Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 11/1015/20. The contractual start date was in April 2012. The final report began editorial review in January 2015 and was accepted for publication in September 2015. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Alex D Tulloch and Graham Thornicroft are employed part-time as consultant psychiatrists for South London and Maudsley NHS Foundation Trust. André Tylee was a director of the Mood Anxiety and Personality Clinical Academic Group and honorary consultant at South London and Maudsley NHS Foundation Trust until October 2014. Catherine Polling has worked as a psychiatrist for South London and Maudsley NHS Foundation Trust since 2014. This included salary support for Alex D Tulloch, Anke Görzig, Sophie Pettit, Leonardo Koeser and Andrew Watson and fees paid on a self-employed basis to BS. Additionally, this study represents independent research part funded by the National Institute for Health Research (NIHR) Biomedical Research Centre at South London and Maudsley NHS Foundation Trust and King’s College London, which maintained the infrastructure used and provided salary support for Alex D Tulloch, Catherine Polling and Mizanur Khondoker. Alex D Tulloch, Diana Rose and Graham Thornicroft are currently supported by NIHR Collaboration for Leadership in Applied Health Research and Care South London at King’s College Hospital NHS Foundation Trust.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2016. This work was produced by Tulloch et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction
This report concerns an organisational change within the South London and Maudsley NHS Foundation Trust (SLaM) associated with its entry into the King’s Health Partners (KHP) Academic Health Sciences Centre (AHSC) in 2009. This change was centred around new structures called Clinical Academic Groups (CAGs), which replaced the directorates through which SLaM had previously managed its operations. Four of these directorates had provided comprehensive adult mental health services to four boroughs in South and Southeast London and the transition to CAGs entailed the loss of these geographically based operational units providing comprehensive adult mental health services to the population within a defined part of SLaM’s geographical catchment. Instead, they were replaced with operational units that divided the work of adult mental services between them by grouping teams and wards with similar functions together and provided services across SLaM’s entire area and, in the case of tertiary services, beyond.
We took a programme evaluation approach to this work. Following Wholey,1 we understand a programme as ‘a set of resources and activities directed towards one or more common goals, typically under the direction of one manager or a management team’ (p. 9). We aimed to define the CAG ‘programme’ straightforwardly enough that another organisation seeking to follow SLaM’s example would know what it would need to do to set itself, at least at the outset, on the same track.
Clarity in relation to the central programme components of the CAG reorganisation was, in reality, achieved only incrementally and over the course of the evaluation. Like many programmes, the CAG reorganisation, especially at first, involved many activities whose relative lack of centrality became evident only over time.
The first programme element was straightforward to identify. This was the CAG restructuring itself, which involved taking a set of geographically based management units and turning them into a new set of service management units in which teams were grouped on the basis of their function or, alternatively, on the basis of the predominant set of problems or diagnoses they treated. As we show in Chapter 3, other NHS trusts in London also undertook this kind of reorganisation around the same time as SLaM; however, unlike SLaM, these other trusts uniformly referred to these new units as service lines, whereas SLaM called them CAGs. This different terminology reflected the special influence in SLaM’s case of the newly formed AHSC.
What we came to see as the second programme element was initially a requirement imposed as part of the initial CAG development process managed by SLaM and KHP, but which over time developed into an evolving and open-ended experiment: the newly formed CAGs were guided to use care pathways to describe, redesign, develop and performance manage their services, and this process extended beyond the initial restructuring period and into the stable operating period of the CAG that we studied. We came to see the use of care pathways as a precept, that is, a general principle that care pathways should, when possible, be used as a resource for managing and changing services. However, as we show in Chapter 3, the way that care pathways were introduced and the exigencies of management led SLaM to a distinctive form of ‘high-level care pathway’, which, although demonstrably effective as a tool for management, deviated in some ways from the usual understanding of care pathways described in the literature. This has the important consequence, we believe, that SLaM’s CAG reorganisation cannot be treated as a case study of the use of care pathways as these are usually understood.
Having identified the core programme components, our intention was to draw on the methods of realistic evaluation2 to explore what happened when SLaM introduced CAGs. For each programme component this would require us to consider the key mechanisms through which change was sought, the changing contexts in which this occurred and the outcomes produced by the combined effect of mechanism and context.
Plan of the report
We do not preface the accounts of our methods and results with a separate review of the literature relevant to each programme component. In the case of the CAG restructuring itself, this was because a scoping review of research into service line management indicated that no truly comparable change has been described and studied in the past; the only apparently similar evaluation studied a quite different higher-level separation between acute, mental health and primary care service lines in the Veterans Administration (VA). 3–5 In the case of the use of care pathways, this is because of the particularities of SLaM’s practices compared with those described in other studies. 6,7 However, relevant literature is cited and discussed in other chapters, especially the qualitative results chapter (see Chapter 3).
Chapter 2 outlines our main research questions and describes the methods adopted in this study. In our qualitative and some of our quantitative data collection, we focused on the Mood Anxiety and Personality CAG (MAP CAG) and also on those users of SLaM’s services who have a non-psychotic diagnosis. This limitation to one CAG was necessitated by the resources available to us and we chose the MAP CAG in preference to the Psychosis CAG only because another large research project affecting the latter was anticipated at the time that research funds were being sought. Studying only a single CAG imposed some limitations of scope, but also allowed us to investigate the organisational process in greater depth than had we attempted to evaluate more than one CAG.
Chapter 3 tells the story of the CAG programme, based on documentary evidence and on evidence from interviews with SLaM staff and service users. We look first at the overall circumstances within which this organisational change took place. We then describe the early development of KHP and its CAG programme, provide a brief history of SLaM and the Institute of Psychiatry (IoP) and outline the immediate context within which SLaM decided to reform its operational units as CAGs. We set out what the interviews and documentary sources suggest were the key mechanisms through which change was initially sought at the time of CAG formation. We then use key themes identified from the interviews to set out what actually happened, here contrasting findings in 2012 (our first wave of data collection) with findings in 2014.
Chapter 4 details our quantitative findings, setting out what we were able to discover about activity and costs, effectiveness, safety and patient centredness and how these had changed across SLaM’s four boroughs (Croydon, Lambeth, Lewisham and Southwark) since 2009.
In Chapter 5 we discuss our findings and consider their implications.
Chapter 2 Research questions and methods
This organisational study explored three main research questions: how the SLaM CAG programme (as exemplified through the MAP CAG) was conceptualised and implemented by SLaM staff; the extent to which there were changes in activity levels and in the quality of patient care over the 5 years since the start of the programme in 2009 and the extent to which those changes could reasonably be attributed to the CAG programme; and the main lessons that could be learned and applied more generally. As noted in the previous chapter, to keep the research to a reasonable scale and scope we studied only one CAG (the MAP CAG) and concentrated on its most important services: those provided through community mental health teams (CMHTs) and psychotherapy teams. The MAP CAG was selected in preference to the other large adult CAG (Psychosis) because a large programme of research was envisaged in the latter at the time that we were seeking research funding for this study.
We used a combination of qualitative and quantitative methodologies and data to inform our understanding of the SLaM CAG programme and the definition and implementation of the MAP CAG. The qualitative work included two sets of semistructured interviews at the start and end of the project as well as document analysis and drew on a realistic evaluation framework. 2 The quantitative work identified and analysed data held in a database of anonymised electronic patient records to examine, test and develop the qualitative findings.
Realistic evaluation aims to test and refine programme theories by establishing clear and measurable relationships between an intervention such as the CAG programme and its outcomes that are explained by an underlying theory of change. It is sensitive to contextual effects, identifying a series of context–mechanism–outcome configurations. The underlying assumption is that all programmes do generate regular patterns of results, but only when broken down into their underlying components, and when the context in which those components operate is taken into account. Without this disaggregation and consideration of context, programmes can appear to generate very different results from one implementation to another. Realistic evaluation has previously been used in the analysis of similar programmes in the NHS; although it does not provide a methodological prescription but instead a set of principles and orientations, the use of a comparative case study approach is typical. For example, Rycroft-Malone et al. 8 reported candidate context–mechanism–outcome mechanisms in the Collaborations for Leadership in Applied Health Research and Care programme, using a comparative case study approach based entirely on qualitative data. Rycroft-Malone et al. 9 used similar approaches to study protocol-based care in a variety of settings, whereas Greenhalgh et al. 10 reported a realistic evaluation of a large-scale change programme for stroke, renal services and sexual health services in inner London and also included a review of the existing – limited – literature on the use of realistic evaluation in health-care contexts. Notably, the latter authors10 reported that core tasks of realistic evaluation – definition of programme goals and definition of programme mechanisms – were far from straightforward to perform. Early in the evaluation we attempted to create logic models linking inputs, activities, outcomes and outputs,11 but it was ultimately more straightforward to present the necessary context–mechanism–outcome configurations either in narrative form or using diagrams that directly represented those relationships. 2
In relation to the SLaM CAG programme our objective was to undertake an evaluation that would (1) be meaningful to the managers, clinicians, academics, service users and commissioners who were involved in or who were affected by implementation of the MAP CAG; (2) take advantage of their detailed knowledge of the multiple contexts into which the CAG programme was introduced; (3) support replication of the programme elsewhere; and (4) support research utilisation. 12 We used the professional, tacit and formal knowledge of various actors in the SLaM CAG programme and the MAP CAG to develop a narrative of change that describes how those involved thought their use of resources (money, authority, expertise, time, etc.) had contributed to the changes identified, and we aimed to develop context–mechanism–outcome configurations to illustrate how specific components of the SLaM CAG programme had achieved that change. Our restriction to a single site to some extent limited our ability to apply these methods, as any given mechanism would at most be observed in a single overall CAG context and four potentially different borough context within that CAG. However, if context is understood as a specific, differentiated element, external to the programme, which determines the outcome in combination with a given mechanism – a formulation that we believe is consistent with the principles of realistic evaluation – then we still observed a plurality of contexts, at least in some cases. For example, the programme was applied across four London boroughs, each of which had pre-existing services that had arisen in different ways and would therefore potentially interact differently with the same programme element; differences could also be observed at the individual team level. Moreover, even with a smaller number of different observed contexts per mechanism, realistic evaluation holds out the hope of better generalisability than standard quasi-experimental methods. Because programmes are typically altered when applied elsewhere, and also introduced into contexts that differ from the original site, the effects of any programme when viewed as a whole appear inconsistent across implementations. However, the component context–mechanism–outcome relationships, if correctly specified, operate consistently between different sites, allowing different overall patterns of effects to be explained.
Qualitative data collection
The qualitative work was undertaken in two phases, during the first 4 months and the last 3 months of the study. In phase 1 (months 1–4, May–August 2012), five group meetings were held: three service user-only meetings, one MAP CAG staff meeting and one final joint meeting with self-selected people from both categories who had attended one of the previous meetings. The service user meetings were co-facilitated by the two service user researchers on the team, who also attended the final joint meeting.
The study team prepared a topic guide before the interviews (see Appendix 1).
The service users who attended these meetings came from different boroughs and were drawn from two key groups: ‘involved’ service users (n = 4), that is, those who had a formal but largely voluntary role within the MAP CAG (such as membership of the MAP CAG Service User Advisory Group), and ‘non-involved’ service users (n = 9) and one carer, who had no formal role within the MAP CAG. These latter respondents were contacted through local service user organisations known to the MAP CAG’s Patient and Public Involvement Co-ordinator. The MAP CAG was relatively new at the start of our evaluation and we anticipated that it might be largely unknown to the non-involved service users, whose interactions with the trust are almost exclusively through contact with clinical teams. We therefore separated these early meetings to ensure that each stakeholder group had sufficient opportunity to develop their potentially contrasting views before coming together.
The staff who attended the group meetings were senior individuals who had played a key role in developing the SLaM CAG programme and in defining and developing the MAP CAG and included clinicians, academics and managers from the MAP CAG. Subsequently, we performed a few further interviews with staff members either alone or in pairs; some of these were respondents who we had already interviewed in the group interviews and others were new respondents whose knowledge of the programme had been indicated to us by the initial set of respondents. All staff respondents were approached on the basis of their closeness to the programme, rather than attempting to recruit a predefined number of people; we aimed to select those people who would be able to explain the programme and its history to us and how it worked.
All of the meetings and interviews were recorded and transcribed following prior permission from the participants.
Again taking a lead from our staff respondents, we also gained access to documentary sources relevant to the history of the MAP CAG. These documents were produced by the MAP CAG, by SLaM or by KHP.
All materials are described in Table 1.
| Activity | Number of participants |
|---|---|
| Group meetings | |
| Service users (non-involveda) | 4 (plus 1 carer) |
| Service users (involveda) | 3 |
| Service users (non-involved and involved) | 6 |
| Senior SLaM/MAP CAG staff (managers, clinicians, academics) | 7 |
| Joint meeting (3 service users and 3 staff) | 6 |
| Other interviews | |
| Senior MAP CAG staff (manager) | 1 |
| Senior MAP CAG staff (managers) | 2 |
| Senior MAP CAG staff (financial managers) | 2 |
| Senior MAP CAG staff (borough services) | 1 |
| KHP, SLaM and MAP CAG document review and analysis | – |
In phase 2 (month 27 of the study), follow-up interviews were undertaken with senior MAP CAG staff – a service manager, a clinical manager and a clinical academic, each of whom had contributed as phase 1 respondents – to consider external and internal developments since the first round of meeting and interviews and to present preliminary findings from the quantitative analysis.
Qualitative analysis
The interview and documentary materials were used in two ways.
First, throughout the project we repeatedly read and considered the available materials to develop an understanding of the CAG programme and its effects. We experimented with the use of logic modelling, which represents a programme as an assembly of inputs, activities, outputs and outcomes. We also experimented with representing the CAG programme as a set of context–mechanism–outcome configurations. Alongside both methods we drafted narrative text about the CAG programme and its effects. At the fourth group meeting in phase 1 and during the phase 2 interviews we presented some aspects of our understanding of the programme to cross-check this with respondents’ understandings. Ultimately, these analyses led to the representations of the CAG programme presented in the project report.
Second, we performed a thematic analysis. This was first applied to the phase 1 interview materials. Transcripts were initially reviewed and discussed by two team members. Subsequently, one researcher used qualitative data analysis software (NVivo 10; QSR International, Warrington, UK) to identify content relating to our research questions and to produce an initial set of themes arising from the data, guided at first by the prompts that had been used for the group interviews (see Appendices 1 and 2). The resulting analyses were cross-checked by the second team member. At a project team meeting during phase 2, three project team members considered the initial set of themes produced during phase 1, taking account of both the phase 2 interviews and he understanding that we had gained through the analysis of documents, and then decided on a modified list of themes for use in the final report (see Appendix 3). One team member recoded the phase 1 transcripts using these codes and this coding was rechecked by the other two team members. These themes and associated quotations were used as the basis for writing up the qualitative results.
Subsequent to the phase 2 interviews in July 2014, transcripts were read through and considered by three project team members, with an initial list of themes developed out of that discussion and to a large extent aiming to code issues that had also been raised in phase 1. These additional themes were also used as the basis for writing up the qualitative results, as noted above.
Quantitative work
Quantitative parts of the evaluation were performed using data held in a database of anonymised electronic patient records that is maintained by SLaM – the Clinical Record Interactive Search (CRIS) system. 13
Data management
We worked using the Structured Query Language (SQL) database version of the CRIS system. All data management was performed using Microsoft SQL Server 2008 (Microsoft Corporation, Redmond, WA, USA) and programmed in Transact-SQL.
Based on a comprehensive list of the names of all of the trust’s teams and wards we classified these teams into groups of similar services. We then used a fully cleaned table of activity data to define a set of periods under the care of a CMHT, including all of the various forms of CMHT that SLaM has operated, both before and after the CAG reorganisation, and including teams within the current MAP CAG and also outside it. This allowed us to analyse individuals with non-psychotic disorders before and after the reorganisation. The same was carried out for the psychotherapy teams, which, after the CAG reorganisation, constituted the other major part of the MAP CAG’s services. We included the integrated psychological treatment teams that the MAP CAG formed subsequent to the CAG restructuring but also the predecessor teams that performed a similar function before the reorganisation. Some highly specialised services that do not predominantly serve clients from SLaM’s four home boroughs were not included, such as the outpatient clinic associated with the inpatient Affective Disorders Unit.
The same cleaned activity table was used in combination with the trust’s own internal accounting data to derive unit costs for all forms of community and inpatient care. This required several rounds of error checking, enabling us to define a group of services for which both the financial and the activity data were adequate. Unit costs were calculated per ward or team and per financial year, using a currency of cost per single contact for community locations and cost per day for inpatient locations.
Data sets
Seven data sets were defined.
The main data set was defined as follows: to the periods of CMHT care and psychotherapy team care, we joined data on (1) demographics, (2) diagnosis, (3) referral date, (4) whether or not the episode had included a face-to-face contact, (5) costs of care delivered by CMHTs during the 365 days after the start of treatment, (6) combined costs of CMHT care, home treatment team care and inpatient care during the 365 days after the start of treatment, (7) previous service use, (8) receipt of secondary care psychotherapy during the episode or within 3 months of its end, (9) receipt of Improving Access to Psychological Therapies (IAPT) individual cognitive–behavioural therapy (CBT) during the episode or within 3 months of its end, (10) the Health of the Nation Outcome Scales (HoNOS)14 score near the beginning and near the end of the episode and (11) the Clinical Outcomes in Routine Evaluation 10-item version (CORE-10)15 score near the beginning and near the end of the episode.
The HoNOS is a 12-item instrument intended for use as a routine outcome measure in community mental health services serving individuals with severe mental illness. It covers symptoms, behaviour and social function. The CORE-10 is a short, 10-item version of a longer instrument, the Clinical Outcomes in Routine Evaluation Outcome Measure (CORE-OM), that may be used as a screening tool and outcome measure in psychology and psychiatric services and specifically addresses symptoms of common mental disorder.
A second data set (the text data set) consisted of 200 randomly selected periods of care under a CMHT, a borough-based psychotherapy team or both with a coded diagnosis of depression [F32–39 in the International Statistical Classification of Diseases, 10th Revision (ICD-10)]. For these episodes, the full anonymised text of the electronic patient record was extracted, allowing manual coding of prescribing and psychotherapy receipt and referral.
A caseload data set was defined containing data on current caseload per borough on any given calendar day, with different totals being calculated for CMHT care and psychotherapy. The counts in the data set were based on individuals with non-psychotic diagnoses who had been accepted for care by the relevant team and who had not been discharged at the census day.
A current waiting time data set was also defined. On any calendar day, a current waiting time was defined for any individual who had been referred to the CMHT or psychotherapy team but who had neither been seen for a face-to-face contact nor already been discharged. The current waiting time was defined as the number of days between the referral date and the census day. Adopting this method allowed us to investigate waiting time throughout the study period in a way that was not subject to bias as a result of censoring.
Next, we defined a data set of self-harm presentations in accident and emergency – the A&E data set. A data set was created that was identical to the main data set above, except that periods of CMHT care were extended by 3 months to create a data set of current or recent CMHT patients. This data set was then joined to a separate data set of psychiatric liaison consultations in A&E extending from April 2009 to November 2011, selecting only those consultations that had been manually coded as following an episode of self-harm (this A&E data set had been prepared for another study16). The data set was divided into 3-month time bands, for each of which we defined whether or not care co-ordination was in place, whether there was a change of care co-ordinator or care co-ordination was ended, whether or not there was a change in team and whether or not discharge occurred.
We also produced a data set – the acute admission data set – that was identical to the A&E data set except for being based on a data set of acute hospital admissions taken from Hospital Episode Statistics, selecting only those admissions coded as intentional self-injury using the appropriate ICD-10 X chapter headings.
Finally, we extracted a data set – the IAPT data set – including records of IAPT individual CBT treatment within each borough IAPT service.
Quantitative analysis
Initially, we performed descriptive analyses of clinical, demographic and service use variables, both for CMHT episodes and psychotherapy episodes, based on the main data set. These analyses included graphs showing the distribution of scores on each item of the HoNOS (for CMHT episodes) and the CORE-10 (for psychotherapy episodes).
The precise details of the analyses aimed at establishing the effects of the CAG restructuring were not decided in the original study protocol; we hoped that the qualitative interviews would give clear guidance as to the changes in activity and in quality of care that we should expect. Subsequent to the first wave of interviews, which did not in fact provide much clear guidance in this area, we decided to choose a series of indicators that would at least in part cover most domains of quality of care. 17 We grouped these under the following headings: cost and activity, effectiveness (subdivided into process and outcome), safety and patient centredness. Generally, quantitative analyses were guided by preliminary graphical analyses; for example, when the shape of the curve describing a particular indicator could not clearly be fitted by one or two straight lines we did not attempt to fit a trend line but instead simply compared values pre and post the CAG restructuring. Because of differences at baseline in the configuration of services within boroughs and because commissioning intentions also varied by borough we assumed that there were likely to be differences between boroughs. Therefore, all quantitative analyses either analysed boroughs separately or included interaction terms allowing per-borough effects to be examined separately. The choice to analyse by borough was made independently of the attempt to define specific context–mechanism–outcome configurations in the qualitative part of the study.
Activity and costs
First, we took the caseload data set and plotted daily CMHT caseload for each borough over time. Inspection of these plots suggested that a regression of daily caseload against time, possibly allowing the slope of the fitted line to vary after CAG implementation, would provide a meaningful fit of the data. Each borough was analysed separately. Models in which caseload was regressed only against time (γ = βtimeXtime + β0 + ε) were compared using likelihood ratio (LR) testing with models in which caseload was regressed against time, a pre-/post-CAG indicator variable and an interaction term between the latter and time (γ = βtimeXtime + βCAGXCAG + βCAGxtimeXCAG × time + β0 + ε). We applied Durbin’s alternative test to the initial analyses to test for the presence of autocorrelation and reran them using Newey–West standard errors as necessary.
Turning to the main data set, we went on to investigate the number of episodes of CMHT care for those with non-psychotic disorders starting per month. Data were analysed from 1 April 2009 to 31 March 2014. For this analysis, and all other analyses based on this data set, we included only episodes during which there was at least one face-to-face contact. After graphing these monthly counts, we applied a t-test to examine whether or not the mean count of new episodes per month differed before and after CAG implementation.
Next, we analysed the length of CMHT episodes, still working with the main data set. We analysed centile values rather than means as this allowed us to include unfinished as well as finished episodes without necessarily introducing bias; by having a follow-up period longer than the centile value of interest, any episode that is unfinished at the point of data extraction will necessarily fall within a higher centile. We analysed episodes starting between 1 April 2009 and 30 September 2013 and extracted data on 5 March 2015; this allowed us to be confident that any centile point below 521 days would be safely unaffected by censoring. After inspection of plots of key centile values over time, we used a non-parametric test for equality of medians to compare median values before and after CAG implementation.
We went on to analyse the number of contacts per CMHT episode during the year subsequent to the start of the episode, again working with the main data set. The mean number of contacts per episode was calculated and plotted per 6-month time band. We also performed a linear regression to test the effect of calendar time on the number of contacts, including a random effect to allow for person-level clustering and testing whether or not any linear trend altered before and after CAG implementation. For this, and the analyses of costs (see below), we studied episodes starting between 1 April 2009 and 31 March 2013.
Building on the previous analysis, we analysed CMHT costs on their own and CMHT costs added to inpatient costs and home treatment team costs (a more comprehensive measure of the costs of adult mental health services). We began by graphing mean costs in the first 365 days following the beginning of the episode, aggregating these over 6-month time bands, and graphing each borough separately. Having inspected the curves, we regressed whole-year costs against the pre-/post-CAG indicator variable, including a random effect at person level. The first (unadjusted) analysis did not include other covariates. The second (adjusted) analysis included age, gender, ethnicity, marital status, diagnosis and the number of inpatient days in the preceding year, the regression model being as follows:
Analogous analyses were performed for psychotherapy episodes, although we were unable to investigate numbers of contacts and costs per year of treatment as the recording of activity in psychotherapy teams was very incomplete. This would have affected our results directly (through contacts themselves) and indirectly (through the calculation of unit costs). Analysis of psychotherapy episode length was restricted to the period from 1 April 2009 to 30 September 2012 to ensure that the median episode length was not subject to censoring.
Finally, we used the IAPT data set to graph counts of new episodes of individual CBT within the four boroughs’ IAPT teams against time.
Effectiveness: process measures
Using the text data set we attempted to assess how far treatment for depression followed accepted treatment guidelines such as those produced by the National Institute for Health and Care Excellence (NICE). 18 Initial exploration of the free-text data indicated that it would be impossible to assess the duration of antidepressant treatment and therefore whether switching or augmentation of an antidepressant had happened at a particular point. We therefore adopted the less ambitious aim of documenting patterns of antidepressant use and change in prescribing at the first assessment, alongside documenting whether psychotherapeutic treatment was already in use at the time of the first assessment or if a referral for psychotherapeutic treatment was made at that point.
We calculated the proportions taking antidepressants at the initial consultation, started on antidepressants at that consultation or not taking antidepressants after that consultation and compared these proportions before and after CAG implementation. Among those already taking antidepressants, we compared the proportions given an additional treatment, the proportions with a dose increase and the proportions with a dose decrease. We also calculated the proportions already receiving psychotherapy at the first appointment, the proportions not receiving psychotherapy and not referred for it and the proportions not already receiving psychotherapy and referred for it. Looking at those not already referred, we examined whether or not the proportion referred for psychotherapy had changed since CAG implementation. The significance of any differences was tested using the chi-squared test.
The structured data on prescribing in the CRIS system are unreliable because the source electronic patient record does not support electronic prescribing. Therefore, we restricted our analysis of structured data to the receipt of psychotherapy.
Using the main data set, and selecting individuals under the care of CMHTs and with a diagnosis of a depressive disorder (ICD-10 codes F32–39), we calculated the percentage of episodes for which an episode of psychotherapy in secondary care or individual CBT in IAPT started during that episode or within 3 months of its end. The percentage with such an episode was graphed per borough and per 6-month time band. Logistic regression, with a generalised estimating equation approach to within-subject clustering, but otherwise without any added covariates, was then used to assess the presence of any trend in psychotherapy use (lnγ = βtimeXtime + β0 + ε) and whether or not any such trend altered before and after CAG implementation (lnγ = βtimeXtime + βCAGXCAG + βCAG × timeXCAG × time + β0 + ε).
Effectiveness: outcome measures
We used outcome measures collected as part of the trust’s routine outcome measurement programme to assess whether or not the change in outcome measures before and after treatment altered over the period straddling the introduction of the MAP CAG.
For CMHT episodes, we used the total score on the HoNOS, which was the most frequently used measure. We used the nearest score to the start of the episode and the nearest score to the end of the episode, excluding any score more than 2 months away from the reference point as well as any score later than the middle of the episode (for pre-treatment scores) or earlier than the middle of the episode (for post-treatment scores). Each treatment episode could contribute zero, one or two scores to the analysis. Before embarking on regression analysis, we graphed the mean of the pre-treatment scores and the mean of the post-treatment scores, aggregating data over 6-month time bands and per borough. Next, we constructed a series of mixed-effects analyses, including random effects at person and episode level. The dependent variable for the regression was the total HoNOS score and so the treatment effect was estimated by means of an indicator variable. (This method is superior to the direct regression of the difference between pre- and post-treatment scores as it allows individuals with only one measure to contribute to the analysis.) The steps followed were these:
-
We modelled the size of the treatment effect without entering any covariates in the analysis but including random effects:(Model 1)γ=βtreatment effectXtreatment effect+β0+υpersonZperson+υepisodeZepisode+ε.
-
We added a series of covariates (diagnosis, age, sex, ethnicity, marital status, borough within which service was received, calendar time relative to the date of CAG implementation and a post-CAG indicator variable):(Model 2)γ=βtreatment effectXtreatment effect+βdiagnosis1Xdiagnosis1+βdiagnosis2Xdiagnosis2+ βageXage+βsexXsex+βethnicity1Xethnicity1+βethnicity2Xethnicity2+βmarital1Xmarital1+ βmarital2Xmarital2+βborough1Xborough1+βborough2Xborough2+βborough3Xborough3+ βtimeXtime+βMAPXMAP+β0+υpersonZperson+υepisodeZepisode+ε.
-
We constructed a model in which two-way interaction terms between the treatment effect indicator and important covariates were simultaneously added – this tests for stratum-specific treatment effects by borough and diagnosis and also whether or not the basic treatment effect varies with time:(Model 3a)γ=βtreatment effectXtreatment effect+βdiagnosis1Xdiagnosis1+βdiagnosis2Xdiagnosis2+ βageXage+βsexXsex+βethnicity1Xethnicity1+βethnicity2Xethnicity2+βmarital1Xmarital1+ βmarital2Xmarital2+βborough1Xborough1+βborough2Xborough2+βborough3Xborough3+ βtimeXtime+βMAPXMAP+βtreatment_effect × diagnosis1Xtreatment_effect × diagnosis1+ βtreatment_effect × diagnosis2Xtreatment_effect × diagnosis2+βtreatment_effect × borough1Xtreatment_effect × borough1+ βtreatment_effect × borough2Xtreatment_effect × borough2+βtreatment_effect × borough3Xtreatment_effect × borough3+ βtreatment_effect × timeXtreatment_effect × time+β0+υpersonZperson+υepisodeZepisode+ε.
As appropriate, insignificant interactions were removed, yielding model 3b.
-
Assuming that the related two-way interactions were significant, we tested for three-way interactions between (i) treatment effect, diagnosis and time and (ii) treatment effect, borough and time. The aim of this analysis was to examine whether or not the stratum-specific treatment effects of primary interest varied over time. Insignificant effects were removed from a subsequent model (model 4b):(Model 4a)γ=βtreatment effectXtreatment effect+βdiagnosis1Xdiagnosis1+βdiagnosis2Xdiagnosis2+ βageXage+βsexXsex+βethnicity1Xethnicity1+βethnicity2Xethnicity2+ βmarital1Xmarital1+βmarital2Xmarital2+βborough1Xborough1+ βborough2Xborough2+βborough3Xborough3+βtimeXtime+ βMAPXMAP+βtreatment_effect × diagnosis1Xtreatment_effect × diagnosis1+ βtreatment_effect × diagnosis2Xtreatment_effect × diagnosis2+βtreatment_effect × borough1Xtreatment_effect × borough1+ βtreatment_effect × borough2Xtreatment_effect × borough2+βtreatment_effect × borough3Xtreatment_effect × borough3+ βtreatment_effect × timeXtreatment_effect × time+βtreatment_effect × diagnosis1 × timeXtreatment_effect × diagnosis1 × time+ βtreatment_effect × diagnosis2 × timeXtreatment_effect × diagnosis2 × time+βtreatment_effect × borough1 × timeXtreatment_effect × borough1 × time+ βtreatment_effect × borough2 × timeXtreatment_effect × borough2 × time+βtreatment_effect × borough3 × timeXtreatment_effect × borough3 × time+ β0+υpersonZperson+υepisodeZepisode+ε.
-
We looked for evidence that the overall effect of treatment over time altered after CAG implementation. This required the addition of an interaction between the treatment effect and the post-CAG indicator variable, together with a three-way interaction between the treatment effect, the post-CAG indicator and calendar time:(Model 5)γ=βtreatment effectXtreatment effect+βdiagnosis1Xdiagnosis1+βdiagnosis2Xdiagnosis2+ βageXage+βsexXsex+βethnicity1Xethnicity1+βethnicity2Xethnicity2+ βmarital1Xmarital1+βmarital2Xmarital2+βborough1Xborough1+ βborough2Xborough2+βborough3Xborough3+βtimeXtime+ βMAPXMAP+βtreatment_effect × diagnosis1Xtreatment_effect × diagnosis1+ βtreatment_effect × diagnosis2Xtreatment_effect × diagnosis2+βtreatment_effect × borough1Xtreatment_effect × borough1+ βtreatment_effect × borough2Xtreatment_effect × borough2+βtreatment_effect × borough3Xtreatment_effect × borough3+ βtreatment_effect × timeXtreatment_effect × time+βtreatment_effect × borough1 × timeXtreatment_effect × borough1 × time+ βtreatment_effect × borough2 × timeXtreatment_effect × borough2 × time+βtreatment_effect × borough3 × timeXtreatment_effect × borough3 × time+ βtreatment_effect × MAPXtreatment_effect × MAP+βtreatment_effect × timeXMAPXtreatment_effect × timeXMAP+ β0+υpersonZperson+υepisodeZepisode+ε.
-
Assuming that the added effects in model 5 were significant, we tested whether or not the time trend in the borough- or diagnosis-specific treatment effect varied before and after CAG implementation. This required the fitting and testing of a four-way interaction term between treatment effect, time, borough or diagnosis and the post-CAG indicator:(Model 6)γ=βtreatment effectXtreatment effect+βdiagnosis1Xdiagnosis1+βdiagnosis2Xdiagnosis2+ βageXage+βsexXsex+βethnicity1Xethnicity1+βethnicity2Xethnicity2+ βmarital1Xmarital1+βmarital2Xmarital2+βborough1Xborough1+ βborough2Xborough2+βborough3Xborough3+βtimeXtime+ βMAPXMAP+βtreatment_effect × diagnosis1Xtreatment_effect × diagnosis1+ βtreatment_effect × diagnosis2Xtreatment_effect × diagnosis2+βtreatment_effect × borough1Xtreatment_effect × borough1+ βtreatment_effect × borough2Xtreatment_effect × borough2+βtreatment_effect × borough3Xtreatment_effect × borough3+ βtreatment_effect × timeXtreatment_effect × time+βtreatment_effect × MAPXtreatment_effect × MAP+ βtreatment_effect × borough1 × timeXtreatment_effect × borough1 × time+βtreatment_effect × borough2 × timeXtreatment_effect × borough2 × time+ βtreatment_effect × borough3 × timeXtreatment_effect × borough3 × time+ βtreatment_effect × borough0 × time × MAPXtreatment_effect × borough0 × time × MAP+ βtreatment_effect × borough1 × time × MAPXtreatment_effect × borough1 × time × MAP+ βtreatment_effect × borough2 × time × MAPXtreatment_effect × borough2 × time × MAP+ βtreatment_effect × borough3 × time × MAPXtreatment_effect × borough3 × time × MAP+β0+υpersonZperson+υepisodeZepisode+ε.
For psychotherapy episodes, we followed an identical procedure, except that we used total scores on the CORE-10, which was the more frequently used outcome measure within the psychotherapy services.
Safety
We investigated safety only for CMHT patients as these made up the largest group.
As described earlier, we worked first with the A&E data set, which consisted of a set of CMHT episodes, divided into quarterly time bands and joined to a set of psychiatric liaison consultations for self-harm. This was treated as a multiple failure time data set, that is, once a person presented to A&E with self-harm, he or she was treated afterwards as having entered the ‘at-risk’ pool.
First, we calculated raw rates for each quarter and graphed these for each borough, restricting our analyses to those with a non-psychotic disorder.
Next, we constructed a series of exponential regression models:
-
Looking at each borough separately, we regressed the rate of self-harm presentation against time, whether or not the period of CMHT treatment ended in the quarter, whether or not there was a change of team in the quarter, whether there was a change of care co-ordinator or care co-ordination finished in the quarter, age, sex and ethnicity. Following exploration of the data, an interaction term was also fitted between change of team and change/end of care co-ordinator:ln λ(t)=βtimebandXtimeband+βageXage+βsexXsex+βethnicity1Xethnicity1+βethnicity2Xethnicity2+βCMHT_end(t)XCMHT_end(t)+βteam_change(t)Xteam_change(t)+βCC_end(t)XCC_end+ βteam × CC(t)Xteam × CC(t)+β0+ε.
-
We constructed a set of regression models that were identical except that they allowed the trend in the rate of self-harm presentation to vary before and after CAG implementation. We compared the models using LR testing:ln λ(t)=βtimebandXtimeband+βpostCAGXpostCAG+βtimebandXpostCAGXtimebandXpostCAG+βageXage+βsexXsex+βethnicity1Xethnicity1+βethnicity2Xethnicity2+βCMHT_end(t)XCMHT_end(t)+βteam_change(t)Xteam_change(t)+βCC_end(t)XCC_end+βteam × CC(t)Xteam × CC(t)+β0+ε.
We then went on to perform an analogous set of analyses with the acute admission data set, described earlier.
Patient centredness
As only a very small proportion of trust service users complete Patient Experience Data Information Centre (PEDIC) satisfaction questionnaires and the use of these questionnaires began around the same time as CAG implementation, we did not attempt to analyse patient satisfaction data. Therefore, our analysis of patient centredness consisted of an analysis of waiting time or, more precisely, current wait time among patients accepted for treatment but not yet seen for a face-to-face appointment.
As with previous analyses, we analysed each borough separately and began with a graphical analysis. For each day, 25th, 50th and 75th centile values of current waiting time were calculated and graphed against calendar time for each borough. Following visual inspection of plots, we performed a t-test of mean current waiting time, comparing waiting time before and after CAG implementation. This analysis was performed for CMHT episodes and for psychotherapy episodes.
Overall project timetable
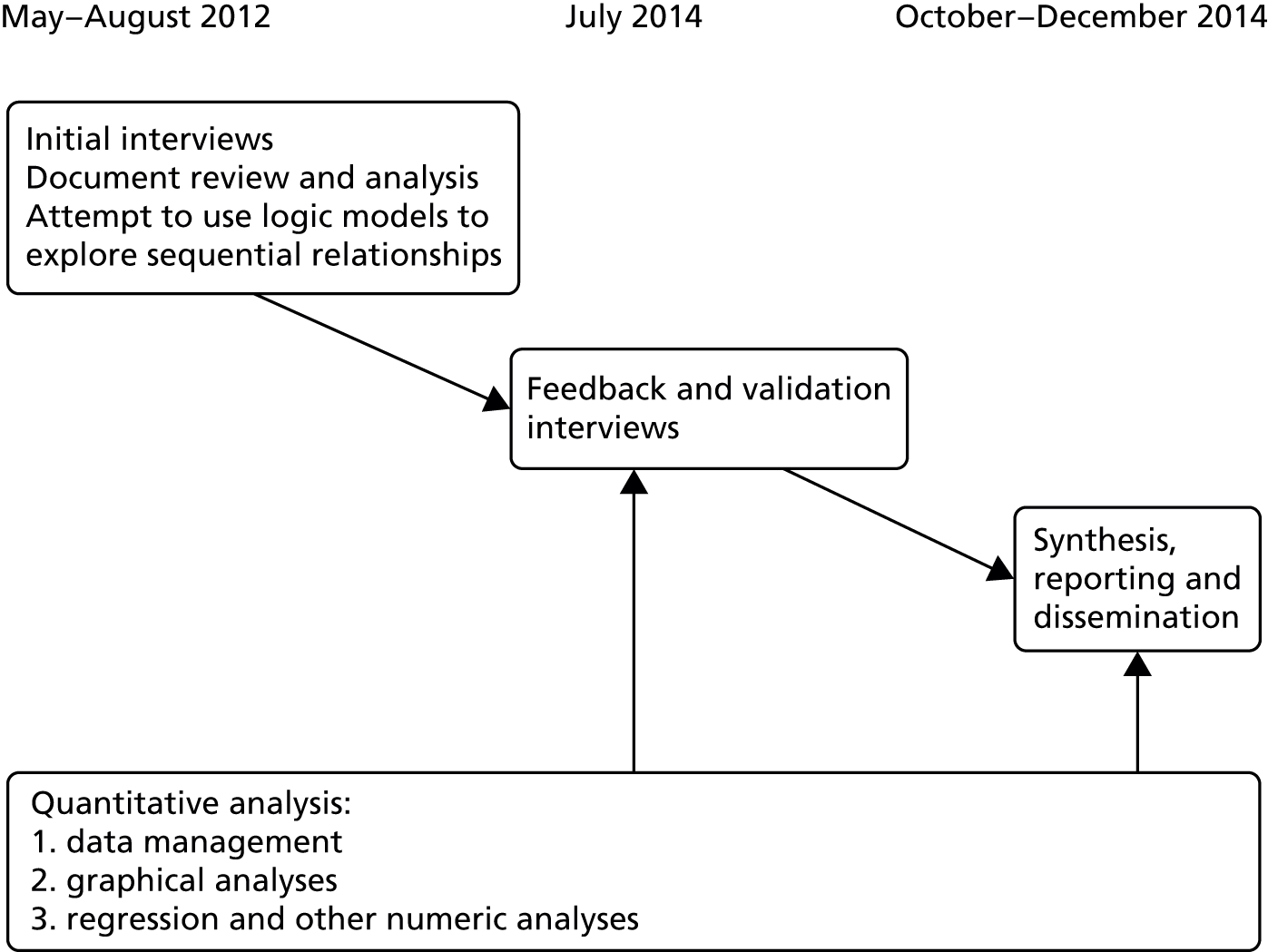
The timing of data collection and analysis for the project as a whole is set out in Figure 1.
FIGURE 1.
MAPLE study design and timeline.
Ethics and research governance
Neither ethical nor research governance approval was required for the quantitative analysis, which was based on fully anonymised data. The qualitative component of the study was considered and approved by the London (Harrow) Research Ethics Committee (12/LO/0363) and was approved by SLaM’s Research and Development Office. Consent forms and information sheets are provided in Appendix 4.
Chapter 3 Qualitative results
In this chapter we set out the results of our qualitative investigation, which was based on a combination of documentary sources, an initial literature review and interviews with a range of stakeholders.
Background to the changes begins by outlining the history of the organisations involved in or impacted by the CAG restructuring, before moving on to describe how these organisations embarked on the formation of a new AHSC, a process that was the starting point for SLaM’s decision to restructure with CAGs. We then consider what it was intended that the CAG restructuring would achieve, looking at documentary sources, but also setting out what our respondents saw as the need for change, and how their perspectives did or did not align with the public KHP vision. We introduce the topic of the financial climate within the NHS by considering how this may have influenced the decision to restructure and the timing of that restructuring.
In The Clinical Academic Group restructuring we then move on to the CAG restructuring itself, that is, the process of the transfer of services from the borough directorates to the new CAGs. We set out the details of the structural changes and the rationale provided for them. We make reference to similar service-line reorganisations in other London mental health service providers. Finally, we set out, based on our respondents comments, what appeared to be the key context–mechanism–outcome configurations associated with the CAG restructuring.
In Care pathways we look at SLaM’s motivations for using care pathways, before an excursus into the literature on care pathways. The remainder of the section describes the MAP CAG’s work to develop and use care pathways, examining which aspects of this work appeared to succeed and why.
In Influences originating outside the Clinical Academic Group programme we consider the other contextual influences that were of critical importance in determining what changes the MAP CAG made and why. In particular, we examine financial issues and the influence of relationships with commissioners. Having set out the mechanisms through which change was sought, and the other contextual factors, we then proceed to look at the major changes that the MAP CAG made and consider the balance of influences over these changes. Finally, we consider briefly what effects being part of the KHP might have had over the MAP CAG.
In Views of service users we look at what service users knew about the CAG programme, what their priorities and preferences were and how the CAG programme related to these.
Finally, in The situation in 2014 we summarise evidence from our second wave of data collection in 2014, looking at ongoing issues and examining what developments there had been since our original investigation.
Background to the changes
The trust and the Institute of Psychiatry: origins and development
The organisational change whose results we attempt to evaluate here most centrally involves an NHS foundation trust – SLaM – whose history is inextricably linked to a predominantly postgraduate research and teaching institute, the IoP at King’s College London (KCL).
The South London and Maudsley NHS Foundation Trust as an organisation dates from 1999, when it was formed by a merger between the Bethlem and Maudsley NHS Trust, the mental health services provided by Lambeth Healthcare NHS Trust and Lewisham and Guy’s Mental Health NHS Trust. Although the last two trusts operated services that mainly served their local populations, the Bethlem and Maudsley NHS Trust had less typical features; indeed, its two constituent hospitals have a unique place in the history of mental illnesses and their treatment: the Bethlem Royal Hospital is the oldest psychiatric hospital in Europe, having operated continuously since 1247, whereas the Maudsley Hospital and its associated medical school (now the IoP) were established expressly to support research into mental disorders and their treatment19 and became pre-eminent in this field in the post-war period. 20 Before the formation of the NHS, the Bethlem Hospital operated as a voluntary hospital, whereas the Maudsley was supported by the London County Council. After the formation of the NHS, the two hospitals were merged under one board, an arrangement that persisted until the formation of SLaM. Although over time the Bethlem and Maudsley acquired greater responsibility for local service provision, especially in the Camberwell area, spanning the London boroughs of Lambeth and Southwark, and later in Croydon, to some extent the hospitals retained their original position as providers of specialised tertiary health care. At the point of the merger between the three trusts, a directorate structure was adopted that in part recognised the unusual nature of many of the services provided by the Bethlem and Maudsley as well as the fact that some services served local populations that extended beyond a single borough. Therefore, as well as borough directorates serving Croydon, Lambeth, Lewisham and Southwark, a National and Specialist Directorate was established that included some services of a tertiary nature as well as some services that served more than one local borough; notably, this included the Maudsley Psychotherapy Department.
The South London and Maudsley NHS Foundation Trust became the 50th NHS foundation trust in 2006. 21 By 2010 (the year in which the CAG structure was adopted) it had come to provide services to a population of around 1,200,000 people resident across the London boroughs of Croydon, Lambeth, Lewisham and Southwark. The structure of those services was in many cases determined by national policy, for example home treatment teams and early-onset teams in line with the National Service Framework. 22 It also continued to provide a range of tertiary services.
The Maudsley Hospital was associated from its inception with a postgraduate medical school, which, since 1948, has been called the IoP. Initially, the IoP was administered on behalf of the University of London by the British Postgraduate Medical Federation. In August 1997 the British Postgraduate Medical Federation was disbanded and the IoP was absorbed as a separate faculty into KCL, but remained apart from KCL’s School of Medicine, which itself subsequently merged with the United Medical and Dental Schools of Guy’s and St Thomas’ Hospitals. The links between SLaM and the IoP have always been very close, with many IoP staff also holding contracts with SLaM and much research being carried out within SLaM. (In 2014, the IoP was renamed as the Institute of Psychiatry, Psychology and Neuroscience, but it is referred to here under the name current during the study period.)
