information about progress (no. 15), and they could draw on their knowledge of how a condition affected their relative or friend in deciding when and where to seek information from practitioners. Patients’ and carers’ communication styles varied, and they could present themselves as collaborative, knowledgeable or vulnerable when interacting with practitioners (no. 14).
Whether through differences of opinion or different expectations of the acute system, the approach of carers could differ markedly from that of patients (no. 3). However, this was more complex than carers simply advocating for hospital admission: many carers could recognise when a patient’s needs were better addressed through rehabilitation than through acute inpatient care (no. 67). While the goals of patients, carers and practitioners were diverse and not always congruent, there were usually sufficient shared goals for collaborative decision-making provided that all parties perceived the others to be fulfilling ‘their end of the bargain’.
Collaborative decision-making about admissions
Admission decisions could be influenced by the preferences and views of patients and carers (no. 11). These expectations could be raised by what acute care and community practitioners said (no. 8), and patients could feel frustration if their expectations about admission or returning home were not met (no. 79). What patients and carers considered to be appropriate actions could differ, requiring practitioners to negotiate a mutually acceptable decision that balanced medical, social and personal factors (no. 6; no. 84). The involvement of a consultant often resulted in patients being less likely to be admitted to hospital (no. 59), through the assertive use of skills and authority, and recognition of the risk of iatrogenic harm (no. 10). However, these skills and authority were not sufficient without the backing of a supportive wider urgent care system.
A common thread ran through the decision-making process. If the concerns and fears of patients (and carers) were elicited and addressed, and if knowledge of their (or their relatives’) health and social care needs was taken into account, then the patients/carers were more likely to be satisfied with the decision (no. 13; no. 37). This was the case even where the decision was different from that expected (no. 13; no. 37). However, practitioners’ goal of ‘efficiently processing’ patients through the system could sometimes lead to patients and carers being viewed primarily as sources of information rather than equal partners in decision-making (no. 1; no. 12; no. 96), and this goal could limit staff communication with patients and carers (no. 37). Communication could also be limited when practitioners assumed that patients had the same level of understanding and tolerance for uncertainty as themselves (no. 100). The involvement of patients and carers in decision-making was often the first element that diminished when work pressure increased.
Interprofessional communication
Within acute care, a range of professional communication issues affected the decision-making process:
-
a lack of clarity about which medical team was responsible for the care of a patient, leading to confusion about who was responsible for patient care (no. 30) or a delay while a specialist response was obtained (no. 33)
-
disagreements between medical teams about the patient’s clinical pathway, for example where specialist teams’ views on patient management differ (no. 74) or where ED practitioners do not follow a specialist team’s preferred pathway (no. 75)
-
weak communication between ED doctors and new, evolving multidisciplinary teams (such as an ACE team), often limiting use of these teams (no. 64)
-
strained working relationships between junior ED doctors and specialists within the hospital, which inhibit quality of communication (no. 85)
-
the availability of specialist teams to interrupt planned work on wards or in clinics to attend to unscheduled care (no. 31).
Acute care system
Patients travelled through a sometimes disjointed community and hospital system that aimed to provide safe, efficient and patient-centred care. This journey was facilitated or constrained by the actions of practitioners (including GPs, the 111 service, acute care doctors and nurses, and social care practitioners) and the decisions that they made regarding patient care and referrals.
Information sharing and differentiation
While practitioners often mentioned the problems caused by a suboptimal primary care system in failing to stem the flow of patients to the ED, many examples of best practice were observed and reported. Clear and concise communication between primary and acute care could optimise resource use, facilitate decision-making and enable timely access to assessment and services (no. 57; no. 80). This could act at two levels. First, decision-making could be supported by systems that enabled differentiation of patients’ needs, so that a greater proportion of those entering the ED were patients with urgent care needs that could not be managed by other community services (no. 89), outpatient clinics (no. 42) or hospital specialties (no. 61; no. 80).
Second, communication between GPs and hospital doctors about alternative inpatient or outpatient services could allay practitioners’ fears about the appropriateness of referrals and the ongoing care of patients (no. 82). For example, if GPs knew of, and trusted in, hospital ‘hot’ clinics, or ED doctors knew of and trusted in GPs and other community services to have the skills and resources to proactively follow up in the community, then each had a greater confidence in decision-making that made use of these services.
Knowledge about local pathways and resources
Pathways that provided alternatives to, or alternative routes through, the acute care system were a valued resource for admission avoidance (no. 61; no. 104; no. 106). Knowledge and communication about local systems and pathways was vital for their use (no. 39). Local knowledge about services offering alternatives to hospital admission (such as community specialist nurses or community beds), and about referral processes, was valued but unevenly distributed (no. 39). Staff turnover could contribute to the loss of local knowledge, as there was insufficient time for such knowledge to be communicated to new members of staff (no. 58). Practitioners’ lack of knowledge or confidence in the quality and role of services, particularly in the community, could lead to a reluctance to refer (no. 49). Knowledge about alternatives to hospital admission involved ‘knowing that’ (a service exists) as well as ‘knowing how’ (to access it) and ‘trusting in’ the service to provide appropriate care. Key to this knowledge was referral to appropriate ‘discharge’ teams, whose remit was to identify social and functional needs and match these with community resources, thereby avoiding admission where possible. These teams were highly knowledgeable about resources, but frequently frustrated by the patchy, ‘postcode lottery’ nature of community response within the regions served by the hospitals (no. 110).
Responses to the 4-hour target
The 4-hour target acted as an overarching context for decision-making in acute care, driving a need to process patients and keep up the flow.
While practitioners perceived this target as having achieved positive effects as a collective goal for service delivery (no. 73; no. 78), in the context of resource constraints it was also perceived as driving inappropriate admissions (no. 40; no. 102). This was a particular problem for patients who required ‘watchful waiting’ on account of diagnostic uncertainty (no. 72), who needed their mobility or home care conditions assessed (no. 44) or who had complex health and social issues that could nevertheless be resolved without hospital admission (no. 41; no. 73).
Patients were often observed to act less as ‘customers’ of a service and more as collaborators in managing limited resources. Patients often demonstrated self-care and acted in a way that optimised practitioners’ time and the use of available acute beds (no. 4). Patients ‘rationed’ their own care by not making requests to practitioners they perceived to be busy, or to those who were attending to patients whose needs they judged to be greater than their own (no. 5).
The timely availability of hospital beds (no. 20), hospital transport (no. 86) or home care services (no. 9) routinely impinged on decision-making (no. 71). Waiting times for these services significantly increased staff costs within EDs (no. 105). The peak in admissions that occurred shortly before the 4-hour target indicated that avoidable admissions were occurring as a result of efforts to comply with the 4-hour standard.
Resources and initiatives to support decisions and flow
The speed with which diagnostic investigation, checking and reporting could be completed and communicated had a significant impact on when informed decisions could be made in acute care (no. 54). Reduced availability or non-availability of services outside office hours could slow this process (no. 66; no. 69); case studies suggest this led to more admissions as a way of managing risk (no. 112).
In addition to a focus on diagnostics, a number of new spaces and teams had been developed across all sites to improve flow and reduce admissions. New spaces were used to take patients ‘off the clock’ while waiting for results or while being watched, cared for or prepared for going home, in a less pressured environment. In Porthaven, which had the greatest array of new spaces, the co-ordinating senior ED consultant was said to have confidence in the roles of the AGPS, CDU and ambulatory care pathway in the locality (no. 102).
Specialist teams with responsibility for admission decisions about complex, elderly patients could contribute to preventing unnecessary admissions, for example by organising timely specialist outpatient appointments not available to acute care practitioners. However, these new teams could also be a source of frustration for some practitioners, who viewed the existence of such initiatives as adding a step to the care pathway rather than contributing to the overall care of the patient (no. 46). They also stressed that the service was not consistently available to them out of normal working hours (no. 111). Practitioners also perceived that it was more difficult to make arrangements for community support outside normal working hours, again leading to admission as a way of managing risk (no. 112).
Initiatives designed to optimise the flow of patients through the acute care system could be perceived by practitioners as tactical service reconfigurations to meet a target rather than as actions to address the root cause of issues in acute care (no. 101).
Use of seniors’ time
So that they could use their ‘clinical eye’ (no. 26), even senior clinicians might want to see a patient in person before making any complex decision about care (no. 70). However, this could also reflect senior clinicians’ uncertainties about the capacity and ability of the wider urgent care system to provide care. However, at the site incorporating the most senior involvement clinically, a consultant ‘controller’ did not routinely see patients but instead both provided advice and monitored the system. At Underbridge, a conceptually related innovation was a nurse practitioner-led emergency unit overseen by senior medical staff.
Practitioners judged how they used their time, as highlighted in the tension experienced between meeting targets and providing patient-centred care (no. 48) and/or teaching staff (no. 63). A desire to avoid ‘failures’ pulled practitioners towards meeting the demands of the system and away from the needs of patients, optimal communication and the learning requirements of staff.
Towards principles of practice in acute care
The problems described in the previous section reflect several dilemmas that may be deemed applicable to other NHS services:
-
whether to invest in triage to onward pathways or to carry out most care at the first contact
-
whether to ‘step up’ care when needed or involve senior input at the start
-
whether to have protocolised pathways or empower practitioners to respond creatively to patient need
-
whether to facilitate patient choice or make decisions based on objective need
-
whether to take an individual or population/system view.
The heterogeneity of patient need and resource constraints means that it is important to consider how each need/resource may be reconciled or balanced in different situations. The following types of patient illustrate the variety of need:
-
individuals requiring time-consuming diagnostic skill and investigations to rule out – or diagnose and provide immediate treatment for – life-threatening illness (Porthaven case 10, see Appendix 12)
-
individuals with functional impairment or social difficulties who have new care needs resulting from their illness or living situation (Porthaven case 7, see Appendix 12)
-
individuals (or carers) with anxieties about their health or care (Underbridge case 5, see Appendix 12)
-
individuals with an undifferentiated and uncertain diagnosis (Churchtown case 1, see Appendix 12).
Many individuals with multimorbidity may present with all four types of need, and an ideal acute care system will be able to manage expectations, provide diagnosis, treatment and care, and involve patients in the decisions.
Principles for optimum practice were identified from the problems described in the first part of the synthesis. These principles are summarised in Figure 17, which depicts how they are relevant to the wider system (hospital and community), the internal design of the acute care settings and the interactions between patients, carers and practitioners. This second part of the synthesis presents a series of positive statements which indicate how the principles for avoiding inappropriate admissions and unsafe discharges in acute care settings might have an effect. The statements have been generated by combining analytic statements that relate to best practice as observed, reversing negative statements and drawing on inferences related to silences in the data (these last indicated by *).
FIGURE 17.
Principles of decision-making for avoiding inappropriate admissions and unsafe discharges in acute care settings.
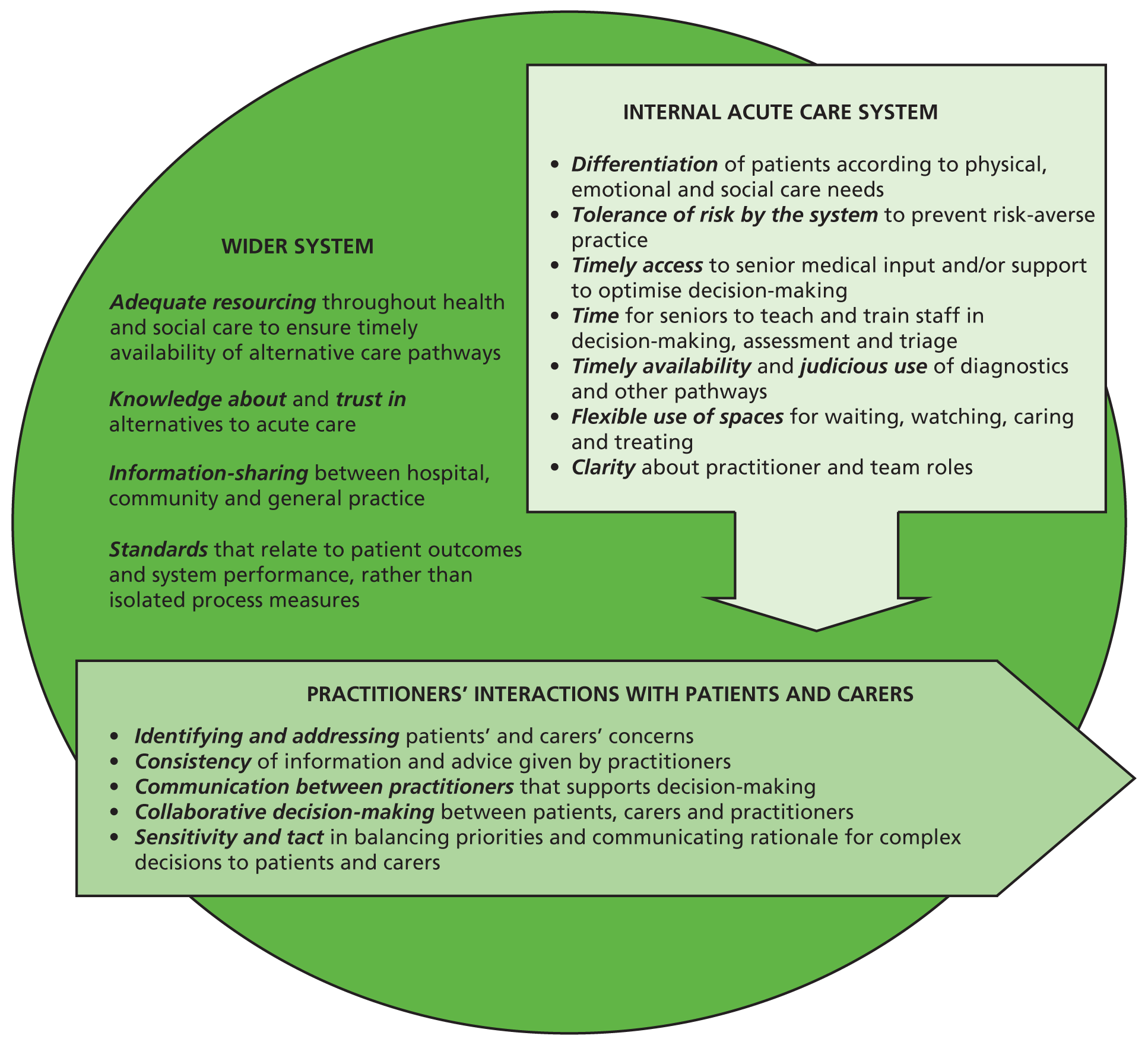
Practitioner interactions
The experience and engagement of patients and carers/families may be optimised by:
-
demonstrating understanding about the patient’s discomfort, distress and predicament
-
eliciting his/her goals and preferences as well as information about the patient’s condition and valuing patient and carer knowledge
-
making the decision-making process explicit and giving viable choices
-
ensuring they feel they can ask questions and make suggestions
-
providing information about progress through the system even if it is only to inform people about uncertainty
-
practitioners taking over decision-making for those who are the most confused or unwell
-
establishing a routine practice of attending to care needs while in acute care – communication, allaying fears and concerns, provision of food and drink, attending to toileting needs, etc.
Patient expectations about being admitted may be managed by:
-
GPs and paramedics stressing the possibility or likelihood that patients will go home, when making referrals
-
making initial assessments at a desk with patients clothed (more like a GP or outpatient clinic)
-
providing an ‘ambulatory space’ when patients are waiting for results or being observed, which allows individuals to be seated and clothed and access food and drinks themselves.
Patients’ and carers’ (sometimes different) anxieties about illness being managed at home may be addressed by:
-
eliciting and giving value to concerns
-
talking through the risks to create understanding about drawbacks and benefits of care in hospital versus the community
-
negotiating compromises
-
providing safety net advice about what to do if discharged
-
involving senior practitioners when needed to check and support decisions.
The ability of junior doctors to make good decisions may be enhanced by:
-
pathways to specialist teams and diagnostics being clear, known, easy and reliable, but sufficiently focused so that all patients are not routinely referred
-
ensuring availability of senior doctors
-
encouraging senior nurses to provide supportive advice
-
being respected by doctors from specialty teams.
Junior doctors’ learning may be enhanced by:
-
seniors expecting that juniors may seek advice about a preferred plan rather than wait to be told what to do
-
receiving ‘micro’ training in relation to difficult cases.
Seniors may deploy their clinical expertise regarding individual patients in a variety of ways, by:
-
selecting cases they may discharge or admit much more rapidly than juniors
-
selecting cases with clinical complexity and uncertainty, or anxiety
-
advising juniors on decisions without seeing the patient
-
advising juniors on decisions by reviewing the patient briefly and advising on tests and referral pathways.
System factors: using resources to manage flow within and out of acute care settings
During the pre-hospital phase, patients may be directed to the appropriate place/team by:
-
GPs making themselves available and trusted by patients at risk of admission
-
GPs referring patients to specialist teams, where clinically appropriate, rather than signposting to the ED
-
hospitals providing referral systems involving clinician–clinician conversations (such as Porthaven AGPS) to differentiate and direct GP referrals to the correct hospital or community team
-
ambulance staff liaising with GPs or the admission avoidance team prior to the decision to transfer to the ED.
Overall flow and capacity within EDs may be managed by:
-
having a senior doctor and nurse oversee all patients within a unit while others care for individuals
-
having information systems in place that allow capacity and flow in the ED and the whole hospital to be visible
-
having patient areas visible from central positions, while also guarding privacy
-
having easy access to the AMU, radiology and other acute care spaces
-
having easy access to past clinical records from hospital and primary care systems.
Relations between specialty teams and practitioners in EDs may be enhanced by:
-
ensuring an understanding of each team’s remit and contact details
-
making space to work together collaboratively.
Rushed decisions to admit as the 4-hour deadline approaches may be avoided by:
-
identifying and managing patients who are likely to need a more prolonged decision-making time period soon after arrival
-
involving teams specialising in discharge at an early stage in the pathway
-
utilising ambulatory units or CDUs that are ‘off the clock’ for those needing time-consuming investigations or ‘watchful waiting’.
Discharges may be made more safely by:
-
liaising with GPs about concerns and plans*
-
arranging for GPs to follow up patients the next day*
-
having specialist ‘hot’ clinics or diagnostics (plus follow-up) available within days
-
support from community teams able to provide social care and/or treatment at home*
-
transfers to nursing homes with the facility to monitor and provide rehabilitation*
-
encouraging juniors to consider the discharge option, though also checking with a middle-grade or senior doctor
-
involving hospital teams specialising in discharge
-
providing clear information to patient, family and community teams on safety netting.
The specific components above are more likely to be successful when incorporated into systems where:
-
the culture is positive, engendering learning and flexibility
-
risk is ‘named’ but managed positively
-
teams are stable with minimal use of locums (optimising local knowledge of context and how to get things done efficiently).
Although the ED environment may be stressful, we have indicated several measures that may be employed to mitigate this pressure, and specific features of the clinical environment and communication with patients that could enhance the safety of patients and optimise their experience. The different elements of the acute care system, both in the community and in secondary care, need to collaborate more closely and generate joined-up pathways though a blend of flexibility and management of flow.
Chapter 8 Discussion
Introduction
The 3A study has investigated emergency medical admission decision-making in four diverse sites and revealed similar interactional but diverse organisational responses to common pressures on time, space and practitioners. Time pressure limits the extent to which patients and carers are enabled to share in decision-making, and gives little opportunity for full information to be obtained, or alternatives to admission identified and arranged. The complexity of medical and social issues, the importance of patient safety, practitioners’ risk aversion and the need to maintain flow through busy departments are all factors that contribute to admission by default. Each organisation responded with contrasting spatial and organisational infrastructures, different staffing models, and a variety of innovations.
Organisation of emergency care at the four sites
Variations across sites included alternative entry points to ED and ways of triaging or negotiating ‘planned’ GP referral. Observation wards, or areas where it was possible to ‘stop the clock’, observe and plan treatment and discharge, were not always present, and were configured differently in each site. However, each new entry point and/or space could both reduce and increase pressures on capacity: for example, pressures on one AMU regularly resulted in ‘overflow’ into the ED.
In 3A, the site with the lowest admission rate included a hospital-based AGPS, which managed and sent home all seven of the patients observed in the VSM study. While further research is required, this finding supports previous research suggesting that GP services may play a role in reducing admission of ambulatory patients. 36–38 This is also in agreement with the idea that many ambulatory care-sensitive conditions may be managed without hospital admission. 41–43
By providing trusted alternative pathways with greater capacity in the community and at the entry point to hospital assessment – including ED observation areas, ACUs and ‘hot’ clinics – admissions could be reduced. This supports the suggestions made by the Royal College of Emergency Medicine17 that a range of community and hospital initiatives are required to tackle crowding. The diversity of organisational structures and experiences uncovered by the 3A study also endorses the concept of whole-system redesign. 10 Our findings highlight important innovations in care models, but caution that local monitoring and evaluation, and national sharing of models are required so that learning from ‘bottom-up’ innovation may be accumulated.
Reasoning and communication
Reasoning of patients and carers
The reasoning of patients and carers begins with concerns that prompt the decision to seek urgent care. For patients in our study, the principal value of hospital EDs was rapid access to assessment and treatment that was not available elsewhere. However, the use of emergency services was influenced by the way in which individuals were directed to use them. GPs or out-of-hours services, community nurses or the 111 service could quickly escalate to ambulance call-out, even if this was not necessarily what the patient wanted. This finding adds a further dimension to the results of a study that considered why patients with primary care problems called for ambulances, which concluded that poor knowledge of alternatives, anxieties of carers and attitudes to risk were important. 52
While higher rates of avoidable admissions have been reported in urban areas with greater deprivation,3 the site in our study with the lowest admission rate had the largest and most deprived urban population, suggesting that the multiple initiatives there could be effective in avoiding admissions.
Reasoning of practitioners
Senior practitioners held the view that EDs operated in a ‘take all’ fashion, and that the absence of alternative options, or inability to access them, resulted in unnecessary hospital referral and admission. Higher hospital referral rates are a significant problem in themselves because they are associated with higher rates of conversion to admission. 8 This could be because appropriate decision-making may quickly diminish in overstretched departments under 4-hour target pressure. At times of high pressure, faced with the competing demands of a safe decision for a complex patient – often with limited background information – and maintaining patient flow, the default decision was to admit. While the 3A study observed this phenomenon frequently, cases where junior ED doctors actively considered and tried to set up community-based care were far less common.
