Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 11/1015/09. The contractual start date was in August 2012. The final report began editorial review in May 2015 and was accepted for publication in October 2015. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2016. This work was produced by Ingram et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction, summary of study design and research objectives
Introduction
The improvements in survival of preterm infants over the past 20 years mean that > 90% of all infants born at ≥ 27 weeks’ gestation will survive and go home. For nearly all such infants, a relatively short period in intensive care will be followed by a longer period in ‘high-dependency care’ and then ‘special care’ before discharge to home.
For parents of such infants there is a need to learn how best to look after them following discharge and to prepare themselves and their home environment to care for the baby. There is increasing evidence that ex-preterm infants make a disproportionate demand on emergency and out-of-hours health services, and many parents have expressed concern and uncertainty about how best to respond to minor illness or changes in routine in these very vulnerable infants.
In a preliminary survey of neonatal units in the UK, we found that in most neonatal units the process of preparing families for discharge home with their preterm infant is relatively unstructured and is commonly left until relatively late in the hospital stay. The emphasis is usually on informing the parents about issues that the nursing and medical staff feel are important, rather than addressing the parents’ identified needs and anxieties.
In many other areas of medicine it has been shown that a structured approach to discharge planning, with the use of a pathway of care and predictable timing for discharge, improves the quality of care after discharge, and reduces the need for unexpected readmission after discharge, as well as improving patient satisfaction.
Many parents of preterm infants are routinely informed by medical and nursing staff that their baby will be discharged home at or around the time the baby was due to be born – that is, around 40 weeks’ postmenstrual age (the estimated date of delivery, EDD). This is despite increasing evidence in recent years that improvements in neonatal care were leading to progressively shorter stays in hospital and earlier discharge home. Using EDD as the expected discharge date means that the process of preparing parents to take their baby home is often left until very shortly before the baby is to be discharged, commonly leaving parents feeling unprepared and lacking in confidence in caring for their baby.
In an audit of the length of stay (LOS) of preterm infants in neonatal units in the South West region, we found that almost all infants born at 27–33 weeks’ gestation (see Chapter 4) were discharged home well before their original EDD, and around 50% were discharged home at ≥ 1 month before this date.
We have developed an approach to improving parents’ preparedness to take their baby home – the Train-to-Home package – utilising a number of tools to help increase parents’ involvement in the care of their baby from an early stage, to develop their understanding of their baby’s needs, and to provide, soon after the baby is admitted to hospital, an accurate estimate of when the baby is likely to be discharged from hospital. The pack is parent centred and provides a means of improving communication between staff and parents throughout the baby’s hospital stay.
The aim of this approach was to improve parents’ self-confidence and knowledge about how to care for their baby after discharge, with the potential aim of facilitating earlier discharge to home and reducing the use of emergency or out-of-hours services after discharge.
Study design
The study took place in four local neonatal units (LNUs) in South West England. We used a before-and-after study design, with initial baseline data collection over an 11-month period before the Train-to-Home package was introduced. This was followed by a 1-month ‘washout’ period during which the Train-to-Home package was introduced and intensive staff-teaching in its use was carried out. Then there was a further period of data collection in an 11-month period, during which the Train-to-Home package was routinely used for all infants of 27–33 weeks’ gestation who were admitted to the units. Details of the study methodology are given in Chapter 5 of this report.
Research objectives
The aim of the study was to assess whether the introduction of the parent-centred neonatal discharge package (Train-to-Home) could increase parental confidence in caring for their infant, reduce the LOS of infants in neonatal care and reduce health-care resource use after discharge from hospital.
The primary objective and outcome measure was a comparison of changes in maternal and paternal confidence when caring for a premature baby from just after birth, to around the time of discharge from hospital, and at home 8 weeks after discharge, before and after the introduction of the Train-to-Home package in four LNUs (formerly known as level II units) in South West England.
The secondary objectives were to:
-
measure the LOS of infants born before and after the introduction of the Train-to-Home package, and assess whether this intervention was associated with any reduction in overall LOS in hospital
-
estimate the potential cost savings associated with the introduction of the Train-to-Home intervention in terms of UK NHS and other health-care resources used by parents and infants in the 8-week period after discharge from hospital, before and after introduction of the Train-to-Home package
-
explore parents’ and staff’s views of the intervention and its delivery in greater detail using qualitative interviews.
Chapter 2 Context and background
The organisation of neonatal intensive care
The survival of preterm infants has improved significantly over recent years, with survival rates of 91% for infants born at 28 weeks’ gestation and 98% at 33 weeks’ gestation. 1 This improved survival has resulted in more infants requiring intensive or high-dependency care for longer periods, and increasing the pressure on the scarce resources of neonatal care.
The improved survival rate has brought to the fore the problems associated with infant discharge home after long periods in hospital. It has also raised awareness of the particular needs of such infants and their families in coping successfully with the transition from hospital to home. This transition and community-based follow-up care is an increasing focus of investigation, with attempts to facilitate the processes and reduce the adverse effects of recurrent emergency health-care contacts, which commonly lead to hospital readmission. 2,3 Relatively little attention has been given to the impact and potential importance of this aspect of neonatal care, despite the huge volume of published literature on improving outcomes for preterm infants. 4 Improved education and information provided to families of preterm infants might improve the appropriate use of hospital and community health services after discharge, and reduce the numbers of babies readmitted to hospital,5 although few studies have shown such a relationship.
In the UK, neonatal care is delivered in three types of neonatal unit working together in managed clinical networks. Neonatal intensive care units (NICUs) – formerly referred to as level III neonatal units – provide the full range of intensive care for infants with complex problems, including extreme prematurity drawn from a wide geographical area. They also provide high-dependency and special care services for their local population (similar to LNUs). NICUs commonly function as regional referral centres for infants with complex conditions, and may be linked to other tertiary infant health-care services, including paediatric cardiology, paediatric surgery and other specialist paediatric services. LNUs provide high-dependency care, special care and limited intensive care for their own catchment population. They generally provide the majority of care for infants born at ≥ 27 weeks’ gestation. Special care units provide special care for only their local population. 6
Neonatal care is an expensive and limited health resource, with prematurely born infants occupying the majority of neonatal hospital bed-days. 7 The median LOS for infants born at < 34 weeks’ gestation in South West England LNUs during 2010 was 38 days [audit figures from the ‘Badger’ neonatal data collection system (BadgerNet) – a live patient data management system used by the majority of neonatal units in the UK].
Approximately 70,000 babies born in England each year (10% of all births) require additional medical care after delivery and are admitted to neonatal units. 8 Infants requiring neonatal unit admission are categorised as needing intensive care, high-dependency care or special care. The British Association of Perinatal Medicine (BAPM) have defined the care categories based on the therapeutic and monitoring needs of the baby. 9 Of the 70,000 infants admitted for neonatal care annually, 19,500 are admitted to intensive care. 8 The 2010 BAPM standards recommend that one nurse should provide care to one infant in intensive care, two infants in high-dependency care or four infants in special care. 10 The cost of care is determined mainly by nursing-staff requirements, with intensive care thus costing more than high-dependency or special care. For most infants of < 34 weeks’ gestation, a relatively short period in intensive care is followed by a much longer period in high-dependency care and then special care before discharge home.
The economic cost of neonatal care
Petrou and Khan11 have recently reviewed studies conducting predictive economic modelling of the economic consequences (economic burden) of moderate and late preterm birth. Costs associated with initial hospitalisation were estimated from 10 studies. Mean hospital costs varied between US$1334 for a surviving term infant and US$32,153 for a surviving moderate or late preterm infant (US$ 2008 prices). Studies varied substantially in terms of their methodology, sample size and location. Costs following initial hospital discharge were estimated from 13 studies. 11 Of these studies, 11 focused on a funder perspective, looking at hospital costs after discharge, and excluded costs to other economic sectors, families and carers, and society. Petrou and Khan11 argue that these costs, and the indirect costs associated with days off work and lost productivity, are potentially large in comparison with the perspective for costs taken in most studies. This suggests that most identified studies underestimate the economic cost burden of medium and late preterm babies in the immediate period after discharge. Two studies12,13 within the Petrou and Khan review took a broad perspective on the full range of costs associated with initial hospital discharge and included funder, families and carers, and society. They demonstrated a differential range in cost estimates of 1.3- to almost 10-fold difference between those infants born at between 32 and 36 weeks’ gestation and those born at term. 11
Johnston et al. 14 recently estimated the economic burden of prematurity in Canada by describing and characterising the economic cost burden of premature birth over the first 2 years of life. They accessed high-quality and comprehensive data to populate the parameters of the Markov state–transition decision model and included resource use, direct medical costs, parental out-of-pocket expenses, education costs and mortality. 13 The cost per infant from discharge to age 2 years ranged from CA$9280 to CA$2228 for early preterm births of < 28 weeks’ gestation to late preterm births of 33–36 weeks’ gestation, and total economic cost from discharge to age 2 years was CA$94,081,058 (n = 27,308). They estimated the average number of inpatient hospital days and associated standard error (SE), outpatient costs, and associated indirect costs incurred due to lost productivity by caregivers of preterm infants from discharge to age 2 years. Mean inpatient days [standard deviation (SD)] from discharge to age 2 years were 17.5 (3.32) days, 8.75 (1.27) days and 2.40 (0.17) days for early, moderate and late preterm infants, respectively. Outpatient mean costs for the same groups were CA$2403 (CA$223), CA$1453 (CA$103) and CA$734 (CA$13) respectively. These findings provide a useful basis for this current study for comparison, albeit the period after discharge in our study was only 8 weeks, although it is likely that the consequences of improved parental confidence in caring for their infant will be most easily seen in the first few weeks after discharge, a period during which collection of detailed information from parents is least difficult. The published studies outlined above emphasise the importance of accurate recording of inpatient days post discharge and inclusion of costs associated with emergency department (ED) visits, but, to date, there is very little evidence for the costs related to post-discharge emergency admission of preterm infants.
The average LNU cost in the UK for each very-low-birthweight baby (birthweight of < 1500 g, which is the mean birthweight at 30 weeks’ gestation) is > £13,000. Any increase in parental confidence to care for their infant at this stage could reduce their LOS, and possibly reduce health-care resource use after discharge, making potentially significant health-care savings. 11
The need for discharge planning
Preterm infants of gestational ages 27–33 weeks, inclusive, have a > 90% probability of survival but usually spend a prolonged period in a LNU. Their progress is relatively predictable, which makes a discharge planning process easier because outcomes are anticipated, and parents may be informed ahead of time about expected events and changes over time. Infants born more prematurely will usually be born in a NICU or be transferred to one soon after birth. They will spend a considerable period there before either being transferred to a LNU or discharged directly home.
Infants born at ≥ 33 weeks’ gestation, who develop serious medical problems or have complex anomalies or conditions (e.g. severe intrapartum asphyxia), have extremely variable LOS and a need for tertiary NICU facilities. The range of conditions and the very wide range of possible outcomes, in terms of in-hospital clinical course, make infants outside the 27–33 weeks’ gestation range much less suitable for anticipatory care planning as a group.
The capacity for care of low-birthweight infants is limited by the lack of intensive care cots in NICUs and LNUs. Experience from several UK neonatal networks suggests that moving infants from intensive care to high-dependency or special care cots is a major limitation to the appropriate use of intensive care. This is caused by delays in discharging infants from high-dependency/special care cots. A relatively small reduction in special care or high-dependency care LOS provides a relatively small cost saving, but has a disproportionately greater effect in improving intensive care cot availability and allowing the most effective use of scarce resources.
In the UK, individual health visitors (HVs) are routinely allocated to all infants soon after birth. They carry out a support, advisory and monitoring role for preterm infants after discharge from hospital, which is an important component of routine health care. Changes to NHS workforce planning and commissioning processes have altered HV workload patterns and changed their involvement with mothers and preterm babies. 15 HVs have shifted from providing a generic health promotion/maintenance service for all infants to a focused role concentrating on families at highest risk, namely monitoring, preventing and identifying child neglect and abuse. In many areas this role change has been accompanied by a significant reduction in overall HV numbers, and a loss of expertise in the care and support of preterm infants. This has led many LNUs and NICUs to develop hospital-based outreach teams to provide support, advice and monitoring to families of preterm infants for several weeks after discharge. They also address some of the parents’ psychological and practical needs with individualised support and care programmes. Our unpublished survey of UK neonatal units in 2010 showed the importance that staff attached to having post-discharge care of preterm infants co-ordinated by a team with knowledge and experience of hospital neonatal care.
The importance of involving parents in the discharge planning process
Parents with preterm babies in a neonatal care unit have particular psychological and practical needs, which may be met with individualised developmental and behavioural care programmes. 16–19 Moyer et al. 5 highlight the need to capture and report which types of interventions might support a multidimensional approach to transition from neonatal units to home for this group of infants.
Evidence indicates that early discharge programmes and integrated health-care approaches in neonatal units substantially shorten LOS without increasing health resource use. This approach complements strategies used in adult health-care settings, for which the discharge process is a key part of the patient experience. Hesselink et al. 20 report on a programme to improve adult health-care transitions from hospital to primary care across five European countries. They identified barriers to, and facilitators of, these transitions, which include low prioritisation of discharge consultations by health-care teams owing to busy workloads, insufficient preparation for going home, care at home not meeting individual requirements, and a range of discharge mechanisms from instructing patients and their families to shared decision-making. They conclude that patient and family involvement when preparing for home is determined by the extent to which health teams are patient focused and build discharge around patient wishes, needs and abilities. Further evidence suggests that involving patient carers in patient treatment, and setting provisional discharge dates early in the hospital stay, motivates and prepares them for discharge. 7 When the patient is a child, in this case a preterm baby, involvement and support of the mother, the father and other family members is of vital importance.
The POPPY (Parents of Premature babies Project) systematic review and report of parental experience described the key elements of family-centred care in neonatal units. 21 It found that transition between different levels of care, including hospital to home, was difficult for parents; families valued consistent communication, support in developing readiness for home and improved discharge information when making the transition home. 21 A number of possible cost benefits include reduction in readmission to hospital; reduction in non-scheduled attendance at EDs; increase in attendance at scheduled outpatient appointments after discharge; and reduction in unscheduled use of community health resources, in addition to improving parental confidence and reduced LOS. A risk factor for increased use of health services is parental perception of prematurely born infant vulnerability. 22
The transition from the LNU to home involves a complex process of adaptation by parents and systematic multidisciplinary approaches to families. 23 Discharge home needs to be planned, and families need to be supported by preparation, overnight stays in the unit, HV contact details, and having home visiting/outreach in place. Discharge planning, and the way in which discharge and adjustment to home takes place, are key elements in supporting this transition, especially when vulnerable babies have been very sick. In 2010, we contacted neonatal units across the UK to gain insight into existing discharge practice. This indicated that all participating units had nurse-led documentation, and existing discharge processes were rarely planned and were mainly reactive. These findings mirror Redshaw and Hamilton’s findings24 that family-centred care is inconsistent, despite being emphasised in Department of Health Neonatal Toolkit documents6 and National Institute for Health and Care Excellence (NICE) guidance. 25 Discharge planning has been shown to work best when it is mutually shared by neonatal unit teams and families. 3
Understanding and improving the discharge planning process for parents and their infants in neonatal units: the importance of parental confidence
McGrath3 noted that parents of infants in neonatal units focus on discharge and the care they need to deliver to facilitate this, even when their infants are in the early and acute phase of care. Parents’ ability to take in and retain complex and frequently changing messages from neonatal health professionals is limited under conditions of stress and anxiety during their baby’s stay on the neonatal unit. Few messages are perceived to be relevant to what parents need to learn and do on discharge from hospital. There is evidence that early practical involvement by parents in providing baby care in neonatal units leads to increased parental confidence and competence in their parenting skills, and greater willingness to take full responsibility for their infant’s care. 3
In the USA, the use of a health-coach programme to prepare families of infants with complex medical problems or born prematurely was explored. 5 The programme sought to help them to act as advocates for their infants. Families receiving health coaching were more likely to view the transition from hospital to home as positive within a few days of discharge, and to report confidence in knowing how to care for their baby.
Raines26 reported on the nature of stress experienced by mothers as they prepare to take their infants home from the NICU, in particular, mothers’ self-perceived ability to assume their maternal role. This challenge to mothers assuming their maternal role is echoed by Finlayson et al. 27 in their report of mothers’ perceptions of family-centred care in three English NICUs, where they describe mothers feeling unable to assume their role. Raines26 suggested that the mothers’ levels of stress impede their learning. She recommended that NICU staff should create low-stress environments where discharge education can be most effective when readying families for home.
Work in the USA and Canada on early educational interventions for parents in neonatal units has shown that parent–infant interactions may be enhanced and LOS reduced. 17 Parents’ concerns evolve as they move from NICU to home, and these may be addressed by providing timely discharge information and early anticipatory guidance to help build parental confidence as they move towards taking their baby home. 22 Supporting and involving parents in the process of preparing to leave neonatal units for home provides them with opportunities for confidence building in their abilities to care for their preterm infant at home. 23 In addition to uncertainty about their ability to care for their baby, a range of parental concerns have been identified when low-birthweight infants make the transition from NICU to home. These include breastfeeding proficiency and losing care from unit staff. 22,28,29
Parenting stress30 undoubtedly affects maternal self-efficacy. Furthermore, parental self-efficacy and parenting competence have been found to be moderated by parent knowledge of development31 and as a possible predictor of child functioning. 32 Teti and Gelfand33 have suggested that maternal efficacy beliefs mediate the effects of depression, social support and infant temperament on parenting behaviours. 33 Studies using infants within the first year of life have found that maternal prior experience34 and social support35 are positively related to maternal self-efficacy. Also, several authors have investigated the longer-term impact of low maternal self-efficacy. For example, Leerkes and Crockenberg36 found that mothers who had low self-efficacy were more likely to display less sensitive behaviour towards their infant (especially when their infant was highly distressed), were more likely to give up when trying to soothe their infant and also exacerbate infant distress.
Self-efficacy tools based on Bandura’s Social Learning Theory may be used to indicate the level of belief and confidence about one’s perceived ability to plan and carry out specific tasks. 37–39 Behaviour-specific scales have been developed to identify people with high or low confidence. Examples of such scales include the Breastfeeding Self-Efficacy Scale,40 Childbirth Self-Efficacy Inventory41 and the Perceived Maternal Parenting Self-Efficacy tool (PMPS-E)42 for mothers of infants receiving neonatal care. The PMPS-E tool is a psychometrically robust, reliable and valid measure of parenting self-efficacy for mothers of relatively healthy preterm neonates. We planned to use this to measure maternal and paternal confidence in caring for their baby at three time points. The developers of the PMPS-E agreed that it would be appropriate to use with fathers in our study, and one of the original authors of this measure (Barnes) was a member of the project steering group for the present study.
Development of parent-orientated approaches to planning for infant discharge from neonatal units
The UK development of focused, hospital-based outreach care rather than generic community-based care is similar to the system that has been developed over many years in Canada. McMaster Neonatal Unit in Canada developed an interactive discharge planning tool to achieve timely transfers between the various levels of care and to give families permission to speak and engage with the process. 43 When using the tool in neonatal units, parents asked more questions than before and the tool opened up dialogue between parents and staff. The Canadian project prepared families for transfer from NICUs to LNUs nearer their home. The Canadian tool emphasised the importance of communicating with parents and focusing on their needs and understanding rather than being driven by clinical staff perception of infant needs. Other features include helping parents to read their baby’s changing cues, and keeping baby and parental readiness as the focus of unit practice. Implementing the approach improved parental involvement in, and understanding of, the discharge planning process; however, a number of barriers to successful implementation were identified, notably a lack of direct engagement by neonatologists. Also some nursing staff thought the newly established discharge planning pathways were redundant because the constituent actions and information were documented elsewhere or formed part of normal nursing care. Despite these limitations, the implementation was successful, as parents and families in the NICU accepted it and engaged with the process.
In 2010, a research team member was seconded to the McMaster University neonatal unit to gain experience in using the intervention tool and investigate the feasibility of developing a UK version for an intervention study. In Chapter 4 of this report we present the outcome of this secondment and our subsequent development of a tool using the same principles but orientated to UK families and neonatal unit staff needs.
Summary and conclusions
Improved survival over the past few years means that large numbers of preterm infants spend long periods of time in neonatal care before being discharged home. There has been increasing awareness of the problems experienced by infants and their parents in the process of preparing for, and dealing with, the consequences of discharge from hospital.
There is growing understanding of infant and family needs for structured discharge preparation, early parental involvement in infant care, and support, before, during and after discharge; however, few neonatal units have structures in place to facilitate these processes and many families feel unprepared to take their baby home. This may contribute to delays in hospital discharge and/or inappropriate use of health-care resources after discharge, with recurrent infant readmissions and overuse of out-of-hours or other urgent care resources by families after infants go home.
Studies show the potential value of parent-orientated practical approaches to involving and educating parents about discharge planning during the infant’s hospital stay. Unfortunately, discharge planning and parental education remains poorly organised and unstructured in most UK neonatal units.
We have developed a UK version of a Canadian approach to preparing families for home using a parent-orientated approach to discharge planning based on underpinning principles of early involvement and empowerment of parents.
This report documents the implementation of this approach in four UK LNUs, and the effects of that implementation on parental self-efficacy scores, patterns and costs of health and social care resources use after discharge from hospital, and infants’ LOS in LNUs.
Literature search
Literature searches were completed by a University of the West of England Faculty Librarian and a Research Fellow in November 2009, and rerun in January 2010, with final searches being rerun in February 2015.
No specific date limitations were applied to the search on either occasion.
Databases: EMBASE; Health Management Information Consortium (HMIC); Maternity and Infant Care (MWIC); Ovid MEDLINE®; PsycINFO; Cumulative Index to Nursing and Allied Health Literature (CINAHL) Plus; and Alternative Medicine British Nursing Index 3 (AMED).
Key words used:
neonatal unit* or scbu or special care baby unit* or nicu or neonatal intensive care unit*
prematur*) adj3 baby) or prematur*) adj3 babies) or prematur*) adj3 neonate*) or 32 week*) adj3 baby) or ‘32’) adj3 babies) or 32 week*) adj3 infant*) or 32 week*) adj3 neonate*).
discharg* adj3 plan*) or discharg*) adj3 meet*) or discharg*) adj3 manag*) or going home or leav*).
Chapter 3 Development and implementation of the intervention materials and approaches
The intervention materials used in this study were developed in three closely related, but separate, processes. The materials and innovative approaches to working with the parents of preterm infants were implemented in four LNUs. In this chapter we describe the background, development and implementation of the documentation, together with the approach we used to implement the intervention in LNUs:
-
development of a UK version of the McMaster University ‘train to home’ package
-
development of locally appropriate LOS estimates for infants at each gestational age included in the study
-
development of pathways of care for infants of gestational ages 27–30 weeks’ and 31–33 weeks’ gestation
-
implementation of the interventions in the four LNUs included in the study.
Development of a UK version of the McMaster University ‘Train-to-Home’ package
The original Canadian version of the ‘Train-to-Home’ tool used a visual image of a train with five windows, each representing an area of infant condition or care. The five windows represented ‘Tests’, ‘Jaundice’, ‘Growing’, ‘Feeding’ and ‘Breathing’. Each of the windows could be coloured green, yellow or red, depending on the medical condition of the baby. The medical and nursing staff at McMaster University had determined the criteria for colouring the windows in green, yellow or red. 43
Our initial feedback from UK medical and nursing staff who were shown the Canadian documentation was that it had a North American style and approach, and did not reflect the way in which UK medical and nursing staff discussed clinical problems with parents. We established a Parent Advisory Group (PAG) to support the project, whose members all had experience of having a baby in NICU. They also had strong views that certain parts of the Canadian documentation, particularly the emphasis on laboratory tests and neonatal jaundice, were not in line with their perception of how communications between staff and parents worked in UK neonatal units.
Developing a UK form of the ‘Train-to-Home’ package acceptable to the staff in the participating LNUs was the first stage of the study. We needed to ensure that LNU staff would use the documentation and to maximise the chances of that happening, we needed them to have a sense of ownership of this central part of the project.
One way of achieving this was to use a Delphi consensus approach to facilitate development. We considered this to be an appropriate way to maximise project participation by a large group of LNU professionals. Using a Delphi approach has been shown to minimise the risk of a single opinion or senior individual influencing group projects, in our case the content of the final document. It allowed suggestions to be assessed and considered for inclusion regardless of the person from whom they originated: that is, suggestions are viewed in their own right and on the basis of their own merits rather than in the light of who made the suggestion.
Development of the UK Train-to-Home package by a multiple iteration Delphi review process by the Parent Advisory Group and the Clinical Advisory Group
In order to develop a culturally appropriate and acceptable form of the train for use with UK families, nursing and medical staff, we set up two advisory expert panels, a PAG and a Clinical Advisory Group (CAG). The CAG included at least one experienced neonatal nurse and one consultant neonatologist from each of the four participating LNUs. CAG membership also included additional neonatal nurses and consultant neonatologists working in South West England but not in the four study LNUs.
In the first phase we consulted with CAG members individually by e-mail, seeking comments and suggestions on the content and wording of the McMaster ‘Train-to-Home’ documents. In particular, we sought relevant labels for each window, and the criteria to be used to determine window colour: that is, red, yellow or green. The initial responses from each CAG member were not shared with other group members. CAG members were asked open-ended questions on the content and wording of the original McMaster documents, and asked to suggest alternatives to those parts of the documentation that they felt were not appropriate for use in UK neonatal units.
The responses received were collated, categorised and included as a series of unattributed suggestions attached to the original McMaster documentation. These were then forwarded to CAG members individually. Responses from the second round of the Delphi process were collated and a new version of the documentation was constructed using the majority of suggestions received. Where there were significant differences of opinion between CAG members about aspects of the revised documentation (e.g. about how best to categorise types and levels of ventilatory support), these were identified as alternatives and were again forwarded to each CAG member with specific requests for them to consider which approach or wording was the most appropriate. Again, the individual responses from each CAG member were not initially shared with other members of the group. The differences of views were predominantly related to the most appropriate cut-points to use to distinguish between different levels of support that might represent points of change between the different coloured windows, for example the combination of level of inspired oxygen and the use of continuous positive airway pressure to separate ‘red’ from ‘yellow’, and all were easily resolved at this stage.
After the third Delphi round, the documentation was revised in line with the suggestions received, and e-mailed to each member of the PAG for comments and suggestions about content and wording. Delphi methodology was used to involve PAG members individually and seek their comments and suggestions before convening a full PAG meeting to discuss the documentation and suggestions from parents already received. PAG suggestions were incorporated into the third iteration of the documentation. Medical and nursing members of the Project Steering Group reviewed the third iteration, and appropriate comments and suggestions were incorporated into the documentation.
At this stage the proposed documentation was sent, for review, to the senior nurse and a nominated consultant neonatologist in each of the four participating neonatal units, and to ensure that the proposed boundaries defining the red, yellow or green windows on the train were compatible with current management of infants within the defined gestational limits in each of the neonatal units. This process led to a number of relatively minor changes to the definitions of levels of care used in several of the categories, and these changes underwent a further iterative process of refinement to ensure that the wording and definitions used were compatible with current management in all four units.
Finally, a meeting was convened of all members of the CAG, together with the other medical and nursing staff in the participating units who had been involved in the process of developing this documentation who were able to attend – either in person or by telephone conference call. At this meeting the structure, content and presentation of the proposed modified Train-to-Home documentation was discussed and a final version agreed.
This final version (Figure 1; for further details see Appendix 1) was then sent to the lead consultant neonatologist in each of the four participating neonatal units for formal approval. Once this approval had been received the documentation was adopted by the Project Management Group and the Project Steering Group for use in the study.
FIGURE 1.
The ‘Train-to-Home’ package (© University of Bristol and University of the West of England).

Development of locally appropriate length of stay estimates for infants at each gestational age included in the study
Estimating the likely date of discharge for preterm infants from 27 to 33 weeks’ gestation inclusive
We collected data from the routine neonatal database used in South West England (‘BadgerNet’) to estimate the likely discharge date for infants in the study’s gestational age range. Data were collected on all infants in the gestational age range of 27 weeks 0 days to 33 weeks 6 days, who were born in the four study LNUs from 1 April 2011 to 31 March 2013 (a few months before the planned implementation date for the intervention used in the study). We included only those infants who were born in, and discharged to home from, the same LNU. Those infants who were transferred to a regional NICU but transferred back to the LNU in which they had been born, and subsequently discharged to home from the original LNU, were included. Infants who were transferred from the original LNU to another unit from which they were then discharged home and those who did not survive to discharge home were excluded. The ‘Badger’ database provided information on gestation at birth (in weeks and days) and age in days at the time of discharge to home for all infants in the target gestational age range.
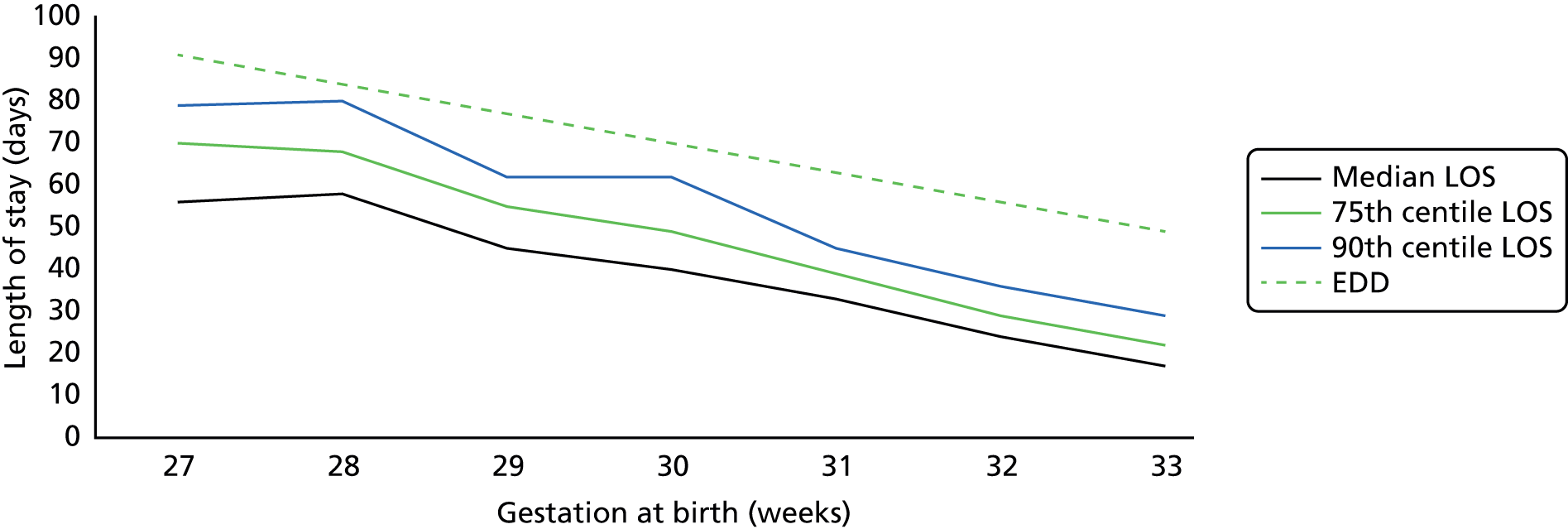
Overall, 531 infants met the criteria and were included in the study. In order to achieve large enough groups of infants to assess LOS, we aggregated the data into weeks of gestational age rather than weeks and days. We then calculated the median (50th centile), 75th and 90th centiles for LOS for each week of gestational age within the study range. The numbers of infants at each week of gestational age are given in Table 1, together with the median, 75th and 90th centiles for LOS for infants in each gestational age group.
| Gestation (weeks) | Number of infants | Median LOS (days) | 75th centile for LOS (days) | 90th centile for LOS (days) |
|---|---|---|---|---|
| 27 | 26 | 56 | 70 | 79 |
| 28 | 40 | 59 | 68 | 80 |
| 29 | 39 | 45 | 55 | 62 |
| 30 | 55 | 42 | 49 | 62 |
| 31 | 82 | 33 | 39 | 45 |
| 32 | 118 | 24 | 29 | 36 |
| 33 | 171 | 18 | 22 | 29 |
These data are shown graphically in Figure 2. There was considerable random variation in the 90th centile for LOS because of marked variation in the condition and progress of a small number of infants at each gestation, but for infants of all gestations the 90th centile gave a discharge date considerably sooner than the baby’s EDD, equal to 40 weeks’ gestation. The 75th centile showed a more consistent pattern of change with increasing gestational age, although still showed some week-to-week variation. Overall, the 75th centile for the infant’s postmenstrual age (gestation plus postnatal age) at the time of discharge home was between 36 and 37 weeks for all gestations, except for babies born at 28 weeks, for whom it was 37 weeks and 5 days. In other words, the great majority of preterm infants went home 3–4 weeks before the mother’s original EDD, which is the measure that, until now, has been the one most commonly used by neonatal staff to estimate the likely date of discharge for preterm infants.
FIGURE 2.
Median, 75th centile and 90th centile for LOS and estimate date of delivery for preterm infants, 2011–13.
We needed a consistent and usable chart to allow medical and nursing staff to give parents – within 7–10 days after an infant’s birth – an estimated range of dates for discharge from hospital to home. We decided to use the 75th centile, and to smooth the data to avoid the likely random variations in recorded LOS over only a 2-year period. To make the chart usable and avoid staff making time-consuming calculations for each baby, we included estimated LOS in whole weeks for immature infants of < 31 weeks’ gestation. The more mature infants would mostly be discharged home in < 5 weeks, so we gave the estimated LOS in weeks and days. For simplicity and ease of use, we gave a 2-week range of dates for the less mature infants and 5 days for the more mature infants.
Consultation with the CAG and PAG during the development phase indicated that the range of estimated dates should be no wider than 2 weeks for less mature infants, and should be < 1 week for the more mature infants to be helpful in infant discharge planning. The project aim was to refine the initial range of estimated dates for discharge as the infant progressed through the LNU. As more information became available about each infant’s progress, the estimated dates could be adjusted and the window narrowed.
Figure 3 shows the upper estimate of the LOS, based upon the smoothed 75th centile line (representing the initial estimate of the date by which most infants would have been discharged) together with the earlier limit of the estimated date of discharge, superimposed upon the median and 75th centile lines shown on Figure 2. For all gestations the lower estimate of likely discharge date was just below the median LOS.
FIGURE 3.
Median, 75th centile and estimated LOS for preterm infants based on data from 2011 to 2013.