Academic Health Science Centres
Academic Health Science Centres are partnerships between one or more universities and health-care providers that aim to break down barriers and increase co-operation, and which combine basic and translational health research, clinical care and education to improve health care. In 2007 a review of health care in London recommended that a number of AHSCs should be created,23 and in 2009 five NHS/university partnerships were designated as AHSCs by the Department of Health in England. One of these was KHP, which brings three NHS foundation trusts – Guy’s and St Thomas’, King’s College Hospital and SLaM – together with KCL, which includes the IoP as well as KCL’s School of Medicine. Guy’s and St Thomas’, King’s College Hospital and SLaM together provide almost all secondary health care across the London boroughs of Lambeth and Southwark and provide a significant portion of secondary and tertiary health care across the rest of south and south-east London.
King’s Health Partners and Clinical Academic Groups
To transcend the traditional distinction between a hospital and its associated medical school, AHSCs typically require new bodies to be created that allow for joint working between the hospital and the university; this may require the modification of existing departmental structures. 24,25 While preparing for its application for accreditation as an AHSC, KHP developed the concept of a CAG as the means by which the AHSC would operate. To demonstrate the practicality of the concept, four pilot CAGs were established in advance of the initial bid for accreditation. It is clear from documentary sources that CAGs have been, and continue to be, central to KHP’s operation. Thus, first among KHP’s stated objectives was to ‘drive the integration of research, education and training, and clinical care for the benefit of patients through our new CAGs’. 26 In more recent documents, CAGs are described as the ‘integration engines’ of the AHSC. 27
An early KHP document describes the structure and rationale of the KHP CAGs as follows:
CAGs will bring together, within a single management structure, academics, clinicians and managers whose work is focused on a single specialty or group of related specialties. Each CAG will be responsible for developing a strategy which addresses the tripartite mission of clinical care, research and education and the CAG leaders will be accountable to KHP for delivery of this tripartite agenda. The CAG model allows the partners to maintain their independent external accountabilities (for clinical delivery by the NHS Foundation Trusts and for academic performance by KCL) which the partners are not permitted to delegate. The CAG leaders will be the principal change agents required to achieve the necessary cultural transformation through supporting changes in structures, policies and incentives. 28
The relationship between CAGs and the broader KHP governance structure was defined from the outset. Broadly, these governance arrangements consisted of a partnership agreement between the partner trusts and KCL, a Partnership Board and an Executive. In relation to the CAGs:
[The Executive] will [. . .] be responsible for the development, co-ordination and performance of CAGs, which will progressively be brought within the formal governance framework through an internal approval process that will ensure they are fit for purpose. This process, which will be managed by the Executive on behalf of the Partnership Board, will require each CAG to demonstrate that it has strong leadership, a coherent strategy and a credible business plan to deliver that strategy. 28
In line with these principles, KHP devoted a small project team to support partner trusts in developing CAGs and preparing submissions for CAG accreditation. This team was complemented within SLaM by the creation of a team dedicated to CAG development, with the two teams working closely together. KHP’s original intention was that each CAG should complete three modules with progress documented in three documents (the accreditation submission) that corresponded to each of the modules. In the end, module 3 was never requested and remained on hold. However, each CAG did make submissions for module 1 and module 2. For module 1, each CAG was required to (a) define an Executive ‘which will be involved in delivering CAG accreditation and the development of the CAG following this’29 and (b) define a communication and engagement plan for internal and external use. For module 2, each CAG was required to (a) set out a clinical strategy addressing quality and productivity and describing CAG innovations, and to (b) set out a research strategy and (c) set out an education and training strategy.
A point that is of critical importance for the present evaluation is that CAGs were innovations that proved to be susceptible to different modes of implementation. As noted in the description of CAGs reproduced above,28 the scope of the KHP CAG programme was explicitly limited so that each hospital partner would retain responsibility for the governance of its clinical services. At Guy’s and St Thomas’ and King’s College Hospital, CAGs were developed as additional structures that supported collaboration between clinicians and academics and between clinicians in different trusts, but which did not take responsibility away from the existing management structure for service delivery. However, SLaM elected to develop CAGs as new organisational units that entirely replaced the existing management structures for clinical services. It is this decision and its consequences that are the focus of our evaluation. Each SLaM CAG was incorporated as a separate internal unit that was charged with responsibility for all aspects of the delivery of defined services within a defined budget and that replaced the operational units that had previously had these responsibilities. This meant that responsibility for both clinical delivery and the development and implementation of a strategy to deliver KHP’s tripartite agenda of research, education and clinical service was devolved to the same managerial units.
This decision was not solely influenced by the need for SLaM to meet its commitments to the AHSC. Rather, it was intended that the restructuring into CAGs would also lead directly to improvements in clinical services. How this might occur was stated most clearly and succinctly in a ‘Frequently Asked Questions’ document distributed to SLaM staff in 2009, in which the question ‘How will mental health Clinical Academic Groups actually work?’ was answered as follows:
Our aim is to provide more specialist services and more focused interventions. We have been discussing for some time the need to improve consistency and have greater clarification about what we are providing and for whom. Care pathway development is an important cornerstone for Clinical Academic Group development.
Other key themes include promoting the integration of physical, psychological and social care, the emphasis on recovery and the interface between acute and mental health services. Our Clinical Academic Groups will be based on a multi-disciplinary approach to care and treatment.
Finally, and crucially, Clinical Academic Groups will empower teams to be innovative. One of the ways we will achieve this is through the development of Service Line Management at SLaM where teams have detailed information about the services they are providing, how effective they are and how much they cost. 30
As noted in Chapter 1, our view is that the key elements of the CAG restructuring were (1) the restructuring itself and (2) the development of a way of working with care pathways. This early document does not entirely reflect this. In our interviews we saw little evidence of the CAG restructuring having led to the changes listed in the second and third paragraph quoted above, including the development of service line management at team rather than CAG level. In contrast, the notion of care pathways being the ‘cornerstone’ of CAG development was fully borne out by interview and other documentary evidence and, moreover, the linkage between care pathway and CAG development postulated here reflects exactly the later course of development, in which care pathways became intertwined with the management of the CAG.
Having sketched out what SLaM’s CAG restructuring was, and how the entry into KHP provided an opportunity for it to happen, we will next consider why SLaM’s leadership might have decided to undertake the restructuring at that particular time. This was a topic that we discussed with our staff respondents. In the next sections we set out why those respondents thought that there was a need for change, the extent to which the KHP vision aligned or could be made to align with what was perceived to be the right strategic direction for SLaM, and what elements of the external environment might have favoured SLaM’s decision to embark on the CAG programme at the time that it did.
The need for change
In mid-2012, around 18 months after the CAG ‘go live’ date of 1 October 2010, we asked our respondents to reflect on the reasons why SLaM had undergone the CAG programme. Broadly, and for a variety of reasons, our respondents (identified as R1, R2, etc.) told us that the old system simply wasn’t working any more:
We had to look at some other way of delivering services that could meet more needs or a wider range of needs. And we weren’t going to do that with the old model.
R6
Fleshing out what this meant in relation to the MAP CAG, interviewees told us that:
-
the local services that the MAP CAG covered had developed in different boroughs in ‘very diverse ways that were not always very rational’ (R5)
-
central psychotherapy services had been managed by a National and Specialist Directorate that took referrals from the boroughs but were not linked to them managerially, with the result that ‘nobody had a coherent vision of psychological therapies in the Trust as a whole’ (R5)
-
many service users were being maintained within the secondary services when they did not need to be:
[Y]ou had an awful lot of people who would have been singularly maintained on depot medication in small doses or something to that effect and might have been seen once every six months or once every twelve months at an outpatient clinic. That was a hangover from previous generations, and, even amidst all the changes, that group had been maintained within the secondary services when they didn’t actually need to be.
R6
These problems were very long-standing and often related to issues that had not been resolved when SLaM was created from its three predecessor trusts. Overall, this situation was described by one interviewee (R5) as a ‘very mixed bag of parallel and incoherent services’.
Managers and senior clinical staff working in SLaM were well aware of these problems. They had sought to implement various changes at various times prior to the CAG programme and, indeed, one reason why SLaM was able to restructure rapidly with CAGs as operational units (as required by the KHP timetable) was that senior people in SLaM and the IoP had been considering approaches such as service line management and care pathways for some time and were therefore ready to embrace this new initiative. As one interviewee said:
a number of us were very involved in the London mental health group . . . so we already had quite a bit of information around the care pathway approaches, pros and cons . . . so we weren’t starting from scratch . . . The timing was perfect.
R2
That level of preparation notwithstanding, the organisational and managerial context into which the CAG programme was introduced was complex and somewhat fluid and the challenges faced were considerable. In the psychotherapy services, which it will be recalled had been divided between the borough directorates and the National and Specialist Directorate prior to the CAG restructuring, previous attempts to make changes had not succeeded:
The whole issue of the psychological therapies has been the elephant in the room for years. It’s the only part of the trust that was never really sorted out at the time [when SLaM was formed].
R1
In the case of Croydon, where the introduction of CAGs would require significant reorganisation of the generic CMHTs existing at that point to create assessment and treatment teams and support and recovery teams:
It was something that was being talked about – an option of what was available and where it could go in context of how we could provide services . . . I suppose, if you look across the other boroughs, most of them had already been working that way in some form or fashion.
R6
Similarly, the difficulty in recasting the relationship between primary care and secondary care was recognised as a long-standing problem in need of a solution, at least in some parts of the trust:
there’s been a bit of a history with the GP practices insofar as there has always been a reluctance to take cases back.
R6
In all, this meant that the reorganisation was seen as a natural next step:
It was a natural progression is the truth of it and it was almost strengthened and restarted but it was the next logical progression and so it didn’t feel odd to anyone.
R2
And the perceived inevitability of this change also meant that, regardless of whether particular individuals were enthusiastic or sceptical about the new structures being implemented, most worked positively towards the progression of this unavoidable reorganisation:
People are determined to make the change work.
R6
And this was partly driven by competition between CAGs to make their own section a success:
[Name] would have been influenced by what was happening in all the directorates because he would not want his directorate to fail, he would want it to get as far down the road as possible.
R6
In summary, there was pre-existing awareness of the need for change within SLaM, but previous attempts to make changes had not worked well. The general view was that the CAG programme provided a chance to overcome these difficulties and had come along at an appropriate time.
The King’s Health Partners vision and its relevance
The decision to form the AHSC and to use CAGs as the ‘integration engines’ of the new partnership was one that had been taken at high level in KCL and the partner NHS trusts in 2008 and 2009. However, the sense in which CAGs were critical to KHP and the sense in which they were critical to SLaM were not necessarily identical. Our respondents reflected in various ways on the relevance of the KHP vision of integrating research, education and clinical service. As we have noted earlier, there was, from the start, a contrast between KHP’s vision of CAGs as the means of advancing its ‘tripartite mission’ and the vision espoused by SLaM wherein CAGs would be the vehicles for other desirable changes to services. None of our respondents opposed the vision of clinical and academic integration espoused by KHP:
It is a sort of vision you can’t quarrel with, anybody would think, yeah that sounds good.
R3
However, it was clear that some leaders and senior managers within SLaM had additional and different reasons for supporting SLaM’s CAG restructuring. Even so, when our respondents discussed the practicalities of clinical work or management or even the work of transforming evidence into practice, they also described the challenges of relating the KHP vision to the everyday reality of their work. For example, one respondent working mostly in a clinical service told us:
[a] lot of people also felt: How does this relate to us on the ground and what we’re struggling with? So there was that, and a lot of real enthusiasm in a group of people but a lot of cynicism in another bit.
R3
A similar view was expressed by another respondent who informed us that:
the overarching rationale of King’s Health Partners . . . I mean that’s not something that feels terribly important to us on a day-to-day basis.
R5
Individual CAGs were required to report regularly to a KHP Performance Council and these sessions, especially, seemed to have been occasions that brought home the difference between the KHP vision and each CAG’s own aim to provide the best possible service within the resources available:
It’s interesting when we go to the KHP Performance Council and talk about what we’ve been doing, and the balance between talking about the KHP vision and talking about our external realities.
R1
Most strikingly, one of our respondents questioned whether or not KHP and CAGs were the best structures to take research and put it into practice:
We’ve already got in the IAPT services an excellent example of how research has been put into practice, it was done quickly and effectively and attracted a huge amount of money and it didn’t require King’s Health Partners to do any of it.
R5
In summary, the KHP agenda was generally seen as important as a driver of the SLaM CAG programme, but it was not the only factor. As one interviewee put it:
There were different voices when the CAGs were set up, there were clearly the KHP voice with their tripartite mission, there was also an internal voice which was very much about, is there a different way we can operationally manage services that might help us get through the next few years?
R1
The financial environment and the decision to restructure
The financial and economic crisis faced by the world economy in 2007–8 and its subsequent impact on NHS finances formed the wider background to the KHP CAG programme and SLaM’s decision to restructure using CAGs. In May 2009, the Chief Executive of the NHS, David Nicholson, made it clear that the recent era of increasing growth and capacity had come to an end and warned about the urgent need to plan for a much tighter financial environment: the NHS would need to release unprecedented levels of efficiency savings between 2011 and 2014 – between £15B and £20B across the service. 31
This was a contextual factor that was of decisive significance for the MAP CAG once established – a point to which we will return – but it was also important in securing support for the initial reorganisation and, most of all, for the decision to implement CAGs during the 2010–11 financial year rather than at a later date. Senior staff within SLaM and the IoP saw the CAG programme as an opportunity to look at services in a new way, and borough directors saw it as helpful because they were running out of ideas about how to maintain quality while continuing, as required, to take 3% per annum out of the budget for clinical services:
[T]hey seem to feel that they run out of ideas of how to do that on a borough basis and maybe having new structures that went across boroughs would help with making efficiencies and reorganising services in a different way.
R3
Overall, the harsh financial climate also increased pressure to make changes rapidly before things got even worse. In a sense, the KHP requirement that the CAG programme be implemented quickly was seen as fortuitous for SLaM; despite the rush, several interviewees believed that CAGs were introduced at the correct time:
We went into CAGs in quite a rushed manner . . . There was a decision taken that we’d either get on and do it now or we’d leave it for a year later. We were anticipating the degree of disruption about to come through with large efficiency savings and if we’d been trying to do it this year on top of the large amounts of money to come out then we would have been in quite a difficult position.
R1
The Clinical Academic Group restructuring
The South London and Maudsley NHS Foundation Trust’s approach to Clinical Academic Group definition
In the preceding section we described why the change to CAGs was seen as desirable, the extent to which the KHP ‘vision’ was relevant to the everyday reality of running services and how SLaM staff may have had a different view of the purpose of CAGs; we also identified the worsening financial climate as relevant to the decision to reorganise into CAGs as soon as possible. Now we move on to the CAG restructuring itself – the taking of a set of services and their recasting into groups of services managed by CAGs – asking why it took the form that it did. At the end of the section, based on our respondents’ comments, we set out how we see the CAG restructuring as the first element of the CAG programme and describe the context–mechanism–outcome configurations associated with it.
The decision about how areas of clinical and academic activity would be defined as CAGs was devolved from KHP to the partner trusts. As noted earlier, the additional challenge for SLaM was how to define CAGs in such a way that they would both meet the requirements set by KHP and be fit for the purpose of managing SLaM’s clinical services.
Some existing directorates, such as Mental Health of Older Adults, Child and Adolescent Mental Health and Addictions, already had responsibility for a defined area of practice throughout the trust and could be reshaped relatively easily as CAGs; indeed, the Mental Health of Older Adults Directorate was rapidly transformed into a pilot CAG. But SLaM’s adult mental health services were organised geographically, with borough directorates (in Croydon, Lambeth, Lewisham and Southwark) dividing work in adult mental health between four separate management units, each of which was responsible for a different geographical area. The solution to transforming these borough directorates into CAGs was sought primarily in the functionally specialised team types that had already developed at borough level. In some cases, these functional teams had arisen because of government policy and especially the NHS Plan,22 which mandated the creation of home treatment teams and first-episode psychosis teams; these teams were present across the four boroughs. Other forms of specialisation had arisen because of local initiatives, leading to differences between the boroughs. Most notably, Croydon had continued to operate generic CMHTs whereas the other boroughs had for several years prior to the CAG restructuring operated assessment and treatment teams, which mostly dealt with short-term treatment and therefore had a user population with a variety of diagnoses, including many with non-psychotic disorders, and support and recovery teams, which predominantly served people with severe mental illness. Croydon was also the only borough that operated a single psychotherapy service, with the other boroughs either using more than one service (Lambeth and Southwark) or being reliant on services provided outside the borough (Lewisham). However, despite the differences between boroughs, and the variable extent to which functional specialisation had occurred, it was reasonably accurate to present the eventual CAG structure as first and foremost ‘[b]uilding on differentiation and specialisation which has already taken place – e.g. Early Intervention in Psychosis and IAPT’. 32 When teams were divided between CAGs, a degree of correspondence was ensured between the nature of the population served and the name of the CAGs, for example the Psychosis CAG acquired responsibility for those inpatient wards and community services whose users mostly have severe mental illness, whereas the Psychological Medicine CAG became responsible for those services physically based in acute hospitals.
However, there were a number of other relevant considerations. The first of KHP’s stated objectives was to drive the integration of research, education and training. Reflecting this, the SLaM CAG groupings were also determined by the need to link to the IoP departments. Turnover and therefore financial viability of the proposed CAGs were also important, meaning that there were many cases in which teams could conceivably have been allocated differently but for the need to ensure that each CAG was of an adequate size. It also seemed that persuasive argumentation had had a role, as had political considerations. As one interviewee told us:
one of the reasons why we had Psych Med and MAP CAG separate was there was a lot of interest across KHP about the integration of physical and mental . . . so politically I think that CAG [Psychological Medicine] had to be developed as a separate entity. And of course it’s a very odd CAG because it’s also got all the crisis services in it, and they had to go there to make it a reasonable size.
R1
Why SLaM had chosen to create multiple adult mental health CAGs rather than a single adult mental health CAG was a question that it was difficult to satisfactorily address 2 years after the decision was taken. We understood that a major limiting factor had been size: a single adult mental health CAG would have been too large to manage.
The seven CAGs that SLaM finally decided on were:
-
Addictions
-
Child and Adolescent Mental Health
-
Developmental and Behavioural Medicine
-
Mental Health of Older Adults and Dementia
-
Mood, Anxiety and Personality Disorder
-
Psychological Medicine
-
Psychosis.
Of these seven CAGs, three together (Mood, Anxiety and Personality Disorder, Psychological Medicine and Psychosis) covered the adult mental health services that were previously managed by the four borough directorates, alongside some related services previously managed by the National and Specialist Directorate. The division of adult mental health services between three CAGs, and the functionally specialised nature of SLaM’s teams, meant that it was inevitable that many service users would move not just between teams but also between CAGs, whereas under the previous arrangements most service users would access services provided by a single directorate. For example, someone treated within an assessment and treatment team who was admitted via an A&E attendance to an inpatient ward would be the responsibility of three CAGs over that period.
Our present evaluation focuses mainly on the services provided by the MAP CAG. At the time of CAG formation these services consisted of:
-
Assessment and treatment teams in Lambeth, Lewisham and Southwark. (As noted above, these did not exist in Croydon.) These teams provided an entry point to community mental services for primary care referrals, initial assessment and, for those with non-psychotic disorders, some ongoing management. Longer-term case management for psychotic disorders was provided by the support and recovery teams that came to be managed by SLaM’s Psychosis CAG.
-
Other services previously managed by the borough directorates and primarily catering for users with non-psychotic disorders, for example psychotherapy services at St Thomas’ Hospital, serving many Lambeth service users, the Croydon psychology service and the intensive psychological treatment service at Guy’s Hospital, serving many Southwark service users.
-
Tertiary referral services for mood, anxiety and personality disorders previously managed within SLaM’s National and Specialist Directorate, for example the Affective Disorders Unit and the Crisis Recovery Unit.
-
Services mainly commissioned by local boroughs but, for historic reasons, managed within SLaM’s National and Specialist Directorate, for example the Traumatic Stress Service and the Maudsley Psychotherapy Service.
-
The IAPT services for Croydon, Lambeth, Lewisham and Southwark.
These services were, however, only the starting point for the operation of the MAP CAG; indeed, as we shall see, there was substantial change in the first years of operation of the MAP CAG.
The decision to appear to use psychiatric diagnosis as the basis for the names of two of the adult mental health CAGs did not have universal support:
I remember thinking very strongly at the beginning that using psychiatric diagnosis to make any division of anything is manifestly stupid because psychiatric diagnosis is such a feeble construct.
R5
The debate about what the CAG names meant and whether or not they were helpful was, for these reasons, a difficult and contentious one, and it went on long after the SLaM CAGs had been formally defined:
We had lots and lots of debates about the fact that the names of the CAGs were unhelpful and we would review it and change it at some point and of course no one has got round to doing that because what else you call them is really tricky. But a very common theme is the names aren’t helpful. The CAGs aren’t about diagnoses, they’re actually around needs and functions and trying to find a sensible way of grouping people together and providing something sensible and standardized.
R2
However, an interpretation of what CAGs are about in terms of needs and functions does not escape the difficulties associated with the imprecision of psychiatric diagnosis. The precise nature of peoples’ mental health needs is often not clear. This was a particular problem for the MAP CAG because, as we saw above, the services it covered included the initial assessment of people referred from primary care, or presenting as emergencies, with undiagnosed problems:
A good example is the group of people that come to us when we’re not even sure yet and indeed have as many social and other difficulties as they might have mental health difficulties . . . they are a large group . . . how do you standardise what you do for those people and indeed how do you make decisions about when they should be on one of the other defined pathways.
R2
To this extent the ‘MAP’ CAG was misnamed. As another respondent said:
[The MAP CAG] is providing the assessment function, the front door to primary care for everything . . . I spend a lot of time engaging with people with psychosis because you can’t pass them on to the psychosis CAG until they are engaged and assessed and stabilised which is often a very lengthy and time-consuming process. It would be a complete mistake to think that we are services for common mental disorders or even for mood, anxiety and personality, we do all sorts of stuff.
R5
Clinical Academic Groups and service lines
The South London and Maudsley NHS Foundation Trust was not the only mental health service provider that decided around the same time to recast its borough-based structure into a structure of operational units based on diagnosis or need or the nature of the service provided. In London alone, several other mental health NHS trusts underwent similar reorganisations during the same period, discarding borough-based management structures in favour of structures that were similar to SLaM’s CAGs. 33–36 This underlying similarity is disguised by the fact that all of these other trusts called their new operational units service lines, whereas SLaM called them CAGs. Yet, with the exception of their having academic as well as managerial and clinical leadership, SLaM’s CAGs conform just as closely to the concept of a service line and it would be reasonable to describe SLaM’s CAGs as service lines modified because of the process of entering an AHSC.
Service line management has been defined as:
a system in which a hospital trust is divided into specialist clinical areas that are then managed, by clinicians, as distinct operational units. SLM enables clinicians and managers to plan service activities, set objectives and targets, monitor financial and operational activity and manage performance. Service-line reporting provides the necessary data on financial performance, activity, quality and staffing
Foot et al. (p. 2)37
Service lines have also been described as ‘the units from which the trust’s services are delivered, each with their own focus on particular medical conditions or procedures and their own specialist clinicians. Each unit also has clearly identified resources, including support services, staffing and finances’ (p. 2). 38 Service line management was introduced into health care in the 1980s in the USA and since the mid-2000s it has been extensively promoted in the NHS by Monitor, the foundation trust regulator, who have sponsored national conferences on the topic and published a set of toolkits intended to support foundation trusts on its introduction. 39
Why then did SLaM and these other London mental health trusts attempt to introduce service lines at the same time? The context common to SLaM and the other trusts was twofold: the support of the foundation trust regulator Monitor for service line management and the structure of the payment mechanisms being developed for mental health services in England. For example, a presentation to Monitor by SLaM’s then Chief Executive (Stuart Bell) noted that mental health Payment by Results (PbR), at that time under development, would provide funding on a per diem basis at ‘needs-based cluster’ level, with these needs-based clusters roughly representing different levels of service need. 32 Reorganisation by service line would group patients according to a single funding stream, matching service expenditure to revenue for each stream.
Despite the similar motivation for trusts to adopt service lines, the resulting structures showed considerable variation (Table 2) and we assume that local factors were a major determinant, as was true of SLaM when it defined its CAG structure. There was, however, a consistent difference between SLaM and the other London providers in the treatment of inpatient services and other crisis services, including home treatment teams: all other providers managed these through a single service line whereas SLaM instead divided these acute services between the Psychological Medicine CAG and the Psychosis CAG.
| South London and Maudsley CAGs | Camden and Islington service lines | Central and North West London service lines | Barnet, Enfield and Haringey service lines |
|---|---|---|---|
| Mood, Anxiety and Personality | Community Mental Health | Assessment and Brief Treatment | Common Mental Health Problems |
| Community Recovery | Severe and Complex Non-Psychotic | ||
| Psychosis | Rehabilitation and Recovery ± Outreach | Rehabilitation | Psychosis |
| Psychological Medicine | Acute | Acute Mental Health | Crisis and Emergency |
| Psychological Medicine | Common Mental Health Problems | ||
| Eating Disorders | Severe and Complex Non-Psychotic | ||
| Behavioural and Developmental | Offender Care | Forensic | |
| Learning Disability | |||
| Child and Adolescent | Child and Adolescent | Common Mental Health Problems | |
| Severe and Complex Non-Psychotic | |||
| Addictions | Substance Misuse | Addictions | |
| Mental Health of Older Adults and Dementia | Ageing and Mental Health | Older People and Healthy Ageing | Dementia/Cognitive Impairment |
Mechanisms of change associated with the Clinical Academic Group restructuring itself
Finally, we turn to the question of the mechanisms through which we anticipated that the CAG restructuring itself might lead to change. Ultimately, we approached this question, and the related question of the effects of care pathways, through the framework of context–mechanism–outcome configurations provided by realistic evaluation. 2 The structure of inputs, activities, outcomes and outputs provided by logic modelling11 did not seem to provide a helpful framework for our developing thinking.
The main mechanism through which our respondents suggested that the CAG restructuring would lead to change was simply expressed as more effective oversight: similar services would be managed together and viewed as a whole, as well as individually. This theory is very similar to that proposed in the literature on service line management, in which the new structures give clinicians and managers joint control over production processes that have previously been separated between different management divisions of the health-care provider. 40 How context determines the outcomes of this mechanism really inheres in the idea of oversight: what is seen determines what is done. For example, in the case of SLaM’s psychological therapy services:
nobody had a coherent vision of psychological therapies in the Trust as a whole and of course as soon as we acquired this very mixed bag of parallel and overlapping and incoherent services, we were faced with an immediate management challenge to bring some order and rationality into that.
R5
A second mechanism was the initial CAG restructuring precipitating change through the need for ‘CAG compliance’. Because the CAG management structures were based on a particular model of team structure, in those cases in which the local team structure did not fit with that model it was inevitable that further team-level restructuring would occur. This applied to the services in Croydon, which had continued to operate as generic CMHTs up until the introduction of CAGs. These teams needed to be reorganised into separate MAP and support and recovery teams (the latter being operated by the Psychosis CAG). The literature on team configurations in adult mental health services is limited to the Psychiatric Research in Service Management (PRiSM) study performed in the 1990s, which compared an area that established separate acute and continuing care teams with an area that established a generic CMHT. 41,42 Patients in the sector served by the acute and continuing care teams had slightly greater increases in met needs, satisfaction and quality of life than patients in the sector served by the generic CMHT, but this was associated with costs that were 10% greater relative to the other sector, although overall costs declined in both sectors. Overall, this suggests that the effects to be expected from changing from generic CMHTs to separate teams are limited. Despite this, SLaM was not alone in making such changes. As one of our respondents pointed out:
this kind of move is happening across the country sort of connected with service line management, so most Trusts are developing services that primarily see a group of patients with similar . . . umm . . . kind of PbR clusters.
R1
Again, the role of context here is fairly straightforward: only because SLaM had a particular group of services that did not fit with its chosen structure was it necessary to reorganise at team level. Had SLaM chosen differently in relation to its CAG structure or had the existing team structure been different, this mechanism would not have generated the same outcomes.
A third, and final, mechanism was through changes to accounting arrangements. In essence, the CAG restructuring led to a reassembly of teams that, in the case of the MAP CAG, made financial difficulties at team level and CAG level obvious in a way that they had not been before, with the contextual factor of team-level deficits interacting with new CAG-level accounting arrangements to precipitate a major reorganisation of psychology and psychotherapy services. Again, the interaction between context and mechanism was essential: had the MAP CAG not encompassed teams that had received long-standing cross-subsidies from other services now outside the MAP CAG, this mechanism would not have operated.
Care pathways
Introduction
In the preceding section we considered the CAG restructuring itself as the first programme element within the CAG reorganisation and suggested three mechanisms through which the CAG restructuring itself might have led to change. As previously noted, both documentary sources30 and our respondents placed particular stress on the role of care pathways as the means through which CAGs might bring about desirable change. In this section it is to this second programme element that we turn.
Care pathways and consistency of care
A key aim of the SLaM CAG programme was to improve the consistency of the services being offered. This was seen as a matter of principle:
There were very general principles about consistency of care, consistency of standards, saying to service users this is what you should expect from us, being able to say to commissioners this is what you’re getting or in some cases this is what you should be getting but you’re not and so all those principles were there and I suppose care pathways was always a shorthand for that . . . and it does link with service line management in a way because it’s saying a group of services, a service line this is what’s in it.
R1
But in practice these principles were not easily applied. The four boroughs had different histories and different levels of resources, and their commissioners had different intentions. Initially, there were some unrealistic expectations:
There were lots of fantasies around when MAP CAG came about . . . that the borough boundaries are gone and everyone is going to have the same. So boroughs that have felt they’ve not been able to provide the level of service they wanted to would find themselves able to. Clearly that was never going to be the case because of differing investment levels and commissioning intentions.
R1
In the longer term the different boroughs continued to have different models of care, albeit within the overall framework of the CAG programme. Interviewees suggested that in some ways this was useful because it helped to retain local ownership of the service:
From an organisational development point of view that one has to be very careful about trying to drive single sets of standards across a large area because we run the risk of alienating local staff and local systems and there’s probably a lot of theory around which will say successful services and ones that are generated through local problem-solving, local application and owned by the local system.
R1
It also meant that practice in one borough could be compared with that in another and the model that worked better could then be promoted:
So for example in our community services in [Borough A] we separated out assessment from treatment into two separate services and we pragmatically said OK, let’s see how that works and we’ll do it differently elsewhere. Interestingly and this is very interesting is that I think we believe that the [Borough A] model works better and we’re now going to unpick [Borough B].
R1
The complex nature of mental health needs also created other difficulties for the CAG. Many psychiatric service users have multiple needs. In practice, what this meant was that the patient groupings associated with each CAG were not, and could not be, completely discrete. Service users often needed to receive services across different CAGs and this meant that there were inevitable interfaces and overlaps between the CAGs:
inevitably when you divide services into chunks then you still get interface issues, or competitiveness between the new structures. Of course we are experiencing that now and even though we have various CAGs who apparently are discrete in what they’re trying to achieve, there are significant overlaps because patients move between them.
R1
The care pathways that were developed in each SLaM CAG following CAG definition were intended to provide ‘a clear and thorough description of every stage that is involved in receiving care and treatment at SLaM’,30 that is, across SLaM services as a whole, and were quite explicitly intended to address ‘interface issues’ that were potentially increased by the creation of CAGs. Thus:
Many people have mixed needs and will need to receive services across different Clinical Academic Groups. We need to make sure that this happens as smoothly as possible. In order to help us do this, we are developing ‘care pathways’ across all of our services. This involves developing a clear and through description of every stage that is involved in receiving care and treatment at SLaM. This will make it easier for people to understand what they can expect from our services, what happens next and what treatment options are available to them. And it means that there will be a clear process for moving between different services and different Clinical Academic Groups if that is what someone needs. 30
What are care pathways?
The last 20 years has been about putting building blocks of services in place, community teams, home treatment teams and different types of services. I think what we’re going to be concentrating on for the next 20 years and beyond, is what actually goes on within those teams, what treatment will be available, what’s the pathway of care that people are going to have on offer?
Stuart Bell, SLaM Chief Executive, 201143
Although care pathways are mentioned in KHP’s application for accreditation as an AHSC28 and also in the MAP CAG’s accreditation submission to KHP,29,44 their prominence was largely a SLaM-specific element of the transition to CAGs, rather than a requirement imposed by KHP. Our respondents were clear about the importance of the work of developing care pathways:
the work was around the care pathways as being a really important part of operationalising a new way of working . . . the CAGs were structures and they set a framework, the care pathways were actually about how we were going to organise things differently and operationalise.
R2
But as one interviewee (R5) reminded us, ‘the term care pathway is not adequately defined and it’s used in lots of different ways’ and ‘the care pathways have been used as the vehicle for rationalising services, but used in a very particular sense’.
However, before describing how SLaM set about defining and using care pathways we will review what care pathways are or, more precisely, the variety of understandings that there are of care pathways in the literature. Care pathways have been widely used in the USA, the UK and elsewhere for many years as a means of monitoring processes and processing times in a wide range of health-care systems, primarily to improve the efficiency of hospital care while maintaining or improving quality. 45,46 They also have a potential use as a basis for calculating costs for commissioning or reimbursement of service use, as with the PbR system currently in place in England. 6
However, the literature on care pathways also reports confusion about what they should be called (they have been variously referred to as ‘clinical pathways’, ‘integrated care pathways’, ‘critical pathways’, ‘care plans’, ‘care paths’ and ‘care maps’47). Evidence to support their effectiveness has, to date, been weak,7 particularly in mental health,6 but the disparate nature of the literature and the wide variety of interventions subsumed under the one description may make evidence synthesis difficult. A summary of the available evidence published in 2011 reported that some systematic reviews show that care pathways can improve some outcomes compared with usual care in some hospital settings, but there were no systematic reviews of their effectiveness in mental health care and there was a weak primary evidence base. 48
Care pathways have been defined differently by different commentators. The European Pathway Association (EPA), launched in 2004 [see www.e-p-a.org (accessed 8 October 2015)], defines care pathways as ‘complex intervention[s] for mutual decision making and organisation of predictable care for a well-defined group of patients during a well-defined period’ (p. 1)49 and lists five defining characteristics (Table 3). Kinsman et al. 50 built on the work of the EPA and others when preparing for a Cochrane systematic review on the impact of care pathways7 and similarly identified five defining characteristics. Not all had to be met when care pathways were identified for the review but the first characteristic was essential, along with three out of the other four (Table 3).
| EPA definition51 | Cochrane definition50 |
|---|---|
| Care pathways are complex interventions for mutual decision making and organisation of predictable care for a well-defined group of patients during a well-defined period They have the following characteristics:
|
Clinical pathways are tools used to guide evidence-based healthcare; an intervention is defined as a clinical pathway if it is a structured multidisciplinary plan of care and at least three of the remaining four criteria are met:
|
Overall, and as their common origins would suggest, there are many similarities between the EPA and the Cochrane definitions. But a key point of difference is whether or not care pathways should be regarded as complex interventions, leading to ongoing debate about how their impact should be assessed. 7,46 These debates about the nature and value of care pathways are matched by other debates about how they should be developed and implemented. These include discussion about the need to develop different care pathway models in different settings45 and about the importance of working on pathway development at different levels and balancing organisational and system requirements and patient involvement. 52
In the UK, care pathways were introduced in the 1990s, initially mainly in hospitals53 and as tools for designing care processes, implementing clinical governance and improving the quality of clinical care. 54 In 2007 the Darzi review of health care in London23 emphasised the importance of community services [‘The hospital is not always the answer’ (p. 4)] and of patient involvement and highlighted the need for care pathways for long-term conditions, including in psychiatric care ‘to enable service users and staff to know what is expected of different services and service users at each point in their care’ (p. 58). Given all this, senior staff in SLaM and the IoP were clear about the potential of care pathways and aware of the importance of implementation:
Care pathways can serve as a useful tool to reduce unacceptable variations in service provision and improve quality (e.g. reduce length of stay or multiple assessments, improving multi-disciplinary collaboration, increasing evidence based practice, providing a strategic approach to cost efficiency, enhancing user empowerment and putting recovery & social inclusion principles at the heart of services) but only if they are actually implemented [bold added for emphasis].
South London and Maudsley NHS Foundation Trust (p. 1)55
The KHP CAG programme provided a practical opportunity for SLaM and the IoP to introduce care pathways into everyday practice across the trust.
The South London and Maudsley NHS Foundation Trust’s way of developing care pathways: ‘high level’ to ‘implementation’
The SLaM-wide CAG development team anticipated that care pathway development would reflect the same principles that guided the CAGs and saw it as important that this exercise should be standardised across the SLaM CAGs:
So there’s thousands of bit of paper basically saying to CAGs this is what you’ve got to do in this kind of format, trying to make them kind of do something vaguely similar and we got as far as high-level care pathway.
R2
To this end a series of briefing documents was placed on the CAG development intranet site during 2009/10, which, taken together, illustrate what the CAG development team intended to happen during the initial stages of care pathway development.
An initial Framework for CAG Care Pathway Development55 stressed the need for a holistic approach that built on what had already been done (in SLaM as well as elsewhere) while identifying the processes that would work best in SLaM. It was therefore important to involve local stakeholders, including SLaM’s commissioners. The framework also provided guidance on what it described as an ‘appropriate’ level of standardisation of the care pathway development process. This included the need to balance a top-down and bottom-up approach, be in line with best practice, support the implementation of PbR and service line management and demonstrate delivery through an appropriate set of quality and outcome indicators for the care packages. As this document noted, ‘there needs to be a common framework for care pathway development but with sufficient flexibility so that there is local ownership’. 55 A set of brief guidance notes for the CAG care pathway working groups was also produced at the start of the care pathway development programme. 56 These notes described a ‘common chain’ of linked stages that was intended to apply to all of the care pathways that would be developed, namely (a) entry, (b) assessment, (c) diagnosis/formulation, (d) service and treatment options, (e) review and reassess and (f) exit. For each of these stages the guidance provided detailed advice about the information that should be sought when developing the pathway. Notably, this guidance explicitly intended SLaM’s care pathways to specify the evidence-based treatment options that should be available within any care pathway. However, and very importantly, there was a assumption from 2009 onwards that the care pathways that would be produced initially would be ‘quite high level in the first iteration and there will be much further work undertaken to refine and robustly implement them’. 55 This distinction between ‘high-level’ pathways (those limited to ‘common chain’ processes described above) and ‘implementation’ pathways (those including specific elements of treatment and care) continued to be an important feature of SLaM’s approach to care pathway development. It was included in the timetable set out for CAG development up to December 2010, 6 months before the withdrawal of the additional resources made available to support CAG development. The production of high-level pathways was required to be complete by September 2010, at which point these would be published on the trust intranet, and these high-level pathways would be required to be able to support contract negotiations with commissioners by the end of 2010,57 whereas the iterative process of transforming high-level into implementation pathways was not explicitly timetabled. Therefore, from the outset, the possibility was created that the development of care pathways at SLaM would not progress beyond high-level pathways, which, as they did not specify treatment options and were not intended as a guide for the delivery of individual care, significantly departed from the definitions of care pathways set out in Table 3.
A further briefing document of 10 ‘must-dos’ was also produced. 58 This encapsulated the ambitions of the care pathway development exercise, calling it ‘a radical agenda to transform services’, and also identified the constraints under which it was operating:
Care pathways must:
Not simply describe how we do things now – this is a radical agenda to transform services in the most innovative way possible.
Deliver efficiencies and increase productivity (no waste, no duplication, no delays) – in short, we need to provide quality services with fewer resources (20% to 30%).
Reflect the views and preferences of service users and their families as much as possible – ‘Lean’ services are built around what users value and they are evaluated according to user satisfaction.
Describe the level of consistency required across Trust services and eliminate inequities – we need to identify core standards that are reflected in compliance and target requirements.
Reflect commissioner requirements as set out in the developing PbR framework – we can’t provide what we don’t get paid for.
Describe service users’ journeys across organisational boundaries (internal & external) so that interfaces are managed effectively – working in partnership with primary care is a key issue.
Make the best use of research and best practice knowledge – local solutions making the best use of available resources (both people & money).
Integrate monitoring and evaluation so that there is a continual cycle of review and development – articulate standards in ways that can be measured using ePJS [SLaM’s electronic clinical record] (e.g. waiting times, duration of interventions, review frequency, assessment & outcome measures).
Reflect the guiding principles for CAG development within the overarching strategic framework for the Trust/KHP – including a significant focus on a holistic approach that integrates health and social care interventions and promotes recovery and social inclusion.
Work in practice – no point having a gold standard care pathway on paper and inadequate services on the ground. 58
Many of the messages in the earlier guidance were re-emphasised in this less formal document. But this less formal document was more trenchant, especially about the need to be pragmatic and ensure that the care pathways worked in practice and interacted with other components of the CAG programme, such as service line management and reporting.
Reflecting the stage that care pathway development had reached across SLaM’s CAGs by June 2011 when SLaM’s team dedicated to CAG development was dissolved, the final report to SLaM’s board at that stage recommended that the board consider how to continue the care pathway development process and, in particular, oversee a transition from high-level to detailed care pathway development. 59 For the most part, and looking across all of the CAGs, the report recognised that this work had not yet been undertaken at that point and that the high-level care pathways were the only outputs from the process of care pathway development that were in regular use. The sense at that time, therefore, was that the process of development was incomplete: ‘the high level pathways provide the framework but this now needs to be followed through in implementation pathways setting out the detailed guidance and protocols and based on appropriate service configuration’. 60 As noted above, this implied that the stage of development of care pathways at that time differed importantly from the ways that care pathways are ordinarily conceptualised.
Care pathway development in the Mood, Anxiety and Personality Clinical Academic Group
In contrast to the step-wise development process supported by the SLaM CAG development team, there was a very early effort in the MAP CAG to develop detailed clinical protocols for MAP services in a way that diverged quite markedly from the SLaM CAG programme detailed above. One interviewee (R1) told us that ‘when the [MAP]CAG started the care pathways were probably better described as clinical protocols; very, very detailed, very [inaudible] about what NICE said’.
In line with a recommendation in the 2007 review of health care in London,23 this exercise used the format used for the Map of Medicine as a basis [see http://mapofmedicine.com/ (accessed 1 December 2015)], but the content of the protocols was new or revised. The task was directed by the original academic director of the MAP CAG and involved vigorous discussion among clinical and academic staff. It resulted in the production of a 223-page manual of clinical protocols covering depression, depression in long-term medical conditions, panic disorder, generalised anxiety disorder, phobia, post-traumatic stress disorder, obsessive compulsive disorder and personality disorder. 61 They bore little resemblance to the common chain of stages referred to in the guidance above;56 instead, they seemed to have more in common with the detailed care pathways whose elaboration was intended to follow that of the high-level pathways.
At that early stage (late 2010 and early 2011) only one MAP pathway conformed to the model set out by SLaM’s CAG development team. This was developed from scratch to describe and manage the activity of assessment and treatment teams and looked very much like the high-level pathways produced by the other CAGs. As the 2011 progress report noted:
It is distinct from other [MAP] pathways in that it is non-diagnostic and non-evidence based, and aims to provide a helpful descriptor of the processes provided by the MAP CAG for referrals at a point when they [the patients] necessarily do not have a diagnosis and cannot be offered evidence based treatment. 59
By way of illustration, Figure 2 shows the panic disorder pathway and Figure 3 shows the engagement, assessment and stabilisation pathway. Later care pathway development occurred alongside service redevelopment, following the principle that care pathways should ‘[n]ot simply describe how we do things now’58 but should also be the basis for redesign. So the reorganisation of the borough-based psychology services in Lambeth, Lewisham and Croydon that took place in 2012 also involved the design of a high-level care pathway (Figure 4) at a similar level of abstraction to the engagement, assessment and stabilisation pathway. We were not aware of the MAP CAG having created any ‘before and after’ pathways; in the case of the integrated psychological treatment team pathway, it seemed that the preceding situation was too diverse to represent in this way. Therefore, the best guide to how care processes changed over time was provided by the quantitative data (see Chapter 4).
FIGURE 3.
Engagement, assessment and stabilisation pathway. SLaM 2012. 61 ADL, activity of daily living; AMHP, approved mental health practitioner; FACS, fair access to care services; HoNOS, Health of the Nation Outcome Scale; MCHT, Mental Health Clustering Tool; PHQ-9, Patient Health Questionnaire-9 items; SDS, self-directed support.
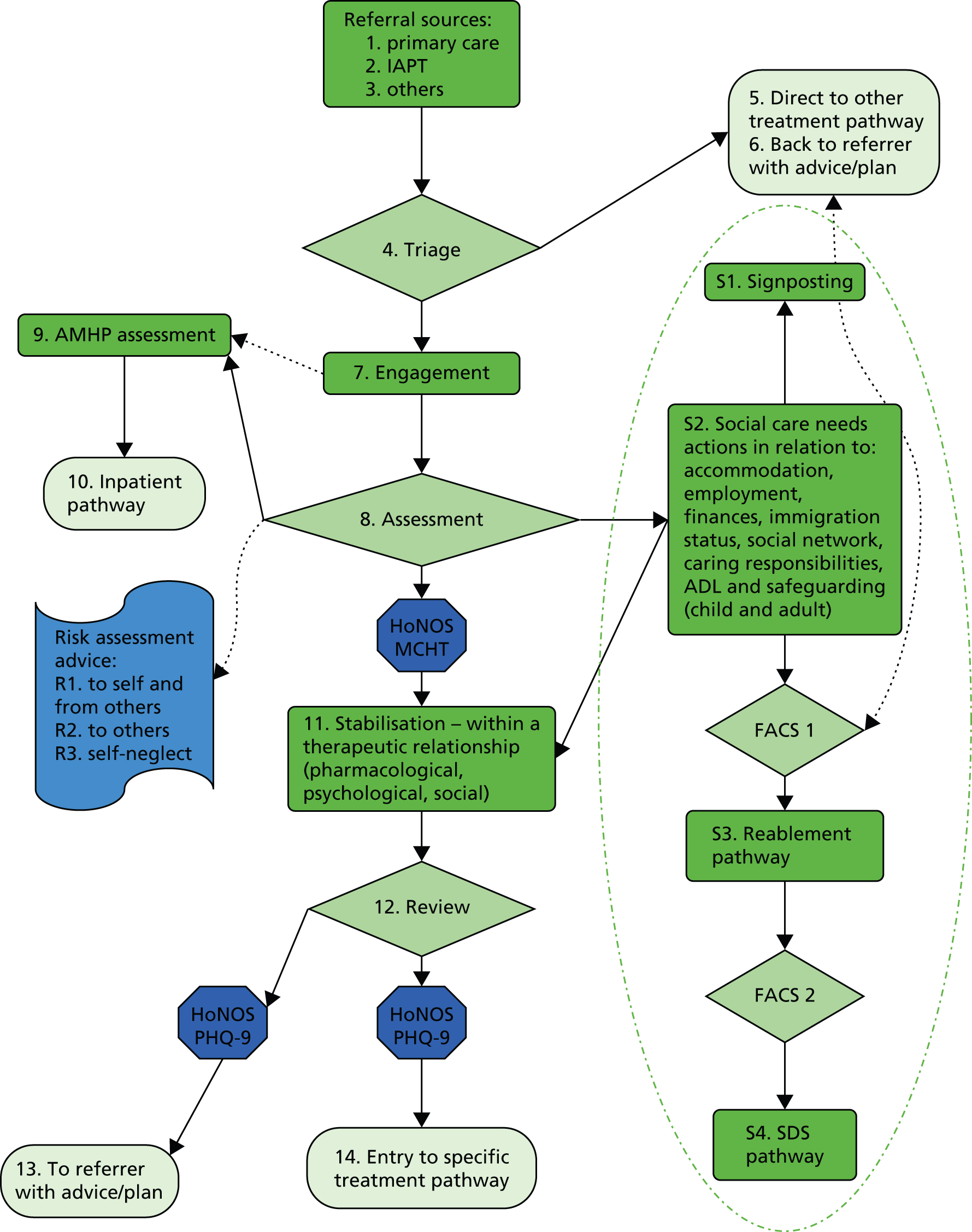
FIGURE 4.