Practitioners were aware of the potential clinical risks as well as the social risks arising from the decisions they made. More senior and experienced practitioners was observed to be more tolerant of uncertainty and risk; ED seniors show great understanding of medical risk, and GP involvement both before and after arrival at hospital may provide additional understanding of community capacity. 51
This 3A study has provided insight into the role played in admission avoidance by experience and seniority. More experienced practitioners demonstrated better insights into the risks associated with different decisions. Our findings support the idea that early ‘senior first’ involvement in decisions results in reduced likelihood of admission. 28,31–33 However, ‘senior first’ involvement was not associated with a shorter overall patient journey; this may be because seniors became concurrently involved in more complex cases. Other studies have found that early involvement of physicians in screening reduces time spent in the ED29 and time to treatment and discharge30 but, owing to multiple modes of involvement and small numbers, the results of our study did not show that this was the case. Senior staff expressed the view that the impact of senior input was related to experience, a good knowledge of local services and alternatives, and individual attitudes to uncertainty and risk.
Communication between practitioners
The importance of effective communication between primary and secondary care was repeatedly voiced. A patient who arrived expeditiously with no clinical information was much harder to manage than one whose pathway had been negotiated with the patient’s own GP and who arrived with an informative letter and copy of key clinical information. The Porthaven AGPS’s low admission rate was perhaps unsurprising. Underbridge and Waterbury had some provision to access primary care records from ED, although in our study it was too early to assess the impact of these innovations. However, our observations suggest that systems that incorporated pre-hospital review, facilitated information sharing and employed service models such as the AGPS and ACUs that allow more ‘planned’ care for selected patients, as opposed to unscheduled emergency care, were more likely to find alternatives to admission.
The impact of the 4-hour target on practitioner behaviour
While the 4-hour standard was intended to improve patient experience and outcomes by ending lengthy waits, the 3A study captured the effects of this target from the perspective of appropriate decision-making. The majority of admissions and discharge occurred around the 4-hour target, suggesting that this target may have considerably influenced decision-making. This raised the question of whether or not a quick decision was necessarily the best, even if it maintained flow. These findings support the views of Cooke, who considered that the 4-hour target was a crude tool to drive quality improvement in emergency care and that it could detract from patient-centred care. 9 We found that involvement in decision-making was valued by patients, and that viable alternatives to hospital admission were often preferred. In showing how patients’ preferences could be unvoiced or unheard, while priority was given to avoiding breaches, the 3A study presents a counterperspective to the premise that fastest is necessarily best.
Strengths and limitations of the study
The principal strength of 3A is its broad examination of the views and expectations of patients and carers, the reasoning of practitioners, and the role of system factors in the decision-making process. Deep insights were gained from observing and interviewing some 500 patients, carers and practitioners. The ethnographic data provided insights into the range of new initiatives, and the experience and participation of patients, and allowed us to generate hypotheses about how to safely reduce unnecessary admissions.
Although EDs and associated units accept patients with unselected conditions, and the ethnography sampled a broad range of ‘uncertain’ medical cases, the VSM study focused on recruitment of patients in two categories that had been identified as typical of ‘grey’ admission decision areas and that were known to account for a high proportion of acute medical admissions. Although the study data cannot claim to be representative, the two groups are typical of these important types of presentation.
There are several limitations in the design of 3A. We studied only four sites, chosen because of contrasting care models. We recruited and followed patients after arrival at hospital, and only interviewed patients, carers and relatives, limiting our observational study to the period of decision about admission.
The VSM study was a unique component of the 3A project. While the Lean concepts of maintaining quality and eliminating waste may be translated from the manufacturing industry into health services, there are inherent differences. The primary weakness of the approach is in the number of variables to be accommodated, including individual patients, practitioners of different types and grades, models of care, resources available and other competing demands and pressures on the system. Caution is therefore required in drawing inferences from the limited statistical analyses we undertook. It is important to acknowledge that ‘value’ was predominantly interpreted as contact time with the patient, and we did not discriminate between the value of staff with varying levels of experience or seniority. There were also some practical challenges in making VSM measurements at different times and in different places. While it proved relatively straightforward to undertake VSM measurements in the ED pathway, it was less so in the associated acute care units at Porthaven and Waterbury, owing to the longer time frame for assessment and larger areas to be observed.
Another limitation of the VSM study was that recruitment was only during weekday, daytime hours and not outside working hours. Consequently, the services are represented responding to peak daytime demand.
There are also limitations to the staff cost estimates based on the VSM data, which should be treated with caution. It was not possible to accurately estimate the time different grades spent on individual patients, or the proportion of staff members’ time that was dedicated to acute care. This partly related to the sheer number and variety of staff seen and tests received by some patients, which could not be fully captured through the VSM data collection methods (in which the observer stays with the patient). The care models differ somewhat, with non-ED services not costed into the model. Also, basing costs on ‘top-down’ assessments, based on each department’s staff rotas or overall staffing profiles, generated widely different total cost estimates and it was difficult to transparently correct these estimates for things such as unfilled posts and differences in actual current mix of staff grades. Ultimately, however, the cost analysis that was proposed and undertaken was not designed to provide a comparative cost-effectiveness study.
The use of a critical realist framework allowed us to use ethnographic data to theorise about causation and to combine data sets to generate analytic statements for use in the synthesis. We were able to focus on how and why patients and practitioners responded to each other and to the resources and constraints of the acute care system. The product of the synthesis, written in the form of positive practice pointers, is, however, limited by being generated inductively. Each statement is a tentative hypothesis, generated from empirical evidence, rather than an intervention of proven effectiveness. The synthesis provides material for researchers using a range of methods to evaluate these ‘candidate theories’ and innovations.
Implications of the study for policy and practice
The questions of how best to configure emergency medical care, and for which patients hospital admission is appropriate, continue to dominate debate in the NHS. The 3A study, while recognising that further research is needed to test these models, may be able to inform future policy decisions that will affect practice.
What does patient-centred care mean in emergency medicine?
One definition of patient-centred care is ‘to put the patient first in everything that is done’,56 and this may be said to hold in the context of emergency medicine. The 3A study may help to inform the optimal shape of patient-centred care in emergency medicine:
-
practitioners communicating clearly and in a timely fashion with patients and carers
-
better information exchange, allowing greater patient and carer participation in decision-making at all stages of the patient journey
-
not imposing unrealistic restrictions on time for more complex decision-making
-
improving knowledge of, and access to, alternatives to admission at all levels of the system.
We contend that all of the above would increase the likelihood of avoiding unnecessary admissions as well as improving patient experience.
Implications for service design
While the plethora of new initiatives was, at times, confusing for researchers as well as practitioners, we concluded that both new spaces and new teams, as well as ‘differentiation’, could be part of the solution to the problem of escalating admissions:
-
The availability of clinical decision/observation units with sufficient capacity at busy periods may allow time for safe decision-making, thereby reducing admission rates and decreasing the risk of inappropriate discharge.
-
If patients with complex needs (who may not be the most unwell) are identified and managed early in their journey, by specialist teams where these exist, there is a better chance of avoiding admission.
-
ACUs supported by a ‘discharge team’ may be well placed to set up care in the community.
-
Sharing clinical information between primary care, secondary care and social care may enhance decision-making.
-
Specialist pathways for certain patient groups (e.g. stroke, chest pain) may reduce time in the unscheduled care department and avoid unnecessary admissions.
-
Given the predominance of admissions not preceded by GP contact, there may be scope for active liaison between the ED and both GPs and emerging community-based acute care teams in the planning of treatment and care, as a means of avoiding admissions.
In summary, a flexible acute admissions pathway with multiple entry points and subsequent pathways may be better able to meet the needs and expectations of patients and carers. Whether this model is constructed under the overarching umbrella of the ED or is run as separate pathways may be a secondary consideration.
New ways of working
The observation that approximately 50% of training posts in emergency medicine are unfilled poses a significant challenge to aspirations for 24/7 senior-led emergency medicine services. 2 Therefore, creative ways of working that optimise the deployment and flexibility of the whole workforce are needed.
Consultants in EDs, rather than being ‘protocolised’ to see all unwell patients early, need time to take on a range of roles:
-
‘Cherry picking’ cases where their skills, experience and authority will have most benefit – i.e. patients with complexity or anxiety or who may be rapidly ‘shipped on’.
-
Adoption of the ‘controller’ system of Porthaven, in which a senior physician is consulted by other staff, including junior and middle-grade medical staff, triage nurses and nurse practitioners, and other professionals. This role of ‘training in action’ may be a feasible way of having senior and specialist advice suggested at the hospital front door. 70
-
Involvement in system redesign. We were impressed by the dedication, patient-centred focus, thoughtfulness and energy of seniors in the acute care setting. These attributes were often put to use in devising and modelling new ways of solving the admissions problem.
While our study focused more on the medical role, a potentially important innovation was the nurse practitioner-led emergency care unit, as developed at Underbridge. However, the findings of 3A support the view that whole-system redesign is appropriate to develop new ways of working, better integrate medical and social care, and improve pathways and alternatives to the ED. 10,69
In conclusion, the 3A study has generated a rich narrative description of the acute admission decision-making process and the reasoning behind it, based on observation and accounts of a substantial sample of patients and practitioners. The VSM method was applied in a novel way to examine value, waste and system bottlenecks at four sites with contrasting models of care. The findings, interpreted through a critical realist lens, give considerable insight into why and how patients find themselves being admitted to hospital. These findings may signpost features of care models and service design that are required to safely reduce avoidable acute admissions.
Recommendations for further research
The design of services and role of practitioners in the acute care setting is recognised internationally to be an under-researched area. This study has pointed to some specific areas requiring further research, particularly within the ED. It also points to the need for research in relation to care before and after the admission assessment within the acute care setting. The full range of study types is likely to be required, from further in-depth observational qualitative studies through to quantitative intervention studies. This research will be facilitated by the availability of a standard definition of a hospital admission.
First, there is an important need for further research to value and capture the experience of patients who use emergency care, since this is a fundamental indicator of quality of care, and not simply to see patients as passive recipients of emergency care regardless of its quality. As models of care are refined and evolve, the patient experience should be a central outcome indicator. This study found that, while patients were generally uncomplaining, they and their carers had significant concerns. Our research suggests that the experience of patients and carers could be significantly improved, particularly by improving shared decision-making and being more explicit in communication about risk. Therefore, there is a need for research to identify ways to optimise communication, including the study of communication-training interventions. Experience of care was also at times disjointed and bewildering, and therefore research that identifies how teams may work together, involving patients and carers, to provide a better experience is also required. Interventions to support practitioners in dealing with the pressures of admission avoidance, risk aversion and the 4-hour standard, and simultaneously improving experience, are a related area requiring further work.
This study identified a series of specific care components that should be prioritised for more formal research to identify the optimum configurations for admission avoidance. These include greater GP involvement in pre-hospital and hospital care, improved flow of information from primary to secondary care, a range of different ways of ED working, and pathway configurations and entry routes that all contribute to safely controlling avoidable acute admissions.
The principles outlined in Chapter 7 provide a list of potential areas for both further in-depth investigation and development of interventions. There will inevitably be a tension between the evaluation of single components and of redesigning whole systems, incorporating multiple elements from the list of principles outlined. While the reconfiguration of whole services incorporating improved pathways, deployment of seniors and teams is theoretically possible, the reconfiguration of spaces is likely to be highly context-dependent and difficult to evaluate with comparators or controls. Even for the design of new pathways, teams and deployment of seniors, running cluster randomised controlled trials of EDs will require considerable feasibility work, and it is likely that alternative types of study design will be required. Involving researchers working alongside services to develop theory-based models for this range of interventions may be preferable to researchers imposing ideas on services and expecting services to comply with randomised designs. Such implementation alongside innovation may allow simultaneous building of theory and development of practice.
Our research also emphasises an important need for further research on initial access to emergency care in the community, and on whole-system integration. New models of integrated care with care navigators or case managers need to incorporate the function of foreseeing and managing acute crisis for frail individuals with multimorbidity; this will require evaluation. There is also scope for further research into ambulance teams attending individuals for potential admission, liaising with GPs or carrying out elements of assessment prior to arrival at hospital. Links between ambulance and triage or assessment units, and teams such as the AGPS in Porthaven easing pressure on busy EDs, are models that were not seen initially in any of our four sites, but are being developed in one of them now. We saw little evidence of communication between the ED and general practice for those individuals attending without seeing their GP first. One site had intermittent access to GP records, but a range of other communication and shared management options could be deployed with GPs, both in hours and ‘out of hours’ services. The range of community-based teams aiming to provide diagnostics and care in order to avoid admissions merits considerable research.
Lastly, given the tentative nature of many of our theories [and the multifaceted complexity of the system(s)], implementation research in this area should focus on collaboratively developing models of care that incorporate principles of practice at individual, team and system levels. These would incorporate nuanced understandings of the multiple contexts in which care is delivered and empower practitioners to use evidence to inform their practice while judiciously modifying such models so that they are appropriate, acceptable and effective in local contexts.
Conclusions
This project has revealed the contrasting strategies developed by four acute hospitals to provide timely urgent care, including their diverse approaches and many innovations to avoid unnecessary hospital admissions and make safer discharge decisions. There are multiple opportunities to avoid unnecessary admission to hospital, starting from the time the concerned patient or carer first seeks help. If admission is not necessary, the outcome rests upon the ability of the hospital to identify a safe and appropriate alternative arrangement in a short space of time. Patients’ and carers’ immediate needs, and their understanding of the urgent care system, influence how it is accessed. In consequence, alternatives to hospital attendance need to be clear and accessible. Clear signposting and confidence in the pre-hospital phase of care, more routine involvement of GPs, provision of better community-based and outpatient alternatives, and improved communication with secondary care ED and specialties all have roles to play.
The current dichotomy of admission or discharge driven by the 4-hour target is conducive to rapid decision-making and maintenance of flow, but it does not necessarily support optimal decision-making or patient-centred care. Once patients arrive at secondary care, however, hospital admission becomes much more likely. With insufficient time, unnecessary admissions may occur by default. Basic patient care may also suffer.
This research provides further evidence that services which allow space and time to gather information, observe, investigate and plan are likely to produce more patient-centred care. We have shown that authoritative, experienced, skilful practitioners may and do play a key role in safely reducing admissions through early clinical senior input as well as through supporting juniors, taking an overview of all patients and contributing to service design. Safe discharge from hospital acute care settings may also be supported by community teams and beds, access to GP notes, ‘hot’ clinics, ACUs and collaboration from medical specialists.
Some further gains can probably be made in the hospital setting by optimising the flexible use of space, time and experienced practitioners from different professions. However, we still end up concluding that new community-based models of care are also required to contribute to safe reduction of avoidable admissions. In particular, if more complex patents with multiple needs were assessed by community teams with medical input, coming to hospital acute care settings if they required investigations, then numbers of unscheduled attendances could be reduced, dissipating the current extreme pressures on the hospital system and delivering more person-centred care.
In conclusion, the 3A study has generated a rich narrative description of the acute admission decision-making process and the reasoning behind it, based on observation and first-hand accounts of a substantial sample of patients and practitioners. The VSM method was successfully applied to examine value, waste and system bottlenecks at four sites with contrasting models of care. The findings, interpreted through a critical realist lens, provide considerable insight into why patients find themselves being admitted to hospital. These insights enable us to point to the hospital-based models of care that are best suited to safely reducing unnecessary hospital admissions. They also point to the need for a renewed focus on developing and evaluating the community-based response to the urgent needs of individuals with multimorbidity.
Acknowledgements
We would like to thank all the participants involved in this research for their time and contributions. In particular, we are grateful to the four NHS hospital trusts for agreeing to participate in this study and allowing researchers into their EDs and AMUs to observe infrastructure, staff at work and patients receiving treatment. We are very grateful to the medical directors of these four organisations for agreeing to allow busy frontline staff to be interviewed at length in the workplace, and to all the managers and staff of the EDs and associated medical units for accepting the presence of researchers in their departments and observing their clinical practice.
Most of all, we are grateful to the many people who were patients receiving emergency treatment, and to their relatives and carers, for being so willing to talk to the researchers at such a sensitive time and in a vulnerable place. We also thank the many members of the PPI group for their time and invaluable contribution to the study.
We are also indebted to the clinicians at the four hospitals for their willing collaboration, without which the project would have been impossible. We are particularly grateful to Dr Jason Smith (consultant in emergency medicine), Dr Annabel Carter (consultant in acute medicine), Dr Bill Lusty (consultant in acute medicine), Dr Mark Daly (associate medical director), Dr Victoria Stacey (consultant in emergency medicine) and Dr Dominic Williamson (consultant in emergency medicine).
We are grateful to the members of the project steering group, who gave generously of their time and were a constant source of invaluable advice and suggestions throughout the project. In particular we express our gratitude to the chairman, Professor Suzanne Mason (University of Sheffield, School of Health and Related Research), and Professor Catherine Pope (University of Southampton).
We thank Mike Williams, who contributed to the VSM study design but then had to withdraw from the study team.
Steering group members
Jonathan Pinkney (principal investigator, Centre for Clinical Trials and Population Studies, Plymouth University).
Richard Byng (principal investigator, Centre for Clinical Trials and Population Studies, Plymouth University).
Susanna Rance (Senior Research Fellow in urgent care research, Centre for Clinical Trials and Population Studies, Plymouth University).
Suzanne Mason (Professor of Emergency Medicine, University of Sheffield).
Catherine Pope (Professor of Medical Sociology, University of Southampton).
Andy Collen (South East Coast Ambulance Service NHS Foundation Trust).
Derek Bell (Director of NIHR Collaboration for Leadership in Applied Health Research and Care, Imperial College London).
John de Pury (NHS Confederation Research Networks, Universities UK, London).
Margaret Turley (lay representative).
Other contributors
We are also grateful to the following contributors:
Siobhan Sharkey (Lecturer in Methodology, Plymouth University Peninsula Schools of Medicine and Dentistry). Design and methods for ethnographic study.
Anne Murphy (Independent Learning Advisor, Innovation in Learning). Learning sets methodology, facilitation and reporting.
Andrew Gibson (Research Fellow in Patient and Public Involvement, University of Exeter). PPI groups. Design and methods. Data collection and interpretation.
Contributions of authors
Jonathan Pinkney (Professor of Medicine, Plymouth University Peninsula Schools of Medicine and Dentistry). Co-chief investigator. Design of project. Liaison with NHS sites, managers and clinicians. Project management, clinical panel set-up and facilitation, quantitative analyses, data interpretation and main report author.
Susanna Rance (Senior Research Fellow, Plymouth University Peninsula Schools of Medicine and Dentistry; current post senior research fellow, Institute for Health and Human Development, University of East London). Ethnographic methodology, data collection, analysis, PPI, learning sets, literature review process, reading groups and main report author.
Jonathan Benger (Professor of Emergency Medicine, University of the West of England). Design of project, site lead and project management, identification of suitable hospitals for inclusion in the study, strategic advice, data interpretation and contributor to main report.
Heather Brant (Research Fellow in emergency care, University of the West of England). Ethnographic and VSM fieldwork, data collection, site description data, data interpretation, data analysis of ethnographic data and contributor to main report.
Sian Joel-Edgar (Associate Research fellow in health service research, University of Exeter Business School). VSM study, design, data collection, analysis, interpretation and main report author.
Dawn Swancutt (Research fellow, Plymouth University Peninsula Schools of Medicine and Dentistry). Ethnographic study, data collection, analysis, interpretation of ethnographic and VSM data and main report author.
Debra Westlake (Research Fellow, Plymouth University Peninsula Schools of Medicine and Dentistry). Ethnographic study, data collection, analysis and interpretation, set-up and analysis of clinical panel data and contributor to main report.
Mark Pearson (Senior Research Fellow in Evidence Synthesis, University of Exeter Medical School). Synthesis of findings from component studies and main report author.
Daniel Thomas (GP Academic Clinical Fellow, Plymouth University Peninsula Schools of Medicine and Dentistry). Analysis of VSM data, data collection, interpretation and main report author.
Ingrid Holme (Lecturer in Sociology, University of Ulster). Ethnographic data collection and analysis.
Ruth Endacott [Professor of Clinical Nursing (critical care), Plymouth University]. Design and methods, data interpretation and main report author.
Rob Anderson (Associate Professor of Health Economics and Evaluation, University of Exeter). Project management. Economic analysis – design, data collection, analysis, interpretation – and main report author.
Mike Allen (Senior Modeller, University of Exeter). HES data extraction, analysis, interpretation and advice, and main report author.
Sarah Purdy (Professor in Primary Care, University of Bristol). Research design, data interpretation, expert advice on literature and main report author.
John Campbell (Professor of Primary Care, University of Exeter). Idea for project, author, project management, data interpretation and main report author.
Rod Sheaff (Professor of Health Services Research, Plymouth University). Idea for project. Project management, advice on health service policy, data interpretation and main report author.
Richard Byng (Professor of Primary Care, Plymouth University Peninsula Schools of Medicine and Dentistry). Co-chief investigator. Conceived project, design and methodology, project management, data interpretation and main report author.
Data sharing statement
Requests for data sharing should be submitted to the corresponding author. The authors will consider sharing data after the primary publications of this research.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
References
- Blunt I, Bardsley M, Dixon J. Trends in Emergency Admissions in England 2004–2009: Is Greater Efficiency Breeding Inefficiency?. London: The Nuffield Trust; 2010.
- Department of Health . Emergency Admissions to Hospital: Managing the Demand 2013.
- O’Cathain A, Knowles E, Maheswaran R, Pearson T, Turner J, Hirst E, et al. A system-wide approach to explaining variation in potentially avoidable emergency admissions: national ecological study. BMJ Qual Saf 2014;23:47-55. http://dx.doi.org/10.1136/bmjqs-2013-002003.
- McDonagh MS, Smith DH, Goddard M. Measuring appropriate use of acute beds: a systematic review of methods and results. Health Policy 2000;53:157-84. http://dx.doi.org/10.1016/S0168-8510(00)00092-0.
