Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 12/209/59. The contractual start date was in April 2014. The final report began editorial review in April 2015 and was accepted for publication in January 2016. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Paul Aylin reports grants and other from Dr Foster (company has included an analysis of weekend mortality in previous ‘Hospital Guide’ and have paid travel expenses to biannual conference on Global Comparators in Healthcare), outside the submitted work. Alex Bottle reports that The Dr Foster Unit at Imperial College London, where he is based, is part-funded by Dr Foster Intelligence, a private health-care information company (wholly owned by Telstra Corporation Ltd).
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2016. This work was produced by Aylin et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Background and research objectives
Patient concerns
Our study arose as a direct result of questions posed in the high-risk obstetric anaesthetic clinic by patients who were scheduled to undergo cancer surgery while pregnant. Patients wanted to know the statistical risks of an adverse outcome to the pregnancy, including miscarriage, stillbirth, premature delivery or problems following birth such as admission to neonatal intensive care. Unfortunately, the current evidence base is not sufficient to answer these questions and, therefore, this constitutes a ‘knowledge gap’.
A postal survey of women who had undergone non-obstetric surgery during pregnancy in our maternity unit over a 5-year period was then conducted. All respondents (75% response rate) expressed concern regarding the lack of availability of statistical data that could guide their decision. Although they felt that they were adequately counselled, they all agreed that, if there had been more information available, they would have been more confident in their decision-making and less anxious regarding the pregnancy outcome.
Previous literature
Previous literature suggested that non-obstetric surgery is carried out in approximately 1–2% of pregnancies,1 with common operations being appendectomy, cancer surgery and orthopaedic procedures. In this situation, women and their doctors are understandably anxious about the risk of harm to the fetus. However, there is limited available evidence quantifying the risks of miscarriage (fetal loss before 24 weeks’ gestation), stillbirth (fetal loss after 24 weeks’ gestation), premature labour or infant death post delivery.
A Canadian study investigated data from 2656 women between 1971 and 1978. 2 Patients were matched to controls by age and geographical area. There was no statistically increased risk of fetal loss among the group as a whole. However, there was an increased risk of fetal loss in women undergoing a general anaesthetic, which was most marked for women undergoing general anaesthesia for obstetric or gynaecological procedures. Some of these obstetric procedures were cervical cerclages, procedures to prevent recurrent fetal loss, and some bias will therefore have resulted. The study did not differentiate between fetal loss at different stages of pregnancy, did not look at prematurity and did not control for coexisting illness, parity or smoking.
Mazze and Källén et al. 3 analysed outcomes of 5405 Swedish women who had undergone surgery during pregnancy between 1973 and 1981 (during which period there were a total of 720,000 births in Sweden). There was no increase in rates of congenital malformations or stillbirth; however, there were significant increases in death within 7 days of delivery and in prematurity.
The other Swedish studies involved subsets of the original data – specifically investigating appendicectomy4 and laparoscopic surgery (here the data were expanded to include 2,015,000 deliveries from 1973 to 1993). 5 Sixteen per cent of women undergoing appendectomy after 24 weeks’ gestation delivered on the day of their operation, with 22% delivering within 1 week. This resulted in a significant increase in prematurity and death within 7 days of delivery, but not in stillbirth.
A systematic review of the literature from 1966 to 2002 identified 54 papers, involving a total of 12,452 patients. 6 The miscarriage rate among patients undergoing surgery during pregnancy was 5.8% (10.5% if surgery took place in the first trimester); stillbirth occurred in approximately 2% of surgeries and premature delivery in 8.2%. There were, however, no controls for comparison. The clearest data (although still poorly controlled) exist for appendicitis, with surgery-induced delivery occurring in 4.6% of women undergoing appendectomy and stillbirth in 2.6%, compared with 1.2% for other surgical procedures (p < 0.001). Fetal loss in the presence of peritonitis was 10.9%, which suggests that the condition itself rather than the operation may lead to fetal harm.
There are a number of problems with the currently available evidence. It all dates back 20–40 years and is therefore unlikely to be representative of current outcomes given the improvements in anaesthetic drugs, surgical techniques and neonatal care. Furthermore, the Swedish data4,5 were collected with the aim of studying births and, therefore, patients who miscarry, the largest group of adverse birth outcomes, are unrecorded in these studies. The studies are also, in general, poorly controlled and have conflicting results regarding the risk of surgery. Duncan et al. 2 suggest that surgery is associated with an increased risk of fetal loss (including miscarriage), and the Swedish studies4,5 suggest that there is no increase in stillbirth but that there is an increase in prematurity and early neonatal death, particularly in the case of appendectomy. Furthermore, although it is clear from the data on appendectomy that the risk to the fetus when a pregnant woman undergoes surgery is not uniform, there have been few attempts to quantify the risk by other types of surgery.
Nonetheless, of the evidence that is available, none relates directly to NHS outcomes, and there is no current NHS policy regarding carrying out non-obstetric surgery in pregnant women.
The project had three main objectives:
-
to carry out a descriptive analysis of the data, describing counts of each adverse outcome by year, maternal age, procedure type, socioeconomic status and trimester of pregnancy
-
to calculate the absolute risk and the relative odds of each adverse outcome in those women who have undergone surgery compared with those who have not
-
to independently analyse broad groups, such as elective and emergency operations, as well as common procedures such as appendectomy, cholecystectomy, specific cancer surgeries and orthopaedic surgery.
Chapter 2 Methods
Hospital Episode Statistics database
Hospital Episode Statistics (HES) is an administrative database that includes records of all patient admissions and day cases in all English NHS hospital trusts (www.hscic.gov.uk/hes). In HES, each record contains data on patient demographics (e.g. age, ethnicity and socioeconomic deprivation based on postcode of residence), the episode of care (e.g. hospital name, date of admission and discharge) and clinical information. 7,8 Diagnoses for each patient are recorded using the International Classification of Diseases, Tenth Edition (ICD-10). Procedures performed during an episode are coded using the Office of Population, Censuses and Surveys’s Classification of Surgical Operations and Procedures (OPCS), version 4 (OPCS-4). In addition, each episode relating to the delivery of a baby contains details about the labour and delivery (e.g. parity, mode of delivery, gestational age, birthweight) in supplementary data fields known as the HES ‘maternity tail’.
In HES, each patient is assigned a unique identifier. This makes it possible to link historical medical records.
Each record represents the continuous period of time during which patient is under the care of a consultant and is called an ‘episode’. Episodes can be linked into admissions (also called a ‘spell’) to one hospital provider.
Selection of the cohort
We examined 10 years of HES maternity data from 2002–3 to 2011–12. Pregnancy records were defined as those that contained information about a delivery in either the OPCS procedure fields or the maternity tail9 (Table 1), or information about a spontaneous abortion in the ICD-10 diagnosis fields (Table 2).
| Code | OPCS-4 code | Delmeth code | Method of delivery description |
|---|---|---|---|
| 1 | R17 | 7 | Elective caesarean section |
| 2 | R18, R25.1 | 8 | Emergency caesarean section |
| 3 | R19, R20 | 5, 6 | Breech vaginal delivery |
| 4 | R21 | 2, 3 | Forceps delivery |
| 5 | R22 | 4 | Vacuum delivery |
| 6 | R23, R24 | 0, 1 | Cephalic vaginal delivery without instruments |
| 7 | R25.2 | 9 | Other methods of delivery, including destructive operation to facilitate delivery |
| 8 | R25.8, R25.9 | X | Unknown |
| Outcome | Definition |
|---|---|
| Spontaneous abortions associated with hospitalisation | Pregnancy episodes with an ICD-10 code for spontaneous abortion (O03, O05, O06) |
| Preterm delivery | Pregnancy episodes with an ICD-10 code for preterm delivery (O60) or using length-of-gestation field in the HES maternity tail |
| Maternal death | Method of discharge field (value: 4 = ‘died’) in delivery or spontaneous abortion admission |
| Caesarean section | Pregnancy episodes with an OPCS code or using delivery method field in the HES maternity tail (see Table 1) |
| Long inpatient stay (delivery admission only) | Upper quartile of length of stay plus 1.5 times the interquartile range (separate values for caesarean and vaginal delivery)10 |
| Stillbirth | ICD-10 code that identifies the outcome of delivery in the mother’s record (Z37.1, Z37.3, Z37.4, Z37.6, Z37.7) or using birth status field in the HES maternity tail. Values were recoded into three categories: one or more stillborn; all live; unknown |
| Low birthweight | Birthweight field in the HES maternity tail. Values were recoded into three categories: one or more newborn with low birthweight (< 2500 g); all newborns weighed > 2500 g; unknown |
Duplicate records were identified on the basis of the date of admission, the date on which the episode started, provider code, HES identification number and consultant code. 11,12 The resulting sample was restricted to women aged between 15 and 49 years. 11,13–15
Definition of outcomes and risk factors
In our original proposal we aimed to examine six outcomes: miscarriage, stillbirth, preterm labour, low birthweight, prolonged length of neonatal stay and neonatal death prior to discharge from hospital. Following receipt of data, it became clear that the linkage process on which the maternity tails were derived did not allow prolonged length of neonatal stay and neonatal death prior to discharge from hospital to be determined. We therefore substituted three new outcomes related to delivery: caesarean section, maternal death in hospital and a long inpatient stay (maternal). Our final list of adverse outcomes, based on mothers’ records, was spontaneous abortion (associated with hospitalisation), preterm delivery, caesarean section, maternal death and long maternal inpatient stays. Our adverse outcomes based on infants’ records were low birthweight and stillbirth. The definitions of these outcomes are listed in Table 2.
Adjustment for potential confounders is important to account for any differences between those women who received non-obstetric surgery during pregnancy and those who did not. We examined risk factors identified from previous research literature16–23 and these are defined in Table 3.
| Risk factors | Definition |
|---|---|
| Maternal age | Age at start of delivery admission field in HES. Values were recoded into six categories: 15–19 years, 20–24 years, 25–29 years, 30–34 years, 35–39 years and ≥ 40 years |
| Multiple pregnancy | ICD-10 code in any diagnosis field (O30) derived from delivery or spontaneous abortion admission |
| Parity | Number of previous pregnancies ‘numpreg’ field in the HES maternity tail; however, where this value was missing, we identified previous pregnancies by linking historical health records using the woman’s HES identification number back to 1997. Values were recoded into two categories: primiparous and multiparous |
| Previous emergency admission (year prior to pregnancy) | Method of admission field in HES (value: 21–28) from admission records in the previous year |
| Socioeconomic deprivation | Carstairs deprivation quintile24 based on postcode from delivery or spontaneous abortion admission |
| Comorbidities | Charlson Comorbidity Index score25 derived from secondary diagnosis fields in delivery or spontaneous abortion admission |
| Comorbidities (prior to pregnancy) | Charlson Comorbidity Index score25 (from admissions within 3 years prior to pregnancy) |
| Gestational diabetes | ICD-10 code in any diagnosis field (from delivery or spontaneous abortion admission): O24 – diabetes mellitus in pregnancy |
| Hypertension/pre-eclampsia | ICD-10 code in any diagnosis field (from delivery or spontaneous abortion admission):
|
| Cardiac diseases | ICD-10 code in any diagnosis field (from delivery or spontaneous abortion admission):
|
| Operations on amniotic cavity | OPCS code in any procedure field (R10) from admissions within pregnancy |
| Obstetric surgery | OPSC code in any diagnosis field (from admissions within pregnancy):
|
| Previous caesarean section | Previous pregnancy episodes with an OPCS code or using the delivery method field in the HES maternity tail (from 1997–8 to 2011–12) (see Table 1) |
| Non-obstetric surgery | An operating theatre procedure based on OPCS procedure field defined in previous research.26 From the list we excluded obstetric and male-associated procedures. Furthermore, after discussion with clinicians, two OPCS codes were excluded (K66.1 – cardiotachyography, S06 – other excision of skin) |
Risk factors such as maternal age, multiple pregnancy, socioeconomic deprivation, gestational diabetes, comorbidities, hypertension/pre-eclampsia and cardiac diseases were identified using information recorded within the hospital episode relating to the delivery or spontaneous abortion. Operations on the amniotic cavity and obstetric surgery were included in the analyses if they occurred during pregnancy (not during delivery or spontaneous abortion admission). Comorbidities (prior to pregnancy) were identified using women’s historical admission records for 3 years prior to pregnancy. The list of non-obstetric procedures, based on operating theatre procedures defined in previous research,26 was derived from the OPCS procedure fields. A non-obstetric procedure was included in the analysis if it occurred during pregnancy.
We estimated the beginning of pregnancy as:
-
for delivery: admission day minus gestational age (if available) or admission day minus 36 weeks (if gestational age not available, but diagnosis field indicates preterm delivery) or admission day minus 40 weeks (otherwise)
-
for spontaneous abortions: 3 months prior to admission day.
We assumed that the procedure was related to cancer or acute appendicitis if the ICD-10 code in any diagnosis field in the procedure admission was C00–C97 or K35, respectively.
From this point onwards, when we describe pregnancies in which surgery was or was not carried out we are referring specifically to non-obstetric surgery.
Statistical methods
We carried out a descriptive analysis of the data, describing total number and rates of risk factors, outcomes and missing data, and counts of each adverse outcome by year. We described counts of outcomes by common surgery groups and trimester of surgery.
We calculated the crude risk, odds ratio (OR), relative risk (RR), attributable risk, numbers needed to harm (NNHs) and associated 95% confidence intervals (CIs) of adverse birth outcomes in pregnancies in which surgery was carried out compared with pregnancies in which surgery was not carried out. 27 All pregnancy records were included in the analysis when spontaneous abortion associated with hospitalisation and maternal death were the outcomes of interest. For the remaining outcomes, only pregnancy records that ended in delivery were included. In addition, we made some comparisons of risk between surgical groups. We independently analysed broad groups of procedure (see detailed definition of groups in Appendix 1) and estimated RR and associated 95% CIs, attributable risk and NNHs of adverse birth outcome in pregnancies where surgery occurred compared with pregnancies where surgery did not occur. We also repeated these analyses by trimester of procedure.
We calculated adjusted ORs, RR and attributable risk using two approaches:
-
We calculated the adjusted RR using a simple relationship:28
where P0 denotes the proportion of untreated subjects who experience the outcome of interest and ORadj denotes the OR obtained from a logistic regression model. The 95% CIs for the RR were estimated by substituting the upper and lower CIs for the OR from the multivariate logistic regression model. 29 It is a simple method that approximates a risk ratio from the adjusted OR and derives an estimate of an association or treatment effect that better represents the true RR. We used backwards elimination regression, and only explanatory variables with a p-value < 0.05 were considered significant. The overall model evaluation was presented by the Akaike information criterion, the R2 and c-statistic.
-
We calculated the adjusted RR, attributable risk and NNH using Austin’s method. 30 We assumed that a dichotomous outcome variable Y is observed for each subject (with Y = 1 denoting success and Y = 0 denoting failure). Furthermore, let Ti denote treatment status of the ith subject (with T = 1 denoting treatment and T = 0 denoting no treatment), whereas X1i, X2i . . . Xki denotes the value of k confounding variables. The following logistic regression model relates the odds of the outcome to treatment status and baseline confounding variables:
where β denotes the log-OR and eβ denotes the OR. Using this formula, one can determine the probability of the outcome if a given subject were treated and the same subject were untreated. The probability of the outcome if a subject were treated is:
If a subject were not treated, then the probability of the outcome is:
The mean probability (p¯T=1) of success in the cohort if all patients were treated and the mean probability (p¯T=0) of success in the cohort if all patients were untreated is then calculated. These are also referred to as the marginal probabilities of success for treated and untreated subjects. The risk difference and the RR can be estimated as p¯T=0−p¯T=1 and p¯T=1/p¯T=0, respectively. The NNH is defined as the inverse of the risk difference. 31,32
The CIs for each measure of effect were estimated using a non-parametric bootstrap method. 33 A bootstrap sample is a random sample drawn with replacement from the original sample such that the random sample has the same size as the original sample. We created 1000 bootstrap samples and estimated the quantity of interest in each of them. The end points of the non-parametric 95% CIs would be the 2.5th and 97.5th percentiles of that quantity across the bootstrap samples. This method allows for comparison of outcomes between two populations whose only difference was the exposure (non-obstetric surgery during pregnancy). It permits an estimate of the adjusted attributable risk and NNH.
We carried out two-level logistic regression to investigate the effects of hospitals on the adverse birth outcome. 34 To test for significant differences between proportions we used chi-squared tests. Data were analysed using the SAS 9.2 software package (SAS Institute, Cary, NC, USA).
Missing data and sensitivity analysis
Our analysis assumed a live birth where the birth status in the maternity tail was unknown and there was no Z37 diagnosis code to indicate a stillbirth. We assumed a weight of > 2500 g if the birthweight was not recorded. Furthermore, we assumed that pregnancy was full term (40 weeks) where the gestational age in the maternity tail was unknown and there was no O60 diagnosis code to indicate preterm delivery. In a sensitivity analysis, we excluded all records with missing data in these fields and recalculated the adjusted RR, attributable risk and NNH. We also examined the effect of excluding gestational diabetes, obstetric surgery and operations on the amniotic cavity from the risk adjustment model for spontaneous abortion (associated with hospitalisation).
Chapter 3 Results
The following section provides the descriptive characteristics for the study sample. The unadjusted risks are then reported. Finally, we present the adjusted risk of each adverse outcome in pregnancies in which surgery was carried out compared with pregnancies in which no surgery was carried out, together with the attributable risk and the NNH.