Integrated psychological treatment team (IPTT) pathway, SLaM 2012. 62 ATT, assessment and treatment team; MH, mental health; PD, personality disorder.
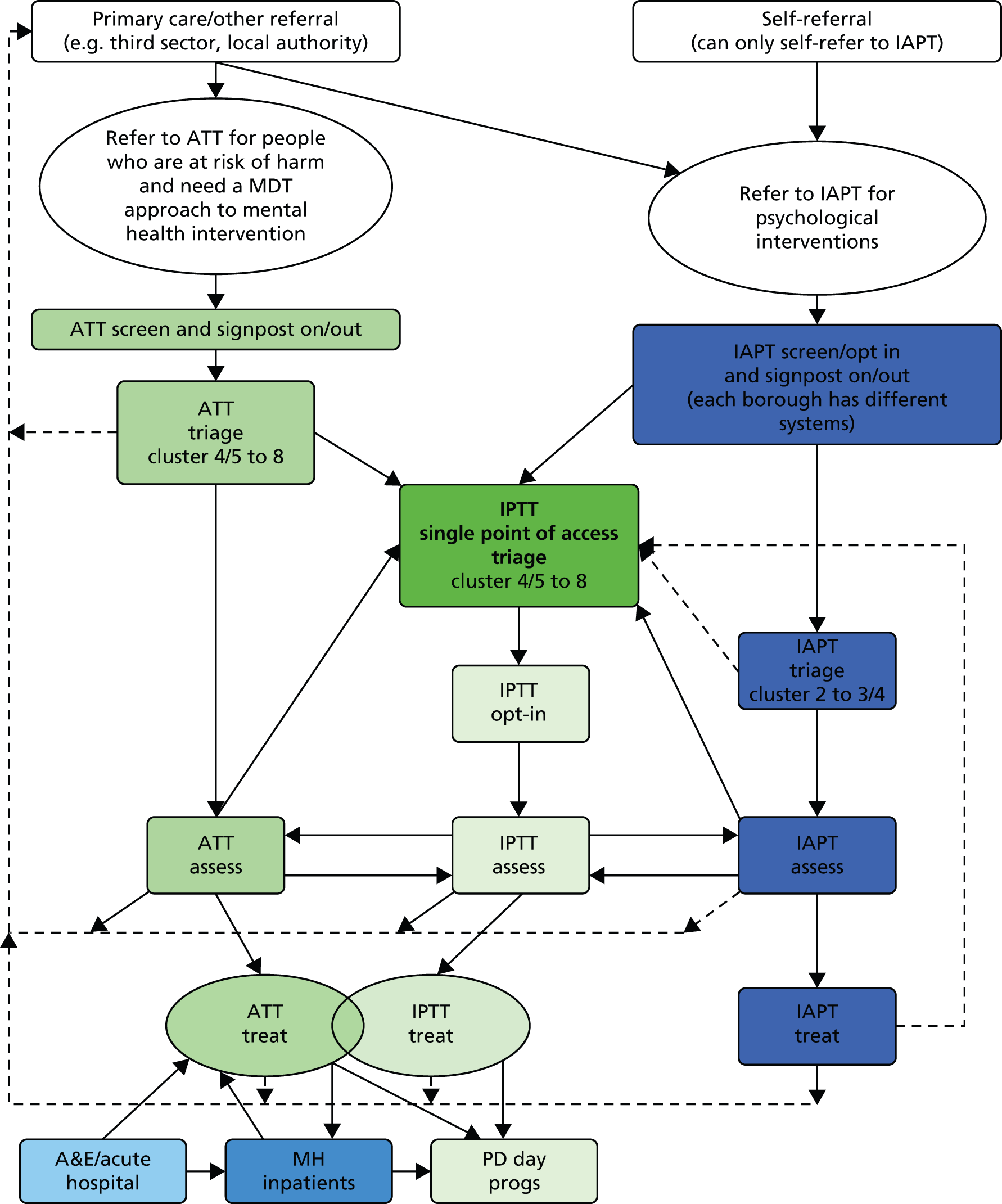
When our evaluation was first envisaged in 2011, the detailed pathways based on the Maps of Medicine were presented by key respondents as an important part of what the CAG was doing. By 2012, it was clear that substantial time and energy had gone into their development:
what was absolutely most fundamental was getting groups of people together that represented the tripartite perspective and there being massive disagreements and just genuine differences of opinion about what the evidence said or not.
R2
We were told that the MAP CAG:
had just the most amazing workshops we ran with lots of very experienced and very knowledgeable people disagreeing with each other and it was fascinating. And I thought that’s what this is all about the process of having the conversations, trying to develop a shared ownership of a piece of work that was, we have to make compromises of ourselves to make this work.
R2
But there was also debate about the use of the Maps of Medicine detailed clinical protocols and how difficult it was to take ‘NICE guideline-type high-level stuff and just slot it into place. It just doesn’t work with the complexity’ (R5).
And as our interviews proceeded it became clear that these detailed pathways had not been implemented at all on the ground. One interviewee told us:
We have care pathways which are written documents saying these are NICE guidelines, treatments for different conditions, on the whole they’ve not been implemented . . . we’re not on the whole yet going around saying here is a care pathway that describes the psychological treatments.
R5
One suggestion was that the detailed pathways might be useful in the psychotherapy reorganisation that was then gathering pace, but it turned out instead that it was the production of a new ‘high-level’ pathway for the new integrated psychological therapy teams that appeared to have been important. Similarly, the development of the high-level engagement, assessment and stabilisation pathway was viewed as important, for example, without it, CAG managers would have found it more difficult to represent the work of the assessment and treatment teams to external audiences, especially commissioners.
Overall, therefore, the MAP CAG’s use of care pathways over time began to resemble more and more the early-stage process of care pathway development set out by the SLaM CAG development team, that is, it developed and used a small number of high-level care pathways mainly as a tool for operational management and service development. It seemed to some extent that the earlier developments based on the Maps of Medicine had been driven by the greater commitment of some clinical and academic stakeholders to guidelines and treatment protocols and, possibly, the personal commitment of those stakeholders to particular therapy modalities and services, but this enthusiasm had not been sufficient to drive implementation beyond the production of the pathways themselves.
More generally, MAP CAG managers and clinicians were acutely aware of the tension between the two kinds of care pathway, and significant thinking had been done to theorise it. One respondent talked about conflicting discourses:
[S]ervice people think along functional lines and so you have got your two conflicting kinds of discourse in play. One is about what do patients need and for how long will they need it and in what way do they need it? And that conflicts with the diagnostic discourse which talks about what’s the correct evidence based treatment for you and it is interesting watching people struggle with trying to hold that together really.
R1
Several interviewees made a distinction between three linked attributes of care pathways: function, form and content. The high-level care pathways were about function. They were schematic functional descriptions of specific services. In the MAP CAG care pathways of this type were the Engagement, Assessment and Stabilisation care pathway and, once the relevant reorganisation was under way, the integrated psychological therapy team care pathway. Describing these high-level pathways one interviewee said:
In our CAG work we use these terms form and function, and what the care pathways were about was function . . . about saying we want some definable process whereby the patient can go along a track.
R1
‘Form’ referred to the teams and services. In the MAP CAG, form necessarily differed between the boroughs because they came from different starting points:
The form is how you do it, what team it is, community mental health teams or something else and that was secondary because that would always be different across the Trust because historically things developed in different ways.
R1
As this respondent also pointed out, these inevitable differences belied earlier expectations that the care pathways would achieve complete consistency in specific services:
That was quite an important bit of learning for us at the beginning because you go out on this journey thinking, right we’re being told that everything should be the same of course very soon very obviously things are not the same.
R1
In relation to content, another interviewee told us:
we’ve had a long debate about when a care pathway is about form and when it’s about content and the original [Map of Medicine] care pathways are, they’re all content and no form, so these are the evidence-based treatments and they make no statements whatsoever about where you can get the treatment if you happen to live in south Lambeth, so we’ve made no connection between our theoretical pathway and the actual thing that happens to a patient who is referred.
R5
However, referring to the need for implementation, this respondent added, ‘I think our challenge now is to bring those together’ (R5).
The language used at this stage in the MAP CAG’s development was therefore one of bringing together these three aspects of care pathway work and aggregating function, form and content within each care pathway over time as they developed and were implemented in particular contexts. A similar pattern has been described in the literature45 and we will return to this point in Chapter 5.
Mechanisms of care pathways
The picture that we have sought to paint up to this point is of a set of borough directorates transformed into a group of CAGs, with clinical and general managers learning through practice about care pathways and the ways in which they would and would not be helpful as a tool. The incremental way in which the MAP CAG developed these ways of working in relation to care pathways suggested to us that the use of care pathways in the CAG programme should best be considered as a precept. That is, the CAG programme entailed, alongside the CAG restructuring itself, a general principle that, whenever possible, care pathways should be used as a tool to solve the problems faced by clinical and service managers as they attempted to maintain, improve and develop the services for which they were responsible. The fact that the Maps of Medicine project work had been effectively abandoned by 2012 whereas the use of high-level care pathways was extended represented organisational learning on the part of the MAP CAG. How far this learning had gone, even by 2012, was strikingly put by one of our informants:
[F]rom when we were accredited, we ran in within a few months to enormous financial problems, so actually I think what we’ve been doing over the last year is using the care pathways as a way of trying to recover the CAG position and I think we have worked with nearly every team in the CAG now to do some form of restructure, there’s very little that’s part of the CAG that hasn’t been touched.
R1
What we think underpinned these important effects that high-level care pathways had on the ways that general and clinical managers in the MAP CAG worked was the way that the term ‘care pathway’ came to indicate not just the schematic representation of the work of a particular group of teams – the ‘abstract’ care pathway – but also those teams themselves, and their work – the ‘concrete’ care pathway. In line with this second, concrete understanding, each pathway, once established, also had a corresponding management team, with reporting lines ultimately to the CAG directors. For example, the April 2014 MAP organisation chart63 shows the engagement, assessment and stabilisation pathway’s ‘clinical pathway lead’ (a clinical manager) and ‘head of pathway’ (a general manager). The melding of these two aspects yielded two main mechanisms by which change occurred.
The first mechanism was the use of care pathways to support service redesign, most notably in the case of the creation of assessment and treatment teams in Croydon and integrated psychological treatment teams in Lambeth, Lewisham and Southwark; these changes were discussed above and are discussed again below. Having a care pathway meant that these services started operating with a clear vision of how they would be expected to deploy their resources, rather than developing policy and practice ad hoc. Because the MAP CAG’s high-level care pathways described a required sequence of clinical activities at a high level of abstraction, this mechanism is consistent with more marked effects on activity and therefore cost rather than on aspects of health-care quality such as safety and effectiveness. (To anticipate somewhat, this was, very broadly, what our quantitative analyses demonstrated.)
The second mechanism was the use of high-level pathways for ongoing performance management and smaller service alterations. High-level pathways provided a basis for selecting performance indicators and targets that could be used to develop systems for performance measurement. New CAG performance and activity spreadsheets were produced; a summary CAG scorecard was produced; an entirely new outcomes framework for the new integrated psychological treatment teams was produced; and trading accounts were introduced across SLaM. Building management structures around high-level pathways (1) increased the number of meaningful comparisons made between teams; (2) prompted more, and better informed, explanations of the sources of variation; and (3) suggested where changes to managerial and/or clinical activity might lead to improved performance. One early piece of evidence in support of the use of the new performance information was an early revision of the Croydon reorganisation in which the busier MAP West team was split into separate assessment and treatment teams; results had seemed to suggest that the Southwark assessment team was proving better able to cope with a large volume of referrals and so this system was replicated in Croydon. Again, the operation of this mechanism would be consistent with greater effects on activity and cost than on other aspects of health-care quality.
In the case of the CAG restructuring itself, the lack of comparator sites did not prevent us from considering what might have happened had different teams been put together under different management arrangements, had pre-existing teams been differently structured or had team finances been different. Therefore, we were able to gain some view of the context–mechanism–outcome configurations associated with the CAG restructuring. This style of analysis, relying on programme participants’ reasoning about counterfactuals, could not be applied in the case of our examination of how the MAP CAG applied care pathways. Therefore, we leave open the question of how context interacted with mechanism to generate the outcomes observed.
Influences originating outside the Clinical Academic Group programme
In The Clinical Academic Group restructuring and Care pathways we have attempted to identify the context–mechanism–outcome configurations associated with CAG restructuring and with the use of care pathways. However, we also postulate three mechanisms outside of the CAG programme that, coupled with aspects of the broader context around the programme, and sometimes combined with the effects of the CAG programme itself, had observable effects on managerial actions during the study period. The first mechanism was the managerial responsibility to balance the books. The second mechanism was the influence of borough commissioners, including the need to follow through on initiatives that had been agreed with commissioners but which were not part of the CAG’s overall strategy. The third mechanism was the influence of KHP itself. In this short section we attempt to sketch these phenomena.
Balancing the books
Our interviews suggested that the most important non-CAG influence was the managerial responsibility to balance the books, combined with a financial situation in which this was particularly challenging. Statements such as ‘we are trying to provide the best possible service within the financial envelope’ occurred frequently in the initial interviews and appeared to apply regardless of the organisational structure within which managers and clinicians worked. One of our respondents told us that:
[T]he number one priority of the CAG is to have a financially viable and coherent set of services to act as a vehicle for anything else because actually it doesn’t make sense to talk about doing more research, delivering outcome measures and so on if you’ve actually got a bunch of services that don’t make sense or are on the verge of collapse.
R5
Another respondent put it like this:
If we were working in a CAG pre our financial problems, we would be probably thinking primarily about how do we actually use the evidence-based therapy, make sure it’s there in all services. What we’re trying to do now is say how can we pragmatically get a better quality to people within a reduced envelope of money and try and see as many people as we were before.
R1
And in relation to the relative importance of the local compared with the national situation:
Far more important than anything that’s going on at the King’s Health Partners level is the fact that we are now trying to make the biggest reduction in health care resources in the history of the health service and actually that’s what dictates a large amount of what we do on a day-to-day basis.
R5
In practice, there had been ongoing financial cuts in SLaM’s services (nationally and at borough level) for some considerable time before the CAG restructuring:
we were doing three per cent [cuts] year on year for probably five years before the CAGs started.
R1
But the scale of the cuts being predicted in 200930 was of a very different order. These requirements created a huge challenge for the new CAGs:
All of the CAGs have got very big savings targets and some of the CAGs have not managed to reach balanced budgets this year so an enormous amount of stress, so the CAGs have got very, very large targets and they’re nowhere near them.
R1
The full extent of the difficulties that the MAP CAG was facing was not clear until after the ‘go-live’ date in October 2010. The MAP CAG had inherited a comprehensive set of business plans from the predecessor directorates, along with information on whether these business plans had been carried out or not. All too often they had not:
we went into CAGs just as the money pressures were [starting], looking back on business plans, none of these services had been held to account for savings plans for years.
R1
The new team running the MAP CAG inherited business plans from other directorates that had not been fulfilled and savings plans that had not been met:
[W]e inherited a massive cost when we arrived.
R1
The business plans also revealed considerable cross-subsidy of services:
When I looked at the budget statements for the very first time I was aghast at how many of the services are subsidised and didn’t break even.
R1
In Background to the changes we emphasised how some of these financial problems were made more obvious by the CAG restructuring; however, what made these problems something that needed to be sorted out was not anything particular to the CAG programme but rather a general responsibility on the part of the CAG’s managers that would have operated regardless of the specifics of the MAP CAG’s situation.
The influence of the commissioners
The SLaM commissioners are borough based; they expect a certain level of service delivery and outcome for a certain level of investment, and this investment differs between boroughs. As a result, what is achievable in some boroughs is not necessarily achievable in others; it depends on the level and direction of investment. Interviewees were well aware of this and we were given one example of how it had worked in practice:
Psychosis in some boroughs will have much easier access to earlier interventions because it’s been specifically commissioned.
R1
Although commissioners were not involved in the initial process of defining and forming CAGs, they had a large say in how they wanted services to perform and what they expected as outcomes:
No matter how we might believe in having consistent pathways or services it’s actually our commissioners’ intentions which will drive what we do.
R1
Well-informed dialogue with them was therefore important.
Generally, managers had to follow through on actions originating before the CAG formation, especially when these actions had been negotiated and agreed by borough commissioners. This applied to a reorganisation into separate assessment and treatment teams in Southwark and a reorganisation in Lambeth, led by the commissioners, which aimed to shift mental health care out of secondary health care (the Lambeth Living Well Collaborative). In itself, the influence of commissioners on reorganisations also continued to be important after CAG formation. For example, an internal restructuring of the assessment and treatment teams in Lewisham and their caseloads to make them fully ‘CAG compliant’ had to wait several years until the agreement of the commissioners had been gained.
The King’s Health Partners’ contribution to the Mood, Anxiety and Personality Clinical Academic Group
We have focused mainly on how the transition to CAGs affected the way that SLaM operated its mental health services. However, as we noted at the outset, CAGs were structures intended initially to be the means through which KHP would influence research, training and activity. How then did being part of KHP affect what the SLaM CAGs did?
Being part of KHP meant that each CAG was committed to a set of governance and performance management arrangements additional to those internal to SLaM; as noted earlier, there was the KHP accreditation process and there was also the requirement to report regularly to the KHP Performance Council. Not surprisingly, there was some concern about potential duplication between these two sets of requirements, and even those running these two systems worried that they might be seen simply as a matter of ‘having the same conversation with a different group of people’ (R4).
As the same interviewee suggested, the key question was therefore:
What did the formal CAG accreditation process [and presumably by extension the ongoing performance management arrangements] truly add over and above what [CAG staff member] was mobilising with the CAG?
R4
What was clear from the MAP CAG interviews was that the answer to this question was twofold: the influence of KHP requirements on the performance management processes within SLaM and the strategic oversight that the KHP processes themselves offered.
As reported earlier, the SLaM CAGs submitted two accreditation modules to KHP. The second submission concerned the development of strategy in the three areas brought together in the KHP CAGs – clinical strategy, research strategy and training strategy – and this new emphasis on strategy across three dimensions had considerable influence on the pre-existing performance processes within SLaM. The SLaM CAGs were now being asked to look at the bigger, strategic picture, and to do so they needed not only the routine clinical and financial data that had traditionally been the main focus of data collection and performance measurement within SLaM, but also data on research and on education and training:
The performance processes in SLaM have changed drastically as a result of KHP because SLaM now is expecting to . . . see the bigger scheme of things around strategy, interfaces and specifically being very upfront about the expectations of the research, education and training as well as the real operational service delivery.
R2
However, achieving this change was far from straightforward. On one hand, there were already well-established SLaM performance measures for service delivery and it proved possible to upgrade these rapidly post the CAG reorganisation. But measures for research and education and training were less well established and it proved harder to identify and collect usable routine data about these activities. The ongoing efforts to do so were described to us as work in progress. As one interviewee put it:
the machinery on the service side is obviously really well developed and so that clunks away on its own. If you actually want to get the training, education and research information out it’s obviously collected in different places in slightly different ways.
R2
The KHP Performance Council was intended to bring together information on all three aspects of each CAG’s work and, in the light of that data (taken together), get senior people from each CAG to think strategically about what it was achieving, both as an individual CAG and also in collaboration with other CAGs, for example at the interface of physical and mental health care:
If we’re going to add any value we will find some ways of bringing together information that didn’t used to be brought together and it makes sense to me that of course at this stage it would be the most senior people wanting to do that, look at it, make something of it.
R2
Again, achieving this result was far from straightforward. In principle, the KHP Performance Council provided a forum for that value-added conversation. In practice, interviewees told us, this did not always work well, especially early on. In large part this was because these conversations depended on a good understanding of each CAG and on good data from each CAG (the latter being derived from the CAGs’ own reporting systems), and neither of these was available at the start:
It’s only now as the CAGs are coming back for the second and third appearance that I think we’re really getting into so the Performance Council have some knowledge, some corporate memory of the CAG . . . so the work that we’ve started to do over the last two years on the score card, on pulling out where the highlights in terms of clinical service, teaching and research could be covered at the Performance Council has all been groundwork but we’re still not yet at the point where the CAG comes in and we’ve go right you’re on red for this in clinical service, this in academia, this in teaching. Those will be the three elements in today’s conversation.
R4
Again, this was work in progress.
However, and despite these imperfections, interviewees thought that the discussions with the KHP Performance Council had worked better in the SLaM CAGs than in the acute CAGs and attributed this to the fact that the former had managerial responsibilities for their services whereas the acute CAGs did not:
So how do you connect that thought-time back into what difference does it make to patients? And I think in the SLaM CAGs you’ve got a much better chance really of seeing that because there’s a much stronger thread between the leadership and the people who are doing the work on the ground because at least they’re in the same accountability line. Whereas in the acute side we have lots of marvellous conversations about mental health for cardiac patients, but we can’t then go, alright, can you do it?
R4
In summary, much of the work on performance measurement and management for KHP is still work in progress, but it was possible to see how, over time, and in combination with the performance measurement systems being developed by SLaM, it might build into a system covering all three parts of the KHP agenda.
Views of service users
In the preceding sections, we sketched a picture of SLaM’s CAG programme, its two key programme components and some other influences emanating outside the programme. We based this account on documents produced by KHP, SLaM and the MAP CAG and on responses from staff in the MAP CAG. Here, we present the contrasting results of our interviews with MAP CAG service users before bringing the story of the CAG programme up to date based on staff interviews performed in 2014.
During 2012 we interviewed 13 MAP CAG service users and one carer supporting a service user in a series of four group interviews. Although this was a small sample and cannot be said to represent the ‘service user view’ across SLaM, these service users did come from different boroughs and were drawn from two key groups. They included four ‘involved’ service users, that is, those who had a formal but largely voluntary role within the MAP CAG (such as membership of the MAP CAG Service User Advisory Group) and nine ‘non-involved’ service users and one carer who had no formal role within the MAP CAG. We asked both groups what they wanted from SLaM and SLaM services and we also explored their understanding of the MAP CAG, sought their views on the information they had been given about the changes and their opportunities to provide feedback and asked them about their own experience during the reorganisation. Levels of agreement on different issues varied between and within the two groups and in what follows we note where there was general agreement and where opinions differed, although otherwise we have not attributed the remarks quoted to any particular respondent. Overall, these interviews were very different from the interviews that we performed with staff; as noted earlier in this chapter, the decision to form CAGs and the decision to reorganise SLaM using CAGs were taken at high level within KHP and SLaM, with any consultation with service users occurring later in the process.
Understanding of the Mood, Anxiety and Personality Clinical Academic Group
All of the service users reported initial confusion about the aims and objectives of the MAP CAG; they also noted that this appeared to be shared by some MAP CAG clinical staff. However, it was also clear that some, but not all, of this confusion had abated by the time the interviews were conducted in 2012. The involved service users demonstrated a good understanding of the CAG reorganisation and what it was seeking to achieve and recognised the possibilities of moving from wide-ranging services that were geographically based to more specialist care within the CAGs. One member of this group told us:
I think it’s a good idea to specialise in different aspects of mental illnesses, different things . . . do one thing well rather than many things sort of not so well.
Involved service user
On the other hand, the non-involved service users were more inclined to say that, despite a lot of talk about the changes, they were still uncertain about what those changes really meant on the ground. This group also reported confusion about the relation between the CAG programme and the NHS-wide budget cuts that were introduced at the same time:
I just thought this was just part of, because the new government had come in, it was just a way of cutting costs and just redistributing teams in a new way . . . I didn’t realise that it was part of an ongoing programme.
Non-involved service user
Getting information about the changes
During the development of the CAG programme a considerable volume of information was made available through the SLaM website and there was widespread consultation with relevant stakeholders, including service users. This communication was therefore a two-way process. There were also ongoing formal opportunities for service users to provide feedback about their own experiences of SLaM services through a variety of mechanisms, many of which were already in place before the CAG programme. These included SLaM Service User Advisory Groups, a yearly SLaM-wide patient survey and ongoing data collections related to the PEDIC data collection and the Patient Experience Tracker. Within the MAP CAG there were the local service user groups and networks in the four boroughs [such as the Touchstone Centre and the Service User Network (SUN) group in Croydon] and their associated websites. There were also informal opportunities for exchange of information between staff, service users and carers during service delivery.
As a group, the involved service users were aware of the efforts to tell people about the CAG programme and, in particular, cited the large-scale meetings designed to inform stakeholders. But they were concerned about the costs of this additional communication and about whether or not such efforts could be maintained at a time of financial constraint. They also thought that the patient view might have been somewhat lost in all of the managerial change. The non-involved service users provided a more mixed message about the information they had been given. Non-involved service users without a care co-ordinator appeared to fare worst. One had received no official communication about the changes and, as a result, became anxious:
The communications I received about services, I didn’t actually get anything. It was quite, it can provoke quite a bit of anxiety actually because it makes you think that you’ve dropped through the net and nobody will, you won’t have any help and support.
Non-involved service user
Others were told by their care co-ordinator, sometimes during their last meeting before a change was made. This seems to have worked better:
[M]y CPN [community psychiatric nurse] . . . clearly told me, I don’t remember receiving a letter but he clearly told me that he was moving, changing me over to the mood anxiety and I was quite happy. So I was more than happy to be changed over and it was really done cleanly and he sat in and said his goodbyes to me.
Non-involved service user
Service user needs
There was general agreement among the service users that they needed more clarity about what services were available. This, they argued, was essential for patient confidence and could encourage compliance and recovery and limit stress in a crisis:
I want a pathway to access where I know where I can go and what will happen. Now, I don’t want to be floundering or when I’m in a state, I’m in no fit mind to go and seek any help anyway. Somebody else will have to do it so actually the carers should know where we should go.
Service user
There is some difficulty in interpreting what this informant meant by ‘a pathway to access’. Service users tended to use the terms ‘care pathway’ and ‘care plan’ interchangeably, and generally in the context of remarks about the services that were available to an individual patient. In this sense, there was (in 2012) no evidence of any familiarity with the high-level, functional care pathways that the SLaM CAGs had been encouraged to develop. But it was clear that the service users were familiar with, and concerned about, care plans. There was general agreement that care plans were important, that service users should be actively involved in developing their own care plans and that this should be an ongoing exercise:
What people need is continuity of care if they are to stabilise. They need collaboration, negotiation and partnership, an opportunity to talk on an equal basis. It is detrimental to therapy to have things done to you. There needs to be an understanding of what the patient needs.
Service user
It was also evident that these ideals were not, at that stage, being met for all MAP CAG service users.
Developing user-led services
One constructive suggestion was that it might be possible to build capacity for treatment and support by capitalising on innovative self-help projects, such as the SUN group in Croydon and the Lambeth Living Well Collaborative. Service users generally agreed that these initiatives offered much potential. Of SUN they said:
it breaks this cycle that systems actually perpetuate because you’ve got people coming to SUN who are coping in different ways but who are also extending that capacity of resource to others and that peer support, it’s not entirely service user led and all those old categories, this is actually something different that is an active partnership.
Service user
The key, service users suggested, was co-production (and render any other co-productions similarly):
SUN is about self-referral . . . they have quite a lot of input and active input, they call it coproduction . . . that is possibly where the capacity is because there isn’t any more new money . . . It’s in these grassroots projects that these things might come about.
Service user
Providing feedback
We also asked about the flow of information from service users. By definition, the involved service users had more opportunities to raise general issues of concern through formal mechanisms such as the Service User Advisory Groups and both groups had the same access to interactive websites and the same opportunities to respond to SLaM-wide patient surveys. But there was evidence that some of these formal mechanisms were not as widely used as they might have been:
Of course, then you get the patient survey every year . . . but then the numbers in the patient survey are terribly low.
Involved service user
Moreover, the non-involved service users identified other mechanisms that were, in principle, available to individual patients to provide feedback on their own experiences but which did not, in practice, work well. One specific problem was too much staff oversight. One non-involved service user said:
[The hospitals have] got the machine where patients can give information back – and what transpired was they had no information whatsoever because they expected patients to give feedback on the staff and it was right in front of the staff . . . People are frightened to use them.
Non-involved service user
And, even when feedback was specifically sought, staff oversight could constrain what people felt able to say:
Sometimes they give you a feedback form to fill in, the person who has done the training . . . You’ve got to fill it in and give it back to the same person. How can you say anything negative? . . . I usually tick the nice box because I might need them again.
Non-involved service user
In addition, there was a perception that service user views were not valued:
Staff are asked to make sure they tick the box, care plans to reach a target. What it says about service users’ experiences doesn’t matter.
Service user
Service users’ experiences within the Mood, Anxiety and Personality Clinical Academic Group
Confusion among service users about the reorganisation persisted as the MAP CAG was implemented. Some questioned why they were allocated to MAP CAG rather than another CAG. One non-involved service user told us:
I didn’t understand it at all but I looked it up . . . I read that ‘M’ is for mood and ‘A’ is for anxiety and ‘P’ is for personality disorder then I thought, I haven’t got personality disorder, I don’t really want to go to that kind of thing, you know . . . it’s misunderstood.
Non-involved service user
Other non-involved service users provided evidence of confusion (among staff as well as service users) about how the new arrangements operated:
When you went through the switchboard at [XXX] to speak to the secretary who dealt with your team, it took them about a month to six weeks to know which team to actually put you through to.
Non-involved service user
A specific concern raised by several non-involved service users was that the new discharge policies would mean that they would be ‘dropped’ by the system and would not be able to get back:
[XXX] discharged me back to my GP but about four or five months later I was getting ill again so they actually had to refer me back to the psychiatric system, it took nine months to even send a letter to me for an appointment.
Non-involved service user
More generally, it was apparent that many, if not all, of the service users who were interviewed continued to believe that the real driver behind the changes was the financial situation rather than the CAG programme. This belief shaped concerns about care in the longer term:
I think it’s going to get worse, you know because what’s going on now with all these cutbacks and things like that, benefits and things like that, it’s going to get harder.
Non-involved service user
In summary, many service users did not fully understand the rationale behind the changes and had concerns about the cuts they were experiencing and the direction the services were taking. They were sceptical about what the CAG programme could achieve:
[CAGs] seem like a good idea. I don’t know how the actual strategy behind it all, you know, in the higher echelons of the sort of psychiatric departments of the NHS, I don’t know how it will all filter through to the patients.
Non-involved service user
On the other hand, it was clear that it would be possible to convey a persuasive narrative in support of CAGs. As one of our respondents put it, some way into a discussion of the MAP CAG:
Today is the first time I’ve ever heard about what the actual driving force of this MAP CAG reconfiguration is about and I’ve been involved with the Trust for four and a half years . . . basically what you’re trying to do is get effective management so you can monitor and manage what you do and have effective accountability, that’s what you actually do isn’t it? That would have been a much more positive narrative than some of the other narratives that are mentioned.
Non-involved service user
The situation in 2014
The final round of interviews with senior MAP CAG staff in 2014 provided further evidence about the changes that had been made and also about several unresolved and inter-related issues. These included the basis on which the MAP CAG had been defined, the overlaps between the SLaM CAGs, the interface between the MAP CAG and primary care, MAP CAG influences on commissioning and vice versa and the impact of all of these factors on patient care.
How Clinical Academic Groups were defined and operated alongside each other
The debate about how the MAP CAG was defined vis-à-vis the other CAGs continued throughout the period of our review. Informants noted that the CAGs for children and young people and for dementia and older adults had worked well. The behavioural and developmental CAG had also worked well. In all cases this was because these CAGs ‘make perfect sense and always did . . . that was always how life was configured’ (R1).
It was a different story for the adult mental health CAGs that were carved out of the original borough-based services. Informants told us that borough-based differences persist within the CAGs, driven by the different requirements and investment levels of borough-based commissioners and by the different traditions of service in each borough. Further complications arose because the nature of psychiatric illness, the lack of certainty in psychiatric diagnosis and the number of service users with multiple problems led, inevitably, to numerous interfaces and overlaps between the SLaM CAGs. One respondent, who now favours the creation of a single adult mental health CAG, told us that he thought that the initial configuration of multiple adult mental health CAGs had been too much influenced by the wish to preserve links to specific departments at the IoP. Overall, our respondents continued to question the CAG structures that had been created for adult mental health services. It also appeared that the CAGs had caused difficulties in relationships with commissioners and in ensuring that services in geographical localities were properly integrated and that these difficulties were not unique to SLaM. One informant said:
It is interesting looking across London as well because I’ve looked at the different service lines that have been developed and, quite different to the way we have done our CAGs in a way and a lot of other trusts are beginning to return to the borough question as well.
R1
The CAG programme provided an opportunity to have a fresh start, look at whole systems and make tough decisions about the viability of areas that had been ‘haemorrhaging money’. As a result, we were told, the MAP CAG finances had become stable, a significant achievement given the central importance of finances in the reorganisation of the borough psychotherapy services and the ultimately unsuccessful attempt to restructure the Affective Disorders Unit and the Crisis Recovery Unit. But the pressure to find savings continued and, to explore further economies, in 2014–15 the adult mental health CAGs developed an adult mental health plan, initially implemented in services in Lambeth and Lewisham. The changes suggested in the adult mental health plan were intended to make the service work better by, for example, having discharge co-ordinators with a specific role to negotiate the transition out of acute care, upgrading the importance of home treatment teams in an attempt to get fewer people admitted and to get them out of hospital quicker and making changes to the support and recovery teams, such as reducing their caseload. The adult mental health plan is a mixture of activities that are intended to be directly cost saving and initiatives that are meant to save money because they are meant to make the service more effective but in a co-ordinated way. As the adult mental health plan was being developed a crisis occurred over inpatient admissions and this became a particular focus of attention. Although the changes made as part of the adult mental health plan occurred after the end of our study period, and we cannot therefore comment on their effectiveness, we took the plan itself as evidence that within SLaM’s adult services there was a perception that the current CAGs were not able to effect the necessary changes by working as separate entities on their own.
In all, the issue of whether or not the adult mental health CAGs are in the right alignment is an active question within SLaM:
So the discussion going on in the trust at the moment is how we get back into clearer borough relationships with the caveat of not allowing boroughs to go native. . . . the proposal is almost you have operational units but they are intersected by CAG standards, CAG strategy, the outcomes, evidence . . . the kind of KHP priorities so one doesn’t invent a new service because that’s what you feel like doing.
R1
Broadly, the adult mental health plan perhaps indicated a tendency towards greater and greater centralisation of decision-making for adult mental health services existing alongside a persisting recognition that boroughs needed to be adequately recognised as a level at which some decisions would inevitably be made.
Overlaps between the Clinical Academic Groups
The development and implementation of care pathways clarified the extent to which there was overlap between the SLaM CAGs. They also, in principle, provided a framework within which service users could move between the CAGs as necessary. But, we were told, in practice these overlaps are not always well handled. Service users can get stuck in one particular pathway:
[In] personality disorder we think there’s more and more of an overlap with psychosis which is not being picked up and this is a real problem for CAGs because of silo working. We’ve seen examples of people with schizophrenia being pushed up the pathway in terms of cost and complexity because they’ve got a personality issue within their psychosis rather than trying to find ways of managing across.
R1
There was concern about this tendency towards ‘silo working’, not only because of its impact on patient care but also because of its impact on staff attitudes and behaviour. As the same respondent said:
Broadly so everyone’s lost some general psychiatry principles whereby you apply a little bit of everything to this person in front of you who actually has quite a few strands to how they are presenting.
R1
Interface with primary care
Before the CAG programme many service users were being maintained within secondary services when they did not need to be and they had become accustomed to these arrangements. But the idea behind the changes was that service users would not necessarily be held all the time in the mental health services. Instead, they would come in for an episode of treatment as they needed it and would then be discharged back to their general practitioner (GP) with a clear care pathway so that if things started to go wrong again they could go back to their GP and be rapidly rereferred. This depended on GPs having the competence and willingness to play their part. But this assumption was questioned by SLaM staff:
[W]e talk about discharging to primary care as if they are a group of people waiting to receive these referrals and – (a) I don’t think they’ve got the capacity, (b) I am not sure that the political will is there.
R1
And the new arrangements worried service users who (as we described earlier) saw people being discharged more rapidly and finding it harder to get referred back; they were concerned about being ‘dropped’ by the service.
Effective liaison with primary care is a particular problem for the MAP CAG because it includes the assessment and liaison teams and hence has a large interface with primary care. Staff told us that, over the years, they have considered the various models for working at the interface that are described in the literature. 64 But the evidence base to support service development is still weak and it is not yet clear how to build the necessary capacity within primary care:
[O]ver the years we have done different GP models; all of them have been about secondary clinicians going in and largely carrying on behaving as if they are secondary clinicians and they never build the capacity.
R1
Approaches now being considered include SLaM employing GPs to work half-time in a practice and half-time in a SLaM assessment and liaison team, enabling them to develop confidence and special skills in mental health, and discharging people back into a network of services in the community rather than just to GPs.
In this context, we discovered that a small but significant change was under way in relation to the MAP assessment teams that had previously been split off from the MAP treatment teams. As noted earlier, the ‘MAP’ part of the name of these teams had caused confusion because the case mix actually encountered by any team responsible for accepting all referrals from primary care was much wider than just mood, anxiety and personality disorders. In recognition of this, and building on the engagement, assessment and stabilisation pathway, whose main points of entry and exit are to and from primary care, these teams were in the process of being renamed assessment and liaison teams.
Commissioning
As we found in the first round of interviews in 2012, relationships with commissioners continued to be complicated by the CAGs. Although the stress on high-level care pathways meant that the MAP CAG was inevitably focused on a trust-wide template for providing services, differing commissioning intentions and historic levels of investment led to a degree of tension. On occasion the MAP CAG had acted irrespective of commissioners’ views to provide services in the way that it thought best:
In [named borough] . . . the costs of community mental health teams have gone up because we deliberately put more money in there. We’ve subsidised because the quality was worrying . . . [but] [w]hat’s inadvertently happened is we have bunged loads of extra money from both CAGs into [named borough] to try and sew up the gaps but of course it is not commissioned. So one technically is subsidising it from elsewhere. And then when you go to the commissioners and say ‘By the way, you owe us all this money’, that’s kind of, ‘well, it’s your choice to put it in there’.
R1
Some aspects of interactions with commissioners appeared to have been somewhat simplified with the appointment of a Chief Operations Officer, whose responsibilities include dialogue with commissioners, meaning that borough commissioners no longer have to interact directly with multiple CAGs. As with the adult mental health plan, this appeared to be an indication that some early problems with the CAG structure were being addressed through greater centralisation. However, what we were told very clearly was that the commissioners, including GP commissioners, continue to dislike dealing with the CAGs rather than with the previous borough directorates.
Using the care pathways in practice
Informants told us that the detailed MAP CAG care pathways that were linked to NICE guidelines had not been revisited. Instead, the MAP CAG has developed, or is in the process of developing, four pathway groupings for engagement, assessment and stabilisation (which includes the interface with primary care), recurrent affective disorders, personality disorders and anxiety disorders. In the case of personality disorders and recurrent affective disorders, new services had been established corresponding to these pathways, with the mood disorder pathway being associated with the appointment of a new chair in mood disorders. Clinical leads, academic leads and management leads have been appointed to take each pathway forward:
So that process . . . has morphed from this huge document that was disease focused into four groupings now.
R7
This was associated with an important change of thinking in which this smaller number of new pathways – not just the engagement, assessment and stabilisation pathway – had become associated with defined clinical services. As one of our informants put it:
I mean, when the CAG started the care pathways were probably better described as clinical protocols; very, very detailed, very layered about what NICE said, what someone else said, and the process going through them was fairly tortuous because they were actually more around different professionals rivalling with each other as to what intervention to be included, so we kind of moved out of that and we have pragmatists leading it so for example the PD [personality disorder] leader will say well yes, these are all relevant. But actually what is important for this pathway is how they are put together and how they are delivered so I think that there are certain points of tensions still but I think by aligning the clinical guidance with services we have more purchase and more happens. Otherwise it becomes a rather academic exercise.
R1
This pragmatic approach has also been demonstrated in the way that the high-level pathways, both on paper and also embodied in other ways (e.g. in clinical dashboards), have continued to be used to support other components of the CAG programme. The possibility that they might support a clearer interface with primary care continued to be held out, despite the difficulties described above:
One of the things that pathways do is make it really clear why someone is in secondary care and if they are not receiving the interventions that they need then perhaps they should be in primary care. Community mental health teams have historically for years kept people in secondary services who might not need to be there . . . one of the things about the CAG and the pathways is about tightening up what actually are we providing. Are we doing it well? Are we doing it in the way that we’ve said we’ll do it? That then begins to start a different dialogue with primary care and with the commissioners.
R1
Overall, the fact that care pathways continued to be a prominent part of the way that our respondents talked about so many aspects of the MAP CAG, 5 years after the transition to CAGs began, indicates that they had become institutionalised as part of the vocabulary through which senior MAP staff thought about and discussed the ‘business’ of the MAP CAG.
Summary
As part of its entry into KHP, SLaM reorganised its directorates to form a set of CAGs, which may be thought of as service lines modified to meet the needs of an AHSC. Among the changes associated with this, borough directorates were abolished and responsibility for adult mental health services was split between three CAGs, of which we studied one in depth: the MAP CAG. Our qualitative interviews indicated that the need for change in SLaM’s services was widely accepted among managers and senior clinicians and academics, even though their reasons may have differed from the KHP vision. Going into CAGs was seen as an opportunity to sort out long-standing difficulties with some parts of the trust’s operations. It was also seen as an opportunity to embark on major change while the financial climate was comparatively benign and before such change was forced on the trust by worse conditions. Furthermore, it was an opportunity for SLaM to implement a long-held ambition to start using care pathways.
We identified two elements within the CAG programme. The first was the CAG restructuring itself, which we judged had promoted change through increased oversight, by generating a need for services to be ‘CAG compliant’ and by altering accounting arrangements in ways that promoted change. The second programme element was the use of care pathways. Over the 5 years of operation of the MAP CAG that we surveyed, significant developments were made in the use of care pathways. We view the use of care pathways in SLaM as a precept, that is, there was a general principle that care pathways should be used whenever possible to solve the problems faced by clinical and service managers as they attempted to maintain, improve and develop the services for which they were responsible. What the MAP CAG discovered was that its Maps of Medicine care protocols, which conformed more closely to the definitions of care pathways found in the literature, were of little practical use in the everyday work of managing the CAG. However, high-level pathways, which simply described in schematic flow the sequences of processes within a particular service, were helpful for performance measurement and management and for discussions with commissioners and others, including discussions about transforming or redesigning services. Care pathways, in this very specific sense, had become part of the everyday vocabulary of clinical and service managers in SLaM. By 2014, when we performed our follow-up interviews, the use of high-level pathways was being extended: new pathways were being developed for recurrent affective disorders, personality disorders and anxiety disorders, each of which was associated with ‘bricks and mortar’ services. In the case of the recurrent affective disorders pathway, the new service had entailed the appointment of new senior academic and clinical staff. Care pathways, from the outset, were seen in part as a way of defining the relationships between CAGs, but this was an area that seemed to have been problematic. Interface issues between teams had continued to cause problems in patient care and, at the organisational level, the adult mental health plan had now been developed between the CAGs as an attempt to jointly reorganise community and inpatient care to promote efficiency and effectiveness.
All of this change occurred in a broader context outside the CAG programme, and in many cases that context over-rode how the CAG programme would otherwise have progressed. During the early part of the MAP CAG’s life, financial considerations determined which parts of the service needed to be urgently reformed and, in the end, outranked any other consideration. Arguably the most important result of the whole CAG programme was that this process of ‘recovering the CAG position’ had been negotiated successfully: by 2014, when we performed further data collection, the MAP CAG’s finances were in order, with the main cost being the loss of two specialised but non-viable inpatient services. We perceived that the managerial imperative to balance the books was a very important influence over action.
Similarly important were the views of commissioners. Even after the introduction of the CAG, changes came about and other changes were delayed because of the views of commissioners; SLaM was not able to act autonomously. KHP also had some influences over the MAP CAG, although these seemed somewhat marginal to its main clinical activities.
An additional point that came out, especially in the 2014 interviews, was that SLaM had found some aspects of the loss of borough structures difficult to deal with. Our respondents told us that they had heard that similar difficulties had affected other mental health providers who had reorganised using service lines. However, there was a very clear preference for boroughs not to be allowed to ‘go native’ again and for the gains in consistency and the notion of a SLaM standard to be preserved.
Figures 5 and 6 show in graphical form the two programme elements that we identified, their mechanisms and the context in which those mechanisms operated and, in summary form, the outcomes observed or expected. The external contextual factors that we identified are also shown. As we noted earlier, we did not ultimately find logic models to be a helpful tool and therefore these diagrams attempt to depict context–mechanism–outcome configurations as per the model provided by realistic evaluation. 2
FIGURE 5.
