Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 12/5001/55. The contractual start date was in January 2013. The final report began editorial review in November 2014 and was accepted for publication in September 2015. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Gavin D Perkins, Frances Griffiths, Anne-Marie Slowther, Robert George, Philip Satherley, Barry Williams, Norman Waugh and Matthew W Cooke received a grant to conduct this work from the National Institute for Health Research Health Services and Delivery Research programme (grant number 12/5001/55). Gavin D Perkins reports serving on the Resuscitation Council (UK) Executive Committee and Health Services and Delivery Research programme researcher-led panel. Anne-Marie Slowther received funding from the General Medical Council and serves as a Trustee of the UK Clinical Ethics Network Charity. Zoe Fritz was involved in developing and evaluating the Universal Form of Treatment Options.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2016. This work was produced by Perkins et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction
Background
Cardiac arrest
Cardiac arrest is the term used to describe the cessation of cardiac mechanical activity and is diagnosed clinically by the absence of signs of circulation. 1 Cardiac arrest may occur suddenly and unexpectedly in someone who was otherwise fit and healthy and in whom prompt initiation of treatment has the potential to be lifesaving. By contrast, cardiac arrest is also the final common pathway of the dying process, which occurs as someone reaches the end of his or her natural life.
Resuscitation
The act of attempting to revive somebody from death is termed resuscitation. The first description of resuscitation is widely attributed to biblical times, when the prophet Elisha restored the life of a boy through a form of mouth-to-mouth resuscitation. 2 The concept of resuscitation then lay largely dormant until the mid-17th century, when the Dutch Humane Society recommended the use of expired air ventilation to resuscitate victims of drowning. 3 The first successful attempts at defibrillation (the application of electric shocks directly to the heart through an open chest) to treat cardiac arrest due to the disordered heart rhythm known as ventricular fibrillation were reported in the 1940s,4 followed by reports of successful external defibrillation (defibrillation electrodes applied to the outside of the chest wall) becoming available in the 1950s. 5
The landmark paper by Kouwenhoven et al. ,6 published in the Journal of the American Medical Association in 1960, is widely regarded as the birth of modern-day cardiopulmonary resuscitation (CPR). In this paper the authors described a case series of 20 patients in whom the combination of external chest compressions and expired air ventilation was used to resuscitate mostly victims of witnessed, in-hospital cardiac arrest with potentially reversible causes of cardiac arrest. The permanent survival rate was reported as 70%. The authors concluded that ‘Anyone, anywhere, can now initiate cardiac resuscitative procedures. All that is needed are two hands’.
A further report describing their experience in 118 patients provided further detail on the indications and contraindications for resuscitation. 7 The authors noted:
Not all dying patients should have CPR attempted. Some evaluation should be made before proceeding. The cardiac arrest should be sudden and unexpected. The patient should not be in the terminal stages of a malignant or other chronic disease and there should be some possibility of a return to a functional existence.
So, CPR developed to deal with very acute situations – people drowning, or having arrhythmias such as ventricular fibrillation after an acute myocardial infarction. In these cases, the underlying organs (lungs or heart) were capable of sustaining life after a short period of resuscitation. The success of these early cases encouraged the widespread dissemination of resuscitation techniques. Hospitals started having ‘crash teams’ which included a resuscitation trolley with electrocardiogram defibrillators and equipment for ventilating people. These teams would be called to wherever in the hospital a cardiac arrest occurred, although in coronary care units, where many arrests occurred, staff would defibrillate at once, alerted by continuous electrocardiogram monitors with alarm devices.
Do-not-attempt-cardiopulmonary-resuscitation orders
Cardiopulmonary resuscitation can be very successful, especially if used after heart attacks, where a mostly healthy heart may arrest as a result of arrhythmias. However, CPR can also cause harm. A systematic review of injuries following CPR attempts identified rib fractures with a frequency of up to 97% and sternal fractures with a frequency of up to 43% in cases of attempted resuscitation. 8 There is also a risk of internal injuries, with the systematic review noting a frequency of 1–5% of cases sustaining cardiac, pulmonary or intra-abdominal organ injuries. 8 Even if the heart is initially restarted, fewer than half of those who survive initially will survive to go home from hospital. 9
A do-not-attempt-resuscitation (DNAR) order, or, as it has more latterly been known, a do-not-attempt-cardiopulmonary-resuscitation (DNACPR) order, provides a mechanism for making a decision to withhold CPR prior to a cardiac arrest occurring. DNACPR decisions have been recorded in medical records since the early 1970s. 10 Despite the fact that processes to record resuscitation decisions have been in place for almost 40 years, their application is variable. The Office for National Statistics reports that over 500,000 people die each year in England and Wales. The majority (approximately 285,000) deaths occur in hospital, with the remaining deaths occurring in public places, community care settings or the patient’s own home. The UK National Cardiac Arrest Audit indicates that hospital-based resuscitation teams attempt resuscitation in about 20,000 patients annually. 9 As current practice is to resuscitate all patients unless they have a DNACPR decision recorded, this implies that the majority (90%) of in-hospital deaths occur with a DNACPR decision in place.
A multicentre cohort study conducted in the UK examined the case records of over 500 patients who sustained an in-hospital cardiac arrest during a 2-week period in November 2011. 11,12 Reviewers found that one-quarter of patients who received CPR had substantial functional limitations and two-thirds had an underlying fatal disease. 11 The independent reviewers suggested that a DNACPR decision could have been made prior to cardiac arrest in 85% of cases. 11 There were also 52 cases in which CPR was commenced despite a DNACPR decision being in place. 11 In addition to this report, other research has demonstrated deficiencies in several aspects surrounding DNACPR decisions, including failure to recognise patients for whom resuscitation is not appropriate and failure to make a timely DNACPR decision. 13,14 Even when decisions are made there is unclear communication of the decision both within the health-care team and to patients/surrogates. 13–15 In addition, documentation is often suboptimal and there are misunderstandings about what a DNACPR decision means. 13,14,16 This highlights a major gap in current approaches to making and applying DNACPR decisions. There is significant regional and international variation in how DNACPR orders are approached, with many institutions initiating changes to improve DNACPR practice. 17,18 DNACPR decisions are broadly based around three categories; these are:
-
perceived futility of CPR (CPR is unlikely to restore spontaneous circulation)
-
refusal of CPR by the patient with capacity or through an advance decision to refuse treatment
-
when the burdens of the resuscitation attempt are thought to outweigh the benefits.
In the UK and many other countries there is no legal obligation for a doctor to provide CPR if they consider that doing so would be futile. However, in some countries it would be illegal to make such decisions without patient consent. Irrespective of international differences in decision-making, DNACPR decisions form part of an essential framework to enable a dignified death which is uninterrupted by a futile resuscitation attempt.
Aims and objectives
Aims
This research aims to identify the frequency with which and reasons why conflict and complaints arise, identify inconsistencies in implementation of national guidelines across NHS acute trusts, understand the experience of health professionals in relation to DNACPR, its process and ethical implications, and summarise the research evidence around DNACPR decisions.
A stakeholder group comprising health-care users, providers, ethicists, legal personnel and policy-makers maintained oversight during the project to ensure that the project remained focused on the issues that are important to patients and their families and relevant to NHS staff, and incorporated relevant ethical and legal frameworks.
Objectives
The objectives are to:
-
review and summarise the published evidence base informing DNACPR policy and practice
-
identify the themes of current complaints/conflict in relation to DNACPR decisions and explore local solutions developed to tackle these problems
-
examine current acute hospital, community and ambulance service policies to identify inconsistencies and examples of best practice across NHS organisations
-
explore health professionals’ experiences of DNACPR policy and practice
-
summarise and disseminate findings from this research.
Overview
Chapter 2 presents the results of the review of published literature concerning two aspects of DNACPR decisions: first, a review of published studies that have used interventions to improve DNACPR decision-making practice, and, second, a review of the published evidence concerning barriers to and facilitators of good DNACPR decision-making practice.
Chapter 3 aims to establish the size of problems associated with DNACPR decision-making in the UK by exploring evidence from complaints made to the NHS and incidents reported by the NHS to the National Learning Reporting System, from Parliamentary and Health Service Ombudsman and coroners’ reports involving DNACPR decisions and by reviewing the nature of calls from the general public to a national helpline related to DNACPR.
The review of NHS trust policies (see Chapter 4) evaluates similarities and differences between a sample of DNACPR policies from acute, community and ambulance service NHS trusts and identifies examples of good practice.
Chapter 5 considers health professionals’ experiences, reporting on a focus group study exploring service providers’ perspectives of DNACPR decisions.
At several stages throughout the study, stakeholders were invited to contribute to the study. Chapter 6 reports on this engagement, including a final event at which they recommended priorities for future research.
Chapter 7 brings together findings from all of the data sources through a discussion of the key issues identified and concludes with implications for practice and recommendations for research.
Chapter 2 Review of published evidence
Overview
A systematic review of the worldwide literature sought to synthesise existing research evidence for the processes, barriers and facilitators related to DNACPR decision-making and the implementation of DNACPR decisions (PROSPERO CRD42012002669). The review was conducted in two phases. First, a scoping review was undertaken to explore the literature for evidence of interventions that improved the process or recording of DNACPR decisions. 19 Second, a more in-depth review of the international literature was undertaken to explore the literature for evidence of barriers to and facilitators of DNACPR decision-making. 20 Overall, 84 papers were included in the review (37 in the scoping review and 47 in the full review).
Introduction to the scoping review
The purpose of the scoping review was to evaluate evidence about systems for improving the appropriate use of DNACPR decisions.
Method of the scoping review
Identification of studies
We identified recent studies (2001–February 2014) investigating interventions designed to improve how DNCAPR policies are applied in practice. An initial search for the scoping study was conducted in 2011, covering 10 years, and this study updated that search.
Medical subject heading (MeSH) terms and text words covering different terms used for DNACPR and for systems used to implement them were used and combined to develop the search strategy. These included the MeSH term Resuscitation Orders (covering Do-Not-Resuscitate Orders; Resuscitation Decisions; Resuscitation Policies; Withholding Resuscitation) and do not resuscitate, do not attempt resuscitation, not for resuscitation, allow natural death (AND), DNR, DNAR, NFR (not for resuscitation) and DNACPR as text words. Results were limited to English-language articles.
Information sources
Predetermined relevant databases were searched: MEDLINE (Ovid), EMBASE (Ovid) and Cumulative Index to Nursing and Allied Health Literature (CINAHL) (EBSCOhost). MEDLINE was searched first, followed by EMBASE and then CINAHL.
Inclusion criteria
The inclusion criteria for studies were:
-
randomised controlled trials, before-and-after studies and observational studies with a control group
-
studies that involved DNACPR decisions on adults in hospitals, nursing homes or the community
-
studies that tested an intervention designed to improve the application of DNACPR policy into practice.
Study selection
Two reviewers independently screened the search results titles and abstracts for relevance. The full text of eligible and potentially eligible articles were retrieved and independently reviewed during a second phase of study selection by both reviewers. Disagreements between reviewers were resolved by discussion.
Data extraction
Four randomly selected studies were used to test and refine a data extraction form developed specifically for this review. Data were extracted by one reviewer and checked by a second, with disagreements resolved through discussion. Information extracted was on:
-
country/countries of origin
-
study design
-
population studied, including number in each group (unless otherwise stated it was assumed that all participants were adults)
-
the type of intervention used
-
details on the control group
-
outcome measure used
-
the effect of the intervention.
Risk of bias and quality assessment
The studies were assessed for risk of bias using the criteria given by Thomas et al. 21 This tool assesses selection bias, study design, confounders, blinding, data collection methods and withdrawals and dropouts. Each element was rated as strong, moderate or weak to give an overall global rating. Two reviewers independently rated all studies and any discrepancies were settled by consensus.
Evidence synthesis
A meta-analysis of included studies was planned, determined by assessment of heterogeneity of setting, participant, intervention and outcome. Where meta-analysis was not possible, a narrative thematic analysis of the studies’ findings was planned.
Results of the scoping review
Study selection
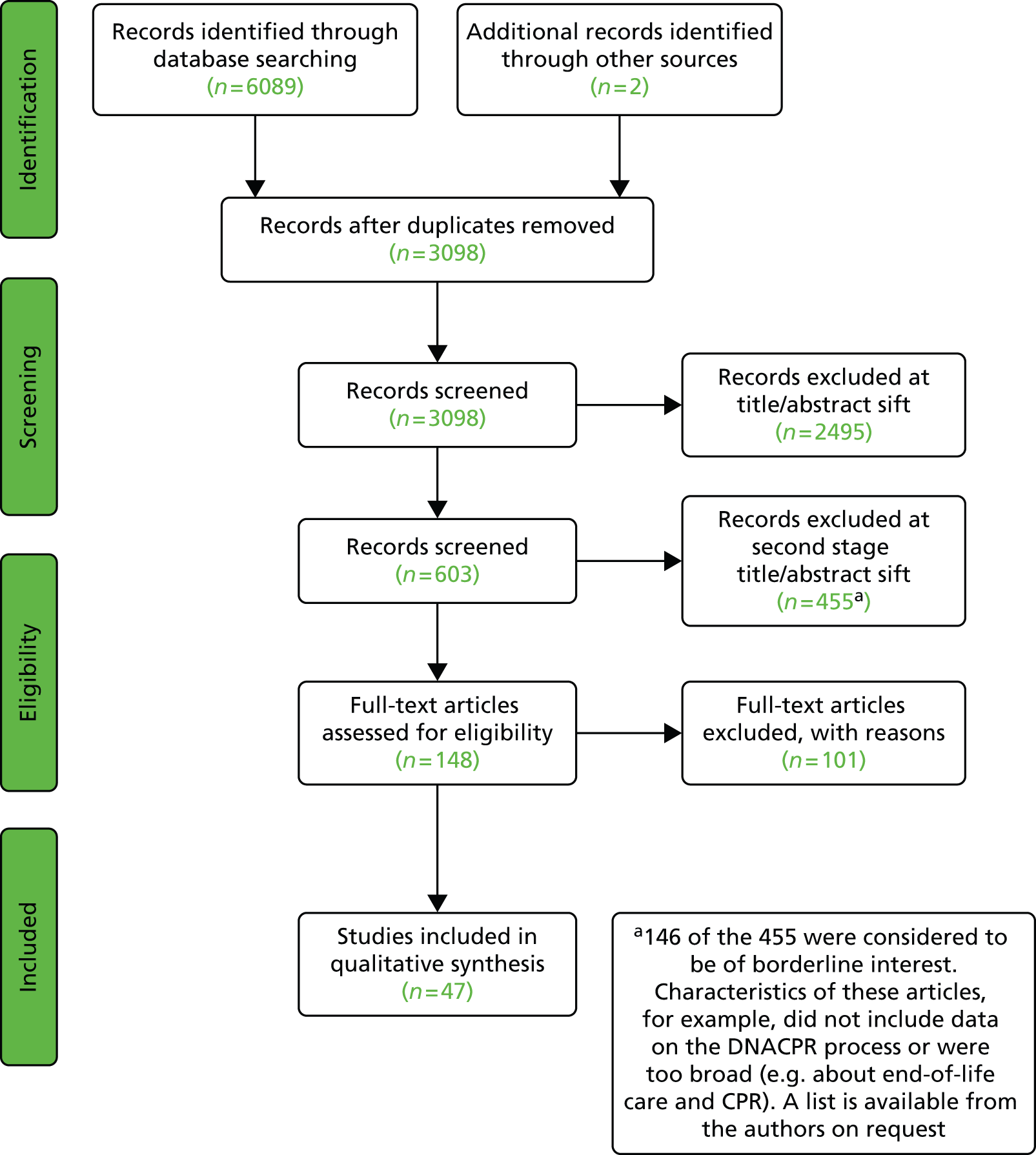
Thirty-seven studies were identified for inclusion in the review (see Appendix 1). 16,22–57 The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram (Figure 1) shows the numbers of studies identified at each stage of the selection process.
FIGURE 1.
The PRISMA flow diagram: scoping review.

Setting
Over half (20/37) of the studies were conducted in the USA,22,25,28–31,39,41,42,45,47–50,52–57 nine were conducted in the UK,26,32–35,37,40,43,44 two were conducted in Australia23,24 and one study was conducted in each of Germany,46 Belgium,38 Switzerland,51 the Netherlands,16 Singapore36 and Saudi Arabia. 27
Quality of evidence
Of the 37 studies, eight were randomised controlled trials,22–24,30,45,54,55,57 27 were before-and-after studies16,25–29,31–44,48–53,56 and two were cluster controlled studies. 46,47 Two studies were assessed as providing strong evidence,24,40 12 were assessed as providing moderate evidence16,22,23,29,30,35–38,54,55,57 and 23 were assessed as providing weak evidence. 25–28,31–34,39,41–53,56
Synthesis of findings
The settings and outcomes were too heterogeneous to allow meta-analysis. Studies were, therefore, grouped into four themes. See Appendix 1 for characteristics and results of the studies for each of the themes: (1) structured communication and specialist teams, (2) DNACPR documentation, (3) nursing home and community interventions and (4) education (physician and patient). One paper, investigating a change in legislation, did not fall into these themes.
Structured communication
In a prospective randomised trial,22 general medical patients were randomised to a scripted intervention (involving talking about what resuscitation involves and asking the patients’ preferences with regard to resuscitation status) or standard clerking. There was significant improvement in documentation in the intervention arm. Patients (98%) in the intervention group reported being happy to take part in a discussion about resuscitation. In a second study,23 patients with advanced cancer were randomised to either a combination of a patient information leaflet and a resuscitation discussion with a psychologist or standard care. DNACPR decisions were placed earlier in the intervention group but the overall frequency of decisions was the same.
Introducing specialist teams
Medical emergency teams (METs) have been introduced to respond to acute deterioration in patients admitted to hospital. Four studies investigated the relationship between MET and DNACPR decisions. 24,58,25,26,27 Chen et al. 24 and Hillman et al. 58 assessed the role of the MET on the issuing of DNACPR orders as part of the MERIT cluster randomised study involving 23 hospitals in Australia. Issuing a DNACPR order at time of appropriate call-out was 10 times higher per 1000 admissions in hospitals with a MET, although this represented only 5% of total DNACPR activity. Two retrospective audits of the impact of the MET on the number of patients dying with DNACPR decisions in place had conflicting results: Smith et al. 25 found there to be a significant increase, while Kenward et al. 26 found no significant differences between the two periods. They did, however, observe that 24% of patients (not in cardiac arrest at time of call) seen by the MET received DNACPR decisions within 24 hours of review. 26 Finally, Al-Qahtani et al. 27 found the introduction of an intensivist-led rapid response team significantly increased the number of ward-based DNACPR decisions initiated by the intensive care team.
Three studies (two cohort and one quasi-randomised) demonstrated that specialist teams such as palliative care, acute care for the elderly and ethics were associated with an increased proportion of patients with documented resuscitation decisions. 28–30 A further cohort study31 evaluated the effect of 24-hour intensivist cover on DNACPR processes: there was an improvement in the time taken to document DNACPR decisions but no significant differences in the number of patients receiving CPR within 24 hours prior to death.
Do-not-attempt-cardiopulmonary-resuscitation documentation
Two prospective chart audits and three retrospective chart audits evaluated the introduction of pre-printed DNACPR forms compared with hand-written notes in the medical records. 32–36 Butler et al. 32 found significant improvement in recording a valid reason, consultant authorisation, consultant review and patient involvement. There were also increases in surrogate involvement and documentation in nursing notes. 32 By contrast, Lewis et al. 33 found no difference in the number of resuscitation attempts, demographics and survival to discharge. In retrospective studies, Castle et al. 34 found improvements in clarity of decision, date, clinician name and signature and reason for decision. No significant improvement in patient or surrogate involvement was observed. 34 Diggory et al. 35 found that the introduction of a clerking pro forma to record patients’ resuscitation status on admission was associated with an increased documentation of decisions. Tan et al. 36 showed the introduction of a physician order form for DNACPR decisions was associated with fewer patients receiving CPR within the 24 hours prior to death and more patients dying with a DNACPR decision in place.
Five studies examined modifications to existing DNACPR forms. Diggory’s team37 continued the audit cycles from their 2003 study and found that removing the statement indicating that all DNACPR decisions should be discussed with the patient increased the recording of resuscitation status and the number of DNACPR decisions issued. Piers et al. 38 updated the DNACPR form to emphasise the reason for the DNACPR decision and involvement of others (surrogates, nurses) in the decision-making process. In addition, they provided a 45-minute briefing on patient rights. 38 There was improved completion of reason for decision, nurse involvement and surrogate involvement. 38 However, there was no improvement in number of deaths occurring with DNACPR decisions. 38
Reducing complexity of the DNACPR form from a seven-page to a one-page document increased junior doctors’ confidence, reduced stress and improved the number of DNACPR decisions per 100 admissions. 39 Changing to a form [the Universal Form of Treatment Options (UFTO)] which contextualises the DNACPR decision within overall treatment plans was associated with a reduction in harms per 100 admissions as well as a reduction in the harms contributing to patient death. 40 Thematic interviews were suggestive of increased clarity of goals of care, better communication between clinicians and earlier decision-making with the UFTO than with the standard DNACPR form. 40
Finally, linkage between the electronic patient record and printing of DNACPR wristbands reduced the number of discrepancies between patients’ documented wishes and resuscitation-status wristband. 41
Nursing home and community interventions
Six studies42–47 identified interventions which increased the proportion of nursing home residents with DNACPR decisions. Interventions included the introduction of a palliative care team, end-of-life care pathways and staff training/education. The introduction of structured advanced care planning in the community moved preferences towards less invasive levels of care at life’s end and increased compliance with participants’ wishes and deaths at home (including DNACPR). 48
Legislation
Baker et al. 49 evaluated the impact of the American 1991 Patient Self-Determination Act59 on the number of early and late DNACPR decisions for six medical conditions 1 year either side of the Patient Self-Determination Act. There were increases in the percentage of early DNACPR decisions for four of the six conditions, while patients with chronic obstructive pulmonary disease (COPD) showed a significant increase in late DNACPR decisions; overall, there was little change in the use of DNACPR decisions. 49
Physician education
Six studies assessed educational interventions. 50–55 Study participants included 44 medical students and 269 junior doctors. 50–54 Studies typically used multifaceted interventions including role play (n = 350,52), provision of information (n = 250,51), reflective practice (n = 351–53) and case-based discussions (n = 252,53).
Two linked studies randomised first-year postgraduate residents to a multimodal educational intervention to improve code status discussions. 54,55 The multimodal package included a 2-hour teaching with deliberate practice of communication skills, online modules and self-reflection in addition to assigned clinical rotations. Control group residents completed clinical rotations alone. Residents’ performances were rated using an 18-point behavioural checklist during a standardised patient encounter with an actor. 54,55 Residents randomised to the educational intervention had significantly higher scores in the simulated discussion with a standardised patient both at 2 months and at 1 year than those who received routine education alone. 54 Residents rated the education programme positively. 54,55
Two studies assessed self-reported changes in comfort and/or confidence in discussing CPR decisions: Seoane et al. 53 found that house officers rated their self-confidence in this area more highly at the end of a rotation which involved a specialised teaching component, while Kahn et al. 52 found that participants reported significantly improved understanding of the legality of DNACPR decisions (but not in comfort of discussing them) after attending a workshop with simulated patients centred on end-of-life discussion skills.
Two studies assessed changes in patients’ outcomes/experiences after training. 50,51 Furman et al. 50 found no change in the number of resuscitation discussions with patients on admission following a half-day training session (including role-playing exercises) for medical residents. Junod Perron et al. 51 trained nine junior doctors on the meaning of and ethics surrounding DNACPR decisions in parallel with introducing a new DNACPR policy and form. The doctors self-reported their performance in DNACPR decision-making. The doctors reported better patient involvement and improved understanding of the scope of the DNACPR decisions post intervention. 51
Patient/surrogate education
Five studies were identified. 16,22,23,56,57 Three studies addressed patient/surrogate education,16,56,57 while two studies evaluated structured communication with patients. 22,23 The overall quality assessment was weak for one study56 and moderate for four. 16,22,23,57
In a large (n = 2517) before-and-after study,16 introduction of a patient information leaflet and provision of written information for doctors in a tertiary hospital in the Netherlands had no effect on the frequency of DNACPR documentation. Showing a short video of CPR to relatives of patients in intensive care improved their knowledge about resuscitation but did not influence their preference about DNACPR decisions. 56 Finally, in a randomised controlled crossover trial,57 cancer patients’ choices about whether they preferred to be asked about their opinion or informed of a DNACPR decision were unchanged after watching two short videos.
Summary of the scoping review
This scoping review suggests that structured discussions at the time of admission to hospital and review by specialist teams at the point of an acute deterioration served as useful triggers to review DNACPR decisions. Linking DNACPR decisions to discussions about overall treatment plans provided greater clarity about goals of care, aided communication between clinicians and reduced harms. Standardised documentation proved helpful for improving the frequency and quality of recording DNACPR decisions. Studies into patient and clinician education were limited in scope and did not provide compelling evidence that education in isolation improved clinical processes or patient outcomes.
Introduction to the full review
The findings of the scoping review were extended in the main review. The objectives of the main review were:
-
to identify factors that influence DNACPR decision-making and who makes the decisions
-
to identify the barriers to and facilitators of the decision-making process
-
to identify factors that influence implementation of DNACPR orders
-
to identify barriers and facilitators to the implementation process.
Method of the full review
Identification of studies
The starting point for this review was 2003; this was influenced by a government publication, Choice, Responsiveness and Equity,60 which supported patient equity in being given, and making choices with health-care professionals about, their health care. This included being consulted and given a choice about where patients would like to die, whether or not their treatment should be withdrawn and whether or not they should be resuscitated. The period of the search was from January 2003 to July 2013.
An iterative procedure was used to develop the search strategy, with input from the stakeholder group, known articles identified in earlier work and the sifting of 200 titles/abstracts randomly selected from results of an initial scoping search undertaken in June 2013. The final search strategy was designed to capture generic terms for DNACPR. The strategy was deliberately sensitive in order to capture all relevant study types including qualitative studies and articles with uninformative titles and no abstracts. The search strategy was developed for MEDLINE® and adapted as appropriate for other databases. All searches were undertaken between 12 and 19 July 2013. The final strategies used are available (see Appendix 2).
Information sources
Studies were identified by searching predetermined relevant electronic databases, scanning reference lists of included studies and contacting key experts in the field. The databases searched were MEDLINE (Ovid), MEDLINE In-Process and Other Non-Indexed Citations (Ovid), EMBASE (Ovid), Applied Social Sciences Index and Abstracts (ASSIA) (ProQuest), all sections of The Cochrane Library (Wiley) including Cochrane Database of Systematic Reviews, Database of Abstracts of Reviews of Effects, Cochrane Central Register of Controlled Trials, NHS Economic Evaluation Database, Health Technology Assessment Database, CINAHL, EBSCOhost, PsycINFO (ProQuest), Science Citation Index and Social Science Citation Index (Web of Science), and The King’s Fund library database.
All bibliographic records identified through the electronic searches were collected in a managed reference database.
Inclusion criteria
All types of study were included which reported decision-making and implementation of DNACPR orders, for example qualitative studies, randomised controlled trials, observational designs and systematic reviews. Participants comprised any health-care professional who was involved in decision-making and implementation of DNACPR orders. Any type of intervention for decision-making or implementation and any type of outcome measurement were included, although the review was not limited to outcome measures but included all outcomes if they were reported. International studies were included, although papers were limited to those published in the English language.
Exclusion criteria
Papers were excluded if they were abstract/conference proceedings, editorials, letters, think pieces or commentaries; patient or surrogate experiences; pre-existing patient-led decision-making on DNACPR such as advanced decision-making (this review focuses on decisions made by physicians and other staff members such as paramedics where the patient’s pre-determined wishes regarding CPR are not known. It does, however, touch on patient decision-making from the physicians’ perspective in Communicating the decision to patients and relatives); individual case studies; simulations for training, hypothetical situations and vignettes; pre-2003 data (unless it crossed into 2003 and beyond); studies in which DNACPR was not the primary focus of the study; studies including children (under 18 years of age); and non-English-language publications.
Study selection
References (n = 3098 after deduplication) were screened independently for eligibility by four reviewers (two pairs), who assessed either the MEDLINE abstracts (CM and BC) or the abstracts from other databases (AG and RC). Disagreements were resolved by consensus (between AG and RC or between CM and BC). Titles and abstracts for retrieved studies were screened for eligibility and full texts were obtained when the abstract was unclear. Studies that could not be decided on by one pair of reviewers were deliberated by a reviewer from the other pair.
One reviewer (RC) and one independent reviewer (NW) checked 20% and 100% (respectively) of the second sift of abstracts (n = 603) prior to obtaining full-text papers for inclusion.
Agreement was reached on 146 of the papers to be set aside as of borderline interest. These were records that did not include data on the DNACPR process or were too broad, for example they were about end-of-life care and CPR. Full-text papers (n = 148) were further assessed for eligibility and 101 were excluded with reasons, for example the data were collected prior to 2003.
Data extraction
Using provisional themes, which had emerged from the second sift of abstracts, a broad framework was devised for data extraction and checked with stakeholders by e-mail for any other expert input. This framework was comprehensive and allowed for additional themes to emerge from the data extraction. A data extraction sheet was developed and pilot tested on randomly selected studies (BC) and refined accordingly. One review author (CM) extracted the following data: aims and objectives, research methods, participant characteristics, intervention, data collection and analysis, and results based on the framework. Fifteen papers (32%) had data extracted by other reviewers (RF, RC, BC and ZF) and checked by the main reviewer (CM).
Risk of bias in individual studies and quality assessment
The risk of bias was considered across all studies and results were examined for missing data. Study quality and risk of bias were evaluated in individual studies guided by the Critical Appraisal Skills Programme tool61 for qualitative studies. Owing to the heterogeneity of the research methods and to provide a common comparison of studies, this tool was adjusted slightly to accommodate all other research methods included in papers, by removing the word qualitative and references to only qualitative research methods; for example, ‘is a qualitative methodology appropriate?’ was changed to ‘is the methodology appropriate to the study?’. Other quality assurance checklists were considered but the Critical Appraisal Skills Programme provided the basis for a simple and straightforward check across all study types and enabled studies to be compared for quality throughout the data extraction process.
Half of the studies in the review were perceived to be of low quality: that is, of little value or not generalisable to a wider community. Many of the studies were cross-sectional, and small population samples were included. Studies commonly utilised self-reported non-validated questionnaires which only occasionally were piloted for face and content validity.
The following quality criteria were used:
-
Low: poor quality – not well designed, biased, few if any aims and objectives, data collection tool is not tested or described, small local study.
-
Medium: medium quality – some attempt to test the data collection tool, the study has some robustness, not generalisable, can be a small study.
-
High: good quality – robust methodology, aims and objectives, unbiased, could be generalisable.
Planned methods of analysis
The diversity of the research methods used in the review studies did not lend itself to a meta-analysis. Throughout the title and abstract sifting stage of 3098 hits, a list was compiled of the major recurring categories emerging from the literature. Twelve key categories formed a broad framework for data extraction from the final 47 studies. The stakeholders were invited to comment on or add their expert input to the 12 categories. If other categories emerged during data extraction these would also be incorporated into the framework. Data were extracted which addressed the following 12 categories: (1) staff members and their roles in DNACPR decision-making; (2) information about DNACPR forms; (3) clinical and patient factors considered in decision-making; (4) consultations with patients, surrogates or team members; (5) timing of decision-making, for example early, late or emergency orders; (6) compliance with guidelines or policies, including a brief description of these; (7) following on from consultations with patients and surrogates; (8) skills and characteristics of decision-makers; (9) other outcomes such as resources and costs; (10) description of the implementation of the order, for example who does this and how; (11) description of the documentation used or how decisions are communicated; and (12) interpretation of the DNACPR order, for example levels of care. No further categories were added.
The framework used in data extraction was compiled from 12 key categories; these 12 categories broadly addressed the study’s objectives (objectives 1 and 2 were addressed by categories 1–9 and objectives 3 and 4 were addressed by categories 10–12). Analysis involved familiarisation with and comparison of the studies. Interrogation of the extracted data was conducted for each of the research questions. A narrative synthesis, using similar principles to those described by Thomas and Harden,62 was developed to examine relevant themes, identifying patterns and anomalies across the studies.
Results
Forty-seven studies were included in the final review (see Appendix 3). The study flow diagram is provided below (Figure 2). From the extracted data there were four emerging overarching themes which were categorised into four key domains: considering the decision, discussing the decision, implementing the decision and the consequences of DNACPR orders. Each domain was synthesised into subcategories.
FIGURE 2.
The PRISMA flow diagram.
Considering the decision
The evidence here is mostly descriptive. It identifies key staff members included in the discussion and decision-making of a DNACPR order. It illustrates the variation in the timing, setting and epidemiology – particularly (a) older people, (b) prognosis, (c) quality of life, (d) other considerations of patients – which affects and influences decision-making regarding DNACPR orders. Thirty-seven articles contributed to this theme and 17 included a questionnaire or survey design. 38,63–78 Of these 17 articles, 12 were deemed low-quality studies,63–68,72–77 two were deemed medium quality38,71 and three were deemed high quality. 69,70,78
Twelve articles included reviews or audits of medical records, registry of deaths or MET calls,16,75,79–88 of which two were of high quality16,86 two were of medium quality85,87 and eight were of low quality. 75,79–84,88
Eight articles included qualitative designs of interviews, focus groups and observations;14,15,40,67,89–92 of these, three were deemed high quality,15,89,92 three were deemed medium quality14,40,91 and two were deemed low quality. 67,90
Key decision-makers
The studies reported that the key decision-maker was usually a senior physician, often the person in charge of the patient63–65,71,79,88 who would either make a lone decision66,79,81,88 or involve other physicians. 63,82 Several studies reported that the nurse may be the first person who broaches the subject of a DNACPR order with the patient, after developing a rapport with them,14 and they are consulted by the physician about DNACPR status38,63,67,69,89 and may follow up the physician’s discussion to check their understanding. 68 Generally, nurses felt that the overall responsibility should lie with the medical consultant or treating physician14,63,70 but specialist registrars in one English study93 had differed in their opinion from that of their consultant at some point (n = 126/235, 54%), with many (n = 198/235, 84%) feeling that the decision should not lie solely with the consultant. Further evidence shows that nurses may have a different approach to CPR and DNACPR from physicians14 and may place more power with the patient and relatives. 71 One study70 reported that nurses felt that decisions were often made by medical staff in the patients’ best interest but another63 found that 80% of nurses felt that the patient’s view should be the decisive factor. Nurses felt that they should be part of the decision-making process. 69,70 Patient and family wishes for resuscitation were sometimes reported as key to decision-making. 83,93 Although patient autonomy played an important role,72,75,89 particularly among nurses,73 one study64 found that it did not significantly change the physician’s decision. However, the presence of family, particularly adult children as surrogate decision-makers,72,84,85 often aided decision-making.
Timing
The studies illustrated a variation in the timing of DNACPR decision-making. The timings were described as days to death or days from admission, so it was difficult to identify commonalities of the timings of decision-making. DNACPR order decision-making ranged from admission or within 24 hours of admission15,74,75,84,88,94 to less than 7 days before death. 79,84,85 Sometimes there were less than 24 hours before death,84,85 with many emergency teams having to decide moments before death whether or not there was a DNACPR order already in place. 66,76,86,90,91 In one Scottish study,87 consultants on general adult wards and those in old-age psychiatry differed in their opinions about whether or not a DNACPR order should be issued at all: some would discuss this with the family in cases where the patient may live for many more years and others would raise it only if the patient was clearly at the end of his or her life. There were indications that the longer the duration of the stay in hospital the more DNACPR orders were documented,16 sometimes after a prolonged stay and aggressive therapeutic measures. 79
Setting
Evidence revealed variations among different specialties over decision-making. 87 There were more DNACPR orders written in acute wards than in planned admissions such as surgical wards. 70 This is illustrated by one study16 which found more DNACPR orders in acute admissions (n = 99/119) than in planned admissions (n = 20/119; p < 0.05); the most frequently written DNACPR orders came from internal medicine and pulmonology, with fewer from cardiology, thoracic surgery and neurosurgery wards. It was found that an inappropriate setting, such as a busy ward with a lack of privacy, could limit DNACPR discussions. 77
Epidemiology
The evidence from these studies showed that a number of factors were considered in DNACPR decision-making. A study of doctors in Germany72 found that decisions were mostly influenced by the patient’s age, underlying disease, chronic malignant disease, previous resuscitations and expected quality of life, and this is reflected in other studies. It was evident from the review that attitudes towards older patients were changing. One study73 found that, between 1989 and 2003, staff attitudes towards DNACPR changed, with fewer staff over this time considering a person’s age as important in DNACPR decision-making; in 2003, an increasing number of staff also felt that the chances of successful CPR were higher, which might have underpinned their change in attitude towards age as a factor. Another study85 appeared to support this, as it found that the significance of age in a bivariate analysis lost significance in a multivariable analysis. Despite this, many other studies indicated that older age was still a key consideration. 16,64,72,79,80,83,85,86,88 The age of the older patient was differently defined but started as young as 67 years. 16 One study66 explained this more broadly, in that the proportion of patients undergoing CPR decreased with increasing age and was significantly lower for patients over 80 years of age; in one example,78,93 it was found that younger patients were more likely to have CPR and longer attempts at CPR, whereas older patients in similar circumstances would have a DNACPR order in place.
Prognosis
A poor prognosis is frequently mentioned as a contributor to a DNACPR decision; this includes cancer (advanced, terminal or untreatable), heart failure, COPD, psychiatric diagnoses75,79,83,92 and other comorbidities. 72,75,79,80,83,93 The frequency of intensive care unit (ICU) stays83 and previous resuscitations64,72 were also important contributors to DNACPR decision-making.
Quality of life
Quality of life was frequently mentioned when making decisions, although the term remained undefined by staff;87 factors staff considered included poor quality of life of the patient prior to cardiopulmonary arrest and expected quality of life after resuscitation. 72,87,93 Similarly mentioned were terms such as futility,77,86 withholding potentially harmful treatment77 and the likelihood of successful CPR. 77,93
Other considerations
Other considerations included race/ethnicity (white compared with African Americans, with African Americans having fewer DNACPR orders, which appeared to be a cultural choice). 80,85 Being unmarried,84 having pastoral care,85 a lack of bystander basic life support at cardiac arrest and ineffectiveness of basic life support66 were also mentioned.
Discussing the decision
The evidence from this review illustrates several challenges in discussions of DNACPR between physicians, patients and relatives. Of the 26 articles in this theme, 16 included cross-sectional questionnaires or surveys,38,39,63–65,68,70,74,75,77,78,83,93,95–97 of which six were deemed high quality,70,78,93,95–97 two were deemed medium quality38,39 and eight were deemed low quality. 63–65,68,74,75,77,83 Eight articles included qualitative methods,13–15,89,91,97–99 of which three were of high quality,15,89,98 four were of medium quality13,14,91,97 and one was of low quality. 99 The remaining three articles are reviews of records or audits,80,81,87 of which two were of medium quality81,87 and one was of low quality. 80 These articles include reported challenges posed by communicating decisions to patients and to relatives, discussion of prognosis and a preference for discussing CPR rather than DNACPR. Limitations were found to include personal hurdles for staff members and a lack of specific skills and training among decision-makers.
Communicating the decision to patients and relatives
Consensual decision-making included patient views, medical expertise and a team approach,89 but often the level of involvement of the patient varied. Key factors for involvement appeared to be that the patient was able to communicate and was competent. 63,95 In those studies which reported on the DNACPR discussion process, it was found that some physicians would normalise the need to discuss resuscitation by explaining that it was something they discussed with all patients. 15,75 Examples were given in which physicians would ease into the conversation by asking about, for example, the patient or surrogate’s understanding of their condition, their understanding of CPR and previous conversations they might have had. 75 One evaluation of a new form, which was more than a DNACPR order, found that doctors thought that following the instructions on this new form made conversations with patients easier. 40 In one study,97 86% of physicians reported that they would normally or always involve the patient or their family before completing a DNACPR order.
These approaches, however, are not consistent. Examples were found which illustrate that findings varied in reporting how often patients were involved in decision-making. One study77 found that hospital-based clinicians reported discussing resuscitation decisions with patients less than 25% of the time but still thought that it was important to do so. In a study in Norway,95 findings reported that of 40 out of 176 patients who were able to take part in a discussion, only 28 out of the 40 (70%) actually did. There were various reports on the different challenges physicians faced with patient discussions which may explain these variations. In countries where patient autonomy was a priority,15,96 sometimes to the point of excluding families,15 physicians could experience difficulties if the patient made a decision that they did not agree with, particularly when they felt that a DNACPR order was appropriate but the patient requested CPR. Other examples included reports that some patients did not want to discuss their resuscitation status65 or be involved in the DNACPR decision-making. 65,75 Clinicians felt that they would not want to enter into discussion if the patient had poor health status65 or if they thought that they would cause the patient anxiety or distress. 70,75,77 Holland et al. 77 reported a participant’s response that it would take away ‘hope’, further pushing the patient into decline, and that it was ‘kinder’ to involve patients only if there was an expected positive outcome to CPR. Patients in one study in Hong Kong68 reported finding it difficult to accept stopping the treatment they were on, with some believing that DNACPR is equivalent to euthanasia.
There is evidence to show that relatives are mostly consulted in DNACPR decision-making,79,93,95 often as a proxy to the patient93 and sometimes without the patient’s involvement. 81 One study found that there were only a small number of cases in which the family was not involved. 79 The number of families consulted increased (n = 34/78, 44%, to n = 46/73, 63%) in one Belgian study after the introduction of a new DNACPR form. 38 Families were frequently involved when the patient lacked capacity (e.g. because of dementia)87 or were unable to communicate. 63 In emergency situations such as those outside hospital, paramedics reported that challenges in interaction with relatives could normally be solved by good communication;91 one Irish study65 reported physicians referring a disagreement with relatives to another medical colleague (n = 73; 42%), a medical defence organisation (n = 41; 24%), the Medical Council (n = 18; 10%) or an ethics board/forum (n = 3). Families, often unaware of the terminal care diagnosis, could demand excessive care, insist on intensive care and act aggressively towards staff. 63 In some cases, it was reported that relatives could become physically or verbally aggressive and threaten legal action, particularly when the patient had requested DNACPR. Attempts to over-rule the patient’s wishes were sometimes successful. 78 Relatives can also change the patient and physicians’ decisions; for example, when a patient’s wife, who disagreed with the patient’s expressed desire for no life support, responded on the patient’s behalf, the physician did not write a DNACPR order. 98
Discussion of prognosis
Information about prognosis and likelihood of survival beyond CPR varied across disciplines. 99 This information is required for patients and families14,99 to gain a realistic understanding of the choices to be made. It was noted that patients often had a poor understanding of the decision they had to make and up to half of physicians in one study15,96 were concerned about this. Patients were reported as focusing on life-sustaining therapies rather than on long-term goals. 99
The evidence illustrated the ways in which physicians communicated to patients and relatives; several studies found that sometimes discussion was delivered in a non-patient-specific15,99 or impartial way,15 contained too much medical jargon and terminology, which the patient might not understand, or might have a different understanding of a term compared with the physician’s meaning of that same term. 15,75,99 In one study,15 discussions were described as scripted, depersonalised and procedure focused, and sometimes came with a disclaimer. The review found a disconnection in communication between physicians, patients and relatives, which was underpinned by differences in the use of patients’ language; for example, ‘vegetable’, ‘invalid’ or ‘quality of life’99 were commonly used phrases but, without further explanation, they could lead to confusion for patients about what CPR or DNACPR is and can do. 15 Patients can have fluctuating preferences or might not fully understand clinical phrases such as ‘life support’; in one example, a patient had not wanted to be on life support until the physician explained the term, after which the patient had a better understanding and changed their mind. 98 Physicians often lacked the time for discussions99 or follow-up for patients to express their views or ask questions. 68 Discussions of DNACPR could be brief, with a median time of between 199 and 10 minutes. 74
Preference for discussing cardiopulmonary resuscitation rather than do not attempt cardiopulmonary resuscitation
Some of the evidence indicated a patient’s lack of understanding of CPR and its success rate77 but also that physicians did not always clarify the unpredictability of CPR. 99 CPR was more readily discussed with patients than DNACPR, as illustrated by one Swiss study75 in which it was found that resident physicians initiated more discussions for CPR than DNACPR (83% and 68%, respectively) but patients initiated more discussions for DNACPR than CPR (16% and 8%, respectively). One example found that during discussion a physician changed the minds of 3 out of 4 of patients in this study from DNACPR to CPR. 99 Conversely, the discussion was sometimes framed in such a way that the patient did not request CPR. 15
Limitations
Personal hurdles for staff
Some of the evidence describes a range of negative personal feelings reported by medical staff which may illustrate why patients are not always included in discussions; this includes staff feeling inexperienced and uncomfortable,83,93 being too embarrassed to broach the subject of DNACPR with patients75 and finding it difficult to make decisions by themselves,83 thereby rejecting or avoiding the responsibility of decision-making altogether. 13 This is illuminated further by two studies in which nurses described how they perceived a physician’s reluctance to discuss DNACPR as stemming from physicians’ personal fears, a fear of harming the patient14 and not having enough courage to withdraw treatment as a result of their inability to tolerate medical uncertainty. 63 Nurses, particularly those who often cared for seriously ill patients, appeared to find it easier than physicians to approach a dying patient; the nurses’ particular traits were that they found it rewarding and felt that they were responsible for the physical and emotional support of the patient, and wanted to spend as much time with the patient as they could. 63 The evidence shows that patients felt that it was acceptable to be involved in DNACPR discussions68 and that physicians may underestimate the numbers of patients who want to discuss DNACPR status even though they would find the discussion upsetting. 75 There sometimes appeared to be a discrepancy between a physician’s assessment of the patient’s interest and the patient’s wishes and priorities. 75 One study found that physicians were worried about complaints being made against them. 93
Lack of specific skills and training
The reported lack of adequate skills is illustrated by evidence which found that nearly one-third of physicians in one study96 reported low skills in DNACPR discussions (measured as < 4 on a 5-point scale), with others reporting low satisfaction with the outcome of the discussion and low confidence levels. 39 The latter study describes a significant improvement in house officers’ confidence levels after an intervention (24% to 7%; p = 0.002) but no significant change was seen at the comparison hospital (20% to 15%; p = 0.45). A lack of, or inadequate, training in resuscitation discussions was raised in three studies,77,96,98 with 92% of resident physicians in one study74 reporting a need for formal training to help improve their skills; another study found that medical students’ skill development appeared to stagnate in the latter years of training. 96 Some evidence shows that training can influence physicians’ sensitivity to patients’ autonomy in decision-making. 64
Implementing the decision
Local guidelines, policies and laws variously apply to decision-making but there is no consistent approach to the implementation and review of a DNACPR order. Thirty-four articles are included here,13,14,16,38,39,41,63–65,67–70,73,75,76,78–84,87,89–91,93,95,97,98,100–102 of which 18 are questionnaire or survey studies; six of these are high-quality studies,69,70,78,93,95,102 one is of medium quality38 and 11 are of low quality. 63–65,67,68,73,75,83,90,100,101 Ten articles included chart or medical record audits16,39,41,76,79,80,82–84,87 of which one was of high quality,41 three were of medium quality16,39,87 and six were of low quality. 76,79,80,82–84 Eight included qualitative methods;13,14,39,41,89,91,97,98 of these, three were of high quality41,89,98 and five were of medium quality. 13,14,39,91,97 Staff are alerted not to initiate CPR in a multitude of ways: by written form, electronically or word of mouth. However, these are prone to a breakdown in communication, incomplete documentation, lack of clear reasoning and variation in treatment and care, particularly concerns about suboptimal care, responsibility for changes to care and treatment, and whether the patient should have palliative care or be admitted to an ICU. Staff can be unsure of their actions and have reported having to overcome moral and ethical dilemmas as a result.
