Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 12/64/118. The contractual start date was in December 2013. The final report began editorial review in June 2015 and was accepted for publication in March 2016. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Sir Liam Donaldson was the chairperson of the National Patient Safety Agency (NPSA) (2010–12) and is currently involved in the programme of research associated with the National Reporting and Learning System (NRLS). He is also the World Health Organization’s patient safety envoy. Sukhmeet Panesar is a former clinical adviser at the National Patient Safety Agency (2008–10), a former special adviser to Sir Liam Donaldson (2010–12) and a former academic clinical fellow at Imperial College London working for the NRLS research programme. Peter Hibbert has undertaken paid consultancy with Power Health Solutions (PHS), St Vincent’s Health Australia and for the Australian Commission on Safety and Quality in Health Care, all regarding incident reporting. Amy Butlin obtained a Cardiff University Research Opportunities (CUROP) scholarship to undertake this work. Gareth Parry received funding to attend the Advisory Group Meetings.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2016. This work was produced by Carson-Stevens et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Background
This chapter sets the scene for our research, giving key background information about characterising patient safety incident reports from general practice in the National Reporting and Learning System (NRLS). It describes the emerging international interest towards patient safety in primary care, and the opportunities and challenges for using the NRLS to inform patient safety efforts and, finally, outlines the structure of our detailed report that follows.
Patient safety in primary care
Internationally, over the past two decades there has been growing realisation that health-care provision can inadvertently result in harm to patients, known as ‘health care-related harm’. Around 1 in 10 hospital inpatients experience a patient safety incident during their care. 1 Unsafe care is thus responsible for a substantial, potentially preventable, burden of disease. 2,3 Over the past decade, most of the research on patient safety has been based in secondary care, where it has been demonstrated that it is possible to identify patterns in errors and determine those most frequently leading to major harm and isolate those most amenable to prevention. Informed by these epidemiological studies,4 patient safety in secondary care is now in an era of implementing interventions and monitoring their effectiveness in different settings. There is now recognition that similar work is needed in primary care, and in February 2012, the World Health Organization (WHO) convened its first Safer Primary Care Expert Group in Geneva, Switzerland, to stimulate international action to support the delivery of safer primary care. 4
Despite the fact that in most developed nations the majority of health-care interactions with health-care professionals (HCPs) occur in primary care settings, little is known about the possible risks to patients and their impact on patient health. 3,5
Primary care poses unique challenges for the design of better-quality systems of care delivery. 3,5,6 Given the different case-mix considerations and the approach to care provision between hospitals and general practice, the ability to transfer lessons to primary care from efforts in hospital settings is limited. 5 Challenges facing modern primary care could also inadvertently create greater risks of health care-related harm; for example, patients are discharged from hospital earlier than before, and receive episodic and decentralised care; clinicians prescribe and monitor high-risk drugs; consultations are time-pressured; and continuity of care relies on co-ordination between many care providers and services. 7
The Francis Report8 states that general practitioners (GPs) must play a greater role in quality monitoring, and reaffirmed the responsibility of HCPs to report patient safety incidents and suboptimal care. Demonstrating the benefits for learning from reported patient safety incidents is considered essential to establishing a patient safety culture within health-care organisations. 9
Patient safety research in primary care
The discipline of patient safety is predicated on the theory that harm is caused by a multifactorial chain of events. 10,11 The underlying assumption is that if systems (i.e. organisations and networks of organisations), and working conditions within these, can be optimised, then patient safety incidents would be less likely to occur. Determining the most frequent and most harmful safety incident types will support advances in agenda-setting needed for patient safety in primary care. Established methods for examining health-care safety, for example case note review, root cause analysis or incident reporting, provide different and incomplete observations of those underlying problems.
Our WHO-commissioned systematic review of the world literature (up until January 2015) determined that patient safety incidents are a relatively frequent occurrence in primary care (around 2–3% of consultations), although only around 4% of those result in severe harm. 12 The review identified that few studies have hypothesised or explored the relationship between cause (error) and effect (harm), and the underlying system failures in primary care. 7,13–18 Typically such insights about contributory factors can be found in studies that have investigated root causes of patient safety incidents (i.e. root cause analyses) as well as analysis of free-text descriptions of safety incidents in incident-reporting systems. No such studies have occurred within general practice in the UK. Although around 6% of patient safety incidents are reported in hospital settings,19 the figure is likely to be considerably lower in primary care, which contributes < 1% of reports to the NRLS from England and Wales. 20 Given the similarities of challenges faced by primary care services in developed nations identified by an international Delphi consensus study, a detailed analysis of (to our knowledge) the largest repository of general practice safety incidents could support action in priority areas of patient safety in primary care. 6
Patient safety incident reporting in England and Wales
Incident-reporting systems have previously been used to identify priority areas and generate recommendations to improve care quality and safety at a local and national level. 21–24 In 2003, a major investment was made in the NRLS to better understand incidents occurring in England and Wales. Each hospital and health-care facility has a reporting system that collects paper or electronically submitted incident forms. Since 2004, NHS organisations in England and Wales have uploaded their incidents to the NRLS central database. Around 100,000 incidents a month are uploaded, making it the most comprehensive system in the world. The NRLS has informed multiple learning outputs, including rapid response reports, patient safety alerts, and safer practice notices. 20 Despite these initiatives, incident-reporting systems have gained little respect from the health information and research and clinical communities. 23,25
The NRLS contains information about incidents with ‘free-text’ descriptions of the events, perceived contributing factors and plans to minimise risk of reoccurrence. Over 40,000 reports from general practice in England and Wales have been submitted to the NRLS in the past decade, and these have never previously been systematically analysed. The under-representation of general practice within the NRLS suggests that there has been a poor reporting culture among staff in England and Wales in the past decade and is probably a reflection of the national emphasis placed on patient safety in hospital settings. 26 Paradoxically, despite the large number of incident reports received by patient safety-reporting systems like the NRLS, a mismatch exists between what actually occurs in clinical care and what HCPs report as a patient safety incident. 19 A characterisation of how HCPs in general practice interpret ‘patient safety incident’ is needed if efforts can be undertaken to advance the agenda around what gets reported for system learning.
Incident reports permit a retrospective window on the health-care system, providing an opportunity for directing improvement initiatives by identifying weaknesses in the system that lead to errors and harms experienced by patients. 27 Large-scale incident analysis is an underexploited area within primary care patient safety and should serve to demonstrate the value of safety monitoring, as well as emphasise the benefits of an effective reporting system for HCPs, managers, leaders and patients.
Learning from patient safety incidents
Supporters of patient safety-reporting systems believe that they are not being used to their full potential to benefit patients. 28 Patient safety incidents can have a major impact on patients’ lives downstream, with potential for litigation claims. Having a system in place to advance understanding through learning about the magnitude and nature of preventable harm can offer insights into how best to protect patients, clinicians and health-care organisations.
Leading experts recognise that despite limitations of reporting systems (under-reporting, incomplete view of incident and reporting biases), they provide multiple perspectives over time and form an integral part of routine monitoring in clinical practice. 29 The NRLS has provided insight into understanding underlying system failures and has helped identify areas for intervention in secondary care, including: (1) prescribing and monitoring lithium therapy;30 (2) reliable administration of insulin;31 (3) early detection of complications in surgical care;32–34 and (4) essential care after an inpatient fall. 35 Furthermore, clinical researchers have explored descriptions of patient safety incidents in anaesthesia and identified system deficiencies relating to practical procedures, communication of information to patients, verbal and written communication practices, and continuity of care. 36 Their analysis also led to the development of an anaesthesia-specific incident report data collection form. 37
There has been minimal development of methods for maximising the potential of learning from incident reports. National systems rely on patient safety experts methodically trawling through patient safety incidents by severity and frequency. For example, each incident reported as leading to death or severe harm is reviewed individually by trained clinical staff at the NHS Commissioning Board (formerly the National Patient Safety Agency) and a range of outputs are produced to provide solutions to patient safety problems. These include one-page reports called rapid response reports, quarterly data summaries and topic-specific information on issues such as preventing inpatient falls in hospitals. NRLS staff will frequently consult subject matter experts from professional organisations, such as the Royal Colleges. NHS organisations are also subject to deadlines by which they are expected to implement key findings from such reports. These have offered important insights that have helped shape national policy – for example, demonstrating the risks of bone cement implantation syndrome associated with use of cement in hip fracture surgery, and the potential for information technology (IT)-based interventions to reduce many cases of drug allergy-related morbidity. 26,38
Although there is substantial evidence that the NRLS can identify priority issues for intervention, there is a risk that the opportunity for learning is confined to England and Wales; a major limitation exists for comparison between health-care systems, as there is no widely used standardised taxonomy for classifying incidents in primary care settings. 39–41 This means that studies currently define and measure incidents differently, resulting in variations in the estimated proportions of incidents and harms.
The structure of this report
After this introduction, Chapter 2 gives the aims and objectives of our characterisation of patient safety incident reports from general practice in England and Wales, followed by an overview of the mixed-methods approach that was developed to achieve this (see Chapter 3). An overview of our findings is included in Chapter 4, followed by a report of our analysis of all severe harms and deaths occurring in general practice in Chapter 5, and a report of analyses for each major safety incident category in Chapter 6. Chapters 7 and 8 explore the implications of this work in relation to existing literature within the field and present the conclusions and recommendations that can be drawn from this study. Relevant supporting material is presented in the appendices.
Chapter 2 Aims and objectives
We undertook a mixed-methods study to characterise the nature and range of incidents reported from general practice in England and Wales.
The objectives were to:
-
develop a classification using empirical evidence from reports
-
describe the frequency of different types of incidents
-
describe incident characteristics such as gender, ethnicity, geography, time of day and level of patient harm
-
determine which characteristics are associated with different levels of patient harm using exploratory data analysis (EDA)
-
map relationships between themes (i.e. categories of incidents and potential contributory factors) and elicit possible areas with opportunity for intervention by corroborating findings from EDA and thematic analysis.
Chapter 3 Overview of methods
A mixed-methods study was undertaken to characterise the nature and range of incidents reported from general practice in England and Wales, to identify priority issues for the development of patient safety in primary care. The Aneurin Bevan University Health Board (ABHB) Research Risk Review Committee classed the study as a service evaluation (ABHB research and development reference number: SA/410/13; see Appendix 1). This chapter provides a detailed description of the methods used in the study.
Our analytical plan deviated from our original study protocol following support from the funder and guidance provided by the study’s Professional Advisory Group (PAG), which comprised methodological experts in qualitative and quantitative analysis, health-care organisational leaders and policy-makers. Given the intrinsic biases of incident report data, largely the unknown denominator and minimal primary care patient safety literature base to fill in the gaps generated by those uncertainties, the PAG advised us to use EDA methods in preference to harm susceptibility ratios and network analyses to determine the key relationships. 42 The PAG proposed that the development of EDA methods for incident report analysis could be more readily adopted by organisations seeking to make sense of their own local incident report data. These methods have enabled us to achieve all study outcomes, which include development of a classification system (objective 1) to generate a detailed description of primary care. Patient safety incidents from general practice in England and Wales were characterised (objectives 2–4) to identify candidate areas of development for patient safety in primary care (objective 5). Our recent outputs using these methods have been accepted for publication in the journals Pediatrics, Vaccine and the British Journal of General Practice.
Study method
Data source
The definition of a patient safety incident in the NRLS is ‘any unintended or unexpected incident that resulted in or could have resulted in harm to one or more patients’. 20 Reporting incidents that resulted in severe harm or death of a patient became mandatory in June 2010; however, before this all reporting was voluntary, and remains so for incidents resulting in no, low or moderate harm.
Health-care professionals have a duty to report incidents to health-care organisations’ incident management systems. These are anonymised and uploaded to the NRLS. Each report contains structured categorical information about location, patient demographics and reporter perception of severity of harm. This is collected in a report that also contains unstructured free-text descriptions of the incident, potential contributory factors and planned actions to prevent recurrence. The free-text description, where the reporter is asked to describe what happened and why they think it happened, offers a rich body of qualitative data for identification of areas for improvement. These descriptions provide insight into the harms occurring or detected by HCPs working in general practice from their perspective.
Donaldson et al. 43 have described the NRLS in detail, including its current management in England and Wales.
Study design
We undertook a cross-sectional mixed-methods evaluation of reports that included a thematic analysis informed by an EDA. 44,45
Study setting
Incident reports were included from 571 different locations, such as health boards (formerly local health boards) in Wales and clinical commissioning groups (formerly primary care trusts) in England.
Sample selection
Incident reports received by the NRLS between April 2005 and September 2013 from general practice were considered as the complete data set (n = 42,729 reports). Given the inductive and exploratory nature of the study, we analysed all incidents resulting in severe harm or death and a random sample of 12,500 non-fatal reports. To ensure that results in our sample were current, a weighting was applied to the random sample so that recent reports (from 2012 onwards) were given a higher priority than reports from previous years (2005–11); increasing proportions from no harm, low harm and moderate harm were also selected. Following removal of all reports with a severe level of harm and death, approximately 15%, 30% and 60% of each stratum were drawn using a simple random sample without replacement. The probability of drawing a report from group 2 was twice the probability of drawing a report from group 1 (least recent and increasing proportions of level of harm, from no harm to moderate harm), and four times more likely in group 3 (most recent and increasing proportions of level of harm, from no harm to moderate harm) than in group 1; this resulted in a data set with 12,500 reports. The frequencies for each combination can be seen in Table 1.
| Reporting period | Group | Group size (n) | Level of harm | Total | ||
|---|---|---|---|---|---|---|
| None | Low | Moderate | ||||
| April 2005–9 | 1 | 17,238 | 2162 | 846 | 631 | 3639 |
| 2010–11 | 2 | 12,588 | 2237 | 894 | 770 | 3901 |
| 2012–September 2013 | 3 | 10,413 | 2292 | 1721 | 947 | 4960 |
| TOTAL | 6691 | 3461 | 2348 | 12,500 | ||
Classification system and reviewer training
The analysis of safety incident reports has largely been organised and managed using safety classification systems called taxonomies. 46–62 Several patient safety classifications were reviewed and considered for inclusion,20,63–66 including those developed for general practice. 7,65,67–70 These classification systems provided considerable guidance for shaping the scope of the system needed; however, we did not judge that they would support detailed coding of patient safety incidents from general practice. Therefore, we empirically developed our own classification system to undertake a detailed description of incidents, including those that are complex in nature, which involve a sequence of events that culminate in, and contribute to, the incident.
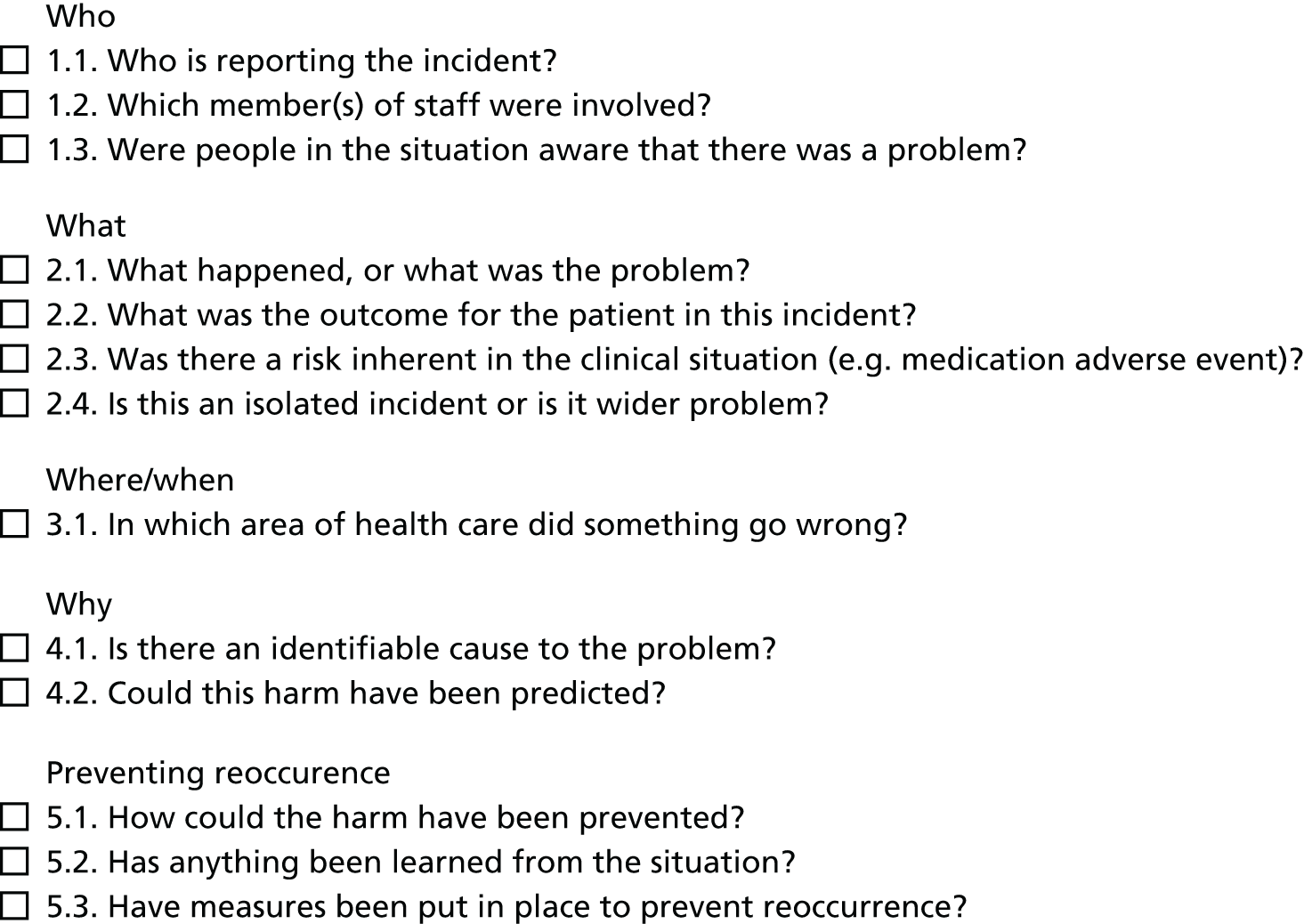
We developed a classification system that incorporated multiple coding frameworks, and utilised existing patient safety incident classification rules (see Appendix 2), to enable chronological coding (see Figure 1). 71 Based on the WHO’s International Classification for Patient Safety (WHO ICPS),63 four independent classes to describe the incident, its contributory factors, and type and level of harm were developed using an iterative approach. 71,72 The WHO ICPS descriptions of level of harm63 were used (see Appendix 3 for examples of excerpts of the classification system codes).
A multidisciplinary team of clinicians were recruited as incident reviewers. Preparatory online modules on patient safety provided by the Institute for Healthcare Improvement Open School were completed by all reviewers. Next, a human factors expert delivered training in incident analysis, classification, root cause analysis and human factors in health care and supported reviewers via weekly calls to undergo simulation with a practice data set. During the training period, to focus reviewers on the relevant content of interest, they were required to identify in each incident the criteria outlined in Figure 1. These criteria were developed by content analysis of 500 randomly sampled incidents by a junior and senior investigator.
FIGURE 1.
Criteria for orientation to incident report content. Reproduced with permission from Carson-Stevens et al. 73 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/.
Framework development for each class was guided by a priori codes generated from pilot work. 74 The reviewers’ interpretations were informed by tacit knowledge, clinical expertise and the human factors training received to guide sensemaking, defined as ‘the active process of assigning meaning to ambiguous data’, in order to identify the learning that can be used to inform improvements in clinical care. 75,76 Once > 70% agreement (kappa statistic) between reviewers and an experienced coder (HW) was achieved, the reviewers were eligible to code the study data.
Coding management system
To ensure that our process was replicable for health-care organisations to consider adopting the classification system, we decided not to use an existing qualitative data analysis management software tool. In addition, given the distributed and international nature of the project (members of the research team in the UK, the USA and Australia), we developed a bespoke solution to support the iteration of frameworks and provide secure access to numerous concurrent reviewers regardless of geographical location. The system comprised a back-end database system and a web-based portal. The back-end database was built on Microsoft SQL Server 2014 (Microsoft Corporation, Redmond, WA, USA), with custom SQL algorithms to provide, for example, live concordance checks of reviewers’ double-coding. The web front end was produced using a customised version of Portofino 4.1.1 (Many Designs, Genoa, Italy), an open-source web framework written in JavaScript (Netscape Communications Corporation, Mountain View, CA, USA).
Data analysis
There were three stages of analysis:
-
stage 1: familiarisation and data coding, which involved reading the free text of the report and applying codes to describe incident type, potential contributory factors and level and type of harm
-
stage 2: generation of data summaries, using EDA methods
-
stage 3: interpretation of themes and learning; seeking to understand the most commonly identified patient safety incidents, events leading up to incidents and reported contributory factors, and the contexts within which they occurred.
Each stage will now be considered in more detail.
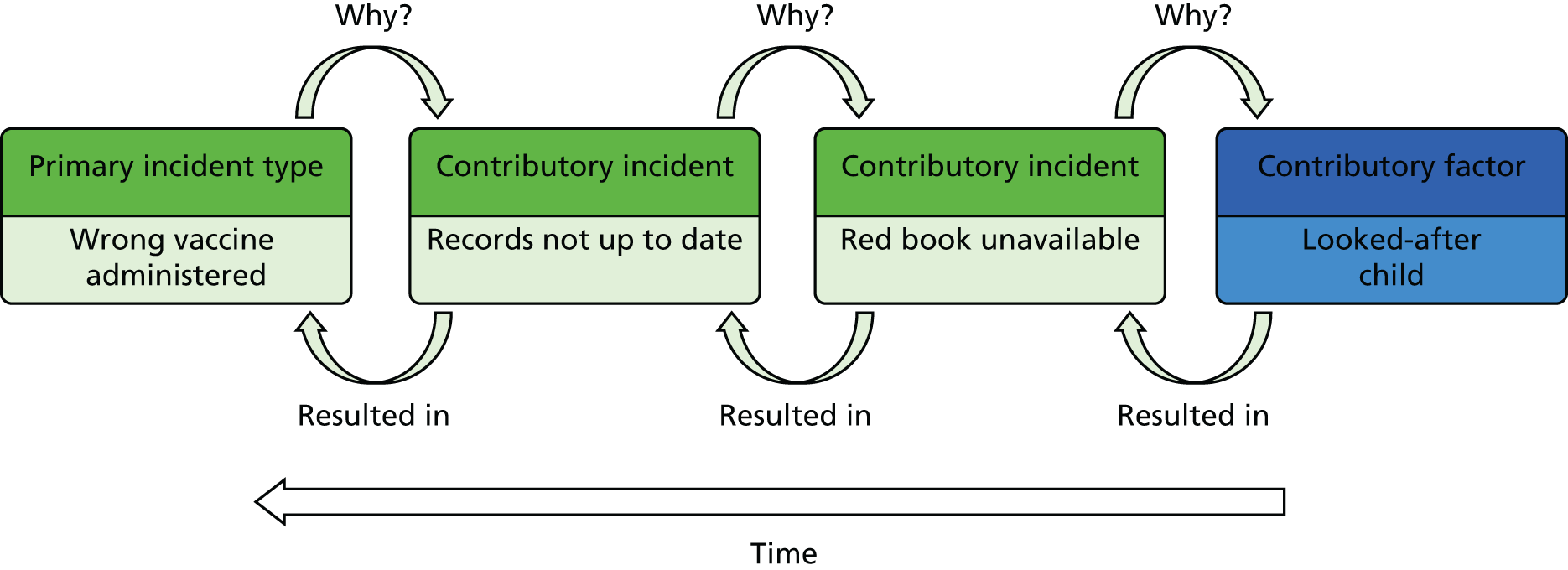
Stage 1: data familiarisation and coding
Reviewers orientated themselves to the content by reading the incident report, which comprised several structured categorical variables and three unstructured categories of free-text data. The reviewer was required to objectively choose the codes, with no inferences made, that represented the content described in each report from the four classes: incident type, contributory factors and type and degree of harm. The nine rules for applying the Australian Patient Safety Foundation ‘recursive model for incident analysis’71 (see Appendix 2) were used to guide chronological ordering of coded data (Figure 2).