Context–mechanism–outcome configurations for the CAG restructuring. Note: programme elements (on the left) and outcomes (on the right) are shown in dark green and mechanisms are shown in blue. Context proper to each context–mechanism–outcome configuration is shown in light green next to a line linking a mechanism to an outcome, whereas wider context appears in plain text inside the enclosing line.
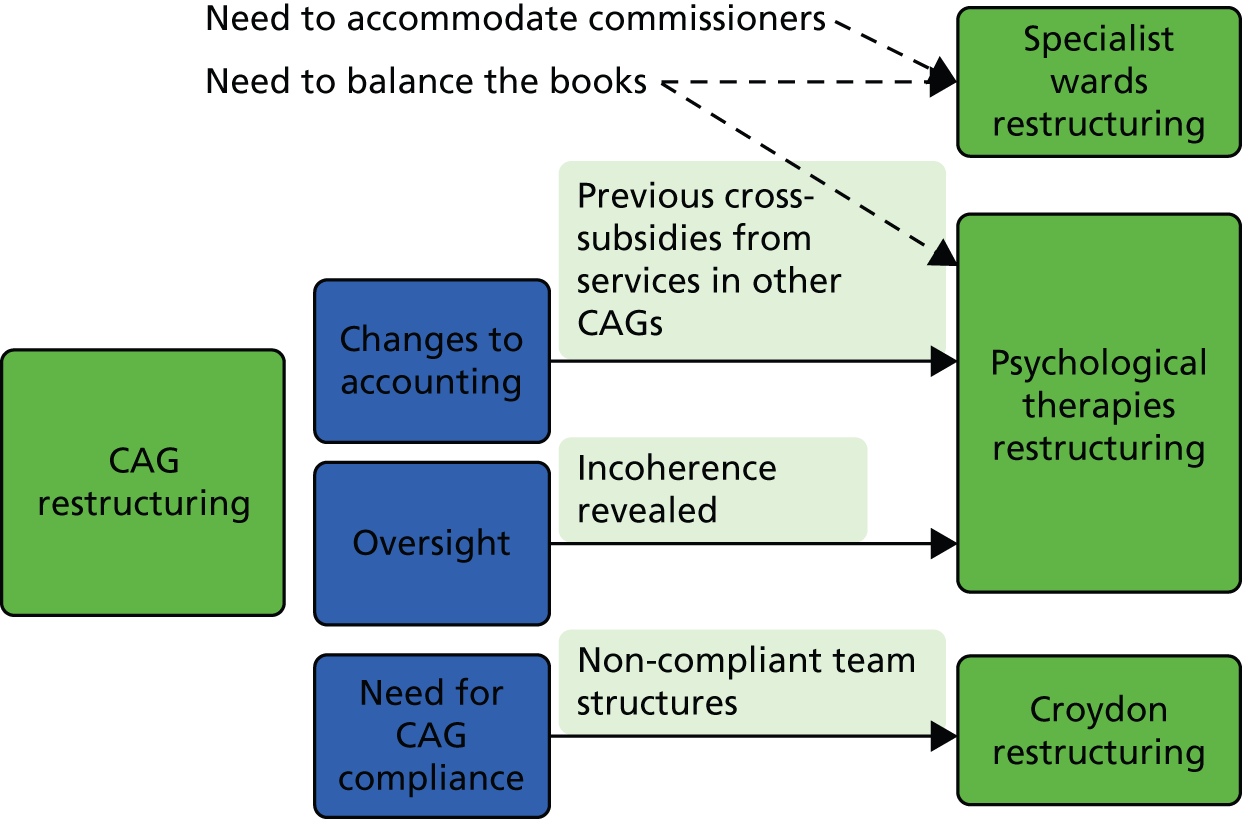
FIGURE 6.
Context–mechanism–outcome configurations for the use of high-level pathways. See Figure 5 for explanatory note. We did not postulate specific effects of context.
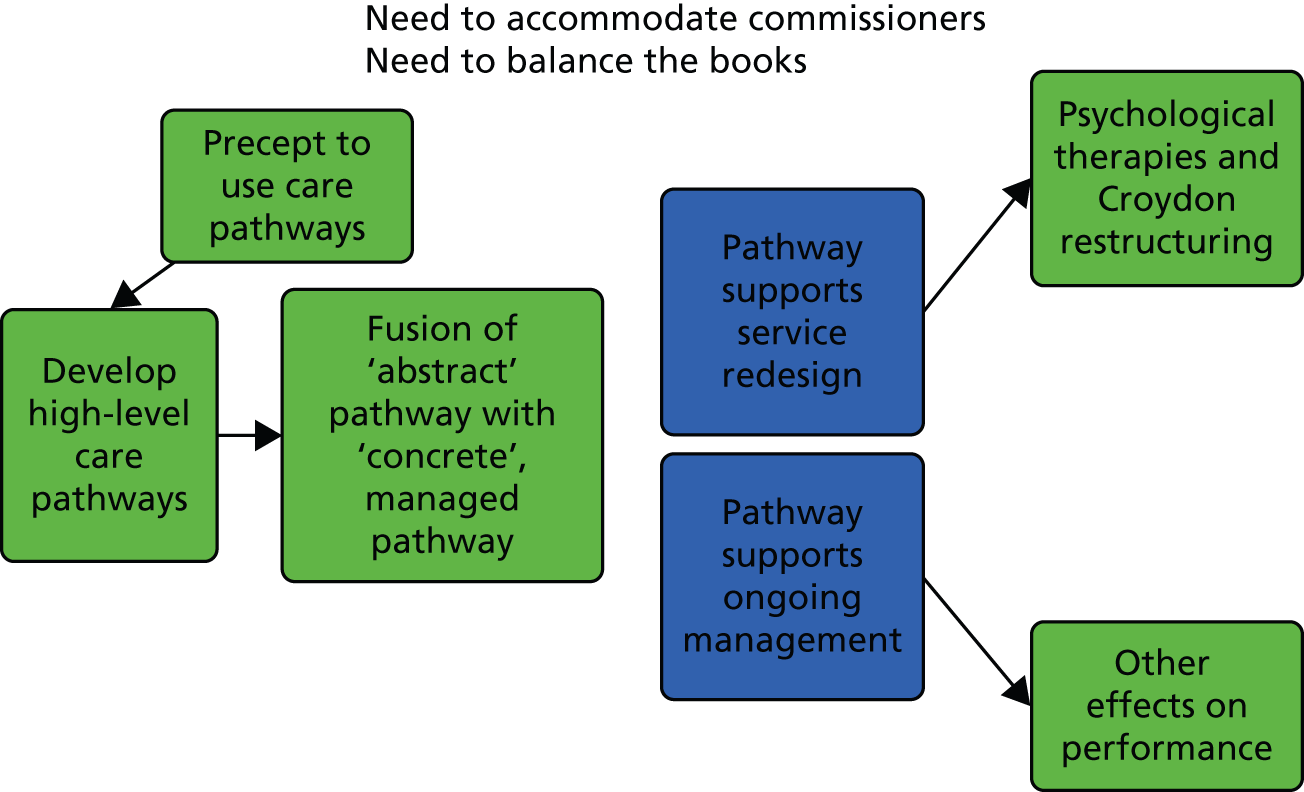
To summarise Figure 5, we postulated three mechanisms by which the CAG restructuring itself had effects: changes to accounting (by which we mean the grouping of team-level finances at the level of CAGs rather than directorates), oversight (by which we mean the CAG having an overview of all teams carrying out ostensibly similar work) and the need for CAG compliance (by which we mean the necessity for teams not ‘fitting’ the CAG template to be reformed). The respective contextual elements were the existence of significant cross-subsidies, the existence of incoherence in a group of similar services and the existence of non-compliant team structures. Outside the CAG programme itself we postulated the mechanisms of needing to balance the books and accommodate commissioners. (We leave KHP influences out here as these did not affect clinical service management.)
In the case of the psychological therapies restructuring, which took a set of borough-facing psychotherapy services and turned them into integrated psychological treatment teams for Lambeth, Lewisham and Southwark, the availability of the concept of a high-level care pathway helped with the redesign (see Figure 6) but the major influences are shown in Figure 5. The separation of the chronically loss-making psychotherapy services, which were placed in the MAP CAG, from the profitable services that had also been in the National and Specialist Directorate but which were now placed in other CAGs meant that a directorate which had, at aggregate level, broken even gave way to several CAGs, one of which, the MAP CAG, had a recurring deficit. At the more abstract level of context–mechanism–outcome configurations, the CAG restructuring and resulting changes in accounting arrangements generated a context of undisguised financial difficulty that triggered the mechanism of cost-cutting aimed at balancing the books.
In the case of the Croydon reorganisation to create separate MAP assessment and treatment teams, the high-level care pathways were a tool used in the setting up of the teams (see Figure 6) but did not themselves precipitate change. Financial considerations did not appear to have been important. Because the MAP CAG, and the other CAGs, were team-based structures, this meant that Croydon had to have teams that fitted into the new structure. Therefore, it was the CAG restructuring itself which was the main mechanism that led to the Croydon restructuring; the services had to become ‘CAG compliant’. In addition to this, we were told that the division of Croydon’s generic CMHTs was a change that would have happened anyway, and possibly faster, without the CAG restructuring; therefore, the CAG restructuring should be regarded as a sufficient, but not a necessary, cause of the Croydon reorganisation.
In the case of the Affective Disorders Unit and Crisis Recovery Unit, no amount of restructuring, whether using care pathways or not, was able to overcome the financial problems that the units were experiencing because of loss of cost per case income, a problem that was itself mainly a result of the difficult environment in the rest of the NHS. Therefore, it was the need to balance the books that was of decisive significance in the initial decision to restructure the units by merging them together, as well as the ultimate decision to close the services. The mechanisms of the CAG programme were not important.
Figure 6 indicates how the precept to use care pathways first led to the development (on paper) of high-level pathways and then to a fusion of these abstract pathways with the teams to which each pathway applied, such that any pathway could be seen as referring to both the pathway and the real work to which that pathway related. Subsequently, we postulated two mechanisms whereby the pathway might have effects: first, by supporting service redesign (this was evident in the psychological therapies and Croydon restructurings and also in the later redesign of personality disorder and recurrent affective disorder services) and, second, by supporting ongoing management of services (an effect that would potentially encompass effects on all of the CAGs’ services). In the case of these mechanisms, we did not identify particular contextual effects, other than the trivial sense (not depicted in the diagram) in which service redesign required the existence of a service needing to be redesigned.
The main lesson from our interviews with service users was that the CAG programme was poorly understood outside a relatively small circle of service users who were part of the Service User Advisory Group for the MAP CAG. For those who had been through the reorganisation process, it had not been clear what the rationale for the changes had been. Indeed, in the absence of other information, service users had been inclined to see the CAG programme as a cost-cutting exercise. Despite this, it seemed to us, and our respondents, that it would have been possible to justify CAGs to service users by focusing both on how care pathways could lead to the creation of predictable ‘patient journeys’ and on how CAGs would lead to managers having a better overview of services and making sure that these operated and interoperated in rational and understandable ways.
Chapter 4 Quantitative results
In this chapter we investigate whether or not the changes described in Chapter 3 led to measurable changes in the services and among the service users affected. We concentrate again on the MAP CAG and specifically on patients treated in CMHTs (including all forms of CMHT, before and after the CAG reorganisation) as well as the borough-based psychotherapy teams (the integrated psychological treatment teams and their predecessors). As noted in Chapter 3, the management of both of these sets of teams came to be guided by a high-level care pathway in the period after the introduction of the CAG in October 2010.
As noted in Chapter 2, the selections of data used data from April 2009, 18 months before the ‘go-live’ date for the CAG on 1 October 2010. The end dates for each analysis vary slightly depending on the time needed for follow-up, but we aimed to use data collected up to the end of March 2014.
Descriptive analyses
Community mental health teams
Demographic, clinical and service use characteristics of the sample are shown in Table 4. Data were entirely complete for service use and largely complete for demographic variables. A diagnosis was available in 90.4% of episodes. Completeness for the HoNOS was 61.9% at the start of the episode and 27.4% at the end of the episode. Overall, 30.6% of those episodes with a recorded diagnosis were associated with a psychotic or bipolar diagnosis; 61.8% of episodes were associated with a non-psychotic diagnosis (depression, anxiety disorders, stress-related and somatoform disorders and various other diagnoses including eating disorders, organic disorders, learning disability and developmental disorders).
| Variable | Complete, n (%) | Measure |
|---|---|---|
| Age (years), mean (SD) | 28,060 (100.0) | 38.5 (12.4) |
| Gender, n (%) | ||
| Male | 28,059 (100.0) | 13,389 (47.7) |
| Female | 14,670 (52.3) | |
| Ethnicity, n (%) | ||
| White British | 26,781 (95.4) | 14,749 (55.1) |
| Black African or Caribbean | 6860 (25.6) | |
| Other | 5172 (19.3) | |
| Marital status, n (%) | ||
| Single | 26,681 (95.1) | 18,606 (69.7) |
| Divorced/separated/widowed | 3369 (12.6) | |
| Married | 4706 (17.6) | |
| Diagnosis, n (%) | ||
| Schizophrenia (F20) | 25,355 (90.4) | 3039 (12.0) |
| Other psychotic (F21–9) | 2566 (10.1) | |
| Bipolar disorders (F30–1) | 2183 (8.6) | |
| Depression (F32–9) | 7732 (30.5) | |
| Neurotic and anxiety (F40–9) | 4173 (16.5) | |
| Personality and related (F60–9) | 2216 (8.7) | |
| Drug and alcohol disorders (F1x) | 1898 (7.5) | |
| Other disorders | 1548 (6.1) | |
| Total days in treatment with SLaM in the preceding year, n (%) | ||
| None | 28,062 (100.0) | 13,819 (49.2) |
| 1–182 | 9295 (33.1) | |
| 183–364 | 3119 (11.1) | |
| 365 | 1829 (6.5) | |
| Number of admissions to SLaM wards in the preceding year, n (%) | ||
| None | 28,062 (100.0) | 23,445 (83.5) |
| 1 | 3894 (13.9) | |
| 2 | 554 (2.0) | |
| ≥ 3 | 169 (0.6) | |
| HoNOS score at start of episode, mean (SD) | 17,374 (61.9) | 10.8 (5.6) |
| HoNOS score at end of episode, mean (SD) | 7694 (27.4) | 8.0 (5.5) |
Distributions of item scores on the admission HoNOS scale for CMHT service users with a diagnosis of a mood, anxiety or personality disorder are shown in Figure 7. In general, there was a preponderance of scores of 0 (none) or 1 (mild); the only items for which a majority scored above this level were items 7 and 8, representing depressed mood and other mental and behavioural symptoms respectively.
FIGURE 7.
Distribution of admission HoNOS scale item ratings for people with mood, anxiety and personality disorders treated by CMHTs. Sample covers the period from 1 April 2009 to 31 March 2014. The content of each item is as follows: item 1, overactive, aggressive, disruptive or agitated behaviour; item 2, non-accidental self-injury; item 3, problem drinking or drug taking; item 4, cognitive problems; item 5, physical illness or disability problems; item 6, problems associated with hallucinations and delusions; item 7, problems with depressed mood; item 8, other mental and behavioural problems; item 9, problems with relationships; item 10, problems with activities of daily living; item 11, problems with living conditions; item 12, problems with occupation and activities.
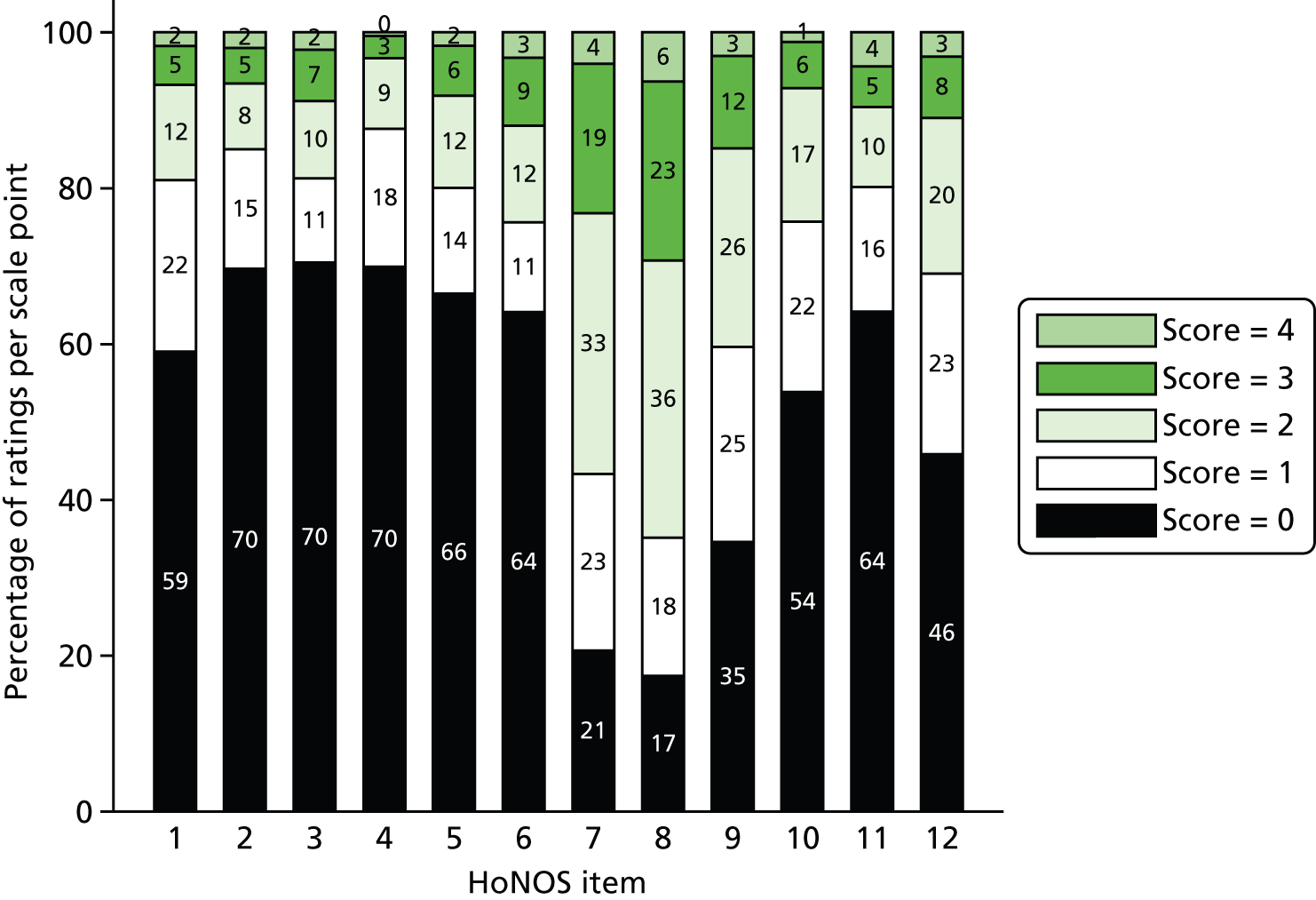
Outpatient psychotherapy teams
Demographic, clinical and service use characteristics of the sample are shown in Table 5. Data were entirely complete for service use and largely complete for demographic variables. A diagnosis was available in 89.1% of episodes. Completeness for the CORE-10 was 53.7% at the start of the episode and 20.6% at the end of the episode. Overall, 11.1% of those episodes with a recorded diagnosis were associated with a psychotic or bipolar diagnosis; 86.4% of episodes were associated with a non-psychotic diagnosis (depression, anxiety disorders, stress-related and somatoform disorders and various other diagnoses including organic, learning disability and developmental disorders).
| Variable | Complete, n (%) | Measure |
|---|---|---|
| Age (years), mean (SD) | 6041 (100.0) | 40.3 (13.1) |
| Gender, n (%) | ||
| Male | 6041 (100.0) | 2234 (37.0) |
| Female | 3807 (63.0) | |
| Ethnicity, n (%) | ||
| White British | 5796 (95.9) | 3896 (67.2) |
| Black African or Caribbean | 830 (14.3) | |
| Other | 1070 (18.5) | |
| Marital status, n (%) | ||
| Single | 5640 (93.4) | 3627 (64.3) |
| Divorced/separated/widowed | 793 (14.1) | |
| Married | 1220 (21.6) | |
| Diagnosis, n (%) | ||
| Schizophrenia (F20) | 5380 (89.1) | 166 (3.1) |
| Other psychotic (F21–9) | 115 (2.1) | |
| Bipolar disorders (F30–1) | 315 (5.9) | |
| Depression (F32–9) | 1794 (33.3) | |
| Neurotic and anxiety (F40–9) | 1570 (29.2) | |
| Personality and related (F60–9) | 798 (14.8) | |
| Drug and alcohol disorders (F1x) | 140 (2.6) | |
| Other disorders | 482 (9.0) | |
| Total days in treatment with SLaM in the preceding year, n (%) | ||
| None | 6041 (100.0) | 1736 (28.7) |
| 1–182 | 2177 (36.0) | |
| 183–364 | 951 (15.7) | |
| 365 | 1177 (19.5) | |
| Number of admissions to SLaM wards in the preceding year, n (%) | ||
| None | 6041 (100) | 5502 (91.1) |
| 1 | 418 (6.9) | |
| 2 | 84 (1.4) | |
| ≥ 3 | 37 (0.6) | |
| CORE-10 score at start of episode, mean (SD) | 17,374 (61.9) | 21.7 (6.4) |
| CORE-10 score at end of episode, mean (SD) | 7694 (27.4) | 18.1 (7.0) |
Distributions of item scores on the admission CORE-10 scale for outpatient psychotherapy service users with a diagnosis of a mood, anxiety or personality disorder are shown in Figure 8.
FIGURE 8.
Distribution of item scores from CORE-10 administered at the episode start for people treated in outpatient psychotherapy teams. Sample covers the period from 1 April 2009 to 31 March 2014. The content of each item is as follows: item 2, tension, anxiety and nervousness; item 3, having someone to turn to; item 7, ability to cope when things go wrong; item 10, talking to people felt too much; item 15, panic and terror; item 16, plans for suicide; item 18, sleep difficulties; item 23, hopelessness; item 27, unhappiness; item 28, unwanted images or memories.
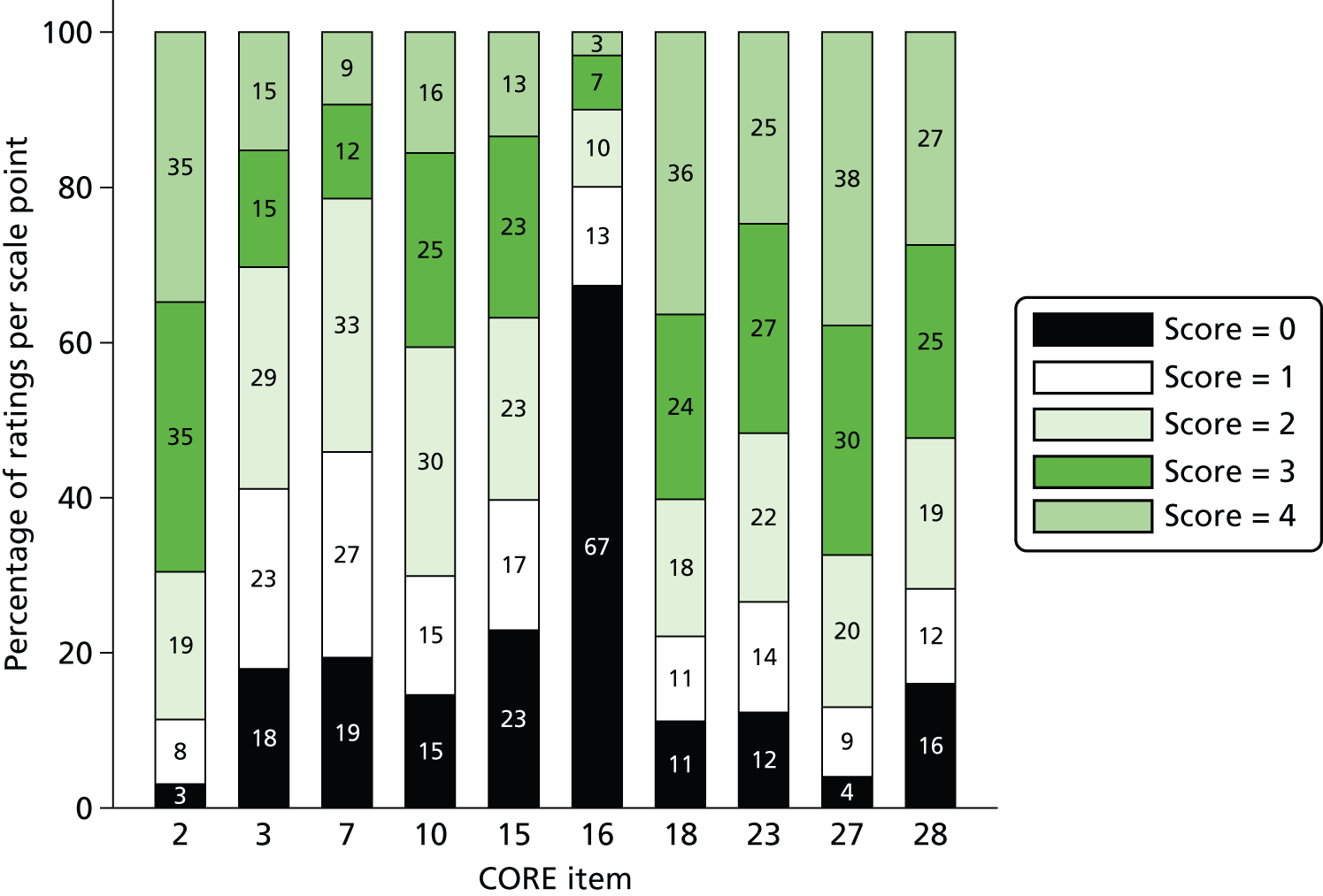
Activity and costs
The following section details analyses of activity and costs, first looking at CMHT episodes and moving on to psychotherapy episodes.
Community mental health team caseload, episode counts and episode duration
The total number of individuals with a non-psychotic diagnosis under the care of each borough’s CMHTs was calculated for every day between April 2009 and March 2014 (Figure 9).
FIGURE 9.
Daily CMHT caseload for episodes starting between April 2009 and March 2014 in (a) Croydon; (b) Lambeth; (c) Lewisham; and (d) Southwark. Non-psychotic diagnoses only, with at least one face-to-face contact per episode. Smoothed daily figures are shown.
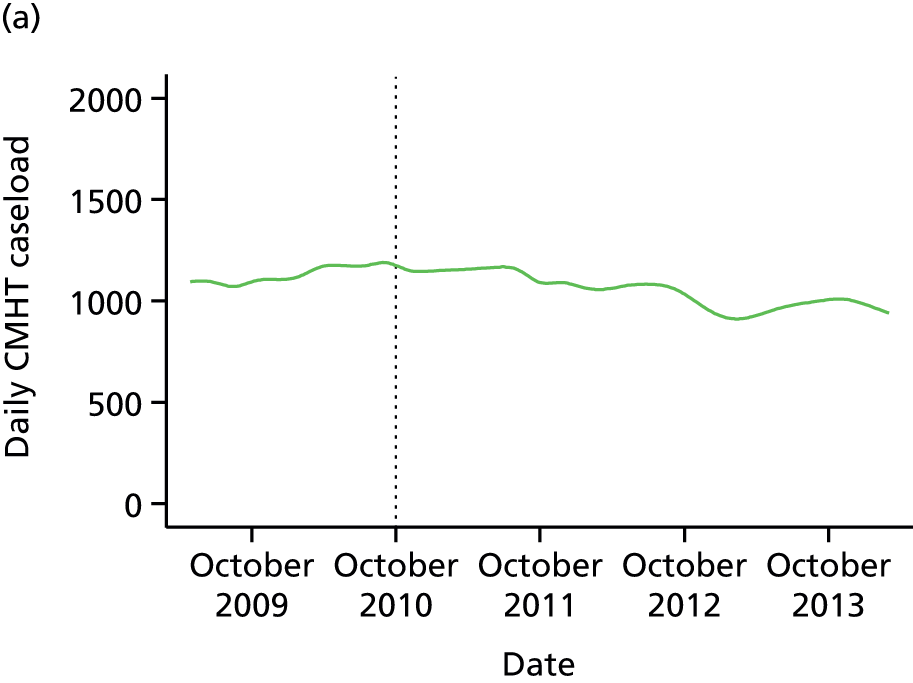
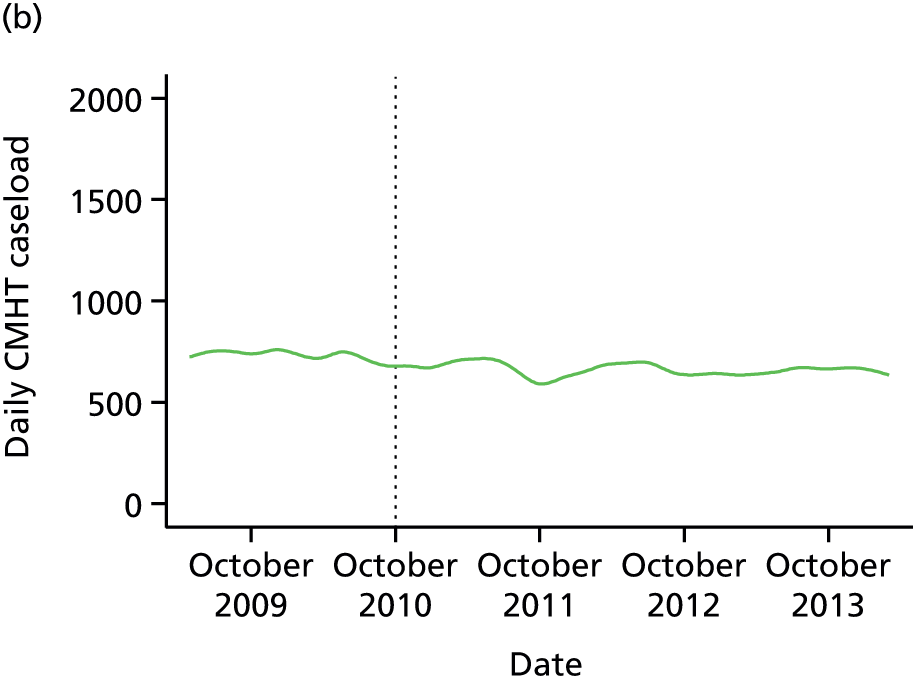
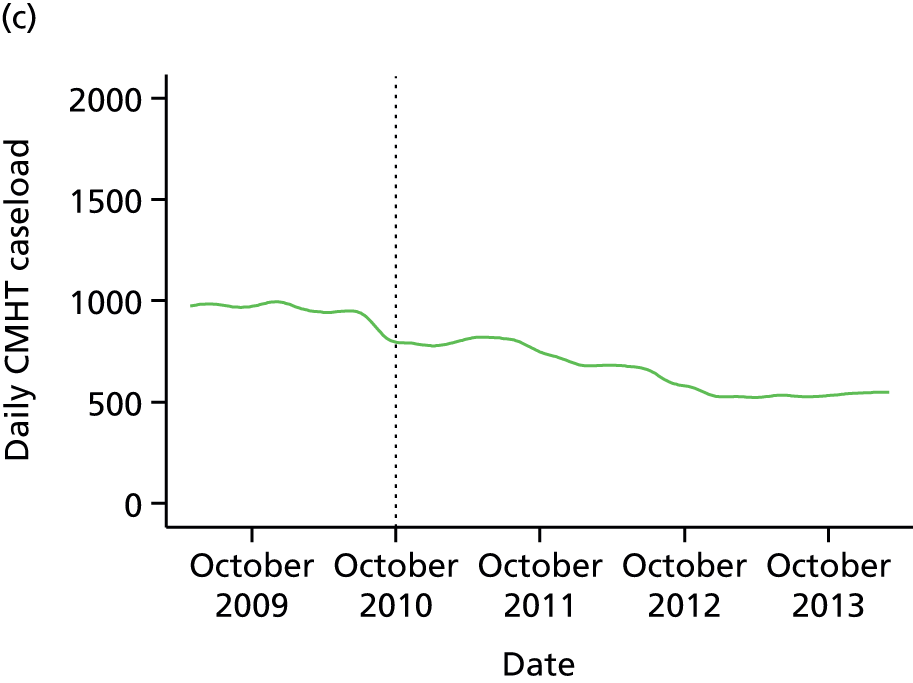
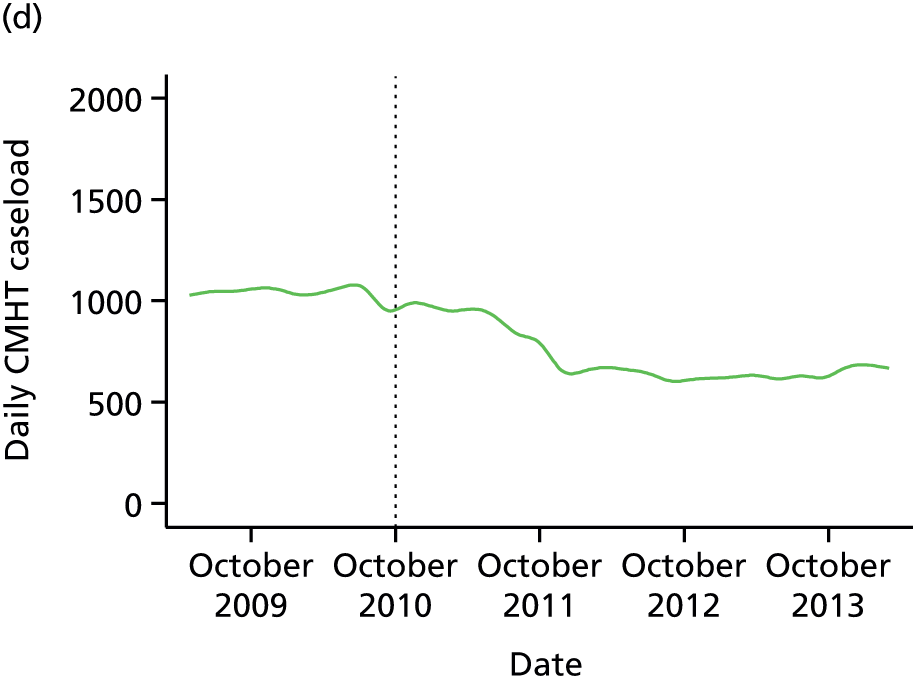
Visual inspection of the plots in Figure 9 indicated that a regression of the daily caseload figures against time, possibly allowing the slope of the fitted line to vary after CAG implementation, would provide a meaningful fit of the data. Each borough was analysed separately. Models in which caseload was regressed only against time (γ = βtimeXtime + β0 + ε) were compared using LR testing with models in which caseload was regressed against time, a pre-/post-CAG indicator variable and an interaction term between the latter and time (γ = βtimeXtime + βCAGXCAG + βCAG × timeXCAG × time + β0 + ε). Durbin’s alternative test indicated that serial autocorrelation was present (p < 0.0001 in all boroughs). This was attributable to the fact that one day’s caseload can differ from the next only by the difference between the number of new patients and the number of discharges that day. Therefore, Newey–West standard errors were used for the final analyses.
In all four boroughs, rates of change differed before and after CAG implementation (p < 0.0001 in all cases). All CMHT caseloads reduced in the post-CAG period and only in Lambeth did the caseload reduce more slowly in the post-CAG period than in the pre-CAG period (Table 6).
| CMHT | Rate of change per day (95% CI; Wald test p-value) | |
|---|---|---|
| Pre CAG | Post CAG | |
| Croydon | 0.24 (0.23 to 0.25; 0.001) | –0.26 (–0.27 to –0.25; 0.001) |
| Lambeth | –0.08 (–0.10 to –0.06; 0.001) | –0.02 (–0.03 to –0.02; 0.001) |
| Lewisham | –0.20 (–0.23 to –0.17; 0.001) | –0.28 (–0.29 to –0.27; 0.001) |
| Southwark | –0.05 (–0.08 to –0.03; 0.001) | –0.29 (–0.31 to –0.27; 0.001) |
Counts of episodes per month and median episode length are graphed in Figures 10 and 11 respectively. Considering borough CMHT caseloads together with counts of new episodes per month and episode length pre- and post-CAG implementation, it appeared that the reduction in caseload in Croydon was attributable to a reduction in episode length (median 266 days before vs. 239 days after; χ2 p = 0.052) rather than any difference in the number of new episodes starting per month (mean 61 episodes per month pre CAG vs. 58 episodes per month post CAG; t-test p = 0.38). In Lambeth the reduction in caseload post CAG was probably attributable to a reduced number of new episodes (67 episodes per month pre CAG vs. 61 episodes per month post CAG; t-test p = 0.06) rather than a reduction in episode length (median 160 days before vs. 166 days after; χ2 p = 0.31). In Lewisham the reduction in caseload post CAG was attributable to both effects (70 episodes per month pre CAG vs. 58 episodes per month post CAG; t-test p = 0.0007; median 142 days pre CAG vs. 121 days post CAG; χ2 p = 0.007); this was also the case in Southwark (85 episodes per month pre CAG vs. 75 episodes per month post CAG; t-test p = 0.02; median 143 days pre CAG vs. 100 days post CAG; χ2 p < 0.001).
FIGURE 10.
Counts of new CMHT treatment episodes per month for episodes starting between April 2009 and March 2014 in (a) Croydon; (b) Lambeth; (c) Lewisham; and (d) Southwark. Non-psychotic diagnoses only, with at least one face-to-face contact per episode. The vertical line represents the point that the MAP CAG was established in October 2010.
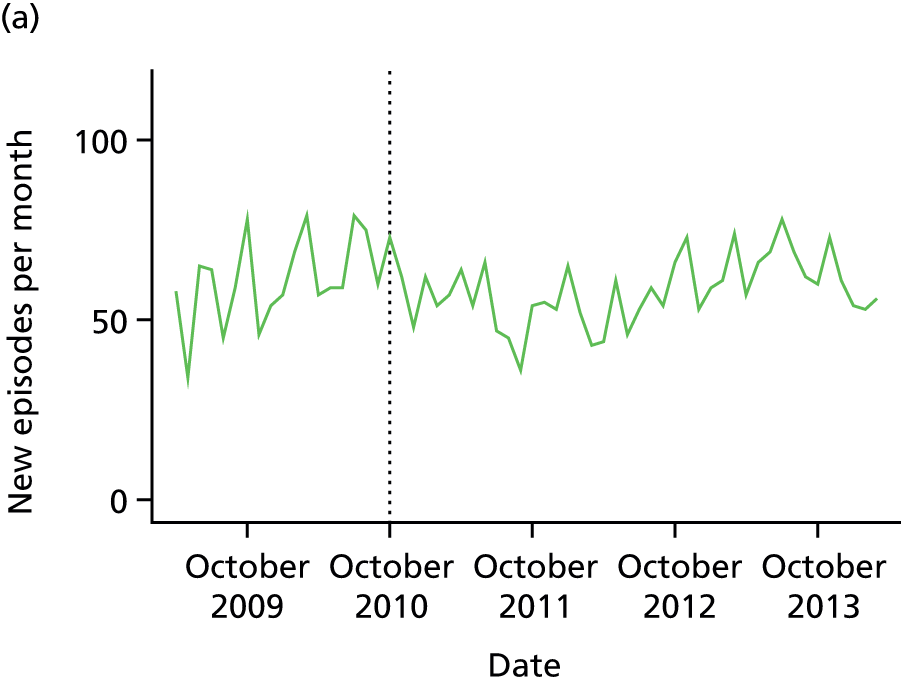
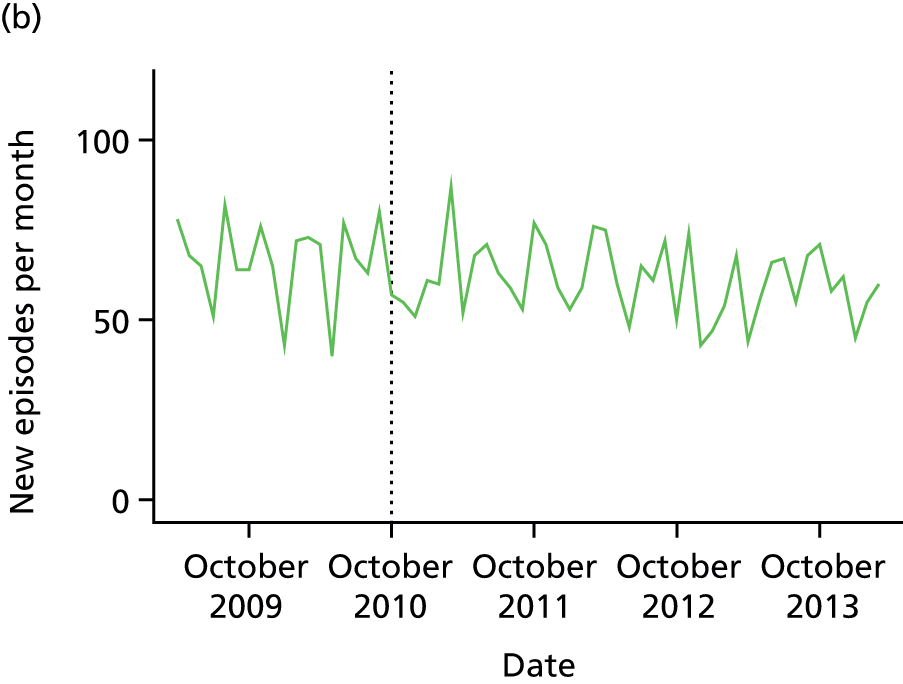
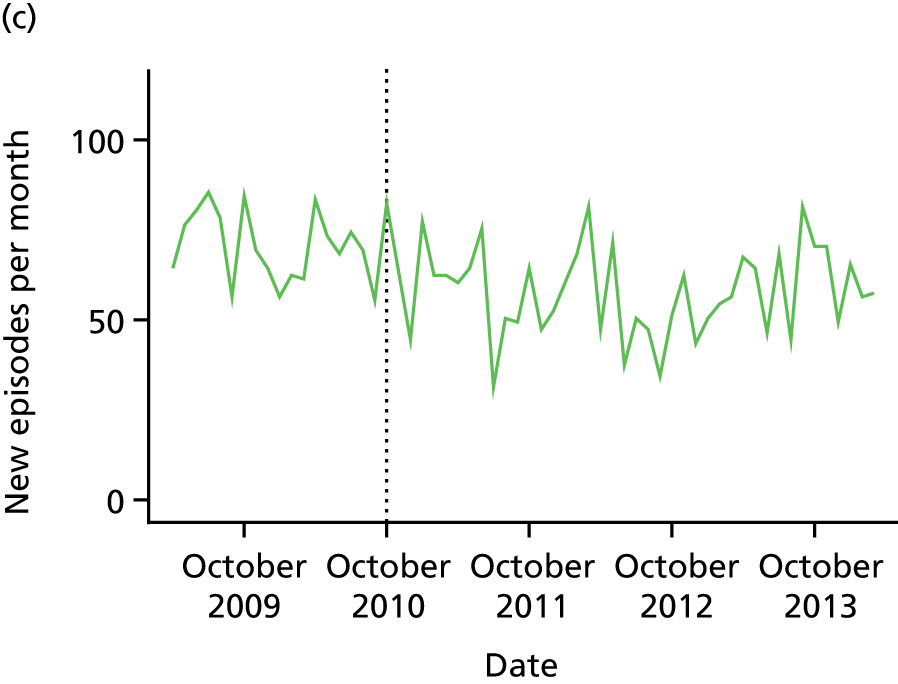
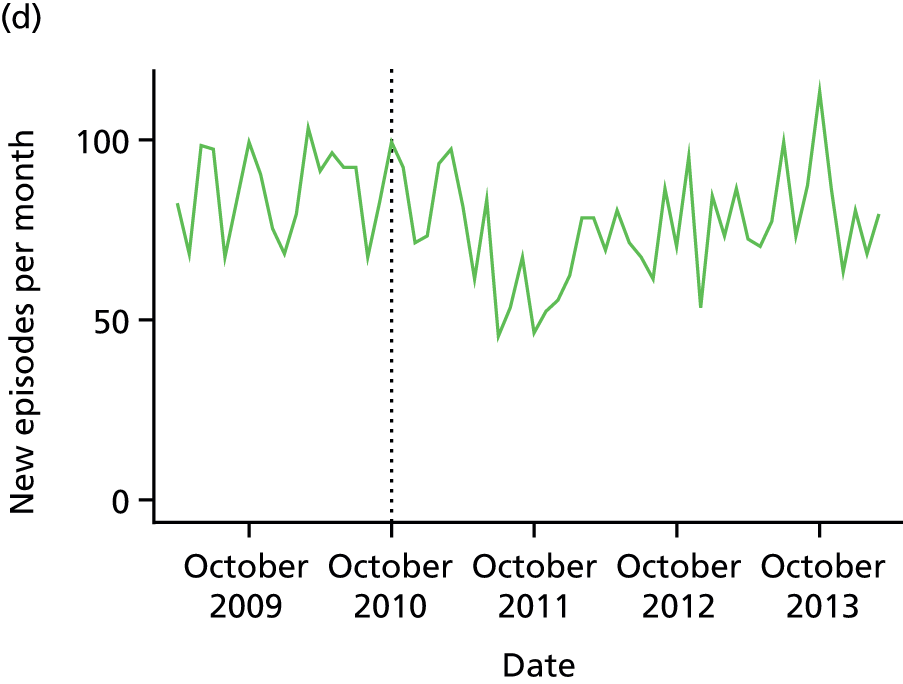
FIGURE 11.
Community mental health team episode duration (days) for episodes starting between April 2009 and September 2013 in (a) Croydon; (b) Lambeth; (c) Lewisham; and (d) Southwark: 25th, 50th and 75th centile values. Non-psychotic diagnoses only, with at least one face-to-face contact per episode. Data aggregated over 6-month time bands, with each data point plotted at the start of its related time band.
