Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 12/135/02. The contractual start date was in April 2013. The final report began editorial review in October 2014 and was accepted for publication in February 2015. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2016. This work was produced by Winpenny et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction
Background
It is important to make the most cost-effective use of NHS resources; inappropriate overuse of resources wastes money and may expose patients to harm, while inappropriate underuse of resources deprives patients of treatments from which they could benefit. General practitioners (GPs) generate cost in three main ways: by prescribing drugs, by referring patients to outpatients (which may generate elective admissions) and by admitting patients to hospital as emergencies. In this report we address the second of these: outpatient referral. There is known to be wide and unexplained variation in the referral rates of individual GPs. 1 There is inappropriate overuse and inappropriate underuse of specialist resources, and specialist services may be organised in ways which are neither cost-effective nor convenient for patients. As a consequence, there have been many attempts to improve the effectiveness and efficiency of the outpatient referral process, which we summarised in a previous review for the National Institute for Health Research (NIHR) Service Delivery and Organisation programme. 2
In recent years, the requirement to improve efficiency has been stronger than ever. Through the QIPP (Quality, Innovation, Productivity and Prevention) challenge, the NHS was expected to make £20B worth of efficiency savings by 2015. However, research from the Nuffield Trust suggests that, even were this challenge to be achieved, a potential shortfall of £28–34B would remain by 2021–2. 3
One initiative intended to encourage more efficient use of resources was the transfer of commissioning responsibility to Clinical Commissioning Groups (CCGs), introduced through the 2012 Health and Social Care Act. 4 As CCGs take over responsibility for commissioning, they need to balance their responsibility to their patients with a responsibility to manage NHS budgets.
This report sets out findings from a scoping review of the literature to update what we know about interventions designed to improve the effectiveness and efficiency of the outpatient referral system. We also provide substudies on a range of more recent innovations taking place in England, which are not yet adequately covered in the published literature. Finally, we include data on international experiences in this area, which may provide lessons for the UK.
Aims and objectives
-
Identify and review what is currently known about strategies involving primary care that are designed to improve the effectiveness and efficiency of outpatient services.
-
Comment on the impact of such schemes on the organisation of primary care, the primary care workforce, access, clinical outcomes for patients and patient experience.
-
Identify and comment on the potential for innovative models of care to be replicated more widely.
-
Identify the needs for future research in this area in terms of both primary research and systematic reviews that might be needed.
-
Summarise the findings in a way that will be readily accessible to policy-makers and managers.
Structure of the report
The main part of the report relates to a scoping review of the literature in which we identify what is currently known about strategies involving primary care that are designed to improve the effectiveness and efficiency of outpatient services.
This is followed by reports of five smaller substudies, in which we investigate referral management centres (RMCs), in-house review of referrals, financial incentives to reduce referrals, consultants with novel types of employment contracts and international experience of improving care at the primary–secondary interface.
Chapter 2 Scoping review (main study)
Introduction
This scoping review aims to update the review undertaken by Roland et al. in 2006. 2,5 That review found that transferring services from secondary to primary care and strategies intended to change the referral behaviour of primary care practitioners were often effective in improving outpatient effectiveness and efficiency. However, relocating specialists to primary care and developing joint working arrangements between primary and secondary clinicians were largely ineffective. Strategies not involving primary care that had the potential to improve outpatient effectiveness and efficiency included the introduction of intermediate care services and the redesign of hospital outpatient services.
As outpatient services have been the focus of considerable attention in the intervening years, the NIHR Health Services and Delivery Research (HSDR) programme commissioned an update of this review.
Aims
The aims of this current scoping review were to:
-
identify and review what is currently known about strategies involving primary care that are designed to improve the effectiveness and efficiency of outpatient services
-
comment on the impact of such schemes on the organisation of primary care, the primary care workforce, access, clinical outcomes for patients, patient experience and cost.
Methods
Scoping review
The definition of a scoping review is a review which ‘aims to map rapidly the key concepts underpinning a research area and the main sources and types of evidence available’,6 with the basic approach following that of a systematic review: defining the research question, identifying relevant references and screening references for eligibility for inclusion. 7
Defining the scope of the review
Our previous review conceptualised interventions designed to reduce hospital outpatient attendance in four categories:
-
transfer – the substitution of services delivered by hospital clinicians for services delivered by primary care clinicians
-
relocation – shifting the venue of specialist care from outpatient clinics to primary care without changing the people who deliver the service
-
liaison – joint working between specialists and primary care practitioners to provide care to individual patients
-
professional behaviour change – interventions intended to change the referral behaviour of primary care practitioners, including referral guidelines, audit and feedback, professional education and financial incentives.
The previous review included two additional categories that did not directly involve primary care but reflected important changes at the primary–secondary interface. These were:
-
Intermediate care services including community mental health teams (CMHTs) and hospital at home. We did not include intermediate care in the current review, mainly because research on hospital at home is not primarily focused on outpatient attendance. We did, however, include the previous category of community-based mental health teams, but described these in the more appropriate category of ‘Relocation of secondary care to primary care settings – the provider remains a specialist’.
-
Hospital redesign of outpatient services (e.g. the substitution of nurses for doctors in outpatient clinics). We did not include interventions in this review if they solely involved the reorganisation of services within hospital, but we did include studies if they involved some new interface with primary care. These were then included in one of the categories above.
We used these categories in the current scoping review, but also introduced the following three changes from the previous review:
-
Owing to recent advances in the area, we included a new topic of telecare – in particular, remote sensing technology in patients’ homes. We define telecare as ‘offering remote care, often using sensing devices, of old and physically less able people, enabling them to remain living in their own homes’. We did not include admissions as an outcome of telecare interventions in our analysis, keeping to the study’s focus on outpatient attendance. This fits within the broader definition of telemedicine as ‘the use of medical information exchanged from one site to another via electronic communications to improve a patient’s clinical health status’. 8 However, we restricted the definition of telemedicine for the purpose of this review to interventions involving some form of direct contact between specialists (doctors or nurses) and patients. We added telecare and telemedicine under the category of relocation.
-
We included a specific topic for RMCs within the category of professional behaviour change; these are a new approach to demand management for outpatient referrals.
-
We included a new topic of patient education, which involves the use of decision aids and aids to patient choice within a new category of patient behaviour change. This aspect of the review was restricted to decisions about referral to and discharge from outpatients (e.g. not the use of a decision aid used in a specialist clinic to help a patient decide whether or not to have an operation).
The framework for this current scoping review is shown in Table 1.
| Model | Type of working arrangement |
|---|---|
| Transfer: substitution of primary care for secondary care | Surgical clinics (e.g. minor surgery) |
| Medical clinics (e.g. diabetes, asthma) | |
| GPwSIs | |
| Discharge from outpatient to primary care | |
| Direct access to diagnostic tests/investigations | |
| Direct access to services | |
| Relocation: relocation of secondary care to primary care settings – the provider remains a specialist | Shifted outpatient clinic |
| Specialist attachment to primary care teams | |
| CMHTs | |
| Telemedicine (‘the use of telecommunication and information technologies in order to provide clinical health care at a distance’) | |
| Telecare (‘offering remote care, often using sensing devices of old and physically less able people, enabling them to remain living in their own homes’) | |
| Liaison: joint management of patients by primary and secondary care clinicians | Shared care including consultation liaison |
| Professional behaviour change: interventions intended to reduce rates of referral from primary to secondary care | Guidelines, including referral pro formas |
| Audit and feedback | |
| Professional education including academic detailing | |
| In-house review (i.e. second opinion) | |
| Financial incentives | |
| Advice requests – including e-mail advice, sending patient details for ‘paper consultation’, and telephone advice | |
| Patient behaviour change | Decision aids and aids to patient choice designed to influence decisions about referral to and discharge from specialist clinics |
Search strategy
We reran the previous search strategy, adding search terms for the new categories. The literature was searched from February 2005 to April 2014, starting with the end date for each of the previous searches.
The databases searched in the current review were:
-
MEDLINE® (via Ovid) (February 2005 to April 2014)
-
EMBASE (via Ovid) (February 2005 to April 2014)
-
Health Management and Information Consortium Health Management and Policy database (via Ovid) (February 2005 to April 2014)
-
The King’s Fund database of grey literature (http://kingsfund.koha-ptfs.eu/) (February 2005 to April 2014).
The previous review included a search in the Cochrane Database of Systematic Reviews and a search in the Campbell Collaboration Library of Systematic Reviews. We did not replicate those searches in this update, as we found that references from those databases were picked up in the other searches.
The detailed search strategies can be found in Appendix 1.
We became aware that many primary care trusts (PCTs) have produced guidelines to reducing referrals, often drawing on common sources such as the NHS Institute and The King’s Fund. These were not included in the review as, on investigation, we discovered that they reiterated advice on managing referrals without any evaluative component and did not, therefore, meet our inclusion criteria (see the following section).
Inclusion and exclusion criteria
Type of study
Any type of observational study was eligible for inclusion in the scoping review. Editorials and modelling studies were also included. Conference abstracts, letters, commentaries, vignette studies, hypothetical cases and articles which were simply referral guidelines were, however, excluded. Only studies conducted in high-income countries were included.
Interventions
To be eligible for inclusion, studies had to evaluate schemes in primary care settings that were designed to improve the effectiveness and efficiency of outpatient services. The categories of interventions that were eligible are described in Table 1. The interventions could also involve direct access of GPs to physiotherapy, osteopathy and alternative medicine (under direct access of primary care providers to specialist services), as long as there was an evaluation of referral to outpatients.
Eligible studies had to report on an intervention that was potentially transferable to the NHS. For example, we excluded studies of interventions led by hospitalists, which are implemented in the USA but have little applicability to the NHS context. 9
Interventions that were excluded included:
-
pharmacist interventions in primary care which did not have outpatient referral as an outcome
-
services where an outpatient clinic (usually in a hospital) is developed as an alternative to hospital admission
-
studies which simply looked at the quality or appropriateness of referrals, that is studies that did not suggest or evaluate a new model
-
hospital-at-home interventions, as these are designed as an alternative to inpatient management rather than to outpatient referral
-
optometry services in primary care
-
support services in the home
-
medical homes (as this is mainly a US concept and does not relate to outpatient referral in the NHS)
-
services which delivered screening or delivered preventative care in GP practices in order to reduce illness later in life, unless they had an evaluative component relating to outpatient services.
Comparators
The studies did not need to include a comparator intervention. If more than one type of intervention was included, these were described.
Outcomes
The interventions had to have some impact on specialist/secondary care, and had to report an evaluation of the outpatient interface rather than provide a simple description of a service. For the purposes of this review, CMHTs were also considered as secondary/specialist care. Outcomes of interest included, but were not limited to, access, including waiting times, referral rates, patient outcomes (clinical and patient experience), service outcomes, physician outcomes and costs.
Outcomes excluded from the scoping review were:
-
self-referral
-
inpatient admission
-
dental and orthodontic referrals
-
studies that evaluated solely accident and emergency or emergency room attendance.
Quality
We did not formally assess the quality of the studies, nor did we exclude studies based on quality criteria. When we had concerns about the quality of a study (e.g. when the study design or the definition of the intervention were not clearly reported), this was noted in the relevant findings section or in the table of included studies (see Appendix 2).
Study selection
Records identified by the searches were assessed for inclusion by scanning titles and abstracts against the inclusion and exclusion criteria. Screening was undertaken by three researchers. Initially, the researchers independently screened the same 500 records and compared their results. This was repeated with a further set of 250 records to ensure consistency in deciding both which studies to include and which categories to place them in. All of the remaining titles and abstracts were then screened by one researcher (EW or CM), who deliberately kept in any records for which there was any doubt. This list was then assessed by a second researcher (MR) to determine the final list of papers for inclusion. Full texts were then retrieved of potentially eligible studies and reassessed against the inclusion and exclusion criteria. Disagreements or uncertainties between reviewers were resolved by discussion within the research team.
Data extraction
Data from studies identified as eligible were extracted into a Microsoft Excel® spreadsheet template (Microsoft Corporation, Redmond, WA, USA). Data were extracted on study design and objective(s), intervention(s) and reported outcomes. The data extraction template was piloted on a small number of studies and refined. Data extraction was undertaken by three researchers, with some duplicate extraction to check for consistency of approach.
Data synthesis
As the purpose of a scoping review is to demonstrate what is presented in the literature and to identify gaps in the literature without a formal synthesis, we did not attempt formally to synthesise the data. Within each category, key messages were extracted initially by MR, and then checked against the references by other members of the research team. We also commented on the implications of the findings for the NHS in each section.
Advisory board and patient and public involvement
We convened an advisory board with representatives from primary care, secondary care and national and local commissioning, and two patient and public representatives. The advisory board commented on the research protocol at the beginning of the study and on a draft report of findings in March 2014. In addition to comments by e-mail, patient and public representatives attended a meeting in March 2014, to help to think through the implications of the study and to provide ideas for dissemination.
Findings
This chapter presents the findings of the scoping review. The data are presented by the type of working arrangement for each of the five models presented above.
Description of studies
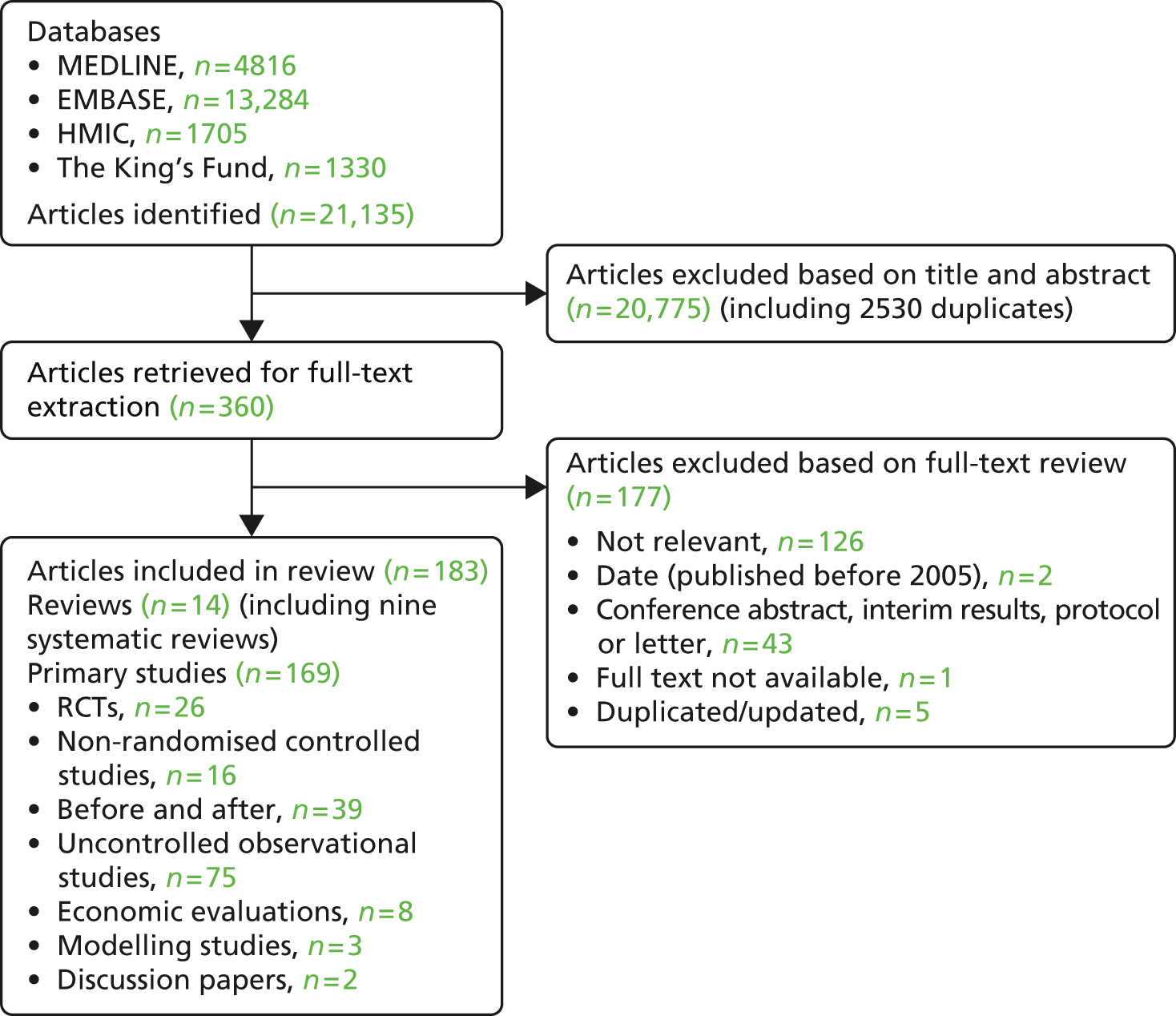
Our search identified a total of 21,135 records across the four databases searched; of these, after removal of duplicates and initial screening of titles and abstracts, we considered 360 references for further evaluation. Of these, 184 studies were identified as eligible for inclusion in the review (Figure 1). Further details of individual studies are presented in Appendix 2. Appendix 3 provides an overview of studies which we excluded from our review based on full-text review.
FIGURE 1.
Peer-reviewed literature included in the study. HMIC, Health Management Information Consortium; RCT, randomised controlled trial.
Transfer (substitution of primary for secondary care)
Surgical clinics
Surgical clinics refer to GPs carrying out minor surgery in primary care.
Key summary points:
-
Minor surgery carried out in general practice can be safe and effective, but this depends, critically, on the skill and training of the operator.
-
The cost-effectiveness of minor surgery carried out in general practice is likely to depend on local payment/contractual arrangements.
Minor surgery principally became of interest because the 1990 GP contract included financial incentives for GPs to carry out minor surgery in their own practices.
Nine studies (10 papers) were included in our previous review, from which we concluded that ‘some evidence suggests that the quality of care provided in general practice was initially poor due to inadequacies in GP training, problems in maintaining surgical skills given the low patient volume, and inadequacies in the equipment and/or procedures used to sterilise surgical implements’. We also suggested that ‘many of the additional patients receiving minor surgery under the conditions of the 1990 contract may not have previously been referred to hospital, and that GPs may have used minor surgery in place of cheaper, equally effective treatments’.
Since then, the policy context has changed in that the financial incentives for GPs to carry out minor surgery have reduced. However, some general practitioners with a special interest (GPwSIs) are contracted specifically to carry out minor surgery.
An additional six papers were found in our updated scoping search (Table 2). 10–15
| Article | Country | Study type | Aim/intervention |
|---|---|---|---|
| Dhumale (2004)10 | UK (England) | Prospective observational study | To assess the feasibility of performing hernia surgery in a general practice (n = 4965), involving a GPwSI in surgery, a theatre nurse and a surgical administrator |
| Dhumale et al. (2010)11 | UK (England) | Retrospective case review | To reduce waiting times and relieve pressure on local hospital waiting lists by setting up a surgical centre which offers hernia repair (n = 1164) carried out by two GPwSIs in a practice |
| George et al. (2008)12 | UK (England) | Prospective randomised controlled equivalence trial | To compare competence of GPs and hospital doctors across a range of elective minor surgical procedures, in terms of the safety, quality and cost of care for patients (n = 568) |
| Nelson et al. (2014)13 | USA | Economic modelling | To measure the cost-effectiveness of training rural primary care providers to perform knee injections in community-based outpatient clinics instead of referring patients to specialised care in hospital |
| Olah et al. (2005)14 | UK (England) | Observational study | To test whether or not endometrial thermal ablation is suitable for use in primary care settings (n = 87 women) |
| Van Dijk et al. (2011)15 | The Netherlands | Audit | To examine the association between surgical interventions in general practices (n = 48) and hospital referrals for four skin conditions (n = 14,203 patients) |
One study was a randomised controlled trial (RCT) which concluded that patient satisfaction was high, access to care was improved and costs were lower when procedures were carried out in primary care (the mean cost for hospital-based minor surgery was £1222 and for primary care was £449). However, the quality of minor surgery carried out in general practice was not as high as the quality of that carried out in hospital. 12 This related in particular to the incomplete excision of skin cancers. Using completeness of excision of malignancy as an outcome, hospital minor surgery was more cost-effective than surgery in primary care. However, another study of highly trained GPs (GPwSIs) found no difference in the incomplete excision rate between GPwSIs and hospital doctors. 16
Studies in the past have suggested that, with adequate training, GPs may safely perform procedures such as hernia repairs11 and endometrial thermal ablation14 in primary care.
There is little additional information on the cost-effectiveness of minor surgery in general practice. Van Dijk et al. 15 found that Dutch practices which carried our minor surgery referred fewer patients with those conditions to hospital, but did not carry out a formal cost-effectiveness analysis. In practices in rural USA, Nelson et al. 13 found that it was cost-effective to train primary care doctors to carry out knee injections for patients with osteoarthritis.
Conclusion
Minor surgery carried out in general practice can be safe and effective, but this depends, critically, on the skill and training of the operator, with some studies suggesting that the technical quality of surgery may be lower when operations are carried out by GPs. The cost-effectiveness of minor surgery carried out in general practice is likely to depend on local payment/contractual arrangements. The effect on outpatient utilisation of doing surgery in general practice is also likely to depend on local care pathways. If GPs have incentives to carry out minor surgery, for example through local contracts, there is the potential for ‘supply-induced demand’: that is, minor procedures being carried out that would not necessarily have been referred before. In some cases, these may address previously unmet patient need, but item-of-service fees to GPs to carry out procedures could also lead to unnecessary operations being carried out.
We note that recent National Institute for Health and Care Excellence (NICE) guidance is that ‘all GPs and GPs with a Special Interest who diagnose, manage and excise low-risk basal cell carcinomas (skin cancers) in the community are fully accredited to do so, and undergo continuous professional development in the diagnosis and management of skin lesions to maintain their accreditation’. 17 NICE also advises that all patients with suspected malignant melanoma should be referred to a specialist.
Medical clinics
Medical clinics refer to the provision of continued treatment and management of specific conditions within a general practice setting.
Key summary points:
-
With adequate supervision and training, a wide range of conditions can be managed in primary care both safely and effectively.
-
Few studies examine the cost-effectiveness of transferring care into primary care.
In our previous scoping review, we concluded that ‘there was a marked dearth of research comparing general practice care with hospital care’ for major chronic diseases. However, we concluded that ‘If care is well structured – there is a disease register and recall system, with clinical reviews conducted in accordance with evidence-based guidelines – then short-term health outcomes for patients appear to be as good as those achieved in hospital outpatient clinics’. However, there was insufficient evidence to draw conclusions about costs of primary versus secondary care of chronic conditions.
The policy context of the earlier review was the 2004 GP contract which included major financial incentives for GPs to monitor chronic conditions in general practice [the Quality and Outcomes Framework (QOF)]. These changes have become firmly embedded in the structure and practice of primary care since then.
An additional 16 papers were identified in our updated scoping search (Table 3). 18–33
| Article | Country | Study type | Aim/intervention |
|---|---|---|---|
| Berger et al. (2007)18 | Norway | Economic modelling | To examine the expected outcomes and costs associated with the treatment of patients with painful neuropathies (n = approximately 35,000), and the consequences of shifting care from secondary to primary care |
| van Boeijen et al. (2005)19 | The Netherlands | RCT | To compare the effectiveness and feasibility of three different types of care for patients (n = 154) with diagnosis of panic disorder or generalised anxiety disorders across 46 practices |
| Briggs et al. (2008)20 | UK (England) | Observational study | To measure the impact of a combined nurse-/pharmacist-led clinic in primary care for patients (n = 120) with chronic pain |
| Chew et al. (2010)21 | Australia | Cost-effectiveness analysis (simulation) | To evaluate the cost-effectiveness of a general practice-based programme for managing coronary heart disease patients |
| Coetzee (2011)22 | UK (England) | Observational pilot study | To evaluate a structured clinic supported by a GP in a primary care setting for patients with mild to moderate alcohol dependency (n = 76 treatment episodes) |
| Courtenay et al. (2006)23 | Multiple | Literature review | To identify the impact and effectiveness of nurse-led care in dermatology |
| Dusheiko et al. (2011)24 | UK (England) | Observational study | To examine if the better management of 10 chronic diseases (asthma, CHD, CKD, COPD, dementia, diabetes, hypertension, hypothyroidism, mental health and stroke) is associated with reduced hospital costs in England |
| Johnson et al. (2006)25 | UK (England) | Observational study | To assess a new model of integrated diabetes care in a primary care setting (n = 4 practices) |
| Kuethe et al. (2011)26 | The Netherlands | RCT | To compare outcomes of provision of asthma care by a GP, paediatric pulmonologist or a hospital-based specialist asthma nurse for children (n = 107) with moderate asthma |
| Mahmalji et al. (2010)27 | UK (England) | Observational study | To assess the knowledge, capability and interest of GPs (n = 75) in urology provision |
| Martin et al. (2011)28 | UK (England) | Observational study | To assess the impact on hospital costs and mortality of the QOF to UK general practice in 2004 (population: 50 million) |
| Maruthachalam et al. (2006)29 | UK (England) | Prospective observational study | To assess the impact of a nurse-led flexible sigmoidoscopy clinic established in a GP practice for patients (n = 1000) with colorectal cancer |
| Newman et al. (2005)30 | USA | Retrospective case review | To assess the competency and safety of outpatient colonoscopy by family physicians (n = 2) in an outpatient office setting (n = 731 colonoscopy procedures) |
| Tuomisto et al. (2010)31 | Finland | Retrospective before-and-after study | To report on outcomes after a national asthma programme was launched, establishing a new division of labour between primary and secondary care with asthma co-ordinators (one physician and at least one nurse) nominated at each health-care centre (n = 198 patients) |
| van Dijk et al. (2010)32 | The Netherlands | Observational study | To evaluate referral rates for hospital treatment of patients (n = 6101) with diabetes after the introduction of primary care nurses |
| Zwar et al. (2012)33 | Australia | Cluster RCT | To evaluate a nurse–GP partnership model (including a home visit and an individualised care plan) of care for patients (n = 451) with COPD in 44 general practices |
The additional studies we found confirm that high-quality care can be provided for patients in primary care, including for diabetes,21,25,32 adult asthma,31 childhood asthma,26 colonoscopy,29,30 alcohol dependence22 and chronic obstructive pulmonary disease (COPD). 33 Providing additional resources in primary care can also reduce secondary care utilisation, for example through the use of a nurse-/pharmacist-led clinic for patients with chronic pain. 20
In some studies, the primary care alternative to specialist referral is a different and less intensive approach to management. For example, van Boeijen et al. 19 found that two management approaches in primary care (guided self-help and structured guidelines) were as effective for patients with anxiety as referral to a psychologist for cognitive–behavioural therapy. This study emphasises that, although a common assumption is made that the same care will be provided whether in a primary or a secondary care setting, this may not in fact be the case, either by design or by default.
The support and training for primary care staff is important. For example, in the case of urological conditions, GPs did not feel that they had the skills to take on the additional roles,27 and primary care nurses in primary care did not feel confident in dealing with some of the skin conditions they were managing. 23 However, the additional studies found in this review support the earlier conclusion that a wide range of conditions can be managed effectively in primary care if adequate training and support is given to staff.
However, there are few studies of the cost-effectiveness of transferring chronic disease management from secondary to primary care. The potential for cost saving by moving services from specialist to primary care was emphasised in a modelling study by Berger et al. ,18 who found that even small increases in the number of patients with neuropathic pain managed in primary rather than secondary care in Norway could result in substantial overall cost savings. Economic analyses depend in part on whether care improves (or gets worse) as a result of transfer to primary care. Two reports of the same study, Dusheiko et al. 24 and Martin et al. ,28 suggested that, for stroke care, improvements in management since the 2004 GP contract had led to a reduction in hospital expenditure (significant for both outpatients and admissions), but they did not find evidence of this for other conditions they studied. 24,28 Several studies report lower rates of secondary care utilisation when care is moved from secondary to primary care but there is a striking absence of studies which estimate the impact of transferring care on the overall health budget (i.e. primary and secondary care combined). For example, in a study of colonoscopy in general practice,29 the cost of the procedure was lower in primary care, but the authors did not report a full economic analysis taking into account the total number of referrals for colonoscopy to hospital and primary care-based clinics combined or referrals from the primary care clinic to secondary care.
Conclusion
The long-term management of major chronic diseases has become routine in UK general practice and the evidence suggests that, with adequate supervision and training, a wide range of conditions can be managed in primary care effectively. However, there is a paucity of studies looking at the cost-effectiveness of transferring care, for example for chronic disease management, from secondary to primary care. Although there is evidence that routine management in primary care reduces the use of specialist care, cost savings will be made only if money is actually transferred from secondary to primary care.
General practitioners with a special interest
A GPwSI is a GP who supplements their core professional role by undertaking advanced procedures not normally done by a GP.
Key summary points:
-
GPwSIs were introduced principally to increase capacity to provide specialist advice.
-
GPwSIs can provide an effective addition to specialist outpatient associated with high levels of patient satisfaction.
-
Whether or not they provide a cost-effective alternative to outpatient clinics remains unclear and may depend on local service configuration and contractual arrangements.
General practitioners with a special interest were developed in the early 2000s principally to increase the capacity of the NHS to provide specialist advice and to reduce outpatient waiting times. In our previous review, we concluded that GPwSIs provided care that was of an equivalent standard to that provided in hospital outpatient clinics, although systems for monitoring quality and outcomes varied, with data on long-term follow-up of patients largely absent. GPwSIs appeared to be costlier than outpatient clinics in part because the rates of pay for GPwSIs are higher than for non-consultant doctors in outpatient clinics. However, we commented that the costs were highly likely to be context specific. It should also be noted that GPwSIs were introduced without there necessarily being an intention to reduce cost, as a main aim was to increase capacity to reduce outpatient waiting times.
We identified 10 additional studies and relevant commentaries in this updated scoping review (Table 4). 10,34–42
| Article | Country | Study type | Aim/intervention |
|---|---|---|---|
| Baker et al. (2005)34 | UK (England) | RCT | To determine whether there are differences in clinical outcomes or patient satisfaction among patients attending GPwSI-run orthopaedic clinics based in hospital outpatient departments and general practices (n = 321 patients) |
| Coast et al. (2005)35 | UK (England) | Cost-effectiveness analysis within RCT | To compare the economic cost of GPwSI service with hospital outpatient care for dermatology patients (n = 556) in 29 primary care practices |
| Dhumale (2004)10 | UK (England) | Prospective observational study | To assess the feasibility of performing hernia surgery in a general practice with local anaesthesia performed by a GPwSI in surgery, a theatre nurse and a surgical administrator (n = 4965 patients) |
| Gilbert et al. (2005)36 | UK (England) | Retrospective case review | To examine the proportion of GP referrals to a hospital respiratory medicine clinic, which might be suitable for a GPwSI respiratory clinic (n = 96 referrals) |
| Jones et al. (2006)37 | UK (England) | Discussion paper | To discuss role of GPwSIs in improving access to specialties with long waiting times |
| Levell et al. (2012)38 | UK (England) | Observational study | To assess the impact of the introduction of dermatology intermediate care services |
| Nocon et al. (2004)39 | UK (England) | Observational study | To evaluate models of diabetes care in 19 clinics with range of organisational models including clinics run by GPs in own practice, clinics run by a community diabetologist and clinics run by specialist nurses |
| Ridsdale et al. (2008)40 | UK (England) | Observational study | To evaluate the outcomes of training GPwSIs (n = 61) for a headache clinic |
| Salisbury et al. (2005)41 | UK (England) | RCT | To evaluate a GPwSI service for dermatology patients (n = 556) |
| Sibbald et al. (2008)42 | UK (England) | Observational study | To evaluate the impact on patients and local health economies of shifting specialist care from hospitals to the community in 30 demonstration sites |
Salisbury et al. 41 randomised dermatology patients to being seen either in a hospital outpatient clinic or by a GPwSI in primary care. They found no difference in clinical outcomes, but waiting times for the GPwSI were shorter and patients preferred being seen in the primary care setting. However, an economic analysis suggested that referrals randomised to the GPwSI were 76% more expensive than the hospital equivalent (£208 vs. £118). 35 In a non-randomised study of a GPwSI for headache compared with a neurology outpatient appointment, there were again no differences in clinical outcomes and patients again preferred the GPwSI setting. However, in this case the costs of the GPwSI appointment were lower than those for the hospital clinic. 40
One study randomised patients to seeing GPwSIs in either a hospital or a practice setting. 34 There were no differences in clinical outcomes, but patients again preferred being seen in primary care settings.
Overall, it is clear that appropriately trained and supported GPwSIs can provide a high-quality service that is valued by patients, and patients generally prefer to be seen in community settings. GPwSIs are now operating in a wide range of specialty areas37 and there is clearly significant potential for patients currently seen in outpatient clinics to be seen by GPwSIs; for example, Gilbert et al. 36 estimated that 23% of patients seen in a chest clinic could be seen by a GPwSI.
When interpreting the impact of GPwSIs on waiting times and costs from studies in the early 1990s, it is important to appreciate that these clinics were generally introduced as additional services designed to reduce waiting times at a time of major investment in the NHS. Now that the NHS faces reduced additional investment, GPwSI services are more likely to be intended as a substitute for hospital care. However, it does not necessarily follow that the introduction of GPwSIs will reduce demand on hospital services, although they have the potential to do so; the provision of additional services could result in ‘supply-induced demand’ if GPs’ referral thresholds change. For example, in an earlier study described in our previous review, Nocon et al. 39 reported that although outpatient attendances reduced following the introduction of GPwSIs, overall attendances rose. Indeed, we found one report in which hospital attendances increased after the introduction of GPwSIs in the community. 38 In an evaluation of practitioners with special interests among a range of ‘closer to home’ demonstration sites set up by the Department of Health in England in the mid-2000s, Sibbald et al. 42 suggested that the difference in cost per patient for commissioners may be lower for GPwSIs than hospital care national tariffs but that this might be explained by GPwSIs seeing less complex cases. They similarly cautioned that GPwSIs may increase demand for outpatient services.
It is, therefore, not clear whether or not GPwSIs provide a cost-effective alternative to outpatient clinics. In addition to the potential for ‘supply-induced demand’ referred to in the previous paragraph, there are two reasons why GPwSI clinics could be more expensive. The first is that hospital clinics are staffed by a mixture of consultants and cheaper subconsultant grades, whereas GPwSIs are paid at the equivalent of consultant grade. There are also economies of scale in hospitals which may allow consultants working in a hospital clinic to give opinions on a larger number of patients when they are supported by junior staff.
Conclusion
General practitioners with a special interest can provide an effective addition to specialist outpatient associated with high levels of patient satisfaction. Whether or not they provide a cost-effective alternative to outpatient clinics remains unclear and may depend on local service configuration and contractual arrangements.
Discharge from outpatients to primary care
Patients may be discharged early from secondary care to be followed up in primary care, instead of receiving continued follow-up in an outpatient clinic.
Key summary points:
-
GPs can follow up patients across a range of diagnostic groups as an alternative to hospital follow-up.
-
It is important to ensure than general practices have the administrative support and resources to ensure that follow-up protocols can be reliably followed, and that there is adequate support from specialists when queries or problems arise.
-
More use could be made of providing patients with information on what to expect from follow-up arrangements.
In our previous review, we found that both patient-initiated outpatient follow-up and transfer of follow-up to primary care are plausible strategies for reducing outpatient attendance rates and overall NHS costs without adverse effects on the quality of care or health outcomes. Patients in general found GP visits more convenient, less time-consuming and less expensive than outpatient attendance. However, the acceptability of alternative discharge arrangements to patients, specialists and GPs was variable and far from universal.
An additional 13 studies43–55 including one systematic review54 were identified in our updated search (Table 5).
| Article | Country | Study type | Aim/intervention |
|---|---|---|---|
| Augestad et al. (2013)43 | Norway | RCT | To reduce the number of hospital visits for respiratory patients (n = 100) through pre-clinic telephone consultation |
| Choudhury et al. (2013)44 | UK (England) | Observational study | To evaluate the impact of LES for patients with diabetes (n = 21,026) through which GPs receive training and monetary incentives |
| Grunfeld et al. (2006)45 | Canada | Multicentre RCT | To assess whether or not follow-up by the patient’s family physician is a safe and acceptable alternative to follow-up in specialist clinics for patients (n = 968) diagnosed with breast cancer in Ontario |
| Hall et al. (2011)46 | UK (Scotland) | Observational study | To explore the views of potential recipients (n = 23) and providers (n = 6) of shared follow-up of cancer and conduct a modelling exercise of shared follow-up |
| Hennessey et al. (2013)55 | UK (Northern Ireland) | Audit | To assess the impact of monitoring stable prostate cancer patients (n = 65) in primary care rather than hospital, using a computerised system to monitor PSA |
| Hewlett (2005)47 | UK (England) | RCT | To determine the impact of a direct access patient initiated review for rheumatoid arthritis vs. rheumatologist initiated review every 3–6 months for patients (n = 209) in a teaching hospital |
| Lau et al. (2010)48 | UK (England) | Retrospective case review | To audit the transfer of patients (n = 134) with successful suppression of recurrent anogenital herpes simplex virus infection to their GPs |
| Lu et al. (2012)49 | The Netherlands | Modelling (simulation) | To assess the impact of three alternatives to current guidelines for breast cancer follow-up |
| Lund et al. (2013)50 | Denmark | Audit | To assess the transfer of prostate cancer patients (n = 2585 patients, including 530 transferred to follow-up with a GP) follow-up consultations from hospital to primary care |
| Meeuwsen et al. (2012)51 | The Netherlands | Multicentre RCT | To measure the cost-effectiveness of a follow-up care delivered by memory clinic or GP for patients (n = 175) with a new diagnosis of mild to moderate dementia living in the community |
| Meran et al. (2011)52 | UK (Wales) | Observational study | To measure the risk associated with a renal patient care pathway for patients (n = 88) discharged from a renal outpatient clinic trust |
| Torregrosa-Maicas et al. (2013)53 | Spain | Observational study | To assess the impact of a quick consultation intervention for CKD patients |
| Thompson-Coon et al. (2013)54 | Multiple | Systematic review (n = 5) | To compare the effectiveness of face-to-face consultations with telephone consultations for surgery follow-up (n = 865 adults across four studies) |
Five of the 13 studies involved cancer patients. 45,46,49,50,55 In one RCT in Canada, there was no difference in outcome at follow-up (for a mean of 3.5 years) when patients (968 women with breast cancer) were seen in an oncology clinic compared with a family practice. 45 Likewise, in a trial in Norway there were no significant differences for a range of outcomes in 110 patients with colon cancer randomised to specialist or GP follow-up, which included a decision support tool for patients and GPs. However, costs were reduced in the GP follow-up arm. 43 The acceptability of follow-up in primary care was assessed by Hall et al. 46 in a qualitative interview study. They found that patients would generally be willing to have GPs share their cancer follow-up, with the caveat that the GPs had received extra training and were appropriately supported by secondary care specialists. GPs in the study stressed the importance of maintaining their own clinical skills and having reliable clinical and administrative support from secondary care. In a modelling study, Lu et al. 49 showed the considerable cost savings that could accrue from transferring follow-up of cancer patients to primary care, with no significant difference in patient outcomes. With the limited evidence on cancer follow-up from our previous review, there is clearly potential for the routine monitoring of patients who have had cancer to be carried out in primary care, provided that clear protocols and training are available to primary care physicians.
Two other studies looked at the follow-up of people, the first following a diagnosis of dementia51 and the second a limited study of patients with renal failure,52 both concluding that patients could be discharged to primary care without adverse consequences. One-third of patients with recurrent anogenital herpes48 could also be successfully be transferred to care from their GPs, although a proportion of patients did not want to be transferred as they did not want their GP to know about their diagnosis.
The systematic review54 related to telephone consultations by the specialist (surgeon or specialist nurse) as an alternative to outpatient clinic attendance following surgery. Because of the poor methodological quality of the studies included, the authors felt unable to draw any firm conclusions about the role of telephone follow-up in this situation.
The additional studies found in this scoping review, although limited in number, support the ability of GPs to follow up patients across a range of diagnostic groups as an alternative to hospital follow-up. Although many of the procedures and investigations required during follow-up may be available to GPs, general practices are not currently as well organised for ongoing follow-up of many conditions as they are, say, for the routine monitoring of diabetes or asthma. Therefore, if patients requiring ongoing follow-up are to be discharged back to primary care, it is important to ensure that general practices have the administrative support and resources to ensure that follow-up protocols can be reliably followed, and that there is adequate support from specialists when queries arise or problems occur. One option is to involve patients more closely in the decision. For example, in the studies by Augestad et al. 43 of colon cancer and Lund et al. 50 of prostate cancer, leaflets were given to the patients explaining what sort of follow-up they should expect from their GP and when to expect particular tests, etc. This information was also provided in leaflets for GPs.
Where the need for follow-up relates to patients’ symptoms, the patient may be able to assess the need for hospital follow up. For example, in a 6-year randomised trial of patients with rheumatoid arthritis47 patients were discharged and allowed to make follow-up appointments when they felt they needed one, rather than being given routine appointments. All outcomes (clinical, patient experience and economic) were in favour of patient-directed follow-up.
The availability of electronic records shared between hospitals and GPs could increase the availability of decision support when patients are no longer seen regularly in the specialist clinic. For example, Hennessey et al. introduced an electronic decision support system into their clinic which decided when prostate cancer patients needed to have their next outpatient appointment and/or prostate-specific antigen (PSA) test. 55 This was based on the computer’s assessment of a PSA test which had been carried out by their GP. Patients were not formally discharged from the clinic, but the authors reported that the number of outpatient attendances was greatly reduced.
One question which this review does not answer is how many patients are being followed up in hospital clinics who could be discharged to primary care. In a study in Birmingham, UK, GPs were given a financial incentive among other things to review the records of patients being followed up in hospital diabetic clinics and discharge those who did not meet specified referral criteria. A substantial reduction in both new and follow-up referrals was reported (odds ratios 0.69 and 0.77, respectively), although there were no data for comparators in this simple before-and-after analysis. 44
Conclusion
The studies found in this scoping review support the ability of GPs to follow up patients across a range of diagnostic groups as an alternative to hospital follow-up. If patients requiring ongoing follow-up are to be discharged back to primary care, it is important to ensure that general practices have the administrative support and resources to ensure that follow-up protocols can be reliably adhered to, and that there is adequate support from specialists when queries or problems arise. More use could be made of providing patients with information on what to expect from follow-up arrangements. It is not known what proportion of patients currently followed up in outpatients could be discharged.
Direct access to diagnostic tests and investigations
GPs may be permitted to directly order or conduct diagnostic tests, rather than having to refer patients to outpatient departments for such procedures.
Key summary points:
-
Patients value being able to have tests ordered directly by their GP, especially where tests are locally available.
-
The costs of providing services in the community compared to in hospital are uncommonly reported.
-
Especially for complex tests such as MRI and CT, increased convenience to patients may need to be balanced against the greater efficiency of tests being carried out in a centralised location.
CT, computerised tomography; MRI, magnetic resonance imaging.
In our previous study, we described studies evaluating GPs’ access to electrocardiograms (ECGs), echocardiography, ultrasound, upper gastrointestinal endoscopy, sigmoidoscopy and various types of radiology, including five studies of direct access to magnetic resonance imaging (MRI) or computerised tomography (CT). We concluded that GPs having direct access to these tests was popular with patients and that a significant proportion of investigations (varying between studies and types of investigation) were thought to save an outpatient referral. Although there were differences in the types of patients referred, the diagnostic yield was similar when comparing tests ordered by GPs and specialists. We found few data to assess whether or not direct access to investigations led to a net reduction in NHS costs (i.e. whether or not the increased costs of testing in primary care were offset by reduced costs of attendance at outpatient clinics).
Since our first review was published, GPs have gained more or less universal direct access to ECGs, echocardiography, ultrasound, upper gastrointestinal endoscopy and, in places, MRI. Sometimes access to these investigations requires a range of criteria to be met, usually contained in a referral pro forma.
In this scoping review, we identified 25 additional papers (Table 6). 56–80 These included direct access to MRI (three studies),63,64,72 CT (three studies),57,70,74 diagnosis and management of deep-vein thrombosis (DVT) (four studies),59,60,73,75 retinal photography for diabetic retinopathy (six studies),56,61,62,67–69 ultrasound (one study)79 and gynaecological ultrasound (two studies),65,78 siascopy for suspicious moles (one study),76 respiratory tests (two studies),66,80 lung cancer diagnostic (one study),58 cardiac arrhythmia monitoring (one study)71 and computer-aided cardiac auscultation (one study). 77
| Article | Country | Study type | Aim/intervention |
|---|---|---|---|
| Andonegui et al. (2012)56 | Spain | Observational study | To assess the appropriateness of diabetic retinopathy diagnosis in general practice (four trained GPs; 2750 referrals) |
| Benamore et al. (2005)57 | UK (England) | Retrospective case review | To assess the effectiveness of primary care access to CT head examinations (n = 1403) for managing common neurological conditions in primary care |
| Bjerager et al. (2006)58 | Denmark | Observational study | To investigate diagnostic delay in primary care for patients with lung cancer (n = 84) |
| Buller et al. (2009)59 | The Netherlands | Prospective management study | To evaluate the safety and efficiency of a new management strategy for patients with suspected DVT (n = 1028), which would reduce unnecessary investigations and treatments |
| Campbell et al. (2008)60 | Canada | Observational study | To help family physicians (n = 80) assess the risk of DVT, and potentially decrease the use of D-dimer tests in hospital |
| Castro et al. (2007)61 | Spain | Retrospective case review | To assess the agreement of digital fundus images between primary care physician and specialist for patients with retinopathy (n = 776 digital fundus images of 194 patients) |
| Cuadros et al. (2009)62 | USA | Observational study | To describe a telemedicine system for diabetic retinopathy screening (EyePACS) |
| DAMASK Trial Team (2008)64 | UK | Pragmatic randomised trial | To evaluate a new referral pathway for patients with continuing knee problems (n = 533 in 11 sites) |
| DAMASK Trial Team (2008)63 | UK | Cost-effectiveness within pragmatic randomised trial | To evaluate a new referral pathway for patients with continuing knee problems (n = 533 in 11 sites) |
| Jawad and Robinson (2009)65 | UK (England) | Retrospective observational study | To assess the feasibility of a gynaecological ultrasound service in the community (n = 327 women) |
| Lucas et al. (2007)66 | The Netherlands | Observational study | To assess a model of care in which GPs refer patients (n = 80) suspected for obstructive pulmonary disease to an asthma/COPD service in which lung function assistants perform spirometry and collect patient data |
| Massin et al. (2008)67 | France | Observational study | To report on a regional telemedical ophthalmology network in which fundus photographs of diabetic patients (n = 13,777) are taken by technicians in 16 screening centres, and then sent to a reference centre where ophthalmologists grade them |
| Newman et al. (2012)68 | USA | Before-and-after study | To assess the impact on screening rates of digital retinal imaging for retinopathy screening in family residency programme (n = 1106 patients) |
| Olayiwola et al. (2011)69 | USA | Observational study | To assess the impact on screening rates of telemedicine diabetic retinopathy screening for at-risk patients (n = 568) |
| Pallan et al. (2005)79 | UK (England) | Observational study | To measure the impact of an independent radiographer-led community diagnostic ultrasound service (n = 373 patients) |
| Simpson et al. (2010)70 | UK (Scotland) | Retrospective case review | To assess the outcomes of direct-access CT for patients with chronic headaches (n = 4404) |
| Skipsey et al. (2012)71 | UK (Scotland) | Prospective audit | To assess the outcomes of direct-access cardiac arrhythmia monitoring for GPs (n = 289 referrals) |
| Starren et al. (2012)80 | UK (England) | Audit | To review the service provided by the Community Respiratory Assessment Unit to primary care health professionals (n = 1156 referrals) |
| Taylor et al. (2012)72 | UK (England) | Retrospective case review | To compare a primary care imaging pathway for neurology outpatients (n = 100) with traditional outpatient referral |
| Ten Cate-Hoek et al. (2009)73 | The Netherlands | Cost-effectiveness analysis | To assess a diagnostic strategy for DVT which employed a clinical decision rule and a point-of-care D-dimer assay, compared with hospital-based strategies (n = 1002 patients) |
| Thomas et al. (2010)74 | UK (Scotland) | Prospective observational study | To evaluate whether or not primary care access to brain CT referral for chronic headache reduced referral to secondary care (n = 232 referrals) |
| van der Velde et al. (2011)75 | The Netherlands | Observational study | To compare the diagnostic performance of two clinical decision rules to rule out DVT in primary care patients (n = 1002) |
| Walter et al. (2012)76 | UK (England) | RCT | To assess the impact of adding a computerised diagnostic tool to current best practice and whether or not it resulted in more appropriate referrals for patients (n = 1297) with pigmented skin lesions |
| Watrous et al. (2008)77 | USA | Observational study | To evaluate the impact of computer-assisted auscultation on physicians’ (n = 7) accuracy of murmur detection as well as their decisions to refer asymptomatic patients with heart murmurs (n = 100 pre-recorded heart sounds) |
| Williams et al. (2007)78 | UK (England) | Audit | To assess the effectiveness of a new referral system for women (n = 277) with post-menopausal bleeding |
Imaging studies
Studies of MRI related to patients with knee pain (two studies)63,64 and headache (one study). 72
The DAMASK (Direct Access to Magnetic Resonance Imaging: Assessment for Suspect Knees) trial team63,64 reported a RCT in which patients with knee problems were randomised to early MRI and a provisional orthopaedic appointment, compared with referral to an orthopaedic specialist without prior MRI. The ‘early MRI’ group showed small but clinically insignificant (as defined by the authors) improvements in quality of life at 24 months and there was no significant difference in the number of patients eventually referred to an orthopaedic surgeon (82% intervention and 86% control). The ‘early MRI’ group were more likely to have had knee surgery during the 2-year follow-up period. Early MRI was associated with increased overall NHS costs, but the authors concluded that the small improvement in quality of life represented a worthwhile investment [£5840 per quality-adjusted life-year (QALY)].
One concern about giving GPs direct access to MRI and CT is that large numbers of patients might get investigations without really needing them, resulting in a very low rate of positive findings. In an observational study, Taylor et al. 72 evaluated MRI scanning in patients with headache, using a locally agreed care pathway for determining eligibility for direct-access MRI scans. Significant abnormalities were found in 7 out of 100 cases but there was no evaluation of the impact of the service on outpatient attendance. Benamore et al. 57 found a significant pick-up rate when GPs had direct access to CT for patients with headache who had defined clinical features. In contrast, GPs in Tayside were given open access to CT for patients with chronic headache and had a very low pick-up rate of abnormalities (1.4%). Nevertheless, these GPs reported that the CT scan had avoided a referral in 86% of cases. 74 Simpson et al. 70 reported similar results for open access to CT for patients with chronic headache: a low pick-up rate of significant abnormalities but a high rate of potentially avoided referrals. It is difficult to draw firm conclusions about the value of negative investigations from these studies, whether in terms of helping the GPs’ management, reassuring patients or avoiding referrals.
Williams et al. developed a protocol in which women with post-menopausal bleeding were referred to a gynaecologist only if their transvaginal ultrasound was abnormal. 78 The study did not consider the absolute impact of the intervention, but rather a change in the radiological criterion for normality (from 3 mm to 4 mm endometrium requiring specialist referral). The introduction of the protocol was associated with a 15.7% increase in referrals for ultrasound, and the change in protocol resulted in 27 fewer women (10%) requiring referral to a gynaecologist without any missed cancers. In a separate study, Jawad and Robinson65 showed that nearly half of women referred for pelvic ultrasound were managed entirely in the community through a community gynaecological ultrasound service, although this ultrasound service also included the removal of intrauterine contraceptive devices with ‘lost strings’ and difficult intrauterine contraceptive device fittings.
Neither of these ultrasound studies shows what proportion of women with these problems would have been referred to specialists in the absence of tests; indeed, they underline the absence of this type of evaluation in the literature. However, the study by Williams et al. shows that when a protocol is developed for the use of a test and onward referral, the details of the protocol may have a significant impact on the effectiveness (and probably cost-effectiveness) of the pathway. 78 It is also important to realise that investigations are not without unintended consequences. Not only are false positives common, especially for investigations such as spinal MRI, but false negatives are common, too; for example, Bjerager et al. 58 found that a normal chest radiograph was a common reason for delay in referring patients with lung cancer.
Other studies of access to tests and investigations
Four papers (two studies)59,60,73,75 examined the use of D-dimer as a blood test to avoid urgent referral to hospital to exclude a diagnosis of DVT, a condition which used to be managed by inpatient admission but now is increasingly managed as outpatient, and hence is included in this review. In the Netherlands, Buller et al. 59 found that 49% of patients with suspected DVT could be managed without hospital referral, with only 1.4% of those not referred developing a DVT over the following 3 months. However, seven DVTs were missed, although none was fatal. A cost-effectiveness analysis showed that the protocol had a 66% chance of being cost-effective at a threshold of €40,000 per QALY (£33,000 per QALY, slightly more than the NICE threshold of £30,000 per QALY). 73 In a parallel analysis of the same study, van der Velde et al. 75 showed that two decision rules on the D-dimer protocol resulted in a similar number of referrals being avoided (45% and 49%) – a result which, although not different in this study, shows the potential for different referral protocols to influence the performance of a test. Indeed, in a study of a similar D-dimer protocol in Canada60 there was a considerable increase in D-dimer tests in primary care without any reduction in the number of patients referred for onward investigation.
Studies of non-mydriatic retinal photography (combined with telemedicine in one study) suggest that it can be used to screen for diabetic eye disease in general practice settings. 56,61,62,67–69 However, these studies are now of relatively limited relevance to the UK, as such screening is now largely contracted to high-street opticians.
Other studies show that GPs can refer appropriately when given direct access to cardiac arrhythmia monitoring71 and respiratory tests,80 with the latter study showing that a substantial number of incorrect provisional diagnoses could be rectified with access to tests. Likewise, computer-assisted auscultation of heart murmurs appeared helpful to GPs in deciding when to refer patients with heart murmurs. 77 However, none of these studies examined what would have happened to these patients without the availability of the tests, or was able to document either improvement in management or the effect on cost (i.e. increased cost of testing vs. potential reduction in cost of referral). Indeed, novel tests are not always beneficial; Walter et al. 76 showed that a siascopic approach to assessing pigmented lesions performed no better than a validated clinical checklist, although the latter was an improvement on what, for many GPs, was routine practice.
A model to assess cost-effectiveness of direct access to tests and investigations
Direct access to tests has the following potential benefits:
-
increased convenience for patients, especially when the investigation is located in the community
-
increased speed of diagnosis/pathway to correct management, avoiding waits for outpatient clinics, especially where the same test is likely to be ordered by the specialist
-
increased diagnostic accuracy in primary care where patients would not otherwise have been referred
-
avoidance of unnecessary outpatient referral (with the potential harms associated with unnecessary investigation).
It also has the following potential disbenefits:
-
overall increase in cost (owing to additional testing)
-
additional referrals (from false-positive testing)
-
false reassurance (from false-negative testing).
The studies reviewed in this and our previous review show that virtually no studies examined all of these potential costs and benefits. They also demonstrated that crude questions (e.g. ‘Is MRI cost-effective?’) are too simplistic, as these tests are often not made available on their own, but are more often combined with a locally agreed protocol with referral criteria for the test.
Where the purpose of a test is simply to expedite one that would be ordered by the specialist, the efficiency of the GP arranging the test in advance is clear, and a proportion (maybe a substantial proportion) of referrals may be avoided. However, the availability of testing in primary care will almost certainly increase the overall number of tests carried out and the net benefit to the NHS in many cases remains unclear.
Conclusion
An overarching issue is the policy context that NHS services should be provided ‘closer to home’ in order to increase convenience for patients. In this case, at least, the results are clear: patients in many studies valued being able to have tests ordered directly by their GP, especially when tests could be conveniently arranged and/or made locally available. However, the costs of providing services in the community compared with in hospital are not commonly reported. Pallan et al. 79 found that an ultrasound service was 39% more expensive per test when provided in the community. Although this difference was not statistically significant, it serves as a reminder that, especially for complex tests such as MRI and CT, the increased convenience to patients may need to be balanced against the greater efficiency of tests being carried out in a centralised location.
Direct access to services
In some areas GPs can refer patients directly to particular services rather than referring to a consultant who would then refer the patient on to the service.
Key summary points:
-
In some cases (e.g. direct access to audiology for hearing aids) the benefits of bypassing an unnecessary specialist referral are clear-cut.
-
Direct access to some services (e.g. physical therapies for musculoskeletal problems) produces a substantial increase in demand. Although popular with patients, their cost-effectiveness as an alternative to referral (or non-referral) is less clear.
-
Rational use of services can be addressed by locally agreed pathways which need to be followed in order for services to be accessed.
In our previous review, we concluded that GPs generally refer appropriately to direct-access services, but that there was inconsistent evidence on the impact on the overall demand for services, with savings in hospital costs sometimes offset by an overall increase in demand.
An additional seven studies81–87 were identified in our updated scoping search (Table 7).
| Article | Country | Study type | Aim/intervention |
|---|---|---|---|
| Bernstein (2011)81 | UK (England) | Audit | To assess the outcomes of a ‘see and treat’ interface for musculoskeletal referrals (audit of > 30,000 referrals each year) |
| Eley and Fitzgerald (2010)82 | UK (England) | Audit | To assess the impact on referrals of a direct referral audiology clinic for patients aged over 60 years old with hearing loss (n = 353) |
| Gurden et al. (2012)83 | UK (England) | Observational study | To describe and evaluate a community-based musculoskeletal service, in terms of patient-reported outcomes and satisfaction for patients (n = 696) consulting for back or neck pain |
| Julian et al. (2007)87 | UK (England) | Prospective observational study | To compare outcomes of integrated care pathway (led by the GP) with a one-stop consultant-led menstrual clinic (n = 99) for women with menstrual disorders, compared with traditional referral (n = 94) |
| Maddison et al. (2004)84 | UK (Wales) | Before-and-after study | To assess new strategies for musculoskeletal problems, including a common pathway for all referrals, a central clinical triage of patients to the appropriate clinical service, a new back-pain pathway led by extended scope physiotherapists and three community-based multidisciplinary clinics run by specially trained GPwSIs and extended scope physiotherapists |
| Ryan et al. (2010)85 | UK (Wales) | Before-and-after study | To evaluate the provision of low-vision service in community through accredited low-vision practitioners (n = over 14,000 appointments) |
| Thomas et al. (2005)86 | UK (England) | RCT | To assess outcomes of referrals to an acupuncture service (n = 159) for patients with persistent non-specific low-back pain (n = 241) in three non-NHS acupuncture clinics, with referrals from 39 GPs working in 16 practices |
For some services, there appears to be a clear-cut benefit in streamlining a manifestly inefficient referral pathway. For example, patients for whom a hearing aid is needed can be referred directly to an audiology clinic without first being seen by an ear, nose and throat (ENT) surgeon. 82 The audiologist is able to pick up those patients requiring assessment by a specialist (in this case, 16%) and it is unlikely that many patients are prescribed hearing aids unnecessarily, making this a highly cost-effective alternative to consultant referral.
Referrals to a service may increase when direct access is provided, and then there is a question of whether or not this addresses an unmet need. For example, the provision of a direct-access low-vision aid service in Wales increased the number of low-vision aid assessments by 51% and identified what the authors described as a ‘considerable unmet burden of need’. 85 There were major reductions in waiting times, significant reductions in visual disability in patients referred and very high patient satisfaction.
Musculoskeletal services are more complex. Many areas have introduced referral pathways to reduce referrals to orthopaedic clinics. These pathways may include direct access to physiotherapy (face to face or by telephone), osteopathy, chiropractic and acupuncture. The difficulty in evaluating these services is that referrals are often for conditions which are themselves self-limiting. For example, RCTs88,89 suggest that the effect of manual therapies for back pain is generally small and shortens the duration of disability rather than curing patients who would otherwise have remained disabled (although one RCT in this review suggested a long-lasting effect of direct access to acupuncture for low-back pain86). In other reports, which indicate high patient satisfaction and improvements in symptoms following direct access to new services (e.g. Bernstein81 and Gurden et al. 83), it is hard to attribute improvements in patients’ symptoms to the new service in the absence of any comparison group.
The issue the NHS faces with musculoskeletal problems is a huge burden of morbidity and a limited specialist resource. Where the patient requires physiotherapy and the only route to this is to see an orthopaedic surgeon (which is no longer commonly the case), is it clearly more efficient to provide direct access to physiotherapy for those patients. However, the provision of direct access also increases demand; for example, a study described in our earlier review showed that when direct access to a musculoskeletal service was introduced in Wales, referrals more than doubled. 84
We found other studies recommending direct access to services but with little comparative evaluation. For example, Julian et al. 87 found that women with menstrual problems could be effectively managed by GPs using a protocol which allowed access to investigations and direct listing for surgery, with no significant differences in patient outcomes compared with a consultant-led menstrual clinic. Studies of direct access to services generally show high patient satisfaction and a decrease in waiting times. However, almost all of these services were introduced at a time of major increases in NHS funding and top-down initiatives to reduce outpatient waiting times between 2000 and 2010. The additional services were often funded in addition to existing outpatient services, with this increase in supply generating its own additional demand. It therefore remains very hard to comment in general on the cost-effectiveness of direct access to services.
Perhaps the most promising change during this period, but one which was addressed only tangentially in the studies we found, was the increasing tendency for locally agreed pathways between GPs and specialists to be used as the basis for access to services (e.g. criteria which need to be met in order for a patient with back pain to be referred directly for MRI). We note also that during this period (though maybe less widespread), specialists have been introducing similar types of criteria for outpatient referrals also. These are often articulated in electronic referral forms which require certain criteria to be met (or tests carried out) before the referral is accepted. We discuss these further in Professional behaviour change, Guidelines, including referral pro formas.
Conclusion
In some cases (e.g. direct access to audiology for hearing aids) the benefits of bypassing an unnecessary specialist referral are clear-cut. However, in other cases – musculoskeletal services being a common example – the benefits are less certain. Direct access to physical therapies for musculoskeletal problems produces a substantial increase in demand for such services and, although they are very popular with patients, their cost-effectiveness as an alternative to referral (or non-referral) is less clear. The rational use of services, including investigations, treatment services such as physiotherapy, and specialist referral, can be addressed by locally agreed pathways which need to be followed for services to be accessed.
Relocation
Shifted outpatient clinics
Shifted outpatient clinics involve hospital specialists providing care in community settings.
Key summary points:
-
Community clinics are popular with patients but may be more expensive than hospital outpatient clinics.
-
Current policies to move consultant clinics into the community can be justified only if (a) high value is given to patient convenience or (b) community clinics can run at a scale to enable the efficiencies of patient throughput in a hospital clinic to be realised.
Shifted outpatient clinics involve hospital specialists visiting premises outside the hospital site to provide care. Instead of travelling to hospital clinics, patients visit specialists in these community settings. In our previous review we found that these clinics were popular with patients. However, specialists generally see fewer patients in a community clinic (partly because they are less likely to be working alongside junior staff) and a significant proportion of patients seen in community-based clinics needed to be seen again in the hospital, and community clinics may, therefore, be more expensive than hospital outpatient clinics. A benefit expected of some clinics was that interaction between specialists and GPs would help to educate GPs, but this did not generally occur. A Cochrane review included in the previous review drew similar conclusions. 90
The four additional studies identified in this review did not, in general, add to these conclusions (Table 8). 39,42,91,92
| Article | Country | Study type | Aim/intervention |
|---|---|---|---|
| Frost et al. (2012)91 | Canada | Discussion paper | To discuss shifted outpatient models of care which aim to enhance collaboration between family physicians and specialists in Ontario |
| Nocon et al. (2004)39 | UK (England) | Observational study | To evaluate models of diabetes care in 19 clinics with a range of organisational models including clinics run by GPs in their own practice, clinics run by a community diabetologist and clinics run by specialist nurses |
| Sibbald et al. (2008)42 | UK (England) | Observational study | To evaluate the impact on patients and local health economies of shifting specialist care from hospitals to the community in 30 demonstration sites through interviews of a range of stakeholders and economic case studies |
| Wiedemer et al. (2007)92 | USA | Prospective observational study | To evaluate the impact of a structured opioid renewal programme for chronic pain run by a nurse practitioner and clinical pharmacist in a primary care setting (n = 335 patients) |
In most cases, the community-based specialist service was provided as an addition rather than an alternative to outpatient clinics: patient satisfaction was high and waiting times were reduced. However, it was not possible to determine whether or not reductions in waiting time were simply as a result of increased specialist capacity, or what effect a new locally based service had on demand. A study by Nocon et al. 39 showed that when a community-based diabetes service was introduced (some run by specialists, some run by specialist nurses and some run by GPs), referrals to hospital outpatients reduced, though overall the number of referrals rose.
Issues which are clear in relation to community-based specialist clinics are:
-
They are popular with patients and often associated with reduced travelling time.
-
They may reduce waiting times when they are part of an expansion of specialist capacity.
-
The ready availability of specialist opinion in local clinics may increase referrals, with uncertain benefits to patients.
Key issues which remain unanswered in relation to community-based consultant clinics include:
-
Whether or not community-based clinics can ever be cost-effective from the perspective of the NHS, bearing in mind the smaller number of patients generally seen in community clinics. The reduced number of patients seen in community clinics results in part because specialists are often accompanied (or even outnumbered) by junior staff in hospitals, enabling the consultant to supervise the management of a larger number of patients.
-
How community clinics can be used to improve interaction with GPs, potentially leading to the upskilling of GPs and fewer referrals in future. There is little evidence that this potential benefit of moving consultants into the community has been realised to date.
In our view, current policies to move consultant clinics into the community can be justified only if (a) high value is given to patient convenience in relation to NHS costs or (b) community clinics can run at a scale to enable the efficiencies of patient throughput in a hospital clinic to be realised.
Alternative models may, however, be used to bring specialist expertise into primary care. For example, Wiedemer et al. 92 described a nurse practitioner and a pharmacist who ran a clinic for patients with chronic pain on opiates. There was no evaluation of the impact of the scheme on specialist referral outside the practice, but management by primary care physicians improved over time (e.g. greater use of treatment agreements). We describe in the other sections models in which non-medical specialists may contribute expertise to primary care. Sibbald et al. 42 also looked at a range of relocation services, where the venue of specialist care shifted from hospital to the community and, in some cases, the consultants provided community-based outpatient clinics with GPs or other practitioners with a special interest. However, in their evaluation of these services, the impact on interaction between consultants and GPs or upskilling in community was still not clear. The impacts on waiting time and satisfaction were in line with other studies.
Conclusion
Specialists generally see fewer patients in community clinics (partly because they are less likely to be working alongside junior staff), and a significant proportion of patients seen in community-based clinics needed to be seen again in the hospital. Community clinics may, therefore, be more expensive than hospital outpatient clinics. Current policies to move consultant clinics into the community can be justified only if (a) high value is given to patient convenience in relation to NHS costs or (b) community clinics can run at a scale to enable the efficiencies of patient throughput in a hospital clinic to be realised.
Specialist attachment to primary care teams
A specialist physician is attached to a primary care team and works with that team to provide services in their particular field.
Key summary points:
-
Specialist attachment to primary care teams have a stronger educational focus than shifted outpatient clinics.
-
Few formal evaluations of this type of attachment have been reported: they appear costly and often have depended on the enthusiasm of individual specialists to undertake this type of work.
-
New types of appointment in future (e.g. community-based geriatricians) will need to be evaluated against traditional approaches to specialist employment.
Although bearing some similarities to shifted outpatient clinics, this group of studies involves active participation of both specialist and generalist in the clinic, and hence includes elements (particularly educational elements) which are absent from the shifted outpatient model. In our previous review, we included practice-based physiotherapy in the category (and concluded that primary care-based physiotherapy services were more cost-effective than hospital-based physiotherapy). We have not included physiotherapy as a ‘specialist resource’ in this review as physiotherapy has, since our first review, become an established part of the primary care environment. In our previous review, we also included CMHTs in this section. Because of the diversity of mental health team models, we now consider these separately (see the following section).
An additional two studies93,94 were identified in our updated scoping search (Table 9).
| Article | Country | Study type | Aim/intervention |
|---|---|---|---|
| Levy et al. (2009)93 | UK (England) | Observational study | To evaluate a primary care based allergy service (n = 151 patients referred to the clinic), run by a specialist allergy nurse and a GPwSI in respiratory disease and allergy |
| Moffatt et al. (2012)94 | Australia | Observational study | To assess the outcomes of the education of GPs (n = 15) by an endocrinologist conducting patient consultations jointly with the GP at the GP’s rooms |
Levy et al. 93 describe a clinic in which a GPwSI ran an allergy clinic with a specialist allergy nurse. Ninety-one per cent of patients could be managed without onward referral and, even taking into account the referring GPs’ own estimates that one-third of patients referred to the community clinic would not have been referred to a hospital clinic, the authors still estimated a significant cost saving compared with referral to a consultant clinic in the hospital.
Moffatt et al. 94 describe a different model in which an endocrinologist visits practices on a regular basis, carrying out joint consultations with selected patients and their GP, and discussing cases with the GPs after the clinic session. Moffatt describes substantial educational benefits for the GPs, including self-reported reductions in referrals. Although no formal economic evaluations have been reported, these approaches appear costly and in general have depended on the enthusiasm of individual specialists to undertake this type of work. Their potential benefits in terms of longer-term improvements in quality of primary care and reduction in specialist referrals have not, to our knowledge, been evaluated. We describe other models of specialist liaison later under CMHTs, academic detailing and professional education. The potential for this type of arrangement to develop in future is uncertain, but there is interest in developing more formal arrangements, for example through the appointment of community geriatricians. It will be important to evaluate such arrangements in future in comparison with the appointment, for example, of hospital-based specialists.
Community mental health teams
Multidisciplinary specialist mental health teams are now commonly located in community settings.
Key summary points:
-
Collaborative models of mental health care are effective across a wide spectrum of disorders.
-
CMHTs are likely to be most effective when there are regular opportunities for face-to-face contact between mental health and primary care teams and the practice team.
-
There is little evidence on the cost-effectiveness of different models of care and, especially given the diversity of local arrangements, little to guide local commissioners on the optimum configuration of services.
In our previous review we commented on a 1998 Cochrane review comparing CMHTs with standard hospital-based care for patients with severe mental illness. This review found that CMHTs had reduced mortality rates, especially for suicide, fewer patients dropped out, there were reduced hospitalisations and CMHTs appeared to lead to reduce health service costs. 95 A broader review suggested that, compared with hospital-based clinics, CMHTs led to increased user satisfaction and improved adherence to treatment. 96
The NHS landscape has changed considerably since those reviews, with a multiplicity of models of mental health teams working in the community, mostly multidisciplinary, sometimes clearly specialist in orientation (e.g. for early-episode psychosis) and sometimes including more generic staff, including a category known as ‘primary care mental health worker’. These models operate in different ways in different localities and it is, therefore, difficult to describe and evaluate such services. The difficulty is compounded by the fact that, in many areas, an outpatient ‘referral’ has been replaced by referral to the local CMHT, when the patient may be seen by a range of possible professionals depending on the presenting problem. Bower and Gilbody97 described different models of specialist–primary care interaction and concluded that:
-
Training of primary care staff was ineffective in improving outcomes unless intensive.
-
Consultation-liaison could affect the behaviour of primary care clinicians but was difficult to generalise (note that consultation-liaison in this review refers to mental health specialists entering into an ongoing educational relationship with primary care clinicians. It differs from the use of the term in secondary care, which refers to psychiatrists working at the interface with acute general medicine, e.g. in the management of suicide attempts).
-
Collaborative care (which had a number of definitions) led to small to medium-sized improvements in patient outcomes, patient satisfaction and patient compliance. These models generally involved drug treatment for patients with more severe disorders.
-
Replacement/referral, including to a range of psychological therapies, were generally effective, at least in the short term.
-
There was limited evidence on the cost-effectiveness of the models.
In the current review, we identified 10 papers,97–106 including four systematic reviews,98,99,101,102 which add to these findings (Table 10).
| Article | Country | Study type | Aim/intervention |
|---|---|---|---|
| Bower and Gilbody (2005)97 | Multiple | Meta-review (review of reviews) | To use conceptual models to bridge the gap between research findings and policy development with regard to the treatment of common mental health disorders in primary care (service structure, burden and quality improvement) |
| Cape et al. (2010)98 | Multiple | Systematic review | To assess the effectiveness of consultation-liaison services (mental health professionals advising/supporting primary care in the management of depression but not delivering care) for primary care patients with a diagnosis or symptoms of depression |
| Christensen (2008)99 | Multiple (mostly USA and UK) | Systematic review | To determine the effective components of depression care in primary care. Interventions comprised various types, including audit and feedback, education, multidisciplinary teams, etc. |
| Fickel et al. (2007)100 | USA | Literature review and interviews | To assess usual practice and potential barriers within the relationship between primary care and mental health |
| Gilbody et al. (2006)101 | Multiple | Systematic review | To review enhancement strategies aiming to improve the quality and outcome of care for depression in primary care settings |
| Harkness and Bower (2009)102 | Multiple | Systematic review | To measure the effect of on-site mental health workers delivering psychological therapy and psychosocial interventions in primary care practices |
| Kates et al. (2011)103 | Canada | Observational study | To report on the Family Health Team Mental Health Programme, a shared care model in which family physicians or nurses work with part-time specialists to provide treatment in primary care settings in Ontario |
| Kendrick et al. (2005)104 | UK (England) | RCT | To evaluate community mental health nurse care as an alternative to GP care for patients (n = 247) with a new episode of anxiety, depression or reaction to life difficulties |
| Morgan et al. (2013)105 | Australia | RCT | To evaluate a model of collaborative care with practice nurse acting as case manager to identify depression, review pathology results, lifestyle risk factors and patient goals and priorities for patients (n = 400) with depression |
| Younes et al. (2008)106 | France | Retrospective observational study | To evaluate a consultation-liaison intervention between psychiatry and primary care which provided GPs (n = 118) support for mental health patients (n = 181), without referring them to specialty care |
Christensen et al. 99 reviewed 55 controlled trials of treatments for depression. They concluded that a key predictor of successful treatment was a case manager providing direct feedback to the primary care physician, delivering psychological therapy and delivering an intervention that incorporated patient preferences. Nurse-, psychologist- and psychiatrist-delivered care were effective, but pharmacist-delivered care was not. Morgan et al. 105 confirmed that practice nurses could act as effective case managers for depression, this time in patients with comorbid diabetes or heart disease. However, Kendrick et al. 104 found that specialist mental health nurse support was no better than support from GPs for patients with ‘anxiety, depression and reactions to life difficulties’ in terms of patient outcomes, although patient satisfaction was greater in the mental health nurse group than in the GP group. A feature of this trial was that patients were enrolled with relatively minor symptoms (minimum score of 3 on the General Health Questionnaire; duration of symptoms at least 4 weeks but less than 6 months). It may be that specialist intervention is more effective for those with more severe symptoms.
Harkness and Bower102 conducted a systematic review of 42 studies on the evidence for the effectiveness of programmes in which on-site mental health workers, such as counsellors or psychiatrists, worked alongside physicians to provide therapy to patients. They found that primary care mental health works delivering psychological therapy and psychosocial interventions caused a significant reduction in consultations, prescribing and referrals to specialist care. However, they found that the changes were modest, not always consistent and did not generalise to the wider practice population. They commented that the economic significance of their work was unclear, but their results lent no support to the suggestion at the time that providing mental health care in primary care would lead to a substantial reduction in the cost of referrals.
A systematic review of 11 economic evaluations of enhanced primary treatment for depression found that these treatments, although effective, were associated with increased cost. 101 The authors estimated the benefit at between £7 and £13 per depression-free day.
A systematic review and meta-analysis of five evaluations of consultation-liaison psychiatry found no evidence of effectiveness of this intervention on antidepressant use or depression outcomes. 98 Although consultation-liaison models do have the potential to reduce referral, as in Younes et al. ,106 they are often dependent on the commitment of an individual psychiatrist, are hard to generalise and have not generally been subjected to economic analysis.
The siting of mental health workers and teams may be important in promoting collaboration, with Fickel et al. 100 commenting that collaborative care was often suboptimal, with the ‘collaboration’ occurring a most basic level. Kates et al. 103 found that the colocation of mental health workers in Canadian primary care practice improved collaboration.
We excluded a number of American papers from our review because the health-care system for mental health care is so different from that of the UK. We noted, however, the conclusion of one systematic review of US trials of integrated approaches to the management of depression involving primary care and mental health services. 107 They concluded that ‘Although most trials showed positive effects, the degree of integration was not significantly related to depression outcomes. Integrated care appears to improve depression management in primary care patients, but questions remain about its specific form and implementation’.
Conclusion
Collaborative models of mental health care are probably effective across a wide spectrum of disorders. They are enhanced by an identified case manager who can come from a range of disciplines including some found within the primary care team. CMHTs are likely to be most effective when there are regular opportunities for face-to-face contact between members of the mental health team and the practice team. In some cases this might be achieved by colocation and in others by regular meetings. Services associated with improved outcomes are likely to cost more but there is little evidence on the cost-effectiveness of different models of care and, especially given the diversity of local arrangements, little to guide local commissioners on the optimum configuration of services.
Telemedicine
Telemedicine can be used to provide health care at a distance, replacing or complementing outpatient care. It may involve video consultations or transmission of electronic images.
Key summary points:
-
In countries with very remote rural areas, video consultations will continue to be a viable alternative to patients or specialists having to travel long distances.
-
In England it is unlikely that video consultations will be a cost-effective alternative to outpatient clinics.
-
‘Store-and-forward’ services for images of skin conditions shows promise, though may be of less value in suspected skin cancer.
-
Telemedicine services are often established by local enthusiasts without any formal evaluation, and in particular without adequate economic evaluation.
There is a large literature on telemedicine, and in our previous review we included five systematic reviews and 20 studies. We concluded that few studies were designed in a way that allowed the overall impact of telemedicine interventions on health service use to be assessed. There were many anecdotal reports of outpatient visits being reduced by teleconsultations, and it seemed clear that a substantial proportion of teleconsultations do not need to be followed by a visit to the hospital for a face-to-face consultation. However, the cost-effectiveness of individual telemedicine interventions was highly context specific, and examples are available in the literature of instances in which telemedicine consultations were both substantially more expensive and substantially less expensive than conventional outpatient visits.
An additional 32 studies were identified in our updated scoping search,66,108–138 including three literature reviews108,116,136 (Table 11).
| Article | Country | Study type | Aim/intervention |
|---|---|---|---|
| Backman et al. (2010)108 | UK | Literature review | To discuss the current status of cardiac care in the community, and how telecardiology can help to support GPs in the diagnosis and management of cardiac disease |
| Borve et al. (2012)109 | Sweden | Observational feasibility study | To compare diagnosis outcomes of MMS consultation (picture) and face-to-face consultation for patients with skin lesion or condition (n = 40 patients) |
| Bowns et al. (2006)110 | UK (England) | RCT | To assess the feasibility of store-and-forward technology for dermatology patients (n = 208) |
| Borooah et al. (2013)111 | UK (Scotland) | Before-and-after study | To reduce waiting times and inefficiencies in the referral pathway for ophthalmology patients (n = 17,528) through an electronic referral unit using digital images for clinical decision-making |
| Butler and Yellowlees (2012)112 | USA | Retrospective cost analysis | To evaluate the costs of store-and-forward, or asynchronous telepsychiatry in a primary care setting (125 consultations) for patients with non-urgent psychiatric problems |
| Chong and Moreno (2012)113 | USA | RCT | To assess the feasibility and acceptability of clinic-based telepsychiatry (webcam) for low-income Hispanic patients with major depression (n = 167) |
| Colven et al. (2011)114 | South Africa | Observational study | To assess effect of a teledermatology network on diagnostics by primary care providers (n = 7) for patients in underserved areas (n = 120) |
| Crompton et al. (2010)115 | UK (Wales) | Observational study | To report on an e-mail-based teledermatology service, providing GPs with rapid access to a hospital-based consultant dermatologist (n = 40 general practices) |
| Diamond and Bloch (2010)116 | USA | Literature review | To review the evidence on telepsychiatry assessment of children and adolescents |
| Eikelboom et al. (2005)117 | Australia | Observational study | To determine the feasibility of teleotology consultations for children (n = 66) in remote communities |
| Eminovic et al. (2009)118 | The Netherlands | Multicentre cluster randomised trial | To assess the impact of teledermatologic consultations on referral for patients (n = 631) from 35 practices in two regions (n = 85 GPs) |
| Eminovic et al. (2010)119 | The Netherlands | Economic evaluation based in multicentre cluster randomised trial | To assess the impact of teledermatologic consultations on referral for patients (n = 631) from 35 practices in two regions (n = 85 GPs) |
| Ferrer-Roca et al. (2010)120 | Spain | Non-RCT | To assess the impact of a telemedicine scheme on quality of life for patients referred (n = 800) to hospital in dermatology, traumatology, psychiatry, internal medicine, pain-relief unit, X-ray department, endocrinology and rheumatology specialties |
| Hilty et al. (2006)121 | USA | Observational study | To evaluate the impact of utilisation of telepsychiatric services by individual primary care providers and clinics in rural areas in California (n = 400 patients) |
| Hsiao and Oh (2008)122 | USA | Retrospective case review | To examine the time intervals in which cancer patients (n = 169), referred conventionally or by store-and-forward teledermatology, were evaluated, diagnosed and treated |
| Knol et al. (2006)123 | The Netherlands | Observational study | To assess a store-and-forward dermatology service (n = 505 teleconsultations) |
| Lasierra et al. (2012)124 | Spain | Observational study | To assess the impact of provision of teledermatology service (n = 120 consultations), based around a web application for patients accessing dermatology |
| Lucas et al. (2007)66 | The Netherlands | Observational study | To assess a model of care where GPs refer patients (n = 80) suspected for obstructive pulmonary disease to an asthma/COPD service in which lung function assistants perform spirometry and collect patient data |
| Mahendran et al. (2005)125 | UK (England) | Observational study | To evaluate the impact of store-and-forward teledermatology, including a pro forma and a photograph, for patients (n = 163) with skin lesion |
| MacFarlane (2006)126 | Ireland | Observational study | To evaluate the feasibility and acceptability of joint teleconsultations involving specialists, GPs and their patients |
| Moreno-Ramirez et al. (2005)127 | Spain | Observational study | To assess the feasibility a teledermatology service for patients with pigmented lesions (n = 219 consultations) |
| Moreno-Ramirez et al. (2007)128 | Spain | Observational study | To evaluate a store-and-forward teledermatology service for routine triage of patients (n = 2009) with skin cancer in primary care centres (n = 12) |
| Moreno-Ramirez et al. (2009)129 | Spain | Economic evaluation | To evaluate a store-and-forward teledermatology service for routine triage of patients (n = 2009) with skin cancer in primary care centres (n = 12) |
| Morton et al. (2011)130 | UK (Scotland) | Observational study | To assess the outcomes of a store-and-forward teledermatology service (n = 188) vs. usual care (n = 289) on pathways and costs |
| Myers et al. (2010)138 | USA | Observational study | To assess the feasibility and acceptability of a telepsychiatry service (n = 701 patients) |
| Summerhayes et al. (2012)131 | UK (England) | Before-and-after study | To evaluate the impact of introducing a telemedicine system on conventional leg ulcer care in a rural general practice for patients (n = 54) with a non-healing wound |
| Tadros et al. (2009)132 | UK (Scotland) | Prospective observational study | To assess the use of a digital image referral service where GPs send digital images of skin lesions to a plastic surgery department (n = 300 patients) |
| Tan et al. (2010)133 | New Zealand | Observational study | To assess teledermoscopy as a triage tool for a hospital skin lesion clinic through the use of store-and-forward teledermatology (n = 491 lesions in 200 patients) |
| Thind et al. (2011)134 | UK (Scotland) | Audit | To assess the feasibility of a teledermatology service (n = 230 patients) |
| van der Heijden et al. (2011)135 | The Netherlands | Prospective observational study | To investigate the effect of teledermatology on the efficiency, quality and costs of care when integrated in daily practice and applied following patient (n = 37,207 teleconsultations) selection by a GP (n = 1820) |
| Wade et al. (2010)136 | Multiple | Systematic review | To assess the economic value of using real-time video communication |
| Weatherburn et al. (2009)137 | UK (England) | Audit | To present the outcomes of undertaking ECGs (n = 373) in general practice (n = 8 general practices and n = 2 walk-in centres) |
Many of the additional papers we identified had minimal evaluative components, but often showed the enthusiasm of the authors for a new development they had piloted. We have not reviewed each study in detail, because in large part they do not add greatly to the conclusions of the previous review and systematic reviews. However, we draw some conclusions from studies in the following areas.