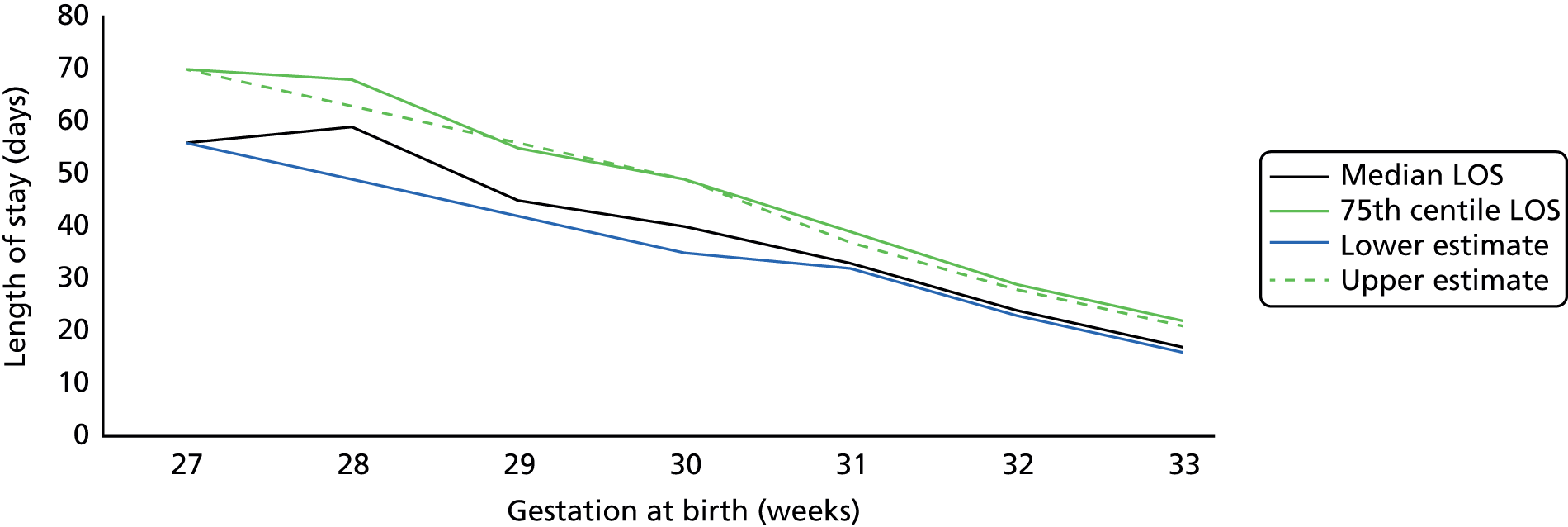
Using 2011–13 data, this range of estimated dates indicates that 77% of infants born at 27–30 weeks’ gestation inclusive would have been discharged home by the later estimated date based on the smoothed 75th centile, and 75% of infants born at 31–33 weeks’ gestation would have been discharged home by this date. The irregularity in the LOS at each gestation meant that there was a larger variation in the proportion of infants discharged home by the later estimated date for some gestational ages (Figure 4). This is inevitable when using a small database derived from a cohort of infants born in a 2-year period. The proportion of infants still in hospital at the later estimated date of discharge was < 25% for all gestations with the exception of 28 weeks (35%) and 31 weeks (27%). For infants born at 27 and 29 weeks the figures were 19% and 15%, respectively.
FIGURE 4.
Numbers of infants at each gestation who had been discharged or were still in hospital by the later estimated discharge date based on data from 2011 to 2013.
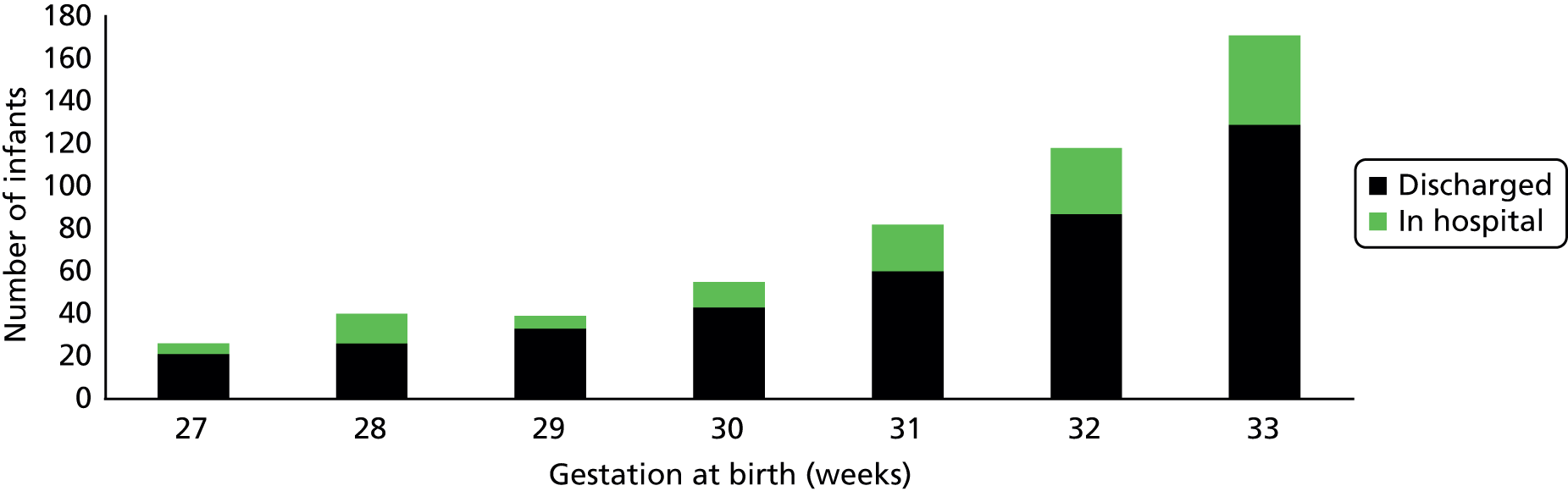
The proportion of infants who had been discharged before the first of the two estimated dates of discharge varied between 50% (at 27 weeks’ gestation) and 27% (at 33 weeks’ gestation).
The final version of the tool that was used in the study is shown in Appendix 2.
Summary
We developed a reliable and simple tool to estimate the likely date of discharge home for infants of 27–33 weeks’ gestation born in the four study LNUs. This was based on the LOS of all infants born in the four units over the preceding 2-year period. We used the smoothed 75th centile for LOS as the later estimate of likely discharge date, with a 2-week window of likely discharge date for less-mature infants (< 31 weeks’ gestation) and a 5-day window for more mature infants.
This easy-to-use tool was applied to all infants within the target gestational age range within 7–10 days of birth, and gave estimated dates of likely discharge that were correct for > 75% of infants. The intention was to refine the initial estimated date of discharge on a 1- to 2-weekly basis as the infant progressed through the LNU (see Appendix 2).
Actual length of stay by gestation for infants included in the study
Figure 5 shows the median (50th centile) and 75th centile of LOS for infants enrolled in the study from the four study LNUs. It shows that the median and 75th centiles for LOS recorded for each gestation for the study period were similar to those in the 2-year period used to develop the tool. However, for infants born at 27 weeks’ gestation, the previously collected data suggested shorter LOS than for infants in the study, although these differences did not reach statistical significance. At all gestations, between 50% and 75% of infants in the study were discharged by the later of the two dates suggested by the tool.
FIGURE 5.
Media and 75th centile for LOS for preterm infants prior to (2011–13), and during, stay period.
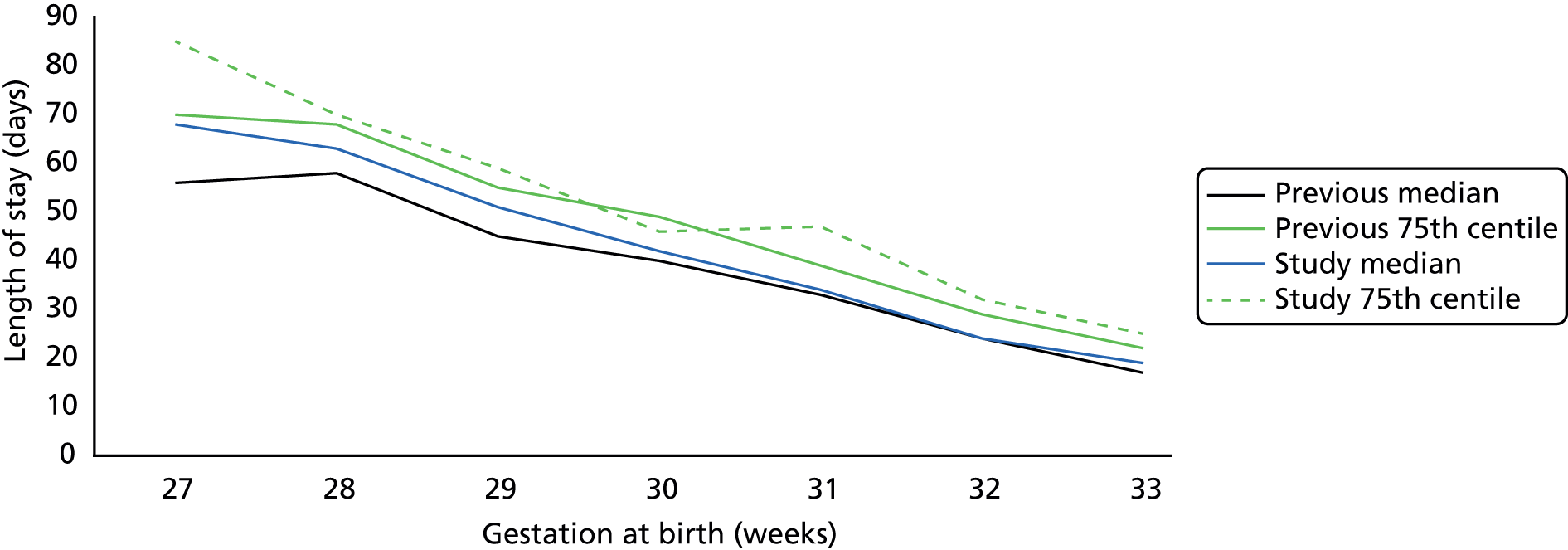
Despite considerable variation in infant LOS in the target gestational age range, the tool predicted a likely discharge date for all gestations, by which time close to 75% of the infants had been discharged home. The mean postmenstrual age (i.e. gestation at birth plus postnatal age) at discharge for infants during the study period and during the preceding period from which the above graphs were developed were 36 weeks/4 days and 36 weeks/3 days, respectively – a non-significant difference.
Development of pathways of care for infants of gestational ages 27–30 weeks’ gestation and 31–33 weeks’ gestation
During the development of the UK Train-to-Home package, PAG members said that, in addition to parents having some indication of when their baby would be going home, it would be very helpful for them to have some indication of the pathway the baby might follow during their hospital stay. From our contact with Canadian neonatal units, we were aware that a number of Canadian ‘pathways to home’ had been developed and used to give parents an understanding of likely events and changes that might occur at each stage of a baby’s stay in Canadian NICUs. Unfortunately, the cultural difference in language used in these documents was unsuitable for use in the UK, as the information concentrated on technical aspects of infants’ care. With considerable input from PAG members we developed two pathway documents using the main subject areas described in the UK Train-to-Home package as a template: one for babies of 27–30 weeks’ gestation and one for babies of 31–33 weeks’ gestation.
A number of milestones that were likely to occur during a baby’s stay in a LNU were matched to each of the five areas of care and development symbolised by the train windows (breathing, feeding, growth, temperature and sleeping). In partnership with the PAG members, we linked questions about these milestones to the approximate time during the baby’s stay in LNU when they were likely to be raised or be relevant to parents. Each pathway covered the period from birth to discharge from hospital.
The draft pathway documents were reviewed and modified by CAG members. This iterative process was repeated, with a further review by PAG and CAG members until a form of wording acceptable to both groups was achieved. The final versions of the parent pathway booklets used in the study are shown in Appendix 3.
Implementation of the interventions in the four local neonatal units included in the study
We arranged a number of interactive briefing and training sessions for LNU staff in close consultation with lead clinicians, lead nurses and educational leads from each of the four study LNUs to explain the intervention, the documentation and the approach to be used during the intervention. LNU lead nurses identified two dates for the briefing and training sessions to be run to minimise operational disruption. Two briefing and training sessions per day were delivered.
Throughout the briefing and training events we emphasised that the intervention package was being introduced as a change to routine LNU policy for all infants in the target gestational age range 27–33 weeks inclusive, and was not itself a research intervention. All babies and families were to be involved in the changed approach, rather than only those who gave consent to take part in the study.
Briefing and training sessions: before and during the intervention
Pre-implementation briefing and training sessions took place in September 2013. The intervention started on 1 October 2013. During each session, the background to the project was introduced, as well as the nature and purpose of the intervention. Time was spent going through and explaining the documentation, and how it had been developed. Information was presented using a PowerPoint® (2010) (Microsoft Corporation, Redmond, WA, USA) presentation supplemented by paper examples of each of the relevant documents. A project documents pack was given to each LNU attendee. Sessions lasted for between 45 and 60 minutes, with questions taken during the presentations and at the end. LNU attendee feedback was captured by immediate verbal feedback and anonymous written feedback. Feedback was reviewed after each session and used to improve the quality of subsequent presentations.
There was a 15-minute period in between sessions, which allowed for specific detailed discussion with individuals who had particular questions about the project.
The briefing and training sessions were delivered by PJF (a neonatologist) and HB (an experienced neonatal nurse). LNU attendees included a mixture of neonatal nurses, junior medical staff, ancillary staff and consultant neonatologists. Copies of the PowerPoint presentation were made available to each LNU lead clinician to facilitate ‘cascade’ teaching of other LNU medical and nursing staff. A copy of the PowerPoint presentation is given in Appendix 4.
Between 5 and 18 LNU members of staff attended the pre-implementation briefing and training sessions in each unit. At the end of the initial run of sessions we asked LNU lead nurses and lead clinicians to contact us when, and if, further sessions were needed. PJF and HB also visited the LNUs during the first 2 months of implementation to talk informally with LNU staff, answer questions from staff and parents, and arrange further sessions as required. HB delivered a further two to four briefing and training sessions in each LNU during December 2013 and January 2014. PJF delivered two additional sessions each – mostly to LNU junior medical staff in three of the four units. Other planned sessions were cancelled because of heavy LNU workload.
In total, 18 additional sessions were delivered in the four LNUs during the intervention period in addition to the 16 pre-implementation sessions. HB and PJF were available by phone and e-mail to LNU senior staff at each unit to answer queries arising during the intervention process during the period 1 October 2013 to 31 August 2014.
Feedback on the briefing and training session provided for the intervention implementation
A semistructured telephone interview with five of the six LNU lead consultant neonatologists on the briefing and training sessions was carried out at the end of the study. Comments are given below and identities anonymised:
The medical staff found the concepts interesting but the process was ‘not exciting’ to them. Nurses found the initial teaching helpful but it was difficult to cascade the teaching to other nursing staff.
This was really helpful. It was particularly helpful to be able to understand how the estimated discharge dates had been derived.
The teaching was well presented and well explained, but we (i.e. the staff on the unit) were probably too optimistic about how well we would be able to cascade the training to other staff – this was a problem at times.
It was difficult to keep staff up to speed with this because of the rapid turnover of staff – it would probably have been better if we could have made one or possibly two members of the middle grade medical staff responsible for ongoing teaching to ensure all staff understood the project.
The training provided was good and got everyone up and running but cascading training was very difficult – especially for nursing staff. Nurses (or at least some nurses) found it particularly hard to ‘hand over control’ of parts of the process to parents – though this improved as the study progressed.
Chapter 4 Research methods
Design
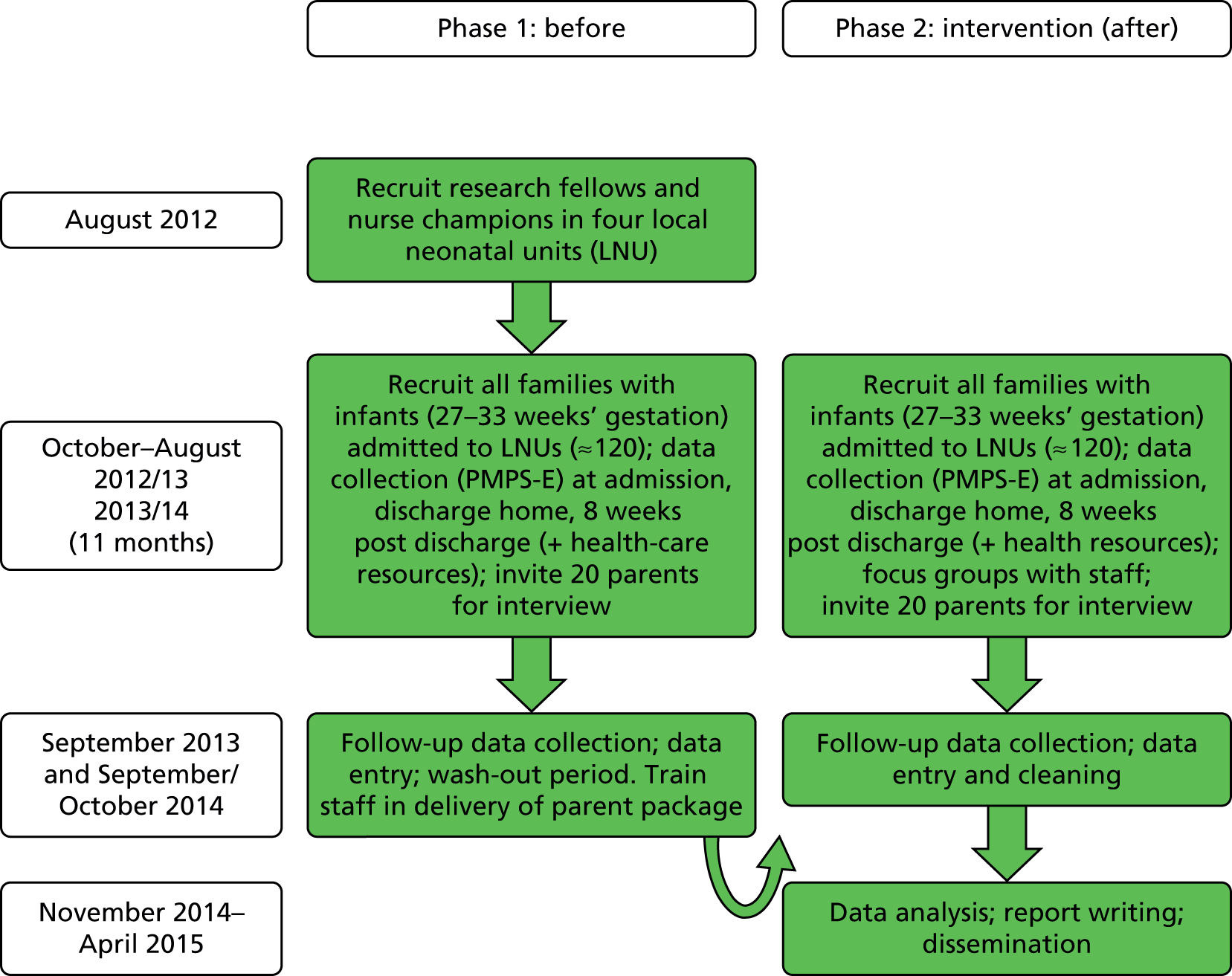
The Preparing for Home study used the PMPS-E (see Appendix 5) to measure parental perception of self-efficacy when caring for their infant soon after birth, at discharge home, and 2 months after discharge home. Parents were recruited to the study before and after the introduction of the parent-centred neonatal discharge Train-to-Home package, as shown in Figure 6. This was designed to facilitate and improve parental confidence in caring for their infant and their experience of discharge home.
FIGURE 6.
Study flow diagram.
Participant inclusion/exclusion criteria
Parents of infants born between 27 weeks 0 days and 33 weeks 6 days were recruited in four LNUs in South West England (Exeter, Taunton, Bath and Swindon). They were recruited during two 11-month periods (October to August in 2012–13 and 2013–14) before and after the introduction in the LNUs of the Train-to-Home package and parent pathways. Infants with major congenital anomalies, those from triplet or higher-order births, or mothers who were aged < 16 years were not eligible for the study.
Description of local neonatal units
The four units involved each had:
-
three or four intensive care cots, four high-dependency cots and 10–14 special care cots
-
between 30 and 53 nursing whole-time equivalents
-
shift patterns, with a combination of 12- and 7.5-hour early/late shifts
-
medical staffing comprising five to seven consultants on a rota, six to eight registrars and two to eleven senior house officers.
All units had experienced organisational change during the study period, some of which had effects on staff workload. All of the units were also working towards World Health Organization (WHO)/United Nations Children’s Fund (UNICEF) Baby Friendly accreditation breastfeeding awards.
The Perceived Maternal Parenting Self-Efficacy and sample size required
The PMPS-E uses 20 statements and a four-point Likert scale (strongly agree to strongly disagree) to generate a minimum score of 20 (indicating a low level of self-efficacy) and a maximum score of 80 (indicating a very high level of self-efficacy). It has been validated using mothers (n = 165) of hospitalised preterm neonates (average age 31.9 weeks’ gestation) with a mean score of just under 60, and a SD of around 10, measured 10 days after birth. 42 A preliminary controlled study conducted by Barnes44 on potential changes in score over a 10-day period (using an intervention such as encouraging the mother to hold and stroke the baby) yielded a 10-point improvement compared with a higher than expected 5-point improvement among the controls (placebo effect). This suggests a potential medium effect size of 0.5 SD. Assuming a more moderate effect size of 0.4 SDs (equivalent to a 4-point improvement more than the controls) and 80% power with a 5% significance level and two-sided test we would need 100 parents in each group (200 in total).
Potential sample size available for the study
In 2010, 181 singletons and 81 twins were born between 27 weeks and < 34 weeks and admitted to the four intervention LNUs within the first week of life over an 11-month period (audit data from the Badger system). This suggested that we would have in excess of 220 mothers to invite into the study for each of the 11-month recruitment periods, of which at least 80% (n = 176) would be eligible for inclusion. If we recruited 70% of mothers with 20% loss to follow-up, we would recruit around 100 mothers per group. Our experience in previous similar work suggested very high uptake and relatively few families lost to attrition. If we achieved higher recruitment rates and lower loss to follow-up rates (i.e. 90% and 5%, respectively), we could recruit 150 mothers per arm, which would increase the power of the study to 93%.
Data collection
In each LNU, research nurses, or ‘nurse champions’, for the study screened all admitted babies for eligibility and gained parental assent to pass their details to the research team. Parental consent was sought by one of the study researchers and demographic information collected. Both parents were invited to take part in the study and they completed the PMPS-E tool within a few days of their baby’s admission to the LNU. A discharge pack was left in the LNU towards the end of each baby’s stay to be given to parents before they took their baby home. The researcher collected discharge information on LOS and feeding method. Parents were encouraged to complete their discharge PMPS-E questionnaires and leave them in a study box in the LNU. Their discharge pack also contained four 2-week health-care resource-use questionnaires and a further PMPS-E questionnaire to take home. The health-care resource-use sheets recorded all contacts (planned and unplanned) with primary and secondary health-care services fortnightly over the 8-week period from discharge.
Soon after discharge home, the study co-ordinator telephoned each family to check the discharge information, alert them to future calls to be made 4 and 8 weeks later and checked their preferred contact method (phone, text, e-mail or post). At the 4- and 8-week contacts, health-care resource-use data were collected for the previous 4 weeks. At the 8-week contact, the final PMPS-E questionnaire was completed, and families were asked if they would be happy to be contacted one final time for an interview. Data were double-entered on to a Microsoft Access® (Office 14) (Microsoft Corporation, Redmond, WA, USA) database and, when data entry was complete, exported into Microsoft Excel® (Office 14) (Microsoft Corporation, Redmond, WA, USA) for uploading into statistical packages.
Statistical methods
For proportional data, chi-squared tests were used to n – 1 degrees of freedom (df), and a Fisher’s exact test if the expected cell was < 5. Test of normality on continuous data was conducted using the Shapiro–Wilk test and observing the Q–Q plots. The Mann–Whitney U-test was used to compare unpaired data that were not normally distributed and both medians and interquartile ranges (IQRs) were reported to describe these distributions.
Multivariable linear regression modelling was used for all variables with valid values to assess the mean differences in PMPS-E scores and 95% confidence interval (CI) between phase 1 and phase 2 at discharge and 8 weeks after discharge; the dependent variable was PMPS-E score at discharge or home and independent variable was the group effect, adjusted for baseline scores. A number of family factors, maternal factors (including pregnancy history) and infant factors were collected for modelling, to be used only if significant differences were identified between the two time periods. As this was not a randomised controlled trial (where differences at baseline could be considered as random), we included any differences in the model if significant at the 5% level. The primary analysis (maternal PMPS-E scores) was conducted on an intention-to-treat basis.
For the primary analysis, multiple imputation techniques were used as a sensitivity analysis to account for missing values. A multivariable imputation model was used to predict missing PMPS-E score values. The standard errors (SEs) of the predicted mean values at each time point were corrected using Rubin’s rule. A per-protocol analysis was conducted as part of the exploratory analysis, which also included an investigation of paternal PMPS-E scores, maternal PMPS-E subscale scores and an investigation of between-centre variation.
Statistical analysis was performed using Statistical Package for Social Sciences (SPSS) version 21 (IBM Corporation, Armonk, NY, USA) and Stata v13 (StataCorp LP, College Station, TX, USA).
Qualitative methods
Parent interviews
Semistructured telephone interviews were carried out with a sample of parents. They explored their experiences of time spent on the LNU caring for their infant, perceptions of communication with staff about their infant’s condition, their infant’s discharge to home, and contact with health services after discharge. Two months after discharge, parents were contacted by phone to complete the final PMPS-E and health resource-use questionnaires. At the end of this call, parents were invited to take part in a semistructured telephone interview at a time of their choice. The researcher explained that they would be contacted once more by phone to answer more in-depth questions about their experiences of having an infant in the LNU, preparation for discharge and contact with health services since discharge.
Parents were purposively selected for interview from those who had agreed to further contact and could be contacted by phone. Maximum variation sampling was used to interview parents from different ethnic and socioeconomic groups, with babies of different gestational ages from single and multiple births. Theoretical sampling was used to develop emerging findings by targeting participants with characteristics of interest (such as younger or first-time mothers).
Interviewers used a topic checklist so that similar areas were covered during each study phase, but with flexibility so that parents could raise issues of importance to them (see Appendix 6 for topic guides). Interviews in phase 2 were also used to explore and understand parents’ views and use of the parent package. The topic checklist was developed with the PAG using relevant literature and insights from study management team meetings.
Nursing and medical staff focus groups and interviews
After family recruitment was completed in phase 2, arrangements were made with the LNUs for researchers to run focus groups with nursing staff in each unit. Visit dates were advertised widely throughout the LNUs several weeks in advance to encourage good attendance. Managers arranged the focus group timings to fit in with staff rotas, usually early afternoons. One-to-one interviews were arranged after the focus groups for staff unable to attend the groups. Short telephone interviews were carried out by a senior researcher with consultant neonatologists from each LNU in early 2015. These interviews were not audio-recorded, but detailed and careful notes were taken and transcribed immediately after the interview.
Qualitative analysis
Parent interviews and nursing staff focus groups were audio-recorded and transcribed verbatim. Data items were systematically assigned codes using the qualitative data organisation package NVivo 2010 (QSR International Pt, Warrington, UK). Thematic analysis used constant comparative techniques so that emerging themes could be tested in subsequent interviews. 45 Data analysis was an iterative process that informed further sampling and data collection. Three members of the research team analysed 10% of the data independently to compare coding and enhance its rigour: two researchers independently both analysed most of the interview transcripts and the third researcher selected two early interviews from each phase and from different units to check the coding. Descriptive accounts were produced, and theoretical explanations for behaviours, opinions and decisions were developed.
Health-economic methods
Rationale for approach to design of economic analysis
Our research study evaluated an intervention that the units had all agreed to adopt as a unit policy. Although we provided (unfunded) assistance and training in achieving this, the aim of the study was not to implement the package but to evaluate its efficacy in neonatal units that had implemented it as a part of routine infant and parent care. Thus analysing the costs of developing the intervention and training the staff using a standard costing approach was not appropriate or relevant information for decision-makers. It is important to recognise that commissioners/sponsors of interventions want to see cost savings demonstrated before they will consider rollout of an intervention that is feasible to implement and acceptable to service users. One of the tensions throughout this project was that some staff in the units were unclear about the nature of the study, and some assumed that they needed to use it only with families who agreed to take part in the research. However, delivery of the Train-to-Home intervention was separate from involving families in answering our questionnaires (the PMPS-E and health-care resource-use tool in the 8 weeks after discharge). The changes associated with use of health-care resources before and after implementation of the Train-to-Home intervention using before-and-after samples, 1 year apart, were costed and did not consider the cost of implementation of the intervention.
Development of the health-care resource-use tool
Resource-use data tools are often designed by developing new questionnaires for each study or modifying questionnaires from a previous study. They are not necessarily validated in their current form, unlike patient-reported measures of health outcome. 46 They need to be appropriate, study specific and easily understood so that participant recall and self-report is accurate. We designed a short data collection tool so that parents could complete it during a busy and stressful time as they were caring for preterm infants during an 8-week post-discharge period. It also needed to be long enough to collect data for estimating cost changes from the perspective of the NHS primary and secondary care, society, and families and carers. Our resource-use data collection tool was piloted with the PAG to check ease of completion and understanding before submission for ethical approval (see Appendix 7). The questions were in four blocks: unplanned use of, and contact with, secondary care services; planned outpatient follow-up contacts; family costs from using those services; and use of primary care and other therapists.
Data preparation and cost estimation
Health resource-use data were entered into the Access database, downloaded into Excel spreadsheets and prepared for cost analyses. The data were reviewed manually to identify low coverage or no-response items, and to clean the data for analysis. There were significant numbers of low-/no-response items in question 2 regarding use of trains, buses, overnight accommodation and number of days off work; these variables were removed from the database. Contact with a health professional – face to face and by telephone, and duration of contact time – was separated out and combined, so that each case had one entry indicating the frequency and duration of contact time by each health professional and contact type. This allowed resource-use volumes and the price of those resources to be treated separately in estimating costs when this was applicable.
Costing the care provided in the LNUs is complex because different tariffs or prices are attached to each care level and recent price information to estimate costs at each level of prematurity is not accessible. This mirrors the costing difficulties reported in the Toolkit for High Quality Neonatal Services. 6 Therefore, we have used proxy prices and recorded their sources, and listed assumptions, unit cost estimates and sources of prices used to calculate costs in Appendix 8.
These data were checked against the health resource-use database and added and/or corrected. Resource-use data in volume units were combined with price and unit cost information from published sources47 to estimate costs per item in pounds sterling (2014 prices). All variables were named and defined (see Appendix 8).
Health-economic data analysis
Cost analysis was performed using SPSS version 21. The reasons for infant inpatient readmission to hospital, outpatient and ED attendance, and hospital centres attended were analysed and compared across the two phases using chi-squared tests. Data were graphed when this was more useful. Continuous data were tested using the Shapiro–Wilk test of normality in distribution (see Appendix 9). These data were not normally distributed, so the Mann–Whitney U-test was applied to test for statistically significant differences in costs during the two phases. We costed the changes associated with use of health-care resources before and after implementation of the Train-to-Home intervention, using before-and-after samples, which were exactly 1 year apart, so we did not adjust for month of discharge or seasonal effects.
Parent Advisory Group input
The PAG was established in 2012 to assist with the study application and comprised six parents who had previous experience of having a baby cared for in a NICU. PAG members met four times (January 2013, June 2013, June 2014 and November 2014) to contribute to study project management. They made extensive comments on the design and content of intervention materials, reviewed training topics and resource-use questionnaire content. PAG members have discussed recruitment issues and how to involve more parents, qualitative interview results, dissemination of findings to parent groups, and future use and format of the intervention including the use of technology (apps and websites). They also contributed extensively by e-mail on the content of the parent pathways, and helped to develop and focus the booklet questions and statements.
The Neonatal Critical Care Service specification document, which sets out what NHS England expects from Trusts providing neonatal services, emphasises the need to provide family-centred care and to help parents understand their baby’s needs. Neonatal staff are required to provide support to enable parents to make informed choices and play an active part in their baby’s care. PAG members felt that the Train-to-Home package was an innovative way to engage parents and assist staff in their efforts to communicate with and encourage parents.
The chairperson of the group, Joanne Ferguson (JF), and another parent, Catherine Miles (CM), are members of the Trial Steering Group and contributed to those discussions from a parent perspective. As a lay member of the Neonatal Clinical Reference Group, JF provided input on national neonatal standards and issues, and, as a champion for the charity Bliss, CM provided input on local experiences and issues. As members of online parent support groups, they also provided details of, and insights from, support networks for parents with babies in neonatal care.
Ethics approval
The study was given National Research Ethics Service (NRES) ethics approval by the NRES Committee London – City & East in June 2012: 12/LO/0944.
Chapter 5 Results: part 1 – study population and quantitative data
Ascertainment
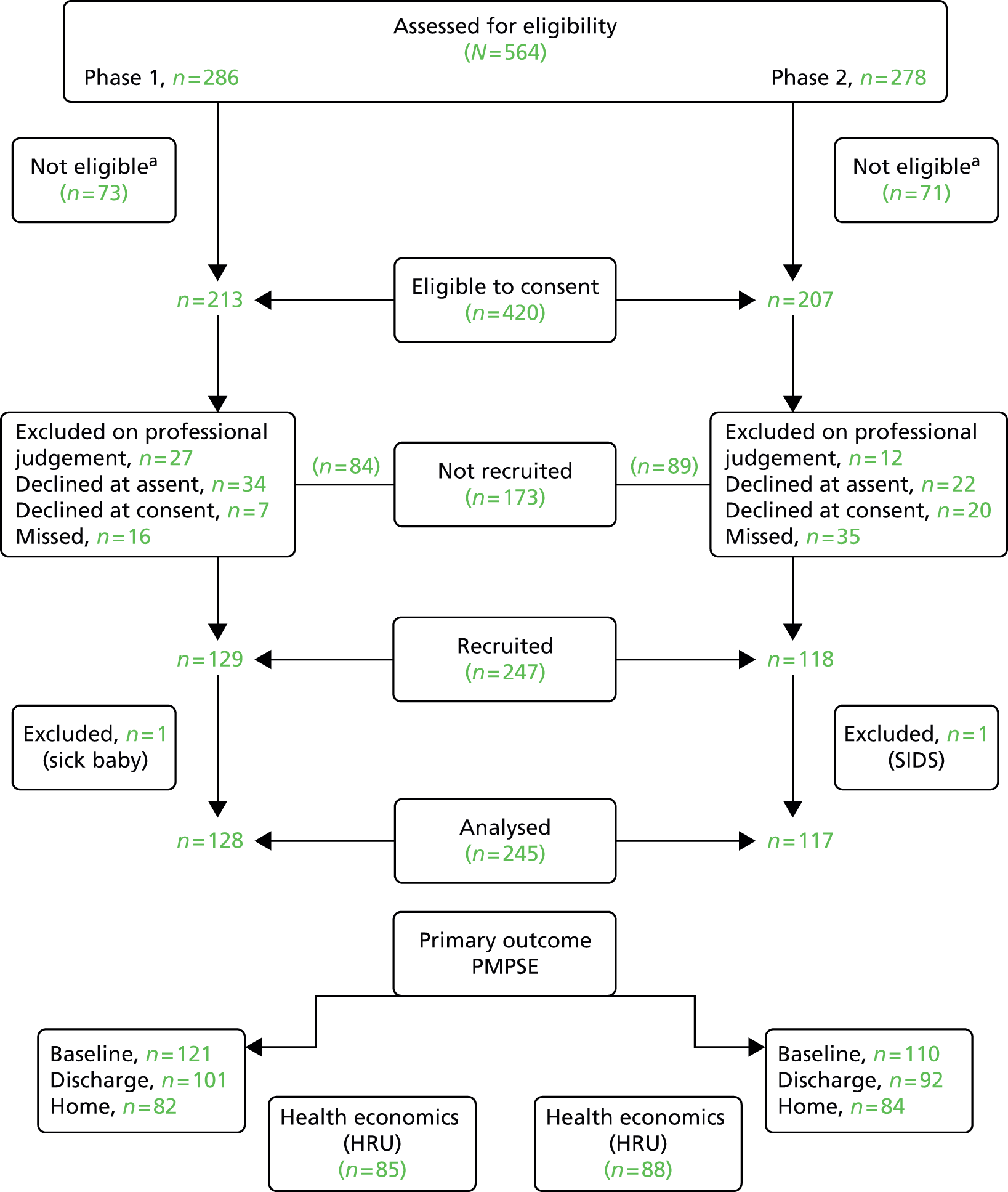
We recruited 247 families in total: 129 received usual care in the first 11-month study period (phase 1, October 2012 to August 2013) and 118 received the intervention in the subsequent 11-month study period (phase 2, October 2013 to August 2014), as shown in Figure 7. We had two withdrawals: one from phase 1 (baby very unwell) and one from phase 2 [baby died of sudden infant death syndrome (SIDS)]. The analysis is thus based on 245 infants, 128 receiving usual treatment and 117 receiving the intervention. Table 2 shows the breakdown across units; the contribution from each unit across the two time periods was evenly split (chi-squared on 3 df; p = 0.99).
FIGURE 7.