Compliance with guidelines, law or local policies
Some countries require compliance with guidelines, law or local policies. In the UK, guidelines include taking into account the wishes of the patient and family, the expected quality of life and prognosis,87 broadly reflecting factors of importance to nurses. 73 A hospital DNACPR policy might be known widely by doctors and nurses101 but less well known by others, for example administrative staff. Guidelines, however, were often not read or known about, and sometimes lacked consensus among medical staff. One example of this was found in a Welsh study of hospital and practice nurses,67 in which it was found that a fraction of hospital nurses (11/49) had read the acute trust policy and national guidelines and most practice nurses had not read them at all. Half of the practice nurses in this study were also unsure if there was a local policy that applied to their place of work. Myint et al. 93 reported that nearly all specialist registrars in their study (n = 227, 97%) were aware of the absence or presence of local trust guidelines and two-thirds of respondents thought that the guidelines were helpful in day-to-day practice; however, there was a discrepancy when they were asked what document or guidance they would recommend. Only one-fifth (n = 48, 21%) would recommend their own trust guideline, with fewer recommending the British Medical Association (BMA) guidelines (n = 45, 19%); 29 (n = 29, 12%) would recommend the BMA/Resuscitation Council (UK) [RC(UK)]/Royal College of Nursing (RCN) guidelines and fewer still (n = 27, 11%) would recommend the General Medical Council (GMC) guidelines.
Other examples from outside the UK indicated little difference. In a study in Ireland,65 only 21% knew that there was a formal resuscitation policy in their hospital, while 54% did not think there was one and 24% did not know. Only 4% reported that the policy was publicly displayed. A study in Norway95 found that more than half of nurses were not aware of any guidelines or policies in their unit; conversely, in another study the participants were adamant about the importance of following legal requirements and nurses’ ethical guidelines related to resuscitation. 14 Swiss guidelines required a senior clinician to be responsible for making DNACPR decisions but, in reality, it was found that interns and resident physicians were involved in the decision-making on a daily basis, and one study found that there was not always consensus among staff, which could lead to non-compliance with an order. 89
In other countries there did not appear to be any common approach to the implementation of DNACPR orders but there was some alignment to European regulations. The default position by the Clinical Ethics Committee in Switzerland75 was one of resuscitation except in cases where there was a refusal by a patient who was competent and informed, or where the patient was in end-of-life care, or where CPR would be considered futile. Patients were included in decisions, unless they were incapable of making decisions, in end-of-life care or if CPR would be futile for them. Hungarian law64 is reputed to reflect European regulations on the limitation of therapy, and patient autonomy is accepted, in certain cases, as more important than the right to life. Outside Europe, legislation varied over DNACPR policy; for example, in Korea, DNACPR was not legal practice and so institutions had individual policies, particularly concerning written or verbal consent by the family which was recorded in notes following a discussion with the family. 81 In Taiwan,84 legislation had been in effect since 2007 and patients were able to forego CPR independent of any physiologic futility, and, once a DNACPR order was signed by a patient or surrogate, the physician was allowed to withhold complete or partial CPR, which included endotracheal intubation, cardiac massage, cardiac defibrillation, resuscitative drugs, pacemakers and mechanical ventilation. Two studies mentioned regular reviewing of DNACPR orders. 75,101 Recommendations required a regular review of CPR or DNACPR orders,75 with one study suggesting that reviews of DNACPR orders in acute hospitals should take place 24-hourly. 101 Ongoing reviews often took place without the patient’s knowledge68 and they took place less urgently for continuing-care patients. 87
Communicating the decision to the wider health team
Highly visible documentation or symbols were commonly used to alert staff to the DNACPR status of a patient and were recorded in the patient’s medical notes. 13,87 However, the colours used to denote this were not consistent (e.g. red and black,13 orange82 or blue). 87 In addition, the content of pre-printed DNACPR order forms varied widely.
High visibility of do-not-attempt-cardiopulmonary-resuscitation orders
In some Scottish wards, blue forms identified which patients had a DNACPR order; however, an audit found that this procedure had broken down for about one-third of patients who should have had blue forms but did not. However, decisions were clearly noted in the notes and staff were clear about which patients were to be resuscitated and which were not. 87 Various visual symbols were used to denote which patients had a DNACPR order, such as a red heart or other symbol,63 armbands,41 a black circle written on a whiteboard or an encircled ‘R’ recorded on an electronic record,13 or ‘resus minus’ (R-minus) was recorded in the patients’ records. 91 In the main, decisions were documented in records and/or nurses’ notes,13,70,79,87 and clarified at staff handover. 70 However, audits had found that this was not always consistent. 16,79,80,102
Pre-printed do-not-attempt-cardiopulmonary-resuscitation order forms
The content of pre-printed DNACPR forms varied widely but those forms described in studies included the date83 and time of the decision,81 discussion with the patient and/or relatives83 or anyone involved in the process,102 nature of the discussion81 and justification of the decision. 83 There might be space for the physician’s formal confirmation of the DNACPR decision81,83,102 and patient and family signatures,81 although this was not always the case where a verbal decision was recorded on the form or just recorded in notes. 81,102
Some studies reported that levels of ceilings of care or objectives of care pre-recorded on the form38,40,82,83,102 listed variously; for example:
-
code one – abstention of CPR (full treatment)
-
code two – no escalation of therapy
-
code three – comfort treatment (sedation, mechanical ventilation, nutrition, intravenous perfusion)
-
code four – no treatment (active therapy removal) in confirmed brain death82
-
0 – full therapy
-
one – no CPR
-
two – withholding of therapy such as dialysis
-
three – withdrawal of life-sustaining therapy
-
four – withdrawal of mechanical ventilation (active dying process had started). 38
One English study40 described the development and evaluation of a form which listed and focused on treatments to be given rather than those to be withdrawn and made a distinction between whether active or supportive care is in the best interest of the patient. Several of the studies described the evaluation of differently designed forms to improve the process of documentation38,40 and some were designed to be completed on admission to hospital. 16,40,83 One US study39 described reducing seven different forms, which covered all aspects of the law in New York (e.g. adults without capacity, adults without surrogates), to a single form including only the relevant detail. Some studies described what had not been included on the forms, including the patient’s condition (e.g. there was nowhere to record fluid and food administration),81,82 documentation of discussion with the patient or relatives and an assessment that CPR would not be beneficial. 82 One study found that there was no consistent approach to patient involvement across several different types of forms. 102
Breakdown in communication
Lack of clear reasoning
The evidence illustrates that reasons for the DNACPR order are not always fully documented, if at all,16 or are inconsistently recorded in different places; for example, 60% of documentation did not record a clear reason why a DNACPR decision had been taken but some information was recorded in clinical notes instead. 87 Very generalised reasons using phrases such as ‘futility’, ‘frailty’ or ‘comorbidities’13 were used with no further explanation. Forty per cent of recorded decisions in one study87 were simply recorded as an advanced state of illness contributing to a poor quality of life, meaning CPR was unlikely to be successful.
Missing, incorrect or incomplete documentation
Several reasons were given for non-documentation of patient discussions, which included the lack of capacity, potential distress, time pressure and the patient not wanting to discuss the topic. 13 Decision-making with patients and/or their relatives was variously documented in the evidence. Most decisions were documented by relatives, particularly when the patient was comatose;84,87 others reported that just a few were documented. 13,16
Although there was little way of knowing if a lack of documentation was an oversight or had been forgotten,13 the impact on the patient could be devastating; for example, one study reported the consequences of not completing documentation in a case where a ‘95-year-old patient’ was resuscitated by a crash team when a doctor forgot to complete an order. 13 Discrepancies in documentation can also have devastating results for the patient. Evidence shows that incorrect documentation arising from discussions with patients can result in resuscitation being withheld or administered when the opposite was requested by the patient. 98
Treatment and care
Interestingly, the review studies clearly illustrate variations in the meaning of a DNACPR order to health-care staff. An English study40 found that doctors believed that a DNACPR order referred to reduced care (e.g. reduced out-of-hours medical escalation, contacting the outreach team, frequency of nursing observations, reduced pain relief and altered fluid intake), despite clear guidelines that DNACPR orders applied only to CPR. Other examples of the misinterpretation of care for patients with DNACPR orders included where some doctors and nurses believed that nursing observations would be reduced63,97 or remain unchanged,100 that contact with outreach teams and other medical staff and out-of-hours medical escalation would be less frequent, although nurses less often felt that this occurred than doctors. 97 It was also suggested that pain relief and amounts of fluids would be altered97 and one Finnish study63 noted that basic care was reduced for patients with a DNACPR order. One Taiwanese study84 reported that patients with a DNACPR order in an ICU were less likely than patients without a DNACPR order to receive life-support therapies at the end of their life, such as vasopressors, resuscitative drugs, cardiac massage, pacemakers, cardiac defibrillation, mechanical ventilation and supplemental oxygen, but were as likely to receive blood transfusions, intravenous fluids, haemodialysis, endotracheal intubations, total parenteral nutrition and nasogastric tube feeding.
Concerns regarding suboptimal care
Concerns were raised regarding the implications of poor care after a DNACPR order was implemented. Examples have been reported where less-experienced staff (< 1 year) reported that they may unknowingly reduce care to patients,68 and many doctors and nurses (n = 16/23, 69.5%) felt a DNACPR order would have negative consequences for the patient and result in suboptimal care. 13 The possibility of the implementation of substandard care led to a refusal by physicians to complete documentation in one study. 78
Responsibility for changes to care and treatment
Responsibility for change in care and treatment was explained differently: junior doctors thought that nursing care would be affected, nurses thought that it would be the responsibility of out-of-hours doctors and consultants gave a mixed response which did not include them. 13 Cohn et al. 13 suggested that although care may be differential, it is not explicit or tangible.
Palliative care or intensive care unit?
Although studies reported on decision-making and implementation of DNACPR orders, there was little evidence comparing the settings in which this took place. The current review raised questions about what type of treatment and care should be stopped in connection with a DNACPR order, and whether or not staff should instigate a palliative care pathway. In a comparison study of the perspectives of doctors and nurses it was found that they differed in their approach to a DNACPR order; most doctors regarded it as not undertaking CPR in the case of cardiopulmonary arrest and nurses regarded it as a ‘new’ phase in which health was deteriorating and a palliative care approach was needed to allow for death with dignity. 89
One study63 found that those working in internal medicine interpreted DNACPR orders as simply not offering resuscitation, whereas those in oncology interpreted it in terms of holistic and palliative care. In a cardiology department,79 therapeutic efforts were limited in the 24 hours preceding death in 34.5% (n = 39/113) of its patients and treatment and care was reduced to morphine chloride and spiritual support but involved little palliative care. The evidence also shows variation in whether or not patients with a DNACPR order should be admitted to an ICU. Patients with a DNACPR order were less likely to survive and be discharged from the ICU (87.2% to 46.4%). 84 One study38 found that half of all patients who died had an ICU admission near the end of their life, while only 17% (n = 66/396) of patients died in a palliative care unit; the authors suggested that the transition from curative to palliative care is suboptimal.
Staff dilemmas
A lack of complete or updated documentation, or poor decision-making, could leave doctors on call and nurses uncertain about what to do in an emergency event. 13,14,79 Performing CPR by default can raise moral and ethical issues for staff and has life-and-death consequences for the patient. 91
Updated documentation is also imperative where a DNACPR status has been reversed, as one example shows: one paramedic91 found that although the records stated ‘resus minus’, this should have been reviewed, as the patient’s health had improved.
Difficulties arise with the implementation of DNACPR orders if the wider health team is unsure of the decision or if they disagree with it. Evidence illustrates how staff may have to perform CPR when they feel that it is inappropriate, particularly in the case of medical teams who work in emergency situations, such as arrest teams78 or paramedics outside the hospital who are obliged to perform CPR if the patient is still alive. 76,90 The last two of these studies described how in 2007 the law was changed in Los Angeles, USA, meaning that paramedics were allowed to forego CPR in certain circumstances (if there was a verbal request, if there was an unwitnessed arrest, if the time to resuscitation was longer than 10 minutes or if the patient met the criteria for irreversible death, i.e. asystole).
Nurses, in particular,69 reported that they would allow the patient’s preferences to influence non-initiation of CPR (n = 97, 83%) or refuse to sign a DNACPR order if they disagreed with it; one example was given of a nurse who would not countersign an order given by an out-of-hours doctor. The order was later stated as incorrect and cancelled by a regular consultant. 13
Consequences of do-not-attempt-cardiopulmonary-resuscitation orders
The practical aspects of not issuing a timely DNACPR order can be prolonged and costly, and just a small amount of evidence from two low-quality studies addresses this:76,79 one study was an audit of the registry of deaths79 and one included a focus group, a survey and patient notes. 76 The evidence reported here is not overly reliant on these two studies but reports on the key findings. The evidence reports on the extra medical and technical costs of keeping a patient alive when perhaps a DNACPR order would be more appropriate. One example in particular illustrated this,79 in which most patients had had a prolonged stay in the department and had undergone aggressive and expensive treatment prior to a DNACPR order; the treatment included orotracheal intubation (n = 49, 43.4%), coronary angiography (n = 27, 23.9%), inotropic drugs (n = 55, 48.7%) and intra-aortic balloon counterpulsation (n = 15, 13.3%). Martinez-Selles et al. 79 argued that physicians find it harder to withdraw treatment than to start it and that they need a tool to help them decide which patients would not benefit from aggressive management.
The evidence also shows that resources can be used unnecessarily when staff are prevented from making a decision not to resuscitate, particularly outside hospital. One example of this is described in an evaluation of a new policy for paramedics in Los Angeles, previous to which unnecessary costs and resources were incurred as paramedics were required to resuscitate a patient and transport them to hospital even when it would have been more appropriate not to resuscitate. However, after the implementation of the new policy allowed them to withhold CPR in certain circumstances, unnecessary costs were still incurred, as paramedics could spend several hours waiting for the police to arrive rather than being free to attend other emergency events. 90
Summary
The objectives of this review were to identify the factors, facilitators of and barriers to DNACPR decision-making and implementation of DNACPR orders. The review found many variations in DNACPR decision-making and implementation processes, in particular who is ultimately responsible for the decision-making, how the decision is made and communicated, in which setting, how the DNACPR order is implemented and who does this.
Overall, the studies did not provide a robust evidence base owing to the low quality of many of the studies, and there was sparse evidence of the cost and resources involved in resuscitating patients who might have been more suitable for a DNACPR order.
The key messages from the analysis indicate that there is good practice in DNACPR decision-making and implementation but there is also a wide variation which is cause for concern. This review of international literature has identified many different practices yet similar problems in DNACPR decision-making and implementation.
The two themes, considering and discussing the decision, illustrate how the facilitators of good practice in DNACPR decision-making included a whole-team approach including the patient, if he or she is able, or their family,89 a professional supporting body,65 early decision-making which is regularly reviewed40,75,83 at a time and in a setting which is amenable to discussion,74,99 and using commonly understood language. 75,98,99 However, examples of good practice were lacking in the literature.
There were several barriers to consider for a DNACPR order to be carried out satisfactorily; these included large variation in the timing, time pressure and setting in which DNACPR orders take place, which limited decision-making and discussion. 74,99 Patients’ wishes may fluctuate over time and they may reconsider their choice when faced with death. 98 Relatives’ wishes could be powerful and were sometimes allowed to over-ride those of the patient. 98 Conflicts63,78 and ethical confusion can arise. 77 The review also found that there were communication challenges between the decision makers, and patients and relatives. 15,99 There was a preference for introducing the discussion of CPR rather than DNACPR with the patient,75 which it was felt encouraged hope, to avoid upsetting the patient or to avoid a difficult conversation. 70,75,77 Poor delivery of the decision and the misunderstanding of language could lead to devastating consequences for the patient. There is a reported need for specialist training and skill development in DNACPR processes. 74,75,77,83,93,96,98
The final two themes considered the implementation and consequences of DNACPR orders. The review illustrated how facilitators of good practice in implementation of the order included a consistent approach to following and understanding local and national policy, clearly recorded reasoning underpinning the decision and complete and immediately available documentation. 13,14,40,41,82,83,87 The review found a variation in staff understanding and support of local and national policy, and a lack of consensus in decision-making. Where documentation was available, this was inconsistent across and within countries, and the review found a variation in recording of the decision and poor reasoning for the decision. 13,14,79,91,98 Ward staff and staff working outside a hospital were often left unsure about what to do with a patient experiencing a cardiac arrest and had to make their decisions which usually defaulted to CPR. 90 The review found that there were common variations in the treatment and care of patients who had a DNACPR order, with some patients experiencing suboptimal care whether this was consciously or unconsciously delivered by staff. 63,78,84,97 The financial costs of decision-making and implementation of CPR or DNACPR were only alluded to in the literature. 64,68,90
DNACPR decision-making and implementation can be complex, as it is dependent on context, policy, people and resources. Decision-making can be long or short term and regularly reviewed; it affects patients, families, staff and organisations, raises a barrage of emotions in patients, relatives and health professionals; and affects the type of care and support provided. There are also financial implications to decision-making. Heterogeneous documentation and policies can cause misunderstandings and a repeat of distressing conversations. Health professionals and researchers are beginning to raise awareness of improving the process of DNACPR decision-making and implementation and some studies have reviewed and evaluated new systems for making the process easier. 16,38–41,90,102 Placing CPR/DNACPR within broader goals of care has the potential to aid discussions, decision-making and implementation processes, and reduce the negative impact of DNACPR orders on other aspects of patient care.
Chapter 3 The size of the problem
Introduction
Failures in DNACPR policy, and gaps between policy and practice, are likely to lead to adverse consequences for patients and their families. Our previous systematic review of lay press reports (covering 1 January to 30 June 2010) sought primarily to examine the epidemiology and outcome from press reports of attempted resuscitation. 103 The study found DNACPR to be one of eight resuscitation-related themes. Review of these cases includes examples of patient stories in which resuscitation was either withheld (without discussion) or provided (when the patient had expressly declined CPR). More recently, the Court of Appeal judgement in the case of Janet Tracey104 has highlighted the potential harm to, as well as the infringement of the rights of, patients and families, from the failure of health-care professionals to discuss DNACPR decisions. The National Confidential Enquiry into Patient Outcome and Death (NCEPOD) ‘Time to Intervene?’ report identified a range of cases in which patients had potentially been harmed as a result of inappropriate or lack of DNACPR decision-making. 105 This work package sought to assess the extent of adverse consequences relating to DNACPR decisions as an indication of the extent of the problem with current DNACPR policy and practice.
Methods
Following our initial stakeholder meeting, we expanded our proposed sources of information for this study to include the following sources of data:
-
NHS trusts (record of incidents, complaints and Ombudsman investigations)
-
National Reporting and Learning System (NRLS) patient safety incident reports
-
coroners’ Rule 43 reports
-
Parliamentary and Health Service Ombudsman investigation reports
-
NHS Litigation Authority
-
Compassion in Dying’s End-of-Life Rights Information Line.
NHS trusts
Individual NHS trusts have local policies and processes for recording patient safety incidents and patient complaints based on the National Patient Safety Agency Reporting Framework. 106 Incidents are usually identified and investigated by the NHS organisation involved. There are two tiers of classification, incidents and serious incidents, defined as follows:
-
Incident: an event or circumstance which could have resulted in, or did result in, unnecessary damage, loss or harm such as physical or mental injury to a patient, staff, visitors or members of the public.
-
Serious incident: an incident that occurred in relation to NHS-funded services and care resulting in one of the following:
-
unexpected or avoidable death of one or more patients, staff, visitors or members of the public
-
serious harm to one or more patients, staff, visitors or members of the public or where the outcome requires life-saving intervention and major surgical/medical intervention, or results in permanent harm or shortened life expectancy or in prolonged pain or psychological harm (includes incidents graded under the National Patient Safety Agency’s definition of severe harm).
-
We sought to identify the frequency of incidents, serious incidents, complaints and Ombudsman investigations from NHS trusts. Using the NHS service directory, we obtained care trust lists and identified a random sample of 60 NHS trusts (47 acute hospital trusts, eight community trusts and four ambulance trusts). Freedom of information (FOI) requests were sent to all trusts in the sample, seeking information on:
-
how many incidents, serious untoward incidents and Ombudsman investigations the trust had in the period April 2010–April 2012
-
how may incidents, serious untoward incidents, complaints and Ombudsman investigations were related to DNAR/DNACPR decisions over this time frame
-
a summary of the investigation findings and any recommendations for practice/change in policy that occurred as a consequence.
National Reporting and Learning System
The NRLS is part of the NHS Commissioning Board Special Health Authority and receives confidential reports on patient safety incidents from health-care staff and organisations across the UK. The reports are analysed to identify common risks to patients and opportunities to improve patient safety (www.nrls.npsa.nhs.uk/). The NRLS publishes summary reports annually. We requested a data search from NRLS for the period 1 January 2010–31 December 2012 with the following parameters:
-
total number of incidents in the period and number of incidents that include DNACPR
-
DNACPR incidents by organisation type (acute hospital trust, community trust, ambulance trust)
-
severity grading of DNACPR incidents, compared with severity grading of all incidents
-
DNACPR incidents by clinical specialty.
To identify reports relating to DNACPR, the following search terms were used: ‘dnacpr’, or ’dnar’, or ’dnr’, or (‘resus’ or ‘cpr’), and (‘not attempt’, or ‘do not resus’).
Coroners’ Rule 43 reports
Coroners investigate deaths that have been reported to them if they have reason to think that the death was violent or unnatural or if the cause of death is unknown, or if the deceased died while in prison, police custody or another type of state detention such as an immigration centre or while detained under the Mental Health Act 1983. 107,108
The Coroners (Amendment) Rules 2008109 amended Rule 43 of the Coroners Rules 1984110 with effect from 17 July 2008 and require that if inquest evidence suggests that there might be a risk of future deaths and action is needed to prevent recurrence, the coroner must prepare a report under Rule 43 which suggests actions to prevent future deaths. These reports can be served to all involved or to those with an interest in the incident and requires a response by the recipients stating whether or not the suggested actions will be taken and, if not, indicating the reason why. The response must be received within 56 days of notification. Rule 43 notices and responses were reported to the Lord Chancellor, who produced a biannual summary of Rule 43 notices. 111
The Coroners and Justice Act 2009112 saw changes to the reporting process which came into force in July 2013. 108 These changes altered the terminology used from ‘Rule 43 reports’ to ‘Prevention of Future Death reports’. Reports are now sent to the Chief Coroner, who produces a written summary on the Judiciary website at www.judiciary.gov.uk.
Summary reports of Rule 43 and Prevention of Future Death reports were accessed via the Ministry of Justice111 and the Chief Coroner’s Office. 113 We extended our initial plans of reviewing Rule 43 notices from 2011 to include all reports since inception of the new-style reporting up to the currently published reports (2013). We electronically searched each report for the keywords ‘resuscitation’, ‘DNAR’ and ‘DNACPR’. Full details of the Rule 43 and Prevention of Future Death reports were applied for from the Lord Chancellor and Chief Coroner. Requests were first made in September 2013, with follow-up contacts with the Chief Coroner’s Office in March 2014, April 2014, June 2014 and July 2014.
Parliamentary and Health Service Ombudsman investigation reports
The role of the Parliamentary and Health Service Ombudsman is to investigate complaints that individuals have been treated unfairly or have received poor service from the NHS in England. The legal authority and responsibilities of the Ombudsman are mainly drawn from the Health Service Commissioners Act of 1993. 114 Reports on examples of individual or systemic failures of service are published on the Parliamentary and Health Service Ombudsman website (www.ombudsman.org.uk/reports-and-consultations/reports). We submitted a FOI request to the Parliamentary and Health Service Ombudsman’s office for details of any complaints the health services Ombudsman had received between 2008 and 2013 relating to DNACPR, DNAR or ‘AND’ orders.
Compassion in Dying’s End-of-Life Rights Information Line
Compassion in Dying is a national charity that supports people at the end of life to have what they consider to be a good death by providing advice and information about their rights and choices. The charity runs a free telephone helpline, the End-of-Life Rights Information Line, which is available during office hours to the general public. The majority of calls and e-mails are received from individuals who are currently ‘well’ but want to plan for their future. However, patients about to go into hospital for treatment, carers, solicitors and health- and social-care professionals also make regular contact. The Information Line has in place a system for monitoring the number of calls they receive, the initial reason given for the call, other topics discussed and the type of caller. One of the conversation topics recorded on their monitoring form is DNACPR. The Information Line team enters the data from their monitoring form into a spreadsheet. For this study the team recorded additional entries for each call during which topics related to DNACPR were discussed. The topic list for the recording spreadsheet was developed by the research team based on a summary of the issues raised in a sample of 10 consecutive calls in which DNACPR had been mentioned; evidence from the literature; and the experience of the study team regarding DNACPR and qualitative methodology. The agreed list of topics was added to the telephone line data collection spreadsheet and the collected data were reviewed at regular intervals by members of the study team and the person responsible for the telephone line service at Compassion in Dying. At 4 months the topics were reviewed and minor adjustments were made to refine the topics. The data collection took place from November 2013 to June 2014.
The Information Line team provided the research team with a summary of the number of calls:
-
during the period of data collection
-
during which DNAR was raised
-
during which each topic related to DNAR was raised.
Results
NHS trust data
A majority of trusts (45/62 or 73%) responded to the FOI request. The quality of data was mixed owing to variability in recording systems. Not all trusts coded data in relation to DNACPR status. One trust (44) provided data for 2012–13 only. The responses from trusts are presented in Table 1.
| Trust identifier | Type of trust | Incidents | SUI | Complaints | Ombudsman reports | DNACPR incidents | DNACPR SUI | DNACPR complaints | DNACPR ombudsman reports |
|---|---|---|---|---|---|---|---|---|---|
| 01 | Acute | 16,114 | 37 | 139 | 12 | 0 | 0 | 0 | 0 |
| 02 | Acute | 15,393 | 440 | NR | UPI | 0 | 0 | 1 | 0 |
| 05 | Community | 15,450 | 595 | 428 | 4 | 2 | 0 | 2 | 0 |
| 06 | Acute | 66 | INP | INP | INP | 3 | UPI | UPI | INP |
| 08 | Acute | INP | 76 | 2609 | 0 | INP | 0 | 3 | 0 |
| 09 | Acute | 31,911 | 132 | 947 | 12 | 26 | 0 | 0 | 0 |
| 11 | Acute | 35,589 | 81 | 1789 | UPI | 4 | 0 | UPI | UPI |
| 13 | Community | 15,164 | 238 | 1178 | 1 | 1 | 0 | 0 | 0 |
| 14 | Acute | 1069 | 35,249 | 324 | 6 | 23 | 1 | 4 | 0 |
| 15 | Acute | 59 | 39 | 697 | 5 | UPI | UPI | UPI | UPI |
| 16 | Acute | INP | 78 | 479 | 0 | INP | INP | INP | INP |
| 17 | Acute | 23,103 | 157 | 976 | 40 | 38 | 0 | 9 | 0 |
| 18 | Acute | 6886 | 172 | 966 | 27 | UPI | UPI | UPI | UPI |
| 19 | Acute | 8126 | 220 | 2 | 0 | UPI | UPI | UPI | UPI |
| 21 | Community | INP | 304 | 423 | 24 | 0 | 0 | 0 | 1 |
| 22 | Community | 5322 | 45 | UPI | UPI | 2 | 0 | 0 | 0 |
| 24 | Community | 18,672 | 165 | 599 | 0 | 2 | 0 | 0 | 0 |
| 25 | Acute | UPI | 132 | 1003 | 59 | INP | 0 | 0 | INP |
| 28 | Ambulance | 11,173 | 35 | 1658 | 43 | UPI | 0 | 4 | 0 |
| 30 | Acute | 12,486 | 192 | 823 | 23 | 24 | 24 | 0 | UPI |
| 31 | Acute | 23,063 | INP | 1489 | INP | 5 | INP | 9 | INP |
| 33 | Ambulance | 4696 | INP | 859 | 9 | 6 | INP | INP | INP |
| 34 | Acute | INP | 223 | 749 | 19 | 4 | 8 | 5 | 0 |
| 36 | Acute | 23,758 | 90 | 760 | 5 | 42 | INP | 3 | INP |
| 37 | Acute | 3508 | 35 | 117 | 0 | 0 | 0 | 0 | 0 |
| 38 | Acute | 23,754 | 1578 | 501 | 0 | 0 | 0 | 0 | 0 |
| 40 | Acute | 20,192 | 57 | 969 | 52 | 2 | 0 | 2 | 0 |
| 42 | Ambulance | INP | INP | 578 | 2 | INP | INP | 0 | 0 |
| 44 | Acute | 18,088 | 74 | INP | INP | 0 | 0 | UPI | UPI |
| 46 | Community | 6140 | 279 | 258 | 5 | 0 | 0 | 0 | 0 |
| 48 | Acute | 13,052 | 84 | 608 | 29 | 8 | 0 | 1 | 0 |
| 49 | Acute | 28,535 | 448 | 783 | 15 | 22 | 0 | 1 | 0 |
| 50 | Acute | 27,677 | 296 | 0 | 0 | 0 | 0 | 0 | 0 |
| 51 | Acute | INP | INP | 1075 | 26 | INP | INP | 2 | 0 |
| 52 | Ambulance | INP | 48 | 783 | 15 | 22 | 0 | 1 | 0 |
| 53 | Acute | 8284 | 139 | 599 | 14 | UPI | 2 | 0 | 0 |
| 54 | Acute | INP | 315 | INP | INP | 20 | INP | INP | INP |
| 55 | Acute | 9004 | 80 | 476 | 6 | 7 | 0 | 1 | 0 |
| 56 | Acute | 30,113 | 77 | 1214 | 46 | 19 | 0 | 8 | 0 |
| 57 | Acute | 24,188 | 20 | INP | INP | INP | 0 | INP | INP |
| 58 | Acute | 70,555 | 54 | 705 | 17 | INP | 0 | 2 | 0 |
| 59 | Acute | 41,991 | 465 | 3237 | 12 | INP | INP | UPI | UPI |
| 60 | Acute | 89 | INP | INP | INP | 0 | 0 | 0 | 0 |
| 61 | Acute | 33,732 | 293 | 696 | 5 | 0 | 0 | 2 | 0 |
| 62 | Community | 20,638 | 45 | 158 | 7 | 2 | 0 | 2 | 0 |
| Total | 647,640 | 43,087 | 31,654 | 540 | 284 | 35 | 62 | 1 |
The data obtained through this exercise were variable. Individual trusts interpreted the request in different ways. For example, several trusts did not code serious untoward incidents or complaints for DNACPR events; some of these trusts therefore did not provide data for any serious incidents or complaints, while others provided total numbers but not numbers relating to DNACPR. It was not always clear from the return whether an absence of a response in any one field indicated no events or simply no response. There was a striking difference in the total numbers of reported incidents across trusts, which suggests substantial variability in the processes for recording and coding these events. Some trusts identified any incident where DNACPR was mentioned as a related incident but review of the summaries indicated that several of these incidents were not related to DNACPR and the existence of a DNACPR form was incidental.
However, across all trusts that responded, the number of incidents/complaints relating to DNACPR was a very small percentage of the total numbers of incidents and complaints (Table 2).
| Type of trust | Incidents | Serious incidents | Complaints | Ombudsman |
|---|---|---|---|---|
| All | 0.04 | 0.08 | 0.19 | 0.18 |
| Acute | 0.04 | 0.08 | 0.21 | 0 |
| Ambulance | 0.17 | 0 | 0.12 | 0 |
| Community | 0.1 | 0 | 0.13 | 2.43 |
Where responders provided information about the issues raised or actions taken in response to incidents, the following themes were identified.
Failure to make a do-not-attempt-cardiopulmonary-resuscitation order
This included cases where clinical review concluded that a DNACPR order should have been in place but was not, and so resuscitation was commenced, and cases where either a general practitioner (GP) or a family member reported that the patient had expressed a wish not to be resuscitated but, because a DNACPR order had not been in place, resuscitation had continued. Several cases described a terminally ill patient (one who had a Liverpool Care Pathway document in place) having CPR initiated because there was no DNACPR form completed.
Lack of clarity and plan regarding end-of-life care. Lack of joined up care between specialties. Patient not for intensive care and received lifesaving treatment in the absence of a clear documented plan of care.
Young patient with terminal metastatic cancer brought to hospital following resuscitation by paramedics. Care provided by Macmillan nurses and GP. No DNAR order initiated within primary care.
Resuscitation on patient started when nurse identified that patient wanted DNR but form not completed.
Failures of documentation
This was a major theme and included a range of problems with documentation, including failure to complete the form correctly; failure to use the current version; orders filed in the wrong patient’s notes; failure to transfer documentation along with the patient during his or her transfer to another ward or institution; and DNACPR order recorded in error.
. . . it was discovered that the patient’s documentation was not appropriate and therefore the ambulance crew had to continue with resuscitation and bring the patient into hospital.
999 call to patient with cancer. Advised that patient had a DNAR in situ. Family advised this was not true and that previous crews had also asked for a DNAR which the family found upsetting. Crew requested this be removed from the ambulance computer system as soon as possible.
Patient was deemed not for resuscitation and appropriate form completed. Patient transferred to another ward and when the patient returned back to original ward DNR form could not be located.
Failure to communicate with patients and/or family
This was the most common reason for complaint related to DNACPR. Examples included a patient finding a DNACPR form in her discharge documents; families complaining that a DNACPR had not been discussed with them; and families distressed because the reasons for DNACPR had not been explained to them.
Although in agreement with DNAR, family of deceased patient unhappy that this was not discussed with them – Findings indicate that this was not discussed as it should have been and it has been agreed within the Specialty that in future where these circumstances arise, the DNAR will only be valid for 48 hours until discussed with family.
Patient found a permanent DNAR order in notes which noted discussion with patient. This was refuted by the patient.
Conflict with families over do-not-attempt-cardiopulmonary-resuscitation
Some complaints involved the patient’s family disagreeing with the DNACPR order, including a case in which the patient had capacity to make a decision and had agreed to DNACPR.
Family unaware of DNR in place and wanted resuscitation to take place against wishes of patient.
Patient’s son felt that the decision to not resuscitate his mother was inappropriate. He wanted an explanation as to why the decision was rescinded later without any explanation.
Lack of communication between staff
There were several issues identified in relation to communication about DNACPR between staff in different organisations (ambulance service/community care/hospital units) as well as communication within a unit (e.g. nursing handover).
. . . patient arrested on a Patient Transport Service’s (PTS) vehicle whilst travelling home from hospital. Confusion over the presence of a valid DNAR – GP unaware but advised ward had a record that patient did not wish to be resuscitated.
Ward unsure of DNAR plan for patient on ward transfer.
Delay in clinicians being advised patient had a DNAR in place – resuscitation attempt made with ROSC (return of spontaneous circulation) . . . Crew concerned not advised of DNAR in a timely manner.
Poor process
Poor process included issues regarding the seniority of the person completing the DNACPR form, the need for the person completing the form to be the clinician responsible for the patient’s care and the need for appropriate review of DNACPR orders.
DNAR order not reviewed by GP, therefore nursing staff at nursing home rang emergency services for admission into hospital due to community DNAR running out.
A further recommendation was that there was to be a roll out of new DNAR forms. . . . These forms should only be completed by a doctor of an adequate grade, i.e. ST3 and above and that the doctor should have been involved in the patient’s care.
Failure to implement a do-not-attempt-cardiopulmonary-resuscitation order
This included examples in which DNACPR orders were in a patient’s notes but were not found until after resuscitation had been initiated or completed.
NHS Concern identified several ambulance attendances where DNAR’s have been in place, but have not been accepted by the crews.
. . . the patient was admitted onto the ward and condition acutely deteriorated. Nursing staff called for assistance and health care assistant (HCA) showed the DNR form to show patient is not for resuscitation.
Some trusts had reviewed their DNACPR policies or developed training for staff in response to the incident reports. The focus of changes were on improved documentation and communication between staff; regular review of documents, particularly at the time of transfer or discharge; and improved communication with patients and families.
National Recording and Learning System
Aggregate data provided by NRLS are presented in relation to the degree of harm ascribed to the reported incident (Table 3) and clinical specialty (Table 4).
| Type of organisation | Total incidents | DNACPR incidents | No harm/not recorded | Low harm | Moderate harm | Severe harm | Death |
|---|---|---|---|---|---|---|---|
| Acute/general hospital | 2,863,210 | 3527 | 2371 | 584 | 392 | 74 | 106 |
| Ambulance service | 15,995 | 157 | 93 | 54 | 7 | 2 | 1 |
| Community/general dental service | 2182 | 3 | 3 | 0 | 0 | 0 | 0 |
| Community nursing/medical/therapy service | 459,657 | 722 | 367 | 172 | 130 | 25 | 28 |
| Community optometry/optician service | 152 | 1 | 1 | 0 | 0 | 0 | 0 |
| Community pharmacy service | 28,677 | 1 | 0 | 0 | 1 | 0 | 0 |
| General practice | 16,822 | 35 | 18 | 9 | 4 | 2 | 2 |
| Learning disabilities service | 78,466 | 3 | 1 | 2 | 0 | 0 | 0 |
| Mental health service | 519,472 | 79 | 41 | 11 | 13 | 3 | 11 |
| Total | 3,984,633 | 4528 | 2895 | 832 | 547 | 106 | 148 |
| Specialty | Total incidents | Incidents fitting search terms (DNACPR) |
|---|---|---|
| Accident and emergency | 181,494 | 380 |
| Anaesthesia pain management and critical care | 37,280 | 37 |
| Dentistry general and community | 1116 | 1 |
| Diagnostic services | 138,989 | 94 |
| Learning disabilities | 6200 | 14 |
| Medical specialties | 1,182,831 | 1869 |
| Mental health | 5207 | 6 |
| Obstetrics and gynaecology | 375,674 | 72 |
| Primary care/community | 16,525 | 35 |
| Patient transport services | 2053 | 21 |
| Surgical specialties | 594,311 | 769 |
| Other specialties | 68,073 | 23 |
| Children’s specialties | 485 | 0 |
| Other | 206,827 | 13 |
| Not applicable | 15,235 | 13 |
| Unknown | 27,360 | 19 |
The number of incidents in acute trusts is significantly greater than in other organisations but the percentage of total incidents related to DNACPR is of a similar, very small order across all organisations (≤ 0.01%). The number of incidents categorised as causing moderate or severe harm was 653 out of a total number of DNACPR-associated incidents of 4528 (25%) and there were 148 deaths.
Within acute trusts the majority of DNACPR-related incidents occur in medical and surgical specialties and emergency care. This is likely to reflect the type and severity of illness seen in patients in these specialties, and the age range of the patient cohort.
Coroners’ Rule 43 reports
Summary reports of Rule 43/Prevention of Future Death reports were obtained covering October 2008–September 2013. The frequency of issuing Rule 43 or Prevention of Future Death notices in relation to DNACPR was relatively infrequent, representing only 0.5% of the total number of notices issued since the revised legislation in 2008. The total number of reports and the number of reports potentially related to DNACPR issues are summarised (Table 5).
| Date | Report | Total number of reports | DNACPR issue |
|---|---|---|---|
| October 2008–March 2009 | 1 | 207 | 0 |
| April 2009–September 2009 | 2 | 164 | 1 |
| October 2009–March 2010 | 3 | 195 | 1 |
| April 2010–September 2010 | 4 | 175 | 0 |
| October 2010–March 2011 | 5 | 189 | 0 |
| April 11–September 2011 | 6 | 210 | 1 |
| October 2011–March 2012 | 7 | 233 | 2 |
| April 2012–September 2012 | 8 | 186 | 0 |
| October 2012–March 2013 | 9 | 235 | 5 |
| April 2013–September 2013 | 10 | 244 | 1 |
| Total | 2038 | 11 (0.5%) | |
The notices each involved single incidents and were served on eight NHS trusts, the Department of Health (n = 2), private health-care providers (n = 2), the Care Quality Commission (n = 1) and the Ministry of Justice (n = 1). Table 6 summarises the circumstances leading to the issuing of a Rule 43/Prevention of Future Deaths notice. The overall frequency of issuing Rule 43 or Prevention of Future Death notices in relation to DNACPR was relatively low, representing only 0.5% of the total number of notices issued since the revised legislation in 2008. 109 The focus of notices on NHS trusts could be broadly categorised into problems with communication (between health-care staff and the patient/relatives n = 3), documentation (n = 2), staff training (n = 2) and problems with transferring DNACPR decisions between the hospital and community settings (n = 1). Two coroners served notices on the Secretary of State for Health suggesting the need for a national DNACPR policy to be considered.
| Date | Recipient | Description |
|---|---|---|
| April–September 2009 | NHS trust | To consider a review of the hospital’s use of DNAR authority forms and the effectiveness of inpatient dietary risk assessments |
| October 2009–March 2010 | NHS trust | To consider a review of how forms indicating a patient’s wishes for resuscitation can be better annotated to ensure that changes are easily identified |
| April–September 2011 | Ministry of Justice | To consider a review of the ‘do not resuscitate’ policy and to ensure that decisions not to resuscitate are made only following consultation with the prisoner/patient themselves or with members of their family |
| October 2011–March 2012 | NHS trust | To consider improving communication between clinicians and patient family members and the arrangements for DNAR orders |
| Private provider | To consider reviewing procedures and training at [name of provider and location] in relation to ‘do not resuscitate’ orders and first aid | |
| October 2012–March 2013 | NHS trust and Department of Health | To consider reviewing the trust’s resuscitation policy so that the DNAR form clearly states the plan of care (NHS trust) |
| To consider whether or not there is merit to having a national policy on DNAR orders (Department of Health) | ||
| NHS trust | To consider reviewing policies and training of staff in the use of DNACPR orders | |
| NHS trust | To consider ways of ensuring adherence to the trust’s policies on DNAR orders | |
| NHS foundation trust | To consider making it an absolute requirement to communicate with relatives when decisions are made not to resuscitate | |
| (1) Care Quality Commission; (2) private provider; (3) NHS primary care trust | To consider the need for [private provider] and NHS [primary care trust] to review their policies, service-level agreements and guidance to staff in nursing homes and primary health care when making do not resuscitate orders for patients transferring from hospitals to nursing homes | |
| April–September 2013 | Secretary of State for the Department of Health | To consider a review of the resuscitation policy |
Full details of the Rule 43 requests were provided for four cases.
