Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 11/2004/12. The contractual start date was in October 2012. The final report began editorial review in December 2014 and was accepted for publication in May 2015. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Ms Alison Faulker received consultancy fees for her role in the project. The authors declare no other competing interests.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2016. This work was produced by Simpson et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction, background and aims
The context and delivery of mental health care are diverging between the countries of England and Wales, although they retain points of common interest and hence provide a rich geographical comparison for research. Across England, the key vehicle for the provision of recovery-focused, personalised, collaborative mental health care is the care programme approach (CPA). The CPA is a form of case management introduced in England in 1991, then revised and refocused. 1 In Wales, the CPA was introduced in 20032 but it has now been superseded by The Mental Health [care and treatment planning (CTP)] Regulations (Mental Health Measure), a new statutory framework. 3 Data for England show that 403,615 people were on the CPA in 2011/12. 4 Centrally held CPA numbers supplied by the Corporate Analysis Team at the Welsh Government indicate 22,776 people in receipt of services as of December 2011, just 6 months prior to the introduction of CTP under the Mental Health Measure.
In both countries, the CPA/CTP requires providers to comprehensively assess health/social care needs and risks; to develop a written care plan (which may incorporate risk assessments, crisis and contingency plans, advanced directives, relapse prevention plans, etc.) in collaboration with the service user and carer(s); to allocate a care co-ordinator; and to regularly review care. Both the CPA and CTP processes are now also expected to reflect a philosophy of recovery and to promote personalised care,1,5 although interpretations of personalisation may vary between countries. 6
The concept of recovery in mental health was initially developed by service users and has led to disparate conceptualisations7 but broadly refers to ‘a way of living a satisfying, hopeful, and contributing life even with limitations caused by illness,’ while developing new purpose or meaning. 8(p. 527) The importance of addressing service users’ personal recovery alongside more conventional ideas of clinical recovery9 is now supported in guidance for all key professions. 10–13 To this has been added the more recent idea of personalisation. Underpinned by recovery concepts, this aims to see people and their families taking much more control over their own support and treatment options, alongside new levels of partnership and collaboration between service users and professionals. 14 Recovery and personalisation in combination require practitioners to tailor support and services to fit the specific needs of the individual and enable social integration through greater involvement of local communities.
Cochrane systematic reviews of case management including the CPA15 did not consider recovery-oriented outcomes and few studies are explicitly conducted into the practices of the CPA care planning and co-ordination. Early investigations in England prior to the refocus on recovery drew attention to the bureaucracy associated with care co-ordination which, combined with high caseloads, deflected practitioners from therapeutic interventions linked to positive outcomes. 16,17
National audits in England reported considerable local variation in implementation of the CPA, and despite improvements in performance, significant numbers of service users were not receiving care in line with guidelines. 18 A review conducted in Wales reflected concerns in risk assessment, care planning, unmet need and service planning, training, information requirements and systems, transfer of care arrangements, and leadership. 19 The authors concluded that there was a high risk that services were not effectively meeting users’ and carers’ needs and that significant improvement was required.
Service users appear to remain largely mystified by care planning and review processes. In a national quality survey of over 17,000 community mental health (CMH) service users across 65 English NHS trusts, 42% said that their care was co-ordinated under the CPA. 20 Over 90% of all respondents described their care as well organised and 83% of those on the CPA knew who their care co-ordinators were. Despite this, over half did not understand their care plans; only 16% had written copies; 20% said that their care plans did not set out their goals; and 11% said that their views had not been taken into account during care planning. In Wales, 310 users of NHS/local authority (LA) mental health services responded to a similar survey. 21 Only 58% knew who their care co-ordinator was; just half were given or offered copies of their care plans, with only 51% ‘definitely’ understanding the content of care plans and 43% ‘definitely’ involved in ‘co-producing’ the content.
The need for greater co-production has also been found in the area of risk management. Research for the Joseph Rowntree Foundation22 on service users’ views on risk reported that perceptions of risk and rights were significantly different for mental health service users. Practitioners tended to perceive service users as a source of risk first rather than to consider them potentially at risk in vulnerable situations; they appeared to be overlooked by adult safeguarding practices; and their individual rights were compromised by mental health legislation.
This evidence, which points to the relative lack of genuine service-user involvement in CPA/CTP processes, is significant in the context of what we know about therapeutic relationships and recovery. The therapeutic relationship is a reliable predictor of patient outcomes in mainstream psychiatric care. 23,24 Strong, collaborative, working alliances between case managers and people with long-term mental health difficulties have been shown to reduce symptoms, improve levels of functioning and social skills, promote quality of life, enhance medication compliance and raise levels of satisfaction with care received. 25 Yamashita et al. 26 describe negotiating care within a trusting relationship as key in case management and this relationship may influence users’ perceptions of stigma. 27
In summary, the limited available evidence contrasts with the aspiration that CPA/CTP care planning and related processes should be collaborative, personalised and recovery-oriented. In addition, the current approach to assessing and managing risk under the CPA may not be satisfactory for either service providers or service users.
Aims
In this multisite, cross-national comparative study we aimed to identify and describe the factors that ensure CPA/CTP care planning and co-ordination is personalised, recovery-focused and conducted collaboratively.
As an exploratory study guided by the Medical Research Council Complex Interventions Framework28 we aimed to generate empirical data, new theoretical knowledge and greater understanding of the complex relationships between care planning, recovery and personalisation. It was the intention that this study would produce theory and empirical evidence that will inform commissioners, service managers, practitioners and service users and provide the rationale for a future intervention and evaluation.
In order to develop studies to examine interventions aimed at improving patient experience and outcomes, we aimed to collate and synthesise theoretical and empirical data using a range of methods in order to inform and develop a pragmatic and feasible intervention likely to be acceptable to service users, families/carers, practitioners and service managers. Our study will also provide lessons for similar, equally problematic, care planning and co-ordination processes for people with long-term conditions in a range of other health/social care settings. 29,30
Research question
What components need to be in place in order to ensure that care planning and co-ordination for people with severe mental illness are personalised, collaborative and recovery-focused?
Objectives
-
To review the international peer-reviewed literature on personalised recovery-oriented care co-ordination, and compare and contrast the English and Welsh contexts for recovery-based mental health care.
-
To conduct a series of case studies to examine in detail how the needs of people with severe mental illness using CMH services are assessed, planned and co-ordinated.
-
To investigate service users’, informal carers’, practitioners’ and managers’ views of these processes and how to improve them in line with a personalised, recovery-oriented focus.
-
To measure service users’ and staffs’ perceptions of recovery-oriented practices.
-
To measure service users’ views of the quality of therapeutic relationships and empowerment.
-
To identify methods, measures and processes for successfully evaluating a complex intervention aimed at delivering personalised, recovery-focused care planning and co-ordination and improved patient outcomes.
Structure of report
This report presents the key findings of our empirical research building upon a meta-narrative policy and literature review within the context of continuing developments in the organisation, structure and delivery of community mental health care in England and Wales.
In Chapter 2 we outline the methodology and design of the study, including public and patient involvement and ethical issues. In Chapter 3 we outline the methods and findings of the comparative policy analysis and meta-narrative literature review. In Chapter 4 we present the results from the within-case analysis, with findings from quantitative and qualitative analyses for both meso- and micro-level data presented for each case-study site. Then, in Chapter 5 we draw out comparisons and contrasts across sites set within the cross-national policy contexts and provide summary charts of the factors identified from this cross-case analysis that appear to function as facilitators of and barriers to the provision of recovery-focused, personalised care planning and delivery. Finally, in Chapter 6, we consider the limitations of the study and then explore the findings in relation to our aims and objectives and recent and ongoing research in relevant and overlapping areas. We end by outlining some tentative implications for mental health care commissioning, service organisation and delivery, clinical practice and health-care professional education and training, and recommendations for future research.
Chapter 2 Methods
Design
We conducted a cross-national comparative study of recovery-focused care planning and co-ordination in community mental health care settings, employing a concurrent transformative mixed-methods approach with embedded case studies. 31(p. 15) Concurrent procedures required us to collect quantitative and qualitative data at the same time during the study and then integrate that data in order to provide a comprehensive analysis of the research problem. One form of data is nested within another larger data collection procedure in order to analyse different questions or levels of units in an organisation.
In this study, in-depth micro-level case studies of everyday ‘frontline’ practice and experience with detailed qualitative data from interviews and reviews of individual care plans are nested within larger meso-level survey data sets, senior-level interviews and policy reviews in order to provide potential explanations and understanding.
At the macro-level is the national context. Cross-national comparative research involves ‘comparisons of political and economic systems . . . and social structures’32(p. 93) where ‘one or more units in two or more societies, cultures or countries are compared in respect of the same concepts and concerning the systematic analysis of phenomena, usually with the intention of explaining them and generalising from them’. 33(pp. 1–2) In this study, devolved government and the emergence of similar but distinct health policy, legislation and service development in England and Wales provided a fascinating backdrop for the investigation of community mental health care.
Such an approach fits well with a case-study method34 that allows the exploration of a particular phenomenon within dynamic contexts where multiple influencing variables are difficult to isolate. 35 It allows consideration of historical and social contexts36 and is especially useful in explaining real-life causal links that are potentially too complex for survey or experimental approaches. 37 So, in this study, we have conducted a detailed comparative analysis of ostensibly similar approaches to recovery-focused care planning and co-ordination within different historical, governmental, legislative, policy and provider contexts in England and Wales.
In our study the definitions of the case studies were predetermined,38 focusing on six selected NHS trust/health boards. Data collection at this level included identifying local policy and service developments alongside empirical investigations of care planning and co-ordination, recovery, personalisation, therapeutic relationships and empowerment, employing mixed quantitative and qualitative methods.
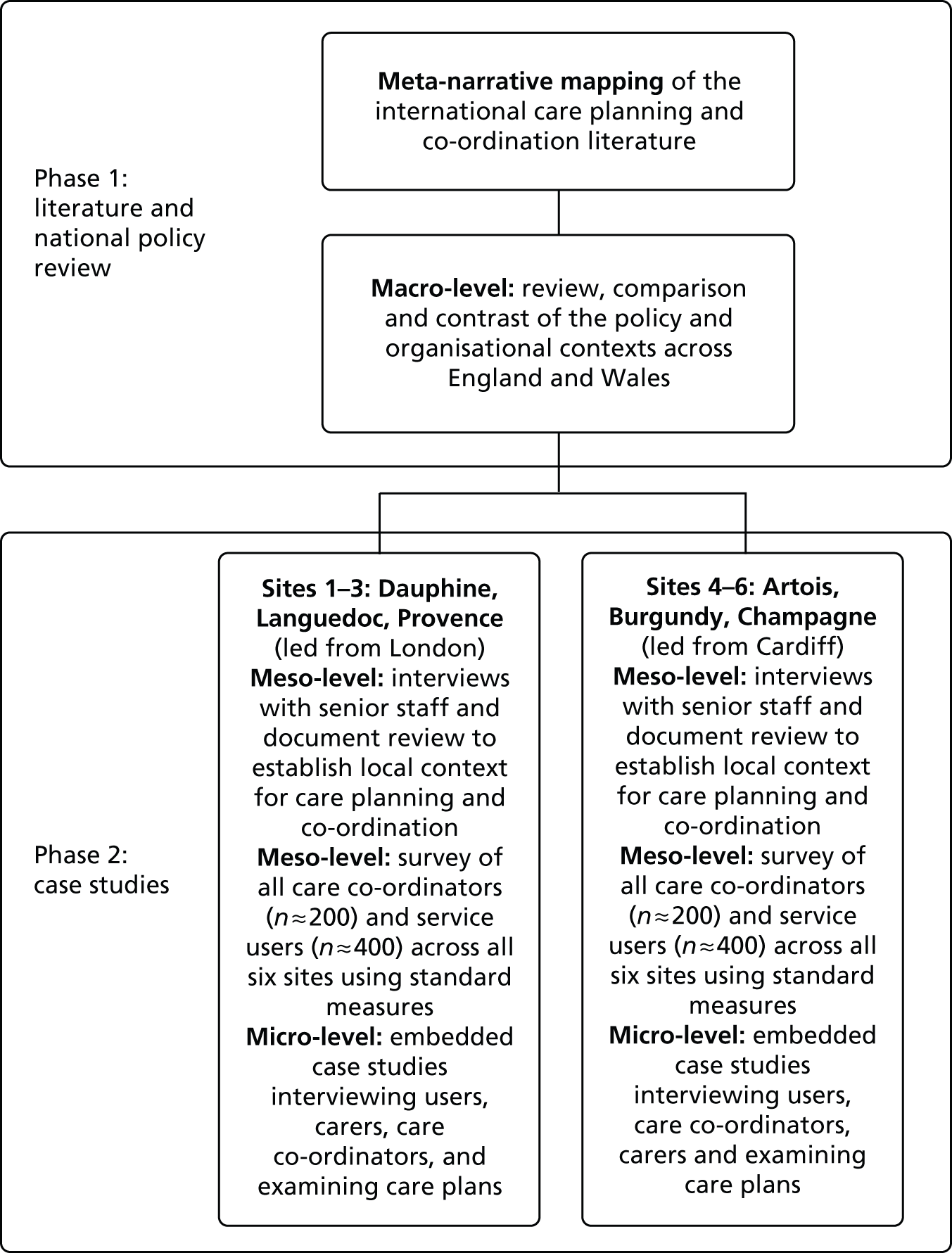
Within each of the six case-study sites we attempted to recruit participants within six embedded case studies made up of a service user, carer/family member and care co-ordinator triad. These explored the views and experiences of care planning and co-ordination from the triangulated perspectives of service users, carers and care co-ordinators. This design is represented in Figure 1.
FIGURE 1.
Diagram of study design with embedded case studies.

Theoretical/conceptual framework
Transformative research seeks to include an explicit ‘intent to advocate for an improvement in human interests and society through addressing issues of power and social relationships’. 39(p. 441) In line with this, transformative procedures require the researcher to employ a transformative theoretical lens as an overarching perspective. 40 This lens provides a framework for topics of interest, methods for collecting data, and outcomes or changes anticipated by the study. In our study, our choice of methods, data collection and approach to analysis is guided by a theoretical framework emphasising the connections between different ‘macro/meso/micro’ levels of organisation41 and concepts of recovery and personalisation that foreground the service-user perspective and, arguably, may challenge more traditional service/professional perspectives. Furthermore, our research team and processes involve mental health service users throughout.
Methodology
Phase 1: literature and policy review and synthesis
Literature review on mental health care planning and co-ordination processes
We employed Greenhalgh et al. ’s42 meta-narrative mapping method (MNM), which focuses on providing a review of evidence that is most useful, rigorous and relevant for service providers and decision-makers and that integrates a wide range of evidence. 43 Our MNM review provides a preliminary map of current mental health care planning and co-ordination by addressing four points: (1) how the topic is conceptualised in different research traditions; (2) what the key theories are; (3) what the preferred study designs and approaches are; and (4) what the main empirical findings are. The methods employed are described in Chapter 3 where we also bring together our broad narrative synthesis.
Comparative analysis of policy and service frameworks
Through searching English and Welsh Government websites we also identified all key, current, national-level policy and guidance documents directly relating to mental health care planning and co-ordination across the two countries, along with those that relate directly to the promotion of recovery and the delivery of personalised care. Drawing on these we produce a narrative synthesis identifying major themes and areas of policy convergence and divergence (see Chapter 3), and use these materials to lay out the large-scale (or ‘macro-level’) national policy contexts to inform our case-study research interviews (see Chapter 4).
Phase 2: case studies
In Phase 2, we conducted six in-depth case-study investigations34 across six contrasting NHS trust/health board case-study sites in England (n = 4) and Wales (n = 2) (meso-level) employing mixed quantitative and qualitative methods. Then, in each site, access was secured to a single Community Mental Health Team (CMHT) from which up to six service users, their care co-ordinators and informal carers were sampled as embedded micro-level case studies. 31 Qualitative data were generated related to care planning and co-ordination processes in each (Figure 2).
FIGURE 2.
Diagram of study plan.
Sampling
We selected six case-study sites: four NHS trusts in England and two local health boards (LHBs) in Wales that are commissioned to deliver CMH services. These sites were identified to reflect variety in geography and population and include a mix of rural, urban and inner city settings in which routine community care is provided to people with complex and enduring mental health problems from across the spectrum of need. The six trusts and health boards initially approached were all within 3 hours’ travelling distance of the two lead universities to facilitate data generation. Selection of the six sites followed advice from the reviewers and was a pragmatic decision, balancing a variety of settings and populations with logistical and data management pressures in the time available.
Within each meso-level trust/health board site we aimed to survey a large sample of service users and care co-ordinators (Figure 3). Survey questionnaires focused on recovery-oriented practices (both groups), and quality of therapeutic relationships and feelings of empowerment (service users only). Interview data were also generated relating to local contexts, policies, practices and experiences from senior managers and senior practitioners, purposively selected to include psychiatrists, senior nurses, psychologists, social workers and occupational therapists (OTs).
FIGURE 3.
Sample size and data collection targets.
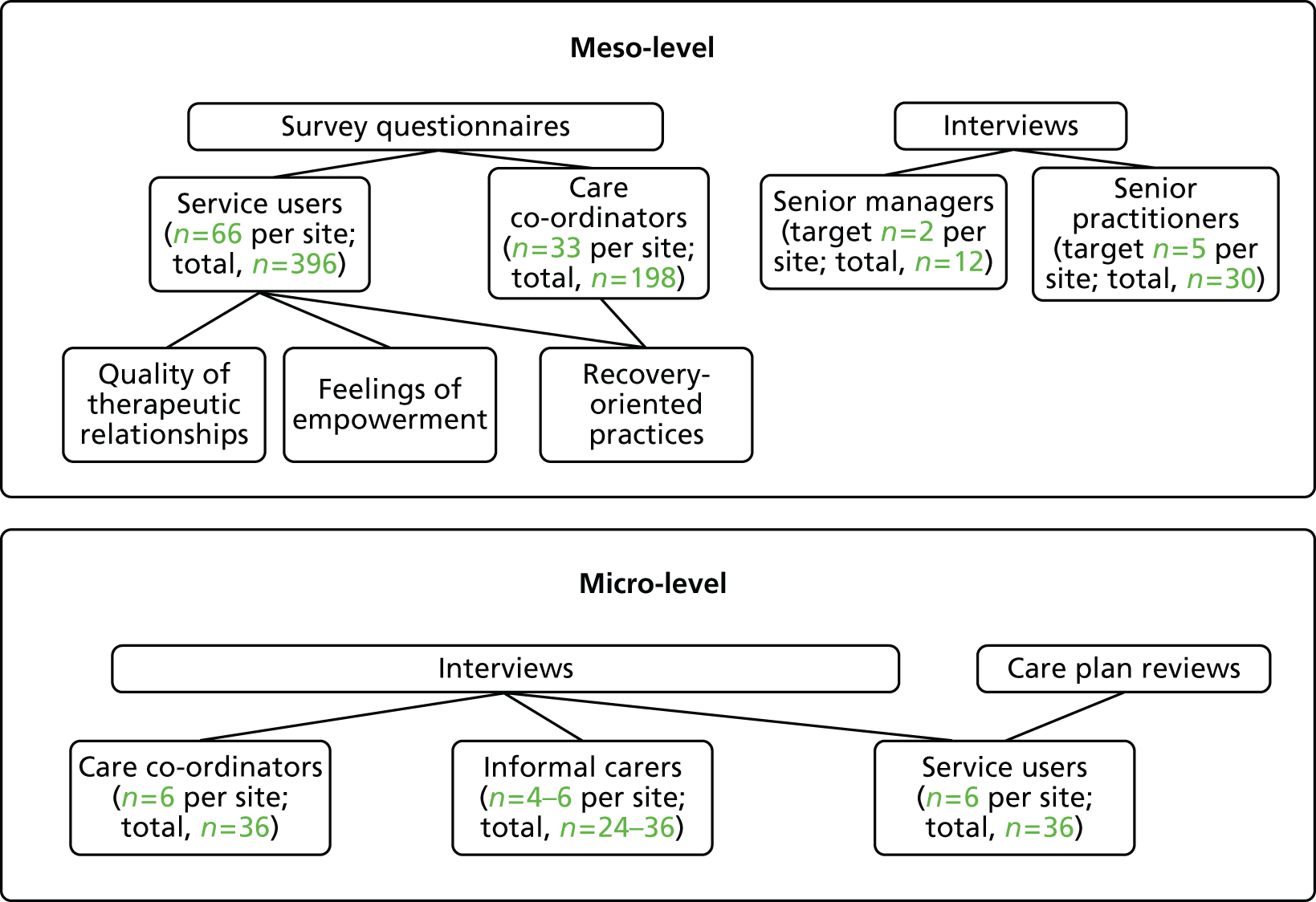
In each trust/board site we also selected a single team providing routine CMH care that met our inclusion criteria (i.e. providing CMH care to adults; team manager in post; reasonably stable staffing; not due for merger or closure). We then invited a sample of six service users under the care of that CMHT to become the starting point for a series of embedded case studies nested within each larger (meso-level) organisational case study. To generate knowledge of how care is planned, co-ordinated and experienced at the ‘micro-level’, each service user, their informal carer and their care co-ordinator were invited to be interviewed and (with appropriate permissions) their written care plans reviewed (see Figure 3).
Sample size calculations
The key variables of interest for this study were the responses of service users and health-care staff in relation to the extent to which recovery-oriented practices were evident in the services surveyed. An established measure, the Recovery Self-Assessment (RSA) scale44 was used for this purpose, and prior investigations among US mental health services provided mean and standard deviation (SD) values on which to base estimates using the standard formula for scaled and categorical items. 45 Findings from the prior study provided a range of mean values for the RSA summary score from mean (SD) 3.87 (0.62) (providers) to 4.06 (0.69) (people in recovery). Applying a 0.69 SD value and an error margin or precision level of 3% provided a total sample size of 127. Anticipating a potential non-response rate of 40% requires inflation of the sample size to 250 to allow for this. In our study, we planned to seek RSA scale responses from service users (n = 400) and care co-ordinators (n = 200); these calculations indicate that generalisability to the target population and appropriate precision in findings is likely, even in the event of a poor survey response rate.
Sample size calculations for the interviews were based on informed estimations of the number of care co-ordinators per CMHT (six). Assuming half agreed to take part, this then gave us a suggested number of service users to randomly select from care co-ordinator caseloads (approximately 25 per care co-ordinator with a predicted response rate of 10%) for research interviews and care plan reviews, giving us a total of seven service users per CMHT. We aimed to recruit six service users per team and where possible their associated informal carer and care co-ordinator.
Instrumentation
-
Documentation and officially collected data. Local meso-level CPA policy and procedure documents, Care Quality Commission, national and local audits and reviews were collated where possible.
-
The RSA44 scale is designed to measure the extent to which recovery-oriented practices are evident in services. It is a 36-item self-administered questionnaire completed in this study by service users and care co-ordinators. The scale addresses the domains of life goals, involvement, treatment options, choice and individually tailored services. The RSA scale has been tested for use with people with enduring and complex mental health problems and across a range of ethnic backgrounds.
-
The Scale to Assess the Therapeutic Relationship – Patient version (STAR-P)46 is a specifically developed, brief (12-item) scale that assesses therapeutic relationships in community psychiatry. It has good psychometric properties and is suitable for use in research and routine care. The subscales measure positive collaborations, positive clinician input and non-supportive clinician input in the patient version. It was completed by service users.
-
The Empowerment Scale (ES)47 is a 28-item questionnaire with five distinct subscales: self-esteem, power, community activism, optimism and righteous anger. Empowerment is strongly associated with recovery and this is the most widely used scale, with good psychometric properties. It was completed by service users (see Appendix 1 for all questionnaires).
-
Structured interviews with senior managers, senior practitioners, care co-ordinators, service users and carers. Interview schedules were developed by the study team in consultation with our Project Advisory Group (PAG) and Lived Experience Advisory Group (LEAG) and drawing on relevant literature. All interviews aimed to explore participants’ views and experiences of care planning and co-ordination, safety and risk, recovery and personalisation and the context within which these operated. Interview schedules for each group of respondents included 15 lead questions with numerous prompts suggested for the interviewer (see example question below and full schedule in Appendix 2). Schedules were slightly amended following piloting with our service user researchers.
Example question: Q1. What does the CPA/CTP mean to you?
Prompts: What is the purpose of care planning? What are the most important aspects of the CPA/CTP? What works/does not work? Have your views about the CPA/CTP changed at all over time? In what way/why?
-
CPA care plan review: within each ‘embedded case study’, the six purposively selected service users’ written care plans were systematically reviewed and appraised against a structured template incorporating the identified key concepts of personalisation and recovery (see Appendix 3). Care plans were also used to collate demographic, diagnostic and service use data.
Research ethics
The study received NHS Research Ethics approval from the National Research Ethics Service Committee Yorkshire and The Humber – Sheffield (Ref.: 13/YH/0056 A) on 13 February 2013. A major amendment was approved on 7 May 2013 to allow a reminder letter to be sent to service users for the questionnaire component and for the interview invitation letter to include information about interviewees receiving a £15 payment.
Considerable attention was given to ensuring the welfare of the service user, carer and other participants and of the researchers. This included providing opportunities to pause or withdraw from interviews, assurances of anonymity and confidentiality and responding to concerns for people’s welfare. Careful arrangements were made for the location and conduct of interviews and all researchers received training, supervision and opportunities for debriefing.
Procedure
Provisional agreement to participate in the study was obtained in writing from senior trust/health board managers (e.g. Chief Executive) prior to submission of the research proposal for funding. Following commissioning of the study, a formal invitation to take part in the study was communicated to a senior manager, such as the Chief Executive, in each organisation and all accepted and identified a principle investigator/link person to facilitate research ethics and governance approvals and contacts with other staff.
Suitable local CMHTs meeting inclusion criteria were identified with the assistance of local NHS trust principal investigators. Team leaders were approached by a researcher who explained the study, responded to any queries and invited them to participate. Nobody declined to take part. Key personnel were identified using purposive sampling and were invited to participate in interviews and to forward local policies and information. Researchers with help from clinical studies officers and research nurses distributed information sheets, consent forms and questionnaires to CMHT care co-ordinators and collated completed questionnaires. Where the identified CMHT had insufficient numbers of care co-ordinators, a second (or third) team was approached within the host site with the questionnaire survey.
Questionnaire packs and invitations to participate in the survey were distributed by post to service users following discussions with the PAG and the LEAG, who wanted to prevent undue pressure or paternalistic ‘gate keeping’ by clinicians. Service users from CMHT caseloads were randomly selected for invitation to participate via the service provider team using agreed criteria (e.g. under care of the CPA/CTP, minimum of 6 months of contact with service). With the help of the Mental Health Research Network (MHRN) and the National Institute for Social Care and Health Research Clinical Research Centre (NISCHR CRC) clinical studies officers, and after checks with the clinical team to prevent inappropriate mailings (e.g. to recently deceased patients), service users were posted the survey pack. The pack included a covering letter, an invitation to participate, the patient information sheet, the pack of three questionnaires and a demographic information sheet. The envelope also included a brief description of the study in numerous languages with details of who to contact for more information in other languages (we received no contact in response to this insertion). A freepost return envelope was included. In line with evidence-based recommendations to maximise returns of postal surveys,48 questionnaires were printed single-sided and some envelopes were stamped with ‘Private and Confidential’ and the University logo. Reminder letters were posted out to all recipients 2–3 weeks after the initial mail-out.
For the service user interviews, again with the help of the MHRN/NISCHR CRC clinical study officers and research nurses, lists of service users under the care of the selected CMHT and subject to the CPA/CTP, were checked with the responsible psychiatrist or team leader to prevent inappropriate mailings.
In each setting the final list of service users for sampling were grouped into care co-ordinator categories to enable us to gain different service user/carer/care co-ordinator triads. Any care co-ordinators already interviewed as senior practitioners were excluded. From the remaining lists, up to four service users per care co-ordinator were randomly selected and letters were posted inviting them to contact the research team by phone, post or e-mail if they wished to participate in an interview about their experiences of care planning and co-ordination. Once a service user contacted the team, a researcher would explain the study, answer any questions and arrange a date, time and venue for the interview. If insufficient responses had been received within 4 weeks of the mail-out, a second batch of invitations was posted. This was repeated until the target number was met or time ran out.
When a service user agreed to be interviewed, they were asked for the name of anyone they considered to be an informal carer that we might contact for interview, and their care co-ordinator was identified. It was made clear that there would be no disclosure of shared information between parties and the care co-ordinator would not be told which specific service user had taken part in the interview. Service users were also asked for permission to review their care plans.
Senior manager, senior practitioner and care co-ordinator interviews were conducted by academic researchers (SB, JE, JV, BH, MC) and clinical study officers. Service user and carer interviews were conducted by service user researchers (JT, DH, KB, BE, AM) with one of the academic researchers in attendance, or occasionally by academic researchers (BH, MC). Care plan reviews were undertaken by clinical study officers using the template provided.
Public and patient involvement
The study was developed and designed with full involvement of co-investigator and independent service user researcher Alison Faulkner (AF) and in consultation with the Service User and Carer Group Advising on Research (SUGAR), based at City University London and facilitated by the Chief Investigator (AS). In addition, a LEAG was established, consisting of 10 service users and one carer with direct experience of mental health care planning and co-ordination. This separate advisory group for ‘experts through experience’ ensured that more time could be spent exploring the service user and carer views and ensuring that their perspectives were able to inform the study. Members were recruited via MHRN, Involving People and other patient and public involvement networks and came from London, the north of England, south-east England, and South and North Wales.
The group was facilitated by AF and met with members of the research team five times during the course of the study. The LEAG:
-
drew on personal lived experiences of care planning, care co-ordination and mental health services to inform the interview topic guide and advise the research team
-
suggested changes to the design, ordering and wording of questions on the interview schedules (adopted)
-
suggested changes to the method of inviting service users to participate in the study (adopted)
-
advised on the participant information sheets before these were submitted for NHS ethics review (adopted)
-
suggested relevant literature to inform the literature review (adopted)
-
explored and discussed initial analysis of interview transcripts
-
discussed with the service-user researchers their experiences of interviewing service users and using the interview schedules
-
explored possible reasons for low response rates in some areas (language, literacy, stigma, poor experiences of services so low motivation to help)
-
explored tentative findings from initial framework analysis.
The PAG consisted of representatives with a clinical or research background from each of the participating NHS trusts/health boards, as well as independent academics. One service user and one carer member also represented the LEAG on the PAG, with input from the LEAG timetabled on the agenda of all meetings, which were chaired by John Larsen, then Head of Research and Evaluation at Rethink Mental Illness.
Five service user researcher assistants/service user project assistants were employed to work on the study on a temporary contract basis, three of whom were based in London, and two of whom were based in Cardiff. All received training and ongoing support throughout the study.
Analytical framework
We framed our data analysis by drawing on social scientific ideas and the findings of our Phase-1 evidence and policy review, an approach used by co-investigators in previous studies. 49 Our concern to explore commonplace practices in CMH is congruent with interactionist interests in social processes and human action. 50 This perspective also recognises the importance of social structures, so that in any given setting person-to-person negotiations are shaped by features of organisational context. 51 The immediate context for frontline practitioners/care co-ordinators in this study is the CMHT workplace, each of which we view as a complex open system. Each participating team also sits within a larger meso-level NHS trust/health board site, which in turn is located within a national-level system of mental health services. This idea of ‘nested systems’ is a feature of complexity thinking,41 and informed our plan to generate, analyse and connect data at different (but interlocking) macro/meso/micro ‘levels’ of organisation. Analysis and interpretation of the case-study data were informed by a conceptual framework that emphasised the connections between different (macro/meso/micro) levels of policy and service organisation, and that drew on the findings of the literature and national policy review in relation to care planning, recovery and personalisation.
Quantitative analysis
Preparation of the data
Data from the questionnaires were entered into SPSS package, version 21 (Armonk, NY, USA). The data were checked and cleaned by a second researcher prior to statistical analysis. The distribution of the questionnaire data was assessed for normality by exploring the data graphically. Comprehensive sensitivity analyses were completed in order to determine what parameters to use when dealing with missing data. The service-user version of the RSA scale questionnaire in particular had a moderate number of missing data and therefore the parameters that were used for calculating the subscales were based on 50% completion levels.
Exploring the data
Descriptive statistics were calculated for the three questionnaires (the RSA scale, STAR-P and ES). The total scores, subscale means and SDs were derived to produce a ‘recovery profile’ for each site. Where appropriate, these scores were compared against reference values (STAR-P and ES) or the participant groups (the RSA scale). Some further detailed analysis at a descriptive level was completed on the primary outcome scale (the RSA scale) to aid with the triangulation of the qualitative and quantitative data. This was completed at an individual item level on the scale by ranking the mean responses for each question to determine where the most agreement was for the participant groups. The top five items were selected from the questionnaire and presented as a recovery profile for the site.
Inferential statistics
Several one-way analyses of variance (ANOVAs) were conducted to compare differences between the six sites on the RSA scale, STAR-P and ES measures. Subsequent Tukey post-hoc tests were conducted to ascertain which measures differed between which locations. A series of one-way analyses of covariance (ANCOVAs) were completed to adjust the analyses for potential confounders. The variables that were chosen for service users were: age; gender; ethnicity; relationship status and time in mental health services. The variables that were chosen for staff were: age, gender, ethnicity, time working in mental health services and time as a care co-ordinator. The criteria for adjusted analysis between the ANOVA and ANCOVA were the p-value from the omnibus test, the adjusted means and the p-value from the post-hoc test. If the p-value from the omnibus test for the ANCOVAs were not substantively different from the ANOVAs then no further post-hoc analyses were completed.
Correlations
Correlations were carried out to identify if there was a relationship between the outcome measures and to determine if there were relationships among the patients on recovery-oriented focus, empowerment and the quality of therapeutic relationship. Three Pearson’s correlations were completed on the mean total scores for the measures RSA scale and STAR-P, RSA scale and ES, and STAR-P and ES for all participants and by individual site. Cohen’s effect sizes were used to describe the data (small r = 0.10, medium r = 0.30, and large r = 0.50).
For all analyses the significance level was set at a level of 0.05.
Qualitative analysis
All digital interview recordings were professionally transcribed and transcripts checked against original recordings for accuracy, and any identifying information redacted, before being imported into QSR International’s NVivo 10 (QSR International, Doncaster, VIC, Australia) qualitative data analysis software for analysis using framework method. 52,53
In this study, numerous transcripts were read by all members of the research team to familiarise themselves with the data. The framework matrix was developed a priori from the interview schedules, with sections focusing on organisational background and developments, care planning, recovery, personalisation and recommendations for improvement. Each matrix section also had an ‘other’ column for the inclusion of data-led emergent categories.
Summarising and charting of 10 transcripts using the matrix was undertaken by two researchers (JV, SB), and was then checked and discussed by AS, BH and MC. Slight amendments to the matrix were made before summarising and charting of all transcripts ensued (by RC, SB, JV, NA, AT, BH and MC), following an agreed format for notation and linking to text. Researchers read and checked 10% of each other’s summarising against transcripts to ensure accuracy and consistency of approach.
Once all charting was completed, second-level summarising was undertaken (by BH, MC, AS, AF and RC) to further precis data and to identify commonalities and differences within trust/health board sites and groups (e.g. senior managers).
In addition, summarised data from the embedded micro-level case studies at each site were subject to further comparison of the views expressed by linked service users, carers and care co-ordinators. These data were then compared against the review of the care plan. This allowed us to tease out agreements and disagreements in the perspectives of the participants within these triads.
Integration and synthesis of data sets
The framework method was also employed to bring together charted summaries of qualitative data alongside summary statistics of the quantitative measures for each case-study site, noting points of comparison and contrast between what we found in our analysis of each type of data.
Armed with our set of six within-case analyses we then conducted a cross-case analysis to draw out key findings from across all sites. We then considered the relationships between stated orientations to recovery and personalisation in national and local policy and senior staff interviews, and what we have found by studying the accounts of users, carers and care co-ordinators and by reviewing written care plans. In this way we were able to investigate the data to identify ‘evidence’ at the intersections between macro-meso-micro levels and CPA/CTP care planning, recovery and personalisation; hence the ‘transformative’ nature of the study design. 31 This is represented in Table 1.
| Level of analysis | Local context/background | CPA/CTP care planning | Recovery | Personalisation |
|---|---|---|---|---|
| Macro-level (national policy, regional drivers, etc.) | ||||
| Meso-level (trust/board policies; senior manager/practitioner interviews, etc.) | ||||
| Micro-level (service delivery: user/carer/care co-ordinator experiences) |
The results of these within-case and across-case analyses are presented in Chapters 4 and 5. We have then drawn on these findings to produce charts identifying the key facilitators and barriers to the delivery of recovery-focused, personalised care planning and co-ordination (see Chapter 5).
Chapter 3 Meta-narrative review and comparative cross-national policy analysis
Literature review
Introduction
It has long been recognised that patients with a variety of chronic and complex health conditions often require long-term care from different health and social care professionals working across community and hospital settings. However, those living with multiple health and social care needs often experience a highly fragmented service, leading to suboptimal care experiences, outcomes and costs. 54,55 Many countries have developed strategies to enable better co-ordination of care; however, evidence suggests that these have often not achieved their objectives. 56
The aim of this literature review is to give an account of care co-ordination and care planning in CMH settings. The question underpinning the review is: ‘What interventions have proved more or less effective in promoting personalised recovery-oriented care co-ordination for CMH service users?’. The focus of the review is care co-ordination in UK CMH contexts, but some research from non-UK settings will also be discussed.
Background and context setting
High-profile failures in mental health care in the UK during the 1980s led to an unprecedented evaluation of care co-ordination between hospital and community services to ensure better quality care. The most immediate trigger was the recommendations of the Spokes Inquiry57 into the killing of a hospital social worker by a psychiatric patient. At the time of the inquiry, care for people with severe mental illness in the community had been described as haphazard and unco-ordinated,58 a view reinforced within the Spokes report,57 which described how, prior to the killing, the patient had been able to ‘drop out of sight’ of mental health services whenever she was discharged from hospital. This, allied to fears about high levels of mental illness among the homeless and in the criminal justice system,59 led to the introduction of a raft of strategies and policies to improve the organisation and delivery of mental health care in the late 1980s to early 1990s.
However, the deterioration in standards of mental health care evidenced in the 1980s can be seen as a culmination of public policy decisions over previous decades. This included a reduction in inpatient mental health beds in the UK from 150,000 in the early 1950s to approximately 50,000 in the early 1990s,55 and the medicalisation and professionalisation of mental disorder, which were key themes of the Royal Commission on the Law Relating to Mental Illness and Mental Deficiency. The subsequent Percy Commission Report60 concluded that mental disorder should be regarded ‘in much the same way as physical illness and disability’ (paragraph 5) and that mental hospitals should be run as much as possible like hospitals for physical disorders. In addition, the 1959 Mental Health Act61 separated health and social care for people who did not need inpatient treatment by handing over responsibility for social care to LAs and councils.
The shifts described above created ideal incubating conditions for subsequent failures in care co-ordination that became increasingly evident in the 1980s. Such was the disarray that some commentators at the time described CMH care in England as an ‘unwieldy dinosaur with its health and social care brains working independently’. 62(p. 2)
In the context of an accelerating, policy-driven shift away from hospital care, the CPA was introduced in England in 1991 and in Wales in 2004 to provide case management and to give shape and coherence to the delivery of CMH services. Case management is a method of working designed to ensure that service users are provided with services that are co-ordinated, effective and efficient. However, the CPA was not developed with a particular model of case management in mind and therefore lacked a single or coherent underpinning philosophy of care. 58 As a result, the introduction of the CPA was very much shaped by the local context, and differences in local approaches were tolerated provided that the fundamental features of the CPA were implemented.
The fundamental features included systematic assessments of health and social care needs; the provision and regular review of a written care plan; close monitoring and co-ordination by a named key worker; the involvement of users and carers in planning and provision of care; and inter-professional and inter-agency collaboration. A CPA register was also established to record details of those cared for under the CPA.
The role of the care co-ordinator and effective teamwork were identified at the time of the CPA’s inception as key to successful implementation,63 given the previous repeated failures of agencies and professionals to communicate and successfully deliver co-ordinated care.
Search strategy
Initial literature searches were undertaken using the following key words and terms: ‘mental health’, ‘care planning’, ‘care co-ordination’ (and ‘co-ordination’), ‘collaborative care’, ‘recovery’, ‘recovery focus(ed)’, personali*. JE ran a preliminary search from which a random sample of articles was assessed by BH and MC, to identify relevant papers and possible additional search terms/phrases. Further discussions were carried out by BH, AJ and JE on the modification of the search strategy.
As a result, additional key words/search terms were included: ‘mental illness’, ‘care collaboration’, ‘patient care planning’ and ‘person-centred care’. We also included proximity indicators (such as ADJ or N- as appropriate of each database), truncation ($) and wildcard (*) symbols as well as Boolean commands (AND and OR) where appropriate. Key search terms were searched by their subject (MeSH headings) and by keyword. The following databases were searched: Applied Social Sciences Index and Abstracts (ASSIA), Cumulative Index to Nursing and Allied Health Literature (CINAHL), Allied and Complementary Medicine Database, EMBASE, The Cochrane Library, MEDLINE, PsycINFO, Education Resources Information Center, British Humanities Index, Scopus, Social Care Online and Web of Science. The search was limited to the period 1990 to date and included articles in the English language only. This search was rerun on the databases ASSIA and CINAHL and the search strategy was verified by a health and social care librarian working for the Information Sciences service at Cardiff University.
During a meeting on the 20 November 2012 with the LEAG and the PAG, it was suggested that the term ‘user experience’ be included in the search strategy. Further discussions among the PAG advised that the addition of terms such as ‘recovery’ or ‘recovery focused’ to the search strategy would narrow the focus too much and that research covering these topics in CMH settings should be captured by using the existing search terms. The issue of rejecting papers where research was considered low quality was weighed against an interest in a broad representation of approaches and views. However, some studies were excluded on the grounds of insufficient detail about the research process undertaken within each study. 64,65
Following removal of duplicate cases, 811 references were retrieved and entered into an EndNote version X7 (Thomson Reuters, New York, NY, USA) library. These references were then screened by BH and MC to identify key papers for the meta-narrative synthesis focusing on papers about care planning and co-ordination in mental health in the community. The papers were labelled as Y (Yes), N (No) and M (Maybe). In the end, there were 45 papers labelled Y, 617 labelled N, and 94 labelled M. There was an agreement among the team on the papers excluded. A further snowball search on the web and using Google Scholar (Google, Mountain View, CA, USA) produced 81 references. From this there were none labelled Y, 69 labelled N and 12 labelled M. A final review of the M papers and back-chaining revealed a further three papers that were added to the original 45, giving a final total of 48.
Meta-narrative review
Meta-narrative review looks historically at how particular research traditions have unfolded over time and shaped the kind of questions being asked and the methods used to answer them. As outlined by Greenhalgh and Wong, a research tradition is a ‘series of linked studies, each building on what has gone before and taking place within a coherent paradigm (that is, within a shared set of assumptions and preferred methodological approach shared by a group of scientists)’. 66(p. 4)
Given the wider social, political and historical context outlined above it is unsurprising that the ‘unfolding plot of the research’67(p. 423) from the UK is dominated by researchers’ efforts to understand whether or not the CPA has led to changes in management, service organisation and delivery (Tradition 1). Although our searches were limited to the period 1990 onwards (when the CPA came in), there is little history of research into care planning and co-ordination within CMH settings prior to this date. There are no pre- and post-evaluation studies of the introduction of the CPA, comparing changes, if any, in care planning and co-ordination in CMH settings.
Instead, researchers initially framed their studies within the findings of public inquiries or governmental reviews into difficulties and failures within CMH settings. It seems reasonable to conclude, therefore, that the CPA resulted in changes both to working practices within clinical CMH settings, and also to research priorities and practices within the UK, creating a hitherto unseen tradition of research within mental health services with a focus on care planning and co-ordination.
Another narrative and tradition of research focuses on service-users’ and carers’ experiences of CMH provision (Tradition 2). Although its emergence may not be surprising given that one of the primary aims of the CPA was to increase the involvement of service users and carers in care planning and provision, this focus was rare in the context of the early to mid-1990s. Another notable feature of this tradition is the emphasis on involving service users and carers in the design and execution of research projects68–71 at a time where both government policy promoting service user involvement and the ‘service user movement’ were in their infancy. 72,73 It is within this tradition that the current study most comfortably sits.
Service-user involvement within this tradition includes involvement in some aspects of conventional research projects (such as question setting or data collection) as well as collaborative research where service users work on most if not all aspects of projects as co-investigators alongside academic researchers. There is less evidence of there being user-controlled research in which service users set the agenda, design and conduct the research. 73
Finally, several studies have sought to determine whether interventions have improved the functioning and performance of the CPA (Tradition 3) in terms of improved care co-ordination and care planning. This tradition of research focuses on processes and outcomes of care, and the prevailing language positions the CPA and CMH work as being driven by requirements to demonstrate organisational efficiency. For example, some studies frame mental health work as requiring standardisation owing to its complex nature and the mental health workforce as having a deficit of knowledge as regards effective care co-ordination and planning.
The three research traditions identified are summarised in Table 2.
| Research traditions | Explanation |
|---|---|
| Tradition 1: CMH care co-ordination and planning, the CPA and the organisation, management and delivery of services | A tradition of research that explores the organisation and delivery of CMH services that has come about since the inception of the CPA |
| Tradition 2: Service-users’ and carers’ experiences of CMH care co-ordination and planning and their involvement in research | A tradition of research that focuses on service users’ and carers’ experiences of CMH services. A tradition that also involves these groups directly as researchers in some or all aspects of the research process |
| Tradition 3: Improvement to the functioning and performance of co-ordination and care planning in CMH services | A tradition of research from the UK and internationally that aims to determine whether or not improvements to planning and co-ordination of CMH services occur following interventions |
Striking in the review was the increase in non-UK research into care planning and co-ordination in community settings with only two studies appearing before 2005, at which point the number increases and surpasses UK research output. These non-UK studies were also aligned with the three research traditions described above but are not included here due to space restrictions.
Tradition 1: community mental health care co-ordination and planning, the care programme approach and the organisation, management and delivery of services
The first tradition of research consists of a series of studies primarily from the 1990s that seek to understand the impact of the CPA on the organisation and delivery of CMH services. This tradition of research draws on a range of methodological approaches (see Appendix 4). The CPA is often discussed as a uniform approach, yet it is noticeable that the earliest study of the CPA68 undertaken in three English health districts demonstrates clear variation in CPA interpretation and implementation. Adherence to the principles of care programming within each district’s community care plans ranged from minimal mention of care programmes to the wholesale adoption of the concept into mental health planning and service evaluation. Later published studies also draw attention to the degree of variation in the implementation of the CPA between different trusts within the same health authority and within the same trust. 16,74–78
Variable implementation of the CPA may well contribute to inconsistency in research findings within and across sites. For example, Schneider’s68 study of three health authorities describes how staff perceived the CPA as offering ways of working that were both creative and flexible as well as rigid and lacking flexibility. Similarly, more rigorous documentation and better care planning are reported in some studies,68,79,80 whereas others report a lack of coverage of psychosocial aspects16,77 or risk assessments not completed fully or jointly. 76 Claims that the CPA led to improved continuity of care,68 better team-working across professions16,68,79 and overall effectiveness of care68,70,81,82 also need to be balanced with findings that most general practitioners (GPs) had not heard of the CPA,83 that the role and function of the CPA had not been explained properly to staff,16,70,83 leading to managers not knowing which patients were on the CPA. 81
Uncertainty also exists in terms of the relationship between the CPA and inpatient bed occupancy rates, with Tyrer et al. ’s62 claims of increased admission to hospital following the introduction of the CPA being contradicted elsewhere. 82 The use of hospitalisation as an outcome measure has been criticised as inadequate for assessing programme success in this population, given that rates of hospital admission and length of inpatient stay can be influenced by other factors, such as local service configuration and bed availability. 84
Such uncertainty and variability raise crucial questions regarding the use and effectiveness of the CPA in practice, especially where researchers attempt to make judgements on programme outcome or cause–effect comparisons across more than one research site. The lack of clarity regarding the exact nature of the CPA in practice reflects a similar vagueness globally about the concept of care co-ordination. For example, a review of research found over 40 heterogeneous definitions and models of care co-ordination to be in existence. 85 The lack of clarity and homogeneity has also been identified as an explanatory factor for the failure of many strategies that seek to improve care co-ordination. 56
Sociopolitical factors partly explain the large variations in the way organisations adapted or assimilated the CPA’s requirements. For example, the CPA was introduced with no or limited additional resources,68,83,86 at a time when health and social care spending was being cut and the vast majority of resources for mental health services were allocated to inpatient care rather than day and community services. 87 As a result, little or no staff training was provided, no particular philosophy of care emerged to underpin CPA implementation and employees were left to manage a change in process as best they could. 58
In an era of increased managerialism in the NHS, the introduction of the CPA was experienced by practitioners as a ‘top-down’ policy imposition that failed to build on the existing knowledge, skills and abilities of the workforce, and resulted in tensions over clinical values and cultures. Staff perceived the CPA as leading to more work16,68,82,83 and a sense of being overworked16,68 especially owing to increasing levels of bureaucracy. 16,68,71 Staff also reported that the additional burden of work that accompanied the implementation and day-to-day operation of the CPA led to increased time being spent away from patients. 16,68,83
The unintended consequence of a lack of detailed, national policy implementation strategy for the CPA was a considerable variation in the delivery of services, as well as variation in staff and patient experiences both within and across health authorities. A review of CPA implementation links the ‘paradoxical effect’ (p. 24) of burgeoning levels of local bureaucracy to the national policy decision not to be overly prescriptive about CPA documentation. 1
Overall, this tradition of research has been firmly focused on developing a better understanding of how the introduction of the CPA influenced the organisation and delivery of nascent and arguably inadequate CMH services. Researchers frame the CPA as a policy intervention that attempted to reverse several decades of deteriorating mental health services characterised by, among other things, inadequate co-ordination and organisation of care within and across different professional groups. There is little research that seeks to delineate or explore developments in multiprofessional and multiagency working in the wake of CPA implementation; studies undertaken in this tradition perpetuate the status quo of multiprofessional working at that time, failing to mention or merely hinting at different ways of working within and across teams. However, Simpson’s16 study describes some of the effects of team working in CMHTs, such as finding that care co-ordination was enhanced within teams when members demonstrated respect for co-workers.
The combination of three decades of profound changes in the policy definition of mental health and illness, together with the broader context of large-scale change towards managerialism within the health and social care sector during the late 1980s and early 1990s, leaves the impression that the CPA was destined to fail before it had been launched.
Tradition 2: service users’ and carers’ experiences of community mental health care co-ordination and planning and their involvement in research
Until the 1990s there were few attempts to involve service users in the planning and delivery of their care and treatment. As Perkins and Repper88 point out, service users were excluded from service planning meetings and were only involved via demonstrating their symptoms and hearing the doctor’s prescription. Implementation of the CPA was fairly novel in responding to service user and carer demands for greater involvement in the care planning process, both of which began to be more explicitly promoted as indicators of good practice. 80
Alongside these developments, a view also emerged that service user involvement in research could make an important contribution to the empowerment of mental health service users. For example, service users have long argued that dominant research approaches to mental illness can perpetuate patients’ inequality and disempowerment. 89 Consequently, the coproduction of new knowledge and the transformation of the terms and concepts used by mental health researchers have been promoted as a potentially influential means to achieve broader social and political change. 90
A tradition of undertaking research that involves service users and carers is rooted in the origins of research into care co-ordination and care planning in CMH work (see Appendix 5). Early studies not only focused on service user and carer experiences of CMH but also involved service users and carers as collaborators in the design and implementation of research studies. For example, Carpenter and Sbaraini80 involved service users and a carer in a PAG and in formulating a questionnaire to explore users’ perceptions of the extent to which the CPA empowered user and/or carer involvement. Rose et al. 71 not only involved service users in designing a data collection instrument (semistructured interview schedule) but also extended service user involvement to data collection, with 12 service users being trained to undertake interviews alongside researchers.
Interestingly, Rose et al. 71 describe how, on many occasions, the project team were warned about the potential negative consequences of service users’ involvement in research. In particular, care co-ordinators worried that users were unable to sustain confidentiality about other users. No such difficulties emerged during the study, leading the authors to conclude that ‘users can be successfully interviewed by other users who have been trained to do this. We argue that, in fact, the user interviewers elicit more open and honest responses than professionals do.’71(p. 29) Subsequent studies in this tradition of service-user involvement in research have since reached similar conclusions. 91–94 The narrative within this research tradition positions service users and carers as having much ‘insider knowledge’ to share and that, as a result, questions are framed and studies conducted in ways that are most relevant to users of CMH services.
A moot question is whether or not this makes any difference in terms of the quality and relevance of data collection and interpretation. For example, Rose et al. 95 conclude that the literature is ambivalent about whether or not service-user researchers obtain different quantitative data to conventional mental health researchers (e.g. Rose91 suggesting differences but Rose et al. 96 finding none). However, there is evidence that service-user researchers both collect and interpret qualitative data differently from conventional researchers and in a way that is more in tune with the priorities of service users themselves. 94,97
It is also important to note that most studies of service users’ and carers’ experiences did not involve them in study design and implementation. 70,80,81,86,98–102 However, a commitment to learning more about service users’ and carers’ experiences resonates throughout these studies. This research tradition has also contributed significantly to the debate about whether or not policy changes that were meant to embed principles aimed at increasing service user and carer involvement in CMH practices actually resulted in the desired changes to carers’ and service users’ experiences.