Recruitment chart. a, Reasons for no-eligibility as per protocol: transfer; language problems; abnormality; triplets, out of area; age. SIDS, sudden infant death syndrome.
| Unit | Phase 1 | Phase 2 | ||
|---|---|---|---|---|
| n | % | n | % | |
| 1 | 32 | 25.0 | 29 | 24.8 |
| 2 | 25 | 19.5 | 24 | 20.5 |
| 3 | 34 | 26.6 | 29 | 24.8 |
| 4 | 37 | 28.9 | 35 | 29.9 |
| Total | 128 | 100 | 117 | 100 |
Infant characteristics
Table 3 shows infant characteristics at birth. There was no significant difference between the two groups. In phase 1, there was a higher proportion of twins (only one of the twins was used in the analysis) but this was not quite significant at the 5% level. There were slightly more males in phase 2 and a lower proportion in both groups born during the autumn months because of the September ‘washout period’ of the study. The proportion of infants was similar when split by gestational age pathway and there was no difference in gestational age overall. The mean birthweight was also similar among the two groups. Similarly, there was no significant difference between phases in the month during which infant discharge occurred (p = 0.86).
| Characteristic | Group of interest | Phase 1 | Phase 2 | p-value | ||
|---|---|---|---|---|---|---|
| n/N | % | n/N | % | |||
| Gender | Male | 64/128 | 50.0 | 62/117 | 53.9 | 0.64 |
| Twin | Yes | 16/128 | 12.5 | 25/117 | 21.4 | 0.06 |
| Month of birth | December to February | 28/128 | 21.9 | 37/117 | 31.6 | |
| March to May | 43/128 | 33.6 | 31/117 | 26.5 | ||
| June to August | 36/128 | 28.1 | 29/117 | 4.8 | ||
| September to November | 21/128 | 16.4 | 20/117 | 17.1 | 0.32 (3 df) | |
| Gestational agea | 27–30 weeks | 37/128 | 28.9 | 35/117 | 29.9 | |
| 31–33 weeks | 91/128 | 71.1 | 82/117 | 70.1 | 0.86 | |
| Units | Mean | N, SD | Mean | N, SD | p-value | |
| Birthweight | kg | 1.70 | 128,0.50 | 1.65 | 114, 0.45 | 0.44 |
| Gestational age | weeks (w)/days (d) | 31w 5d | 128w 13d | 31w 4d | 117w 12d | 0.59 |
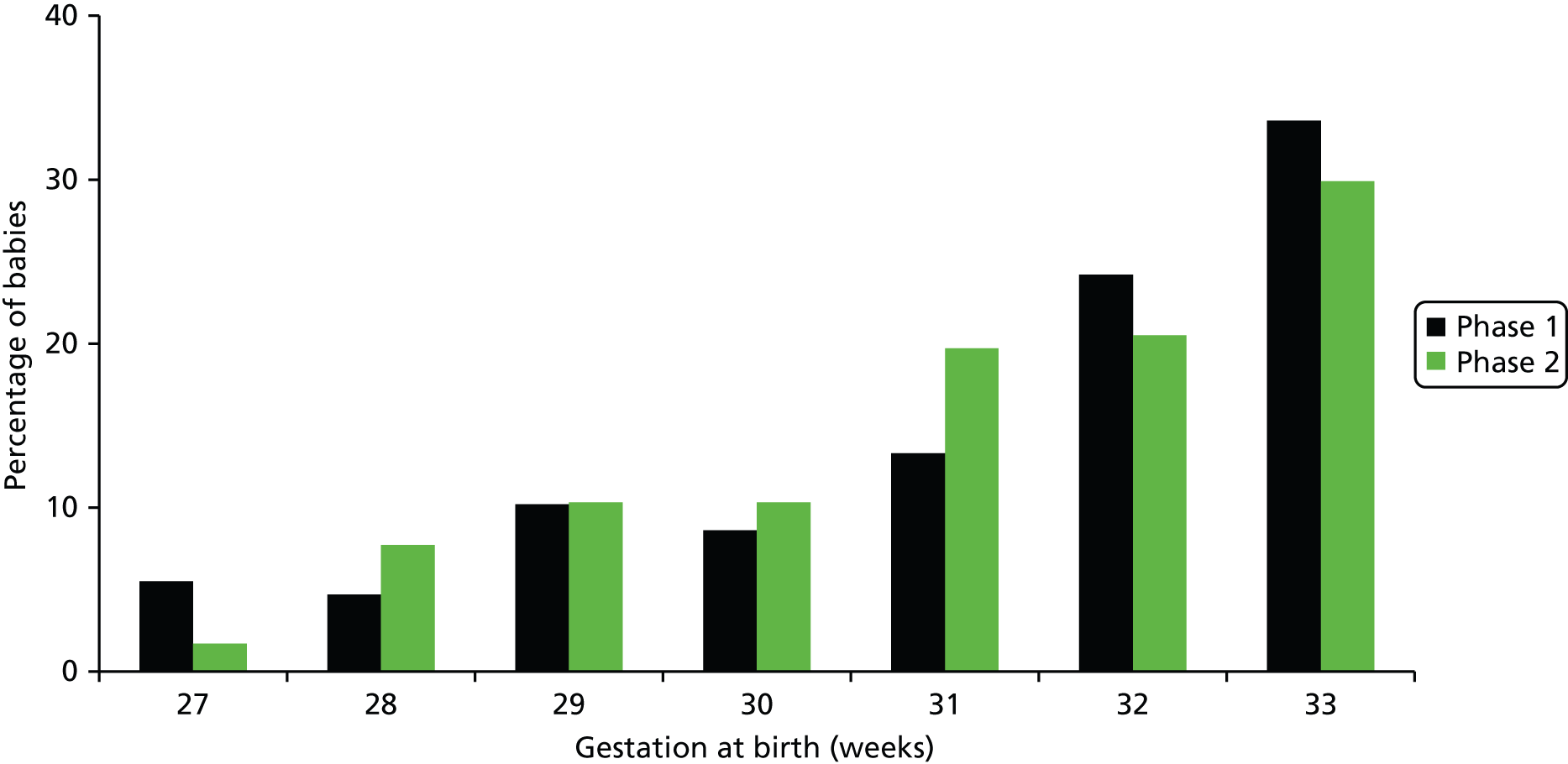
The proportion of children in the study increased with gestational age (Figure 8); fewer than one-third were between 27 and 30 weeks’ gestation but there was no significant difference between gestational ages at birth of infants between phase 1 and phase 2 (Mann–Whitney U-test; p = 0.59).
FIGURE 8.
Gestational age rounded down to whole weeks. Note: n = 128, phase 1; n = 117, phase 2.
Family characteristics
Table 4 shows family characteristics. There was no significant difference between the two groups. There were no significant differences in family size, maternal and paternal education, parental age or deprivation score; more of the mothers had a supporting partner in phase 2 but this was not quite significant at the 5% level. There was no significant difference in maternal or paternal ethnicity, and only one mother and two partners in the study had language difficulties (not shown in table), all of whom were in phase 2.
| Characteristic | Group of interest | Phase 1 | Phase 2 | p-value | ||
|---|---|---|---|---|---|---|
| n/N | % | n/N | % | |||
| Mother has partner | Yes | 112/124 | 90.3 | 108/112 | 96.4 | 0.06 |
| Other | None | 70/117 | 59.8 | 37/117 | 31.6 | 0.32 (3 df) |
| Dependent | One other child | 28/117 | 19.4 | 31/117 | 26.5 | |
| Childrena | Two other children | 14/117 | 28.1 | 29/117 | 24.8 | |
| Three or more children | 5/117 | 16.4 | 20/117 | 17.1 | ||
| Highest maternal qualification | < GCSEb | 13/107 | 12.1 | 6/103 | 5.8 | 0.19 (3 df) |
| GCSEb | 23/107 | 21.5 | 23/103 | 22.3 | ||
| Advanced level | 25/107 | 23.4 | 35/103 | 34.0 | ||
| Degree | 46/107 | 43.0 | 39/103 | 37.9 | ||
| Highest paternal qualification | < GCSEb | 6/71 | 8.5 | 7/93 | 7.5 | 0.46 (3 df) |
| GCSEb | 22/71 | 31.0 | 24/93 | 25.8 | ||
| Advanced level | 19/71 | 26.8 | 36/93 | 38.7 | ||
| Degree | 24/71 | 33.8 | 26/93 | 28.0 | ||
| Maternal ethnicity | British | 109/119 | 91.6 | 98/106 | 92.5 | 0.18 (2 df) |
| Other whitec | 2/119 | 1.7 | 5/106 | 4.7 | ||
| Otherd | 8/119 | 6.7 | 3/106 | 2.8 | ||
| Paternal ethnicity | British | 73/77 | 94.8 | 86/99 | 86.9 | 0.19 (2 df) |
| Other whitec | 3/77 | 3.9 | 8/99 | 8.1 | ||
| Otherd | 1/77 | 1.3 | 5/99 | 5.1 | ||
| Units | Mean | N, SD | Mean | N, SD | p-value | |
| Maternal age | In years | 30.7 | 120, 5.7 | 30.7 | 111, 5.9 | 0.98 |
| Paternal age | In years | 33.2 | 77, 6.4 | 32.5 | 101, 6.8 | 0.46 |
| Deprivation score | IMD units | 17.6 | 126, 11.7 | 16.2 | 115, 12.4 | 0.36 |
In Figure 9, the Index of Multiple Deprivation score is split into quintiles based on UK national data (http://tools.npeu.ox.ac.uk/imd). If the population under study was representative of the national profiles, then the distribution would be uniform around the 20% level. The families involved in this study included fewer families than the general population from the most deprived quintiles, but there were no significant differences between phases 1 and 2 (chi-squared on 4 df; p = 0.46). Overall, 26% of families were in the least deprived quintiles and 10% were in the most deprived quintiles.
FIGURE 9.
Index of Multiple Deprivation score split into quintiles. Note: n = 126, phase 1; n = 115, phase 2.

Pregnancy characteristics
Table 5 compares the pregnancy history between the two phases. The proportion of infants from previous pregnancies admitted to a neonatal unit was higher in phase 1 (16.3% vs. 10.6%) but this difference was not significant (p = 0.42). The proportion of previous pregnancies and live births was slightly higher in phase 2 but, again, not significantly so.
| Characteristic | Group of interest | Phase 1 | Phase 2 | p-value | ||
|---|---|---|---|---|---|---|
| n/N | % | n/N | % | |||
| Previous | Never | 87/104 | 83.7 | 93/104 | 89.4 | 0.42 (3 df) |
| Admission to NICU | Once | 13/104 | 12.5 | 8/104 | 7.7 | |
| Twice | 4/104 | 3.8 | 3/104 | 2.9 | ||
| Previous pregnancies | None | 55/105 | 52.4 | 50/105 | 47.6 | 0.57 (4 df) |
| 1 | 20/105 | 19.0 | 18/105 | 17.1 | ||
| 2 | 17/105 | 16.2 | 15/105 | 14.3 | ||
| 3 | 5/105 | 4.8 | 7/105 | 6.7 | ||
| ≥ 4 | 8/105 | 7.6 | 15/105 | 14.3 | ||
| Previous live births | None | 65/103 | 63.1 | 58/105 | 55.2 | 0.14 (3 df) |
| 1 | 23/103 | 22.3 | 21/105 | 20.0 | ||
| 2 | 12/103 | 11.7 | 15/105 | 14.3 | ||
| ≥ 3 | 3/103 | 2.9 | 11/105 | 10.5 | ||
Table 6 compares the details of this pregnancy at baseline and at discharge.
| Characteristic | Interest group | Phase 1 | Phase 2 | p-value | ||
|---|---|---|---|---|---|---|
| n/N | % | n/N | % | |||
| At baseline | ||||||
| Mum inpatient at baselinea | Yes | 13/110 | 11.8 | 11/97 | 11.3 | 0.95 |
| Family transferred from another unit | Yes | 27/128 | 21.1 | 24/117 | 20.5 | 0.91 |
| At discharge | ||||||
| Baby went home with oxygen? | Yes | 3/96 | 3.1 | 6/94 | 6.4 | 0.33b |
| Baby went home with tube feeds | Yes | 2/96 | 2.1 | 0/95 | 0 | 0.50b |
Just over 10% of mothers in both groups were inpatients and just over 20% of families in both groups transferred from another unit; there was no difference between groups. There was no significant difference in the proportion of infants given oxygen or tube feeds to take home. Although slightly more infants went home on a Friday in phase 1, and on a Monday in phase 2, these differences were not significant (chi-squared on 6 df; p = 0.39), as illustrated in Figure 10.
FIGURE 10.
Day of week on which discharge occurred. Note: n = 104, phase 1; n = 98, phase 2.

Infant medical conditions
Table 7 shows broadly grouped infant medical conditions for the two phases of the study.
| Medical conditions | Phase 1 | Phase 2 | p-value | ||
|---|---|---|---|---|---|
| n/N | % | n/N | % | ||
| Cardiorespiratory conditions | 46/128 | 35.9 | 39/117 | 33.3 | 0.67 |
| Infections | 26/128 | 20.3 | 25/117 | 21.4 | 0.84 |
| Metabolic, endocrine, nutritional, gastroenterological | 28/128 | 21.9 | 12/117 | 10.3 | 0.01 |
| Neurological | 6/128 | 4.7 | 0/117 | 0 | 0.03a |
There was no significant difference in the prevalence of cardiorespiratory conditions or infections but significantly more of the infants in phase 1 had metabolic, endocrine, nutritional or gastroenterological conditions or neurological conditions. Grouping these last two types of conditions together was also significant (p = 0.006). Although the infants may have had more than one of the listed conditions, a comparison of the number of conditions was not significant (p = 0.16 on 4 df).
Infant feeding
Table 8 shows the mode of feeding and type of milk given to the infant at discharge and 8 weeks post discharge. Data are limited in phase 1 for this latter period.
| Characteristic | Group of interest | Phase 1 | Phase 2 | p-value | ||
|---|---|---|---|---|---|---|
| n/N | (%) | n/N | (%) | |||
| Feeding at discharge | ||||||
| Mode of feeding at discharge | Breast | 40/92 | 43.5 | 41/94 | 43.6 | |
| Bottle | 32/92 | 34.8 | 24/94 | 25.5 | ||
| Both | 18/92 | 19.6 | 29/94 | 30.9 | ||
| Tube | 2/92 | 2.2 | 0/94 | 0 | 0.13a | |
| Type of milk at discharge | Breast | 52/92 | 56.5 | 57/92 | 62.0 | |
| Formula | 22/92 | 23.9 | 17/92 | 18.5 | ||
| Both | 18/92 | 19.6 | 18/92 | 19.6 | 0.65b | |
| Feeding at 8 weeks post discharge | ||||||
| Mode of feeding at 8 weeks | Breast | 16/54 | 29.6 | 18/81 | 22.2 | |
| Bottle | 31/54 | 57.4 | 40/81 | 49.4 | ||
| Both | 7/54 | 13.0 | 23/81 | 28.4 | ||
| Tube | 0/54 | 0 | 0/94 | 0 | 0.10b | |
| Type of milk at 8 weeks | Breast | 16/52 | 30.8 | 26/81 | 32.1 | |
| Formula | 26/52 | 50.0 | 35/81 | 43.2 | ||
| Both | 10/52 | 19.2 | 20/81 | 24.7 | 0.69b | |
Two infants in phase 1 were tube fed when discharged. The proportion of infants given breast milk either from the breast or via a bottle fell from 78.8% at discharge to 54.1% at 8 weeks post discharge in the whole cohort.
Bottle-feeding was more common at discharge in phase 1, and the proportion given breast milk (by breast or bottle) at discharge was more common in phase 2 (phase 1, 76%; phase 2, 82%) but none of these differences were significant. At 8 weeks post discharge, bottle-feeding was still more common in phase 1 and the proportion given breast milk (by breast or bottle) at discharge was slightly more common in phase 2 (phase 1, 50%; phase 2, 57%) but again none of these differences was significant.
Being told discharge dates
Table 9 shows the proportion of families that were given a rough idea or an exact date of discharge and when this was given. This question was asked of families at baseline and prior to discharge.
| Characteristic | Phase 1 | Phase 2 | p-value | |||
|---|---|---|---|---|---|---|
| At baseline | ||||||
| n/N | % | n/N | % | |||
| Given rough idea of discharge at baseline | Yes | 80/114 | 70.2 | 92/103 | 89.3 | 0.001 |
| Given exact date of discharge | Yes | 4/104 | 3.0 | 8/94 | 8.5 | 0.17 |
| Given rough or exact date | Yes | 81/114 | 71.1 | 92/103 | 89.3 | 0.001 |
| Units | Median | N, IQR | Median | N, IQR | ||
| Days after admission given a rough idea of discharge date | Days | 1 | 0–2.5 | 3 | 1–6 | 0.0002 |
| Prior to discharge | ||||||
| n/N | % | n/N | % | |||
| Given rough idea of discharge | Yes | 70/91 | 76.9 | 81/91 | 89.0 | 0.03 |
| Given exact date of discharge | Yes | 30/86 | 34.9 | 49/89 | 55.1 | 0.007 |
| Given rough or exact date of discharge | Yes | 71/86 | 82.6 | 83/89 | 93.3 | 0.03 |
| Was discharge date ever brought forward? | Yes | 36/58 | 62.1 | 18/75 | 24.0 | < 0.0001 |
| Units | Median | N, IQR | Median | N, IQR | ||
| Days since admission: rough idea | Days | 18 | 7–32 | 10 | 2–21 | 0.08 |
| Days since admission: exact date | Days | 21 | 17–44 | 22 | 12.5–38 | 0.40 |
Around 70% of parents in phase 1 received a rough idea of discharge at the time of the baseline questionnaire, usually on the first day in the unit. In phase 2, parents received a rough idea of the likely discharge date a little later (3 days), although the proportion (89%) receiving this information was significantly higher (p = 0.001). This reflects the intervention protocol of giving parents a settling in period before suggesting probable discharge dates and then giving them a date range during which time their baby might be discharged. Few parents received an exact discharge date at baseline. The proportion of parents receiving either a rough idea or exact discharge date discharge was 71% in phase 1 and 89% in phase 2 (p = 0.001).
Shortly before discharge, 77% of families in phase 1 reported receiving a rough discharge date compared with 89% in phase 2, a significant difference (p = 0.03). Parents received an exact date more often in phase 2 (55%) than in phase 1 (35%), and again this was significant (p = 0.007). Most parents in both groups received either a rough idea or exact discharge date, but again this was significantly higher (p = 0.03) in phase 2 (93%) than in phase 1 (83%). According to the pre-discharge questionnaires, parents in phase 2 received a rough idea of discharge date earlier than parents in phase 1; for both groups receiving an exact date, this had happened, on average, around 3 weeks after the birth. The discharge date was also brought forward from that given initially for a much larger proportion of families in phase 1 (62%) than those in phase 2 (24%), and this was highly significant (p < 0.0001).
Length of stay
This analysis excludes 10 infants transferred from the study LNUs to another unit before discharge.
The LOS ranged from 12 days to 89 days (Figure 11) and was slightly longer in phase 2 [median = 32 days (IQR 20–46 days)] compared with phase 1 [median = 29 days (IQR 19.5–43.5 days)], although this difference was not significant (Mann–Whitney U-test; p = 0.32).
FIGURE 11.
Length of stay comparison between the two groups. Note: n = 121, phase 1; and n = 114, phase 2.

Table 10 shows some variation when split by unit, for example unit 4 LOS seems to be around 1–2 weeks shorter than that of unit 2, but the difference between phase 1 and phase 2 is fairly consistent at each site with the overall result above.
| Unit | Phase 1 | Phase 2 | ||
|---|---|---|---|---|
| Median (days) | IQR | Median (days) | IQR | |
| 1 | 30 | 25.5–52 | 34 | 24–60 |
| 2 | 34 | 10.5–48 | 37 | 23–45 |
| 3 | 28.5 | 21.5–45.5 | 34 | 19.5–47.5 |
| 4 | 22 | 16–35.5 | 27 | 20–38 |
Splitting by gestational age does not produce a significant difference, the median LOS for those infants born between 27 and 30 weeks’ gestation was 51 days (IQR 41.5 to 60.5 days) for phase 1 and 52 days (IQR 45.0 to 63.5 days) for phase 2 (Mann–Whitney U-test; p = 0.42). For infants born between 31 and 33 weeks’ gestation, median LOS was 23 days (IQR 17–30 days) for phase 1, and 24 days (IQR 18.5–33.5 days) for phase 2, a difference that was again not significant (Mann–Whitney U-test; p = 0.33).
Maternal Perceived Maternal Parenting Self-Efficacy scores (primary analysis)
The data for days taken from birth to various time points to measure maternal PMPS-E were not normally distributed. Figure 12 shows a typical Q–Q plot from birth to discharge and it does not follow a linear trend. The Shapiro–Wilk test suggests significant departure from normality at all three time points (p < 0.0001).
FIGURE 12.
The Q–Q plot to test whether days from birth to discharge PMPS-E are normally distributed. Normal Q–Q plot of days from birth to discharge-completed mother.
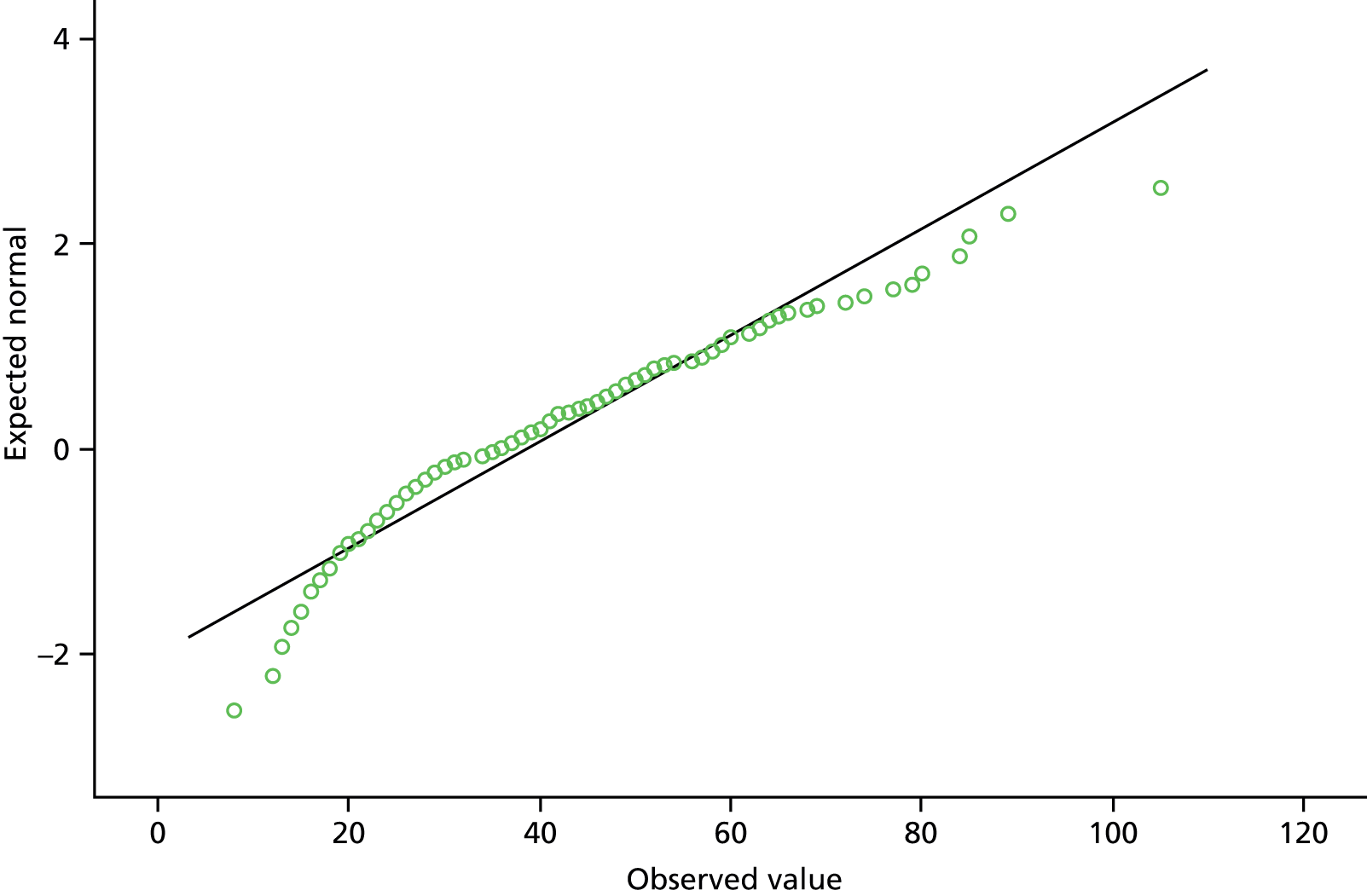
Table 11 suggests there was no significant difference between the days taken to measure maternal PMPS-E from birth to baseline, discharge or 8 weeks post discharge between the two groups.
| When measured | Phase 1 | Phase 2 | p-valuea | ||||
|---|---|---|---|---|---|---|---|
| n | Median | IQR | n | Median | IQR | ||
| Baseline | 120 | 10 | 7–13 | 108 | 11 | 6–14 | 0.76 |
| Discharge | 99 | 34 | 24–51 | 89 | 37 | 23–49.5 | 0.85 |
| Home | 82 | 101.5 | 82.75–117.25 | 115 | 94.5 | 83–110.75 | 0.16 |
Maternal Perceived Maternal Parenting Self-Efficacy distribution
The Shapiro–Wilk test suggests a significant departure from normality at baseline (p = 0.002), at discharge (p < 0.0001), at home (p < 0.0001), between discharge and baseline (p < 0.0001), and was borderline between home and baseline (p = 0.052). Figure 13 shows a typical distribution of PMPS-E scores using maternal scores at discharge for all mothers from both trial phases, therefore a non-parametric analysis approach was adopted.
FIGURE 13.
Distribution of maternal PMPS-E scores at discharge.
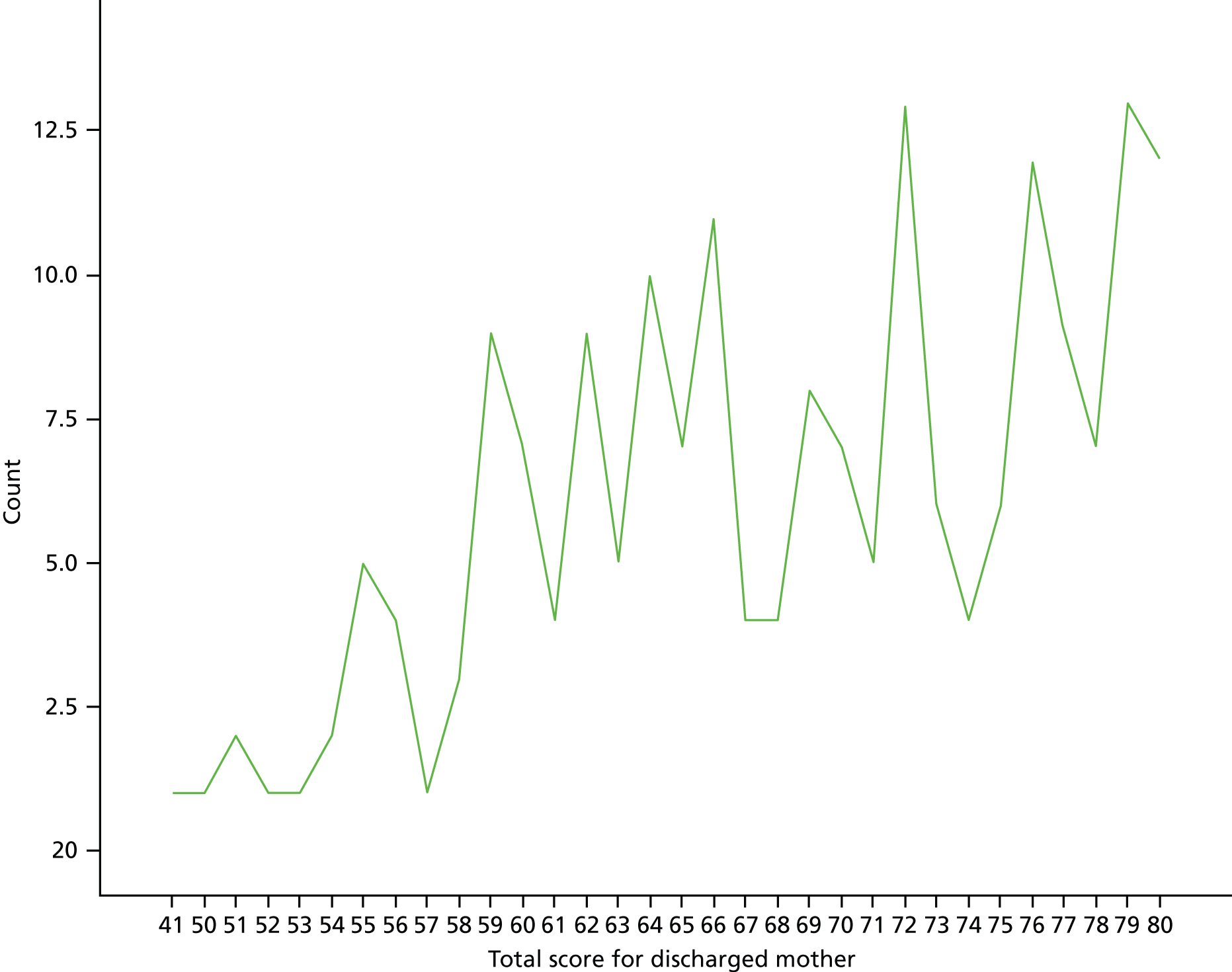
Maternal Perceived Maternal Parenting Self-Efficacy scores
Table 12 shows the median PMPS-E score of mothers at baseline, discharge and 8 weeks post discharge. The primary analysis was powered to compare scores for around 100 mothers per group, thus the comparison at home 8 weeks post discharge was slightly underpowered.
| When measured | Phase 1 | Phase 2 | p-value | ||||
|---|---|---|---|---|---|---|---|
| n | Median | IQR | n | Median | IQR | ||
| Baseline | 121 | 60.0 | 54.0–69.5 | 110 | 59.0 | 54.0–67.0 | 0.33 |
| Discharge | 101 | 70.0 | 61.5–76.5 | 92 | 69.0 | 64.0–74.75 | 0.77 |
| Home | 82 | 74.0 | 66.0–79.0 | 84 | 74.0 | 70.25–78.0 | 0.52 |
Again, there was no significant difference between groups at each time point. The median improvement in maternal PMPS-E score from baseline to discharge taken at an individual level (i.e. subtracting the individual baseline score from the individual discharge score and summing these differences over each group) was slightly higher in phase 2 (+8) than in phase 1 (+7) but this difference was not significant (p = 0.60). The difference in individual improvement was more marked from baseline to home with a median improvement of +14 in phase 2 compared with +11 in phase 1, but this was not quite significant (p = 0.10). Data from Table 12 are illustrated in Figure 14.
FIGURE 14.
Median maternal PMPS-E scores at baseline, discharge and home. The minimum score is 20, indicating poor self-efficacy; the maximum score is 80, representing high self-efficacy.

Regression model
The difference in maternal PMPS-E scores between the two phases at discharge and 8 weeks post discharge were tested using linear regression. The dependent variable for each of the two models was maternal PMPS-E score at discharge and 8 weeks post discharge. The independent variable being tested (Table 13) was the group effect adjusted for the baseline PMPS-E score. Thus the coefficient reported was the mean difference (i.e. phase 2 – phase 1) in PMPS-E score at discharge or home between the two groups.
| Dependent variable maternal PMPS-Ea | Coefficient | 95% CI | p-value |
|---|---|---|---|
| At dischargeb | |||
| Difference between phase 2 and phase 1 | –0.07 | –2.05 to 1.91 | 0.95 |
| At 8 weeks post dischargec | |||
| Difference between phase 2 and phase 1 | +1.48 | –0.47 to 3.42 | 0.14 |
On average, mothers in phase 2 at discharge scored 0.07 points lower in the PMPS-E score than mothers in phase 1: virtually no difference between the two groups (p = 0.95) with an effect size of 0.005. At 8 weeks post discharge, mothers in phase 2 scored 1.48 points higher in the PMPS-E score than mothers in phase 1, with an effect size of 0.12, although this difference was not significant (p = 0.14).
Exploratory analyses
Imputation of missing values for the primary analyses
Variables predicting missing PMPS-E scores at discharge and 8 weeks post discharge included the number of children in the family, maternal education, gestational age in weeks and maternal age. Table 14 compares the results of the primary analysis given in Table 13 with the results after imputing data for mothers with missing PMPS-E data to include all 245 mothers in the model.
| Dependent variable maternal PMPS-E | Coefficient | 95% CI | Phase 1 | Phase 2 | p-value | ||||
|---|---|---|---|---|---|---|---|---|---|
| n | Mean | SE | n | Mean | SE | ||||
| At discharge | |||||||||
| Initial model | |||||||||
| Phase 2 | –0.07 | –2.05 to 1.91 | 97 | 68.66 | 0.84 | 91 | 68.32 | 0.82 | 0.95 |
| Imputed model | |||||||||
| Phase 2 | +0.11 | –1.78 to 2.01 | 128 | 68.87 | 0.79 | 117 | 68.46 | 0.79 | 0.91 |
| At 8 weeks post discharge | |||||||||
| Initial model | |||||||||
| Phase 2 | +1.48 | –0.47 to 3.42 | 80 | 71.88 | 0.82 | 84 | 73.07 | 0.65 | 0.14 |
| Imputed model | |||||||||
| Phase 2 | +1.26 | –0.64 to 3.17 | 128 | 72.07 | 0.74 | 117 | 73.09 | 0.67 | 0.19 |
The results are quite similar. At discharge, the group effect still centred around zero [–0.07 points in the initial model (p = 0.95) and +0.11 points in the imputed model (p = 0.91)]. At 8 weeks post discharge, the group effect suggested an increase in scores for those mothers in phase 2 [+1.48 points in the initial model (p = 0.14) and +1.26 points in the imputed model (p = 0.19)], but neither finding suggested significant differences. The mean values and SEs were similar using both approaches.
Adjusting for significant factors
The only significant difference between infants in phase 1 and phase 2 was a higher prevalence of infants in phase 1 having conditions related to the metabolic, endocrine, nutritional, gastroenterological or neurological systems (p = 0.006). Adjusting for this in the models presented in Table 13 made little difference to the comparison of PMPS-E scores between the two groups. At discharge, the association between infant medical conditions and the PMPS-E score was not significant (p = 0.28) and the influence on the group effect was minimal (phase 2 mothers scored 0.15 points higher; p = 0.89). At 8 weeks post discharge, again the association between infant medical condition and PMPS-E score was not significant (p = 0.71), and the influence on the group effect was to slightly reduce the difference to 1.39 points (p = 0.18).
Maternal Perceived Maternal Parenting Self-Efficacy subscales
The 20 questions of the PMPS-E score can be split into four mutually exclusive subscales. These are:
-
Caretaking procedures (mother’s perceptions of her ability to perform the activities and tasks related to the baby’s basic needs such as feeding).
-
Evoking behaviour(s) (perceptions in her ability to elicit a change in the baby’s behaviour, e.g. soothing the baby).
-
Reading behaviour(s) or signalling (perceptions in her ability to understand and identify changes in her baby’s behaviour, e.g. ‘I can tell when my baby is sick’).
-
Situational beliefs (mothers’ beliefs about her ability to judge her overall interaction with the baby).