Parliamentary and Health Service Ombudsman investigation reports
Currently, the Ombudsman service does not record DNACPR as a keyword in recording complaints. Therefore, it is not possible to determine the number of complaints received that relate to DNACPR. However, the Ombudsman’s Clinical Advice Directorate (which provides advice on some but not all cases referred to the Ombudsman) has a clinical tag for DNACPR orders which was introduced in August 2012. Data from the Clinical Advice Directorate are summarised in Table 7.
| Categories | August–December 2012 | January–July 2013 |
|---|---|---|
| DNAR (theme in complaint) | 12 | 19 |
| DNAR (identified by clinical advisor) | 0 | 2 |
Although no detail could be provided regarding individual complaints, the Ombudsman’s office was able to say that complaints about DNACPR orders were usually one part of the overall complaint. The complaints about DNACPR orders included complaints about poor communication, non-consultation with family members, discussing the DNAR with the patient against the family’s wishes and ignoring verbal requests from the patient to enforce the DNAR order.
Compassion in Dying Information Line
Between 1 November 2013 and 30 June 2014, 110 callers to the information line raised issues regarding DNACPR. The most frequent concern expressed by callers (n = 58, 53%) was that they (or their friend/family member) would be resuscitated against their wishes, or that their wishes would not be known by the professional caring for them at the time (n = 19, 17%). This theme of concern about loss of autonomy or control was reinforced by a number of callers enquiring specifically about how they could avoid resuscitation (17%). Several callers expressed fear that there would be adverse consequences of resuscitation leading to severe impairment, while lack of information about or understanding of the process of DNACPR orders was the main reason for enquiry by others. Two callers were concerned about the fact that their relatives had a DNACPR order in place when they felt that the relative should be resuscitated instead. Table 8 summarises the range and frequency of topics covered.
| DNACPR-related topic | ||||||
|---|---|---|---|---|---|---|
| Worried about resuscitation against their wishes | Worried their wishes will not be known | Fear of consequences of resuscitation | Clarification of terminology/process | Experience with friend or family member ill/dying | Direct question on how to avoid resuscitation | |
| Number of callers raising topic | 58 | 19 | 16 | 29 | 21 | 19 |
Summary
Do-not-attempt-cardiopulmonary-resuscitation decisions were a relatively rare (< 0.5%) source of incidents and complaints in the NHS. However, when such events occurred they were often serious and, in some cases, resulted in deaths. Data from the helpline suggest that some members of the public are concerned that health-care professionals do not or will not respect their wishes with regard to resuscitation. There is a lack of understanding among the public about what a DNACPR order is and how it relates to an advance directive. Health-care professionals do not discuss DNACPR with patients and their families and they do not communicate adequately with each other about a patient’s DNACPR status. Doctors either avoid discussing with patients/making the decision or do not see this as a priority. There is a lack of knowledge about process and confusion over documentation within and between health-care organisations.
Chapter 4 Evaluation of NHS trusts’ do-not-attempt-cardiopulmonary-resuscitation policies
Introduction
In England and Wales the Human Rights Act 1998115 and the Mental Capacity Act 2005116 provide the legal basis for DNACPR decision-making. The Human Rights Act 1998115 covers fundamental rights, such as the right to life and the right to be free from inhuman and degrading treatment, and The Mental Capacity Act 2005116 works under the assumption that every adult is able to make their own decisions unless a mental capacity assessment shows otherwise. The latter act sets out how to carry out an assessment of capacity, describes who can make decisions for people who lack capacity and provides a checklist to ensure that any decision taken on behalf of a person without capacity is in his or her best interest. Based on these laws, national guidelines117 in England describe the context, setting and process for making informed decisions to omit CPR and provide a framework to support decisions relating to CPR.
Local policy-makers are responsible for ensuring that effective systems are in place for recording and communicating decisions related to resuscitation. DNACPR decisions may apply across a number of settings, including hospitals, patients’ homes, nursing homes and hospices as well as during transfer between these settings. The RC(UK) recommends that DNACPR decisions travel with the patient and should be recognised and accepted by all health-care services. To support the standardisation of DNACPR recording, the RC(UK) has developed a model DNACPR form (Figure 3).
FIGURE 3.
Resuscitation Council (UK)-recommended DNACPR decision form. Reproduced with permission.
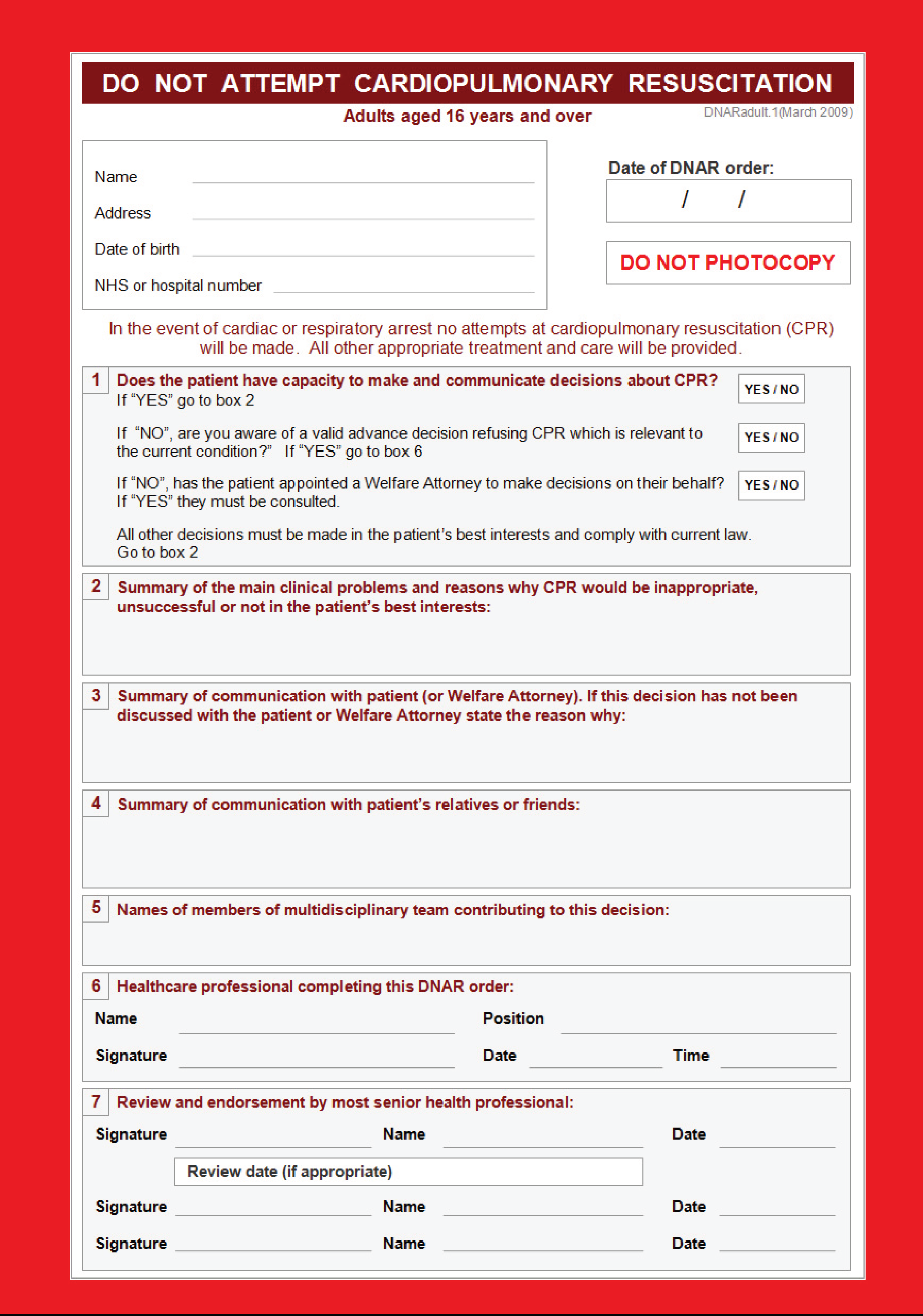
Recent high-profile cases in the media suggest that issues exist in terms of DNACPR decision-making in English health-care settings claiming lack of consistency in approach across England. It is, therefore, of interest to understand the impact that the national guidelines have on local policies, which, in the absence of a national DNACPR policy, determine local practice.
We therefore reviewed a random sample of local DNACPR policies from acute, community and ambulance service trusts across England and mapped them against aspects from national guidelines to identify variation and consistencies between and within trust types and inconsistencies in implementation of national guidelines. 118
Methods
Using the NHS service directory, we obtained NHS care trust lists of acute, community and ambulance service trusts. We identified a random sample of 20 acute hospital trusts for review. After mapping, a further six trusts were chosen to ensure geographical coverage. All 10 ambulance service trusts and a random sample of 12 community health trusts were further included. FOI requests for adult DNACPR policies were sent to the sample of English acute trusts, ambulance service trusts and community trusts. If a separate DNACPR policy was not available, then the trust’s resuscitation policy was requested. Follow-up e-mails were sent once if (1) the wrong policy was sent, (2) it was inferred on reading the policy that additional information was available, or (3) the health trust had not responded after 2 months.
Additional information given in the accompanying e-mails by the trust on further policies and the validity of the policy was considered in the data extraction process, as was information on the back of the DNACPR form, if this was provided.
A data extraction form was established using aspects of decision-making from the joint statement by the RC(UK), the BMA and the RCN on decisions relating to CPR. 117 The resulting extraction form was piloted by two reviewers and was subsequently adjusted. The final form comprised 26 questions on aspects taken from the national guidelines, including documentation, ethical and legal issues, DNACPR decision-makers and the involvement of others in DNACPR decisions, as well as practical considerations such as validity, review period and portability of decisions. Policies were then read in their entirety by one researcher (Karoline Freeman) and data were extracted using the agreed form. Queries during the data extraction process were discussed and agreed with Gavin Perkins. The first 30% of data extractions were checked by a second reviewer (Richard Field) and confirmed as accurate.
Data were synthesised quantitatively as frequencies of responses per question (documentation of DNACPR decisions, implementation of legal and ethical aspects, decision-makers and involvement of others) and narratively (practical considerations). For the qualitative synthesis, policies were coded using descriptive coding. The main categories of topic areas were identified by discussion through clustering of the codes.
Results
A total of 48 local DNACPR policies were reviewed (100% response rate). The 26 acute trusts consisted of 6 teaching hospitals, 19 district general hospitals and 1 specialist centre. Good geographical coverage of England was achieved, with the reviewed policies from 26 acute and 12 community trusts. All 10 English ambulance services were considered.
Documentation
The trusts produced specific local documents referred to as policies (85%), procedures (6%) or guidelines (8%) (Table 9). There was variation in the terms used to describe resuscitation decisions, with two-thirds of trusts referring to the term ‘DNACPR’, one-quarter referring to ‘DNAR’ and the remainder referring to ‘not for CPR’ or ‘AND’.
| Policy type item | Acute trusts (n = 26), n (%) | Community trusts (n = 12), n (%) | Ambulance trusts (n = 10), n (%) | Total (N = 48), N (%) |
|---|---|---|---|---|
| Type of document | ||||
| Policy | 22 (85) | 12 (100) | 7 (70) | 41 (85) |
| Procedure | 2 (8) | 0 | 1 (10) | 3 (6) |
| Guideline | 2 (8) | 0 | 2 (20) | 4 (8) |
| Terminology | ||||
| DNAR | 6 (23) | 3 (25) | 3 (30) | 12 (25) |
| DNACPR | 16 (62) | 8 (67) | 7 (70) | 31 (65) |
| Not for CPR | 3 (12) | 0 | 0 | 3 (6) |
| AND | 1 (4) | 2 (17)a | 0 | 3 (6) |
How frequently are policies reviewed?
The time since last review of policies varied across local trusts, from less than 1 month to 47 months. Figure 4 shows that 17 trusts reviewed their policy within the past 12 months, 17 did so within the past 2 years and 6 did so within the past 3 years. Three policies did not include dates of review.
FIGURE 4.
Time elapsed since last review of policy.

Although review generally takes place after 2 or 3 years, five policies had not been reviewed for over 3 years and 13 (27%) policies were not within their review cycle. Of these, only (12%) were known to be under review (Figure 5). Three-quarters of policies were reported as having undergone an equality and diversity assessment.
FIGURE 5.
Proportion of policies within/outside their policy review cycle.
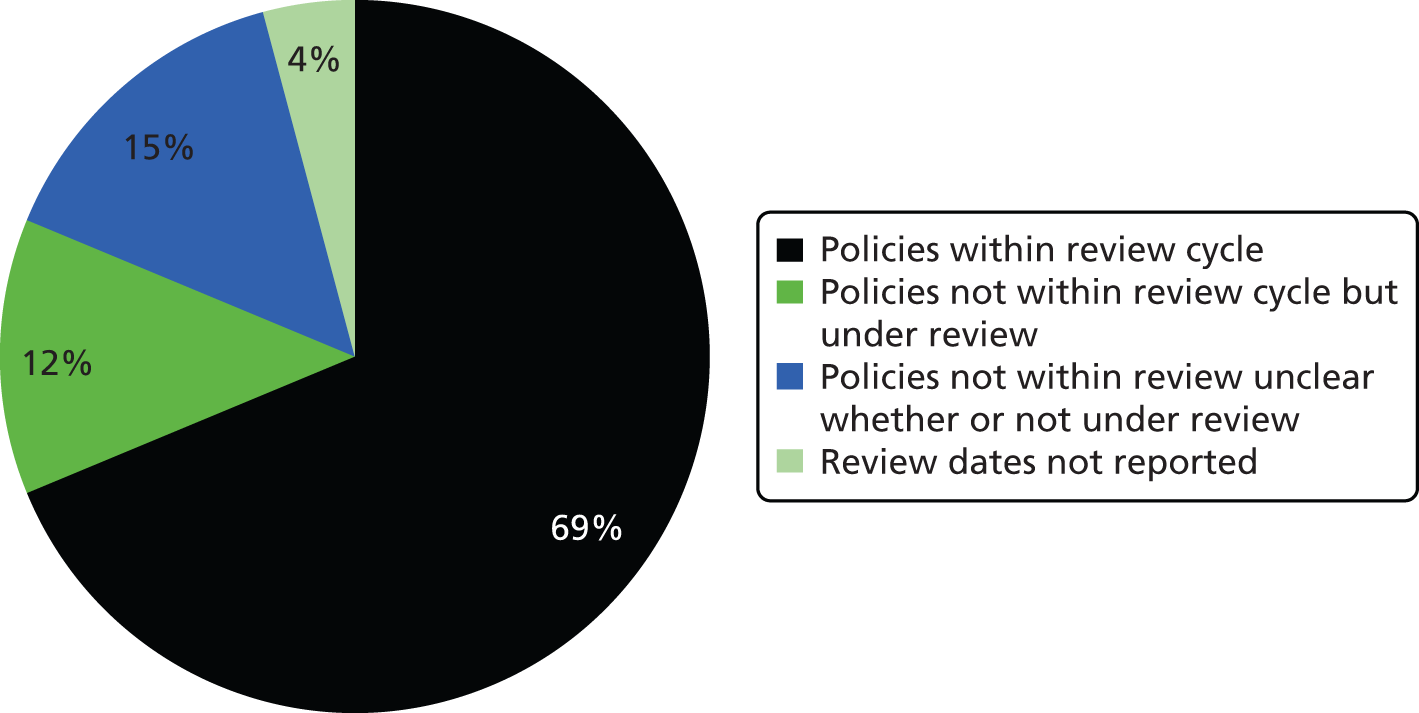
Relationship with other policies
The review identified that all of the reviewed acute and community trusts are primary decision-makers for DNACPR decisions, while ambulance service trusts do not make lasting DNACPR decisions. Policies varied in their level of commitment, terminology, visibility and extent (Table 10). Noticeably, standalone policies tended to be used more by acute and community trusts, while ambulance service trusts mostly integrated their DNACPR policy into policies dealing with patients at the end of life or recognising life-extinct policies.
| Policy type item | Acute trusts (n = 26), n (%) | Community trusts (n = 12), n (%) | Ambulance trusts (n = 10), n (%) | Total (N = 48), N (%) |
|---|---|---|---|---|
| Standalone | 21 (81) | 9 (75) | 3 (30) | 33 (69) |
| Integrated into resuscitation policy | 5 (19) | 3 (25) | 3 (30) | 11 (23) |
| Mentioned in other policies | 0 | 0 | 4 (40) | 4 (8) |
| Coverage | ||||
| Local | 23 (88) | 9 (75) | 8 (80) | 40 (83) |
| Regional | 3 (12) | 3 (25) | 2 (20) | 8 (17) |
Ethical and legal basis for do-not-attempt-cardiopulmonary-resuscitation decisions
The joint statement ‘Decisions relating to Cardiopulmonary Resuscitation’ from the BMA, the RC(UK) and the RCN117 was the most frequently cited source of national guidance for acute and community NHS trusts. Reference to relevant legislation (Mental Capacity Act 89%, Human Rights Act 78%) was common. GMC guidelines were highlighted less frequently (50%). Nine out of 10 ambulance service trusts additionally cited the Joint Royal College Ambulance Liaison Committee.
Acute and community trust policies universally correctly identified the circumstances in which a DNACPR decision could be considered (futility, overall benefit and patient refusal) and most clarified that the DNACPR decision related only to the act of resuscitation and did not apply to other aspects of care (Table 11).
| Item from national guidelines | Acute trusts (n = 26), n (%) | Community trusts (n = 12), n (%) | Ambulance trusts (n = 10), n (%) | Total (N = 48), N (%) |
|---|---|---|---|---|
| Does the policy describe all three situations (futility, burden and refusal) in which DNACPR decisions are appropriate? | 26 (100) | 12 (100) | 6 (60) | 44 (92) |
| Does the policy clarify the relationship between DNACPR and other aspects of care? | 25 (96) | 11 (92) | 9 (90) | 45 (94) |
| Does the policy contain the RC(UK) flow diagram to guide DNACPR decisions yes or modified? | 20 (42) | 10 (83) | 3 (30) | 33 (69) |
| Does the policy contain information on audit? | 26 (100) | 12 (100) | 9 (90) | 47 (98) |
| Has an equality and diversity assessment been carried out? | 17 (65) | 10 (83) | 9 (90) | 36 (75) |
Decision-makers and involvement of others in do-not-attempt-cardiopulmonary-resuscitation decisions
All acute and community trusts were responsible for primary DNACPR decisions while ambulance service trusts were not primary decision-makers of lasting DNACPR decisions. The review identified variation in the grade of clinical staff authorised to make an initial DNACPR decision (Figure 6).
FIGURE 6.
Grade of staff authorised to make DNACPR decisions.
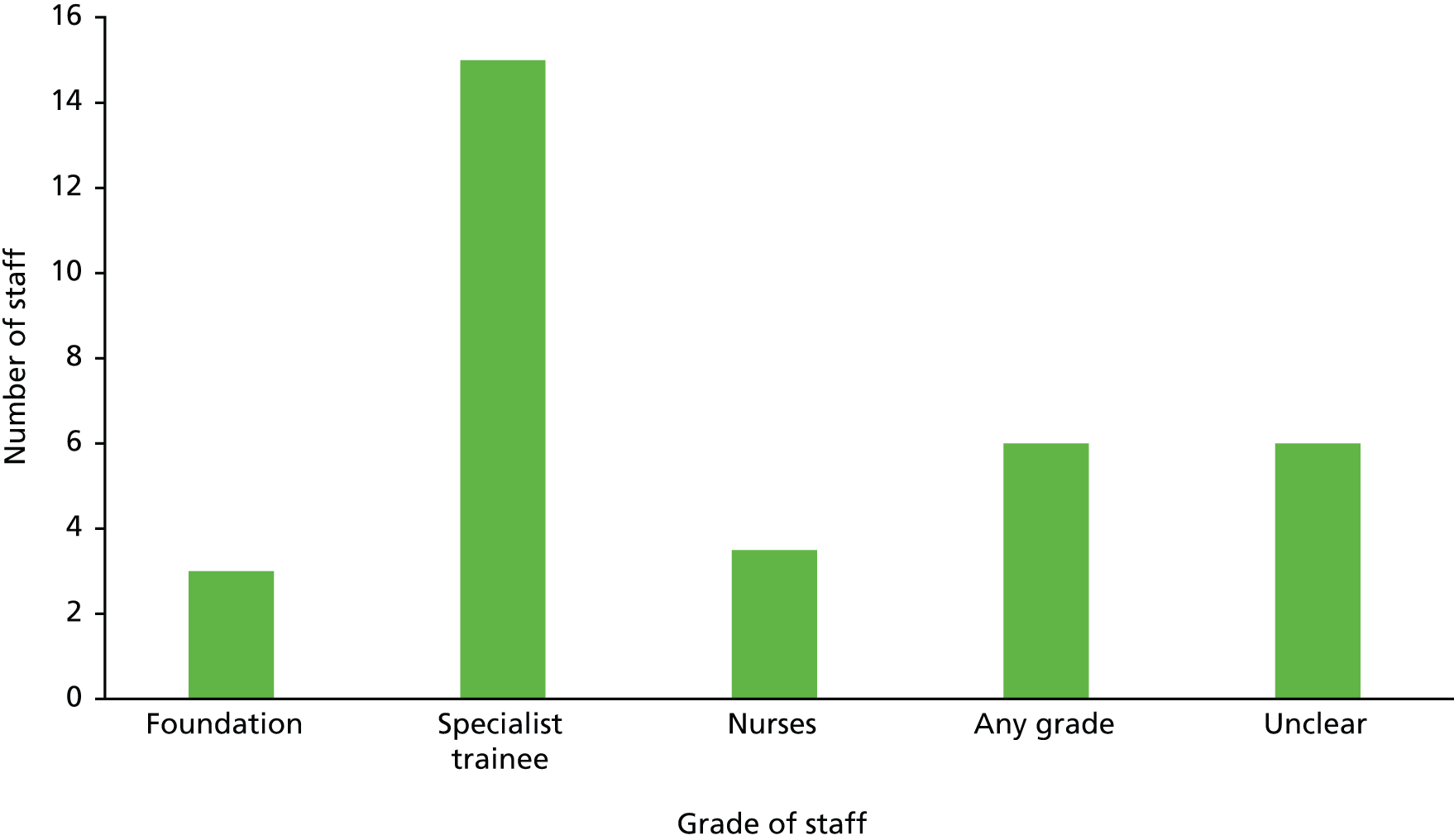
Authority was delegated to senior nursing staff at seven trusts (one limited to MacMillan Nurses, three for community decisions only and three appropriately qualified nurses) or junior medical staff [foundation year doctors (n = 3), specialist trainee doctors (n = 15), most senior available/any grade (n = 6) or undefined/unclear (n = 3)]. At all acute trusts accountability for DNACPR decisions rested with consultants, and at community trusts it rested with the most senior clinician, who may be a GP, consultant or nurse, depending on the circumstances. Few (8%) trusts mandated medical staff to discuss decisions with others within the multidisciplinary team, although most (74%) recommended discussion; one-fifth made no such recommendations (Table 12).
| Consultation of multidisciplinary team | Acute trusts (n = 26), n (%) | Community trusts (n = 12), n (%) | Total (N = 38), N (%) |
|---|---|---|---|
| Must | 1 (4) | 2 (17) | 3 (8) |
| Should | 22 (85) | 6 (50) | 28 (74) |
| Not mentioned | 3 (12) | 4 (33) | 7 (18) |
In 100% of reviewed policies, acute trusts recommended that staff talk to patients and relatives; community trusts recommended that staff talk to patients in 100% of policies and to relatives in 92% (Table 13). Guidance requiring clinical staff to assess the patient for capacity and guidance about when to consult a lasting power of attorney or independent mental capacity advocate occurred less commonly. Fifty per cent of trusts recommended the use of a patient information leaflet. Fewer than 1 in 10 trusts provided practical guidance on how to approach DNACPR decision-making for patients of different cultures.
| Content of the policy | Acute trusts (n = 26), n (%) | Community trusts (n = 12), n (%) | Ambulance service trusts (n = 10), n (%) | Total (N = 48), N (%) |
|---|---|---|---|---|
| Does the policy contain guidance relating to cultural differences? | 3 (12) | 1 (8) | 0 | 4 (8) |
| Does the policy refer to a patient information leaflet for DNACPR? | 12 (46) | 9 (75) | 1 (10) | 22 (46) |
| n (%) of these that are the RC(UK) information leaflet | 1 (4) | 0 | 0 | 1 (2) |
| Does the policy require staff to assess patient capacity? | 15 (58) | 9 (75) | 1 (10) | 25 (52) |
| Does the policy tell staff when to consult/inform patients or relevant others? | ||||
| Patients | 26 (100) | 12 (100) | 6 (60) | 44 (92) |
| LPA | 20 (42) | 11 (92) | 3 (30) | 34 (71) |
| Relatives | 26 (100) | 11 (92) | 5 (50) | 42 (88) |
| IMCA | 18 (69) | 8 (67) | 2 (20) | 28 (58) |
Recording do-not-attempt-cardiopulmonary-resuscitation decisions
There was variation in how DNACPR decisions were recorded (Table 14). One-quarter of trusts used the RC(UK) DNACPR form or a modified version. As a general guide, modifications included adding or changing a couple of questions but required the general layout to be the same as the RC(UK) form while any more substantial changes would make the form bespoke. The majority of forms were paper forms (81%) with only 8% of trusts using electronic versions. None of the forms required the patient to give consent. Health-care professionals making the DNACPR decision were obligated to sign the form, which also had room for a countersignature by the consultant if a junior doctor initiated the decision, which would need endorsement. In one specific case the form required the doctor’s signature to be witnessed by the registered nurse who was involved in the discussion about the DNACPR decision.
| DNACPR form | Acute trusts (n = 26), n (%) | Community trusts (n = 12), n (%) | Ambulance trusts (n = 10), n (%) | Total (N = 48), N (%) |
|---|---|---|---|---|
| RC(UK) | 2 (8) | 3 (25) | 0 | 5 (10) |
| Modified | 4 (15) | 3 (25) | 1 (10) | 8 (17) |
| Bespoke | 16 (62) | 4 (33) | 4 (40) | 24 (50) |
| Form not sent | 4 (15) | 2 (17) | 5 (50) | 11 (23) |
| Type of forma | ||||
| Paper | 24 (92) | 10 (83) | 5 (50) | 39 (81) |
| Electronic | 1 (4) | 0 | 0 | 1 (2) |
| Both | 1 (4) | 2 (17) | 0 | 3 (6) |
Practical issues of do-not-attempt-cardiopulmonary-resuscitation decision-making
Review
Policies on review ranged from regular review required with or without specification of a review date to regular review not recommended. The majority of policies included specific prompts that required clinicians to initiate review. These prompts included admission/readmission, transfer/discharge, surgery/anaesthesia and the change of the patient’s condition or of the patient’s mind.
A review period was given in 7 out of 26 (27%) policies from acute trusts which ranged from 24 hours to 6 months. Six policies (23%) recommended regular review but did not specify a particular time period, while four (15%) policies did not recommend regular review. One stated that review was not required and eight (31%) did not mention regular review. Specific prompts for review were admission/readmission (n = 17), transfer/discharge (n = 16) and surgery/anaesthesia (n = 16). Clinical discretion would prompt a review in 22 out of 26 (85%) policies and a change in the patient’s condition or patient’s expressed wishes as a reason for review was mentioned in 24 out of 26 (92%) policies.
Similarly, regular review was mentioned in 5 out of 12 policies from community trusts, which ranged from weekly (n = 2) to 6 monthly (n = 1); the time period was not specified in two policies. One trust did not recommend regular review. The frequency of the review period was determined by clinical judgement and the change in patient status/patient change of mind in the majority of policies (8/12 and 11/12, respectively). Specific situations that prompted review were admission/readmission (7/12), transfer/discharge (9/12) and surgery/anaesthesia (4/12).
Five out of 10 policies from ambulance services did not mention anything about review. Three out of 10 policies stated that if a review date is specified on the form, ambulance service staff need to check whether or not their decision is within the review period. Five out of 10 policies stated that decisions without review date, including decisions for terminally ill patients, should be considered indefinite. For other patients regular review is recommended in three of these five policies, while one policy does not recommend regular review. In 5 out of 10 policies review is required at clinical discretion. Situations that should prompt a review were change in the patient’s condition or change in his or her expressed wishes (n = 3), admission/readmission (n = 1) and transfer/discharge (n = 1). One policy recognised that review dates on forms will vary across the region according to different local policies. Another policy included a form that stated that no decision should be regarded as indefinite and that the review period must be no longer than 3 months.
Validity
The duration of time over which a DNACPR decision was considered valid varied widely. DNACPR decisions from acute trusts ranged from valid indefinitely (54%) to valid for the duration of one hospital admission only (31%), to valid until a specific point in time (8%) and to up until a specified review date (4%). Similarly, in community trusts validity ranged from valid indefinitely (42%) to valid up until a specified review date (42%). Two community trusts had no information in the policies about the validity of decisions and in one acute trust the duration of validity was unclear. There was similarly wide variation in trusts’ approach to reviewing DNACPR decisions, with time points ranging from 24 hours to months.
Ambulance services focused on the requirements to recognise a valid DNACPR decision from other organisations. The level of proof required ranged from the original DNACPR form being acceptable only (n = 1) to photocopies with an ink signature/legible signature being acceptable (n = 2) to the form not necessarily needing to be seen (n = 1). Six policies did not specify the requirements regarding the level of proof of a valid DNACPR decision. Acceptable formats of DNACPR decisions varied considerably. Two trusts recognised that DNACPR decisions came in a variety of formats and were willing to accept verbal and written DNACPR decisions (including letters, entries in patient notes and pro formas). Another two trusts accepted any kind of written decisions, while one trust stated that a decision had to be presented on a DNACPR form. Three more trusts required specific forms only. Seven out of 10 policies specified details that staff were required to check in order to establish the validity of the document. These included the patient’s details, the review date, a list of items (if the decision was not on a pro forma) and the completeness of transport-specific sections on the DNACPR form.
Portability
The portability of DNACPR decisions between organisations and health-care settings (community/acute care) was one of the greatest sources of inconsistency and variation. DNACPR decisions were portable in 13 out of 26 acute trusts and 8 out of 12 community trusts. An additional six acute trusts’ DNACPR decisions extended to include ambulance transport. The remaining acute trusts (n = 7), but only one community trust, had a system in place through which non-portable DNACPR decisions could be communicated between providers. The level of portability of DNACPR decisions in the remaining three community trusts was unclear. The level of detail in which handover systems were described in the policies was generally greater in the community trusts than in the acute trusts.
Exemplars of best practice
Deciding Right
The North-East region’s ‘Deciding Right’ is presented as an exemplar of best practice. 119 This regional policy has been implemented across all health-care settings in the region. It integrates the principles of making care decisions, including DNACPR decisions, in advance, thereby providing a tool for overall treatment plans.
The authors provide context to the tool:
Individuals have the right to make decisions in advance about their care and for that to happen as a shared partnership with health and social care professionals. Individuals who lack capacity have the right to have decisions made in their best interests in the way required by the Mental Capacity Act. Health and social care professionals have a duty to follow national legislation and guidance. They also need clear instructions about what the individual wants to happen.
Deciding right empowers the individual and the professional to make the right decisions.
Reproduced with permission from www.nescn.nhs.uk/deciding-right and the Deciding right app on Google Play and the Apple store
Portability checklist
An example of a clear, unambiguous pathway, describing the transfer of a fully portable DNACPR form between and within acute and community care settings, is provided in Box 1.
If, on review, the DNACPR is still considered appropriate, carry decision over to the patient’s care setting/home on discharge, including the following considerations:
-
Liaise with the patient’s GP and identify an agreed, appropriate community review date (ideally within 24 hours), which should be documented on the DNACPR form.
-
Send the original DNACPR form (top white copy) with a review date in place with the patient.
-
Communicate and discuss sensitively with the patient.
-
Leave the yellow copy (second copy) in the front of the patient’s medical hospital notes facilitating early consideration of resuscitation issues on any potential subsequent readmission.
Communication with ambulance service and/or ongoing care setting must take place.
Before ambulance transfer complete appropriate section on the DNACPR form.
When booking transport for DNACPR patient from acute trust, fax DNACPR form to ambulance control contact centre.
Within community settings, hand DNACPR forms directly to the attending crew on arrival or fax to ambulance service contact centre.
The DNACPR status must also be recorded by the attending ambulance service crew on the ambulance service patient report form.
Summary
This review identified significant variation in English NHS trusts’ approaches to DNACPR decision-making. Gaps identified included practical guidance around when and how to communicate DNACPR decisions and in relation to the portability/transferability of decisions between health-care settings. There is a need for greater consistency in trusts’ approaches to DNACPR decision-making.
Chapter 5 Obtaining service providers’ perspectives on do-not-attempt-cardiopulmonary-resuscitation decisions
Introduction
The purpose of this activity was to explore health professionals’ experiences with DNACPR policy and practice.
Methods
We used focus groups to explore service-provider perspectives on DNACPR decisions as they are an established method for collecting data from health professionals on their experiences of policy and practice and on their opinions, and how through discussion health professionals develop or construct their knowledge and understanding of an issue. 120,121 In relation to decisions concerning the end of life, Dalkin et al. 122 used health professional focus groups to investigate how a new integrated care pathway for individuals with life-limiting illnesses requiring palliative care worked in practice; Gélinas et al. 123 used focus groups to explore the stressors faced by nurses providing end-of-life care in ICUs; and Thompson et al. 124 used focus groups to explore health professionals’ views on advanced directives. Health professionals’ experiences of DNACPR will rarely occur in isolation, and, particularly where there have been difficulties with the decision-making process, DNACPR is discussed with health professional colleagues, formally or informally. Focus groups facilitate similar discussions by encouraging the sharing of and reflection on experiences and the development of ideas and views on policy and practice. When policy and practice have particular ethical significance, as in the case of DNACPR, the integration of ethical analysis with standard qualitative data analysis can provide both descriptive and normative insights. 125
Design
We undertook multiple relatively brief focus groups to maximise participation of clinicians from the relevant health service contexts, to ensure that we included clinicians with a range of experience of DNACPR and to preserve anonymity for the participants. Focus group attendees were assured that the discussion would be kept confidential to the research team. They were also assured that their data would not be recognisable in the research report, including any quotations from the focus group data. With a small number of focus groups which aim for extensive discussion of an issue, it can be difficult to preserve anonymity while also demonstrating the provenance of the research. We undertook focus groups until we were confident that we achieved both diversity of participants and contexts and data saturation based on initial analysis.
Ethical and governance issues
Approval to conduct the study was granted by the University of Warwick Biomedical and Scientific Research Ethics Committee and permission was obtained from the trust research and development departments for access to their staff when the research took place on NHS premises. The study was registered with the Clinical Research Network Portfolio system.
Recruitment processes
Our recruitment aim in focus groups was to engage clinicians from a range of disciplines who had professional experience of DNACPR decision-making and were interested in discussing DNACPR decisions. We recruited participants from among attendees at conferences that had relevance to DNACPR, holding the focus groups in the conference venue. We included focus group discussions within existing educational sessions for health professionals. We advertised for participants at clinical meetings and contacts in NHS trusts, such as resuscitation leads, identified participants.
Development of vignettes to stimulate focus group discussion
We constructed 10 vignettes in which DNACPR decisions were problematic based on cases reported in NCEPOD’s report ‘Time to Intervene?’. 105 This set of vignettes included at least one vignette relevant to each clinical role and context from which participants were drawn. Drawing on the legal and ethical regulatory framework for professional practice in the UK (Mental Capacity Act 2005116 and GMC guidance for end-of-life decision-making126) and the ethics literature on end-of-life decision-making, we identified key ethical principles and issues that should be addressed when considering DNACPR decisions. Three members of the research team (SC, AMS and FG) coded the first 10 vignettes using the identified principles/issues. For the vignettes and a table indicating the ethical principles/issues represented by each vignette, see Appendix 4.
The allocation of vignette to focus group was sequential to ensure that all vignettes were used in rotation. The exception was the GP focus group. As this was part of a planned educational session, we tailored vignettes to the learning needs of the participants in collaboration with the GP tutors.
Focus group process
Each focus group was led by a trained facilitator who had clinical knowledge of CPR and DNACPR decisions. Most focus groups were audio recorded. Detailed field notes were taken where audio recording was not possible as a result of the noisy environment – usually the case when multiple groups were meeting in one room. Consent was collected from participants before the focus group started. The facilitator introduced the purpose of the focus group and offered assurances regarding confidentiality and anonymity. Focus group members were asked their role, the length of time they had worked in their current role and the length of time they had been working as a health professional (total). Participants read the first vignette and were asked if the scenario was one they recognised from their own experience. Views were sought about where DNACPR decisions might fit into the given scenario, measures that could have been taken to avoid the difficult situation described in the vignette and reasons why this might not happen (see Appendix 4). Discussion was facilitated until the group had no new comments. The facilitator prompted for background to the experiences and opinions expressed. If time permitted a further vignette was discussed. Focus groups’ durations ranged from 15 minutes to 1 hour (see Appendix 5).
Data management and initial analysis
Focus group data were transcribed verbatim, checked for accuracy and uploaded into the analysis software NVivo 10.0 (QSR International, Warrington, UK) to aid data handling. Data from early focus groups were read by FG, AMS, GDP, ZF and SC to consider whether or not the data collected were on topic, were in sufficient depth, covered the range of ethical issues and included the range of health professionals. This resulted in the development of further vignettes and the seeking of focus group participants from missing professions. Data saturation was quickly reached with professionals working in palliative care. SC undertook an initial thematic analysis. This informed further review of the data by the team and the development of analysis plans (1) to explore issues related to the process of making DNACPR decisions and (2) to explore ethical issues related to DNACPR.
Analysis of the process of making do-not-attempt-cardiopulmonary-resuscitation decisions
Our approach to the data assumed that the views people articulate in language map onto their experience,127–129 in contrast to a constructionist approach in which meaning and experience are believed to be created through language. 130 Transcripts were analysed inductively, by which process the derivation of themes is data driven rather than theory driven. 131 After the initial thematic analysis, coded data and new data were reviewed by the research team and a coding scheme was developed. This was then further reviewed and developed. At least 40% of the data were read by other analysis team members (FG, GDP, AMS and ZF) who contributed to code development. Codes included knowledge of DNACPR decision-making, how decisions were made, engagement with the family, changes to DNACPR decisions when a patient is transferred, barriers and enablers to DNACPR decisions and explicit mention of ethics or values. Coding was undertaken by SC, and independent coding was undertaken by Sarah Owen on 25% of transcripts; coding was compared and discrepancies discussed to improve the consistency of coding. Coded data were then extracted theme by theme. Extracted data were read, discussed and further analysed by the analysis team (SC, FG, AMS, GDP and ZF). The outcome of this was presented to the wider research team, along with the initial results of all work packages, and discussed. A final analysis was developed.
Ethical analysis
In the ethical analysis we were looking for implicit rather than explicit articulation of ethical principles, values and conflicts. Thematic coding identified very little explicit recognition of ethical issues. Transcripts were allocated to members of the analysis team (FG, AMS, SC, GDP and ZF), with each transcript being read by two people. Readers were asked to identify examples of explicit articulation of ethical issues; areas of conflict or disagreement; expressions of discomfort with current or perceived practice; or examples of avoidance of an ethical issue. All allocated transcripts were discussed in depth at an analysis meeting during which consensus was reached on the ethical interpretation of the data. Ethical issues and values identified were considered in relation to ethical, professional and legal normative frameworks. The discussion was recorded and transcribed to ensure that we had captured the range and nuance of the ethical issues identified. The process was repeated with a further sample of transcripts to look for any new themes/issues arising and to consolidate consensus on the initially agreed themes. The initial analysis was presented to the wider research team along with the results of initial analysis of all work packages and discussions. From this, a final analysis was developed. For a summary of themes, see Appendix 6.
Results
Focus group participants
A total of 223 clinicians participated in 34 focus groups. Clinical disciplines represented included acute medicine, critical care, emergency medicine, geriatrics, palliative care, general practice, cardiology and surgery. Participants included doctors, nurses, and paramedics from junior to senior (Table 15). Participants were drawn from across the UK. Aspects of the vignettes used to stimulate discussion were readily recognised by all participants. Although discussion focused on the vignette for the first few minutes of discussion, participants soon started describing their own experiences that were in some way related to the vignette or to DNACPR more widely. We focused our analysis on what they said about their own experiences.
| Specialty | Total number | Profession/grade | Length of time in current role | Gender | ||
|---|---|---|---|---|---|---|
| Range | Median | Male | Female | |||
| General practice | 30 | Includes one registrar, one ED doctor, two FY2 doctors | 2 months to 35 years | 11.5 (6 values) | Data not available | |
| Community | 8 | One clinical director, one head of service improvement, one child psychologist, five nurses (two matrons, one heart failure, one district, one lead) | 4 months to 8 years | 2.5 | 2 | 6 |
| Geriatricians | 7 | Six consultants (one locum, one lead), one FY2 doctor | 6 months to 20 years | 8 | 4 | 3 |
| Acute medicine | 15 | Eight consultants, six registrars, one lead nurse gastroenterology | 4 months to 27 years | 3 (10 values) | 10 | 5 |
| Cardiology | 6 | One consultant, one registrar, four nurses (one cardiac arrest prevention, two CNSs, one ward manager) | 3 to 18 years | 5.5 (5 values) | 2 | 4 |
| Palliative care | 23 | Five consultants, one registrar, 17 nurses (one consultant, nine CNSs,a one matron, one lead for cancer, four research, one other) | Newly appointed to 18 years | 3 (21 values) | 5 | 18 |
| Surgical specialties, mainly orthopaedic | 11 | Two consultants, one SPR, one staff grade, two CT2, one CT1, one SHO, one FY2 doctor, two nurse practitioners | 6 months to 27 years | 2 | 9 | 2 |
| Emergency department | 10 | Two consultants, one staff grade doctor, one FY1 doctor, one AMP, one night matron, four nurses | 2 weeks to 18 years | 3 (9 values) | 2 | 8 |
| Critical care | 30 | One ICU director, 19 consultants (13 ICU, three anaesthetists, three nurses), two research fellows, two registrars, one FY1 doctor, five nurses (four critical care outreach, one senior clinical) | 2 weeks to 40 years | 8 (25 values) | 20 | 8 |
| Resuscitation officers | 31 | Includes three resuscitation managers and six trust resuscitation leads, director of independent training company | 1 to 19 years | 5 (27 values) | 10 | 18 |
| Paramedics | 19 | Includes one senior advisor, three supervisors, one research fellow, one training officer | 4 months to 33 years | 5 (19 values) | 13 | 4 |
| Non-specialty | 33 | One SPR, 16 FY2 doctors, four FY1 doctors, one SHO research fellow, 11 nurses (one matron, three ward managers, three ward sisters, one night practitioner, one staff nurse, two clinical educators) | 2 weeks to 12 years | 6 months (31 values) | 10 | 23 |
The analysis of focus group data is presented in two distinct sections. The first is an analysis of the process of making DNACPR decisions with no normative judgement; the second is an ethical analysis of DNACPR decision-making. To illustrate the results we include quotes from focus group discussions. There are few quotes from GP discussions as these were not audio recorded, and so our analysis is based on field notes with few quotations. After each quote we have indicated the focus group source of the quote. Table 16 indicates the composition of each focus group.
| Focus group ID | Group composition |
|---|---|
| 4 | Four paramedics |
| 5 | Three paramedics; one advanced medical practitioner |
| 6 | Three paramedics (one instructor, one research fellow and one lecturer) |
| 7 | Two nurses (one armed forces and one emergency department); two paramedics |
| 8 | Two resuscitation managers; one clinical director; one head of service improvement; one staff grade doctor, one child psychologist |
| 9 | Four research nurses (one non-clinical, one academic); one medical director; one registrar (all palliative care) |
| 10 | Eight resuscitation training officers; one consultant geriatrician; one cardiac arrest prevention nurse |
| 11 | Six resuscitation officers; two critical care outreach nurse/resuscitation officers; one end-of-life care lead/resuscitation officer; one GP/emergency department doctor |
| 12 | Four resuscitation officers; two paramedics; one hospital night matron; one independent CPR training company director |
| 13 | One hospice worker; three resuscitation officers; two consultants (one emergency department and one anaesthetics); one cardiologist; one emergency department nurse |
| 14 | Three consultants (two anaesthetics and one ICU); three resuscitation officers |
| 15 | Four ICU consultants; one nurse consultant; one senior nurse ICU |
| 16 | One consultant; one critical care outreach nurse; one registrar; two ICU research fellows |
| 17 | Two ICU nurse consultants |
| 18 | Two Foundation Year 1 doctors; two registrars; one senior house officer; one ward manager; one clinical educator |
| 19 | Two resuscitation officers; one ICU consultant; one Foundation Year 1 doctor |
| 20 | One emergency department consultant; one lead nurse community; one nurse clinical teacher |
| 21 | One clinical educator; one staff nurse; two lead nurses (one cancer and one gastroenterology) |
| 22 | Two consultants (one palliative care and one geriatrician); one Foundation Year 1 doctor; one registrar; one cardiac nurse |
| 23 | Six ICU consultants; one registrar |
| 24 | Three consultants (one nurse); seven clinical nurse specialists; one community matron (all from palliative care) |
| 25 | Three consultants (two physicians and one palliative care) |
| 26 | Five paramedics |
| 27 | Two ward mangers; one senior house officer |
| 28 | One palliative care consultant; two matrons; one ward manager; one community cardiac nurse |
| 29 | Two ward sisters; one night practitioner; one emergency department nurse; two clinical nurse specialists (all nurses) |
| 30 | One Foundation Year 1 doctor; 21 Foundation Year 2 doctors |
| 31 | Two nurse practitioners; one matron; one district nurse; one critical care outreach nurse; one resuscitation officer; one clinical sister; one cardiac specialist nurse |
| 32 | Six consultants (four medical consultants and two geriatricians); three GPs; three medical registrars |
| 33 | Four consultants (three medical consultants and one geriatrician); one GP; one ICU director |
| 34 | Two orthopaedic consultants; two registrars; four senior house officers |
Analysis 1: the process of do-not-attempt-cardiopulmonary-resuscitation decision-making
The nature of the do-not-attempt-cardiopulmonary-resuscitation decision
Focus group participants recognised DNACPR decisions as complex and difficult. Participants described DNACPR decisions as one of the following: signing a DNACPR order, revoking a DNACPR order or not making a decision about a DNACPR order when it might be considered appropriate to make a decision (e.g. in the community or hospital when a patient is very frail).
