Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 10/1007/02. The contractual start date was in September 2011. The final report began editorial review in October 2014 and was accepted for publication in April 2015. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2016. This work was produced by Mannion et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction
Policy context
The UK NHS is widely acknowledged as providing some of the best health care in the world, with the vast majority of patients receiving care which is safe and effective. 1 However, as in every other health system, not all care is as safe as it could be and, although estimates vary, there is growing evidence to suggest that about 1 in 10 patients admitted to hospital may be harmed as a result of their care. 2 This harm is not limited to minor events but is often serious, including major iatrogenic disability, health-care-associated infection (HCAI) and avoidable deaths. In addition to human suffering, this results in significant financial costs, with prolonged hospital stays alone costing over £2B per year. 3 In response to evidence of widespread harm there has been a concerted effort to make health care safer, and numerous initiatives and significant resources are being invested in developing national and local strategies to improve patient safety in NHS organisations. However, change has proved difficult to effect and the optimal mix of strategies remains unclear, with the NHS acknowledging that it is not yet able to prevent errors and major service failures recurring. 4,5
Over the past decade it has become increasingly recognised that most harm to patients in hospital settings is not deliberate, negligent or the result of serious incompetence. Instead, harm more usually arises as an emergent outcome of a complex system in which typically competent clinicians, professionals and managers interact in inadequate systems and unsafe organisational environments. Yet we still know very little about the role of organisational and governance processes in developing safer health-care environments. More specifically, we know very little about how hospital trust boards can contribute to safer patient care, although such boards have been the focus of increasing scrutiny for shortcomings in its governance role. Most recently, the report of the public inquiry into Mid Staffordshire NHS Foundation Trust concluded that unnecessary suffering and neglect of patients was primarily caused by a serious failure on the part of the hospital trust board, which ‘did not listen sufficiently to its patients and staff or ensure the correction of deficiencies brought to the trust’s attention. Above all, it failed to tackle an insidious negative culture involving a tolerance of poor standards and disengagement from management and leadership responsibilities’. 4 Similar failures in hospital board leadership and governance are a recurring theme of earlier inquiries into hospital scandals in the English NHS, including the tragic events at Bristol Royal Infirmary in the 1990s, and date as far back as the late 1960s, with the inquiry into the mistreatment of long-stay patients at Ely hospital. 6
The changing role of hospital boards in the English NHS
Hospital trust governing boards, as corporate entities with statutory oversight responsibilities, are accountable for the overall quality and safety of the care its organisations provide. These boards therefore have a fundamental governance role in the oversight of quality and safety, which involves defining priorities and objectives, crafting strategy, shaping culture and designing systems of organisational control. Hospital boards in the English NHS have traditionally shared many similarities with the Anglo-Saxon private sector unitary board model, which typically comprises a chairperson, chief executive, executive directors and non-executive directors (NEDs). 7 All board members share corporate responsibility for key strategic decisions, including the effective oversight of health-care quality and patient safety. Members of the board have specific duties, with the chairperson leading the board [for foundation trusts (FTs), the chairperson also chairs the Council of Governors]. Alongside the chairperson, the chief executive leads the executive arm of the organisation and takes lead responsibility for service delivery.
Within the English NHS, FTs now make up the majority of organisations, with an expectation that all other trusts will follow in due course. At the end of 2013, 147 out of 230 NHS providers in England (64%) (including acute and mental health hospitals and ambulance services) operated as NHS FTs, which have greater freedoms than other types of hospitals and are based on co-operative and mutual traditions. 8 Governance arrangements in FTs are locally determined within a national framework and non-executive board members are appointed by the governors of the hospital, rather than by the NHS Appointments Commission.
The FT ‘social ownership’ model of governance incorporates three tiers of accountability: (1) the membership, (2) the board of governors and (3) the management board. Eligibility criteria for membership include residency (‘the membership community’), patients in the preceding 3 years, staff and representatives of partner agencies on the board of governors. Members have voting rights for electing representatives to the board of governors and have the right to be consulted on key strategic issues. The management board is accountable to members for ensuring developments consistent with the needs of its community of stakeholders across ‘the local health economy and wider NHS’ and for ensuring that a trust’s activities comply with the terms of its licence. The board of governors is charged with acting as a vehicle for influencing change and development – essentially a strategic rather than an operational role. Governors are required to represent communities and hold a responsibility for feeding back discussion to these communities, serving a twofold role of community liaison and linking with members (downwards) and oversight and accountability of FT activities (upwards). There has been no previous research exploring the relative role and influence of boards versus boards of governors in FTs with regard to patient safety.
Recent years have witnessed a stream of formal guidance designed to strengthen NHS board governance in the light of lessons learned from private sector corporate scandals and failures, including:
-
The Healthy NHS Board: Principles for Good Governance 9
-
The NHS Integrated Governance Handbook: a handbook for executives and non-executives in health-care organisations10
-
The Intelligent Commissioning Board: understanding the information needs of Strategic Health Authorities and primary care trust (PCT) boards11
-
Governing the NHS: A Guide to NHS Boards. 12
Despite a plethora of guidance available to NHS boards on effective leadership and governance arrangements, both in general terms and with specific reference to safe care, we nonetheless still have a meagre evidence base (i.e. drawn from empirical study) on which to offer guidance of effective board practice of patient safety.
Previous work in this area
Prior to this study, what limited evidence existed on board roles and impacts in terms of patient safety and service quality originated mostly from the USA, where several studies have investigated the relationship between governance practices and quality processes and clinical outcomes (see Chapter 3 for a detailed review of the literature and evidence). However, a degree of caution is required when attempting to extrapolate recommendations for effective governance to the NHS context. First, hospitals in the USA operate within a very different economic and political environment, which will necessarily impact on the relative priorities and objectives of boards. Second, all these studies are based on large-scale questionnaire surveys and, although they provide an overview of broad patterns and trends in board practice, they nevertheless fail to capture fully the messy internal processes and behavioural dynamics through which board governance is actually played out and which are best explored through more interpretive and qualitative research designs. Third, these studies have tended to be purely empirical and lack clear theoretical and conceptual frameworks for guiding the collection, analysis and interpretation of data. Finally, these studies focus on the more generic topic of ‘service quality’ rather than the more narrowly defined topic of patient safety.
Contemporary issues and challenges
Effective hospital board oversight in the English NHS currently faces a number of challenges. Changes in the policy landscape, particularly in response to the first Francis public inquiry13 and the Darzi review in 2008,14 have seen quality and safety move up the political agenda. However, the oversight of patient safety is often compromised by the number of competing priorities faced by boards. Recent reports conclude that board discussions concerning patient safety often take second or third place after efforts to ensure that hospital finances and central performance targets are met. 15 Within this context, a key challenge facing board oversight of patient safety is the use of risk-based ratings and measures, which are set by Monitor and the Care Quality Commission (CQC). This has the potential to ‘dilute the message’ of patient safety for boards, in being effectively reduced to a series of national standards and priorities or specific issues and campaigns related to infection control, such as meticillin-resistant Staphylococcus aureus (MRSA) and Clostridium difficile infection rates. 16 Challenges to effective board oversight may also be attributed to boards’ limited knowledge and understanding of patient safety issues and concepts, and many boards currently lack the necessary skills and understanding to make sense of emerging trends in patient safety. Limited knowledge and understanding of patient safety among board members, particularly non-executives, also means they are often inhibited when challenging and posing critical questions about safety issues and concerns. This is particularly the case for NEDs who tend not to have a clinical or operational background in health-care quality. 17
In light of these current challenges facing boards, discussions with key informants in the scoping phase of this study (see Appendix 1 for details) raised a number of suggestions about how board oversight of patient safety could be improved. At the centre of these proposals were concerns about strengthening and building trust through the development of better interpersonal connectedness within its organisation. Rather than a ‘tick-box’ focus on meeting particular targets, it was suggested that oversight needed to become ‘value driven’ in the development of relationships that were more sensitive and responsive to organisational needs and concerns. To accomplish this, particular board activities and practices were highlighted for enhancing trust in organisational relationships. These included providing a greater amount of time and emphasis on board discussions and dialogue about patient safety, developing enhanced leadership skills that allow patient safety to be more visible and seeing board members as ‘stewards’ with a responsibility for developing a culture of partnership within the organisation. Leadership here was seen as critical to ‘set the tone’ for the organisation with regard to prioritising the quality of care.
Moreover, although board oversight was seen as a collective effort, individual board members with specific roles were noted as being key catalysts for action. For example, the chief executive is central in setting the tone, and the chairperson is key to facilitating open discussion. Medical and nurse directors, acting as custodians for clinical governance, also have an important role to play in setting the patient safety culture of the organisation, as do finance directors in supporting patient safety initiatives. Using NEDs to actively challenge executive decisions and to hold the board to account provides important checks and balances. Some boards needed greater input from NEDs in providing the necessary critical reflection in ‘holding up a mirror’ to the organisation by asking critical and probing questions. An additional suggestion for fostering greater interconnectedness with the wider organisation was opening up board business to greater staff, patient and public scrutiny. This is seen as having the potential, not only to further hold the board to account but also to create connections and interactions with the organisation and the community that the hospital served.
Scoping discussions also raised a number of points about the potential over-reliance on formal quantitative performance measures in relation to patient safety, which possibly came at the expense of ignoring insights gleaned through soft intelligence networks. Boards need to have access to different types of information concerning patient safety in order to increase its intelligence about the issues at hand. Greater reliance on dashboards could help to disaggregate information about particular trends within the organisation rather than simply relying on an aggregated picture of the organisation as red, amber or green ratings. For example, the Quality Risk Profiles (QRPs) capturing mortality data, readmission data, and outlier data combined with data on patient outcomes in relation to dignity, nutrition and privacy can provide a useful basis for hospital board discussions. In addition, scorecards and metric-based approaches can be supplemented with narrative or ‘reality checks’ that connect staff concerns and patient experience to quantitative data.
Collectively, these observations demonstrate the potential to support the development of internal board dynamics to facilitate greater dialogue related to patient safety, alongside external board communications to improve the connection with patients and staff. The insights gathered in the scoping discussions thus informed the development and refinement of the research design and the research questions as set out below.
Defining patient safety
As the focus of this study is on patient safety, it is important that we are clear about how we have interpreted the term and used it in our research design and analysis and how it differs from other quality-of-care issues. Charles Vincent defines patient safety as ‘The avoidance, prevention and amelioration of adverse outcomes or injuries stemming from the process of healthcare’. 18 This definition clearly differentiates patient safety from more generic quality-of-care issues by focusing on the ‘dark side of quality’18 and highlighting care that causes harm to patients rather than merely being of a poor or inadequate standard. It also draws attention to attempts to prevent and reduce errors and adverse patient outcomes in recognition that simply trying to avoid error is not in itself enough and one must seek to reduce errors of all kinds. In this study, we have adopted an approach based on Vincent’s definition of patient safety. We also recognise that safety resides in health-care systems (at all levels) as well as people working within such systems. During the fieldwork for this study, and in particular the case studies, it was often difficult to clearly distinguish patient safety from the broader concept of quality. Indeed, the two are synonymous and often conflated in common usage and expression. Although in our analysis we have attempted to separate out issues related to patient safety, in some areas we have found it very difficult to provide a clear-cut distinction between issues specifically related to quality and those specifically related to safety. This should not necessarily be viewed as a deficiency of the study but rather as a reflection of the complexity and ambiguity inherent in the concept and the many ways in which it can be interpreted and applied in health-care contexts.
Aims and objectives of the study
Against this background, our study aimed to generate theoretically grounded empirical evidence on the associations between board practices, patient safety processes and patient-centred outcomes with the aim of improving NHS hospital boards’ understanding, effectiveness and accountability in relation to safeguarding care. The study was undertaken between October 2011 and September 2014.
The specific aims were:
-
to identify the types of governance activities undertaken by hospital trust boards in the English NHS with regard to ensuring safe care in its organisation
-
in FTs, to explore the role of boards and boards of governors with regards to the oversight of patient safety in its organisation
-
to assess the association between particular hospital trust board oversight activities and patient safety processes and clinical outcomes
-
to identify the facilitators and barriers to developing effective hospital trust board governance of safe care
-
to assess the impact of external commissioning arrangements and incentives on hospital trust board oversight of patient safety
-
on the basis of findings relating to points 1–5, to make evidence-informed recommendations for effective hospital trust board oversight and accountability and board member recruitment, induction, training and support.
Research design and project overview
In essence, the study comprised three distinct but interlocking strands:
-
a literature review of the theoretical and empirical literature relating to hospital board oversight of patient safety (undertaken between December 2011 and December 2014)
-
in-depth mixed-methods case studies in four organisations to assess the impact of hospital board governance and external incentives on patient safety processes and outcomes (undertaken between September 2012 and September 2014)
-
two national surveys of hospital board oversight of patient safety which were then linked to routine data on patient safety processes and outcomes (undertaken between March 2012 and April 2013).
Structure of the report
Chapter 2 provides a detailed explanation of the theories and research methods underpinning the study. Chapter 3 presents the findings from the literature review of theoretical and recent empirical work in this area. The next five chapters present the main findings from fresh empirical studies in the NHS: first from case study work in four purposefully selected NHS foundation hospital trusts (see Chapters 4–7) and then from national quantitative surveys of board activity/competence and patient safety performance linkages across English NHS hospital trusts (see Chapter 8). The report concludes (see Chapter 9) with an integration and discussion of the findings and a look forward at the emerging research agenda around these issues.
Chapter 2 Theories of board behaviour and research design
This chapter outlines the theories of board behaviour that underpinned the study and sets out the research design and methods of data gathering and analysis used in the empirical part of the study.
Theories of board behaviour
Several theoretical frameworks of board governance have been developed,19,20 and here we make the distinction between whether boards are conceptualised in either instrumental or symbolic terms. Guidance on the role and conduct of NHS boards is most usually informed by instrumentalist assumptions of the role of boards as forums for deliberation, conciliation and decision-making. On these terms a ‘successful’ board is one that is able to take decisions on corporate strategy in an efficient and effective manner and can monitor its implementation through to organisational success. Four key instrumentalist frameworks can be discerned in the literature:
-
Agency theory is based on the assumption that, unless scrutinised, staff will seek to pursue their own interests rather than wider organisational objectives (opportunism). Here the board is conceptualised as a monitoring device set up to ensure compliance by developing systems of checking, monitoring and control to hold staff accountable for their actions. This approach has previously been used to understand and classify clinical governance strategies in UK hospitals. 21
-
Stewardship theory works on the assumption that staff are motivated by more than their own narrow self-interests and that managers want to do a good job and serve as effective stewards of an organisation’s resources. 22 The theory assumes a high degree of trust, with the focus of the board being on creating a framework for shared values and enabling staff, rather than monitoring and coercing performance.
-
Stakeholder theory assumes a multiplicity of competing and co-operative interests within organisations and focuses on how various stakeholder interests can be addressed, integrated and balanced. 23 The role of board members within this framework is to understand and represent the views of all those with a stake in the organisation, and it is recognised that the board may need to manage complex trade-offs between stakeholders, including staff, patients and the public.
-
Resource dependency theory derives from the strategic management literature and Zahra and Pearce played a significant part in its original development. 24 From this perspective the organisation is seen as an amalgam of tangible and intangible assets and dynamic capabilities. The main function of the board is to successfully manage internal and external relationships to leverage influence and resources. Board members are selected for their background, contacts and skills in mediation and boundary spanning.
In spite of their differences, all four of these instrumentalist theories assume that board members are able to exercise influence over staff and that, via this influence, they lever beneficial change and enhance organisational performance. Garratt25,26 has integrated the insights from both agency and stewardship theories and posits two main areas of board foci, which he terms ‘conformance’ and ‘performance’ (Table 1). Conformance has both external and internal dimensions: external accountability includes compliance with regulatory and legal requirements, as well as accountability to external stakeholders. In contrast, the internal dimension is associated with management control. The conformance dimension, therefore, shares many similarities with the agency theory perspective on governance. The performance dimension, according to Garratt,25 involves governing the organisation to enhance its achievement of goals and objectives. This, again, consists of two main functions: policy formulation and strategic thinking. The performance dimension is thus closely linked to the stewardship theory of corporate governance. This framework (illustrated in Table 1) suggests that boards need to focus on both conformance and performance aspects of corporate governance and that blended perspectives on agency/stewardship may be necessary.
| Focus | Short-term focus on ‘conformance’ | Long-term focus on ‘performance’ |
|---|---|---|
| External | Accountability Ensuring external accountabilities are met, e.g. to stakeholders, funders, regulators Meeting audit, inspection and reporting requirement |
Policy formulation Setting and safeguarding the organisation’s mission and values Deciding long-term goals Ensuring appropriate policies and systems are in place |
| Internal | Supervision Appointing and rewarding senior management Overseeing management performance Monitoring key performance indicators Monitoring key financial and budgetary controls Managing risks |
Strategic thinking Agreeing strategic direction Shaping and agreeing long-term plans Reviewing and deciding major resource decisions and investments |
A number of board assessment tools have been developed and used in empirical research to assess the instrumental activity of boards and to guide and inform board development programmes. 19,27 For example, the 65-item Board Self-Assessment Questionnaire (BSAQ) has recently been used in studies of hospital boards in the USA28 and a small-scale study of FTs in England. 29 The benefit of theoretically informed instruments such as the BSAQ is that they have predictive power and can be used to assess the implications of adopting different board strategies (rather than merely taxonomic uses). The BSAQ instrument was used in the national surveys of NHS boards (see below).
Although popular management literature and government documents tend to idealise board members’ activities through the use of ‘heroic’ narratives,30 there is considerable debate over the extent to which boards undertake the classic instrumentalist functions of establishing objectives and core strategies. Within the empirical and critical theory literature, boards have been characterised as performing largely non-instrumental roles by acting primarily as legitimating institutions that formally declare decisions negotiated elsewhere. 31 These perspectives indicate the potential importance of the symbolic and ceremonial value of boards and the need to explore efficacy of board performances in a more dramaturgical sense. In this regard, Hajer32,33 and Hajer and Versteeg34 have outlined a framework for the analysis of the performative dimension of board governance. The approach opens up the day-to-day interactions of board members for analysis through consideration of the setting in which deliberation takes place; the scripting in terms of the actors involved in the decision-making forum; the staging in terms of deliberate attempts to organise the interaction between participants by drawing on existing symbols; and the performance in terms of the way in which the interaction constructs new knowledge, understandings and power relationships that project forward to shape future interactions and provide opportunities for challenge and change over time.
These diverse theories provide multiple and complementary perspectives on board governance and each has been used at various times in the analysis to make sense of the data gathered.
Research design for the empirical work
The empirical strand of the study was informed by a review of the theoretical and empirical literature relating to board governance of quality and safety, and explores both instrumentalist and performative aspects of boards. Given the diversity of views and approaches to understanding board governance of patient safety, and the intrinsic complexity of any relationships between board governance and patient safety processes and outcomes, we adopted a multimethod approach, integrating qualitative and quantitative elements in order to examine these relationships in both breadth and depth in the empirical strand of the study. In order to capture the breadth of any associations between board activity and patient safety we conducted a national survey of board practice with regard to patient safety. This was linked to routine national performance data sets on patient safety processes and outcomes. The combined data set was used to explore board practice–patient safety associations at the organisational level. In addition, to contribute depth and richness to our understandings, we used comparative case study methods and qualitative approaches to explore board dynamics and the governance of patient safety in four hospital trusts. We next elaborate on each of these strands in turn, beginning with the case studies, followed by the national quantitative survey and analysis.
Case studies: sampling, data gathering and analysis
We utilised a comparative case study design across multiple study sites to generalise theoretically within and between cases. 35 Although each case has its own integrity in terms of theory building and generating policy implications, we developed common themes across case study sites using comparative case study methods. 36
Case selection
As we intended to consider the enactment of internal governance arrangements and the effects of external financial and regulatory mechanisms with reference to patient safety, each case study had as its centre of investigation an acute foundation hospital trust through which links between governance and patient safety were explored. We selected FTs because this organisational form was the policy direction for acute sector organisations at the time of planning the study. The unit of analysis is thus the FT rather than the wider health economy, with a focus on the operation of the board and its effects within the specific ‘tracer condition’ area of infection control.
It is important to acknowledge that FT boards operate within a national and regional context, and for this reason we undertook some scoping of context with key commissioners and stakeholders. However, our focus on the board as the seat of governance ensured a focus on the formal enactment of governance within board structures.
In addition to normal requirements of ethical approval, cases were selected on the basis of their performance trajectory over the last 3 years on a range of safety and quality indicators selected from the Dr Foster (Dr Foster Limited, London, UK) database. Every year Dr Foster publishes a hospital guide that uses publicly available statistics to measure and assess what is happening in hospitals in England to increase the transparency around variations in performance. The data focuses on indicators in three domains of quality obtained from the available statistics, combined with information from self-reporting of safety aspects from an annual questionnaire, and is informed by the National Patient Safety Agency organisational feedback reports and CQC ‘alert’ lists. We used these data to select case study sites that were indicated to be getting worse (in the light of overall improvement of other hospitals) or getting better, as follows:
-
two foundation hospital trusts with a ‘downwards’ performance trajectory, as indicated above
-
two foundation hospital trusts with an ‘upwards’ performance trajectory, as indicated above.
We then made sure that the sample was drawn from across the country and included large teaching hospitals (THs) and a district general hospital. Throughout the analysis and reporting, trust sites have been anonymised by being renamed after Scottish islands. The two upwards-performing trusts are identified as Lewis and Arran, and the two downwards-performing trusts are known as Islay and Skye. Appendix 2 contains the case study invitation letter and Appendix 3 contains the participant information sheet.
Brief description of the four selected case studies
Lewis is one of the bigger NHS trusts in the UK, delivering services across several sites within a single city. It offers many specialist services, with a large consultant body seen as being at the cutting edge of clinical care. Its long-standing reputation for high-quality clinical care is reflected in it consistently being in the upper quartile of hospital ratings.
Arran is a renowned TH providing general and specialist services across multiple sites. Over the last 5 years the board has been characterised by relative stability, with low levels of turnover. The trust aims to continue to build its ‘brand’ as a provider of leading specialist services, and it is undertaking large-scale redevelopment in order to deal with excess demand within accident and emergency (A&E) services. Organisational performance against the Hospital Standardised Mortality Ratio (HSMR) is very good, but the trust has faced some performance issues with regard to expressed staff satisfaction and, more recently, infection control rates.
Islay is an integrated provider of hospital, community and primary care services. It has a well-documented profile for its achievements in relation to quality and safety, with the board in particular receiving a number of awards and plaudits for these efforts. The trust holds high scores for both patient and staff satisfaction.
Skye is a district general hospital trust providing services across two sites. It was one of the earlier NHS trusts to be awarded foundation status. Over the past 5 years, the board has been characterised by continuous change, with the arrival and departure of several chief executive officers (CEOs), medical directors (MDs) and two nursing directors (NDs) during this period. The trust has one of the highest patient demands in the country and has faced a number of challenges related to bed capacity. Organisational performance is currently a cause for concern, with the HSMR above average, high A&E demand and increasing infection rates.
Data collection in the case studies
In the context of board governance, the focus of our data collection in the case studies was to explore the following areas:
-
to examine board of director oversight of patient safety
-
to understand the relationship between the board of directors and governors with respect to overseeing patient safety issues
-
to understand how the board complies with a particular patient safety issue (conformance)
-
to understand how the board responds to a specific patient safety issue during the course of fieldwork (performance)
-
to explore the commissioning relationships related to patient safety.
Data gathering consisted of interviews and observations at management boards and the governing board.
Exploring board oversight of patient safety
Our research carried out semistructured interviews with the board of directors at each site. This included the executive and NEDs as well as other board directors deemed relevant to the research and included directors of quality and risk. These interviews built on what was understood to be the key themes and issues related to the subject area17 (see Chapter 3) in examining how board members understood their role in terms of strategic vision and leadership activities, to understand how members understood particular board mechanisms associated with effective oversight, to understand how board members understood, analysed and interpreted the information they provided, and to understand how board members understood their relationship with the wider health economy in terms of commissioning and regulation associated with patient safety.
In addition to these interviews, overt non-participant observation was undertaken by the research team at four management board meetings at each case study site. This totalled nearly 50 hours of observation (Table 2). Descriptive free-text field notes were taken by both observers at each meeting, supplemented with documentary data including the agenda, supporting papers and (retrospectively on completion) the minutes of each meeting. Data included an overview of comments made and questions raised and by whom, and a log of the time spent on each agenda item. These have been summarised to provide an overview of patient safety issues within the context of all board activity. Data from field notes were compiled across multiple board meetings within each trust to detail board operations and identify the manner in which patient safety-related issues were discussed.
| Case study site | Number of board meetings | Time observed |
|---|---|---|
| Islay | 4 | 12 hours 46 minutes |
| Skye | 4 | 14 hours 52 minutes |
| Arran | 4 | 6 hours 1 minute |
| Lewis | 4 | 14 hours 5 minutes |
| Total | 16 | 47 hours 44 minutes |
We supplemented our instrumentalist analysis of conformance and performance with a dramaturgical analysis of observation field notes following the framework developed by Hajer33,34 and previously used by members of the team in a study of partnership boards. 37 Reported in Chapter 7, this analysis explores the scripting, setting, staging and performance of patient safety governance, revealing the manner in which such work was conducted and the ability (or otherwise) of board members to ensure action.
Exploring board of governors’ oversight of patient safety
Interviews were undertaken with a variety of governors across the case study sites in order to understand their experiences of working with their board and holding the executive to account in relation to patient safety matters. These interviews asked governors to reflect on their abilities to exercise this function and also explore different ways in which the role of governors could be improved.
In addition to these interviews, overt non-participant observation was undertaken at nine board of governor meetings, totalling over 21 hours of observation (Table 3). This total number was less than the board of directors observation owing to practical difficulties, as board of governor meetings tended to take place only once every 3 months or so. Such a length of time between meetings meant it was difficult to capture four meetings at each site within the study time frame.
| Case study site | Number of board of governor meetings | Time observed |
|---|---|---|
| Islay | 1 | 2 hours 21 minutes |
| Skye | 2 | 4 hours 16 minutes |
| Arran | 2 | 3 hours 43 minutes |
| Lewis | 4 | 11 hours 7 minutes |
| Total | 9 | 21 hours 27 minutes |
As with the board observations, descriptive free-text field notes were taken by both observers at each meeting, supplemented with documentary data including the agenda, supporting papers and (retrospectively on completion) the minutes of each meeting.
Following ‘tracer’ issues in the trusts
In each trust we followed two ‘tracer’ issues on patient safety from board to ward. One of these (called a ‘board conformance issue’) was the same in each trust and reflected a patient safety issue requirement for all trusts imposed by external regulators. The second (called a ‘board performance issue’) was different in each trust and reflected the board’s response to a local issue requiring performance improvement.
This approach was informed by the work of Garratt. 26 As discussed in Chapter 6, Garratt suggests that an effective board is able to balance tasks simultaneously, with a ‘learning board’ having two sides: board conformance (sometimes termed compliance) and board performance. Conformance itself involves two aspects: ‘ensuring accountability’ through appropriate regulation and ‘supervision of management’ through conformance to key performance indicators. Similarly, performance also involves two aspects: ‘policy formulation and foresight’ and ‘strategic thinking’ to drive the enterprise forward by allowing it to survive and grow by maintaining, learning and developing its position in its energy niches.
The tracer condition analysis looked to analyse the different ways in which these four board tasks (policy formulation, strategic thinking, supervision of management and ensuring accountability) interacted with each other.
Board ‘conformance issue’ analysis
In order to explore conformance to requirements within the governance of patient safety, each case study focused on a specific ‘tracer’ related to patient safety activity. The selection of this tracer condition was inductively derived from our initial observations of board and governor meetings, as well as our interviews with board members. What became apparent from these observations and interviews was how boards were required to conform to a range of performance indicators devised by the regulator Monitor. One of the central targets related to patient safety was the monthly performance in relation to cases of C. difficile infection. Across all of the sites, C. difficile infection rate was the central patient safety performance indicator that boards were required to conform to.
As a result, our analysis of board ‘conformance’ related to the management of C. difficile infections as a key performance indicator of infection prevention and control. Such a focus allowed us to explore the manner in which the case study site incorporated patient safety requirements from external agencies within its governance structures (i.e. how it undertook compliance).
Data collection for our conformance analysis built on a series of semistructured interviews with a variety of stakeholders involved in the oversight and delivery of C. difficile infection prevention and control. To achieve this, our research team contacted members of the infection prevention and control (IPC) committees within each of the sites. A purposive sample of stakeholders was interviewed from each committee, which included board members, managers, doctors, nurses and microbiologists. The selection of these stakeholders was made on the basis that they had detailed understanding of the C. difficile infection issue and were in charge of working with the board to successfully achieve the required level of performance.
Board ‘performance issue’ analysis
In order to explore the performance aspect of governance, our research analysed how each case study site dealt with a patient safety issue or incident identified during fieldwork, from ‘board to ward’. As with our board conformance data collection, these issues were inductively derived from our observations of board and governor meetings, as well as interviews with board members. From these we were able to ascertain a number of examples of ‘policy formulation and foresight’ and ‘strategic thinking’ by the board, which looked to respond to and improve patient safety. The eventual selection of issues and interventions would be wide ranging and provided our analysis with the additional benefit of exploring in real-time board development and response to patient safety issues. The selected issues were as follows:
-
board development of a ‘staff stores’ initiative
-
board development of the ‘bed plan’
-
board development of the ‘After Francis’ initiative
-
board development of junior doctors’ dissatisfaction.
A purposive sample was used to identify key stakeholders who were involved in the oversight and delivery of these initiatives. This tended to start with the particular board members who were leading these initiatives. Following on, our research then identified key stakeholders involved within each initiative across the organisation. The eventual sample for each of these ‘performance’ tracers included managers, nurses, doctors and allied health professionals.
Commissioning for patient safety
Where possible, interviews with commissioners were carried out to further understand the external environment in relation to the governance of patient safety. These interviews reflected on the experience of commissioners in their interactions with the FT boards regarding patient safety issues and concerns, as well as documenting any important issues regarding the governance processes associated with commissioning for patient safety.
Investigation of all of these issues entailed numerous interviews in each trust, as detailed in Table 4.
| Case study site | Executive board interviews | Conformance tracer issue (C. difficile infection) | Performance tracer issue (local board initiative) | Governors | Commissioners | Totals |
|---|---|---|---|---|---|---|
| Skye | 16 | 4 | 10 | 2 | 3 | 35 |
| Lewis | 15 | 9 | 7 | 4 | 4 | 39 |
| Islay | 13 | 5 | 3 | 2 | 2 | 25 |
| Arran | 13 | 1 | 3 | 0 | 0 | 17 |
| Case study totals | 57 | 19 | 23 | 8 | 9 | 116 |
| Scoping interviews | 11 | |||||
| Grand total | 127 |
Manchester Patient Safety Framework
We had originally intended to administer the Manchester Patient Safety Framework (MaPSaF) to provide further supporting information on the maturity of board safety culture within each case study site. Designed as a diagnostic and development tool, the MaPSaF identifies dimensions related to working practices, such as risk management training, the investigation of patient safety incidents and staff education. However, during the course of fieldwork it became evident that most of the case study sites were undertaking assessments of patient safety culture commissioned by external third parties, and the decision was taken to avoid the risk of ‘culture assessment overload’ occasioned by further summary assessment.
Approach to qualitative data analysis
Our approach to qualitative data analysis proceeded through the three flows of activity, as outlined by Miles et al. 38 Here, a ‘data condensation’ process was used to select, focus, simplify and abstract data from field notes of observations and interviews transcripts. A thematic approach to qualitative data analysis was taken, whereby the data were coded, labelled and clustered into themes that both emerged from data as well as directly related to our research questions and theoretical frameworks influencing the study. 39
Approach to thematic analysis
For the interviews with board members, our analysis built on our literature review,17 which highlighted a number of issues for boards in relation to the governance of patient safety. These would form the central codes for the analysis (deductive); however, our analysis was also open to a variety of emerging themes that occurred during the course of the fieldwork (inductive). The response to the Francis Inquiry findings was an example of a code which emerged from the interview data.
Data analysis for the observation of board meetings was informed by Hajer33 and Hajer and Versteeg’s34 governance framework; their analytic dimensions of scripting, setting, staging and performance were used as a deductive, a priori template (‘code book’) against which qualitative material within field notes were organised. Thematic analysis revealed patterns (similarities and differences) within the data that were important to the operation of governance,40,41 showing the divergent dramaturgies at play within each specific site.
The tracer condition interviews were analysed using a combination of deductive and indicative approaches. Our analysis was informed by the research questions (deductive); for example, our conformance data analysis was particularly interested in the role of performance targets and measurement for C. difficile infections. Our analysis was also inductive, particularly for the ‘performance’ interviews, as this sample of interviews was one that emerged from the fieldwork as examples of board activity in relation to patient safety.
The interviews with governors and commissioners would also proceed through a thematic approach, whereby codes were generated specifically from the research questions (deductive); for example, from analysing the experience of these groups in holding each hospital board to account. Our analysis would also generate a selection of emergent codes (inductive) from the data. For example, the dynamic and often turbulent environment of recent changes to the commissioning environment was something that emerged as important to our research area. Our approach to these interviews was also iterative in that our fieldwork had already carried out many of the board interviews and observations. These caused a number of points worthy of further investigation to surface, which we then looked to explore.
Our ‘data display’ organised and compressed the transcribed interviews using the NVivo software programme (QSR International, Warrington, UK). An example of each of our interview coding frames can be found in Appendix 4. To provide inter-rater reliability, two members of the research team independently coded data and discussed the application of the coding frames.
The case study analysis presents data drawn from multiple sources (interviews with a range of internal and external stakeholders, observations and secondary documents), with a reporting structure organised in relation to our main research questions. Data analysis proceeded in parallel with collection to iteratively inform subsequent collection and refine the emerging analysis. Data from multiple sources was initially coded against our main research questions drawn from the literature, the coding categories for individual case study analysis being strategic vision; leadership activity; board mechanisms; governor relations; assessment of performance; relationships with commissioners and regulators. These concerns are presented as detailed individual case studies, with the initial research questions used as a point of departure to explore the range of concerns revealed inductively within each case. The individual case studies were then aggregated thematically to provide a summary overview chapter, with a subsequent analysis offered of emergent themes across the case studies – principally concerning getting and using hard and soft intelligence (as opposed to data) and exploring resulting concerns and tensions between conformance and performance.
Our purposive sampling strategy meant that decisions regarding data saturation point were made based on practical purposes.
For the board interviews, our sample was the executive board. Saturation point was reached when all of these interviews were included, with the exception of those members who declined to participate.
For the governor interviews, our sample criteria were built on capturing a subsection of governors who could outline the central issues facing governors. We spoke to a selection of public governors at each site. We did try to contact staff governors; however, we were unsuccessful in getting any to agree to participate.
For the tracer condition interviews, our purposive samples and decisions about saturation point varied. The conformance tracer condition (C. difficile infection) saturation point was reached when we had interviewed all or near to all members of the IPC teams. The performance tracer condition would reach a saturation point when we had spoken to range of stakeholders.
Surveying English NHS boards
Given the paucity of information available on English NHS boards, we used the BSAQ tool (discussed shortly) along with other survey instruments as a means of providing an account of board composition, activities and orientations. Our goals were as follows: first, to provide a basic descriptive account of English NHS boards in acute hospitals, which is currently lacking in the literature; second, we wanted to provide a snapshot of the BSAQ six-dimensional structure applied to English NHS boards; and, finally, we sought to explore whether there were major differences between different types of hospitals, looking at FTs versus non-FTs and THs versus non-THs.
Two national surveys were undertaken about board management in NHS acute and specialist hospital trusts in England. The first of these surveys was issued to 150 trusts in the financial year 2011/12 as part of the annual trust survey carried out by Dr Foster. The questionnaire was completed online via a dedicated web tool. This survey gathered data on each trust’s board and activities related to the oversight of patient safety; 145 replies were received, making for an overall response rate of 97%. We believe that this response rate is unusually high because of the levels of engagement of NHS trusts with Dr Foster (in some cases responses were omitted from individual questions, making the effective response rate slightly lower for some data items). The national survey questions are contained in Appendix 5.
The second survey targeted individual board members from these trusts. We used an adapted version of the BSAQ questionnaire that had been tested previously with a small sample of FTs in the English NHS29 (see Appendix 6 for the BSAQ questions). This survey was also completed through online means and data were gathered between May 2012 and April 2013. By this time period, trust numbers were reduced to 144 because of merger activity in the sector. A total of 334 responses were received from 165 executive and 169 non-executive board members, providing at least one response from 95 of the 144 NHS trusts then in existence (66%). In order to gain trust-based estimates on each of the six BSAQ dimensions, replies from individuals from the same trust were aggregated.
For all of the main indicators calculated across both surveys we explored differences between FTs and non-FTs and between THs and non-THs.
Assessing boards with the Board Self-Assessment Questionnaire
As interest has grown in understanding the effectiveness of boards, both inside and outside health care, a range of board assessment tools have been developed and applied. Most prominent among these, and a tool that has seen some use in health care, is the 65-item BSAQ. The BSAQ is derived from research highlighting the characteristics of effective non-profit governing boards in the USA. 42,43
The initial research on the BSAQ examined the practices of boards identified by a panel of experts on board development as either reputedly very effective or reputedly very ineffective. On the basis of this dichotomy of board development, the researchers isolated observable behaviours that were distinctive to the more effective boards and, using the critical incident technique as part of a qualitative study, identified six dimensions or competencies of effective board performance. 42 Following the qualitative phase, structured interviews with boards of trustees were used to aid the development of a self-administered 65-item questionnaire, in which each item is answered using a 4-point Likert-type scale. The BSAQ has subsequently been subject to extensive testing for validity, reliability and sensitivity, and this process confirmed that the six theoretically derived dimensions also had some empirical distinctiveness. 44,45
These six dimensions are labelled: contextual, educational, interpersonal, analytical, political and strategic (Box 1 provides more details). Four of these dimensions relate directly to Garratt’s instrumental board tasks (located in Table 1) and the remaining two (educational and interpersonal) are more behavioural, reflecting recognition of the need for boards to develop group cohesion, reflection and development.
-
Contextual dimension. The board understands and takes into account the culture, values and norms of the organisation it governs.
-
Educational dimension. The board takes the necessary steps to ensure that all board members are well informed about the organisation and the professions working there, as well as the board’s own roles, responsibilities and performance.
-
Interpersonal dimension. The board nurtures the development of board members as a group, attends to the board’s collective welfare and fosters a sense of cohesiveness.
-
Analytical dimension. The board recognises complexities and subtleties in the issues it faces and draws upon multiple perspectives to dissect complex problems and to synthesise appropriate responses.
-
Political dimension. The board accepts as one of its primary responsibilities the need to develop and maintain healthy relationships among key stakeholders.
-
Strategic dimension. The board helps envisage and shape institutional direction and helps ensure a strategic approach to the organisation’s future.
Evaluating the Board Self-Assessment Questionnaire in the English NHS context
Because the BSAQ has seen only limited use in the UK context, we revalidated the data structure of the instrument using the data from English NHS boards. Factor analysis was performed at the respondent level to explore underlying factors that characterise boards. This analytic strategy is more fully explored in Chapter 8, in which the eigenvalues and item loadings are also presented.
Relating board-level variables to organisation-level quality and safety
After constructing the factor scores representing the six BSAQ dimensions and the total BSAQ score, we explored whether or not these were correlated with patient safety measures (although we did not explore a priori hypotheses). In doing so, we estimated various multivariate models regressing patient safety measures (from Dr Foster) and measures of hospital ability to handle errors, near-misses and incidents, taken from the National NHS Staff Survey (NSS) for 2012 on the total BSAQ score, controlling for a number of hospital-level characteristics. The full range of dependent variables are described and presented in Chapter 8 and more fully in Appendix 7.
Integrating quantitative and qualitative data
The implications of the findings from the literature review, qualitative case studies and the national surveys were discussed at meetings of the whole research team. The original research objectives were used to structure the discussion; for each of the five keys objectives the relevant qualitative data were discussed and a consensus achieved regarding how to interlock the findings relating to each objective. Chapter 5 presents the ‘integrated’ findings relating to each research objective.
Concluding remarks
In this chapter we have set out the basic theoretical framings used to shape data collection and interpret the findings, and we have laid out the various stages of qualitative and quantitative data gathering. Subsequently, Chapters 4–7 present various aspects of the qualitative data and Chapter 8 provides a full account of the quantitative data. The qualitative data have been structured in the following way: Chapter 4 provides an overview of findings across all four case sites; Chapter 5 provides more detailed analysis on a case-by-case basis; Chapter 6 displays the findings from our tracer issues (two for each trust site); and, finally, Chapter 7 takes a dramaturgical view of board performance to explore the more symbolic aspects of board practice(s).
First, however, we turn to the literature that underpins the work: Chapter 3 provides a synthesis of existing empirical work and a systematic narrative review exploring board composition and activities alongside organisational performance.
Chapter 3 Systematic narrative review and synthesis
Introduction
Although standards and guidance on board oversight have been produced, as have summaries of evidence of the effectiveness of board oversight of quality and safety, the research base in relation to board oversight of patient safety has not yet been fully exploited. The purpose of this chapter is to review and synthesise this evidence base. It begins with an overview of the literature review methods employed, before presenting the results, which are connected to four discernible storylines regarding board governance of patient safety.
Review methods
The research carried out a narrative systematic review in order to describe, interpret and synthesise key findings and debates concerning board oversight of patient safety. 46 We also produced a synthesis of these findings with the intention of supporting the development of our empirical work and contributing to wider debates regarding policy and practice within this area.
An initial systematic search of the area (Table 5) enabled us to map the broad parameters of the literature and map their development over time. To ensure rigour, we followed accepted practice in identifying the review focus, specifying the review question, searching for and mapping the available evidence and identifying studies for inclusion. 46 In selecting papers, we focused on those that considered board oversight in the context of quality and safety, and the research team and expert panel suggested seminal works and advised on search terms. The team drew up a list of key terms and searched the published literature from 1991 to 2012 across a number of databases, excluding non-English-language articles.
| Search title and abstract from 1991 to 2012 | |
|---|---|
| Board governance Hospital board Board of trustees Boards of management Management boards Board members Board chairpersons AND patient safety or safety AND quality |
|
| Database searched | Number of results |
| HMIC | 11 |
| EMBASE | 103 |
| MEDLINE | 32 |
| ASSIA | 20 |
| EBSCOhost (CINAHL and Business Premier) | 52 |
| SSCI | 39 |
| Total with duplicates removed | 187 |
The team then reviewed titles and abstracts for relevance, using broad inclusion criteria to identify studies of hospital board directors’ or boards of trustees’ oversight of quality and patient safety. Our initial search uncovered 187 articles and, after reviewing the titles and abstracts, we identified a subset of 66 papers for detailed study, which we added to those identified by earlier reviews,47 removing duplicates. Disagreements about whether or not to select a reference for full review were resolved by discussion within the team. Finally, we used snowballing techniques to augment papers for review – manually, by searching references of included papers, and electronically, by using citation-tracking software to identify papers that cited already included papers. These searches were adapted iteratively to ensure maximum capture of empirical work; at the end of the process 124 publications were deemed relevant.
We followed guidance on narrative synthesis from Popay et al. 48 in our data extraction and appraisal of study quality. Our key concern was to understand the effectiveness of oversight in terms of board composition and interventions with boards, such as the setting of standards and benchmarks. In particular, we were keen to explore any evidence for improved performance and patient outcomes, such as reductions in mortality and morbidity, from board interventions, as well as identifying factors that impact on the effective implementation of those board interventions. The synthesis phase of the review explored key aspects of board oversight of quality and patient safety and identified four common storylines:
-
leading for safer care
-
measuring safe care
-
internal board oversight
-
external regulation and accountability.
After a brief historical account of the growth of the field, we will examine each storyline in turn and present a narrative synthesis.
The literature uncovered
A growing field of enquiry
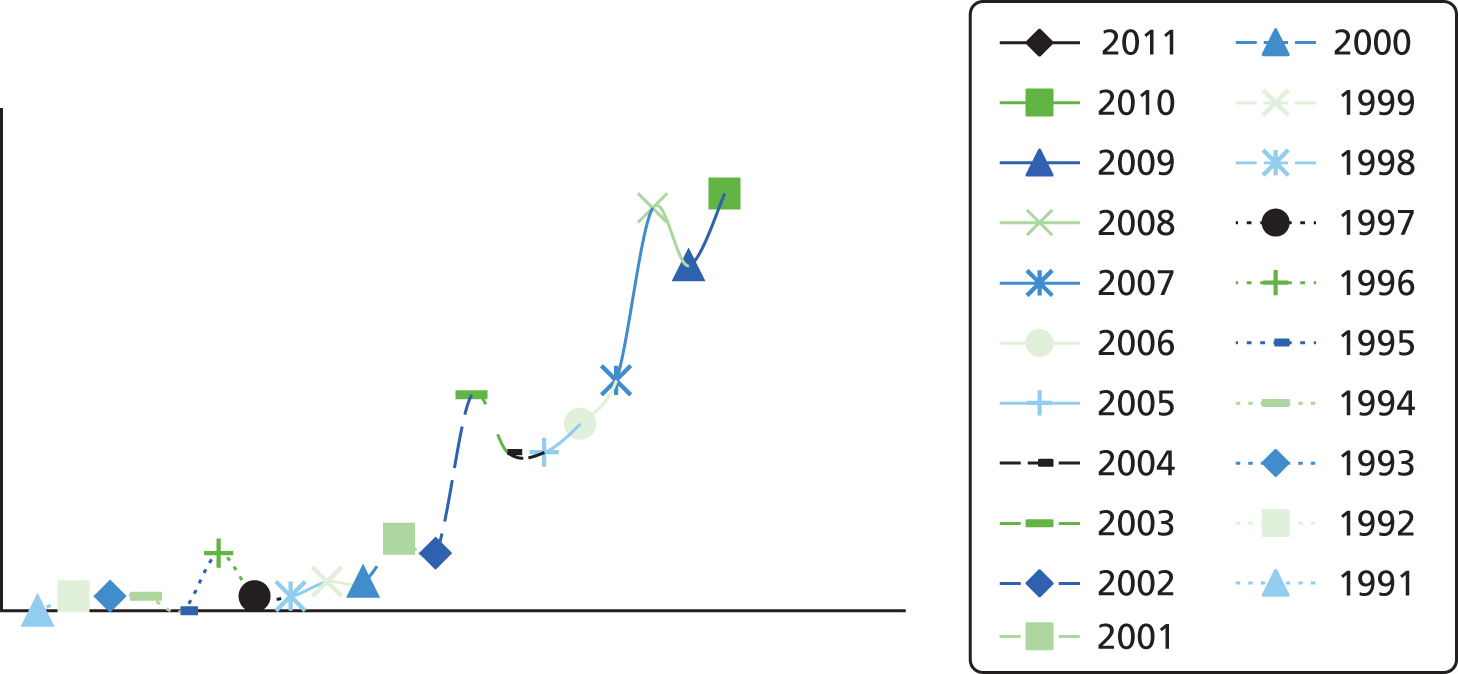
The US Institute of Medicine’s reports, To Err Is Human: Building a Safer Health System49 and Crossing the Quality Chasm: A New Health System for the 21st Century,50 and the UK Chief Medical Officer’s report into learning from adverse events, An Organisation with a Memory,51 were hugely influential in calling for changes to health-care systems and organisations that would improve quality and safety. It is, therefore, unsurprising that our results show large and rapid growth since 2000 in the number of published articles that relate to hospital board oversight of quality and patient safety (Figure 1), a trend that reinforces the increased policy salience of board oversight of safety.