Descriptive analysis
We identified 6,486,280 pregnancies in the period April 2002 to March 2012. Two-thirds of the study population were aged between 20 and 34 years (73.4%) and the majority were multiparous (55.5%) (Table 4). Twenty-seven per cent of women were living in the most socioeconomically deprived area based on the Carstairs measure of socioeconomic deprivation quintile. More than 10% of our population had an emergency admission to hospital a year prior to pregnancy and nearly 10% had previously had a caesarean delivery. Table 4 also includes information about maternal complications such as gestational diabetes (1.5%), hypertension/pre-eclampsia (3.4%) and cardiac disease (0.3%).
| Risk factor | Frequency (%) | ||
|---|---|---|---|
| Total pregnancies | Pregnancies in which surgery was not carried out | Pregnancies in which surgery was carried out | |
| Total number of pregnancies | 6,486,280 (100) | 6,438,652 (100) | 47,628 (100) |
| Maternal age (years)* | |||
| 15–19 | 423,482 (6.5) | 420,045 (6.5) | 3437 (7.2) |
| 20–24 | 1,228,398 (18.9) | 1,217,961 (18.9) | 10,437 (21.9) |
| 25–29 | 1,702,845 (26.3) | 1,690,140 (26.3) | 12,705 (26.7) |
| 30–34 | 1,830,026 (28.2) | 1,817,982 (28.2) | 12,044 (25.3) |
| 35–39 | 1,049,786 (16.2) | 1,042,638 (16.2) | 7148 (15.0) |
| ≥ 40 | 251,743 (3.9) | 249,886 (3.9) | 1857 (3.9) |
| Multiple pregnancy** (yes) | 70,758 (1.1) | 70,198 (1.1) | 560 (1.2) |
| Parity* | |||
| Primiparous | 2,888,248 (44.5) | 2,867,468 (44.5) | 20,780 (43.6) |
| Multiparous | 3,598,032 (55.5) | 3,571,184 (55.5) | 26,848 (56.4) |
| Previous emergency admission* | 672,946 (10.4) | 664,019 (10.3) | 8927 (18.7) |
| Carstairs deprivation quintile* | |||
| 1 = least deprived | 1,054,232 (16.3) | 1,047,238 (16.3) | 6994 (14.7) |
| 2 | 1,064,704 (16.4) | 1,057,376 (16.4) | 7328 (15.4) |
| 3 | 1,195,999 (18.4) | 1,187,080 (18.4) | 8919 (18.7) |
| 4 | 1,371,638 (21.2) | 1,360,905 (21.2) | 10,733 (22.5) |
| 5 = most deprived | 1,754,815 (27.0) | 1,741,297 (27.0) | 13,518 (28.4) |
| 6 = unknown | 44,892 (0.7) | 44,756 (0.7) | 136 (0.3) |
| Charlson Comorbidities Index score* | |||
| 0 | 6,254,984 (96.4) | 6,210,332 (96.4) | 44,652 (96.8) |
| 1+ | 231,296 (3.6) | 228,320 (3.6) | 2976 (3.2) |
| Charlson Comorbidities Index score* (prior pregnancy) | |||
| 0 | 6,375,029 (98.3) | 6,329,356 (98.3) | 45,673 (95.9) |
| 1+ | 111,251 (1.7) | 109,296 (1.7) | 1955 (4.1) |
| Gestational diabetes* (yes) | 98,196 (1.5) | 97,179 (1.5) | 1017 (2.1) |
| Hypertension/pre-eclampsia* (yes) | 222,312 (3.4) | 220,481 (3.4) | 1831 (3.8) |
| Cardiac diseases* (yes) | 16,951 (0.3) | 16,626 (0.3) | 325 (0.7) |
| Other operations on amniotic cavity* (yes) | 32,491 (0.5) | 32,214 (0.5) | 277 (0.6) |
| Obstetric surgery* (yes) | 327,050 (5.0) | 325,036 (5.1) | 2014 (4.2) |
| Previous caesarean deliveries* (yes) | 640,405 (9.8) | 635,174 (9.8) | 5231 (11.0) |
| Non-obstetric surgery | 47,628 (0.7) | 0 | 47,628 (100) |
Spontaneous abortions associated with hospitalisation accounted for 5.8% of all pregnancies (Table 5). The numbers of maternal deaths following spontaneous abortion associated with hospitalisation or delivery were very small; only 235 cases were identified, and this corresponds to a maternal death rate of 4 per 100,000 pregnancies. Among our cohort there were more than 450,000 (7.5%) preterm deliveries and nearly 1.5 million (23.9%) elective or emergency caesarean deliveries.
| Outcome | Frequency (%) | ||
|---|---|---|---|
| Total pregnancies | Pregnancies in which surgery was not carried out | Pregnancies in which surgery was carried out | |
| Total number of pregnancies | 6,486,280 (100) | 6,438,652 (100) | 47,628 (100) |
| Spontaneous abortion associated with hospitalisation | 376,323 (5.8) | 373,203 (5.8) | 3120 (6.6) |
| Preterm delivery | 457,793 (7.5) | 452,877 (7.5) | 4916 (11.1) |
| Preterm delivery by weeks | |||
| 22–27 | 37,968 (8.3) | 37,630 (8.3) | 338 (6.9) |
| 28–33 | 87,557 (19.1) | 86,509 (19.1) | 1048 (21.3) |
| 34–37 | 190,703 (41.7) | 188,707 (41.7) | 1996 (40.6) |
| Unknown | 141,565 (30.9) | 140,031 (30.9) | 1534 (31.2) |
| Maternal death | 235 (0.004) | 223 (0.003) | 12 (0.025) |
| Caesarean section | 1,461,707 (23.9) | 1,448,871 (23.9) | 12,836 (28.8) |
| Long inpatient stay | 578,709 (9.5) | 573,471 (9.5) | 5238 (11.8) |
| Stillbirth | |||
| One or more stillborn | 33,774 (0.6) | 33,363 (0.6) | 411 (0.9) |
| All live | 5,996,017 (98.1) | 5,952,658 (98.1) | 43,359 (97.4) |
| Unknown | 80,166 (1.3) | 79,428 (1.3) | 738 (1.7) |
| Low birthweight | |||
| ≥ 1 child with a low birthweight | 342,631 (5.6) | 338,800 (5.6) | 3831 (8.6) |
| All newborns weighing > 2500 g | 4,499,574 (73.6) | 4,468,782 (73.7) | 30,792 (69.2) |
| Unknown | 1,267,752 (20.8) | 125,7867 (20.7) | 9885 (22.2) |
Table 6 presents total number and rates of missing records for gestational age, socioeconomic deprivation, birth status and birthweight. In nearly 40% of all pregnancies, no information about gestational age was available. Less than 1% of records included no information about socioeconomic deprivation.
| Outcome | Frequency (%) | ||
|---|---|---|---|
| Total pregnancies | Pregnancies in which surgery was not carried out | Pregnancies in which surgery was carried out | |
| Gestational age | 2,550,455 (39.3) | 2,530,344 (39.3) | 20,111 (42.2) |
| Socioeconomic deprivation | 44,892 (0.7) | 44,756 (0.7) | 136 (0.3) |
| Birth status | 80,166 (1.3) | 79,428 (1.3) | 738 (1.7) |
| Birthweight | 1,267,752 (20.8) | 125,7867 (20.7) | 9885 (22.2) |
We identified 47,628 pregnancies in which surgery had been carried out at some time (0.7%). Of these surgeries, 25,445 (53.4%) were elective procedures and 22,183 (46.6%) were non-elective. The most common type of surgical procedure was abdominal (12,493, 26.2%), followed by dental (5365, 11.3%), nail and skin (4762, 10.0%), musculoskeletal (4563, 9.6%), ear, nose and throat (ENT) (3060, 6.4%) and perianal (2977, 6.2%) (Table 7). There were 3062 cases of appendectomy and 1306 cases of cholecystectomy. The most frequent procedures were diagnostic endoscopic examination of the peritoneum (5518), drainage of a lesion of the skin (1662) and emergency excision of an abnormal appendix (1448) (Table 8).
| Outcome | Common operation group (%) | |||||||
|---|---|---|---|---|---|---|---|---|
| Abdominal | Breast | Dental | ENT | Nail and skin | Perianal | Musculoskeletal | Other | |
| Number of procedures (%) | 12,493 (26.2) | 1884 (4.0) | 5365 (11.3) | 3060 (6.4) | 4762 (10.0) | 2977 (6.2) | 4563 (9.6) | 12,524 (26.3) |
| Spontaneous abortion associated with hospitalisation | 46.8 | 2.9 | 10.8 | 7.0 | 5.6 | 3.4 | 8.5 | 15.0 |
| Preterm delivery | 27.4 | 5.2 | 8.9 | 5.4 | 8.9 | 3.9 | 7.8 | 32.5 |
| Caesarean section | 25.4 | 4.0 | 9.3 | 5.3 | 9.2 | 6.4 | 9.0 | 31.4 |
| Long inpatient stay | 26.5 | 3.7 | 9.7 | 6.1 | 9.8 | 6.0 | 9.1 | 29.1 |
| Stillbirth | 28.0 | 2.9 | 11.0 | 6.6 | 8.8 | 2.4 | 8.5 | 31.8 |
| Low birthweight | 26.5 | 4.9 | 10.0 | 6.2 | 9.0 | 4.2 | 8.5 | 30.7 |
| OPCS-4 code | Description | n (%) |
|---|---|---|
| Abdominal | ||
| T43.9 | Diagnostic endoscopic examination of peritoneum, unspecified | 5518 (44.2) |
| H01.2 | Emergency excision of abnormal appendix NEC | 1448 (11.6) |
| J18.3 | Total cholecystectomy NEC | 1091 (8.7) |
| Breast | ||
| B28.3 | Excision of lesion of breast | 663 (35.2) |
| B33.1 | Drainage of lesion of breast | 220 (11.7) |
| B35.3 | Extirpation of lesion of nipple | 148 (7.9) |
| Dental | ||
| F09.1 | Surgical removal of impacted wisdom tooth | 1344 (25.1) |
| F09.3 | Surgical removal of wisdom tooth NEC | 1329 (24.8) |
| F10.4 | Extraction of multiple teeth NEC | 594 (11.1) |
| ENT | ||
| F34.1 | Bilateral dissection tonsillectomy | 637 (20.8) |
| E03.6 | Septoplasty of nose NEC | 167 (5.5) |
| D02.1 | Excision of lesion of external ear | 177 (5.8) |
| Nail and skin | ||
| S47.2 | Drainage of lesion of skin NEC | 1662 (34.9) |
| S42.1 | Primary suture of skin NEC | 276 (5.8) |
| F02.1 | Excision of lesion of lip | 230 (4.8) |
| Perianal | ||
| H60.3 | Drainage of pilonidal sinus | 1062 (35.7) |
| H58.2 | Drainage of perianal abscess | 707 (23.7) |
| H52.4 | Rubber band ligation of haemorrhoid | 138 (4.6) |
| Musculoskeletal | ||
| A65.1 | Carpal tunnel release | 769 (16.9) |
| T67.6 | Primary simple repair of tendon | 338 (7.4) |
| A64.2 | Primary repair of peripheral nerve NEC | 207 (4.5) |
The proportions of common procedure groups for different outcomes were similar to the overall proportions, except for abdominal procedures and spontaneous abortion associated with hospitalisation (see Table 7).
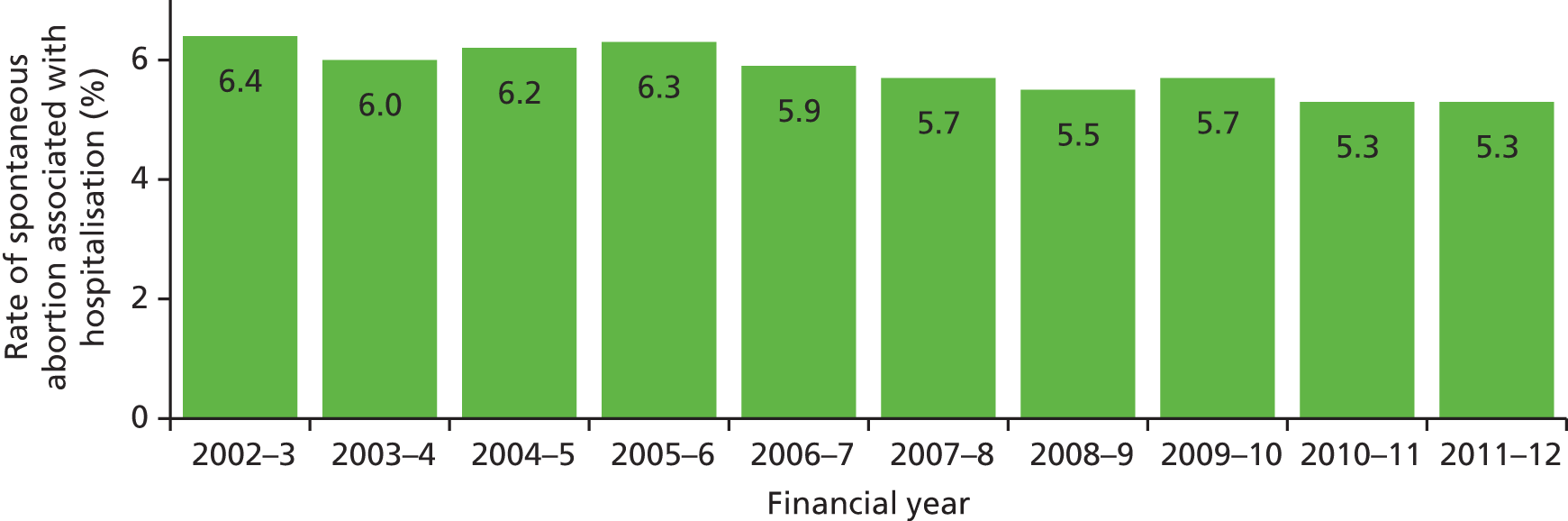
Spontaneous abortion associated with hospitalisation
Among our cohort, we identified 376,323 (5.8%) spontaneous abortions associated with hospitalisation, 3120 of which occurred in women who had undergone surgery during their pregnancy. The percentage of spontaneous abortions associated with hospitalisation has decreased from 6.4% to 5.3% since 2002–3 (Figure 1).
FIGURE 1.
Rate of spontaneous abortion associated with hospitalisation per year in England.
Preterm delivery
Of the 457,793 (7.5%) preterm deliveries between 2002–3 and 2011–12 in England, 1.1% were to women who had undergone surgery during pregnancy. The percentage of all deliveries that occurred preterm increased from 6.7% in 2002–4 to 8.0% in 2011–12 (Figure 2).
FIGURE 2.
Rate of preterm delivery per year in England.

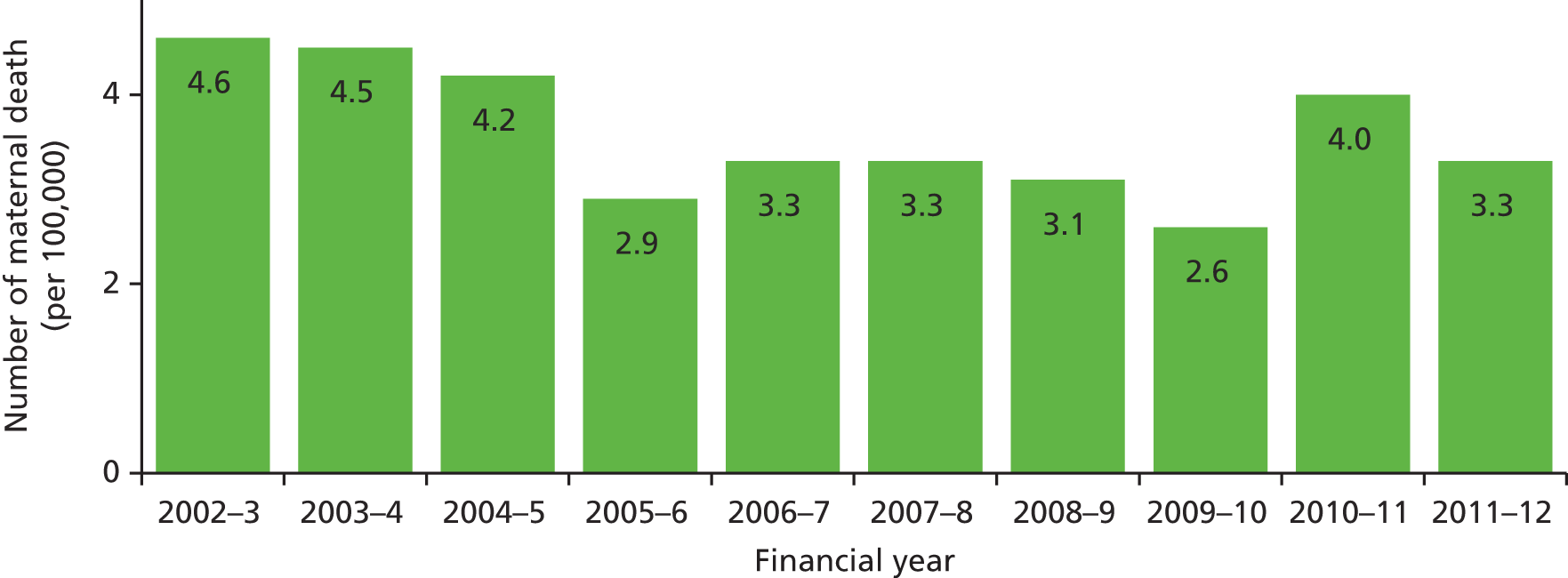
Maternal death
The number of maternal deaths following delivery (or spontaneous abortion associated with hospitalisation) was small. Only 235 cases were identified, and this corresponded to a maternal death rate of 4 per 100,000 pregnancies (Figure 3). Moreover, only 12 of these women had undergone surgery during pregnancy.
FIGURE 3.
Number of maternal deaths per 100,000 pregnancies per year in England.