Telecardiology involved ECGs being transmitted electronically and reported back to the GP by telephone by a cardiologist or nurse specialist. 137 With the increasing sophistication of automated analysis by the ECG machine itself, it is not clear that this is the ‘revolution’ claimed in the commentary by Backman et al. 108
With regard to teledermatology, the majority of evaluations were telemedicine for skin conditions, mainly of ‘store-and-forward’ services in which the GP sends a digital image of the skin lesion with a clinical description of the patient and the specialist responds with a diagnosis and management plan. In general, there is a reasonably high concordance between diagnoses made face to face and ones made from a good digital image, better concordance in terms of management plan and often sufficiently good concordance to be able to manage the patient with the potential to reduce referrals. 109,114,115,123,124,130,135 Telemedicine consultations may also reduce the need for outpatient attendance. 118,119
The clinical case for sending digital images for suspected skin cancer (teledermoscopy) is less clear, with two studies reporting that 49% and 70% of patients would require a face-to-face consultation110,127 and a high proportion of telemedicine diagnoses which were unclear or incorrect when compared with a face-to-face assessment. 125 A study by Tan et al. 133 reported discordance in diagnosis of 12.3% between teledermoscopy and face-to-face assessments for patients referred with possibly malignant skin lesions, with one malignant lesion missed by using teledermoscopy. Other authors reported safe and effective use of teledermatology for diagnosis of skin lesions,122,128 with the potential for significant reductions in the intervals between referral and diagnosis. 132 However, this result may not be relevant to the UK, where there is a maximum 2-week wait for outpatient appointments for suspected cancer.
Ophthalmology referrals were reduced in Scotland in a scheme which enabled optometrists to send a digital image along with a referring e-mail. Along with a redesign of the system pathway, a reduction of 37% in referrals was claimed, though it was not clear how much of this related to the pathway redesign and how much to the ability to send digital images. 111
In terms of teleotology, transmission of digital images of the eardrum along with audiometry and tympanometry enabled ENT specialists in Australia to give confident management advice. 117 This is perhaps most relevant to very rural locations, as audiometry and tympanometry are not currently widely available for children in UK primary care; they are provided in Australian primary care because of the very large distances that some patients would otherwise need to travel for the tests to be carried out.
For diabetes, Siriwardena et al. 139 identified 27 studies aimed at improving care. These mostly involved some form of behavioural therapy through videoconferencing or telephone calls. The sole outcome they reported was improvement in haemoglobin alpha 1 (HBA1), which they found improved in 12 studies (44%). However, the magnitude of change in HBA1 was not reported, and no economic evaluation was reported.
Telepsychiatry consultations have been widely reported with the aim of reducing travelling times in remote areas, but also to reduce the stigma associated with attending a psychiatric clinic, which may deter some patients from attending. Sometimes the primary care practitioner may be present at the consultation, an approach which is uncommon but may enhance the education value of the medium. Alternatively, the GP may present the patient at the start and discuss the specialist’s opinion at the end. 121 One RCT reported no differences in overall depression or in the number of days that were lost or unproductive owing to depression when telepsychiatry was compared with treatment as usual and for follow-up care. 113 A review of telepsychiatry for children and adolescents pointed to the weakness of the evidence base and could draw only the rather limited conclusion that ‘there are no data that suggest that this process contributes to negative outcomes’. 116
Live video consultations are reported in other disciplines, too, and are particularly likely to be favoured in very rural areas. 120 These studies appear to have been designed without a specific educational component, unlike the study reported by Thind et al. ,134 in which teleconsultations were established specifically to support a GPwSI in dermatology working in a remote area of Scotland.
Economic analyses are reported infrequently. A systematic review of economic analyses of real-time video communication concluded that teleconsultations, where the GP and specialist were both present, were likely to be more expensive than conventional outpatient clinics and not cost-effective for local delivery of services. 136 Our previous review included the only major UK study of ‘virtual outreach’, in which telemedicine consultations across a range of disciplines were found to be more expensive than conventional outpatient visits (£724 and £625 per patient, respectively). 140 In an economic analysis of a study in the Netherlands,118 the authors found that teledermatology became cost-effective when the patient was more than 75.1 km from a dermatologist, or when more than 37% of outpatient referrals could be prevented (which was judged to be unlikely). Likewise, van der Heijden found that 68% of dermatology referrals could be prevented by a telemedicine consultation (in which the GP was normally present) but costs were reduced by only 18%, and the authors were able to conclude only that the service could ‘probably’ be provided at lower cost. 135
Economic analysis of video consultations cannot be applied to the more common ‘store-and-forward’ approach of sending digital images to a dermatologist, which should, in principle, be cheaper. A number of authors, including Moreno-Ramirez et al. 129 and Butler and Yellowlees,112 have reported that patients can be managed more cheaply by ‘store-and-forward’ telemedicine than by conventional outpatient appointments. 112,121 However, the cost of establishing telemedicine services is not always included in published analyses. Furthermore, the logistics of setting up telemedicine services are significant and may make them difficult to maintain. 124 Sometimes the continuation of a service depends on the availability of enthusiasts. 138
One potential benefit of video consultations is the learning opportunity that they offer for the health professionals involved. However, although some studies report educational benefits (e.g. Hilty et al. 121), these are not always realised, and MacFarlane et al. 126 reported disappointing results in terms of GPs learning from the joint consultations.
The majority of applications conventionally associated with telemedicine require significant investment in fixed devices (e.g. video cameras). Quinn et al. 141 described the use of smartphones by district nurses to transmit images from the patient’s home. Although more a proof of concept that a formal evaluation, the authors suggest that smartphones have the potential to reduce clinic visits substantially. Two recent reviews of mobile phone technology in health care142,143 point to substantial opportunities for using smartphones in health care, well beyond the scope of this review.
Conclusion
Physical location is likely to be a major determinant of the use of telemedicine as an alternative to outpatient clinics. In countries with very remote rural areas, video consultations will continue to be a viable alternative to patients or specialists having to travel very long distances. In England it is unlikely in general that video consultations will be a cost-effective alternative to outpatient clinics. ‘Store-and-forward’ services for images of skin conditions, however, show promise, though they may be of less value in cases of suspected skin cancer. Too often, however, the establishment of these services appears to depend on local enthusiasts and lacks any economic evaluation.
Telecare
Telecare is remote care which uses sensing devices to allow older and physically less able people to remain living in their own homes.
Key summary points:
-
Although there are many studies of telecare, they generally focus on avoiding admissions rather than outpatient attendance. We did not find sufficient evidence to comment specifically on the impact of telecare on the use of outpatient services.
Telecare, defined as ‘offering remote care, often using sensing devices, of old and physically less able people, enabling them to remain living in their own homes’, did not form a major part of this review. As we commented in our previous review, ‘no wider conclusions can be drawn on the impact on outpatient attendance of telecare interventions, as this outcome was not generally reported’.
This remained the case because virtually all of the studies identified in our literature search focused on avoidance of hospital admission and did not report on outpatient attendance. For example, a recent major RCT of telecare in England (the ‘Whole System Demonstrator’) was focused on admission reduction, although they also reported that there was no difference in outpatient attendances between control and intervention groups. 144
We found that one study by Willems et al. 145 compared reorganisation of a hospital service to provide nurse monitoring of asthma through telecare with conventional outpatient appointments. They concluded that there was no significant difference in clinical outcome or secondary care usage between groups, although the type of professional accessed changed and there was no economic evaluation. We found no studies that specifically aimed to provide telecare as an alternative to outpatient attendance. Overall, we do not think it is appropriate to report on the impact of telecare interventions as an alternative to outpatient services, as that is not the target of the interventions, and outcomes relating to outpatients are commonly not reported.
Liaison
Shared care
Shared care is a model of working in which a hospital specialist and a primary care practitioner agree a joint management plan that specifies which elements of care for a particular patient are to be delivered by each clinician.
Key summary points:
-
Care can be given in primary care using shared care protocols across a wide range of conditions without loss of quality.
-
Compared with outpatient visits, cost savings to patients can be considerable, but savings to the health service are less clear-cut. Some studies show net savings by moving care from outpatient clinics to a shared-care model, but such savings are not universal.
-
Shared care may not improve care or reduce duplication where there is lack of agreement as to who will be doing what.
In our earlier review, we concluded that shared-care arrangements generally produced similar outcomes to conventional outpatient care but that evidence on cost-effectiveness was mixed, with some evaluations showing cost savings and others finding increased costs. We commented that successful operation of shared-care schemes depended on good communication between specialists and generalists.
Among the eight additional studies identified in this review (Table 12),98,146–152 we found one Cochrane review152 on the effectiveness of shared care in chronic disease management which identified 20 studies, including 19 RCTs. In this review Smith et al. identify five models of shared care:
-
Basic model: a specific, regular communication system is set up between specialty and primary care. This may be enhanced by an administrator who organises appointments and follows up and recalls defaulters from care.
-
Community clinics: specialists attend or run a clinic in a primary care setting with primary care personnel. Communication is informal and depends on the specialists and primary care team members meeting on site.
-
Liaison: a liaison meeting attended by specialists and the primary care team in which the ongoing management of patients within the service is discussed and planned.
-
Shared care record card: a more formal arrangement for information sharing where an agreed data set is entered onto a record card which is usually carried by the patient.
-
Computer-assisted shared care and electronic mail: a data set is agreed on and collected in both the specialty and primary care setting and is circulated between the two sectors using computer systems such as a central repository or e-mail. This system may also include centrally co-ordinated computerised registration and recall of patients.
| Article | Country | Study type | Aim/intervention |
|---|---|---|---|
| Cape et al. (2010)98 | Multiple | Systematic review | To assess the effectiveness of consultation-liaison services (mental health professionals advising/supporting primary care but not delivering care) for primary care patients with a diagnosis or symptoms of depression |
| Crowe et al. (2010)146 | UK (England) | Observational study | To explore the challenges facing GPs’ adherence to shared-care arrangements for specialist drugs |
| Davies et al. (2007)147 | UK (England) | RCT/economic evaluation | To assess the cost-effectiveness and acceptability of treating patients with rheumatoid arthritis (n = 460) in shared care. Management of patients in primary care with annual hospital review, instead of management in hospital specialist clinic |
| DeMiglio and Williams (2012)148 | Canada | Observational study | To explore the views and experiences of community-based palliative care team members and key informants regarding the barriers involved using a shared-care model to provide care in the community |
| Fleury et al. (2012)149 | Canada | Observational study | To assess the state of collaboration among GPs (n = 60), psychiatrists and psychosocial mental health-care professionals and to develop a new model of collaboration |
| Jha et al. (2007)150 | UK (England) | Observational study | To assess the outcomes of an integrated care pathway for women (n = 65) with continence problems |
| McCrone et al. (2004)151 | UK (England) | Observational study | To assess service use and costs depending on level of shared care for patients (n = 349) with severe mental illness in general practices (n = 50) |
| Smith et al. (2009)152 | Multiple | Systematic review | To evaluate the effectiveness of shared-care interventions designed to improve the management of chronic diseases (including asthma and COPD, cancer, congestive cardiac failure, depression, diabetes mellitus, hypertension, opiate misuse and chronic mental illness) across the primary–specialty care interface |
Smith et al. ’s review152 specifically excludes structured disease management programmes and specialist outreach clinics, which we also cover elsewhere. The comparator of ‘usual care’ was most frequently management delivered in primary care but in four studies the comparator was a secondary care clinic and we focus on these four studies in this review. They show no significant differences between shared care and outpatient care for clinical or psychosocial outcomes apart from recording risk factors which was better in the shared care model in two of the studies. For treatment satisfaction there were no differences, apart from one study of asthma care in which patients preferred hospital follow-up. Generally, the results support Smith et al. ’s overall conclusion from their review, which is that there were few identifiable differences between shared care and usual care. They interpret this as ‘no case for shared care’, but, in the context of the present review, ‘no difference’ between hospital follow-up and shared care with primary care is a positive result which shows the potential of the model. Costs are, therefore, key to interpretation of the findings; here, three out of the four studies in which outpatient care was the comparator show cost savings for the health service and one showed an increase in health service costs. In the three studies in which they were measured, cost savings for patients were substantial in the shared-care arms of the trials.
The majority of additional studies identified in this review provide a generally low level of evaluation, but in the main support the use of shared care in the management of long-term conditions. Only two of these present significant information on costs. The first of these presents the results of the economic evaluation of a RCT of intensive hospital outpatient management of patients with rheumatoid arthritis. 147 The mean cost per patient was slightly higher in the shared-care group, but a small gain in quality of life in that group means that the shared care intervention was likely to be cost-effective (at £2000 per QALY). In an earlier economic evaluation of the follow-up of people with serious mental illness,151 the costs of the shared-care model were critically dependent on the ‘amount’ of shared care offered, with complex patients receiving ‘medium’ or ‘high’ levels of shared care being significantly more expensive than those receiving ‘low’ levels of shared care.
We included consultation-liaison models in this review also, where there are typically joint consultations with specialist, patient and GP. All five studies identified were in mental health care, including the systematic review by Cape et al. 98 which we have already described in Community mental health teams and which found no evidence of effectiveness of the intervention on antidepressant use or depression outcomes. Given the significantly increased costs of this model, it does not present a cost-effective form of shared care, quite apart from the logistic difficulties of sustaining the model that we have commented on before.
Three qualitative studies looked at the problems which health-care teams experienced in developing shared-care models. The first related to a model of shared care in which a consultant wishes the GP to prescribe a specialist drug with which the GP may not be familiar. This type of shared-care model usually involves a protocol, for example detailing blood checks which need to be carried out. In this study, Crowe et al. 146 found that the GPs reported uncertainty and confusion surrounded the sharing of test results between primary and secondary care, which resulted in test duplication and omission. The GPs complained particularly about the lack of compliance of other staff in their practices and hospital colleagues with these arrangements (hospital specialists were not interviewed as part of the study). In a study in a very different setting, DeMiglio and Williams148 explored the problems in setting up shared-care arrangements for palliative care teams in Canada. Here, they found that working arrangements were inhibited by rules and regulations in the various organisations and by inflexibility in funding arrangements. In another Canadian study, numerous factors were found to inhibit shared care, including lack of resources, lack of time and incentives for collaboration and inappropriate GP payment models. 149
Conclusion
The results of studies of shared care suggest that care can be given in primary care using shared care protocols across a wide range of conditions without loss of quality. Cost savings and convenience to patients can be considerable, but savings to the health service are less clear-cut. There are studies which show net savings by moving from outpatient clinics to a shared-care model, but such savings are not universal and may depend on the nature of the shared-care arrangement. Shared care may not improve care or reduce duplication where it lacks clear agreement and assent between the parties as to who will be doing what, or lacks full support from the relevant organisations involved.
Professional behaviour change
The section on professional behaviour change is the one which has undergone greatest expansion since our previous review, in which the same section took up only three pages of the final report. This was in part because the field had been covered by a recent Cochrane review. We concluded that ‘referral guidelines, supplemented by structured referral sheets or local educational interventions from secondary care specialists, are the only interventions shown to reduce referral rates without compromising the quality of care. Financial incentives also change referral rates but their impact on the appropriateness of referral is unknown; unselected reductions in both necessary and unnecessary referrals may occur. Newer innovations, such as obtaining an “in-house” second opinion prior to referral, appear promising but require further investigation’.
This recent Cochrane review153 has been updated by the same authors,154 though with conclusions that remained substantially unaltered. They concluded: ‘Active local educational interventions involving secondary care specialists and structured referral sheets are the only interventions shown to impact on referral rates based on current evidence. The effects of “in-house” second opinion and other intermediate primary care based alternatives to outpatient referral appear promising’.
In this review we have expanded this section and dealt separately with eight different approaches to professional behaviour change. This is in part because of increased interest and number of publications in the area, and partly because of a number of innovative changes in practice that have taken place since our previous review was published. These include the widespread use of electronic referral pro formas, the establishment of RMCs, the incentivisation of in-house review of referrals and the ability to seek advice from specialists by e-mail.
Guidelines, including referral pro formas
Clinical guidelines for GPs are written with the aim of helping GPs with diagnosis and treatment decisions. These may include guidance on the conditions for which it is appropriate to refer patients to secondary care.
Key summary points:
-
Guidelines, audit and feedback, and professional education programmes are all relatively ineffective on their own but may be combined, or linked with other interventions.
-
Guidelines are increasingly incorporated into referral pro formas which have to be completed as part of the referral process.
-
Guidelines may increase or reduce numbers of referrals: interventions aimed at changing professional behaviour should be aimed at increasing the appropriateness of referrals rather than as a crude form of demand management.
In this review we included two additional systematic reviews154,155 and 18 additional studies,75,156–172 shown in Table 13.
| Article | Country | Study type | Aim/intervention |
|---|---|---|---|
| Akbari et al. (2008)154 | Multiple | Systematic review | To estimate the effectiveness and efficiency of interventions (including professional educational interventions, financial interventions and organisational interventions) targeting outpatient referral rates or outpatient referral appropriateness |
| Bridgman et al. (2005)156 | UK (England) | Prospective controlled study | To evaluate the effect of a new referral management model for orthopaedic patients (n = 14,006) |
| Clarke et al. (2010)155 | Multiple | Systematic review | To assess the effectiveness of guidelines for referral to elective surgical assessment |
| Elwyn et al. (2007)157 | UK (Wales) | Before-and-after study | To assess the impact of a guideline adherence intervention on referrals (n = 1730) of patients in three endoscopy units in two hospital trusts |
| Emery et al. (2007)158 | UK (England) | Cluster RCT | To evaluate a computer decision support system for the management of familial cancer risk in primary care (n = 45 general practice teams) |
| Fleuren et al. (2010)159 | The Netherlands | Observational study | To assess the impact of the introduction of a shared care guideline for back-pain referrals (n = 723 patients) |
| Garcia Garcia et al. (2011)160 | Spain | Observational study | To assess the impact of a co-ordinated pathway between nephrology care and primary care (n = 559 referrals) |
| Glaves (2005)161 | UK (England) | Before-and-after study | To determine if the use of request guidelines can achieve a reduction in the number of radiographic examinations of the cervical spine, lumbar spine and knee joints performed for GPs for patients referred (n = 7026) to three community hospitals and a district general hospital |
| Hamilton et al. (2013)162 | UK (England) | Observational study | To provide GPs (n = 614) with risk assessment tools applicable to patients aged ≥ 40 years with bowel or respiratory symptoms in 7 of 28 English cancer networks and to evaluate those tools |
| Jani et al. (2012)163 | UK (England) | Audit | To assess use of standardised referral pro forma (n = 586 referrals) in compliance to NICE guidelines and cancer diagnosis rates in a Cancer Network |
| Jiwa et al. (2006)164 | UK (England) | Cluster RCT | To measure the change in referrals (n = 716) for colorectal pathology, following practices (n = 44) being offered an electronic interactive referral pro forma and/or an educational outreach visit by a local colorectal surgeon |
| Kennedy et al. (2012)165 | UK (Scotland) | Retrospective case review | To assess the effect of referral guidelines (electronic referral system) for patients (n = 190) with suspected head and neck cancer |
| Kim-Hwang et al. (2010)166 | USA | Before-and-after study | To evaluate electronic referral system that facilitates iterative pre-visit communication between referring and specialty clinicians to improve the referral process (n = 505 questionnaires) |
| Menon and Larner (2012)167 | UK (England) | Observational study | To assess the impact of the publication of the NICE guidance, National Dementia Strategy, and Department of Health/Alzheimer’s Society resource pack for patients (n = 213) referred to a Cognitive Function Clinic |
| Meeuwissen et al. (2008)168 | The Netherlands | Before-and-after study | To assess the outcomes of a stepped-care programme for depression in primary and secondary care for patients (n = 164) with a mild, moderate or severe major depression |
| Melia et al. (2008)169 | UK (England) | Retrospective before-and-after study | To assess the Prostate Cancer Risk Management Programme launched in November 2002 that includes guidelines for GPs on PSA cut-off levels for urological referral in asymptomatic men (n = 1747 referrals) |
| Slade et al. (2008)170 | UK (England) | RCT | To assess whether or not the Threshold Assessment Grid for referral to specialist mental health services could improve agreement between primary care and CMHT on suitability of referral (n = 1061 patients) |
| Spatafora et al. (2005)171 | Italy | Prospective observational study | To assess whether or not adopting a shared protocol between urologists and GPs might change diagnostic procedures and referral patterns in the management of men (n = 1759) with lower urinary tract symptoms |
| van der Velde et al. (2011)75 | The Netherlands | Observational study | To compare the diagnostic performance of two clinical decision rules to rule out DVT in primary care patients (n = 1002) |
| West et al. (2007)172 | UK (England) | Observational study | To assess the impact of easy-to-follow written referral guidelines on GP referrals to an orthopaedic outpatient department (n = 471 letters of referral) |
In their Cochrane review, Akbari et al. 154 concluded that passive dissemination of guidelines was ineffective, but that guidelines associated with structured referral sheets were associated with improved pre-referral management of patients. A second systematic review of the effect of guidelines on referral found that, in four RCTs, guidelines improved the appropriateness of pre-referral care, and in another trial included in the same systematic review there was an improvement in the appropriateness of referrals, although there was no measurable effect on practitioner knowledge, rates of referral or costs. 155 However, in none of these five studies was the guideline development ‘passive’; in each case it was combined with another intervention such as a structured referral sheet or an investigation pathway developed locally between GPs and specialists.
The limited effect of guidelines on their own is consistent with the wider literature on quality improvement. 173 Perhaps mindful of this, the great majority of the studies we identified combined guidelines with other interventions, for example referral pro formas,163,166 outreach or liaison visits by consultants,164,168,171 feedback on referrals,157 professional education,158 a more rapid appointment with the specialist if guidelines were followed159 and returning referrals which did not meet the guidelines. 161 All of these studies showed some impact of the intervention, although in some cases the improvement was confined to better information in the referral letter. Guidelines may also improve the quality of care provided without necessarily changing patterns of referral as, for example, in the urology shared-care protocol described by Spatafora et al. 171 The limited impact of guidelines on their own is not surprising, especially bearing in mind Clarke et al. ’s conclusion from an empirical survey of GPs that referral guidelines were ‘rarely used in practice’. 155
However, there were other studies which did not report any change, for example incorporation of guidelines into a pro formas for head and neck cancer165 or for mental health problems,170 and three studies of passive dissemination of referral guidelines showed them to be ineffective. 167,169,172 Slade et al. 170 commented on a number of reasons why the pro formas in their study may have been ineffective. These included GPs feeling that the pro formas were oversimplistic, did not reflect the complexity of patients’ problems and were seen as a means of reducing referrals.
Guidelines can also be used to reject referrals. Garcia Garcia et al. 160 reported a study in Spain in which nephrologists rejected referrals which did not adhere to guidelines, sending 28.5% of referrals back with ‘an explanatory report including suggestions for patient management’. They found that the GPs included in the programme ‘showed great interest and no complaints were registered’.
Although some guidelines have been developed to reduce the number of inappropriate referrals, it should not be assumed that the aim or outcome is always a reduction in secondary care utilisation. Hamilton et al. 162 provided practices with risk assessment tools to assist GPs in selecting patients for cancer investigation and found that their use resulted in an increase in the number of chest radiographs ordered, the number of referrals and the number of cancers diagnosed.
Bearing in mind the well-established literature on the relative ineffectiveness of passive use of guidelines in changing clinical practice, guidelines should in general be regarded as part of other interventions. Indeed, they are an essential part, and it would not be realistic to conceive of many of the interventions considered in this section unless they were underpinned by clinical or organisational guidelines. The place of referral pro formas as a way of reinforcing guidelines has increased rapidly in recent years as electronic record systems have become more sophisticated. These pro formas are sometimes used as a way of requiring information from the GP before a referral request can be accepted, and this may include the results of tests that locally agreed guidelines indicate should be done before referral for a particular condition. An example might be that the result of a partner’s sperm count should be available when referring a woman with infertility. Depending on whether information in a referral pro forma is advisory or mandatory, pro formas can be used to require adherence to guidelines. An example of a guideline being used to incentivise particular professional behaviours was reported by Fleuren et al. :159 if Dutch GPs adhered to an agreed protocol for the first 6 weeks of back pain, a priority referral and MRI were guaranteed if the patient was subsequently referred. This led to a reduction in referrals judged as inappropriate against national guidelines for referral from 15% to 8%. 159
Conclusion
Guidelines, audit and feedback, and professional education programmes are all relatively ineffective on their own but may be combined, or linked with other interventions. Of these, professional education programmes probably have the greatest potential to change behaviour, although we noted that some positive studies involved very intensive interventions (e.g. biweekly visits by specialists to general practices). Guidelines are increasingly incorporated into referral pro formas which have to be completed as part of the referral process. A number of studies of professional education and of guidelines had the effect of increasing referrals. In our view all interventions aimed at changing professional behaviour should be aimed at increasing the appropriateness of referrals rather than as a form of crude demand management.
Audit and feedback
Commissioning bodies audit rates of referral and provide feedback on these referrals to GPs.
Key summary points:
-
Despite the widespread use by PCTs and CCGs of feedback to GPs on their referral data, we did not find sufficent evidence to draw conclusions about the value of such feedback.
We found few relevant papers157 on the impact of audit and feedback on referral behaviour. In our previous review, we concluded that simple feedback of rates of referral had no impact on referral practice.
In the present review, no studies of simple audit and feedback were included in the Akbari et al. Cochrane review. 154 Elwyn et al. 157 reported a study in which feedback was sent to GPs on the appropriateness of their referrals to endoscopy against NICE referral guidance (but with no referrals being denied). The intervention was associated with an increase in the appropriateness of future referrals.
Despite the limited support from research findings, feedback of rates of referral without any indication of appropriateness remains common, and probably ubiquitous, across PCTs and CCGs in England. If such feedback is to have any effect, it probably relies on GPs having the time and the inclination to review the clinical appropriateness of their referrals.
Professional education, including academic detailing
Education for primary care professionals may take a number of forms including provision of written information, single educational events and ongoing support from a specialist.
Key summary points:
-
Professional education is described in one major review as ‘potentially effective’: a reasonable summary of a literature where both studies and interventions are highly varied, ranging from intensive specialist support to single educational events.
-
There is a clear tension between education at an intensity (e.g. monthly practice visits from specialists) which could not be mounted or sustained across a range of specialist disciplines, and more modest interventions that appear less effective.
In this section we include all forms of professional education, including ‘academic detailing’, which is a term used to define a particular type of face-to-face engagement between an expert (e.g. a specialist) who may visit a practice on one or more occasions. It has most commonly been used in relation to prescribing, with the term ‘academic’ principally indicating that there is no pharmaceutical company involvement.
We identified 18 studies154,164,174–189 which assessed the effect of professional education schemes (Table 14).
| Article | Country | Study type | Aim/intervention |
|---|---|---|---|
| Akbari et al. (2008)154 | Multiple | Systematic review | To estimate the effectiveness and efficiency of interventions (including professional educational interventions, financial interventions and organisational interventions) targeting outpatient referral rates or outpatient referral appropriateness |
| Azuri et al. (2009)174 | Israel | RCT | To investigate the effect of raising awareness of erectile dysfunction diagnosis and treatment in a community setting by training physicians (n = 39) |
| Batinac et al. (2009)175 | Croatia | Prospective before-and-after study | To measure the impact of GP continuous medical education on outcomes for patients with iron deficiency anaemia (n = 1586) |
| Cameron et al. (2010)176 | USA | Observational study | To evaluate academic detailing as a strategy to increase early detection of dementia in primary care practices (104 physicians and 248 office/clinic staff) |
| Eide et al. (2013)177 | USA | Before-and-after study | To develop an interactive web-based course to improve the skills of primary care providers (n = 54) in skin cancer detection |
| Evans (2009)178 | UK (Wales) | Observational study | To assess the impact of a retrospective peer review of referral models for patients of 32 practices (n = about 7000 referrals) |
| Evans et al. (2011)179 | UK (Wales) | Observational study | To assess the impact of a retrospective peer review of referral models for patients of 32 practices (n = about 7000 referrals) |
| Grassini et al. (2008)180 | Italy | Prospective before-and-after study | To assess the impact on referrals (n = 1017) of a 1-day training course on appropriateness of indications in digestive endoscopy, followed by letter containing a summary of the lectures and a copy of selection criteria for colonoscopies |
| Jiwa et al. (2006)164 | UK (England) | Cluster RCT | To measure the change in referrals (n = 716) for colorectal pathology, following practices (n = 44) being offered an electronic interactive referral pro forma and/or an educational outreach visit by a local colorectal surgeon |
| Lester et al. (2009)181 | UK (England) | Cluster RCT | To evaluate educational intervention for GPs on first-episode psychosis for patients (n = 179) referred from general practices (n = 110) |
| Power et al. (2007)182 | UK (England) | Cluster RCT | To evaluate the impact of an onset team from secondary care providing education to GPs on discussing early signs of psychosis (46 practices, n = 150 patients) |
| Shariff et al. (2010)183 | UK (England) | Before-and-after study | To assess the impact of giving GPs a 12-page illustrated guide to common skin lesions on referrals (n = 470) |
| Suris et al. (2007)184 | Spain | Before-and-after study | To analyse the influence of a primary care rheumatology consultancy programme on referrals (n = 2793) to rheumatology unit |
| Ulrik et al. (2010)185 | Denmark | Before-and-after study | To evaluate the impact of an educational programme for GP-diagnosed COPD patients (n = 3058) |
| Vernacchio et al. (2013)186 | USA | Before-and-after study | To evaluate a quality improvement programme consisting of (a) physician education, (b) decision support tools available at the point of care, and (c) longitudinal feedback of data on physician referrals for adolescent idiopathic scoliosis (n = cohort of about 30,000 patients) |
| Westwood et al. (2006)187 | UK (England) | Observational study | To test the feasibility of providing genetic nurse counsellor clinics in primary care to develop a questionnaire, to evaluate patients’ satisfaction with their genetics appointments and to establish patient and provider costs (n = 36 practices) |
| Westwood et al. (2012)188 | UK (England) | Cluster RCT | To assess whether or not a primary care genetic-led education improves both non-cancer and cancer referral rates, and whether or not primary care-led genetic clinics improve the patient pathway (n = 73 practices) |
| Willigendael et al. (2005)189 | The Netherlands | Before-and-after study | To evaluate the effectiveness of combined education training for GPs (n = 53) and practice assistants (n = 65) for the management patients (n = 100) with peripheral artery disease |
Akbari et al. 154 included three RCTs of specialist-led educational strategies, one of which was highly intensive, involving monthly visits by orthopaedic surgeons to discuss cases in which the GPs were uncertain of diagnosis or management and were considering referral (the others were less intensive). The most intensive of the interventions was associated with a near halving in the number of orthopaedic referrals. Of the other two, both interventions were associated with higher rates of referral following the educational intervention (though the reviewers note a unit of analysis error in one of the studies which might have led to an overestimate of statistical significance). Both of these results were against the hypothesised direction of effect.
Evans et al. 178 described a scheme in north Wales in which GPs had weekly protected time to discuss the appropriateness of their referrals, with regular input from local consultants. For orthopaedics the scheme was associated with a reduction in referrals by up to 50% and an increase in use of other local services, with a better understanding of other local management options for common orthopaedic conditions. An observational study by Cameron et al. 176 in the USA evaluated academic detailing as a strategy to increase the early detection of dementia in primary care practices. In a follow-up evaluation, 55% of the doctors said that they had increased referrals to community resources, 24% said that they were already making satisfactory referrals prior to the visit and 21% said that they had not increased referrals but intended to do so.
Suris et al. 184 described an intensive biweekly programme of support by rheumatology specialists which was associated with a 31% reduction in referrals. Other studies also reported a reduction in number or an increase in the appropriateness of referrals following educational programmes. 175,177,180,182,186,188,189 However, some studies found little or no impact of education on the rates or appropriateness of referrals. 164,174,181,183 It should be noted that some of these involved a relatively modest intervention, for example a lecture or a single outreach visit, and in one case GPs were simply sent a 12-page illustrated guide to common skin lesions. 183 A study by Ulrik et al. 185 demonstrated that the focused education of GPs and their staff improved the diagnosis and management of COPD, but did not significantly alter the percentage of referrals. It is probably important to distinguish programmes whose main aim is to improve quality of care without any specific aim to reduce (or increase) referrals.
Most of the interventions described here were aimed at increasing the appropriateness of referrals or reducing the number of referrals, or both. However, we note that in two of the three trials included in the Cochrane review, referrals were increased following the educational intervention. It is important to acknowledge that better clinical management in primary care will sometimes result in an increase in specialist referral. We noted some time ago that GPs with greater knowledge in a clinical area tended to refer more patients to hospital in that area,190 and this possibility should not be ignored at a time when local pressures are likely to be exclusively focused on reducing referrals.
In their review, Akbari et al. 154 described professional education as ‘potentially effective’, and this is probably a reasonable summary of a literature in which studies and interventions are very varied, ranging from intensive specialist support to single educational events and, although we have not analysed this in detail, the more intensive or multifaceted interventions appear to be more effective. 154 There is a clear tension between education at an intensity which is unlikely to be sustained (e.g. monthly practice visits from specialists) and could not be mounted across a range of specialist disciplines, and more modest interventions that appear less effective. There is a question of whether or not the impact of an intensive intervention can be sustained over time, thus allowing rotation of specialists into an ongoing set of educational programmes. We found no evidence on the long-term sustainability of changes associated with educational interventions.
In-house review of referrals
In-house review refers to GP referrals being checked by other members of the same GP practice.
Key summary points:
-
Evidence on in-house referral schemes (which provide for systematic review of referrals by other GPs in the practice) is very limited.
-
The weak evidence that exists supports this approach in terms of reducing referrals and acceptability to patients.
In our previous review, we commented that ‘newer innovations, such as obtaining an “in-house” second opinion prior to referral, appear promising but require further investigation’. Akbari et al. 154 drew the same conclusion, but still based on only one study. 191,192 In our current review, we identified four additional studies that examine in-house review of referrals (Table 15). 178,179,193,194
| Article | Country | Study type | Aim/intervention |
|---|---|---|---|
| Cox et al. (2013)193 | UK (England) | Retrospective time-series analysis | To assess the impact of three RMCs and two internal peer-review approaches to referral management on outpatient visits (n = 376,000) |
| Evans (2009)178 | UK (Wales) | Observational study | To assess the impact of a retrospective peer-review of referral models for patients of 32 practices (n = about 7000 referrals) |
| Evans et al. (2011)179 | UK | Observational study | To assess the impact of a retrospective peer review of referrals models |
| Imison and Naylor (2010)194 | Multiple | Literature review and observational study | To examine the evidence on the current quality of GP referrals and to assess the impact of different types of referral management |
We identified four additional studies in our review. Two papers by Evans178 and Evans et al. 179 reported on an intervention in which GPs discussed the appropriateness of their referrals on a weekly basis, observing a reduction in the variability of rates of referral between doctors in the practice, and a reduction in the overall mean rate of referral. The approach also appeared to be acceptable to patients. The arrangement described by Evans et al. is not the same as either that in the previous study, in which referrals were routinely seen by another GP before the decision to refer was confirmed, or the model which has been taken up and incentivised by a number of PCTs/CCGs, in which referral letters are scrutinised by other GPs in the practice before being sent to the hospital.
In a report on referral management published by The King’s Fund in 2010,194 including a literature review and case studies, the authors concluded, based on limited evidence, that, of the referral management strategies considered, a strategy ‘built around peer review and audit, supported by consultant feedback, with clear referral criteria and evidence-based guidelines is most likely to be both cost- and clinically-effective’. However, more recently, a retrospective time-series analysis of outpatient attendances from practices which started implementing internal peer review of referrals showed no significant changes in outpatient attendance rates. 193
Because of the interest in these models and the lack of published literature, we conducted a substudy of in-house referrals as part of this project, and this is reported elsewhere in this report (see Chapter 4).
Referral management centres
Referral management centres manage the process of referral from primary to secondary care, often with an aim of reducing referral volume.
Key summary points:
-
There is very limited evidence published on the effectiveness of RMCs.
-
The evidence that exists is equivocal and suggests that reduction in referrals by RMCs is less likely to represent value for money than the use of more passive alternatives such as in-house peer review.
In-house referral schemes discussed in the previous section involve some form of scrutiny of referrals within the referring GP’s own practice. RMCs involve the scrutiny of referrals outside the practice. They have been introduced in an attempt to ensure that referrals are appropriately directed and (though not always explicitly) to produce downward pressure on GPs’ rates of referral. These organisational interventions are new and they are not mentioned either in our previous review or in the systematic review by Akbari et al. 154
In our current review, we identified six studies193–198 about RMCs (Table 16).
| Article | Country | Study type | Aim/intervention |
|---|---|---|---|
| Cox et al. (2013)193 | UK (England) | Retrospective time-series analysis | To assess the impact of three RMCs and two internal peer-review approaches to referral management on outpatient visits (n = 376,000) |
| Davies and Elwyn (2006)195 | Multiple | Literature review | Commentary on RMCs |
| Ferguson and Cook (2011)196 | UK (England) | Observational study | To investigate the sustainability of a primary care orthopaedic interface service looking at referrals |
| Fischer et al. (2010)197 | USA | Observational study | To report on an electronic referral system containing algorithms based on clinical practice guidelines (n = 23 primary care organisations) |
| Imison and Naylor (2010)194 | Multiple | Literature review and observational study | To examine evidence on the current quality of GP referrals and to assess the impact of different types of referral management |
| National Leadership and Innovation Agency for Healthcare (2007)198 | UK (Wales) | Literature review and observational study | To ensure appropriate referral of patients to relevant services through seven referral management pilot programmes |
Referral management centres were first introduced for orthopaedic problems in order to deal with the large number of referrals to orthopaedic surgeons which they felt could be better managed by other practitioners (e.g. physiotherapists). GPs did not refer to these other services either because they were unable to or because they were unaware of them, and so some RMCs were established with the extra capacity to provide additional care in the community (i.e. they did more than just triage referrals). For example, the Bath and North East Somerset Orthopaedic Interface Service retained 50% of referrals passed to their system, sending only 21% on to see an orthopaedic surgeon. 196
However, other RMCs have been established to screen all referrals, with an explicit or implicit aim of reducing hospital outpatient attendance. The aim of these services is to identify inappropriate referrals, which can be considered in terms of three broad categories:
-
referrals made to the wrong service or specialist
-
referrals containing insufficient information, making it difficult to assess urgency or relevance
-
referrals that do not conform to accepted clinical guidance.
Referrals may be ‘accepted’ by the RMC and passed on to the hospital clinic, diverted to a service judged more appropriate or returned to the GP as inappropriate. Considerable concerns have been expressed about these centres in terms of introducing delays in treatment, interfering with the GP’s clinical judgement, making inappropriate triaging decisions based on information in the letter without seeing the patient, breaching patient confidentiality and restricting patient choice. 195
Although we found studies describing concerns about these centres,194,198 we found only one published article in the academic literature of an evaluation of RMCs. This involved three centres which were set up to reduce referrals from GP practices in Norfolk. 193 The introduction of two of these had no impact on numbers of outpatient referrals, whereas the third was associated with an increase in referrals. Comparison with two schemes involving within-practice peer review of referrals indicated that RMCs were more expensive but not more effective than these schemes.
Although not strictly relevant to the UK context, one American study was also noted, in which all referrals from primary care were directed through an internet-based ‘branching logic that required a series of clinical responses regarding the patient’s diagnosis or symptoms’. This resulted in the rejection of 22% of referrals as inappropriate. 197
In addition to these peer-reviewed articles, two further reports on RMCs were identified in the grey literature. The first, a report on an evaluation of seven referral management pilots in Wales,198 reported that although there was significant variation in the quality and potential sustainability of the initiatives, which were diverse in their scope and operational details, the majority of pilots provided some ‘hard’ evidence of the impact of their referral management diversions. Pilots that were designed to tackle single issues or groups of related problems were considered to be more successful than those using an all-specialty generic model of referral management, which was not considered to be cost-effective. The second report, on a study conducted for The King’s Fund,194 examined approaches to referral management, including RMCs, more broadly. This study included a literature review, two phases of qualitative research (interviews with 21 commissioners and case studies of four schemes, including two RMCs) and quantitative analysis of outpatients attendances. The authors that concluded that RMCs were less likely to represent value for money than more passive approaches such as peer review.
Because of the interest in these models and the lack of published literature, we conducted a substudy of RMCs as part of this project, and this is described elsewhere in this report (see Chapter 3).
Financial incentives
GPs may be given financial incentives directly to reduce outpatient referrals. Other financial incentives provided to GPs may also impact on referrals indirectly.
Key summary points:
-
A number of financial incentives have been introduced through the QOF which indirectly increased the number of referrals made by GPs for specific conditions.
-
No studies were found that reported on the direct incentive introduced through the QOF to avoid inappropriate outpatient referrals.
Interest in financial incentives in relation to referrals falls into two areas:
-
direct financial incentives for GPs to reduce referrals
-
secondary effects on referrals of other financial incentives.
We do not consider here the effect of fundamental changes in remuneration systems for doctors in primary care, for example changing from fee for service to capitation.
We included six studies in our review (Table 17). 154,199–203
| Article | Country | Study type | Aim/intervention |
|---|---|---|---|
| Aghaie-Jaladerany et al. (2007)199 | UK (Scotland) | Retrospective case review | To assess the early impact of the implementation of the UK CKD guidelines on new patient attendances (n = 160) at nephrology clinics |
| Akbari et al. (2008)154 | Multiple | Systematic review | To estimate the effectiveness and efficiency of interventions (including professional educational interventions, financial interventions and organisational interventions) targeting outpatient referral rates or outpatient referral appropriateness |
| Minshall and Smith (2008)200 | UK (England) | Audit | To conduct an audit of practice records of patients (n = 610) with epilepsy in general practices (n = 13), followed by an education session led by a neurologist |
| Phillips et al. (2009)201 | UK (Wales) | Before-and-after study | To assess the impact of revised renal QOF accompanied by a rigorous process of assessing referrals and supported by an education and management pathway within a NHS trust |
| Pockney et al. (2004)202 | UK (England and Wales) | Observational study | To evaluate the introduction of fee-for-service for minor surgery procedures by GPs in six health authorities over 8 years |
| Srirangalingam et al. (2006)203 | UK (England) | Before-and-after study | To determine the impact of the new General Medical Services contract on referral patterns to a secondary care diabetes clinic (n = 647 referrals) |
The Cochrane review by Akbari et al. 154 described two studies of the impact of GP fundholding on referrals in the 1990s. In this scheme, GPs had a direct financial incentive to reduce referrals for conditions for which they had a budget (e.g. elective surgery). There appeared to be a small reduction in rates of referral in fundholding practices. In our previous review, we also suggested that financial incentives introduced for GPs to conduct minor surgery in the early 1990s led to them carrying out operations for relatively trivial conditions that would not previously have been referred to hospital or where non-operative treatments were available, a conclusion supported by a more recent study. 202
A second set of studies assessed the impact of the QOF on hospital utilisation. 199–201,203 This pay-for-performance scheme did not (initially) have any incentives related to outpatient referrals but did provide incentives for chronic disease management that could have impacted on referrals. The evidence is clear that it did, with a step increase in referrals to renal clinics after the introduction of an incentive to identify and manage patients with renal failure,199,201 and an increase in referrals to a diabetic clinic when tighter targets for blood sugar control were introduced into the QOF. 203 Referrals also increased to neurology clinics following an incentive to provide better seizure control for patients with epilepsy,200 although in this study a neurologist provided additional educational support to practices at the same time.
More recently, an incentive has been introduced into the QOF for GPs to:
-
review data on secondary care outpatient referrals
-
participate in an external peer review with other GPs in the CCG to compare its secondary care outpatient referral data with those of the other contractors
-
engage with the development of and follow care pathways to improve the management of patients in primary care in order to avoid inappropriate outpatient referrals.
No data are available on the impact of this incentive on patterns of referral and there are currently no incentives to actually reduce rates of hospital referral.
Specialist advice as an alternative to referral
GPs seek advice from specialists about the management of individual patients, without making a referral.
Key summary points:
-
Studies in which GPs can obtain specialist advice by telephone or e-mail suggest that there is substantial opportunity to reduce the number of patients who are seen in outpatient clinics.
The traditional model of outpatient referral in the NHS is for the patient’s GP to write a referral letter, after which the patient is given an appointment and seen in the outpatient clinic. In this section we review ways in which GPs can seek advice about the management of individual patients without the patient actually being seen by the person giving that advice. These developments are relatively new and were not covered in our previous review or in the systematic review by Akbari et al. 154
A number of studies have reported interventions in which the GP seeks advice by letter or e-mail but without an expectation of the patient being seen by the person giving that advice (Table 18). 204–211
| Article | Country | Study type | Aim/intervention |
|---|---|---|---|
| Oliva et al. (2013)204 | Spain | Before-and-after study | To report on a virtual referral system between specialised endorinological care and primary care (n = 1947 virtual consultations) aiming to improve the resolution of endocrine diseases in primary care; to decrease inadequate visits to secondary care; and to establish a direct communication system between primary and secondary care |
| Patterson et al. (2010)205 | UK (Northern Ireland) | Observational study | To evaluate the impact of an e-mail triage system for new referrals to neurologist (n = about 2400 referrals) |
| Scalvini et al. (2011)206 | Italy | Observational study | To evaluate a telemedicine service for care of hypertensive patients (n = 1719) from 399 randomly selected GPs |
| Stoves et al. (2010)207 | UK (England) | Before-and-after study | To assess the impact of electronic consultations on nephrology referrals for patients with CKD in 85 practices |
| Sved Williams et al. (2006)208 | Australia | Observational study | To evaluate outcomes and satisfaction with a consultation-liaison service to GPs (n = 77), provided by a cohort of private and public psychiatrists |
| Walker et al. (2009)209 | UK | Observational study | To describe an e-mail enquiry service for endocrinology and diabetes established in one hospital |
| Wegner et al. (2008)210 | USA | Observational study | To assess the estimated savings from paid telephone consultations between paediatric subspecialists and primary care physicians (n = 306 consultations) |
| Williams et al. (2012)211 | Ireland | Observational study | To assess an internet neurology referral system for GPs (n = 710 electronic referrals) |
Patterson et al. 205 described a system by which GPs could e-mail neurologists for advice, which they found safe and effective in reducing face-to-face outpatient appointments. There was some increase in overall referrals (i.e. e-mail and appointment requests combined) but an overall reduction in cost, with small increases in GPs’ time outweighed by reductions in specialist time. Similarly, Williams et al. 211 assessed an internet neurology referral system (Neurolink) for GPs in Ireland. The authors reported that 19% (127/662) of patients did not require a neurology outpatient appointment and, instead, the GP was given advice, treatment and investigation options for those patients.
In endocrinology, Oliva et al. 204 reported that 88% of queries from GPs could be resolved without the need for a physical consultation, and Walker et al. 209 also reported the success of an e-mail advice service for diabetes and endocrinology.
Stoves et al. 207 described a system by which the GP requested advice by e-mail on patients with mild to moderate chronic kidney disease but in a situation where the specialist had access to the GP’s electronic medical record. Ninety-two per cent of requests for advice could be managed without the specialist needing to see the patient, and, when the GP did request a face-to-face consultation, the majority could still be managed in primary care with the provision of appropriate advice.
The telephone may also be an underused resource. In an Australian example, psychiatrists saw patients only if it was judged necessary after a telephone conversation between the psychiatrist and the GP,208 and in the USA a telephone conversation between the primary care physician and a paediatric subspecialist meant that referral was avoided in 32% of cases. 210
There is overlap between the studies of electronic communication and some of the studies we describe in Relocation, Telemedicine, especially the use of store-and-forward images for skin problems and diabetic retinopathy. Sometimes a teleconsultation has been used to give advice to GPs. For example, Scalvini et al. 206 describe how a 10-minute teleconsultation with a specialist was able to resolve half of the problems in a group of hypertensive patients at high risk of cardiovascular disease.
Seeking advice from specialists by letter or by telephone is not a new approach. Indeed, over 20 years ago Roland and Bewley212 described an advice line (‘Boneline’) through which GPs could seek advice from orthopaedic surgeons by telephone. However, a number of things have changed which make it likely that telephone and electronic communication between GPs and specialists will play a much larger role in future. Telephone is perhaps the least easy method of communication to use, simply because it requires the availability of both the specialist and the GP at the same time. E-mail, however, provides the opportunity for asynchronous communication and can also be used to transmit test results, images, etc. Doctors, along with others in society, are used to getting rapid responses to queries using e-mail in their personal life. There is no reason why medicine should be different from other sectors in its use of this technology, and we note that a number of NHS trusts are already offering an electronic advice service with an agreed tariff with local commissioners.
There are a number of potential consequences of the ability to communicate more easily with specialists. One is that the need for face-to-face referrals could diminish, and several of the studies quoted above suggest that this could happen. However, easy access to specialist opinion could also increase the number of patients eventually seen in clinic. The potential benefits of this for patient care (i.e. seeking specialist advice which would not otherwise have been sought) are unknown, and this would be an important area for future research.
Conclusion
A number of studies have evaluated interventions which enable GPs to get e-mail or telephone advice from specialists without the need for a face-to-face consultation. E-mail may provide an easier form of contact and includes the opportunity to include test results, images, etc. Some NHS trusts are now providing a tariff for e-mail enquiries. Studies in which GPs can obtain specialist advice by telephone or e-mail suggest that there is substantial opportunity to reduce the number of patients who are seen in outpatient clinics.
Patient behaviour change
Decision aids
Patient decision aids are designed to influence decisions about referral to and discharge from specialist clinics.
Key summary points:
-
Insufficent evidence was found to draw conclusions.
Patient decision aids were not considered in our previous review or in the systematic review on interventions to improve outpatient referrals. 154 In this review we identified one relevant RCT in which patients with a range of chronic conditions were offered coaching on how to discuss their condition with their primary care physician. Patients in the coaching group were much more likely to be referred to a specialist in subsequent consultations with their primary care physician than those who had not received coaching (51% vs. 28%). 213
Although the results of this study in the USA may not be directly applicable to the UK, they raise an important question of what the ‘correct’ level of referral is. The studies described in earlier sections of this review use professional benchmarks for assessing the appropriateness of referrals (e.g. NICE guidance). Even where professional opinion is the gold standard we noted some interventions in which improvements in care were associated with increases in hospital referral.
This study raises the additional issue of what patients would prefer, and it was beyond the scope of this review to identify whether patients think they are referred to specialists too often or not often enough. In making referral decisions, GPs assess the clinical need for referral, but they are also influenced by the patient’s wishes. 214 They are, therefore, balancing clinical need with the wishes of the patient and the availability of health-care resources.
Discussion
This scoping review updates our previous review published in 2006. 2 Our broad conclusions are similar to those of the previous review, but with some significant new sections and findings. Below we summarise these findings and make suggestions for their future relevance in the changing policy environment.
Transfer: substitution of primary for secondary care
The evidence found in this review suggests that substition of primary care for secondary care may be both safe and effective for long-term chronic disease management and for minor surgical interventions. However, the safety and efficacy of these services will depend on the competency of the individuals providing the care, and the support available to them. In all cases of transfer of services from secondary to primary care, it is important to ensure that general practices (or ‘GPs with a special interest’) have the administrative support and resources to ensure that protocols can be reliably followed, and that there is adequate support from specialists when queries arise or problems occur.
There is little evidence available on the wider effect of such arrangements, including the impact on outpatient referrals. In addition, there is little evidence on the cost-effectiveness of these transfer arrangements, and this is likely to depend on local payment and/or contractual arrangements. Although many of these changes were introduced with the aim of decreasing waiting times, the policy environment has now changed, with a much greater emphasis on cost reduction and increasing cost-effectiveness. As such, the focus is now likely to be on CCGs needing to reduce expenditure on outpatient services and seeing the provision of primary care follow-up for chronic conditions or GP minor surgery as one way of doing this. Further cost-effectiveness evidence will be required to assess whether or not such changes are cost-effective in practice.
A large number of studies have now been carried out on the effects of giving GPs access to a wider range of diagnostic tests. Earlier studies were of access to tests and investigations which have now become generally available to GPs (e.g. ultrasound and endoscopy). More recent studies evaluate GPs’ use of a wider range of investigations, including MRI and CT. Especially when combined with a referral protocol, it is clear that GPs can make effective use of a wide range of diagnostic facilities, although it is striking how few studies look at all of the costs and benefits of widening access to diagnostic tests, including the net impact on referrals to outpatient clinics. Moreover, the costs of providing services in the community compared with in hospital are not generally reported and the desire to provide services ‘closer to home’ may conflict with the economies of scale that can be achieved by centralising complex investigations.
In some cases (e.g. direct access to audiology for hearing aids) the benefits of bypassing an unnecessary specialist referral are clear-cut. However, in other cases the benefits of direct access to services – musculoskeletal services being the most common example – are less certain. Direct access to physical therapies for musculoskeletal problems produces a substantial increase in demand for such services and, although they are very popular with patients, their cost-effectiveness as an alternative to referral (or non-referral) is less clear.
In several of the types of service transfer interventions discussed above, there is the potential for supply-induced demand or for the new service to address previously unmet need. For example, if incentives are introduced for GPs to conduct minor surgery, minor surgical procedures may be carried out which would not have previously been done. In addition, direct access of GPs to tests or services may result in increased use of diagnostic tests or use of particular services. In the case of direct access to services, rational use of services including investigations, treatment services such as physiotherapy, and specialist referral is increasingly being addressed by locally agreed pathways which need to be followed for services to be accessed, and such protocols and pathways may also be useful for determining whether tests or procedures are required.
Relocation
In shifted outpatient models, hospital specialists visit premises outside their hospitals to provide care, and these clinics are popular with patients. However, a significant proportion of patients seen in community-based clinics need to be seen again in hospital and specialists may see fewer patients in community clinics, and community clinics may, therefore, be more expensive than hospital-based outpatient clinics. Current policies to move consultant clinics into the community can be justified only if (a) high value is given to patient convenience in relation to NHS costs or (b) community clinics can run at a scale to enable the efficiencies of patient throughput in a hospital clinic to be realised.
Community mental health teams are a particular example of moving specialist care into the community, and these teams appear effective across a wide spectrum of disorders. They are enhanced if patients have an identified case manager, who can come from a range of disciplines, including some found within the primary care team. CMHTs are likely to be most effective when there are regular opportunities for face-to-face contact between members of the mental health team and the primary care team. In some cases this can be achieved by colocation and in others this can be done by regular meetings. Services associated with improved outcomes are likely to cost more but there is little evidence on the cost-effectiveness of different models of care and, especially given the diversity of local arrangements, there is little to guide local commissioners on the optimum configuration of services.
For telemedicine, physical location is likely to be a major determinant of its use as an alternative to outpatient clinics. In countries with very remote rural areas, video consultations will continue to be a viable alternative to patients or specialists having to travel very long distances. In England it is unlikely, in general, that video consultations will be a cost-effective alternative to outpatient clinics. ‘Store-and-forward’ services for images of skin conditions show promise, although they may be of less value in cases of suspected skin cancer. Too often, however, the establishment of these services appears to depend on local enthusiasts. It would be helpful if more economic evaluations were reported. We did not report on the outcome of telecare interventions, as the focus of these was almost exclusively on avoiding admissions rather than on the interventions as an alternative to outpatient consultations.
Liaison
Shared-care protocols are now used across a wide range of conditions without loss of quality of care. Cost savings to patients can be considerable if they do not have to travel to outpatient clinics, but savings to the health service are less clear-cut. There are studies which show net savings from moving from outpatient clinics to a shared-care model, but such savings are not universal and may depend on the nature of the shared-care arrangement.
Professional behaviour change
Since our last review, a substantial number of studies have been published aiming to change referral behaviour by GPs. Guidelines, audit and feedback, and professional education programmes are all relatively ineffective on their own, but may be combined, or linked with other interventions. Of these, professional education programmes probably have the greatest potential to change behavior, although we noted that some positive studies involved very intensive interventions (e.g. biweekly visits by specialists to general practices). Guidelines are increasingly incorporated into referral pro formas which have to be completed as part of the referral process. A number of studies of professional education and of guidelines had the effect of increasing referrals and, in our view, all interventions aimed at changing professional behaviour should be aimed at increasing the appropriateness of referrals rather than becoming a form of demand management. From a very limited evidence base, programmes which involve GPs obtaining a second opinion from one of their colleagues prior to referral (in-house referral) have the potential to reduce referrals. We also found a few studies with inconclusive results of external review of referrals (‘referral management centres’). Because of the very limited information on both of these interventions, we undertook limited primary data collection on each of these interventions, reported as separate substudies in Chapters 3–7.
A number of studies have evaluated interventions which enable GPs to get e-mail or telephone advice from specialists without the need for a face-to-face consultation. E-mail may provide an easier form of contact and includes the opportunity to include test results, images and so on. Some NHS trusts are now providing a tariff for e-mail enquiries. Studies in which GPs were able to obtain specialist advice by telephone or e-mail suggest that there is substantial opportunity to reduce the number of patients who are seen in outpatient clinics.
In this review, we have not addressed interventions which are about the internal reorganisation of outpatient clinics in hospitals. Many such studies exist, often evaluating staff substitution, for example providing a nurse specialist or physiotherapist as an alternative to seeing a doctor. As in primary care, there is likely to be substantial opportunity for role substitution in hospitals. However, in the absence of robust economic evaluations, it should not be assumed that the cost of care is reduced just because the salary of the person first seen is reduced. A range of other interventions have been described to increase the efficiency of hospital throughput, including ‘one-stop clinics’ and a pre-clinic telephone call from the specialist to arrange investigations in advance; O’Byrne et al. 215 reported that this more than halved the number of patients requiring multiple attendances.
Overall, we identified a wide range of new approaches which substitute for conventional outpatient clinics and have the potential to provide high-quality care in community settings. However, robust economic evaluations were rarely reported and the cost-effectiveness of many interventions remains unclear. However, it is also important to note that most cost-effectiveness studies look at the cost of interventions to the provider rather than the price that the purchaser charges. We note that the value of many interventions will depend on local contracts, and we anticipate that CCGs, when letting contracts for community services, will ensure that the price they pay is lower than for comparable services delivered in hospital. We also note the potential for ‘supply-induced demand’ when services are made locally available to GPs. A ‘cheaper’ primary care-based service will save the purchaser money only if there is corresponding disinvestment in hospital services.
Limitations of the review
In this scoping review we aimed to map the key concepts pertaining to strategies involving primary care that are designed to improve the effectiveness and efficiency of outpatient services, and the main sources and types of evidence available. We developed an inclusive search strategy based on that used in the previous review. Our review begins from 2005, as it is an update of the previous review.
The main aim of the literature review was to provide evidence that is useful to those working in the NHS, whether as managers, commissioners or practitioners. Thus, our review focuses on those papers which are applicable to the current English context. We have not included studies which address other forms of health system, or which address strategies already commonly used in the English NHS.
Given the nature of the evidence which addressed disparate outcomes and used a wide variety of designs and analysis methods, it was not possible to carry out any meta-analysis or other quantitative synthesis of findings. In addition, as this is a scoping review, we do not formally assess the quality of the included studies.
Gaps in the literature and recommendations for future research
Across the areas addressed in this review there remain both gaps in the evidence and areas in which the evidence available is of a very poor quality. Although there are a large number of papers which report on the reorganisation of health-care provision, many of these do not look at the wider impacts on the health-care system and, thus, do not address the effect on the effectiveness and efficiency of outpatient services. For example, although a number of studies demonstrate that the transfer of service provision from secondary to primary care is safe and effective in itself, it is unclear if the assumed reduction in secondary care service provision is achieved in reality, or if this is a more cost-efficient method of service provision.
In many of the areas covered, there was a clear need for further evidence on cost-effectiveness. While this may depend on local arrangements for reimbursement for service delivery, or tariffs set up for new initiatives such as ‘advice referral’, this information will be important to those designing service models and commissioning services.
Finally, there is a continued need for further high-quality evidence. We reported in our previous study that more robust studies are required, and this remains the case in many areas. Studies are needed which employ rigorous experimental designs, supported by qualitative studies which assess the factors that may impact on future successful implementation in other settings.
Chapter 3 Referral management centres: substudy of four centres (substudy 1)
Introduction
The introduction of RMCs is one of a range of measures taken to tackle rising demand for outpatient appointments, by seeking to manage the process of referral from primary to secondary care. RMCs lie at the active end of a continuum of such approaches, which also includes the use of referral guidelines and the peer review of referrals. 194 Broadly, the role of RMCs is to act as an external arbiter to review referrals and to perform some action with respect to them (i.e. to reject, divert, or provide advice or some additional function), but considerable diversity in their form and organisation is acknowledged in the literature. 195 Although some RMCs are designed primarily to manage bookings or facilitate patient choice, many have among their aims the clear implicit or explicit goal of reducing referrals. This substudy focuses on this subset of initiatives.
Widespread concerns have been expressed in the academic, GP and UK national press195,216–220 regarding the potential negative effects of RMCs, such as the introduction of error and delay into the referral process and the undue interference of managers in clinical decisions. In addition, the limited evidence published on their effectiveness is equivocal and suggests that reduction in referrals by RMCs is less likely to represent value for money than the use of more passive alternatives such as peer review. 193,194,198 Despite this, RMCs still represent a widely used approach and new schemes continue to be developed across the UK. Around one-quarter of CCGs were reported to be using a RMC in 2014, of which 64% had been set up since 2010 and 21% since CCGs took control of commissioning in 2013. 221 Their continued popularity in the absence of supportive evidence raises questions regarding the rationale behind their implementation.
The epitome of a complex intervention, RMCs rely on human agency and the actions of multiple stakeholders to make them work, require a sequence of intervening processes to occur before they achieve their ultimate outcome and, furthermore, have a tendency to adapt and evolve over time. 222 Indeed, a recent review of demand management interventions demonstrated that such programmes require concomitant changes at all levels of the health system to make them work effectively, and that they inevitably evolve over time as stakeholders make changes in response to experiences of what does and does not work on the ground. 223
This study sought to gain a better understanding of the inner workings of RMCs and the factors contributing to the achievement of their goals. To begin to understand this complexity, we have drawn on the principles of realist evaluation,224 an approach premised on the idea that complex interventions represent theories (held by those designing and implementing them) regarding about how best to remedy a particular problem and how participants are likely to respond to the solutions offered. Although a full-scale realist evaluation of RMCs (involving developing, testing and refining theories, to explain why they work in some circumstances and not others) was beyond the scope of this study, we sought to engage in the first stage of this process, that of eliciting programme theories (the ideas and assumptions about what a programme is intended to achieve and how it is supposed to work). In so doing, we aimed to identify the key issues to be considered when establishing or evaluating such schemes.
Methods
The study took place at four RMC sites in dispersed geographic areas in England. Sites were identified through speculative e-mails based on an internet search. Advertisement in the GP press yielded no further responses. All sites expressing interest were included.
Sampling and data collection
Purposive sampling was used to select participants involved in the commissioning, set-up and running of the identified RMCs and GP referrers. The study sought to include clinicians and managers with a variety of roles to gain a wide range of perspectives. Individuals fulfilling these roles were approached via an e-mail describing the purpose of the study and inviting them to participate. In-depth interviews were conducted by two researchers (SB and MR) at the participant’s workplace or by telephone, between July 2013 and May 2014. Verbal consent was sought for participation and audio-recording of interviews. A common interview guide was used for each interview, although emphasis was placed on allowing participants to talk from their own perspective. The questions were designed to understand the intended aims of the schemes, how stakeholders felt about the schemes and what had worked well and less well with respect to their implementation. The topics covered included the design of the RMC; its aims; changes in the scheme since it was initiated; acceptability to a range of stakeholders; outcomes; and local context. The interviews took the form of a guided conversation, during which programme theories relating to RMCs (identified through relevant literature and through preceding interviews) were explored. The interview schedule therefore developed iteratively (for the interview topic guide see Appendix 4). The interviews were transcribed verbatim and anonymised through the removal of references to identifiable names and places.
Data analysis
Thematic analysis of the data was conducted based on the principles outlined by Boyatzis. 225 The transcripts were read and reread and ‘codes’ were applied to meaningful sections of text. Codes were derived inductively from the data and as analysis progressed these were organised into overarching or organising themes using NVivo 10 software (QSR International, Warrington, UK). Data within themes were scrutinised for disconfirming and confirming views across the range of participants. Analysis was led by SB in regular discussion with MR. Emerging findings were also shared with members of the study advisory group for comment.
Based on advice from the National Research Ethics Service and Cambridgeshire Local Research Ethics Committee, the study was deemed a service evaluation and we did not obtain formal ethics approval, although we sought to adhere to good research ethics practice throughout.
Results
Two interviewers conducted 18 interviews relating to four sites. Between three and six respondents were interviewed at each site, drawing from the groups described above. Table 19 provides a summary of the characteristics of the schemes included and the candidates interviewed.
| RMC | Key features | Interview number | Interviewee characteristics | Role in RMC |
|---|---|---|---|---|
| A | Functions: clinical triage by GPs with additional expertise and allied health professionals; reviews referrals from 30 specialties; referrals diverted to community service, returned to GP with advice or sent on to acute trust; manages patient bookings through ‘Choose and Book’ process; provides individual-level advice and guidance to GPs, monthly referral reports and live access to referrals data; broader educational function Organisation: provided by existing out-of-hours provider and software specialist; covers three CCGs, 95+ practices, 70,000 referrals; practices pay based on patient list size; operating 2010–present; patient booking originally provided out of area but now commissioned locally |
A1 | GP with managerial responsibility, director of RMS provider organisation | Set-up and running |
| A2 | Manager, CCG | Commissioning | ||
| A3 | Two managers (joint interview), RMS provider | Set-up and running | ||
| A4 | GP | User only | ||
| A5 | GP | User only | ||
| B | Functions: clinical triage by GPs; referrals diverted to community service, returned to GP with advice or sent on to acute trust; reviews referrals from selected specialties; manages appointments booking (not linked to ‘Choose and Book’); collects data to inform commissioning; limited individual-level feedback; educational sessions and newsletters Organisation: provided by existing out-of-hours provider; covers one CCG, 70+ practices; funded by CCG – cost per letter triaged; operating 2010–present; began as purely administrative with later introduction of GP triaging |
B1 | Manager, CCG | Running (contract monitoring) |
| B2 | GP with managerial responsibilities | Commissioning/set-up | ||
| B3 | GP with managerial responsibilities | Running (contract monitoring) and user | ||
| B4 | GP with managerial responsibilities | Development, running and user | ||
| B5 | GP with managerial responsibilities, also employed by RMS provider | Set-up and running, GP triager and user | ||
| B6 | GP | User only | ||
| C | Functions: no clinical triage by RMC staff; consultant triage commissioned from secondary care; following consultant triage referrals to selected specialties diverted to community service, returned to GP with advice or accepted by acute trust; non-clinical staff at RMC manage patient bookings through ‘Choose and Book’ and the process of sending referrals for selected specialties for consultant triage; collects data to inform commissioning; data reports at GP/practice level; internal peer-review and educational sessions Organisation: provided by existing educational services provider; covers one CCG, < 20 practices; funded by CCG – unit cost per triaged and non-triaged referral; operating 2012–present; began as purely administrative with later introduction of consultant triage element |
C1 | Manager, RMS provider organisation | Set-up and running |
| C2 | Manager, CCG | Commissioning and set-up | ||
| C3 | GP with managerial responsibility | Set-up, running and user | ||
| C4 | Practice manager, also involved in management of RMS provider organisation | User, set-up and running | ||
| D | Functions: clinical triage by GPs and nurses under supervision; focus on changing referral behaviour through feedback and education; no diversion of referrals, GP retains responsibility for referral destination; no management of patient bookings; collects rich data; provides individual-level feedback on referrals, weekly ‘top-tips’, access to detailed referral data; broader educational function Organisation: provided by Community of Interest Company set up specifically to deliver RMS; covers one CCG, opt-in required – 16/24 participated; operating 2010–13 – contract not continued |
D1 | Manager, RMS provider | Set-up and running |
| D2 | GP with managerial responsibility, CCG | Commissioning | ||
| D3 | GP, also employed by RMS provider | GP triager and user |
The four interventions included in the study all had among their aims the reduction of referrals to secondary care and shared a number of features: providing a central point of contact for GPs and service providers with regard to referrals; managing referrals to a wide range of specialties; collecting and analysing data; and providing feedback and education to GPs. There were also considerable differences between the schemes with respect to scale, the model used for clinical triage and the role played in managing appointment bookings and in diverting referrals.
The interviews conducted provided a rich source of data. Stakeholders described a range of different aims (programme theories) that were often present in the same RMC, and both aims and functions evolved or were reprioritised over time (see the following section). In addition, three themes were identified that related to the context in which the programmes were implemented: the impact of practical and administrative difficulties; the importance and challenge of stakeholder buy-in; and the dependence of perceived effectiveness on the aims and priorities of the scheme (see The impact of practical or administrative difficulties, The importance and challenge of stakeholder buy-in and sustaining relationships and The dependence of perceived effectiveness on the aims and priorities of the scheme).
The diversity and evolving nature of the aims and functions of referral management centres
Referral management centres had a wide range of aims and programme theories
The RMCs included in this study were selected on the basis that they aimed to reduce referrals. In all cases, however, this was just one of many inter-related aims articulated (summarised in Figure 2). At the highest level, interview data indicated that the broad aim of the schemes was to ensure the best use of limited resources, under which three chains of more specific subaims were described, highlighting the ways in which this could be achieved: quality improvement, reduction in referrals to secondary care and increased efficiency in the referral process.
FIGURE 2.
The aims and functions of RMCs, based on interview findings.

With respect to quality improvement, interviewees described how RMCs aimed to collect and analyse data on referral quality and, based on the understanding gained, to standardise referral processes, educate GPs and implement primary care pathways. Desired outcomes included improvement in the quality (and reduction in the variability) of referrals and, in turn, improvements in the quality of patient care, with patients seen ‘in the right place, at the right time, and by the right clinician or specialty’ (B4, GP with managerial responsibilities), ensuring that ‘when they’re sitting in front of that person, that person has everything that it’s reasonable and possible for them to have in order for them to treat that patient appropriately’ (B1, manager).
In order to change patterns of referral, interviewees described how RMCs aimed to collect rich data on referral patterns, to inform the development of alternative, more cost-effective models of service delivery to meet identified local needs, to divert referrals to alternative services (such as lower tariff community services) and, in so doing, to reduce referrals to secondary care. Also described was the expectation that improving referral quality would also result in fewer referrals, with the aim of educating GPs to provide ‘better quality letters where more information was there, and therefore justifying more effectively, the reason for the referral’ leading to GPs ‘doing more in the general practice setting’ (D3, GP triager).
Finally, to make the referral process more parsimonious, RMCs aimed to centralise referral and appointment booking processes, to hold comprehensive and up-to-date knowledge on available provider services, to reduce the (administrative and knowledge seeking) burden on referring GPs and, through these measures, to increase the efficiency of the referral process.
Interviewees described a complex network of aims and underlying tacit assumptions regarding how the achievement of one aim depends on the delivery of another.
[The aim was] to improve the quality of referrals, to reduce unwanted variation and to trust that by doing those two things an unplanned consequence would be [. . .] a reduction in unnecessary expenditure.
D1, manager, RMC provider
Yeah, certainly my thrust has always been about improving the quality [of referrals] [. . .] They can’t try and address the referral problem and not raise the quality of primary care.
A2, manager, commissioning, CCG
The weight given to the different aims varied significantly, not only between schemes but also between stakeholders within the schemes. While one GP user of a scheme (B6) perceived the aim to be to ‘save money on referrals into secondary care’, a manager involved in its commissioning (B1) was clear that it aimed ‘to collect data on why patients are referred’ to inform how best to ‘shape services for the future’. Similarly, a manager for a RMC provider organisation described a mismatch between commissioner and provider expectations.
[The CCG] saw the RMC as a way of reducing referrals, therefore reducing costs. So I had to explain to them ‘you’re not going to reduce costs by just commissioning a RMC in isolation’, for starters. [. . .] you will only reduce costs by commissioning community pathways at a reduced tariff. [. . .] I have to be very clear when commissioners come to us about what their expectations are of a referral management centre [. . .].
C1, manager, RMC provider
Referral management centres evolved substantially over time
Not only did the aims of the schemes (or the weighting of them) vary between sites and between stakeholders, but interviewees also reported that they had evolved over time, dependent on changing local priorities and on the successes already achieved.
So the idea has changed as the service changed. They were initially collecting that data [on referral quality] and being able to present that [to practices] and want to possibly performance manage GPs. [. . .] but more recently it’s been about making sure that patients, are seen in the right place, so not going into inappropriate clinics. Not going to clinics with investigations that could have been done in primary care, having to be done again in secondary care. It’s about improving the patient experience, that’s the intention.
B3, GP with managerial responsibilities
Interviewees described how the functions of RMCs had evolved considerably since their initial implementation, in response to changes in aims and local context. For example, for two of the schemes (RMCs B and C), data collected were reported to have informed the development of new community services, which in turn led to a need for the introduction of clinical triage (to divert referrals appropriately).
. . . first of all [. . .] we’d look at which specialties we thought would benefit from a community pathway, then we had to bring in the triage so it could be agreed which patients went into that community pathway. [. . .] No changes have been made because the Gateway wanted change if you see what I mean, they were all changes that were going on in the landscape with the CCG and the GPs, the providers, and then the Gateway responds.
C1, manager, RMC provider
Also highlighted was the fact that evolution in the functions and processes of RMCs resulted from efforts made to overcome identified challenges, for example to respond to GP concerns or iron out administrative glitches. For RMC A, for example, the bookings management element of the scheme was originally provided by an administrative team some distance away from the CCGs served, but, for issues of cost and the acknowledged benefits and increased acceptability of using staff with local knowledge, this was relocated in the CCG area.
The capacity to evolve was described by several participants as key to the success of RMCs.
[. . .] if it’s going to be a success, it needs to evolve, [. . .] you can start off with something but if it stays the same, then I think in the case of ours, we’d be having problems with it; whereas as it’s evolved it’s been able to respond to the needs of firstly the PCT and now the CCG.
B2, GP with managerial responsibilities
One interviewee acknowledged that, by encouraging appropriate referral behaviour on the part of GPs, RMCs might find that they were no longer needed.
[. . .] once the provider landscape has settled down, and people are much clearer about what they should be managing, and what they shouldn’t be managing, and what they should be sending, and what they shouldn’t be sending. If all that were in place, we might not need an RMS [. . .] it might not be something that we’ll have forever.
B1, manager, CCG
The impact of practical or administrative difficulties
Participants reflected on how practical issues had a profound impact on the functioning of the schemes, with difficulties often attributed to the need to manage evolving or unclear aims and functions.
Software and system limitations
System design and information technology (IT) compatibility issues were reported to present a major challenge. Both a lack of clarity in aims and changes in the primary function of RMCs (e.g. from administrative to clinical function) presented IT challenges, with adaptations of software for new purposes causing difficulties for data capture and issues with the subsequent quality (and hence the utility) of the data collected.
I think that the problem was that the original set-off of the RMS, being admin managed, had a database that was designed to manage from the admin point of view. [. . .] So the clinical steps that were taken have been put on top of the old admin database. [. . .] the impact that that made meant that data protection was a bit harder, but also that audit of clinical information was harder.
B5, GP with managerial responsibilities, and GP triager
[. . .] it was an aspiration really, saying ‘we will use this data for commissioning intentions, commissioning purposes’. However, on looking at it, we’ve seen a few issues in the data quality, so we’re not prepared to use that as a reliance really. It’s good at giving a ball-park at the moment but we’ve tasked our data teams [at the CCG] to start, well, continue looking at it with them and get them up to speed as to what exactly we’re wanting to get out of it.
C2, manager, CCG
Some features of clinical and administrative IT systems were highlighted as being important enablers of the schemes and, conversely, their absence was highlighted as disadvantageous. For RMC B, the lack of a facility for GPs to carry out triage remotely was cited as a reason for difficulties experienced in recruiting local GP triagers, which in turn was reported to reduce the credibility of the scheme, thereby affecting GP buy-in.
Contract and capacity issues
A number of interviewees described difficulties with successful contracting of RMC services and managing capacity within RMCs, in the context of continual and unpredictable changes in service structure and demand, with the potential to have a negative impact on both the sustainability of the scheme and the quality of patient care.
[. . .] more triage specialties were brought in [. . .] That did result in a number of changes to process [. . .] The team kept saying ‘you are adding extra steps in, you are increasing the risk of delays’, because it took longer to invest the time to do each referral. [. . .] But that was the way the commissioners wanted it. So we were taking longer to process the referrals, the [RMC] team doubled in size [. . .], which meant a lot of new members joined it and then it’s a 5-week training programme, so that hindered progress. And the activity levels started to rise too. So the combination of all those factors made it very difficult for the team to keep up with the volume that was coming in and a backlog started to generate.
C4, practice manager also involved with RMC
The importance and challenge of stakeholder buy-in and sustaining relationships
The most frequently cited challenge to the success and sustainability of RMCs was the need to achieve and sustain buy-in from the various stakeholders (commissioners, RMC providers, acute and community service providers and, perhaps most importantly, referring GPs) on whose collaboration the proper functioning of the schemes depends.
Establishing shared vision
Both commissioners and providers of RMCs described a lack of clarity in the aims at the outset, with one interviewee commenting that those developing the RMC had been ‘shooting in the dark’ (C1, manager, RMC provider). Also highlighted was the challenge of managing the differing priorities of commissioners and referring GPs, and communicating effectively to sell the concept to all involved.
We had to speak a little bit with fork tongue [. . .] They [the CCG] were most interested in reducing the referrals but we said to them that, ‘if we speak to our constituency [GPs] about that subject we will get yawns and non-participation’.
D1, manager, RMC provider
Unclear and poorly communicated aims were associated with a perceived lack of awareness among referring GPs regarding the purpose of the intervention and of their role in it.
If I was going to do this again, there would be a huge advertising campaign [targeting referring GPs], so to speak, actually saying what the intentions are [. . .] I don’t really think that many of my colleagues really had a grasp of that at the beginning.
B5, GP with managerial responsibilities, employed by RMC as triager
As time’s gone on I think I’ve understood the aims, but it hasn’t been clearly set out by the RMS. I think I’ve learnt through the process what the aims are, but that’s my idea of what it is. I haven’t ever received anything from the RMS to say this is what we’re trying to do.
B6, referring GP
A lack of early and effective involvement of GPs in the development of the aims of RMCs and a perception of being ‘told what to do’ (B6, GP) was reported to contribute to misinformation and distrust and, consequently, resistance to engagement with RMC processes.
[. . .] if I had a conversation with doctors about actually what it is that we’re trying to do, then I often find that people are much more ready to come on board, more aware of the process. And that one-to-one dialogue, it would be much better if that dialogue had been done at an earlier phase. When you have misinformation out there, then it pollutes what people actually think and turns it into a purely financial-driven motive and actually the points about improving patient care, reducing waiting times and saving money at the same time will get missed.