FIGURE 2.
Example of codes from the classification system using the recursive model for incident analysis. Reproduced with permission from Carson-Stevens et al. 73 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/. This figure was based on the work of Hibbert P, Runciman W, Deakin A. A Recursive Model of Incident Analysis. Adelaide, SA: Australian Patient Safety Foundation; 2007. 71
Coding large data sets required effective teamwork in order to utilise the tacit knowledge and experience of multiple coders. 77 To ensure validity and reliability of coding throughout the study, regular intercoder reliability checks were undertaken on a 20% random sample of each reviewer’s coding quota for every 250 reports coded. 78 Kappa statistics were calculated for each principal incident type, defined as the incident that occurred just before the harm or potential harm. A kappa of > 0.7 was sought and is consistent with previous studies of a similar nature. 66 The reviewers met to discuss discordant reports and where discrepancies could not be resolved by discussion between reviewers, third-person arbitration was sought from a senior investigator (ACS). 78
Learning from discussions about discordance was shared at weekly coding meetings and informed the inductive amendment of codes and their definitions throughout the study process. The study team comprised professionals from medicine, nursing, physiotherapy and mixed-methods researchers, and also benefited from the participation of a pharmacist and dentist present via teleconference. A human factors expert attended weekly meetings and advised the team on classification development and analysis of complex incident reports. These meetings were also used to discuss intercoder agreement and attempted to resolve any issues that related to the understanding and application of specific codes, as well as for wider discussion among a multidisciplinary team. Ideally, a code book (a collection of coding classes) should be ‘all inclusive’ with codes with definitions that are ‘mutually exclusive’. 79 When an existing code was not available to describe the incident characteristics, at the weekly coding meetings, the study team discussed whether a new code was needed or the definition of an existing code should be amended to be more inclusive.
Hypotheses emerged from each step of analysis and were noted by reviewers during coding and analysis via electronic memos that were also discussed at weekly coding meetings. For example, as codes were assigned (e.g. ‘wrong dose administered’ and ‘wrong drug administered’) and the code book was developed, the study team observed how cases clustered around particular codes or sets of related codes and thematic groups emerged, such as ‘administration errors’, which informed the development of each class. 80 Implications of changes to the code book were considered on a case-by-case basis; given the structured nature of the coding process, it was possible to isolate reports that would be impacted by new codes or changes to the definition of existing codes.
Stage 2: generation of descriptive summaries
We described and summarised the data, in order for them to inform hypothesis formation. The analysis aimed to describe the most frequent incident types, contributory factors and incident outcomes. Moreover, the analysis explored high-level associations among these features. The nature of our inquiry was inductive and was guided by clinical expertise. Therefore, EDA methods were used to produce, for example, frequency tables, cross-tabulations and bar charts, ready for interpretation and refinement through expert clinical guidance. 42 As the purpose of our study was to generate learning to support HCPs to improve the safety of care delivery, we recognised that it was essential for the outcomes of the EDA to be both accessible and provide a logical account of how we identified the priority issues for possible intervention.
Frequency tables enabled us to identify the most common and most harmful reported incident types. Cross-tabulations between data variables (e.g. age group, incident type, contributory factor and incident outcomes), and between incident codes and contributory factor codes, helped to identify priorities (e.g. vaccine errors in children) and clusters of reported contributory events or factors for further inquiry by thematic analysis.
Stage 3: interpretation of themes and learning
The purpose of our thematic analysis44 was to deepen the analysis and interpretation gained in stage 1 (description of characteristics of incidents) and stage 2 (identifying patterns in the data) to identify and prioritise the most important patient safety problems. Thematic analysis enabled identification and description of recurring themes, not captured by the quantitative data, that could be targeted to mitigate events.
Exploratory data analysis enabled us to collate relevant codes and explore the relationships between the most common and most harmful reported safety incidents and contributory factors and outcomes. Re-examination of these incidents in clusters of similar incidents provided an opportunity to identify contextual issues within each subset of data (e.g. all reports describing moderate harms or worse following issues relating to access of clinical services for urgent assessment). The subsets of reports were independently reread by two clinicians. The clinician reviewers were encouraged to identify any relevant clinical contextual issues that might not have been explicit in the report that could help explain the relationships identified from the EDA in more detail. At this stage, interpretation of report content and the identification of stand-alone and cross-cutting themes about reported causes and opportunities to prevent recurrence within the data were encouraged. Themes and their supporting data, including clinical vignettes, were discussed by the study team and recommendations were agreed.
Ethics considerations
The ABHB Research Risk Review Committee waived ethics approval (ABHB research and development reference number SA/410/13; see Appendix 1). No issues were identified from the information within reports that raised serious professionalism or ongoing patient safety issues.
Chapter 4 Overview of study findings
In this chapter, we provide a summary of our analysis of all included incident reports and discuss the reports that have been excluded from the analysis in the interests of highlighting how the incident-reporting system is misused or the purpose of the system is misinterpreted. In Chapter 5, we summarise all reports describing serious harms and deaths, and describe inherent themes relating to the underlying reported preventable causes of such incidents. In Chapter 6, we will explore each of the five categories of safety incident outlined in Chapter 5. Recommendations for research and development are proposed in Chapter 7.
Overview
A total of 13,699 reports from general practice were coded. Five high-level, incident-type categories summarise the majority of safety incidents described within the reports:
-
communication with and about patients
-
timely diagnosis and assessment
-
medication and vaccine provision
-
errors in investigative processes
-
treatment and equipment provision.
Of the 9031 reports included in the analysis, the severity of harm could be determined in 5755 cases. This was unclear for the remainder (n = 3276 incidents). Table 2 shows the number of incidents for each category of harm severity and also gives an example of an incident with different levels of severity of harm.
| Severity of harm | Description | Example | Reports, n (%) |
|---|---|---|---|
| Unclear | It is unclear from the free-text description what level of harm has occurred | Patient given medication to which they had a documented allergy, but no mention of an allergic reaction | 3276 (36.3) |
| None | Patient outcome is not symptomatic or no symptoms detected and no treatment is required | Patient given medication to which they had a documented allergy, but did not develop an allergic reaction | 1210 (13.4) |
| Low | Patient outcome is symptomatic, symptoms are mild, loss of function or harm is minimal or intermediate but short term, and no or minimal intervention (e.g. extra observation, investigation, review or minor treatment) is required | Patient given medication to which they had a documented allergy and developed a minor rash which did not require any additional treatment | 3549 (39.3) |
| Moderate | Patient outcome is symptomatic, requiring intervention (e.g. additional operative procedure or additional therapeutic treatment), an increased length of stay, or causing permanent or long-term harm or loss of function | Patient given medication to which they had a documented allergy and required hospital admission for further treatment and observation | 631 (7.0) |
| Severe | Patient outcome is symptomatic, requiring life-saving intervention or major surgical/medical intervention, shortening life expectancy or causing major permanent or long-term harm or loss of function | Patient given medication to which they had a documented allergy and subsequently had an anaphylactic reaction requiring intubation and admission to intensive care | 122 (1.4) |
| Death | On balance of probabilities, death was caused or brought forward in the short term by the incident | Patient given medication to which they had a documented allergy and subsequently had an anaphylactic reaction from which they died | 243 (2.7) |
Just over half of the included reports (50.3%, n = 4545) described harm to one or more patients.
Severity of harm by incident category
Table 3 reports the number and proportion of incidents in each category and the proportions resulting in no harm, harm or serious harm (all incidents resulting in moderate harm, severe harm or death).
| Incident category | Harm, n (%) | No harm, n (%) | Serious harm or death, n (%) | Harm not specified, n (%) | Total, n (%) |
|---|---|---|---|---|---|
| Communication with and about patients | 82 (46) | 463 (17) | 172 (6) | 1061 (38) | 2805 (21) |
| Medications and vaccines | 1280 (52) | 425 (17) | 238 (10) | 779 (31) | 2484 (18) |
| Investigative processes | 536 (40) | 84 (6) | 38 (3) | 719 (54) | 1339 (10) |
| Treatment and equipment provision | 515 (68) | 64 (9) | 116 (15) | 175 (23) | 754 (6) |
| Diagnosis and assessment | 575 (79) | 33 (5) | 366 (50) | 120 (17) | 728 (5) |
| No harm from primary care (excluded reports) | 4668 (34) | ||||
| Othera | 921 (7) | ||||
| TOTAL | 13,699 (100) | ||||
Incidents related to communication with and about patients were most frequently reported safety issues (n = 2805, 21%), followed by incidents related to medications and vaccines (n = 2484, 18%) and investigative processes (n = 1339, 10%). Incidents relating to timely diagnosis and assessment (n = 728, 5%) and treatment and equipment provision (n = 754, 6%) were less frequently reported. However, diagnosis and assessment-related incidents were most likely to cause harm to the patient; although 79% of incidents in this category resulted in a harmful outcome, two out of three of all harmful outcomes were serious harms or deaths (n = 366, 50%). This was followed by incidents relating to treatment and care equipment (68%, n = 515), and then medications and vaccines (52%, n = 1280). Although communication with, and about, the patient was the most frequently reported incident category, 46% (n = 1282) of these incidents resulted in harm and 6% (n = 172) resulted in serious harm or death.
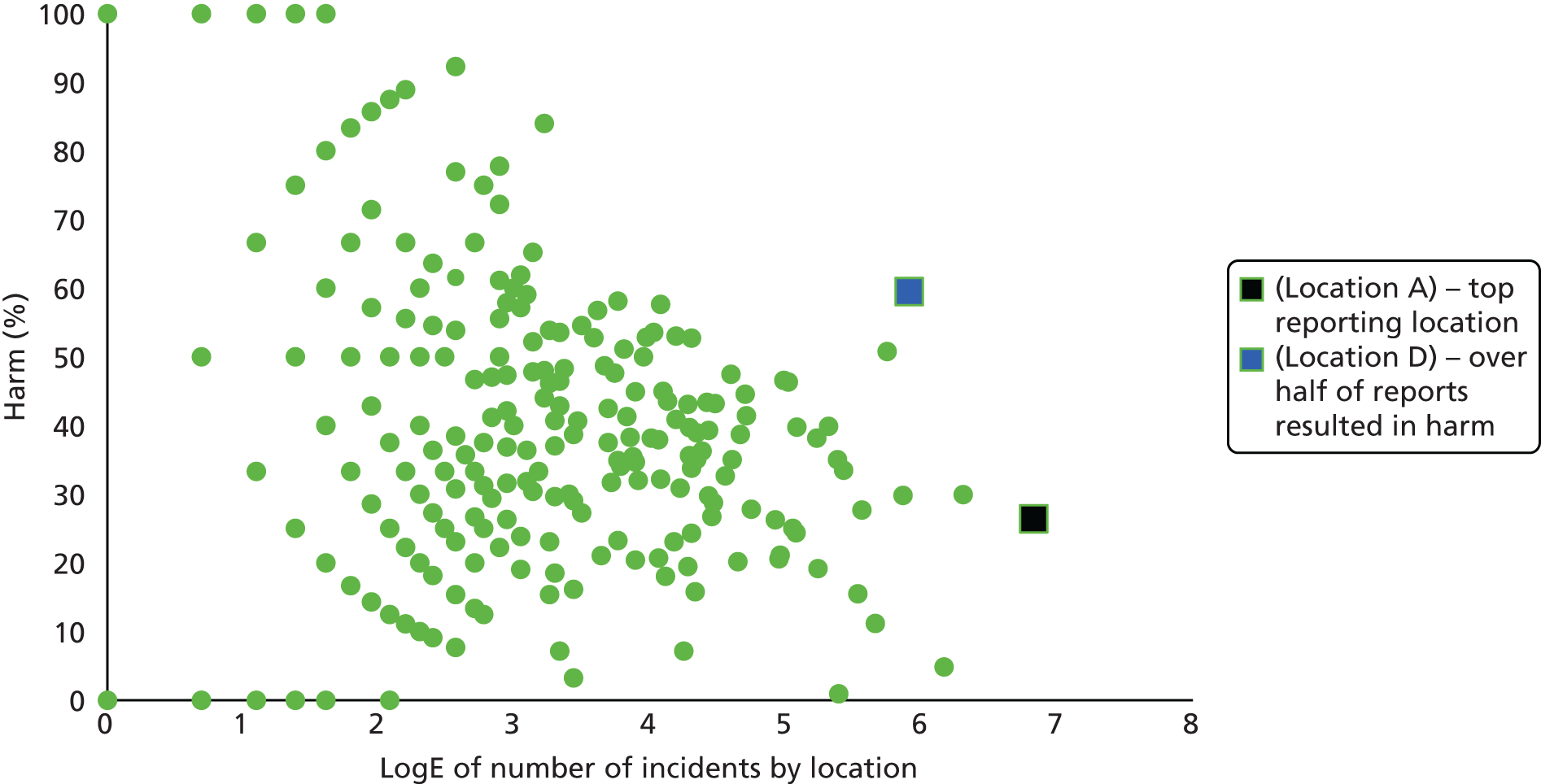
Reporting locations
Although 462 separate locations provided at least one report, over half of the reports originated from only 30 locations (n = 7071, 52%). Sixty-seven locations reported only one incident. Figure 3 demonstrates the variation in reporting across locations. This implies that some organisations do not report general practice safety incidents to the NRLS or do not have a mechanism for receiving local incident-reporting system from general practice in its organisation. The top reporting location (shown in black) reported 920 incidents, of which 26% (n = 243) resulted in harm and 4% (n = 40) in serious harm. Other locations are similar to the organisation in blue where, of the 368 incidents reported, over half (60%, n = 219) resulted in harm. Where they do report, different thresholds for receiving reports (i.e. only serious harms or deaths), as well as different mechanisms or thresholds for uploading incident reports to the NRLS, could explain the variation identified (see Figure 3).
FIGURE 3.
Scattergraph of the percentage of harmful incidents by the frequency of reports per location.
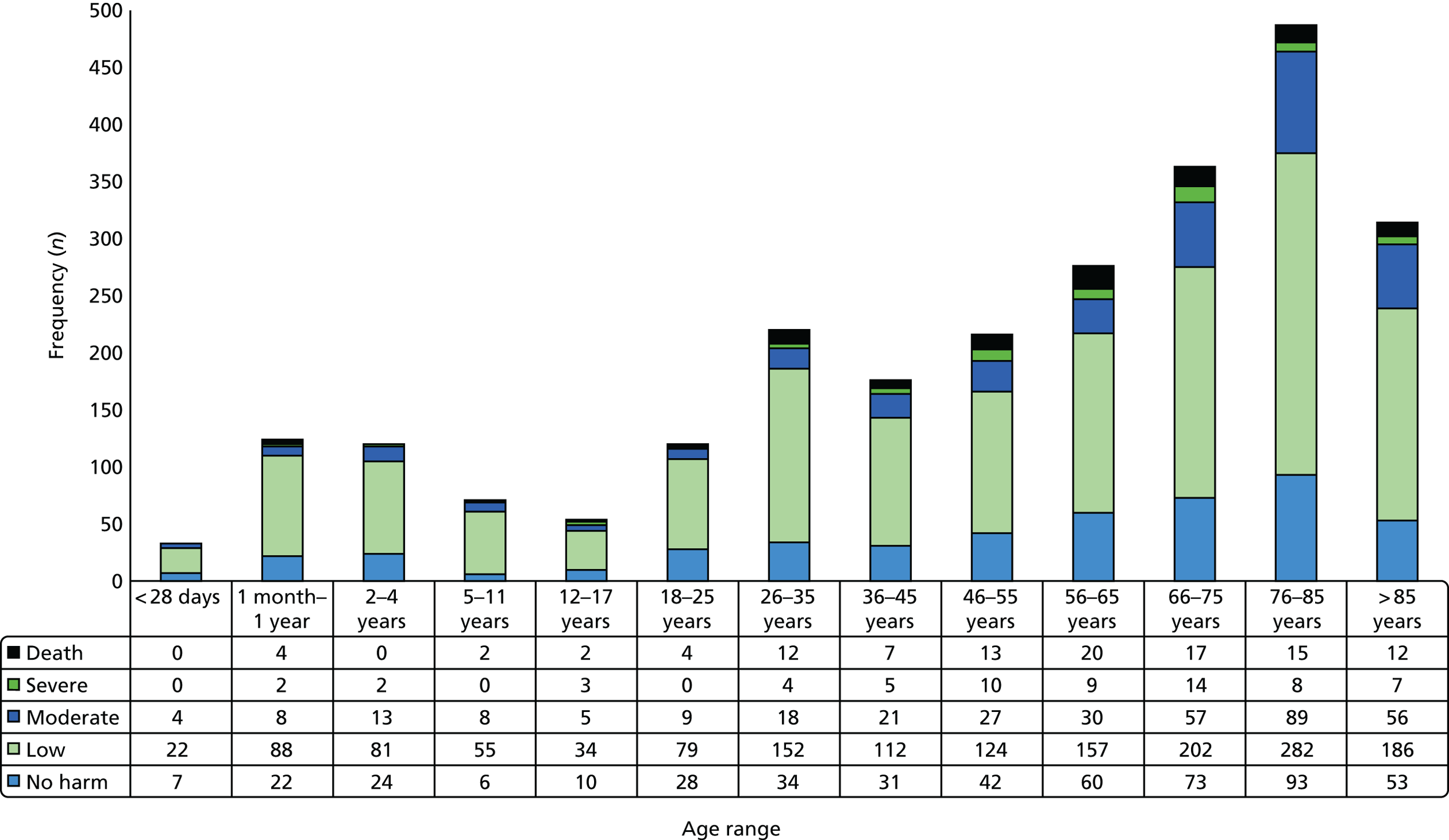
Reported age of patients
The age of the patient was provided in 6472 incident reports. Figure 4 demonstrates the frequency of reports by age group. The age group accounting for the highest proportion of incident reports was 76–85 years (n = 1403, 22%), and 53% (n = 3417) of all reports involved a patient aged > 65 years while 9% (n = 576) involved patients aged < 4 years. The frequency distribution of incident reports shows peaks at both extremes of age (children and elderly patients), consistent with the expected number of contacts with general practice in these age groups. This pattern was apparent across all the incident categories (see Chapter 6).
FIGURE 4.
Frequency of reports by age group.

In 2574 cases, both the level of harm and patient age were reported. Figure 5 demonstrates the clustered frequencies of each level of harm outcome per age group. Figure 5 also shows that those aged > 65 years feature most within incident reports describing serious harms (moderate harm or worse). The age group with the highest proportion of reports that resulted in serious harm was the 66–75 years age group (24%).
FIGURE 5.
Frequency of level of harm by age group.
Reported contributory factors
In total, 4862 contributory factors, defined as issues that did not directly cause, but contributed to, the occurrence of an incident, were identified. Only around one-third of incident reports described reasons why the incident occurred, which significantly inhibits learning to improve future practice. Staff-related factors (n = 1792) were most frequently identified, followed by service- (n = 1505) and patient-related factors (n = 1383). A breakdown of those classes is included in Table 4 for patient- and staff-related factors, and Table 5 for equipment- and service-related contributory factors.
| Contributory factors | Contributory factor subtheme | Examples of frequently described contributory factors | Total (n) |
|---|---|---|---|
| Patient-related factors (N = 1383) | Patient characteristics (n = 1051) | Patient pathophysiology | 127 |
| Patient is a child | 89 | ||
| Patient frailty | 83 | ||
| Rare disease or rare presentation | 69 | ||
| Language or patient decision-making (n = 258) | Patient behaviour | 117 | |
| Non-compliance with instructions from HCPs | 82 | ||
| Patient speaks a language other than English | 21 | ||
| Geography (n = 74) | Patient new to area | 51 | |
| Access difficulties | 12 | ||
| Staff-related factors (N = 1792) | Staff decision-making (n = 806) | Failure to follow protocol | 460 |
| Inadequate skill set or knowledge | 266 | ||
| Wrong professional carries out task | 44 | ||
| Mistake(n = 986) | Not otherwise specified | 552 | |
| Misread/did not read | 96 | ||
| Distraction/oversight | 25 |
| Contributory factors | Contributory factors subtheme | Examples of frequently described contributory factors | Total (n) |
|---|---|---|---|
| Equipment-related factors (N = 182) | Design and usability(n = 142) | Poor equipment design | 110 |
| Inadequate medication storage or packaging | 32 | ||
| Service-related factors (N = 1505) | Inadequate protocols (n = 520) | Investigation-related protocols | 155 |
| Medication-related protocols | 87 | ||
| Referral-related protocols | 82 | ||
| Continuity of care (n = 412) | Out-of-hours services | 98 | |
| Transfer of information between secondary and primary care | 86 | ||
| Continuity of care within primary care | 59 | ||
| Working conditions (n = 420) | Inadequate provision of health-care staff | 261 | |
| Busy/overloaded by work | 126 | ||
| Education and training (n = 95) | Knowledge of others’ roles | 53 | |
| Service availability (n = 58) | Long wait for service | 37 | |
| Service unavailable | 21 |
Although staff mistakes, defined as a deficiency or failure in judgement or inferential processes, were described in 986 reports, additional information that could yield any insight into ways to improve future practice was minimal. However, reports describing failures in staff decision-making processes (n = 806) included failure to follow protocols (n = 460) such as for international normalised ratio (INR) monitoring or an inadequate skill set or knowledge (n = 266), for example relating to patients at risk of acute deterioration.
Unavailability or inadequate protocols (n = 520), pressures from low staffing levels (n = 420) and operational challenges to ensure continuity of care (n = 412) were the most common service-related contributory factors (see Table 4 for further details). Lack of familiarity of different staff member roles was also described in 53 reports.
The patient-related factors included the physical and physiological characteristics of children and elderly people, as well as behaviour-related issues such as compliance. Several patient groups were discussed in terms of their potentially vulnerable status, particularly those with pre-existing pathophysiology or disability (n = 127), children (n = 89) and the frail elderly (n = 83). Non-compliance with instructions from HCPs (n = 82) was described in a small number of incidents.