Senior nursing staff have experience to know whether a patient is likely to survive CPR. They cannot complete the DNACPR form but they and FY2 or FY1 can discuss it and make a note that they have discussed it. If a senior doctor is not available to come down, if the FY2 has discussed it with the senior doctor by phone the FY2 can sign the form but the senior doctor has to sign within 24 hours.
13
I want to give you an instance where this person had a DNR order from the emergency department. The patient came to my ward. I went to see his wife and wife said, they have put a red form in. My husband has got early dementia, he is independent, he has got pneumonia and they have put a red form on this man. That is wrong. I had to reverse that order. He had antibiotics and the patient went home independent, walked out of the hospital.
22
Some consultants, even if you asked them, on a respiratory ward to see a very frail patient, even if you ask them to do a DNACPR sometimes they get distracted or they won’t do it, it won’t be their priority. Whereas others, you know, others it’s the first thing they think about.
19
Participants rarely talked about considering signing a DNACPR order and deciding not to do so, although they did talk about getting on with treatment as their priority for patients in acute situations.
The FY2 or even the registrar automatically just says, yes the patient is for full escalation, and it is not until they get to the next morning and post take round by the consultant who then might make that (make a DNACPR order) decision.
15
You’ve got a patient who is down, they’ve just found this woman, it’s cardiac arrest. I haven’t got time to mess around for 5 minutes waiting for paperwork (a DNACPR order) because that’s 5 minutes I’ve not started resuscitating. So I’ve got to start and when the paperwork turns up I can stop.
4
This sense of urgency and commitment to deal with an acute illness in a timely way formed the context for the discussion about DNACPR for all clinicians working in ambulance services, emergency departments, acute care and critical care. This contrasted with the longer time perspective of general practice. GPs discussed how patients with long-term conditions should be considered for DNACPR orders. The example was given of patients with COPD who have had numerous hospital admissions and in whom treatment is becoming ineffective. The GPs discussed that they were in a position to raise the issue of DNACPR incrementally each time they saw the patient.
When talking about DNACPR orders in the acute care setting, some participants talked, with some concern, about DNACPR orders that specified resuscitation only if the patient had a shockable heart rhythm.
You’ve actually got to get a monitor on and say, okay let’s see if we can do something.
13
A few participants described how a decision not to give CPR might be made but without the paperwork required by local policy.
I’ve come across certainly unfortunate irregularity particularly in our other hospital where it’s apparent from the notes what is right and what’s been decided, but they don’t have the DNAR form. And the form seems to have some sort of biblical quality, if it’s not on that form it doesn’t really count, which to me I don’t think that is correct. The form is there to make it easier to communicate, but the message remains the same. But it doesn’t necessarily specify whether they filled out their local DNAR form . . . If you’ve written clearly, if you’ve said she had capacity and she clearly stated her wishes with the appropriate consultant and it’s handwritten in the notes that to me is as valid as a piece of paper. But I’ve certainly found that if it’s not on the right form it doesn’t get acknowledged.
23
The health professionals involved with do-not-attempt-cardiopulmonary-resuscitation decisions
Many different types of health professionals are involved in DNACPR decisions or have their clinical practice affected by these decisions. Senior nurses on wards commonly initiate the process of a DNACPR order being put in place.
Like last week we had a lady who came to me and said, I’ve thought about CPR and discussed it with my daughter and I’d like to be made not for resuscitation. So then at the earliest opportunity I discussed it with my consultant and then put it in place.
29
Signing a DNACPR order was frequently described as something undertaken by the admitting team on or soon after admission to hospital.
I work in a trust that is actually quite good at identifying patients where it might not be appropriate for this course of treatment. We don’t very often have, the only emergencies we have come in are primary and they often are already in a pretty poor state when they come in, obviously depending on the down time that they had. So our teams are generally pretty good and would either make a decision pretty immediately they come through the door depending on how the ambulance has delivered them, or very quickly within about 1 to 2 hours of treatment whether they would be appropriate, it would be appropriate to have a DNR in place or not.
11
Junior doctors described observing that a patient was deteriorating, and so, in order to avoid having to start CPR inappropriately, going to find a senior clinician to make the DNACPR decision even though that senior clinician might not know the patient.
Not infrequently that it comes to a situation where you see the patient in front of you going down pretty quickly and you know that they’re going to arrest and you need that red form signing quickly otherwise you’ve got an obligation to start doing chest compressions when you know that it’s really not appropriate. And it’s not fair on the patient to start doing things like that. That’s the situation where you ask a consultant . . . that doesn’t know the patient, but you need to get that form signed otherwise we’re going to have to start the process.
34
Many participants commented that junior doctors would seek advice from the critical care team about a patient if their own senior was not available. If the critical care team advised that the patient would not be a candidate for the intensive therapy unit (ITU), the junior doctor was more confident about making a DNACPR decision.
Paramedics were most commonly described as in the position of undertaking CPR in a situation in which there was uncertainty about its appropriateness.
Within the community sector, when we’re looking at commencing CPR, we are taught within our mandatory training that unless we have actually got the signed sheet in front of us to say, DNAR we are to start CPR . . . So if we don’t have that piece of paper right in front of us at that point we start resuscitation. And that’s where we come from. So the discussions have to be obviously before you get to the point where the patient collapses.
20
Revoking a DNACPR order was described, for example, when a patient went to theatre for an operation.
Patients who have palliative care can have palliative procedures but anaesthesia increases the risk involved. One increases the risk of respiratory arrest . . . [but] recovery from an arrest in theatre is better than in-hospital arrest . . . because you get them in time. So you would stop the order for . . . the duration of the surgery and for the immediate recovery period.
12
There are other procedures that increase risk and which create a dilemma for health professionals if it is not well established that a DNACPR order should be revoked.
And also a lot of the intervention we may do apart from anaesthetics [that] increase the risk of arrest . . . the thing that people are worried about is giving him analgesia because you may do something that causes an arrest and then well are you then morally obliged to try and treat that if he arrests because it is iatrogenic rather than the patient’s disease?
12
General practitioners were identified most commonly as the health professionals who would not make a decision about a DNACPR order when it might be considered appropriate.
The GP should have discussed DNACPR at an early stage. The patient had chronic lung disease and home oxygen and attempts at CPR are likely to have been unsuccessful. Even if a DNACPR decision was in place the patient may still have been admitted to hospital but it may have prevented futile attempts at CPR.
7
However, GP participants indicated that GPs are beginning to undertake DNACPR decisions more routinely.
As a GP we are actually doing this proactively with our integrated plans, but that’s for the over 75s. Certainly if we get a patient where the consultant writes and says Mr Smith is now palliative because there is nothing more we can do his ischemic cardiomyopathy that is a conversation we would try and engage in . . . [we say] it doesn’t mean we withdraw treatment it simply is in this event, if your heart stopped would you want us to try and get it going again, bearing in mind particularly for this gentleman, the chance of success are almost nil.
32
For patients in nursing homes, GPs work with senior nurses to ensure that DNACPR orders are put in place where appropriate.
I myself being a GP . . . I look after an EMI [elderly mental infirm] nursing home . . . We have got things in place where as soon as the resident gets admitted the senior nursing staff . . . and one of the next of kin, whoever is around at the time of admission, [discuss] about DNAR straight away. She [senior nurse] makes the provisional decision, obviously the form needs to be signed by myself because I am the primary GP looking after the nursing home. If I don’t agree then I don’t sign for various reasons, but 99% are signed because they are elderly, they have got other comorbidity conditions, they are frail, they have got dementia, that’s the reason they are in the nursing home. So I’m sure my colleagues try to do the same out in the community. And things are changing.
33
Health professional knowledge of the law and policy related to do-not-attempt-cardiopulmonary-resuscitation
Although sufficiently interested in DNACPR to attend a focus group, participants were not always clear about the DNACPR decision-making process in relation to the law and policy. Although the decision not to undertake CPR is established as a clinical decision, not all participants were clear about this.
I have one question, if somebody says that I want CPR . . . and . . . you are making the decision that no you are not for CPR, this is a medical decision. If somebody insists that they want to have CPR, what is the legal situation?
32
Participants thought that the patient had the right to request CPR.
But the patient still has the right to say, I want you to try, and that’s the point.
32
Field notes taken during a GP discussion (GP notes 01) captured uncertainty within the group. The group were discussing a vignette about a man with an aortic aneurysm that was not operable owing to his poor respiratory function from his COPD. Most participants thought that if they discussed DNACPR with the patient they would be giving that patient a choice about whether or not he wanted to be resuscitated. When challenged by one of the GPs, who stated that it was a clinical decision, most of the group disagreed, emphasising respect for the patient’s autonomy and right to choose: ‘It is his and his wife’s decision’. The participants went on to suggest that if the patient would not agree to a DNACPR order, then, were he to develop an acute illness, it would be up to the paramedics or hospital consultant (if the patient was admitted) to make a decision.
This confusion among health professionals is considered further in Duty of care to the patient, where we consider how our focus group participants considered DNACPR in relation to patient autonomy as a core ethical principle underlying current health-care practice.
Health professionals’ distress in relation to do-not-attempt-cardiopulmonary-resuscitation decisions
During the focus groups participants recounted stories related to DNACPR decisions that had caused distress to themselves or their colleagues. However, when we examined these systematically we found that the distress was related to a problem regarding the processes around the clinical decision rather than about making the clinical decision itself, for example where the family disagreed with the clinical decision, had not been involved in the decision or had made a complaint.
One patient who was seen by the registrar and was DNACPR’d and then the family came in and were absolutely livid . . . the DNR order was retracted . . . I ended up seeing the family when I picked this patient up a day or two later. We had a long discussion and at the end of it they understood what it was all about.
12
Things can often go wrong massively, especially if somebody does go into cardiac arrest. And it’s very stressful and if they make a decision and families aren’t involves or discussed it can often cause a lot of issues with the family.
29
You are talking about very time-pressured situations, you have somebody who is critically unwell. In a lot of these situations they haven’t discussed that he is expected to die or that the heart is going to stop very soon. It should all be about this patient’s best interests but equally it’s not the patient who is having a go at you for the next few months as all the complaints go through. And I can easily see that that’s going to figure in your mind, and in everybody’s mind . . . these discussions should have happened at a calmer time and place.
12
Although our participants did not express discomfort with making a DNACPR decision, they described other clinicians who avoided making DNACPR decisions.
[A doctor treating an] elderly patient with bad medical history fails at that point to make a decision, at the moment, because they know when things are going to happen they probably won’t be there.
19
Our participants had volunteered for the focus groups and so they might have been more comfortable with DNACPR decisions or might have not wanted to admit to discomfort with this aspect of their clinical practice. In Professional integrity and responsibility we consider further the distress of health professionals related to DNACPR and how this relates to challenges to professional integrity.
The timing of a do-not-attempt-cardiopulmonary-resuscitation decision
The timing of the DNACPR decision was a theme that ran throughout all focus group discussions. It was the key issue underlying most of the discussion and debate about the process of making a DNACPR decision. The problem of deciding when to consider a DNACPR order was linked to clinical uncertainty of prognosis. Many participants recognised the uncertainty inherent in predicting future health and how rapidly a patient’s clinical condition can change. This uncertainty about prognosis for individual patients is inherent to all clinical practice and can be difficult to discuss with patients. 132,133 Coping with this fundamental uncertainty can be compounded by other uncertainties such as lack of knowledge of the patient, which we will discuss later. Our data suggest that health professionals vary in terms of their recognition and understanding of clinical uncertainty about individual patients. Some participants expressed this uncertainty very clearly.
It’s almost impossible to define when something will be absolutely futile. The best you can do is based on your experience of what is likely to happen with a patient . . . You could say, . . . think it’s very unlikely that this lady is going to pull through, she’s profoundly acidotic, we think part of her bowels just died she’ll only get worse from here, I can’t see her getting better . . . But to say exactly what’s going to happen, you can’t . . . Say we’re not going to take you to theatre to try and repair your bowel, we’re going to make you comfortable. At that point she will almost inevitably die. But to say that’s what would happen anyway you can’t. She may just be dehydrated. She might be. She might pick up.
12
I suppose the only other thing I would want to add is about the temporal nature of this . . . just because we have said right now that’s how we feel [about CPR not being appropriate] and the family understands, things could change in 12 hours or 24 hours. So my anxiety . . . is that you suddenly find that order is still in place 3 days later and the patient is having their breakfast, you know.
16
Clinical uncertainty was sometimes illustrated by stories of patients whom the clinical team considered to be dying but, against expectations, survived and left hospital.
I’m reminded of a patient I saw where the intensivists didn’t want to resuscitate. This was a lady with dreadful asthma who was literally going to stop breathing, and I persuaded him to in fact ventilate her and she went home, no problem.
33
However, these clear expressions of clinical uncertainty were the exception. Most participants talked about uncertainty but without expressing an understanding of how and why it is inherent to clinical practice.
The level of uncertainty about patient prognosis expressed varied across clinical contexts. Participants from palliative care expressed most certainty about imminent death and the need for a DNACPR order.
From a hospice point of view, it is something that needs to be discussed for every single patient that comes in . . . If the CPR form isn’t filled in by the time it gets to within 12 hours [of admission] the nurses are on top of it . . . putting the form in front of doctors and saying, you haven’t made this decision.
9
However, there were participants working in palliative care who talked about potential uncertainty even when a patient was known to have a life-limiting condition.
If we know they’re end of life, and obviously with a cancer trajectory you do, you know the outcome, these long-term condition patient the trajectory isn’t quite so clear, and this chap may have been dipping because of some treatable cause and he may have come out of that and come home. So making a DNAR decision with somebody with a long-term condition I think is more difficult.
20
Some participants working with acutely ill patients expressed considerable confidence about the likely outcome of clinical scenarios.
You should decide only whether or not if at this moment of time when you’re making that decision, do you think that [based on] the information that you have is that going to be a successful resuscitation or not. If the answer is no this person is not going to be able to be successfully resuscitated then I think you should put that order, and that order can be reviewed if you get new information to say that this is an incorrect [decision] . . . you are most likely to make a right decision rather than a wrong decision.
22
Senior nursing staff have experience to know whether a patient is likely to survive CPR.
13
However, other participants were more cautious about making a DNACPR decision in an acute situation and preferred to wait a few days both to see how the clinical condition of the patient developed and to have time to talk to the patient/family when they were less pressured.
I think there’s a lot of pressure to make very quick decisions, and actually sometimes making the decision after a few days can be helpful because everyone can see where things are moving. And I think it’s very hard to make a decision at the front door [of the hospital] because it’s hard to spend enough time in the middle of an acute emergency to have those discussions in an effective and non-directive way.
32
General practitioners see patients over many years during which time the patient’s deterioration may be very gradual. In their discussions GPs talked about how this gradual deterioration could make it difficult to know at what point a DNACPR decision should be considered: when is the patient close enough to death for it to be appropriate to talk about DNACPR (e.g. for patients with dementia or COPD) (GP notes 02 and GP notes 03). Another example given was cancer: a patient can appear fit and well even though they have cancer that is likely to be life limiting. The GPs discussed the difficulty of raising the issue of DNACPR in this situation (GP Notes 03) as it seems to make the terminal nature of the illness certain whereas the apparent health of the patient gives hope that it is not terminal. This problem of deciding when to initiate discussion about a DNACPR order and to sign it, for patients with chronic illness deteriorating gradually over a long time course, was not discussed by participants working in acute care. They talked about DNACPR decisions as if they would be straightforward for GPs to undertake. They suggested that DNACPR orders should be put in place before an acute illness and that, if they were, their problems related to DNACPR would be solved.
This [signing DNACPR order] needs to be done before the acute phase of this episode happens, let’s do it before it’s happened at all; let’s do it months, years before it’s happened but knowing that at some point this person with this many problems is going to have a cardiac arrest and they’re not going to be any better off.
7
The people that are coming in through our doors are acutely unwell and that’s probably not, for some of our patients, that’s not the right time to making the decision . . . it’s a decision hopefully best made or discussed within the community setting
19
Discussions should be initiated early while the patient still has full mental capacity. Often on admission to hospital they lack mental capacity because they are too ill and then the situation is not reviewed as their condition improves.
11
The certainty expressed here, that it is possible to know when patients are sufficiently unwell for CPR to be inappropriate and to know this before an acute event, runs counter to the expressed understanding of clinical uncertainty discussed at the start of this section. These participants want the best for their patients and in their desire for this they are forgetting that uncertainty is intrinsic to clinical practice. It may be that it is possible to improve on current practice in relation to DNACPR but that clinical uncertainty will remain.
The frequency of review of do-not-attempt-cardiopulmonary-resuscitation decisions
The frequency of review of DNACPR decisions is another way in which participants talked about the timing of DNACPR decisions. A number of triggers for review of a DNACPR decision were identified. Change in the patient’s clinical condition was commonly mentioned. For example, patients deteriorating in hospital might have a DNACPR order put in place.
As a night matron we get called to a lot of poorly patients in the night . . . We come across a lot of patients who are you’ve said, not for ITU but you flick to the front of their notes and no DNACPR has been done, and the patient’s deteriorating in front of you. We will actively encourage the doctors to come and do [the DNACPR form] do it now please.
13
Only a few participants mentioned a patient’s recovery prompting the review of a DNACPR order.
The policy is that when they arrive [in hospital] that it’s up to the registrar to re-evaluate that document in light of the current situation. Because if that patient’s gone away and you know, had a heart transplant, kidney transplant, he’s doing marvellously thank you very much.
13
A few participants did talk about their concern that DNACPR orders were not always reviewed when the patient’s condition improved.
An acute event such as a myocardial infarction would also precipitate review of a DNACPR order.
It depends how long before the admission the DNR was issued and how relevant is it to the current scenario. So you know, a patient goes into hospital with an acute event and therefore you have to reassess everything that day when they come in with an acute event.
34
A change in health setting was discussed as precipitating a DNACPR order or reviewing one already in place, for example admission to hospital, hospice or nursing home. A change of ward was also mentioned as a reason for review, although the participants suggested that this was not always done.
In my hospital if you go from one ward to another you’re supposed to have your DNR order reassessed anyway. Not cancelled but there’s an obligation to reassess it. I suspect this is a piece of guidance that we don’t keep to [laughs]. But I mean it’s there for a good reason that something may have changed as the patients move from one ward to another so it should precipitate a review.
15
There was very little discussion about reviewing DNACPR decisions on discharge from hospital except in the GP groups where there was uncertainty as to whether they or the consultant following up a patient was responsible for making or reviewing a DNACPR decision.
A DNACPR order would be reviewed after it had been over-ridden, for example for a patient having an operation in theatre. A few participants mentioned revoking a DNACPR order if a patient had an acute event that could be treated. The example given by a GP was someone having an anaphylactic reaction which precipitated an arrest (GP notes 01).
In order for the family of the patient to have time to accept that their relative was dying, one participant delayed signing a DNACPR order.
You turn up and the family expects you, do something, do something, sometimes, sometimes not . . . Even though it probably isn’t going to work, the family are desperate for attempts to be made, and then when it doesn’t work at least they can say, everything was done, and it helps them accept and cope with the death in the long term. Even though in reality it’s probably not the best for the patient because even if you got them back the family might then say, oh I got that extra 2 days, where although they weren’t with it they could maybe hear and I could hold their hand and they were still alive even though they weren’t really. And that makes perfect sense. I think that it is really important for the family to be able to say goodbye and accept that everything was done.
6
Most participants emphasised the importance of involving the patient, where possible, and their family in the decision to sign a DNACPR order. In acute clinical situations, participants described the difficult timing of this decision-making for the patient, who might not have mental capacity as a result of being severely ill, and for the family in their distress.
And the relatives as well. Especially in her situation where she’s unarousable. I know it’s distressing for the son and it’s not really the best time to have that conversation. It’s one of the worst times you could have that conversation.
19
Reasons for making a do-not-attempt-cardiopulmonary-resuscitation decision
Participants in the focus groups talked about many reasons for DNACPR decisions. We categorised these into reasons related to the patient, the family, the clinician, the organisation and society more generally.
The patient
The futility of attempting CPR, and the importance of making a DNACPR order in this situation, was identified particularly by participants working with acutely ill patients.
If we get a patient where the consultant writes and says the patient is now palliative because there is nothing more we can do for his ischemic cardiomyopathy . . . we would say . . . if your heart stopped would you want us to try and get it going again, bearing in mind . . . the chances of success are almost nil.
32
Rather than say [to a patient] I wouldn’t do CPR . . . I talk about not sending you to intensive care or putting you on a ventilator because if you had a successful CPR event unless you are a cardiac patient who has had an arrhythmia, the chances are extremely high that you’re going to land up on a ventilator . . . I say, it wouldn’t be appropriate with your pulmonary fibrosis to put you on a ventilator.
32
Participants talked about the desire to do no harm and to allow a dignified death through avoiding what they considered inappropriate attempts at CPR. We consider the ethical dimension of this in Duty of care to the patient. Here, we focus on what participants said about who was experiencing the harm and loss of dignity. A few participants talked about the potential harm that patients told them they wanted to avoid.
Some patients with chronic long-term medical conditions . . . are happy to know that they’re going to have active treatment but not necessarily being brought back from the dead unnecessarily.
13
More commonly, participants talked about the harm to patients – or about DNACPR not being in the patient’s best interest – but without indicating whether they understood this from patients or if it was based on their own judgement.
I mean the person had a lot of other medical problems, had leg problems and then you’re just going to increase the suffering, and you’re not offering any, you’re not being fair to the patient because it’s not in their best interest to be resuscitated from that.
19
The family was also mentioned as experiencing harm from an inappropriate attempt at CPR.
I think it’s important to acknowledge obviously, I mean we’re here for the patient and it’s about their best interests, but inappropriate resuscitations also have a very detrimental or negative effect on the family because you’re taking that time away from, you know, they’re possibly sitting with that patient, because it’s not really possible. And also for the staff that are involved in resuscitation, you know when you’ve got no hope of actually getting this patient back, you know, it’s quite a damaging thing really I think to be doing.
19
However, when talking about avoiding harm for patients, participants commonly referred to the harm they themselves experienced, either personally or in terms of their professional practice.
The case that affected me most was the man who had metastatic cancer. We didn’t know what the primary was so we had no idea of prognosis. The consultant for one reason or other hadn’t put a DNACPR on him even though he was on oxygen all the time and he had very widespread cancer. He arrested and he didn’t have a DNACPR. So they brought him back and then he came back to the ward and then he died 2 hours later.
19
It hurts me when I read things like fractured ribs as a consequence of chest compressions, because I think that’s poor practice.
11
A few participants questioned if futile attempts at CPR were poor practice.
I’m beginning to feel that sometimes we’re so hooked up on it and it’s the intensivists often who get very angry . . . Does it actually matter that much if there are a few patients in the hospital, who want resuscitating for whom it’s not been the right time to have the conversation. We do do futile resuscitation, you know, is that actually such bad practice as we think? I am not sure.
32
These comments were not taken up and discussed further by the other members of the group, suggesting that the idea that futile CPR should be avoided has become so pervasive that the group were not able or willing to contemplate it.
Participants discussed whether and how they would consider the patient’s quality of life when deciding whether or not to sign a DNACPR order. In their discussions, GPs suggested that although it might be appropriate to discuss quality of life for someone with dementia, clinicians should not consider quality of life from their own perspective. For example, people with dementia can enjoy life (GP notes 03). This concern about avoiding judging the quality of a patient’s life was also mentioned by participants working in hospital settings.
She has multiple comorbidities and it’s unlikely she has what I would consider a decent quality of life but she and her family may disagree with that. And I’m looking at it from being 41 [years old] as opposed to being 88 [years old].
12
You ask yourself is this going to be successful resuscitation, do you think that there is a possibility that this person . . . what we actually cloud ourselves with is the quality of life, right, that is not a judgement that you and I should be making.
22
However, the discussions suggested that these comments were made mainly to counter a tendency for clinicians to make a judgement about a patient’s quality of life. In the following quotation, the participant seems to suggest that quality of life is an important factor when considering a DNACPR order.
You can refuse to resuscitate somebody who even demands resuscitation, so you haven’t got to discuss resuscitation, if you think that the chances of restarting their heart are impossible. You should discuss resuscitation if it’s a more of a judgement call, qualitative call, i.e. we could restart your heart but your longer-term function might not be adequate, etc., etc. But of course then you have quality issues about what I might judge somebody’s quality of life as opposed to what they might judge somebody’s quality of life and there’s no black and white there. And so that’s a much more difficult situation I think.
18
The nature of the patient’s illness(es) is at the centre of why a DNACPR decision is made. Where the patient has certain types of heart or lung disease, clinicians expressed considerable confidence about the futility of CPR and so would sign a DNACPR order.
DNACPR is something that you think about for every patient that comes in, but obviously in this case you’ve got ‘an 88-year-old’ with multiple comorbidity, so it would definitely be higher on your priority to make that decision at the point of admission. You would hope perhaps as well with history of previous heart failure and with comorbidities that he might already have a DNAR decision in place.
19
The GP should have discussed DNACPR at an early stage. The patient had chronic lung disease and home oxygen and attempts at CPR are likely to have been unsuccessful. Even if a DNACPR decision was in place the patient may still have been admitted to hospital but it may have prevented futile attempts at CPR.
7
However, a decision to sign a DNACPR order was also seen as something that would be based on multiple factors, where each individual factor would not in itself be an indication for an order.
If you go back to this lady when she was in her nursing home and perhaps doing okay, and you look at what we know about her, we discover I would suggest a number of things we’re told about her don’t necessarily preclude CPR. Her age is not a factor, that’s quite explicit that to use age would be prejudicial. The fact she’s in a nursing home by itself might tell us something about her state of health and ability to look after herself, but in itself is arguably not quite enough to say nursing home, no CPR, that would again be prejudicial. So then abdominal pain. Well is that an indication for not doing CPR? No. Vomiting? No. Diabetes? No. Atrial fibrillation? No. Ischemic heart disease? No. So then we move onto dementia and needing help with activities of daily living. Well clearly when you start to look at, I mean you start to do something else which we don’t always remember to do which is cluster all of these things together to build up a more meaningful multifactorial profile, then maybe the case against CPR starts to come into focus, but it’s perhaps one that does require further discussion, in this case with the son because we’re led to believe from the story that this lady doesn’t have sufficient mental capacity herself. The son might be remote, there may be issues getting together to have that appropriate discussion. There are cases of course where the case against CPR is so strong that for clinical reasons you could say, well this is not in the patient’s interest, this isn’t an appropriate thing to be offered and therefore we don’t necessarily need to raise it as a subject and you can make that decision. I’m not convinced from this that that would be a terribly good way to go forward I think this would need some discussion.
9
The age of the patient was commonly mentioned as one factor among many in decisions about DNACPR. Some participants took care to say that in itself age was not a factor. However, participants expressed concern that age did influence a decision to sign a DNACPR order.
I do worry about age. I worry about it as I’m getting older, but my mother and my father are early 70s and actually they’re really, really fit, but then see ‘some 40-year-olds’ . . . It’s not just age though, it’s age plus comorbidity.
15
Although most participants considered DNACPR decisions to be part of overall care, making the decision was mostly talked about as a separate process from that for making other decisions. However, several participants suggested that a decision about CPR should not be the focus for discussion but rather be a part of the overall discussion about prognosis and management of the health conditions.
The first is that actually I think it’s impossible to hold a CPR conversation as an isolated conversation. Certainly in the work that I do, if I say to anybody, shall I resuscitate your mother, the answer is yes. But if I say your mother’s got this wrong, this wrong, this wrong . . . and these are things we’re trying to make better, but if we can’t make things better before her heart stops, we are not going to make it better afterwards. So I don’t think, I think we’ve got a bit of a misconception that we’re trying to discuss CPR, we’re trying to discuss prognosis and management.
32
Clinicians used the ‘surprise question’ to help them to make a decision about whether or not sign a DNACPR order.
Treatment escalation decisions are always made before a patient leaves our ED or AMU [acute medical unit]. We ask the question, would you be surprised if the patient died in the next 3 weeks? If no then need to talk about DNACPR, if we would be surprised then no need to think about DNACPR.
13
It’s that question, it’s not do you expect them to die, it’s would you be surprised, yes. They’re not saying you’ve only got 6 months or 12 months to live, they’re saying if somebody rang you up and said by the way they died, would you be surprised?
13
By the surprise question and by the scoring system, this patient would be considered at risk of dying within 12 months.
2
Participants also described finding it helpful to think through whether or not a patient would be admitted to critical care when considering whether or not to sign a DNACPR order.
You end up getting them to a point where you’ve got cardiac output back and you’re bagging them, and then you get [the] ITU [clinical team] to come down and they say, well I’m not taking the patient, and you’re sitting there going, well now what do I do, you know, and that is the worst position to be in.
32
The intensivist will consider whether there is the potential to get the patient off a ventilator if they do survive CPR.
13
Some participants described how clinicians called the critical care team to assist them with thinking this through.
I think junior doctors are reluctant to make this kind of decision and take the responsibility for the decision without having some more senior experience as [name] said. The middle grade cover is becoming ever more junior since the doctors’ hours went down, and we get a lot more referrals to ICU to make the end of life decision on behalf of the clinical team. And it is in part because the trainee doctors are less experience and also some consultant physicians who are uncomfortable making that decision without support from another colleague.
15
The family of the patient
Participants recognised the importance of discussing the signing of a DNACPR order with the family of the patient. Some of the dilemmas encountered in doing this are discussed in Role of the family, including clarifying for the family when a clinician is consulting them about the patient’s wishes rather than about the family’s own views, and the influence of families on the decision. Participants talked of experiences where the patient’s family had thought that they were taking responsibility for the decision. One participant explained:
I clearly explain to them [the patient’s family] that I am taking that burden of responsibility on myself, I’m not putting [responsibility on to the family] I’m just letting you know why I am taking this decision. You must put yourself as the person in charge.
32
There were no instances in which participants talked about discussing revoking a DNACPR order with the family, but the vignettes we used had been unlikely to prompt this discussion.
The individual clinician
The most commonly mentioned reason given related to the individual clinician for making DNACPR decisions was their level of competence to make the decision. The more junior clinician participants talked about their own level of competence; some were more comfortable than others with making DNACPR decisions.
I can imagine in some cases it might be people don’t want to. But also it’s always supposed to be a senior decision, but because I’ve had a little bit of experience on the ward I feel quite comfortable discussing these things. Like last week we had a lady who came to me and said, I’ve thought about CPR and discussed it with my daughter and I’d like to be made not for resuscitation. So then at the earliest opportunity I discussed it with my consultant and then put it in place. But I know that the juniors aren’t allowed to put a DNAR in place. Now I think that’s probably right because it’s quite a lot of responsibility for them.
29
Maybe it is a decision that we’re not comfortable as junior doctors making, but there’s no system in place that the more senior people are contacted.
16
A critical care clinician talked about changes over time he had observed in the confidence of middle-grade doctors in making DNACPR decisions and that some consultants also sought support when making these decisions.
I think junior doctors are reluctant to make this kind of decision and take the responsibility for the decision without having some more senior experience. The middle grade cover is becoming ever more junior since the doctors’ hours went down and, we get a lot more referrals to ICU to make the end-of-life decision on behalf of the clinical team. And it is in part because the trainee doctors are less experienced and also some consultant physicians who are uncomfortable making that decision without support from another colleague.
15
One clinician talked about their experience of making DNACPR decisions for everyone admitted to the hospital where they worked.
We are talking about being a medical registrar on call. Probably we are in touch with these situations more often than anybody else. My experiences in my place about a year back, we actually encouraged that a DNACPR decision needs to be made on the point of entry so that everybody is clear whether this patient is for resuscitation or not.
32
This approach was problematised by other participants concerned that a DNACPR decision may be made too readily, an issue we discuss further in Duty of care to the patient. Most participants were somewhat aware of the policy or guidance within their own health-providing organisation including the grades of clinician considered competent to make DNACPR decisions. However, only a few participants talked about whether or not their organisations were supportive of their clinical approach to DNACPR decisions. These participants were in focus groups held at conferences likely to attract innovators in the field.
Participants also talked about their competence to make a DNACPR decision in terms of whether or not they considered that they knew enough about the patient. This varied from expressing confidence that a decision should be based on what was currently known, with no delay for seeking further information about the patient, through to taking time to gather information about the patient even if this delayed the DNACPR decision and so risked a potentially futile attempt at CPR.
Some participants mentioned taking into account their competence in relation to dealing with the family of the patient. This was mentioned by clinicians of all types and grades but was most clearly expressed by this paramedic.
I think the difficulty of being placed in those situations is, do the staff go for basic life support or do they go for full advanced life support? The danger with the advanced life support is if I give this table [pointing to the table in front of him] enough adrenalin I’ll get a pulse out of it. So the danger you’ve got is that you get some form of return of spontaneous circulation in a patient you know in your heart of hearts you shouldn’t really be resuscitating. And if you’re on your own, crews are often put in (this situation), it’s very difficult even when you know exactly what you should and shouldn’t be doing, the pressure from families can be very difficult to put off and say, well actually I’m really, really sorry I’m not going to do it, it’s not appropriate, etc., etc. Sometimes you’ll be able to do that, you’ll be able to say, I’m terribly sorry but this is not appropriate, there’s nothing more that can be done now, your husband/wife, has died. There are other situations where you think, if I go down that route I’m going to get a clip round the ear hole. And that then gives all of us the problem of do I, OK fine, do I just do BLS [basic life support] so I’m doing something, or do I go for advanced life support and just hope to god I don’t get ROSC [return of spontaneous circulation].
26
Several participants expressed the view that the most important competence for DNACPR decision-making was communication.
These doctors . . . are quite junior and they can’t make decisions. But I’m not sure I agree with that actually because of all the decisions made in medicine this is one of the least kind of scientific/medical decisions you make, it’s much more cultural and social and about the patient’s views. And I’m not sure you necessarily need a senior doctor, you need someone who can communicate well with the family . . . [A DNACPR decision] is often not a complex senior medical decision, it’s about communication and it’s much more about the social aspects of not resuscitating people.
16
The wider clinical team and organisation
Some participants mentioned the policy of their health-care organisation and guidelines from their professional organisations. Most paramedics mentioned their guidelines.
I have guidelines as a paramedic and I can’t just decide off my own back that I’m not going to do the following, I have to at least begin to do until I can establish the facts.
6
Among other clinicians, few talked clearly about professional guidance shaping their approach to DNACPR, but some did.
I think that the GMC make it very clear that as doctors we have to defend, you know, the complex decisions we’re making. I think you’re right, it’s pretty clear-cut, but I still think that the institution should have a clearly defined process . . . there is going to be a medico-legal case that transpires later . . . I’m being a bit defensive here, but having been in a number of these situations you kind of think, well as a system we should be taking these decisions seriously, and it’s a quick call, you know. Phone your medical consultant and say, I’m going to present you with a quick scenario and this is what I am doing, are you comfortable with that.
16
A few NHS trusts were described as good or supportive in terms of DNACPR decisions, although this did not necessarily reduce variation in clinical practice.
I work in a trust that is actually quite good at identifying patients where it might not be appropriate for this course of treatment.
11
Luckily our trust is quite supportive in that [DNACPR decisions] but I don’t know what the other trusts are doing. But there is a lot of personal variation as well.
32
Most participants did not describe their organisations as supportive. A lack of support was a factor in clinicians avoiding making a DNACPR order. DNACPR orders were more likely to be made where clinicians were able to contact senior doctors or discuss with colleagues, particularly those working in critical care. The time available to talk as clinical teams and to talk to family members about a DNACPR decision was considered by many to be insufficient and difficult to organise.
Nurses are less able to join ward rounds with medical teams on some wards, it’s a real challenge, especially when a number of consultants are doing different rounds multiple times in a day. But it is simply also making sure the doctors and nurses are talking to each other anyway and the nurses and doctor are bringing back relevant information to the patient and their relatives. Because I guess not everybody is there at the time the relatives are there.
25
It [talking to family members] might not happen . . . if they can only visit in the evening . . . you’ve got consultants or senior doctors with other time commitments.
29
In almost every focus group the experience of seeing the quality of care for patients reduced when a DNACPR order was signed was described and discussed. We consider this further in Consequences of a DNACPR order on overall patient care. Participants observing this in their clinical setting avoided signing DNACPR orders because of the effect it might have on patient care.
Reasons for making a do-not-attempt-cardiopulmonary-resuscitation decision: society
Participants talked about the use of resources for health care and the role of DNACPR decisions in preventing resources being diverted to futile CPR and subsequent intensive care if the prognosis was poor.
It also helps us with resources. If resus is full we can move someone into a side room, into one of the cubicles where they can have a bit of dignity and a bit of peace and some privacy. Whereas if we’re not aware of it [DNACPR order] we can essentially hold a bed, block a bed, which is unacceptable. Also do unnecessary and perhaps invasive investigations.
29
Senior clinicians in particular were clear that it was their responsibility to make DNACPR decisions on clinical grounds and that this was part of their professional responsibility within the guidance provided by organisations such as the GMC and the Royal Colleges. These clinicians are therefore acting on behalf of society in making these decisions.
Analysis 2: ethical analysis
During the focus groups participants rarely explicitly referred to ethical principles, although their conversations reflected underlying ethical difficulties and tensions either experienced by an individual about what was the right thing to do or observed as conflicts between individuals, for example between different health professionals or between clinicians and family members. Here we present the ethical themes identified in the data and reflect on how ethical tensions shape DNACPR decision-making.
Duty of care to the patient
The concept of a duty of care to an individual patient is enshrined in professional codes such as the GMC’s Good Medical Practice134 and The Duties of a Doctor Registered with the General Medical Council. 135 Participants in all focus groups articulated this sense of duty in a range of ways, often expressed as a concern that they were failing in their duty of care by action or inaction around DNACPR decision-making. An intrinsic element of a health professional’s duty of care is to protect their patient from harm. (In the Reasons for making a do-not-attempt-cardiopulmonary-resuscitation decision we have considered harm to family and health-care staff.) Participants talked about the harm of performing CPR on a patient when there was little chance of the patient surviving or when survival was likely to result only in a postponement of death and significant suffering for the patient.
doing CPR on such a patient I think is really brutal and torturing rather than doing anything good.
33
And it’s then to then find when you’ve already started CPR and broken numerous ribs and everything to then find out this poor patient was meant to die with dignity and not like that. That’s horrible as well.
29
The concept of respect for dignity was also seen as important and there was a concern among participants that in attempting CPR on patients with little chance of survival clinicians were denying their patients a dignified death, and thus failing in their duty to respect their patient’s dignity. Respect for dignity is distinct from avoiding physical or psychological harm. Even when death is inevitable, or has actually occurred, there is still an obligation to treat a person with dignity and respect.
If I was this patient’s consultant I would have considered myself failed in my duty to ensure a dignified death.
22
And for me that is a horribly undignified death if when the patient arrests CPR is . . . And everybody’s view is it was always going to be a non-event really. Yes. With ejection fraction of 10%.
27
This is wrong. We see this every day in all NHS hospitals all over the country, and that is the wrong thing to do. You have denied or we have actually . . . I’m very passionate about this, you have denied a good death to this patient by not putting in the DNR order.
22
However, there was also clearly a concern among participants that initiating a DNACPR order, and discussing a DNACPR decision with a patient, could also cause harm. The potential psychological harm to a patient of being told that they would not be considered for resuscitation was clearly a concern to participants, sometimes supported by their own experience.
. . . when she was on her own and quite breathless, she was asked about DNAR and she was told, there’s no point resuscitating you. So she was told that she would not be resuscitated, but with nobody around . . . But because she was explained all this when she was very ill and on her own late at night, it frightened her and it changed how she behaved forever, but she was alive for another year. And when she did come in on her admission where she died she was dreading coming in here because of that DNACPR. It absolutely changed her outlook on coming into hospital.
25
People can react in unexpected ways, such as ‘the 90-year-old’ who was becoming more frail. She was furious when the GP – who had known her for years – raised DNACPR, as was her son who lived in the same house (GP notes 02).
Participants expressed concern that a DNACPR decision generated a perception in patients that they were being abandoned in their hour of need by those who had a duty to care for them.
The patient wants you to do everything for them, they don’t want to be left to die and we need to reassure them on that, that we’re not going to leave them to die.
13
Yes, it’s last hope. And they want every little last bit. They don’t want the decision. They don’t want to say, yes that’s fine, don’t do it. They feel like they’re signing their death warrant.
12
A further potential harm of making a DNACPR decision is that the decision is incorrect and that a patient will die who would have survived resuscitation. Some participants expressed concern that DNACPR decisions were in fact being made precipitately, and indeed questioned whether or not it was necessarily such a bad thing if futile resuscitation attempts were made occasionally. This argument appeared to be based on an assessment that attempting resuscitation inappropriately is less ethically problematic than failing to attempt to resuscitate someone when one should.
Looking at it from the opposite side and they have a number of patients who had had DNARs made on them which have been made very easily. Made the decision just based on what standard of life is. And so although I’m sure we all see where we definitely want them to make DNACPR, there is the opposing side where there’s a number of organisations that are quite concerned at the ease in which DNARs are being made as well.
13
A key problem for clinicians when trying to fulfil their duty of care towards a patient in these situations is the uncertainty that permeates the decision-making process. As discussed earlier, this uncertainty is intrinsic to clinical practice but is compounded by, for example, information not being available. In the emergency or acute care situation, information on prognosis, previous quality of life and likely response to initial treatment may all be difficult to assess, making a decision about what is in the best interests of the patient with regard to CPR much more difficult.
Would we get him back to what he was like before he came in? Because you could possibly do that if he responded to the antibiotic and . . . Well he’s got carers three times a day and a lot of previous medical history of comorbidity, but he might have . . . we’ve just presumed he’s a poorly chap, but he might have quite a nice life generally.
13
Respect for patient autonomy
This is a core ethical principle underpinning the patient–doctor relationship as understood in current health-care practice, with its emphasis on shared decision-making and patient-centred care. It is also the principle that underpins the legal doctrine of informed consent and the realisation of Article 8 of the European Convention on Human Rights: the right to respect for private and family life. 136 It is, therefore, not surprising that respect for autonomy and what it means in the context of DNACPR decision-making was a dominant theme in our focus group discussions. One conception of autonomy is that a person, in this case a patient, should be free to make decisions about his or her life, including decisions about his or her medical treatment, without interference from others; patient choice should be respected. However, in order to make choices, a patient needs to have the relevant information to inform that choice and a key concern for many participants was that health professionals were not giving patients that relevant information. The lack of open and honest discussion about CPR by clinicians, at all stages of the patient journey, was a recurring theme in our data.
I think you know, in this case for this gentleman he’s been unwell for a long time, and the ideal opportunity is to talk to this gentleman early on in his diagnosis and get some ideas and get him and his family discussing end of life and what his wishes are. So that by the time he comes into hospital extremely poorly . . . it hasn’t been fair on this gentleman or his family that it hasn’t been discussed in hospital, but actually the conversation hasn’t happened before he’s even got there . . . it should have happened much earlier.
28
And what should have been done in this case and may even have been done, is that in the nursing home somebody would have discussed with her at leisure, before a crisis occurred as to what she wanted if she was unable to make a decision.
33
You would imagine that the consultant that’s told him that, or the team that have told him that would have had some forward planning, or I would have thought they would have some forward planning in terms of what to do if and when it did leak or rupture. And if that’s not the case then that’s certainly a conversation that needs to be had.
17
One person we’re not really involving in here is the patient themselves. So I think what we often do, and I’m sure we’re all probably guilty of it, is not actually asking the patient. So we ask the family, we talk to our team, but it’s very difficult to actually sit down with a patient and say, how would you feel if your heart stopped beating, what would you like me to do. And often if you have a frank discussion with the patients they will say, do not . . . do not ever try CPR, I do not want that to happen. So I think the emphasis on . . . so we need to re-educated I guess and actually speak to the patients because a lot of elderly patients find the thought of being resuscitated horrifying.