B5, GP with managerial responsibilities, employed by RMC as triager
Sustaining engagement
Participants described a wide range of measures implemented to keep GPs on board (Table 20).
| Challenges | Approaches to achieving and sustaining buy-in from referring GPs |
|---|---|
| Lack of awareness among referring GPs of the aims and purpose of the scheme | Engaging GPs in dialogue during the development of the scheme |
| Practice outreach through roadshows/practice visits | |
| Opportunity to be involved as a triager | |
| Regular newsletters/educational sessions on common referral issues | |
| Cynicism and mistrust among GPs with respect to the achievements of the scheme | Piloting systems and presenting evidence of success |
| Performance management of RMCs to ensure that quality of patient care is not affected | |
| Resistance to changing referral behaviour | Offering incentives for referring through the RMS |
| Presenting bespoke data to practices at level of individual GPs to enable benchmarking | |
| Frustration with bureaucracy | Ensuring parsimony in administrative processes, e.g. evolving to include all specialties |
| Ensuring GPs are kept up to date with changes to processes through regular communication/newsletters, etc. | |
| Challenge to clinical autonomy | Moving from purely administrative to clinical triage [based on the assumption that feedback from a fellow clinician would be better received than that from ‘some manager or clinical person’ (interview B4)] |
| Taking the approach of changing referral behaviour through education alone (with GPs retaining ultimate responsibility for referral destination) | |
| Providing feedback to GPs on their referrals that supports education and learning | |
| Ensuring that the tone of this feedback is moderate and advisory |
The evolving nature of RMCs, however, was reported to present significant challenges, with rapid and widespread changes occurring simultaneously in many different referral pathways, leading to frustration among referring GPs unable to keep up.
[. . .] the rules changed. I think, initially, it was some clinics, then it was other clinics and then it was everything and it was keeping up with their change [. . .] As they were developing, we were trying to understand what they were doing.
B6, referring GP
Clarity and parsimony of referral processes were described as important factors influencing GP support.
[. . .] the advantage is that now we don’t do Choose and Book it is a lot more straightforward at that interface with the patient; [. . .], so we saved a lot of time.
A4, referring GP
[. . .] as a GP I don’t want to be thinking about a lot of different pathways. Ideally I want to try and keep it down to as little as possible, so you know the more the RMC does, the better, because you just, you end up sending 90–95% of your referrals to the RMC and you don’t have to think about it after that.
C3, GP with managerial responsibility
Maintaining quality and safety in patient care was considered paramount to ensuring continued engagement. The potential for introducing delay into the referral process was acknowledged as a serious threat to the acceptability of the schemes.
We knew that the whole systems would start falling apart if clinical safety and quality fell apart [. . .] When GPs heard about it [breaches in agreed turnaround times for referrals] . . . I mean it wasn’t kept secret . . . then it was that loss of faith in something [. . .].
B2, GP with managerial responsibilities
Respecting general practitioner autonomy and responsibility
A major stumbling block in selling the concept of RMCs to GPs was the perception that such schemes present a challenge to clinical autonomy, the avoidance of which was cited by interviewees across all the included schemes as an important consideration in the design, implementation and sustainability of the initiatives (as outlined in Table 20). Even with respect to the RMC, however, this took a purely educational approach, with GPs retaining responsibility for the referral destination; interviewees described the challenges associated with GPs’ resistance to negative feedback.
[T]he tone in which the triagers rattled their notes into the computer, when they were finding a referral not as good as it might be, was not always as diplomatic as it could be. [. . .] we had to put that text through a moderator who would change all the language so that there were no [. . .] unnecessary spikes in it, [. . .] We train them [GP triagers] all in how to do that.
D1, manager, RMC provider
[T]here is rivalry in primary care. We all like to feel our practices are the best practice [. . .]. I know that a number of practices were being contacted fairly frequently [. . .] they hadn’t done this, that or the other; and I think that some practices didn’t like that and left, which were the very practices one could say that really required that support.
D2, GP with managerial responsibilities
The dependence of perceived effectiveness on the aims and priorities of the scheme
All interviewees reported that the RMC they described was successful with respect to at least one of its aims. The perceived effectiveness of the schemes, however, varied by stakeholder and according to how the aims and priorities were specified.
[. . .] if you say that the initial thing that a referral management service set out to achieve [was] the information, and where were the key areas that had the highest number of referrals, actually it achieved that [. . .] [I]t was then set up to say ‘well, if you have that data is there actually anything that you can do?’ Now it didn’t say you’ve got to do this, ‘cause actually that would have tied its hands and you would have had either failure or success. So because it wasn’t tied down too much, you were then able to move into the next phase [. . .].
B2, GP with managerial responsibilities
Different measures of success for different stages of referral management centre development
Perceived success achieved in relation to the aims set out in Figure 2 could be seen to reflect, to some degree, the maturity of the scheme, as, for example, effective data collection and analysis was a prerequisite for the implementation of processes to achieve the specified intermediate and desired outcomes and move towards the overarching aim to ensure best use of NHS resources. Interviewees tended to report greater difficulties in measuring achievements against (and were less confident in their claims with respect to) higher-level goals, with success claimed less consistently, reflecting marked disagreements between stakeholders (as illustrated in Table 21).
| Focus of aim | Outcome | RMC A | RMC B | RMC C | RMC D |
|---|---|---|---|---|---|
| Overarching aim | Better use of resources | ✓ (A1, A2, A3) | ? (B1, B3) Too soon to draw conclusions |
? (C2) Too soon to draw conclusions |
✓ (D1, D3) |
| ✗ (D1, D2, D3) Commissioner not convinced by figures |
|||||
| Desired outcomes | Improved quality of patient care | ✓ (A1, A3, A5) Patients generally unaware |
✓ (B2, B5) Community clinics offer convenience and shorter waiting times |
✓ (C1, C2) Quicker referral times More time and information available to support patient choice |
✓ (D1, D3) Patients unaware RMC highlights cases that should be upgraded to urgent |
| ✗ (A2, A5) Occasional restricted choice for patients Concern about quality of community service provision |
✗ (B2, B3, B4, B6) Reduced patient choice Referrals sometimes get lost |
||||
| Reduced referrals to secondary care | ✓ (A1, A2, A4) Up to 15% reduction |
✓ (B4) 8% reduction |
? (C2) Not a significant impact but too soon to tell |
✓ (D1, D3) | |
| ✗ (D2) Commissioner not convinced by figures |
|||||
| Improved efficiency of referral process | ✓ (A2, A3, A4, A5) | ✓ (B3, B6) | ✓ (C1, C2, C3, C4) | N/A | |
| ✗ (A1, A2, A5) Some duplication of work due to administrative glitches Teething trouble with IT/systems |
✗ (B1, B2, B3, B4) Some issues with undercapacity and turnaround times Some duplication of work |
✗ (C1, C3, C4) Some issues with undercapacity and turnaround times Issues with booking management system |
|||
| Intermediate outcomes | Improved referral quality | ✓ (A2, A3) | ? (B1, B4) Believed to be reducing variability in referrals |
? (C1) Anecdotally, fewer rejections from providers |
✓ (D1, D3) |
| Diversion of referrals to alternative services | ✓ (A2, A4) | ✓ (B3, B5) | ✓ (C3) | N/A | |
| Reduced burden on GPs and practice staff | ✓ (A4, A5) | ✓ (B3) | ✓ (C1, C2, C3, C4) | N/A | |
| Process implementation | Standardised referral processes | ✓ (A2, A3) | Not mentioned in data | ✓ (C1, C2) | N/A |
| GP education/culture change | ✓ (A1, A3) | ✓ (B2, B4, B5, B6) | ✓ (C1, C2, C3, C4) | ✓ (D1, D2, D3) | |
| Implementing primary care pathways | ✓ (A2) | ✓ (B1) | ✓ (C2) | ✗ (D2) Did not effect pathway change as expected |
|
| Centralising referral/booking processes | Not mentioned in data | ✓ (B4, B6) | ✓ (C1, C2) | N/A | |
| Providing up-to-date service knowledge | ✓ (A1, A2, A4) | ✓ (B1, B3) | ✓ (C1, C2) | ✓ (D3) | |
| Informing service development | Not mentioned in data | ✓ (B2, B4, B5, B6) | ✓ (C1) | Not mentioned in data | |
| ✗ (C2) Some concerns regarding data quality |
|||||
| Data | Collection and analysis of data | ✓ (A2) | ✓ (B2, B3, B4) | ✓ (C3, C4) | ✓ (D2, D3) |
For all schemes, RMC providers and commissioners expressed with varying degrees of confidence that referrals to secondary care were being curbed by the schemes. The calculation of efficiency savings, however, was reported to be a highly complex process, requiring sophisticated analysis, the factoring in of costs of running the RMC, the provision of alternative services to which referrals were diverted and possible disinvestments in secondary care. Providers and commissioners described the challenges of both calculating savings and communicating the findings, which were, thus, open to interpretation.
[. . .] we’ve got a schedule [for calculating savings] [. . .], in the absence of anything more specific, we’re trying to quantify it that way. Now whether there’s a better or more sophisticated way of doing it, I don’t know [. . .] I think we’ll always be looking at our data, and how it’s presented, and whether there’s a more accurate way of looking at things. But, I think on the whole it’s convincing people that it’s a good thing, and it’s the right thing.
B1, manager CCG
The trouble with differing priorities
Effectively communicating success and a shared vision of what this looks like for a particular scheme was held by many to be essential for the scheme’s survival. The provider of one scheme recounted how its failure to meet the commissioner’s aim to centralise and standardise referral processes (owing to a number of practices opting out), combined with a lack of confidence in the figures demonstrating cost-effectiveness, meant that despite strong evidence of success (from the perspective of the providers) the contract for the scheme was not renewed.
[The CCG] took the decision [. . .] that it was more important to bring all the practices together under a common denominator, even if it was the lowest common denominator, rather than to [. . .] look at the evidence and purchase that which is known to be effective. We were bitterly, bitterly disappointed . . . [. . .] we were very well resourced, we fulfilled all our expectations, we got going, we saw the curve beginning to bend [. . .] The big, big problem was that we as leaders didn’t operate in such a way that others felt drawn in [. . .].
D1, manager, RMC provider
Discussion
Summary of findings
Professionals involved in the commissioning and provision of RMCs, and GP users of the schemes, described the wide range and evolving nature of their aims and functions. Practical and administrative difficulties, compounded by the need for schemes to evolve to meet changing needs, were reported to have a significant impact on their successful functioning. Achieving buy-in from, and sustaining relationships between, RMC stakeholders was both challenging (partly as a result of a lack of clarity in aims and implementation issues) and key to success. The perceived effectiveness of schemes, however, was dependent on their aims and priorities. Many schemes were judged successful by those involved, with reference to a range of outcomes (e.g. the collection of useful data, GP education and centralised and streamlined referral processes), despite limited evidence of reduced referral rates or cost savings.
Strengths and limitations
This is the first qualitative study to focus specifically on functioning RMCs. Building on work exploring approaches to referral management more broadly,194,198 this study includes successful and less successful schemes and a wide range of stakeholders, sampled across and within RMCs of varying scope and operational structure, allowing access to a broad range of perspectives, to explore the ways in which RMCs are intended to work and to seek to understand challenges to implementation and factors influencing perceived success. There are, however, a number of limitations. As only a small number of participants were interviewed in relation to each of the schemes, some of the findings may represent idiosyncratic views. In particular, it is important to note that many of the stakeholders interviewed had considerable investment in the success of their scheme. Furthermore, the fact that our sites were essentially self-selected means that they may not represent the experiences of a wider range of RMCs.
Discussion of findings
The wide range of aims and diverse models of operation of RMCs highlighted in this study is in keeping with observations previously reported in the literature. 194,195,198 The evolving nature of RMCs has also been noted. 194,198 One effect may be that there is a feedback loop between the context in which the programme occurs and the programme itself; so, being educated by the RMC on what is or is not appropriate to refer, GPs learn what constitutes an ‘appropriate’ referral or learn about additional facilities available in the community, and begin to send referrals that are more in line with what providers perceive they should be receiving. This in turn means that fewer referrals are diverted or rejected by the RMC, which can lead to a revision of the aims and function of the RMC. 223 The evolution of aims was also reported to influence the type of information that the RMC required, so, as functions evolved, IT systems sometimes made it more difficult to collect the data that RMCs needed to fulfil their renewed functions. Our finding that the aims of RMCs evolved over time is consistent with the tenet of realist evaluation that complex interventions are not universally successful but have a pattern of different outcomes depending on context. The consequence of this is that it may be difficult to precisely measure whether or not the intervention was a success if it is not clear either what the criteria for success are or that there are multiple criteria for success, some of which are more valued by one set of interests than by another. This means that one group of stakeholders can describe the RMC as a success by selectively focusing on one set of criteria and ignoring others.
The importance and challenge of stakeholder engagement in ensuring the success of RMCs has been highlighted in previous studies, with a clear focus on quality194 and the provision of good data198 identified as important ways to overcome cynicism and mistrust and to generate support. A key difference between the findings of this and other studies, however, is that concerns expressed about the centres with respect to issues such as introducing delays in treatment, interfering with the GP’s clinical judgement and restricting patient choice194,195,198 emerge as challenges to be overcome rather than inherent flaws in the functioning of the schemes. Our findings are consistent with those of Pawson et al. ,226 which show that clinical buy-in is gained if clinicians are given the power to have significant control over the aims and functioning of the RMC, which in turn means that the RMC’s remit meets clinical interests rather more than managerial ones. Our findings are also consistent with work that shows the tension between the managerial and clinical roles being adopted increasingly by clinicians following the most recent NHS reforms. 227 Sometimes, two sets of interests appeared to jar against each other, leading to a lack of clarity and confusion about the aims of the RMCs and potentially hindering their functioning. While GPs were in general sceptical and sometimes resistant to feedback, how feedback was given appeared to have a significant impact on how GPs responded to RMCs. Feedback could foster GP engagement when provided in a constructive or educational way, but lead to disengagement if provided in a critical or punitive manner.
With respect to the success or effectiveness of RMCs, this study was not designed to identify the impact of RMCs on patterns of referral. Nevertheless, reflecting the limited and equivocal published evidence from elsewhere on the effectiveness of RMCs,194,195,198 in most sites we found that interviewees were hesitant to draw conclusions with respect to the ability of the schemes to deliver on the aim to make better use of resources. This hesitancy appeared to result, in the main part, from the difficulties described in calculating, interpreting and communicating efficiency savings, requiring complex analysis, taking into account a broad range of outcomes and associated costs and savings (costs of running the RMC, the provision of alternative services to which referrals were diverted, and possible disinvestments in secondary care). For all of the RMCs, at least one stakeholder described improved patient care as an outcome, and a reduction in referrals to secondary care was reported for three out of four schemes. However, the leap required to explain how this represented better use of resources overall was seldom made, despite this being reported as an explicit aim by one or more stakeholders for all of the RMCs. In addition, the common sentiment that it was too soon to draw conclusions could be seen to reflect the fact that it takes time for the effects of the RMC to filter through to the wider use of resources in the health system and that a number of schemes had been up and running for only a relatively short period of time.
As well as considering the impact of RMCs on referral patterns, previous research has also suggested that such schemes improve referral quality;228 in keeping with this, our data suggest that the perception that RMCs improved referral quality was widely held by a range of stakeholders. This is an area in which further research is clearly needed. In addition to understanding the overall impact of RMCs on patterns of referral, it is important to determine their impact on GPs’ decisions on whether or not to refer, which type of clinician the person needs to be referred to and which local services can provide that care.
Implications for practice
The findings of this study have a number of implications for the development of similar schemes. First, clarity of aims and shared understanding between stakeholders are essential to get engagement and buy-in, and this necessitates the early involvement of GPs in the development of the schemes. Second, although indicators of success should be agreed between stakeholders from the outset, it needs to be acknowledged that schemes are likely to change over time. Third, the evolution of schemes needs to be anticipated and plans need to be made for potential modifications to referral processes, including IT systems, and for the effective communication of changes to relevant stakeholders.
Chapter 4 In-house review of referrals (substudy 2)
Introduction
In-house referral systems rely on some form of internal peer scrutiny of referrals within a general practice before the referrals are sent on to secondary care. These schemes have some elements in common with the other two types of scheme described in Chapters 3 and 5, in that they are designed to limit referrals and practices may receive a financial incentive to take part in the scheme. However, they differ in that the process is internal to the practice and involves discussion of referrals between GPs working in the same practice.
Peer review of referrals can take a number of forms, including obtaining a second opinion on the patient from another GP prior to referral,191,192 discussing the appropriateness of referrals on a weekly basis179 and individual GP reviews of each other’s referral letters. 229 Based on the evidence available, comparing a number of different referral management approaches, Imison and Naylor concluded that ‘Peer review and feedback alongside the use of guidelines and structured referral sheets appears to offer the greatest hope of a cost-effective approach to referral management’. 194 However, as set out in Chapter 2, there is limited published literature on this topic.
Give the paucity of published literature, our aims in undertaking this substudy were to study a number of schemes currently in operation in GP practices. The specific aims of this substudy were:
-
to describe the schemes which have been implemented and the aims of these schemes
-
to describe the positive and negative outcomes from such schemes, as perceived by those working in the practice
-
to describe the potential effectiveness of the schemes in reducing unnecessary referrals to secondary care.
Methods
The purposive sampling of CCGs or practices operating peer review of referral schemes was done through searching the internet and recommendations from members of the project team, advisory board and interviewees to whom we had already spoken. We also invited responses from those involved in such schemes by advertising in Pulse magazine; however, we received no response to this advertisement.
In each CCG or practice identified, we contacted a CCG or practice manager with the request to interview three participants in the scheme, including, ideally, someone with management responsibility for setting up or running the scheme and two GPs who took part in the scheme. Participants were informed by e-mail about the study, and consented to take part in an interview. Interviews were conducted face to face (n = 2) or by telephone (n = 8) according to convenience and participant preference, with each interview lasting approximately 30 minutes. Permission was sought to audio-record the interview and informed consent was recorded verbally. The interviews were conducted following an interview schedule, which included questions about the design of the system of peer review of referrals, the aims of the scheme, any changes in the scheme since it was initiated, acceptability, outcomes and local context. The full interview topic guide is included in Appendix 5.
The interviews were transcribed verbatim and transcripts were kept on a secure server with restricted access only to the core research team. The transcripts were read and reread and coded manually by a single researcher. Initial codes were drawn from the interview topic guide and additional codes were added as they emerged from the data. As analysis progressed these codes were organised into overarching themes.
Based on advice from the National Research Ethics Service and the Local Research Ethics Committee, the study was deemed service evaluation and we did not obtain formal ethics approval, although we sought to adhere to good research ethics practice throughout.
Results
The peer-review schemes
We interviewed stakeholders of three different peer review of referral schemes. Schemes 1 and 2 were implemented at GP practice level, and, in each of these, three interviews were conducted with GPs working at the practice. The third scheme studied was discussed at the CCG level, and here peer review of referrals within individual practices was one element of a wider CCG-level referral management initiative which also included the introduction of a RMC. In this third scheme, four interviews covered the referral management initiative as a whole, and discussion of peer review of referrals formed a section of these interviews. These four interviews were conducted with a manager at the RMC provider organisation, a manager at the CCG, a GP with managerial responsibility at one practice and a practice manager at a second practice.
Each of the three schemes studied conducted peer review of referrals in a different way. The key characteristics of the approaches to peer review of referrals at the three schemes are summarised in Table 22.
| Referral scheme design | Scheme 1 | Scheme 2 | Scheme 3 |
|---|---|---|---|
| Initial referral decision | Made by consulting GP | Made by consulting GP | Made by consulting GP |
| Referral decision documented | Referral letter | Referral letter and pro forma | Not known |
| Referrals reviewed | All referrals not categorised as urgent or 2-week wait referrals | All referrals not categorised as urgent or 2-week wait referrals | Only those referrals for which the referrer has doubts about the need for referral |
| Referral review format | Lunchtime meeting twice per week, more flexible review by partners between meetings | Two GPs review the referrals from the previous day each morning | Informally on a daily basis or in weekly practice meetings, depending on the practice |
| Reviewers | All present in practice meeting | All GPs, two on each day | Other GPs present at informal meetings, e.g. coffee time, or all present in practice meetings, depending on the practice |
| Final decision-maker | Reviewers | Consulting GP | Consulting GP |
| Time scheme has been in operation | 3–4 years | 7–8 years | 1–2 years |
Across all of the schemes, the management of the patient was discussed with GP colleagues, and changes to the initial referral plan were suggested where needed. Changes might include a change to the referral pathway such as referral to a local GPwSI or another GP in the practice, or suggestions of further treatment by the GP before referral. The peer review also allowed the team to make sure that referrals were in line with the local system guidance and any pre-set thresholds, for example conditions that needed be met before patients would be considered for surgery.
Aims
Although the aims of the schemes were relatively similar, there were differences in the way in which these aims were perceived and communicated. In all schemes there was an aim to ensure that referrals were appropriate. In some cases this was due directly to pressure from the CCG (formerly PCT) to reduce referrals. In scheme 3 an additional aim of the overall referral management initiative was to increase referral to community services, where appropriate, rather than referring to secondary care services.
The primary aim was to look at the pathways of care but particularly with a financial focus on it of commissioning community pathways that were only at two-thirds of the tariff of the traditional secondary care pathway.
Scheme 3, participant 1
In other cases, together with the need to use NHS resources appropriately, there were explicit aims of improving quality for the patient, of ensuring that patient referrals went down the right route in order to improve patient care and, possibly, of reducing delays.
Benefits
In addition to the reduction of inappropriate referrals, and hence cost containment, interviewees reported a number of benefits from the peer review of referrals.
One major area of benefit of doing the scheme was in learning from the review process. GPs reported that it enabled them to share experience between doctors and that it was educational, not only in terms of understanding alternatives for addressing the patients’ needs, but also in that the process helped with understanding the options for places to refer ‘it gets us better at sending them to the right place’ (scheme 1, participant 2). GPs were also able to learn more about the skills of others in their practice. For some GPs it also ‘helped me appreciate that part of my responsibility is to manage the resources’ (scheme 1, participant 1).
A particular benefit was seen for trainees in the practice. The schemes enabled trainees to receive feedback on the referrals that they made and was ‘another way of them being exposed to more and more patients and the outcomes from looking after them’ (scheme 1, participant 2). One interviewee reported that as a registrar she had found attending referral meetings very educational.
A further benefit was the increase in interaction with other GPs making for a more open atmosphere in which people felt happy to ask one another’s advice. In scheme 1, in which referrals were discussed in the practice meeting, the process had encouraged many more informal conversations, with doctors discussing their patients with one another. It was suggested that this was in part because people wanted to avoid their referrals being rejected at the meeting stage.
I think one thing that’s probably happening is a lot more corridor conversations, discussions in the clinical meetings certainly; I’m thinking of referring this patient, what do you suggest I do; so on a rather much more informal basis things get discussed.
Scheme 1, participant 2
In addition to the above benefits, in all schemes the GP practices were incentivised in some way to take part in the referral scheme through a local enhanced service or other agreement with the CCG or Local Commissioning Group (LCG).
Disadvantages
There were a number of disadvantages to introducing peer-review of referrals scheme, although most interviewees appeared to feel that the advantages outweighed these. One disadvantage was the time taken to review referrals. The time needed depended on the way in which the peer review of referrals was set up, with estimates of approximately 30 minutes of time for each GP each week, as well as the additional administrative time required to process the referrals.
I often get home very late and I think to myself ‘well if we didn’t have this special meeting, I would be able to get home to read my son a bedtime story’; and that’s the downside.
Scheme 1, participant 3
Another concern was the delay between making a referral and the letter being sent out. This delay depended on the method used for review. In the case where all referrals were reviewed the following day (scheme 1) the delay would be only 1 day, but it could be up to 1 week where referrals were reviewed at meetings. However, this delay was thought to be low in comparison with the typical waiting time for the outpatient appointment to take place.
In schemes 1 and 2, GPs reported that they sometimes felt a little uncomfortable, or simply that it was daunting, making suggestions to a more senior partner.
[I]t was uncomfortable and really quite difficult to turn round to a senior partner and say, ‘well actually have you tried this or that?’.
Scheme 1, participant 3
Impact of the scheme on patients
The impact of the scheme on the patient differed between the scheme in which the discussion of the review group was final (scheme 1) and the other two schemes (schemes 2 and 3) in which the final decision on whether or not to refer lay with the initial referring doctor. In scheme 1 GPs felt that the application of the peer-review scheme meant that the process was not very patient centred, and they described patients occasionally being upset when they were ultimately not referred: ‘probably once a month or more patients get upset’ (scheme 1, participant 2). However, another GP commented that patients generally understood when the process was explained. Interviewees also described how referring to a decision made in a practice review meeting could be used to help maintain the relationship with the patient, as the patient realised that decision came not from the individual GP alone, but from the colleagues who had discussed the referral. One doctor commented, ‘I’ve learned some specific communication skills around referral decision-making’ (scheme 1, participant 1).
In schemes 2 and 3, in which the review of referrals was used to provide advice and suggestions only, and the decision to refer lay, ultimately, with the individual GP, there was much less of an impact on patients and there was no mention of complaints from patients. GPs commented that patients were largely unaware of the scheme unless it became necessary to suggest changes to their referral: ‘majority probably not aware that there is a referral system in place’ (scheme 2, participant 1). In these cases patients were often pleased that they were receiving additional attention: ‘They quite like the idea that their problem is worth maybe a second or third opinion from another GP’ (scheme 3, participant 3).
Effectiveness
Interviewees’ opinions on the effectiveness of the scheme were obtainable for schemes 1 and 2, which had been in place for several years. In both of these schemes, benefits were reported. In the opinion of one of the interview participants from scheme 2, when the review scheme was initiated up to 20% of referrals received useful comments through the review, and in scheme 1 up to 20% of referrals were reportedly diverted or stopped. However, as the scheme has continued referral behaviour has changed and the effectiveness of the scheme in terms of changing behaviour or making alternative suggestions about referrals has gradually dissipated. In both cases the interviewees reported that < 5% of referrals now needed advice about alternative procedures. A GP from scheme 2 commented that the process ‘could be something that you don’t need to do forever’ (scheme 2, participant 1) once you had built in the self-discipline of referring based on guidelines, referral thresholds and not referring unnecessarily.
Integration with other referral management systems
In none of our cases was peer review of referrals the only referral management scheme in place. In scheme 1, some referrals could be passed to GPwSIs, for example a musculoskeletal pathway and a mental health pathway. In scheme 2, interviewees reported that musculoskeletal referrals were triaged by a musculoskeletal group and ENT referrals were looked at by a GPwSI. In scheme 3, the peer review of referrals preceded the direction of a large proportion of referrals to a RMC.
Discussion
This substudy showed potential benefits from in-house review of referrals. These included ensuring that the most appropriate referral pathway had been selected and that local guidelines had been met, in both cases by sharing knowledge of local options among GPs within the practice. In-house review of referrals also had the benefit of increasing communication between GPs and opportunities to learn from each other’s clinical practice. Interview participants reported that the main impact on referrals was in the early stages of the schemes, with less impact as time went on (possibly because GPs gradually adopted common standards and guidelines for referral).
There is a significant cost to in-house review due to the time required for review, especially where all referrals are reviewed by another GP before being sent out of the practice. The three schemes considered all included specific financial incentives for the practices to take part. However, the review of referrals studied in this substudy would be less resource intensive than in-house referral of patients for a second opinion, as tested previously. 191,192
One of the benefits of group practice is the ability for GPs to learn from each other. However, opportunities are limited during the busy working day. In-house reviews of referrals are one opportunity for this learning to take place, either through discussion at team meetings or through the review of outgoing referral letters.
Strengths and limitations
This was a small exploratory study of only three purposively sampled peer review of referral schemes. The schemes investigated were found to work in different ways, and there may also be other variations to the models presented here. We conducted three or four interviews per scheme, which included those who had been responsible for setting up the scheme as well as those working within each scheme; however, the small number of study participants means that the views reported here may not be representative of other schemes. Future research would benefit from further examination of the data on changes in referral numbers and destination over time (as well as other potential benefits such as education), together with a more thorough assessment of the cost-effectiveness.
Chapter 5 Financial incentives to reduce referrals (substudy 3)
Introduction
In our original application, we identified a need to determine whether or not practices had explicit financial incentives to reduce referrals, as this would present them with potential conflicts of interest in terms of providing optimal care for their patients. We indicated at the time of the grant application that we were not sure if such schemes would come into operation, although they have existed in other countries in the past, for example during the initial introduction of the managed care schemes Health Maintenance Organisations in the USA. 230,231 However, the issue was important, as it was at least possible that general practice incomes would in future in some way relate to the financial performance of CCGs. So, even if there were no direct incentives to reduce referrals, it was possible that indirect incentives would exist as they did in the time of GP fundholding, when individual practitioners were able to benefit financially from reducing referrals, even though, in principle, ‘savings’ had to be spent on improving patient care.
Methods
When Quality Premium: 2013/14 Guidance for CCGs232 was published in 2013, it became clear that none of the performance indicators being passed down from NHS England related to outpatient attendance (in contrast to a focus on reducing inpatient care). It was, therefore, unlikely that we would find direct financial incentives to reduce outpatient referrals being passed down to GPs.
We therefore contacted 12 CCGs to ask about financial incentives for GPs to reduce referrals. Four replied, and two were willing to share the actual agreements they made with practices so that we could see how referrals were being addressed in formal CCG–practice contracts.
Based on advice from the National Research Ethics Service and Cambridgeshire Local Research Ethics Committee, the study was deemed service evaluation and we did not obtain formal ethics approval, although we sought to adhere to good research ethics practice throughout.
Findings
The CCGs that replied all fed back information on patterns of referrals to their GP practices. This is a continuation of feedback that all PCTs have been providing for several years. Feedback may or may not include statistical analysis, such as funnel plots to identify practice outliers. None had or were planning to have financial penalties or rewards relating specifically to reductions in outpatient attendance. However, they all encouraged practices to look critically at their referrals, for example by regular in-house review, though they were not generally associated with financial incentives.
Most frequently, the requirement to review referrals is not written into an agreement with the practice, but we identified six LCGs within one CCG in which there were specific financial agreements relating to reviews of referrals. We reproduce a summary of the criteria from these agreements in Box 1 as examples of the types of behaviour which CCGs are trying to encourage.
-
Practices are required to comply with the CCG clinical thresholds policies for referrals, including, where required, the proactive use of clinical pro formas. Practices should refer to the clinical thresholds policies prior to referral, to ensure compliance.
-
In addition, practices are required to actively review referral/secondary care utilisation data and to develop specific action plans or submit queries via the LCG management team as appropriate. Trend over time data will be provided by the LCG team on a monthly basis.
The practice agrees to:
-
receive and review practice specific referral, activity and budget monitoring reports each month, including prescribing budget and performance information
-
adhere to the LCG Prior Approval Policy for low-priority treatments/procedures, including completion of threshold checklists and pro formas for conditions/procedures covered by the LCG referral policies, where they exist.
Member practices undertake to:
-
develop and sustain a referral review system within the practice and be able to demonstrate that such a system exists
-
review monthly budget reports and data, validate as far as possible with the advice/support of LCG data analysts and send queries to the LCG
-
in the event of the data showing that a practice is an outlier, the practice should take action with the collaboration of the LCG to analyse the data and produce remedial action plan if there is evidence of inappropriate variation
-
ensure that locally agreed referral pathways/thresholds and pro formas are readily available and used by all clinicians working in the practice.
-
Member practices undertake to develop and sustain a referral review system within the practice and be able to demonstrate that such a system exists.
-
The practice will be set an objective based on their referral activity and will be asked to produce and implement a plan to fulfil the objective as part of their Annual Plan.
-
Through prospective referral meetings in practice, GPs should review the appropriateness of referrals with a view to reducing variation in referral rate through clinical engagement. The aim is to reduce the variation in GP referrals across the LCG.
-
Ensure that the most appropriate local pathway is used when referring a patient to another health professional by using the Advice and Guidance clinical decision and referral software, once available.
-
The practice will provide the referral lead with a practice plan (2013–14) for referral review and monitoring.
-
The practice will undertake prospective, systematic and regular practice-based peer review of referrals. The practice will code all referrals using the codes as specified by the CCG board.
-
The practices will meet every 2 months with the referral lead and will send an e-mail report to the referral lead before each meeting to update him or her on any referral management work done.
The GP practice agrees to:
-
receive and review practice specific referral, activity and budget monitoring reports each month, including prescribing budget and performance information
-
adhere to the LCG Prior Approval Policy for low-priority treatments/procedures, including completion of threshold checklists and pro formas for conditions/procedures covered by the LCG referral policies, where they exist.
Discussion
At present there appear to be no direct or indirect financial incentives for practices to reduce outpatient referrals. The focus of the CCGs’ approach is to encourage practices to review data on patterns of referral. This appears to be a common pattern across the NHS, encouraging clinical audit but without any incentives that would result in clear conflicts of interest or present a significant risk of serious unintended consequences.
In Chapter 4 we described schemes in which practices have been given a financial incentive to undertake formal in-house review of referrals.
Chapter 6 Specialist services in the community: a qualitative study of consultants holding novel types of employment contracts in England (substudy 4)
Introduction
There are strong policy and service drivers in England to prevent avoidable hospital referrals and admissions and treat people closer to home. 233 In England specialists traditionally work in hospitals for both inpatient and outpatient work and are employed by hospitals (called ‘acute trusts’ in the English NHS). Traditional attempts to relocate specialist services in the community and reduce demand for hospital outpatients have included shifted outpatient clinics and attachment of specialists to primary care teams. Evidence suggests that such arrangements can improve access to care but that the impact on hospital use and health outcomes is less clear. 5,39,90 In the case of specialist attachment to primary care teams, few evaluations have been reported but evidence suggests that they may be costly and depend greatly on the enthusiasm of individual specialists. 93,94 One of the limitations of the traditional means of relocation of secondary care to primary care is that specialists have, in general, remained employed by acute trusts and as such may have little real incentive to reduce referrals. In practice, they have become drawn back into hospital work, reducing the extent to which they develop new means of working with primary, secondary and social care providers to improve care pathways. 21
There are an increasing number of novel arrangements for consultants in England, whereby consultants are contracted solely or for the majority of their time by a community trust. To our knowledge such arrangements have not been the subject of previous research and the extent to which consultants are working in these ways and the impact of these contractual arrangements may have on patient care, the consultants themselves and the wider workforce are not well understood. Given this lack of research, this exploratory study had the broad aim to understand the potential benefits and limitations of these new contractual arrangements. We sought to focus on the perceptions and experiences of community employed consultants rather than to measure their effectiveness. Increasing understanding in this area may provide important learning, particularly at a time of financial pressures to reduce referrals and increased focus of health services on community-based care and on integrated care. 234
Methods
A qualitative approach using semistructured interviews was adopted, with interviews conducted between November 2013 and May 2014.
We focused on specialties that have to date been largely hospital-based specialties in England. There is no routine source from which to identify consultants who hold at least part of their contract with a community organisation, either as direct employees or through subcontracts from an acute trust, which was our primary eligibility criterion. Hence we used opportunistic sampling to identify individual consultants and snowballed from there, asking participants to suggest other potentially eligible consultants. This led to an initial focus on geriatric and respiratory medicine (RM). We then deliberately sought palliative medicine (PM) as a third specialty, anticipating that there would be sufficient numbers of consultants in PM with a community-based contract, to see whether or not themes arising from the initial interviews would apply to another specialty. These consultants were recruited by means of an advert placed in the Association of Palliative Medicine’s newsletter. In our sampling, we attempted where possible to ensure a range of participants according to employer organisation, geographic setting and stage of consultant career.
The purpose of the study was explained to all potential participants at point of first contact and again before commencing the interview. Verbal consent was sought to participate and to audio-record the interview. Interviews, conducted by EP or MR, were typically conducted by telephone. A common interview guide was used in each interview, although emphasis was placed on allowing participants to talk from their own perspective. Driven by the research aims, questions were designed to understand the nature of the role, what works well or less well with the post, experience of working with colleagues in the community and acute trust, and training and recruitment. The interviews were transcribed verbatim and the names of participants were removed. The transcripts were read and reread and ‘codes’ were applied to meaningful sections of texts. As analysis progressed, these were organised into overarching or organising themes using the qualitative software NVivo. Analysis was led by one researcher (EP) but discussed frequently between EP and MR while data collection was ongoing so that themes arising could be probed further during interviews. Where it was not possible to audio-record the interviews, full notes were taken. As agreed, we checked the use of quotations with participants before publishing these findings. Quotations are presented with participant number and clinical specialty (given as GM for geriatric medicine, RM for respiratory medicine and PM for palliative medicine).
Based on advice from the National Research Ethics Service and Cambridgeshire Local Research Ethics Committee, the study was deemed service evaluation and it was not deemed necessary to obtain formal ethics approval; however, we sought to adhere to good research ethics practice throughout.
Results
We completed 14 interviews (3 in person and 11 by telephone), 12 of which were audio-recorded (all except GM 01 and RM 10). All participants were consultants (full- or part-time), with seven working in geriatrics, three in RM and four in PM. Employment arrangements varied by individual and in many instances these had undergone different iterations with changes in community organisations over time. In general the interviews were a very rich source of information. The consultants were eager and willing to talk about their experiences, reflecting their commitment to community posts, challenges encountered and concerns for sustainability. A number of themes arose in the analysis, which we outline below.
Origin and development of posts
A clear theme was the importance of individual commitment and motivation to both creating and shaping posts which were often largely unspecified at outset. For most of the consultants we spoke to, the motivation reported for taking up a community-held contract was part of a wider vision that more community management would better meet the needs of patients and a view that a population perspective was preferable to a disease or condition focus, which they felt was more prevalent in acute care.
For a number of years we’d been developing the community service . . . and that’s what my interest was, the repetitive and, I felt, rather fruitless nature of acute care, we don’t actually fix anything. The patients just come back again and again and again because you never actually address the underlying issues and you patch them up and you send them out with very little result. Also, a lot of patients you get admitted, you think, ‘Well, had I known about this patient 6 months ago, I would have done something so they wouldn’t be here now’, and so the trust over the last 10 years has been developing community service to meet those needs of frail, older people and having set up the services to supply them, I was then able to transfer my contract across in order to provide the consultant leadership and medical specialist input to those services.
GM 08
This said, in addition to the motivation of consultants who created the posts, what they wanted had to fit with the agendas of the organisations with whom they were negotiating. In the case of several geriatricians, the creation of posts was agreed only when community trusts had calculated that it was financially preferable to directly employ consultants in community roles rather than pay the capitation fees associated with acute trust employees providing community sessions. Other examples from RM were where trusts were particularly committed to a larger vision of integrated care and creating new pathways for patients.
It’s got to be part of the organisation agenda, it can’t just be, you can’t be individual people kind of swimming against the tide . . . yes I think it’s all about whichever organisation it is, investing in this is the right way to do things and supporting it.
GM 04
It was similarly evident that consultants had a lot of scope in shaping and developing individual posts once these were created, often speaking of the notion of starting ‘with a blank sheet of paper’.
Well when I first started I had this sort of, I had a telephone and blank diary, that’s how much they knew what to do with me. No induction, no thinking, nothing in the diary, just that was it.
PM 14
I think that just depends on your attitude really. My experience is that when I first came I wasn’t at all busy because nobody quite knew how to use me as you rightly say and now I’m incredibly busy ‘cause you do literally have to go looking for work.
GM 02
Although consultants described having a free rein to develop their posts, the main components of posts, developed over time, were similar for consultants across the three specialties: clinical, strategic and educational. These are shown in more detail in Table 23.
| Area of responsibility | Description of role | Examples of implementation |
|---|---|---|
| Clinical | Clinical responsibility for own caseload or managing others with caseload | In-reach ward rounds |
| Outpatient/community clinics (single specialty or joint with other specialties) | ||
| Domiciliary visits | ||
| Hotline service for patients | ||
| Supporting nurse specialists holding caseload | ||
| Multidisciplinary team meetings/complex case reviews | ||
| Strategic | Developing pathways or models of care | Development of patient pathways |
| Improving working practices between GPs and nursing homes | ||
| Developing strategic partnerships, e.g. across specialties or with third sector | ||
| Educational | Educating GP and wider community-based workforce in what community consultant can do | Visiting individual GP practices |
| Providing specialty-specific education to GPs and others to improve management in primary care | Condition-specific review of diagnoses and management in GP practices |
A number of consultants reflected that the lack of specification for their roles was, potentially, liberating and that they could often achieve a lot without the organisational constraints that might normally be present.
I had nobody bearing down on you saying, I need you to do this by next week, or you know, you’re accountable for that, nobody had a clue, so I just did what everybody’s obviously very pleased with now, so it was, in a way, it was completely unsupported and on the other hand totally free, and the pressure came from within ourselves to do a good job.
PM 14
Significance of where contract was held
Some interviewees reflected that it did not matter where their contract was held – ‘Who holds your contract is much less relevant than the job that you do’ (GM 02) – but for others it made a key difference. One consultant was able to directly compare being a community geriatrician contracted to an acute trust with being contracted to a community organisation and the fundamental difference in these roles.
I think at that time [when contracted to acute trust] I would say, one still felt like a hospital doctor because one was based at the hospital and did all the same tasks and roles that all the other hospital consultants were doing so it was really like a sessional commitment to the community work, if you like . . . it’s [the new post with the community trust] not just about turning up and doing a service, a lot of it is about changing culture, upskilling people, you know, looking at attitudes and the belief statures in community workers, the rehab teams, the nurses, the GPs.
GM 06
The tension that could be created as a result of where contracts were held was further evident in instances where consultants were still employed by an acute trust but subcontracted to a community trust.
So the main problem is that you’re working for two diametrically opposed trusts. So on the one hand what I’m doing is keeping people out of the acute trusts as much as I can and if you . . . I was given a free rein I could really, you know, decimate their income. Whereas, on the other hand I actually am fully employed, my contract is held by the acute trust and they’re telling me all the time to be mindful that I actually work for them. And that I have to be careful that I don’t, sort of, disrupt the apple cart too much, that I don’t want to take away too much work.
RM 09
Centrality of relationships and understanding of role
As noted, consultants described that an important part of their role was in educating GPs and the wider community workforce. It was clear from the interviews that forming good relationships, particularly with the GPs, was central to the success of the community consultant role and could be one of the more challenging and rewarding aspects of the role. In doing this the right balance had to be sought between supporting GPs and ensuring that they were aware of what a community consultant could offer and, at the same time, being careful not to cross professional boundaries.
I really regard myself and my service as a supplementary service, it’s a, sort of, complementary service to general practice, it’s not parallel and we mustn’t be seen . . . we mustn’t, (a) be seen to set up a parallel service to primary care because we need primary care to make it work and (b) if it’s . . . There isn’t enough of capacity in community geriatrics to do primary care as well.
GM 03
I think it’s working alongside your referrers, understanding what they need from you, understanding their challenges, their constraints and valuing their skills very much. Certainly, in the community, you have very skilled GPs and it’s understanding their skills. They don’t want people to come and take over, they want people to help and support them and skill them and help them with the complex cases and I think it’s about building up those relationships.
PM 11
Consultants reported a range of different strategies that they might adopt to try to build such relationships, including regular visits to GPs, providing GPs with own mobile number and using opportunities such as national initiatives or changes in guidelines to build educational events for colleagues in primary care. These strategies were generally adopted and adapted over time by individual consultants, although one reported that their local CCG had instigated a pairing scheme between consultants and GPs that was a useful forum to build relationships and plan more proactively and strategically.
For some, relationships with hospital-based colleagues were as important but also challenging. Among the consultants in GM and RM whom we spoke to, there was often a perception of a ‘them and us’ mentality and a perceived lack of understanding among hospital-based colleagues of what community-based consultants could do, and also, in some cases, that community consultants were not accorded the same status.
Community is like being . . . they would say it’s like being a GP. They feel perhaps that you’re not a proper . . . it doesn’t have the buzz and the adrenaline and the status of being a secondary care doctor, I think but I think that’s got to change because in actual fact I think that what I do is far more influential than what they do now.
RM 09
Consultants often reported that relationships with the acute trust were helped when they had previously worked for the trust or where they knew colleagues well. These consultants often made deliberate efforts to interact with hospital-based colleagues to maintain these links, though this was considered more challenging for new consultants.
The perceived gap between community and acute services was reported to a far lesser extent among the palliative care consultants we spoke to, perhaps because PM has traditionally had closer relationships with community-based services. In some cases, very close working relationships were reported with hospital-based colleagues.
Potential professional isolation
A common theme across the three specialties was that community consultant roles could be potentially isolating; the relative freedom to work on one’s own and shape the role was countered by feelings of professional isolation.
It’s quite [an] isolated job and isolating. It’s very much I think you have to be quite self-contained because actually I’m pretty much on my own. So there are no other doctors as such around me which can be tough sometimes.
GM 03
You know, I was lonely. I had another colleague who was working the other end of the patch and we obviously used to see each other, but I didn’t have that buzz of having lots of people around. I’m surprised at that, that was one of the challenges, I think, to be a bit more isolated.
GM 07
Particular difficulties that consultants faced was not having a similar colleague close by with whom they could check decisions, the opportunity to attend educational meetings regularly and, for some, the ‘buzz’ associated with working in a specialist team. However, interestingly, one consultant (GM 06) reflected that, having established relationships within the community, this provided a more stable and a closer team than she thought could be achieved in a hospital setting. The degree to which consultants felt isolated varied, but a common idea coming from the interviews was that ‘resilience’ was a key characteristic needed in the role. Most of the strategies adopted to try to mitigate isolation were individually driven. For example, consultants would arrange to meet regularly with colleagues in neighbouring areas or in acute trusts, would identify educational opportunities, or would seek to do some on-call duties to keep them in touch with consultant colleagues. In some cases, where community teams had become established, these arrangements had become more formalised over time. Often, consultants would go to considerable lengths to travel to meetings because of the benefit and interaction that they brought.
I could probably get [the substance of the meeting] from somebody else telling me in 10 minutes, but actually I go because other consultant colleagues go, which is a bit sad, essentially it’s my only opportunity in a week to hopefully, they’ll be somebody else there, and I might just speak to them for well, 1 or 2 minutes but at least you’re hearing what other people are saying about various clinical situations, you’re kind of making sure that you’re staying up to date, and you know, having the same challenges . . .
PM 14
In one case, the potentially isolating nature of the community consultant role had partly contributed to a decision to move the main contract of employment from a community trust to the acute trust so that more support was available.
Training, preparedness and sustainability
In trying to understand how the skill and training requirements of community-based consultants might differ from those needed in more traditional hospital-based roles, participants consistently identified three things that were perhaps not unique to community roles but areas in which greater emphasis was needed. These were (1) having a greater acceptance of and ability to manage risk, as access to investigations is often limited; (2) having the ability to build and work effectively in diverse teams covering specialty care, primary care, social services and others; and (3) managing a patient holistically, often in his or her home, rather than by the nature of their diagnosis (Table 24).
| Skills areas | Quotation (interview ID) |
|---|---|
| Acceptance and management of risk | [Y]ou’re having to accept that you’re taking greater risks in some ways. And also I think it’s almost going back to your basics, your clinical skills cause that’s what you rely on. Because you can’t always get everything else around you to say well actually it’s not x, y and z. Which might not be a bad thing but it’s a different way of workingGM 03 |
| Team work | Communication is a huge one, managing a team is another big one, you know, being able to work well within a team environment and being able to trust your other team members is absolutely keyRM 09 |
| Holistic management of patients at home | . . . the biggest point of learning is to think much more broadly than simple medicine. So it’s dealing with the whole psychosocial components of a presentation because in frail older people living in the community simply fixing the medicine doesn’t solve their issues, doesn’t solve the problem, more broad base problem-solving approach, than you would traditionally get in acute medicine, so it’s much more challenging. That’s what makes it interestingGM 08 |
| And I have a much better insight into, you know, how difficult it is assessing somebody at home sometimes. You know you’ve got the dog or you’ve got whatever and trying to examine abdomens, it’s very hard at home. Yes, all of those things is very difficultGM 03 |
Of the three specialties we covered, PM training routinely involves a community-based component, and it was evident from the interviews that consultants in PM generally felt better prepared for work as a community consultant than did the consultants in geriatrics and RM.
I think I did feel prepared to work in a community post because of the experience that I’ve had. So, you know, when I started I was already very clear how I would work, how I would write to GPs . . . how it would all be set up. So I think that felt a very easy transition . . .
PM 13
Despite this, challenges remained in maintaining training positions in community organisations for palliative care, particularly in a financial climate where trusts had to make efficiency savings. The other two specialties, however, seemed to face more fundamental challenges to creating training posts and in attracting high-quality candidates. In some cases it had been possible to set up a purely community-based training opportunity, whereas in others consultants were reliant on trainees choosing to spend some of their training in the community, which could depend on their acute trust releasing them to do this. One of the challenges that participants thought was preventing more interest in community-based posts was the perception of the low status of community-based consultants within the professions.
So one of the other main challenges that you have of course, is overcoming the perception that community care or integrated care is a Cinderella-type specialty, sort of, a bit tree huggy and a bit, you know, this isn’t really respiratory medicine it’s all primary care type nonsense. In the past there has been a perception that the people that do these sort of roles are the ones that can’t get a proper job.
RM 09
The consultants we spoke to were clear that where there was a lack of training opportunities this had a knock-on effect on recruitment, and raised real concerns about the sustainability of community-based posts, even in areas where there was good support for the posts and where they were highly valued.
It’s a huge, huge problem for us and when my colleagues in [neighbouring area] wanted to recruit some similar sorts of post to do the same thing for their service . . . they advertised several times with no success at all . . . So we have tempered our expectations and are trying to advertise posts sort of half and half, with limited success . . . So they’re [trainees] comfortable in the hospital, they feel that’s what their training has provided them with and they don’t know what to do in the community.
GM 08
Discussion
Directly employing or subcontracting consultants to community organisations offers, in theory, a number of potential benefits over more traditional means of relocating specialist services in the community. Our exploratory study showed that consultants believed that such working arrangements offered greater potential to take a population perspective, to treat patients in a holistic sense and to form good working relationships with GPs and other community-based colleagues in order to improve care for patients. However, our findings also highlight a number of challenges to these new models of working. Community consultant posts are often idiosyncratic. Consultants, particularly within geriatrics, reported that they had often taken forward the vision to create their own post and were responsible for shaping their post. Although this offered flexibility and a certain degree of freedom that consultants welcomed, the lack of clarity regarding roles clearly presented challenges. Consultants could feel isolated, as it took time for community-based professionals to work out how to work with them, while at the same time they experienced isolation from hospital-based colleagues. Concerns were also raised around the longer-term development and sustainability of community-based posts because of the lack of training opportunities or recognition of such posts within career development opportunities. The experience of consultants in PM, in contrast to those in GM and RM, was that a community-based component within their specialist training prepared them well for the requirements of community-based posts and added legitimacy to their career choice.
In literature drawing on sociology of the professions, issues of identity and negotiation of boundaries has highlighted some of the challenges with previous policies around workforce modernisation in the NHS in England. 235,236 In terms of increasing specialist provision of care in the community, these have typically provided for role expansion through vertical substitution of tasks,237 for example through GPwSIs or specialist nurses. 235,238,239 These studies suggest that it may be particularly important to understand inter- and intraprofessional boundaries and that the reconfiguration of professional roles may be limited or slow to take place in the NHS if professional identity is threatened too strongly and the development of new roles is not supported institutionally, for example by professional bodies. 235 In our case, the concern was less to do with vertical substitution and more with regard to ‘diversification’ within selected specialties, as consultants with community-held contracts represent a novel approach to practice, providing services in new ways and in a different setting. 237 Contrary to more traditional models of relocating specialist services, consultants in our sample did seem to feel that they had developed new ways to collaborate with GPs which acknowledged their expertise, and that they were not looking to merely extend a model of hospital care in a community setting. 237,240,241 This said, our findings suggest that issues around professional identity may also be important and that inter- and intraprofessional, including intraspecialty, relationships may be crucial to understand. Previous research has highlighted the perceived status and superiority gap between generalists and specialists in the community but, in the context of community-based contracts, our findings suggest that this gap may be equally significant between hospital and community-based specialists. 240 Similar to the studies of the early introduction of nurse specialists, our interviews showed that consultants, particularly in GM and RM, may themselves be unusual and individually driven to create or move into these diversified roles. 235 Similarly, too, in these specialties, they appeared at times to be unsupported by their collective profession and had to be very self-driven in terms of seeking education, supervision and development opportunities. PM provided an interesting example of where community roles had been more formalised into career development and training. Yet still, even for consultants in this specialty, isolation could be a factor. Interestingly, the consultants we spoke to often consciously traded off this isolation with perceived freedom from organisational constraint. As these posts continue to develop, it will be important in future research to further understand consultants’ professional roles and the degree to which these may be compromised or strengthened by their location in the community, and the impact this has on practice.
Although exploratory, our research suggests that the idiosyncratic nature of some of these posts and the lack of clarity around roles may create challenges in the long term, and without any kind of ‘blueprint’ for how these posts should develop there may be missed opportunities for learning and building on experience. There are benefits from these posts remaining relatively unbounded in terms of developing a more flexible workforce. Yet greater formalisation or codification of these roles, for example by professional bodies, may help to overcome some of the challenges created by the lack of understanding and to develop these posts as a targeted and desirable career choice for upcoming trainees. Recent research into the role of integrated respiratory specialists in the UK by the British Thoracic Society suggests that this has started to be taken on board by professional bodies and highlights similar findings in that integrated specialist roles are currently taken by passionate individuals but that a lack of forward planning, job description and clear career pathways raises concerns going forward. 234
There are a number of limitations to our study. It is exploratory in nature and points to areas for further investigation rather than providing definitive evidence. We are unsure how our sample of consultants may differ from the wider pool of community-based consultants in these specialties. Therefore, findings such as the dependence on individual enthusiasm in creating and shaping posts may be a function of our sample, although we deliberately sought to widen our study sample through the inclusion of consultants from three specialties. We also limited our study to understanding the perspectives of consultants themselves and acknowledge that future research would benefit from understanding the perspectives of the wider workforce, including management, GPs and hospital-based specialists as well as patients.
Conclusion
In seeking to understand the experience of community-based consultants, this substudy suggests that although these posts are often driven or taken up by highly motivated individuals who report the benefits in terms of being able to provide more appropriate care for patients, the long-term development of these posts is likely to be constrained by a number of factors. Their idiosyncratic nature, the lack of clarity around the role, challenges to professional identity and the lack of training opportunities or continued professional development may all need to be addressed.
Chapter 7 Moving care from hospital into the community: international experiences (substudy 5)
Introduction
Managing demand at the interface between primary and secondary care has been at the centre of a range of policy initiatives in the English NHS since at least the mid-1990s, and various attempts have been made to address GPs’ referral behaviour,242 to introduce alternatives to hospital referral and, so, to reduce the reliance on secondary care more broadly. 243 Better balancing primary and secondary care is expected to enhance allocative efficiency,244,245 which is core to countries’ efforts to meet the challenge of growing cost pressures and concerns about the financial sustainability of health-care systems in the light of ageing populations, advances in medical technology and increasing patient expectations. 246 Similar to the NHS, health-care systems elsewhere have been experimenting with different approaches of shifting specialist services away from hospital into the community, with an expectation that this will increase accessibility of services and so the responsiveness of the system, and, potentially, reduce costs. 247 This chapter seeks to explore these experiences, focusing on a small sample of high-income countries and on approaches and models of care designed to enhance the effectiveness of services at the primary–secondary care interface. We include systems that have a strong primary care gatekeeping system in place in order to enable lesson learning for the NHS in England.
Methods
Country selection
The original proposal for this work to the NIHR HSDR programme foresaw including a range of high-income countries with different approaches to health-care organisation, governance and financing. On the basis of our earlier work247–249 we further suggested including Australia, Germany, the Netherlands, New Zealand and the USA. However, in the light of the issues which we explored in the scoping review and substudies, as presented in the preceding chapters, we refocused the international component so that it was restricted to high-income countries that operate a (strict) gatekeeping system.
Country selection was informed by recent work by Kringos250 and Kringos et al. 251 on primary care in 31 European countries. Of these, we considered a sample of 23 countries that are members of the Organisation for Economic Co-operation and Development (OECD) and are classified as high income. 252 In 2009–10, 11 of these 23 countries had at least partial gatekeeping in place (i.e. patients cannot directly access specialist physicians within the publicly funded system but require a referral from their GP or family physician); of these 11, eight have been rated, on the basis of a range of dimensions considered to be core for primary care (including access, continuity, co-ordination and comprehensiveness), to have strong primary care systems (see Appendix 6, Table 26): Denmark, Estonia, Finland, the Netherlands, Portugal, Slovenia, Spain and the UK. 253 Of these, we selected a subsample of countries, considering geographical location, economic performance (gross domestic product per capita), level of health-care spending and principal approach to health-care funding. On this basis, we identified four countries for detailed review: Denmark, Finland, the Netherlands and Spain.
Approach
We developed a structured data collection template that sought to capture, for each of the countries reviewed, information on care approaches that have been implemented in order to enhance access to specialist care while maintaining the general principles of the primary care gatekeeping system, and so improve the effectiveness of services at the primary–secondary care interface. The data collection template was informed by the general conceptualisation of interventions designed to reduce hospital outpatient attendance that guided the overall evidence review presented in this report: transfer (substitution of services delivered by hospital clinicians for those delivered in primary care), relocation (of specialist services into the community), liaison (joint working between specialists and primary care practitioners) and professional behaviour change (changing referral behaviour of primary care practitioners). We further distinguished specific interventions and approaches as previously identified by Roland et al. 2 and those that have emerged from the present evidence review (see Chapter 2). For each of the interventions and care approaches we sought to understand the extent to which these were implemented in the country under review and are available routinely. The full data collection template is shown in Appendix 7.
Data collection was undertaken by experts in each of the countries reviewed. Country experts were identified from the International Healthcare Comparisons network established within an ongoing project that provides systematic internationally comparative health policy analyses to the Department of Health in England254,255 and from the authors’ professional networks. Experts were asked to complete the data collection template by making use of the best data available and using all relevant sources, such as ongoing or completed research projects, policy documents, or routine statistics, surveys and census data related to primary care.
Data were grouped according to broad intervention categories and informed by the categories that led data collection. The completed data collection templates are presented in Appendix 8; we describe these by means of a narrative account. To place country experiences in context, we further provide basic descriptive information about the key characteristics of the health system in each country, drawing on existing data sourced from a targeted review of the evidence. As part of this overview we also included data on England for comparison.
Findings
Principal features of primary care in Denmark, Finland, the Netherlands and Spain
Table 25 provides an overview of the public primary care systems in place in each of the four countries reviewed, with England included for comparison (or the UK where data for England were not available).
| Features | Denmark256 | Finland257,258 | The Netherlands259 | Spain260 | England261 |
|---|---|---|---|---|---|
| Population size (2012)262 | 5.59 million | 5.41 million | 16.75 million | 46.15 million | 53.5 million263 |
| Health system financing | |||||
| GDP per capita current prices (US$ PPP, 2012)262 | 41,949 | 38,389 | 42,295 | 31,919 | 34,773 (UK) |
| Health expenditure total (% of GDP, 2012)262 | 11.0 | 9.1 | 11.8 | 9.4 | 9.3 (UK) |
| Health expenditure per capita (US$ PPP, 2012)262 | 4698 | 3559 | 5099 | 2998 | 3289 (UK) |
| Main sources of funding for health care (% of total health expenditure in 2012)262 | Taxation (85.8), OOP (12.4) | Central and local (municipal) taxes (60.7), social security (14.4), OOP (18.7) | SHI (71.8), taxation (7.7), OOP (5.5) (2011) | Central and local taxes (68.3), social security (4.7), OOP (20.7) (2011) | Central taxes (84%), OOP (9%) (UK) |
| Health system governance | Shared by central government, regions and municipalities; regions and municipalities are largely responsible for organising health care | Central government directs health services at the national level and defines general health policy; organisation of health care is the responsibility of municipalities | Shared by the government and the corporatist (self-governance) sector | Central government sets principles of Spanish national health service; 17 autonomous communities are responsible for organisation of health services | Central level by government and agencies at arm’s length from government; local organisations organise health-care delivery |
| Principles of health-care provision outside hospital | |||||
| Provision of primary care | GP practices; practice structure is gradually shifting from solo to group practices; practices are increasingly employing nurses | Municipal health centres which comprise a range of professionals: GPs, nurses, midwives, social workers, dentists, physiotherapists, psychologistsa | GPs in group practices of 2–7 doctors; practices are increasingly employing nurses | Primary care teams in health centres, which may include dentists, stomatologists, paediatricians as well as midwives | Primary care team in GP practices or health centres; comprises GPs, nurses and other health professionals such as midwives or health visitors |
| Choice of primary care provider | Yes, within specified local area; registration with GP required (‘group 1’)a | From 2012 registration with health centre of choice in municipality of residence; from 2014 choice of any centre in the country | Yes; registration with GP required | Varies across regions; typically limited to GPs available in the region of residence | Within specified small area only; registration with GP required |
| GP gatekeeping | Yes; direct access to certain specialists, e.g. ophthalmologists, ENT specialists and dentists | Yesb | Yes | Yes; direct access to certain specialists in some regions, e.g. gynaecologists, paediatricians | Yes |
| Payment of physicians in primary care | A combination of capitation per patient (one-third) and fee-for-service (two-thirds) for consultations, home visits, out-of-hours services, minor surgery, etc. | A combination of basic salary and variable added payments and bonuses | Combination of capitation and fee-for-services, plus additional funding for activities that substitute for secondary care and for providing out-of-hours care | Basic salary for individual physician plus performance related payment (up to 15% of salary in some regions) | Combination of capitation and fee-for service based on centrally negotiated contract; voluntary pay-for-performance element (‘Quality and Outcomes Framework’) |
In all four countries, the provision of primary care is principally GP-led, while the level of involvement of other health professionals varies. For example, at the time of writing Denmark had only recently begun to move to group practices that also include nurses,256 whereas multiprofessional teams in health centres have traditionally formed the core of primary care in Finland and Spain. 257,260
In each country, concerns about rising health-care costs, in particular those associated with hospital care, have prompted reform efforts that include measures to reduce the dependence on hospital- or specialist-based service delivery. 256,257,260 Data collected in this study showed that countries are using approaches such as transfer, relocation, liaison and professional behaviour change, or elements thereof, to varying degrees (see Appendix 8). However, the range of measures and interventions that have been or are being implemented is shaped, to a large extent, by the specific features of the organisation and delivery of primary care and their evolution over time in each country. For example, in Finland, services offered within primary care can include those that elsewhere would be considered specialist care. 265 In part, this has its origins in the historical development of the health-care sector before the 1972 primary care reform, which introduced municipal health centres that partly evolved from small local hospitals. As a result, health centres offer a wide range of services, including GP-led inpatient units, and they are well equipped with medical technology, including facilities for minor surgery and diagnostic equipment. 257 This means that interventions that elsewhere were introduced to specifically reduce referrals to specialist care, such as performing minor surgery or making available equipment for near patient diagnostic testing in general practice,2 by definition form a core part of primary care in Finland.
Against this background, approaches used by countries to improve the effectiveness of services at the primary–secondary care interface and to reduce referrals to specialist care in hospital can be broadly classified into financial mechanisms and incentives; transfer; relocation; and guidelines and protocols. We discuss these in turn.
Financial mechanisms and incentives
All four countries have some form of financial incentive in place which may be directly or indirectly used to control referral patterns from primary to secondary care or to move care into the community more broadly. The types of financial mechanism include incentives targeted at the provider (Denmark, the Netherlands and Spain) or the purchaser of services (Finland).
In Denmark, the paying of GPs was changed in the 1980s, moving away from capitation-only to also include a fee-for-services element, which accounts for around two-thirds of a GP’s payment. 266 This move was in part motivated to reduce referrals to secondary care, and the negotiation of fees, undertaken by the Board for Wages and Tariffs of the Regions and the Association of General Practitioners in Denmark, seeks to create incentives for the GPs to treat patients who could be treated in general practice rather than refer them on to hospital. 256 Fees apply to a range of services, including minor surgery, out-of-hours services and home visits.
Following the 2006 health-care reform, the Netherlands has introduced a range of incentives impacting on referrals. These include fees for ‘modernisation and innovation procedures’, which incentivise primary care physicians to perform procedures that are potentially substituting for secondary care, including for minor surgery. 267,268 This scheme also incentivises guideline adherence269 and selected telecare interventions. 270 A further approach is the use of a bundled payment for selected chronic conditions such as diabetes, COPD and vascular risk, involving care groups that are often exclusively led by GPs. 271 Care groups are responsible for the organisation, co-ordination and delivery of care for these conditions; they negotiate the price for a defined care package in line with national standards with health insurance funds.
In Spain, the relationships between regional health services authorities and public providers are regulated by mix of salary and contractual agreements. Referral protocols and targets have been in place since the late 1980s, largely in order to avoid any saturation of specialised care institutions,272,273 and most regional health authorities have established referral rates audit and feedback systems, with standards based on the average rate of referral in the region (autonomous community) concerned. More recently, regional authorities have attached more explicit monetary incentives to objectives set out in agreements, including referrals from primary to secondary care. 274 These incentives typically take the form of a ‘productivity bonus’, although only three regions are operating an actual financial penalty system in the form of withholding the bonus when objectives are not achieved.
Finland does not use explicit financial incentives targeted at individual GPs; however, there is an inherent incentive to control the number of referrals, as primary and specialist services are funded through the same route. This followed the 1993 state subsidy for public services reform, which made local municipalities responsible for all secondary and tertiary care costs. 275 It has prompted the introduction of alternatives to specialist care in hospital, such as the contracting of specialists to provide clinics in primary care (see Transfer). The 1993 reform also permitted municipalities to purchase services from private providers, both in primary and in secondary care, and contractual agreements tend to incorporate ceilings on referrals. However, the proportion of municipal health services that is currently purchased from private providers has remained low. 257
Evidence of effect
There is some evidence from the countries reviewed that the use of financial mechanisms has impacted referral rates and the dependence on hospital-based service delivery more broadly. However, much of the evidence pertains to evaluations of local or pilot initiatives, and there are few robust data on their long-term impacts at the system level. For example, there is evidence from Denmark that following the change by Copenhagen municipality from a mostly capitation-based system to one that combines capitation and fees in the 1980s, there was an increase in the volume of activities that were specifically remunerated and referrals to specialists decreased,276 although it is unclear if this reduction has been observed elsewhere across the country and whether or not it was sustained long term.
In the Netherlands, a small number of evaluations of interventions are linked to fee payments under ‘modernisation and innovation procedures’. For example, one observational study of 70 GP practices of the substitution effect of transferring minor surgery to primary care found evidence of a significantly lower referral rate for minor surgery for patients with sebaceous cysts over the period 2006–10, although the overall effect was small (odds ratio 0.98, 95% confidence interval 0.97 to 0.99). 277 An evaluation of a teledermatology service involving over 37,000 teleconsultations conducted between 1820 GPs and 166 dermatologists over a period of 3.5 years found that 68% of referrals to a dermatologist could be prevented (see also Chapter 2, Findings, Relocation). 135 The estimated cost reduction was 18%. However, related work also suggested that GPs were facing challenges in identifying suitable patients for this approach. 270 Available evidence on teleconsultation in eye care and cardiology in the Netherlands has pointed to reductions of referral rates of around 50% for patient selected by the GP for telemedicine;270 similar observations were made for telepulmonology consultations. 278 However, in Chapter 2 (see Findings, Relocation, Telemedicine), there is a general lack of economic evaluations which take a whole-system perspective.
The evidence on the impact of bundled payment for selected chronic conditions through mostly GP-led care groups remains generally mixed. Care groups in the Netherlands subcontract GPs, medical specialists, nurses and other disciplines, and approximately 78% of GPs are members of such a group. 279 Recent evaluations indicate that the system of bundled payments improves the organisation and co-ordination of care. 280 However, thus far there is little robust evidence on the impacts of care groups on referral patterns. 281
In Spain, there is very little robust evaluation of the impacts of financial mechanisms and incentives on secondary care referral. Primary care providers have argued that the effectiveness of such incentives has decreased because of successive reduction of the incentives. 282
For Finland, the 1993 state subsidy reform formed part of a larger move to create economic incentives for municipalities to improve the efficiency of services. 257 A number of changes have occurred in the organisation of primary care as a consequence of these reforms but there are few robust data that would allow for the assessment of its impacts on secondary care referrals.
Transfer
All four countries have interventions in place that involve the substitution of services delivered by hospital clinicians for those delivered in primary care (see Appendix 8, Transfer). In some these are linked to explicit financial incentives, such as the provision of minor surgery in Denmark and the Netherlands, as noted above. In Finland and Spain they form part of the common basket of services provided in primary care,257,283 and, for example, proposals by the Spanish Ministry of Health to transfer all ambulatory minor surgery to the primary care level are currently being considered by the Inter-territorial Council of the national health system. 284
Countries are also increasingly using nurses or practice assistants to provide specialised services in primary care, in particular for chronic diseases. For example, in the Netherlands, only approximately 10% of all diabetes patients are treated in secondary care as a consequence of a range of measures, including the introduction of practice assistants or nurses in primary care. 269 The Netherlands has also introduced new professional roles to better link the interface between secondary and primary care. These include ‘skin therapists’ seeking to (part) substitute for dermatologists and optometrists or ophthalmic technicians to (part) substitute for ophthalmologists, and both new roles work closely with the GP and with the relevant specialist.
Evidence of effect
In Spain, measures such as transferring minor surgery to primary care settings and offering direct access to tests and investigations are generally seen to be effective approaches in reducing the referral of patients to specialists. 284 However, anecdotal evidence suggests that, although widely available, minor surgery procedures in primary care do not seem to have reduced pressure on hospital surgery departments but instead might have led to an increase in service utilisation, by uncovering a previously unmet need for minor ailments (such as warts or verrucae).
The use of practice assistants or nurse-led diabetes treatment in the Netherlands has been linked to a reduction of 40% in referrals to hospital. 269 However, this transfer has not led to a reduction in total diabetes-related hospital costs; instead, these costs increased, which has been attributed to efforts by hospitals to compensate for their financial losses. 285 Regarding mental health, the introduction of practice assistants or nurses in primary care from 2008 has yet to be fully implemented; people with mild mental health problems continue to be treated by specialists and are not quickly referred back to primary care. 286 Empirical evidence on the effectiveness of new professionals such as skin therapists in reducing referrals to dermatologists is currently lacking,287 although the introduction of optometrists or ophthalmic technicians has been linked to a reduction in referrals to eye specialists. 288
Relocation
There are examples of relocation of specialist services into the community in all four countries, such as CMHTs, or the use of telecare and telemedicine interventions, although the range and scope of such approaches varies, reflecting to large extent the general features of primary care in the countries under review (see Appendix 8, Relocation). Finland is the only one of the four countries in which specialist services have been relocated into primary care as a consequence of the transformation of several smaller specialist hospitals to share premises with municipal health centres. 247,289 Finland also provides an example in which the attachment of specialists to primary care teams, such as paediatricians, ENT specialists and ophthalmologists, is common following the colocation of primary care teams and specialists in newly integrated organisations. 265 Some health centres directly employ geriatricians as internal consultants, while in other cases a visiting consulting doctor will perform this task in the health centre. There is little systematic evidence of the frequency and volume of these types of approaches in Finland, although a monitoring system is being implemented. There is a common belief that including a specialist as a (flexible) consultant in primary care teams or organisations reduces pressure on outpatient services, and many larger cities take this approach in an expectation of saving costs.
Decision support, guidelines and protocols
All countries use some form of decision-support mechanism in the form of guidelines, pathways or treatment protocols at national, regional or local levels to enhance co-ordination along the primary–secondary care interface and so reduce unnecessary referrals (see Appendix 8, Liaision and Professional behaviour change). In the Netherlands, referral guidelines for GPs generally recommend that patients should be referred only in exceptional circumstances,290 and there is evidence that general practices that adhere to referral guidelines have lower referral rates to secondary care. Finland has also established criteria, at national level, for referral to non-urgent elective care,291,292 and although there is wide confidence in the appropriateness of such criteria, there is little empirical evidence as to their effect on referral rates. Similarly, in Spain, although guidelines for specialist referral are used across the country, and agreed by primary care teams and specialists, there is little systematic evaluation of their effectiveness.
As indicated earlier, some settings are using financial incentives to enhance guideline adherence, such as the ‘Modernisation and Innovation procedures’ in the Netherlands,269 or, in Spain, through contractual agreements between regional health authorities and primary care providers. 274 Nominally, objective achievement is assessed by external or internal audit. Some regions have introduced ‘integrated care processes’ that specify the roles of different providers along the care pathway for a range of conditions and population groups (Andalusia, Asturias, Catalonia and Valencia); as part of these pathways they have also introduced audit mechanisms and associated incentives or penalties, at least in principle. 293 There is, however, little robust evidence of their effectiveness.
Other decision-support mechanisms include consultation liaison. For example, in Finland, where health centres employ or contract with a specialist to deliver clinics, the visiting specialist may offer a joint consultation with the GP to review a patient’s case. The Netherlands introduced a consulting secondary care specialist in mental health care in 2013, following experiences with the aforementioned practice assistant- or nurse-led mental health care in primary care, which was found to insufficiently substitute for mental health care at specialist level. 290 Further, a number of GPs in some regions team up with specialists for joint consultations in primary care. Joint consultations have been linked to fewer referrals to secondary care and fewer diagnostics in secondary care. On average, 15% of patients who receive a joint consultation are referred to secondary care. 294,295
Discussion
This paper has explored experiences in Denmark, Finland, the Netherlands and Spain of approaches and models of care designed to enhance the effectiveness of services at the primary–secondary care interface. Similar to England, these countries operate fairly strict primary care gatekeeping and have recently been rated to provide strong primary care systems. 251 All four countries have engaged in reform efforts to reduce reliance on hospital-based service delivery and have put approaches and mechanisms in place to reduce referrals from primary to secondary care. Although several common approaches have emerged, such as the use of financial mechanisms and incentives, transfer, relocation, and guidelines and protocols, the nature and scope of these approaches has varied, reflecting, to a great extent, the specific features of the organisation and delivery of primary care and their evolution over time in each country. With the possible exception of financial incentives, the relative lack of robust evidence of effect of approaches that are being implemented elsewhere challenges our ability to draw lessons for the English NHS. It is notable that comparatively ‘interventionist’ approaches targeting referral rates,194 such as in-house review and RMCs, which are implemented in England are not common or being considered in any of the countries reviewed here.
Available data on the use of targeted financial incentives for the delivery of specific services, such as minor surgery,277 as implemented in Denmark and the Netherlands point to a reduction in referral rates. However, similar to experience in the UK, which introduced financial incentives for GPs to conduct minor surgery in the 1990s, there remains a question about whether or not this presents a true substitution effect. Other evidence, again from the Netherlands, finds considerable effects of selected (incentivised) telehealth interventions, such as in dermatology, eye care and cardiology, with data on teledermatology further highlighting the potential for cost reductions. 270 However, there is a need to better understand the impact on the system more broadly both in terms of generalisability across the country and sustainability of observed effects. Overall, and again drawing on data for the Netherlands, financial incentives appear to be more likely to be effective if introduced alongside other measures, such as the use of nurse-led chronic care. In the case of diabetes, this was associated with a marked reduction in the number of referrals to hospital, although it did not result in a reduction in costs for hospitals. 285 This suggests that reducing referrals on its own may not be sufficient to save costs in secondary care if not accompanied by other measures that compensate hospitals for the associated loss of income. More system-wide approaches, such as those introduced in Finland which bring together financial responsibility for primary and secondary care, or bundled payments making GP-led care groups responsible for selected chronic conditions, as introduced in the Netherlands, may provide more promise for better balancing the primary–secondary care interface. 280 These include the systematic colocation or contracting of specialists alongside or into primary care teams, and it will be important to systematically monitor the impact of such approaches on specialist service utilisation and cost.
Chapter 8 Conclusions and recommendations
We have studied, through literature review or empirical research, a wide range of interventions aimed at changing care at the primary–secondary interface. Our review was driven by the framework of categories of interventions presented in Table 1. Under each of these categories we have found further evidence on a number of topics discussed in the previous review, as well as evidence on new interventions not previously captured. Below we present the new evidence from this study in each of the review categories, comparing the present study findings from both the literature and the five substudies with the conclusions of the previous review.
Transfer
The 2006 review noted two key areas in which there was positive evidence that the transfer of outpatient services to primary care would result in reduced demand on outpatient services. These were (1) the earlier discharge of outpatients to no follow-up, patient-initiated follow-up or GP follow-up; and (2) direct access for GPs to hospital-based diagnostic tests and investigations or hospital-provided treatments. This review found additional evidence that discharge from outpatients to follow-up in primary care did not impact on patient outcomes, and may be cost saving compared with hospital follow-up. By contrast, although direct access of GPs to hospital-based diagnostic tests and services has increased in recent years and a large number of new papers were found on this topic, the impact of these changes on outpatient services and the cost-effectiveness of such an approach remains unclear.
The previous review also noted two promising interventions that were judged to merit further investigation. These were the (1) role of GPwSIs and (2) the transfer of medical care for common chronic conditions from secondary to primary care. This review found additional evidence to support the ability of GPwSIs to provide a high-quality service that is valued by patients, but evidence on cost-effectiveness remains inconclusive. In this review we found additional studies that confirm that high-quality care can be provided for patients in primary care for a wide range of chronic conditions and may result in lower secondary care utilisation. Again, there are few data available on cost-effectiveness.
The previous review found that transfer of minor surgery from outpatient to primary care, although effective at reducing outpatient attendances, was associated with important reductions in quality and safety of care. This review found further evidence leading to a more promising overall conclusion, suggesting that minor surgery carried out in general practice can be safe and effective, but, crucially, this depended on the skill of the operator. However, there is, again, little evidence on whether or not this approach is cost-effective.
Relocation
The previous review found that the relocation of specialist services to primary care settings, although associated with improved access, was not effective in reducing outpatient attendances. In this review we found further evidence on this topic, suggesting that community-based specialist clinics are popular with patients and may reduce waiting times when associated with an expansion in specialist capacity. However, the overall effect on efficiency and effectiveness of outpatient services was unclear. We also found two studies of specialist attachment to primary care teams, which included a strong educational focus. Although the initial findings appeared promising, these approaches appeared very costly and there is a need for further evaluation of the long-term costs and benefits of such schemes.
Owing to the paucity of published evidence on relocation of specialist services to primary care, we conducted a substudy to understand the experience of consultants directly employed or subcontracted to community organisations. Such consultants reported benefits in provision of more appropriate care for patients, but we identified a number of constraints to bear in mind in the future development of such posts. Such posts are often dependent on the enthusiasm of individual consultants and they face a number of problems in their new roles. The ways in which these models currently work could not simply be expanded into the new models of care envisaged in the NHS Five Year Forward View. 296
We found a number of papers on the interactions between CMHTs and primary care. The majority of studies noted benefits from close working between primary care and specialist mental health teams for the treatment of common mental health conditions and in some cases this may reduce specialist referrals. However, there is a wide diversity of different models and little evidence of the cost-effectiveness of particular approaches.
A number of papers set out the benefits of telemedicine video consultations as an alternative to patients or specialists travelling long distances, particular in very remote rural areas. However, in England it is unlikely that video consultations will be cost-effective. More promising were studies of store-and-forward services for skin conditions, where remote diagnosis may reduce the need for outpatient attendance.
Liaison
Evidence from the previous review suggested that although joint working between primary and secondary care clinicians might improve quality of care, there was little impact on outpatient attendance. Although this review surfaced a number of new studies, the conclusions remain largely the same. Although cost savings to patients can be considerable, there is no consensus as to cost implications to the health service from implementation of shared-care practices.
Professional behaviour change
The 2006 review suggested that the only intervention with good evidence of reducing demand and increasing efficiency of outpatient services was the provision of structured referral sheets to prompt GPs to conduct necessary tests or treatments before referral. Obtaining a second opinion in the GP practice prior to referral was also judged to be promising, although this was based on only one study. Other behaviour-change strategies were concluded to be ineffective, including passive dissemination of referral guidelines, audit and feedback of referral rates and discussion of referral behaviour with an independent medical advisor. Financial incentives to reduce outpatient referrals were judged to be effective but risky in that necessary referrals may also be reduced.
In this review we found a substantial amount of additional evidence of interventions to change professional behaviour in ways which might reduce the number or improve the appropriateness of outpatient referrals. The studies found indicated that guidelines, audit and feedback on referrals may be relatively ineffective on their own but have more potential when combined together or linked with other interventions. Unsurprisingly, the more intensive professional education programmes appeared to have most effect in terms of behaviour change.
Owing to limited available literature, we conducted substudies on the use of RMCs and in-house review of referrals within primary care. Our substudy on in-house review of referral showed reported benefits of the sharing of knowledge among GPs to improve the selection of appropriate referral pathways and ensure that local guidelines had been followed. Interviewees suggested that owing to the educational component of such work, improvement in the quality and overall reduction of outpatient referrals might be greatest at the beginning of the initiative and that the effect then dissipated over time. Further research will be required to understand whether or not such a strategy is cost-effective. RMCs are an opportunity for further scrutiny of outpatient referrals beyond the GP practice. There is little consensus from the literature as to the impact of RMCs on numbers of outpatient referrals and some suggestion that these are less cost-effective than in-house review schemes. In our own study those interviewed reported some improvement in the quality of referrals. However, again, owing to the education of GPs over time, the impact on number of referrals reduced over time.
It is clear that financial incentives can change behaviour, as shown by the effect of QOF incentives on increasing referrals to renal, diabetic and neurology clinics. However, in our literature review and substudies we did not find any evidence of direct or indirect financial incentives being used to encourage practices to reduce outpatient referrals.
One promising intervention not described in the previous review is the provision of specialist advice to primary care doctors by e-mail or telephone. The papers reviewed describe a safe and effective system which reduces outpatient appointments and provides a concomitant reduction in cost.