Overall, this corpus of research demonstrates that the introduction of the CPA has mostly failed to deliver on the promises of increasing service-user understanding70,71,86,91 and involvement71,75,77,86,91,92,94,98,101 in care planning and care co-ordination. Research also suggests that other fundamental aspirations of the CPA have similarly had a limited effect on the actual practices of CMH workers. For example, studies show that service users were not aware of, or not allocated, key workers or care co-ordinators70,71,81,92 and had not seen or were not in possession of a care plan or CPA documentation. 70,71,81,86,92,98,101,103
However, the variation in approaches to CPA implementation noted earlier is also apparent when reviewing research findings in this tradition. For example, a small number of studies running counter to the findings listed above have suggested that service users were well informed about their care and treatment plans92,98,103 leading to service users having more trust in staff68,80 and influence and choice in their care. 68,80,103 However, it is worth noting that a considerable weight of evidence suggests the lack of desired impact made by the CPA on service-users’ experiences.
A similar picture emerges in research on carers’ experiences. Studies demonstrate that carers lacked information about the CPA70,100,103 and that carers felt frustrated and isolated70 by not having their views sought or taken seriously. 70,75,86 These findings are not surprising in light of evidence that suggests health authorities often had no formal policy for carer involvement, instead relying upon ad hoc arrangements. 70,75,100 On a more positive note, the CPA had the effect of generating more contact with carers in some areas,68,80 which resulted in greater levels of carer satisfaction. 68,100
None of the studies reports overt organisational and professional strategies of resistance that served to suppress the involvement of service users and carers. Instead, indicators of professional or medical dominance are more subtle but arguably just as profound in diminishing the opportunities for user or carer involvement. For example, Newbigging et al. 77 describe how Independent Mental Health Advocates (IMHA), who play an important part in representing and advocating for service users’ best interests in CPA meetings, are frequently not invited to CPA meetings through apparent lapses in effective communication and diary planning by care teams.
Similarly, when IMHAs were invited, the CPA meetings were poorly organised and often overrun, with the result that IMHAs had to leave meetings before they had finished owing to other commitments. Foucault neatly captures the fact that subtlety is often an overlooked essential for the effective operation of power, stating that ‘Power is tolerable only on condition that it masks a substantial part of itself. Its success is proportional to its ability to hide its own mechanisms’. 104(p. 86)
The CPA has been described as encouraging a focus on service users’ problems rather than their strengths71,92 and as a way of working that prioritises a preoccupation with illness,16,82,94 which is indicative of an approach to caring that creates patient dependency on practitioners through ‘pathologising’ individuals. It is also an approach that means illness comes to define the totality of the person. The nature of the CPA has arguably reinforced a reluctance in some practitioners to move away from an illness model towards a more person-centred and participative mode of mental health practice.
Very few studies explored whether aspects of workplace culture or organisation were prevalent in resisting, frustrating or promoting policy objectives to increase service-user and carer involvement. How far underlying cultural change has kept pace with the more obvious structural reforms in CMH care remains a matter of debate 20 years after the introduction of the CPA. A number of important questions remain about the conditions responsible for promoting or suppressing service-user and carer involvement, the relationship between hierarchies and power structures within CMH workplaces, and the most conducive ways of navigating these to ensure greater participation.
Although those who introduced the CPA deserve praise for encouraging and promoting the development of service-user and carer involvement, this research tradition demonstrates that taking action to involve users requires a willingness to change attitudes and practice, not merely the introduction of policy or best practice imperatives. The danger otherwise is that, without a genuine commitment, calls for greater involvement merely become ‘an exercise in rhetoric’ that leaves existing power relations between professionals and service users/carers untouched.
Many in this research tradition have pioneered approaches to service-user and carer involvement. As a result, service users and carers have contributed greatly to changing how mental ill health is conceptualised and have aided in the production of new knowledge, which has led to a better understanding of methods for improving the lives and advancing the rights of people with mental health problems. It has challenged a model of mental illness as simply deficit and pathology of a psychiatric diagnosis as a ‘master status’105 that swamps any other aspects of the person.
Tradition 3: interventions to improve the care programme approach
The demonstration of clinical effectiveness of health-care interventions has had an increasing role in the UK and devolved governments’ health strategy since the mid-1990s. 106 At the same time, national policy at the macro-level has focused on the CPA as a means of systematically assessing the health and social care needs of those in greatest need, leading to the development of an individual care plan, co-ordinated by a keyworker. As already discussed, however, very different versions of the CPA were implemented at the level of service delivery within and across regions of England. A tradition of research therefore emerged during the late 1990s that reflected both the perceived need to demonstrate and improve clinical effectiveness, as well as capturing the early difficulties and variation in the implementation of the CPA (see Appendix 6).
As already discussed, the CPA led to diverse, often time-consuming, bureaucratic practices that meant staff spent less time with patients. 16,68,83 CPA documentation is framed by researchers and clinicians as problematic, since poor documentation increases the risk of vital patient and treatment information being missing when planning and co-ordinating care. Consequently, the third research tradition describes how the elimination of variation in documentation processes can lead to improved performance and reliability in care planning and outcome measurement.
Macpherson et al. 106 provide an example of a study that encompasses issues related to variation and effectiveness; stating that standardised documentation for individual care planning should be combined with outcome measurement, to give a meaningful measure of the effectiveness of care. To better understand the relationship between care planning and patient outcomes, a formalised space was introduced to the CPA documentation for establishing and standardising treatment goals. Goals were set within a care planning assessment and review meeting and agreed with patients (n = 139), relatives, professionals and advocates prior to the meeting’s conclusion. One year later a clinical review meeting found that 68% of goals were fully and 11% partially achieved (43% of goals were partially or not achieved). Goals targeting drug treatment of psychiatric syndromes were most likely to be fully successful (84%), whereas approaches to self-care skills, side effects, physical/medical problems and family relationships were moderately successful.
Recent UK mental health policy has emphasised the need for services to adopt a ‘recovery orientation’ to improve service users’ experience of care, social inclusion and recovery. An attempt to standardise outcome measurements for recovery was undertaken by Killaspy et al. 102 who assessed a measure of recovery, the Mental Health Recovery Star (MHRS) for acceptability, reliability and convergent validity. Recovery was defined by the authors as ‘a personal and dynamic process of adjustment and growth following the development of a mental health problem’ (p. 65).
Although the MHRS was relatively quick and easy to use and had good test–retest reliability, inter-rater reliability was inadequate. Furthermore, convergent validity suggests that MHRS assesses social function more than recovery, leading to the conclusion that it cannot be recommended as a routine clinical outcome tool but may facilitate collaborative care planning. Interestingly Gould’s94 study reviewed in Tradition 2 also suggested that the MHRS operated more as a measure of social functioning than recovery. Others saw the MHRS as too complicated, putting too much pressure on service users with long-term problems to find employment and being a rigid tool.
Both Lockwood and Marshall107 and Marshall et al. 108 researched interventions aimed at standardising patients’ needs assessments; the first of these studies was a pilot study, which led to the second study. The intervention in both studies is relatively convoluted and complex, initially involving a research nurse undertaking a baseline assessment of the patient to identify needs. Data from these assessments were then entered into computer software to determine which of the practitioner-identified needs or problems required action. When needs required action, the research nurse and consultant psychiatrist considered a list of pre-defined interventions provided by the software, before deciding whether or not the patient was likely to benefit from any of the interventions. The research nurse then provided the keyworker with a report of the needs identified, which were then used to guide care plan discussions between the keyworker and the patient.
In the pilot study significant reductions were seen in ‘unmet’ needs and the level of anxious/depressive symptoms, suggesting that needs feedback improved the quality of nursing assessment and care planning within the CPA. However, the follow-up study108 found that standardised needs assessment did not substantially enhance care planning. The process of using an independent registered nurse, who was not a keyworker or a member of the clinical team to undertake the needs assessment, allied to having to search a computer database for interventions associated to needs, would have made transferability of these findings into clinical practice difficult, as the trial intervention differed greatly from usual practices.
The CUES-U tool (Carers’ and Users’ Expectations of Service – User version) tested by Blenkiron et al. 99 consisted of a 17-item service user outcome scale in booklet form developed by academics, clinicians and service users. CUES-U was described as an ‘important tool’ (p. 334) because it focuses on issues of quality of life and satisfaction that mental health service users (rather than professionals) identified as priorities. Service users (n = 86) completed the CUES-U booklet before returning and discussing the contents of the booklet with care co-ordinators, who then recorded changes made to care plans as a result of receiving the CUES-U feedback.
The CUES-U mediated discussion led to a change in clinical care for 49% of respondents. Care co-ordinators rated CUES-U as a good use of their time in 64% of cases. A large proportion (84%) of service users were satisfied with the level of control and consultation they received; 87% were satisfied with their relationships with mental health workers and > 70% were satisfied with levels of information and advice and access to services. However, a significant limitation of high levels of satisfaction was that patients knew that their care co-ordinator would see their replies, although many did write negative comments in free text boxes. The authors concluded that CUES-U can be an effective and practicable tool for increasing users’ involvement in their care and for service benchmarking.
A move from paper documentation towards electronic CPA (eCPA) records was proposed by Howells and Thompsell. 109 The eCPA consisted of a computer-based CPA system for care planning and documentation – using a Microsoft Word template – designed to improve the quality of information in CPA care plans in a CMH team in London. Completed eCPA care plans were e-mailed to the acute ward, the hospital’s emergency clinic and any other agencies. The CPA manager received the original signed copy, a copy was filed in the case notes and the GP, the patient and carer were given a copy. The eCPA was welcomed by staff with a take-up rate of almost 100%. Patients welcomed the legibility and detail of the forms and expressed no concerns about the change to the eCPA. Care plans were longer and more detailed, being no longer constrained by fixed-size boxes on paper forms. Care plans were also adjusted more frequently by CMHT staff, who did not have to completely rewrite the forms by hand. As a result, the plans better reflected the changing needs of patients.
To summarise, attempts to improve needs assessment and/or care planning processes by changing documentation featured in all of the interventions, either through amending features of existing documentation106,109 or introducing new assessment and planning documentation and processes. 99,102,107,108 Some of the interventions were described as leading to more collaboration with service users during care planning,99,102,106 whereas Howells and Thompsell109 reported greater collaboration within CMH teams. However, Lockwood and Marshall107 and Marshall et al. 108 reported marginal or no improvements in needs assessment and care planning during a pilot study and trial of an intervention that bore little resemblance to usual clinical practice.
Interestingly, those who developed the interventions via an inclusive, multidisciplinary and/or service-user involvement approach reported most success,99,102,106,109 although the quality of research in this tradition is generally weak with no long-term studies of the effects of these interventions on improving care planning and patient outcomes.
Conclusion
This study clearly sits within and across the first two traditions of research into the CPA: the organisation, management and delivery of mental health services and service-users’ and carers’ experiences of community mental health care co-ordination and planning. In particular, it builds on earlier work where service users are involved in the research process.
Policy overview
In this section we provide a narrative overview of the key policy developments in England and Wales in relation to care planning and co-ordination. A list of key policy documents referred to in this review can be found in Appendix 7. A ‘diagrammatic map’ of key policies and relevant literature is shown in Appendix 8.
The political devolution of power to the Scottish Executive and the Welsh Assembly Government has often been identified as a trigger for the unravelling of a UK-wide NHS. Some commentators dispute the description of a unified pre-devolution NHS, stating that not insignificant differences between the three countries existed long before political devolution,110 particularly in the field of community care. 111 In the context of CMH services the image of a cohesive pre-devolution policy landscape is dealt a blow when we consider that the CPA, first introduced in England in 1990, was only formally introduced into Wales in 2003, 4 years after devolution.
It is also worth noting that the findings from our literature review clearly demonstrate that major differences existed in terms of implementation of the CPA within England, as health regions were afforded total autonomy in how they chose to introduce changes to CMH working practices. In terms of the CPA, we conclude, therefore, that no unified ‘English’ policy approach existed at the outset, making any intra- or cross-national policy comparisons difficult.
Health policy from 1990: changes to community mental health working in England and Wales
Initial moves towards a different way of organising and delivering CMH services can be located within a brief health and LA circular policy document for England. 112 Produced in the context of an accelerating, policy-driven shift away from hospital care, the circular emphasised the importance of ‘systematic arrangements for deciding whether a patient referred to the specialist psychiatric services can, in the light of available resources and the views of the patient and, where appropriate, his/her carers, realistically be treated in the community’. To this end, the document specified that health and social care needs should be assessed and planned and a ‘keyworker’ appointed to oversee and review the delivery and co-ordination of interagency and interprofessional services.
The circular appeared shortly after the publication of plans for an across-the-board reorganisation of community care via the White Paper Caring for People. Subsequently incorporated within the NHS and Community Care Act,113 this placed a responsibility on LAs to implement ‘care management’. With their parallel systems of care co-ordination, for many years thereafter the health-led CPA, and the social care-led care management, ran in unhelpful parallel.
Uppermost in the minds of policy-makers in the early 1990s was the management of the risks associated with the community care of people with severe, long-term, mental health problems. As a result, ‘supervision registers’ were introduced, this again being an initiative within England only, where they were implemented as an add-on to locally structured CPA arrangements. 114 Supervision registers promoted care planning and co-ordination as a mechanism for risk assessment and its management. However, as with the introduction of the CPA, no additional resources were provided to support those appearing on supervision registers.
Building Bridges115 was a detailed document produced for NHS England in 1995, which promoted the importance of interprofessional CMH teams and the CPA as the ‘cornerstone’ of care. 115(p. 45) A year later guidance on the community care of people with mental health problems in Wales was published,116 which formally introduced into the Welsh mental health system the ideas of health and social care assessment, care planning, review and key-working. Neither this nor subsequent additional guidance117 mentioned this as the introduction of the CPA into Wales.
Meanwhile, the election of New Labour to government in 1997 coincided with a significant raising of the profile of mental health as an area for policy action in England, with new guidance on ‘modernising’ the CPA being introduced towards the end of the decade. 118 This reaffirmed the central place of the CPA in modern systems of care but also highlighted where changes needed to be made, noting professionals’ complaints that the CPA resulted in a significant administrative burden for time-pressed care co-ordinators and service users’ views on patchy and inconsistent experiences of care planning.
In post-devolution Wales, a new national strategy for adult mental health services included a section on care planning and co-ordination and on the imperative for all users to have a written plan of care overseen by a ‘keyworker’. 119 Two years later came the formal introduction, for the first time in Wales, of something directly referred to as the CPA. 2 This talked, very clearly, about the CPA as a vehicle assisting service users towards recovery, supporting empowerment and the embracing of holistic care.
The current situation in England and Wales
In England, a further review and ‘refocusing’ of the CPA was undertaken1 which was strong on minimising bureaucracy and on simultaneously driving up the quality of care planning via a commitment to national-level consistency. The CPA was presented as a values-based process through which care is tailored uniquely to the individual and serves to promote social inclusion and recovery. For the first time a set of approved training materials were produced to support practitioners. 120 In current mental health policy for England, represented most completely in the cross-government No Health Without Mental Health121 and its ancillary documents, the CPA takes something of a back seat as the focus shifts to cross-sector and cross-government action to improve mental health across the board.
Meanwhile, in Wales, care planning and co-ordination have taken a distinct turn in recent years. An influential, critical, review of the CPA122 contributed to the power to make new mental health law devolved to the National Assembly for Wales. This process led to the eventual passing of the Mental Health (Wales) Measure [MH(W)M] and its attendant documents, including a code of practice123 and a raft of training material. Part 2 of the Measure obliges health and LA services to produce CTPs for all users of secondary mental health services. The phrase ‘CTP’ supersedes ‘CPA’, although each is required to be developed by a care co-ordinator working collaboratively with the service user and other providers. CTPs must be in writing, and kept actively under review by care co-ordinators who must now be drawn from a prescribed range of professional groups. Since the passing of the Measure, a new overarching strategy for mental health across the lifespan in Wales has been produced,5 along with an initial plan for delivery. 124
Current policy frameworks across both England and Wales emphasise the importance of mental health services in promoting recovery and tailoring care to the needs of the individual. Where the biggest difference remains is in the context of arrangements for care planning and co-ordination, and in the use of a statutory instrument in Wales within which CMH care is overseen. Current mental health policy in England also heavily features the term ‘personalisation’, with no use of this term appearing within current mental health policy in Wales.
Personalisation, through service users holding personalised budgets, is portrayed in policy documents from England as a means of ‘giving people greater choice and control over their care and treatment’. 121(pp. 32–3) In Wales, an Independent Commission on Social Services rejected this view of personalisation, stating that ‘We believe that the label ‘personalisation’ has become too closely associated with a market-led model of consumer choice’. 6(p. 15) The Commission is clear that the focus instead should be on personalised budgets offering the means of establishing patient and public ‘voice’ as a force for improving services that meets the diverse needs of the population of Wales, rather than promoting individualised consumerist choice as a means of improving services through market forces. Peckham et al. 125 similarly identify that different political ideologies are increasingly apparent in policy rhetoric, objectives and mechanisms introduced within devolved national policy, although the question of how visible such differences are at the level of mental health service organisation and service delivery remains to be seen. Such is the focus of this study.
Chapter 4 Results: within-case analysis
Summary of chapter
This results chapter is divided into a number of sections. First, we provide brief summary data of recruitment rates and an explanation of our naming policy for case-study sites. Second, for each site we provide a brief introduction followed by a detailed breakdown of service user and care co-ordinator participants in the survey study and results of the questionnaire data. This is followed by narrative summaries of meso-level organisational policies, approaches and values in relation to care planning and co-ordination, recovery and personalisation, drawing on interview data from senior managers and practitioners. These are illustrated with very brief quotations throughout. This in turn is followed by detailed narrative summaries of micro-level perspectives on care planning and co-ordination, recovery and personalisation, drawing on interview data from service users, carers and care co-ordinators, again with brief illustrative quotations throughout.
Where data were available, detailed embedded case-study comparisons were also conducted, comparing the perspectives of ‘linked’ service user, carer and care co-ordinator, along with a review of the service user’s care plan. This close examination further enriched and expanded our understanding of the within-case analyses but cannot be presented in full, owing to the limited space available in this report. Each site case study includes a brief summary of the data included. An example of the tables created for each of the themes used for our framework analysis is included in Appendix 9.
Quotations are labelled with the initial of the site pseudonym; then SM, SP, SU, CA or CC for senior manager, senior practitioner, service user, carer or care co-ordinator, respectively; and their unique number [e.g. B-SM-001 (Burgundy-Senior Manager-001)].
Recruitment and case-study sites
Recruitment
Across the six sites, 449 service users completed questionnaires (against a target of 400) and 201 care co-ordinators completed questionnaires (against a target of 200).
A total of 117 interviews were completed (against a target of 138), consisting of 12 out of a target of 12 senior managers; 27/30 senior practitioners; 33/36 service users; 28/36 care co-ordinators and 17/24 carers. A total of 33/36 care plans were reviewed. More detail is provided under each case-study site and a demographic breakdown of all interviewees by site is given in Appendix 10.
Case-study sites
Each site was given a pseudonym to help maintain anonymity of participants. French names were chosen to avoid any accidental connection with English or Welsh sites or regions. The site names are: Artois,* Burgundy,** Champagne,** Dauphine,* Languedoc* and Provence* (*sites in England; **sites in Wales).
The quantitative and qualitative data analyses will be combined and presented for each site in alphabetical order.
Meso-level and micro-level analysis by site
Artois
Artois Trust provides both primary and secondary mental health services to a population of around 1.6 million people. It covers a large geographical area, which is predominantly rural, and serves six LAs. Owing to the large catchment area, ethnicity and deprivation rates vary. According to the 2011 census, in one area 16% of the population were from a non-white background, whereas elsewhere this figure was only 7%. Equally, deprivation rates vary from high in the more densely populated urban areas to low in the rural communities of affluence. Adult psychiatric admissions are provided in seven hospitals and six rehabilitation units with 149 beds, 23 of which are accessible to the principal recovery team that data were collected from. Community services are provided through 13 CMHTs. Adult psychiatric admissions are provided in seven hospitals and six rehabilitation units with 149 beds, 23 of which are accessible to the principal recovery team that data were collected from.
Participant characteristics: care co-ordinators
A total of 38 care co-ordinators from two CMHTs in Artois completed the questionnaires. The majority of the respondents had been working in mental health for at least 4 years (97.4%) and 84.2% had worked as a care co-ordinator > 4 years (Table 3).
| Variable | n (%)a |
|---|---|
| Sex | |
| Female | 20 (52.6) |
| Male | 17 (44.7) |
| Age (years) | |
| Median | 45 (range 27–61) |
| Ethnicity | |
| White British/Irish | 27 (71.1) |
| Indian | 4 (10.5) |
| Indo-Caribbean | 3 (7.9) |
| Black African | 1 (2.6) |
| White other | 1 (2.6) |
| Profession | |
| Mental health nurse | 15 (39.5) |
| Social worker | 10 (13.2) |
| Psychiatrist | 5 (13.2) |
| OT | 5 (2.7) |
| Employment/recovery worker | 3 (7.9) |
| Education | |
| Degree | 16 (42.1) |
| Diploma/similar | 12 (31.6) |
| Postgraduate diploma/certificate | 6 (15.8) |
| Master’s degree | 3 (7.9) |
| Doctorate | 1 (2.6) |
| Time working in mental health services | |
| 10+ years | 29 (76.3) |
| 7–9 years | 5 (13.2) |
| 4–6 years | 3 (7.9) |
| 7–9 years | 3 (7.9) |
| 1–3 years | 1 (2.6) |
| Time working as a care co-ordinator | |
| 10+ years | 21 (55.3) |
| 4–6 years | 8 (21.1) |
| 1–3 years | 3 (7.9) |
| < 1 year | 3 (7.9) |
Participant characteristics: service users
In total, 484 questionnaires were sent to service users to invite them to take part in the study. We received 70 responses, which gave us a response rate of 14.5%. Further details of the demographic characteristics can be found in Table 4.
| Variable | n (%)a |
|---|---|
| Sex | |
| Female | 46 (65.7) |
| Male | 20 (28.6) |
| Age (years) | |
| Median | 46 (range 18–72) |
| Ethnicity | |
| Asian | None |
| White British/Irish | 61 (87.1) |
| White other | 3 (4.3) |
| Black (African/Caribbean/other) | 2 (2.8) |
| Mixed race | None |
| Mental health problem | |
| Psychosis/schizophrenia/bipolar-type disorder | 22 (31.4) |
| Depression/anxiety | 14 (20) |
| Dual diagnosis | 3 (4.3) |
| Other | 3 (4.3) |
| Two or more of above | 25 (35.7) |
| Time in mental health service | |
| < 1 year | 5 (7.1) |
| 1–3 years | 14 (20) |
| 4–6 years | 12 (17.1) |
| 7–9 years | 6 (8.6) |
| 10+ years | 30 (42.9) |
| Living status | |
| Independent as single | 35 (50) |
| Independent in relationship | 12 (17.1) |
| Living with family | 12 (17.1) |
| Living with friends/other | 5 (7.2) |
| Supported accommodation | 1 (1.4) |
| Other | 1 (1.4) |
| Daytime activity | |
| Full-time employment | 4 (5.7) |
| Part-time employment | 7 (10) |
| Education/training | 3 (4.2) |
| Unemployed | 27 (38.5) |
| Voluntary work | 7 (10) |
| Other | 17 (24.2) |
| Time with care co-ordinator | |
| Daily | 1 (1.4) |
| Weekly | 20 (28.6) |
| Monthly | 24 (34.3) |
| Other | 22 (31.4) |
| Time with carer | |
| Daily | 28 (40) |
| Weekly | 23 (32.9) |
| Fortnightly | 5 (7.1) |
| Monthly | 4 (5.7) |
| Other | 7 (10) |
Summary scores for the questionnaires
Summary scores for three measures (ES; STAR-P and the RSA scale) were completed by service users. A provider version of the RSA scale was completed by the care co-ordinators.
There was a loss of participant numbers within each of the subscales owing to missing data. The number of participants is presented alongside the subscales. In particular, the RSA subscale for the service users was subject to significant attrition; this will be discussed in Chapter 5.
Empowerment Scale
A total empowerment score for each respondent was obtained by summing the scores of individual items (Table 5). The overall mean score for the sample was above the midpoint for the instrument. Out of a possible score of 4, indicating a higher perceived level of empowerment, the mean ± SD score was 2.62 ± 0.37, which is slightly lower than the reference value. 126 Mean subscale scores were also calculated for the five subscales; a breakdown of the subscales are provided in Appendix 1. The subscale values were slightly lower than the reference group, apart from community activism and righteous anger which were comparable. The Wowra and McCarter126 values relate to data collected in South Carolina and, therefore, relate to different health-care systems. Overall, the trend in scores aligns well with the report by Rogers et al. ,127 demonstrating that the subscale items with the lowest scores were internally oriented relating to self-esteem, power–powerlessness (social isolation) and the expression of anger. Items with the highest scores were externally oriented, relating to community activism.
| Subscales | N | Service-user scorea | Reference valuea |
|---|---|---|---|
| Self-esteem–self-efficacy | 67 | 2.57 (0.71) | 2.82b |
| Power-powerlessness | 65 | 2.43 (0.50) | 2.51b |
| Community activism and autonomy | 66 | 3.13 (0.44) | 3.12b |
| Optimism and control over the future | 67 | 2.62 (0.62) | 2.72b |
| Righteous anger | 66 | 2.34 (0.70) | 2.34b |
| Total Score | 67 | 2.62 (0.37) | 2.74 (0.34)b |
Scale to Assess the Therapeutic Relationship
The mean total score for the STAR-P was 34.51 (10.79), 17.37 (6.26) for ‘positive collaboration’, 8.12 (3.31) for ‘positive clinician input’, and 8.90 (2.35) for ‘non-supportive relationships’. These values are lower than the reference values obtained from the validation paper (Table 6). 46
| Subscales | N | Service-user score | Reference valuea |
|---|---|---|---|
| Positive collaborationb | 68 | 17.37 (6.26) | 19.9 (6.7) |
| Positive clinician inputc | 69 | 8.12 (3.31) | 9.3 (3.0) |
| Non-supportive relationshipsc | 69 | 8.90 (2.35) | 9.3 (3.3) |
| Total score | 68 | 34.51 (10.79) | 38.4 (12.0) |
Recovery Self-Assessment Scale
Mean scores and SDs for the RSA scale are provided in Table 7. Mean scores from service users and care co-ordinators on the subscales fell in the moderate to high range (2.96/5 to 3.76/5). The difference in mean total RSA scores was only marginal, care co-ordinators had the highest ratings (µ = 3.35, SD = 0.68), followed by service users (µ = 3.27, SD = 0.96). The lowest scoring subscales were ‘Involvement’ and ‘Diversity of treatment options’ for both participant groups. Within these subscales the scores demonstrate indifference.
| Subscales | N | Service users (N = 58–69)a | Care co-ordinators (N = 38)a |
|---|---|---|---|
| RSA total | 66 | 3.27 (0.96) | 3.35 (0.68) |
| Life goals | 65 | 3.48 (1.00) | 3.68 (0.72) |
| Involvement | 58 | 2.89 (1.11) | 3.01 (0.81) |
| Diversity of treatment options | 67 | 2.99 (1.20) | 2.96 (0.87) |
| Choice | 69 | 3.66 (0.90) | 3.76 (0.64) |
| Individually tailored services | 64 | 3.27 (1.00) | 3.18 (0.77) |
Recovery Profile from the Recovery Self-Assessment Scale
Below we include a recovery profile for the site based on individual item analysis of the five highest rated recovery-orientated practices. This is based on the mean scores of all of the respondents and is presented from the perspective of the service user and service provider.
The five highest rated items for the service users and care co-ordinators were within the choice, life goals and individually tailored services subscales (Table 8). Other high-rated items by the service users were also within the life goal domain, such as staff knowledge of special interest groups, encouragement to take risks and try new things, staff use of recovery language and staff diversity in terms of culture, ethnicity, lifestyle and interests. In addition to this, strengths were seen in the area of choice such as monitoring personal goals and staff listening to and following choices and preferences. Other highly rated items for care co-ordinators were in the area of life goals such as assisting people to develop career and life goals (including education and employment) and accessing activities and other programmes and services. Other strengths were involving significant others and goals around choice such as listening to preferences and choosing practitioners.
| Rank | Service users (mean of 3.84–4.38 on Likert scale) | Care co-ordinators (mean of 3.97–4.22 on Likert scale) |
|---|---|---|
| 1 | Staff do not use threats, bribes, or other forms of coercion to influence my behaviour or choices Choice |
Staff believe that people can recover and make their own treatment and life choices Life goals |
| 2 | Most of my services are provided in my natural environment (i.e. home, community, workplace) Choice |
Staff do not use threats, bribes, or other forms of coercion to influence the behaviour or choices Choice |
| 3 | The role of staff is to assist me and other people in recovery with fulfilling my individually defined goals and aspirations Life goals |
The role of agency staff is to assist a person with fulfilling their individually defined goals and aspirations Life goals |
| 4 | My service provider makes every effort to involve my significant others (spouses, friends, family members) and other sources of natural support (i.e. clergy, neighbours, landlords) in the planning of my services, if this is my preference Individually tailored |
Every effort is made to involve significant others (spouses, friends, family members) and other natural supports (i.e. clergy, neighbours, landlords) in the planning of a person’s services, if so desired Individually tailored |
| 5 | Agency staff believe that I can recover and make my own treatment and life choices Life goals |
Most services are provided in a person’s natural environment (i.e. home, community, workplace) Choice |
Narrative summary of interview data: senior managers and senior practitioners
We conducted interviews with one senior manager and four senior practitioners. The senior practitioners consisted of two mental health nurses, a psychiatrist and a social worker.
Local context: Artois
In the period prior to the commencement of data generation the trust had been through significant restructuring. Some expressed concern over the costs of this and the impact on the morale of staff who had to reapply for their jobs. For example, a senior practitioner described the service redesign as a ‘. . . massive expense. Nurses had to reapply for their posts. Doctors did not. They just got switched. Massive upheaval now with managers, some not being appointed and skulking off somewhere or, very, very difficult for everyone’ (A-SP-005). A view was that reorganisation had also caused confusion over the trust’s overarching aims, and concern was also expressed relating to external quality reviews. Part of this restructuring had seen CMH services move to what was described as a more ‘functional’ model. This involved the setting up of separate access/assessment teams and recovery teams providing ongoing care. Positive and negative views of this change were given. Greater integration between health and social care was cited as a benefit, but lack of continuity for service users was noted with individuals having to repeat their stories as they moved through the system. Recovery team staff were said to feel as though they were entering half-way through the user’s journey. A senior professional said, ‘one criticism is there’s a disruption of continuity of care [previously] . . . we would stay with the patient through different phases of his problems [from admission through to discharge and community follow-up] . . . but that is no longer the case’ (A-SP-002). Participants also talked of discontinuity of psychiatrist care.
Other changes were taking place alongside these internal restructurings. Participants talked of their concerns over an increasing fragmentation of services, with ‘any qualified provider’ charities and private sector organisations taking on increasing amounts of work. This was viewed as likely to create a more complicated system of services, making it harder to share information and records and leading to a loss of relational continuity with people using services. A senior manager suggested that, ‘whilst very attractive and trendy at the moment, I think after a couple of homicide reports or suicide reports, high profile, that says people cannot talk to each other, people do not talk to each other because they work for different organisations, I think there’ll be demand for people to be brought back into one organisation’ (A-SM-002). Welcome shifts towards a recovery approach were counterbalanced by the use of community treatment orders (CTOs). Social care funding was described as having been ‘decimated’, leading to tighter criteria for access and greater prioritisation.
Care planning and co-ordination
The CPA was described as the framework for all care and interventions and as underpinning the service-user journey. The care of > 80% of the adults using local mental health services was organised using the CPA, with the principles being applied to the remainder. Clarity was needed when moving people from CPA to non-CPA care, with risk assessment ‘integral’ to care planning for A-SP-001 and ‘the topmost heading . . . irrespective of anything else really’ for A-SP-002.
Local policies had been produced, addressing the overall operation of the CPA, how care should be delivered across transitional points and the competencies required of care co-ordinators. Involvement of service users in the CPA was seen as a positive, as was its structure and its capacity to evidence care and individuals’ relative contributions. Welcome shifts were described to the use of the first person in care plans, and to use of a more narrative format. The CPA was also described as a ‘necessary evil’. Negative comments included its bureaucratic and time-consuming character, the plethora of forms associated with it, contributing to staff disengagement, and its use for the purpose of performance review rather than recording users’ needs and subsequent plans. One senior manager observed, ‘it’s almost like it’s [the CPA] been hijacked’ (A-SM-002). Participants also talked of connections being made between the CPA, Payment by Results (PbR) and clustering.
The incorporation of CPA templates into an electronic record system also attracted positive and negative views. This was structured and accessible but also not user-friendly, with separate sections for different activities. Standard templates existed but could not be tailored, and printouts for service users were described as unwieldy. The shift to all-electronic records had also compromised the ability of care co-ordinators to work directly on care plans in people’s homes, with one senior practitioner seeing a solution through investment in mobile technology: ‘I’m hopeful that the introduction of the laptops will support more collaborative care planning’ (A-SP-001).
Recovery team care co-ordinators managed caseloads of up to 25, and increases in demand were described. The work was described as all-consuming and generic, and responsibilities were said to have doubled or tripled over the years. Allocation was based on fit between care co-ordinator and user needs, tempered by allocation sometimes having to be made on the basis of capacity. A senior manager summarised this in the following way:
Whatever discipline you are if you’re that person’s care co-ordinator the expectation would be that you would do everything a care co-ordinator is expected to do [. . .] sometimes people will be allocated a care co-ordinator because of availability and capacity rather than best fit. That can be a problem.
A-SP-005
Being a care co-ordinator could involve responsibilities at the edge of the usual scope of professional practice, and a participant gave the example of nurses struggling with involvement in child protection work.
It was not necessary for care co-ordinators to be registered mental health professionals. Some were concerned at this practice, with one asking if non-professional care co-ordinators would be tolerated in cancer services, for example. Disputes were also described over the allocation of service users to staff without professional qualifications, and a general practice was outlined of never allocating people with significant risk to Band-4 staff. Reviews were convened at least annually (and often more frequently), and a flexible approach to these was encouraged. Carer involvement was seen as starting from a low base with variations in practice, and tensions were observed around service-user consent. Training had recently been reviewed and included the CPA and risk as a mandatory minimum for care co-ordinators. Initiatives also included the involvement of a carer and a service user in training, which was welcomed.
Recovery
Recovery was spoken of in different ways. It was seen as a helpful concept bridging medical and social models of care, and as offering welcome hope to people using services. Participants also spoke of recovery as a personal journey involving collaborations between workers and users, and as an idea having a profound impact on ways of working. As examples, A-SP-001 described recovery as ‘supporting the service user with their family to get to a point where they are achieving the best possible life they can and achieving their own goals with the support they need’ and A-SP-004 spoke of, ‘seeing people as individuals, seeing that actually there is potential’. A shift to a narrative format was said to facilitate recovery-oriented care plans, although these were seen as hard to accomplish at certain stages of the service user’s journey (e.g. during a period of compulsory treatment).
Another view was that recovery has become de rigueur, with senior practitioner A-SP-005 saying that ‘it’s about language, isn’t it? And it’s also that terms kind of get trendy . . . I sometimes feel that there’s quite a lot of rhetoric around these sorts of things and that it’s a fashionable thing and then it goes’. Wellness Recovery Action Plans (WRAPs), recovery plans and the Recovery Star were all mentioned, although views of tools of this type were mixed. One view was that the Recovery Star had been imposed, and another that recovery was inhibited by the CPA which served to manage and control people. Recovery ideas were also spoken of as justifying the discharge of reluctant service users and of transferring people back to primary care. Commitments to recovery ideals were also seen as not universal, with a view being that not all psychiatrists were persuaded.
Personalisation
Personalisation attracted a number of views. It was about moving away from a ‘blanket one size fits all’ (AB-SM-001) approach, with the shift towards first person terminology in care plans an expression of this. ‘Personalisation’ was also described as being to LAs what ‘recovery’ was to the NHS. Uptake of personal budgets was slow, their use surrounded by complex administrative procedures, and for one person ‘there’s tensions about how it works within mental health particularly with CTOs [compulsory treatment orders] being a big thing’ (A-SP-004). Personalisation also involved significant form-filling, and one senior professional spoke of concerns over risk in the context of people having personal budgets. Personalisation was also seen as a precursor to more profound changes for A-SM-002, who said, ‘I think it means privatisation personally, but I’m a cynic’.
Suggestions for improvements
Standards and quality were believed to have improved, which was reflected in the language used about people. A participant wanted a flexible workforce competent and confident to work with the CPA, with care co-ordinators having time to sit and discuss terms which may mean different things to professionals and to service users. This was extended to a request for space for care co-ordinators to co-create care plans. An electronic record system that worked for staff rather than the other way round was asked for, as was a reduction in paperwork. Adequate staffing for adequate roles and increased resources was described as being needed, along with a stronger organisation-wide commitment to the idea of recovery that included training and supervision. Attention to improving continuity of care was also sought.
Narrative summary of interview data: service users, carers and care co-ordinators
We conducted interviews with four service users and two care co-ordinators. Unfortunately, we were unable to interview any carers for this site.
Care planning and co-ordination
Service users expressed powerfully polarised views of their care planning and co-ordination. Positive feedback described this as carefully thought out, with high levels of communication – even sometimes too much of this – observed amid the health-care team in question. The mere fact of having details written down was also deemed to be helpful. This can be contrasted with the opposite view of a confusing, rigidly structured and unhelpful care planning experience, which was seen as little more than an obligatory task. CPA meetings were, however, felt to be more collaborative. Care co-ordinators also conceptualised care planning as a useful way of recording care planning activity and progress, an efficient means of liaising with GPs, and as enabling the ‘sharing [of] information with other people in short hand’ (A-CC-001). This corresponds with the significance attributed to inter-professional communication by service users at this particular site.
Interestingly, although service users agreed in general that care plans are easy to understand, clear and use straightforward language, care co-ordinators felt strongly that the CPA document is not user friendly. The information technology (IT) systems used to produce care plans were seen by both categories of respondent to be problematic: a hindrance for staff, and resulting in the inclusion of duplicated, if not irrelevant, information for service users. The latter were keen to attribute this to the systems used – ‘that’s just what forms are like in databases and the like isn’t it? . . . I understand why so it’s not a biggie’ (A-SU-002) – rather than finding it indicative of any other shortcoming in the CPA process. It was also suggested that care plans function primarily as a checklist for staff: ‘the form is a prompt for them to make sure they’ve covered everything rather than a personalised summary for me . . .’ (A-SU-002). Various suggestions were made as to how matters might be improved. Respondents cited a need for the CPA process to be generally ‘less prescriptive’ and more recovery-focused, with ‘less of an . . . emphasis on trying to fix the problem and more of an emphasis on trying to learn how to deal with the problem’ (A-SU-004), suggesting that a more active role and a greater sense of personal agency would be preferred. Service users also felt that they would benefit from being better informed about the overall aims and objectives of the CPA, and it was mentioned that out-of-hours services could also be improved.
No particular inclination towards a specific care plan format was mentioned by service users, but care co-ordinators were more aware of potential problems in this respect, acknowledging that existing formats struggle to meet such a wide range of needs and expectations. It was posited that phone apps might be more accessible and friendlier for service users, although service user respondents did not raise this as a point of concern. Most respondents had received copies of their written care plans, but these were regarded as almost completely insignificant – ‘I don’t know where I’ve put it’ (A-SU-004) – and often cast aside: ‘[I] stick them in a drawer somewhere’ (A-SU-002). Throughout the responses provided by both service users and care co-ordinators, there was no mention of any inclination to refer regularly to existing care plans, indicating that they were seen to be largely inconsequential. Service users did, on the whole, feel satisfactorily involved in the planning of their care and felt this to be a collaborative process. Although care co-ordinators seemed to agree with this – also describing care as person-centred – they nevertheless acknowledged that the level of involvement is largely determined by the service user for whom the care is being planned. The Recovery Star approach was cited as a means of facilitating greater service-user involvement, although it should be noted that none of the respondents for this site discussed any personal experiences of these. Care co-ordinators also recognised that, in some cases, the CPA is primarily a formality.
For both categories of respondent, safety and risk were understood to be important elements of care planning and, overall, service users were satisfied that these issues had been discussed with them. Care co-ordinators recognised risk assessment to be fundamental to the CPA, and acknowledged the complexity of the factors that need to be considered in relation to this, also observing that sensitivity is crucial to the process. The potential benefits of positive risk taking were also discussed by both care co-ordinators and service users.
Recovery
Few wholly positive definitions of the term were given and, at best, most respondents associated this with the development of helpful coping strategies. Service users, in particular, found the concept unhelpful, ambiguous and subjective. One respondent vehemently voiced an objection – ‘I hate that word’ (A-SU-002) – and felt that the term itself to be deceptive because it implies that ‘the end result is being fixed and I believe you don’t get fixed’ (A-SU-002). The connotations of a possible ‘happy ending’ (A-SU-002) implicit in the term were also found to be inappropriate, since this is not a viable goal in this particular context. Interestingly, respondents from both categories understood that recovery should mean enabling choice and independence – ‘finding the best way to live with whatever you’re going through and adapting better to it’ (A-SU-002), and should ‘mean that you are leading your life in a meaningful and fulfilling way’ (A-CC-001). The ‘journey’ metaphor was not mentioned here. Fewer than half of service user respondents felt that their care plans had helped with their recovery. Where they had, this was attributed to the inclusion of concrete and practical steps that can be followed closely, as well as the exposition of plans that might bring about helpful change and progress. Other respondents maintained that conversations with their care co-ordinator had been far more useful for their recovery than the care plan itself and that this provided valuable support.
Wellness Recovery Action Plans were used extensively by service users at this site and were championed accordingly. The completion of these plans was described as a helpful process – a ‘thought provoking exercise’ (A-SU-002) – that encouraged self-reflection and functioned as a uniquely personal document that cannot properly be completed without the service user’s full involvement: ‘Nobody can write a WRAP plan for me but a care plan can be written without someone’ (A-SU-002). WRAPs were also distinguished from care plans in this respect: ‘it’s the WRAP plan that belongs to me and it’s the care plan that belongs to the professionals’ (A-SU-002). Service users felt that WRAPs offered a useful way for professionals to get to know them and to hear their thoughts.
Less enthusiasm emerged among care co-ordinator responses, and, although respondents acknowledged making good use of WRAPs and relapse plans, they did not evaluate the usefulness of these either for themselves or for service users. It was acknowledged that staff are now expected to use the Recovery Star approach as a means of assessing outcomes in relation to care plans. It was generally agreed that professional approaches have always been recovery focused, but respondents did also recognise that the requirement to meet current organisational targets often stands in tension with the delivery of recovery-oriented practices.
Personalisation
Not all service users were able to define the term but those who did recognised that it can have different meanings; this notion of multiple meanings was also reflected in care co-ordinators’ responses, incorporating factors such as individualised, service-user led services, and the importance of choice. Powerful links were also drawn with personal budgets, although only one service user actually received direct payment funding. The fluidity of the concept was acknowledged by service users, as was the importance of tailoring care to suit individuals’ specific needs:
It means putting the person at the centre of what you do, so not forgetting that you’re dealing with human beings and that every human being is an individual and that what works for one person will not necessarily work in exactly the same way for another person.
A-SU-002
Achieving a balance between structure and flexibility was felt to be important for service users. Most felt that their care was personalised and that individualised, tailored services were currently being provided. For one service user, however, this has not always been the case: ‘before [my current CC] I would probably have laughed at [the idea] frankly’ (A-SU-004). In keeping with this, care co-ordinators recognised that the scope of personalised care is necessarily limited by the availability of particular facilities and opportunities and that some services may be unavailable or inaccessible. It was also noted that new service users are typically allocated to whichever care co-ordinator has space on their caseload (rather than in consideration of the person most appropriate for the case), meaning that relationships are not always personalised in this respect. The opportunity for service-user creativity was viewed as a positive aspect by care co-ordinators, although they recognised that service users sometimes have a limited knowledge of additional services that might be available and useful to them.
Embedded case-study comparisons
Detailed case-study comparisons were made for two cases, with dyads consisting of service user and care co-ordinator only (there were no carers interviewed for this site). Tables were drawn up for each of the themes used for our framework analysis: an example is presented in Appendix 1.
Burgundy
Burgundy LHB serves approximately 500,000 people, of whom 1.6% are from black and minority ethnic (BME) groups. It covers a wide geographical area with a mix of urban and rural communities, some of which are densely populated. Twenty-four per cent of the small areas measured in the largest urban part of the locale, and almost 30% of a second part are in the most deprived 20% of areas in Wales. 128 Mental health services are provided in three hospital sites and one community rehabilitation unit with 85 adult psychiatric beds, from eight CMHTs and from a range of specialist services. The main CMHT that data were collected from has 20 psychiatric beds available to them.
Participant characteristics: care co-ordinators
Thirty-seven care co-ordinators from four CMHTs within the locality completed questionnaires. All the respondents had spent > 4 years working in mental health services and the majority had spent > 4 years working as a care co-ordinator (93.6%). Further details of the demographic characteristics can be found in Table 9.
| Variable | n (%)a |
|---|---|
| Sex | |
| Female | 25 (67.6) |
| Male | 12 (32.4) |
| Age (years) | |
| Median | 45 (range 26–64) |
| Ethnicity | |
| White British/Irish | 31 (83.8) |
| White other | 2 (5.4) |
| Indo-Caribbean | 2 (5.4) |
| Pakistani | 1 (2.7) |
| Profession | |
| Mental health nurse | 22 (59.5) |
| Social worker | 12 (32.4) |
| Psychologist | 2 (5.4) |
| OT | 1 (2.7) |
| Education | |
| Degree | 13 (35.1) |
| Diploma/similar | 8 (21.6) |
| Postgraduate diploma/certificate | 8 (21.6) |
| Master’s degree | 4 (10.8) |
| Doctorate | 2 (5.4) |
| Time working in mental health services | |
| 10+ years | 26 (70.3) |
| 4–6 years | 6 (16.2) |
| 7–9 years | 5 (13.5) |
| Time working as a care co-ordinator | |
| 10+ years | 18 (48.6) |
| 4–6 years | 10 (27) |
| 7–9 years | 4 (10.8) |
| < 1 year | 4 (10.8) |
| 1–3 years | 1 (2.7) |
Participant characteristics: service users
In total, 544 questionnaires were sent to service users to invite them to take part in the study. We received 75 responses, providing a response rate of 13.8%. Further details of the demographic characteristics can be found in Table 10.
| Variable | n (%)a |
|---|---|
| Sex | |
| Female | 37 (49.3) |
| Male | 33 (44) |
| Age (years) | |
| Median | 49 (range 23–69) |
| Ethnicity | |
| Asian | 1 (1.3) |
| White British/Irish | 60 (80) |
| White other | 10 (13.3) |
| Mental health problem | |
| Psychosis/schizophrenia/bipolar-type disorder | 23 (30.7) |
| Depression/anxiety | 8 (10.7) |
| Other | 5 (6.7) |
| Two or more of above | 38 (50.6) |
| Time in mental health service | |
| 10+ years | 49 (65.3) |
| 7–9 years | 8 (10.7) |
| 4–6 years | 6 (8) |
| 1–3 years | 5 (6.7) |
| < 1 year | 3 (4) |
| Living status | |
| Independent as single | 31 (41.3) |
| Independent in relationship | 16 (21.3) |
| Living with family | 21 (28) |
| Living with friends | 1 (1.3) |
| Supported accommodation | 4 (5.3) |
| Daytime activity | |
| Full-time employment | 2 (2.7) |
| Part-time employment | 3 (4) |
| Education/training | 2 (2.7) |
| Unemployed | 32 (42.7) |
| Voluntary work | 8 (10.6) |
| Other | 25 (33.3) |
| Time with care co-ordinator | |
| Daily | 2 (2.7) |
| Weekly | 24 (32) |
| Monthly | 22 (29.3) |
| Other | 27 (36) |
| Time with carer | |
| Daily | 50 (66.7) |
| Weekly | 8 (10.7) |
| Fortnightly | 5 (6.7) |
| Monthly | 2 (2.7) |
| Other | 9 (12) |
Summary scores for the questionnaires
The information presented here will be in the same format as that presented for the previous research site.
Empowerment Scale
A total empowerment score for each respondent was obtained by summing the scores of individual items (Table 11). The overall mean score for the sample was above the midpoint for the instrument. Out of a possible score of 4, indicating a higher perceived level of empowerment, the mean ± SD score was 2.62 ± 0.34, which is slightly lower than the reference value. 126 The subscale values were slightly lower than the reference group, apart from power–powerlessness, which was comparable.
| Subscale | N | Service-user scorea | Reference valueb |
|---|---|---|---|
| Self-esteem–self-efficacy | 74 | 2.60 (0.73) | 2.82 |
| Power–powerlessness | 71 | 2.51 (0.54) | 2.51 |
| Community activism and autonomy | 70 | 3.07 (0.56) | 3.12 |
| Optimism and control over the future | 74 | 2.63 (0.60) | 2.72 |
| Righteous anger | 73 | 2.24 (0.69) | 2.34 |
| Total score | 73 | 2.62 (0.43) | 2.74 (0.34) |
Scale to Assess the Therapeutic Relationship
The mean total score for the STAR-P was 38.49 (8.55), 19.81 (4.85) for ‘positive collaboration’, 9.46 (2.45) for ‘positive clinician input’, and 9.23 (2.83) for ‘non-supportive relationships’. These values closely align with the reference values obtained from the validation paper (Table 12). 46
| Subscale | N | Service-user score | Reference valuea |
|---|---|---|---|
| Positive collaborationb | 73 | 19.81 (4.85) | 19.9 (6.7) |
| Positive clinician inputc | 74 | 9.46 (2.45) | 9.3 (3.0) |
| Non-supportive relationshipsc | 73 | 9.23 (2.83) | 9.3 (3.3) |
| Total Score | 73 | 38.49 (8.55) | 38.4 (12.0) |
Recovery Self-Assessment Scale
Mean scores and SDs for the RSA scale are provided in Table 13. Mean scores from service users and care co-ordinators on the subscales fell in the moderate to high range (2.90/5 to 3.92/5). The difference in mean total RSA scores was only marginal, care co-ordinators had the highest ratings (µ = 3.41, SD = 0.61), followed by service users (µ = 3.33, SD = 0.95). The lowest scoring subscales were ‘involvement’ and ‘diversity of treatment options’ for both participant groups. Within these subscales the scores demonstrate indifference.
| Subscale | N | Service users (N = 66–74)a | Care co-ordinators (N = 37)a |
|---|---|---|---|
| RSA total | 71 | 3.33 (0.95) | 3.41 (0.61) |
| Life goals | 70 | 3.55 (1.06) | 3.73 (0.70) |
| Involvement | 69 | 2.96 (1.12) | 2.90 (0.66) |
| Diversity of treatment options | 71 | 3.06 (1.08) | 3.23 (0.76) |
| Choice | 74 | 3.65 (0.89) | 3.92 (0.65) |
| Individually tailored services | 66 | 3.27 (1.06) | 3.10 (0.80) |
Recovery Profile from the Recovery Self-Assessment Scale
The five highest rated items for the service users and care co-ordinators were within the choice and life goals subscales (Table 14). Other highly rated items by the service users related to life goals, such as staff knowledge of special interest groups, encouragement to take risks and try new things and staff diversity in terms of culture, ethnicity, lifestyle and interests. In addition to this, respondents reported that participants that are doing well get as much attention as those with difficulties, and that effort is made to include significant others and other sources of support. Other highly rated items for the care co-ordinators were in the area of life goals, such as using language of recovery, knowledge of special interest groups and activities, assisting with development of career and life goals (including education/employment). In addition to this, other strengths were involving significant others, discussing sexual and spiritual needs and interests and listening to the choices and preferences of participants.
| Rank | Service users (mean of 3.86–4.34 on Likert scale) | Care co-ordinators (mean of 4.14–4.43 on Likert scale) |
|---|---|---|
| 1 | Agency staff do not use threats, bribes or other forms of coercion to influence my behaviour or choices Choice |
Agency staff do not use threats, bribes or other forms of coercion to influence the behaviour or choices Choice |
| 2 | The role of agency staff is to assist me and other people in recovery with fulfilling my individually defined goals and aspirations Life goals |
Progress made towards goals (as defined by the person in recovery) is monitored on a regular basis Choice |
| 3 | Most of my services are provided in my natural environment (i.e. home, community, workplace) Choice |
The role of agency staff is to assist a person with fulfilling their individually defined goals and aspirations Life goals |
| 4 | Staff use a language of recovery (i.e. hope, high expectations, respect) in everyday conversations Life goals |
Most services are provided in a person’s natural environment (i.e. home, community, workplace) Choice |
| 5 | Staff at this agency help to monitor the progress I am making towards my personal goals on a regular basis Choice |
Agency staff believe that people can recover and make their own treatment and life choices Life goals |
Narrative summary from interviews: senior managers and senior practitioners
We conducted interviews with two senior managers and three senior practitioners. The senior practitioners consisted of a mental health nurse, a psychiatrist and a social worker.
Local context: Burgundy
Community Mental Health Teams had a long history of integrating health and social care staff, exemplified by a senior professional’s commitment to ‘bringing [together] the skills of each person, whether they are health or social care. . . and helping and growing from that’ (B-SP-002). Recent and ongoing local developments included the setting up of assertive outreach, crisis resolution and primary mental health services along with reconfigurations of existing teams. Drivers for developments had included the introduction of CTOs and the desire from within to take the initiative to improve services. High levels of demand and limited resources were promoting closer collaboration with third-sector organisations. Local commitments to recovery and meeting needs in individualised, collaborative and interdisciplinary style were expressed, although no clear service philosophy was said to exist at CMHT level. The MH(W)M attracted differing views. A senior manager said that the Measure had ‘provided the impetus for everything else that’s come’ including a ‘regional approach to everything. . .[which] clearly identifies how the priorities are the same across the footprint’ (B-SM-001). This granted representatives of the LHB and its three neighbouring LAs space to agree and address common priorities. A LA view was that the Measure was promoting a more systematic approach to gathering information but a LHB view was that the larger integration of health and social care had not gone far enough. A senior professional saw the Measure as a driver for positive changes in practice, with CTP being ‘far more holistic’ (B-SP-002) than their predecessors. CMHTs, however, were also said to face additional administrative demands through the introduction of CTP, with no additional resources being available and IT systems not being shared. A senior professional, for example, described the following:
Extra demands of doing the [CTP] paperwork within a specific time . . . the job has become much more desk orientated, rather than face to face work.