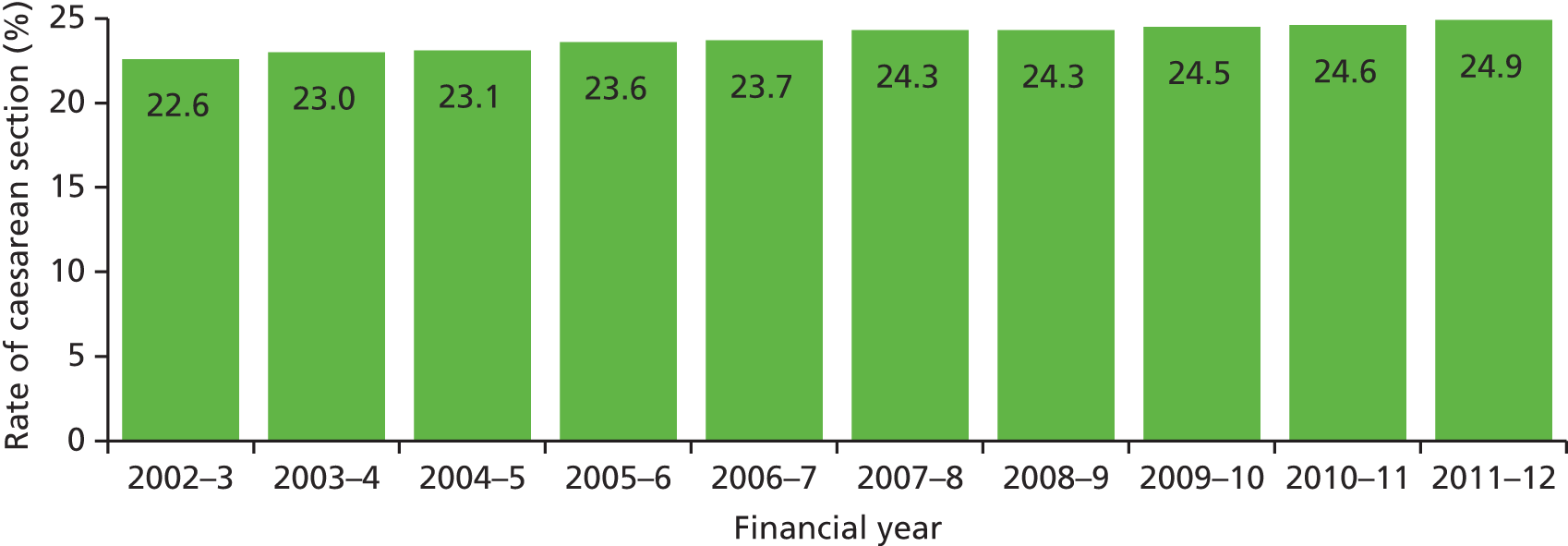
Caesarean section
We identified 1,461,707 (23.9%) pregnancies resulting in delivery by caesarean section over the 10-year period of the study; 12,836 of these caesarean sections were carried out in women who had undergone surgery during that pregnancy. Figure 4 shows that the proportion of caesarean deliveries slightly increased from 22.6% (in 2002–3) to 24.9% (in 2011–12).
FIGURE 4.
Rate of caesarean section per year in England.
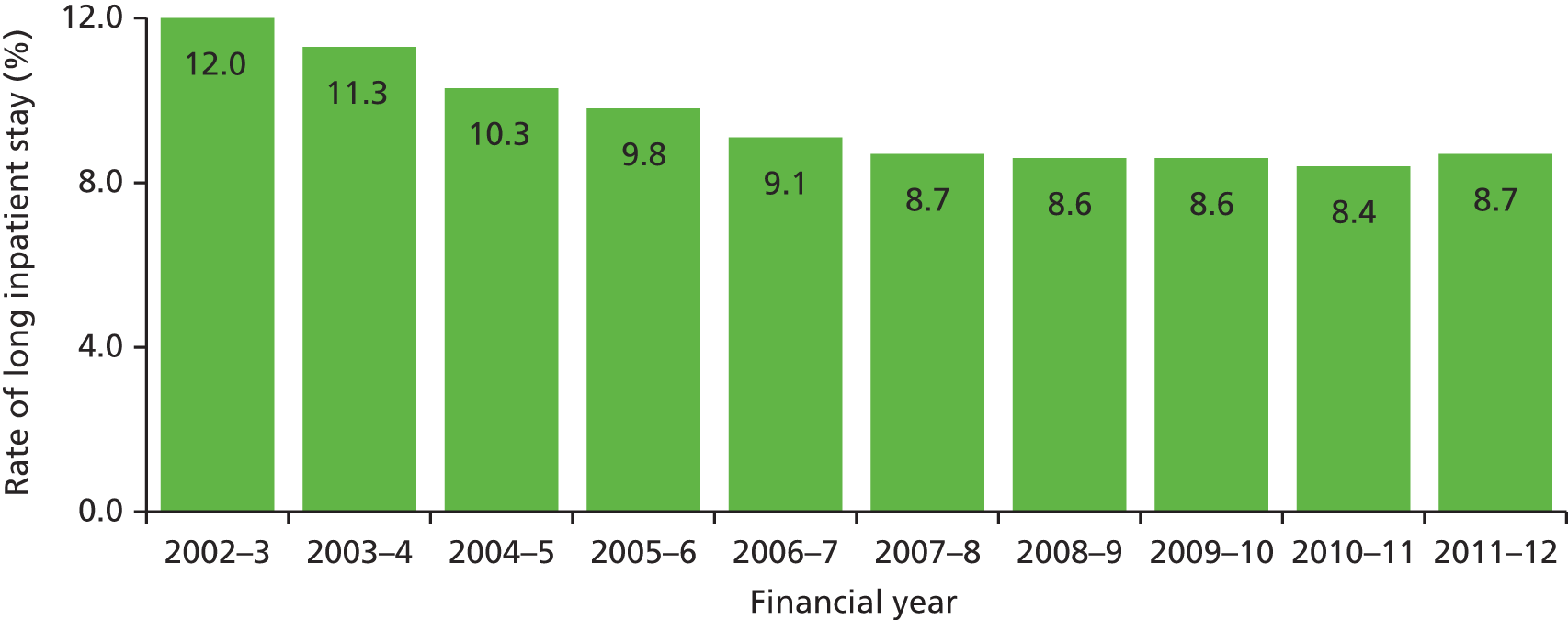
Long inpatient stay
A long inpatient stay for a delivery episode was defined as the upper quartile of length of stay plus 1.5 times the interquartile range (10 days or longer for a caesarean delivery, 4 days or longer for a vaginal delivery). Figure 5 represents the trends in long inpatient stays from 2002–3 to 2011–12.
FIGURE 5.
Rate of long inpatient stay per year in England.
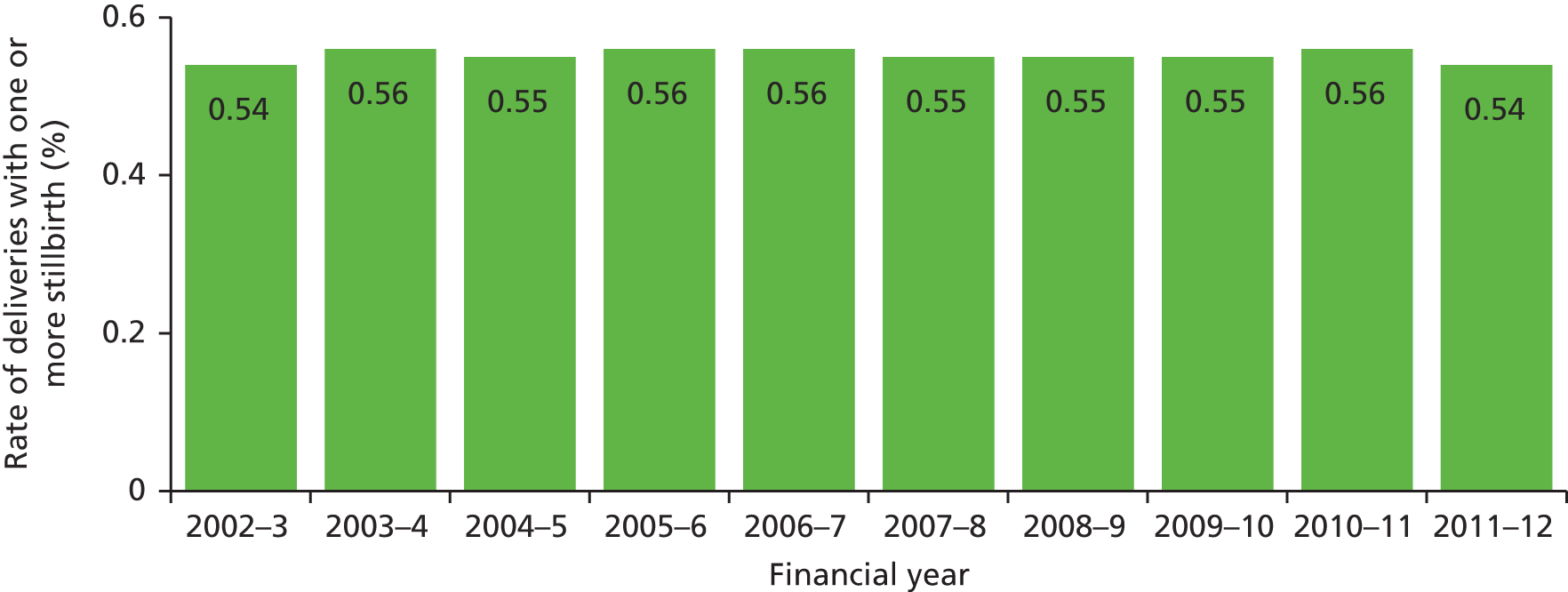
Stillbirth
Over the past 10 years, the stillbirth rate has remained relatively stable, at 0.54% (Figure 6). In our study population, 33,774 pregnancies resulted in stillbirth, of which only 411 occurred in women who had undergone surgery during their pregnancy. Not all records contained information about stillbirth; however, the percentage of missing data decreased from 2.8% in 2002–3 to 0.15% in 2011–12.
FIGURE 6.
Proportion of deliveries resulting in one or more stillborn child per year in England.
Low birthweight
A total of 342,631 (5.6%) pregnancies between 2002–3 and 2011–12 in England resulted in the delivery of one or more low-birthweight newborns, of which 3846 were to women in whom surgery had been performed. There was little change in the proportion of low-birthweight deliveries over the 10-year period (Figure 7). A notable decrease in 2007–8 can be explained by a high percentage of missing birthweight fields for that year. The proportion of birthweight values that are missing has fallen greatly over the period: from 26.0% (in 2002–3) to 10.0% (in 2011–12).
FIGURE 7.
Proportion of deliveries resulting in one or more low-birthweight newborns per year in England.

Unadjusted analyses
Table 9 gives the crude risk for each outcome by risk factor. Almost 6% of all pregnancies resulted in spontaneous abortion associated with hospitalisation. A higher risk was estimated for women aged > 40 years (14.5%) or women who had cardiac disease (11.4%). The risk of spontaneous abortion associated with hospitalisation was higher if surgery was carried out during pregnancy (6.6%). The risk of a spontaneous abortion associated with hospitalisation in pregnancies in which surgery occurred was 13% higher than in pregnancies in which surgery did not occur (RR 1.13, 95% CI 1.09 to 1.17).
| Risk factor | Spontaneous abortion associated with hospitalisation (%) | Preterm delivery (%) | Caesarean section (%) | Long inpatient stay (%) | Stillbirth (%) | Low birthweight (%) |
|---|---|---|---|---|---|---|
| Crude risk | 5.8 | 7.5 | 23.9 | 9.5 | 0.6 | 5.6 |
| Maternal age (years) | ||||||
| 15–19 | 7.2 | 8.2 | 13.4 | 11.5 | 0.6 | 6.8 |
| 20–24 | 5.2 | 7.5 | 17.1 | 9.6 | 0.5 | 6.1 |
| 25–29 | 4.7 | 7.3 | 21.7 | 9.5 | 0.5 | 5.4 |
| 30–34 | 4.9 | 7.1 | 26.7 | 9.3 | 0.5 | 5.1 |
| 35–39 | 7.1 | 7.8 | 32.0 | 8.9 | 0.6 | 5.6 |
| ≥ 40 | 14.5 | 9.1 | 38.4 | 9.4 | 0.9 | 6.7 |
| Multiple pregnancy | ||||||
| Yes | 1.8 | 49.9 | 64.7 | 17.9 | 2.6 | 51.8 |
| No | 5.9 | 7.0 | 23.5 | 89.3 | 0.5 | 5.1 |
| Parity | ||||||
| Primiparous | 7.4 | 7.6 | 25.0 | 12.8 | 0.6 | 5.9 |
| Multiparous | 4.5 | 7.5 | 23.1 | 6.9 | 0.5 | 5.4 |
| Previous emergency admission | ||||||
| Yes | 6.7 | 9.0 | 69.7 | 10.8 | 0.6 | 6.9 |
| No | 5.7 | 7.3 | 19.0 | 9.3 | 0.6 | 5.5 |
| Carstairs deprivation quintile | ||||||
| 1 | 5.1 | 6.3 | 26.3 | 8.9 | 0.4 | 4.2 |
| 2 | 5.3 | 6.6 | 25.4 | 9.1 | 0.5 | 4.6 |
| 3 | 5.6 | 7.0 | 24.5 | 9.3 | 0.5 | 5.0 |
| 4 | 5.8 | 7.8 | 23.1 | 9.5 | 0.6 | 5.8 |
| 5 | 6.3 | 8.8 | 21.7 | 10.1 | 0.7 | 7.3 |
| Unknown | 23.9 | 11.4 | 28.1 | 10.7 | 1.3 | 7.5 |
| Charlson Comorbidities Index score | ||||||
| 0 | 5.8 | 7.5 | 23.8 | 9.4 | 0.5 | 6.9 |
| 1+ | 6.0 | 8.6 | 28.5 | 10.6 | 0.6 | 5.6 |
| Charlson Comorbidities Index score (prior pregnancy) | ||||||
| 0 | 5.8 | 7.4 | 23.8 | 9.4 | 0.7 | 8.3 |
| 1+ | 7.1 | 11.8 | 30.0 | 11.4 | 0.6 | 5.6 |
| Gestational diabetes | ||||||
| Yes | 0.6 | 16.6 | 54.4 | 19.7 | 1.0 | 7.9 |
| No | 5.9 | 7.4 | 23.4 | 9.4 | 0.6 | 5.6 |
| Hypertension/pre-eclampsia | ||||||
| Yes | 0.1 | 13.2 | 41.2 | 19.3 | 1.1 | 11.9 |
| No | 6.0 | 7.3 | 23.3 | 9.1 | 0.5 | 5.4 |
| Cardiac diseases | ||||||
| Yes | 11.4 | 11.6 | 36.6 | 13.4 | 0.8 | 9.0 |
| No | 5.8 | 7.5 | 23.9 | 9.5 | 0.6 | 5.6 |
| Operations on amniotic cavity | ||||||
| Yes | 1.2 | 12.2 | 30.9 | 10.8 | 3.1 | 10.9 |
| No | 5.8 | 7.5 | 23.9 | 9.5 | 0.5 | 5.6 |
| Obstetric surgery | ||||||
| Yes | 0.4 | 6.3 | 6.2 | 13.0 | 0.4 | 4.2 |
| No | 6.1 | 7.6 | 24.9 | 9.3 | 0.6 | 5.7 |
| Previous caesarean section | ||||||
| Yes | 6.6 | 9.1 | 69.7 | 3.4 | 0.6 | 6.1 |
| No | 5.7 | 7.3 | 18.9 | 10.1 | 0.6 | 5.6 |
| Non-obstetric surgery | ||||||
| Yes | 6.6 | 11.1 | 28.8 | 11.8 | 0.9 | 8.6 |
| No | 5.8 | 7.5 | 23.9 | 9.5 | 0.6 | 5.6 |
| Crude RR (95% CI) | 1.13 (1.09 to 1.17) | 1.48 (1.44 to 1.52) | 1.21 (1.19 to 1.23) | 1.24 (1.21 to 1.28) | 1.68 (1.53 to 1.86) | 1.57 (1.52 to 1.62) |
A little over 6 million deliveries took place in NHS hospitals in England between 2002–3 and 2011–12, 7.5% of which were preterm. In approximately half of pregnancies with multiple gestations (i.e. more than one baby), delivery occurred preterm. Women with gestational diabetes, hypertension/pre-eclampsia or cardiac diseases were at higher risk of a preterm delivery. Pregnancies in which surgery occurred had a 48% higher risk of a preterm delivery (RR 1.48, 95% CI 1.44 to 1.52) than in pregnancies in which surgery did not occur.
Nearly 24% of all deliveries were by caesarean section. Previous caesarean delivery was associated with a higher risk of caesarean section. Moreover, two-thirds of women (69.7%) who had an emergency admission in the year prior to their pregnancy had a caesarean delivery. Furthermore, women who had gestational diabetes during pregnancy, or hypertension/pre-eclampsia, had a higher risk of caesarean delivery. Women had a 21% higher risk of a caesarean delivery (RR 1.21, 95% CI 1.19 to 1.23) if they had undergone surgery during their pregnancy.
Nearly 10% of women had a long hospital stay following delivery, and the risk was higher for women with gestational diabetes, hypertension/pre-eclampsia or cardiac diseases (19.7%, 19.3% and 13.4%, respectively). The risk of a long inpatient stay was similar in women who underwent obstetric or non-obstetric surgery (13.0% and 11.8%, respectively). Women had a 24% higher risk of a caesarean delivery (RR 1.24, 95% CI 1.21 to 1.28) if they had undergone non-obstetric surgery during their pregnancy.
The percentage of deliveries ending in a stillbirth was 0.6%. Multiple pregnancy and surgery on the amniotic cavity were associated with a higher risk of stillbirth. The risk of stillbirth was 68% higher if the woman had undergone surgery during pregnancy than if she had not (RR 1.68, 95% CI 1.53 to 1.86).