Overarching conclusions
There are two prime motivations commonly reported to be behind interventions to change care at the primary–secondary interface, namely:
-
to provide care in locations which are more convenient to patients (‘care closer to home’)
-
to reduce the amount of care delivered in hospital outpatient clinics as part of a drive to limit the rise in overall health-care costs.
Alongside these two aims is a narrative that care in the community is cheaper than care in hospitals, an assumption which may be flawed, as there are a number of reasons why care in the community may be more expensive than conventional outpatient care. This may be because there is a loss of economies of scale (e.g. in the case of specialist clinics relocated to community settings), an increased cost of staff (e.g. GPwSIs when compared with hospital clinic staff which include trainees), and the possibility that providing more convenient access to care may increase the amount of care provided, either because of supply-induced demand or because previously unmet need is addressed. In addition, for some things (e.g. minor surgery) GPs may have a direct financial incentive to increase the volume of care provided.
There is no doubt that care in the community is popular with patients, and this has been demonstrated in a wide range of evaluations, from the follow-up of chronic medical conditions to GPwSIs to consultant outreach clinics. What is, therefore, extremely disappointing is the very limited number of robust economic evaluations, especially those which look at the whole system, for example to determine whether or not moving care into the community without disinvestment in hospital services results in an overall increase in health-care utilisation and cost. Therefore, against the two prime motivations identified above, we conclude the following:
-
High-quality care in the community can be provided for many conditions and is popular with patients.
-
The provision of care in the community may not be cheaper than outpatient services. The limited cost-effectiveness evidence we found was inconclusive, with a number of studies suggesting that interventions might increase the cost of care provision. Evaluations of new forms of community-based care (whether formal research studies or local evaluations) need to take account of the impact of changes on overall health-care utilisation (i.e. primary and secondary care costs combined).
-
The assumption that care moved into the community is cheaper may be incorrect, because of supply-induced demand, because unmet need is addressed by new forms of care or because there is a loss of efficiencies of scale found when services are provided in hospitals. Evaluations of new forms of community-based care (whether formal research studies or local evaluations) need to take account of the impact of changes on overall health-care utilisation (i.e. primary and secondary care costs combined). Evidence from this study suggests that further shifts of care into the community can be justified only if (a) high value is given to patient convenience in relation to NHS costs or (b) community care can be provided in a way that reduces overall health-care costs.
A number of studies have looked at whether or not care provided by GPs is safe and can be delivered to a high standard (e.g. medical clinics, surgical clinics, discharge from regular outpatient follow-up). In general, care provided by GP practices can be provided to a high standard provided there is clear guidance and the appropriate training of staff. Additional resources may also be needed in primary care as increasing amounts of work are shifted from hospitals to GP surgeries. GP practices have shown that they can provide effective monitoring of conditions such as heart disease and diabetes. However, as an increasing number of patients with less common conditions are discharged to GP care, better models may be needed of providing regular high-quality follow-up for these patients. Part of this may depend on agreed follow-up protocols which can be shared among the specialist, GP and patient. The main area in which specific concerns have been raised about the safety of care provided by GPs is minor surgery, where a number of studies show that inadequate care (e.g. the incomplete excision of skin cancers) is more common in GP surgeries than in hospitals. This emphasises the need for the training and ongoing support of GPs who take on additional roles. Simply transferring care into the community and hoping that quality is maintained is not acceptable.
One of the barriers to change at the primary–secondary interface is the historically poor communication between GPs and specialists. Both can be hard to reach via the telephone, and communication traditionally remains by means of a referral letter from the GP and a reply from the specialist when he or she has seen the patient some weeks later. There are many opportunities for better communication; for example, some studies suggest that a substantial proportion of referrals could be avoided by using e-mail (including the transmission of results and images). This aspect of NHS care seems to have stayed rooted in the 20th century when many other professions have moved on to using more modern methods of communication. Other developments to improve interactions between specialists and generalists locate (and sometimes employ) GPs within community organisations. This occurs commonly in Finland, but the cost-effectiveness of these new arrangements are largely untested, and they present significant uncertainties around professional roles for the doctors involved.
Limitations of this study
Our review of the literature identified a number of areas which we thought were poorly represented in the existing literature and where we undertook additional substudies. However, these were of necessity small in scale and cannot present comprehensive evaluations of, for example, the future role of RMCs. The general absence of cost data in the literature was a serious problem in terms of trying to draw conclusions about the cost-effectiveness of most of the interventions studied.
Our approach to literature review was a scoping review, with the aim of rapidly mapping the key concepts underpinning the research area and the main sources and types of evidence available, rather than a thorough synthesis of all available evidence. Our framework for this review was based on the framework developed for the 2006 review, and although we conducted a systematic search for literature, we did not formally assess the quality of the studies. We restricted our articles to those which were judged by the reviewers to be relevant to the NHS, excluding a small number of studies from the USA which would not be applicable to the NHS context.
For the substudies on RMCs, in-house review of referrals and community consultants, we relied on reports from a small number of interviewees at purposively sampled practices and RMCs. For the substudy on international experiences, we used a structured data collection template which was completed by experts in each of the countries reviewed. Although the findings were not validated by a second set of experts, these experts work within the International Healthcare Comparisons network and this method has been used for many previous internationally comparative health policy analyses through this network.
Although we have presented a range of interventions at the primary care interface as if they were discrete and separate, in reality they often overlap. So, for example, a move to discharge patients from a particular clinic to primary care could involve the development of local guidelines and educational visits from consultants to GP practices.
We are also very aware that a number of interventions are initially developed and promoted by enthusiastic clinicians. Examples that stand out are telemedicine (specialists with an interest in technology), community-based consultants (posts often developed by committed specialists for themselves) and consultation liaison models (again often developed by enthusiastic individual clinicians). In many of these cases, there are questions about how the interventions can be rolled out more widely into routine practice.
Research recommendations
It is clear that while the strong policy steer to move care into the community continues, the NHS will continue to respond to these pressures, sometimes in the belief that they will be cost saving. A second rhetoric is around the importance of integrated care, particularly important as the number of frail elderly with multiple medical conditions increases. Bearing this in mind we were struck by the inflexibility of the continuing divide between primary and secondary care. With this in mind our two general research recommendations are:
-
Priority should be given to evaluations of interventions that reduce the artificial divide between primary and secondary care. These might include exploiting electronic methods of communication between GPs and specialists, specialists working in community-based roles, and the development of shared pathways of care between primary and secondary care.
-
All evaluations of interventions at the primary–secondary care interface should include an economic evaluation which takes a whole-system approach and takes into account the possibility that interventions designed to save money may do the reverse, through supply-induced demand, addressing unmet need or loss of efficiencies of scale that may be found in hospitals.
Acknowledgements
We would like to thank a number of people who contributed to this study. Isla Kuhn, Deputy Medical Librarian, Medical Library, Cambridge University Library, conducted the literature searches for the scoping review. Dionne S Kringos, Peter Vedsted, Simo Kokko and Antonio Duran contributed to Chapter 7, providing input on the comparison countries. Members of our advisory board, Mark Friedberg, Christine Emerson, Martin McShane, Jonathan Fuld, Joanne Greenhalgh, Kate Massey and Roger Hughes, provided comments on both the research protocol and the draft report. Finally, we would like to thank all of our study participants who contributed to this study through their participation in interviews.
Contributions of authors
Eleanor Winpenny (analyst, RAND Europe) contributed to the scoping review, conducted the substudy on in-house review of referrals and co-ordinated the preparation of this report for publication.
Céline Miani (analyst, RAND Europe) contributed to the scoping review and the substudy on in-house review of referrals, and contributed to the preparation of this report for publication.
Emma Pitchforth (research leader, RAND Europe) contributed to the scoping review, conducted and prepared for publication the substudy on specialist services in the community.
Sarah Ball (analyst, RAND Europe) conducted and prepared for publication the substudy on RMCs.
Ellen Nolte (Director of Health and Healthcare, RAND Europe) conducted and prepared for publication the chapter on international comparisons.
Sarah King (senior analyst, RAND Europe) contributed to the scoping review.
Joanne Greenhalgh contributed to the substudy on RMCs.
Martin Roland (Professor of Health Services Research, University of Cambridge) oversaw the whole study, contributed to the scoping review, contributed to the substudy on specialist services in the community, conducted the substudy on financial incentives to reduce referrals and reviewed all other sections.
Disclaimer
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
Publication
Winpenny EM, Miani C, Pitchforth E, King S, Roland M. Improving the effectiveness and efficiency of outpatient services: a scoping review of interventions at the primary – secondary care interface. J Health Serv Res Policy 2016: in press.
Data sharing statement
All available data are included as an appendix to the report.
References
- O’Donnell CA. Variation in GP referral rates: what can we learn from the literature?. Fam Pract 2000;17:462-71. http://dx.doi.org/10.1093/fampra/17.6.462.
- Roland M, McDonald R, Sibbald B. Outpatient Services and Primary Care: A Scoping Review of Research Into Strategies For Improving Outpatient Effectiveness and Efficiency. Southampton: NIHR Trials and Studies Coordinating Centre; 2006.
- Roberts A, Marshall L, Charlesworth A. A Decade of Austerity. London: Nuffield Trust; 2012.
- Health and Social Care Act 2012. Chapter 7. London: The Stationery Office; 2012.
- Sibbald B, McDonald R, Roland M. Shifting care from hospitals to the community: a review of the evidence on quality and efficiency. J Health Serv Res Policy 2007;12:110-17. http://dx.doi.org/10.1258/135581907780279611.
- Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol 2005;8:19-32. http://dx.doi.org/10.1080/1364557032000119616.
- CRD’s Guidance For Undertaking Reviews In Healthcare. York: CRD; 2009.
- American Telemedicine Association . What Is Telemedicine? n.d. www.americantelemed.org/about-telemedicine/what-is-telemedicine#.VL0xttKsV8E (accessed 19 January 2015).
- Halasyamani LK, Valenstein PN, Friedlander MP, Cowen ME. A comparison of two hospitalist models with traditional care in a community teaching hospital. Am J Med 2005;118:536-43. http://dx.doi.org/10.1016/j.amjmed.2005.01.027.
- Dhumale R. Feasibility study of hernia surgery in a general practice setting. Br J Gen Pract 2004;54:604-7.
- Dhumale R, Tisdale J, Barwell N. Over a thousand ambulatory hernia repairs in a primary care setting. Ann R Coll Surg Engl 2010;92:127-30. http://dx.doi.org/10.1308/003588410X12518836439281.
- George S, Pockney P, Primrose J, Smith H, Little P. A prospective randomised comparison of minor surgery in primary and secondary care. The MiSTIC trial. Health Technol Assess 2008;12. http://dx.doi.org/10.3310/hta12230.
- Nelson RE, Battistone MJ, Ashworth WD, Barker AM, Grotzke M, Huhtala TA, et al. Cost effectiveness of training rural providers to perform joint injections. Arthritis Care Res 2014;66:559-66. http://dx.doi.org/10.1002/acr.22179.
- Olah KS, Alliston J, Jones J, Stewart G, Mavrommatis R. Thermal ablation performed in a primary care setting: the South Warwickshire Experience. BJOG 2005;112:1117-20. http://dx.doi.org/10.1111/j.1471-0528.2005.00635.x.
- van Dijk CE, Verheij RA, Spreeuwenberg P, Groenewegen PP, de Bakker DH. Minor surgery in general practice and effects on referrals to hospital care: observational study. BMC Health Serv Res 2011;11. http://dx.doi.org/10.1186/1472-6963-11-2.
- Twist M. Rate of incomplete excision of basal cell carcinomas by General Practitioners with Special Interest. Br J Dermatol 2009;161. http://dx.doi.org/10.1111/j.1365-2133.2009.09129.x.
- NICE Updates its Guidance on the Treatment and Care of People with Skin Cancer. London: NICE; 2010.
- Berger A, Kramarz P, Kopperud GS, Edelsberg J, Oster G. Economic impact of shifting the locus of care for neuropathic pain from specialists to general practitioners. Eur J Health Econ 2007;8:245-51. http://dx.doi.org/10.1007/s10198-006-0025-2.
- van Boeijen C, van Oppen P, van Balkom A, Visser S, Kempe P. Treatment of anxiety disorders in primary care practice: a randomised controlled trial. Br J Gen Pract 2005;55:763-9.
- Briggs M, Closs SJ, Marczewski K, Barratt J. A feasibility study of a combined nurse/pharmacist-led chronic pain clinic in primary care. Qual Prim Care 2008;16:91-4.
- Chew DP, Carter R, Rankin B, Boyden A, Egan H. Cost effectiveness of a general practice chronic disease management plan for coronary heart disease in Australia. Aust Health Rev 2010;34:162-9. http://dx.doi.org/10.1071/AH09742.
- Coetzee J. GP-led services for alcohol misuse: the fresh start clinic. London J Prim Care (Abingdon) 2011;1:11-5. http://dx.doi.org/10.1080/17571472.2011.11493322.
- Courtenay M, Carey N. Nurse-led care in dermatology: a review of the literature. Br J Dermatol 2006;154:1-6. http://dx.doi.org/10.1111/j.1365-2133.2005.06979.x.
- Dusheiko M, Gravelle H, Martin S, Rice N, Smith PC. Does better disease management in primary care reduce hospital costs? Evidence from English primary care. J Health Econ 2011;30:919-32. http://dx.doi.org/10.1016/j.jhealeco.2011.08.001.
- Johnson M, Baird W, Goyder E. Understanding issues involved in the transfer of diabetes care to general practice: the patient perspective. Qual Prim Care 2006;14:247-52.
- Kuethe M, Vaessen-Verberne A, Mulder P, Bindels P, van Aalderen W. Paediatric asthma outpatient care by asthma nurse, paediatrician or general practitioner: randomised controlled trial with two-year follow-up. Prim Care Respir J 2011;20:84-91. http://dx.doi.org/10.4104/pcrj.2011.00003.
- Mahmalji W, Mukerji G, Abel P, Raza A. A community urology service: fact or fiction?. BJU Int 2010;106:1428-30. http://dx.doi.org/10.1111/j.1464-410X.2010.09731.x.
- Martin S, Smith PC, Dusheiko M, Gravelle H, Rice N. Do Quality Improvements In Primary Care Reduce Secondary Care Costs?. London: The Health Foundation; 2011.
- Maruthachalam K, Stoker E, Nicholson G, Horgan AF. Nurse led flexible sigmoidoscopy in primary care--the first thousand patients. Colorectal Dis 2006;8:557-62. http://dx.doi.org/10.1111/j.1463-1318.2006.00973.x.
- Newman RJ, Nichols DB, Cummings DM. Outpatient colonoscopy by rural family physicians. Ann Fam Med 2005;3:122-5. http://dx.doi.org/10.1370/afm.268.
- Tuomisto LE, Erhola M, Luukkaala T, Puolijoki H, Nieminen MM, Kaila M. Asthma Programme in Finland: did the use of secondary care resources become more rational?. Respir Med 2010;104:957-65. http://dx.doi.org/10.1016/j.rmed.2010.01.018.
- van Dijk CE, Verheij RA, Hansen J, van der Velden L, Nijpels G, Groenewegen PP, et al. Primary care nurses: effects on secondary care referrals for diabetes. BMC Health Serv Res 2010;10. http://dx.doi.org/10.1186/1472-6963-10-230.
- Zwar NA, Hermiz O, Comino E, Middleton S, Vagholkar S, Xuan W, et al. Care of patients with a diagnosis of chronic obstructive pulmonary disease: a cluster randomised controlled trial. Med J Aust 2012;197:394-8. http://dx.doi.org/10.5694/mja12.10813.
- Baker R, Sanderson Mann J, Longworth S, Cox R, Gillies C. Randomised controlled trial to compare GP-run orthopaedic clinics based in hospital outpatient departments and general practices. Br J Gen Pract 2005;55:912-17.
- Coast J, Noble S, Noble A, Horrocks S, Asim O, Peters TJ, et al. Economic evaluation of a general practitioner with special interest led dermatology service in primary care. BMJ 2005;331:1444-8. http://dx.doi.org/10.1136/bmj.38676.446910.7C.
- Gilbert R, Franks G, Watkin S. The proportion of general practitioner referrals to a hospital respiratory medicine clinic suitable to be seen in a GPwSI respiratory clinic. Prim Care Respir J 2005;14:314-19. http://dx.doi.org/10.1016/j.pcrj.2005.04.006.
- Jones R, Rosen R, Tomlin Z, Cavanagh MR, Oxley D. General practitioners with special interests: evolution and evaluation. J Health Serv Res Policy 2006;11:106-9. http://dx.doi.org/10.1258/135581906776318929.
- Levell NJ, Penart-Lanau AM, Garioch JJ. Introduction of intermediate care dermatology services in Norfolk, England was followed by a 67% increase in referrals to the local secondary care dermatology department. Br J Dermatol 2012;167:443-5. http://dx.doi.org/10.1111/j.1365-2133.2012.10850.x.
- Nocon A, Rhodes PJ, Wright JP, Eastham J, Williams DRR, Harrison SR, et al. Specialist general practitioners and diabetes clinics in primary care: a qualitative and descriptive evaluation. Diabet Med 2004;21:32-8. http://dx.doi.org/10.1046/j.1464-5491.2003.01063.x.
- Ridsdale L, Doherty J, McCrone P, Seed P. Headache Innovation and Evaluation Group. A new GP with special interest headache service: observational study. Br J Gen Pract 2008;58:478-83. http://dx.doi.org/10.3399/bjgp08X319440.
- Salisbury C, Noble A, Horrocks S, Crosby Z, Harrison V, Coast J, et al. Evaluation of a general practitioner with special interest service for dermatology: randomised controlled trial. BMJ 2005;331:1441-4. http://dx.doi.org/10.1136/bmj.38670.494734.7C.
- Sibbald B, Pickard S, McLeod H, Reeves D, Mead N, Gemmell I, et al. Moving specialist care into the community: an initial evaluation. J Health Serv Res Policy 2008;13:233-9. http://dx.doi.org/10.1258/jhsrp.2008.008049.
- Augestad KM, Norum J, Dehof S, Aspevik R, Ringberg U, Nestvold T, et al. Cost-effectiveness and quality of life in surgeon versus general practitioner-organised colon cancer surveillance: a randomised controlled trial. BMJ Open 2013;3. http://dx.doi.org/10.1136/bmjopen-2012-002391.
- Choudhury S, Hussain S, Yao G, Hill J, Malik W, Taheri S. The impact of a diabetes local enhanced service on quality outcome framework diabetes outcomes. PLOS ONE 2013;8. http://dx.doi.org/10.1371/journal.pone.0083738.
- Grunfeld E, Levine MN, Julian JA, Coyle D, Szechtman B, Mirsky D, et al. Randomized trial of long-term follow-up for early-stage breast cancer: a comparison of family physician versus specialist care. J Clin Oncol 2006;24:848-55. http://dx.doi.org/10.1200/JCO.2005.03.2235.
- Hall SJ, Samuel LM, Murchie P. Toward shared care for people with cancer: developing the model with patients and GPs. Fam Pract 2011;28:554-64. http://dx.doi.org/10.1093/fampra/cmr012.
- Hewlett S. Patient initiated outpatient follow up in rheumatoid arthritis: six year randomised controlled trial. BMJ 2005;330. http://dx.doi.org/10.1136/bmj.38265.493773.8F.
- Lau L, French P. Anogenital herpes simplex suppressive therapy: an audit of transfer of care to general practitioners. Int J STD AIDS 2010;21:441-2. http://dx.doi.org/10.1258/ijsa.2010.010003.
- Lu W, Greuter MJW, Schaapveld M, Vermeulen KM, Wiggers T, De Bock GH. Safety and cost-effectiveness of shortening hospital follow-up after breast cancer treatment. Br J Surg 2012;99:1227-33. http://dx.doi.org/10.1002/bjs.8850.
- Lund L, Jonler M, Graversen PH, Borre M, Bro F. Shared care is a model for patients with stable prostate cancer. Dan Med J 2013;60.
- Meeuwsen EJ, Melis RJF, Van Der Aa GCHM, Golüke-Willemse GAM, De Leest BJM, Van Raak FHJM, et al. Effectiveness of dementia follow-up care by memory clinics or general practitioners: randomised controlled trial. BMJ 2012;344. http://dx.doi.org/10.1136/bmj.e3086.
- Meran S, Don K, Shah N, Donovan K, Riley S, Phillips AO. Impact of chronic kidney disease management in primary care. QJM 2011;104:27-34. http://dx.doi.org/10.1093/qjmed/hcq151.
- Torregrosa-Maicas I, Juan-Garcia I, Solis-Salguero MA, Ramos-Tomas C, Puchades-Montesa MJ, Gonzalez-Rico M, et al. Advancing in the management of chronic kidney disease: the results of implementing a quick resolution consultation. Nefrologia 2013;33:93-8. http://dx.doi.org/10.3265/Nefrologia.pre2012.Oct.11560.
- Thompson-Coon J, Abdul-Rahman A-K, Whear R. Telephone consultations in place of face to face out-patient consultations for patients discharged from hospital following surgery: a systematic review. BMC Health Serv Res 2013;13. http://dx.doi.org/10.1186/1472-6963-13-128.
- Hennessey DB, Lynn C, Templeton H, Chambers K, Mulholland C. The PSA tracker: a computerised health care system initiative in Northern Ireland. Ulster Med J 2013;82:146-9.
- Andonegui J, Zurutuza A, de Arcelus MP, Serrano L, Eguzkiza A, Auzmendi M, et al. Diabetic retinopathy screening with non-mydriatic retinography by general practitioners: 2-year results. Prim Care Diabetes 2012;6:201-5. http://dx.doi.org/10.1016/j.pcd.2012.01.001.
- Benamore RE, Wright D, Britton I. Is primary care access to CT brain examinations effective?. Clin Radiol 2005;60:1083-9. http://dx.doi.org/10.1016/j.crad.2005.05.010.
- Bjerager M, Palshof T, Dahl R, Olesen F. Delay in diagnosis of lung cancer in general practice. Br J Gen Pract 2006;56:863-8.
- Buller HR, Cate-Hoek AJT, Hoes AW, Joore MA, Moons KGM, Oudega R, et al. Safely ruling out deep venous thrombosis in primary care. Ann Intern Med 2009;150:229-35. http://dx.doi.org/10.7326/0003-4819-150-4-200902170-00003.
- Campbell S, MacDonald M, Carr B, Anderson D, MacKinley R, Cairns S. Bridging the gap between primary and secondary care: Use of a clinical pathway for the investigation and management of deep vein thrombosis. J Health Serv Res Policy 2008;13:15-9. http://dx.doi.org/10.1258/jhsrp.2007.007015.
- Castro AF, Silva-Turnes JC, Gonzalez F. Evaluation of retinal digital images by a general practitioner. Telemed J E Health 2007;13:287-92. http://dx.doi.org/10.1089/tmj.2006.0046.
- Cuadros J, Bresnick G. EyePACS: an adaptable telemedicine system for diabetic retinopathy screening. J Diabetes Sci Technol 2009;3:509-16. http://dx.doi.org/10.1177/193229680900300315.
- DAMASK (Direct Access to Magnetic Resonance Imaging: Assessment for Suspect Knees) Trial Team . Cost-effectiveness of magnetic resonance imaging of the knee for patients presenting in primary care. Br J Gen Pract 2008;58:e10-16. http://dx.doi.org/10.3399/bjgp08X342660.
- DAMASK (Direct Access to Magnetic Resonance Imaging: Assessment for Suspect Knees) Trial Team . Effectiveness of GP access to magnetic resonance imaging of the knee: a randomised trial. Br J Gen Pract 2008;58:e1-8.
- Jawad R, Robinson G. Gynaecological ultrasound in community sexual and reproductive health clinics. J Fam Plann Reprod Health Care 2009;35:35-7. http://dx.doi.org/10.1783/147118909787072207.
- Lucas A, Smeenk FJWM, van Schayck O, Smeele I, Brouwer T. The validity of diagnostic support of an asthma/COPD service in primary care. Br J Gen Pract 2007;57:892-6. http://dx.doi.org/10.3399/096016407782317883.
- Massin P, Chabouis A, Erginay A, Viens-Bitker C, Lecleire-Collet A, Meas T, et al. OPHDIAT: a telemedical network screening system for diabetic retinopathy in the Ile-de-France. Diabetes Metab 2008;34:227-34. http://dx.doi.org/10.1016/j.diabet.2007.12.006.
- Newman R, Cummings DM, Doherty L, Patel NR. Digital retinal imaging in a residency-based patient-centered medical home. Fam Med 2012;44:159-63.
- Olayiwola JN, Sobieraj DM, Kulowski K, Hilaire DS, Huang JJ. Improving diabetic retinopathy screening through a statewide telemedicine program at a large federally qualified health center. J Health Care Poor Underserved 2011;22:804-16. http://dx.doi.org/10.1353/hpu.2011.0066.
- Simpson GC, Forbes K, Teasdale E, Tyagi A, Santosh C. Impact of GP direct-access computerised tomography for the investigation of chronic daily headache. Br J Gen Pract 2010;60:897-901. http://dx.doi.org/10.3399/bjgp10X544069.
- Skipsey DA, Dawson FM, Breen C, Leslie SJ. Evaluation of a direct access cardiac arrhythmia monitoring service. Cardiol J 2012;19:70-5. http://dx.doi.org/10.5603/CJ.2012.0010.
- Taylor TR, Evangelou N, Porter H, Lenthall R. Primary care direct access MRI for the investigation of chronic headache. Clin Radiol 2012;67:24-7. http://dx.doi.org/10.1016/j.crad.2011.02.006.
- Ten Cate-Hoek AJ, Toll DB, Buller HR, Hoes AW, Moons KGM, Oudega R, et al. Cost-effectiveness of ruling out deep venous thrombosis in primary care versus care as usual. J Thromb Haemost 2009;7:2042-9. http://dx.doi.org/10.1111/j.1538-7836.2009.03627.x.
- Thomas R, Cook A, Main G, Taylor T, Galizia Caruana E. Primary care access to computed tomography for chronic headache. Br J Gen Pract 2010;60:426-30. http://dx.doi.org/10.3399/bjgp10X502146.
- van der Velde EF, Toll DB, Ten Cate-Hoek AJ, Oudega R, Stoffers HEJH, Bossuyt PM, et al. Comparing the diagnostic performance of 2 clinical decision rules to rule out deep vein thrombosis in primary care patients. Ann Fam Med 2011;9:31-6. http://dx.doi.org/10.1370/afm.1198.
- Walter FM, Morris HC, Humphrys E, Hall PN, Prevost AT, Burrows N, et al. Effect of adding a diagnostic aid to best practice to manage suspicious pigmented lesions in primary care: randomised controlled trial. BMJ 2012;345. http://dx.doi.org/10.1136/bmj.e4110.
- Watrous RL, Thompson WR, Ackerman SJ. The impact of computer-assisted auscultation on physician referrals of asymptomatic patients with heart murmurs. Clin Cardiol 2008;31:79-83. http://dx.doi.org/10.1002/clc.20185.
- Williams SC, Lopez C, Yoong A, McHugo JM. Developing a robust and efficient pathway for the referral and investigation of women with post-menopausal bleeding using a cut-off of < or = 4 mm for normal thickness. Br J Radiol 2007;80:719-23. http://dx.doi.org/10.1259/bjr/87219886.
- Pallan M, Linnane J, Ramaiah S. Evaluation of an independent, radiographer-led community diagnostic ultrasound service provided to general practitioners. J Public Health (Oxf) 2005;27:176-81. http://dx.doi.org/10.1093/pubmed/fdi006.
- Starren ES, Roberts NJ, Tahir M, O’Byrne L, Haffenden R, Patela IS, et al. A centralised respiratory diagnostic service for primary care: a 4-year audit. Prim Care Respir J 2012;21:180-6. http://dx.doi.org/10.4104/pcrj.2012.00013.
- Bernstein I. Integrated musculoskeletal service design by GP consortia. London J Prim Care (Abingdon) 2011;1:16-2. http://dx.doi.org/10.1080/17571472.2011.11493323.
- Eley KA, Fitzgerald JE. Quality improvement in action. Direct general practitioner referrals to audiology for the provision of hearing aids: a single centre review. Qual Prim Care 2010;18:201-6.
- Gurden M, Morelli M, Sharp G, Baker K, Betts N, Bolton J. Evaluation of a general practitioner referral service for manual treatment of back and neck pain. Prim Health Care Res Dev 2012;13:204-10. http://dx.doi.org/10.1017/S1463423611000648.
- Maddison P, Jones J, Breslin A, Barton C, Fleur J, Lewis R, et al. Improved access and targeting of musculoskeletal services in northwest Wales: targeted early access to musculoskeletal services (TEAMS) programme. BMJ 2004;329:1325-7. http://dx.doi.org/10.1136/bmj.329.7478.1325.
- Ryan B, White S, Wild J, Court H, Margrain TH. The newly established primary care based Welsh Low Vision Service is effective and has improved access to low vision services in Wales. Ophthalmic Physiol Opt 2010;30:358-64. http://dx.doi.org/10.1111/j.1475-1313.2010.00729.x.
- Thomas KJ, MacPherson H, Ratcliffe J, Thorpe L, Brazier J, Campbell M, et al. Longer term clinical and economic benefits of offering acupuncture care to patients with chronic low back pain. Health Technol Assess 2005;9. http://dx.doi.org/10.3310/hta9320.
- Julian S, Naftalin NJ, Clark M, Szczepura A, Rashid A, Baker R, et al. An integrated care pathway for menorrhagia across the primary–secondary interface: patients’ experience, clinical outcomes, and service utilisation. Qual Saf Health Care 2007;16:110-15. http://dx.doi.org/10.1136/qshc.2005.016782.
- Furlan AD, Yazdi F, Tsertsvadze A, Gross A, Van Tulder M, Santaguida L, et al. A systematic review and meta-analysis of efficacy, cost-effectiveness, and safety of selected complementary and alternative medicine for neck and low-back pain. Evid Based Complement Alternat Med 2011;2012. http://dx.doi.org/10.1155/2012/953139.
- Rubinstein SM, van Middelkoop M, Assendelft WJ, de Boer MR, van Tulder MW. Spinal manipulative therapy for chronic low-back pain: an update of a Cochrane review. Spine (Phila Pa 1976) 2011;36:E825-46. http://dx.doi.org/10.1097/BRS.0b013e3182197fe1.
- Gruen R, Weeramanthri T, Knight S, Bailie R. Specialist outreach clinics in primary care and rural hospital settings (Cochrane Review). Community Eye Health 2006;19.
- Frost DW, Toubassi D, Detsky AS. Rethinking the consultation process: optimizing collaboration between primary care physicians and specialists. Can Fam Physician 2012;58:825-28.
- Wiedemer NL, Harden PS, Arndt IO, Gallagher RM. The opioid renewal clinic: a primary care, managed approach to opioid therapy in chronic pain patients at risk for substance abuse. Pain Med 2007;8:573-84. http://dx.doi.org/10.1111/j.1526-4637.2006.00254.x.
- Levy ML, Walker S, Woods A, Sheikh A. Service evaluation of a UK primary care-based allergy clinic: quality improvement report. Prim Care Respir J 2009;18:313-19. http://dx.doi.org/10.4104/pcrj.2009.00042.
- Moffatt J, Hossain D, Hansford G. Physician in practice clinic: educating GPs in endocrinology through specialist-outreach. Rural Remote Health 2012;12.
- Simmonds S, Coid J, Joseph P, Marriott S, Tyrer P. Community mental health team management in severe mental illness: a systematic review. Brit J Psychiatry 2001;178:497-502. http://dx.doi.org/10.1192/bjp.178.6.497.
- Thornicroft G, Tansella M. Components of a modern mental health service: a pragmatic balance of community and hospital care overview of systematic evidence. Brit J Psychiatry 2004;185:283-90. http://dx.doi.org/10.1192/bjp.185.4.283.
- Bower P, Gilbody S. Managing common mental health disorders in primary care: conceptual models and evidence base. BMJ 2005;330:839-42. http://dx.doi.org/10.1136/bmj.330.7495.839.
- Cape J, Whittington C, Bower P. What is the role of consultation-liaison psychiatry in the management of depression in primary care? A systematic review and meta-analysis. Gen Hosp Psychiatry 2010;32:246-54. http://dx.doi.org/10.1016/j.genhosppsych.2010.02.003.
- Christensen H. Models in the delivery of depression care: a systematic review of randomised and controlled intervention trials. BMC Fam Pract 2008;9. http://dx.doi.org/10.1186/1471-2296-9-25.
- Fickel JJ, Parker LE, Yano EM, Kirchner JE. Primary care – mental health collaboration: an example of assessing usual practice and potential barriers. J Interprof Care 2007;21:207-16. http://dx.doi.org/10.1080/13561820601132827.
- Gilbody S, Bower P, Whitty P. Costs and consequences of enhanced primary care for depression: systematic review of randomised economic evaluations. Brit J Psychiatry 2006;189:297-308. http://dx.doi.org/10.1192/bjp.bp.105.016006.
- Harkness EF, Bower PJ. On-site mental health workers delivering psychological therapy and psychosocial interventions to patients in primary care: effects on the professional practice of primary care providers. Cochrane Database Syst Rev 2009;1. http://dx.doi.org/10.1002/14651858.cd000532.pub2.
- Kates N, McPherson-Doe C, George L. Integrating mental health services within primary care settings: the Hamilton Family Health Team. J Ambul Care Manage 2011;34:174-82. http://dx.doi.org/10.1097/JAC.0b013e31820f6435.
- Kendrick T, Simons L, Mynors-Wallis L, Gray A, Lathlean J, Pickering R, et al. A trial of problem-solving by community mental health nurses for anxiety, depression and life difficulties among general practice patients. The CPN-GP study. Health Technol Assess 2005;9. http://dx.doi.org/10.3310/hta9370.
- Morgan MAJ, Coates MJ, Dunbar JA, Reddy P, Schlicht K, Fuller J. The TrueBlue model of collaborative care using practice nurses as case managers for depression alongside diabetes or heart disease: a randomised trial. BMJ Open 2013;3. http://dx.doi.org/10.1136/bmjopen-2012-002171.
- Younes N, Passerieux C, Hardy-Bayle MC, Falissard B, Gasquet I. Long term GP opinions and involvement after a consultation-liaison intervention for mental health problems. BMC Fam Pract 2008;9. http://dx.doi.org/10.1186/1471-2296-9-41.
- Butler M, Kane RL, McAlpine D, Kathol R, Fu SS, Hagedorn H, et al. Does integrated care improve treatment for depression? A systematic review. J Ambul Care Manage 2011;34:113-25. http://dx.doi.org/10.1097/JAC.0b013e31820ef605.
- Backman W, Bendel D, Rakhit R. The telecardiology revolution: improving the management of cardiac disease in primary care. JRSM 2010;103:442-6. http://dx.doi.org/10.1258/jrsm.2010.100301.
- Borve A, Holst A, Gente-Lidholm A, Molina-Martinez R, Paoli J. Use of the mobile phone multimedia messaging service for teledermatology. J Telemed Telecare 2012;18:292-6. http://dx.doi.org/10.1258/jtt.2012.120206.
- Bowns IR, Collins K, Walters SJ, McDonagh AJG. Telemedicine in dermatology: a randomised controlled trial. Health Technol Assess 2006;10. http://dx.doi.org/10.3310/hta10430.
- Borooah S, Grant B, Blaikie A, Styles C, Sutherland S, Forrest G, et al. Using electronic referral with digital imaging between primary and secondary ophthalmic services: a long term prospective analysis of regional service redesign. Eye 2013;27:392-7. http://dx.doi.org/10.1038/eye.2012.278.
- Butler TN, Yellowlees P. Cost analysis of store-and-forward telepsychiatry as a consultation model for primary care. Telemed J E Health 2012;18:74-7. http://dx.doi.org/10.1089/tmj.2011.0086.
- Chong J, Moreno F. Feasibility and acceptability of clinic-based telepsychiatry for low-income Hispanic primary care patients. Telemed J E Health 2012;18:297-304. http://dx.doi.org/10.1089/tmj.2011.0126.
- Colven R, Shim M-HM, Brock D, Todd G. Dermatological diagnostic acumen improves with use of a simple telemedicine system for underserved areas of South Africa. Telemed J E Health 2011;17:363-9. http://dx.doi.org/10.1089/tmj.2010.0163.
- Crompton P, Motley R, Morris A. Teledermatology – the Cardiff experience. J Vis Commun Med 2010;33:153-8. http://dx.doi.org/10.3109/17453054.2010.525447.
- Diamond JM, Bloch RM. Telepsychiatry assessments of child or adolescent behavior disorders: a review of evidence and issues. Telemed J E Health 2010;16:712-16. http://dx.doi.org/10.1089/tmj.2010.0007.
- Eikelboom RH, Mbao MN, Coates HL, Atlas MD, Gallop MA. Validation of tele-otology to diagnose ear disease in children. Int J Pediatr Otorhinolaryngol 2005;69:739-44. http://dx.doi.org/10.1016/j.ijporl.2004.12.008.
- Eminovic N, De Keizer NF, Wyatt JC, Ter Riet G, Peek N, Van Weert HC, et al. Teledermatologic consultation and reduction in referrals to dermatologists: a cluster randomized controlled trial. Arch Dermatol 2009;145:558-64. http://dx.doi.org/10.1001/archdermatol.2009.44.
- Eminovic N, Dijkgraaf MG, Berghout RM, Prins AH, Bindels PJ, de Keizer NF. A cost minimisation analysis in teledermatology: model-based approach. BMC Health Serv Res 2010;10. http://dx.doi.org/10.1186/1472-6963-10-251.
- Ferrer-Roca O, Garcia-Nogales A, Pelaez C. The impact of telemedicine on quality of life in rural areas: the Extremadura model of specialized care delivery. Telemed J E Health 2010;16:233-43. http://dx.doi.org/10.1089/tmj.2009.0107.
- Hilty DM, Yellowlees PM, Nesbitt TS. Evolution of telepsychiatry to rural sites: changes over time in types of referral and in primary care providers’ knowledge, skills and satisfaction. Gen Hosp Psychiatry 2006;28:367-73. http://dx.doi.org/10.1016/j.genhosppsych.2006.05.009.
- Hsiao JL, Oh DH. The impact of store-and-forward teledermatology on skin cancer diagnosis and treatment. J Am Acad Dermatol 2008;59:260-7. http://dx.doi.org/10.1016/j.jaad.2008.04.011.
- Knol A, van den Akker TW, Damstra RJ, de Haan J. Teledermatology reduces the number of patient referrals to a dermatologist. J Telemed Telecare 2006;12:75-8. http://dx.doi.org/10.1258/135763306776084365.
- Lasierra N, Alesanco A, Gilaberte Y, Magallon R, Garcia J. Lessons learned after a three-year store and forward teledermatology experience using internet: strengths and limitations. Int J Med Inform 2012;81:332-43. http://dx.doi.org/10.1016/j.ijmedinf.2012.02.008.
- Mahendran R, Goodfield MJD, Sheehan-Dare RA. An evaluation of the role of a store-and-forward teledermatology system in skin cancer diagnosis and management. Clin Exp Dermatol 2005;30:209-14. http://dx.doi.org/10.1111/j.1365-2230.2005.01735.x.
- MacFarlane A. A qualitative study of the educational potential of joint teleconsultations at the primary–secondary interface. J Telemed Telecare 2006;12:22-4. http://dx.doi.org/10.1258/135763306777978399.
- Moreno-Ramirez D, Ferrandiz L, Bernal AP, Duran RC, Martin JJR, Camacho F. Teledermatology as a filtering system in pigmented lesion clinics. J Telemed Telecare 2005;11:298-303. http://dx.doi.org/10.1258/1357633054893364.
- Moreno-Ramirez D, Ferrandiz L, Nieto-Garcia A, Carrasco R, Moreno-Alvarez P, Galdeano R, et al. Store-and-forward teledermatology in skin cancer triage: experience and evaluation of 2009 teleconsultations. Arch Dermatol 2007;143:479-84. http://dx.doi.org/10.1001/archderm.143.4.479.
- Moreno-Ramirez D, Ferrandiz L, Ruiz-de-Casas A, Nieto-Garcia A, Moreno-Alvarez P, Galdeano R, et al. Economic evaluation of a store-and-forward teledermatology system for skin cancer patients. J Telemed Telecare 2009;15:40-5. http://dx.doi.org/10.1258/jtt.2008.080901.
- Morton CA, Downie F, Auld S, Smith B, van der Pol M, Baughan P, et al. Community photo-triage for skin cancer referrals: an aid to service delivery. Clin Exp Dermatol 2011;36:248-54. http://dx.doi.org/10.1111/j.1365-2230.2010.03960.x.
- Summerhayes C, McGee JA, Cooper RJ, Ghauri ASK, Ranaboldo CJ. Introducing leg ulcer telemedicine into rural general practice. Wounds UK 2012;8:28-36.
- Tadros A, Murdoch R, Stevenson JH. Digital image referral for suspected skin malignancy – a pilot study of 300 patients. J Plast Reconstr Aesthet Surg 2009;62:1048-53. http://dx.doi.org/10.1016/j.bjps.2008.02.005.
- Tan E, Yung A, Jameson M, Oakley A, Rademaker M. Successful triage of patients referred to a skin lesion clinic using teledermoscopy (IMAGE IT trial). Br J Dermatol 2010;162:803-11. http://dx.doi.org/10.1111/j.1365-2133.2010.09673.x.
- Thind CK, Brooker I, Ormerod AD. Teledermatology: a tool for remote supervision of a general practitioner with special interest in dermatology. Clin Exp Dermatol 2011;36:489-94. http://dx.doi.org/10.1111/j.1365-2230.2011.04073.x.
- van der Heijden JP, de Keizer NF, Bos JD, Spuls PI, Witkamp L. Teledermatology applied following patient selection by general practitioners in daily practice improves efficiency and quality of care at lower cost. Br J Dermatol 2011;165:1058-65. http://dx.doi.org/10.1111/j.1365-2133.2011.10509.x.
- Wade VA, Karnon J, Elshaug AG, Hiller JE. A systematic review of economic analyses of telehealth services using real time video communication. BMC Health Serv Res 2010;10. http://dx.doi.org/10.1186/1472-6963-10-233.
- Weatherburn G, Ward S, Johnston G, Chisholm S. Off-site expert support for nurses undertaking ECGs in primary care. Br J Nurs 2009;18. http://dx.doi.org/10.12968/bjon.2009.18.9.42258.
- Myers KM, Vander Stoep A, McCarty CA, Klein JB, Palmer NB, Geyer JR, et al. Child and adolescent telepsychiatry: variations in utilization, referral patterns and practice trends. J Telemed Telecare 2010;16:128-33. http://dx.doi.org/10.1258/jtt.2009.090712.
- Siriwardena LSAN, Wickramasinghe WAS, Perera KLD. A review of telemedicine interventions in diabetes care. J Telemed Telecare 2012;18:164-8. http://dx.doi.org/10.1258/jtt.2012.SFT110.
- Wallace P, Barber J, Clayton W, Currell R, Fleming K. Virtual outreach: a randomised controlled trial and economic evaluation of joint teleconferenced medical consultations. Health Technol Assess 2004;8. http://dx.doi.org/10.3310/hta8500.
- Quinn EM, Corrigan MA, O’Mullane J, Murphy D, Lehane EA, Leahy-Warren P, et al. Clinical unity and community empowerment: the use of smartphone technology to empower community management of chronic venous ulcers through the support of a tertiary unit. PLOS ONE 2013;8. http://dx.doi.org/10.1371/journal.pone.0078786.
- Leslie I, Sherrington S, Dick D, Gray N, Chang T-T. Mobile Communications for Medical Care. Cambridge: Universtiy of Cambridge & China Mobile; 2011.
- Free C, Phillips G, Watson L, Galli L, Felix L, Edwards P, et al. The effectiveness of mobile-health technologies to improve health care service delivery processes: a systematic review and meta-analysis. PLOS Med 2013;10. http://dx.doi.org/10.1371/journal.pmed.1001363.
- Steventon A, Bardsley M, Billings J, Dixon J, Doll H, Hirani S, et al. Effect of telehealth on use of secondary care and mortality: findings from the Whole System Demonstrator cluster randomised trial. BMJ 2012;344. http://dx.doi.org/10.1136/bmj.e3874.
- Willems D, Joore M, Hendriks J, Nieman F, Severens J, Wouters E. The effectiveness of nurse-led telemonitoring of asthma: results of a randomized controlled trial. J Eval Clin Pract 2008;14:600-9. http://dx.doi.org/10.1111/j.1365-2753.2007.00936.x.
- Crowe S, Cantrill JA, Tully MP. Shared care arrangements for specialist drugs in the UK: the challenges facing GP adherence. Qual Saf Health Care 2010;19. http://dx.doi.org/10.1136/qshc.2009.035857.
- Davies LM, Fargher EA, Tricker K, Dawes P, Scott DL, Symmons D. Is shared care with annual hospital review better value for money than predominantly hospital-based care in patients with established stable rheumatoid arthritis?. Ann Rheum Dis 2007;66:658-63. http://dx.doi.org/10.1136/ard.2006.061234.
- DeMiglio L, Williams A. Shared care: The barriers encountered by community-based palliative care teams in Ontario, Canada. Health Soc Care Community 2012;20:420-9. http://dx.doi.org/10.1111/j.1365-2524.2012.01060.x.
- Fleury MJ, Imboua A, Aube D, Farand L. Collaboration between general practitioners (GPs) and mental healthcare professionals within the context of reforms in Quebec. Ment Health Fam Med 2012;9:77-90.
- Jha S, Moran P, Blackwell A, Greenham H. Integrated care pathways: the way forward for continence services?. Eur J Obstet Gynecol Reprod Biol 2007;134:120-5. http://dx.doi.org/10.1016/j.ejogrb.2006.07.028.
- McCrone P, Fitzpatrick NK, Mathieson E, Chisholm D, Nourmand S. Economic implications of shared care arrangements. A primary care based study of patients in an inner city sample. Soc Psychiatry Psychiatr Epidemiol 2004;39:553-9.
- Smith SM, Allwright S, O’Dowd T. Effectiveness of shared care across the interface between primary and specialty care in chronic disease management. Cochrane Database Syst Rev 2009;3.
- Grimshaw JM, Winkens RAG, Shirran L, Cunningham C, Mayhew A, Thomas R, et al. Interventions to improve outpatient referrals from primary care to secondary care. Cochrane Database Syst Rev 2005;3.
- Akbari A, Mayhew A, Al-Alawi MA, Grimshaw J, Winkens R, Glidewell E, et al. Interventions to improve outpatient referrals from primary care to secondary care. Cochrane Database Syst Rev 2008;4. http://dx.doi.org/10.1002/14651858.cd005471.pub2.
- Clarke A, Blundell N, Forde I, Musila N, Spitzer D, Naqvi S, et al. Can guidelines improve referral to elective surgical specialties for adults? A systematic review. Qual Saf Health Care 2010;19:187-94. http://dx.doi.org/10.1136/qshc.2008.029918.
- Bridgman S, Li X, Mackenzie G, Dawes P. Does the North Staffordshire slot system control demand of orthopaedic referrals from primary care? A population-based survey in general practice. Br J Gen Pract 2005;55:704-9.
- Elwyn G, Owen D, Roberts L, Wareham K, Duane P, Allison M, et al. Influencing referral practice using feedback of adherence to NICE guidelines: a quality improvement report for dyspepsia. Qual Saf Health Care 2007;16:67-70. http://dx.doi.org/10.1136/qshc.2006.019992.
- Emery J, Morris H, Goodchild R, Fanshawe T, Prevost AT, Bobrow M, et al. The GRAIDS trial: a cluster randomised controlled trial of computer decision support for the management of familial cancer risk in primary care. Br J Cancer 2007;97:486-93. http://dx.doi.org/10.1038/sj.bjc.6603897.
- Fleuren M, Dusseldorp E, van den Bergh S, Vlek H, Wildschut J, van den Akker E, et al. Implementation of a shared care guideline for back pain: effect on unnecessary referrals. Int J Qual Health Care 2010;22:415-20. http://dx.doi.org/10.1093/intqhc/mzq046.
- Garcia Garcia M, Valenzuela Mújica MP, Martinez Ocaña JC, Otero Lopez Mdel S, Ponz Clemente E, López Alba T, et al. Results of a coordination and shared clinical information programme between primary care and nephrology. Nefrologia 2011;31:84-90.
- Glaves J. The use of radiological guidelines to achieve a sustained reduction in the number of radiographic examinations of the cervical spine, lumbar spine and knees performed for GPs. Clin Radiol 2005;60:914-20. http://dx.doi.org/10.1016/j.crad.2005.02.013.
- Hamilton W, Green T, Martins T, Elliott K, Rubin G, Macleod U. Evaluation of risk assessment tools for suspected cancer in general practice: a cohort study. Br J Gen Pract 2013;63:e30-6. http://dx.doi.org/10.3399/bjgp13X660751.
- Jani A, Jenner L, Ma F, Dutton S, Stevens R, Sharma RA. Referral proformas improve compliance to national colorectal 2-week wait targets: does this affect cancer detection rates?. Colorectal Dis 2012;14:1351-6. http://dx.doi.org/10.1111/j.1463-1318.2012.03010.x.
- Jiwa M, Skinner P, Coker AO, Shaw L, Campbell MJ, Thompson J. Implementing referral guidelines: lessons from a negative outcome cluster randomised factorial trial in general practice. BMC Fam Pract 2006;7. http://dx.doi.org/10.1186/1471-2296-7-65.
- Kennedy AM, Aziz A, Khalid S, Hurman D. Do GP referral guidelines really work? Audit of an electronic urgent referral system for suspected head and neck cancer. Eur Arch Otorhinolaryngol 2012;269:1509-12. http://dx.doi.org/10.1007/s00405-011-1788-3.
- Kim-Hwang JE, Chen AH, Bell DS, Guzman D, Yee HF, Kushel MB. Evaluating electronic referrals for specialty care at a public hospital. J Gen Intern Med 2010;25:1123-8. http://dx.doi.org/10.1007/s11606-010-1402-1.
- Menon R, Larner AJ. Use of cognitive screening instruments in primary care: the impact of national dementia directives (NICE/SCIE, National Dementia Strategy). Fam Pract 2012;28:272-6. http://dx.doi.org/10.1093/fampra/cmq100.
- Meeuwissen JAC, van der Feltz-Cornelis CM, van Marwijk HWJ, Rijnders PBM, Donker MCH. A stepped care programme for depression management: an uncontrolled pre-post study in primary and secondary care in The Netherlands. Int J Integr Care 2008;8.
- Melia J, Coulson P, Coleman D, Moss S. Urological referral of asymptomatic men in general practice in England. Br J Cancer 2008;98:1176-81. http://dx.doi.org/10.1038/sj.bjc.6604291.
- Slade M, Gask L, Leese M, McCrone P, Montana C, Powell R, et al. Failure to improve appropriateness of referrals to adult community mental health services – lessons from a multi-site cluster randomized controlled trial. Fam Pract 2008;25:181-90. http://dx.doi.org/10.1093/fampra/cmn025.
- Spatafora S, Canepa G, Migliari R, Rotondo S, Mandressi A, Puppo P. Effects of a shared protocol between urologists and general practitioners on referral patterns and initial diagnostic management of men with lower urinary tract symptoms in Italy: the Prostate Destination study. BJU Int 2005;95:563-70. http://dx.doi.org/10.1111/j.1464-410X.2005.05340.x.
- West YR, Kendrick BJL, Williamson DM. Evaluation of the impact of orthopaedic guidelines on referrals from primary care to a specialist department. Qual Prim Care 2007;15:27-31.
- Giguère A, Légaré F, Grimshaw J, Turcotte S, Fiander M, Grudniewicz A, et al. Printed educational materials: effects on professional practice and healthcare outcomes. Cochrane Database Syst Rev 2012;10. http://dx.doi.org/10.1002/14651858.cd004398.pub3.
- Azuri J, Gelerenter R, Dushinat M, Friedman N, Kokia E. Raising awareness for the diagnosis and treatment of erectile dysfunction in patients with high risk to develop ED. Int J Impot Res 2009;21:249-52. http://dx.doi.org/10.1038/ijir.2009.15.
- Batinac T, Petranovic D, Duletic-Nacinovic A, Troselj-Vukic B, Jelovcic-Barbic B. Significance of continuous medical education of general practitioners about common diseases – iron deficiency anemia. Coll Antropol 2009;33:1191-6.
- Cameron MJ, Horst M, Lawhorne LW, Lichtenberg PA. Evaluation of academic detailing for primary care physician dementia education. Am J Alzheimers Dis Other Demen 2010;25:333-9. http://dx.doi.org/10.1177/1533317510363469.
- Eide MJ, Asgari MM, Fletcher SW, Geller AC, Halpern AC, Shaikh WR, et al. Effects on skills and practice from a web-based skin cancer course for primary care providers. J Am Board Fam Med 2013;26:648-57. http://dx.doi.org/10.3122/jabfm.2013.06.130108.
- Evans E. The Torfaen referral evaluation project. Qual Prim Care 2009;17:423-9.
- Evans E, Aiking H, Edwards A. Reducing variation in general practitioner referral rates through clinical engagement and peer review of referrals: a service improvement project. Qual Prim Care 2011;19:263-72.
- Grassini M, Verna C, Battaglia E, Niola P, Navino M, Bassotti G. Education improves colonoscopy appropriateness. Gastrointest Endosc 2008;67:88-93. http://dx.doi.org/10.1016/j.gie.2007.05.019.
- Lester H, Birchwood M, Freemantle N, Michail M, Tait L. REDIRECT: cluster randomised controlled trial of GP training in first-episode psychosis. Br J Gen Pract 2009;59:e183-90. http://dx.doi.org/10.3399/bjgp09X420851.
- Power P, Iacoponi E, Reynolds N, Fisher H, Russell M, Garety P, et al. The Lambeth Early Onset Crisis Assessment Team Study: general practitioner education and access to an early detection team in first-episode psychosis. Brit J Psychiatr 2007;51:S133-9. http://dx.doi.org/10.1192/bjp.191.51.s133.
- Shariff Z, Roshan A, Williams AM, Platt AJ. 2-week wait referrals in suspected skin cancer: does an instructional module for general practitioners improve diagnostic accuracy?. Surgeon 2010;8:247-51. http://dx.doi.org/10.1016/j.surge.2010.03.004.
- Suris X, Cerda D, Ortiz-Santamaria V, Ponce A, Simon JL, Calvo E, et al. A rheumatology consultancy program with general practitioners in Catalonia, Spain. J Rheumatol 2007;34:1328-31.
- Ulrik CS, Hansen EF, Jensen MS, Rasmussen FV, Dollerup J, Hansen G, et al. Management of COPD in general practice in Denmark – participating in an educational program substantially improves adherence to guidelines. Int J Chron Obstruct Pulmon Dis 2010;5:73-9. http://dx.doi.org/10.2147/COPD.S9102.
- Vernacchio L, Trudell EK, Hresko MT, Karlin LI, Risko W. A quality improvement program to reduce unnecessary referrals for adolescent scoliosis. Pediatrics 2013;131:e912-20. http://dx.doi.org/10.1542/peds.2012-2359.
- Westwood G, Pickering RM, Latter S, Lucassen A, Little P, Karen Temple I. Feasibility and acceptability of providing nurse counsellor genetics clinics in primary care. J Adv Nurs 2006;53:591-604. http://dx.doi.org/10.1111/j.1365-2648.2006.03760.x.
- Westwood G, Pickering R, Latter S. A primary care specialist genetics service: a cluster-randomised factorial trial. Br J Gen Pract 2012;62. http://dx.doi.org/10.3399/bjgp12X630089.
- Willigendael EM, Teijink JAW, Bartelink ML, Langenberg M, Welten RJTJ, Buller HR, et al. Combined training of GPs and practice-assistants on peripheral arterial disease: positive effects after six months. Fam Pract 2005;22:520-2. http://dx.doi.org/10.1093/fampra/cmi041.
- Reynolds G, Chitnis J, Roland M. General practitioner outpatient referrals: do good doctors refer more patients to hospital?. BMJ 1991;302:1250-2. http://dx.doi.org/10.1136/bmj.302.6787.1250.
- Maggs-Rapport F, Kinnersley P, Owen P. In-house referral: changing general practitioners’ roles in the referral of patients to secondary care. Soc Sci Med 1998;46:131-6. http://dx.doi.org/10.1016/S0277-9536(97)00154-8.
- Kinnersley P, Rapport F, Owen P, Stott N. In-house referral: a primary care alternative to immediate secondary care referral?. Fam Pract 1999;16:558-61. http://dx.doi.org/10.1093/fampra/16.6.558.
- Cox J, Steel N, Clark A. Do referral-management schemes reduce hospital outpatient attendances? Time-series evaluation of primary care referral management. Br J Gen Pract 2013;63:e386-92. http://dx.doi.org/10.3399/bjgp13X668177.
- Imison C, Naylor C. Referral Management: Lessons For Success. London: The King’s Fund; 2010.
- Davies M, Elwyn G. Referral management centres: promising innovations or Trojan horses?. BMJ 2006;332:844-6. http://dx.doi.org/10.1136/bmj.332.7545.844.
- Ferguson S, Cook F. Is a primary care orthopaedic interface service sustainable in a continually changing political and healthcare environment?. Clin Govern Int J 2011;16:137-47. http://dx.doi.org/10.1108/14777271111124491.
- Fischer BS, Martinez E, Driscoll M, Conway T. Practice profile. Chicago: using evidence-based rules to make smarter referrals. Health Aff (Millwood) 2010;29:972-5. http://dx.doi.org/10.1377/hlthaff.2010.0068.
- Referral Management Pilots in Wales: Follow Up Review: Final Report. Cardiff: NLIAH; 2007.
- Aghaie-Jaladerany H, Cowell D, Geddes CC. The early impact of the United Kingdom Chronic Kidney Disease (CKD) guidelines on the number of new attendances at renal clinics. Scott Med J 2007;52:28-31. http://dx.doi.org/10.1258/rsmsmj.52.4.28.
- Minshall I, Smith D. The impact of a citywide audit with educational intervention on the care of patients with epilepsy. Seizure 2008;17:261-8. http://dx.doi.org/10.1016/j.seizure.2007.08.002.
- Phillips LA, Donovan KL, Phillips AO. Renal quality outcomes framework and eGFR: impact on se1ondary care. QJM 2009;102:415-23.
- Pockney P, George S, Primrose J, Smith H, Kinley H. Impact of the introduction of fee for service payments on types of minor surgical procedures undertaken by general practitioners: observational study. J Public Health 2004;26:264-7. http://dx.doi.org/10.1093/pubmed/fdh152.
- Srirangalingam U, Sahathevan SK, Lasker SS, Chowdhury TA. Changing pattern of referral to a diabetes clinic following implementation of the new UK GP contract. Br J Gen Pract 2006;56:624-6.
- Oliva X, Micalo T, Perez S, Jugo B, Solana S, Bernades C, et al. Virtual referral system between specialized endocrinological care and primary care. Endocrinol Nutr 2013;60:4-9. http://dx.doi.org/10.1016/j.endonu.2012.09.004.
- Patterson V, Humphreys J, Henderson M. Email triage is an effective, efficient and safe way of managing new referrals to a neurologist. BMJ Qual Saf 2010;19:1-4. http://dx.doi.org/10.1136/qshc.2009.038513.
- Scalvini S, Rivadossi F, Comini L, Muiesan ML, Glisenti F. Telemedicine: the role of specialist second opinion for GPs in the care of hypertensive patients. Blood Press 2011;20:158-65. http://dx.doi.org/10.3109/08037051.2010.542646.
- Stoves J, Connolly J, Cheung CK, Grange A, Rhodes P, O’Donoghue D, et al. Electronic consultation as an alternative to hospital referral for patients with chronic kidney disease: a novel application for networked electronic health records to improve the accessibility and efficiency of healthcare. Qual Saf Health Care 2010;19. http://dx.doi.org/10.1136/qshc.2009.038984.
- Sved Williams A, Dodding J, Wilson I, Fuller J, Wade V. Consultation-liaison to general practitioners coming of age: the South Australian psychiatrists’ experience. Australas Psychiatry 2006;14:206-11. http://dx.doi.org/10.1080/j.1440-1665.2006.02276.x.
- Walker JN, Rourke D, Allen K, Karavitaki N, Levy J. An e-mail GP advisory service: a more efficient way of dealing with clinical enquiries. Br J Hosp Med (Lond) 2009;70:532-3. http://dx.doi.org/10.12968/hmed.2009.70.9.43872.
- Wegner SE, Humble CG, Feaganes J, Stiles AD. Estimated savings from paid telephone consultations between subspecialists and primary care physicians. Pediatrics 2008;122:e1136-40. http://dx.doi.org/10.1542/peds.2008-0432.
- Williams L, O’Riordan S, McGuigan C, Hutchinson M, Tubridy N. A web-based electronic neurology referral system: a solution for an overburdened healthcare system?. Ir Med J 2012;105.
- Roland M, Bewley B. Boneline: evaluation of an initiative to improve communication between specialists and general practitioners. J Public Health Med 1992;14:307-9.
- Leveille SG, Huang A, Tsai SB, Allen M, Weingart SN, Iezzoni LI. Health coaching via an internet portal for primary care patients with chronic conditions a randomized controlled trial. Med Care 2009;47:41-7. http://dx.doi.org/10.1097/MLR.0b013e3181844dd0.
- Ringberg U, Fleten N, Forde O. Examining the variation in GPs’ referral practice: a cross-sectional study of GPs’ reasons for referral. Br J Gen Pract 2014;64:e426-33. http://dx.doi.org/10.3399/bjgp14X680521.
- O’Byrne L, Roberts N, Partridge M. Preclinic telephone consultations: an observational cohort study. Clin Med 2012;12:140-5. http://dx.doi.org/10.7861/clinmedicine.12-2-140.
- Anon . Gateways using Nurses to Screen GP Referrals. Pulse n.d. www.pulsetoday.co.uk/gateways-using-nurses-to-screen-gp-referrals/12511567.article (accessed 19 July 2014).
- Anon . Gatekeeper Job is One for Trained GP. Pulse n.d. www.pulsetoday.co.uk/gatekeeper-job-is-one-for-a-trained-gp/12511735.article (accessed 19 July 2014).
- Anon . Almost Half of GPs Say Delays Caused by Referral Management Schemes Have Harmed Patients. Pulse n.d. www.pulsetoday.co.uk/almost-half-of-gps-say-delays-caused-by-referral-management-schemes-have-harmed-patients/14685668.article#.U8wIJVRwbIU (accessed 20 July 2014).
- Robinson S. Exclusive: Scrutiny of GP Referrals Has Delayed Care and Breached Patient Confidentiality. GP n.d. www.gponline.com/exclusive-scrutiny-gp-referrals-delayed-care-breached-patient-confidentiality/article/1299680?HAYILC = RELATED (accessed 20 August 2014).
- Anon . NHS Managers are Blocking Hospital Referrals to Save Money, Say GPs. Daily Mail n.d. www.dailymail.co.uk/health/article-1359919/NHS-managers-blocking-hospital-referrals-save-money-say-GPs.html (accessed 19 July 2014).
- Robinson S. Is the Scrutiny of GP Referrals Justified?. GP n.d. www.gponline.com/scrutiny-gp-referrals-justified/article/1299525 (accessed 20 August 2014).
- Pawson R. The Science of Evaluation: A Realist Manifesto. London: Sage; 2013.
- Pawson R, Greenhalgh J, Brennan C, Glidewell E. Do reviews of healthcare interventions teach us how to improve healthcare systems?. Soc Sci Med 2014;114:129-37. http://dx.doi.org/10.1016/j.socscimed.2014.05.032.
- Pawson R, Tilley N. Realistic Evaluation. London: Sage; 1997.
- Boyatzis RE. Transforming Qualitative Information: Thematic Analysis and Code Development. Thousand Oaks, CA, London and New Delhi: Sage Publications; 1998.
- Pawson R, Greenhalgh J, Brennan C. Demand management for planned care: a realist synthesis. Health Serv Deliv Res 2016;4.
- McDermott I, Checkland K, Harrison S, Snow S, Coleman A. Who do we think we are? Analysing the content and form of identity work in the English National Health Service. J Health Organ Manag 2013;27:4-23. http://dx.doi.org/10.1108/14777261311311771.
- Xiang A, Smith H, Hine P, Mason K, Lanza S, Cave A, et al. Impact of a referral management ‘gateway’ on the quality of referral letters; a retrospective time series cross sectional review. BMC Health Serv Res 2013;13. http://dx.doi.org/10.1186/1472-6963-13-310.
- Rowlands G. ‘Within practice’ review of referrals significantly alters referral rates – a pilot project. Br J Gen Pract 1997;47:124-5.
- Armour BS, Pitts MM, Maclean R, Cangialose C, Kishel M, Imai H, et al. The effect of explicit financial incentives on physician behavior. Arch Intern Med 2001;161:1261-6. http://dx.doi.org/10.1001/archinte.161.10.1261.
- Levinson DF. Toward full disclosure of referral restrictions and financial incentives by prepaid health plans. N Engl J Med 1987;317. http://dx.doi.org/10.1056/NEJM198712313172708.
- Quality Premium 2013/14 – Guidance for CCGs. Leeds: NHS England; 2013.
- Iacobucci G. GPs put the squeeze on access to hospital care. BMJ 2013;347. http://dx.doi.org/10.1136/bmj.f4351.
- The Role of the Respiratory Specialist in the Integrated Care Team. London: British Thoracic Society; 2014.
- Currie G, Finn R, Martin G. Role transition and the interaction of relational and social identity: new nursing roles in the English NHS. Organization Stud 2010;31:941-61. http://dx.doi.org/10.1177/0170840610373199.
- Hunter B, Segrott J. Renegotiating inter-professional boundaries in maternity care: implementing a clinical pathway for normal labour. Sociol Health Ill 2014;36:719-37. http://dx.doi.org/10.1111/1467-9566.12096.
- Nancarrow SA, Borthwick AM. Dynamic professional boundaries in the healthcare workforce. Sociol Health Ill 2005;27:897-919. http://dx.doi.org/10.1111/j.1467-9566.2005.00463.x.
- Currie G, Finn R, Martin G. Professional competition and modernizing the clinical workforce in the NHS. Work Employ Soc 2009;23:267-84. http://dx.doi.org/10.1177/0950017009102858.
- Martin GP, Currie G, Finn R. Reconfiguring or reproducing intra-professional boundaries? Specialist expertise, generalist knowledge and the ‘modernization’ of the medical workforce. Soc Sci Med 2009;68:1191-8. http://dx.doi.org/10.1016/j.socscimed.2009.01.006.
- Berendsen A, Benneker W, Schuling J, Rijkers-Koorn N, Slaets J, Meyboom-de Jong B. Collaboration with general practitioners: preferences of medical specialists – a qualitative study. BMC Health Serv Res 2006;6. http://dx.doi.org/10.1186/1472-6963-6-155.
- Dagneaux I, Gilard I, De Lepeleire J. Care of elderly people by the general practitioner and the geriatrician in Belgium: a qualitative study of their relationship. J Multidiscip Healthc 2012;5:17-25. http://dx.doi.org/10.2147/JMDH.S27617.
- Coulter A. Managing demand at the interface between primary and secondary care. BMJ 1998;316. http://dx.doi.org/10.1136/bmj.316.7149.1974.
- Roland M, McDonald R, Sibbald B. Can Primary Care Reform Reduce Demand on Hospital Outpatient Departments. Research Summary. Manchester: University of Manchester, National Primary Care Research and Development Centre; 2007.
- Appleby J, Ham C, Imison C, Jennings M. Improvements in Productivity: Doing More With The Same, Not More Of The Same. London: The King’s Fund; 2010.
- Hurley E, McRae I, Bigg I, Stackhouse L, Boxall A-M, Broadhead P. The Australian Health Care System: The Potential For Efficiency Gains. Canberra, ACT: National Health and Hospitals Reform Commission; 2009.
- Thomson S, Foubister T, Mossialos E. Financing Health Care in the European Union: Challenges and Policy Responses. Copenhagen: World Health Organization on behalf of the European Observatory on Health Systems and Policies; 2009.
- Ettelt S, Nolte E, Mays N, Thomson S, McKee M. Health Care Outside Hospital. Accessing Generalist and Specialist Care in Eight Countries. Copenhagen: World Health Organization on behalf of the European Observatory on Health Systems and Policies; 2006.
- Nolte E, Hinrichs S. DISMEVAL. Developing and Validating Disease Management Evaluation Methods for European Healthcare Systems. Final Report. Santa Monica, CA: RAND Corporation and DISMEVAL Consortium; 2012.
- Nolte E, Knai C, McKee M. Managing Chronic Conditions – Experience in Eight Countries. Observatory Studies Series No. 15. Copenhagen: World Health Organization on behalf of the European Observatory on Health Systems and Policies; 2008.
- Kringos D. The Strength of Primary Care in Europe. Utrecht: Nivel; 2012.
- Kringos D, Boerma W, van der Zee J, Groenewegen P. Europe’s strong primary care systems are linked to better population health but also to higher health spending. Health Aff (Millwood) 2013;32:686-94. http://dx.doi.org/10.1377/hlthaff.2012.1242.
- The World Bank . Country and Lending Groups n.d. http://data.worldbank.org/about/country-and-lending-groups#OECD_members (accessed June 2014).
- Kringos D, Boerma W, Bourgueil Y, Cartier T, Dedeu T, Hasvold T, et al. The strength of primary care in Europe: an international comparative study. Br J Gen Pract 2013;63:e742-50. http://dx.doi.org/10.3399/bjgp13X674422.
- International Healthcare Comparisons . About Us n.d. www.international-comparisons.org.uk/about-us/ (accessed June 2014).
- Nolte E, Ettelt S, Thomson S, Mays N. Learning from other countries: an on-call facility for health care policy. J Health Serv Res Policy 2008;13:58-64. http://dx.doi.org/10.1258/jhsrp.2007.007146.
- Olejaz M, Juul Nielsen A, Rudkjøbing A, Okkels Birk H, Krasnik A, Hernández-Quevedo C. Denmark: health system review. Health Syst Transit 2012;14:1-192.
- García-Armesto S, Abadía-Taira M, Durán A, Hernández-Quevedo C, Bernal-Delgado E. Spain: health system review. Health Syst Transit 2010;12:1-295.
- Vuorenkoski L, Mladovsky P, Mossialos E. Finland: health system review. Health Syst Transit 2008;10:1-168.
- Vrangbæk K, Thomson S, Osborn R, Squires D, Jun M. International Profiles Of Health Care Systems. 2013. New York, NY: The Commonwealth Fund; 2013.
- Organisation for Economic Co-operation and Development . OECD.StatExtracts n.d. http://stats.oecd.org/ (accessed July 2014).
- Office for National Statistics . Population Estimates for UK, England and Wales, Scotland and Northern Ireland, Mid-2011 and Mid-2012 n.d. www.ons.gov.uk/ons/rel/pop-estimate/population-estimates-for-uk--england-and-wales--scotland-and-northern-ireland/mid-2011-and-mid-2012/index.html (accessed June 2014).
- Miani C, Pitchforth E, Nolte E. Choice of Primary Care Provider: A Review of Experiences in Three Countries. London: London School of Hygiene and Tropical Medicine, Policy Innovation Research Unit; 2013.
- Schäfer W, Kroneman M, Boerma W, van den Berg M, Westert G, Devillé W, et al. The Netherlands: health system review. Health Syst Transit 2010;12:1-229.
- Boyle S. United Kingdom (England): health system review. Health Syst Transit 2011;13:1-486.
- Kokko S. Integrated primary health care: Finnish solutions and experiences. Int J Integr Care 2009;9.
- OECD Reviews of Health Care Quality: Denmark 2013: Raising Standards. Paris: OECD; 2013.
- Vogelaar E. Voorstel Van Ella Vogelaar, Onafhankelijke Voorzitter Van Het Overleg Tussen LHV, VWs En ZN, Aan Genoemde Partijen Voor Een Beleidsagenda En Bekostigingssystematiek Huisartsenzorg Voor 2006 En 2007 2005. www.medischcontact.nl/home.htm (accessed 19 January 2016).
- Regeling initiatiefruimte ziekenfondsverzekering. Leiden: Zorg en Zekerheid; 2004.
- van Dijk C, Verheij R, Hansen J, van der Velden L, de Bakker D. Effect van praktijkondersteuner n diabetesbegeleiding op het verwijsgedrag van huisartsen bij diabetici. Utrecht: NIVEL; 2010.
- van der Heijden J, Schepers I. Teledermatologie en andere succesvolle teleconsultatiediensten in de dagelijkse huisartsenpraktijk. Bijblijven 2011;27. http://dx.doi.org/10.1007/s12414-011-0065-0.
- Effects of Bundled Payment on Curative Health Care Costs in The Netherlands: An Analysis for Diabetes Care and Vascular Risk Management Based on Nationwide Claim Data, 2007–2010. Bilthoven: RIVM; 2012.
- Guía de gestión de los servicios de admisión y documentación clínica. Madrid: Ministerio de Sanidad y Consumo, Instituto Nacional de la Salud; 2000.
- Cartera de servicios de Atención Primaria Definiciones, criterios de acreditación, indicadores de cobertura y normas técnicas. Madrid: Instituto Nacional de la Salud Subdireccion General De Coordinacion Administrativa; 2001.
- National Health System of Spain. Annual Report 2009. Madrid: Ministerio de Sanidad, Política Social e Igualdad; 2010.
- Tynkkynen L, Keskimäki I, Lehto J. Purchaser-provider splits in health care-the case of Finland. Health Policy 2013;111:221-5. http://dx.doi.org/10.1016/j.healthpol.2013.05.012.
- Krasnik A, Groenewegen PP, Pedersen PA, von Scholten P, Mooney G, Gottschau A, et al. Changing remuneration systems: effects on activity in general practice. BMJ 1990;300:1698-701. http://dx.doi.org/10.1136/bmj.300.6741.1698.
- van Dijk CE, Korevaar JC, Koopmans B, de Jong JD, de Bakker DH. The primary-secondary care interface: does provision of more services in primary care reduce referrals to medical specialists?. Health Policy 2014;118:48-55. http://dx.doi.org/10.1016/j.healthpol.2014.04.001.
- Thijssing L, van der Heijden J, Chavannes N, Melissant C, Jaspers M, Witkamp L. Telepulmonology: effect on quality and efficiency of care. Respir Med 2014;108:314-18. http://dx.doi.org/10.1016/j.rmed.2013.10.017.
- van Til de Wildt T, Struijs J. De organisatie van zorggroepen anno 2010. Huidige stand van zaken en de ontwikkelingen in de afgelopen jaren. Bilthoven: National Institute for Public Health and the Environment; 2010.
- de Bakker D, Raams J, Schut E, Vrijhoef B, de Wildt J. Evaluatiecommissie Integrale Bekostiging. Eindrapport van de Evaluatiecommissie Integrale Bekostiging. Integrale bekostiging van Zorg: werk in uitvoering. Den Haag: ZonMw (The Netherlands Organisation for Health Research and Development); 2012.
- Struijs J, De Jong-Van Til J, Lemmens L, Drewes H, De Bruin S, Baan C. Bundled Payments of Diabetes Care: Effects on Care Delivery Process and Quality of Care at Three-Year Follow-Up. Bilthoven: National Institute for Public Health and the Environment; 2012.
- Confederación Estatal de Sindicatos Médicos (CESM) . Primaria Y Especializada Creen Que debería Reducir Derivaciones n.d. www.cesm.org.es/index.php/profesion/3606-primaria-y-especializada-creen-que-deberia-reducir-derivaciones (accessed 28 October 2015).
- Marco Estratégico para la mejora de la Atención Primaria en España: 2007–2012. Proyecto AP-21. Estrategias para la mejora de la Atención Primaria. Análisis de situación de la Atención Primaria. Madrid: Ministerio de Sanidad y Consumo; 2007.
- Anon . Sanidad Estudia Trasladar Toda La cirugía Menor Ambulatoria a Atención Primaria n.d. www.redaccionmedica.com/noticia/sanidad-estudia-trasladar-toda-la-cirugia-menor-ambulatoria-a-primaria-6882 (accessed 28 October 2015).
- Struijs J, Mohnen S, Molema C, de Jong van Til J, Baan C. Effect van integrale bekostiging. Bilthoven: RIVM; 2012.
- Advies functie eerstelijns Geestelijke GezondheisZorg (GGZ). Utrecht: NZa; 2011.
- Hansen J, Schepman S. Op de huid. Inventarisatie zorgvraag en marktgebied huidtherapie. Utrecht: NIVEL; 2009.
- Batenburg R, van Hassel D. De omvang en potentiële filterwerking van de optometrist binnen de oogzorg in Nederland: een verkennende analyse op basis van cliëntgegevens van optometriepraktijken en LINH. Utrecht: NIVEL; 2012.
- Kokko S. Towards fragmentation of general practice and primary healthcare in Finland?. Scand J Prim Health Care 2007;25:131-2. http://dx.doi.org/10.1080/02813430701576482.
- van Dijk C, Korevaar J, de Jong J, Koopmans B, van Dijk M, de Bakker D. Kennisvraag. Ruimte voor substitutie? Verschuivingen van tweedelijns- naar eerstelijnszorg. Utrecht: NIVEL; 2013.
- Pelttari H, Minna K. Kiireettömään hoitoon pääsyn selvitys. Nykytila ja toimenpide-ehdotuksia. Helsinki: Sosiaali-Ja Terveyministeriö; 2014.
- Yhtenäiset kiireettömän hoidon perusteet. Sosiaali- ja terveysministeriön oppaita. Helsinki: STM; 2005.
- Cartera de servicios de atención primaria. Desarrollo, organización, usos y contenido. Madrid: Ministerio de Sanidad y Política Social; 2010.
- Carrousel . Carrousel Gezamenlijke Consulten n.d. www.carrousel.azm.nl/ (accessed 28 October 2015).
- Vlek H, van Leeuwen Y, Crebolder H. Het gezamenlijk consult: een effectieve methode om de ervaringskennis van de huisarts te vergroten. Huisarts Wet 2003;46:164-6. http://dx.doi.org/10.1007/BF03083235.
- NHS England . Five Year Forward View 2014. www.england.nhs.uk/wp-content/uploads/2014/10/5yfv-web.pdf (accessed 31 December 2015).
- Blanco Franco M, Bruzos González E, Canedo L, González Fernández M, Martínez Quiroga M, Martínez Villanueva A, et al. Guía De práctica clínica De cirugía Menor En Atención Primaria 2010.
- Delgado Zafra S, Casas Nicot B, Gavira Iglesias J. Análisis de un programa de salud: cirugía menor en Atención Primaria. Med Fam Andal 2012;13:28-33.
- González Cano J, Sellés Dechent R, Guinot Martínez E, Belenguer Tarin V. Cirugia Menor. Guía De Actuación Clínica En A. P n.d. www.san.gva.es/documents/246911/251004/guiasap010cma.pdf (accessed June 2014).
- Grupo de Cirugía Menor de la Asociación Gallega de Medicina Familiar y Comunitaria . Curso De Cirugia Menor n.d. www.agamfec.com/pdf/Grupos/Ciruxia_menor/Curso_Cirugia_menor.pdf (accessed 28 October 2015).
- Guerrero Francisca D, del Rosario G, Marin Concepción P, Bouza Mónica R. Cirugía Menor 2011. www.juntadeandalucia.es/servicioandaluzdesalud/library/plantillas/externa.asp?pag = . /. /contenidos/gestioncalidad/estratcuidados/PracAvCirugiaMenor24052011.pdf (accessed 2014).
- Pérez Vega F, Domínguez Romero M, Galiana Martínez J, Lorenzo Peñuelas J. Cirugía Menor. Programa de Cirugía Menor en Atención Primaria. Cadiz: Grupo Andaluz para el Desarrollo y la Investigación de la Cirugía Menor; 2008.
- Protocolo de cirugía menor en atención primaria. Santa Cruz de Tenerife y Las Palmas de Gran Canaria: Gobierno de Canarias, Consejería de Sanidad, Servicio Canario de la Salud, Dirección General de Programas Asistenciales; 2010.
- Manual práctico de cirugía menor. Valencia: Societat Valenciana de Cirugía Menor y Comunitaria; 2012.
- Cuñat V. Cirugía menor y otros procedimientos en las consultas de atención primaria. Semergen 2002;28:71-2. http://dx.doi.org/10.1016/S1138-3593(02)74039-2.
- Heiligers P, Noordman J, Korevaar J, Dorsman S, Hingstman L, van Dulmen A, et al. Kennisvraag: praktijkondersteuners in de huisartspraktijk (PoH’s), klaar voor de toekomst?. Utrecht: NIVEL; 2012.
- León A. Primaria pedirá a Educación y Sanidad la segunda especialidad. Diario Médico n.d. www.diariomedico.com/2007/09/24/area-profesional/profesion/primaria-pedira-a-educacion-y-sanidad-la-segunda-especialidad (accessed August 2014).
- Saaresranta T, Anttalainen U, Brander P, Lojander J, Polo O. Follow-up of the CPAP treatment for patients with sleep apnea is commonly being transferred to primary health care: a review. Suomen lääkärilehti 2012;67:3001-5.
- Eugenia Lauret Braña E, Parra Blanco A, Suárez González A, López Rivas L, Blay Albors P, Rodríguez Gordaliza F, et al. Protocolo de detección precoz de cáncer colorrectal en personas de riesgo elevado. Guia de Uso Adecuado de Colonoscopia en Asturias. Oviedo: Servicio de Salud del Principado de Asturias; 2010.
- Vedsted P, Olesen F, Hollnagel H, Bro F, Kamper-Jørgensen F. [General Practice in Denmark]. Copenhagen: TPL; 2005.
- Vedsted P, Olesen F. Are the serious problems in cancer survival partly rooted in gatekeeper principles? An ecologic study. Br J Gen Pract 2011;61:e508-12. http://dx.doi.org/10.3399/bjgp11X588484.