Excluded reports
Around one in five reports (n = 3147, 23%) contained insufficient detail or did not describe a patient safety incident, defined as ’any unintended or unexpected incident which could have led (or did lead) to harm for one or more patients receiving NHS-funded healthcare’. 20 Of note, although pressure ulcers can represent the outcome of poor care, the majority of reports relating to pressure ulcers contained little descriptive or contextual information or had not occurred in the community setting (e.g. incident report simply stated ‘pressure ulcer, grade 3′) and were therefore also excluded from the analysis. Table 6 shows a summary of excluded reports.
| Reason for exclusion | Frequency |
|---|---|
| Inappropriate use of system | |
| Irrelevant – did not describe a patient safety incident | 784 |
| Insufficient detail – report did not contain sufficient detail about what happened | 810 |
| Incident not related to health care, for example a fall in the GP surgery car park or patient has self-harmed despite appropriate intervention from GP | 762 |
| Defensive reporting – reporting system being used by professionals to defend their involvement in events other than a safety incident | 97 |
| Reporting death – a patient death with no apparent health-care-related cause was reported | 233 |
| Act of violence by patient – violence from a patient to HCPs | 105 |
| Complaint/coroner investigation – detail about a complaint and the need for, or outcome of, a coroner investigation | 118 |
| Outcomes from secondary care or unclear | |
| Pressure ulcer – grade of pressure ulcer stated but no description of how it occurred within community | 1703 |
| Health-care-associated infection – a hospital-acquired infection | 56 |
| TOTAL | 4668 |
National Reporting and Learning System data limitations
One of our study objectives was to describe characteristics of the patient and incident such as gender, ethnicity, geography, time of day, and level of patient harm. Rather than amend our objectives as a result of various limitations, we have included them in order to highlight opportunities to improve the quality of data uploaded to the NRLS.
-
Gender is inconsistently provided as a structured variable to the NRLS and present in < 40% of reports.
-
Ethnicity is not captured via a structured classification system.
-
Time of day is an inconsistent and unstructured variable that can be identified by free-text analysis; we have therefore highlighted where it is important as a contextual issue.
Chapter 5 Serious harms and death in general practice
In this chapter, we provide a summary of all reports describing serious harm and deaths in incident reports received from general practice.
Overview
Of the total 13,699 incident reports, 996 incidents resulted in moderate or severe harm to, or death of, a patient. Moderate and severe harms, using the WHO ICPS definitions,63 were considered to be permanent loss of function, conditions necessitating hospital admission or disability. We called these serious harms.
An overview of level of harm outcome by incident category is provided in Table 7.
| Incident category (N, % of total) | Incident type | Serious harm or death, n |
|---|---|---|
| Diagnosis and assessment (N = 366, 37%) | Diagnosis | 217 |
| Assessment | 149 | |
| Medication and vaccine provision(N = 238, 24%) | Adverse event | 63 |
| Prescribing | 45 | |
| Clinical decision-making | 26 | |
| Dispensing | 24 | |
| Monitoring | 22 | |
| Administration | 15 | |
| Immunisation-related | 12 | |
| Provision of treatment and care equipment(N = 116, 12%) | Treatment | 89 |
| Equipment | 27 | |
| Communication with and about patients(N = 172, 21%) | Referrals | 70 |
| Accessing clinical services | 60 | |
| Information transfer | 22 | |
| Miscommunication | 18 | |
| Inaccurate knowledge about patients | 2 | |
| Investigative processes (N = 38, 4%) | ||
| Others(N = 66, 7%) | Transporting patients | 20 |
Priority contributory themes
Fewer than half of the 996 reports (n = 431, 43%) contained descriptions of contributory factors. Combined with insights generated by thematic analysis, the four main contributory themes underpinning serious harm- and death-related incidents were:
-
communication errors in the referral and discharge of patients
-
physician decision-making
-
delays in cancer diagnosis associated with unfamiliar symptom presentation and/or inadequate administration
-
delayed management or mismanagement following failures to recognise signs of clinical (medical, surgical and mental health) deterioration.
Table 8 highlights the proportion of serious harms and death outcomes by each theme.
| Theme | Harm (n) | |||
|---|---|---|---|---|
| Subtheme | Moderate | Severe | Death | Total |
| Communication errors in the referral and discharge of patients complicated by failures in IT systems | 72 | 11 | 17 | 100 |
| Referral not performed when indicated | 27 | 8 | 12 | 47 |
| Premature and poor discharge planning | 27 | 2 | 2 | 31 |
| Information transfer between care providers | 18 | 1 | 3 | 22 |
| Physician decision-making | 64 | 18 | 14 | 96 |
| Prescribing | 40 | 5 | 5 | 50 |
| Treatment decisions | 12 | 8 | 4 | 24 |
| Monitoring | 12 | 5 | 5 | 22 |
| Delayed cancer diagnosis associated with unfamiliar symptom presentation and/or inadequate assessment | 30 | 42 | 21 | 93 |
| Delayed management or mismanagement following failures to recognise signs of clinical (medical, surgical and mental health) deterioration | 26 | 5 | 30 | 61 |
| Errors in the process of triaging patients | 14 | 1 | 13 | 28 |
| Identifying acute clinical conditions | 6 | 2 | 15 | 23 |
| Diagnosis of emergency condition delayed | 6 | 2 | 2 | 10 |
| TOTAL | 192 | 76 | 82 | 350 |
Factors contributing to incidents describing serious harm and death
In this section, we provide a summary of the contributory factors identified in all serious harm and death reports.
Patient-related factors were the most frequently reported (n = 215) contributors to incidents resulting in serious harm and death. These included patient characteristics, such as patient pathophysiology (n = 51) or frailty (n = 21). For example, one patient without a care package following discharge from hospital, and with poor eyesight, self-administered the wrong dose of insulin. Rare presentations, such as for an atypical cancer presentation, or a rare disease such as bladder cancer in a young child, may have made diagnosis more challenging in 43 incidents. Service-related contributory factors were also frequently described (n = 190). The out-of-hours primary care services (n = 48) were often implicated; for example, some incidents were attributed to the failure of HCPs to share information. In one case, the out-of-hours service failed to pass on urgent blood test results to the patient’s GP and thereby delayed further assessment. Forty-one incidents were attributed to inadequate protocols; for example, inadequate protocols regarding the handling of referrals by mental health teams resulted in some cases delays in assessment, and led to deterioration in the patient’s mental health or death by suicide. Working conditions, such as staff being too busy to spend sufficient time assessing a patient, were described in 17 reports. Staff-related factors were described in 108 reports and included failure to follow protocols (n = 38), such as those for warfarin dosing, and staff members having an inadequate skill set or knowledge to assess acutely unwell patients, resulting in missed emergency diagnoses (n = 36).
Examination of priority themes
In this section, we will define each priority theme by considering the role of identified contributory factors, and, when relevant, the events leading up to the incident, and other contextual issues identified by thematic analysis.
Communication errors in the referral and discharge of patients
Errors in the processes involved in transferring patient information compromised the continuity of care between primary and secondary care. The most frequently reported error, mentioned in 47 reports, was the failure of referral to take place as intended. These resulted in delays in management for 18 patients and in the death of 10 patients. For example:
Discharge home with pressure sore on sacrum and × 2 heels from [community hospital]. Unable to mobilise and/or eat and drink – district nurse was not informed.
Errors relating to referrals not being made were sometimes preceded by another incident, including poor discharge planning, for example failure to refer to community practitioners such as district nurses for wound reviews (n = 10), missed diagnoses (n = 7) or failure to transfer patient information (n = 5), such as failure to send patients’ discharge summaries to their GP.
Premature or incomplete discharge planning was described in a further 31 reports. In 27 cases this resulted in the patient being readmitted to hospital; two patients died. One report described a frail elderly gentleman who could not cope without additional support at home following discharge and, as a result of self-neglect, developed cellulitis from leg wounds. He was eventually readmitted to hospital but later died. Of the 21 incidents in which patient age was reported, nearly three-quarters (n = 15) of patients were aged ≥ 66 years.
A further 22 incidents involved errors in the transfer of patient information between different health-care settings, with 10 resulting in the patient’s admission to hospital. These included incomplete discharge summaries (n = 5), failure to send discharge summaries (n = 5) and delay in sending discharge summaries (n = 4). In four cases, the patient’s GP failed to action recommendations included in the discharge summary. For example:
Patient attended GP appointment with a new resident GP. Enquired about the referral to urology department at acute hospital that should have been made by the long-term locum GP 3 months previous. On investigation, it was found unsent in the records.
Few contributory factors were reported in relation to incidents involving poor communication between health-care providers. Of note, poor continuity of care between health-care providers was only explicitly reported as a potential contributory factor in five cases.
Physician decision-making
In total, 96 incidents were identified as resulting from physician decision-making: 24 reports described errors in the clinical treatment decision process, 50 reports described errors in prescribing medications and 22 recorded errors in monitoring dose-dependent medications. For example:
Patient discharged from [hospital] on [date]; no warfarin dose or INR results sent to GP. INR checked and information added to INRstar (or did not enter dose was changed in hospital). Patient given 2 mg daily (subsequently found dose in hospital was 0.5 mg). Patient suffered GI [gastrointestinal] bleed and died on [date].
Over half (n = 56, 58%) of the reports were preceded by another incident. The interface between physicians, existing paper-based and/or computer-based systems and patients was the apparent underlying issue in a number of these incidents. Errors in the transfer of patient information between health-care settings were recorded in 17 reports, and errors in the process of recording, storing and accessing patient documentation in a further seven reports. Inadequate communication with patients was described in eight reports. For example, one report detailed a district nurse missing the opportunity to check the immunisation status of a patient; the patient did not receive the required pneumococcal vaccine and subsequently developed pneumococcal sepsis. In another example, the GP failed to act on discharge advice:
Practice notified that patient was being discharged following 10-day admission for treatment of iatrogenic hypercalcaemia caused by a high dose of alfacalcidol. GP did not change dose of alfacalcidiol as stated in letter.
At least one contributory factor was identified in over half (n = 54, 56%) of physician-related medication errors. Twelve reports described how patient behaviour or actions contributed to the development of incidents, for example non-compliance with instructions from the patient’s physician in some cases resulted in adverse drug events and recurrence of the patient’s illness.
A further 15 incidents were due, at least in part, to staff members failing to follow protocols or having an inadequate skill set or knowledge. For example, one GP prescribed 10 times the recommended dose of trimethoprim for an 8-week-old baby. Service-related factors included poor continuity of care between different HCPs (n = 8); for example, one patient received the wrong doses of insulin as a result of the lack of communication between the discharging medical team and the district nurses. Four incidents arose, at least in part, because the patient received care from an out-of-hours service. For example, one patient was prescribed a large quantity of amitriptyline by an out-of-hours GP despite a history of overdose, and was found dead 2 days later. This highlights the lack of background clinical information available to out-of-hours service doctors when making clinical decisions. Of particular note, 17 adverse events followed an error in the process of monitoring medications, of which 14 involved staff failing to follow protocol or having an inadequate skill set or knowledge. This included one case in which a patient’s INR was not monitored despite the patient being prescribed anti-tuberculosis medications known to interact with warfarin. The patient subsequently developed a pontine cerebrovascular event and was found to have an INR of 10. Another staff-related factor was mistakes in prescribing medications (n = 8), such as confusing drugs with similar names or appearances. For example:
A locum GP diagnosed tonsillitis and prescribed [p]enicillamine instead of [p]enicillin. The patient was unaware of the mistake and took the tablets as prescribed. He sought further medical advice as symptoms were not improving.
Delays in cancer diagnosis associated with unfamiliar symptom presentation and/or inadequate administration
Communication process errors commonly underpin missed and delayed cancer diagnoses. Missed or delayed cancer diagnosis accounted for 9% (n = 93) of reports describing serious patient harm or death. In 25 cases, these were preceded by an incident involving investigative processes, such as an error in reporting of diagnostic imaging results. In 16 cases, communication process errors were preceded by a referral error. For example, an elderly patient with an identified lung opacification on a chest radiograph was given a routine rather than an urgent referral. By the time adenocarcinoma was diagnosed, the cancer had metastasised and the patient developed carcinomatosis. Another 59 reports recorded a delay in the assessment or management of a cancer diagnosis, and 18 of those described the death of a patient. For example:
Patient attended surgery with symptoms of irritable bowel syndrome. Given prescription, over next few months came back for telephone advice. Told had colitis and given further medication. Patient was not given a PR [per rectal] examination at any visit. Referred to endoscopy 7 months later and found to have bowel tumour. Patient undergoing chemotherapy at the time of report.
In over half of incidents involving a delay in cancer diagnosis, the patient’s age was recorded (n = 24, 62%), and missed cancer diagnoses were reported for a broad range of age groups. Symptoms of a rare presentation was the most common contributory factor for a delayed cancer diagnosis. Other factors included non-disclosure of symptoms (n = 9) and visiting different HCPs for the same symptoms (n = 6). For example:
Patient’s mother contacted the Patient Advice and Liaison Service, stating that her adult daughter died. For 6 months prior to her daughter’s death, the GP had been treating her for migraine, anxiety, depression and panic attacks. In addition, she had been losing her eyesight but the GP had insisted that she see an optician who had referred her back to the GP, stating that something else was amiss. The patient had been told that the GP was in touch with the optician. After the patient died, two brain tumours were discovered.
Failures to recognise signs of clinical deterioration
Missed or delayed diagnosis of an acute clinical condition (n = 61) frequently resulted from errors during telephone triage (n = 28), of which seven involved out-of-hours services. For example:
Call passed from NHS Direct to out-of-hours service with a ‘less urgent’ priority. 10-week-old baby with central cyanosis, increased respiratory rate, and ‘noisy’ breathing.
Acute clinical conditions were missed in 23 reports, and a further 10 reports described the delayed diagnosis of an emergency condition, such as bowel perforation, which resulted in a delayed hospital admission and the death of a patient. Another example includes:
2-month-old baby taken to A&E [accident and emergency] as Sudden Unexpected Death of Infancy having died at home. Baby had been seen by GP on previous evening with temperature of 38 Celsius; diagnosed with possible chest infection and prescribed amoxicillin. NICE guidance states that fever ≥ 38 Celsius in child less than 3 months is a red flag and a child should be admitted to hospital. Preliminary results from post-mortem suggest that infection is likely cause of death.
Involvement of out-of-hours services was described in 10 of these incidents. For example:
Patient seen on home visit. Advised had been seen with symptoms strongly suggestive of an acute stroke at home by out-of-hours service at approximately 2015 hours yesterday evening and told to contact her GP the next morning. Policy is that patient suspected of suffering an acute stroke should be admitted as a 999 to hospital for appropriate diagnosis and treatment.
In eight cases, the HCP did not appreciate the severity of illness, leading to delays in escalating concerns and co-ordinating urgent transport to hospital. Of the 36 reports that described emergency transport delays, 10 stated that the delay was preceded by failures in triaging patients or in the assessment of acutely unwell patients. In addition, four incidents were preceded by inadequate verbal communication between HCPs.
Errors in the process of identifying patients at risk of deterioration as a result of mental health problems were largely fatal, with 27 out of 29 incidents resulting in the death of a patient. The majority of these involved the patient taking an overdose of medication. Patient behaviour, such as not attending a planned review with their GP, contributed to these incidents in five cases.
Chapter 6 Patient safety incidents in general practice
In this chapter, we explore each of the five categories of safety incidents described in reports received from general practice and the inherent themes relating to the underlying reported causes.
The five categories of incident type, in descending order of frequency, are:
-
communication with and about patients
-
medication and vaccine provision
-
errors in investigative processes
-
treatment and equipment provision
-
timely diagnosis and assessment.
Communication with and about patients
Overview
Over one-fifth (n = 2805) of the reports described problems relating to communication with, and about, patients. Five themes were evident from synthesis of the reported descriptions of events and contributory factors:
-
barriers to accessing clinical services
-
errors in information transfer between care providers
-
up-to-date patient records
-
delays in referral decision-making and administrative processes
-
miscommunication with patients and between professionals.
Barriers to accessing clinical services (n = 636) and delays in referral (n = 746) were the most frequent incidents and were also associated with the most harm.
Table 9 provides an overview of themes and subthemes associated with levels of harm for communication-related safety incidents.
| Incident theme | Harm, n (%) | Total (%) | |||
|---|---|---|---|---|---|
| Subtheme | Yes | No | Serious | Not specified | |
| Barriers to accessing clinical services | 412 (65) | 85 (13) | 60 (9) | 139 (22) | 636 (100) |
| Message handling and telephone calls | 24 | 9 | 3 | 16 | 49 |
| Arranging appointments | 88 | 37 | 3 | 42 | 167 |
| Accessing a clinician | 300 | 39 | 54 | 81 | 420 |
| Errors in information transfer between care providers | 235 (31) | 135 (18) | 22 (3) | 386 (51) | 756 (100) |
| Communication not acted on | 17 | 8 | 4 | 6 | 31 |
| General transfer of information between care providers | 19 | 13 | 2 | 39 | 71 |
| Information errors between secondary and primary care | 177 | 104 | 15 | 340 | 621 |
| Information errors within primary care | 22 | 10 | 1 | 1 | 33 |
| Availability and accuracy of patient records | 56 (15) | 95 (26) | 2 (1) | 276 (74) | 427 (100) |
| Availability of medical records | 214 | 29 | 0 | 188 | 243 |
| Accuracy of medical records | 27 | 63 | 2 | 77 | 167 |
| Other documentation | 3 | 3 | 0 | 11 | 17 |
| Delayed referrals | 466 (62) | 90 (12) | 70 (9) | 190 (25) | 746 (100) |
| Delayed decision | 213 | 29 | 34 | 64 | 306 |
| Delayed referral | 87 | 15 | 12 | 20 | 122 |
| Erroneously completed referrals | 27 | 20 | 2 | 25 | 72 |
| Office-based errors | 139 | 26 | 22 | 81 | 246 |
| Miscommunication | 113 (47) | 58 (24) | 18 (8) | 69 (29) | 240 (100) |
| With patients | 78 | 36 | 11 | 38 | 152 |
| Between HCPs | 35 | 22 | 7 | 31 | 88 |
| TOTAL | 1282 | 463 | 172 | 1060 | 2805 |
Further examination of communication themes
Barriers accessing clinical services
Problems accessing clinical services were identified in 636 reports, and 65% of those described a harm outcome. Reported incidents related to difficulties in arranging appointments with GPs, statutory assessment services (e.g. ‘new-baby check’ or cervical smears), or for message handling by, or telephone calls with, receptionists and delays in presentation or timely advice as a result of involvement of NHS Direct.
Barriers to accessing acute care services were the type of incident most likely to result in serious harm (n = 60).
Patients experienced difficulties or delays in accessing home visits or telephone call assessments with a triage nurse or GP, or in securing a primary care appointment. In addition, reports described patients not receiving visits from community-based HCPs, such as health visitors, because of a lack of information transfer from secondary care. For example:
Notification of birth details not faxed through to surgery. Health visitor only aware on day 14 when discharge summary faxed through to surgery. Discharge summary telephone number of client incorrect. Midwife made aware by client but still no communication with Health visitor so no birth visit scheduled.
Errors in information transfer between care providers
Incidents arising from ineffective or inadequate transfer of clinical information from one provider to another were identified in 756 reports. Over one-quarter of these incidents led to harm (n = 235, 31%), and few incidents led to serious harm (n = 22). The majority of incidents occurred at the interface between primary and secondary care (n = 621).
Reports described patients receiving letters intended for the GP from the hospital consultant, for example:
Copies of neurology results not sent with letter concerning serious diagnosis – instead, sent to direct to patient. No details in letter as to further treatment or follow-up. Information and copy results eventually obtained from secretary to consultant.
Some discharge and clinic letters were delayed, incorrect or incomplete, or indeed never sent, sometimes after long and complex inpatient stays leading to primary care doctors and nurses struggling to make sense of management plans. Often the error was identified before the patient experienced any harm, for example:
Discharge summary had bisoprolol 10 mg daily and atenolol 50 mg daily (both beta-blockers). Medication should have been bisacodyl tablets 10 mg and atenolol 50 mg. Patient went to see the doctor 4 days later, blood pressure was low: 96/76.
These incidents caused distress to patients and carers, and HCPs spent a lot of time mitigating possible harmful clinical outcomes by chasing up the hospital team. Once errors occur, the consequences for the patient can escalate quickly, as in the following example:
Discharge summary for patient received from ward on [Date]. Seven new medications on the discharge summary with no indication why they were started. Contacted the ward and spoke to consultant. He checked the notes and rang back the following day. He confirmed that the patient should not be taking the medications and they were not prescribed in hospital. A new discharge summary was agreed to be issued. We tried to contact the patient but he had been readmitted. Senior house officer on the admitting ward confirmed the patient has been receiving the seven medications since readmission. The patient is still in hospital.
Availability and accuracy of patient records
Reports describing unavailable or inaccurate patient records (n = 427, 15%) resulted in multiple communication incidents. Around 10% of reports involved patients aged < 1 year, which perhaps reflects the complexity of medical records for this age group, which include parent-held records (the Red Book), GP surgery records and public health vaccine records. Inaccurate or unclear medical records were often caused by filing errors (n = 58). For example:
Patient presented with stepmother for preschool booster. Written consent from father was brought but parental held record was not available. Nurse explained she was giving REPEVAX and MMR [measles, mumps and rubella]. The following day stepmother called expressing concern that MMR had already been given in 2004. Incomplete documentation of initial dose of MMR booster.
Other reports described cases of patient notes being unavailable and thus delaying or hampering child protection meetings or case conferences, and others reported that notes were unavailable because of IT connection problems, highlighting IT system failure consequences:
A loss of IT connection due to a loose connection at a surgery resulted in two surgery sessions without access to computer appointment or patient notes.
Delays in referral decision-making and administrative processes
Delayed referrals account for 40% of the described serious harm outcomes for all communication-related incidents. Referrals were most commonly delayed by clinician decision-making (n = 306), or a clinician forgetting to send referral letters or awaiting further information before doing so (n = 122). For example:
Dr failed to send 2-week-rule cancer referral for patient. The training implication has been addressed with the doctor in the practice.
Erroneously completed referrals, either from primary to secondary care services or from secondary to primary care, were described in 72 reports. Reports described practitioners’ confusion about the correct referral method to select from several available (especially out of hours or at weekends and public holidays). Ineffective protocols were identified as the most common contributory factor described in these reports (n = 49). Across the reports, it was apparent that staff found it difficult to identify the appropriate referral protocol or form or the correct fax number to use when sending referral letters:
Attended surgery [Date] with symptoms, which warranted a 2-week cancer referral (upper GI [gastrointestinal] cancer). Secretary not at surgery Friday afternoon so form faxed by reception staff to fax number on form. Secretary checking referrals [1 month later] + noted no acknowledgement. Realised wrong fax number on form. The number of the fax on the cancer referral form is now for a fax machine in the Orthopaedic dept. Presumably they received the first fax but it wasn’t passed on or taken further.
As a result of these communication failures, patients did not receive medication (such as warfarin or insulin), dressings were not changed and surgical wounds or pressure ulcers were left untended for days. Failures to reinstate care packages also left vulnerable patients without basic care that led to a worsening of their condition and readmission.
Miscommunication with patients and between professionals
Reports in this theme could be divided into failures of communication between professionals and patients (n = 152) and failures of communication between HCPs (n = 88). Around half of these incidents were harmful (n = 113, 47%), and of these incidents one in six led to serious harm. For example, a patient was given erroneous advice about insulin that could have resulted in a fatal outcome:
Patient sought advice from OOH [out of hours] about his insulin – his insulin pens had accidentally been frozen and he was due to go away on holiday and needed to take meds with him. He was advised to leave pens out for 1.5 hours and they would be OK.