The percentage of women who gave birth to one or more low-birthweight babies was 5.6%. Moreover, among women with multiple pregnancy the risk of low-birthweight babies was much higher (51.8%). The risk of delivering a baby with a low birthweight was 57% higher for women who underwent a procedure during pregnancy than for those who did not (RR 1.57, 95% CI 1.52 to 1.62).
Tables 10 and 11 present information about the timing of surgery. In almost half of cases (42.0%), information about when in pregnancy the procedure was carried out (i.e. gestational age) was not provided. Only 4% of surgeries and 0.2% of elective operations occurred during the same admission as the delivery or spontaneous abortion (associated with hospitalisation). Of the surgeries carried during pregnancy for which gestational age was recorded, 45% were carried out in the first trimester, 26% in the second trimester and 29% in the third trimester.
| Outcome | First trimester | Second trimester | Third trimester | Trimester unknown | Same admission |
|---|---|---|---|---|---|
| Number of surgical operations (%) | 12,544 (26.3) | 7160 (15.0) | 7942 (16.7) | 19,982 (42.0) | 1696 (3.6) |
| Planned surgery | 8185 | 3273 | 2806 | 11,181 | 49 |
| Spontaneous abortion associated with hospitalisation | – | – | – | 3120 | 56 |
| Preterm delivery | 1483 | 873 | 1133 | 1427 | 396 |
| Maternal death | 1 | 1 | 1 | 9 | 6 |
| Caesarean section | 3338 | 1975 | 2628 | 4895 | 893 |
| Long inpatient stay | 1402 | 829 | 973 | 2034 | 190 |
| Stillbirth | 85 | 59 | 70 | 197 | 62 |
| Low birthweight | 1322 | 769 | 948 | 792 | 280 |
| Time period | All (%) | Abdominal (%) | Abdominal laparoscopic (%) | Abdominal open (%) | Appendectomy (%) |
|---|---|---|---|---|---|
| Deliveries | |||||
| 24 hours | 1872 (4.2) | 462 (4.2) | 53 (0.7) | 409 (10.3) | 51 (1.7) |
| 48 hours | 1913 (4.3) | 463 (4.2) | 54 (0.8) | 409 (10.3) | 51 (1.7) |
| 1 week | 2407 (5.4) | 484 (4.4) | 59 (0.8) | 425 (10.7) | 61 (2.1) |
| Total | 44508 | 11041 | 7073 | 3968 | 2925 |
| Spontaneous abortion | |||||
| 24 hours | 65 (2.1) | 27 (1.9) | 15 (1.2) | 12 (7.6) | 3 (2.2) |
| 48 hours | 85 (2.7) | 38 (2.6) | 26 (2.0) | 12 (7.6) | 3 (2.2) |
| 1 week | 340 (10.9) | 231 (15.9) | 209 (16.1) | 22 (14.0) | 11 (8.0) |
| Total | 3120 | 1452 | 1295 | 157 | 137 |
A closer examination of timing between delivery (or spontaneous abortion associated with hospitalisation) and surgery suggests that < 6% of operations occurred within 1 week of the end of the pregnancy. In the case of pregnancies ending in spontaneous abortion associated with hospitalisation, 11% of operations occurred during the week prior to the abortion. Among women who underwent abdominal surgery and whose pregnancy ended in spontaneous abortion associated with hospitalisation, 16% of procedures occurred in the week prior to the abortion (see Table 11).
Table 12 shows the numbers of adverse birth outcomes in pregnant women undergoing laparoscopic and open abdominal surgeries. Approximately two-thirds of all abdominal operations were laparoscopic. Where gestational age was known, the number of abdominal operations in the first trimester that were laparoscopic was nearly five times (3102) the number of open procedures (643). This ratio was reversed in the second trimester (606 laparoscopic vs. 995 open), and by the third trimester 2.5 times as many procedures were open (698) as were laparoscopic (284).
| Outcome | Abdominal laparoscopic | Abdominal open |
|---|---|---|
| Total | 8368 | 4125 |
| Spontaneous abortion | 1295 | 157 |
| Preterm delivery | 1421 | 683 |
| Caesarean section | 3243 | 1469 |
| Long inpatient stay | 1580 | 667 |
| Maternal death | 0 | 2 |
| Stillbirth | 75 | 41 |
| Low birthweight | 754 | 1106 |
Regression analysis
We used a logistic regression model to determine the relationship of surgery with adverse birth outcomes, while adjusting for other risk factors. Tables 13–20 give the ORs and total numbers of cases (n) of the final model for each outcome of interest. The choices of explanatory variables were constrained by previous studies and by their significance (with p < 0.05) in each model, and are given as follows.
-
Multiple pregnancy, parity, previous emergency admission, gestational diabetes, hypertension/pre-eclampsia, cardiac disease, operation on amniotic cavity, obstetric and non-obstetric surgery – binary coded with ‘NO’ as reference group.
-
Maternal age, in six categories: 15–19 years, 20–24 years, 25–29 years (reference group), 30–34 years, 35–39 years and ≥ 40 years.
-
Socioeconomic deprivation (Carstairs deprivation quintile), in six categories: 1 (least deprived, reference group), 2, 3, 4, 5 (most deprived) and 6 (unknown).
-
Comorbidities (Charlson Comorbidities Index score): 0 (reference group) and 1+.
-
Tables 13–20 show that, after adjusting for risk factors, pregnancies in which surgery was carried out compared with pregnancies in which surgery was not carried out had significantly higher odds of a spontaneous abortion associated with hospitalisation (OR 1.14, 95% CI 1.10 to 1.18); preterm delivery (OR 1.48, 95% CI 1.44 to 1.53); caesarean section (OR 1.30, 95% CI 1.27 to 1.33); long inpatient stay (OR 1.25, 95% CI 1.21 to 1.28); maternal death (OR 4.72, 95% CI 2.61 to 8.52); stillbirth (OR 1.65, 95% CI 1.50 to 1.82); and low birthweight (OR 1.53, 95% CI 1.48 to 1.59).
| Risk factors | Value | OR (95% CI) | p-value |
|---|---|---|---|
| Maternal age (years) | 15–19 | 1.17 (1.15 to 1.18) | < 0.0001 |
| 20–24 | 0.98 (0.97 to 0.99) | ||
| 25–29 | 1 | ||
| 30–34 | 1.14 (1.13 to 1.15) | ||
| 35–39 | 1.80 (1.78 to 1.82) | ||
| ≥ 40 | 4.03 (3.98 to 4.09) | ||
| Multiple pregnancy | Yes | 0.27 (0.26 to 0.29) | < 0.0001 |
| Parity | Yes | 0.53 (0.52 to 0.54) | < 0.0001 |
| Previous emergency admission | Yes | 1.22 (1.21 to 1.24) | < 0.0001 |
| Carstairs deprivation quintile | 1 (least deprived) | 1 | < 0.0001 |
| 2 | 1.08 (1.07 to 1.09) | ||
| 3 | 1.17 (1.16 to 1.19) | ||
| 4 | 1.27 (1.26 to 1.29) | ||
| 5 (most deprived) | 1.46 (1.44 to 1.48) | ||
| 6 (unknown) | 5.97 (5.82 to 6.12) | ||
| Charlson Comorbidities Index score | 1+ vs. 0 | 1.03 (1.01 to 1.05) | 0.0039 |
| Previous Charlson Comorbidities Index score | 1+ vs. 0 | 1.32 (1.28 to 1.35) | < 0.0001 |
| Gestational diabetes | Yes | 0.083 (0.077 to 0.091) | < 0.0001 |
| Pre-eclampsia/hypertension | Yes | 0.021 (0.018 to 0.023) | < 0.0001 |
| Cardiac disease | Yes | 1.93 (1.84 to 2.03) | < 0.0001 |
| Operation on amniotic cavity | Yes | 0.16 (0.14 to 0.18) | < 0.0001 |
| Obstetric surgery | Yes | 0.057 (0.054 to 0.06) | < 0.0001 |
| Year (or per year since 2002–3) | 1.008 (1.007 to 1.009) | < 0.0001 | |
| Non-obstetric surgery | Yes | 1.14 (1.10 to 1.18) | < 0.0001 |
| AIC | 2,873,160.1 | ||
| R 2 | 0.24 | ||
| c-statistic | 0.66 |
| Risk factors | Value | OR (95% CI) | p-value |
|---|---|---|---|
| Maternal age (years) | 15–19 | 1.19 (1.17 to 1.21) | < 0.0001 |
| 20–24 | 0.99 (0.98 to 1.00) | ||
| 25–29 | 1 | ||
| 30–34 | 1.13 (1.12 to 1.14) | ||
| 35–39 | 1.77 (1.76 to 1.79) | ||
| ≥ 40 | 3.91 (3.86 to 3.96) | ||
| Multiple pregnancy | Yes | 0.28 (0.26 to 0.29) | < 0.0001 |
| Parity | Yes | 0.54 (0.53 to 0.55) | < 0.0001 |
| Previous emergency admission | Yes | 1.22 (1.21 to 1.24) | < 0.0001 |
| Carstairs deprivation quintile | 1 (least deprived) | 1 | < 0.0001 |
| 2 | 1.08 (1.07 to 1.09) | ||
| 3 | 1.17 (1.16 to 1.19) | ||
| 4 | 1.28 (1.26 to 1.29) | ||
| 5 (most deprived) | 1.46 (1.44 to 1.48) | ||
| 6 (unknown) | 5.71 (5.82 to 6.12) | ||
| Charlson Comorbidities Index score | 1+ vs. 0 | 1.02 (1.01 to 1.05) | 0.0011 |
| Previous Charlson Comorbidities Index score | 1+ vs. 0 | 1.27 (1.24 to 1.30) | < 0.0001 |
| Pre-eclampsia/hypertension | Yes | 0.020 (0.018 to 0.022) | < 0.0001 |
| Cardiac disease | Yes | 1.93 (1.84 to 2.03) | < 0.0001 |
| Year (or per year since 2002–3) | 0.98 (0.97 to 0.99) | < 0.0001 | |
| Non-obstetric surgery | Yes | 1.14 (1.10 to 1.18) | < 0.0001 |
| AIC | 2,755,361.3 | ||
| R 2 | 0.18 | ||
| c-statistic | 0.64 |
| Risk factors | Value | OR (95% CI) | p-value |
|---|---|---|---|
| Maternal age (years) | 15–19 | 1.12 (1.11 to 1.14) | < 0.0001 |
| 20–24 | 1.01 (1.00 to 1.02) | ||
| 25–29 | 1 | ||
| 30–34 | 0.99 (0.98 to 1.00) | ||
| 35–39 | 1.06 (1.05 to 1.07) | ||
| ≥ 40 | 1.18 (1.16 to 1.20) | ||
| Multiple pregnancy | Yes | 13.12 (12.92 to 13.33) | < 0.0001 |
| Parity | Yes | 0.98 (0.97 to 0.99) | < 0.0001 |
| Previous emergency admission | Yes | 1.18 (1.17 to 1.19) | < 0.0001 |
| Carstairs deprivation quintile | 1 (least deprived) | 1 | < 0.0001 |
| 2 | 1.06 (1.05 to 1.08) | ||
| 3 | 1.14 (1.13 to 1.15) | ||
| 4 | 1.28 (1.27 to 1.30) | ||
| 5 (most deprived) | 1.47 (1.46 to 1.49) | ||
| 6 (unknown) | 1.83 (1.76 to 1.89) | ||
| Charlson Comorbidities Index score | 1+ vs. 0 | 1.02 (1.01 to 1.04) | 0.0118 |
| Previous Charlson Comorbidities Index score | 1+ vs. 0 | 1.43 (1.40 to 1.46) | < 0.0001 |
| Gestational diabetes | Yes | 2.23 (2.19 to 2.27) | < 0.0001 |
| Pre-eclampsia/hypertension | Yes | 1.78 (1.76 to 1.81) | < 0.0001 |
| Cardiac disease | Yes | 1.52 (1.45 to 1.60) | < 0.0001 |
| Operation on amniotic cavity | Yes | 1.68 (1.62 to 1.74) | < 0.0001 |
| Obstetric surgery | Yes | 0.77 (0.75 to 0.77) | < 0.0001 |
| Year (or per year since 2002–3) | 1.023 (1.021 to 1.024) | < 0.0001 | |
| Non-obstetric surgery | Yes | 1.48 (1.44 to 1.53) | < 0.0001 |
| AIC | 3,129,848.1 | ||
| R 2 | 0.20 | ||
| c-statistic | 0.60 |
| Risk factors | Value | OR (95% CI) | p-value |
|---|---|---|---|
| Maternal age (years) | 15–19 | 0.528 (0.523 to 0.534) | < 0.0001 |
| 20–24 | 0.74 (0.73 to 0.75) | ||
| 25–29 | 1 | ||
| 30–34 | 1.30 (1.29 to 1.31) | ||
| 35–39 | 1.66 (1.65 to 1.67) | ||
| ≥ 40 | 2.27 (2.24 to 2.29) | ||
| Multiple pregnancy | Yes | 6.74 (6.63 to 6.85) | < 0.0001 |
| Parity | Yes | 0.389 (0.387 to 0.391) | < 0.0001 |
| Previous emergency admission | Yes | 1.18 (1.17 to 1.19) | < 0.0001 |
| Carstairs deprivation quintile | 1 (least deprived) | 1 | < 0.0001 |
| 2 | 1.00 (0.99 to 1.01) | ||
| 3 | 1.03 (1.02 to 1.04) | ||
| 4 | 1.04 (1.03 to 1.05) | ||
| 5 (most deprived) | 1.03 (1.02 to 1.04) | ||
| 6 (unknown) | 1.38 (1.34 to 1.41) | ||
| Charlson Comorbidities Index score | 1+ vs. 0 | 1.24 (1.23 to 1.26) | < 0.0001 |
| Previous Charlson Comorbidities Index score | 1+ vs. 0 | 1.15 (1.13 to 1.17) | < 0.0001 |
| Gestational diabetes | Yes | 3.12 (3.08 to 3.17) | < 0.0001 |
| Pre-eclampsia/hypertension | Yes | 2.18 (2.16 to 2.20) | < 0.0001 |
| Cardiac disease | Yes | 1.68 (1.62 to 1.74) | < 0.0001 |
| Previous caesarean delivery | Yes | 15.07 (15.00 to 15.17) | < 0.0001 |
| Operation on amniotic cavity | Yes | 1.12 (1.09 to 1.15) | < 0.0001 |
| Obstetric surgery | Yes | 0.152 (0.150 to 0.154) | < 0.0001 |
| Year (or per year since 2002–3) | 1.026 (1.025 to 1.027) | < 0.0001 | |
| Non-obstetric surgery | Yes | 1.30 (1.27 to 1.33) | < 0.0001 |
| AIC | 5,654,992.0 | ||
| R 2 | 0.30 | ||
| c-statistic | 0.75 |
| Risk factors | Value | OR (95% CI) | p-value |
|---|---|---|---|
| Maternal age (years) | 15–19 | 0.96 (0.94 to 0.97) | < 0.0001 |
| 20–24 | 0.94 (0.93 to 0.95) | ||
| 25–29 | 1 | ||
| 30–34 | 1.02 (1.01 to 1.03) | ||
| 35–39 | 1.03 (1.02 to 1.04) | ||
| ≥ 40 | 1.08 (1.06 to 1.10) | ||
| Multiple pregnancy | Yes | 2.13 (2.09 to 2.17) | < 0.0001 |
| Parity | Yes | 0.501 (0.498 to 0.504) | < 0.0001 |
| Previous emergency admission | Yes | 1.24 (1.23 to 1.25) | < 0.0001 |
| Carstairs deprivation quintile | 1 (least deprived) | 1 | < 0.0001 |
| 2 | 1.03 (1.02 to 1.04) | ||
| 3 | 1.05 (1.04 to 1.06) | ||
| 4 | 1.10 (1.09 to 1.11) | ||
| 5 (most deprived) | 1.24 (1.23 to 1.25) | ||
| 6 (unknown) | 1.13 (1.09 to 1.17) | ||
| Charlson Comorbidities Index score | 1+ vs. 0 | 1.14 (1.12 to 1.16) | < 0.0001 |
| Previous Charlson Comorbidities Index score | 1+ vs. 0 | 1.18 (1.16 to 1.21) | < 0.0001 |
| Gestational diabetes | Yes | 1.62 (1.59 to 1.65) | < 0.0001 |
| Pre-eclampsia/hypertension | Yes | 2.13 (2.11 to 2.15) | < 0.0001 |
| Cardiac disease | Yes | 1.46 (1.39 to 1.53) | < 0.0001 |
| Operation on amniotic cavity | Yes | 1.20 (1.16 to 1.24) | < 0.0001 |
| Obstetric surgery | Yes | 1.81 (1.79 to 1.83) | < 0.0001 |
| Year (or per year since 2002–3) | 0.938 (0.937 to 0.939) | < 0.0001 | |
| Non-obstetric surgery | Yes | 1.25 (1.21 to 1.28) | < 0.0001 |
| AIC | 371,889.6 | ||
| R 2 | 0.18 | ||
| c-statistic | 0.63 |
| Risk factors | Value | OR (95% CI) | p-value |
|---|---|---|---|
| Maternal age (years) | 15–19 | 0.27 (0.10 to 0.76) | < 0.0001 |
| 20–24 | 0.76 (0.48 to 1.18) | ||
| 25–29 | 1 | ||
| 30–34 | 1.32 (0.93 to 1.89) | ||
| 35–39 | 1.53 (1.04 to 2.25) | ||
| ≥ 40 | 2.23 (1.34 to 3.69) | ||
| Multiple pregnancy | Yes | 4.19 (2.33 to 7.55) | < 0.0001 |
| Carstairs deprivation quintile | 1 (least deprived) | 1 | < 0.0001 |
| 2 | 1.81 (1.07 to 3.06) | ||
| 3 | 1.78 (1.07 to 3.03) | ||
| 4 | 2.23 (1.35 to 3.68) | ||
| 5 (most deprived) | 2.70 (1.67 to 4.36) | ||
| 6 (unknown) | 4.20 (1.44 to 12.25) | ||
| Charlson Comorbidities Index score | 1+ vs. 0 | 5.05 (3.62 to 7.04) | < 0.0001 |
| Pre-eclampsia/hypertension | Yes | 3.54 (2.42 to 5.18) | < 0.0001 |
| Cardiac disease | Yes | 79.23 (57.36 to 109.44) | < 0.0001 |
| Year (or per year since 2002–3) | 0.90 (0.86 to 0.95) | < 0.0001 | |
| Non-obstetric surgery | Yes | 4.72 (2.61 to 8.52) | < 0.0001 |
| AIC | 4721.4 | ||
| R 2 | 0.001 | ||
| c-statistic | 0.58 |
| Risk factors | Value | OR (95% CI) | p-value |
|---|---|---|---|
| Maternal age (years) | 15–19 | 1.05 (1.00 to 1.10) | < 0.0001 |
| 20–24 | 0.97 (0.94 to 1.00) | ||
| 25–29 | 1 | ||
| 30–34 | 1.03 (1.00 to 1.07) | ||
| 35–39 | 1.23 (1.19 to 1.27) | ||
| ≥ 40 | 1.53 (1.46 to 1.61) | ||
| Multiple pregnancy | Yes | 4.63 (4.41 to 4.87) | < 0.0001 |
| Parity | Yes | 0.82 (0.81 to 0.84) | < 0.0001 |
| Carstairs deprivation quintile | 1 (least deprived) | 1 | < 0.0001 |
| 2 | 1.10 (1.06 to 1.15) | ||
| 3 | 1.21 (1.16 to 1.26) | ||
| 4 | 1.44 (1.39 to 1.50) | ||
| 5 (most deprived) | 1.79 (1.73 to 1.86) | ||
| 6 (unknown) | 2.96 (2.68 to 3.27) | ||
| Charlson Comorbidities Index score | 1+ vs. 0 | 0.79 (0.74 to 0.84) | < 0.0001 |
| Previous Charlson Comorbidities Index score | 1+ vs. 0 | 1.33 (1.24 to 1.44) | < 0.0001 |
| Gestational diabetes | Yes | 1.51 (1.42 to 1.62) | < 0.0001 |
| Pre-eclampsia/hypertension | Yes | 1.85 (1.77 to 1.93) | < 0.0001 |