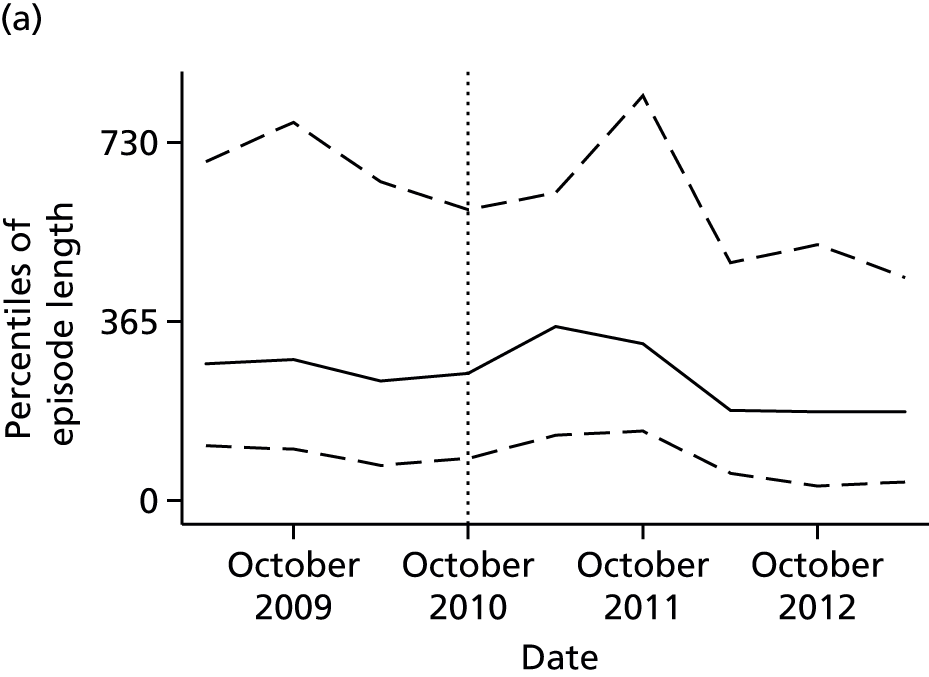
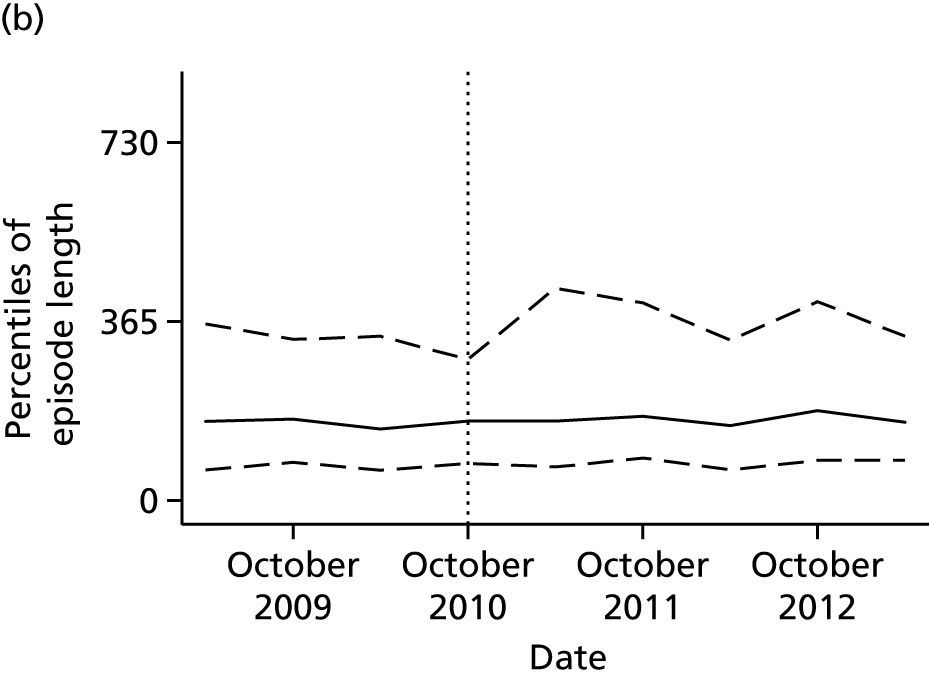
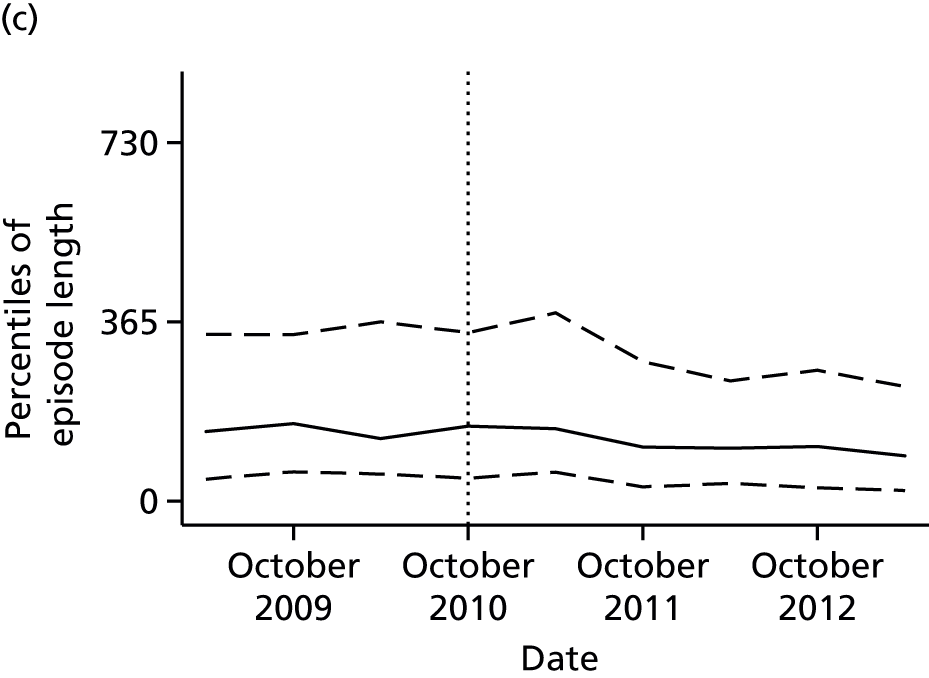
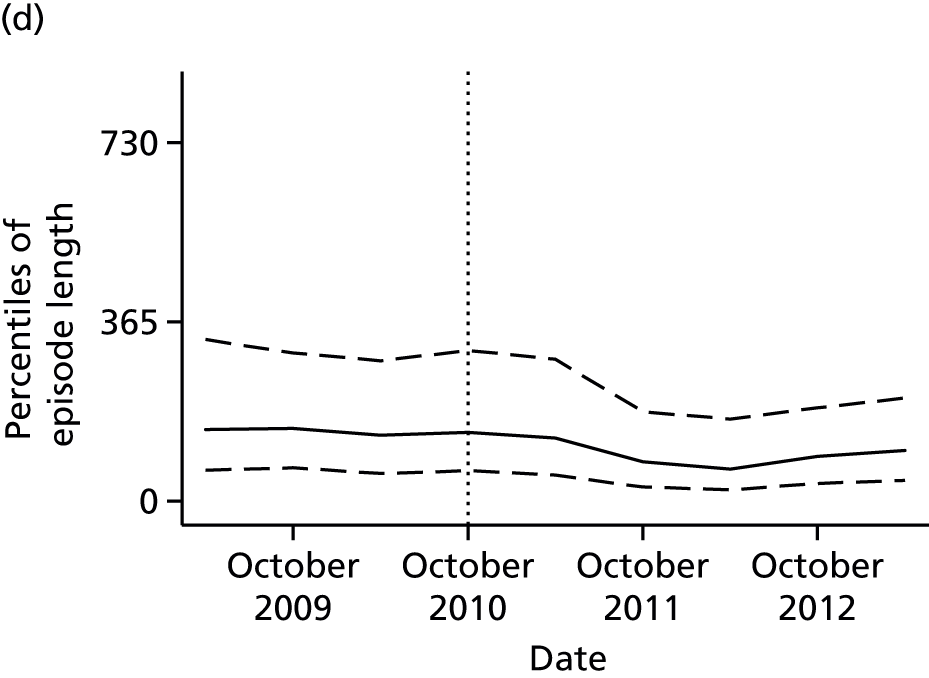
Number of contacts within a year of the start of a community mental health team episode
Figure 12 demonstrates the 25th, 50th and 75th centile values of the number of contacts per episode in the year after the first contact, covering CMHT episodes starting in the period from 1 April 2009 to 31 March 2013 and therefore including activity up to 31 March 2014.
FIGURE 12.
Number of contacts over the first 365 days of a CMHT episode for episodes starting between April 2009 and March 2013 in (a) Croydon; (b) Lambeth; (c) Lewisham; and (d) Southwark: 25th, 50th and 75th centile values. Non-psychotic diagnoses only, with at least one face-to-face contact per episode. Data aggregated over 6-month time bands, with each data point plotted at the start of its related time band.



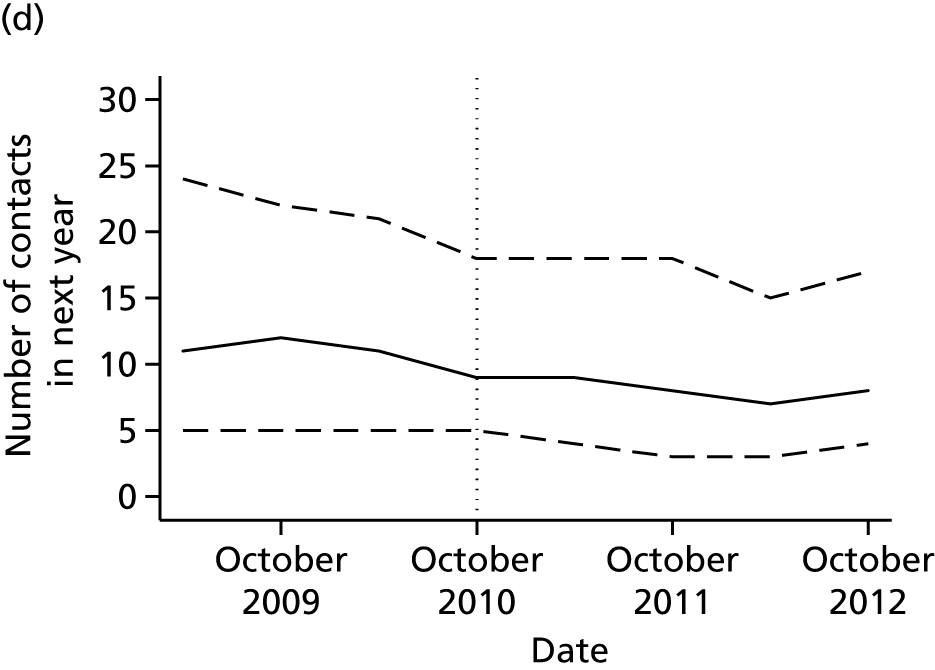
As with episode length, inspection of the plots indicated that the number of contacts did not alter in linear fashion with time across all four boroughs. Therefore, we used linear regression with a random effect at individual level to test whether or not the mean number of contacts in the first year of an episode was altered after CAG implementation. In Croydon, there was a borderline significant increase in the mean number of contacts after CAG implementation [b = 1.03, 95% confidence interval (CI) –0.10 to 2.17; p = 0.075]; in Lambeth, there was a non-significant decrease in the mean number of contacts (b = –0.95, 95% CI –2.12 to 0.22; p = 0.11); in Lewisham, there was a significant increase in the mean number of contacts (b = 0.85, 95% CI 0.03 to 1.67; p = 0.042); and in Southwark, there was a larger significant decrease in the number of contacts (b = –2.99, 95% CI –4.2 to –1.8; p < 0.001).
Costs associated with community mental health team episodes
Figure 13 demonstrates the mean unadjusted costs of CMHT care over the 365 days subsequent to the start of an episode of CMHT care.
FIGURE 13.
Unadjusted CMHT costs for episodes starting between April 2009 and March 2013 in (a) Croydon; (b) Lambeth; (c) Lewisham; and (d) Southwark. Individuals with non-psychotic diagnoses only, with at least one face-to-face contact per episode. Data aggregated over 6-month time bands, with each data point plotted at the start of its related time band.
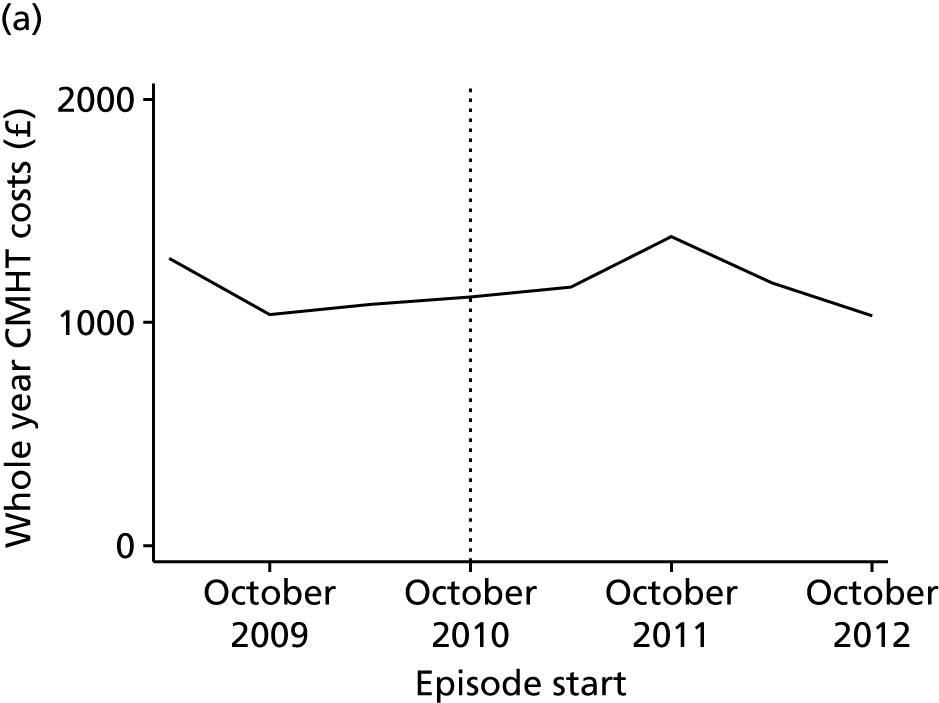

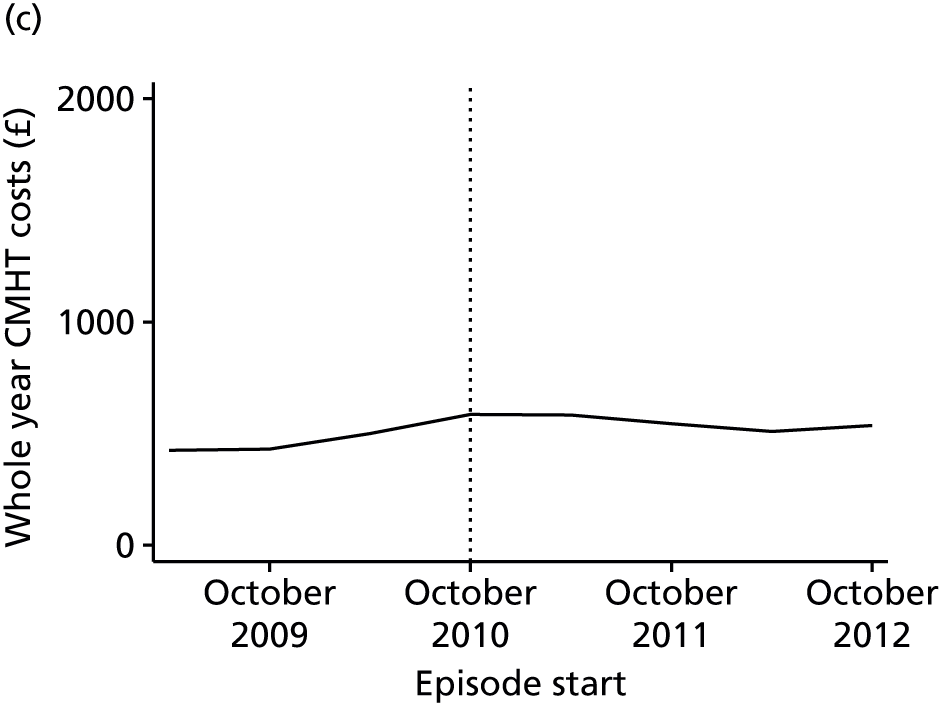

We performed raw and adjusted analyses of the costs and how they changed over time. In view of the appearance of the graphical plots of costs, we simply compared costs in the pre-intervention period with costs in the post-intervention period.
Looking at unadjusted CMHT costs in Croydon, there was no evidence that these differed pre and post intervention (b = 16.9, 95% CI –114.1 to 147.9; p = 0.80). This was also the case for adjusted CMHT costs (b = –3.2, 95% CI –134.2 to 127.8; p = 0.96). In Lambeth, unadjusted costs were similarly unchanged (b = –54.8, 95% CI –216.8 to 107.3; p = 0.51), as were adjusted costs (b = –55.3, 95% CI –230.2 to 119.6; p = 0.54). In Lewisham, unadjusted costs increased after the introduction of the CAG (b = 135.6, 95% CI 66.6 to 204.7; p< 0.001), as did adjusted costs (b = 114.6, 95% CI 43.5 to 185.8; p = 0.003). In Southwark, there was a borderline significant reduction in unadjusted costs (b = –113.5, 95% CI –233.8 to 6.9; p = 0.065), which was just significant when adjusted (b = –121.7, 95% CI –242.2 to –1.2; p = 0.048).
In a second set of analyses we examined costs for core adult mental health services, defined as the sum of inpatient costs, home treatment costs and CMHT costs. Figure 14 depicts these costs, aggregated over 6-month time bands and graphed separately per borough.
FIGURE 14.
Unadjusted costs of core adult mental health services for CMHT episodes starting between April 2009 and March 2013 in (a) Croydon; (b) Lambeth; (c) Lewisham; and (d) Southwark. Individuals with non-psychotic diagnoses only, with at least one face-to-face contact per episode. Data aggregated over 6-month time bands, with each data point plotted at the start of its related time band.
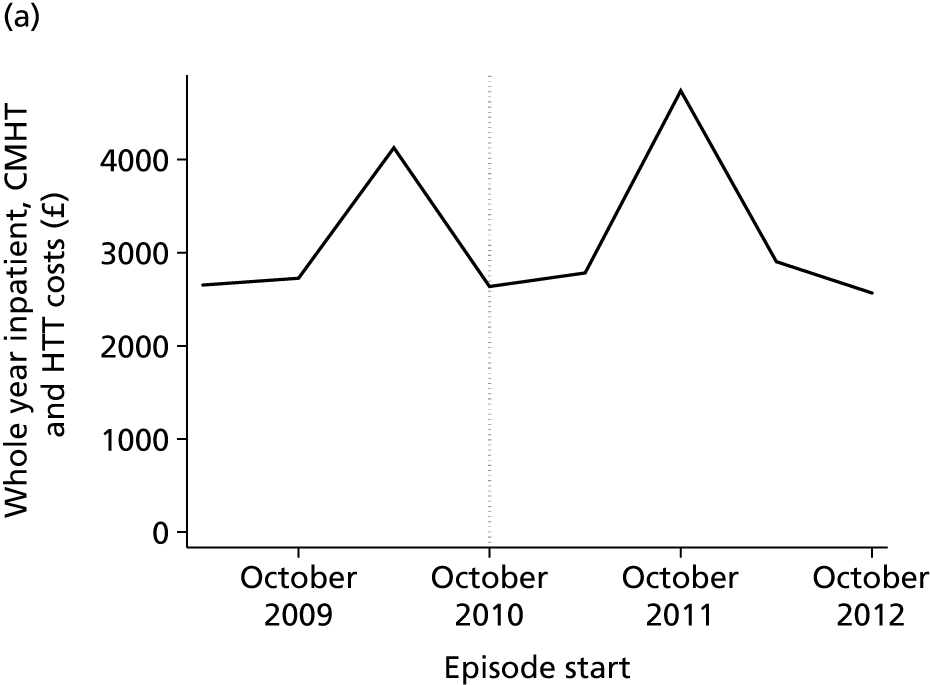
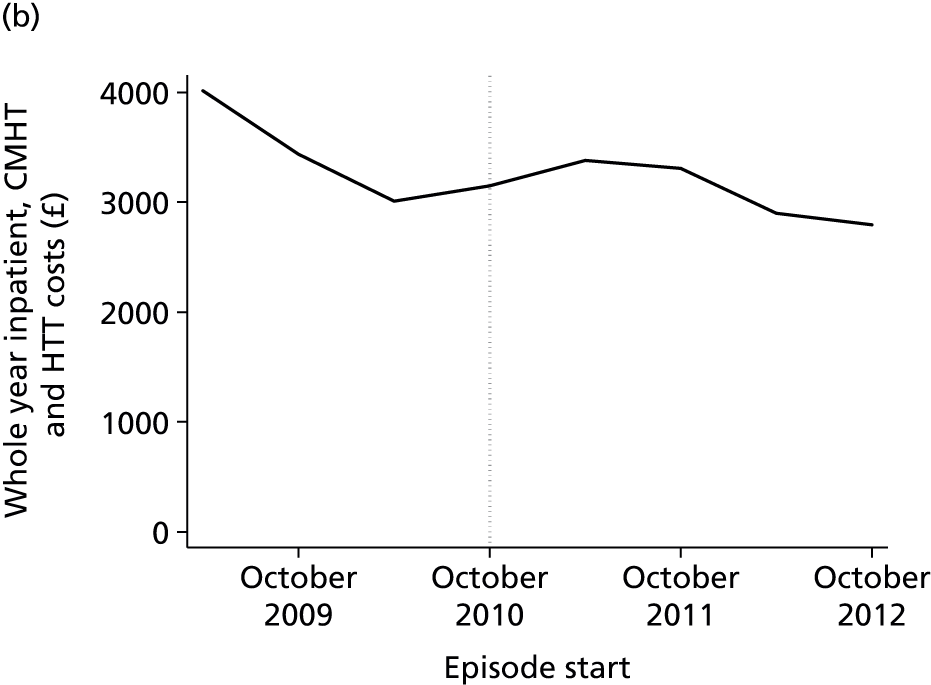
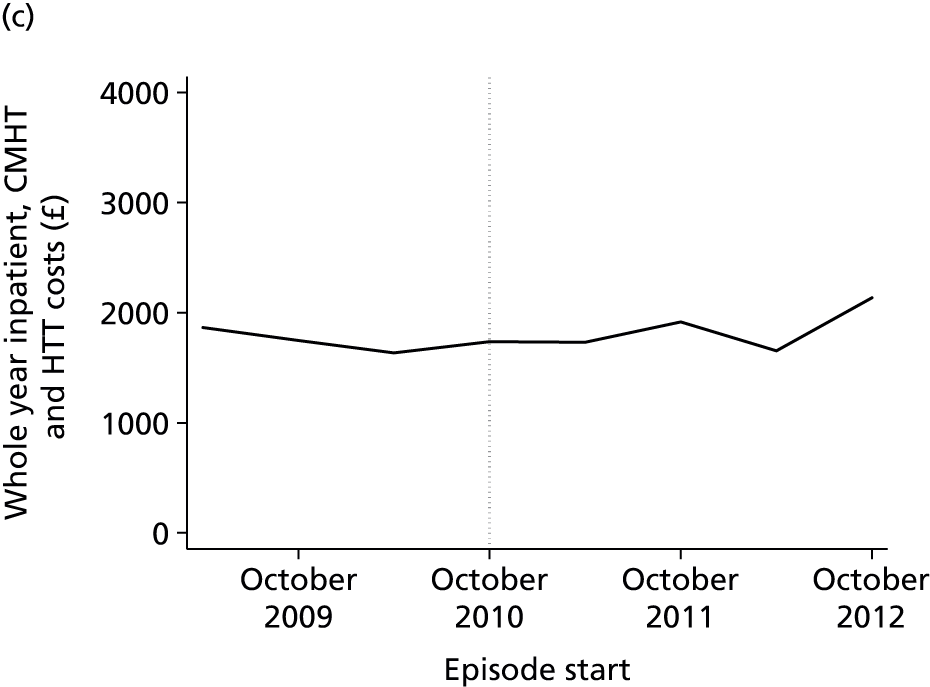
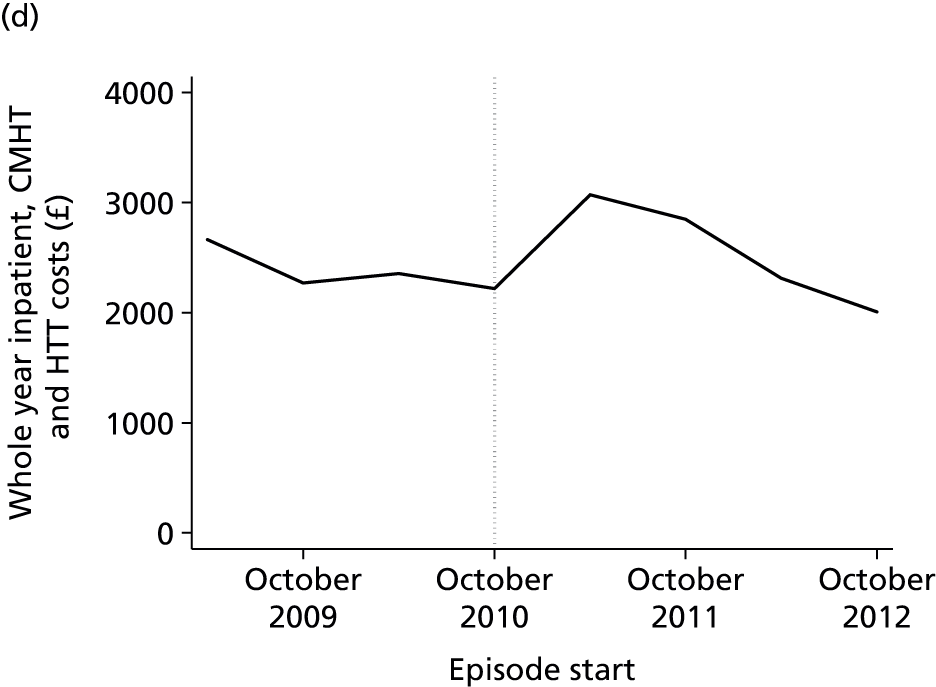
Again, we compared costs before and after the introduction of the CAG. Analyses were unadjusted and adjusted as described above. In all four boroughs there was no difference in unadjusted or adjusted costs (Croydon: unadjusted: b = 57.1, 95% CI –836.6 to 950.8, p = 0.90; adjusted: b = –207.4, 95% CI –1029.3 to 614.5, p = 0.62; Lambeth: unadjusted: b = –659.2, 95% CI –1525.1 to 206.7, p = 0.14; adjusted: b = –417.8, 95% CI –1269.9 to 434.4, p = 0.34; Lewisham: unadjusted: b = –119.3, 95% CI –623.9 to 385, p = 0.60; adjusted: b = –334.2, 95% CI –862.9 to 193.7, p = 0.22; Southwark: unadjusted: b = 218.1, 95% CI –319.5 to 755.7, p = 0.43; adjusted: b = 202.7, 95% CI –341.5 to 747.0, p = 0.47).
Psychotherapy caseload, counts of new episodes and episode duration
Daily borough caseloads within psychotherapy teams for individuals with non-psychotic diagnoses are displayed in Figure 15.
FIGURE 15.
Psychotherapy team daily caseloads for episodes starting between April 2009 and March 2014 in (a) Croydon; (b) Lambeth; (c) Lewisham; and (d) Southwark. Individuals with non-psychotic diagnoses only, with at least one face-to-face contact per episode. Smoothed daily figures are shown.
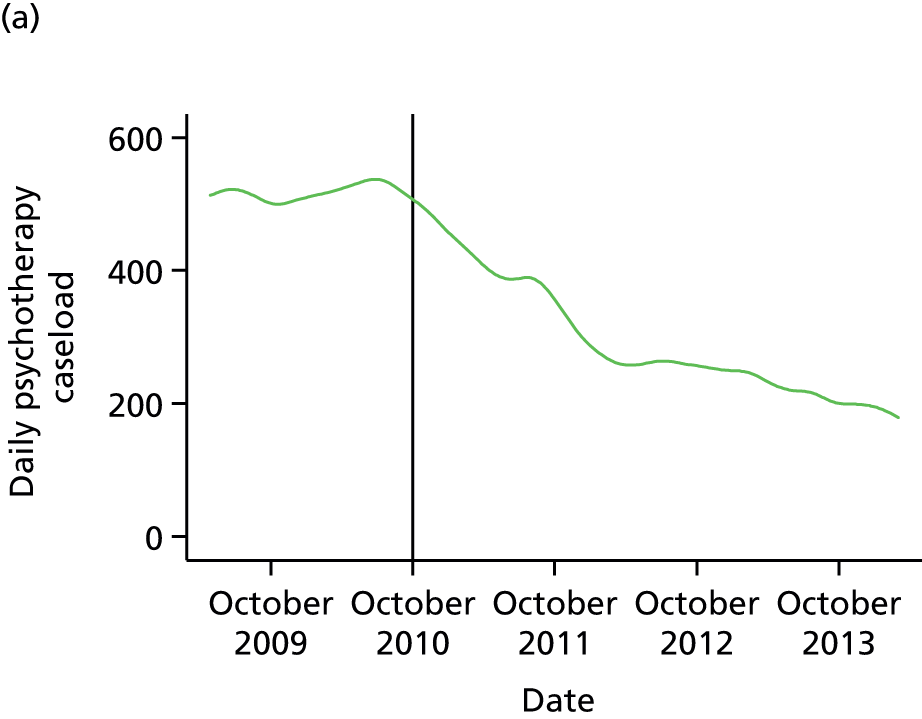
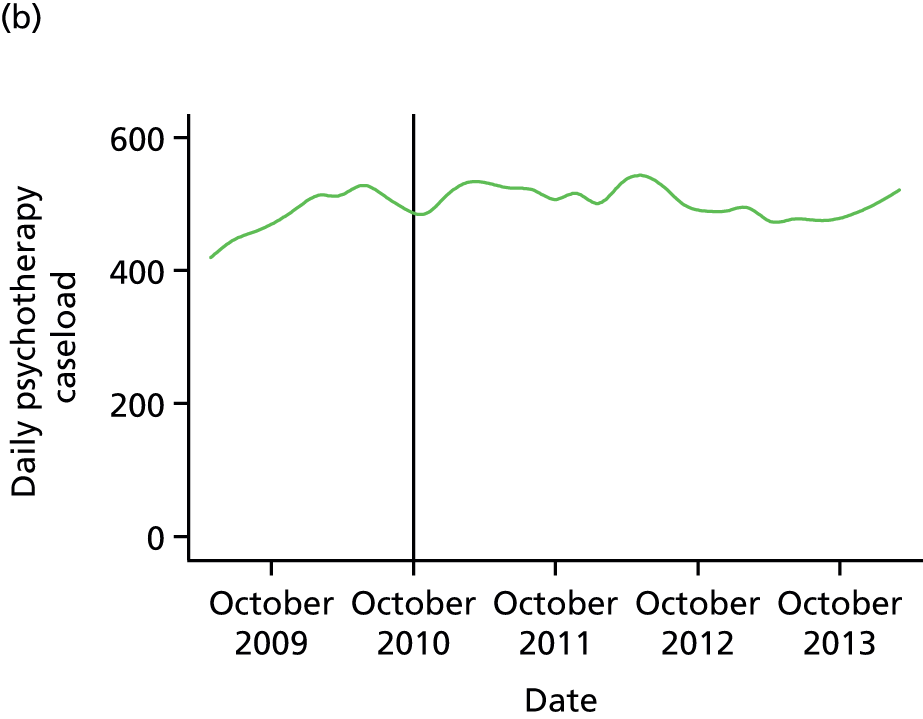
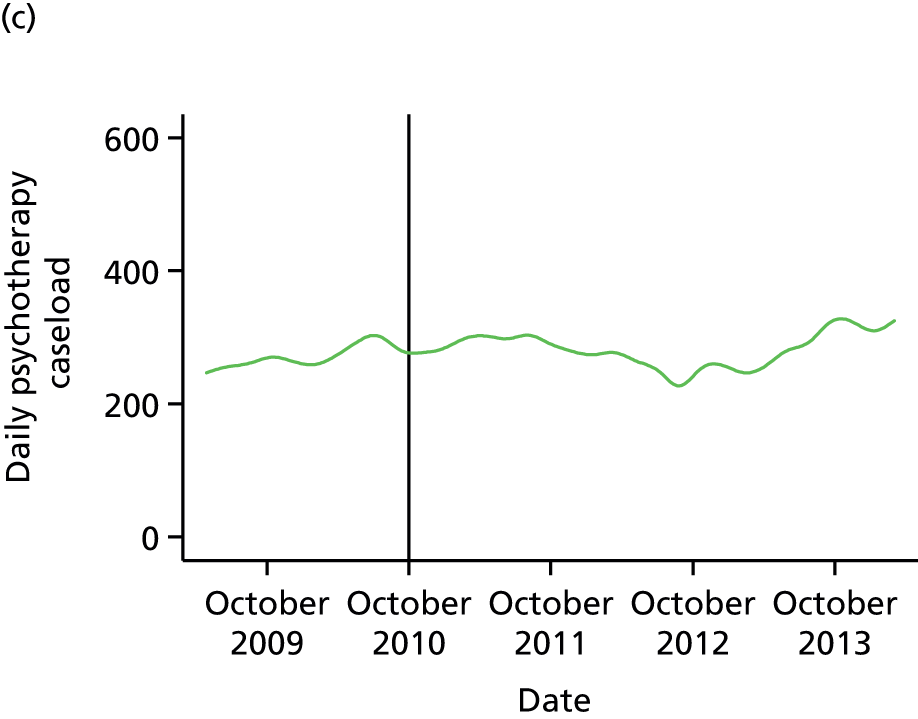

As with the CMHT data, visual inspection of the plots in Figure 15 indicated that a regression of the daily caseload figures against time, possibly allowing the slope of the fitted line to vary after CAG implementation, would provide a meaningful fit of the data. Each borough was analysed separately. Models in which caseload was regressed only against time (y = βtimeXtime + β0 + ε) were compared using LR testing with models in which caseload was regressed against time, a pre-/post-CAG indicator variable and an interaction term between the latter and time (y = βtimeXtime + βCAGXCAG + βCAG × timeXCAG × time + β0 + ε). Durbin’s alternative test indicated that serial autocorrelation was present (p < 0.0001 in all boroughs). As with the CMHT data, this was attributable to the fact that one day’s caseload can differ from the next only by the difference between the number of new patients and discharges that day. Therefore, Newey–West standard errors were used for the final analyses.
In all four boroughs, rates of change in the daily caseload altered in the post-CAG period (p < 0.0001 in all cases), with an increasing caseload before CAG implementation being followed by a reducing, or less strongly increasing, caseload (Table 7).
| Borough | Rate of change per day (95% CI; Wald test p-value) | |
|---|---|---|
| Pre CAG | Post CAG | |
| Croydon | 0.04 (0.03 to 0.05; < 0.001) | –0.23 (–0.24 to –0.23; < 0.001) |
| Lambeth | 0.19 (0.17 to 0.20; < 0.001) | –0.03 (–0.03 to –0.02; < 0.001) |
| Lewisham | 0.08 (0.08 to 0.09; < 0.001) | 0.01 (0.00 to 0.02; < 0.001) |
| Southwark | 0.04 (0.03 to 0.05; < 0.001) | –0.08 (–0.08 to –0.07; < 0.001) |
Counts of episodes per month and the 25th and 50th centiles of episode length are shown in Figures 16 and 17 respectively. Considering these alongside the caseload analyses it appeared that changes in caseload were generally driven by opposing effects of episode count and duration. In Croydon, the mean number of new episodes per month pre CAG was 29; post CAG it was 11 (t-test p < 0.0001). This outweighed the effect of episode length, with the median length increasing from 398 to 490 days (χ2 p = 0.015). In Lambeth, there were 24 new episodes per month pre CAG and 21 post CAG (t-test p = 0.28), with an increase in median episode length from 517 to 600 days (χ2 p = 0.039); in Lewisham, there were 20 new episodes per month pre CAG and 21 post CAG (t-test p = 0.50), with a non-significant reduction in episode length (pre CAG 354 days vs. post CAG 316 days; χ2 p = 0.09); and in Southwark, there were 18 new episodes per month pre CAG and 14 post CAG (p = 0.02), with an increase in median episode length from 450 to 505 days (χ2 p = 0.025).
FIGURE 16.
Counts of new treatment episodes for psychotherapy teams for episodes starting between April 2009 and March 2014 in (a) Croydon; (b) Lambeth; (c) Lewisham; and (d) Southwark. Individuals with non-psychotic diagnoses only, with at least one face-to-face contact per episode.

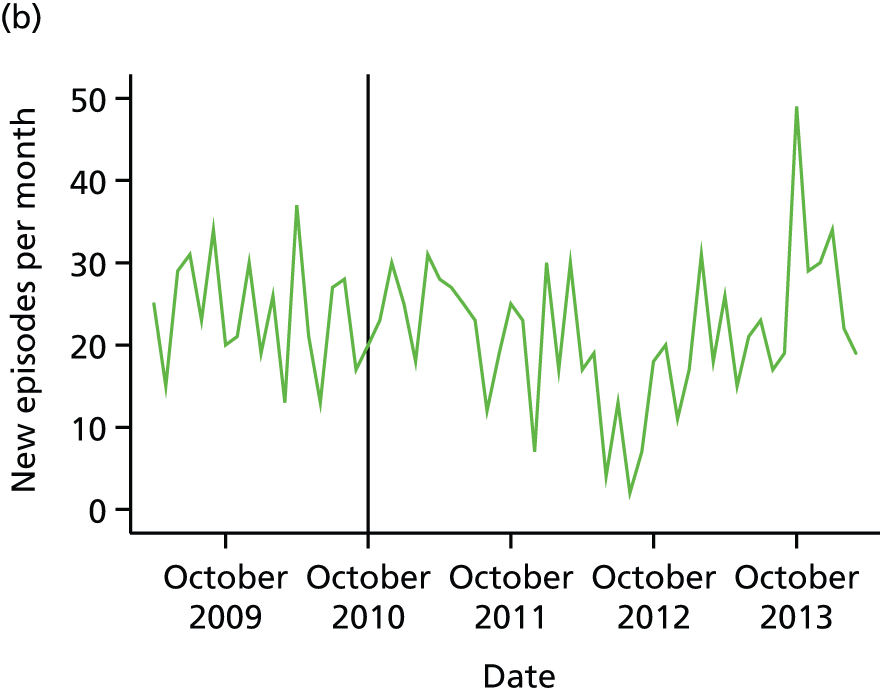
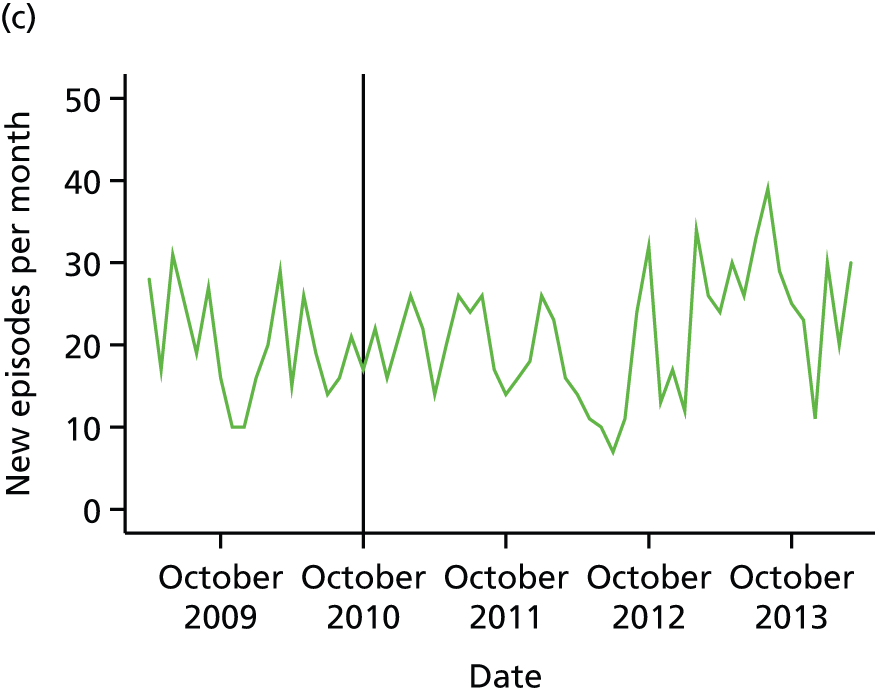
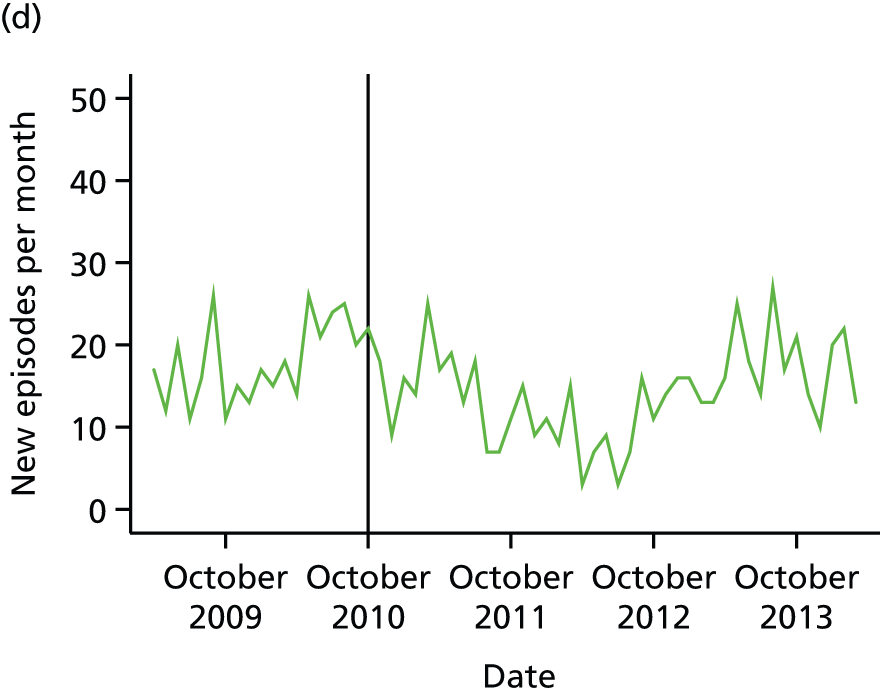
FIGURE 17.
Psychotherapy episode duration for episodes starting between April 2009 and March 2013 in (a) Croydon; (b) Lambeth; (c) Lewisham; and (d) Southwark: 25th and 50th centile values. Individuals with non-psychotic diagnoses only, with at least one face-to-face contact per episode. Data are aggregated over 6-month time bands, with each data point representing episodes starting in the 6 months after the point indicated on the x-axis.
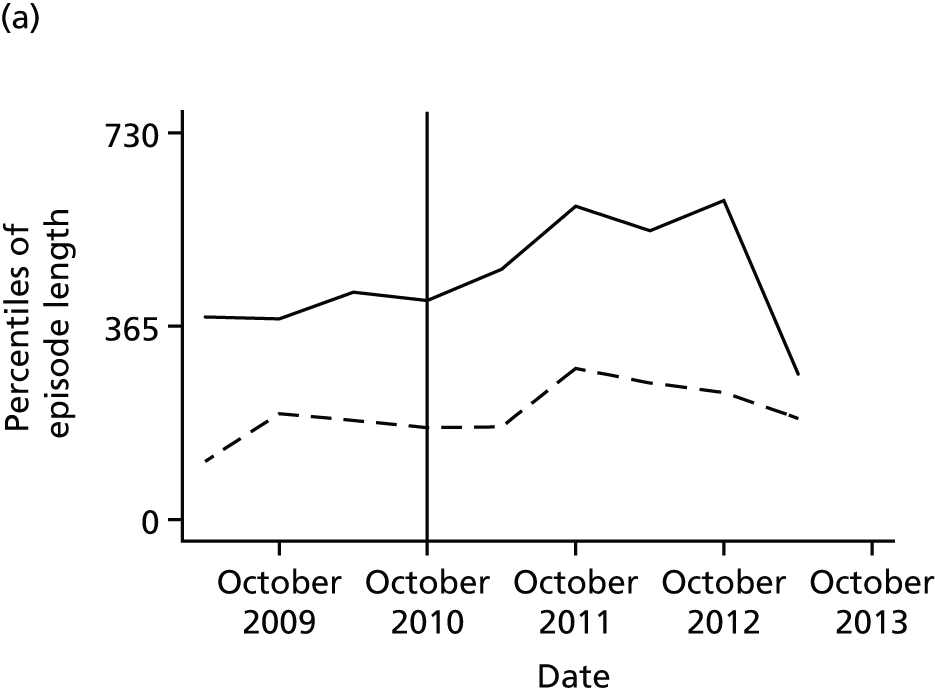
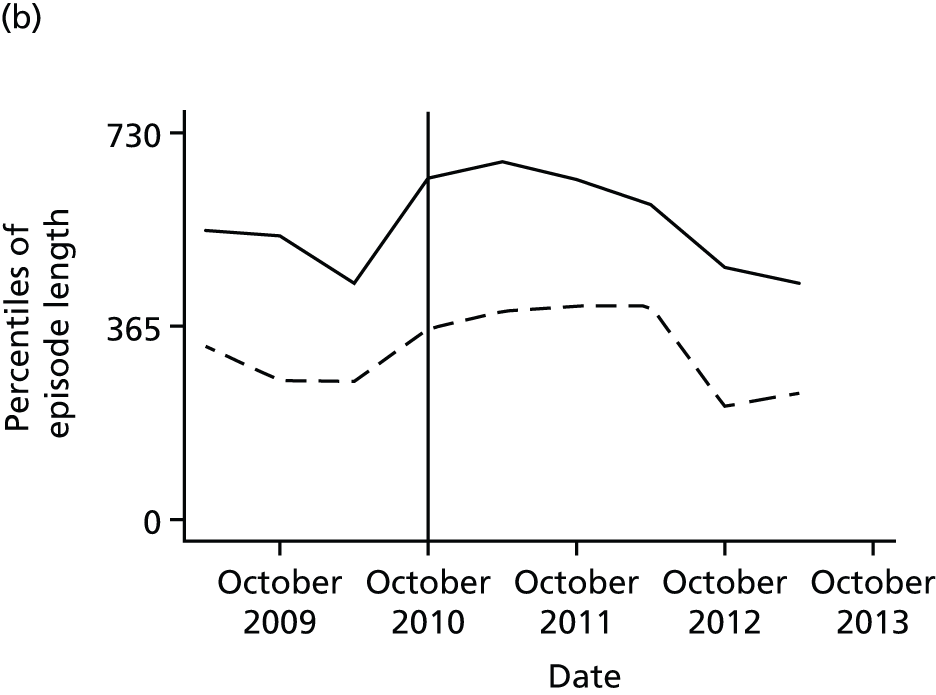

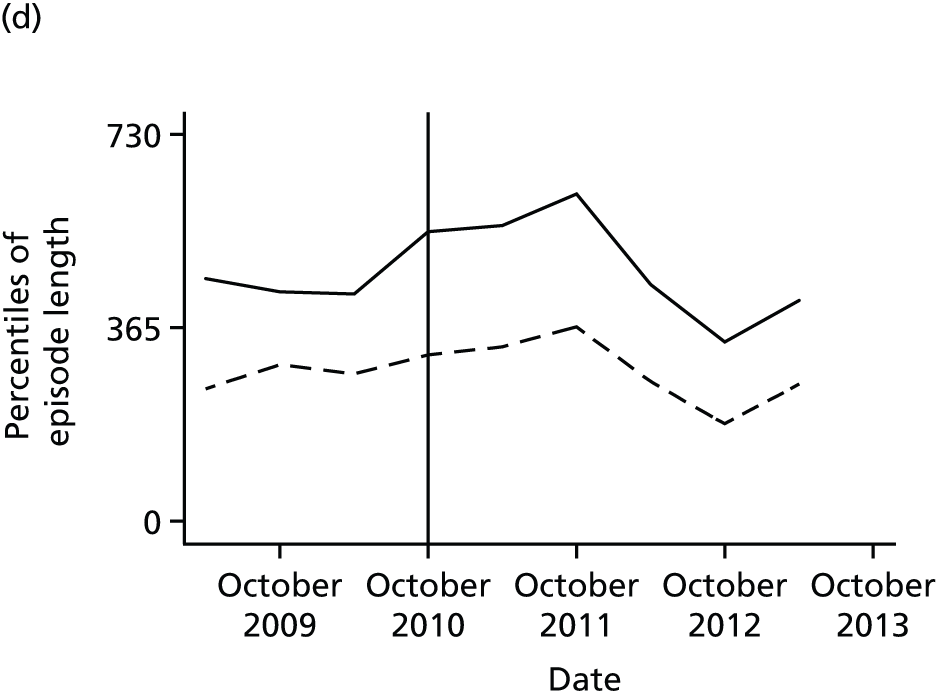
Number of psychotherapy contacts and costs
Analysis of costs and events indicated that there was under-recording of activity within the psychotherapy teams, especially prior to the most recent period. Therefore, we did not analyse either of these variables.