Reports described doctors, nurses or reception staff giving patients incorrect advice with regards to taking medication, where to attend for medical attention or how to access other services. This led to patients being seen in an inappropriate setting, taking medication in incorrect doses or at an incorrect frequency, or being unclear as to when they should seek attention in the event of deterioration. Others described a lack of clear communication over the telephone or face to face between professionals with regard to how seriously unwell a patient was and how urgently they needed to be assessed, leading to an inappropriate delay in their assessment.
Medication and vaccine provision
Overview
Almost one-fifth of reports (n = 2484) described medication- and vaccine-related incidents. Five themes were evident from synthesis of the reported descriptions of events and contributory factors:
-
safer medication provision
-
reliable therapeutic drug-level monitoring processes
-
avoidable adverse drug reactions
-
immunisation-related errors for children, elderly and the immunocompromised
-
clinician decision-making about treatments.
Table 10 provides an overview of themes and subthemes associated with described levels of harm for medication- and vaccine-related incidents. The themes are also summarised by level of harm severity in a clustered bar chart in Figure 6.
| Theme | Harm, n (%) | Total (%) | |||
|---|---|---|---|---|---|
| Subtheme | Yes | No | Serious | Not specified | |
| Safer medication provision | 559 (38) | 327 (22) | 84 (6) | 543 (40) | 1429 (100) |
| Prescribing | 293 | 181 | 45 | 289 | 763 |
| Dispensing | 143 | 94 | 24 | 172 | 409 |
| Administering | 123 | 52 | 15 | 82 | 257 |
| Therapeutic drug monitoring | 79 (65) | 9 (8) | 22 (18) | 32 (27) | 120 (100) |
| Avoidable adverse drug reaction | 130 (94) | 2 (1) | 63 (45) | 7 (5) | 139 (100) |
| Immunisation-related errors | 321 (69) | 32 (7) | 12 (3) | 111 (24) | 464 (100) |
| Prescribing | 9 | 4 | 1 | 3 | 16 |
| Dispensing | 4 | 4 | 0 | 5 | 13 |
| Administering | 267 | 20 | 1 | 99 | 386 |
| Other | 41 | 4 | 10 | 4 | 49 |
| Clinician decision-making | 70 (58) | 18 (15) | 26 (21) | 33 (27) | 121 (100) |
| Other | 121 (57) | 37 (18) | 31 (15) | 53 (25) | 211 (100) |
| TOTAL | 1280 | 425 | 238 | 779 | 2484 |
FIGURE 6.
Clustered bar chart of medication- and vaccine-related incidents by level of harm.
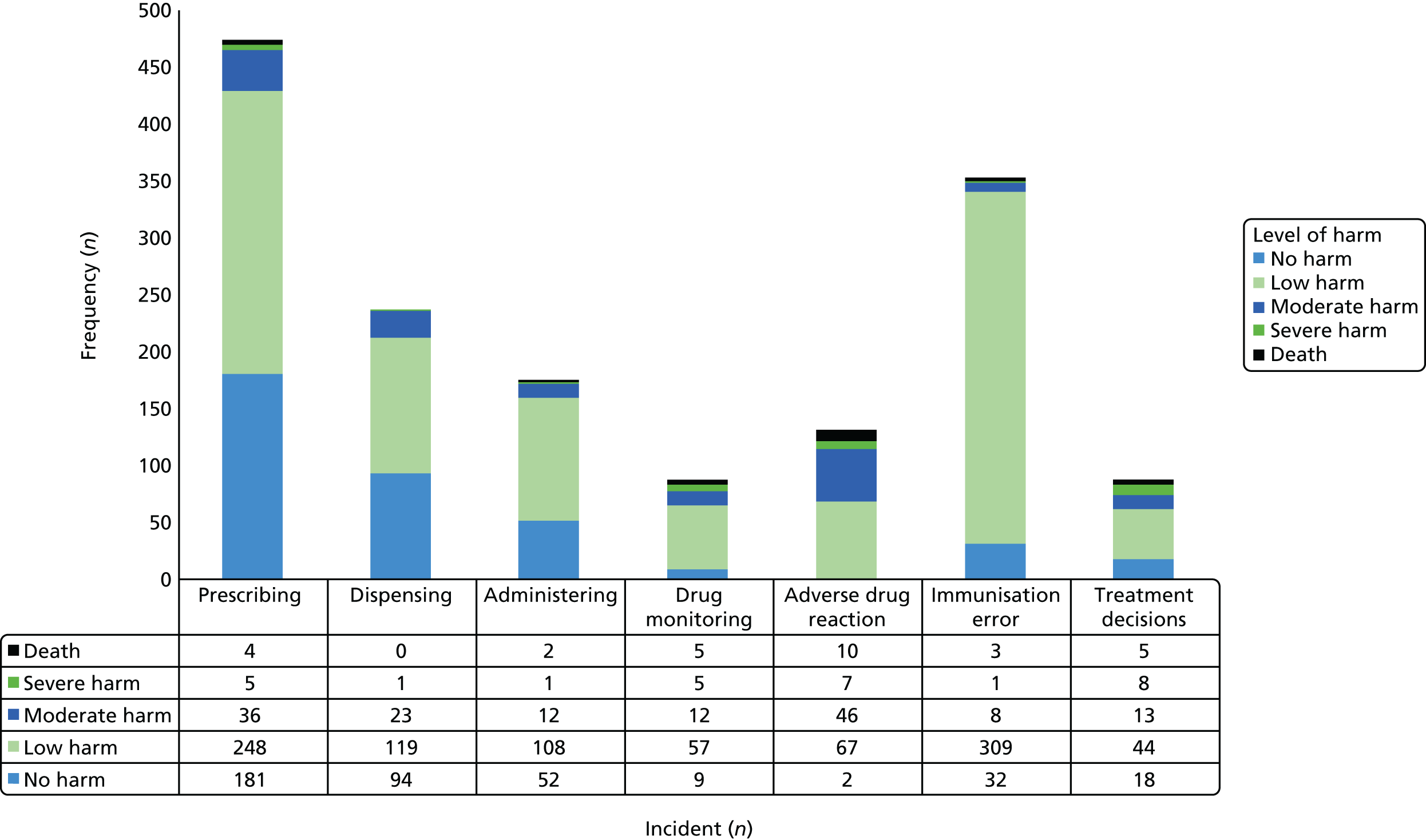
Prescribing incidents were most frequently described (n = 763, 31% of all medication- and vaccine-related incidents), followed by dispensing incidents (n = 409, 16%) and immunisation-related errors (n = 464, 19%).
Avoidable adverse drug reactions were less common (n = 139), although they were the reports with the highest proportion of serious harm (n = 63, 45%).
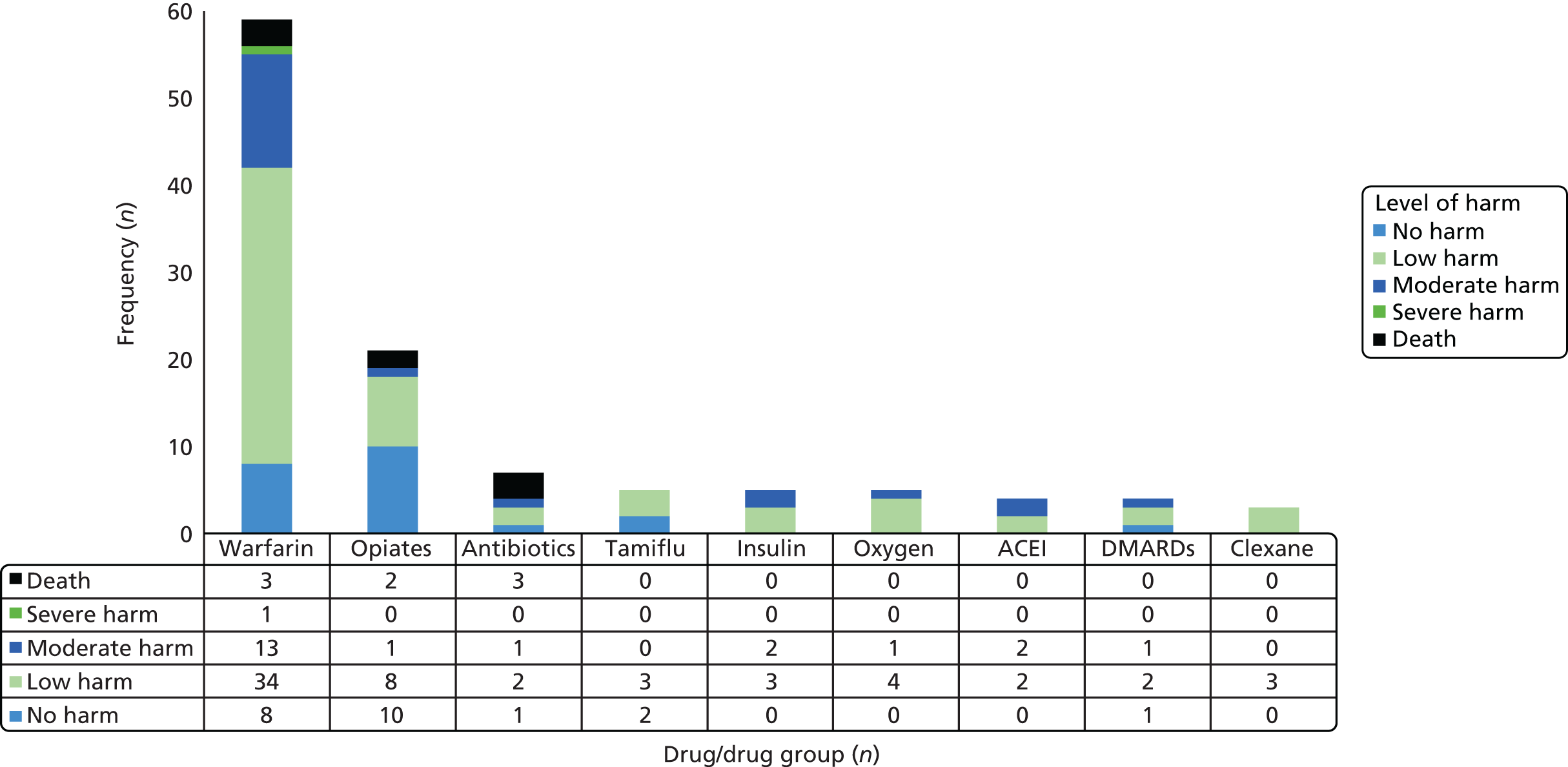
Warfarin (n = 59) and opiates (n = 21) were the drugs most often described in reports; inadequate monitoring or hospital admissions as a result of avoidable complications were described as contributory factors. Opiate-related incidents were often related to drug-seeking behaviour, unintentional drug overdoses or failure to treat symptoms in palliative care patients in a timely manner. Other drugs described in reports are summarised in Figure 7.
FIGURE 7.
Clustered bar chart of drugs/drug groups by level of harm. ACEI, angiotensin-converting enzyme inhibitor; DMARD, disease-modifying antirheumatic drug.
Further examination of medication and vaccine themes
Safer medication provision: prescribing
Prescribing errors were the most frequent (n = 763, 31%) of all medication- and vaccine-related incidents; they included prescribing the wrong dose (n = 226) or even the wrong medication (n = 151). Illegible prescriptions, wrong formulations and prescription of wrong routes of administration were also reported.
The most frequent events preceding a prescribing-related incident were errors of administration (n = 99, 43% of such reports), documentation (n = 36, 16%) or communication (n = 39, 17%). Errors in transfer of information from secondary to primary care were described in 90 reports; this was often because of a delay in receiving the information or incomplete/inaccurate information.
Staff mistakes were the most frequently described contributory factor and were linked to other contributing factors such as IT failures (n = 17, 4%), disruptions to continuity of care (n = 51, 11%) and non-adherence to protocols for repeat prescribing (n = 26, 5%). Being a child made up 7% (n = 34) of described patient-related contributory factors, and was also associated with non-continuity of care and staff failure to follow protocol.
Safer medication provision: dispensing
Dispensing errors were described in 409 reports (15% of all medication- and vaccine-related incidents). The wrong drug was described in 114 reports (29% of dispensing-related reports), and seven reports described serious harm outcomes. The wrong dose of medication dispensed was the next most frequent incident type (n = 91, 22%), and nine of those incidents resulted in serious harm outcomes.
Descriptions of staff mistakes featured often (n = 84), and 32 reports identified confusion between similar medication names, such as Buccastem® (Alliance Pharmaceuticals Limited, Chippenham, UK) and bisoprolol; trazodone and tramadol; amisulpride and amitriptyline; and pregabalin and Pregaday® (Wülfing Pharma GmbH, Gronau, Germany). For example:
53-year old man dispensed trazodone 50 mg instead of tramadol 50 mg, sticker said tramadol on the trazodone box. Patient saw GP 5 days later complaining of dry mouth, blurred vision and feeling ‘spaced out’.
Safer medication provision: administering
Errors in the administering of drugs or vaccines (including oxygen) were described in 257 reports (9% of all medication- and vaccine-related incidents). Failure to administer medication at the correct time was the most frequently described error (n = 53, 21%), with five reports describing serious harm outcomes, including one patient death. For example:
The nurse in a nursing home left the enoxaparin injection on the bedside table in preparation to inject the patient but the patient administered it orally because she thought it was analgesia.
Administration of the wrong dose of medication was the next most frequent type of incident (n = 62, 24% of administration-related incidents) with seven of those reports describing serious harm outcomes and one resulting in death. Cases of administration of the wrong medication (n = 44, 17%) or at the wrong time (n = 41, 16%) were also reported.
Prior incidents that led to an administering error included a prescribing error (n = 21), inability to access a HCP (n = 10) and poor communication between HCPs and patients (n = 13). Reported contributory factors included staff mistakes (n = 60), including distraction (n = 9) or misreading labels (n = 12) and similar medication names (n = 7); and staff failure to follow protocol (n = 11); inadequate skill set/knowledge (n = 6); and patient behaviour factors (n = 9), including non-compliance.
Reliable therapeutic drug-level monitoring
Incidents related to therapeutic drug monitoring were described in 120 reports (only 4% of all medication- and vaccine-related incidents); 22 reports described serious harm and included five patient deaths. Subthemes identified included monitoring not commenced (n = 24) and doses not adjusted following monitoring (n = 12); warfarin was the most frequently involved drug (n = 17) and resulted in two patient deaths.
Prior incidents that led to drug monitoring-related incidents included inadequate transfer of information from secondary to primary care (n = 11), referrals not made when appropriate (n = 5) and miscommunication between the HCP and the patient (n = 6). In contrast to other medication incidents, staff mistakes rarely contributed to therapeutic drug monitoring incidents, being cited in only two such reports. Staff failing to follow protocol was described in 12 reports, for example failure to request a repeat INR for a patient when a new treatment was commenced. Inadequate organisational protocols contributed to 13 incidents, of which six related to protocols about transferring patients between secondary and primary care. Patient factors were also reported (n = 19), 10 of which resulted from patient non-compliance. Several reports made reference to patients on warfarin who were non-compliant with monitoring. Some reports described the ethical issues doctors faced, knowing that withdrawal of treatment would also put the patient at risk of life-threatening events such as pulmonary embolism or stroke.
Avoidable adverse drug reactions
Avoidable adverse drug reactions were described in 139 reports (6% of all medication- and vaccine-related incidents), and 63 of those (45%) resulted in serious harm outcomes, with 10 reports recording patient death. For example:
Patient was given a script by a community matron for Oramorph[®, Boehringer Ingelheim Limited, Bracknell, UK] 2.5 ml 4–6 hourly as required but the label on the bottle said take 2.5 5-ml spoons, result in a total of 12.5 ml. This is five times the prescribed amount on the script. The patient had three doses over 12 hours and passed away at 6.00 a.m.
Twenty-six reports described patient-related contributory factors, such as pre-existing pathophysiology and frailty; seven reports involved patients with known allergies and 22 related to patients on drugs that necessitated patient monitoring (not mutually exclusive). Warfarin was the most frequently involved medication, and 16 reports described a serious outcome resulting in hospital admission, for example epistaxis, vaginal bleeding, haemoptysis or cerebrovascular accident.
Immunisation-related errors for children, the elderly and the immunocompromised
Immunisation-related incidents were described in 464 reports (19% of all medication- and vaccine-related incidents). The majority concerned vaccine administration (n = 386, 83%) and resulted in low harm, although three deaths were reported, and two incidents related to the pneumococcal vaccine not being administered at the appropriate time. Incidents in which either the wrong vaccine was administered (n = 138, 30%) or the wrong number of doses were administered (n = 122, 26%) were also recorded. Incidents relating to administration of the wrong number of doses often involved children and occurred because the medical documentation was inaccurate and not checked, resulting in the child receiving an additional, unnecessary, vaccine that could potentially cause an adverse event.
Immunisation administration errors involving medical records (n = 49) included discrepancies in GP records or personal records (Red Book) and/or other child-health records. Frequent contributory factors were staff mistakes (n = 105), for example staff unaware of the new immunisation programme, staff confusing vaccinations with similar names or staff not checking the medical records, resulting in administration of a vaccine that was not indicated.
Clinician decision-making about treatments
Issues underpinned by clinician decision-making about treatments in acute and chronic situations were described in 121 reports (4% of the total medication- and vaccine-related incidents), with 24 reports recording serious harm outcomes including four patient deaths. Specifically, these reports described no treatment given (n = 37), insufficient treatment given (n = 19) and the wrong treatment given (n = 16). See examples in Box 1.
A patient with central chest pain radiating to her jaw saw the GP (after ECG), who wrote a letter querying a MI and sent the patient home to pack a bag and wait for the ambulance. He noted in the letter that the patient lived alone and had no help. When the ambulance arrived, the patient was packing a bag in her bedroom still suffering chest pain. She had received no medications and was thrombolysed in her bedroom. She was then transferred to a CCU.
Example 2A patient with poorly controlled asthma visited a GP who did not change treatment or provide any steroids, resulting in respiratory arrest and resuscitation.
Example 3A GP arranged for CTPA of an outpatient basis. The patient received no treatment while awaiting a CTPA, contrary to definitive guidelines for outpatient management.
CCU, critical care unit; CTPA, computed tomography pulmonary angiography; ECG, electrocardiography; MI, myocardial infarction.
A range of incidents preceded clinician decision-making errors, including inaccurate medical records (n = 6); poor discharge planning (n = 3); and delays in responding to results (n = 3). These low numbers perhaps reflect the fact that reasons for errors in clinical decision-making are multifactorial. Lack of continuity of care was the most frequently cited issue (n = 18), and was attributed to issues with out-of-hours care (n = 5), lack of communication between secondary and primary care (n = 2) and locum staff (n = 3). Within reports, poor communication between HCPs that contributed to the GP not seeing the ‘whole patient’ was a frequent cross-cutting issue.
Errors in investigative processes
Overview
A total of 1339 reports described safety issues related to clinical investigations. Four themes were evident from synthesis of the reported descriptions and contributory factors:
-
ordering incorrect investigations to inform differential diagnosis
-
practical and administrative barriers for collection and transfer of specimens
-
administrative failures leading to delays, wrong results or failure to receive results
-
misinformed clinical decision-making and incorrectly interpreted investigative results.
Table 11 provides an overview of each theme and the harm outcomes described in reports. There were few reports of serious harm (n = 38, 3% of investigative process-related incidents). Practical and administrative barriers to the collection and transfer of specimens were implicated in 866 reports (66%); of these, mislabelling clinical samples accounted for the majority of incidents (n = 486, 56%).
| Theme | Frequency, n (%) | ||||
|---|---|---|---|---|---|
| Subtheme | Harm | No harm | Serious harm | Not specified | Total |
| Ordering incorrect investigations to inform differential diagnosis | 66 (61) | 10 (9) | 7 (6) | 32 (30) | 108 (100) |
| Wrong diagnostic imaging test ordered or not ordered | 15 | 6 | 3 | 10 | 31 |
| Wrong investigation ordered or not ordered | 51 | 4 | 4 | 22 | 77 |
| Practical and administrative barriers for collection and transfer of specimens | 279 (32) | 44 (5) | 8 (1) | 543 (56) | 866 (100) |
| Mislabelled request form | 4 | 2 | 0 | 25 | 31 |
| Mislabelled sample | 123 | 26 | 2 | 337 | 486 |
| Errors in the process of obtaining or processing a laboratory specimen | 121 | 12 | 3 | 140 | 273 |
| Errors in the process of obtaining or processing of a diagnostic image | 11 | 3 | 1 | 17 | 31 |
| Errors in the process of obtaining or processing of other diagnostic investigation | 5 | 0 | 0 | 1 | 6 |
| Lost specimens | 5 | 0 | 1 | 7 | 12 |
| Other | 10 | 1 | 1 | 16 | 27 |
| Administrative failures leading to delays, wrong results or failure to receive results | 109 (45) | 22 (9) | 9 (4) | 109 (45) | 240 (100) |
| Error in the process of physician receiving accurate laboratory test results including errors of delay | 77 | 19 | 6 | 77 | 173 |
| Error in the process of physician receiving accurate diagnostic imaging test results including errors of delay | 27 | 1 | 3 | 23 | 51 |
| Error in the process of physician receiving accurate other test results including errors of delay | 5 | 2 | 0 | 9 | 16 |
| Misinformed clinical decision-making and incorrectly interpreted results | 82 (66) | 8 (6) | 14 (11) | 35 (28) | 125 (100) |
| Response to a laboratory result | 63 | 6 | 10 | 25 | 94 |
| Response to a routine laboratory result | 3 | 0 | 2 | 4 | 7 |
| Response to imaging result | 7 | 1 | 2 | 4 | 12 |
| Response to drug level | 3 | 1 | 0 | 2 | 6 |
| Response to other investigations | 6 | 0 | 0 | 0 | 6 |
| TOTAL | 536 | 84 | 38 | 719 | 1339 |
Further examination of investigative process themes
Ordering correct investigations to inform the differential diagnosis
Diagnoses were often delayed or missed because of mistakes in the investigative process. The wrong laboratory test was ordered, or not ordered at all, when it would have been appropriate, in 77 reports. In 51 cases, this led to harmful outcomes. For example:
A patient attended with abdominal pain and was advised they had irritable bowel syndrome but investigations recently have revealed late stage ovarian cancer with spread to the lymph nodes. If an ultrasound scan had been done earlier this could have been detected sooner.
Reports also described situations in which, if clinicians had organised further investigations or put in place a safety net for the patient to return, serious diagnoses could have been detected sooner. For example:
Patient presented with frank haematuria from which a renal carcinoma was identified. It was noted that patient had presented last year with another incident of haematuria urinalysis * 2 positive for blood microscopy negative not investigated further.
Delays in undertaking investigations, largely because of waiting lists, carry a risk of delayed treatment for preventable illness and worsening of the condition. It was apparent, however, that if the patient did not demand to be seen or undergo an investigation, then such delays would not be identified. For example:
2-week-rule referral made by GP for suspected pancreatic cancer due to jaundice and deranged bloods. Seen in clinic and urgent scan was requested [by hospital team]. Patient re-attended surgery several times and scan date was chased. GP chased scan report as now 5 weeks post referral and still no [date]. Eventual diagnosis made of pancreatic cancer.