18
However, the occurrence of a discussion with the patient is not in itself sufficient to enable the patient to make an autonomous decision. The quality of the information provided and the ability of the patient to understand the information and to set it in the context of his or her own experience and values is also required. Several participants identified significant challenges in providing appropriate information in a way that patients would understand, particularly in an acute medical setting.
Yes, you need to have the rapport with the patient and that’s the problem we have. We meet the patient 5 to 10 minutes, they are scared, they are sitting in resus, there’s lots going around them, they might not comprehend everything that’s going on, and then make such a hard decision is a very difficult thing to do I think.
18
So now we have to discuss all the DNACPR decisions with the patient, but it’s very difficult to discuss with the patient, he may not have capacity. He’s barely able to talk and he’s quite distressed, he might actually be much more interested in whether his daughter’s coming in or whether the dog’s been fed or, you know, it can be . . .
8
The need to start the conversation about resuscitation and DNACPR much earlier in the patient journey was raised in several of the focus groups. Participants suggested that GPs may be better placed to discuss this with the patient because they are likely to know the patient better and be able to initiate the discussion at a time and in a setting in which the patient can reflect on the information and make a considered decision. Advance directives were seen as helpful to clinical decision-making in the acute and emergency situation.
I guess that’s part of the point of advance care planning in people who have irreversible conditions, whatever that condition may be and at whatever stage that may be at. Because then you’ve got in black and white what that person wants. Having power of attorney is all well and good but it’s another person’s opinion of what they think that person would want. The advanced care planning is to try and get the individual’s actual wishes.
22
I think in an ideal world if you are having routine follow-up for comorbidities in the community and you’re seeing your GP, that is really in an ideal world where these decisions should be made, at a less vulnerable time, and then that document and that order follows you rather than it being made at vulnerable times.
18
I would probably go one step further than that and say that she lives in a nursing home and that should probably have been addressed in the nursing home, and she should have come to hospital with that decision in place where there was time to have made that decision before it became an acute situation.
16
However, even in these more controlled situations it can be difficult to ensure that decisions are appropriately informed and to take account of the uncertainty of future events. One GP described having such a conversation with an older patient.
. . . although I have said to ’a 92-year-old’, if you collapse in front of me what would you like me to do? To which his reply was, if I have a heart attack don’t bother, but if it’s my appendix I want to be resuscitated.
20
This quote illustrates the importance of seeing CPR as one element in a holistic view of future care: if my heart stops because of a heart attack I would not want resuscitation but I would want it if there was a remedial cause for my cardiac arrest. Advance directives allow for a more nuanced approach to these decisions than a DNACPR form. However, any meaningful discussion with a patient about resuscitation, whether in hospital or in the community, requires time and several participants identified pressure on time as a reason why these conversations were not had or properly recorded.
There’s not the time in the day for GPs to go and have that discussion with people . . . I mean at 88 you don’t know necessarily that she’s in her last year of life, you know, that’s very difficult.
33
Yes. Time constraints, you’re called away and then you forget to go back and document what you have discussed. That does happen. I have to remind myself often enough to go back and record something.
17
Some participants suggested that DNACPR discussions should become a routine part of all hospital admissions to normalise the process and thus reduce patient and clinician anxiety about the subject and again remove it from the acute situation. However, such approaches raise questions about the level of information provided to patients in this context and to what extent this is true respect for patient autonomy.
. . . it should be just on the admission form, you know, name, date birth, do you wish to be resuscitated, yes or no. I think a bit more matter-of-fact rather than aiming this big decision, you know.
18
Adding to that, as a medical student I’ve seen a few departments in district general hospitals they had the medical registrar walked around and actually, like we ask for allergies, it became normal. I found it a bit frightening at the beginning, but then looking back there were a surprising amount of people saying actually, oh I would never want this.
18
Prior discussions and advance directives may help to facilitate autonomous decision-making but respect for autonomy also means respecting a person’s right to change his or her mind. Some participants reflected on the difficulties of predicting what one would want to happen at a future date, giving examples of patients who had changed their mind about an advance directive when faced with the reality of a life-threatening situation.
. . . having said that I’ve been an ITU sister I’ve seen people come in with living wills and then ripped them up and said I’ve changed my mind, oh I feel different now.
18
Accepting the difficulties of facilitating autonomous decision-making there was general consensus among participants in our focus groups that clinicians have a responsibility to have these discussions with patients, reflecting the strong sense that patients should be involved in and informed about all aspects of their care. However, respect for patient autonomy also implies respect for decisions that a patient makes about his or her care and this aspect of autonomy raised significant ethical tensions for participants, namely to what extent does a patient have a right to request CPR (or refuse a DNACPR order) when the clinician considers CPR futile or likely to cause harm to the patient. Some participants were very clear that this was a clinical decision and that the purpose of discussion with the patient or his or her family was to explain the reasons for the decision or simply to inform them of the decision.
And it’s like any other treatment, patients and families can request but they can’t insist and at the end of the day a DNACPR order is our responsibility and our decision. They can express an opinion but it’s ultimately our responsibility.
22
. . . because my understanding is legally that patient cannot demand treatment. They have every right to refuse treatment but my understanding is that actually legally a doctor does not need a patient’s permission to sign a DNACPR. Good practice is to have a discussion with that patient, but ultimately that doctor can say, I understand that but actually I still want to sign it.
21
I think the other thing is that, I don’t know what your approach is, but in some ways you’re not asking a family member to make a decision, you’re saying that this is my professional opinion that this futile or it isn’t, this inhumane it isn’t, and do you understand that I am communicating that to you, and that’s what we’re intending to do. I mean I think the wrong approach is to say, well here’s the scenario, what you want us to do.
16
Others were less sure of both the legal and the moral weight of such a position. Some participants thought that if a patient had capacity and requested resuscitation then a clinician must respect their wishes. One nurse participant referred to a dictatorial attitude exhibited by some doctors in discussing DNACPR with patients and relatives.
The difficulty then comes with if the patient says, I want to be resuscitated, but you feel it’s inappropriate, then that’s difficult and they have to be resuscitated providing they’ve got capacity to make that decision.
18
Participants struggled with their desire to take into account both their patient’s wishes and values and their clinical obligation to minimise harm to their patient. This dilemma highlights the ethical challenge of interpreting and defining the limits of patient autonomy. Does respect for autonomy require that the patient be informed, that the patient is involved/consulted in the decision or that the patient should consent to the decision?
Role of the family
Many patients for whom decisions about resuscitation are made will lack capacity and may be too ill to participate in a discussion with clinicians. In the UK the Mental Capacity Act 2005116 and Adults with Incapacity (Scotland) Act137 provide a clear legal framework for decision-making in these situations. This framework, echoed by professional guidance such as the GMC’s guidance on end-of-life decision-making,126 emphasises the importance of consulting families about the wishes and values of the patient to inform a best-interest decision. GMC guidance also advises that families should be supported in these situations.
It is important that you and other members of the health care team acknowledge the role and responsibilities of people close to the patient. You should make sure, as far as possible, that their needs for support are met and their feelings respected, although the focus of care must remain on the patient. 126
Focus group participants recognised the importance of involving family members in decisions about resuscitation, although most talked about involving and informing family members to prevent their distress rather than to seek their views about the patient’s wishes. Even when clinicians were clear about the reason for seeking the views of the family, they found that this was a difficult concept for families to take on board. There was some uncertainty among participants about how to respond when a family member had a lasting power of attorney.
. . . it’s very disturbing and things can often go wrong massively, especially if somebody does go into cardiac arrest. And it’s very stressful and if they make a decision and families aren’t involved or discussed it can often cause a lot of issues with the family.
29
My difficulty I have in these discussions is that when you explain it to the relatives they often tell you what they want and not what they think the patient wants. And trying to distinguish those two in a relative’s head when you’re explaining to them that a family member is very ill and probably going to die, is a very difficult thing to do.
33
This one’s slightly different from a lot of the ones that we see in health care because the health and welfare has lasting power of attorney in there, and that puts an extra, probably a little . . . not a spanner but a little bit more of a confusion on people’s heads about what can we and can’t we do. It’s just a case of all you’ve got to do is communicate that to the son and ask his consent . . .
10
Participants described facing difficult decisions when family members were expecting or demanding resuscitation for the patient when the clinician thought it was either futile or not in the patient’s interest. These situations were often distressing for both clinicians and the patient’s family.
I’ve had lots of examples recently where the patient themselves have wanted the DNAR to be put in place and then the families have put pressure on medical staff and it’s then very difficult isn’t it for medical staff to then say, what do we do, do we go with the family?
13
But then some of the younger patients with cerebral palsy, it can be very difficult, you know for some people who had severe contractures all their lives and bed bound, no cognition and you discuss the CPR and yes we definitely want everything, and you think damn you! . . .
12
We had a similar scenario on neuro quite recently relatively young but had hypoxic brain injuries and we twice had this conversation with [the family]. I was constantly fighting, his sats was below 50 at one point, trying to rectify it, and the family were adamant he was not to be DNAR. And in the end I just had to keep battling away through the night shift to try and keep this man remotely alive. They weren’t actually happy to make that decision; they were very angry and very distressed.
12
Participants described different responses to family pressure to perform CPR or refusal to allow a DNACPR order to be initiated. Some were very clear that the medical interests of their patient were paramount, while others appeared to take into account the impact on family members of seeing their loved ones apparently being left to die.
I have put my foot down and said, this is . . . like you have a duty of care towards your mother, I have a duty of care towards my patient, and I will not do what is wrong for . . . but I offered them a second opinion, that is always, you always . . . and what you must remember is that it’s not us against them, it’s trying to arrive at a consensus.
22
In our case what we did, we . . . we did make him for resus, that was eventually done. Although we thought it’s not going to be successful but the pressure of the family and the patient, we said, OK, that’s fine.
22
. . . even though it probably isn’t going to work, the family are desperate for attempts to be made, and then when it doesn’t work at least they can say, everything was done, and it helps them accept and cope with the death in the long term. Even though in reality it’s probably not the best for the patient because even if you got them back the family might then say, oh I got that extra 2 days, where although they weren’t with it they could maybe hear and I could hold their hand and they were still alive even though they weren’t really sort of thing. And that’s perfect, makes perfect sense, and I think that’s really important for the family to be able to say goodbye and accept that everything was done.
6
Paramedics described sometimes being faced with a relative who was unaware of a patient’s previous advance refusal of CPR. They faced an ethical tension between respecting the patient’s previous wishes, and their interests, and trying to respond sensitively to a family member in extreme distress.
The problem is when I arrived the family didn’t know anything about this when I talked to them and they wanted me to resuscitate. So, on my own, so I started . . . During this time I sort of chatted to the family a little bit more as well . . . in effect we did everything we could and we decided at a certain time to stop. The family were happy, it was like the final thing had been done, you know, they’d seen we’d done our best and we stopped and everybody was sort of happy with that.
26
Patient-centred care
The concept of patient-centred care is central to good clinical practice. This concept recognises the patient as a unique person with his or her own values, life narrative, relationships and physical response to disease. The ethical principle of respect for persons requires recognition of the whole person and the context of an individual case or situation informs and shapes ethical decision-making. Many participants expressed concerns about the tension between DNACPR decision-making and patient-centred care, which manifested in a number of ways.
There was concern that initial decisions for DNACPR were made in the acute situation without sufficient information about the patient’s personal and medical history, leading to assumptions being made based on generalities such as age and comorbidity. Examples were given of these assumptions leading to inappropriate DNACPR decisions.
I would like, when people say, oh this person has got dementia, what degree of dementia because I want to give you an instance where this person had a DNR order put in from emergency department, the patient came to my ward, wife. I went to see his wife and wife said, they have put a red form in. My husband has got early dementia, he is independent, he has got pneumonia and they have put a red form on this man. That is wrong. I had to not only reverse that order, had antibiotics and the patient went home independent, walked out of the hospital.
22
Everybody’s individual aren’t they? . . . a ‘96-year-old lady’ the other day who was telling me she’s just done two parachute jumps for her birthday, and she is . . . and I just . . . I admire that woman so much and I’m thinking . . . basically you know, everybody is individual.
13
And I think there is a duty on the part of the clinical team to ensure that they know who this woman is in the context of her life, and a life that looks like it’s drawing to a close. So to isolate a decision such as if your heart stops beating we will not restart it because it won’t work, has to be done in the context of who she is rather than a cold clinical legal conversation with a patient.
24
A further concern was that resuscitation, and to a certain extent DNACPR decisions, were becoming divorced from a holistic assessment of a patient’s care needs. This could mean that the focus on a DNACPR decision distracted clinicians from the more fundamental need to focus on escalation of care to prevent the need for CPR, or on palliative care when resuscitation was not appropriate. Alternatively, decisions to resuscitate (or failure to make a decision) could be made without consideration of whether other interventions necessary as a consequence of CPR (such as ICU care) would be appropriate or available for the patient.
. . . because we want them to escalate treatment before they make the decision not to resuscitate. Treatment escalation is a priority; making sure this patient doesn’t die, not, what you are going to do when they do die.
13
But we wouldn’t know that on scene, I mean we’ve got abdominal pain and vomiting and that could be anything, and that could be treatable as much as it might not be treatable . . . There’s a lot going on there that we need to do that actually I think actually negates the decision on, well she’s very sick and she’s going to die in the next hour or two, let’s not bother going anywhere, let’s just stay. We don’t get to make that decision.
4
And it wouldn’t . . . I mean just thinking about our own kind of upper GI practice, in this institution it would not be that unusual that a person who had been stented with this diagnosis would not have been referred at that point to palliative care suddenly things move on very quickly and you know, you can see everybody stumbling over themselves around decision-making . . . or the family would say, well we’re not having that form in the notes and, oh okay, well the form is taken away . . . You can see how this all happens, can’t you?
24
And actually what usually happens, the registrars I think will back me up, is that you end up getting them to a point where you’ve got cardiac output back and you’re bagging them, and then you get ITU come down and they say, well I’m not taking the patient, and you’re sitting there going, well now what do I do, you know, and that is the worst position to be in. so if you make it quite . . . so what I often do as a sort of step that says effectively I’m not doing CPR but I’m not putting it that way, I say, it wouldn’t be appropriate with your pulmonary fibrosis to put you on a ventilator.
32
Consequences of a do-not-attempt-cardiopulmonary-resuscitation order on overall patient care
There was real concern expressed by many participants that a DNACPR decision had a range of adverse consequences in terms of patient care. Rather than seeing DNACPR as one decision on a continuum of decisions required to provide optimum care for a patient, the DNACPR decision seemed to categorise a patient as ‘not for active treatment’. The DNACPR label coloured all other interactions between health-care professionals and the patient.
when the nurses hand over to each other they will say, this is patient Joe Bloggs who is a DNA, and then they will talk about him. But the first thing, the very first thing they mention about the patient in their handover, after they have said the name of the patient is the DNA. And I think that’s so wrong in the order of priorities of how a patient should be seen.
25
But you’re assuming then that that patient’s DNARd and not for treatment. A lot of them are DNAR and for active treatment until the point that their heart stops, so you shouldn’t remove . . . necessarily be moving them [into a side room to allow to die].
29
No I think there’s . . . certainly within medical consultant colleagues some of those feel uncomfortable with the idea of having to write a ceiling of care document on a patient because they fear that if they write DNAR nothing will happen to the patient. And a lot of work has had to go into supporting them to make those decisions, but also to I suppose empower the staff to realise that it doesn’t mean palliative care.
15
Most of the trust do a ceiling a care form as a separate from DNAR but in most of the situations within most of the trusts that I’ve worked in the staff, the nursing staff will take a DNACPR as a no-go area and they will not even do the doables, they will probably try to de-escalate from the observations chart, which is from 1-hourly maybe to 4-hourly, or they will pressurise the junior doctors when the consultant has already left to do an end of life discussion with the patients and the consultant was astonished to see the next morning that this was not what was said and why didn’t you treat the treatable cause, which is probably pneumonia or, or maybe even a palliative procedure which could have been done.
32
The data revealed the importance of seeing DNACPR decision-making as one element in a process of assessment and management of the overall care of an individual patient and highlighted a potential danger of treating DNACPR decisions as fundamentally different from other decisions about patient care. Identifying DNACPR decisions as an integral part of holistic patient care means that they are less likely to be avoided or forgotten. However, it also requires recognition of the complexity of these decisions and the need for clinical judgement.
Professional integrity and responsibility
Participants talked about the importance of clinicians taking responsibility for making resuscitation decisions and linking this to their professional integrity. The challenges to professional integrity and the emotional impact of these challenges were recognised, but participants suggested that this was not a reason for avoiding difficult decisions.
Again it’s getting the medics . . . to realise that the buck stops with us regardless of whatever or whoever . . .
13
. . . when I see that someone is just being unreasonable, after having explained everything and is not acting in the best interest of that patient then it becomes my duty if I have not done my duty to make sure that I don’t do the wrong thing for my patient. I will not be browbeaten or basically cowed down to do what is wrong.
22
Professional responsibility included the responsibility for having an honest discussion with the patient and/or their family. Several participants referred to the difficulty of having these conversations and the variation in practice depending on the particular views or the communication skills of the doctors involved. The responsibility to acknowledge the need for training in making these decisions and having the associated conversations was also highlighted.
From my point of view, having sat on many occasions with families and doctors just quietly because I don’t have to do the talking in those situations, it’s not my responsibility, it’s not my decision. And it is very much about the approach of the team, and what the consultants specifically always say. What I think happens is that the doctors who don’t want to have that discussion with the family, they’re the ones that don’t make the decisions about do not resuscitate, they leave it for somebody else to do. And they’re generally the ones that are more uncomfortable with having that discussion. It’s not because they can’t see that it’s the right thing to do, but would prefer to avoid having that discussion. That’s mainly what I’ve observed.
16
But I also would say there is something about individuals recognising an inadequacy in their ability and however much training can we put on actually if those individuals are avoiding having those conversations because they’re difficult. And something about that person identifying their own learning needs as well, but that’s hard.
25
Several participants commented on the importance of having an experienced clinician making these decisions and having the conversations with patients and relatives. There were a range of views on whether or not this doctor needed to be senior and in this context a distinction emerged between ‘informing discussions’ and ‘consenting discussions’. Participants appeared to think that for preliminary discussions, particularly in the community or for patients with established life-limiting diseases, the clinician who had an established professional relationship with the patient and knew them well would be best placed to discuss this with the patient. However, the actual decision as to whether or not an individual patient should have a DNACPR order (except in cases where there was an advance directive refusing CPR) was seen as a clinical decision and one that should, therefore, be made by the doctor responsible for the patient’s care. Participants expressed some concern that this responsibility was not always accepted, with some consultants avoiding making the decision or leaving it to juniors, and GPs not initiating a conversation at an appropriate point in a patient’s illness trajectory.
At the end of the day it’s my responsibility to the patient to relay what information I have and if I think that patient is peri-arrest I have a duty of care to that patient to escalate that to my seniors so that somebody with more experience can help me make a decision.
22
I think from my point of view we have patients who are really quite sick, similar sort of . . . you know, we’ve done investigations and we know they’re not going to be for intensive care. So we . . . I try and highlight those patients to the consultant to say, do we need to think about a resus status here. And depending which consultant is on the ward will depend on what type of discussion we have about that. And I think one of the consultants is saying, well I’m not going to go and have this discussion with the patient, I don’t think it’s appropriate that we have to tell all the patients and all their relatives that this is what we’re doing. So he won’t go and discuss it . . . I’ve had a discussion with him and he told me it’s a medical decision; and if that’s the case then we do need to, you know, if appropriate talk to the patient in an appropriate manner.
29
I think the interesting thing with this scenario . . . these types of scenarios are that if we’re called to nursing homes where is a registered health, or should be, a registered health-care professional on the scene, very often they’re calling us for us to be the decision-makers when actually they should have stepped up to the plate and said actually, OK, fine, our patient has now died, I’ve got the DNACPR, I’ve got the diagnosis, etc., that’s it, OK fine, the patient’s died, we’ll do the rest. But we do get called quite a bit purely to shove the problem to us, for us to sort out.
26
Participants referred to an ethical tension that had been created inadvertently by policies and processes to improve DNACPR decision-making. Rigid policies and requirements for documentation sometimes placed staff in a position of resuscitating a patient when their professional and clinical instinct was not to do so.
I think . . . I think the issues about DNACPR I think to some extent we’ve taken steps backwards because of . . . because of the documentation being much more in some ways clear cut, but also perhaps taking out some of the subtleties. I think there would have been in the past instances where that sort of scenario the staff would have felt comfortable in interpreting what was written without the DNACPR document. And I think people don’t feel now trust in the organisation, so if they’re not covered by a form, they feel obliged to go ahead with something.
28
I mean this is a little bit clearer, we’ve been called, there is something wrong with this patient, we need to deal with . . . the jobs that I dread going to are nursing homes or residential homes. You know you’re going to a cardiac arrest, you turn up and they’ve found them in the morning or what have you, or they’ve just come across them and it’s a case of, right OK, they’ve quite clearly passed away, they’ve been not known necessarily to have been ill, you know, life has taken its natural course. But because we’ve been called we don’t know necessarily when they were last seen, they are warm or what have you, you end up having to do a 20-minute protocol on a patient. And you just think, well you know, the family don’t necessarily want this but there’s no formal DNR in place, no one’s discussed what they need to do with these patients if they are found to have passed away during the night or found to not be breathing. It’s difficult, those are the jobs that I dread.
4
Participants viewed acting with professional integrity and fulfilling their duty of care to their patients in the face of clinical uncertainty and perceived or actual external constraints as major challenges. These challenges generated emotions of anxiety, self-doubt and fear of censure through complaints, professional regulatory bodies or legal proceedings. Participants described a range of fears and anxieties about DNACPR decisions including fear of getting it wrong (do we have enough information to make a decision); fear of harming the patient and failing to do their best for the patient by either upsetting them with conversation or performing inappropriate CPR; fear of upsetting the family; and fear of organisational censure. One striking anxiety or fear that participants identified, which often precipitated action that conflicted with their professional duty of care, was that of litigation or complaints by patients’ families. Few examples of experience of complaints or litigation were given but the threat of it was cited in several focus groups as a reason for not initiating a DNACPR order or resuscitating when it was considered clinically inappropriate.
I think sometimes when families are really angry, I think sometimes doctors back off a little bit because it’s frightening. And so it may be that actually . . . because actually it’s like, oh it’s easier just to say, actually okay we don’t want them to get angry, we don’t want them to make a complaint, rather than actually kind of like tackling the difficult conversations. Because actually at that point there should have been a really good in depth explanation as to why it wasn’t appropriate to resuscitate her and what her wishes were.
24
I think they are taught. I think there is a bit of a fear around making DNACPR decisions and it can be a very grey area, and I think that . . . and it’s affected greatly by the media because what we’ll see is, you know, like a headline in the newspaper, you know, death warrant or death sentence applied to the patient. And you see just this sort of a bit of a biased report, but then, you know, when people are sort of looking to be challenged possibly legally or, you know, for there to be litigation it makes people then afraid of making those decisions. Whereas actually what we need to is keep our focus on the patient and what’s right for the patient at that time.
19
I think the main thing is what is people’s expectations of resuscitation and a fear of medico-legal liability and . . . because I think people perceive it as like oh, would somebody look at me and say I have not done anything. So again that comes with the confidence and that’s where you need kind of more senior people in those types of decision-making.
20
Societal values/responsibilities
Health professionals work within a legal and professional ethical framework that is determined by societal norms, and in recent years there has been a shift in normative emphasis towards respect for patient autonomy and the obligation to involve patients in all decisions about their care. As noted above, autonomous decision-making requires appropriate and accurate information on which to make a decision. A strong theme emerging from our data was health professionals’ concern that patients and their families had received misleading information about CPR from media portrayals, and that societal expectations of the extent to which medicine can save and prolong life create difficulties in discussions around DNACPR.
It’s difficult for patients as well because I mean if you have this conversation about resus with people in clinic they know that Holby City all got resuscitated, and they will survive. Of course that’s what they want.
23
I’m sure you’ve read it – where they’re looking at televised and dramatised where-76% of patients survive. So that tells the public that resuscitation works where we all know it doesn’t in the vast majority of people. But yet, it’s offered to everybody.
10
And actually relatives do get anxious because they think with CPR means it’s a magic thing which just brings everyone back to life, because that’s what they’re shown on Holby City, you know, they do two compressions and then they’re back and normal and functioning and walking and running, you know.
19
The use of society’s health-care resources for the resuscitation of those nearing the end of their life is another concern raised by our participants, as discussed earlier.
Summary
Our research participants described do-not-attempt-cardiopulmonary-resuscitation decisions as ones that, by their very nature, are difficult, although ones that clinicians could become skilled in making. There is no certainty about clinical prognosis and so a DNACPR decision will always be, to some extent, based on uncertainty. Clinicians varied in their level of understanding of this uncertainty.
There is no straightforward approach to knowing when to make a DNACPR decision. Those working in the acute setting suggested that it should be done before an acute event or deterioration in the patient’s condition. However, those working in the community were unsure when it would be appropriate to broach the issue with patients who are deteriorating gradually.
There were other uncertainties, in addition to clinical uncertainty, which made decision-making difficult. Participants described a range of information that they would like to have when making or revoking a DNACPR order: patient expectations and desires for life/death, usually obtained from the family; diagnoses and prognosis; current quality of life for the patient; and the views of others, including other clinicians, the patient themselves and the patient’s family.
Although some mentioned age, participants also questioned whether or not it should be considered a factor in itself rather than as part of the other factors. Participants, however, described signing DNACPR orders without the information that they would ideally like to have, usually in the context of a patient with an acute illness. There was a diversity of responses on this topic, from making a decision based on the information available to avoid delay in making the DNACPR decision, to waiting to gather the information with potential delay in signing a DNACPR order. The availability of resources was not mentioned as information needed to make a decision for a particular patient, although the lack of resources such as critical care beds was mentioned as causing a problem if a patient was resuscitated.
Most of the discussion was about signing a DNACPR order. There was little discussion of revoking orders, although concern was expressed that it was important to consider this.
The ease with which a decision to sign a DNACPR order was made varied by clinical condition and specialty. There are also situations in which undertaking CPR would be appropriate even if, overall, CPR would be considered inappropriate. Participants in all focus groups talked about the importance of involving the patient and/or family where possible, despite their concerns that this was difficult to do. The main reason given by participants for signing a DNACPR order was to avoid a futile attempt at CPR and the harm that this can cause. However, the harm described was mostly that experienced by the health professionals. The participants were less clear about the harm that would be caused to the patient or his or her family. A few participants mentioned harm caused to society through the inappropriate use of resources.
With uncertainty inherent in many aspects of a DNACPR decision and different people affected by the decision (different types of clinician, the patient, the patient’s family), tensions related to these decisions are perhaps not unexpected; however, they can cause distress to all those involved. However, the decision, although a complex clinical one, was not in itself considered distressing but, rather, as part of normal professional clinical practice.
Despite this, there was concern expressed about the variation in how DNACPR decisions were made and variation in the prevalence of DNACPR orders between health-care settings that were otherwise similar. This variation was attributed to variation in professional competence, including the influence of personal factors on professional practice, and to variation in the clinical context including support, guidance and policy for the professionals.
Many participants were concerned about DNACPR decisions being considered separately from the overall care of individual patients. There was also concern expressed about the reduction in quality of care received by patients when a DNACPR order has been signed.
The wide range of health professionals across our focus groups shared a common feeling of ethical discomfort about DNACPR decision-making as it currently happens in practice. This discomfort arose from difficulties in interpreting specific ethical principles such as duty of care or respect for autonomy in the particular context of resuscitation decisions, and from the need to balance conflicting duties and interests in situations of uncertainty and time constraint. These ethical challenges are not unique to DNACPR decisions; health professionals make decisions every day that require them to assess what is in their patient’s best interests (often with limited information), negotiate the limits of patient autonomy and take into account the interests of families and other patients. However, DNACPR decision-making appears to generate particular ethical discomfort and uncertainty for health professionals. Many, if not all, of our participants strongly supported the principle of respecting patient autonomy by acknowledging the importance of discussing the risks and benefits of resuscitation with patients and informing them of any decision made. They also recognised that doctors had a duty to sign a DNACPR order when not to do so would cause significant harm to a patient. However, numerous examples were given in which discussions with patients were not had and decisions were not made. Doctors reported avoiding these conversations out of fear that the patient would ask for resuscitation and struggling to negotiate the limits of patient autonomy in these situations. However, they recognised that in doing so they are denying some patients their right to refuse CPR. It would seem that these decisions and conversations are so difficult for some health professionals that they lead to a failure of their professional responsibility.
The interests of the family were a source of ethical concern for clinicians both in making and in implementing DNACPR decisions. There were different views among our participants about the role of the patient’s family in the decision-making process and, in some cases, there was a lack of knowledge regarding the legal position. Some clinicians articulated a clear sense of a duty to take into account the interests of the family, in some cases balancing these with the interests of the patient. Many clinicians indicated that fear of family complaints influenced their decision regarding CPR.
The singularity of CPR, and the associated DNACPR decision, compared with the numerous other treatment decisions made for patients who are very sick, is reinforced by the fact that trusts have specific DNACPR policies and forms to record the decision. Our participants in general welcomed policies or guidance on DNACPR but also recognised that policies could limit professional judgement and shift the clinical focus from care of the patient to compliance with the policy. A further concern arising from our data was the unintended consequence of making DNACPR such a singular decision rather than an integral part of an overall care plan. A key theme across all of our focus groups was the negative impact on overall patient care of having a DNACPR order and the conflation of ‘do not resuscitate’ with ‘do not provide active treatment’. Overall, the strongest ethical message to come out of our data was that decisions about CPR were complex and context specific, and should be seen as one aspect of the holistic care of an individual patient.
Chapter 6 Stakeholder engagement
Introduction
The project was structured to ensure that the views and opinions of stakeholders remained central tothe initiation and progression of the project. Stakeholders were defined as patients and the public, policy-makers, health-care professionals and professional organisations representing the interests of each of those groups.
Methods
Membership of stakeholder groups
The stakeholder groups were consulted at three phases during the project: at the start of the project, 6 months into the project and at the end of the project. The core group comprised patient and public members, health-care professionals from acute hospital and ambulance service settings, and a solicitor. The group included representatives from the organisations listed in Box 2.
Age UK. a
BMA. a
Clinical Commissioning Groups.
College of Paramedics. a
Compassion in Dying. a
DAC Beachcroft Solicitors. a
Department of Health.
Faculty of Intensive Care Medicine. a
GMC. a
Hempsons Solicitors.
Hospices.
Intensive Care Foundation. a
Intensive Care Society Patient and Relatives Committee. a
NCEPOD. a
National Council for Palliative Care. a
National Institute for Health Research.
National Outreach Forum. a
Nursing and Midwifery Council.
NHS acute trusts. a
NHS ambulance services. a
NHS community trusts.
NHS England. a
Patient and public representatives.
RC(UK). a
RCN. a
Royal College of Anaesthetists. a
Royal College of Physicians (London). a
University/User Teaching and Research Action Partnership (UNTRAP). a
Core group.
Initial and follow-up meetings
The project initiation meeting took place in June 2013 at the University of Warwick. It was attended by 19 members of the stakeholder group plus nine members of the project team. The meeting was chaired by Barry Williams from the Intensive Care Society Patient and Relatives Committee.
The initial part of the meeting focused on introductions and bringing the group up to speed on the contemporary issues in relation to DNACPR. The meeting received an update from David Pitcher from the RC(UK) in relation to the NCEPOD report into cardiac arrest and plans for revision for the Joint Statement for DNACPR decisions. Patient and public members shared their personal experiences in relation to DNACPR decisions which broadly included (a) failures to consult or inform the patient or those close to the patient that a DNACPR decision had been made, (b) failure to place a DNACPR decision leading to a futile resuscitation attempt in the final moments of a patient’s life, (c) concerns about public understanding of DNACPR decisions and (d) problems with the process of implementing DNACPR decisions between hospital and community settings.
The remainder of the meeting allowed the research team to present and refine the methodology for the various work packages for the project in consultation with the stakeholder group. The meeting provided a useful introductory platform from which the research team were able to feed in to the development of the revised Joint Statement by the RC(UK), the BMA and the RCN.
The group met for a second time in May 2014 and received an update on the completed work packages. A conceptual model outlining the decision-making process (considering, discussing, implementing and consequences) was introduced and refined. Focus groups in the afternoon highlighted the importance of public awareness, patient involvement, consistent processes and tools to aid best practice. This meeting allowed the structure for the main dissemination event to be tested and refined.
Final stakeholder meeting and dissemination event
The final stakeholder meeting was co-hosted with Dr Bee Wee, National Clinical Director for End-of-Life Care, Dr David Pitcher [chairperson of the RC(UK)] and the research team. It took place on 13 October 2014 at the Royal Society of Medicine and was attended by 140 patients, doctors, nurses, policy-makers and representatives from an expanded stakeholder group.
The meeting was structured to provide an overview of the research findings, to review some exemplars of best practice, to consider relevant medico-legal matters and to receive an update on the RC(UK)/RCN/BMA Joint Statement, which was published on 7 October 2014.
The group were invited to provide written comments during the morning sessions about important clinical and research topics for discussion in the afternoon session. The written comments were grouped into topic areas by the research team and then presented back to the wider group for discussion. When possible delegates were asked to vote to express a preference on the topic being discussed. The discussion was audiotaped and reviewed by SC, who produced a detailed written summary of the focus of discussions. The results of voting were captured by an electronic voting system. The main areas of discussion are summarised below.
Standardised policies and improved transferability of decisions
There was strong support for the development of national (68%) or regional (25%) policies. Most attendees (88%) supported the use of a standardised national form to record decisions. A key driver for national/regional policies was to ensure better transferability of decisions between health-care settings and to reduce variation.
Overall treatment plans
Virtually all (98%) of the attendees supported a more holistic approach to DNACPR decision-making through considering DNACPR decisions as part of overall treatment plans. It was proposed that a group consider working together to explore pulling together the best elements of existing tools as a starting point. It was suggested that integrating DNACPR as part of overall treatment plans might mitigate the reported negative impact of DNACPR on overall care.
Communication and shared decision-making
Involvement of the patient and those close to the patient as central partners in decision-making was encouraged. There were requests for practical tools to assist clinicians in the best ways to approach discussing DNACPR decisions in the acute and community settings and how to promote wider involvement of the multidisciplinary team (particularly where access to such a team may be more difficult, e.g. in primary care). It was suggested that experts with experience in DNACPR decision-making might provide support to those who are less experienced (‘best practice champions’). It was noted that, in many organisations, individual clinicians may refuse to participate in DNACPR decision-making and a there was a request for guidance on how best to manage such situations.
Greater information and guidance was requested about how religious and cultural differences may affect patient and family requests for CPR and how clinicians should respond to these requests.
Public awareness
There were calls to promote a greater public awareness about DNACPR, particularly about the burden and benefits of CPR and the limits of modern medicine. A national information leaflet was suggested as a starting point. How best to achieve change in awareness and attitudes was identified as a future research need.
Priorities for future research
Identified priorities for future research were identifying the impact of DNACPR decisions on other aspects of care and the effectiveness of different strategies to improve public education about DNACPR.
Reflections
We had public and patient involvement throughout the project. Barry Williams and Phillip Satherley were members of the Study Management Group and helped to maintain focus on the important issues. We worked with UNTRAP (University/User Teaching and Research Action Partnership) which is a partnership between service users, carers and academics based at the University of Warwick and supports public involvement with research and teaching. Members of UNTRAP came to three meetings at which they shared personal stories about DNACPR and the effects on them and their families. We were able to use these experiences to focus the research questions and the methodology and interpret the results.
Chapter 7 Discussion and conclusion
This study had several objectives which have been addressed through different research methods reported in the preceding chapters, as indicated:
-
to review and summarise the published evidence base informing DNACPR policy and practice (see Chapter 2)
-
to identify the themes of current complaints/conflict in relation to DNACPR decisions and explore local solutions developed to tackle these problems (see Chapter 3)
-
to examine current acute hospital, community and ambulance service DNACPR policies to identify inconsistencies and examples of best practice across NHS organisations (see Chapter 4)
-
to explore health professionals’ experiences of DNACPR policy and practice (see Chapter 5).
Together with the final stakeholder meeting, dissemination event and published papers, this discussion chapter contributes to the final study objective: ‘to summarise, prioritise and disseminate findings from this research.’ It provides a discussion of the key issues synthesised from the results of each section of the study.
This study found evidence of variation and suboptimal practice in relation to DNACPR across health-care settings, reduced quality of care for patients with DNACPR orders and inappropriate expectations of the outcome of CPR among family members and the general public. DNACPR decisions are considered difficult clinical decisions. We will first consider the legal and policy context for DNACPR decisions in the UK and then the nature of the decision itself. We will then discuss why variation and suboptimal practice occurs and how this could be improved, by considering each of the stages in making DNACPR decisions: considering, discussing and implementing the decision. We will then discuss widely recognised unintended consequences of DNACPR decisions and lay expectations of CPR outcomes.
The legal and policy context for do-not-attempt-cardiopulmonary-resuscitation decisions in the UK
All health-care practice takes place within a legal and professional regulatory framework that evolves over time and in response to developments in medical practice and societal expectations. At the time of this study there was a range of legal and professional guidance in the UK relating to end-of-life decision-making in general and to DNACPR in particular.
Decisions about whether to provide or withhold CPR must comply with the principles contained in the Human Rights Act 1998. 115 Specific articles invoked by the resuscitation decision-making process include the right to life (Article 2), the right to be free from inhuman or degrading treatment (Article 3), the right to respect for privacy and family life (Article 8), the right to freedom of expression, which includes the right to hold opinions and to receive information (Article 10), and the right to be free from discriminatory practice in respect of these rights (Article 14).
It is established in common law, reiterated in the case of Ms B,138 that a person with capacity can refuse any treatment, including life-sustaining treatment, but that a person cannot demand a treatment that a doctor considers not to be in the person’s best interests. 139 The Mental Capacity Act 2005116 and the Adults with Incapacity (Scotland) Act137 set out the process by which decisions should be made for a person lacking capacity, emphasising the requirement to make the person the centre of the decision-making process, taking into account their wishes and values where known and consulting with those close to the person to determine these. The Mental Capacity Act also enshrines in law the right of a person to make an advance refusal of treatment, including life-sustaining treatment, to come into effect if the person should lose capacity; this would include a refusal of CPR. The landmark case of Bland in 1993140 established that withholding (or withdrawing) a life-sustaining medical treatment may be lawful if the treatment is not considered to be in the patient’s best interests. The legal position could thus be summarised as follows: an adult person with capacity has the legal right to refuse (either contemporaneously or in advance) life-sustaining treatment, including CPR, and a doctor may lawfully withhold life-sustaining treatment, including CPR, based on a considered judgement that the treatment is not in the patient’s best interests.
Specific professional guidance on DNACPR was available to clinicians at the time of our study. 117,126 The GMC’s guidance on end-of-life decision-making published in 2010126 has a specific section on DNACPR which includes guidance on making the decision, involving the patient and family and communicating and recording the decision. The principles informing this guidance are echoed in the Council of Europe’s guidance on end-of-life decision-making in 2014. 141
Our review of trust policies indicated that the relevant legal and ethical principles, which were current at the time of the study, were incorporated almost universally into acute and community trust policies. There was less consistency in the translation of national guidance in to policies, but no more so than in the use of terminology used to describe the decision to withhold CPR. Terminology used included DNACPR, DNAR, AND and ‘not for CPR’. This may in part explain the observations in our study that some clinicians involved in making DNACPR decisions are unclear about the relevant law and guidelines. There are many more care staff who are not responsible for DNACPR decision-making but who have an interest in DNACPR as they are responsible for making the decision to call or not to call a clinical team able to perform CPR when a patient’s heart stops. These staff are likely to be less familiar with the current law and guidance in this area. This knowledge gap can create a sense of confusion about what is a clear legal position in the UK.
Immediately following the data collection period of our study, the Court of Appeal judgement in the case of R (Tracey) v Cambridge University Hospitals NHS Foundation Trust was published. 104 The judgement made it a legal requirement to consult with the patient and his or her family when making a DNACPR decision, save in exceptional circumstances. 142 In October 2014 the RC(UK) issued new guidance on decisions relating to CPR, which took into account recent changes in the law. 143 At the time of our review the median age of policies was 24 months. One-third of policies had time expired in relation to the internal review date set in the policy. This creates uncertainty about the timeliness with which the change in UK law and professional guidance will permeate policies and professional practice.
The nature of the do-not-attempt-cardiopulmonary-resuscitation decision
Do-not-attempt-cardiopulmonary-resuscitation decisions are, by their nature, difficult, although clinicians can become skilled in making these decisions with patients. Most attention is paid to the decision to sign a DNACPR order with little consideration of reviewing or reversing DNACPR orders as a patient’s condition changes. Decisions not to sign a DNACPR order when it might be considered appropriate are often made by omission but can be part of a planned delay in decision-making while information is gathered about the patient, including their response to treatment.
Uncertainty is recognised as inherent to clinical practice133,144–146 particularly when trying to determine prognosis at the individual patient level. Clinicians have to make DNACPR decisions despite this inherent uncertainty. Care planning is difficult particularly towards the end of life because of uncertainty. 147 In contrast to DNACPR decisions, undertaking CPR is highly routinised and the decision-making follows pre-specified guidance to ensure that everyone knows exactly what to do and when to do it. So, at the time of undertaking CPR decisions are relatively low in uncertainty. However, there is evidence from our study that some clinicians do not perceive this difference. They do not understand the relatively high uncertainty inherent in DNACPR decisions. This is important, as the approach to clinical tasks involving a relatively high level of uncertainty needs to be different from the approach to those with a relatively low level. Where there is high uncertainty, clinicians need the opportunity to refer to other clinicians and to deroutinise the task to allow capacity to handle the uncertainty, and any evaluation of the task needs to be qualitative. 148 Our study provides examples of clinicians who approach DNACPR decisions in this way. In contrast, medical tasks with relatively low uncertainty can be routinised within a formal structure and evaluated quantitatively. Our study provides examples of clinicians who talk about CPR in this way. However, there are also worrying examples of clinicians who routinise DNACPR decisions. Further, when the processes for supporting DNACPR decisions were discussed, there was considerable attention paid to the task of identifying whether or not a DNACPR order has been made. This is a task involving relatively low uncertainty and so requires processes and support quite different from those for making a DNACPR decision. The nature of the DNACPR decision itself as a difficult clinical decision, owing to its inherent uncertainty, needs to be clearly recognised and distinguished from related low-uncertainty tasks when considering DNACPR policy, practice and education.
Clinical uncertainty creates ethical dilemmas for clinicians who have a moral duty to minimise harm to the patient as a result of their treatment and to provide treatment that will be of benefit to that individual. 149 However, the uncertainty for clinicians in making DNACPR decisions is not limited to clinical factors such as prognosis, likely outcomes of CPR and patient comorbidities. In many instances there will be uncertainty about the patient’s wishes and values regarding CPR. Clinicians in our study described the difficulty of ascertaining patients’ wishes in acute situations and the risk of making assumptions about patients’ wishes based on limited information. Current legal frameworks, bioethics literature and clinical practice emphasise the priority given to patient autonomy in treatment decisions. 116,149–152 Uncertainty regarding patients’ wishes and values constrains clinicians’ ability to fulfil their obligation to respect patient autonomy in these situations. Many clinicians in our focus groups expressed concern that their patients’ views about CPR had not been explored at a time when they were able to express them. Critiques of advance refusals of treatment highlight the difficulties of a person predicting in advance what treatment they would wish to have or not to have in a hypothetical future situation. 153,154 Some of our clinicians reported this as a difficulty in practice. The challenge of ascertaining patients’ wishes in advance while not closing down appropriate future discussion of treatment options must be recognised.
As noted above, many treatment decisions are complex and involve inherent uncertainty, and many decisions are made in situations in which it is not possible to ascertain the patient’s wishes with certainty. However, DNACPR decisions appear to create particular ethical difficulties for clinicians. Additional factors contributing to this may include the separation of the decision from its consequence and the irreversible consequence of the decision if enacted. A DNACPR decision is an advance decision which may or may not be put into effect at a later time. The clinician making the decision will probably not be there at the time the decision is enacted and will therefore not have the opportunity to change his or her mind, unlike, for example, a decision not to ventilate or commence dialysis if the patient’s clinical condition deteriorates. If a DNACPR order is acted on then the immediate consequence is death of the patient and hence DNACPR decisions can be seen as the paradigm ‘life-or-death’ decision. There is evidence to suggest that patients see this decision as a choice between life and death, disregarding the fact that in the majority of cases death will be the outcome even if CPR is attempted. 155
A further feature of the apparent singularity of DNACPR decisions relates to the roles of the clinician and the patient in the decision-making process. The recent trend in UK clinical practice and medical education has been to promote a shared decision-making model for treatment decisions. 156–158 The doctor brings knowledge of treatment options, their risks and benefits and likelihood of success, the patient brings their personal values and self-knowledge and a joint decision is reached regarding the most appropriate course of action. With regard to DNACPR decisions, the legal framework and professional guidance makes it clear that the decision ultimately rests with the doctor because this is essentially a decision not to treat and a doctor cannot be required to provide a treatment that he or she does not think is clinically appropriate or considers is not in the patient’s best interests. 126 Our focus group data suggest that this distinction is not understood (or concurred with) by all clinicians and the data from NHS complaints suggest that patients’ families may also have different views about who is the decision-maker. The distinctive nature of DNACPR decisions compared with other decisions to withhold treatment was noted in the Tracey judgement (paragraph 55). 104 This nature contributes to the ethical difficulties faced by clinicians in making these decisions.