Activity in borough Improving Access to Psychological Therapies teams
The numbers of new treatment episodes of IAPT individual CBT (a treatment equivalent in intensity to that provided within the borough psychotherapy teams) are shown in Figure 18.
FIGURE 18.
Counts of new IAPT individual CBT treatment episodes between April 2009 and March 2014 in (a) Croydon; (b) Lambeth; (c) Lewisham; and (d) Southwark.
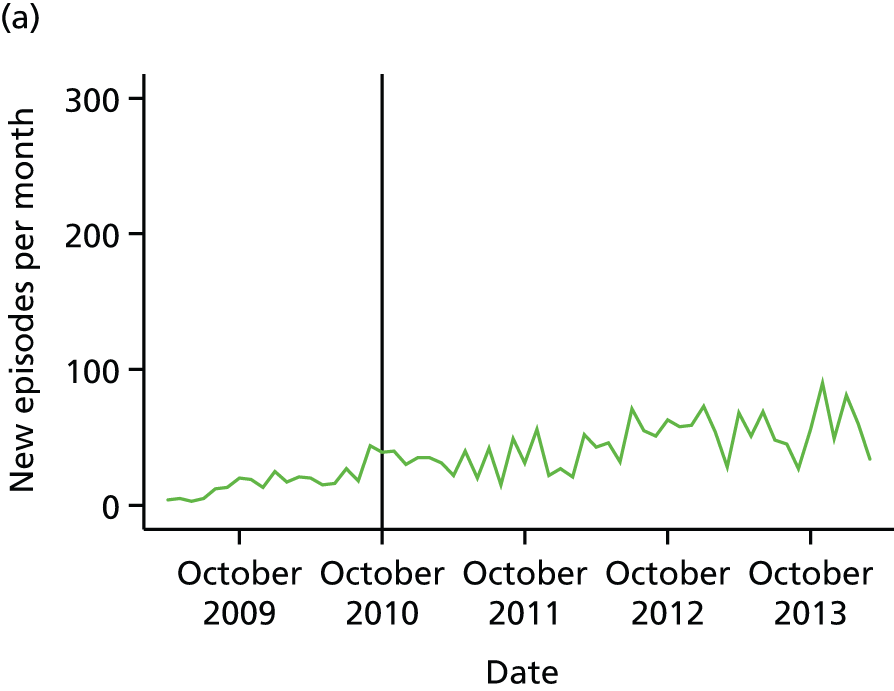
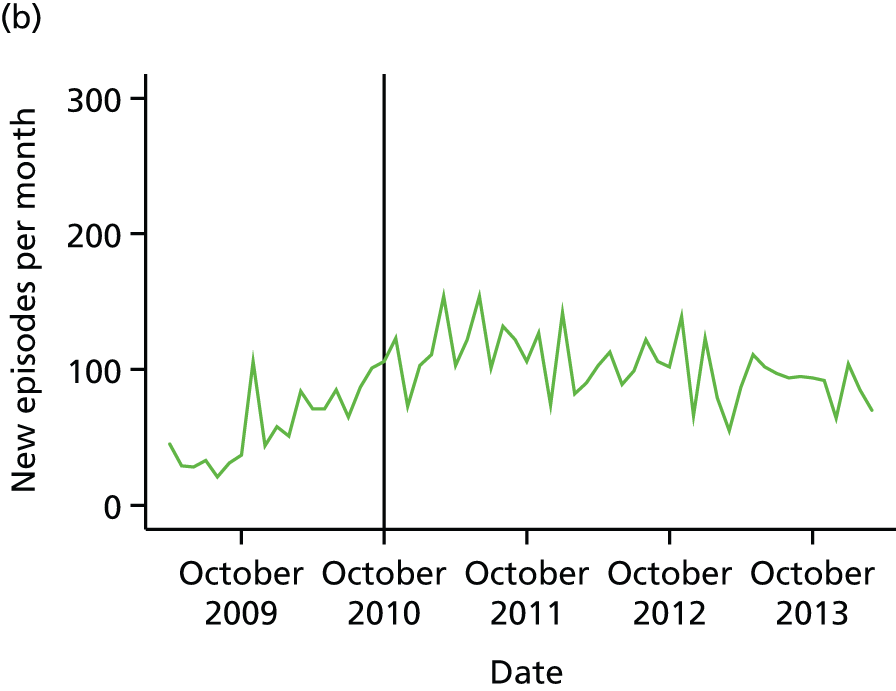
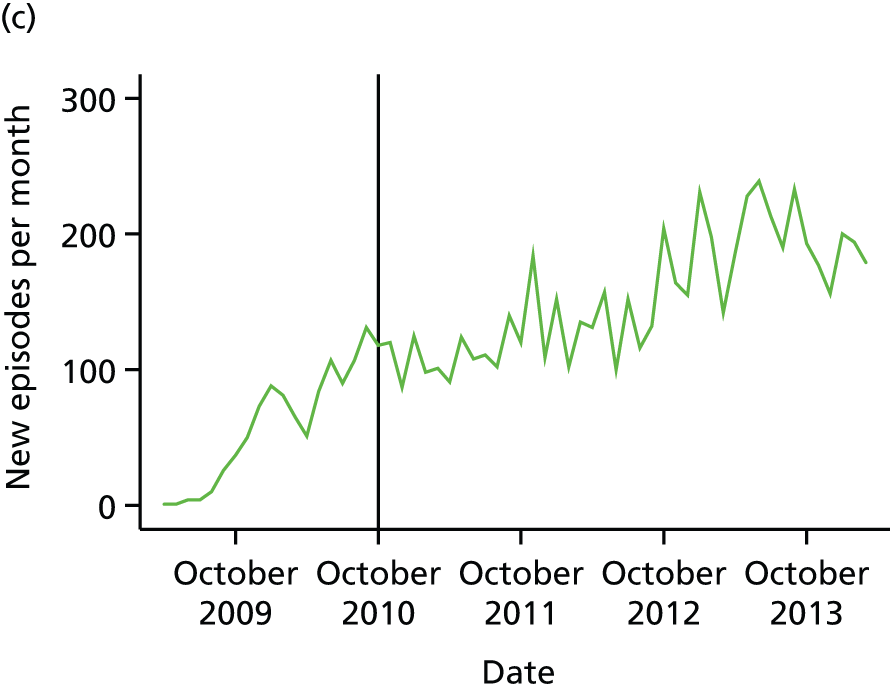
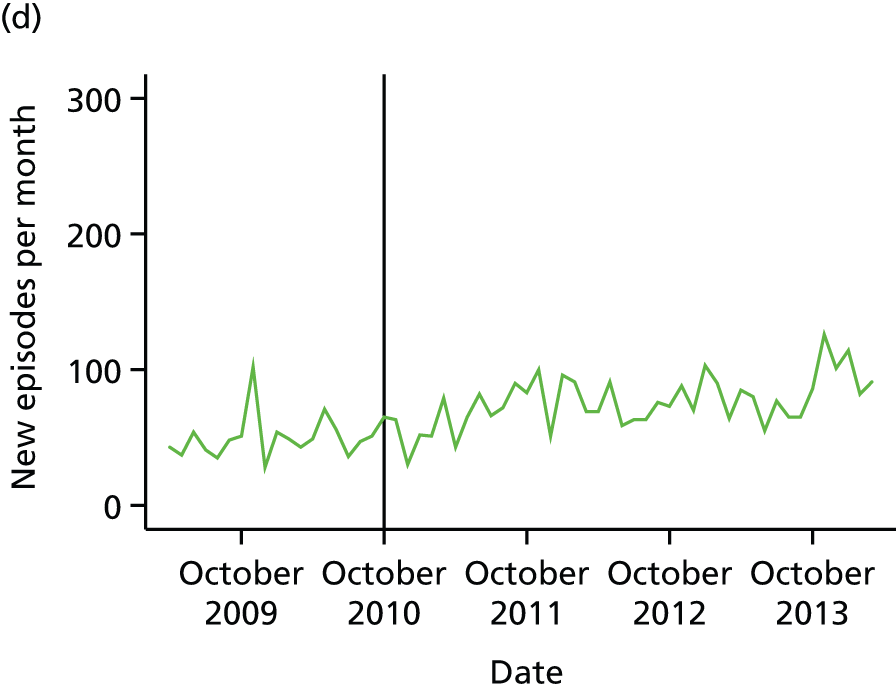
Regression analyses of monthly counts against time indicated that activity increased over time in all four boroughs. (There was significant autocorrelation in two boroughs according to Durbin’s alternative test and so Newey–West standard errors were calculated; the source of this autocorrelation was unclear but it may have been because of the use of explicit targets for new episodes per month in services that were just beginning to operate and were gradually increasing their capacity). In Croydon, the increase per month was 0.92 (95% CI 0.71 to 1.13; p < 0.001); in Lambeth, it was 0.75 (95% CI 0.21 to 1.29; p = 0.007); in Lewisham, it was 3.17 (95% CI 2.63 to 3.71; p < 0.001); and, finally, in Southwark, it was 0.82 (95% CI 0.57 to 1.08; p < 0.001). Because of collinearity between the pre-/post-CAG indicator and the time variable it was not possible to test whether or not this trend altered over time.
Effectiveness
Effectiveness of processes in community mental health teams assessed using case notes
Table 8 shows the results of the analysis of treatment processes in the sample of MAP patients taken from before and after the implementation of the CAG, and whose free-text notes were used to code various indicators of treatment. There was no evidence that treatment processes for depression have changed since the introduction of the CAG, at least as assessed by antidepressant use, the use of other medications or referral for psychotherapy.
| Treatment process | Before CAG implementation (n = 77), n/N (%) | After CAG implementation (n = 123), n/N (%) | Chi-squared p-value |
|---|---|---|---|
| Antidepressant use at first contact | |||
| Antidepressant already prescribed at first contact | 38/77 (49) | 76/123 (62) | 0.22 |
| Antidepressant prescribed at first contact | 7/77 (9) | 9/123 (7) | |
| No antidepressant prescribed | 32/77 (42) | 38/123 (31) | |
| Addition of other treatment at first contact among those already taking an antidepressant | 8/38 (21) | 14/76 (18) | 0.74 |
| Dose increase at first contact among those already taking an antidepressant | 16/38 (42) | 29/76 (38) | 0.68 |
| Dose decrease at first contact among those already taking an antidepressant | 8/38 (21) | 10/76 (13) | 0.28 |
| Referral for psychotherapy at first appointment | |||
| Already referred/receiving psychotherapy | 15/77 (19) | 16/123 (13) | 0.40 |
| Referred for psychotherapy | 37/77 (48) | 59/123 (48) | |
| Not referred | 25/77 (32) | 48/123 (39) | |
Effectiveness of processes in community mental health teams using structured data on receipt of psychotherapy during community mental health team treatment or within 3 months of its ending
The percentages of CMHT patients with a diagnosis of depression and who were treated by one of the borough-based psychotherapy teams or who received individual CBT in the local IAPT service are shown in Figure 19, with data aggregated over 6-month time bands.
FIGURE 19.
Proportion of CMHT episodes with depression receiving psychological treatment (in secondary care or IAPT individual CBT) for episodes starting between April 2009 and March 2014 in (a) Croydon; (b) Lambeth; (c) Lewisham; and (d) Southwark. Episodes with at least one face-to-face contact per episode. Diagnosis of depression according to ICD-10 code F32. Data are aggregated over 6-month time bands, with each data point plotted at the start of its related time band.

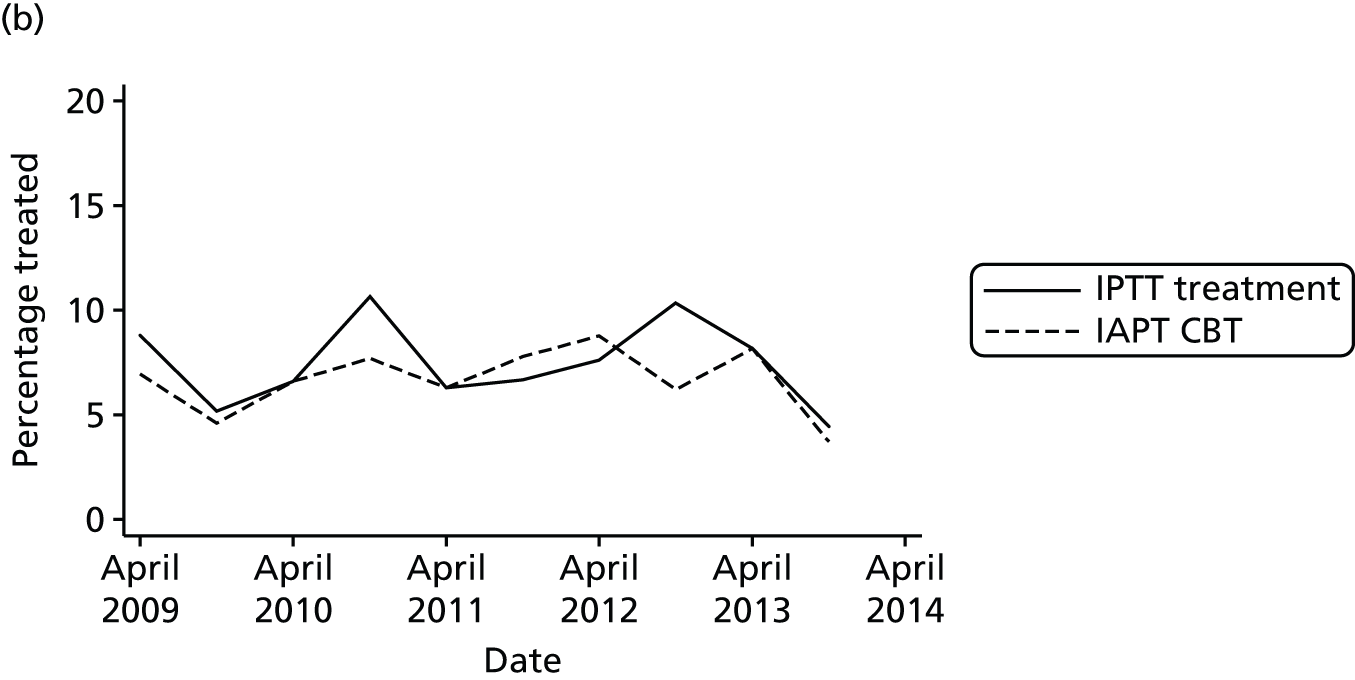
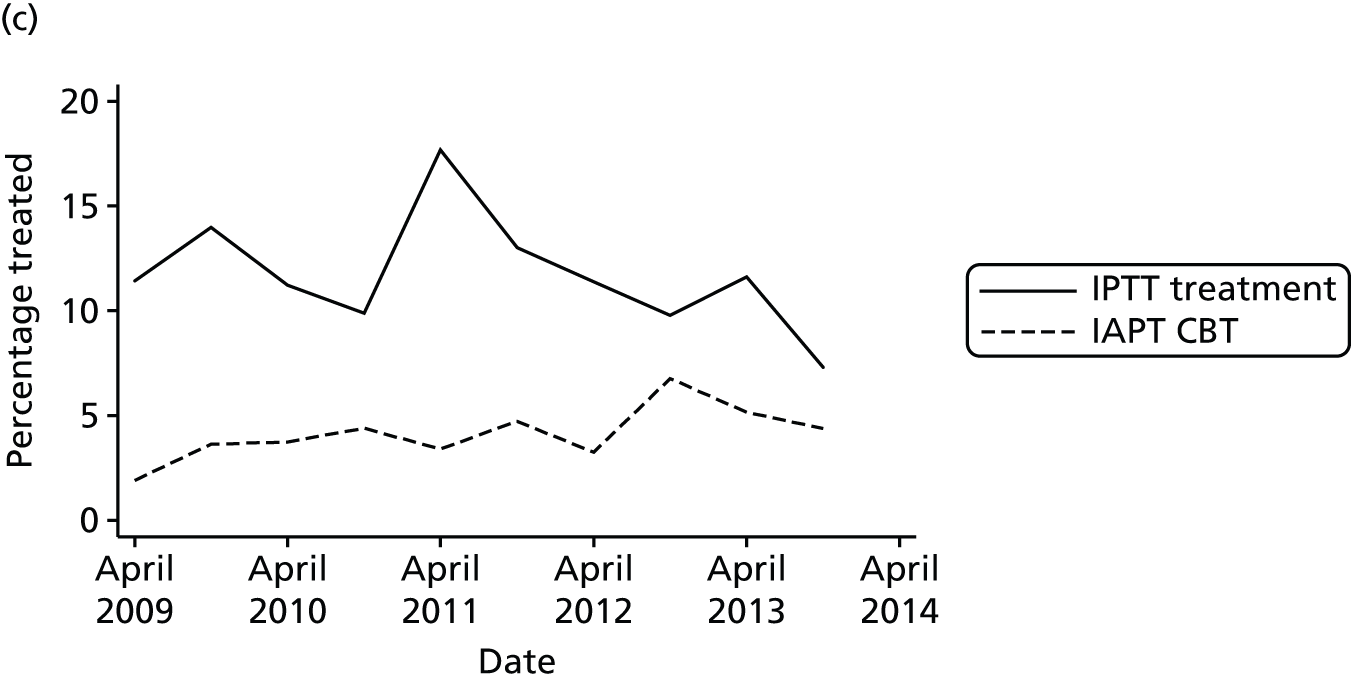
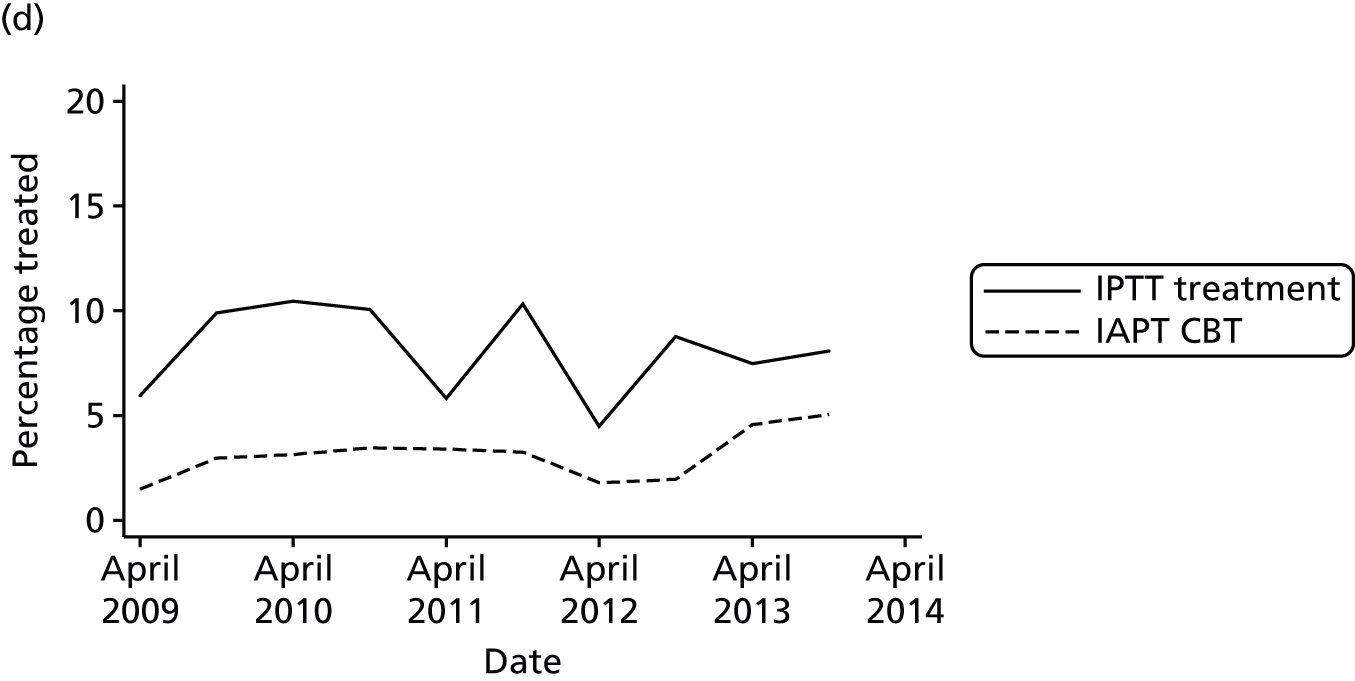
The logistic regression model demonstrated that the odds ratio (OR) for receipt of psychological therapy per month was 0.96 in Croydon (95% CI 0.95 to 0.97; p < 0.001). This implies that the odds of being treated were multiplied by 0.96 for each additional calendar month. A LR test comparing with a model also including a post-CAG indicator variable and an interaction between that indicator and time suggested that this trend did not alter after CAG implementation (p = 0.56). In Lambeth, there was no change in the odds of treatment over time (OR 1.00, 95% CI 0.99 to 1.01; p = 0.90) and again there was no evidence of an altered trend with time (p = 0.51). Similarly, in Lewisham, there was no change in the odds of treatment over time (OR 1.00, 95% CI 1.00 to 1.01; p = 0.85) and no evidence that this changed post-CAG implementation (p = 0.36). Finally, in Southwark, there was also no change in the odds of treatment receipt over time (OR 1.00, 95% CI 0.99 to 1.01; p = 0.89) and no evidence that this trend altered after CAG implementation (p = 0.18).
Effectiveness of community mental health teams judged by change in Health of the Nation Outcome Scales total score between the start and the end of treatment
Figure 20 demonstrates the mean total HoNOS scores at the start and end of treatment over time and by borough. Treatment effect by borough over time is plotted in Figure 21.
FIGURE 20.
Community mental health team episodes starting between April 2009 and March 2014 in (a) Croydon; (b) Lambeth; (c) Lewisham; and (d) Southwark: mean HoNOS total scores at the start and end of treatment. Individuals with non-psychotic diagnoses only, with at least one face-to-face contact per episode. Data aggregated over 6-month time bands, with each data point plotted at the start of its related time band.
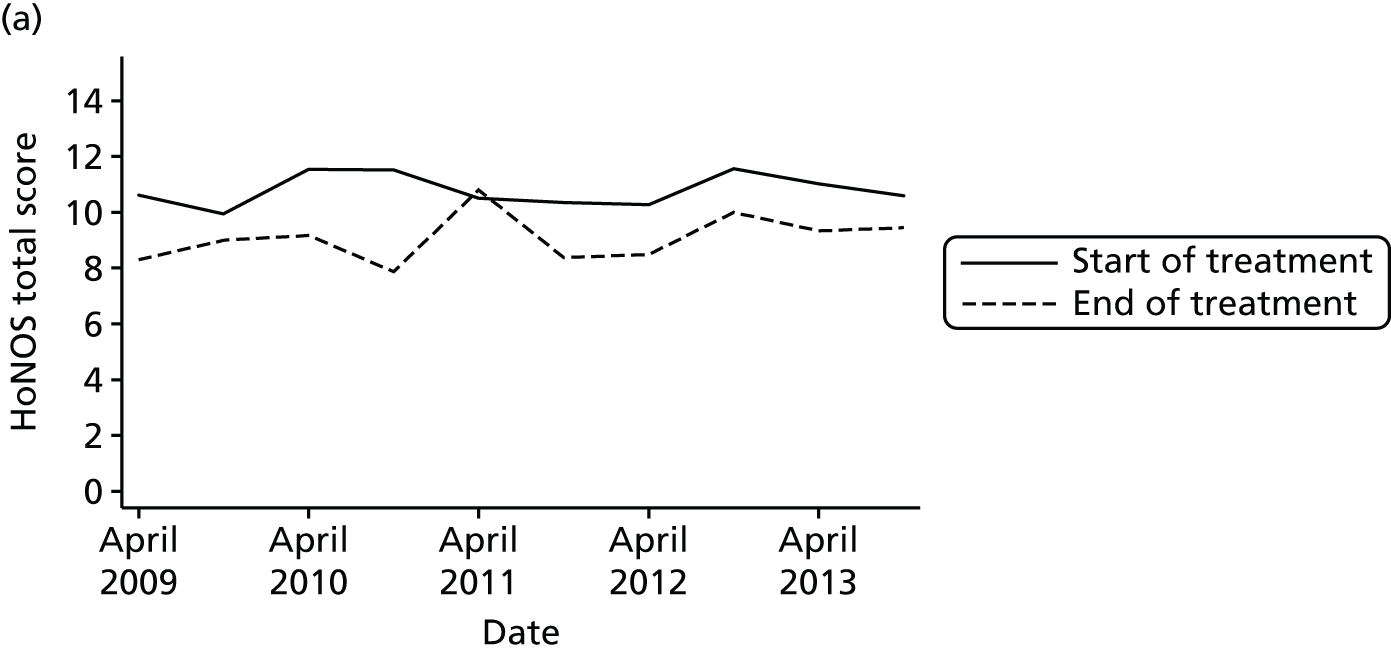
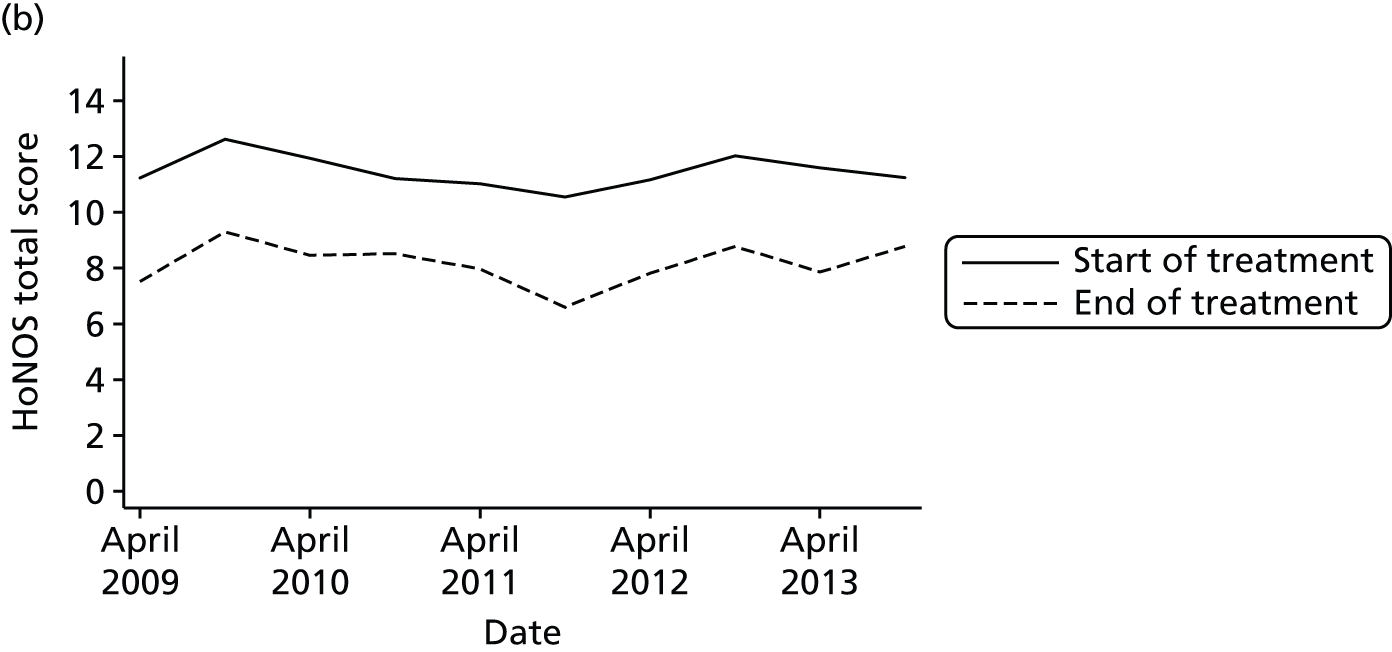
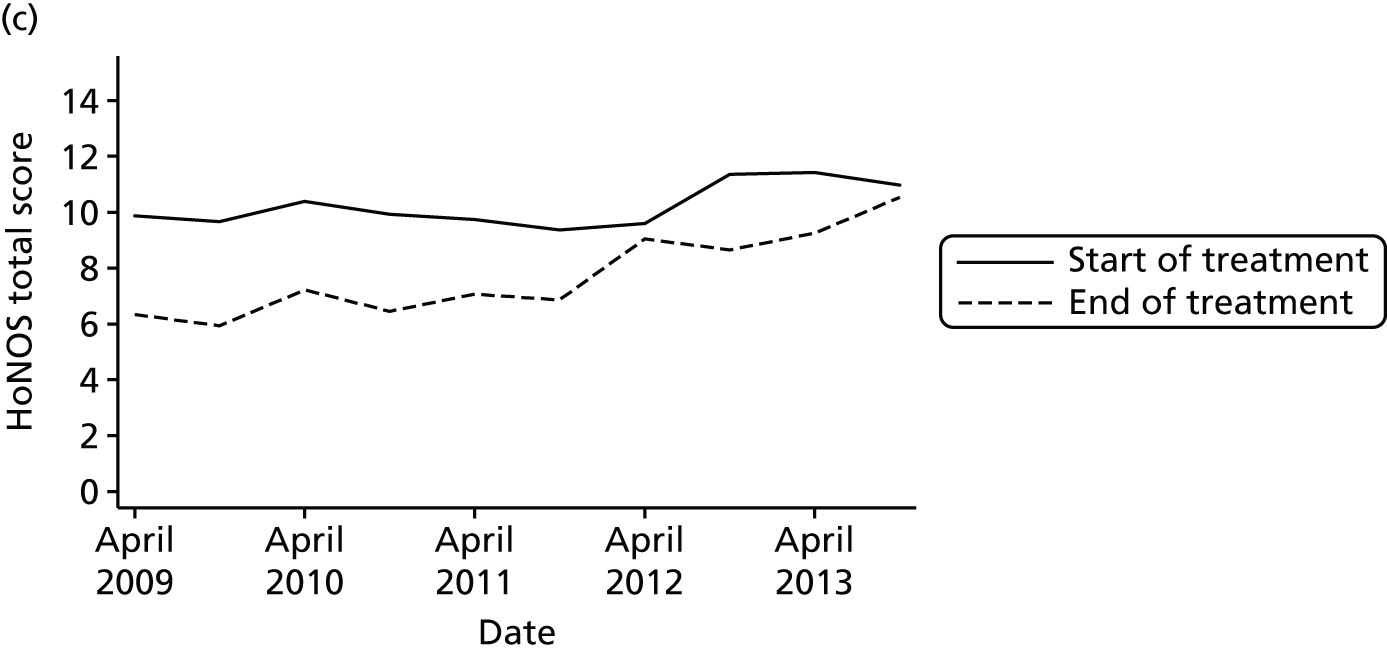

FIGURE 21.
Community mental health team episodes starting between April 2009 and March 2014 with a diagnosis of mood, anxiety or personality disorder: predicted treatment effect. The slope in the treatment effect for Croydon pre month was –0.01 (95% CI –0.03 to –0.01; p = 0.33); in Lambeth it was 0.00 (95% CI –0.01 to 0.02; p = 0.54); in Lewisham it was 0.06 (95% CI 0.04 to 0.07; p < 0.001; and in Southwark it was 0.01 (95% CI 0.00 to 0.03; p = 0.049).
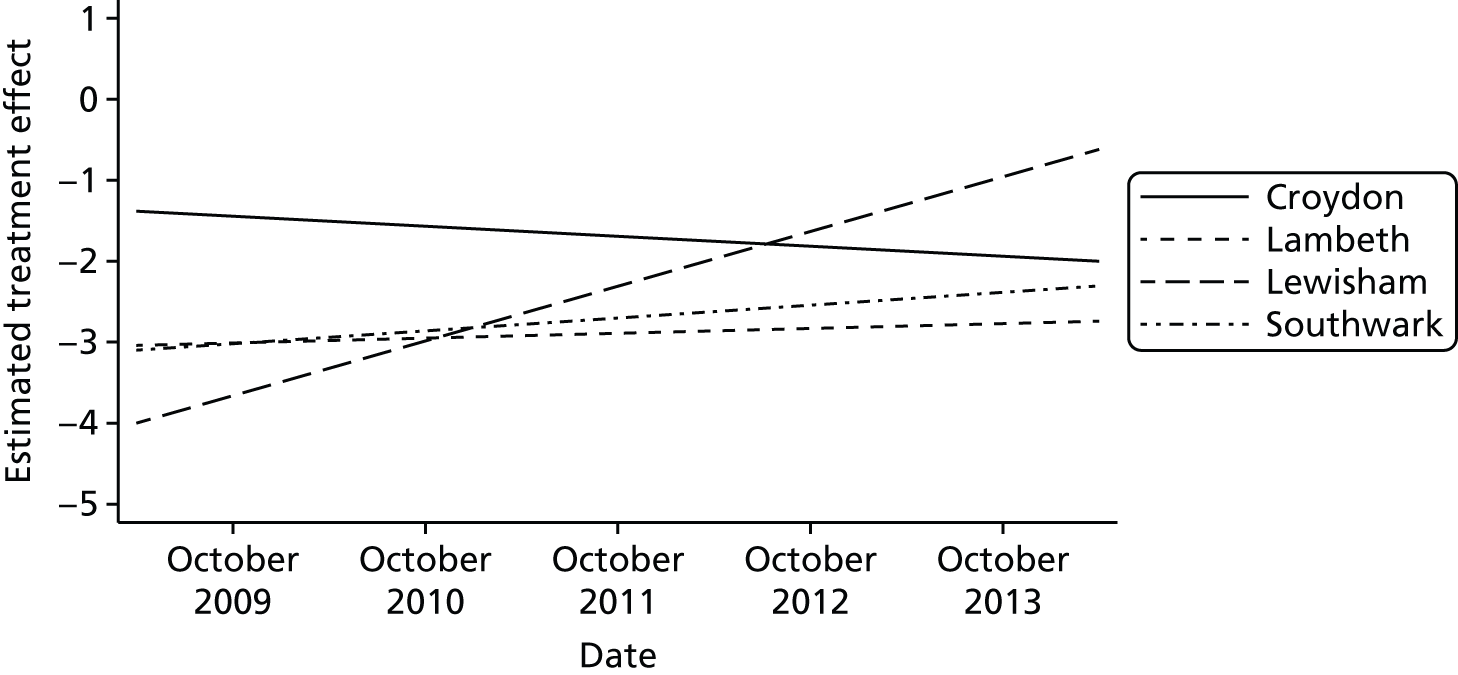
Effectiveness of psychotherapy teams judged by change in Clinical Outcomes in Routine Evaluation total score between the start and the end of treatment
Figure 22 demonstrates the mean total scores on the CORE-10 at the start and end of treatment over time and by borough.
FIGURE 22.
Mean CORE-10 total score before and after psychological treatment for episodes starting between April 2009 and March 2014 in (a) Croydon; (b) Lambeth; (c) Lewisham; and (d) Southwark. Individuals with non-psychotic diagnoses only, with at least one face-to-face contact per episode.
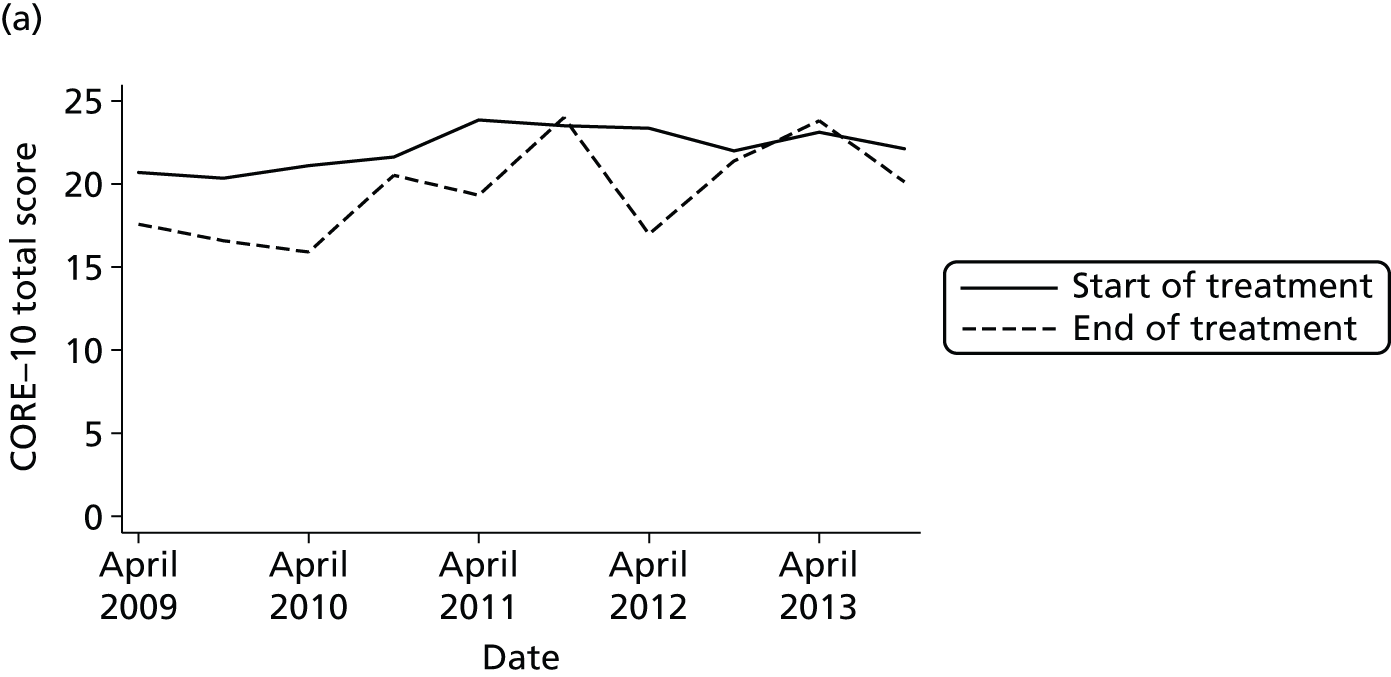
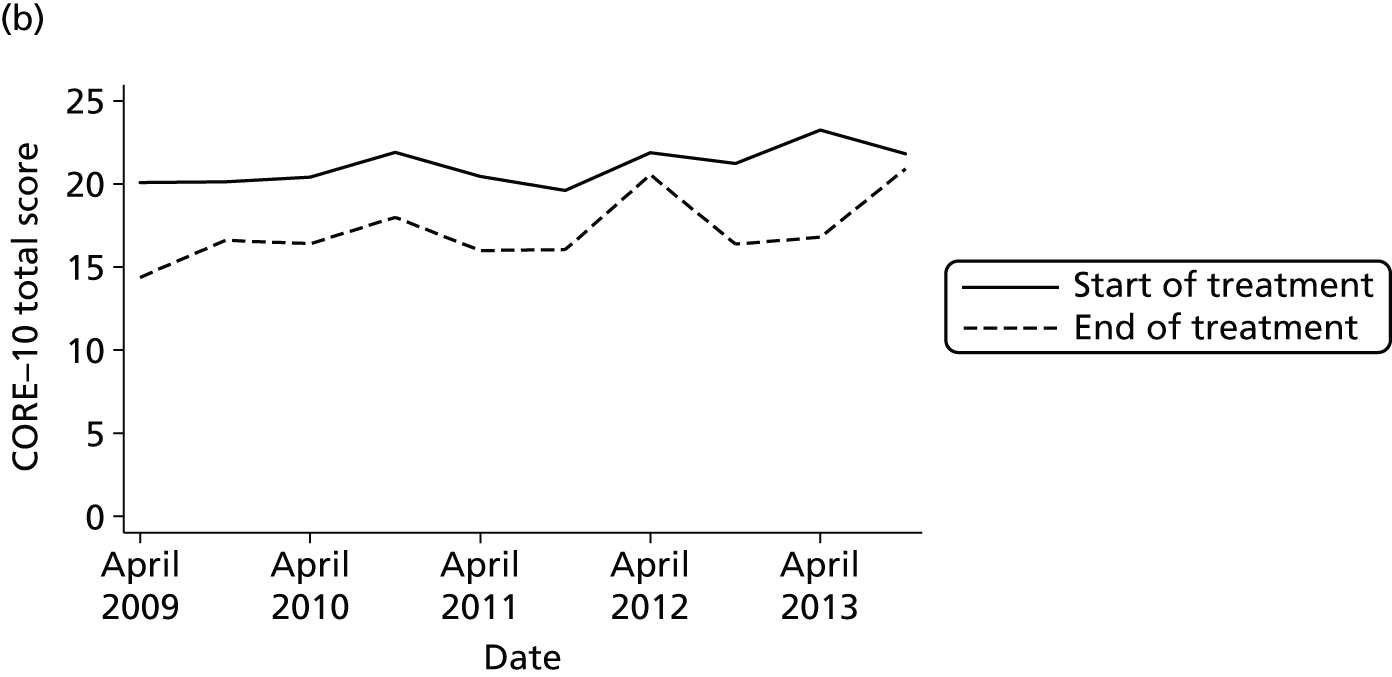
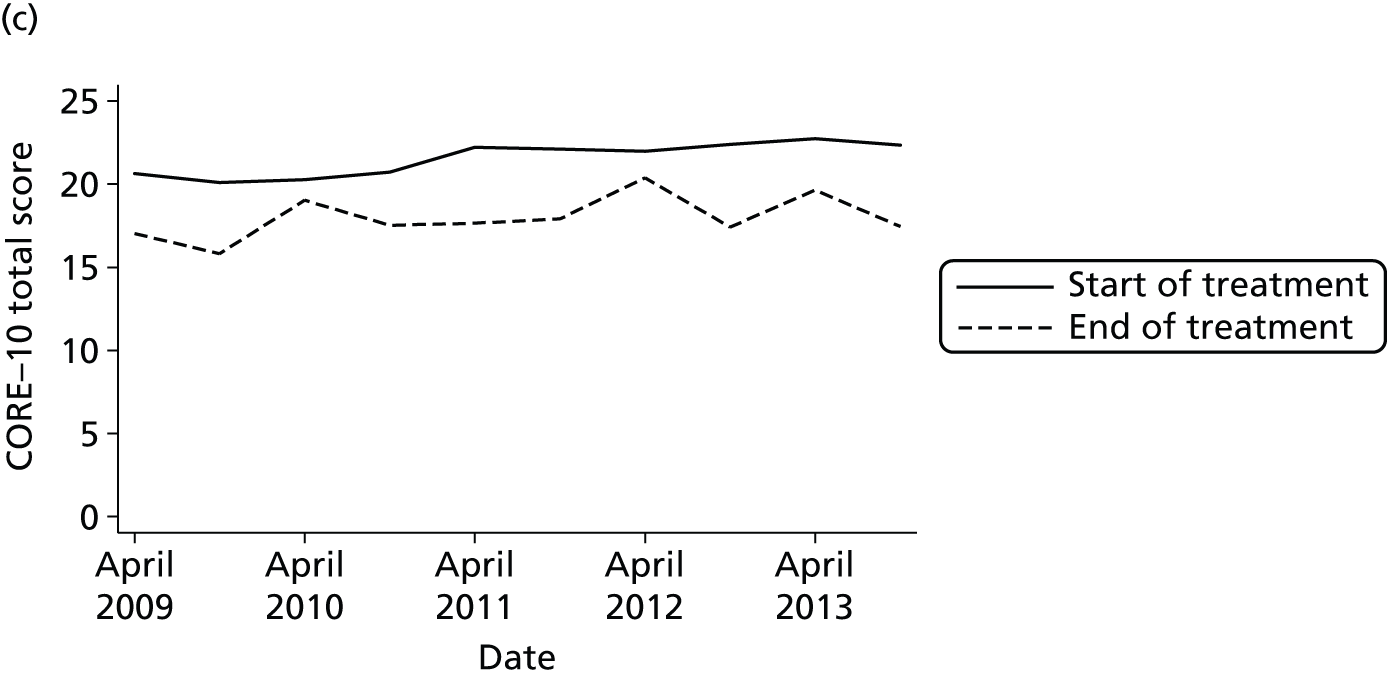
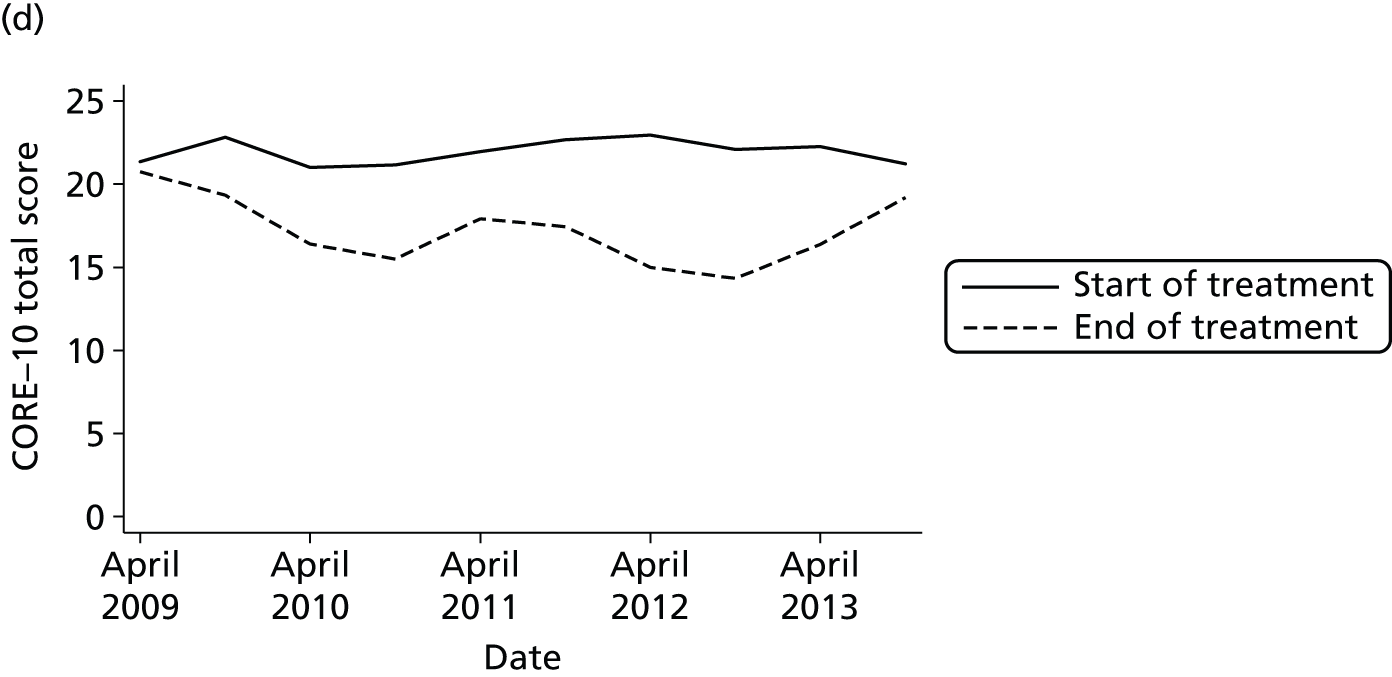
Of the 5774 total observations, 2658 (46%) had a pre-treatment rating along with the necessary covariates and 1052 (18%) had a usable post-treatment rating, giving a sample size of 3710. A model unadjusted for any other variable gave an estimated value for the treatment effect of b = –3.8 (95% CI –4.2 to –3.4; p < 0.0001), indicating an average reduction in the total score of 3.8 points (model 1). This effect was not altered (b = –3.8) by the addition of diagnosis, age, sex, ethnicity, marital status, borough and time as covariates (model 2). Fitting models with the same set of covariates, but including interactions with treatment effect (model 3a), there was evidence that the treatment effect increased with time (p = 0.0154) and was affected by diagnosis (p = 0.0470) but not by borough (p = 0.19), so the latter was omitted from the resulting model (model 3b). The three-way interaction between treatment effect, time and diagnosis included in model 4a was not significant (p = 0.0934). The LR test comparing model 3b with the model containing interactions with the post-CAG indicator variable (model 5) was also not significant (p = 0.74). In summary, the effectiveness of psychotherapy appeared to increase over time, but this trend was not affected by CAG implementation. Figure 23 shows the predicted treatment effect over time based on Model 3b.