Table 15 compares the median maternal PMPS-E score at baseline, discharge and at home between the two phases, broken down by each of these four subscales.
| Time period | Subscale | Phase 1 | Phase 2 | ||
|---|---|---|---|---|---|
| Median | IQR | Median | IQR | ||
| Baseline | Caretaking procedures | 12 | 10–14 | 12 | 10–13 |
| Evoking behaviour(s) | 21 | 19–26 | 21 | 18–24 | |
| Reading behaviour(s) | 17 | 15–19 | 17 | 15–19 | |
| Situational beliefs | 10 | 9–12 | 10.5 | 9–12 | |
| Discharge | Caretaking procedures | 14 | 12–15 | 14 | 12–15 |
| Evoking behaviour(s) | 25 | 21–27 | 23.5 | 21–27 | |
| Reading behaviour(s) | 20 | 18–23 | 20 | 18–22 | |
| Situational beliefs | 12 | 10–12 | 12 | 10–12 | |
| Home | Caretaking procedures | 15 | 14–16 | 15 | 14–16 |
| Evoking behaviour(s) | 25 | 21–28 | 26 | 23–28 | |
| Reading behaviour(s) | 22 | 20–24 | 22 | 20–24 | |
| Situational beliefs | 12 | 10–12 | 12 | 11–12 | |
There was little difference between phases 1 and 2 at the subscale level. Mothers in phase 2 scored slightly less on the evoking behaviour subscale at discharge but slightly more than those in phase 1 at 8 weeks post discharge.
Maternal Perceived Maternal Parenting Self-Efficacy between-centre variation
Figure 15 illustrates the differences in maternal PMPS-E scores at baseline, discharge and home between each LNU. In unit 1, the scores at baseline were lower for mothers in phase 2, although the difference decreased over time. In unit 2, the scores at baseline were exactly the same but increased more among phase 2 mothers over time. In unit 3, the baseline scores were higher among phase 2 mothers but decreased over time, whereas in unit 4 (like unit 1) the baseline scores were lower for phase 2 mothers but were much higher at discharge and at home 8 weeks post discharge.
FIGURE 15.
Median maternal PMPS-E scores at baseline, discharge and home by centre. (a) Unit 1; (b) unit 2; (c) unit 3; and (d) unit 4.

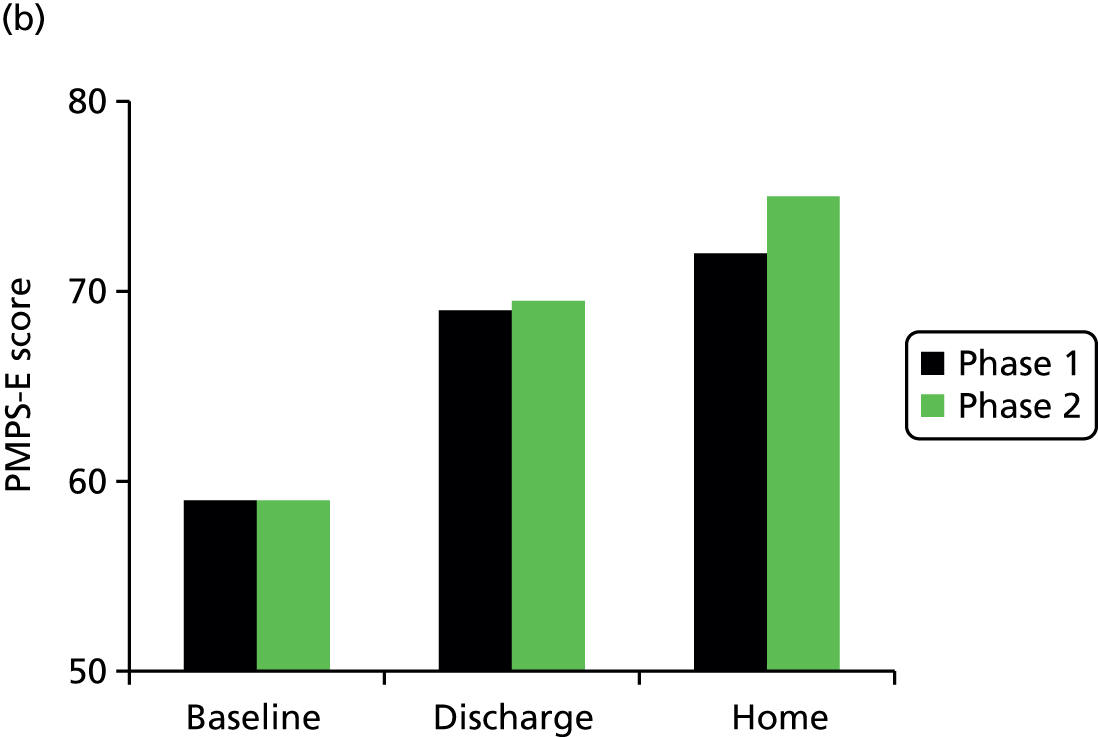
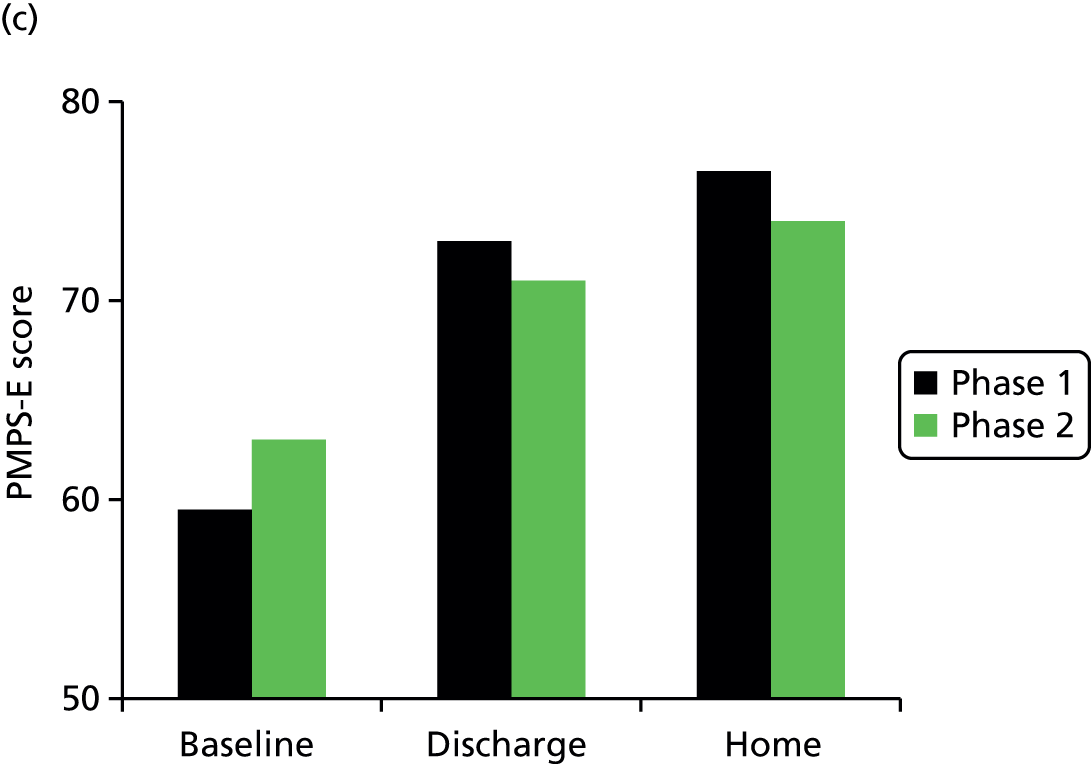
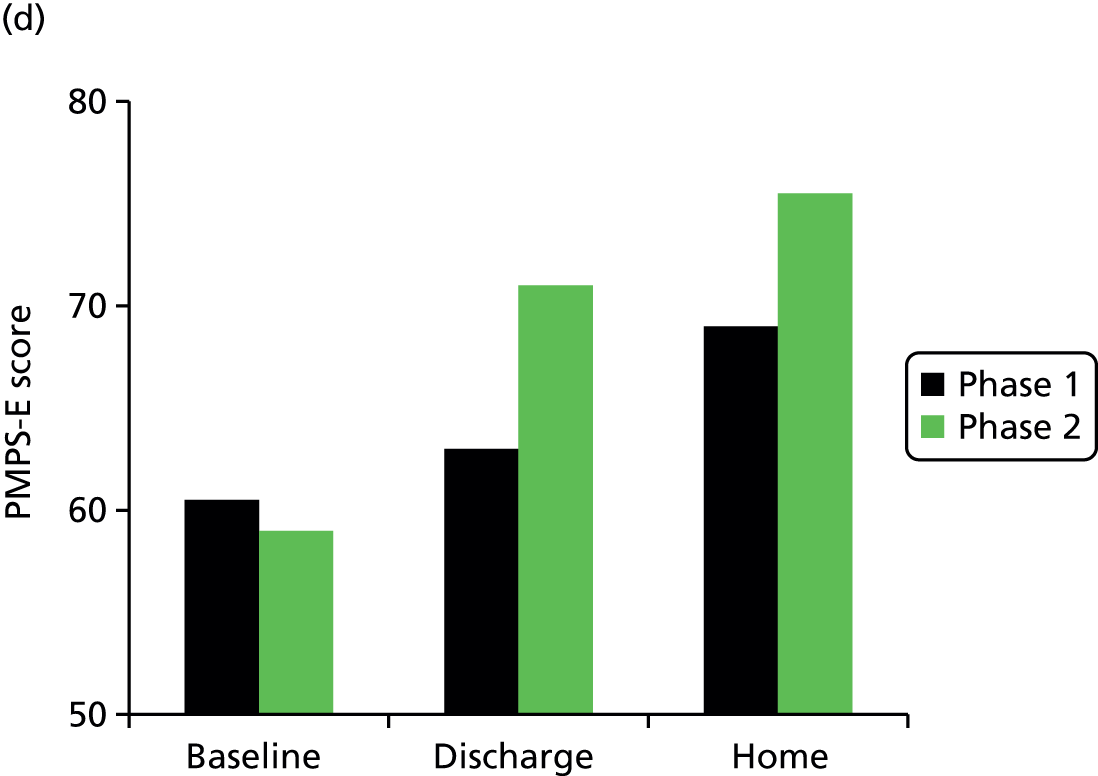
Table 16 shows the median difference in maternal PMPS-E from baseline to home comparing phase 1 with phase 2 for each of the units.
| Unit | Phase 1 | Phase 2 | p-value |
|---|---|---|---|
| Median difference | Median difference | ||
| 1 | 11 | 14 | 0.45 |
| 2 | 12 | 16 | 0.13 |
| 3 | 17 | 10 | 0.61 |
| 4 | 8.5 | 18 | 0.11 |
Adjusting the primary analysis models in Table 13 for centres made little difference to the group effect.
Per-protocol analysis
There was evidence when the researchers visited units, and confirmed in subsequent qualitative interviews, that staff from one particular unit were less engaged with the intervention and there were questions about whether or not the intervention was delivered properly. Dropping this unit from the analysis, Table 17 shows the median PMPS-E score of the mother at baseline, discharge and 8 weeks after discharge from just three units.
| Time point | Phase 1 | Phase 2 | p-value | ||||
|---|---|---|---|---|---|---|---|
| n | Median | IQR | n | Median | IQR | ||
| Baseline | 91 | 60.0 | 54.0–68.0 | 85 | 59.0 | 54.0–68.0 | 0.19 |
| Discharge | 74 | 67.0 | 60.0–76.0 | 70 | 67.5 | 60.0–76.0 | 0.98 |
| Home | 60 | 72.5 | 65.0–78.0 | 63 | 74.0 | 65.0–78.0 | 0.34 |
Again there was no significant difference between groups at each time point when restricted to three units. The median improvement in maternal PMPS-E score from baseline to discharge taken at an individual level (i.e. subtracting the individual baseline score from the individual discharge score and summing these differences over each group) was slightly higher in phase 2 (+9) than in phase 1 (+7) but this difference was not significant (p = 0.27). This difference in individual improvement was more marked from baseline to home, with a median improvement of +16 in phase 2 compared with +11 in phase 1, and this difference was significant (p = 0.02).
Figure 16 illustrates the data from Table 17.
FIGURE 16.
Median maternal PMPS-E scores at baseline, discharge and home (three units).
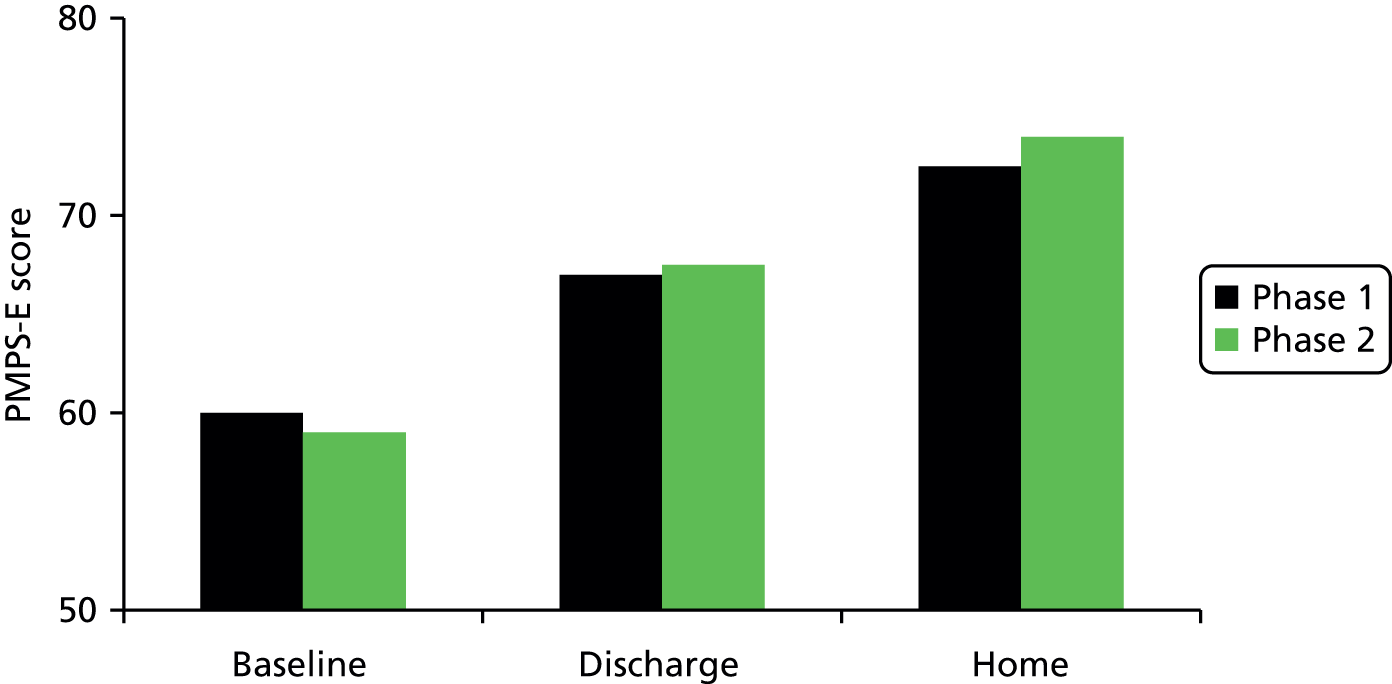
The difference in maternal PMPS-E scores for the three units between the phases at discharge and 8 weeks post discharge (Table 18) were tested using linear regression similar to Table 13.
| Dependent variable, maternal PMPS-Ea | Coefficient | 95% CI | p-value |
|---|---|---|---|
| At dischargeb | |||
| Intervention (phase 2) | +0.21 | –2.17 to 2.60 | 0.86 |
| At 8 weeks after dischargec | |||
| Intervention (phase 2) | +1.79 | –0.55 to 4.12 | 0.13 |
On average, mothers in phase 2 at discharge scored 0.21 points higher in the PMPS-E score than mothers in phase 1, a difference that was not significant (p = 0.86). At 8 weeks post discharge, mothers in phase 2 scored 1.78 points higher in the PMPS-E score than mothers in phase 1; again, this difference was not significant (p = 0.13). As Figure 15 shows, there appears to be a slightly larger difference in PMPS-E scores when restricting the analysis to three units but the smaller numbers used yield wider CIs and a similar p-value, suggesting that this study may be underpowered to test the significance of this finding.
Paternal Perceived Maternal Parenting Self-Efficacy score
As anticipated, fewer fathers participated in the study, so, given the lack of power, the assessment of paternal PMPS-E scores will be exploratory in nature.
The data for the days taken from birth to various time points to measure paternal PMPS-E were not normally distributed at baseline (p < 0.0001) or discharge (p = 0.002), thus, although means could be reported for days from birth to home (p = 0.44), medians have been presented for consistency. Table 19 suggests there was no significant difference between the days taken to measure the paternal PMPS-E from birth to baseline, discharge or 8 weeks post discharge between the two groups. The relatively large difference in median days at discharge reflects the small numbers observed and was not significantly different between phases 1 and 2.
| Time point | Phase 1 | Phase 2 | p-value | ||||
|---|---|---|---|---|---|---|---|
| n | Median (days) | IQR (days) | n | Median (days) | IQR (days) | ||
| Baseline | 49 | 10 | 8–13 | 40 | 9.5 | 5–14.75 | 0.76 |
| Discharge | 40 | 30 | 22.25–49 | 28 | 42.5 | 22.25–52.75 | 0.40 |
| Home | 20 | 96.5 | 82–114.5 | 23 | 102 | 88–120 | 0.50 |
The paternal PMPS-E scores were borderline normally distributed at birth and discharge but not the home scores (Shapiro–Wilk test; p = 0.046). For consistency, Table 20 shows the median PMPS-E score of the partner at baseline, discharge and 8 weeks post discharge.
| Time point | Phase 1 | Phase 2 | p-value | ||||
|---|---|---|---|---|---|---|---|
| n | Median | IQR | n | Median | IQR | ||
| Baseline | 49 | 60.0 | 52.5–68.5 | 39 | 61.0 | 46.0–69.0 | 0.87 |
| Discharge | 41 | 63.0 | 59.0–70.5 | 29 | 63.0 | 57.0–73.0 | 0.91 |
| Home | 20 | 69.0 | 64.0–75.0 | 24 | 67.5 | 62.5–75.75 | 0.85 |
The paternal PMPS-E scores were similar to maternal PMPS-E scores at baseline but tended to be lower at discharge and home for both groups. There was no significant difference between groups at each time point. The median summed individual difference in paternal PMPS-E score from baseline to discharge was slightly higher in phase 2 (+6) compared with phase 1 (+5) but this difference was not significant (p = 0.57). The median improvement from baseline to home was lower in phase 2 (+12) compared with phase 1 (+13), but, again, this difference was not significant (p = 0.75).
The difference in paternal PMPS-E scores was modelled in the same way as the maternal PMPS-E scores.
Table 21 shows that on average fathers in phase 2 at discharge scored 0.92 points higher in the PMPS-E score than fathers in phase 1, a difference that was not significant (p = 0.62). At 8 weeks post discharge, fathers in phase 2 scored 0.54 points higher in the PMPS-E score than fathers in phase 1; again, this difference was not significant. The numbers in both models were very low.
| Dependent variable, paternal PMPS-Ea | Coefficient | 95% CI | p-value |
|---|---|---|---|
| At dischargeb | |||
| Intervention (phase 2) | +0.92 | –2.77 to 4.62 | 0.62 |
| At 8 weeks post dischargec | |||
| Intervention (phase 2) | +0.54 | –3.53 to 4.62 | 0.79 |
Summary
-
Of 247 families recruited, 245 took part: 128 in phase 1 and 117 in phase 2 after introduction of the intervention.
-
The number of families taking part was similar in each of the two phases across the centres and there was no significant difference in infant or family characteristics.
-
Compared with UK national quintiles of deprivation, the less deprived groups were over-represented; 26% of the families were from the least deprived quintile and 10% from the most deprived.
-
There was no significant difference in pregnancy history, the proportion of families transferred from another unit, mothers who were inpatients or the day of the week discharge occurred.
-
There was no significant difference in mode of feeding or type of milk given to the infants but fewer bottle-feeding infants were discharged in phase 2.
-
The only significant difference between the two groups was a higher prevalence of infants in phase 1 having metabolic, endocrine, nutritional, gastroenterological or neurological conditions (p = 0.006).
-
There was no difference in maternal PMPS-E scores between baseline and discharge (p = 0.95). At 8 weeks post discharge, mothers in phase 2 scored 1.48 points higher in the PMPS-E score than mothers in phase 1, although this difference was not significant (p = 0.14).
-
Imputing the missing PMPS-E scores yielded similar results.
-
There was some suggestion that maternal PMPS-E scores improved more from baseline to 8 weeks post discharge in LNUs in which staff engaged with the intervention, but there was insufficient power in this study to test whether or not this was truly significant.
-
There was little difference in these findings when adjusting for infant medical conditions or conducting a per-protocol analysis of those units that successfully implemented the intervention.
-
There was little difference between phase 1 and phase 2 at the PMPS-E subscale level. Mothers in phase 2 scored slightly less on the evoking behaviour subscale at discharge but slightly more than those in phase 1 at 8 weeks post discharge.
-
There was no significant difference in paternal PMPS-E at discharge (p = 0.62) or 8 weeks post discharge (p = 0.79), although the numbers for these scores were quite low.
-
The discharge date was more commonly brought forward (p < 0.0001) for families in phase 1 (62%) than those in phase 2 (24%), and significantly more of the mothers in phase 2 (p = 0.03) received approximate or exact information on the anticipated discharge date.
-
There was variation in LOS by unit but no significant difference (p = 0.32) between families in phase 1 (median 29 days) or phase 2 (median 32 days).
Chapter 6 Results: part 2 – qualitative interviews with parents and staff
One-to-one interviews and analysis of the audio-recordings of these provide an opportunity to gain insights about the experience of being a parent in a neonatal unit, including planning for discharge home. Similarly, insights can be gained by interviewing staff about their role and attitudes towards parental needs, particularly in relation to giving parents information about the changing situation of their baby and discharge from the unit. For both groups, collecting and analysing data on the experience in their own words has the potential to illuminate some of the processes underlying what has been found in the quantitative analyses.
Parent interviews
Thirty-seven telephone interviews were conducted with parents: 16 interviews in phase 1 and 21 in phase 2 following the introduction of the intervention. Fathers took part in three of the interviews and both parents contributed to these discussions. Interviews varied in length from 30 to 60 minutes. The parents had babies of all gestational ages from 27 to 33 weeks, some had twins, and both first-time and subsequent parents were represented in the sample across all four LNUs. Family demographics are shown in Table 22.
| Demographic | Phase 1 (n = 16) | Phase 2 (n = 21) | Total (n = 37) |
|---|---|---|---|
| Gestation 27–30 weeks | 5 | 9 | 14 |
| Gestation 31–33 weeks | 11 | 12 | 23 |
| Male : female baby | 7 : 9 | 12 : 9 | 19 : 18 |
| First baby : second/third baby | 10 : 6 | 14 : 7 | 24 : 13 |
| Mother’s age, years (median) | 32 | 32 | 32 |
In both phases, parents were asked to describe their time in the unit, which members of staff were easy to talk to and who provided them with support and advice. Further questions explored how prepared they felt for going home, and who provided support and gave them advice when at home. Finally, they were asked if there were things that they would have liked to have been told to prepare them better. We compared the themes developed in phase 1 with findings in phase 2 to illustrate any differences or core issues. Parents in phase 2 were also asked about their views on the Train-to-Home materials (train and booklets) and how they and the staff used them.
Life in the neonatal unit
Parents described their experiences in a similar way over the 2-year period as ‘feeling stressed and concerned, but staff were helpful and friendly’. Themes describing their journey are shown in Box 1.
‘Rollercoaster of emotions.’
‘You learn a lot in there.’
‘They were approachable and listened to me.’
‘Conflicting advice about feeding.’
The ‘NICU family’: support from other parents.
‘Rollercoaster of emotions’
Emotional upheaval marked parents’ experience of the admission of their baby to a neonatal unit. Overall, they recalled mixed feelings about having a baby in the LNU. Their feelings became increasingly positive with the improvements in their baby’s health and with the passage of time.
Well I suppose it was a mixture of like, well it was a worrying time, but also it was in the end a more positive time to be able to watch your baby grow, and know that she was doing well.
Mother #305 phase 1
How would I describe my time? Very emotional, very up and down like a rollercoaster of emotions. And I suppose the biggest thing: every minute felt like an hour, an hour felt like a day, a day felt like a week; it just seemed to go on and on. But um obviously the staff were very supportive and helped us to feel, you know, confident that [baby] would come home and he’d be fine, so yeah.
Mother #315 phase 1
A spectrum of emotions was described by parents across the different LNUs from ‘hell’ to ‘comforting’ and ‘reassuring although still scary’. Even although one unit was described as ‘relaxing’ by parents, they still experienced traumatic and negative feelings.
We found it really, strangely relaxing. Once we got over the initial um shock of seeing her with – with all the wires and everything around, which was always stressful, it was really nice and relaxing.
Mother #514 phase 1
Parents talked about the distress of being separated from their newborn baby, and later the stress of having to leave their baby on the LNU when they went home.
It was just the fact that my baby was in the unit and I wasn’t there with him, and I had to go home every night; that was the worst thing ever. It was fine when I was there in the day um with him, but leaving and going home was awful. But the staff at the unit were very positive and reassuring and helpful and brilliant really.
Mother #719 phase 1
They also talked about the feelings of emotional isolation as they felt that staff didn’t want to give them false or unrealistic hopes about their baby’s condition.
They never say to you ‘Don’t worry it’s all going to be fine,’ because they can’t give you any of that false hope, and they don’t know if everything will be fine, so he might be fine today but then by tomorrow you know as I said they can get infections so quick. So you do feel quite, um, like emotionally isolated with it all.
Mother #213 phase 2
Positive experience was linked to support from LNU staff, primarily the nursing team. The physical environment is challenging – it was very hot, light levels were low and parents spent a long time doing very little other than being with their baby. In phase 2, parents commented that having Wi-Fi would have helped pass the time and relieved the boredom.
They keep the lights very low, and it’s very hot, the environment is quite depressing, they have tried to keep the colours brighter, staff are really friendly as well, even small things like Wi-Fi access would have made a massive difference . . . I think it is quite hard as a parent, or like the mum who has to go and sit there all day every day, and if you don’t you feel bad, then if you do you’re bored.
Mother #213 phase 2
‘You learn a lot in there’
In both phases, parents talked about the LNU as a place where they learnt parenting skills. This opportunity would not be available to parents of term babies as they are in hospital for much shorter periods.
I think in some ways, and this sounds silly, but having a premature baby is almost a bit of a better benefit than actually having a full-term baby. Because having a full-term baby you’re suddenly thrown into the world of, ‘Oh my God, we’ve got a baby: what do we do now?’ With a premature baby, obviously they needed that specialist care for the time till they’re able to go home, and in that time you’re taught so many things that you would have to just learn on the spot at home.
Father #307 phase 1
‘They were approachable and listened to me’: establishing relationships with nurses
Mothers mostly found nurses and midwives easy to talk to, and they described most staff as helpful and supportive. Staff with a friendly approachable manner were valued, and they appreciated having ‘a normal everyday conversation’ with them. Support for parents included ‘being listened to’, ‘staff knowing about their family’ and having continuity of care for them and their baby. Mothers commented on the importance of the shift handover between staff as a way of ensuring that information was passed thoroughly and appropriately. They also commented on the advantages of having the same staff caring for their baby in building relationships with the family. Both of these aspects supported parents in their communication with the staff.
Approachable and supportive
We certainly found all the nurses in high dependency very approachable . . . I think, because we built up a relationship with them over a long period of time. Um and um it’s nice when we – if we bump into them. Um, you know, we felt part of the family, put it that way, part of the unit family.
Mother #315 phase 1
I found them really supportive when I was there . . . Um I found they were really good with regard to the rest of my family, because obviously one of the biggest issues for me was being there with [baby] and leaving my other two, and then vice-versa, and I felt so guilty all the time. And they were really supportive about that and really understanding.
Mother #112 phase 1
I actually found them supportive, and I think they’ve got vast knowledge . . . I don’t feel like I am asking a stupid question, like why is she asking those kinds of questions? Might be obvious but they do just respond. So yeah I find that very helpful . . . Yes, I think they were very approachable.
Mother #823 phase 2
Being listened to
Yeah I found it quite friendly, you know, there was always help at hand if needed, professional or um, you know, someone to listen, you know, someone to listen to me, which was quite good.
Mother #521 phase 1
A normal conversation
But others were very good, and they kept like asking, and like the ones I liked, they would ask things about you as well, and not constantly about [baby], like they would remember if you’d said that you were going shopping or something, and they’re remember to ask, and things like that which was quite nice.
Mother #206 phase 2
I found, um, quite a lot of the nurses had very good people skills . . . they just came across better.
Mother #608 phase 2
Hand over and continuity of care
And their handovers were good, they reckoned to have like about a half hour handover every time they swapped shifts. So you knew what was happening. The communication that they have with each other from like the night to the day staff, and day staff to night staff.
Mother #307 phase 1
‘Conflicting advice about feeding’
Less positive support was recalled by some mothers trying to express breast milk or learning to breastfeed their baby. A lack of consistent advice, and the attitude of some staff, made them feel apprehensive and lacking in confidence about caring for their baby.
There was one nurse, I think she was a sister, and she basically made my life hell. She did it with other mums who had the same problem, in as far as if I wasn’t expressing enough [breast milk] that was my fault and I’m not feeding or looking after my baby properly. Whereas the other nurses were, ‘Look, don’t worry. You’ve got formula we can mix. You need to relax to be able to do this’ . . . but whenever this other nurse came up it was just hellish.
Mother #320 phase 1
I would have to ask specifically for them to come and help. I was encouraged every time to put him to the breast (when) I tube fed. But if I actually wanted some help with latching on or positioning or anything I would have to sort of say, ‘Can you give me a hand?
Mother #719 phase 1
I was getting different advice . . . because you kind of get moved on to nursery nurses, and health-care workers rather than neonatal nurses, and they all do things differently, because the level of experience or the training they have had, and I had one there say to me, ‘Stop expressing now in between feeds,’ then the next night another nurse said, ‘Are you still expressing?’ And I said no I was told to stop, and she went, ‘Oh that’s strange, I don’t know why because we’re told to tell you to carry on.
Mother #213 phase 2
It was actually, the breast feeding was one of the issues of why we had to wait to go, because [twin 1] was breastfeeding and [twin 2] wasn’t, and we actually had a lot of pressure on me, um, from the nurses to get [twin 2] to breast feed, so much so like they would you know really be kind of forceful about putting her to the breast. Um, and so we never talked about bottles or formula or anything, because they you know were . . . we doing breast feeding . . . Then the day I got home I stopped producing milk, I had no idea what to do with bottles and formula, because no one taught us as a backup. That was hard.
Mother #617 phase 2
Medical staff were mentioned too, but they were less visible on the LNUs. Some mothers linked communication with the consultant to receiving good or bad news about the baby’s condition. In phase 2, particularly at one LNU, parents reported that doctors had been very helpful and supportive.
The baby doctors were always there, the neonatal doctors, there was always a doctor around in either side of the unit. Um so you didn’t – if you wanted to find something out you could always approach one of them, you didn’t have to go searching for someone.
Mother #307 phase 1
I mean obviously the doctors are very busy, um, but they certainly . . . if you had concerns they would definitely come and it might not be straight away but they would definitely come and spend some time talking things over with you, . . ., but they very much wanted to put you at your ease . . . and take you through it slowly . . . you know, he was happy to sit and talk to us again once we’d thought about actually the things that we wanted to ask him.
Mother #819 phase 2
‘The ‘Neonatal Intensive Care Unit family’: support from other parents
These new friendships were valued and they felt part of a NICU family. They talked about developing their ideas with other families and learning from those who were ahead of them in their progress to going home. Some families kept in touch after they had gone home, too.
We were talking to lots of other parents who were going through the stage just ahead of us . . . I think we just bounced off ideas all the time about what we were thinking of . . . the dilemmas we had about whether to continue trying breastfeeding or just to go to bottle feeding.
Mother #315 phase 1
Every day we would have lunch together and sit there together expressing and everything, so like they know exactly, you don’t have to explain anything to them because they know exactly what’s going on.
Mother #206 phase 2
I thought it was a great experience, um, at the end of the nine weeks we felt like we were almost like part of a NICU family, not just with, um, not just with the staff, but also with the other parents that we had met there.
Mother #617 phase 2
Preparing to go home
Themes developed under this section are ‘practical preparation’, ‘emotional preparation’ and ‘the role of breastfeeding’, as shown in Box 2.
‘Knowledge and skills transfer, but not enough notice.’
Emotional preparation‘Uncertainty, feeling rushed, motivation to get home.’
Role of breastfeeding‘Breastfeeding is the harder way to do it.’
Practical preparation: ‘knowledge and skills transfer, but not enough notice’
Parents considered the knowledge they received practically prepared them for going home and most recalled the practical skills they had been taught, including holding their baby, sleeping positions, first aid emergency and resuscitation (cardiopulmonary resuscitation), bathing, bottle-feeding and nappy changing. The nurses trained the parents in readiness for going home with their baby. There was no reported systematic information delivery using checklists or going home packs throughout the LNUs in phase 1. One LNU identified that they had a pre-existing checklist; however, parents reported that processes seemed to be reactive rather than proactive.
In phase 1, many mothers were very concerned about the lack of notice about discharge and not having a date to go home or any structured or meaningful discussion about going home. This made it difficult for them to alert other family members about their imminent departure if they needed to make family arrangements.
It was all very quick in the end . . . we didn’t really talk about going home and then all of a sudden it was, ‘Let’s try demand feeding. You could go home in 2 days,’ um very, very sudden.
Mother #719 phase 1
I did actually, admittedly, think we would have a bit more notice to ‘er – to get some stuff in.
Mother #713 phase 1
We didn’t actually know we were going home until sort of the very last minute.
Mother #221 phase 1
Because my parents were looking after my other children, so it was important that they were highly involved in what was going on. I texted them all – well we had to wait for the paediatrician to do his round on the day that we were discharged, and I texted them all going, ‘Yeah we’re coming home today’.
Mother #112 phase 1
In phase 2, some mothers were irritated about the inconsistency between staff about the timing of messages about discharge, particularly between doctors and nurses. They reported that the decision about whether they would go home at the planned date lay with the doctors. Nevertheless, mothers mostly reported being quite well prepared for going home.
They [the nurses] just made decisions on you know upping the milk and things like that, they didn’t make any major decisions.
Mother #808 phase 2
As far as the standard like training or procedure that the unit goes through for parents I do feel, it was good, and I didn’t get home and think oh my goodness what do I do with this baby.
Mother #213 phase 2
Yeah, it was quite good that I was very hands on, um, from as early on as I could be really, um, so yeah things like changing nappies, getting her changes, giving her a wash, giving her a bath, all those sort of things . . . so after all that I don’t think there was anything else they could have really done.
Mother #807 phase 2
Emotional preparation: ‘uncertainty, feeling rushed, motivation to get home’
Mothers described their uncertainty about going home as a mixture of feeling scared, nervous and excited. Some felt that they were not well supported by staff in this preparation and they needed more reassurance. In phase 1, a few families from two LNUs felt that they were not ready for home for various reasons, including the health of the baby. The scariness of taking home a ‘tiny baby’ was raised by a small number of mothers, but this was overcome by the desire to have the family under one roof. For others, the thought of putting in place the routines learnt at hospital supported their preparation.
It came to the point where we, yeah, we were getting prepared to do it and, yeah, nervous, scared, but excited at the same time . . . mentally kind of preparing how we were going to do things you know, continuing it at home rather than having the hospital around to help.
Mother #521 phase 1
These concerns were also echoed in phase 2. A few mothers felt their family needed to be all together, other mothers felt they would never be ready. However, more parents in phase 2 commented that they felt mentally prepared to take their baby home.
I just got on with it . . . it did help me feel mentally prepared by the train date.
Mother #814 phase 2
I was feeling ready to go home.
Mother #623 phase 2
Me too . . . we couldn’t wait to come home actually to be honest . . . yeah, we could bring the babies home.
Father #623 phase 2
The role of breastfeeding: ‘breastfeeding is the harder way to do it’
Breastfeeding was supported and encouraged by nurses across all four LNUs. In two LNUs mothers identified a nurse who functioned as a breastfeeding advisor. In the other LNUs, mothers said they could approach almost any nurse with varying degrees of ease depending on their relationship. They mentioned having advice about expressing breast milk regularly and frequently, various ways to position a baby for feeding, and how to ensure that the baby was latched on, but there was conflicting advice about on some points, particularly using nipple shields.