- Holtzer-Goor K, van Sprundel E, Lemij H, Klazinga N, Koopmanschap M. Cost-effectiveness of monitoring glaucoma patients in shared care: an economic evaluation alongside a randomized controlled trial. BMC Health Serv Res 2010;10. http://dx.doi.org/10.1186/1472-6963-10-312.
- Pautas de actuación conjunta de los Equipos Básicos de Atención Primaria y los Dispositivos de Apoyo a la Rehabilitación. Patologia del Aparato Locomotor. Sevilla: Servicio Andaluz de Salud, Consejería de Salud and Junta de Andalucía; 2005.
- Protocolo de derivación a tención temprana en neonatos en riesgo. Madrid: Comunidad de Madrid; 2013.
- Olesen F, Bro F, Vedsted P. The role of NHS gatekeeping in delayed diagnosis. BMJ 2014;348. http://dx.doi.org/10.1136/bmj.g2633.
- Arroyo A, Andreu J, García P, Jover S, Arroyo M, Fernández A, et al. Análisis de un programa de derivación directa entre atención primaria y especializada en pacientes potencialmente quirúrgicos. Aten Primaria 2001;28:381-5. http://dx.doi.org/10.1016/S0212-6567(01)70399-X.
- Cerdán Carbonero M, Sanz López R, Martínez Ramos C. Improving communication between levels of health care: Direct referral of patients to a ‘one-stop’ service for major outpatient surgery. Aten Primaria 2005;35:283-8. http://dx.doi.org/10.1157/13073412.
- Fernández Aguirre M, Emparanza Knorr J, Gómez Fraga I, González Osinalde M, Madruga Carpintero F, Mugica Iriondo O. Direct vs. indirect referrals to rehabilitation from primary care. Rehabilitacion 2010;44:211-15. http://dx.doi.org/10.1016/j.rh.2010.01.007.
- Kringos D, Klazinga N. The Composition of Primary Care Teams. Canada, England, France, Germany, The Netherlands, United States. Amsterdam: Academisch Medisch Centrum; 2014.
- González-Ramallo V, Segado-Soriano A. Twenty five years of hospital at home in Spain. Med Clin (Barc) 2006;126:332-3. http://dx.doi.org/10.1157/13085746.
- Brotons C, Falces C, Alegre JB, E, Casanovas J, Catà T, Martínez M, et al. Randomized clinical trial of the effectiveness of a home-based intervention in patients with heart failure: the IC-DOM study. Rev Esp Cardiol 2009;62:400-8. http://dx.doi.org/10.1016/S0300-8932(09)70897-8.
- Mendoza H, Martín M, García AA, F, Aizpuru F, Regalado De Los Cobos J, Belló M, et al. ‘Hospital at home’ care model as an effective alternative in the management of decompensated chronic heart failure. Eur J Heart Fail 2009;11:1208-13. http://dx.doi.org/10.1093/eurjhf/hfp143.
- SaludMadrid . Servicios médicos. Servicio De Hospitalización a Domicilio n.d. www.madrid.org/cs/Satellite?cid = 1142635532242&language = es&pagename = HospitalGregorioMaranon/Page/HGMA_contenidoFinal (accessed June 2014).
- Puig-Junoy J, Casas A, Font-Planells J, Escarrabill J, Hernández C, Alonso J, et al. The impact of home hospitalization on healthcare costs of exacerbations in COPD patients. Eur J Health Econ 2007;8:325-32. http://dx.doi.org/10.1007/s10198-006-0029-y.
- Grenzner V, Olivet M, Lacasa C, Fernández FG, A, Torras M, Lemonche C, et al. Reorganising specialist care in the Ciutat Vella Health Sector: analysis of an experience. Aten Primaria 1998;21:377-82.
- Grupo para la Asistencia Médica Integrada Continua de Cádiz (GAMIC) . The consulting of internal medicine in primary care improves the efficacy of medical care. Med Clin (Barc) 2004;122:46-52. http://dx.doi.org/10.1016/S0025-7753(04)74138-X.
- Implementing Transnational Telemedicine Solutions . Finland n.d. www.transnational-telemedicine.eu/countries/finland/ (accessed 28 October 2015).
- Nikkanen T, Timonen M, Ylitalo K, Timonen O, Keinänen-Kiukaanniemi S, Rajala U. Quality of diabetes care among patients managed by teleconsultation. J Telemed Telecare 2008;14:295-9. http://dx.doi.org/10.1258/jtt.2008.080313.
- Hautala N, Aikkila R, Korpelainen J, Keskitalo A, Kurikka A, Falck A, et al. Marked reductions in visual impairment due to diabetic retinopathy achieved by efficient screening and timely treatment. Acta Ophthalmol 2014;92:582-7. http://dx.doi.org/10.1111/aos.12278.
- Hautala N, Hyytinen P, Saarela V, Hägg P, Kurikka A, Runtti M, et al. A mobile eye unit for screening of diabetic retinopathy and follow-up of glaucoma in remote locations in northern Finland. Acta Ophthalmol 2009;87:912-13. http://dx.doi.org/10.1111/j.1755-3768.2009.01570.x.
- Sensire . Zorg Op Afstand n.d. www.sensire.nl/onze_diensten/zorg_op_afstand/telesens.aspx (accessed 28 October 2015).
- Pazio . Vernieuwen, Versnellen, Versterken n.d. www.pazio.nl/pazio-bouwsteen-voor-regionale-eonomische-agenda-ebu/ (accessed 28 October 2015).
- ZonMw . Zorg Op Afstand in Almere n.d. www.zonmw.nl/nl/projecten/project-detail/zorg-op-afstand-in-almere/samenvatting/ (accessed 28 October 2015).
- Dinesen B, Huniche L, Toft E. Attitudes of COPD patients towards tele-rehabilitation: a cross-sector case study. Int J Environ Res Public Health 2013;10:6184-98. http://dx.doi.org/10.3390/ijerph10116184.
- Dinesen B, Seeman J, Gustafsson J. Development of a program for tele-rehabilitation of COPD patients across sectors: co-innovation in a network. Int J Integr Care 2011;11.
- Telemedicine – A Key to Health Services of the Future. National Action Plan for Dissemination of Telemedicine – In Brief. Copenhagen: The Danish Agency for Digitisation; 2012.
- MedCom . Dissemination and Technological Future-Proofing 2012–2013 n.d. www.medcom.dk/dwn5323.pdf (accessed 28 October 2015).
- Udsen F, Heyckendorff Lilholt P, Hejlesen O, Ehlers L. Effectiveness and cost-effectiveness of telehealthcare for chronic obstructive pulmonary disease: study protocol for a cluster randomized controlled trial. Trials 2014;15. http://dx.doi.org/10.1186/1745-6215-15-178.
- Region Syddanmark . The Ulcer Project. Telemedicine Consultations for the Treatment of Diabetic Foot Ulcers n.d. www.renewinghealth.eu/documents/28946/396054/Treatment+of+Diabetic+Foot+Ulcer+project.pdf (accessed 28 October 2015).
- Doupi P, Renko E, Hämäläinen P, Mäkelä M, Giest S, Dumortier J. eHealth Strategies. Country Brief: Finland. Bonn and Brussels: empirica Gesellschaft für Kommunikations- und Technologieforschung mbH; European Commission, DG Information Society and Media; 2010.
- Hyppönen H, Reponen J, Lääveri T, Kaipio J. User experiences with different regional health information exchange systems in Finland. Int J Med Inform 2014;83:1-18. http://dx.doi.org/10.1016/j.ijmedinf.2013.10.002.
- Lopez-Bastida J, Cabrera-Lopez F, Serrano-Aguilar P. Sensitivity and specificity of digital retinal imaging for screening diabetic retinopathy. Diabet Med 2007;24:403-7. http://dx.doi.org/10.1111/j.1464-5491.2007.02074.x.
- Martinez-Ramos C. Telemedicina en España. II. Comunidades Autónomas. Sanidad Militar, Marítima y Penitenciaria. Proyectos Humanitarios. Reduca (Recursos Educativos), Serie Medicina 2009;1:182-20.
- Martín-Lesende I, Orruño E, Bilbao A, Vergara I, Cairo M, Bayón J, et al. Impact of telemonitoring home care patients with heart failure or chronic lung disease from primary care on healthcare resource use (the TELBIL study randomised controlled trial). BMC Health Serv Res 2013;13. http://dx.doi.org/10.1186/1472-6963-13-118.
- Martín-Lesende IO, E, Cairo C, Bilbao A, Asua J, Romo M, Vergara IB, et al. Assessment of a primary care-based telemonitoring intervention for home care patients with heart failure and chronic lung disease. The TELBIL study. BMC Health Serv Res 2011;11. http://dx.doi.org/10.1186/1472-6963-11-56.
- Segrelles Calvo G, Gómez-Suárez C, Soriano J, Zamora E, Gónzalez-Gamarra A, González-Béjar M, et al. A home telehealth program for patients with severe COPD: the PROMETE study. Respir Med 2014;108:453-62. http://dx.doi.org/10.1016/j.rmed.2013.12.003.
- Pedrón-Giner C, Navas-López V, Martínez-Zazo A, Martínez-Costa C, Sánchez-Valverde F, Blasco-Alonso J, et al. Analysis of the Spanish national registry for pediatric home enteral nutrition (NEPAD): implementation rates and observed trends during the past 8 years. Eur J Clin Nutr 2013;67:318-23. http://dx.doi.org/10.1038/ejcn.2013.8.
- Martínez-Ramos C, Cerdán M, López R. Mobile phone-based telemedicine system for the home follow-up of patients undergoing ambulatory surgery. Telemed J E Health 2009;15:531-7. http://dx.doi.org/10.1089/tmj.2009.0003.
- Galiano-Castillo N, Ariza-García A, Cantarero-Villanueva I, Fernández-Lao C, Díaz-Rodríguez L, Legerén-Alvarez M, et al. Telehealth system (e-CUIDATE) to improve quality of life in breast cancer survivors: rationale and study protocol for a randomized clinical trial. Trials 2013;14. http://dx.doi.org/10.1186/1745-6215-14-187.
- Dutch College of General Practitioners . National Primary Care Collaboration Agreement on Malnutrition n.d. www.nhg.org/sites/default/files/content/nhg_org/uploads/lesa_malnutrition_eng_24_3_11_0.pdf (accessed 28 October 2015).
- Meijer L, Schellevis F. Referring patients with chronic renal failure: differences in referral criteria between hospitals. Ned Tijdschr Geneeskd 2012;156.
- Consejería de Igualdad SyPs . Procesos Asistenciales Integrados (PAI) n.d. www.juntadeandalucia.es/salud/sites/csalud/contenidos/Informacion_General/p_3_p_3_procesos_asistenciales_integrados/listado_procesos?perfil = org (accessed 28 October 2015).
- Calidad y Seguridad . Procesos Asistenciales Integrados, Protocolos De atención Y Vías clínicas n.d. www.san.gva.es/web/calidad/protocolos-de-atencion (accessed June 2014).
- Pérez Gortari P, Diez Andrés A, Ruiz Téllez A, Martínez Ferrer J, Almeida Llamas V, Santos Larregola L. El Especialista Consultor Integrado En El Centro De Salud 2001. www.elmedicointeractivo.com/ap1/emiold/publicaciones/centrosalud9/553–556.pdf (accessed June 2014).
- Anonymous . La figura de la enfermera gestora de casos cobra protagonismo en el SNS. GazetaMedica n.d. www.gacetamedica.com/noticias-medicina/2014–01–17/politica/la-figura-de-la-enfermera-gestora-de-casos-cobra-protagonismo-en-el-sns/pagina.aspx?idart=807251 (accessed August 2014).
- Pérez Hernández R, López Alonso S, Lacida Baro M, Rodríguez Gómez S. La Enfermera Comunitaria de Enlace en el Servicio Andaluz de Salud. Enferm Comun 2005;1:43-8.
- Duodecim . Duodecim n.d. www.duodecim.fi/web/kotisivut (accessed 28 October 2015).
- GuíaSalud . Catalogue of Clinical Practice Guidelines in the Spanish National Health System (NHS) n.d. http://portal.guiasalud.es/web/guest/catalogo-gpc (accessed 28 October 2015).
- SemFYC . Guías clínicas n.d. www.semfyc.es/es/informativo/guias_clinicas_profesionales/ (accessed 28 October 2015).
- Netherlands Institute for Health Services Research . Netherlands Information Network of General Practice (LINH) n.d. www.nivel.nl/en/netherlands-information-network-general-practice-linh (accessed 28 October 2015).
- Ros C, Hutten J, Groenewegen P. Centra centraal: onderzoek naar kwaliteitskenmerken van gezondheidscentra en de produktiecijfers van huisartsen. Utrecht: NIVEL; 1996.
- Wijkel D. Lower referral rates for integrated health centres in The Netherlands. Health Policy 1986;6:185-98. http://dx.doi.org/10.1016/0168-8510(86)90007-2.
Appendix 1 Search strategy
General search strategy terms and limitations
Language limitations: English, French, German, Spanish and Dutch.
Date limitations: 2005 to present.
Type of document limitations: include only randomised trials (RCTs), controlled clinical trials, controlled before-and-after studies and interrupted time series, systematic reviews, meta-analyses, observational studies.
Country limitations: high-income countries only.
Search terms
| Length of stay | Length of stay OR length of hospital stay OR length of hospitalisation OR length of hospitalization OR bed days OR hospital stay |
| Interventions | Day surgery OR comprehensive geriatric assessment OR enhanced recovery OR short-acting anaesthetics OR discharge planning OR patient discharge OR case management OR care management OR early discharge OR hospital at home OR post-discharge care OR clinical pathway OR service (re)design OR home ward OR virtual ward OR staffing OR staff OR organisation OR organisational OR admissions OR follow-up OR discharged OR discharge OR model of care OR payment(s) OR contract(s) OR contracting OR commission(ing) OR procure(ment) OR fees OR incentive OR management OR managerial |
| Settings | Hospital OR Primary care OR community care OR care home OR nurse care OR nursing care OR nursing home OR home care OR home OR outpatient OR secondary care OR clinic OR telecare OR tele care OR telemedicine OR telehealth OR intermediate care OR family practice OR general practitioner OR GP OR specialist physician OR specialist care OR social care OR local authority care OR long-term care |
| Outcomes: general | Outcome OR impact OR efficiency OR effectiveness OR efficacy |
| Patient outcomes | OR Patient satisfaction OR patient experience OR patient preference OR quality of life OR patient health OR health status OR acceptability |
| Service outcomes | Quality of care OR safety OR emergency re(-)admissions OR re-admissions OR readmissions OR service utilisation OR service utilization OR waiting times OR waiting list OR outpatient attendance OR acceptability to clinicians OR bed occupancy OR utilisation rate OR utilization rate OR referral |
| Costs | Costs OR spending OR saving(s) OR expense OR economy OR cost-effectiveness OR spend OR cut OR expenditure |
The logic links between the different categories should be the following:
1 AND 2 AND 3 AND 4 AND 5 (general OR a OR b OR c)
Search terms should be found in the title or the abstract.
Details of search strategies
MEDLINE
Date of search: April 2014.
Search strategy
-
primary health care/
-
family practice/
-
physicians, family/
-
primary care.ti,ab.
-
primary health care.ti,ab.
-
general practice$.ti,ab.
-
family practice$.ti,ab.
-
general practitioner$.ti,ab.
-
(gp or gps).ti,ab.
-
(family adj (physician$ or doctor$)).ti,ab.
-
primary care practitioner$.ti,ab.
-
or/1-11
-
gatekeeping/
-
gpwsi$.ti,ab.
-
((gp$ or practitioner$) adj2 special adj2 interest$).ti,ab.
-
((outreach or specialist$ or satellite) adj clinic$).ti,ab.
-
(liaison adj3 (service$ or provid$ or provision or organis$ or organiz$ or deliver$ or attachment$)).ti,ab.
-
gatekeep$.ti,ab.
-
shared care$.ti,ab.
-
(integrated adj2 care).ti,ab.
-
(discharge adj (guideline$ or procedure$ or arrangement$ or routine$)).ti,ab.
-
((primary or gp or gps) adj3 secondary care).ti,ab.
-
((practice$ or practitioner$) adj3 incentive$).ti,ab.
-
(‘model of care’ or ‘models of care’).ti,ab.
-
“referral management”.mp.
-
exp Health Care Rationing/ or “health care ration*”.mp.
-
or/13-26
-
12 and 27
-
limit 28 to (english language and yr=“Feb 2005 - current”)
-
outpatients/
-
ambulatory care facilities/
-
pain clinics/
-
surgicenters/
-
exp ambulatory care/
-
outpatient clinics, hospital/
-
ambulatory surgical procedures/
-
surgical procedures, minor/
-
outpatient$.ti,ab.
-
day surgery.ti,ab.
-
day case surgery.ti,ab.
-
day care surgery.ti,ab.
-
exp Telemedicine/ or telemonitor*.mp.
-
exp Remote Consultation/ or “remote consult*”.mp.
-
or/30-43
-
‘referral.mp. and consultation’/
-
referral$.ti,ab.
-
waiting lists/
-
(waiting adj (time or times or list or lists)).ti,ab.
-
appointment$.ti,ab.
-
patient admission/
-
exp “Appointments and Schedules”/
-
admission$.ti,ab.
-
or/45-52
-
12 and 44 and 53
-
limit 54 to (english language and yr=“Feb 2005 - current”)
-
“decision making”.mp. or exp Decision Making/
-
“decision support”.mp.
-
exp Choice Behavior/ or choice.mp.
-
“choose and book”.mp.
-
“choose & book”.mp.
-
exp “Appointments and Schedules”/ or appointment*.mp.
-
exp Decision Support Techniques/
-
exp Patient Preference/
-
exp Patient Participation/
-
“health litera$”.mp.
-
exp Health Literacy/
-
exp Patient Education as Topic/
-
exp Consumer Health Information/
-
“shared decision making”.mp.
-
or/56-69
-
12 and 53 and 70
-
limit 71 to (english language and yr=“Feb 2005 - current”)
-
29 or 55 or 72
EMBASE
Date of search: April 2014.
Search strategy
-
primary health care/
-
family practice/
-
physicians, family/
-
primary care.ti,ab.
-
primary health care.ti,ab.
-
general practice$.ti,ab.
-
family practice$.ti,ab.
-
general practitioner$.ti,ab.
-
(gp or gps).ti,ab.
-
(family adj (physician$ or doctor$)).ti,ab.
-
primary care practitioner$.ti,ab.
-
or/1-11
-
gatekeeping/
-
gpwsi$.ti,ab.
-
((gp$ or practitioner$) adj2 special adj2 interest$).ti,ab.
-
((outreach or specialist$ or satellite) adj clinic$).ti,ab.
-
(liaison adj3 (service$ or provid$ or provision or organis$ or organiz$ or deliver$ or attachment$)).ti,ab.
-
gatekeep$.ti,ab.
-
shared care$.ti,ab.
-
(integrated adj2 care).ti,ab.
-
(discharge adj (guideline$ or procedure$ or arrangement$ or routine$)).ti,ab.
-
((primary or gp or gps) adj3 secondary care).ti,ab.
-
((practice$ or practitioner$) adj3 incentive$).ti,ab.
-
(‘model of care’ or ‘models of care’).ti,ab.
-
“referral management”.mp.
-
exp Health Care Rationing/ or “health care ration*”.mp.
-
or/13-26
-
12 and 27
-
limit 28 to (english language and yr=“Feb 2005 - current”)
-
outpatients/
-
ambulatory care facilities/
-
pain clinics/
-
surgicenters/
-
exp ambulatory care/
-
outpatient clinics, hospital/
-
ambulatory surgical procedures/
-
surgical procedures, minor/
-
outpatient$.ti,ab.
-
day surgery.ti,ab.
-
day case surgery.ti,ab.
-
day care surgery.ti,ab.
-
exp Telemedicine/ or telemonitor*.mp.
-
exp Remote Consultation/ or “remote consult*”.mp.
-
or/30-43
-
‘referral.mp. and consultation’/
-
referral$.ti,ab.
-
waiting lists/
-
(waiting adj (time or times or list or lists)).ti,ab.
-
appointment$.ti,ab.
-
patient admission/
-
exp “Appointments and Schedules”/
-
admission$.ti,ab.
-
or/45-52
-
12 and 44 and 53
-
limit 54 to (english language and yr=“Feb 2005 - current”)
-
“decision making”.mp. or exp Decision Making/
-
“decision support”.mp.
-
exp Choice Behavior/ or choice.mp.
-
“choose and book”.mp.
-
“choose & book”.mp.
-
exp “Appointments and Schedules”/ or appointment*.mp.
-
exp Decision Support Techniques/
-
exp Patient Preference/
-
exp Patient Participation/
-
“health litera$”.mp.
-
exp Health Literacy/
-
exp Patient Education as Topic/
-
exp Consumer Health Information/
-
“shared decision making”.mp.
-
or/56-69
-
12 and 53 and 70
-
limit 71 to (english language and yr=“Feb 2005 - current”)
-
29 or 55 or 72
Health Management and Information Consortium
Date of search: April 2014.
Search strategy
-
primary health care/
-
primary health care.ti,ab.
-
primary health care.ti,ab.
-
general practice$.ti,ab.
-
family practice$.ti,ab.
-
general practitioner$.ti,ab.
-
(gp or gps).ti,ab.
-
(family adj (physician$ or doctor$)).ti,ab.
-
primary care practitioner$.ti,ab.
-
or/1-9
-
gatekeeping/
-
gatekeep$.ti,ab
-
gpwsi$.ti,ab.
-
((gp$ or practitioner$) adj2 special adj2 interest$).ti,ab.
-
((outreach or specialist$ or satellite) adj clinic$).ti,ab.
-
(liaison adj3 (service$ or provid$ or provision or organis$ or organiz$ or deliver$ or attachment$)).ti,ab.
-
shared care$.ti,ab.
-
(integrated adj2 care).ti,ab.
-
(discharge adj (guideline$ or procedure$ or arrangement$ or routine$)).ti,ab.
-
((primary or gp or gps) adj3 secondary care).ti,ab.
-
((practice$ or practitioner$) adj3 incentive$).ti,ab.
-
(‘model of care’ or ‘models of care’).ti,ab.
-
“referral management”.mp.
-
exp Health Care Rationing/ or “health care ration*”.mp.
-
or/11-24
-
10 and 25
-
outpatients/
-
ambulatory care facilities/
-
pain clinics/
-
surgicenters/
-
exp ambulatory care/
-
outpatient clinics/
-
ambulatory surgical procedures/
-
outpatient$.ti,ab.
-
day surgery.ti,ab.
-
day case surgery.ti,ab.
-
day care surgery.ti,ab.
-
exp Telemedicine/ or telemonitor*.mp.
-
exp Remote Consultation/ or “remote consult*”.mp.
-
or/27-39
-
‘referral.mp. and consultation’/
-
referral$.ti,ab.
-
waiting lists/
-
(waiting adj (time or times or list or lists)).ti,ab.
-
appointment$.ti,ab.
-
appointment*.mp.
-
patient admission/
-
admission$.ti,ab.
-
or/41-48
-
10 and 40 and 49
-
“decision support”.mp.
-
“choose and book”.mp.
-
“choose & book”.mp.
-
exp Patient Participation/
-
“health litera$”.mp.
-
exp Health Literacy/
-
exp Consumer Health Information/
-
“shared decision making”.mp.
-
choice.mp.
-
or/51-60
-
10 and 49 and 61
-
26 or 50 or 62
-
limit 63 to yr=“Feb 2005 –Current”
The King’s Fund library (OvidSP)
Date of search: May 2014.
URL: http://kingsfund.koha-ptfs.eu/
Search strategy
Search 1
(Telemedecine AND review) OR (telehealth AND review) OR (telecare AND review) (2005 - 5 May 2014)
Search 2
(Referral AND management) (2005 - 5 May 2014)
Search 3
Outpatient (2005 - 5 May 2014)
Appendix 2 Studies included in the review
| Reference | Country | Study design | Study aims and intervention | Outcomes |
|---|---|---|---|---|
| Aghaie-Jaladerany et al. (2007)199 | UK (Scotland) | Retrospective case review | Aim: to assess the early impact of the implementation of the UK CKD guidelines on new patient attendances at nephrology clinics Population: adult patients with CKD Sample size: 160 patients Interventions: introduction of CKD guidelines and laboratory eGFR reporting. The CKD guideline recommends that all patients with stage 4 and 5 CKD are either referred to or discussed with a nephrologist. For stage 3 CKD the majority of patients can be managed in primary care but referral is recommended if there is a progressive fall in eGFR, heavy proteinuria, suspected systemic illness or uncontrolled blood pressure |
Number of referrals: the introduction of eGFR reporting and the CKD guideline was associated with an abrupt rise of 48% in the overall number of new attendances to the renal clinic from 333 in the 6 months before June 2006 to 492 patients in the 6 months after June 2006. Comparing the second 6 months of 2005 with the second 6 months in 2006, the proportion of females (43.4% vs. 56.3%, p < 0.0001) and average age (61.3 vs. 66.4 years) of new patients attending renal clinics increased Patient outcomes: NR Patient satisfaction: NR Access to care: NR Costs: NR |
| Akbari et al. (2008)154 | Multiple | Systematic review | Aim: To estimate the effectiveness and efficiency of interventions to change outpatient referral rates or improve outpatient referral appropriateness Population: Primary care physicians and specialists Sample size: 17 studies, 23 separate comparisons Interventions: The reviews looked at multiple types of interventions, including professional educational interventions, financial interventions, and organisational interventions |
Passive dissemination of guidelines Number of referrals Jones 1993: increase in the number of referrals for upper gastrointestinal problems, referrals for endoscopy and upper gastrointestinal radiology investigations. The statistical significance of these findings is uncertain Grimshaw 1998: no significant changes in referral patterns or appropriateness of referral Costs Jones 1993: there were statistically significant increases in prescribing costs for upper gastrointestinal drugs and ulcer-healing drugs Dissemination of referral guidelines with structured management sheets Number of referrals Abu-Ramadan 2002: a reduction of over 50% in the number of referrals to the eye hospital post-intervention. However, it is very difficult to interpret which aspect of the intervention contributed most to the change in the number of referrals Bennett 2001: no effect of the interventions on referral rates. However, the authors analysed data from 68% of the practices to determine ‘quality of referrals’. In the group of physicians who saw the video and had access to the checklist, the percentage of appropriate referrals increased following the intervention; in all other groups, including the control group, it decreased Morrison 2001: no difference in referral rates per 1000 registered women aged 20 to 44 years. There were improvements in five items of pre-referral investigations/advice, with a median improvement in post-intervention absolute difference of +7.3%, but none of the improvements in individual tests was statistically significant. However, there was a statistically significant improvement in the proportion of couples receiving all appropriate investigations/advice (improvement in post-intervention absolute difference +9.6%, odds ratio 1.324, 95% CI 1.001 to 1.752; p = 0.025) Thomas 2003: 48.2% of eligible patients were referred through the new system, freeing up the equivalent of 350 new outpatient slots over a 12-month period. No differences in referral patterns or case mix of the patients referred. Compliance with referral guidelines increased significantly Vierhout 1995: increase in GPs use of injection therapy (30.6% study vs. 11.7% control, p < 0.001), a reduction in subsequent referral to orthopaedic surgeons (35.4% study vs. 68.0%; p < 0.001) and an increase in proportion of patients disorder-free after 1 year (35.4% study vs. 23.7% control; p < 0.05) Banait 2000: study practices had higher endoscopy referral rates, increased appropriateness of referral, marginally higher diagnostic yields and higher serology testing rates. However, there was no reduction in prescriptions for acid-suppressing drugs Grimshaw 1998: significant increase in the number of tracer referrals following the intervention against the hypothesised direction of effect; no significant improvements in referral following feedback on referral rates or discussion with an independent adviser Access to care Thomas 2003: waiting times for first appointments for the tracer conditions decreased (ratio of means of waiting times 0.7, 95% CI 0.55 to 0.89) although the post-intervention difference is likely to underestimate the true effect of the intervention as there was a substantial fall in waiting times for control patients probably as a result of the freed-up new outpatient appointments. There was also a reduction in waiting times for all urology patients of 11 weeks (95% CI 7.1 to 15 weeks) Costs Thomas 2003: the annual cost of the intervention was estimated to be £9555 (representing the total costs of guideline development and dissemination; however, in many settings these costs would be subsumed into normal running costs). There were non-significant reductions in post-referral general practice costs (for prostatism only) and the travel costs of patients attending health services. There were significant reductions in the mean hospital management costs per patient of £80.26 for prostatism and £44.79 for haematuria Other outcomes Morrison 2001: no differences in the time from first appointment to establishing a management plan or in the proportion of couples with a management plan after 1 year of referral. There were 8% fewer pregnancies within 12 months in the study group. General practice and hospital costs were greater in the study group (unfortunately there was a unit of analysis error and the statistical significance of these findings is unclear) Emslie 1993: observed improvements in: eliciting five items of sexual history (median improvement in post-intervention absolute difference +16.0%); undertaking five pre-referral examinations and investigations in the female partner (median improvement in post-intervention absolute difference +24%); and undertaking two pre-referral examinations and investigations in the male partner (median improvement in post-intervention absolute difference +18%). There was also an increase in the number of referrals in which the male partner had been seen prior to referral (improvement in post-intervention absolute difference +17%) Organisational interventions Number of referrals Bertakis 1987: fewer referrals and a lower annual per-patient cost of laboratory tests for those patients seen in family practice; fewer primary care attendances, fewer acute care visits and fewer emergency room visits for patients receiving primary care from family physicians O’Cathain 1995: more physiotherapy referrals, fewer orthopaedic referrals and fewer rheumatology referrals Kinnersley 1999: approximately 70% of patients having an in-house second opinion were judged to need referral to the same hospital discipline immediately (63.0%) or within 12 months (9.8%) Bridgman 2005: relative reductions in the monthly referral rate per 10,000 population of 22% in the intervention group and 10% in the control group. No significance levels were reported Financial interventions Number of referrals Davidson 1992: reduction in the number of non-primary care referrals by providers receiving capitation based remuneration but little effect in providers receiving increased fee-for-service Coulter 1993: referral rates were higher in fundholding practices during phase 1 but fundholding and non-fundholding practices had similar referral rates during phase 2 Kammerling 1996: reductions in the fundholding practices compared with controls but these were modest at best Linnala 2001: at baseline the rates of referral to a specialist were higher in the experimental group (5.7% age/sex adjusted) than in the control group (4.4% age/sex adjusted), increasing to 6.8% on the experimental group and 5.5% in the control group. The percentage of referrals sent to private specialists by the GPs in the control group increased from 5.7% to 33.6% in the experimental group but decreased slightly (8.8% to 5.6%) in the control group, suggesting that there was a change in the destination rather than number of referrals |
| Andonegui et al. (2012)56 | Spain | Observational study | Aim: to assess the appropriateness of diabetic retinopathy diagnosis in general practice Population: patients with diabetes under the care of all GPs in a geographic area sent for retinal imaging on suspicion of diabetic retinopathy Sample size: 2750 patients referred for retinal imaging Interventions: over a 2-year period the digital retinography images were sent to four GPs who had received training in the interpretation of retinal photographs to decide whether or not patients had diabetic retinopathy. Patients whose images were judged as normal had a new examination scheduled for the following year, while those whose image was judged to be abnormal were referred to an ophthalmologist for further investigation |
Number of referrals: NR Patient outcomes: NR Patient satisfaction: NR Access to care: NR Costs: NR Appropriateness of referral: of the 2750 patients sent for imaging, the four trained GPs referred 714 to an ophthalmologist for further investigation. Of the 714, 55% did not have diabetic retinopathy, 34% did have diabetic retinopathy and 11% had images that were not considered to be suitable for diagnosis. Among the 2672 patients whose images were considered normal by the trained GPs, 7% had some degree of diabetic retinopathy |
| Augestad et al. (2013)43 | Norway | RCT | Aim: to assess whether colon cancer follow-up can be organised by GPs without a decline in the patient’s quality of life and increase in cost or time to cancer diagnoses, compared with hospital follow-up Population: patients surgically treated for colon cancer Sample size: 110 patients (55 intervention and 55 control), followed by 78 GPs (942 follow-up months) and 70 surgeons (942 follow-up months), respectively Interventions: 24-month follow-up according to national guidelines at the community GP office. To ensure a high follow-up guideline adherence, a decision support tool for patients and GPs was used |
Number of referrals: there were 185 face-to-face surgeon outpatient consultations in the intervention, compared with 227 in the control group. There were 33 surgeon telephone consultations in the intervention, compared with 41 in the control group. A total of 778 trips (consultations, radiological investigations and colonoscopy) to the hospital were registered: 528 in the surgeon group and 250 in the GP group Patient outcomes: there was no significant effect on the main QoL outcome measures. However, on the EORTC QLQ-C30 subscales, there were significant effects in favour of GP follow-up, i.e. role functioning (p = 0.02), emotional functioning (p = 0.01) and pain (p = 0.01). There were no differences in time to recurrent cancer diagnosis (GP 35 days vs. surgeon 45 days; p = 0.46) Patient satisfaction: NR Access to care: NR Costs: the mean cost of follow-up per patient per follow-up cycle was £292 in the GP group and £351 in the surgeon group (p = 0.02) |
| Azuri et al. (2009)174 | Israel | RCT | Aim: to investigate the effect of raising awareness of erectile dysfunction diagnosis and treatment in a community setting by training physicians Population: primary care physicians Sample size: 78 physicians (two intervention groups of 19 and 20 vs. 39 controls), 3862 patients (1959 in both intervention groups and 1903 in control group) Interventions: the 39 physicians in the intervention group all attended three lectures by an experienced sexologist which covered issues regarding erectile dysfunction, epidemiology, treatment and training on how to approach these patients. In addition, 20 of these physicians received a computerised list of their own patients considered to be at high risk |
Number of referrals: there was no significant change in the number of patients referred to urologists for consultation between the intervention and control group after implementation of the intervention (27.3 vs. 24.9%; p = 0.088) Patient outcomes: There was no significant difference between the intervention and control in the percentage of new diagnoses of erectile dysfunction after implementation of the intervention (1.0% vs. 1.2%; p = 0.57) Patient satisfaction: NR Access to care: there was no significant difference between intervention and control in the number of new patients who received PDE5-inh medications after implementation of the intervention (1.6% vs. 2.2%; p = 0.19) Costs: NR |
| Backman et al. (2010)108 | UK | Literature review | Aim: to discuss the current status of cardiac care in the community, and how telecardiology can help to support GP in the diagnosis and management of acute and chronic cardiac disease Population: primary care Sample size: NR Interventions: telecardiology care |
Number of referrals: evidence is presented from one study (Molinari et al. 2002) which looked at the use of telecardiology services to reduce the number of hospital referrals. The study demonstrated that of 134 patients with suspected coronary events and who would otherwise have been referred, 84 had no abnormalities and unnecessary hospitalisation was avoided. A pilot study in the UK trialled a local telecardiology service found that secondary care referrals were prevented in 65.8% of cases Patient outcomes: NR Patient satisfaction: NR Access to care: NR Costs: in the Molinari et al. 2002 study, the authors estimated that the telecardiology service could have saved $504,000 (based on an average hospital stay of 3 days per patient, and a daily hospitalisation cost of $2000 per patient). The UK pilot study estimated saving to the NHS in excess of £300,000. A second report estimated that if the service was rolled out across England as a whole it would save £45M per year |
| Baker et al. (2005)34 | UK (England) | RCT | Aim: to determine whether there are differences in clinical outcome or patient satisfaction among patients attending orthopaedic clinics run by GPwSIs based in primary care or in hospital Population: patients aged 18 years or older, in two urban PCTs in the Leicester area, referred to orthopaedic departments who can be managed by GPwSIs. Conditions included lower-back pain, shoulder, elbow, wrist, ankle conditions, etc. Sample size: 321 patients (168 practice based and 153 hospital based) Interventions: patients referred to orthopaedic department were randomly allocated to see a GPwSI in primary care practice or a GPwSI in outpatient clinic in hospital |
Number of referrals: there was no difference in the proportion of practice-based vs. hospital-based patients referred to an orthopaedic specialist (2.4%, 95% CI 0.7 to 6.0 vs. 4.6%, 95% CI 1.9 to 9.2) or physiotherapist (22.0%, 95% CI 16.0 to 29.1 vs. 26.1%, 95% CI 19.4 to 33.9) Patient outcomes: there was no significant difference between groups in 10 clinical symptoms at 3-month follow-up Patient satisfaction: significantly higher levels of satisfaction were reported for patients in practice-based consultations for 2/15 measures: getting an appointment (median 75 vs. 66.7; p = 0.024) and level of information received (median 75.0 vs. 71.9; p = 0.031). For the remaining 13 measures there was no significant difference between locations of consultation Access to care: NR Costs: NR |
| Batinac et al. (2009)175 | Croatia | Prospective before-and-after study | Aim: to measure the impact of continuous medical education on the outcomes of care delivery Population: patients referred to a haematology outpatient clinic with iron deficiency anaemia Sample size: 1586 patients Interventions: a year-long education campaign on the diagnosis and management of iron deficiency anaemia, including publications, lectures and anaemia management guidelines targeting primary care physicians |
Number of referrals: NR Patient outcomes: NR Patient satisfaction: NR Access to care: following intervention there was a significant decrease in the proportion of patients starting iron therapy before diagnostic confirmation (55.24% vs. 12.60%; p < 0.001) Costs: NR Appropriateness of referrals: following education the number of patients incorrectly referred (i.e. patients wrongly referred with a diagnosis of iron deficiency anaemia) significantly decreased, compared with before the education intervention (67.24% vs. 24.71%; p < 0.001) |
| Benamore et al. (2005)57 | UK (England) | Retrospective case review | Aim: to assess the effectiveness of primary care access to CT head examinations for managing common neurological conditions within primary care Population: patients referred from primary care to radiology department for a CT head examination Sample size: 1403 patients Interventions: improving primary care access to CT head examinations |
Number of referrals: using data from the first 8 years’ experience of the service demonstrated that the most common reason for referral was investigations of headache (46.6%). 60% of secondary care referrals were for normal CT scans. In patients with focal neurology, 90/314 (29%) were referred, allowing 71% to be managed in primary care or referred directly to tertiary care. The authors also noted that only 30% of patients with an infarct were referred, and thus the results above may represent effective use of resources, but may not reflect best practice Patient outcomes: NR Patient satisfaction: NR Access to care: NR Costs: NR |
| Berger et al. (2007)18 | Norway | Economic modelling | Aim: to examine expected outcomes and costs associated with the treatment of painful neuropathies, and the consequences of shifting care from secondary to primary care Population: patients aged over 18 years old experiencing neuropathic pain (equivalent to about 1% of the population) Sample size: approximately 35,000 individuals Interventions: authors modelled two scenarios to compare standard care in which most patients are assumed to be referred for specialist care against a hypothetical care model in which patients were treated in primary care |
Number of referrals: the authors estimated that the number of visits to a specialist would decrease by 12,123 from 42,773 to 30,651 per year and visits to a pain clinic would decrease by 7,967 from 17,990 to 10,023 if the hypothetical model of care was implemented Patient outcomes: NR Patient satisfaction: NR Access to care: NR Costs: shifting care from specialists and pain clinics was estimated to result in a potential saving of NOK 74.1M ($11.9M) from NOK 251.1M to NOK 175.7M |
| Bernstein (2011)81 | UK (England) | Audit | Aim: to assess the outcomes of a ‘see and treat’ interface for musculoskeletal referrals Population: patients with musculoskeletal issues Sample size: approximately 30,000 referrals in the Ealing area Interventions: a ‘see and treat’ model in which triage occurs at the point of GP referral. The referring GP chose general physiotherapy, interface clinic or secondary care. Their decision was aided by referral guidance and an educational programme |
Number of referrals: the proportion of referrals to secondary care decreased from 100% in 2005 to 73% in 2010 as GPs chose to refer patients to the interface service instead. The introduction of the referral guidance and an educational campaign in 2009 led to a sustained 10% reduction in GP referrals into musculoskeletal services Patient outcomes: NR Patient satisfaction: NR Access to care: it is reported that patients start treatment earlier after the intervention because triage happens before referral, not after Costs: author states that the programme is cost-effective but no details are reported |
| Bjerager et al. (2006)58 | Denmark | Observational study | Aim: to investigate reasons for diagnostic delay in primary care for patients with lung cancer Population: patients with a newly histologically verified diagnosis of lung cancer (median age 66 years; 35.7% female) Sample size: 84 patients Interventions: N/A |
Number of referrals: NR Patient outcomes: overall, 64 patients (76.2%) presented lung-related symptoms to the GP (coughing, haemoptysis or thoracic pain). These patients experienced a median delay of 29 days. Fourteen (16.7%) had atypical symptoms (arthralgia, muscle pain, pain in back or shoulder, or vague symptoms such as fatigue). These patients experienced a median delay of 104 days. Four patients (4.8%) with symptoms related to brain metastases had a median delay of 24 days, and two patients (2.4%) who were diagnosed by chance had 1 and 9 days of delay, respectively. One-third of the patients contacting their GP with signs and symptoms of lung cancer were referred to secondary care on their first contact, but they experienced a 2-week median delay due to system delay. Patients not diagnosed by the GP’s initial actions had a median delay of > 6 weeks. The median delay for patients with a false-negative chest radiograph was nearly six times longer for patients with a first chest radiograph raising suspicion of cancer. Other important reasons for delay in primary care were comorbidity, waiting times for investigations and lack of explicit follow-up appointment Patient satisfaction: NR Access to care: NR Costs: NR |
| van Boeijen et al. (2005)19 | The Netherlands | RCT | Aim: to compare the effectiveness and feasibility of three different types of care Population: patients aged over 18 years old diagnosed with panic disorder or generalised anxiety disorders across 46 practices in urban and rural areas Sample size: 154 patients (59 manual, 67 CBT, 28 guidelines) Interventions: compared three models of care. A self-help manual for anxiety disorders used by the patient under the direction of the GP, CBT provided by behaviour therapist in secondary care and care from GP following College of General Practitioners’ guidelines for the treatment of anxiety |
Number of referrals: NR Patient outcomes: all three treatments resulted in improved patient outcomes. However, there was no significant difference in patient outcomes between the three treatment types. The self-help manual was considered by GPs to be more feasible to carry out than the less structured College of General Practitioner guidelines. This suggests that treating patients in primary care with the manual is a safe alternative to secondary care treatment Patient satisfaction: NR Access to care: NR Costs: NR |
| Borooah et al. (2013)111 | UK (Scotland) | Before-and-after study | Aim: to reduce waiting times and inefficiencies in the referral pathway for ophthalmology patients through an electronic referral unit using digital images for clinical decision-making Population: patients eligible for ophthalmic referral Sample size: 17,528 patients referred Interventions: centralised ophthalmic electronic referral unit, which uses digital images for clinical decision-making |
Number of referrals: no significant difference in new patients referred, but lower number of new patients seen (7462 vs. 8714). There were also fewer casualty patients seen (1984 vs. 2671) and fewer new patient DNAs (503 vs. 635). There was an increased number of follow-up patients seen (13,879 vs. 11,390) Patient outcomes: the authors reported that the reduction in waiting times resulted in fewer emergencies Patient satisfaction: patient satisfaction reported at 97% in the pilot study Access to care: median waiting time was reduced from 14 to 4 weeks Costs: estimated saving of £239,580 per annum for new appointments. Additional savings suggested for travel costs (including an estimate of £13,068 for hospital transport costs for new appointments). Financial benefits may be offset by increased numbers of follow-up appointments, but unclear whether this relates to this intervention or other changes |
| Borve et al. (2012)109 | Sweden | Observational feasibility study | Aim: to compare diagnostic outcomes from MMS containing digital photographs of dermatological conditions with face-to-face consultation Population: patients aged over 18 years old with skin lesion or condition who would otherwise be referred to a dermatologist Sample size: 40 patients (23 women and 17 men) Interventions: GPs sent a picture of the skin lesion via MMS to two dermatologists, who both provided a diagnosis within 48 hours. Clinical diagnosis and management was verified in a face-to-face consultation with the dermatologists |
Number of referrals: NR Patient outcomes: NR Patient satisfaction: NR Access to care: NR Costs: NR Diagnosis accuracy: when making a diagnosis via MMS both dermatologists made the correct diagnosis in 78% of cases. Concordance between dermatologists was 68%, which increased to 88% after the face-to-face consultation. Adequate triage decisions were made in 85% of cases for one dermatologist and 95% for the other via MMS. Concordance between the dermatologists was 65% increasing to 73% after the face-to-face consultation. When comparing MMS with face-to-face a concordant diagnosis was made in the same diagnostic category in 80% compared with 98% of patients. Picture quality was judged sufficient to excellent in 37/40 cases |
| Bower and Gilbody (2005)97 | Multiple | Meta-review (review of reviews) | Aim: to use conceptual models to bridge the gap between research findings and policy development Population: mental health patients and providers Sample size: 17 reviews Interventions: conceptual models concerning service structure, burden and quality improvement in the context of mental health in primary care |
Number of referrals: identified eight reviews of replacement/referral involving several different psychological therapies. Evidence of impact on referrals is NR Patient outcomes: two reviews on training showed that only intense training in psychosocial interventions for GPs can have positive impact on patient outcomes. Two reviews on consultation liaison suggested that it fails to deliver benefits. Five reviews on collaborative care found that it was more likely to have benefits for patients, and to impact positively on patient satisfaction. The eight reviews on replacement/referral found it to be generally clinically effective Patient satisfaction: one review suggested that patient satisfaction increases with collaborative care Access to care: NR Costs: limited information on cost-effectiveness is presented |
| Bowns et al. (2006)110 | UK (England) | RCT | Aim: to assess the feasibility of (1) store-and-forward technology in dermatology and (2) digital photography and dermoscopy Population: for store-and-forward dermatology patients aged 16 years and over from eight general practices in Sheffield requiring a new consultant opinion. For digital photography adults requiring a consultant opinion due to a suspicion of malignant melanoma or squamous cell carcinoma Sample size: Store-and-forward 208 patients (111 intervention and 97 control) Interventions: patients were managed using teledermatology, in which text and digital images were forwarded electronically to the consultant, compared with conventional hospital outpatient consultation. Patients referred to the 2-week wait clinic were invited to have a series of digital photographs, with and without dermoscopy, immediately before their face-to-face consultation. A second consultant viewed these and outlined a diagnosis and management plan. This was compared with the actual management. Both were compared with the definitive diagnosis (either the final clinical or histological diagnosis) |
Number of referrals: for store-and-forward 58% (95% CI 47% to 67%) were judged to require a face-to-face consultation in order to establish a diagnosis. For digital photography 30% of cases would not have needed face-to-face consultations, but two severe cases would have been missed Patient outcomes: NR Patient satisfaction: NR Access to care: NR Costs: NR Accuracy of diagnosis: store-and-forward concordance in 55% of telemedicine cases and 78% face-to-face. In 55% of telemedicine and 84% of face-to-face consultations, management plan concurred. For digital photography concordance was 68% when both standard and dermoscopic images were employed |
| Bridgman et al. (2005)156 | UK (England) | Prospective controlled study | Aim: to evaluate the effect of a new orthopaedic referral management model, ‘slot system’, on GP orthopaedic referral rates Population: patients aged over 16 years old orthopaedic referrals in North Staffordshire Sample size: 99 practices (12 intervention, 24 control, 63 all other practices in North Staffordshire), 14,006 patients Interventions: practices were provided with locally developed guidelines on appropriate referrals and routes of referrals for musculoskeletal problems. GPs referred patients through a ‘slot system’ using a specially designed pro forma |
Number of referrals: mean monthly referral rate (per 10,000 population per month) decreased from 9.4 at baseline to 7.29 after the first year, and remained at 7.3 the year after. In the control group, referral rates decreased from 10.99 to 9.9 but increased to 11.7 the year after. The rate of referrals in all other practices in the area remained relatively constant across the time period (9.5, 9.31 and 10.33). The relative reduction in mean referral rates between the control and the treatment groups after introduction of the slot system was –23.7% after 1 year and –39.5% after 2 years. The difference in reduction of referral rates is equivalent to 2–4 referrals per 10,000 patients per month Patient outcomes: NR Patient satisfaction: NR Access to care: NR Costs: NR |
| Briggs et al. (2008)20 | UK (England) | Observational study | Aim: to measure the impact of a combined NPLC in primary care Population: patients referred by GPs to the pain service in a PCT in the north of England Sample size: 120 patients Interventions: patients referred to the hospital pain service were triaged by a trained district nurse and a hospital pain consultant to either the NPLC or the hospital clinic. In the NPLC, a nurse and a pharmacist worked together. The nurse completed a training programme with the hospital pain team, and clinic guidelines and referral pathways were agreed with the pain team |
Number of referrals: only 13 of the 120 patients treated in the NPLC were referred to secondary care over a 1-year period Patient outcomes: clinical data were collected for 65 patients. Mean pain scores on referral were 8 (median: 8) and 6.3 (median: 6) on discharge Patient satisfaction: 92% of the 24 patients who were asked for feedback said they were satisfied or very satisfied with the NPLC Access to care: NR Costs: NR |
| Buller et al. (2009)59 | The Netherlands | Prospective management study | Aim: to evaluate the safety and efficiency of a new management strategy, ‘clinical decision rule’, for patients with suspected DVT, which has the potential to reduce unnecessary investigations and treatments Population: patients with suspected DVT in 300 primary care practices in three regions of the Netherlands (Amsterdam, Maastricht and Utrecht). 1002 patients Sample size: 1028 patients Interventions: a clinical decision rule was provided on a worksheet. The decision rule included seven clinical items associated with DVT and a D-dimer assay result each with a corresponding score. A total score was calculated for each patient, and those with a score of ≥ 4 were referred |
Number of referrals: NR Patient outcomes: NR Patient satisfaction: NR Access to care: NR Costs: NR Appropriateness of referrals: 500 patients (49%) had a score of ≤ 3, which means that they were not referred. Of those, 1.4% were misdiagnosed as they developed DVT within 3 months. 502 patients (51%) were referred for an ultrasonography, 374 of whom had a normal ultrasonogram. Based on scenario analysis if the physician used only clinical items on decision rule and did not refer patients with a score of ≤ 3, DVT would be missed in 9.6% of patients. If physician used only the D-dimer assay and did not refer patients with a normal score, DVT would be missed in 3.4% of patients |
| Butler and Yellowlees (2012)112 | USA | Retrospective cost analysis | Aim: to evaluate the costs of store-and-forward, or asynchronous telepsychiatry in a primary care setting Population: patients were identified by primary care providers as having non-urgent psychiatric problems Sample size: 125 asynchronous telepsychiatry consultations were performed Interventions: an asynchronous telepsychiatry intervention in a rural primary care setting. Asynchronous telepsychiatry patients’ interviews were videotaped and electronically sent, along with medical records and notes, to psychiatrists |
Number of referrals: NR Patient outcomes: NR Patient satisfaction: NR Access to care: NR Costs: the fixed costs of asynchronous telepsychiatry were US$7000, of which US$4000 consisted of development costs for the web-based consultation software. The remaining US$2000 consisted of equipment costs, and US$1000 for provider training costs. The marginal cost was $68.18. The time spent per consultation by the psychiatrist was 30 minutes, and time spent per consultation by other providers was 64 minutes. The break-even point between the asynchronous telepsychiatry and the in-person consultations was 249 patient encounters |
| Cameron et al. (2010)176 | USA | Observational study | Aim: to evaluate academic detailing as a strategy to increase early detection of dementia in primary care practices Population: primary care physicians Sample size: 104 physicians, 248 office/clinic staff Interventions: this method involved a 15-minute educational session by a physician, an Alzheimer’s Association representative and an Area Agency on Ageing representative |
Number of referrals: in a follow-up evaluation, 55% physicians said that they had increased referrals, 24% said that they were already making satisfactory referral prior to the visit and 21% said that they had not increased referrals but intended to Patient outcomes: NR Patient satisfaction: NR Access to care: NR Costs: NR Other: 77.4% of physicians rated the visit as very effective |
| Campbell et al. (2008)60 | Canada | Observational study | Aim: to help family physician assess the risk of DVT Population: patients with suspected DVT in family practices Sample size: not clear. A pilot group of 80 family physicians participated Interventions: introduction of a DVT clinical pathway from primary to secondary care, including an evidence-based scoring system to calculate the probability of DVT |
Number of referrals: referrals to the hospital DVT clinic increased by 14% overall Patient outcomes: NR Patient satisfaction: 96% of patients were very satisfied or satisfied with the scheme. Physicians were also generally satisfied with the pathway Access to care: after introduction of the pathway the number of D-dimer tests being ordered increased by 42%. The proportion of patients undergoing subsequent tests did not change. The length of stay in the emergency department fell from 379 minutes before the pathway was introduced to 285 minutes after Costs: NR Appropriateness of referrals: the proportion being appropriately referred from the emergency department to the clinic for 1-week follow-up increased by 35.9% |
| Cape et al. (2010)98 | Multiple | Systematic review | Aim: to assess the effectiveness of consultation-liaison services, involving mental health professionals advising and supporting primary care professionals in the management of depression Population: adult primary care patients with a diagnosis or symptoms of depression Sample size: five studies. Sample size in included studies ranged from 375 to 92 patients Interventions: patients were seen once or twice by a mental health professional for assessment (consultation) and advice to the GP about management (liaison), but no treatment was provided by the specialist. This is in between collaborative care and education and training models |
Number of referrals: NR Patient outcomes: no significant effect on patient outcomes. No significant effect on the rate of use of antidepressants Patient satisfaction: NR Access to care: NR Costs: NR |
| Castro et al. (2007)61 | Spain | Retrospective case review | Aim: to assess concordance between diagnoses made by primary care physician and specialist using digital fundus images Population: adult patients with retinopathy Sample size: 776 digital fundus images of 194 patients Interventions: images that were diagnosed by an ophthalmologist were retrospectively sent to a GP for diagnosis. The GP was aware of the patients’ medical history |
Number of referrals: NA Patient outcomes: NR Patient satisfaction: NR Access to care: NR Costs: NR Diagnostic accuracy: inter-rater reliability was measured using kappa statistic. Kappa ranges from 0 to 1, with 1 indicating maximum reliability. Concordance between ophthalmologist (considered standard) and GP for patients with diabetes kappa was 0.8, for patients with hypertension kappa was 1 and for patients with both diseases kappa was 0.79 |
| Chew et al. (2010)21 | Australia | Cost-effectiveness analysis (simulation) | Aim: to evaluate the cost-effectiveness of a general practice-based programme for managing CHD patients Population: NA Sample size: NA Interventions: establishment of a practice-specific patient register of CHD patients with recall mechanisms and provision of care assessment |
Number of referrals: NA Patient outcomes: NA Patient satisfaction: NA Access to care: NA Costs: based on 2006 estimates, 263,487 DALYs were attributable to CHD in Australia; it is estimated that the CHD programme would add an additional AU$115,650,000 to the annual national heath expenditure. Using an estimated 15% reduction in deaths and disability and a 40% estimated programme uptake, the programme’s incremental cost-effectiveness ratio would be AU$8081 per DALY averted. With more conservative estimates of effectiveness and uptake, estimates of up to AU$38,316 per DALY averted were observed in the sensitivity analysis |
| Chong and Moreno (2012)113 | USA | RCT | Aim: to assess the feasibility and acceptability of telepsychiatry for low-income Hispanic patients Population: adult Hispanic patients with major depression recruited from a community health centre Sample size: 167 patients (80 intervention and, 87 control) Interventions: psychiatry services were delivered via a video webcam, compared with standard face-to-face care. Patients who received treatment via webcam received monthly telepsychiatry sessions at a community health centre for 6 months |
Number of referrals: NR Patient outcomes: although depression severity decreased faster among web-based patients than face-to-face patients, no differences were found in the overall depression score. There was no difference between groups in the number of days that were lost or unproductive owing to depression Patient satisfaction: patients who received web-based care were significantly more satisfied with their visits with the psychiatrists (p < 0.01) and reported significantly higher alliance with the psychiatrist than patients who received face-to-face care when asked to rate their visits with their primary care provider (p < 0.001). When asked to rate (on a scale of 1 to 10) the care they received mean rating for face-to-face based care was 8.8 (±2.4), compared with 9.4 (±1.1) for web-based care Access to care: patients who received the web-based care were significantly more likely to use antidepressant medications than patients who received face-to-face care (p < 0.05) Costs: NR |
| Choudhury et al. (2013)44 | UK (England) | Observational study | Aim: to evaluate the impact of LES for patients with diabetes through which GPs receive training and monetary incentives Population: patients with diabetes in a large PCT area in Birmingham between 2009 and 2010 Sample size: 21,026 patients from 76 general practices Interventions: LES for diabetes, including additional training for GPS (and a monetary incentive). To evaluate the impact of LES to improve management of patients with diabetes |
Number of referrals: there was a significant difference between LES and non-LES practices, with LES practices referred fewer patients for hospital appointments, both for a new appointment and for follow-up appointments Patient outcomes: no differences were observed between LES and non-LES practices for lipid and blood pressure outcomes. LES practices were, however, significantly more likely to achieve better glycaemia levels (p < 0.001) Patient satisfaction: NR Access to care: NR Costs: NR |
| Christensen (2008)99 | Multiple (mostly USA and UK) | Systematic review | Aim: to determine which components of interventions for depression in primary care are most effective Population: adult patients suffering from depression Sample size: 55 studies. Sample size in included studies ranged from 15 to 2730 patients Interventions: various interventions, including audit and feedback, education and multidisciplinary teams |
Number of referrals: NR Patient outcomes: case management and tracking of patients was associated with improved patient outcomes, e.g. case management may improve adherence to treatment and allow deliver of enhanced care. Maximum benefit, though, will be attained if providers are professionally trained in mental health. The training of GPs in depression care and the provision of clinical practice guidelines were not associated significantly with improved outcomes. Community interventions appeared to be as beneficial as general practice interventions Patient satisfaction: NR Access to care: NR Costs: NR |
| Clarke et al. (2010)155 | Multiple | Systematic review | Aim: to assess the effectiveness of guidelines for referral for elective surgical assessment Population: patients aged over 16 years old with a non-urgent surgical condition Sample size: 24 studies. The number of referrals within included studies ranged from 100 to 5000 Interventions: the referral guidelines were defined by the authors as ‘a set of rules, an algorithm or a protocol which gives guidance on the circumstances in which a formal elective request is made from primary care on behalf of a patient for treatment or consultation by a surgical specialist’ |
Number of referrals: no overall conclusion can be made as studies used different measures. Four studies reported a reduction in crude numbers, three reported no change and one suggested that guidelines would increase the number of referrals. Two well-designed randomised trials reported no change, and one reported a reduction in referral rates in the intervention arm Patient outcomes: two studies reported on health outcomes using a SF-36 and found no difference between the intervention and control groups Patient satisfaction: NR Access to care: three studies reported reductions in waiting times, one reported mixed results and one reported no change Costs: the review did not include a formal economic evaluation. One cohort study reported a reduction in costs of between £1.45 and £49.54 per patient (2000 prices) compared with historical controls for lower urinary tract symptoms. Another study found a non-significant increase in costs for treatment group Appropriateness of referrals: appropriateness of referrals improved. All studies that assessed appropriateness of investigations and diagnostic evaluations before referral showed improvements after use of guidelines |
| Coast et al. (2005)35 | UK (England) | Cost-effectiveness analysis within a RCT | Aim: to compare the economic cost of a GPwSI service with hospital outpatient care for dermatology Population: adults referred to dermatology service for non-urgent skin problem, covering 29 primary care practices in Bristol Sample size: 556 patients (354 intervention, 202 control) Interventions: care provided by a GPwSI in dermatology instead of regular hospital outpatient care |
Number of referrals: NR Patient outcomes: patients who received GPwSI care had slightly better health outcomes Patient satisfaction: patients who received GPwSI care reported greater satisfaction with the care they received Access to care: on average, waiting times were lower for patients who saw the GPwSI (72 days, on average, vs. 113 days) Costs: the costs to the NHS of the GPwSI were about 75% higher than for standard outpatient care (£208 vs. £118), with a higher unit cost associated with the GPwSI consultation than with the outpatient consultation (provided by consultant, or registrar, or clinical assistant). The average cost to the patient and carer was slightly lower in the intervention group |
| Coetzee (2011)22 | UK (England) | Observational pilot study | Aim: to identify the most effective models for delivering treatment for alcohol dependency in the primary care setting Population: patients suffering from mild to moderate alcohol dependency, in primary care setting in Wandsworth, UK Sample size: six treatment episodes in LES and 76 treatment episodes in the Fresh Start Clinic Interventions: two models of care. First, the LES agreement for screening, brief interventions and treatment. All GPs involved in this service were required to attend training in the management of alcohol withdrawal and had access to the support of a specialist alcohol nurse. Second, a structured GP-led clinic supported by a full-time specialist nurse prescriber. The clinic was promoted as the ‘Fresh Start Clinic’. It offered planned alcohol withdrawal within a pre-agreed structured treatment plan, and signposts to aftercare |
Number of referrals: NR Patient outcomes: data were available only for the Fresh Start Clinic. The mean number of lost working days was 19.2. There was reported to be a 100% completion rate, with 57% of patients abstaining at 3–6 months. There was a 50% improvement in mental well-being, and an improvement in serum gamma-glutamyl transferase and mean corpuscular volume levels Patient satisfaction: patients in the Fresh Start Clinic reported positive feedback; data were not reported for LES Access to care: the mean waiting time to treatment was 7 days for patients in the Fresh Start Clinic; data were not reported for the LES Costs: NR |
| Colven et al. (2011)114 | South Africa | Observational study | Aim: to understand whether or not using a teledermatology network improves diagnosis in primary care in underserved areas Population: dermatology patients from six primary care physicians and one dermatology-trained nurse Sample size: 120 referrals Interventions: primary care clinicians were provided with a camera and training in dermatological photography and image file handling. They then sent their images and patient medical records to teleconsultants who responded with care recommendations |
Number of referrals: NR Patient outcomes: NR Patient satisfaction: both patient and provider satisfaction was reported to be very high (> 90%) Access to care: NR Costs: NR Diagnostic accuracy: concordance in diagnosis between primary care physician and specialist increased as the number of referrals increased, from 13% for the first four referrals, to 50% by the ninth to twelfth referrals |
| Courtenay et al. (2006)23 | Multiple | Literature review | Aim: to identify the impact and effectiveness of nurse-led care in dermatology Population: N/A Sample size: 14 studies Interventions: any kind of nurse-led care in dermatology |
Number of referrals: NR Patient outcomes: two studies looking at nurse education showed reduction in the severity of eczema. Four studies examined impact on QoL, with two reporting marginal improvements in QoL and two reporting no improvement. However, one study showed that patients were more likely to have better knowledge about treatment and care, and that number of follow-ups by dermatologists reduced Patient satisfaction: seven studies suggest that patients are satisfied with nurse-led services. Patients feel that they receive more information about their condition and its management Access to care: one study reported that access to care with a nurse is quicker than with a GP. Two studies reported increased use of emollients, although one of them found an increase in the use of topical steroids Costs: NR |
| Cox et al. (2013)193 | UK (England) | Retrospective time-series analysis | Aim: to assess the impact of three RMCs and two internal peer-review approaches to referral management on outpatient visits Population: NHS Norfolk patients, between 2006 and 2011 Sample size: retrospective analysis of 376,000 outpatient attendees Interventions: 85 practices formed five groups to improve referral management. Three RMC groups and two groups carried out internal peer review of referrals groups (monthly peer review of selected referrals, plus guidelines and feedback) |
Number of referrals: there was no reduction in hospital attendance rates or attendance rate ratios (group attendance rate divided by equivalent English attendance rates) in any group. The group that had the largest budget and the widest range of activities (one of the RMC groups) actually saw a significant increase in both measures Patient outcomes: NR Patient satisfaction: NR Access to care: NR Costs: RMCs were more expensive than peer-review initiatives (£6.23, £6.13 and £3.22 for RMCs vs. £0.55 and £2.54 peer-registered patient for peer review) |
| Crompton et al. (2010)115 | UK (Wales) | Observational study | Aim: to report on the development of an e-mail-based teledermatology service which aimed to provide GPs in the metropolitan area of Cardiff with rapid access to a hospital-based consultant dermatologist Population: GPs in Cardiff, UK Sample size: Implemented in stages. Pilot stage 5 GPs, now includes 40 out of 71 practices Interventions: a ‘store-and-forward’ intervention, in which GPs e-mail a brief clinical history and digital image for diagnosis by a consultant. E-mails were reviewed by two teledermatology consultants. Information contained in the replies include provisional and differential diagnoses, advice on further investigations, outline treatment plans (including suggested topical and systemic therapies), advice for in-practice minor surgery and recommendations for referral to the hospital outpatient clinic for face-to-face consultation with the dermatologist |
Number of referrals: the number of teledermatology referrals increased year on year over the 4 years from 283 referrals from 19 practices in year 1 to 8948 from 40 practices in year 4. The percentage of patients being referred to hospital stayed relatively constant over the 4 years, at around 19% Patient outcomes: NR Patient satisfaction: NR Access to care: NR Costs: NR Other: only 10% of the teledermatology referrals during the 4 years of service were considered too poor and unfit to make a diagnosis. The vast majority, average 88%, did not receive any comment from the dermatologist |
| Crowe et al. (2010)146 | UK (England) | Observational study | Aim: to explore the challenges facing GPs’ adherence to shared-care arrangements for specialist drugs Population: three PCT in one Strategic Health Authority in the north-west of England Sample size: 47 interviews were conducted with a range of practice PCT and Strategic Health Authority staff and other relevant stakeholders Interventions: shared care is the joint participation of hospital consultants and GPs in the planned delivery of care for patients with a chronic condition informed by an enhanced information exchange over and above routine discharge and referral letters |
Number of referrals: NR Patient outcomes: NR Patient satisfaction: NR Access to care: NR Other: GPs faced multiple challenges in adhering to shared-care arrangements for specialist drugs, including ambivalence around the management of psychiatric patients, the sharing of test results, compliance with the shared care arrangement and the dependence on specialist advice |
| Cuadros et al. (2009)62 | USA | Observational study | Aim: to describe a telemedicine system (EyePACS) for diabetic retinopathy screening Population: patients with diabetic retinopathy Sample size: During pilot phase (2005–6), 3562 patients. From 2006 to 2008, 34,100 patients in 120 primary care sites Interventions: primary clinic personnel (i.e. nursing, technical or administrative staff) were trained and certified by the EyePACS programme to acquire retinal images from standard digital retinal cameras. Images were interpreted by certified EyePACS reviewers or local eye care providers certified through the EyePACS Retinopathy Grading System |
Number of referrals: The overall rate of referral was 8.21% for sight-threatening retinopathy and 7.83% for other conditions (no other results were reported) Patient outcomes: NR Patient satisfaction: NR Access to care: NR Costs: NR |
| DAMASK (Direct Access to Magnetic Resonance Imaging: Assessment for Suspect Knees) Trial Team (2008)63 | UK | Cost-effectiveness within pragmatic randomised trial | Aim: to investigate the cost-effectiveness of GP referral to early MRI for patients with continuing knee problems Population: adult patients aged 18–55 years old, consulting their GP about a continuing knee problem recruited from 163 practices at 11 sites across the UK (between November 2002 and October 2004) Sample size: 386 patients (206 intervention and 180 control) Interventions: direct referrals by GPs to the local radiology department for a MRI examination. GPs also received an educational seminar about MRI, clinical diagnosis, and conservative management, compared with standard care control referral to the local orthopaedic department for consultation with a specialist, who may or may not subsequently request a MRI examination |
Number of referrals: NR Patient outcomes: patients randomised to intervention also had mean KQoL-26 physical functioning scores that were better by 3.65 (1.03 to 6.28; statistically significant; p = 0.007) Patient outcomes: NR Patient satisfaction: NR Costs: estimated from the NHS perspective, over 2 years’ direct referrals by GPs for MRI was found to be associated with an increase of cost of £294 (95% CI £31 to £573) per patient. However, overall referral to GPs was considered cost-effective, as it was associated with a greater gain in the number of QALYs (0.05, 95% CI 0.0225 to 0.118), so overall mean differences in cost and QALYs generated an incremental cost per QALY gained of £5840. The authors reported that, at a cost-per-QALY threshold of £20,000, referral by GPs for MRI was associated with a 0.81 probability of being cost-effective to the NHS |
| DAMASK (Direct Access to Magnetic Resonance Imaging: Assessment for Suspect Knees) Trial Team (2008)64 | UK | Pragmatic randomised trial | Aim: to evaluate a new referral pathway of GP referral to early MRI for patients with continuing knee problems Population: adult patients aged 18–55 years old, consulting their GP about a continuing knee problem recruited from 163 practices at 11 sites across the UK (between November 2002 and October 2004) Sample size: 533 patients (279 intervention and 274 control) Interventions: direct referrals by GPs to the local radiology department for a MRI examination. GPs also received an educational seminar about MRI, clinical diagnosis and conservative management, compared with standard care control referral to the local orthopaedic department for consultation with a specialist, who may or may not subsequently request a MRI examination |
Number of referrals: in the intervention group, 230 (82%) patients had an orthopaedic consultation, compared with 236 (86%) patients in the control group: mean difference 3.7% (95% CI –2.4% to 9.8%). In the intervention group, 112 (40%) patients had an arthroscopy, compared with 77 (28%) patients in the control group: mean difference 12% (95% CI 4.1% to 19.7%) Patient outcomes: over 24 months, patients randomised to intervention had a mean SF-36 physical functioning scores that were better by 2.81 (95% CI –0.26 to 5.89) than those directly referred to orthopaedics, but the result was not significant. Patients randomised to intervention also had mean KQoL-26 physical functioning scores that were better by 3.65 (95% CI 1.03 to 6.28) (the authors did not consider this to be clinically significant). Over the previous 12 months, the median number of days patients took off work or were prevented from normal activities was zero in both groups Patient satisfaction: NR Access to care: the median waiting time from randomisation to MRI was 41 days in the intervention group and 79 days in the control group; from randomisation to arthroscopy was 337 days in the intervention group and 294 days in the orthopaedic group Costs: NR |
| Davies et al. (2007)147 | UK | RCT/economic evaluation | Aim: to assess the cost-effectiveness and cost-effectiveness acceptability of treating rheumatoid arthritis in shared care Population: patients aged over 18 years old with rheumatoid arthritis in England Sample size: 460 patients (228 intervention and 232 control) Interventions: management of patients in primary care with annual hospital review, instead of management in hospital specialist clinic |
Number of referrals: NR Patient outcomes: over 3 years, the mean number of QALYs was 1.67 for intervention group and 1.6 for control group Patient satisfaction: NR Access to care: NR Costs: over 3 years, the mean cost was £4540 for intervention group and £4440 for control group. If policy-makers are prepared to pay £2000 per QALY, the intervention would be cost-effective in 50% of cases. If policy-makers are prepared to pay £13,000 or more per QALY, the intervention would be cost-effective in 80% of cases |
| Davies and Elwyn (2006)195 | Multiple | Literature review | Aim: to discuss RMCs and whether or not there is any evidence that they can deliver | The authors discussed problems and benefits of RMCs, concluding that they ‘do not know whether referral management centres will increase or decrease risk, efficiency, or choice, and little research evidence exists to support predictions of performance’ |
| DeMiglio and Williams (2012)148 | Canada | Observational study | Aim: to explore the views and experiences of community-based palliative care team members and key-informants regarding the barriers involved using a shared-care model to provide care in the community Population: physicians and nurses working in community-based palliative care teams Sample size: five community-based palliative care teams and six key informants were interviewed Interventions: community-based palliative care teams which are based on collaborative partnerships (shared care) between primary care physicians and community nurses |
Number of referrals: N/A Patient outcomes: N/A Patient satisfaction: N/A Access to care: N/A Costs: N/A Other: barriers to collaboration were of three types – institutional barriers (including funding issues), interest-related barriers (including time-management issues) and idea-related barriers (including difficulties in understanding the concept of shared care and in capturing evidence of its impact) |
| Dhumale (2004)10 | UK (England) | Prospective observational study | Aim: to assess the feasibility of performing hernia surgery in a general practice Population: patients in one general practice in north-west Norfolk Sample size: 4965 surgical procedures, including 286 inguinal hernia repairs Interventions: hernia surgery with local anaesthesia performed by a GPwSI in surgery, a theatre nurse and a surgical administrator |
Number of referrals: NR Patient outcomes: complication rates compared favourably with published literature Patient satisfaction: NR Access to care: average waiting time for hernia repair decreased from 18 months to 4 months Costs: NR |
| Dhumale et al. (2010)11 | UK (England) | Retrospective case review | Aim: to reduce waiting times for patients in order to relive pressure on local hospital waiting lists for other surgical procedures Population: patients who underwent abdominal wall hernia repair at a dedicated ambulatory hernia service Sample size: 1164 patients Interventions: set-up of an ambulatory hernia service at Probus Surgical Centre in Cornwall in 2005. Mesh hernia repairs were carried out by one of two GPwSIs and tissue repairs by the associate surgeon. All procedures were performed as day cases |
Number of referrals: NR Patient outcomes: complications recorded were three recurrences, three haematoma, one bowel perforation, one wound bleeding, one superficial wound infection, one hydrocele and two chronic pain Patient satisfaction: 98% found the information given before the operation adequate, 100% were happy with the overall care received on the day of operation and 95% would recommend hernia operation under local anaesthetic to their friends. On an overall satisfaction score of 1–10, 91% gave a score of 10 and 100% gave a score of ≥ 8 Access to care: all patients were seen within 4 weeks Costs: NR |
| Diamond and Bloch (2010)116 | USA | Literature review | Aim: to review the literature on telepsychiatric assessment of children and adolescents Population: studies focusing on child and adolescent psychiatric assessment Sample size: NR Interventions: telepsychiatry assessment of children and adolescents |
Number of referrals: NR Patient outcomes: no data were found to suggest that telepsychiatry leads to negative outcomes. Several studies reported that there was no difference in outcomes between telepsychiatry and face-to-face consultation Patient satisfaction: author reports data showing that participants in videoconferencing were satisfied with its use Access to care: NR Costs: NR Other: all participants found useful a second-opinion child-telepsychiatry service providing access to expertise to outlying mental health staff in Australia. Concerns with telepsychiatry: the camera may not show the whole room and some things may happen off-camera. The position of the camera (e.g. on top of the screen) may make it look as though the psychiatrist is not looking the patient in the eye. Conducting one-off consultation and not knowing the outcomes of their treatment may reduce the job satisfaction of the psychiatrist. One review reported that telepsychiatry may not be adequate for assessing teenage depression and for ‘difficult teenagers who refused to cooperate’ |
| Dusheiko et al. (2011)24 | UK (England) | Observational study | Aim: to examine whether or not better primary care management of 10 chronic diseases is associated with reduced hospital costs Population: patients in 8000 English general practices Sample size: 5 million patients Interventions: none. Use of QOF data to build index of quality of disease management and assess the impact of better management on use of hospital services. Ten conditions are asthma, CHD, CKD, COPD, dementia, diabetes, hypertension, hypothyroidism, mental health and stroke |
Number of referrals: NR Patient outcomes: NR Patient satisfaction: NR Access to care: NR Costs: only better management of stroke is associated with reduced hospital costs. A 10% improvement in the general practice stroke care over 3 years has resulted savings of £130M in 2007–8. This decrease in expenditure comes from reductions in emergency admissions and subsequent follow-up visits mainly |
| Eide et al. (2013)177 | USA | Before-and-after study | Aim: to develop an interactive web-based course (INFORMED) to improve the skills of primary care providers in skin cancer detection Population: primary care providers at two different sites assessing patients with suspected skin cancer Sample size: 54 primary care providers Interventions: 1- to 2-hour interactive, web-based course in skin cancer detection for primary care providers |
Number of referrals: at site one, there was a slight decrease in referrals for possible skin cancer (630 referrals before the course vs. 607 6 months after the course); in the other site, the number of referrals to dermatology decreased from 727 to 266 (statistical tests were not reported) Patient outcomes: the mean score for appropriate diagnosis and management increased from 36.1% to 46.7% (OR 1.6, 95% CI 1.4 to 1.9), with greatest improvement in benign lesions, from 32.1% to 46.3% (OR 1.9, 95% CI 1.6 to 2.4) Patient satisfaction: NR Access to care: NR Costs: NR |
| Eikelboom et al. (2005)117 | Australia | Observational study | Aim: to determine whether or not the use of teleotology consultations is feasible to make an assessment of a patient Population: children aged under 16 years old with ear disease in remote communities Sample size: 66 children Interventions: a paediatric otolaryngologist assessed children’s ear during a normal consultation. Over 1 month later, the same consultant made an assessment based on digital images, audiometry data and clinical data of the same children |
Number of referrals: rate of recommendation for referral was slightly higher for the teleotology assessments (up to 15.4%) Patient outcomes: NR Patient satisfaction: NR Access to care: NR Costs: NR Appropriateness of diagnosis: there was significant agreement between the two types of consultations (p < 0.01) |
| Eley and Fitzgerald (2010)82 | UK (England) | Audit | Aim: to assess the impact of DRACs on ENT appointments and appropriate GP use of clinic Population: patients aged over 60 years old with hearing loss referred to the DRACs Sample size: 353 patients Interventions: direct referral by GPs to audiology clinics (DRACs) for the assessment and the provision of hearing aids are offered to patients aged over 60 years old with long-standing hearing loss, instead of ENT referral |
Number of referrals: of the 353 DRAC referrals, 16% of patients were referred to an ENT specialist, before being sent back to DRAC Patient outcomes: NR Patient satisfaction: NR Access to care: NR Costs: excluding those patients who had an ENT appointment, had the 298 patients had an ENT appointment instead of DRAC, the additional cost to the system would have been £18,774. This represents a large cost saving |
| Elwyn et al. (2007)157 | UK (Wales) | Before-and-after study | Aim: to assess the impact of a guideline adherence intervention on referrals Population: patients referred to three endoscopy units in two hospital trusts who had a complaint of dyspepsia Sample size: 1730 patients (1118 before referrals, 612 after referrals) Interventions: referrals were assessed against the NICE guidelines for the management of dyspepsia by two part-time GPs. Where requests did not adhere to the referral guidelines, feedback was sent to GPs |
Number of referrals: there was a decline in the number of referrals for gastroscopy by hospital doctors for dyspepsia from 26.6 to 18.4 referrals per week and for GPs from 13.3 to 12.1 referrals per week. After adjusting for seasonal variation, an estimated drop of 10 referrals a week (p < 0.001) was found for hospital doctors; the drop of 3.2 referrals per week for GPs was not significant (p = 0.065) Patient outcomes: NR Patient satisfaction: NR Access to care: the mean interval referral-to-procedure interval for gastroscopy reduced from 52.1 days to 39.4 days (p < 0.001) Costs: NR Other: mean adherence rates was higher among hospital doctors than GPs. There was a significant increase in adherence to guidelines among GPs after implementation of the intervention (55% vs. 75%; p < 0.001). No change over time was observed for hospital doctors’ adherence |
| Emery et al. (2007)158 | UK (England) | Cluster RCT | Aim: to evaluate a computer decision support system (GRAIDS) for the management of familial cancer risk in primary care Population: patients in primary care who expressed concerns about their family history of breast or colorectal cancer. A total of 45 general practice teams in East Anglia, UK Sample size: 246 patients (162 patients and 23 practices in the intervention group, 84 patients and 22 practices in the control group) Interventions: training in the new assessment strategy and access to the GRAIDS software was conducted, compared with an educational session and guidelines about managing familial breast and colorectal risk |
Number of referrals: GRAIDS practice teams referred a mean 6.2 (±3.1) per 10,000 registered patients per practice per year compared with 3.2 (±2.8) per 10,000 registered patients per practice per year in comparison practices (mean difference 3.0; 95% CI 1.2 to 4.8; p = 0.002) Patient outcomes: there were no significant differences in knowledge scores between patients referred from intervention and those referred from comparison practices. Cancer worry scores were significantly lower in patients from intervention practices than in those from comparison practices (mean difference −1.44, 95% CI −2.64 to −0.23; p = 0.02) Patient satisfaction: NR Access to care: NR Costs: NR Appropriateness of referrals: there were 162 relevant referrals made by the GRAIDS practices and 84 referrals by the comparison practices to the Regional Genetics Clinic for familial cancer risk assessment. Referrals from GRAIDS practices were more likely to be consistent with referral guidelines (odds ratio = 5.2, 95% CI 1.7 to 15.8; p = 0.006) |
| Eminovic et al. (2009)118 | The Netherlands | Multicentre, cluster randomised trial | Aim: to assess the impact of teledermatologic consultations (‘store-and-forward’) on dermatology referrals Population: dermatology patients from 35 practices in the catchment area of two Dutch general district hospitals in Almere and Zeist Sample size: 631 patients (327 intervention and 304 control), from 85 GPs Interventions: GPs in treatment practices used teledermatologic consultations in which four pictures of each skin condition were sent via e-mail with structured form to a dermatologist, who replied within 48 hours with recommendations; this was compared with normal referral to an outpatient clinic |
Number of referrals: NR Patient outcomes: at the 1-month dermatologist visit 20% of patients in the interventions had recovered or partially recovered, compared with 4.1% in the control group Patient satisfaction: no significant difference between groups Access to care: NR Costs: NR Appropriateness of referral: dermatologists considered a face-to-face consultation to be unnecessary in 39% of cases in the intervention group and 18.3% of cases in the control group, a difference of 20.7% (95% CI 8.5% to 32.9%). Estimated differences in proportion of preventable consultations ranged from 19% to 25.5% (sensitivity analyses). Full or partial recovery before specialist consultation was the most common reason for judging the consultation preventable. Differences represent the potential for a reduction in face-to-face referrals if teledermatologic consultations were to be adopted |
| Eminovic et al. (2010)119 | The Netherlands | Economic evaluation based in multicentre cluster randomised trial | Aim: to understand under which conditions ‘store-and-forward’ teledermatology can reduce costs from a societal perspective Population: dermatology patients from 35 practices in the catchment area of two Dutch general district hospitals in Almere and Zeist Sample size: 631 patients (327 intervention and 304 control), from 85 GPs Interventions: GPs in treatment practices used teledermatologic consultations in which, four pictures of each skin condition was sent via e-mail with structured form to a dermatologist, who replied within 48 hours with recommendations, compared with normal referral to outpatient clinic |
Number of referrals: NR Patient outcomes: authors cite Pak et al. 2007 to further confirm authors’ previous findings that there is no difference in clinical outcomes between conventional care and teledermatology. On this basis a cost minimisation study design was chosen Patient satisfaction: NR Access to care: NR Costs: costs considered included investments (set-up costs), GP care, dermatology care, out-of-pocket expenses by patients and employer costs (owing to patient working-days lost). Mean costs of teledermatology compared with conventional care per care episode were €387 (95% CI €281 to €502.5) vs. €354 (95% CI €228 to €484), giving a total mean difference of €32.5 (95% CI –€29 to €74.7). Monte Carlo simulation showed that conventional care was less expensive than teledermatology in 89% of all simulations. Scenario analysis showed that costs for teledermatology and conventional care would have been similar if 37% of referrals by the GPS were prevented. Increasing the proportion of prevented referrals decreased the costs of teledermatology. Teledermatology also becomes less expensive relative to conventional care when the distance to the dermatologist is further. Teledermatology and conventional costs would also be similar if the distance to the hospital is 75.1 km Appropriateness of referral: results reported in earlier study (Eminovic 2009), suggested that 20.7% of face-to-face dermatological consultations could be avoided if teledermatology was used |
| Evans (2009)178 | UK (Wales) | Observational study | Aim: to assess the impact of a retrospective peer review of referrals models Population: patients from three practices in south-east Wales Sample size: NR Interventions: GPs funded for weekly protected time to retrospectively discuss referrals by peer review. Six–weekly cluster meetings are also organised with hospital consultants to discuss appropriateness of and alternatives to referrals. Feedback was given to practices on their referral rates |
Number of referrals: no clear direction of effect on referral rates (some GPs referred more after scheme, some less), but variation in referral rates across GPs decreased. Orthopaedic referrals decreased by up to 50% in the three practices. Patients were directed instead to alternatives such as physiotherapy, podiatry and local multidisciplinary teams. Overall reduction in emergency referrals was 17.4% over 1 year Patient outcomes: NR Patient satisfaction: NR Access to care: NR Costs: NR Quality of referrals: the quality of referrals improved, including better information included in the referral letter, better use of guidelines, etc. Appropriateness of referrals: for one practice, the hospital provided data on emergency referrals which showed that the proportion of referrals sent home without admission fell from 60% to < 20% |
| Evans et al. (2011)179 | UK (Wales) | Observational study | Aim: to assess the impact of a retrospective peer review of referrals models Population: patients from 32 practices in south-east Wales (implemented in two phases; in phase 1, 2008 to 2009, 10 practices, in phase 2, 2009 to 2010, 22 practices) Sample size: approximately 7000 referrals Interventions: GPs funded for weekly protected time to retrospectively discuss referrals by peer review. Six–weekly cluster meetings are also organised with hospital consultants to discuss appropriateness of and alternatives to referrals. Feedback was given to practices on their referral rates |
Number of referrals: the highest referrers show a decrease while the lowest referrers may show an increase in referrals rates. The variation in referral rates between GPs decreased from 2.6 to 7.7, to 3.0 to 6.5 per 1000 patients per quarter. Overall, there was a decrease in the number of referrals to secondary care, from 5.5 to 4.3 per 1000 patients per quarter Patient outcomes: NR Patient satisfaction: NR Access to care: NR Costs: NR Quality of referrals: GPs’ own assessment of referrals showed an improvement in quality. Consensus was reached over many referral pathways |
| Ferguson and Cook (2011)196 | UK (England) | Observational study | Aim: to investigate the sustainability of a primary care orthopaedic interface service looking at referrals Population: patients with orthopaedic problems Sample size: total sample size not reported Interventions: a primary care musculoskeletal interface service (OIS) was set up in 2003 to provide efficient and timely management for patients with orthopaedic problems. An orthopaedic physiotherapist specialist delivers services, supported by an orthopaedic consultant and his or her medical team |
Number of referrals: the interface service processes (OIS) from 179 to 256 referrals per month. Around 50% are retained to be seen in the OIS, the rest passed on to secondary care. Of those seen in OIS, 58% of patients were discharged, 21% were followed up within the service and 21% were referred to secondary care Patient outcomes: NR Patient satisfaction: the author states that ‘of the 115 patients surveyed the results were overwhelmingly positive’, although the data are not presented. Hospital non-attendance rate was low, at 4–7% Access to care: not reported directly. The service was in part developed to reduce long waiting times for orthopaedic appointments in secondary care Costs: the author states that ‘because up to 30% of patients from the OIS go onto secondary care, there is an additional first contact charge for them. In spite of this, significant savings are realised because of the proportion of patients that are seen in the OIS and discharged’, although data are not reported |
| Ferrer-Roca et al. (2010)120 | Spain | Non-RCT | Aim: to assess the impact of a telemedicine scheme on quality of life Population: patients referred to hospital from primary care to the following specialties: dermatology, traumatology, psychiatry, internal medicine, pain-relief unit, X-ray department, endocrinology and rheumatology Sample size: 800 referrals (380 teleconsultations, 420 face-to-face consultations) Interventions: patients had the option to see a specialist face to face or by teleconsultation. Teleconsultations were arranged by nurses using a videoconferencing system |
Number of referrals: NR Patient outcomes: no difference in patient outcomes Patient satisfaction: added advantages of teleconsultation as reported by patients was less travelling (p = 0.0001) Access to care: for teleconsultation, time required for examination, diagnosis and treatment was significantly less (p = 0.0001) Costs: NR |
| Fickel et al. (2007)100 | USA | Literature review and interviews | Aim: to assess the extent of collaboration and potential barriers to the relationship between primary care and mental health Population: primary care and mental health clinical leaders Sample size: 22 interviews with clinical leaders from 10 outpatient facilities Interventions: primary care–mental health collaboration |
Number of referrals: NR Patient outcomes: NR Patient satisfaction: NR Access to care: NR Costs: NR Collaboration: both primary care and mental health leaders were generally pleased with the relationships between the two services Barriers: mental health leaders were more likely to identify barriers than primary care leaders. Barriers included inadequate numbers of mental health providers and physical distance between primary care and mental health clinics |
| Fischer et al. (2010)197 | USA | Observational study | Aim: to report on the implementation of an electronic referral system, introduced to improve the organisation of referrals Population: 23 organisations providing primary and specialty care to uninsured and Medicaid patients in the Chicago area, including Cook County Health and Hospitals System, community health centres, several community hospitals and the local health department Sample size: 195 clinical sites with 2226 active providers are connected to the referral system Interventions: an electronic referral system was introduced in 2003. The software contains algorithms based on clinical practice guidelines. Following these rules the referral is either approved or denied. Denials include an explanation, and can be appealed for clinical review. A referral support centre, staffed by nurses and clerks, supports the computerised system. In 2008, the referral system was expanded to allow patients in specialty care to be referred back to primary care providers |
Number of referrals: on average more than 15,000 referrals are processed through the system per month Patient outcomes: NR Patient satisfaction: NR Access to care: the referral processing time was reduced from an average of 3 months to 5.5 days, with priority referrals processed in 2.5 days. Most priority patients received appointments within 1–3 weeks. Waiting times for non-urgent referrals varied from a few days to a few months, depending on the specialty Costs: a full cost–benefit analysis was not conducted. The project cost close to US$2M over 4 years. Approximately 70% of funds were spent on initial design and development. Reduction in Referral Support Centre staff saved US$1M in salaries and benefits per year. Other benefits assumed due to reduction in inappropriate referrals Appropriateness of referrals: in the first year 23,000 referrals, or 22%, of total requests were screened out as inappropriate during the first year of operation |
| Fleuren et al. (2010)159 | The Netherlands | Observational study | Aim: to assess the impact of the introduction of a shared care guideline from national guidelines for back pain on referrals Population: patients with lumbosacral radicular syndrome (LRS) referred to the hospital neurologist by a GP from the Eindhoven and Helmond region Sample size: 723 patients from 360 GPs Interventions: implementation of shared-care guideline, which consisted of a trade-off. If the GP agrees to conservative management approach in the first 6 weeks, the patient was guaranteed a priority consultation with neurologist and MRI if symptoms persist |
Number of referrals: NR Patient outcomes: NR Patient satisfaction: Access to care: duration of the total diagnostic procedure (number of days between referral by the GP and the consultation by the neurologist) decreased from an average of 44.5 days to 41.8 days 2 year later in Eindhoven and from 53.7 days to 47.5 days in Helmond Costs: Total costs of implementation over the 2 years were €42,600 for the two regions (94% of the cost were personnel costs) Appropriateness of referrals: the percentage of unnecessary referrals significantly decreased from 15% before implementation to 9% 1 year after (adjusted OR 0.52, 95% CI 0.28 to 0.96), and 8% 2 years after (adjusted OR 0.48, 95% CI 0.27 to 0.86) |