- O’Cathain A, Knowles E, Maheswaran R, Turner J, Hirst E, Goodacre S, et al. Hospital characteristics affecting potentially avoidable emergency admissions: national ecological study. Health Serv Manage Res 2013;26:110-18. http://dx.doi.org/10.1177/0951484814525357.
- A&E Clinical Quality Indicators Implementation Guidance. London: DH; 2010.
- Weber EJ, Mason S, Carter A, Hew RL. Emptying the corridors of shame: organizational lessons from England’s 4-hour emergency throughput target. Ann Emerg Med 2011;57:79-88. http://dx.doi.org/10.1016/j.annemergmed.2010.08.013.
- O’Cathain A, Knowles E, Turner J, Maheswaran R, Goodacre S, Hirst E, et al. Explaining variation in emergency admissions: a mixed-methods study of emergency and urgent care systems. Health Serv Deliv Res 2014;2:1-13. http://dx.doi.org/10.3310/hsdr02480.
- Cooke MW. Intelligent use of indicators and targets to improve emergency care. Emerg Med J 2014;31:5-6. http://dx.doi.org/10.1136/emermed-2013-202391.
- Acute and Emergency Care: Prescribing the Remedy. London: The Royal College of Emergency Medicine; 2014.
- Higginson I. Emergency department crowding. Emerg Med J 2012;29:437-43. http://dx.doi.org/10.1136/emermed-2011-200532.
- Boreham NC, Shea CE, Mackway-Jones K. Clinical risk and collective competence in the hospital emergency department in the UK. Soc Sci Med 2000;51:83-91. http://dx.doi.org/10.1016/S0277-9536(99)00441-4.
- Moore L, Deehan A, Seed P, Jones R. Characteristics of frequent attenders in an emergency department: analysis of 1-year attendance data. Emerg Med J 2009;26:263-7. http://dx.doi.org/10.1136/emj.2008.059428.
- Hunt KA, Weber EJ, Showstack JA, Colby DC, Callaham ML. Characteristics of frequent users of emergency departments. Ann Emerg Med 2006;48:1-8. http://dx.doi.org/10.1016/j.annemergmed.2005.12.030.
- Richardson DB. Increase in patient mortality at 10 days associated with emergency department overcrowding. Med J Aust 2006;184:213-16.
- Higginson I, Whyatt J, Silvester K. Demand and capacity planning in the emergency department: how to do it. Emerg Med J 2011;28:128-35. http://dx.doi.org/10.1136/emj.2009.087411.
- Crowding in Emergency Departments. London: The Royal College of Emergency Medicine; 2012.
- Nugus P, Forero R. Understanding interdepartmental and organizational work in the emergency department: an ethnographic approach. Int Emerg Nurs 2011;19:69-74. http://dx.doi.org/10.1016/j.ienj.2010.03.001.
- Flowerdew L, Brown R, Russ S, Vincent C, Woloshynowych M. Teams under pressure in the emergency department: an interview study. Emerg Med J 2012;29. http://dx.doi.org/10.1136/emermed-2011-200084.
- Patterson PD, Pfeiffer AJ, Weaver MD, Krackhardt D, Arnold RM, Yealy DM, et al. Network analysis of team communication in a busy emergency department. BMC Health Serv Res 2013;13:1-12. http://dx.doi.org/10.1186/1472-6963-13-109.
- Kilner E, Sheppard LA. The role of teamwork and communication in the emergency department: a systematic review. Int Emerg Nurs 2010;18:127-37. http://dx.doi.org/10.1016/j.ienj.2009.05.006.
- Jeffcott SA, Ibrahim JE, Cameron PA. Resilience in healthcare and clinical handover. Qual Saf Health Care 2009;18:256-60. http://dx.doi.org/10.1136/qshc.2008.030163.
- Jeffcott SA, Evans SM, Cameron PA, Chin GS, Ibrahim JE. Improving measurement in clinical handover. Qual Saf Health Care 2009;18:272-7. http://dx.doi.org/10.1136/qshc.2007.024570.
- Sujan M, Spurgeon P, Inada-Kim M, Rudd M, Fitton L, Horniblow S, et al. Clinical handover within the emergency care pathway and the potential risks of clinical handover failure (ECHO): primary research. Health Serv Deliv Res 2014;2.
- Aylin P, Yunus A, Bottle A, Majeed A, Bell D. Weekend mortality for emergency admissions: a large, multicentre study. Qual Saf Health Care 2010;19:213-17. http://dx.doi.org/10.1136/qshc.2008.028639.
- Kane RL, Keckhafer G, Flood S, Bershadsky B, Siadaty MS. The effect of Evercare on hospital use. J Am Geriatr Soc 2003;51:1427-34. http://dx.doi.org/10.1046/j.1532-5415.2003.51461.x.
- Meislin HW, Coats SA, Cyr J, Valenzuela T. Fast Track: urgent care within a teaching hospital emergency department – can it work?. Ann Emerg Med 1988;17:453-6. http://dx.doi.org/10.1016/S0196-0644(88)80235-X.
- Wanklyn P, Hosker H, Pearson S, Belfield P. Slowing the rate of acute medical admissions. J Roy Coll Physicians Lond 1997;31:173-6.
- Russ S, Jones I, Aronsky D, Dittus RS, Slovis CM. Placing physician orders at triage: the effect on length of stay. Ann Emerg Med 2010;56:27-33. http://dx.doi.org/10.1016/j.annemergmed.2010.02.006.
- Soremekun OA, Capp R, Biddinger PD, White BA, Chang Y, Carignan SB, et al. Impact of physician screening in the emergency department on patient flow. J Emerg Med 2012;43:509-15. http://dx.doi.org/10.1016/j.jemermed.2012.01.025.
- Sen A, Hill D, Menon D, Rae F, Hughes H, Roop R. The impact of consultant delivered service in emergency medicine: the Wrexham Model. Emerg Med J 2012;29:366-71. http://dx.doi.org/10.1136/emj.2010.107797.
- Subash F, Dunn F, McNicholl B, Marlow J. Team triage improves emergency department efficiency. Emerg Med J 2004;21:542-4. http://dx.doi.org/10.1136/emj.2002.003665.
- White AL, Armstrong PA, Thakore S. Impact of senior clinical review on patient disposition from the emergency department. Emerg Med J 2010;27:262-5. http://dx.doi.org/10.1136/emj.2009.077842.
- CEM Standard for Senior Review Prior to Discharge (‘Consultant Sign-Off’). London: The Royal College of Emergency Medicine; 2010.
- Emergency Medicine Consultants Workforce Recommendations. London: College of Emergency Medicine; 2010.
- Dale J, Lang H, Roberts JA, Green J, Glucksman E. Cost-effectiveness of treating primary care patients in accident and emergency: a comparison between general practitioners, senior house officers, and registrars. BMJ 1996;312:1340-4. http://dx.doi.org/10.1136/bmj.312.7042.1340.
- Carson D, Clay H, Stern R. Primary Care and Emergency Departments: Report from the Primary Care Foundation 2010.
- Rogers P, Ward L, Salisbury C, Purdy S. Does a general practitioner support unit reduce admissions following medical referrals from general practitioners?. Qual Prim Care 2011;19:23-3.
- Cooke M, Oliver D, Burns A. Quality Care for Older People with Urgent and Emergency Care Needs: The ‘Silver Book’. London: British Geriatrics Society; 2012.
- Wright PN, Tan G, Iliffe S, Lee D. The impact of a new emergency admission avoidance system for older people on length of stay and same-day discharges. Age Ageing 2014;43:116-21. http://dx.doi.org/10.1093/ageing/aft086.
- Tian Y, Dixon A, Gao H. Emergency Hospital Admissions for Ambulatory Care-Sensitive Conditions: Identifying the Potential for Reductions. London: The King’s Fund; 2012.
- Ham C, Imison C, Jennings M. Avoiding Hospital Admissions: Lessons from Evidence and Experience. London: The King’s Fund; 2010.
- Purdy S, Griffin T, Salisbury C, Sharp D. Prioritizing ambulatory care sensitive hospital admissions in England for research and intervention: a Delphi exercise. Prim Health Care Res Dev 2010;11:41-50. http://dx.doi.org/10.1017/S1463423609990211.
- Carter A. The Ambulatory Care Unit at Derriford Hospital. Clin Med 2014;14:250-4. http://dx.doi.org/10.7861/clinmedicine.14-3-250.
- Lattimer V, Burgess A, Knapp F, Dalton S, Brailsford S, Junior E, et al. The Impact of Changing Workforce Patterns in Emergency and Urgent Out-of-Hours Care on Patient Experience, Staff Practice and Health System Performance 2010. www.nets.nihr.ac.uk/projects/hsdr/08151997 (accessed 23 December 2015).
- Müller-Engelmann M, Keller H, Donner-Banzhoff N, Krones T. Shared decision making in medicine: the influence of situational treatment factors. Patient Educ Couns 2011;82:240-6. http://dx.doi.org/10.1016/j.pec.2010.04.028.
- O’Hara R, O’Keeffe C, Mason S, Coster JE, Hutchinson A. Quality and safety of care provided by emergency care practitioners. Emerg Med J 2012;29:327-32. http://dx.doi.org/10.1136/emj.2010.104190.
- Adams RJ, Smith BJ, Ruffin RE. Patient preferences for autonomy in decision making in asthma management. BMJ 2001;56:126-32. http://dx.doi.org/10.1136/thorax.56.2.126.
- Campbell J. Inappropriate admissions: thoughts of patients and referring doctors. J R Soc Med 2001;94:628-31.
- Pearson SD, Goldman DL, Orav J, Guadagnoli E, Garcia TB, Johnson PA, et al. Triage decisions for emergency department patients with chest pain. J Gen Intern Med 1995;10:557-64. http://dx.doi.org/10.1007/BF02640365.
- Hensher M, Fulop N, Coast J, Jefferys E. The hospital of the future: better out than in? Alternatives to acute hospital care. BMJ 1999;319:1127-30. http://dx.doi.org/10.1136/bmj.319.7217.1127.
- Booker MJ, Simmonds RL, Purdy S. Patients who call emergency ambulances for primary care problems: a qualitative study of the decision-making process. Emerg Med J 2014;31:448-52. http://dx.doi.org/10.1136/emermed-2012-202124.
- Nairn S, Whotton E, Marshal C, Roberts M, Swann G. The patient experience in emergency departments: a review of the literature. Accid Emerg Nurs 2004;12:159-65. http://dx.doi.org/10.1016/j.aaen.2004.04.001.
- Patient-Centred Leadership. London: The King’s Fund; 2013.
- Mid Staffordshire NHS Foundation Trust . Report of the Mid Staffordshire NHS Foundation Trust Public Inquiry Executive Summary; February 2013 n.d. http://webarchive.nationalarchives.gov.uk/20150407084003/http://www.midstaffspublicinquiry.com/sites/default/files/report/executive%20summary.pdf (accessed 29 June 2015).
- Future Hospital: Caring for Medical Patients. London: Royal College of Physicians; 2013.
- Pawson R, Tilley N. Realistic Evaluation. London: Sage Publications; 1997.
- Stake R, Denzin NK, Lincoln YS. Handbook of Qualitative Research. Thousand Oaks, CA: SAGE Publications; 1994.
- Savage J. Ethnography and health care. BMJ 2000;321:1400-2. http://dx.doi.org/10.1136/bmj.321.7273.1400.
- Leslie M, Paradis E, Gropper MA, Reeves S, Kitto S. Applying ethnography to the study of context in healthcare quality and safety. BMJ 2015;23:99-105. http://dx.doi.org/10.1136/bmjqs-2013-002335.
- McEvoy P, Richards D. A critical realist rationale for using a combination of quantitative and qualitative methods. J Res Nurs 2006;11:66-78. http://dx.doi.org/10.1177/1744987106060192.
- Ohno T. The Toyota Production System: Beyond Large-Scale Production. Portland: Productivity Press; 1988.
- Ritchie J, Lewis J. Qualitative Research Practice: A Guide for Social Science Students and Researchers. London: Sage Publications; 2003.
- Bhaskar R. A Realist Theory of Science. London: Verso; 2008.
- Pawson R. The Science of Evaluation: A Realist Manifesto. London: Sage Publications; 2013.
- Sayer A. Realism and Social Science. London: Sage Publications; 2000.
- Maxwell JA. A Realist Approach for Qualitative Research. London: Sage Publications; 2012.
- Archer MS. Making Our Way through the World: Human Reflexivity and Social Mobility. Cambridge: Cambridge University Press; 2007.
- Walley P. Designing the accident and emergency system: lessons from manufacturing. BMJ 2003;20:126-30. http://dx.doi.org/10.1136/emj.20.2.126.
- Ham C. Emergency department pressures need to be tackled through integrated urgent and emergency care. BMJ 2015;350. http://dx.doi.org/10.1136/bmj.h322.
- Womack JP, Jones DT. Lean Thinking: Banish Waste and Create Wealth in Your Corporation. London: Simon & Schuster; 2003.
- Hines P, Found P, Griffiths G, Harrison R. Staying Lean: Thriving Not Just Surviving. New York, NY: Productivity Press; 2011.
- Dart R. Can Lean thinking transform American healthcare?. Ann Emerg Med 2011;57:279-81. http://dx.doi.org/10.1016/j.annemergmed.2010.11.027.
- Holden RJ. Lean Thinking in emergency departments: a critical review. Ann Emerg Med 2011;57:265-78. http://dx.doi.org/10.1016/j.annemergmed.2010.08.001.
- Radnor ZJ, Holweg M, Waring J. Lean in healthcare: the unfilled promise?. Soc Sci Med 2012;74:364-71. http://dx.doi.org/10.1016/j.socscimed.2011.02.011.
- Womack JP, Jones DT. Lean consumption. Harvard Bus Rev 2005;83:58-6. http://dx.doi.org/10.1049/me:20050411.
- Bicheno J, Holweg M. The Lean Toolbox 4th Ed: The Essential Guide to Lean Transformation. Buckingham: Picsie Books; 2009.
- Radnor Z. Review of Business Process Improvement Methodologies in Public Services. London: Advanced Institute of Management Research; 2010.
- Rich N, Bateman N, Esain A, Massey L, Samuel D. Lean Evolution: Lessons from the Workplace. Cambridge: Cambridge University Press; 2006.
- George ML. Lean Six Sigma for Service. New York, NY: McGraw Hill; 2003.
- Kollberg B, Dahlgaard JJ, Brehmer P-O. Measuring Lean initiatives in health care services: issues and findings. Int J Prod Perform Manag 2007;56:7-24. http://dx.doi.org/10.1108/17410400710717064.
- Young T, Brailsford S, Connell C, Davies R, Harper P, Klein JH. Using industrial processes to improve patient care. BMJ 2004;328:162-4. http://dx.doi.org/10.1136/bmj.328.7432.162.
- Young TP, McCLean SI. A critical look at Lean Thinking in healthcare. Qual Saf Health Care 2013;17:382-6. http://dx.doi.org/10.1136/qshc.2006.020131.
- Bicheno J. The Lean Toolbox for Service Systems. Buckingham: Picsie Books; 2008.
- Fillingham D. Can Lean save lives?. Leadersh Health Serv 2006;20:231-41.
- Robinson S, Radnor ZJ, Burgess N, Worthington C. SimLean: utilising simulation in the implementation of Lean in healthcare. Eur J Oper Res 2012;219:188-97. http://dx.doi.org/10.1016/j.ejor.2011.12.029.
- Hines P, Holweg M, Rich N. Learning to evolve: a review of contemporary Lean thinking. Int J Oper Prod Man 2004;24:994-1011. http://dx.doi.org/10.1108/01443570410558049.
- Rother M, Shook J. Learning to See: Value Stream Mapping to Add Value and Eliminate Muda. Brookline, MA: Lean Enterprise Institute; 2003.
- Jimmerson C. Value Stream Mapping for Healthcare Made Easy. New York, NY: CRC Press; 2010.
- Allder S, Silvester K, Walley P. Managing capacity and demand across the patient journey. Clin Med 2010;10:13-5. http://dx.doi.org/10.7861/clinmedicine.10-1-13.
- Walley P. Managing variation in demand: lessons from the UK National Health Service. J Healthc Manag 2006;51:309-21.
- Womack JP, Jones DT. Lean Solutions. New York, NY: Simon and Schuster; 2009.
- Brandao de Souza L. Trends and approaches in Lean healthcare. Leadersh Health Serv 2009;22:121-39. http://dx.doi.org/10.1108/17511870910953788.
- Jacobs SM, Pelfrey S. Applying just-in-time philosophy to healthcare. J Nurs Adm 1995;25:2-9. http://dx.doi.org/10.1097/00005110-199501000-00009.
- Heinbuch SE. A case of successful technology transfer to health care: total quality materials management and just-in-time. J Manag Med 1995;9:48-56. http://dx.doi.org/10.1108/02689239510086524.
- Whitson D. Applying just-in-time systems in healthcare. IIE Solutions 1997;29:32-7.
- Ideal Design and Emergency Access (IDEA) Programme. London: NHS Modernisation Agency; 2002.
- The Big Referral Wizard: A Guide to Systems Management in Healthcare. London: NHS Modernisation Agency; 2002.
- Bushell S, Mobley J, Shelest B. Site visit: discovering Lean thinking at Progressive Healthcare. J Qual Participation 2002;25:20-5.
- Feinstein KW, Grunden N, Harrison EI. A region addresses patient safety. Am J Infect Control 2002;30:248-51. http://dx.doi.org/10.1067/mic.2002.122645.
- Joint Commission on Accreditation of Healthcare Organisations . Doing More With Less: Lean Thinking and Patient Safety in Health Care 2006. www.jointcommissioninternational.org/assets/1/14/sisp01_sample_pages2.pdf (accessed 29 June 2015).
- Zidel T. A Lean Guide to Transforming Healthcare. Milwaukee, WI: American Society for Quality; 2006.
- Smith AC, Barry R, Brubaker CE. Going Lean: Busting Barriers to Patient Flow. Chicago, IL: Health Administration Press; 2008.
- Allway M, Corbett S. Shifting to Lean service: stealing a page from manufacturers’ playbooks. J Organ Excel 2002;21:45-54. http://dx.doi.org/10.1002/npr.10019.
- Miller D. Going Lean in Health Care. Cambridge, MA: Institute for Healthcare Improvement; 2005.
- Jones D, Mitchell A. Lean Thinking for the NHS. London: NHS Confederation; 2006.
- Spear SJ. Fixing health care from the inside. Harv Bus Rev 2005;83:78-91.
- Condel JL, Sharbaugh DT, Raab SS. Error-free pathology: applying Lean production methods to anatomic pathology. Clin Lab Med 2004;24:865-99. http://dx.doi.org/10.1016/j.cll.2004.07.001.
- Massey L, Williams S. CANDO: implementing change in an NHS trust. Int J Public Sector Manage 2005;18:330-49. http://dx.doi.org/10.1108/09513550510599256.
- King DL, Ben-Tovim DI, Bassham J. Redesigning emergency department patient flows: application of Lean Thinking to health care. Emerg Med Australas 2006;18:391-7. http://dx.doi.org/10.1111/j.1742-6723.2006.00872.x.
- Fillingham D. Lean Healthcare: Improving the Patient’s Experience. Chichester: Kingsham Press; 2008.
- Brandao de Souza L, Pidd M. Exploring the barriers to Lean health care implementation. Public Money Manage 2011;31:59-66. http://dx.doi.org/10.1080/09540962.2011.545548.
- Dahlgaard J, Pettersen J, Dahlgaard-Park S. Quality and Lean health care: a system for assessing and improving the health of healthcare organisations. Total Qual Manag Bus 2011;22:673-89. http://dx.doi.org/10.1080/14783363.2011.580651.
- Ng D, Vail G, Thomas S, Schmidt N. Applying the Lean principles of the Toyota Production System to reduce wait times in the emergency department. CJEM 2010;12:50-7.
- Ford AL, Williams JA, Spencer M, McCammon C, Khoury N, Sampson T, et al. Reducing door-to-needle times using Toyota’s Lean manufacturing principles and value stream analysis. Stroke 2012;43:3395-8. http://dx.doi.org/10.1161/STROKEAHA.112.670687.
Appendix 1 The Avoidable Acute Admissions literature review reading group
A novel form of reading group was developed to aid the literature review process for the project. This method allowed 68 papers to be reviewed in eight meetings with participation from a total of 11 researchers (Table 13). The reading group was found to be more efficient and engaging than a traditional form of review, and it enabled ongoing dissemination of texts and discussion with the wider team.
| Topic | Date | Number of papers discussed | Number of researchers participating |
|---|---|---|---|
| Decision-making | 1 October 2013 | 6 | 4 |
| Patient experience | 15 October 2013 | 6 | 3 |
| Senior input | 1 November 2013 | 10 | 5 |
| Teaching, training, learning | 26 November 2013 | 7 | 4 |
| VSM | 13 March 2014 | 10 | 4 |
| User groups | 27 June 2014 | 11 | 5 |
| Teamwork | 13 August 2014 | 9 | 6 |
| Safety and efficiency | 1 October 2014 | 9 | 4 |
The initial literature review was carried out in a traditional way, with individual researchers reviewing papers and presenting the findings at a meeting that took the style of a journal club. It was found that the amount of work and time this entailed would not be sustainable for the project, and the rest of the research team was not informed of the wide range of literature being reviewed.
In the new form of reading group, the research team identified topics for which a literature review was required. A lead team member was nominated for each topic, and this person identified a number of papers in this area that were especially relevant to the project. They contacted experts in that topic area to ensure that key papers were included. The list of readings was circulated to the team and each member chose one or two papers to review in detail. The team then met in a reading group to discuss the papers. Participants also referred to the relevance of each paper in the light of their previous experience or project fieldwork, to add further insight and context.
This approach allowed for a broad literature review to be undertaken in time that could be made available, with the workload shared. The findings from each reading group meeting led on to discussion about further topics, and helped to identify further questions or areas to be reviewed. In some cases, authors of the papers were contacted for further information about their research which was relevant to the 3A study. The meetings were audio-recorded, transcripts were created and edited versions including the details of texts discussed were made available to all, for ease of reference later in the project.