B-SP-003
The number of people on CTOs was also seen as significant, creating pressure on resources.
Care planning and care co-ordination
The Measure was described as underpinning all the work that was done. The legal context was said to have encouraged care co-ordinators to pay closer attention to paperwork and (compared with the CPA) had promoted a more standardised approach. One senior practitioner captured this thus:
. . . historically, people might have been a little bit blasé about their paperwork, and the pressures that we all face, isn’t it? It’s easy to get lost, the paperwork’s easy to get lost. But I think having a legal framework is binding really.
B-SP-002
In practice, the all-Wales CTP was used by care co-ordinators alongside pre-existing local templates for holistic and risk assessments, but a local culture was described of service users not always being involved in assessments of risk. A senior manager, for example, said how risk assessment was ‘one thing . . . you never discuss with service users just in case it alarms them’ (B-SM-001).
For some, the CTP was praised for driving a more integrated and collaborative approach, illustrated by its completion in the first person. Care and treatment plans were also praised for capturing the service-user journey in an evolving way, and for encouraging staff to think about potential discharge of service users. Conversely, the Measure was described as having made little real difference in practice, with care planning still not user-led and a paper exercise in the hands of some staff with a senior professional saying how ‘in most cases, they see it [the CTP] as a paper exercise’ [B-SP-003]. This same participant also stated that, ‘my understanding is that the psychiatrists are refusing to write care and treatment plans which has brought a little bit of conflict among ourselves’ and that a ‘hidden group’ of people who had care and treatment plans but were not recorded as such also existed.
The work of care co-ordination was seen as generic, with a senior manager saying that ‘. . . we do something very similar, whether you’re a social worker, OT or nurse’ (B-SM-002). It was undertaken by any mental health professional, with the three groups mentioned by B-SM-002 (all holding caseloads of around 30) usually fulfilling the role. Psychiatrists were said to be resisting and this was causing tension. Participants talked of the value of matching care co-ordinators to service users based on need, but also that allocation often reflected workload, as B-SM-002 explained: ‘when you’re looking to allocate somebody within the team it quite often goes to the person who’s got the space rather than the best person for the person, and I’m being totally honest there’. Once appointed, care co-ordinators were said to carry out most of the necessary work identified in the care plan, although nurses were also described as ‘providing’ as well as ‘coordinating’ where social workers did less of the former. Reviews were usually 6-monthly (with a range from 3 months to 1 year). Differing accounts were given of involvement in these; one said carers were routinely invited, whereas another said that they were rarely asked based on assumptions that users and carers would have opposing views. Another view was that carers could become over-involved.
Carer assessments were offered, but not consistently, and for one participant the only time carers were consulted was when use of the Mental Health Act61 was being considered. Monitoring of reviews was achieved through care co-ordinator supervision. Improving user and carer involvement was described as necessary for the future, with one senior manager saying that:
we can’t work in the community without carers and relatives, end of story, so we have to get them on board, we have to get them involved, we have to listen to them, but I don’t think we do enough, I think we could listen to them better.
B-SM-002
Other improvements that participants said were needed included investment in joint IT systems, reductions in the duplication of documentation, training in outcome-focused care planning and more people able to fulfil the care co-ordinator role.
Initial in-house training following the implementation of the MH(W)M was described as being either uni-professional or whole-team, meaning (for one participant) that preparation for care and treatment plans reflected team culture and the relative value it placed on the care planning and co-ordination process. Staff in post were now advised to consult the Welsh Government website for further information, with care co-ordination included in a general induction for new starters.
Recovery
The MH(W)M was seen as having placed a recovery approach high on the national agenda, with a senior manager saying how:
Recovery is very much the underpinning philosophy [of care planning and co-ordination] if you like [and adding that in the locality] I wouldn’t say that there’s actually a protocol or a policy.
B-SM-002
However, understanding, views and experiences of recovery were mixed. Recovery was described as service users being empowered to manage their own illness and to be more informed. It was about people making choices, knowing what they wanted and having ownership. A senior professional said:
I’ve got a couple of people on my caseload and I’m working with that recovery ethos, and I think it, it’s about the person taking responsibility and being included in the decisions that are being made, but it’s about that person making the decisions as well.
B-SP-002
Recovery was also described as service users returning to previous levels of functioning. Incorporation of recovery ideas in practice was seen as patchy even within single teams, although a hope was expressed that care was now being collaboratively planned. A participant talked of needing two versions of the CTP: one for service users with detail, and one for staff. Some had only heard of recovery plans, whereas one senior professional said they actively used them. Tensions were seen in a recovery approach between what users and professionals wanted, and participants spoke of the need for training in recovery along with changes in ethos to better recognise the expertise of people using services.
Personalisation
Personalisation was described by a LA manager as being at the heart of everything which is done:
It’s what we should be doing, it’s at the heart of everything we do which is just putting the person central to everything . . . engaging with the person, finding out what they want, being very honest about what we can provide . . . It is about outcomes for people . . . outcomes for them, not outcomes for us, not how many cases we can discharge from secondary care.
B-SM-001
Personalisation was also described as care that was individualised and, as such, something that was already in place. It was also a concept that senior manager B-SM-001 said was just thrown at people and was in danger of being misunderstood (this being possibly compounded by differences in emphasis across Wales and England). Personalised care was seen as compromised by the current state of the economy and of services, and that ‘realism’ meant being clear about what services can and should do. A crucial view was that personalisation needed to be tested, given practitioners’ views that this is what they already did. Having control over care did not feature strongly, with a senior professional saying that little has changed in this area over a period of 6–8 years. Direct payments but not personal budgets were discussed by health-care staff.
Suggestions for improvements
Participants spoke of the work to be done to better integrate services and to fully involve service users and carers from the very beginning via good relationships and engagement. Variation in the quality of written care and treatment plans needed addressing, along with a clearer focus on achieving outcomes with service users. Whole-team training in recovery was requested, along with training to enable practitioners to make big decisions (e.g. on discharge). Many participants spoke of having insufficient time and of pressure on resources.
Narrative summary of interview data: service users, carers and care co-ordinators
We conducted interviews with five service users, four carers and three care co-ordinators in Burgundy.
Care planning and co-ordination
Very mixed feelings were expressed in relation to care planning and co-ordination, seeming to vary widely from individual to individual. For some service users, it helped them to feel in control – ‘It’s to keep me on an even keel basically and to make sure that I am well most of the time’ (B-SU-001) – whereas others felt obliged to accept unsatisfactory arrangements and did not feel sufficiently empowered to change them. Some respondents observed a lack of structure in their care planning and a fear of (re)admission to hospital was recounted. It was, however, acknowledged that where service users find it difficult to talk to their carers, they are comfortable talking with care staff instead, seeing this as a valuable means of support.
The extent to which service users felt staff ought to be involved also varied, although there was some tension apparent between a wish for more professional proactivity or more substantial help in some cases, and reluctance towards intrusion in another. These same inconsistencies were experienced by carers: feelings of frustration were caused by the poor standard of care provided, and a lack of meaningful engagement was described. At best, carer respondents felt satisfied with the responsiveness of care. A desire was expressed for ‘action not words’ (B-CA-003); a dislike of dismissive attitudes among professionals was also voiced, as was a need for faster access to psychiatrists. It was also suggested that some GPs have an inadequate comprehension of psychiatric medication. Rural locations (and therefore limited transport) were cited as a problem, and there was some concern among carers that service users may tend on occasions to agree with professionals simply because that is ‘what they want to hear’ (B-CA-003). Although care co-ordinators were on the whole more positive – conceptualising care plans as individualised, tailored to service users’ needs, and outcome-focused – they nevertheless agreed that the successful delivery of this depends largely upon the care co-ordinator involved. Where care plans were written in the first person, this was deemed to be helpful, although service users did not draw attention to this themselves.
For most respondents, care plans were primarily used as a ‘record’ of care co-ordinator and CMHT decisions and actions, for example, although it was also understood by some carers as a contract, detailing procedures to be followed in the event of structural CMHT changes. There was widespread agreement that care plans had little, if any, meaningful impact on care or relevance for service users or carers. Although service users were satisfied that care co-ordinators were looking out for them and monitoring their progress, they described their own role primarily in passive terms (i.e., simply requiring them to sign care plans produced on their behalf). One respondent had never received a care plan at all until their participation in this research was disclosed. Care co-ordinators conceded that they tend to take a flexible approach to the CTP process – which they see as ‘open to interpretation’ – preferring not to adhere to it rigidly. Approaches to CTP seemed to vary significantly between care co-ordinators, with some fully engaged in building relationships with service users and working towards definite goals, whereas others were more concerned with administering medication and monitoring progress. Lack of time, limited administrative support and inadequate IT training were also cited as problematic in this regard.
The document itself held hardly any value for service users and carers; most felt indifferent about them, some describing them as meaningless pieces of paper: ‘it makes no difference to us’ (B-CA-004). Paper plans were typically read once and then discarded or disposed of altogether. Care co-ordinators corroborated this view that care plans may not mean anything at all to some service users, especially longer-term clients. They, too, rarely refer to care plans, using them mainly for review purposes, but otherwise preferring to rely on their professional skills and their knowledge of the service user as a person.
Some care co-ordinators recounted jointly developing care plans with service users and encouraging them to write their own plans, whereas others acknowledged the aforementioned passive role experienced by service users themselves. Once again, the success of this was determined by the individual care co-ordinator in question. It was also acknowledged that where CTOs exist, these necessarily result in less choice and control for service users. A continuum of opinions and feelings about ownership and involvement emerged in our data for this site. For service users, this ranged from greater involvement and decision-making, through to co-production. Others were happy for care co-ordinators to take a dominant role, although one respondent in particular voiced strongly opposing views:
I don’t understand why I can’t adjust my medication. But they said if I did, it would affect other medication, and so, just grin and bear it.
B-SU-004
Similarly, among carers, there was some appreciation of involvement in care planning and reviews, although a need for greater continuity was reported, as well as a wish for more definite action to be taken as a result of their input.
Respondents expressed various different views on the consideration of safety and risk. For this service this was especially disparate; individual experiences ranged from no consideration at all, to inadequate emphasis of key issues, and even the notion of these being used as a threat:
[My community psychiatric nurse (CPN)] said if you do anything wrong you will be sectioned. And I don’t want to be sectioned again because I didn’t like it. It was a bad place.
B-SU-002
Carers recounted fewer overall concerns and did not give significant emphasis to safety and risk as part of CTP. Risk assessments were, however, thought to be useful in the event of a crisis. From the care co-ordinator’s perspective, however, risk was far more of a focal point: the adequate signposting of vulnerability and recognition of the potential for exploitation was of particular concern. It was also suggested that service users and carers may have difficulty self-identifying with risk and safety from their own points of view.
Recovery
There was no general agreement on definitions of the term, and thoughts were different across all three categories of respondent. For service users, this was closely linked to their own agentic capacity (i.e. their ability to function as agents of change): some understood recovery to mean taking control and self-management, or establishing set goals, and striving to reach them. Others, in contrast, focused on the importance of accepting their illness and being willing to receive help and support. For some, however, recovery was a meaningless term, and merely implied a sense of resignation: ‘[I] just keep taking the tablets’(B-SU-005). Understanding among carers was similarly disparate, ranging from gaining control to maintaining ‘some sort of life’ (B-CA-003), right through to seeing recovery as ‘just an idea’ (B-CA-004). Some respondents had not heard the term at all. Neither service users nor carers referred to the standard ‘journey’ metaphor for recovery, and yet this definition was the primary one given by care co-ordinators, as were notions of maintaining the best quality of life possible. This was felt to be in tension with a separate management agenda – not thought to be helpful – which focuses on moving service users through the system. Care co-ordinators also noted that different professional disciplines have different ideas about the concept and meaning of recovery.
Neither carers nor care co-ordinators attributed any significance to the role of the care plan in, or its impact on, recovery. There were mixed feelings among service users; respondents reported that the care plan had helped them accept their illness, or had at least helped by encouraging them to talk about it, but these benefits were not universally agreed. For some service users, the care plan had been of no help at all, and their relationship with the care co-ordinator was thought to be far more important in this regard.
None of the service users interviewed had ever heard of recovery plans or WRAPs and all claimed not to have these. One carer did, however, explain that, although a WRAP was in place, the service user’s illness had prevented any discussion of strengths and abilities, thereby rendering it ineffective at the current time. WRAPs were not discussed by care co-ordinators for this site at all.
From care co-ordinator perspectives, there was overall agreement that current care is recovery-focused. Nevertheless, it was acknowledged that there is often a tension between focusing on service users’ needs and desired achievements and the necessary implementation of particular care-planning strategies. Respondents agreed that the recovery approach can present challenges for service users with longer term problems, and it was also noted that services are now sometimes too focused on diagnoses, discharge, referrals and caseload management, and that pressures to work in this way can cause problems for staff.
Only one service user mentioned that their care co-ordinator’s recognition of their own strengths and abilities had helped with their recovery – these aspects were not discussed by carers or care co-ordinators. Two service users spoke about becoming aware of service user-led support groups through their own efforts, although only one felt able to get involved:
I’ve taken it on my own back to seek help in that way, possibly through a bipolar support group in town . . . they [care co-ordinators] haven’t suggested anything . . . this treatment or care is purely off our own backs.
B-SU-003
Similarly, one carer said that the service user had tried to attend an alcohol support group, but this had not been through the CMHT:
He went there on his own . . . but he wouldn’t stay amongst all the people – although this wasn’t offered by the CMHT: he had to do this on his own initiative.
B-CA-003
There was some evidence to suggest that, in some cases, service users rely very heavily on their carers for support: one respondent described how their partner had ‘saved my life’ and given them something to live for, whereas the weight of this responsibility was felt to be overwhelming for some carers.
Personalisation
There was very little familiarity with, or comprehension of, the term ‘personalisation’ among interviewees, although various service users did understand it to mean ‘tailoring the plan around me’ (AB-SU-001) or, quite simply, being ‘treated as a person’ (B-SU-004). Carers, in contrast, were not aware of the term at all, and some care co-ordinators had never heard it. Of those who had, personalisation was not a meaningful concept, and one respondent described it as ‘playing with words’ (B-CC-004).
The extent to which current care planning and co-ordination might be described as personalised also varied, although there was a general sense of ambiguity and ambivalence about this for all three categories of respondent: carers and care co-ordinators in particular described personalised approaches as vague. Service users’ experiences were polarised – some felt that they recognised themselves in their care plans and were able to make amendments to them; others suggested that ‘it fits my life very well’ (B-SU-002). These positive descriptions were, however, offset by alternative ones in which care was defined as definitively not personalised, but simply as ‘a collection of statements’ (A-SU-003) so generic that they could belong to anyone at all. These responses were mirrored by those of carers, among whom only one respondent reported feeling satisfied that care was adequately tailored. Others were ambivalent, and some felt strongly that the care received followed a traditional model that was absolutely not personalised under any circumstances: ‘[it’s] rubbish. . . what care? What personalisation?’ (B-CA-003). Mention was also made of a wish for services to be communicated in Welsh as a means of easing interactions and boosting service users’ confidence.
Carers note that the kind of care received is entirely dependent upon what is on offer (rather than what service users actually need), and this was substantiated by care co-ordinators, who admitted that what service users can get is entirely dependent upon what is locally available. Some felt that it was possible to personalise within the framework provided by CTP, but this was not unequivocally agreed, and consideration was given to the fact that some service users ‘may not be mentally well or well enough to call the shots’ (B-CC-003) in relation to their own care plans. Only one care co-ordinator mentioned having access to direct payments, but was not familiar with any particular model, and does not use the facility. Neither service users nor carers discussed this.
Embedded case-study comparisons
Detailed case-study comparisons were made for four cases consisting of three triads of service user, carer and care co-ordinator, and one dyad of service user and carer only. Tables were drawn up for each of the themes used for our framework analysis: an example is presented at Appendix 9.
Champagne
Champagne LHB serves approximately 500,000 people living in two contrasting areas: one urban and fairly ethnically diverse (20% of people from BME groups), the other rural and predominantly white British (96%). Twenty-seven per cent of the small areas measured in the urban part of the locale are among the most deprived 20% of areas in Wales. 128 The site provides adult acute mental health services from two hospital sites with 69 psychiatric adult and 5 intensive care beds. They also provide CMH services from eight CMHTs. The principle CMHT that data were collected from has approximately eight psychiatric beds available to them.
Participant characteristics: care co-ordinators
Thirty-one care co-ordinators from four CMHTs within the locality completed the questionnaires. The majority of respondents had spent > 4 years working in mental health services (83.9%) and two-thirds had spent > 4 years working as a care co-ordinator (67.7%). Further details of the demographic characteristics can be found in Table 15.
| Variable | n (%)a |
|---|---|
| Sex | |
| Female | 16 (51.6) |
| Male | 15 (48.4) |
| Age (years) | |
| Median | 42 (range 25–60) |
| Ethnicity | |
| White British/Irish | 27 (87.1) |
| White other | 1 (3.2) |
| Indo-Caribbean | 1 (3.2) |
| Indian | 1 (3.2) |
| Pakistani | 1 (3.2) |
| Profession | |
| Mental health nurse | 11 (35.5) |
| Psychiatrist | 9 (29) |
| Social worker | 7 (22.6) |
| OT | 2 (6.5) |
| Psychologist | 1 (3.2) |
| Other | 1 (3.2) |
| Education | |
| Degree | 9 (29) |
| Master’s degree | 8 (25.8) |
| Postgraduate diploma/certificate | 7 (22.6) |
| Doctorate | 4 (12.9) |
| Diploma/similar | 3 (9.7) |
| Time working in mental health services | |
| 10+ years | 18 (58.1) |
| 7–9 years | 4 (12.9) |
| 4–6 years | 4 (12.9) |
| 1–3 years | 4 (12.9) |
| < 1 year | 1 (3.2) |
| Time working as a care co-ordinator | |
| 10+ years | 11 (35.5) |
| 7–9 years | 5 (16.1) |
| 4–6 years | 5 (16.1) |
| 1–3 years | 7 (22.6) |
| < 1 year | 3 (9.7) |
Participant characteristics: service users
In total, 500 questionnaires were sent to service users to invite them to take part in the study. We received 72 responses, which gave us a response rate of 14.4%. Further details of the demographic characteristics can be found in Table 16.
| Variable | n (%)a |
|---|---|
| Sex | |
| Female | 41 (56.9) |
| Male | 27 (37.5) |
| Age (years) | |
| Median | 44 (range 18–69) |
| Ethnicity | |
| Asian | 2 (2.8) |
| White British/Irish | 54 (75) |
| White other | 8 (11.1) |
| Black (Afro/Caribbean/Other) | None |
| Mixed race | 5 (6.9) |
| Mental health problem | |
| Psychosis/schizophrenia/bipolar-type disorder | 23 (31.4) |
| Depression/anxiety | 18 (25) |
| Dual diagnosis | 4 (5.6) |
| Other | 3 (4.2) |
| Two or more of above | 24 (33.3) |
| Time in mental health service | |
| 10+ years | 36 (50) |
| 7–9 years | 9 (12.5) |
| 4–6 years | 11 (15.3) |
| 1–3 years | 11 (15.3) |
| < 1 year | 3 (4.2) |
| Living status | |
| Independent as single | 31 (43.1) |
| Independent in relationship | 10 (13.9) |
| Living with family | 21 (29.2) |
| Living with friends | 1 (1.4) |
| Supported accommodation | 2 (2.8) |
| Other | 5 (6.9) |
| Daytime activity | |
| Full-time employment | 6 (8.3) |
| Part-time employment | 3 (4.2) |
| Education/training | 4 (5.5) |
| Unemployed | 36 (50) |
| Voluntary work | 3 (4.1) |
| Other | 15 (20.8) |
| Time with care co-ordinator | |
| Daily | 1 (1.4) |
| Weekly | 15 (20.8) |
| Monthly | 23 (31.9) |
| Other | 30 (41.7) |
| Time with carer | |
| Daily | 42 (58.3) |
| Weekly | 19 (26.4) |
| Fortnightly | 1 (1.4) |
| Monthly | 4 (5.6) |
| Other | 5 (7) |
Summary scores for the questionnaires
The information presented here will be in the same format as that presented for the previous research sites.
Empowerment Scale
The overall mean score for empowerment was above the midpoint for the instrument (Table 17). Out of a possible score of 4, indicating a higher perceived level of empowerment, the mean ± SD score was 2.56 ± 0.38 this is slightly lower than the reference value. 126 The subscale values were slightly lower than the reference group.
| Subscale | N | Service-user scorea | Reference valuea |
|---|---|---|---|
| Self-esteem–self-efficacy | 72 | 2.50 (0.73) | 2.82b |
| Power-powerlessness | 72 | 2.44 (0.53) | 2.51b |
| Community activism and autonomy | 71 | 3.05 (0.58) | 3.12b |
| Optimism and control over the future | 72 | 2.51 (0.60) | 2.72b |
| Righteous anger | 72 | 2.32 (0.60) | 2.34b |
| Total score | 72 | 2.56 (0.38) | 2.74 (0.34)b |
Scale to Assess the Therapeutic Relationship
The mean total score for the STAR-P was 34.09 (10.13), 17.13 (5.79) for ‘positive collaboration’, 8.01 (3.05) for ‘positive clinician input’, and 9.09 (2.80) for ‘non–supportive relationships’ (Table 18). These values are slightly lower than the reference values obtained from the validation paper. 46
| Subscale | N | Service-user score | Reference valuea |
|---|---|---|---|
| Positive collaborationb | 69 | 17.13 (5.79) | 19.9 (6.7) |
| Positive clinician inputc | 70 | 8.01 (3.05) | 9.3 (3.0) |
| Non-supportive relationshipsc | 70 | 9.09 (2.80) | 9.3 (3.3) |
| Total score | 70 | 34.09 (10.13) | 38.4 (12.0) |
Recovery Self-Assessment Scale
Mean scores and standard deviations for the RSA scale are provided in Table 19. Mean scores from service users and care co-ordinators on the subscales fell in the middle to moderate range (2.70/5 to 3.79/5). The difference in mean total RSA scores was only marginal; care co-ordinators had the highest ratings (µ = 3.35, SD = 0.56), followed by service users (µ = 3.18, SD = 0.87). The lowest scoring subscales were ‘Involvement’, ‘Diversity of treatment options’ and ‘Individually tailored services’ for both participant groups. Within these subscales, the scores demonstrate indifference.
| Subscale | N | Service users (N = 56–70)a | Care co-ordinators (N = 31)a |
|---|---|---|---|
| RSA total | 63 | 3.13 (0.87) | 3.35 (0.56) |
| Life goals | 63 | 3.38 (0.97) | 3.79 (0.52) |
| Involvement | 56 | 2.70 (1.11) | 2.92 (0.73) |
| Diversity of treatment options | 65 | 3.05 (1.12) | 2.94 (0.7) |
| Choice | 70 | 3.66 (0.83) | 3.70 (0.62) |
| Individually tailored services | 60 | 2.99 (1.06) | 3.11 (0.75) |
Recovery Profile from the Recovery Self-Assessment scale
The five highest rated items for the service users and care co-ordinators were within the choice and life goals subscales (Table 20). Other highly rated items by the service users related to life goals such as ‘staff use a language of recovery and believe that I can recover’. In addition to this, respondents reported that most of the services are provided in their natural environment. Other highly rated items for the care co-ordinators were in the area of life goals, such as using language of recovery, assisting the person to fulfil their goals and aspirations, and with development of career and life goals (including education/employment). In addition to this, other strengths were discussing sexual and spiritual needs and interests, listening to the choices and preferences of participants, and actively involving service users to give back to their community.
| Rank | Service users (mean of 3.69–4.65 on Likert scale) | Care co-ordinators (mean of 4.07–4.31 on Likert scale) |
|---|---|---|
| 1 | Staff do not use threats, bribes or other forms of coercion to influence my behaviour or choices Choice |
Staff do not use threats, bribes or other forms of coercion to influence the behaviour or choices Choice |
| 2 | The role of staff is to assist me, and other people in recovery with fulfilling my individually defined goals and aspirations Life goals |
Procedures are in place to facilitate referrals to other programmes and services if the agency cannot meet a person’s needs Life goals |
| 3 | Staff listen to and follow my choices and preferences Choice |
Agency staff believe that people can recover and make their own treatment and life choices Life goals |
| 4 | Staff help to monitor the progress I am making towards my personal goals on a regular basis Choice |
Staff are knowledgeable about special interest groups and activities in the community Life goals |
| 5 | Staff are knowledgeable about special interest groups and activities in the community Life goals |
Every effort is made to involve significant others (spouses, friends, family members) and other natural supports (i.e. clergy, neighbours, landlords) in the planning of a person’s services, if so desired Individually tailored |
Narrative summary from interview data: senior managers and senior practitioners
We conducted interviews with two senior managers and five senior practitioners. The senior practitioners consisted of a mental health nurse, psychiatrist, social worker, psychologist and ward manager.
Local context: Champagne
Local developments in the period immediately preceding and during data generation included the introduction of integrated LHB/LA management within CMHTs and the setting up of assertive outreach and primary mental health care services. Newly integrated managers were described as knowing what needed to be done while simultaneously carrying significant responsibilities, lacking wider influence and having to work to two organisations. Separate IT systems and lack of higher-level management integration were given as examples of the progress still to be made in inter-agency working.
A senior manager (C-SM-001) said how expectations of service users and third sector organisations were high following the introduction of Together for Mental Health5 and now the MH(W)M. The Measure, in particular, was seen as highly significant and as exerting an impact. A senior professional said how the Measure ‘is massive’ (C-SP-003), and at the highest level, a partnership board with LHB and LA representation shared responsibility for the creation and implementation of new policies and procedures following its passing. National aspirations were reflected in local expressions of commitment to recovery, user involvement, personalised care, dignity, respect, safety and outcome-focused interventions. These were tempered (for some) by accounts of a lack of senior management vision, gaps between policy aspiration and practice reality, and everyday pressures for staff. For example, one senior professional expressed the view that, ‘There are service user involvement protocols in place across the board, but I don’t think it’s been grasped and led at a senior management level, middle management level’ (C-SP-001). Other concerns included increases in demand and levels of acuity, high caseloads for community workers, cuts in training and development opportunities, and rising administrative workloads.
Care planning and care co-ordination
Implementation of the MH(W)M had placed care planning and care co-ordination on a statutory footing for ‘relevant patients’ accepted by secondary mental health services, and local policy was being developed outlining the expectations of care co-ordinators. Care co-ordinators used the template all-Wales CTP addressing eight areas of life, but lacked an equivalent national template for the conduct of general, and risk, assessments. The CTP format was positively appraised in providing structure and a framework for recording the service-user journey, and in requiring staff to attend to a wide range of needs. It was also described as reductionist and bureaucratic, and as insufficiently weighted towards psychological, occupational and medical domains consistent with the provision of mental health care. A senior professional said how the questions on the CTP forms are:
pretty reductive . . . it would be nice to have a question about, why would you want to do this, because then you can capture a bit of the person’s motivation, and some of their values . . . and also I suppose something about what difference would that make.
C-SP-003
An ongoing challenge, described as a cultural one, was the local determination of what constitutes a ‘good’ care plan.
Only mental health professionals could act as care co-ordinators, and contrasting figures were given for average caseload sizes. The upper range stated for nurses and social workers was 30–40+. Once appointed, care co-ordinators carried significant, formal, responsibilities, including the recognition and management of risk, which was described as sitting at the heart of everything. A senior professional described this as ‘very much at the forefront of what we do . . . safety and risk, rightly or wrongly drives what we do, very much, and a lot of the time’ (C-SP-002). An expectation was that newly created care and treatment plans be reviewed after one month in the first instance, with all care and treatment plans subject to review on at least an annual basis. Widespread support was given to the involvement of users and carers in reviews, but carer involvement varied, reflecting both service users’ wishes and differences in practice among professionals. Here, a senior professional referred to some of the tensions:
I think carers’ needs are always high on, in everyone’s mind . . . we do where appropriate, ask people and support them. But again, our views probably completely differ to that of carers . . . I’m aware that we probably are not delivering the service that they want.
C-SP-001
More integrated records and IT, better cross-agency sharing of information and greater administrative support were all seen as improvements needed to support care co-ordinators in their work, along with more people able to fulfil the role. One view was that care and treatment plans could be completed by people with less training.
Welsh Government-commissioned learning materials supporting the implementation of the MH(W)M were available, and an all-Wales approach to training in risk assessment and management was in place. However, senior professionals talked of a lack of care co-ordinator training opportunities, including in the use of recovery principles and in the competencies needed for the role. Where local training was available, participation could be difficult given prior clinical commitments.
Recovery
Recent policy and legislation set an agenda for the provision of care informed by recovery principles, echoed locally in the creation of an inter-agency charter underpinned by commitments to recovery values. Widespread support was found for recovery ideas, and participants spoke of the importance of hope, choice, empowerment and holism, and of people being enabled to live meaningful lives with or without symptoms. Exemplifying this, a senior professional talked of:
providing hope, and delivering a service that actually makes that person feel hopeful that they can recover in the first instance . . . [and] that they will get out of life what they want to get out of life while living with an illness’, and that recovery should be a ‘whole system view.. [and] should come right from the top and . . . be written into every operational policy, into people’s job descriptions . . . written in every policy, every job description.
C-SP-001
Anecdotal evidence was said to exist of shifts away from paternalism and from exclusively biomedical approaches. A senior manager (C-SM-001) also talked of necessary cultural and professional change to fully realise this values-based aspiration, and that rebranding existing ways of working would not be enough. Recognition of organisational commitments to recovery and of greater user involvement was tempered by concerns that recovery practice was developing at an uneven rate, with teams moving at a different pace. One view was that ‘warm words’ (C-SP-003) had been grafted onto a medical model, and another was that training in recovery and in the use of recovery tools needed to take place. Recovery plans and strengths approaches barely featured in participants’ talk, and the use of care and treatment plans for this purpose was hampered by the CTP template wording, which lacked a clear recovery focus. The idea that cultural change was needed was also extended to people using services, as well as to those providing them.
Personalisation
Participants saw personalisation as referring to care that was individually tailored, and (for some) as care that additionally gave people the freedom to lead or develop services for themselves in potentially idiosyncratic ways. A senior manager commented that, ‘It means making sure that we’re striving to make sure that the person’s at the centre of their case’ (C-SM-001) and a senior professional talked of, ‘the person leading, and having control over what happens to them within the services’ (C-SP-001). Reference was made to the importance of acknowledging potential differences in view between people using, and people providing, services. Tension was seen as a possibility when wanting to adopt a personalised approach with people who were very unwell and not wanting contact. Risk was seen as a challenge to personalisation. Another concern was that personalised care could raise expectations for help in areas in which health and social care services were ill-suited to respond.
Care and treatment plans were thought to be helpful in the promotion of personalised care, and personalisation as an ideal was seen to fit with recovery as part of the overall aim of the service. One participant (C-SP-001) said this aim was already being achieved. This was not a uniform view, however, and others were clear that personalisation was not happening: ‘Personalisation is at the moment a concept but it hasn’t really been put in practice’ (C-SP-002). Differences were found by background, with senior social care professionals demonstrating greater awareness of personalisation than senior health-care professionals. Professionals were also not sure if LHB policies existed in this area, and training opportunities did not feature. Moves towards direct payments were described, but participants recognised that the use of personal budgets was not well developed. It was suggested that one way that more personalised practices could be developed was to establish a forum where staff and service user experts might share and learn from each other’s experiences.
Suggestions for improvements
Participants spoke of the importance of having vision, and of being able to offer choice, to instil hope and to involve people in their own recovery. Having the time to provide high-quality care was important, but people spoke of a demanding system that inhibited practitioners’ best intentions. Closer integration between health and social care agencies was proposed with a view to harmonising procedures, along with interprofessional and interagency training to support recovery-focused services and personalisation. Brave decisions were asked for to support the shift to personal budgets, and managers were asked to renew their focus on leading the incorporation of recovery ideals into practice. Professionals spoke of wanting encouragement for more positive risk-taking and of risk trumping the focus on recovery. The experience of under-resourcing was described as dispiriting, and of care plans pointing to services that are not available. Specific new initiatives, which service users were said to have asked for, included investment in peer support and resource centres. Change across the whole system was seen as applying to third-sector organisations that with statutory services might need to change their ways of working.
Narrative summary of interview data: service users, carers and care co-ordinators
We conducted interviews with six service users, four carers and five care co-ordinators in Champagne.
Care planning and co-ordination
On the whole, care planning was felt to be useful, especially as a means of monitoring personal progress: ‘[knowing] how far I’ve come from where I was and how far I’m going to go’ (C-SU-001). It was, however, acknowledged that this usefulness was also contingent upon other factors, such as the implementation of regular updates, the scheduling of structured activities and a consistent level of regular personal contact from staff. Carers, in particular, were appreciative of the CMHT support that accompanies the care-planning process. Although most service user respondents had not received copies of their care plans, and some had not seen a care plan at all, their potential usefulness was nevertheless recognised. The one respondent who did have a copy described referring to it on a regular basis, and feeling a sense of ownership in relation to it. Importantly, service users also emphasised that, for some, it may be difficult to admit that mental health care is required and that, in such situations, help may not be welcomed. With the exception of one service user, respondents understood their care plans fairly well. The inclusion of emergency contact details was also considered important by service users. There was some suggestion from service users that electronic formats might be useful. This possibility was not mentioned by carers, and care co-ordinators preferred written (paper) formats, with one respondent noting that there have been changes to the language used to describe care-planning work.
For care co-ordinators, care plans are considered useful as long as sufficient time is available to work on them properly; the need for more time was a shared concern within this group. The function of care plans as providing a valuable timeframe within which they could work was recognised, although some respondents were unclear whether or not service users had copies of current plans. For these respondents, care planning was associated with collaboration, risk management and recovery, although there were mixed feelings about the importance of regularly referring to the documents. One respondent considered care planning to be a helpful way of monitoring service users’ progression, whereas another felt that it was more important to have a good knowledge of exactly what is happening at any given time with a service user’s care. One respondent conceptualised the care plan as ‘a bit of a contract’ (C-CC-004), facilitating the development of an agreement with service users about the content of their plan. The variability of service-user engagement was felt to be challenging in some cases, and an example was given of one service user who hides their care plan so that it cannot be easily located or read.
Overall, care co-ordinators were keen to emphasise that the usefulness and effectiveness of care planning is dependent upon the specific individuals involved. Interestingly, although one respondent suggested that the care-planning process could work in the absence of care plan documents, another felt that care plans were crucial unless service users could be seen on a daily basis. It was also mentioned that care plans should be conceptualised as an ongoing, continual process, rather than as a task that ought to be completed and ‘signed off’. Another hindrance to effective care planning included the ‘cumbersome’ (C-CC-002) IT systems currently in use.
Most service users were satisfied with their level of involvement and felt that they were adequately listened to. One respondent without a care plan expressed a wish for greater involvement and noted that the provision of care plans without the appropriate follow-up process was unhelpful. Carers did not describe a high level of involvement themselves – although some did attend meetings – and this did not seem to be a major area of concern. For some, a purposeful choice was made not to be involved, such that service users were given full scope to speak for themselves: ‘I wanted him to speak his mind alone and then I would come in afterwards’ (C-CA-003). Care co-ordinators, meanwhile, felt that they encouraged involvement from service users and carers wherever possible: ‘I think I can speak for everybody in the team where it’s patient centred’ (C-CC-005). Respondents emphasised that informal involvement – ‘on a walk and talk basis’ (C-CC-002) – ought to be recognised as valuable. From a care co-ordinator perspective, then, ‘it’s very much [the service user’s] . . . as much as possible we put the onus on the patient’ (C-CC-005).
Mixed feelings about the consideration of safety and risk were expressed by respondents. Most service users agreed that these aspects had been adequately addressed. It was however acknowledged that such issues were not always explicitly discussed and that even where they were, discussions usually centred primarily on the identification of emergency contact information. Some service users were uncertain whether risk assessments were included in their CTP, and one respondent mentioned that they were still able to ‘get away with’ self-harming [C-SU-004], and another described feeling neglected since their discharge from hospital: ‘[at home] nobody’s checked up on me or anything’ [C-SU-005]. There were no serious concerns expressed among carers, who were on the whole fairly satisfied with the management and consideration of risk and safety, but did feel that perhaps these matters could be discussed more thoroughly with CMHT staff.
For care co-ordinators, however, thorough risk assessment was acknowledged to be ‘paramount’ [C-CC-004] to the care planning process, and it was suggested that it can sometimes be difficult to establish the necessary balance between safety and positive risk taking, especially given the shift among practitioners away from a risk averse culture and towards embracing positive risk taking more generally. Respondents described the importance of knowing service users’ individual limitations in this latter respect, and noted the importance of considering possible risk to both self and others. It was suggested that the awareness of risk was often an intuitive matter: for one respondent, it was a continual focus – ‘it’s in the back of your mind constantly, I guess’ [C-CC-004]. Another respondent described their approach as ‘very safety conscious’ [C-CC-005], and also explained that current working practices are underpinned by a ‘very low tolerance of any sort of verbal abuse or . . . physical intimidation’ [C-CC-005].
Other than one service user respondent who recounted a traumatic experience of having been poorly treated at a local Accident and Emergency department, this group did not express strong feelings about possible improvements to care planning. Carers, meanwhile, although generally satisfied with their current situations, suggested that better communication between different services would be helpful, and felt that some services were inadequately funded, resulting in a lack of available staff and limited contact. Better access to respite care was also cited as a possible improvement, as well as increased help from out-of-hours services, more face-to-face contact with staff, and a greater number of structured activities for service users.
Care co-ordinators were similarly concerned about the current lack of resources in mental health services and felt that, as a consequence of this, existing work necessarily involves more crisis management than ought to be the case. It was also noted that medical practitioners, in particular, have very little time available for the CTP process, and that perhaps it would be better assigned to staff in other professions. More training for the drawing up of care plans was deemed necessary, and it was suggested that peer support workers would be useful for service users in helping them to write their care plans themselves. The duplication of information observed in care plan formats was considered unnecessary, and it was emphasised that generic templates do not work effectively: ‘one size fits no-one’ [C-CC-002].
Recovery
On the whole, service users were less certain than carers or care co-ordinators in terms of defining recovery, with some respondents more knowledgeable than others. Responses were very mixed: two respondents associated recovery with the notion of ‘getting better’, being symptom free and remaining out of hospital. Others acknowledged that, although they will not make a full recovery, they are keen to be symptom free without having to take medication. The ability to engage in structured activities (e.g. work, hobbies) was indicative for some service users of a shift towards recovery, and some respondents felt that a healthy mind, a positive outlook and the ability to function socially were key objectives.
Some service users had been introduced by their care co-ordinators to various day centres and other local facilities or helped to access suitable courses. Some took up these opportunities but others tried them briefly but felt unable to continue owing to the inhibiting nature of their mental condition:
I’ve been told about [NAME OF LOCAL CENTRE] . . . I’ve been there a few times, but I don’t particularly like it there, and there’s one in [PLACE NAME] . . . I went there for a very short time, a period . . . It was all right, but I think you know your limits, like. If you feel a bit paranoid or panicky you just withdraw, so that’s why I didn’t bother going again see, yeah.
C-SU-001
Another service user said that she had not really been given information about support groups but her co-ordinator had ‘got me weekly art therapy for up to two years. . . and I start a 12 week Mindfulness course in a couple of weeks’ time’ (C-SU-002).
Most carers, meanwhile, seemed to have a good understanding of recovery, acknowledging that the recovery process is necessarily a wholly individual one, that the primary objective is to manage life within the boundaries of mental illness, and that this will necessarily mean living a different kind of life than previously experienced pre-illness. These views were mirrored in care co-ordinators’ responses, which were similarly knowledgeable and also focused upon the significance of individualisation. The re-establishment of a meaningful day-to-day life was considered important here, and the process of empowerment – building upon service users’ strengths and abilities – was recognised to be valuable for recovery purposes. One carer said that the service user had been helped to undertake ‘a lot of activities’ (C-CA-003) and proceeded to list positive thinking, cognitive–behavioural therapy, table tennis, a gym and a local centre that provided numerous activities and support. Service users agreed strongly that their own strengths and achievements were recognised. Some association of recovery with a drive towards discharge targets was made, but this was not a dominant tendency.
There was a general uncertainty among respondents over whether or not care plans were helpful for recovery, and no strong opinions were voiced in relation to this. Some service users, in particular, felt that the structured goals incorporated into their care plans had been useful, whereas others valued their implicit function as a ‘safety net’ alongside other support networks, for example, friends and family, as well as structural support such as benefit payments and financial assistance. Other respondents suggested that a more ‘active’ care plan would be beneficial in striving for recovery. Carers’ responses on this point were equally diverse; medication was felt to be important in some cases, and the value of psychological therapies – with a desire for greater availability – was also mentioned. Support from the appropriate professional at the right time was described as being crucial to the recovery process. Less emphasis was given by carers to the identification of personal strengths, and one respondent was unsure whether or not these would actually be recorded in the care plan document upon their recognition. None of the service users had a recovery plan, and although one carer assumed that such a document had been drawn up, they were unclear about this. Although there was a general awareness of the existence of additional help and support networks, carers indicated that such resources were often difficult to find, and that more guidance was required in this respect.
Most care co-ordinators felt that they did already work in a recovery-focused way, and there were suggestions here about the ways in which CTP provides a good structure for visualising the recovery process. Limited resources and risk adversity were cited as hindrances to the delivery of recovery-oriented care, as were the demands of detailed documentation. There was a sense that as a consequence, work often involves a great deal of ‘firefighting’ (i.e. dealing with emergencies rather than advance planning). It was noted by some respondents that longer-term service users might find the drive towards recovery upsetting at times, and also that the implicit emphasis on discharge can be challenging for staff.
Personalisation
Most service user and carer respondents did not have a clear understanding of the term ‘personalisation’. Several had never heard it at all, and the concept had never been explained to them. Care co-ordinators, meanwhile, were all at least familiar with the term, but many were unable to provide a clear definition, and felt the concept to be an ambiguous one. As a consequence of this ambiguity, two respondents described feeling uncomfortable about using the term at all. For some care co-ordinator respondents, personalisation was associated with choice, bespoke services and the unique tailoring of care provisions, but this was not universally recognised. It was also acknowledged that, although the concept of personalisation may be useful in principle, a lack of relevant services and support systems renders it less valuable in practice.
For service users, there were mixed feelings about the extent to which care was currently tailored to their own individual needs. Some felt that this was the case, whereas others were less convinced. Similarly diverse feelings were expressed in terms of whether or not respondents felt in charge of their care; this was not the case for all. There was also some sense among service users that they preferred to defer to the knowledge of carers and professionals when making key decisions. Carers were similarly ambivalent; some respondents felt that services were personalised, whereas others cited a need for more comprehensive help and support. There was also some acknowledgement of the fact that service users’ expectations for personalised care cannot always be met, and that some services (especially psychological therapy) are simply not available.
Care co-ordinators maintained that their approaches are as personalised as possible in the face of budget constraints, time limitations and demanding workloads. It was widely acknowledged that there is often a disparity between the concept of personalisation as an ideal and the reality of the care that can actually be delivered. For one respondent, the flexibility and creativity encouraged by a personalised approach were seen as positive qualities, although many others recognised that lack of service-user engagement, and the reluctance of some to embrace choice in their care planning, were significant hindrances. It is notable that, although personal budgets were mentioned by care co-ordinators, neither carers nor service users referred to these.
Embedded case-study comparisons
Detailed case-study comparisons were made for six cases consisting of three triads of service user, carer and care co-ordinator; two of service user and care co-ordinator only; and one of service user and carer only. Tables were drawn up for each of the themes used for our framework analysis; an example is presented in Appendix 9.
Dauphine
Dauphine Trust provides mental health and community services to a population of around 750,000 people. It covers an extremely densely populated urban area, which is very multicultural. Figures from the 2011 census showed that this site’s catchment area had one of the most ethnically diverse communities in the UK. For example, one area had 45% Asian (Indian, Bangladeshi, Pakistani, Chinese and other Asian), 27% white British/white other, 19% black African/Caribbean and the remaining 9% split between mixed, Arab and other backgrounds. According to the 2010 English Indices of Deprivation (EID), a high percentage of the areas covered by this site are among the top 10% of the country’s most deprived boroughs. Inpatient mental health services are provided from three hospital sites with 297 acute inpatient beds, and community services from 10 CMHTs. For this study, the CMHT that data were collected from had 14 psychiatric beds accessible to them.
Participant characteristics: care co-ordinators
Thirty-three care co-ordinators from four CMHTs within the locality completed the questionnaires. All of the respondents had spent > 4 years working in mental health services and the majority had spent > 4 years working as a care co-ordinator (81.8%). Further details of the demographic characteristics can be found in Table 21.
| Variable | n (%)a |
|---|---|
| Sex | |
| Female | 18 (39.4) |
| Male | 13 (54.5) |
| Age (years) | |
| Median | 46 (range 29–57) |
| Ethnicity | |
| White British/Irish | 10 (30.3) |
| Bangladeshi | 4 (12.1) |
| Black African | 4 (12.1) |
| Black Caribbean | 4 (12.1) |
| Indo-Caribbean | 2 (6.1) |
| Pakistani | 2 (6.1) |
| Asian other | 2 (6.1) |
| Black other | 2 (6.1) |
| White other European | 1 (3) |
| White other | 1 (3) |
| Profession | |
| Mental health nurse | 17 (51.5) |
| Social worker | 12 (36.4) |
| Profession continued | |
| Psychiatrist | 1 (3) |
| OT | 1 (3) |
| Employment/recovery worker | 1 (3) |
| Education | |
| Degree | 12 (36.4) |
| Postgraduate diploma/certificate | 7 (21.2) |
| Diploma/similar | 6 (18.2) |
| Master’s degree | 6 (18.2) |
| Time working in mental health services | |
| 10+ years | 21 (63.6) |
| 7–9 years | 7 (21.2) |
| 4–6 years | 4 (12.1) |
| Time working as a care co-ordinator | |
| 10+ years | 9 (27.3) |
| 7–9 years | 5 (15.2) |
| 4–6 years | 11 (33.3) |
| 1–3 years | 2 (6.1) |
| < 1 year | 4 (12.1) |
Participant characteristics: service users
In total, 666 questionnaires were sent to service users to invite them to take part in the study. We received 62 responses, which gave us a response rate of 9.2%. Further details of the demographic characteristics can be found in Table 22.
| Variable | n (%)a |
|---|---|
| Sex | |
| Female | 23 (37.7) |
| Male | 35 (57.4) |
| Age (years) | |
| Median | 47 (range 21–66) |
| Ethnicity | |
| Asian | 19 (31.1) |
| White British/Irish | 20 (32.8) |
| White other | 6 (9.8) |
| Black (Afro/Caribbean/Other) | 13 (21.3) |
| Mixed race | 2 (3.3) |
| Mental health problem | |
| Psychosis/schizophrenia/bipolar-type disorder | 31 (50.8) |
| Depression/anxiety | 4 (6.6) |
| Dual diagnosis | 1 (1.6) |
| Other | 2 (3.3) |
| Two or more of above | 21 (34.4) |
| Time in mental health service | |
| 10+ years | 37 (60.7) |
| 7–9 years | 6 (9.8) |
| 4–6 years | 4 (6.6) |
| 1–3 years | 8 (13.1) |
| < 1 year | 2 (3.3) |
| Living status | |
| Independent as single | 35 (57.4) |
| Independent in relationship | 2 (3.3) |
| Living with family | 13 (21.3) |
| Living with friends | 1 (1.6) |
| Supported accommodation | 5 (8.2) |
| Hostel/no fixed abode | 2 (3.3) |
| Other | 1 (1.6) |
| Daytime activity | |
| Full-time employment | 1 (1.6) |
| Part-time employment | 3 (4.9) |
| Education/training | 5 (8.2) |
| Unemployed | 31 (50.8) |
| Voluntary work | 8 (13.1) |
| Other | 11 (18) |
| Time with care co-ordinator | |
| Daily | 0 |
| Weekly | 14 (23) |
| Monthly | 32 (52.5) |
| Other | 13 (21.3) |
| Time with carer | |
| Daily | 28 (45.9) |
| Weekly | 14 (23) |
| Fortnightly | 4 (6.6) |
| Monthly | 4 (6.6) |
| Other | 9 (14.7) |
Summary scores for the questionnaires
The information presented here will be in the same format as that presented for the previous research site.
Empowerment Scale
The overall mean score for empowerment was above the midpoint for the instrument (Table 23). Out of a possible score of 4, indicating a higher perceived level of empowerment, the mean ± SD score was 2.64 ± 0.40; this is slightly lower than the reference value. 126 The subscale values were also slightly lower than the reference group, apart from ‘community activism’, which was comparable.
| Subscales | N | Service-user scorea | Reference valueb |
|---|---|---|---|
| Self-esteem–self-efficacy | 55 | 2.63 (0.72) | 2.82 |
| Power–powerlessness | 54 | 2.42 (0.56) | 2.51 |
| Community activism and autonomy | 55 | 3.12 (0.58) | 3.12 |
| Optimism and control over the future | 57 | 2.70 (0.70) | 2.72 |
| Righteous anger | 56 | 2.31 (0.71) | 2.34 |
| Total score | 56 | 2.64 (0.40) | 2.74 (0.34) |
Scale to Assess the Therapeutic Relationship
The mean total score for the STAR-P was 33.53 (9.23); 17.29 (6.03) for ‘positive collaboration’, 8.22 (2.79) for ‘positive clinician input’, and 8.02 (3.45) for ‘non-supportive relationships’. These values are lower than the reference values obtained from the validation paper (Table 24). 46
| Subscales | N | Service-user score | Reference valuea |
|---|---|---|---|
| Positive collaborationb | 58 | 17.29 (6.03) | 19.9 (6.7) |
| Positive clinician inputc | 58 | 8.22 (2.79) | 9.3 (3.0) |
| Non-supportive relationshipsc | 58 | 8.02 (3.45) | 9.3 (3.3) |
| Total score | 58 | 33.53 (9.23) | 38.4 (12.0) |
Recovery Self-Assessment scale
Mean scores and SDs for the RSA scale are provided in Table 25. Mean scores from service users and care co-ordinators on the subscales fell in the moderate range (2.93/5 to 3.69/5). The mean total RSA scores were very similar for care co-ordinators (µ = 3.31, SD = 0.75) and service users (µ = 3.31, SD = 0.96). The lowest scoring subscales were ‘Involvement’ and ‘Diversity of treatment options’ for both participant groups. Within these subscales, the scores demonstrate indifference. Service users also gave low scores on the ‘Individually tailored services’ subscale, which falls within the range of indifference.
| Subscales | N | Service users (N = 46–55)a | Care co-ordinators (N = 33)a |
|---|---|---|---|
| RSA total | 52 | 3.31 (0.96) | 3.31 (0.75) |
| Life goals | 53 | 3.46 (1.00) | 3.54 (0.83) |
| Involvement | 46 | 2.93 (1.09) | 2.99 (0.84) |
| Diversity of treatment options | 53 | 3.21 (1.12) | 2.98 (0.91) |
| Choice | 55 | 3.69 (0.98) | 3.46 (0.68) |
| Individually tailored services | 52 | 3.21 (1.07) | 3.49 (0.86) |
Recovery Profile from the Recovery Self-Assessment scale
The five highest rated items for the service users and care co-ordinators were within the choice and life goals subscales (Table 26). Other highly rated items by the service users were ‘staff members use a language of recovery’, ‘they monitor progress on personal goals’, and ‘there is the opportunity to discuss sexual and spiritual needs and interests’. Other highly rated items for the care co-ordinators were in the area of individually tailoring services, such as involving family and friends, offering specific services and programmes for individual interests, and helping people to build connections in their neighbourhoods. In addition to this, other strengths were related to life goals; staff agreed that their primary role was to help people in recovery to develop career and life goals, and fulfil aspirations. Staff also agreed that they were knowledgeable about special interest groups and activities in the community, and that progress was monitored on a regular basis.
| Rank | Service users (mean of 3.67–4.64 on Likert scale) | Care co-ordinators (mean of 3.79–4.23 on Likert scale) |
|---|---|---|
| 1 | Staff do not use threats, bribes or other forms of coercion to influence my behaviour or choices Choice |
Staff do not use threats, bribes or other forms of coercion to influence the behaviour or choices Choice |
| 2 | Most of my services are provided in my natural environment (i.e. home, community, workplace) Choice |
Agency staff believe that people can recover and make their own treatment and life choices Life goals |
| 3 | The role of staff is to assist me and other people in recovery with fulfilling my individually defined goals and aspirations Life goals |
Staff are diverse in terms of culture, ethnicity, lifestyle and interests Life goals |
| 4 | Staff believe that I can recover and make my own treatment and life choices Life goals |
Staff routinely assist individuals in the pursuit of their educational and/or employment goals Life goals |
| 5 | Staff listen to and follow my choices and preferences Choice |
Procedures are in place to facilitate referrals to other programmes and services if the agency cannot meet a person’s needs Life goals |
Narrative summary of interview data: senior managers and senior practitioners
We conducted interviews with two senior managers and five senior practitioners. The senior practitioners consisted of two approved mental health professionals, a psychiatrist, a social worker and a mental health nurse.
Local context: Dauphine
Local developments in the period prior to data generation included the setting up of primary care liaison services and proving improved physical health care, as well as better training for care co-ordinators and investment in IT. Integration between health and social care workers via colocation in community teams was described as a major move forward, and more medical practitioner input had been secured. However, participants also spoke of austerity-driven savings targets, meaning the loss of posts at the same time as demand was increasing, and of the challenges of providing services to a diverse and mobile community.