| Fleury et al. (2012)149 | Canada | Observational study | Aim: to assess the state of collaboration among GPs, psychiatrists and psychosocial mental health-care professionals and to develop a new model of collaboration Population: 60 GPs in 5 (of 18) Quebec regions Interventions: N/A. The article reviews different models of collaboration |
Number of referrals: approximately half of GPs referred their patients to psychologists in private practice of the public system. Referrals to psychiatrist were requested for complex common mental disorders Patient outcomes: N/A Patient satisfaction: N/A Access to care: N/A Costs: N/A GP satisfaction: GPs favoured a model in which a team of psychosocial professionals and psychiatrists would be working with them, practising in the GPs’ own settings. They also favoured training, financial incentives, appropriate mode of compensation (payments) and wide access to care |
| Frost et al. (2012)91 | Canada | Discussion paper | Aim: a discussion of an alternative model, termed the ‘shifted outpatient model’, which could enhance collaboration between family physicians and specialists Population: all patients attending primary care services in Ontario, Canada Sample size: N/A Interventions: a shifted outpatient model, in which consultants are invited into primary care practices for regularly scheduled, dedicated sessions, during which the consultants make themselves available to assess patients, communicate directly with primary care providers, and participate in the clinic’s educational initiatives |
Number of referrals: the authors refer to literature suggesting that primary care-based specialist programmes lead to reduction in referral rates to specialists in secondary or tertiary settings Patient outcomes: the authors refer to a review which found that (when part of more complex interventions) specialist outreach clinics resulted in improved outcomes, compared with usual care Patient satisfaction: the author reports that the model is preferable for patients, but cites no evidence gathering from patients themselves Access to care: the authors refer to a review which found that specialist outreach clinics in primary care improve access to care Costs: NR |
| Garcia Garcia et al. (2011)160 | Spain | Observational study | Aim: To enable better collaboration and co-ordination between primary and secondary care nephrology centres, and, consequently, reduce unnecessary referrals to secondary care Population: patients treated within the Parc Taulí Health and University Corporation Sample size: programme implemented in an area with 426,000 inhabitants and 230 GPs Interventions: development and implementation of a consensus document and protocol for management of arterial hypertension in primary care and referral of patients to specialists. In addition, unnecessary referrals were returned with an explanation and recommendations. In-person and electronic clinical consultations for primary care doctors with a reference nephrologist. A continuous training programme in kidney disease and arterial hypertension was implemented in the in-person consultation sessions. Use of a clinical information system. The programme was implemented over a 3-year period from 2007 to 2010 |
Number of referrals: the number of first nephrology visits requested by primary care providers continued to rise for the first 2 years of the programme from a baseline of 417 requests in 2004. By the third year of the programme the number of requests for referrals appeared to have stabilised at 544 requests. The number of denied referral requests increased from 0 in 2004 to 155 in 2009. By 2009 denied referral rates made up 28.49% of the total number of referrals Patient outcomes: NR Patient satisfaction: NR Access to care: NR Costs: NR GP satisfaction: GPs were generally satisfied with the improvement in communication and the continuous training programme |
| George et al. (2008)12 | UK (England) | Prospective randomised controlled equivalence trial | Aim: to determine whether or not GPs are able to perform a range of elective minor surgical procedures, in terms of the safety, quality and cost of care, as competently as hospital doctors Population: consenting patients presenting at general practices and needing minor surgery in the south of England Sample size: 568 patients (637 skin procedures, 17 ingrowing toenail procedures) Interventions: on presentation to their GP, patients were randomised to either treatment in primary care or treatment at their local hospital. Evaluation was by assessment of clinical quality and safety of outcome, supplemented by examination of patient satisfaction and cost-effectiveness |
Number of referrals: NR Patient outcomes: mean visual analogue scale score (for quality of surgery) was significantly higher for procedures carried out in hospital than those carried out in primary care (mean difference = 5.46 on 100-point scale, 95% CI 0.925 to 9.99), but the clinical importance of the difference was uncertain. Hospital doctors were better at achieving complete excision of malignancies, with a difference that approached statistical significance [15/20 (75%) hospital vs. 7/16 (44%) GP, χ2 = 3.65; p = 0.056]. The proportion of patients with postoperative complications was similar in both groups Patient satisfaction: no global score of patient satisfaction was reported. Few significant differences between arms, except in matters relating to convenience and knowing the doctor, where the primary care arm has lower scores than the hospital arm. The hospital arm scored better on provision of information following the operation Access to care: all access to care items in the patient questionnaire favour treatment in primary care. Ease of making appointment mean difference = 0.203 (95% CI –0.055 to 0.461); not kept waiting mean difference = 0.496 (95% CI 0.177 to 0.816) Costs: the mean cost for hospital-based minor surgery was £1222.24 and for primary care was £449.74. Using postoperative complications as an outcome, both effectiveness and costs of the alternative interventions are uncertain. Using completeness of excision of malignancy as an outcome, hospital minor surgery becomes more cost-effective |
| Gilbert et al. (2005)36 | UK (England) | Retrospective case review | Aim: to examine the proportion of GP referrals to a hospital RM clinic which might be suitable for a GPwSI respiratory clinic Population: referrals to the Department of Respiratory Medicine at the Norfolk and Norwich University Hospital Sample size: 96 referrals Interventions: two GPs and one consultant respiratory physician assessed all GP referral letters to the RM department of a teaching hospital, to determine the patient’s suitability to be seen in a GPwSI respiratory clinic, assuming that such a clinic had a predetermined range of investigative facilities. Assessors considered whether the referrals suitable for a GPwSI clinic could be seen in either a community-based or a hospital-based clinic |
Number of referrals: NR Patient outcomes: NR Patient satisfaction: NR Access to care: NR Costs: NR Appropriateness of referral: out of 96 referrals covering a wide range of respiratory conditions, except lung cancer, 22 (23%) were considered by all assessors to be suitable for a GPwSI clinic and 40 (42%) referrals were considered unsuitable. For the remaining 34 referrals (35%), there was varying degrees of agreement on suitability. The largest groups of patient referrals considered suitable for a GPwSI clinic were those with COPD or cough as the main presenting clinical problem. The most common groups considered unsuitable were referrals of patients with an abnormal chest radiograph, haemoptysis and possible interstitial lung disease |
| Gilbody et al. (2006)101 | Multiple | Systematic review | Aim: to review enhancement strategies aiming to improve the quality and outcome of care for depression in primary care settings Population: patients with depression in primary care Sample size: 11 studies Interventions: economic studies were included that examined the cost-effectiveness of organisational interventions to improve the quality and outcome or care for depression in primary care settings (i.e. clinical education; dissemination and implementation of treatment or management guidelines; reconfiguration of roles within primary care; case management or active follow-up; consultation liaison; or other methods of improving working relationships between primary care and specialist/secondary services) |
Number of referrals: NR Patient outcomes: NR Patient satisfaction: NR Access to care: NR Costs: the authors found a near-uniform finding that the interventions based on collaborative care/case management resulted in improved outcomes but were also associated with higher costs. When considering primary care depression treatment costs alone, incremental cost-effectiveness ratio estimates ranged from £7 to £13 per additional depression-free day. Educational interventions alone were associated with increased cost and no clinical benefit |
| Glaves (2005)161 | UK (England) | Before-and-after study | Aim: to determine if the use of request guidelines can achieve a sustained reduction in the number of radiographic examinations of the cervical spine, lumbar spine and knee joints performed for GPs Population: patients referred by GPs to three community hospitals and a district general hospital (Buxton, Whitworth, Newholme, Chesterfield) Sample size: 7026 referrals in the year before the intervention Interventions: GPs were asked to comply with referral guidelines for radiography of the cervical spine, lumbar spine and knee, and all requests for these three examinations were checked. Requests that did not fit the guidelines were returned to the GP with an explanatory letter and a further copy of the guidelines. Where applicable, a large-joint replacement algorithm was also enclosed. If the GP maintained the opinion that the examination was indicated, she or he had the option of supplying further justifying information in writing or speaking to a consultant radiologist |
Number of referrals: across all sites and for all three examinations, the total number of examinations fell by 68% in the first year (95% CI 67% to 69%), achieving a total reduction compared with baseline in the second year of 79% (95% CI 78% to 80%) Knee radiographs fell by 64% in the first year (95% CI 62% to 65%), achieving a 77% reduction in the second year (95% CI 75% to 79%). Lumbar spine radiographs fell by 69% in the first year (95% CI 68% to 71%), achieving a 78% reduction in the second year (95% CI 77% to 80%). Cervical spine radiographs fell by 76% in the first year (95% CI 74% to 78%), achieving an 86% reduction in the second year (95% CI 84% to 88%). All reductions were highly significant (p < 0.0001) Patient outcomes: NR Patient satisfaction: NR Access to care: NR Costs: NR |
| Grassini et al. (2008)180 | Italy | Prospective before-and-after study | Aim: to combat rising colonoscopy demand by reducing inappropriate colonoscopies Population: outpatients referred for colonoscopy by primary care physicians to a single endoscopy unit Sample size: 1017 patients Interventions: an education programme consisting of a one-day training course on appropriateness of indications in digestive endoscopy. Followed by letter containing a summary of the lectures and a copy of the ASGE/SIED selection criteria for colonoscopies, with the recommendation to keep it for reference, and consult it when considering prescribing a colonoscopy |
Number of referrals: absolute number of referrals may not be comparable Patient outcomes: NR Patient satisfaction: NR Access to care: estimated a reduction in waiting list from 70 to 58 days (15%) Costs: estimated an annual saving of €19,000 through reduction of inappropriate colonoscopies Appropriateness of referrals: the number of inappropriate referrals was reduced following the intervention. Before the intervention, 23% of colonoscopies were inappropriate, whereas after the training course only 7.1% were inappropriate. After the course, of colonoscopies prescribed by those physicians who had attended the course only 2.6% were inappropriate, whereas those physicians who had not attended the course (but had received the letter) prescribed 8.9% of colonoscopies inappropriately (p < 0.025) |
| Grunfeld et al. (2006)45 | Canada | Multicentre RCT | Aim: to test the hypothesis that follow-up by the patient’s family physician is a safe and acceptable alternative to follow-up in specialist clinics for women diagnosed with breast cancer Population: patients with early-stage breast cancer who had completed adjuvant treatment, were disease free, and were between 9 and 15 months after diagnosis, in Ontario, Canada Sample size: 968 patients (483 intervention and 485 control) Interventions: follow-up was provided by a family physician, who were provided with a one-page guideline on follow-up that provided management and care recommendations. Family physicians were instructed to refer patients back to the cancer centre if a recurrence or new primary breast cancer developed. Outcomes compared against to follow-up in the cancer centre according to usual practice |
Number of referrals: NR Patient outcomes: in the family physician group, there were 54 recurrences (11.2%) and 29 deaths (6.0%). In the cancer centre group, there were 64 recurrences (13.2%) and 30 deaths (6.2%). In the family physician group, 17 patients (3.5%) compared with 18 patients (3.7%) in the cancer centre group experienced a serious clinical event (0.19% difference, 95% CI –2.26 to 2.65). No statistically significant differences (p < 0.05) were detected between groups on any of the health-related quality-of-life questionnaires Patient satisfaction: NR Access to care: NR Costs: NR |
| Gurden et al. (2012)83 | UK (England) | Observational study | Aim: to describe and evaluate a community-based musculoskeletal service, commissioned by NHS North East Essex PCT, in terms of patient-reported outcomes and satisfaction Population: adult patients consulting their GP for at least 4 weeks for back or neck pain in North East Essex PCT Sample size: 696 patients Interventions: patients consulting their GP for at least 4 weeks for back or neck pain were referred according to their preference to a chiropractor or osteopath or physiotherapist working in the independent sector |
Number of referrals: the authors conclude that ‘evaluation by the PCT demonstrated that the service reduced primary care consultations, imaging and inappropriate referrals to secondary care. Referrals to spinal surgeons reduced by more than 25%’ Patient outcomes: using the Bournemouth Questionnaire, the Bothersomeness scale and the Global Improvement Scale, approximately two-thirds of patients (64.6%, 67.8% and 69.9%, respectively) reported an improvement at discharge, and approximately 65% a significant reduction in medication. 97% of patients were discharged from the service with advice on self-management; the remainder were recommended for secondary care referral Patient satisfaction: almost all (99.5%) patients were satisfied with the service Access to care: NR Costs: NR |
| Hall et al. (2011)46 | UK (Scotland) | Observational study | Aim: study 1 – to explore the views of potential recipients of shared follow-up of cancer; study 2 – to conduct a modelling exercise for shared follow-up and to explore the opinions and experiences of both the patients and GPs involved Population: patients with a range of cancers currently attending for structured follow-up in secondary care in north-east Scotland Sample size: study 1 – 18 patients; study 2 – six GPs and five patients Interventions: six GPs were trained to deliver shared follow-up, which involved follow-up protocols and a system of specialist support for participating GPs. GPs were also given the opportunity to shadow consultants as they conducted follow-up appointments |
Number of referrals: N/A Patient outcomes: N/A Patient satisfaction: many rural patients, and some urban patients, would appreciate follow-up being available near to home with the associated benefits of time saved and easier parking and continuity of care. Patients have concerns related to the level of extra training received by the GP and loss of contact with their consultant. GPs have concerns about gaining and maintaining the clinical skills needed to conduct follow-up, especially if the numbers of patients seen are small. They also have concerns about lack of support from other GPs, and some administrative and organisational issues Access to care: NR Costs: NR |
| Hamilton et al. (2013)162 | UK (England) | Observational study | Aim: to help GPs to select patients for cancer investigation, and reduced extra cancer deaths due to diagnostic delay Population: patients attending GP practices in 7 of 28 English cancer networks Sample size: 614 GPs Interventions: GPs were provided with risk assessment tools applicable to patients aged 40 years and older with bowel or respiratory symptoms |
Number of referrals: compared with the preceding 6 months, there were 292 more chest radiographs, 104 extra 2-week chest clinic appointments and 47 additional diagnoses of lung cancer. For suspected colorectal cancer, there were 304 more 2-week referrals, 270 more colonoscopies and 10 more cancers identified Patient outcomes: a 37% increase in new lung cancer diagnoses and a 7% increase in new colorectal cancers, comparing 6 months during the intervention period with a 6-month period before the intervention Patient satisfaction: NR Access to care: NR Costs: NR Other: a total of 2593 risk assessment tools (1160 lung and 1433 colorectal) were completed |
| Harkness and Bower (2009)102 | Multiple | Systematic review | Aim: to assess the effectiveness of on-site mental health workers delivering psychological therapy and psychosocial interventions in primary care on the clinical behaviour of primary care providers Population: studies of mental health workers working alongside primary care providers Sample size: 42 studies Interventions: on-site mental health workers delivering psychological therapy and psychosocial interventions in primary care practices (replacement model) |
Number of referrals: the presence of mental health workers significantly reduced the rates of mental health referral (relative risk 0.13, 95% CI 0.09 to 0.20) for the patients they were seeing (taken from seven studies). There was no consistent pattern as to the impact on referrals in the wider patient population Patient outcomes: NR Patient satisfaction: NR Access to care: the presence of mental health workers significantly reduced the number of primary care providers consultations (standardised mean difference –0.17, 95% CI –0.30 to –0.05) (taken from 10 studies) Costs: there was evidence that mental health workers resulted in significant reductions in prescribing costs (standardised mean difference –0.22, 95% CI –0.38 to –0.07). Mixed results were found in changes to total costs |
| Hennessey et al. (2013)55 | UK (Northern Ireland) | Audit | Aim: to assess the impact of monitoring patients in primary care rather than hospital, using a computerised system to monitor PSA Population: patients with stable prostate cancer Sample size: 65 patients Interventions: implementation of a computerised system to monitor PSA in primary care – automatic letters are sent to the patient when PSA test is due, the patient attends his local health centre for test and then the GP forwards results to nurse specialist in hospital, where they are analysed |
Number of referrals: between 2006 and 2012, a total of 274 outpatient appointments were saved (median of three appointments per patient) Patient outcomes: each patient avoided having to travel a median of 126 miles and 228 minutes. This amounts to a total of 21,700 miles and 30,400 minutes saved Patient satisfaction: NR Access to care: the urology consultant saved 4090 minutes of consultations, which is the equivalent of 12 full outpatient clinics Costs: avoiding 274 hospital consultations potentially saved £32,000 |
| Hewlett (2005)47 | UK (England) | RCT | Aim: to determine the impact of a direct-access scheme compared with usual reviews Population: rheumatology patients in a teaching hospital Sample size: 209 randomised patients (105 intervention and 104 control; after 6 years, 68 intervention and 52 control) Interventions: direct access patient initiated review for rheumatoid arthritis compared to rheumatologist initiated review every 3–6 months |
Number of referrals: 38% fewer hospital appointments in the intervention group, median number of appointments was 8 vs. 13 (p < 0.0001) Patient outcomes: no significant difference across 13/14 clinical outcomes. Deterioration in range of movement in elbow was smaller in the intervention group Patient satisfaction: patient and GP satisfaction with and confidence in the system was higher in the intervention group Access to care: NR Costs: suggestions that the scheme could free up some resources, as an average of 11% each year do not request a review in the intervention group |
| Hilty et al. (2006)121 | USA | Observational study | Aim: to assess changes over time in the utilisation of telepsychiatric services by individual primary care providers and linics in rural areas, specifically: (a) types of referrals for telepsychiatry service; (b) primary care providers’ knowledge and skills related to medication dosing; and (c) primary care providers’ satisfaction with telepsychiatry Population: those attending 15 rural clinics, served by The University of California-Davis Health System, in California Sample size: 400 consecutive initial telepsychiatric consultations Interventions: patients received an initial telepsychiatric consultation delivered from the academic medical centre to rural or suburban primary care sites from July 1996 to December 2002. Primary care providers also received educational interventions – regular continuing medical education lectures, primary care providers’ participation in consultations, consultation notes for primary care providers from the psychiatrist, telephone consultations from primary care provider to psychiatrist |
Number of referrals: the psychiatrist was asked to evaluate what would have happened if the telepsychiatric consultation were not available. Estimated alternatives were local care by primary care provider in medical clinic (30.2%), local mental health outpatient services (46.5%), refer out of community for mental health outpatient services (14.2%), refer out of community for mental health inpatient services (3.4%), other (5.7%). Over time the proportion of the alternatives changed, with provision of care locally by the primary care provider in the medical clinic without delay increasing (35.9% from 24.5%), provision of local mental health outpatient services with delay decreasing (21.8% from 35.6%) and referral out of community for mental health outpatient services decreasing (10.4% from 18.0%) Patient outcomes: primary care providing improved. Among the first 200 consultations, only 47.4% of the medication doses for depressive and anxiety disorders were adequate, according to national guidelines. Among the second 200 consultations, dosing adequacy improved to 63.6% (p < 0.001) Patient satisfaction: NR Access to care: NR Costs: the total capital cost of the videoconferencing units was US$6000–9000, and the hourly rate for lines ranged from US$20–40 (depending on distance and long-distance carrier) |
| Hsiao and Oh (2008)122 | USA | Retrospective case review | Aim: to examine the time intervals in which skin cancer patients referred conventionally or by store-and-forward teledermatology were evaluated, diagnosed and treated Population: all patients who had been treated for skin cancer in a Veterans Affairs medical centre’s dermatological surgery clinics as a result of a conventional dermatology or teledermatology referral from three remote primary care clinics over a 4.5-year period (1 January 2003 to 31 July 2007) Sample size: 169 patients (92 intervention and 77 control) Interventions: teledermatology referral, in which the electronic medical record system permits exchange and images among health providers. Teledermatologist reviews the images and responds with a consult note that includes a diagnostic assessment and management recommendations. Compared with conventional face-to-face consultation |
Number of referrals: N/A Patient outcomes: NR Patient satisfaction: NR Access to care: for conventional and teledermatology referrals, respectively, the overall mean time intervals for initial consult completion were 48 and 4 days (p < 0.0001), for biopsy were 57 and 38 days (p = 0.034) and for surgery were 125 and 104 days (p = 0.006). Teledermatology consults were also associated with fewer dermatology clinic visits before surgery (p = 0.02) Costs: NR |
| Imison and Naylor (2010)194 | Multiple | Literature review and observational study | Aim: to examine evidence on the current quality of GP referrals and to assess the impact of different types of referral management Population: not specified Sample size: personnel from 21 PCTs and four case studies sites (75 interviews) Interventions: use of clinical guidelines; peer review and audit; clinical assessment and triage services; RMCs; financial incentives. The literature review aimed to examine evidence on the current quality of GP referrals and to assess the impact of different types of referral management |
This literature review largely describes the research conducted in the Wales study (an evaluation of seven referral management pilots) – which comprised a variety of approaches including triage, audit and the use of a RMC. The authors also reported results from other reviews and papers included in our review. Overall, they summarised the information and concluded: ’A referral management strategy built around peer review and audit, supported by consultant feedback, with clear referral criteria and evidence-based guidelines is most likely to be both cost- and clinically-effective
|
| Jani et al. (2012)163 | UK (England) | Audit | Aim: to assess the use of a standardised referral pro forma in compliance with NICE guidelines and cancer diagnosis rates Population: those referred for suspected cancer under ‘2-week wait referral’ to six acute NHS trusts in the Thames Valley Cancer Network in June 2010 Sample size: 586 referrals Interventions: use of pro forma compared with no use of pro forma |
Number of referrals: NR Patient outcomes: no information provided on relationship between use of pro forma and cancer detection rates Patient satisfaction: N/A Access to care: N/A Costs: N/A Appropriateness of referrals: paper suggests a statistically significant correlation between higher levels of NICE compliance in referrals received at each trust and higher cancer detection rates among referrals at the trust level (no stats data given) |
| Jawad and Robinson (2009)65 | UK (England) | Retrospective observational study | Aim: to investigate the feasibility of providing an ultrasound scanning service for certain gynaecological problems in the community Population: women attending a community gynaecological ultrasound service in Southwark PCT over 2 years (January 2006 to December 2007) Sample size: 327 patients Interventions: provision of a gynaecological ultrasound service in the community. Service was originally provided for women with intrauterine device and intrauterine system problems and has expanded to include other conditions. The service can also prescribe for immediate health needs |
Number of referrals: of 327 women who attended for ultrasound examination, 152 were managed entirely in the community. Estimate saved at least 80 referrals that would have otherwise been sent to hospital ultrasound units. Also likely to have avoided many gynaecology outpatient referrals, but does not estimate a number Patient outcomes: NR Patient satisfaction: authors infer that service is acceptable to patients based on low ‘Did not attend’ rate of 10% Access to care: sexual and reproductive health clinics are a walk-in service, no restrictions on access Costs: NR |
| Jha et al. (2007)150 | UK (England) | Observational study | Aim: to assess whether or not an integrated care pathway improves the services provided for continence care Population: women presenting in primary care with incontinence problems or related urinary symptoms Sample size: 65 patients referred to intervention. Comparisons in study made between 20 patients referred to intervention and 20 to control Interventions: an integrated care pathway, where patients were seen initially in a nurse-led clinic, compared with women referred directly to outpatients |
Number of referrals: of 40 patients seen in the nurse-led clinic, 12 referred directly for urodynamic studies, seven referred directly to the hospital for physiotherapy and six referred to the continence advisors. Seven patients seen in the nurse led clinic were discharged either on anticholinergics or following physiotherapy without needing to see a doctor for further management as they were symptom free Patient outcomes: NR Patient satisfaction: NR Access to care: shorter time from referral to first medical contact, diagnosis, physiotherapy/Continence Advisory Service, treatment/discharge for the integrated care pathway group, as compared with the outpatient gynaecology clinic. The differences in each of the outcomes was significant (p < 0.05) Costs: NR |
| Jiwa et al. (2006)164 | UK (England) | Cluster RCT | Aim: to reduce unnecessary referrals and increase the proportion of those referred who had significant colorectal pathology Population: patients with lower-bowel symptoms referred from 44 general practices in North Trent Sample size: 716 referrals from 44 practices (12 software, 11 educational outreach, 9 both, 12 control) Interventions: included software for an electronic interactive referral pro forma, which prompts for the assessment of patients with lower-bowel symptoms, an educational outreach visit by a local colorectal surgeon. Practices selected one, both or neither intervention |
Number of referrals: no statistical differences in proportion of cases referred which have significant colorectal pathology Patient outcomes: NR Patient satisfaction: NR Access to care: NR Costs: NR Other: low clinician satisfaction with the software |
| Johnson et al. (2006)25 | UK (England) | Observational study | Aim: to explore the views and experiences of patients with type 2 diabetes whose diabetes care had been transferred from the hospital clinic to the patient’s GP Population: patients whose diabetes care had moved to their GP practices in Sheffield Sample size: 12 interviews with patients from four GP practices Interventions: specialist-supported diabetes care services, which encourage collaboration with specialist practitioners from local hospitals to provide GP and practice nurse-led care for people requiring uncomplicated management of type 2 diabetes |
Number of referrals: NR Patient outcomes: NR Patient satisfaction: patients valued the time that could be dedicated by the GP and practice nurses, in comparison with hospital visits. Consultation quality was a key factor in patient satisfaction Access to care: a variety of opinions on comparison of GP with hospital care. GP is more convenient and takes less time, but there is a lack of out-of-hours access and GP reviews are not frequent. Chiropody services are more fragmented Costs: NR |
| Jones et al. (2006)37 | UK (England) | Discussion paper | Aim: to improve access to specialties with long waiting times Population: N/A Sample size: N/A Interventions: GPwSIs |
Number of referrals: the authors report that there is no evidence available, but suggest that establishing new services may uncover previously unmet demand Patient outcomes: the authors report that there is no information available on clinical outcomes for patients seen by GPwSIs compared with comparable patients seen by hospital specialists Patient satisfaction: NR Access to care: NR Costs: the authors highlight set-up costs |
| Julian et al. (2007)87 | UK (England) | Prospective observational study | Aim: to facilitate patient access to diagnostic and therapeutic facilities within secondary care, eliminating the need for a traditional referral Population: a large teaching hospital and GP practices in one PCT Sample size: 193 patients (99 intervention and 94 control) Interventions: the Bridges integrated care pathway involved the use of shared evidence-based guidelines for the management of patients in both primary and secondary care which determined timing for investigations and surgical treatment. Management decisions were made by GPs in all but atypical or complex cases. Compared with a one-stop consultant-led menstrual clinic for women with menstrual disorders |
Number of referrals: significantly fewer hospital outpatient visits in integrated care pathway group than in clinic group. This was due to lower number of visits for an initial consultation (23% vs. 100%; p < 0.001) and reduced follow-up visits (85% in integrated care pathway had no outpatient follow-up, compared with 70% in hospital clinic group; p = 0.006) Patient outcomes: health status was measured at baseline and at 8 months using SF-36 version 2. No statistically significant differences were seen between the groups apart from the role-emotional score, which was higher in the clinic than the integrated care group (although not entirely clear from the paper). There were no significant differences between the two groups for menstrual questionnaire score Patient satisfaction: patient experience was measured using the patient career diary. Significant improvements were seen in integrated care pathway group compared with the clinic group, at point of arrangements made for patient to attend hospital (score 69.2 vs. 64.2; p = 0.095), at time of first outpatient or specialist clinic visit (score 72.9 vs. 67.4; p = 0.007) but not for overall health care (score 68.8 vs. 63.2; p = 0.075) Access to care: At 8-month follow-up there were no significant differences in number of women not receiving treatment, those receiving medical treatment, and those who had undergone or were awaiting surgery (p = 0.789) Costs: NR |
| Kates et al. (2011)103 | Canada | Observational study | Aim: this article reviews the evolution of the Hamilton Family Health Team Mental Health Program and the changes made by practices with key lessons learnt. The programme aims to expand access, increase skills of primary care physicians, smooth care transitions, improve patient experience and clinical outcomes, and use health resources more effectively and efficiently Population: patients treated by family physicians in Ontario Sample size: N/A Interventions: the Family Health Team Mental Health Programme. A shared care model where family physicians or nurses work with part-time specialists to provide treatment. Counsellors work in physician offices, psychiatrists visit the practices, two addiction specialists and three child and youth mental health professionals support the 150 family physicians providing training and support and some direct care as needed |
Based on early quantitative evidence Number of referrals: the Hamilton Family Health Team Mental Health Program has improved access to mental health and addictions care for children (14% of referrals) and adults aged > 65 years (8% of referrals) who may otherwise experience lengthy waiting lists for services Patient outcomes: no clear outcomes were reported Patient satisfaction: the programme has improved patient comfort in seeking and receiving mental health and addictions care from a health location that is more convenient and has fewer stigmas attached Access to care: the programme has improved access to mental health care, particularly for individuals who come from communities that may traditionally underutilise mental health services. This includes ethnocultural groups in which family physicians or practice nurses may speak a person’s language or understand their culture, something that may not happen in standalone mental health clinics. The programme has also resulted in reduced waiting times for an initial assessment Costs: NR |
| Kendrick et al. (2005)104 | UK (England) | RCT | Aim: may save GP time, reduce GP prescribing of psychotropic medication, may reduce referrals to psychiatric outpatient clinics, and increase access to care quickly Population: GP patients attending practices in two southern English counties, aged 18–65 years with a new episode of anxiety, depression or reaction to life difficulties and scoring at least 3 points on the General Health Questionnaire-12 screening tool. Symptoms had to be present for a minimum of 4 weeks but no longer than 6 months Sample size: 247 patients (90 problem-solving CMHN, 79 generic CMHN, 78 control) from 98 GPs in 62 practices Interventions: CMHN care problem-solving therapy, which was a brief structured treatment designed to be given in primary care to help resolve problems, generic CMHN treatment compared usual with GP care |
Number of referrals: NR Patient outcomes: no significant differences were found between the groups at 8 weeks or 26 weeks in symptoms (Clinical Interview Schedule – Revised), social functioning (Social Adjustment Scale), problem severity (Problem Appraisal Scale), or health-related quality of life (EuroQol-5 Dimensions instrument) Patient satisfaction: greater satisfaction with treatment was found in both the CMHN groups than in the GP group Access to care: N/A Costs: a cost–utility analysis showed that CMHN care represented a significant additional health service cost. There were no savings in sickness absence and hence total cost was increased in the CMHN groups, compared with GP care. CMHN care is, therefore, unlikely to be cost-effective compared with GP care |
| Kennedy et al. (2012)165 | UK (Scotland) | Retrospective case review | Aim: to facilitate appropriate and prompt referral Population: patients referred to the Combined Head and Neck Oncology Clinics at Aberdeen Royal Infirmary Sample size: 190 patients Interventions: referral guideline for suspected head and neck cancer, made into an electronic referral system from primary care to the appropriate hospital-based multidisciplinary cancer team |
Number of referrals: only 15 of 190 (8%) of referrals had a confirmed diagnosis of head and neck cancer. During the same period 89 new cases of primary head and neck cancer were diagnosed independently of the online system, through referrals made through other routine non-urgent channels Patient outcomes: NR Patient satisfaction: NR Access to care: NR Costs: NR |
| Kim-Hwang et al. (2010)166 | USA | Before-and-after study | Aim: to improve communication between primary care providers and specialists for more efficient use of specialist services Population: referrals to San Francisco General Hospital Sample size: 505 clinicians Interventions: an electronic referral system that facilitates iterative pre-visit communication between referring and specialty clinicians to improve the referral process |
Number of referrals: NR Patient outcomes: NR Patient satisfaction: NR Access to care: NR Costs: NR Appropriateness of referrals: it was difficult to identify the reason for referral in 19.8% of medical and 38.0% of surgical visits using paper-based methods vs. 11.0% and 9.5% of those using eReferral (p = 0.03; p < 0.001). Of paper methods, 6.4% of medical and 9.8% of surgical referrals were deemed inappropriate vs. 2.6% and 2.1% using eReferral (p = 0.21; p = 0.03). Follow-up was requested for 82.4% of medical and 76.2% of surgical patients with paper-based referrals vs. 90.1% and 58.1% of eReferrals (p = 0.06; p = 0.01). Of those where a follow-up visit was requested, follow-up was considered avoidable for 32.4% of medical and 44.7% of surgical follow-ups with paper-based methods vs. 27.5% and 13.5% with eReferral (0.41 and < 0.001) |
| Knol et al. (2006)123 | The Netherlands | Observational study | Aim: to assess a store-and-forward dermatology service Population: dermatology patients of participating GPs in the province of Friesland, the Netherlands Sample size: 505 teledermatology consultations, 503 patients from 29 GPs Interventions: an overview and two detail digital photographs of the skin problems were taken on a digital camera and attached to an e-mail message containing standard clinical information. These e-mail messages were sent to a dermatologist, who replied by e-mail after evaluation |
Number of referrals: NR Patient satisfaction: NR Access to care: NR Costs: NR Appropriateness of referrals: of 306 patients who GPs would have referred to secondary care, 163 (53.27%, 95% CI 47% to 58%) were not referred owing to the teledermatology. Of the 144 who GPs would not have referred, 24 (16.67%) were referred to secondary care following teledermatology consultation Patient outcomes: NR |
| Kuethe et al. (2011)26 | The Netherlands | RCT | Aim: to test whether or not the provision of care by an asthma nurse can relieve the time pressure on paediatricians or GPs Population: children aged 6–16 years, recruited from a hospital outpatient department and from GPs in the same region, who had moderate asthma and who were treated by continuous use of an inhaled corticosteroid Sample size: 107 patients (45 recruited from GP, 62 recruited from hospital) Interventions: follow-up asthma care provided by a GP, a paediatrician or a hospital-based specialist asthma nurse |
Number of referrals: NR Patient outcomes: no difference between the three groups based on lung function tests, asthma control, medication requirements and number of severe exacerbations Patient satisfaction: NR Access to care: NR Costs: NR |
| Lasierra et al. (2012)124 | Spain | Observational study | Aim: to assess the accuracy of diagnosis made using teledermatology Population: patients accessing dermatology services in the Spanish region of Aragon Sample size: 120 consultations Interventions: provision of teledermatology service, based around a web application |
Number of referrals: NR Patient outcomes: NR Patient satisfaction: NR Access to care: NR Costs: NR Accuracy of diagnosis: high degree of concordance between diagnosis by teledermatology and face-to-face consultation. Total agreement for adult patients was seen in 62% of inflammatory dermatoses, 83% of infections and infestations, 80% of tumours and 100% of other dermatoses. Total agreement for paediatric patients was seen in 76% of inflammatory dermatoses, 75% of infections and infestations, 79% of tumours and 55% of other dermatoses. Teledermatology was able to provide a first reliable diagnosis in 64% of cases. In 42% of cases teledermatology was used to give a first reliable diagnosis and no second visit was required Physician time: the dermatology invested 6 minutes per consultation using teledermatology, compared with 10 minutes per consultation in a face-to-face visit. However, GPs had to spend 19 minutes per teledermatology consultation, whereas they would invest in 10 minutes for a normal dermatology consultation |
| Lau et al. (2010)48 | UK (England) | Retrospective case review | Aim: to assess the appropriateness of shifting care from a sexual health clinic to GP for suppressed herpes Population: patients attending a central London genitourinary medicine clinic in 2007 Sample size: 134 patients Interventions: transfer of patients with successful suppression of recurrent anogenital HSV infection to their GPs. a detailed letter was sent to the GP including information on diagnosis, treatment and rationale for transfer of care. The clinic continued to act as a resource for advice and guidance |
Number of referrals: N/A Patient outcomes: of the 106 patients attending for suppressive therapy, transfer of care was initiated in 69 (65%), all of whom were successfully suppressed Patient satisfaction: 11 of 128 patients did not want to transfer as did not want their GP to know their diagnosis Access to care: NR Costs: NR |
| Lester et al. (2009)181 | UK (England) | Cluster RCT | Aim: to increase detection and referral of first-episode psychosis Population: young people aged 14–30 years with first-episode psychosis referred from practices in three inner-city PCTs in Birmingham to early intervention services with a diagnosis of psychosis over a 3-year period from April 2004 to February 2007 Sample size: 179 referrals (97 intervention and 82 control) from 110 practices Interventions: educational intervention for GPs on first-episode psychosis |
Number of referrals: no difference in number of referrals of young people with first-episode psychosis to early-intervention services between intervention and control practices. Relative risk of referral 1.20 (95% CI 0.74 to 1.95) Patient outcomes: no difference was seen between the groups in terms of health outcomes, measured using a number of scales: the Early Signs Scale, the Insight Scale, the Premorbid Adjustment Scale. No difference was seen between the groups measured using the PANSS at baseline, but a significant difference was seen in total PANSS (difference –11.89; p = 0.04), general PANSS (–6.23; p = 0.03) and negative PANSS (difference –3.79; p = 0.04) but not positive PANSS (difference –1.88; p = 0.16) between intervention and control practices at 4-month follow-up Patient satisfaction: NR Access to care: there was a reduction in delay in reaching early-intervention services in the intervention compared with control group (difference of 222.03 days, 95% CI 83.54 to 360.52 days) Costs: NR |
| Leveille et al. (2009)213 | USA | RCT | Aim: To test the effectiveness of an internet portal-based coaching intervention to promote discussion about chronic conditions between the patient and their primary care physician (PCP) Population: Adult patients (aged ≥ 20 years old) with chronic musculoskeletal pain, mobility difficulty or depression Sample size: 241 patients (121 in the intervention group and 120 in the control group), recruited from the patient list of 57 primary care physicians Intervention: PatientSite is a secure internet portal that enables patients to communicate with their health-care team through electronic messaging and to schedule appointments, request prescriptions and referrals, and review sections of their medical records. For patients to be eligible to access the portal, their physicians must be registered PatientSite users Each intervention group patient received a standardised PatientSite message from a nurse e-coach that provided a brief description of the screened condition(s) and general tips on how to communicate more effectively with one’s PCP. The e-coach note also emphasised that patients’ active participation in the patient–physician relationship may enhance their health-care experience. The message encouraged patients to use a link to the intervention website for additional communication tools and to correspond with the e-coach via PatientSite if they wished Control group patients received a general message through PatientSite containing links to US Government websites with general health information |
Number of referrals: Intervention group patients were more likely to report that their PCP referred them to a specialist (51% vs. 28%; p = 0.002) Patient outcomes: the intervention group patients were more likely to report that their PCP gave them specific advice to improve their health or prevent illness (94% vs. 84%; p = 0.03) On the other hand, control patients reported more medication changes than intervention patients (29% vs. 15%; p = 0.03) Otherwise, intervention and control participants reported similar experiences, including comparably high rates of discussing their screened condition with their PCP The 3-month follow-up survey did not show any significant differences between treatment groups Medical record reviews did not show evidence of differences in diagnosis or management of the screened conditions between treatment groups Patient satisfaction: the intervention patients rated the medical care received in their visit as slightly better than did the control group [9.4 vs. 9.1 on a 0 to 10 scale (where 10 is best), p = 0.07] Access to care: NR Costs: NR Other: no PCP reported that participants seemed more prepared than other patients, and only one PCP reported that the intervention improved patient–PCP communication |
| Levell et al. (2012)38 | UK (England) | Observational study | Aim: to assess the effect of introducing dermatology integrated intermediate care services on the number of dermatology referrals to secondary care Population: those requiring dermatology services in Norfolk Sample size: serves approximately 600,000 people Interventions: introduction of dermatology intermediate care services in April 2005. Involved training and governance supervised by secondary care in accordance with government guidelines |
Number of referrals: 67% increase in the mean number of new patients per year seen in secondary care dermatology in 2008–10, compared with 2004–6. This is compared with a 23% increase in dermatology new patients over the same period in England. These numbers do not include those patients seen in the intermediate care services Patient outcomes: NR Patient satisfaction: NR Access to care: NR Costs: NR Other: following the increase in referrals, three new consultants were recruited at the Norfolk and Norwich University Hospital (NNUH) during 2008–10 |
| Levy et al. (2009)93 | UK (England) | Observational study | Aim: to reduce referrals from primary to secondary care Population: patients at a UK NHS-funded primary-care based allergy service in Harrow PCT Sample size: 151 patients Interventions: referral by GPs to a primary-care based allergy service in north-west London, run by a specialist allergy nurse and GPwSI in respiratory disease and allergy |
Number of referrals: NR Patient outcomes: NR Patient satisfaction: patients rated their satisfaction with the service with an overall median score of 75% (IQR 65.64–82.32%) Access to care: on average, patients waited 15.7 days (SD 16.67 days) from referral to an offer of an appointment and were seen 18.11 days (SD 18.07 days) from the date of referral Costs: estimated saving to the local health economy of £13,580 over 9 months, through reduction in secondary care referrals Appropriateness of referrals: GPs were asked to state on the referral pro forma whether or not they would have referred the patient elsewhere if the clinic did not exist. GPs stated that they would have referred 66% of the patients to secondary/tertiary care. Following assessment, 9% of patients were recommended for onward referral to tertiary allergy specialists by the two clinicians running the clinic |
| Lu et al. (2012)49 | The Netherlands | Modelling (simulation) | Aim: to evaluate the clinical effects and costs of four different strategies for follow-up after breast cancer treatment Population: input population for the model was based on a database of women diagnosed with breast cancer between January 1989 and January 2003 and treated in four hospitals in the north Netherlands Sample size: 5073 patients Interventions: the model compared the current guidelines in the Netherlands with three alternative strategies. Current guidelines recommend hospital follow-up for 5 years with yearly mammography for all, followed by continued hospital follow-up with yearly mammography for those aged 60 years or under, referral to the National Screening Programme for mammography every second year for those women aged over 60 years who have undergone mastectomy, and referral to GP for yearly physical breast examination and mammography every second year for those women aged over 60 years who have undergone breast-conserving therapy. The first alternative strategy involved shortening the time of initial hospital follow-up from 5 to 2 years before movement to the appropriate aftercare; the second alternative strategy involved shortening the time of hospital follow-up from 5 to 2 years and lowering the age of referral to National Screening Programme/GP aftercare from 60 to 50 years; the third alternative strategy involved shortening the time of hospital follow-up from 5 to 2 years and lowering the age of referral to National Screening Programme/GP aftercare from 60 to 50 years and terminating yearly physical examination in general practice |
Number of referrals: NR Patient outcomes: no substantial differences was observed in the number of secondary tumours detected, in the programme sensitivity and in the sensitivity of physical examination or mammography Patient satisfaction: NR Access to care: NR Costs: total screening costs with current guidelines were estimated at €4.3M (95% CI €4.26M to €4.34M). The three alternative strategies were associated with lower mean screening costs: €3.98M (95% CI €3.94M to €4.02M), €3.52M (95% CI €3.48M to €3.56M) and €3.16M (95% CI €3.14M to €3.18M), respectively |
| Lucas et al. (2007)66 | The Netherlands | Observational study | Aim: to determine the validity of the diagnosis and advice when assessed using only written information Population: all patients suspected of an obstructive pulmonary disease referred to an asthma/COPD service in Eindhoven, the Netherlands Sample size: 80 patients Interventions: GPs refer patients suspected for obstructive pulmonary disease to an asthma/COPD service where lung function assistants perform spirometry and collect patient data. These data are assessed by a pulmonologist at a local hospital |
Number of referrals: NR Patient outcomes: NR Patient satisfaction: NR Access to care: NR Costs: NR Accuracy of diagnosis: good concordance in diagnosis between patients in the paper and face-to-face assessments (κ = 0.82). Good concordance in assessment of reversibility (κ = 0.76). Good concordance in diagnostic subcategories ‘normal’ and ‘about normal’ (κ = 0.78). Good concordance in advising for additional tests (κ = 0.65). Poor concordance in assessment of stability of the pulmonary condition (κ = 0.39) |
| Lund et al. (2013)50 | Denmark | Audit | Aim: to report on the transfer of patients from hospital to primary for follow-up consultations Population: patients with prostate cancer Sample size: 2585 patients, including 530 patients transferred to follow-up with a GP Interventions: transferring follow-up of stable prostate cancer patients to GPs in primary care using a treatment plan to keep the patient informed and a discharge template (with patient summary) to be shared with the GP |
Number of referrals: 1 in 5 patients regularly seen for follow-up could be transferred to primary care. The main reasons for not transferring the patients to primary care were patient’s wish and unstable patient’s health status Patient outcomes: NR Patient satisfaction: 99% of transferred patients reported that they were satisfied with the information they received with regard to follow-up process. 69% felt safe ‘to a great extent’ and 27% felt safe to some degree Access to care: NR Costs: NR |
| MacFarlane (2006)126 | Ireland | Observational study | Aim: to explore participants’ views on the educational aspect of joint teleconsultations, and to seek examples of learning that had taken place Population: GPs and specialists taking part in an RCT of teleconsultation in London and Shropshire Sample size: 39 semistructured interviews with GPs and specialists, two focus groups with specialists and six focus groups with GPs Interventions: joint teleconsultations involving specialists, GPs and their patients |
Number of referrals: N/A Patient outcomes: NR Patient satisfaction: NR Access to care: NR Costs: NR Other: the study reported on the educational benefits for GPs of conducting joint teleconsultations with specialists and their patients. Although some learning was reported, GPs and specialists felt that the educational benefit was, overall, disappointing and that more education would be achieved by direct discussion between GP and specialist without the patient present |
| Maddison et al. (2004)84 | UK (Wales) | Before-and-after study | Aim: to review the impact the impact of the targeted early access to musculoskeletal services programme on accessibility to musculoskeletal services. The programme aimed to ensure patients are referred to the appropriate services, to minimise duplicate referrals, to reduce waiting times, and to offer more services locally Population: those referred to musculoskeletal services in north-west Wales NHS Trust from 2001 to 2003 Sample size: unclear, but includes all patients referred to musculoskeletal services (between 300 and 900 patients per month) Interventions: strategies for change included a common pathway for all referrals for musculoskeletal problems, central clinical triage of patients to the appropriate clinical service, a new back pain pathway led by extended-scope physiotherapists and three community-based multidisciplinary clinics run by specially trained GPwSIs and extended-scope physiotherapists |
Number of referrals: the total number of referrals for musculoskeletal problems increased by 116%. The number of orthopaedic referrals slightly reduced Patient outcomes: no change in surgery conversion rate Patient satisfaction: questionnaires showed that 88% of patients rated the service as good or excellent and 75% were completely satisfied with the service provided Access to care: reduction in waiting times reported Costs: NR |
| Mahendran et al. (2005)125 | UK (England) | Observational study | Aim: to investigate the value of store-and-forward teledermatology system in the diagnosis and management of lesions suspicious of skin cancer. To compare the accuracy of diagnosis and appropriateness of management of teledermatology consultations with face-to-face consultations Population: patients with a lesion suspicious of skin cancer who would normally have been referred to the dermatology department Sample size: 163 patients from six practices Interventions: local GPs referred patients using store-and-forward teledermatology, using a pro forma and a photograph. Teledermatology results as assessed by a consultant and a trainee dermatologist (specialist registrar year 3) were compared with a subsequent face-to-face diagnosis made in the outpatient clinic |
Number of referrals: N/A Patient outcomes: NR Patient satisfaction: NR Access to care: NR Costs: NR Appropriateness of diagnosis: there was concordance between teledermatology and face-to-face consultations in 48% of cases. 17% the teledermatology diagnoses included the clinical diagnosis as a possibility. 20% the teledermatology diagnosis were incorrect or could not be made; 15% the digital image was of insufficient quality for assessment. Analysis of the telemedicine management plans indicated that the management plan was appropriate in 55% of the teledermatology referrals (13% required reassurance only and did not need to be seen in a face-to-face consultation; 9% did not need any action but needed a further review appointment by the dermatologist; 33% could have been sent directly for a minor operation). 45% of the teledermatology referrals were not adequately managed (15% had a poor-quality image; 20% needed to be seen in clinic to make a diagnosis or plan best management; 10% would have been inappropriately booked for surgery using teledermatology) |
| Mahmalji et al. (2010)27 | UK (England) | Observational study | Aim: to assess the knowledge, capability and interest of GPs in urology provision Population: GPs in the north-west Thames region Sample size: 75 GPs Interventions: GP management of urological conditions |
Number of referrals: NR Patient outcomes: NR Patient satisfaction: NR Access to care: NR Costs: NR Other: fewer than half of GPs were happy to manage common urological problems: erectile dysfunction 49%, female voiding difficulties 45%, benign prostate hyperplasia 43%, female incontinence 16%, family planning 28%, haematuria 2%. Very few GPs (< 10%) reported that they carry out urological procedures or interpret urological investigations, apart from digital rectal examination, which was performed regularly by 62% of GPs. There was low interest from GPs in furthering their urological knowledge |
| Martin et al. (2011)28 | UK (England) | Observational study | Aim: to assess the impact on hospital costs and mortality of the QOF to UK general practice in 2004 Population: 50 million English citizens Sample size: data cover 50 million patients Interventions: introduction of the QOF to UK general practice in 2004 |
Number of referrals: NR Patient outcomes: across a population of 50 million people, a one-unit increase in the stroke QOF score for 2007–8 would be associated with 2385 ( = 50 m × 0.0000477) fewer deaths in that year Patient satisfaction: NR Access to care: NR Costs: various models are reported. Using the preferred model, the impact of a 1-point increase in the stroke achievement rate will be associated with a fall of £0.33 per person in hospital costs (coefficient of –0.330). With a population of 50 million people, this implies that a 1-point increase in the stroke QOF score is associated with a reduction in annual total hospital costs of £16.5M |
| Maruthachalam et al. (2006)29 | UK (England) | Prospective observational study | Aim: to establish a nurse-led flexible sigmoidoscopy clinic that would provide a patient orientated service in a primary care setting Population: Patients with lower GI symptoms referred to the endoscopy department of Newcastle upon Tyne NHS Trust who were capable of self-administering a home enema Sample size: 1000 patients Interventions: a nurse-led flexible sigmoidoscopy clinic established in a GP practice in Newcastle upon Tyne in order to reduce delays in the diagnosis and treatment of patients with colorectal cancer |
Number of referrals: NR Patient outcomes: NR Patient satisfaction: 99% of patients surveyed (447 of 788 patients who returned the questionnaire) were satisfied with the service provided. Waiting time was reduced in community clinic compared with secondary care Access to care: median time for referral to the community clinic was 35 days, compared with 87 days before establishment of the community clinic. Median time increased through the study owing to the increased number of referrals made to the clinic. For those patients found to have colorectal cancer, the median time from referral to histological diagnosis of colorectal cancer was 26 days, compared with 65 days in secondary care Costs: average cost of performing a flexible sigmoidoscopy in primary care was calculated to be £270, compared with £396 in secondary care |
| Massin et al. (2008)67 | France | Observational study | Aim: to facilitate regular annual funduscopic evaluations of patients with diabetes while saving medical time Population: diabetic patients living in the Ile-de-France area and screened between 1 September 2004 and 31 December 2006 Sample size: 13,777 patients Interventions: regional telemedical network developed, named OPHIDAT. Fundus photographs were taken by technicians in 16 screening centres, then sent to a reference centre where ophthalmologists grade the images. Screening centres can be in primary or secondary care |
Number of referrals: retinal photographs of at least one eye were non-gradable in 9.7% of patients. After screening, 25.2% of patients were referred to an ophthalmologist for diabetic retinopathy, cataract and/or non-gradable photographs Patient outcomes: NR Patient satisfaction: NR Access to care: NR Costs: NR |
| McCrone et al. (2004)151 | UK (England) | Observational study | Aim: to assess service use and costs depending on level of shared care Population: patients attending practices in an inner-London health authority with severe mental illness Sample size: 349 patients from 50 practices Interventions: Shared Care Assessment Schedule used to measure shared care between professionals |
Number of referrals: higher use of psychiatrist services in participants with medium and high levels of shared care, compared with low shared care. Medium shared care OR 3.27 (p = 0.006), high shared care OR 3.92 (p = 0.002) Patient outcomes: the high-shared-care group saw a mean increase in the Comprehensive Psychopathological Rating Scale score of 1.53 above the change for the low-shared-care group (so high shared care less effective, but CIs not reported) Patient satisfaction: NR Access to care: NR Costs: total costs for medium-shared-care group higher than for low-shared-care group (regression coefficient 2606, (90% CI 452 to 4923). No significant difference in total costs between low- and high-shared-care groups. When split down by service, costs were higher in residential care, for medium and high shared care compared with low shared care, social worker costs were higher in medium (but not high) share care compared with low shared care, CMHN costs were higher in high shared care (but not medium shared care) than in low shared care (all comparisons used a 90% CI) |
| Meeuwissen et al. (2008)168 | The Netherlands | Before-and-after study | Aim: to evaluate the implementation of a stepped care programme for depression in primary and secondary care Population: patients in the Zeeuws-Vlaanderen area of the Netherlands who sought care from a general practice or mental health institution for a mild, moderate or severe major depression (according to DSM-IV criteria) January 2000 to June 2002 Sample size: 164 patients and 28 caregivers Interventions: a stepped care programme for depression in primary and secondary care, which aims to initiate interventions at the right time and adequate intensity, with good follow-up care. Consists of a five-step algorithm for the diagnostics and treatment of depression supported by a liaison-consultation function, in which interventions are considered based on the Dutch Multidisciplinary Guideline for Depression and the General Practitioners Standard for Depressive Disorders |
Number of referrals: no change in total number of referrals, but significant decrease in the proportion referrals for depression of all referrals from 26% pre intervention to 21% post intervention (p = 0.02) Patient outcomes: the caregivers were asked in interview about the perceived clinical implications of the programme. They reported that the shared care programme improved appropriate treatment of patients, improved collaborative care and improved quality of care Patient satisfaction: NR Access to care: the caregivers reported shorter waiting times and accessible care for the patient Costs: NR |
| Meeuwsen et al. (2012)51 | The Netherlands | Multicentre RCT | Aim: to examine the effectiveness of post-diagnosis dementia treatment Population: patients with a new diagnosis of mild to moderate dementia living in the community and their informal caregivers. Receiving care in nine memory clinic from 159 GPs in the Netherlands Sample size: 175 patient–caregiver pairs (78 in memory clinic, 75 in GP group) Interventions: usual care provided by memory clinic or GP. Memory clinic provided care based on the specialist Dutch dementia guideline of the Dutch Institute for Healthcare Improvement, whereas the GPs provided care based on the Dutch general practice and homecare dementia guidelines |
Number of referrals: NR Patient outcomes: there was no difference in patient outcomes between the memory clinic group and the GP group on quality of life, behavioural disturbance, activities of daily living or depression. There was no difference in caregiver outcomes between the memory clinic group and the GP group on self-perceived caregiving burden, quality of life, emotional problems or life control. At 12 months, but not at 6 months, there was a statistically significant increase in anxiety and depression scores in the memory clinic group when compared with the GP group. Anxiety trait was 2.1 (95% CI 0.24 to 4.03) points higher, anxiety state was 2.4 (95% CI 0.35 to 4.36) points higher and depression was 2.1 (95% CI 0.15 to 4.02) points higher for the memory clinic group compared with the GP group. At 6 months’ follow-up, but not at 12 months ,there was a statistically significant increase in anxiety state and inventory for measuring social involvement in the memory clinic group compared with the GP group. Anxiety state was 3.6 (95% CI 1.29 to 5.81) points higher and social involvement was –0.8 (95% CI –1.54 to –0.14) points lower for the memory clinic group than for the GP group Patient satisfaction: NR Access to care: NR Costs: NR |
| Melia et al. (2008)169 | UK (England) | Retrospective before-and-after study | Aim: to investigate whether or not there was an increase in the rate of referral of asymptomatic men with a raised PSA Population: data retrieved from pathology laboratories at the main hospital in Chichester, Sutton and Merton, Truro and York on PSA requests between 1 December 2001 and 31 May 2004. Data collected from GP partners on demographic data of the GP partner, membership of the RCGPs and awareness of receiving the PCRMP pack. Data collected from GPS on referrals from 1 December 2001 to 31 May 2002 and 1 December 2003 and 31 May 2004 Sample size: 2494 pre- and 3209 post-PSA requests from 48 practices with 200 GPs Interventions: Prostate Cancer Risk Management Programme was launched in November 2002 and includes guidelines for GPs on the age-specific PSA cut-off levels for urological referral in asymptomatic men |
Number of referrals: there was no significant increase in referrals among asymptomatic men with raised PSA levels before compared with after the launch of the PCRMP (13.7% vs. 18.2%). The most frequent management alternative to referral was retesting Patient outcomes: NR Patient satisfaction: NR Access to care: NR Costs: NR |
| Menon and Larner (2012)167 | UK (England) | Observational study | Aim: to measure the frequency of cognitive screening instrument use reported in referrals from primary care to a dedicated secondary care service. In order to improve dementia awareness, diagnosis and management Population: those referred to the Cognitive Function Clinic in Liverpool, over two periods, October 2004–September 2006 and February 2008–February 2010 Sample size: 231 referrals Interventions: publication of NICE guidance, National Dementia Strategy and Department of Health/Alzheimer’s Society resource pack ‘Understanding dementia. A resource pack for GPs and patients’ |
Number of referrals: total number of referrals increased from 231 (October 2004–September 2006) to 477 (February 2008–February 2010). However, over this period the proportion of these patients receiving a dementia diagnosis fell from 50.6% to 31.2% (χ2 = 24.6; p < 0.001). Much of the increase in referrals came from primary care. Primary care referrals made up 53.2% of referrals in October 2004–September 2006, compared with 64.2% of referrals in February 2008–February 2010. Of primary care referrals the proportion of dementia diagnoses fell from 36.6% to 22.9% (χ2 = 8.36; p < 0.01) Patient outcomes: NR Patient satisfaction: NR Access to care: NR Costs: NR |
| Meran et al. (2011)52 | UK (Wales) | Observational study | Aim: to examine whether or not there was a risk associated with increased discharge to primary care supported by the patient pathway Population: all patients discharged from the renal outpatient clinic of a NHS Trust in South East Wales between June 2007 and July 2008 Sample size: 88 patients Interventions: introduction of a renal patient care pathway |
Number of referrals: initial number of referrals not reported. Of the 88 patients discharged into primary care, six were rereferred back to the nephrology clinic. Three of these patients were rapidly redischarged back to primary care, two remain under nephrology follow-up and one patient is now on dialysis Patient outcomes: of the 88 patients, 70 had no significant decline in eGFR post discharge, 15 had no eGFR measurement post discharge (one of whom died from dilated cardiomyopathy) and three patients had a decline in eGFR > 15% post discharge and were rereferred Patient satisfaction: NR Access to care: NR Costs: NR |
| Minshall and Smith (2008)200 | UK (England) | Audit | Aim: to describe the results of a 2-year reaudit of care patients with epilepsy Population: Patients of all ages, with epilepsy on treatment, in 13 general practices serving Chester and the surrounding area completed the first audit Sample size: 610 patients Interventions: an audit of practice records of patients with epilepsy, followed by education. The audit followed a comprehensive audit template and concluded with individualised categorisation of each patient leading to recommendations for future care. Audit was followed by an educational session led by a neurologist. A second audit was carried out 2 years after the initial audit |
Number of referrals: there were 77 referrals made which related to issues highlighted in the audit Patient outcomes: admissions to A&E fell (43 pre first audit and 19 post audit care; p = 0.0026). There were clear health gains in 62 (13%) individuals from referrals and practice interventions related to the audit. The authors reported that there was little evidence of improved seizure control Patient satisfaction: NR Costs: NR |
| Moffatt et al. (2012)94 | Australia | Observational study | Aim: to explore the perceived benefits of Physician in Practice Clinic, as a measure of the effectiveness of the programme Population: GPs involved in the clinic Sample size: 15 semistructured interviews Interventions: education of the GPs by an endocrinologist conducting patient consultations jointly with the GP at the GP’s rooms. The intervention was implemented in a Division of General Practice. Expectation that would lead to improved patient outcomes in the long-term due to better educated GPs and improved access. It was also thought that would lead to reduced waiting time to specialist care by means of more targeted referrals |
Number of referrals: the GPs interviewed reported making fewer referrals Patient outcomes: NR Patient satisfaction: NR Access to care: NR Costs: NR Other: the GPs reported benefits including educational benefits in the short term such as acquisition of new knowledge, interactive learning and applying new knowledge quickly. In the longer term GPs reported improved relationships with specialist department at hospital |
| Moreno-Ramirez et al. (2005)127 | Spain | Observational study | Aim: to report on the first month of implementation of a teledermatology facility in a pigmented lesion clinic Population: patients with pigmented, circumscribed lesions Sample size: 219 teleconsultations Interventions: GPs in 16 primary care centres took two pictures of lesion and sent them via e-mail, along with clinical information to the pigmented lesion clinic. A report was then submitted to the GP, with suggestion of a diagnosis and management (referral or no referral) |
Number of referrals: 49% of the patients were referred to the face-to-face clinic Patient outcomes: NR Patient satisfaction: 86% of patients said they were very satisfied, and 97% of the GPs were very satisfied Access to care: reports were sent to GPs in a mean time of 44 hours and patients were seen by a dermatologist within 8 days on average Costs: NR Appropriateness of referrals: concordance of decisions was checked between observers (several dermatologists looking at the cases), within observers (the dermatologist seeing the patient face to face after teleconsultation) and between teleconsultation diagnosis and final dermatopathological diagnosis. Agreement within observers was κ = 0.91 (95% CI 0.87 to 0.96), agreement within observers was κ = 0.93 (95% CI 0.93 to 0.96) and accuracy of diagnosis was κ = 0.79 (95% CI 0.70 to 0.89) |
| Moreno-Ramirez et al. (2007)128 | Spain | Evaluation | Aim: to evaluate a store-and-forward teledermatology system aimed at the routine triage of patients with skin cancer Population: patients with circumscribed lesions fulfilling at least one of the following criteria: changes in ABCD criteria (asymmetry, border irregularity, colour variegation, and diameter 6 mm), recent history, multiple melanocytic lesions, symptoms and/or patient’s application for surgical treatment and concern about moles Sample size: 2009 teleconsultations from 12 primary care centres Interventions: store-and-forward teledermatology in which two digital pictures were taken of patients and sent with clinic information by e-mail to clinic. The case was evaluated by a teleconsultation and report with possible diagnosis and management of case returned to GP |
Number of referrals: teleconsultations demonstrated a filtering percentage of 51.20% (95% CI 49.00% to 53.40%) with 980 out of 2009 (48.80%) were referred to face-to-face clinic Patient outcomes: NR Patient satisfaction: NR Access to care: teleconsultation reports were available to the GP in a mean of 61.06 hours (95% CI 33.83 to 88.29 hours). For patients referred to the face-to-face clinic the mean time interval to attendance was 12.31 days for teledermatology vs. 88.62 days for letter referral system (p < 0.001) Accuracy of diagnosis: concordance between intraobserver agreement management decision was κ = 0.91 (95% CI 0.89 to 0.93), management options κ = 0.83 (95% CI 0.78 to 0.88); diagnosis κ = 0.85 (95% CI, 0.79 to 0.91), agreement with gold standard κ = 0.81 (95% CI 0.78 to 0.84) Costs: NR |
| Moreno-Ramirez et al. (2009)129 | Spain | Economic evaluation | Aim: to conduct an economic analysis of a store-and-forward teledermatology system Population: patients with circumscribed lesions fulfilling at least one of the following criteria: changes in ABCD criteria (asymmetry, border irregularity, colour variegation, and diameter 6 mm), recent history, multiple melanocytic lesions, symptoms and/or patient’s application for surgical treatment and concern about moles Sample size: 2009 teleconsultations from 12 primary care centres Interventions: store-and-forward teledermatology in which two digital pictures were taken of patients and sent with clinic information by e-mail to clinic. The case was evaluated by a teleconsultation and report with possible diagnosis and management of case returned to GP |
Number of referrals: NR Patient outcomes: NR Patient satisfaction: NR Access to care: NR Costs: significantly lower unit cost for patients receiving teledermatology than for those receiving conventional care (€79.89 vs. €129.37 per patient; p < 0.005). Incremental cost was €49.59 in favour of teledermatology. The cost ratio between teledermatology and conventional care was 1.6 |
| Morgan et al. (2013)105 | Australia | RCT | Aim: to determine the effectiveness of collaborative care in reducing depression in primary care Population: patients with depression and type 2 diabetes, coronary heart disease or both Sample size: 400 patients (206 intervention and 194 control) Interventions: collaborative care in which a practice nurse acts as a case manager to identify depression, review pathology results, lifestyle risk factors and patient goals and priorities. Patients attend a series of visits to the practice nurse and GP over 3 months for 12-month period. Compared with usual care |
Number of referrals: for patients receiving the intervention there was a significant increase compared with baseline in patients referred to (16%; p < 0.001) and attending an exercise programme (7%; p = 0.041) and referrals to mental health workers (7%; p = 0.022) and visits by mental health workers (17%; p < 0.001) at 6 months with intervention, whereas for the control group only referrals to mental health worker significantly increased over the same time period (12%; p < 0.001). The difference between groups was significant for referrals to an exercise class and mental health worker (p < 0.001) and visits by mental health worker (p = 0.044) Patient outcomes: for patients in the intervention there was a significantly greater reduction in the mean depression scores (for patients with moderate to severe depression) after 6 months than for those in the control, 5.7 (±1.3) vs. 4.3 (±1.2) (p = 0.012). The improvements were maintained at 12 months. Significant decrease in 10-year cardiovascular disease risk from 27.4% (±3.4) to 24.8% (±3.8) (p = 0.015) Patient satisfaction: NR Access to care: NR Costs: NR |
| Morton et al. (2011)130 | UK (Scotland) | Observational study | Aim: to compare the outcomes and costs of conventional and photo-triage referral pathways Population: patients referred for an urgent appointment, where the GP suspected skin cancer Sample size: 477 patients (289 intervention, 188 control) Interventions: store-and-forward teledermatology in which patients were offered the opportunity to attend for screening photographs at one of two community locations close to region’s main population foci. During photography session, up to four high-quality images, including dermatoscopic images, were taken for each patient. Images and electronic referral letter available for consultants to view. Consultant records diagnosis and makes referral to appropriate clinic. Compared with conventional letter referral |
Number of referrals: the photo-triage diverted 72% of referrals away from conventional consultant-led skin cancer clinic Patient outcomes: NR Patient satisfaction: NR Access to care: 91% of photo-triage patients received definitive care at initial visit compared with 63% via conventional pathway. The waiting time was reduced for photo-triage patients for three types of lesions studied Costs: there was reported to be a small cost saving, £1.70 per patient using photo triage, compared with conventional referral Accuracy of diagnosis: photo-triage correctly identified 95% of benign naevi, 93% of seborrhoeic keratosis, 100% angiomas and 83% of acitinic keratoses (although total numbers of all outcomes was very low) |
| Myers et al. (2010)138 | USA | Observational study | Aim: to assess the feasibility and acceptability of a telepsychiatry service Population: children and adolescents Sample size: 701 patients Interventions: Seattle Children’s Hospital telepsychiatry service. After the initial assessment, the telepsychiatrist determined whether the patient would receive a single consultation and return to the referring primary care practitioner with treatment recommendations, additional consultative sessions or ongoing care |
Number of referrals: a total of 190 primary care practitioners referred patients to telepsychiatry, with paediatricians referring to the service more frequently than family physicians (p < 0.05) Patient outcomes: information from previous studies is summarised Patient satisfaction: NR Access to care: NR Costs: NR |
| National Leadership and Innovation Agency for Healthcare (2007)198 | UK (Wales) | Literature review and observational study | Aim: to ensure appropriate referral of patients to relevant services through seven referral management pilot programmes Population: N/A Sample size: N/A Interventions: seven referral management pilot programmes (they were diverse in their scope and operational details) |
The following conclusions were made in this report: ’1) Other LHBs and Trusts which have looked at rolling out RMC activity across the board have concluded that the overhead is disproportionate to the benefit. Their targeted efforts have been successful and it may be they did not have the scale of generic problems inherited by VoG [Vale of Glamorgan] 2) Clinical led triage seems to be one of the most successful methods of diverting cases to more appropriate services and offering greater accountability. Findings from the literature review would also support this view. The principle of accessing flows, directing where marginal (if clinically led), does appear to generate efficiencies if not cost savings 3) There are tensions around using the GPwSI as an alternative service. It appears that unless the GPwSI is trained and supported by consultants in hospitals their development is not encouraged. They are not necessarily a cheaper service; however they may provide a better or timelier service. Of course, the reluctance of consultants to be involved in GPwSI development may just be protectionism, but consultants do have genuine concerns over safety as well as being sceptical about changes which involve them losing control 4) The literature review provided evidence for the view that, in England, PCTs see RMCs at best as a temporary measure. Demand management is best accomplished through market interventions such as Choose and Book and practice-based commissioning (PBC). Wales is not going to introduce Choose and Book or to have PBC so the ‘market’ is not going to produce the changes anticipated in England. We have commented previously on the lack of influence LHBs have in relation to Trusts and this is a major obstacle to service reconfiguration. Whether market led or not, commissioning needs to become more ‘intelligent’ and joined up between primary and secondary sectors so that sound data and independent analysis generate genuine questions about ways to provide the most appropriate service – spotting opportunities for new, more localised services, supporting primary care to do more The present balance of power does not promote this. 5) Whilst not wishing to advocate the ‘free for all’ competition which is emerging in England with the setting up of hybrid assessment and treatment arrangements it has to be acknowledged that incentives and market mechanisms exist there that do not exist in Wales. Whilst these now, emerging, arrangements are as yet unproven, they do demonstrate that, given some incentive, primary care providers can effect change and redirect secondary care activity away from traditional forms of provision’ |
| Nelson et al. (2014)13 | USA | Economic modelling | Aim: to measure the cost-effectiveness of training rural primary care providers to perform knee injections in community-based outpatient clinics Population: use of cost, probability and utility data (modelling only) Sample size: N/A Interventions: trained primary care providers giving injection in outpatient clinics instead of referring patients to specialised care in hospital |
Number of referrals: NR Patient outcomes: from the patient’s perspective, the intervention was cost-effective in the majority of simulations at a willingness-to-pay threshold above US$300/QALY and was cost-effective in 93.6% of the simulations at a threshold of US$50,000/QALY Patient satisfaction: NR Access to care: NR Costs: from the perspective of the payer (the Veterans Affairs), the intervention was cost-effective in the majority of simulations at a willingness-to-pay threshold above US$19,500 per QALY and was cost-effective in 74.4% of the simulations at a threshold of US$50,000 per QALY |
| Newman et al. (2005)30 | USA | Retrospective case review | Aim: to assess competency and safety of family physicians in outpatient office setting, in the context of inadequate number of trained colonoscopists, particularly, in rural areas Population: patients from a rural family practice office who had a colonoscopy Sample size: 731 patients Interventions: each physician attended a formal training course and referral gastroenterologist initially supervised them when performing colonoscopy |
Number of referrals: 29 (4%) of patients were referred, 10 to colorectal surgery and 19 for resection of large polyps Patient outcomes: caecal intubation rates increased significantly from 89.5% to 94.6% following training (χ2 = 6.682; p = 0.008) Patient satisfaction: 281 patients reported a mean satisfaction score of 8.8 (10 max.); 92% patients would have another examination in the family medicine clinic Access to care: NR Costs: NR Accuracy of diagnosis: correlation of findings at referral with initial examination were reported as high |
| Newman et al. (2012)68 | USA | Before-and-after study | Aim: to assess the feasibility of using non-mydriatic digital retinal imaging for retinopathy screening in a busy family medicine residency programme at the point of care using a nurse-driven protocol Population: all adult patients with an established diagnosis of diabetes mellitus, being seen during 2-year study period at academic family medicine centre site Sample size: 1106 patients (659 intervention and 447 control) Interventions: digital retinal imaging for retinopathy screening in family residency programme, used in collaboration with nurse-driven protocol. Nurses were trained in the collection of digital images which were sent for evaluation by a retinal specialist. A standing order was developed that mandated all staff nurses and medical assistants review the electronic medical record of all diabetic patients to check if screening documented. If screening had not been carried out in the past 12 months then patient was referred from digital retinal imaging |
Number of referrals: NR Patient outcomes: patient satisfaction: Limited evidence of satisfaction with imaging at point of care is reported, average score 8.6 (±3.2) out of 10 Access to care: screening rates increased from 161 patients per year to 330 patients per year after implementation of digital retinal imaging. Only 58% of patients referred to the local ophthalmologist following the digital retinal imaging kept and completed appointment Costs: NR |
| Nocon et al. (2004)39 | UK (England) | Observational study | Aim: to evaluate an innovative approach to the provision of primary-care based diabetes services Population: all patients in the Bradford area Sample size: questionnaire sent to 19 specialist clinic providers, 142 GPs outside specialist clinic practices. Interviews with 24 specialists, 8 GPs, 2 practice nurses and 55 patients Interventions: specialist diabetes clinics led by GPwSIs 19 clinics with range of organisational models including clinics run by GPs in own practice, clinics run by a community diabetologist and clinics run by specialist nurses. GPs received training which initially consisted of a 2-day workshop, sessions for GPs to discuss individual cases with consultants and others open to other health-care professionals |
Number of referrals: from April 1998 to September 2001 2451 referrals made to clinics. There was a significant reduction in the mean monthly hospital attendance of 25% from year preceding to 2 years after (p < 0.0001). No significant reduction in numbers of new referrals to or new attendances at hospital. Mean monthly number of attendances in hospital and specialist clinics combined increased by 35% from 1997–8 to 2001 Patient outcome: NR Patient satisfaction: patients reported a range of advantages with the clinics, including improved accessibility and personal care. However, some criticism around quality of care and organisational aspects Access to care: NR Costs: there is little difference in reported costs. In 2000 the average cost per patient attending the specialist clinics was £165 (range £111–239) compared with £194 (with overhead) or £136 (without overheads) for hospital clinic attendance |
| Olah et al. (2005)14 | UK (England) | Observational study | Aim: to test whether the simplicity of thermal ablation and lack of associated major complications makes it suitable for use in primary care settings Population: women referred to the thermal ablation clinic in a peripheral hospital unit run by GPs by gynaecologists from the local hospital and by GPs across South Warwickshire Sample size: 166 patients Interventions: thermal ablation unit was established with two ablation practitioners from primary care. The overall responsibility for the unit, including training was with the consultant gynaecologist. The clinic also involved a radiographer with special interest and a nurse with training in thermal ablation technique was always present |
Number of referrals: of the 166 women referred to the clinic, 87 were treated. No women required admission to hospital following the procedure Patient outcomes: thermal ablation resulted in significant reduction in the number of women having no premenstrual syndrome symptoms, 24% vs. 10% (p < 0.001). Severity of premenstrual syndrome symptoms also reduced with reduction in women having severe symptoms, 9% vs. 35% (p < 0.001). Increased number of women with no dysmenorrhoea following ablation (27% vs. 7%). No major complications experienced. Four women went on to have a hysterectomy within the 2-year follow-up period Patient satisfaction: the majority of women (96%) were satisfied or very satisfied at 1 month after surgery and levels of satisfaction were maintained in the following 2 years Access to care: NR Costs: NR |
| Olayiwola et al. (2011)69 | USA | Observational study | Aim: that telemedicine initiative would help to improve screening rates for an at-risk population of patients compared with conventional referrals for specialist care Population: diabetic patients attending a Community Health Centre in Connecticut, 60% of who are racial/ethnic minorities and > 90% are below the federal poverty line Sample size: 568 patients Interventions: telemedicine diabetic retinopathy screening, in which patients seen by nurse for wider education and self-management and retinal screening by trained camera operator. Images were sent for review by a retina specialist who provided consultation within 48 hours. Imaging was part of broader comprehensive diabetes care approach based on chronic care model |
Number of referrals: 13% of patients required a referral to an eye specialist, the rest were cleared for follow-up 1 year later Patient outcomes: diabetic retinopathy was identified in 25% of patients screened Patient satisfaction: NR Access to care: the proportion of diabetic patients screened increased after the introduction of the programme from 10–12% to 20%. 60% of patients screened were racial/ethnic minorities and 24% were uninsured Costs: preliminary data suggests that the programme saved US$25.00 per patient using telemedicine |
| Oliva et al. (2013)203 | Spain | Before-and-after study | Aim: to improve the resolution of endocrine diseases in primary care using communication and IT to establish a direct communication system between primary and secondary care through which they can provide rapid and effective advice to primary care doctors Population: patients attending primary care subdivision of Baix Llobregat Litoral, in the province of Barcelona Sample size: 1947 virtual consultations Interventions: a virtual referral system between specialised endocrinological care and primary care. The specialist has a datebook in software used by healthcare centres (e-CAP) where the family physician includes the patients who want to consult the endocrinologist without a personal visit. All consultations are answered in the clinical history, where the specialist’s opinion is recorded. If the patient needs assessment in person, the specialist makes an appointment for him/her in their datebook. The primary care doctor then makes another appointment for the patient in the telephone visit section to notify the patient. It was not possible for primary care doctors to make a direct referral without first using the virtual consultation system |
Number of referrals: 88% of virtual consultations were resolved virtually without requiring hospital visit Patient outcomes: NR Patient satisfaction: NR Access to care: NR Costs: NR Appropriateness of referrals: there was a reduction in the proportion of inappropriate first visits referred to specialist, after introduction of virtual consultation, 25% vs. 10% (p < 0.001) |
| Pallan et al. (2005)79 | UK (England) | Retrospective observational study | Aim: to assess the benefits and disadvantages of a radiographer-delivered, primary care-based mobile diagnostic ultrasound service Population: patients who underwent diagnostic ultrasound in a primary care area in the West Midlands Sample size: 373 patients (189 intervention, 184 control) Interventions: independent radiographer-led community diagnostic ultrasound service provided to GPs compared with ultrasound services offered by the local NHS Trust |
Number of referrals: NR Patient outcomes: NR Patient satisfaction: patients were more satisfied with mobile clinic than hospital care, 86% satisfied/very satisfied vs. 76% Access to care: the mean waiting time for an appointment after GP referral was lower for referrals to the mobile clinic than for hospital, 17.44 days (95% CI 15.85 to 19.02 days) vs. 44.53 days (95% CI 38.83 to 50.23 days) Costs: there was a non-significant increase in cost per abnormality detected associated with the mobile clinics, £107.69 (95% CI £90.61 to £132.71) vs. £77.35 (95% CI £63.76 to £98.30) Other: there is some evidence of increased GP satisfaction with community service |
| Patterson et al. (2010)205 | UK (Northern Ireland) | Observational study | Aim: to analyse the effects of an e-mail triage system on waiting times, cost of care and safety over 5 years Population: patients being referred by their GP to the neurological clinic at two rural hospitals, Tyrone County Hospital in Omagh and the Erne Hospital in Enniskillen Sample size: 120,000 people in hospital catchment Interventions: e-mail triage, in which GPs e-mailed neurologist using template. Consultant replied to GP to ask for further information, give advice about diagnosis and management, arrange for GP to undertake further investigations, or arrange a hospital appointment |
Number of referrals: the total number of referrals to consultant (both via e-mail and conventional) increased over 6 years. There was no evidence of increased referrals to conventional neurology as the e-mail system became more widely used Patient outcomes: the majority of patients, around 75%, receiving an e-mail consultation did not attend their GP again with original symptoms Access to care: the waiting time for e-mail neurologist fell from 72 weeks in 2002 to 4 weeks in 2007. Waiting time for conventional referral fell to 13 weeks (in line with NHS target from 2007) Costs: e-mail consultations resulted in a cost saving of £52.56 per patient compared with conventional referral. Cost savings were largely as a result of time savings in secondary care. The cost of GP time input was higher for e-mail referral system, £9.75 vs. £3.70 |
| Phillips et al. (2009)201 | UK (Wales) | Before-and-after study | Aim: to determine the impact of eGFR reporting and the incorporation of CKD in the revised QOF on referral numbers and appropriateness to a nephrology service and the impact of a newly introduced Map of Medicines-based patient care pathway coupled to the systematic screening of all new referrals Population: a single NHS trust in south-east Wales Sample size: 560,000 people in the catchment area of the trust Interventions: the revised QOF in 2006 requires GPs to keep a register of patients with CKD with estimated eGFR below 60 ml/minute/1.73 m. The Map of Medicine is a web-based visual representation of evidence-based patient care journeys introduced in 2007. The renal patient pathway brought together all the guidelines currently available to primary care physicians and the recommendations of the Welsh National Service Framework to provide clear guidelines on referral together with the minimal clinical data required to prioritise outpatient appointments. Additionally, the pathway provided the appropriate support and education to facilitate the discharge of uncomplicated cases back into primary care. GPs and practice nurses received training at launch of pathway |
Number of referrals: there was a rapid increase of 61% in new patient referral following introduction of QOF. The rate of referral was similar between local health boards despite fact that prevalence of CKD varied. Following the introduction of the pathway in the number of inadequate (lack of adequate clinical information in referral letter) and the total number new referrals reduced (data presented graphically) Patient outcomes: NR Patient satisfaction: NR Access to care: the mean number of outpatient visits after the first visit was reduced from 4.1 (±4.4) to 1.5 (±0.8). Number of follow-up patients discharged from clinics increased from 4.6% to 8.4%. The increase in referrals led to an increase in the number of patients waiting to be seen Costs: NR Appropriateness of referrals: following introduction of the pathway the proportion of inappropriate referrals slightly increased |
| Pockney et al. (2004)202 | UK (England and Wales) | Observational study | Aim: to encourage GPs to provide minor surgery services in primary care and therefore reduce referrals to secondary care Population: patients undergoing minor surgery in primary care in England and Wales Sample size: 3,758,320 in 1993 to 3,875,668 in 2000 total population covered by six health authorities Interventions: a fee for service for minor surgery procedures was introduced in the 1990 contract for GPs in England and Wales. GPs could claim up to 60 procedures annually, drawn from a prescribed list, and received £20 per procedure (1990 prices) |
Number of referrals: NR Patient outcomes: NR Patient satisfaction: NR Access to care: the only type of procedure that increased was cautery, from a rate of 8.16 per 1000 population (95% CI 8.07 to 8.25) to 11.34 (95% CI 11.23 to 11.44). Incisions decreased and others remained quite stable over time. Authors conclude that little evidence of transfer of workload from secondary to primary care Costs: NR |
| Power et al. (2007)182 | UK (England) | Cluster randomised trial | Aim: to evaluate the effectiveness of a GP education programme and an early detection assessment team (LEO CAT) in reducing delays in assessing treatment for first-episode psychosis patients Population: all patients aged 16–35 years living in Lambeth and presenting to local mental health services between June 2003 and August 2005 for the first time with first-episode psychosis Sample size: 46 GP practices (23 intervention, 23 control), 150 patients (50 registered with intervention GP, 63 with control GPs, 37 not registered with GP in study) Interventions: a GP education programme provided by LEO CAT on discussing early signs of psychosis. Education provided through video, discussion and leaflets. Follow-up provided on case-by-case basis. Direct access to LEO CAT for new referrals. Compared with standard local mental health services |