Appendix 2 Clinical panel complete appendix
Executive summary
Panel composition
Two clinical panels were assembled, one in the two northern sites and one in the southern sites. The clinical panels comprised four experienced clinicians working in emergency medicine and two patient representatives recruited through the local Collaboration for Leadership in Applied Health Research and Care. The northern panel comprised three ED consultants, a senior trainee in emergency medicine who had completed her training, a nurse practitioner in emergency care and the two patient representatives. The southern panel comprised one ED consultant, one AMU consultant, a senior trainee in acute medicine, a senior nurse/ward manager in the AMU and a GP representing an AGPS and ambulatory care pathway.
Stage 1: case review and selection
Stage 1 of the panel process was undertaken as set out in the terms of reference document. Briefly, batches of ethnographic and VSM case studies were specially prepared for the clinical panels by the research team. Batches of cases were emailed in advance to panel members, who then scored to what extent the admit/discharge decision appeared appropriate, and further described the principal grounds for their opinion. The research team selected from these cases those for which there appeared some difference of opinion between scorers about the likely appropriateness of the decision, or cases considered by the scorers as interesting and representative, to discuss in stage 2. The cases reviewed by the northern panel at both stage 1 and stage 2 were from the southern sites, and vice versa for the southern panel.
Stage 2: consensus discussion
In stage 2, both panels were convened and facilitated in the same way by one of the principal investigators (JP). The northern panel was convened at Underbridge hospital on 6 November 2014, and the southern panel at Porthaven hospital on 9 December 2014. Ten selected cases including ethnographic and VSM studies were discussed in depth by each clinical panel. The discussions were tape-recorded and transcribed.
Summary
-
The clinical panel exercise confirmed that most of the cases reviewed were considered typical of patients referred to ED and associated emergency medical units. Most of the clinical decisions for the patients reviewed were deemed appropriate and understandable by these clinicians and patients.
-
In stage 1, most reviewers were consistent in their independent responses, but would often express caveats relating to circumstances and availability of alternative management options.
-
In stage 2, the principal area of potential disagreement and debate centred on the extent to which the admissions could have been avoided, and these discussions highlighted the extent to which it is possible to identify the optimal solutions to medical and social complexity, especially when faced with a 4-hour target.
-
A considerable degree of mutual understanding of the patient and professional perspectives, and systems factors constraining decision-making, was apparent in the stage 2 panel meetings, generating consensus.
-
There were no instances where there was strong disagreement about the admit/discharge decisions; rather the different voices on the panels graphically illustrated the challenges of avoiding hospital admission, even when it was not always the most appropriate course of action and admission might have been avoided.
-
The discussions highlighted the extent to which admit decisions are constrained by organisational and structural differences in emergency care pathways. The ED unit not infrequently appeared to be the wrong place for the patient’s health-care needs to be assessed and optimal decisions made, whereas alternative pathways, both in the community and within secondary care (including AMU, ACU or CDU), can be more appropriate.
-
The professional composition of the two review panels, as well as the site-specific models of care adopted by their hospitals, may have had an effect on the suggestions made by the panels for alternative pathways to admission for the cases reviewed. The panel reviewers from the north site were exclusively from emergency medicine, whereas the southern site reviewers included medical specialists and a GP. Southern panel reviewers particularly emphasised the potential merits of the ambulatory care pathway and AGPS as an alternative to medical admissions in the cases reviewed; those services are available at one of the hospitals.
How the data have been used
The results of the clinical panels have been used to interpret several other streams of data in the project, including practitioner and patient ethnography and the VSM study. The data were also used as source material for the realist synthesis.
| Process | North | South |
|---|---|---|
| Recruitment of participants | Four clinicians recruited from Site C | Five clinicians recruited from site A |
| Two local PPI members via PenCLAHRC, Exeter University | Two local PPI members via PenCLAHRC, Exeter University | |
| Stage 1: the following were e-mailed to clinical participants | Covering letter describing process and requirements | Covering letter describing process and requirements |
| Blank score sheet | Blank score sheet | |
| Protocol for clinical panel | Protocol for clinical panel | |
| VSM cases sites A and B: 60 cases; four batches of 15; two batches (2 × 15) for each participant | VSM cases sites C and D: 48 cases; four batches of 12; two batches (2 × 12) for each participant | |
| Ethnography cases sites A and B: 11 cases; four batches of two or three; two batches (2 × 3 or 2) for each participant | Ethnography cases sites C and D: 12 cases; four batches of three; two batches (2 × 3) for each participant | |
| Stage 1: the following were sent to PPI team, Exeter, for selection for stage 2 | 11 ethnography cases (all); 4 VSM cases (purposively sampled for variation in length of time in department and/or cases that demonstrated particular features of the patient journey) | 12 ethnography cases (all); 4 VSM cases (purposively sampled for variation in length of time in department and/or cases that demonstrated particular features of the patient journey) |
| Criteria for batching (stage 1) | Ethnography cases purposively sampled for a spread of age/gender/site/morbidity/outcome; VSM cases divided to give an even spread representing each site/presenting condition/complexity of care process/outcome | Ethnography cases purposively sampled for a spread of age/gender/site/morbidity/outcome; VSM cases divided to give an even spread representing each site/presenting condition/complexity of care process/outcome |
| Criteria for selection of cases for stage 2 face-to-face meeting |
|
|
| Stage 2: meeting in north and south sites chaired and recorded by JP | 10 cases discussed: seven ethnography, three VSM | 10 cases discussed: seven ethnography, three VSM |
FIGURE 18.
Avoidable Acute Admissions clinical panel admission decision score sheet.
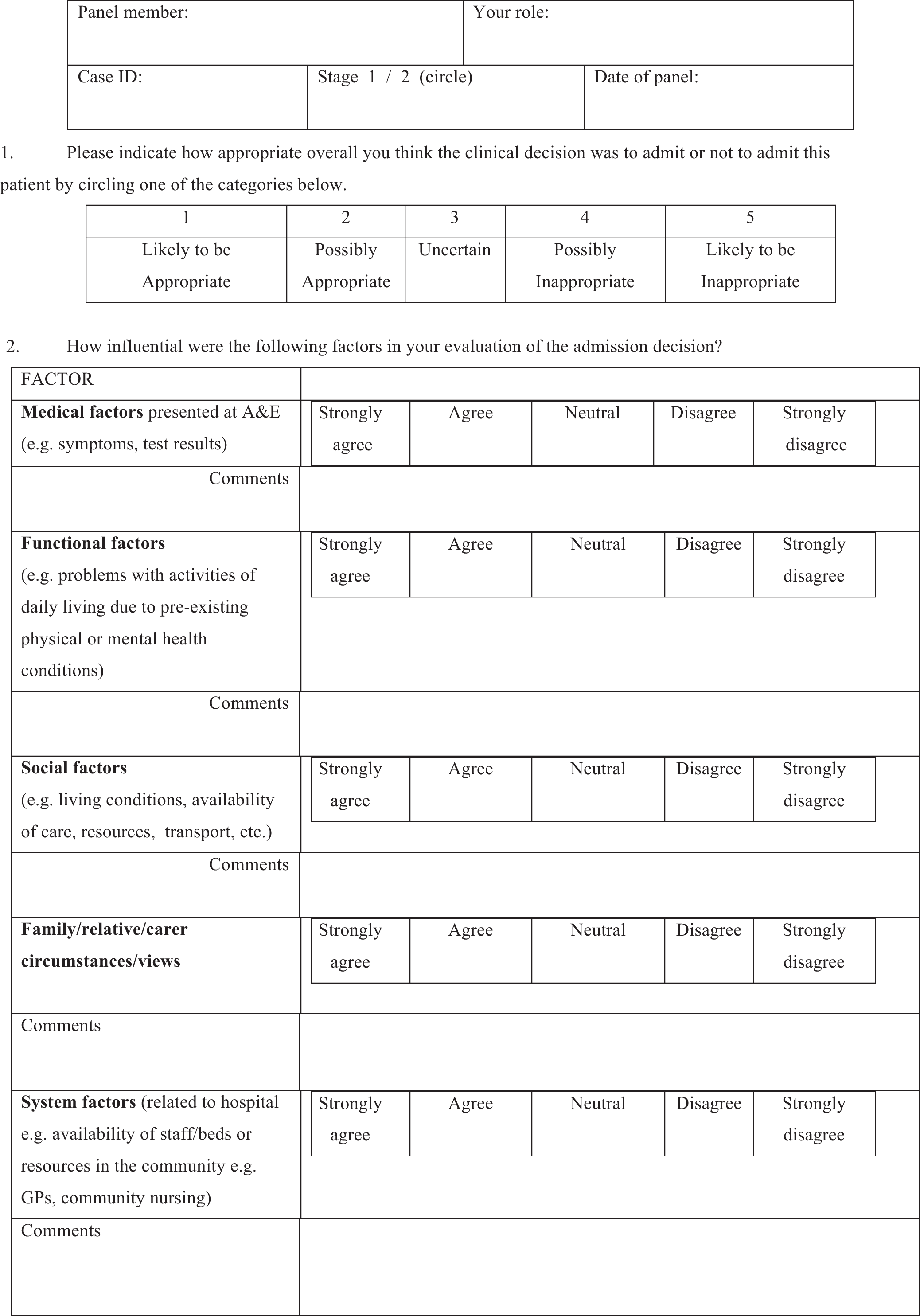

Data sources and coding method for clinical panel case studies
The case identifiers that were used to identify the Clinical Panel case studies presented here were different in order to ensure anonymity of both patients and hospitals. Otherwise, it may have been possible for clinical panel members to guess the identity of member of hospital, members of staff, and potentially identify patients. Thus, these cases were deliberately recoded for anonymity according to study identifiers in which P = patient, FC = family/carer and S = staff member. The dates were also used in the identifier to allow researchers to trace the cases, while preserving anonymity of study site and person. Using a different identification system from the main report also made it less likely that any panel participants could retrospectively identify individual cases from the main report.
Thus, interview S013–110614 (1) denotes interview number 013 with a staff member on the date 110614. The number in brackets refers to the number of individual observations. Interview FC001,FC002–110614 (3) denotes family/carer interviews 1 and 2 on 110614. Field notes 110614 (1) denotes an observation from field notes recorded on 110614. When more than one interview was conducted with a given individual on a specific date, the number of the interview is denoted by an additional suffix. For example, FC002_110614.3 was the third interview with Family and Carer 2 on 11 June 2014.
| Case | Admit/discharge decision | Influence of these factors on the decision | ||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Medical | Functional | Social | Family/relative/carer | System | ||||||||||||||||||||||||||
| Reviewer 1 | Reviewer 2 | Reviewer 1 | Reviewer 2 | Reviewer 1 | Reviewer 2 | Reviewer 1 | Reviewer 2 | Reviewer 1 | Reviewer 2 | Reviewer 1 | Reviewer 2 | |||||||||||||||||||
| 1 | 1 | 5 | 1 | 3 | 3 | 2 | 1 | 2 | 2 | 2 | 3 | 2 | ||||||||||||||||||
| 2 | Omitted but comment indicates disagreement | 3 | 5 | 2 | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | ||||||||||||||||||
| 3 | 4 | 2 | 2 | 2 | 5 | 5 | 5 | 5 | 5 | 5 | 1 | 1 | ||||||||||||||||||
| 4 | 1 | 1 | 2 | 3 | 2 | 4 | 2 | 4 | 2 | 2 | 1 | 2 | ||||||||||||||||||
| 5 | 1 | 1 | 1 | 2 | 3 | 3 | 4 | 3 | 4 | 4 | 3 | 2 | ||||||||||||||||||
| 6 | 1 | 1 | 1 | 1 | 5 | 4 | 5 | 4 | 5 | 4 | 2 | 2 | ||||||||||||||||||
| 7 | 2 | 5 | 3 | 3 | 2 | 1 | 1 | 2 | 1 | 2 | 1 | 1 | ||||||||||||||||||
| 8 | 2 | 1 | 2 | 2 | 3 | 4 | 2 | 4 | 4 | 4 | 3 | 1 | ||||||||||||||||||
| 9 | 1 | 1 | 2 | 2 | 4 | 3 | 5 | 3 | 2 | 2 | 2 | 3 | ||||||||||||||||||
| 10 | 2 | 5 | 2 | 2 | 4 | 3 | 4 | 3 | 2 | 3 | 1 | 2 | ||||||||||||||||||
| 11 (omitted)a | ||||||||||||||||||||||||||||||
| 12 | 5 | 1 | 4 | 3 | 4 | 3 | 4 | 3 | 3 | 3 | 1 | 3 | ||||||||||||||||||
| Number of cases in which reviewers show disagreement with original decision | 3 | 3 | ||||||||||||||||||||||||||||
| Key12345DecisionLikely to be appropriatePossibly appropriateUncertainPossibly inappropriateLikely to be inappropriateFactorsStrongly agreeAgreeNeutralDisagreeStrongly disagree | Key | 1 | 2 | 3 | 4 | 5 | Decision | Likely to be appropriate | Possibly appropriate | Uncertain | Possibly inappropriate | Likely to be inappropriate | Factors | Strongly agree | Agree | Neutral | Disagree | Strongly disagree | ||||||||||||
| Key | 1 | 2 | 3 | 4 | 5 | |||||||||||||||||||||||||
| Decision | Likely to be appropriate | Possibly appropriate | Uncertain | Possibly inappropriate | Likely to be inappropriate | |||||||||||||||||||||||||
| Factors | Strongly agree | Agree | Neutral | Disagree | Strongly disagree | |||||||||||||||||||||||||
In five cases the original decision was considered likely to be appropriate or possibly appropriate by both reviewers. In six cases, at least one reviewer considered the decision possibly inappropriate or likely to be inappropriate. In three cases the reviewers differed by at least 2 points and in two cases they differed by 4 points. In one case the reviewer had omitted to give a Likert score, but had indicated in comments that the decision was possibly inappropriate.
| Case | Admit/discharge decision | Influence of these factors on the decision | ||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Medical | Functional | Social | Family/relative/carer | System | ||||||||||||||||||||||||||
| Reviewer 1 | Reviewer 2 | Reviewer 1 | Reviewer 2 | Reviewer 1 | Reviewer 2 | Reviewer 1 | Reviewer 2 | Reviewer 1 | Reviewer 2 | Reviewer 1 | Reviewer 2 | |||||||||||||||||||
| 1 | 1 | 1 | 1 | 1 | 1 | 4 | 1 | 4 | 1 | 3 | 3 | 1 | ||||||||||||||||||
| 2 | 4 | 5 | 4 | 1 | 4 | 3 | 4 | 3 | 4 | 2 | 4 | 3 | ||||||||||||||||||
| 3 | 1 | 1 | 1 | 1 | 4 | 4 | 4 | 4 | Omitted | 4 | 1 | 2 | ||||||||||||||||||
| 4 | 1 | 1 | 1 | 1 | 4 | 5 | 3 | 5 | 4 | 4 | 2 | 3 | ||||||||||||||||||
| 5 | 1 | 1 | 4 | 2 | 1 | 4 | 3 | 5 | 2 | 4 | 2 | 5 | ||||||||||||||||||
| 6 | 1 | 3 | 4 | 2 | 4 | 4 | 4 | 2 | 5 | 2 | 1 | 2 | ||||||||||||||||||
| 7 | 1 | 1 | 2 | 1 | 2 | 2 | 2 | 2 | 4 | 5 | 2 | 1 | ||||||||||||||||||
| 8 | 4 | 2 | 2 | 2 | 4 | 1 | 4 | 1 | 4 | 2 | 4 | 1 | ||||||||||||||||||
| 9 | 2 | 1 | 2 | 1 | 2 | 2 | 4 | 3 | 2 | 4 | 2 | 2 | ||||||||||||||||||
| 10 | 1 | 4 | 1 | 2 | 4 | 5 | 4 | 5 | 4 | 5 | 1 | 1 | ||||||||||||||||||
| 11 | 1 | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 1 | 1 | 1 | ||||||||||||||||||
| 12 | 1 | 3 | 1 | 2 | 2 | 5 | 4 | 5 | 4 | Omitted | 4 | 2 | ||||||||||||||||||
| Number of cases in which reviewers show disagreement with original decision | 2 | 2 | ||||||||||||||||||||||||||||
| Key12345DecisionLikely to be appropriatePossibly appropriateUncertainPossibly inappropriateLikely to be inappropriateFactorsStrongly agreeAgreeNeutralDisagreeStrongly disagree | Key | 1 | 2 | 3 | 4 | 5 | Decision | Likely to be appropriate | Possibly appropriate | Uncertain | Possibly inappropriate | Likely to be inappropriate | Factors | Strongly agree | Agree | Neutral | Disagree | Strongly disagree | ||||||||||||
| Key | 1 | 2 | 3 | 4 | 5 | |||||||||||||||||||||||||
| Decision | Likely to be appropriate | Possibly appropriate | Uncertain | Possibly inappropriate | Likely to be inappropriate | |||||||||||||||||||||||||
| Factors | Strongly agree | Agree | Neutral | Disagree | Strongly disagree | |||||||||||||||||||||||||
In six cases both reviewers were in absolute agreement with the original decision. In three cases one reviewer thought the decision was likely to be appropriate and the second reviewer deemed it likely to be appropriate or was neutral. In two cases one reviewer believed the decision to be possibly inappropriate but the other reviewer found the decision was likely to be appropriate or possibly appropriate. In one case both reviewers found the decision inappropriate.
Case study for clinical panel: case 1 (AA)
Case summary
Patient profile/social data
AA is a 73-year-old white British man, retired van driver, with wife and daughter (present during interviews); in residential care home for less than a year.
Medical history
History of falls, bleed on brain due to fall 11 months ago, minor fall 1 week ago, cellulitis, sepsis, alcohol abuse, urinary tract infections, osteoarthritis, gout, similar confused episode 6 months ago, from which he recovered after antibiotics for urine infection; GP visit 2 days ago, antibiotics prescribed.
Pathway into emergency department
Care home called the rapid response service, taken by paramedics to hospital.
Reason for coming to hospital today
AA presented to ED this morning in a confused state, off legs and not communicating.
Diagnostic tests
Blood tests, chest X-ray, urine sample requested but patient unable to give while on ED.
Diagnosis
None reached while on ED.
Treatment
None given on ED.
Admit/discharge decision
Admission to medical assessment ward.
Time in the department
AA entered ED at 10.14 on a Wednesday. Decision made in less than 2 hours that he should be admitted. Spent just over 4 hours on ED, 2 hours waiting for bed and 6 hours on medical assessment ward before transfer to acute elderly ward.
Stages of decision-making
1: Accessing information
On initial rapid assessment by a consultant, AA presents as a patient from a care home with a possible urinary tract infection whose admission may be avoided: ‘it may be that he’d be able to go, erm, back to the home, I guess, if he’s got a mild urinary tract infection, we’ll want to get him home, so he might be an avoidable admission’ [S013_110614]. A case history and full assessment is made by a junior doctor, who then hands over to a middle-grade doctor, who takes over responsibility for his case.
Gaining information on AA’s history and current problems is difficult, since he cannot communicate for himself. His relatives are asked to provide information about current medication and symptoms, but AA is in a care home and has recently seen a doctor in the home who is not the family GP. His relatives do not know what the GP was treating with a recent course of antibiotics and therefore feel they are not ‘as helpful and involved as you should be’ and ‘not 100% sure of everything’ [FC002_110614.3]. This makes decision-making difficult for ED staff, who do not have a complete picture of the patient. Because of his complex history, AA’s daughter comments that they feel ‘whenever you’re in this situation you always think you’d be more prepared. We need like an emergency booklet on Dad’s medical history really’ [FC002_110614.3]. However, the relatives’ view is that AA’s current symptoms are caused by an infection, similarly to a previous episode, and they are expecting him to be admitted.
2: Investigation of a complex patient
The middle-grade doctor responsible for AA is looking for underlying causes and trying to find something to treat, while also recognising that the care home has limited provision for his safety:
Well basically he has some kind of infection that causes him to be more confused, because he’s more confused he has probability [sic] that makes falling over more likely. He therefore needs more looking after and the rest home don’t have the facilities to look after him 24 hours a day. So he’s more likely going to, doing himself a harm, plus we don’t know what the reason is why he is like that. So he needs blood tests to find out is there underlying infection. If we find something then we can treat that.
[S006_110614]
He reflects on the circular nature of AA’s presentation – infection leading to confusion leading to falls leading to further symptoms – but without a clear diagnosis the clinician feels he cannot offer treatment. Concerns over level of care mean he weighs up the risks and benefits of returning the patient to the community. In this case, he is aided in that process by the specialist nurse from the care of the elderly team, who makes her own assessment and contacts the care home.
3: The care situation – the package that a residential home offers
AA’s relatives see the care home as a provider of basic ‘caring’ but not meeting his needs while he is unwell: he no longer fits ‘the package that they [care home] offer’ and ‘he is not safe’ [FC002_110614.3]. The specialist nurse assesses whether the care home can cope with AA’s changing needs and establishes that they have concerns about taking him back in his current condition.
Sometimes when people come in from the residential homes and they’ve got an infection the residential homes are happy to have them back [. . .] But in this case, in this chap’s case, it’s because he’s . . . he’s got erm, a history of sepsis and the residential home are a bit concerned about his mobility. He will have to come in and get probably treated with IV [intravenous] antibiotics I would have thought.
Specialist nurse [S039_110614]
4: The relatives’ role in decision-making
AA’s relatives are aware that there are risks to him being admitted, but believe the benefits of availability of X-ray and other tests and speed of test results compared with resources offered by the community services outweigh the risks. AA’s daughter mentions that he may be ‘deskilled’ by being in hospital:
so you just hope that he will be able to, erm, you know, regain those walking skills and the ability to converse and be as independent as he was before he was admitted [. . .] obviously he’s a vulnerable person as well, so there is a possibility he could catch something else while he’s in here. But, erm – I think it is necessary that he is here.
[FC002_110614.3]
Ultimately a consensus is reached between the ED doctor, the specialist team nurse and the family that AA should be admitted.
Key elements of carer experience
AA’s wife and daughter were pleased that their relative would be admitted, as they felt he needed swift assessment and treatment that the care home and community services could not provide. They were appreciative that their viewpoint about what is ‘normal’ for AA had been taken into account, and particularly that their knowledge of his previous symptoms and treatment were considered:
How do you, you know, how do you feel about what’s happened today?