Practical and administrative barriers for labelling and transfer of specimens
Errors in administration (i.e. form filling, labelling, completing the form), although common (n = 796, 59%), largely resulted in low harms, such as the need for retesting. Transport errors were also reported; the issue of ‘sample deterioration’ was highlighted and concern was raised about result accuracy and impact on correct interpretation when needless delays in transfer had occurred.
Administrative failures leading to delays, incorrect results or failure to receive results
Issues with the administrative (electronic and paper-based) processes enabling the timely receipt of test results were described in 240 reports. These issues were varied and included not receiving the results, delays in receiving the results and receiving inaccurate results. Communication issues between professionals and inconsistent message-handling procedures within GP surgeries were also implicated. Failures in practice processes to review results that did not occur on the same day as investigation, or those being processed out of hours and noted as urgent, was a recurring issue. For example:
. . . lab phoned through a result early afternoon giving a high potassium level, they said it needed to be reported to a GP asap but with no other indication of urgency GP on call was already out on visits and could not be contacted by phone, there were no other GPs in the building. Unfortunately the patient died whilst packing his bag to go to hospital.
Most test results are sent electronically to practices, with paper copies often sent afterwards as a safety net. However, although the GP might read an electronic report, over-reliance on the software for planning next steps for management in the clinical record system does highlight the need for parallel (possibly manual) processes when the findings are potentially so serious. For example:
The patient presented with cough, bloody sputum . . . known smoker and heavy drinker. A chest X-ray was ordered and patient given [a]moxil 500 mg × 21. [software] mailbox showed that the GP had read the X-ray report but there was no direction shown, it was left unedited, no action taken, The X-ray was not ‘sent to anyone‘ it appears to have dropped from the active mailbox into a ‘bucket‘ awaiting action. (WORSE [sic] than this the GP did not know about the ‘bucket‘.) . . . The chest X-ray showed an early lung tumour which was not picked up until the patient presented 1 year later. His condition is now advanced and probably terminal. The GP had 10 minutes training on [software] with 4 GPs around one computer.
Misinformed clinical decision-making and incorrectly interpreted investigation results
Errors in responding to test results in a timely manner were cited in 125 reports (10% of all investigative process errors), of which 82 described harm outcomes. For example:
Elderly male patient . . . attended surgery with recent but not current chest pain. Given ECG [electrocardiography], which was misread. Patient advised to return home but should have been sent to hospital urgently. Patient died at home from heart attack within 24–48hrs . . . Evidence the machine may have given GP undue confidence in his diagnosis, as it gave a reading of normal sinus rhythm.
Unreliable or non-existent processes underpinned failures to review patients’ notes before the end of the general practice day or rerouting results to the wrong doctor for review.
Timely diagnosis and assessment
Overview
Seven hundred and twenty-eight reports (5% of total reports) described issues with diagnosis and assessment of patients; three themes were evident from synthesis of the reported descriptions of events and contributory factors:
-
timely triage and assessment of patients
-
patient assessment for safe discharge
-
missed or wrong diagnosis.
The majority of reports described harm, and 3 in 5 of those incidents resulted in serious harm outcomes (n = 366, 64%). Table 12 provides a summary of incident themes and subthemes.
| Theme | Harm, n (%) | Total (%) | |||
|---|---|---|---|---|---|
| Subtheme | Yes | No | Serious | Not specified | |
| Missed or delayed diagnosis | 297 (86) | 8 (2) | 217 (63) | 40 (11) | 345 (100) |
| Missed/delayed diagnosis | 285 | 7 | 207 | 39 | 331 |
| Wrong diagnosis | 12 | 1 | 10 | 1 | 14 |
| Timely triage and assessment of patients | 189 (78) | 12 (5) | 118 (49) | 41 (17) | 242 (100) |
| Triage process | 39 | 6 | 28 | 11 | 56 |
| Identifying acute conditions | 30 | 1 | 23 | 1 | 32 |
| Identifying risk of deterioration | 3 | 0 | 2 | 0 | 3 |
| Delayed assessment for care | 27 | 1 | 3 | 0 | 28 |
| Identifying vulnerable patients | 9 | 1 | 4 | 9 | 19 |
| Refusal to do home visit | 9 | 0 | 4 | 2 | 11 |
| Examination of patient | 7 | 1 | 4 | 2 | 10 |
| History taking | 0 | 1 | 0 | 3 | 4 |
| Identifying mental health issues | 29 | 0 | 29 | 1 | 30 |
| Other | 36 | 1 | 21 | 12 | 49 |
| Discharge risk assessment | 89 (63) | 13 (9) | 31 (22) | 39 (28) | 141 (100) |
| TOTAL | 575 | 33 | 366 | 120 | 728 |
Four in 10 reports had identifiable contributory factors (n = 292, 40%). Reports largely described four key contributory issues: lack of continuity of care (n = 56, 19%); staff decision-making processes, mainly related to a failure to follow protocols or insufficient knowledge (n = 52, 18%); patient characteristics such as age, frailty or not having English as a first language (n = 51, 17%); and disease characteristics such as rare conditions or a rare presentation of a condition (n = 48, 16%).
Further examination of diagnosis and assessment themes
Timely triage and assessment of patients
Timely triage and assessment issues were described in 242 reports; they included failures to recognise acutely unwell patients (n = 32) and those at risk of deterioration (n = 29), patients who were vulnerable to abuse or being abused (n = 19), and those at risk of harm from mental health problems (n = 30). For example:
Call received regarding a child who had died, the mother reported that she had sought assessment and advice from NHS Direct. The call was prioritised as a P2 and placed in the First Advice Queue. It was picked up by X 24 minutes later. The child was assessed using the ‘Breathing problems toddler Age 1–4 years Algorithm’ and a disposition of self care was recorded. Boards have reviewed the call and concerns raised regarding the quality of assessment and appropriateness of the disposition.
Problems with triage processes were described in relation to HCPs in 13 reports and non-HCPs in eight reports. In another example involving telephone triage, the severity of the patient’s condition was not ascertained:
Patient telephoned NHS Direct following aches in her shoulders and experiencing excess wind. After clinical assessment they advised the patient she was probably suffering from trapped wind and received information relating to indigestion. Following the call to NHS Direct the patient symptoms worsened and her husband telephoned 999 for an ambulance. Whilst the patient husband was on the telephone, the patient collapsed, lost consciousness and subsequently died. The post mortem report stated that the cause of death was ischaemic heart disease and coronary artery atheroma.
A failure to recognise signs of abuse was preceded by poor information transfer from secondary to primary care in 22 reports, and by a failure to refer for nursing care on discharge from hospital in nine reports. Contributory factors included lack of continuity of care with out-of-hours services (n = 14), and 10 reports queried whether or not the HCP cited in the report had sufficient professional knowledge. Serious harm outcomes were described in 86 reports (61%).
Patient assessment for safe discharge
Issues with risk assessment for discharge were described in 141 reports. Analysis of linked incidents showed that this resulted in multiple problems following discharge, including poor information transfer to primary care (n = 51), failure to refer patients for emergency care when indicated (n = 9), failure to refer patients for nursing care at home (n = 8), prescribing errors (n = 7) and problems with the provision of care equipment (n = 28). Such issues described in reports are reflected in the following example:
Message received from GP [Date] – patient was discharged from . . . ward [day before] late pm – no referral sent to child district nurse. Urinary catheter (long term) in situ. No advice given to family re changing bags/care of catheter and no bags supplied on discharge. No information whether DN [district nurse] can change catheter.
The next example describes the discharge of twin babies with a complex in-hospital history:
The health visitor carried out a primary birth visit following the twins’ discharge from the SCBU (Special Care Baby Unit). There was no discharge letter with information for the service or medications required. No discharge plan. No resuscitation training given to the parent. The mother stated that she was told it would be given prior to discharge, but that it was not received. Twins discharged on oxygen therapy. No apnoea monitor. No risk assessment surrounding the twins’ care. No official referral to the paediatric community nurse and no involvement pre-discharge. The paediatric community nurse was not informed of the discharge. The twins had been cared for over the past seven weeks in the SCBU (Special Care Baby Unit). No liaison had been made with the community staff.
Most (75%) patients affected were aged ≥ 66 years, possibly reflecting the complex needs of the elderly on discharge. Not all reports highlighted so many opportunities to improve clinical care as the previous example. Only 21% of reports (n = 30) documented a contributory factor, of which the majority (n = 17) discussed the complexity of the patient in terms of comorbidities. This may be because the reports were written in primary care and, therefore, the report writer was not involved in planning the discharge.
Missed or delayed diagnosis
Problems with diagnosis were identified in 345 reports, with 86% (n = 297) describing a harm outcome. A total of 331 reports described a missed or delayed diagnosis. The conditions that were missed were wide-ranging and included fractures, tuberculosis, diabetes mellitus, infection, pregnancy and myocardial infarction. These cases illustrate the difficulty of clinical decision-making in complex patients with undifferentiated presentations, for example, delineating between known side effects from a prescribed drug and a possible red flag for a more serious diagnosis:
The patient was an 85-year-old man with dementia and Parkinson disease who had symptoms of diarrhoea and was taking Aricept[®, Pfizer Inc., New York, NY, USA]. The diarrhoea was attributed to being a side effect of his Aricept and the doctor failed to diagnose his progressed colon carcinoma.
A missed or delayed cancer diagnosis was described in 128 reports. Diagnostic problems were preceded by insufficient assessment in seven reports, by insufficient examination in eight reports and by failure to recognise acute conditions in seven reports, which suggests that missed or delayed diagnoses are underpinned by lack of clinical skills. This is also suggested by the 16 reports in which the knowledge or skill of the HCP was described as a contributory factor. For example, a lack of prior knowledge of the patient’s history would make it more difficult to interpret test results and determine if they were normal, as was evident in the following example:
Patient had undergone radical prostatectomy for cancer. Had follow up PSA [prostate-specific antigen] levels – which should be undetectable. Any detectable PSA level, even in ‘normal’ range, is abnormal. Previous detectable level passed as normal result. The patient noticed this.
In 31 cases, the rare presentation of a condition was a contributory factor, and in 18 reports, the continuity of care between primary HCPs was discussed. The latter contributory factor was associated with high rates of harmful outcomes, as 72% (n = 207) of cases led to serious harm.
Fewer reports (n = 14) described a wrong diagnosis. These reports related to wide variety of conditions, some of which were more serious than others. Wrong diagnoses were largely, although not exclusively, due to failures of professional competence, such as failing to examine a patient fully; however, some were attributed to unusual clinical presentations (undifferentiating signs or symptoms) and these cases accounted for a high proportion of serious harm incidents (n = 10, 71%).
Treatment and care equipment
Overview
Incidents involving treatment and care equipment provided for community care were described in 754 reports (6% of total reports). Three themes were evident from synthesis of the reported descriptions of events and contributory factors:
-
decisions about methods of administering treatments
-
complications of therapeutic procedures
-
functioning and availability of care equipment.
Table 13 provides an overview of themes and subthemes related to treatment and care equipment and associated levels of harm.
| Theme | Harm, n (%) | Total (%) | |||
|---|---|---|---|---|---|
| Subtheme | Yes | No | Serious | Not specified | |
| Decisions about methods of administering treatments | 95 (76) | 8 (6) | 32 (26) | 22 (18) | 125 (100) |
| No treatment | 14 | 1 | 3 | 4 | 19 |
| Insufficient treatment | 62 | 6 | 20 | 16 | 84 |
| Incorrect treatment | 17 | 1 | 7 | 2 | 20 |
| Other | 2 | 0 | 2 | 0 | 2 |
| Complications of treatment procedures | 230 (79) | 21 (7) | 57 (20) | 40 (14) | 291 (100) |
| Ordering treatment | 1 | 0 | 0 | 0 | 1 |
| Implementation | 48 | 13 | 9 | 18 | 79 |
| Complication | 135 | 2 | 38 | 15 | 152 |
| Timeliness | 39 | 4 | 9 | 6 | 49 |
| Choosing correct procedure | 5 | 2 | 0 | 1 | 8 |
| Wrong site/side | 1 | 0 | 0 | 0 | 1 |
| Other | 1 | 0 | 1 | 0 | 1 |
| Functioning and availability of care equipment | 190 (56) | 35 (10) | 27 (8) | 113 (33) | 338 (100) |
| Lack of functioning therapeutic equipment | 72 | 7 | 13 | 18 | 97 |
| Insufficient supply of care adjunct | 5 | 6 | 0 | 12 | 23 |
| Failure of equipment | 104 | 21 | 11 | 71 | 196 |
| Stolen | 0 | 0 | 2 | 5 | 5 |
| Other | 9 | 1 | 1 | 7 | 17 |
| TOTAL | 515 | 64 | 116 | 175 | 754 |
Harm was identified in the majority of reports (n = 515, 68%). Serious harm was caused by 15% of these incidents (n = 116). The unavailability of functioning care equipment (n = 338), such as beds to prevent pressure sores or catheter replacements, was the most common incident, followed by problems carrying out treatments in the community (n = 291).
A large proportion of reports (n = 55, 21%) were related to patient characteristics such as age, frailty or pregnancy. Other contributory factors included patients not following advice or having sufficient knowledge for safe self-care (n = 48, 18%), or making mistakes such as misreading information (n = 27, 10%).
Further examination of treatment and care equipment themes
Decisions about methods of administering treatments
An error in the clinical decision of what, if any, treatment to give a patient was identified in 125 reports, with 95 (76%) describing a harm outcome. These decisions were subdivided into three subthemes.
-
No treatment was given (n = 19, 15%). Treatments not administered varied but included insulin, dressings and emergency contraception. In 15 cases, another incident was involved, for example a pregnant patient was not treated for herpes infection because her laboratory results were not acted on and another patient’s pressure ulcer was not treated because the equipment that was ordered was not in stock. Only three (16%) of these reports resulted in serious harm.
-
Insufficient treatment or monitoring was undertaken (n = 84, 68%). Pressure ulcers developed or deteriorated in 33 reports, often because of the lack of equipment, patients choosing not to use suggested treatment or poor care. Other reports described GPs calling an ambulance for sick patients, but not monitoring them or starting basic treatment while waiting for the ambulance. Twenty incidents in this category (24%) led to serious harm.
-
Incorrect treatment (n = 20, 16%) following clinical assessment. This was a diverse group, with reports describing the wrong type of dressing used on leg ulcers, insertion of contraindicated intrauterine contraceptive coils and cauterising a cancerous ‘wart’.
Complications of treatment procedures
Complications arising during procedures were described in 291 (39%) reports. Minor infections following minor surgery and needle-stick injuries were described. More serious outcomes highlight the major risks associated even with commonplace procedures performed in general practice, which included uterine perforation following coil insertion, a fragment of a needle remaining in the shoulder joint after injection and an abscess forming at an injection site. These incidents were generally considered a complication of a procedure rather than being attributed to poor technique; thus, only 29 reports (10%) had an identifiable contributory factor, of which 10 were related to the patient’s pathophysiology, and only three were considered to be due to a HCP’s lack of skills.
Incidents in which a procedure was not carried out correctly, resulting in poor infection control, needle-stick injuries, dressings adherent to wounds, new leg wounds from incorrect bandaging or urinary retention, were described in 79 reports. Contributory factors included failure to follow protocol (n = 9), inadequate skill set (n = 8) and staff mistakes (n = 8).
The other apparently important group was incidents related to timeliness of treatment (n = 49, 17%). Many of these involved the care of catheters, but incidents related to the emergency care of patients and wound care were also reported. For example:
Patient called *** as catheter had fallen out during the night. *** called district nurse and left a message at 03:40 giving details of the problem and asking if they could attend in the morning to re-catheterise. Patient was wearing a pad. It was a Sunday and worker alone got a message just after 08:00 and was unable to attend immediately.
In 40 of the 49 reports, the incident occurred because the district nurses did not receive a referral on discharge. Of those, nine reports (18%) described serious harm outcomes.
Functioning and availability of care equipment
Errors around the provision and operation of equipment involved in patient care were described in 338 (45%) reports. Failure of equipment was common (n = 196, 58%), and the most frequently reported types of incident involved malfunctioning of pressure-relieving equipment, fridges going above the recommended temperature range and power cuts compromising IT systems’ functioning.
Issues directly related to access to care equipment such as dressings, insulin needles or catheters were identified in 97 reports. For example, some patients were sent home from hospital without the necessary equipment and in other cases pharmacies incorrectly dispensed a short-term rather than a long-term catheter. In 28 reports, poor discharge planning preceded problems with care equipment provision. Insufficient supply of care equipment was reported 23 times, and was generally related to not having the right equipment in the surgery or central stores. Items included electrocardiography paper, blood bottles, dressing packs and continence pads.
Chapter 7 Discussion of findings and recommendations
Main findings
This is the largest analysis of general practice patient safety incident reports undertaken. We have developed a method to derive learning from general practice patient safety incident reports to identify priority issues to guide future improvement efforts.
We will first discuss our main findings in relation to the methods development needed to undertake this study and observations about the completeness and accuracy of the incident reports reviewed. We will then consider the implications of the recommendations for research and development identified within, and between, the themes from each incident category.
Quality of National Reporting and Learning System reports
Development of a comprehensive classification system to characterise safety incident reports in general practice has permitted the description of events leading up to patient safety incidents, their reported contributory factors (human and system issues), and patient- and system-level outcomes. We propose that four independent classes (a description of the incident, its contributory factors and the type and level of harm) should provide sufficient minimal information for practising HCPs to identify learning for improvements in future practice from the reports.
The manual coding of reports was a resource-intensive process in terms of the application of codes and the development of the code book. Codes within each class were inductively added and amended throughout the study, with fewer iterations needed towards the end of the study. We consider that the regular team meetings we held to discuss such changes would need to be emulated by those responsible for the analysis of incident reports within health-care organisations.
Our methods of analysis (EDA and thematic analysis) were designed to permit future adoption in health-care organisations by HCPs with minimal training. Further work is now needed to develop and test the content and delivery of such training. Outcomes from analysis (e.g. clustered bar charts) were also chosen to provide a logical account of how priority issues for possible intervention were identified. In addition, clinical expertise supported interpretation of context and identification of the implications of the described safety incidents on patients and their families. Our findings are hypothesis generating, inductive in nature and require testing and development by further research and clinical practice improvement.
At best, around one-third of reports contained descriptions of contributory factors. This represents a major missed opportunity to learn from patient safety incidents. Descriptions of contributory factors, when considered in relation to the type of incident and context, can provide a steer on potential causes of patient safety incidents and inform the conceptual design of interventions to mitigate future harms. A total of 462 discrete NHS organisations uploaded at least one incident report, although over half of the reports originated from just 30 organisations (n = 7071, 51.6%). This implies that some organisations do not report general practice safety incidents to the NRLS, or do not have mechanisms for receiving reports from general practice in its organisation.
The number of reports excluded from the analysis suggests a misguided use of local reporting systems in terms of knowledge and understanding of its purpose.
Crosscutting issues for research and development
Our discussion of key findings from incident report analysis is focused on the themes informed by the most frequent and most harmful reports. Identifiable contributory factors, interpreted in terms of the incident type, the context in which they occurred and patient outcomes, support the basis of our recommendations. Our recommendations are exclusively focused on systems improvement since there was no apparent focus on human-specific recommendations from our analyses. When human error was described as an implicated contributing factor to the developing incident, the professional involved was usually working within a complex system with less than optimal work processes. However, we stress that the focus on systems does not negate the HCP’s duty to report a safety incident. We also recognise the need to enable practitioners to be provided with regular updates of learning from safety incidents that examine human factors.
We will focus our recommendations for research and development on four broad areas:
-
maximising opportunities to learn from patient safety incidents via mandatory data capture and a national, co-ordinated effort to support organisations to build the capacity and capability of their workforces to report data for learning
-
testing methods to identify and manage vulnerable patients at risk of deterioration, unscheduled hospital admission or readmission following discharge from hospital
-
building IT infrastructure to enable details of all health-care encounters to be recorded in one system, aid communication between professionals and services and support safer administrative practices (e.g. prescribing, referral and discharge communication)
-
activating the patient, parent and carer role in preventing patient safety incidents.
Improvement efforts to develop, test and implement solutions across these four broad areas of recommendation will address the prevention of the vast majority of safety incidents analysed within this study.
Maximise opportunities to learn from patient safety incidents
Confront the blame culture
A culture of blame within NHS organisations is often described when a patient safety incident occurs. 81–84 For over a decade, seminal patient safety policy documents and initiatives have highlighted that patient safety incidents are largely the result of poorly designed systems. 85 Several public inquiries have highlighted the detrimental consequences of a workforce that practises in fear of reprimand and punitive action following a medical error. 10,81,84,86
The UK policy document An Organisation with a Memory signalled the need to learn lessons from medical errors in order to prevent future, similar events. 87 Patient safety incident reporting was heralded as an important mechanism to create learning, as part of an ongoing commitment to support a safe culture with a learning ethos, in which individuals acknowledge and learn from patient safety incidents. 88,89 Reporting and learning systems rely on HCPs to report, and be open about, patient safety incidents that they witness or are involved in. 90 Fear of blame, however, poses a significant barrier to staff fulfilling this duty and creates missed opportunities for system learning and improvement, often at a huge cost to the individual staff members. 86,88,91–94
Previous studies have demonstrated that when HCPs report incidents, the narrative often reflects the fact that responsibility for the incident is placed on an individual through ‘person-blaming,’ rather than blaming the organisation or failings in the system. 95 This is, however, contrary to the mantra encouraged by patient safety initiatives worldwide. It is well acknowledged that uncertainty about the implications of reporting, not least the personal shame about involvement in a medical error, fuels barriers to incident reporting. 92,96 The ‘second victim’ concept describes the experience of HCPs who are involved in safety incidents and suffer psychological distress in the aftermath of a medical error. Loss of confidence, low self-esteem and self-doubt are well-documented issues. 86
The term ‘whistleblowing’ has traditionally been coined to describe situations in which HCPs speak up about major system failures, malpractice, wrongdoing or fraud. 8 The term often conjures negative professional connotations as a result of high-profile cases within medicine of clinicians who have been disgraced as a result of speaking up in the interests of patient safety. 97,98 This has become evident in organisations where undue emphasis has been placed on the ‘active failure’ aspect of the incident in which an acute error has played a role in the event evolution, whereas the ‘latent system conditions,’ in which poor system defences act as predisposing weaknesses, receive less consideration. Although both of these components are important and frequently occur in combination, active errors are unduly emphasised, with blame, in the majority of cases, falling on individuals and teams. 99 This is often apparent in media coverage of patient safety incidents.