| Cardiac disease | Yes | 1.38 (1.15 to 1.65) | 0.0005 |
| Operation on amniotic cavity | Yes | 5.63 (5.28 to 6.01) | < 0.0001 |
| Obstetric surgery | Yes | 0.66 (0.63 to 0.70) | < 0.0001 |
| Non-obstetric surgery | Yes | 1.65 (1.50 to 1.82) | < 0.0001 |
| AIC | 410,495.3 | ||
| R 2 | 0.13 | ||
| c-statistic | 0.60 |
| Risk factors | Value | OR (95% CI) | p-value |
|---|---|---|---|
| Maternal age (years) | 15–19 | 1.18 (1.16 to 1.20) | < 0.0001 |
| 20–24 | 1.07 (1.06 to 1.08) | ||
| 25–29 | 1 | ||
| 30–34 | 0.97 (0.96 to 0.98) | ||
| 35–39 | 1.05 (1.04 to 1.06) | ||
| ≥ 40 | 1.20 (1.18 to 1.23) | ||
| Multiple pregnancy | Yes | 20.98 (20.66 to 21.32) | < 0.0001 |
| Parity | Yes | 0.91 (0.90 to 0.92) | < 0.0001 |
| Previous emergency admission | Yes | 1.22 (1.21 to 1.23) | < 0.0001 |
| Carstairs deprivation quintile | 1 (least deprived) | 1 | < 0.0001 |
| 2 | 1.11 (1.09 to 1.13) | ||
| 3 | 1.23 (1.22 to 1.25) | ||
| 4 | 1.47 (1.45 to 1.49) | ||
| 5 (most deprived) | 1.89 (1.87 to 1.92) | ||
| 6 (unknown) | 1.72 (1.65 to 1.80) | ||
| Charlson Comorbidities Index score | 1+ vs. 0 | 1.13 (1.11 to 1.15) | < 0.0001 |
| Previous Charlson Comorbidities Index score | 1+ vs. 0 | 1.32 (1.28 to 1.34) | < 0.0001 |
| Gestational diabetes | Yes | 1.23 (1.20 to 1.26) | < 0.0001 |
| Pre-eclampsia/hypertension | Yes | 2.26 (2.23 to 2.30) | < 0.0001 |
| Cardiac disease | Yes | 1.60 (1.51 to 1.70) | < 0.0001 |
| Operation on amniotic cavity | Yes | 2.15 (2.07 to 2.23) | < 0.0001 |
| Obstetric surgery | Yes | 0.72 (0.71 to 0.74) | < 0.0001 |
| Year (or per year since 2002–3) | 1.007 (1.005 to 1.008) | < 0.0001 | |
| Non-obstetric surgery | Yes | 1.53 (1.48 to 1.59) | < 0.0001 |
| AIC | 2,483,423.9 | ||
| R 2 | 0.25 | ||
| c-statistic | 0.64 |
Final analysis
This section presents the final results: adjusted RR and attributable risk and NNH for pregnancies in which surgery occurred compared with pregnancies in which surgery did not occur (Table 21). The risk of an adverse birth outcome for pregnancies with specific types of operations is also presented.
| Outcome | Baseline, % | RR (95% CI) | RR (95% CI)a | Attributable risk, % (95% CI)a | NNH (95% CI)a |
|---|---|---|---|---|---|
| Non-obstetric surgery vs. no non-obstetric surgery | |||||
| Spontaneous abortion associated with hospitalisation | 5.8 | 1.13 (1.09 to 1.17) | 1.12 (1.08 to 1.16) | 0.7 (0.4 to 0.9) | 143 (107 to 230) |
| Preterm delivery (missing values considered as full term) | 7.5 | 1.43 (1.39 to 1.47) | 1.42 (1.39 to 1.46) | 3.2 (2.9 to 3.4) | 31 (29 to 34) |
| Preterm delivery (missing values excluded) | 11.3 | 1.48 (1.44 to 1.51) | 1.45 (1.42 to 1.50) | 5.0 (4.7 to 5.6) | 20 (18 to 21) |
| Maternal death | 0.004 | 4.72 (2.61 to 8.52) | 4.67 (1.79 to 8.93) | 0.013 (0.003 to 0.028) | 7692 (3571 to 33,333) |
| Caesarean section | 23.9 | 1.21 (1.19 to 1.23) | 1.17 (1.15 to 1.19) | 4.0 (3.6 to 4.5) | 25 (22 to 28) |
| Long inpatient stays | 9.5 | 1.22 (1.19 to 1.25) | 1.21 (1.18 to 1.26) | 2.0 (1.7 to 2.4) | 50 (41 to 60) |
| Stillbirth (missing values consider as live) | 0.6 | 1.64 (1.50 to 1.81) | 1.64 (1.47 to 1.80) | 0.4 (0.3 to 0.4) | 287 (227 to 386) |
| Stillbirth (missing values excluded) | 0.6 | 1.65 (1.50 to 1.82) | 1.65 (1.48 to 1.81) | 0.4 (0.3 to 0.5) | 275 (220 to 369) |
| Low birthweight (missing values consider as birthweight > 2500 g) | 5.6 | 1.49 (1.44 to 1.54) | 1.46 (1.43 to 1.53) | 2.6 (2.5 to 2.9) | 39 (37 to 42) |
| Low birthweight (missing values excluded) | 7.1 | 1.54 (1.49 to 1.59) | 1.50 (1.47 to 1.55) | 3.5 (3.3 to 3.8) | 28 (27 to 30) |
After adjusting for potential confounders, the RR associated with hospitalisation was 1.13 (95% CI 1.09 to 1.17) for spontaneous abortion, 1.43 (95% CI 1.39 to 1.47) for preterm delivery, 4.72 (95% CI 2.61 to 8.52) for maternal death, 1.21 (95% CI 1.19 to 1.23) for caesarean section and 1.22 (95% CI 1.19 to 1.25) for long inpatient stay in pregnancies in which surgery was carried out compared with pregnancies in which it was not. The RR for maternal death was high but was based on very small numbers with very wide CIs. The RR for stillbirth and low birthweight was 1.64 (95% CI 1.50 to 1.81) and 1.49 (95% CI 1.44 to 1.54), respectively. Using Austin’s method,30 we found little or no difference in our estimated RRs except for caesarean section (which is a relatively common outcome). NNH represents the number of operations associated with one additional adverse birth outcome. We estimated that, for every 143 pregnancies in which a surgical operation was carried out, compared with pregnancies in which a surgical operation was not carried out, there was one additional spontaneous abortion (associated with hospitalisation); for every 31 operations during pregnancy there was one additional preterm delivery; for every 25 operations there was one additional caesarean section; for every 50 operations there was one additional long inpatient stay; for every 287 operations there was one additional stillbirth; for every 39 operations there was one additional newborn with low birthweight; and for every 7692 operations there was one additional maternal death. Again, this estimate came with very wide 95% CIs (3571 to 33,333 operations); see Table 21. We repeated our analysis excluding records with missing values for preterm delivery, stillbirth and low birthweight, and found little difference in RR, but attributable risk and NNH changed more because of the differences in baseline incidence.
We identified 47,628 pregnancies in which surgery was carried out (0.7% of all pregnancies); in 25,445 cases (53.4%) the procedure was elective and in 22,183 (46.6%) it was non-elective. In general, the risks of adverse outcomes were higher for non-elective surgery than for planned surgery, although non-elective surgery was not associated with a significantly higher risk of spontaneous abortions associated with hospitalisation. Twenty-six per cent (12,493) of all surgical operations were abdominal. The RR of adverse birth outcomes (excluding maternal death) was higher for pregnancies in which surgery was carried out than for pregnancies in which it was not. The RR of spontaneous abortion associated with hospitalisation was 1.90 (95% CI 1.81 to 1.99), with a NNH of 20 (Table 22). Laparoscopic abdominal surgery was associated with an even higher RR for spontaneous abortion associated with hospitalisation (RR 2.47, 95% CI 2.34 to 2.60) and seemed to contribute most of the risk associated with abdominal surgery, as open abdominal surgery was not associated with a raised risk (RR 0.65, 95% CI 0.56 to 0.76). Appendectomy was not associated with an increased risk of spontaneous abortion associated with hospitalisation, but was associated with a raised risk of preterm delivery (RR 1.49, 95% CI 1.34 to 1.64), caesarean section (RR 1.13, 95% CI 1.06 to 1.21), long inpatient stay (RR 1.32, 95% CI 1.20 to 1.46) and low birthweight (RR 1.43, 95% CI 1.26 to 1.62).
| Outcome | RR (95% CI) | RRa | Attributable riska (%) | NNHa |
|---|---|---|---|---|
| Elective surgery vs. no surgery | ||||
| Spontaneous abortion associated with hospitalisation | 1.12 (1.08 to 1.18) | 1.12 | 0.7 | 141 |
| Preterm delivery | 1.31 (1.25 to 1.35) | 1.29 | 2.2 | 46 |
| Caesarean section | 1.15 (1.12 to 1.17) | 1.12 | 2.8 | 36 |
| Long inpatient stay | 1.12 (1.08 to 1.16) | 1.11 | 1.1 | 92 |
| Stillbirth | 1.35 (1.17 to 1.55) | 1.34 | 0.2 | 531 |
| Low birthweight | 1.38 (1.32 to 1.43) | 1.41 | 2.3 | 43 |
| Non-elective surgery vs. no surgery | ||||
| Spontaneous abortion associated with hospitalisation | 1.00 (0.95 to 1.06) | N/A | N/A | N/A |
| Preterm delivery | 1.57 (1.51 to 1.62) | 1.54 | 4.0 | 25 |
| Caesarean section | 1.28 (1.25 to 1.32) | 1.23 | 5.4 | 18 |
| Long inpatient stay | 1.33 (1.28 to 1.37) | 1.32 | 3.0 | 33 |
| Stillbirth | 1.87 (1.63 to 2.13) | 1.86 | 0.5 | 210 |
| Low birthweight | 1.60 (1.53 to 1.67) | 1.56 | 3.1 | 32 |
| Abdominal surgery vs. no surgery | ||||
| Spontaneous abortion associated with hospitalisation | 1.90 (1.81 to 1.99) | 1.87 | 5.0 | 20 |
| Preterm delivery | 1.62 (1.54 to 1.70) | 1.51 | 3.6 | 28 |
| Caesarean section | 1.27 (1.23 to 1.30) | 1.21 | 5.0 | 20 |
| Long inpatient stays | 1.30 (1.24 to 1.37) | 1.29 | 2.8 | 36 |
| Stillbirth | 1.76 (1.47 to 2.11) | 1.76 | 0.4 | 240 |
| Low birthweight | 1.61 (1.51 to 1.71) | 1.57 | 3.2 | 32 |
| Abdominal laparoscopic surgery vs. no surgery | ||||
| Spontaneous abortion associated with hospitalisation | 2.47 (2.34 to 2.60) | 2.41 | 8.2 | 12 |
| Preterm delivery | 1.52 (1.43 to 1.62) | 1.50 | 3.7 | 27 |
| Caesarean section | 1.21 (1.16 to 1.26) | 1.17 | 4.0 | 25 |
| Long inpatient stay | 1.29 (1.21 to 1.37) | 1.28 | 2.7 | 37 |
| Stillbirth | 1.72 (1.37 to 2.16) | 1.72 | 0.3 | 253 |
| Low birthweight | 1.54 (1.43 to 1.66) | 1.51 | 2.8 | 35 |
| Abdominal open surgery vs. no surgery | ||||
| Spontaneous abortion associated with hospitalisation | 0.65 (0.56 to 0.76) | 0.66 | –1.9 | N/A |
| Preterm delivery | 1.80 (1.67 to 1.96) | 1.77 | 5.8 | 17 |
| Caesarean section | 1.37 (1.30 to 1.44) | 1.29 | 7.0 | 14 |
| Long inpatient stay | 1.32 (1.22 to 1.43) | 1.31 | 2.9 | 34 |
| Stillbirth | 1.84 (1.36 to 2.50) | 1.84 | 0.4 | 217 |
| Low birthweight | 1.72 (1.57 to 1.89) | 1.67 | 3.8 | 26 |
| Appendectomy vs. no surgery | ||||
| Spontaneous abortion associated with hospitalisation | 0.78 (0.66 to 0.92) | 0.79 | –1.2 | N/A |
| Preterm delivery | 1.49 (1.34 to 1.64) | 1.46 | 3.5 | 28 |
| Caesarean section | 1.13 (1.06 to 1.21) | 1.11 | 2.6 | 39 |
| Long inpatient stays | 1.32 (1.20 to 1.46) | 1.32 | 3.0 | 33 |
| Stillbirth | 1.05 (0.65 to 1.68) | N/A | N/A | N/A |
| Low birthweight | 1.43 (1.26 to 1.62) | 1.40 | 2.2 | 44 |
| Abdominal surgery vs. other surgery | ||||
| Spontaneous abortion associated with hospitalisation | 2.52 (2.36 to 2.69) | 2.48 | 7.0 | 14 |
| Preterm delivery | 1.19 (1.12 to 1.26) | 1.18 | 1.9 | 52 |
| Caesarean section | 1.08 (1.04 to 1.12) | 1.06 | 1.7 | 58 |
| Long inpatient stays | 1.10 (1.04 to 1.16) | 1.10 | 1.2 | 86 |
| Stillbirth | 1.24 (1.00 to 1.54) | 1.24 | 0.2 | 477 |
| Low birthweight | 1.14 (1.05 to 1.22) | 1.13 | 1.1 | 90 |
| Musculoskeletal surgery vs. no surgery | ||||
| Spontaneous abortion associated with hospitalisation | 0.94 (0.84 to 1.07) | N/A | N/A | N/A |
| Preterm delivery | 1.18 (1.08 to 1.30) | 1.18 | 1.3 | 75 |
| Caesarean section | 1.11 (1.05 to 1.17) | 1.09 | 2.1 | 47 |
| Long inpatient stays | 1.19 (1.09 to 1.29) | 1.18 | 1.7 | 57 |
| Low birthweight | 1.34 (1.21 to 1.49) | 1.32 | 1.8 | 56 |
| Cholecystectomy vs. no surgery | ||||
| Spontaneous abortion associated with hospitalisation | 1.36 (1.12 to 1.64) | 1.31 | 1.8 | 56 |
| Preterm delivery | 1.12 (0.93 to 1.34) | N/A | N/A | N/A |
| Caesarean section | 1.07 (0.95 to 1.19) | N/A | N/A | N/A |
| Long inpatient stays | 1.18 (1.00 to 1.39) | 1.09 | 0.8 | 122 |
| Stillbirth | 1.17 (0.58 to 2.32) | N/A | N/A | N/A |
| Low birthweight | 1.04 (0.82 to 1.32) | N/A | N/A | N/A |
| ENT surgery vs. no surgery | ||||
| Spontaneous abortion associated with hospitalisation | 1.07 (0.93 to 1.23) | N/A | N/A | N/A |
| Preterm delivery | 1.22 (1.09 to 1.36) | 1.22 | 1.6 | 63 |
| Caesarean section | 1.01 (0.94 to 1.07) | N/A | N/A | N/A |
| Long inpatient stay | 1.15 (1.05 to 1.27) | 1.15 | 1.4 | 71 |
| Stillbirth | 1.52 (1.04 to 2.21) | 1.51 | 0.3 | 356 |
| Low birthweight | 1.39 (1.22 to 1.57) | 1.36 | 2.0 | 49 |
| Breast surgery vs. no surgery | ||||
| Spontaneous abortion associated with hospitalisation | 0.74 (0.60 to 0.91) | 0.74 | –1.5 | N/A |
| Preterm delivery | 1.94 (1.74 to 2.17) | 1.90 | 6.7 | 15 |
| Caesarean section | 1.17 (1.08 to 1.27) | 1.14 | 3.4 | 30 |
| Long inpatient stay | 1.13 (0.98 to 1.27) | N/A | N/A | N/A |
| Stillbirth | 1.19 (0.67 to 2.08) | N/A | N/A | N/A |
| Low birthweight | 1.94 (1.70 to 2.21) | 1.87 | 4.9 | 20 |
| Dental surgery vs. no surgery | ||||
| Spontaneous abortion associated with hospitalisation | 1.01 (0.91 to 1.12) | N/A | N/A | N/A |
| Preterm delivery | 1.13 (1.04 to 1.24) | 1.12 | 1.1 | 91 |
| Caesarean section | 0.97 (0.92 to 1.02) | N/A | N/A | N/A |
| Long inpatient stay | 1.12 (1.04 to 1.21) | 1.12 | 1.3 | 77 |
| Stillbirth | 1.62 (1.23 to 2.16) | 1.62 | 0.3 | 292 |
| Low birthweight | 1.32 (1.20 to 1.46) | 1.30 | 1.7 | 59 |
| Nail and skin surgery vs. no surgery | ||||
| Spontaneous abortion associated with hospitalisation | 0.58 (0.50 to 0.67) | 0.59 | –2.4 | N/A |
| Preterm delivery | 1.24 (1.14 to 1.36) | 1.24 | 1.8 | 56 |
| Caesarean section | 1.09 (1.03 to 1.15) | 1.08 | 1.9 | 53 |
| Long inpatient stay | 1.16 (1.07 to 1.26) | 1.18 | 1.7 | 58 |
| Stillbirth | 1.33 (0.96 to 1.84) | N/A | N/A | N/A |
| Low birthweight | 1.29 (1.17 to 1.43) | 1.27 | 1.5 | 65 |
| Perianal surgery vs. no surgery | ||||
| Spontaneous abortion associated with hospitalisation | 0.56 (0.46 to 0.67) | 0.56 | –2.5 | N/A |
| Preterm delivery | 0.86 (0.75 to 0.99) | 0.89 | –0.8 | N/A |
| Caesarean section | 1.17 (1.10 to 1.25) | 1.18 | 3.9 | 25 |
| Long inpatient stay | 1.08 (0.97 to 1.20) | N/A | N/A | N/A |
| Stillbirth | 0.59 (0.32 to 1.11) | N/A | N/A | N/A |
| Low birthweight | 0.93 (0.80 to 1.08) | N/A | N/A | N/A |
| Cancer-related surgery vs. no surgery | ||||
| Spontaneous abortion associated with hospitalisation | 0.53 (0.36 to 0.78) | 0.54 | –2.7 | N/A |
| Preterm delivery | 5.31 (4.82 to 5.82) | 5.09 | 30.5 | 3 |
| Caesarean section | 1.66 (1.50 to 1.83) | 1.53 | 12.6 | 10 |
| Long inpatient stay | 1.48 (1.23 to 1.79) | 1.47 | 4.5 | 22 |
| Stillbirth | 3.12 (1.73 to 5.60) | 3.11 | 1.2 | 86 |
| Low birthweight | 4.44 (3.86 to 5.08) | 4.16 | 17.7 | 6 |
| Acute appendicitis-related surgery vs. no surgery | ||||
| Spontaneous abortion associated with hospitalisation | 0.62 (0.35 to 1.08) | N/A | N/A | N/A |
| Preterm delivery | 2.03 (1.57 to 2.62) | 1.99 | 7.4 | 14 |
| Caesarean section | 1.13 (0.92 to 1.36) | N/A | N/A | N/A |
| Long inpatient stay | 1.49 (1.13 to 1.93) | 1.47 | 4.5 | 22 |
| Stillbirth | 1.08 (0.27 to 4.27) | N/A | N/A | N/A |
| Low birthweight | 1.71 (1.21 to 2.39) | 1.66 | 3.7 | 27 |
Approximately 2.5% (1306) of all surgeries during pregnancy were cholecystectomy. A comparison with no surgery during pregnancy showed a difference only in spontaneous abortions associated with hospitalisation (RR 1.36, 95% CI 1.12 to 1.64).