National-level policy aspirations were reflected in participants’ talk. Senior managers and professionals spoke of the use of a recovery approach, and of care that was personalised and focused on the individual, the family and the community. For example, a professional said, ‘we do try and involve service users . . . and make them to be active participants within their care planning’, and ‘participation’s something I think we do. I think we are respectful of clients, and that we try to have genuine relationships with them’ (D-SP-002). People also talked of commitments to tackling discrimination and stigma and promoting physical health. One senior professional, however, also spoke of values having been lost in service reorganisation:
I think that’s lost in a lot of logistics and bureaucratic stuff . . . because of a lot of things happening, restructuring and so forth.
D-SP-004
Care planning and care co-ordination
Not all users of the service had their care organised using the CPA, with inclusion determined by various criteria including severity and complexity of need and legal status. Decisions on the use of the CPA were taken by members of the wider multidisciplinary team (MDT). The CPA itself was described as meaning different things to different people. Recognition of the CPA as something that should be holistic, person-centred and client-led contrasted with descriptions of it as a means of defensively detailing services made available. One senior professional described the care co-ordinator role as one aimed at helping people ‘on the paths of recovery, or to at least reduce their mental distress and the impact that that distress has on their everyday life’ (D-SP-002), and another said that the CPA was ‘more to do with collaborative care for clients in a community setting’ (D-SP-003). However, a third also talked of the care plan as a document to which professionals could point as a record of what was on offer: ‘professionals can say, well this is what we have agreed that we are going to do’ (D-SP-001).
Frequent redesign of CPA documentation (three times in 5 years) had increased care co-ordinator workload, with the current CPA template comprising a series of forms. This was ‘fairly straightforward’ (D-SM-002), but was also very lengthy, at 14 pages. People spoke approvingly of the appearance of first-person care plans, and this same senior manager indicated that:
A certain number of our care plans are written in the first person because that’s really the way that we should be doing it with CPA because it’s all about the service user’ . . . Risk assessment was also described as ‘our number one [priority].
D-SM-002
Assessments in this area were described as happening collaboratively, with users and others as necessary. Challenging moves to person-centred care had been the introduction of PbR and clustering, which was said to have led to ‘cluster-focused’, rather than individualised, care plans. PbR was also described as adding ‘another layer of paperwork that needs to be completed and another target that needs to be met’ (D-SP-005).
Different care co-ordinator caseload sizes were given by different participants, with 40 the uppermost number. A suggestion made was that significant numbers of people would be discharged in the future. The work of care co-ordination was undertaken by any professional, but usually by nurses and social workers. Caution was taken not to overcommit psychologists and OTs to the role for fear of losing their capacity to provide specialist interventions. Although efforts were made to allocate the most appropriate care co-ordinators to service users, professional background was not seen as important to the work of care co-ordination itself. This was variously described as vast, and as carrying considerable responsibility, with a senior professional adding that ‘the role is so complex and there’s so much uncertainty’ (D-SP-001). Another view (from D-SM-002) was that the generic character of care co-ordination threatened the professional identity of all who did it.
Reviews for people whose care was organised under the CPA took place every 3–6 months, with a traffic light system alerting care co-ordinators to when to conduct reviews. Reviews were usually organised around psychiatrists’ diaries, and were described as often being medically led, whereas more user, carer and cross-professional control would be desirable. One professional said, ‘rather [than] it being consultant led, I think it should be service user led or carer led, and then the consultant sort of comes in terms of medication and so forth’ (D-SP-004). Carers were actively encouraged to participate, even if for part of the meeting only, and efforts to engage with carers included carers’ assessments and support plans and the availability of a carers’ centre. Some carers, it was suggested, were either overinvolved with or abusive of service users.
Mixed views were given on training. A general view was that care co-ordinators were given no training for the role, although a new 3-month course requiring attendance for one afternoon per week had recently commenced. This was seen as largely a medic-led course but also a step in the right direction. Training was said to have helped improve poor standards of care co-ordination in the past. External supervision had once been offered, but was now reduced to management supervision centred on caseloads.
Recovery
Different views were expressed of recovery. A senior manager (D-SM-001) said how the trust had traditionally been concerned with minimising and managing risk, with its move towards a recovery and user-centred approach emerging over the last 2–3 years. A senior professional spoke of progress, with people ‘now talking about recovery in a more open kind of way, it has now become mainstream, compared to when it first started in 2004’ (D-SP-001). Others spoke of resistance to the shift towards recognising individuals’ strengths and abilities, instead tending towards more conservative practice and an attitude of ‘if it’s not broken, do not fix it’ (D-SP-SM-002). Recovery was talked of as the taking of steps towards independence and fulfilment, with workers assisting in the identification of interests and life plans. A variety of practices were offered as examples of a recovery approach in action: employment coaches to help people find work; personal budgets to get gym membership; laptops and Skype™ (Microsoft Corporation, Redmond, WA, USA) to contact family overseas. Personal recovery plans and personal budgets were talked about, along with commitments to the instilling of hope, the setting of goals and involvement in communities. Contrasting views included the idea that service users could be ‘mollycoddled’ by services (D-SP-004) and that recovery planning was adequately addressed in the CPA. People spoke of the need for recovery training, and one of a need for a recovery approach to be imposed from the centre of the organisation. Some services users were also described as unprepared for the change in ethos associated with this way of thinking and working. One senior professional said that since arriving in the locality they ‘have not heard the word recovery mentioned, not even once’ (D-SP-001).
Personalisation
Widespread agreement existed that the trust was endorsing a personalised approach, which was sometimes linked to the idea of individualised care, although different service users’ experiences of this were said to reflect different styles of care co-ordination. For example, one senior professional said how the trust’s approach was ‘definitely’ personalised, as ‘all my care plans have always been personalised because the patient is the centre of what you’re doing and you can’t plan care unless you involve the patient [. . .]’ (D-SP-005). There was awareness of personalising care through the purchasing of care packages/services, and of putting the person in control through having a personal budget. The trust was said to be encouraging CMHTs to use personal budgets and large numbers of service users (as many as 50%) were signed up. Difficulties included the extensive paperwork required to apply for budgets, and of long delays (up to 12 months) in actually getting money once approved. Tensions were identified with clustering, which is, according to a senior professional, ‘not personalised and I’m not sure why we’re moving in that direction [. . .]’ (D-SP-005). Reference was also made to documents recommending that service users buy their care co-ordination from charities, with participants worried about the sharing of information outside of current services.
Suggestions for improvements
Participants had pride in their service, its staff and the range of what was provided. Changes were also thought to be needed, on the part of agencies, workers and users. A social work manager said the LA had ‘abandoned’ mental health services, and a view was that a stronger shared vision across health and social care organisations was needed. Closer ties to third-sector organisations were also suggested. Training (including in recovery, for service users as well as staff) and supervision were given as areas needing investment, with staff and service users needing to embrace more recovery-oriented ways of working. An example was for service users to take the lead in writing their care plans. Administrative workloads and paperwork need reducing, as one way of freeing up time to be with users and to thus be more personalised. Changes in ethos required included shifts away from orientations to crisis management and the management of risk. Limited resources were a major barrier.
Narrative summary of interview data: service users, carers and care co-ordinators
We conducted interviews with six service users, two carers and six care co-ordinators in Dauphine.
Care planning and co-ordination
Both service users and carers had mixed feelings towards – and varying levels of knowledge about – care planning, although there was an overall awareness of the process being carried out. Not all service user respondents possessed a copy of their care plan, which partly explains the inconsistent levels of engagement observed within this group in relation to care plans and their content. Some respondents had simply not felt motivated to read their plans properly. A similar ambivalence was apparent for carers in this respect: ‘You can write anything on a piece of paper but if nothing is getting done practically, it doesn’t mean anything’ (D-CA-002). Some carers were not involved at all and had never received copies of care plans, whereas others knew very little about the care planning process more generally. There were also concerns raised about the dictatorial nature of some plans and, consequently, the potential impact upon service users of being given personal copies. These views stand in contrast to those expressed by care co-ordinators, which are characterised by rich detail and extensive knowledge, and are framed in far more positive terms. For most care co-ordinators, care planning enables an individualised, holistic and multidisciplinary approach, which encourages collaborative work with service users. From this perspective, the CPA is a means of ensuring that care is adequately planned and clearly structured, and also that continuity of engagement between inpatient and outpatient services is maintained. Care co-ordinators also felt that the CPA was a valuable way of monitoring service users and facilitating continuity of care, especially when there are changes to the staff involved. Despite this mostly optimistic point of view, concerns were raised about the impact of increasing administrative demands, which necessarily reduce clinical contact time. Respondents were also aware of the potential danger of reducing care planning to a box ticking procedure, thereby compromising its individualised quality.
Among service users, there were disparate reports about the recognition of personal strengths, although this was not mentioned by either carers or care co-ordinators in relation to care planning. Some service users described their care plans as useful, especially where structured activities were included, and carers were even less forthright about this, perhaps in line with their apparent lack of involvement in the process, as observed in data for this site. One service user also suggested that their care plan had changed very little in the past decade.
Service users reported mixed levels of involvement in their care plans, and one carer declined to attend planning meetings for fear of the service user in question becoming irate with their care co-ordinator. Despite the powerful extent to which carers seemed to feel uninvolved in care planning, care co-ordinators maintained that it was useful to have their involvement. As far as care co-ordinators were concerned, ownership of care plans resides with service users themselves. It was also suggested that, for some service users, delaying decision-making pending improvements in their mental health could perhaps help to increase the likelihood of greater input on their part.
Various critiques of care plans – and challenges therein – were voiced; these differed depending on the type of respondent. For service users, key issues included a lack of choice about medication, insufficient contact with practitioners, and immigration status as a barrier to accessing additional services. Care co-ordinators, meanwhile, acknowledged the interruptions to continuity of care caused by staff changes, and also emphasised the challenges brought about by the reluctance of some service users to engage (and work) with staff. This was felt to be a major challenge from a professional perspective, not least because of the time-consuming nature of such relationships. It was emphasised that these difficulties vary in scope, depending upon the severity of service users’ particular illnesses.
Time pressures were also cited as a hindrance to collaborative care planning, a consequence of this being that professionals may simply write care plans in advance and ask service users to sign them, rather than involving them fully from the outset. Interestingly, disagreements between service users and care co-ordinators over care plan content – which subsequently have to be resolved within the MDT more widely – were a significant concern for the latter group of respondents, and it was noted that involvement does not necessarily equate to agreement. This particular issue was not a central one for carers or service users themselves. Care plan format was discussed by service users only, among whom there was a general preference for paper formats for ease of reference, and a sense of distrust towards other technologies.
Improvements suggested by service users included more clearly structured meetings and the provision of better information about the availability of other services in the community. The involvement of a wider range of professionals and more comprehensive consideration of additional needs (e.g. housing, work, social contact) was seen to be preferable, and the importance of focusing on individuals, and not simply their diagnoses, was foregrounded. Carers, meanwhile, expressed a wish for more support all around, from staff, families and the community more widely. For care co-ordinators, more training and increased personal supervision and support were deemed necessary, as well as increased contact time with service users, a reduction in current administrative demands, and some simplification of care plan content. The provision of advocates for all service users was also thought to be beneficial.
There were significant differences in service users’ awareness of how, or indeed if, safety and risk were considered in their care plan. The quality of relationships with staff were felt to be hugely influential on safety management, with poor relationships seen as a barrier to help-seeking, and good ones as supportive and encouraging in this respect. There was also an overall sense that risk and safety were not proactively managed, and a lack of regular check-ins from staff was a particular concern for one respondent, especially as this resulted in a significantly increased reliance upon carers during periods of illness. Carers gave less emphasis to such issues, but acknowledged that safety ought to be conceptualised in emotional (not just physical) terms, and also that risk needed to be equally well considered in relation to self and others.
Service users were also aware of the fact that they may also lack insight in relation to risk and safety when they are unwell. It was acknowledged that housing arrangements – the difference between supported housing and hostels, for example – can have a significant bearing on service users’ safety. There was on the whole agreement among care co-ordinators that the current working culture is a risk averse one, with positive risk taking rarely considered in care plans. It was felt that risks to staff and others were likely to be discussed more comprehensively than service users’ risk to themselves. One respondent also noted that risk is sometimes categorised depending on the diagnostic symptoms, rather than in accordance with service users’ own experiences of the symptoms.
Recovery
All respondents defined recovery primarily in terms of coping with and managing illness, as well as associating the term with ideas about making progress and moving forward. One service user respondent also suggested that recovery requires active participation on their part: ‘I think it should be more . . . proactive than about sustaining’ (D-SU-006). Carers were the only respondent group to use the ‘journey’ metaphor in this context. For care co-ordinators, listening to service users – as opposed to being overly prescriptive – was important in recovery-focused work.
There were differing opinions as to the helpfulness of care planning in relation to recovery. Carers and care co-ordinators were uncertain about this, whereas service users did not feel that it was especially helpful at all, citing contact with staff and medication as more useful.
Recovery plans did not appear to be widely used, and not all respondents were familiar with them. Care co-ordinators also had different views about the extent to which these are used.
Among service users and carers, there was a sense that achievements are not adequately recognised by staff, and this was reflected in the lack of emphasis given to the matter in care co-ordinators’ responses. One service user maintained that this was not particularly important, and that ongoing support and help were of greater value.
Personalisation
There was a notable disparity at this site in the definitions given by the three categories of respondent. Although service users demonstrated a full spectrum of understanding, there was a lack of general knowledge among carers. For care co-ordinators, meanwhile, personalisation is inextricably linked to personal budgets, which were the focal point of their discussions here, and which they felt to be a positive means of ensuring service user-led care, and the meeting of individual needs.
Other than one respondent, most service users and carers felt that current services are not personalised. This stands in direct opposition to the views of care co-ordinators, who consider services to be quite highly personalised. The primary hindrance identified was lack of time, which interferes with the extra effort required for personalisation:
I suppose often care co-ordinators, myself included, sometimes we get slightly panicked when people talks about personalisation because we think . . . that’s going to generate a lot of work.
D-CC-004
Care co-ordinators also emphasised that service users’ capacity (for decision-making and ‘leading’ their own care planning) necessarily determines the extent to which services can be personalised.
Among service users in particular, this shortcoming was attributed to funding problems, the lack of flexibility in staff outlooks and inadequate clarity around the decision-making processes that underpin the approval or rejection of claims. Both service users and carers felt that more support was required in order to ensure personalised care. Frustrations were expressed towards the complexity of application processes and a lack of staff support for such activities.
Despite the focus on personal budgets throughout care co-ordinators’ responses, only half of the respondents actually used them, and only one service user was actually engaged in managing their own budget. Among carers, budgets were either not discussed at all, or were an unfamiliar concept. The positivity of care co-ordinators’ views notwithstanding, there was a general professional acknowledgement of how a current lack of resources limits the possibility of meeting service users’ requests. It was also mentioned that the comparisons sometimes drawn between budgets awarded to individual service users can cause tension and difficulty. Service users’ reluctance to engage with the care-planning process (attributed mainly to those with substance misuse problems) was also identified as being a hindrance to the delivery of personalised care.
Embedded case-study comparisons
Detailed case-study comparisons were made for six cases consisting of two triads of service user, carer and care co-ordinator; and four of service user and care co-ordinator only. Tables were drawn up for each of the themes used for our framework analysis; an example is presented in Appendix 9.
Languedoc
The trust provides mental health, learning disabilities, and drug and alcohol services to a population of around 735,000 people. It covers an area that is largely rural with very few urban pockets. According to the 2010 EID, this site includes 19 areas that are within the country’s top 10% of the most deprived areas. These deprived areas are typically densely populated, urban and with a younger population, although two of them are officially classified as rural. Around 93% of the population are from White British backgrounds, and the remaining 7% are from BME groups. The trust provides both community and inpatient services and operates from two hospital sites. It has around 150 adult psychiatric beds and there are seven CMHTs. The main CMHT that data were collected from has around 42 psychiatric beds available to them.
Participant characteristics: care co-ordinators
Twenty-eight care co-ordinators from three CMHTs within the locality completed the questionnaires. The majority of respondents had spent > 4 years working in mental health services (92.8%) and had spent > 4 years working as a care co-ordinator (85.7%). Further details of the demographic characteristics can be found in Table 27.
| Variable | n (%)a |
|---|---|
| Sex | |
| Female | 19 (67.9) |
| Male | 9 (32.1) |
| Age (years) | |
| Median | 49 (range 27–59) |
| Ethnicity | |
| White British/Irish | 26 (92.9) |
| Indo-Caribbean | 1 (3.6) |
| White other | 1 (3.6) |
| Profession | |
| Mental health nurse | 19 (67.9) |
| Social worker | 4 (14.3) |
| OT | 4 (14.3) |
| Psychiatrist | 1 (3.6) |
| Education | |
| Degree | 9 (32.1%) |
| Diploma/similar | 8 (28.6) |
| Postgraduate diploma/certificate | 5 (17.9) |
| Master’s degree | 3 (10.7) |
| Time working in mental health services | |
| 10+ years | 24 (85.7) |
| 7–9 years | 2 (7.1) |
| 1–3 years | 1 (3.6) |
| < 1 year | 1 (3.6) |
| Time as care co-ordinator | |
| 10+ years | 15 (44.1) |
| 7–9 years | 7 (25.0) |
| 4–6 years | 2 (7.1) |
| 1–3 years | 1 (3.6) |
| < 1 year | 3 (10.7) |
Participant characteristics: service users
In total, 477 questionnaires were sent to service users to invite them to take part in the study. We received 92 responses, which gave us a response rate of 19.2%. Further details of the demographic characteristics can be found in Table 28.
| Variable | n (%)a |
|---|---|
| Sex | |
| Female | 48 (52.2) |
| Male | 40 (43.5) |
| Age (years) | |
| Median | 49 (range 20–68) |
| Ethnicity | |
| Asian | 2 (2.2) |
| White British/Irish | 79 (85.9) |
| White other | 5 (5.4) |
| Black (Afro/Caribbean/Other) | 1 (1.1) |
| Mixed race | 1 (1.1) |
| Mental health problem | |
| Psychosis/schizophrenia/bipolar-type disorder | 33 (35.9) |
| Depression/anxiety | 18 (19.6) |
| Dual diagnosis | 2 (2.2) |
| Other | 3 (3.3) |
| Two or more of above | 34 (36.9) |
| Time in mental health service | |
| 10+ years | 55 (59.8) |
| 7–9 years | 5 (5.4) |
| 4–6 years | 10 (10.9) |
| 1–3 years | 18 (19.6) |
| < 1 year | 2 (2.2) |
| Living status | |
| Independent as single | 46 (50) |
| Independent in relationship | 15 (16.3) |
| Living with family | 16 (17.4) |
| Living with friends | 2 (2.2) |
| Supported accommodation | 7 (7.6) |
| Other | 2 (2.2) |
| Daytime activity | |
| Full-time employment | 5 (5.4) |
| Part-time employment | 8 (8.7) |
| Education/training | 3 (3.3) |
| Unemployed | 39 (42.4) |
| Voluntary work | 16 (17.4) |
| Other | 18 (19.6) |
| Time with care co-ordinator | |
| Daily | 2 (2.2) |
| Weekly | 30 (32.6) |
| Monthly | 28 (30.4) |
| Other | 32 (34.8) |
| Time with carer | |
| Daily | 49 (53.3) |
| Weekly | 27 (29.3) |
| Fortnightly | 7 (7.6) |
| Monthly | 4 (4.3) |
| Other | 4 (4.3) |
Summary scores for the questionnaires
The information presented here will be in the same format as that presented for the previous research sites.
Empowerment Scale
The overall mean score for empowerment was above the midpoint for the instrument (Table 29). Out of a possible score of 4, indicating a higher perceived level of empowerment, the mean ± SD score was 2.62 ± 0.44; this is slightly lower than the reference value. 126 The subscale values were all lower than the reference group.
| Subscale | N | Service-user scorea | Reference valueb |
|---|---|---|---|
| Self-esteem–self-efficacy | 90 | 2.60 (0.78) | 2.82 |
| Power–powerlessness | 90 | 2.45 (0.55) | 2.51 |
| Community activism and autonomy | 90 | 3.09 (0.47) | 3.12 |
| Optimism and control over the future | 91 | 2.61 (0.65) | 2.72 |
| Righteous anger | 91 | 2.21 (0.72) | 2.34 |
| Total score | 91 | 2.62 (0.44) | 2.74 (0.34) |
Scale to Assess the Therapeutic Relationship
The mean total score for the STAR-P was 36.07 (9.03), 18.62 (4.92) for ‘positive collaboration’, 8.46 (2.75) for ‘positive clinician input’, and 9.14 (2.87) for ‘non-supportive relationships’. These values fall slightly below the reference values obtained from the validation paper; however, one of the subscales, non-supportive relationships, is very close (Table 30). 46
| Subscale | N | Service-user score | Reference valuea |
|---|---|---|---|
| Positive collaborationb | 90 | 18.62 (4.92) | 19.9 (6.7) |
| Positive clinician inputc | 91 | 8.46 (2.75) | 9.3 (3.0) |
| Non-supportive relationshipsc | 91 | 9.14 (2.87) | 9.3 (3.3) |
| Total score | 91 | 36.07 (9.03) | 38.4 (12.0) |
Recovery Self-Assessment Scale
Mean scores and SDs for the RSA scale are provided in Table 31. Mean scores from service users and care co-ordinators on the subscales fell in the middle to high range (2.70/5 to 4.04/5). For the mean RSA total score, the care co-ordinators score higher (µ = 3.57, SD = 0.56) than the service users (µ = 3.12, SD = 0.94). There is some variability between responses for the service users and the care co-ordinators. For the service users, the lowest scoring subscales were ‘Involvement’, and ‘Diversity of treatment options’. Within these subscales the scores demonstrate indifference. The highest rated subscale score is for the ‘Choice’ subscale; in particular the care co-ordinators scored highly on this, indicating that this is seen as an area of priority by the clinicians.
| Subscale | N | Service users (N = 81–87)a | Care co-ordinators (N = 28)a |
|---|---|---|---|
| RSA total | 86 | 3.12 (SD = 0.94) | 3.57 (SD = 0.56) |
| Life goals | 81 | 3.31 (1.00) | 3.82 (0.60) |
| Involvement | 81 | 2.66 (1.12) | 3.23 (0.63) |
| Diversity of treatment options | 83 | 2.70 (1.04) | 3.24 (0.64) |
| Choice | 87 | 3.72 (0.86) | 4.04 (0.50) |
| Individually tailored services | 84 | 3.05 (1.12) | 3.42 (0.69) |
Recovery Profile from the Recovery Self-Assessment Scale
The five highest rated items for the service users and care co-ordinators were within the choice and life goals subscales (Table 32). Other items rated highly by the service users were that staff members listened to them and followed their choices and preferences, used a language of recovery and encouraged them to take risks and try new things. Other highly rated items for the care co-ordinators were in the area of choice, such as listening to choices and preferences, choosing practitioners and monitoring progress on goals. In addition to this, other strengths were related to life goals; staff agreed that their primary role is to help people in recovery to be knowledgeable about specialist interest groups, use a language of recovery, develop career and life goals, and fulfil aspirations. Staff also strongly agreed with the importance of their role in helping people to become involved with activities to connect with communities, and in developing personal leisure interests and hobbies.
| Rank | Service users (mean of 3.67–4.64 on Likert scale) | Care co-ordinators (mean of 4.21–4.79 on Likert scale) |
|---|---|---|
| 1 | Staff do not use threats, bribes or coercion to influence my behaviour or choices Choice |
Staff do not use threats, bribes or coercion to influence the behaviour or choices Choice |
| 2 | Most of my services are provided in my natural environment (i.e. home, community, workplace) Choice |
Most services are provided in a person’s natural environment (i.e. home, community, workplace) Choice |
| 3 | The role of staff is to assist me and other people in recovery with fulfilling my individually defined goals and aspirations Life goals |
The role of staff is to assist a person with fulfilling their individually defined goals and aspirations Life goals |
| 4 | Staff believe that I can recover and make my own treatment and life choices Life goals |
Staff believe that people can recover and make their own treatment and life choices Life goals |
| 5 | Staff at this agency help to monitor the progress I am making towards my personal goals on a regular basis Choice |
People in recovery are given the opportunity to discuss their sexual and spiritual needs and interests Diversity of treatment options |
Narrative summary of interview data: senior managers and senior practitioners
We conducted interviews with three senior managers and five senior practitioners. The senior practitioners consisted of two mental health nurses, a psychiatrist, a social worker and an OT.
Local context: Languedoc
Local developments in the period immediately prior to data generation included the restructuring of community services and changes to the interprofessional composition of teams. Assertive outreach and early intervention, once provided through separate teams, had both been brought back into CMHTs. Social workers had been withdrawn from teams in order to concentrate exclusively on eligibility assessments, personalisation and personal budgets. A senior manager explained how (as a consequence) care co-ordinators are generally:
a registered nurse, a doctor, or a qualified OT. Very rarely you would find a social worker, because under the Section 75 agreement then they’re no longer expected to be a care co-ordinator.
L-SM-001
Budget cuts had led to the loss of up to five support worker posts, and the workload of those remaining was said to be increasing. In this context of retraction and reorganisation, staff morale was described as low.
Mixed views were expressed on values and goals: participants talked of recovery, individualised care, respect, involvement and having a community focus. They also talked of making a difference and the ‘6Cs’ in the post-Francis report129 era. The ‘6Cs’ consist of care, compassion, courage, communication, commitment and competence and are the central components of the Compassion in Practice paper as articulated by the Chief Nursing Officer. 130 Where one saw continuous improvement, others spoke of managers concerned with reputation, targets and protecting their jobs, and of national policies and aspirations having little impact on practice locally. A senior manager said how, at a management level, ‘the values and principles would all be very much around meeting targets, protecting the reputation of the trust . . . I don’t want to sound too cynical, but it’s difficult not to’ (L-SM-002). The trust was variously described as ‘working within a business model’ (L-SP-005), and as being paternalistic and medically dominated. Other views were that quality varied and that some people received a service which they would not if they lived elsewhere.
Care planning and care co-ordination
The CPA was used to organise care for people with serious mental illnesses and complex needs, and attracted a variety of views. It was described as a structure for making sure that needs were assessed and a recovery-focused programme of care offered and reviewed, overseen by a care co-ordinator who had a good relationship with the service user. For example, a senior manager said how the CPA was:
to ensure that people are offered a needs-based recovery focused programme of care that meets their individual needs, their family’s needs. And that spans all different types of care that they might need.
L-SM-001
A senior professional said how the CPA has a:
number of features, these would include a named care co-ordinator, having regular reviews and having a written care plan, which is normally shared with all the people, all the agencies, who are delivering care to this person.
L-SP-001
The CPA was also talked of as a monitoring system to reduce the risk of serious incidents, and as being different things to different people. Distinctions were drawn between what the CPA was and what it could be, with patchy implementation across the locale.
In the trust, a general structured assessment tool was used, with the specific assessment of risk said to be more important than other areas (e.g. crisis and contingency planning). A senior manager said how:
the thing that we score best on in . . . audits is the risk assessment, simply because people think that that’s more important . . . and to some extent they’re probably right.
L-SM-002
Information technology systems across the trust and LA were not compatible, and the trust’s package was said to lack functionality, forcing staff also to use paper records. Staff were unable to print documents for people in their own homes, and one senior professional spoke of a need to make the CPA less service-centred and more like the user-owned approach found in maternity care. PbR and clustering attracted different views. One view, from a senior manager (L-SM-001), was that it helped the CPA with costing and quality. Another, from a professional, was that the clustering tool increased financial pressures, reduced contact time between service users and practitioners and used out-of-date language: ‘words fail me on that one, how they’ve used this tool that’s about . . . 25, 30 years old, the wording in it is appalling’ (L-SP-001).
Local authority participants saw the CPA as something done by health staff within the trust. The CPA was not something that social workers were involved with, as following local arrangements they were not expected to fulfil the role of care co-ordinator. Caseloads were said to be rising but different estimates were given of caseload numbers, with an upper figure of 40 cited for nurses. They, plus OTs and psychiatrists, were the professionals most likely to fulfil the care co-ordinator role. Becoming a care co-ordinator reflected the service user’s presentation and assessment, but also local capacity. Some described the CPA as medically dominated, leading to poor teamwork and poor reviews, in which people’s voices were not heard. A senior professional said how the CPA is ‘weighted very heavily [in favour of doctors]’, and how ‘everybody in those CPA meetings should have the opportunity to have their point of view. They’re not meetings where the doctors give their orders out and say what they want to have happen’ (L-SP-002).
Reviews were usually 6-monthly and organised around the diaries of psychiatrists, who also determined the precise frequency of meetings and (according to one participant) vetoed the involvement of some people. Meetings sometimes happened in people’s homes, and participants talked of experimenting with video chat technology as a way of involving service users. Carers and people working outside of statutory services were usually invited, and one participant expressed a view that carers should be at reviews even where the service user did not want this. Others talked of tensions around confidentiality and consent, with carers’ assessments routinely offered.
Training involved a mandatory day (which was either every 1 or 3 years) addressing the CPA, clinical risk, diversity and electronic systems. One senior professional talked of having no specific care co-ordination training, and one saw care co-ordination as an expected and everyday part of the work of a nurse.
Recovery
Broad understandings were given of a recovery approach. This was described as highly personalised and individual, and about valuing strengths, independence and goals. A senior manager emphasised the change from traditional services this demanded ‘when everybody started to talk about recovery, people thought it’s something that we do anyway . . .I don’t think that there’s always been appreciation of the depth of it’, and how ‘people in some respects underestimated the level of investment that you have to make as an organisation and as a practitioner to work in a true recovery focused way’ (L-SM-001).
Evidence of recovery ideals in action cited by participants included co-produced care plans, some use of WRAPs and plans for a Recovery College. Resistance to recovery was also discussed. Participants talked of conservative medical practices, partly in response to work pressures and worries over risk and blame. At the highest level, managers were said to lack ‘passion’ for changing established ways of working, and at least some practitioners and service users were said to want to continue working in established ways. One senior manager said that:
The principles that are behind the recovery model are the same principles that are behind a lot of stuff that AMHPs [approved mental health professionals] and social workers and people would do anyway, and most decent nurses and OTs.
L-SM-002
In the case of tools (e.g. the Recovery Star), concerns over additional paperwork were given as reasons for their underuse. A view given by some participants was that if service users have capacity and decline therapies or other interventions then there is little else that can be offered.
Personalisation
There was a general awareness of personalisation being about people taking more control over their lives. Service users setting their own outcomes was cited as a way of helping this, but the process for achieving this could be relatively superficial (e.g. asking users to provide signatures). A senior professional view was that what people did was personalised because ‘I think it is by its very nature, in what we do’, and that ‘care planning is very personalised in itself, specific to each person’ (L-SP-005). Participants also pointed to the large numbers of people who the trust could not be sure had received copies of their care plan. Another view was that personal budgets brought about greater personalisation. The set up of these formed a large part of the work of social workers under local arrangements, who were said to have specific targets to meet. Varying estimates were given on the uptake of personal budgets, and requests for service users to make contributions to their own care were given as reasons why some services were turned down. Personal budgets were also seen as difficult to deliver, being surrounded by administrative processes described by one professional as ‘absolutely dire [because they turn a] simple process . . . into an absolute mass of paperwork [. . .]’ (L-SP-002).
Suggestions for improvements
Leadership was seen as important, along with cultural change. This was said to require a move away from a predominantly medical, paternalistic approach towards one which was more oriented towards recovery, personalised care and service user involvement. Training for staff on personalisation and recovery was said to be needed, along with helping service users to also better understand these concepts. Less bureaucracy was asked for. Challenges included staff inertia and budget cuts, and staff feeling that jobs were insecure.
Narrative summary of interview data: service users, carers and care co-ordinators
We conducted interviews with six service users, two carers and six care co-ordinators in Languedoc.
Care planning/co-ordination
There was a general awareness among service users and carers of care being planned and co-ordinated. For most, care plans were felt to be useful as a means of sharing information, recording key details and keeping track of progress, as well as for recording important contacts (e.g. emergency numbers). For service users, care plans themselves were deemed to constitute only a small part of the care planning process, with more priority and significance attributed to relationships and medication, and were thus felt to be relatively unimportant. Carers agreed that regular CPN visits were especially valuable. It was also noted that care plans sometimes fail to meet all relevant needs and may not cover specific elements such as contingency arrangements.
There was a similar emphasis among care co-ordinators upon the usefulness of care plans in terms of ‘keeping track’ – not only of service user individuals, but also of public safety. Efficient assessment and individualised care planning with a view to meeting personal needs were also considered to be of central importance. Interestingly, the information sharing practices foregrounded by service users and carers were, for care co-ordinators, associated with overwhelming quantities of paperwork and time pressures, which can result in rushed work. It was also acknowledged by this group of respondents that some service users see little value in care plans and are sometimes disinterested in them. Observations were made, too, about the difficulties sometimes experienced in finding ‘common ground’ between care co-ordinators and service users, which can be a hindrance to good care planning.
Levels of engagement with care plans varied widely among service users, although this was apparently less of a focal point for carers, who raised few concerns. Some service users had been given care plans whereas others had not; some took little notice of them, whereas others found the scrutiny of their engagement with their own personal details uncomfortable: ‘like being under a microscope’ (L-SU-003). It was generally felt that care plans are primarily important and useful for staff – something that staff are obliged to do. Service users and carers were keenly aware of this and agreed that the main function of the document was to facilitate effective intra-staff communication and to demonstrate that staff are able to maintain a clear picture of what is happening at any given time. Despite care co-ordinators’ insistence that involvement is the most important aspect of care planning, and that service users should own their care plans, they nevertheless recognised that this is not always the case in practice. One care co-ordinator said, ‘I think if it isn’t well understood it can just become a paper exercise and also what sometimes makes it not work is the pressures of the job, which a lot of the times is about, well meeting targets and it becomes more like a tick box sometimes’ (D-CC-002). Reflecting service users’ views, one respondent described the care plan document as being owned by care co-ordinators and written for service users, rather than truly belonging to them. Care co-ordinators also suggested that the level of involvement likely to be experienced by service users was partly dependent upon the extent to which their needs and expectations were seen as ‘realistic’ (L-CC-002). In such circumstances, there was said to be scope for significant input.
Service users described mixed experiences of involvement, along a continuum from fully involved, to good collaboration, through to no input at all. One example was given in which a service user was given scope to write their own care plan, but then staff added additional or missing details on their behalf. Some respondents observed that there was a general shift towards more collaborative work, although this was clearly not a universal experience. One respondent reported that their existing care plan had changed very little in the last decade. Although the paper format was preferred overall, most service users admitted that once the care plan is written, they do not refer to it again, and it was often seen as a piece of paper that they did not take particularly seriously. Similarly, carers used care plans primarily as an aide memoire, as a summary of meetings, or around review times, and did not feel that care plans functioned as ongoing ‘active’ documents:
You can give all the copies [of a care plan] out in the world, you know, but if it doesn’t mean anything in reality. You can write anything on a piece of paper but if nothing is getting done practically, it doesn’t mean anything.
L-CA-002
There was some preference among carers for more comprehensive care plans, and the notion of a portfolio of consecutive care plans (as a means of following progression more closely and incorporating updates more clearly) was also mooted. Care co-ordinators were also of the opinion that care plans are more a function of meetings than they are an active day-to-day document. Recognition was made of the fact that, as a consequence of this, omissions or oversights tend to be identified and addressed only when reviews are carried out.
Care co-ordinators raised concerns, too, about the existing format and structure of care plans, with most of the opinion that these could be shorter and simpler. The time-consuming nature of care plan documentation was mentioned:
Paperwork for instance takes probably up to like 75% of the care co-ordinator’s time . . . you probably see somebody here for an hour and [the paperwork] . . . ends up taking probably half of your day and that then is not useful at all . . . [because] that time you could have been using to see other people.
L-CA-002
It was suggested that any information included solely for the purpose of meeting targets – rather than as a means of enhancing service users’ experiences – ought to be removed from the document altogether. On the whole, service users seemed to understand their care plans, although it was mentioned that a clearer explanation of some headings might be beneficial. Care co-ordinators agreed that a simplification of existing paperwork would benefit all involved, and would also make documentation more accessible for all readers. Feelings were mixed about the usefulness of alternative (e.g. electronic) formats; this was seen to be dependent upon the skills and abilities of individual service users, but not thought to be suitable for all. Care co-ordinators were ambivalent about the IT systems used in their work. Assessments were described as comprehensive (despite being a little repetitive), and respondents complained that they had limited access to two of the systems used which, in turn, are not mutually compatible.
There was noticeable uncertainty among service users over whether or not issues around safety and risk had been assessed, discussed or incorporated into their care plans, and these did not seem to be major areas of concern here. Only one respondent described having a very helpful crisis and contingency plan and felt confident about using this as and when needed. Concerns were also raised about the sensitivity of risk-based discussions in a home visit environment where there are children present. Carers were more confident that safety and risk had been adequately considered by care co-ordinators, although they acknowledged that this was not always reflected in the care plans themselves. One respondent also noted that the existing risk assessment does not include provision for admission to hospital, or any contingency plan, despite care co-ordinators’ emphasis upon the importance of such inclusions. In contrast, risk assessment was felt to be a priority for care co-ordinators, and risk was understood to be more important from a practitioner’s perspective in general. ‘They’re always paramount . . . [my risk] radar is always very high up, yeah, and I always take risk very seriously’ (L-CC-002). Risk is assessed on an ongoing, continual basis, and care co-ordinators described a willingness to prioritise these, sometimes to the detriment of care plans or well-being plans. The main concerns raised in this context were in relation to blame, and the consequences of this for staff. Care co-ordinators also acknowledged the difficulties inherent in sharing the full details of risk assessments with service users, who would struggle with knowing exactly what information was held by the staff.
For service users and carers in particular, the relationship with their care co-ordinators was felt to be fundamentally important. One service user said:
[CPN is] supposed to see you every fortnight but . . . Sometimes they’re not in for weeks so you might not see anyone for a month or six weeks . . . My care co-ordinator is part time anyway, so she’s very, very busy all the time, and when she does come to see you, she’s literally, sits there, and she’s not even in my house ten minutes . . . I can’t tell her how I’m feeling or, and get into an in depth conversation that, in couple of minutes. You’re not programmed to talk like that. You have to feel, you know what I mean?
L-SU-004
Although care co-ordinators seemed to be less emphatic about this, they were very concerned about having to compromise time spent with service users in the face of ever increasing administrative tasks. There was also some discussion of a harsh compromise between demands for standardisation on one hand, and individualised care planning processes on the other.
The fluidity of care planning processes, frequent changes of care co-ordinator, and interruptions in continuity more widely, were cited as challenging by all three categories of respondent, with most emphasising the disruption that this creates. Similarly, some respondents felt insecure about the possibility of having support systems taken away as a consequence of structural and organisational changes; this was felt to have a negative impact on their sense of control over their care planning. Many felt that such issues could be better managed, ensuring that contact and support are actively maintained at all times, rather than having to be pursued by service users and carers during periods of change. Carers also recounted problems with continuity and high care co-ordinator turnover, and some expressed a wish for greater recognition of their role in relation to – and the scope of their relationships with – service users. Concerns were raised about feelings of isolation for some service users under community care. Better communication between care co-ordinators and GPs was also desired, and this was mirrored in care co-ordinators’ suggestions for better connections with physical health services via the use of well-being plans. There was some doubt expressed over whether or not GPs actually read the care plans that they are sent.
Recovery
Definitions of recovery varied across and within all categories of respondent, with one service user stating that the concept had not been discussed with them at all. There was, however, general acknowledgement of the complexities involved. Some service users rejected the notion of recovery altogether, although this was typically where it was understood in relation to the idea of a medical ‘cure’. Most respondents associated recovery with managing illnesses and symptoms, and (re-)establishing a satisfactory quality of life:
What I understand now, it’s for managing my illness. Recovery also involves knowing when you’re at risk, finding support, or, it’s hard to deal with it. And being able to access professionals who will be able to help me deal with new things.
L-SU-001
Although service users and care co-ordinators mentioned hope as a significant factor – it was also suggested that this would be a preferable term – this was not discussed by carers, who were in turn more focused upon the possibility of regaining independence, and who emphasised that only gradual progress ought to be expected. The ‘journey’ metaphor was mentioned only by service users, but this was not the dominant definition. Care co-ordinators also mentioned that difficulties may arise in situations where practitioners’ views of achievable progress or achievements sit in conflict with service users’ personal views of the same.
Service users at this site were unsure about the impact of recovery on care planning, and some did not make a clear connection between the notion of recovery and strategies of coping and self-management. Their relationships with care co-ordinators and/or support workers were instead felt to be very important in terms of recovery. For care co-ordinators, the recovery-oriented approach has resulted in a greater focus in care plans upon specific goals, as well as more of a drive towards referral and discharge; this was not seen to be a positive development. In general, care co-ordinators described working in a recovery-focused way; there were mixed feelings on whether or not procedures have changed as a consequence of this, although some respondents did feel that care planning had become less prescriptive and more collaborative overall. One care co-ordinator tried to explain the desire to provide a personal, responsive approach:
The definition of recovery from A to B is different. So, and as such you have to have the resources to tailor the care you are providing to meet that very aspiration of that very particular person . . . it’s an issue you have to keep on reminding yourself [about].
L-CC-006
There was some suggestion among care co-ordinators that the concept of recovery was perhaps for the benefit of organisational goals, as well as a sense that the intention for new clients is to move them on through services and reduce their level(s) of dependence.
Not all service users use recovery plans. Some respondents had not heard of WRAPs, whereas others had used them at various points, even if not continuously. Only one respondent felt that the Recovery Star had been helpful with care planning. Similar inconsistencies emerged in carer responses, although several did feel that WRAPs would, in principle, be useful. Carers also recognised the period immediately following hospital discharge to be especially challenging in relation to the formulation of recovery plans. There were also mixed responses among care co-ordinators; some indicated that WRAPs were used only occasionally, whereas others maintained that service users were encouraged to develop them.
All care co-ordinators emphasised the importance of taking a strengths-based approach to care planning, and this was mirrored in the responses of most respondents across the three categories. Carers did, however, note that the recognition of strengths and abilities does not necessarily mean that these will be recorded in care plan documents per se.
Among the criticisms made by service users of care received were the side effects of medication, which have resulted in weight gain and a loss of creativity as a consequence of adhering to the ‘chemical cosh’ (L-SU-001). Some also expressed sadness at being unable to regain the life that they had lived pre-illness. Carers were especially concerned about support around medication, noting that amendments to this can be traumatic, such that service users sometimes remain on unsuitable prescriptions, fearful of the possible consequences of any changes. For care co-ordinators, meanwhile, long waiting lists (especially for psychological therapies) and inconsistent levels of service-user engagement were cited as hindrances to the delivery of recovery-focused care. A perceived lack of organisational support for recovery, and an overemphasis on meeting targets, was seen as similarly challenging in this respect.
Most service users and some carers and care co-ordinators spoke about help being provided to access local voluntary services, day centres and activities and there seemed to be quite a lot available. One service user attended an art group and pottery class and said:
We get a lot of support there through other service users and that from that [which is helpful because] you get your distraction, but there’s also, from whatever you’re doing but there’s also people, other people there that you can keep in contact with . . . You just keep going, you just meet people, you start talking and I’ve still got friends from when I was on the day ward in 2009.
L-SU-005
There was some confusion among carers and care co-ordinators about what was available, and the need for an updated directory was mentioned: ‘Yeah we could do with a directory really of everything that’s around but that’s updated and I mean in real time, really, but things are changing that much, what’s here today might not be here next month’ (L-CC-006).
Personalisation
There was a significant degree of ambiguity around the term, with no unequivocal definition provided, although almost all respondents linked this to the notion of individualised care plans, rather than generic ones. This was the case even for care co-ordinators, some of whom – despite having received dedicated training – were not familiar with the term and others of whom had no clear sense of its meaning. Both service users and care co-ordinators also drew links between personalisation and ownership or ‘control’ of care planning, although this was not mentioned by carers. Most respondents across the three categories described their existing care as adequately personalised, with care co-ordinators in particular maintaining that service users’ needs are heard, and that that their contributions are recognised. There is much emphasis among care co-ordinators upon the likelihood of service users having ‘unrealistic’ expectations, which may not be matched by, for example, the availability of therapies or hospital beds. There was also some mention of the workload involved:
I suppose often care co-ordinators, myself included, sometimes we get slightly panicked when people talks about personalisation because we think, oh shit, God that’s going to generate a lot of work. And therein lies the problem that’s fundamentally wrong with the system.
L-CC-004
Embedded case-study comparisons
Detailed case-study comparisons were made for six cases consisting of two triads of service user, carer and care co-ordinator; and four of service user and care co-ordinator only. Tables were drawn up for each of the themes used for our framework analysis; an example is presented in Appendix 9.
Provence
Provence Trust provides both community and inpatient mental health services to a population of around 1.5 million people. The catchment area is predominantly rural with some urban localities, within which are provided specialist services. According to the 2011 census, > 90% of the population are from White British backgrounds. The EID reported that some of the areas within the catchment are affluent and among the least deprived 10% of areas in the country. Adult inpatient services are provided from six hospital sites, with approximately 30 CMHTs and 225 adult psychiatric beds, of which 34 beds are allocated to the principal CMHT that data were collected from.
Participant characteristics: care co-ordinators
Thirty-four care co-ordinators from three CMHTs within the locality completed the questionnaires. The majority of respondents had spent > 4 years working in mental health (85.3%) and two-thirds had spent > 4 years working as a care co-ordinator (67.6%). Further details of the demographic characteristics can be found in Table 33.
| Variable | n (%)a |
|---|---|
| Sex | |
| Female | 25 (73.5) |
| Male | 8 (23.5) |
| Age (years) | |
| Median | 45.5 (range 25–63) |
| Ethnicity | |
| White British/Irish | 24 (70.6) |
| White other | 3 (8.8) |
| Black African | 1 (2.9) |
| Bangladeshi | 1 (2.9) |
| Asian other | 1 (2.9) |
| Profession | |
| Mental health nurse | 13 (38.2) |
| Social worker | 10 (29.4) |
| OT | 7 (20.6) |
| Psychiatrist | 2 (5.9) |
| Psychologist | 1 (2.9) |
| Other | 1 (2.9) |
| Education | |
| Postgraduate diploma/certificate | 5 (14.7) |
| Doctorate | 1 (2.9) |
| Degree | 14 (41.2) |
| Diploma/similar | 8 (23.5) |
| Master’s degree | 6 (17.6) |
| Time working in mental health services | |
| 10+ years | 20 (58.8) |
| 4–6 years | 6 (17.6) |
| 7–9 years | 3 (8.8) |
| 1–3 years | 3 (8.8) |
| < 1 year | 2 (5.9) |
| Time working as a care co-ordinator | |
| 10+ years | 15 (44.1) |
| < 1 year | 7 (20.6) |
| 7–9 years | 5 (14.7) |
| 1–3 years | 4 (11.8) |
| 4–6 years | 2 (5.9) |
Participant characteristics: service user
In total, 398 questionnaires were sent to service users to invite them to take part in the study. We received 78 responses, which gave us a response rate of 19.6%. Further details of the demographic characteristics can be found in Table 34.
| Variable | n (%)a |
|---|---|
| Sex | |
| Female | 46 (59) |
| Male | 30 (38.5) |
| Age (years) | |
| Median | 50 (range 20–72) |
| Ethnicity | |
| Asian | 1 (1.3) |
| White British/Irish | 65 (83.3) |
| White other | 7 (9) |
| Black (Afro/Caribbean/other) | 1 (1.3) |
| Mixed race | 2 (2.6) |
| Mental health problem | |
| Psychosis/schizophrenia/bipolar-type disorder | 28 (35.9) |
| Depression/anxiety | 14 (17.9) |
| Dual diagnosis | 3 (3.8) |
| Other | 5 (6.4) |
| Two or more of above | 25 (32) |
| Time in mental health service | |
| < 1 year | 7 (9) |
| 1–3 years | 12 (15.4) |
| 4–6 years | 3 (3.8) |
| 7–9 years | 7 (9) |
| 10+ years | 45 (57.7) |
| Living status | |
| Independent as single | 29 (37.2) |
| Independent in relationship | 24 (30.8) |
| Living with family | 8 (10.3) |
| Living with friends | 3 (3.8) |
| Supported accommodation | 11 (14.1) |
| Other | 2 (2.6) |
| Daytime activity | |
| Full-time employment | 6 (7.7) |
| Part-time employment | 6 (7.7) |
| Education/training | 2 (2.6) |
| Unemployed | 39 (50) |
| Voluntary work | 13 (16.7) |
| Other | 11 (14.1) |
| Time with care co-ordinator | |
| Daily | 0 (0) |
| Weekly | 13 (16.7) |
| Monthly | 32 (41) |
| Other | 29 (37.2) |
| Time with Carer | |
| Daily | 38 (48.7) |
| Weekly | 16 (20.5) |
| Fortnightly | 4 (5.1) |
| Monthly | 7 (9) |
| Other | 7 (9) |
Summary scores for the questionnaires
The information presented here will be in the same format as that presented for the previous research sites.
Empowerment Scale
Table 35 shows that the overall mean score for the sample was above the midpoint for the instrument. Out of a possible score of 4, indicating a higher perceived level of empowerment; the mean ± SD score was 2.73 ± 0.39; this is aligned with the reference value. 126 The subscale values align extremely well with those from the reference group and are all above the midpoint for the scale, suggesting that service users in this site have moderate levels of empowerment.
| Subscale | N | Service-user scorea | Reference valueb |
|---|---|---|---|
| Self-esteem–self-efficacy | 76 | 2.73 (0.73) | 2.82 |
| Power–powerlessness | 76 | 2.57 (0.48) | 2.51 |
| Community activism and autonomy | 76 | 3.14 (0.52) | 3.12 |
| Optimism and control over the future | 76 | 2.77 (0.65) | 2.72 |
| Righteous anger | 76 | 2.35 (0.56) | 2.34 |
| Total score | 77 | 2.73 (0.39) | 2.74 (0.34) |
Scale to Assess the Therapeutic Relationship
Table 36 shows that the mean total score for the STAR-P was 32.33 (11.91), 16.15 (6.57) for ‘positive collaboration’, 7.83 (3.49) for ‘positive clinician input’, and 8.53 (3.11) for ‘non-supportive relationships’. The service user scores for this site are a lot lower than those of the reference value. 46 The respondents scored particularly low on the positive collaboration and positive clinician input, suggesting that care planning did not score highly in terms of collaboration in this site.
| Subscale | N | Service-user score | Reference valuea |
|---|---|---|---|
| Positive collaborationb | 74 | 16.15 (6.57) | 19.9 (6.7) |
| Positive clinician inputc | 75 | 7.83 (3.49) | 9.3 (3.0) |
| Non-supportive relationshipsc | 75 | 8.53 (3.11) | 9.3 (3.3) |
| Total score | 75 | 32.33 (11.91) | 38.4 (12.0) |
Recovery Self-Assessment scale
Mean scores and SDs for the RSA scale are provided in Table 37. Mean scores from service users and care co-ordinators on the subscales fell in the moderate to high range (2.91/5 to 3.70/5). The difference in mean total RSA scores was only marginal; care co-ordinators had the highest ratings (µ = 3.25, SD = 0.46), followed by service users (m = 3.10, SD = 1.03). The lowest scoring subscale was ‘Involvement’ and ‘Diversity of treatment options’ for both participant groups. Interestingly, care co-ordinators scored lower on the ‘Diversity of treatment options’ than the service users. Both participant groups scored highly on the ‘Life goals’ and ‘Choice’ scales.
| Subscale | N | Service users (N = 68–74)a | Care co-ordinators (N = 34)a |
|---|---|---|---|
| RSA total | 73 | 3.10 (SD = 1.03) | 3.25 (0.46) |
| Life goals | 68 | 3.30 (1.10) | 3.70 (0.55) |
| Involvement | 69 | 2.86 (1.23) | 2.86 (0.56) |
| Diversity of treatment options | 73 | 2.91 (1.16) | 2.74 (0.51) |
| Choice | 74 | 3.39 (0.98) | 3.58 (0.74) |
| Individually tailored services | 71 | 2.89 (1.24) | 3.08 (0.64) |
Recovery profile from the Recovery Self-Assessment scale
The five highest rated items for the service users and care co-ordinators were within the ‘Choice’ and ‘Life goals’ subscales (Table 38). Service users did not identify any other items strongly enough for there to be a strong agreement (> 3.5) across the mean responses. Other highly rated items for the care co-ordinators were in the area of ‘Choice’, such as listening to choices and preferences, monitoring progression towards goals and providing services in the natural environment. In addition to this, other strengths were related to ‘Life goals’, with staff agreeing that their primary role is to help people in recovery to be knowledgeable about specialist interest groups, to use the language of recovery, and to ensure that procedures are in place for referring service users to services. Staff also strongly agreed that every effort is made to involve significant others in care.
| Rank | Service users (mean of 3.49–4.11 on Likert scale) | Care co-ordinators (mean of 3.91–4.18 on Likert scale) |
|---|---|---|
| 1 | Staff do not use threats, bribes or other forms of coercion to influence my behaviour or choices Choice |
Staff believe that people can recover and make their own treatment and life choices Life goals |
| 2 | Most of my services are provided in my natural environment (i.e. home, community, workplace) Choice |
The role of staff is to assist a person with fulfilling their individually defined goals and aspirations Life goals |
| 3 | Staff believe that I can recover and make my own treatment and life choices Life goals |
Staff actively assist people in recovery with the development of career and life goals that go beyond symptom management and stabilisation Life goals |
| 4 | The role of agency staff is to assist me and other people in recovery with fulfilling my individually defined goals and aspirations Life goals |
Staff routinely assist individuals in the pursuit of their educational and/or employment goals Life goals |
| 5 | Agency staff are diverse in terms of culture, ethnicity, lifestyle and interests Life goals |
Staff do not use threats, bribes or other forms of coercion to influence the behaviour or choices Choice |
Narrative summary of interview data: senior managers and senior practitioners
We conducted interviews with two senior managers and five senior practitioners. The senior practitioners consisted of a mental health nurse, psychiatrist, social worker and two approved mental health professionals.