Some recent studies have attempted to reduce some of the uncertainty associated with predicting poor outcomes after resuscitation. Using data from over 50,000 in-hospital cardiac arrests contained in the American Heart Association’s ‘Get with the Guidelines’ registry project, Ebell et al. 159 developed a scoring system to identify patients who were unlikely to benefit from a resuscitation attempt. The Good Outcome Following Attempted Resuscitation (GO-FAR) scoring system was able to identify a cohort of patients (approximately 10% of acute admissions) who had a very low chance of a good outcome (< 1% survival with intact brain function). Seventy per cent of acute admissions had intermediate outcomes (2–10% survival with intact brain function) and approximately 20% had a > 25% chance of a good outcome. The generalisability of these findings should be assessed in the NHS. If the findings are reproduced, the utility of this clinical prediction rule to inform patient-centred decision-making about resuscitation should be further evaluated.
Understanding variation in the practice of do-not-attempt-cardiopulmonary-resuscitation decision-making
The nature of DNACPR decisions is likely to lead to some variation. Our study demonstrates strategies used by clinicians to reduce this variation. This includes talking to other clinicians, having expert role models and taking time to collect and consider relevant information. In this section we explore why the variation expected due to the nature of the decision can become amplified to unacceptable levels. We start at the beginning of the process, when a DNACPR decision is being considered, and then move on to the discussion of the decision with patients and/or family members and the implementation of the decision.
Considering the do-not-attempt-cardiopulmonary-resuscitation decision
Timing the decision as well as the decision itself is difficult in the face of clinical uncertainty. In this section we explore why variation occurs in how DNACPR decisions are considered, beyond that expected as a result of uncertainty. We explore what influences the timing of DNACPR decisions and what prevents clinicians using well-established strategies for managing the uncertainty inherent in the decision-making.
The ability to predict end of life is important for timing the initiation of a discussion about DNACPR. Patterns of decline have been identified towards the end of life160,161 and it has been demonstrated that experienced clinicians can predict when a majority of patients are nearing the end of life. 162 Failure to anticipate the need to consider DNACPR, particularly when patients were deteriorating gradually, such as in primary care, was reported in our study, and this is similar to other research findings. 163 Some clinicians wait for the patient to initiate the conversation but research suggests that not all patients wish to have conversations about the end of life. 163 In the acute sector there was variation between clinicians as to how quickly after admission they thought a DNACPR decision should be made, and service providers varied in what they expected of their clinicians. Increased community health-care worker engagement in advance care planning (including DNACPR), identifying triggers to consider resuscitation status (e.g. change in health status, acute admission deterioration,24,58 transfer between health-care settings) and discussions with multidisciplinary teams including intensive care24,25–27,58 and palliative care clinicians28–30 may act as facilitators to improved practice.
Experienced clinicians described that for the majority of patients, despite the uncertainty, they are able to judge when a patient is nearing the end of life: when medical treatment including CPR is futile. Medical futility has been defined164 and examples have been identified,165 although as treatments change such examples require review. Where a patient has a life-limiting illness and treatment is futile, even where this is not directly related to the condition of the cardiorespiratory system, CPR is usually considered inappropriate and, similarly, when the condition of the cardiorespiratory system indicates that CPR is unlikely to be successful. Experienced clinicians use what has been termed practical certainty for managing uncertainty in relation to end-of-life care planning. 147 This is where clinicians are as certain as they can be about patient prognosis and about patient wishes. As described by experienced clinicians in our study, reaching practical certainty about prognosis requires drawing on clinical experience, often involving discussion with other clinicians and observing the response of the patient to treatment over time. Similarly, reaching practical certainty about patient wishes requires spending time with the patient or, where this is not possible, the patient’s family. Although clinicians reported trying to take time and to consult with other clinicians, this was not easy in busy clinical settings, and the evidence from our study indicates that there is variation in how persistent clinicians are in trying to take time over DNACPR decisions when time is such a limited resource.
The strategy of considering decisions as provisional, allowing for changes in patient condition and patient and family priorities, can be used to cope with uncertainty,132 although few study participants discussed DNACPR decisions as provisional.
There is evidence that, although patients might prefer to make their own decisions about DNACPR, where they have developed a relationship of trust with the clinician, for example while in hospital, they will endorse the clinician as decision-maker. However, this endorsement is withheld from doctors who are not considered rational, knowledgeable and compassionate. 166 This again suggests that it is important for clinicians to take time when making DNACPR decisions – providing care for the patient over time, observing treatment response over time and taking time to discuss with patients and their family. However, the evidence suggests that many clinicians have insufficient time for this process.
Cardiopulmonary resuscitation that is apparently futile caused distress to some of our study participants. A commentary on this suggests that this is at least in part because clinicians see it as the infliction of physical abuse on the dead or dying patient,13,167 and this would be in direct contradiction to their professional ethical duty not to harm their patients. Some clinicians are very anxious to avoid witnessing futile CPR or allowing it to happen through not ensuring that a DNACPR order is in place. This anxiety was a source of pressure on DNACPR decision-makers to write DNACPR orders without taking time over the decision. In contrast, there were clinicians in our study who questioned whether the patient experienced futile CPR as distressing or as physical abuse. These clinicians were less concerned about undertaking potentially futile CPR. The potential harm arising from not providing CPR when it might be successful, and the psychological harm to a patient of being told that CPR would not be attempted, were sources of concern for some clinicians in our study. How clinicians balance these perceived harms will vary depending on their experience, their knowledge of and relationship with the patient and their own values.
Discussing the decision
Although the DNACPR decision in the UK is a clinical decision, there is an expectation, and since the Tracey judgement a legal requirement, that the decision is discussed where possible with the patient, and, where this is not possible, with the patient’s family. 104 Although there is evidence that many clinicians are conscientious in undertaking these discussions, the review of incidents and complaints indicated that a failure to discuss DNACPR decisions with patients and their relatives was a common cause of concern. This section considers the causes of these failures and how they could be avoided.
The absence of practical tools to guide clinicians on how best to approach discussions, limited guidance in trust policies on decision-making in those that lack capacity, time pressures,68,74,99 difficulty in scheduling discussions in a timely manner, lack of training in relevant communication skills,15,86,96 discomfort with discussions about dying83,93 and concerns that such discussions may cause patient or family distress14 were barriers to effective discussion and led to variations in the quality of the DNACPR decision-making process.
Person-centred health care has appropriately become the accepted norm in the UK. The presence of family, particularly adult children, often aids communication and decision-making. The Mental Capacity Act116 requires clinicians making significant treatment decisions about patients who lack capacity to consult with family and those who know the person in order to ascertain the person’s wishes and values. Although clinicians may be fully committed to this approach, in practice clinicians are finding it hard to follow consistently. Guidance within policies and decision forms can serve as useful prompts to assist with communication and decision-making. 113 This may also contribute to promoting a culture within the organisation in which time spent in discussion with patients and family is highly valued, along with engagement with developing skills in communication.
While there is general agreement that the focus of decision-making should be on what is in the patient’s best interests, clinicians in our study also described being influenced by the expressed wishes of the patient’s family regarding DNACPR decisions. Some clinicians reported modifying their decisions to avoid distress to the family by taking their interests into account. Others reported that their decisions could be influenced by concerns that the family would complain or take legal action if they disagreed with the decision. Developing skills in communication and conflict resolution, together with time to provide adequate explanation and support for families, is likely to refocus these discussions on the interests of the patient.
The published evidence and information from focus groups indicated that focusing discussions on treatment that would be provided (i.e. for CPR rather than DNACPR)16 and discussing CPR decisions in the context of overall treatment plans were received more positively than those focusing on not attempting resuscitation. 17 The provision of tools to aid structured discussion18 and the normalising of discussions about resuscitation so that it was part of an overall discussion of treatment were also helpful. During discussions care is required to ensure that the use of medical jargon does not lead to misunderstandings. 15,99
The evidence suggests that there is need for training, support and practical guidance and tools to help clinicians engaging with patients and families to discuss DNACPR. Embedding the DNACPR decision within the discussion of treatment plans has the potential to normalise the decisions as part of considered treatment plans so that patients come to expect it. It can also support the development of trust between patients and their families and clinicians. Patients do not feel abandoned when a DNACPR decision is made as part of a plan that focuses on treatments that will be provided rather than those that will be withheld.
Implementing the decision
There was wide variation in the systems used for recording DNACPR decisions across NHS providers in England. This might contribute to why clinicians in the literature report a lack of specific knowledge120,121 and disagreements with local DNACPR policies. It may also contribute to the variation in quality of DNACPR decision-making.
Clinicians often felt the DNACPR form limited their ability to apply judgement – specifically unless there is clear and up-to-date documentation, doctors and nurses respond to cardiac arrest assuming CPR is appropriate although there is often uncertainty. They take this action to ensure patients who can benefit do so, and to avoid potential criticism from their employing organisation or family members. The review of incidents, complaints and Ombudsman’s and coroners’ reports identified that occasionally process failure causes catastrophic consequences for the patient with CPR being withheld where indicated. Process failure also led to instances of CPR being provided where it was recognised to be futile and/or against the patient wishes.
There was generally poor communication and lack of transferability of DNACPR decisions between health-care settings. A participant in the stakeholder group meeting described a patient having to keep three different DNACPR forms at home because they received treatment from three different health providers. The data from the Compassion in Dying information line indicate that there is concern among some members of the public that they will be resuscitated against their wishes, or that clinicians will not be aware of their wishes in relation to resuscitation.
Unlike the DNACPR decision itself or the discussion of DNACPR with patients and families, implementing the DNACPR decision is relatively low in uncertainty and should be relatively straightforward. It is likely to require a national commitment to a seamless system and a willingness of individual trusts to amend their own processes. A national system would enable a joined-up system from the patient perspective. It will also have benefit for clinicians when moving jobs between NHS trusts as it will remove the need for them to learn a new set of forms and policies for each trust, reduce confusion about the process and allow them to concentrate on making good clinical decisions.
Consequences of variation in do-not-attempt-cardiopulmonary-resuscitation decision-making
Although some variation in DNACPR decision-making is to be expected, this variation is amplified at each stage of the decision-making process. Variation in the decision-making process means that patients nearing the end of life have very different experiences in relation to DNACPR depending on where they are, how well they know their clinician, the expertise of the clinician, the support available to the clinician, including time and access to clinical colleagues for discussion, and organisational policy and practice. We consider how the NHS might reduce this variation in practice in our suggestions for future developments.
Consequences of the decision
A key theme emerging from the focus groups was the negative impact that a DNACPR decision either had or was perceived to have on the overall quality of care and treatment provided. This concern was emphasised by the reference during the stakeholder group to the common observation of nursing handovers beginning with a statement about a patient’s DNACPR status rather than their clinical condition and care plan. The literature reviewed similarly noted associations between DNACPR decision and evidence of reduced escalation of medical/nursing care68,78,84,97 such as altered pain relief, fluid administration and reduced basic nursing and medical care. 13,14,63 This observation suggests that the DNACPR decision is viewed by clinicians as having a broader and more profound message than the narrow parameters intended. The decision is interpreted as a decision that attempts to preserve life are not to be undertaken. This perception is also seen in patients who consider that a DNACPR decision is a decision about life and death rather than a decision about a particular treatment. 155 Providing clearer guidance through the use of individualised overall treatment plans might change this perception among clinicians and patients and reduce this negative impact on patient care.
Expectations of cardiopulmonary resuscitation
Our study participants were concerned about the unrealistically high expectations of CPR among patients and families. These add a further issue for clinicians when they are engaging patients and/or families in what is already a difficult conversation. Such unrealistic expectations have been documented and a public education intervention has been shown to reduce them. 168
Only a small number of our study participants expressed concern about the inappropriate use of health-care resources in providing or following up on inappropriate CPR. Desmond Tutu, when reflecting on the death of Nelson Mandela, questioned why resources were used to prolong life at the end of life. 169 This observation is concordant with the large body of literature reporting that substantial health-care costs are consumed in the final year of life. 170,171 The balance of benefit, burdens and costs of such interventions and the role of advanced care planning is an area that would benefit from further research.
Strengths and limitations
Reviewing the evidence about DNACPR decision-making has presented some challenges because decision-making itself and its impacts involve complex processes which are not straightforward to observe or quantify. An overall limitation of this study is the variable quality of some of the data synthesised, meaning that the evidence for good or poor practice and their impacts could be under- or overstated. However, by drawing together so many different sources of evidence the synthesis presented paints a picture of repeated issues common to different data sources indicating that there is room for improvement.
It is interesting that many of the topics researched in studies reviewed in the literature were echoed in the other data used in this project. The scoping review noted that a large number of studies reviewed focused on interventions to improve documentation and its use. The main literature reviews’ domains covered the decision itself, communication, the system for implementing the decision and consequences. These themes were similar to, and the perspectives in the literature were supplemented by, those that emerged from the other data sources used in this study, giving a more nuanced picture.
The quality of data provided by trusts through the FOI requests was mixed due to variability in recording systems and local interpretation of our request for information. There was a striking difference in the total numbers of reported incidents across trusts, which suggests substantial variability in the processes for recording and coding these events. The lack of a specific coding variable for DNACPR in the Ombudsman’s database meant that it was not possible to determine the number of complaints received that related to DNACPR or to independently verify the observations reported by the Clinical Advice Directorate.
It could be argued that some of the data synthesised in this study focused on problems and negative experiences (e.g. incident reporting, complaints, coroners’ and Ombudsman’s reports), and present two problems. We cannot access unreported incidents, which means that the scale of the problem could be larger than we report. Good practice is difficult to access from existing data sources and is not usually quantified other than by the absence of incidents of harm or complaints. So, although we did look for best practice in the NHS DNACPR policies reviewed, our findings concerning good practice may be limited.
We had a 100% response rate for our sample of trusts’ DNACPR policies, which covered acute trusts, community trusts and ambulance service trusts, providing. While it could be argued that the focus for the different services DNACPR policies could make comparison difficult, the finding that there was so much variability/variation between policies within this sample is a concern. With so many different systems in place, the already complex communication of decisions between staff within and across different trusts with different roles and focuses for patients in their care is made more challenging than is perhaps necessary.
Taking a broad approach to the literature reviews revealed a limited amount of work in a number of different areas related to DNAR decisions, but it meant that combining results other than narratively was not possible. The finding that the quality of studies reviewed was often low does not mean that practice is necessarily poor; rather, it could mean that high-quality evidence or the reporting thereof is lacking. The literature reviews’ results are limited by their search strategies (e.g. being restricted to English-language publications), which means that there is a possibility that some evidence may have been missed.
Although the data used in several of the different strands of this study were variable in quality, it was clear that several important themes were repeated in the different data sources and reiterated in the focus group results. These themes can be broadly grouped into communication problems and DNACPR system issues. Communication issues between clinicians, patients and families resulted in DNACPR decisions not being made when they should have been, patients’/families’ wishes not being respected, and clinicians having to deal with conflict between patients’ and families wishes’ or between their clinical decision and patients’/families’ wishes. System issues relating to documentation and the lack of staff training to provide a unified system led to confusion and problems in implementing the decisions.
A strength of using so many data sources for this evidence synthesis is that while one or two sources could have provided some information and each on their own would have presented challenges for the reliability/credibility of the results, common issues emerged from each source, giving different perspectives and thus insights into the problems.
Conclusions and implications for practice and research
This study found evidence of variation and suboptimal practice in relation to DNACPR across health-care settings, reduced quality of care for patients with DNACPR orders and inappropriate expectations of the outcome of CPR among family members and the general public. Together, the findings from this study suggest that there is scope to improve the approach to DNACPR decision-making in the NHS.
Published evidence suggests benefit in moving from the paradigm of DNACPR decisions which focus on withholding treatments to one which contextualises resuscitation decisions within a broader framework of overall care and treatment that will be provided. Such an approach received broad support from clinicians interviewed in our focus groups and was universally endorsed at the stakeholder meeting.
A shift in focus from DNACPR to overall care and treatment plans provides an opportunity for policy-makers to align local/regional approaches to produce a joined-up national system which will enable improved consistency in approach as well as portability of decisions between health-care settings.
Experienced clinicians are best placed to make decisions in partnership with patients and families. Education in initiating and promoting early discussions on emergency treatment plans (including resuscitation) must recognise the potential complexity and uncertainty of decision-making and the importance of having sufficient time to engage in discussions and come to a decision. Early engagement with patients and the public, including education to empower them to initiate discussions and to be well informed when involved in the decision-making, is important. The utility of clinical prediction tools for reducing uncertainty and variation requires further research. The complexity of the decision-making task must be recognised as quite different from the routinised completion of a form and implementation of the decision.
Our recommendations are for research into:
-
identifying effective training strategies that will equip clinicians to make DNACPR decisions, including an understanding of the nature and the complexity of the decisions together with the associated communication skills
-
the utility of clinical prediction tools to reduce uncertainty and variation in decision-making
-
robustly evaluating a national system for DNACPR decisions within overall care and treatment plans should there be such an initiative.
The stakeholder group’s recommendations for research were:
-
research to identify the impact of DNACPR decisions on other aspects of care
-
evaluation of different strategies to improve public education about DNACPR.
Acknowledgements
Core stakeholder group
Bob Ewings (patient/public representative), David Pitcher [RC(UK)], David Whitmore (College of Paramedics, London Ambulance Service), Elyas Khalif (patient/public representative), James Beattie (National Council for Palliative Care), Jane Harper (Faculty of Intensive Care Medicine), Jacky Roy (patient/public representative), Tom Genry (Age UK), Jasmeet Soar (Royal College of Anaesthetists), JP Nolan (RCN), Mark Temple (Royal College of Physicians), Rebecca Mussell (BMA), Sarah Quinton, critical care nurse (National Outreach Nurse Forum), Sarah Woods (DAC Beachcroft), Sharon Burton (GMC), Steve Brett (Intensive Care Foundation), Sue Williams (patient/public representative) and Marrisa Mason (NCEPOD).
Dissemination meeting external speakers
Steph Garfield-Birkbeck (NIHR HSDR programme), Claud Regnard (Deciding Right), David Gabbott (Gloucester Hospitals), Sarah Woods (DAC Beachcroft), Stephen Evans (Hempsons Solicitors), David Pitcher [RC(UK)] and Bee Wee (National Clinical Director, End of Life Care Programme, NHS England).
Contributions of authors
Gavin D Perkins (Professor of Critical Care Medicine) designed and led the project, contributed to all work packages and drafted, revised and approved the final report.
Frances Griffiths (Professor of Medicine in Society) designed the project, led the focus group work, contributed to the ethics analysis and drafted, revised and approved the final report.
Anne-Marie Slowther (Associate Professor of Clinical Ethics) designed the project, led the assessment of the size of the problem and ethics work streams, contributed to the focus group work and drafted, revised and approved the final report.
Robert George (Professor of Palliative Care) designed the project, contributed to the systematic review and drafted, revised and approved the final report.
Zoe Fritz (Bioethics Fellow) contributed to the systematic review, focus groups and ethics analysis and drafted, revised and approved the final report.
Philip Satherley (Lay Representative, Compassion in Dying) designed the project, obtained and contributed to the analysis of the patient information line data, contributed to the stakeholder groups and approved the final report.
Barry Williams (Lay Representative, Intensive Care Foundation) contributed to the design and oversight of the project, chaired the stakeholder group meetings and approved the final report.
Norman Waugh (Professor of Public Health & Health Technology Assessment) designed the project and the systematic review and drafted, revised and approved the final report.
Matthew W Cooke (Professor of Emergency Medicine) designed the project, attended stakeholder meetings and approved the final report.
Sue Chambers (Research Nurse) co-ordinated the project, led the focus group work, contributed to the ethical analysis and drafted, revised and approved the final project.
Carole Mockford (Senior Research Fellow, RCN Institute) led the main systematic review and drafted, revised and approved the final report.
Karoline Freeman (Research Fellow, Warwick Evidence) led the review of DNACPR policies and drafted, revised and approved the final report.
Amy Grove (Research Fellow, Warwick Evidence) contributed to the systematic reviews and approved the final report.
Richard Field (Foundation Year Doctor) led the scoping review and drafted, revised and approved the final report.
Sarah Owen (Specialist Trainee Doctor) contributed to the focus group coding and analysis and approved the final report.
Ben Clarke (Medical Student) contributed to the systematic reviews and approved the final report.
Rachel Court (Information Scientist, Warwick Evidence) designed and ran the search strategies, contributed to the systematic review and approved the final report.
Claire Hawkes (Senior Research Fellow Emergency Care, Warwick Clinical Trials Unit) contributed to the synthesis of the findings from the different work packages and the discussion section, and approved the final report.
Publications
Field RA, Perkins GD, Baker A. Systematic review of interventions to improve outcomes associated with do-not-attempt-resuscitation orders. Resuscitation 2012;83(Suppl. 1):e122.
Field RA, Fritz Z, Baker A, Grove A, Perkins GD. Systematic review of interventions to improve appropriate use and outcomes associated with do-not-attempt-cardiopulmonary-resuscitation decisions. Resuscitation 2014;85:1418–31.
Freeman K, Field R, Perkins GD. Variation in local trust do not attempt cardiopulmonary resuscitation (DNACPR) policies: a review of 48 English health care trusts. BMJ Open 2015;5:e006517.
Mockford C, Fritz Z, George RM, Court R, Grove A, Clarke B, et al. Do not attempt cardiopulmonary resuscitation (DNACPR) orders: a systematic review of the barriers and facilitators of decision-making and implementation. Resuscitation 2015;88:99–113.
Data sharing statement
Enquiries about the availability of data should be addressed to the corresponding author.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
References
- Jacobs I, Nadkarni V, Bahr J, Berg RA, Billi JE, Bossaert L, et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update and simplification of the Utstein templates for resuscitation registries. A statement for healthcare professionals from a task force of the international liaison committee on resuscitation (American Heart Association, European Resuscitation Council, Australian Resuscitation Council, New Zealand Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Council of Southern Africa). Resuscitation 2004;63:233-49. http://dx.doi.org/10.1016/j.resuscitation.2004.09.008.
- Colorado Springs, CO: Biblica; 2011.
- Cooper JA, Cooper JD, Cooper JM. Cardiopulmonary resuscitation: history, current practice, and future direction. Circulation 2006;114:2839-49. http://dx.doi.org/10.1161/CIRCULATIONAHA.106.610907.
- Beck CS, Pritchard WH, Feil HS. Ventricular fibrillation of long duration abolished by electric shock. J Am Med Assoc 1947;135. http://dx.doi.org/10.1001/jama.1947.62890150005007a.
- Zoll P, Linenthal A, Gibson W, Paul M, Norman L. Termination of ventricular fibrillation in man by externally applied electric countershock. N Engl J Med 1956;254:727-32. http://dx.doi.org/10.1056/NEJM195604192541601.
- Kouwenhoven WB, Jude JR, Knickerbocker GG. Closed-chest cardiac massage. JAMA 1960;173:1064-7. http://dx.doi.org/10.1001/jama.1960.03020280004002.
- Jude JR, Kouwenhoven WB, Knickerbocker GG. Cardiac arrest. Report of application of external cardiac massage on 118 patients. JAMA 1961;178:1063-70. http://dx.doi.org/10.1001/jama.1961.03040500005002.
- Hoke RS, Chamberlain D. Skeletal chest injuries secondary to cardiopulmonary resuscitation. Resuscitation 2004;63:327-38. http://dx.doi.org/10.1016/j.resuscitation.2004.05.019.
- Nolan JP, Soar J, Smith GB, Gwinnutt C, Parrott F, Power S, et al. Incidence and outcome of in-hospital cardiac arrest in the United Kingdom National Cardiac Arrest Audit. Resuscitation 2014;85:987-92. http://dx.doi.org/10.1016/j.resuscitation.2014.04.002.
- Rabkin MT, Gillerman G, Rice NR. Orders not to resuscitate. N Engl J Med 1976;295:364-6. http://dx.doi.org/10.1056/NEJM197608122950705.
- National Confidential Enquiry into Patient Outcome and Death . Time to Intervene? A Review of Patients Who Underwent Cardiopulmonary Resuscitation As a Result of an In-Hospital Cardiopulmonary Arrest 2012.
- Perkins GD, Temple RM, George R. Time to intervene: lessons from the NCEPOD report. Resuscitation 2012;83:1305-6. http://dx.doi.org/10.1016/j.resuscitation.2012.08.332.
- Cohn S, Fritz ZB, Frankau JM, Laroche CM, Fuld JP. Do not attempt cardiopulmonary resuscitation orders in acute medical settings: a qualitative study. QJM 2013;106:165-77. http://dx.doi.org/10.1093/qjmed/hcs222.
- Saevareid TJ, Balandin S. Nurses’ perceptions of attempting cardiopulmonary resuscitation on oldest old patients. J Adv Nurs 2011;67:1739-48. http://dx.doi.org/10.1111/j.1365-2648.2011.05622.x.
- Deep KS, Griffith CH, Wilson JF. Communication and decision making about life-sustaining treatment: examining the experiences of resident physicians and seriously ill hospitalized patients. J Gen Intern Med 2008;23:1877-82. http://dx.doi.org/10.1007/s11606-008-0779-6.
- Meilink M, van de Wetering K, Klip H. Discussing and documenting (do not attempt) resuscitation orders in a Dutch Hospital: a disappointing reality. Resuscitation 2006;71:322-6. http://dx.doi.org/10.1016/j.resuscitation.2006.05.013.
- Clements M, Fuld J, Fritz Z. Documentation of resuscitation decision-making: a survey of practice in the United Kingdom. Resuscitation 2014;85:606-11. http://dx.doi.org/10.1016/j.resuscitation.2014.02.005.
- Richardson DK, Zive DM, Newgard CD. End-of-life decision-making for patients admitted through the emergency department: hospital variability, patient demographics, and changes over time. Acad Emerg Med 2013;20:381-7. http://dx.doi.org/10.1111/acem.12112.
- Field RA, Fritz Z, Baker A, Grove A, Perkins GD. Systematic review of interventions to improve appropriate use and outcomes associated with do-not-attempt-cardiopulmonary-resuscitation decisions. Resuscitation 2014;85:1418-31. http://dx.doi.org/10.1016/j.resuscitation.2014.08.024.
- Mockford C, Fritz Z, George R, Court R, Grove A, Clarke B, et al. Do not attempt cardiopulmonary resuscitation (DNACPR) orders: a systematic review of the barriers and facilitators of decision-making and implementation. Resuscitation 2015;88:99-113. http://dx.doi.org/10.1016/j.resuscitation.2014.11.016.
- Thomas BH, Ciliska D, Dobbins M, Micucci S. A process for systematically reviewing the literature: providing the research evidence for public health nursing interventions. Worldviews Evid Based Nurs 2004;1:176-84. http://dx.doi.org/10.1111/j.1524-475X.2004.04006.x.
- Nicolasora N, Pannala R, Mountantonakis S, Shanmugam B, DeGirolamo A, Amoateng-Adjepong Y, et al. If asked, hospitalized patients will choose whether to receive life-sustaining therapies. J Hosp Med 2006;1:161-7. http://dx.doi.org/10.1002/jhm.78.
- Stein RA, Sharpe L, Bell ML, Boyle FM, Dunn SM, Clarke SJ. Randomized controlled trial of a structured intervention to facilitate end-of-life decision making in patients with advanced cancer. J Clin Oncol 2013;31:3403-10. http://dx.doi.org/10.1200/JCO.2011.40.8872.
- Chen J, Flabouris A, Bellomo R, Hillman K, Finfer S. MERIT Study Investigators for the Simpson Centre and the ANZICS Clinical Trials Group . The Medical Emergency Team System and not-for-resuscitation orders: results from the MERIT study. Resuscitation 2008;79:391-7. http://dx.doi.org/10.1016/j.resuscitation.2008.07.021.
- Smith L, O’Sullivan P, Lo B, Chen H. An educational intervention to improve resident comfort with communication at the end of life. J Palliat Med 2013;16:54-9. http://dx.doi.org/10.1089/jpm.2012.0173.
- Kenward G, Castle N, Hodgetts T, Shaikh L. Evaluation of a medical emergency team one year after implementation. Resuscitation 2004;61:257-63. http://dx.doi.org/10.1016/j.resuscitation.2004.01.021.
- Al-Qahtani S, Al-Dorzi HM, Tamim HM, Hussain S, Fong L, Taher S, et al. Impact of an intensivist-led multidisciplinary extended rapid response team on hospital-wide cardiopulmonary arrests and mortality. Crit Care Med 2013;41:506-17. http://dx.doi.org/10.1097/CCM.0b013e318271440b.
- Lustbader D, Pekmezaris R, Frankenthaler M, Walia R, Smith F, Hussain E, et al. Palliative medicine consultation impacts DNR designation and length of stay for terminal medical MICU patients. Palliat Support Care 2011;9:401-6. http://dx.doi.org/10.1017/S1478951511000423.
- Shuman AG, McCabe MS, Fins JJ, Kraus DH, Shah JP, Patel SG. Clinical ethics consultation in patients with head and neck cancer. Head Neck 2013;35:1647-51. http://dx.doi.org/10.1002/hed.23204.
- Wald HL, Glasheen JJ, Guerrasio J, Youngwerth JM, Cumbler EU. Evaluation of a hospitalist-run acute care for the elderly service. J Hosp Med 2011;6:313-21. http://dx.doi.org/10.1002/jhm.906.
- Wilson ME, Samirat R, Yilmaz M, Gajic O, Iyer VN. Physician staffing models impact the timing of decisions to limit life support in the ICU. Chest 2013;143:656-63. http://dx.doi.org/10.1378/chest.12-1173.
- Butler JV, Pooviah PK, Cunningham D, Hasan M. Improving decision-making and documentation relating to do not attempt resuscitation orders. Resuscitation 2003;57:139-44. http://dx.doi.org/10.1016/S0300-9572(03)00029-7.
- Lewis KE, Edwards VM, Hall S, Temblett P, Hutchings H. ‘Do not attempt resuscitation’ – do standardised order forms make a clinical difference above hand-written note entries?. Resuscitation 2009;80:113-19. http://dx.doi.org/10.1016/j.resuscitation.2008.08.009.
- Castle N, Owen R, Kenward G, Ineson N. Pre-printed ‘do not attempt resuscitation’ forms improve documentation?. Resuscitation 2003;59:89-95. http://dx.doi.org/10.1016/S0300-9572(03)00176-X.
- Diggory P, Cauchi L, Griffith D, Jones V, Lawrence E, Mehta A, et al. The influence of new guidelines on cardiopulmonary resuscitation (CPR) decisions. Five cycles of audit of a clerk proforma which included a resuscitation decision. Resuscitation 2003;56:159-65. http://dx.doi.org/10.1016/S0300-9572(02)00349-0.
- Tan A, Seah A, Chua G, Lim TK, Phua J. Impact of a palliative care initiative on end-of-life care in the general wards: a before-and-after study. Palliat Med 2014;28:34-41. http://dx.doi.org/10.1177/0269216313484379.
- Diggory P, Shire L, Griffith D, Jones V, Lawrence E, Mehta A, et al. Influence of guidelines on CPR decisions: an audit of clerking proforma. Clin Med 2004;4:424-6. http://dx.doi.org/10.7861/clinmedicine.4-5-424.
- Piers RD, Benoit DD, Schrauwen WJ, Van Den Noortgate NJ. Do-not-resuscitate decisions in a large tertiary hospital: differences between wards and results of a hospital-wide intervention. Acta Clin Belg 2011;66:116-22.
- Sulmasy DP, Sood JR, Texiera K, McAuley RL, McGugins J, Ury WA. A prospective trial of a new policy eliminating signed consent for do not resuscitate orders. J Gen Intern Med 2006;21:1261-8. http://dx.doi.org/10.1111/j.1525-1497.2006.00612.x.
- Fritz Z, Malyon A, Frankau JM, Parker RA, Cohn S, Laroche CM, et al. The Universal Form of Treatment Options (UFTO) as an alternative to Do Not Attempt Cardiopulmonary Resuscitation (DNACPR) orders: a mixed methods evaluation of the effects on clinical practice and patient care. PLOS ONE 2013;8. http://dx.doi.org/10.1371/journal.pone.0070977.
- Schiebel N, Henrickson Parker S, Bessette RR, Cleveland EJ, Neeley JP, Warfield KT, et al. Honouring patient’s resuscitation wishes: a multiphased effort to improve identification and documentation. BMJ Qual Saf 2013;22:85-92. http://dx.doi.org/10.1136/bmjqs-2012-000928.
- Hanson LC, Reynolds KS, Henderson M, Pickard CG. A quality improvement intervention to increase palliative care in nursing homes. J Palliat Med 2005;8:576-84. http://dx.doi.org/10.1089/jpm.2005.8.576.
- Hockley J, Watson J, Oxenham D, Murray SA. The integrated implementation of two end-of-life care tools in nursing care homes in the UK: an in-depth evaluation. Palliat Med 2010;24:828-38. http://dx.doi.org/10.1177/0269216310373162.
- Livingston G, Lewis-Holmes E, Pitfield C, Manela M, Chan D, Constant E, et al. Improving the end-of-life for people with dementia living in a care home: an intervention study. Int Psychogeriatr 2013;25:1849-58. http://dx.doi.org/10.1017/S1041610213001221.
- Morrison RS, Chichin E, Carter J, Burack O, Lantz M, Meier DE. The effect of a social work intervention to enhance advance care planning documentation in the nursing home. J Am Geriatr Soc 2005;53:290-4. http://dx.doi.org/10.1111/j.1532-5415.2005.53116.x.
- Schmitten J, Lex K, Mellert C, Rotharmel S, Wegscheider K, Marckmann G. Implementing an advance care planning program in German nursing homes: results of an inter-regionally controlled intervention trial. Deutsch Arztebl Int 2014;111:50-7. http://dx.doi.org/10.3238/arztebl.2014.0050.
- Wenger NS, Citko J, O’Malley K, Diamant A, Lorenz K, Gonzalez V, et al. Implementation of physician orders for life sustaining treatment in nursing homes in California: evaluation of a novel statewide dissemination mechanism. J Gen Intern Med 2013;28:51-7. http://dx.doi.org/10.1007/s11606-012-2178-2.
- Schamp R, Tenkku L. Managed death in a PACE: pathways in present and advance directives. J Am Med Dir Assoc 2006;7:339-44. http://dx.doi.org/10.1016/j.jamda.2006.01.022.
- Baker DW, Einstadter D, Husak S, Cebul RD. Changes in the use of do-not-resuscitate orders after implementation of the Patient Self-Determination Act. J Gen Intern Med 2003;18:343-9. http://dx.doi.org/10.1046/j.1525-1497.2003.20522.x.
- Furman CD, Head B, Lazor B, Casper B, Ritchie CS. Evaluation of an educational intervention to encourage advance directive discussions between medicine residents and patients. J Palliat Med 2006;9:964-7. http://dx.doi.org/10.1089/jpm.2006.9.964.
- Junod Perron N, Morabia A, de Torrenté A. Evaluation of do not resuscitate orders (DNR) in a Swiss community hospital. J Med Ethics 2002;28:364-7. http://dx.doi.org/10.1136/jme.28.6.364.
- Kahn MJ, Sherer K, Alper AB, Lazarus C, Ledoux E, Anderson D, et al. Using standardized patients to teach end-of-life skills to clinical clerks. J Cancer Educ 2001;16:163-5.
- Seoane L, Bourgeois DA, Blais CM, Rome RB, Luminais HH, Taylor DE. Teaching palliative care in the intensive care unit: how to break the news. Ochsner J 2012;12:312-17.
- Szmuilowicz E, Neely KJ, Sharma RK, Cohen ER, McGaghie WC, Wayne DB. Improving residents’ code status discussion skills: a randomized trial. J Palliat Med 2012;15:768-74. http://dx.doi.org/10.1089/jpm.2011.0446.
- Wayne DB, Moazed F, Cohen ER, Sharma RK, McGaghie WC, Szmuilowicz E. Code status discussion skill retention in internal medicine residents: one-year follow-up. J Palliat Med 2012;15:1325-8. http://dx.doi.org/10.1089/jpm.2012.0232.
- McCannon JB, O’Donnell WJ, Thompson BT, El-Jawahri A, Chang Y, Ananian L, et al. Augmenting communication and decision making in the intensive care unit with a cardiopulmonary resuscitation video decision support tool: a temporal intervention study. J Palliat Med 2012;15:1382-7. http://dx.doi.org/10.1089/jpm.2012.0215.
- Rhondali W, Perez-Cruz P, Hui D, Chisholm GB, Dalal S, Baile W, et al. Patient-physician communication about code status preferences: a randomized controlled trial. Cancer 2013;119:2067-73. http://dx.doi.org/10.1002/cncr.27981.
- Hillman K, Chen J, Cretikos M, Bellomo R, Brown D, Doig G, et al. Introduction of the medical emergency team (MET) system: a cluster-randomised controlled trial. Lancet 2005;365:2091-7. http://dx.doi.org/10.1016/S0140-6736(05)66733-5.
- Omnibus Budget Reconciliation Act of 1990 2002.
- Choice, Responsiveness and Equity. London: Department of Health; 2003.
- Critical Appraisal Skills Programme . Critical Appraisal Skills Programme 2007. www.casp-uk.net/ (accessed 1 October 2014).
- Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol 2008;8. http://dx.doi.org/10.1186/1471-2288-8-45.
- Hildén HM, Louhiala P, Honkasalo ML, Palo J. Finnish nurses’ views on end-of-life discussions and a comparison with physicians’ views. Nurs Ethics 2004;11:165-78. http://dx.doi.org/10.1191/0969733004ne681oa.
- Elo G, Dioszeghy C, Dobos M, Andorka M. Ethical considerations behind the limitation of cardiopulmonary resuscitation in Hungary – the role of education and training. Resuscitation 2005;64:71-7. http://dx.doi.org/10.1016/j.resuscitation.2004.08.001.
- Butler M. Dissatisfaction with do not attempt resuscitation orders: a nationwide study of Irish consultant physician practices. Ir Med J 2006;99:208-10.
- Duchateau FX, Burnod A, Ricard-Hibon A, Mantz J, Juvin P. Withholding advanced cardiac life support in out-of-hospital cardiac arrest: a prospective study. Resuscitation 2008;76:134-6. http://dx.doi.org/10.1016/j.resuscitation.2007.06.018.
- Jepson J. Do not attempt resuscitation decisions: the nursing role. Br J Nurs 2003;12:1038-42. http://dx.doi.org/10.12968/bjon.2003.12.17.11719.
- Abby T. Do not resuscitate: how is it perceived?. J Pain Man 2012;5:61-7.
- De Keyser Ganz F, Kaufman N, Israel S, Einav S. Resuscitation in general medical wards: who decides?. J Clin Nurs 2013;22:848-55. http://dx.doi.org/10.1111/j.1365-2702.2012.04240.x.
- Giles H, Moule P. Do not attempt resuscitation’ decision-making: a study exploring the attitudes and experiences of nurses. Nurs Crit Care 2004;9:115-22. http://dx.doi.org/10.1111/j.1362-1017.2004.00065.x.
- Yang GM, Kwee AK, Krishna L. Should patients and family be involved in ‘do not resuscitate’ decisions? Views of oncology and palliative care doctors and nurses. Indian J Palliat Care 2012;18:52-8. http://dx.doi.org/10.4103/0973-1075.97474.
- Dobos M, Dioszeghy C, Hauser B, Elo G. Determinant role of education in the ethical aspects of resuscitation: a German/Hungarian comparison. Bull Med Ethics 2005;211:25-30.
- McAdam C, Barton A, Bull P, Rai G. An audit of nurses’ views on DNR decisions in 1989 and 2003. Br J Nurs 2005;14:1061-5. http://dx.doi.org/10.12968/bjon.2005.14.20.20047.
- Siddiqui MF, Holley JL. Residents’ practices and perceptions about do not resuscitate orders and pronouncing death: an opportunity for clinical training. Am J Hosp Palliat Care 2011;28:94-7. http://dx.doi.org/10.1177/1049909110374599.
- Hurst SA, Becerra M, Perrier A, Perron NJ, Cochet S, Elger B. Including patients in resuscitation decisions in Switzerland: from doing more to doing better. J Med Ethics 2013;39:158-65. http://dx.doi.org/10.1136/medethics-2012-100699.
- Grudzen CR, Hoffman JR, Koenig WJ, Boscardin J, Lorenz KA, Asch SM. The LA story: what happened after a new policy allowing paramedics to forgo resuscitation attempts in prehospital cardiac arrest. Resuscitation 2010;81:685-90. http://dx.doi.org/10.1016/j.resuscitation.2010.02.011.
- Holland CL, Bowker LK, Myint PK. Barriers to involving older people in their resuscitation decisions: the primary–secondary care mismatch highlights the potential role of general practitioners. Int J Clin Pract 2013;67:379-84. http://dx.doi.org/10.1111/ijcp.12067.
- Myint PK, Rivas CA, Bowker LK. In-hospital cardiopulmonary resuscitation: trainees’ worst and most memorable experiences. QJM 2010;103:865-73. http://dx.doi.org/10.1093/qjmed/hcq129.
- Martinez-Selles M, Gallego L, Ruiz J, Fernández Avilés F. Do-not-resuscitate orders and palliative care in patients who die in cardiology departments. What can be improved?. Rev Esp Cardiol 2010;63:233-7. http://dx.doi.org/10.1016/s1885-5857(10)70043-8.
- Messinger-Rapport BJ, Kamel HK. Predictors of do not resuscitate orders in the nursing home. J Am Med Directors Assoc 2005;6:18-21. http://dx.doi.org/10.1016/j.jamda.2004.12.006.
- Kim do Y, Lee KE, Nam EM, Lee HR, Lee KW, Kim JH, et al. Do-not-resuscitate orders for terminal patients with cancer in teaching hospitals of Korea. J Palliat Med 2007;10:1153-8. http://dx.doi.org/10.1089/jpm.2006.0264.
- Janssen van Doorn K, Diltoer M, Spapen H. Do-not-resuscitate orders in the critically ill patient – an observational study with special emphasis on withholding of renal replacement therapy. Acta Clin Belg n.d.;63:221-6. http://dx.doi.org/10.1179/acb.2008.041.
- Becerra M, Hurst SA, Junod Perron N, Cochet S, Elger BS. ‘Do not attempt resuscitation’ and ‘cardiopulmonary resuscitation’ in an inpatient setting: factors influencing physicians’ decisions in Switzerland. Gerontology 2011;57:414-21. http://dx.doi.org/10.1159/000319422.
- Chang Y, Huang C, Lin C. Do-not-resuscitate orders for critically ill patients in intensive care. Nurs Ethics 2010;17:445-55. http://dx.doi.org/10.1177/0969733010364893.
- Bailey FA, Allen RS, Williams BR, Goode PS, Granstaff S, Redden DT, et al. Do-not-resuscitate orders in the last days of life. J Palliat Med 2012;15:751-9. http://dx.doi.org/10.1089/jpm.2011.0321.
- Mendes A, Carvalho F, Dias C, Granja C. In hospital cardiac arrest: factors in the decision not to resuscitate. The impact of an organised in-hospital emergency system. Rev Port Cardiol 2009;28:131-41.
- Chakraborty N, Creaney W. Do not resuscitate’ decisions in continuing care psychiatric patients: what influences decisions?. Psychiatr Bull 2006;30. http://dx.doi.org/10.1192/pb.30.10.376.
- Brizzi M, Abul-Kasim K, Jalakas M, Selariu E, Pessah-Rasmussen H, Zia E. Early do-not-resuscitate orders in intracerebral haemorrhage; frequency and predictive value for death and functional outcome. A retrospective cohort study. Scand J Trauma Resusc Emerg Med 2012;20. http://dx.doi.org/10.1186/1757-7241-20-36.
- Imhof L, Mahrer-Imhof R, Janisch C, Kesselring A, Zuercher Zenklusend R. Do not attempt resuscitation: the importance of consensual decisions. Swiss Medical Wkly 2011;141. http://dx.doi.org/10.4414/smw.2011.13157.
- Grudzen CR, Timmermans S, Koenig WJ, Torres JM, Hoffman JR, Lorenz KA, et al. Paramedic and emergency medical technicians views on opportunities and challenges when forgoing and halting resuscitation in the field. Acad Emerg Med 2009;16:532-8. http://dx.doi.org/10.1111/j.1553-2712.2009.00427.x.
- Nordby H, Nohr O. The ethics of resuscitation: how do paramedics experience ethical dilemmas when faced with cancer patients with cardiac arrest?. Prehosp Disaster Med 2012;27:64-70. http://dx.doi.org/10.1017/S1049023X1200026X.