Approximately 1.5% (710) of all operations were in patients with a diagnosis of cancer. The RR of adverse birth outcomes was higher for pregnancies in which cancer-related surgery was carried out than for pregnancies in which surgery was not carried out, with the exception of spontaneous abortion associated with hospitalisation (RR 0.53, 95% CI 0.36 to 0.78). The RR was 5.31 (95% CI 4.82 to 5.82) for preterm delivery, 1.66 (95% CI 1.50 to 1.83) for caesarean section, 1.48 (95% CI 1.23 to 1.79) for long inpatient stay, 3.12 (95% CI 1.73 to 5.60) for stillbirth and 4.44 (95% CI 3.86 to 5.08) for low birthweight.
Our analysis comparing outcomes following laparoscopic and open appendectomy (RR 2.36, 95% CI 1.71 to 3.26) and all abdominal surgery (RR 3.82, 95% CI 3.29 to 4.41) further illustrates the apparent increased associated risk of spontaneous abortion with laparoscopic procedures (Table 23).
| Outcome | RR (95% CI) | RRa |
|---|---|---|
| Laparoscopic appendectomy vs. other appendectomy | ||
| Spontaneous abortion | 2.36 (1.71 to 3.26) | 2.38 |
| Laparoscopic surgery vs. open abdominal surgery (any kind) | ||
| Spontaneous abortion | 3.82 (3.29 to 4.41) | 3.73 |
| Preterm delivery | 0.85 (0.77 to 0.94) | 0.85 |
| Caesarean section | 0.88 (0.83 to 0.94) | 0.90 |
Tables 24–26 present adjusted RRs and their 95% CIs, attributable risks and NNHs for pregnancies in which surgery was or was not carried out, by trimester. The RR of preterm delivery, caesarean section, stillbirth and low birthweight was between 20% and 30% higher for operations carried out in the third trimester than for those carried out in the first trimester. There was little difference by trimester of operation in the RR of a long inpatient stay.
| Outcome | First trimester | Second trimester | Third trimester |
|---|---|---|---|
| Preterm delivery | 1.51 (1.44 to 1.58) | 1.57 (1.48 to 1.68) | 1.82 (1.72 to 1.93) |
| Caesarean section | 1.13 (1.10 to 1.17) | 1.17 (1.12 to 1.21) | 1.39 (1.34 to 1.44) |
| Long inpatient stay | 1.22 (1.16 to 1.28) | 1.26 (1.19 to 1.35) | 1.29 (1.21 to 1.37) |
| Stillbirth | 1.21 (0.98 to 1.50) | 1.47 (1.13 to 1.90) | 1.56 (1.23 to 1.97) |
| Low birthweight | 1.83 (1.73 to 1.92) | 1.89 (1.77 to 2.03) | 2.21 (2.06 to 2.38) |
| Outcome | First trimester | Second trimester | Third trimester |
|---|---|---|---|
| Preterm delivery | 3.6 | 4.1 | 5.9 |
| Caesarean section | 2.5 | 3.1 | 7.4 |
| Long inpatient stay | 2.1 | 2.4 | 2.7 |
| Stillbirth | – | 0.2 | 0.3 |
| Low birthweight | 4.3 | 4.7 | 5.6 |
| Outcome | First trimester | Second trimester | Third trimester |
|---|---|---|---|
| Preterm delivery | 28 | 24 | 17 |
| Caesarean section | 40 | 32 | 13 |
| Long inpatient stay | 49 | 42 | 37 |
| Stillbirth | – | 394 | 330 |
| Low birthweight | 23 | 21 | 18 |
Table 27 presents the results of two-level logistic regression for adverse birth outcomes. The intraclass correlation coefficients were close to 0 (from 0.0939 for spontaneous abortion associated with hospitalisation to 0.008 for low birthweight), meaning that only 1.0–10.0% of the variance is attributable to trust level. Random parameters of level 2 for stillbirth and maternal death were even smaller, and these are not presented here.
| Fixed coefficients or random parameters | Multilevel models (SE) | ||||
|---|---|---|---|---|---|
| Spontaneous abortion associated with hospitalisation | Preterm delivery | Caesarean section | Long inpatient stay | Low birthweight | |
| Fixed coefficients | |||||
| Maternal age | 0.0141*** (0.0001) | 0.0008*** (0.0001) | 0.0412*** (0.0001) | 0.0019*** (0.0001) | –0.0002** (0.0001) |
| Multiple pregnancy | –0.0414*** (0.0009) | 0.4234*** (0.001) | 0.3784*** (0.0015) | 0.0831*** (0.0011) | 0.4647*** (0.0009) |
| Parity | –0.0391*** (0.0002) | –0.0054*** (0.0002) | –0.1413*** (0.0003) | –0.0597*** (0.0002) | –0.0083*** (0.0002) |
| Previous emergency admission | 0.0099 *** (0.0003) | 0.0157*** (0.0003) | 0.0273*** (0.0005) | 0.0181*** (0.0004) | 0.0114*** (0.0003) |
| Carstairs deprivation quintile | 0.0068*** (0.0001) | 0.0054*** (0.00008) | 0.0003** (0.0001) | 0.0029*** (0.0001) | 0.0069*** (0.0001) |
| Charlson Comorbidities Index score | 0.0007* (0.0005) | 0.0059*** (0.0006) | 0.0359*** (0.0009) | 0.0113*** (0.0007) | 0.0073*** (0.0005) |
| Charlson Comorbidities Index score (prior to pregnancy) | 0.0161*** (0.0007) | 0.0316*** (0.0008) | 0.0229*** (0.0013) | 0.0159*** (0.001) | 0.0184*** (0.0007) |
| Gestational diabetes | –0.0571*** (0.0007) | 0.0811*** (0.0008) | 0.2071 (0.0012) | 0.0494*** (0.0009) | 0.0133*** (0.0007) |
| Hypertension/pre-eclampsia | –0.0638*** (0.0005) | 0.0488*** (0.0005) | 0.1437*** (0.0008) | 0.089*** (0.0006) | 0.0576*** (0.0005) |
| Cardiac disease | 0.0524*** (0.0018) | 0.039*** (0.0020) | 0.0887*** (0.0031) | 0.0335*** (0.0024) | 0.0293*** (0.0018) |
| Other operations on amniotic cavity | –0.0528*** (0.0013) | 0.0502*** (0.0014) | 0.0237*** (0.0022) | 0.0139*** (0.0016) | 0.0496*** (0.0013) |
| Obstetric surgery | –0.06*** (0.0004) | –0.0185*** (0.0005) | –0.1964*** (0.0007) | 0.0518*** (0.0006) | –0.0155*** (0.0004) |
| Year | 0.0005*** (0.00003) | 0.0007*** (0.00004) | 0.0039*** (0.0001) | –0.0052*** (0.0001) | 0.0002*** (0.00003) |
| Previous caesarean section | 0.5406*** (0.0006) | ||||
| Non-obstetric surgery | 0.0071*** (0.0011) | 0.0366*** (0.0049) | 0.0426*** (0.0018) | 0.0202*** (0.0014) | 0.0266*** (0.0011) |
| Random parameters | |||||
| Level 1: pregnancies | 0.0531 (0.00003) | 0.06178 (0.00004) | 0.1475 (0.0001) | 0.0836 (0.00004) | 0.0498 (0.00003) |
| Level 2: trust | 0.0055 (0.0007) | 0.004299 (0.00045) | 0.0028 (0.0003) | 0.0008 (0.0001) | 0.0004 (0.00004) |
| Intraclass correlation | 0.0939 | 0.0651 | 0.0186 | 0.0095 | 0.008 |
Chapter 4 Discussion
We aimed to estimate the risk of adverse birth outcomes in pregnancies in which surgery was carried out and to compare this with the risk in pregnancies in which no surgery was recorded, and, also, to estimate the risk associated with common procedure groups.
In this chapter we summarise the main results and their relation to previous studies. We then note the strengths and limitations of our analysis and suggest future work.
Key findings
-
We identified 6,486,280 pregnancies, among which non-obstetric surgery was carried out in 47,628 (0.7%), in the period April 2002 to March 2012.
-
The most common surgical procedure group was abdominal (26.2%), followed by dental (11.3%), nail and skin (10.0%), musculoskeletal (9.6%), ENT (6.4%) and perianal (6.2%). There were 3062 cases of appendectomy and 1306 cases of cholecystectomy.
-
Non-obstetric surgery during pregnancy was associated with a higher risk of adverse birth outcomes than if no surgery was carried out. We estimated that for every 143 pregnancies in which a surgical procedure was performed, there was one additional spontaneous abortion (with a hospital admission); for every 31 procedures there was one additional preterm delivery; for every 7692 procedures there was one additional maternal death in hospital; for every 25 procedures there was one additional caesarean section; for every 50 procedures there was one additional long inpatient stay; for every 287 procedures there was one additional stillbirth; and for every 39 procedures there was one additional low-birthweight baby.
-
Dental, perianal, breast, cancer, abdominal, ENT and musculoskeletal procedures were associated with a higher risk of adverse birth outcomes than no surgery.
-
For almost half of operations (42.0%), no information about when in pregnancy the procedure was carried out was recorded.
-
For pregnancies in which gestational age was recorded, the RR for preterm delivery, caesarean section, stillbirth and low birthweight was between 20% and 30% higher for those operations carried out in the third trimester than for those performed in the first trimester. There was little difference by trimester of operation in the risk of a long inpatient stay.
Findings in relation to other studies
Spontaneous abortion associated with hospitalisation and preterm delivery
We found a high RR (1.13) for spontaneous abortion associated with hospitalisation for surgery during pregnancy. Duncan et al. 2 found an even higher RR (1.58) of abortion associated with a general anaesthetic in their 1986 Canadian study of 2565 pregnant women. Our study is much larger and more recent, perhaps reflecting improvements in surgery, but (like Duncan et al. ’s2 study) is unable to dissociate the risk of surgery from the risk of anaesthesia or the underlying condition for which the procedure was carried out. Other studies have focused on abdominal surgery. We found that, compared with no surgery, abdominal surgery was associated with an even higher risk of spontaneous abortion (associated with a hospital admission) (RR 1.90, 95% CI 1.81 to 1.99) and of preterm delivery (RR 1.62, 95% CI 1.54 to 1.70). Our study’s definition of spontaneous abortion is limited by the information that is held in administrative databases which includes spontaneous abortion only if this is recorded during a hospital admission. A large number of women whose pregnancies end in spontaneous abortions are never hospitalised. Gerstenfeld et al. 35 performed a retrospective review of all non-obstetric abdominal procedures in a women’s hospital at the University of Southern California School of Medicine during a 7-year period from 1991 to 1998. They found no significant difference in preterm delivery rates between women who underwent abdominal surgery and those who did not (OR 1.13, 95% CI 0.56 to 2.25; p = 0.84), and only two cases of spontaneous abortion following surgery. The post-surgical follow-up period in this study was short (a maximum of 4 weeks) and only 67% of subjects were followed up. The study was small and included only 106 women who underwent surgery. We found a significant difference between laparoscopic and open abdominal surgery for risk of spontaneous abortion (RR 3.82, 95% CI 3.29 to 4.41). Gerstenfeld et al. 35 found no significant difference, but, again, their study was limited by small numbers. There may be reluctance by surgeons to perform laparoscopic surgery beyond 26–28 weeks’ gestation because of previous evidence which suggests that ‘A gestational age of 26 to 28 weeks seems to be the limit for successful completion of laparoscopic surgery’36 and, although this evidence has since been refuted,37 the perception and practice may persist. Our analysis of open versus laparoscopic abdominal procedures by trimester (where gestational age at delivery was recorded) confirms that this remains the case, as the number of laparoscopic operations performed during the first trimester was nearly five times the number of open operations, whereas, in the third trimester, the number of open operations was 2.5 times the number of laparoscopic procedures. Unfortunately, in the case of spontaneous abortion, gestational age was frequently not recorded, so we were unable to examine the relationship between timing of procedures and outcome. However, there is no reason to doubt that the pattern would be similar. Within our definition of spontaneous abortion (associated with hospitalisation), we look only for operations 3 months prior to the event (which, by definition, occurs before week 24 of pregnancy) and women are likely to be admitted to hospital only during the second trimester. We are, therefore, picking up selected cases that are more likely to have a higher proportion of laparoscopies. We are unable to identify women who suffer spontaneous abortions who are not admitted. In addition, as is true for other studies and all our outcomes, we have no means of disentangling the effect of the surgery from the effect of the underlying condition itself.
For abdominal surgery, we found a reduced risk of preterm delivery (RR 0.85, 95% CI 0.77 to 0.94); Gerstenfeld et al. 35 found no significant difference in preterm delivery rate, but we suspect that, again, the small sample size and period from which their cohort was drawn may explain this difference. Two other studies compared pregnancy outcomes following laparoscopic and open appendicectomy38,39 and found no difference in the rates of preterm delivery. Sadot et al. 38 performed a hospital-based retrospective review of 65 pregnant women who underwent appendectomy for presumed appendicitis from 1999 to 2008. They calculated the overall preterm delivery rate and the rate of preterm delivery within 1 month of operation. In neither case was there any statistically significant difference between the laparoscopic and open groups. The authors did not analyse rates of spontaneous abortion.