FIGURE 1.
Results of the systematic search of board oversight and patient safety.
The study of board oversight in relation to quality and patient safety can be situated within the broader literature that addresses the role of leadership in improving quality in US hospitals. 52–56 With variable successes achieved by hospitals in implementing quality improvement programmes and initiatives,57,58 the publication of empirical studies of US hospitals emerges from 2004 onwards, revealing variation in the adoption of board practices that are thought to be associated with higher performance and better patient outcomes (Table 6). 53,66 These cross-sectional surveys of predominantly non-profit hospitals indicate the importance of examining the leadership actions that are thought to influence the effectiveness of quality improvement activities in hospital settings. 71
| Author (year) country | Participants | Context (aims) | Board assessment (methods) | Summary of findings |
|---|---|---|---|---|
| Baker et al. (2010),59 Canada and the USA | 15 governance experts, average of 10 board members across four case studies, survey of Quebec and Ontario health economies | To identify governance practices and improve governance related to patient safety | Semistructured interviews, documentary analysis and survey | Effective governance is in its early stages. Better information, expertise, plans, skills and relationships still required |
| Grey and Weiss (2004),60 USA | 98 CEOs and trustees from 16 non-profit hospitals in the New York area | To learn about how trustees define their responsibilities, how they relate to hospital activities and their decision-making processes | Structured, open-ended interviews with trustees and CEOs | Governance by boards was a strength and weakness for non-profit hospitals. Fundamental ambiguities in the ethical significance of the trustee role were identified |
| Goeschel et al. (2011),61 USA | 35 boards from cross-section of hospitals across Tennessee and Michigan | To identify effective measures to monitor quality | Survey and voluntary site request for safety scorecards | Measures varied widely with uncertain validity. More valid outcome measures required |
| Jha and Epstein (2010),57 USA | 722 chairpersons from non-profit acute care hospitals | To determine board engagement and activities in relation to quality of care | Survey and composite measures of hospital performance | Quality of care often not a top priority. Differences in quality-related activities between high- and low-performing institutions |
| Jha and Epstein (2012),62 USA | 722 chairpersons from ‘black-serving’ and ‘non-black-serving’ non-profit hospitals | To compare how boards at black-serving and non-black-serving hospitals engage in quality-of-care issues | Survey and composite measures of hospital performance | Board chairpersons of black-serving hospitals report fewer expertise and priorities regarding quality issues than chairpersons of non-black serving hospitals |
| Jha and Epstein (2013),63 UK | 132 chairpersons from a cross-section of English hospitals | To compare governance practices among English and US hospital boards | Survey and composite measures of hospital performance | English board chairpersons report more expertise and emphasis on quality-of-care issues than the USA; however, hospital performance against quality metrics not as substantial as the USA |
| Jiang et al. (2008),52 USA | 562 hospital presidents/CEOs across 50 states selected from the 2006 TGI survey | To examine the prevalence and impact of particular board activities | Survey and composite measures of hospital performance | Governing boards are engaged in quality oversight, particularly through internal data and national benchmarks |
| Jiang et al. (2009),64 USA | Based on a data set from Jiang et al. (2008)52 | To examine differences in hospital quality performance associated with particular practices | Based on Jiang et al. (2008)52 | Better performance associated with having a board quality committee, strategic goals, a quality agenda, safety dashboards/benchmarks and involvement of physician leaders |
| Jiang et al. (2011),65 USA | 445 hospitals selected from the 2007 TGI survey | To explore the practices of governing boards in quality oversight through the lens of agency theory | Survey and composite measures of care and mortality | Regular review of quality performance is the most common practice |
| Joshi and Hines (2006),66 USA | 47 CEOs and board chairpersons from cross-section of 30 hospitals across 14 states | To determine whether or not hospital leaders understand safety and quality issues and activities | Interview survey and composite measures of clinical quality | Overall level of knowledge low. Significant differences between perceptions. Mild association between board engagement and hospital performance |
| Kroch et al. (2006),53 USA | Convenience sample of 139 hospitals across nine states | To analyse hospital board dashboards and its relationship to leadership engagement | Online dashboard implementation survey and performance data analysis using composite measures | Variation and commonalities in the way dashboards are created and used. Improved quality linked to shorter, more focused dashboards |
| Machell et al. (2010),15 UK | Nurse executives and boards in six English NHS hospital trusts | To examine board focus on clinical quality and nurse executives in supporting this | Observations | Clinical quality occupied a fragile position. Nurse executives are well placed to help |
| Mastal et al. (2007),67 USA | 73 hospital chief executives, CNOs and chairpersons from 63 hospitals | To analyse board engagement in quality and safety and the role of nursing within this | Telephone interviews and focus group | Significant differences in perceptions between CNOs, chairpersons and CEOs. Boards had limited comprehension of salient nursing quality issues |
| Prybil et al. (2010),68 USA | CEOs from 123 non-profit community health systems | To examine oversight of patient quality at non-profit community health systems and compare with benchmarks of good governance | Survey and benchmark analysis | Activities associated with effective governance include standing committees and safety targets/reports. Gaps continue between present reality and current benchmarks |
| Prybil et al. (2013),69 USA | Senior trustees and CEOs from 14 private non-profit health systems | To examine board oversight of quality in private non-profit health systems and compare with benchmarks of good governance | Documents, interviews and benchmark analysis | Effective governance identified in majority of boards with presence of standing committees, system wide quality measures and action plans directed at improving quality |
| Ramsay et al. (2010),70 UK | Case study of 21 personnel, including board members from a hospital trust in England | To describe the external and internal governance systems for HCAIs and medication errors in a NHS trust | Documentary analysis and interviews | Nationally, HCAIs a higher priority than medication errors. Governance of medication errors took place at divisional or ward level |
| Vaughn et al. (2006),71 USA | CEOs and senior executives from a cross-section sample of 413 hospitals in eight states | Identify characteristics of hospital leadership engagement in quality improvement | Survey and composite measures of clinical quality | Better quality associated with boards spending more than 25% of time on quality issues; that received formal measurement reports; and communicating a quality strategy to medical staff |
From 2008, larger-scale studies covering wider geographical areas begin to feature. Building on the cross-sectional survey of the prevalence and impact of board activities in US hospitals,52 Jiang et al. 64 developed the scope of their evaluation of board oversight to include impact on clinical outcome measures such as mortality, morbidity and complications, as well as differences in the processes of care. Jha and Epstein57 carried out the first national survey of board chairpersons in the USA to analyse board engagement with clinical quality and identify differences between board activities in high- and low-performing organisations.
From 2010, studies have emerged that seek to differentiate and explore board activities related to patient safety in specific socioeconomic, organisational and geographical contexts. Jha and Epstein62 pursued an explicitly socioeconomic focus to compare boards of directors’ priorities and practices in serving the interests of minority-group patients. Prybil et al. 68 examined specific board structures, practices and cultures that relate to good governance in US non-profit community health systems. Baker et al. 59 carried out the first significant study of board governance and quality and safety in Canadian health-care organisations, and studies from the UK have emerged that analyse the formal governance arrangements for HCAIs and medication errors. 70 More recently, Jha and Epstein63 conducted the first national survey of English hospital board activities, providing an international comparison with their survey of non-profit acute care hospital boards in the USA. In addition, studies have also been published examining health board oversight of quality and safety in the Netherlands,72 Scotland73 and Australia. 74
The theoretical and conceptual dimensions of board oversight have also received more explicit attention. Jiang et al. 65 employ the agency theory perspective as a lens through which to explore the role and practices of hospital governing boards, while Ford-Eickoff et al. 75 explore how concepts such as complexity absorption and requisite variety can support hospital board governance and oversight, hypothesising that boards with greater variety and breadth of expertise among its membership can better respond to complex environments and have greater potential for sense-making and learning.
Emerging storylines
Our review of board oversight of patient safety identifies a variety of empirical evidence and expert advice that suggests that specific board activities are associated with improvement in the quality and safety of hospital care. However, the results also suggest that the adoption of such activities remains variable and that our understanding of boards’ impact on patient safety is currently limited. We present the findings thematically, as four storylines derived from the narrative review: (1) leading for safer care, (2) measuring safe care, (3) internal board oversight and (4) external regulation and accountability.
Leading for safer care
Board oversight of patient safety tends to reflect a key message from the quality improvement literature as a whole; that is, that strong and committed leadership from the CEO and the board is vital to the success of quality improvement and safety programmes. 56,76–79 A review by Clarke et al. 80 suggests that leadership on patient safety should learn from the characteristics and behaviours of high-reliability organisations, such as those found in the nuclear and aviation industries. In health care, leadership is associated with perceiving lapses in patient safety to be a problem of the system rather than individual employees, and with words and actions that promote a culture that encourages the identification of mistakes, emphasises system improvements that reduce variability and makes safety a given.
Empirical evidence from cross-sectional surveys in the USA suggests that boards that demonstrate such leadership have a positive impact on the safety performance of its organisations. Boards that place a high priority on quality and safety are associated with higher performance,64 as are boards that set strategic goals for quality improvement and demand reports on the progress of action in response to adverse events. 52,72,81 A US national survey of 722 chairpersons in 2007 and 2008 by Jha and Epstein found that respondents from high-performing non-profit hospitals were more likely than respondents from low-performing non-profit hospitals to establish and publicly disseminate goals and to perceive themselves as influential throughout the organisation. 57
Although such practices have been found to be associated with effective leadership on patient safety, empirical evidence suggests significant variation in the implementation. Drawing on the 2006 TGI (The Governance Institute, San Diego, CA, USA) survey of 562 chairpersons and CEOs from hospitals across the USA, Jiang et al. 52 found that fewer than half the CEOs regarded their organisations’ governing boards as very effective in overseeing quality. Similarly, Baker et al. 59 found in case studies of Canadian and US health-care organisations that, although most boards had established strategic goals for quality improvement, many did not have specific objectives with clearly defined targets, which suggests that words are not necessarily backed up by actions. Observational research by Machell et al. 15 of how nurse executives and boards work in acute care hospitals and mental health trusts across England found that many chief nursing officers (CNOs) perceived board members to be only moderately engaged in quality improvement initiatives. This was attributed to members’ lack of knowledge about quality and patient safety issues, the limited time available for participating in quality initiatives and to a lack of quality champions at board level. Such a view is echoed in qualitative research of non-profit hospitals in the USA. Interviews with CEOs and trustees by Grey and Weiss60 in 1998 and 1999 found that the two most important issues for local non-profit hospital boards in the New York area were mergers/acquisitions and financial management, with hospital quality and safety receiving far less attention. These findings are consistent with US national survey data from Jha and Epstein,57 which revealed that approximately half of the non-profit hospital boards did not rate quality of care as a top priority for board oversight or for CEO performance evaluation. Most boards were primarily focused on financial issues, assuming that its quality of care was adequate.
Measuring safe care
Board oversight of quality and patient safety rests on directors’ ability to obtain, process and interpret information, assess current performance and set strategic direction using a range of metrics that are tailored to local circumstances. A variety of expert advice has been produced to encourage boards to understand the big picture on quality and safety performance through the use of checklists and dashboards. 82–87 Reinertsen88 summarises the steps that trustees can take to manage quality in their organisations by focusing on a limited number of internal quality measures, or ‘dots’, and argues that such an approach can generate significant improvements, particularly in terms of building organisational buy-in, maintaining constancy of purpose and nurturing collaborative effort.
Empirical evidence from US hospital surveys suggests that boards that engage in reviewing and tracking its organisation’s performance through the collection and analysis of internally generated data (quality dashboards or scorecards) and national benchmarks are likely to have better outcomes in relation to quality. 52,64,65 This finding is supported by US research by Kroch et al. ,53 whose analysis of hospital board dashboard composition found that higher-performing organisations were more likely than their lower-performing counterparts to have dashboards that were shorter and more frequently reviewed and that focused on areas that are critical for quality. In England, single case study research conducted in 2008 by Ramsay et al. 70 found that scorecard data in a hospital offered a view of the organisation as a whole and facilitated division- and ward-specific analysis and feedback on the governance of HCAIs. Empirical studies and expert advice also emphasise, alongside the use of formal performance metrics and quantitative data sets, the role of soft intelligence in capturing the qualitative experience of patients and staff, which often defies simple coding and quantification. 59,89 In the USA, interviews with board chairpersons and CEOs by Joshi and Hines66 identified measurement of patient centredness as a key issue for board oversight of quality of care and recommended tapping into informal and soft intelligence channels as a key means for safeguarding care, including through executive walkabouts, patients telling their stories at board meetings and board members shadowing clinicians so that they might better understand frontline challenges in delivering safe care.
Patient safety metrics are clearly important in any strategy that is designed to improve care, but the empirical evidence suggests a need for considerable effort to increase board members’ proficiency in the use and interpretation of metrics and to improve the credibility, validity and reliability of data. Baker et al. 59 found that many Canadian health-care organisations had struggled to develop useful measurements for board oversight of quality and patient safety. Their survey of board chairpersons from hospital, as well as regional and community, organisations reported that, despite boards receiving and discussing a range of quantitative indicators, only half rated the information as good or excellent in enabling them accurately to assess its organisation’s performance. In England, research found that the information that was accessible to hospital boards generally fell short of the then NHS regulator’s recommended range of quantitative and qualitative material90 and that more needed to be done to cascade information about safety performance to frontline staff. 78 The recent survey of 132 chairpersons in England by Jha and Epstein63 also reported variable use of quality metrics among English hospital boards and found that boards of hospitals with foundation status were more likely than non-profit boards in the USA to use quality dashboards, request quality reports and review specific quality data as part of its oversight activities. Variation in the use of metrics by US boards is illustrated by the survey and scorecard analysis of Goeschel et al. ,61 which show significant differences in the use of scorecards across the participating hospitals in Michigan and Tennessee. In contrast, interview and documentary research by Prybil et al. 69 found a high degree of consistency in measurement, with 11 of 14 large, non-profit health systems in the USA formally adopting system-wide quality measures and standards.
Expert advice has sought to address the need for board members to have greater awareness of and understanding about quality and safety, recommending that quality expertise be included in board member competency profiles and suggesting that boards receive training and continuing education in areas to do with quality and safety. 90 Evans91 suggests that exams for board members on the use and implementation of quality measures could improve quality and accountability of care in hospitals.
Empirical studies have assessed the quality literacy of hospital boards by considering members’ participation in formal training programmes and setting time aside to develop knowledge and capability in relation to improving patient safety. 73,74 Some of this work has revealed the limited time and resources that many boards devote to such activities. US and Canadian research found a ‘remarkably low’ degree of knowledge among hospital boards about published quality reports and best-practice guidance in relation to safe care,66 with many board members having only limited expertise in using and implementing such information. 59 Formal training for boards on clinical quality also appears to be underdeveloped. 57 Reflecting on the findings of the 2006 TGI survey in the USA, Jiang et al. 64 suggest that the lack of formal training poses specific difficulties for board members who are drawn from sectors outside health care, who are less likely to have the technical skills that would enable them adequately to address clinical quality issues. More recently, comparative research by Jha and Epstein63 has found that chairpersons in NHS hospitals make a higher assessment of their own expertise in relation to quality than do their US counterparts. Moreover, the surveys suggest that board chairpersons’ assessments of their hospitals’ quality performance (in both England and the USA) are over-rated when compared with the external assessments undertaken by the Hospital Quality Alliance (in the USA) and the CQC (in England).
Internal board oversight
The role of hospital board members in overseeing quality of care has been characterised as being to monitor the strategic plans that senior management develop or to act as advisors and work at the periphery of the decision-making process. 75,92 Baker et al. 59 note that health boards historically tended to delegate the oversight function to medical staff and did not consider quality and safety issues to be its top priority, which might reflect a recognition on the part of board members of clinical leaders’ expertise and the traditional separation between the responsibilities of administrative and medical staff.
The increasing interest in board oversight of patient safety has also focused on formal organisational structures and processes for safeguarding care, as well as the informal relationships and dynamics between boards and professional groups. One aspect of this is board agendas and the extent to which patient safety is discussed at board meetings. 73,74 Findings from US hospital settings suggest that having quality and safety as standing items on the board agenda provides a critical lever for engagement in quality and safety issues. 57,66 Jiang et al. 52 found that most board meetings had agenda items on quality, but only 41% of boards indicated that they spent > 20% of meeting time on quality. Hospitals in which boards spent ≥ 20% of meeting time on quality had better process-of-care rates than hospitals in which boards spent less time on quality. 64 This research supports earlier findings on variability between hospitals in relation to the amount of time that boards give to quality and safety. In England, qualitative research from the Healthcare Commission90 found that safety is rarely the first item on the board agenda. This is supported by the observational research of English hospital boards by Machell et al. ,15 whose main conclusion was that considerations of clinical quality were accorded a low priority in boardrooms, compared with financial matters, organisational restructuring and the need to meet central government performance targets.
The formal structure of boards has also been found to be related to the effective oversight of patient safety. 93 US national survey data show that boards with a separate quality committee are more likely than those without to be high performing. High-performing organisations are more likely to use quality dashboards or scorecards, issue written policy throughout the organisation and establish strategic goals for quality improvement. 52,63,64 However, qualitative research into a hospital trust in England by Ramsay et al. 70 found differing opinions about the effectiveness of subcommittees. Although there was concern about potential duplication of messages, which might lead to mistakes in reporting, duplication of key messages was also seen as necessary to sustain staff engagement in safety-related issues.
Effective board oversight of safety also requires attention to be paid to dynamics and tensions within and between boards, medical staff and senior leaders. 94 In particular, expert advice advocates having a physician leader on a board quality committee to enhance performance by facilitating communication and building trust and confidence. 88,92,94 The empirical analysis of the 2007 TGI survey by Jiang et al. 64 found that hospitals in which representatives with clinical expertise served on the board quality committee performed significantly better on process and outcomes of care than did hospitals that had no such expertise on its boards. Collaborative retreats with multidisciplinary staff groups95 and internal collaboratives, built around safety initiatives, have also been found to enhance safeguarding processes. 55
Although such intergroup dynamics are associated with benefits, expert advice and empirical research highlight the need for board development in the area. Nursing leadership, for example, remains conspicuously absent from many board deliberations and decision-making. 15,67,96–99 Grey and Weiss60 note that further discussion is required about the ethical conflicts and ambiguities that can arise when board members combine professional and clinical interests with corporate roles and duties. Boards’ relationships with the wider patient community also need consideration. A survey of US non-profit hospitals by Jha and Epstein,57 conducted in 2008, suggested that board chairpersons in hospitals that predominantly serve black populations reported less expertise and prioritisation of quality issues than chairpersons of boards in non-black-serving hospitals.
External regulation and accountability
Our primary focus has been on internal processes for board oversight of patient safety, but we also considered research into the external accountability of boards. Case study research by Baker et al. 59 found that Canadian organisations grappled with the challenge of reconciling the information needed for external accountability with that required to inform local improvements. One dilemma was about whether or not to make performance data publicly available. Some hospitals had made available information on incidence of C. difficile, MRSA and vancomycin-resistant enterococci (VRE) infections, while others were approaching the issue more cautiously.
In the English NHS, a case study of a hospital by Ramsay et al. 70 considered the board’s accountability in relation to national targets and regulatory bodies for HCAIs and medication errors. Although the researchers could not categorically conclude that stronger external governance resulted in more effective local governance, they found that, at the time of data collection in 2008, rates of HCAIs such as MRSA and C. difficile infections were amenable to meta-regulation, for example through target setting. Medication error data based on incident reports were identified as being more difficult to govern, because such events tended to be more open to interpretation and to suffer from substantial under-reporting.
Qualitative research by the Healthcare Commission90 in England found that, despite the onus on commissioners or purchasers of services to drive up quality and safety through contracting and payment systems, there were local variations in the extent to which commissioners had robust information systems in place for holding hospitals to account for the quality of care that they provided. Commissioning practice in holding provider organisations to account varied across health economies from ad hoc requests to providers for reports of serious untoward incidents to the systematic benchmarking of providers against indicators of quality and safety. The research found that the most effective accountability arrangements between commissioners and providers were those that were supported through ‘relational contracting’ and which built on strong personal relationships and collaborative, rather than competitive, partnerships between organisations.
Synthesis and discussion of findings
Studies of board governance and patient safety have identified a wide range of governance practices that are associated with higher performance. Some are to do with routine feedback and monitoring in the corporate board environment, such as spending time on quality issues, using quality performance reports, reviewing dashboard indicators regularly to monitor quality and setting quality goals at the theoretical ideal level rather than average levels or national benchmarks. Others are more strategic in focus, such as involving medical staff in the quality strategy, having a quality subcommittee and developing new clinical programmes and services to meet quality-related criteria. Finally, approaches to do with wider systems of governance have a part to play, such as the exploration of different ways of producing public reports to enhance transparency and accountability to the community, and the equal involvement of board (corporate) and medical (professional/collegiate) staff in setting the agenda. 57,64,65,71
Taken together, the findings suggest that empirical studies of patient safety governance are informed by the broad assumption that failures in safety (adverse events) are not brought about solely by individual human error but are conditioned, precipitated and exacerbated by wider systemic and latent factors in the work environment and organisational context,100 and are therefore amenable to control and prevention. This assumption functions as a latent programme theory in the field of enquiry, and its influence is clearly seen in the nature of the dependent and independent variables selected in the more recent large-scale quantitative studies considered above. To summarise, empirical studies of board governance of patient safety are clearly situated within a quality and safety paradigm. 18
Methodological and theoretical development
Despite such apparent coherence in a relatively new and emergent empirical literature, the field remains methodologically and theoretically underdeveloped. The empirical study of board governance and patient safety consists largely of cross-sectional surveys, predominantly undertaken in US acute health-care settings. The limitations of this study design are acknowledged and include poor generalisability and an inability to substantiate causal relationships between study variables, as opposed to statistical correlations. Although cross-sectional empirical studies have increasingly specified board processes and reporting arrangements in addition to expected outcomes of good patient safety governance, such as low readmission rates and avoidance of adverse events,52,64 hypothesised relationships between dependent and independent variables generally remain ill-defined. The implicit assumption that aspects of board oversight lead to high-performing organisations66 is plausible, but this relationship is likely to be multidirectional and is potentially confounded by a variety of factors that are currently not well described in the literature or elaborated within multivariate empirical models.
Although empirical studies document the structural characteristics of hospitals in terms of size, ownership, teaching status, urban/rural location and region within its respective samples, the cross-sectional design has often left implicit or been unable to attribute differences in processes and outcomes of patient care quality and safety between different types of hospitals (e.g. for profit/non-profit/community/acute care) and hospital boards (e.g. local/multiunit systems). The analysis of these causal relationships is likely to be important when we consider the current environmental and organisational pressures facing hospitals, particularly those in the USA, given the increasing consolidation of hospitals into multiunit systems noted earlier.
Theory could play a much more explicit role in the development of hypothesised relationships between independent and dependent variables for empirical testing in this field of enquiry. In addition, a closer relationship between theory and empirical work would strengthen the credibility of advice on how best to govern for patient safety. This is an important consideration, given that the corporate governance literature makes conflicting normative claims about how board members should behave, some of which originate in the assumptions of the theoretical model rather than in empirical verification of the behaviour’s ability to achieve a specified outcome. In short, although plenty of advice is available to boards regarding what they should do, the advice is conflicting because of different expectations of what boards are for. The rival theoretical traditions that inform competing schools of corporate governance are summarised well by Chambers and Cornforth,19 but it might be helpful briefly to consider the rival theoretical framings of agency and stewardship perspectives on corporate governance, to illustrate its potential for explicit hypothesis generation to underpin empirical enquiry and to provide an example of how the implicit use of theory may lead to conflicting advice on what boards ought to do.
Agency theories of corporate governance require the board to develop processes to ensure the effective scrutiny of executives, on the assumption that the interests of citizens and officials are not aligned and officials will act to secure their own interests. In contrast, stewardship models assume greater alignment of interests between executives and citizens and emphasise the importance of board processes in improving performance. 19 From an agency perspective, one might reasonably hypothesise that boards that hold executives to account through elaborate systems of audit (checking) will achieve better patient safety outcomes. Alternatively, from a stewardship perspective one might hypothesise that such systems are likely to reduce the creativity that committed executives require if they are to drive superior performance (trusting). 101 Agency and stewardship framings are both found in the patient safety literature, the former in the study by Jiang et al. 65 and the latter by Prybil et al. 68 where it is suggested that boards appear to be embracing the stewardship of quality and safety as a fundamental duty. However, in neither case are these models explicitly used to generate testable hypotheses that underpin the empirical work.
Although we strongly argue for more explicit use of the corporate governance literature to guide empirical work, we also encourage greater attention to be paid to the potential limits of the corporate governance literature in relation to patient safety. Specifically, we draw attention to the implications of cultural theory102 for governance for patient safety. Hood’s model identifies markets and professional clans as bases of authority (modes of governance) that potentially compete with the corporate board, the implication being that the operation of insurance markets and/or professional bodies may limit a board’s ability to govern. Contextual differences are important in terms of the institutional arrangements that characterise health-care systems. Comparative evidence of such differences is emerging, most notably Jha and Epstein’s63 recent observation of substantial differences between boards of directors in England and the USA, which were accounted for by the different roles and resources allocated to board members, as well as the different health-care systems in each country.
Therefore, board governance as a mechanism for change is likely to lead to different outcomes according to the context. Critical reflection is required on the extent to which the current field of corporate governance is appropriately conceptualised and applicable to the complex quasi-markets, multiunit systems and professional bureaucracies that tend to characterise health care. In short, greater attention to the theoretical and conceptual basis of board governance would help the development of the empirical field and help to prevent, for example, the making of simple prescriptions for strong leadership without first defining such leadership, how it is to be obtained and the nature of the causal mechanisms that lead to its desired effects.
Given the methodological and theoretical limitations noted, it is clear that the quantitative study of board oversight for patient safety requires further work, in terms of developing new measures and relationships, underpinned by crisper theorising. It is especially important to test assumed causal relationships between practices that are associated with good governance and desired outcomes in terms of safer care; moreover, evaluation programmes will need to assess the extent to which interventions are implemented as intended, as well as to search for unintended consequences. In addition, further study of the microprocesses associated with board governance is required. 103 Although qualitative and case study research is beginning to emerge in this area,59,70 further study of the practices undertaken in the boardroom would provide much-needed insight into exactly how patient safety governance is exercised and experienced.
Concluding remarks
Despite growing pressures for boards to improve and emerging evidence that more effective board oversight is associated with higher quality of care, efforts to create effective governance for quality and patient safety are in its early stages. Many boards have focused largely on financial performance and access issues and are still developing the broader skills needed to assume a more corporate role while assembling the necessary expertise in quality and patient safety.
In the context of increasing expectations and pressure to deliver better care more safely, it is more urgent than ever that hospital governing boards take action to strengthen its oversight of patient safety. The review has captured some of the key areas where boards may be able to develop greater expertise, for example through the provision of better information and education for board members in the use of data to inform decision-making. However, our review also suggests that efforts to create effective governance for quality and patient safety remain variable and are in the early stages of development. The findings from the review, including the emerging storylines, were used to inform the theoretical basis of the study and structure the empirical work undertaken as part of the present study and outlined in Chapters 4–8.
Chapter 4 Overview of cases and emerging themes
Introduction and guiding research questions
This is the first of five chapters presenting new empirical findings, the first four of which cover the qualitative case study work, and the fifth and final of which explores findings from the quantitative surveys.
This opening chapter presents a synthesis of material from all four case study sites to address each of our five main research objectives in turn:
-
identify the governance activities undertaken by hospital trust boards with regard to ensuring safe care in its organisation
-
explore the role of boards and boards of governors in FTs with regard to the oversight of patient safety in the organisation
-
assess the association between particular hospital trust board activities and patient safety processes and clinical outcomes
-
identify the facilitators and barriers to developing effective hospital trust board governance of safe care
-
assess the impact of external commissioning arrangements and incentives on hospital trust board oversight of patient safety.
For each research question, a brief summary of similarities and differences between case study sites is provided and important emergent themes within the data explored.
Governance activities
In this section, we present an account of the governance activities of the board, examining strategy, leadership and attention given to patient safety issues by boards.
Strategic activity
In our study sample, all the trusts were greatly exercised by strategic concerns, but case study sites were highly differentiated in the robustness of its strategic approaches to the governance of patient safety. Skye was perhaps the least developed, lacking a coherent strategy because of extensive recent periods of turnover in executive board membership and beset with financial difficulties which, understandably, focused the attention of the board during the period of observation. Although there was much scope for development at this site, there was also cause for optimism given more recent board membership reconfiguration and the potential for strategic focus that this brings. In contrast, Islay had developed a patient safety and quality improvement strategy that was closely integrated into the business of the trust. The board saw themselves as quality and safety strategy pioneers; this was reflected in highly developed leadership activities (see below) as well as more strategically in its translation of strategic goals into summary indicators and reporting systems which were reviewed within board meetings. Therefore, although the trust was able to track its compliance with performance indicators related to patient safety monitored by regulatory agencies, this was done in the context of the quality monitoring and improvement activity required to meet internal strategic goals. This emphasis was reflected in the structure of the board meeting agenda, which was designed to support a focus on continuous improvement to meet internal strategic goals.
Lewis and Arran are both widely acknowledged as elite organisations, a significant proportion of their work involving the provision of specialist clinical services. Consequently, both have highly organised medical workforces who inform strategic developments within their fields. At Lewis, the overall strategic direction of the trust is built on a very strong CEO who effectively personifies the trust. The emphasis is on securing the legacy of the organisation as the local and regional provider of choice, and board meetings during the period of observation firmly focused on issues of estates and finance to support this legacy. Performance indicators of patient safety monitored by external regulators were routinely reported to the board. However, board discussions centred on the need to challenge targets set for reductions in infection rates and the associated penalties for failure to comply, rather than the service redesign required for compliance under the regulatory regime.
Strategic planning arrangements at Arran are undergoing development, moving away from emergent and evolutionary processes of strategic decision-making towards more formalised approaches, envisaged as an annual process. These more formal arrangements have developed in response to an acknowledged lack of team cohesion with regard to strategic direction; although the global aspirations of the trust were always clear, there was perhaps less clarity or shared understanding in relation to its strategic implications. These more formal arrangements are designed to increase coherence and shared understandings between staff, with the intention of securing actions to address identified difficulties. The trust has a highly detailed performance indicator reporting framework (see below) which is used to monitor performance in relation to external regulatory requirements.
Leadership activities
Given the highly turbulent nature of board membership over recent years, it is perhaps unsurprising that leadership at Skye is experienced as ‘staccato’. Board dynamics were acknowledged as troubled; although NDs were often vocal in their challenges to executives, this was not universally the case, with some concern expressed over possible scapegoating and the existence of ‘favourites’ who were challenged less often. The adversarial nature of the board was experienced negatively by some participants and was felt to foster defensiveness and covert behaviour, with the consequence of continued uncertainty over clinical practice. This feeling of unease was exemplified in the operation of the infection control strategy; although it had helped to identify and address a long-standing quality issue, concerns continued to be raised over the engagement of medical staff because of the frequent non-attendance of executives at infection control meetings, to the extent that, following a breach of Monitor targets, they were unaware of the issues. Limited staff engagement was also evident in planning to address the ‘bed crisis’, which was hampered by a lack of involvement of medical and nursing staff, both at consultant and ward staff levels.
In contrast, leadership of patient safety activity at Islay was clearly attributed to the board and principally to the CEO, who had ensured that quality improvement infrastructure and methodologies were embedded within the organisation to the point that coaching and these methodologies were ‘mainstream’ activities within the trust for all levels of staff. The board had been developed over a period of 10 years, with a stable membership and the support of external quality improvement specialists over the long term. Board dynamics were experienced as ‘supportively challenging’; that is, depersonalised and intended to stimulate further improvement in patient services. This dynamic was supported by charging NEDs with free-ranging scrutiny roles, rather than the more usual committee roles. High staff engagement and an improvement-oriented approach were exemplified in the trust’s response to C. difficile infection, which was characterised by division-based (local) targets to drive internal competition; charging the MD with responsibility for infection control; and the direct involvement of quality improvement personnel in planning reductions. Similarly, the use of ‘staff stories’ (an extension of the quality improvement approach of ‘patient stories’) of experience of care within the trust fostered staff engagement and trust that their insights and contributions were valued.
At Lewis, board leadership of patient safety, as with strategy, was dominated by the CEO, who was highly visible within the organisation and known for ‘unannounced’ inspections, an approach also favoured by other directors. Although the benefits of this approach were acknowledged, some concern was expressed over the limited scope for clinical presence within the board, especially in light of the level of responsibility given to the medical and nursing directors with regard to patient safety. The limited nature of clinical engagement in patient safety issues was identified within the infection control strategy implementation, particularly in relation to work at the interface of primary and secondary care. Although the monitoring of external infection control targets had driven interest in and support for infection control in some quarters, many senior clinicians remained unengaged, which was hampering improvement in C. difficile infection management. Similarly, some resistance had been noted to the medical appraisal systems that had been instituted in the wake of the Francis report. The concern was that without increased engagement, the trust risked sanctioning disrespectful behaviour to patients, with inevitable negative consequences for patient experience.
Arran has devolved considerable responsibility for patient safety into its clinical boards, each of which is supported by a single medical directorate for quality and safety that brings together activity across the clinical boards and reports upwards to the board. This structure reflects clinical leadership for patient safety and charges the board with oversight. Given this arrangement, board anxieties chiefly related to the extent to which staff feel able to report incidents within the devolved structure, the concern being the extent to which staff feel that it is safe to do so (i.e. that their concerns will be heard and acted on and that no negative reputational consequences will follow from expressing such concerns). This possibility is at least tacitly acknowledged by a number of respondents at various tiers within the organisation; cultural interventions concerning values have been made to address such fear and incorporated into staff appraisal systems to provide a means of raising and challenging such behaviours. Although these interventions have been welcomed, fears over the possible negative consequences of raising issues continue to be expressed, and there is evidence from junior doctors’ responses to the General Medical Council (GMC) survey of a fear of bullying by some senior medical staff. The main issue is that this constitutes a latent patient safety problem, with potentially damaging consequences for patients (and, indeed, the trust). Similarly, in relation to infection control, although the trust has a clear, well-resourced system and a specialist team to co-ordinate activity across clinical boards, fear of negative reputational damage associated with identifying problems is reported as hampering the reporting of issues. This has led to the development of specific practices in reporting of routine data to identify potential future problems and thus speak a language of ‘response required’ that can be heard at board level before problems arise.
Allocation of board time to patient safety
Observational and documentary data identified the time spent on patient safety, the supporting information provided and the nature of these discussions. Detailed summary tables are presented for each board meeting observed at each site in Appendix 8, and narratively summarised here. Across all four observed board meetings, Skye allocated 379 minutes out of 892 (42% of the total time) to matters directly concerned with service quality, patient safety, performance measurement and risk; considerably more than that allocated to strategy and capacity (185 minutes, 21% of time), human resources (HR) (79 minutes, 9% of time) and finance (55 minutes, 6% of time). Detailed supporting information was provided to board members within their briefing materials, including internal and external benchmarking data, line graphs of monthly and quarterly trends and ‘traffic-light’ indication of breaches of targets. This information was used by board members to frame their discussions, with much time being taken up in ascertaining the accuracy of the information presented and its implications for service delivery.
In contrast, the board at Lewis spent comparatively less of its time on matters of service quality, patient safety, performance measurement and risk. Of a total of 845 minutes over four board meetings, 236 minutes (28% of time) was spent on these matters. Although this was longer than other topics, time allocation was more evenly allocated between priorities, with 198 minutes (23% of time) allocated to estates, 158 minutes (19%) to capacity and strategy, 105 minutes (12%) to finance and 13 minutes (2%) to HR. Extensive documentation was provided in relation to quality and safety, as at Skye. However, in contrast, this was often not directly referred to in discussions or used to frame discussion/debate/challenge by directors; discussion was largely framed narratively by the CEO, with little direct recourse to the documentation provided. Indeed, some materials included within directors’ briefing materials were not discussed at all including the staff survey, patient-reported outcome measures, the National Institute for Health and Care Excellence (NICE) guidelines, quarterly monitor returns, a red–amber–green (RAG)-rated end-of-life care outcomes report, a safeguarding review in learning disabilities services, minutes from the complaints panel, pressure ulcers, patient falls and, on one occasion, the previous board minutes for approval. This reflects the more narrative style of the board at Lewis, and the dominance of the CEO in board meetings. The overall impression is one of a stark contrast with Skye, with hardly any reference to the different information provided in directors’ briefing packs and limited direct discussion of performance targets except concerning C. difficile infections, which focused mostly on the financial consequences of breaching compliance, rather than the quality improvement needed to ensure it. Many of the documents included in directors’ briefing packs but not discussed cover patient experience, human dimensions and safety, which only Islay discussed in any detail.
Board meetings at Arran were considerably shorter than at the other sites, owing in part to the continuation of a closed (private) part of the meeting to which the research team was not granted access. In total, the four board meetings lasted for 421 minutes. Most of this time was spent on quality, safety and performance (252 minutes, 60% of the total time), the vast majority of which was spent in relation to assurance activity against external performance targets and frameworks. In total, 83 minutes (20%) were spent on finance, 56 minutes (13%) on HR and only 30 minutes (7%) on strategy and capacity. All of the time allocated to strategy was spent during a single board meeting; typically, strategic discussions were not held within the public board meeting. Although a wide range of performance data were made available to directors, attention tended to be concentrated closely on those showing shortfall and the board had a very ‘assurance-heavy’ feel. Furthermore, there was little discussion of quality improvement activity in relation to these indicators.
Islay board meetings lasted 830 minutes in total. Of this, 448 minutes (54% of total time) was spent on quality, safety, performance management and risk. Of the remainder, 315 minutes (38%) was spent on strategy and capacity, 31 minutes (4%) on HR, 28 minutes (3%) on finance, and 8 minutes (1%) on estates. Board meetings were split into two halves, the first of which was open to the public. Much of the strategic discussion was done in the second (closed) half of the meeting because of commercial sensitivities; consequently, the two halves had a very different balance of material. In contrast to the other sites, directors discussed the human dimensions of patient safety explicitly, each meeting starting with a ‘patient story’ narrative to focus attention. A wide range of statistical data in addition to performance management indicators were discussed, including quality improvement data from run charts. Indeed, the emphasis was largely on quality improvement (improve performance further) than assurance (conform to standards).
The roles of trust boards and trust boards of governors
The common narrative at all sites in relation to the board of governors was of a largely ineffective, if well-meaning, body that received information from the executive. Indeed, all sites indicated a largely educative environment with limited challenging or holding to account; meetings tended to resemble seminars rather than board meetings. Although governors typically indicated cordial relations with the board, there was often a sense of bemusement from board members concerning the governor contribution beyond acting as the ‘eyes and ears’ of the board within governors’ constituencies. Skye and Lewis both reported engagement of governors in assurance work in relation to NED appraisal and committee work, respectively, but the latter was experienced as frustrating by governors, despite the availability of training to support the process, with little engagement from NEDs. Overall, governor meetings appeared to contribute little to effective governance of patient safety at any of our sites.
Oversight activities, patient safety processes and clinical outcomes
All sites were subject to external oversight by Monitor and, predictably, this external regulatory framework informed internal mechanisms at each of our sites. However, a range of orientations towards the use of performance indicators associated with patient safety (and the systems and practices adopted) was evident.
Although Skye had adopted a ‘RAG’ indicator reporting system to the board, concerns were expressed over the validity and reliability of data presented, with ongoing concerns over inconsistencies in measurement between clinical service areas which made aggregations of indicator data difficult and hampered escalation of issues to the board. Standardisation of performance measurement indices formed part of an ongoing pathway redesign process that was intended to address the issue. In contrast, board members at Lewis expressed greater confidence in the validity and reliability of data embedded into assurance mechanisms, which incorporated a wide range of clinical indicators beyond those required for Monitor compliance, including a modified Clinical Assurance Toolkit (CAT). Indicators were also benchmarked against ratings of other Shelford Group Trusts (10 multispecialty academic health-care organisations). Although indicator summaries were thus valued, it was expressed that there was concern over the lack of contextual (qualitative) information in relation to specific issues, such as the HSMR, and that presentations and/or briefings would be welcomed. Similar concerns about the over-reliance on quantitative summaries were expressed at Arran; high-level performance data, supplemented with lower-level clinical ‘care-thermometer’ information, was well developed. The concern was that such aggregated data could be used to respond to risks only after problems had manifested; what was required was more qualitative contextual analysis of performance indicator data that enabled potential risks to be predicted before they manifested. This difference lies at the heart of distinctions between assurance and improvement-oriented behaviour; reacting to solve problems once they manifest rather than redesigning systems to avoid unnecessary risk. Islay was attempting to combine the requirements of external assurance with ongoing quality improvement through development of national- and local-level data sets, quality improvement data from projects linked to strategic priorities and qualitative information from reports by clinical service areas. Despite these efforts, respondents indicated the need for further training of NEDs to understand the implications of run-chart data, and the need for further disaggregation of data at ward level.
Facilitators and barriers to board governance
Facilitators
The main facilitator at Islay was understood to be a clear strategic mission (5-year plan) focused on care quality, which had been translated and codified into performance measures and incorporated in an organisational quality dashboard. Objectives were clearly identified against the plan, with risk assessment of the likelihood of the delivery and devolution of responsibility for achievement to service areas. This ensured continuous focus on organisational objectives, notwithstanding the requirements of external performance management regimes. The strategic focus was buttressed by board dynamics characterised by ‘supportive challenge’; airing of issues was not interpreted as disloyalty and openness was valued (always subject to respectful framing) in order to maintain focus and momentum towards strategic objectives. At Lewis and Arran, the stability of board membership over time was considered to be an important facilitator of patient safety governance; the detailed knowledge and connection with staff of the CEO was accorded a high value. At Arran, the extent of clinical leadership was considered an important factor in board governance, notwithstanding persistent concerns (identified above) about the bullying of juniors by senior medical staff. In contrast, it was accepted at Skye that facilitators were relatively weak; the focus here was on optimism regarding the possible impact of recent board reconfigurations and the increased emphasis on care quality over finance evident in board meetings.
Barriers
All sites faced considerable barriers to the appropriate escalation of issues, that is, how best to act following identification of a potential concern. At Skye, this was primarily caused by disputes over the validity/reliability of summary indicator data (information deficit) and communication difficulties between clinical units and the board, and between board members (executives and non-executives), leading to a sense of confusion over the meaning of indicator data received at the board. At Lewis, the difficulties were mainly caused by perceived lack of engagement of senior medical staff, resulting in little communication between corporate teams and ward level staff in many parts of the organisation. Although reporting systems for major events at Arran were judged to be robust, respondents indicated concern that staff may not come forward with issues related to patient safety for fear of negative implications for their career; this was in relation to an acknowledged problem of bullying of junior medical staff to the extent that staff were not prepared to speak out. An additional issue at Arran concerned fears of oversensitivity to financial considerations, leading to poor decisions over safety, such as failure to provide adequate cover to meet a financial target exposing patients to unnecessary risk, rather than acting as a trigger for redesign work to make efficiency savings safely. Islay also manifested concerns over appropriate escalation at point of concern, in its failure to identify a hygiene problem within its kitchens (rather than directly in clinical services). This raises the prospect that, while its planning arrangements are well developed, it risks being caught out in services areas that do not feature within the planning schedule.
Impact of external commissioning arrangements and incentives
Commissioning
Relationships with commissioners at Islay were acknowledged by all to be excellent, and the trust was considered an exemplar provider in terms of the depth and subtlety of its documentation and analysis. The only reported difficulty concerned managing the reactions of other local providers who did not always believe their reported outcomes. Skye reported cordial relationships with commissioners and good involvement of commissioners in clinical governance committee work, although closer working was required over proposed reconfigurations to reduce secondary care demand that would have negative repercussions for the trust. Similarly, relationships with commissioners at Lewis were coloured by the trust’s ambitions for expansion and large capital development projects, in the context of proposed expansion of integrated care. Commissioners indicated that they found the trust to be aggressive with regards to defending its interests, yet had reached accommodation of the financial consequences of breaches in infection control targets.