Local context: Provence
A major restructuring had taken place across the trust in the period prior to data generation. Inpatient and CMH services had separated. Services had centralised and been designated as ageless. This meant that community staff worked with anyone over the age of 18 years, with no upper limit and no separate older adult services. This reorganisation attracted mixed views. Participants spoke of service users having longer distances to travel, and of the change as being top-down. Staff were described as lacking skills and confidence to work with older people with complex physical health needs. A senior professional said how:
We’re not specialists in their needs, their needs can be very complex because often they have got physical health problems alongside. Sometimes there’s, it’s maybe signs of organic problems as well, so we don’t necessarily know if their loss of memory might be to do with depression or whether they have early signs of dementia or something. So there’s a lot of other complexities and we’ve had no training yet.
P-SP-005
Across the locale a high degree of health and social care integration was reported, with NHS and LA staff co-located in CMHTs, staff being seconded in from other organisations and practitioners fulfilling shared roles. An example was nurses working as approved mental health professionals (with responsibilities during the operation of the Mental Health Act61). Integration was seen as a good thing, although participants also talked of having to use different IT systems for health and social care activities.
The trust claimed strong values. These were described as centring on the provision of high-quality mental health services and the improvement of service user and staff experience, on financial viability, choice, recovery, partnership, inclusion, advocacy, individualised care and involvement. Participants also described commitments to the use of evidence and to outcomes, and to being an active site for the conduct of research. However, some participants drew contrasts between public statements and reality, citing service reconfiguration as an example of imposed change. Participants also spoke of difficulty meeting financial targets, and a sense of constant urgency in meeting timescales and targets set by commissioners.
Care planning and care co-ordination
Accounts were given of the history of the CPA and of its current constituent elements. These included assessment, care planning (including for crises and contingencies), the appointment of a care co-ordinator and review. People talked of the importance of care co-ordinators knowing the people using their services, and of risks being assessed in collaboration with service users using a two-level risk assessment approach. ‘Risk’ was described by a senior professional as ‘core, it’s central, integral to care planning’ (P-SP-001). Local distinctions were made between the ‘standard’ and ‘enhanced’ CPA, with the extension of CPA principles to people with less complex needs seen as important for the purposes of identifying responsible care co-ordinators. For a senior manager the most important element was ‘the collaborative approach with patients really, in that they have some ownership of their care plan [. . .] with rather than for them’ (P-SM-001).
A variety of views were given of the local care plan format and the electronic record system supporting this. Documentation was praised for being user-friendly with good use of language emphasising needs and recovery, but was also said to be insufficiently lay. A senior manager talked of the difficulties associated with the CPA having to serve multiple ends: ‘obviously, you’re pleasing two beasts, performance commissioners, as well as trying to balance that with making sure your paperwork is service user friendly, which is challenging’ (P-SM-002).
Two versions of the electronic record existed: one for people whose care was organised using the full CPA, and one for all other users of the service. A further electronic system existed for LA-related work, such as safeguarding and carer assessments. In the trust system, all relevant information was contained about service users, and a care planning module existed with sections to be printed for service users to sign. Staff could straightforwardly move information from old care plans to new, where this was appropriate to do so. The format was also described as very linear. Challenges included the need to change whole care plans if the care co-ordinator changed and overcoming the unintended consequences of investing in electronic records. Electronic records were said to have created barriers by removing people from their actual plans and reducing creativity in favour of reliance on the local CPA template. Participants talked of laptop and tablet computers as having the potential to address this. For managers, the electronic system was a tool to check notes. The trust was said to be retendering for its IT support, and one hope was for a system of electronic records containing care plans that service users could edit.
Mental health nurses, social workers and OTs all provided care co-ordination, with psychiatrists acting as co-ordinators for people using outpatient services only. Psychologists were said to be less involved and more concerned with specialist provision. Differing estimates were given of typical caseload sizes, with an upper limit given at 50. Although staff specialised in certain tasks (e.g. Mental Health Act61 work, medication administration), care co-ordination was described as entirely generic. One senior professional said how:
Roles though have been merged, so roles which traditionally would have been seen as being a social worker role or social services role have been picked up by health staff who increasingly, so pretty well every aspect, in fact it probably is every aspect of work that traditionally a social worker would do now, health employees would do as well.
P-SP-001
Differing accounts were given on care co-ordinator allocation. One view was that, historically, social workers had co-ordinated services for people with predominantly social care needs, but that allocation of care co-ordinators to service users based on distinctions between ‘health care’ and ‘social care’ were now unfeasible. Another was that alignment was attempted based on need.
Local commissioning arrangements meant that stable, long-term users of residential care, for example, were able to access the trust’s services. Commissioning requirements created unwanted bureaucracy surrounding reviews, and care co-ordinators now needed to produce additional ‘support plans’. Some care plans were said not to have changed for 4 years and others were described as ‘paltry’, with participants speaking of some staff who paid lip service only to the CPA system. Reviews were described as sometimes happening at arbitrary times, forced by the electronic record system. Linking reviews to clustering was suggested by one. Typically, reviews occurred 6-monthly, but sometimes occurred annually. Meetings took place in psychiatrists’ offices and were organised by care co-ordinators, whose capacity to prepare could be inhibited by time constraints. Mixed views were expressed on degrees of user and carer involvement, with variance described at the level of individual care co-ordinator. A general approach towards carer involvement was indicated, with targets set for carer assessments. The possibility of tensions between service users and carers was noted, as well as the potential for overinvolvement.
Participants spoke of periodic training for the CPA, which had been obligatory when the CPA was first introduced. A view was that as people have been care co-ordinating for so long, there is no training for it: ‘I think there should be better training and better guidance on how to write the risk assessments and care plans, because I have had none’ (P-CC-003). Another participant talked of having taken part in a 9-week, user-led course on care co-ordination.
Recovery
Recovery was described as the maximisation of potential, and of people with lived experience of mental health difficulties having meaning, purpose and hope in ways defined by themselves. There was widespread support for these principles, and enthusiasm:
I think the principles around recovery are brilliant and it’s fantastic that we are incorporating it into the way the Trust works and really we, they should be more evident in everybody’s care plan, the recovery focus.
P-SP-001
One senior practitioner said that the people they worked with would not ‘recover’ at all and that ‘recovery’ was not an appropriate word:
I’ve got people on care packages and the actual wording is, ‘please demonstrate how they’re going to require less input next year as they will improve’ and you just think that they won’t. This recovery is actually a bit of a misnomer.
P-SP-002
Generally, services were said to be more focused on recovery despite ‘cultural lag’ in some places and resistance from some staff (P-SP-002). Resistance was particularly noted from medical practitioners (with some versions of ‘recovery’ being perceived as oppositional to the medical model) and from older nurses. Changes were nonetheless described in the use of language and approach towards more collaborative care planning, in the growth of peer support, in service users joining interview panels and in the setting up of Recovery Colleges. However, the CPA was said to need to become more recovery-focused in its operation. This required a culture change from staff and also from service users, who (one person said) needed to take greater responsibility for their care. Tensions were also observed between aspirations of recovery and the loss of liberty some users experienced.
No clear picture emerged of the use of recovery tools. A local tool existed, and at least some staff were said to use WRAPs and/or the Recovery Star. A view was that specific tools were always less important than the approach used. Paperwork and orientations to targets were given as reasons why care co-ordinators struggled to find time to engage in face-to-face recovery-promoting activities.
Personalisation
Examples of personalisation in action given by participants included self-management, self-directed support packages (or direct budgets) and personal health budgets. Personalisation was also described as a more general approach, which was concerned with the person as an individual: ‘there’s much more flexibility, individualism and actually in great depth and detail, and people’s care packages are set up very much tailored for the individual’ (P-SP-001). The local system for realising personalised care was described as difficult to navigate, being bureaucratic and characterised by a proliferation of external providers. Service users were said to experience uncertainty in this context, and services were said to lack flexibility in key areas (e.g. out-of-hours support was limited, and no anger-management service could be purchased). Specific examples were given of budgets being used to support peer workers accompanying people to social activities. Commissioners’ targets for self-directed support had reportedly been exceeded, but achieving this had increased administrative burdens on staff to deliver ‘micro-commissioning’. Staff had also needed to develop new skills (e.g. in negotiating with providers). Where personalisation had been achieved this was (in one view), despite the processes and structures, rather than because of them. For practitioners, the use of external providers was said to involve a handing over of responsibility, raising concerns for some over the management of risk. Personal budgets were said to be widely used, with up to 50% of people on care co-ordinator caseloads involved in one estimate.
Suggestions for improvements
Quality of work, rather than quantity, was seen as an important focus. Caseload supervision and active caseload management was said to be necessary, along with training for staff to use the right language and right forms. More time for the work needing to be done was needed, along with more staff and improved IT resources. Staff and service users were said to need to take greater ownership of both the CPA and the idea of recovery. Centralised services and excessive administration were both cited as barriers.
Narrative summary of interview data: service users, carers and care co-ordinators
We conducted interviews with six service users, five carers and six care co-ordinators in Provence.
Care planning and co-ordination
There was an overall awareness among service users and carers of care being planned and co-ordinated. Fewer than half of respondents actually had a copy of their current care plans, however, and fewer still felt actively engaged with them. Non-possession of the document notwithstanding, there was universal agreement that care plans should function primarily as a guide or structure for service users and carers; this mirrors care co-ordinators’ conceptualisation of it as a guiding framework or system: ‘I think the thing I found most helpful was having a structure to. . . my care plan and a weekly timetable to follow. So it’s helped me stay stable and build a structure using weekly timetables to add full range of activities’ (P-SU-001). For most service users and carers, having a strong sense of being ‘looked after’ – even where this is not demonstrated in active delivery of the same – was felt to be valuable, and care co-ordinators suggested that care plans themselves are not particularly important from a service user’s perspective.
On the whole, all three categories of respondent agree that, in practice, the main value of care plans is to keep a record of information, progress and key contact details, although few actually refer to them regularly because they are not felt to be dynamic, active or responsive documents. The written format was preferred by most – a ‘life written down on a piece of paper’ (S-CA-004) – and no strong feelings were reported about alternative formats, although care co-ordinators expressed a general opinion that most service users would not have the necessary skills for phone apps or other such alternatives, for example. Care co-ordinators describe the electronic systems that they use as labour-intensive, overcomplicated and a hindrance to regular updates:
The CPA computer system’s awful. It makes things a lot more difficult, and it’s not just with care plans, risk assessments, you have to lock them, and then you have to go and pull the whole thing through, you can’t just edit it, go in and edit it, so it’s really time-consuming.
P-CC-002
Although they feel that care plans use too much jargon and need simplifying, however, neither service users nor carers are especially concerned by this.
The experiences of care planning/co-ordination reported by service users range from empowering, collaborative and facilitative of independent living, right through to feeling as though they have been cast aside: ‘[my psychiatrist] wants to offload me because psychiatrists don’t like being care co-ordinators, they’ve got too much else to do’ (S-SU-002). The varying levels of involvement experienced by both service users and carers also reflect this, with some being fully and actively involved and able to make contributions, whereas others had neither involvement nor influence. For service users, this level of involvement seemed also to determine their subsequent sense of care plan ownership. Among care co-ordinators, there was much divergence about ownership, which was variously attributed to service users and professionals, with some describing shared ownership between the two parties:
The most important aspect of it for me is that it is a way of recording and delivering treatment for service users, that is done in a way that it allows partnership working with all the, with the service user and the care co-ordinator and other professionals but it also allows to, a framework for recording the way that is going to be done.
P-CC-001
There was an overall wish for greater involvement for both service users and carers, although care co-ordinators feel that there is an inherent tension between giving service users plenty of scope for involvement and simply relying on them to voice any disagreements they have about the written content.
Regular contact with professionals was cited as important for most respondents, although this was acknowledged to be contingent upon services users’ willingness to engage, and was sometimes difficult to achieve given current limitations in terms of staffing and resources. Much emphasis was given to the importance of consistency and coherence over time, to create an ongoing support system, but most respondents state that this has not been adequately established. Carers, in particular, seem dissatisfied with their experiences. This sense of inconsistency is also evident in care co-ordinators’ widely disparate views, with some championing the consistency achieved, and others describing it as ‘appalling’ (P-CC-003). It was noted that the obligatory inclusion of risk assessments does not necessarily mean that service users or carers have been fully involved in discussions about risk and safety, nor does it ensure that adequate actions will be taken in the event of a crisis. Among care co-ordinators, concerns were expressed about the quality and consistency of risk assessments. Few respondents focused on the value of setting goals and objectives, and no significant emphasis was given to the recognition and use of strengths and abilities.
Recovery
Various definitions were provided, but all predominantly focused on being able to manage illness and developing coping skills, aiming for gradual improvement. The ‘journey’ metaphor was hardly used by respondents. Among care co-ordinators, there was no major significance given to a drive towards discharge. It was also understood by many that recovery may not necessarily be a primary objective for some service users.
Radically different feelings were expressed among service users and carers about the role and impact of the care plan in relation to recovery, from some finding it no help at all in some cases, to others finding it pivotal. Its centrality in this regard was powerfully linked to respondents’ wider experiences of care planning, depending upon whether these were positive or negative. On the whole, care co-ordinators were ambivalent about this. All respondents acknowledged that good additional support from family friends was important for recovery. Overall, carers attributed more value to the development of individual strengths than did service users, whereas care co-ordinators recognised the value of working with strengths and abilities:
[Focusing on strengths and abilities is] . . . the most important part . . . everyone, however shit they feel, everyone, you can drag some little positive out of them or something that would be a good, something they once liked or they once did. It might take a while but you can normally get there, and if you can find that just little tiny seed of interest in something and build on it, then I think that makes a difference.
P-CC-003
However, they noted that this was not necessarily translated into any specific actions or interactions carried out with service users or carers.
None of the respondents used WRAPs, and most service users had never heard of them at all. Care co-ordinators were mostly familiar with WRAPs – describing these as useful ‘tools’ – but had chosen not to use them because they are too time-consuming, lengthy and intricate.
Personalisation
Not all service users and carers were familiar with the term, but there was general agreement that personalisation means focusing on individuals and their unique needs. All care co-ordinators were familiar with the term, but most conceded that it is a term they do not actually use. For service users and carers, neither positive nor negative connotations were associated with the term, although there was some apprehension among care co-ordinators that it might have negative consequences by virtue of creating unrealistic expectations for service users. Most service users and care co-ordinators felt that care was personalised, whereas carers were more ambivalent about and less assured of this. For service users, the degree to which care is felt to be personalised is inextricably linked to the help and support they have received from professionals and friends/family. Service users described personalised care from a passive perspective; it is something that happens to them, rather than involving any active processes (e.g. choice, ownership) on their part. In contrast, carers evaluate personalisation in terms of how much choice and ownership service users have in relation to their care. Care co-ordinators acknowledged that the extent to which service users feel in charge of their care is variable but some also voiced concerns about personalisation leading to ‘unrealistic’ expectations:
I think again if you give someone complete full reins to go ahead and design their care plan it just becomes unrealistic so I think it’s just about being realistic all the time . . . And being realistic isn’t, I don’t think, it’s not a bad thing. It’s about what’s available to us, and that’s not because I don’t want to help my client get whatever they want but it’s what’s available to us as a service and resources that are available to us.
P-CC-002
Lack of resources, inadequate training and increased paperwork were seen by care co-ordinators as powerful hindrances to the delivery of personalised care: ‘Well, the trouble is you do the training but it’s the same training that gets churned out every year, so, no, I don’t think it’s adequate, personally’ (P-CC-004). Accordingly, some service users viewed deficits in personalised care as a structural/systemic problem rather than as a professional inadequacy.
Embedded case-study comparisons
Detailed case-study comparisons were made for six cases consisting of five triads of service user, carer and care co-ordinator; and one of service user and care co-ordinator only. Tables were drawn up for each of the themes used for our framework analysis; an example is presented in Appendix 9.
Chapter 5 Results: cross-case analysis
Summary of chapter
In this chapter, we conduct a comparison across the six sites. The chapter is in three sections. Section 1 contains cross-case analysis of scores on the quantitative measures. In Section 2 we draw on the within-case analysis of the qualitative data presented in the previous chapter and focus on four key areas: local context and developments; CPA/CTP care planning and co-ordination; recovery; and personalisation. Section 3 ends the chapter with tables identifying potential facilitators and barriers to the delivery of recovery-focused, personalised care planning and co-ordination. These are then discussed in more detail in Chapter 6.
Section 1: cross-case analysis of the quantitative data
Inferential statistics were used to determine if there were any differences across sites for the three questionnaires. Cross-site analyses will be presented for the three service-user questionnaires (the RSA scale, STAR-P and ES) followed by a cross-site analysis of the care co-ordinator questionnaire (the RSA scale). In addition, several correlations were conducted to determine associations between the questionnaire subscales and totals globally and on a site-specific basis.
Service users
One-way ANOVAs of all subscales were conducted and subsequent Tukey’s post-hoc tests demonstrated some areas of significant differences between research sites on the STAR-P measure of therapeutic relationships. There were significant differences across sites in the mean total STAR-P score [F(5,429) = 3.45; p-value = 0.005], the positive collaboration subscale [F(5,426) = 3.75; p-value = 0.002] and the positive clinician input subscale [F(5,431) = 2.80; p-value = 0.017]. There are no global differences across the sites for the RSA scale and ES. Table 39 shows the mean item scores, alongside the parameters of significance.
| Survey measure | One-way ANOVA parameters | Artois mean (SEM) | Burgundy mean (SEM) | Champagne mean (SEM) | Dauphine mean (SEM) | Languedoc mean (SEM) | Provence mean (SEM) |
|---|---|---|---|---|---|---|---|
| RSA scale | |||||||
| Life goals | F(5,394) = 0.65; p = 0.659 | 3.48 (0.12) | 3.55 (0.13) | 3.38 (0.97) | 3.43 (0.14) | 3.31 (0.11) | 3.30 (0.13) |
| Involvement | F(5,373) = 0.81; p = 0.543 | 2.89 (0.15) | 2.96 (0.13) | 2.70 (0.15) | 2.93 (0.16) | 2.66 (0.13) | 2.86 (0.15) |
| Diversity of treatment options | F(5,406) = 1.67; p = 0.139 | 2.99 (0.15) | 3.06 (0.13) | 3.05 (0.14) | 3.21 (0.15) | 2.70 (0.11) | 2.91 (0.14) |
| Choice | F(5,423) = 1.27; p = 0.277 | 3.66 (0.11) | 3.65 (0.10) | 3.66 (0.10) | 3.69 (0.13) | 3.72 (0.09) | 3.39 (0.11) |
| Individually tailored services | F(5,418) = 1.72; p = 0.129 | 3.27 (1.00) | 3.34 (0.13) | 2.95 (0.13) | 3.23 (0.14) | 3.04 (0.12) | 2.89 (0.14) |
| Mean total score | F(5,405) = 0.86; p = 0.509 | 3.27 (0.12) | 3.33 (0.11) | 3.13 (0.11) | 3.31 (0.13) | 3.12 (0.10) | 3.10 (0.12) |
| STAR-P | |||||||
| Positive collaboration | F(5,426) = 3.75; p = 0.002** | 17.37 (0.76) | 19.81 (0.57) | 17.13 (0.70) | 17.29 (0.79) | 18.62 (0.52) | 16.15 (0.76) |
| Positive clinician input | F(5,431) = 2.80; p = 0.017* | 8.12 (0.40) | 9.46 (0.28) | 8.01 (0.36) | 8.22 (0.37) | 8.46 (0.29) | 7.83 (0.40) |
| Non-supportive clinician input | F(5,430) = 1.66; p = 0.142 | 8.90 (0.28) | 9.23 (0.33) | 9.09 (0.33) | 8.02 (0.45) | 9.14 (0.30) | 8.53 (0.36) |
| Mean total score | F(5,429) = 3.45; p = 0.005** | 34.51 (1.31) | 38.49 (1.0) | 34.09 (1.21) | 33.53 (1.21) | 36.07 (0.95) | 32.33 (1.37) |
| ES | |||||||
| Self-esteem–self-efficacy | F(5,428) = 0.78; p = 0.563 | 2.57 (0.09) | 2.60 (0.09 | 2.50 (0.09) | 2.63 (0.10) | 2.60 (0.08) | 2.73 (0.09) |
| Power–powerlessness | F(5,422) = 0.81; p = 0.542 | 2.43 (0.06) | 2.51 (0.06) | 2.44 (0.06) | 2.42 (0.08) | 2.45 (0.06) | 2.57 (0.05) |
| Community activism and autonomy | F(5,422) = 0.32; p = 0.901 | 3.13 (0.05) | 3.07 (0.07) | 3.05 (0.07) | 3.12 (0.08) | 3.09 (0.05) | 3.14 (0.06) |
| Optimism and control over the future | F(5,431) = 1.36; p = 0.238 | 2.62 (0.08) | 2.63 (0.07) | 2.51 (0.07) | 2.70 (0.09) | 2.61 (0.07) | 2.77 (0.08) |
| Righteous anger | F(5,428) = 0.58; p = 0.718 | 2.34 (0.09) | 2.24 (0.08) | 2.32 (0.07) | 2.31 (0.10) | 2.21 (0.08) | 2.35 (0.06) |
| Total score | F(5,294) = 1.41; p = 0.221 | 2.62 (0.05) | 2.62 (0.05) | 2.56 (0.04) | 2.64 (0.05) | 2.62 (0.05) | 2.73 (0.04) |
Burgundy in particular performs well on the STAR-P scale (Figure 4). If Burgundy is used as a reference site, other research sites may be considered in relation to this. Languedoc also performs well on the perceived therapeutic relationship; however, Provence and Dauphine do not perform as well on this scale. Tukey’s post-hoc tests revealed that service users in Burgundy (38.49 ± 8.55) score higher on the mean total STAR-P than those in Provence (32.33 ± 11.91; p-value = 0.003). Burgundy also performs particularly well in comparison to perceptions of therapeutic relationships in Dauphine; however, this does not reach statistical significance (33.53 ± 9.23; p-value = 0.056).
FIGURE 4.
Mean positive collaboration subscale score for service users ± 95% confidence interval. Scoring range for the scale from 0–24. **p-value < 0.01.
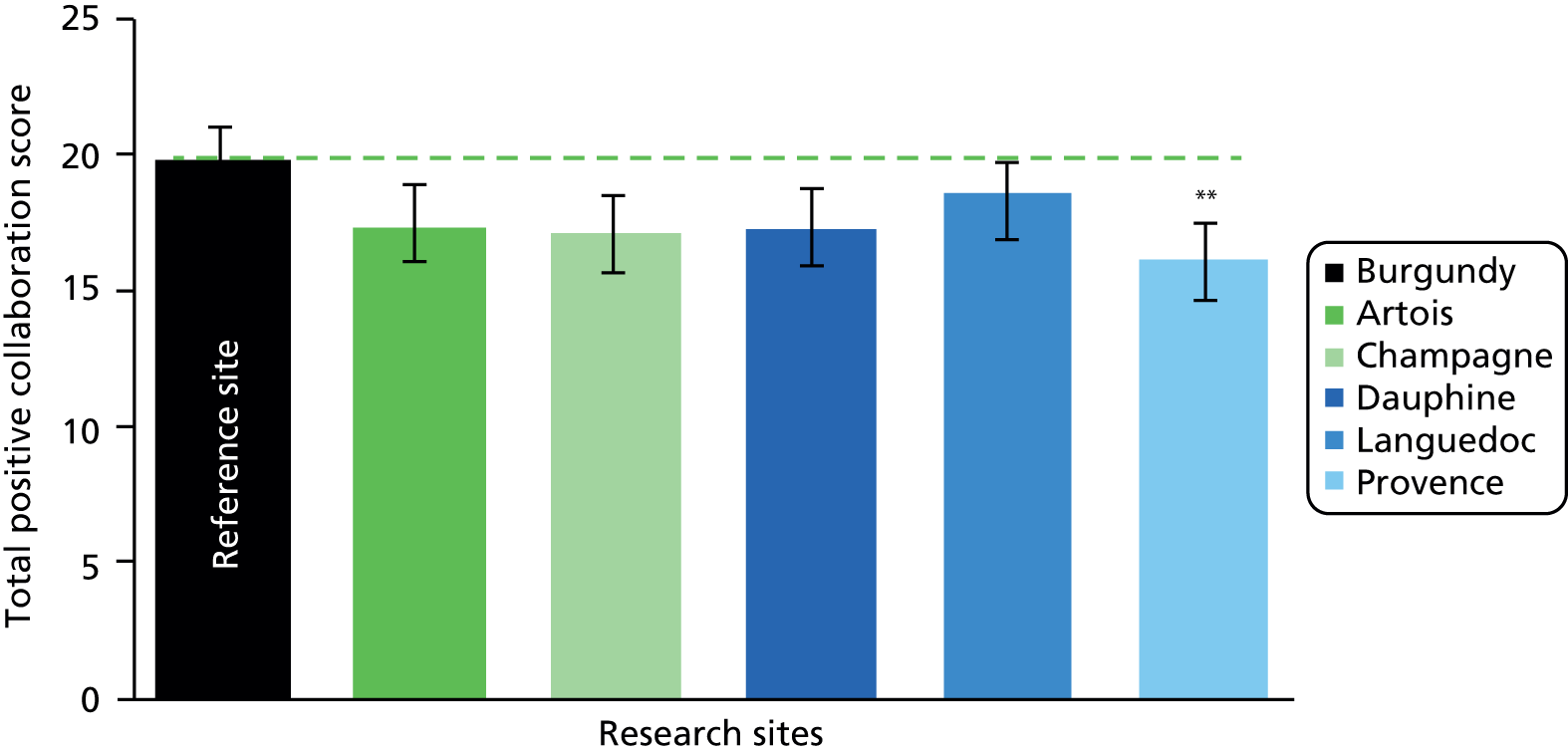
Subscales of the Scale to Assess the Therapeutic Relationship
Tukey post-hoc tests revealed that service users in Burgundy (19.81 ± 6.57) score higher on the ‘Positive Collaboration’ subscale than those in Provence (16.15 ± 6.57; p-value = 0.002) and Champagne (17.13 ± 5.79; p-value = 0.062); however, this does not reach significance. There were no significant differences between Burgundy and the other sites on this subscale. Figure 5 shows the mean positive collaboration subscale with Burgundy as a reference site to the other sites.
FIGURE 5.
Mean total STAR-P score for service users ±95% confidence interval. Scoring range for the scale from 0–48. **p-value = 0.01.

Further Tukey post-hoc tests revealed that responses on the ‘Positive Clinician Input’ subscale are different across the research sites. The reference site, Burgundy (9.46 ± 2.45), performs significantly better than Provence (7.83 ± 3.49; p-value = 0.012) and Champagne (8.01 ± 3.05; p-value = 0.45). Burgundy and Champagne are the two Welsh research sites, which suggests that the differences within this subscale may be appearing at a local level rather than as a result of macro-level policy and the implementation of CTP and processes surrounding it (Figure 6).
FIGURE 6.
Mean positive clinician input subscale score for service users ± SEM. Scoring range for the scale from 0–12. **p-value < 0.01.
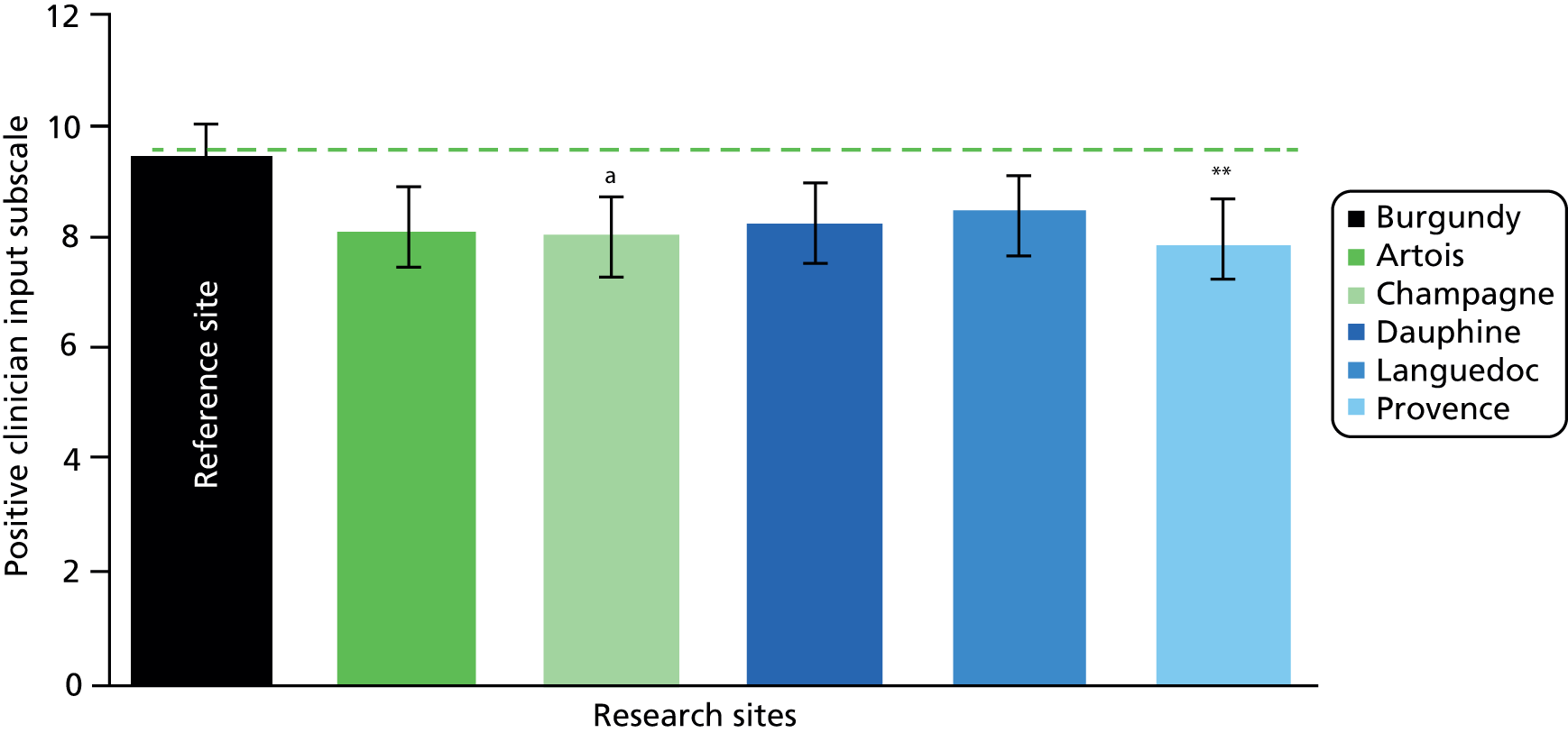
Care co-ordinators
One-way ANOVAs were conducted for the mean RSA total score and the five RSA subscales for the care co-ordinators (Table 40). There was a significant difference between the research sites in the ‘Choice’ subscale [F(5,195) = 3.40; p-value = 0.006]. There were no significant differences found in the mean total RSA score and the other four subscales; however, the ‘Diversity of treatment options’ subscale was approaching significance [F(5,195) = 2.10; p-value = 0.068].
| RSA scale | One-way ANOVA parameters | Artois | Burgundy | Champagne | Dauphine | Languedoc | Provence |
|---|---|---|---|---|---|---|---|
| Mean (SEM) | Mean (SEM) | Mean (SEM) | Mean (SEM) | Mean (SEM) | Mean (SEM) | ||
| Life goals | F(5,195) = 0.71; p = 0.617 | 3.68 (0.12) | 3.73 (0.11) | 3.79 (0.09) | 3.54 (0.15) | 3.82 (0.11) | 3.70 (0.09) |
| Involvement | F(5,195) = 0.98; p = 0.429 | 3.01 (0.13) | 2.91 (0.11) | 2.92 (0.13) | 2.99 (0.15) | 3.23 (0.12) | 2.87 (0.10) |
| Diversity of treatment options | F(5,195) = 2.10; p = 0.068 | 2.96 (0.14) | 3.23 (0.13) | 2.94 (0.13) | 2.98 (0.16) | 3.24 (0.12) | 2.74 (0.09) |
| Choice | F(5,195) = 3.40; p = 0.006** | 3.76 (0.10) | 3.92 (0.11) | 3.70 (0.11) | 3.46 (0.10) | 4.04 (0.10) | 3.58 (0.13) |
| Individually tailored services | F(5,195) = 1.74; p = 0.126 | 3.18 (0.13) | 3.10 (0.13) | 3.11 (0.13) | 3.49 (0.15) | 3.42 (0.15) | 3.42 (0.13) |
| Mean total score | F(5,195) = 0.997; p = 0.421 | 3.35 (0.11) | 3.41 (0.10 | 3.35 (0.11) | 3.31 (0.13) | 3.57 (0.11) | 3.25 (0.08) |
When using Dauphine as the reference site (the site with the lowest score on this subscale), it is apparent that other sites are performing significantly better around the subscale of ‘Choice’ (Figure 7).
FIGURE 7.
Mean item response ‘Choice’ subscale score for care co-ordinators ±95% confidence interval. Scoring range on a scale of 1–5. *p-value < 0.05, **p-value < 0.01.
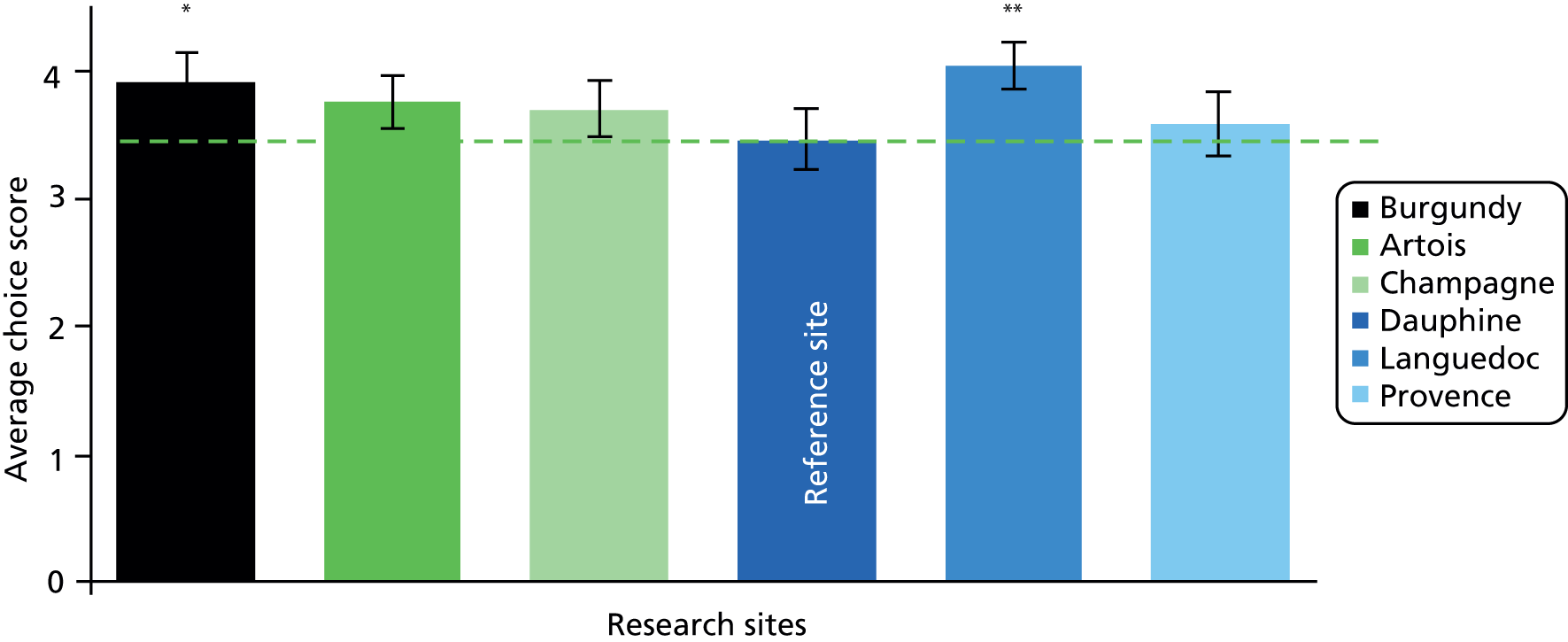
This scale measures some important perceptions that may have a significant effect on patient outcomes, concordance to care and collaboration with clinicians. Subsequent Tukey’s post hoc revealed that service users in Dauphine (3.46 ± 0.68) score significantly lower on the subscale than Languedoc (4.04 ± 0.50; p-value = 0.008) and Burgundy (3.92 ± 0.65; p-value = 0.041). There were no significant differences between Dauphine and the other sites on this subscale. A summary table for the five highest scoring items on the RSA scale for each site is included in Table 41 for the service users and Table 42 for the care co-ordinators.
| Rank | Artois (mean of 3.84–4.38 on Likert scale) | Burgundy (mean of 3.86–4.34 on Likert scale) | Champagne (mean of 3.69–4.65 on Likert scale) | Dauphine (mean of 3.67–4.64 on Likert scale) | Languedoc (mean of 3.67–4.64 on Likert scale) | Provence (mean of 3.49–4.11 on Likert scale) |
|---|---|---|---|---|---|---|
| 1 | Choice Staff do not use threats, bribes or other forms of coercion to influence my behaviour or choices |
Choice Staff do not use threats, bribes or other forms of coercion to influence my behaviour or choices |
Choice Staff do not use threats, bribes or other forms of coercion to influence my behaviour or choices |
Choice Staff do not use threats, bribes or other forms of coercion to influence my behaviour or choices |
Choice Staff do not use threats, bribes or coercion to influence my behaviour or choices |
Choice Staff do not use threats, bribes or other forms of coercion to influence my behaviour or choices |
| 2 | Choice Most of my services are provided in my natural environment (i.e. home, community, workplace) |
Life goals The role of staff is to assist me and other people in recovery with fulfilling my individually defined goals and aspirations |
Life goals The role of staff is to assist me and other people in recovery with fulfilling my individually defined goals and aspirations |
Choice Most of my services are provided in my natural environment (i.e. home, community, workplace) |
Choice Most of my services are provided in my natural environment (i.e. home, community, workplace) |
Choice Most of my services are provided in my natural environment (i.e. home, community, workplace) |
| 3 | Life goals The role of staff is to assist me and other people in recovery with fulfilling my individually defined goals and aspirations |
Choice Most of my services are provided in my natural environment (i.e. home, community, workplace) |
Choice Staff listen to and follow my choices and preferences |
Life goals The role of staff is to assist me and other people in recovery with fulfilling my individually defined goals and aspirations |
Life goals The role of staff is to assist me and other people in recovery with fulfilling my individually defined goals and aspirations |
Life goals Staff believe that I can recover and make my own treatment and life choices |
| 4 | Individually tailored My service provider makes every effort to involve my significant others and other sources of natural support in the planning of my services, if this is my preference |
Life goals Staff use a language of recovery (i.e. hope, high expectations, respect) in everyday conversations |
Choice Staff help to monitor the progress I am making towards my personal goals on a regular basis |
Life goals Staff believe that I can recover and make my own treatment and life choices |
Life goals Staff believe that I can recover and make my own treatment and life choices |
Life goals The role of staff is to assist me and other people in recovery with fulfilling my individually defined goals and aspirations |
| 5 | Life goals Staff believe that I can recover and make my own treatment and life choices |
Choice Staff help to monitor the progress I am making towards my personal goals on a regular basis |
Life goals Staff are knowledgeable about special interest groups and activities in the community |
Choice Staff listen to and follow my choices and preferences |
Choice Staff help to monitor the progress I am making towards my personal goals on a regular basis |
Life goals Staff are diverse in terms of culture, ethnicity, lifestyle and interests |
| Rank | Artois (mean of 3.97–4.22 on Likert scale) | Burgundy (mean of 4.14–4.43 on Likert scale) | Champagne (mean of 4.07–4.31 on Likert scale) | Dauphine (mean of 3.79–4.23 on Likert scale) | Languedoc (mean of 4.21–4.79 on Likert scale) | Provence (mean of 3.91–4.18 on Likert scale) |
|---|---|---|---|---|---|---|
| 1 | Life goals Staff believe that people can recover and make their own treatment and life choices |
Choice Staff do not use threats, bribes or other forms of coercion to influence the behaviour or choices |
Choice Staff do not use threats, bribes or other forms of coercion to influence the behaviour or choices |
Choice Staff do not use threats, bribes or other forms of coercion to influence the behaviour or choices |
Choice Staff do not use threats, bribes or coercion to influence the behaviour or choices |
Life goals Staff believe that people can recover and make their own treatment and life choices |
| 2 | Choice Staff do not use threats, bribes or other forms of coercion to influence the behaviour or choices |
Choice Progress made towards goals (as defined by the person in recovery) is monitored on a regular basis |
Life goals Procedures are in place to facilitate referrals to other programmes and services if the agency cannot meet a person’s needs |
Life goals Staff are diverse in terms of culture, ethnicity, lifestyle and interests |
Choice Most services are provided in a person’s natural environment (i.e. home, community, workplace) |
Life goals The role of staff is to assist a person with fulfilling their individually defined goals and aspirations |
| 3 | Life goals The role of staff is to assist a person with fulfilling their individually defined goals and aspirations |
Life goals The role staff is to assist a person with fulfilling their individually defined goals and aspirations |
Life goals Staff believe that people can recover and make their own treatment and life choices |
Life goals Staff believe that people can recover and make their own treatment and life choices |
Life goals The role of staff is to assist a person with fulfilling their individually defined goals and aspirations |
Life goals Staff actively assist people in recovery with the development of career and life goals that go beyond symptom management and stabilisation |
| 4 | Individually tailored Every effort is made to involve significant others and other natural supports in the planning of a person’s services, if so desired |
Choice Most services are provided in a person’s natural environment (i.e. home, community, workplace) |
Life goals Staff are knowledgeable about special interest groups and activities in the community |
Life goals Staff routinely assist individuals in the pursuit of their educational and/or employment goals |
Life goals Staff believe that people can recover and make their own treatment and life choices |
Life goals Staff routinely assist individuals in the pursuit of their educational and/or employment goals |
| 5 | Choice Most services are provided in a person’s natural environment (i.e. home, community, workplace) |
Life goals Staff believe that people can recover and make their own treatment and life choices |
Individually tailored Every effort is made to involve significant others and other natural supports in the planning of a person’s services, if so desired |
Life goals Procedures are in place to facilitate referrals to other programmes and services if the agency cannot meet a person’s needs |
Diversity of treatment options People in recovery are given the opportunity to discuss their sexual and spiritual needs and interests |
Choice Staff do not use threats, bribes, or other forms of coercion to influence the behaviour or choices |
Adjusted analysis
The advantage of using unadjusted ANOVAs to examine the data is that this retains the maximum number of participants in the analysis; the disadvantage is that case-mix differences between the sites could potentially bias the findings. In contrast, the strength of using ANCOVAs is that they adjust for the potential confounders but this is achieved at the cost of losing participants in the analysis owing to missing data on the covariates. This reduces the statistical power of the analysis and changes the composite of the sample, which poses a problem for the interpretation. Analysing the data using unadjusted and adjusted analyses offers a check on the robustness of the original (unadjusted) findings.
The ANOVAs reported above are not adjusted for potential confounders (i.e. variables that are potentially associated with the outcome variables and which may be differentially distributed across sites). For service users, three demographic variables (age; gender; ethnicity) and two care-related variables (relationship status; time in mental health services) were identified as potential confounders. These variables were used as covariates in a series on ANCOVAs to determine whether or not they substantively change the findings from the unadjusted analyses. For care co-ordinators, three demographic variables (age, gender and ethnicity) and two measures of clinical experience (time working in mental health services and time as a care co-ordinator) were identified as potential confounders for a further series of ANCOVAs. To determine whether the adjusted findings were different from the original findings, we compared the p-values for the omnibus ANOVA/ANCOVA, the p-values for the post-hoc comparisons, and the unadjusted and adjusted means for each scale and subscale for each site.
Service users
For the service users there were no substantive differences in the adjusted analysis for any of the subscales or the total scores of the RSA scale and the ES. Similarly, there were no substantive differences for two of the three STAR-P subscales or the total STAR-P score. However, for the ‘Positive clinician input’ subscale of the STAR-P there were minor differences in the adjusted means and this resulted in the difference between Burgundy and Champagne becoming non-significant (p-value = 0.285). The observed difference between Burgundy and Provence in the unadjusted analysis remained significant in the ANCOVA (p-value = 0.040).
Overall, the ANCOVA analyses for service users show that, although there were marginal changes in the adjusted means, these changes were not substantive and did not affect the overall pattern of findings. Consistency between the adjusted and unadjusted analyses suggests that the findings are robust.
Care co-ordinators
For the care co-ordinators, two of the five subscales of the RSA scale suggested no substantive differences in the adjusted analysis. However, for the ‘Choice’ subscale, some previously non-significant post-hoc comparisons become significant in the adjusted analyses. Figure 8 shows that the difference between Burgundy and Dauphine and the difference between Languedoc and Dauphine remained significant, but, in addition, Burgundy (4.00 ± 0.12) and Languedoc (4.07 ± 0.14) were now also significantly different from Provence (3.44 ± 0.14) (p-value = 0.034 and p-value = 0.024, respectively). As the graph shows, these new differences emerged because the adjusted mean for Provence was marginally reduced and became closer to the reference site of Dauphine. It should be noted that the changes in the means are marginal and that the overall pattern of findings remains essentially the same.
FIGURE 8.
Adjusted mean item response on Choice subscale score for care co-ordinators ± 95% confidence interval. Scoring range on a scale of 1–5. **p-value < 0.01. a, identifies a significant difference compared with Dauphine; b, identifies a significant difference compared with Provence.
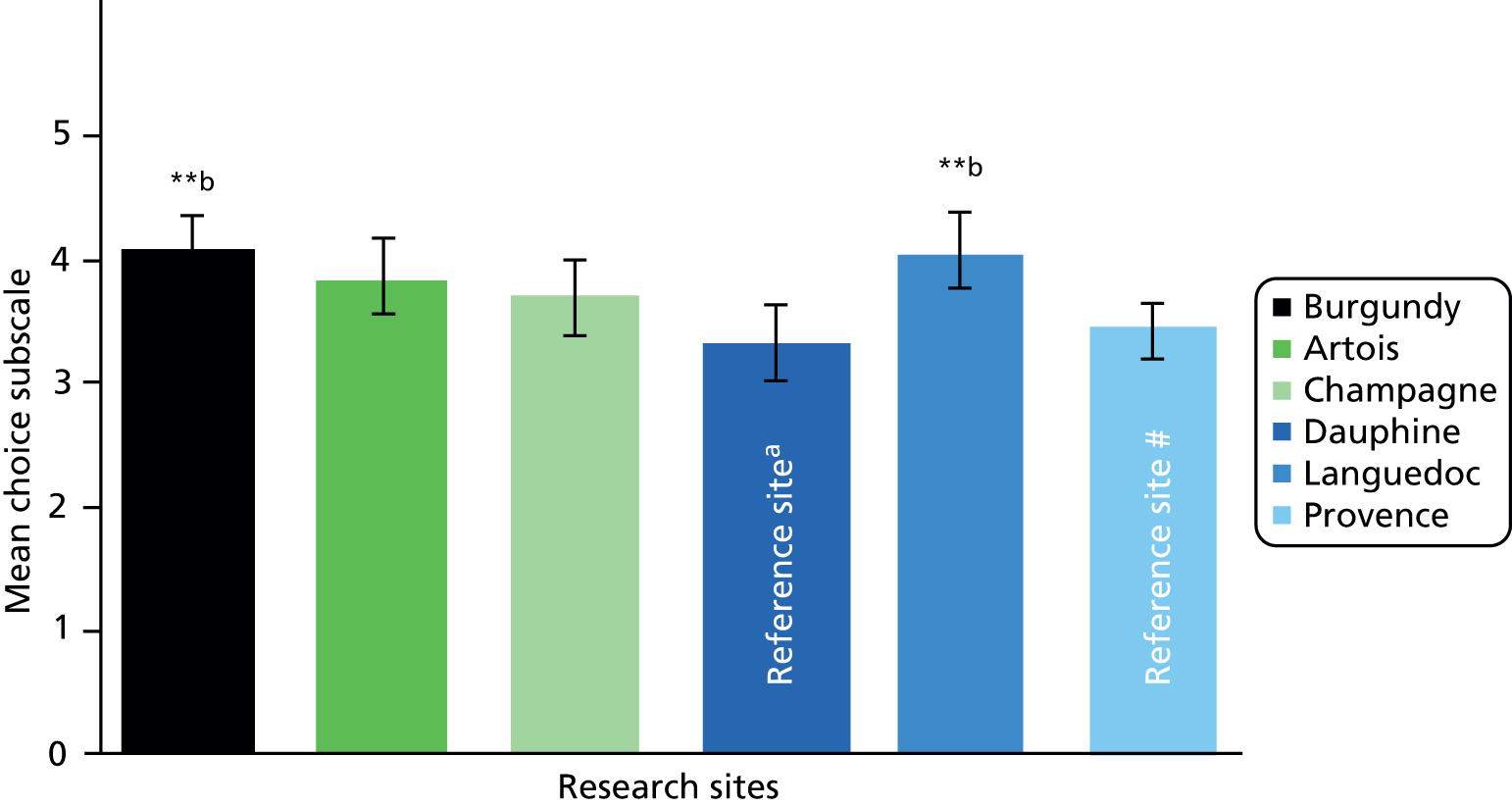
For the total RSA score, changes in the adjusted means resulted in an emergent significant difference between Dauphine (2.99 ± 0.14) and Languedoc (3.65 ± 0.13; p-value = 0.019) (Figure 9a). For the ‘Diversity of treatment options’ subscale the difference between Dauphine (2.84 ± 0.86) and Burgundy (3.24 ± 0.78) became statistically significant (p-value = 0.035) (Figure 9b). For the ‘Life goals’ subscale, the differences between Dauphine (3.21 ± 0.15) and two other sites also became significant: Languedoc (3.92 ± 0.14; p-value = 0.024) and Champagne (3.86 ± 0.13; p-value = 0.029) (Figure 9c).
FIGURE 9.
Adjusted mean scores for care co-ordinators ± 95% confidence interval. (a) RSA total score; (b) diversity of treatment options; and (c) life goals subscale. *p-value < 0.05.