- Micallef S, Skrifvars MB, Parr MJ. Level of agreement on resuscitation decisions among hospital specialists and barriers to documenting do not attempt resuscitation (DNAR) orders in ward patients. Resuscitation 2011;82:815-18. http://dx.doi.org/10.1016/j.resuscitation.2011.02.048.
- Myint PK, Miles S, Halliday DA, Bowker LK. Experiences and views of specialist registrars in geriatric medicine on ‘do not attempt resuscitation’ decisions: a sea of uncertainty?. QJM 2006;99:691-700. http://dx.doi.org/10.1093/qjmed/hcl096.
- Fritz Z, Malyon A, Frankau JM, Parker RA, Cohn S, Laroche CM, et al. The Universal Form of Treatment Options (UFTO) as an alternative to do not attempt cardiopulmonary resuscitation (DNACPR) orders: a mixed methods evaluation of the effects on clinical practice and patient care. PLOS ONE 2013;8. http://dx.doi.org/10.1371/journal.pone.0070977.
- Naess M. ‘Do-not-attempt-resuscitation’-orders in ICCUs: a survey of attitudes and experiences of nurses in Norway. Intensive Crit Care Nurs 2009;25:140-6. http://dx.doi.org/10.1016/j.iccn.2008.05.001.
- Deep KS, Green SF, Griffith CH, Wilson JF. Medical residents’ perspectives on discussions of advanced directives: can prior experience affect how they approach patients?. J Palliat Med 2007;10:712-20. http://dx.doi.org/10.1089/jpm.2006.0220.
- Fritz Z, Fuld J, Haydock S, Palmer C. Interpretation and intent: a study of the (mis)understanding of DNAR orders in a teaching hospital. Resuscitation 2010;81:1138-41. http://dx.doi.org/10.1016/j.resuscitation.2010.05.014.
- Deep KS, Griffith CH, Wilson JF. Discussing preferences for cardiopulmonary resuscitation: what do resident physicians and their hospitalized patients think was decided?. Patient Educ Counsel 2008;72:20-5. http://dx.doi.org/10.1016/j.pec.2008.01.017.
- Anderson W, Chase R, Pantilat S, Tulsky J, Auerbach A. Code status discussions between attending hospitalist physicians and medical patients at hospital admission. J Gen Intern Med 2010;26:359-66. http://dx.doi.org/10.1007/s11606-010-1568-6.
- Park Y, Kim J, Kim K. Changes in how ICU nurses perceive the DNR decision and their nursing activity after implementing it. Nurs Ethics 2011;18:802-13. http://dx.doi.org/10.1177/0969733011410093.
- Smith GB, Poplett N, Williams D. Staff awareness of a ‘do not attempt resuscitation’ policy in a district general hospital. Resuscitation 2005;65:159-63. http://dx.doi.org/10.1016/j.resuscitation.2004.11.019.
- Zhukovsky DS, Hwang JP, Palmer JL, Willey J, Flamm AL, Smith ML. Wide variation in content of inpatient do-not-resuscitate order forms used at National Cancer Institute-designated cancer centers in the United States. Support Care Cancer 2009;17:109-15. http://dx.doi.org/10.1007/s00520-008-0490-5.
- Field RA, Soar J, Nolan JP, Perkins GD. Epidemiology and outcome of cardiac arrests reported in the lay-press: an observational study. J R Soc Med 2011;104:525-31. http://dx.doi.org/10.1258/jrsm.2011.110228.
- R (Tracey) V Cambridge University Hospitals NHS Foundation Trust &Amp; Ors 2012.
- Findlay G, Shotton H, Kelly K, Mason M. Time to Intervene? A Review of Patients Who Underwent Cardiopulmonary Resuscitation as a Result of an In-Hospital Cardiorespiratory Arrest. London: NCEPOD; 2012.
- National Framework for Reporting and Learning from Serious Incident Requiring Investigation. London: NRLS, National Patient Safety Agency; 2010.
- Mental Health Act 1983. London: The Stationery Office; 1983.
- Guide to Coroner Services. London: Ministry of Justice; 2014.
- The Coroners (Amendment) Rules 2008. London: The Stationery Office; 2008.
- The Coroners Rules 1984. London: The Stationery Office; 1984.
- The Lord Chancellor . Summaries of Rule 43 Reports n.d. www.justice.gov.uk/publications/policy/moj/summary-of-reports-and-responses-under-rule-43-of-the-coroners-rules (accessed 1 July 2014).
- Coroners and Justice Act 2009. London: The Stationery Office; 2009.
- The Chief Coroner . Prevention of Future Death Reports (Previously Known As Rule 43) n.d. www.justice.gov.uk/coroners-burial-cremation/coroners/rule-43 (accessed 10 November 2014).
- Health Service Commissioners Act 1993. London: The Stationery Office; 1993.
- Human Rights Act 1998. London: The Stationery Office; 1998.
- Mental Capacity Act 2005. London: The Stationery Office; 2005.
- Decisions Relating To Cardiopulmonary Resuscitation: A Joint Statement by the BMA, RC(UK) and RCN. London: BMA; 2007.
- Freeman K, Field RA, Perkins GD. Variation in local trust do not attempt cardiopulmonary resuscitation (DNACPR) policies: a review of 48 English healthcare trusts. BMJ Open 2015;5. http://dx.doi.org/10.1136/bmjopen-2014-006517.
- Northern England Strategic Clinical Networks . Deciding Right n.d. www.cnne.org.uk/end-of-life-care---the-clinical-network/decidingright (accessed 25 January 2016).
- Griffiths F. Research Methods for Health Care Practice. London: Sage; 2009.
- Pope C, Mays N. Qualitative Research in Health Care. Oxford: Blackwell; 2006.
- Dalkin SM, Jones D, Lhussier M, Cunningham B. Understanding integrated care pathways in palliative care using realist evaluation: a mixed methods study protocol. BMJ Open 2012;2. http://dx.doi.org/10.1136/bmjopen-2012-001533.
- Gelinas C, Fillion L, Robitaille MA, Truchon M. Stressors experienced by nurses providing end-of-life palliative care in the intensive care unit. Can J Nurs Res 2012;44:18-39.
- Thompson TD, Barbour RS, Schwartz L. Health professionals’ views on advance directives: a qualitative interdisciplinary study. Palliat Med 2003;17:403-9. http://dx.doi.org/10.1191/0269216303pm784oa.
- Ives J, Draper H. Appropriate methodologies for empirical bioethics: it’s all relative. Bioethics 2009;23:249-58. http://dx.doi.org/10.1111/j.1467-8519.2009.01715.x.
- Treatment and Care Towards the End of Life: Good Practice in Decision Making (Online Version). Manchester: GMC; 2010.
- Potter J, Wetherell M. Discourse and Social Psychology: Beyond Attitudes and Behaviour. London: Sage; 1987.
- Widdicombe S, Wooffitt R. The Language of Youth Subcultures: Social Identity in Action. London: Harvester Wheatsheaf; 1995.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77-101. http://dx.doi.org/10.1191/1478088706qp063oa.
- Burr V. An Introduction to Social Constructionism. London: Routledge; 1995.
- Boyatzis R. Transforming Qualitative Information: Thematic Analysis and Code Development. Thousand Oaks, CA: Sage; 1998.
- Griffiths F, Green E, Tsouroufli M. The nature of medical evidence and its inherent uncertainty for the clinical consultation: qualitative study. Brit Med J 2005;330:511-15. http://dx.doi.org/10.1136/bmj.38336.482720.8F.
- Fox RC, Bendelow G, Carpenter M, Vautier C, Williams S. Gender, Health and Healing: The Public/Private Divide. London: Routledge; 2002.
- General Medical Council . Good Medical Practice (2013) 2013. www.gmc-uk.org/guidance/good_medical_practice.asp (accessed 1 November 2014).
- General Medical Council . The Duties of a Doctor Registered With the General Medical Council 2014. www.gmc-uk.org/guidance/good_medical_practice/duties_of_a_doctor.asp (accessed 1 November 2014).
- European Convention on Human Rights. Strasbourg: European Court of Human Rights; 2002.
- Adults with Incapacity (Scotland) Act 2000. London: The Stationery Office; 2000.
- Ms B V An NHS Hospital Trust 2002.
- Burke R (on the Application Of) V General Medical Council &Amp; Ors 2005.
- Airedale NHS Trust V Bland 1993.
- Guide on the Decision-Making Process Regarding Medical Treatment in End-of-Life Situations. Strasbourg: Council of Europe; 2014.
- Fritz Z, Cork N, Dodd A, Malyon A. DNACPR decisions: challenging and changing practice in the wake of the Tracey judgment. Clin Med 2014;14:571-6. http://dx.doi.org/10.7861/clinmedicine.14-6-571.
- Resuscitation Council (UK) . Decisions Relating to Cardiopulmonary Resuscitation. Guidance from the British Medical Association, the Resuscitation Council (UK) and the Royal College of Nursing 2014.
- McWhinney IR. An acquaintance with particulars. Fam Med 1989;21:296-8.
- Gorovitz S, MacIntyre A. Toward a theory of medical fallibility. J Med Philosophy 1976;1:51-7. http://dx.doi.org/10.1093/jmp/1.1.51.
- Tanenbaum S. What physicians know. N Engl J Med 1993;329:1268-71. http://dx.doi.org/10.1056/NEJM199310213291713.
- Fisher M, Ridley S. Uncertainty in end-of-life care and shared decision making. Crit Care Resusc 2012;14:81-7.
- Holmberg L. Task uncertainty and rationality in medical problem solving. Int J Qual Health Care 2006;18:458-62. http://dx.doi.org/10.1093/intqhc/mzl043.
- Beauchamp TL, Childress JF. Principles of Biomedical Ethics. New York, NY: Oxford University Press; 2009.
- General Medical Council . Patients and Doctors Making Decisions Together 2008.
- O’Neill O. Autonomy and Trust in Bioethics. Cambridge: Cambridge University Press; 2002.
- Gillon R. Ethics needs principles – four can encompass the rest--and respect for autonomy should be ‘first among equals’. J Med Ethics 2003;29:307-12. http://dx.doi.org/10.1136/jme.29.5.307.
- Fagerlin A, Schneider CE. Enough. The failure of the living will. Hastings Cent Rep 2004;34:30-42. http://dx.doi.org/10.2307/3527683.
- Puchalski CM, Zhong Z, Jacobs MM, Fox E, Lynn J, Harrold J, et al. Patients who want their family and physician to make resuscitation decisions for them: observations from SUPPORT and HELP. Study to understand prognoses and preferences for outcomes and risks of treatment. Hospitalized Elderly Longitudinal Project. J Am Geriatr Soc 2000;48:S84-90. http://dx.doi.org/10.1111/j.1532-5415.2000.tb03146.x.
- Eliott J, Olver I. Choosing between life and death: patient and family perceptions of the decision not to resuscitate the terminally ill cancer patient. Bioethics 2008;22:179-89. http://dx.doi.org/10.1111/j.1467-8519.2007.00620.x.
- Elwyn G, Frosch D, Thomson R, Joseph-Williams N, Lloyd A, Kinnersley P, et al. Shared decision making: a model for clinical practice. J Gen Intern Med 2012;27:1361-7. http://dx.doi.org/10.1007/s11606-012-2077-6.
- Stiggelbout AM, Van der Weijden T, De Wit MP, Frosch D, Legare F, Montori VM, et al. Shared decision making: really putting patients at the centre of healthcare. Brit Med J 2012;344. http://dx.doi.org/10.1136/bmj.e256.
- Coulter A, Collins A. Making Shared Decision-Making a Reality: No Decision About Me, Without Me. London: The King’s Fund; 2011.
- Ebell MH, Jang W, Shen Y, Geocadin RG. Development and validation of the Good Outcome Following Attempted Resuscitation (GO-FAR) score to predict neurologically intact survival after in-hospital cardiopulmonary resuscitation. JAMA Intern Med 2013;173:1872-8. http://dx.doi.org/10.1001/jamainternmed.2013.10037.
- Lunney JR, Lynn J, Foley DJ, Lipson S, Guralnik JM. Patterns of functional decline at the end of life. JAMA 2003;289:2387-92. http://dx.doi.org/10.1001/jama.289.18.2387.
- Murray SA, Kendall M, Boyd K, Sheikh A. Illness trajectories and palliative care. Brit Med J 2005;330:1007-11. http://dx.doi.org/10.1136/bmj.330.7498.1007.
- Abarshi EA, Echteld MA, Van den Block L, Donker GA, Deliens L, Onwuteaka-Philipsen BD. Recognising patients who will die in the near future: a nationwide study via the Dutch Sentinel Network of GPs. Br J Gen Pract 2011;61:e371-8. http://dx.doi.org/10.3399/bjgp11X578052.
- Barclay S, Momen N, Case-Upton S, Kuhn I, Smith E. End-of-life care conversations with heart failure patients: a systematic literature review and narrative synthesis. Br J Gen Pract 2011;61:e49-62. http://dx.doi.org/10.3399/bjgp11X549018.
- Schneiderman LJ, Jecker NS, Jonsen AR. Medical futility: its meaning and ethical implications. Ann Intern Med 1990;112:949-54. http://dx.doi.org/10.7326/0003-4819-112-12-949.
- Doty WD, Walker RM. Medical futility. Clin Cardiol 2000;23:II6-16. http://dx.doi.org/10.1002/clc.4960231404.
- Eliott JA, Olver I. Dying cancer patients talk about physician and patient roles in DNR decision making. Health Expect 2011;14:147-58. http://dx.doi.org/10.1111/j.1369-7625.2010.00630.x.
- Curtis JR, Burt RA. Why are critical care clinicians so powerfully distressed by family demands for futile care?. J Crit Care 2003;18:22-4. http://dx.doi.org/10.1053/jcrc.2003.YJCRC5.
- Marco CA, Larkin GL. Public education regarding resuscitation: effects of a multimedia intervention. Ann Emerg Med 2003;42:256-60. http://dx.doi.org/10.1067/mem.2003.285.
- Tutu D. Desmond Tutu: a dignified death is our right – I am in favour of assisted dying. The Guardian 2014.
- Dixon J, Matosevic T, Knapp M. The economic evidence for advance care planning: systematic review of evidence. Palliat Med 2015;29:869-84. http://dx.doi.org/10.1177/0269216315586659.
- Tanuseputro P, Wodchis WP, Fowler R, Walker P, Bai YQ, Bronskill SE, et al. The health care cost of dying: a population-based retrospective cohort study of the last year of life in Ontario, Canada. PLOS ONE 2015;10. http://dx.doi.org/10.1371/journal.pone.0121759.
Appendix 1 Scoping review
Structured communication
| Author and country | Study quality | Study type | Population (patient), n | Intervention | Control | Outcome (tool used) | Effect |
|---|---|---|---|---|---|---|---|
| Nicolasora et al. (2006) (USA)22 | Moderate | Prospective randomised trial | 297 patients admitted to the department of medicine | Scripted intervention detailing life-sustaining interventions and advance directives (3 months). n = 136 | Routine clerking (3 months). n = 161 | Number of patients who welcomed the intervention, number who made a decision regarding resuscitation | 98% in the intervention group willingly discussed CPR; eight patients requested DNACPR orders. Resuscitation status was documented by discharge in 61 (38%) patients (control) vs. 125 (92%) patients (intervention) |
| Stein et al. (2013) (Australia)23 | Moderate | Prospective randomised trial | Patients with advanced metastatic cancer with no further curative treatment based in two hospitals over a 17-month period. n = 120 | A patient information leaflet on living with advanced cancer and a discussion with a psychologist used a shared decision-making model including a question about resuscitation wishes. n = 55 | Standard care. n = 65 | DNACPR order in place at time of death. Median time between documented DNACPR decision and death | DNACPR order at time of death: control = 44/58 (76%) vs. 26/38 (68%) intervention (p = 0.4). Medium time DNACPR order placed before death: control group = 12.5 days vs. 27 days intervention group (p = 0.03) |
Introducing specialist teams
| Author and country | Study quality | Study type | Population (patient) n | Intervention | Control | Outcome (tool used) | Effect |
|---|---|---|---|---|---|---|---|
| Chen et al. (2008) (Australia)24 | Strong | Cluster randomised controlled trial | 6780 patients who required an emergency team response at 23 hospitals | MET (6 months). n = 4161 | Non-MET hospitals (6 months). n = 2619 | Difference in issuing DNACPR orders between MET and non-MET emergency teams | For adverse event free calls the proportion of DNACPRs made at the call (3.05% non-MET vs. 7.96% MET; p = 0.048). DNACPR issued 1 in every 33 calls non-MET vs. 1 in every 12 MET hospitals; however, this subset represented only 5% of all DNACPR activity. Per hospital admission METs were 10 times more likely to issue a DNACPR |
| Kenward et al. (2004) (UK)26 | Weak | Before-and-after comparison | Patients in a 700-bed district general hospital with approximately 53,500 admissions per year | Introduction of a MET | Audit data for 1 year prior to the introduction of the MET | Percentage of deaths with a DNACPR order | Deaths with a DNACPR order 87.1% pre intervention vs. 87.6% post intervention. No significant difference [24.6% (32/130) of patients seen by the MET were made DNACPR within 24 hours of review] |
| Al-Qahtani et al. (2013) (Saudi Arabia)27 | Weak | Before-and-after comparison | 256,195 patients admitted to a tertiary care academic hospital | Introduction of an intensivist-led RRT. n = 157,804 | Data obtained over a 2-year period pre RRT implementation. n = 98,391 | Incidence of ward-based DNACPR orders initiated by the intensive care team | Pre-intervention DNACPR incidence was 0.7 per 1000 admissions vs. 1.7 per 1000 admissions post intervention (p < 0.0001) |
| Smith et al. (2013) (USA)25 | Weak | Before-and-after comparison | Patients in tertiary referral centre over a 13-year period | Introduction of a MET. Data were collected from a 5-year period | Retrospective audit data for 8 years prior to introduction of the MET | Ratio of number of new DNACPR orders placed to the number of in-hospital deaths (DNR-to-death ratio) | The DNR-to-death ratio was 0.53–0.58 pre intervention; this increased by 0.10 over the intervention period (p < 0.001) |
| Wald et al. (2011) (USA)30 | Moderate | Quasi-randomised controlled trial | Medical inpatients aged ≥ 70 years admitted to a 425-bed tertiary care hospital. n = 217 | A hospital-run acute care for the elderly (ACE) service an interdisciplinary team approach to identify and address geriatric syndromes in patients aged ≥ 70 years. n = 122 | Patients randomised to usual care on the general medical services. n = 95 | Percentage of patients with DNACPR orders | 26.3% of control patients had a DNACPR order vs. 39.3% of intervention patients (p = 0.04) |
| Lustbader et al. (2011) (USA)28 | Weak | Before-and-after comparison | Patients who died following admission to the medical ICU. n = 1208 | A palliative care consultation with the palliative care team and the patient and/or legal surrogate. Treatment preferences and goals of care were discussed (42 months). n = 693 | Control data from patients who died prior to the introduction of the palliative care team (18 months). n = 515 | Percentage of patients with DNACPR orders at time of death | The intervention group contained a significantly higher percentage of patients with a DNR designation at death than did the control group (86% vs. 68%, chi-squared test, p < 0.0001). 68% of patients in the control group had DNACPR orders at time of death vs. 86% of patients post intervention (p < 0.0001) |
| Shuman et al. (2013) (USA)29 | Moderate | Before-and-after comparison | Patients with head and neck cancer receiving ethics consultations between 2007 and 2011. n = 14 | Ethics consultation which are designed to enable to patient to make informed choices about their medical care including resuscitation status | Percentage with DNACPR orders before consultation | Change in number of patients with DNACPR orders | Percentage of patients with DNACPR orders: 21% (3/14) pre vs. 79% (11/14) post consultation |
| Wilson et al. (2013) (USA)31 | Weak | Before-and-after comparison | Patients dying on the medical ICU over two 6-month periods. n = 150 | 24-hour on-site intensivist cover. n = 65 | Intensivist on call from home 7 p.m. to 7 a.m. with residents on-site. n = 85 | Time from admission to document DNACPR status CPR performed within 24 hours of death | Pre-intervention median (IQR) time to document DNACPR status 3 (1–8) days vs. 1 (0–6) day post-intervention (p = 0.03). CPR was performed within 24 hours of death in 22/85 (26%) pre vs. 15/65 (23%) cases post intervention (p = 0.69) |
Do-not-attempt-cardiopulmonary-resuscitation forms
| Author | Study quality | Study type | Population (patient), n | Intervention | Control | Outcome (tool used) | Effect |
|---|---|---|---|---|---|---|---|
| Lewis et al. (2009) (UK)33 | Weak | Before-and-after comparison | 280 adults sustaining an in-hospital cardiac arrest | Introduction of standard DNACPR forms (workshops and discussions on DNACPR in training courses) (2 years). n = 147 | Pre-interventional data (no form) (2 years). n = 133 | Primary: number of CPR attempts. Secondary: patient demographics, survival to discharge (STD) | No difference in the numbers of CPR attempts, or demographics and STD. However, return of spontaneous circulation decreased 42.9% pre vs. 30.6% post intervention (p = 0.033) |
| Castle et al. (2003) (UK)34 | Weak | Before-and-after comparison | 37 adult inpatients who had died without undergoing resuscitation in a large district general hospital | Introduction of a pre-printed DNACPR form which included briefing on the new form as part of the junior doctors’ induction (1 week). n = 20 | Audit pre-introduction of the form (1 week). n = 17 | Clear documentation in notes; decision, date, signed, clinician name, reason, patient involvement | Clarity of decision 65% pre vs. 100% post (p = 0.05). Date 71% pre vs. 100% post (p = 0.014). Signed 53% pre vs. 100% post (p = 0.001). Clinician name 29% pre vs. 100% post (p ≤ 0.001). Reason 18% pre vs. 90% post (p ≤ 0.001). Patient involvement 6% pre vs. 20% post (not significant p = 0.348). No change in surrogate involvement (24% vs. 25%) |
| Butler et al. (2003) (UK)32 | Weak | Before-and-after comparison | All patients who died at the hospital pre intervention and patients with a DNACPR in the post-intervention period | Introduction of a standardised DNACPR form (4 months). n = 62 | Audit pre-introduction of the form (DNACPR order written in patients notes) (8 months). n = 94 | Deaths with a DNACPR order. Improved documentation and decision-making, reason, consultant authorisation and review | Deaths which had a DNACPR: 94/193 (48.7%) pre vs. 37/65 (59.6%) post intervention. Valid reason for DNACPR: 81 (86.1%) pre vs. 61 (98.4%) post (p > 0.01). Consultant authorised: 35 (37.2%) pre vs. 56 (90.3%) post. Decision reviewed: 35 (37.2%) pre vs. 50 (80.6%) (p < 0.001).Patient involvement: 1.1% pre vs. 14.5% post (p < 0.001). Relatives involved: 69 (74%) vs. 52 (83.9%) post. Documentation in nursing notes: 64 (68.1%) pre vs. 58 (93.5%) post |
| Diggory et al. (2003) (UK)35 | Moderate | Before-and-after comparison | 184 patients admitted and clerked on an elderly care unit | Audit 2 pro forma to record resuscitation status decision (1 month). n = 109 | Audit 1 pre-introduction of pro forma (1 month). n = 75 | Increased documentation of resuscitation status decision | Documentation increased from 36% pre vs. 94% post intervention |
| Tan et al. (2014)36 (Singapore) | Moderate | Before-and-after comparison | 1397 adult deaths on the general wards of a large tertiary hospital | Introduction of a physician order form, staff education and a palliative consult period (1 year). n = 714 | Pre-interventional audit data (1 year). n = 683 | Deaths with DNACPR order. CPR attempt in the last 24 hours of life | Deaths with a DNACPR decision: 452/683 (66%) pre vs. 571/714 (80%) post (p < 0.001). CPR in last 24 hours of life: 64/683 (9.4%) pre vs. 37/714 (5.2%) post (p = 0.003) |
| Piers et al. (2011) (Belgium)38 | Moderate | Before-and-after comparison and cross-sectional | 228 consecutive deaths in a tertiary hospital and a cross-sectional study carried out on a single day in the pre- and post-intervention period | Staff education and new DNACPR form (16 weeks). n = 113 | Pre interventional data (12 weeks). n = 115 | Documented surrogate involvement; nurse involvement; reason for DNACPR; deaths without a DNACPR form. Number of DNACPRs on a single day | Surrogate involved: 34/78 (44%) pre vs. 46/73 (63%) post (p = 0.022). Nurses involved: 11/78 (14%) pre vs. 20/73 (27%) post (p = 0.047). Documented reason: 25/78 (32%) pre vs. 43/73 (59%) post (p = 0.001). Deaths without a DNACPR: 7/89 (8%) pre vs. 11/88 (13%) post (p = 0.332). Patients with DNACPR: 117/676 (17%) pre vs. 75/624 (12%) post intervention (p = 0.008) |
| Diggory et al. (2004) (UK)37 | Moderate | Before-and-after comparison | 259 patients admitted and clerked on an elderly care unit | Audit 6 removal of the mandatory patient/relative discussion from the DNACPR policy (1 month). n = 119 | Audit 5 (1 month). n = 140 | Increased documentation of resuscitation status decision and DNACPR rate | Resuscitation status documented: 96 (81%) pre vs. 148 (94%). Number of patients with DNACPR orders: 25 (45%) pre vs. 73 (68%) post |
| Sulmasy et al. (2006) (USA)39 | Weak | Before-and-after comparison with a comparison site | Patients/surrogates approached for consent for DNACPR orders | Change in DNACPR policy in which a single-sided consent form was used instead of seven separate forms | A control site in which no intervention was given | % of house officers lacking confidence in consenting; DNACPR orders per hospital admission; surrogate stress (Horowitz impact of event scale) | Percentage of house officers who lacked confidence: 24% pre vs. 7% post intervention site (p = 0.002). Control site: 20% pre vs. 15% post (p = 0.45). Incidence of DNACPR orders: 4.53 per 100 admissions pre vs. 7.22 per 100 admissions post (p < 0.001) intervention site. Control site incidence: 3.85 per 100 pre vs. 1.95 per 100 admissions post (p < 0.001). Surrogate stress: 23.6 ± 10.1 pre vs. 17.3 ± 15.9 post (p = 0.02) intervention site |
| Fritz et al. (2013) (UK)40 | Strong | A prospective mixed-methods before-and-after study with contemporaneous case controls | Adult patients admitted to two wards of a 480-bed acute hospital in two 3-month periods. n = 1090 | Introduction of a UFTO which includes a resuscitation status decision. The UFTO was to be completed for all admissions. Patients who had a ‘not for attempted CPR’ decision were included. n = 118 | Pre-intervention data. Patients with a standard DNACPR order. n = 103 | Harm rate using the Global Trigger Tool. Results of thematic interviews with clinicians | Harm rate per 100 admissions pre (DNACPR group) 68.9 vs. 37.3 post intervention (UFTO) p = 0.001. Harms contributing to patient death pre (DNACPR group) 66/71 (93%) vs. 4/44 (9.1%) post intervention (UFTO) p = 0.006. Key findings from interviews suggested that there was increased clarity of goals of care, better communication between clinicians and earlier decision-making with the UFTO than the standard DNACPR form |
| Schiebel et al. (2013) (USA)41 | Weak | Before-and-after comparison | Patients with DNACPR status in 2059-bedded academic tertiary care hospital over a 3-year period. n = 299 | Implementation of an electronic DNACPR system which clearly displayed active DNACPR orders on the patient’s electronic medical record. The system was linked to the automated printing of a newly designed DNACPR wristband. n = 103 | Audit of patients’ medical records pre intervention to look for discrepancies between patient wishes and electronic medical record. n = 196 | Primary: discrepancies between documented patient wishes and resuscitation status wristband. Secondary clear identification of current resuscitation status in the electronic record. Recognition of DNACPR wristband by resuscitation team | Pre-intervention 37/196 (19%) patients vs. 2/103 (2%) post intervention had discrepancies between wristband and documented wishes (p < 0.001). In simulated scenarios correct identification of wristband occurred 12/36 (33%) vs. 14/24 (58%) with new wristband (p = 0.056). Pre-intervention multiple resuscitation statuses were present in 8% of electronic patient records; following intervention no patients had multiple resuscitation orders |
Nursing home and community interventions
| Author and country | Study quality | Study type | Population (patient), n | Intervention | Control | Outcome (tool used) | Effect |
|---|---|---|---|---|---|---|---|
| Hanson et al. (2005) (USA)42 | Weak | Before-and-after comparison | 458 nursing home residents in eight nursing homes | Introduction of palliative care leadership teams into six nursing homes. n = 346 | Pre-intervention baseline data. n = 345 | Percentage of residents with a DNACPR order and percentage of residents with a DNACPR order flag on their chart | DNACPR orders 58% (pre) vs. 65% (post) p ≤ 0.05, DNACPR chart indicators 45% (pre) vs. 60% (post) (p ≤ 0.05) |
| Hockley et al. (2010) (UK)43 | Weak | Before-and-after comparison | Residents in seven nursing homes. n = 228 | Introduction of two end-of-life care tools (Gold Standards Framework for Care Homes and adapted Liverpool Care Pathway for Care Homes). n = 133 | Pre-intervention data. n = 95 | Increase in percentage of residents with a DNACPR order in their notes | 14/95 (15%) residents had a DNACPR order pre vs. 96/133 (72%) post intervention (p < 0.001) |
| Morrison et al. (2005) (USA)45 | Weak | Randomised controlled clinical trial | Adults admitted to a long-term bed in a 514-bed nursing home. n = 139 | Training of nursing home social workers in advanced care planning; structured advance care planning discussions with residents; and completion of a care plan with regular review. n = 43 | Training of nursing home social workers in legal aspects of advance directives only. n = 96 | Documentation of CPR preference | CPR preference recorded 20% (control) vs. 40% (intervention) (p = 0.05) |
| Livingston et al. (2013) (UK)44 | Weak | Before-and-after comparison | Adults with dementia who died in a 120-bed Jewish nursing home. n = 98 | A 10-session interactive staff educational training programme on end-of-life care including advance care planning and communication about end of life. Managers also underwent training in the gold standards framework post intervention (12 months). n = 42 | Pre-intervention review of records (12 months). n = 56 | Number of residents who died with a DNACPR order in place. Number of residents whose advanced care wishes (DNACPR and/or hospitalisation) were met | Residents with dementia dying with a documented DNACPR decision 4/28 (14%) pre intervention vs. 16/22 (73%) post intervention (p < 0.001). Residents without dementia dying with a documented DNACPR decision: 2/20 (10%) pre intervention vs. 6/7 (86%) post intervention (p < 0.001). Residents whose advanced care wishes were met 5/7 (71%) pre intervention vs. 13/13 (100%) post intervention p = 0.04 |
| Wenger et al. (2013) (USA)47 | Weak | Cluster controlled trial | Nursing homes in coalition and non-coalition areas. n = 555 | The formation of community coalitions which were to provide grassroots, education and training to nursing homes in order to improve implementation of POLST (physician orders for life sustaining treatment). Nursing homes in coalition areas. n = 143 | Nursing homes in non-coalition areas. n = 140 | Percentage of residents with a POLST; POLST completed with resident; staff education; structural implementation of POLST; difficulties in implementation | Percentage of residents with a POLST were 59.8% in coalition areas vs. 48.0% non-coalition areas (p = 0.02). Percentage of POLST forms completed with resident were 92.1% in coalition areas vs. 76.5% in non-coalition areas (p = 0.015). Use of case discussions and role-play in staff education was 53% in coalition areas vs. 36% in non-coalition areas (p = 0.01). Other educational measures were none significant. No significant difference in percentage of nursing homes reporting difficulties in POLST use or in structural factors |
| Schmitten et al. (2014) (Germany)46 | Weak | Prospective cluster controlled trial | Nursing home residents in nine nursing homes in one German state. n = 1582 | The establishment of regional advanced care planning programme in four nursing homes consisting of. 20 hours of training of non-physician facilitators. 4 hours of training of primary medical care physicians and 4 hours of staff education of other key medical/nursing staff. n = 136 | Five control nursing homes. n = 439 | Number of new ADs over the 16.5-month period. Number of ADs stating current resuscitation status and if a prominent note for DNACPR was on their file. Total number of ADs at the end of the study period. Total number of AD stating resuscitation status at the end of the study period | Numbers of new ADs were 49/136 (36%) intervention vs. 18/439 (4.1%) control (p < 0.001). Numbers of new ADs stating current resuscitation status 47/49 (95.9%) intervention vs. 7/18 (38.9%) control (p = 0.001). Prominent DNACPR note of file 40/49 (81.6%) intervention vs. 0/18 control (p = 0.001). Total numbers of ADs at end of study were 71/136 (52.2%) intervention vs. 109/439 (24.8%) control (p < 0.001). Total ADs with current resuscitation decision were 51/71 (71.8%) intervention vs. 11/98 (11.2%) control (p < 0.001) |
| Schamp et al. (2006) (USA)48 | Weak | Before-and-after comparison | Adults enrolled in a urban community outpatient PACE site (aged at least 55 years and frail enough to qualify for a nursing home placement). n = 160 | Enrolment in PACE which involved confirmation of current health-care wishes and advance directive | Documented health-care wishes prior to enrolment on the PACE programme | Change in present DNACPR documentation | 77 (48%) of patients had DNACPR orders pre intervention vs. 61 (38%) post intervention (p < 0.05) |
Legislation
| Author and country | Study quality | Study type | Population (patient), n | Intervention | Control | Outcome (tool used) | Effect |
|---|---|---|---|---|---|---|---|
| Baker et al. (2003) (USA)49 | Weak | Before-and-after comparison | Medicare patients admitted to 29 non-federal hospitals between 1991 and 1997 with myocardial infarction, heart failure, gastrointestinal haemorrhage, COPD, pneumonia or stroke. n = 91,539 | Passage of the Patient Self-Determination Act in December 199159 (requiring hospitals to develop policies on advance directives, ask new patients if they had an advance directive, provide patients with information on advance directives and educate the staff on advance directives) | Chart data of patients before the Patient Self-Determination Act (1991 data) | Percentage of early DNACPR orders (first or second day of hospital stay) and percentage of late DNACPR orders (day 3 or later) | Myocardial infarction early DNACPR orders 10.4% (1991) vs. 13.1% (1992); p = 0.02; heart failure early DNACPR orders 8.6% (1991) vs. 13.0% (1992); p = 0.03; gastrointestinal haemorrhage early DNACPR orders 8.9% (1991) vs. 11.8% (1992); p = 0.02; COPD early DNACPR orders 6.9% (1991) vs. 9.7% (1992); p = 0.05. There were no significant changes for patients with pneumonia or stroke. No significant changes in late DNACPR orders except for COPD: COPD late orders 4.3% (1991) vs. 6.4% (1992); p = 0.01 |
Physician education
| Author and country | Study quality | Study type | Population (patient), n | Intervention | Control | Outcome (tool used) | Effect |
|---|---|---|---|---|---|---|---|
| Furman et al. (2006) (USA)50 | Weak | Before-and-after comparison | Eight medicine residents serving 79 patients on at internal medicine unit | Medical residents received a half-day training session intervention involving didactic training and a role-play exercise (5 days). n = 35 | Pre-intervention documentation of a resuscitation discussion (10 days). n = 44 | Increased documentation of a resuscitation status discussion | Pre intervention, 44 (32%) patients had discussions. Post intervention, 35 (34%) patients had discussions. No significant difference |
| Junod Perron et al. (2002) (Switzerland)51 | Weak | Before-and-after comparison | Nine junior doctors serving 255 patients with a DNACPR order on an internal medicine unit | Information given to the doctors about DNACPR meaning, ethics, patients’ rights and futility (5 months). n = 115 | Pre-intervention data (5 months). n = 140 | Accurate understanding, interpretation and use of DNR orders (survey attached to DNACPR form). Patient involvement in the decision | Pre-intervention correct physician understanding 62/140 (44%) vs. 107/115 (93%) post intervention (p < 0.001). Patient involvement 17.1% pre vs. 47.8% post (p < 0.01). Nurse and surrogate involvement non-significant |
| Kahn et al. (2001) (USA)52 | Weak | Before-and-after comparison | 44 third-year medical students | A half-day workshop using standardised simulated patients with two end-of-life scenarios. n = 44 | Pre-test of self-efficacy to deal with end-of-life issues using a 5-point Likert scale. n = 44 | Improvement in pre- and post-test scores on being comfortable discussing DNACPR orders and understanding the legal issues surrounding DNACPR orders | More students felt comfortable discussing DNACPR orders: mean Likert score 2.5/5 (pre) vs. 2.7/5 (post) (p = 0.54). Improved understanding of legal issues: 2.6/5 (pre) vs. 3.6/5 (post) (p < 0.01) |
| Seoane et al., (2012) (USA)53 | Weak | Before-and-after comparison | 214 medical ICU house officers | Teaching throughout a 1-month rotation involving role modelling, tutorials and case-based discussions | Pre-rotation survey using a 4-point Likert scare to rate confidence in nine aspects of palliative care including discussion DNACPR orders | Improvement in pre- and post-test scores on being comfortable discussing DNACPR orders | Mean confidence was 3.1(0.9)/4 pre intervention and 3.6(0.6)/4 post intervention (p < 0.001) |
| Szmuilowicz et al. (2012) (USA)54 | Moderate | Prospective randomised controlled trial | 38 post-graduate year 1 medical residents at a large academic medical centre. n = 38 | Extra multimodal educational intervention consisting of seminars, self-directed learning, e-learning modules, reflective practice and a booster session at 4 months. n = 19 | Residents undergoing the 6-month rotation without any of the extra educational interventions. n = 19 | Score of a resuscitation status decision with a simulated patient after 2 months after the booster session | Mean resuscitation status discussion scores were 53.2 ± 16.2% for control group vs. 75.1 ± 8.9% for intervention group (p < 0.001) |
| Wayne et al. (2012) (USA)55 | Moderate | As above | As above | As above | As above | Score of resuscitation status decision with a simulated patient 12 months after first simulated discussion test | Mean resuscitation status discussion scores were 54.7 ± 17.1% for control group vs. 71.9 ± 16.0% for intervention group (p < 0.001) |
Patient/surrogate education
| Author and country | Study quality | Study type | Population (patient) n | Intervention | Control | Outcome (tool used) | Effect |
|---|---|---|---|---|---|---|---|
| Meilink et al. (2006) (the Netherlands)16 | Moderate | Before-and-after comparison | 2517 admission notes on all clinical admissions to a tertiary referral hospital | Introduction of a DNACPR patient information sheet and informing (in writing) consultants and residents about the DNACPR order documentation (1 month). n = 1281 | Pre-intervention audit data (1 month). n = 1237 | Documentation of resuscitation status decision in the medical record | Pre intervention, 132 (10.7%) patients had a resuscitation decision. Post intervention, 119 (9.3%) had a decision. No improvement |
| McCannon et al. (2012) (USA)56 | Weak | Before-and-after comparison | Surrogate decision-makers of medical ICU patients. n = 50 | A 3-minute video depicting a simulated CPR attempt followed by a four-question CPR knowledge assessment. n = 27 | A four-question CPR knowledge assessment without the video. n = 23 | Primary: score on CPR knowledge Secondary: percentage of surrogates making a DNACPR decision for patients |
Pre-intervention average surrogate score was 2.0 ± 1.2 vs. 2.9 ± 1.2 out of 4 post intervention (p = 0.008). Pre intervention, 22% of surrogates chose DNACPR status vs. 59% post intervention (p = 0.23) |
| Rhondali et al. (2013) (USA)57 | Moderate | Randomised controlled crossover trial | Patients with advanced cancer attending a supportive care clinic. n = 80 | Patients watched two similar videos showing a simulated resuscitation status discussion. Video 1 ended the discussion with a question asking the patient their preference for resuscitation. Video 2 ended the discussion with a recommendation of DNACPR from the doctor. n = 80 | The patients were split into two groups. The first group watched video 1 followed by video 2. The second group watched video 2 followed by video 1 in order to minimise bias. n = 80 | Patients were asked at the end of each video what resuscitation status they would choose for the patient (CPR or DNACPR) | There was no difference in patients choosing DNACPR between the question (video 1) and the recommendation (video 2). 58/80 patients chose DNACPR for the video patient. After watching the first video DNACPR was chosen 34/58 (59%) for video 1 (question) vs. 24/58 (41%) for video 2 recommendation (p = 0.49). Overall percentage of patients choosing DNACPR for the video patient was 74% for question (video 1) vs. 73% recommendation (video 2) |
Appendix 2 Full review: search strategies
MEDLINE (Ovid) (1946 to week 1 July 2013)
Date range searched: 1 January 2003 to July 2013.
Date of search: 12 July 2013.
| 1 | Resuscitation Orders/ | 3068 |
| 2 | “do not attempt resuscitation”.tw. | 123 |
| 3 | “do not attempt cardiopulmonary resuscitation”.tw. | 3 |
| 4 | “do not resuscitate”.tw. | 1345 |
| 5 | “not for resuscitation”.tw. | 50 |
| 6 | “resuscitation order*”.tw. | 108 |
| 7 | (“cardiopulmonary resuscitation” adj2 decision*).tw. | 43 |
| 8 | “CPR decision*”.tw. | 39 |
| 9 | DNAR.tw. | 103 |
| 10 | DNACPR.tw. | 2 |
| 11 | ((DNR or NFR) and (resuscitat* or CPR)).tw. | 699 |
| 12 | (DNR order* or DNR discussion* or NFR order* or NFR discussion*).tw. | 601 |
| 13 | allow natural death.tw. | 9 |
| 14 | allow dignified death.tw. | 0 |
| 15 | (advance care planning/ or advance directives/ or living wills/) and exp Resuscitation/ | 916 |
| 16 | ((advance* care plan* or patient care plan* or advance* directive* or living will*) and (resuscitat* or CPR)).tw. | 458 |
| 17 | 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 | 4095 |
| 18 | limit 17 to (english language and yr=“2003 -Current”) | 1616 |
MEDLINE In Process & Other Non-Indexed Citations (Ovid) (11 July 2013)
Date range searched: 1 January 2003 to July 2013.
Date of search: 16 July 2013.
| 1 | “do not attempt resuscitation”.tw. | 7 |
| 2 | “do not attempt cardiopulmonary resuscitation”.tw. | 2 |
| 3 | “do not resuscitate”.tw. | 77 |
| 4 | “not for resuscitation”.tw. | 4 |
| 5 | “resuscitation order*”.tw. | 10 |
| 6 | (“cardiopulmonary resuscitation” adj2 decision*).tw. | 3 |
| 7 | “CPR decision*”.tw. | 2 |
| 8 | DNAR.tw. | 4 |
| 9 | DNACPR.tw. | 2 |
| 10 | ((DNR or NFR) and (resuscitat* or CPR)).tw. | 37 |
| 11 | (DNR order* or DNR discussion* or NFR order* or NFR discussion*).tw. | 26 |
| 12 | allow natural death.tw. | 3 |
| 13 | allow dignified death.tw. | 0 |
| 14 | ((advance* care plan* or patient care plan* or advance* directive* or living will*) and (resuscitat* or CPR)).tw. | 19 |
| 15 | 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 | 104 |
| 16 | limit 15 to (english language and yr=“2003 -Current”) | 81 |
EMBASE (1974 to week 28 2013)
Date range searched: 1 January 2003 to July 2013.
Date of search: 17 July 2013.
| 1 | “do not attempt resuscitation”.mp. | 192 |
| 2 | “do not attempt cardiopulmonary resuscitation”.mp. | 9 |
| 3 | “do not resuscitate”.mp. | 1730 |
| 4 | “not for resuscitation”.mp. | 69 |
| 5 | “resuscitation order*”.mp. | 213 |
| 6 | (“cardiopulmonary resuscitation” adj2 decision*).mp. | 50 |
| 7 | “CPR decision*”.mp. | 46 |
| 8 | DNAR.mp. | 172 |
| 9 | DNACPR.mp. | 6 |
| 10 | ((DNR or NFR) and (resuscitat* or CPR)).mp. | 1118 |
| 11 | (DNR order* or DNR discussion* or NFR order* or NFR discussion*).mp. | 768 |
| 12 | allow natural death.mp. | 18 |
| 13 | allow dignified death.mp. | 0 |
| 14 | (patient care planning/ or living will/ or medical order/ or medical documentation/) and resuscitation/ | 1243 |
| 15 | ((advance* care plan* or patient care plan* or advance* directive* or living will*) and (resuscitat* or CPR)).tw. | 577 |
| 16 | 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 | 3643 |
| 17 | limit 16 to (english language and yr=“2003 -Current”) | 1827 |
Cumulative Index to Nursing and Allied Health Literature via EBSCOhost
Date range searched: 1 January 2003 to July 2013.
Date of search: 17 July 2013.