Incentives
Commissioning for Quality and Innovation (CQUIN) was experienced at both Islay and Lewis as too unwieldy in operation to act as effective incentives, and negatively perceived as ‘taking money off’ rather than incentivising improvement activity. At Skye, CQUIN were perceived as having a positive impact on stroke pathway redesign, but a distraction from other areas that also required redesign work. Although compliance frameworks were generally welcomed for the effect on focusing attention on aspects of patient safety, concerns were raised in relation to the negative unintended consequences, such as reduced focus on areas not covered under the framework (e.g. environmental health). Penalties also proved difficult to apply at both Skye and Lewis, as they could have potentially bankrupted the former and led to bitter dispute with commissioners at the latter.
Emergent themes
Our summary of data in relation to the research questions above identifies four important analytic themes related to patient safety governance: (1) the identification and attribution of patient safety issues, (2) escalation of concerns over patient safety, (3) the dynamics of whistleblowing and (4) the tensions between assurance and improvement. We consider each in sequence.
Identification and attribution of patient safety issues
Detailed reporting of summary performance indicator data related to patient safety is common to all of our sites, informed by the requirements of external regulatory regimes and, in some instances (Islay and Arran), considerably exceeding them in scope and scale. Although such summary reporting concentrates board members’ attention and allows breaches to be clearly indicated, a number of factors were identified which caution against over-reliance on such systems. Experience at Skye shows the importance of the perceived validity and reliability of the underlying data if action is to follow, otherwise time may be spent on debating what the data reveals, feeding tensions between board members rather than acting upon the implications of summary measures. Similarly, detailed observation of board activity at Arran showed that, even where there are clear breaches of targets in RAG summary indicators accepted as appropriate, it does not necessarily follow that the data will be interpreted as showing a patient safety failure requiring action; rather, the attribution ‘patient safety problem’ is dependent on acceptance that the breach really is a breach and not a misinterpretation. Respondents at Arran and Lewis also draw attention to the important role of qualitative data in contextualising and making subtle judgements in relation to summary data. Specifically, ‘green’ indicator ratings may conceal manifesting failures in risk management that will, if left unchecked, eventually result in ‘red’ figures. Summary reporting of ‘traffic lights’ on a single page of A4 paper may offer assurance that all is well, but such assurance will be illusory.
Escalation of concerns over patient safety
In addition to accurate identification of performance shortfalls, service improvement requires the engagement of staff to identify underlying problems and implement changes. Where staff engagement is lacking, initiatives may not embed or embed only partially; this is a particular problem where there are concerns about the bullying of staff. Escalation requires the existence of a reporting structure, conditions of trust and support between staff and a quality improvement orientation to address underlying problems.
Dynamics of whistleblowing
Despite the acknowledged importance of whistleblowing for preventing unsafe clinical practice, staff reporting such events face a dilemma where they fear negative repercussions for their career for doing so, placing the individual in the invidious position of ‘damned if you do, damned if you don’t’. Such fears are more likely to flourish in an environment in which such action is considered to be an act of disloyalty to the organisation or profession; this is especially the case within elite organisations where such action threatens the self-image of high performance. Where such practices exist, the fear is that formal policies in relation to whistleblowing will prove ineffective and opportunities for identifying safety issues before they manifest will be lost.
Tensions between assurance and improvement
Despite the availability of quality improvement infrastructure, three of our sites operationalised the governance of patient safety largely in terms of assurance, in which performance indicator systems were used to alert the board about poor performance in relation to specific clinical indicators ‘after the fact’. Major problems with this approach include that it may foster non-reporting to avoid the blame and shame that goes with underperformance, that disputes may arise over the reliability and validity of the indicators on which judgements of performance are made and that it does not provide guidance on how best to address the manifesting poor performance. In short, in seeking to identify problems it may paradoxically make it harder to report them. Islay sought to counter such negative unintended consequences through strategic focus on service improvement and embedding performance indicator reporting systems within quality improvement cycles, even to the extent of structuring the board agenda around strategic quality improvement.
Concluding remarks
This chapter has begun the analysis of the four case study sites by examining board dynamics against our pre-specified research questions. In doing so, a number of key issues have emerged that highlight the challenges for boards in getting and interpreting information (as opposed to data) on quality and safety issues. In particular, the balance and congruence between ‘hard’ quantitative data and ‘softer intelligence’ (staff and patient accounts) remains poorly determined. Core concerns in this latter category are the risks and challenges of staff raising concerns, either through formal clinical governance channels or through whistleblowing. Finally, in developing appropriate responses, boards struggle to balance quality assurance needs (conformance attainment) with more proactive improvement (performance enhancement).
Chapter 5 digs deeper into each case, building on these cross-case emerging themes.
Chapter 5 Site-by-site case study narratives
Introduction
This second of four chapters on the qualitative findings presents an in-depth account of each of the four case study organisations. The discussion is structured around seven key themes that emerged from the cross-case analysis (see Chapter 4) and the review of the theoretical literature (see Chapter 3). These are:
-
Strategic vision. This theme explores how boards seek to develop and deploy a range of resources (e.g. intellectual, financial, social, technological and political) to oversee safe care.
-
Leadership activities. This relates to the way in which board members interact and engage with the wider organisation, patients and the public as part of their approach to governing patient safety.
-
Board meetings and mechanisms. Here we outline the specific practices that were seen as being integral to board governance.
-
Governor relations. Observations here relate to the relationships seen between the management boards and its respective boards of governors.
-
Assessing organisational performance. This theme explores how board members perceive, interpret and react to patient safety performance information.
-
Relationship with commissioners. We explore the relationships between the board and its key commissioners.
-
Relating to regulation. This final theme gathers insights into the regulatory environment and how boards react to externally set performance targets and incentives.
Each of these themes is now discussed as they played out within each of the four case study sites: Islay, Skye, Lewis and Arran.
Islay
Islay is an integrated provider of hospital, community and primary care services. It has a reputation for its achievements in relation to promoting quality and safety and the organisation has received several awards in recognition of its performance in this area. The trust is also a leading organisation in terms of both patient and staff satisfaction.
Strategic vision
The Islay ‘success story’ was attributed to the fact that they had a clear a strategic vision ‘to be become one of the safest hospitals in the NHS’. Inspired by the CEO and ND, the strategic vision was triggered by ‘a road to Damascus moment’ during a visit in 2004 to the Institute of Healthcare Improvement (IHI) based in the USA. This subsequently led to the adoption of the IHI quality collaborative methodology in the trust, including signing up to the Saving 1000 Lives programme and the introduction of patient stories at board meetings. The board attributed its high performance in quality/safety in part to the ability to translate its mission into hard performance measures, which were summarised in a quality dashboard. The board’s 5-year strategy was linked to specific performance objectives that were disseminated across organisational divisions. These objectives were also subject to risk assessment to determine the extent to which they could be delivered:
We launched our quality improvement strategy 4 years ago and we were, as I say, ahead of the game for what that was worth . . . with clear aims and objectives, time frames, responsible officers . . . And we’ve demonstrated that time and time again.
Board members appeared confident that they had nurtured a strong patient safety culture across the organisation. Indeed, they were so confident about this that it was reported that external patient safety improvement initiatives, such as the implementation of recommendations for the Francis Inquiry, had little impact in changing its ongoing strategy. The introduction of a Nursing Assessment and Accreditation System (NAAS) in 2008, which was used to assess hospital ward-level quality and patient experience, was cited as an example of the organisation being ‘ahead of the curve’ in its efforts to improve quality and safety. The successful adoption of the quality improvement (QI) collaborative methodology, which was responsible for the elimination of high-grade pressure ulcers, was another reported example of the way in which continuous quality improvement methods were embedded within the organisation.
Despite these much vaunted successes, there remained scepticism among some board members as to whether or not the high performance could be attributed to the approach to quality improvement taken in the organisation. The director of development, for example, suggested that the performance was not the result of the quality improvement programmes but rather of wider factors and, in particular, of the income generated from a mixture of tariff and non-tariff services:
I think we’ve been lucky again that we haven’t had financial problems like a lot of other places. Now, part of that is down to good management . . . But part of it is down to luck. We’ve got a service profile and income profile that puts us in a good position, so we’ve a good mix of general hospital-type services and specialist services.
Board members believed a number of factors could stall the momentum that had been built up around quality improvement. The difficult economic environment was cited as a key factor, particularly the tensions associated with funding the ‘7-day week’ agenda. Hospital reconfiguration in the region was also viewed as a threat to ensuring safe care. It was reported that Islay was in a unique position to lead the necessary system changes across the local health economy, yet organisations did not always want to engage with them. Islay had a reputation ‘for wanting to take everything’ and there was a feeling among some board members that they needed to build better relationships with key stakeholders across the region, otherwise they risked isolation. It was believed that being isolated within the local health economy might have serious negative consequences for the organisation. For example, it was felt that if neuroscience services were to be moved to another organisation this would precipitate serious financial difficulties for the organisation.
Leadership activities
Successful board oversight of patient safety was often linked to the leadership style of the CEO and the ND, and in particular to their efforts to invest in quality improvement programmes and embed these across the organisation. The executive directors were described as an experienced team who worked well together and who believed collectively in the strategic approach being taken.
Central to board strategy was the focus on consulting and engaging staff at all levels of the hierarchy in key decisions. This was cited as key to them, being one of the organisations with the highest engagement scores in the NHS for two consecutive years. Specific leadership styles that were frequently mentioned related to ‘asking questions’, ‘getting the best out of that individual’ and obtaining ‘rich information from that individual’. The CEO described that what made Islay different from other organisations was that the board did not have a chief operating officer (COO). The rationale was that they wanted each executive director to have a specific domain of responsibility for a division of the organisation. The role of the executive was therefore cast as one of striving to encourage, advise, motivate and coach the management staff within their particular divisions. This close contact with staff lower down the organisation meant that the board’s vision became ‘something that everyone believed in’:
I firmly believe that if you continue to chase the dollar, you will be chasing the wrong thing. You need to chase the quality and safety, and what brings quality and safety for me is deep staff engagement, and that costs you not a penny.
Although staff engagement was noted as a particular success, there was also recognition among some board members that engagement policies could be variable. Despite achieving high NSS satisfaction scores, recent qualitative research undertaken by the trust had highlighted significant variability across the divisions in terms of staff feeling that they were a member of a team, that they could speak out if they saw something untoward and that managers supported them. This breakdown in board communication was illustrated by a poorly graded environmental health inspection which, it was reported, had exposed the limitations of staff engagement in the organisation:
We’ve got a bit of a less robust connection . . . and that was brought into stark relief by the experiences in the patient kitchen . . . I would say the engagement is more variable than it might first appear.
The existence of ‘closed’ and ‘hard-to-reach’ areas of the organisation was challenging. For example, engaging with staff working in one or two specific departments and in the operating theatres was raised as an area where there was thought to be ‘room for improvement’ in terms of embedding the desired behavioural and cultural changes and, in particular, inculcating new approaches to working among senior consultant medical staff. The NEDs also noted that the board did not have the same visibility in the community services that they ran as they had in the hospital and that they needed to think of different ways of better engaging staff in care homes, intermediate care providers and the private sector. The CEO also raised the challenge of developing better engagement with the public, as he felt the board had yet to develop an effective way of gathering patient, family and carer views about the services the trust provided.
Board meetings and mechanisms
Quality and safety issues were described as being the core business of the board meetings at Islay, with the first part of meetings given over to presentations about the progress of ongoing quality improvement activities and typically ‘over one-third’ of board meetings being spent discussing and debating quality and safety issues. A feature of board meetings at Islay was the participation of all divisional directors in the first part of board meetings. The purpose of involving them was to create an opportunity for the board to cascade messages down the organisation and to hold the divisional directors to account for the quality/safety performance of their divisions.
Islay was unique among the case study sites in having a ‘patient story’ at the start of each board meeting. The aim was to ‘set the tone’ for discussion and to focus the immediate attention of board members on service quality and patient safety matters. The ND had ‘championed’ this approach, but there were conflicting views about its usefulness, with the business director questioning the overly emotional connections that could be engendered by such stories. Criticism was also made regarding the lack of time available for the board members to discuss fully the implications of the patient’s story.
The fieldwork uncovered that, out of the almost 13 hours of board discussion observed across the four meetings, a total of 160 minutes was spent discussing patient safety issues (just over 20% of the total time). Compared with the other case study sites, there was less discussion about C. difficile infection issues and attainment of external performance targets. Patient safety discussions tended to be connected to wider quality improvement activities. The only patient safety-specific issues discussed at length were those relating to issues around mortality coding in orthopaedics (just under 30 minutes) and the environmental health inspection (50 minutes). The majority of time spent at the four board meetings observed tended to be focused on broader strategic issues, such as hospital reconfiguration, developing strategic partnerships and strengthening links with the community sector.
Governor relations
A number of board members described their support for governors as an effective means for FTs to engage their local community. It was also thought that governors provided ‘a voice of the people’, along with providing important intelligence about the organisation in terms of ‘what people are feeling and thinking’. NEDs talked about the additional education and training programmes they had developed for governors to help them in their role. The board chairperson described developing a close relationship with governors where he would feed back the outcomes of executive board meetings and give his ‘own honest opinion’ of what was happening:
I meet with the council of governors personally and in private, and I go through the board papers with them . . . I wouldn’t drop that meeting because they think it is so valuable to be able to ask tough questions privately and for me to be able to give an honest and open and sometimes a personal opinion about them. They get it unvarnished.
However, some board members suggested that the role of governors in the organisation was still not clear and questioned the competencies and capabilities of governors to successfully fulfil their role. It was also noted that the time needed to volunteer meant that governors were overwhelmingly of retirement age and that there was less representation from younger social groups in the population.
Governors described being engaged with the governance of patient safety at a number of levels. These included the Quality Subgroup, where governors were to able talk and challenge NEDs about the day-to-day operational issues related to quality and safety. Governors also described generally good relationships between the board and the council of governors. Governors felt that they were able hold the board to account through a variety of channels, including involvement in the chairperson’s appraisal and being able to actively challenge NEDs at the Quality Subgroup. The main issues of concern for governors related to the ‘steep learning curve’ and the time needed to fulfil the role effectively. It was thought by some that the ‘enforced’ election process and the potential removal of governors at the end of their 3-year term resulted in a ‘loss of key talent and organisational memory’.
Fieldwork observation of governor meetings supported many of the issues raised in the interviews. Governors rarely participated in discussions, which were dominated by the CEO and the chairperson. The focus of the discussions was one of education about particular issues (in this case hospital reconfiguration) in order to seek support from governors to continue the position the board was currently taking.
Assessing organisational performance
The organisation had been a forerunner in developing a quality assurance framework that combined national-level data regarding the HSMR and standardised health mortality indicators with additional local data, such as the NAAS, and Quality Improvement projects using Statistical Process Control run charts. Board members described triangulating these data with additional and softer intelligence obtained through walkabouts, board briefings (project managers presenting reports), and the complaints panel. Walkabouts, in particular, were highlighted as a good way to make the board visible and as an opportunity to engage with frontline staff and to respond immediately to their concerns:
I think that regular attendance on the shop floor gives us a level of information and knowledge that we otherwise wouldn’t get . . . and I think that that gets pulled back into the discussions that we have at board level.
Although the current performance information and quality indicator dashboard was in large part supported, comments were made, particularly by NEDs, calling for a greater narrative interpretation and analysis of the bold statistics and graphs provided and for a greater allowance of time for the board to ‘think about the implications’ of what the information was ‘saying’. The chairperson made the point that, although disaggregation of the data was the ultimate goal, this information needed to be presented in an accessible way:
People would probably like the graphs, but I couldn’t give two hoots about the graphs because words mean more to me. So to tell me what that actually means. Is it good, bad or indifferent? Have we gone up? Have we gone down? What is the trend?
. . . looking at these graphs are leaving us cold. We’ve been doing it for 3 years, we see eight data points above or below, and then it drops down, great, what does that tell us?
Frustrations were raised by the ND about NEDs still struggling with interpreting run charts, despite the board having used them since 2007. However, rather than more training, NEDs reported that they wanted more time to develop relationships within the organisation and also between fellow NEDs.
Relationships with commissioners
Board members described good relations with commissioners that have continued during the transition from the local PCT to the local Clinical Commissioning Group (CCG). The experience of the MD supported the move to CCGs in facilitating greater clinical involvement in commissioning decisions, and it was seen as an opportunity to have ‘mature’ discussions about the current economic environment. An example of this was the recent collaboration around unscheduled care, which brought organisations across the local health economy together in an attempt to save several million pounds. Alongside these positive experiences, some board members reported that commissioners were ‘suspicious of their success’ and that this led to ‘mistrust’ in negotiations. Frustrations were also expressed about commissioners being overly focused on hospital oversight at the expense of the wider health economy, with community care settings in particular described as ‘very loose’ in relation to patient safety:
I think there is a recognition across the health economy that we’re one of the ambitious organisations who are at the top . . . but I think that also brings with it a level of unhelpful scrutiny and unhelpful, what’s the word I’m looking for, mistrust. It can’t all be good. Trying to find a problem, if you like, which is irritating, to say the least.
Interviews with commissioners suggested that they felt ‘very fortunate’ to have such a high-performing trust. Islay’s strong emphasis on quality and safety meant that they tended to ‘shine out of the information’ that was being presented. Islay was seen as ‘slick’, with their success being attributed in large part to a very stable board and a very strong chief executive. Islay had been open and transparent in sharing performance information. This was supplemented with regular meetings and conversations about issues or incidents that were reported:
I get a lot of comparative data . . . compared to other organisations across the region, and there are a range of indicators where it is performing better . . . the mortality rates are low, infection control rates are much lower; so a range of indicators where it gives us a level of assurance compared to similar organisations. It’s doing very well.
The only ongoing issue specific to Islay was where rival providers thought the organisation’s performance was ‘too good to be true’. For example, it was reported that clinical quality managers in the health economy could not believe that Islay had failed to report any grade III or IV pressure ulcers. The recent ‘absolutely excellent’ CQC inspection rating was cited as a case in point, as Islay had been inundated with requests nationally for help but there were few requests from within the local health economy. To improve relationships, the CCG was working with the MD and ND of Islay to try and encourage local general practitioners (GPs) and its own medical consultants to collaborate around a quality improvement programme. The goal was for both parties to use the same incident reporting system to encourage dialogue and the sharing of information between primary and secondary care about incidents.
Board members reported that the CQUIN mechanisms being used were not really impacting on service delivery as much as expected. Interviews with commissioners raised similar issues for example, although the CQUIN for dementia services was seen to have had an impact in terms of raising awareness, greater local ownership was needed in order to maximise impact. CQUIN targets, it was thought, were in danger of becoming ‘a bit of a tick box’ as a way of securing finance, but with little long-term service impact. As a result, the CCG was trying to take a more collaborative approach in identifying areas where they wanted to try and secure improvement. Recent examples of this were the agreement of two CQUINs around developing 7-day working in surgery and acute medicine. There appeared to be a shared interest for both parties for quality improvements in this area:
I do believe it needs to be done and in a collaborative way. It’s not good us as Commissioners saying, ‘we want you to improve by X in area Y’ if they haven’t got the appetite to do that.
Relating to regulation
The Monitor compliance framework was supported by board members in terms of ‘focusing the mind’ in relation to key performance areas. The introduction of infection control targets exemplified this, with the development of targets for MSRA and C. difficile infections seen as changing the way infection control was governed. The CQC criteria were also reported as being helpful in supporting the board to identify problems related to cleanliness and infection control:
You’ve got to take that as being a success. You know, there’s no other way of saying that . . . when we started with MRSA, we were probably having 80 [cases] a year . . . [but] we haven’t had any this year . . . So that, in part, has to be the fact that targets have been set.
The first thing I look at in the board pack is the infection control! And then I look at all the data, you know. So I think we are incredibly mindful of that.
However, the point was made that the experience of Mid Staffordshire NHS Trust highlighted the unintended consequences of focusing on performance indicators as an end in themselves. The recent case of an environmental health breach was use to illustrate where those service areas (kitchens) not covered by Monitor or CQC compliance frameworks often went unnoticed. On this basis, it was reported that the board needed to be ‘brave’ in balancing the interests of Monitor and the wider interests of the organisation and patients. The ND raised the point that central targets needed to be backed up with a supportive local culture and that the leadership of the organisation needed to be focused on quality improvement. The Islay board was therefore seen as good at combining a locally driven agenda on quality alongside the national agenda and centrally set performance standards.
CQC inspections are getting more and more focused on the minutia of the documentation, and yet you know you could have the entire documentation perfect, but the patients could be not being treated kindly.
Skye
Skye is a district general hospital trust providing services across two sites. It was one of the early NHS trusts to be awarded foundation status. Over the past 5 years the board has been characterised by continuous change, with the arrival and departure of several CEOs, MDs and NDs. The trust has one of the highest patient demands in the country and has been faced with a number of challenges related to bed capacity. Organisational performance is currently a cause for concern, with the HSMR above average, high A&E demand and increasing infection rates. Skye had struggled to successfully implement governance activities to ensure safe care because of a continuous turnover of board members and the priority placed on finance by successive board regimes.
Strategic vision
Interviews with board members at Skye suggested that the continuous change of executive board members in recent years had prevented the development of an effective strategy for patient safety. In what was described as a ‘jigsaw puzzle of piecemeal activities’, bed capacity was cited as a case in point where previous board decisions to remove beds were linked to a variety of problems facing the trust, including poor A&E performance, poor C. difficile infection management rates, high pressure ulcer rates and a demoralised workforce:
If there’d been someone in the executive with a longer term sort of organisational memory, they might have put some connections together.
Points were also raised about previous board configurations that promoted cost control over quality improvement. The dominant influence of the finance director was seen as a feature during this time, described as ‘a 100% focus on short-term financial issues’. One example of finance seen as overriding patient safety decisions related to the protracted attempt by the IPC committee to purchase a fogging machine to improve deep cleaning. Vacancies, recruitment and pathway redesign were also issues where finance would challenge progress being made.
Criticisms regarding the lack of strategy were also directed at the current board. The director of HR described it as ‘a very functional board’, with no deeper discussions about the evolution of service delivery. The style of the chairperson was also mentioned as a contributory factor, being described as ‘more hands-on than strategic’. An example of this was the proposed ‘quality day’, which was a response to pleas for more dedicated time for discussion. Although this initiative was supported, concerns were also raised about the style of the chairperson, who was described as trying to ‘cram everything in’ and focus on targets rather than developing more informal open discussions about strategy and moving forward:
I had originally thought oh good, because that means we’ll be able to stand back and look at our organisational purpose . . . Actually what it’s turned out to be now is a list of things that just looks like a long board day, so we’re going to talk about C. diff . . . it’s probably partly because the chair doesn’t like blank spaces on agendas.
Despite this lack of strategic thinking, notable improvements were connected to the latest board configuration. The appointment of a new director of finance and a new CEO were seen as improving relations within the organisation and with commissioners. The dynamic was also improving in light of the Francis Report, which was switching the board on to quality. The recent bed plan exemplified how the clinical drivers outweighed the finance issue, as decisions were taken ‘before the financial answer had been found’.
Leadership activities
The continuous turnover of board members at Skye had created a form of ‘staccato leadership’, characterised by interruptions and hiatuses. The new CEO was a case in point: it took him time to find his feet, and this ‘created gaps’, which meant the chairperson had ‘to do a bit more leading than might be expected’. Despite this turbulence, the board was aware that they needed to set the tone in promoting a culture of openness and transparency. Being visible was central to these activities, which were exemplified by the chairperson holding regular meetings with large groups of senior nurses to talk to them about the key issues of the moment. Executive and non-executive involvement in a variety of governance committees, including the mortality review group and the ‘safer care’ group within the clinical governance subcommittee, provided further examples of leadership activities.
It’s the visibility of the leadership I think is the key thing. And I mean they go on to wards to basically look around and talk to staff and actually say, ‘I’m a non-executive director, do you want to raise anything? What are the issues that you’re concerned about?’ So I think on an individual level, ours are very good.
Board leadership was also associated with challenge by creating an environment where certain behaviours were not tolerated. This was particularly the case for NEDs, who were noted for their vocal challenge in holding the executive to account. For example, the acting ND, new to the position, reflected on the difficulties of responding to the challenge from NEDs. Being in an acting position, she noted, ‘made it a hugely vulnerable and exposed place to be’ as the NEDs attacked her inexperience. NEDs very much believed that challenging the executive was key to their role; however, the point was made that they struggled to hold the MD to account because they lacked the necessary clinical knowledge. ‘Second-guessing clinicians’ was an ongoing struggle; therefore, having greater clinical knowledge in the boardroom was seen as necessary. The chairperson was particularly frustrated at holding individual clinicians to account, and described the disproportionate amount of trust given to them as particularly unhelpful as the board sought to understand and investigate any quality and safety issues. Things were changing, with the board now doing more work via the clinical directors who could then provide a peer-to-peer approach to scrutinising clinical practice.
It surprised me when I first got involved in the health sector that pretty serious things can go wrong, and accountability doesn’t seem to be as strong as it would be in other industries. A ‘never’ event should be a ‘never’ event, and people who were involved it, I would take a much stronger line than it appears the health, well the NHS certainly take at the moment.
Issues were also raised about the boards’ ability to engage staff. The board was improving the engagement mechanisms with notable updates to appraisals as well as the introduction of weekly briefings to promote communication; however, the point was raised by a NED that staff were feeling ‘underinformed’ about what was happening:
We don’t generally engage with staff too well. You can see from the survey results . . . [that] a theme running through this is the performance appraisal. There were people who’d do it in groups, so the ward manager would just do all the nurses together. I mean, absolutely dreadful, and that was if it was done [at all].
Board meetings and mechanisms
Although some board members, notably the chairperson, described how meetings over recent years had become more focused on quality and patient care, others were frustrated with the way the agenda was covered, with the chairperson seen as being driven by action plans and timescales. The chairperson, in turn, was aware of these frustrations; however, he believed that the right approach was being taken, and described how a recent action plan related to mortality was being delivered:
I could understand the frustrations on some of my colleagues . . . I’m a bit more in the ‘doing’ rather than the ‘talking’ camp here. You know, we can talk about things for forever and a day . . . but there is a time when the talking has to stop and the doing has to start.
The observations of board meetings highlighted that out of almost 15 hours of discussion across four board meetings, 4.5 hours of the discussion related directly to patient safety issues (30% of the total time). Most of this time was spent on the mortality review across patient pathways (95 minutes) followed by discussions about the breach of C. difficile infection rate performance targets and the resulting financial penalty (80 minutes). Other issues included discussions regarding performance related to patient falls, complaints and pressure ulcers, along with policy updates concerning patient safety, such as the CEO’s summary of the Francis Inquiry (which in in one board meeting lasted for around 30 minutes).
Governor relations
Board members had mixed opinions about the role of governors. On the one hand, the board understood the need to have governors holding NEDs to account and providing a voice for patients, the public and staff. The trust secretary described how the board proactively worked with governors in holding quarterly time-out sessions to brief them on any current issues, and NEDs suggested that they did feel that governors were holding them to account through being involved in their performance appraisal, as well as through governor observations of their performance in chairing different subcommittees.
However, other board members pointed to limitations of the governor role in the (perceived as poor) quality of their contribution to patient safety walk-rounds, productive wards and various other initiatives. One senior executive suggested that governors did not properly hold the board to account, and the quarterly time-out sessions were seen as a ‘bit of a hassle’. Despite well-meaning questions, the capability of governors was seen as mixed and as often diluted by personal agendas, pet topics and minor issues:
We can give a 5-minute spiel about something and talk with intent, hopefully. And people think, ‘Oh, that’s okay,’ and then you get another quarter.
There are some who are not confident to speak up and we try and encourage them but they’re not confident at all. There’s some who are very confident but actually kind of miss the point or misunderstand their role.
Interviews with governors described how they supported the latest board efforts, particularly in helping the chairperson and CEO to respond to patient safety issues. They were also impressed with the NEDs describing their observation of subcommittees where (for example) infection control reports would ‘get some hammer’. This was in contrast with the previous board, which was described as being ‘very entrenched in the old way’, that had ‘not got a grip’ of patient safety. The current board also seemed far more receptive to governors. This was evidenced by greater strategic involvement included drawing up the annual report, sitting on the Clinical Governance Committee, getting access to ‘never event’ explanations, setting the agenda of meetings, going on walkabouts and providing an opportunity to raise issues from a patient perspective.
Having spoken to other governors from other organisations, we’re better off here . . . We participate to a greater extent than any of the others I know I’ve met. And we’re not just a talking shop. We don’t just have governors’ meetings where we talk about things then go away and forget about them.
Despite this, there were still some issues with the current board. As a relatively inexperienced board, some felt that they needed to develop better relationships with the organisation and be more open to staff feedback about service improvements. Concerns were also raised about the quality reports that they received having inaccurate information, particularly in relation to finance. Furthermore, issues were also raised related to the governor role itself and the time needed to develop this properly. The first 3 years following election were seen as a very steep learning curve and it was often only in the second term that governors felt that they had real influence.
Observation of governor meetings found that the majority of discussions centred on governor education about the latest policy developments and the provision of summary performance information. As with the other sites, dialogue was mostly led by the CEO, who would summarise his report, providing a number of updates regarding policy. There were also PowerPoint® (Microsoft Corporation, Redmond, WA, USA) presentations by the CEO about the Francis Inquiry, along with the COO, who presented a business intelligence report detailing the key performance indicators related to activity and infection control. The result of this was that there were limited contributions from the other board members, apart from the chairperson. The chairperson was, however, influential in encouraging governors to question the business intelligence report. The question and answer sessions in response to this report did tend to be active and, in one meeting, this led to a short but significant discussion that challenged the COO about poor C. difficile infection management performance. Points were made about performance being ‘not good enough’. At these times the MD and ND would enter the conversation, allaying concerns and suggesting that things were being done to improve the situation.
Assessing organisational performance
Board member interaction and analysis of performance information was, again, mixed. Some positive aspects were raised, particularly by the trust secretary, about the quality dashboard and how the board was ‘ahead of the game’ in some of the information it was collecting related to HR and the disaggregation of the HSMR broken down on a monthly basis. However, the stronger opinion, particularly from NEDs and the COO, described the current benchmarking as poor, with mistakes in the reports often being found. More work was needed to improve the methodology, as the accuracy of the data was currently being questioned.
I think the business intelligence report isn’t quality controlled brilliantly well. I’m fed up with spotting reds that should be green . . . that needs to be tightened.
Patient safety performance was seen as worrying, with both the HSMR and the standardised health mortality indicators being above average. One of the ways the board was looking to respond to these trends was by paying particular attention to the way that different directorates input information into the Corporate Risk Register. The CEO raised the point that there was currently some disconnect between the information systems used by the directorates and that used by the board, with directorates lacking a consistent structure, leading to people measuring things in different ways. This meant that when issues escalated up to board levels, not all staff were receiving consistent messages. The trust secretary described how directorates viewed the Corporate Risk Register as ticking the box rather than as an opportunity to raise any issues they had with the data. In looking to resolve the disconnect between central support units and board-level measurement systems, the MD and COO at the time of writing were undertaking a pathway redesign that was looking to standardise performance measures across central support units, which will then be reported to the executive team.
Alongside the review of quantitative data, board members described how they gathered soft intelligence through the review of patient complaints, the carrying out of mock CQC assessments and walkabouts. Board briefings provided opportunities for people to be invited or to offer a presentation to the board. A recent example of this was bringing people in who were involved in an investigation of a recent serious incident. Having a patient come to speak to the board was suggested, as well as having a commissioner on the board providing the ‘client voice’. A note of caution was raised, however, that there was a danger that board business could become diluted, with other people coming in and taking over the agenda: there are certain things that have got to be done. Connected to this point the ND, with the support of the CEO, was looking to introduce patient stories to board meetings as a way for the board to interact with more qualitative material at board level. Despite her enthusiasm, fellow board members decided that it was not appropriate. Reasons for opposition included:
It ends up with ‘Woe is me’ and we end up spending 30 minutes to three-quarters-of-an-hour on a patient’s story and it didn’t actually make any difference to the patient, right? And the one thing that concerned me through all this was: ‘Where is the learning? Where is the continuous improvement? Where is the will to not make that mistake again? Where is the will to plug that hole and say, that will not happen again?’.
The touchy-feely stuff . . . Yes. I’m a surgeon by trade, so I’m not good on touchy-feely.
In Skye, NEDs raised a number of personal challenges in relation to measuring performance. As it often took up to 6 months to get a handle on the job, understanding and processing the volume of information was an ongoing challenge. Walkabouts were mentioned as a good way for NEDs to triangulate the information and yet they were also problematic for NEDs, as they were not necessarily prepared with enough information about the area they were going into. Despite these concerns, other NEDs believed that they were starting to tap into the organisational realities. A NED, who was female, stressed the need for a greater female presence on the board, particularly when it came to connecting with female staff. In this sense, rather than further statistical training in this area, more attention should be dedicated to developing relationships and managing situations:
Actually seeing with your own eyes is difficult. The difficulty I think, that it becomes a box-ticking exercise, that you’re looking at a list which somebody’s prepared for you and you tick the boxes and say yeah, it’s really fine.
Relationships with the commissioners
Relationships with commissioners were described as cordial and constructive in working through the current pressures in the system. Despite this, there were calls for the board to have a closer relationship with the CCGs, particularly in relation to what commissioners were doing in the community to help reduce hospital demand. Having a commissioner as a NED on the board or attending regularly was tabled as an option to facilitate further communication and interaction. The COO also called for commissioners to spend more time in the hospital, particularly to see how A&E worked:
[we need to get] closer to these guys and we’ve got to, you know, have sometimes some difficult conversations like, ‘Hey guys, you’re throwing everybody into A&E because you’re not really making yourselves available to people, so come on, let’s play fair here’ . . . we need to have a chat about this because this is not how we need to do things.
The arrival of the new CE improved communication, with regular meetings now taking place. Furthermore, the board had recently witnessed a ‘very sensible approach’ by commissioners to support the investment of a fogging machine to encourage the prevention and control of C. difficile infections. Such a ‘joined-up approach’ was linked to the Francis Inquiry recommendations, to which commissioners were now looking for a more transparent and collegiate relationship with provider organisations.
Interviews with commissioners revealed positive relations with Skye. Since Skye had become a FT, commissioners commented on how progress had been made in terms of openness and communication about patient safety issues. The relationship was now at a point where it felt more like a partnership. This was exemplified by commissioners recently being invited to attend and contribute to their Clinical Governors Standards Committee and attend their mortality review group:
If we turn the clock back 6 years, for example, we weren’t allowed to be in any of their groups. They used to occasionally invite our medical director – our clinical governance leader was a GP – to the odd one, but they basically didn’t invite us as a matter of course.
A key driver for this openness was the events at Mid Staffordshire NHS Foundation Trust, which had driven a realisation that they needed to be open. Commissioners had witnessed the trust become more proactive at handling, reflecting on and reporting serious incidents. Commissioners had been impressed with the NED who was chairing the Clinical Governors’ Standards Committee in the way he challenged the committee and called for a drive to improve standards. Commissioners had also seen the trust become more open to collaboration in working together on patient pathways:
From our perspective, the fact that they then reported 4 months late, we have to take a good view of that. We have to say, ‘Well okay, you should have picked it up at the time but are we going to flog you for it when you’ve actually been open and said we’re reporting it now?’
Although it was reported that Skye had a positive baseline with high patient satisfaction, there were also ongoing problems with several issues, such as the management of the emergency care pathway, clinical rota covers and admissions at the weekend. This meant that the trust were in a high-risk category for quality and safety. This was likely to receive ongoing attention; however, commissioners had been working with the trust to resolve these issues. In doing so, commissioners were pleased and supportive of the way the trust were responding, particularly concerning urgent admissions:
We have to make sure we stick by the line with them, that they’ve done what we asked them to do, and if we didn’t then I think that would be a bit of a breach of trust between the two organisations because they’ve really tried their best on it.
Interviews with board members recognised that CQUIN payments did provide a lever by which commissioners could encourage certain behaviours and practices within the trust. The use of CQUIN to inform the stroke pathway was a good example of CQUIN being used as a carrot to encourage best practice. The CEO also suggested that the CQUIN target for a needs assessment for dementia patients was ‘absolutely the right thing to do’ and was forming part of the board’s dementia strategy. That said, the director of risk suggested that CQUIN was also presented as a double-edged sword: it was good to have such payments, but it could provide a distraction from other activities. Further issues cited included the point that any payments went into a trust ‘black hole’ rather than to the teams and departments who were delivering. As such, it became all sanction and no reward, which led some staff to become apathetic.
For commissioners, CQUIN had provided an incentive for the trust to claim significant additional monies, as well as being a driver for good practice. Falls was a case in point, with the commissioners incentivising reductions in serious falls. The introduction of a falls risk assessment scheme was correlated to a reduction in serious falls. CQUIN was also credited with reductions in pressure ulcers and with supporting Skye to fund service changes and encourage further discussions with community services.
Relating to regulation
Board members suggested that the previous emphasis on finance and cost control were connected to the fact that Monitor was financially driven in its focus, and that that skewed board behaviours towards the ‘financial baseline rather than worrying too much about quality’. Having targets attached to the regulatory framework and financial costs attached to these did focus the mind and being held to account through the Monitor compliance framework was a ‘reasonable way’ of doing so. However, the current compliance framework continued to create dysfunctional consequences, as attention and energy moved from one target to the next. VRE was mentioned as a case in point where the board invested energy to hit a national standard which then slipped as the ‘searchlight goes onto something else like C. difficile’.
As the organisation was in breach of its C. difficile infection rate target, the financial penalties that followed represented a key issue for the board. A number of frustrations were outlined, including the lack of consultation regarding how the target was formulated and the relatively small margins of error (a handful of cases can lead to multimillion pound fine). The lack of dialogue regarding the target negotiation was having a demotivating effect and potentially turning people off infection prevention as ‘we’ve been set up to fail’. The trust was eventually able to negotiate the penalty with the CCGs, but the maximum fine would have completely wiped out their surplus and put them into deficit.
Financial penalties had also driven safety improvements in response to changes in insurance premiums set by the NHS Litigation Authority (LA). The money lost to litigation payments was a cause for concern, as the premium was likely to increase based on the number of claims made over the past 12 months. Further detailed analysis of litigation claims by the board was therefore needed:
We’ve been running on no claims, unprotected no claims discount, if you like, since the inception of the NHS LA and now they’re moving to relating your premium to how many accidents you’ve had. And again that will hopefully focus all boards, including ours, on understanding how that we can prevent those accidents, if you want to call them that, and obviously the costs that arise for the system for that.
Changes to the local authority funding formula from weighted deprivation age were also highlighted as problematic in reducing the amount of funding because of the high deprivation in the area. The local health economy was expected to lose a large sum of its revenue as a result of these changes. Thus, the external environment had a number of conflicting effects on the discussion of quality and safety by the board.
Lewis
Lewis is a large NHS trust that delivers services across several sites. It offers one of highest number of specialist services in the NHS, with a large consultant body, and is described as being at the ‘cutting edge’ of clinical care. Its long-standing reputation for high-quality clinical care is reflected in its consistently being in the upper quartile of hospital performance and quality ratings. Board members at Lewis attributed their success to the leadership of the CEO, who had shaped the strategy and culture of the organisation.
Strategic vision
Board members described how a culture of quality and safety was built into the vision and mission of the organisation and how this was led by the CEO. As one of the longer-serving CEOs in the NHS, his style of leadership was described as ‘one that reigned’ but also ‘one that people aligned to’. Other board members spoke critically of his style being ‘abrupt and antagonistic’:
I think absolutely culture is determined right from the top . . . He sort of determines the strategy and we run round after him doing the sums, improving the governance, you’ve got to work with somebody a long time, haven’t you, to get that kind of confidence? So, I think we are a little bit different here in how strategy’s determined in organisations where the chief exec’s been there for a long time.
Alongside the CEO’s power and influence, the chairperson strongly believed that success was attributed to ‘sticking close’ to the annual plan by holding the organisation to account against the corporate goals that had been set. Furthermore, both the chairperson and the CEO emphasised that success was linked to developing and nurturing a culture of clinical leadership, as a well as a research-centred culture:
Compared to some places, we’ve actually got very high calibre senior staff . . . We’ve got a lot of longstanding senior medical staff. We’ve also got the dimension of the academic and the medical school and the students. That actually brings a little bit of a different flavour to things . . . The academics . . . they have a fresh dimension and challenge because they’re not completely service imbued.
Despite quality and safety being expressed as ‘everywhere’ in driving strategy, some of the board members described how more work was required to better translate these messages across the organisation. The ND reported a ‘power gradient’ with the board not as in-control as they perhaps thought they were. The MD alluded to areas of the organisation that were ‘sweeping issues under the carpet’, while the trust secretary suggested communication and translation of board objectives was a particular issue in the large TH within the trust where the ‘old guard’ of senior medics still had ‘too much control’.
I think what we have become aware of, over the last year or 18 months, is that we’ve achieved a lot of change in some parts of the organisation, and in a few areas, very little change . . . it’s probably not fair to single them out, but other disciplines where the culture remains very much that of sweeping things under the carpet, of not learning.
The board had received lots of feedback about how the trust was a ‘good place to work’; however, an emerging theme was apparent that people felt inhibited to speak up or ‘whistleblow’ when there were problems in terms of quality and safety. The ‘listening events’ in response to the Francis Inquiry highlighted (through anonymous voting) that one-third of staff did not feel confident about raising concerns for fear of being disciplined. As in all NHS trusts a formal whistleblowing policy was in place, yet it was felt that further work was needed develop a culture where staff felt comfortable about raising concerns.
Leadership activities
As with strategic vision, board leadership of patient safety was dominated by the CEO. His long tenure meant that he was highly visible and had developed strong relationships across the organisation. His ‘organisational memory’ was seen as a key factor in driving organisational success. The ND and the MD had also worked at the organisation for many years.
You’ve got that stability at a very senior level . . . I think there is a bit of a benefit there . . . these very small trusts don’t have the critical mass, the financial stability, and therefore that then knocks on to quality and being able to, sort of, flex your muscles a bit and challenge the system. Whereas, when you’re big and you’ve got a bit of cash in the book, you can tend to, you know, be a little bit more arrogant maybe, but just say, ‘No, we’re fixing that. We don’t need your help, but, you know, we’ll call you in if needed’.
The CEO had a reputation for carrying out unannounced inspections, and the ND also exemplified this ‘leading by example’ style of leadership by doing a nightshift once a month. Of the CEO, the trust secretary said:
It’s his nature, it’s his personality, he knows the guys scrubbing pans in the kitchens, he knows the porters by name, he knows the cleaners who run the corridors around here by name and he takes a personal interest in them. It’s not just a bit of grandstanding, he genuinely does. And he gets out on the shop floor and I think that’s a big difference . . . pretty often, he informally pops up in peculiar places, he’s quite often got his camera with him and people then get a sheaf of embarrassing photographs slapped on their desks the next day, you know, ‘why is this corridor filled with all this equipment?’ ‘Who left all these rubbish bags there?’ So, it sets the standard very high.
Board members described how they addressed patient safety by being actively involved in the governance structures of the organisation. A NED described how chairing the clinical governance and standards committee made it clear that the board takes patient safety very seriously. The complaints process was seen as a good example. This was described as ‘very exec-led’ and ‘taken extremely seriously’, with the CEO scrutinising every single complaint. Further scrutiny was also undertaken at the complaints panel, which comprised governors, the director of quality and effectiveness, the ND and the MD.
Although some members of the board commented on how the CEO had created the right balance and skill mix, the dominance of the CEO was also mentioned as a potentially inhibiting factor. The MD felt that the chairperson could be stronger ‘in reining him at times’ in order to facilitate better discussion. One NED also suggested that too much of the patient safety brief ‘fell on the laps’ of the ND and MD and that these roles were already overstretched. The ND’s remit, in particular, was described as ‘colossal’. Indeed, the MD herself suggested that further support here would be helpful.
Board meetings and mechanisms
Board meetings were described as being predominantly focused on quality and safety issues. A NED described how the quality report containing MRSA and C. difficile infection rates and hospital mortality statistics (and similar) tended to occupy about one-quarter of the whole meeting.
That said, both the ND and MD still thought that more discussion could be given to the quality and safety papers rather than having protracted discussions about finance and business matters, which were thought to sometimes dominate the board agenda. The board agenda had been restructured, with a section now dedicated at the start to discuss quality and clinical effectiveness. This view was questioned by the chairperson, who was less in favour of the change, suggesting that it was leading to duplication with the governors’ meeting agenda and that the first part of an executive board meeting was starting to resemble a board of governors’ meeting. Others disagree:
I don’t think that there’s enough discussion at the board about the clinical issues and quality issues. I think there’s far too much concentration on politics and buildings and arguments about the office block and all this sort of stuff, which are important from the organisation’s point of view – there’s a lot of money associated with them – but I think the board agenda is dominated by those issues.
Non-executive directors were confident that they challenged and held the executive to account in board meetings. Despite NEDs’ confidence that they effectively challenged the board, in contrast, the ND’s experience of meetings was that there was not enough challenge. In her view, meetings tended to be dominated by the CEO. This was connected to views suggesting that the chairperson had a key role in encouraging contributions from other board members:
I don’t think the challenge is there. And I think that’s because it’s so dominated by the chief executive. Please don’t get me wrong – I’m not saying he’s not right or that he’s bad for the organisation. You can see very well that he isn’t bad for the organisation. I just . . . I think the board would be healthier if there was more challenge from the whole spectrum of board members rather than it being so dominated by one person. And I think some of that comes down to his personality, some of it comes down to relatively weak chairing.
The observation of board meetings found that out of just over 14 hours of discussion observed across the four meetings, a total of 200 minutes were directly related to patient safety issues, around 24%. This time was predominantly spent on discussions about C. difficile infections (about 70 minutes), and covered the target being set and the financial penalty imposed if the target was breached. A wide range of shorter discussions were directly linked to the Quality Report agenda item, containing performance indicators (falls, sharps, needles) as well as clinical risk factors, such as clinical negligence, and environmental health. The majority of these board meetings were based around monologues by the CEO, who provided a commentary on the ‘matters arising’ that the board faced, particularly in relation to estates and service reconfiguration.