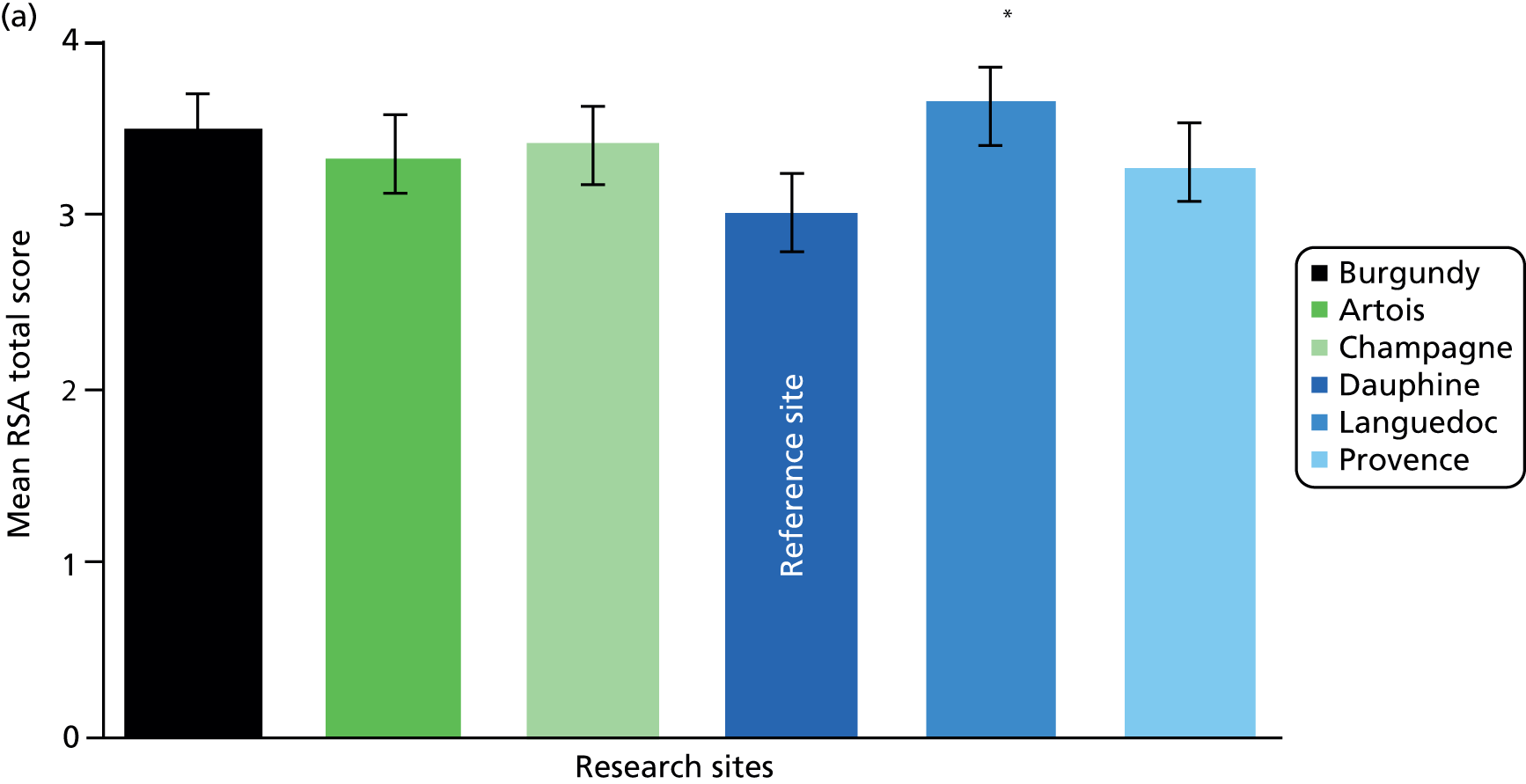
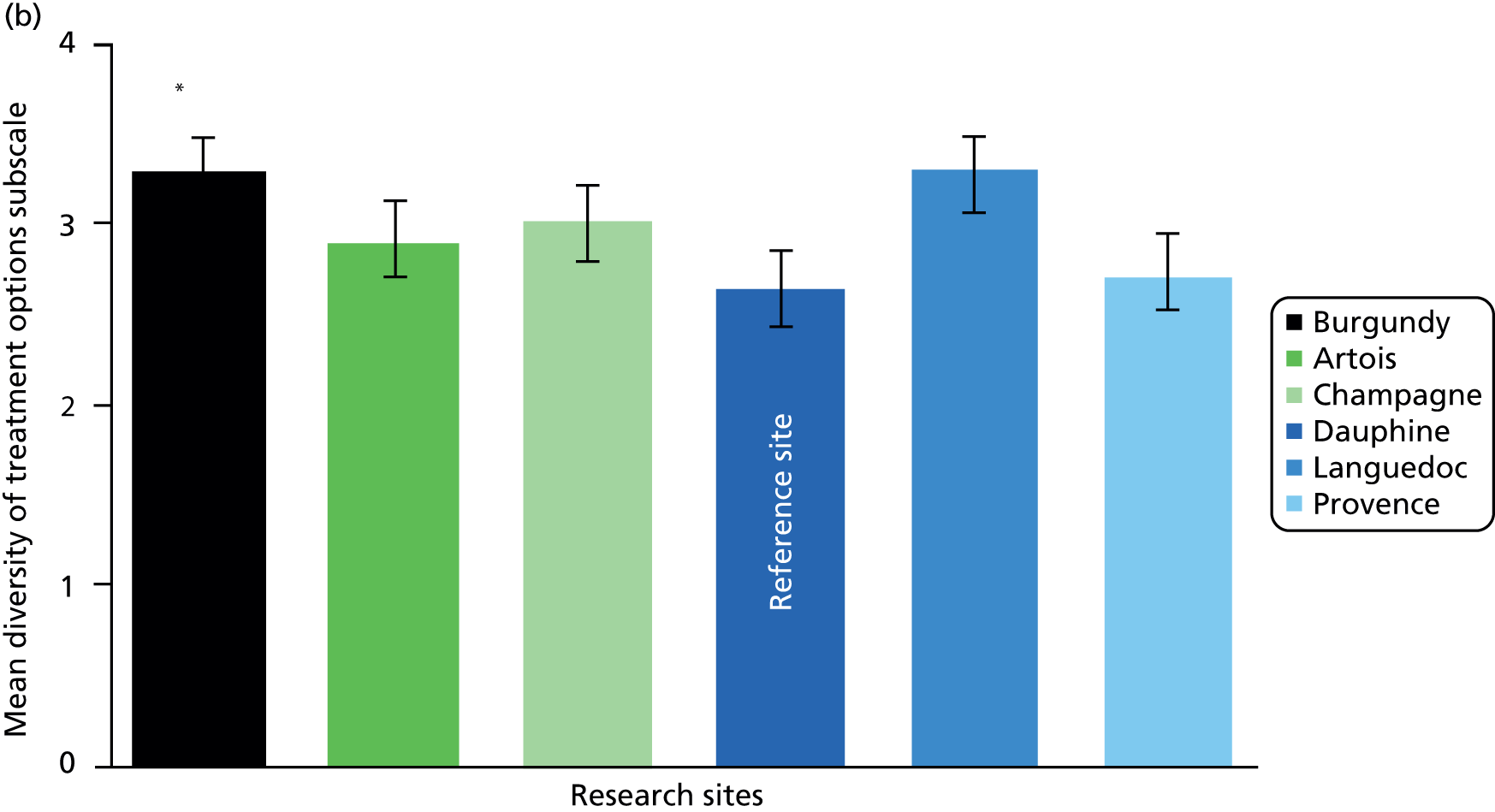
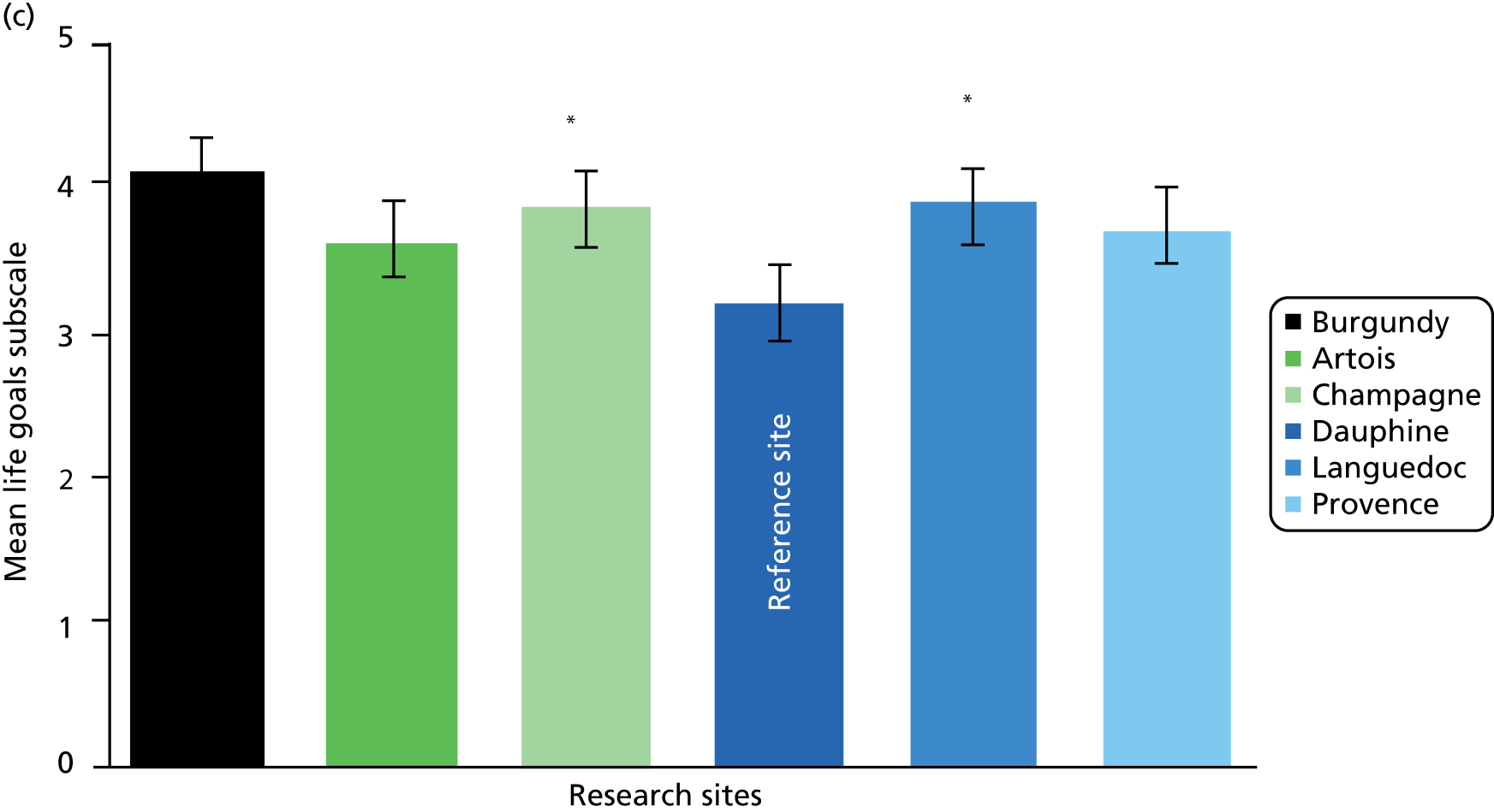
In terms of statistically significant differences between sites, the findings for care co-ordinators changed more than the findings for the service users in the adjusted analyses. Proportionally, the observed number of changes in significance was small compared with the number of post-hoc comparisons conducted, and changes in significance were predicated on relatively small absolute changes in the adjusted means across the various sites and outcome measures. The vast majority of the post-hoc comparisons did not change in terms of statistical significance in the adjusted analyses. The findings from the ANCOVAs therefore are suggestive of potential site differences on particular measures between specific sites, but these findings should be interpreted cautiously as there were no specific a priori hypotheses about site differences, and the loss of participants as a result of missing data on the covariates changes the sample composition.
Correlations between the outcome measures
Pearson’s correlations were completed at the global level with all participants to determine if there were associations between the responses on the questionnaire scales. Table 43 shows that there is a strong positive correlation between the RSA scale and the STAR-P (r = 0.61, N = 409; p-value < 0.001). There is an association between the recovery-oriented focus and ratings of the quality of therapeutic relationships among service users. There is a weak relationship between the RSA scale and ES and a negligible relationship between the STAR-P and the ES.
| Measures | Parameters | Total sample |
|---|---|---|
| RSA scale and STAR-P | r | 0.607 |
| Sig. | 0.000** | |
| N | 409 | |
| RSA scale and ES | r | 0.204 |
| Sig. | 0.000 | |
| N | 406 | |
| STAR-P and ES | r | 0.138 |
| Sig. | 0.004 | |
| N | 431 |
To explore the pattern of the higher correlation between the RSA scale and STAR-P, subsequent correlations were completed at the subscale level. There were positive associations found between the ‘positive collaboration’ and ‘positive clinician input’ subscales and the five RSA subscales (Table 44). There were small to medium correlations between the ‘non-supportive clinician input’ subscale and the five subscales of the RSA scale. This is expected, as this subscale is a negatively framed subscale and, therefore, it is less likely to correlate with the RSA scale.
| Psychometric scale | Subscale | Parameters | RSA scale | ||||
|---|---|---|---|---|---|---|---|
| Life goals | Involvement | Diversity of treatment options | Choice | Individually tailored services | |||
| Scale to Assess Therapeutic Relationships STAR-P |
Positive Collaboration | r | 0.636** | 0.518** | 0.578** | 0.602** | 0.560** |
| Sig. | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | ||
| N | 395 | 377 | 407 | 420 | 415 | ||
| Positive clinician input | r | 0.569** | 0.502** | 0.525** | 0.533** | 0.524** | |
| Sig. | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | ||
| N | 398 | 379 | 409 | 425 | 420 | ||
| Non-supportive clinician input | r | 0.252 | 0.096 | 0.214 | 0.303 | 0.210 | |
| Sig. | 0.000 | 0.062 | 0.000 | 0.000 | 0.000 | ||
| N | 398 | 379 | 409 | 424 | 419 | ||
Although it appears that these questionnaire scales have a strong positive correlation, the results should be interpreted with caution. There is the possibility that a ceiling effect in the data may have negatively skewed the data. When assessing the correlations by trust/health board it is apparent that there is some variability (Table 45).
| Measures | Artois | Burgundy | Champagne | Dauphine | Languedoc | Provence |
|---|---|---|---|---|---|---|
| RSA scale and STAR-P | 0.724** | 0.389 | 0.537** | 0.652** | 0.624** | 0.71** |
| 0.000 | 0.001 | 0.000 | 0.000 | 0.000 | 0.000 | |
| 65 | 71 | 63 | 52 | 86 | 72 | |
| RSA scale and ES | 0.082 | –0.005 | 0.133 | 0.32 | 0.328 | 0.355 |
| 0.525 | 0.969 | 0.300 | 0.023 | 0.002 | 0 | |
| 63 | 71 | 63 | 50 | 86 | 72 | |
| STAR-P and ES | 0.071 | 0.123 | 0.187 | 0.179 | 0.184 | 0.173 |
| 0.574 | 0.301 | 0.121 | 0.188 | 0.08 | 0.137 | |
| 66 | 73 | 70 | 56 | 91 | 75 |
The RSA scale and STAR-P demonstrate the strongest and most consistent correlations compared with the overall analyses. There is, however, some variability across sites. All correlations demonstrate at least medium effects, and most are classed as large effect sizes.
With the RSA scale and ES, the sites are demonstrating greater variability, with some sites showing medium effects (Dauphine, Languedoc and Provence) and other sites showing smaller effects (Champagne and Artois); one site shows no relationship (Burgundy). The discontinuity across these sites suggests that some of these scales are behaving differently across the sites; however, further exploration of this is beyond the scope of this report.
The STAR-P and ES show less variability, with all sites showing a small to moderate association.
Section 2: cross-case analysis of the qualitative data
The following is a narrative summary of the cross-case analysis of the interview data. Tables charting summaries of the within-case analyses, allowing cross-case comparisons, are available in Appendix 11.
Local context and developments
Across all six sites there was an acknowledgement that services had been or were still undergoing a significant process of restructuring. The nature and impact of this period of flux appeared to vary, in particular between the two countries but also in relation to the integration of health and social care. Overall, there appeared to be moves towards greater integration of health and social care staff within teams, with colocation of NHS and LA personnel. Staff in Provence in particular stressed the strong shift towards generic mental health roles. Languedoc appeared to be moving in a different direction, with social workers being removed from CMHTs to focus on social care assessments and personal budget applications. This reportedly led to higher workloads within CMHTs and lower morale; this was also the only site in which medical domination of services was cited as an issue. Greater uncertainty about developments seemed to be expressed where more adventurous, wide-ranging restructuring had taken place, such as in Provence, where services were being centralised and teams now worked across age groups. This was accompanied by strongly articulated recovery-focused values, but there were acknowledgements by senior staff that staff morale had been hard hit by the upheaval, and the anticipated gains remained uncertain.
Development of new services in primary (e.g. primary care liaison roles) and secondary (setting up or merging of assertive outreach or crisis teams with CMHTs) care were reported, often alongside concerns over the impact of cuts in budgets, reductions in social care services and the challenges of providing continuity of care and effectively managing risks across an increasing range of third sector providers under the ‘any provider’ legislation in the Health and Social Care Act 2012. 131
In the two Welsh sites, the Mental Health Measure was clearly a strong driver for developments with senior managers and practitioners in both Burgundy and Champagne extolling its virtues, although the impact on everyday practice was less clear. Integration of health board and LA managers and teams was high on the agenda, although integration in the Champagne site appeared to be frustrated by continuing differences at the most senior levels and the absence of shared and accessible IT systems. Similar frustrations with IT were articulated across all sites.
Often strong commitments to the recovery agenda on all sites appeared to be frustrated by seemingly contrary policies (e.g. CTOs) and the related administrative demands; high acuity, high demands on services, high caseloads and the inadequacies and/or inflexibility of IT systems. Moreover, other organisational targets were skewing care co-ordination work, with recovery being interpreted as through-put and discharge, targets for PbR, personal budgets and organisational prioritising of particular types of support all working to standardise rather than personalise care or place recovery at the centre of things.
Care planning and co-ordination
The core aspects of the CPA were simply and straightforwardly expressed by senior managers and practitioners in terms of assessment, care plan, care co-ordinator and regular reviews. However, there appeared to be greater difficulty in articulating the implementation of the policy. There were major challenges in trying to make the CPA meet the very different needs of service users, practitioners, managers and commissioners. It continues to be administratively heavy and is insufficiently oriented towards recovery. There was widespread reporting of and often dissatisfaction with changes to documentation and some lack of clarity over CPA eligibility. In England, there were some concerns that the introduction of clustering and PbR was resulting in care plans being less individualised (Artois, Dauphine, Languedoc).
In Wales, the Measure was seen as very important, but there was no consensus on its actual impact. Views regarding the CTP were more mixed. In both sites, it was agreed that the All Wales CTP provides the structure or a framework to work within, but it was seen by some as reductionist. In Burgundy, it was claimed that not all psychiatrists used the CTP.
The introduction of electronic CPA documentation appeared to bring some benefits in terms of accessing and sharing information, but it also brought unwieldiness and a greater distancing from service users, as working collaboratively with people on care plans in their homes became more difficult. The solution, paradoxically, may lie in the development of more integrated IT systems and the use of modern, mobile technology.
Care co-ordinator caseloads reportedly ranged from 25 (Artois) to 40 or more (Champagne, Dauphine, Languedoc) or even 50 (Provence), and in most sites these were increasingly attributable to growing demands and tighter staff budgets. The care co-ordinator role was now held by any mental health professional, most often mental health nurses, social workers and OTs, less often psychologists, and rarely psychiatrists. Artois now also employed ‘non-professional’ staff (on Band 4) as care co-ordinators, with some concerns being expressed following incidents.
The care co-ordinator role was seen as a ‘generic’ role, with staff taking on increasingly similar co-ordinator duties, but one that was also complex, carrying significant responsibilities and often tasked with delivering most of the direct care. However, this genericism contained a tension when allied with capacity pressures within teams and attempts to allocate care co-ordinators to service users based on degree of fit. The desire to be responsive and provide a more personalised approach to care co-ordination was often frustrated by the lack of capacity within a team’s or individual’s caseload. Hence, a newly referred service user that might benefit from social worker input as s/he has predominantly social care needs is allocated a mental health nurse as care co-ordinator. The co-ordination tasks are similar but the therapeutic or supportive interventions are shaped, and at times limited, by the disciplinary background of the co-ordinator. There were widespread calls for more training on the CPA and specifically for care co-ordinators.
Efforts to increase the involvement of carers were mentioned occasionally (Dauphine), but more often it was the challenges and continuing tensions around issues such as service users’ consent and confidentiality that were mentioned (Artois, Languedoc), or uncertainty around how to involve people (Burgundy). There were varied experiences of care planning and care co-ordination from the viewpoints of service users, carers and care co-ordinators across all six sites, with no distinct differences identified. At best, care is planned in a structured and collaborative way with clear communication and opportunities for service users to influence and feel some ownership of the process. At worst, service users say that they feel cast aside, not involved, or that their care is planned as an obligatory task and in ways that are confusing and rigid.
Care co-ordinators are sometimes more positive about care being planned in individualised, collaborative ways than are service users and carers. They tend to welcome collaboration, but some also worry over how to address differences in view or believe strongly that some service users, particularly those with longer contact with services, are unwilling or unable to engage in such a process.
Risk was consistently seen as central to the CPA/CTP process by senior staff across all six sites. Similarly, safety and risk were paramount for care co-ordinators, but service users and carers were hardly involved in the assessment of these and many care co-ordinators expressed concerns over sharing their views, or those of their colleagues, around issues of risk. Service users and carers were often unaware of risk assessments being documented. Perhaps as a consequence, some service users and carers are largely unaware of risk management taking place and can feel that risk is not managed sufficiently or proactively. Risk aversion limits positive risk-taking and sits at odds with recovery ideals and practices.
Care plans are useful for staff and are recognised as having to be created; they have value as records of what has been decided and for including contact details and, sometimes, crisis and contingency plans. For a handful of people care plans are like a contract. But, for the majority of people, care plans are not highly valued and are not seen as active documents; many people (care co-ordinators and service users included) do not routinely refer to care plans once they have been created. Many service users do not have care plans, or have received and quickly discarded them. Others file them in a drawer, never to look at them again. Interestingly, care co-ordinators often thought that care plans were difficult to understand, but most service users did not agree; they just thought that they were of limited utility. Some care co-ordinators mentioned the development of first person care plans but service users rarely, if ever, mentioned this. There is clearly a tension between standardisation of documentation and individualised approaches to care planning. There was some, but not much, evidence of care planning addressing service users’ strengths and accomplishments.
As has been reported previously, care co-ordinators find care planning and care co-ordination administratively burdensome and complain that they have insufficient time for face-to-face work with service users and their families. Therapeutic relationships, however, are seen as very important; along with the care co-ordinator’s skills and knowledge of the service user. Service users and carers want to see more of their care co-ordinator and recognise discontinuity (e.g. when care co-ordinators leave or when there is organisational change) as a barrier to good care. There is no clear appetite for electronic care plans: service users and care co-ordinators repeatedly reported that current IT systems (which are often incompatible within sites, and between NHS and LA services) are frequently inflexible and a hindrance to collaborative care planning.
Carers have varied experiences within sites, but many are not engaged with care planning and co-ordination. Some do not see this as problematic, instead seeing it as something that occurs primarily between the service user and their care co-ordinator.
Surprisingly little was said about review meetings, although experiences varied; at best these meetings are collaborative, with good preparation and involvement of the service user and others. Often, care co-ordinators described difficulties arranging multidisciplinary involvement and ad hoc meetings with perhaps just the service user and psychiatrist.
Across all sites, the lack of sufficient staff, resources and time to work more collaboratively with service users and carers was reported by care co-ordinators.
Recovery
Among senior personnel there was some clear articulation of what recovery and recovery-focused values might be, but varying degrees of sign-up to recovery and frequent talk of resistance among some staff. In Languedoc, for example, there was a broad understanding and evidence of a Recovery College, co-produced care plans and some use of recovery tools (e.g. Recovery Star, WRAP) but a reported lack of passion among senior managers, and conservative medical staff content to retain more traditional approaches. Similar resistance among medical staff and some older nursing staff was also reported in Provence, alongside a belief that ‘not all service users will recover’. Nonetheless, managers in Provence also cited the introduction of peer workers and greater use of ‘recovery language’.
In Artois, recovery was seen as a ‘bridge between medical and social models’ and also something ‘we have always been doing’. It was also seen as being about discharging service users reluctant to move on. Barriers to the implementation of a greater focus on recovery in Artois included the need for more staff, more time, improved IT systems and a stronger organisational commitment.
Senior staff in Dauphine acknowledged that the move towards recovery had been fairly recent and had been met by some resistance among some staff, and that the CPA alone ‘was enough’. However, there was a drive to increase the use of personal budgets, and help with obtaining employment was much more commonplace. Some recovery-focused tools were being introduced (Artois, Languedoc), but this was much less clear elsewhere (Burgundy, Champagne, Dauphine, Provence).
In Wales, the Measure had placed recovery high on the agenda for senior staff, with good understandings of recovery seen in Champagne but more mixed understandings of recovery expressed in Burgundy. For some in Champagne, the CTP did not have a clear focus on recovery and it was felt that greater training was needed for both staff and service users to bring about a change in culture.
More training around recovery working and the use of recovery tools, and perhaps a better understanding of the new ways of working to deliver recovery-focused care, were suggested for both staff and service users (Champagne, Dauphine).
As with care planning, service users, carers and care co-ordinators had varied views and experiences in relation to recovery across all sites, with the term itself often having different meanings for different people. Different views between professional groups were also mentioned. For some care co-ordinators it was even seen as unhelpful or deceptive, as it appeared to be more about discharging service users from caseloads. Across sites, many service users used terms commonly found in recovery literature, such as choice, independence, hope, fulfilment; but, for many, recovery is primarily about managing and coping better with their illness. Very few talked about recovery as a ‘journey’.
There were no clear views that care planning helped recovery, unless care plans included practical steps or helped service users to accept or talk about their mental health. Some service users and carers said that strengths were acknowledged. For service users and carers in particular, conversations and relationships, along with families and friends, were identified as being far more important than care plans in promoting recovery.
Even within single sites there is variable use of, experience in, and enthusiasm for recovery tools. At best, WRAPs are seen as very personalised and helpful, but some care co-ordinators worry about the extra work required. Some care co-ordinators say they have always worked in a recovery-focused way, and what hindered them were organisational targets and issues such as adversity to risk, documentation, limited resources and ‘firefighting’. There were also the challenges of negotiating over sometimes competing views between service users and care co-ordinators on achievable progress and managing medication side-effects, which can seriously impair recovery.
Personalisation
Across the case-study sites, personalisation was not understood as consistently as the concept of recovery among senior personnel, and definitions tended to include person-centred care plans and the use of first-person terminology in care plans (Artois); placing the person at the heart of social care (Artois); and the use of personal budgets (Artois, Dauphine) and direct payments (Champagne).
In relation to personal budgets, there was a clear lack of uniformity and this was also the one area where there was a marked difference between the two countries, perhaps reflecting the different policy emphases. Some sites saw the use of personal budgets as a key tool in the move towards a focus on recovery and personalisation of care (e.g. Dauphine, Languedoc, Provence). In both sites in Wales, there was much less emphasis on the use of personal budgets, which were seen very much as part of a creeping ‘marketisation’ of health care and, as a consequence, were subject to more resistance and a more limited move towards the use of direct payments (Champagne).
Even where personal budgets were promoted, it was recognised that they were accompanied by extremely heavy administrative loads, which took practitioners away from face-to-face contact with service users and their families (Artois, Dauphine, Languedoc). There were also often severe delays in actually receiving funds, which impacted on service users and staff (Dauphine). Elsewhere, service users often failed to meet the strict approval criteria against which they were judged, or were reluctant to make a contribution (Languedoc). Senior staff also spoke of there being tensions when service users were unwell and suggested that talk of a more personalised approach could ‘raise expectations’ that could not always be met (due to tight budgets and restricted local services and options) (Champagne).
There was also an articulation of some of the tensions that exist in the supposed move towards greater personalisation, with CTOs (Artois) and clustering cited as a counterpoint (Dauphine). Being able to purchase services from any provider also increased difficulties around sharing information and issues of confidentiality (Dauphine). Uniquely, in Languedoc, under an agreement made under Section 75 of the National Health Services Act 2006 between the LA and the trust, social workers were removed from CMHTs to focus on assessments and processing of direct payments and personal budgets. 132 The aim was to increase the move towards the use of personal budgets by service users to purchase care and support, which was seen as a key tool in the move towards personalisation of services. It appeared that, although the success of this approach was still to be determined, the impact on remaining staff within CMHTs was less than positive, with caseloads and workloads increasing with the loss of the social workers from the teams.
Commissioners of services in Provence also saw personal budgets as key drivers towards greater self-directed support. The Trust had exceeded initial targets, but senior staff spoke of the significant administrative burden. Staff also needed to develop new skills and understanding to negotiate with providers. Concerns had also emerged about the potential increased risk when dealing and communicating with multiple providers following recent serious incident enquiries. Nonetheless, personal budgets were now being used widely, according to senior managers and practitioners.
Among service users, carers and care co-ordinators, personalisation was understood in very different ways across sites. Often it was equated with individualised care, choice, service user-led services, tailoring care, and balancing structure and flexibility. More specifically, it was used to refer to new practices: personal budgets and direct payments. A number of people in all sites had no idea what personalisation is about.
Service users and carers variously described care as being personalised, or as very much not personalised, depending on personal experiences, with no distinct differences between sites emerging. Some service users saw their care plans as very personalised, others most definitely did not. Similar feelings were expressed by carers. Personalisation was constrained by lack of resources and availability of local services, by service users not always being aware of the options available to them, and by service users deferring to professionals. Gaps were observed between the ideal and the reality, with staff reporting high administrative workloads and the complexity of actually accessing and using personal budgets. As with recovery, some care co-ordinators reported that personalisation can raise unrealistic expectations.
It was also apparent that services across sites often allocate care co-ordinators to service users on the basis of caseload space rather than appropriateness, further challenging personalised relationships or more personalised approaches to strengths, interests and goals. In terms of personalisation, care planning and co-ordination it was not clear that personalisation can be achieved consistently using current templates and approaches.
Section 3: potential facilitators and barriers to the delivery of recovery-focused, personalised care planning and co-ordination
This chapter ends with two tables in which we draw on the detailed within-case and cross-case analyses above to identify potential facilitators and barriers to the delivery of recovery-focused, personalised care planning and co-ordination (Tables 46 and 47). These are discussed in more detail in Chapter 6.
| Level of analysis | CPA/CTP care planning | Recovery | Personalisation |
|---|---|---|---|
| Macro-level (national policy, regional drivers, etc.) | Clearly articulated national-level policy goals (which may or may not be enshrined in statute) Commissioning indicators/goals linked to those policies |
||
| Meso-level (trust/board policies, etc.) | Focused implementation of national policy Management of caseload size and stronger caseload management Integrated, flexible IT support Simplify documentation |
Senior organisational commitment to and promotion of recovery High level of staff understanding/engagement in recovery model MDT approach to holistic care/recovery goals Provision of and access to training on new recovery working, recovery tools, etc. Recovery training for service users (and carers?) Employment coaches, peer support workers in teams |
Staff training in personalisation Simplify administrative processes surrounding use of personal budgets and direct payments Examples of innovative use of personal budgets |
| Micro-level (service delivery-user/carer experience/care co-ordinator) | Good relationship between service user (carer, where applicable) and care co-ordinator | Strong therapeutic relationships Continuity in relationships Family/friend support Safety and risk discussed |
Service users aware of services, options, choices available Staff and service user understanding of personalisation and personal budgets |
| Level of analysis | CPA/CTP care planning | Recovery | Personalisation |
|---|---|---|---|
| Macro-level (national policy, regional drivers, etc.) | Reductions in health and social care budgets | National policies at odds with recovery (e.g. clustering/PbR; CTOs) | No clear policy or national policy at odds with personalisation (e.g. clustering/PbR) |
| Meso-level (trust/board policies, etc.) | Restructuring, causing confusion and low staff morale Job insecurity (owing to cuts or restructuring) High caseloads Lack of training Poor IT support and incompatible IT systems across health/social care interface |
Senior/medical staff missunderstanding of or resistance to recovery Removal of social workers from MDT High caseloads Lack of training |
Personal budget processes cumbersome, lengthy Lack of staff awareness, training |
| Micro-level (service delivery-user/carer experience) | Limited collaboration or involvement in care plans Limited or absent involvement in risk assessment decisions |
Staff resistance to recovery approach Lack of shared understanding of the term recovery |
Limited or overly rigid definition of term Personal budget processes cumbersome and lengthy Lack of information for and understanding among service users |
Chapter 6 Discussion
Introduction
In this chapter, we draw out the key implications from the findings from both the within-case and the cross-case analyses and discuss some of the key issues that have emerged in relation to recovery-focused personalised care planning. We make connections between the interconnected macro/meso/micro levels, summarise the impact of public and patient involvement in the study and identify the strengths and limitations of the work. We conclude with a review of the implications of our findings for services, and make several recommendations in line with our macro/meso/micro framework.
Making connections: macro, meso and micro in community mental health care planning and co-ordination
In our comparative review of the prevailing mental health policy contexts across England and Wales we elected to highlight points of divergence. We emphasised in particular the shift towards the use of legislation in Wales [with the introduction of statutory care and treatment plans following the passing of the MH(W)M], and the contrast between this and the continued use of the CPA as guidance in England. Many managers and practitioners in the two Welsh sites spoke at length of the significance of the Measure and how this was raising awareness of the absolute centrality of care planning and co-ordination processes. However, comparisons of survey results across sites, and our analysis of micro-level interview data, cause us to question the extent to which the Measure is being ‘felt’ by service users at the frontline.
We make only cautious claims of significant differences in scores on our three measures across the six sites, and such differences as can be detected follow no national pattern. For example, Burgundy (a Welsh site) performed relatively well on service users’ perceptions of therapeutic relationships, but Champagne (the second Welsh site) did not. Differences in the degrees of service-user involvement in care planning qualitatively described by participants varied within and across sites, with no discernible national pattern. One tentative interpretation of this is that meso-level characteristics of individual locales may be more important than cross-national macro-level policy and legal differences in shaping people’s experiences of receiving (and providing) care. An alternative is that longer periods of time need to elapse before legal and policy change can be expected to be seen in local organisations and at the face-to-face level. For their part, legislators in Wales are actively reviewing the Measure and recommendations have been made by the National Assembly’s Health and Social Care Committee that training is needed to improve the quality of care and treatment plans and the level of service-user involvement. 133
Large-scale policy in both England and Wales places considerable emphasis on both the process and the product of care planning. However, across all sites participants described various difficulties with care planning and with the content and utility of completed care plans as documents. Divergent macro-level policies, when drawn on at local level, are capable of creating unintended consequences within interconnected mental health systems. 134 In our interpretation, the extent to which care planning and co-ordination is being shaped by national policy drivers is leading to the appearance of a gap between national aspirations and actual practices and everyday experiences. We found evidence of care planning and co-ordination being shaped by large-scale imperatives to adhere to mental health-specific law and policy but also to ‘clustering’ and PbR, to commissioners’ demands for monitoring data and to services managers’ needs to review and improve professional performance. For many, care planning and co-ordination was primarily about the assessment and management of risk, involving the construction of professional judgements made with little collaboration with people using services. In the face of competing macro- and meso-level pressures, at the micro-level we heard of care plans being constructed and then forgotten about by service users and practitioners unsure or unable to make active, day-to-day, use of them. Frequently, service user participants were unable to talk knowledgeably about the way their care plans were produced or subsequently used.
Across all sites we found evidence that austerity, as an explicit macro-level response to economic collapse, was being felt. Caseloads were described as rising and services in many areas had undergone major reconfiguration in an effort to reduce costs. Opportunities to match care co-ordinators to service users on the basis of need were challenged by practical contingencies, including care co-ordinators’ caseloads being full. If care co-ordinators are likely to become de facto providers of most care, as some participants said was the case, then the degree of fit between user and practitioner is an important consideration. Here, ‘fit’ refers to the particular constellation of skills and knowledge possessed by staff reflecting, to some degree, professional backgrounds but also the degree of ‘fit’ at the interpersonal level. Teams in which staff are overworked have less capacity to make optimal alignments between people using services and those co-ordinating and providing these. 135 Such restrictions are distinctly at odds with new legislation offering greater choice to mental health service users. 136 Care co-ordinators were not universally professionally trained, nor necessarily trained in care co-ordination, raising further questions about preparedness to take on a significant and challenging role.
Recovery is a theme found in macro-level mental health policy equally across England and Wales, with personalisation making rather less of an explicit appearance (and being differently interpreted) in the two countries. At the meso-level, significant within- and across-site differences were found in people’s understandings of, and orientations to, recovery ideals. Our data suggest that national aspirations that recovery is seen as a cultural and values-based approach to improve mental health care, as understood and drawn on by practitioners universally, are not yet being realised. Risk, in contrast, was described as driving processes of care planning and co-ordination more than any other consideration. In an era of large-scale service retrenchment, we also heard of recovery being described as a means of shifting responsibilities from service providers back to individuals and families.
Personalisation, as a macro-level idea found in recent policy and guidance, was understood (if at all) in different ways by different people. We detected different macro-level approaches across England and Wales, with Welsh policy-makers concerned about some versions of personalisation being a cover for service privatisation. Large-scale aspirations that care be uniquely tailored to individuals’ needs clashed with micro-level evidence that setting up, for example, personal budgets was bureaucratic and exceptionally time-consuming.
Recovery and care planning
Recovery as a concept is well discussed in the academic literature, and within service-user research and activist circles,137 but its filtering into practice has been a less consistent affair. In parallel to the literature,138 we encountered little in the way of shared understanding of recovery in our study sites. More worryingly perhaps, we found a creeping cynicism towards some of the perceived organisational motives behind the promotion of recovery.
In the current study we have demonstrated a close correlation between scores for therapeutic relationships provided by people using mental health services, and the recovery-oriented nature of those services. It has been known for some time that people using services value the relationships they have with workers, as much and if not more so, than the purely biomedical elements of their care. 139–141 Time and again our research interviews with people using services make this point; it is the relationship with their worker that they value. It goes further than this, however; it is relationships more widely that are reported as being helpful in recovery. Family, friends and people with whom the person can reciprocally share experiences and support feature strongly in our research interview data.
We cannot be sure, however, of the direction of the association between recovery and quality relationships. Are these relationships a fundamental element leading to recovery-oriented services or are they the consequence of recovery-focused service delivery? In relation to worker–service user relationships our detailed analysis of the research interviews suggests that it is the former rather than the latter. We draw this conclusion based on various data. For example, recovery as a concept means different things to different people. The absence of a shared understanding implies no universal agreement on the focus for recovery, what recovery will mean for the individual or how services should be provided to achieve this outcome. Lack of a shared understanding is not confined to the worker–service user relationship; it extends right through organisations too. Care planning is seen as an artefact of this process rather than central to it by many service users and often care co-ordinators themselves. Care co-ordination brings significant administrative burdens upon workers, and service users for the most part may have had some awareness of their care being co-ordinated but little understanding of how this might have related to something called recovery. Care plans are largely not valued or seen as instrumental in achieving recovery by service users. In Wales, where there is now a legal obligation on health boards and LAs to provide recovery-oriented care plans, we heard a subtle shift as some service users and particularly carers began to expect more from services and perhaps now see a potential legal recourse to achieving this if services do not meet their expectations. Workers too have adopted the language of recovery and articulated clear understanding of the new legal requirements in this respect. We detected, however, that across all sites burdensome administration and increased service demand was offered as part explanation from workers for an approach in which old practices could be dressed up to show adherence to new requirements embodied in supposedly recovery-focused care and treatment plans.
Despite all of this, the relationship with the worker endures and is seen as one of the few constants in an ever changing landscape of health and social care provision. It is notable that in our Burgundy site this stability of relationships between workers and service users is perhaps the key element in the high scores achieved for quality of the therapeutic relationship and outcomes on recovery orientation of the service. We could not see any other fundamental difference in service delivery in this site when compared with our other research sites that could account for these outcomes.
Recovery-focused care co-ordination works well for people when there is a sense of shared effort or collaboration in which the person feels involved, has a significant say in the services that are provided and where their independence and autonomy are respected by workers. Care plans are not seen as being instrumental in this process for many but they do help some when they are focused on practical steps or where they help people talk about their health care with workers.
A concern that arises from our data is the inherent risk that recovery could easily come to mean something other than what was originally conceived as its meaning is subverted in a drive towards achieving organisational ends. In many settings workers refer to organisational imperatives to increase through-put of cases and discharge people or move them onto personal budgets all in the name of recovery. This can be seen as a reasonable, and even admirable, attempt to prevent people getting stuck in the system of care and enabling them to maintain or regain their independence.
However, organisational pressure to achieve targets in this area generates its own resistance, as seen elsewhere when frontline staff are required to implement policy in real-world settings. 142 This results in staff and service users displaying some cynicism towards the perceived ‘re-conceptualisation’ of recovery by organisations seeking to trim costs while demand is increasing. Our data show that the concerns of professionals and service users centre on people being moved towards discharge or independence sooner than they would choose or perhaps is indicated by their level of need; workers and service users refer to the recovery ‘agenda’ and express scepticism about the real purposes to which it is being put. Were these concerns borne out, the goodwill and sense of optimism that surrounds the concept of recovery could itself be lost and the ground never recovered in a hasty (and, we would suggest, unlikely) attempt to achieve cost savings. Therefore, it is imperative in our view that shared understandings of the concept and goals of recovery are fully understood and appreciated at all levels of mental health organisations. Board-level responsibility and understanding of recovery and how it can and should be achieved may be a reasonable place to start. These understandings need to involve those people using these services as well as their carers. They must be shared with external organisations and appear in operational policies so that it is clear what is meant by recovery and how it will be achieved.
Personalisation
Drawing on the evidence presented here, personalisation is not yet a concept fully understood or accepted by people using and working in mental health services; lack of consistency and even of recognition of the term was apparent within sites and within the different groups of interviewees. Recently introduced mechanisms that claimed to promote personalisation, principally personal budgets and direct payments, were seen by staff as administratively burdensome and bureaucratic. There was also evidence of major difficulties in ensuring that personal budgets were agreed, and once agreed that monies were received. Lengthy delays created frustrations for service users and staff alike, and there were reports of these frustrations harming the therapeutic relationship. There is an increasing literature on personal budgets that suggests that this may be a great force for personalisation and empowerment,143 but unless the processes are improved, our data suggest that they may appear suspiciously like another laborious, hugely bureaucratic process – rather like the CPA was seen on its introduction. 58 Yet ‘personalisation’ of public services is very much the ‘new policy orthodoxy’,144(p. 2) broadly accepted across the political parties and seen as central to improving service delivery and empowering service users. Much greater attention needs to be afforded this topic by health and social care researchers, perhaps particularly for those service users with severe mental illness, to ensure that their needs are being met and their lives really are being improved by such an approach.
Safety and risk
Our data show that care co-ordinators are focused on concerns centred on requirements for risk assessment asserting that, for example ‘we are assessing risk continuously’. For service users, however, there is less awareness of risk assessments taking place and often no direct involvement or collaboration in the process. Carers have some awareness of safety and risk being considered and in some cases greater knowledge than the person receiving care themselves. Some service users see the presence of contingency or crisis plans as evidence of risk being considered. Care plans may be shared but risk assessments apparently much less so. This raises considerable issues of justice and fairness in mental health care delivery but also, crucially, militates the notion of recovery, which regards positive risk taking as fundamental. Additionally, the predictive accuracy of risk assessment in mental health care is fraught with problems such that even the best actuarial tools perform substantially below those acceptable in other areas of health care. 145 Workers devote considerable time and effort to these processes and appear to have significant faith in practices surrounding risk. However, as Langan146 cogently argues, much risk assessment practice is concerned only with risks for which workers will be held accountable. This focus on accountability excludes a broader consideration of risks to people in receipt of health care, including those occurring as a result of contact with services.
Iatrogenic risks, meaning those linked with the provision of care, are infrequently considered in the delivery of mental health services. The most obvious and perhaps most frequently cited iatrogenic risks are those posed by psychotropic medicine such as irreversible side-effects. 147,148 Kelly and McKenna149 further noted those risks presented by the community itself in the form of discrimination, stigma and possible physical attack. Recent figures suggest that 40% of mental health patients were victims of crime in the last year, and that 19% were victims of assault. Figures among women were even higher. 150 Risks presented by intense scrutiny and follow-up by workers151 may also result from failure to discuss these risks openly with people using services and their families or carers. Risk assessment practice may also inform the unexpectedly high use of CTOs152 and other forms of more subtle monitoring of people by services suggesting that a failure to inform and involve people in these processes places them at a significant risk of continued restrictions on their liberty.
Risk in mental illness is chiefly presented from the perspective of workers without reference to alternative views that may be available. This ‘professional’ perspective also pervades the face-to-face practice of risk assessment work to the extent that people are often unaware that a risk assessment has taken place. 153 The phenomenon of risk, however, suggests that there are competing bodies of knowledge about the concept itself. 154 Risk is a socially constructed concept that is positioned by much of the mental health literature as a binary opposition between the rationalist professional view and non-professional versions. Lupton notes that ‘risk perspectives of experts are privileged as objective and factual over those of lay people’154(pp. 56–57) whose perceptions are found wanting and contaminated by cultural influences. Professional perspectives are somehow seen as immune from these very same influences. An alternative is for care co-ordinators to have risk conversations with people they work with, thus allowing service user and professional accounts to stand side by side as credible versions of the day-to-day realities of living risky lives. This will not only allow service users to benefit from the expert opinion of care co-ordinators but will also help workers see the range of risk concerns that people encounter in their everyday lives.
Langan146 has noted, for instance, that risk assessment practices in mental health often overplay individual factors at the expense of structural, social and interactional causes. An alternative is to develop care co-ordination for individuals to benefit from social bonding, adjustment and integration with the aim of sustaining community living in the absence of overt measures of social control such as ongoing intrusive monitoring. More direct involvement of people in their own risk assessments may lead to much better informed assessments and open the possibility of focusing on micro-level relationships (individuals, family, household, community) that enable people to benefit from supports that in themselves can successfully manage or reduce risk behaviours. 155
Training interventions
Unsurprisingly, the findings of our study included a strong call for more training in recovery-focused care planning and co-ordination. Our data would support the need for training to include exploration of the different understandings of recovery; coproduction and joint working, including around care planning, goal setting, risk assessment and management, and the choice and use of recovery tools. Similarly, training could include a greater focus on personalisation and in particular the use of personal budgets. This might include training in conducting assessments and developing a ‘recovery support plan which identifies the goals a person has for his or her recovery and how those goals could be met’. 143(p. 4) But it also needs to explore some of the tensions identified in our study around negotiating with multiple providers on issues of risk, communication and confidentiality.
Unfortunately, training brings as many challenges as answers. First, there are great difficulties for health service managers to provide time and support for training alongside all the mandatory training required of staff and the ever-increasing demands placed on practitioners. Second, there is also little evidence that training alone leads to any significant change in practice.
The impressive THORN training programme156 in psychosocial interventions for clinicians who work with people with serious mental illness and their families included case management, cognitive–behavioural therapy and family therapy. Despite a lengthy training programme, back-filled posts and highly positive evaluations of the training, there is very little evidence of this leading to major changes in clinical practice. 156 In particular, attempts to increase work with families was a dismal failure, with often as little as one extra family receiving input within a year of training. Stanbridge and Burbach157 suggest a strategic and whole-team training approach shaped to the particular needs and interests of the team to maximise impact.
Just such a whole-team approach in relation to delivering recovery-focused working within CMHTs has been adopted in Slade et al. ’s REFOCUS programme of research. 158 The aim of the intervention was to give community-based mental health professionals the skills they needed to work in a more recovery-focused way. It comprised team training for 12 months to help professionals understand more about personal recovery and how they can better support people on their individual recovery journeys. The intervention encourages team members to focus more on service users’ values, strengths and personal goals, and helps professionals develop and practise coaching skills. It encourages mental health professionals to work more collaboratively with people who are unwell and to make sure that care plans emphasise personal goals and reflect a service user’s preferences for treatment.
The REFOCUS trial158 was a cluster randomised controlled trial involving 29 community-based teams; 15 of the teams were trained in the REFOCUS intervention. The study compared the recovery journey of service users who have been supported by professionals working in these teams with the recovery journeys of service users supported by professionals working in the other 14 teams, who have not had the specialist REFOCUS training (the control arm). Unfortunately, despite great efforts, the results from this study have been disappointing (see Appendix 12):159
The REFOCUS Trial shows that implementation within mental health systems is more challenging than simply introducing a new intervention, and requires organisational commitment. However, we did show that where REFOCUS was fully implemented, a positive impact on recovery was found. So the major challenge is implementation, which starts but does not end with training.
Professor M. Slade, Institute of Psychiatry, Psychology and Neuroscience, Kings College London, 2014, personal communication
Another programme of research that holds out hope is Lovell et al. ’s Enhancing the Quality of User Involved care Planning (EQUIP) in mental health services programme. 160,161 This programme is now delivering user- and carer-led training to CMHTs in a cluster randomised controlled trial designed to bring about more user-focused care planning. We keenly await the results.
The Implementing Recovery through Organisational Change (ImRoc) programme led by the Centre for Mental Health162 is also a major driver in trying to bring about recovery-focused organisations and practice in mental health in England. A key part of their strategy sees the introduction of peer workers in the workplace as a key driver of recovery-focused work. 163 The lead author of this report is involved in a new NIHR programme of research (RP-PG-1212–20019) aimed at evaluating the impact of mental health peer support workers. This 5-year programme of research began on 1 March 2015. Although not specifically focused on care planning, it will be interesting to see whether or not the presence of peer workers within teams influences work culture.
In Wales, the National Institute for Social Care and Health Research (NISCHR)-funded Plan4Recovery164 study is examining social approaches to promote recovery. In particular, it is asking how people share in decisions about their care and how they make links with others in their communities for support and friendship. The aim is to assess how these are related to recovery and quality of life. The study is measuring involvement in decision-making, social contacts, recovery and quality of life with a cohort of people using a range of statutory and non-statutory services. Again, we keenly await the results.
The challenge of bringing about and maintaining change in practice is well-recognised and has led to the growth of Improvement Science, with a focus on implementing and sustaining evidence-based change within organisations and practice. 165,166 Simply delivering more training, even if possible, is unlikely to be enough and the challenge is to develop and evaluate innovative quality improvement approaches that also include a focus on the meso-level context of organisations, as they attempt to bring about a meaningful shift in mental health care culture. 167 Training and related interventions aimed at care co-ordinators and bringing about change should draw on the best evidence available and be delivered as part of a high-quality programme of research. 168
Public and patient involvement
This study was developed and conducted with a high level of service-user and carer involvement from the start, including an independent service-user researcher as co-investigator. Regular consultations throughout the study with both SUGAR, the in-house service user and care advisory group on research169 and the project’s specially convened LEAG ensured that the study was conducted with a clear focus on the views and experiences of service users and carers, and that the methods used reflected this.
Additionally, five service-user researchers were employed to work alongside the research team, helping with recruitment and interviewing service users and carers. Training and support was provided and structured reflection methods employed to help both the service users and academic researchers to learn from the joint experience and improve their ways of working. A blog post was published, and the service-user and academic researchers jointly produced and gave a presentation on their work at an international psychiatric nursing research conference. They will jointly produce a paper for publication exploring the benefits and some of the challenges for both parties in the near future.
Strengths and limitations
Data were collected from a wide range of participants using a mix of methods from across a reasonable spread of teams and service providers in geographically varied locations in two countries. The interview data in particular are rich, and the framework method provided a time-consuming but structured and visible method of organising, analysing and comparing these data within and across sites. We believe that the framework method and detailed presentation of results supports the transferability of these findings to other similar services.
However, there remains the possibility that within each sub-group of service users, carers, practitioners and managers, there may have been an element of self-selection or inherent biases not immediately apparent to the researchers. There appears to be a wide selection of professions and viewpoints identified among the staff interviews but the service-user sample may be weighted more towards those with long-standing contact with services. This may have been reflected in more limited experiences of a more recovery-focused approach from clinicians who may feel longer-term service users are less likely to respond to a focus on recovery. Similarly, such a population may have different expectations of care co-ordinators and mental health services than a younger sample less habituated to the familiarities of mental health service delivery.
Overall, the postal survey response rate of service users surveyed was low, ranging between 9% and 19%, which may introduce bias. Owing to the nature of the survey, it is not possible to make comparisons between responders and non-responders, as we had no access to data for non-participants. There was a moderate level of missing data for the RSA scale completed by service users, possibly owing to some of the difficult language used. As a consequence, more detailed analysis of covariance within these data was restricted by lack of power. The RSA scale was selected for use after consideration of several organisational-focused measures of recovery. Nonetheless, this was not a satisfactory measure as too many participants found some of the language and North American terminology unfamiliar and unclear. Adaptation and re-validation of this measure to a British population or the identification of a more suitable measure would be recommended for future studies. Mindful of not taking up too much of the time of busy health care staff, the care co-ordinators were asked to complete the RSA scale only. On reflection, this was perhaps a wasted opportunity, as once practitioners had consented to participate, it might have been beneficial to have requested their views on other aspects of services and their work with service users and carers, with minimal additional time burden.
The involvement of service users and carers throughout the study as researchers and advisors has also provided added value to the study through additional viewpoints and interpretations. However, greater involvement of service users and carers in the analysis may have provided even greater insight and may be something that can be explored in a further analysis.
Conclusions
The results of this cross-national, multisite, mixed-methods study suggest that there is a gap between the macro-level national policy aspirations for recovery-focused, personalised care planning and co-ordination and the meso-/micro-level ‘street-level’ practices and everyday experiences of service users, carers and care co-ordinators. Of particular concern was evidence of a perhaps widening discrepancy between policy and practice and the indications of an emergent cynicism among participants as recovery concepts and ideals are subverted by higher order organisational needs, directives and ends. There is a serious risk that the hope and optimism that recovery approaches can offer often much-maligned mental health services is being dampened and perhaps snuffed out by the ‘re-conceptualisation of recovery’ at a macro-level. Clearly, among participants in this study within and across the six sites, there was a lack of consensus about what recovery means. This may be expected with such a relatively nascent and contested concept. But a loss of focus and legitimacy at a time when services are and will continue to be under enormous pressure to respond to the increasing demands placed upon them at a time of continued austerity is worrying and could have serious ramifications for the engagement, safety and well-being of local populations and communities and the retention of top-quality staff. Mental health service commissioners and providers need to ensure that there is clarity and consistency in establishing and communicating with partners and recipients of services what is meant by recovery and to ensure that the aims and operations of the organisation are designed to support staff and service users in realising that vision.
Care planning itself was seen by care co-ordinators and managers as a useful way of recording and evidencing plans and actions but were largely deemed irrelevant thereafter by most frontline staff and the majority of service users. However, the processing, completing, updating and uploading of care plan documentation is (again) reported to require considerable time and energy away from direct contact with services users, families and wider networks, while appearing to have a minimal role in aiding recovery. IT may provide some assistance in accessing and sharing information but paradoxically appears more often to require even yet more time away from the service user as care co-ordinators grapple with inflexible, unwieldy systems and, from the service user’s viewpoint, depersonalised outputs. After 25 years of the CPA and its more recent siblings and repeated accounts of bureaucratic overload, it really is time for innovative, more flexible, genuinely person-centred solutions to this dilemma. It is clear from service users and carers in this study that the key instrument in helping and enabling people towards recovery is the therapeutic relationship with empathic, respectful and skilful care co-ordinators and wider family and social support networks. The allocation or choice of care co-ordinator and care planning processes must be redesigned to support rather than hinder that. WRAPs and similar approaches, as often discussed in our data, may provide a more individualised and recovery-focused method that merits more detailed investigation, especially in light of recent evidence. 170
Issues of safety and risk go hand-in-hand with mental health service delivery, perhaps more than in any other area of health care. Our data showed clearly that for managers, senior practitioners and front-line clinicians, risk assessment and management is central to their work and a key component in care planning and co-ordination. However, for the majority of service users and some carers, this was far less evident and there was a clear disjuncture between these experiences. Most service users did not feel that their safety had necessarily been considered, or that perceptions of their risk towards others had been discussed with them. In order to provide genuinely personalised, recovery-focused care planning and to ensure the safety and well-being of all, attention must be given to how greater openness, partnership working and shared decision-making can be developed in this important area.
The findings from this study will inform our sister project, commissioned by NIHR HS&DR (13/10/75), in which we undertake to employ a similar design and methodology to investigate recovery-focused care planning in acute inpatient mental health settings. It is anticipated that the combined outcomes will help us design and evaluate a whole-system intervention that helps bring about more personalised, collaborative care planning and co-ordination across settings. In the interim, the following recommendations are presented, including those for research.
Recommendations (by macro-, meso- and micro-level)
-
Commissioners and providers of mental health services should aim to ensure that there is clarity and consistency in establishing and communicating with partners and recipients of services what is meant by recovery and to ensure that the aims and operations of the organisation are designed to support staff and service users in realising that vision. These understandings need to be developed through the involvement of people using these services and frontline practitioners. They need to be shared with external organisations and appear in operational policies so that it is clear what is meant by recovery and how it will be achieved (macro-level).