Number of referrals: significantly more intervention group GPs referred their patients directly to mental health services, 86.1% vs. 65.7% (p < 0.05). 47.6% of patients in the control group were referred to mental health services from A&E, compared with 12% in the intervention (p < 0.05) Patient outcomes: overall, there was no impact on the duration of untreated psychosis between intervention and control group, 239.9 days (±537) vs. 245.3 days (±526.9) Patient satisfaction: NR Access to care: intervention GPs referred their patients to mental health services on average 12.2 days (median 1 day; ±30.6) after first seen, compared with 78.1 days (median 6 days; ±26.8) in controls. Intervention patients were assessed by mental health services on average 14.0 days (median 7 days; ±26.8) after the referral, compared with 31.2 days (median 7 days; ±53.5). Intervention patients started medication on average 53.1 days (median 36 days; ±79.5) after first seeing their GP, compared with 114.1 days (median 37 days; ±264.1) for control Costs: NR |
| Ridsdale et al. (2008)40 | UK (England) | Observational study | Aim: to describe the training of GPwSIs in headache and the setting up of a GPwSI clinic in general practice Population: patients with a headache who had attended a specialist or GPwSI clinic in inner London Sample size: 211 patients (61 intervention and 56 control) Interventions: training of GPwSIs to run a headache clinic. Training consisted of 6 half-days of teaching involving 12 sessions of clinics with neurologist, 12 sessions of clinic with a second doctor interested in headache and 6 sessions of clinics with other neurologists in locality. For clinics GPs worked one session on alternate weeks providing specialist clinics. Compared with hospital neurology service |
Number of referrals: NR Patient outcomes: there was no significant difference in headache impact between GPwSI clinic and hospital attendees, mean score 64.3 (±93) vs. 61.2 (±10.4), or the frequency of severe headache pain (adjusted OR 10.5, 95% CI 0.47 to 2.32) or in how often headaches limited daily activities (adjusted OR 1.57, 95% CI 0.72 to 3.41) Patient satisfaction: patients attending GPwSI clinic reported significantly higher satisfaction scores than those attending hospital, 64.2 (±6.2) vs. 60.2 (±7.6). GP clinic attenders were more likely to agree with the statement that it was the kind of service they wanted, 97% vs. 80%, adjusted OR 3.5 (95% CI 1.4 to 8.8) Access to care: NR Cost: the GPwSI clinic costs were lower than hospital costs for both first attendance £136 vs. £203 and follow-up £68 vs. £121 |
| Ryan et al. (2010)85 | UK (Wales) | Before-and-after study | Aim: to determine whether or not the primary care-based Welsh Low Vision Service improve access to low-vision rehabilitation services and whether or not it was effective Population: all potential providers of low-vision services in Wales Sample size: before 5692 appointments (5472 provided by secondary care, 22 primary care) and after 8636 (4704 in secondary care, 3932 primary care) Interventions: Provision of low-vision service (Welsh Low Vision Service) in community through accredited low-vision practitioners. Practitioners provided with a low-vision aid kit and used standard reporting tools to be recorded centrally. This service existed alongside secondary care service but was funded through government primary care budget |
Number of referrals: NR Patient outcomes: there was a significant reduction in visual disability of 0.79 logits (p < 0.001) Patient satisfaction: of patient who had been prescribed magnifiers, 98% found the service helpful Access to care: low-vision services provided by an additional 127 optometry practices following implementation of programme. Number of NHS funded low-vision appointments increased by 51.7% with increase in primary care settings. The proportion of patients seen for an initial low-vision assessment within 2 months increased from 11% before Welsh Low Vision Service introduced to over 70% for those attending the primary care Welsh Low Vision Service (and 60% elsewhere). The modal response category for waiting times for a low-vision assessment in primary care remained the same in both periods, for secondary care it reduced from 6–12 months to 2 weeks-2 months Cost: NR |
| Salisbury et al. (2005)41 | UK (England) | RCT | Aim: to assess the effectiveness, accessibility and acceptability of a GPwSI for skin problems Population: adults referred to a hospital dermatology clinic, with non-urgent skin problems Sample size: 556 patients (354 intervention, 202 control) Interventions: patients with skin problems are referred by GP to outpatient dermatology clinic as usual. Suitability for management in the GPwSI service was assessed on basis of referral letter. Suitable patients would see and be followed up by GPwSI or specialist nurse, or referred to hospital outpatient care |
Number of referrals: NR Patient outcomes: there was no significant difference in the disease-related quality of life between services Patient satisfaction: overall patient satisfaction was significantly higher for patients who attended the GPwSI service than those who attended the hospital service, 71.05 vs. 65.93 (p = 0.01). Patients reported that the GPwSI was more accessible, mean access score 76.1 vs. 60.5 (p < 0.001) Access to care: the mean waiting time between referral letter being received and first appointment was significantly shorter for GPwSI service, 72 days vs. 113 days (mean difference 40, 35 to 46; p < 0.001). The proportion patients followed up for first-appointment was greater for GPwSI service, 59% vs. 44% Cost: NR |
| Scalvini et al. (2011)206 | Italy | Observational study | Aim: to evaluate the feasibility of a second-opinion consultation in supporting GPs during the daily diagnosis and therapeutic management of patients with hypertension Population: symptomatic (teleconsultation for symptoms) and asymptomatic (teleconsultation for control) hypertensive patients attending their GP Sample size: 1719 patients from 399 practices Interventions: telemedicine. GPs recorded and transferred, either by mobile or fixed line, an ECG tracing to specialist for cardiological second opinion. GPs also reported to the specialist on patient’s blood pressure values, medical history and other information. Specialists available 24 hours per day, 365 days per year could advise on diagnosis and therapeutic treatment |
Number of referrals: for patients attending a routine visit, suggested referral to A&E in 0.4% of cases, compared with 16.0% of patients with symptoms Patient outcomes: NR Patient satisfaction: NR Access to care: the second opinion provided through teleconsultation quickened and helped GPs in presenting a possible solution in about 50% of cases. Comparing teleconsultation for symptoms and control, therapeutic intervention (33.3% vs. 23.4%) and need for new examination (19.6% vs. 8.6%) were significantly higher in patients referred for symptoms (p < 0.05 for both). The length of the teleconsultation was on average 8.83 (±6.47) minutes per patient Cost: NR |
| Shariff et al. (2010)183 | UK (England) | Before-and-after study | Aim: to quantify the effect of a targeted continuing medical education module on improving diagnostic accuracy Population: all referrals for dermatology and plastic surgery under the 2-week wait rule to Castle Hill Hospital, Hull, between July and September 2006 and August and October 2007 Sample size: 237 patients before intervention, 233 patients after Interventions: GPs in area covered by the teaching hospital were sent a 12-page illustrated guide to common skin lesions positively highlighting common diagnostic pitfalls in the diagnosis of cutaneous melanoma and squamous cell carcinomas |
Number of referrals: there was no difference in the number of specialist referrals made in under 24 hours (94.5% vs. 94.2%) or delayed referrals (13% vs. 13%) after implementation of the intervention Patient outcomes: NR Patient satisfaction: NR Access to care: the number of specialist appointments made within 14 days did not change (90.7% vs. 90.5%), nor did the number of patients receiving their first treatment within 62-day target (97.9% vs. 97.8%) Costs: NR Diagnostic accuracy: there was no overall change in the accuracy of diagnosis after implementation of the intervention (23.5% vs. 21.2%) |
| Sibbald et al. (2008)42 | UK (England) | Observational study | Aim: to evaluate the likely impact on patients and local health economies of shifting specialist care from hospitals to the community Population: service providers at 30 community sites in England Sample size: interviews with service managers at the 30 sites, plus 58 interviews with commissioners, GPs and hospital doctors at 12 sites; economic case studies in six sites; and 1058 patients surveyed at the 30 sites and 9 conventional outpatient services Interventions: ‘Closer to Home’ services which use specially trained community staff such as GPwSIs, nurses and other practitioners with special interests to increase the provision of diagnostic and treatment facilities in community sites |
Number of referrals: service providers considered that the service had resulted in a reduction in referrals to secondary care, although noted that the closer-to-home service is potentially seeing only the less complex cases Patient outcomes Patient satisfaction: the patient survey reported higher overall satisfaction than for outpatient care: 88.2 vs. 85.4 (p = 0.04) Access to care: patients reported shorter waiting times to attend demonstration services (6.7 vs. 10.1 weeks; p = 0.001); higher technical quality of care (96.2 vs. 94.5; p < 0.001); and better access (72.2 vs. 65.8; p = 0.001) than for conventional services, but there was no significant difference in co-ordination or interpersonal quality of care Costs: the authors stated that the services would cost less (from the commissioner perspective) than they would have cost under the national tariff prices if they had been provided in hospitals. This was largely because the new services saw patients with less complex conditions, which meant that new services undercut the price tariff applied to hospitals, thus providing a cost saving to commissioners. There was some concern that expansion of new services might destabilise hospitals. The authors concluded that moving specialist care into the community can improve patient access, particularly when new services are added to existing hospital services Other: some service providers expressed concerns about service quality |
| Simpson et al. (2010)70 | UK (Scotland) | Retrospective case review | Aim: to assess the significance of pathology, impact of the service and GP satisfaction for GPs who have direct access to CT Population: all patients, and their GPs, who had been referred from primary care for direct access CT in Greater Glasgow from February 1999 to March 2007 with chronic headaches for longer than 3 months Sample size: 4404 CT scans Intervention: a service which gives GPs direct access to CT |
Number of referrals: the direct access to CT service resulted in an 80% reduction in initial referrals to neurology and a 94% reduction in initial referrals to general medicine. Of patients screened, 86% did not require specialist referral; 47% of GPs surveyed indicated that direct access CT would be their preferred choice of referral for investigation of patients with chronic headache Patient outcomes: of the scans, 10.5% were found to be abnormal. There were no false negatives but two false positives (0.05%) Patient satisfaction: NR Access to care: 98% of reports were received by GP within 1 week of the patient’s CT scan Costs: the direct-access CT service resulted in a cost saving of approximately £86,681.81 |
| Skipsey et al. (2012)71 | UK (Scotland) | Prospective audit | Aim: to describe the clinical outcomes from a novel direct-access arrhythmia monitoring service Population: patients considered to be at low risk of arrhythmia in the north of Scotland from 18 June 2008 to 8 November 2010 Sample size: a total of 289 patients from 47 GP practices (165 intervention, 72 control) Interventions: GPs were offered direct access to an arrhythmia monitoring service. Compared with patients initially referred by GP to consultant and then redirected by consultant to monitoring service as appropriate |
Number of referrals: a total of 96.2% (230) patients were returned directly to be managed by requesting GP Patient outcomes: there was no systematic difference in the patients referred via either route (p = 0.14) Patient satisfaction: NR Access to care: the median waiting time was 84 days (range 0–285 days) Costs: NR Appropriateness of referral: the request for monitoring was deemed appropriate in 78.7% of cases, while 17.2% were considered inappropriate |
| Slade et al. (2008)170 | UK (England) | RCT | Aim: to see whether or not a standardised assessment, Threshold Assessment Grid, of the severity of mental health condition could improve agreement between primary care and CMHT on suitability of referral to a specialised mental health service Population: all GP practices that provided care for residents in the study catchment areas: one London borough and three areas in Manchester Sample size: 73 GP practices (36 intervention and 37 control) Interventions: GPs completed a standardised referral form, Threshold Assessment Grid, to assess the severity of mental health problems, which was sent with usual referral request to specialist mental health services. Compared with usual referral process |
Number of referrals: a total of 517 patients in intervention practices and 544 in control practices were referred to the CMHT Patient outcomes: NR Patient satisfaction: NR Access to care: NR Costs: in the Croydon study site, patients in in intervention practices had significantly higher contact with primary care use post referral (incidence rate ratio 1.36, 95% CI 1.08 to 1.70; p = 0.008), which resulted in an extra cost of £42 per annum, extrapolated over 1 year Appropriateness of referrals: no difference in the appropriateness of referrals made by GPs in intervention and control practices, 64% vs. 60% (OR 1.18, 95% CI 0.91 to 1.53). There was no significant difference in the ease of identifying urgency of referral, 81% vs. 76% (p = 0.22), or in the ease of identifying appropriate profession for assessment, 89% vs. 87% (p = 0.65) |
| Smith et al. (2009)152 | Multiple | Systematic review | Aim: to evaluate the effectiveness of shared-care health service interventions designed to improve the management of chronic disease across the primary–specialty care interface Population: studies included participants with a range of chronic disease including asthma, COPD, cancer, congestive cardiac failure, depression, diabetes mellitus, hypertension, opiate misuse and chronic mental illness Sample size: 20 studies Interventions: the majority of the included studies involved a multifaceted shared-care intervention. Shared care is the joint participation of GPs and specialists in the planned delivery of care, informed by an enhanced information exchange over and above routine discharge and referral notice |
Number of referrals: data from seven studies suggested that the effect of shared care on hospital admissions was mixed, with shared care being associated with a reduction in hospital admissions in older patients and in those with higher levels of baseline morbidity Patient outcomes: of seven RCTs, only one found a statistically significant benefit of shared care on physical health outcomes. The results were mixed for mental health outcomes (eight studies) Patient satisfaction: four studies reported no significant differences between shared care and control groups in mean treatment satisfaction scores; five additional studies reported the proportions of patients either moderately or very satisfied with care or rating care as ‘very good to excellent’ Access to care: nine studies reported measures of service utilisation and three of these indicated significantly increased disease-related visits in the shared-care group Costs: the authors stated that cost data were limited and difficult to interpret |
| Spatafora et al. (2005)171 | Italy | Prospective observational study | Aim: to assess whether or not adopting a shared protocol between urologists and GPs might change diagnostic procedures and referral patterns in the management of men with lower urinary tract symptoms Population: men aged ≥ 50 years in general good health presenting to GPs who used the participating urological centre with a history of lower urinary tract symptoms of more than 2 months, between October 2000 and December 2002 Sample size: 45 urology centres; 263 GPs; 1759 patients (903 before and 856 after) Interventions: urologists developed a diagnostic algorithm to aid GPs in making a diagnostic decision |
Number of referrals: implementation of the protocol did not change referral patterns. Both before and after implementation of the protocol 51.2% of patients were managed entirely by the GP and 44.3% were referred to the urologist after some diagnostic procedures and the remainder (4.5% before and 4.6% in after) were referred before starting a diagnostic evaluation Patient outcomes: NR Patient satisfaction: NR Access to care: the use of a digital rectal examination by GPs increased from 32% to 41%, the use of transrectal and suprapubic ultrasonography decreased from 33% to 23% and 53% to 44%, respectively, (all p < 0.001) and use of the International Prostate Symptom Score increased from 4.5% to 23.1% (p < 0.001) Costs: the direct costs per patient incurred in before compared with after were €71.82 vs. €61.93 |
| Srirangalingam et al. (2006)203 | UK (England) | Before-and-after study | Aim: to determine the impact of the new General Medical Services contract on referral patterns to a secondary care diabetes clinic Population: patients referred to consultant-led diabetes clinic in Tower Hamlets, London, with type 1 diabetes Sample size: 328 referrals pre contact, 319 post contact Interventions: the QOF of the new General Medical Services provides financial reward for achieving diabetes-related quality indicators |
Number of referrals: there was no significant change in referrals in the 6 months after implementation of the General Medical Services contract. There was an increase in referrals for poor glycaemic control after implementation (54% vs. 77%; p = 0.001) and the glycaemic threshold for referral with poor glycaemic control was reduced (9.7% vs. 10.6%; p = 0.006; mean difference = 0.9%, 95% CI 0.4% to 1.3%) Patient outcomes: NR Patient satisfaction: NR Access to care: NR Costs: NR |
| Starren et al. (2012)80 | UK (England) | Audit | Aim: to review the service provided by the CRAU to primary care health professionals Population: GP referrals Sample size: 1156 patients Interventions: the CRAU was established to provide diagnostic support to GPs. The CRAU is a nurse-led facility and access to a respiratory specialist was always available. All local GPs had access to the service. It provided focused history-taking, quality-assured spirometry and evidence-based guideline-derived management advice |
Number of referrals: from 1156 referrals, 666 were referred for one of five common reasons: suspected asthma, confirmed asthma, suspected COPD, confirmed COPD or unexplained breathlessness. COPD was the most prevalent referral indication (445/666, 66.8%). Half of the first appointment referrals (430/878) would have been referred to a respiratory specialist if the services of the CRAU were not available. The authors stated that this would suggest that GPs are looking for support to help them to obtain accurate respiratory diagnoses in a significant proportion of cases, and it suggests that the CRAU was recognised as a suitable alternative to secondary care in these cases Patient outcomes: NR Patient satisfaction: NR Costs: NR Accuracy of diagnosis: one-third of suggested diagnoses of COPD by the GP were found to be incorrect (161/445, 36%) with inappropriate prescribing of inhaled therapies resulting from this misdiagnosis |
| Stoves et al. (2010)207 | UK (England) | Before-and-after study | Aim: to compare nephrology referrals following the introduction of electronic consultations (e-consultations) for CKD Population: patients with mild to moderate CKD in primary care Sample size: 85 practices (17 intervention and 68 control) Interventions: the service allowed GPs to send electronic referrals and share patient electronic health records with a renal specialist to request advice. Specialist reviews the electronic record and records their clinical decision. GPs received training about the new service |
Number of referrals: there was a significant reduction in paper referrals from implementation practices Patient outcomes: NR Patient satisfaction: NR Access to care: waiting times between referral and consultation were considerably reduced for e-consultations, mean number of days 7 (±0.8) vs. 55.1 (±1.6). The mean (SE) time to perform an e-consultation was 15.5 (0.4) minutes. E-consultations provided the renal specialist with access to more clinical information. Recommendations made by e-consultation were adhered to in 82% of cases for additional tests, 97% for treatment change and 89% for monitoring schedule Costs: NR Appropriateness of referral: of GPs requesting referral by letter only 56% were appropriate (71% in implementation practices and 52% control practices) but 98% of referrals requested were approved for review by the hospital clinic. 90% of e-consultations who questioned need for clinic review were deemed appropriate and 27% were sent for assessment Other: e-consultation provided nephrologists with access to more clinical information. GPs reported that the service was convenient, provided timely and helpful advice, and avoided outpatient referrals. Specialist recommendations were well followed, and GPs felt more confident about managing CKD in the community |
| Summerhayes et al. (2012)131 | UK (England) | Before-and-after study | Aims: to evaluate the impact of introducing a telemedicine system on conventional leg ulcer care in a rural general practice Population: all patients presenting with a non-healing wound on their lower leg of at least 1 month’s duration in a semirural general practice between December 2006 and December 2007 Sample size: 54 patients (29 before and 25 after) Interventions: digital images of ulcer is imported into the leg ulcer telemedicine by GPs and along with care records is sent to a specialist for consultation; the system is also used to map treatment plans and healing rates |
Number of referrals: the number of secondary care appointments increased from 27 to 31 Patient outcomes: the median time for the healing for leg ulcers was reduced from 105 to 70 days Patient satisfaction: NR Access to care: GP input fell from 83% to 24% of patients and secondary care involvement rose from 45% to 60% of patients. The number of primary care appointments fell from 751 to 472 and the mean time from referral to a secondary care appointment fell from 47 to 18 days Costs: after the introduction of leg ulcer telemedicine, patient travel cost fell from £68 to £49 per patient. Primary care cost remained unchanged, £357.46 per patient to £353.52 per patient, while secondary care cost increased from £226 to £263 per patient and the procedure cost remained the same. The total cost per patient slightly increased from £651.41 to £665.27 |
| Suris et al. (2007)184 | Spain | Before-and-after study | Aim: to analyse the influence of a primary care rheumatology consultancy programme on referrals to a rheumatology unit Population: GPs and rheumatologists in 15 health-care areas, covering a population of over 360,000 Sample size: four rheumatologists delivered the training, and 117 GPs attended Interventions: rheumatologists delivered 120 training sessions over 1 year, discussing cases of musculoskeletal disorders and approaches to case management |
Number of referrals: at the end of the pilot year, the number of GP referrals was 31% lower than the previous year. The number of new visits in the rheumatology unit increased slightly during the program (3.34% increase compared with the previous year). The referral rate to the rheumatology unit decreased significantly from 8.13 per 1000 (1652 out of 203,206) to 5.53 per 1000 (1141 out of 206,285), a difference of 2.59% (95% CI 2.09% to 3.10%; p < 0.0001) Patient outcomes: NR Patient satisfaction: NR Access to care: the waiting time to be seen by a rheumatologist dropped by a mean of 15 days per person per month (95% CI 119.7 to 9.2 days per person per month) over the whole period of study. Similar findings were observed for the number of people waiting to see a rheumatologist which decreased by a rate of 61 persons per month (95% CI –113 to –5 persons per month) Costs: NR Other: GP satisfaction with regard to rheumatology referrals and services increased significantly (p < 0.0001) |
| Sved Williams et al. (2006)208 | Australia | Observational study | Aims: to evaluate outcomes and satisfaction with a consultation-liaison service to GPs, provided by a cohort of private and public psychiatrists Population: all psychiatrists in southern Australia Sample size: 27 psychiatrists and 77 GPs Interventions: psychiatrists made themselves available approximately 1 day per month to participate in a roster and be on call to answer telephone calls from GPs and to provide them with advice within 24 hours. In addition, when GP, patient and psychiatrist agreed on this pathway, participant psychiatrists were prepared to see patients for one-off face-to-face assessments within 14 days, with feedback to the GP in a short time frame, preferably by an immediate telephone call, with written feedback within 14 days |
Number of referrals: although no data were reported by the study authors, GPs noted a reduction in the need to refer patients on to further management Patient outcomes: NR Patient satisfaction: NR Access to care: the mean call-back time was 1.7 hours. The average reported time for telephone calls from psychiatrist to GP as recorded by the psychiatrists was 11.1 minutes Costs: NR Other: common issues on which advice was sought were psychopharmacology, the treatment of depression, particularly resistant depression, diagnostic issues and suicidality. Ninety-five per cent of GPs found the advice that was provided be helpful, with 100% of calls being returned within the 24 hours promised time frame. Of the GPs, 59% noted improved knowledge about mental health, 27% reported increased knowledge of mental health services and 64% noted increased confidence in managing patients with mental health problems |
| Tadros et al. (2009)132 | UK (Scotland) | Prospective observational analysis | Aim: to assess the use of a digital image referral service where GP’s send digital images of skin lesions to a plastic surgery department Population: all referrals for suspected skin cancers as well as non-malignant symptomatic skin lesions to Ninewells Hospital, Dundee Sample size: 300 patients Interventions: GPs used an existing electronic referral service to send digital images relevant medical history and current medication to the plastic surgery department. The consultant on call was responsible for screening and vetting the referrals received. All electronic referrals should be assessed in 24 hours |
Number of referrals: NR Patient outcomes: NR Patient satisfaction: all patients were happy to have photographs taken in GP surgery and sent electronically to the hospital. None of the patients was unhappy about the overall treatment Access to care: digital image referral for skin malignancy and other cutaneous lesions reduced the interval between referral and diagnosis by 81% and referral to commencement of treatment in suspect lesions by 30% Costs: NR Accuracy of diagnosis: the mean overall correct diagnosis between the four consultants was 83.25%; 90.25% of malignant lesion and 76.58% of benign lesions were correctly identified by the four clinicians Other: 88% of GPs felt that the feedback received from the plastic surgeons following electronic referral had been educationally valuable and 84% of GPs thought that it had enhanced the patient journey |
| Tan et al. (2010)133 | New Zealand | Observational study | Aim: to assess teledermoscopy as a triage tool for a hospital skin lesion clinic Population: patients who had been referred by their GP to a hospital specialist skin lesion clinic for diagnosis and management of one or more skin lesions Sample size: 200 patients Interventions: a store-and-forward teledermatology which involves taking photo images or video files and sending them to a consultant dermatologist who provided a diagnosis and management advice. The same patients were seen in face-to-face consultations and outcomes were compared |
Number of referrals: N/A Patient outcomes: NR Patient satisfaction: NR Access to care: NR Costs: NR Appropriateness of diagnosis: of referrals to clinic, 74% could have been managed by the GP following advice from the teledermoscopist Accuracy of diagnosis: concordance between face-to-face diagnosis and teledermoscopy was 74% for both dermatologists. Kappa value for concordance was 0.95 (95% CI 0.91 to 0.98) for dermatologist A and 0.95 (95% CI 0.91 to 0.99) for dermatologist B. Only 12.3% of lesions had disparate diagnoses of clinical significance when teledermoscopy and face-to-face diagnosis were compared. Twelve of 491 (2.4%) lesions appeared to have been under-reported by teledermoscopy when compared with face-to-face diagnosis. When histopathology became available, one malignant lesion had been missed (a basal cell carcinoma diagnosed as solar keratosis) by teledermoscopy. Concordance between dermatologists using teledermoscopy was 72.3%, while for face-to-face consultations concordance ranged from 75.5% to 82.2%. Kappa values for interobserver agreement were > 0.90 |
| Taylor et al. (2012)72 | UK (England) | Retrospective case review | Aim: to compare a primary-care imaging pathway for neurology outpatients with traditional outpatient referral Population: patients referred for a MRI scan for investigation of headaches Sample size: 200 patients (100 intervention and 100 control) Interventions: guidelines were generated providing specific pathways for diagnosis and treatment of common causes of headache, highlighting ‘red flag’ features indicating urgent referral to neurology secondary care, and selecting those patients with chronic headache resistant to medical treatment who could be referred directly for MRI by their GPs. Compared with usual neurology referral |
Number of referrals: in the GP cohort, there was an onward outpatient clinic referral rate of 17%; 8% of these referrals were following advice from the reporting radiologist. Of the remaining 9%, two were referrals to ENT clinics for possible sinus disease described on MRI and seven were referrals to general neurology or headache clinics. In addition, one patient had simultaneous referral for GP-access MRI and outpatient referral Patient outcomes: no statistically significant difference in rates of major abnormalities, incidental findings or ischaemic lesions was identified between the two cohorts Patient satisfaction: NR Access to care: 91% of patients waited < 4 weeks from GP appointment to MRI examination, with 53% waiting < 2 weeks Costs: NR Other: of the GP patients surveyed, 86% agreed or strongly agreed that the referral process was smooth and uncomplicated |
| Ten Cate-Hoek et al. (2009)73 | The Netherlands | Cost-effectiveness analysis | Aim: to assess the incremental cost-effectiveness of a diagnostic strategy for DVT used by the AMUSE study Population: patients presenting to primary care with complaints suspected of being DVT Sample size: 1002 patients Interventions: a score was calculated for each patient with suspected DVT using a clinical decision rule and a rapid point-of-care D-dimer assay. Patients with a score of ≥ 4 were referred for ultrasound. Compared with hospital-based strategies |
Number of referrals: NR Patient outcomes: NR Patient satisfaction: NR Access to care: NR Costs: adherence to the AMUSE strategy on average resulted in savings of €138 per patient at the expense of a very small health loss (0.002 QALYs) compared with the best hospital strategy. The incremental cost-effectiveness ratio was €55,753. The cost-effectiveness acceptability curves showed that the AMUSE strategy had the highest probability of being cost-effective. Results are sensitive to decreases in sensitivity of the diagnostic strategy, but are not sensitive to increase in age (range 30–80 years), the costs for health states, and events |
| Thind et al. (2011)134 | UK (Scotland) | Audit | Aim: to assess the feasibility of a teledermatology service to provide remote supervision to a trainee GPwSI in order to reduce face-to-face consultations with a consultant dermatologist and to provide appropriate diagnosis and care Population: patients referred from primary to secondary care with a request for diagnosis of a photographable lesion or eruption, in a community hospital Sample size: 230 patients; 50 were given a satisfaction questionnaire Interventions: patients were seen by a GPwSI in dermatology for diagnosis and treatment. A digital image, current history, clinical details and the GPwSI assessment and management plan were forwarded for review to a consultant dermatologist |
Number of referrals: 31% of patients had a face-to-face consultation with the consultant following teledermatology consultation Patient outcomes: NR Patient satisfaction: 90% of patients were ‘very’ or ‘completely’ satisfied. Similar percentages of patients preferred to see a dermatologist or a GPwSI (42% for both; 16% had no preference) Access to care: the waiting time for a clinic appointment was shorter, with an average of 3 months to see the GPwSI. More time per patient was spent for teledermatology consultations than in conventional face-to-face consultations Costs: the time saved in medical staff travelling time was 4 hours per month, but any saving in consultant travel was offset by the additional GPwSI resources used Accuracy of diagnosis: there was concordance in diagnosis between the GPwSI and consultant in 60% of cases (95% CI 53% to 67%). For 21% of cases there was a disagreement and in the remaining 19% of cases it was not possible to assess agreement. It was reported in the discussion that there were some conditions for which teledermatology worked well; however, for skin cancer teledermatology was less accurate than face-to-face consultations Other: it was reported that educational feedback and supervision are easily incorporated into teledermatology consultations. The GP felt supported with a consequent increase in confidence to a point where teledermatology was not required in every case |
| Thomas et al. (2005)86 | UK (England) | RCT | Aim: to compare the efficacy of treatment options for persistent lower-back pain Population: patients aged 18–65 years with persistent non-specific low-back pain assessed as suitable for primary care management by their GP Sample size: 241 patients (159 intervention, 80 control), from 39 GPs in 16 practices Interventions: patients were allowed up to 10 acupuncture treatment;, content and frequency was determined by the acupuncturist. Compared with usual care from GP, which commonly consisted of a mixture of physiotherapy, medication and recommended back exercises |
Number of referrals: NR Patient outcomes: analysis of covariance, adjusting for baseline score, found an intervention effect of 5.6 points on the SF-36 pain dimension (95% CI –1.3 to 12.5) in favour of the acupuncture group at 12 months, and 8 points (95% CI 0.7 to 15.3) at 24 months. Patients receiving acupuncture care reported a significantly greater reduction in worry about their back pain at 12 and 24 months, compared with the usual care group. At 24 months, the acupuncture care group was significantly more likely to report 12 months pain free and less likely to report the use of medication for pain relief Patient satisfaction: NR Access to care: NR Costs: the acupuncture service was found to be cost-effective at 24 months. The estimated cost per QALY was £4241 (95% CI £191 to £28,026) using the SF-6D scoring algorithm based on responses to the SF-36, and £3598 (95% CI £189 to £22,035) using the European Quality of Life-5 Dimensions health status instrument. The NHS costs were greater in the acupuncture care group than in the usual care group. However, the additional resource use was less than the costs of the acupuncture treatment itself, suggesting that some usual care resource use was offset |
| Thomas et al. (2010)74 | UK (Scotland) | Prospective observational study | Aim: to evaluate whether or not primary care access to brain CT referral for chronic headache reduced referral to secondary care Population: patients aged ≥ 18 years with a normal neurological examination, with chronic headache attending GPs in Tayside and north-east Fife, Scotland Sample size: 215 patients Interventions: GPs were given access to refer patients directly to brain CT |
Number of referrals: based on questionnaires given to the referring GPs, it was estimated that the scan had stopped a referral to secondary care in 88% of cases. In 5% of cases the scan had resulted in a referral. GPs referred 14% scanned patients to a neurologist because of headache. It is estimated that imaging reduced referrals to secondary care by 86% in the follow-up period (mean follow-up period of 1.3 years per patient) Patient outcomes: significant abnormalities were noted in three (1.4%) patients; there were 22 (10.2%) non-significant findings and 190 (88.4%) normal scans Patient satisfaction: NR Access to care: NR Costs: NR |
| Thompson-Coon et al. (2013)54 | Multiple | Systematic review | Aim: to compare the effectiveness of face-to-face consultations with telephone consultations for surgery follow-up Population: patients discharged from hospital following surgery Sample size: four studies (from five papers). Sample size of included studies ranged from 48 to 364 Interventions: telephone consultations. Compared with face-to-face outpatient consultations |
Number of referrals: NR Patient outcomes: NR Patient satisfaction: the authors stated that the results seem to suggest that patients were happy to receive routine follow-up care by telephone, and in some cases preferred this method Costs: two studies reported on costs. Uppal et al. in 2004 estimated the direct and indirect health care related costs of telephone follow-up consultations at £50 per patient, compared with £106.11 for those conducted face to face. A simple cost calculation in the paper by Mandal et al. estimated the cost of a telephone review at between £1 and £2 (it is not clear which costs have been included in these calculations) |
| Torregrosa-Maicas et al. (2013)53 | Spain | Observational study | Aim: to assess the impact of a quick consultation intervention for CKD patients Population: patients with slow-progressing CKD in the catchment area of the University Clinical Hospital of Valencia Sample size: 385 patients Interventions: stable CKD patients of the hospital nephrology department are referred to a quick consultation clinic within 2 weeks. During the quick consultation, it is decided through a rapid evaluation process if the patients can be monitored in primary care or should remain in specialised care |
Number of referrals: 28.05% of patients were initially evaluated through high-resolution consults. Of those, 70% were referred over to primary care for monitoring and the remaining 30% were given specialist appointments Patient outcomes: NR Patient satisfaction: NR Access to care: NR Costs: NR |
| Tuomisto et al. (2010)31 | Finland | Retrospective before-and-after study | Aim: to evaluate the profile of newly diagnosed adult asthma cases and the approach adopted to secondary care management at the launch of the Finnish asthma programme in 1994 and 7 years later Population: non-acutely referred patients with asthma Sample size: 298 patients (165 before, 133 after) Interventions: during and after the programme, a new division of labour between primary and secondary care was defined. Asthma co-ordinators (one physician and at least one nurse) were nominated at each health-care centre, and asthma nurses took an active role in primary care and later also in secondary care in the management of asthma, both before and after diagnosis |
Number of referrals: NR Patient outcomes: the asthma patients in 2001 were significantly older, more obese and had more comorbidities than in 1994. The proportion of obese asthmatics (BMI > 30 kg/m2) increased significantly from 19% in 1994 to 33% in 2001 (p = 0.011) Patient satisfaction: NR Access to care: the percentage of asthma diagnosis made at an out-patient visit increased from 73% to 92% (p < 0.001). The number of secondary care visits per new case of asthma decreased from 7.3 to 5.4, and the number of days in hospital decreased from 3.6 to 0.95 Costs: NR |
| Ulrik et al. (2010)185 | Denmark | Before-and-after study | Aim: to ascertain whether or not participating in an educational programme could improve adherence to guidelines Population: patients with COPD in primary care Sample size: 124 GPs (1716 patients before and 1342 after) Interventions: an educational programme based on the GOLD guidelines and designed by a group of Danish pulmonologists and GPwSIs. It involved meetings between GPs and consultants to discuss the GOLD guidelines and training on how to correctly perform and interpret a spirometry test |
Number of referrals: the number of patients referred for COPD rehabilitation non-significantly increased after the education programme: 12% vs. 16% Patient outcomes: NR Patient satisfaction: NR Access to care: NR Costs: NR Other: results show improved adherence to COPD guidelines |
| van der Heijden et al. (2011)135 | The Netherlands | Prospective observational analysis | Aim: to investigate the effect of teledermatology on the efficiency, quality and costs of care when integrated in daily practice and applied following patient selection by a GP Population: all GPs in the Netherlands. GPs undertook a teledermatology consultation for patients with new or existing skin conditions for who they felt it was suitable Sample size: 1820 GPs, 166 dermatologists, 37,207 teleconsultations Interventions: GPs sent patient data, clinical photographs, the patient’s history and an optional more detailed patient history based on a questionnaire to their regional dermatologist who would provide response within 2 working days |
Number of referrals: in total, 8578 (23%) of patients were referred for a face-to-face consultation after teledermatology consultation. Of patients who the GP would have sent for referral to the dermatologist 74% were avoided as a result of the teledermatology consultation. In the group of patients where the GP used teleconsultation for a second opinion and had not planned on referring the patient, 16% were consequently referred following teleconsultation (n = 10,611). The overall reduction in the number of face-to-face consultations was 68% Patient outcomes: NR Patient satisfaction: NR Access to care: the mean response time of the dermatologist in the first round of a teledermatology consultation was 4.6 hours Costs: the estimated cost reduction was 18%, compared with conventional face-to-face care, weighted mean outpatient costs €157.06 vs. €192.00 per patient Other: GPs indicated that there was a beneficial educational effect in 85% of the teleconsultations (helpfulness of the dermatologist’s response was ‘a lot’ in 25% of the teledermatology consultations) |
| van der Velde et al. (2011)75 | The Netherlands | Observational study | Aim: to compare the diagnostic performance of two clinical decision rules to rule out DVT in primary care patients Population: patients > 18 years old with clinically suspected DVT indicated by one or more of the following symptoms: swelling, redness or pain of the lower extremity Sample size: 1086 patients Interventions: GPs entered data into two decision rules: (1) Wells rule and (2) primary care rule. In all patients, D-dimer testing was performed using a rapid point-of-care assay. The rules were used to calculate a score, with patients who score ≥ 4 referred for ultrasonography |
Number of referrals: significantly more patients would have been referred using the Wells rule than the primary care rule, 55% vs. 51% (p < 0.001) Patient outcomes: NR Patient satisfaction: NR Access to care: NR Costs: NR Accuracy of diagnosis: confirmed DVT was slightly higher among patients according to the primary care rule than the Wells rule, 25% vs. 23% (p = 0.40). Both decision rules missed seven thromboembolic events which occurred during 3 months of follow-up in patients with a low score on the clinical items and a negative D-dimer. Of these, four were missed by both rules, whereas the results of the decision rule were discordant for three patients |
| Van Dijk et al. (2010)32 | The Netherlands | Observational study | Aim: to evaluate referral rates for hospital treatment of patients with diabetes after the introduction of primary care nurses Population: patients newly diagnosed or with pre-existing diabetes being managed in primary care attending practices that participate in the Netherlands Information Network of General Practice Sample size: 2004 25 GP practices, 301 newly diagnosed patients and 2124 known type 2 diabetes patients. 2006 29 GP practices, 450 newly diagnosed patients, 3226 known type 2 diabetes patients Interventions: the introduction of primary care nurses |
Number of referrals: the overall referral rate for newly diagnosed patients to all secondary care specialists decreased by > 50% between 2004 and 2006 in all practices (OR 0.44, 95% CI 0.22 to 0.88; p < 0.05). There was no difference in referral rates between general practices with and without primary care nurses. For patients with pre-existing diagnosis of type 2 diabetes, there was no overall change in referral rates to secondary care specialists between 2004 and 2006 (p = 0.23). However, referral rates to one specialist (internists) decreased in general practices with a primary care nurse (OR 0.59, 95% CI 0.31 to 1.11; p < 0.1); there was no difference between referral rates to other specialists Patient outcomes: NR Patient satisfaction: NR Access to care: the presence of a primary care nurse had no impact on the number of diabetes-related contact with GP for either newly diagnosed or pre-existing patients Costs: NR |
| Van Dijk et al. (2011)15 | The Netherlands | Audit | Aim: to examine the association between surgical interventions in general practice and hospital referrals Population: patients eligible for minor surgery for laceration/cut, neoplasm skin benign/unspecified, naevus/mole and sebaceous cyst in 48 practices that participated in the Netherlands Information Network of General Practice in 2006–7 Sample size: 14,203 patients, 15,923 care-episodes Interventions: GPs conducting minor surgery in their own practice |
Number of referrals: referrals rates differed between diagnoses: for care-episodes with a laceration/cut, 1.0% of patients were referred to hospital care; for benign neoplasm skin/naevus 10.2% were referred, and for sebaceous cyst 8.2% were referred. Regression analyses demonstrated that GP practices that performed more minor surgery interventions had a lower referral rate for patients with a laceration/cut (correlation –0.38, 95% CI –60 to –0.11) and those with a sebaceous cyst (correlation –0.42, 95% CI –0.63 to –0.16), but not for people with benign skin/naevus. The absolute difference in referral rate appears to be relevant only for sebaceous cysts (from 9.4% to 5.1%) Patient outcomes: NR Patient satisfaction: NR Access to care: GP practices performed minor surgery in 8.9% of the care-episodes with laceration/cut, 27.4% for benign neoplasm skin/naevus and 26.4% for sebaceous cyst Costs: NR |
| Vernacchio et al. (2013)186 | USA | Before-and-after study | Aim: to evaluate a quality improvement programme designed to reduce unnecessary specialty referrals for adolescent idiopathic scoliosis Population: all patients aged 10–18 years of age on the records of two large not-for-profit insurers in Massachusetts Sample size: monthly mean of 30,539 patients Interventions: the quality improvement programme was developed with the Pediatric Physicians’ Organization. It comprised (a) physician education, (b) decision support tools available at the point of care and (c) longitudinal feedback of data on physician referrals for adolescent idiopathic scoliosis |
Number of referrals: initial visits to orthopaedic surgery for adolescent idiopathic scoliosis declined from 5.1 to 4.1 per 1000 adolescents per year, a reduction of 20.4% (p = 0.01). Process control chart analysis showed a rapid change in referral patterns after the initiation of the programme which was sustained over the 2-year post-intervention period and demonstrated that 66 initial and 131 total adolescent idiopathic scoliosis specialty visits were avoided as a result of the programme Patient outcomes: NR Patient satisfaction: NR Access to care: the number of patients with scoliosis receiving a brace within 30 days increased from 4.4% to 9.3% (p = 0.02). The number of patients receiving surgery within 6 months decreased from 1.9% to 0.8% (p = 0.30) Costs: NR |
| Wade et al. (2010)136 | Multiple | Systematic review | Aim: to assess the economic value of using one type of telehealth delivery: synchronous (real-time) video communication Population: studies with patient outcome data and a non-telehealth comparator were included. Cost analyses, non-comparative studies and those where patient satisfaction was the only health outcome were excluded. Clinical disciplines were diverse including dermatology, mental health, paediatric cardiology, home nursing, intensive care, emergency medicine, neurology and medical disciplines Sample size: 36 studies Interventions: telehealth services which used synchronous video communication as the major mode of delivery and telehealth services which directly delivered patient care either provided to patient or provider to provider |
Number of referrals: NR Patient outcomes: 12 (33%) of studies reported improved health outcomes, 21 (58%) reported outcomes that were not significantly different, 1 (3%) reported that outcomes differed according to patient group and 2 (6%) reported that telehealth was less effective Patient satisfaction: NR Access to care: NR Costs: 22 (61%) out of 36 eligible studies found telehealth to be less costly than the non-telehealth alternative; 11 (31%) found greater costs, 2 (6%) gave mixed results and 1 (3%) gave the same result. Twenty-three of the studies took the perspective of the health services, 12 were societal, and 1 was from the patient perspective. In three studies of telehealth to rural areas, the health services paid more for telehealth, but due to savings in patient travel, the societal perspective demonstrated cost savings. With regard to health outcomes, 12 (33%) of studies found improved health outcomes, 21 (58%) found outcomes were not significantly different, 2 (6%) found that telehealth was less effective and 1 (3%) found outcomes differed according to patient group. The organisational model of care was more important in determining the value of the service than the clinical discipline, the type of technology or the date of the study |
| Walker et al. (2009)209 | UK | Observational study | Aims: to describe an e-mail enquiry service for endocrinology and diabetes established within one hospital and assess its benefits Population: GPs and their patients within the Oxfordshire region Sample size: NR. A figure shows that the number of enquiries was about 200 in 2005, about 450 in 2006, about 550 in 2007 and > 700 in 2008. 250 GPs have participated in the scheme Interventions: GPs e-mail a specialist registrar about endocrinology and diabetes patients (intervention not clearly defined). In the previous system, they used to call the registrar via switchboard |
Number of referrals: a formal referral was suggested in < 10% of cases Patient outcomes: NR Patient satisfaction: NR Access to care: in 2008, in 80% of the cases, registrars replied to queries within 48 hours Costs: NR Other: e-mails allow more time for reflection and discussion of the cases with specialists, there is a record of interactions between GP and registrar and the registrar working day is not interrupted by telephone calls. In 2008, in 4% of the cases, the query was not clear enough, which led to some delays |
| Walter et al. (2012)76 | UK (England) | RCT | Aim: to assess whether or not adding a computerised diagnostic tool, the MoleMate system (SIAscopy with primary care scoring algorithm), to current best practice (clinical history, naked eye examination, 7-point checklist) resulted in more appropriate referrals Population: adults with pigmented skin lesions not immediately diagnosed as benign Sample size: 1297 patients (643 intervention, 654 control) Interventions: patients were assessed by trained primary care clinicians using best practice using the MoleMate system. Compared with usual GP assessment |
Number of referrals: a higher proportion of lesions were referred in the intervention group, 29.8% vs.22.4% (p = 0.001) Patient outcomes: NR Patient satisfaction: compared with the control group, more patients in the intervention group ranked their consultation as very good or excellent for thoroughness, 83.1% vs. 71.2% (p < 0.001), communication 82.1% vs. 70.6% (p < 0.001) and reassuring care 77.2% vs. 66.4% (p < 0.001). Anxiety scores were similar between groups Access to care: NR Costs: NR Appropriateness of referral: the appropriateness of referral did not differ significantly between the intervention or control groups: 56.8% vs. 64.5%, difference 8.1% (95% CI −18.0% to 1.8%). The proportion of benign lesions appropriately managed in primary care did not differ (intervention 99.6% vs. control 99.2%) Accuracy of diagnosis: there was no difference in the accuracy in the decision to take a biopsy or monitor skin lesions between the GP diagnosis and MoleMate system when verified by an expert, 95.7% vs. 98.5% (p = 0.26). However, the percentage agreement with expert assessment that the lesion was benign was significantly lower with MoleMate, 84.4% vs. 90.6% (p < 0.001). Thirty-six histologically confirmed melanomas were diagnosed; 18/18 were appropriately referred in the intervention group and 17/18 in the control group |
| Watrous et al. (2008)77 | USA | Observational study | Aim: to evaluate the impact of CAA on physicians’ accuracy of murmur detection as well as their decisions to refer asymptomatic patients with heart murmurs Population: primary care physicians Sample size: seven primary care physicians. Pre-recorded 100 heart sounds recordings of patients with and without heart disease (55 innocent murmurs, 30 pathological murmurs and 15 without a murmur) Interventions: the CAA tool performs spectral and temporal analysis of heart sounds, graphically displays murmur energy profiles and relates the data statistically to referral guidelines. Physicians were provided with a 15-minute orientation on how to use the CAA |
Number of referrals: N/A Patient outcomes: N/A Patient satisfaction: N/A Access to care: N/A Cost: NR Appropriateness of referral: the average physician referral accuracy increased from 70.4% to 82.9% using CAA (p < 0.001); referral sensitivity increased from 86.7% to 92.9%, while specificity increased from 63.5% to 78.6% using CAA (p < 0.001) Accuracy of diagnosis: sensitivity for detection of murmurs significantly increased with use of CAA from 76.6 to 89.1% (p < 0.001), while specificity remained unaffected (80.0 vs. 81.0%). CAA improved sensitivity of correctly identifying pathological murmur cases from 82.4% to 90.0% (p < 0.001), and specificity of correctly identifying benign cases (with innocent or no murmurs) from 74.9% to 88.8% (p < 0.001) |
| Weatherburn et al. (2009)137 | UK (England) | Audit | Aims: to present the outcomes of undertaking ECGs in general practice Population: Patients with acute cardiac symptoms or long-term conditions, and practice nurses who undertake ECGs Sample size: 373 ECGs from eight general practices and two walk-in centres Interventions: for each patient, the recorded ECG was stored in the memory of the device and sent to the Broomwell Call Centre where it was displayed for interpretation by cardiac physicians. Call centre staff, who were available 24 hours per day, then discussed results by telephone with the referring nurse and followed up with a written report sent to the practice |
Number of referrals: there were 76 changes in care pathways – 18 patients for whom admissions were not anticipated had acute admission, 24 were referred to hospital, and in 14 cases medical assessment within primary care with amendment of treatment resolved the problem, avoiding hospital visits Patient outcomes: NR Patient satisfaction: NR Access to care: NR Costs: NR Appropriateness of referrals: for the admissions to hospital these were appropriate as hospital intervention was necessary because the ECGs identified serious conditions |
| Wegner et al. (2008)210 | USA | Observational study | Aim: to assess the estimated savings from paid telephone consultations between paediatric subspecialists and primary care physicians Population: Medicaid-insured patients under 22 years of age attending primary care clinics in North Carolina Sample size: 47 paediatric subspecialists from six academic centres, 306 consults to 292 patients Interventions: Telephone consultations between primary care physicians and paediatric specialists |
Number of referrals: paediatric subspecialists reported that telephone consultations led to avoidance of specialist visits 32% (n = 98), hospital transfers 11% (n = 35), hospital admissions 5% (n = 14) and emergency department visits 5% (n = 14). Fewer than 3% of forms indicated avoidance of more than one service Patient outcomes: NR Patient satisfaction: NR Access to care: telephone consultations were generally < 15 minutes in length and exceeded 30 minutes in < 7% of calls Costs: after adjusting for the reimbursed costs of providing telephone consultations, an estimated US$477,274 was saved, equivalent to US$39 saving per dollar spent on teleconsultation |
| West et al. (2007)172 | UK (England) | Observational study | Aim: to assess the impact of written guidelines on GP referrals to an orthopaedic outpatient department Population: referrals for patients with orthopaedic conditions Sample size: 471 referral letters to 1 orthopaedic department at a district general hospital (304 before intervention and 167 after) Interventions: provision of easy-to-follow written referral guidelines for GP referrals to an orthopaedic outpatient department. The recommendations were based on the current evidence in the orthopaedic literature for managing the various conditions |
Number of referrals: in the first period without the referral guidelines, 64% of the referral letters did not meet the criteria for referral, while in the second period it was 61% (p = 0.49). There was no evidence to suggest that the implementation of guidelines significantly affected the numbers of referrals Patient outcomes: NR Patient Satisfaction: NR Access to care: NR Costs: NR |
| Westwood et al. (2006)187 | UK (England) | Prospective observational study | Aim: to test the feasibility of providing genetic nurse counsellor clinics in primary care in the UK, to develop a questionnaire to evaluate patients’ satisfaction with their genetics appointments and to establish patient and provider costs Population: new patients referred to the CGS between July 2002 and May 2003 Sample size: 122 referrals across 36 general practices Interventions: referral letters were passed to a genetic counsellor for triage and an appointment was arranged in the primary care genetic counsellor clinics. Patients could request an appointment in secondary care instead |
Number of referrals: 58 of the 122 patients referred were not sent a clinic appointment for various reasons. Sixty-four appointment letters were sent and seven people cancelled their appointments, only one because he wished to be seen in secondary care clinic as this was closer to his workplace than the allocated clinic. A total of 22 of the 45 patients who kept their appointments were dealt with by the genetic counsellor without the need to be referred to the medical team in secondary care Patient outcomes: NR Patient satisfaction: 90% of the 37 patients who returned a satisfaction questionnaire were either quite or very satisfied with their clinic visit. 10% were very or a bit dissatisfied. Patients were most satisfied with the affective aspects (relating to the counsellor’s behaviour towards them) and the information given, and were least satisfied with the procedural aspects of the appointment Access to care: For the 57 patients who were sent an appointment and who did not cancel, the mean waiting time was 79 days (11–218) or 11 weeks (15–31 weeks) Costs: NR |
| Westwood et al. (2012)188 | UK (England) | Cluster RCT | Aim: to assess whether or not a primary care genetic-led education improves both non-cancer and cancer referral rates, and whether or not primary care-led genetic clinics improve the patient pathway Population: new patients referred to the CGS between 1 June 2003 and 30 November 2004 and registered with a GP in an area covering three PCTs in the south of England Sample size: 73 general practices (36 intervention and 37 control) Intervention: GPs in the intervention practices received education on CGS referral pathways, received electronic referral guidelines and example case scenarios illustrating inheritance patterns, recurrence risks and ethical issues. A NHS intranet secure website with access to cancer referral guidelines and a referral form was developed. The practices were randomised to one of four groups: (1) education and primary care clinic; (2) education and secondary care clinic; (3) no education and primary care clinic; and (4) no education and secondary care clinic |
Number of referrals: there was no difference in the total referral rates among GPs (RRR 1.34, 95% CI 0.89 to 2.02; p = 0.161). The number of non-cancer referral rates did not differ between practices (RRR 1.15, 95% CI 0.72 to 1.84; p = 0.567); however, the number of cancer referrals was significantly higher in the intervention practices (RRR 2.02, 95% CI 1.01 to 4.03; p = 0.046) Patient outcomes: NR Patient satisfaction: there was no difference in patients’ satisfaction between groups. Overall, 90% of patients were either quite or very satisfied with their clinic visit and 79% of respondents felt that the visit had been helpful Access to care: it took 33% less time to attend a primary than a secondary care appointment, 39.7 vs. 57.7 minutes (p < 0.001) Costs: overall, no difference in NHS excess treatment costs was identified, £45.57 vs. £44 (p = 0.369) Appropriateness of referrals: GPs who had received educational training made more appropriate cancer referrals (RRR 2.36, 95% CI 1.07 to 5.24; p = 0.035) |
| Wiedemer et al. (2007)92 | USA | Prospective observational study | Aim: to measure the impact of a structured opioid renewal programme for chronic pain run by a nurse practitioner and clinical pharmacist in a primary care setting Population: patients with a chronic non-cancer pain managed with opioid therapy in primary care clinic at an urban veterans hospital Sample size: 335 patients Interventions: a structured opioid renewal programme for chronic pain, the Opioid Renewal Clinic, run by a nurse practitioner and a clinical pharmacist in a primary care setting |
Number of referrals: initially, 335 patients were referred to the Opioid Renewal Clinic. Of these 335 patients, 13% were referred for addiction treatment. The preliminary analysis suggests that Opioid Renewal Clinic has resulted in a decline per patient of 72.7% in emergency room visits and 59.6% of unscheduled primary care provider visits Patient outcomes: of the 171 patients referred for aberrant drug-taking behaviours 45% adhered to the Opiod Treatment Agreement, but 38% self-discharged from the practice when the structured programme was offered. Of the 164 referred for no aberrant drug-related behaviour all adhered to the Opiod Treatment Agreement Patient satisfaction: NR Access to care: NR Costs: the cost of oxycontin for the pharmacy was reduced from US$129,793 to US$5236 but the number of prescriptions per month remained constant so that this reduction was due to a shift from oxycodone sustained action to other, less costly, long-acting opioids Other: of the primary care providers who responded to questionnaires, the majority found the programme helpful in their practice, both in changing abnormal illness behaviour and in freeing up more time to deal with important medical problems |
| Willems et al. (2008)145 | The Netherlands | RCT | Aim: to evaluate the effects of a nurse-led telemonitoring intervention for patients with asthma Population: asthmatic patients aged 7 years and over from the University Hospital Maastricht Sample size: 109 patients (55 intervention and 54 control) Interventions: instead of regular outpatient appointments with lung specialists, patients in the intervention arm were managed through a telemonitoring device registering lung function values and symptoms and had a nurse as the main caregiver |
Number of referrals: no significant difference in medical consumption/health-are utilisation Patient outcomes: no statistically significant difference in asthma-specific quality of life scores and no statistically significant differences in improvements in any symptoms Patient satisfaction: NR Access: NR Costs: NR |
| Williams et al. (2012)211 | Ireland | Observational study | Aim: to assess an internet neurology referral system (Neurolink) for GPs Population: patients referred to neurology services Sample size: 710 electronic referrals Interventions: neurology electronic referral system (Neurolink) which allowed GPs direct online access to consultant neurologists for initial diagnosis and advice whether their patient should attend specialist consultation in person and/or what tests should be completed prior to meeting the neurologist |
Number of referrals: 19% (127/662) of patients did not require a neurology outpatient appointment and the GP was given advice, treatment and investigation options instead Patient outcomes: NR Patient satisfaction: NR Access to care: of 662 referrals with available data, the average time taken for a neurologist consultant to reply to a GP referral was 19 hours and 8 minutes Costs: NR Other: all GPs surveyed (n = 19) said they preferred Neurolink compared with ‘regular mail.’ This was because of the quick response time and the additional treatment advice provided. Twelve GPs felt more comfortable dealing with neurological conditions as a result of using Neurolink and 12 said that they would be happy if only Neurolink referrals were accepted by the neurology department in the future |
| Williams et al. (2007)78 | UK (England) | Audit | Aim: to assess the effectiveness of a new referral system for women with post-menopausal bleeding Population: women with post-menopausal bleeding Sample size: 277 patients Interventions: the introduction of a new protocol. Patients were referred to a gynaecologist following an abnormal transvaginal ultrasound |
Number of referrals: during the 6-month study period, there was a 15.4% increase in referrals for ultrasound compared with the same period 2 years previously. The change in protocol resulted in 27 fewer women (10%) requiring referral to a gynaecologist without any missed cancers Patient outcomes: NR Patient satisfaction: NR Access to care: NR Costs: NR |
| Willigendael et al. (2005)189 | The Netherlands | Before-and-after study | Aim: to measure the effect of GPs and practice assistants combined training on the management of patients with PAD Population: patients with PAD Sample size: 100 patients (50 before and 50 after), from 53 GPs and 65 accompanying practice assistants Interventions: combined education training for GPs and practice assistants to management patients with PAD |
Number of referrals: after training, the number of patients referred for PAD to the vascular outpatients clinic with a (correct) ankle–brachial index measurement increased from 5 (10%) before training to 29 (58%) after training Patient outcomes: NR Patient satisfaction: NR Access to care: NR Costs: NR Accuracy of diagnosis: the ability to refer patients with actual PAD increased from 30% before training to 70% after training (showing an improvement in the GP diagnostics) |
| Younes et al. (2008)106 | France | Retrospective observational study | Aim: to explore long-term GP opinions (relating to impact on their management and on patient medical outcome) and to determine the secondary referral rate, after a sufficient time lapse following the intervention to reflect a ‘real-world’ primary care setting Population: Patients with mental health problems Sample size: 181 patients, 139 GPs Interventions: a specialist consultation centre (composed of mental health professionals) which provided GPs support for mental health patients who they considered posed a problem, without transferring the main responsibility to specialty care |
Number of referrals: 44.2% of cases Patient outcomes: 58.9% of GPs reported that the intervention had a positive impact on patient medical outcomes Patient satisfaction: NR Access to care: NR Costs: NR Other: 91.2% of GPs evaluated effects as positive for primary care management (mainly as support). Two years post intervention, management was shared care for 79.7% of patients (the GP as the psychiatric care provider) and care by a psychiatrist for 20.3% patients |
| Zwar et al. (2012)33 | Australia | Cluster RCT | Aim: to evaluate a nurse–GP partnership model of care for patients with a diagnosis of COPD Population: patients with a diagnosis of COPD aged 40 to 80 years Sample size: 451 patients (234 intervention and 217 control) in 44 general practices (22 intervention and 22 control) Interventions: home visitation by a registered nurse with specific training in COPD care who worked with the GP, the patient and other health professionals to develop and implement an individualised care plan. Patients in the control group practices received usual care |
Number of referrals: NR Patient outcomes: at 12 months, there was no statistically significant difference in disease-related QoL scores measured using the SGRQ between intervention and control groups, 38.7 vs. 37.6 (difference 1.1 (95% CI –1.53 to 3.74; p = 0.41) or in measures of quality of life, lung function and smoking status Patient satisfaction: NR Access to care: compared with the control group, attendance at pulmonary rehabilitation was more frequent in the intervention group, 31.1% vs. 9.6% (p = 0.002) Costs: NR Accuracy of diagnosis: of the 451 patients included in the study, 57.8% were confirmed as having COPD based on results from post-bronchodilator spirometry Other: compared with the control group, mean COPD knowledge score was higher in the intervention group, 10.5 vs. 9.8 (difference 0.70, (95% CI 0.10 to 1.2; p = 0.02) |
Appendix 3 Table of studies excluded at full-text review stage
| Abdelhamid AS, Mooney J, Walker AA, Barton G, MacGregor AJ, Scott DGI, et al. An evaluation of rheumatology practitioner outreach clinics: a qualitative study. BMC Health Serv Res 2012;12:119 |
| Abdel-Kader K, Fischer GS, Li J, Moore CG, Hess R, Unruh ML. Automated clinical reminders for primary care providers in the care of CKD: a small cluster-randomized controlled trial. Am J Kidney Dis 2011;58:894–902 |
| Agvall B, Alehagen U, Dahlström U. The benefits of using a heart failure management programme in Swedish primary healthcare. Eur J Heart Fail 2013;15:228–36 |
| Allard M, Jelovac I, Léger PT. Treatment and referral decisions under different physician payment mechanisms. J Health Econ 2011;30:880–93 |
| Allder S, Walley P, Silvester K. Is follow-up capacity the current NHS bottleneck? Clin Med 2011;11:31–4 |
| Almaawiy U, Pond GR, Sussman J, Brazil K, Seow H. Are family physician visits and continuity of care associated with acute care use at end-of-life? A population-based cohort study of homecare cancer patients. Palliat Med 2014;28:176–83 |
| DAMASK (Direct Access to Magnetic Resonance Imaging: Assessment for Suspect Knees) Trial Team. Cost-effectiveness of magnetic resonance imaging of the knee for patients presenting in primary care. Br J Gen Pract 2008;58:775–8 |
| DAMASK (Direct Access to Magnetic Resonance Imaging: Assessment for Suspect Knees) Trial Team. Effectiveness of GP access to magnetic resonance imaging of the knee: a randomised trial. Br J Gen Pract 2008;58:767–74 |
| Angeles RN, Guenter D, McCarthy L, Bauer M, Wolfson M, Chacon M, et al. Group interprofessional chronic pain management in the primary care setting: a pilot study of feasibility and effectiveness in a family health team in Ontario. Pain Res Manag 2013;18:237–42 |
| Aniff M, et al. Two year impact of a home based primary care program on hospitalizations, emergency room and office visit utilization on patients with diabetes. J Am Geriatr Soc 2013;61:S170 |
| Bakhai M, Hopster D, Wakeel R. A retrospective study comparing the accuracy of prehistology diagnosis and surgical excision of malignant melanomas by general practitioners and hospital specialists. Clin Exp Dermatol 2010;35:63–7 |
| Bal R, Mastboom F, Spiers HP, Rutten H. The product and process of referral. Optimizing general practitioner-medical specialist interaction through information technology. Int J Med Inform 2007;76(Suppl. 1):28–34 |
| Banks J, Sharp DJ, Hunt LP, Shield JP. Evaluating the transferability of a hospital-based childhood obesity clinic to primary care: a randomised controlled trial. Br J Gen Pract 2012;62:e6–12 |
| Barnes K, Longfield P, Jones K, Littlemore G, McDonough C, McIntyre A, et al. Evidence based commissioning: calculating shift potentials for paediatric services. Clin Governance 2013;18:39–48 |
| Barr DA, Seaton RA. Outpatient parenteral antimicrobial therapy (OPAT) and the general physician. Clinical Medicine. J R Coll Phys Lond 2013;13:495–9 |
| Beaulieu MD. Primary and secondary care: breaking down barriers for our patients with chronic diseases. Can Fam Physician 2013;59:221 |
| Beaver K. Comparing hospital and telephone follow-up after treatment for breast cancer: randomised equivalence trial. BMJ 2009;338 |
| Benoiton LA, Schmidt E, Tarr GP, Thomson IA, Rennie SC, van Rij AM. Assessment and management of leg ulcers in the community and an outpatient clinic. N Z Med J 2013;126:26–34 |
| Bergus GR, Emerson M, Reed DA, Attaluri A. Email teleconsultations: well formulated clinical referrals reduce the need for clinic consultation. J Telemed Telecare 2006;12:33–8 |
| Bermingham S, et al. Does continuity of care matter? Value Health 2013;16:A257 |
| Bikou O, Licka M, Kathoefer S, Katus HA, Bauer A. Cost savings and safety of ICD remote control by telephone: a prospective, observational study. J Telemed Telecare 2010;16:403–8 |
| Bird JH, Biggs TC, Schulz C, Lower N, Faris C, Repanos C. Implementation of an evidence-based acute tonsillitis protocol: our experience in one hundred and twenty-six patients. Clin Otolaryngol 2013;38:410–15 |
| Bogucki P, Charman C. ‘Choose and Book’ teledermatology: a service overview. Br J Dermatol 2013;169:4 |
| Bunce C. Surgeon gives GPs direct access. |
| Butler M, Kane RL, McAlpine D, Kathol R, Fu SS, Hagedom H, et al. Does integrated care improve treatment for depression? A systematic review. J Ambulatory Care Manag 2011;34:113–25 |
| Butler S, Klepacka K, Agius M, Zaman R. Depression treatment by Bedford East Community Mental Health Team an audit to assess how many patients in a Bedfordshire Community Mental Health Team might safely be transferred to primary care. Psychiatria Danubina 2010;22:317–22 |
| Camps C, Iranzo V, Caballero C, Blasco A, Godes MJ, Safont MJ, et al. Oncology outside hospital: a new experience for the benefit of longer survivors. Clin Translat Oncol 2011;13:249–53 |
| Carrier E, Dowling MK, Pham HH. Care coordination agreements: barriers, facilitators, and lessons learned. Am J Managed Care 2012;18:e398–404 |
| Carroll JC, Wilson BJ, Allanson J, Grimshaw J, Blaine SM, Meschino WS, et al. GenetiKit: a randomized controlled trial to enhance delivery of genetics services by family physicians. Fam Pract 2011;28:615–23 |
| Cerimele JM, Katon WJ, Sharma V, Sederer LI. Delivering psychiatric services in primary-care setting. Mount Sinai J Med 2012;79:481–9 |
| Cerimele JM, Strain JJ. Integrating primary care services into psychiatric care settings: a review of the literature. Prim Care Comp J Clin Psychiatry 12:2010 |
| Chamley M, Atkinson R, Azille J, Camfield E, McGowan D, Basudev N, et al. The establishment of a patient-centred outcome-based community diabetes service in southeast London. Diabetic Med 2013;30:196 |
| Cherryman G. Imaging in primary care. Br J Gen Pract 2006;56:563–4 |
| Cheshire A, Polley M, Peters D, Ridge D. Is it feasible and effective to provide osteopathy and acupuncture for patients with musculoskeletal problems in a GP setting? A service evaluation. BMC Famy Pract 2011;12:49 |
| Chomienne MH, Grenier J, Gaboury I, Hogg W, Ritchie P, Farmanova-Haynes E. Family doctors and psychologists working together: doctors’ and patients’ perspectives. J Eval Clin Pract 2011;17:282–7 |
| Cigrang JA, Dobmeyer AC, Becknell ME, Roa-Navarrete RA, Yerlan SR. Evaluation of a collaborative mental health program in primary care: effects on patient distress and health care utilization. Prim Care Commun Psychiatry 2006;11:121–7 |
| Clarke A, Musila N, Le Maistre N, Black N, van der Meulen. The REFER Project: Realistic Effective Facilitation of Elective Referral for Elective Surgical Assessment. Southampton: NIHR Service Delivery and Organisation Programme; 2010 |
| Clemensen J, Larsen SB, Kirkevold M, Ejskjaer N. Telemedical teamwork between home and hospital: a synergetic triangle emerges. Stud Health Technol Inform 2007;130:81–9 |
| Conlin M, Herman L, Mouton M, Wilson L, Patel R, McPherson J. The use of a personalized gene expression test to improve decision making in the evaluation of women with suspected coronary artery disease. J Womens Health 2013;22:7–8 |
| Cook N, George C. GP direct access CT KUB for suspected urinary tract calculi: initial experience at a university hospital. Clin Radiol 2013;68(Suppl. 1):3 |
| Croft P, Porcheret M, Peat G. Managing osteoarthritis in primary care: the GP as public health physician and surgical gatekeeper. Br J Gen Pract 2011;61:485–6 |
| Csiba L. Is the outpatient management of acute minor stroke feasible and safe? J Neurol Neurosurg Psychiatry 84:243 |
| Davies M, Elwyn G. Referral management centres: promising innovations or Trojan horses? BMJ 2006;332:844–6 |
| Dewan B, Skrypak M, Moore J, Wainscoat R. A service evaluation of the feasibility of a community-based consultant and stroke navigator review of health and social care needs in stroke survivors 6 weeks after hospital discharge. Clin Med 2014;14:134–40 |
| Dhar A, Lee SH, Borthwick H, Nair P, White C. PTU-057 point-of-contact faecal calprotectin (FC) testing in diarrhoea helps decision making for referral to gastroenterologists: a primary care pilot study in north east England. Gut 2013;62(Suppl. 1):67–8 |
| Dijksman L, Dinant GJ, Spigt MG. eDiagnostics: a promising step towards primary mental health care. Fam Pract 2013;30:695–704 |
| Docherty MJ, Choudhury M, Littlejohns P. NICE ‘referral advice’ recommendations database. BMJ 2011;342:123 |
| Doull I. Shared care – is it worth it for the patient? J R Soc Med 105(Suppl. 2):25–9 |
| Dowswell T, Carroll G, Duley L, Gates S, Gülmezoglu AM, Khan-Neelofur D, et al. Alternative versus standard packages of antenatal care for low-risk pregnancy. Cochrane Database Syst Rev 2010;10:CD000934 |
| Dusheiko M, Gravelle H, Jacobs R, Smith P. The effect of financial incentives on gatekeeping doctors: evidence from a natural experiment. J Health Econ 2005;25:449–78 |
| Evans NR, Richardson LS, Dhatariya KK, Sampson MJ. Diabetes specialist nurse telemedicine: admissions avoidance, costs and casemix. Practical Diabetes 2012;29:25–8 |
| Finley A. The value of understanding patient referral flow. Healthc Financ Manage 2013;67:84–9 |
| Fisken RA. Putting more specialist physicians into the community is not answer to primary-secondary care divide. BMJ 2012;345:e4730 |
| Flannery F, Adams D, O’Connor N. A community mental health service delivery model: integrating the evidence base within existing clinical models. Australas Psychiatry 2011;19:49–55 |
| Fleury MJ, Imboua A, Aubé D, Farand L, Lambert Y. General practitioners’ management of mental disorders: a rewarding practice with considerable obstacles. BMC Fam Pract 2012;13:19 |
| Fortney JC, Maciejewski M, Tripathi SP, Deen TL, Pyne JM. A budget impact analysis of telemedicine-based collaborative care for depression. Med Care 2011;49:872–80 |
| Foster NL, Jagust WJ, Fox NC. A peek behind the curtain: amyloid imaging, referrals, and specialist memory evaluations. Alzheimer Dis Associated Disord 2013;27:1–3 |
| Fox KF, Tenkorang J, Rogers A, Wood DA. Are rapid access cardiology clinics a valued part of a district cardiology service? Int J Cardiol 2009;137:42–6 |
| Foy JM, Kelleher KJ, Laraque D, for the American Academy of Pediatrics Task Force on Mental Health. Enhancing pediatric mental health care: strategies for preparing a primary care practice. Pediatrics 2010;125:S87–108 |
| Free C, Phillips G, Watson L, Galil L, Felix L, Edwards P, et al. The effectiveness of mobile-health technologies to improve health care service delivery processes: a systematic review and meta-analysis. PLOS Med 2013;10:e1001363 |
| French SD, McKenzie JE, O’Connor DA, Grimshaw JM, Mortimer D, Francis JJ, et al. Evaluation of a theory-informed implementation intervention for the management of acute low back pain in general medical practice: the IMPLEMENT cluster randomised trial. PLOS ONE 2013;8:e65471 |
| Gask L, Khanna T. Ways of working at the interface between primary and specialist mental healthcare. Br J Psychiatry 2011;198:3–5 |
| Gask L, Joseph S, Hampson M. Polyclinics and psychiatry: risks and opportunities. Psychiatrist 2010;34:106–9 |
| Glaser A, Levitt G, Morris P, Tapp J, Gibson F. Children and Young People workstream of the National Cancer Survivor Initiative (NCSI), UK. Enhanced quality and productivity of long-term aftercare of cancer in young people. Arch Dis Child 2013;98:818–24 |
| Goeree R, von Keyserlingk C, Burke N, He J, Kaczorowski J, Chambers L, et al. Economic appraisal of a community-wide cardiovascular health awareness program. Value Health 2013;16:39–45 |
| Gomez Caballero ME, Corominas H, Narvaez J, Torrente V, de la Fuente de Dios D, Campoy E, et al. Diagnostic and therapeutic delay of rheumatoid arthritis patients in Catalonia (Spain) and their relationship with specialized healthcare units. The audit study. Ann Rheum Dis 2013;71:715 |
| Goonewardene SS, Symons M, McCormack G, Makar A. The Worcestershire prostate cancer survivorship programme: a new concept for holistic long-term care and follow-up. BJU Int 2014;113:116–17 |
| Grimshaw JM, Winkens RA, Shirran L, Cunningham C, Mayhew A, Thomas R, et al. Interventions to improve outpatient referrals from primary care to secondary care. Cochrane Database Syst Rev 2005;3:CD005471 |
| TOMBOLA Group. Cytological surveillance compared with immediate referral for colposcopy in management of women with low grade cervical abnormalities: multicentre randomised controlled trial. BMJ 2009;339:b2546 |
| Gruen RL, Weeramanthri TS, Knight SE, Bailie RS. Specialist outreach clinics in primary care and rural hospital settings (Cochrane Review). J Community Eye Health 2006;19:31 |
| Haggarty JM, Jarva JA, Cernovsky Z, Karioja K, Martin L. Wait time impact of co-located primary care mental health services: the effect of adding collaborative care in Northern Ontario. Can J Psychiatry 2012;57:29–33 |
| Hands LJ, Clarke M, Mahaffey W, Francis H, Jones RW. An e-health approach to managing vascular surgical patients. Telemed J E-Health 2006;12:672–80 |
| Hansson J. Coordination in networks for improved mental health service. Int J Integrated Care 2010;10:e52 |
| Harma C. Review of open-access colonoscopy referrals (ROAR study). J Gastroenterol Hepatol 2013;(28):124–5 |
| Harrison R, Macfarlane A, Murray E, Wallace P. Patients’ perceptions of joint teleconsultations: a qualitative evaluation. Health Expect 2006;9:81–90 |
| Harvey ST, Fisher LJ, Green VM. Evaluating the clinical efficacy of a primary care-focused, nurse-led, consultation liaison model for perinatal mental health. Int J Mental Health Nurs 2012;21:75–81 |
| Health Quality Ontario. Continuity of care to optimize chronic disease management in the community setting: an evidence-based analysis. Ont Health Technol Assess Ser 2013;13:1–41 |
| Holtzer-Goor KM, Plochg T, Lemij HG, van Sprundel E, Koopmanschap MA, Klazinga NS. Why a successful task substitution in glaucoma care could not be transferred from a hospital setting to a primary care setting: a qualitative study. Implement Sci 2013:8:14 |
| Houston Y, Rawle M, Patterson D, Rook L. Inflammatory bowel disease telephone helplines an audit of 9 sites across Yorkshire and Humber region, United Kingdom. J Crohn Colitis 2013;7:S295–6 |
| Iecovich E, Biderman A. Use of adult day care centers: do they offset utilization of health care services? Gerontologist 2013;53:123–32 |
| Iles R. A physiotherapy telephone assessment and advice service for patients with musculoskeletal problems can improve the process of care while maintaining clinical effectiveness. J Physiother 2013;59:130 |
| Johnson G, White A, Livingstone R. Do general practices which provide an acupuncture service have low referral rates and prescription costs? A pilot survey. Acupuncture Med 2008;26:205–13 |
| Jones J, Dunkley I, Maddocks J. OC-077 Is the referral appropriate? Gut 2013;62(Suppl. 1):33–4 |
| Kantarevic J, Kralj B, Weinkauf D. Enhanced fee-for-service model and physician productivity: evidence from family health groups in Ontario. J Health Econ 2010;30:99–111 |
| Katon W, Russo K, Lin EH, Schmittdiel J, Ciechanowski P, Ludman E, et al. Cost-effectiveness of a multicondition collaborative care intervention. Arch Gen Psychiatry 2012;69:506–14 |
| Kessler R. Mental health care treatment initiation when mental health services are incorporated into primary care practice. JABFM 2012;25:255–9 |
| Kim SE, Michalopoulos C, Kwong RM, Warren A, Manno MS. Telephone care management’s effectiveness in coordinating care for Medicaid beneficiaries in managed care: a randomized controlled study. Health Serv Res 2013; 48:1730–49 |
| Klotz J, Muir L, Cameron C, Delaney L. Monitoring a remote phototherapy unit via telemedicine. J Cutaneous Med Surgery 2005;9:47–53 |
| Laforme A, Cossette P, Nugyen DK, Bérubé AA. Epilepsy clinic hotline audit: expectations, performance, satisfaction and impact. Epilepsy Currents 2013;(13):315–16 |
| Laiteerapong N, Kirby J, Gao Y, Yu TC, Sharma R, Lee SM, et al. Health centers care for a sicker population with fewer clinic visits and fewer hospitalizations. J Genl Intern Med 2013;(28):S84 |
| Lam TP, Chow RW, Lam KL, Lennox IM, Chan FH, Tsoi SL. Evaluation of the learning outcomes of a year-long postgraduate training course in community geriatrics for primary care doctors. Arch Gerontol Geriatrics 2011;52:350–6 |
| Lau Y, Fleming C. Teledermatology service in Tayside, Scotland: a snapshot. Br J Dermatol 2013;169:138–9 |
| Lee L, Hillier LM, Stolee P, Heckman G, Gagnon M, McAlney CA, et al. Enhancing dementia care: a primary care-based memory clinic. J Am Geriatrics Soc 2010 58:2197–204 |
| Legido P, Lanzeta I, Begiristain M, Iza I, Rodriguez J, Centeno J, et al. Results of the introduction of a comprehensive health care model for plurypathological patients. Eur Intern Med 2013;24:e231 |
| Lewis R, Hendry M. A review comparing the effectiveness of nurse-led follow up for cancer with conventional care. Nurs Times 2009;105:25–7 |
| Lewis RA, Neal RD, Hendry M, France B, Williams NH, Russell D, et al. Patients’ and healthcare professionals’ views of cancer follow-up: systematic review. Br J Gen Pract 2009;59:e248–59 |
| Lineker SC, Husted JA. Educational interventions for implementation of arthritis clinical practice guidelines in primary care: effects on health professional behaviour. J Rheumatol 2010;37:1562–9 |
| Lithgo K, et al. N006 Supported Self Help and Management–SSHAMP. J Crohn Colitis 2013;7(Suppl. 1) |
| Madhan KK, Chamberlain M, Anderson E. Anaemia in patients with chronic kidney disease: Management with epoetin beta in primary care setting in New Zealand. Nephrology 2008;13:428–32 |
| McConnochie KM. Potential of telemedicine in pediatric primary care. Pediatr Rev 2006;27:e58–65 |
| Meadows GN, Harvey CA, Joubert L, Barton D, Bedi G. Best practices: the consultation-liaison in primary-care psychiatry program: a structured approach to long-term collaboration. Psychiatric Serv 2007;58:1036–8 |
| Meyer F, Peteet J, Joseph R. Models of care for co-occurring mental and medical disorders. Harvard Rev Psychiatry 2009;17:353–60 |
| Miraz S, Chetwood A. Follow-up rates: is there potential for reduction? Br J Healthc Manag 2012;18:49–50 |
| Mistry H. Systematic review of studies of the cost-effectiveness of telemedicine and telecare. Changes in the economic evidence over twenty years. J Telemed Telecare 2012;18:1–6 |
| Murphy S, Blake C, Power CK, Fullen BM. The role of clinical specialist physiotherapists in the management of low back pain in a spinal triage clinic. Irish J Med Sci 2013;182:643–50 |
| Najera C, Ivorra J, Chalmeta I, Grau E, Valero JL, Garcia-Armario MD, et al. AB0817-HPR Activity of telephone consultation to nursing by request in rheumatology. Ann Rheumatic Dis 2013;72(Suppl 3):A1090 |
| Ooi J, Vinayaga-Pavan M, Koh DCK, Morgan V, Wong VS. PTH-075 You’ve gut mail: a gastroenterology e-mail helpline is efficient and cost-effective in resolving patient queries and reducing non-elective inpatient bed-days. Gut 2013;62(Suppl. 1):A241–2 |
| O’Reilly R, Bishop J, Maddox K, Hutchinson L, Fisman M, Takhar J. Is telepsychiatry equivalent to face-to-face psychiatry? Results from a randomized controlled equivalence trial. Psychiatric Serv 2007;58:836–43 |
| Osborn N, Welch J. Providing HIV services in a GP practice. HIV Med 2013;(14):13–4 |
| Ovens L, Louison P, Elliot P. Auditing the benefits of a complex wound clinic. Wounds UK 2007;3:30–43 |
| Palmer NB, Myers KM, Vander Stoep A, McCarty CA, Geyer JR, DeSalvo A. Attention-deficit/hyperactivity disorder and telemental health. Current Psychiatry Reports 2010;12:409–17 |
| Pandor A, Thokala P, Gomersall T, Baalbaki H, Stevens JW, Wang J, et al. Home telemonitoring or structured telephone support programmes after recent discharge in patients with heart failure: systematic review and economic evaluation. Health Technol Assess 2013;17(32) |
| Parab CS, Cooper C, Woolfenden S, Piper SM. Specialist home-based nursing services for children with acute and chronic illnesses. Cochrane Database Syst Rev 2013;6:CD004383 |
| Parfitt N, Smeatham A, Timperley J, Hubble M, Gie G. Direct listing for total hip replacement (THR) by primary care physiotherapists. Clin Governance 2012;17:210–16 |
| Patel NG. Telephone follow-up in elective versus emergency surgery. Surg Endoscopy Other Interventional Techniques 2013;(27):S70 |
| Patterson V. Teleneurology. J Telemed Telecare 2005;11:55–9 |
| Peguero A, Courville C, Lamarche J. Implementation of videotelenephrology clinics: a seamless health care and role model in chronic kidney disease. Blood Purification 2013;35:155 |
| Peters AH, de Leeuw RJ. Integrating care for people with depression: developments in the Netherlands. Int J Integrated Care 2009;9 |
| Pinnock H, Netuveli G, Price D, Sheikh A. General practitioners with a special interest in respiratory medicine: national survey of UK primary care organisations. BMC Health Serv Res 2005;5 |
| Poots J, Kennedy R, Dennison T, Gatt M, Blair PH, McKinley M, et al. Nurse-led rapid access vascular examination clinic triage reduces inappropriate referrals for peripheral arterial disease. Irish J Med Sci 2011;180:363–7 |
| Pottle A. A nurse-led rapid access chest pain clinic-experience from the first 3 years. Eur J Cardiovasc Nurs 2005;4:227–33 |
| Price T, Lithgo K, Johnson MW. OC-078 Cost savings and outpatient clinic appointments saved: a 2 year review of a nurse led telephone advice line for inflammatory bowel disease. Gut 2013;62(Suppl. 1):A34 |
| Quinn EM, Corrigan MA, O’Mullane J, Murphy D, Lehane EA, Leahy-Warren P, et al. Clinical unity and community empowerment: The use of smartphone technology to empower community management of chronic venous ulcers through the support of a tertiary unit. PLOS ONE 2013;8:e78786 |
| Rabey M, Morgans S, Barrett C. Orthopaedic physiotherapy practitioners: surgical and radiological referral rates. Clin Governance 2009;14:15–19 |
| Rivas C, Abbott S, Taylor SJ, Clarke A, Roberts CM, Stone R, et al. Collaborative working within UK NHS secondary care and across sectors for COPD and the impact of peer review: qualitative findings from the UK National COPD Resources and Outcomes Project. Int J Integrated Care 2010;10:e58 |
| Roberts A, Garrett L, Godden DJ. Can telehealth deliver for rural Scotland? Lessons from the Argyll & Bute Telehealth Programme. Scott Med J 2012;57:33–7 |
| Roland M. General practitioners with special interests – not a cheap option. BMJ 2005;331:1448–9 |
| Roth MT, Ivey JL, Esserman DA, Crisp G, Kurz J, Weinberger M. Individualized medication assessment and planning: optimizing medication use in older adults in the primary care setting. Pharmacotherapy 2013;33:787–97 |
| Ryan T, Hatfield B, Sharma I. Outcomes of referrals over a six-month period to a mental health gateway team. J Psychiatric Mental Health Nurs 2007;14:527–34 |
| Saario S. Managerial reforms and specialised psychiatric care: a study of resistive practices performed by mental health practitioners. Sociol Health Illn 2012;34:896–910 |
| Sadatsafavi M, FitzGerald M, Marra C, Lynd L. Costs and health outcomes associated with primary vs. secondary care after an asthma-related hospitalization: a population-based study. Chest 2013;144:428–35 |
| Salahuddin S, Paisley A, Young B. The use of remote technology in delivering care during pregnancy in patients with pre-pregnancy diabetes. Diabetic Med 2013;30:169 |
| Salam MA, Matai V, Salhab M, Hilger AW. The facial skin lesions ‘see and treat’ clinic: a prospective study. Eur Arch Oto-Rhino-Laryngol 2006;263:764–6 |
| Salazar-Fernandez CI, Herce J, Garcia-Palma A, Delgado J, Martin JF, Soto T. Telemedicine as an effective tool for the management of temporomandibular joint disorders. J Oral Maxillofacial Surg 2012;70:295–301 |
| Salisbury C, Montgomery AA, Hollinghurst S, Hopper C, Bishop A, Franchini A, et al. Effectiveness of PhysioDirect telephone assessment and advice services for patients with musculoskeletal problems: pragmatic randomised controlled trial. BMJ 2013;346:f43 |
| Salles N, Jenn J, Barateau M, Sarry O, Libery M, Baudinet M, Rainfray M. Telemedicine consultation for patients with chronic wounds especially pressure ulcers. Eur Geriatric Med 2013;4:S113 |
| Schou M, Gustafsson F, Videbaek L, Tuxen C, Keller N, Handberg J, et al. Extended heart failure clinic follow-up in low-risk patients: a randomized clinical trial (NorthStar). Eur Heart J 2013;34:432–42 |
| Serginson J. Asthma management in a respiratory nurse practitioner outpatient clinic. Respirology 2013;18:11 |
| Shanley S, Myhill K, Doherty R, Ardem-Jones A, Hall S, Vince C, et al. Delivery of cancer genetics services: the Royal Marsden telephone clinic model. Fam Cancer 2007;6:213–19 |
| Shore JH. Telepsychiatry: videoconferencing in the delivery of psychiatric care. Am J Psychiatry 2013;170:256–62 |
| Sibbald B. Direct access to diagnostic services. Br J Gen Pract 2009;59:e144–5 |
| Siddique K, El-Abyed S, Basu S. One-stop cholecystectomy clinic: a way forward for the future? Surg Endoscopy Other Interventional Techniques 2013;27:S34 |
| Siriwardena LS, Wickramasinghe WA, Perera KL, Marasinghe RB, Katulanda P, Hewapathirana R. A review of telemedicine interventions in diabetes care. J Telemed Telecare 2012;18:164–8 |
| Smellie WSA, Robson CA. Use of a parallel clinical advisory service to support lipid lowering in primary care. Qual Prim Care 2003;11:199–203 |
| Health Quality Ontario. Specialized nursing practice for chronic disease management in the primary care setting: an evidence-based analysis. Ont Health Technol Assess Ser 2013;13:1–66 |
| Spierings N, et al. The 5-year itch: comparison of walk-in vs. choose-and-book emergency dermatology clinics in 2007 and 2012. Br J Dermatol 2013 |
| Steventon A, Bardsley M, Billings J, Dixon J, Doll H, Beynon M, et al. Effect of telecare on use of health and social care services: findings from the Whole Systems Demonstrator cluster randomised trial. Age Ageing 2013;42:501–8 |
| Steventon A, Tunkel S, Blunt I, Bardsley M. Effect of telephone health coaching (Birmingham OwnHealth) on hospital use and associated costs: cohort study with matched controls. BMJ 2013;347:f4585 |
| Taleb AC, Böhm GM, Avila M, Wen CL. The efficacy of telemedicine for ophthalmology triage by a general practitioner. J Telemed Telecare 2005;11(Suppl. 1):83–5 |
| Tappin D, Nawaz S, McKay C, MacLaren L, Griffiths P, Mohammed TA. Development of an early nurse led intervention to treat children referred to secondary paediatric care with constipation with or without soiling. BMC Pediatrics 2013;13:193 |
| Taylor R, Marley A. An integrated model for community COPD care. Aust J Prim Health 2006;12:45–50 |
| Taylor SJC. Effectiveness of innovations in nurse led chronic disease management for patients with chronic obstructive pulmonary disease: systematic review of evidence. BMJ 2005;331:485 |
| Teegala P, Mackay V. Primary infertility referrals to the gynaecology clinic in Glasgow South – can we improve the patient journey? BJOG 2013; Wiley-Blackwell, NJ USA |
| Thompson E, Pearson MG, Davies L, McKnight E, Trusdale A, Sargeant K, et al. S71 Computer-guided consultation in COPD practice. Thorax 2013;68(Suppl 3):38–9 |
| Twist M. Rate of incomplete excision of basal cell carcinomas by general practitioners with special interest. Br J Dermatol 2009;161:187 |
| Ukena C, Bohm M. Management of heart failure: are specialists really needed? Eur Heart J 2013;34:416–18 |
| Vahidi RG, Mojahed F, Jafarabadi MA, Gholipour K, Rasi V. A systematic review of the effect of payment mechanisms on family physicians service provision and referral rate behavior. J Pakistan Med Students 2013;3:54–60 |
| van de Pol AC, van der Gugten AC, van der Ent CK, Schilder AG, Benthem EM, Smit HA, et al. Referrals for recurrent respiratory tract infections including otitis media in young children. Int J Pediatr Otorhinolaryngol 2013;77:906–10 |
| Van Der Feltz-Cornelis CM, van Oppen P, Adèr HJ, van Dyck R. Randomised controlled trial of a collaborative care model with psychiatric consultation for persistent medically unexplained symptoms in general practice. Psychother Psychosom 2006;75:282–9 |
| van Dijk P, Hogervorst W, ter Riet G, van Dijk F. A protocol improves GP recording of long-term sickness absence risk factors. Occupational Med 2008;8:257–62 |
| van Gurp N, Boonman-De Winter LJM, Meijer Timmerman Thijssen DW, Stoffers HEJH. Benefits of an open access echocardiography service: a Dutch prospective cohort study. Neth Heart J 2013;21:399–405 |
| van Orden M, Hoffman T, Haffmans J, Spinhoven P, Hoencamp E. Collaborative mental health care versus care as usual in a primary care setting: a randomized controlled trial. Psychiatric Serv 2009;60:74–9 |
| Vigen R, et al. Patterns of outpatient follow-up after acute myocardial infarction: follow-up frequency is associated with utilization of evidence-based therapies. Circulation 2013;6(Suppl.):A184 |
| Vincent MW, Brown D, Tulloch D. Does allowing GPs direct access to CT KUB decrease emergency attendances or outpatient referrals? BJU Int 2013 |
| Watson J, McDonnell V, Bhaumik S. Valuing people: evaluating referral systems: a study of a multidisciplinary single point of referral system to dedicated adult learning disability health services in Leicester, UK. Br J Develop Disabil 2005;51:155–70 |
| Wilkinson OM, Duncan-Skingle F, Pryor JA, Hodson ME. A feasibility study of home telemedicine for patients with cystic fibrosis awaiting transplantation. J Telemed Telecare 2008;14:182–5 |
| Willems D, Joore M, Hendriks J, Nieman F, Severens J, Wouters E. The effectiveness of nurse-led telemonitoring of asthma: results of a randomised controlled trial. J Eval Clin Pract 2008;14:600–9 |
| Williams L, Fryer J, Andrew R, Powell C, Pink J, Elwyn G. Setting up a paediatric rapid access outpatient unit: views of general practice teams. BMC Fam Pract 2008;9:54 |
| Wootton R, Tait A, Croft A. Environmental aspects of health care in the Grampian NHS region and the place of telehealth. J Telemed Telecare 2010;16:215–20 |
| Wootton R, Bloomer SE, Corbett R, Eedy DJ, Hicks N, Lotery HE, et al. Multicentre randomised control trial comparing real time teledermatology with conventional outpatient dermatological care: societal cost–benefit analysis. BMJ 2000;320:1252–6 |
| Wootton R. Realtime telemedicine. J Telemed Telecare 2006;12:328–36 |
| Wootton R. Twenty years of telemedicine in chronic disease management--an evidence synthesis. J Telemed Telecare 2012;18:211–20 |
| Yeung RO, Oh M, Tang TS. Does a 2.5-year self-management education and support intervention change patterns of healthcare use in African-American adults with type 2 diabetes? Diabet Med 2014;31:472–6 |
Appendix 4 Referral management centres: interview topic guide
Introduction
We are conducting this interview as part of a research study designed to identify and review what is currently known about strategies involving primary care that are designed to improve the effectiveness and efficiency of outpatient services.