Got loads of support with breastfeeding. You just felt able to, you know, ask questions. They were particularly useful, very supportive, yeah.
Mother #305 phase 1
Yeah, sort of positive spin, because I had difficulty, um, producing enough breast milk, um, and they were always sort of really helpful and positive about it, they just sort of you know said, ‘keep trying,’ so really sort of supportive.
Mother #814 phase 2
There was mixed opinion on nipple shields: some people said it might help and other people said ‘no don’t’.
Mother #719 phase 1
She suggested that I try some nipple shields, and another nurse on the day shift helped me use them, and between the two of those nurses, that’s what got the breastfeeding going. Whereas – one nurse was like, ‘Why are you using nipple shields? You haven’t got flat nipples,’ but it wasn’t the point. And because she just came in she didn’t have a clue.
Mother #305 phase 1
All of us who are friends all had to use the nipple shields, we always had to use it, and then we all went home with them, and I just found it too hard, but some of the mums have kept on with it and stuff. But I just found it [breastfeeding] . . . he found it too hard.
Mother #408 phase 2
When mothers encountered issues with breastfeeding, nurses continued to support them. For some nurses, this involved supporting a mother’s decision to switch to formula feeding or suggesting topping up with formula to ensure that the baby could go home sooner.
So that we could go home they said, ‘Why don’t you just do top-ups with formula? Because then we know that she’s got a means of having enough milk when you go home.’
Mother #514 phase 1
I was expressing for about eight weeks, um, so we were using that, and then gradually I think it was probably about a week before we thought she might go home they started introducing a bit of formula with my milk, um, to get her used to the taste, and then I think we were on about 50/50 when we went home, and then when we got home we just used formula straight away which she was fine with, um, because that was always my plan to do formula anyway. So it was like a bonus that she’d had my milk.
Mother #206 phase 2
There was a sense in the interviews that breastfeeding was difficult for this group of babies but it is not clear how nurse to parent conversations or mother to mother conversations contributed or improved this.
I understand breast is best, and I’m completely aware of that; I didn’t realise how difficult it would be though.
Mother #320 phase 1
Mothers were also aware of the delays that could be associated with breastfeeding and weight gain.
Everybody acknowledged that breastfeeding is the harder way of doing it. And a lot of babies that were bottle-fed left sooner than us. Like there was a baby that was only 1 day older, and he went home a week sooner because he went home on a bottle.
Mother #305 phase 1
What ended up stopping us from going home . . . was his weight because we were breastfeeding. He was tube fed with breast milk which is then fortified . . . and then they stopped fortifying it, so his weight took a sudden drop, because all of a sudden it wasn’t being fortified. So then they needed to see that weight go back on, to ensure he could home healthy, so we’re struggling to put the weight back on, and he was losing maybe like a couple of grams each time, so I found that very frustrating, it was very upsetting, because they weigh every other day, and then it was quite disappointing every time we didn’t get to go home.
Mother #213 phase 2
Train-to-Home intervention in phase 2
The Train-to-Home intervention was introduced against this background of a lack of notice about the expected discharge date and parents feeling rushed just before babies were discharged home. The train was designed to be kept up to date by parents in discussion with staff, so that staff were aware of the parents’ perceptions of their baby’s progress. This would then provide staff and parents with opportunities for engagement and education to support parental confidence. The gestational age-appropriate booklets gave parents some questions to ask and aspects of their baby’s care and development to focus on as their baby progressed.
All of the parents interviewed in phase 2 spoke English. For some, English was not their first or native language, and the train window colour system indicating baby progress worked well for them as they understood the movement between red, yellow and green as a clear marker.
Parent-reported positive comments about the Train-to-Home package
Many parents responded positively to the Train-to-Home package. Mothers, fathers and siblings found the visual representation of their baby’s progress helpful and enjoyable. Positive themes were the ‘value of staff engagement’, ‘giving us hope’, ‘something you can visually see’, ‘fathers and families loved it’, ‘the dates prepare you for home’, ‘feeling in control’ and ‘do it right at the beginning’, as shown in Figure 17.
FIGURE 17.
Themes generated about the Train-to-Home intervention in phase 2.
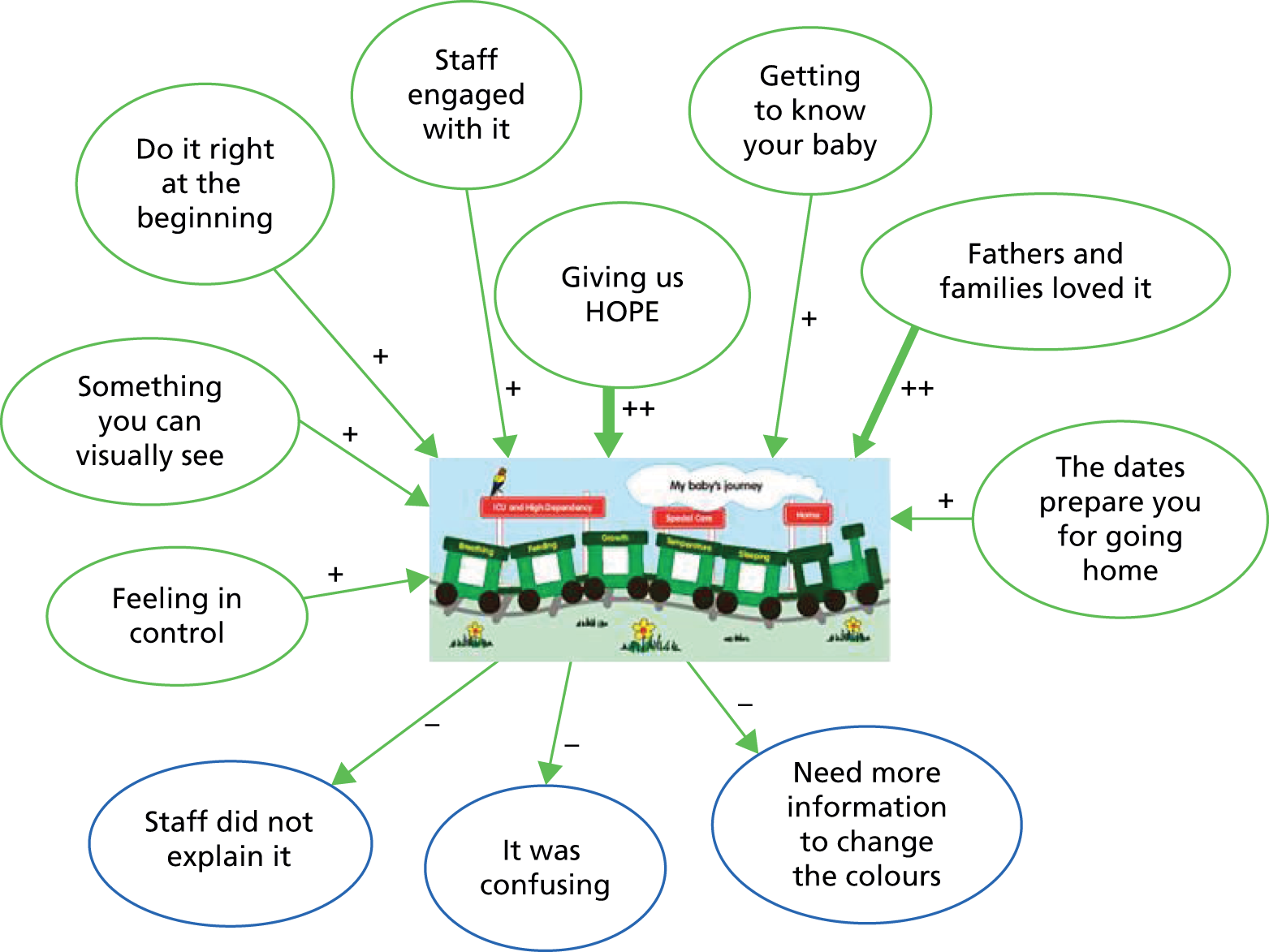
‘The value of staff engagement’
Where staff engaged with the intervention and delivered care through the intervention, parents responded positively and felt that it helped them understand what was going on around them.
It was one of the nursery nurses sat down with me and explained what it [Train-to-Home] all was, um, and did the first kind of round of stickers and everything, and then the, um, nurse that had been the most kind of trying to get us home she went through it again a bit later, updated it with a different discharge date and everything.
Mother #219
We loved it [Train-to-Home], we felt like it made us feel like a part of it, and we loved getting the little booklet out, and you know we would discuss it between the two of us and discuss it with the nurses, and you know we would get excited, we would take pictures of it, and, um, we enjoyed it.
Mother #617
‘Giving us hope’
An impression of progress, an end in sight, and of moving towards home indicated by the changing of the stickers on the train from red, through yellow to green, was reflected in the parents comments captured in most LNUs.
The train date was earlier obviously, [than due date] and so it made us kind of think well actually there’s no reason why he won’t be out earlier, um, if he achieves all of these things, um, which obviously are on the train. So I think, um, it gave us that sort of encouragement really.
Mother #223
It was such a long process that it made it feel like you know there was an end in sight.
Mother #617
It’s good because it shows you the progress that your baby is having.
Father #623
The train was one of the only things I remember from those first couple of days . . . I was in shock, pain, emotional and very tired . . . I remember the train, remember thinking – OK so he works his way along until he leaves.
Mother #802
Yeah, it was, it was really helpful, because what happened is even when we got there and we were given a day I always looking forward to that day, and I was happy that the date didn’t move as in she went home within that day, I was really, really glad that I had a date to look up to.
Mother #823
The train is meant to give you like a bit of hope for when your baby is coming home. We all knew it’s not definite, but it’s meant to give you that bit of hope.
Mother #808
‘Something you can visually see’
Some parents took more ownership of the process and explained it to their wider families. The system of colours also provided parents with an ‘at-a-glance’ affirmation that their baby was improving in health.
I really liked it, I thought it was a great idea, because it’s a quick easy way of seeing where they are and showing . . . when my parents came, instead of having to explain everything I could show them the little train, and they had their colours on there.
Mother #219
It helped, um, us visually see how sort of much progress he’d made, and it was sort of quite encouraging to see him going from a red to an amber, and then an amber to a green. So that was useful, and also it was quite useful to show relatives and friends, sort of how far he was progressing, and sort of provide pointers on what to go through with them and what to explain and things. It helped provide it in a bit more simplistic terms really.
Mother #223
Well it was good information because they were giving you, um, the colour they would say that’s a red it means the baby is not ready, so you could just see day by day if the baby is . . . the problems with the baby’s health. It was very helpful because when I came the next day I was just like oh she’s got more green than red, it was just very optimistic saying, you were like oh my God, it won’t take long to go home with the baby.
Mother #622
It is a bit more involvement, obviously it’s not a lot, but it’s something, and it’s something you can visually see, because looking at your child in an incubator and that, the only difference you can really see is maybe a few tubes are coming, um, but when you can look at a chart, and look at colours and obviously going from red to green and that it’s all positive. So a little bit helps really.
Mother #807
‘Fathers and families loved it’
Looking at the train, reviewing the criteria, changing the stickers and taking photographs to send to their family were all mentioned by mothers as helpful activities for fathers and siblings when in the LNU.
Visually, um, for my partner especially he could just see how well he was doing. Obviously I had put the stickers, I would talk to people and then I would put the stickers on, um, but it’s also something nice to take home as well. Just say look, you know, this is how well he came on.
Mother #608
My partner he really got into it for the first, um, week or so, he read all through the booklet and he wanted to do stickers and he wanted to update it. I think for him it was like something he could look at, you know, focus on.
Mother #225
Yes, um, one of the nurses sat down and sat through it all with . . . and, um, we went through everything so that myself and my partner completely understood, um, it, and it was great because we’ve got a four year old, so when he came in he could . . . he loved the train, he thought the train was fantastic, and it was great for him to be able to understand a bit more. He used to stand there hoping that it would turn green in front of his eyes, he thought it was magic.
Mother #418
It made us feel good when he got an amber [sticker]. I took pictures of the train and showed it to friends, to the grandparents and colleagues at work. Towards the end I was able to say that he’d got four greens and we were just working on the feeding. I thought it made it visual – it was really excellent.
Father #816
Weirdly enough my husband loved it, um, I liked it, but he wanted to put the new stickers on as soon as physically possible, whereas I wanted to not put the upper stickers until we were absolutely sure that was the level that she was at, because there was a couple of times where it felt like back tracking if you had to change the colours of your stickers. My husband couldn’t wait.
Mother #819
‘The dates prepare you for going home’
Parents confirmed that the package helped them to prepare for taking their baby home by giving them a time window in advance that they could work towards.
It just says the date you will be going home, it’s just a rough idea about how you can be prepared for it.
Mother #622
And you know like roughly when he can go home, so it’s quite helpful as well.
Mother #623
‘Feeling in control’
A few parents spoke of the control that they felt about engaging with the Train-to-Home package.
It was great because it put me even more in control, and I felt like I was doing more, so it was great.
Mother #418
Well actually the doctors came round one point while I was there early and they said that I could do the stickers myself. So, um, that was quite good. Something so small actually makes a big impact, you kind of feel quite good about being able to sort of put a different colour sticker in, because you can see how she is improving really.
Mother #807
‘Do it right at the beginning’
Some parents had not received the train at the beginning of their LNU stay and this impeded their chance to engage with their baby’s progression.
We did think it was a really good idea that you can see him progressing, but it’s just unfortunate that we didn’t do it right at the beginning . . . So we didn’t actually see much of a progress . . . so that’s the only one thing I do suggest . . . is to do it right at the beginning so that you can see a change . . . more consistent with it, and like right from the beginning, because I think it’s fantastic that you can see the change and see the progress.
Mother #408
It might have been [nurse], who I think, um, you know, went through it in quite a lot of depth with us, which was helpful. But that did happen a bit later down the line . . . maybe just, um, I don’t know whether to be done slightly sooner?
Mother #621
So I would definitely say within the first week, you need to know that’s an option, that’s a good idea, but sort of 3/4 days onwards I think.
Mother #814
Using the booklets: ‘questions to ask and getting to know your baby’
Over half of the parents who were interviewed used the booklets. Those who used them found the questions helpful and ‘loved getting the booklet out’ to use. Both mothers and fathers found the booklet useful, it facilitated engagement and understanding, helped them to ask questions and many of parents wrote comments or observations in it.
Fathers’ engagement
He did go through that and write down yeah his thoughts and questions I think.
Mother #225
My partner did more of that to be honest than I did, so yeah . . . I think he thought that was quite helpful actually. It gives guidance and things, doesn’t it?
Mother #621
Getting to know your baby
It kind of gave us a guide to what we should be doing and what we should be learning and looking for, um, with our own children, and it kind of gives you a guide, okay next week, you know, we can look forward to this.
Mother #617
It was good being able to sort of chart her progress to see sort of where she’s at in the bigger scheme of things, um, on a daily basis, so yeah that was quite useful.
Mother #819
Discussion with staff
I did find it useful, like when we looked for the questions, and especially going through with the nurses, when you went through with the nurses, and they went through each stage and like talked us through it, and it was helpful, you know it was useful to look at. Especially the questions in there that you probably didn’t think yourself about the questions to ask. So it was good to look in there, and then you think oh yes, I would like to ask that question, and then you know we felt that we could ask them.
Mother #408
Parent-reported negative comments
Negative or critical comments during the interviews mainly focused around nursing staff attitudes, confused messages and an apparent lack of understanding or engagement with the package, as shown in Figure 17.
‘Staff didn’t explain it’
Some parents in three LNUs reported that the train was not always introduced or fully explained to them to enable them to engage with the intervention.
Yeah, nobody ever explained that train to us, like, and then one day I was like I’m going to stick some stickers on there, so I did, because everyone else I knew had put their stickers on, and everyone was like looking at [baby]’s, because it had nothing on, so um yeah nobody went through that like booklet or anything . . . it didn’t really mean as much for us. But it was quite nice, when I put all the green stickers on, I took a photo of it and I put it in her baby book. Um, yeah it is quite nice to have it in there.
Mother #206
The train appeared one day with some dates on it, um, and . . . it must have been that I wasn’t around when the nurse came to do it, and then I didn’t know what it meant for quite some time, I think it was another couple of weeks before it was explained to me.
Mother #213
They didn’t really use the stickers or anything. I didn’t really get explained what to do with that . . . mine didn’t really get used to be honest.
Mother #417
‘It was confusing’
The parents mentioned being confused by nursing staff comments about the materials developed for the study or when they appeared not to use them. This included not explaining the criteria for changing train window colours, challenging the going home dates, and being advised to use ‘due date’ as the date when their baby would be going home. In half of the LNUs, nursing staff told parents to use the due date as the target for going home, and then added a different, earlier, date to the train.
I was talking it through with one of the other nurses, and she was explaining it to me, and she was saying actually some of the, um, the things there that are written down to get each spot could be changed around really.
Mother #221
I think nearly all of them [nurses] said that, it [going home date range] was unrealistic. It seemed very strange, because when it [the train] was first presented to us we were kind of like ‘oh wow that’s really soon’, because the consultant, the first thing they said was you have to go with his due date . . . So that was very confusing.
Mother #225
You always get told to wait until due date.
Mother #418
‘Give me more information to change the colours’
Some parents reported that nursing staff handed over responsibility for maintaining the train to them but did not give them enough information to use it correctly. This meant that stickers were not updated as parents did not understand the basis on which to change them.
Perhaps it didn’t get updated often enough, because we had it done initially, and then it was only updated when they’d got to all green, um, and there were a couple of things that I felt, um, [baby] in particular had . . . she’d kind of moved on, she had achieved it, but it wasn’t updated particularly . . . wasn’t sure if I was supposed to touch the train, um, it kind of seemed like that was something that they did, um, and it wasn’t for me to do, because they would determine whether they had met all the little targets.
Mother #219
I think it just needs a little bit more work around explaining it to parents, and, you know, who is leading on it really, and at what point, you know, what’s the criteria so that you can make judgements about where your baby is. Because things like for example sleeping, I thought well does that mean . . . you know what does that mean? Does that mean she is sleeping lots so that’s a good thing?
Mother #621
At home
By using the Train-to-Home package to help parents to understand their baby’s needs while in hospital, it was hoped that it would support their empowerment further after taking their baby home. Themes in this section cover the interviews in both phases and are shown in Box 3. They describe the type of help and support that parents received following discharge home with their baby.
‘Health visitor support was either fantastic or a bit vague.’
‘Neonatal outreach team is a great support.’
‘GPs helpful for medical things.’
‘Staying in contact with other parents met on the unit.’
‘Wider family support is most helpful.’
‘Using the internet and Facebook to get information.’
‘I would have liked to have known more about . . .’
‘Health visitor support was either fantastic or a bit vague’
Once at home, parents had a range of services they could turn to for support and advice. Many parents from all the LNUs regarded their HV as most useful, helpful and knowledgeable in discussing a variety of routine problems that they encountered, including breastfeeding and tongue tie.
My health visitor has been fantastic. She’s been coming out weekly and has been really, really good support . . . More with the breastfeeding side because I was having problems, obviously [baby] was tongue-tied and I was having real doubts whether or not I could actually carry on breastfeeding when I first brought her home, because it was just so wearing. And she was really, really supportive in, ‘Well let’s look beyond the problem. Let’s see what’s causing it.’ And, you know, she was absolutely fantastic.
Mother #318 phase 1
The health visitor has been very good. Unfortunately she’s retired now, which is a shame because I would have liked to have had her for a bit longer. She was very good because she noticed the tongue tie. I think just her sheer experience was really helpful, um, and she was like . . . she’s referred us to the cranial osteopath and then she gave me some advice about, um, foods and things to avoid and stuff like that. So she’s been really good.
Mother #213 phase 2
My health visitor is amazing, um, yeah she’s really friendly, she’s really easy to get hold of, um just need to send her a text and she rang me back when I had a problem . . . I mean I haven’t had many problems, um, but I have she’s been really, helpful, really happy to answer any questions.
Mother #219 phase 2
However, there were other parents who had concerns about the lack of direction they received from their HV, the lack of specific understanding about premature babies, and a focus on child protection aspects of the role rather than parental support.
Um the health visitor was good for some basic stuff, but I did find that she was – she’s quite vague. I almost got the impression that she didn’t want to give me too much information because she didn’t want to be wrong, like she didn’t want to give advice and just say, ‘Well you could try this or you could try that,’ but, I don’t know, I found her a bit vague in what she was saying. I don’t know if that’s just her. I don’t know what other health visitors are like.
Mother #109 phase 1
When the health visitor came round she didn’t have a great deal of experience with prem babies, so I found that what she was saying was contradicting special care, what they told us before we came home. So I kind of ignored what she said.
Mother #418 phase 2
‘Neonatal outreach team is a great support’
One unit supported mothers with a hospital neonatal outreach team after leaving the LNU. This support was sometimes preferred over community-based HVs because the outreach team gave advice specific to premature babies.
My health visitor actually used to do NICU herself in the past, which actually helped. But she did more practical – rather than [outreach team] were solely giving knowledge and information regarding NICU and prematurity. Whereas the health visitor was more, I suppose, generalised of how things would be going normally. So any more worries and concerns I had, it was easier to speak to neonatal outreach team members regarding things about her being early, asking them rather than the health visitor.
Mother #521 phase 1
Yeah, the NICU health visitor and my own health visitor . . . found them really helpful . . . all three of them, they’ve been there for me as well as [baby], obviously that’s what they’re there for, but I found them a great support.
Mother #608 phase 2
‘GPs helpful for medical things’
General practitioner (GP) knowledge seemed to be more mixed. Some parents felt supported by their GP in terms of routine illnesses, but as with HVs, most do not have specific preterm knowledge and advise parents to contact the LNU or in one situation go to an ED.
My doctor was brilliant, because obviously she was the one that was saying, you know, ‘Let’s get this [hernia] sorted, and bring him back tomorrow, or bring him back in two days’ time and let me have a look then.’ So . . . she was fantastic.
Mother #315 phase 1
Actually the GP has been very helpful from a baby point of view, the sort of reassurance about just generally having a baby, when I’ve been to see them, but not really about a premature baby.
Mother #719 phase 1
Also my GP . . . it’s literally the medical, illness side, then it’s definitely the GP.
Mother #807 phase 2
‘Staying in contact with other parents met on the unit’
Several parents remained in contact with other parents that they met on the LNU and one unit had started a support group for recently discharged parents.
Well I’ve kept contact with the friends I made on the ward, we meet up every four weeks and we talk. Also the [name] group have got the Facebook page, they also come to the unit, they’ve been really good actually when I’ve had any sort of questions, just posted it on there and then loads of other mums have replied saying, ‘I was in exactly the same situation, I tried this’ so it’s been quite nice.
Mother #206 phase 2
I have joined the support group that runs out of [the unit], I’ve been to one of their community meet ups, and met some mums that way, so yeah we just chat to a few . . . If you’ve got any questions really, all mums from the unit, and I think they let you stay for about 2 years, so if you’re experiencing something they’ve been through they can help out. It’s a big Facebook group as well, so that’s quite nice, so it’s really easy to get hold of somebody.
Mother #219 phase 2
‘Wider family support is most helpful’
Families in phase 2 identified the support they receive from their wider family (grandparents and sisters) as being helpful and having the most useful knowledge. Understanding the baby’s needs while in the unit was also important for the wider family in knowing how to help after discharge.
Family really that has given most of the help . . . it’s two babies feeding is quite difficult isn’t it? . . . this is the most important thing I think, that’s why we get help from family.
Mother #623 twins phase 2
[My sister] she’s got a baby who is, I think just 11 weeks older than [baby], so she’s kind of recently been through the kind of stuff that I’m about a couple of months behind on. So it’s good to have that . . .
Mother #814 phase 2
Yeah, definitely my mum [most helpful knowledge] because I don’t really see my health visitor.
Mother #808 phase 2
‘Using the internet and Facebook to get information’
Mothers described using the internet cautiously to find more information on a range of issues specific to premature infants, which they would have liked to have been given before going home. They mentioned using Facebook, Mumsnet and Netmums, NHS websites for illness and BLISS for support. They looked for information about how their baby would be followed up, how many routine appointments they will have, when to use corrected age, why certain tests/scans are necessary and the long-term implications of prematurity. Mothers described feeling stranded in the community and that other people did not understand.
We’ve got like a chat on Facebook, so we put our things on there as well. I’d probably say those mums have been the most helpful, um, because our babies were all premature and very similar age, and if somebody said, ‘My baby is doing this, what do you think I should do?’ And then another mum will say, ‘I tried this, it seems good,’ and it’s you know we’ve all sort of had each other for support. So I would probably say that’s the best really.
Mother #206 phase 2
Because I’ve read things that if they’re not gaining weight . . . that can have effects on their general development. Yeah you see that was me being naughty and Googling. But I was reading articles, research articles, because I have access to the BMJ and stuff for my own job so . . . yeah as opposed to just junk like . . . think we’ve been quite anxious recently.
Mother #112 phase 1
We avoided it [using the internet] when she was in hospital, um, for obvious reasons, um, but it’s more to you know find out what milestones she should be doing, um, for her current actual age, of her corrected age as well. So just sort of see we’re in the right ballpark area of what she’s supposed to be doing, so just for that sort of thing really.
Mother #819 phase 2
There’s only one main website for premature babies, and that’s the BLISS website, but I think again it’s more for support rather than actual information, and I think it is because the ranges are so large, so they can’t give you . . . so you go on the NHS website about weaning and it will say around average of 6 months, but you can’t do that with premature babies, because also they then develop at different rates as well, so everything is just a bit up in the air with them.
Mother #213 phase 2
I felt actually quite stranded about having a premature baby. All my antenatal friends’ babies were all full-term. They’re younger in chronological age than [my baby] but gestationally they were full-term, so it’s all different, and they don’t quite understand.
Mother #719 phase 1
‘I would have liked to have known more about . . .’
There was practical information that parents thought would be helpful in advance such as how to establish a routine at home, how much medicine a premature baby can have, understanding weight and feeding. In phase 2, several mothers mentioned baby tongue tie not being identified before going home, which had contributed to feeding difficulties.
. . . with the breastfeeding side because I was having problems, obviously [my baby] was tongue-tied and I was having real doubts whether or not I could actually carry on breastfeeding when I first brought her home, because it was just so wearing. And she [HV] was really, really supportive in, ‘Well let’s look beyond the problem. Let’s see what’s causing it’.
Mother #318 phase 1
What I did find quite strange, because also, he had tongue tie, which my health visitor only picked up three weeks ago, and she said, ‘I’m surprised they didn’t pick up on it in hospital’.
Mother #213 phase 2
[twin 1] was showing no interest in breastfeeding, and he was really struggling. We have since found out that he had a tongue tie that wasn’t picked up, so he had that cut last week, so he may have been able to feed had it been picked up earlier, but I don’t know, he didn’t seem interested.
Mother #219 phase 2
Well there’s one medical thing, [twin 1] was tongue tied and it was not caught. [When was it caught?] Two weeks after discharge, and it was, found by the cranial osteopathy that we went to, and it’s caused like a lot of feeding problems. If that would have been found a lot sooner I think that we could have probably prevented some of the issues we’re having today with her feedings.
Mother #617 phase 2
Summary
Parents described their time in the LNU as a ‘roller coaster emotional journey’, where ‘they learnt a lot’, ‘established relationships with nurses’ and received ‘support from the ‘NICU family’. They felt prepared practically for going home but in phase 1 many were very concerned about the lack of notice about the expected discharge date and a lack of structured, meaningful discussion about going home. In phase 2, mothers mostly reported being quite well prepared for going home. Mothers expressed emotional uncertainty about going home and some felt that they needed more reassurance. In phase 2, more parents said they felt mentally prepared to take their baby home. In both phases it was acknowledged that breastfeeding was often difficult and getting it right could delay the timing of their baby’s discharge home.
Set against this background of a lack of notice and feeling rushed just before babies were discharged home, the Train-to-Home intervention was introduced. Many parents responded positively to the Train-to-Home package and found it helpful for showing them in a visual way that their baby was progressing. Mothers, fathers and siblings enjoyed using it. Any negative comments were focused around nursing staff attitudes, confusing messages and an apparent lack of understanding or engagement with the package.
Once home, parents had a range of services they could turn to for support and advice including HVs, hospital neonatal outreach nurses and GPs. Several parents remained in contact with others whom they had met on the LNU, and one unit had started a support group for parents discharged from the unit. Mothers described a cautious use of the internet to find more information on a range of issues specific to premature infants, which they would have liked to have been given before going home. They mentioned using Facebook, Mumsnet and Netmums, NHS websites for illness and BLISS for support.
Nursing staff focus groups and interviews
Eighteen nursing staff were interviewed in person across the four sites, in groups of three or four and a few as individuals. We included two managers, seven sisters, four staff nurses, two health-care assistants and three nursery nurses. The primary aim was for the groups to discuss their views on the intervention materials and how they had used them. Quotes are attributed to the different units rather than particular individuals. Interviews and groups varied in length from 30 to 60 minutes.
Preparing parents to take their baby home: ‘gaining weight, feeding and maintaining temperature’
During the focus groups and interviews we initially discussed nursing staff views on preparing parents for discharge home and what they thought were the main issues for parents. They all used basic criteria for discharge home from the neonatal unit highlighting that they told parents that babies had to gain weight, feed well (particularly if breastfed), and maintain their temperature before they could go home. They thought that parents worried about coping and feared taking their baby home.
They discussed the factors that facilitated earlier discharge or delayed discharge home. Although they mentioned using ‘aim for your due date’ as a guide, they said that now they advise parents that around 37 weeks’ gestation is a more realistic expectation.
We used to say that babies go home about their due date and anything before is a bonus. We know that they don’t go home on their due date, so now we tend to say . . . it will probably be between 37 and 38 weeks in most cases. Term is anything from 37 weeks. The focus here would be to get them breastfeeding, establish breastfeeding.
There is a perceived feeling that if they bottle feed they will get home quicker. For a mum who is breastfeeding they get frustrated with that last hurdle and they will switch to bottle if most of the others around them are bottle feeding.
The whole communication with parents and working with them has changed quite dramatically really over the last sort of 4 or 5 years really . . . we’re much more focused on their gestation, where they are in their gestational developmental journey and their nutrition. This is linked in with a Trust-wide tool looking at discharge planning.
Unit #1
It’ll be your due date, but we’re not very specific about setting that date. We expect babies to be going home now at 35 weeks. A few years ago they weren’t going home till 38/39 weeks, so our expectations are that we build the parents up to going a bit earlier than that. If they end up staying a bit longer it becomes harder doesn’t it.
Unit #2
Clinical and other justifications for not setting discharge dates were provided by some staff:
Infection keeps them longer, problems with breastfeeding, reflux, poor feeding.
The thing is though when you’re going home receiving breast milk you will have a longer stay. You do get home more quickly when you’re bottle feeding, um, and you have to look very carefully at the support that parents need in the last few days before they go home if they’re breastfeeding, and it’s actually huge.
Babies need to be 35 weeks, feeding well, keeping warm.
There’s a good guide in our admission booklet.
I think mainly breastfeeding, it can take a lot longer for the feeding.
Parents lose all their confidence initially and we have to build that back up again.
Unit #3
Feeding keeps them in a bit longer, but you know when you need to establish breastfeeding it does take that bit longer than if they were going home bottle feeding, and it’s the baby itself though really.
We get quite a few social issues, so they’re ready to go home on a Thursday or Friday but we can’t send them home until Monday so there’s a full care package available.
Unit #4
Using the intervention materials
Themes generated from the staff reports of using the intervention are shown in Box 4.
‘A visual representation to explain baby’s progress.’
‘A chance to sit down with the parents.’
‘Intensive care may be too early.’
‘Some parents used the booklet like a diary.’
‘A visual representation to explain baby’s progress’
We sought staff views on having visual materials to help parents understand that discharge is approaching. Staff agreed that this was a good idea but there were very mixed views about using the package on the LNUs. Using it to help explain a baby’s progress was welcomed by some and most acknowledged that it helped to start a discussion:
I think it definitely helped discussion and it did promote conversation, so as a tool it engaged I think people and actually made you focus more on discharge planning and targets and actually engaging conversation. That visual is great isn’t it? And I know for some parents it’s absolutely fantastic, but for others it’s not been.
Unit #1
It looks good, it looks nice and some parents love it, and then they get really cross because they can’t take it home and they say what’s the point? It starts off a discussion. But to be honest some people love it, some people hate it.
Unit #2
A lot of people talk about their journeys really, so why can’t it be a train? I think if you’re going to get a family that, like that way, that visual way of seeing stuff . . . I think it would work. Anything we can provide for parents that is going to make their journey easier, that’s good. I think there’s a place for it but not for every family though.
Unit #3
Thus, although the value of the intervention package was acknowledged by many staff, for some it was implemented in a less than wholehearted way, and a degree of ambivalence was reflected in their responses.
In contrast, staff in the fourth unit really embraced the materials and appreciated the principles involved.
I think traditionally we’ve always told parents that they will go home around the time they had been due, but actually babies don’t . . . they’re going home around that 35/36 week mark, much sooner. By having a more structured plan to prepare them for home . . . they’ve got a date to work for. It’s the first question they always ask, ‘When can we go home? When can we take our baby home?’ It’s one you can’t properly answer, but this gives them a bit more of an idea when to expect them home. It allows them to prepare at home, so family coming to support them, that sort of thing.
Unit #4
Seeing that visual representation that their baby is getting better; that they are making that journey towards home. It’s fantastic; it’s been a really good way of engaging the parents with their baby’s progress. It’s definitely a good sort of starting point for communication with them. Dads love it. They also appear with the parents talking to the relatives, and they’re explaining it and they feel empowered.
I think it should be used with all our parents. They can all understand it and because it’s quite visual you can explain it to them in a way that they understand. Once they’ve been given it they’ve all been really interested.
‘A chance to sit down with the parents’: using the train on the unit and explaining the dates
The dates on the Train-to-Home package were usually changed following a discussion with doctors. Most nurses struggled with explaining the dates to parents but in one LNU nurses found that talking about the dates and changing the window colours helped them to promote discussion with parents and explain how their baby was progressing.
I think initially the parents really like the train, they see it as something quite positive, and they like the dates. But the problem we get is that as it comes nearer the time and they don’t necessarily meet their dates, I know that you can change the dates, but there’s no guidance on how to change them. So it’s quite hard to know what to change them to, because it’s almost a guess, because feeding is a bit you can’t tell, you can’t predict how long it’s going to take somebody to feed, and when they don’t reach those dates or you change the dates then they get quite disappointed. So initially it’s quite positive, and for the babies that become unwell during their journey and go backwards, that’s really difficult for them. We’ve only had a few of these though.
Unit #1
The first date is always very optimistic for what happens in our unit. I found the dates difficult as there was no guidance on how to extend them rather than narrow the dates.
The uncertainty was emphasised and the big differences between individual babies. Some staff expressed a need for more guidance on changing the dates, with some feeling that this was not their role.
It’s a huge difference between each individual child. So once you start writing the date on there then the parents are like glued to that date, and it’s a bit difficult to then try and move it. The consultant would actually write the dates and explain to the parents.
Unit #2
We tend to do it quite often on the doctor’s round, often the doctors will alter the date or put a date on if there isn’t one and sometimes speak to the parents about it as well.
Unit #3
Others relied on a shared discussion and emphasised the ‘rough guide’ aspect of initial dates, with a more flexible and reflective attitude to changes in the likely timing of discharge home.
We change the dates in discussion with the doctors. Sometimes the frame is just a little bit too narrow. I don’t think the doctors have been so on board. I think we are because we’re face to face and there’s so many things that . . . and for me it’s an excuse to sit down with the parents and discuss the train and feeding plan.
Unit #4
I think it’s been lovely to be able to give them an idea right from the word go. I really liked that, because that is the one thing that they always ask is you know, ‘When will my baby be going home?’ It’s like, ‘Well, this is a rough guide,’ and what I do feel we haven’t done well is to reassess it nearer the time that they’re going home, yeah, keep reassessing it.