Note: search reads from bottom to top.
| S18 | S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 OR S9 OR S10 OR S11 OR S12 OR S13 OR S16 Limiters – Published Date from: 20030101-; Language: English |
1119 |
| S17 | S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 OR S9 OR S10 OR S11 OR S12 OR S13 OR S16 | 2080 |
| S16 | S14 OR S15 | 210 |
| S15 | AB ((advance* N1 care N1 plan*) OR (patient N1 care N1 plan*) OR (advance* N1 directive*) OR (living N1 will*)) AND (resuscitat* OR CPR) | 190 |
| S14 | TI ((advance* N1 care N1 plan*) OR (patient N1 care N1 plan*) OR (advance* N1 directive*) OR (living N1 will*)) AND (resuscitat* OR CPR) | 29 |
| S13 | ((MH “Advance Care Planning”) OR (MH “Advance Directives”) OR (MH “Living Wills”)) AND (“Resuscitation Orders+”) | 376 |
| S12 | TI “allow dignified death” OR AB “allow dignified death” OR MW “allow dignified death” | 0 |
| S11 | TI “allow natural death” OR AB “allow natural death” OR MW “allow natural death” | 16 |
| S10 | TI ( (DNR N1 order*) OR (DNR N1 discussion*) OR (NFR N1 order*) OR (NFR N1 discussion*) ) OR AB ( (DNR N1 order*) OR (DNR N1 discussion*) OR (NFR N1 order*) OR (NFR N1 discussion*) ) OR MW ( (DNR N1 order*) OR (DNR N1 discussion*) OR (NFR N1 order*) OR (NFR N1 discussion*) ) | 320 |
| S9 | TI ( (DNR OR NFR) AND (resuscitat* OR CPR) ) OR AB ( (DNR OR NFR) AND (resuscitat* OR CPR) ) OR MW ( (DNR OR NFR) AND (resuscitat* OR CPR) ) | 311 |
| S8 | TI ( DNAR OR DNACPR ) OR AB ( DNAR OR DNACPR ) OR MW ( DNAR OR DNACPR ) | 44 |
| S7 | TI CPR N1 decision* OR AB CPR N1 decision* OR MW CPR N1 decision* | 31 |
| S6 | TI “cardiopulmonary resuscitation” N2 decision* OR AB “cardiopulmonary resuscitation” N2 decision* OR MW “cardiopulmonary resuscitation” N2 decision* | 40 |
| S5 | TI (resuscitation N1 order*) OR AB (resuscitation N1 order*) OR MW (resuscitation N1 order*) | 1744 |
| S4 | TI ( “do not resuscitate” ) OR AB ( “do not resuscitate” ) OR MW ( “do not resuscitate” ) | 643 |
| S3 | TI ( “do not attempt cardiopulmonary resuscitation” ) OR AB ( “do not attempt cardiopulmonary resuscitation” ) OR MW ( “do not attempt cardiopulmonary resuscitation” ) | 3 |
| S2 | TI ( “do not attempt resuscitation” ) OR AB ( “do not attempt resuscitation” ) OR MW ( “do not attempt resuscitation” ) | 55 |
| S1 | MH “Resuscitation Orders” | 1731 |
The Cochrane Library (all sections) searched via Wiley
Date range searched: 1 January 2003 to July 2013.
Date of search: 19 July 2013.
| #1 | MeSH descriptor: [Resuscitation Orders] this term only | 16 |
| #2 | “do not attempt resuscitation”:ti,kw,ab | 2 |
| #3 | “do not attempt cardiopulmonary resuscitation”:ti,kw,ab | 0 |
| #4 | “do not resuscitate”:ti,kw,ab | 34 |
| #5 | “not for resuscitation”:ti,kw,ab | 2 |
| #6 | resuscitation next order*:ti,kw,ab | 24 |
| #7 | “cardiopulmonary resuscitation” near/2 decision*:ti,kw,ab | 4 |
| #8 | CPR near/3 decision*:ti,kw,ab | 1 |
| #9 | DNAR:ti,kw,ab | 0 |
| #10 | DNACPR:ti,kw,ab | 0 |
| #11 | ((DNR or NFR) and (resuscitat* or CPR)):ti,kw,ab | 22 |
| #12 | (DNR next order* or DNR next discussion* or NFR next order* or NFR next discussion*):ti,kw,ab | 21 |
| #13 | “allow natural death”:ti,kw,ab | 0 |
| #14 | “allow dignified death”:ti,kw,ab | 0 |
| #15 | MeSH descriptor: [Advance Care Planning] this term only | 48 |
| #16 | MeSH descriptor: [Advance Directives] this term only | 69 |
| #17 | MeSH descriptor: [Living Wills] this term only | 12 |
| #18 | #15 or #16 or #17 | 111 |
| #19 | MeSH descriptor: [Resuscitation] explode all trees | 3325 |
| #20 | #18 and #19 | 10 |
| #21 | ((advance* next care next plan* or patient next care next plan* or advance* next directive* or living next will*) and (resuscitat* or CPR)):ti,kw,ab | 35 |
| #22 | #1 or #2 or #3 or #4 or #5 or #6 or #7 or #8 or #9 or #10 or #11 or #12 or #13 or #14 or #20 or #21 | 57 |
| #23 | #22 from 2003 | 25 |
Science Citation Index and Social Sciences Citation Index via Web of Science
Date range searched: 1 January 2003 to July 2013.
Date of search: 19 July 2013.
Note: search reads from bottom to top.
| # 16 | 1053 | (#15) AND Language=(English) Databases=SCI-EXPANDED, SSCI Timespan=2003-2013 |
| # 15 | 2199 | #1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14 Databases=SCI-EXPANDED, SSCI Timespan=All years |
| # 14 | 758 | TS=(((advance* NEAR/1 care NEAR/1 plan*) OR (patient NEAR/1 care NEAR/1 plan*) OR (advance* NEAR/1 directive*) OR (living NEAR/1 will*)) AND (resuscitat* OR CPR)) Databases=SCI-EXPANDED, SSCI Timespan=All years |
| # 13 | 0 | TS="allow dignified death" Databases=SCI-EXPANDED, SSCI Timespan=All years |
| # 12 | 14 | TS="allow natural death" Databases=SCI-EXPANDED, SSCI Timespan=All years |
| # 11 | 453 | TS=((DNR NEAR/1 order*) OR (DNR NEAR/1 discussion*) OR (NFR NEAR/1 order*) OR (NFR NEAR/1 discussion*)) Databases=SCI-EXPANDED, SSCI Timespan=All years |
| # 10 | 567 | TS=((DNR OR NFR) AND (resuscitat* OR CPR)) Databases=SCI-EXPANDED, SSCI Timespan=All years |
| # 9 | 3 | TS=DNACPR Databases=SCI-EXPANDED, SSCI Timespan=All years |
| # 8 | 106 | TS=DNAR Databases=SCI-EXPANDED, SSCI Timespan=All years |
| # 7 | 109 | TS=(CPR NEAR/2 decision*) Databases=SCI-EXPANDED, SSCI Timespan=All years |
| # 6 | 138 | TS=(“cardiopulmonary resuscitation” NEAR/2 decision*) Databases=SCI-EXPANDED, SSCI Timespan=All years |
| # 5 | 214 | TS=(resuscitation NEAR/1 order*) Databases=SCI-EXPANDED, SSCI Timespan=All years |
| # 4 | 46 | TS=“not for resuscitation” Databases=SCI-EXPANDED, SSCI Timespan=All years |
| # 3 | 1161 | TS=“do not resuscitate” Databases=SCI-EXPANDED, SSCI Timespan=All years |
| # 2 | 3 | TS=“do not attempt cardiopulmonary resuscitation” Databases=SCI-EXPANDED, SSCI Timespan=All years |
| # 1 | 126 | TS=“do not attempt resuscitation” Databases=SCI-EXPANDED, SSCI Timespan=All years |
Applied Social Sciences Index and Abstracts via ProQuest
Date range searched: 1 January 2003 to July 2013.
Date of search: 19 July 2013.
| S1 | SU(“do not resuscitate orders”) | 74 |
| S2 | “do not attempt resuscitation” | 14 |
| S3 | “do not attempt cardiopulmonary resuscitation” | 0 |
| S4 | “do not resuscitate” | 137 |
| S5 | “not for resuscitation” | 8 |
| S10 | resuscitation PRE/2 order* | 16 |
| S11 | “cardiopulmonary resuscitation” NEAR/2 decision* | 13 |
| S12 | CPR NEAR/2 decision* | 12 |
| S13 | DNAR | 11 |
| S14 | DNACPR | 0 |
| S15 | ((DNR OR NFR) AND (resuscitat* OR CPR)) | 65 |
| S16 | (DNR PRE/1 order*) OR (DNR PRE/1 discussion*) OR (NFR PRE/1 order*) OR (NFR PRE/1 discussion*) | 46 |
| S17 | “allow natural death” | 0 |
| S18 | “allow dignified death” | 0 |
| S19 | ((advance* PRE/1 care PRE/1 plan*) OR (patient PRE/1 care PRE/1 plan*) OR (advance* PRE/1 directive*) OR (living PRE/1 will*)) AND (resuscitat* OR CPR) | 55 |
| S20 | S1 OR S2 OR S3 OR S4 OR S5 OR S10 OR S11 OR S12 OR S13 OR S14 OR S15 OR S16 OR S17 OR S18 OR S19 | 187 |
| S22 | S20 AND la.exact(“ENG”) AND pd(>20030101) | 97 |
PsycINFO via ProQuest
Date range searched: 1 January 2003 to July 2013.
Date of search: 19 July 2013.
| S2 | (“do not attempt resuscitation” OR “do not attempt cardiopulmonary resuscitation” OR “do not resuscitate” OR “not for resuscitation” OR (resuscitation PRE/2 order*) OR (“cardiopulmonary resuscitation” NEAR/2 decision*) OR (CPR NEAR/2 decision*) OR DNAR OR DNACPR OR ((DNR OR NFR) AND (resuscitat* OR CPR)) OR ((DNR PRE/1 order*) OR (DNR PRE/1 discussion*) OR (NFR PRE/1 order*) OR (NFR PRE/1 discussion*)) OR “allow natural death” OR “allow dignified death” OR (((advance* PRE/1 care PRE/1 plan*) OR (patient PRE/1 care PRE/1 plan*) OR (advance* PRE/1 directive*) OR (living PRE/1 will*)) AND (resuscitat* OR CPR))) AND la.exact(“ENG”) AND pd(>20030101) | 271 |
The King’s Fund Library database
Date range searched: 1 January 2003 to July 2013.
Date of search: 19 July 2013.
Note: this is a small database and complex searching is not possible. The results were sifted online.
Keyword: resuscitation
OR
Subject: resuscitation
OR
Title: resuscitation
Publication Date Range: 2003 –
Language: English
Number 36
Appendix 3 Full review: studies reviewed
| Authors | Quality of study | Country (year data collected) | Purpose of study | Study design | Setting | Participants |
|---|---|---|---|---|---|---|
| Abby 201268 | Low | Hong Kong (2009) | Perceptions of DNACPR order | Cross-sectional questionnaire | One hospital | 16 physicians, 33 nurses, 25 patients, 27 relatives |
| Anderson et al. 201099 | Low | USA (2008–9) | Do physicians’ DNACPR/CPR discussions meet recommendations? | Cross-sectional observational study; questionnaires | Two university hospitals | 32 physicians, 80 patients |
| Bailey et al. 201285 | Medium | USA (2005) | To ascertain DNACPR practice, timing of orders | Prospective chart abstraction | Six Veteran’s Affairs Medical Centres | 1069 records of deceased veterans |
| Becerra et al. 201183 | Low | Switzerland (2004–5) | To determine the prevalence of DNACPR/CPR orders; associated factors; how decisions are made and documented | Prospective review of DNACPR/CPR orders. Retrospective face-to-face survey of physicians | The medical wards of a large tertiary university teaching hospital | 106 patients, 61 residents |
| Brizzi et al. 201288 | Low | Sweden (2007–9) | Frequency and predictive factors for DNACPR orders and association to prognosis | Medical record review; computed tomography scans | One hospital | 197 ICH patients |
| Butler et al. 200665 | Low | Ireland (2003) | How DNACPR orders are made in practice | Cross-sectional survey | 38 general hospitals with acute admission facilities | 173 consultant physicians |
| Chakraborty and Creaney 200687 | Medium | UK: Scotland (2004) | Reasons contributing to DNACPR orders in psychiatric patients | Audit; nurses were asked for missing data for the audit | Psychiatric wards of Ayrshire and Arran | 35 DNR orders for elderly patients |
| Chang et al. 201084 | Low | Taiwan (not given) | To compare differences in care for those with a DNACPR order; to determine clinical factors which influence DNACPR decision-making | Prospective data collection | ICUs in two Taipei area hospitals | 202 patients |
| Cohn et al. 201313 | Median | UK: England (2010) | To determine the influence of a DNACPR order on the care of patients | Primarily direct observation; semistructured interviews; 3-month ‘notes review’ of nominal 100 decisions | Two acute wards in a typical middle-sized NHS hospital | 13 doctors; 14 nursing staff; two patient interviews; 103 DNACPR decisions/581 admissions |
| Deep et al. 200796 | High | USA (2005) | How do physicians approach DNACPR/CPR discussions; what do they find most challenging? | Survey | Teaching hospital | 55 resident physicians |
| Deep et al. 200815 | High | USA (not given; probably as ID12) | How do discussions occur and what factors influence physicians’ communicative practice? | Qualitative semistructured interviews | Two medical centres served by one training programme | 28 resident physicians; 28 patients; 12 surrogates |
| Deep et al. 200898 | High | USA: Kentucky (2006) | How discussions around DNACPR/CPR are interpreted by patients, relatives, and physicians | Semistructured interviews after consultation about CPR | Two medical centres served by one training programme | 28 resident physicians; 28 patients |
| De Keyser Ganz et al. 201369 | High | Israel: Jerusalem (not given) | To explore the reasons nurses do not initiate CPR in cases they consider futile | Questionnaire survey | Five adult internal medicine wards in two hospitals | 122 nurses |
| Dobos et al. 200572 | Low | Germany (2003) | To determine if bioethical principles are linked to the education of doctors and to compare results with another study (see Elo et al.,64 below) | Cross-sectional questionnaire | Two medical centres in Hungary and Germany | 36 doctors in Ulm |
| Duchateau et al. 200866 | Low | France (12-month period: no dates given) | Factors contributing to refraining from CPR in a pre-hospital setting | Prospective, descriptive study | Physician-staffed emergency medical service | Emergency medical technician (EMTs) staffed ambulances; physician-staffed emergency medical service. 227 patients |
| Elo et al. 200564 | Low | Hungary (2003) | To recognise the ethical factors limiting resuscitation in Hungary (rules vs. everyday practice) | Face-to-face cross-sectional survey | ICUs in Hungary | 72 doctors |
| Fritz et al. 201097 | High | UK: England (over the course of 2 weeks) | Doctors’ and nurses’ perceptions of care received by patients with a DNACPR order | Anonymous questionnaire: one for physicians and one for nurses | One hospital | 50 doctors in general medicine; 25 ward nurses from general medicine; 10 ward nurses from care of the elderly wards; five did not identify which area they worked in |
| Fritz et al. 201340 | Medium | UK: England (2010–11) | To develop a new version of the DNACPR order; to assess its impact on patient care; and to compare its use against the DNACPR form used before the intervention (UFTO) | Face-to-face semistructured interviews; direct observation; field notes; medical records; case studies Modified early warning score on admission and Charlson comorbidity scores; The Institute for Health Care Improvement Global Trigger Tool A mixed-methods before-and-after study with contemporaneous case controls |
480-bed acute hospital on two wards | n = 47 consultants, nurses, junior doctors; 247 patients (for DNACPR) records; 26 (for palliative or optimal supportive care within 72 hours of admission); 168 case–control studies |
| Giles and Moule 200470 | High | UK: England (not given) | Nurses’ attitudes, experiences and factors contributing to DNACPR decision-making | Questionnaire | One hospital; 11 ward areas including critical care, general medical and surgical ward | 78 registered nurses |
| Grudzen et al. 201076 | Low | USA: Los Angeles (not given) | Following introduction of a new policy – to determine the rate of change in foregoing resuscitation attempts by paramedics | Described as observational but is a records study – quasi experimental before-and-after study | Pre hospital | 1656 patients who experienced a cardiac arrest: 897 before and 759 after the policy change |
| Grudzen et al. 200990 | Low | USA: Los Angeles (2006–8) | Following introduction of a new policy – paramedics and EMT perspectives and decision-making afterwards | Focus groups, survey, field notes (in first session) | Geographically diverse group of large (more than four fire stations in their catchment area) and small EMS agencies (with four or fewer fire stations) | 36 paramedics or EMT |
| Hildén et al. 200463 | Low | Finland (not given) | To compare nurses’ experiences and views with doctors’ views on end-of-life discussions | Postal questionnaire | At random from the registers of the Finnish Nurses Association and the Finnish Union of Practical Nurses | 51% (no numbers given) so approximately 408 |
| Holland et al. 201377 | Low | UK: England (not given) | To determine current clinical practice for patient involvement in resuscitation decisions; and to explore perceived barriers | Questionnaire: specifically designed, not validated | Two hospitals; GPs at University of East Anglia-affiliated teaching practices | Hospital clinicians: nine male and three female GPs: seven male and six female |
| Hurst et al. 201375 | Low | Switzerland (2004–5) | Physicians’ justification for DNACPR orders; decisions regarding patient inclusion; and how they initiated discussions | Face-to-face questionnaire with physicians on an ad hoc basis; patient records | Six wards of the General Internal Medicine Department of the Geneva University Hospitals | No numbers of physicians are given (those who were in their offices at data collection times to a maximum of 61 resident physicians); 106/1446 patient cases after screening for CPR/DNAR orders in the study period |
| Imhof et al. 201189 | High | Switzerland (not given) | To describe the involvement of physicians and nurses in DNACPR/CPR decision-making; analyse decision patterns; and understand practical implications | ‘Grounded theory’ interviews | Acute care settings of seven different hospitals | 92 comprising 52 nurses and 40 doctors |
| Janssen van Doorn et al. 200882 | Low | Belgium (3-month period) | To examine the process, consequences and impact of writing DNACPR orders, particularly withholding renal replacement therapy | Prospective review of all DNR orders | The Department of Intensive Care | 43 patients |
| Jepson 200367 | Low | UK: Wales (not given) | To examine the roles of hospital and practice nurses in DNACPR decision-making | Described as an audit but included a questionnaire and semistructured interview designed for hospital and community nurses | Hospital and community nursing | 45 practice nurses working in the ‘same area’; 49 acute hospital nurses |
| Kim et al. 200781 | Medium | Republic of Korea (2001–5) | To examine current practices relating to DNACPR orders for terminal patients with cancer | Retrospective medical chart review | Four major teaching hospitals in urban areas of Korea | 387 patients |
| McAdam et al. 200573 | Low | UK: England (1989–2003) | To ascertain any change in nurses’ attitudes towards DNACPR orders between 1989 and 2003 | Questionnaire | Two hospitals of a district general hospital complex in 1989:acute medical wards or in A&E (not ICU), and the same hospital trust in 2003: acute general medicine (no mention of ICU or A&E) | 1989: 81 nurses practising in acute medical wards or in A&E (not ICU) 2003: 110 nurses practising in acute general medicine in the same trust |
| Martinez-Selles et al. 201079 | Low | Spain (2007–9) | To evaluate the use of DNACPR orders and palliative care in cardiac patients | Retrospective data collection from registry of deaths | Cardiology department of a tertiary hospital | 113 medical records |
| Meilink et al. 200616 | Medium | The Netherlands (2005) | To improve documentation of DNACPR orders in medical records by introducing a patient information sheet | Retrospective chart review | Isala Clinics, a tertiary hospital | 119/1281 records with a DNAR order on the admission form (9.3%) 83 of these orders were positive resuscitation orders and 36 were DNAR decisions |
| Mendes et al. 200986 | Low | Portugal (2002–6) | To identify factors associated with DNACPR orders in patients who suffer cardiac arrest | Retrospective data collection from recorded MET calls | Hospital | 277 in hospital deaths from cardiac arrest with MET intervention |
| Messinger-Rapport 200580 | Low | USA (not given) | To determine prevalence and predictors of DNACPR orders in nursing home | Cross-sectional chart review study | 899-bed academic long-term care facility | 177 patient records but the code status could not be ascertained from 15 of the records and so these were excluded |
| Micallef et al. 201192 | High | Australia (2009–10) | To assess level of agreement on DNACPR/CPR orders between intensive care doctors, specialist physicians and surgeons; barriers to documenting decisions during MET calls | 11 month prospective single-centre observational study | 650-bed tertiary referral university teaching hospital | 129 patients referred to the MET between 1 July 2009 and 30 May 2010; patients who had in-hospital cardiac arrests |
| Myint et al. 200693 | High | UK: England (2003) | Experience, practice and opinions of SpRs in geriatric medicine regarding DNACPR decisions | Cross-sectional postal questionnaire | Multiple settings trainee members of the British Geriatrics Society | 235 specialist registrars |
| Myint et al. 201078 | High | UK: England (2003) | To examine the personal experiences of SpRs in geriatric medicine and DNACPR decision-making | Postal questionnaire survey | Multiple settings trainee members of the British Geriatrics Society | 198 responses included |
| Naess 200995 | High | Norway (not given) | Attitudes and experiences of nurses in intensive coronary care units | Cross-sectional questionnaire: web based | Intensive coronary care units in five hospitals (one for each health-care region) | 176 nurses completed the questionnaire |
| Nordby and Nohr 201291 | Medium | Norway (2009) | How paramedics experience difficult ethical dilemmas regarding DNACPR/CPR of cancer patients | Semistructured interviews | National ambulance services | 15 paramedics |
| Park et al. 2011100 | Low | South Korea (2008) | To determine the perceptions and attitudes of nurses towards DNACPR; changes in their nursing activities after the order is decided | Questionnaire | Six university general hospitals | 252/300 ICU nurses after exclusions |
| Piers et al. 201138 | Medium | Belgium (2007–8) | Introduction of a new DNACPR form: with emphasis on motivation of the decision and description of participants in the decision-making process | Audit pre and post intervention; questionnaires sent to doctors and nurses | 1062-bed tertiary hospital in Ghent | 330 patient deaths, 228 included, 115 pre-intervention, 113 post-intervention |
| Saevareid and Balandin 201114 | Medium | Norway (2009–10) | Nurses’ perspectives about DNACPR/CPR in the oldest old | Semistructured, in-depth interviews | Three hospitals: acute geriatric, cardiology, surgical rheumatology, lung and infection wards, ICU and an anaesthetic department | Nine female nurses and one male nurse agreed to participate |
| Schiebel et al. 201341 | High | USA: Minnesota (2006–9) | Introduction of armbands to indicate resuscitation status | (1) Electronic audit; (2) observation; and (3) pre- and post-intervention audits | Academic, tertiary care hospital with 2059 beds | Phase 1:First 50/210 charts with DNACPR orders Phase 2: 5775 orders for 4288 patients of which 1162 were DNACPR orders Phase 4: 316 active DNACPR orders pre intervention and 199 post intervention |
| Siddiqui and Holley 201174 | Low | USA: Illinois (2008) | To analyse internal medicine resident physicians’ training and comfort in discussing DNACPR and pronouncing death | Online survey | 18 internal medical residency programmes | 176 (22%) residents in training |
| Smith et al. 2005101 | Low | UK: England (2003) | To determine the level of knowledge about the hospital’s DNACPR policy among a range of staff | Cross-sectional questionnaire by e-mail and internal mail | UK district general hospital | 677: nurses, health-care support workers (n = 396); doctors (n = 37); administrative and support staff (n = 244) |
| Sulmasy et al. 200639 | Medium | USA: New York (2002–4) | DNACPR consent form transformed into an order form with witness verbal consent. To assess house officers’ attitudes and confidence obtaining informed consent; if process improved; decrease in surrogate stress levels | Intervention and control hospitals: mixed-methods before-and-after study: questionnaire; chart review Validated instrument |
Two hospitals | House officer: n = 277 Physician and nursing attitudes: not reported; patient charts n = 429 (intervention hospital n = 269; comparison hospital n = 160) Surrogate stress: n = 120 |
| Yang et al. 201271 | Medium | Singapore (2011) | To determine the views of oncology and palliative care doctors and nurses on DNACPR orders | Questionnaire survey | A tertiary specialist cancer centre and an inpatient oncology ward located within the same campus | 37 doctors and 109 nurses |
| Zhukovsky et al. 2009102 | High | USA (2002–3) | A descriptive study to inform revisions of the current inpatient DNACPR form | Survey by mail | The National Cancer Institute-designated cancer centres | 60% of institutions participated: 30 DNACPR forms |
Appendix 4 Vignettes used in focus groups
Do-not-attempt-cardiopulmonary resuscitation vignettes for acute care groups
Vignette 1
Following a domiciliary visit by the GP, an 88-year-old gentleman was admitted to a medical assessment unit because of shortness of breath. The patient had a long past medical history including life-long smoking, diabetes, ischaemic heart disease, previous coronary artery surgery, heart failure and chronic kidney disease. The patient lived alone and was unable to care for himself independently. A social care package was in place, with carers visiting 3 times a day. The patient had a grade 2 pressure ulcer on his sacrum.
On admission to hospital the patient was assessed promptly by a FY2 (Foundation Year 2) doctor who made a differential diagnosis of heart failure or chest infection and started treatment with antibiotics and increased diuretics. At the time the patient was distressed and unable to speak, oxygen saturations were 84% on high flow oxygen, respiratory rate was 32 breaths per minute, blood pressure was 85/45 mmHg, pulse rate was 140 beats per minute (atrial fibrillation) and arterial blood gasses showed a compensated metabolic acidosis.
Six hours after admission to the medical assessment unit the patient had a cardiac arrest. CPR started promptly. After 10 minutes of CPR there was a return of circulation and spontaneous respiratory effort. However, the patient remained obtunded and unresponsive. He sustained two fractured ribs as a consequence of chest compressions. After discussion with the consultant in charge it was decided that further investigation or escalation of care was not appropriate. The patient survived for a further 36 hours but never regained consciousness.
Vignette 2
An 88-year-old lady was admitted to hospital from a nursing home with abdominal pain and vomiting. Past medical history included diabetes, atrial fibrillation, ischaemic heart disease and dementia. The patient was very dependent on help with activities of daily living. On assessment the patient was noted to be very frail. Blood pressure was unrecordable and the patient was unrouseable. Biochemistry revealed severe renal impairment (urea 32 mmol/l, creatinine 507 µmol/l), a profound metabolic acidosis (pH 7.05) and raised lactate (12 mmol/l). The nursing home contacted the patient’s son who was present and had lasting power of attorney to make welfare decisions for his mother.
The patient was reviewed jointly by specialist trainee doctors year 2 from medicine and surgery who decided that at that time the patient was not stable enough to have CT (computed tomography) of the abdomen but that ischaemic bowel was the most likely diagnosis. The plan was to commence fluid resuscitation and reassess. It was noted that the outcome was likely to be poor but no decision about CPR status was documented.
The patient had a cardiac arrest 4 hours later and underwent 10 minutes of CPR. This was unsuccessful.
Vignette 3
Mary was 43 years old and admitted to a medical assessment unit after suffering an acute, severe asthma attack. On admission to hospital she was extremely breathless, unable to complete sentences in one breath, wheezing and cyanosed. Her vital sign were recorded as peak expiratory flow rate of 33–50%, respiratory rate of ≥ 25 breaths/minute, heart rate of 110 beats/minute and SpO2 (peripheral capillary oxygen saturation) of 94%.
Mary had a long history of drug dependency and was frequently abusive and aggressive to the nursing staff during repeated hospital admissions for episodes of self-harm, drug overdoses and acute asthma. Three years ago while under the influence of a recreational hallucinogenic substance Mary walked into the path of an oncoming bus and sustained serious leg injuries which caused permanent disability and restricted mobility. This incident acted as a catalyst for both Mary and her family to review her lifestyle. At the time of admission to hospital she was enrolled on a drug rehabilitation programme and was complying with her planned regime of treatment.
Following an initial assessment by the medical staff, Mary was prescribed nebulised ipratropium bromide 0.5 mg, oral prednisolone 40 mg and supplementary oxygen. After a satisfactory response to medication Mary was accompanied to the X-ray department by a health-care assistant. Mary’s condition deteriorated while in the X-ray department where she suffered a respiratory arrest.
Before the emergency call was made it was noted that Mary had a tattoo across her chest clearly stating ‘do not resuscitate’. Mary had been known to make comments in the past about not wanting to live and the staff decided to clarify the situation with the medical assessment unit before commencing CPR. They were instructed to immediately commence CPR and summon the emergency team. Mary was successfully resuscitated and transferred to ICU where she made a full recovery and was eventually discharged home.
Vignette 4
A 65-year-old gentleman was admitted to hospital with severe chest pain. The patient was known to have a thoraco-abdominal aortic aneurysm and surgical or radiological intervention had previously been ruled out following multidisciplinary team assessment. The patient had chronic lung disease and home oxygen therapy had been prescribed. The patient was hypotensive and appeared pale. Fluids, oxygen and analgesia were prescribed while basic investigations were started. The impression was that this was a leaking aneurysm. Little analgesia was given due to concerns over respiratory depression and the patient continued to complain of severe pain.
Four hours after admission to the surgical assessment unit the patient had a cardiac arrest. CPR was commenced and continued for 20 minutes until the on-call surgical consultant arrived. CPR was stopped after assessment of the situation at that time and death confirmed.
Vignette 5
Mr Smith is a 65-year-old man with severe ischaemic cardiomyopathy. His mobility is very restricted due to breathlessness and cyanosis. Mr Smith has his bed downstairs and uses a commode at the bedside.
Mr Smith lives with his wife and has a son who lives nearby. Their daughter lives further away and is due to be married in 3 months’ time. Both siblings visit their parents regularly. A social care package is in place to assist Mr Smith with activities of daily living.
Following a home visit from the GP Mr Smith is admitted to hospital due to worsening breathlessness. He is admitted to a ward and cared for by the cardiology team who ware familiar with the patient’s history and treatment. Over the next 6 days in hospital changes are made to drug treatment to try to optimise cardiovascular function. However, Mr Smith remains very breathless and repeat echocardiography shows global severe impairment of left ventricular systolic function (estimated ejection fraction of 10%).
The consultant discusses progress with Mr Smith and his family, explaining that there are limited options for further treatment but that active therapy would continue in the hope that things may improve. Mr Smith tells the consultant that he has every faith in him and knows that he will do the best he possibly can to help him. The consultant does not discuss CPR status with the patient but an entry is made in the medical notes stating ‘in the event of a cardiac arrest CPR will not be effective and should not be performed’.
One day later the patient has a cardiac arrest and CPR is initiated and continued for 15 minutes. It is not successful and the patient is certified dead.
Vignette 6
A 66-year-old gentleman was admitted to hospital with an infective exacerbation of chronic lung disease. This was the fourth admission within the previous 12 months. At home, the patient was housebound and unable to walk more than 10–15 metres due to breathlessness. He lived alone and had a daughter who lived in Australia. A social care package was in place with carers visiting twice daily and neighbours providing additional support.
The admission process and initial treatment were excellent and confirmed at consultant review which occurred within 12 hours of admission to hospital. At this review, after discussion with the patient, it was agreed that care would not be escalated to tracheal intubation and ventilation should the patient fail to respond to treatment. CPR status was not discussed or documented.
The patient had a cardiac arrest 48 hours after hospital admission and underwent a 25-minute period of unsuccessful CPR.
Vignette 7
Lucinda is an 86-year-old lady who has metastatic colonic carcinoma. The patient is on an end-of-life care pathway and understands that she is nearing the end of life. All therapeutic options have been explored. The patient lives with her daughter who has lasting power of attorney for welfare decisions. Carers visit twice a day. Pain was well controlled with regular doses of oral morphine, anti-emetics and sedatives. However, over the last week the pain has increased in severity and Lucinda has required morphine more frequently. She remains lucid but is sometimes drowsy during the day.
Following a visit from the GP Lucinda is admitted to hospital with ascites. Paracentesis is performed to ease the symptoms of pain and breathlessness.
Forty-eight hours after hospital admission Lucinda has a PEA (pulseless electrical activity) cardiac arrest. The cardiac arrest team is summoned and CPR starts promptly. After 10 minutes of CPR there is a return of circulation and spontaneous respiratory effort. However, Lucinda remains obtunded and unresponsive. After discussion with the consultant in charge it is decided that further investigation or escalation of care is not appropriate. The patient survives for a further 36 hours but does not regain consciousness.
Vignette 8
Linda is a 67-year-old lady with advanced inoperable pancreatic carcinoma. She is a widow who lives with her 26-year-old son who has Down syndrome. Her daughter lives nearby and is aware of Linda’s diagnosis but is not always on hand if needed.
A biliary stent was inserted 2 months ago to provide symptomatic relief from bile duct obstruction and jaundice. Linda’s condition has remained reasonably stable until 3 days ago when she became more jaundiced and began to complain of pain and nausea. Following a home visit by the GP Linda was admitted to hospital with suspected sepsis. Ultrasound examination showed biliary tree dilatation. Chest X-ray showed consolidation at the right lung base. All treatment options were discussed with Linda who declined further invasive procedures or escalation of care. Linda understood the severity of the situation but was content to be treated with antibiotics, fluids, oxygen and analgesia. Resuscitation status was discussed with Linda by her consultant and it was agreed that CPR would not be initiated and this is documented in the notes.
The following day Linda’s condition deteriorated further and she became increasingly drowsy with periods of confusion. Her daughter was contacted and arrived at the hospital with her brother. They were informed by the registrar of the DNACPR decision which made them very angry and they demanded that this decision is overruled.
Two days later Linda had a cardiac arrest and CPR was initiated. After 10 minutes of resuscitation spontaneous return of circulation was obtained. Linda was intubated, had poor respiratory effort and remained obtunded. She was transferred to the ICU. No consultants were involved in this process. Her daughter was several miles away at this time and was urgently summoned.
Vignette 9
Mrs B is 70 years old and has moderately severe dementia. She lives with her daughter who is her main carer. Mrs B recognises her daughter but has difficulty in remembering other members of the extended family. She eats if reminded to do so and enjoys being driven around the local area but is reluctant to walk further than the garden gate. She watches television and particularly likes game shows although she probably does not understand them. She has been physically fit all her life and the only medication she is taking is Arisept for her dementia. Mrs B has been admitted for investigation of ‘blackouts’ with a provisional diagnosis of intermittent arrhythmia. During the admission process the registrar raises with Mrs B’s daughter the question of CPR in the event of Mrs B having a cardiac arrest while on the ward. She explains that CPR will have a low chance of success and the even if successful she would require intensive care. Her daughter is very clear that her mother should be resuscitated if this should happen. She accuses the registrar of disregarding her mother because she has dementia.
Vignette 10
Doris Jones is an 88-year-old lady who is admitted to hospital from a nursing home with a suspected fractured neck of femur following a fall. Mrs Jones is very dependent on help with activities of daily living and her mobility is limited due to breathlessness. Past medical history includes diabetes, atrial fibrillation, ischaemic heart disease and dementia.
On assessment in the emergency department Mrs Jones is noted to be very frail, breathless and cyanosed. Following administration of analgesia radiological examination reveals a displaced intracapsular hip fracture together with an enlarged heart. The nursing home contacted the patient’s son who is present and has lasting power of attorney to make welfare decisions for his mother.
Over the next 48 hours Mrs Jones is reviewed by a geriatrician and an anaesthetist with a view to arranging either internal fixation or hemiarthroplasty. Changes are made to drug treatment to try to optimise cardiovascular function. However, Mrs Jones remains very breathless and an echocardiography shows global severe impairment of left ventricular systolic function (estimated ejection fraction of 10%).
The consultant discusses progress with Mrs Jones’ son, explaining that the outcome of surgery is likely to be poor. However, the son requests that every attempt should be made to improve his mother’s quality of life. Surgery was performed later that day under spinal anaesthesia. Post-operative recovery was initially uneventful but during the night Mrs Jones’ became increasingly breathless and confused. Her oxygen saturations were 89%, blood pressure 210/110 mmHg, a pulse rate of 124 per minute (thready and irregular). Following review by the on-call registrar intravenous diuretics and supplementary oxygen was administered to relieve the dyspnoea.
Mrs Jones had a cardiac arrest 4 hours later and underwent 10 minutes of CPR. This was unsuccessful.
Do-not-attempt-cardiopulmonary resuscitation vignettes for general practitioner groups
Vignette 1
Mr D is a 65-year-old gentleman with a history of COPD first diagnosed 10 years ago. He is on maximum therapy and home oxygen. He lives with his wife and has two children who live nearby. Three months ago he was diagnosed with an abdominal aortic aneurysm and following multidisciplinary team assessment surgical and radiological intervention was ruled out because of the high risk of mortality due to his poor respiratory function.
You are Mr D’s GP. You have received a letter from the MDT (multidisciplinary team) stating the outcome of their discussion and discharging Mr D from follow-up. There is a home visit request from Mrs D because Mr D has an increased cough and she thinks he may have a chest infection. When you visit you find that apart from a slight cough his respiratory function is much the same as usual. After you have examined him Mr D asks what the letter from the hospital said.
Questions
-
In explaining what the MDT has said and its implications would you discuss what might happen if his aneurysm began to leak?
-
Would you raise the question of DNACPR in the event of something like this happening to him in the future?
-
If yes how would you go about it?
-
What might stop you discussing this with Mr D? What might make it difficult?
-
If you did discuss it with him and he agreed to DNACPR who would you inform?
-
If Mr D did not have an aortic aneurysm would you discuss DNACPR with him?
Vignette 2
Mrs B is 80 years old and has moderately severe dementia. She lives with her daughter who is her main carer. Mrs B recognises her daughter but has difficulty in remembering other members of the extended family. She eats if reminded to do so and enjoys being driven around the local area but is reluctant to walk further than the garden gate. She shows little interest in any activities and needs help with personal hygiene. Her daughter books an appointment to see you to talk about her mother and asks whether she should have ‘one of those do not resuscitate orders’. She says she wants her mother to be able to go peacefully but is afraid that if she calls the out-of-hours service if her mother becomes ill they will ignore her wishes because ‘they have to do everything don’t they?’
Questions
-
How do you respond to Mrs B’s daughter? (Note questions re: advance refusal of treatment/lasting power of attorney/best interests/assessment of patient.)
-
If you agree with the daughter that a DNACPR order should be completed how do you allay her fears that it will be ignored?
-
Is there anything else that you would discuss with her daughter? (Other treatments that might not be appropriate? Planning for terminal care?)
Vignette 3
Mr W is 70 years old and has moderately severe dementia. He lives in a nursing home which has a dementia care wing and has been there for 6 months. Mr W needs care with personal hygiene and help with feeding. He has settled well into the home and wanders around the lounge and garden talking to the other residents and staff, although his speech is difficult to understand. In the past 6 weeks he has had two chest infections which have responded to oral antibiotics but since the last episode the staff have noticed that he seems frailer. The manager of the home has suggested to you that a DNACPR order would be a good idea. At a visit to review his medication you see that his daughter, who visits him every day, is present. You raise the question of DNACPR and she responds very angrily, accusing you and the home of discriminating against her father because of his age and disability. She wants him to receive all treatment if he becomes ill including admission to hospital and CPR if necessary. Her brother calls you later that day to support his sister’s view.
Questions
-
How do you respond to Mr W’s daughter? (Exploring reasons/explaining DNACPR/who has the responsibility for making the decision?)
-
What do you say to the nursing home manager?
-
If Mr W’s daughter had a lasting power of attorney would this make a difference to your response to her?
-
If Mr W’s son was a barrister or journalist would that alter your response?
Ethical principles and issues raised by each vignette
| Vignette | Respect autonomy | Capacity | Voluntary decision/coercion | Balance of benefits and harms | Benefit/harm from patient perspective | Benefit/harm from clinical perspective | Benefit/harm from carer/family perspective | Is family sought to help with decision | Lasting power of attorney surrogate decision-maker | Respect for family | Prompting review with patient when patient is able to communicate |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ||||
| 2 | ✗ | ✗ | ✗ | ✗ | ✗ | ||||||
| 3 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | |||||
| 4 | ✗ | ✗ | ✗ | ||||||||
| 5 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | |
| 6 | ✗ | ✗ | ✗ | ✗ | ✗ | ||||||
| 7 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ||||
| 8 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ||||
| 9 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | |||
| 10 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ||
| GP1 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | |
| GP2 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ||
| GP3 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ |
Appendix 5 Focus group schedule
Introduction to focus group
Welcome.
Facilitator to introduce self.
Introduce project
You will have received information about the project, but just to remind you the project involves undertaking focus groups – like this one – to explore DNACPR decisions. We are undertaking focus groups with health professionals in hospitals and the community across the West Midlands and London. We will write up the findings as a report to inform future policy and practice.
Introduce focus group process
-
Give vignettes to discuss.
-
Finish by [TIME].
Introductions of group
Name.
Professional role.
Length of time in current role.
Who in the focus group they currently work with (team/ward/clinic).
Show part 1 of a vignette
Is this situation similar to a situation you have experienced?
If everyone says yes – continue to next question.
If anyone says no, talk through with them at what point in the patient pathway they might encounter this type of patient.
Tell me about where DNACPR decisions fit in this situation?
Prompts:
Tell me more
Why?
I am interested to hear from you ‘name’.
Thank you, that was a helpful contribution ‘name’, I would now like to hear from others.
Show part 2 of vignette
Tell me about the steps that could have been taken to avoid this situation.
Prompts:
-
What about outside/inside the acute hospital situation?
-
Tell me why it does not happen.
-
Prompt for when a participant has gone off topic: ‘Thank you – please clarify that relates to DNACPR decisions’.
Use further vignettes.
Finish on time.
Coding scheme for the process of making do-not-attempt-cardiopulmonary-resuscitation decisions
Examples of using or potentially using the DNACPR process, where it is problematic or non-problematic. The examples are of a particular situation or type of situation experienced by the participant.
-
Making the DNACPR decision:
How this is done at any one time/place/patient (there is not a lot about this but what there is seems important such as ‘surprise’ question).
-
Difficulties/barriers and enablers to making a DNACPR decision:
For example: no seniors available, policy that everyone follows.
-
Treatment/treatment decisions:
How these relate to or are influenced by DNACPR decisions. Examples include change in the care provided; not for admission to ICU therefore should be for DNACPR.
-
Staff training:
Issues and processes.
-
Transferability of DNACPR decisions.
-
Across organisational boundaries, e.g. between hospital and GP, between ward and operating department, etc.
-
Across time, e.g. does a DNACPR decision from last year still apply?
-
Across illness states.
-
Across patient contexts.
-
What the health professional (participant) wants to know/needs to know/does know/does not know/cannot find out at the time of making a decision about CPR or not.
Personal knowledgeKnowledge about DNACPR guidelines and processes as expressed by participants about themselves; specifically where health professionals are expressing concern about DNACPR such as the inclusion of patient/family in the decision, changing circumstances and changing DNACPR decisions.
Patient and carer knowledgePublic/family carer knowledge as perceived by the health professionals in the focus groups.
Family influence on cardiopulmonary resuscitation decisionParticipant’s perception of family influence/action/non action at the time of the DNACPR decision that has affected/not affected the health professional’s decision about CPR. Accounts of interactions between families/carers and health professionals as perceived by the health professionals in the focus groups.
Ethical issuesEthical issues explicitly identified/discussed by participant(s) in relation to DNACPR policy, process, guidelines, experience or potential experience.
ValuesInstances where a participant explicitly expresses a value in relation to DNACPR policy, process, guidelines or DNACPR/CPR experience or potential experience.
Appendix 6 Ethical analysis themes and definitions
Duty of care
Includes acting in a patient’s best interests and protecting patients from harm, either harm from CPR or harm from having the conversation.
Patients’ rights
Includes reference to patients’/families’ expectations of care or participants’ views on whether or not patients have a right to demand treatment.
Patient-centred care
Includes references to holistic care, seeing the patient as a person, treating the whole patient and seeing CPR as just one aspect of the treatment of the patient.
Respect for patient autonomy
Includes reference to what the patient wants and the need to explore the beliefs and values of the patient.
Equity of care
Includes concerns about variability in care and the impact of personal values on clinical decisions.
Role of the family
Includes references to the interests, views, wishes of the family and how much weight they are given or should be given.
Professional integrity and responsibility
Includes taking responsibility for making resuscitation decisions, fear of censure and working within organisational constraints.
Societal values/responsibilities
Includes the influence of societal values on DNACPR decision-making, and the obligations and responsibilities of society and policy-makers.
List of abbreviations
- AND
- allow natural death
- BMA
- British Medical Association
- CINAHL
- Cumulative Index to Nursing and Allied Health Literature
- COPD
- chronic obstructive pulmonary disease
- CPR
- cardiopulmonary resuscitation
- DNACPR
- do not attempt cardiopulmonary resuscitation
- DNAR
- do not attempt resuscitation
- FOI
- freedom of information
- GMC
- General Medical Council
- GP
- general practitioner
- ICU
- intensive care unit
- ITU
- intensive therapy unit
- MET
- medical emergency team
- NCEPOD
- National Confidential Enquiry into Patient Outcome and Death
- NRLS
- National Reporting and Learning System
- PRISMA
- Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- RCN
- Royal College of Nursing
- RC(UK)
- Resuscitation Council (UK)
- UFTO
- Universal Form of Treatment Options