Governor relations
Governors were emphasised as a key priority for the CEO and the chairperson. The CEO described how they were given ‘top-level’ information with which to scrutinise the board and to enable them to ‘drill down’ and ask critical questions. For the CEO, this had led to a number of challenging questions, particularly in relation to high levels of patient falls and difficult staffing levels. In contrast, other board members, particularly the finance director, supported the view that governors were not particularly effective. He felt that governor meetings tended to be ‘easily distracted’ from the key issues and got ‘bogged down’ in personal interests and issue campaigns.
Interviews with governors revealed a great deal of support for the board, with particular praise for the trust secretary, chairperson and chief executive. Governors interviewed were happy with the type and amount of information they received. Governors were involved in a variety of subcommittees, including the complaints panel. The lead governor described how she worked very closely with the chairperson and the trust secretary. The majority of quality and safety issues were covered in the Quality of Patient Experience working group.
Ongoing issues were raised about improving the relationship with NEDs. They described how NEDs tended to lack interest in governors, which was manifest in NEDs often not turning up to meetings and having little direct contact. The difficulties of finding members of the public with the required competencies to be a governor were also raised. It was reported that governors were often happier to do the softer things (‘potter round and do patient food testing’), with the general public having little understanding as to the complicated reality of the role.
The majority of discussion at board of governors’ meetings was built around governor education regarding the latest policy developments alongside the provision of summary information about performance. There were a variety of PowerPoint presentations covering issues about improving patient experience, workforce development and infection control. The CEO was central to these discussions, with his report occupying a significant part of the meeting agenda. Here, the CEO provided a summary of the key issues facing the trust and sought to mobilise governor support. Governors made only a limited contribution to the meetings, other than largely supporting the CEO and chairperson in their current negotiations. In relation to C. difficile infection rates, they supported the CEO in his criticism of the financial penalty being imposed for a breach of target. Some questions and challenges were raised regarding patient and staff experience. For example, a governor consistently made the point in the meetings that the board needed to improve hospital food by providing healthier options.
Assessing organisational performance
Board members expressed confidence and support in the ‘good reports and regular dashboards’ that were provided. In addition to the mandated performance measures, board members described other ways in which safety performance was measured. They had recently adopted the CAT, which was being adapted to the needs of the local context and used to provide a monthly online survey covering a variety of clinical quality assurance measures. The board also benchmarked their performance against other FTs.
Although the overall message was one of support for the board, concerns were raised about the amount of information that board members had to read in advance of and during board meetings. Both the MD and a NED suggested that more detailed ‘deep-dive’ analysis of particular issues was needed, as there was a danger with ‘high-level reports’. Other concerns were raised about the danger of looking at serious risks at the expense of more everyday ‘average’ issues.
The corporate governance committee spends quite a lot of time fretting about the Corporate Risk Register. Are we looking at the right things? . . . What about the stuff in the middle ground? . . . Something ticking away there that’s been running for months or even years, that might actually be more of a concern . . . and I worry about some of those things from a governance perspective because people tend not to keep their eye on those so much.
Walkabouts were cited as something the board regularly carried out, but again there were anxieties expressed by a NED who held the view that they were ‘never quite sure of what’s going on’ therefore a ‘certain amount of wit’ was needed to understand the high-risk areas. The MD wanted the board to build-in walkabouts as part of the board meeting in order to gain further soft intelligence. A NED also supported the view that further work was needed with the organisation in relation to communication and engagement with different members.
I, personally, feel that there should be more board-to-ward communication . . . some of them, I think, don’t actually . . . They’re a bit frightened of it . . . I think some of them feel out of place. It’s a bit like putting a barrister in an operating theatre – they’re fine in a courtroom, but you put them in an operating theatre and it’s a different ball game.
Relationships with commissioners
There was reported to be a problematic relationship between the trust and local commissioner. A NED, for example, described how relations with the former PCTs were based around ‘tick-box exercises of patient safety rather than looking at the bigger picture’. Relations had improved with the introduction of CCGs and the board had quality meetings with CCGs, which were described as being positive and constructive. Board members described having good professional relationships; however, there were some points of contention in relation to capital investments within the local health economy. Here, local ‘rivalries and egos’ created strained relationships, particularly regarding to the decision to build a new hospital.
Reflecting on their experiences, the interviews with commissioners suggested that the board was at times too ‘aggressive in its ambitions’ for business expansion and in its attempts to seek control of the local health economy. Despite these tensions, they recognised that there had been a lot of work within the trust to promote quality and safety issues. From this standpoint, Lewis was described as an excellent trust providing excellent care:
My opinion of the trust is they’re a trust that absolutely puts patients at the centre of everything it does and wants to do the right thing, and if things go wrong, hands in the air and tells us it’s gone wrong, this is what we’ll do to put it right.
In relation to the CQUIN, board members suggested that the financial incentive did make the trust ‘stop and think’ about quality issues. For example, the CQUIN for dementia had worked in driving improvements. However, there was a fear that within the new commissioning arrangements there was a danger that incentives such as the CQUIN would get less attention. In contrast, commissioners suggested that the CQUIN had not driven quality improvement. Rather than acting as a financial incentive, the CQUIN tended to be perceived as a sanction or penalty for trusts with ‘money being taken off them’. There was a feeling that the CQUIN therefore needed to be redesigned if it was to deliver its intended outcomes. Options proffered for improvement included redesigning the CQUIN so that they ‘joined up across the pathway’ and for the CQUIN to apply across ‘hospital stay experience as well as in the community’.
They see it as their money, it’s extremely difficult to negotiate stretching targets and you know we are sort of working on that and we certainly don’t give them all of the money up front.
Relating to regulation
For the CEO, Monitor was valued as being a ‘genuine independent regulator’ built on a ‘constructive relationship of guidance and opinion’. Having the same relationship manager for 5 years had helped to nurture informal dialogue on what was described as a need-to-know basis. In contrast, the MD suggested that, because Monitor was primarily set up as a financial regulator, this largely framed the discussions. Although the Monitor compliance targets had driven improvements, the point was raised that the threat of the financial penalty per case of C. difficile infection over the target trajectory had negative consequences for services delivery. Problems were also raised regarding the CQC. The CEO suggested that it was up to the CQC to better communicate emerging issues. The MD also characterised the CQC as ‘very much a box-ticking apparatus’ that did not ask the right questions or ‘talk to people on the ground’.
Arran
Arran is a TH providing general and specialist services across multiple sites. Over the last 5 years the board has been characterised by relative stability, with low levels of turnover of board members. The trust aims to continue to build its global brand as a provider of specialist services and is undertaking large-scale redevelopment in order to address excess demand for local A&E services. Organisational performance as measured by the HSMR is higher than average, but the trust has faced some performance issues with regard to levels of staff satisfaction and, more recently, infection control rates. Arran’s ambition is to be a world leader in clinical excellence, and innovation appears to have distracted attention from the board oversight of patient safety.
Strategic vision
As a large specialist TH, Arran’s strategic vision was focused on supporting clinical excellence and securing a drive for further funding for research and development. This was particularly the case in clinical areas, where the trust was seen as being a leader in the field. There was a clear aspiration to further enhance the ‘global brand’ of the organisation.
In striving for clinical excellence, the fluidity that characterised the trust meant that board members often associated more with a ‘vision’ of clinical excellence than a corporate plan. The board had not yet translated this vision into operational plans, as one NED observed:
Some people want a very detailed strategy document written and [others are] of the view that so long as we broadly know where we’re going, we don’t need it, because it changes so much; it’s hard to be definitive about where we’re going, even though we think we want to know where we want to go. So writing it down, it would be out of date as soon as you’d written it.
One board member explained that the reason for the lack of strategy by the board was in large part connected to a preference for a ‘crisis management’ style of governance. The point was also raised that safety and quality improvements tended to be patchy across the organisation or merely bolted on to local initiatives at the division level rather than being seen as an organisation-wide approach:
We are much better when we’ve got a crisis, a burning platform to deal with rather than seeing a problem and dealing with it in a structured, planned way. I’m overstating the distinction but I just think that things tend to be quite operational, crisis driven rather than improvement focused.
Some board members expressed concerns that the drive for innovations to increase efficiency could compromise service quality and patient safety. This view was further supported by the observation that the trust had a ‘strong audit culture’ and was ‘strongly focused on research’ but less focused on continuous quality improvement:
I do hear stories about people making perhaps not very well advised shortcuts because they thought that they had to hit the budget overall . . . a more able manager will find a creative way of spending what they need to deliver the service. Your less creative, innovative or less financially enabled person will hide behind the fact of, ‘Oh I didn’t think I’d got the budget to do that’ but it’s not an acceptable behaviour.
However, other board members disputed this view and suggested that the Quality and Safety Agenda was given priority, with ‘the days of having finance at number one long gone’. Discussions about patient safety were said to have had high visibility throughout the board and the Quality and Safety Committee. The strong clinical presence running throughout the organisation also ensured that issues around finance did not compromise quality and safety.
Leadership activities
Interviews with board members in Arran highlighted how the leadership associated with patient safety contrasted with other organisations. In support of its strategic vision of clinical excellence, the governance structures of the trust were led by medical professionals, with the trust having multiple medical directors each operationally responsible for the financial, workforce and patient safety issues within their own directorate. These MDs formed part of ‘clinical boards’, consisting of divisions that reported upwards to the executive board through a range of feedback and audit systems. In addition, the trust had a medical directorate, which provided forums for sharing quality and patient safety information across the various clinical boards:
It’s a clinically led organisation with nursing, doctor and AHP (allied health professional) feed-in to specialty and division . . . If you believe that the right systems and processes will stop mal-alignment and errors, we have a number of checks on that.
Although board members generally expressed confidence in the medically led assurance mechanisms with regard to patient safety, some concerns were expressed about the underlying culture around incident reporting. This was acknowledged as ‘suboptimal’ and was connected to deeper staff concerns about the reputational and career consequences of reporting in an environment perceived as being hierarchical and where people could be ‘scapegoated’ for raising issues about poor quality and unsafe care:
We still have a way to go about developing a really positive reporting culture; for everyone to feel that we’ve got a just reporting culture that’s flexible, that then acts effectively. So we still get ‘never events’, we still get serious incidents.
It’s a matter of record that we have a less-than-fantastic record on bullying and harassment which we’ve tried to address over the last 3 or 4 years, but it’s a fact.
In response to these issues and concerns, considerable effort was being made by the board to encourage a more open and responsive organisational culture. The ‘Making a Difference Together’ initiative was set to support staff in translating the values of kindness, teamwork, safety and improvement into their working values and practice. This initiative was incorporated into all appraisals and consultant appointment panels in an attempt to spread these values throughout the organisation:
Whereas before if you were a UK leading surgeon with some good R&D [research and development] behind you and the support of the university I think you could have been pretty assured you’d get a clinical place. Here, we’re starting to get to the place now where we’re saying, ‘Actually no. If you don’t appreciate the importance of kindness, if you don’t appreciate the importance of working in a team . . .’
Although this development was considered to be important and a priority, some concern was expressed over the extent to which these cultural changes were embedded within the organisation. An issue of significant ongoing tension was raised by a board member, which related to his perception of the corporate culture of the trust. As an ambitious organisation which promoted the view that ‘we want to be the best’, it was felt that this had been a distraction from the day-to-day business of providing ‘the best things for patients’. It was also felt that more needed to be done to translate the ‘high-level vision’ into something that could ‘change behaviour on the front line’:
My concern has been when we say we want to be the best at the same time as we’re taking a defensive position on a safety issue or an access issue: I’m suspicious because it’s just who appears to be the best rather than actually [who is] providing the best service.
An example of this was the introduction of the World Health Organization’s ‘Safe Surgical Checklist’. Theatre teams were taken out for a half-day at a time as it became apparent that there were cultural issues with staff feeling that they were unable to speak out openly if there were any issues about the quality of care, as well as being unable to address problems associated with clinical teams not working well together.
Board meetings and mechanisms
It was reported that over recent years there has been an increase in time spent on quality and safety at the expense of finance. This was driven in large part by the arrival of new NEDs, many of whom had extensive clinical experience. In addition to increased time devoted to patient safety, the manner in which these issues were addressed was also changing, from previously ‘noting requirements and ensuring compliance’ to attempting to understand such requirements and integrate them within organisational routines and practice:
I mean [patient safety has] certainly changed in terms of profile, as I’ve already indicated. I think it’s changed in terms of not just ticking the box that we do it, if you see what I mean, but actually people genuinely trying to assure themselves that it is done.
Openness was identified by some members of Arran as an important feature of the organisation’s culture. This was exemplified by the first part of board meetings being open to the public (before this was made mandatory post Francis Inquiry). Board members described how this had facilitated honest exchanges between executives and non-executives. This was particularly the case for the NEDs, who could ‘always speak absolutely freely and without consequence’. NEDs did not ‘pull their punches’, which meant that the executive was ‘held to account’:
What I would say is that [NEDs are] pretty well empowered here. They are seen and treated with a lot of respect by the executive. We don’t always agree with everything they say, but when they say ‘jump!’ to quite a large extent we jump.
Although many NEDs were confident that they could challenge other board members in meetings, some raised questions about their ability to challenge executives, especially in relation to the availability of detailed information on quality. A NED described his experience over the past 6–12 months of watching the increase in C. difficile infections. He had had to trust professionals that ‘the matter was in hand’, but was anxious that he had not seen data to support this view and had not seen a consistent action plan being formulated.
Overall, board relations were described as being good, with healthy challenge and debate alongside ‘friendly fun and banter’. Indeed, some board members welcomed the way that ‘challenge’ was starting to increase. This was seen as a positive shift from the ‘incredibly stage-managed’ meetings of the past, as ‘executives and non-executives were increasingly looking to resolve ongoing organisational problems’:
I think we’re only starting to get to a place where execs can question one another, but I would say that’s definitely an evolution. Previously, I’d have said that was almost unheard of, that would have been seen as being disloyal and, not career threatening, but just not done. That’s – I would say that’s definitely changed. So it’s better than it was but I’d say it’s got a way to go before you can speak freely.
Observations of board meetings revealed that, of the almost 14 hours of discussions across the four meetings, a total of just over 4 hours was directly related to issues of patient safety, representing almost 30% of board time. The largest amount of time spent on any single issue related to an environmental health risk involving contamination at the kitchens (just under 1 hour) – an issue which was not part of the trust strategy and, thus, was not included in proactive quality improvement work. Other notable issues included safety in operating theatres (about 30 minutes), orthopaedic performance (30 minutes) and patient falls (just over 10 minutes). Considerable additional time was devoted to more general discussions about quality improvement, including ‘patient story’ narratives (30 minutes) and quality improvement presentations related to specific service areas, such as community nursing (almost 1.5 hours).
Governor relations
Governors were viewed as ‘the eyes and ears’ of the trust. Governors were involved in the Quality and Safety Committee, where they could hold board members and managers to account. Board members described being impressed by their ‘penetrating questions’. Governors were also represented on the clinical quality review group and had their own high-quality patient care group, which carried out focus groups or interviews.
Governors and the board had a good relationship, with the board providing governors with information and the governors providing the board with patient journeys. Although some suggested that governors were ‘pretty good’ at holding the trust to account as a ‘critical friend’, it was also expressed that it would be very difficult for governors to actually hold the board members and managers properly to account with regard to the ‘bigger picture stuff’ as they lacked detailed information and knowledge about board issues. As with other sites, issues were also raised about individual governors having their own ‘hobby-horses’ and interests rather than putting forward a more rounded view.
Analysis of governor meetings found that the majority of time centred on governor education and the provision of summary information regarding trust performance. These meetings tended to have three central parts running throughout: a PowerPoint presentation about a particular topic (in this case a junior doctors survey and service line reporting); the chairperson’s report, providing a summary of recent activities and events (such as charity work, visits and any latest developments); and the CEO’s report, which provided a summary of the latest performance ratings. The meetings were largely driven by the contributions from the chairperson and the CEO. The NEDs did not contribute to any of the discussions. Overall, governor contributions were limited to questions for further information regarding the presentations, further clarification about particular trends related to hospital activity, providing updates about working group activities and discussion and reflections directly related to patient experience. There was no discussion of patient safety at the meetings outside of the CEO’s summary of progress regarding IPC.
Assessing organisational performance
Arran had developed information systems and an information pack that concentrated on safety as well as the other key aspects of performance, which were broken down across divisions within each clinical board. With access to detailed information from across all of the divisions, an executive described how her exposure to board information illustrated that they were functioning well in relation to quality and safety:
. . . it gives us a pointer in terms of who we should be speaking to, and there’s some commentary in there as well and I place a lot of reliance on this, as I think many other people do.
To complement the RAG ratings, board information was supplemented by ‘Care Thermometer’ clinical data, which provided more fine-grained information at ward level. Although this was welcomed, some concern was expressed that these disaggregated data were currently used in a largely reactive manner, with the view that the board was a little slower than they should be at addressing particular issues:
For the most part, we look back at what has happened and try and learn from it and then try and quickly apply, ‘Oh if that’s happened, what must we do looking forward’? If we were to aspire to the absolute best practice, which we do, there’s something about tracking non-safety trends in an intelligent way that you can now do with the level of data capture and using it to predict where the might be a problem.
There was also some concern about an over-reliance on quantitative summaries. To balance this, board members used a number of techniques for gathering soft intelligence, including unannounced visits, ongoing review of all complaints and walkabouts:
The secret of it all is to talk to a lot of people because people will often tell you in conversation what they wouldn’t tell you if they had to write a report about it or if it had to go through their line management process, wherever that line management process may apply.
There was some support for the use of ‘patient stories’ to provide additional qualitative information and soft intelligence on patient experience. However, this was not universally supported by board members and consequently patient stories were not routinely used:
We’ve done [a patient story] once and the board were quite staggered at the story that was told. But they were staggered and then they were sort of – ‘so what’? Well the ‘so what?’ is that we developed the whole ‘Making a Difference’ campaign as a result of it. So the board are starting to see that this is important. But I think they don’t want to be just hit with a sledgehammer every month and yet I think there’s nothing wrong with that! [Laughs.]
Relationships with commissioners
Arran relies heavily on specialist commissioning contracts. The majority of their income comes from specialist commissioners, especially the Nationalist Specialist Group (NSG). Although, on the whole, relations with commissioners were described as cordial, it was reported that the fragmentation in the commissioning landscape made it difficult to have meaningful discussions. However, it was thought that the NSG were helpful allies in promoting safety within the organisation:
We’re a much bigger client of National Specialist Group than most other hospitals. That will probably be a good thing for safety because I think for the first time . . . the people on the other side of the table really know what they’re talking about . . . The CCG are less likely to get hold of the Safety Agenda.
In relation to patient safety, the Clinical Quality Review group within the trust provided an opportunity for commissioners and the trust to meet and review matters related to quality and safety. Commissioners would scrutinise their performance, looking at serious incidents, infection control and waiting times and pressures ulcers, etc. Commissioners and the trust were currently in discussions about the financial penalties regarding the breach of C. difficile infection rate targets.
Relating to regulation
Monitor was well regarded for ‘keeping the board on their toes’. One result of external performance targets was that the board began to invest time and energy into developing their own performance indicators. However, questions were raised about the regulatory frameworks and the targets established in relation to C. difficile and MRSA infections. The board was in discussion with Monitor about the recent breach in this area: it was thought that Monitor did not take into consideration the specialist, tertiary nature of the trust and its policy of admitting patients from other hospitals that already had infections.
Concluding remarks
The case study findings highlight a variety of activities, practices, supporting tactics and relationships associated with the effective board governance of patient safety. The findings suggest that different board behaviours can be identified across different organisations and governance contexts. They also relate to the various models of board governance outlined in Chapter 2.
The case studies provide links to agency theory through the ways in which boards established processes to measure patient safety performance to ensure compliance and to hold staff accountable for their actions. Agency theory thus appears particularly relevant in terms of understanding board governance at Arran, in particular the way the board focused on the use of audit and performance measurement to support its ‘clinical board’ governance structure.
The case studies link to stewardship theory in the way that boards have sought to create a framework of shared values, built on trust, within their organisations. The relationships developed between the board and staff through initiatives such as such ‘walkabouts’ exemplified attempts by boards to improve their relationships with the broader organisation. Stewardship theory was particularly relevant in terms of understanding behaviour at Islay in relation to the board’s engagement of staff and patients in the development of strategies for quality and safety.
The case studies also show evidence of practices that can be understood through stakeholder theory, where boards have attempted to manage complex trade-offs between stakeholders, including staff, patients and the public. The documented involvement and interaction with governors across the sites represents an illustration of this, where boards recognised, to varying degrees, the need to engage governors in the oversight of patient safety. Similar engagement and trade-offs were seen in the relationships between several of the case study trusts and their commissioners.
Finally, the case studies link to resource dependency theory in the way boards attempted to manage internal and external relationships in order to leverage influence and resources. The relationship with commissioners was an example of this in terms of the boards’ attempts to negotiate influence and resources. The negotiation between Lewis and Monitor regarding the imposition of financial penalties for a breach of targets represents a good example of this.
These data, therefore, provide specific insights into the challenges of enacting board governance, as well as showing how the different theoretical ‘lenses’ discussed in Chapter 2 can provide complementary insights into the complex processes at play. The next analysis (see Chapter 6) seeks to drill down into the trusts by following key safety issues ‘from board to ward’. In this way we seek to extend our reach from the activities and processes at executive level to the impacts and actions at mid-tier management and frontline clinical services.
Chapter 6 Case study analysis of tracer issues
Introduction
The purpose of this chapter is to present a qualitative analysis of board activities in our case study sites, associated with two tracer issues and informed by the theoretical framework of conformance and performance, as developed by Garratt26 and explained in Chapter 2. In order to explore conformance, we followed board involvement in the management of C. difficile infections; control of C. difficile infection is a key requirement by the external regulator in IPC. To explore performance aspects of governance we examined how each case study site dealt with a specific patient safety issue or incident, identified during fieldwork, from ‘board to ward’.
We first provide a brief overview of the Garratt framework before exploring the findings from the case study sites relating to conformance (the issue of C. difficile infection control) and then performance (issues specific to each site).
Background to Garratt’s ‘learning board’ model
In exploring the effect of board directors, Garratt26 posits four tasks that require sufficient diversity within a board for it to cope with the ongoing intellectual and operational challenges: policy formulation, strategic thinking, supervising management and ensuring accountability (for more details, see Chapter 2). For Garratt, an effective board is able to balance these four tasks simultaneously, combining external, internal, long-term and short-term perspectives. Garratt compares an effective board to a brain which is engaged in continuous learning, a ‘learning board’ being the centre of a learning organisation’s business brain. 26 There are two sides to learning boards: board conformance, sometimes termed compliance, and board performance. Conformance itself involves two aspects: ‘ensuring accountability’ through conformance to regulation, audits and stakeholder rights, and ‘supervision of management’ through conformance to key performance indicators, budgets, projects and organisational capability. Similarly, board performance also involves two aspects: ‘policy formulation and foresight’ and ‘strategic thinking’ to drive the enterprise forward by maintaining learning and developing its position in its energy niches to allow it to survive and grow. Garratt suggests that these four board tasks (policy formulation, strategic thinking, supervision of management and ensuring accountability) feed naturally into each other as interactive elements of an annual cycle of the board’s learning. This structured way of thinking about board tasks was used to inform the analysis of tracer issues.
Tracer issue 1: board attention to ‘conformance’
The following subsection presents findings from each of our case study sites in relation to board conformance, analysing the board’s role and subsequent activities in relation to an IPC issue, specifically C. difficile infections.
Islay’s response to C. difficile infections
Islay was seen as high performing in terms of C. difficile infection containment. Interviews with IPC committee members reflected pride in their achievements, and they expressed their support of board members’ forward thinking in relation to infection control. The Quality Improvement Strategy was central to progress, as it made infection control a key priority from the outset. The very first quality improvement collaborative undertaken by the trust was related to C. difficile infection control, with results showing significant reductions in the participating patient group.
The board provided financial support and encouragement to the infection control team; C. difficile infection control was well resourced, with six HPV (human papillomavirus) fogging machines to hand, a team of 24/7 domestics available to move patients at all times and side rooms also available. The IPC team were also able to draw on a relatively advanced electronic patient record system to manage and track patients with infections.
The team suggested that they had a slightly different dynamic to other trusts, as the MD was the director of IPC and considered to be a ‘crucial driving force’, providing strong leadership and accountability in relation to IPC performance. The MD supported the IPC team in situations where directorates were underperforming, providing the necessary ‘clout’ that meant audits and reports were taken seriously. A further example given was that of ‘antibiotic stewardship’, in which the MD was central to a ‘Green for Go’ campaign concerned with changing compliance with the antibiotic guidelines from ‘red’ to ‘green’. The ND was also important, keeping in regular contact with the IPC team and creating a direct reporting link to the board.
The arrival of performance targets was cited as crucial in shaping board behaviour, as the financial cost for breaching the C. difficile infection rate target raised its corporate profile. Building on these mandated performance targets, IPC committee members described how the board seized the moment very early to develop division-based targets to increase competition across the divisions, to reflect on progress and to ensure that divisions were held accountable.
Ongoing issues in the governance of C. difficile infection rate management were identified. Although targets had driven a number of improvements, there was now recognition that the C. difficile infection rate targets needed to be revised – continuing reduction to a point of zero tolerance was not realistic and difficult to communicate to staff groups. IPC committee members did, however, suggest that more could be done in relation to preventing and controlling C. difficile infections, including improvements in the translation and accessibility of antibiotic guidelines, availability of web-based guidelines and other IT resources for the workforce, such as apps.
There was still work to be done regarding joined-up working with the community. Despite the availability of a regional collaborative for all infection control leads to meet and discuss key issues, collaboration between hospital and community infection control teams could be improved. The fact that community and acute trusts had separate targets caused friction between teams. Maintaining the focus and resources for C. difficile infection control was also presented as a challenge given the existence of ‘rival’ infections. For example, a recent outbreak of CPE (carbapenemase-producing Enterobacteriaceae) infection in a neighbouring hospital highlighted the likelihood of more pressure on resources such as side rooms used to treat C. difficile-infected patients in the future.
Skye’s response to C. difficile infections
At the time of the fieldwork, C. difficile infections had gone up from being undertrajectory to a point where acceptable levels had been breached. The cause of this trend related to continuing problems with matching capacity with demand as bed occupancy levels were running at 90%. Such levels prevented the opportunities to carry out deep cleaning, as wards were full and essential isolation facilities, such as side rooms and en-suite rooms, were not available.
Historically, members of the IPC committee suggested that board approaches to infection control had been ‘hit and miss’, with frustrations expressed about the time taken to make decisions, putting costs before quality and a culture described as ‘ticking a box but missing the point’. The IPC team provided evidence to show one of the effective ways to control C. difficile infection through good environmental decontamination, but this had taken 3 years:
[D]eep cleans: we have been trying to get that in place for 3 or 4 years. It has gone to the finance group, it’s essentially been said ‘Oh well, yes we support it’ but there’s no money, so essentially it didn’t happen.
It was noted that responses had improved recently, with the latest board proactively looking to involve the IPC committee and placing them at the forefront of the strategic plan. The team were now in regular contact with the CEO, who had also recently decided that there should be an executive member taking part in every root cause analysis. Despite this increase in engagement, questions were still raised about the MD who, despite being a member of the IPC committee, never attended the meetings. This lack of engagement was linked to wider problems with medical involvement in infection control. The COO also tended not to attend IPC committee meetings. Embarrassingly, when the trust breached its target and was asked to report to Monitor, key personnel were not able to explain what the issues were.
Although targets were supported in getting infection control funded and recognised, questions were raised about unintended consequences and equity, as elsewhere. First, board focus on targets such as C. difficile infection rates had the potential to distract from other important issues. Second, as the organisation was already starting from a low baseline, continuous reduction in the C. difficile infection rate target meant they were more likely to get penalised when compared with a trust starting from a much higher threshold. The trust managed to negotiate a reasonable financial outcome with CCGs after they breached the target. Indeed, there were positive (unintended) consequences in that the penalty enforced further investment to reduce infections.
We’ve probably reached the stage where most organisations have probably reached the irreducible minimum. And it’s no coincidence that rates have probably plateaued or, if anything, are slowly creeping up.
Although policies and guidance were available, further education about antibiotic stewardship was needed, as knowledge of microbiology among nursing and medical staff was described as poor. While junior doctors were a problem in this regard, the introduction of consultant champions had improved antibiotic prescribing. The trust also needed to find new ways to translate information. Information technology was tabled as a solution. The trust had an electronic prescribing system which was good in flagging up resistant antibiotics on patients but it needed to be improved to build in more ‘red flags’, such as whether someone was C. difficile toxin negative. Developing an antibiotic website along with the use of apps were ways in which the trust was making information more accessible.
The IPC team was collaborating with the local health economy to deliver training around C. difficile infection control and antibiotic prescribing and was part of a clinical governance forum where old cases of C. difficile and MRSA infections were discussed. However, more work needed to be done at CCG level to fill the big gaps within nursing (residential) homes.
Lewis’s response to C. difficile infections
Interviews with IPC committee members revealed overwhelming support for the board in relation to its oversight of C. difficile infections. All IPC members commented on how the CEO, ND and MD were receptive to and supportive of organisational efforts related to IPC. Support at board level was demonstrated by successful business cases, which funded the organisational response to C. difficile infections. It was also demonstrated by CEO and MD attendance at serious infection review meetings (SIRM), which gave further power to the infection control team by signalling the backing of the board. The CEO was particularly important here in terms of knowing the different roles at each level and managing interactions between different parts of the organisation. The ND was also a member of the IPC committee and its operational review group, and her involvement was welcomed:
I’m involved in preparing the report for the board on a monthly basis, so I know the questions that they are asking on the basis of the information that we are providing. They do want to know what is happening and what we are doing to try and change the current situation and improve our rates as much as possible.
The introduction of infection control targets has driven interest in C. difficile infection and led to investment, enthusiasm and support for infection control. As a result, questions and concerns raised by the board tended to focus on the targets at the expense of wider factors affecting patient safety. Although targets have undoubtedly raised awareness, IPC committee members suggested that a different strategy was now required, as continuing reduction in C. difficile infections was considered to be no longer achievable. They were also concerned about securing greater recognition of the fact that a tertiary, specialist trust such as Lewis tended to receive the most complicated patients with existing problems (i.e. C. difficile carried from elsewhere).
At the moment it’s all about C. difficile so people are prepared to throw money at it . . . but things that are not quite so high profile and like E. coli maybe don’t get the same attention.
The board mind-set was changed to ‘we’ve got to meet these targets, we’ve got to reduce the numbers . . . we don’t want Monitor on our back, we don’t want the Care Quality Commission on our back and we certainly don’t want fines.
More work was needed to engage the workforce in IPC issues, particularly those related to C. difficile. Although information dissemination via e-mail or the intranet was considered good, staff engagement was acknowledged to be low for junior and senior clinical staff alike. This was particularly so in relation to antimicrobial stewardship (getting clinical staff to prescribe the right antibiotics). Things were improving as the IPC team were starting to apply more pressure to medical staff, but they required more support from senior medical staff, including the MD. Compulsory attendance at patient reviews, particularly those concerning C. difficile infection, was suggested as way to improve the situation. Further issues concerned how best to educate junior medics and change the practices of senior medics to be consistent with new guidance; initiatives included an induction package for junior medics, additional support from pharmacy teams and ‘antibiotic champions’ in each directorate.
Concerns were also expressed about the epidemiology of C. difficile, with focus moving to community settings and patient profiles. It was felt that more community involvement with C. difficile was required. The trust formed part of a region-wide HCAI partnership that concentrated on C. difficile and MRSA, and had a subgroup sharing best practice, experiences and lessons learned. Despite good relations, further joined-up working between primary and secondary care was called for, as the approach to managing C. difficile infections was to look at C. difficile carriage in the patient population. As it stood, the key issue was a lack of clarity over who was responsible for infection control in primary and community settings such as GP surgeries and care homes. A ‘great deal of work’ was needed in terms of education and awareness at the interface between community and secondary care.
C. difficile is much more widespread in the greater community than we had thought and that carriage of C. difficile by patients or carers or visitors is probably a much greater risk for transmission than using an antibiotic.
Arran’s response to C. difficile infections
The IPC team at Arran outlined an extensive infection control infrastructure supported by ‘infection control link practitioners’ (mainly nurses) who were trained to act as ‘the eyes and ears on wards and within departments’ for audit purposes and charged with embedding infection control training into practice.
One IPC nurse suggested that, although some of the education was relatively simple for some audiences (e.g. educating those nurses in charge of cleaning wards), the challenges came when trying to engage the wider clinician audience to changing particular practices. Recently the approach by the IPC team has changed towards providing a more customised ‘tailor-made’ education programme for particular clinical groups. This approach has gained a number of successes, including ‘transforming hand hygiene’ within A&E by developing a series of must-do rules:
[Y]ou need to go into the silos and actually see, you know, who are the champions there, who are the opinion leaders, how can we influence them to get them involved and then recruit them and try and get them to join in.
In contrast to other sites, the IPC team described having a distant relationship with the board: although the IPC committee had relatively good relationships with staff, the relationship with the board proved to be challenging, particularly when attempting to escalate problems; one IPC described being told by the CEO ‘to stop coming to him with bad news’. This opinion exemplified a reluctance to engage with underlying systems and process problems within the organisation, with a preference for ‘good news’ headlines. Such a perspective was linked to wider issues with the incident reporting systems of the trust. This included ‘a culture of bullying and intimidation’ prevalent throughout the organisation, which meant that there was a tendency for middle managers to project the image of being ‘seen to be doing okay’ by achieving targets and making sure none of the issues was escalated up to board level:
In the lower ranks we have a joke about how only good news goes through and none of the bad; so that you know you’ve got a problem on the ground but by the time it gets to the chief exec people are all saying everything’s okay . . .
. . . if you do pick up on anything you will find that people will be too nervous to tell you about all the intimidation that goes on because even when the CQC came in . . . it wasn’t said but the implication was that nobody should really go over there and tell anybody about the bullying culture. It wasn’t picked up here at all but it does exist.
Although the trust had historically made significant achievements in relation to C. difficile infection control, recent trends suggested that occurrence of C. difficile infections was increasing, with a breach in the performance target likely to happen. An IPC committee member explained that this increase was in large part caused by the distorted picture that the board received in relation to C. difficile infection management performance. The lack of systems to effectively govern C. difficile infections meant the response only happened in times of crisis. Although the organisation did respond to infection control issues, it did so reactively, once an external target had been breached.
. . . suddenly people become aware of it and say, ‘Why didn’t anybody tell us?’ I’m very cynical about it.
. . . it’s not just me, it’s organisationally, they’re not a listening organisation, not to the staff that are working inside them.
Tracer issue 2: board attention to ‘performance’
The following subsection presents findings from our four case study sites in relation to board performance aspects of governance, analysing board responses and subsequent actions in dealing with emerging patient safety issues.
The Islay board’s development of the ‘staff stories’ initiative
Board members were looking to further develop staff engagement as part of the Quality Improvement Strategy. To do so they carried out what was described as a series of ‘Berwick sessions’ to identify staff concerns in relation to quality and safety. These Berwick sessions had two objectives: to raise staff awareness of achievements currently being made and to enable staff to raise previously unidentified concerns, thereby developing emerging themes.
Building on the idea of patient stories as a way of providing a voice to untapped intelligence about the organisation, the board developed the idea of ‘staff stories’ about their past experiences of being a patient within the organisation. The board requested volunteers to ‘have a cup of tea’ and speak to them about their patient journey and to rate particular aspects of the service. The questions asked by the board built on CQC inspection questions such as ‘Did you feel safe? Did you feel that your treatment was resourceful? Was it effective? Was the outcome what you expected it to be?’ These questions were supplemented with a self-reported visual analogue scale ranking experience in terms of safety, effectiveness, resourcefulness and caring.
Feedback from participating staff identified positive and negative experiences of the initiative. One staff member described the positive experience of being listened to:
[T]hey were quite transparent throughout the whole thing and admitted that, you know, if there were any faults in the services they wanted to rectify them . . . it wasn’t about pointing blame towards anyone, it was about learning from mistakes . . . and putting strategies in place to improve the services that they offer.
However, this respondent also stated that it could have been further enhanced by having a clinical perspective from someone involved in the patient journey under discussion to triangulate patient experience with a frontline staff perspective and initiate a dialogue with the service under review. Greater transparency of dissemination of feedback across departments would also have been welcomed, as would evaluation of the extent to which lessons were being learned and applied.
if they’d had someone there as a representative from that service that might have kind of helped them to understand things a little bit more . . . I came away in some ways feeling not bad but, you know, oh I feel like I’ve just been really negative there about that part of the service . . . Whereas if the person from the service had been there, then perhaps that might have been giving the board a bit of a better understanding of how it operates and why they do things in a certain way.
The Skye board’s development of the ‘Bed Plan’
In a context of ever-rising demand for services, the trust was unable to match capacity and demand or successfully manage patient flow. Faced with a bed crisis, the COO developed proposals to redesign bed management. The key proposal was to close emergency admissions and open an additional rehabilitation ward at one of the trust sites in an attempt to reduce the number of outliers and ward transfers, improving efficiency and quality by having patients on the right wards with the staff skills.
Even on the heady days of summer we still seemed to have patients who weren’t in a bed belonging to medicine. It wasn’t entirely correct . . . that seemed to give us a signal that there was something amiss.
. . . [the bed plan] gives us a better patient experience by . . . not moving anybody overnight and, making sure people aren’t in acute beds who don’t need to be there.
Interviews with staff involved in the formulation and implementation of the bed plan indicated that the proposals had improved the situation, reducing the number of outliers. Investment in additional bathrooms and bays had also improved infection control, as it was now possible to isolate cases and provide decamp facilities. Yet despite these successes interviewees were critical of the amount of time needed to make these changes. The Bed Plan was described as ‘the outcome of a discussion many times over’, where continuous changes at executive level led to protracted negotiations over the plan.
Managers and nurses identified limitations in the engagement processes associated with the plan: consultation processes had largely failed to engage nurse and ward managers in the key admission areas of A&E. Further, consultant physicians had each been nominated a number of beds spread across up to six different parts of the trust; one manager described their anxiety with the possible implications for patient care of making physicians ‘homeless’ as a result of the changes, and suggested a need for a dialogue with the executive team.
It was further suggested that better links were needed between the board and the clinical support unit management team, clinical directors, and senior nurses if engagement was to be improved. Suggestions to enable this included staff invitations into boardroom decision-making processes and increased visibility of board members on wards. The board needed to ‘get their faces known out there in clinical practice’.
If you went round an organisation and you asked most of the matrons, who are obviously heavily involved and impacted by the Bed Plan . . . if you asked all of them for details there’d be a very different range of answers and some people wouldn’t be able to answer. We all know the new ward is opening . . . but when you go into the details of that and what that actually means and where patients . . . it gets a little bit fuzzy, especially around how we’re going to staff those wards.
Despite these difficulties there was cause for optimism. Some interviewees noted that the board should be given credit for the huge effort involved and also their increased openness, visibility and enhanced communication via team briefings. The new CEO was perceived to be working in the right direction as the forthcoming strategic plan built on a consultation process.
The Lewis board’s development of the ‘After Francis’ initiative
In response to the Francis Inquiry, the MD, the ND and the director of quality scrutinised all 290 recommendations of the Francis Inquiry and RAG rated the organisation against those recommendations. For those areas deemed less than fully compliant, a series of working groups and listening events were set up to explore issues related to communication and staff awareness of how to raise concerns. The 3000 staff who attended the listening events were asked to anonymously vote ‘Would you recommend this as a place to look after your friends and family and if you had concerns would you know how to raise them and what mechanisms are in place to do so?’ Although over 96% of attendees said they would recommend the trust, the board wanted to know why 4% would not; to do so they invited staff to express their concerns and make suggestions for improvements via an anonymous electronic survey.
The 960 responses were largely positive but a significant proportion (20%) stated they were not confident to raise concerns: specifically, a consistent theme was the inability to raise concerns about senior medical staff. Suggestions for improvement included helping staff build their own confidence to be able to raise a concern, and reassurance that they would be listened to and taken seriously, and that reported inappropriate behaviour would be challenged. Themes around communication, attitude, hierarchy and the conduct of some groups of staff were raised.
[W]hile the vast majority of our medical staff are fantastic, absolutely superb, would willingly go to any of them for referral or care, but we have a small group who have been brought up in a particular style and they manifest that, and other people think it’s OK to behave in that way.
Although the trust had a whistleblowing policy under which concerns could be managed confidentially, areas of improvement were required in relation to reporting and ensuring feedback of action to those raising issues. Strategies in response to these findings included the incorporation of a ‘core professional and leadership behaviours’ dimension into all staff appraisals to ‘talk through with you how you feel your role fits into that bigger trust vision and strategy’.
Although the introduction of the new appraisal system received good feedback from staff, some resistance to staff appraisals has been made by doctors; some ‘difficult conversations’ led by the MD were needed with a small cohort of clinicians who, although clinically competent, displayed disrespectful behaviour which negatively impacted on staff morale and patient care.
The slight concern I have in this organisation is some of the badly behaved are very, very able and competent clinicians – probably you would describe them as exceptional – and because of that their behaviour has been tolerated and appears to be tolerated and they appear to be protected . . . That person continues to be protected and I feel very uncomfortable with that, and I’m in a senior role and I am aware of the difficult individual and feel completely unable to do anything about it. And I don’t like that; I think that’s not good.
I don’t get the sense that consultants . . . see themselves as managers and leaders in the organisation. They’re here to do a job . . . You know it’s a good job, it’s a technical job, it’s a challenging job, and it’s a very skilled job. But it’s – the responsibility – I just don’t get the sense that there’s that kind of commitment to the organisation and they’re here for life any more.
Francis Inquiry feedback and listening events also indicated poor communication between corporate teams and ward-level staff in many parts of the organisation. In response, proposals for new means of communication were developed, in order to standardise operating procedures. These included inviting all staff groups to feedback events at specific places and times, consistent publication of information bulletins and increases in the ‘presence’ of board members within staff information bulletins.
[W]e want to take that back a step, refresh the standard operating procedure around that to make it much more ‘Right, that will come out on a Friday lunch-time’.
On reflection, further engagement of senior medical staff at the outset would have improved the initiative. Because of time constraints, senior clinicians were not able to come away from their clinical commitments to attend, and therefore a more proactive approach was required. Some staff members also suggested increased involvement from the MD and NEDs was required:
I suppose I’m seeing much more from the nursing taking the lead, from quality and effectiveness taking the lead – and instinctively I feel that you almost shouldn’t be able to see any light between the medical and the nursing director on this.
The Arran board’s developments on junior doctors’ dissatisfaction
The board was made aware that the annual GMC national survey had indicated junior doctors’ concerns about the possible negative consequences of reporting a colleague’s inappropriate practice. The survey also identified that ‘undermining’ (a term for bullying) was indicated in a handful of the 40 specialties within the trust. This was acknowledged as a potentially serious problem:
Junior doctors not feeling empowered, not feeling able to challenge their seniors – that’s a problem. If that led to an occasion where a junior doctor had a concern about patient care or about safety and they felt unable to say because of perceived repercussions that’s a serious issue.
In moving forward the board was described as ‘significantly sighted’ on the junior doctors’ issue. This translated into the chairperson and the governing body implementing an ongoing review of this issue with the aim of developing long-term cultural change. The executive board was also reviewing junior doctors as a standing item at the HR subcommittee, which had developed an action list of 10 things that needed improvement. Agreement was also secured from the MDs that this was something that they would support within their board. Progress would be reported on after a year. Although it was stated that the action plan was getting stuck on administrative issues, progress was being made:
It’s been very trustee proactive at a trust-wide level but firefighting in individual departments. Hopefully in the future we’ll move to a point where it will be very proactive on both fronts but at the moment that’s pretty much how it is really.
Concluding remarks
The tracer issue analysis presented above shows the extent to which these hospitals could be characterised as the ‘learning boards’ envisaged by Garratt. The case studies of board conformance highlight that boards have been reasonably effective in ensuring ‘accountability’ through IPC committee members engaged in regular audits and education initiatives related to the control and prevention of C. difficile infections. The findings also point to limitations within these efforts in relation to ongoing challenges, such as engagement of the medical workforce. IPC committee members also indicated the extent to which the introduction of external performance targets had driven board behaviours, but again these findings suggest limitations, with performance targets having reached a point where they were no longer relevant to the organisation.
The case studies of board performance showcase how boards have looked to formulate policy and strategy in relation to patient safety governance. The ‘After Francis’ initiative in Lewis represents a case in point, in which the board have looked to respond to quality and safety issues and develop new approaches to patient safety governance. Yet as with board conformance, notable gaps appear within these efforts as the boards struggle to engage particular areas of the workforce. These findings also point to notable ‘blind spots’ in board policy formulation, where particular areas of the workforce were not as engaged as they could or should have been, subsequently leading to difficulties in policy implementation. Fears of raising concerns or being seen as outspoken remain a significant problem in some areas.
Having drilled down in each of the trusts, we now move to a different framing for the final chapter in this qualitative analysis: a dramaturgical view of board performance to explore the more symbolic aspects of board practice(s).
Chapter 7 Hospital boards: a dramaturgy perspective
Introduction
This chapter draws on qualitative data from the overt non-participant observation in board meetings at the same four NHS hospital FT boards explored in Chapters 4–6. It seeks to address explicitly the performative aspects of trust boards (i.e. what board members say and do to discharge their accountabilities for patient safety). Applying a dramaturgical framework and using the dimensions ‘scripting’, ‘setting’, ‘staging’ and ‘performance’, we found important differences between case study sites in the performative dimensions of processing and interpretation of safety information. This was most clearly seen in the use of infection control data. In this chapter we detail the board rituals and practices associated with these differences, including the legitimation of current progress, the querying of data classification and the naming and shaming of executives, and consider their implications for the governance of patient safety.