Erm . . . Well, I think it’s been swift hasn’t it, the service that we’ve been given? I think what’s been good is that the doctors have actually listened to what we’ve said, because obviously one concern is that Dad had a fall Thursday night and with his previous brain injuries they could have thought he would have needed those sorts of scans and all those sort of things but we, from our previous experience as a family, think it’s more related to some sort of infection [. . .]
You know, it’s good that they have gone down that route –
Took it on board . . .
[FC001/002_110614.3]
Key elements of health professional experience
Practitioners weigh up AA’s clinical and caring needs in making their decision. While the consultant in charge initially suspected that the patient might receive treatment and go back to the care home, the middle-grade doctor considered that it would take time to get to the bottom of AA’s symptoms and that the care home would not cope with his current needs. The specialist team chanced to come into the ED at the moment at which decisions were being made and took the initiative in confirming the situation with the care home, thus consolidating AA’s admission decision.
Data sources
Interviews with medical practitioners S013_110614, S006_110614 and S039_110614 and carers FC001/FC002_110614.3. Observation of interaction between medical practitioners and patient/carers P003_110614; S037_110614, S006_110614, S039_110614. Fieldnotes FN_4_110614.
Summary of clinical panel review of case 1 (AA)
In the scoring of decision-making on the Likert scale (stage 1), there was significant disagreement between reviewers about this patient’s admission. Reviewer 1 thought this was likely to be an appropriate admission, whereas reviewer 2 thought it was an inappropriate admission, believing that a community solution would have been more beneficial for AA: preferably a bed in a community hospital.
During stage 2 discussion, the reviewers pointed out that there was insufficient medical information on which to make a sound decision, since investigations were not carried out in the ED. The implication was that the responsibility of ED is to follow through on as many investigations as possible and achieve a diagnosis before making a decision:
But the thing that struck me really about this was it doesn’t seem clear why they’re medically admitting him, so there’s, you know, a lot of greyness and uncertainty, as you said [CP4].
Why has this guy been admitted to an acute medical bed, what’s the reason for him coming in, is it because he needs care, nursing care, or is it he needs medical treatment?
Lack of information about previous care was also seen as a barrier to making a confident discharge decision, and even though a specialist team had been instrumental in discovering the reluctance of the care home to take AA back that day, which was thought to be ‘a bit of a decision-maker, swayer for the middle-grade doctor’ (CP4), no significant medical or care history had been investigated.
But, you know, as you said, it’s very difficult because actually he’s in a care home and they will have lots of information about him, but we’re not very good at getting that information from care environment to hospital.
CP3
Picking up on AA’s relatives comments, that they needed a booklet to explain his history, a PPI member pointed out that the burden often falls on patients themselves to carry their own medical history, believing that ‘it becomes a responsibility of a patient to be able to give doctors information that they need’ (PPI1). Her practical suggestion was that ‘in a care home or nursing home situation I would think that that information should be in a booklet in his room or where he stays, that if he leaves that just goes with him wherever he goes’ (PPI1).
However, the reviewers were also pragmatic in their assessment of the case, realising that the ideal does not often exist in their working environment, and that system factors of time and limitations of community resources weigh heavily on decision making:
They didn’t quite manage to get to that within the 4 hours that he was in the emergency department.
So you’re feeling it was probably appropriate on . . .
On what they managed to achieve in the time. I guess if, in an ideal world if they had achieved a diagnosis and treated something, and they felt happy that they sort of knew why he was confused, he could potentially, if the local area was set up for that, got him to a community hospital bed rather than an acute medical bed in an acute hospital. But that would have depended on them being confident medically that there wasn’t something else they needed to treat or investigate. We don’t know whether he’s fallen [again?], bumped his head, and it was in a context of his recent, um . . . injuries.
Reviewers found this case typical of many presentations to their ED department and summed up the view that system factors are most likely to determine whether or not this type of patient is admitted.
Case study for clinical panel: case 11 (BC)
Case summary
Patient profile/social data
BC is a 66-year-old white British woman, retired, who is being treated for bowel cancer with chemotherapy elsewhere. She was brought in by her husband, with whom she lives independently, and who is profoundly deaf.
Medical history
Bowel cancer, left hemicolectomy (bowel section removed), liver metastases (cancer spread to liver) and osteoarthritis.
Reason for attending the emergency department
BC was referred to the medical team with chest pain that she had been experiencing for the past 2 days by her GP who queried a PE (blood clot to lung).
Pathway into emergency department
BC had experienced retro-sternal pain and had rung her chemotherapy nurse, who had advised that she see her GP, who assessed her, completed an ECG, measured her blood pressure and then referred her to the medical team. She was driven to the hospital by her husband.
Diagnostic tests
Bloods, urinalysis, two ECGs and a chest X-ray.
Diagnosis
Query a PE (a clot on the lung).
Admit/discharge decision
Initial decision was to admit but following a discussion with the patient the consultant was persuaded to discharge her with an appointment to return the next day for a CT scan and review in ambulatory care.
Time in the department
BC arrived at 15.52 on a Monday afternoon and was seen by the medical SHO at 17.30. Reviewed by the medical consultant at 18.19. Time of departure not recorded.
Treatment
Pain relief (paracetamol) and anticoagulant injection (prevention of clots).
Stages of deciding on discharge
1: The role of other health professionals in the decision
BC had been experiencing increasing pain for the last 2 days and was unsure how to manage the pain so she sought advice from her current health care providers: the oncology nurse, the oncologist and her GP.
Yes, well, I phoned, um, I phoned the [name of clinic] where I was, where I’m having the chemo to say I was having the chest pains and they were quite uncomfortable. There was nobody in the clinic so I phoned the senior oncology nurse, I had got her mobile number, and, um, she was working at the [name of hospital], she wasn’t there, so, um, then she phoned my consultant’s secretary, who said that all in all, the, the, um, resident medical officer at the [name of hospital] said it wasn’t suitable for me to go in, um, if I had chest pains and to go down to my GP. So I got an appointment at the GP for ECG and blood pressure and the doctor said it was all fine but, but it was all fast, it was too high, um, and hence he phoned here.
Interview with patient [P022_020913]
The medical consultant was unhappy to discharge BC without discussing her case with her oncologist, which he did, and they both agreed that she could be discharged on the proviso she returned the next day for further investigations:
He [the medical consultant] agreed that if the cardiac blood test was normal then he would begin anti-coagulant treatment overnight and arrange for her to return to the ambulatory care unit the next day for her scan if her oncologist was happy. He spoke to the oncologist who agreed the plan.
Fieldnotes [FN_13_020913]
2: Role of patient in decision-making
BC had made it abundantly clear to the health professionals that she did not like being in hospital and did not feel that her current condition warranted admission:
The medical SHO was told by the patient that she did not want to stay. The SHO decided to keep the patient in ED as he was hoping that she may be suitable to discharge. The patient was reviewed by the medical consultant [. . .]. The patient responded by saying that she did not want to come into hospital. As a result the consultant offered a compromise that if the cardiac blood test was normal then he would begin anti-coagulant treatment overnight and arrange for her to return to the ambulatory care unit the next day for her scan if her oncologist was happy [. . .] The patient was very happy to be going home, as was her husband.
Fieldnotes [FN_13_020913]
3: Admitting reduces risk and helps to speed process up
One of the primary reasons behind choosing to admit a patient is to weigh up the risks associated with not admitting. In the case of BC the medical consultant initially thought that admission was the safest option:
The patient was reviewed by the medical consultant who said that he was confident that this was not a cardiac event but would like to see the blood results to exclude this. He was more concerned however by a blood result that is raised and this can be due to her having a clot but also as a result of her cancer treatment which makes her more vulnerable and as a result she would require a scan to exclude a clot and wanted to admit her.
Fieldnotes [FN_13_020913]
When the medical SHO was asked why he would have preferred to admit BC he replied: ‘Admitting patients can help ‘speed things up’ (fieldnotes; FN_13_020913).
4: The availability of an alternative to admission
Having a service such as the ACU allowed the consultant to offer the patient an alternative pathway to admission while being reassured that the same level of care and access to investigations could be guaranteed.
Key elements of patient experience
BC and her husband shared an acute dislike of hospitals and desire to not be admitted:
They told me that they ‘hated being in hospital’ and would ‘rather not be here’, because of recent events and time spent as a patient . . . Her husband also felt that hospitals were not run well and were dirty and there was a lot of hanging around.
Fieldnotes [FN_13_020913]
So what did you feel when you heard you were coming in here?
Oh, disappointed. I mean, last time I came in . . . I wanted to go home, but it was about, I don’t know, obviously at night, and they wouldn’t let me go home, and I felt absolutely fine, and I stayed overnight and I didn’t have anything with me, and it was a complete, you know, it was horrid, because I wanted to get home, because the consultant didn’t come round until quarter past twelve the next morning, and, um, I just didn’t know what to do with myself, so not a good experience. One to be avoided.
Interview with patient [P0_22_020913]
However, there was also a sense of disappointment that her primary reason for attending, her pain, had been overlooked and not addressed:
BC complained to the medical consultant that her reason for attending was to address her pain which had not been resolved and that she was disappointed that she was till in pain despite telling everyone that was what she was experiencing.
Fieldnotes [FN_13_020913]
Key elements of health professionals’ experience
The nurse practitioner from the ACU felt that:
Patients were given unrealistic expectations by the referring practitioner and then it is up to the NP to unpick these expectations and is left to explain that yes they had been told one thing but they had been misled . . . and of course the patients and their families get cross.
Fieldnotes [FN_14_020913]
Data sources
Fieldnotes transcript (FN_13_020913 and FN_14_030913), incorporating notes on observation, informal conversations, and unrecorded interview with medical SHO and MNP, transcript of recorded interview with patient (P022_020913) and field jottings (2 and 3 September 2013).
Summary of clinical panel review of case 11 (BC)
At stage 1 of the clinical panel the clinician reviewers both judged this to be an appropriate decision (1 on the Likert scale), although one reviewer commented that from the patient’s viewpoint BC’s primary symptom, her pain, had not been addressed. PPI review suggested that from a patient experience perspective this case was worthy of fuller discussion at stage 2.
During stage 2 discussion, the reviewers suggested a number of ways in which, while it was an appropriate decision to discharge the patient with an outpatient appointment for the next day in ambulatory care, the patient experience could have been better.
The clinician discussion centred around the risk stratification protocols for diagnosis of chest pain and whether this process serves the patient well in such a case as BC’s, where the presence of low levels of cardiac enzyme in the blood and presentation of pain may indicate an admission, but where her medical history and preference for discharge are mediating factors:
We can risk-stratify them [. . .] to whether it’s safe for a patient to go home with a query pulmonary embolism, but a lot of the time it comes down to patient choice. Some patients just don’t want to stay in hospital, and they’re willing, when given the risks and benefits of waiting an investigation or going home, they choose to go home.
But occasionally there’s a patient who does have a raised troponin who you say, ‘Hang on a minute, I was going to send you home, but you’ve got a raised troponin and the pathway says that I should admit you to hospital.’ And sometimes the patient says, ‘I don’t want to come in’, in which case I say, ‘Well . . .’ [indicates that he would go with patient wishes].
The medical physicians discuss that this comes down to the doctor’s individual levels of risk aversion. CP4 (medical registrar) commented: ‘it’s a high-cost strategy for a relatively low risk, but I think because in our patient population [hard to hear] tend to be young, the adverse outcome is massive, so I tend to be relatively risk averse.’
The panel were in agreement that an ambulatory pathway was beneficial for BC, but believed that her route to this decision could have been more direct had a different service been available at the hospital:
I just wondered what CP1 [AGPS] thought about the pathway of this poor patient ringing the oncology nurse [. . .] round the whole hospital and then told to go to your GP?
I mean we would probably get the oncology nurse ringing us actually [. . .] we would never say, ‘Go and see your GP’ for a pulmonary embolism. But I guess if that pathway doesn’t exist in this establishment [. . .] the best way to get them into hospital was probably through their GP.
The panel also pointed out there was an element to BC’s care which was suboptimal and which is commonly experienced by patients in ED:
I think that’s something we’re really bad at, because we . . . admit people to ambulatory care or to our clinical decision unit and it’s normally us that go round and review all the investigations and say to the patient at the end of their, er . . . their visit, ‘So, all good news, everything’s normal, you can go home, it’s all fine,’ and they go ‘Can you give me some painkillers? No one gave me any painkillers, I’ve been here 6 hours.’ ‘Oh, well we were ruling out heart attack.’ ‘Well I haven’t had a heart attack, [hard to hear] some painkillers!’
There was reflection from a PPI member that failure to address patient comfort could have been due to handover between different professionals, a fact that was acknowledged as something that ‘we still can’t get 100% right at the moment’ (CP3, senior nurse ambulatory care) given the strain on the system from numbers coming through ED: ‘I think mistakes happen and things get, don’t get communicated as well as they should be’ (CP3).
Appendix 3 Mid-project workshop
Appendix 4 Patient and public involvement in the Avoidable Acute Admissions study
Introduction
A PPI group advised the project from its beginning. Members of the group had a variety of backgrounds including people with physical health problems, visual impairments, carers and people with multimorbidities. The membership of the group has fluctuated across the life of the project but in total 14 lay members have been involved. PPI members were paid travel expenses and £25 per half-day involvement as a ‘thank you’ payment.
There have been a number of different ways that people have been involved. These include participation in four half-day workshops on specific topics during the course of the project. These were:
-
ethics application preparation
-
introduction to the Acute Avoidable Admissions project and ethnographic research
-
analysis of qualitative data 1
-
analysis of qualitative data 2 and introduction to VSM.
Patient and public involvement members were also actively involved in both the mid-term and end-of-project workshops and in the two external clinical panels that examined case study material from the project.
Aim of the involvement
The aim of the involvement was to ensure that the patient and carer perspective was addressed in answering our three key RQs. These questions were:
-
What influences operate on the acute admissions decision process?
-
How is the whole admissions process experienced by patients and practitioners?
-
In the four hospitals studied, how are the models of care similar and different?
Impact of patient and public involvement on the research
Input from the PPI group helped sensitise the research team to a number of key issues. These included the following:
-
It strengthened our ethics application and in particular our strategy for engaging with patients and carer participants during the fieldwork. The PPI group were particularly concerned that sufficient account be taken of the fact that that potential participants may well be under considerable stress, in pain or anxious. The contribution that PPI made in this area was something specifically mentioned in the ethics committee’s positive response to our application.
-
It increased our awareness of accessibility issues encountered by people with a physical or sensory disability in negotiating their way through an A&E department.
-
Patients and carers make efforts to avoid admissions that they perceive to be unnecessary. This is not something that the research team had foreseen.
-
Some patients learn to use the emergency system to get speedy checks and tests.
-
Patients and carers fear that staff will go too much by the book rather than focusing on their needs.
-
During the VSM process it was noticeable that patients tended to highlight waiting times while professionals tended to note the points of assessment or treatment.
-
Issues of communication between health professionals and patients and patients’ supporters were a key issue. The PPI group were particularly concerned that patients might be left in A&E not even knowing basic information such as whether or not they could eat or drink.
Conclusion
Patient and public involvement has made a positive impact on both quantitative and qualitative aspects of this project, helping to keep the research as a whole grounded in the concerns of the people who use hospitals. This was made possible by the fact that PPI was planned and fully costed into the bid from the beginning, with a named person responsible for leading the PPI activities.
Appendix 5 Patient and public involvement poster presented at the INVOLVE conference
Appendix 6 Learning sets reports
Appendix 7 An overview of Lean theory and value stream mapping
The Lean concept originated from the Toyota production system and was initially applied to manufacturing industry, where it has been used to improve the efficiency and effectiveness of process performance. 71,72 Lean has been described variously as a philosophy, an approach, a technique and a transformational management strategy with a number of tools that can be used to achieve improvement in production processes. 71,73–76 The Lean methodology aims to maximise value for customers (or patients in the case of health care) while minimising waste (relevant examples are shown in Figure 19).
By eliminating the processes and steps that do not give value to the customer, it is proposed that production processes will be more efficient, save money and provide an improved customer experience. The same concept may be applied to the delivery of health care.
The principles and tools associated with Lean are widely described in the literature. 71,72,77–79 The Lean philosophy is underpinned by five key principles (Box 1).
-
Identify customers and specify value.
-
Identify and map the value stream.
-
Create flow by eliminating waste.
-
Respond to customer pull.
-
Pursue perfection.
Value
The underlying assumption of the Lean concept is that the delivery of a product or service should give value to customers. 71 Thus, Lean tools and methods are used to critically examine processes to reduce wasteful activities that add no value for the customer. 80
Understanding customer value in health care raises the question: who is the customer? In general, the customer is the patient, although there are several different perspectives on this issue. 81,82 Radnor et al. 75 argue that Lean in health care breaches the view that the patient is the sole customer and that the customer and commissioner (the one who pays) are the same. Equally, in public funded services the patient does pay, albeit indirectly through taxation. However, in health-care delivery systems there may be ambiguity in the definition of ‘value’. 83
Value stream
The value stream is defined as the processes or activities required to design, order and provide a specific product or service. 71 This requires identification of the individual components of the process. Womack and Jones71 describe actions that clearly create value, actions that create no value but are required because of the design of current processes (necessary non value adding) and activities that create no value (waste). Examples of wasteful activities for manufacturing, service and health care have been identified. 77,84–86 However, Lean thinking is not solely about waste reduction but also about increasing activities that add customer value without additional costs. 87
Creating value stream maps of a process is a key step in understanding how processes work and identifying value and waste from the customer’s perspective. VSM enables visualisation of information and physical flows. 77,88 In health care VSM is often at a high level that can miss operational complexity. 89 Furthermore, it is not always easy to define waste because of the complexity of the parts of the pathway and supporting functions. Robinson et al. 86 and Radnor et al. 75 described different types of waste in the UK NHS using the framework of Ohno. 62
Flow
A further principle of Lean is ‘flow’. 71 The traditional approach in manufacturing was to maximise the efficiency of individual parts of the process. Work is undertaken in batches and then passed on to the next part of the process. Variation in demand created by batch working or random variation can create queues with waiting time that detracts from value. Lean seeks to achieve continuous and seamless flow essentially through reduction in variation of demand and standardisation of processes.
When patients wait in queues at different points in the pathway it is wasteful. As Radnor et al. 75 observed, health care is usually capacity based, whereby demand is ‘pushed’ into the system rather than ‘pulled’ as advocated by Lean thinking. Therefore, because of both random and non-random patterns of demand, large variations are the norm for many health-care pathways such as an ED, and it is hard to achieve a balance between demand and capacity at certain times. 90,91 The ability of health-care providers to manage demand in order to reduce variation in care is limited, particularly in urgent and emergency care.
Customer pull
‘Pull in simplest terms means that no one upstream should produce a good or service until the customer downstream asks for it’ (p. 67). 71 The Lean concept maintains that the pull approach is desirable, whereby a service is delivered to order rather than being pushed onto the customer. However, this approach is hard to implement, particularly when demand variability is high (such as in health care). In order to achieve a pull-based system an organisation needs firstly to understand the customer and their pull demands (real and created). To reduce the difficulty of applying a pull-based system, there also needs to be a reduction in the variability of demand where possible. 72 Again this is hard to achieve in health care, as there are few indicators (apart from seasonal variations year on year, such as winter demand levels) that foretell demand fluctuations. Attempts to reduce demand variability require accurate demand measurements over time, assessing multiple sources of information that predict demand levels and standardising certain aspects of customer demand.
Perfection
As organisations begin to accurately specify value, identify the entire value stream, make the value-creating steps for specific products flow continuously, and let customers pull value from the enterprise, something very odd begins to happen . . . suddenly perfection doesn’t seem like such a crazy idea.
p. 2571
The pursuit of perfection requires a standardised process of benchmarking in order to ascertain improvements over time. Often, however, this is difficult, as measures of performance tend to be outputs (e.g. length of hospital stay and admission rates) rather than quality measures (e.g. patient experience). It is also often confused with a comparison between companies where contextual factors may make comparisons void. The pursuit of perfection should use metrics that look at how individual companies (or hospital departments in the case of health care) progress against their own performance measurements. Furthermore, those metrics should not be the end of the Lean process but rather a process of continual improvement with suggestions that form future state maps and with Lean being a cultural way of life.
Lean in health care
The principles of Lean, although first developed by Toyota and applied to manufacturing processes, have subsequently been applied to many different industries. It is an approach that has been quickly adopted by other car and manufacturing companies, with Womack and Jones92 arguing that it could be applied to any kind of company or system, including health care.
Literature reviews of Lean health care are showing that it is growing in popularity and implementation. 93 It has been suggested that this is because Lean health care is more in tune with staff empowerment and the concept of gradual and continuous improvement intrinsic to Lean theory than other types of service improvement strategies. Initial applications of Lean such as by Jacobs and Pelfrey,94 Heinbuch95 and Whitson96 sought to apply the manufacturing principles of just in time to health care, but did not refer to Lean specifically. Their research focused on areas of supply chain and stock inventory in particular. 94–96 The first explicit use of Lean in health care appeared in the works of the NHS Modernisation Agency97,98 in which it was used to understand patient flows within the hospital in order to increase efficiencies in a time of increasing financial pressures. This was followed by Bushell et al. 99 and Feinstein et al. ,100 who reported positive results in implementing a Lean approach. More recently, Joint Commission on Accreditation of Healthcare Organisations,101 Zidel102 and Smith et al. 103 have given some example cases of using Lean in a health-care setting and some guidance on how to carry out Lean research in practice.
There are numerous examples of Lean principles being applied to health care but Brandao de Souza93 noted that the academic literature surrounding the use of Lean principles in health care centred on three areas:
Speculative: literature which speculates about the benefit of Lean in health-care environments. For example, Allway and Corbett104 used hospitals to exemplify the potential of Lean and its potential use for performance objectives.
Methodological: new approaches or further developments to a Lean approach in health care. For example, Miller105 looked at the similarities between manufacturing and health care, and Jones and Mitchell106 reflected on the benefits and challenges to Lean health care. Additionally, this includes the discussion of barriers to implementation, such as by Spear,107 who looked at specific reasons for a delay in Lean health-care adoption.