‘Intensive care may be too early?’: when to introduce the package
A number of staff on three LNUs thought that it would be better to use the package in the lower-dependency areas after the first weeks of intensive care. However, following the implementation and use of the Train-to-Home package, the fourth LNU was keen to use the package as soon as babies were admitted and wanted to continue with its use.
There’s that anxiety of moving from high dependency to low dependency where there’s less nurses and, you know, babies aren’t monitored as much, but it gives them a focus they’re actually going home. And actually what would be really nice is thinking of when we’re working with parents and actually empowering them beginning to sort of hand over the reins, because that’s actually a really difficult transition for some parents, especially when they have been in for a long time, there’s actually that nervousness of going home, and taking over that sort of care, and we’re obviously trying to empower at an earlier stage with teaching parents to tube feed and take on more sort of in high dependency. But as they come round the unit, having that tool where they could actually start to share some decision-making.
Unit #1
Use of the train as a signal to parents was preferred by some staff once a baby was moving on from intensive care and in some instances from high-dependency care, and they saw the train and the booklet as a way of providing information for parents at, what they perceived as, a more appropriate time, bearing in mind the needs of the baby and staff workload:
I think there’s more time in low dependency. You’ve got also more of an idea of when that baby is likely to go home, because you don’t know if his journey in high dependency is going to be two or three days or a long time. Whereas once they have gone into low dependency normally it’s just growing and just getting . . . so they’re heading towards home. And parents relax more about it don’t they? They start enjoying their baby rather than being worried about it. To start you’d almost give them something different to focus on wouldn’t it? Once the baby went to low dependency, right we can start thinking about discharge now.
Unit #2
They have a lot going on in the first week or couple of weeks and they don’t remember the peripheral stuff, so intensive care is too early.
Unit #3
I think when they get into the special care side it’s probably good . . . to introduce them, only because in ITU and high dependency there’s quite a lot going on, and things changing quite quickly. When they get to special care they can be there for a couple of days, but some could be there for a couple of weeks.’
There is that negativity built up about it, because some staff have felt that, obviously it’s an important thing, but to staff who are trying to save lives actually it comes way down on the list. So it’s getting . . . I think we need to sort of be allowed to use it and introduce it when it’s appropriate, and it’s getting the timing right for the parents and for the workload of the staff to be quite honest. If we did take this forward I think the intensive care side is too early.
However, not all staff saw it that way, particularly those in the fourth unit:
I think overall it’s worked really well, it’s been quite positive for the parents, which is the main thing really. We just do it every day now, you kind of get used to doing it, so it’s part of the daily thing you do with the parents where we’ve figured oh we’ve got to get the train, need to do this, need to do that, we just do it now.
Unit #4
The parent pathway booklets: ‘some parents used it like a diary’
Nursing staff did not report seeing parents using the booklets much. It was also clear that most of them did not offer parents guidance on using them.
It’s interesting looking at the moment at some of the developmental work that’s being looked at and they’ve got the pathway there which is a similar sort of pathway over how you would expect a journey to take place. And I think the whole pathway idea working with parents is a really positive one. But I felt that it sort of almost made it over simplified . . . I think you almost needed to have a more individualised approached, so to use the pathway as an overarching goal, target, but to be able to have individualised it a little bit more.
Unit #1
Some parents would look in the book and literally they would have essays written on every question. Other parents would never write in it. They might have read it but they never wrote in it. So it just was an individual thing really. But some parents literally would write everything down. It got better with the booklets, and the booklets were quite useful I think.
Unit #2
I haven’t actually, no I haven’t actually seen them [parents] use them [booklets]. Um, I’ve seen them, but my knowledge on them is not the best. Is that something that would be kept . . . would usually be kept on the cot side with them?
Unit #3
I think they’ve asked about the temperature more and things like that. They feel they’re able to ask, because they’re involved in this idea of the colour stickers. It’s almost like they need the verification of the book to say to you, ‘In the book it says . . .’ so does that mean that I can? . . . Some of them used them daily and read you know questions out, or underlined things, and wrote how their babies were doing, like a diary really.
Unit #4
Ongoing use of the Train-to-Home materials
Responses to continued use of the materials after phase 2 of the study was mixed: one LNU was negative, another was very positive and the others were ambivalent. There was some discussion about possible formats for future versions including a website or an app for parent use.
I think having a generic tool that you can then adapt and working with your own individual unit culture or own flow, or design is actually really helpful. So I think any electronic system that you’re talking about, or apps or things like . . . are going to be really useful because then actually you can mould it slightly can’t you and make it individualised.
Unit #1
Others were satisfied with what they already had in place:
I personally think we are really good at our discharge planning. I think because of our tick lists we go through all those things, and I think that works really well. We’re good at our planning, I don’t say we’re necessarily good at our dates. We are not using the trains any more, I haven't seen any around.
Unit #2
However, some staff recognised the value of this kind of innovation for new staff and as a way of working with parents:
I think if I was a new member of staff, obviously I’m not, but I would actually almost use this as, well as a learning tool, to have those conversations with people, and you know, if you don’t know the answer, if a parent asks you something then you find out somebody who does know that. So, you know, there’s quite a good learning tool I feel for new members of staff.
Unit #3
I would be quite upset if they were taken away. Because it’s been so positive, and I have seen that, and that’s really nice, you do feel you’re making a difference for the parents.
Unit #4
We’d really like to keep the trains. The visual aspect of it and actually find a way of extending that to all our babies, not just those babies that fall inside the criteria. That would be our ideal. There’s a lot in the NHS at the moment about all patients having this journey card and having the discharge dates, and knowing what’s going to happen next and that sort of thing. We would really like the train to be ours rather than it being an odd bit of like postcard that gets tatty and forgotten. This is just a really good way of us doing that with our parents and giving them a way forward to work towards going home. It’s been brilliant, and they love changing those stickers and going to the next colour.
Unit #4
The NHS initiative on discharge planning was mentioned by two groups of nursing staff and they considered the Train-to-Home package fitted well with this approach because the pathways focused on developmental care. Staff told us that they have started to focus on babies’ stages in their gestational developmental journey and our approach seemed to fit with this. They thought that having more time to embed the materials into each LNU was needed. This normalisation period would allow more individuals to be trained and promote optimal delivery of the package.
Consultant paediatrician interviews
Six consultant paediatricians based at the four LNUs were invited to take part in a short telephone interview and five agreed. The interviews took place in January and February 2015 and lasted from 15 to 45 minutes. They were not recorded, but careful notes were taken during the course of the interviews.
All five were positive about the Train-to-Home project, but in some LNUs they highlighted the difficulties of getting the nursing staff to adopt an approach that the nurses felt the LNU did not need to use. The consultants had not anticipated this. They mentioned that some nurses thought the estimated discharge dates on the train were too early, and were worried about effect on parents of the colours returning to red when a baby’s condition deteriorated. However, from the clinician perspective, as well as the nursing staff, the fourth LNU was very positive about the intervention and underlying concepts, and wished to adopt this approach to discharge planning.
At the start of the interview they were asked for their overall impressions of the project and intervention materials without any interviewer prompts. These first responses summarised the content of the rest of the interview well and have been included verbatim, to illustrate their views.
There was real value in the process of thinking clearly about discharge planning; we need to do more work on improving information exchange and supporting parents. . . . It was very difficult to get nurses to ‘buy in’ to the process – the nurses thought it was ‘too simplistic’. When one or two babies took longer to be ready for home than our initial estimate the nurses became very hostile about the estimates – said they were ‘too optimistic’ – did not like having to give parents the ‘bad news’ that their baby would be in hospital longer than the initial estimated date . . .many of the medical staff ‘kept their heads down’ and avoided talking to nurses about it after this, though in general the doctors liked having an idea of when the baby was likely to go home from early in the hospital stay – this allowed better communication with families . . . the families were almost all very positive about it.
Unit #1
I found this gave me a much better focus on discharge planning. The early parent involvement was very helpful in improving communication and parents’ understanding. There was better continuity of the process from initial time on the ward to going home. Some nurses thought it was condescending for parents. It focused attention on the baby’s overall progress when we were discussing the baby on ward rounds.
Unit #2a
This was a very helpful approach that improved communication between us (the medical staff) and parents about the planning for sending the baby home. The information for parents was very helpful and parents really appreciated being involved in this from an early stage.
Unit #2b
The idea was very good. It ‘normalised’ the process of going home from early in the hospital stay. It was good to start these conversations sooner than we usually do. The process did however unmask some ‘chain of command’ problems – some nurses felt very negative about it and we were ‘too democratic’ about how we implemented this – we were not forceful enough in pushing this when certain nurses seemed unwilling. At times it seemed as if this project was in competition with NIDCAP training (Newborn Individualized Developmental Care and Assessment Program) – though both involved many of the same ideas about empowering parents.
Unit #3
The unit found it an extremely interesting and valuable study and we were happy to be involved with it. There was a lot of positive feedback following this study. Both the medical and nursing staff found this tool extremely helpful. The underlying concept of using visual images using the ‘train’ was very appealing to both healthcare professionals and parents. Many doctors found it easy to explain to parents what is going on with their baby’s progress using the train.
Unit #4
Nursing staff were more focused on what matters most to parents, which is having their baby discharged as quickly and as safely as possible.
Many parents appreciated being told when to expect their baby to be discharged at the time of admission with a specific ‘timeline’ assigned it. The inclusion of the actual dates of discharge made it easier for parents to prepare at home for the arrival of their baby and staff to appreciate the anticipated duration of each individual patient’s admission. The very nature of setting a timeline gave parents and staff some sort of ‘working time schedule’. This allowed the team to schedule none urgent communication interventions in a timely fashion. In other words this study greatly enhanced communication between healthcare practitioners and parents.
Parents appreciated the visual nature of this tool and its precision. They felt more empowered in the care of their baby and this tool made it easier for them to understand the clinical course of their baby’s admission. This tool makes it easier for parents to understand the concept of a baby being ‘physiologically ready for discharge’ i.e. what physiological maturation that must occur before their baby can go home.
Summary
The nursing and medical staff mostly agreed that the visual nature of the intervention materials was helpful in explaining a baby’s progress to parents, but nursing staff had varied views about using the package on the LNUs. Doctors reported that it helped improve their communication with parents and some nurses felt that it gave them a chance to sit down and have a conversation with parents on how their baby was likely to progress, explaining the dates, using the train and discussing their baby’s developmental changes and needs. For nurses in three LNUs, introducing the package to intensive care was too early, whereas doctors in all LNUs wanted early introduction to normalise the discharge process and help parents understand when their baby was physiologically ready for discharge. Both nursing and medical staff in one LNU were very positive about the Train-to-Home intervention and were keen for it to continue.
Chapter 7 Results: part 3 – economic analysis
Characteristics of the sample
Cost analysis is based on 173 infant cases – 85/128 in phase 1 and 88/117 in phase 2 – giving response rates of 66% in phase 1 and 75% in phase 2 respectively. Table 23 shows the breakdown of responses across four LNUs and infant gestational age.
| Characteristic | Group of interest | Phase 1 | Phase 2 | ||
|---|---|---|---|---|---|
| n/N | Total n (%) | n/N | Total n (%) | ||
| Centre | Unit 1 | 21/32 | 24.7 | 19/29 | 21.6 |
| Unit 2 | 22/25 | 25.9 | 24/24 | 28.4 | |
| Unit 3 | 20/34 | 23.5 | 23/29 | 26.1 | |
| Unit 4 | 22/37 | 25.9 | 22/35 | 23.9 | |
| Total | 85/128 | 100.0 | 88/117 | 100.0 | |
| Gestational age,a weeks | 27–30 | 24/37 | 28.2 | 30/35 | 34.1 |
| 31–33 | 61/91 | 71.8 | 58/82 | 65.9 | |
| Total | 85/128 | 100.0 | 88/117 | 100.0 | |
Missing data
We have not used multiple imputation methods for missing data in the economic analysis as our response rates and completeness and coverage of the hospital attendance and health-care resource-use data are robust considering the context of our approach to data collection and situation of the families participating in the study. Families have been discharged from hospital with a preterm baby and a high percentage completed the health-care resource-use tool every 2 weeks over the 8-week discharge period in both phases of the study.
Of 247 families recruited 245 took part: 128 in phase 1 and 117 in phase 2 after implementation of the intervention. Of these, 85 of 128 in phase 1 and 88 of 117 in phase 2 completed the health-care resource-use tool. These are good response rates.
Economic analysis assumes that missing data in the phase 1 8-week period are similar to the phase 2 8-week period.
Table 24 demonstrates that completeness and coverage of responses for hospital attendance in the post-discharge period across both phases of the study is good; 74% of the families reported attendance at hospital as an inpatient, outpatient or attendance at ED. Data on appointments at outpatients and attendance at ED were missing for 27% and 20% of infants in phases 1 and 2, respectively. These proportions need to be borne in mind when reading the findings below.
| Type of health-care use | Yes, n (%) | No, n (%) | Total (%) |
|---|---|---|---|
| Hospital attendance | 132 (74.2) | 39 (22.8) | 171/173 (99) |
| Inpatient readmission after discharge | 31 (18.0) | 141 (82.0) | 172/173 (99) |
| Outpatient appointment | 119 (91.5) | 11 (8.5) | 130/173 (75) |
| ED attendance | 34 (23.8) | 109 (76.2) | 143/173 (83) |
Table 25 presents a comparison of the frequency and duration of 24-hour periods in hospital after readmission as an inpatient, frequency of outpatient appointments and frequency of ED attendance across all cases in phases 1 and 2.
| Secondary care user | Phase 1 | Phase 2 | Total babies | Difference, units | p-valuea | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Babies, n | Units, n | Median | IQR | Babies, n | Units, n | Median | IQR | ||||
| Inpatient days | 16 | 78 | 2.5 | 4.5 | 15 | 85 | 3 | 12 | 31 | +7 | 0.78 |
| Outpatient appointments | 56 | 115 | 2 | 2 | 63 | 117 | 1 | 1 | 119 | +2 | 0.34 |
| ED attendances | 16 | 31 | 1 | 1 | 15 | 20 | 1 | 0 | 31 | –11 | 0.03b |
Table 25 suggests that there were no significant differences in use of inpatient services connected with readmission of infants after discharge and the frequency of outpatient appointments between each phase. There was, however, a statistically significant difference in frequency of attendance at ED (p < 0.05), as measured by the Mann–Whitney U-test. The number of babies was equal in both phases (phase 1, n = 16; phase 2, n = 15; overall, n = 31), but frequency of attendances at ED across cases in phase 2 fell compared with phase 1. Figure 18 depicts the comparative phase 1 and phase 2 pattern of frequencies of inpatient, outpatient and ED attendances across the cases. The findings concerning the fall in frequency of ED attendance across cases in phase 2 must be interpreted with caution, as the number of cases in each phase was < 20 per group (see Table 25).
FIGURE 18.
Comparison of secondary care use by phase. (a) Hospital inpatient days; (b) hospital outpatient appointments; and (c) ED attendance.

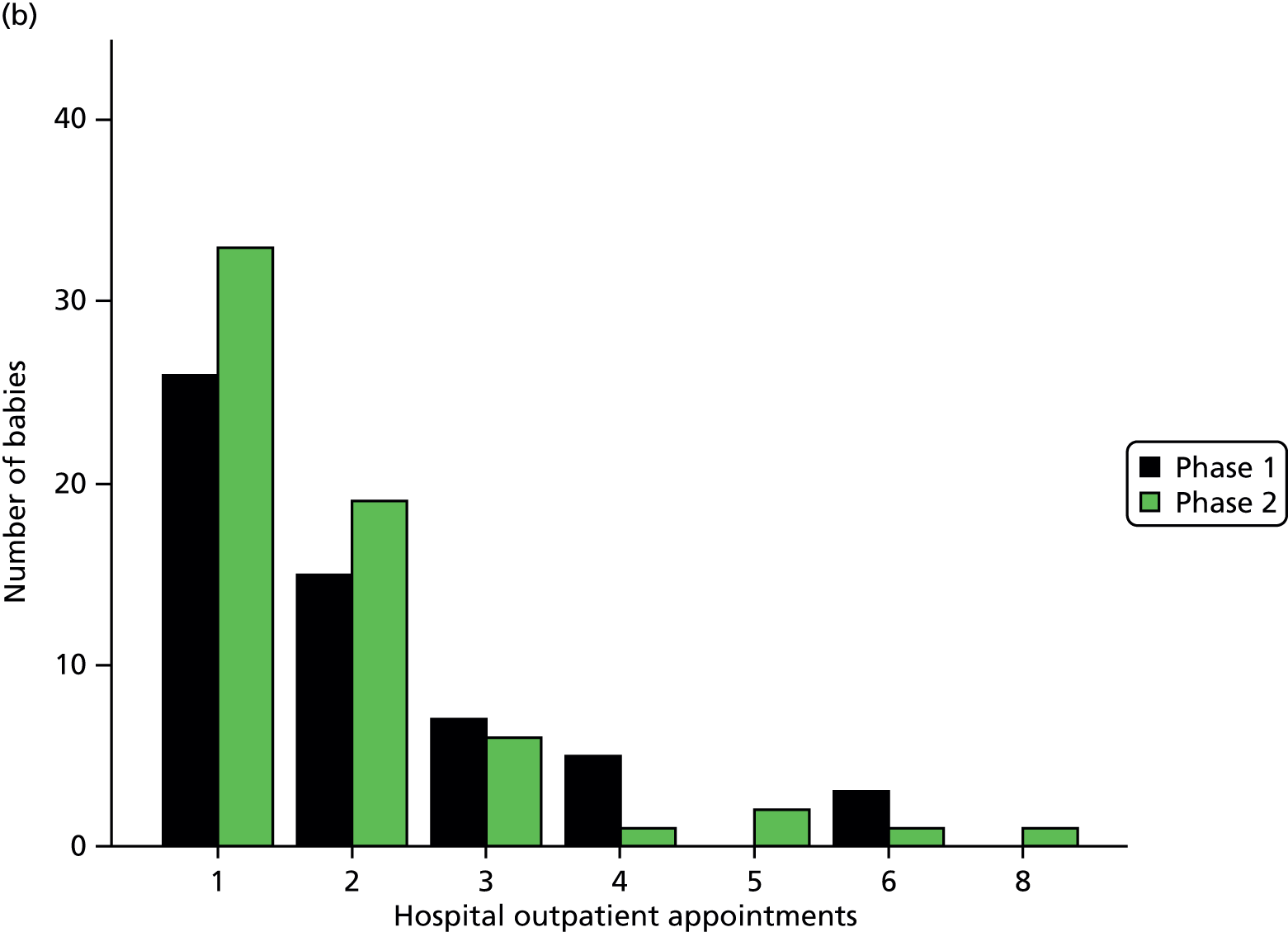
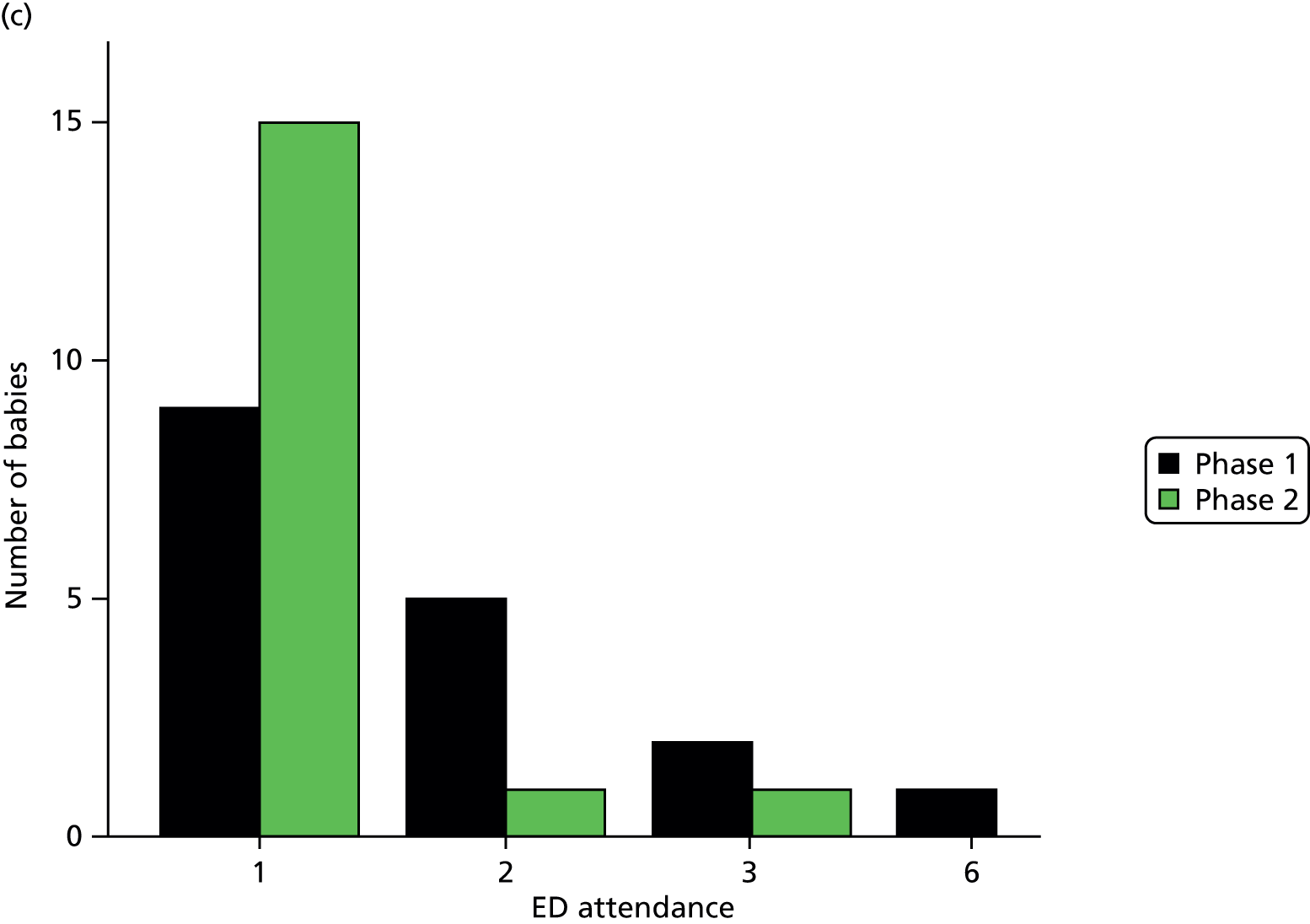
Table 26 presents the cost changes associated with the use (frequency and duration) of inpatient care as a result of readmission after discharge, the frequency of outpatient appointments and the frequency of attendances at ED across all cases over an 8-week discharge period in phases 1 and 2 from a funder perspective.
| Cost | Phase 1 | Phase 2 | Total cases | Cost change | p-valuea | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Number of cases | Cost, £000 | Median, £ | IQR, £ | Number of cases | Cost, £000 | Median, £ | IQR, £ | ||||
| Inpatient days | 16 | 25.4 | 815 | 1467 | 15 | 27.7 | 978 | 3912 | 31 | +163 | 0.84 |
| Outpatient appointments | 56 | 12.5 | 218 | 204 | 63 | 13 | 109 | 109 | 119 | –109 | 0.48 |
| ED attendance | 16 | 3.4 | 111 | 111 | 15 | 2.22 | 111 | 0 | 31 | – | 0.03* |
Figure 19 suggests the reasons for readmission after discharge and attendance at ED largely fall into areas covered by the Train-to-Home package and provide some support for the possible influence of the package on frequency of ED attendance in phase 2.
FIGURE 19.
Reasons for admission. (a) Inpatients; (b) outpatient attendance; and (c) ED attendance by gestational age. GI, gastrointestinal.

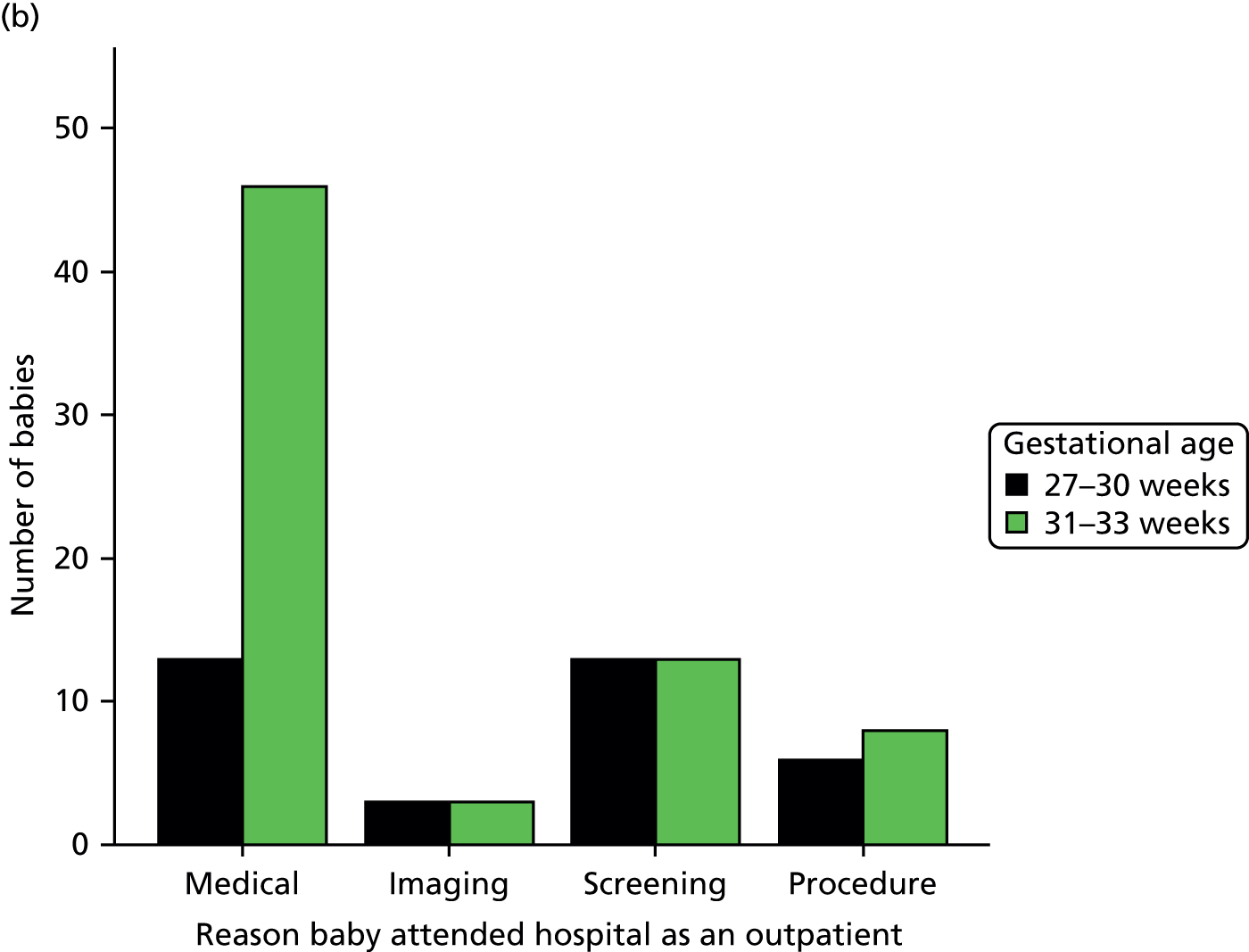
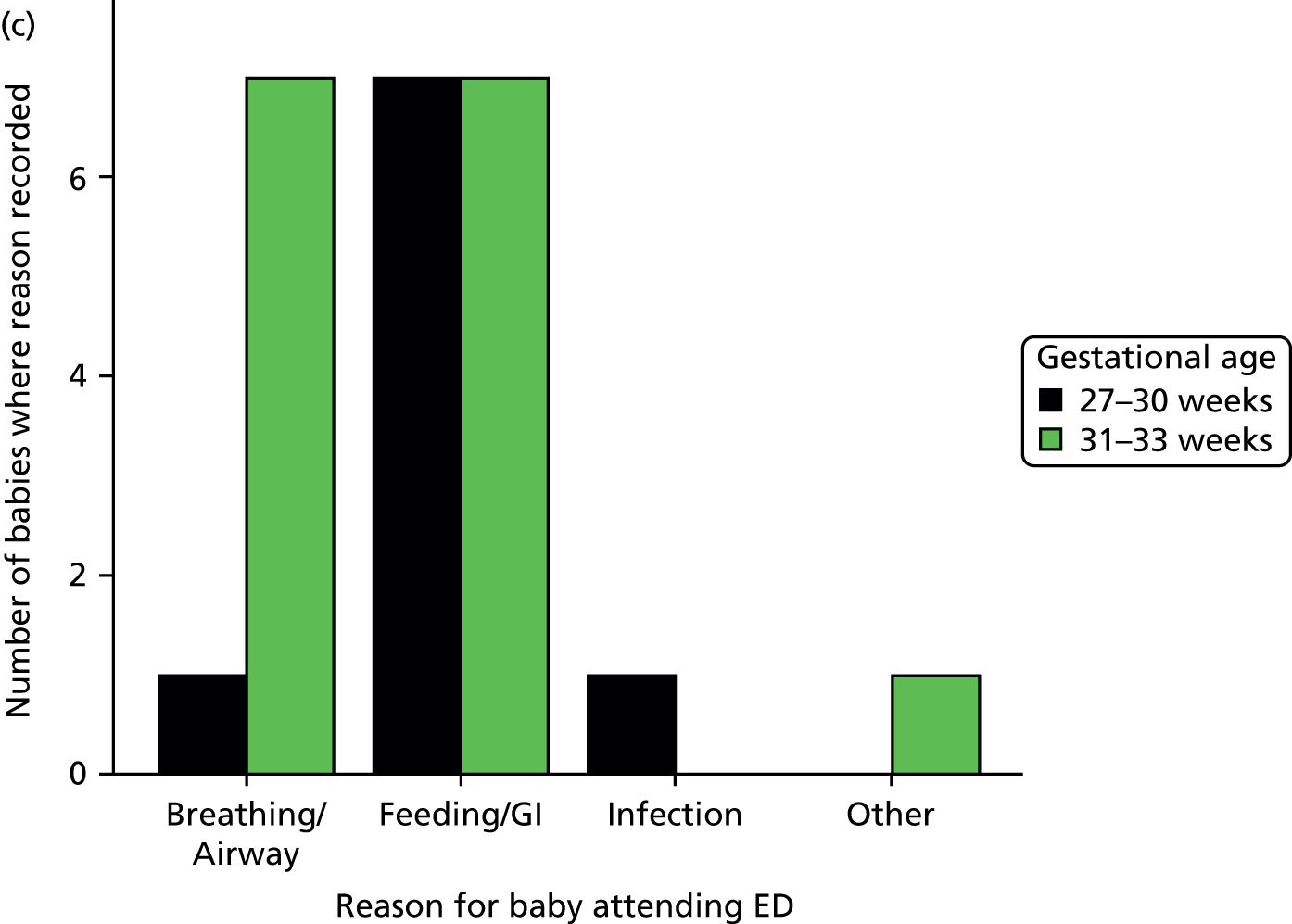
Table 27 shows there are no significant differences in costs associated with use of primary and secondary health services from the family’s perspective in the discharge period across phases 1 and 2.
| Cost, pounds sterling 2014 prices | Phase 1 | Phase 2 | Total N | p-valuea | ||||
|---|---|---|---|---|---|---|---|---|
| n | Median, £ | IQR, £ | n | Median, £ | IQR, £ | |||
| As inpatient: cost of car | 10 | 145 | 486 | 3 | 25 | 204 | 13 | 0.27 |
| Hospital visit: cost of taxi | 84 | 6 | 40 | 87 | 12 | 46 | 171 | 0.72 |
| Hospital visit: parking fee | 84 | 1.4 | 6.75 | 87 | 2.00 | 4 | 171 | 0.57 |
| ED visit: car mileage | 9 | 20 | 24.50 | 7 | 26 | 51 | 16 | 0.87 |
| GP visit: car mileage | 16 | 4.5 | 8.25 | 6 | 5 | 9.75 | 22 | 0.88 |
Table 28 and Figure 20 show that there was no significant difference in cost from a funder perspective, although there was a slight, but non-significant, reduction in the number of contacts with a community health professional in the post-discharge period between the phases.
| Cost, pounds sterling 2014 prices | Phase 1 | Phase 2 | Total N | p-valuea | ||||
|---|---|---|---|---|---|---|---|---|
| n | Median, £ | IQR £ | n | Median, £ | IQR, £ | |||
| GP | 85 | 117 | 128.70 | 88 | 117 | 112.13 | 22 | 0.90 |
| Practice nurse | 85 | 7.30 | 14.60 | 88 | 7.30 | 14.60 | 173 | 0.29 |
| Neonatal nurse | 85 | 0 | 10.70 | 88 | 0 | 53.50 | 173 | 0.37 |
| HV | 85 | 129.60 | 148.50 | 88 | 129.60 | 125.28 | 173 | 0.98 |
| Out of hours | 85 | 0 | 0 | 88 | 0 | 0 | 173 | 0.14 |
| Walk-in centre | 85 | 0 | 0 | 88 | 0 | 0 | 173 | 0.34 |
| Number of contacts, of all types, with community health professional over 8 weeks | 83 | 9 times | 5 times | 86 | 8 times | 7 times | 169 | 0.10 |
FIGURE 20.
Number of contacts with community health professionals by phase.
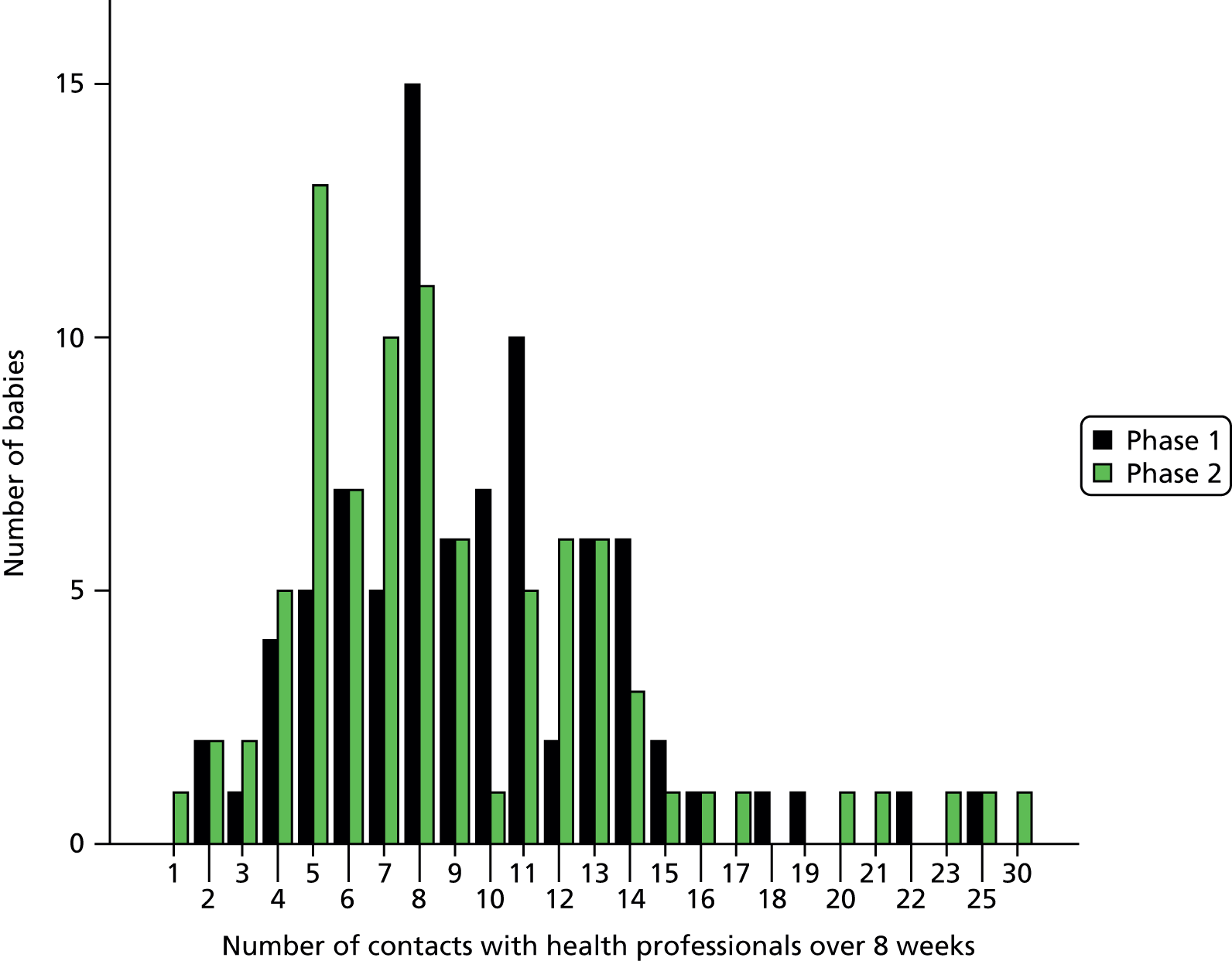
Summary
Health-economic data were available for 66% and 75% of cases in phases 1 and 2, respectively. There were no significant differences in inpatient readmissions, outpatient appointments or use of primary care health services between the two phases.