As explored briefly in Chapter 2, boards are most often considered instrumentally, whereby a ‘successful’ board is one able to take decisions on corporate strategy efficiently and effectively. 19 However, attention may also be given to symbolic approaches which understand boards in terms of the implicit social aspects of board practice. 37,104 From this perspective, boards undertake important organisational work outside of the formal agenda in terms of conventions and ritual activity, in which participants construct narratives about who they collectively are. It is in this regard that the concept of performativity may prove particularly helpful, and the purpose of this chapter is to explore the application of performativity empirically. Below, we introduce performativity and consider the breadth of its influence within the study of organisational life, trace its foundations within the seminal work of Austin105 and Goffman106 and consider its empirical application in the context of participatory governance. 32 We then employ the framework of scripting, setting, staging and performance developed by Hajer to the dynamics and processes of hospital executive board meetings in relation to patient safety. We consider the insights such an approach can bring, and their implications for the study of patient safety governance more widely.
The rise of ‘performativity’
From its inception within linguistic philosophy,105 the reach of performativity has grown in many different ways. Early areas of influence include theoretical development in the emergence of order in complex interactive systems,107 the framing, staging and (re)creation of social life106 and the ‘language games’ that structure performative utterances. 108 Later applications include the performative constitution of gendered identity through interactions,109,110 the continuous construction of society through ongoing performance111,112 and the effects of economic theory on action. 113 Organisationally, performativity has informed analysis of the continuous change present in the enactment of organisational routines,114 the enactment of technology within social settings,115,116 the role of storytelling in co-ordinating within and between organisations117 and organisational change as active translation rather than passive diffusion. 118
The foundations of performativity: Austin and Goffman
Austin105 coined the neologism performativity to describe those instances in which the utterance of a phrase constitutes an action which changes reality rather than describes it; a simultaneous ‘saying’ and ‘doing’ with creative potential that, once the intention of the utterance is recognised, requires others to act in accordance with its implications. Austin’s paradigmatic case is the phrase ‘I do’ when spoken within the context of a marriage ceremony; a phrase with implications beyond indicating acceptance and requiring the people exchanging the vows to act, and be acted on by others, as a married couple from that point forward. Austin additionally stipulates that performative utterances are meaningful actions that are neither true nor false; rather, they create a social reality.
Although Austin provides a working definition of performativity, Goffman’s106 dramaturgy of social interactions applies a theatrical metaphor to indirectly explore its operation, principally through framing. For Goffman, the framing of the stage – the separation of front of stage, backstage and audience, and the reciprocal acceptance of the roles of audience and players – shapes the performativity of utterances onstage. In an extension of earlier work on the presentation of self,119 he applies this metaphor to the operation of social life, in which performativities are made possible through framing. Frames are essentially classification systems that actors use to order and make sense of diverse social phenomena, so that the performative potential of an utterance depends upon the frames available to actors within specific settings.
The performativity of governance: Hajer
Applying Goffman’s work106,119 to the arena of public governance, Martin Hajer33 and others have advocated the placing of a greater emphasis on the symbolic and performative dimensions of governance, focusing attention on the setting(s) in which deliberation takes place and the norms expressed during the process. Organisational life is conceived as a series of staged performances in which interactions of scene and acts produce a particular staging of decision-making. 33,34 Hajer33 operationalises Goffman’s approach, outlining a dramaturgical governance framework for the analysis of the performative dimension of board governance. Practice is explored through consideration of the setting(s) in which deliberation takes place and the enactment of organisational frames, operationalised through a consideration of the scripting, setting, staging and performance of board governance.
Scripting refers to the determination of actors involved in the decision-making forum and, by implication, those who are excluded. Consistent with the generative potential of performativity, it considers the way in which participatory practices construct participants as either active or passive, collaborators or protesters and competent or incompetent. In contrast, setting concerns the physical environment in which interaction takes place, additionally including artefacts (e.g. minutes of previous meetings, tabled reports) that participants bring to the physical environment and which shape the performance. Deliberate attempts to organise the interaction between participants is identified as staging. It is achieved by drawing on existing symbols and the invention and use of new ones, together with conventions governing distinctions between active players and passive audiences; what might be termed the unwritten rules of engagement. The final category, performance, concerns the way in which interaction constructs new knowledge/understandings/power relationships that shape future interactions and provide opportunities for change over time.
Crucially, if Goffman is correct that reality is mediated through the application of frames to make sense of the mass of available information, then it follows that all accounts of reality are shaped. The implication then, in the context of patient safety governance, is that the examination of safety could be framed in many ways with radically different consequences for action. For example, in presenting data that indicates a breach of an infection control performance target, is this an instance of unreliable data requiring a defence of organisational practice to an external regulator, a worrying event requiring detailed diagnostic work to uncover systemic problems and institute quality improvement activity or an impossibly harsh target imposed by regulators that needs to be robustly challenged?
Given the above framing, we exploited the opportunities presented by our observational data to examine the dramaturgy of board performance(s).
Board overviews as a background to dramaturgy
In presenting findings we first outline the operation of the board at each site to retain the integrity of each organisational setting. We then offer a comparative analysis of Hajer’s dramaturgical categories, scripting, setting and staging, in sequence across sites, indicating the scope and scale of differences between sites in board enactment of patient safety governance (these are summarised in Table 7). We then explore the fourth of Hajer’s dramaturgical categories, ‘performance’, in relation to board deliberation of indicators associated with infection control; a key component of the external performance management regime within the English NHS at the time of the study.
| Dramaturgical category | Case study site | |||
|---|---|---|---|---|
| Arran | Skye | Lewis | Islay | |
| Scripting | CEO shaped events through ‘CEO report’ agenda item; low levels of NED challenge; opportunities to challenge ‘managed’ | Chairperson dominant; NEDs forthright challenges; adversarial (agency) model with execs lauded or shamed | CEO a dominant personality; much deferral to his experience; NEDs able to question; ‘embattled’ narrative of CEO the main coda | NEDs’ robust yet respectful challenge; endemic, framed and legitimated as ‘improving patient experience’ |
| Setting I: physical | Large, airy meeting room in trust headquarters education centre; non-adversarial ‘horse-shoe’ arrangement of tables at the front of the room, space for many observers as required; high-quality projection facilities routinely used | Rotating venue, typically cramped, dated and poorly equipped; no consistent seating arrangement; ‘audience’ very close to board tables | Boardroom at main site – imposingly furnished (dark wood, large tables); a place ‘where important decisions are made’. Separate table for those invited to present to the board – adversarial; calls to mind the layout of an ‘inquiry’ | Rotating venue, always in well-furnished, low-key ‘office’ environment. Spacious, with room for a wide range of attendees to observe as required |
| Setting II: artefacts | Presentations modelled on medical lectures; routinely used to summarise main points of reports in board papers and frame discussion. Successfully limited the scope for alternative challenges | Detailed information presented using software tools; typically ‘dry’ delivery; used by NEDs to facilitate challenge | Not used other than in ‘special’ presentations by external speakers – and then not supported by software or projection; relied on orations from presenters and challenges made with reference to supporting information in board papers | Presentations routinely used in clinical updates – supported by presentation software and projection facilities |
| Staging | Highly structured and formal; CEO’s report placed early in agenda affording scope to craft an over-arching narrative which reinforced the self-image of the organisation as a high performer even where there were difficulties (e.g. infection control); performance data summarised to one page of A4 and used to identify ‘red’ areas for development work – assurance mode | Highly structured and formal; chairperson steered focus on breach of targets in summary indicators to facilitate robust challenge | CEO dominance of ‘matters arising’, placed early in the agenda, set the tone. Most of the time spent on these items; the ‘CEO show’ | Highly structured, yet ‘permission to speak’. Opens with a narrative patient story ‘to concentrate our minds’ – patient experience a guiding principle, invoked routinely. Performance data reported within a ‘quality improvement strategy’ section – improvement mode |
| Performing: infection control | Despite existence of summary A4 ‘traffic light’ indicators showing breach on infection control, CEO used their report to frame perceptions (successful reclassification with commissioners and Monitor) to remove the breach. There was no non-executive challenge | Chairperson adopts tone of ‘disappointment’ at data presented on C. difficile infection target breach to demand action by the ND. No attempt to ‘explain away’ or contextualise the breach | C. difficile infection targets presented as unobtainable by CEO; legal challenge threatened to commissioners as part of ‘embattled’ narrative | Infection control target (reported in QI strategy section) is met, but CEO warns against complacency. Data are disaggregated to identify potential ‘hot spots’ to further drive performance |
Arran: a world-class provider
Arran has a strong research culture and a global reputation for service innovation and development. The board acts strategically and is externally oriented, seeking to secure compliance with central policy directives while safeguarding and further developing its global reach and status as a pre-eminent provider and academic research centre. In operation, board meetings are highly formal and structured to enable the CEO to ‘steer’ interpretations of events. The executive team are experienced, with low turnover and a strong medical presence. NEDs exhibit very low levels of challenge, even when performance difficulties are under discussion; indeed, the dynamic of board meetings could be summarised as maintenance of the narrative of ‘world class’ status while engaging with potential performance difficulties evident in summary indicator data.
Skye: a local service under pressure
In marked contrast, Skye presents as a trust with high levels of turnover in the executive team in recent years and overt recognition of many problems in service provision. This had led to a focus on internal problems rather than the development of organisational strategy in relation to the wider external environment. Board meetings were steered strongly by the chairperson, who dominated a newly appointed CEO. Strong challenges from NEDs were common, and included expressions of disappointment at poor service performance, as well as strong support for those executives considered to be performing well. During the period of observation, one of the executives, who was considered to be performing poorly, stepped down, to be replaced by a deputy who received similarly high levels of challenge. The dynamic of the board could be summarised as routine non-executive challenge with limited long-term strategic direction.
Lewis: an embattled regional powerhouse
Protective of its reputation as a regional ‘leading light’, board meetings were structured to ensure that issues of strategic importance to the trust received due consideration and events were considered as they unfolded over successive meetings. The image of the trust revealed through board operation is that of a guardian of the interests of the locale and wider region, requiring continued political influence to secure those interests. The trust has an experienced and longstanding executive team; indeed, the CEO personifies the organisation, dominating board meetings and acting as a political antagonist to defend local interests. During observation the majority of time was spent on a small number of financial and estate issues and related legal disputes. NEDs were typically involved in clarifications related to their specific areas of interest rather than challenges over strategy or performance. Overall, the board dynamic could be characterised as one of defending its status as regional champion.
Islay: faith in quality improvement methodologies
The overwhelming impression of this site is of one in which board structures and processes focus attention on the reconfiguration of integrated care strategies through the lens of service quality improvement defined as ‘patient experience’. Central to this approach was the consideration of performance issues related to external regulatory requirements (e.g. infection control, reduction in incidence of pressure sores), and these were directly linked to improvement work to support the strategic plan. Patient experience was routinely invoked and normalised by the presentation of a patient experience narrative at the start of each board meeting. NEDs were encouraged to question and the executive team actively sought their contributions. This board could be characterised as drawing on a wide range of soft and hard intelligence, seeking to maintain strategic focus while discharging external regulatory accountabilities.
A dramaturgy of board governance in patient safety
Scripting
Sites demonstrated distinctive variations with regard to scripting. Although often commenting on information presented to the board, at Arran NEDs were limited in their challenges to executives; collectively, the tone was one of ‘low challenge’ without overt conflict. This was achieved principally through agenda shaping by the CEO, who used his ‘CEO report’ agenda item to reframe potential performance issues.
In marked contrast, the chairperson and NEDs at Skye confidently challenged executives, particularly in relation to poor performance in infection control and capacity/demand issues, challenging the CEO to improve standards and the finance director to increase investment in capacity. There was clear differentiation in the way that executives were seen and treated. The MD was widely seen as competent and dependable, with NEDs formally acknowledging his pathway development work. In contrast, the ND received tougher questioning and her hesitancy was drawn to attention. In this manner, executives were either lauded or shamed, and such public shaming had a negative reputational impact within subsequent board meetings.
At Lewis, board meetings could be summarised as ‘the CEO show’, characterised by political statements defending organisational interests. There was much deferral to his experience, political influence and judgement. Central to this performance was the crafting of a narrative of an embattled trust fighting for local interests. Board meetings gave the impression of a trust under fire, enmeshed in structural, legal and financial disputes. The CEO’s views were rarely challenged, in large part because the board supported his position, but also because they accepted that his performance was part of the ritual, crafted with humour, emotion and political point scoring. In this context, the chairperson had a supportive presence, summarising issues as appropriate.
At Islay the board maintained a clear focus on strategy and service improvement, with positive roles for each member. The CEO projected a calm manner, as a moderniser and believer in quality improvement methodology, with a similarly oriented executive team. The CEO had heavily invested in board development in relation to quality improvement and this training clearly informed board practice. Robust yet respectful challenge was the norm among NEDs, framed and legitimated as ‘improving patient experience’. Board dynamics were driven by this central narrative, which granted permission for depersonalised challenge.
Setting I: physical
Board meetings at Arran were held within the education centre at trust headquarters in a large room with high-quality presentation facilities used in formal presentations by invited speakers to address specific agenda items. The location reinforced a sense of ‘information transmission’ rather than deliberation: a passive process. The room was large, bright and airy and could have accommodated up to 30 observers with ease. The audience for the public board meeting typically consisted of five governors and/or members of the public, ordered into rows of (sparsely populated) chairs facing presentation screens and set back from board members, who were themselves seated in a ‘horseshoe’ arrangement of three tables at the front of the room; a non-adversarial framing consistent with a ‘common purpose’.
Meetings at Skye were held at different locations across the trust. With one exception, meeting rooms were poor environments in which to facilitate discussion: cramped, hot and lacking air circulation. Because of the cramped conditions, the audience (3–5 governors) tended to split into two groups at opposite sides of the room, very close to the board table. The chairperson, CEO, trust secretary and trust minute-taker always sat together, with other seats haphazardly assigned with no consistency across meetings.
Board meetings at Lewis were held at the boardroom at the main trust site, whose décor, original to the building, consisted of dark-wood tables and chairs with red leather covers: an imposing environment reflecting civic pride. The seating arrangement was stable across meetings. The chairperson, CEO and observers sat together, the business development director and NEDs together on an adjacent table to the ND and finance director, with some spaces for guest speakers and observers. The trust secretary, MD and more NEDs sat at an adjacent table. One important feature was that those invited to present to the board faced an experience akin to an inquiry or investigation; waiting in an anteroom for the appointed time on the agenda, invited in when required and positioned on a table in front of the board to face questions.
Although the venue for Islay’s board meetings rotated, they were always held in well-furnished, low-key ‘office’ environments. Rooms were spacious and able to accommodate observers as required. Seating was arranged around a large single table on an ad hoc basis. Attendees included members of the QI team and clinical leads who attended to report updates regarding specific clinical reviews.
Setting II: artefacts
All sites provided board members with ‘board papers’, a briefing pack for information consisting of a formal, standardised agenda and appended reports for each agenda item in sequence, ahead of the board meeting. The format and contents was very similar across sites. Two frames of reference were identified that underpinned these board papers: RAG ratings and ‘narrative’ executive summaries. Patient safety performance information contained within the board papers was assigned red, amber or green (RAG) ratings to document performance. Additional quantitative material would include line graphs, along with run charts and bar charts to present performance. In addition, board papers presented information in the form of an executive summary of the ‘key issues’ over the past month and the options for moving forward.
At some sites, notably Arran, special presentations were typically undertaken by medical staff in response to specific issues highlighted within previous board meetings. The format of these presentations broadly adhered to conventions associated with academic medical lectures: presenters using the electronic facilities available to display detailed presentations, summarising the main points of associated reports appended within the compendium of board papers and then responding to questions from the floor. Presentations anticipated likely questions and were generally of a high standard. While affording non-executive board members the opportunity to raise detailed questions, the presentation format provided the opportunity for prior framing material to create the desired effect.
Although similar conventions operated at Skye, the presentations were generally more informal in tone and lacked vibrancy. They typically afforded NEDs the opportunity to raise questions in relation to detail rather than broader framing.
Staging
Very formal in operation, the ordering of the agenda at Arran was significant in affording the CEO scope to craft an over-arching narrative that reinforced the perception of the organisation as a high performer. A separate ‘performance report’ delivered by the director of strategy provided a high-level summary and narrative overview of key performance indicator (KPI) data related to activity, efficiency, access, cancer, infection, quality and safety, workforce, finance and the Monitor compliance framework. Performance data were presented for the current month and year to date, disaggregated by subdivision (medicine, surgery and cancer and specialist) on a range of indicators for each of the performance areas listed above, summarised on a single A4 page, with additional supporting data for each performance area on subsequent pages. Presentation adopted a traffic-light system in which performance against each indicator is colour coded: green for ‘good’, amber for ‘attention’ and red for ‘breach’. This summary of performance acts as a strong visual cue of actual and potential performance shortfalls, drawing the eye to patterned clusters of ‘red’ and ‘amber’ on the page. Consequently, board attention was often drawn to, and time was spent on, those performance indicators with ‘red’ and/or ‘amber’ status. Executive behaviour at the board seemed strongly influenced by the need to publicly demonstrate performance against standards as indicated by the performance indicators (‘conformance’), and account for any observed shortfall.
The structure (KPIs) and form (‘traffic-light’ RAG indication of performance against targets) of reporting used to inform the board potentially facilitates the discharge of public governance in the form of assurance (‘conformance’). Although such a system could be used by non-executives in a bullish manner to vociferously challenge executives on performance shortfalls, this was not done at any of the observed board meetings. Rather, the CEO drew attention to shortfalls in his CEO report, recontextualising the figures and outlining ongoing work to diagnose and/or address shortfall. Non-executives seemed generally supportive of these reassurances.
The CEO’s report was wide-ranging, provided opportunities for clarification and discussion and, consequently, took a considerable amount of time. The CEO used this composite section, delivered very early in the board meeting, to consider multiple items related to trust activity/performance and its implications, in the light of external policy directives and/or the strategic opportunities they provided. Examples include Dr Foster performance rankings, Monitor KPI governance ratings, CQC visit outcomes and implications for the trust of the Francis Report into patient safety. This section was not delivered as a monologue – rather, the CEO outlined his perspective and invited others (typically executive members, also notably the chairperson) to comment in the light of this analysis and/or to clarify issues. Although there was opportunity for NEDs to ask questions during proceedings, contributions invited by the CEO came from executive board members, with minimal NED input.
In contrast to the close executive control exhibited above, at Skye the staging was typified by the chairperson’s dominance of the agenda. The chairperson exercised his non-executive role in challenging the executive and largely supporting the views of other non-executives. His steering of the agenda, and of contributions from other non-execs, focused principally on the breach of targets (particularly C. difficile infections) and issues related to coding and validity of information provided, with very limited external horizon scanning or evidence of facilitating strategic thinking. The chairperson was active throughout, but particularly in relation to quality and patient safety, as evinced in steering challenge to the ND about infection control and the failure to achieve the C. difficile infection target. There was a sense (picked up by an audience member in an aside to the researchers) that he dominated the meeting; by controlling the staging and encouraging the NED performance the chairperson prevented other narratives from unfolding.
Staging at Lewis was shaped by an extensive ‘matters arising’ section, placed immediately after the opening item of ‘apologies’. This was by far the longest section and invariably consisted of the following issues considered most important: a major capital investment project, ‘safe and sustainable’; paediatric cardiac surgery; any Qualified Provider procurements; an Academic Health Science Network and commissioner penalties in relation to C. difficile infections.
Board meetings at Islay were strategically focused and tightly structured around the agenda. The tone of each meeting was set by an opening ‘patient story’ narrative, introduced by the chairperson as ‘something to focus our minds’. These narratives, collected by the improvement team and presented in the patient’s own words, concerned issues such as the fears, anxieties and negative experiences following diagnosis, processes of care and treatment outcomes. They were emotive and used by the chairperson to legitimate challenge and concern with service improvement, and this language of ‘patient experience’ was available to, and used by, board members to depersonalise challenging questions. The strategic focus on service improvement was also supported by the structure of the agenda, which considered ‘service improvement’ to be a standing agenda item placed immediately after the ‘patient story’ opening, and led by members of the quality improvement team presenting data and updating progress on strategically important projects, such as intensive care, community services, falls and infections. The incorporation of indicators for infections into this section is important, as it ties external regulatory requirements to internal strategy in an agenda item specifically oriented to service improvement.
Performance(s): board governance of infection control
Board meetings at Arran were dominated by the CEO and typified by a need to present trust performance in a favourable light, consistent with a ‘world-class’ reputation. This dominance was not exercised through explicit force of personality, but principally through careful structuring of the agenda and the use of framing in the ‘CEO report’ agenda item to shape perceptions of, and thus actions in relation to, items which appeared later in the agenda.
As outlined above, the CEO’s report often drew attention to shortfalls in performance. Notable examples in relation to patient safety included failure to achieve reduction in C. difficile infection targets for three quarters in succession and a potential breach of A&E waiting time target in quarter 4 (and thus for the whole year). Although both of these topics could have elicited vociferous challenges from NEDs, no such challenges were made. Rather, in relation to the former, the CEO announced that he had successfully argued with commissioners for a waiver of penalties for 10 cases, and once this had been agreed he argued with the relevant external regulatory body for reclassification as ‘green’ (healthy) under their governance performance indicator, which had been flagged as amber, placing the trust under external scrutiny. This was presented by the CEO as evidence of oversensitivity to borderline non-compliance. His analysis drew support for an internal review of antibiotic prescribing habits (supported by comments from a NED and one of the MDs). In the case of the A&E issue, the seriousness of the potential breach was minimised by reference to the ubiquity of such problems nationally (‘everyone faces such difficulties’), addressed with reference to current plans to expand A&E provision (‘we are already dealing with this’) and attention focused on the role of limited out-of-hours cover by GPs in increasing demand on A&E services (‘the problem lies elsewhere’).
In both instances, the CEO’s report identified poor performance against indicators that could have been addressed within the latter ‘performance’ report section as ‘breaches’ and subtly interpreted the data in a misleading way. That these analyses were convincing is clear from the positive reception they received and that fact that neither of these issues were referred to in the latter presentation of the ‘performance’ report or picked up by NEDs for further exploration. Given the important work involved in framing these issues in such a way that possible poor performance is acknowledged, while simultaneously offering reassurance that ‘all is well’, the CEO report was typically one of the longer, and on one occasion the longest, agenda item(s), at 46 minutes out of a total of 110 (42% of the total time).
At Skye, board performances were typified by high levels of NED activity. In relation to breach of a C. difficile infection target, the chairperson adopted a tone of disappointment at failure to reach the target, presenting it as a serious issue that needed to be tackled and required explanation by the ND and active discussion by NEDs. Although there is some acceptance that there are widespread difficulties in meeting the target, there is no serious attempt by the chairperson or any executive to reframe the target breach. The ND (and later the acting ND) is held responsible. A ‘red’ trajectory against A&E performance led to NED involvement in discussions concerning historical failures of the board. NEDs also challenged finance report data showing an operating surplus despite underperformance of general medicine and lower than anticipated emergency admissions; a downwards trajectory from amber to red in summary performance data was also used by NEDs to challenge performance.
At Lewis, the CEO’s dominance and use of humour, emotion and politics is exemplified in discussions of a breach of infection control targets. Discussion was dominated by the financial penalties associated with breach of the target, particularly regarding how the trust would pay the financial penalty if its target were breached. As it stood, the trust faced a fine of over £1M per case in breach of the target. Disputes with commissioners ensued and legal proceedings developed. The issue of discussion centred on ‘proportionality’ and perceived unfair treatment in comparison with their regional neighbours, whose targets were considered far easier to reach. Mediation was the next step, with the trust taking the commissioners to court. The CEO suggested they had no choice and he was forced to make a stand.
Although board consideration of infection control at Islay was also framed in relation to external targets, the service improvement orientation of the board was very evident. The MD presented data showing that the trust was meeting its target – although it was close to the limit. This was warmly welcomed by a NED, who praised the effort, and then quickly considered the interventions required to ensure continuous compliance, prompting a discussion of the educational interventions being made to embed infection control in staff behaviour, including associating high-risk cases with reinforcement of requirements to junior doctors.
Reading across the cases then, we see very different emphases and approaches to the performative aspects of governance. These are summarised in Table 6, and further discussed below.
Discussion
Obtaining, processing and interpreting performance information are acknowledged as important aspects of boards’ oversight role. 120 Although there is some empirical support for the assertion that those hospital boards which prioritise the collection and analysis of performance, data tend to have improved quality outcomes. 64 We draw attention to the importance of processing and interpreting this information and to the performativities at play: the social practices involved in realising the potential of patient safety performance indicators121 and, perhaps even more importantly, how ‘warning signals’ provided by such information systems may be muted, deflected or even silenced.
Although the same level of performance indicator data relating to infection control was available in all of our case study sites, differences in use were significant and related to the practices legitimated within each setting. At Skye, board activities were underpinned by agency theories of governance,19 in which the interests of board members were framed in adversarial terms and identified the primary responsibilities of NEDs as seeking assurance of conformance to standards. Consequently, infection control data were used to ‘name and shame’ executives by a dominant non-executive cadre led by a strong chairperson. In contrast, board activities at Lewis were informed by stewardship theories of governance,19,122 in which board members’ interests were framed as compatible and built on a shared set of values related to regional position and protection of the locale. Thus, infection control data indicating similar levels of underperformance to that at Skye was framed by the CEO as an ‘unattainable target’ and a threat of legal challenge was issued to commissioners. To similar effect, at Arran the CEO drew on resource dependence models of governance,24 in which board members seek to manage internal and external relationships to leverage influence. Board members’ shared values in relation to the position of the trust as a world-leading organisation were mobilised by the CEO to forestall challenge to his interpretation of the meaning of infection control rates; not through force of personality so much as through use of the agenda structure of the ‘CEO report’ to reframe the breach of target as ‘a data difficulty’ and by exerting influence over local commissioners to secure a reclassification to reduce the number of ‘cases’ below the regulatory threshold then discussing the reclassification with the regulatory agency. The early placement of the CEO report provides an opportunity for reframing poor performance against indicators and minimising the challenge related to it, even though the traffic-light reporting makes it plain to see. This is chilling in the light of the reaction to concerns about mortality indicators in the Mid Staffordshire NHS Foundation Trust case, in which (seemingly) efforts were made to reinterpret poor performance against mortality indicators. 4
It is important to state here that we do not claim privileged status for our own analysis; that our perspective somehow reflects a single underlying objective ‘truth’ to which we had special access and that remained unavailable to the board members observed. We do not claim that the performance indicator data presented at these board meetings showed deficiencies in patient safety that were inappropriately interpreted away. Indeed, the very value of a performative approach is that it seeks to trace the way in which words both ‘say’ and ‘do’; to consider those meaningful actions that are neither true nor false but that create a social reality that is then acted upon by others. Our analysis shows the use of data to create a social reality in relation to infection control rates, which guided future actions. The value of performative analysis is also evident in relation to board activity at Islay, in which the chairperson nevertheless used data showing compliance with infection control targets as an opportunity to consider how to improve practice.
Our findings have important implications for the governance of patient safety. The very different performances observed in relation to infection control data evident in our case study sites has implications for the nature of advice and training made available to boards. Crucially, while the availability of information may be a necessary precursor for improvement, it is clear from the data presented above that it is not in itself sufficient. A set of behaviours/practices that use such information to support cycles of improvement activity is also required. This draws attention to additional lines of inquiry that explore the relational or trust-based dynamics associated with board governance. For example, when there is a common set of strong values, NED challenge runs the risk of being framed as disloyalty. In these cases and scenarios it is important for boards to reflect critically on existing relationships and ensure that they create conditions for openness and transparency.
Concluding remarks
It is acknowledged that studies of statistical associations between organisational structures and patient safety outcomes are not able to explore the dynamic and messy lived reality of board governance practices related to patient safety. 17 Our analysis of such practices at four hospital boards indicates the importance of local processes of organising in relation to governance of patient safety. Although the availability of summaries of quality indicators to board members is undoubtedly important, so equally is the operation of processes of organising that make it possible for local actors to use such information to make interventions to hold executives to account with regard to patient safety processes and outcomes. In this regard, our findings indicate the challenges faced by board members in terms of the artefacts at their disposal and the limitations of the scripts and stages associated with board practices. Encouragingly, in drawing attention to practices associated with the enactment of safety and quality they also indicate possibilities and opportunities for enhanced deliberation of information with which to improve the corporate governance of safety and quality, and we encourage the additional applications of performativity-based approaches in order to further develop our understanding of patient safety governance enacted by boards.
This chapter concludes our analysis and presentation of the qualitative data, and we move next to a consideration of the quantitative data, exploring any relationships between boards and wider organisational performance.
Chapter 8 National survey of NHS boards
Introduction
This chapter presents the key findings drawn from the two national surveys of NHS boards (see Chapter 2, Methods). These survey data have been linked to nationally available routine data to begin to explore some of the analytic questions set out in Chapter 1.
The findings are presented here in three main parts. First, a descriptive account of NHS boards which also examines differences between hospitals of different types, specifically FTs versus non-FTs and THs versus non-THs. Given the different governance arrangements for FTs and the greater scale and complexity of TH activities, it seemed worthwhile to make this exploration, but we had no specific prior hypotheses that we were testing. Within this descriptive account of NHS boards we examine two key areas: (1) board size, structure and composition, including clinical representation on the board, and (2) board engagement with patient safety issues, including the use of diverse sources of hard and soft information.
Second, we present an analysis of the Board Self-Assessment Questionnaire (or BSAQ) that revalidates the data structure of the BSAQ instrument alongside a descriptive account of aggregate trust board responses in the six dimensions that make up the BSAQ.
Finally, we present an analytic account that explores correlations between various descriptive variables of boards (including BSAQ) and numerous routinely available quality and safety parameters aggregated to organisation level.
The nature of NHS boards
Board size and composition
Given the range and diversity of roles required of NHS trust boards, it follows that they need to be of sufficient size and diversity. The smallest board in our sample had eight members and, in general, boards were tightly clustered in size with between 10 and 15 members. Around 42% of boards had 10–12 members and around 51% had 13–15 members, with the largest board counting only 17 members. We found no significant difference in board size between trusts of different types (FT/non-FT; TH/non-TH).
In our study, around 62% of boards had three or fewer serving board members with clinical backgrounds. For about two-thirds of the trusts (63%), board members with a clinical background constituted < 30% of the board. We found no significant differences between FT/non-FT and TH/non-TH trusts in the distribution of board members with clinical backgrounds. Our findings chime with recent work that focused on NEDs, which found that only half of trusts (52%) had any NED with health-care leadership experience, with the overwhelming majority of NEDs (86%) being drawn from a commercial, financial or managerial background (non-clinical).
Board engagement with patient safety
In this study, boards appear to give considerable time to safety and quality issues. Only one-fifth of trust boards (21%) reported that ≤ 30% of their time was spent discussing safety and quality issues, but only one-quarter (26%) reported that > 60% of their board time was spent on these issues.
Board practices around patient safety
A very high proportion of the trusts in our survey reported the kinds of desirable characteristics and board-related processes that research says may be associated with higher performance (Box 2). On only two of these questions (safety measures in the CEO’s performance review, and formal training for board members on quality and safety) did affirmation fall at or below 90%. There was a small (but still non-significant) difference between FT/non-FT boards with respect to board members receiving formal training in relation to patient safety, with 90% of FT boards versus 83% of non-FT boards reportedly receiving training. Other differences between trusts of different types on the raft of measures in Box 2 were minimal. These generally high (or very high) ‘desirable responses’ by trusts may represent considerable board attention being paid to quality and safety, especially in the light of scandals such as that of Mid Staffordshire NHS Foundation Trust, and/or they may reflect a growing awareness of the importance of signalling that such issues are being taken seriously. These uniformly high affirmative response rates made correlational analysis of any relationships between board responses in these areas and organisational outcomes inappropriate.
Does the board have a formal subcommittee that discusses patient safety issues? (Yes: 100%.)
Are there procedures for proactively responding to the reporting of staff concerns about patient safety? (Yes: 100%.)
Has the board set explicit measurable goals for improving performance in relation to patient safety? (Yes: 98%.)
Does the board have formal procedures for reporting inappropriate behaviours in relation to patient safety on a regular basis? (Yes: 98%.)
Have strategic goals and objectives related to patient safety been distributed to staff groups within the last 12 months? (Yes: 99%.)
Are patient safety measures included in the CEO performance review? (Yes: 90%.)
Have board members received formal training in relation to patient safety? (Yes: 87%.)
Board use of information on patient safety
In our national survey we found that hospital boards were using a wide range of hard performance metrics and soft intelligence to monitor their organisation with regard to patient safety. Quantitative data, including a range of clinical outcomes measures, infection rates and process measures, such as medication errors and readmission rates, were reportedly used at every board meeting across most hospital trusts (> 80%). It is noteworthy, however, that fewer trusts reported routine reporting of patient safety surveys (81%) and implementation of patient safety alerts (79%). A much smaller proportion of trusts (57%) routinely report morbidity rates at every board meeting. There was no appreciable difference between FT/non-FT boards and TH/non-TH boards on most reporting of explicit performance metrics except for ‘formal morbidity reporting’, for which 52% of non-FTs compared with 60% of FTs routinely presented these at board meetings.
There were some (generally small) differences between FT and non-FT boards, and also between TH and non-TH trusts, in their use of softer intelligence, but these differences were not marked and nor were they consistent. For example, the difference between FTs and non-FTs in their use of patients’ stories was 8% (80% vs. 88%); the same difference seen in their use of board members engaging with clinicians (91% vs. 83%), but with the direction of difference reversed.
In general, then, despite a very high level of desirable characteristics being reported (see Box 2), there remained considerable variation in the use of diverse sources of hard and soft information. Explicit metrics (such as morbidity rates), in particular, were used only intermittently in a considerable number of trusts.
The application of the Board Self-Assessment Questionnaire in English boards
The BSAQ instrument123 was developed to assess board performance in non-profit organisations in the USA in six areas (Box 3). Since its development, it has undergone extensive analysis of reliability, validity, and sensitivity. 43,44 It has also been used to assess board effectiveness in non-profit US hospitals45 and in one small study of UK NHS trusts. 29 As this was the first major study using BSAQ in the UK context, we first tested the data structure of the instrument in that setting.
-
Contextual dimension. The board understands and takes into account the culture, values and norms of the organisation it governs.
-
Educational dimension. The board takes the necessary steps to ensure that all board members are well informed about the organisation and the professions working there, as well as about the board’s own roles, responsibilities and performance.
-
Interpersonal dimension. The board nurtures the development of board members as a group, attends to the board’s collective welfare and fosters a sense of cohesiveness.
-
Analytical dimension. The board recognises complexities and subtleties in the issues it faces and draws upon multiple perspectives to dissect complex problems and to synthesise appropriate responses.
-
Political dimension. The board accepts as one of its primary responsibilities the need to develop and maintain healthy relationships among key stakeholders.
-
Strategic dimension. The board helps envisage and shape institutional direction and helps to ensure a strategic approach to the organisation’s future.
Testing the structure of the Board Self-Assessment Questionnaire
The BSAQ online survey was conducted over two periods: between 21 May and 20 August 2012 (phase 1) and between 30 January and 5 April 2013 (phase 2). A total of 334 responses were received from 165 executive and 169 non-executive board members representing 95 NHS trusts (of the 144 that were sent the BSAQ questionnaire). Of these 95 trusts, 51 are FTs. Board composition by foundation status is shown in Table 8.
| Board composition | Non-FT (n = 42) | FT (n = 51) | ||||
|---|---|---|---|---|---|---|
| Mean | Minimum | Maximum | Mean | Minimum | Maximum | |
| Respondents | 3.62 | 1 | 8 | 3.57 | 1 | 13 |
| Board size | 12.57 | 8 | 17 | 13.10 | 10 | 16 |
| Proportion of respondents | 0.30 | 0.06 | 0.88 | 0.27 | 0.06 | 0.87 |
| Clinicians | 3.50 | 2 | 7 | 3.37 | 2 | 8 |
| Proportion of clinicians | 28.27 | 0.13 | 0.64 | 25.79 | 0.14 | 0.53 |
| Executives | 1.74 | 0 | 4 | 1.80 | 0 | 9 |
| Proportion of executives | 0.14 | 0 | 0.40 | 0.13 | 0 | 0.60 |
Table 8 shows that non-FTs had a slightly higher response rate and a slightly smaller board size, but a higher proportion of clinicians on the board. However, differences were not found to be statistically significant.
The 65 questions on the BSAQ are scored by respondents on a 4-point Likert scale as one of strongly disagree, disagree, agree or strongly agree. Each of the questions corresponds to one of the six dimensions of board performance.
Factor analysis
We perform factor analysis at the respondent level to explore underlying factors that characterise board performance in each of the six dimensions. We find that there is a single underlying factor for each dimension that can be expressed as a BSAQ score. This continuous score summarises the inter-relationships among the ordinal 4-point scale questions in the dimension. A total BSAQ score is also derived and is used to explore whether or not there are associations between board performance and patient safety measures. Specifically, our analysis comprises the following steps:
-
We carry out ordinal factor analysis on each of the six dimensions of board performance individually. Based on the extracted factors, for each respondent we construct six scores, one for each dimension.
-
We apply factor analysis on the factor scores representing the six BSAQ dimensions to construct a total BSAQ score.
-
We explore correlations between the constructed BSAQ scores and a number of patient safety measures.
-
We estimate multivariate models regressing patient safety measures and measures of hospital ability to handle errors, near-misses and incidents on the total BSAQ score and a number of hospital-level characteristics.
Purpose of factor analysis
Each BSAQ dimension consists of a number of questions (items). Factor analysis assumes that the variance in a given item can be explained by one or more common underlying factors and by variance that is unique to the item. The amount of variation in the item that is caused by the common factors is known as communality. Our purpose is to establish whether or not each of the pre-determined BSAQ dimensions is unidimensional. The process, known as factor extraction, is iterative. First, the squared multiple correlation for each item (a measure of how much variance an item shares with the other items) is initially placed on the diagonal of the correlation matrix to approximate communalities (how much the items share with the factors). Then factors are extracted successively, with the first factor accounting for the maximum amount of common variance. The second factor is extracted from the residual correlation matrix after factoring out the influence of the first factor, and the process continues until some criteria are met.
Revealing the latent factors
In factor analysis, eigenvalues represent the amount of common variance among all items that is explained by a particular factor. The larger the eigenvalue, the more total common variance in the items that is explained by the factor. Table 9 presents six sets of eigenvalues obtained from factor analysis performed in each of the six BSAQ dimensions. In the first dimension, the contextual dimension, there are six negative eigenvalues, which are not acceptable in factor analysis and, therefore, only factors 1–6 are further examined for this dimension. Similarly, in the other dimensions, only the positive factors are examined. The amount of common variation explained by the first factor is 3.30, significantly larger than the variance explained by the other factors. One of the criteria for determining the end of the extraction process is to select only those factors for which the eigenvalues are > 1 (Kaiser–Guttman criterion). In all six dimensions, only the first factor meets this condition. Although the criterion is criticised as being inappropriate for factor analysis, two other commonly used criteria confirm the existence of a single factor within each dimension. Unlike principal component analysis, the eigenvalues in factor analysis do not sum up to 1; therefore, values > 1 do not necessarily imply that the factor accounts for more than its share of the total variance in the items. 124 The percentage of variance extracted by the first factor exceeds 85% in all six dimensions (much higher than commonly used thresholds in social sciences).
| Item | BSAQ dimension | |||||
|---|---|---|---|---|---|---|
| Contextual | Educational | Interpersonal | Analytical | Political | Strategic | |
| 1 | 3.30 | 2.99 | 2.37 | 2.72 | 2.47 | 4.58 |
| 2 | 0.58 | 0.59 | 0.45 | 0.30 | 0.22 | 0.53 |
| 3 | 0.29 | 0.26 | 0.24 | 0.24 | 0.10 | 0.26 |
| 4 | 0.11 | 0.20 | 0.13 | 0.11 | 0.07 | 0.11 |
| 5 | 0.07 | 0.04 | 0.04 | 0.03 | –0.03 | 0.06 |
| 6 | 0.02 | 0.00 | –0.05 | –0.04 | –0.04 | 0.02 |
| 7 | –0.02 | –0.03 | –0.09 | –0.08 | –0.13 | –0.06 |
| 8 | –0.13 | –0.11 | –0.13 | –0.14 | –0.19 | –0.08 |
| 9 | –0.15 | –0.17 | –0.17 | –0.19 | –0.11 | |
| 10 | –0.17 | –0.20 | –0.19 | –0.23 | –0.23 | |
| 11 | –0.26 | –0.27 | –0.22 | –0.24 | ||
| 12 | –0.33 | –0.31 | –0.27 | |||
Scree plots125 identified in all cases show distinct breaks between the slope of the larger eigenvalue (which corresponds to the first factor) and the trailing off of the other eigenvalues, suggesting the use of one factor. Figure 2 shows the scree plot for the contextual scale as an example.
FIGURE 2.
Scree plot for the 12 items of the contextual scale.

The results of finding a single factor for each of the six BSAQ dimensions supports the validity of the BSAQ dimensions and is also found in previous studies. 29,42,44,45
Contribution of items in the common factor
Each of the dimensions in BSAQ has a number of questions that load onto that dimension; for example, there are 12 questions/items in the contextual domain, but only eight questions/items in the political domain. The factor loadings presented in Table 10 indicate the extent to which each of the items correlate with the underlying factor. The square of an item’s loading represents the item’s communality. For instance, 26% of the common variance that item 1 shares with the other 11 items within the contextual domain can be explained by the common factor. In all six dimensions, items load reasonably strongly, exceeding the commonly used threshold of 0.3 for communality,124 with only few exceptions.
| Item | BSAQ dimension (loading/loading2) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Contextual | Educational | Interpersonal | Analytical | Political | Strategic | |||||||
| 1 | 0.51 | 0.26 | 0.53 | 0.28 | 0.48 | 0.23 | 0.56 | 0.31 | 0.48 | 0.23 | 0.69 | 0.48 |
| 2 | 0.65 | 0.42 | 0.58 | 0.34 | 0.18 | 0.03 | 0.54 | 0.29 | 0.50 | 0.25 | 0.56 | 0.31 |
| 3 | 0.58 | 0.34 | 0.54 | 0.29 | 0.55 | 0.31 | 0.56 | 0.31 | 0.47 | 0.22 | 0.60 | 0.36 |
| 4 | 0.43 | 0.19 | 0.45 | 0.20 | 0.40 | 0.16 | 0.63 | 0.40 | 0.69 | 0.47 | 0.77 | 0.59 |
| 5 | 0.52 | 0.28 | 0.33 | 0.11 | 0.58 | 0.34 | 0.40 | 0.16 | 0.60 | 0.35 | 0.48 | 0.23 |
| 6 | 0.57 | 0.33 | 0.38 | 0.15 | 0.39 | 0.15 | 0.37 | 0.14 | 0.66 | 0.43 | 0.56 | 0.32 |
| 7 | 0.56 | 0.32 | 0.59 | 0.35 | 0.47 | 0.22 | 0.68 | 0.47 | 0.60 | 0.36 | 0.66 | 0.43 |
| 8 | 0.55 | 0.30 | 0.51 | 0.26 | 0.52 | 0.27 | 0.37 | 0.13 | 0.39 | 0.16 | 0.66 | 0.43 |
| 9 | 0.58 | 0.33 | 0.62 | 0.39 | 0.55 | 0.30 | 0.53 | 0.28 | 0.48 | 0.23 | ||
| 10 | 0.43 | 0.19 | 0.38 | 0.14 | 0.41 | 0.17 | 0.47 | 0.22 | 0.60 | 0.36 | ||
| 11 | 0.26 | 0.07 | 0.35 | 0.13 | 0.43 | 0.19 | 0.69 | 0.48 | ||||
| 12 | 0.54 | 0.29 | 0.60 | 0.36 | 0.61 | 0.37 | ||||||
Scores
We generate a score on the common factor for all respondents. We do this for all six dimensions, following two approaches.
The more sophisticated approach is to estimate factor scores. In the context of BSAQ, an estimated factor score is a linear composite of the optimally weighted individual responses on the items that comprise a particular dimension. In common factor analysis, there is no unique solution to estimate factor scores. 126 We apply the following method, which is implemented in SAS version 9.2 (SAS Institute Inc., Cary, NC, USA), to calculate factor scores.
-
All of the individual’s responses on the items are standardised to form a new k × 1 vector, where k is the number of items.
-
The PROC FACTOR procedure in SAS coupled with the SCORE option produces a k ×1 vector of factor score coefficients following a multiple regression approach. These coefficients are the weights to be used in step 3.
-
The standardised individual’s scores on the items are weighted by the generated factor score coefficients and summed across all items to produce the individual’s factor score. This is a standardised score with a mean of zero and a variance equal to the squared multiple correlation between the estimated factor scores and the true factor values (which are not known).
The second approach is to create factor-based scales. This less sophisticated method does not use weights but has the advantage of allowing use of only the items that load satisfactorily on a factor. Because all items in BSAQ dimensions load reasonably well, this is not relevant for our analysis.