Case studies: the results of the application of Lean approaches to health care. Case studies are subcategorised as:
-
akin to manufacturing (e.g. Condel et al. ’s108 case study in pathology)
-
managerial and support (e.g. Massey and Williams’s109 report on the evaluation of a single tool implementation in the training and development department in a NHS trust)
-
organisational and patient flow [e.g. King et al. 110 on the Flinders Medical Centre in Australia and Fillingham (2008)111 on the Bolton Hospitals NHS Trust].
Brandao de Souza93 described the quantity of speculative literature in the field as high in comparison with methodological and case-study-based research. Furthermore he went on to say that there was a need for more concrete works on Lean health care and that in his literature review he found no work that criticised the use of Lean in health care. More recently, however, there has been a growing number of critical studies that have evaluated the application of Lean thinking to complex social environments such as health care. 73–75,78,86,112,113
Lean thinking and value stream mapping in emergency medical care
There have been several previous applications of Lean analysis of emergency medicine case studies to understand and improve processes. Walley69 described a study of two EDs in the UK where researchers directly observed staff over 6 weeks to understand sources of, and responses to, demand, and identify ways to improve patient care. This approach identified the problem of complex queuing of patients by triage category leading to waits. The author suggested ways to improve flow and future challenges that might occur with these changes. King et al. 110 undertook a case study in an Australian ED, triggered by severe overcrowding. During three sessions with a Lean consultant, the multidisciplinary team used their experiences of working in the ED to create a schematic representation of how the department functioned. Changes to the schematic were suggested to improve patient flow, particularly focusing on the large group of patients who were thought likely to be discharged from ED at triage. A before-and-after study of the changes found a reduction in waiting times to be seen and time in department, and a decrease in patients leaving without being seen. A similar study was undertaken by Ng et al. 114 in a Canadian ED, prompted by long waits and decreasing satisfaction. This study also identified those patients deemed ‘dischargeable’ at triage to be a key group upon which to focus improvements. A similar exercise with a Lean consultant was undertaken to identify potential improvement. The current departmental value stream map was developed from staff experience, a future state map of ideal ED process was developed, and improvements that would lead to this ideal were produced. Following implementation, a before-and-after study found a reduction in wait to be seen, shorter length of stay, fewer patients leaving without being seen and increased patient satisfaction. For both King et al. 110 and Ng et al. ,114 value was assessed from the perspective of the staff, or the perceived perspective of the patient. Both studies showed that the interventions coincided with improved waiting times and no change in safety metrics. Ng et al. 114 also showed improved patient satisfaction, although there was no ‘shop floor’ data collection or direct patient input. Lean thinking and VSM have also been applied to improve time to thrombolysis treatment for stroke patients in an ED. 115 Following VSM the implementation of specific changes was shown to reduce door-to-needle time without compromising safety. This study also did not consider patient experience in mapping or discuss any effects the interventions may have had on other aspects of the ED (e.g. use of resources from other areas of patient care). Overall, these various studies suggest a likely benefit from applying Lean theory to the study and improvement of processes in emergency medical care.
Finally, Holden undertook a critical review of 18 studies of the implementation of Lean specifically in EDs. These results also confirmed a general trend of improvement in waiting times and journey times in departments, and reductions in numbers of people leaving before being seen. 74 In summary, application of Lean theory, using the methodology of VSM, has emerged as an important tool to investigate potential inefficiencies and waits in patient flow in a variety of health-care settings including emergency medicine.
Appendix 8 Steering group
The steering group members are:
Jonathan Pinkney.
Richard Byng.
Susanna Rance.
Suzanne Mason.
Catherine Pope.
Andy Collen.
Derek Bell.
John de Pury.
Margaret Turley.
Dates of meetings held
9 April 2013.
9 July 2013.
8 October 2013.
23 January 2014.
7 May 2014.
Appendix 9 Amendments to protocol design
The study has been completed broadly in line with the protocol submitted to the funders. A number of minor changes have been made.
Value stream mapping
Within the VSM study, it was not possible to develop consistent site-based value stream maps for ED and acute medicine admission pathways, given the complexity and heterogeneity demonstrated within the patient pathways.
It was not possible for non-clinical researchers to develop clinical summaries from the clinical records.
The clinical panel judged the appropriateness of VSM but in the results there were insufficient cases where pathways were judged inappropriate to incorporate these into the analysis.
Although we had gained permission to revise down estimates of numbers in the VSM study to 60, in the end we were able to collect 108 cases, near the original ambition of 120.
Ethnography
Within the ethnography there had been a plan to use diaries to contribute to mini case studies, but this was not feasible.
Learning sets
Although we employed an expert in learning sets and spent considerable time engaging with participants and planning the procedures, it was not possible to ensure adequate attendance at these meetings. Instead of a second round of learning sets, the procedures were adjusted to have brief meetings with larger numbers of participants at each site to consider the results. Additionally, site leads were identified and invited to both mid-term and end-of-project workshops, and one clinician from each site committed to work together as a team to respond to the results of the research.
Workshop
Lastly, rather than have a workshop at the end of the study with all of the completed results, we held a workshop at the start of the synthesis process involving practitioners from each site, carers and patients, and internal and external researchers, to start the process of developing hypotheses about the ways to improve the organisation of emergency care.
Appendix 10 Interview topic guides
Appendix 11 NVivo coding framework
Appendix 12 Summaries of ethnographic case studies (A–D)
| Weekdays | Weekends and bank holidays | ||||
|---|---|---|---|---|---|
| Case 12 | Case 11 | Case 7 | Case 8 | Case 9 | Case 10 |
| Patient factors | |||||
| 60-year-old rural woman with stroke-like symptoms. Felt she was not ill enough to go in. Did not want to take an ambulance from someone who needed one | 66-year-old woman with two falls. Reluctant to go to hospital. GP gave counselling for anxiety rather than pain relief she wanted. Once in ED, unclear about tests being done | 82-year-old woman living in retirement complex, with two falls in a week. Wants independence. Concerned about clogging a bed | 69-year-old woman living alone. Funny turn. Reluctant to seek help and make a fuss. Once in ED, feels she is there under false pretences, wants to go home, concerned about wasting staff time | 83-year-old man, chest pain. Concerned about delays experienced in the past. Sympathetic to demands of busy system but clear about answers wanted and results pending | 83-year-old man, two heart attacks, strokes. Sudden bad turn. Patient and wife flexible, recognising demands on hospital system |
| Influence of others | |||||
| Relatives’ influence | |||||
| Detected worrying symptoms | Daughter dismissed GP view. Called 999 | Son prefers admission; wants to avoid frequent readmissions | Concerned neighbour and friend advises ED | Wife is retired nurse. Uses knowledge of system to get patient seen urgently | Wife active participant. Called 999. Expected patient to be in overnight. Happy to be guided by staff about length of stay |
| Practitioner actions | |||||
| Doctor, experienced junior, talks to neurology registrar, who happens to be in ED. Provisional diagnosis: small stroke | Ambulance paramedic facilitated contact with GP, who instructed going to ED. ANP discussed with senior. Referred for X-ray just in case. Hip fracture | ED consultant handled sensitively. Admitted patient for social reason, though not sick | Junior doctor and consultant admit to MAU to wait for second troponin test. Refer to neurology specialist. Lack of clarity about what was being investigated | Careful assessment by ‘more senior junior doctor’: high-risk patient. Made early provisional decision before handing to medics | ‘More senior junior doctor’ (same as in Case 9) had uncertainties about condition. Ordered tests to aid decision |
| System factors | |||||
| Monday. Confusing referral process to neurology: GP advised going through ED. Long wait for scans. Problem about transport home for ‘well’ patient | Monday p.m. ANP, experienced but new to hospital, has to discuss each case with senior. Unforeseen X-ray result dictated patient pathway | Saturday. ED and MAU picked up slack in community services, which were known to be slow | Primary care alternatives not available on holiday weekend. Overnight stay needed to wait for test. Long neurology delay. Patient slipped off cardiac radar | Bank holiday Sunday affected time lapse. Timely cardiology review could have avoided admission. No consultant available | Weekend delays. Low availability of diagnostics on a Bank holiday Sunday. High demand on scanner. No consultant available |
| Outcome | |||||
| Discharge with urgent outpatient appointment for CT scan the next day. Patient not happy about travelling home alone late in the day and having to return the next day | Admitted to surgical ward. Patient and daughter viewed ED care positively: busy but they make time for you | Admitted to MAU to speed up OT assessment and ensure safety at home | Admitted to MAU. Patient fell in gap of care between medical and neurology. Negative patient experience: lack of information on what was being investigated, results of tests and why waiting to see different specialist | Admitted to MAU. Referred to medical ward. Patient and wife pleased that he would stay in hospital | Admitted to MAU. Next steps pending test results |
| Learning | |||||
| Care was expedient for system but not patient centred | GP’s assumption of overanxiety was unfounded. Paramedic’s intervention, senior support for new ANP and caution with X-ray ensured safe outcome with positive experience for patient | Patient-centred care, where ED and MAU take on extra work to get patient speedily through system and safely back home | Lack of clear decision-maker. Negative commodification and poor patient experience. Frustrating for patient and annoying to consultant | Case well managed by ‘more senior junior’ going with ‘gut instinct’ in absence of consultant. Referring to medical ward acted as safety net | The ‘more senior junior’ had sufficient judgement to know which cases did (not) need senior input. Caution applied through testing |
| Weekday daytime | |||||
|---|---|---|---|---|---|
| Case 1 | Case 2 | Case 3 | Case 4 | Case 5 | Case 6 |
| Patient factors | |||||
| 73-year-old man living in care home. History of falls. Multiple comorbidities. Recent GP visit. Confused, off legs | 86-year-old woman living with 90-year-old partner. Dementia; fall; pain. Once in ED, wants to go home. Feels she has no choice. Perceives long process. Not offered food or drink. Distressed that partner is unable to visit | 40-year-old man. Left side pain. Called 111. In ED, does not know what is happening. Wonders about fluids; hungry. Unsure why sent to surgical ward. Wanted a named person in charge | 70-year-old woman living alone. Dizzy spells. Failing memory. In ED, stated preference to go home. Accepts doctor’s authority | 67-year-old man. Discharged a week before after bypass operation. Breathless, trouble sleeping. Saw GP, surprised at referral to MAU. Preference to go home | 31-year-old man. History of palpitations. Thunderclap headache. Wanted pain relief to return to work. Locum GP referred to hospital. Patient accepted, thinks doctors know better. Did not mind being in waiting area |
| Influence of others | |||||
| Carers’ and relatives’ influence | Partner’s influence | Unaccompanied | Relatives’ influence | Unaccompanied | Unaccompanied |
| Care home called rapid response. Relatives provided information, thought infection, expected and were happy with admission. Considered patient to be unsafe in care home. Wanted speedy test results | Called 999. Concerned about managing at home. Relieved at admission. Told patient she is one of hundreds of people in ED | Daughter complements information about patient. Concern about falls. Doubt about safety of discharge | |||
| Practitioner actions | |||||
| Considered possible urinary tract infection and avoidable admission. Junior doctor handed to mid-grade. Decision-making difficult with insufficient information, concerns for patient’s safety in community. Specialist ACE nurse contacted care home. Consensus in favour of admission reached between ED doctor, specialist nurse, family | Mobility and fitness to return home were key factors in assessment. Fracture detected, not requiring surgery. Admitted to MAU under care of specialist team | CT kidney, ureter and bladder scan; renal colic; kidney stone, surgery not indicated. Junior doctor handed care to mid-grade. Pain was a major factor. Consultant tried to expedite treatment in ED to make hospital stay shorter. Discharge decision was made and then missed so patient was admitted | Junior doctor thought of admission for more tests. Senior geriatrician arrived unexpectedly with ACE team. Convinced family about discharge and organising home care; arranged outpatients appointment | Pleural effusion as result of heart surgery. Risk assessment by junior doctor. Senior agrees. No treatment. Explanation to patient | Brain scan, lumbar puncture to exclude bleed on brain. Diagnosis: tension headache. Analgesia |
| System factors | |||||
| Decision in 2 hours. Patient spent 4 hours on ED, 6 hours on MAU before transfer to ward | Patient was 3 hours 20 minutes in ED, 13 hours 40 minutes in MAU. Admitted though did not need an acute bed. Rehab in community would have been preferable; no bed available. Transferred to surgical ward as outlier at 02.26 | Surgical bed sought; no beds. Patient was 7 hours in ED. Two patients on ED were already ‘AFO’, no more space | ACE team available but little known about by doctors | Doctors felt diagnosis could have been dealt with as non-emergency: unnecessary GP referral | Patient wrongly sent to ED; redirected to MAU triage. Timely decision depended on availability of appointments for urgent scans. Patient spent 4 hours in ambulatory triage area, 6 hours on ward |
| Outcome | |||||
| Relatives pleased that their contribution was acknowledged, and with swift service. Patient admitted to MAU. Transfer to acute ward | Patient moved to surgical ward. Still there, far from home and with partner unable to visit, 3 weeks later | Discharged 22.00 after 12.5 hours in hospital. In open holding space, patient found it hard to rest. Happy with initial care but felt doctors lost the plot about communication | Discharged after 3 hours on ED, with outpatients appointment due to ACE team intervention | Discharge after 3 hours in MAU. Patient to return to GP if problem persists. Patient very satisfied with MAU care: dealt with quickly, in depth. Asked for and received clarification. Happy to be discharged | Discharge at 23.00 after 10 hours. Patient very satisfied with quick CT scan, consultant’s explanation, access to drinks and food in waiting area, being kept informed, polite staff, staff patient-focused, not too rushed |
| Learning | |||||
| Clinical and caring needs balanced; family involvement | OT perturbed at limited options for community discharge. Very unsatisfactory outcome for patient | No observation unit. Had there been observation facilities on ED, patient would not have been referred to ward; could have been discharged earlier. Suboptimal nursing re fluids/food | Post hoc reflections by doctors: ACE team nurses and OTs have less decision-making confidence and authority; ACE team’s role not really understood; senior input was key here, not necessarily specialist. PPI comment: patient should not have been in ED; a secondary care facility in community would be preferable | Junior doctor makes confident provisional diagnosis and prediction of outcome. Feels patient got a good service. Senior doctor considered it important to prevent admissions like this, which waste staff time, tests and patient time | Consultant weighed up risks and benefits to patient and service of doing tests. Aware of colleagues’ different attitudes to risk. One would have batted patient out of door. Ultimate concern: patient safety. Gut feeling OK, but have to exclude |
| Weekday daytime | |||||
|---|---|---|---|---|---|
| Case 1 | Case 2 | Case 3 | Case 4 | Case 5 | Case 6 |
| Patient factors | |||||
| 56-year-old woman working in health sector. Central chest pain. Called GP, who said ring for ambulance. She felt ‘terrified’ and thought there were more deserving cases | 74-year-old man. Self-dialyses. Hot and dizzy; optician called 999. Ambulance crew gave choice but advised hospital. Patient did not want to go; once in, felt he would ‘look a fool’ if he went home and collapsed there | 65-year-old man. Slurring of speech. Saw GP, who referred to ED for assessment: query TIA. Patient concerned about difficulty talking, crucial to his business. Sensed possibility of serious condition | 23-year-old man, driver, living 80 miles from hospital. Sudden onset left flank pain. Patient felt vulnerable far from home; work pressure to get sorted | 24-year-old woman. Previous attendance; previous admission to another hospital, headaches, query seizures. Patient in hurry to get sorted as unable to drive until attending clinic appointment 15 weeks later. Unwilling to wait, and reluctant to visit GP as felt would be unable to help | 40-year-old woman. Acute medical nurse: clinical knowledge fed her concern. 4 days’ fever, aches, chest pain. Concern about possible TSS. Rang 111, who advised ambulance |
| Influence of others | |||||
| Partner’s influence | Unaccompanied | Partner’s influence | Workplace influence | Relatives’ influence | Unaccompanied |
| Husband also health sector worker. Surprised at GP’s advice | Wife expected nothing to be wrong but knew condition was suspicious | Manager advised calling ambulance | Patient’s mother brought her to ED based on 111 advice the week before. Patient and mother concerned about seizures | ||
| Practitioner actions | |||||
| Assessed by experienced middle-grade doctor 1 hour after presenting. Doctor quickly formalised plan: two ECGs, repeated Triple Marker, chest X-ray. Decided safe to go home but ‘on radar as a risk’ | Junior doctor saw patient, guided by consultant. Senior irritated by lack of information. Junior thought discharge likely. Senior thought something underlying. Disagreements among professionals | Patient seen in first instance by ED consultant, who assessed time and possible delay over weekend; wanted patient to be seen that afternoon (Friday). Aided by reliable information from patient and wife; comprehensive GP letter; senior assisted by nurse able to pull strings with TIA clinic | Suspected kidney infection or PE. Mid-grade doctor discussed with consultant. Plan agreed on basis of several tests. For non-confident junior, case carried uncertainty and risk. Thorough but lengthy process: overinvestigation. Consultant questioned relevance of additional tests | Patient seen by junior doctor, who read notes and checked on computer system. Case discussed in doctors’ handover. Senior doctor not convinced about TIA | Junior not familiar with TSS; guided by patient. Wanted to observe temperature. Cautious approach, prolonged time. Senior advised TSS very rare |
| System factors | |||||
| Delays with repeat ECG and sourcing medication to take home. 4 hours 20 minutes in ED | Patient was 3 hours 40 minutes in ED | Quick and efficient pathway. TIA clinic open | 3 hours 51 minutes in ED | 3 hours 39 minutes in ED. Availability of notes: they often ring GP and request notes to be sent through | Patient’s suitability for ambulatory care was noted but missed. AEC communication not effective, staff frustrated. IV fluids were prescribed but overlooked |
| Outcome | |||||
| Not admitted. Further investigations needed. Referred to clinic for early outpatient follow-up | Patient admitted to acute medical ward. Observation, no treatment. Admitting medical consultant discharged him 40 minutes later. Patient irritated at lack of information about tests, doctors’ repeated questioning, time taken for results and decisions | Patient discharged from ED, seen in TIA clinic that afternoon. Admission avoided | Discharge. Patient felt vulnerable far from home, and was worried about work and vehicle, and transport home | Discharge. Referral to fit clinic. Symptoms suggested not safe to allow patient to drive | 3 hours 6 minutes in ED. Diagnosis: urine infection. Discharged. Antibiotics. Patient happy to have diagnosis, but surprised. Doubtful if she would get prompt GP appointment |
| Learning | |||||
| GP urgent referral was appropriate. Middle-grade doctor acted decisively with tests, risk assessment, decision to discharge and early follow-up clinic appointment | Opinions can differ between similarly qualified doctors from different specialties. Repeated questioning and delays can prove annoying for patients. Acute medical consultant felt that, if acute medical expertise had been available earlier, admission could have been avoided | ‘Senior first’ consultant acted speedily, aware of alternatives to admission thanks to experience and knowledge of system. A junior would have been more likely to admit. Unusually, in this case everything fitted into place, avoiding all contingencies | Junior doctor was reassured by tests that patient was safe, but his self-questioning and overinvestigation lengthened the patient’s stay and was potentially costly for the hospital. Decision made quickly with senior input; patient left 45 minutes later | Patient came to ED to speed up process, dissatisfied with GP and future clinic appointment options. Access to GP notes aided decision despite doubtful diagnosis | New ambulatory care initiative insufficiently informed to staff. Communication and action problems about this and IV fluids. Full screening due to junior doctor’s doubts led to unexpected diagnosis. Patient was not confident of timely GP access |
| Weekends and bank holidays | Weekdays | ||||
|---|---|---|---|---|---|
| Case 1 | Case 2 | Case 8 | Case 3 | Case 4 | Case 5 |
| Patient factors | |||||
| 35-year-old woman. Single parent reliant on neighbour. History of migraines. Family history of aneurysm. Was having clinic treatments. Severe sudden pain. Did not want to stay in hospital, concern for daughter. Fear of lumbar puncture pain and effects | 52-year-old woman. Previous TIA, panic attacks, anxiety. Dizzy, chest ache. Called 111, who sent ambulance. Query TIA. Patient sought reassurance. Repeat attender. Relieved to be checked out but doubts about ‘being silly’ | 86-year-old man. Central chest pain. Patient adamant that hernia caused pain and did not require hospital visit | 41-year-old woman living alone, disabled with chronic neck pain, on basic benefits, children living apart. Attended ED 2 days before, fourth time with this problem. Called GP, 111 arranged ambulance | 77-year-old man. Bleed on brain 8 months ago. Sudden severe headache. Saw GP, who checked well and referred to medical team. Query haemorrhage. Patient wanted autonomy, disliked having ambulance transport | 51-year-old woman, works on farm. Chest pain for 2 weeks. Called GP, referred to 111, advised ED by ambulance. Patient reluctantly accepted admission after dodgy ECGs: ‘You’d be stupid not to’ |
| Influence of others | |||||
| Neighbour’s influence | Unaccompanied | Relatives’ influence | Unaccompanied | Partner’s influence | Unaccompanied |
| Advised patient to call ambulance | Wife followed daughter’s advice to call ambulance if symptoms recurred | Wife concerned about symptoms. Both fearful after past experience of 2 weeks of being admitted and readmitted | |||
| Practitioner actions | |||||
| ED SHO contacted neurology registrar, who advised cautionary approach and lumbar puncture | Patient seen at 21.00 by SHO, who thought symptoms anxiety related. Discussed with ED consultant, who urged caution: possibility of TIA with non-classic symptoms. SHO followed TIA pathway; used electronic referral to TIA clinic (no specialist sign-off needed) | Query acute coronary syndrome. SHO saw patient, referred to medical team, discussed with middle-grade doctor. Staff nurse expected discharge. Doctor put as high risk: comorbidities and intuition. Disagreement between patient and doctor concerned about possible serious event. Chest infection diagnosed | Initially admitted to observation ward, then acute medical ward for pain relief. Nurse questioned her need to attend, with sudden improvement after treatment. Consultant said he would get her in to see pain team and neurologist | Seen by medical SHO. Scan, admitted to acute medical ward after 3 hours 40 minutes in ED. Streamlined review pathway started by GP | Seen by ED registrar, referred to medical team, reviewed in ED in under an hour. Repeated abnormal ECGs |
| System factors | |||||
| ED consultant felt this was a clear case of avoidable admission, which would get more frustrating if bed required later | GP notes should have been available but electronic access not working. Evening, so no GP contact. New intake of junior doctors | Patient waited for bed to become available on MAU | After multiple ED visits, patient had no new tests or diagnosis. Long wait to see pain clinic. Waiting months for neurology appointment. Frustrated to be back in ED. Long, costly journey. Sense of abandonment | GP referral to specialist team relieves pressure on ED but no beds on ward; team see patients in ED. CT scan possible that evening | 111 called ambulance despite patient’s protests. In MAU because of 4-hour target. Staff frustrated at patients being moved during assessment to avoid breaches. Time-wasting and duplication. Ambulatory care not used, chest pain grey area. Avoidable admission? |
| Outcome | |||||
| Admitted to observation ward overnight to await result of lumbar puncture in morning. No biochemistry analysis out of hours | Discharge. Referred to TIA clinic. Patient returned to ED days later; sent home again | Patient admitted to medical short-stay ward (MAU) for IV antibiotics. After resisting admission he enjoyed attention, was happy with care and did not mind waiting for a bed | Patient ‘dismissed’ at 02.00, ‘dramatic’, high on drugs, crawling upstairs | Discharged from medical ward later that evening. Poor patient experience: no explanation re delays; nurse mentioned awful lot of sick people; sense of injustice | Admitted to acute medical ward. Diagnosis unclear. Discharged with appointment to return for tests. Patient unhappy at conflicting information. Wanted to self-mobilise, did not feel at risk of heart attack |