FIGURE 23.
Community mental health team episodes starting between April 2009 and March 2014 with a diagnosis of mood, anxiety or personality disorder: predicted effect of psychotherapy on CORE-10 total score. The slope of the treatment effect over time per month was –0.025 (95% CI –0.048 to –0.003; p = 0.027).

Safety
Rates of accident and emergency consultations for self-harm among current or recent community mental health team patients
Figure 24 demonstrates the unadjusted rates of A&E consultations for self-harm among current CMHT patients or those discharged from a CMHT no more than 3 months previously. Rates are calculated separately for quarterly time bands and graphed separately by borough. Only those individuals with non-psychotic diagnoses are included.
FIGURE 24.
Unadjusted rates of A&E consultation for self-harm for CMHT episodes starting between April 2009 and November 2011 in (a) Croydon; (b) Lambeth; (c) Lewisham; and (d) Southwark. Individuals with non-psychotic diagnoses only, with at least one face-to-face contact per episode. Estimated rates per 3-month time band. Whiskers indicate 95% CIs for each estimate. q, quarter.
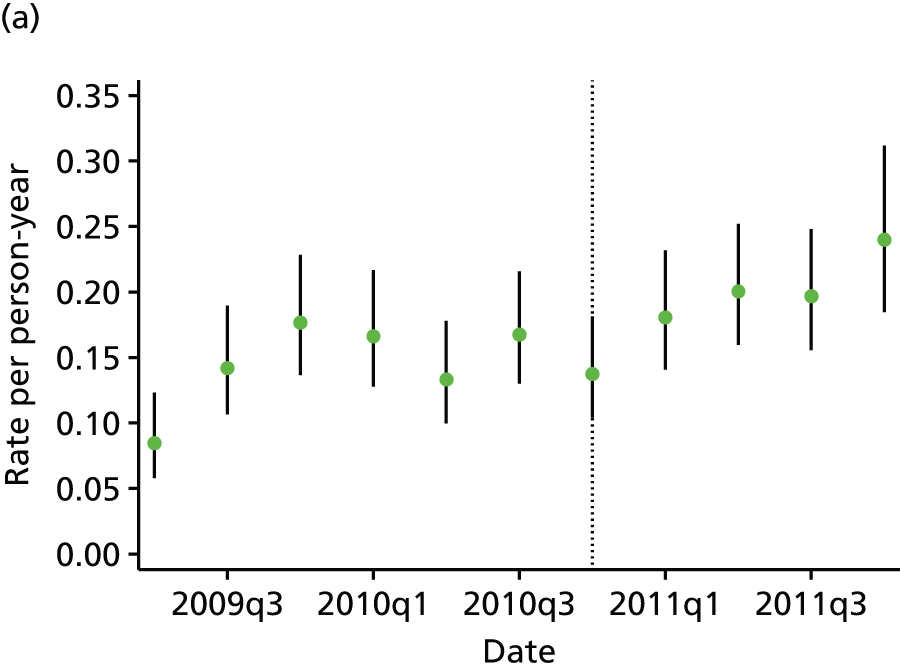
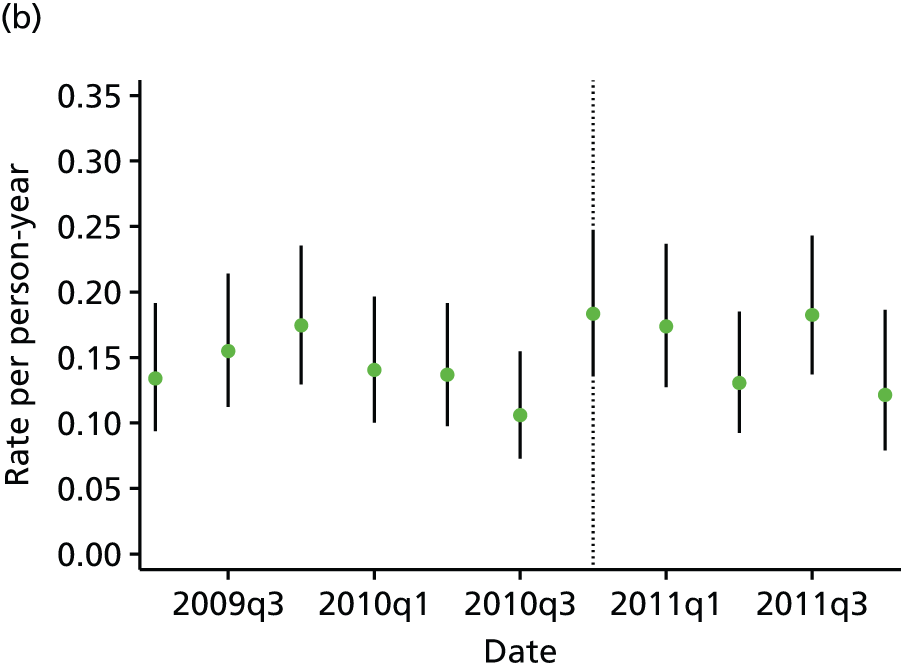
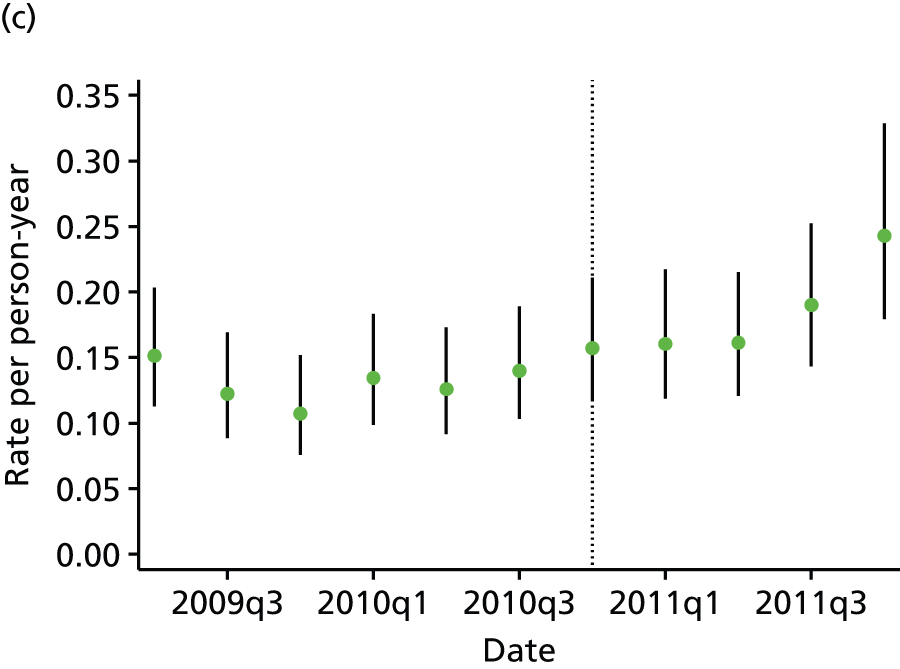
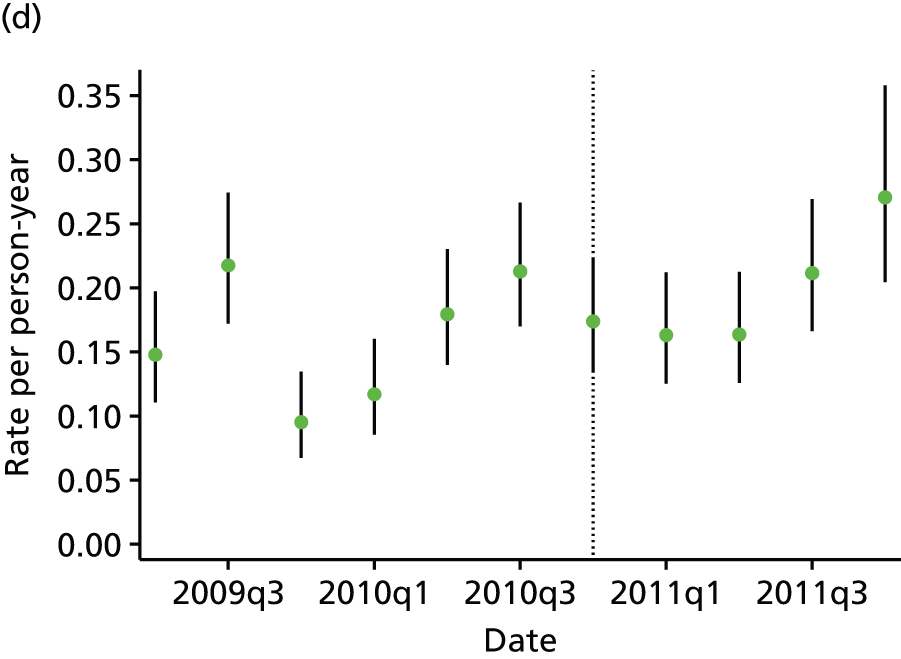
In Croydon, there was an upwards trend in the adjusted rate of self-harm throughout the study period [hazard ratio (HR) per quarter 1.07, 95% CI 1.04 to 1.10; p < 0.0001]; however, there was no evidence that this trend was different before and after CAG implementation (LR test p = 0.47). Findings were similar in Lewisham, where there was an overall increasing trend (HR per quarter 1.08, 95% CI 1.05 to 1.11; p < 0.0001) and the LR test comparing the varying trend model with the constant trend model was non-significant (p = 0.94), and also in Southwark, where the HR per quarter was 1.08 (95% CI 1.05 to 1.11; p < 0.0001) and the LR p-value comparing the varying trend model and the constant trend model was 0.35. In Lambeth, the trends in the rate of self-harm were better modelled by an altered trend before and after CAG implementation (LR test p = 0.0076). However, neither the trend before CAG implementation nor the trend after implementation was significant: the HR per quarter before CAG implementation was 0.97 (95% CI 0.89 to 1.06; p = 0.48) whereas the HR per quarter after CAG implementation was 0.91 (95% CI 0.82 to 1.01; p = 0.09).
Rates of acute hospital admission for self-harm among current or recent community mental health team patients
Figure 25 shows the unadjusted rates of admission to an acute hospital with an ICD-10 code indicating a primary diagnosis of self-harm. This data series extends to March 2013.
FIGURE 25.
Unadjusted rates of acute hospital admission for self-harm for CMHT episodes starting between April 2009 and March 2013 in (a) Croydon; (b) Lambeth; (c) Lewisham; and (d) Southwark. Individuals with non-psychotic diagnoses only, with at least one face-to-face contact per episode. Estimated rates per 3-month time band. Whiskers indicate 95% CIs for each estimate. q, quarter.
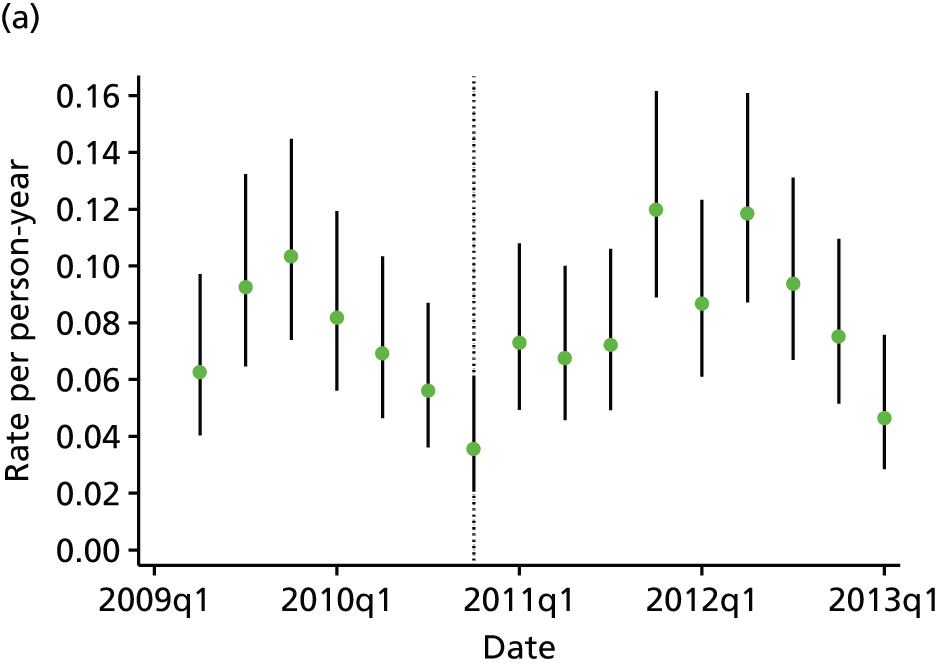
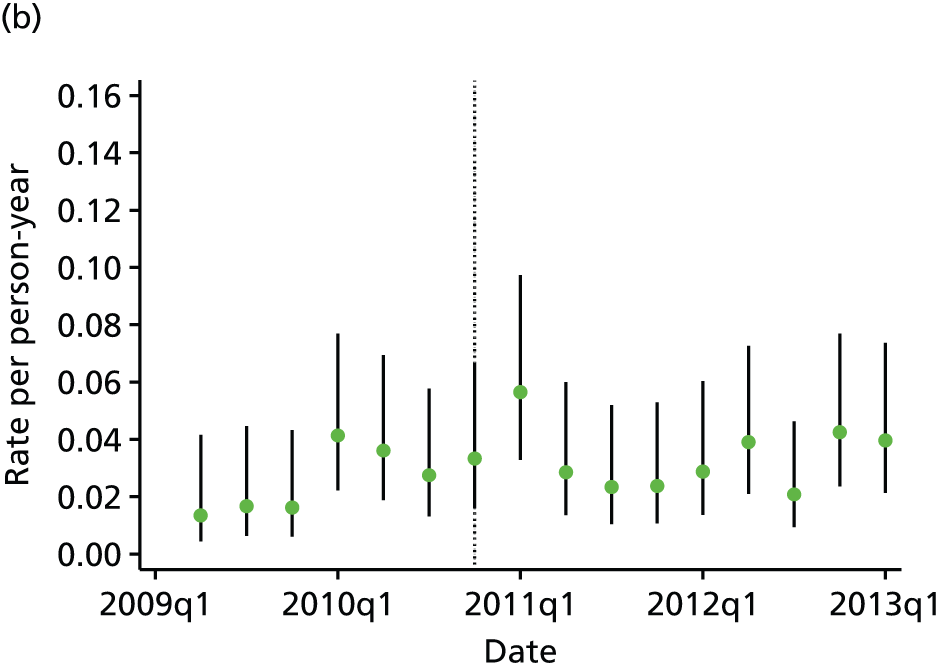
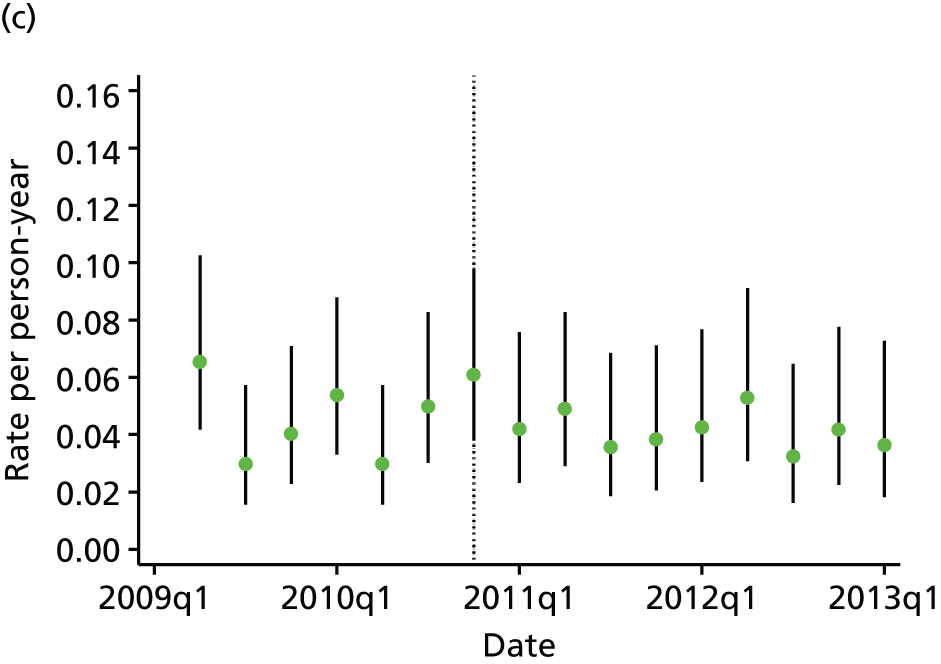
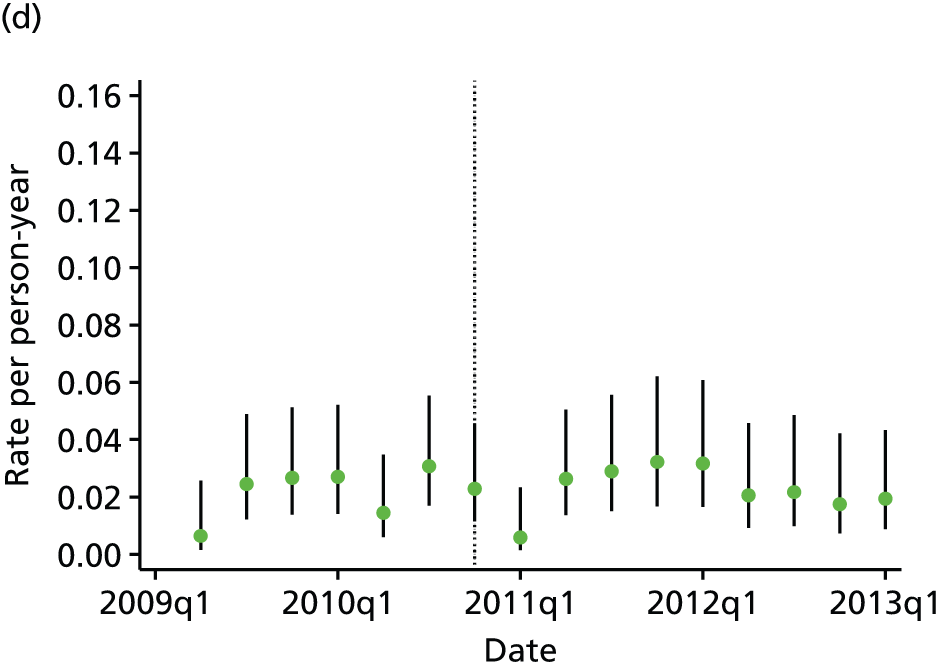
In Croydon, there was no trend in the adjusted rate of self-harm over time (HR per quarter 1.01, 95% CI 0.99 to 1.03; p = 0.53) and no evidence that there were different trends before and after CAG implementation (LR test p = 0.59). Findings were similar in Lewisham, where there was no trend (HR per quarter 1.01, 95% CI 0.98 to 1.05; p < 0.0001) and the LR test comparing the varying trend model with the constant trend model was non-significant (p = 0.54), and also in Southwark, where the HR per quarter was 1.03 (95% CI 0.99 to 1.11; p = 0.17) and the LR p-value comparing the varying trend model and the constant trend model was 0.17. In Lambeth, there was an upwards trend in the rate of self-harm (HR per quarter 1.05, 95% CI 1.01 to 1.09; p = 0.0186) and no evidence that this trend altered before and after CAG implementation (LR test p = 0.0076).
In view of the apparently non-linear shape of the curve for Croydon, we also compared the overall rate after CAG implementation with the overall rate before CAG implementation. The relative rate of admission was 1.03 in Croydon (95% CI 0.84 to 1.26; p = 0.77), 1.56 in Lambeth (95% CI 1.05 to 2.31; p = 0.03), 1.18 in Lewisham (95% CI 0.88 to 1.58; p = 0.27) and 1.22 in Southwark (95% CI 0.83 to 1.81; p = 0.31).
In summary, there was evidence of increasing self-harm presentations in Croydon, Lewisham and Southwark and of increasing self-harm admissions in Lambeth. There was no evidence that any positive or negative trend had altered after CAG implementation.
Patient centredness
Current waiting time for community mental health teams
In Croydon, the mean current waiting time was reduced by 14.0 days after CAG implementation (95% CI –15.7 to –12.2 days; p < 0.001) and in Lewisham it was reduced by 10.5 days (95% CI –12.5 to –8.6 days; p < 0.001). However, in Lambeth it was increased by 10.8 days (95% CI 8.3 to 13.2 days; p < 0.001) and in Southwark it was increased by 10.3 days (95% CI 6.5 to 14.2 days; p < 0.001). The variation in current waiting time over time is shown in Figure 26.
FIGURE 26.
Daily current waiting time for CMHTs for episodes starting between April 2009 and March 2013 in (a) Croydon; (b) Lambeth; (c) Lewisham; and (d) Southwark: 25th, 50th and 75th centile values.
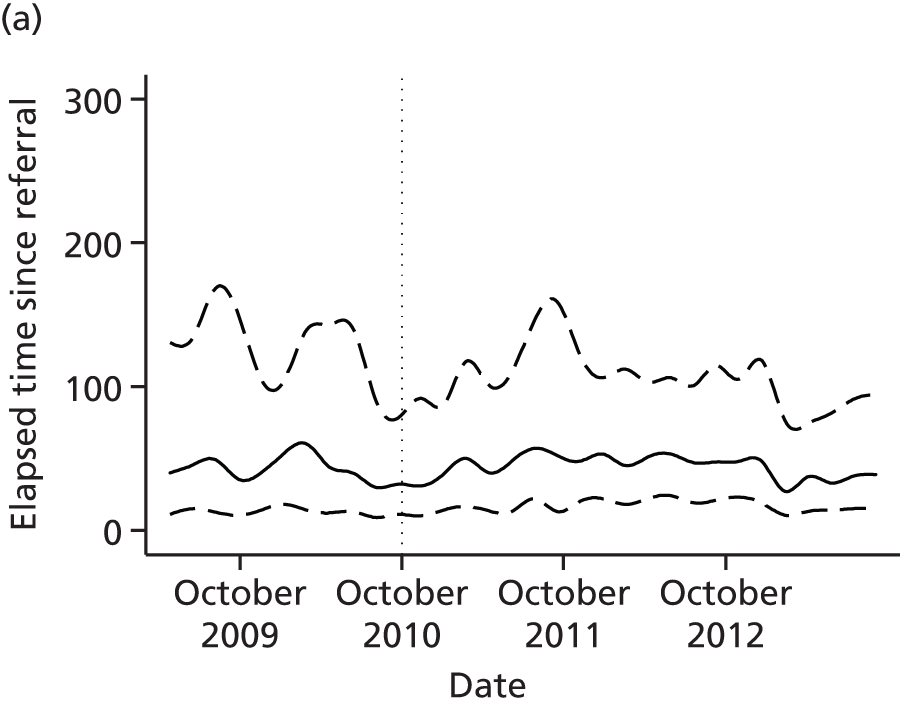

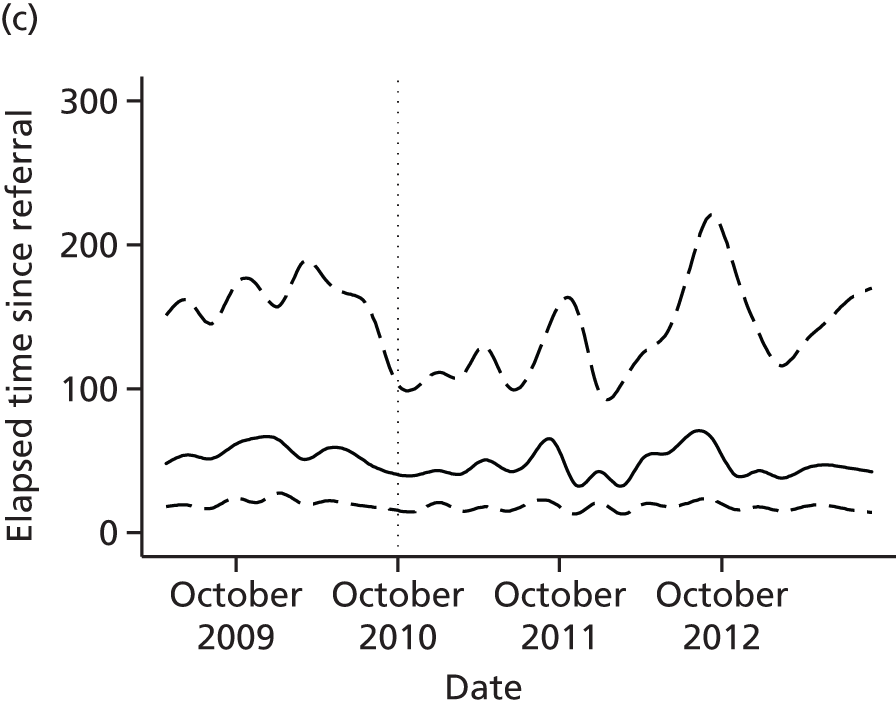

Current waiting time in psychotherapy teams
In Croydon, the mean current waiting time increased by 45.0 days post-CAG implementation (95% CI 37.5 to 52.5 days; p < 0.001); in Lambeth it reduced by 33.2 days (95% CI –36.3 to –30.1 days; p < 0.001); in Lewisham it reduced by 55.3 days (95% CI –63.6 to –47.1 days; p < 0.001); and in Southwark it reduced by 67.7 days (95% CI –75.1 to –60.2 days; p < 0.001). The variation in current waiting time over time is shown in Figure 27.
FIGURE 27.
Daily current waiting time in psychological teams for episodes starting between April 2009 and March 2013 in (a) Croydon; (b) Lambeth; (c) Lewisham; and (d) Southwark: 25th, 50th and 75th centile values.
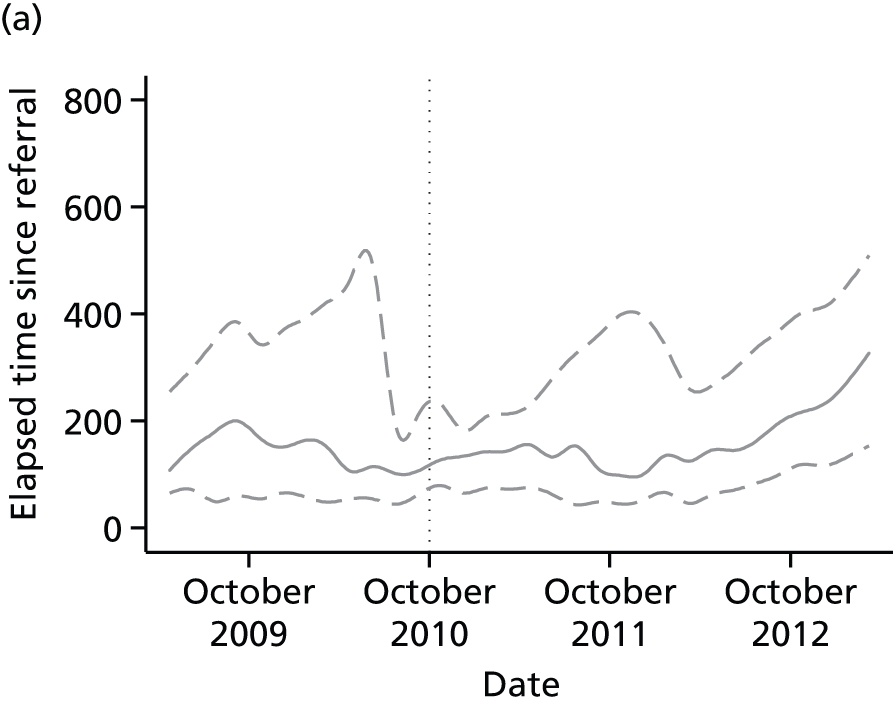
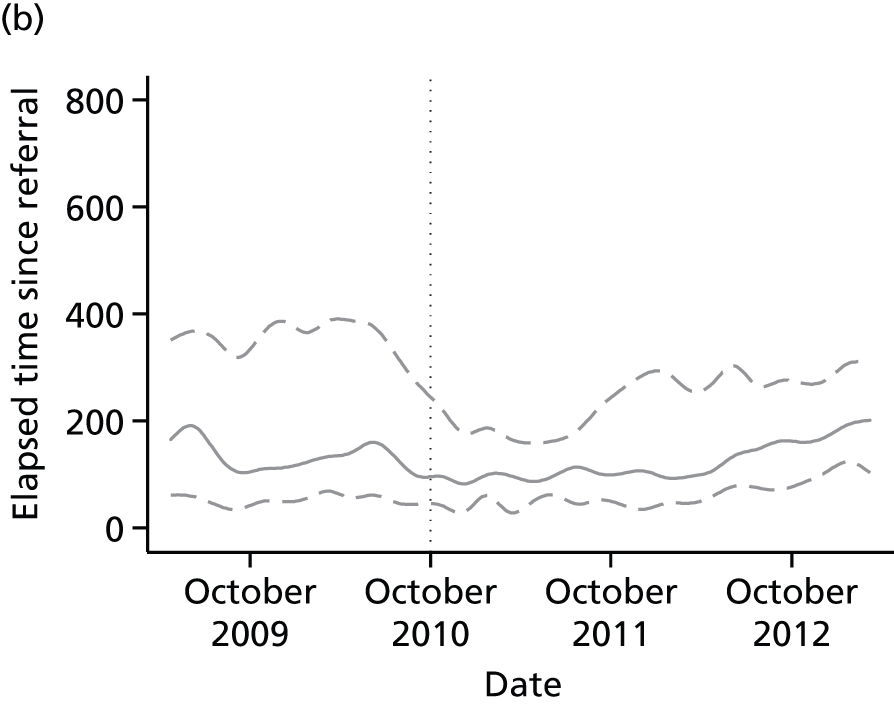
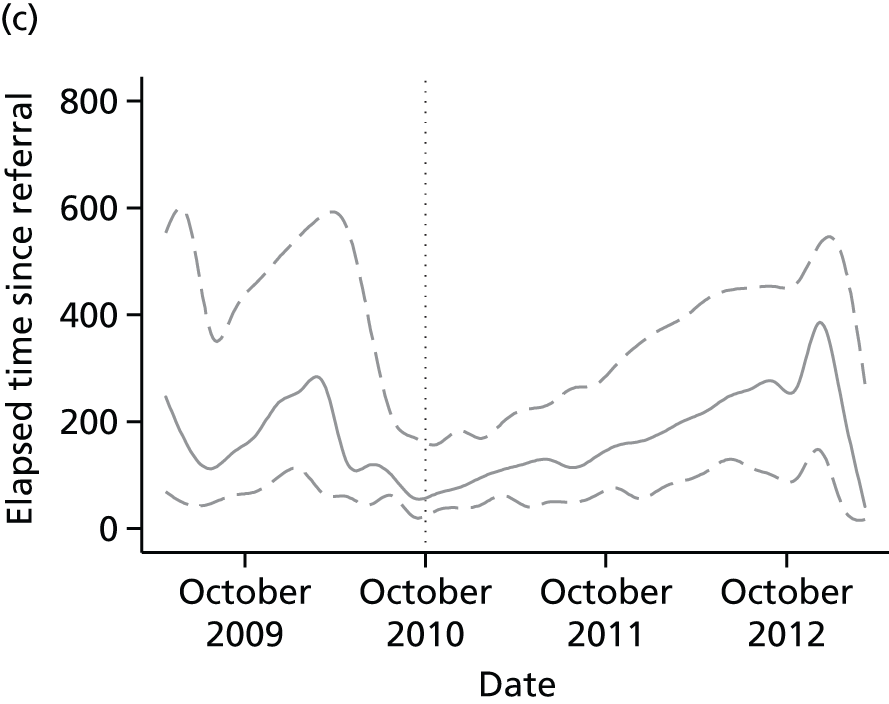
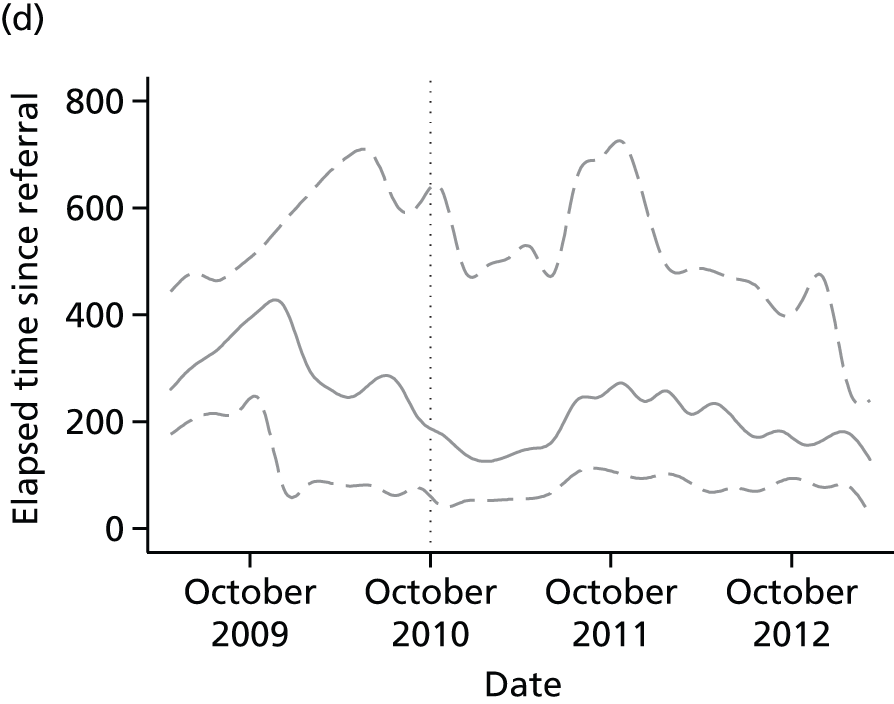
Summary of quantitative findings
The quantitative findings are summarised in Table 9.
| Analysis | Croydon | Lambeth | Lewisham | Southwark |
|---|---|---|---|---|
| Costs and activity | ||||
| CMHTs | ||||
| Caseload | Increasing pre CAG; decreasing post CAG | Decreasing pre CAG; decreasing more slowly post CAG | Decreasing pre CAG; decreasing more rapidly post CAG | Decreasing pre CAG; decreasing more rapidly post CAG |
| Number of new episodes starting per month | No change post CAG | Borderline significant reduction post CAG | Reduced post CAG | Reduced post CAG |
| Length of new episodes | Borderline significant reduction in median post CAG | No change in median post CAG | Reduction in median post CAG | Reduction in median post CAG |
| Number of contacts per episode | Borderline significant increase post CAG | No change post CAG | Increased post CAG | Reduced post CAG |
| CMHT costs per episode | No change post CAG | No change post CAG | Increased post CAG | Reduced post CAG |
| CMHT, inpatient and home treatment costs per CMHT episode | No change post CAG | No change post CAG | No change post CAG | No change post CAG |
| Psychotherapy teams | ||||
| Caseload | Increasing pre CAG; reducing post CAG | Increasing pre CAG; reducing post CAG | Increasing pre CAG; increasing less strongly post CAG | Increasing pre CAG; reducing post CAG |
| Number of new episodes starting per month | Reduced post CAG | No change post CAG | No change post CAG | Reduced post CAG |
| Length of new episodes | Increased median length post CAG | Increased median length post CAG | No change in median post CAG | Increased median length post CAG |
| IAPT teams | ||||
| Number of new episodes starting per month | Increasing over time | Increasing over time | Increasing over time | Increasing over time |
| Effectiveness | ||||
| Patterns of treatment for depression | No evidence of change post CAG | No evidence of change post CAG | No evidence of change post CAG | No evidence of change post CAG |
| Psychotherapy use by CMHT patients with depression | Reducing use over time | No change over time | No change over time | No change over time |
| Reduction in HoNOS score (CMHT patients) | No change over time | No change over time | Reduction in effect over time; trend not altered by CAG implementation | Reduction in effect over time; trend not altered by CAG implementation |
| Reduction in CORE score (psychotherapy patients) | Greater reduction over time; no effect of CAG implementation | Greater reduction over time; no effect of CAG implementation | Greater reduction over time; no effect of CAG implementation | Greater reduction over time; no effect of CAG implementation |
| Safety | ||||
| A&E deliberate self-harm presentations (CMHT patients) | Upward trend, unaltered post CAG | Non-significant trends pre and post CAG | Upward trend, unaltered post CAG | Upward trend, unaltered post CAG |
| Deliberate self-harm admissions (CMHT patients) | No trend | Upward trend, unaltered post CAG | No trend | No trend |
| Patient centredness | ||||
| Current waiting time (CMHTs) | Reduced post CAG | Increased post CAG | Reduced post CAG | Increased post CAG |
| Current waiting time (psychotherapy teams) | Increased post CAG | Reduced post CAG | Reduced post CAG | Reduced post CAG |
This summary table may be further summarised as follows. In all but one borough there was evidence of a more rapid reduction in CMHT caseload after CAG implementation. Episode costs altered only in Lewisham (where they increased in association with an increased number of events per episode) and Southwark (where costs decreased in association with a reduced number of events per episode), but when home treatment and inpatient costs were included there was no difference.
Changes in psychotherapy activity were more variable. Croydon, Lambeth and Southwark changed from an increasing caseload pre-CAG implementation to a reducing caseload post-CAG implementation. There was evidence in all boroughs of increased numbers of IAPT episodes throughout the study period. We were unable to look at costs in the psychotherapy services; our presumption, given the much better financial health of these services by 2014, was that these had reduced.
We found no evidence that treatment effectiveness had increased, although generally it was unaltered. In Croydon, there seemed to have been a reduction in the proportion of people with depression receiving psychotherapy. In Lewisham and Southwark, the two boroughs in which there had been the clearest reduction in the length of episodes, effectiveness as measured by HoNOS score appeared to have slightly reduced, but this trend appeared not to have altered at the point of CAG implementation.
Safety appeared not to have been altered pre and post CAG. There were trends in some boroughs but these trends had not altered pre and post CAG.
Waiting time in CMHTs had either increased or reduced (there was no consistent pattern) but the three new IAPT teams all seemed to have reduced waiting times compared with the pre-CAG service for the same borough.
Chapter 5 Discussion
Introduction and overview
In the preceding chapters we have analysed SLaM’s reorganisation of its adult mental health services from a structure based on borough directorates to a structure based on CAGs, which, broadly, we have characterised as a service line structure modified to account for the important local contextual factor of the formation of the local AHSC – the KHP. Based on our interviews in the MAP CAG, the most significant mechanisms through which change occurred were (1) the restructuring itself, which placed similar and related teams together under unified management, sometimes disclosing problems that were not so obvious under the previous arrangement, and (2) the precept to use care pathways as the means of managing and transforming services, which, over time, developed into a precept to use what came to be called high-level pathways. The extent of change that has happened since October 2010 (a full-scale reorganisation in Croydon, the complete redevelopment of all borough-facing psychotherapy services, an attempted restructuring of two specialist inpatient services followed by their closure, the development of new personality disorder and recurrent affective disorder pathways, etc.) indicates that the MAP CAG had engendered very significant and far-reaching change. It was also clear that the use of high-level pathways, in particular, represented an important shift in the culture of management within SLaM.
However, our attempt to survey activity, costs, effectiveness, safety and patient centredness in the MAP CAG showed a pattern of mixed results. Overall, there was most evidence of altered patterns of activity, although the details of changes differed between boroughs and services. In very broad outline, there was less activity both in the CMHTs and in the psychotherapy services. There was little evidence of altered treatment effectiveness and no evidence that the introduction of CAGs had altered any trends in treatment effectiveness. There was no evidence of altered safety. There was some evidence of increased patient centredness in the reformed psychotherapy services in the form of reduced waiting times, but some other services had increased waiting times. Costs in some of the CMHTs had altered, but not consistently, and there were no effects on care costs when other aspects of adult mental health services such as home treatment team use and inpatient bed use were included.
Overall, therefore, the quantitative results could be taken as showing welcome stability in the face of significant change. Alternatively, and less optimistically, they could be taken as showing two broad sets of changes. First, the restructuring and its sequelae and the development of high-level pathways together had no clear effects on care quality. Second, there was some evidence that less care is being provided, a phenomenon that, falling outside our understanding of the context–mechanism–outcomes of the CAG programme, is presumably related to a tendency towards increased demand management and cost control in a constrained financial environment.
However one looks at this issue, it is certainly worth asking the following question: ‘Can the CAG programme as we have conceptualised it deliver better quality care in future?’ Because of what we shall describe as the non-recurring nature of the effects of the CAG restructuring itself, we suggest that the answer to this question may depend on SLaM’s future approach to the use of care pathways. We might therefore also ask, ‘Can the precept to use care pathways – considered in their full sense – deliver on its promise to deliver better-quality care more reliably and efficiently?’.
Before moving on to our discussion of these questions, we consider the strengths and limitations of the research that we carried out.
Strengths and limitations
Our research used data taken from a 5-year window covering the period before and after SLaM’s CAG restructuring. In some form we were able to use all of the data from SLaM’s CMHTs and psychotherapy teams that had been collected during routine service provision in that period. These data included routine outcome measures and many other measures. By taking advantage of a separate study of self-harm presentations and data collected in acute hospitals we were also able to look at rates of self-harm among CMHT patients. It would therefore have been difficult to improve on the comprehensiveness and size of the data sets that we were able to work with. Moreover, we did not just perform a quantitative study. Had we not collected interview data with multiple respondents and had access to relevant documentary sources, it would have been very difficult for us to make sense of our quantitative findings, which, at first sight, showed a complex picture in which many areas showed no straightforward change. Having two waves of qualitative data collection helped us to make firmer conclusions than had we relied on a single wave; in particular, it was our second wave that showed us how thoroughly embedded the concept of a high-level pathway had become in the management of the MAP CAG.