Construction of factor-based scales is done as follows. A respondent’s score on the factor-based scale is the sum of the individual’s (unstandardised) responses to the items. Because all the items are measured on a 4-point Likert scale, the possible range for the 12 items in the contextual dimension is 12–48, for the 10 items in the analytical dimension it is 10–40, and so forth. Table 11 shows that factor-based scales do not differ by foundation or teaching status. We will not use further factor-based scales, as they do not take into account item loadings.
| Variable | Foundation | Teaching | ||||
|---|---|---|---|---|---|---|
| No (n = 42) | Yes (n = 51) | Difference | No (n = 66) | Yes (n = 27) | Difference | |
| Contextual | 36.13 | 36.91 | –0.77 | 36.32 | 37.13 | –0.81 |
| Educational | 36.49 | 37.18 | –0.69 | 36.87 | 36.87 | 0.00 |
| Interpersonal | 32.05 | 32.53 | –0.47 | 32.00 | 33.08 | –1.08 |
| Analytical | 29.81 | 30.14 | –0.33 | 29.99 | 29.99 | 0.00 |
| Political | 24.65 | 25.02 | –0.36 | 24.84 | 24.88 | –0.04 |
| Strategic | 36.50 | 37.11 | –0.62 | 36.78 | 36.96 | –0.18 |
| BSAQ | 195.63 | 198.87 | –3.24 | 196.80 | 198.91 | –2.11 |
Total Board Self-Assessment Questionnaire score
To develop a composite BSAQ score for all 65 items we performed factor analysis on the factor scores representing the six BSAQ dimensions. One single factor emerges and Table 12 shows the factor loadings. All dimensions load very strongly on the common underlying factor. About 67% of the common variance that the contextual dimension shares with the other five BSAQ dimensions is explained by the common factor.
| Variable | Loading | Loading2 |
|---|---|---|
| Contextual | 0.82 | 0.67 |
| Educational | 0.72 | 0.52 |
| Interpersonal | 0.79 | 0.62 |
| Analytical | 0.82 | 0.68 |
| Political | 0.76 | 0.58 |
| Strategic | 0.81 | 0.66 |
Ordinal factor analysis
Factor analysis applied to ordinal data is criticised for using Pearson’s correlations and therefore relying on the assumption that the variables are continuous and follow a multivariate normal distribution. A more suitable approach might be to perform factor analysis on the matrix of polychoric correlations, which can be thought of as correlations between unobserved continuous variables that represent crudely the ordinal variables. We present the results of ordinal factor analysis in Tables 13 and 14. One common factor emerges and the differences in loadings compared with conventional factor analysis are small.
| Item | BSAQ dimension | |||||
|---|---|---|---|---|---|---|
| Contextual | Educational | Interpersonal | Analytical | Political | Strategic | |
| 1 | 4.38 | 3.91 | 3.09 | 3.66 | 3.31 | 5.88 |
| 2 | 0.71 | 0.75 | 0.54 | 0.35 | 0.28 | 0.64 |
| 3 | 0.34 | 0.33 | 0.33 | 0.31 | 0.11 | 0.33 |
| 4 | 0.12 | 0.26 | 0.16 | 0.15 | 0.07 | 0.13 |
| 5 | 0.10 | 0.04 | 0.04 | 0.06 | –0.02 | 0.08 |
| 6 | 0.02 | –0.01 | –0.07 | –0.05 | –0.04 | 0.02 |
| 7 | –0.02 | –0.04 | –0.12 | –0.10 | –0.18 | –0.09 |
| 8 | –0.15 | –0.14 | –0.16 | –0.17 | –0.22 | –0.10 |
| 9 | –0.19 | –0.21 | –0.21 | –0.24 | –0.13 | |
| 10 | –0.21 | –0.24 | –0.24 | –0.31 | –0.27 | |
| 11 | –0.31 | –0.33 | –0.28 | –0.28 | ||
| 12 | –0.42 | –0.40 | –0.33 | |||
| Item | BSAQ dimension (loading/loading2) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Contextual | Educational | Interpersonal | Analytical | Political | Strategic | |||||||
| 1 | 0.55 | 0.31 | 0.59 | 0.35 | 0.56 | 0.32 | 0.66 | 0.44 | 0.57 | 0.32 | 0.77 | 0.59 |
| 2 | 0.74 | 0.55 | 0.65 | 0.42 | 0.26 | 0.07 | 0.60 | 0.36 | 0.60 | 0.36 | 0.66 | 0.44 |
| 3 | 0.65 | 0.42 | 0.60 | 0.36 | 0.62 | 0.39 | 0.67 | 0.44 | 0.52 | 0.27 | 0.68 | 0.46 |
| 4 | 0.55 | 0.31 | 0.51 | 0.26 | 0.45 | 0.20 | 0.72 | 0.53 | 0.80 | 0.63 | 0.83 | 0.69 |
| 5 | 0.61 | 0.38 | 0.38 | 0.14 | 0.68 | 0.47 | 0.50 | 0.25 | 0.68 | 0.46 | 0.54 | 0.30 |
| 6 | 0.66 | 0.43 | 0.42 | 0.18 | 0.43 | 0.19 | 0.42 | 0.17 | 0.74 | 0.55 | 0.65 | 0.42 |
| 7 | 0.65 | 0.42 | 0.72 | 0.51 | 0.53 | 0.28 | 0.78 | 0.60 | 0.67 | 0.45 | 0.72 | 0.52 |
| 8 | 0.61 | 0.37 | 0.56 | 0.32 | 0.65 | 0.42 | 0.46 | 0.21 | 0.50 | 0.25 | 0.77 | 0.59 |
| 9 | 0.67 | 0.45 | 0.69 | 0.48 | 0.60 | 0.36 | 0.62 | 0.38 | 0.56 | 0.32 | ||
| 10 | 0.51 | 0.26 | 0.48 | 0.23 | 0.45 | 0.20 | 0.53 | 0.28 | 0.69 | 0.48 | ||
| 11 | 0.28 | 0.08 | 0.43 | 0.19 | 0.46 | 0.21 | 0.80 | 0.63 | ||||
| 12 | 0.63 | 0.40 | 0.68 | 0.46 | 0.67 | 0.45 | ||||||
Conclusion regarding the data structure of the Board Self-Assessment Questionnaire score
Overall, then, this analysis supports and replicates the original six-factor structure of the BSAQ and provides reasonable grounds for using the dimensions described with English NHS boards.
Using the Board Self-Assessment Questionnaire to describe and analyse English NHS trust boards
The BSAQ data gathered as part of this study generally showed high or very high levels of agreement with desirable statements of practice in each of the six previously identified dimensions. Aggregate levels of agreement within each dimension ranged from 73% (on the interpersonal dimension) to 85% (on the political dimension). Differences between aggregate levels of agreement for FT/non-FT were generally small: across the six dimensions these difference between trust types ranged from 0% to 4%. For THs/non-THs the differences ranged from 1% to 5%. Nonetheless, there was some consistency in these data, with non-FT boards generally scoring slightly higher than FT boards across all six dimensions except ‘strategic’, and teaching boards generally scoring slightly higher than non-teaching boards across all six dimensions except ‘educational’. However, none of these differences was statistically significant.
Relating Board Self-Assessment Questionnaire scores to patient safety parameters from routine data sets
After constructing the factor scores representing the six BSAQ dimensions and the total BSAQ score, we explored whether or not these are correlated with patient safety measures. We found no strong correlations between any of the six BSAQ dimensions or the total BSAQ score and the various patient safety measures.
Regressions
We estimate multivariate and hierarchical models regressing patient safety measures (see Appendix 7 for a full description of the patient safety measures) and measures of hospital ability to handle errors, near-misses and incidents (taken from the NSS for 2012) based on the total BSAQ score. We control for a number of hospital-level characteristics.
The dependent variables are listed in Table 15 (patient safety measures) and Table 16 (measures of provider ability to handle errors).
| Patient safety metrics | Mean | Minimum | Maximum | |
|---|---|---|---|---|
| Relative risks | ||||
| HSMR | Hospital Standardised Mortality Risk (spells with a primary diagnosis of any of 56 common condition specialty groups) | 99.1 | 67.1 | 120.3 |
| HSMR2 | Hospital Standardised Mortality Risk (spells with any primary diagnosis) | 98.8 | 66.9 | 116.4 |
| VLRM | Very Low Risk Mortality (spells with a primary diagnosis associated with a low mortality diagnosis group – consistently below 0.5%) | 95.3 | 37.3 | 181.3 |
| ASM | After Surgery Mortality (deaths following surgery with complications) | 98.7 | 37.7 | 192.9 |
| HSMR_E | Hospital Standardised Mortality Risk for weekend emergency admissions (in-hospital deaths following weekend emergency admissions) | 97.3 | 68.9 | 117.9 |
| HSMR_EW | Hospital Standardised Mortality Risk for weekday emergency admissions (in-hospital deaths following weekday emergency admissions) | 104.5 | 61.5 | 131.0 |
| READM | Twenty-eight-day readmissions | 99.7 | 6.6 | 83.6 |
| Rates | ||||
| MRSA | [MRSA/(total number of spells)]*10,000 | 0.7 | 0.0 | 2.8 |
| MSSA | [MSSA/(total number of spells)]*10,000 | 1.8 | 0.5 | 6.2 |
| Cdiff | [Cdiff/(total number of spells)]*10,000 | 4.2 | 1.4 | 13.6 |
| Ecoli | [Ecoli/(total number of spells)]*10,000 | 24.0 | 14.8 | 64.4 |
| PSI | Rate of organisational patient safety incidents | 6.9 | 2.0 | 17.6 |
| Count | ||||
| Never events | Total number of never events | 1.7 | 0.0 | 9.0 |
| Variable | Mean | Standard deviation | Minimum | Maximum |
|---|---|---|---|---|
| Treat fair | 47.88 | 5.68 | 33.77 | 59.70 |
| Report | 86.16 | 3.16 | 75.83 | 91.46 |
| Blame | 13.18 | 3.02 | 7.47 | 20.39 |
| Action | 61.96 | 5.82 | 46.08 | 74.08 |
| Safe | 71.79 | 3.94 | 62.22 | 78.97 |
| Confident | 55.23 | 5.67 | 40.91 | 67.76 |
| Confidential | 63.22 | 4.97 | 51.33 | 70.79 |
| Inform | 42.51 | 6.65 | 28.54 | 63.97 |
| Feedback | 42.10 | 6.17 | 29.81 | 61.25 |
We also explored the option of examining patient safety indicators published on the NHS Choices website (www.nhs.uk/NHSEngland/thenhs/patient-safety/Pages/patient-safety-indicators.aspx). These cover measures of safe staffing, infection control and cleanliness, open and honest reporting, patients assessed for risk of blood clots, NHS Safety Thermometer data on pressure ulcers and falls with harm, NHS England patient safety reporting, CQC national safety standards and the percentage of staff who would recommend the hospital, also taken from the NSS.
We did not, however, incorporate these data into the analyses with the BSAQ, as the BSAQ data are reported at trust level and the patient safety data are reported at provider site level. There is a large number of missing data and large variation within trusts across sites in the ratings, making it difficult to aggregate up to trust level.
Measures of hospital ability to handle errors, near-misses and incidents are defined as proportions of NHS staff respondents who responded agree or strongly agree to the following nine statements and questions:
-
My organisation treats staff who are involved in an error, near-miss or incident fairly.
-
My organisation encourages us to report errors, near-misses or incidents.
-
My organisation blames or punishes people who are involved in errors, near-misses or incidents.
-
When errors, near-misses or incidents are reported, my organisation takes action to ensure that they do not happen again.
-
Would you feel safe raising your concern?
-
Would you be confident that your organisation would address your concern?
-
My organisation treats reports of errors, near-misses or incidents confidentially.
-
We are informed about errors, near-misses and incidents that happen in this organisation.
-
We are given feedback about changes made in response to reported errors, near-misses and incidents.
The set of explanatory variables in the regressions includes the total BSAQ score, FT status and three dummy variables indicating hospital size (small, medium and large). The reference category is acute TH.
Regression results are presented in Tables 17a–e for the patient safety measures and Tables 18a–c for the provider measures of effective management of errors.
| HSMR | HSMR2 | VLRM | |
|---|---|---|---|
| Intercept | 91.41*** (2.96) | 91.65*** (3.01) | 100.05*** (9.27) |
| BSAQ score | –1.43 (1.42) | –1.50 (1.44) | –0.20 (4.44) |
| Foundation | 3.63** (2.12) | 4.45** (2.16) | 0.13 (6.65) |
| Respondents/board | –6.96 (5.30) | –7.67 (5.39) | –12.75 (16.60) |
| Small | 9.72*** (3.23) | 8.78*** (3.29) | –5.55 (10.13) |
| Medium | 6.88** (2.93) | 5.73* (2.98) | –1.78 (9.18) |
| Large | 12.42*** (3.11) | 11.65*** (3.16) | 2.00 (9.75) |
| R 2 | 0.20 | 0.19 | 0.014 |
| ASM | HSMR_E | HSMR_EW | |
|---|---|---|---|
| Intercept | 101.64*** (8.14) | 89.92*** (2.88) | 95.97*** (3.64) |
| BSAQ score | –3.84 (3.90) | –1.48 (1.38) | –1.23 (1.74) |
| Foundation | –0.30 (5.84) | 3.46* (2.07) | 4.34 (2.61) |
| Respondents/board | 6.14 (14.59) | –6.18 (5.16) | –9.27 (6.52) |
| Small | –5.96 (8.90) | 9.08*** (3.15) | 11.54*** (3.98) |
| Medium | –9.31 (8.07) | 6.54** (2.85) | 7.85** (3.61) |
| Large | –1.32 (8.57) | 11.88*** (3.03) | 14.13*** (3.83) |
| R 2 | 0.03 | 0.19 | 0.18 |
| MRSA_rate | MSSA_rate | Cdiff_rate | |
|---|---|---|---|
| Intercept | 0.82*** (0.15) | 2.16*** (0.25) | 4.87*** (0.52) |
| BSAQ score | 0.03 (0.07) | 0.07 (0.12) | 0.43* (0.25) |
| Foundation | –0.08 (0.10) | –0.02 (0.18) | 0.01 (0.37) |
| Respondents/board | 0.02 (0.26) | 0.59 (0.46) | –0.09 (0.93) |
| Small | 0.27 (0.16) | –0.52* (0.28) | –0.19 (0.57) |
| Medium | –0.16 (0.14) | –0.68*** (0.25) | –1.32** (0.52) |
| Large | –0.21 (0.15) | –0.61** (0.27) | –0.33 (0.55) |
| R 2 | 0.14 | 0.11 | 0.14 |
| ecoli_rate | Never events | Org_PSI_rate | |
|---|---|---|---|
| Intercept | 21.03*** (2.00) | 2.82*** (0.50) | 5.91*** (0.68) |
| BSAQ score | 0.08 (0.96) | –0.02 (0.24) | –0.01 (0.33) |
| Foundation | –0.54 (1.44) | –0.01 (0.36) | –0.02 (0.49) |
| Respondents/board | 6.41* (3.59) | –2.06** (0.89) | 3.44*** (1.22) |
| Small | 3.38 (2.19) | –1.20** (0.55) | 0.91 (0.74) |
| Medium | 1.66 (1.98) | –0.38 (0.49) | 0.08 (0.67) |
| Large | 0.93 (2.11) | –0.67 (0.52) | –0.60 (0.72) |
| R 2 | 0.07 | 0.06 | 0.12 |
| Day case/inpatient | READM | |
|---|---|---|
| Intercept | 5.10*** (0.53) | 97.15*** (1.95) |
| BSAQ score | –0.02 (0.25) | –0.41 (0.93) |
| Foundation | –0.33 (0.38) | –1.87 (1.40) |
| Respondents/board | –0.97 (0.95) | 4.93 (3.49) |
| Small | –0.30 (0.58) | 2.78 (2.13) |
| Medium | 0.11 (0.52) | 1.86 (1.93) |
| Large | –0.38 (0.56) | 3.87* (2.05) |
| R 2 | 5.10*** (0.53) | 0.11 |
| Treat fair | Report | Blame | |
|---|---|---|---|
| Intercept | 49.03*** (1.67) | 84.97*** (0.93) | 13.72*** (0.85) |
| BSAQ score | 1.19 (0.80) | 0.64 (0.45) | –0.55 (0.41) |
| Foundation | 0.68 (1.20) | 1.10 (0.67) | –0.26 (0.61) |
| Respondents/board | 1.17 (2.98) | 2.22 (1.67) | 0.24 (1.53) |
| Small | –2.37 (1.82) | 0.33 (1.02) | –1.08 (0.93) |
| Medium | –0.96 (1.65) | 0.22 (0.92) | –0.09 (0.84) |
| Large | –4.22** (1.75) | –1.55 (0.98) | –0.13 (0.90) |
| R 2 | 0.11 | 0.14 | 0.005 |
| Action | Safe | Confident | |
|---|---|---|---|
| Intercept | 60.66*** (1.66) | 71.64*** (1.14) | 51.74*** (1.59) |
| BSAQ score | 0.95 (0.79) | 1.26** (0.55) | 1.41* (0.76) |
| Foundation | 2.53** (1.19) | 0.50 (0.82) | 3.14*** (1.14) |
| Respondents/board | 3.76 (2.97) | –0.23 (2.04) | 5.14* (2.84) |
| Small | –1.72 (1.81) | 0.29 (1.25) | 0.27 (1.73) |
| Medium | –0.99 (1.64) | 0.14 (1.13) | 0.44 (1.57) |
| Large | –3.04* (1.74) | –0.60 (1.20) | –1.62 (1.67) |
| R 2 | 0.13 | 0.08 | 0.18 |
| Confidential | Inform | Feedback | |
|---|---|---|---|
| Intercept | 63.48*** (1.42) | 43.59*** (1.92) | 42.96*** (1.80) |
| BSAQ score | 0.74 (0.68) | 0.34 (0.92) | 0.97 (0.86) |
| Foundation | 1.17** (1.02) | 3.10** (1.38) | 2.29* (1.29) |
| Respondents/board | 1.23 (2.54) | 1.25 (3.44) | 0.91 (3.23) |
| Small | –1.93 (1.55) | –3.98* (2.10) | –3.25 (1.97) |
| Medium | –0.65 (1.41) | –3.64* (1.90) | –1.77 (1.79) |
| Large | –2.92* (1.49) | –4.57** (2.02) | –4.03** (1.90) |
| R 2 | 0.10 | 0.13 | 0.12 |
Results are not significant for the total BSAQ score in any of the patient safety measure regressions. For a few of the patient safety measures size is significant, suggesting differences in patient safety outcomes between small, medium and large trusts and acute teaching trusts (the reference category).
Two of the variables show a positive and significant association between total BSAQ score (better board governance) and the proportion of staff feeling safe to raise concerns about errors, near-misses and incidents and also feeling confident that their organisation would address their concern. We ran further regressions on the factor scores representing the six BSAQ dimensions for these two variables to explore which aspects are correlated with staff’s ability to raise concerns over patient safety.
Tables 19a and 19b show results for the six BSAQ dimensions against staff feeling ‘safe’ to raise concerns about errors, near-misses, and incidents, whereas Tables 20a and 20b show the regressions for the six BSAQ dimensions against staff feeling ‘confident’ that their organisation would address their concern.
| Contextual | Educational | Interpersonal | |
|---|---|---|---|
| Intercept | 71.41*** (1.13) | 71.65*** (1.17) | 71.47*** (1.16) |
| BSAQ score | 1.52*** (0.57) | 0.68 (0.60) | 0.94 (0.58) |
| Foundation | 0.48 (0.81) | 0.63 (0.84) | 0.61 (0.83) |
| Respondents/board | 0.37 (2.02) | 0.02 (2.09) | 0.04 (2.07) |
| Small | 0.22 (1.23) | 0.26 (1.28) | 0.32 (1.27) |
| Medium | 0.13 (1.12) | –0.24 (1.14) | 0.12 (1.16) |
| Large | –0.54 (1.19) | –0.85 (1.22) | –0.61 (1.22) |
| R 2 | 0.10 | 0.04 | 0.05 |
| Analytical | Political | Strategic | |
|---|---|---|---|
| Intercept | 71.67*** (1.15) | 71.78*** (1.15) | 71.72*** (1.16) |
| BSAQ score | 1.32** (0.63) | 1.42** (0.66) | 0.98* (0.55) |
| Foundation | 0.57 (0.82) | 0.48 (0.82) | 0.63 (0.82) |
| Respondents/board | –0.23 (2.06) | –0.50 (2.07) | –0.39 (2.09) |
| Small | 0.19 (1.25) | 0.24 (1.25) | 0.25 (1.26) |
| Medium | 0.07 (1.13) | 0.25 (1.15) | –0.09 (1.14) |
| Large | –0.64 (1.21) | –0.78 (1.20) | –0.63 (1.22) |
| R 2 | 0.07 | 0.07 | 0.06 |
| Contextual | Educational | Interpersonal | |
|---|---|---|---|
| Intercept | 51.45*** (1.56) | 51.59*** (1.62) | 51.53*** (1.60) |
| BSAQ score | 2.03** (0.79) | –0.22 (0.83) | 1.23 (0.80) |
| Foundation | 3.07*** (1.12) | 3.45*** (1.16) | 3.23*** (1.14) |
| Respondents/board | 5.85** (2.79) | 5.59* (2.89) | 5.41* (2.85) |
| Small | 0.19 (1.70) | 0.08 (1.77) | 0.33 (1.75) |
| Medium | 0.51 (1.54) | 0.03 (1.59) | 0.49 (1.59) |
| Large | –1.49 (1.64) | –1.86* (1.70) | –1.59* (1.68) |
| R 2 | 0.21 | 0.15 | 0.18 |
| Analytical | Political | Strategic | |
|---|---|---|---|
| Intercept | 51.75*** (1.60) | 51.83*** (1.61) | 51.90*** (1.59) |
| BSAQ score | 1.36 (0.87) | 1.18 (0.92) | 1.53** (0.76) |
| Foundation | 3.23*** (1.14) | 3.20*** (1.15) | 3.24*** (1.13) |
| Respondents/board | 5.17* (2.86) | 5.02* (2.89) | 4.71 (2.85) |
| Small | 0.15 (1.74) | 0.18 (1.75) | 0.26 (1.73) |
| Medium | 0.34 (1.58) | 0.43 (1.60) | 0.25 (1.55) |
| Large | –1.67* (1.68) | –1.83* (1.68) | –1.56* (1.67) |
| R 2 | 0.18 | 0.17 | 0.19 |
Results are positive and significant for staff feeling ‘safe’ in the contextual, analytical, political and strategic domains, though the effect is strongest in the contextual dimension, which focuses on the board taking cognisance of the organisation’s values and norms; for example, it may support a more open and transparent culture around whistleblowing, thereby enabling staff to feel safe to raise concerns.
Results are positive and significant for staff feeling ‘confident’ in the contextual and strategic dimensions, suggesting that a focus on the organisational values and institutional direction gives staff a sense of security and assurance that patient safety concerns will be dealt with.
Concluding remarks
As in previous research,29,42,44,45 this analysis has shown the validity of the six BSAQ dimensions. The study improves on previous analyses by doing a factor analysis applied to ordinal data, calculating both factor scores and factor-based scales and developing a composite BSAQ score from the factor scores. This allows us to obtain an appropriate measure of the underlying latent variable board governance. We test for simple correlations between this composite BSAQ score and various measures of patient safety. Like previous research,29 we found no association between board governance and various measures of patient safety. We ran multivariate regression models, taking account of provider type and size, but again found no association between board governance and any measures of patient safety.
We also ran multivariate regressions and found a positive association between board governance on two measures of staff feeling confident about raising concerns about errors, near-misses and incidents and also feeling confident that their organisation would address their concern. This suggests that there is some association between board governance and staff’s ability to address issues around patient safety, but that board governance does not directly affect patient safety outcomes.
Chapter 9 Conclusions and research implications
Introduction
Hospital trust boards in the English NHS have statutory responsibility for upholding the quality and safety of care delivered by their organisation. However, recent high-profile reports on serious failings in the quality of hospital care in the NHS, most notably the standards of care at Mid Staffordshire NHS Trust, raise serious concerns over the ability of trust boards to discharge these duties effectively. Despite a plethora of guidance available to NHS boards on effective governance, both in general terms (e.g. structure and role) and with specific reference to safer care,76,127 significant gaps remain in our understanding of what board governance looks like and the organisational processes through which safer care is accomplished and sustained. Against this background we wanted to strengthen the theoretical and empirical evidence base that underpins board governance of safe care in the English NHS. In this final chapter we draw together the main findings of the study and look forward at the emerging research agenda in this area. Appendix 9 sets out the current and planned publications arising from this study.
A reminder of the ambitions of this study
Prior to this study, most of the research on hospital board governance originated from the USA, was theoretically underdeveloped, focused on the more generic concept of service quality rather than patient safety and was almost entirely of a quantitative nature. In the design of this study we attempted to address the limitations of previous research and, in so doing, generate new knowledge and evidence to support improved board oversight of safer care. Through reviewing extant literature and theory and through fresh empirical study, involving national surveys across hospital trusts in the English NHS and in-depth qualitative case studies, we have sought to:
-
identify the types of governance activities undertaken by hospital trust boards in the English NHS with regard to ensuring safe care in its organisation
-
explore the role of boards versus boards of governors in FTs with regard to the oversight of patient safety in its organisation
-
assess the association between particular hospital trust board oversight activities and patient safety processes and clinical outcomes
-
identify the facilitators and barriers to developing effective hospital trust board governance of safe care
-
assess the impact of external commissioning arrangements and incentives on hospital trust board oversight of patient safety.
In the rest of this chapter we summarise the main findings of the research relating to each of these research objectives and then, subsequently, we identify the research issues arising from the study. The chapter rounds off with a discussion of some of the study limitations and a note of projected project outputs.
Drawing together the empirical work and conclusions from the findings
This section takes each of the research objectives in turn and integrates findings from across all parts of the study.
Research objective 1: to identify the types of governance activities undertaken by hospital trust boards in the English NHS with regard to ensuring safe care in its organisation
NHS hospital boards as corporate entities have a fundamental strategic role in developing the strategy, systems and cultures for its organisations. These approaches can be ‘hard’, for example the setting and monitoring of polices, standards and procedures, or ‘soft’, for example nurturing appropriate values and beliefs. We uncovered a range of instrumental and symbolic/performative behaviours and activities undertaken by boards in relation to fulfilling its oversight duties with regard to safeguarding care.
In instrumental terms, a ‘successful’ board is one able to take decisions on corporate strategy efficiently and effectively. 19 In the national survey, a very high proportion of trust boards reported the kinds of desirable characteristics and board-related processes that research says may be associated with higher performance, with all having quality subcommittees and proactive procedures in place to address patient safety concerns and almost all having explicit objectives related to improving patient safety. However, given the current focus on patient safety in the NHS, it was surprising that only 87% of trusts reported that board members had actually received any received training in patient safety issues. This, alongside the in-depth case study work, indicates that some members of hospital boards may be struggling to fulfil their roles and responsibilities concerning safety. In this regard it is notable that, in the USA, a number of states have introduced initiatives and legislation around board training, particularly in the form of accreditation, and mandatory induction and orientation programmes for board members. 76 This may also be an area that requires greater attention in the UK.
In the case studies we found that, although each organisation had developed its own unique style of board governance and approaches to safeguarding care, all sought to provide strategic assurance by:
-
establishing organisational structures and processes for reporting safety-related information throughout the organisation and to the board
-
setting the tone for the whole organisation by making patient safety a strategic priority
-
developing and nurturing an ‘open and fair culture’ within the trust which encouraged the reporting of patient safety-related incidents
-
using high-level information to ensure that the trust is complying with safe practices and standards and meeting externally led targets.
However, the degree to which these aspirations were fully met was moot, with persistent reports (away from the board) about the risks and challenges of communicating bad news or of challenging senior management perspectives and actions.
The four case studies exhibited features associated with the range of instrumental theories and models of board governance outlined in Chapter 2. However, it was also clear that the boards adopted different models at different times and in relation to particular aspects of board governance. Governance activities, then, were seen to be contingent on a variety of internal factors, such as board dynamics, and on external factors, such as the regulatory environment and commissioning relationships. The case studies (see Chapters 4–7) show evidence of board governance approaches related to:
-
agency theory, in the way that boards sought to measure its patient safety performance to ensure compliance and to hold staff accountable for their actions
-
stewardship theory, in the way that boards attempted to implement a framework of shared values built on trust–based relationships
-
stakeholder theory, in the way that boards have attempted to manage complex trade-offs between stakeholders, including staff, patients and the public
-
resource dependency theory, in the way that boards attempted to manage internal and external relationships to leverage influence and resources.
In our four case studies, three of the sites operationalised the governance of patient safety largely in terms of assurance and performance data were used retrospectively to alert the board of poor performance. However, such an approach may encourage under-reporting of patient safety matters and does not provide guidance on how best to address past performance deficiencies. In only one case of our four study sites did the board seek to mitigate the potential for such dysfunctional organisational consequences, through a strategic focus on quality improvement (in this case, even to the extent of structuring the board agenda around strategic quality improvement).
Our analysis of the performative and symbolic aspects of board activities highlights the role and differences in local and ritualistic processes of organising in relation to the governance of patient safety. Although each case study identified different performativities at play in different situations, it was clear that the setting(s) in which board decisions and deliberation take place, and the local enactment of organisational frames (operationalised through different approaches to the scripting, setting, staging and performance of board activity), have an important bearing on how organisations approach the oversight of patient safety. These findings highlight the challenges faced by board members in terms of the artefacts that they have available and the key role of scripting and staging, especially when decisions in these areas often pass unchallenged, unremarked or even unnoticed. A better understanding of these issues may feed into revised training and induction processes for board members.
The amount of time boards devote to discussing patient safety-related issues has been identified as a key issue related to performance in this area. 57 In our study we found that most boards do allocate a considerable amount of time to discussing patient safety- and quality-related issues. The NSS obtained responses which indicate that only one-fifth of trust boards reported that ≤ 30% of their time was spent discussing safety and quality issues. In the case studies we found similar evidence, with only one study site allocating < 30% of their board time to debating quality/safety matters. However, we also identified (through the case study sites) that boards used this time rather differently. For example, for some a wide range of performance data were made available to directors and attention tended to be concentrated closely on those showing shortfalls. Such approaches tended to be quality assurance oriented, with less discussion of proactive quality improvement. In other sites, the emphasis was more on the use of quantitative data to support quality improvement rather than secure conformance against externally set standards.
A key issue in the study was the type and amount of information that board members used to help exercise scrutiny over safety issues. In the national survey we found that hospital boards were using a wide range of hard performance metrics and soft intelligence to monitor their organisation with regard to patient safety, including a range of clinical outcomes measures, infection rates and process measures, such as medication errors and readmission rates.
It is noteworthy, however, that fewer trusts reported routine reporting of patient safety surveys and the implementation of patient safety alerts, and a much smaller proportion of trusts routinely report morbidity rates at every board meeting. Softer intelligence, used organisationally and reported at all board meetings, was also more variably reported, with discussions with clinicians and executive walkabouts being most often reported, alongside use of patient stories. However, in only about two-thirds of trusts did board members shadow clinicians and report back to the board. These findings indicate some scope for broadening and enriching board activities with regard to understanding and assessing patient safety.
In the case studies we also identified a range of information and performance data reported to the board, and surfaced some of the key issues and challenges in their use by board members. For example, where RAG indicator reporting systems were used, concerns were expressed about the validity and reliability of the judgements so presented. In contrast, board members who focused on quality assurance data expressed greater confidence in the validity and reliability of these data. One way out of the apparent tension between assurance and improvement seemed to lie in attempts to combine the requirements of external assurance with ongoing quality improvement through the development of national- and local-level data sets and qualitative information from reports by clinical service areas. Despite these efforts, we heard reports of the need for further training of NEDs to understand and interpret standard quantitative data sets and for further disaggregation of data at ward level.
Understanding of these tensions is augmented by our parallel view of board activities as performative and symbolic. This analysis highlighted the important role of setting, scripting and staging in the use and interpretation of information and performance data by the board. For example, although the availability of summaries of quality indicators to board members was a key issue, so equally were the local processes of organising in each board that made it possible for non-executive board members to use such information to hold executives to account. The setting and staging could be seen as working in support of such questioning or (more often) working against any breaking out from set scripting patterns. Thus, the dramaturgical arrangements of boards require greater attention if they are truly to become fora for effective debate, challenge and the instigation of action.
Key actions
-
All board members should undertake training and education in relation to approaches to sustaining and improving health-care quality and patient safety. This should be undertaken as part of induction and orientation programmes for new members, with knowledge and skills in this area regularly updated through continuing professional development programmes.
-
There appears to be a particular need for training and education of board members in relation to understanding and interpreting the quantitative data sets and performance indicators used to report patient safety issues at board level.
-
Boards should regularly review the (hard and soft) information that they use to assess and assure patient safety in their organisation. This includes learning from organisations that have used a range of approaches, such as board members shadowing clinicians and use of patient stories to inform board members about patient safety in their organisation.
-
Efforts should be made to encourage and support senior clinicians to engage and contribute towards board oversight activities with regard to patient safety.
Research objective 2: to explore the role of boards versus board of governors in foundation trusts with regards to the oversight of patient safety in its organisation
A strong theme from across study sites was that, although the board of governors are generally perceived as well-meaning, they were also considered to be largely ineffective in helping to promote and deliver safer care for their organisations. Boards of governors seemed to serve a useful educative and community linkage role, but with limited challenge or holding of executives to account. Meetings frequently resembled seminars for information sharing, rather than a formal board meeting where key organisational strategies were debated and discussed. Thus, while governors typically reported good relations with the executive board, there was often a lack of awareness and understanding of respective roles. Although some sites did report engagement of governors in quality assurance work in relation to, for example, NED appraisal and committee work, there were also frustrations at what was seen as only limited active engagement from NEDs. In summary, therefore, governor meetings appeared to play little active and positive role in the governance and safeguarding of care across the organisations we studied. This is, of course, not to say that boards of governors may not fulfil other important functions beyond the safety and quality remit of this study.
Key action
-
More information, encouragement, support and advice should be provided to boards of governors of FTs to enable them to play a more active role in patient safety activities and to hold board members to account for its oversight of patient safety within the trust.
Research objective 3: to assess the association between particular hospital trust board oversight activities and patient safety processes and clinical outcomes
The national surveys were designed to explore any relationship(s) between board structures, board activities, board competencies (as measured by the BSAQ) and a range of patient safety process and outcome variables. The headline finding is that we did not find any statistically significant relationship between these board attributes and (self-reported) processes and any patient safety outcome measures. However, we did find a significant relationship between two dimensions of the BSAQ and two specific and related NSS organisational ‘process’ measures: staff feeling safe to raise concerns about errors, near-misses and incidents and staff feeling confident that their organisation would address their concerns if raised.
In particular, the correlational results are positive and significant for staff ‘feeling safe’ in the contextual, analytical, political and strategic domains of the BSAQ, although the effect is strongest in the contextual dimension. This context dimension explores how the board takes cognisance of the organisation’s values and norms, and positive orientations here may support a more open and transparent culture around whistleblowing, thus enabling staff to feel safe to raise quality concerns.
Results were also positive and significant for staff ‘feeling confident’ about the contextual and strategic BSAQ dimensions, suggesting that a focus on the organisational values and institutional direction give staff a sense of security and assurance that patient safety concerns will be dealt with.
These findings then suggest some association between board governance and staff ability to address issues around patient safety, but also suggest that board governance may not directly affect patient safety outcomes. To be surer of this last point, however, we would need more complex longitudinal data than were available for this cross-sectional study.
This null finding of the effect of boards on outcomes is at odds with previous empirical work in the USA, which did find an association between board activity and quality outcomes. 17 This difference may be explained in part by a number of factors, not least the focus on different measures of outcome in the US studies and the different economic and political environment in which boards operate in the USA. It may also be the case that there is a lagged effect between current board practice/competencies and patient safety outcomes, which our study would not have picked up as it was cross-sectional rather than longitudinal in design.
The finding linking board orientations to staff attitudes from our large-scale quantitative work are further substantiated when we look at the qualitative findings, especially those that were gleaned from the following of ‘tracer conditions’ from board to ward (see Chapter 6). Here there were persistent worries that calling out quality or safety problems or challenging senior management were unlikely to be welcome actions. Thus, providing an environment safe for challenge remains difficult and may yet be one key area in which boards could have an impact.
The results linking board competencies and organisational policies, associated with the creation of more open cultures and the assurance that patient safety concerns will be dealt with appropriately, are important given the current focus on whistleblowing in the NHS and, in particular, the recently announced independent review into whistleblowing to be chaired by Sir Robert Francis QC, Freedom to Speak Up. Indeed, the terms of reference for the review state that ‘it will consider, in the light of recent policy measures in response to the Public Inquiry into Mid Staffordshire NHS Foundation Trust, what further action is necessary to protect those individual NHS workers who speak out and in doing so make a significant contribution to the open culture that is needed to ensure safe care for patients.’ Later in this chapter, and building on our findings, we outline possible future research into board governance and whistleblowing to explore these issues further.
Key action
-
Boards should review its structures and systems and develop appropriate ‘open cultures’ that encourage staff at all levels to report and act on problems and issues around patient safety. Those staff reporting concerns over poor standards of care through formal channels or whistleblowing to external agencies should be supported and protected from potential bullying and intimidation by managers and others in the organisation.
Research objective 4: to identify the facilitators and barriers to developing effective hospital trust board governance of safe care
Organisational strategies, structures and cultures can potentially serve to enable or attenuate attempts to improve board governance; however, there has previously been little research into this important area of patient safety. In the case studies we explored these dimensions and identified a range of possible organisational facilitators and enablers to effective board governance of safe care. For example, a key facilitator at one of our study sites appeared to have been the development and implementation of a clear corporate strategy and operational plan focused on enhancing the quality and safety of care in the organisation. This plan had been further codified into bespoke performance measures, which were then incorporated in an organisation-wide quality dashboard for board review. Thus, objectives were clearly identified against the plan, which ensured continuous focus, supported by board dynamics characterised as ‘supportive challenge’ (where the open discussion of problematic issues was not interpreted as disloyalty).
At other sites, the stability of board membership over time was considered to be an important facilitator of patient safety governance, and the detailed knowledge of, and connection with, clinical staff by the CEO was thought to be crucial. Strong and committed clinical leadership was also considered to be an important facilitating factor in supporting board governance, even when there were persistent concerns over the so-called bullying of junior professionals by senior clinicians (which were, unsurprisingly, seen as being important barriers to effective governance).
We identified a range of other organisational barriers to effective board governance of safe care across the case study sites. Problems and disputes over the validity and reliability of summary performance indicator data and apparent difficulties in communication between clinical units and the board, for example, led to a sense of confusion over the meaning and the correct interpretation of performance indicator data received and reviewed by the board. In addition, problems were seen to arise because of a perceived lack of engagement among senior medical staff in many parts of the organisation, resulting in impaired communication between corporate teams and ward level.
Research objective 5: to assess the impact of external commissioning arrangements and incentives on hospital trust board oversight of patient safety
Hospital trusts operate within a broader system of incentive and constraints, which necessarily help to shape and influence approaches to board oversight of safe care. In terms of the commissioning environment, there is currently a policy focus on the role of CCGs as a means of improving quality and patient safety through the design of contracting and payment systems, as well as through establishing collaborative relationships with providers. Across the case studies we found that contracting issues appeared to play only a relatively minor role in incentivising quality and safety improvement. Building strong and trustworthy relationships between commissioners and providers was often viewed as a better way of stimulating positive change than focusing on incentives and sanctions. Relationships with commissioners across all four of our study sites were seen as largely positive, notwithstanding a few local difficulties (e.g. around plans for expansion and competition with other providers).
External financial incentives also have the potential to influence board oversight strategies. The CQUIN payment framework makes a proportion of providers’ income conditional on locally agreed goals concerning quality (covering dimensions of safety, effectiveness and experience). During the period of the research the incentive was 0.5% of contract value. The aim of the CQUIN is to support a cultural shift by embedding quality improvement and innovation within commissioner-provider discussions. The CQUIN appear to have had a mixed impact across the case study sites and were generally perceived to be a low-powered incentive for quality and safety improvement, as well as possibly inducing a range of unintended and dysfunctional consequences. For example, the CQUIN was perceived by some to be too unwieldy in operation to act as effective incentives and were negatively perceived as ‘taking money off’ rather than incentivising improvement activity. Reactions were not uniform, however, with the CQUIN being perceived as having a (albeit limited) positive impact in some areas but being a distraction in others.
Although compliance frameworks were generally welcomed for their effect of focusing attention on aspects of patient safety, concerns were raised in relation to their negative unintended consequences, notably ‘tunnel vision’ (a reduced attention and focus on important areas of health-care quality and patient safety that were not covered under the CQUIN framework, e.g. environmental health). The CQUIN penalties also proved difficult to apply in practice, with formal sanctions becoming a subject of negotiation between provider and commissioner. Therefore, external financial incentives in the form of the CQUIN appeared to have had little positive impact on board governance and safeguarding care in the case study organisations, and may even have proved an unwelcome distraction.
Key action
-
External commissioning arrangements and financial incentives such as the CQUIN should be evaluated and reviewed regularly to ensure that they are levering and contributing to quality and safety improvement in NHS organisations and are not inadvertently introducing or perpetuating unintended and dysfunctional consequences for organisations, staff and patients.
Research agenda
This report provides evidence of the importance of board governance in the delivery of high-quality and safe care. Yet, because of the complexity of board governance and the influencing factors on patient safety in modern health systems, there is still much to unravel about these key facets of health-care organisation and delivery in the NHS. Therefore, we suggest that there remains a challenging governance- and management-focused research agenda around safer care. Specific methodological issues and substantive areas that warrant further and more sustained investigation might be considered in the following areas:
Research design
As with all research, a rigourous study design enhances the power and credibility of the findings and future research in this area would benefit from a number of features:
-
Any studies should be mixed-method and multidisciplinary in design, drawing on a range of quantitative and qualitative methods, including detailed ethnographic approaches.
-
As the phenomena under investigation are essentially dynamic (governance, performance and change), longitudinal study will offer important additional insights over cross-sectional designs. Although we achieved excellent response rates, the national surveys of board structure, activity and competency (the BSAQ), which were linked to patient safety-related process and outcomes, used a cross-sectional rather than a longitudinal research design. This means that we can only infer associations rather than estimate causality between the variables. Longitudinal research using repeated cross-sectional data would help to unravel any causal relationships.
-
It is plausible that existing board activity and competencies may take time to impact on patient safety outcomes; therefore, there may be a lagged effect. However, in our study the board-level variables were linked with relatively contemporaneous patient safety variables and so may have failed to pick up any lagged associations. Future research might therefore explore such lagged effects, using patient safety data in the form of a time series.
-
In our study we have shown how both instrumental and symbolic theoretical approaches can yield important insights into board behaviour and provide better opportunities for theoretical transference and generalisability to other contexts. Future research will need also need sound conceptual underpinnings rather than relying on empiricism alone.
Research on board governance, whistleblowing, employee silence and voice
Our finding that board governance/competencies appear to be linked to staff feeling safe to raise concerns about patient safety issues, and also their confidence that their organisation would address their concerns, is worthy of further and more sustained exploration, particularly in the context of the current focus on improving whistleblowing policies in the NHS. Whistleblowing (the disclosure, either to a person in authority or in public, of information concerning unsafe, unethical or illegal practices) is central to current debates about addressing poor standards of care in the NHS. Since the 1998 Public Interest Disclosure Act, all NHS trusts have been required to have policy and procedures in place for dealing with whistleblowing. This is now enshrined in the NHS Constitution, which mandates ‘an expectation that NHS staff will raise concerns about safety, malpractice or wrong-doing . . . as early as possible’. 128 Yet a recent House of Commons Public Accounts Select Committee report on patient safety concluded that ‘the NHS remains largely unsupportive of whistleblowing, with many staff fearful of going outside official channels to bring unsafe care to light’. 129 Indeed, the Francis Inquiry noted that there had been a number of whistleblowing policies in place at Mid Staffordshire NHS Foundation Trust that had ‘the clear objective to empower employees to raise concerns and to ensure that those concerns, where valid, were acted upon’. 4 However, the Inquiry heard that, despite the existence of such policies, no adequate support was given to staff who attempted to raise concerns, with witnesses describing ‘an endemic culture of bullying’, with graphic examples of victimisation of those who did raise concerns. 4 Francis concluded that the culture at the trust militated against health professionals openly raising concerns for two key reasons: they considered that such concerns would not be acted on effectively, or they feared negative repercussions from colleagues and/or victimisation by management. Yet despite these serious concerns about the effectiveness of current whistleblowing polices, we still lack a firm evidence base to guide change.
To help address this gap in knowledge, the government announced an independent inquiry into whistleblowing – Freedom to Speak Up – chaired by Sir Robert Francis QC. 130 The review invited NHS staff to share their experiences of speaking up, as well as ideas for removing the obstacles and creating the right environment for an open and honest reporting culture. The review report calls for all NHS health-care organisations and regulators to adhere to its principles and take actions to develop a safety culture, with calls for the Secretary of State for Health to review the progress at least annually. Within such a context, it will be interesting to see how boards respond to these developments and seek to nurture the cultures of safety and learning advocated by Francis.
Research on the role of systematic group bias in board decision-making
Recent research has highlighted the negative impact of systematic cognitive biases on the quality of clinical decision-making when individuals act alone. Croskerry, in the field of emergency medicine, for example, has documented many such systematic biases and has identified a range of possible remedial strategies. 131 Common cognitive biases that have been shown to afflict individual decision-making in clinical contexts include confirmation bias (where individuals mainly seek out information sources that are likely to confirm, rather than challenge, their existing opinion), hindsight bias (whereby the knowledge of the outcomes of previous decisions erroneously influence the predictability associated with a particular new decision) and the ‘fundamental attribution’ bias that arises from relying on decision problems that are seen as representative of all similar problems.
Boards make many decisions in which such individual biases may be a factor, but they also collectively make decisions that may be open to different biasing processes. 132 Group decisions, too, can be imperfect and result in organisational and clinical errors, which may harm patients. 133
Group decisions typically comprise three sequential stages: orientation (problem definition), evaluation (discussion of decision alternatives) and control (deciding which alternative is selected). Furthermore, each stage may be subject to systematic bias resulting from social influences and group dynamics. However, group-decision-making bias is a hitherto unexplored aspect of board oversight of safe care and it would be useful to undertake empirical research to explore the scope, range and impact of systematic group decision-making bias in board settings on patient safety processes and outcomes. Such work might also explore the potential for ‘de-biasing strategies’ to improve decision-making in this area. Possible systematic biases in group decision-making worthy of exploring include:
-
Groupthink. Highly cohesive groups with strongly connected members may inhibit the expression of (true) opinion; in such cases group harmony and unanimity may be privileged over effective decision-making. Clearly, this militates against the delivery of high-quality and safe care, where board members should feel comfortable in expressing dissenting views and be willing to speak openly about concerns they may have regarding the quality of care.