| Learning | |||||
| Obstetric ward manned by ED staff is used for patients to stay without ‘full admission’. High demand for these beds, increasing at weekends | TIA pathway and clinic referral worked efficiently, usable by new SHO | Diagnosis surprised patient and nursing staff. Resistant patient won over: ‘They want to look after me’ | Implicitly punishing, even inhumane behaviour from staff: to discourage a repeat attender? | Formal streamlined process but some insensitive care. Bad past experiences made patient and wife fearful | Breach avoidance was given priority over time-wasting for staff and poor patient experience |
Appendix 13 Synthesis table
| Number | Analytic statement | Source |
|---|---|---|
| 1 | The place of patients and carers in decision-making is widely treated as informative rather than consultative – more active participation is reliant on nurse or relative advocacy | SSD, p. 2 |
| 2 | Doctors have a preference for social and functional information about patients to be available in notes So, if detailed social and functional information about patients is available to EDs, then better admission/discharge decisions can be made (this info may be from family/carers or in GP letter of referral) |
CP 6 November 2014, pp. 3–4 EPW(A), 20 November 2014 |
| 3 | Relatives under pressure are far less reticent than patients or care workers about challenging decisions made by doctors | SSD, p. 4 |
| 4 | Patients, carers and practitioners collaborate (a ‘pact’ within a resource-constrained system) to make the best use of time, self-help, the acute bed, and teams within and outside the hospital | E1 |
| 5 | If patients or carers perceive that practitioners are busy or that other patients have greater need than their own, then they may effectively ration the care they receive by not making requests from practitioners and therefore receive less than optimal care. However, if patients perceive there is an unfair allocation of time and resources, then they may feel unsatisfied and complain But also There is, broadly stated, a generational gap: people born c. 1960s onwards are more likely to expect (and demand) prompt attention to their care than people born before the 1960s |
E5 Endorsed at EPW(C), 20 November 2014 CP, 9 December 2014, p. 23 |
| 6 | Patients and their families/carers are heterogeneous: there may be differences of opinion within families/between carers, or between families/carers and patients | E1 |
| 7 | Where there is a mismatch between the time that relatives want to talk about a patient and the time a practitioner has available, patients/families can feel they are giving ‘over the odds’ in rationing their own expectations of care | E1 |
| 8 | If patients or relatives expect that they are to be admitted (if the GP, ED department or other practitioner has led them to believe this, or if they hold a strong view on this), then it is more likely the patient will be admitted | E1 Endorsed at EPW(D), 20 November 2014 |
| 9 | In making decisions, staff assess the potential for family contributions to transport and home care against the balance of patient safety and mobility And The distance of the patient’s home from the ED is considered in the admission decision |
E1 CP, 9 December 2014, pp. 28–9 |
| 10 | Seniors are said to be more assertive than juniors in withstanding relatives’ pressure to admit an elderly relative when this is not in the patient’s interest | E1 |
| 11 | If patients and relatives’/carers’ preferences align with practitioners’ views, then it is more likely that these will be taken into consideration in decision-making | E1 |
| 12 | If relatives are treated as a resource (of information) by practitioners, then they are less likely to be treated as equal partners in decision-making | E1 |
| 13 | If patients’ (and carers’) concerns and fears are elicited and addressed then, even where the decision is a change from what was expected, they will be more likely to be satisfied with the decision and leave with a positive ongoing relationship with health care | |
| 14 | Patients and carers adopt different approaches to engaging with practitioners, for example adopting clinical language and self-observation roles (aiming for collegiate level of dialogue with staff) or using lay terms and accentuating their vulnerability and dependence on the system (aiming for consideration and compassion) | E1 |
| 15 | The common aim of patients/relatives engaging with practitioners is for information and regular updates about the patient’s status within the system | E1 |
| 16 | If practitioners explicitly involve patients/carers in decision-making, stating what the options are for treatment plans and admissions, then time in hospital may be reduced or admissions avoided and patients will be more satisfied with their experience. However, this is unlikely to apply to all patients; for example, the very unwell, some older people, and people with confusion are likely to gain more satisfaction through handing over decision-making to others | E1 EPW(A), 20 November 2014 |
| 17 | If reliable information is available from primary care, carers and other sources about the patient’s medical history and care needs, then a more secure diagnosis and decision can be made Whereas If information is not available from primary care and other community resources (e.g. care homes), then patient and relative accounts of need/history are heavily relied on such that patients and carers feel they are responsible as ‘holders of information’ |
CP, 6 November 2014, p. 3 |
| 18 | ED decision-making is pared down, rapid, done assertively with partial information, may be incomplete, and carries a degree of risk But The medical community as a whole is anxious to avoid missing potentially important diagnoses, so diagnostic investigation is often considered necessary from a medical perspective |
SSD, p. 1 LS, 15 October 2014 CP, 9 December 2014, p. 4 |
| 19 | While patient safety is the primary consideration in decision-making, the basis of the decision can also be centred on what is safest for clinicians, the hospital, other patients or the community – but often the default is to admit | E2 |
| 20 | If there is an acute bed shortage and pressure from management to decrease admissions, then clinicians may feel pressurised to discharge inappropriately (potentially causing patients harm) | |
| 21 | Growth in A&E attendance (2009–13) national average 5% per year; 1.8–3.8% in case study hospitals | HES |
| 22 | Nationally, 34.6% of emergency admissions are patients aged over 70 years. In our study hospitals, this figure ranges from 33.3% to 40.0% | HES |
| 23 | All four hospitals in this study had emergency readmission rates (at 2, 7 and 30 days) that were a little lower than the national average | HES |
| 24 | The ED is low status yet highly useful for other departments, simultaneously heroic and disastrous in media representation, and persistently (and rapidly) reconfigured | SSD, p. 2 |
| 25 | The ED never has the option to refuse | SSD, p. 1 |
| 26 | Practitioners develop a ‘clinical eye’ for patient presentation (pathology, dress/demeanour, ability to cope) and attempt to rapidly apply this within resource constraints and desire to deliver patient-centred care | SSD, p. 2 |
| 27 | While making a diagnosis is considered very important by some clinicians, others handle risk by ‘ruling out’ risk factors rather than ‘ruling in’ | E2 |
| 28 | Audit, clinical quality indicators, and a culture of admission avoidance guide decision-making, but almost always tempered by a ‘worst case scenario’ outlook | E2 |
| 29 | Practitioner confidence in decision-making is based on:
|
E2 |
| 30 | If there is more than one team involved in the care of the patient (such as a specialist medical team), then there can be confusion between practitioners about who is responsible for the care of the patient | VSM Endorsed at EPW(C), 20 November 2014 |
| 31 | Teams vary in their readiness to ‘share the burden’ of unscheduled care | SSD, p. 2 |
| 32 | Practitioners become disillusioned by efficiency drive that leads to patients being ‘packaged and shipped’ | SSD, p. 5 |
| 33 | If there is more than one team involved in the care of the patient (such as a specialist medical team), then there can be a delay in decision-making until the specialist can respond to the ED request | VSM |
| 34 | If there were more decision-makers (not necessarily doctors), then patients’ pathways would be smoother | LS, 15 October 2014 |
| 35 | Discussion with colleagues almost always takes place before decisions are made by practitioners | SSD, p. 1 |
| 36 | If the patient is in a seated area, such as an ambulatory unit where they are not ‘packaged as a patient’, then practitioners, patients and relatives are less likely to believe that a decision has been made to admit | |
| 37 | If practitioners explicitly state to patients and carers what the options are for discharge, admissions and related treatment plans early in the process, then time in acute care settings may be reduced or admissions avoided and patients will be more satisfied with their experience But note Practitioners strive for efficiency and speedy passage of the patient through the system. Outside formal patient assessment procedures, a minimum of time is allocated for communication, explanation and provision of the updates that patients and carers require. This can have negative effects on patient experience |
E7 SSD, p. 5 |
| 38 | If practitioners inform patients of the possible length of waiting times and reasons for waiting, then the patients are less likely to feel frustrated about waiting and more likely to express satisfaction about their experience | E7 EPW(A), 20 November 2014 |
| 39 | If a doctor has more experience (of the local system) then that doctor may make use of other services available to him/her to avoid an admission (e.g. hospital ACE team, community specialist nurses, community beds) | VSM EPW(B), 20 November 2014 E8 |
| 40 | Resource and time constraints may sway doctors towards admission as a safer option | SSD, p. 2 LS, 15 October 2014 |
| 41 | If it will be a complex, time-consuming process to arrange for a patient to be discharged (e.g. if community resources are needed) and where there are staffing pressures and a high level of acutely ill patients, then a patient will be more likely to be admitted, as it is the ‘line of least resistance’ | E4 EPW(C), 20 November 2014 |
| 42 | If ED doctors can refer to ‘hot’ clinics, where patients will be seen as an outpatient within a short time frame, then they will feel more confident about discharging | Case studies E8 |
| 43 | 4-hour A&E breaches account for ≈ 6% patients nationally. In the study hospitals, 4-hour breach rates ranged from ≈ 5% to 8%. | HES |
| 44 | If time is required to assess a patient’s mobility and home care conditions, then ‘avoidable’ admissions will occur to avoid breaches | SSD, p. 3 |
| 45 | Many tactics to avoid breaches (e.g. observation and short-stay units, and other initiatives) – so many that staff joke about the proliferation of acronyms | SSD, p. 5 |
| 46 | Specialist teams may ‘add nothing’ other than an additional step | LS, 15 October 2014 |
| 47 | Practitioners feel sanctioned when penalties (for breaches) are incurred | SSD, p. 1 |
| 48 | There can be a tension between meeting targets and providing patient-centred care | LS, 15 October 2014 |
| 49 | Practitioners have negative feelings about uncertainties over which they feel they have little control (e.g. referral possibilities, forward care options, resource constraints) | SSD, p. 3 LS, 15 October 2014 |
| 50 | Practitioners complain about the pressure they are under and at the same time speak of the enjoyment that teamwork and a sense of purpose bring | SSD, p. 1 |
| 51 | Conversion rate from A&E attendance to inpatients is ≈ 22% nationally. In the study hospitals, conversion rates ranged from ≈ 26% to ≈ 38% | HES |
| 52 | Nationally, there has been ≈ 0.4% growth in emergency admissions. Growth rates in our study hospitals ranged from ≈ 2.6% per year to 1.9% | HES |
| 53 | A model incorporating the local deprivation index and the proportion of the population aged over 65 years was created to predict admission rates from the local population; predicted admission rates for an equivalent population size would range from 89% to 107% of the national average | HES |
| 54 | If CT scan and blood test results could be turned around faster in the afternoon, then patients would be less likely to be admitted as they wait for results | VSM |
| 55 | If the test results are highlighted on the computer system when they become available, then clinicians are able to act more quickly on this information | Case studies EPW(A), 20 November 2014 |
| 56 | Different parts of the system have different time frames | SSD, p. 2 |
| 57 | If a GP-referred patient attends the ED (rather than via another acute medical route), then the patient’s first point of contact with a doctor will be sooner. This is because the assessing doctor will have spoken to the patient’s GP on the phone prior to speaking to the patient | VSM |
| 58 | If staff attrition occurs to the extent that there is insufficient time for training and multiple unfulfilled vacancies, then avoidable admissions increase | SSD, p. 5 |
| 59 | If a consultant is involved in the care of a patient, then that patient is less likely to be admitted to hospital | VSM |
| 60 | All of our study hospitals showed a similar weekly pattern in emergency admission: ≈ 15% of all admissions occur each weekday and 12% of all admissions occur on each of Saturday and Sunday. This weekend decline is due to reduced GP referral | HES |
| 61 | If there is an alternative admission or assessment pathway, then this can affect the admission rate for those who attend EDs (e.g. AGPS diverts some patients, so those who end up in the ED with chest pain have a higher admission rate) | VSM |
| 62 | If experienced physicians are involved in a conversation with GPs at the time of referral, then they are more likely to avoid admissions by giving advice and options than if calls are taken by nursing staff | E6 |
| 63 | Teaching junior doctors within the ED leads to more face-to-face time with the patient but longer patient journey time while the junior doctors learn | VSM |
| 64 | If a member of a specialist team (e.g. ACE) becomes involved in a case, then the responsible clinician/doctor may pass decision-making on to this specialist; however, this is not always the case and can cause confusion in the decision-making process | CP, 6 November 2014, p. 2 |
| 65 | Where there is uncertainty about diagnosis, the ability of the patient/carers to cope at home, and community service provision, the default (safest) option is to admit (this uncertainty can be compounded if available information is incomplete) Whereas If clinicians are confident that medical follow-up and nursing/rehabilitative/social care will be provided in the community (e.g. virtual ward), then admission can be appropriately avoided for complex but non-acute patients |
CP, 6 November 2014, pp. 2–3 CP, 6 November 2014, p. 9 |
| 66 | The time of day or week (availability of other services) and current workload within EDs affects the decision-making process | CP, 6 November 2014, p. 3 |
| 67 | Carers are reluctant to ‘waste’ hospital time by advocating admission where nursing or rehabilitative care is (probably) needed but there is not an acute (inpatient) medical need | CP, 6 November 2014, pp. 7–8 |
| 68 | If a patient is brought in to the ED with hospital transport, but cannot be sent home by the same method, avoiding an admission by giving that patient an outpatient appointment and sending the patient home late in the evening may cause distress to the patient and may be a less compassionate solution than admitting the patient | CP, 6 November 2014, p. 13 |
| 69 | If there are restrictions on diagnostics, such as scanning, then decisions on admission/discharge are more difficult | CP, 6 November 2014, p. 15 |
| 70 | (Even senior) clinicians find it difficult to make decisions from the history alone; they also gain valuable information from ‘eyeballing’ the patient and ‘chatting to them’. If they are able to do this then they can make more secure decisions about admission/discharge | CP, 6 November 2014, p. 16 |
| 71 | Clinicians have normalised the view that they are working in an imperfect system where pragmatic decision-making based on the availability of resources has to be made | CP, 6 November 2014, p. 15 |
| 72 | If there is diagnostic uncertainty, if ‘watchful waiting’ is required, and if the management of a patient requires liaison between medical specialties/hospital departments, then the pressure of managing acutely unwell patients in EDs leads to a high risk of overlooking ‘watchful waiting’ patients and making less appropriate admission decisions about them | CP, 6 November 2014, pp. 18–19 |
| 73 | Time targets drive ‘do something now’ decisions rather than enable ‘how can we get this person home?’ decisions But conversely ‘The 4-hour target has helped us immensely to solve a lot of problems’ (because it’s a target to aim for) However If patients are near to the 4-hour target, then inappropriate decisions to admit are more likely |
CP, 6 November 2014, p. 19 CP, 6 November 2014, p. 26 LS, 15 October 2014, p. 2 EPW(C), 20 November 2014 |
| 74 | If a patient falls between two specialist teams and where there is discord between these teams on patient pathway, then the hospital stay may be unnecessarily extended and the patient is frustrated by lack of clear progress on decision-making | CP, 6 November 2014, p. 21 |
| 75 | If practitioners in the ED do not follow the protocol preferred by a specialist department for referrals, then the referral may take longer to be processed and a wait may be incurred for the patient | CP, 6 November 2014, p. 21 |
| 76 | If a patient has a difficult experience of a stay in acute care, then that patient may become averse to using the service in the future | CP, 6 November 2014, p. 21 |
| 77 | If patients are not kept informed about decision-making and plans for their treatment, then they become frustrated and regret the decision to attend the department | CP, 6 November 2014, p. 21 CP, 9 December 2014, pp. 4–6 |
| 78 | If early diagnostic testing is not actioned in the ED, then the process can slow down when other specialties take over and the sense of ‘urgency’ is lost | CP, 6 November 2014, p. 22 |
| 79 | If patients have a certain set of expectations about admission/discharge, they can become frustrated if the expectations are not met | CP, 6 November 2014, p. 23 |
| 80 | It is not the type of setting the patient first goes to (e.g. ED or MAU) that leads to quicker medical assessment, but the communication (e.g. with GP) that has taken place prior to the patient reaching hospital | EPW(A), 20 November 2014 |
| 81 | For GPs, keeping people in the community causes them discomfort, fear, worry, potentially extra work and the ‘jeopardy’ of what happens if things go wrong | EPW(A), 20 November 2014 |
| 82 | If GPs can communicate easily with a specialist regarding acute problems and can access alternatives such as ‘hot clinics’, then admission to hospital and unnecessary use of resources can be avoided And equally If ED doctors can communicate easily with a patient’s GP about specialist (non-acute) outpatient investigation, then admission to hospital and unnecessary use of resources can be avoided |
EPW(A), 20 November 2014 CP, 9 December 2014, p. 10 |
| 83 | GPs share risks with their wider medical community in decision-making, whereas nurses (e.g. in an AGPS) largely have individual accountability for their decisions. This leads to a lower tolerance of risk, as the price of getting it wrong for the individual professional is higher | EPW (group), 20 November 2014, p. 29 |
| 84 | If there are conflicts between patients and relatives or carers about admission decisions, then practitioners may need to negotiate a mutually acceptable decision | E1 |
| 85 | If there were a better relationship between junior doctors in EDs and specialists (outside EDs), then referral and co-ordination processes would be improved | EPW(B), 20 November 2014 |
| 86 | Contingent factors that moderate no. 59
|
EPW(C), 20 November 2014 |
| 87 | Endorse no. 61 – hones service delivery so it is clinically appropriate and delivered in the best location. Note that the following factors can impact on successful implementation:
|
EPW(C), 20 November 2014 |
| 88 | 4-hour target was initially useful (spurred action to address unacceptable waits in EDs), but has now ‘outlived its usefulness’ | EPW(C), 20 November 2014 |
| 89 | No. 62 insufficiently reflects grades/levels of experience of practitioners – reword as: If experienced physicians are involved in a conversation with GPs at the time of referral, then they are more likely to avoid admissions by giving advice and options |
EPW(D), 20 November 2014 |
| 90 | Revision to enhance applicability across different EDs: If the patient is in a seated area, then practitioners, patients and relatives are less likely to believe that a decision has been made to admit |
EPW(D), 20 November 2014 |
| 91 | Addition to no. 55: or if Near Patient Testing, in concert with an appropriately qualified and experienced ‘rapid action’ team (to make decisions and deliver care), is available |
EPW(D), 20 November 2014 |
| 92 | If nurses and OTs feel disempowered to make and act on discharge decisions, then effectiveness of the ACE team is contingent on senior specialist presence | E8 |
| 93 | If carers and relatives were more informed of alternatives to ED attendance, then they could put less pressure on staff to admit them to ED | E8 |
| 94 | No. 70 reflected in the depth of discussion about a ‘patient case summary’ and whether or not investigation was warranted given past history and social context | CP, 9 December 2014, pp. 15–18 |
| 95 | Often a decision is based on a worst-case scenario basis, tempered by the threat of blame or punitive sanctions. These can be governed by audits and guided by clinical quality indicators, particularly where there is a culture of admission avoidance within a strict time frame | SSD, p. 1 |
| 96 | While patients or carers, in line with NHS policy, might aspire to ‘involvement’, practitioners can refer more to the ‘influence’ or ‘impact’ of these parties on decision-making. An example of ‘influence’ could be the practitioner knowing that a patient is anxious, or lives alone, even though the patient has not enunciated this | SSD, p. 3 |
| 97 | Determining whether or not symptoms warrant a visit to the ED can be confusing for patients and carers. The decision is frequently driven by anxiety, but it is often mediated by patients’ and carers’ levels of knowledge and understanding about the symptoms, underlying conditions and the patient’s medical history | SSD, p. 4 |
| 98 | Even in the midst of the pressured environment of emergency services, there are many instances of staff’s sensitive communication with patients and engagement with their personal situations | SSD, p. 4 |
| 99 | A certain proportion of avoidable acute admissions fall within the tolerance zone of ‘boarding’, which is made more elastic by staff in response to limitations in families’ ability to provide timely transport and home care | SSD, p. 4 |
| 100 | Staff sometimes make assumptions about a patient’s level of understanding and tolerance of uncertainty. It is in this area that patient satisfaction and retribution to carers could be improved, through regular checks to ask, listen, inform and receive input at different stages in decision-making | SSD, p. 5 |
| 101 | While striving to attend the flow of patients arriving, professionals also contribute to keeping emergency care systems going by devising and testing new initiatives to reduce avoidable admissions. These are multiplying to such a degree that staff are hard pressed to remember the acronyms, uses, pathways, teams and locations of units created to absorb or deflect some of the flow | SSD, p. 5 |
| 102 | A resource for decision-making that is valued by clinicians – time for observation, to see a case evolving and be better able to assess risk – is made more scarce under the pressure of the 4-hour target. To accommodate this need and to avoid breaches, new units are created (such as observation and short-stay units) to house patients who are thus ‘taken off the clock’ | SSD, p. 5 |
| 103 | Most decisions were made close to the 4-hour target; clinical panel review suggested this could lead to suboptimal decision-making | VSM CP |
| 104 | Early senior involvement can reduce patient journey time, but was not significantly associated with higher discharge rates. The site that exhibited the greatest amount of senior involvement also had supporting factors (dedicated consultant ‘controller’, CDU for observation, ambulatory care pathway, AGPS) | VSM |
| 105 | Differences in waiting times for, for example, hospital transport or a bed in different EDs are associated with significant differences in staff costs | VSM EA |
| 106 | Single-entry-point EDs are associated with longer pre-assessment waits for patients | VSM |
| 107 | Tentatively, longer waiting times for decisions and management planning are associated with shorter overall time in acute care | VSM |
| 108 | Tentatively, within acute care it costs more to discharge than to admit to hospital (although not at all sites – however, sites where it was not more costly had higher postassessment waste) | EA |
| 109 | Patient decisions about attending acute care were often directed by GPs, other health professionals, or ‘111’ service advice | VSM |
| 110 | Analytical statement: If complex, often elderly, patients were referred to practitioners with knowledge of community resources for safe discharge, admissions would be more likely to be avoided (these practitioners would most commonly be OTs, physios or social workers working as part of ‘discharge’ teams) But The availability of these resources were determined by geography/health and social care boundaries, and OTs and physios were accustomed to dealing with a great deal of complexity in determining the provision available to a particular patient within their home locality And If these patients were not identified by the team in ED or AMU, they were in danger of being lost in the system of the general hospital, where the impulse to discharge is dissipated and community solutions take longer to achieve |
E9 |
| 111 | Analytical statement: If seniors (geriatricians) from specialist teams for elderly people reviewed complex, elderly patients in ED and MAU they could organise timely specialist outpatient appointments, thus facilitating a safe discharge But See no. 92 And This service was not widely available out of hours or at weekends |
E10 |
| 112 | If a patient attends an unscheduled care department out of hours (i.e. evening, weekends and bank holidays) then the likelihood of an admission is increased because
|
E11 |
| 113 | If practitioners felt the weight of responsibility was on them to make a difficult decision, they perceived their professional reputation was at stake And If they did not feel sufficiently supported in decision-making they feared an unsafe discharge would impact negatively on their sense of self-worth |
|
| 114 | Practitioners were also more comfortable in making a decision if the patient or carer bore some of the risk themselves |
Appendix 14 Models of care and floor plans
FIGURE 20.