Li et al. 100 examined 64 news articles about medical errors printed in newspapers from six countries and concluded that the articles rarely accounted for system failures or approached the error without bias. Of the studied articles, 60% were reported from the viewpoint of a legal expert or patient with investment in the error, and often demonstrated a ‘person approach’ by blaming individuals, which was the case in 41% of the articles. The study also highlighted that 40% of news reports failed to signpost the importance of system failures in the evolution of the error. 100 In the UK, 53% of articles discussed errors negatively, compared with 14% in the USA. 101,102 These draw public attention to human failures and place blame on individual HCPs. These may all be well-intentioned attempts by health-care organisations to be seen to be acting on concerns raised by patients; however, this blame culture has the effect of reducing clinicians’ motivation to report patient safety incidents and preventing learning from incidents that may help to prevent future health care-related harm to patients. 100
Shift focus from human to system failures
Diagnostic errors, for example, can be described as cognitive, system or ‘no-fault’ errors, and may be errors of commission or omission. Croskerry et al. 103 describe a number of initiatives for mitigating specific cognitive errors in practice,104 in keeping with current literature around improving diagnosis and assessment by reducing dependence on flawless cognitive performance. Schiff et al. 105 described the importance of adopting better multidisciplinary approaches, reducing pressure on clinicians to rely solely on their memory and clinical experience when making diagnoses, and instead supporting them by means of computerised and non-technological aids. 106 This supports our findings, which demonstrate that lack of knowledge, oversights and mistakes were frequently described staff factors contributing to patient safety incidents. Cognitive errors, which are often unexpected active errors of commission, complicate the process of improving patient safety; however, focus on providing safe systems and safety-netting may help minimise patient harm when errors occur. 106
Previous studies have highlighted the importance of streamlining systems for referral and discharge or follow-up, using electronic systems to unify patient records. 107 Electronic systems are being developed to support a number of aspects of the diagnosis and assessment process. There is increasing support for the use of clinician decision support systems, to assist in managing consultations. 108,109 For example, a system proposed by de Wit et al. 110 supports the management of polypharmacy in the elderly patient population.
Vulnerable patients were described within the reports analysed. Elderly patients, patients with acute illness or disability have been associated with an increased risk of patient safety incidents. 111 Such patients often experience multiple comorbidities and run the risk that new pathologies will be overlooked as clinicians focus on existing diagnoses which can undermine the presentation of new pathology. 112–114 In addition, they may be incapable of raising concerns about their care or lack agency in decision-making. Guthrie et al. 112 described polypharmacy and choice of acceptable care strategies as specific issues for patients with comorbidities yet to be addressed in policy. Limited resources exist to guide practitioners in managing this demographic. Involvement of patients in training HCPs, to improve management of the vulnerable, has been associated with improvements in patient satisfaction, with no clear detrimental effects. 115,116 Cross-linking electronic guidelines for the management of related disorders, and to aid recognition of red flags to minimise diagnostic overshadowing, is a further proposal for practice-level improvement to mitigate human error. 112
Build capacity and capability of information technology infrastructure
Building IT infrastructure and functionality capable of sharing data between health- and social-care providers could support identification of predictors of risk and inform interventions to prevent future incidents. 117 In addition, efforts to transition existing written processes, and alignment of existing electronic processes, could support HCPs to have timely and reliable access to health-care data needed for safer consultations and permit continuity of care across different health- and social-care sectors.
Based on our findings, referral and discharge processes require attention. The receipt of poor-quality, and sometimes inappropriate, referrals received by district nursing teams is well described,118–122 and each unclear referral has been estimated to cause 5 hours of extra work for district nurse teams. 123 To overcome variability in referral processes, the development and testing of a single, unified electronic referral process with an agreed baseline of minimal information should be agreed between professionals in primary and secondary care settings.
NHS England and other organisations have previously reported that failures in communication processes can account for up to 33% of discharge-related safety incidents. 124,125 Electronic discharge documentation could prevent most paper-based administration failures,126–128 and, across the UK, a process is under way to support 24-hour electronic discharge. 129–131 However, we believe that electronic discharge summaries should be based on accepted best practices, such as those developed by the Scottish Intercollegiate Guidelines Network,132 as well as consensus agreement by primary and secondary care professionals about the minimal essential information that should be included. In parallel, patient-held records could aid understanding about a recent hospital stay and follow-up plans. 133–135
Identify patients at high risk of harm in the community
Reports describing failures of timely diagnosis and assessment, the availability of treatments and care equipment, and lack of continuity of care following discharge often involved patients with social or medical issues that compromised their ability to access GP services.
Exploring the accessibility of clinical services must be a priority for all health-care organisations, and general practices should determine whether or not their existing telephone call-handling processes meet the needs and expectations of their patient population. In 2015, a randomised controlled trial by Campbell et al. 136 was not sufficiently powered to detect differences in safety outcomes (in terms of patient mortality, emergency hospital admissions, and accident and emergency attendance rates) between same-day consultations with GPs/telephone calls, nurse-led computer-supported services and usual care. However, the accompanying process evaluation recognised the importance of culture, capacity and involvement of all practice staff when introducing such major changes to access. The authors recommended examination of significant event audits to explore safety outcomes. 137 We support this recommendation given the diversity of issues patients face while accessing clinical services, in particular the need to focus future improvement efforts on vulnerable patient populations.
In 2015, Warren et al. 138 highlighted the need to explore the drivers of satisfaction among patients from ethnic minority groups. Our findings support this, and determining what constitutes patient satisfaction, particularly among those seeking urgent medical attention, will be an important informant of the design of future improvement projects that seek to develop an accessible system. 139 How best to determine those estimates of patient satisfaction within general practice should be explored with priority patient groups (e.g. the socially deprived, the elderly or homeless people). Issues identified within incident reports could empirically inform those inquiries.
Patients recently discharged from hospital and those receiving end-of-life care in the community or requiring regular district nursing involvement frequently did not receive timely follow-up by community HCPs. Exploring options to intervene early, to manage patients at home and to mitigate avoidable deterioration through proactive intervention is needed. Different options that could achieve this are described in NHS England’s General Medical Services ‘enhanced service’ for vulnerable groups,140 which describes a complex intervention that includes same-day telephone consultations for patients at risk of unplanned hospital admission and timely follow-up by a HCP in the practice on discharge from hospital. Although we acknowledge the unclear benefits of standalone system changes such as telephone triage,136,137 a synergy might be evident from new models that combine same-day telephone triage and risk stratification (or other options).
Given the failures in care that we have identified, we agree with NHS England that new services are needed to support GPs to develop and test new models of care delivery for the ‘enhanced service’: (1) rapid response community nursing; (2) support from mental health service providers; (3) designated district nursing; (4) additional discharge co-ordinator services; (5) additional support for carers; and (6) targeted social-care services. 136 Given the largely social nature of such interventions and the risk of outcome-based evaluation determining the net effect to be minimal, formative theory-driven evaluation options should be considered. 141,142
Activate the patient role in safety
Cultivating conditions in which patients, parents and carers feel comfortable challenging HCPs is needed and could prevent safety incidents. 143 Encouraging patients and HCPs to co-design new models of care delivery that inform local improvement initiatives should be encouraged; for example, improvement in the parent–provider relationship could increase child safety. 144–146 Public health organisations and researchers must seek to establish what methods of communication work best for different patient and parent groups, and embrace the challenge of undertaking research with and for vulnerable patient populations.
Providing patients with access to their medical records could reduce documentation discrepancies and appointment-related incidents, as well as provide HCPs with a safety net. 143 Such incidents could also be prevented by providing staff with better accessibility to unified records. 147
As care models for different patient groups change, investment is required to maximise patient understanding and empowerment to use those services. There is also a broader need to continue efforts to educate the public on the role of each health-care provider (e.g. general practice, pharmacy, optician, clinical injuries unit), and what the expectations of those services can be, including when and how to access each service.
Implications for future practice and research
Our ‘actionable findings’ provide the basis for improvements and interventions, and should be evaluated in practice as to if, and how, they can best achieve the desired benefits for patient safety. They will be considered under groups of recommendations that apply to general practices and health-care organisations, and for the wider health-care system.
What can general practices do?
Identify at-risk patients
Practices can immediately explore their current processes for identifying patients who could be stratified to be at high risk of deterioration, unplanned admission or readmission following discharge from hospital. This should include multidisciplinary team involvement for undertaking the assessment of these patients to achieve integrated care.
Examine patient satisfaction in relation to perceived accessibility
Perceptions of barriers to clinical services must be explored with patients. First steps could include determining whether or not patients find existing telephone and call-handling processes meet their needs and expectations.
All GP surgeries can immediately seek to appoint a patient representative(s) to attend meetings to discuss process changes that will affect how patients receive and interact with services.
What can health-care organisations do?
Report-assisted improvement
Practices must be supported to develop a learning culture by being encouraged to use their own data (e.g. significant event audits and GP-related patient safety incident reports) to identify potential candidate areas for small, local improvement efforts.
At an organisational level, those responsible for governance could support the identification of similar incident reports between practices in order to identify sources of error and use those ideas to inform system redesign efforts to minimise future risk to patients. For example, if there is a sufficient volume of incident reports around a specific theme, such as vaccination error, Pareto charts can be generated to prioritise immediate next steps for improvement projects. 22
Organisations might also seek to identify the ‘beacons’ for others to aspire to. For example, general practices that have high patient satisfaction scores for different patient groups, including socially and medically vulnerable patients, could be identified and their models of delivery observed to determine whether or not there are best practices that can be shared widely for quality improvement.
Prepare the workforce to report
There is a need to develop a culture of open reporting among HCPs and staff in general practice. This must also extend to patients and carers, and mechanisms for escalating concerns and reporting patient safety incidents must be made clear.
To ensure that future incident reports can inform future improvement efforts, the workforce must be provided with patient safety training that increases understanding about the rationale for reporting and prepares them to identify human factors. This could yield more informative narratives for informing systems improvement.
Education providers such as the Institute for Healthcare Improvement provide free access for student HCPs to undertake courses on patient safety, including human factors and root cause analysis. National efforts include the ‘Improving Quality Together’ programme, which is the national quality improvement learning programme for all NHS Wales staff to develop the skills and gain accreditation in quality improvement methodology. It is anticipated that this will enable a consistent approach to improving the quality of services that will help improvements take place much more quickly and spread effectively throughout the country. Organisations should examine its existing infrastructure for receiving reports and disseminating learning back to practice, and monitoring the success of those mechanisms. Competencies around incident reporting may be best demonstrated via appraisal or revalidation processes, or linked to the Quality and Outcomes Framework requirements.
What can national bodies interested in patient safety do?
Support general practices to contribute to the National Reporting and Learning System
At present, there are numerous channels to report patient safety incidents. These include the NRLS, the National Clinical Assessment Service, the General Medical Council and locally at practice level through significant event analyses. The Care Quality Commission also conducts routine inspections of general practices. These systems do not communicate with each other, resulting in an incomplete national picture on patient safety in primary care. There is a need to create a single mechanism of data capture.
Currently, in terms of mandatory data capture, the only incidents that must be reported are never events. A set of such events relevant to primary care, such as those developed by de Wet et al. ,148 should be implemented.
An opportunity exists to better use the analysis of routinely available health-care data, such as patient safety incident report data, to inform the designs of improvement projects. Incident reports are essentially a collection of change ideas to inform the identification of priority areas for quality improvement in practice.
The Five Year Forward View presents an opportunity to deliver the necessary system changes to bring patient safety in primary care to the fore. 149
Co-ordinated expert analysis at a national level
In order to generate recommendations for practice from patient safety incident reports from primary care in England and Wales, we developed a mixed-methods approach that combined the aforementioned detailed data coding process, descriptive statistical analysis, and a thematic analysis of reports. New ideas and hypotheses emerged throughout each step of analysis. Subject matter experts discussed findings and identified key areas for improvement.
Analysis of incident reports at a national level needs a combined enterprise between clinical, research and patient safety experts to regularly review the output of analyses, to corroborate with existing insights from research studies and improvement initiatives, and to develop potential action-orientated solutions with strong face validity among the profession. Involvement of the Royal Colleges in dissemination of learning will continue to be critical, particularly in terms of advocating the uptake of solutions by members and recognising NRLS contributions for appraisal purposes. However, the future of the England and Wales NRLS must be secured, in terms of providing both a means for national learning and the expertise and resources needed to undertake regular systematic inquiries of these data.
Support the development of global learning registries
To advance and accelerate the primary care quality improvement agenda internationally, a global registry for incident reporting could support the ability to generate action-orientated outputs with strong face validity in the health-care profession.
The WHO has proposed a minimal information model to provide a data set in all countries for sharing patient safety incident reports. 150 Efforts will then need to be made to ensure that incident reports from each country meet an acceptable standard to enable learning.
National (and the proposed international) patient safety incident report systems should be designed to describe care failures and safety incidents, and also be utilised to shape priorities for improvement, corroborate insights from research studies, develop potential solutions for application in practice, and share learning of the context-specific approaches of application of solutions.
Data linkages within and between health- and social-care services
The potential value of data linkage to evaluate the impact of patient characteristics on health-care outcomes was demonstrated in a recent UK-wide enquiry into child mortality. 151 From our characterisation of reports involving children, insights for prioritising and designing future safety interventions could be gained by linking incident-reporting systems with electronic medical records and other public or social-care registries. This would enable the identification of incident reports relevant to specific groups. Sheikh et al. 152 have outlined a strategy for health-care IT in the NHS which has four key components: (1) devolve the decision-making processes about systems procurement to practising professionals; (2) consider offering modest financial incentives and highlight the penalties for non-adopters of such systems in the future; (3) governance to ensure safe sharing of data between providers; and (4) oversight from a national body to co-ordinate national efforts to implement advanced health-care IT systems. Lessons from England’s National Programme for Information Technology suggest that rigorous, independent evaluations of implementation efforts are needed. 153
Further research
Analysis of reports from all primary care disciplines
Our potentially generalisable method for interrogating and identifying learning from incident reports should now be applied to other primary care disciplines. In addition to general practice, there are several other ‘point-of-first-access’ disciplines from primary care that have reported > 200,000 reports, which includes dentistry, pharmacy, health visiting, nursing and midwifery. In the same way that general practice reports were overlooked prior to this study, with the exception of medication- and pharmacy-related reports, these reports have also never been systematically characterised to generate learning for primary care patient safety.
In expectation of the need for this follow-on work, we have established the relevant academic, clinical and policy links in each discipline in order to achieve this. Extending this work beyond the confines of general practice is an important next step to advance the field of primary care patient safety, and there is an obvious opportunity to obtain a more representative view of issues by analysing reports from other disciplines. Each discipline is interested in the discipline-specific outputs from our study; thus, we would propose that a sufficiently large sample be drawn from each discipline and that analysis is led by clinical academics from each discipline.
Scoping reviews to identify potential interventions
To realise the full potential of incident reporting for informing the design of new care models, work must now include scoping reviews to identify interventions and improvement initiatives that address the priority recommendations that we recognise are broad in nature and highlight major cultural challenges that need addressing. Similarly, we must identify solutions to prevent the most harmful and most frequent safety incident types where possible. Determining the acceptability and feasibility of interventions with HCPs in general practice (and wider) is needed with a view to evaluating their effectiveness when implemented. We propose scoping reviews for the most frequent and more harmful incident types. This method would enable us to search and synthesise both the published and grey literature, and utilise our links with world-leading improvement organisations and field experts to identify and study initiatives that are not likely to be described by publication.
Broader characterisation of priority areas in general practice
Our study has provided guidance on the nature and range of safety incident reports from general practice. More focused coding and analysis of general practice reports is now needed. During our preparatory work, we analysed all incident reports on children in general practice, all reports involving an immunisation-related error in children and all discharge-related incidents in general practice. These provided a greater volume of similar reports to generate hypotheses from. These more focused analyses enabled more in-depth insights into the potential contributory issues, and the likely changes (both concepts and ideas) that would be needed to enhance patient safety which in turn gave us a stronger handle on the kinds of interventions needed.
We advocate that representative samples of reports be drawn from all primary care disciplines to undertake characterisation of safety incidents in the following content areas:
-
primary care mental health
-
diagnosis and assessment
-
care of the elderly
-
out-of-hours care
-
unwell children
-
vulnerable patient groups.
Natural language processing
Given that at least 13,699 reports have been manually coded by trained clinicians, the data set now provides an opportunity to develop the technology capable of automating the analysis of incident reports using natural language processing (NLP) methods, taking into consideration that free-text information from incident reports is complex to code. NLP offers a set of informatics tools capable of transforming text into a structured format that can be used for research and improvement. Extraction systems based on NLP have been developed in the medical domain. These are yet to be explored for patient safety incident report purposes.
Develop and test empirically informed care models
We have previously discussed how the outcomes from analysis of incident reports should empirically inform the design of improvement initiatives. 23 The value of incident-reporting systems will be realised by HCPs only when their contributions are acknowledged and acted on. Creating an open culture of incident reporting is needed in all care settings, and we recognise that this is an ongoing challenge in hospital settings too. We believe that primary care can accelerate the pace of its quality improvement agenda by using routine data sources like incident reports to identify local and national-level priorities based on the insights of its HCPs and staff.
Strengths and limitations
This is the first mixed-methods analysis of safety incident reports from general practice in England and Wales.
Role of professionals in reporting incidents
Reporting systems rely on data input (reporting) to generate learning. Safety incident-reporting systems rely on staff to write descriptions of incidents, including what happened and perceived reasons for why an incident occurred. 76 At a local level, these reports can inform the basis of recommendations to mitigate harm in practice, and at a national level these reports may be used to identify issues that would otherwise be overlooked. The information described on these forms can be understood as a form of ‘storytelling’ that represents the reporter’s position, perspective and experience, regardless of whether or not the reporter witnessed the incident first hand. 154–156
Only one-third of reports included in this analysis described potential contributory factors and reporters do not routinely describe the organisational-level factors contributing to incidents. Furthermore, it is recognised that incidents are under-reported, can represent only the ‘tip of the iceberg’ and can be limited in narrative content. 19 Although the NRLS accepts reports from patients and parents, few such reports were apparent in our data set. Furthermore, there was likely to be differential reporting between organisations (i.e. those with good reporting cultures are likely to contribute more than those without such cultures). 26,157
Both the coding process and thematic analysis are open to personal interpretation of the data, and may be subject to confirmation bias. We sought to minimise personal interpretation of the data in stage 1 by adhering to the nine rules of recursive incident analysis and designating codes that represent what was explicitly stated in reports. In addition, methodological rigour was ensured by keeping an audit trail of all coding-related decisions, holding weekly meetings to discuss analysis, and independent double-coding of 20% of reports, indicating a high degree of concordance. 158 The reliability of Cohen’s kappa indicated that researchers were applying the coding frameworks consistently. In stage 3 of the analysis, clinicians were encouraged to use their clinical expertise and judgement for the interpretation of reports aligned with priority issues identified by EDA.
Our analytical process required the rigour of an objective and structured coding process in stage 1 to ensure confidence in the identification of priority issues in stage 2. To augment pragmatic, clinically meaningful learning for improvement, a thematic analysis was undertaken in stage 3 that drew on the clinical expertise of reviewers.
Nature of findings
Our findings are hypothesis-generating, inductive in nature, and require testing and development in further research.
Reporting to the NRLS has increased in the last decade, providing large numbers of data from which to generate learning. 159,160 There may be other harmful incident types occurring in primary care that are under-reported because of a fear of being reprimanded. 157 However, despite limitations from under-reporting and reporting biases, analyses of NRLS data have played an important role in generating lessons to mitigate harmful incidents in other areas of clinical practice. 32,161
Incident-reporting culture
Incident reporting is widely understood to be imperative for generating system learning that improves patient safety,10,89,162 yet the literature demonstrates that patient safety incidents are under-reported. 19,81,104 As a result, there has been a great deal of interest in investigating barriers to medical incident reporting. 81,157,163,164 Fear of blame has been cited as a primary factor in the unwillingness of individual doctors to report incidents. 82,165 Waring93 notes that some doctors ‘referred to the excessive time required for form filling that could be better spent with patients or the menial nature of paperwork that was somehow beneath medical expertise’. Meanwhile, the literature also reports that some staff fail to recognise how completing incident forms will impact on practice- or organisation-level change. 93,166
These sociocultural determinants are broad, and the influence of each will vary between individuals and institutions. However, they illustrate that even when there are procedures in place to encourage incident reporting, and even when those policies clearly define which incidents need to be reported, there may be mitigating factors. These environmental and personal issues may affect whether or not an incident is reported, when an incident is reported and how it is reported. It is evident that there are significant cultural and social factors that affect the processes of incident reporting in health-care settings. Despite these limitations, the study findings highlight important challenges faced by patients and primary care professionals in England and Wales.
Chapter 8 Conclusions
Despite over a decade of patient safety research in the hospital setting, incident-reporting systems have struggled to gain traction with the clinical community. Therefore, if HCPs in general practices are to invest time and effort in reporting patient safety incidents, a robust method to learn about risk and to generate strategies to minimise future patient risk is needed. Those professionals will want to see results. An opportunity exists to support health-care organisations to exploit its local data to generate learning from incident reports and inform its quality improvement agenda. This would enable each organisation to undertake its own diagnostics for improvement and prioritise the issues that matter most to its workforce.
Our study is the first systematic analysis of safety incident reports from general practice in the NRLS. Using mixed methods, we have empirically developed a classification to enable coding of patient safety incident reports for the identification of the most common and frequent safety issues, as well as to understand the underlying clinical context reported by HCPs. Opportunities to prevent the issues underpinning the most commonly reported incidents, as well as those described as resulting in severe harm or death, were identified. Recommendations have been made from this analysis by a multidisciplinary team of clinicians, researchers and patient safety experts.
In order to advance the field of patient safety in primary care, regular interrogation of routine data, such as incident reports, will be needed to inform the development of a national quality improvement agenda. Although there are recognised limitations of safety-reporting system data, this study has generated hypotheses through an inductive process that now requires development and testing through future research and improvement efforts in clinical practice. Using the issues that matter most to professionals to gain traction for buy-in could help to accelerate a culture of quality improvement in primary care.
The four classes of data (incident type, contributory factors, level of harm and outcomes) represent the minimum data needed to identify learning to inform future practice improvement. However, major variation currently exists in terms of report content and its ability to inform. Maximising opportunities to learn from patient safety incidents via mandatory data capture and a national, co-ordinated effort to support organisations to build the capacity and capability of their workforce to report data for learning is needed.
Further work must now build on both deepening and broadening understanding of our study findings through further characterisation of safety incident reports from the wider pool of all 270,000+ primary care reports available. In parallel, scoping reviews must be undertaken to identify interventions for incorporation into new models of care delivery for primary care. Evaluation of their effects on patient safety and experience will be needed.
Acknowledgements
Valuable contributions
We have to thank many people who enabled us to deliver this study in 18 months. We are indebted to those who took the time to report the safety incidents. We have taken each report to be a unique opportunity to learn to improve the quality and safety of care for patients, their families and carers, as well as to improve the experience of HCPs and staff responsible for its compassionate delivery.
Our patient and public involvement team
The co-applicants and the research team would like to extend their sincere thanks to the patient and public involvement (PPI) team composed of three lay representatives (Jill Beggs, Susan Howe and Kausar Iqbal). Our lay co-applicant, Antony Chuter, oversaw the PPI team, and one lay representative joined him at each monthly study management group using a rota system to ensure that everyone contributed. After each meeting, the lay representative produced a report to keep the others in touch with the project. Over the course of the study, the team held three all-day workshops to explore aspects of the study, the methods and the early findings. The lay representatives attended these workshops and kept the research team grounded in the reality of the physical and emotional perspectives of patients. In total, we estimate that each lay representative contributed 144 hours of time to the project. The PPI team was truly an integral part of the overall team and we feel this was a good model for PPI in action. They were integral to the success of the project.