Maternal death in hospital
In our study we identified 235 maternal deaths, which corresponds to a maternal death rate of 4 per 100,000 pregnancies. Our estimate is much lower than national estimates (10 per 100,000 according to the report Saving Lives, Improving Mothers’ Care40) because we identified only maternal deaths occurring in the same admission as the delivery or spontaneous abortion. We were not able to capture maternal deaths of women who did not deliver or deaths occurring following discharge. We estimated the RR of non-obstetric surgery during pregnancy to be 4.72 (95% CI 2.61 to 8.52). The baseline risk of maternal death is fortunately very low and translates into a NNH of 7692, which is the number of procedures associated with one additional maternal death. This number was based on only 12 deaths among pregnant women undergoing surgery in our cohort, and so the CIs are wide. Again, we have no means of disentangling the effect of the surgery from the effect of the underlying condition itself. Only one previous study has reported the maternal death of a woman undergoing non-obstetric surgery during pregnancy. 41 This study compared laparoscopic cholecystectomy with open cholecystectomy in pregnant women during the period 1992–6. During the 5-year period of the study, 46 pregnant women who underwent cholecystectomy were identified. The maternal death occurred in a 27-year-old woman who underwent elective laparoscopic cholecystectomy at 20 weeks’ gestation. On postoperative day 15, she presented to the emergency department and died following a laparotomy.
Stillbirth and low birthweight
Our study revealed that non-obstetric surgery during pregnancy is associated with an increased risk of stillbirth and low birthweight. We found that pregnant women who underwent non-obstetric surgery had an attributable risk of 0.4% for stillbirth and 2.6% for low birthweight compared with women who did not have surgery. However, there were no significant differences in the risk of low birthweight and stillbirth between those women undergoing laparoscopic and those undergoing open abdominal surgery. A Swedish study3 analysed outcomes of 5405 patients who had had an operation during pregnancy, out of a total of 720,000 Swedish births between 1973 and 1981, and concluded that the incidence of stillbirth was not increased in women having an operation. However, the incidence of very low birthweight and low-birthweight infants was increased. Mazze and Källén4 investigated appendectomy and laparoscopic surgery, and did not observe a statistically significant increase in stillbirth. However, the authors concluded that the mean birthweight in the operated group was, on average, 78 g less than the expected birthweight. Furthermore, compared with the general population, women undergoing operations during 3–23 weeks’ gestation demonstrated a shift in distribution towards an excess of infants with a birthweight < 3000 g. Another Swedish study5 found no difference in the birthweight of singleton infants born to women who underwent laparoscopy between 4 and 20 weeks of gestation. More recent studies on appendicectomy39,42 compared the effects of laparoscopic appendectomy with those of open appendectomy during pregnancy. There were no significant differences in the birthweight between the two groups. Moreover, Jenkins et al. 43 reported that general anaesthesia, longer surgery duration and intra-abdominal procedures are associated with lower birthweight.
Caesarean section and long inpatient stays
We found a significant effect in the adjusted RR for caesarean section of 1.21 (95% CI 1.19 to 1.23); however, this reduced to 1.17 (1.15 to 1.19) when the more appropriate Austin method30 was used for common outcomes. We also found a higher risk of long inpatient stays (RR 1.22, 95% CI 1.19 to 1.25). We could not find any previous studies reporting caesarean delivery and long inpatient stays in women who had surgery during their pregnancy.
Study strengths and limitations
This is the first study to report the risk of adverse birth outcomes following non-obstetric surgery during pregnancy across NHS hospitals in England. One important strength of this research is the use of the large and rich administrative data set. We extracted data for nearly 6.5 million pregnancies between 2002–3 and 2011–12, 10 times the total in the published literature to date. Furthermore, our data are much more recent and better represent current outcomes.
Another strength is that we estimated adjusted attributable risk and the NNH. The use of Austin’s analytical method30 was a particular strength here, as this allowed us to compare outcomes between two populations whose only difference was the exposure (non-obstetric surgery during pregnancy). These measures are more useful than an OR to women who want to be informed of the risk associated with a non-obstetric procedure, above and beyond the background risk.
Appropriateness of controls
The absolute key limitation of our study is that we have no means of disentangling the effect of the surgery from the effect of the underlying condition itself. Thus, we are able to compare only women who have surgery during pregnancy with women who do not. The ideal study population would be all women who require surgery during pregnancy to enable us to compare outcomes in women who actually had surgery with those who did not. Ideally, participants would be randomised into each group. However, withholding surgery in pregnant women who require treatment would be ethically challenging. From our study we have no way of determining the risk that the underlying condition would result in an adverse birth outcome. However, we still believe that the NNH, in particular, is a useful reference point for any discussion of risk with prospective patients. A further limitation, although certainly not unique to our study, is that we treat surgery during pregnancy as a homogeneous intervention and are unable to disentangle the independent effects of anaesthesia, pre-/peri- and post-operative care, as well as the surgery itself, all of which may influence the outcome of pregnancy. Therefore, we are not able to estimate the independent contribution to the risks of an adverse outcome during pregnancy of each component of this complex intervention.
Our study arose as a direct result of questions posed in the high-risk obstetric anaesthetic clinic by patients who wanted to know the statistical risks of an adverse outcome to their pregnancy. For some combinations of procedures and outcomes we have found no excess risk, and that may help to reassure mothers and remove barriers to potentially unnecessary delays to treatment.
Data quality
The second limitation relates to data quality and completeness. Submission of HES records is mandatory and, in general, coverage is very high. Most debates around HES data quality concern the primary and secondary diagnostic and procedure field. 9,44–46 Nonetheless, a recent systematic review of discharge coding accuracy in routine UK data found that primary diagnosis accuracy has improved from 73.8% to 96.0% in the 10 years since the introduction of Payment by Results. 47 Not all delivery records contain supplementary information, although the percentage of records with a complete maternity tail has improved over time. 48 We found that the proportion of missing values for the key data items of parity, gestational age, birthweight and stillbirth decreased from 24%, 48%, 26% and 2.8%, respectively, in 2002–3 to 16%, 12%, 10% and 0.15%, respectively, in 2011–12. We also carried out sensitivity analyses, comparing analyses based on assumptions about missing variables with analyses in which we excluded records with missing variables and found no major differences in RR and its 95% CIs. Administrative data have more general limitations in the recording of other potential confounders. It is well known that body mass index, smoking status and environmental factors, such as air pollution, are important risk factors for adverse outcomes in pregnancy. 49–52 However, these variables are not recorded in the HES data set.
There are previously documented missing or invalid values in the HES database for patient identifiers, dates of admission, discharge or procedure, method of admission or other key fields. 24,53 Improvements in the quality of the HES data are visible but, importantly, there are unlikely to be biases in recording for women undergoing non-obstetric surgery during their pregnancy, which means that data incompleteness and inaccuracy are unlikely to wholly account for findings.
Spontaneous abortion
A specific limitation around spontaneous abortion is that many spontaneous abortions will not be associated with a hospital admission and these will not be included in our analysis. It is certain, therefore, that our category of spontaneous abortion associated with hospitalisation is only a small proportion of all spontaneous abortions. A spontaneous abortion may be more likely to be reported if it occurs during the same hospital admission as a procedure, and this could account for the increased risk associated with surgery during pregnancy. However, only 1.8% (56/3176) of spontaneous abortions associated with hospitalisation actually occurred in the same admission as the procedure. Gestational age at delivery was essential to determine the trimester in which the procedure was carried out, but was not present on our records for spontaneous abortions associated with hospitalisation. We have already discussed the probable explanation for the increased risk for laparoscopic versus open abdominal surgery for spontaneous abortion. In addition, some of the risk factors that appear to be protective for this outcome, such as gestational diabetes and obstetric surgery, may simply reflect the fact that most spontaneous abortions occur before there is an opportunity for these potential risk factors to occur or be recorded. We carried out a sensitivity analysis in our logistic regression to exclude gestational diabetes, obstetric surgery and operations on the amniotic cavity from the model for spontaneous abortion associated with hospitalisation and found that the adjusted ORs did not change.
Because of the serious potential for ascertainment bias, temporal issues around the recording of risk factors and other unaccounted for confounding related to gestational age, we urge caution when interpreting the risk of spontaneous abortion associated with non-obstetric surgery during pregnancy.
Statistical analyses
Despite the evident advantage of the method introduced by Austin,30 particularly for common outcomes (e.g. caesarean section), the size of the database meant that the calculation of the CIs for one outcome took several days of computing time to run. We therefore had to be selective and were forced to make a priori judgements about which statistical analysis to present. Consequently, not all CIs were estimated. However, the RRs estimated using adjusted ORs obtained directly from the logistic regression, in most cases, were the same as or only slightly different from the RRs obtained using the Austin method. 30
We carried out two-level logistic regression to investigate the effects of hospitals on the adverse birth outcomes. The interclass correlation coefficients were close to 0, meaning that adjusting for the clustering of pregnancies within each trust would be unlikely to affect our results.
Recommendations for further research
Our study has demonstrated that there is a statistically significant increase in the risk of adverse birth outcomes following non-obstetric surgery during pregnancy in England. However, we have identified a number of limitations that would benefit from further research to usefully inform a variety of medical practitioners and the general public. We offer a small set of recommendations for further research:
-
Further research is required to evaluate the association of non-obstetric surgery and spontaneous abortion.
-
Further research is needed to evaluate the impact of non-obstetric surgery on the baby (e.g. neonatal intensive care unit admission, prolonged length of neonatal stay, neonatal death) and could be assessed by linking the maternal and baby records within the HES database. Use of large clinical databases, such as EuroKing Maternity systems (www.euroking.com/), linked to the HES database could be usefully exploited for this purpose.
Dissemination activity
-
To date, we have disseminated findings from this project as an oral presentation at the Applied Epidemiology Scientific Meeting in Warwick University, March 2015.
-
We presented some results to an international science competition FameLab (Lithuania) in April 2015 (www.famelab.lt/apie/).
-
We shall give an oral presentation at the Dame Hilda Lloyd Congress Medal plenary session at the Royal College of Obstetricians and Gynaecologists (RCOG) World Congress in June 2016.
-
We have written up our findings in an academic peer-reviewed journal. 54
-
We have already engaged with the British Society of Endocrine and Thyroid Surgeons and the Association of Breast Surgery, both of which have guidelines. Both organisations have agreed to consider hosting guidance that we produce on their websites.
-
The data will also be used by institutions such as RCOG and the American College of Obstetricians and Gynecologists (ACOG). We are in contact with the RCOG, and it is supportive of our study and would assist in the dissemination of findings to both health-care professionals and the public.
-
We shall contact the ACOG directly following publication to ensure that they are aware of our study. We shall also discuss the possibility of publishing a British guideline taking into account all available evidence, with the RCOG, the Anaesthetists Association of Great Britain and Northern Ireland and the Royal College of Midwives (RCM).
-
We shall contact the RCM directly to ensure that it is aware of our study, and to make sure that it is included in any joint guidelines produced.
-
We shall ensure that a lay summary of our peer-reviewed findings is available online, initially on the Imperial College London website.
Chapter 5 Conclusions
This is the first study to report the risk of adverse birth outcomes following non-obstetric surgery during pregnancy across NHS hospitals in England. We have no means of disentangling the effect of the surgery from the effect of the underlying condition itself. We found that non-obstetric surgery during pregnancy was associated with a significantly higher risk of all the outcomes we looked at, although, because of the potential for ascertainment bias, we have some reservations over the findings associated with spontaneous abortion. The overall attributable risk of an adverse birth outcome in women who had surgery during their pregnancy compared with women who did not was generally low. We estimated that, for every 287 pregnancies in which a surgical procedure was carried out, there was one additional stillbirth; for every 31 procedures there was one additional preterm delivery; for every 25 procedures there was one additional caesarean section; for every 50 procedures there was one additional long inpatient stay; for every 39 procedures there was one additional low-birthweight baby; and for every 7692 procedures there was one additional maternal death in hospital.
Our observational study can never attribute a causal relationship between surgery and adverse birth outcomes. However, we still believe that our findings and, in particular, the NNHs, improve on previous research, by utilising a more recent and larger data set based on UK practice, and are useful reference points for any discussion of risk with prospective patients.
Acknowledgements
This report represents independent research supported by the National Institute for Health Research (NIHR). The views expressed are those of the authors and not necessarily those of the NHS, NIHR or the Department of Health. The Dr Foster Unit at Imperial is partly funded by a research grant from Dr Foster (an independent health-service research organisation). We are also grateful for support from the NIHR Biomedical Research Centre funding scheme.
We would also like to thank Emma Cooper for her input into the original proposal and her assistance in overseeing the study as a patient representative.
Contributions of authors
Paul Aylin was instrumental in securing the data.
Paul Aylin, Alex Bottle and Violeta Balinskaite carried out the analysis and wrote the first draft.
All authors contributed to the original research proposal, helped to refine the classification of outcomes used and the procedure groups for further analysis, and commented on subsequent drafts of the report.
Ethics
We have permission from the Confidentiality Advisory Group under Section 251 of the NHS Act 2006 (formerly Section 60 approval from the Patient Information Advisory Group) to hold confidential data and analyse them for research purposes [PIAG 2–05(d)/2007]. We have approval to use them for research and measuring quality of delivery of health care from the South East Ethics Research Committee (10/H1102/25).
Publications
Balinskaite V, Bottle A, Sodhi V, Rivers A, Bennett PR, Brett SJ, et al. The risk of adverse pregnancy outcomes following nonobstetric surgery during pregnancy: estimates from a retrospective cohort study of 6.5 million pregnancies [published online ahead of print September 14 2016]. Ann Surg 2016.
Data sharing statement
Under the terms of our contract with the Health and Social Care Information Centre, we are allowed to hold our data only for as long as is specified in our data release agreement (usually 3 years unless renewed) and we are unable to share these data with other organisations. At the end of our contract we are obliged to delete the data. All source data, however, are available on application to the Health and Social Care Information Centre.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
References
- Mhuireachtaigh RN, O’Gorman DA. Anesthesia in pregnant patients for nonobstetric surgery. J Clin Anesthes 2006;18:60-6. http://dx.doi.org/10.1016/j.jclinane.2004.11.009.
- Duncan P, Pope W, Cohen M, Greer N. Fetal risk of anesthesia and surgery during pregnancy. Anesthesiology 1986;64:790-4. http://dx.doi.org/10.1097/00000542-198606000-00019.
- Mazze RI, Källén B. Reproductive outcome after anesthesia and operation during pregnancy: a registry study of 5405 cases. Am J Obstet Gynecol 1989;161:1178-85. http://dx.doi.org/10.1016/0002-9378(89)90659-5.
- Mazze RI, Källén B. Appendectomy during pregnancy: a Swedish registry study of 778 cases. Obstet Gynecol 1991;77:835-40.
- Reedy MB, Källén B, Kuehl TJ. Laparoscopy during pregnancy: a study of five fetal outcome parameters with use of the Swedish Health Registry. Am J Obstet Gynecol 1997;177:673-9. http://dx.doi.org/10.1016/S0002-9378(97)70163-7.
- Cohen-Kerem R, Railton C, Oren D, Lishner M, Koren G. Pregnancy outcome following non-obstetric surgical intervention. Am J Surg 2005;190:467-73. http://dx.doi.org/10.1016/j.amjsurg.2005.03.033.
- Aylin P, Williams S, Bottle A, Jarman B. Counting hospital activity: spells or episodes?. BMJ 2004;329. http://dx.doi.org/10.1136/bmj.329.7476.1207.
- The NHS Information Centre for Health and Social Care . HES Online Hospital Episode Statistics 2010. www.hscic.gov.uk/hes (accessed April 2016).
- Knight HE, Gurol-Urganci I, Mahmood TA, Templeton A, Richmond D, Van der Meulen JH, et al. Evaluating maternity care using national administrative health datasets: how are statistics affected by the quality of data on method of delivery?. BMC Health Serv Res 2013;13. http://dx.doi.org/10.1186/1472-6963-13-200.
- Epstein D, Mason A. Costs and prices for inpatient care in England: mirror twins or distant cousins?. Health Care Manag Sci 2006;9:233-42. http://dx.doi.org/10.1007/s10729-006-9090-4.
- Knight H, Cromwell D, van der Meulen J, Gurol-Urganci I, Richmond D, Mahmood T, et al. Patterns of Maternity Care in English NHS Hospitals. London: Royal College of Obstetricians and Gynaecologists; 2013.
- Methodology for Identifying and Removing Duplicate Records from the HES Dataset. Leeds: Health and Social Care Information Centre; 2014.
- Fantini MP, Stivanello E, Frammartino B, Barone AP, Fusco D, Dallolio L, et al. Risk adjustment for inter-hospital comparison of primary cesarean section rates: need, validity and parsimony. BMC Health Serv Res 2006;6. http://dx.doi.org/10.1186/1472-6963-6-100.
- Erekson EA, Brousseau EC, Dick-Biascoechea MA, Ciarleglio MM, Lockwood CJ, Pettker CM. Maternal postoperative complications after nonobstetric antenatal surgery. J Matern Fetal Neonatal Med 2012;25:2639-44. http://dx.doi.org/10.3109/14767058.2012.704445.
- Main EK, Moore D, Farrell B, Schimmel LD, Altman RJ, Abrahams C, et al. Is there a useful cesarean birth measure? Assessment of the nulliparous term singleton vertex cesarean birth rate as a tool for obstetric quality improvement. Am J Obstet Gynecol 2006;194:1644-51. http://dx.doi.org/10.1016/j.ajog.2006.03.013.
- Arck PC, Rücke M, Rose M, Szekeres-Bartho J, Douglas AJ, Pritsch M, et al. Early risk factors for miscarriage: a prospective cohort study in pregnant women. Reprod Biomed Online 2008;17:101-13. http://dx.doi.org/10.1016/S1472-6483(10)60300-8.