-
Group polarisation. Groups sometimes make more extreme (compound) decisions than the initial position of its (individual) members. Extreme decisions are those in which the group makes either a more risky or more conservative decision rather than take a more balanced appraisal or ‘middle of the road’ approach. For example, a hospital board may decide to commit significant resources, incurring high opportunity and sunk costs, to implement a new policy. Conversely, the group may decide not to commit resources to alternative courses of action because of the uncertainty involved. The term ‘risky shift’ is used to describe situations in which a group exhibits more risk-taking behaviour than the initial average risk-seeking tendencies of individual members. ‘Cautious shift’ refers to situations when group action becomes more risk averse than the initial risk tendencies of the individual members. In both cases, the average response of individual group members becomes more extreme when they are part of the group, which may have a negative impact on patient safety in some situations and contexts.
Research on board governance assessment measurement tools
There is a real need for more and better-tested bespoke instruments and tools for assessing and informing hospital board governance and competencies. In the study we used an adaptation of a US measure (the BSAQ), but there is a need for further development in the UK context. As the key characteristics of desirable board governance emerge from further sustained research, we will then be in a better position to build better instruments. Given the dynamic nature and complexity of board governance in health-care contexts, the building, testing and refining of a variety of board tools and instruments will be an ongoing task.
Research on board reach into organisational cultures and practices
As our work on the ‘tracer issues’ (see Chapter 6) demonstrates, a crucial challenge lies in understanding how different levels of organisational hierarchy articulate together. Activity within boards consists largely of discourse-creating dialogue that needs translation into actions at various levels within the hospital. Understanding how the dialogue and discourse creation at one level informs and influences the cultures and practices at another is key, as is identifying and elucidating the key conduits through which these layers are linked. Only detailed ethnographic work, particularly in well-functioning organisations, is likely to shed much light on these complexes processes.
Study limitations
As with all research projects, it is important to acknowledge the limitations of the study. The first limitation relates to the generalisability of the findings beyond the four case study sites. Although the case study sites were sampled purposefully to include organisations with both an upwards and downwards trajectory in relation to a basket of measures of patient safety performance, as well as being dispersed nationally, we cannot state categorically that our findings are necessarily generalisable to all acute trusts in England. Our intention has been to develop generalisable theories, which may or may not relate to particular trusts, depending on context. The time period over which the case studies were carried out was relatively short and more longitudinal work may have uncovered additional or even, possibly, contradictory findings. Nevertheless, we are reasonably confident that our study has uncovered some important aspects of board governance that are transferable to hospital trusts more generally. This view is strengthened by the results of our quantitative survey data, which reinforced many aspects of the case study findings. It was particularly noteworthy that the only significant correlation of the BSAQ data with organisation variables came in the area of staff ‘safety’ and ‘confidence’ in reporting quality failings, a theme also seen in the case work.
A second limitation is that our national surveys represent a snapshot of a particular time (March 2012–April 2013) and, although we obtained excellent response rates from board members (particularly for the board activity survey linked to the Dr Foster questionnaire), some of the responses may have been those that were viewed as ‘socially desirable’ by board members and, therefore, may not represent respondents’ true perception of the situation nor reflect the growing awareness of the importance of signalling that such issues are being taken seriously. The fact that the study was cross-sectional rather than longitudinal in design also means that we could only state that there may be associations between the variables rather than causal linkages. The structured questionnaires will also have failed to pick up many of the complex and qualitative aspects of board behaviour, which defy simple codification but which we did attempt to explore in the qualitative case studies.
A third limitation of this work may be seen in the only limited reach that we were able to obtain into broader hospital working (including at the care ‘coal face’). Although our use of ‘tracer issues’ did extend our view of the impact and influence of board debates and actions to deeper levels of the organisation hierarchy, we still lack the necessary comprehensive picture of how high-level debate and discourse shapes lower-level debates, discourse and, most importantly, practical actions.
Concluding remarks
Our research is the first large-scale mixed-methods study of hospital board activity and behaviour related to the oversight of patient safety in the English NHS. As such, we believe that it has much to contribute to an understanding of boards, their influence and their operation. We have set out the key findings in this report and believe that these should influence the design of future governance arrangements, as well as the training and support of boards. Notwithstanding the contributions to understanding made by this research, we also believe that research in this area is in its infancy and would more than justify additional investment along the lines described in a preceding section. Without effective governance from ‘board to ward’ it seems unlikely that the goals as laid out in the latest enquiry into NHS failings4 can be met in the context of tight financial settlements for the NHS in the foreseeable future.
Acknowledgements
The financial support of the National Institute for Health Research Health Services and Delivery Research programme is acknowledged (project code 10/1007/02).
Contributions of authors
Professor Russell Mannion (University of Birmingham) led the project, was the first author of the final report and participated in all aspects of the research.
Dr Tim Freeman (University of Middlesex) was the second author of the final report, co-designed the study, carried out qualitative fieldwork and analysis and helped to design the national survey questionnaires.
Dr Ross Millar (University of Birmingham) was the third author of the final report, was the lead on the literature review, carried out qualitative fieldwork and analysis and helped to design the national survey questionnaires.
Professor Huw Davies (University of St Andrews) was the fourth author of the final report, provided methodological advice and contributed to the final report.
We would like to thank colleagues at Dr Foster Intelligence, in particular Clare Aitken and Bethan Jones, for their assistance in collecting the national survey data, as well as providing background information to select the case studies. We would like to acknowledge and thank Rowena Jacobs and Panos Kasteridis for helping to analyse and interpret the national survey data.
We are also grateful to our project advisory board for their helpful advice and support: Richard Lilford, Naomi Chambers, Sarah Woolley, Martin Marshall and Elie Milner.
Public and patient involvement
The involvement of key stakeholders, including representatives from public governors, board-level managers, non-executives and clinical governance staff was integral to this research and provided the focus of our case study work. We interviewed patient representatives in our case study fieldwork on the tracer conditions and Elie Milner was the patient and public representative on the project advisory board.
Publications
Millar R, Mannion R, Freeman T, Davies HT. Hospital board oversight of quality and patient safety: a narrative review and synthesis of recent empirical research. Milbank Q 2013;91:738–70.
Mannion R, Davies H, Freeman T, Millar R, Jacobs R, Kasteridis P. Overseeing oversight: governance of quality and safety by hospital boards in the English NHS. J Health Serv Res Policy 2015;20(Suppl.):9–16.
Millar R, Freeman T, Mannion R. Hospital board oversight of quality and safety: a stakeholder analysis exploring the role of trust and intelligence. BMC Health Serv Res 2015;15:196.
Freeman T, Millar R, Mannion R, Davies HTO. A dramaturgy of hospital board governance in the English NHS [published online ahead of print 4 August 2015]. Sociology Health Ill 2015.
Data sharing statement
Data can be obtained from the corresponding author in such a way which safeguards the confidentiality and anonymity of participants and organisations.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
References
- Mirror, Mirror on the Wall: How the US Healthcare System Compares Internationally. New York, NY: Commonwealth Fund; 2014.
- Braithwaite J, Matsuyama Y, Mannion R, Johnson J. Healthcare Reform, Quality and Safety: Perspectives, Participants, Partnerships and Prospects in 30 Countries. London: Ashgate Press; 2014.
- Patient Safety. London: The Stationery Office; 2008.
- Francis R. The Mid Staffordshire NHS Foundation Trust Public Inquiry. London: The Stationery Office; 2013.
- Keogh B. Review into the Quality of Care and Treatment Provided by 14 Hospital Trusts in England: Overview Report. London: NHS England; 2013.
- Secretary of State . Report of the Committee of Inquiry into Allegations of Ill Treatment of Patients and Other Irregularities at the Ely Hospital, Cardiff n.d.
- Chambers N, Walshe K, Smith J. Healthcare Management. Maidenhead: Open University Press; 2011.
- Delivering on the Foundation Trust Provider Landscape. London: The Stationery Office; 2011.
- The Healthy NHS Board: Principles for Good Governance. London: NHS; 2010.
- The Integrated Governance Handbook. London: NHS; 2006.
- The Intelligent Commissioning Board. London: NHS; 2006.
- Governing the NHS: A Guide to NHS Boards. London: NHS; 2003.
- Francis R. The Mid Staffordshire Foundation Trust Inquiry. London: The Stationery Office; 2009.
- High Quality Care For All. London: The Stationery Office; 2008.
- Machell SP, Gough D, Naylor D, Nath V, Steward K. Putting Quality First in the Boardroom: Improving the Business of Caring. London: The King’s Fund; 2010.
- Millar R, Freeman T, Mannion R. Hospital board oversight of patient safety: a stakeholder analysis exploring the role of trust and intelligence. BMC Health Serv Res 2015;15. http://dx.doi.org/10.1186/s12913-015-0771-x.
- Millar R, Mannion R, Freeman T, Davies HTO. Hospital board oversight of patient safety: a narrative review and synthesis of relevant empirical research. Milbank Q 2013;91:738-70. http://dx.doi.org/10.1111/1468-0009.12032.
- Vincent C. Patient Safety. London: BMJ Books; 2011.
- Chambers N, Cornforth C, Walshe K, Harvey G. From Knowing to Doing: Connecting Knowledge and Performance in Public Services. Cambridge: Cambridge University Press; 2010.
- Chambers N, Harvey G, Mannion R, Bond J, Marshall J. Towards a framework for enhancing the performance of NHS boards: a synthesis of the evidence about board governance, board effectiveness and board development. Health Serv Deliv Res 2013;1.
- Mannion R, Davies HTO, Kernick D. Getting Health Economics into Practice. Oxford: Radcliffe Medical Press; 2002.
- Cornforth C. The Governance of Public and Non-Profit Organisations: What Do Boards Do?. London: Routledge; 2003.
- Penrose E. The Theory of the Growth of the Firm. Oxford: Basil Blackwell; 1959.
- Zahra S, Pearce J. Boards of directors and corporate financial performance: a review and integrative model. J Manage 1989;15:291-334. http://dx.doi.org/10.1177/014920638901500208.
- Garratt B. The Fish Rots from the Head – The Crisis in our Boardrooms: Developing the Crucial Skills of the Competent Director. London: HarperCollins; 1996.
- Garratt B. The Fish Rots from the Head – The Crisis in our Boardrooms: Developing the Crucial Skills of the Competent Director. London: Profile Books; 2010.
- Lee S-YD, Alexander JA, Wang V, Margolin FS, Combes JR. An empirical taxonomy of hospital governing board roles. Health Serv Res 2008;43:12-43. http://dx.doi.org/10.1111/j.1475-6773.2008.00835.x.
- McDonagh K, Limbdenstock R. Hospital governing boards: a study of their effectiveness in relation to organisational performance. J Healthc Manage 2006;51:377-89.
- Emslie S. Exploring the Factors That Measure the Performance of Boards of Directors of NHS Foundation Trusts and the Association Between Board and Organisational Performance 2007. www.lccge.bbk.ac.uk/publications-and-resources/postgraduate-research/mres-dissertations (accessed 21 May 2014).
- Learmonth M. NHS trust chief executives as heroes?. Health Care Anal 2001;9:417-36. http://dx.doi.org/10.1023/A:1013816919776.
- Pahl R, Winkler J, Stanworth PJ, Giddens A. Elites and Power in British Society. Cambridge: Cambridge University Press; 1974.
- Hajer M. Setting the Stage: A Dramaturgy of Policy Implementation. Amsterdam: University of Amsterdam; 2004.
- Hajer M. Setting the stage: a dramaturgy of policy deliberation. Adm Soc 2005;36:624-47. http://dx.doi.org/10.1177/0095399704270586.
- Hajer M, Versteeg W. Performing governance through networks. Eur Polit Sci 2005;4:340-7. http://dx.doi.org/10.1057/palgrave.eps.2210034.
- Yin R. Case Study Research Design and Methods. Beverley Hills, CA: Sage; 2009.
- Ovretveit J. Comparative and Cross-cultural Health Research: A Practical Guide. Abingdon: Radcliffe Medical Press; 1998.
- Freeman T, Peck E. Performing governance: a partnership board dramaturgy. Publ Adm 2007;85:907-29. http://dx.doi.org/10.1111/j.1467-9299.2007.00683.x.
- Miles MB, Huberman MA, Saldana J. Qualitative Data Analysis: A Methods Sourcebook. London: Sage; 2013.
- Robson C. Real World Research. Chichester: John Wiley and Sons; 2011.
- Fereday J, Muir-Cochrane E. Demonstrating rigor using thematic analysis: a hybrid approach of inductive and deductive coding and theme development. Int J Qual Methods 2006;5:80-92.
- Crabtree B, Miller W, Crabtree B, Miller W. Doing Qualitative Research. Thousand Oaks, CA: Sage; 1999.
- Holland TP, Jackson DK. Strengthening board performance: findings and lessons from demonstration projects. Nonprofit Manag Leadersh 1998;9:121-34. http://dx.doi.org/10.1002/nml.9201.
- Holland TP. Self-assessment by nonprofit boards. Nonprofit Manag Leadersh 1991;2:25-36. http://dx.doi.org/10.1002/nml.4130020106.
- Jackson DK, Holland TP. Measuring the effectiveness of non-profit boards. Nonprofit Volunt Sect Q 1998;27:159-82. http://dx.doi.org/10.1177/0899764098272004.
- McDonagh KJ. Hospital governing boards: a study of their effectiveness in relation to organizational performance. J Healthc Manag 2006;51:377-89.
- Greenhalgh T, Robert G, Macfarlane F, Bate P, Kyriakidou O, Peacock R. Storylines of research in diffusion of innovation: a meta-narrative approach to systematic review. Soc Sci Med 2005;61:417-30. http://dx.doi.org/10.1016/j.socscimed.2004.12.001.
- Clough J, Nash DJ. Health care governance for quality and safety: the new agenda. Am J Med Qual 2007;22:203-13. http://dx.doi.org/10.1177/1062860607301285.
- Popay J, Roberts H, Sowden A, Petticrew M, Arai L, Rodgers M, et al. Guidance on the Conduct of Narrative Synthesis in Systematic Reviews. Swindon: Economic and Social Research Council (ESRC) Methods Programme; 2006.
- To Err Is Human: Building a Safer Health System. Washington, DC: National Academy Press; 1999.
- Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press; 2001.
- An Organisation with a Memory. London: The Stationery Office; 2000.
- Jiang HJ, Lockee C, Bass K, Fraser I. Board engagement in quality: findings of a survey of hospital and system leaders. J Healthc Manag 2008;53:121-34.
- Kroch E, Vaughn T, Koepke M, Roman S, Foster D, Sinha S, et al. Hospital boards and quality dashboards. J Patient Saf 2006;2:10-9.
- Meyer JA, Silow-Carroll S, Kutyla T, Stepnick LS, Rybowski LS. Hospital Quality: Ingredients for Success: Overview and Lessons Learned. New York, NY: Commonwealth Fund; 2004.
- Paine LA, Baker DR, Rosenstein B, Pronovost PJ. The Johns Hopkins Hospital: identifying and addressing risks and safety issues. Jt Comm J Qual Saf 2004;30:543-50.
- Sandrick K. One giant leap for quality. When boards get behind quality initiatives, patient care benefits. Trustee 2005;58:22-4.
- Jha AK, Epstein AM. Hospital governance and the quality of care. Health Aff 2010;29:182-7. http://dx.doi.org/10.1377/hlthaff.2009.0297.
- Jha AK, Li Z, Orav EJ, Epstein AM. Care in US hospitals – The Hospital Quality Alliance Program. N Engl J Med 2005;353:265-74. http://dx.doi.org/10.1056/NEJMsa051249.
- Baker GR, Denis JL, Pomey MP, Murray AM. Effective Governance for Quality and Patient Safety in Canadian Healthcare Organizations: A Report to the Canadian Health Services Research Foundation and the Canadian Patient Safety Institute. Ottawa, ON: Canadian Health Services Research Foundation/Canadian Patient Safety Institute; 2010.
- Gray BH, Weiss L, Jennings B, Gray BH, Sharpe VA, Fleischman AR. The Ethics of Hospital Trustees. Washington, DC: Georgetown University Press; 2004.
- Goeschel CA, Berenholtz SM, Culbertson RA, Jin LD, Pronovost PJ. Board quality scorecards: measuring improvement. Am J Med Qual 2011;26:254-60. http://dx.doi.org/10.1177/1062860610389324.
- Jha AK, Epstein AM. Governance around quality of care at hospitals that disproportionately care for black patients. J Gen Intern Med 2012;27:297-303. http://dx.doi.org/10.1007/s11606-011-1880-9.
- Jha AK, Epstein AM. A survey of board chairs of English hospitals shows greater attention to quality of care than among their US counterparts. Health Aff 2013;32:677-85. http://dx.doi.org/10.1377/hlthaff.2012.1060.
- Jiang HJ, Lockee C, Bass K, Fraser I. Board oversight of quality: any differences in process of care and mortality?. J Healthc Manag 2009;54:15-30.
- Jiang HJ, Lockee C, Fraser I. Enhancing board oversight on quality of hospital care: an agency theory perspective. Health Care Manage Rev 2011;37:144-53. http://dx.doi.org/10.1097/HMR.0b013e3182224237.
- Joshi MS, Hines S. Getting the board on board: engaging hospital boards in quality and patient safety. Jt Comm J Qual Patient Saf 2006;32:179-87.
- Mastal MF, Joshi M, Schulke K. Nursing leadership: championing quality and patient safety in the boardroom. Nurs Econ 2007;25:323-30.
- Prybil LD, Peterson R, Brezinski P, Zamba G, Roach W, Fillmore A. Board oversight of patient care quality in community health systems. Am J Med Qual 2010;25:34-41. http://dx.doi.org/10.1177/1062860609352804.
- Prybil LD. Nurses in health care governance: is the picture changing?. J Nurs Care Qual 2013;28:103-7. http://dx.doi.org/10.1097/NCQ.0b013e31827efb8b.
- Ramsay A, Magnusson C, Fulop N. The relationship between external and local governance systems: the case of health care associated infections and medication errors in one NHS trust. Qual Saf Health Care 2010;19:1-8. http://dx.doi.org/10.1136/qshc.2009.037473.
- Vaughn TM, Koepke M, Kroch E, Lehrman W, Sinha S, Levey S. Engagement of leadership in quality improvement initiatives: executive quality improvement surveys. J Patient Saf 2006;2:2-9.
- Botje D, Klazingab NS, Wagnera C. To what degree is the governance of Dutch hospitals orientated towards quality in care? Does this really affect performance?. Health Policy 2013;113:134-41. http://dx.doi.org/10.1016/j.healthpol.2013.07.015.
- Bream E, Jha AK, Epstein AM, Black N. Views of the chairs of Scottish health boards on engagement with quality management and comparisons with English trusts. J R Coll Physicians Edinb 2013;43:215-21. http://dx.doi.org/10.4997/JRCPE.2013.305.
- Bismark MM, Walter SJ, Studdert DM. The role of boards in clinical governance: activities and attitudes among members of public health service boards in Victoria. Aust Health Rev 2013;37:682-7. http://dx.doi.org/10.1071/AH13125.
- Ford-Eickhoff K, Plowman DA, McDaniel RR. Hospital boards and hospital strategic focus: the impact of board involvement in strategic decision making. Health Care Manage Rev 2011;36:145-54. http://dx.doi.org/10.1097/HMR.0b013e3182099f6e.
- Conway J. Getting boards on board: engaging governing boards in quality and safety. Jt Comm J Qual Patient Saf 2008;34:214-20.
- Gautam KS. A call for board leadership on quality in hospitals. Qual Manag Health Care 2005;14:18-30. http://dx.doi.org/10.1097/00019514-200501000-00003.
- Safely Does It: Implementing Safer Care for Patients. London: Healthcare Commision; 2009.
- Schyve PM. What you can do: the trustee, patient safety, and JCAHO. Trustee 2003;56:19-21.
- Clarke JR, Lerner JC, Marella W. The role for leaders of health care organizations in patient safety. Am J Med Qual 2007;22:311-18. http://dx.doi.org/10.1177/1062860607304743.
- Prybil LD, Bardach DR, Fardo DW. Board oversight of patient care quality in large nonprofit health systems. Am J Med Qual 2014;29:39-43. http://dx.doi.org/10.1177/1062860613485407.
- Bader BS. CQI progress reports: the dashboard approach provides a better way to keep board informed about quality. Healthc Exec 1993;8:8-11.
- Goeschel CA, Holzmueller CG, Pronovost PJ. Hospital board checklist to improve culture and reduce central line associated bloodstream infections. Jt Comm J Qual Patient Saf 2010;36:525-8.
- Slessor SR, Crandall JB, Nielsen GA. Case study: getting boards on board at Allen Memorial Hospital, Iowa health system. Jt Comm J Qual Patient Saf 2008;34:221-7.
- Lathrop CB. Using graphs to consolidate reports to the board. J Healthc Qual 1997;19:26-33. http://dx.doi.org/10.1111/j.1945-1474.1997.tb00877.x.
- Meyers S. Data in, safety out: balanced scorecards help the board make patient safety their No. 1 priority. Trustee 2004;57:12-4.
- Pugh M, Reinertsen J. Reducing harm to patients: using patient safety dashboards at the board level. Healthc Exec 2007;22:64-5.
- Reinertsen JL. Hospital Boards and Clinical Quality: A Practical Guide. Toronto, ON: Ontario Hospital Association; 2007.
- Frankel A, Baker EG, Neppl C, Simmonds T, Gustafson M, Gandhi TK. Patient safety leadership walkrounds. Jt Comm J Qual Saf 2003;29:16-2.
- Safe in the Knowledge: How Do NHS Trust Boards Ensure Safe Care for Their Patients?. London: Healthcare Commission; 2009.
- Evans M. This is a test. Exams for governance boards on quality measures could be a way to improve care, accountability in hospitals. Mod Healthc 2009;39:6-7.
- Marren JP, Feazell GL, Paddock MW. The hospital board at risk and the need to restructure the relationship with the medical staff: bylaws, peer review and related solutions. Ann Health Law 2003;12:179-234.
- Bader BS. Best Practices for Board Quality Committees 2006. www.greatboards.org/newsletter/reprints/Board_quality_committees_best_practices.pdf (accessed 10 July 2013).
- Weiner BJ, Shortell SM, Alexander J. Promoting clinical involvement in hospital quality improvement efforts: the effects of top management, board, and physician leadership. Health Serv Res 1997;32:491-510.
- Heenan M, Khan H, Binkley D. From boardroom to bedside: how to define and measure hospital quality. Healthc Q 2010;13:55-60. http://dx.doi.org/10.12927/hcq.2013.21615.
- MacLeod L. Nursing leadership: ten compelling reasons for having a nurse leader on the hospital board. Nurse Lead 2010;8:44-7. http://dx.doi.org/10.1016/j.mnl.2010.01.012.
- Meyers S. Cultivating trust: the board-medical staff relationship. Trustee 2008;61:8-12.
- Prybil LD. Nursing involvement in hospital governance. J Nurs Care Qual 2007;22:1-3. http://dx.doi.org/10.1097/00001786-200701000-00001.
- Prybil LD. Engaging nurses in governing hospitals and health systems. J Nurs Care Qual 2009;24:5-9. http://dx.doi.org/10.1097/NCQ.0b013e31818f55b4.
- Waring J, Rowley E, Dingwall R, Palmer C, Murcott T. A narrative review of the UK patient safety research portfolio. J Health Serv Res Policy 2010;15:26-32. http://dx.doi.org/10.1258/jhsrp.2009.009042.
- Davies HTO, Mannion R, Smith P. Reforming Health Care Markets: An Economic Perspective. Buckingham: Open University Press; 2010.
- Hood C. Regulation Inside Government. Oxford: Oxford University Press; 1999.
- Dixon-Woods M, Leslie M, Bion J, Tarrant C. What counts? An ethnographic study of infection data reported to a patient safety program. Milbank Q 2012;90:548-91. http://dx.doi.org/10.1111/j.1468-0009.2012.00674.x.
- Freeman T, Peck E, Braithwaite J, Hyde P, Pope C. Culture and Climate in Health Care Organizations. Basingstoke: Palgrave Macmillan; 2010.
- Austin JL. How to Do Things with Words. Cambridge, MA: Harvard University Press; 1962.
- Goffman E. Frame Analysis. An Essay on the Organization of Experience. Boston, MA: Northeastern University Press; 1974.
- Bateson G. Steps to an Ecology of Mind: Collected Essays in Anthropology. Chicago, IL: University of Chicago Press; 1972.
- Lyotard J. The Postmodern Condition: A Report on Knowledge. Manchester: Manchester University Press; 1979.
- Butler J. Bodies that Matter: On the Discursive Limits of ‘Sex’. London: Routledge; 1993.
- Butler J. Performative agency. J Cult Econ 2010;3:147-61. http://dx.doi.org/10.1080/17530350.2010.494117.
- Latour B, Law J. Power Action and Belief. London: Routledge and Keegan Paul; 1986.
- Latour B. Science in Action: How to Follow Scientists and Engineers through Society. Cambridge, MA: Harvard University Press; 1987.
- Callon M, McKenzie D, Miniesa F, Siu L. Do Economists Make Markets? On the Performativity of Economics. Princeton: Princeton University Press; 2007.
- Feldman M, Pentland B. Reconceptualizing organizational routines as a source of flexibility and change. Admin Sci Q 2003;48:94-118. http://dx.doi.org/10.2307/3556620.
- Orlikowski WJ, Scott S. Sociomateriality: challenging the separation of technology, work and organization. Acad Manag Ann 2008;2:433-74. http://dx.doi.org/10.1080/19416520802211644.
- Law J, Singleton V. Performing technology’s stories: on social constructivism, performance and performativity. Technol Cult 2000;41:765-75. http://dx.doi.org/10.1353/tech.2000.0167.
- Diedrich A, Walter L, Czarniawska B. Boundary stories: constructing the validation centre in west Sweden. Scand J Public Admin 2011;15:3-20.
- Czarniawska B, Sevon G, Czarniawska B, Sevon G. Translating Organizational Change. Berlin: de Gruyter; 1996.
- Goffman E. The Presentation of Self in Everyday Life. New York, NY: Doubleday; 1959.
- The Healthy NHS Board: Principles for Good Governance. London: NHS Leadership Academy; 2013.
- Freeman T. Using performance indicators to improve health care quality in the public sector: a review of the literature. Health Serv Manage Res 2002;15:126-37. http://dx.doi.org/10.1258/0951484021912897.
- Cornforth CJ, Edwards C. Good Governance: Developing Effective Board–Management Relations in Public and Voluntary Organisations. London: CIMA Publications; 1998.
- Chait RC, Holland TP, Taylor BE. The Effective Board of Trustees. Phoenix, AZ: Oryx Press; 1993.
- Comrey AL, Lee HB. A First Course in Factor Analysis. Hillsdale, NJ: Lawrence Erlbaum Associates, Inc; 1992.
- Cattell RB. The scree test for the number of factors. Multivar Behav Res 1966;1:245-76. http://dx.doi.org/10.1207/s15327906mbr0102_10.
- Pett MA, Lackey NR, Sullivan JJ. Making Sense of Factor Analysis: The Use of Factor Analysis for Instrumental Development in Health Care Research. London: Sage Publications; 2003.
- Ramsay A, Fulop N, Fresko A, Rubenstein S. The Healthy NHS Board 2013: Review of Guidance and Research Evidence. Leeds: NHS Leadership Academy; 2013.
- The NHS Constitution. London: The Stationery Office; 2009.
- Ninth Report: Whistleblowing. London: House of Commons, Parliament; 2014.
- Francis R. Freedom to Speak Up: An Independent Review into Creating an Open and Honest Reporting Culture in the NHS. London: The Stationery Office; 2015.
- Croskerry P. Achieving quality in clinical decision making: cognitive strategies and detection of bias. Acad Emerg Med 2002;9:1184-204. http://dx.doi.org/10.1111/j.1553-2712.2002.tb01574.x.
- Mannion R, Thompson C. Systematic biases in group decision making: implications for patient safety. Int J Qual Health Care 2014;26:606-12. http://dx.doi.org/10.1093/intqhc/mzu083.
- Pagliari CJ, Grimshaw J, Eccles M. The potential influence of small group processes on guideline development. J Eval Clin Pract 2001;7:165-73. http://dx.doi.org/10.1046/j.1365-2753.2001.00272.x.
Appendix 1 Effective board governance of safe care scoping study
Stakeholder interview sample
We interviewed 10 people from the following organisations:
-
Health Foundation: an independent charity working to improve the quality of health care in the UK (n = 1).
-
NHS Confederation: a membership body for organisations that commission and provide NHS services, aiming to bring together, and speak on behalf of, the whole of the NHS (n = 1).
-
Department of Health: contribution from representatives involved in patient safety policy development (n = 2)
-
NHS Litigation Authority: a not-for-profit part of the NHS that manages negligence and other claims against the NHS in England (n = 1).
-
Monitor: an executive non-departmental public body of the Department of Health that particularly oversees and regulates FTs (n = 1).
-
Care Quality Commission: an executive body of the Department of Health that regulates, inspects and reviews all adult social care services in England (n = 1).
-
National Patient Safety Agency: responsible for identifying and reducing risks to patients receiving NHS care and leading on national initiatives to improve patient safety. In June 2012, the Agency became part of the NHS Commissioning Board Special Health Authority (n = 1).
-
Witness and seminar contributors to the Mid Staffordshire NHS Trust Inquiry (n = 2).
Appendix 2 Case study invitation letter
Appendix 3 Participant information sheet
Appendix 4 Coding frameworks used in the case study analysis
Example of coding framework: board-level interviews
For the interviews with board members, our analysis built on a literature review (see Millar et al. 17) that highlighted a number of issues for boards in relation to the governance of patient safety. These would form the central codes for the analysis (deductive); however, our analysis was also open to a variety of emerging themes that occurred during the course of the fieldwork (inductive). The response to the Francis Inquiry findings was an example of a code that emerged from the interview data.
Coding framework
| Tree node | Nodes | Node explanation |
|---|---|---|
| ‘Measurement’: instances where board members described the accumulation, interpretation and analysis of performance information | Soft intelligence | The qualitative dimensions of performance measurement, such as patient stories |
| Hard intelligence | The quantitative dimensions of performance measurement, such as RAG ratings | |
| Dashboards | Board perspectives regarding the use and effectiveness of current dashboards | |
| Training and development | Board perspectives on the extent to which they needed further training and development in relation to performance measurement | |
| ‘Leadership’: instances where board members described examples and practices related to executive directors as leaders | Strategy | Board perspectives on the ability to develop an effective strategy regarding quality and safety |
| Priorities | Board perspectives on the possible competing demands placed on them in terms of where their priorities lie | |
| Behaviours | Board perspectives on the behaviours they believed were expected of them in terms of key board activities, e.g. walkabouts | |
| ‘Internal oversight’: instances where board members reflected on the organisational structures and processes for patient safety, as well as the informal relationships and dynamics between boards and professional groups | Processes | Board perspectives on the governance processes within the hospital, including reflections on subcommittees |
| Relationships | Board perspectives on their relationships with staff | |
| Dynamics | Board perspectives on the dynamics of the current board | |
| Meetings | Board perspectives on their reflections on the board meeting | |
| Governors | Board perspectives on their relationships with governors in the oversight of patient safety | |
| ‘External oversight’: instances where board members reflected on their accountability in relation to national targets and regulatory bodies | Targets | Board perspectives on the nature and impact of delivering performance targets |
| Regulation | Board perspectives on their relationship with regulatory bodies | |
| Policy | Board perspectives on government policy in relation to boards and patient safety | |
| Commissioning | Board perspective regarding their relationships with commissioners | |
| *Additional free node for the Francis Inquiry | Francis | A free node was created for board perspectives regarding the Francis Inquiry |
Excerpt from transcript: Code of Internal Oversight and Dynamics (anonymised)
≤ Internals\\Medical Director ≥ – § 5 references coded (12.69% Coverage)
Reference 1 – 3.86% Coverage
I think things have moved on. I think the board . . . Boards are interesting because they . . . This board, the board in this organisation, has three doctors? . . . when I was made director, I had a limited clinical practice. So those people understand all of these aspects of practice. The rest of the board have no more knowledge of it than any layperson coming into hospital for a procedure. I, personally, feel that there should be more board to ward communication. Some of the board members do make time to do walkabouts and that kind of thing – many of them to it quite assiduously . . . does it pretty regularly. Others of them find it very difficult to do that because of external commitments and time constraints. And some of them, I think, don’t actually . . . They’re a bit frightened of it. The way we set it up, I or one of the senior nursing staff . . . would go with them, so they wouldn’t be sent to a ward . . . They’d go with somebody who knew the organisation and knew what questions should be asked and so on. But I think some of them feel out of place. It’s a bit like putting a barrister in an operating theatre – they‘re fine in a courtroom, but you put them in an operating theatre and it’s a different ball game. And it’s the same thing – if I had to go and give evidence in a court of law, the barrister’s very comfortable, but I’m pretty uncomfortable. So it’s the same thing when the board members go into clinical environments.
Example of NVivo node summary table
| Node summary example for case study site | ||||||
|---|---|---|---|---|---|---|
| Source type | Number of sources | Number of coding references | Number of words coded | Number of paragraphs coded | Duration coded | |
| Node | ||||||
| Nickname: | Nodes\\External | |||||
| Nickname: | Nodes\\External\commissioning | |||||
| Classification: | ||||||
| Aggregated: | No | |||||
| Document | 11 | 11 | 13,289 | 407 | ||
| Nickname: | Nodes\\External\regulation | |||||
| Classification: | ||||||
| Aggregated: | No | |||||
| Document | 5 | 5 | 11,384 | 359 | ||
| Nickname: | Nodes\\External\targets | |||||
| Classification: | ||||||
| Aggregated: | No | |||||
| Document | 8 | 12 | 13,818 | 414 | ||
| Nickname: | Nodes\\Francis | |||||
| Classification: | ||||||
| Aggregated: | No | |||||
| Document | 12 | 13 | 15,238 | 496 | ||
| Nickname: | Nodes\\internal | |||||
| Nickname: | Nodes\\internal\governors | |||||
| Classification: | ||||||
| Aggregated: | No | |||||
| Document | 6 | 7 | 12,595 | 442 | ||
| Nickname: | Nodes\\internal\processes | |||||
| Classification: | ||||||
| Aggregated: | No | |||||
| Document | 8 | 13 | 14,804 | 424 | ||
| Nickname: | Nodes\\internal\relationships | |||||
| Classification: | ||||||
| Aggregated: | No | |||||
| Document | 10 | 13 | 16,061 | 456 | ||
| Nickname: | Nodes\\internal\structures | |||||
| Classification: | ||||||
| Aggregated: | No | |||||
| Document | 9 | 9 | 12,716 | 401 | ||
| Nickname: | Nodes\\leadership | |||||
| Nickname: | Nodes\\leadership\dynamics | |||||
| Classification: | ||||||
| Aggregated: | No | |||||
| Document | 11 | 32 | 20,192 | 648 | ||
| Nickname: | Nodes\\leadership\impact | |||||
| Classification: | ||||||
| Aggregated: | No | |||||
| Document | 12 | 26 | 12,377 | 301 | ||
| Nickname: | Nodes\\leadership\priorities | |||||
| Classification: | ||||||
| Aggregated: | No | |||||
| Document | 12 | 23 | 18,847 | 573 | ||
| Nickname: | Nodes\\leadership\strategy | |||||
| Classification: | ||||||
| Aggregated: | No | |||||
| Document | 9 | 12 | 16,465 | 462 | ||
| Nickname: | Nodes\\measurement | |||||
| Nickname: | Nodes\\measurement\dashboards | |||||
| Classification: | ||||||
| Aggregated: | No | |||||
| Document | 8 | 11 | 14,509 | 475 | ||
| Nickname: | Nodes\\measurement\hard | |||||
| Classification: | ||||||
| Aggregated: | No | |||||
| Document | 4 | 4 | 11,333 | 336 | ||
| Nickname: | Nodes\\measurement\soft | |||||
| Classification: | ||||||
| Aggregated: | No | |||||
| Document | 9 | 14 | 13,677 | 420 | ||
| Nickname: | Nodes\\measurement\training | |||||
| Classification: | ||||||
| Aggregated: | No | |||||
| Document | 6 | 7 | 12,032 | 381 | ||
Appendix 5 The national survey board activity questions
-
How many board members are there in your organisation?
-
Over the course of the last year, what percentage of board meeting time has been devoted specifically to discussing patient safety issues?
-
Over the past year, have board members received formal training in relation to patient safety?
-
What training and development programmes have been attended?
-
-
Have the board set explicit measurable goals for improving performance in relation to patient safety?
-
Please specify these measurable goals?
-
-
Have strategic goals and objectives related to patient safety been distributed to staff groups within the last 12 months?
-
Which staff groups have received these goals and objectives:
-
ambulance
-
allied health professionals
-
doctors
-
Health Informatics
-
management
-
nursing
-
Healthcare Science
-
wider health-care team
-
other (please specify).
-
-
-
Does the board have formal procedures for reporting inappropriate behaviours in relation to patient safety on a regular basis?
-
IF YES, what are these procedures?
-
-
Are there procedures for proactively responding to the reporting of staff concerns about patient safety?
-
IF YES, what are these procedures?
-
-
Which of the following informal sources of information related to patient safety are reported at all board meetings? Please indicate all that apply:
-
executive walkarounds
-
patient stories
-
board members shadowed clinicians to better understand patient safety issues
-
board members engaged clinicians to better understand patient safety issues
-
other (please specify).
-
-
Which of the following quantitative data sources related to patient safety are reported at all board meetings?
-
infection rates
-
mortality rates
-
morbidity rates
-
readmission rates
-
incident rates and levels of harm
-
patient safety surveys
-
formal complaints processes
-
medication errors
-
CQC Quality and Risk Profiles (QRPs)
-
staff safety (injuries and/or sickness)
-
implementation of safety alerts
-
formal written reports about safety performance
-
other (please specify).
-
-
How many members of the board have clinical backgrounds?
-
Does the board have a formal subcommittee that discusses patient safety issues?
-
IF YES, how many times a year does this subcommittee meet?
-
-
Are patient safety measures included in the chief executive officer’s performance review?
-
IF YES, please provide details.
-
-
Does the board use any national reporting measures of patient safety?
-
IF YES, please provide details.
-
-
We are interested in the relative importance of a number of activities within your organisation. Please rank the following in order of importance to the board:
-
financial performance
-
clinical effectiveness
-
patient safety
-
patient experience
-
achieving waiting time targets
-
staff satisfaction.
-
Appendix 6 The Board Self-Assessment Questionnaire
Board Self-Assessment Questionnaire
Question items arranged by board performance dimensions or competencies (contextual, educational, interpersonal, analytical, political and strategic).
Items in italics are reverse scored.
Competency 1: understands context (contextual)
6. Induction programmes for new board members, particularly non-executives, specifically include a segment about both the NHS and the organisation’s history and traditions.
12. In discussing key issues, it is not unusual for someone on the board to talk about what this organisation stands for and how that is related to the matter at hand.
13. Values are seldom discussed explicitly at our board meetings.
30. This board has made a key decision that I believe to be inconsistent with the mission of this organisation.
37. I have been present in board meetings where discussions of the history and mission of the organisation were key factors in reaching a conclusion on a problem.
39. It is apparent from the comments of some of our board members that they do not understand the mission of the organisation very well.
42. There have been occasions where the board itself has acted in ways inconsistent with the organisation’s deepest values.
45. New members are provided with a detailed explanation of this organisation’s mission when they join this board.
50. This board reviews the organisation’s mission at periodic intervals.
56. One of the reasons I joined this board was that I believe strongly in the values of this organisation.
59. Former members of this board have participated in special events designed to convey to new members the organisation’s history and values.
63. This board understands the norms of the professions working in this organisation.
Competency 2: builds learning (educational)
2. I have participated in board discussions about what we should do differently as a result of a mistake the board made.
10. At least once every 2 years, our board has a retreat or special session to examine our performance, how well we are doing as a board.
17. This board periodically sets aside time to learn more about important issues facing NHS Trusts.
18. I can recall an occasion when the board acknowledged its responsibility for an ill-advised decision.
21. Most people on this board tend to rely on observation and informal discussions to learn about their role and responsibilities.
24. When a new member joins this board, we make sure that someone serves as a mentor to help this person learn the ropes.
26. I have participated in board discussions about the effectiveness of our performance.
29. I have participated in discussions with new board members about the roles and responsibilities of a board member.
34. I have participated in board discussions about what we can learn from a mistake we have made
38. I have never received feedback on my performance as a member of this board.
46. This board does not allocate organisational funds for the purpose of board education and development.
51. This board has conducted an explicit examination of its roles and responsibilities.
Competency 3: nurtures group (interpersonal)
3. I have had conversations with other members of this board regarding common interests we share outside this organisation
15. Differences of opinion in board decisions are more often settled by vote than by more discussion.
20. This board is as attentive to how it reaches conclusions as it is to what is decided.
27. At our board meetings, there is at least as much dialogue among non-executive members as there is between non-executive members and executive members.
31. The leadership of this board typically goes out of its way to make sure that all members have the same information on important issues.
32. This board has adopted some explicit goals for itself, distinct from goals it has for the total organisation.
43. This board relies on the natural emergence of leaders, rather than trying explicitly to cultivate future leaders for the board.
52. I am able to speak my mind on key issues without fear that I will be ostracised by some members of this board.
57. This board does not recognise special events in the lives of its members.
60. This board provides biographical information that helps members get to know one another better.
64. This board meets socially as a group.
Competency 4: recognises complexity (analytical)
1. This board takes regular steps to keep itself informed about important trends in the local health economy, and in the wider national healthcare environment, that might affect the organisation.
4. I have been in board meetings where it seemed that the subtleties of the issues we dealt with escaped the awareness of a number of the members.
5. Our board explicitly examines the ‘downside’ or possible pitfalls of any important decisions it is about to make.
11. Many of the issues that this board deals with seem to be separate tasks, unrelated to one another.
22. I find it easy to identify the key issues that this board faces.
23. When faced with an important issue, the board often ‘brainstorms’ and tries to generate a whole list of creative approaches or solutions to the problem.
28. When issues come before our board, they are seldom framed in a way that enables members to see the connections between the matter at hand and the organisation’s overall strategy.
47. Recommendations from the executive directors are usually accepted with little questioning in board meetings.
53. This board tries to avoid issues that are ambiguous and complicated.
61. This board seeks information and advice from leaders of other similar organisations.
Competency 5: respects process (political)
9. This board communicates its decisions to all those who are affected by them.
14. If our board thinks that an important internal or external stakeholder or stakeholder group is likely to disagree with an action we are considering, we will make sure we learn how they feel before we actually make the decision.
19. This board has formed ad hoc committees or task forces that include staff as well as board members.
25. I have been in board meetings where explicit attention was given to the concerns of the local community.
33. The board periodically requests information on the morale of the professional staff.
41. Before reaching a decision on important issues, this board usually requests input from persons likely to be affected by the decision.
48. At times this board has appeared unaware of the impact its decisions will have within our local community.
54. The executive directors rarely report to the board on the concerns of patients.
Competency 6: shapes direction (strategic)
7. This board is more involved in trying to put out fires than in preparing for the future.
8. The board sets clear organisational priorities for the year ahead.
16. This board delays action until an issue becomes urgent or critical.
35. Our board meetings tend to focus more on current concerns than on preparing for the future.
36. At least once a year, this board asks that the chief executive articulate his/her vision for the organisation’s future and strategies to realise that vision.
40. This board has on occasion evaded responsibility for some important issue facing the organisation.
44. This board often discusses where the organisation should be headed five or more years into the future.
49. Within the past year, this board has reviewed the organisation’s strategies for attaining its long-term goals.
55. I have been in board meetings where the discussion focused on identifying or overcoming the organisation’s weakness.
58. The board discusses events and trends in the larger environment that may present specific opportunities for this organisation.
62. This board makes explicit use of the long range priorities of this organisation in dealing with current issues.
65. More than half of this board’s time is spent in discussions of issues of importance to the organisation’s long-range future.
Appendix 7 Patient safety measures
Hospital Standardised Mortality Ratio
Metric
The ratio of the observed number of in-hospital deaths with a HSMR diagnosis to the expected number of deaths, multiplied by 100, at trust level.
Denominator
Spells with a primary dominant diagnosis of any of the 56 clinical classifications software groups that comprise the HSMR basket.
Observed
Denominator superspells with method of discharge as death (DISMETH = 4,5).
Deaths are assigned to every provider within the superspell.
Expected
Expected number of in-hospitals deaths derived from logistic regression, adjusting for factors to indirectly standardise for differences in case mix.
Data sources
Secondary user service – commissioning data sets (SUS–CDS) for the financial year 2012/13 (April 2012 to March 2013).
Statistical methods
-
Logistic regression is used to calculate the expected number of in-hospitals deaths. To indirectly standardise for differences in patient case mix, the model is adjusted for the following factors:
-
sex
-
age on admission (in 5-year bands up to 90+ years)
-
interactions between age on admission (in 5-year bands up to 90+ years) and Charlson Comorbidity Score
-
admission method (non-elective or elective)
-
socioeconomic deprivation quintile of the area of residence of the patient (based on the Carstairs Index)
-
diagnosis/procedure subgroup
-
comorbidities (based on Charlson score)
-
number of previous emergency admissions
-
year of discharge (financial year)
-
palliative care (if any episode in the spell has the treatment function code 315 or contains International Classification of Diseases, Tenth Edition (ICD-10) (code Z515 in any of the diagnoses fields)
-
month of admission
-
source of admission.
-
-
Relative risk: the ratio is calculated by dividing the actual number of deaths by the expected number and multiplying the figure by 100. It is expressed as a relative risk, where a risk rating of 100 represents the national average. If the trust has a HSMR of 100, the number of patients who died was exactly as it would be expected taking into account the standardisation factors. A HSMR above 100 means more patients died than would be expected; one below 100 means that fewer than expected died.
-
Control limits: control limits tell us the range of values that is consistent with random or chance variation. Data points falling within the control limits are consistent with random or chance variation and are said to display ‘common-cause variation’; for data points falling outside the control limits, chance is an unlikely explanation and hence they are said to display ‘special-cause variation’ – that is, where the trust’s rate diverges significantly from the national rate.