Our secretarial support
We wish to thank our clerical officer, Sian Newton, for organising our monthly study management groups and all PAG meetings. This was no easy task given the multiple time zones (PDT, EDT, GMT, ACST and AEST) inhabited by co-applicants, study partners and PAG members. Our thanks to Dr Jenny Cooper, Dr Huw Evans, Dr Huw Williams and Mr Adhnan Omar for critically reviewing drafts of this report.
Our Cardiff-based research team
We express our sincere gratitude to the Cardiff-based study team, which went above and beyond to deliver the outcomes of this study. These are mostly early-career clinical researchers (all listed as authors of this report) who, through their involvement over the past 18 months, have emerged to become champions of primary care patient safety. They have represented our team by presenting preliminary findings at five international and five national conferences, presenting six conference posters and delivering workshops based on methodological learning to leading international patient safety organisations such as the Institute for Healthcare Improvement in Cambridge, MA, USA. They have also contributed to online courses on patient safety and incident reporting via the Institute for Healthcare Improvement Open School and the OPENPediatricsTM learning programme organised by Harvard University and Boston Children’s Hospital. In particular, their energy and commitment towards the classification system development and identifying the learning to improve practice has been inspirational. The study has afforded us an invaluable opportunity to build a movement with committed primary care patient safety clinicians and researchers at Cardiff University as well as build strong, meaningful work relationships between collaborating institutions.
Our generous colleagues
We extend our special thanks to Peter Hibbert (Program Manager at the Australia Institute for Healthcare Innovation, Macquarie University) for contributing his time (no less than 2–3 hours per week over the past 18 months) pro bono to the project. Working with the co-founder of the WHO ICPS, to support the development of our primary care-specific classification system, enabled us to learn fast and produce a system that we hope will be used by health-care organisations to make sense of their own patient safety data. We are grateful for the support and guidance on coding safety reports from Anita Deakin (Patient Safety Report Analyst, Australian Patient Safety Foundation).
Our expert advisors
We are extremely grateful to the expert contributions received from members of our PAG, who provided us with critical guidance on the development of methods to analyse incident report data: Dr Karen Gully (Senior Medical Officer, Welsh Government), Janet Davies (Patient Safety Advisor, Welsh Government), Professor Nigel Sparrow (Senior National GP Advisor, Care Quality Commission), Dr Gareth Parry (Institute for Healthcare Improvement and Harvard Medical School), Dr Donna Luff (Boston Children’s Hospital and Harvard Medical School) and Dr Meredith Makeham (Australian Institute for Healthcare Innovation).
Contributions of authors
Dr Andrew Carson-Stevens (Patient Safety Research Lead, Wales Primary and Emergency Care Research Centre, Cardiff University; Visiting Chair, University of British Columbia) was the co-chief investigator.
Peter Hibbert (Program Manager, Australian Institute for Health Innovation, Macquarie University) was a member of the PAG, provided human factors training to the study team and contributed to classification development.
Dr Huw Williams (Academic GP, Primary Care Patient Safety Research Group, Division of Population Medicine, School of Medicine, Cardiff University) undertook data coding and analysis, and contributed to study team discussions about study findings and policy and practice recommendations.
Dr Huw Prosser Evans (Academic F2 Doctor and Clinical Informatics Lead, Primary Care Patient Safety Research Group, Division of Population Medicine, School of Medicine, Cardiff University) designed and developed the analysis software and undertook data coding and analysis.
Dr Alison Cooper (Academic GP Fellow, Primary Care Patient Safety Research Group, Division of Population Medicine, School of Medicine, Cardiff University) undertook data coding and analysis.
Philippa Rees (Research Assistant, Primary Care Patient Safety Research Group, Division of Population Medicine, School of Medicine, Cardiff University) contributed to the pilot analyses of data and development of the classification system.
Anita Deakin (Patient Safety Report Analyst, Australian Patient Safety Foundation) undertook data coding and contributed to the development of the classification system.
Dr Emma Shiels (Academic F2 Doctor, Primary Care Patient Safety Research Group, Division of Population Medicine, School of Medicine, Cardiff University) undertook data coding and analysis.
Dr Russell Gibson (Academic F2 Doctor, Primary Care Patient Safety Research Group, Division of Population Medicine, School of Medicine, Cardiff University) assisted with the analysis of coded data.
Amy Butlin (Medical Student, Primary Care Patient Safety Research Group, Division of Population Medicine, School of Medicine, Cardiff University) contributed to the pilot analyses of data and development of the classification system.
Dr Ben Carter (Lecturer in Medical Statistics, Division of Medical Education, School of Medicine, Cardiff University) provided statistical advice.
Dr Donna Luff (Instructor in Anesthetics, Harvard Medical School) was a member of the PAG and contributed methodological input.
Dr Gareth Parry (Senior Scientist, Institute for Healthcare Improvement; Clinical Assistant Professor of Pediatrics, Harvard Medical School) was a member of the PAG and contributed methodological input.
Dr Meredith Makeham (Associate Professor, Australian Institute for Health Innovation, Macquarie University) was a member of the PAG and contributed methodological input.
Paul McEnhill (Medical Student, Primary Care Patient Safety Research Group, Division of Population Medicine, School of Medicine, Cardiff University) contributed to pilot analyses of data and the development of the classification system.
Dr Hope Olivia Ward (Research Assistant, Primary Care Patient Safety Research Group, Division of Population Medicine, School of Medicine, Cardiff University) contributed to pilot analyses of data and the development of the classification system.
Dr Raymond Samuriwo (Lecturer in Adult Nursing, Primary Care Patient Safety Research Group, Division of Population Medicine, School of Medicine, Cardiff University) contributed to data analysis.
Professor Anthony Avery (Professor of Primary Health Care, Division of Primary Care, School of Medicine, University of Nottingham, UK) contributed to conceptualisation of the study design and study team discussions about study findings and policy and practice recommendations.
Antony Chuter (Independent patient) contributed to conceptualisation of the study design and study team discussions about study findings and policy and practice recommendations.
Professor Sir Liam Donaldson (Chair in Health Policy, Department of Surgery and Cancer, Imperial College, London) contributed to conceptualisation of the study design and study team discussions about study findings and policy and practice recommendations.
Dr Sharon Mayor (Senior Lecturer in Healthcare Improvement, Division of Population Medicine, School of Medicine, Cardiff University) contributed to conceptualisation of the study design and study team discussions about study findings.
Dr Sukhmeet Panesar (Adjunct Assistant Professor, Department of Medicine, Baylor College of Medicine) contributed to conceptualisation of the study design.
Professor Aziz Sheikh (Co-Director, Centre for Medical Informatics, Usher Institute of Population Health Sciences and Informatics, The University of Edinburgh) contributed to conceptualisation of the study design and study team discussions about study findings and policy and practice recommendations.
Dr Fiona Wood (Senior Lecturer, Division of Population Medicine, School of Medicine, Cardiff University) contributed qualitative methodological input.
Professor Adrian Edwards (Director, Division of Population Medicine, School of Medicine, Cardiff University) was the co-chief investigator.
All co-authors have contributed to the drafting of this report.
Publications
Several publications have arisen from the preliminary studies that informed the development of the classification system for this study (described in more detail in Chapter 3). We appreciate the clinical expertise contributed by collaborating colleagues involved in the publications (published or in press) detailed below:
Rees P, Carson-Stevens A, Williams H, Panesar S, Edwards A. Quality improvement informed by a reporting and learning system. Arch Dis Child 2014;99:702–3.
Rees P, Evans H, Panesar S, Llewelyn M, Edwards A, Carson-Stevens A. Contraindicated BCG vaccination in ‘at risk’ infants. BMJ 2014;349:g5388.
Rees P, Panesar SS, Edwards A, Carson-Stevens A. Child mortality in the UK. Lancet 2014;384:1923–4.
Carson-Stevens A, Edwards A, Panesar S, Parry G, Rees P, Sheikh A, et al. Reducing the burden of iatrogenic harm in children. Lancet 2015;385:1593–4.
Carson-Stevens A, Hibbert P, Avery A, Butlin A, Carter B, Cooper A, et al. A cross-sectional mixed methods study protocol to generate learning from patient safety incidents reported from general practice. BMJ Open 2015;5:e009079.
Omar A, Rees P, Prosser Evans H, Williams H, Cooper A, Banerjee S, et al. Vulnerable children and their care quality issues. A descriptive analysis of a national database. BMJ Qual Saf 2015;24:732–73.
Rees P, Edwards A, Evans H, Powell C, Panesar S, Carson-Stevens A. Disparities in the quality of primary healthcare for socially deprived children. Arch Dis Child 2015;100:299–300.
Rees P, Edwards A, Powell C, Evans H, Carter B, Hibbert P, et al. Paediatric immunisation-related safety incidents in primary care: a mixed methods analysis of a national database. Vaccine 2015;33:3873–80.
Rees P, Edwards A, Powell C, Panesar S, Carter B, Williams H, et al. Safety incidents in the primary care office practice setting. Pediatrics 2015;135:2014–3259.
Rees P, Edwards A, Powell C, Williams H, Hibbert P, Makeham M, et al. Identifying priorities for improved child healthcare: a mixed methods analysis of safety incident reports. BMJ Qual Saf 2015;24:730–31.
Williams H, Edwards A, Hibbert P, Rees P, Panesar S, Carter B, et al. Harms from discharge to primary care – mixed methods analysis of incident reports. Br J Gen Pract 2015;65:e829–37.
Williams H, Cooper A, Carson-Stevens A. Opportunities for incident reporting. BMJ Qual Saf 2016;25:133–4.
Our publication in the Pediatrics journal received press coverage in the The Sunday Times (Scotland). We have developed a press release strategy to aid the reach of our findings to a wide audience, which includes the public.
We are currently working on a number of academic presentations and publications that will draw on, and further develop, the themes covered in this report.
Data sharing statement
All data requests should be discussed with the corresponding author.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
References
- de Vries E, Ramrattan M, Smorenburg S. The incidence and nature of in-hospital adverse events: a systematic review. Qual Saf Health Care 2008;17:216-23. http://dx.doi.org/10.1136/qshc.2007.023622.
- Landrigan CP, Parry GJ, Bones CB, Hackbarth AD, Goldmann DA, Sharek PJ. Temporal trends in rates of patient harm resulting from medical care. N Engl J Med 2010;363:2124-34. http://dx.doi.org/10.1056/NEJMsa1004404.
- Sheikh A, Bates DW. Iatrogenic Harm in Primary Care. Cambridge, MA: Harvard University; 2014.
- Sheikh A, Panesar S, Larizgoitia I, Bates D, Donaldson L. Safer primary care for all: a global imperative. Lancet Glob Health 2013;1:e182-3. http://dx.doi.org/10.1016/S2214-109X(13)70030-5.
- Summary of Inaugural Meeting – The Safer Primary Care Expert Working Group. Geneva: WHO; 2012.
- Cresswell KM, Panesar SS, Salvilla SA, Carson-Stevens A, Larizgoitia I, Donaldson LJ, et al. Global research priorities to better understand the burden of iatrogenic harm in primary care: an international Delphi exercise. PLOS Med 2013;10. http://dx.doi.org/10.1371/journal.pmed.1001554.
- Kostopoulou O, Delaney B. Confidential reporting of patient safety events in primary care: results from a multilevel classification of cognitive and system factors. Qual Saf Health Care 2007;16:95-100. http://dx.doi.org/10.1136/qshc.2006.020909.
- Francis R. Freedom to Speak Up – A Review of Whistleblowing in the NHS. London: Department of Health; 2015.
- Leape LL, Berwick DM. Five years after To Err Is Human: what have we learned?. JAMA 2005;293:2384-90. http://dx.doi.org/10.1001/jama.293.19.2384.
- Kohn LT, Corrigan JM, Donaldson MS. To Err is Human: Building a Safer Health System. Washington, DC: National Academies Press (US); 2000.
- Reason J. Human error: models and management. BMJ 2000;320:768-70. http://dx.doi.org/10.1136/bmj.320.7237.768.
- Panesar SS, deSilva D, Carson-Stevens A, Cresswell KM, Salvilla SA, Slight SP, et al. How safe is primary care? A systematic review. BMJ Qual Saf 2015;25:544-53.
- Bhasale AL, Miller GC, Reid SE, Britt HC. Analysing potential harm in Australian general practice: an incident-monitoring study. Med J Aust 1998;169:73-6.
- Holden J, O’Donnell S, Brindley J, Miles L. Analysis of 1263 deaths in four general practices. Br J Gen Pract 1998;48:1409-12.
- Mitchell ED, Rubin G, Macleod U. Understanding diagnosis of lung cancer in primary care: qualitative synthesis of significant event audit reports. Br J Gen Pract 2013;63:e37-46. http://dx.doi.org/10.3399/bjgp13X660760.
- Britt H, Miller GC, Steven ID, Howarth GC, Nicholson PA, Bhasale AL, et al. Collecting data on potentially harmful events: a method for monitoring incidents in general practice. Fam Pract 1997;14:101-6. http://dx.doi.org/10.1093/fampra/14.2.101.
- Fischer G, Fetters MD, Munro AP, Goldman EB. Adverse events in primary care identified from a risk-management database. J Fam Pract 1997;45:40-6.
- Woolf SH, Kuzel AJ, Dovey SM, Phillips RL. A string of mistakes: the importance of cascade analysis in describing, counting, and preventing medical errors. Ann Fam Med 2004;2:317-26. http://dx.doi.org/10.1370/afm.126.
- Sari AB-A, Sheldon TA, Cracknell A, Turnbull A. Sensitivity of routine system for reporting patient safety incidents in an NHS hospital: retrospective patient case note review. BMJ 2007;13. http://dx.doi.org/10.1136/bmj.39031.507153.AE.
- Organisation Patient Safety Incident Reports. London: NHS; n.d.
- Vincent C. Incident reporting and patient safety. BMJ 2007;334. http://dx.doi.org/10.1136/bmj.39071.441609.80.
- Rees P, Carson-Stevens A, Williams H, Panesar S, Edwards A. Quality improvement informed by a reporting and learning system. Arch Dis Child 2014;99:702-3. http://dx.doi.org/10.1136/archdischild-2014-306198.
- Carson-Stevens A, Edwards A, Panesar S, Parry G, Rees P, Sheikh A, et al. Reducing the burden of iatrogenic harm in children. Lancet 2015;385:1593-4. http://dx.doi.org/10.1016/S0140-6736(14)61739-6.
- Rees P, Edwards A, Panesar S, Powell C, Carter B, Williams H, et al. Safety incidents in the primary care office setting. Pediatrics 2015;135:1027-35. http://dx.doi.org/10.1542/peds.2014-3259.
- Runciman WB. Incident monitoring. Baillière Clin Anaes 1996;10:333-56. http://dx.doi.org/10.1016/S0950-3501(96)80020-1.
- Panesar SS, Cleary K, Sheikh A. Reflections on the National Patient Safety Agency’s database of medical errors. J R Soc Med 2009;102:256-8. http://dx.doi.org/10.1258/jrsm.2009.090135.
- Vincent C. Analysis of clinical incidents: a window on the system not a search for root causes. Qual Saf Health Care 2004;13:242-3. http://dx.doi.org/10.1136/qshc.2004.010454.
- Noble DJ, Panesar SS, Pronovost PJ. A public health approach to patient safety reporting systems is urgently needed. J Patient Saf 2011;7:109-12. http://dx.doi.org/10.1097/PTS.0b013e31821b8a6c.
- Vincent C. Patient Safety. Chichester: John Wiley & Sons; 2010.
- Gerrett D, Lamont T, Paton C, Barnes TR, Shah A. Prescribing and monitoring lithium therapy: summary of a safety report from the National Patient Safety Agency. BMJ 2010;341. http://dx.doi.org/10.1136/bmj.c6258.
- Lamont T, Cousins D, Hillson R, Bischler A, Terblanche M. Safer administration of insulin: summary of a safety report from the National Patient Safety Agency. BMJ 2010;341. http://dx.doi.org/10.1136/bmj.c5269.
- Lamont T, Watts F, Panesar S, MacFie J, Matthew D. Early detection of complications after laparoscopic surgery: summary of a safety report from the National Patient Safety Agency. BMJ 2011;342. http://dx.doi.org/10.1136/bmj.c7221.
- Healey F, Sanders DS, Lamont T, Scarpello J, Agbabiaka T. Early detection of complications after gastrostomy: summary of a safety report from the National Patient Safety Agency. BMJ 2010;340. http://dx.doi.org/10.1136/bmj.c2160.
- Panesar SS, Salvilla SA, Patel B, Donaldson SL. Laparoscopic cholecystectomy: device-related errors revealed through a national database. Expert Rev Med Devices 2011;8:555-60. http://dx.doi.org/10.1586/erd.11.43.
- Healey F, Darowski A, Lamont T, Panesar S, Poulton S, Treml J, et al. Essential care after an inpatient fall: summary of a safety report from the National Patient Safety Agency. BMJ 2011;342. http://dx.doi.org/10.1136/bmj.d329.
- Catchpole K, Bell MD, Johnson S. Safety in anaesthesia: a study of 12,606 reported incidents from the UK National Reporting and Learning System. Anaesthesia 2008;63:340-6. http://dx.doi.org/10.1111/j.1365-2044.2007.05427.x.
- Smith AF, Mahajan RP. National critical incident reporting: improving patient safety. Br J Anaesth 2009;103:623-5. http://dx.doi.org/10.1093/bja/aep273.
- Cresswell KM, Sheikh A. Information technology-based approaches to reducing repeat drug exposure in patients with known drug allergies. J Allergy Clin Immunol 2008;121:1112-17. http://dx.doi.org/10.1016/j.jaci.2007.12.1180.
- Makeham M, Dovey S, Runciman W, Larizgoitia I. Methods and Measures Used in Primary Care Patient Safety Research. Geneva: WHO; 2008.
- Elder NC, Dovey SM. Classification of medical errors and preventable adverse events in primary care: a synthesis of the literature. J Fam Pract 2002;51:927-32.
- Sandars J, Esmail A. The frequency and nature of medical error in primary care: understanding the diversity across studies. Fam Pract 2003;20:231-6. http://dx.doi.org/10.1093/fampra/cmg301.
- Tukey JW. Exploratory Data Analysis. Reading, MA: Addison-Wesley; 1977.
- Donaldson LJ, Panesar SS, Darzi A. Patient-safety-related hospital deaths in England: thematic analysis of incidents reported to a national database, 2010–2012. PLOS Med 2014;11. http://dx.doi.org/10.1371/journal.pmed.1001667.
- Boyatzis RE. Transforming Qualitative Information: Thematic Analysis and Code Development. New York, NY: Sage; 1998.
- Leinhardt G, Leinhardt S. Exploratory data analysis: new tools for the analysis of empirical data. Rev Res Educ 1980;8:85-157. http://dx.doi.org/10.2307/1167124.
- Spittal MJ, Findlay GP, Spencer I. A prospective analysis of critical incidents attributable to anaesthesia. Int J Qual Health Care 1995;7:363-71. http://dx.doi.org/10.1093/intqhc/7.4.363.
- Weingart SN, Callanan LD, Ship AN, Aronson MD. A physician-based voluntary reporting system for adverse events and medical errors. J Gen Intern Med 2001;16:809-14. http://dx.doi.org/10.1046/j.1525-1497.2001.10231.x.
- Astion ML, Shojania KG, Hamill TR, Kim S, Ng VL. Classifying laboratory incident reports to identify problems that jeopardize patient safety. Am J Clin Pathol 2003;120:18-26. http://dx.doi.org/10.1309/8U5D0MA6MFH2FG19.
- Usin MF, Ramesh P, Lopez CG. Implementation of an event reporting system in a transfusion medicine unit: a local experience. Malays J Pathol 2004;26:43-8.
- Voluntary Error Reporting System Focusing on Systems Issues Increases Reporting and Contributes to Reduction in Liability Claims in Outpatient Clinics. Rockville, MD: Agency for Healthcare Research and Quality; 2005.
- Davis M, Rake G, Henriksen K, Battles J, Marks E. Advances in Patient Safety: From Research to Implementation. Rockville, MD: Agency for Healthcare Research and Quality; 2005.
- Desikan R, Krauss M, Dunagan W, Rachmiel E, Bailey T, Fraser V, et al. Advances in Patient Safety. Rockville, MD: Agency for Healthcare Research and Quality; 2005.
- Phillips R, Dovey S, Hickner J, Graham D, Johnson M, Henriksen K, et al. Advances in Patient Safety. Rockville, MD: Agency for Healthcare Research and Quality; 2005.
- Hoffmann B, Beyer M, Rohe J, Gensichen J, Gerlach FM. ‘Every error counts’: a web-based incident reporting and learning system for general practice. Qual Saf Health Care 2008;17:307-12. http://dx.doi.org/10.1136/qshc.2006.018440.
- Kellie S, Battles J, Dixon N, Kaplan H, Fastman B, Henriksen K, et al. Advances in Patient Safety. Rockville, MD: Agency for Healthcare Research and Quality; 2008.
- Silas R, Tibballs J. Adverse events and comparison of systematic and voluntary reporting from a paediatric intensive care unit. Qual Saf Health Care 2010;19:568-71. http://dx.doi.org/10.1136/qshc.2009.032979.
- Subhedar NV, Parry HA. Critical incident reporting in neonatal practice. Arch Dis Child Fetal Neonatal Ed 2010;95:F378-82. http://dx.doi.org/10.1136/adc.2008.137869.
- Zwart DL, Van Rensen EL, Kalkman CJ, Verheij TJ. Central or local incident reporting? A comparative study in Dutch GP out-of-hours services. Br J Gen Pract 2011;61:183-7. http://dx.doi.org/10.3399/bjgp11X561168.
- Zwart DL, Steerneman AH, van Rensen EL, Kalkman CJ, Verheij TJ. Feasibility of centre-based incident reporting in primary healthcare: the SPIEGEL study. BMJ Qual Saf 2011;20:121-7. http://dx.doi.org/10.1136/bmjqs.2009.033472.
- Itoh K, Omata N, Andersen HB, Itoh K, Omata N, Andersen HB. A human error taxonomy for analysing healthcare incident reports: assessing reporting culture and its effects on safety perfomance. J Risk Res 2009;12:485-511. http://dx.doi.org/10.1080/13669870903047513.
- November M, Chie L, Weingart S, Henriksen K, Battles J, Keyes M. Advances in Patient Safety: New Directions and Alternative Approaches (Vol 1: Assessment). Rockville, MD: Agency for Healthcare Research and Quality; 2008.
- West DR, Westfall JM, Araya-Guerra R, Hansen L, Quintela J, VanVorst R, et al. Advances in Patient Safety: From Research to Implementation (Volume 3: Implementation Issues). Rockville, MD: Agency for Healthcare Research and Quality; 2005.
- ‘More than words’ – Conceptual Framework for the International Classification for Patient Safety. Version 1.1. Geneva: WHO; 2009.
- Computer Sciences Corporation . AIMS Incident Management System 2015. www.isofthealth.com/en/Solutions/HospitalsandClinics/AIMS.aspx (accessed 31 May 2015).
- Dovey SM, Meyers DS, Phillips RL, Green LA, Fryer GE, Galliher JM, et al. A preliminary taxonomy of medical errors in family practice. Qual Saf Health Care 2002;11:233-8. http://dx.doi.org/10.1136/qhc.11.3.233.