A similar number of infants visited out-of-hours EDs in each phase, but there was a significant difference in the number of visits, with fewer infant attendances to ED in phase 2 (and associated costs) after the introduction of the Train-to-Home package.
Chapter 8 Discussion and conclusions
Discussion
Parents were overwhelmingly positive about the Train-to-Home package. They described feelings of being given hope, feeling in control, and having something visual to show their baby’s progress. They spoke about the involvement of fathers and families, how predicted discharge dates helped them prepare for home and the ways staff engaged with the materials when communicating with them. Staff reactions were mixed: one LNU was very positive and, in other LNUs, more junior nurses and special care staff were more ready to engage with the principles. Medical staff in all four LNUs were positive about the intervention, as it helped them to communicate better with parents.
Nursing staff mentioned the NHS discharge planning initiative and that the Train-to-Home package fitted well with this approach. Some units have started to focus on where babies are in their gestational developmental journey and our approach seemed to fit well with this. Optimum delivery of the package was hampered by a lack of cascade training to inform staff who were not able to attend the preparatory training sessions. It appears that more time was needed to embed the materials into each LNU and, without this period of normalisation, some staff were uncertain about using the package.
There was no identifiable overall increase in parental confidence in caring for their baby when discharged home (as assessed by the PMPS-E score) after the introduction of the Train-to-Home package in the four study LNUs. A slight increase in PMPS-E scores in the three LNUs in which staff engaged with the package did not reach statistical significance.
Once home, parents’ unplanned use of EDs significantly decreased in the 8 weeks post discharge after the package was introduced in the LNUs, which resulted in a significant reduction in ED costs for the post-intervention group of babies. This is particularly notable in view of an increase in ED attendances nationally over this period, which coincided with the introduction of the ‘111 out of hours’ service, which encouraged more callers to attend ED.
Length of stay for babies in the post-intervention phase increased slightly but not significantly. However, during this phase all of the LNUs were working towards gaining full WHO/UNICEF Baby Friendly Initiative accreditation and were encouraging and supporting mothers to go home breastfeeding. This was confirmed in our study, when fewer babies in phase 2 went home being exclusively bottle-fed with formula and more babies went home mixed fed by breast and bottle. Breastfeeding is more difficult for these preterm babies and is often a reason for a longer stay while mothers and babies learn how to breastfeed.
Comparison with other studies
Relatively few studies have investigated parent-centred approaches to improving parental involvement in the care of their babies while in neonatal care. We are not aware of any studies that have systematically attempted to assess the impact of such an intervention on parental self-efficacy or babies’ LOS.
In the McMaster University study, Gaal et al. 43 observed that a major barrier to effective implementation of the intervention was a ‘failure of physician endorsement through action’. She noted that ‘the neonatologists supported the committee’s efforts, readily shared personal philosophies and practices, and yet remained disengaged from incorporating the train into daily bedside management rounds’.
In our study we found that the consultant medical staff supported the principles underpinning the intervention and were enthusiastic about the study aims and objectives. However, they identified reluctance from nursing staff to engage fully with the intervention and they were unwilling to promote it when nurses were unenthusiastic.
Nursing staff feedback confirmed this. Some of the more experienced nurses did not consider that the intervention materials were significantly different from what they already did for parent education and preparation for home. This echoes the findings of Gaal et al. 43 – that some ‘staff saw the discharge planning pathway as a barrier because of its perceived redundancy’.
Some of these implementation difficulties were recognised by parents, who reported nursing staff ambivalence about the intervention. Parents found the intervention helpful, informative and reassuring as they became more engaged and involved in understanding their baby’s progress through the LNU.
Family-centred care and planning for discharge has been emphasised for several years in Department of Health Neonatal Toolkit documents,6 NICE guidance25 and in the POPPY systematic review. 21 Despite this rhetoric around family-centred care in neonatal units, discharge processes continue to be reactive and poorly planned. 24,27 A recent study in NICUs in England showed that mothers did not report positive family-centred practices. 27 Mothers experienced a state of liminality (a state of uncertainty or ambiguity about their role) and were acutely sensitive to inconsistencies in care. They formed deferential relationships with health professionals and remained in a state of anxious surveillance. 27 The study concludes that it is important to minimise the consequences of the liminal experience in the NICU, improve staff–mother interactions and facilitate mothers’ opportunities to be primary caregivers. 27 Our study implemented a family-centred care package and, where it was adopted by the staff, changes were seen in parental confidence in caring for their baby by the time they left the neonatal unit and in the weeks following discharge home.
Dunn et al. 48 developed a web-based family care map to support family-based care practices in neonatal units in New England, USA. Their web-based tool was felt to be the ideal medium to assist individual care providers and family advisors to provide comprehensive family-centred care to infants and families. They concluded that implementation of the family-centred care map had the potential to affect positively the quality of newborn intensive care and lead to improved long-term outcomes. 48 Our Train-to-Home package would also be enhanced by being web-based, to enable staff and parents to access the parent pathways to facilitate parent communication with staff. It would help parents to ask pertinent questions and promote discussion to increase their confidence about taking their baby home after their extended stay in hospital.
Maternal self-efficacy studies have explored the associations with future maternal behaviour. 33,36 Our study measured maternal self-efficacy at three time points and, although there were no significant changes in measured maternal self-efficacy using the PMPS-E, parents reported feeling more confident and better informed about how to care for their babies in phase 2. This is supported by the observed reduction in unplanned ED attendances. This is an important finding, as reducing ED use can save money for the NHS.
Working with the Parent Advisory Group and Clinicians Advisory Group
Our PAG initially comprised eight mothers with experience of a baby in neonatal care and they were very helpful in designing the parent-focused materials. Their contribution to the Delphi process in the development of the study documentation was invaluable. We managed to keep contact with five of them throughout the study, but the other three moved away from Bristol and were not able to attend. Their interest and involvement with the study progress helped to keep the parent perspective firmly in mind when discussing recruitment difficulties and interpreting the findings of the interviews. Their contributions to Project Steering Group meetings were also very valuable.
Clinicians Advisory Group meetings provided a lively discussion forum for developing and refining the intervention materials, and contributions made by the members of this group were central to the development of the study documentation. The Delphi process undertaken to develop and refine the study materials was time-consuming and we are particularly grateful to the members of the CAG for their enthusiastic involvement in this process.
Implications for practice
This study has shown that the use of the infant’s EDD as the basis for estimating when a preterm infant is likely to go home from hospital is no longer appropriate: almost all infants go home considerably earlier than this. The continued reliance on the EDD as a guide to the likely discharge date is a contributory factor in the lack of well-organised and parent-orientated preparation for home in some neonatal units.
Staff concerns that giving parents an initial estimated date for discharge that might be delayed would cause increased parental anxieties were not borne out by the opinions expressed by the parents in this study. Parents reported that they could easily understand and accept that not every baby would go home exactly on the estimated date, and that problems arising during the hospital stay might lead to delay. Parents were very clear that they welcomed partnership working with the professionals and needed to be informed about their baby’s likely discharge date. They reported that a discussion of the types of problems and questions that might arise at each stage of their baby’s pathway through the neonatal unit was a positive and helpful experience.
Implications for future research
The professional approaches and practices in neonatal units are deeply embedded, and in a specialty in which clinical practice is changing extremely rapidly the retention of such embedded standards and approaches is likely to be very important for staff self-confidence. The Train-to-Home intervention was perceived by some staff (particularly experienced nursing staff) as potentially threatening to these deeply embedded standards. However, others clearly understood and embraced the family-centred care principles. It was also interesting that, for some of the less-experienced staff, the use of the intervention materials was found to be helpful in facilitating explanations of complex concepts and changes in the babies’ clinical conditions to parents.
Future research interventions that seek to make changes in the ways in which nursing staff interact and communicate with parents in neonatal units will require a long period of implementation and routine use before the possible effects of such changes can be assessed or measured. Difficulties that inevitably arise when busy nurses, whose priorities must be to clinical care, are asked to adopt different approaches to communicating with parents, and to spend time teaching parents about a tool (Train-to-Home) must be recognised in any future similar interventions.
Attempts to change communication practices in neonatal units should involve parents as the agents for change, as we showed that, even at times of extreme emotional stress and rapid change, parents will engage positively with an interactive process of data collection and will enthusiastically contribute their experiences. Although fathers were much less involved with the data collection in this study than mothers, they, and the wider family, are important and should not be ignored. This study is the first one to use the PMPS-E tool to measure self-efficacy in both mothers and fathers, and our data, although limited, suggest that this tool is appropriate for use with fathers as well as mothers.
Many parents spontaneously asked if the Train-to-Home package was available as an online tool, and some used their mobile phones to photograph the documentation at each stage to send to their extended families and friends as a way of informing them of their baby’s progress. This suggests that further development and implementation of the Train-to-Home package would best be achieved by the use of a web-based approach with mobile phone access, so that parents could more easily engage with, and make use of, the package as part of their involvement in the care of their baby in hospital and their preparation for discharge home.
Strengths and weaknesses of this study
Strengths
Despite involving families with very young preterm infants, at a time when they were under considerable stress, there was a high level of involvement and commitment to the study by those families taking part.
The level of patient and public involvement – particularly in the development and implementation of the intervention – was high, with a PAG being actively involved at all stages.
The development of the intervention involved staff input from all of the four neonatal units taking part in the study. This ensured that the intervention materials were compatible with existing protocols and practices in all participating units.
The four neonatal units involved were self-selected, all having approached the research team in response to publicity about the proposed implementation of the intervention.
The holistic approach used ensured that we identified a wide range of effects of the intervention, on both staff and families.
Limitations
Despite the involvement of staff in the participating units from an early stage we experienced difficulty in some of the units in obtaining full engagement with the nursing staff. Many of the nursing staff showed poor understanding of the difference between the intervention and the research. These issues may have been related to poor cascading systems for changes in practice. Cascading of learning about the intervention in some of the participating units was patchy and limited, and a longer period of time to embed the intervention into practice would have been helpful.
The use of ‘nurse champions’ recruited from the LNU staff (and funded via the Clinical Research Network) did not work well, as not all had volunteered for this role, and clinical requirements were a much higher priority for all of the nurses involved.
As a consequence of the limited time availability of the nurse champions, there was commonly some delay in obtaining assent from families, which led to variation in timing of the initial PMPS-E questionnaires. This may have been an important contributory effect in the lack of identifiable changes in this measure. It also highlights a significant limitation of using such a measure without dedicated research staff to ensure prompt and effective data collection.
In common with most studies involving families from wide socioeconomic backgrounds, recruitment of families from the more-deprived groups was lower than from the less-deprived groups.
Conclusions
This study has shown that the use of a parent-orientated approach to communication with parents and informing parents about the needs and progress of their preterm infant in hospital is both practical and welcomed by parents and many staff. This approach meets the recommended prioritisation of family-centred care for such families. The predicted discharge dates helped parents prepare for home and the ways that staff engaged with the materials when communicating with them helped them feel more confident, as well as having something visual to show their baby’s progress.
There was similar improvement in the maternal self-efficacy scores from baseline to going home in both study phases. Although this was slightly greater in phase 2, this difference was not statistically significant. A similar number of infants visited out-of-hours EDs in each phase, but there was a significant difference in the number of visits, with fewer infant attendances to ED in phase 2 after the introduction of the Train-to-Home package. This is the first intervention that has been associated with such a change, and is particularly notable in view of an increase in ED attendances nationally over this period, which coincided with the introduction of the ‘111 out-of-hours’ service. Although it is important to be cautious in the interpretation of this change, given the relatively small number of infants involved, this observation offers the possibility that the use of such interventions might have direct beneficial effects on the use of out-of-hours NHS resources.
There was no significant change in LOS, although more than half the infants went home at > 3 weeks before their EDD in both phases. During phase 2, all the LNUs were working towards gaining full WHO/UNICEF Baby Friendly Initiative accreditation and were encouraging and supporting mothers to go home breastfeeding, as reflected by the increased proportion of infants’ breastfeeding at discharge in phase 2. This could also have contributed to slightly increased LOS.
Few studies have investigated parent-centred approaches to improving parental involvement in the care of their babies while in neonatal care. We are not aware of any studies that have systematically attempted to assess the impact of such an intervention on parental self-efficacy or babies’ LOS.
Although our initial primary outcome measure did not show any significant differences, the improvement in preparedness for discharge home reported by the parents, and the measured reduction in ED attendances suggests that the intervention had significant benefits. This approach to educating and involving parents in the care and needs of their preterm baby in hospital has potential value and warrants further study and more widespread adoption.
Acknowledgements
Contributions of authors
Dr Jennifer Ingram [senior research fellow (co-principal investigator)] contributed to the original study design, directed the project and supervised project team members jointly with Professor Peter Fleming, helped to develop the Train-to-Home intervention materials, led the qualitative work (interviews and staff focus groups) and analyses, and drafted the final report.
Dr Peter S Blair (reader in medical statistics) contributed to the original study design, supervised data cleaning and conducted all quantitative statistical analyses.
Professor Jane E Powell (Professor of Public Health Economics) contributed to the original study design, developed the health-economic measures used in the study, supervised data entry of health-economic data, and conducted the health-economic analyses.
Dr Sarah Manns (research fellow) contributed to the original study design, carried out the literature searches, visited the Canadian neonatal units, helped to design the interventions used in this study, made regular visits to LNUs to encourage participation, and conducted and helped with data analysis of qualitative interviews with parents.
Heather Burden (lead neonatal network nurse) helped to develop the interventions used in this study, led the nursing teaching in the implementation of the interventions, and helped to ensure that the interventions were appropriately used in the participating units.
Professor David Pontin (Professor of Community Health) contributed to the original study design, gave expert HV input to the study management group, and contributed to the analysis of qualitative interviews.
Dr Margaret Redshaw (senior research fellow) contributed to the original study design, provided social science expert input to the project management group and advised on the qualitative analyses.
Lucy Beasant (research associate) made regular visits to LNUs to encourage participation, and conducted and helped with data analysis of qualitative interviews with parents.
Dr Claire Rose (Consultant Neonatologist) provided neonatology expertise in the original study design and was a member of the project management group.
Deborah Johnson (study co-ordinator) managed the project, supervised data collection and input, helped to develop the databases used, conducted telephone follow-up of parents and assisted with staff focus groups.
Daisy Gaunt (research assistant) conducted the multiple imputation analysis and assisted in the interpretation of the statistical analysis.
Professor Peter Fleming [Professor of Infant Health and Developmental Physiology (co-principal investigator)] led the original development of the study design, supervised members of the research team jointly with Jennifer Ingram, led the development of the Train-to-Home intervention materials, conducted the Delphi process to refine the intervention materials, collected and analysed the data from BadgerNet to identify and quantify LOS to predict expected dates of discharge used in phase 2, developed the teaching materials for implementation of the interventions and led the staff teaching for the Train-to-Home package.
All of the authors contributed to, have read, and are happy to be identified as contributing authors of, the final report of this study.
Other acknowledgements
We are very grateful to Rosie Thompson for her help setting up the study and during phase 1; Kay Pullen for her advice when developing the intervention; Sarah Wain for expertise and contributions to the parent pathways; and Jane Wathen for graphic design of the intervention materials.
We would also like to thank all the parents and neonatal staff who were involved in the study.
We are very appreciative of the valuable contributions from members of the PAG, CAG and Trial Steering Group.
This report presents independent research commissioned by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the Health Services and Delivery Research programme or the Department of Health. The views and opinions expressed by the interviewees in this publication are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, MRC, CCF, NETSCC, the Health Services and Delivery Research programme or the Department of Health.
Data sharing statement
Enquires related to potential data sharing should be addressed to the corresponding author.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
References
- Office for National Statistics (ONS) . Data for 2007–2008 n.d. www.statistics.gov.uk/downloads/theme_health/gestation-spec-infant-mort-tables-07-08.xls#Table3!A1 (accessed 4 July 2011).
- Boykova M, Kenner C. International connections: transition from hospital to home: post-neonatal intensive care unit discharge: a global perspective. Newborn Infant Nurs Rev 2012;12:184-6. http://dx.doi.org/10.1053/j.nainr.2012.09.004.
- McGrath J. Strategies to support the transition to home. J Perinat Neonat Nurs 2012;26:8-9. http://dx.doi.org/10.1097/JPN.0b013e3182437255.
- Smith V, Young S, Pursley D, McCormick M, Zupancic J. Are families prepared for discharge from the NICU?. J Perinatol 2009;29:623-9. http://dx.doi.org/10.1038/jp.2009.58.
- Moyer VA, Papile L-A, Eichenwald C, Giardino A, Khan M, Singh H. An intervention to improve transitions from NICU to ambulatory care: quasi-experimental study. BMJ Qual Saf 2013;23. http://dx.doi.org/10.1136/bmjqs-2012-001726.
- Toolkit for High-Quality Neonatal Services. London: DH; 2009.
- Rose C, Ramsay L, Leaf A. Strategies for getting preterm infants home earlier. Arch Dis Child 2008;93:271-3. http://dx.doi.org/10.1136/adc.2005.093039.
- Chance of a Lifetime? Bliss Baby Report. London: Bliss; 2010.
- Standards for Hospitals Providing Neonatal Intensive and High Dependency Care. London: BAPM; 2001.
- Service Standards for Hospitals Providing Neonatal Care. London: BAPM; 2010.
- Petrou S, Khan K. Economic costs associated with moderate and late pre-term birth: primary and secondary evidence. Semin Fetal Neonatal Med 2012;17:170-8. http://dx.doi.org/10.1016/j.siny.2012.02.001.
- Clements K, Barfield W, Ayadi M, Wilber N. Preterm birth-associated cost of early intervention services: an analysis by gestational age. Pediatrics 2007;119:e866-74. http://dx.doi.org/10.1542/peds.2006-1729.
- Mangham K, Hall C, Jackson E, Owens O, Mahadevia P. The cost of pre-term birth throughout childhood in England and Wales. Pediatrics 2009;123:e312-27. http://dx.doi.org/10.1542/peds.2008-1827.
- Johnston K, Gooch K, Korol E, Vo P, Eyawo O, Bradt P, et al. The economic burden of prematurity in Canada. BMC Pediatrics 2014;14. http://dx.doi.org/10.1186/1471-2431-14-93.
- Craig I, Adams C. Survey shows ongoing crisis in health visiting. Community Pract 2007;80:50-3.
- Glazebrook C, Marlow N, Israel C, Croudace T, Johnson S, White I. Randomised trial of a parenting intervention during neonatal intensive care. Arch Dis Child Fetal Neonatal Ed 2007;92:F438-43. http://dx.doi.org/10.1136/adc.2006.103135.
- Melnyk B, Feinstein N, Alpert-Gillish L, Fairbanks E, Crean H, Sinkin R. Reducing premature infants’ length of stay and improving parents’ mental health outcomes with the Creating Opportunities for Parent Empowerment (COPE) Neonatal Intensive Care Unit Program: a randomised controlled trial. Pediatrics 2006;118:e1414-27. http://dx.doi.org/10.1542/peds.2005-2580.
- Van Der Pal S, Maguire C, Le Cessie S, Wit J, Walther F, Bruil J. Parental experiences during the first period at the neonatal unit after two developmental care interventions. Acta Paediatr 2007;96:1611-16. http://dx.doi.org/10.1111/j.1651-2227.2007.00487.x.
- Wielenga JM, Smith BJ, Unk LK. How satisfied are parents supported by nurses with the NIDCAP model of care for their preterm infant?. J Nurs Care Qual 2006;21:41-8. http://dx.doi.org/10.1097/00001786-200601000-00010.
- Hesselink G, Flink M, Olsson M, Barach P, Dudzik-Urbaniak E, Orrego C. Are patients discharged with care? A qualitative study of perceptions and experiences of patients, family members and care providers. BMJ Qual Saf 2012;21:39-4. http://dx.doi.org/10.1136/bmjqs-2012-001165.
- Brett J, Staniszewska S, Newburn M, Jones N, Taylor L. A systematic mapping review of effective interventions for communicating with, supporting and providing information to parents of preterm infants. BMJ Open 2011;1. http://dx.doi.org/10.1136/bmjopen-2010-000023.
- Garfield C, Lee Y, Kim HN. Paternal and Maternal Concerns for their very low-birth-weight infants transitioning from the NICU to home. J Perinat Neonat Nurs 2014;28:305-12. http://dx.doi.org/10.1097/JPN.0000000000000021.
- Jefferies AL. Going home: facilitating discharge of the preterm infant. Paediatr Child Health 2014;19:31-42.
- Redshaw M, Hamilton K. Family centred care? Facilities, information and support for parents in UK neonatal units. Arch Dis Child Fetal Neonatal Ed 2010;95:F365-8. http://dx.doi.org/10.1136/adc.2009.163717.
- Specialist Neonatal Care Quality Standard. London: NICE; 2010.
- Raines D. Mothers’ stressor as the day of discharge from the NICU approaches. Adv Neonatal Care 2013;13:181-7. http://dx.doi.org/10.1097/ANC.0b013e318285fa2a.
- Finlayson K, Dixon A, Smith C, Dykes F, Flacking R. Mothers’ perceptions of family centred care in neonatal intensive care units. Sex Reprod Healthc 2014;5:119-24. http://dx.doi.org/10.1016/j.srhc.2014.06.003.
- Zamanzadeh V, Namnabati M, Valizadeh L, Badiee Z. Mothers’ experiences of infants discharge in Iranian NICU culture: a qualitative study. Adv Neonatal Care 2013;13:E1-7. http://dx.doi.org/10.1097/ANC.0b013e318281e06a.
- Forsythe P, Maher R, Kirchick C, Bieda A. Safe discharge for infants with high-risk home environments. Adv Neonatal Care 2007;7:69-75. http://dx.doi.org/10.1097/01.ANC.0000267910.73973.f1.
- Raikes H, Thompson R. Efficacy and social support as predictors of parenting stress among families in poverty. Inf Mental Hlth J 2005;26:177-90. http://dx.doi.org/10.1002/imhj.20044.
- Hess C, Teti D, Hussey-Gardner B. Self-efficacy and parenting of high risk infants: the moderating role of parent knowledge of infant development. J Appl Dev Psychol 2004;25:423-37. http://dx.doi.org/10.1016/j.appdev.2004.06.002.
- Jones T, Prinz R. Potential roles of parental self-efficacy in parent and child adjustment: a review. Clin Psychol Rev 2005;25:341-63. http://dx.doi.org/10.1016/j.cpr.2004.12.004.
- Teti D, Gelfand D. Behavioural competence among mothers of infants in the first year: the mediational role of maternal self-efficacy. Child Dev 1991;62:918-29. http://dx.doi.org/10.2307/1131143.
- Gross D, Rocissano L, Roncoli M. Maternal confidence during toddlerhood: comparing preterm and fullterm groups. Res Nurs Health 1989;12:1-9. http://dx.doi.org/10.1002/nur.4770120103.
- Reich S, Bickman L, Heflinger C. Covariates of self-efficacy: caregiver characteristics related to mental health services self-efficacy. J Emot Behav Disord 2004;12:99-108. http://dx.doi.org/10.1177/10634266040120020401.
- Leerkes E, Crockenberg S. The development of maternal self-efficacy and its impact on maternal behaviour. Infancy 2002;3:227-47. http://dx.doi.org/10.1207/S15327078IN0302_7.
- Bandura A. Toward a unifying theory of behavioral change. Psychol Rev 1977;84:191-215. http://dx.doi.org/10.1037/0033-295X.84.2.191.
- Bandura A. Self-efficacy: The Exercise of Control. New York, NY: WH Freeman; 1997.
- Bandura A. On the functional properties of perceived self-efficacy revisited. J Manag 2012;38:9-44. http://dx.doi.org/10.1177/0149206311410606.
- Dennis C, Faux S. Development and psychometric testing of the breastfeeding self-efficacy scale. Res Nurs Health 1999;22:399-40. http://dx.doi.org/10.1002/(SICI)1098-240X(199910)22:5<399::AID-NUR6>3.0.CO;2-4.
- Lowe N. Maternal confidence for labour: development of the childbirth self-efficacy inventory. Res Nurs Health 1993;16:141-9. http://dx.doi.org/10.1002/nur.4770160209.
- Barnes C, Adamson-Macedo E. Perceived Maternal Parenting Self-Efficacy (PMP S-E) tool: development and validation with mothers of hospitalised preterm neonates. J Adv Nurs 2007;60:550-60. http://dx.doi.org/10.1111/j.1365-2648.2007.04445.x.
- Gaal B, Blatz S, Dix J, Jennings B. Discharge planning utilising the discharge train. Adv Neonatal Care 2008;1:42-55. http://dx.doi.org/10.1097/01.ANC.0000311016.94381.21.
- Barnes C. Cognitive, Emotional and Environmental Mediators of Early Parenting in High Risk Families. 2007.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psycho 2006;3:77-101. http://dx.doi.org/10.1191/1478088706qp063oa.
- Ridyard C, Hughes D. Methods for the collection of resource use data within clinical trials: a systematic review of trials funded by the UK Health Technology Assessment programme. Value Health 2010;13:867-72. http://dx.doi.org/10.1111/j.1524-4733.2010.00788.x.
- Curtis L. Unit Costs of Health and Social Care 2014. Canterbury: PSSRU, University of Kent; 2014.
- Dunn MS, Reilly MC, Johnston AM, Hoopes RDJ, Abraham MR. Development and dissemination of potentially better practices for the provision of family-centred care in neonatology: the family-centred care map. Pediatrics 2006;118:95-107. http://dx.doi.org/10.1542/peds.2006-0913F.
- NHS Reference Costs 2011–12. London: DH; 2012.
Appendix 1 The UK adaptation of the ‘Train-to-Home’ package and supporting documentation
Appendix 2 Final version of the tool for estimating likely date of discharge as used in the study
Estimating the probable date of discharge for babies
1. Babies born at 27–30 weeks’ gestation
In the first week after birth, estimate the likely discharge date, as shown in Table 29.
| Gestation at birth | Suggested initial range for estimated date of discharge (in weeks from the date of birth) | Example | |
|---|---|---|---|
| DOB | Initial range for estimated date of discharge | ||
| 27 weeks | 8–10 weeks | 1 October | 26 November – 10 December |
| 28 weeks | 7–9 weeks | ||
| 29 weeks | 6–8 weeks | ||
| 30 weeks | 5–7 weeks | ||
Then adjust the estimated date of discharge according to the baby’s progress and condition as follows:
-
second or third week after birth: aim to narrow the range of dates slightly to a 5- to 7-day range.
-
by 1 month: aim to narrow the range further to 2–4 days.
2. Babies born at 31–33 weeks’ gestation
For these more mature babies it is may be easier to calculate the estimated date of discharge in days from the date of birth.
In the first week after birth: estimate the likely date of discharge as shown in Table 30.
| Gestation at birth | Suggested initial range for estimated date of discharge in days from the date of birth (weeks given in brackets) | Example | |
|---|---|---|---|
| DOB | Initial range for estimated date of discharge | ||
| 31 weeks | 32–37 days (4 weeks 4 days–5 weeks 2 days) | 1 October | 25 October – 29 October |
| 32 weeks | 23–28 days (3 weeks 2 days–4 weeks 0 days) | ||
| 33 weeks | 16–21 days (2 weeks 2 days–3 weeks 0 days) | ||
Adjust the likely date of discharge according to the baby’s progress and condition as follows:
-
second week: aim to reduce the range of dates
-
third week: aim to narrow the range further to 2–4 days.
How were these discharge dates calculated?
Data on all admissions and discharges of babies from 27 to 33 weeks’ gestation inclusive were collected from the four neonatal units involved in the study for a 2-year period (April 2011 to March 2013). The estimated LOS for each gestation given above are based upon these data and are for babies who go home directly rather than those who go home via a local Special Care Baby Unit (SCBU) (e.g. Barnstaple or Torbay). Transfer to a local SCBU usually occurs 1–2 weeks before discharge home.
(On the back of this sheet we printed a copy of the calendar for 2013 and 2014 to facilitate calculation of discharge dates.)