-
Similarly, there is a need for a simple, accessible and universally understood definition of what personalisation means in the context of mental health service delivery. There is also an urgent need for the methods and processes that support personalisation to be simplified and streamlined (macro-level).
-
Commissioners need to recognise that therapeutic relationships lie at the heart of effective care planning, co-ordination and recovery-focused work and team and care co-ordinator allocation and workloads need to be adapted to support this (macro-level).
-
Care and treatment planning processes must be redesigned to enable care co-ordinators to better support recovery in service users. Serious consideration should be given to introducing and evaluating explicitly personalised, recovery-focused care planning tools and methods, such as WRAPs, instead of existing CPA/CTP documentation (macro- and meso-level).
-
High-quality research should be commissioned to investigate the clinical effectiveness and cost-effectiveness of the following:
-
innovative organisational approaches to freeing up staff time to increase direct contact time with service users, carers and social networks with the aim of providing explicit recovery-focused interventions (macro-, meso- and micro-level)
-
use of mobile IT aimed at increasing staff–service user contact time and delivering more flexible, personalised recovery-focused care (macro-, meso- and micro-level)
-
collaborative working and shared decision-making with mental health service users and carers in risk assessment and management (meso- and micro-level)
-
innovative staff/team training interventions, drawing on best evidence available, designed to enable and support care co-ordinators and teams to provide personalised, recovery-focused care planning and co-ordination (meso-level).
-
Acknowledgements
Many thanks are also due to the following people:
Ms Jennifer Egbunike (Research Assistant in Health Research), who conducted data collection and contributed to the literature review.
Mr David Hindle (Service User Researcher in Mental Health), who conducted data collection.
Ms Katherine Barrett (Service User Researcher in Mental Health), who conducted data collection.
Mr John Tear (Service User Researcher in Mental Health), who conducted data collection.
Ms Bethan Mair Edwards (Service User Project Assistant in Mental Health), who conducted data collection.
Mr Alan Meudell (Service User Project Assistant in Mental Health), who conducted data collection.
Ms Alex Thornton (Research Administrator), who conducted data collation and helped with analysis and collating the final report.
Ms Nafiso Ahmed (Research Assistant in Mental Health), who contributed to qualitative analysis and the final report.
Dr Mark Haddad (Senior Lecturer in Mental Health), who contributed advice on sampling.
Mrs Barbara Keogh (Research Nurse and approved mental health professional).
Ms Tara Harvey (Clinical Studies Officer).
Ms Neelam Laxhman (Research Assistant).
Ms Rebecca Holland (Clinical Studies Officer).
Ms Sue Thomson (Research Nurse).
Ms Bethan Rees (Clinical Studies Officer).
Ms Philippa Case (Senior Clinical Research Co-ordinator).
Ms Serena Gregory (Senior Clinical Research Co-ordinator).
Mr Adam Baxter (Clinical Research Co-ordinator).
Many thanks to all local principal investigators, service managers, staff, service users and carers who took part in or helped with the study.
Contributions of authors
Professor Alan Simpson (Professor of Collaborative Mental Health Nursing) led on the design and overall management of the study; conducted data analysis and contributed to and edited the final report.
Dr Ben Hannigan (Reader of Mental Health Nursing) contributed to the design of the study and managed the study in Wales; contributed to the literature and policy review; contributed to training and support of service user researchers; conducted data collection and analysis and contributed to the final report.
Dr Michael Coffey (Associate Professor in Mental Health Nursing) contributed to the design of the study; contributed to the literature and policy review; contributed to training and support of service user researchers; conducted data collection and analysis and contributed to the final report.
Dr Aled Jones (Senior Lecturer in Nursing) led on the literature and policy review and contributed to the final report.
Dr Sally Barlow (Research Fellow in Mental Health) conducted data collection; contributed to training and support of service user researchers; led on quantitative analysis and write-up; conducted qualitative data analysis; provided project management for end of study and contributed to the final report.
Dr Rachel Cohen (Research Fellow in Health Research) conducted data collection and qualitative analysis and contributed to the final report.
Dr Jitka Všetečková (Lecturer in Nursing) was project manager for the study; conducted data collection and contributed to qualitative analysis; contributed to training and support of service user researchers; and contributed to the final report.
Ms Alison Faulkner (Independent Service User Researcher Consultant) contributed to the design of the study and qualitative analysis; contributed to training and support of service user researchers; facilitated the LEAG; and contributed to the final report.
Publications
Simpson A, Hannigan B, Coffey M, Jones A, Barlow S, Cohen R, et al. Study protocol: cross-national comparative case study of recovery-focused mental health care planning and co-ordination (COCAPP). BMC Psychiatry 2015;15:145.
Simpson A, Hannigan B, Coffey M, Jones A, Všetečková J, Faulkner A, et al. Recovery-focused care planning and coordination in England and Wales: a cross national mixed methods comparative case study. Submitted.
Data sharing statement
Data can be obtained from the corresponding author.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
References
- Refocusing the Care Programme Approach: Policy and Positive Practice Guidance. London: Department of Health; 2008.
- Mental Health Policy Guidance: The Care Plan Approach for Mental Health Service Users. Cardiff: WAG; 2003.
- Mental Health (Wales) Measure 2010: Guidance for Local Health Boards and Local Authorities. Cardiff: WAG; 2011.
- Mental Health Bulletin: Annual Report from MHMDS Returns – England 2011–2012; Initial National Figures. London: HSCIC; 2013.
- Together for Mental Health: A Strategy for Mental Health and Wellbeing in Wales. Cardiff: Welsh Government; 2012.
- Sustainable Social Services for Wales: A Framework for Action. Cardiff: WAG; 2011.
- Le Boutillier C, Leamy M, Bird VJ, Davidson L, Williams J, Slade M. What does recovery mean in practice? A qualitative analysis of international recovery-oriented practice guidance. Psychiatr Serv 2011;62:1470-6. http://dx.doi.org/10.1176/appi.ps.001312011.
- Anthony WA. Recovery from mental illness: the guiding vision of the mental health service system in the 1990s. Psychosoc Rehabil J 1993;16:11-23. http://dx.doi.org/10.1037/h0095655.
- Slade M. Personal Recovery from Mental Illness: A Guide for Mental Health Professionals. Cambridge: Cambridge University Press; 2009.
- Understanding Mental Illness: Recent Advances in Understanding Mental Illness and Psychotic Experiences. Leicester: British Psychological Society; 2000.
- Recovering Ordinary Lives. London: COT; 2006.
- From Values to Action: The Chief Nursing Officer’s Review of Mental Health Nursing. London: Department of Health; 2006.
- Fair Deal for Mental Health. London: Royal College of Psychiatrists; 2008.
- Duffy S. Personalisation in Mental Health. Sheffield: Centre for Welfare Reform; 2010.
- Dieterich MIC, Park B, Marshall M. Intensive case management for severe mental illness. Cochrane Database Syst Rev 2010;10. http://dx.doi.org/10.1002/14651858.cd007906.pub2.
- Simpson A. Community psychiatric nurses and the care co-ordinator role: squeezed to provide ‘limited nursing’. J Adv Nurs 2005;52:689-99. http://dx.doi.org/10.1111/j.1365-2648.2005.03636.x.
- Burns T, Yiend J, Doll H, Fahy T, Fiander M, Tyrer P. Using activity data to explore the influence of case-load size on care patterns. Br J Psychiatry 2007;190:217-22. http://dx.doi.org/10.1192/bjp.bp.106.025940.
- No Voice, No Choice: A Joint Review of Adult Community Mental Health Services in England. London: CHAI; 2007.
- Elias E, Singer L. Review of the Care Programme Approach in Wales. Llanharan: National Leadership and Innovation Agency for Healthcare; 2009.
- Community Mental Health Services Survey 2011. London: Care Quality Commission; 2011.
- Adult Mental Health Services: Follow Up Report. Cardiff: WAO; 2011.
- Faulkner A. The right to take risks. J Adult Prot 2012;14:287-96. http://dx.doi.org/10.1108/14668201211286066.
- Hewitt J, Coffey M. Therapeutic working relationships with people with schizophrenia: literature review. J Adv Nurs 2005;52:561-70. http://dx.doi.org/10.1111/j.1365-2648.2005.03623.x.
- McCabe RP S. The therapeutic relationship in the treatment of severe mental illness: a review of methods and findings. Int J Soc Psychiatry 2004;50:115-28. http://dx.doi.org/10.1177/0020764004040959.
- De Leeuw M, Van Meijel B, Grypdonck M, Kroon H. The quality of the working alliance between chronic psychiatric patients and their case managers: process and outcomes. J Psychiatr Ment Health Nurs 2012;19:1-7. http://dx.doi.org/10.1111/j.1365-2850.2011.01741.x.
- Yamashita M, Forchuk C, Mound B. Nurse case management: negotiating care together within a developing relationship. Perspect Psychiatr C 2005;41:62-70. http://dx.doi.org/10.1111/j.1744-6163.2005.00012.x.
- Kondrat DC, Early TJ. An exploration of the working alliance in mental health case management. Soc Work Res 2010;34:201-11. http://dx.doi.org/10.1093/swr/34.4.201.
- Developing and Evaluating Complex Interventions. London: Medical Research Council; 2008.
- Goodwin N, Dixon A, Anderson G, Wodchis W. Providing Integrated Care for Older People with Complex Needs lessons from Seven International Case Studies. London: The King’s Fund; 2014.
- Challis D, Hughes J, Clarkson P, Abendstern M, Sutcliffe C. A Systematic Evaluation of the Development and Impact of the Single Assessment Process in England. Presentation to the Showcasing Social Care Research Event. Department of Health: London; 2007.
- Creswell J. Research Design: Qualitative, Quantitative and Mixed Methods Approaches. London: Sage; 2009.
- Kohn M. Cross-National Research in Sociology. Newbury Park: Sage; 1993.
- Hantrais L, Mangen S. Cross-National Research Methods in the Social Sciences. London: Pinter; 1996.
- Stake RE. The Art of Case Study Research. London: Sage; 1995.
- Fitzgerald L. Case studies as a research tool. Qual Health Care 1999;8. http://dx.doi.org/10.1136/qshc.8.2.75.
- Platt J. Case study in American methodological thought. Curr Sociol 1992;40:17-48. http://dx.doi.org/10.1177/001139292040001004.
- Yin RK. Case Study: Design and Methods. Newbury Park: Sage Publications; 1994.
- Robson C. Real World Research: A Resource for Social Scientists and Practitioners-Researchers. Oxford: Blackwell; 1993.
- Sweetman D, Badiee M, Creswell JW. Use of the transformative framework in mixed methods studies. Qual Inq 2010;16:441-54. http://dx.doi.org/10.1177/1077800410364610.
- Mertens DM. Transformative Research and Evaluation. New York: Guilford Press; 2009.
- Byrne DS. Complexity Theory and the Social Sciences: An Introduction. London: Routledge; 1998.
- Greenhalgh T, Robert G, Macfarlane F, Bate P, Kyriakidou O. Diffusion of innovations in service organizations: systematic review and recommendations. Milbank Q 2004;82:581-629. http://dx.doi.org/10.1111/j.0887-378X.2004.00325.x.
- Wong G, Greenhalgh T, Westhorp G, Buckingham J, Pawson R. RAMESES publication standards: meta-narrative reviews. BMC Med 2013;11. http://dx.doi.org/10.1186/1741-7015-11-20.
- O’Connell M, Tondora J, Croog G, Evans A, Davidson L. From rhetoric to routine: assessing perceptions of recovery-oriented practices in a state mental health and addiction system. Psychiatr Rehabil J 2005;28. http://dx.doi.org/10.2975/28.2005.378.386.
- Cochran WG. Sampling Techniques. New York, NY: Wiley and Sons; 1977.
- Mcguire-Snieckus R, McCabe R, Catty J, Hansson L, Priebe S. A new scale to assess the therapeutic relationship in community mental health care: STAR. Psychol Med 2007;37:85-9. http://dx.doi.org/10.1017/S0033291706009299.
- Rogers ES, Chamberlin J, Ellison ML, Crean T. A consumer-constructed scale to measure empowerment among users of mental health services. Psychiat Serv 1997;48:1042-7. http://dx.doi.org/10.1176/ps.48.8.1042.
- Edwards P, Roberts I, Clarke M, DiGuiseppi C, Pratap S, Wentz R, et al. Increasing response rates to postal questionnaires: systematic review. BMJ 2002;324. http://dx.doi.org/10.1136/bmj.324.7347.1183.
- Hannigan B. Connections and consequences in complex systems: insights from a case study of the emergence and local impact of crisis resolution and home treatment services. Soc Sci Med 2013;93:212-9. http://dx.doi.org/10.1016/j.socscimed.2011.12.044.
- Atkinson P, Housley W. Interactionism. London: Sage; 2003.
- Strauss AL. Negotiations: Varieties, Contexts, Processes, and Social Order. San Francisco, CA: Jossey-Bass; 1978.
- Ritchie J, Lewis J, Nicholls CM, Ormston R. Qualitative Research Practice: A Guide for Social Science Students and Researchers. London: Sage; 2013.
- Ritchie J, Spencer L, Bryman A, Burgess RG. Analyzing Qualitative Data. London: Routledge; 1993.
- Co-ordinated Care for People with Complex Chronic Conditions. Key Lessons and Markers for Success. London: King’s Fund; 2013.
- Bailey D. Interdisciplinary Working in Mental Health. Basingstoke: Palgrave Macmillan; 2012.
- Van Houdt S, Heyrman J, Vanhaecht K, Sermeus W, De Lepeleire J. An in-depth analysis of theoretical frameworks for the study of care co-ordination. Int J Integr Care 2013;13:1-8.
- Report of the Committee of Inquiry into the Care and Aftercare of Sharon Campbell. London: Department of Health and Social Security; 1988.
- Simpson A, Miller C, Bowers L. The history of the Care Programme Approach in England: where did it go wrong?. J Ment Health 2003;12:489-504. http://dx.doi.org/10.1080/09638230310001603555.
- Kingdon D. Care programme approach: recent government policy and legislation. Psychiatric Bull 1994;18:68-70. http://dx.doi.org/10.1192/pb.18.2.68.
- Report of the Royal Commission on the Law Relating to Mental Illness and Mental Deficiency 1954–1957 (Cmnd 169). London: Her Majesty’s Stationery Office; 1957.
- Mental Health Act 1959. London: The Stationery Office; 1990.
- Tyrer P, Morgan J, Van Horn E, Jayakody M, Evans K, Brummell R, et al. A randomised controlled study of close monitoring of vulnerable psychiatric patients. Lancet 1995;345:756-9. http://dx.doi.org/10.1016/S0140-6736(95)90640-1.
- Simpson A. The impact of team processes on psychiatric case management. J Adv Nurs 2007;60:409-18. http://dx.doi.org/10.1111/j.1365-2648.2007.04402.x.
- Akhavain P, Amaral D, Murphy M, Uehlinger KC. Collaborative practice: a nursing perspective of the psychiatric interdisciplinary treatment team. Holist Nurs Pract 1999;13:1-11. http://dx.doi.org/10.1097/00004650-199901000-00003.
- Loveland B. The Care Programme Approach: whose is it? empowering users in the care programme process. Educ Action Res 1998;6:321-35. http://dx.doi.org/10.1080/09650799800200058.
- Greenhalgh T, Wong G. Training Materials for Meta-Narrative Reviews 2013. www.ramesesproject.org/media/Meta_narrative_reviews_training_materials.pdf (accessed 25 November 2015).
- Greenhalgh T, Robert G, Macfarlane F, Bate P, Kyriakidou O, Peacock R. Storylines of research in diffusion of innovation: a meta-narrative approach to systematic review. Soc Sci Med 2005;61:417-30. http://dx.doi.org/10.1016/j.socscimed.2004.12.001.
- Schneider J. Care programming in mental health: assimilation and adaptation. Brit J Soc Work 1993;23:383-40.
- Carpenter J, Sbaraini S. A healthy approach. Community Care 1997;23:32-3.
- Allen C. The care programme approach: the experiences and views of carers. Ment Health Care 1998;1:160-2.
- Rose D, Ford R, Lindley P, Gawith L. In Our Experience: User-Focused Monitoring of Mental Health Services in Kensington & Chelsea and Westminster Health Authority. London: Sainsbury Centre for Mental Health; 1998.
- Telford R, Faulkner A. Learning about service user involvement in mental health research. J Ment Health 2004;13:549-59. http://dx.doi.org/10.1080/09638230400017137.
- Kara H. Mental health service user involvement in research: where have we come from, where are we going?. J Public Ment Health 2013;12:122-35. http://dx.doi.org/10.1108/JPMH-01-2013-0001.
- Bindman J, Beck A, Glover G, Thornicroft G, Knapp M, Leese M, et al. Evaluating mental health policy in England: Care Programme Approach and supervision registers. Brit J Psychiat 1999;175:327-30. http://dx.doi.org/10.1192/bjp.175.4.327.
- Schneider J, Carpenter J, Brandon T. Operation and organisation of services for people with severe mental illness in the UK. A survey of the Care Programme Approach. Brit J Psychiat 1999;175:422-5. http://dx.doi.org/10.1192/bjp.175.5.422.
- Swinson N, Flynn S, Kapur N, Appleby L, Shaw J. The use of the care programme approach in perpetrators of homicide. J Foren Psychi Psych 2010;21:649-59. http://dx.doi.org/10.1080/14789941003739649.
- Newbigging K, Ridley J, McKeown M, Machin K, Poursanidou D. The Right to be Heard. Review of the quality of Independent Mental Health Advocate (IMHA) Services in England: University of Central Lancashire; 2012.
- Rinaldi M, Kuriyan R. No Decision About Me, Without Me. Recovery focused care plan audit: South West London & St George’s Mental Health NHS Trust; 2012.
- Gilleard C. Implementation of the care programme approach in the community. Psychiatric Bull 1995;19:750-2. http://dx.doi.org/10.1192/pb.19.12.750.
- Carpenter J, Sbaraini S. Involving service users and carers in the care programme approach. J Ment Health 1996;5:483-8. http://dx.doi.org/10.1080/09638239619167.
- Brown Z. The care programme approach – the service user’s view. Soc Serv Res 1998;2:55-66.
- Cornwall PL, Gorman B, Carlisle J, Pope M. Ten years in the life of a community mental health team: The impact of the care programme approach in the UK. J Ment Health 2001;10:441-7. http://dx.doi.org/10.1080/09638230120041209.
- Grace J, Steels M, Baruah R. General practitioners knowledge of and views on the care programme approach. Psychiatric Bulletin 1996;20:643-4. http://dx.doi.org/10.1192/pb.20.11.643.
- Holloway F, Oliver N, Collins E, Carson J. Case management: a critical review of the outcome literature (Structured abstract). Eur Psychiat 1995;10:113-28. http://dx.doi.org/10.1016/0767-399X(96)80101-5.
- McDonald KM, Sundaram V, Bravata DM, Lewis R, Lin N, Kraft SA, et al. Closing the Quality Gap: A Critical Analysis of Quality Improvement Strategies (Vol. 7: Care Co-ordination). Rockville, MD: Agency for Healthcare Research and Quality (US); 2007.
- Lawson M, Strickland C, Wolfson P. User involvement in care planning. Psychiatric Bull 1999;23:539-41. http://dx.doi.org/10.1192/pb.23.9.539.
- Finding a Place: A Review of Mental Health Services for Adults. London: Her Majesty’s Stationery Office; 1994.
- Perkins R, Repper J. Dilemmas in Community Mental Health Practice: Choice or Control. Abingdon: Radcliffe Medical Press; 1998.
- Faulkner A, Wallcraft J, Nicholls V, Blazdell J, Treitel R. The right to ask questions. Openmind 1998;91.
- Callard F, Rose D. Mental Health Service User Leadership in Research 2010.
- Rose D. Partnership, co-ordination of care and the place of user involvement. J Ment Health 2003;12:59-70. http://dx.doi.org/10.1080/09638230021000058300.
- Rose D. Users’ Voices. The Perspectives of Mental Health Service Users on Community and Hospital Care. London: The Sainsbury Centre for Mental Health; 2001.
- Diamond B, Parkin G, Morris K, Bettinis J, Bettesworth C. User involvement: substance or spin?. J Ment Health 2003;12:613-26. http://dx.doi.org/10.1080/09638230310001627964.
- Gould D. Service Users’ Experiences of Recovery Under the 2008 Care Programme Approach. London: National Survivors User Network/Mental Health Foundation; 2012.
- Rose D, Barnes M, Crawford M, Omeni E, MacDonald D, Wilson A. How do managers and leaders in the National Health Service and social care respond to service user involvement in mental health services in both its traditional and emergent form? The ENSUE study. National Institute for Health Research 2014;2.
- Rose D, Leese M, Oliver D, Sidhu R, Bennewith O, Priebe S, et al. A comparison of participant information elicited by service user and non-service user researchers. Psychiatr Serv 2011;62:210-13. http://dx.doi.org/10.1176/ps.62.2.pss6202_0210.
- Gillard S, Borschmann R, Turner K, Goodrich-Purnell N, Lovell K, Chambers M. ‘What difference does it make?’ Finding evidence of the impact of mental health service user researchers on research into the experiences of detained psychiatric patients. Health Expect 2010;13:185-94. http://dx.doi.org/10.1111/j.1369-7625.2010.00596.x.
- Webb Y, Clifford P, Fowler V, Morgan C, Hanson M. Comparing patients’ experience of mental health services in England: a five-Trust survey. Int J Health Care Qual Assur 2000;13:273-81. http://dx.doi.org/10.1108/09526860010373253.
- Blenkiron P, Cuzen I, Hammill AC, Mo KH. Involving service users in their mental health care: the CUES Project. Psychiatric Bull 2003;27:334-8. http://dx.doi.org/10.1192/pb.27.9.334.
- Wooff D, Brandon T, Carpenter J, Schneider J. Correlates of stress in carers. J Ment Health 2003;12:29-40. http://dx.doi.org/10.1080/09638230021000058274.
- Hanson M. Evaluating user experience of an NHS mental health service. Int J Health Care Qual Assur 2003;16:341-6. http://dx.doi.org/10.1108/09526860310500005.
- Killaspy H, White S, Taylor TL, King M. Psychometric properties of the Mental Health Recovery Star. Brit J Psychiat 2012;201:65-70. http://dx.doi.org/10.1192/bjp.bp.111.107946.
- Carpenter J, Schneider J, McNiven F, Brandon T, Stevens R, Woof D. Integration and targeting of community care for people with severe and enduring mental health problems: users’ experiences of the care programme approach and care management. Brit J Soc Work 2004;34:313-33. http://dx.doi.org/10.1093/bjsw/bch040.
- Foucault M. The History of Sexuality. Vol I: The Will to Knowledge. London: Penguin Books; 1976.
- Goffman E. Stigma: Notes on the Management of Spoiled Identity. Englewood Cliffs, NJ: Prentice-Hall; 1963.
- Macpherson R, Jerrom B, Lott G, Ryce M. The outcome of clinical goal setting in a mental health rehabilitation service. A model for evaluating clinical effectiveness. J Ment Health 1999;8:95-102. http://dx.doi.org/10.1080/09638239917670.
- Lockwood A, Marshall M. Can a standardized needs assessment be used to improve the care of people with severe mental disorders? A pilot study of ‘needs feedback’. J Adv Nurs 1999;30:1408-15. http://dx.doi.org/10.1046/j.1365-2648.1999.01217.x.
- Marshall M, Lockwood A, Green G, Zajac-Roles G, Roberts C, Harrison G. Systematic assessments of need and care planning in severe mental illness: cluster randomised controlled trial. Brit J Psychiat 2004;185:163-8. http://dx.doi.org/10.1192/bjp.185.2.163.
- Howells R, Thompsell A. Service innovations: the eCPA: a computerised care programme approach planning system. Psychiatric Bull 2002;26:266-8. http://dx.doi.org/10.1192/pb.26.7.266.
- Smith P, Pearson PH, Ross F. Emotions at work: what is the link to patient and staff safety? Implications for nurse managers in the NHS. J Nurs Manag 2009;17:230-7. http://dx.doi.org/10.1111/j.1365-2834.2009.00980.x.
- Hunter DJ, Wistow G. Community Care in Britain: Variations on a Theme. London: King Edward’s Hospital Fund for London; 1987.
- The Care Programme Approach for People with a Mental Illness Referred to the Specialist Psychiatric Services. London: Department of Health; 1990.
- The National Health Service and Community Care Act. London: Her Majesty’s Stationery Office; 1990.
- Introduction of Supervision Registers for Mentally Ill People from 1st April 1994. London: Department of Health; 1994.
- Building Bridges: A Guide to Arrangements for Interagency Working for the Care and Protection of Severely Mentally Ill People. London: Department of Health; 1995.
- Guidance on the Care of People in the Community with a Mental Illness. Cardiff: Welsh Office; 1996.
- Care Planning, Process and Documentation. Cardiff: Welsh Office; 1998.
- Effective Care Co-Ordination in Mental Health Services: Modernising the Care Programme Approach. London: Department of Health; 1999.
- Adult Mental Health Services for Wales: Equity, Empowerment, Effectiveness, Efficiency. Cardiff: National Assembly for Wales; 2001.
- Refocusing the Care Programme Approach (CPA): A Learning Resource for Care Co-Ordinators. Lincoln: University of Lincoln; 2010.
- No Health Without Mental Health: a Cross-Government Mental Health Outcomes Strategy for People of All Ages. London: Department of Health; 2011.
- Elias E, Singer L. Review of the Care Programme Approach in Wales. Llanharan: National Leadership and Innovation Agency for Healthcare; 2009.
- Code of Practice to Parts 2 and 3 of the Mental Health (Wales) Measure 2010. Cardiff: Welsh Government; 2012.
- Together for Mental Health. Delivery Plan: 2012–16. Cardiff: Welsh Government; 2012.
- Peckham S, Mays N, Hughes D, Sanderson M, Allen P, Prior L, et al. Devolution and patient choice: policy rhetoric versus experience in practice. Soc Policy Admin 2012;46:199-218. http://dx.doi.org/10.1111/j.1467-9515.2011.00831.x.
- Wowra SA, McCarter R. Validation of the empowerment scale with an outpatient mental health population. Psychiat Serv 1999;50:959-61. http://dx.doi.org/10.1176/ps.50.7.959.
- Rogers ES, Ralph R, Salzer M. Validating the empowerment scale with a multisite sample of consumers of mental health services. Psychiat Serv 2010;61:933-6. http://dx.doi.org/10.1176/ps.2010.61.9.933.
- Welsh Index of Multiple Deprivation (WIMD). Cardiff: Welsh Government; 2014.
- Francis R. Report of the Mid-Staffordshire NHS Foundation Trust Public Inquiry. London: The Stationery Office; 2013.
- Compassion in Practice: Nursing, Midwifery and Care Staff. Our Vision and Strategy. London: The Stationery Office; 2012.
- Health and Social Care Act 2012. London: The Stationery Office; 2012.
- National Health Services Act 2006. London: The Stationery Office; 2006.
- Post-Legislative Scrutiny of the Mental Health (Wales) Measure 2010. Cardiff: National Assembly for Wales; 2015.
- Hannigan B, Coffey M. Where the wicked problems are: the case of mental health. Health Policy 2011;101:220-7. http://dx.doi.org/10.1016/j.healthpol.2010.11.002.
- Hannigan B, Allen D. Giving a fig about roles: policy, context and work in community mental health care. J Psychiatr Ment Health Nurs 2011;18:1-8. http://dx.doi.org/10.1111/j.1365-2850.2010.01631.x.
- 2014/15 Choice Framework. London: Department of Health; 2014.
- Kalathil J. Recovery and Resilience: African, African-Caribbean and South Asian Women’s Narratives of Recovering from Mental Distress. London: Mental Health Foundation; 2011.
- Le Boutillier C, Leamy M, Bird VJ, Davidson L, Williams J, Slade M. What does recovery mean in practice? a qualitative analysis of international recovery-oriented practice guidance. Psychiat Serv 2011;62:1470-6. http://dx.doi.org/10.1176/appi.ps.001312011.
- Adam R, Tilley S, Pollock L. Person first: what people with enduring mental disorders value about community psychiatric nurses and CPN services. J Psychiatr Ment Health Nurs 2003;10:203-12. http://dx.doi.org/10.1046/j.1365-2850.2003.00560.x.
- Coffey M, Higgon J, Kinnear J. ‘Therapy as well as the tablets’: an exploratory study of service user views of community mental health nurses (CMHNs) responses to hearing voices. J Psychiatr Ment Health Nurs 2004;11:435-44. http://dx.doi.org/10.1111/j.1365-2850.2004.00740.x.
- Bee P, Playle J, Lovell K, Barnes P, Gray R, Keeley P. Service user views and expectations of UK-registered mental health nurses: a systematic review of empirical research. Int J Nurs Stud 2008;45:442-57. http://dx.doi.org/10.1016/j.ijnurstu.2007.02.008.
- Lipsky M. Street-Level Bureaucracy: Dilemmas of the Individual in Public Services. New York, NY: Russell Sage Foundation; 1980.
- Alakeson V, Perkins R. Recovery, Personalisation and Personal Budgets. London: Centre for Mental Health; 2012.
- Needham C. Personalising Public Services: Understanding the Personalisation Narrative. London: Policy Press; 2011.
- Swanson J. Preventing the unpredicted: managing violence risk in mental health care. Psychiat Serv 2008;59:191-3. http://dx.doi.org/10.1176/ps.2008.59.2.191.
- Langan J. Challenging assumptions about risk factors and the role of screening for violence risk assessment in the field of mental health. Health Risk Soc 2010;12:85-100. http://dx.doi.org/10.1080/13698571003632429.
- Busfield J. Mental health problems, psychotropic drug technologies and risk. Health Risk Soc 2004;6:361-75. http://dx.doi.org/10.1080/13698570412331323243.
- Whitaker R. The case against antipsychotic drugs: a 50-year record of doing more harm than good. Med Hypotheses 2004;62:5-13. http://dx.doi.org/10.1016/S0306-9877(03)00293-7.
- Kelly S, McKenna H. Risks to mental health patients discharged into the community. Health Risk Soc 2004;4:377-85. http://dx.doi.org/10.1080/13698570412331323252.
- Khalifeh H, Johnson S, Howard LM, Borschmann R, Osborn D, Dean K, et al. Violent and non-violent crime against adults with severe mental illness. Brit J Psychiat 2015;206:275-82. http://dx.doi.org/10.1192/bjp.bp.114.147843.
- Coffey M. ‘A risk worth taking? Value differences and alternative risk constructions in accounts given by patients and their community workers following conditional discharge from forensic mental health services. Health Risk Soc 2012;14:465-82. http://dx.doi.org/10.1080/13698575.2012.682976.
- Inpatients Formally Detained in Hospitals under the Mental Health Act 1983, and Patients Subject to Supervised Community Treatment. Annual Report, England, 2013. London: Health and Social Care Information Centre; 2013.
- Langan J. Involving mental health service users considered to pose a risk to other people in risk assessment. J Ment Health 2008;17:471-81. http://dx.doi.org/10.1080/09638230701505848.
- Lupton D. Risk. London: Routledge; 1999.
- Estroff SE, Zimmer C, Lachicotte WS, Benoit J. The influence of social networks and social support on violence by persons with serious mental illness. Hosp Community Psych 1994;45:669-79. http://dx.doi.org/10.1176/ps.45.7.669.
- Brooker C, Brabban A. Effective training in psychosocial interventions for work with people with serious mental health problems. Mental Health Rev 2006;11:7-14. http://dx.doi.org/10.1108/13619322200600014.
- Stanbridge RI, Burbach FR. Enhancing working partnerships with carers and families: a strategy and associated training programme. Mental Health Rev 2004;9:32-7. http://dx.doi.org/10.1108/13619322200400041.
- Slade M, Bird V, Le Boutillier C, Williams J, McCrone P, Leamy M. REFOCUS Trial: protocol for a cluster randomised controlled trial of a pro-recovery intervention within community based mental health teams. BMC Psychiatry 2011;11. http://dx.doi.org/10.1186/1471-244X-11-185.
- Slade M, Bird V, Clarke E, Le Boutillier C, McCrone P, Macpherson R, et al. Supporting recovery in patients with psychosis using adult mental health teams (REFOCUS): a multi–site cluster randomised controlled trial. Lancet Psychiatry 2015;2:503-14. http://dx.doi.org/10.1016/S2215-0366(15)00086-3.
- EQUIP . Enhancing the Quality of User Involved Care Planning in Mental Health Services 2015. www.nursing.manchester.ac.uk/equip/ (accessed 1 May 2015).
- Bower P, Roberts C, O’Leary N, Callaghan P, Bee P, Fraser C, et al. A cluster randomised controlled trial and process evaluation of a training programme for mental health professionals to enhance user involvement in care planning in service users with severe mental health issues (EQUIP): study protocol for a randomised controlled trial. Trials 2015;16:1-3.
- Centre for Mental Health & Mental Health Network NHS Confederation . Implementing Recovery through Organisational Change 2014. www.imroc.org/ (accessed 16 December 2014).
- Repper J, Aldridge B, Gilfoyle S, Gillard S, Perkins R, Rennison J. Peer Support Workers: Theory and Practice. London: Centre for Mental Health; 2013.
- Coffey M, Hamigan B, Mendell A, Fitzsimmons D, Hunt J. Plan4Recovery 2014. http://plan4recovery.org.uk (accessed 16 December 2014).
- Langley GJ, Nolan KM, Norman CL, Provost LP, Nolan TW. The Improvement Guide: A Practical Approach to Enhancing Organizational Performance. San Francisco, CA: Jossey-Bass Publishers; 1996.
- Quality Improvement Made Simple. London: Health Foundation; 2013.
- Bate P, Robert G, Fulop N, Ovretveit J, Dixon-Woods M. Perspectives on Context: A Selection of Essays Considering the Role of Context in Successful Quality Improvement. London: Health Foundation; 2014.
- Grimshaw JM, Eccles MP, Lavis JN, Hill SJ, Squires JE. Knowledge translation of research findings. Implement Sci 2012;7. http://dx.doi.org/10.1186/1748-5908-7-50.
- Simpson A, Barlow S, Cox L, Jones J. SUGAR . Adding SUGAR: collaborating with service users and carers in mental health nursing research. J Psychosoc Nurs Ment Health Serv 2014;52:22-30. http://dx.doi.org/10.3928/02793695-20131126-04.
- Cook JA, Copeland ME, Jonikas JA, Hamilton MM, Razzano LA, Grey DD, et al. Results of a randomized controlled trial of mental illness self-management using Wellness Recovery Action Planning. Schizophr Bull 2012;38:881-91. http://dx.doi.org/10.1093/schbul/sbr012.
- Delivering the Care Programme Approach in Wales: Interim Implementation Guidance. Cardiff: WAG; 2010.
- The Role of Community Mental Health Teams in Delivering Community Mental Health Services: Interim Policy Implementation and Guidance. Cardiff: WAG; 2010.
- Lawn S, Battersby MW, Pols RG, Lawrence J, Parry T, Urukalo M. The mental health expert patient: findings from a pilot study of a generic chronic condition self-management programme for people with mental illness. Int J Soc Psychiatr 2007;53:63-74. http://dx.doi.org/10.1177/0020764007075010.
- Margerison N. Care programme approach in practice. Hosp Med 1998;59:130-3.
- Kingdon D, Amanullah S. Care programme approach: relapsing or recovering?. Adv Psychiatr Treat 2005;11:325-9.
- Hemmings C. Implementation of care programme approach in learning disability. Psychiatrist 2007;31.
Appendix 1 Questionnaires: Recovery Self-Assessment Person in Recovery; Scale to Assess the Therapeutic Relationship; Empowerment Scale
Appendix 2 Interview schedule example (service user)
Collaborative Care Planning Project
Semistructured interview schedule
Service user/patient version 2: 8 February 2013
Introduce yourself and explain nature of the study:
Hi. My name is XXXX. Thank you for meeting with me today.
You kindly agreed to take part in the COCAPP research project and I am here today to ask you a few questions about your experience of care planning and co-ordination. It should take about 45 minutes at most. There are no right or wrong answers. We just want to know what you think about the way your care has been planned and co-ordinated.
Remind the person that they have already given their consent to be interviewed and check that they are still OK with that. Remind them their name will not be used and they will not be identified in any way. They may stop at any time.
Check digital recorder and microphone are working and sound levels are adequate.
I am just going to read out the code number for you in this study so that your name can be left out of it and the interview remains anonymous.
Read out participant code and date
-
Can you tell me how your care is planned by the Community Mental Health Team?
Prompts: Do you have a written care plan? Is it working for you? What did you find helpful? Less helpful? Do you understand your care plan? Would a care plan in different formats be helpful (e.g. as a phone app?) Are you aware of your care being planned? How are you involved in the planning of your care? What would help you to be more involved? Does your care plan include a focus on your abilities, assets, skills, strengths? If so, could you give me some examples? Do you feel ownership of your care plan – is it yours (or the service’s plan for you)? What is important for you? When and how often do you refer to your care plan? Some actions in your care plan may be about things for you to do – how helpful is that?
-
Can you tell me about what happens when your care is reviewed?
Prompts: Do you have care review meetings? How helpful are they? What did you find helpful? Less helpful? Do you have enough time? Who was involved in those reviews? Do you have any choice about the timing, venue or who chairs the meeting? How were you involved? Could you contribute? Were your views listened to? Are your wishes and preferences taken on board? What would help you to be more involved? Have you had any experience of meetings with your care co-ordinator to prepare for review meetings or the use of a prompt list?
-
Please tell me about your care co-ordinator
Prompt: How did you first meet him/her? Do you have a good relationship with him/her? How long have you had this care co-ordinator? Have you had others? Was that similar or different? What did they do well/less well? Do you feel able to be open/express your fears with your care co-ordinator? Do you feel you trust your care co-ordinator?
Are you aware of your care being co-ordinated? What does that mean to you?
-
What sort of support do you get from the care co-ordinator?
Prompt: Do you meet up? Does s/he phone you at all? Anything else? What is most helpful? What do they help you with? Are there things you would like more help with? What sort of things? How often do you see him/her?
-
Did you have help or support from other workers?
Prompt: Like who? Social worker? Mental Health Nurse? Psychologist? Occupational therapist? Support worker? What has that been like? Does there appear to be communication between these different workers? Is your care co-ordinator involved in that? What information have you been given about other forms of support (e.g. support groups, peer support, user groups)?
-
Lots of people talk about recovery in mental health nowadays: what does the term ‘recovery’ mean to you?
Prompt: Thank you, that’s helpful. For many people, recovery is generally seen as a personal journey . . . one that may involve developing hope, a secure base and supportive relationships, being more in control of your life and care, social inclusion, how you develop coping skills, and self-management . . . often despite still have symptoms of mental illness etc. [ask next question]
-
How has the planning of your care helped with your recovery?
Prompt: Have you been encouraged to develop a Personal Recovery Plan? A Wellness Recovery Action Plan (WRAP)? Have there been things that have helped your Recovery? Are there things you think might have helped your Recovery? Are your achievements recognised? If you made a progress is it recognised, valued and recorded?
-
Would you have liked to have had more of anything?
Prompt: What sort of thing would you have liked the Care Co-ordinator to have done more?
-
Was there anything that you did not like about the ways your care was planned?
Prompt: Was there anything that was unhelpful? Intrusive?
-
Another term that is being used a lot is ‘personalisation’ – what does the term ‘personalisation’ mean to you? And was treatment personalised?
Prompt: Did you think your care was tailored towards you and your individual needs? What does personalised care mean to you? Could you give me an example of where you think your care was personalised? In what way was it not focused on you as an individual? Do you feel in charge of your care and support?
-
Do you feel your safety has been considered in your care planning and co-ordination?
Prompts: How has your safety been addressed in your care plan or by your care co-ordinator? Have any other aspects of safety or risk been discussed with you?
-
Is there a family member or friend that provides you with support?
Prompt: Who is that? Are there others? Was s/he involved in the planning of your care? In what way? Would you have liked them to have been involved more? Can you give me an example? Have they been involved too much?
-
Can you suggest anything that would improve care planning, either for you or generally?
Prompt: Anything that could be done differently or a new approach to doing things? Can you tell me more about that idea? How would that improve things?
-
Is there anything else you would like to say that we have not covered?
Prompt: Is there anything we have not asked you that we should have?
OK, that’s the end of the interview. Thank you very much for your time.
Appendix 3 Care plan review structured template
Collaborative Care Planning Project care plan review template
Guidance for completing this form
The aim of this template is to record information on recovery and personalisation in the most recently available care plan for the specified recipient of mental health care. Where possible you should answer all questions. Where there is not sufficient information or clarity then please make a note in the notes box. The content of the care plan section is where we expect there to be some difficulty in completing this template and we offer this guidance to help. All reference to the person in the document should be taken to mean the recipient of mental health care.
Inclusion of the person’s views: look for evidence that the person had a say in the care plan. The ways in which the goals are worded might reveal this. For example ‘John would like to stop taking his medication’ indicates that this is John’s view and it also suggests a view that is not usually evident from workers.
Co-production: is there evidence that goals and treatment plans have been jointly formulated or show a shared ownership of goals and outcomes.
Strengths-based assessment: this can be seen in care plans that formulate goals built upon the strengths, skills or talents of the individual. An example might be ‘Jane would like to build on her analytical skills by enrolling on a systems analyst training course’.
Personalisation: is there evidence of choice and control for the person over their care and treatment? Are these based upon the person or just what is available? A care plan solely focused upon medication, side effects, symptoms or risk should not be considered to show personalisation as this ignores other types of support.
Personal budget: these give people control and choice over the purchase of personal social care services to meet their eligible needs. Is there a reference to this or discussion about the use of personal budgets in the care plan?
Recovery-oriented practice: does the care plan indicate a focus on building recovery such as facilitating new relationships, assistance with education or back to work, finance or money, personal care or physical well-being or developing a new sense of purpose?
Person-centred goals: are the care and treatment goals focused on the person’s assessment of their needs?
System-based goals: in contrast to the above are the care and treatment goals solely or majorly focused on system needs such as compliance with treatment.
The person’s views in risk assessment: frequently people are not asked for their view on risk assessments and many will not be aware that they have occurred; where a risk assessment is included are the person’s views on this evident in the document?
The person’s views in risk management plan: is there evidence that the person has agreed to the risk management plan or has been allowed the opportunity to discuss this and provide their perspective?
The person’s views in crisis plan: is there evidence that the person has had a say in the crisis plan, expressed a view on it or indicated their agreement or disagreement with the plan? Please make a note in the notes section to help us understand your response.
The person’s views in relapse plan: if there is a relapse prevention plan has this included the person’s perspectives?
Orientation to social outcomes: does the plan show a focus on social outcomes such as relationships and social networks or support, housing, work or education? If this is partial please make a note in the notes section.
Orientation to medical outcomes: on balance, is the focus on medical outcomes greater or lesser than the focus on personal or social outcomes? Please make a note in the notes section to help us understand this.
Encouragement for self-management: is there evidence that the care plan is encouraging shared responsibility with the person, for instance are there attempts to provide opportunities for the person to create their own plans or goals?
Recognition of personal relationships: is there evidence of a focus on fostering new or maintaining existing relationships?
Advance directives: are there plans for when the person is unable to make known their wishes for treatment? Is this signed and supported by workers?
Notes: please use the notes box beneath questions for adding detail. In the larger notes box it would be useful to give an impression of preponderance in the care plan, is it more focused on recovery and personalisation overall or does this make up only a small proportion of the whole? Include anything else you feel is directly relevant to the care plan that is not otherwise covered.
Collaborative Care Planning Project care plan review template
| Reviewer: | Date: | |
|---|---|---|
| Client/site study identifier: | ||
| Gender: | Please circle Male Female | |
| Age | . . .. . .. . .. . .. . .. years | |
| Care plan signed by service user? | Please circle Yes No | |
| If no is there a reason given? | ||
| Care plan signed by care co-ordinator? | Please circle Yes No | |
| Care plan given to the person? | Please circle Yes No | Unclear |
| Was the person present at the last care plan review? Was a carer present at the last care plan review? Was an advocate present at the last care plan review? |
Please circle Yes No Please circle Yes No Please circle Yes No |
Unclear Unclear Unclear |
| Date for next review included? | Please circle Yes No | |
| Frequency of contact with care co-ordinator? | Please circle daily weekly fortnightly monthly other . . .. . .. . .. . .. . . |
Unclear |
| Length of time on CPA/CTP? | Please specify . . . . . years . . .. . . months | Unclear |
| Content of care plan | ||
| Care plan shows evidence of: Inclusion of the person’s views Coproduction Strengths-based assessment Personalisation Personal budget Recovery-oriented practice Person-centred goals System-based goals The person’s views in risk assessment The person’s views in risk management plan The person’s views in crisis plan The person’s views in relapse plan Orientation to social outcomes Orientation to medical outcomes Encouragement for self-management Recognition of personal relationships Advance directives |
Please circle Yes No Please circle Yes No Please circle Yes No Please circle Yes No Please circle Yes No Please circle Yes No Please circle Yes No Please circle Yes No Please circle Yes No Please circle Yes No Please circle Yes No Please circle Yes No Please circle Yes No Please circle Yes No Please circle Yes No Please circle Yes No Please circle Yes No |
Unclear Unclear Unclear Unclear Unclear Unclear Unclear Unclear Unclear Unclear Unclear Unclear Unclear Unclear Unclear Unclear Unclear |
Appendix 4 Research tradition 1: organisation, management and delivery of services
| Research tradition 1: organisation, management and delivery of services | |
|---|---|
| Positive findings | Negative findings |
| Helps with continuity of care68 Less likelihood of patients being lost to follow-up62,68 Better teamworking across professions16,68,79 Creative care packages68 Rigorous documentation68,79,80 Better care planning68,79 Improve effectiveness of care68,70,81,82 No increase in hospitalisation82 |
No more/or limited resources to implement CPA.68,83,86 CPA means more work for staff,16,68,82,83 especially increased bureaucracy,16,68,71 which results in time away from patient contact16,68,83 and the perception of staff that they are overworked16,68 leading to staff frustration68 Community psychiatric nurses unclear of role.16 CPA created tensions between/within the workforce16 CPA not explained properly to staff16,70,83 GPs unaware of CPA83 Managers not aware of who is on CPA81 Staff not receiving documentation81 Stifles creativity of staff68 Keyworkers create dependency in patients68 More admissions to hospital61 Variation in implementation of CPA16,74–78 Differences in service users’ satisfaction with staff between rural/inner city areas92 Poorly manages prioritisation, may lead to inequities/conflict over resource74,86 Lack of identification of psychosocial aspects16 Risk assessments not completed fully or jointly76,94 |
| Methodology | Methods/authors |
| Quantitative | Randomised controlled trial;62 audit;78,79 cross-sectional survey and longitudinal follow-up;82 telephone survey and routinely collected NHS data;74 postal survey;75 survey of national and local statistics76 |
| Qualitative | Interviews;68,70 interviews, observations and documents16,86 |
| Qualitative and quantitative mixed methods | Postal questionnaire;80,83 interviews and postal questionnaire;81 survey and interviews;71,94 interviews, documents, surveys77 |
Appendix 5 Research tradition 2: service users’ and carers’ experience of the care programme approach
| Research tradition 2: service users’ and carers’ experience of the CPA | |
|---|---|
| Positive findings | Negative findings |
| Encouraged independence80,103 Service users fully involved103 Service users well informed80,92,98 Service users have more trust/comfort in staff68,80 Service users have more say/choice in their care68,80,103 Generated more contact with carers68,80 Greater carer satisfaction68,100 |
Inadequate service-user involvement71,75,77,78,86,91,92,94,98,101 Service users unaware/little understanding of CPA70,71,86,91 Service users unaware of/not allocated keyworkers70,71,81,92 Service users not seen/or hold care plan or CPA documentation70,71,81,86,92,98,101,103 Carers need more information70,100,103 Frustrated carers70 Carer involvement ad hoc/no policy70,75,100 Carers views not sought or taken seriously70,75,86 Carers isolated70 Overly focused on service user’s problems not strengths71,92 Encouraged more focus/priority on medicalisation, illness and severe illness16,82,94 |
| Methodology | Methods/authors |
| Quantitative | Survey/interview;82,98,100,101,103 audit78 |
| Qualitative | Interviews, observations and documents;16,86 in-depth interviews68,70 |
| Qualitative and quantitative mixed methods | Questionnaire and interview;71,81,91,92,94 postal questionnaire;75,80 interviews, documents, surveys77 |
Appendix 6 Research tradition 3: interventions to improve the care programme approach
| Research tradition 3: interventions to improve the CPA | ||
|---|---|---|
| Author/s | Intervention | Outcome |
| Macpherson et al. (1999)106 | Formal clinical goal setting; standard CPA documentation with formalised space to establish any number of treatment goals. Goals set within meeting and agreed with all. Each patient (n = 139) offered copies of final typed CPA documentation | A total of 68% of goals were fully and 11% partially achieved. Goals were no more likely to be achieved in any care setting (i.e. with professional supervision/living independently), or any particular diagnosis Goals targeting the drug treatment of psychiatric syndromes were most likely to be fully successful (84%), whereas approaches to self-care skills, side effects, physical/medical problems and family relationships were moderately successful. Least successful were the attempts to promote structured day care/activities, and to treat substance abuse, which were fully successful in 39% and 17% of cases, respectively. The study claims that individual care planning can be combined with outcome measurement, to give a meaningful measure of the effectiveness of care |
| Lockwood and Marshall (1999)107 | ‘Needs feedback’ as a technique for enhancing the CPA. Needs feedback begins with a standardised assessment of patients’ psychiatric and social needs by a nurse specialist. The patient’s CPN is then provided with information from the specialist on: (1) the needs identified; (2) why these needs have been identified; (3) the interventions required to meet the identified needs; and (4) how these interventions may be obtained | Significant improvements were seen in the number of ‘unmet’ needs and the level of anxious/depressive symptoms. Improvements approaching significance were seen for social functioning and negative psychiatric symptoms, but not for positive psychiatric symptoms. This pilot study suggests that needs feedback may improve the quality of nursing assessment and care planning within the CPA |
| Howells and Thompsell (2002)109 | eCPA – a computer-based CPA system for care planning and documentation – using a Microsoft Word template. Completed eCPA care plan is e-mailed to the acute ward, the hospital’s emergency clinic and any other involved agencies. The CPA manager is sent the original signed copy, a copy is filed in the case notes and the GP, the patient and/or his/her carer is given a copy | The system is designed to improve the quality of information in CPA care plans and to enable the rapid and standardised adoption of evidence-based good practice by CMHT staff. The eCPA welcomed by staff: take-up rate of almost 100% Patients also welcomed the legibility and detail of the forms. Care plans are longer and more detailed, no longer constrained by the size of boxes on paper forms. Care plans are adjusted more frequently by CMHT staff, who do not have to completely rewrite the forms by hand; the plans better reflect the current needs of patients. Availability of the form on-screen at team meetings directs discussions onto patients’ key needs, and ensures that the CPA form reflects a multi professional consensus approach Being able to e-mail the document improved the transfer of information between different agencies. Assists audit as once in electronic format, the information lends itself to statistical analysis and key words can be searched for |
| Blenkiron et al. (2003)99 | CUES-U: 17-item service-user outcomes scale in booklet form. Covers the issues of quality of life and satisfaction with mental health services that users rather than professionals have identified as priorities | CUES-U can be an effective and practicable tool within CMHTs, both for increasing users’ involvement in their care and for service benchmarking. The CUES-U discussion led to a change in clinical care for 49% of respondents. Care co-ordinators rated CUES-U as a good use of their time in 64% of cases. Women and those with a shorter duration of mental disorder were rated as more engaged in the consultation process 84% of service users were satisfied with the level of control and consultation they have; 87% satisfied with relationship with MH workers, high 70% satisfaction for levels of information and advice and access to services. Limitation of high levels of satisfaction was that service users knew their care co-ordinator would see their replies, although many did write negative comments in free-text boxes |
| Marshall et al. (2004)108 | To determine whether feedback from a standardised assessment of need enhances the effectiveness of care planning and whether exposing care co-ordinators to feedback on some patients improves their care of other patients | The only significant effect of the intervention was on patient satisfaction. Patients cluster-randomised to receive feedback were more satisfied than controls, but patients individually randomised to receive feedback were not. Standardised needs assessment did not substantially enhance care planning in this trial. However, giving care co-ordinators some experience of feedback from a standardised assessment of need could improve satisfaction |
| Killaspy et al. (2012)102 | The MHRS: an outcome measure rated collaboratively by staff and service users assessing 10 life domains. The MHRS ratings are agreed through a collaborative discussion between the service user and mental health worker that lasts approximately 1 hour. But its psychometric properties are unknown. Aim is to assess the MHRS’s acceptability, reliability and convergent validity | The MHRS was relatively quick and easy to use and had good test–retest reliability, but inter-rater reliability was inadequate. Collaborative ratings were slightly higher than staff-only ratings. Convergent validity suggests it assesses social function more than recovery. Conclusions: the MHRS cannot be recommended as a routine clinical outcome tool but may facilitate collaborative care planning |
Appendix 7 Key policy documents from England and Wales relevant to community mental health
| England | ||
|---|---|---|
| Year | Organisation | Document name |
| 2011 | Her Majesty’s Government | No Health without Mental Health: Delivering Better Mental Health Outcomes for People of All Ages 121 |
| 2011 | Department of Health | No Health without Mental Health: A Cross-Government Mental Health Outcomes Strategy for People of All Ages 121 |
| 2011 | Department of Health | No Health without Mental Health: A Cross-Government Mental Health Outcomes Strategy for People of All Ages.121 Supporting document – The Economic Case for Improving Efficiency and Quality in Mental Health |
| 2011 | Department of Health | No Health without Mental Health: A Cross-Government Mental Health Outcomes Strategy for People of All Ages – A Call to Action |
| 2010 | University of Lincoln, Centre for Clinical and Academic Workforce Innovation. Mental Health Foundation. Linking Voices. Care Programme Approach Association. National Mental Health Development Unit | Refocusing the Care Programme Approach: A Learning Resource for Care Co-Ordinators. Trainer’s Manual120 |
| 2008 | Department of Health | Refocusing the Care Programme Approach: Policy and Positive Practice Guidance 1 |
| 2006 | Department of Health | From Values to Action: The Chief Nursing Officer’s Review of Mental Health Nursing 12 |
| Wales | ||
|---|---|---|
| Year | Organisation | Document name |
| 2012 | Welsh Government | Together for Mental Health: A Strategy for Mental Health and Wellbeing in Wales 5 |
| 2012 | Welsh Government | Together for Mental Health. Delivery Plan: 2012–16 124 |
| 2012 | Welsh Government | An overview of the Mental Health (Wales) Measure |
| 2012 | Welsh Government | Mental Health Measure Core Units 1–5; Service users; Relationships, recovery, care and treatment planning; Assessment and outcome planning; Review care and treatment Mental Health Measure Additional Units 3 & 4: Leadership and team development; Care organisation and planning: organisational responsibilities |
| 2011 | Welsh Government | Mental Health (Wales) Measure 2010: Guidance for Local Health Boards and Local Authorities 3 |
| 2010 | Welsh Assembly Government | Delivering the Care Programme Approach in Wales: Interim Implementation Guidance 171 |
| 2010 | Welsh Assembly Government | The Role of Community Mental Health Teams in delivering Community Mental Health Services: Interim Policy Implementation and Guidance 172 |
| 2010 | National Assembly for Wales | Mental Health (Wales) Measure 20103 |
Appendix 8 A diagrammatic map of key policies and relevant literature
FIGURE 10.