Models of care at the time that the sites were recruited to the study.
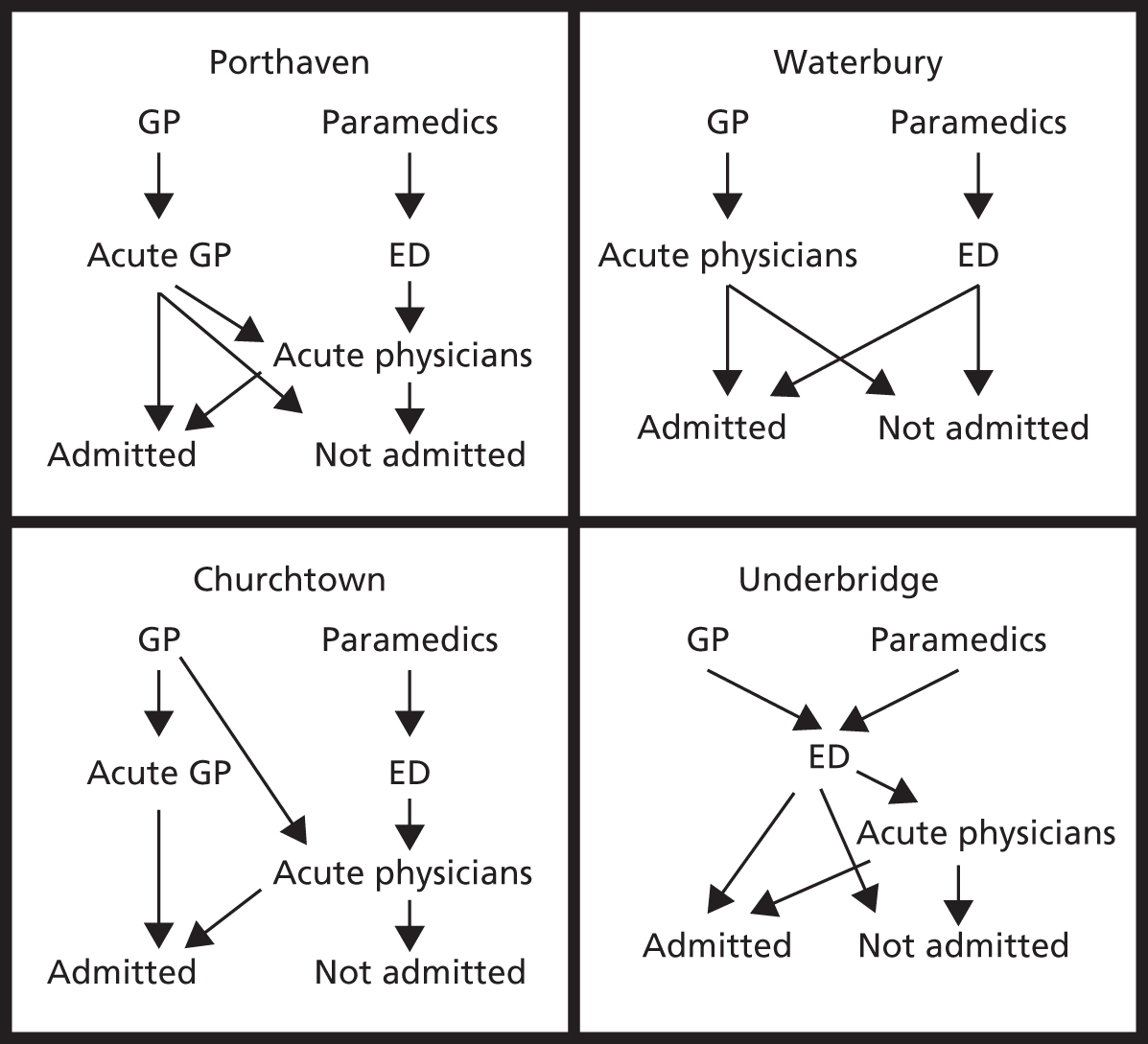
FIGURE 21.
Floor plans of the majors areas of the EDs at the four sites, showing layout of cubicles, beds and staff desks. The red blocks show the central desk areas; beds are shown in blue.
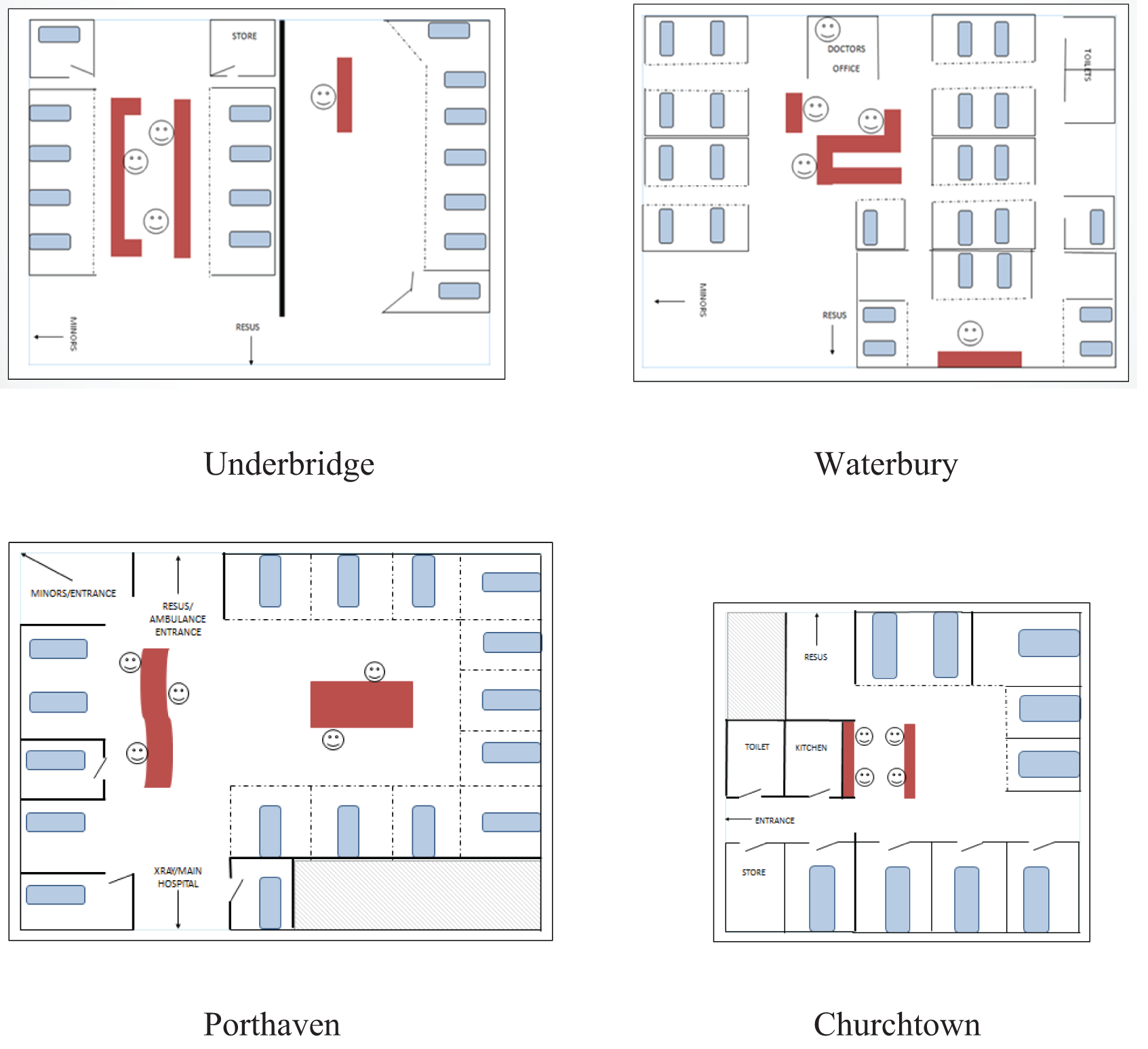
Appendix 15 Value stream maps
FIGURE 22.
Value stream maps for each site: (a) Churchtown; (b) Porthaven; (c) Underbridge; and (d) Waterbury. max., maximum; min., minimum.



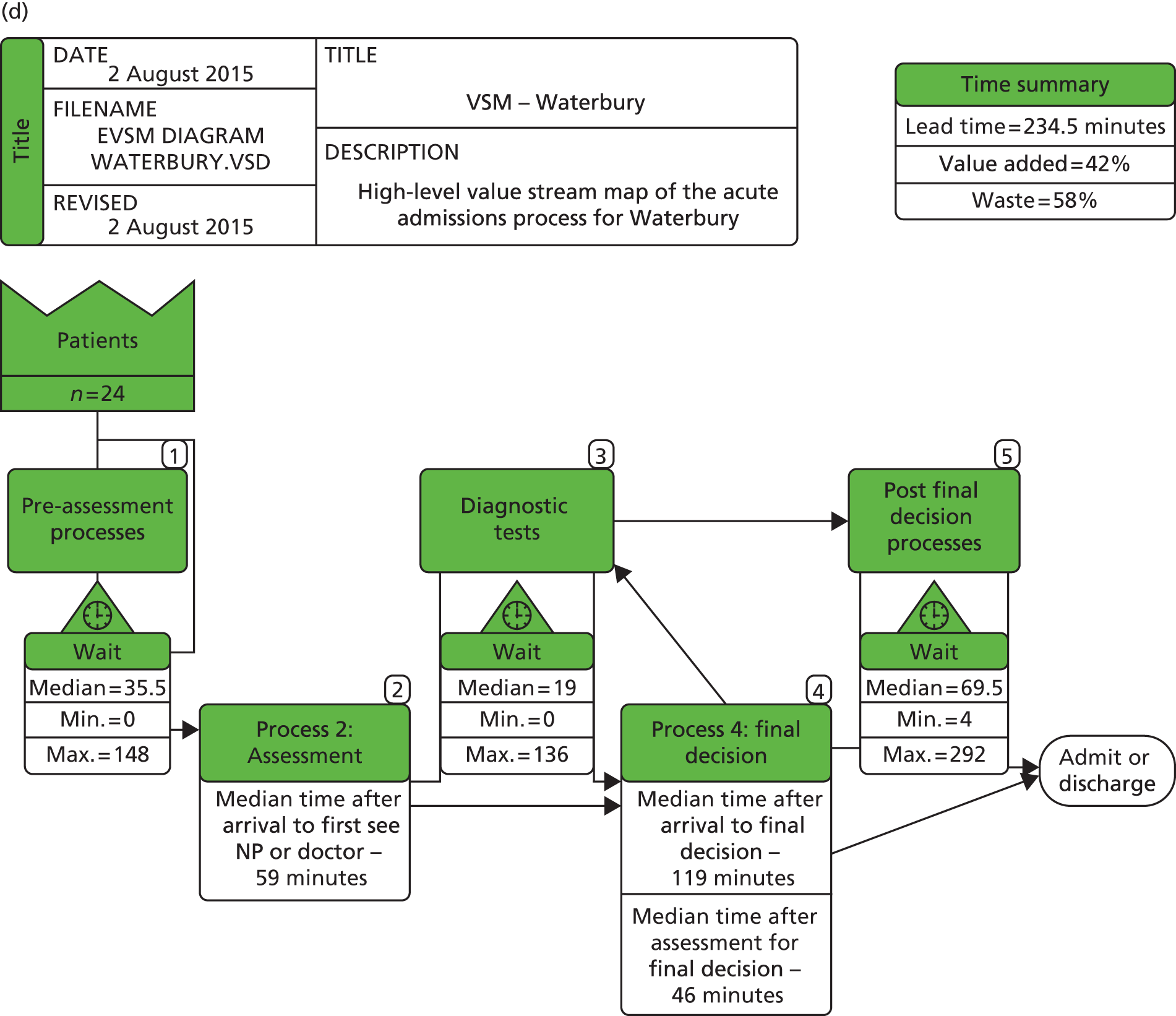
Appendix 16 Value stream mapping timings
Data example 1
On holiday with friends, but had shortness of breath so phoned 111. They sent him to the walk-in medical centre, who called an ambulance to take him the 30 miles to hospital.
| Study ID | Start time | End time | Duration (hours:minutes) | Comment on what is observed |
|---|---|---|---|---|
| VBP107 | 11.00 | 11.00 | Arrival | |
| VBP107 | 11.00 | 11.06 | 00:06 | Wait |
| VBP107 | 11.06 | 11.14 | 00:08 | Junior doctor with patient taking blood sample |
| VBP107 | 11.12 | 11.24 | 00:12 | Senior doctor with patient discussing symptoms |
| VBP107 | 11.19 | 11.20 | 00:01 | Junior doctor with patient |
| VBP107 | 11.20 | 11.36 | 00:16 | Wait |
| VBP107 | 11.36 | 11.44 | 00:08 | Senior doctor finds letter from GP in records |
| VBP107 | 11.44 | 11.47 | 00:03 | Senior doctor with patient discussing letter |
| VBP107 | 11.47 | 11.57 | 00:10 | Wait |
| VBP107 | 11.57 | 12.00 | 00:03 | Senior doctors discussing the patient and arranging AMU transfer |
| VBP107 | 12.00 | 15.02 | 03:02 | Wait and possibly tests |
| VBP107 | 15.02 | 15.02 | Admitted to AMU |
This patient was on a golfing holiday with friends but had shortness of breath very early on so called 111 for advice. He ended up in ED and quickly a decision was made that subject to a clear chest X-ray he could go home because a minor allergic reaction was suspected. However, then the consultant found a GP letter in his file which suggested he may have had a heart attack and put him in a much higher risk group, so the decision was then made to keep him in.
Data example 2
Patient has been having episodes of feeling very sweaty and clammy, and being quite vacant, lasting up to 10 minutes, for last 2–3 weeks. This morning husband was worried she may have been having a stroke. Tried to call GP surgery at 08.45 but unable to get through. Had number of district nurse who had visited a few weeks earlier to do MRSA swab before cataract surgery (does not have regular involvement with the district nurses), who advised him to call 999. Ambulance brought her to hospital with suspected TIA or stroke.
| Study ID | Start time | End time | Duration (hours:minutes) | Comment on what is observed |
|---|---|---|---|---|
| VAP119 | 10.56 | 10.56 | Arrival | |
| VAP119 | 10.56 | 11.08 | 00:12 | Wait |
| VAP119 | 11.08 | 11.15 | 00:07 | HCA with patient doing observations, ECG |
| VAP119 | 11.15 | 11.23 | 00:08 | HCA writing in notes |
| VAP119 | 11.23 | 11.26 | 00:03 | HCA checking blood glucose |
| VAP119 | 11.26 | 11.27 | 00:01 | Wait |
| VAP119 | 11.27 | 11.35 | 00:08 | Doctor 1 (consultant) in with patient |
| VAP119 | 11.35 | 11.37 | 00:02 | Doctor 1 talking to researcher |
| VAP119 | 11.37 | 11.39 | 00:02 | Doctor 1 on computer for old notes – computer not working |
| VAP119 | 11.39 | 11.57 | 00:18 | Doctor 1 reviewing old notes on different computer, writing in notes |
| VAP119 | 11.52 | 11.54 | 00:02 | Nursing staff discussion at desk re need to give IV dextrose as glucose dropping – waiting for consultant to return but no action taken |
| VAP119 | 11.57 | 11.59 | 00:02 | Doctor 1 on phone to diabetes specialist nurse – was told would be down to see patient in less than an hour |
| VAP119 | 11.59 | 12.04 | 00:05 | HCA taking bloods |
| VAP119 | 12.04 | 12.09 | 00:05 | Wait |
| VAP119 | 12.09 | 12.10 | 00:01 | Doctor 1 explaining to patient need for diabetic nurse review and then should be going home |
| VAP119 | 12.10 | 12.12 | 00:02 | Wait |
| VAP119 | 12.12 | 12.12 | 00:00 | HCA in with patient asking re food and drink |
| VAP119 | 12.12 | 12.16 | 00:04 | Wait |
| VAP119 | 12.16 | 12.16 | 00:00 | HCA brought in food and drink for patient |
| VAP119 | 12.16 | 14.10 | 01:54 | Wait |
| VAP119 | 14.10 | 14.12 | 00:02 | Doctor 2 (consultant) in with patient to explain need to go to CDU lounge to await diabetic nurse review, who will also speak to husband when he arrives |
| VAP119 | 14.12 | 14.15 | 00:03 | Wait |
| VAP119 | 14.15 | 14.16 | 00:01 | Nurse in to patient to explain need to get dressed as going to CDU lounge |
| VAP119 | 14.16 | 14.24 | 00:08 | Getting changed behind closed curtains |
| VAP119 | 14.25 | 14.27 | 00:02 | Wait, during which time daughter and husband arrive |
| VAP119 | 14.27 | 14.28 | 00:01 | Travel to CDU lounge |
| VAP119 | 14.28 | 14.38 | 00:10 | In bathroom, then discussion with diabetes nurse |
| VAP119 | 14.39 | 14.46 | 00:07 | Diabetes specialist nurse discuss with husband re change in insulin type and dose, and how to manage hypos |
| VAP119 | 14.46 | 14.47 | 00:01 | Doctor 2 interrupts to explain the prescribed insulin device was not available in the hospital pharmacy |
| VAP119 | 14.47 | 14.55 | 00:08 | Diabetes specialist nurse finishes discussion with husband, she plans to speak to pharmacy about insulin devices |
| VAP119 | 14.55 | 15.45 | 00:50 | Wait for new medications to be organised |
| VAP119 | 15.45 | 15.45 | Discharged |
This patient had experienced a number of short-lived vacant sweaty episodes. Her husband and district nurse were concerned this was due to a stroke, so called an ambulance. When she was seen by a doctor it was felt these were due to hypoglycaemic episodes and that a change in treatment for her diabetes would allow her to be discharged home. The doctor arranged for a diabetes specialist nurse to review the patient, and because of a delay in the nurse’s attendance the patient was moved to the CDU. There was further delay in getting the correct prescription issued, and the patient was then discharged home.
List of abbreviations
- 3A
- Avoidable Acute Admissions
- A&E
- accident and emergency
- ACE
- acute care of the elderly
- ACU
- ambulatory care unit
- ACUA
- acute care unit A
- AEC
- ambulatory emergency care
- AFO
- admit for observation
- AGPS
- acute general practitioner service
- AMU
- acute medical unit
- ANOVA
- analysis of variance
- ANP
- advanced nurse practitioner
- CCG
- Clinical Commissioning Group
- CDU
- clinical decision unit
- CT
- computerised tomography
- ECG
- electrocardiogram
- ECP
- emergency care practitioner
- ED
- emergency department
- EPIC
- Emergency Physicians Integrated Care
- GP
- general practitioner
- HCA
- health-care assistant
- HCP
- health-care professional
- HES
- Hospital Episode Statistics
- IDT
- integrated discharge team
- MAU
- medical admissions unit
- MDU
- medical day unit
- MNP
- medical nurse practitioner
- MTU
- medical triage unit
- NIHR
- National Institute for Health Research
- OPAL
- older person’s assessment and liaison
- PE
- pulmonary embolism
- PenCLAHRC
- Collaboration for Leadership in Applied Health Research and Care South West Peninsula
- PFC
- patient flow co-ordinator
- PPI
- patient and public involvement
- RQ
- research question
- SHO
- senior house officer
- SWAT
- Senior With A Team
- TIA
- transient ischaemic attack
- UTOPIA
- unscheduled treatment of patients in the acute sector
- VSM
- value stream mapping