- Makeham MA, Stromer S, Bridges-Webb C, Mira M, Saltman DC, Cooper C, et al. Patient safety events reported in general practice: a taxonomy. Qual Saf Health Care 2008;17:53-7. http://dx.doi.org/10.1136/qshc.2007.022491.
- Makeham MA, Dovey SM, County M, Kidd MR. An international taxonomy for errors in general practice: a pilot study. Med J Aust 2002;177:68-72.
- Rubin G, George A, Chinn DJ, Richardson C. Errors in general practice: development of an error classification and pilot study of a method for detecting errors. Qual Saf Health Care 2003;12:443-7. http://dx.doi.org/10.1136/qhc.12.6.443.
- Jacobs S, O’Beirne M, Derfiingher LP, Vlach L, Rosser W, Drummond N. Errors and adverse events in family medicine: developing and validating a Canadian taxonomy of errors. Can Fam Physician 2007;53:271-6.
- Buetow S, Kiata L, Liew T, Kenealy T, Dovey S, Elwyn G. Patient error: a preliminary taxonomy. Ann Fam Med 2009;7:223-31. http://dx.doi.org/10.1370/afm.941.
- Hibbert P, Runciman W, Deakin A. A Recursive Model of Incident Analysis. Adelaide, SA: Australian Patient Safety Foundation; 2007.
- Thomas G, James D. Reinventing grounded theory: some questions about theory, ground and discovery. Br Educ Res J 2006;32:767-95. http://dx.doi.org/10.1080/01411920600989412.
- Carson-Stevens A, Hibbert P, Avery A, Butlin A, Carter B, Cooper A, et al. A cross-sectional mixed methods study protocol to generate learning from patient safety incidents reported from general practice. BMJ Open 2015;5. http://dx.doi.org/10.1136/bmjopen-2015-009079.
- Ritchie J, Spencer E, Bryman A, Burgess R. Analyzing Qualitative Data. London: Routledge; 1994.
- Reason J. Human Error. Cambridge: Cambridge University Press; 1990.
- Battles JB, Shea CE. A system of analyzing medical errors to improve GME curricula and programs. Acad Med 2001;76:125-33. http://dx.doi.org/10.1097/00001888-200102000-00008.
- MacQueen KM, McLellan E, Kay K, Milstein B. Codebook development for team-based qualitative analysis. Cultural Anthropol Methods 1998;10:31-6. http://dx.doi.org/10.1177/1525822x980100020301.
- Carey JW, Morgan M, Oxtoby MJ. Intercoder agreement in analysis of responses to open-ended interview questions: examples from tuberculosis research. Cultural Anthropol Methods 1996;8:1-5. http://dx.doi.org/10.1177/1525822x960080030101.
- Gorden R. Basic Interviewing Skills. Itasca, IL: Peacock; 1992.
- Cook A, Scobie S, Hurwitz B, Sheikh A. Analysis of Health Care Error Reports. Oxford: Wiley-Blackwell; 2009.
- Evans SM, Berry JG, Smith BJ, Esterman A, Selim P, O’Shaughnessy J, et al. Attitudes and barriers to incident reporting: a collaborative hospital study. Qual Saf Health Care 2006;15:39-43. http://dx.doi.org/10.1136/qshc.2004.012559.
- Lester H, Tritter JQ. Medical error: a discussion of the medical construction of error and suggestions for reforms of medical education to decrease error. Med Educ 2001;35:855-61. http://dx.doi.org/10.1046/j.1365-2923.2001.01003.x.
- Kreckler S, Catchpole K, McCulloch P, Handa A. Factors influencing incident reporting in surgical care. Qual Saf Health Care 2009;18:116-20. http://dx.doi.org/10.1136/qshc.2008.026534.
- Firth-Cozens J. Barriers to incident reporting. Qual Saf Health Care 2002;11. http://dx.doi.org/10.1136/qhc.11.1.7.
- Batalden PB, Davidoff F. What is ‘quality improvement’ and how can it transform healthcare?. Qual Saf Health Care 2007;16:2-3. http://dx.doi.org/10.1136/qshc.2006.022046.
- Madhok R, Strobl J, Panesar S, Carson-Stevens A, Cross H, McIldowie B, et al. How to protect the ‘second victim’ of adverse events. Health Serv J 2014. www.hsj.co.uk/leadership/how-to-protect-the-second-victim-of-adverse-events/5073269.article (accessed 24 July 2016).
- Donaldson L. An organisation with a memory. Clin Med 2002;2:452-7. http://dx.doi.org/10.7861/clinmedicine.2-5-452.
- An Organisation with Memory: Report of an Expert Group on Learning from Adverse Events in the NHS Chaired by the Chief Medical Officer. London: The Stationery Office; 2000.
- Barach P, Small SD. How the NHS can improve safety and learning. By learning free lessons from near misses. BMJ 2000;320:1683-4. http://dx.doi.org/10.1136/bmj.320.7251.1683.
- Health and Social Care Act 2008 (Duty of Candour) Regulations 2014. London: The Stationery Office; 2014.
- Myketiak C, Curzon P. Medical Incident Reports, Narrative, and Institutional Discourse. Huddersfield: Biannual Troubling Narratives Conference; 2014.
- Vincent C, Stanhope N, Crowley-Murphy M. Reasons for not reporting adverse incidents: an empirical study. J Eval Clin Pract 1999;5:13-21. http://dx.doi.org/10.1046/j.1365-2753.1999.00147.x.
- Waring JJ. Beyond blame: cultural barriers to medical incident reporting. Soc Sci Med 2005;60:1927-35. http://dx.doi.org/10.1016/j.socscimed.2004.08.055.
- Singh H, Sittig DF. Advancing the science of measurement of diagnostic errors in healthcare: the Safer Dx framework. BMJ Qual Saf 2015 n.d.;24:103-10. http://dx.doi.org/10.1136/bmjqs-2014-003675.
- Ottewill M. The current approach to human error and blame in the NHS. Br J Nurs 2003;12:919-24. http://dx.doi.org/10.12968/bjon.2003.12.15.11419.
- O’Connor A. The attitude of staff towards clinical risk management. Clin Risk 1996;2:119-26.
- McDonald S, Ahern K. The professional consequences of whistleblowing by nurses. J Prof Nurs 2000;16:313-21. http://dx.doi.org/10.1053/jpnu.2000.18178.
- White SM. Confidentiality, ‘No blame culture’ and whistleblowing, non-physician practice and accountability. Best Pract Res Clin Anaesthesiol 2006 n.d.;20:525-43. http://dx.doi.org/10.1016/j.bpa.2006.09.002.
- Dasgupta N, Rivera L. When social context matters: the influence of long-term contact and short-term exposure to admired outgroup members on implicit attitudes and behavioural intentions. Soc Cogn 2008;26:112-23. http://dx.doi.org/10.1521/soco.2008.26.1.112.
- Li JW, Morway L, Velasquez A, Weingart SN, Stuver SO. Perceptions of medical errors in cancer care: an analysis of how the news media describe sentinel events. J Patient Saf 2015;11:42-51. http://dx.doi.org/10.1097/PTS.0000000000000039.
- Balasubramanian S. Day of week of procedure and 30 day mortality for elective surgery: retrospective analysis of hospital episode statistics (letter). BMJ 2013;346.
- Aylin P, Alexandrescu R, Jen MH, Mayer EK, Bottle A. Day of week of procedure and 30 day mortality for elective surgery: retrospective analysis of hospital episode statistics. BMJ 2013;346. http://dx.doi.org/10.1136/bmj.f2424.
- Croskerry P, Singhal G, Mamede S. Cognitive debiasing 2: impediments to and strategies for change. BMJ Qual Saf 2013;22:ii65-72. http://dx.doi.org/10.1136/bmjqs-2012-001713.
- de Feijter JM, de Grave WS, Muijtjens AM, Scherpbier AJJA, Koopmans RP. A comprehensive overview of medical error in hospitals using incident-reporting systems, patient complaints and chart review of inpatient deaths. PLOS ONE 2012;7. http://dx.doi.org/10.1371/journal.pone.0031125.
- Schiff GD, Kim S, Abrams R, Cosby K, Lambert B, Elstein AS, et al. Advances in Patient Safety: From Research to Implementation (Volume 2: Concepts and Methodology). Rockville, MD: Agency for Healthcare Research and Quality; 2005.
- Almond S, Mant D, Thompson M. Diagnostic safety-netting. Br J Gen Pract 2009;59:872-4. http://dx.doi.org/10.3399/bjgp09X472971.
- Williams H, Edwards A, Hibbert P, Rees P, Panesar S, Carter B, et al. Harms from discharge to primary care – mixed methods analysis of incident reports. Br J Gen Pract 2015;65:e829-37. http://dx.doi.org/10.3399/bjgp15X687877.
- Murff HJ, Gandhi TK, Karson AK, Mort EA, Poon EG, Wang SJ, et al. Primary care physician attitudes concerning follow-up of abnormal test results and ambulatory decision support systems. Int J Med Inform 2003;71:137-49. http://dx.doi.org/10.1016/S1386-5056(03)00133-3.
- Ramnarayan P, Winrow A, Coren M, Nanduri V, Buchdahl R, Jacobs B, et al. Diagnostic omission errors in acute paediatric practice: impact of a reminder system on decision-making. BMC Med Inform Decis Mak 2006;6. http://dx.doi.org/10.1186/1472-6947-6-37.
- de Wit HA, Mestres Gonzalvo C, Hurkens KP, Mulder WJ, Janknegt R, Verhey FR, et al. Development of a computer system to support medication reviews in nursing homes. Int J Clin Pharm 2013;35:668-72. http://dx.doi.org/10.1007/s11096-013-9827-3.
- Leape LL, Brennan TA, Laird N, Lawthers AG, Localio AR, Barnes BA, et al. The nature of adverse events in hospitalized patients. Results of the Harvard Medical Practice Study II. N Engl J Med 1991;324:377-84. http://dx.doi.org/10.1056/NEJM199102073240605.
- Guthrie B, Payne K, Alderson P, McMurdo MET, Mercer SW. Adapting clinical guidelines to take account of multimorbidity. BMJ 2012;345. http://dx.doi.org/10.1136/bmj.e6341.
- Holland AJ. Ageing and learning disability. Br J Psychiatry 2000;176:26-31. http://dx.doi.org/10.1192/bjp.176.1.26.
- Safeguarding People with Learning Disabilities Within the NHS: An Agenda for the National Patient Safety Agency. London: NPSA; 2004.
- Langton H, Barnes M, Haslehurst S, Rimmer J, Turton P. Collaboration, user involvement and education: a systematic review of the literature and report of an educational initiative. Eur J Oncol Nurs 2003;7:242-52. http://dx.doi.org/10.1016/S1462-3889(03)00033-4.
- Simpson EL, House AO. Involving users in the delivery and evaluation of mental health services: systematic review. BMJ 2002;325. http://dx.doi.org/10.1136/bmj.325.7375.1265.
- Rees P, Edwards A, Powell C, Evans H, Panesar S, Carson-Stevens A. Disparities in the quality of primary healthcare for socially deprived children. Arch Dis Child 2015;100:299-300. http://dx.doi.org/10.1136/archdischild-2014-307618.
- Bowers B, Cook R. Using referral guidelines to support best care outcomes for patients. Br J Community Nurs 2012;17:134-8. http://dx.doi.org/10.12968/bjcn.2012.17.3.134.
- Jarvis A, Mackie S, Arundel D. Referral criteria: making the district nursing service visible. Br J Community Nurs 2006;11:17-22. http://dx.doi.org/10.12968/bjcn.2006.11.1.20280.
- First Assessment a Review of District Nursing Services in England and Wales. London: Audit Commission; 1999.
- Waters KR. Discharge planning: an exploratory study of the process of discharge planning on geriatric wards. J Adv Nurs 1987;12:71-83. http://dx.doi.org/10.1111/j.1365-2648.1987.tb01305.x.
- A District Nursing Service for Today and Tomorrow. A Review of District Nursing in Northern Ireland. Belfast: DHSSPSNI; 2011.
- Clover C. Botched referrals cost district nurses five hours each. Nurs Times 2010. www.nursingtimes.net/whats-new-in-nursing/primary-care/botched-referrals-cost-district-nurses-five-hours-each/5020576.article (accessed 3 Nov 2015).
- Review of National Reporting and Learning System (NRLS) Incident Data Relating to Discharge from Acute and Mental Health Trusts – August 2014. London: Department of Health; 2014.
- Hesselink G, Zegers M, Vernooij-Dassen M, Barach P, Kalkman C, Flink M, et al. Improving patient discharge and reducing hospital readmissions by using Intervention Mapping. BMC Health Serv Res 2014;14. http://dx.doi.org/10.1186/1472-6963-14-389.
- Stainkey L, Pain T, McNichol M, Hack J, Roberts L. Matched comparison of GP and consultant rating of electronic discharge summaries. HIM J 2010;39:7-15. http://dx.doi.org/10.1177/183335831003900302.
- Pocklington C, Al-Dhahir L. A comparison of methods of producing a discharge summary: handwritten vs. electronic documentation. Br J Med Pract 2011;4.
- Maslove DM, Leiter RE, Griesman J, Arnott C, Mourad O, Chow CM, et al. Electronic versus dictated hospital discharge summaries: a randomized controlled trial. J Gen Intern Med 2009;24:995-1001. http://dx.doi.org/10.1007/s11606-009-1053-2.
- Health and Social Care Information Centre . Electronic 24-Hour Discharge Summary Implementation n.d. http://systems.hscic.gov.uk/clinrecords/24hour (accessed 1 February 2015).
- Welsh Clinical Portal. NHS Wales Informatics Service: Cardiff; 2014.
- Scottish Patient Safety Programme . Driver Diagram and Change Package – Safe and Reliable Patient Care Within Practice and Across the Interface 2014.
- The SIGN Discharge Document Edinburgh. Edinburgh: Health Improvement Scotland; 2012.
- Delbanco T, Walker J, Bell SK, Darer JD, Elmore JG, Farag N, et al. Inviting patients to read their doctors’ notes: a quasi-experimental study and a look ahead. Ann Intern Med 2012;157:461-70. http://dx.doi.org/10.7326/0003-4819-157-7-201210020-00002.
- Davies P. Should patients be able to control their own records?. BMJ 2012;345. http://dx.doi.org/10.1136/bmj.e4905.
- The Power of Information: Giving People Control of the Health and Care Information they Need. London: Department of Health; 2012.
- Campbell JL, Fletcher E, Britten N, Green C, Holt T, Lattimer V, et al. The clinical effectiveness and cost-effectiveness of telephone triage for managing same-day consultation requests in general practice: a cluster randomised controlled trial comparing general practitioner-led and nurse-led management systems with usual care (the ESTEEM trial). Health Technol Assess 2015;19. http://dx.doi.org/10.3310/hta19130.
- Campbell JL, Fletcher E, Britten N, Green C, Holt TA, Lattimer V, et al. Telephone triage for management of same-day consultation requests in general practice (the ESTEEM trial): a cluster-randomised controlled trial and cost-consequence analysis. Lancet 2014;384:1859-68. http://dx.doi.org/10.1016/S0140-6736(14)61058-8.
- Warren FC, Calitri R, Fletcher E, Varley A, Holt TA, Lattimer V, et al. Exploring demographic and lifestyle associations with patient experience following telephone triage by a primary care doctor or nurse: secondary analyses from a cluster randomised controlled trial. BMJ Qual Saf 2015;24:572-82. http://dx.doi.org/10.1136/bmjqs-2015-003937.
- Lyratzopoulos G, Elliott M, Barbiere JM, Henderson A, Staetsky L, Paddison C, et al. Understanding ethnic and other socio-demographic differences in patient experience of primary care: evidence from the English General Practice Patient Survey. BMJ Qual Saf 2012;21:21-9. http://dx.doi.org/10.1136/bmjqs-2011-000088.
- A Programme of Action for General Practice. London: NHS England; 2014.
- Ioannidis JP. Why most published research findings are false. PLOS Med 2005;2. http://dx.doi.org/10.1371/journal.pmed.0020124.
- Parry GJ, Carson-Stevens A, Luff DF, McPherson ME, Goldmann DA. Recommendations for evaluation of health care improvement initiatives. Acad Pediatr 2013;13:S23-S30. http://dx.doi.org/10.1016/j.acap.2013.04.007.
- Coulter A, Ellins J. Patient-Focused Interventions: A Review of the Evidence. London: The Health Foundation; 2006.
- Dunston R, Lee A, Boud D, Brodie P, Chiarella M. Co-production and health system reform–from re-imagining to re-making. Aust J Publ Admin 2009;68:39-52. http://dx.doi.org/10.1111/j.1467-8500.2008.00608.x.
- Boyle D, Clarke S, Burns S. Aspects of Co-Production: The Implications for Work, Health And Volunteering. London: New Economics Foundation; 2006.
- Klaber RE, Roland D. Delivering quality improvement: the need to believe it is necessary. Arch Dis Child 2014;99:175-9. http://dx.doi.org/10.1136/archdischild-2012-303563.
- Enabling Patients to Access Electronic Health Records: Guidance for Health Professionals. London: Royal College of General Practitioners; 2010.
- de Wet C, O’Donnell C, Bowie P. Developing a preliminary ‘never event’ list for general practice using consensus-building methods. Br J Gen Pract 2014;64:e159-67.
- Panesar S, Diaper M, Forsyth D, Carson-Stevens A, Ahluwalia S, Rees S, et al. Don’t let primary care patients slip through the nets. Health Serv J 2015. www.hsj.co.uk/sectors/commissioning/dont-let-primary-care-patients-slip-through-the-nets/5078203.fullarticle (accessed 24 July 2016).
- Reporting Patient Safety Incidents. Geneva: WHO; 2014.
- Wolfe I. Why Children Die: Death in Infants, Children and Young People in the UK. London: Royal College of Paediatrics and Child Health and National Children’s Bureau; 2014.
- Sheikh A, Jha A, Cresswell K, Greaves F, Bates DW. Adoption of electronic health records in UK hospitals: lessons from the USA. Lancet 2014;384:8-9. http://dx.doi.org/10.1016/S0140-6736(14)61099-0.
- Sheikh A, Atun R, Bates DW. The need for independent evaluations of government-led health information technology initiatives. BMJ Qual Saf 2014;23:611-13. http://dx.doi.org/10.1136/bmjqs-2014-003273.
- Sanne J. Incident reporting or storytelling? Competing schemes in a safety-critical and hazardous work setting. Saf Sci 2008;46:1205-22. http://dx.doi.org/10.1016/j.ssci.2007.06.024.
- Staender S. Incident reporting in anaesthesiology. Best Pract Res Clin Anaesthesiol 2011;25:207-14. http://dx.doi.org/10.1016/j.bpa.2011.01.005.
- Dixon N. Med QIC Medicare Quality Improvement. Sensemaking Guidelines – A Quality Improvement Tool. Baltimore, MD: Centers for Medicare and Medicaid Services; 2003.
- Lawton R, Parker D. Barriers to incident reporting in a healthcare system. Qual Saf Health Care 2002;11:15-8. http://dx.doi.org/10.1136/qhc.11.1.15.
- Green J, Thorogood N. Qualitative Methods for Health Research. New York, NY: Sage; 2009.
- Panesar SS, Carson-Stevens A, Salvilla SA, Patel B, Mirza SB, Mann B. Patient safety in orthopedic surgery: prioritizing key areas of iatrogenic harm through an analysis of 48,095 incidents reported to a national database of errors. Drug Healthc Patient Saf 2013;5:57-65. http://dx.doi.org/10.2147/DHPS.S40887.
- Pham JC, Gianci S, Battles J, Beard P, Clarke JR, Coates H, et al. Establishing a global learning community for incident-reporting systems. Qual Saf Health Care 2010;19:446-51. http://dx.doi.org/10.1136/qshc.2009.037739.
- Lamont T, Beaumont C, Fayaz A, Healey F, Huehns T, Law R, et al. Checking placement of nasogastric feeding tubes in adults (interpretation of X ray images): summary of a safety report from the National Patient Safety Agency. BMJ 2011;342. http://dx.doi.org/10.1136/bmj.d2586.
- Weiner BJ, Hobgood C, Lewis MA. The meaning of justice in safety incident reporting. Soc Sci Med 2008;66:403-13. http://dx.doi.org/10.1016/j.socscimed.2007.08.013.
- Cullen DJ, Bates DW, Small SD, Cooper JB, Nemeskal AR, Leape LL. The incident reporting system does not detect adverse drug events: a problem for quality improvement. Jt Comm J Qual Improv 1995;21:541-8.
- Pfeiffer Y, Manser T, Wehner T. Conceptualising barriers to incident reporting: a psychological framework. Qual Saf Health Care 2010;19. http://dx.doi.org/10.1136/qshc.2008.030445.
- Wu AW. Medical error: the second victim. The doctor who makes the mistake needs help too. BMJ 2000;320:726-7. http://dx.doi.org/10.1136/bmj.320.7237.726.
- Eland IA, Belton KJ, van Grootheest AC, Meiners AP, Rawlins MD, Stricker BHC. Attitudinal survey of voluntary reporting of adverse drug reactions. Br J Clin Pharmacol 1999;48:623-7. http://dx.doi.org/10.1046/j.1365-2125.1999.00060.x.
Appendix 1 Ethical review
Appendix 2 Rules of recursive model of incident analysis
| Rule | Example |
|---|---|
| 1. An incident has a set of contributing factors | The wrong vaccine was administered (incident) because the child’s ‘Red Book’ was not available (CF) and the computer records were not up to date (CF) |
| 2. An incident can be a contributing factor to another incident | Records not up to date (incident and CF), the wrong vaccine was administered (incident) |
| 3. Some contributing factors cannot be incidents in their own right | A mistake (CF, not an incident) led to the wrong prescribed medication dose (incident) |
| 4. An incident has a set of outcomes | Wrong vaccine administered (incident) requiring the correct vaccine to be administered (outcome) |
| 5. An incident can be an outcome of another incident | Records not up to date (incident) leading to the wrong number of vaccine doses (incident and outcome) |
| 6. Some outcomes cannot be incidents in their own right | Admission to hospital (outcome) after wrong prescribed medication (incident) |
| 7. An outcome of an incident could be a contributing factor to another incident | Communication error between HCPs (incident) led to records not being up to date (incident and outcome) which led to a vaccine-related error (incident) |
| 8. An incident type can be designated the ‘principal incident type’ (i.e. the incident proximal to the descriptive patient outcome) | Communication error (incident) led to inaccurate records (incident) and results in the incorrect vaccine administration (principal incident type) |
| 9. The outcome of a principal incident type cannot be an incident | Admission to hospital (outcome) after failure to access relevant HCP (principal incident type) |
Appendix 3 Primary care patient safety classification (PISA) system
Example of incident descriptor framework
Example of contributory factors framework
Example of outcomes framework
For a full copy of the PISA classification system please contact the corresponding author.
List of abbreviations
- ABHB
- Aneurin Bevan University Health Board
- EDA
- exploratory data analysis
- GP
- general practitioner
- HCP
- health-care professional
- INR
- international normalised ratio
- IT
- information technology
- NLP
- natural language processing
- NRLS
- National Reporting and Learning System
- PAG
- Professional Advisory Group
- PPI
- patient and public involvement
- WHO
- World Health Organization
- WHO ICPS
- World Health Organization’s International Classification for Patient Safety