Data points falling above the upper 99.8% Poisson control limit are said to be significantly ‘higher than expected’, data points falling below the lower 99.8% Poisson control limit are said to be significantly ‘lower than expected’, data points falling between the lower 99.8% Poisson control limit and the upper 99.8% Poisson control limit are said to be ‘within expected range’.
Notes
Superspell, a group of spells linked by transfer.
The HSMR basket of CCS groups accounts for approximately 80% of all in-hospital deaths in England.
See ‘HSMR Toolkit’ for full methodological detail.
Hospital Standardised Mortality Ratio (100)
Metric
The ratio of the observed number of in-hospital deaths to the expected number of deaths for all diagnosis groups, multiplied by 100, at trust level.
Denominator
Spells with any primary dominant diagnosis, linked into superspells.
Observed
Denominator superspells with method of discharge as death (DISMETH = 4,5).
Deaths are assigned to every provider within the superspell.
Expected
Expected number of in-hospitals deaths derived from logistic regression, adjusting for factors to indirectly standardise for differences in case mix.
Data sources
SUS–CDS for the financial year 2012/13 (April 2012–March 2013).
Statistical methods
-
Logistic regression is used to calculate the expected number of in-hospitals deaths. To indirectly standardise for differences in patient case mix, the model is adjusted for the following factors:
-
sex
-
age on admission (in 5-year bands up to 90+ years)
-
interactions between age on admission (in 5-year bands up to 90+ years) and Charlson Comorbidity Score
-
admission method (non-elective or elective)
-
socioeconomic deprivation quintile of the area of residence of the patient (based on the Carstairs Index)
-
diagnosis/procedure subgroup
-
comorbidities (based on Charlson score)
-
number of previous emergency admissions
-
year of discharge (financial year)
-
palliative care (if any episode in the spell has the treatment function code 315 or contains ICD-10 code Z515 in any of the diagnoses fields)
-
month of admission
-
source of admission.
-
-
Relative risk: the ratio is calculated by dividing the actual number of deaths by the expected number and multiplying the figure by 100. It is expressed as a relative risk, where a risk rating of 100 represents the national average. If the trust has a HSMR of 100, the number of patients who died was exactly as it would be expected taking into account the standardisation factors. A HSMR above 100 means more patients died than would be expected; one below 100 means that fewer than expected died.
-
Control limits: control limits tell us the range of values that is consistent with random or chance variation. Data points falling within the control limits are consistent with random or chance variation and are said to display ‘common-cause variation’; for data points falling outside the control limits, chance is an unlikely explanation and hence they are said to display ‘special-cause variation’ – that is, where the trust’s rate diverges significantly from the national rate.
Data points falling above the upper 99.8% Poisson control limit are said to be significantly ‘higher than expected’, data points falling below the lower 99.8% Poisson control limit are said to be significantly ‘lower than expected’, data points falling between the lower 99.8% Poisson control limit and the upper 99.8% Poisson control limit are said to be ‘within expected range’.
Note
Superspell, a group of spells linked by transfer.
Deaths in low risk diagnosis groups
Metric
Deaths per 1000 spells for conditions normally associated with a very low rate of mortality.
Denominator
Spells with a primary diagnosis associated with a low mortality diagnosis group where the mortality rate has been shown to be consistently below 0.5%.
Exclusions:
-
Spells with a diagnosis code for trauma, immunocompromised state or cancer in any diagnosis field.
-
Admission age under 19 (ages 18 and under).
-
Spells with an ICD-10 code R296 (‘Tendency to fall, not elsewhere classified’) in any position.
Numerator
Denominator spells with method of discharge as death.
DISMETH:
4. Died.
Data sources
SUS–CDS (April 2012–March 2013).
Statistical methods
-
To interpret the performance of a trust on a crude rate indicator, the data point is compared against the national crude rate.
-
Control limits: control limits tell us the range of values that are consistent with random or chance variation. Data points falling within the control limits are consistent with random or chance variation and are said to display ‘common-cause variation’; for data points falling outside the control limits, chance is an unlikely explanation and hence they are said to display ‘special-cause variation’ – that is, where the trust’s rate diverges significantly from the national rate.
Data points falling above the upper 99.8% binomial control limit are said to be significantly ‘higher than expected’, data points falling below the lower 99.8% binomial control limit are said to be significantly ‘lower than expected’, data points falling between the lower 99.8% binomial control limit and the upper 99.8% binomial control limit are said to be ‘within expected range’.
Deaths after surgery
Metric
The ratio of the observed number of deaths following surgery with complications of care to the expected number, multiplied by 100.
Denominator
Elective surgical spells, defined by a surgical HRG and an OPCS code for an operating room procedure in any procedure field, for which a diagnosis code indicating potential complications of care is present in any secondary field; and emergency surgical spells, defined by a surgical HRG and an OPCS code for an operating room procedure where the principal operating room procedure took place within 2 days of admission, for which a diagnosis code indicating potential complications of care is present in any secondary field.
Inclusions
Elective admission
ADMIMETH:
11. Elective: from waiting list.
12. Elective: booked.
13. Elective: planned.
Emergency admission where the principal operating room procedure took place within 2 days of admission
ADMIMETH:
21. Emergency: via Accident and Emergency (A&E) services, including the casualty department of the provider.
22. Emergency: via general practitioner (GP).
23. Emergency: via Bed Bureau, including the Central Bureau.
24. Emergency: via consultant outpatient clinic.
28. Emergency: other means, including patients who arrive via the A&E department of another healthcare provider.
Discharge age > 18 years and < 90 years.
Exclusions
Spells where the patient has an immediately subsequent spell in another acute trust or where the spell is the final spell of the superspell and the discharge destination indicates an external transfer
DISDEST:
49. NHS other hospital provider – high security psychiatric accommodation.
50. NHS other hospital provider – medium secure unit (from 1999–2000).
51. NHS other hospital provider – ward for general patients or the younger physically disabled.
52. NHS other hospital provider – ward for maternity patients or neonates.
53. NHS other hospital provider – ward for patients who are mentally ill or have learning disabilities.
When the record is an emergency admission, the following Office of Population and Census Survey codes and Health Resource Groups 3.5 codes do not qualify for the denominator of this metric:
OPCS codes:
K49. Transluminal balloon angioplasty of coronary artery.
K50. Other therapeutic transluminal operations on coronary artery.
K75. Percutaneous transluminal balloon angioplasty and insertion of stent into coronary artery HRG 3.5 codes.
E15. Percutaneous Coronary Intervention.
Observed
Denominator spells with method of discharge as death.
DISMETH:
4. Died.
Expected
Expected number of deaths is derived from logistic regression, adjusting for factors to indirectly standardise for differences in case-mix.
Data sources
SUS – CDS (April 2012 – March 2013).
Statistical methods
-
Logistic regression: expected number of deaths is derived from logistic regression, adjusting for factors to indirectly standardise for differences in case-mix. Adjustments are made for:
-
sex
-
age on admission (in 5-year bands up to 90+ years)
-
admission method (non-elective or elective)
-
socioeconomic deprivation quintile of the area of residence of the patient (based on the Carstairs Index)
-
comorbidities (categorised Charlson Comorbidity Score).
-
-
Relative risk: the ratio is calculated by dividing the actual number of deaths by the expected number and multiplying the figure by 100. It is expressed as a relative risk, where a risk rating of 100 represents the national average. If the trust has a relative risk of 100, the number of patients who died is exactly as it would be expected taking into account the standardisation factors. A relative risk above 100 means more patients died than would be expected; one below 100 means that fewer than expected died.
-
Control limits: control limits tell us the range of values that are consistent with random or chance variation. Data points falling within the control limits are consistent with random or chance variation and are said to display ‘common-cause variation’; for data points falling outside the control limits, chance is an unlikely explanation and hence they are said to display ‘special-cause variation’ – that is, where the trust’s rate diverges significantly from the national rate.
Data points falling above the upper 99.8% Poisson control limit are said to be significantly ‘higher than expected’, data points falling below the lower 99.8% Poisson control limit are said to be significantly ‘lower than expected’, data points falling between the lower 99.8% Poisson control limit and the upper 99.8% Poisson control limit are said to be ‘within expected range’.
Notes
For emergency admissions, the principal operating room procedure date may occur within the first two episodes of the spell, to capture all procedures that took place within two days of the admission date.
Based on Agency for Healthcare Research and Quality Patient Safety Indicators. Translated by the Dr Foster Unit at Imperial College in collaboration with the Care Quality Commission (formerly the Healthcare Commission).
Hospital Standardised Mortality Ratio for emergency admissions (weekend)
Metric
The ratio of the observed number of in-hospital deaths following weekend emergency admissions with a HSMR diagnosis to the expected number of deaths, multiplied by 100, at trust level.
Denominator
Emergency spells with a primary dominant diagnosis of any of the 56 CCS groups that comprise the HSMR basket and an emergency admission on Saturday or Sunday, linked into superspells.
Emergency admissions are defined using the following ADMIMETH codes:
21 Emergency: via A&E services, including the casualty department of the provider.
22 Emergency: via GP.
23 Emergency: via Bed Bureau, including the Central Bureau.
24 Emergency: via consultant outpatient clinic.
28 Emergency: other means, including patients who arrive via the A&E department of another healthcare provider.
Observed
Denominator superspells with method of discharge as death (DISMETH = 4,5).
Deaths are assigned to every provider within the superspell.
Expected
The expected number of in-hospital deaths derived from logistic regression, adjusting for factors to indirectly standardise for differences in case mix.
Data sources
SUS–CDS for the financial year 2012/13.
Statistical methods
-
Logistic regression: expected number of in-hospitals deaths derived from logistic regression, adjusting for factors to indirectly standardise for differences in case mix. Adjustments are made for:
-
sex
-
age on admission (in 5-year bands up to 90+ years)
-
interactions between age on admission (in 5-year bands up to 90+ years) and Charlson Comorbidity Score
-
admission method (non-elective or elective)
-
socioeconomic deprivation quintile of the area of residence of the patient (based on the Carstairs Index)
-
diagnosis/procedure subgroup
-
comorbidities (based on Charlson Comorbidity Score)
-
number of previous emergency admissions
-
year of discharge (financial year)
-
palliative care (if any episode in the spell has the treatment function code 315 or contains ICD-10 code Z515 in any of the diagnoses fields)
-
month of admission
-
source of admission.
-
-
Relative risk: the ratio is calculated by dividing the actual number of deaths by the expected number and multiplying the figure by 100. It is expressed as a relative risk, where a risk rating of 100 represents the national average. If the trust has a HSMR of 100, the number of patients who died was exactly as would be expected taking into account the standardisation factors. A HSMR above 100 means more patients died than would be expected; one below 100 means that fewer than expected died.
-
Control limits: control limits tell us the range of values that are consistent with random or chance variation. Data points falling within the control limits are consistent with random or chance variation and are said to display ‘common-cause variation’; for data points falling outside the control limits, chance is an unlikely explanation and hence they are said to display ‘special-cause variation’ – that is, where the trust’s rate diverges significantly from the national rate.
Data points falling above the upper 99.8% Poisson control limit are said to be significantly ‘higher than expected’, data points falling below the lower 99.8% Poisson control limit are said to be significantly ‘lower than expected’, data points falling between the lower 99.8% Poisson control limit and the upper 99.8% Poisson control limit are said to be ‘within expected range’.
Notes
The HSMR basket of CCS groups accounts for approximately 80% of all in-hospital deaths in England.
See ‘HSMR Toolkit’ for full methodological detail.
Hospital Standardised Mortality Ratio for emergency admissions (weekday)
Metric
The ratio of the observed number of in-hospital deaths following weekday emergency admissions with a HSMR diagnosis to the expected number of deaths, multiplied by 100, at trust level.
Denominator
Emergency spells with a primary dominant diagnosis of any of the 56 CCS groups that comprise the HSMR basket and an emergency admission on Monday, Tuesday, Wednesday, Thursday or Friday, linked into superspells.
Emergency admissions are defined using the following ADMIMETH codes:
21 Emergency: via A&E services, including the casualty department of the provider.
22 Emergency: via GP.
23 Emergency: via Bed Bureau, including the Central Bureau.
24 Emergency: via consultant outpatient clinic.
28 Emergency: other means, including patients who arrive via the A&E department of another healthcare provider.
Observed
Denominator superspells with method of discharge as death (DISMETH = 4,5).
Deaths are assigned to every provider within the superspell.
Expected
The expected number of in-hospital deaths derived from logistic regression, adjusting for factors to indirectly standardise for differences in case mix.
Data source
SUS–CDS for the financial year 2012/13.
Statistical methods
-
Logistic regression is used to calculate the expected number of in-hospitals deaths. To indirectly standardise for differences in patient case-mix, the model is adjusted for the following factors:
-
sex
-
age on admission (in 5-year bands up to 90+ years)
-
interactions between age on admission (in 5-year bands up to 90+ years) and Charlson Comorbidity Score
-
admission method (non-elective or elective)
-
socioeconomic deprivation quintile of the area of residence of the patient (based on the Carstairs Index)
-
diagnosis/procedure subgroup
-
comorbidities (based on Charlson Comorbidity Score)
-
number of previous emergency admissions
-
year of discharge (financial year)
-
palliative care (if any episode in the spell has the treatment function code 315 or contains ICD-10 code Z515 in any of the diagnoses fields)
-
month of admission
-
source of admission.
-
-
Relative risk: the ratio is calculated by dividing the actual number of deaths by the expected number and multiplying the figure by 100. It is expressed as a relative risk, where a risk rating of 100 represents the national average. If the trust has a HSMR of 100, the number of patients who died was exactly as would be expected taking into account the standardisation factors. A HSMR above 100 means more patients died than would be expected; one below 100 means that fewer than expected died.
-
Control limits: control limits tell us the range of values which are consistent with random or chance variation. Data points falling within the control limits are consistent with random or chance variation and are said to display ‘common-cause variation’; for data points falling outside the control limits, chance is an unlikely explanation and hence they are said to display ‘special-cause variation’ – that is, where the trust’s rate diverges significantly from the national rate.
Data points falling above the upper 99.8% Poisson control limit are said to be significantly ‘higher than expected’, data points falling below the lower 99.8% Poisson control limit are said to be significantly ‘lower than expected’, data points falling between the lower 99.8% Poisson control limit and the upper 99.8% Poisson control limit are said to be ‘within expected range’.
Notes
The HSMR basket of CCS groups accounts for approximately 80% of all in-hospital deaths in England.
See ‘HSMR Toolkit’ for full methodological detail.
28-day readmissions
Metric
The ratio of the observed number of non-elective admissions with an emergency readmission within 28 days of discharge to the expected number, multiplied by 100.
Denominator
Non-elective spells where the day of discharge was a weekday, linked into superspells.
Observed
Denominator superspells with a readmission to any provider within 28 days of discharge where readmission is an emergency admission:
ADMIMETH:
21. Emergency – via A&E.
22. Emergency – via GP.
23. Emergency – via Bed Bureau.
24. Emergency – via Outpatient clinic.
28. Emergency – via other means.
Readmission date minus discharge date < 28 days.
Expected
Expected number of 28-day emergency readmissions derived from logistic regression, adjusting for factors to indirectly standardise for differences in case mix.
Data sources
SUS–CDS for the financial year 2012/13.
Statistical methods
-
Logistic regression: the expected number of readmissions is derived from logistic regression, adjusting for factors to indirectly standardise for differences in case mix. Adjustments are made for:
-
sex
-
age on admission (in 5-year bands up to 90+ years)
-
interactions between age on admission (in 5-year bands up to 90+ years) and Charlson Comorbidity Score
-
admission method (non-elective or elective)
-
socioeconomic deprivation quintile of the area of residence of the patient (based on the Carstairs Index)
-
diagnosis/procedure subgroup
-
comorbidities (based Charlson Comorbidity Score)
-
number of previous emergency admissions
-
year of discharge (financial year)
-
palliative care (if any episode in the spell has the treatment function code 315 or contains ICD-10 code Z515 in any of the diagnoses fields)
-
month of admission
-
source of admission.
-
-
Relative risk: the ratio is calculated by dividing the actual number of readmissions by the expected number and multiplying the figure by 100. It is expressed as a relative risk, where a risk rating of 100 represents the national average. If the trust has a standardised readmission ratio of 100, that means that the number of patients who were readmitted is exactly as would be expected taking into account the standardisation factors. A standardised readmission ratio above 100 means more patients were readmitted than would be expected; one below 100 means that fewer than expected were readmitted.
-
Control limits: control limits tell us the range of values that are consistent with random or chance variation. Data points falling within the control limits are consistent with random or chance variation and are said to display ‘common-cause variation’; for data points falling outside the control limits, chance is an unlikely explanation and hence they are said to display ‘special-cause variation’ – that is, where the trust’s rate diverges significantly from the national rate.
-
Data points falling above the upper 99.8% Poisson control limit are said to be significantly ‘higher than expected’, data points falling below the lower 99.8% Poisson control limit are said to be significantly ‘lower than expected’, data points falling between the lower 99.8% Poisson control limit and the upper 99.8% Poisson control limit are said to be ‘within expected range’.
Meticillin-resistant Staphylococcus aureus infections
Data on MRSA infections were obtained from the Health Protection Agency (HPA) mandatory surveillance reports, available at the following website: www.hpa.org.uk/web/HPAweb&HPAwebStandard/HPAweb_C/1254510675444.
Data used for analysis in this study were the sum of MRSA infections reported in financial year 2012/13 for each trust, found in Table 6.
Meticillin-sensitive Staphylococcus aureus infections
Data on Meticillin-sensitive Staphylococcus aureus (MSSA) infections were obtained from the Health Protection Agency (HPA) mandatory surveillance reports, available at the following website: www.hpa.org.uk/web/HPAweb&HPAwebStandard/HPAweb_C/1296684635609.
Data used for analysis in this study were the sum of MSSA infections reported in financial year 2012/13 for each trust, found in Table 8.
C. difficile infections
Data on C. difficile infections were obtained from the Health Protection Agency (HPA) mandatory surveillance reports, available at the following website: www.hpa.org.uk/web/HPAweb&HPAwebStandard/HPAweb_C/1254510678961.
Data used for analysis in this study were the sum of C. difficile infections reported in financial year 2012/13 for each trust, found in Table 3.
Escherichia coli infections
Data on Escherichia coli infections were obtained from the Health Protection Agency (HPA) mandatory surveillance reports, available at the following website: www.hpa.org.uk/web/HPAweb&HPAwebStandard/HPAweb_C/1254510678961.
Data used for analysis in this study were the sum of E. coli infections reported in financial year 2012/13 for each trust, found in Table 10.
Organisation patient safety incidents
Organisation patient safety incidents data were obtained from the NHS National Reporting and Learning System at the following website: www.nrls.npsa.nhs.uk/patient-safety-data/organisation-patient-safety-incident-reports/.
Supporting information about this data set can be found here: www.nrls.npsa.nhs.uk/resources/?entryid45 = 135145.
The data used in this study were for the time period October 2012 to March 2013. Two types of data were included for organisational patient safety incidents:
-
volume of organisational patient safety incidents: the total number of organisational patient safety incidents per trust over the time period
-
rate of organisational patient safety incidents: number of organisational patient safety incidents divided by the number of admissions multiplied by 100 per trust over the time period.
Day case to inpatient conversion rate
Day case to inpatient conversion rates have been calculated by dividing the number of patients who were intended to be managed as a day case but had a length of stay greater than zero by the total number of day cases. This rate was then multiplied by 100.
This metric was calculated for each BSAQ respondent trust for the financial year 2012/13.
Never events
Never-events data are not freely available to the public; however, the BBC published NHS never-events data for calendar years 2009 to 2012 on their website at this address: www.bbc.co.uk/news/health-22466496.
Analysis for this study only used never events from calendar year 2012. The total number of never events that occurred at each trust in 2012 was calculated by summing the number of incidents reported in the spreadsheet. If a trust did not appear in the spreadsheet, it was assumed that no never events occurred at that trust during calendar year 2012.
Appendix 8 Board observations: time spent on different activities
Skye
Meeting 1
| Topic of conversation | Primary coding (foreground) | Secondary coding (background) | Time spent (minutes) |
|---|---|---|---|
| Minutes | Procedure | Board administration | 1 |
| Chairperson report CCGs | Commissioning | Monologue update | 1 |
| Chairperson report ward visits | Quality | Monologue update | 1 |
| CEO report | Reconfiguration | Monologue update | 8, 6 |
| CEO report | Strategy | Monologue update | 1 |
| Waiting times | Capacity and demand | Performance targets | 12, 10 |
| Complaints | Safety | Quality | 15 |
| Falls | Safety | Quality | 3 |
| HSMR coding | Safety | Performance measurement | 3, 3 |
| 24/7 care | Quality | Safety | 10 |
| Staff sickness | HR | Cost savings | 15 |
| C. difficile | Safety | Quality | 15 |
| A&E operational performance | Capacity and demand | Performance targets | 15 |
| Safety performance | Safety | Risk | 10 |
| C. difficile penalties (finance) | Safety | Finance | 4 |
| Tariff emergency admissions | Finance | Performance measurement | 8 |
| Data clarification (finance) | Finance | Performance measurement | 3 |
| HR procedures (interview panels) | HR | Recruitment | 15 |
| Policy summary (CEO report) | Strategy | Monologue update | 6 |
| Expenses policy | HR | Cost savings | 23 |
| Subcommittees | Board administration | 1 | |
| Actions from previous meeting | Board administration | 3 | |
| Governor meeting summary | Public involvement | Quality | 3 |
| Summary of meeting | Board summary of meeting | Board administration | 4 |
| Total (including breaks) | 226 | ||
Meeting 2
| Topic of conversation | Primary coding (foreground) | Secondary coding (background) | Time spent (minutes) |
|---|---|---|---|
| Minutes | Board administration | 6 | |
| Chairperson report | Governor elections | Monologue update | 1 |
| Chairperson report | Commissioning | Monologue update | 2 |
| CEO report | H&SC Act chairperson report | Monologue update | 1 |
| CEO report | Board administration | Monologue update | 5 |
| Appointments | HR | Recruitment | 2 |
| Reconfiguration | Reconfiguration | Strategic partnerships | 5 |
| A&E performance | Capacity and demand | Performance targets | 4 |
| Pathway review | Safety | Performance measurement | 15 |
| Safety performance | Safety | Risk | 10 |
| Friends and family test | Quality | Performance measurement | 8 |
| Call for more in-depth discussion | Strategy | 5 | |
| Pathway review coding process | Safety | Performance measurement | 10 |
| C. difficile | Safety | Performance targets | 23 |
| A&E demand linked to bed plan | Capacity and demand | Patient flow (beds) | 20 |
| A&E demand linked to 30% tariff | Capacity and demand | Finance | 10 |
| Finance underperformance | Finance | Performance targets | 6 |
| Everything Counts policy document | Performance measurement | Strategy | 12 |
| Strategy plan development | Strategy | 10 | |
| Policy and strategy update (monitor) | Performance measurement | Regulation | 6 |
| Subcommittee business (audit) | Board administration | 30s | |
| Actions | Board administration | 3 | |
| Board summary of meeting | Board administration | 7 | |
| Governor response | Public involvement | Board administration | 3 |
| Total (including breaks) | 192 | ||
Meeting 3
| Topic of conversation | Primary coding (foreground) | Secondary coding (background) | Time spent (minutes) |
|---|---|---|---|
| Apologies, minutes | Board administration | 3 | |
| Matters arising | Board administration | 3 | |
| Chairperson report | Board administration | Monologue update | 5 |
| CEO report | Board administration | Monologue update | 1 |
| CEO report | Quality | Risk | 8 |
| CEO report reconfiguration | Reconfiguration | Strategic partnerships | 4 |
| CEO report Francis Inquiry | Quality and safety | Monologue update | 6 |
| Organisational performance no staff cover | Capacity and demand | HR | 13 |
| Mortality performance | Safety | Risk | 12 |
| Complaints data questioned | Quality | Performance measurement | 5 |
| Report summary pressure ulcers | Safety | Performance targets | 2 |
| Report summary FFT | Quality | Performance measurement | 90 |
| HR sickness levels | HR | Workforce | 1 |
| Cancer service development | Strategy | 1 | |
| Staff survey findings | HR | Workforce | 15 |
| C. difficile | Safety | Performance targets | 21 |
| A&E capacity (demand, beds) | Capacity and demand | Patient flow (beds) | 20 |
| Central support unit cash finance | Finance | Performance measurement | 13 |
| Tariff | Finance | Performance measurement | 5 |
| CEO policy summary | Policy update | Monologue | 3 |
| Reconfiguration proposals | Reconfiguration | Risk | 5 |
| Safety at particular sites | Safety | Risk | 9 |
| CEO monitor compliance | Regulation | Performance measurement | 5 |
| Actions | Board administration | 30 | |
| Governor response | Public involvement | Board administration | 15 |
| Total (including breaks) | 104 | ||
Meeting 4
| Topic of conversation | Primary coding (foreground) | Secondary coding (background) | Time spent (minutes) |
|---|---|---|---|
| Minutes | Board administration | 1 | |
| Matters arising staff levels | HR | 3 | |
| Matters arising | Safety | 2 | |
| Chairperson report | Governors | Monologue update | 1 |
| Chairperson report | Quality and safety | Monologue update | 3 |
| Chairperson report | Regulation | Monologue update | 7 |
| CEO report Francis response | Quality | Safety | 30 |
| Coding issues monitor HSMR | Safety | Performance measurement | 15 |
| Quality report | Safety | Performance targets | 10 |
| HR sickness levels | HR | Workforce | 5 |
| HSMR presentation | Safety | Performance measurement | 23 |
| Coding | Safety | Performance measurement | 10 |
| C. difficile | Safety | Performance targets | 15 |
| CQC Quality and Risk profiles | Quality | Performance measurement | 4 |
| A&E beds | Capacity and demand | Patient flow (beds) | 45 |
| C. difficile penalties (finance) | Safety | Finance | 5 |
| Tariff | Finance | Performance measurement | 10 |
| Policy board assurance framework | Risk | Regulation | 10 |
| Monitor compliance | Regulation | Performance measurement | 3 |
| Strategy development | Strategy | Monologue update | 10 |
| Policy information | Strategy | Monologue update | 2 |
| Committee update | Board administration | 5 | |
| Actions | Board administration | 10 | |
| Governors | Public involvement | 7 | |
| Total (including breaks) | 270 | ||
Lewis
Meeting 1
| Topic of conversation | Primary coding (foreground) | Secondary coding (background) | Time spent (minutes) |
|---|---|---|---|
| Pre-board briefing | 30 | ||
| Public Finance Initiative issues | PFI | Estates | 40 |
| Service reconfiguration | Reconfiguration | Risk | 17 |
| Any qualified provider | Commissioning | Procurement | 11 |
| C. difficile target/penalty | Safety | Finance | 9 |
| Academic Health Science Network | Strategic partnerships | 5 | |
| Provider competition | Competition | Risk | 9 |
| Multiprofessional education and training funding reduction | Education | Risk | 4 |
| Women’s services | Quality | Risk | 5 |
| CQC visit to neonatal | Quality | Risk | 2 |
| A&E finance 30% tariff | Finance | Performance measurement | 3 |
| C. difficile (finance) | Safety | Finance | 7 |
| Friends and family | Quality | Performance measurement | 12 |
| Falls | Safety | Risk | 7 |
| Board self-certificate | Regulation | Audit | 3 |
| Health Care Supply Association | Strategy | Board administration | 1 |
| Medical revalidation | Workforce | Board administration | 2 |
| CEO report | Board administration | Monologue update | 9 |
| C. difficile | Safety | Finance | 5 |
| Quality report | Safety | Quality | 11 |
| CQC score card | Quality | Performance measurement | 4 |
| Procurement | Procurement | Commissioning | 2 |
| Finance surplus | Finance | Risk | 14 |
| Land sale | Estates | Finance | 12 |
| Drug funding | Medicines | Finance | 1 |
| Chairperson report | Monologue update | 3 | |
| Total (excluding pre-board briefing) | 211 | ||
Meeting 2
| Topic of conversation | Primary coding (foreground) | Secondary coding (background) | Time spent (minutes) |
|---|---|---|---|
| Apologies, welcome | 2 | ||
| PFI education | PFI | Estates | 18 |
| Car park development | PFI | Estates | 10 |
| Reconfiguration | Reconfiguration | Risk | 10 |
| AQP | Commissioning | Procurement | 2 |
| AHSN | Strategic partnerships | Board administration | 9 |
| C. difficile penalties | Safety | Finance | 8 |
| CQC | Quality | Risk | 1 |
| Reconfiguration | Reconfiguration | Risk | 3 |
| Clinician accused of fraud | Finance | Criminality | 1 |
| Governors | Safety | Risk | 7 |
| Friends and family test | Quality | Performance measurement | 9 |
| 24/7 care | Quality | Safety | 5 |
| Local education and training boards commissioning arrangements | Commissioning | Education | 2 |
| CEO report | Commissioners, reconfiguration | Monologue update | 8 |
| HCAIs: C. difficile and MRSA | Safety | Performance targets | 11 |
| CQC inspection preparation | Quality | Risk | 4 |
| Finance readmissions, RTT | Finance | Performance targets | 5 |
| Quality report, finance falls penalties, sharps needles, ulcers, lost data | Quality | Risk | 10 |
| CQUIN, target performance, dashboard readings | Quality | Performance measurement | 15 |
| Finance CQUIN, C. difficile | Finance | Performance measurement | 4 |
| Finance capital investment | Finance | Risk | 4 |
| Appraisals | HR | Workforce | 2 |
| Land sale | Estates | Finance | 10 |
| Water system problems | Safety | Risk | 5 |
| HSCA | Board administration | Public engagement | 3 |
| Total (including breaks) | 182 | ||
Meeting 3
| Topic of conversation | Primary coding (foreground) | Secondary coding (background) | Time spent (minutes) |
|---|---|---|---|
| Minutes | Board administration | Board administration | 1 |
| Drug costs | Medicines | Finance | 10 |
| PFI building | PFI | Estates | 21 |
| Reconfiguration | Reconfiguration | Risk | 9 |
| Procurement landscape | Procurement | Board administration | 5 |
| AHSN | Strategic partnerships | Board administration | 3 |
| C. difficile | Safety | Performance measurement | 7 |
| HSCA governor elections | Governors | Board administration | 12 |
| Women’s services | Quality | Risk | 3 |
| Research and development presentation and discussion | Research and development | Finance | 20 |
| Commissioning landscape | Commissioning | 28 | |
| GP surgery competition | Competition | Estates | 37 |
| Finance litigation costs | Finance | Litigation | 5 |
| CEO report | Monologue update | 10 | |
| HCAI coding disputes | Safety | Performance measurement | 15 |
| RTT performance (finance) | Capacity and demand | Performance targets | 7 |
| C. difficile penalties (finance) | Safety | Finance | 10 |
| Water system | Safety | Risk | 2 |
| New MD appointed | HR | Recruitment | 8 |
| Total (including breaks) | 210 | ||
Meeting 4
| Topic of conversation | Primary coding (foreground) | Secondary coding (background) | Time spent (minutes) |
|---|---|---|---|
| Pre-board briefing DVD | Patient experience | Quality | 25 |
| Matters arising | Board administration | 1 | |
| PFI building | PFI | Estates | 15, 3 |
| Reconfiguration | Reconfiguration | Risk | 10 |
| AQP | Commissioning | Procurement | 6 |
| AHSN | Strategic partnerships | 3 | |
| C. difficile penalties | Safety | Finance | 11 |
| Land sale | Estates | Finance | 5 |
| Electronic patient record | Information systems | IT | 30 |
| Francis response | Quality | Safety | 28 |
| Information encryption | Data protection | Board administration | 4 |
| Annual plan development | Strategy | Board administration | 1 |
| Contract tariff negotiation with commissioners | Commissioning | Finance | 15 |
| HCAI results | Quality | Safety | 10 |
| Quality report | Safety | Quality | 10 |
| CAT | Quality | Risk | 10 |
| Provider competition | Provider development | Estates | 6 |
| Serious untoward incident | Safety | Risk | 14 |
| CEO report | CCGs, reconfiguration, Health and Wellbeing Board | Monologue for information | 1 |
| Business performance RTT | Capacity and demand | Performance targets | 9 |
| Finance | Finance | 6 | |
| Appointments | HR | Recruitment | 1 |
| Land sale | Estates | Finance | 6 |
| Primary care | Market development | Estates | 21 |
| CEO update | Board administration | Monologue update | 13 |
| Postgraduate training budget reduced | Education | Finance | 8 |
| Total (excluding pre-board briefing) | 242 | ||
Islay
Meeting 1
| Topic of conversation | Primary coding (foreground) | Secondary coding (background) | Time spent (minutes) |
|---|---|---|---|
| Patient story | Patient experience | Quality | 12 |
| QI | Quality | Performance measurement | 45 |
| QI update | Quality (CQI) | Performance measurement | 10 |
| HCAI | Safety | Performance targets | - |
| Chairperson report | Board administration | Monologue update | 5 |
| CEO report | Board administration | Monologue update | 5 |
| CEO report | Capacity and demand | Patient flow (self-referrals) | 11 |
| Strategic Advisory Group | Strategy | Reconfiguration | – |
| Monitor compliance | Regulation | Performance measurement | 1 |
| Finance report | Finance | Cost savings | 8 |
| Finance report (trauma development) | Finance | Recruitment | 5 |
| Corporate Governance Framework | For information | Board administration | 1 |
| Terms of reference | For information | Board administration | 3 |
| Early action research contact | Commissioning | Risk | 5 |
| Audit Committee minutes | For information | 1 | |
| Integrated Care Board update | Integrated care | Strategy | 5 |
| Total (including breaks) | 142 | ||
Meeting 2
| Topic of conversation | Primary coding (foreground) | Secondary coding (background) | Time spent (minutes) |
|---|---|---|---|
| Part one | |||
| Patient story | Patient experience | Quality | 4 |
| Presentation community nursing | Community care | End-of-life care | 35 |
| Operating theatres | Safety | Performance measurement | 25 |
| HCAI report C. difficile | Safety | Performance targets | 85 |
| CEO report | Strategy | Monologue update | 6 |
| CEO report | Staff ratios | Workforce | 4 |
| Annual plan | Strategy | 25 | |
| Board assurance framework | Risk | Performance measurement | 55 |
| Part two | |||
| Matters arising | Commissioning | 5 | |
| CEO report | Reconfiguration | Risk | 33 |
| Firearm found | Risk | Criminality | 2 |
| Change Board meeting frequency | Board administration | Strategy | 49 |
| Finance | Finance | Estates | 8 |
| Away-day Francis reaction | Quality | Safety | 10 |
| SUI | Safety | Risk | 20 |
| Total (including breaks) | 304 | ||
Meeting 3
| Topic of conversation | Primary coding (foreground) | Secondary coding (background) | Time spent (minutes) |
|---|---|---|---|
| Part two | |||
| Patient story | Patient experience | Quality | 12 |
| Chairperson report | Board administration | Monologue update | 6 |
| Minutes | Board administration | Patient experience | 6 |
| Liverpool Care Pathway | Quality | Patient experience | 21 |
| Quality dashboard | Quality | Performance measurement | 14 |
| Falls | Safety | Performance measurement | 11 |
| Infection control | Safety | Performance measurement | 5 |
| CEO report | Quality | Regulation | 4 |
| CEO report | Quality | Strategic partnerships | 4 |
| CEO report | Reconfiguration | Capacity and demand | 16 |
| Integrated care | Strategic partnerships | Reconfiguration | 20 |
| Business development report | Regulation | Quality | 4 |
| Environmental health kitchens | Risk | Quality | 20 |
| Patient discharge letters | Risk | Quality | 5 |
| Finance report | Finance | Performance targets | 4 |
| Finance report | Finance | Income streams | 2 |
| Finance | Capacity and demand | Patient experience | 5 |
| Chair report | Board administration | Monologue update | 3 |
| EARC | Risk | Monologue update | 4 |
| Audit communication | Board administration | Board administration | 2 |
| Part two | |||
| Matters arising | Finance | Estates | 1 |
| Matters arising | Reconfiguration | Risk | 18 |
| Finance report | Finance | Risk | 11 |
| Environmental health | Risk | Quality | 29 |
| Matters arising | Procurement | Contracting | 2 |
| Board action sheet | Strategy | Reconfiguration | 18 |
| Total (including breaks) | 305 | ||
Meeting 4
| Topic of conversation | Primary coding (foreground) | Secondary coding (background) | Time spent (minutes) |
|---|---|---|---|
| Part one | |||
| Patient story | Patient experience | Quality | 5 |
| Introductions | Board administration | Board administration | 1 |
| Chairperson report | Board administration | Monologue | 3 |
| CEO report | Integrated care | Update | 2 |
| CEO report | Kitchens | Update | 7 |
| Nurse presentation end-of-life care | Patient experience | Quality | 14 |
| Orthopaedics update | Quality | Performance measurement | 26 |
| Community care | Performance measurement | Risk | 10 |
| QI presentation | Safety | Performance measurement | 5 |
| MD report | Safety | Performance measurement | 10 |
| CEO report | Regulation | Quality | 13 |
| CEO report | Reconfiguration | Quality | 22 |
| Finance report | Finance | Monologue | 5 |
| HR report | HR | Workforce | 15 |
| People strategy | HR | Strategy | 6 |
| Board assurance | Risk | Estates | 4 |
| Governance | Risk | Safety | 15 |
| Part two | |||
| Monitor | Regulation | Performance measurement | 8 |
| Integrated care | Strategy | Reconfiguration | 43 |
| Integrated care | Strategy | Reconfiguration | 15 |
| Total (including breaks) | 235 | ||
Arran
Meeting 1
| Topic of conversation | Primary coding (foreground) | Secondary coding (background) | Time spent (minutes) |
|---|---|---|---|
| Apologies, minutes | Board administration | 4 | |
| Matters arising | Board administration | 0 | |
| Capacity and demand | Quality | Service reconfiguration | 30 |
| Chairperson report (visit on use of social media) | Monologue update | Miscellaneous | 1 |
| CEO report | |||
| A&E performance | Quality | Performance targets | 7 |
| Dr Foster performance rankings | Quality | Performance targets | 9 |
| Public Accounts Committee | Finance | 5 | |
| National cancer patient experience survey | Quality | Performance measurement | 4 |
| Monitor KPI governance ratings | Safety | Performance targets | 10 |
| Pressure ulcers | Quality | Performance targets | 11 |
| Performance report | |||
| 18-week breaches | Quality | Performance targets | 5 |
| C. difficile | Quality | Performance targets | 3 |
| Workforce | HR | Safety | 1 |
| Quality report | |||
| C. difficile | Quality and risk | Performance targets | 3 |
| Clinical audit | Quality | 1 | |
| Finance and contracting report | 0 | ||
| Financial performance | Finance | Performance measurement | 2 |
| Tariff | Finance | Quality | 0 |
| HR and communication report | 2 | ||
| Review of occupational health services | Service reconfiguration | Quality | 4 |
| Safeguarding | Quality | 0 | |
| Audit report | Finance and performance | 8 | |
| Total (including breaks) | 102 | ||
Meeting 2
| Topic of conversation | Primary coding (foreground) | Secondary coding (background) | Time spent (minutes) |
|---|---|---|---|
| Apologies, minutes | Board administration | 1 | |
| Matters arising | Board administration | 1 | |
| Chairperson report | Monologue update | 2 | |
| CEO report | |||
| Francis report | Quality and safety | 15 | |
| Emergency admissions | Quality | Finance | 3 |
| CQC visit neurology | Quality and safety | Performance monitoring | 2 |
| Clinical negligence scheme for trusts maternity | Risk | Finance | 1 |
| Liverpool Care Pathway | Quality | Service delivery | 6 |
| Information governance | Risk | 4 | |
| Performance report | 15 | ||
| Genitourinary waiting time breaches | Quality | Performance measurement | 8 |
| ‘Safety thermometer’ | Safety | Performance measurement | 5 |
| Quality and safety report | Quality | 2 | |
| Finance and contracting report | Finance | Risk | 17 |
| HR report – consultant revalidation | HR | Appraisal | 5 |
| Audit report | |||
| Internal audit | Finance | 5 | |
| Whistleblowing | HR | Safety | 15 |
| Total (including breaks) | 80 | ||
Meeting 3
| Topic of conversation | Primary coding (foreground) | Secondary coding (background) | Time spent (minutes) |
|---|---|---|---|
| Apologies, minutes | Board administration | 1 | |
| Staff survey report | HR | Workforce | 27 |
| Chairperson report | Quality and safety | External visits | 5 |
| CEO report | Quality and safety | Performance management | 17 |
| Service development | Finance | 6 | |
| Strategy | Performance management | 5 | |
| Finance | Philanthropy | 19 | |
| Executive board report | Service development | Strategy | 6 |
| Research and development strategy | Research and development | Strategy | 19 |
| Maternity services | Service development | 1 | |
| CQC registration | Quality | Patient safety | 1 |
| Workforce | HR | 3 | |
| Performance report | Performance measurement | Patient safety | 12 |
| Quality and safety committee report | Quality | Patient safety | 5 |
| Finance and contracting report | Finance | 2 | |
| Total (including breaks) | 129 | ||
Meeting 4
| Topic of conversation | Primary coding (foreground) | Secondary coding (background) | Time spent (minutes) |
|---|---|---|---|
| Minutes | Board administration | 1 | |
| Matters arising | Board administration | 2 | |
| ND special presentation | |||
| Safe staffing | Patient safety | Quality | 32 |
| Chairperson report | |||
| Education development framework visit | Safety | Quality | 5 |
| Quality and safety report | Quality | Safety | 5 |
| CEO report | |||
| Monitor compliance | Safety | Performance indicators | 25 |
| Quality | Governance | 5 | |
| Executive board | |||
| Quality | Performance indicators | 7 | |
| Performance report | Patient safety | Performance measurement | 8 |
| HR report | HR | Workforce | 5 |
| Finance report | Finance | 10 | |
| Audit committee report | Finance | 5 | |
| Total (including breaks) | 90 | ||
Appendix 9 Project outputs/looking ahead
Alongside this report, four papers have already been prepared for publication and several further are likely to follow.
Papers published or currently under review
Millar R, Mannion R, Freeman T, Davies H. Hospital board oversight of quality and patient safety: a narrative review and synthesis of recent empirical research. Milbank Q 2013;91:738–70.
Mannion R, Davies H, Freeman T, Millar R, Jacobs J, Casteridis P. Overseeing oversight: hospital board governance of quality and safety in the English NHS. J Health Serv Res Policy 2015;20:9–16.
Freeman T, Millar R, Mannion R, Davies HTO. A dramaturgy of hospital board governance in the English NHS [published online ahead of print 4 August 2015]. Sociology Health Ill 2015.
Millar R, Freeman T, Mannion R. Effective hospital board oversight of patient safety: a stakeholder analysis exploring the role of trust and intelligence. BMC Health Serv Res 2015;15:196.
Glossary
- Dramaturgy
- A theatrical metaphor applied to the operation of social life. For Goffman (Frame Analysis. An Essay on the Organization of Experience. Boston, MA: Northeastern University Press; 1974), the framing of the stage – the separation of front of stage, backstage and audience, together with a reciprocal acceptance of the roles of audience and players – shapes the performativity of utterances onstage. In an extension of earlier work on the presentation of self (Goffman E. The Presentation of Self in Everyday Life. New York, NY: Doubleday; 1959) he applies this metaphor to the operation of social life, in which performativities are made possible through framing. Frames are essentially classification systems that actors use to order and make sense of diverse social phenomena, so that the performative potential of an utterance depends upon the frames available to actors within the specific setting.
- Eigenvalues
- Used in factor analysis and explain the proportion of variance explained by a given variable. With five variables, the sum of the eigenvalues will be 5. Sorting the factors by eigenvalue thus results in the first factor having the greatest importance (i.e. explaining the greatest amount of variance).
- Patient safety
- Safety of patients in the context of the presentation of avoidable errors and adverse effects to patients associated with health care.
- Performativity
- A technical term used in sociological analysis. It refers to the capacity of speech or other communication to constitute an action or perform an identity: a simultaneous ‘saying’ and ‘doing’ with creative potential which, once the intention of the utterance is recognised, requires others to act in accordance with its implications. Austin’s (How to Do Things with Words. Cambridge, MA: Harvard University Press; 1962) example is the phrase ‘I do’ when spoken within the context of a marriage ceremony; a phrase with implications beyond indicating acceptance and requiring the people exchanging the vows to act, and be acted upon by others, as a married couple from that point forward. Performative utterances are thus meaningful actions that create a social reality; in themselves they are neither true nor false.
List of abbreviations
- A&E
- accident and emergency
- BSAQ
- Board Self-Assessment Questionnaire
- CAT
- Clinical Assurance Toolkit
- CCG
- Clinical Commissioning Group
- CEO
- chief executive officer
- COO
- chief operating officer
- CQC
- Care Quality Commission
- CQUIN
- Commissioning for Quality and Innovation
- FT
- foundation trust
- GMC
- General Medical Council
- GP
- general practitioner
- HCAI
- heath-care-associated infection
- HR
- human resources
- HSMR
- Hospital Standardised Mortality Ratio
- ICD-10
- International Classification of Diseases, Tenth Edition
- IHI
- Institute for Healthcare Improvement
- IPC
- infection prevention and control
- KPI
- key performance indicator
- LA
- Litigation Authority
- MaPSaF
- Manchester Patient Safety Framework
- MD
- medical director
- MRSA
- meticillin-resistant Staphylococcus aureus
- NAAS
- Nursing Assessment and Accreditation System
- ND
- nursing director
- NED
- non-executive director
- NSG
- Nationalist Specialist Group
- NSS
- National NHS Staff Survey
- PCT
- primary care trust
- QI
- quality improvement
- QRP
- Quality Risk Profile
- RAG
- red/amber/green (traffic-light ratings system)
- SUS – CDS
- secondary user service – commissioning data sets
- TGI
- The Governance Institute (San Diego, CA, USA)
- TH
- teaching hospital
- VRE
- vancomycin-resistant enterococci