Diagrammatic map of key policies and relevant literature. NHWMH, No Health Without Mental Health.
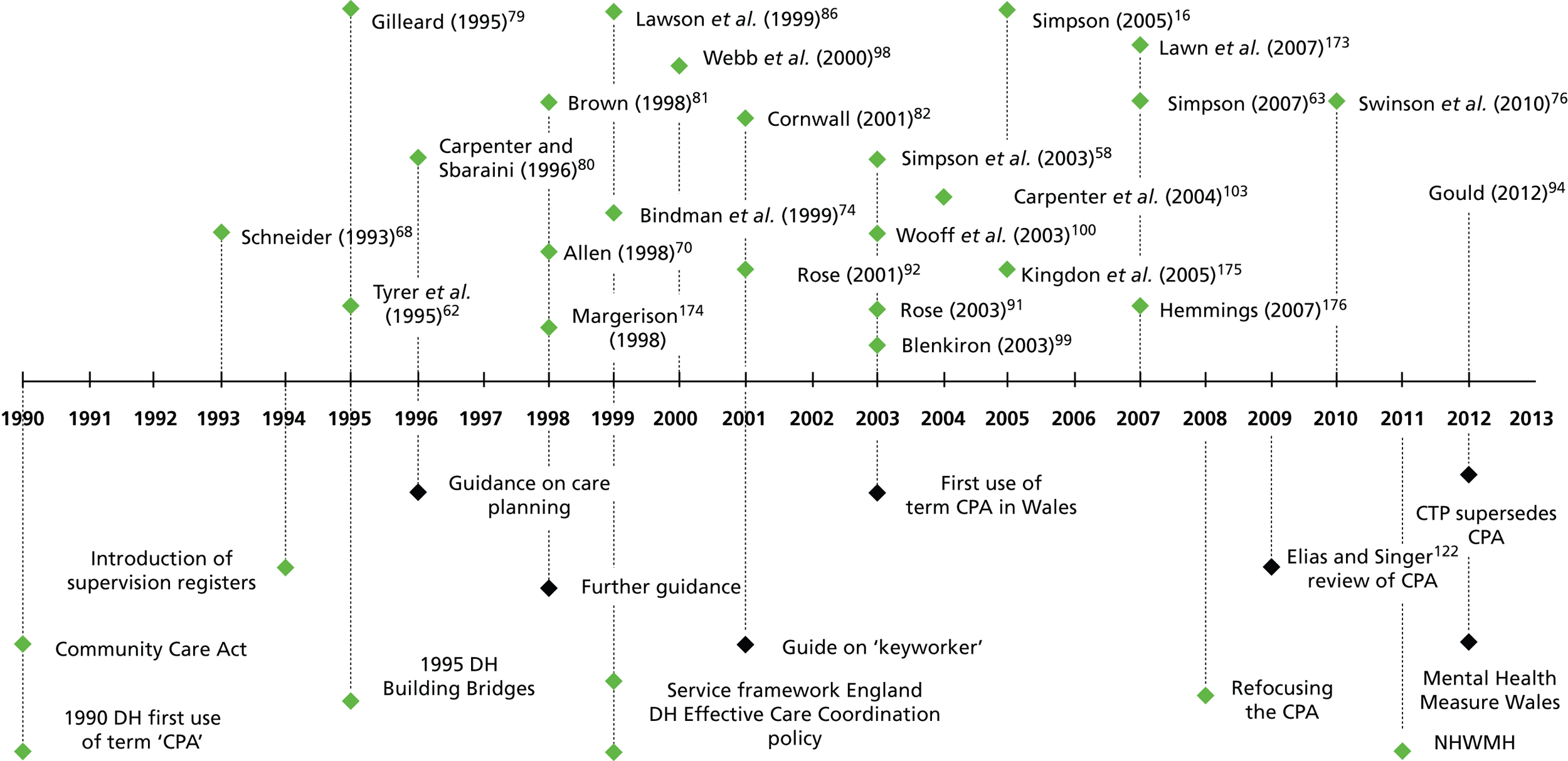
Appendix 9 Example of embedded case study comparison with care plan reviews
| Linked case studies | Agreements | Disagreements | Notes | Care plan reviews |
|---|---|---|---|---|
| SU001, CA001, CC001 | All respondents agree that care planning is collaborative, and agree on the importance and central role of the care plan itself. Care co-ordinator describes it as a ‘live’ document, and service user uses it as a guide. All feel service user and carer are fully involved, and that risk is openly discussed | Service user refers to care plan regularly, whereas carer does not. Service user likes the idea of an app, but care co-ordinator thinks service users are usually not much good with technology and do not like it. Carer feels care plan is not service user-friendly and contains too much jargon: a view not shared by service user and care co-ordinator | This is the only linked case study in which care planning and co-ordination appears wholly collaborative. Care co-ordinator’s positive, active, yet realistic approach (along with their focus on service-user empowerment and shared ownership of the care plan) filters through to carer and service user | Care plan signed by service and care co-ordinator with carer present Service user’s views are included and co-production adhered to Service user not involved in previous risk assessment Service user’s views taken into account in risk management, but not in crisis plan |
| SU002, CA002, CC004 | None | Service user and carer say they have never had nor seen a care plan, but would have referred to one had it existed. They describe their experiences of mental health care as a ‘disappointing service’: service user says safety and risk have never been discussed, and that they have no idea who should be contacted in an emergency Care co-ordinator’s view is the direct opposite: describing care plans as a ‘guide’ – a way of ensuring that the same ‘pathway’ is followed by everyone. Care co-ordinator sees care plans as an important point of reference, a way of keeping service users informed, and feels that service users own their care plans |
Despite care co-ordinator’s seemingly positive attitude towards care plans, they note that they tend to focus on discharge as the ultimate aim of each new referral. They also describe care plans as too vague and lacking in consistency | Most recent care plan completed by crisis resolution team, so is only partly complete: it is suggested that service user ‘lost contact’ and that a full care plan was never drawn up as a consequence Care plan not signed by service user (no reason given) although the notes under coproduction say that service user ‘reports good engagement’ States that service user’s views were considered in risk assessment/management and that they know who to consult in a crisis. Not clear if copy given to service user |
| SU003, CA003, CC002 | Service user and carer both feel that they lack engagement with the care plan, and that it needs a better contingency plan for potential crises. They both agree that current care plan is at least 2 years out of date. Care co-ordinator notes that the current electronic system makes it difficult to keep care plans properly updated; care co-ordinator notes that she has had no adequate guidance for writing risk assessments. Service user, carer and care co-ordinator agree that care plans lack consistency and coherence | Care co-ordinator feels that care plans set out aims and goals for service user, but neither service user nor carer have any sense of this | Care co-ordinator notes that caseloads are too big and that there is too much pressure on staff to discharge service users. Carer says that there is a lack of information sharing between parties involved in care plan | Care plan not signed by service user (no reason given), but signed by care co-ordinator: copy not given to service user Service user’s views included co-production ‘not evidenced’. Service user views in risk assessment not known, no risk management plan evidenced Service user’s views in crisis plan included |
| SU004, CA004, CC005 | Both service and care co-ordinator feel inadequately involved in care planning and relevant discussions, agreeing that care plan is only partly helpful and that more support is needed | Care co-ordinator sees care plan as very important, helpful for aims/goals, and that service user has a say and a choice in writing it | Care co-ordinator suggests that care plans are owned by mental health services, not by service users, and cites limited staff and big caseloads as a hindrance, as well as the duplication of information created by electronic systems | Care plan not signed by service user (no reason given) but is signed by care co-ordinator. Unknown if copy given to service user Notes that service user did not attend risk assessment appointment and that further service-user input is needed in order to do a risk management plan |
| SU005, CC003 | Service user and care co-ordinator seem to agree that care planning is collaborative, although both parties would like more time in which to write it | None | Service user wants more set goals, and feels current care plan focuses on the ‘negatives’ of their illness, rather than on empowerment. This is echoed in care co-ordinator’s description of care planning as ‘firefighting’: they feel that there is too much paperwork and lack of time | Care plan signed by service user and care co-ordinator and copy given to service user Service user’s views are included and service user makes good use of opportunities for co-production No information included about risk assessment management (fields left blank) |
| SU006, CA006, CC006 | Neither service user nor carer have a copy of the care plan, and they agree that they are inadequately involved in care planning/co-ordination | None | Service user and carer describe feeling continually let down by care co-ordinator, who repeatedly fails to set up meetings that have been promised. Carer feels wholly unsupported as service user’s only helper. Care co-ordinator feels that it’s possible to ‘do without’ care plans altogether, and that care co-ordinators (not service users) own them | Care plan not signed by service user: signed by care co-ordinator. Copy not given to service user No coproduction: service user ‘seems not to have been present’ Service user views included on risk assessment and crisis plan but not on risk management Care plan includes service user’s views |
Appendix 10 A demographic breakdown of all interviewees by site
| Demographic information | Burgundy | Artois | Champagne | Dauphine | Languedoc | Provence | ||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| SP | SM | CC | SU | CA | SP | SM | CC | SU | CA | SP | SM | CC | SU | CA | SP | SM | CC | SU | CA | SP | SM | CC | SU | CA | SP | SM | CC | SU | CA | |
| Age (years)/median | 45 | 52 | 44 | 52 | 67 | 43 | 41 | 50 | 26 | – | 42 | 36 | 34 | 52 | 69 | 43 | 50 | 43 | 39 | 50 | 51 | 45 | 49 | 66 | 66 | 51 | 44 | 32 | 42 | 50 |
| Sex | ||||||||||||||||||||||||||||||
| Female | 1 | 2 | 2 | 3 | 2 | 1 | 1 | 2 | 4 | – | 4 | – | 4 | 4 | 2 | 2 | – | 2 | 3 | 1 | 2 | 1 | 5 | 3 | 1 | 3 | 1 | 3 | 5 | 1 |
| Male | 2 | – | 1 | 2 | 2 | 2 | 1 | – | – | – | 1 | 1 | 1 | 2 | 2 | 3 | 2 | 2 | 3 | 1 | 3 | 2 | 1 | 3 | 1 | 2 | 1 | 1 | 1 | 4 |
| Ethnicity | ||||||||||||||||||||||||||||||
| White British/Irish | 1 | 2 | 3 | 2 | 1 | 3 | 1 | 1 | 4 | – | 2 | 1 | 5 | 5 | – | 1 | 1 | – | 2 | 1 | 4 | 3 | 6 | 6 | 2 | 5 | 2 | 2 | 6 | 4 |
| Black Afro-Caribbean/other | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | 1 | – | 4 | 1 | 1 | 1 | – | – | – | – | – | – | 2 | – | 1 |
| Asian | 1 | – | – | – | – | 1 | – | – | – | – | – | – | – | – | – | – | 1 | – | 1 | – | – | – | – | – | – | – | – | – | – | – |
| White other | 1 | – | – | 2 | 2 | – | – | 1 | – | – | 2 | – | – | 1 | 2 | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – |
| Mixed race | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | 1 | – | – | – | – | – | – | – | – | – | – | – | – | – | – |
| Other | – | – | – | – | 1 | – | – | – | – | – | 1 | – | – | – | 1 | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – |
| Profession | ||||||||||||||||||||||||||||||
| Mental health nurse | 1 | 1 | 2 | – | – | 2 | 2 | 1 | – | – | 1 | 1 | 1 | – | – | 1 | 1 | 4 | – | – | 2 | 1 | 6 | – | – | 2 | 2 | 1 | – | – |
| Social worker | – | – | – | – | – | – | – | – | – | – | 1 | – | 2 | – | – | 1 | 1 | – | – | – | 1 | 1 | – | – | – | 1 | – | 2 | – | – |
| OT | – | – | – | – | – | – | – | 1 | – | – | – | – | – | – | – | – | – | – | – | – | 1 | – | – | – | – | 1 | – | 1 | – | – |
| Psychologist | – | – | – | – | – | – | – | – | – | – | 1 | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – |
| Psychiatrist | 1 | – | – | – | – | 1 | – | – | – | – | 1 | – | 1 | – | – | 1 | – | – | – | – | 1 | – | – | – | – | 1 | – | – | – | – |
| Employment/recovery worker | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – |
| Approved Mental Health Professional | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | 2 | – | – | – | – | – | 1 | – | – | – | – | – | – | – | – |
| Other | – | 1 | – | – | – | – | – | – | – | 1 | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – |
| Education | ||||||||||||||||||||||||||||||
| Doctorate | – | – | – | – | – | – | – | – | – | – | 1 | – | – | – | – | – | – | – | – | – | 1 | 1 | – | – | – | – | – | – | – | – |
| Master’s degree | 2 | 1 | – | – | – | – | – | – | – | – | – | – | 2 | – | – | 4 | – | 1 | – | – | – | 1 | 1 | – | – | 1 | 1 | 2 | – | – |
| Postgraduate Diploma/certificate | – | – | 1 | – | – | 1 | – | 1 | – | – | 2 | – | – | – | – | – | 1 | 1 | – | – | 1 | 1 | 2 | – | – | 1 | 1 | 1 | – | – |
| Degree | – | 1 | 2 | – | – | 2 | 2 | 1 | – | – | 1 | 1 | 2 | – | – | – | – | 2 | – | – | 2 | – | – | – | – | 2 | – | – | – | – |
| Diploma/similar | 1 | – | – | – | – | 1 | – | – | – | – | 1 | – | 1 | – | – | 1 | 1 | – | – | – | 1 | – | 3 | – | – | 1 | – | 1 | – | – |
| Length in mental health services | ||||||||||||||||||||||||||||||
| < 1 year | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – |
| 1–3 years | – | – | – | – | – | – | – | – | – | – | – | – | 1 | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – |
| 4–6 years | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | 1 | – | 1 | – | – | – | – | 1 | – | – |
| 7–9 years | 1 | – | – | – | – | – | – | – | – | – | 2 | – | 2 | – | – | – | – | – | – | – | – | – | 2 | – | – | 1 | – | 2 | – | – |
| 10 + years | 2 | 2 | 3 | – | – | 4 | 2 | 2 | – | – | 3 | 1 | 2 | – | – | 5 | 2 | 4 | – | – | 4 | 3 | 1 | – | – | 4 | 2 | 1 | – | – |
| Time as care co-ordinator | ||||||||||||||||||||||||||||||
| < 1 year | 1 | – | – | – | – | – | – | – | – | – | – | – | 1 | – | – | – | – | – | – | – | – | – | – | – | – | – | – | 2 | – | – |
| 1–3 years | – | – | – | – | – | – | 2 | – | – | – | – | – | 1 | – | – | – | – | 1 | – | – | – | – | – | – | – | – | – | – | – | – |
| 4–6 years | – | – | 1 | – | – | – | – | – | – | – | 2 | – | 2 | – | – | 1 | – | – | – | – | 1 | 1 | 2 | – | – | 1 | 1 | 1 | – | – |
| 7–9 years | 2 | – | – | – | – | 2 | – | – | – | – | 2 | – | – | – | – | – | – | 1 | – | – | 1 | 1 | 3 | – | – | – | – | – | – | – |
| 10 + years | – | – | 2 | – | – | 1 | – | 2 | – | – | 1 | 1 | 1 | – | – | 3 | – | 2 | – | – | 1 | – | 1 | – | – | 3 | – | 1 | – | – |
| Living status | ||||||||||||||||||||||||||||||
| Independent as single | – | – | – | – | – | – | – | – | 1 | – | – | – | – | 1 | 2 | – | – | – | 4 | 1 | – | – | – | 2 | – | – | – | – | 1 | – |
| Independent as in relationship | – | – | – | 2 | 1 | – | – | – | 2 | – | – | – | – | – | – | – | – | – | 1 | 1 | – | – | – | 3 | 1 | – | – | – | 2 | 1 |
| Living with family | – | – | – | 3 | 3 | – | – | – | 1 | – | – | – | – | 1 | 2 | – | – | – | – | – | – | – | – | – | – | – | – | – | 1 | 1 |
| Living with friends | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | 1 | 1 |
| Supported accommodation | – | – | – | – | – | – | – | – | – | – | – | – | – | 1 | – | – | – | – | 1 | – | – | – | – | 1 | – | – | – | – | 1 | – |
| Other | – | – | – | – | – | – | – | – | – | – | – | – | – | 2 | – | – | – | – | – | – | – | – | – | – | 1 | – | – | – | – | – |
| Daytime activity | ||||||||||||||||||||||||||||||
| Full-time employment | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | 2 | 1 |
| Part-time employment | – | – | – | – | – | – | – | – | 1 | – | – | – | – | – | – | – | – | – | – | – | – | – | – | 1 | 1 | – | – | – | 1 | – |
| Education/training | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | 1 | – | – | – | – | – | – | – | – | – | – | – |
| Unemployed | – | – | – | 3 | – | – | – | – | 1 | – | – | – | – | 2 | – | – | – | – | 2 | 1 | – | – | – | 3 | – | – | – | – | 2 | 3 |
| Voluntary | – | – | – | – | – | – | – | – | – | – | – | – | – | 1 | 1 | – | – | – | 1 | – | – | – | – | 2 | – | – | – | – | – | – |
| Other | – | – | – | 2 | 4 | – | – | – | 2 | – | – | – | – | 3 | 2 | – | – | – | 2 | 1 | – | – | – | – | 1 | – | – | – | 1 | 1 |
| Time with mental health service | ||||||||||||||||||||||||||||||
| > 1 year | – | – | – | – | 1 | – | – | – | – | – | – | – | – | 1 | 1 | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – |
| 1–3 years | – | – | – | – | – | – | – | – | 1 | – | – | – | – | 1 | 1 | – | – | – | 1 | – | – | – | – | – | – | – | – | – | – | – |
| 4–6 years | – | – | – | 1 | – | – | – | – | 1 | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | 1 | – |
| 7–9 years | – | – | – | – | 1 | – | – | – | 2 | – | – | – | – | – | – | – | – | – | 1 | – | – | – | – | – | – | – | – | – | 1 | – |
| 10 + years | – | – | – | 4 | 2 | – | – | – | – | – | – | – | – | 4 | 2 | – | – | – | 3 | – | – | – | – | 5 | – | – | – | – | 4 | – |
| Mental health problem | ||||||||||||||||||||||||||||||
| Psychosis | – | – | – | 3 | – | – | – | – | – | – | – | – | – | – | – | – | – | – | 1 | – | – | – | – | 4 | – | – | – | – | 3 | – |
| Depression/anxiety | – | – | – | 2 | – | – | – | – | 2 | – | – | – | – | 2 | – | – | – | – | – | – | – | – | – | – | – | – | – | – | 1 | – |
| Dual diagnosis | – | – | – | 1 | – | – | – | – | 2 | – | – | – | – | 2 | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – |
| Other | – | – | – | – | – | – | – | – | – | – | – | – | – | 1 | – | – | – | – | 1 | – | – | – | – | – | – | – | – | – | 1 | – |
| Two or more | – | – | – | 3 | – | – | – | – | – | – | – | – | – | 1 | – | – | – | – | 4 | – | – | – | – | 1 | – | – | – | – | 1 | – |
| Time with care co-ordinator | ||||||||||||||||||||||||||||||
| Daily | – | – | – | – | – | – | – | – | – | – | – | – | – | 2 | – | – | – | – | – | – | – | – | – | – | – | – | – | – | 1 | – |
| Weekly | – | – | – | 2 | – | – | – | – | 3 | – | – | – | – | 2 | – | – | – | – | 1 | – | – | – | – | 2 | – | – | – | – | 2 | – |
| Monthly | – | – | – | 1 | – | – | – | – | 1 | – | – | – | – | 1 | – | – | – | – | 2 | – | – | – | – | 2 | – | – | – | – | 1 | – |
| Other | – | – | – | 2 | – | – | – | – | – | – | – | – | – | 1 | – | – | – | – | 3 | – | – | – | – | 1 | – | – | – | – | 2 | – |
| Time with carer | ||||||||||||||||||||||||||||||
| Daily | – | – | – | 4 | – | – | – | – | 3 | – | – | – | – | 5 | – | – | – | – | 2 | – | – | – | – | 3 | – | – | – | – | 6 | – |
| Weekly | – | – | – | 1 | – | – | – | – | 1 | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – |
| Fortnightly | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – |
| Monthly | – | – | – | – | – | – | – | – | – | – | – | – | – | 1 | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – |
| Other | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | 4 | – | – | – | – | 2 | – | – | – | – | – | – |
Appendix 11 Summaries of within-case analysis for cross-case comparisons
| Site | Local context and background | Care planning and care co-ordination | Recovery | Personalisation | Suggestions for improvements |
|---|---|---|---|---|---|
| Artois | Recent reorganisation: separate assessment and recovery teams Greater health and social care integration Lack of continuity for users Any qualified provider: more providers, more complicated Recovery approach vs. CTOs Social care funding decimated |
CPA for most but not all: unclear on criteria Risk: very important Administrative load Links to PbR Electronic records: standard templates, but unwieldy printouts and difficult to work with services users in their homes Caseloads: to 25 Care co-ordination: all consuming, generic work Allocation of care co-ordinators: degree of fit but also availability Care co-ordinators once allocated do work around the margins Reviews at least annually Tensions re: carer involvement Care co-ordinators could be Band 4s Training recently reviewed |
Recovery: a bridge between medical and social models We have always been doing recovery Recovery is about discharging reluctant service users Some use of tools Standards improving Need more people Need more time Need an electronic system which works Stronger organisational commitment to recovery Need to improve continuity of care |
First person terminology Personalisation is to LA as recovery is to NHS Personalisation vs. CTOs Personal budgets: high administration |
Standards improving Need more people Need more time Need an electronic system which works Stronger organisational commitment to recovery Need to improve continuity of care |
| Burgundy | Long history of integration New teams set up: AOT, CRHT, PHCT The Measure: main impetus for change, but no clear view of impact on the day-to-day CTOs also a driver: extra administration |
The Measure is very important, but no consensus on its actual impact All Wales CTP: captures the journey CTP not used by all psychiatrists CC: generic work by any mental health professional Caseloads: around 30 Try to match care co-ordinators to service users on need, but often workload Reviews: usually six monthly Unclear on extent of carer involvement Need joint IT systems Some training, but has been uni-professional |
Measure: placed recovery high on agenda Mixed understanding and views No clear view on use of recovery plans |
Place the person at the centre: at the heart of social care ‘Thrown’ at the service Not much on budgets, etc. |
Better integration needed Variable quality of CTPs More on outcomes More time |
| Champagne | Integrated NHS/LA management Integrated managers: lack power Lack of shared IT High expectations: policy, the Measure Commitments to recovery but also concern over lack of vision High acuity, high demand, high caseloads |
Statutory footing All Wales CTP: structure, framework but also reductionist Risk Care co-ordinator: mental health professionals, significant work Caseloads: to 40+ Limited training, despite all Wales materials Need more integrated IT |
Good understandings of recovery, some evidence of shifts towards this Uneven progress More training needed, including in approach and tools CTP: no clear recovery focus Culture change needed: staff and service users |
Tailored Tension when people unwell Risk: a challenge to personalisation Raises expectations No consensus on degree of personalisation Limited moves to direct payments |
Need vision Need time System very demanding Closer integration Training Under-resourced |
| Dauphine | PMHC liaison services Co-location of NHS and LA staff Targets and savings Commitments to recovery, but values lost in reorganisation? |
Not all on CPA CPA: different things to different people Frequent changes to format, increasing workload CPAT: lengthy First person care plans Risk: number one PbR: making plans less individual Caseloads: up to 40 Care co-ordinator: vast job, uncertain, high responsibility, generic Efforts to allocate appropriately but generic role 3–6 month reviews, medically led Efforts to involve carers Mixed views on training |
Recent Trust move towards recovery Some resistance, and idea that CPA is enough Variety of practices given: person budgets, employment help Need recovery training, and service users need to change too |
Individualised care Personalised through care packages/services Budgets, but paperwork and delays Clustering: not personalised Buying from any provider: worries over information sharing |
Pride in service Mental health services abandoned by LA Stronger vision needed Training Reduce administration Change in ethos needed |
| Languedoc | Restructuring: AOT and EI in CMHTs Changes to team composition: s75 agreement, so no SWs in teams Loss of posts, increased work Low morale Mixed views on values and goals Trust ‘a business’ Medically dominated, paternalistic |
CPA for most complex A structure Care co-ordinator: needs good relationship with service user Patchy implementation Structured assessment IT: not compatible across NHS and LA CPA service-centred: needs to be more like in maternity care Cannot print in service users’ homes PbR: mixed views Caseloads rising: up to 40 CPA medically dominated Care co-ordinator allocation: try to fit with needs, but also local capacity Reviews 6 monthly, organised around doctors Some use of technology to conduct reviews Carers: invited, tensions around confidentiality Mandatory training |
Broad understanding Evidence: coproduced care plans, some use of tools, recovery college Lack of passion at the top Conservative medics Admin concerns over use of tools |
About taking control The CPA is personalised: but not sure who has their plan Budgets: increased personalisation, and a large part of the work of SWs Budgets: difficult to deliver due to admin, and service users being asked to contribute |
Leadership and cultural change Move away from a medical approach Training on personalisation and recovery needed, along with help for service users to also better understand Less bureaucracy was asked for Challenges: staff inertia and budget cuts, and staff feeling that jobs were insecure |
| Provence | Restructuring: inpatient and CMH separated Services centralised, designated as ageless Mixed views on this High degree of health and social care integration (e.g. shared roles) but different IT systems Strong values claimed by NHS, but unsure about reality |
Standard and enhanced CPA Commitments to collaborative care planning Documentation user friendly, but not lay Two versions of electronic record: full and CPA Lite Electronic records: difficult to work with people in their homes Used by managers to check notes Care co-ordinators: caseloads up to 50 Care co-ordinator: generic task Allocation attempted on need, but workload and capacity Bureaucracy around reviews Some care plans not changed for years Reviews typically 6 monthly Variable carer involvement, tensions with service users possible Periodic training |
Support for principles, but not all will ‘recover’ Cultural lag in places Medics and older nurses resistant Evidence of recovery: use of language, peer support, etc. PA: needs to become more recovery focused No clear picture on use of tools Paperwork and targets barriers to recovery |
Self-management, self-directed support packages (or direct budgets) and personal health budgets A more general approach Local system bureaucratic, lots of providers, service-user uncertainty Commissioners’ targets for self-directed support exceeded, but admin burden Staff: new skills (e.g. negotiating with providers) External providers: concern over risk Personal budgets widely used |
Quality of work important Caseload supervision and active caseload management needed Training More time More staff Improved IT resources Staff and service users: take greater ownership of CPA and recovery Centralised services and excessive administrative barriers |
| Reflections | Lots of restructuring, varying degrees of health and social care integration in teams (IT problems everywhere, but some very different models of attaching SWs), recovery values espoused at the highest level but less sure about action, high demand, cuts to people and other resources, fragmentation of services with any qualified provider, the Measure in Wales | CPA ideas simply and straightforwardly expressed (assess, care plan, care co-ordinator, review) but difficult in its implementation and contested. Attempts to make ‘the CPA’ meet the needs of service users, practitioners, managers, commissioners. Administratively heavy, insufficiently oriented to recovery. Constant format changes, not clear over CPA eligibility CTP: mixed views Care co-ordinators: from any mental health professional background (Band 4s in one site). Complex role, high responsibility. Recognition of value of allocating care co-ordinators to service users based on need/professional fit but across sites compromised by capacity Electronic records: mixed. These get in the way of face-to-face work without mobile technology Caseloads rising PbR and clustering: having an impact Involvement: lots of caveats re: carers Training needed |
Some clear articulation of what recovery might be (values), but varying degrees of sign-up. Cultural lag and resistance on the one hand, ‘we have always been doing this’ on the other. Challenged by dominant medical ethos on one site, challenged by admin workload and lack of time and people Varying use of tools. Admin heavy. Which tool is best? Who knows? How choose? Training needed Tensions re: recovery and compulsion |
Not as uniformly understood as recovery. Everything from individual care (CPA is personalisation in action) to personal budgets and direct payments. Lack of uniformity across sites in budgets, etc. Cross-national differences: personalisation and direct payments not endorsed in the same way (cf. marketisation?) |
Need good leadership, cultural change (staff and SUs), resources, integration across NHS and LA, better tech, improve morale |
| Care planning and care co-ordination | Recovery | Personalisation | |
|---|---|---|---|
| Artois | Polarised views from service users on their care planning and co-ordination. At best, carefully thought out with good communication, helpful to have a written document. At worst confusing, rigid, and an obligatory task Review meetings: seen by service users as collaborative Care co-ordinators saw care planning as useful for recording purposes and drawing in members of the interprofessional team Care plans thought by service users to be easy to understand and clear and a useful prompt for staff, with any shortcomings (e.g. volume of documentation) an inevitable by-product of working with databases Care co-ordinators, however, felt CPA document not user-friendly for them Improvements to the process: less prescriptive, more recovery-focused, more active role for more informed service users, care plans less concerned with fixing than dealing with problems Better out of hours services needed Actual care plans: care co-ordinators saw format as unable to meet all needs and expectations. Service users mostly had copies of care plans but saw these as insignificant. Neither service users nor care co-ordinators regularly refer to care plans Service users mostly satisfied with involvement in care planning, care co-ordinators saw involvement as variable depending on the service user Safety and risk: fundamental to the CPA for care co-ordinators, and service users satisfied with discussions of this |
Service users found the term ambiguous, unhelpful, even deceptive Service users and care co-ordinators: recovery should mean choice, independence, fulfilment No clear service user view that care plans helped with recovery; helpful when including practical steps. Conversations with care co-ordinators more helpful WRAPs used, and seen as helpful, by service users: valued for being very personal (more so than care plans) Care co-ordinators: used WRAPs and relapse plans but less enthusiastic than service users, now expected to use Recovery Star Care co-ordinators: practice always been recovery-focused but organisational targets got in the way of recovery practice |
A term meaning different things to different people (both service users and care co-ordinators): individualised care, service user-led services, choice, personal budgets and direct payments Tailoring care, and balancing structure and flexibility Service users: current care is personalised and tailored Care co-ordinators: saw personalisation as constrained by lack of services New service users allocated to care co-ordinators on the basis of caseload space rather than appropriateness, challenging personalised relationships Service user creativity seen as positive by care co-ordinators, but also that service users not always aware of services available to them |
| Burgundy | Care planning and co-ordination helpful to some service users to feel in control, but others felt unable to influence decisions or that care planning lacked structure Where service users found it difficult to talk to carers, talking to a care co-ordinators was helpful Varied service user views on desired levels of care co-ordinator’s involvement: from wanting more proactivity to wanting less intrusion Carers also had mixed views: satisfaction with quality of care at best, lack of meaningful engagement, dismissive professional attitudes, poor standards, lack of access to psychiatrists at worst Carer concern that service users may acquiesce to professionals Rural locations and limited transport a challenge Care co-ordinators more positive, seeing care plans as individualised and outcome-focused but always dependent on the care co-ordinator’s involved Care co-ordinators saw first person care plans as helpful Actual care plans seen as a ‘record’, but also (for carers) as a contract Care plans seen to have little value, impact or relevance for service users or carers: service users satisfied with care co-ordinators looking out for them, but service users’ role limited to signing care plan Care co-ordinators rarely referred to care plans: reviews only, with work reliant on skills and knowledge of the service users Care co-ordinators: flexible approach to CTPs, with varying practice across different care co-ordinators. Some engaged in building relationships, goals and coproduction but not all Some joint development of CTPs with service users writing their own, but not always Care co-ordinators complained of lack of time and admin support, and lack of IT training Care co-ordinators: CTOs resulted in less choice and control for service users Safety and risk: service users reported different experiences, from risk being used as a threat to not being considered. Carers less concerned with risk, others than during crises. Care co-ordinators saw risk as a focal point, including risk of vulnerability |
No general agreement on the meaning of ‘recovery’ Some service users saw this as linked to self-management, control and goals, others to acceptance of illness. Some saw the term as meaningless, and only one talked of a care co-ordinator recognising their strengths Carers also had disparate understandings Care co-ordinators saw recovery as a journey, and as about quality of life improvement, sitting in tension with management agenda of moving service users through the system Different professional groups have different ideas around recovery Little evidence that care plans have an impact on recovery, and only from service users who said care plans helped them accept or talk about their health WRAPs mentioned only once, by a carer Care co-ordinators: current care is recovery focused, despite tensions with emphasis on (e.g.) diagnosis and caseload management Carer roles considerable in some cases |
Little familiarity with, or comprehension of, ‘personalisation’. Some service users saw this as the tailoring of care plans, but carers and some care co-ordinators not aware of the term Varying reports of care being personalised, with ambivalence across all groups Service user views polarised: some recognised themselves in their care plans and were able to amend them, others saw care definitively not personalised Carers ambivalent, with strong views on non-personalised care reported Wish for services to be communicated in Welsh Personalisation constrained by what is locally available No clear agreement that care could be personalised within the CTP framework Personalisation challenged by service users not being well enough to fully participate Very limited talk of direct payments |
| Champagne | Care planning seen as useful, including in person progress monitoring, but contingent on updates, activities, personal contact Most service users said that they did not have copies of their care plans, but care plans nonetheless useful. Care plans understood by service users, and actively used by one who had ‘ownership’ Service users recognised that some people have difficulty accepting mental health services, and help not welcomed Care plans helpful in including emergency contacts Some service user support for electronic format care plans, but paper form preferred by care co-ordinators Care co-ordinators need more time to work on care plans, emphasising collaboration, risk, recovery Mixed care co-ordinator views on regular referring to care plans: a contract for one, variability in engagement noted on the part of service users by others Care co-ordinators saw usefulness of care planning as reflecting individuals involved Varying care co-ordinator views on care plans as documents Care plans should be seen as continual, not one-offs IT systems a hindrance Most service users happy with level of involvement Carers not highly involved, but this not seen as a problem Safety and risk paramount for care co-ordinators, but service users said risk not explicitly discussed or recorded One service user felt neglected following hospital discharge Care co-ordinators: difficult balance between safety and positive risk taking Improvements needed: communication across services, investment in services, respite care, out of hours, more face-to-face time, structured activities, more psychiatrist involvement in CTPs, training, help from peer support workers |
Service users less certain about ‘recovery’ than other groups, but agreement that their strengths and achievement were recognised Recovery meant different things for different service users (e.g. ‘getting better’, being positive) Carers: recovery a personal process, involving living within the bounds of ill-health Care co-ordinators: recovery as individualisation, meaningful lives, empowerment No clear view on care plans as helping recovery. Structured goals important for some service users, more active care plans important for others Carers: diverse views, including medication, therapies, availability of services Most care co-ordinators described themselves as working in a recovery way, with the CTP a vehicle for capturing this Care co-ordinators: risk adversity, documentation, limited resources, ‘firefighting’ all a hindrance to recovery Recovery as helping people to discharge seen as a challenge for service users and care co-ordinators |
No clear service user or carer understanding Care co-ordinators familiar with the term, but saw this as ambiguous: choice and tailored services mentioned but challenged by lack of services Mixed service user views on the extent of services being tailored Some service users preferred to defer to professionals Carer views on personalisation also mixed: care for some tailored, for others not. Lack of therapies service a challenge Care co-ordinators: care as personalised as possible in conditions of budget constraint, limited time, high workload Gaps between ideal and realities Personal budgets featured in care co-ordinator data only |
| Dauphine | Service users and carers had mixed experiences and knowledge of care planning (e.g. not all service users had care plans, others had not read them in detail, and carers were only partly or not involved) Care plans were also described as having a potentially negative impact if shared with service users Care co-ordinators were far more positive about care planning, as enabling individualised, holistic, collaborative care in a structured and continuous way Care co-ordinators also saw care planning as a way of monitoring service users Care planning hindered by administrative demands Some service users saw their care plans as useful (e.g. where they included structured activities), but one service user said their plan had hardly changed over years Care planning sometimes included a focus on strengths, and service users reported mixed levels of involvement Carers were largely not involved in care planning, but care co-ordinators said it was useful to have carer involvement Ownership of care plans was important for care co-ordinators Service users: lack of choice in medication, insufficient contact with staff, limited services Care co-ordinators: discontinuities of care caused by staff departures, and reluctance of some service users to engage Time insufficient to collaboratively write care plans with all service users, leading to involvement being reduced to signing care plans Care co-ordinators: distinctions between involvement and agreement, which was not an issue for service users Service users happy with paper records, but not the use of new technology Service users asked for more structured meetings and more information on local services, with involvement of wider range of staff to meet wider range of needs Carers wanted more support Care co-ordinators wanted more time, training, support and supervision and less administration Advocates seen as valuable Relationships with staff seen by service users as important in the context of safety and risk, and by carers as needing to focus on self and others Service users: risk not proactively managed, and an awareness of risk in the context of being unwell Care co-ordinators recognised practice as risk-averse, with limited positive risk taking and some risks (to others) more attended to then others (risks to self) |
Recovery seen as coping with illness and managing, with one service user saying it also required service-user participation Care co-ordinators: listening, and not prescribing, seen as important No clear view on care planning as assisting recovery Limited use of recovery plans, and for service users and carers only limited recognition of achievements |
Disparities in views: service users had wide range of understandings of ‘personalisation’, carers lacked knowledge and care co-ordinators linked this to personal budgets Most service users and carers felt services were not personalised, in contrast with care co-ordinators who felt otherwise For care co-ordinators, personalisation challenged by lack of time and extra work involved, by lack of resources and service user reluctance to engage Service users saw complexity in the personal budgets application process, and staff inflexibility and lack of decision-making clarity as hindrances |
| Languedoc | Service users and carers aware of care being planned and co-ordinated, and care plans seen as useful to share information and progress Actual care plans seen by service users as only a small part of the care planning process: relationships and medication more important Care plans not always comprehensive Care co-ordinators also saw care plans as useful to keep track, but as making large administrative and time demands Care co-ordinators: some service users see little value in care plans, and finding common ground can be difficult Service users had varying degrees of engagement (e.g. some had care plans, others not; some took little notice, some felt over-scrutinised) Service users and carers: care plans as important for staff (e.g. to promote communication and to record), but for some service users not owned by service users Care co-ordinators: involvement shaped by service users having realistic needs and expectations Service users described mixed experiences of involvement, and of not referring to care plans once written Carers also saw care plans as not being active documents Care co-ordinators: care plans a function of meetings, and not used actively Care plan format seen by care co-ordinators as needing to be shorted and simpler Service users mostly understood their care plans Mixed feeling about other formats (e.g. electronic) Care co-ordinators not helped by IT incompatibility Safety and risk a priority for care co-ordinators, but service users unsure how these were discussed and incorporated into care plans Carers: risk discussions not always recorded in care plans Care co-ordinators concerned with blame re: risk, and of difficulties in sharing risk details with service users For service users and carers, relationships with care co-ordinators important and for care co-ordinators concern over administrative tasks eroding face-to-face time Tension between standardisation and individualised care Control over care planning and continuity compromised by staff changes and organisational upheaval Better communication with physical health and primary care services needed |
Varied definitions given Recovery not discussed with some service users, or rejected by them (when conflated with medical idea of ‘recovery’) Recovery seen as managing illness and symptoms and improving quality of life, and for service users and care co-ordinators as involving hope Care co-ordinators: difficulties when staff and service users have different ideas around achievable progress No clear links between care planning and recovery, with relationships important for service users Care co-ordinators: recovery has made care planning more focused on goals and (unhelpfully) on moving towards discharge Care co-ordinators felt that they worked in a recovery way, with less prescription and more collaboration, but that recovery also helped organisational goals Inconsistent use of recovery tools, and different levels of endorsement Care co-ordinators valued strengths based approaches, but carers said these were not reflected in care plans Medication side-effects a hindrance to recovery, and (for carers) unsuitable prescriptions sometimes used Targets and lack of organisational support a hindrance to recovery |
Lack of clarity and ambiguity, linked to individualised care plans Care co-ordinators not familiar with personalisation, even following training Service users and care co-ordinators linked personalisation to ‘control’ of care planning Care seen as adequately personalised by all three groups Care co-ordinators: listen to service users, and recognise contributions but also concern over service users having unrealistic expectations not matched by availability |
| Provence | Service users and carers aware of care being planned, though many service users did not have copies of their care plans and others did not feel actively engaged with them Care plans seen as a guide or framework for service users and carers, and a record of information and contact details: but not dynamic or responsive Care co-ordinators: care plans not important from a service user perspective Written care plan format helpful, but no clear appetite for electronic versions Care co-ordinators: hindered by labour-intensive, over-complicated, IT systems for managing care plans Care co-ordinators: care plans full of jargon and need simplifying, but not mentioned by service users or carers Range of service user experiences on involvement, from being empowered to feeling cast aside and unwanted Care co-ordinators: some examples of shared care plan ownership, and overall wish for great service user and carer involvement Tensions for care co-ordinators inviting collaboration and then allowing disagreements Relationships, consistency and coherence important but not uniformly in place in a context of staff and resources limitations Safety and risk very important, but service users and carers not fully involved or actions in the case of crisis not always clear Goals and objectives mentioned by some, but no clear emphasis on strengths |
Various definitions offered, centred on managing illness and coping Recovery not seen as a primary objective for all service users Different experiences described in relation to the impact of care planning on recovery: from no help, to pivotal Families and friends important for recovery Carers more concerned with strengths than service users, and care co-ordinators note that their recognition of strengths is not always mirrored in actions Very little evidence of recovery tools |
Not a familiar term to all, but seen to focus on individuals and their needs Some concern in care co-ordinators that personalisation raises unrealistic expectations Service users and care co-ordinators felt care was personalised, carers less sure Service users describe passive personalisation, with little talk of choice or ownership, but carers emphasise these ideas more and care co-ordinators said service users have variable experiences of being in charge Limited resources and training and excessive administration hindrances to personalised care |
| Reflections | Varied experiences of care planning and care co-ordination within sites. Care co-ordinator and service user variables have a bearing At best, care is planned in a structured and collaborative way with clear communication and opportunities for service user ownership and influencing At worst, service users say they feel cast aside, not involved, or that their care is planned as an obligatory task and in ways which are confusing and rigid Care co-ordinators are sometimes more positive about care being planned in individualised, collaborative, ways than service users and carers sometimes are Care co-ordinators welcome collaboration, but some also worry over how to address differences in view or think some service users will not engage Safety and risk are paramount for care co-ordinators, but service users and carers are hardly involved in the assessment of these and Care co-ordinators have concerns over sharing their views. Some service users and carers feel risk is not managed sufficiently proactively Risk aversion limits positive risk-taking and sits at odds with recovery ideals and practices Care plans are useful for staff and are recognised as having to be created, and have value as records of what has been decided and for including contact details and (sometimes) crisis an contingency plans. For a handful of people care plans are like a contract. Developments are the use of first person care plans But: as documents, care plans are not highly valued, and are not seen as active documents: many people (care co-ordinators and service users included) do not routinely refer to care plans once they have been created. Many service users do not have, or have had and have then discarded or filed away, their care plans. Care co-ordinators think care plans are difficult to understand, but service users do not necessarily agree There is a tension between standardisation and individualised care planning Care co-ordinators find care planning and care co-ordination administratively burdensome, and complain that they have insufficient time for face-to-face work with service users Relationships, however, are seen as very important: along with the care co-ordinators’ skills and knowledge of the service user. Service users and carers want to see more of care co-ordinators, and people recognise discontinuity (e.g. when care co-ordinators leave or when there is organisational change) as a problem There is no clear appetite for electronic care plans for service users, and care co-ordinators report that current IT systems (which are often incompatible within sites, between NHS and LA services) are a hindrance Carers have varied experiences within sites, but many are not engaged with care planning and co-ordination. Some do not see this as problematic Review meetings vary: at best they are collaborative Lack of people and other resources are a problem everywhere There is some, but not much, evidence of care planning addressing service users’ strengths and accomplishments |
Even though ‘recovery’ is everywhere it has ambiguous meanings within all sites. Some even say it is unhelpful or deceptive (e.g. it is about moving people off caseloads) People are clear that recovery should mean choice, independence, fulfilment: but very few talk about the ‘journey’ There is no clear view that care planning and co-ordination helps recovery. Where this is so, it is because care plans include practical steps, or where they help service users to accept or talk about their health. Some service users and carers say strengths are acknowledged Conversations and relationships, more than care plans, promote recovery. Families and friends promote recovery Even within single sites there is variable use of, experience in, and enthusiasm for recovery tools. At best, WRAPs are very personalised and helpful, but some care co-ordinators worry about the extra work Some care co-ordinators say they have always worked in a recovery-focused way, and what hinders them are organisational targets Other hindrances to recovery are adversity to risk, documentation, limited resources, firefighting, different ideas from service users and care co-ordinators on achievable progress, medication side-effects |
Personalisation is understood in very different ways within sites. Often it is equated with individualised care, choice, service user-led services, tailoring care and balancing structure and flexibility. More specifically it is used to refer to new practices: personal budgets and direct payments. Some people have no idea what personalisation is about Care is variously described as being personalised, and as very much not Personalisation is constrained by lack of resources and local services, and by service users deferring to professionals. Gaps are observed between the ideal and the reality, and staff report high administrative workload and complexity using personal budgets, etc. Sites often allocate care co-ordinators to service users on the basis of caseload space rather than appropriateness, challenging personalised relationships Service users are not always aware of services available to them Personalisation and care planning and co-ordination: not clear that personalisation can be achieved using current templates As with recovery, some care co-ordinators say personalisation raises unrealistic expectations |
Appendix 12 REFOCUS results: e-mail correspondence from Mike Slade
Hi Alan
Thanks. Yes, ‘disappointing’ (at least from a REF perspective . . .)
Do refer – summary would be that the REFOCUS Trial shows that implementation within mental health systems is more challenging than simply introducing a new intervention, and requires organisational commitment. However, we did show that where REFOCUS was fully implemented, a positive impact on recovery was found. So the major challenge is implementation, which starts but does not end with training.
Is that enough?
M
ps thanks for reviewing then – we’re almost at the point of re-submission so hopefully it will be accepted soon
From: Simpson, Alan Sent: Tuesday, 16 December 2014 14:27 To: Slade, Mike Subject: REFOCUS results and our COCAPP study
Hi Mike,
I’m just finishing off the report for NIHR on our COCAPP recovery-focused care planning study.
Unsurprisingly, lots of people have called for more training. I’m writing a brief section for the discussion exploring why it ain’t as simple as that.
I’m aware from reviewing your REFOCUS study paper that the results of your superb intervention study were slightly disappointing. I wonder whether you be OK with me making a short reference to that and whether you would suggest a line or two that sums up the results?
Best wishes,
Alan
Alan Simpson
Professor of Collaborative Mental Health Nursing
School of Health Sciences
City University London
Northampton Square
EC1V 0HB
T: + 44 (0)20 7040 5937
Mob: 07852 427816
Twitter: @cityalan
This e-mail and its contents are the property of City University London. If you are not the intended recipient of this message and any attached files, please delete it. Unauthorised copying or distribution of this message, its attachments or parts thereof, is strictly prohibited unless specifically stated otherwise. Please consider the environment before printing this message.
Glossary
- Care co-ordination
- This is the responsibility of a named mental health professional, whose work (under both the care programme approach and the care and treatment plan systems) includes co-ordinating the assessment and planning processes for named individuals using mental health services.
- Care co-ordinator
- The co-ordinator, who is most often a mental health nurse, social worker or occupational therapist, takes responsibility for planning care with the service user’s close involvement and ensures that this care is reviewed regularly.
- Care Plan and Care Planning
- The written care plan lies at the heart of the care planning process and should be collaboratively developed by professionals working in partnership with individual service users and their significant carers. It should include details on goals or intended outcomes, on services to be provided, on plans to be followed in the event of a crisis and on the maintenance of safety.
- Care Programme Approach
- In England, the care programme approach is the framework that underpins how services are assessed, planned, co-ordinated and reviewed for someone with severe mental health problems or a range of related complex needs. The approach requires that health and social services assess need, provide a written care plan, allocate a care co-ordinator and then regularly review the plan with key stakeholders.
- Care and Treatment Plan
- In Wales, with the passing of a new law [the Mental Health (Wales) Measure (2010)], the care and treatment plan is the document that supersedes the care programme approach for all people using secondary mental health services. Care and treatment plans must address at least one of eight areas (accommodation; education and training; finance and money; medical and other forms of treatment, including psychological interventions; parenting or caring relationships; personal care and physical well-being; social, cultural or spiritual; work and occupation).
- Carer
- Anyone who cares, unpaid, for a friend or family member who, as a result of illness, disability, a mental health problem or an addiction, cannot cope without their support.
- Clusters and clustering
- Clusters are the currencies for most mental health services for working age adults and older people in England. Service users have to be assessed and allocated to a cluster by their mental health provider, and this assessment must be regularly reviewed in line with the timing and protocols set out in the mental health clustering booklet. Clusters form the basis of the contracting arrangements between commissioners and providers under Payment by Results.
- Community Mental Health Team
- A Community Mental Health Team provides assessment, care and treatment for people who have one or more types of severe mental illness. They are a multidisciplinary team of community psychiatric nurses, social workers, support workers, psychiatrists, psychologists, occupational therapists and support and administration staff.
- Community treatment orders
- The power given to a Responsible Clinician (usually a psychiatrist) under the Mental Health Act to place certain conditions on the service user which s/he must follow when they have left hospital. Failure to follow the conditions may lead to the service user being compulsorily recalled to hospital.
- Local authority
- Broad term used to describe elected councils in England and Wales with responsibility for the provision of all local government services, including social work, in a specified area.
- Local health board
- In Wales, seven local health boards plan, secure and deliver health-care services in their areas.
- Mental Health Recovery Star
- The Mental Health Recovery Star is a tool for supporting and measuring change in people with mental illness in recovery. It covers 10 key areas, such as managing mental health and social networks and is underpinned by a five-stage model of change.
- Mental Health Research Network and Mental Health Research Network-Cymru
- These research networks in England and Wales (Cymru) (now part of the Clinical Research Network) are made up of research-interested clinicians and practitioners working at both national and local levels to enable studies that are included in the national portfolio of research to receive the right support to ensure that they are delivered successfully in the NHS.
- NHS trusts
- A NHS trust is a public sector corporation within the English NHS generally serving either a geographical area or a specialised function (such as an ambulance service). In any particular location there may be several trusts involved in the different aspects of health care for a resident. Mental health services are usually provided by one NHS trust in an area.
- Payment by Results
- A rules-based payment system recently introduced in England under which commissioners pay health-care providers for each patient seen or treated, taking into account the complexity of the patient’s health-care needs.
- Personalisation
- A way to describe the enhancement of individual choice and control for eligible adults using health and social care services through person-centred planning and self-directed support. Personalisation underpins the idea that health and social care services should be tailored to the particular needs of individuals, and should enable people to live as independently as possible, exercising choice and control. The use of personal budgets to purchase social care support can be a feature of personalisation.
- Recovery
- The contemporary idea of personal (rather than necessarily clinical) recovery in mental health originated in the service-user movement and is now claimed as the philosophical underpinning for many mental health policies and services including care planning. A definition often used is: a way of living a satisfying, hopeful and contributing life even within the limitations caused by illness.
- Service user
- Person who uses health and social care services, or who is a potential user of health and social care services.
- Wellness Recovery Action Plan
- A Wellness Recovery Action Plan is a ‘self-management’ tool used in many countries around the world to help individuals take more control over their own well-being and recovery. A Wellness Recovery Action Plan is underpinned by a number of core principles of recovery, and people work within these principles to create their own plan, which includes a number of components including identification of triggers and early warning signs and associated action plans.
List of abbreviations
- ANCOVA
- analysis of covariance
- ANOVA
- analysis of variance
- BME
- black and minority ethnic
- CMH
- community mental health
- CMHT
- Community Mental Health Team
- CPA
- care programme approach
- CPN
- community psychiatric nurse
- CTO
- community treatment order
- CTP
- care and treatment planning
- ES
- Empowerment Scale
- GP
- general practitioner
- IT
- information technology
- LA
- local authority
- LEAG
- Lived Experience Advisory Group
- LHB
- local health board
- MDT
- multidisciplinary team
- MHRN
- Mental Health Research Network
- MH(W)M
- Mental Health (Wales) Measure
- NISCHR
- National Institute for Social Care and Health Research
- NISCHR CRC
- National Institute for Social Care and Health Research Clinical Research Centre
- OT
- occupational therapist
- PAG
- Project Advisory Group
- PbR
- Payment by Results
- RSA
- Recovery Self-Assessment
- SD
- standard deviation
- STAR-P
- Scale to Assess the Therapeutic Relationship – Patient version
- WRAP
- Wellness Recovery Action Plan