Appendix 3 Parents’ ‘Baby’s Journey’ booklets
Appendix 4 Training materials
PowerPoint presentation to neonatal staff
Slide 1

Slide 2
Slide 3
Slide 4
Slide 5
Slide 6
Slide 7
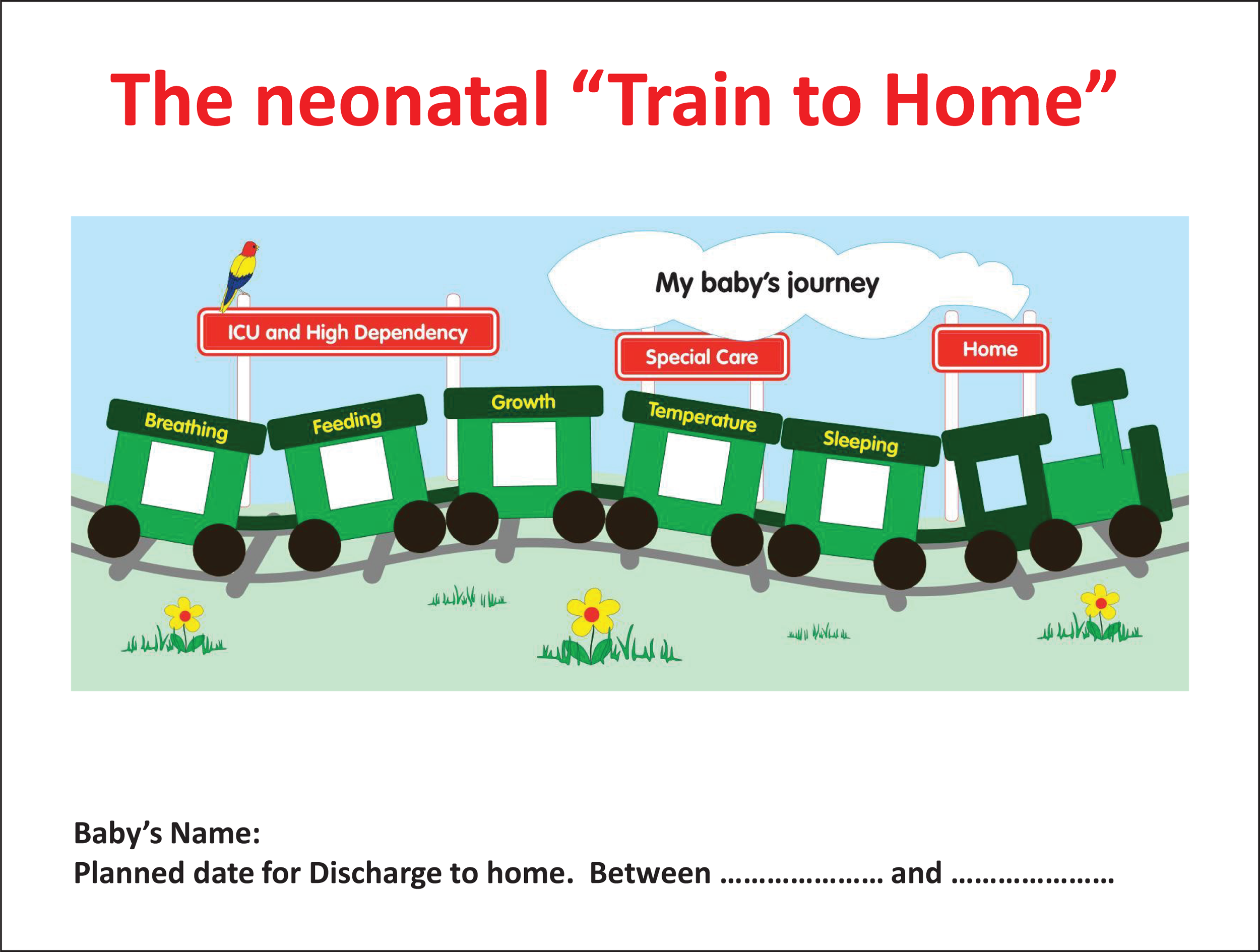
Slide 8
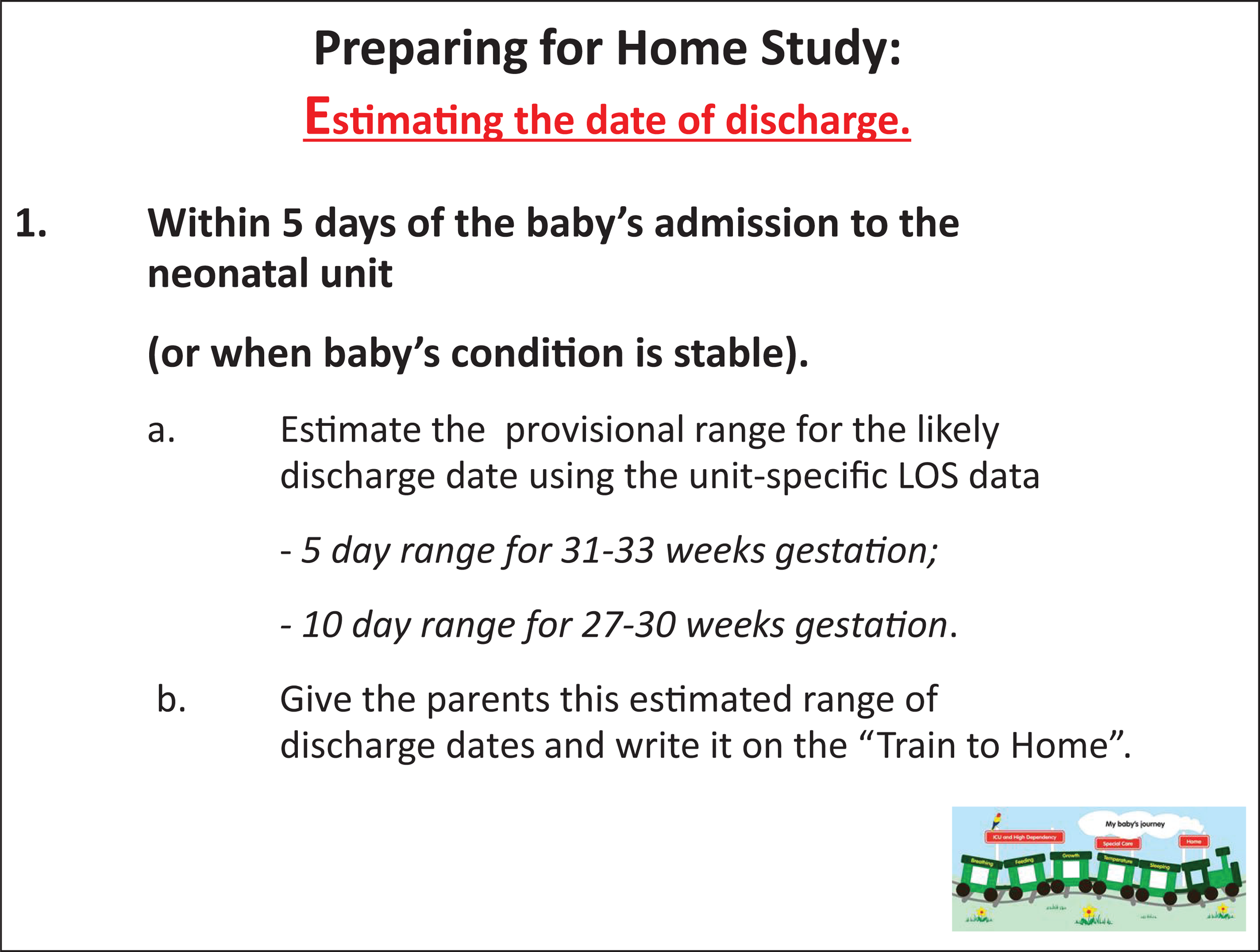
Slide 9
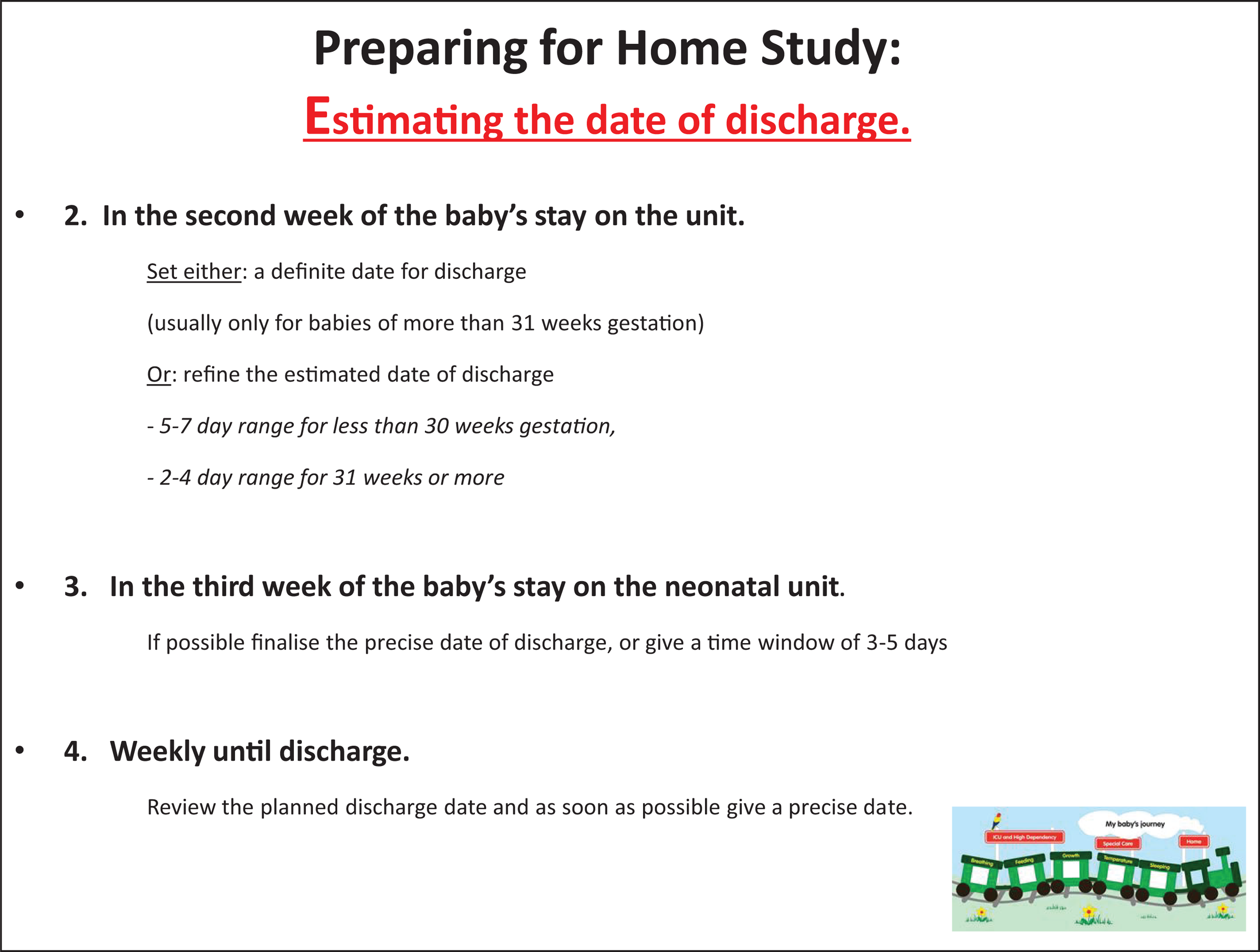
Slide 10
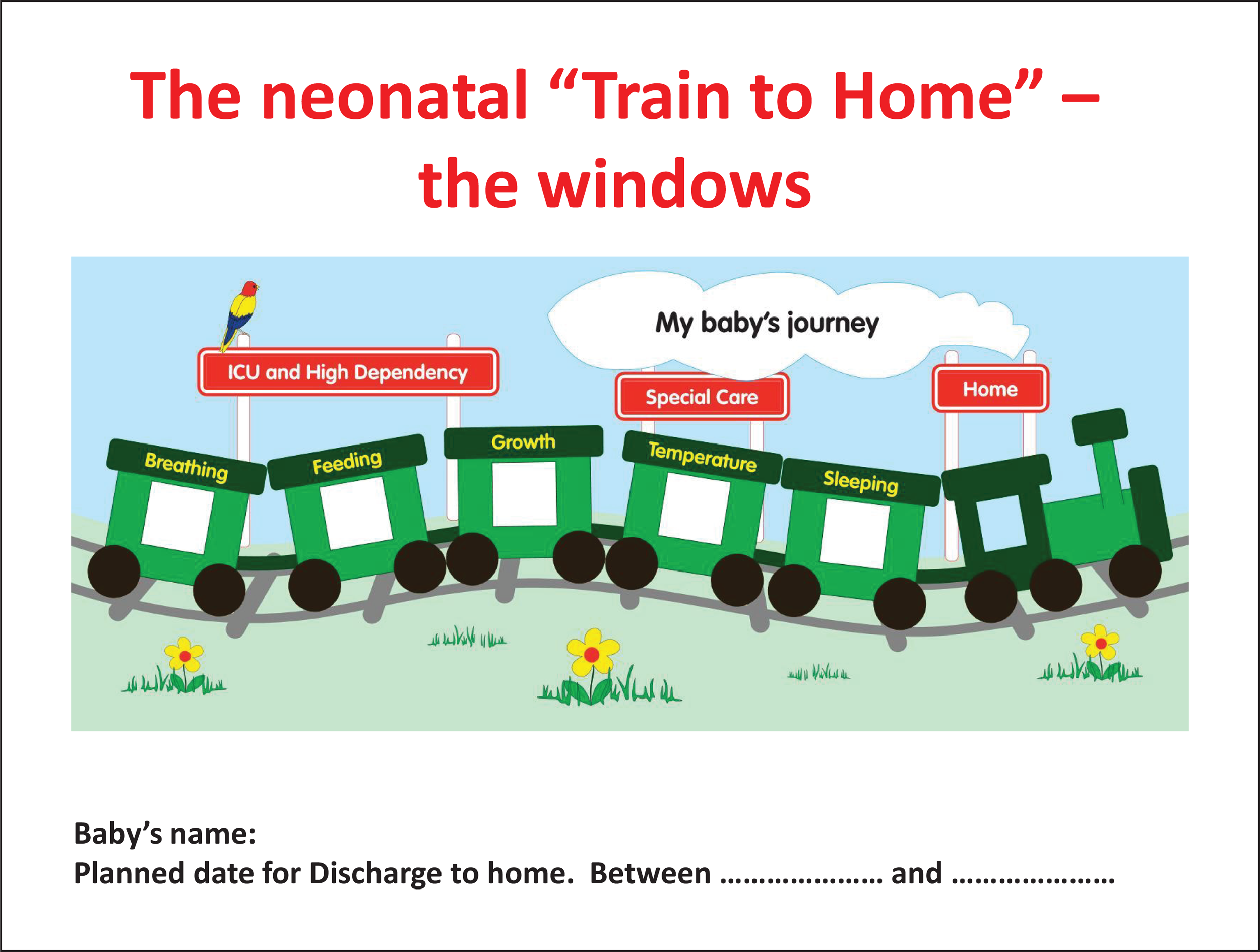
Slide 11

Slide 12
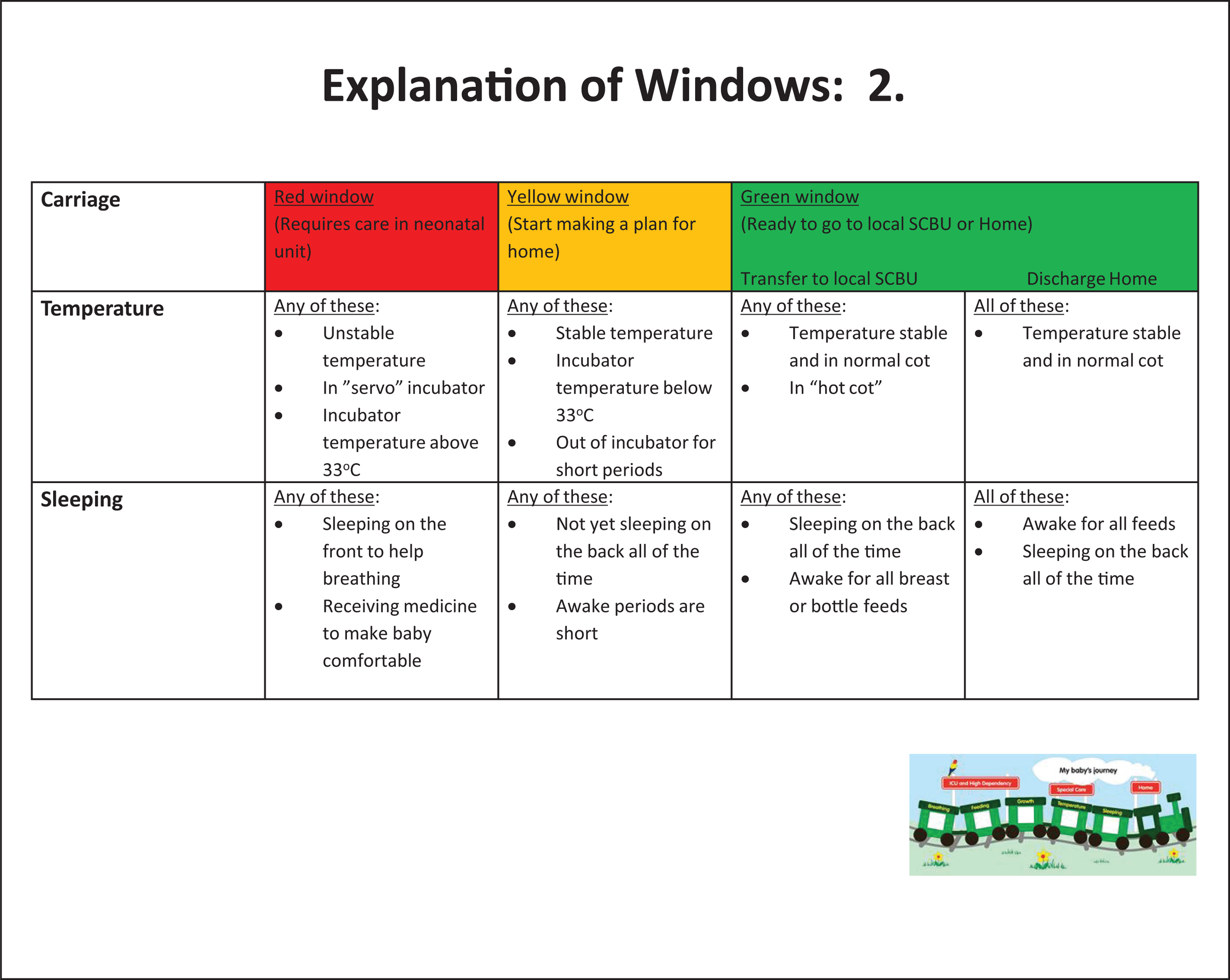
Slide 13
Slide 14
Slide 15
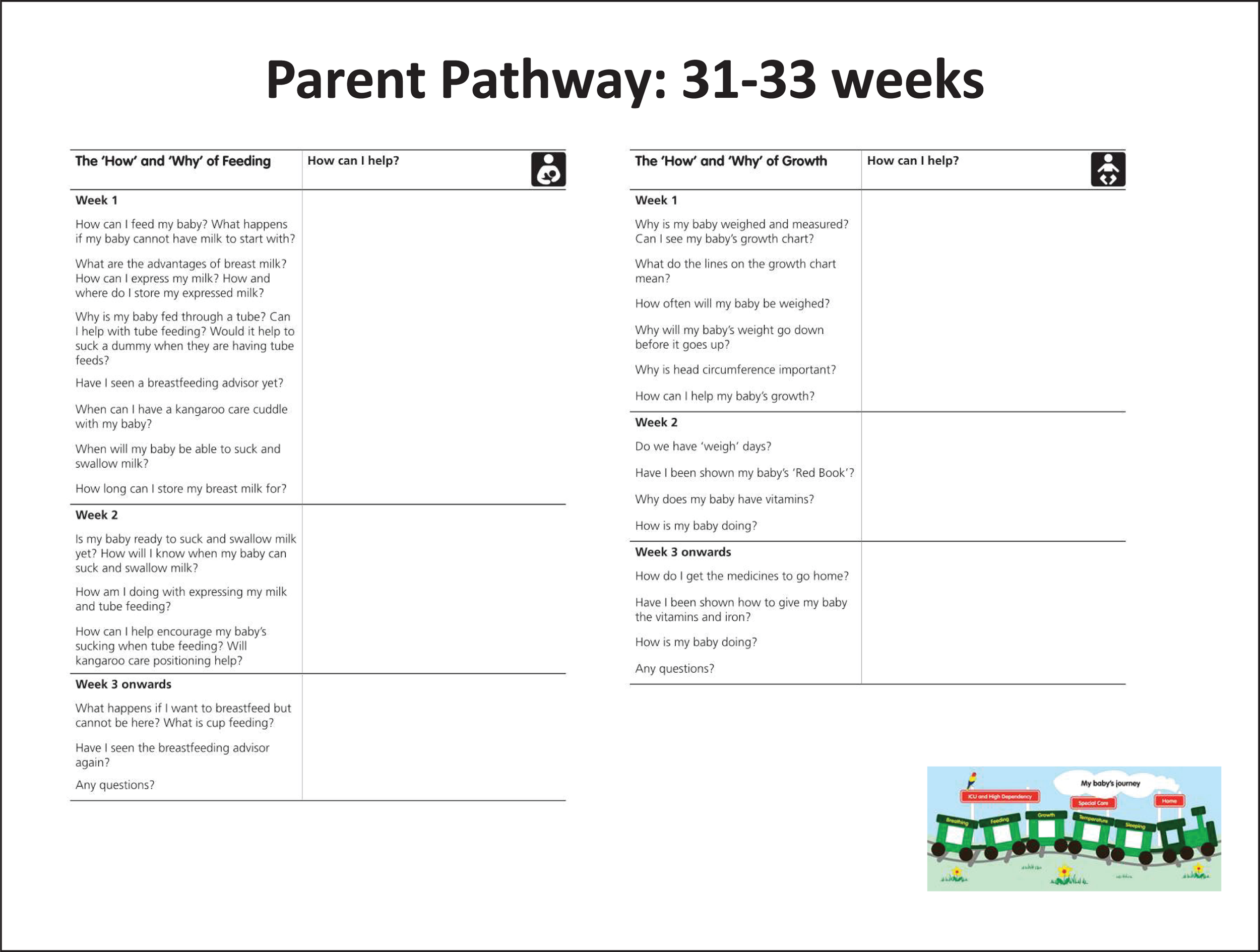
Slide 16
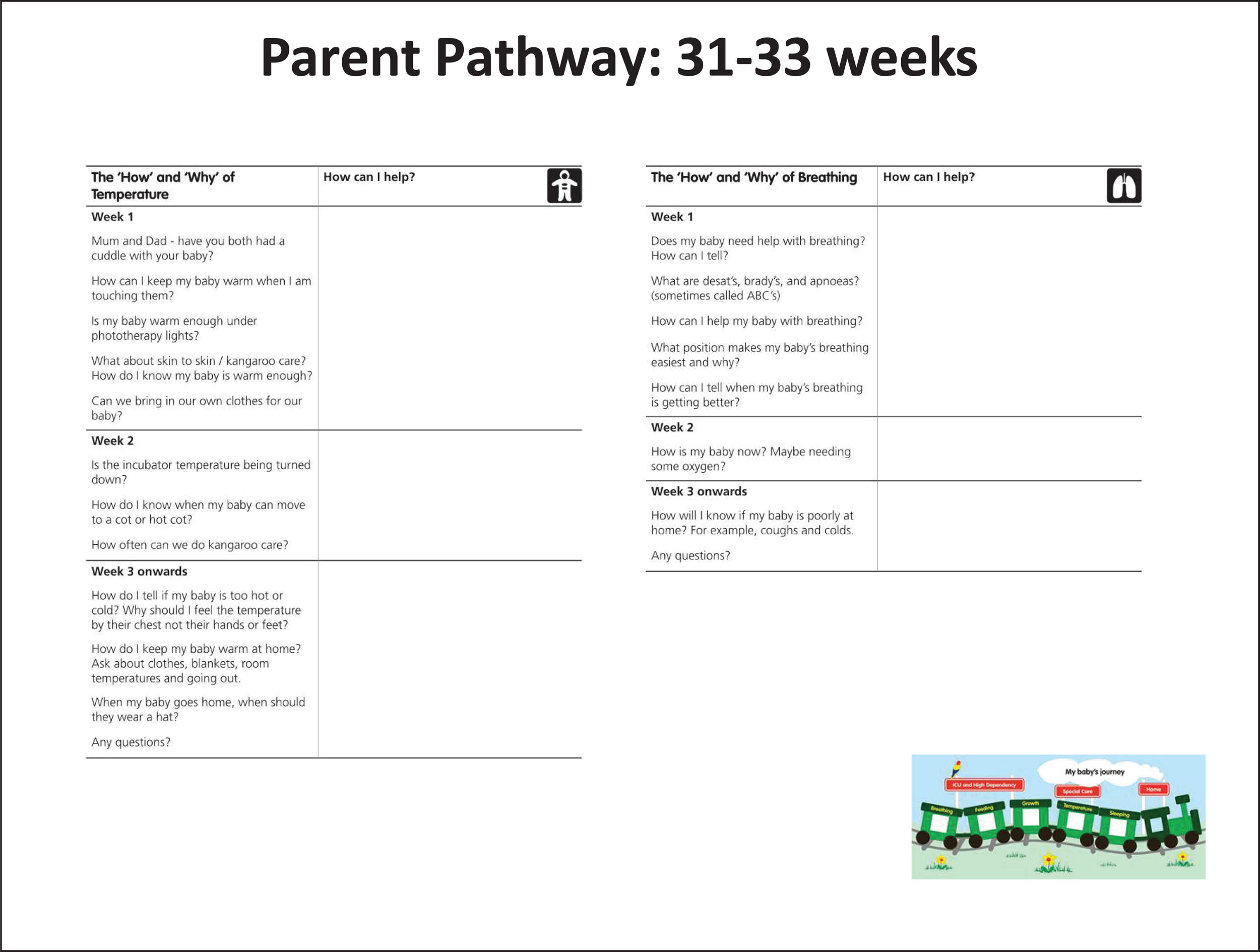
Slide 17

Slide 18
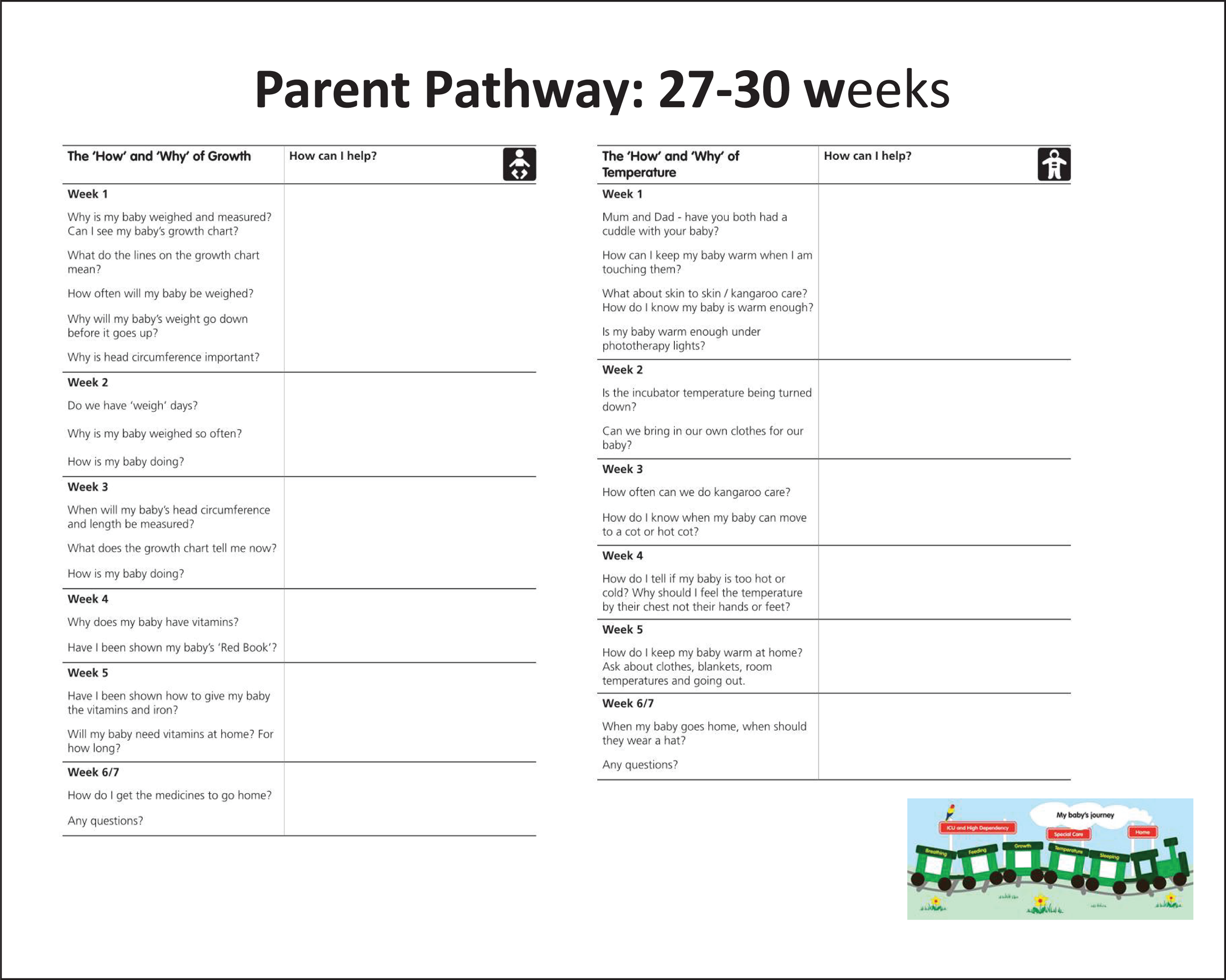
Slide 19

Slide 20
Slide 21
Appendix 5 The Perceived Maternal Parenting Self-Efficacy Questionnaire42
Appendix 6 Qualitative topic guides
Appendix 7 Health-care resource-use tool
Appendix 8 Assumptions, unit cost estimates and sources of prices to calculate costs of health resource use
| Description | Definition | Mean price/unit, pounds sterling 2014 prices | Source |
|---|---|---|---|
| Price of readmission to hospital after discharge | Inpatient – specialist palliative care (adults and children) Average cost per bed-day per patient-day All preterm babies Uplift to 2014 prices |
326 | Curtis,47 p. 111 |
| Price of hospital outpatient appointment for all preterm babies | Per attendance All preterm babies |
109 | Curtis,47 p. 111 |
| Price of hospital accident and emergency admission for all preterm babies | Per attendance All preterm babies Uplift to 2014 prices |
111 | Department of Health reference costs 2011–1249 |
| Price to see GP for 1 minute | Including direct care staff costs – with qualification costs Per minute of patient contact |
3.90 | Curtis,47 p. 195 |
| Price to telephone GP for 1 minute | Per telephone consultation lasting 7.1 minutes £28 | 3.94 | Curtis,47 p. 195 |
| Price to see or telephone practice nurse for 1 minute | £44 (£53) per hour of patient-related work | 0.73 | Curtis,47 p. 192 |
| Price to see or telephone neonatal outreach nurse for 1 minute | £64 (£74) per hour of patient-related work | 1.07 | Curtis,47 p. 190 |
| Price to see or telephone HV for 1 minute | £65 (£76) per hour of patient-related work | 1.08 | Curtis,47 p. 195 |
| Price to see out-of-hours doctor for 1 minute | Including direct care staff costs – with qualification costs Per minute of patient contact |
3.90 | Curtis,47 p. 195 |
| Price to go to walk-in centre for 1 minute | Including direct care staff costs – with qualification costs Per minute of patient contact |
3.90 | Curtis,47 p. 195 |
| Price to ring NHS 111 per minute | Price of call per minute from a BT landline | 0.40 | www.dbh.nhs.uk |
Variables for cost analysis
| Number | Variable | Variable description | Variable coding |
|---|---|---|---|
| 1 | Study_No | Identification of participant | Study number |
| 2 | Gestage | Degree of prematurity | 1 = 27–30 weeks 2 = 31–33 weeks |
| 3 | Group | Before or after parent pack intervention | 1 = phase 1 2 = phase 2 |
| 4 | Centre | Hospital setting | 1 = centre 1 2 = centre 2 3 = centre 3 4 = centre 4 |
| Q1. Has your child gone to hospital in the last 2 weeks? A funder perspective | |||
| 5 | Hosp_attend | Has your child gone to hospital in the last 2 weeks | 1 = yes 2 = no |
| 6 | HospIP_attend | Inpatient care attendance | 1 = yes 2 = no |
| 7 | HospIP_Reason | Reason why attended as inpatient | 1 = breathing/airway 2 = feeding/GI 3 = neurological 4 = infection |
| 8 | HospIP_Which | Which hospital attended as inpatient | Coded 1–7 |
| 9 | HospIPnumdays | Number of 24 hour stays in hospital | Number |
| 10 | Pricereadppd | Price per patient 24 hours All preterm babies |
Pounds sterling 2014 prices |
| 11 | Costreadppd | Cost per patient 24 hours All preterm babies |
Pounds sterling 2014 prices |
| 12 | HospOPattend | Outpatient hospital attendance | 1 = yes 2 = no |
| 13 | HospOPReason | Reason for attending as outpatient | 1 = medical 2 = imaging 3 = screening 4 = procedure |
| 14 | HospOP_Which | Which hospital attended as outpatient | Coded 1–11 |
| 15 | HospOP_Freqapp | Frequency of attendances at outpatients | Number |
| 16 | PriceOPattend | Price of hospital outpatient appointment All preterm babies |
Pounds sterling 2014 prices |
| 17 | CostOPattend | Cost of hospital outpatient appointment All preterm babies |
Pounds sterling 2014 prices |
| 18 | AE_attend | Attended A&E | 1 = yes 2 = no |
| 19 | AE_Reason | Reason for attending ED | 1 = breathing/airway 2 = feeding/GI 3 = infection 4 = other |
| 20 | AE_Which | Which attended ED | Coded 1–7 |
| 21 | AE_Freqattend | Frequency of attendance ED | Number |
| 22 | PriceAEattend | Price of hospital ED admission All preterm babies |
Pounds sterling 2014 prices |
| 23 | CostAEattend | Cost of hospital ED admission All preterm babies |
Pounds sterling 2014 prices |
| Q2. For each health service used by you for your baby in the last 2 weeks, approximately how much did it cost you and/or your family and relatives? A societal perspective and a family-carer perspective | |||
| 24 | HospInP_Car | As inpatient: cost of car | Pounds sterling 2014 prices |
| 25 | HospInP_Park | As inpatient: cost of parking | Pounds sterling 2014 prices |
| 26 | HospVisitTaxi | Hospital visit: cost of taxi | Pounds sterling 2014 prices |
| 27 | HospVisitPark | Hospital visit: parking fee | Pounds sterling 2014 prices |
| 28 | AEAttendTaxi | ED visit: cost of taxi | Pounds sterling 2014 prices |
| 29 | AEAttendCar | ED visit: car mileage | Number of miles |
| 30 | AEAttendPark | ED visit: parking fee | Pounds sterling 2014 prices |
| 31 | GPVisitCar | GP visit: car mileage | Pounds sterling 2014 prices |
| Q3. Please give details for any of the following services that you used for your baby outside hospital in the last two weeks – this should include all telephone contact. A funder and societal perspective | |||
| 32 | NosCon | Number of contacts of all types with health professionals over 8 weeks | Number |
| 33 | GPCost | Minutes’ GP contact, see and telephone Price 1 minute |
Pounds sterling 2014 prices |
| 34 | PNCost | Minutes’ practice nurse contact, see and telephone Price 1 minute |
Pounds sterling 2014 prices |
| 35 | NNCost | Minutes’ Neonatal Outreach Nurse contact, see and telephone Price 1 minute |
Pounds sterling 2014 prices |
| 36 | HVCost | Minutes’ Neonatal Outreach Nurse contact, see and telephone Price 1 minute |
Pounds sterling 2014 prices |
| 37 | OOHCost | Minutes’ contact out-of-hours doctor, see and telephone Price 1 minute |
Pounds sterling 2014 prices |
| 38 | WICost | Minutes’ contact walk-in centre Price of 1 minute |
Pounds sterling 2014 prices |
| 39 | NHS111Cost | Minutes’ contact NHS 111 Price to telephone NHS 111 for 1 minute |
Pounds sterling 2014 prices |
Appendix 9 Analyses of health economic data
Tests of normality
| Tests of normalitya | |||||||
|---|---|---|---|---|---|---|---|
| Variable | Group | Kolmogorov–Smirnovb | Shapiro–Wilk test | ||||
| Statistic | df | p-value | Statistic | df | p-value | ||
| HospIP_Nights | Phase 1 | 0.279 | 16 | 0.002 | 0.580 | 16 | 0.000 |
| Phase 2 | 0.222 | 15 | 0.046 | 0.783 | 15 | 0.002 | |
| Costreadppd | Phase 1 | 0.279 | 16 | 0.002 | 0.580 | 16 | 0.000 |
| Phase 2 | 0.221 | 15 | 0.047 | 0.783 | 15 | 0.002 | |
| HospOP_Nos | Phase 1 | 0.248 | 56 | 0.000 | 0.763 | 56 | 0.000 |
| Phase 2 | 0.283 | 63 | 0.000 | 0.661 | 63 | 0.000 | |
| CostOPattend | Phase 1 | 0.245 | 56 | 0.000 | 0.760 | 56 | 0.000 |
| Phase 2 | 0.282 | 63 | 0.000 | 0.683 | 63 | 0.000 | |
| AE_Nos | Phase 1 | 0.269 | 17 | 0.002 | 0.672 | 17 | 0.000 |
| Phase 2 | 0.513 | 17 | 0.000 | 0.391 | 17 | 0.000 | |
| CostAEattend | Phase 1 | 0.269 | 17 | 0.002 | 0.672 | 17 | 0.000 |
| Phase 2 | 0.513 | 17 | 0.000 | 0.391 | 17 | 0.000 | |
| HospInP_Car | Phase 1 | 0.333 | 10 | 0.002 | 0.707 | 10 | 0.001 |
| Phase 2 | 0.365 | 3 | – | 0.797 | 3 | 0.107 | |
| HospInP_Park | Phase 1 | 0.494 | 84 | 0.000 | 0.198 | 84 | 0.000 |
| Phase 2 | 0.531 | 87 | 0.000 | 0.084 | 87 | 0.000 | |
| HospVisitTaxi | Phase 1 | 0.317 | 84 | 0.000 | 0.484 | 84 | 0.000 |
| Phase 2 | 0.228 | 87 | 0.000 | 0.765 | 87 | 0.000 | |
| HospVisitPark | Phase 1 | 0.485 | 84 | 0.000 | 0.101 | 84 | 0.000 |
| Phase 2 | 0.295 | 87 | 0.000 | 0.541 | 87 | 0.000 | |
| AEAttendTaxi | Phase 1 | 0.532 | 84 | 0.000 | 0.086 | 84 | 0.000 |
| AEAttendCar | Phase 1 | 0.238 | 9 | 0.149 | 0.784 | 9 | 0.013 |
| Phase 2c | 0.207 | 7 | 0.200c | 0.882 | 7 | 0.236 | |
| AEAttendPark | Phase 1 | 0.520 | 84 | 0.000 | 0.251 | 84 | 0.000 |
| Phase 2 | 0.530 | 87 | 0.000 | 0.197 | 87 | 0.000 | |
| GPVisitCar | Phase 1 | 0.256 | 16 | 0.006 | 0.716 | 16 | 0.000 |
| Phase 2 | 0.276 | 6 | 0.170 | 0.879 | 6 | 0.264 | |
| NosCon | Phase 1 | 0.118 | 83 | 0.006 | 0.945 | 83 | 0.001 |
| Phase 2 | 0.170 | 86 | 0.000 | 0.875 | 86 | 0.000 | |
| CostGP | Phase 1 | 0.168 | 85 | 0.000 | 0.842 | 85 | 0.000 |
| Phase 2 | 0.172 | 88 | 0.000 | 0.885 | 88 | 0.000 | |
| CostPN | Phase 1 | 0.228 | 85 | 0.000 | 0.753 | 85 | 0.000 |
| Phase 2 | 0.296 | 88 | 0.000 | 0.488 | 88 | 0.000 | |
| CostNN | Phase 1 | 0.412 | 85 | 0.000 | 0.491 | 85 | 0.000 |
| Phase 2 | 0.388 | 88 | 0.000 | 0.588 | 88 | 0.000 | |
| CostHV | Phase 1 | 0.155 | 85 | 0.000 | 0.894 | 85 | 0.000 |
| Phase 2 | 0.173 | 88 | 0.000 | 0.914 | 88 | 0.000 | |
| CostOOH | Phase 1 | 0.529 | 85 | 0.000 | 0.153 | 85 | 0.000 |
| Phase 2 | 0.512 | 88 | 0.000 | 0.291 | 88 | 0.000 | |
| Costwalkin | Phase 1 | 0.534 | 85 | 0.000 | 0.172 | 85 | 0.000 |
| Phase 2 | 0.509 | 88 | 0.000 | 0.201 | 88 | 0.000 | |
| CostNHS111 | Phase 1 | 0.524 | 85 | 0.000 | 0.100 | 85 | 0.000 |
| Phase 2 | 0.533 | 88 | 0.000 | 0.204 | 88 | 0.000 | |
List of abbreviations
- BAPM
- British Association of Perinatal Medicine
- CAG
- Clinical Advisory Group
- CI
- confidence interval
- df
- degrees of freedom
- ED
- emergency department (formerly known as accident and emergency department)
- EDD
- estimated date of delivery
- GP
- general practitioner
- HV
- health visitor
- IQR
- interquartile range
- LNU
- local neonatal unit
- LOS
- length of stay
- NICE
- National Institute for Health and Care Excellence
- NICU
- Neonatal Intensive Care Unit
- NRES
- National Research Ethics Service
- PAG
- Parent Advisory Group
- PMPS-E
- Perceived Maternal Parenting Self-Efficacy
- POPPY
- Parents of Premature babies Project
- SD
- standard deviation
- SE
- standard error
- SIDS
- sudden infant death syndrome
- SPSS
- Statistical Package for Social Sciences
- UNICEF
- United Nations Children’s Fund
- WHO
- World Health Organization