Our limitations mainly stem from our data collection. In the qualitative work that we undertook we were not able to perform any participant observation and we also left the MAP CAG unobserved for around 2 years between the waves of data collection. We also did not begin to collect data until 18 months after the ‘go-live’ date for the CAG. This meant that we were able to learn about the formative processes of the CAG programme only in retrospect. Because we aimed to interview people who could provide insight into the CAG programme’s mechanisms we opted only to interview people who worked in the MAP CAG or who used its services; this meant that we did not interview GPs or commissioners, meaning that we were reliant on second-hand accounts of their views. Overall, we had to make the best of a modest quantity of qualitative interview data, although this was supplemented by documents. Including service users was made much more complicated by the processes that we were studying; once we began to collect data it became clear that the idea that we would learn about the mechanisms of the CAG programme from service users was not realistic. We had not realised how limited their knowledge of the programme would be, and we overestimated the extent to which the CAG programme would involve changes in service delivery that would be perceptible at the level of individual relationships with clinicians. We probably also overestimated the extent to which, even in the upper managerial, clinical and academic levels, there was a pre-existing, fully articulated theory of what the CAG programme was and how it would work. Arguably, we should have directed more resource at the managerial respondents and less at other groups, but we could not have known this in advance.
In the quantitative work we were limited mostly by data availability. We would have particularly liked to be able to study patient satisfaction, but the data collected for this purpose were so incomplete that they lacked credibility in a research context. In our examination of treatment processes, we were unable to assess whether or not treatment for depression had followed NICE guidelines because data on prescribing and psychotherapy receipt were so partial. In our analyses of treatment effect, the conclusions to be drawn must be tempered by the knowledge that our mixed-effects analyses included post-treatment ratings for no more than 27% of episodes, meaning that the probability of an unbiased estimate effect depends very heavily on the extent to which we were able to include as covariates those other variables that were associated with missingness and which were also associated with the value of the pre- and post-treatment ratings. A conservative view would be that the completeness was so low as to render the analysis unusable, but there was no realistic alternative available to us.
A more general issue, which it is important to acknowledge, is that all of our analyses attempted to estimate causal effects based on observational data, an inherently difficult task yielding results that should be viewed cautiously. One way of assessing the credibility of these analyses is to apply standardised risk of bias criteria, such as those developed by the Cochrane Effective Practice and Organisation of Care (EPOC) group. 65 The analyses of caseload were interrupted time series analyses; our assessment is that these had a low risk of bias according to the EPOC criteria. Other analyses were based on simpler techniques, for example using t-tests to compare monthly counts of episodes pre and post CAG. The EPOC group suggests that this is a weaker design and it is suggested that such studies should not be included in reviews unless the design is fully justified or the data can be reanalysed. In our case we stand by our choice to use these methods as examination of visual plots indicated that fitting straight lines to the data would be misleading (see, for example, Figures 10, 16, 26 and 27). Some other designs that we used are less easy to characterise in standard epidemiological or econometric terms, for example our analyses of rates of self-harm among current or recent CMHT patients pre and post CAG and our mixed-effects analyses of treatment effectiveness. However, we believe that the quality of these analyses is generally good; the main threat to validity is the omission of covariates associated both with the treatment effect and with the exposure of interest (the pre-/post-CAG indicator), and it is difficult to see how any such association could have arisen.
Our most major limitation is the fact that we were able to study only a single organisation and studied only one CAG within that organisation. Although adding further organisations and/or CAGs as study sites would have undoubtedly created a more complex pattern of findings needing interpretation, the combination of different contexts and differences in the programme structure might have made it easier to isolate the key context–mechanism–outcome configurations by comparing contexts and programme elements that did and did not produce a particular outcome. Instead, we were dependent on our respondents’ reasoning about the causal linkages between programme elements and outcomes, such as the Croydon reorganisation and the psychotherapy reorganisation. Because we know little about contextual elements in the other SLaM CAGs or about contextual elements and programme design in other organisations it is difficult to determine to what extent our findings would be predictive of the outcome of the CAG programme in other CAGs or in other organisations. Certainly, we would hope that the closer any other site conforms to the site that we studied, the closer would be the correspondence in results.
The future of the Clinical Academic Group programme
Over the period covered by our investigation (2009–14) it was possible to define two phases of SLaM’s CAG programme. The early phase was the initial management restructuring itself. First, a new set of operational divisions (CAGs) was created based on a preliminary view of the high-level pathways that each would manage; then, over several years in the case of the MAP CAG, each CAG defined iteratively the high-level pathways and corresponding services with which it would proceed. This entailed some major reorganisation and restructuring of services, some of which (the psychological therapies restructuring) was viewed as dealing with an ‘elephant in the room’ that had been allowed to persist too long under the previous structures. The later phase, discernible during our second wave of data collection in 2014, was a period of relatively stable operation in which the definition of a novel high-level pathway became the form in which service development was expressed, and attention was turned more to how CAGs should work together and with primary care while also accommodating the persisting importance of the borough as the level at which commissioning decisions were made and at which most CAG to CAG and CAG to primary care interfacing was carried out.
As we have noted previously, we identified two main programme elements: first, the CAG restructuring and, second, the precept to use care pathways, which developed over time into the consistent use of high-level pathways. These programme elements did not operate equally over both of the phases above. Rather, although care pathways, or what they developed into, were a consistent feature, the effects of the CAG restructuring itself, mediated by the mechanisms of oversight, changes to accounting practices and need for ‘CAG compliance’, were evident only in the early phase.
In an important sense, therefore, the changes that resulted from the CAG restructuring itself were non-recurring: once Croydon’s teams had been reorganised, once the integrated psychological treatment teams had been established and once the specialised inpatient services were restructured and finally closed there were no further novel problems revealed by the MAP CAG’s oversight, no further financial problems revealed and no further non-compliant teams needing to be reorganised. We also note at this point that our study of the MAP CAG suggested that the constitution of SLaM’s CAGs, that is, the teams and wards that went into each and the areas of clinical activity each encompassed, did not seem to us to have contributed directly to the outcomes of the CAG programme that we observed in the MAP CAG. We did not, in other words, think that the MAP CAG achieved anything specifically because of the way that it had been demarcated relative to the other adult mental health CAGs (Psychosis and Psychological Medicine). Indeed, we noted that our respondents, in both phases of the study, harboured some scepticism about the adult mental health CAG structure that had been settled on and identified various problems that had resulted from it. Overall, this has the important consequence that the future of the CAG programme, in our estimation, rests largely on care pathways and how the MAP CAG and, by extension, the other CAGs continue to develop their use of them.
Given its centrality to our argument, the idea of care pathways being used as a resource for service management requires detailed examination. As noted in Chapter 3, a number of ambiguities attend the formal definition of care pathways. Such ambiguities reflect a great deal of diversity in what purports to be a care pathway. As we have seen, SLaM developed local definitions of care pathways during the involvement of SLaM and IoP personnel in the preparation of the London Darzi report in 2008 and 2009 and then subsequently during the early stage of the transformation to CAGs, when it began to articulate a distinction between ‘high-level’ and ‘implementation’ care pathways. This period of thinking and writing about care pathways was then followed by the practical process of implementing them, and in explicating what was meant by the use of care pathways as a management resource for SLaM we relied mainly on what the MAP CAG did. As we set out in the following section, using care pathways as a resource for service management meant the exclusion of one common interpretation of what a care pathway is and the adoption of a contrasting usage.
Consequences of using care pathways as a resource for service management
The precept that care pathways should be used as a resource for service management meant that, quite early on in the CAG’s development, a care pathway ceased to be seen as a protocol, guideline or decision tree or, more generally, as a document that a clinical staff member might use as a resource for decision-making or guidance during the performance of clinical work. This was amply demonstrated by the fate of the majority of care protocols that were developed immediately after the MAP CAG was first set up in 2010. All but one of these protocols did not relate in any specific way to any of the CAG’s services but were instead based on the Maps of Medicine protocols and set out how particular mood, anxiety and personality disorders should be treated. Despite the substantial time and effort involved, the Maps of Medicine pathways were never implemented and the contested process through which they were created came to be seen as part of the founding process of the CAG. In relation to the key issue of whether or not it is possible for the CAG to contribute productively to the clinical management of particular disorders and problems, the main lesson learnt by leaders of the MAP CAG appears to have been that only a combination of direct managerial and clinical (including clinical academic) influence over a discrete service provides sufficient ‘grip’ to motivate change, a conclusion that essentially shaped the new personality disorder and recurrent affective disorder services that were developed in the second phase of the CAG’s operations.
In place of what might be seen as the typical understanding of care pathways (as a form of evidence-based clinical protocol; see Table 3), what developed in SLaM, quite early after the introduction of the CAG programme and certainly by the time of our initial data collection in May 2012, was a situation, still ongoing, in which the term ‘care pathway’ has become, for both service managers and clinical managers, a durable shorthand or ‘gloss’ both for the work of a group of teams operated by the CAG and for the representation of that work in schematic form. This was what was called a ‘high-level care pathway’, to distinguish it from the implementation pathways that were supposed to follow. In this form, the term ‘care pathway’ has become pervasive and ubiquitous within the management layers of the MAP CAG, and it is as a grouping of such high-level pathways that each adult mental health CAG represents itself vis-à-vis the others and to outside agencies such as commissioners. The extent to which these high-level pathways are now essential to the work of the MAP CAG and have proved serviceable is demonstrated amply by their having been the cornerstone of the early and pressing task of reorganising SLaM’s psychotherapy services into integrated psychological treatment teams as well as the recent (post-2012) work of creating new pathways for personality disorder and resistant depressive illness. Furthermore, the engagement, assessment and stabilisation pathway, the only pathway that was developed during the early CAG development work which was not based on the Maps of Medicine work, and which initially was developed ostensibly to be able to describe the work of the MAP CAG’s assessment and treatment teams, has continued to serve the purpose of describing that work and has guided service redesigns in both Croydon and, to a lesser extent, some of the other boroughs.
There are numerous practical consequences of this understanding of a high-level pathway, with its dual meaning of work and the representation of work. All the high-level pathways that are currently in use, whether originating in the early or in the later phase of the development of the MAP CAG, are coterminous with bricks and mortar services and are complemented by lines of reporting and accountability to the CAG Executive and the CAG Directors. Moreover, only to the extent that any of its services deal with patients with a restricted number of clinical problems do the MAP CAG’s care pathways describe the treatment of specific clinical problems, disorders or diagnoses. Crucially, the ambition that the work of defining high-level pathways would lead into a process of defining the low-level ‘content’ of these pathways has not been fulfilled. One suggestion from our respondents was that the lack of attention to the implementation of evidence-based practices since CAG formation has been largely a result of the ongoing severe financial pressures that the CAG has faced. Although this may have been one factor, we suggest that our respondents also raised a more fundamental problem, that is, a lack of fit between pathways based on broadly defined care needs and team functions (what service managers meant when discussing pathways) and pathways based on diagnoses and the details of clinical treatment (what clinicians initially understood by care pathways).
High-level pathways compared with care pathways as generally understood
From our point of view, how SLaM has developed high-level pathways now deviates sufficiently from care pathways as generally defined in the literature that they should be thought of as a distinct phenomenon. Particular points at which high-level pathways do not meet the Cochrane definition of care pathways50 are the fact that they do not in most cases ‘translate guidelines or evidence into local structures’ and do not ‘detail the steps in a course of treatment or care’ (p. 1), other than at a very general and non-specific level. Most of all, it is only possible to state that they ‘standardise care for a specific clinical problem, procedure or episode of healthcare’ (p. 1) by abstracting to a very great extent from the specifics of the care that is given. In relation to the EPA definition of pathways,45 which makes less of the role of care pathways in implementing evidence, it is not possible to argue, we felt, that the high-level pathways actually facilitate communication among team members and with patients and families, nor is it possible to argue that they co-ordinate the care process by ‘coordinating the roles and sequencing the activities of the multidisciplinary care team, patients and their relatives’51 [see also http://e-p-a.org/care-pathways/ (accessed 1 December 2015)], nor were they being used to document variances and outcomes.
The high-level pathways developed by SLaM seem, to us, to have the following characteristics: (1) each pathway describes in outline and at a very general level the activity of staff within a team or teams that are line managed within a particular management subdivision; (2) the operation of the pathway is directed or influenced through line management arrangements; (3) performance management is used, with team leaders being accountable for performance against targets derived from the pathway; (4) the durability of the pathway depends entirely on the durability of the teams and management structure to which it corresponds; if, in particular, there is a team reorganisation, or new teams are formed, the pathway must change.
These high-level pathways appear to us to share important features with how a production process might be conceptualised. In particular, they have the characteristic, noted above, that the pathway can be taken to refer to both the work of a team and the documentary representation of that work. Like a process model of an industrial process, these schematic pathways formulated and used by the SLaM CAG describe the inter-relation between a set of inputs, a set of processes and a set of outputs, exactly in the way that a process model would for a manufacturing process. Equally, the pathway is also taken to indicate that manufacturing process itself and, furthermore, suggests a relationship between that manufacturing process and its model wherein the latter is a simplified version of the same; one might think, for example, of the relation between the activity ‘wrapping chocolate bars’ and the machinery and personnel stationed at a particular part of a production line who together perform that work. This industrial metaphor is exactly that used in the literature on product line management, a literature that had an indirect influence on the decision to restructure into CAGs, but which appeared to have faded into the background in the early stages of the CAG restructuring. For example, Fetter and Freeman39 (pp. 41–2) preface their discussion of product line management in hospitals with the following remarks on what a ‘product’ denotes in health care:
Chase and Aquilano, 1977, p. 2666 define product as ‘the output from a productive system offered for sale (in the case of a business) or otherwise made available (in the case of a governmental or philanthropic organisation) to some consumer.’ In this context, a hospital produces the specific goods and services it provides to patients. These include, for example, the x-rays, medication, and lab tests ordered by physicians as part of the treatment process as well as nursing care, operating room facilities, and certain hotel and social services. But, because the real business of the hospital is to treat individual patients, these are really only intermediate outputs. The specific set of these intermediate outputs provided to each patient is a ‘product’ of the hospital.
Other management theories and approaches that similarly place an emphasis on the understanding of the process by which products are produced, and which have been implemented in the NHS, include business process reengineering67 and Lean, an improvement approach to improve flow and eliminate waste that was originally developed by Toyota. 68,69 Our respondents did not mention these theories as direct influences, although Lean is mentioned in some project documentation. 58 Certainly, descriptions of Lean projects in the literature68,69 make frequent reference to pathways, and it may be that the background influence of Lean and similar techniques promoted a situation in which the understanding of the term ‘care pathway’ was broadened to encompass ideas of pathways taken from these management approaches.
The key point, however, is that this relationship between a production process and its representation, inherent in the idea of the high-level pathways developed by the SLaM CAGs, does not necessarily inhere in the descriptions and definitions of care pathways in the literature. For example, a care pathway could equally be conceived of as a decision tree and therefore as a resource that functions as a much more specific guide to action. Indeed, this latter characterisation appears closer to the EPA definition45 as well as to the approach followed in the MAP CAG’s Maps of Medicine-based protocols.
Why SLaM has focused almost exclusively on high-level pathways is explained by the context in which it sought to use care pathways between 2010 and 2014. Thus, in the MAP CAG, the fact that the Maps of Medicine pathways that were developed in 2010 were not used is explained most economically by their lack of relevance to the project of managing a newly formed division that, shortly after formation, had to embark on a very significant team-level reorganisation, most of all in Croydon and in the psychotherapy services for Lambeth, Lewisham and Southwark, and which has since gone on to develop services further. In a context in which the primary need was to establish a set of viable and manageable services with reporting lines and systems of performance management, high-level pathways were perceived to be, and demonstrably have been, a useful tool. We suggest, in other words, that it was the very context of being used in a management restructuring that led to the important modifications that care pathways underwent in the process of being imported into SLaM. This interdependence between the two major programme components of the CAG reorganisation had the result of making it impossible to draw broader conclusions about the effectiveness of care pathways as these are generally understood, for these are not what came to be implemented.
Importantly, SLaM also did not begin its reorganisation with an explicit definition of health-care quality. Although there was undoubtedly a commitment to provide the best service possible within the available resources, the available documentary sources do not support the view that care pathways were chosen as the essential resource for management because of their likely effectiveness at improving health-care quality, in the terms that this is generally defined. 17,70 Following Donabedian’s classic formulation,70 when we attempt to appraise the quality of care we may distinguish between the demonstration that good outcomes have been achieved, that proper processes of care have been applied and that the structures in place for the delivery of care are those that would be expected to favour good medical care. As we have done in part in our evaluation, assessing the quality of care also entails an examination of the effectiveness, safety, patient centredness, efficiency and equity of care. 17
The high-level pathways developed by the SLaM CAGs are, we suggest, primarily tools to improve some aspects of care processes, but generally leave many aspects of quality of care unexamined and unmanaged. Compared with the typical concept of the care pathway, they even have some important limitations in their ability to affect processes of care. We suggest that these limitations result from the close relationship established between the care pathway and the service managers’ view of the concrete production process: the way that this is documented as a high-level pathway tends towards a generalised view of health-care processes that actually abstracts from the specific details of the care given to a particular individual. It is these details, however, which really determine whether or not good-quality care was provided.
Our suggestion is that now is an opportune time, 5 years on, for SLaM to return to the idea of care pathways and to the concept of health-care quality, and to think again about how care pathways may be of assistance in its continuing efforts to improve the quality of the health care that it provides. Because high-level pathways have proven to be of use to the organisation, we suggest that this examination might usefully focus on how to further develop and use care pathways in ways that complement the existing high-level pathways, that is, further developing the notion of in some way ‘aggregating’ the different aspects of function, form and content that we mentioned in Care pathway development in the Mood Anxiety and Personality Clinical Academic Group. It seems to us that any further use of care pathways, or indeed any related way of standardising clinical work or improving its reliability, would require characteristics that complement those that we have identified for high-level pathways. Therefore, we would expect that these alternative methods (1) define in greater detail how the care process should be carried out or act as an aid to that work process, rather than correspond to a production process considered only in broad outline; (2) be able if required to target staff working in multiple defined services, possibly spanning CAGs and organisations; (3) be capable of influencing or guiding work by means other than line management; (4) not necessarily rely on top-down performance management; (5) be flexible or durable as the situation demands – able to endure when team structures are reformed, for example, but equally able to be introduced, altered, merged with another pathway or ended, and so on, when this is felt to be appropriate; and (6) be capable of use despite the resources relevant to implementation being spread across different CAGs or indeed across different organisations (e.g. SLaM and primary care).
This alternative conception of a care pathway, and its distinction from high-level pathways, is actually rather close to the original concept of product line management,39 which portrays it as a form of matrix management that is introduced in addition to the existing management structures as opposed to replacing them. Fetter and Freeman39 suggest the idea of a ‘patient care team’, which is clinically led and flexibly defined, and which exists to tie together activities necessarily managed within rigid departmental structures – here, we would be thinking of CAGs, but also teams and wards – into a structure that permits management of the production of a particular product. In the case of the MAP CAG, these products might include, for example, episodes of depression care, or episodes of care for someone who has self-harmed. This concept would require the construction of a network of interested individuals who are capable of impacting on the quality problem at hand and who span different management divisions, or indeed span the ‘home’ organisation and other organisations. Because it is clinical work that is being directly targeted, clinical engagement and clinical leadership would be essential. We suggest that such a team would need an internal sponsor – in the case of pathways for diagnoses and clinical problems this would most obviously be the most relevant CAG – and should have agreed objectives on which to report. Such teams would be expected to change and develop over time, guided by progress against objectives and by the setting of new objectives. The use of a matrix structure would avoid an important conceptual difficulty that SLaM struggled with in distinguishing between high-level and low-level care pathways – it would make very clear that care pathways that explicitly cut across the high-level pathways would not in any sense ‘flesh out’ a high-level care pathway operated by one CAG.
One difficulty, already identified by our respondents, is making changes in an organisation that are not backed by line management arrangements and bricks and mortar-managed services. Without tackling this issue there seems little prospect of extending the reach of care pathways into the concrete details of care delivery. However, line management and indeed ‘top-down’ approaches generally are not the only means to motivate change within organisations. For example, in their discussion of how guidelines operate at Intermountain Healthcare, James and Savitz (p. 118)71 note that they ‘didn’t try to control physicians’ practice behaviour by top-down command and control through an employment relationship’, describing this as a ‘classic blunder’. Instead they ‘relied on solid process and outcome data, professional values that focused on patients’ needs, and a shared culture of high quality’. Similarly, in relation to the successes achieved as a result of the radical re-engineering of the VA that was undertaken in the 1990s in the USA, Francis and Perlin72 discuss how the development of clinical guidelines and performance measures was as much a bottom-up as a top-down activity within the VA, ‘belying the common misconception that, as a federal health system with many connections to the military, change occurs through “command and control”’ (p. 65); Kizer and Kirsh73 suggest that it was a combination of ‘VA’s compelling mission, the clarity of performance expectations, healthy intra-organisational competition, substantial local autonomy and a sense of professional fulfilment’ (p. 396) rather than top-down performance management that drove rapid improvement. They also point out that in recent years things have changed: a more centralist approach is being taken in the VA and this has undermined the flexibility to tailor local improvement strategies.
There are also other important issues that would need to be dealt with during any work to further develop care pathways at SLaM. The first is deciding what relationship to establish between clinical work, the documentation of that clinical work and the documentation of a care pathway. A traditional clinical practice guideline exists as a document that, if it gives clear guidance on what action a clinician should take in a particular situation, requires the clinician either to refer to it or to have memorised some part of it. This would be the case for the CAG’s own book of clinical protocols and for the most prominent locally produced guidelines, the Maudsley Prescribing Guidelines. 74 In this situation, documenting health care and documenting the guideline are two completely separate activities. However, care pathways attempt to fuse these activities45,50 so that documenting care is generally seen as a core function of care pathways, alongside their role in standardising care. This would be a major departure from current practice in SLaM. It may also be worth considering some alternative approaches that also attempt some fusion of guidance and clinical documentation. For example, the Standardized Clinical Assessment and Management Plan75 developed at Boston Children’s Hospital is intended to permit documentation of clinical care as well as communicating the elements of the guideline to be followed and recording a clinician’s choices and reasoning for following or not following the recommended course of action. A similar blended approach has been described by Intermountain Healthcare, whose clinical practice guidelines, developed by groups of clinicians, are integrated into documents such as the case record and order sheets for investigations, and where variances from the guidelines are identified based on a sophisticated clinical information system, which are then processed by the project group, often leading to changes in the guideline. 71
The second, and related, issue that would need to be resolved to further develop care pathways are the adaptations that would be necessary to clinical information systems, which in the form of the electronic patient record are used to document nearly every aspect of clinical care. Such changes could be substantial. During the course of our investigation we found that SLaM’s clinical information systems and the related research infrastructure, although sophisticated by British standards, did not suffice to allow us to determine the length of antidepressant treatment, and determining which antidepressant treatment had been given was laborious. Defining psychotherapy receipt was also not straightforward. The outcome measures that we used for our investigations were generally not administered frequently or consistently enough to be of assistance in determining progress in treatment, even though the infrastructure needed to record these measures was sufficient. We were able to cost some treatment episodes, but were only able to use unit costs that did not differentiate between different kinds of contact and intervention. Despite this, our view was that SLaM has great potential to work with its own data, given sufficient time, effort and willingness to modify both systems and the way that they are used in clinical practice.
The third, and perhaps most important, issue is that of clinical engagement. As noted earlier, if the further development of care pathways enters more and more into the domain of clinical activity, it will be essential to engage clinical staff in the process. Among other things, this will require care to ensure that the work of developing and using the new care pathways accords as far as possible with professional norms, that incentives for collaboration are well structured and that a persuasive case is made for change. 76
Implications for practice outside the South London and Maudsley NHS Foundation Trust and for further research
Changes to management structures internal to health-care providers are common, but also diverse, being effected for different reasons within organisations that provide different services in different ways and in different contexts. It is therefore improbable that SLaM’s experience with CAGs provides generalisable lessons other than at some level of abstraction. Certainly, our analysis of the key context–mechanism–outcome configurations for the programme indicated that the effects of the CAG restructuring itself were highly context dependent in a way that should make even mental health NHS trusts changing to service line structures wary of assuming that they will have similar experiences.
We found that SLaM’s CAG reorganisation, 5 years on, had not had clear effects on the quality of care provided, although over the same period there had been modest changes to the quantity of care provided. It might be argued that changes to quality were not to be expected from a management restructuring, but this is to neglect the role in the programme of care pathways, which are a tool precisely intended to improve quality, and also begs the question of what is to be expected of management restructuring if not improvements in the service or products that the organisation provides. The important lesson for other organisations seems to us to be a warning: it is possible to perform a large-scale management restructuring including the use of a recognised technique for quality improvement and not see resulting improvements in quality. Several other implications stem from this. First, if improvements in quality are aimed at, then first of all it would seem advantageous to map out, in a reasonable level of detail and plausibly, how such improvements are to be attained. Second, this model needs to function in an ongoing manner as a template for the changes that are actually made, with alterations to that template made explicitly and in response to learning from the process of change. We found that the work on care pathway development that followed the ending of SLaM’s specific CAG development programme in July 2011 differed from the work that had been sketched out by the CAG development team. For example, a new care pathway for integrated psychological treatment teams was developed, but the proposed fleshing out of high-level pathways into ‘implementation’ care pathways, which did not happen.
Future researchers may find it most fruitful to attempt to answer some related questions, which we touched on but were unable to address in detail. How do plans for change within organisations arise and then change through the process of implementation? Are there differences in how organisational change is thought of at different levels within the organisation, and how do these differences arise? What is the relationship between the abstract vision of a change and the concrete reality of implementation? Another area of interest is care pathways. As we noted above (see High-level pathways versus care pathways as generally understood), the divergence between SLaM’s high-level pathways and care pathways as typically understood is sufficiently wide that SLaM’s experience cannot be taken as indicative of the effects of care pathways in mental health services; this is therefore still a topic requiring further research. 6
Generally, we found it challenging to use programme evaluation techniques. The transition to CAGs was not presented to us as neatly as we have presented here and teasing out what we felt were the two central programme components took considerable effort. Arguably we were not dealing with a programme as this is typically defined; in particular, it was not always clear what the goals of the programme were, or at least the goals of those primarily concerned with implementing the change. This made it impossible to plan the quantitative research on the basis of the qualitative research, which led to a looser connection between the two. One area where the use of realistic evaluation was valuable, however, was forcing us to think very carefully about the interaction between programme mechanisms and contexts. Had we abandoned programme evaluation and adopted a looser case study approach, as, for example, has on occasion been recommended when what is being evaluated does not really seem like a programme,77 we might have lacked the structure necessary to force us to consider those issues.
Our practical experience in carrying out the quantitative research may also be helpful for other researchers. This absorbed most of the resources of the study and was also effectively subsidised by the National Institute for Health Research (NIHR), who fund the infrastructure (the CRIS system) on which we relied. Nearly all of the cost of the quantitative research related to data preparation, which at a rough estimate absorbed 95% of the time of the researchers working on the quantitative analyses. Working with CRIS requires the use of SQL, which is a computer language for databases unknown to most health services researchers, and indeed to many biomedical statisticians. We had those skills within our research team, but most researchers would be dependent on the employment of a SQL programmer or analyst in addition to the other analytical staff required. Furthermore, having the technical programming skills is not sufficient; working with CRIS requires a clear understanding of the contents of the database, encompassing both the logical data model encapsulated in the database and an understanding of the ways in which the data within the database do and do not conform to that model, the latter situation leading to the ‘dirty data’ that are generally endemic in databases, albeit in a small minority of cases. Correcting those dirty data, or at least removing the logical anomalies, itself requires SQL views and stored procedures that must be employed during the extraction of the study data sets. All in all, this is a considerably more difficult proposition than working with preprepared data sets such as the Hospital Episode Statistics. It must also frankly be admitted that the quality of the resulting data is not as high as would be achieved by prospective data collection, although the much greater quantity of data does compensate for this.
Conclusion
Even close to 5 years on, it may be too soon to draw firm conclusions about the effects of SLaM’s CAG restructuring. At this point, it is possible to be clear about the mechanisms through which change was sought – this was not necessarily the case earlier in the programme – and it is also possible to begin to tease out what has and has not changed over the last 5 years. In general, effects on clinical activity are more apparent at this stage than effects on effectiveness and safety. Our view is that the rationale for the CAG programme remains persuasive and many of the abiding difficulties relate to the relationships between the adult mental health CAGs – something that the current adult mental health plan is attempting to address. However, detailed examination of what has come of the experimentation with care pathways indicates that much of what is unique and specific to care pathways has not been taken advantage of – a result, we suggest, of the specific way in which care pathways had to be shaped to serve the needs of an organisation undergoing a thorough reshaping of its internal management structure. We hope that this untapped potential is something that will be addressed in the next phase of CAG development.
Acknowledgements
The CRIS system is supported and maintained by the NIHR Biomedical Research Centre operated by the Institute of Psychiatry, Psychology and Neuroscience and SLaM.
We thank service user and staff respondents and other staff within the MAP CAG.
We thank our external reference group.
The views expressed are those of the author(s) and not necessarily those of the Health Services and Delivery Research programme, the NIHR, the NHS or the Department of Health.
Contributions of authors
Dr Alex D Tulloch led on preparation of the grant application, performed all of the SQL programming, performed a large part of the quantitative analysis and contributed to the qualitative work, report writing and project co-ordination.
Professor Bryony Soper contributed to the grant application, led on the qualitative work and was involved in report writing.
Dr Anke Görzig contributed to the quantitative analyses and edited the draft report.
Dr Sophie Pettit constructed and coded the text data set, developed methods for looking at treatment patterns and edited the draft report.
Mr Leonardo Koeser cleaned and prepared the financial data and performed the cost analyses.
Dr Catherine Polling led on the coding of the self-harm in A&E data set.
Mr Andrew Watson contributed to the collection of qualitative data in phase 1.
Dr Mizanur Khondoker advised on the statistical analysis.
Professor Diana Rose led on the service user component of the qualitative study and edited the draft report.
Professor Paul McCrone supervised the analysis of the cost data and contributed to the grant application.
Professor André Tylee contributed to the grant application and edited the draft report.
Professor Graham Thornicroft was the project sponsor and guarantor, provided project guidance and supervision of Dr Tulloch and edited the draft report.
Data sharing statement
Data from CRIS are not available to external users. Please contact the corresponding author with queries regarding the sharing of qualitative data.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
References
- Wholey JS. Evaluation and Effective Public Management. Boston, MA: Little, Brown; 1983.
- Pawson R, Tilley N. Realistic Evaluation. London: Sage; 1997.
- Charns MP, Wray NP, Byrne MM, Meterko MM, Parker VA, Pucci LG, et al. Service Line Management Evaluation Project: Final Report. Boston, MA: Management Decision and Research Center; 2001.
- Greenberg GA, Rosenheck RA, Charns MP. From profession-based leadership to service line management in the Veterans Health Administration: impact on mental health care. Med Care 2003;41:1013-23. http://dx.doi.org/10.1097/01.MLR.0000083747.57722.4D.
- Byrne MM, Charns MP, Parker VA, Meterko MM, Wray NP. The effects of organization on medical utilization: an analysis of service line organization. Med Care 2004;42. http://dx.doi.org/10.1097/01.mlr.0000102493.28759.71.
- Evans-Lacko SE, Jarrett M, McCrone P, Thornicroft G. Clinical pathways in psychiatry. Br J Psychiatry 2008;193:4-5. http://dx.doi.org/10.1192/bjp.bp.107.048926.
- Rotter T, Kinsman L, James E, Machotta A, Gothe H, Willis J, et al. Clinical pathways: effects on professional practice, patient outcomes, length of stay and hospital costs. Cochrane Database Syst Rev 2010;3. http://dx.doi.org/10.1002/14651858.cd006632.pub2.
- Rycroft-Malone J, Wilkinson J, Burton CR, Harvey G, McCormack B, Graham I, et al. Collaborative action around implementation in Collaborations for Leadership in Applied Health Research and Care: towards a programme theory. J Health Serv Res Policy 2013;18:13-26. http://dx.doi.org/10.1177/1355819613498859.
- Rycroft-Malone J, Fontenla M, Bick D, Seers K. A realistic evaluation: the case of protocol-based care. Implement Sci 2010;5. http://dx.doi.org/10.1186/1748-5908-5-38.
- Greenhalgh T, Humphrey C, Hughes J, Macfarlane F, Butler C, Pawson R. How do you modernize a health service? A realist evaluation of whole-scale transformation in London. Milbank Q 2009;87:391-416. http://dx.doi.org/10.1111/j.1468-0009.2009.00562.x.
- Wholey JS, Hatry HP, Newcomer KE. Handbook of Practical Program Evaluation. San Francisco, CA: Jossey-Bass; 2010.
- McKee M, Figueras J, Lessof S. Research and policy: living on the interface. Eurohealth 2006;12.
- Stewart R, Soremekun M, Perera G, Broadbent M, Callard F, Denis M, et al. The South London and Maudsley NHS Foundation Trust Biomedical Research Centre (SLAM BRC) case register: development and descriptive data. BMC Psychiatry 2009;9. http://dx.doi.org/10.1186/1471-244X-9-51.
- Wing JK, Beevor A, Curtis R, Park S, Hadden S, Burns A. Health of the Nation Outcome Scales (HoNOS). Research and development. Br J Psychiatry 1998;172:11-8. http://dx.doi.org/10.1192/bjp.172.1.11.
- Barkham M, Bewick B, Mullin T, Gilbody S, Connell J, Cahill J, et al. The CORE-10: a short measure of psychological distress for routine use in the psychological therapies. Couns Psychother Res 2013;13:3-13. http://dx.doi.org/10.1080/14733145.2012.729069.
- Polling C, Tulloch A, Banerjee S, Cross S, Dutta R, Wood DM, et al. Using routine clinical and administrative data to produce a dataset of attendances at emergency departments following self-harm. BMC Emerg Med 2015;15. http://dx.doi.org/10.1186/s12873-015-0041-6.
- Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academies Press; 2001.
- Depression in Adults. London: NICE; 2009.
- Allderidge PH. Historical notes on the Bethlem Royal Hospital and the Maudsley Hospital. Bull N Y Acad Med 1971;47:1537-46.
- Jones E. Aubrey Lewis, Edward Mapother and the Maudsley. Med Hist Suppl 2003:3-38.
- Our History. London: South London and Maudsley NHS Foundation Trust; 2012.
- Mental Health Policy Implementation Guide. London: DH; 2001.
- Darzi A. Healthcare for London: A Framework for Action. London: NHS London; 2007.
- Dzau VJ, Ackerly DC, Sutton-Wallace P, Merson MH, Williams RS, Krishnan KR, et al. The role of academic health science systems in the transformation of medicine. Lancet 2010;375:949-53. http://dx.doi.org/10.1016/S0140-6736(09)61082-5.
- Lozon JC, Fox RM. Academic health sciences centres laid bare. Healthc Pap 2001;2:10-36. http://dx.doi.org/10.12927/hcpap.2002.17202.
- King’s Health Partners: An Academic Health Sciences Centre for London. London: King’s Health Partners; 2009.
- Improving Health and Wellbeing Locally and Globally 2014–2019. London: King’s Health Partners; 2014.
- Application to the Department of Health for AHSC Accreditation: Part 2. London: King’s Health Partners; 2009.
- Application for CAG Accreditation: Module 1 – Mobilisation/CAG Formation. London: South London and Maudsley NHS Foundation Trust; 2011.
- Frequently Asked Questions (FAQs) – Clinical Academic Groups. Updated November 2009. London: South London and Maudsley NHS Foundation Trust; 2009.
- Nicholson D. The Year: NHS Chief Executive’s Annual Report 2008/09. London: Department of Health; 2009.
- Bell S. Service Line Management in Mental Health: Monitor Audit Commission Conference 2009. www.monitor-nhsft.gov.uk/home/news-and-events/events/past-events/service-line-management-mental-health-trusts (accessed 28 January 2013).
- Team by Team Guide to Community Services. London: Camden and Islington NHS Foundation Trust; 2011.
- BEH Service Line Chart. London: Barnet Enfield and Haringey NHS Trust; 2010.
- Introduction to Service Lines. 2013. London: Barnet, Enfield and Haringey NHS Trust; n.d.
- CMWL Service Directory: June 2013. London: Central and North West London NHS Foundation Trust; 2013.
- Foot C, Sonola L, Maybin J, Naylor C. Service-Line Management: Can it Improve Quality and Efficiency?. London: King’s Fund; 2012.
- Service-Line Management: An Overview. London: Monitor; 2009.
- Monitor . Service-Line Management: An Approach to Hospital Management 2014. www.gov.uk/government/collections/service-line-management-an-approach-to-hospital-managment (accessed 23 December 2014).
- Fetter RB, Freeman JL. Diagnosis related groups: product line management within hospitals. Acad Manage Rev 1986;11:41-54.
- Thornicroft G, Strathdee G, Phelan M, Holloway F, Wykes T, Dunn G, et al. Rationale and design. PRiSM Psychosis Study I. Br J Psychiatry 1998;173:363-70. http://dx.doi.org/10.1192/bjp.173.5.363.
- Thornicroft G, Wykes T, Holloway F, Johnson S, Szmukler G. From efficacy to effectiveness in community mental health services. PRiSM Psychosis Study. 10. Br J Psychiatry J Ment Sci 1998;173:423-7. http://dx.doi.org/10.1192/bjp.173.5.423.
- 2000–Present. London: South London and Maudsley NHS Foundation Trust; 2014.
- Application for CAG Accreditation: Module 2 – Strategy Development. London: South London and Maudsley NHS Foundation Trust; 2011.
- Vanhaecht K, Panella M, Van Zelm R, Sermeus W. An overview on the history and concept of care pathways as complex interventions. Int J Care Pathw 2010;14:117-23. http://dx.doi.org/10.1258/jicp.2010.010019.
- Vanhaecht K, Ovretveit J, Elliott MJ, Sermeus W, Ellershaw J, Panella M. Have we drawn the wrong conclusions about the value of care pathways? Is a Cochrane review appropriate?. Eval Health Prof 2012;35:28-42. http://dx.doi.org/10.1177/0163278711408293.
- Vanhaecht K, Witte KD, Depreitere R, Sermeus W. Clinical pathway audit tools: a systematic review. J Nurs Manag 2006;14:529-37. http://dx.doi.org/10.1111/j.1365-2934.2006.00705.x.
- Evidence Briefing on Integrated Care Pathways in Mental Health Settings. York: University of York; 2011.
- Panella M, Vanhaecht K. Is there still need for confusion about pathways?. Int J Care Pathw 2010;14:1-3. http://dx.doi.org/10.1258/jicp.2010.010008.
- Kinsman L, Rotter T, James E, Snow P, Willis J. What is a clinical pathway? Development of a definition to inform the debate. BMC Med 2010;8. http://dx.doi.org/10.1186/1741-7015-8-31.
- Vanhaecht K, de Witte K, Sermeus W. The Impact of Clinical Pathways on the Organisation of Care Processes 2007.
- Faber MJ, Grande S, Wollersheim H, Hermens R, Elwyn G. Narrowing the gap between organisational demands and the quest for patient involvement: the case for coordinated care pathways. Int J Care Coord 2014;17:72-8. http://dx.doi.org/10.1177/2053435414540616.
- Campbell H, Hotchkiss R, Bradshaw N, Porteous M. Integrated care pathways. BMJ 1998;316:133-7. http://dx.doi.org/10.1136/bmj.316.7125.133.
- De Luc K, Currie L. Developing and Evaluating Care Pathways in the UK: the Way to Go. Birmingham: Health Services Management Centre, University of Birmingham; 1999.
- Framework for CAG Care Pathway Development. London: South London and Maudsley NHS Foundation Trust; 2009.
- Brief Guidance Notes for CAG Care Pathway Working Groups. London: South London and Maudsley NHS Foundation Trust; 2009.
- Clinical Academic Group Development Programme (October 2010). London: South London and Maudsley NHS Foundation Trust; 2010.
- Top 10 Care Pathway Development Must Do’s. London: South London and Maudsley NHS Foundation Trust; 2010.
- Care Pathway Progress Report June 2011. London: South London and Maudsley NHS Foundation Trust; 2011.
- Review of 2010–2011 CAG Development Objectives. London: South London and Maudsley NHS Foundation Trust; 2011.
- Clinical Protocols (Maps of Medicine) for the Management of Clinical Conditions with the Mood, Anxiety and Personality Clinical Academic Group (MAP CAG). London: South London and Maudsley NHS Foundation Trust; 2012.
- IPTT Operational Policy: Version 4. London: South London and Maudsley NHS Foundation Trust; 2012.
- MAPCAG Organisational Chart: April 2014. London: South London and Maudsley NHS Foundation Trust; 2014.
- Gask L, Khanna T. Ways of working at the interface between primary and specialist mental healthcare. Br J Psychiatry 2011;198:3-5. http://dx.doi.org/10.1192/bjp.bp.109.075382.
- Suggested Risk of Bias Criteria for EPOC Reviews. Oslo: Norwegian Knowledge Centre for the Health Services; 2015.
- Chase RB, Aquilano NJ. Production and Operations Management: A Life Cycle Approach. Homewood, IL: R D Irwin; 1977.
- McNulty T, Ferlie E. Reeingineering Health Care: The Complexities of Organizational Transformation. Oxford: Oxford University Press; 2002.
- Waring JJ, Bishop S. Lean healthcare: rhetoric, ritual and resistance. Soc Sci Med 2010;71:1332-40. http://dx.doi.org/10.1016/j.socscimed.2010.06.028.
- Radnor ZJ, Holweg M, Waring J. Lean in healthcare: the unfilled promise?. Soc Sci Med 2012;74:364-71. http://dx.doi.org/10.1016/j.socscimed.2011.02.011.
- Donabedian A. Evaluating the quality of medical care. Milbank Mem Fund Q 1966;44:166-20. http://dx.doi.org/10.2307/3348969.
- James BC, Savitz LA. How Intermountain trimmed health care costs through robust quality improvement efforts. Health Aff (Millwood) 2011;30. http://dx.doi.org/10.1377/hlthaff.2011.0358.
- Francis J, Perlin JB. Improving performance through knowledge translation in the Veterans Health Administration. J Contin Educ Health Prof 2006;26:63-71. http://dx.doi.org/10.1002/chp.52.
- Kizer KW, Kirsh SR. The double edged sword of performance measurement. J Gen Intern Med 2012;27:395-7. http://dx.doi.org/10.1007/s11606-011-1981-5.
- Taylor D, Paton C, Kapur S. The Maudsley Prescribing Guidelines in Psychiatry. Chichester: John Wiley; 2012.
- Farias M, Jenkins K, Lock J, Rathod R, Newburger J, Bates DW, et al. Standardized clinical assessment and management plans (SCAMPs) provide a better alternative to clinical practice guidelines. Health Aff (Millwood) 2013;32:911-20. http://dx.doi.org/10.1377/hlthaff.2012.0667.
- Dixon-Woods M, McNicol S, Martin G. Ten challenges in improving quality in healthcare: lessons from the Health Foundation’s programme evaluations and relevant literature. BMJ Qual Saf 2012;21:876-84. http://dx.doi.org/10.1136/bmjqs-2011-000760.
- Weiss CH. Evaluation Research: Methods of Assessing Program Effectiveness. Englewood Cliffs, NJ: Prentice-Hall; 1972.
Appendix 1 Interview schedules
Appendix 2 Initial list of themes
-
Addressing problems.
-
Available data.
-
Background.
-
Borough services.
-
Bringing in right people.
-
Business case.
-
CAG as means to an end.
-
CAG development.
-
CAG development groups.
-
CAGs as structures setting a framework.
-
Care pathways.
-
Commissioners.
-
Compromise.
-
Continuity.
-
Co-ordination.
-
Cross-subsidies.
-
Distinction from acute CAGs.
-
Duplication of performance measurement.
-
Efficiency savings.
-
Financial issues.
-
Integrated working.
-
Interface between mental health and acute CAGs.
-
KHP accreditation process.
-
Lines of accountability.
-
Local solutions.
-
Names and scope of CAGs.
-
Natural progression.
-
Need for change.
-
Organisational buy-in.
-
Organising the system.
-
Performance council.
-
Performance measurement.
-
Pre-existing structures and services.
-
Psychological service review.
-
Public health.
-
Role of primary care.
-
Service development.
-
Service line management.
-
Service specifications.
-
Service user view.
-
Standards.
-
Supportive corporate and executive infrastructure.
-
Timing.
-
Translating research into practice.
-
Tripartite mission.
-
Two tensions.
-
Work of assessment teams.
-
Working together.
Appendix 3 Final list of themes and subthemes
(Used as the basis for writing the final report.)
-
Different visions:
-
KHP vision
-
need for change already
-
different agendas.
-
-
Financial stability and the influence of commissioning.
-
Inherited issues.
-
CAGs.
-
Care pathways.
Appendix 4 Ethics
List of abbreviations
- A&E
- accident and emergency
- AHSC
- Academic Health Sciences Centre
- CAG
- Clinical Academic Group
- CBT
- cognitive–behavioural therapy
- CI
- confidence interval
- CMHT
- community mental health team
- CORE-10
- Clinical Outcomes in Routine Evaluation 10-item version
- CRIS
- Clinical Record Interactive Search
- EPA
- European Pathway Association
- EPOC
- Effective Practice and Organisation of Care
- GP
- general practitioner
- HoNOS
- Health of the Nation Outcome Scales
- HR
- hazard ratio
- IAPT
- Improving Access to Psychological Therapies
- ICD-10
- International Statistical Classification of Diseases, 10th Revision
- IoP
- Institute of Psychiatry
- KCL
- King’s College London
- KHP
- King’s Health Partners
- LR
- likelihood ratio
- MAP CAG
- Mood, Anxiety and Personality Clinical Academic Group
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health Research
- OR
- odds ratio
- PbR
- Payment by Results
- PEDIC
- Patient Experience Data Information Centre
- SLaM
- South London and Maudsley NHS Foundation Trust
- SQL
- Structured Query Language
- SUN
- Service User Network
- VA
- Veterans Administration