Within this study we are conducting a literature review, and substudies of different types of scheme, one of which is referral management centres.
This is one of four localities, in each of which we are conducting three or four interviews with clinicians and managers.
We are trying to find out which aspects of these schemes work well and which ones do not work so well, so that people who may be setting up similar schemes can learn from other people’s experience.
Findings of the study will be written up for publication in a report and journal articles. We will not use attributable quotes without your express permission. Interviews may be followed up with e-mail correspondence or by phone, and we will not use quotes from any e-mails or phone calls without your express permission.
See overleaf for questions and key prompts.
Theories to bear in mind in relation to key topics are outlined in green.
Questions and key prompts
Intervention design: Please describe the referral management centre with which you have been involved. [Probe on the following.]
-
What does it consist of?
-
How is it financed?
-
Who initiated it?
-
Who is leading the intervention?
-
Who is involved in running it? Which services are involved?
-
What has your role been in the initiation, and running of the centre?
-
When was it introduced?
Aims: Please describe the aims of the centre. [Probe on the following.]
-
Why was the centre initiated?
-
What were the expected outcomes? [Probe on patient outcomes, financial outcomes, service utilisation, staff outcomes . . . etc.]
-
How did aims and expectations vary between the different stakeholders involved? Did others have different expectations?
THE BASIC THEORY: The ‘theory’ is that: they (the old provider) was profligate, inappropriate, insensitive, unsafe, slow and inaccurate, whilst we (the new structure) will ensure referrals are parsimonious, appropriate, sensitive, safe, delay free, accurate etc., etc.
POSITIVE THEORIES:
-
RMCs offer better matching of demand with capacity by diverting referrals to services with spare capacity, away from those with long waiting lists and, where appropriate, by preventing unnecessary referrals from reaching secondary care.
-
RMCs produce immediate, systematic data on the volume and distribution of referrals and on use of services, which can be used by commissioners to better plan services.
-
Through improved data collection, RMCs enable commissioners to keep a closer eye on costs and challenge the costs associated with them.
-
RMCs can support patient choice because specialist RMC staff, rather than hard pressed physicians, are better placed to discuss a patient’s choice.
-
RMCs provide feedback to GPs on their referrals , which provides a learning opportunity for GPs and can improve the quality of their referrals in the future.
Changes: Please describe how the scheme has changed since it was initiated. [Probe on the following.]
-
Did the initial implementation go to plan?
-
If there were changes, why were they made? Who initiated them?
-
What was the result of these changes?
-
Have there been changes in impact during the life of the scheme?
Outcomes: What do you feel the scheme has achieved? [Probe on the following.]
-
How could success be measured in terms of key outcomes? [Probe on effects on number of referrals, appropriateness of referral destination, health outcomes, cost of health services.]
-
How do you know that you have achieved the (desired) outcomes?
-
Have there been unexpected outcomes?
-
What have been the effects on the local organisation of primary care and the workforce?
Acceptability: Would you recommend a similar scheme to colleagues in other localities?
-
How have patients responded to these changes? Are they aware of them?
-
How have staff responded to the intervention?
-
How do you think that your view might compare to the views of others?
-
What has the wider impact been on the Trust and beyond?
NEGATIVE THEORIES:
-
RMC staff are less able to make appropriate decisions about referrals than GPs because they lack accumulated wisdom on the particular patient or because they lack the clinical skills, knowledge, expertise or experience , which may, at worse, lead to threats to patient safety.
-
RMCs threaten existing relationships between GPs and consultants and the ability of GPs to refer to a consultant of their choice.
-
RMCs are imposed on GPs by managers with the idea of cutting costs, rather than improving care and, as such, GPs may be reluctant to engage with them.
-
RMCs may deskill local GPs as they simply refer to the RMC instead of using their clinical skill and referral guidelines to decide whether the patient needs to be referred.
-
GPs do not value the feedback provided from RMCs as they perceive it is given by someone with less clinical experience/authority than themselves.
-
RMCs may limit patient choice – patients themselves may be unhappy that the referral decision (whether to refer and where to refer) is made by someone other than their GP and may return to their GP to request a referral to their preferred location.
Local context: Please describe the local context in which the scheme has been implemented. [Probe on the following.]
-
What do you consider were the main enablers in implementing the intervention? [Probe on available resources, staffing, commitment, work culture, ring-fenced time . . .]
-
What do you consider were the main challenges to implementing the intervention and what were the consequences of this? [Probe on resources and time constraints, resistance to change, logistics . . .]
REMEDIAL THEORIES – the circumstances in which GPs will engage with RMCs:
-
If GPs are involved in the process of setting up an RMCs.
-
It can be shown to work as a pilot initially.
-
They ensure the smooth flow of referrals rather than prevent referrals.
-
The GPs undertaking the reviewing are senior and well respected so that referring GPs respect the decisions they make.
-
If the reviewers are not GPs, it helps if the referring GP knows who is doing the reviewing and can judge whether they have the experience and expertise to carry out the review.
-
There is a two-way communication between the referring GP and the reviewer.
-
The driver is quality improvement, not reducing referrals or cost cutting.
-
Patients are informed about the ways in which RMCs work and what will happen to their referral.
Wrap up
Thank you for your time and your input.
Are there others we should talk to who would have different perspectives?
Appendix 5 In-house review of referrals: interview topic guide
Introduction
We are conducting this interview as part of a research study designed to identify and review what is currently known about strategies involving primary which are designed to improve the effectiveness and efficiency of outpatient services.
Within this study we are conducting a literature review, and 4 substudies of different schemes, one of which is in-house review of referrals.
We are conducting 3/4 interviews in each locality, which will contribute to the substudy on in-house review of referrals.
We are trying to find out what aspects of these schemes work well and which ones do not work so well, so that people who may be setting up similar schemes can learn from other people’s experience.
No quotes will be attributed without express permission. The draft report will be shared.
Any questions?
Theory to bear in mind shown in green italics.
Questions
Intervention design: Please describe the system for peer review of referrals with which you have been involved. [Probe on the following.]
-
How and when did the scheme originate?
-
What does it consist of?
-
How is it financed? Does the scheme come under a local enhanced service payment?
-
Who is involved in running it?
-
What has your role been in the initiation, and running of the centre?
-
Have there been changes to the way the scheme has operated over time?
-
Are there other things included under the same scheme, e.g. standard format for referral letters, use of guidelines?
Aims: Please describe the aims of the scheme. [Probe on the following.]
-
Why was the scheme initiated?
-
What were the expected outcomes? [Probe on patient outcomes, financial outcomes, service utilisation, staff outcomes . . . etc.]
-
How did aims and expectations vary between the different stakeholders involved? Did others have different expectations?
-
What benefits and opportunities have been created by the implementation of the scheme?
-
What challenges or issues have been created by the implementation of the scheme?
Peer review provides an opportunity to share knowledge and expertise amongst colleagues, enabling GPs to identify alternative management strategies for the patient and thus avoid a referral to secondary care.
Peer review enables GPs to make better referral decisions in the future through increasing their confidence to resist pressure for referral, enhancing their knowledge and skills of current best practice and increasing their tolerance of uncertainty.
Through sharing knowledge and expertise, peer review enables GPs to build up feelings of mutual trust and support from colleagues, which in turn enables them to avoid referrals to secondary care for reassurance.
Peer review and feedback may prompt or motivate GPs to ensure that they have completed the necessary investigations prior to referring and to document these findings more thoroughly in their referral letters.
Changes: Please describe how the scheme has changed since it was initiated. [Probe on the following.]
-
Has the scheme changed in any way since it was first set up?
-
Why were these changes made and what was the result of these changes?
-
Have there been changes in impact during the life of the scheme?
Acceptability: How well has the scheme been received? [Probe on the following.]
-
How acceptable do you find the scheme?
-
How have other practice staff responded to the scheme?
-
Are patients aware of these changes? How have they responded?
Requirements for prospective in-house review may leave patients thinking that their own GP is not capable of making referral decisions.
Outcomes: What do you think the scheme has achieved? [Probe on the following.]
-
How would success be measured in terms of key outcomes?
-
What has been the effect on these outcomes? [Probe on effects on number of referrals, appropriateness of referral destination, health outcomes, cost of health services.]
-
Impact on GP practice, hospital?
-
How do you know that you have achieved the (desired) outcomes?
-
Have there been unintended consequences of the scheme?
-
What have been the effects on the local organisation of primary care and the workforce?
-
How do you think that your view might compare to the views of others?
-
Do you think that the acceptability/effectiveness of the scheme depends on who carries out the review – which GP or other colleague? Specialist versus generalist? GP versus consultant?
-
What elements of the scheme are working better or less well?
-
How could the scheme be improved?
-
Preferences between this scheme and other referral management schemes.
Peer review may improve the knowledge, skills and confidence of GPs but does not change their referral behaviour.
Prospective in-house review may cause delays for patients in being referred.
Peer review does not change GP behaviour because GPs do not trust the validity of the data/feedback.
Peer review is more likely to change behaviour if it is undertaken by consultants as they have more clinical expertise in particular specialist areas.
However, as consultants may also vary and therefore the consistency of their review and decision making can be improved by using referral guidelines to make their decisions.
Peer review is more likely to change GP referral behaviour if there are supportive relationships amongst colleagues and a shared culture and sense of ownership of the peer review process.
Prospective peer review may be more likely to change referral behaviour because it challenges behaviour in real time.
Prospective peer review is more likely to change behaviour if it also accompanied by an educational component involving feedback and discussion of the decision amongst peers.
Local context: Please describe the local context in which the scheme has been implemented. [Probe on the following.]
-
What do you consider were the main enablers in implementing the intervention? [Probe on available resources, staffing, commitment, work culture, ring-fenced time . . .]
-
What do you consider were the main challenges to implementing the intervention and what were the consequences of this? [Probe on resources and time constraints, resistance to change, logistics . . .]
Peer review is more likely to change behaviour if is incentivised , for example, with CPD points or with QOF payments.
Peer review is more likely to be effective if protected time for participation is resourced , for example, under a Local Enhanced Service Directive.
Peer review is particularly useful for in areas where there are unusually high variations in referral rates amongst practices.
Peer review may be particularly useful in supporting referral decision making for patients with repeat visit to their GP with the same problem.
Wrap up
Thank you for your time and your input.
Are there others we should talk to who would have different perspectives?
Appendix 6 International experiences: country selection
To identify countries for inclusion in this report, we used the definition of primary care gatekeeping proposed by Kringos250 and Kringos et al. ,251 which conceptualised gatekeeping in relation to the degree to which referral would be required for patients to access a range of medical, paramedical and nursing disciplines, namely gynaecologist/obstetrician; paediatrician; specialist of internal medicine; ophthalmologist; ENT specialist; cardiologist; neurologist; surgeon; primary care or GP practice nurse; specialised nurse (e.g. for diabetes); home care nurse; physiotherapist (ambulatory); midwife (ambulatory); occupational therapist; speech therapist; and dentist.
Based on this conceptualisation, the authors distinguished four categories of gatekeeping systems:251
-
No gatekeeping system in place: patients have direct access to the majority of specialist physicians.
-
No gatekeeping system, but there are incentives in place: patients have direct access to the majority of specialist physicians but will have to pay the costs of the visit.
-
Partial gatekeeping system in place: patients require referral for some specialist physicians.
-
Gatekeeping system in place: patients normally require a referral for the majority of specialist physicians.
Table 26 provides an overview of European high-income OECD countries252 in relation to primary care gatekeeping as described by Kringos, which also classifies countries by whether or not GPs have a patient list system in place: that is, a list of residents registered with their practice. 250
| Country | Direct access to majority of specialist physiciansa | Direct access to majority of specialist physicians, additional paymenta | (Partial) gatekeeping: referral for some/majority of specialist physiciansa | Patient list system in placea | Strength of primary care system (Kringos et al. 2013)b |
|---|---|---|---|---|---|
| Austria | ✗ | No | Weak | ||
| Belgium | ✗ | No | Strong | ||
| Czech Republic | ✗ | Medium | |||
| Denmark | ✗c | Strong | |||
| Estonia | ✗ | Strong | |||
| Finland | ✗d | Strong | |||
| France | ✗ | No | Medium | ||
| Germany | ✗ | No | Medium | ||
| Greece | ✗ | Weak | |||
| Iceland | ✗ | Weak | |||
| Ireland | ✗ | No | Weak | ||
| Italy | ✗ | Medium | |||
| Luxembourg | ✗ | No | Weak | ||
| The Netherlands | ✗ | Strong | |||
| Norway | ✗ | Medium | |||
| Poland | ✗ | Medium | |||
| Portugal | ✗ | Strong | |||
| Slovak Republic | ✗ | Weak | |||
| Slovenia | ✗ | Strong | |||
| Spain | ✗ | Strong | |||
| Sweden | Varies across regions | No | Medium | ||
| Switzerland | ✗ | No | Medium | ||
| UK | ✗ | Strong |
Appendix 7 International experiences: data collection template
Background
Health systems vary in relation to the provision of primary and secondary care and the ways patients and users access these. At the same time, the nature of the delivery of health-care services itself is changing, slowly in some instances and more rapidly in others, increasingly blurring the traditional boundaries between what used to be considered primary and secondary care. 242 For example, new developments in medical technology have made it possible to provide many services closer to the patient, with diagnostic or therapeutic interventions that would previously have required a hospital environment now being carried out in ambulatory settings. 242 Elsewhere, advances in medical devices and telemonitoring technology allow for the monitoring and control of many chronic conditions in people’s homes.
Although the acute hospital will always play an important role in the provision of health care, both as a key locale for teaching, training and research as well as in the management of complex and rare disorders, there have been increasing concerns about health systems’ dependence on hospital-based delivery and the efficiency of such services given the changing disease burden and related demand for services. 242 There are also concerns about the (perceived) high costs of hospital care and the notion of moving care into the community as a means to increase accessibility of services and thus the responsiveness of the system, and, potentially, reduce costs.
Consequently, health-care systems have been experimenting with new ways of shifting specialist services from hospital into the community, for example by transferring or relocating diagnostic services, access to which is often considered a crucial bottleneck in NHS-type systems in particular, into the primary care setting. 242 An example is the ‘Closer to Home’ initiative in England which sought to substitute community for hospital care through making greater use of specially trained community staff (‘practitioners with special interests’) and through the increased provision of diagnostic and treatment facilities in community settings. 242 Approaches such as this have been found to be effective in improving access to specialist care for patients and reducing the demand on acute hospitals. 242 However, there is concern about the quality of care while evidence of the impact on cost has remained inconclusive.
In this project we have been commissioned by the NIHR’s HSDR programme in England to update an earlier scoping review by Roland et al. of strategies involving primary care that are designed to improve the effectiveness and efficiency of outpatient services. 2
In order to focus the review, we conceptualise interventions designed to reduce hospital outpatient attendance in four categories:
Transfer: the substitution of services delivered by hospital clinicians for services delivered by primary care clinicians.
Relocation: shifting the venue of specialist care from outpatient clinics to primary care without changing the people who deliver the service.
Liaison: joint working between specialists and primary care practitioners to provide care to individual patients.
Professional behaviour change: interventions intended to change the referral behaviour of primary care practitioners, including referral guidelines, audit and feedback, professional education and financial incentives.
As part of this review we are interested in learning about experiences in a range of high-income countries of innovative approaches and models of care designed to enhance the effectiveness of services at the primary–secondary care interface. We focus on systems that have a strict primary care gatekeeping system in place in order to enable lesson learning for the NHS in England.
How to complete the data collection template
The following sections I–IV provide a template for collection of information on specific activities/approaches in each of the four categories described above. We would like to ask you to consider the situation in your country and provide for each of the activities/approaches data on whether these are:
-
routinely available/offered in primary care (or equivalent settings)
-
available/offered in selected regions/GP practices (or equivalent settings)
-
considered for implementation/currently piloted
-
not available at all.
We ask you to adopt an evidence-based approach as far as possible, by making use of the best data available, using all relevant sources. Suitable data sources include completed/ongoing research projects; policy documents; or routine statistics, surveys and census data related to primary care.
Where appropriate and necessary, additional information may be gathered through interviews with key stakeholders and reviews of work in progress such as pilot projects, Green/White Papers, consultation documents, committee reports, parliamentary hearings, proposals, etc.
Please follow the list of points as closely as possible by inserting the requested information in the space provided. Use additional space where necessary.
Please provide definitions where relevant.
Please provide references for data sources used, where relevant.
Where data are not available and/or not reliable or where a particular point/question is not answerable, please describe where and why this is the case.
Transfer of services
Under this heading we consider the transfer of services or elements of services from secondary to primary care practitioners.
Which of the following working arrangements are provided in primary care in your country:
| Routinely available across primary care | Routinely available in selected regions/GP practices | Considered for introduction/currently piloted | Not available in primary care | Comment | |
|---|---|---|---|---|---|
| Please provide examples for each category where applicable | |||||
| I.1 Minor surgery clinics operated by GPs instead of hospitals Examples: injections (joint and soft tissue), cautery incorporating cryotherapy (e.g. warts and verrucae), excisions (e.g. cysts, skin lesions for histology), incisions (abscesses, cysts) |
|||||
| I.2 Medical clinics run by general practice teams that substitute for hospital outpatient clinics in the management of patients with chronic diseases such as diabetes Examples: GP or nurse-led diabetes clinic in primary care |
|||||
| I.3 GPs with special interests (UK: GPwSIs) who substitute for outpatient specialists in receiving referrals from other GPs These GPs will normally have received special training and therefore have skills beyond those normally expected of a GP |
|||||
| I.4 Discharge of outpatients to (i) no follow-up, (ii) patient-initiated follow-up or (iii) general practice follow-up, as alternatives to routine follow-up in hospital outpatient clinics These constitute a significant change from traditional patterns of follow up in specialist clinics. They may involve long-term follow up or surveillance, for example GP follow-up of cancer patients in remission/following initial therapy, or shorter-term follow-up, for example patients post-inpatient surgery. These approaches are systematically implemented in a move to reduce follow up by specialists |
|||||
| I.5 Direct access for GPs to hospital-based diagnostic tests and investigations Direct-access diagnostic services providing test results that assist the GP in selecting an appropriate course of treatment. Examples include echocardiography, electrocardiography; gastroscopy/sigmoidoscopy, radiology and ultrasound |
|||||
| I.6 Direct access for GPs to hospital-provided treatments, without the prior approval of a specialist in an outpatient clinic Direct-access treatment services are targeted to conditions where the diagnosis can easily be made by a primary care professional and the treatment is routine. We distinguish (i) direct access to physiotherapy; (ii) direct referral to routine or minor surgery; or (iii) direct referral to hearing aid or orthopaedic appliance fitment |
|||||
Relocation to primary care
Under this heading we consider shifting the location of specialist care from outpatient clinics to primary care without changing the people who deliver the service.
Which of the following working arrangements are provided in primary care in your country:
| Routinely available in primary care | Routinely available in selected regions/GP practices | Considered for introduction/currently piloted | Not available in primary care | Comment | |
|---|---|---|---|---|---|
| Please provide examples for each category where applicable | |||||
| II.1a Shifted outpatient (or outreach) services – in which outpatient clinics are relocated to primary care settings We here refer to services provided in a clinic setting, for example by a specialist doctor or a specialist nurse |
|||||
| II.1b Shifted outpatient (or outreach) services – in which outpatient clinics are relocated to the community In contrast to I.1a this refers to services where the location may be less well defined – e.g. follow-up by phone or home visit from a specialist COPD nurse, home visits from a specialist palliative care team |
|||||
| II.2a Telemedicine: ‘the use of telecommunication and information technologies in order to provide clinical health care at a distance’ Examples: telemedicine consultation with/without GP present; teledermatology/photo-triage for suspected skin cancer; digital data transmission from primary care (or patient) to hospital specialist, etc. |
|||||
| II.2b Telecare: ‘remote care, often using sensing devices, of old and physically less able people, enabling them to remain living in their own homes’ Examples: home monitoring of patients and transmission of results (e.g. blood pressure, detectors for falls, bed and chair occupancy sensors, epilepsy sensors) to specialist base |
|||||
| II.3 Attachment of specialists to primary care teams In contrast to II.1 (shifted outpatient clinics) the specialist is integrated within the primary care team, and often employed by the primary care team. We distinguish (i) specialist doctors from (ii) other health-care professionals (for example psychologists) |
|||||
| II.4 Community mental health teams Multidisciplinary teams based in the community (drawn from nurses, psychiatrists, psychologists, and social workers) that aim largely to replace hospital-based care for patients with mental illness |
|||||
Liaison with primary care
Under this heading we consider joint working between primary and secondary care clinicians in the management of individual patients.
Which of the following working arrangements are provided in primary care in your country:
| Routinely available across primary care | Routinely available in selected regions/GP practices | Considered for introduction/currently piloted | Not available in primary care | Comment | |
|---|---|---|---|---|---|
| Please provide examples for each category where applicable | |||||
| III.1 Shared care (joint management plans) Model of working in which a hospital specialist and a primary care practitioner agree a joint management plan that specifies which elements of care for a particular patient are to be delivered by each clinician. Examples: regular communication system between the specialty and primary care |
|||||
| III.2 Consultation liaison (joint consultations and management plans) Examples: on-site mental health workers providing support to primary care providers in managing patients with mental health or other problems; psychiatric key worker working in collaboration with primary care, etc. |
|||||
Professional behaviour change
Under this heading we consider interventions intended to change the referral behaviour of primary care practitioners, including referral guidelines, audit and feedback, professional education and financial incentives.
Which of the following arrangements are commonly found in primary care in your country:
| Routinely used across primary care | Routinely used in selected regions/GP practices | Considered for introduction/currently piloted | Not used in primary care | Comment | |
|---|---|---|---|---|---|
| Please provide examples for each category where applicable | |||||
| IV.1 Guidelines for specialist referral | |||||
| IV.2 Audit and feedback on patterns of referral | |||||
| IV.3 Academic detailing – individual education or coaching by specialists, e.g. by visiting primary care practices | |||||
| IV.4 Professional education aimed at improving the quality of outpatient referrals | |||||
| IV.5 In-house referral This may be one of the following: (a) a systematic approach which uses a second GP to review referrals before they leave the practice (b) One or more GPs in a practice having an interest in a particular clinical area and informally being asked to see patients who might otherwise be referred to a specialist |
|||||
| IV.6 Referral management centres These are administrative facilities outside general practice that assess referrals from GPs to specialists, normally resulting in one of three actions: (a) Onward transmission of the referral to a specialist (b) Diversion of the referral to a community facility (e.g. diversion of orthopaedic referrals to a physiotherapist (c) Return of the referral to the GP, e.g. because it does not meet referral guidelines |
|||||
| IV.7 Financial incentives These would be schemes where there is a direct financial benefit to GPs to reduce referrals to specialists |
|||||
Appendix 8 International experiences: summary overview of country surveys
This appendix provides a summary overview of data collected in Denmark, Finland, the Netherlands and Spain on the range of approaches designed to enhance the effectiveness of services at the primary–secondary care interface, including transfer, relocation, liaison and professional behaviour change.
Transfer
Minor surgery clinics operated by general practitioners
The provision of minor surgery clinics in primary care is common in all four countries reviewed, although the range and scope of surgical interventions varies (Table 27).
| Denmark | Finland | The Netherlands | Spain |
|---|---|---|---|
| Routinely available across primary care There is specific remuneration (fee-for-services) for minor surgery,266 which includes:
|
Routinely available across primary care Covers procedures carried out under local anaesthesia, including (but not limited to) the following: Dermatology
|
Routinely available across primary care In place since 2002.267,268 The frequency with which different procedures are performed by GPs or primary care practice nurses varies:253 Always
|
Routinely available across primary care Dermatology
Piloted
|
Medical clinics
The provision of medical clinics in primary care is common in all four countries reviewed but similar to surgical clinics, their range, scope and availability vary (Table 28).
| Denmark | Finland | The Netherlands | Spain |
|---|---|---|---|
| Routinely available across primary care Basic (and also in some instances more advanced) follow-up is performed by GPs. This includes follow-up for diabetes, COPD, asthma, hypertension and other conditions GPs have an electronic record supporting them in following the guidelines; e.g. anticoagulation is now best treated in general practice |
Routinely available across primary care Larger health centres provide ‘mini-clinics’ for diabetes, asthma, anticoagulant therapy, rheumatoid arthritis, common mental health and problems. In smaller health centres, these are typically provided by nurses One example is Alzheimer’s disease and other dementias: larger health centres have consulting neurologists or geriatricians; most health centres have nurses with special training or skills for both detection and support after diagnosis |
Routinely available across primary care Practice nurse- or assistant-led diabetes treatment programmes Practice assistant- or nurse-led care for COPD, cardiac risk management, depression, financed through (integrated) reimbursement (‘bundled payments’)280 Practice assistant- or nurse-led care in mental health: in place since 2008, with practice assistants or nurses working in primary care to support GPs in diagnosis and patient support, so moving treatment of patients with relatively mild mental health problems into primary care306 |
Routinely available across primary care There are numerous clinics although not necessarily all primary care centres provide services in the field of:
|
General practitioners with a special interest
Although in all four countries reviewed here the notion of GPwSIs in a given area is common, a formalised role such as that conceptualised in the present study is not common in countries outside the UK. For example, in Denmark there are GPwSIs, but they do not formally receive referrals or substitute for hospital-based doctors. However, some GPs are very experienced, for example, in cognitive therapy.
Similarly, in Spain it is common that GPs in different primary care centres have a special interest in particular diseases, procedures or specialties, such as mental health, diabetes, dermatology, cardiovascular disease or children’s and women’s health. However, they have not necessarily received special and regular training in the related field and the focus is also not necessarily on substituting outpatient specialist care or reducing hospital referrals. There was some interest, for instance, from the Spanish Royal College of Physicians in introducing the concept of a ‘general practitioner with a special interest’ in Spain following its introduction in the UK in the early 2000s. It was seen to increase low motivation among some GPs, implicitly addressing the suggestion that many family medicine specialists would rather be hospital specialist. However, this proposal was not taken up. 307
In Finland, especially in larger health centres with 12–16 GPs, some GPs can be more experienced in given areas of medical care such as diagnostics of asthma, diabetes complications, psychiatric problems or dementia. One other example includes gynaecological and obstetric skills, with some GPs having worked for a time in specialist clinics to acquire relevant skills; they may then take on broader responsibilities in the health centre, such as performing obstetric ultrasound examinations, which can, at times, extend further into a wider range of areas, such as abdominal, urological or DVT. In those settings, internal referral is likely to occur frequently, but there are few data on how common this is.
There have been proposals by Finnish specialists that GPs should develop a form of ‘mini-specialty’, to be acquired through training in a specialist clinic for 1–2 years to thoroughly learn certain skills and so become ‘specialists’ inside their organisations. 289 This, it was argued, would enable GPs to see all patients with the disease in question and so reduce the need to refer these to specialist services. GPs as a profession have been reluctant towards this proposal, believing that although GPs with special skills could be beneficial, their core role should remain that of a resource inside their organisation and help others to maintain and broaden their skills while refraining from building lists of patients with given diseases only.
Discharge from outpatients to primary care
Discharge from outpatients to primary care constitutes a considerable change from traditional patterns of follow-up in specialist clinic and the way which such approaches are being pursued (or, indeed, understood) in different countries varies (Table 29).
| Denmark | Finland | The Netherlands | Spain |
|---|---|---|---|
| For some conditions GPs are responsible for follow-up but for others (such as cancer) GPs are not involved. However, nearly all patients discharged from hospital are ‘referred’ back to their GP for further follow-up | Patients with many types of cancer in remission: patients who use some prophylactic cancer medications and that require follow-up Psychiatric patients requiring support in daily living (these patients were moved to primary care in large numbers in the 1990s) Growing number of type 1 diabetes patients using insulin Many health centres have trained their nurses to take care of patients with special devices which previously would be considered to be the responsibility of the specialist clinic |
Co-location of general practice office at with a hospital emergency department. This is intended to prevent people from using the emergency department for conditions that should be provided within primary care259 | This type of outpatient service follow-up is not generally available in most Spanish regional health services. There are some experiences in routine follow-up in physiotherapy units that are established in primary care in some regions (e.g. Madrid, Andalusia, Castilla León, Castilla La Mancha) |
In Denmark and Finland, discharge from outpatients to primary care is common practice, although in Denmark this typically excludes cancer. In Finland, hospital outpatient follow-ups are systematically transferred to primary care as a means to reduce pressure on outpatient services, unless there are specific reasons to keep the responsibility at the specialist level. Examples for the latter include cancers and many less common neurological diseases (Parkinson’s disease, multiple sclerosis) but even in these cases there may be a shared responsibility, in which the primary care level would see the patient in between specialist appointments and consult the specialist if required. One recent example is an ongoing pilot of the provision of continuous positive airway pressure therapy for sleep apnoea patients in primary care. 308
Direct access to diagnostic tests and investigations
All four countries allow for direct access to selected diagnostic services which can then assist the GP in selecting an appropriate course of treatment. But, as with other services, the range of what is being made available in primary care varies across countries, ranging from simple diagnostic tools and tests such as otoscopy, glucose tests and peak flow meter (e.g. the Netherlands) to more sophisticated tools and equipment such as electrocardiography, radiology and ultrasound (e.g. Spain) (Table 30).
| Denmark | Finland | The Netherlands | Spain |
|---|---|---|---|
| Patients suspected to have a serious condition (cancer, heart, rheumatological) can be referred to the relevant diagnostic investigations on a daily basis (e.g. echocardiogram) but the GP will remain responsible for the patient pathway ECGs are performed electronically in all GP practices and can be forwarded to the hospital In some regions GPs can refer for diagnostic tests for a specific condition, e.g. MRI scans for knee problems, or where a patient shows signs of a discus prolapse Ultrasound and endoscopies are starting to become more accessible in primary care or the GP practice; this was informed by research on cancer diagnosis, for example |
The following models are available, but should be seen as ‘exceptional’ rather than routine: Patients who are being examined for a diagnosis of Alzheimer’s disease or other dementias can be referred to brain CT; the clinical examination can be performed by a neurologist or a geriatrician Endoscopy, echocardiography, exercise ECG: the patient may be referred for the diagnostic test to the hospital outpatient department only; the GP retains responsibility for the patient pathway (except in case of complications) Patients with symptoms of common nerve entrapments can be referred to electroneuromyography to confirm the clinical diagnosis |
Routinely available
|
Electrocardiography Basic radiology (e.g. chest radiographs) Blood tests (ESR/CRP, haematology, chemistry; culture and serology) spirometry Pulse oximetry and maximum respiratory flux measure Oscillometry and/or Doppler Otoscopy Indirect laryngoscopy and qualitative audiometry Reflectometry Visual acuity tests and eye fundus exam Social and psychoaffective tests Morbidity tests and quality of life tests (Source283) In some autonomous communities primary care centres have ultrasound available In Asturias, primary care professionals can refer patients to the hospital for colonoscopy309 Routine access to CT and MRI scans is being considered for introduction |
In Denmark, GP practices are typically equipped to undertake a variety of routine tests such as urine and blood tests and physiological tests such as spirometry, peak flow, audiometry and electrocardiography, as well as some biological (bacterial, fungal) and microscopy diagnostics. 310 Indeed, ECGs are performed electronically in all GP practices and can be forwarded to the hospital. In both Denmark and Spain, direct access to ultrasound and endoscopy in primary care is gradually becoming more common. In Denmark, this was prompted, in part, by ongoing research on early cancer diagnosis. 311 In Spain, the Spanish Society of General Practitioners and Family Physicians (one of three GP/family physician associations) has recommended training in ultrasound techniques for their members and, as a result, the use of this equipment has expanded, usually on the margins of regional health services, and against the resistance from hospital specialties (especially urology, obstetrics or gastroenterology).
In Finland, direct access to a range of diagnostic tests and investigations is possible but its implementation varies among health centres. Direct access provides the opportunity for rapid diagnosis and prevents delay which may lead to inappropriate treatment. However, not all health centres have been able or willing to set up such arrangements. One concern about permitting direct access is the potential risk that (younger and less experienced) doctors might be using this route more frequently, which would thus change the usual threshold for referring. At the same time, GPs regard health centres that allow for direct access as providing good and GP-friendly workplaces.
Direct access to services
Direct access to treatment services such as physiotherapy or direct referral to routine or minor surgery or to hearing aid or orthopaedic appliance fitting is available in Denmark, Finland and in some regions in Spain (Table 31).
| Denmark | Finland | The Netherlands | Spain |
|---|---|---|---|
| GPs can directly refer to physiotherapy and for the fitting of hearing aids | Patients with atrial fibrillation requiring electric cardioversion; the hospital special clinic may follow-up on some background clinical findings, but would not request seeing the patient Patients requiring certain types of surgical interventions; this practice is now expanding and specialists assume that GPs can diagnose hernias, wrist ganglions, suspicious moles, etc. In some cases they may receive confirmation for diagnosis from the regional database of X-rays Termination of pregnancy or sterilisation |
‘Skin therapist’: a new professional in the area of dermatology intended to substitute for the dermatologist; works at the interface between secondary and primary care Optometrist/ophthalmic technicians in outpatient settings: new professional who part-substitutes for ophthalmologists, for example, as part of a ‘glaucoma follow-up unit’ in which the optometrist/ophthalmic technician provides follow-up care to stable patients, and collaborates closely with the GP and the specialist312 |
Varies by region: Andalusia: direct referral from primary care to hospital traumatology rehabilitation treatment for selected conditions313 Madrid: direct referral to neonatology treatments from primary care314 Direct access to physiotherapy is routinely available in those autonomous communities that offer physiotherapy services depending on the primary health-care district. Elsewhere, physiotherapy services are available only through orthopaedic surgery departments |
In Denmark, treatments other than physiotherapy and for the fitting of hearing aids are ‘double-gatekept’ by specialists, that is specialists require repeat consultation before a patient can access investigations required by the GP. 315 There is a perceived general lack of trust among hospital-based specialists with regard to GPs.
Conversely, in Finland GPs or primary care centres generally appear to have access to a greater range of treatments provided in hospital compared with those in Denmark (see Table 31), mostly relating to procedures undertaken as day surgery. For example, the GP may refer a patient for a hernia operation, minor orthopaedic or other intervention for which there are clear diagnostic criteria. In such cases, the hospital would expect that the patients do not have complicating chronic illnesses and the diagnostic signs are established using given algorithms. However, where this is not the case, a planned operation will have to be cancelled or postponed, which then creates inefficiency. But there are few empirical data on the frequency with which such cancellations may take place.
In Spain, direct access to orthopaedic appliance fitting is routinely available in those autonomous communities that offer physiotherapy services, but otherwise physiotherapy services are available only through orthopaedic surgery departments. Direct referral to specialist care for potential surgery patients is being considered. 316–318
Relocation
Shifted outpatient clinics
All countries have or are in the process of implementing care models that involve a relocation of selected specialist services to the wider community setting, most commonly home care or hospital at home type models, as well as the systematic use of community or district nurses (Table 32).
| Denmark | Finland | The Netherlands | Spain |
|---|---|---|---|
| Routinely available: Palliative specialist care Oxygen nurse for COPD There is a possibility for GPs, district nurses from the municipality and the hospital to arrange for care planning meetings about older patients Some regions or cities have introduced home-follow-up psychiatric teams Some regions have also introduced geriatric teams |
Some of the larger cities have run pilots of ‘hospital at home for children’ models to, e.g. minimise the risk of infection among specific groups (where intravenous treatment is required). For adults, such services would typically be provided in the community Similarly, adult palliative specialist care is commonly provided in the community setting, while for children it would be provided in specialist settings |
The national ‘Visible Link’ Programme deploys additional community nurses to better link patients, informal carers, health-care providers and official bodies. The programme makes it possible for a general practice to employ a community nurse. Some pioneer projects also start pilot projects with task distribution between (community) nurses and social workers within a community, to link the health and social domain of a health system. However, task distribution tends to have a dominant monodisciplinary focus319 | Family care/family at social risk care Education for health Group education for diabetic patients Education for health (specific social groups) Education for health (home care givers) (Source293) Hospital at home innovations have existed in Spain for more than 30 years,320 with examples established in some autonomous communities (Madrid, Catalonia, Valencia, Basque Country).321–323 These are usually targeted at terminally ill patients or patients with serious chronic diseases |
One cost analysis of home-hospitalisation of just over 100 patients with COPD following admission to the emergency room in two tertiary hospitals in Barcelona found that the average direct cost per patient was significantly lower for those receiving home care by a specialised respiratory nurse than for the comparison group (hospitalised patients), with a difference of €810 (95% CI €418 to €1169) in the mean cost per patient. 324 However, overall there are few robust evaluations of the effectiveness of home care in Spain.
Specialist attachment to primary care teams
Similar to the relocation of outpatient clinics to primary care settings, the integration of specialists within the primary care team is not widely implemented across countries reviewed. One exception is Finland, where attachment of specialists to primary care teams is common and the boundary between specialists and primary care teams has increasingly blurred, following colocation of primary care teams and specialists in newly integrated organisations. 265 For example, health centres contract directly with a specialist to provide clinics on a regular basis, such as paediatricians, ENT specialists and ophthalmologists. This tends to be common in some of the larger cities where there is a high volume of referrals to these services, and where direct contracting of specialists or the placement of specialists in primary care is anticipated to reduce pressures on outpatient departments. Other examples include maternity care provided in health centres by obstetricians based at a nearby hospital. Furthermore, some health centres directly employ geriatricians as internal consultants, while in other cases a visiting consulting doctor will perform this task in the health centre.
The frequency and volume of these types of approaches have so far not been routinely monitored or evaluated; a monitoring system is being implemented but not yet developed to a degree that would allow for precise and comparable data. There is a common belief that including a specialist as a (flexible) consultant in primary care teams or organisations reduces pressure on outpatient services, as a large number of common conditions would be first seen in primary care settings, while only the more complex cases would require referral to the specialist level hospitals and outpatient clinics and many larger cities take this approach in the expectation of cost savings.
Conversely, in Denmark the attachment of specialists to primary care teams is very unusual, although there are some pilots in which psychologists or social workers are attached to a general practice. In the Netherlands, specialists can be subcontracted by primary care groups which are often led by GPs.
In Spain, the attachment of specialists to primary care teams as is also unusual. Spanish primary health-care centres include family physicians (GPs), paediatricians, nurses and other staff. 293 In some regions, centres may also include midwives, dentists or physiotherapists. There have been ongoing efforts to introduce specialist outreach in primary care, integrated and co-ordinated into GPs’ activities. These involve patients attended by specialists in primary care centres but scheduled by the primary care physicians, or patients who are seen by GPs together with specialists. Examples include Catalonia325 and Andalusia. 326 In some of the larger cities (Madrid, Barcelona, Seville, etc.) specialist outpatient services share the same premises with a primary care team, although this does not necessarily imply improved co-ordination between primary and secondary care, as sharing premises is largely designed to optimise infrastructures. There is, however, little empirical evidence on this issue.
Community mental health teams
Multidisciplinary CMHTs form a routine part of primary care service provision in Denmark, Finland and Spain. For example, in Denmark public services for patients with mental health disorders are provided through cross-sector collaboration between the health and social care sectors. 256 Psychiatric treatment is located in general practice and the treatment of those with psychosis is located in community-based psychiatry; admission to hospital is only for severe cases. Community-based psychiatry includes nurses, psychiatrists and psychologists.
In Finland, until the 1990s, outpatient mental health services were provided by specialist level organisations but these teams were subsequently transferred into the community, administered by health centres in about 60–70% of the country. 257 Likewise, in Spain the majority of regional health services have mental health centres that are linked to primary care; such centres include psychiatrists, psychologists, social workers and nurses specialists in mental health; these are located outside hospital. 260
The Netherlands have implemented practice assistant- or nurse-led care in mental health from 2008 as described in Table 32. These work in primary care to support GPs in diagnosis and patient support, thus moving treatment of patients with relatively mild mental health problems into primary care. 306
Telemedicine and telecare
All four countries reviewed for the present study have implemented or are trialling a wide range of telemedicine and telecare approaches. As these terms are frequently used interchangeably, we describe the principal models and approaches together.
The most common approaches that are being or have been implemented are teledermatology and teleconsultation and Table 33 provides a summary overview of a range of services that are being tested or implemented in the different countries. For example, in Finland and the Netherlands teledermatology is available routinely across primary care, whereas in Denmark such approaches are implemented only in remote or underserved regions. In Spain, teledermatology is being trialled but approaches are at different stages of implementation. 323,324
| Denmark | Finland | The Netherlands | Spain |
|---|---|---|---|
| Teledermatology is available in remote/underserved regions Some of the larger hospitals have introduced ‘wound nurses’ that are made available to GPs. They can also send in images, with a specific wound-record available |
Patients with skin lesions raising questions of malignancy: the GP can add a digital photograph to the digital referral and ask for advice on referral vs. treatment in primary care Diabetes care in some health centres: examples include teamwork-based teleconsultation models in health centres that involve a specialist in diabetes care, a diabetes nurse and a patient attended by videoconference;327,328 one other example is the use of mobile eye unit for screening of diabetic retinopathy and follow-up of glaucoma in remote locations in northern Finland which involve the digital transmission of images to specialists329,330 Telematic mental health care in northern Finland |
Teledermatology: reimbursable as ‘modernisation and innovation procedure’. It is aimed at reducing the number of referrals to dermatologists Teleconsultation in the areas of eye care, cardiology, lung care and nephrology |
There are pilots in some of the regions, but these are at different stages of implementation. Many are related to teledermatology323,324 Other experiences include remote video-electroencephalography consultation in La Rioja325 and telemedicine specialised care in Extremadura326 |
In the Netherlands, teledermatology is linked to a financial incentive, a ‘modernisation and innovation procedure’. The intention was to reduce referrals to dermatologists and a prospective study of over 37,000 teleconsultations conducted between 1820 GPs and 166 dermatologists over a period of 3.5 years found that 68% of referrals to a dermatologist could be prevented (see also Chapter 2, Findings, Relocation). 135 The estimated cost reduction was 18%. However, related work also suggested that GPs were facing challenges in identifying suitable patients for this approach. 270 Available evidence on teleconsultation in eye care and cardiology in the Netherlands has pointed to reductions in referral rates of around 50% for patients selected by the GP for telecare;30 similar observations were made for telepulmonology consultations. 278
The Netherlands is also experimenting with a wide range of telecare projects across the country; examples are shown in Box 2.
-
Technology-based connection of patients with nurses via a television screen: the Telesens project aims to connect patients with nurses via a television screen. 331
-
The deployment of a national health-care portal: the PAZIO project in the Province of Utrecht aims at developing a national healthcare portal to facilitate, for example, online appointments, self-management activities for chronically ill patients, or prescription requests by patients; it will also allow patients to access their own medical records. 332
-
A television-based communication system connecting patients at home with health-care providers and their social network: in 2008, the municipality of Almere initiated the Zorg.tv pilot, which is part of a large-scale telecommunication project. The target population of the pilot are patients of local (mental and social) health-care organisations, their carers and family members. Each participant can communicate with each other and their health-care providers via their television. 333
In Denmark, there are a number of pilot projects across the country involving telemedicine or telecare elements. One example is the TELEKAT project in northern Denmark, a telerehabilitation programme taking place in the patients’ own homes and in collaboration with different health professionals including district nurses, GPs, nurses and doctors at the health-care centre and hospital. 334,335 In 2012, the national and regional governments published a national action plan for telemedicine, allocating DKK 80M (approximately €11M) to (part-)finance the various initiatives under the plan and further supported by the regions and municipalities (Box 3). 336 The action plan is part of the Danish eGovernment Strategy 2011–15, and is expected to lead to what has been referred to as a ‘future digital welfare reform’.
As part of the national action plan for telemedicine, there are currently five initiatives being piloted:336
-
Clinically integrated home monitoring involving some 2000 patients with COPD, diabetes or inflammatory bowel disease and pregnant women during 2012–14; patients’ homes are fitted with IT equipment to measure and register relevant data that are transmitted to health-care providers for them to follow up where necessary; the system also allows for video consultations. 337
-
Home monitoring for COPD patients in northern Denmark, implemented as a cluster RCT (‘TeleCare North’) in 2014 and 2015 involving some 1200 participants. 338
-
Telepsychiatry: videoconferencing and virtual cooperation between psychiatry departments and district psychiatric departments to be introduced in all five Danish regions from autumn 2012. 336
-
Demonstration project ‘internet psychiatry’ using an online IT programme targeting people with depression in the Region of Southern Denmark from autumn 2012.
-
Telemedical assessment of ulcers implemented at national level from September 2012 by 2017 (currently tested in Southern Denmark). 339
Similarly, in Finland, a wide range of telemedicine applications have been implemented and are operated as regular services including telemonitoring, telediagnosis, teleconsultation and telelaboratory. 340 Data exchange between health-care organisations in Finland is reported to be increasing rapidly. 341 This has been linked to the introduction of a national electronic health records archive (eArchive) in 2006,340 enabling the access and exchange of patient information across organisations using secure data connections. This allows for the exchange of referrals, feedback, X-rays and laboratory results through the web.
One important sector in telecare is home care or nursing services for older people. Telecare and other new technology applications are used to provide security and also easy contact with the home care staff. The home care staff is in most cases under the administration of primary care, while in some smaller municipalities the local municipality or social service department is in charge.
In Spain, as with many other aspects of the Spanish national health system, telemedicine programmes and projects are implemented at regional or local levels by regional health authorities. 342,343 Regarding telecare, a number of relevant approaches or interventions are currently being trialled or piloted, with the most advanced region in this field seen to be the Basque country (Box 4).
A telemonitoring intervention aimed at home care for patients with heart failure or chronic lung disease implemented as a RCT in Bilbao primary care region. 344,345
A home telehealth programme for patients with severe COPD, implemented as a cluster RCT in the Madrid region. 346
Home enteral nutrition support for children with chronic diseases across Spain. 347
A mobile phone-based telemedicine system for the home follow-up of patients undergoing ambulatory surgery implemented as a pilot project in the Madrid region. 348
A telerehabilitation service for breast cancer survivors implemented as a RCT in the Granada region. 349
Liaison
Shared care
Shared care, in which a hospital specialist and a primary care practitioner agree a joint management plan that specifies which elements of care for a particular patient are to be delivered by each clinician, is only partly implemented in the four countries reviewed. For example, in Denmark, joint care management is in place for many chronic diseases as well as for maternal care. In Finland, the principle of shared care is built into most of the patient pathway guidelines, defining the roles of the GP before and after the specialist consultation or intervention. However, actual joint management plans are not common. Examples may include rare diseases or cancer, which are principally managed by specialists, but some aspects of the care pathway, such as regular monitoring of laboratory results, may be managed by the health centre.
In the Netherlands, it is common for GPs to ask telephone advice on the treatment of specific patients from the following specialists: paediatrician, internist, gynaecologist, surgeon, neurologist, dermatologist and geriatrist. 253 National-level agreements seek to enhance collaboration across medical practitioners in specific clinical fields, with National Primary Care Agreements covering collaboration agreements among different primary care professionals in a region while National Transmural Agreements constitute collaboration agreements among GPs and medical specialists in a region. 319 Examples include a National Primary Care Agreements on malnutrition, which provides recommendations for co-operation and suggestions for working agreements between GPs, dieticians and nurses. 350 An assessment of referral criteria set out in a National Transmural Agreements on chronic renal failure found variation among hospitals in the use of criteria, potentially leading to unnecessary hospital referrals. 351
In Spain, shared-care models of the type in place in the UK have not been tested as such in any of the regional health services, although shared-care models were proposed as a strategic development driver for the Spanish NHS, including a shared vision between primary care and specialist care, specific missions for both levels, shared-care objectives between levels, specific activities and responsibilities for either level, co-ordinated follow-up of patients, shared-care protocols and guidelines, and shared incentives. 283 Joint management plans for selected conditions have been implemented in Andalusia, Asturias, Catalonia and Valencia (Box 5). 283
The ‘procesos asistenciales integrados’ (integrated care processes) defined for the Andalusia region include a wide range of conditions and care populations, such as anaemia, stable angina (chest pain), asthma, COPD, diabetes mellitus; a range of cancers (colorectal, cervix, breast, skin, lung); dementia, anxiety, depression; multimorbidity, newborn at risk, palliative care, non-oncologic chronic pain, maternal health; etc. 352
Integrated care processes have been defined as a ‘tool for quality improvement’ that set out a detailed schedule of patients and all actions, decisions, activities and tasks that are linked sequentially to address a specific health-care problem. 353 They are agreed between professionals as an ‘agreement to comply’ and adapt to the environment and available resources.
One notable example includes the co-ordination in the city of Seville between the internal medicine department at the Virgen del Rocio Hospital and primary care centres. 354 However, this type of approach has not spread to other cities or regions.
Consultation liaison (joint consultations and management plans)
Consultation liaison may include on-site mental health workers providing support to primary care in managing patients with mental health or other problems, or a psychiatric key worker working in collaboration with primary care, among others. Such approaches have been implemented to differing degrees, except in Denmark, where such an approach is currently not documented.
In Finland, as noted in earlier sections of this appendix, where health centres have specialist services under their administration, this would typically involve a range of mechanisms for liaison and consultation. Where health centres employ or contract with a specialist to deliver clinics, the visiting specialist may offer a joint consultation with the GP to review a patient’s case. In addition, there are less formal forms of support for primary care providers delivered by specialists such as telephone advice or through written consultations.
In the Netherlands, the introduction of a consulting secondary care specialist in mental health care was launched from 2013, following experiences with practice assistant or nurse-led mental health care in primary care (see Table 28), which was shown to insufficiently substitute for mental health care at specialist level. 290 Further, a number of GPs in some regions, such as in Limburg, team up with a different specialism each year for joint consultations of the GP and medical specialist in general practice (face to face). Joint consultations have been linked to fewer referrals to secondary care, and fewer diagnostics in secondary care. On average, 15% of patients who receive a joint consultation are referred to secondary care. 294,295
Conversely, in Spain, some regional health services have implemented an ‘internist liaison’, but such models are not common and have not been evaluated. Some regional health services introduced nurse liaison services (enfermeras de enlace) more than a decade ago, and such roles are now formally or informally established across all health regions,355 but approaches have not been evaluated in a robust way. The first initiative was implemented by the Canary Islands health services but perhaps the most important example is the introduction of nurse liaison in the Andalusian health services, which covers the entire region and which has been considered an important investment by the Andalusian government. 356
Professional behaviour change
Guidelines, including referral pro formas
All countries reviewed have guidelines in place for a range of conditions and processes (Table 34).
| Denmark | Finland | The Netherlands | Spain |
|---|---|---|---|
| There are guidelines in place for heart disease, cancer, joints and some chronic diseases | There is a system of national guidelines developed by the Finnish College of Physicians (Duodecim).357 These may then be developed further into regional or local guidelines. The national guidelines apply to all health services, including private services | Referral guidelinesLocal guidelines and protocols: interprofessional or multidisciplinary collaboration is organised at a community level in a community health centre that bring together different disciplines [e.g. GP, physiotherapists, dieticians, social work, pharmacist, (community) nurse, midwife]. The degree of structural collaboration seems to depend on the level of financial reimbursement319 | Clinical guidelines, care plans or protocols are routinely used across primary care in Spain, with an equivalent to a National Guidelines Clearinghouse ‘GuiaSalud’358 The most important Spanish family medicine associations (‘societies’) have their own guidelines359 The most important experience of guidelines for specialist referral are the ‘Procesos Assitenciales Integrados’, established in Andalusia in 2001, which cover almost 100 groups (one for each disease) and are considered the gold standard related to the diseases.352 However, implementation has been uneven and there is a lack of robust evaluation of the approach |
In Finland, in addition to the national and local guidelines, specialists or clinics that detect inappropriate referrals or deviations from the guidelines may contact the head physician in charge of the health centres or in some cases individual doctors to bring about change. Such observations can also lead to organising special training events to clarify the guidelines.
In the Netherlands, the referral guidelines for GPs generally recommend referring patients only in exceptional circumstances,290 and there is evidence that general practices that adhere to referral guidelines have lower referral rates to secondary care.
In Spain, although guidelines for specialist referral are used across the country, with primary care teams and corresponding specialists reaching agreement, there is a deficit of implementation and, especially, evaluation.
Audit and feedback
Formal audit and feedback mechanisms related to referral patterns are not common among countries reviewed. In Finland, in some health centres, the (clinical) head of the centre might have adopted the practice of reading through referrals issued by junior doctors which could then be used as material for in-house training. In some cases, local specialists may send circulars or organise special training events for health centres to guide specialist referral. In the Netherlands, only GPs who participate on a voluntary basis in a research network that is dedicated to regularly collecting information on GP referrals, procedures, patients, etc., may have the chance to be provided with structural feedback information on their referrals in comparison to peers. An example of such a network is the Netherlands Information Network of General Practice, in which around 150 GPs participate and register their required information. 360
In Spain, regions that have introduced joint management plans (Andalusia, Asturias, Catalonia and Valencia) have also introduced audit mechanisms and associated incentives or penalties, at least in principle. There is, however, little robust evidence of their effectiveness. Health authorities in most Spanish regional health services have established referral rates audit and feedback systems from the mid-1990s onwards, with standards based on the average rate of referral in the autonomous community concerned. All centres or physicians with referral rates above the average are ‘penalised’ in some way by having their annual incentives reduced (see Financial incentives).
Professional education, including academic detailing
Individual education or coaching by specialists was found to be common only in the Netherlands. 253 In Spain, coaching or individual education by specialists is the exception, although there is some training of individual GPs in selected hospital departments in some regional health services but this does not occur on a regular basis.
Professional education aimed at improving the quality of outpatient referrals is not used in any of the four countries reviewed for this study.
In-house review
Formal in-house review of referrals by a second GP is not common in countries reviewed. In Denmark, an informal second opinion would often be used in general practice but GPs do not review referrals. Likewise, in Finland, systematic in-house referral review is not usually performed in health centres although informal review mechanisms might be in place. Examples include where the potentially referring doctor is inexperienced compared with the regular GP specialist who is asked to review the case before referring, or in relation to some specific groups of patients for whom special discretion is recommended (e.g. arthroscopy of the knee or shoulder, or for nuclear magnetic resonance or CT scans); there may be also be a guideline in place stating that an experienced GP specialist must be consulted before referring. Finally, in cases where one or several GPs have acquired special skills in some clinical areas there may be an internal rule that these GPs should usually be consulted first. Overall, these systems are not very systematic or mandatory.
In the Netherlands, GPs (particularly in shared practices) have regular face-to-face meetings with the following professionals in which specific patients are discussed, and in which referral decisions may also be a topic of discussion: other GPs, primary care assistant/nurse, nurse practitioner, home care nurse, midwife, physiotherapist, community pharmacist, social worker and community health worker. 253
In Spain, systematic in-house referral review is not used; GPs try to resolve concerns or problems by consulting informally with other colleagues.
Referral management centres
None of the four countries reviewed has RMCs in place. In Denmark, specialists may return referrals because of time pressures but this is not an official approach. In Finland, there have been some proposals to initiate related processes to reduce growing volumes of referrals but there are concerns that such systems may be unacceptable to doctors and could also be perceived to violate patients’ rights. The receiving outpatient clinic has the right to decline the referral or offer advice on next steps, but having an organised outside review body or centre would raise concerns.
Financial incentives
All four countries have some form of financial incentive in place which may be directly or indirectly used to control referral patterns from primary to secondary care.
For example, as mentioned earlier, in Denmark, a number of services provided by GPs are paid for on a fee-for-services basis, such as minor surgery. 266 GPs’ fees are negotiated by the Board for Wages and Tariffs of the Regions and the Association of General Practitioners in Denmark. Negotiations seek to create incentives for the GPs to treat patients who could be treated in general practice, rather than refer them on to hospital. There is evidence that following the change by Copenhagen municipality from a mostly capitation-based system to one that combines capitation and fees, there was an increase in the volume of activities that were specifically remunerated and referrals to specialists decreased. 276
The Netherlands has introduced a range of fees affecting referrals. These include the following:
-
‘Modernisation and innovation procedures’, which incentivise primary care physicians performing procedures that are potentially substituting for secondary care. 267,268
-
Integrated health care centres receive extra funding because they have been shown to reduce referrals to secondary care. 361,362
-
Bundled payments for chronic disease care – care groups (often exclusively led by GPs) are responsible for the organisation, co-ordination and delivery of care for conditions such as diabetes, COPD and vascular risk. Care groups negotiate the price for a defined care package in line with national standards with the health insurance fund. 271
-
Care groups subcontract GPs, medical specialists, nurses and other disciplines. Approximately 78% of GPs in the Netherlands are members of a care group. 279 Recent evaluations indicate that the system of bundled payments is conducive to the organisation and co-ordination of care. 280 However, thus far there is little robust evidence on the impacts of care groups on referral patterns. 281
In Finland, there is an inherent incentive to control the number of referrals, as primary and specialist services are funded through the same route. The lead clinician in the health centre receives regular data on the frequency and cost of the use of specialist services. The payment to individual GPs does not include special incentives for reducing referrals.
In Spain, the relationships between regional health service authorities and public providers are regulated by a mix of salary and contractual agreements. In most regions these agreements contain objective-linked incentives as part of the amounts paid to providers; referral-related objectives are common in such agreements. 274
Appendix 9 Patient and public involvement
Two patients were involved in the development of this proposal. One is actively involved in a general practice patient participation group and has past experience of NHS management, with posts involving acute and primary care settings, primary care service redesign, and contracting both as a purchaser and as a provider. The second is a member of Cambridge University Hospitals Patient Panel with extensive experience both as a patient and through contributions to patient advisory groups.
Both individuals agreed to be members of a Patient Advisory Group which met once over the course of the study to consider a draft report and the progress on the various aspects of the study.
A number of the points made by the patients during the meeting related more generally to the relevance and accessibility of the work to patients and members of the public. The patient representatives felt that interest in our work would have heightened, even in the time since the work began, because of changes in commissioning and budgetary constraints. In order to ensure more patients could be informed of the findings, they suggested that we consider existing local and regional groups when disseminating results. Specific suggestions included Patient Participation Groups, Health and Well-being Boards, Health Watch, local disability groups and Primary Care Research Networks. We discussed preparing a one-page briefing from the study and a plan for dissemination through these and other relevant groups. We asked our patient representatives specifically about the language used in our current draft and they felt that it was appropriate and accessible to a lay audience. We will endeavour to ensure that this is maintained in all outputs from the project, and the patients have offered to read and, where required, revise further material from the project.
The patients also commented on each individual component of the study, highlighting issues that seemed particularly important and seeking clarification from the research team in some cases. We noted all of these points for development of the next draft. Particularly helpful suggestions included (i) to give greater explanation of the change in context, for example commissioning arrangements, from the time of the initial review to this review; and (ii) that there are repeating themes in the findings across strategy type and this could be brought out more in the analysis, for example, around supply-induced demand.
Towards the end of the study we shared drafts of the outputs from the project with the Patient Advisory Group and followed up individually for comment and suggestions, which were useful in finalising our report.
Glossary
- Academic detailing
- A method of service-oriented educational outreach for doctors involving one-to-one or group interaction with a more experienced or knowledgeable health professional, for example general practitioners interacting with a specialist physician.
- Clinical Commissioning Groups
- Replaced primary care trusts in April 2013 as the commissioners of most services funded by the NHS in England.
- Computerised tomography
- Uses X-rays and a computer to create detailed images of the inside of the body. [Definition reproduced from NHS Choices (www.nhs.uk/conditions/ct-scan/pages/introduction.aspx); contains public sector information licensed under the Open Government Licence v3.0 (www.nationalarchives.gov.uk/doc/open-government-licence/version/3/).]
- Magnetic resonance imaging
- A type of scan that uses strong magnetic fields and radio waves to produce detailed images of the inside of the body. [Definition reproduced from NHS Choices (www.nhs.uk/conditions/mri-scan/pages/introduction.aspx); contains public sector information licensed under the Open Government Licence v3.0 (www.nationalarchives.gov.uk/doc/open-government-licence/version/3/).]
- Shared care
- A model of working in which a hospital specialist and a primary care practitioner agree a joint management plan that specifies which elements of care for a particular patient are to be delivered by each clinician.
- Store-and-forward telemedicine
- Technologies that involve the collection of still images (e.g. photographs of skin lesions) and subsequent electronic transmission (e.g. to a specialist dermatologist for advice).
- Subconsultant grades
- Permanent medical posts in the NHS for doctors who do not hold consultant status. Most doctors progress through training grades to a consultant post but some doctors choose to take up permanent subconsultant posts.
List of abbreviations
- CCG
- Clinical Commissioning Group
- CMHT
- community mental health team
- COPD
- chronic obstructive pulmonary disease
- CT
- computerised tomography
- DVT
- deep-vein thrombosis
- ECG
- electrocardiogram
- ENT
- ear, nose and throat
- GM
- geriatric medicine
- GP
- general practitioner
- GPwSI
- general practitioner with a special interest
- HBA1
- haemoglobin alpha 1
- HSDR
- Health Services and Delivery Research
- IT
- information technology
- LCG
- Local Commissioning Group
- MRI
- magnetic resonance imaging
- NETSCC
- NIHR Evaluation, Trials and Studies Coordinating Centre
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health Research
- OECD
- Organisation for Economic Co-operation and Development
- PCT
- primary care trust
- PM
- palliative medicine
- PSA
- prostate-specific antigen
- QALY
- quality-adjusted life-year
- QOF
- Quality and Outcomes Framework
- RCT
- randomised controlled trial
- RM
- respiratory medicine
- RMC
- referral management centre