- de Bernabé JV, Soriano T, Albaladejo R, Juarranz M, Calle ME, Martínez D, et al. Risk factors for low birth weight: a review. Eur J Obstet Gynecol Repro Biol 2004;116:3-15. http://dx.doi.org/10.1016/j.ejogrb.2004.03.007.
- Dempsey JC, Ashiny Z, Qiu C-F, Miller RS, Sorensen TK, Williams MA. Maternal pre-pregnancy overweight status and obesity as risk factors for cesarean delivery. J Matern Fetal Neonatal Med 2005;17:179-85. http://dx.doi.org/10.1080/14767050500073456.
- García-Enguídanos A, Calle M, Valero J, Luna S, Domínguez-Rojas V. Risk factors in miscarriage: a review. Eur J Obstet Gynecol Reprod Biol 2002;102:111-19. http://dx.doi.org/10.1016/S0301-2115(01)00613-3.
- Flenady V, Koopmans L, Middleton P, Frøen JF, Smith GC, Gibbons K, et al. Major risk factors for stillbirth in high-income countries: a systematic review and meta-analysis. Lancet 2011;377:1331-40. http://dx.doi.org/10.1016/S0140-6736(10)62233-7.
- Gardosi J, Madurasinghe V, Williams M, Malik A, Francis A. Maternal and fetal risk factors for stillbirth: population based study. BMJ 2013;346. http://dx.doi.org/10.1136/bmj.f108.
- Goldenberg RL, Culhane JF, Iams JD, Romero R. Epidemiology and causes of preterm birth. Lancet 2008;371:75-84. http://dx.doi.org/10.1016/S0140-6736(08)60074-4.
- Flores PL, Gonzalez Perez G, Trejo FJ, Vega LG, Cabrera Pivaral C, Campos A. Risk factors in cesarean section. Ginecol Obstet Mex 2008;76:392-7.
- Carstairs V, Morris R. Deprivation and Health in Scotland. Aberdeen: Aberdeen University Press; 1991.
- Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987;40:373-83. http://dx.doi.org/10.1016/0021-9681(87)90171-8.
- Bottle A, Aylin P. Application of AHRQ patient safety indicators to English hospital data. Qual Saf Health Care 2009;18:303-8. http://dx.doi.org/10.1136/qshc.2007.026096.
- Altman DG. Practical Statistics for Medical Research. Boca Raton, FL: CRC Press; 1990.
- Zhang J, Kai FY. What’s the relative risk? A method of correcting the odds ratio in cohort studies of common outcomes. JAMA 1998;280:1690-1. http://dx.doi.org/10.1001/jama.280.19.1690.
- Daly LE. Confidence limits made easy: interval estimation using a substitution method. Am J Epidemiol 1998;147:783-90. http://dx.doi.org/10.1093/oxfordjournals.aje.a009523.
- Austin PC. Absolute risk reductions, relative risks, relative risk reductions, and numbers needed to treat can be obtained from a logistic regression model. J Clin Epidemiol 2010;63:2-6. http://dx.doi.org/10.1016/j.jclinepi.2008.11.004.
- Schechtman E. Odds ratio, relative risk, absolute risk reduction, and the number needed to treat – which of these should we use?. Value Health 2002;5:431-6. http://dx.doi.org/10.1046/J.1524-4733.2002.55150.x.
- Cook RJ, Sackett DL. The number needed to treat: a clinically useful measure of treatment effect. BMJ 1995;310:452-4. http://dx.doi.org/10.1136/bmj.310.6977.452.
- Efron B, Tibshirani RJ. An Introduction to the Bootstrap. Boca Raton, FL: CRC Press; 1994.
- Goldstein H. Multilevel Statistical Models. Hoboken, NJ: John Wiley & Sons; 2011.
- Gerstenfeld TS, Chang DT, Pliego AR, Wing DA. Nonobstetrical abdominal surgery during pregnancy in women’s hospital. J Matern Fetal Neonatal Med 2000;9:170-2. http://dx.doi.org/10.1002/1520-6661(200005/06)9:3<170::AID-MFM4>3.0.CO;2-P.
- Fatum M, Rojansky N. Laparoscopic surgery during pregnancy. Obstet Gynecol Surv 2001;56:50-9. http://dx.doi.org/10.1097/00006254-200101000-00025.
- Pearl J, Price R, Richardson W, Fanelli R. Guidelines for diagnosis, treatment, and use of laparoscopy for surgical problems during pregnancy. Surg Endosc 2011;25:3479-92. http://dx.doi.org/10.1007/s00464-011-1927-3.
- Sadot E, Telem DA, Arora M, Butala P, Nguyen SQ, Divino CM. Laparoscopy: a safe approach to appendicitis during pregnancy. Surg Endosc 2010;24:383-9. http://dx.doi.org/10.1007/s00464-009-0571-7.
- Rollins M, Chan K, Price R. Laparoscopy for appendicitis and cholelithiasis during pregnancy: a new standard of care. Surg Endosc 2004;18:237-41. http://dx.doi.org/10.1007/s00464-003-8811-8.
- Knight M, Kenyon S, Brocklehurst P, Neilson J, Shakespeare J, Kurinczuk JJ. Saving Lives, Improving Mothers’ Care – Lessons Learned to Inform Future Maternity Care from the UK and Ireland Confidential Enquires into Maternal Deaths and Morbidity 2009–2012. Oxford: National Perinatal Epidemiology Unit, University of Oxford; 2014.
- Barone JE, Bears S, Chen S, Tsai J, Russell JC. Outcome study of cholecystectomy during pregnancy. Am J Surg 1999;177:232-6. http://dx.doi.org/10.1016/S0002-9610(99)00007-0.
- Carver TW, Antevil J, Egan JC, Brown CV. Appendectomy during early pregnancy: what is the preferred surgical approach?. Am Surg 2005;71:809-12.
- Jenkins TM, Mackey SF, Benzoni EM, Tolosa JE, Sciscione AC. Non-obstetric surgery during gestation: risk factors for lower birthweight. Aust N Z J Obstet Gynaecol 2003;43:27-31. http://dx.doi.org/10.1046/j.0004-8666.2003.00001.x.
- Evans R, Zorlu G, Boseley S. Flaws in hospital episode statistics revealed by FoI requests. Guardian 2010.
- Kirkman MA, Mahattanakul W, Gregson BA, Mendelow AD. The accuracy of hospital discharge coding for hemorrhagic stroke. Acta Neurol Belg 2009;109:114-19.
- Haliasos N, Rezajooi K, O’Neill K, Van Dellen J, Hudovsky A, Nouraei S. Financial and clinical governance implications of clinical coding accuracy in neurosurgery: a multidisciplinary audit. Br J Neurosurg 2010;24:191-5. http://dx.doi.org/10.3109/02688690903536595.
- Burns E, Rigby E, Mamidanna R, Bottle A, Aylin P, Ziprin P, et al. Systematic review of discharge coding accuracy. J Public Health 2012;34:138-48. http://dx.doi.org/10.1093/pubmed/fdr054.
- Murray J, Saxena S, Modi N, Majeed A, Aylin P, Bottle A. Quality of routine hospital birth records and the feasibility of their use for creating birth cohorts. J Public Health 2012;35:298-307. http://dx.doi.org/10.1093/pubmed/fds077.
- Padula AM, Mortimer K, Hubbard A, Lurmann F, Jerrett M, Tager IB. Exposure to traffic-related air pollution during pregnancy and term low birth weight: estimation of causal associations in a semiparametric model. Am J Epidemiol 2012;176:815-24. http://dx.doi.org/10.1093/aje/kws148.
- Olsson D, Mogren I, Forsberg B. Air pollution exposure in early pregnancy and adverse pregnancy outcomes: a register-based cohort study. BMJ Open 2013;3. http://dx.doi.org/10.1136/bmjopen-2012-001955.
- Liu X, Du J, Wang G, Chen Z, Wang W, Xi Q. Effect of pre-pregnancy body mass index on adverse pregnancy outcome in north of China. Arch Gynecol Obstet 2011;283:65-70. http://dx.doi.org/10.1007/s00404-009-1288-5.
- Hackshaw A, Rodeck C, Boniface S. Maternal smoking in pregnancy and birth defects: a systematic review based on 173 687 malformed cases and 11.7 million controls. Hum Reprod Update 2011;17:589-604. http://dx.doi.org/10.1093/humupd/dmr022.
- Hansell A, Bottle A, Shurlock L, Aylin P. Accessing and using hospital activity data. J Public Health 2001;23:51-6. http://dx.doi.org/10.1093/pubmed/23.1.51.
- Balinskaite V, Bottle A, Sodhi V, Rivers A, Bennett PR, Brett SJ, et al. The risk of adverse pregnancy outcomes following nonobstetric surgery during pregnancy: estimates from a retrospective cohort study of 6.5 million pregnancies. Ann Surg 2016.
Appendix 1 Office of Population, Censuses and Surveys’s Classification of Surgical Operations and Procedures, codes and descriptions of procedures of common surgical groups
| Description | Code |
|---|---|
| Other specified excision of peripheral nerve | A598 |
| Radiofrequency controlled thermal destruction of peripheral nerve | A604 |
| Injection of destructive substance into peripheral nerve | A605 |
| Selective denervation of peripheral nerve | A606 |
| Other specified destruction of peripheral nerve | A608 |
| Unspecified destruction of peripheral nerve | A609 |
| Excision of lesion of peripheral nerve | A611 |
| Cryotherapy to lesion of peripheral nerve | A612 |
| Secondary microsurgical graft to peripheral nerve | A622 |
| Primary microsurgical repair of peripheral nerve NEC | A624 |
| Microsurgical repair of multiple peripheral nerves NEC | A627 |
| Unspecified microsurgical repair of peripheral nerve | A629 |
| Primary repair of peripheral nerve NEC | A642 |
| Unspecified other repair of peripheral nerve | A649 |
| Carpal tunnel release | A651 |
| Unspecified release of entrapment of peripheral nerve at wrist | A659 |
| Cubital tunnel release | A671 |
| Other specified release of entrapment of peripheral nerve at other site | A678 |
| Primary neurolysis of peripheral nerve and transposition of peripheral nerve | A681 |
| Neurolysis of peripheral nerve and transposition of peripheral nerve NEC | A683 |
| Primary neurolysis of peripheral nerve NEC | A684 |
| Unspecified other release of peripheral nerve | A689 |
| Revision of carpal tunnel release | A692 |
| Implantation of neurostimulator into peripheral nerve | A701 |
| Biopsy of lesion of peripheral nerve | A731 |
| Decompression of peripheral nerve NEC | A733 |
| Exploration of peripheral nerve | A734 |
| Transfer and reimplantation of peripheral nerve NEC | A736 |
| Other specified other operations on peripheral nerve | A738 |
| Endoscopic excision of infrapatellar fat pad | O192 |
| Unspecified prosthetic replacement of head of radius using cement | O249 |
| Other specified other prosthetic replacement of head of radius | O268 |
| Extra-articular ligament reconstruction for stabilisation of joint | O271 |
| Repair of capsule and anterior labrum for stabilisation of glenohumeral joint | O273 |
| Subacromial decompression | O291 |
| Excision of lesion of chest wall | T013 |
| Correction of pectus deformity of chest wall | T021 |
| Removal of prosthesis from chest wall | T024 |
| Removal of wire from chest wall | T054 |
| Other specified other operations on chest wall | T058 |
| Palmar fasciectomy | T521 |
| Plantar fasciectomy | T523 |
| Other specified excision of other fascia | T528 |
| Excision of lesion of fascia | T531 |
| Destruction of lesion of fascia | T532 |
| Division of palmar fascia | T541 |
| Unspecified division of fascia | T549 |
| Release fasciotomy of forearm | T552 |
| Release fasciotomy of anterior compartment of lower leg | T554 |
| Release fasciotomy of posterior compartment of lower leg | T555 |
| Release fasciotomy of leg NEC | T556 |
| Other specified release of fascia | T558 |
| Unspecified release of fascia | T559 |
| Dermofasciectomy | T561 |
| Biopsy of lesion of fascia | T572 |
| Repair of fascia | T573 |
| Excision of ganglion of wrist | T591 |
| Excision of ganglion of hand NEC | T592 |
| Excision of ganglion of knee | T593 |
| Excision of ganglion of foot | T594 |
| Other specified excision of ganglion | T598 |
| Unspecified excision of ganglion | T599 |
| Re-excision of ganglion of wrist | T601 |
| Re-excision of ganglion of hand NEC | T602 |
| Re-excision of ganglion of foot | T604 |
| Total excision of bursa | T621 |
| Excision of bursa NEC | T622 |
| Aspiration of bursa | T624 |
| Injection into bursa | T625 |
| Other specified operations on bursa | T628 |
| Multiple transfer of tendon to tendon | T641 |
| Transfer of tendon to tendon NEC | T642 |
| Insertion of tendon into bone NEC | T644 |
| Tenodesis | T645 |
| Other specified transposition of tendon | T648 |
| Excision of lesion of tendon | T652 |
| Other specified excision of tendon | T658 |
| Primary repair of tendon using tendon transfer procedure | T671 |
| Primary repair of tendon using lengthening procedure | T672 |
| Primary repair of tendon using permanent prosthesis | T673 |
| Primary repair of tendon using temporary prosthesis | T674 |
| Primary repair of tendon using graft | T675 |
| Primary simple repair of tendon | T676 |
| Other specified primary repair of tendon | T678 |
| Unspecified primary repair of tendon | T679 |
| Secondary repair of tendon using tendon transfer procedure | T681 |
| Secondary repair of tendon using temporary prosthesis | T684 |
| Secondary repair of tendon using graft | T685 |
| Primary tenolysis | T691 |
| Other specified freeing of tendon | T698 |
| Tenotomy NEC | T702 |
| Adjustment to muscle origin of tendon | T703 |
| Lengthening of tendon | T705 |
| Tenosynovectomy | T711 |
| Other specified excision of sheath of tendon | T718 |
| Reconstruction of sheath of tendon | T721 |
| Biopsy of lesion of sheath of tendon | T722 |
| Release of constriction of sheath of tendon | T723 |
| Exploration of sheath of tendon | T724 |
| Other specified other operations on sheath of tendon | T728 |
| Exploration of tendon NEC | T743 |
| Injection of therapeutic substance into tendon NEC | T744 |
| Other specified other operations on tendon | T748 |
| Microvascular free tissue transfer of flap of muscle | T761 |
| Unspecified transplantation of muscle | T769 |
| Excision of whole muscle group | T771 |
| Wide excision of muscle | T772 |
| Partial excision of muscle NEC | T773 |
| Debridement of muscle NEC | T774 |
| Other specified excision of muscle | T778 |
| Plastic repair of rotator cuff of shoulder NEC | T791 |
| Other specified repair of muscle | T798 |
| Unspecified repair of muscle | T799 |
| Other specified release of contracture of muscle | T808 |
| Biopsy of neuromuscular junction | T812 |
| Biopsy of lesion of muscle NEC | T813 |
| Other specified biopsy of muscle | T818 |
| Unspecified biopsy of muscle | T819 |
| Exploration of muscle | T834 |
| Catheter manometry of muscle compartment | T835 |
| Other specified other operations on muscle | T838 |
| Excision of lesion of soft tissue NEC | T962 |
| Other specified other operations on soft tissue | T968 |
| Primary anterior decompression of cervical spinal cord and fusion of joint of cervical spine | V221 |
| Other specified primary decompression operations on cervical spine | V228 |
| Primary decompression of thoracic spinal cord NEC | V242 |
| Other specified decompression operations on thoracic spine | V248 |
| Primary posterior decompression of lumbar spine and intertransverse fusion of joint of lumbar spine | V253 |
| Primary posterior laminectomy decompression of lumbar spine | V254 |
| Primary posterior decompression of lumbar spine NEC | V255 |
| Primary lateral foraminotomy of lumbar spine | V256 |
| Other specified primary decompression operations on lumbar spine | V258 |
| Unspecified primary decompression operations on lumbar spine | V259 |
| Other specified revisional decompression operations on lumbar spine | V268 |
| Primary insertion of lumbar interspinous process spacer | V281 |
| Primary anterior excision of cervical intervertebral disc and interbody fusion of joint of cervical spine | V294 |
| Primary anterior excision of cervical intervertebral disc NEC | V295 |
| Primary microdiscectomy of cervical intervertebral disc | V296 |
| Other specified primary excision of cervical intervertebral disc | V298 |
| Revisional excision of thoracic intervertebral disc, unspecified | V329 |
| Primary laminectomy excision of lumbar intervertebral disc | V331 |
| Primary fenestration excision of lumbar intervertebral disc | V332 |
| Primary anterior excision of lumbar intervertebral disc NEC | V334 |
| Primary microdiscectomy of lumbar intervertebral disc | V337 |
| Other specified primary excision of lumbar intervertebral disc | V338 |
| Unspecified primary excision of lumbar intervertebral disc | V339 |
| Revisional laminectomy excision of lumbar intervertebral disc | V341 |
| Revisional microdiscectomy of lumbar intervertebral disc | V347 |
| Primary fusion of joint of thoracic spine | V381 |
| Other specified primary fusion of other joint of spine | V388 |
| Revisional transforaminal interbody fusion of joint of lumbar spine | V397 |
| Posterior attachment of correctional instrument to spine | V411 |
| Anterior attachment of correctional instrument to spine | V412 |
| Removal of correctional instrument from spine | V413 |
| Other specified instrumental correction of deformity of spine | V418 |
| Excision of lesion of cervical vertebra | V431 |
| Excision of lesion of thoracic vertebra | V432 |
| Biopsy of cervical vertebra | V471 |
| Biopsy of lumbar vertebra | V473 |
| Radiofrequency controlled thermal denervation of spinal facet joint of cervical vertebra | V481 |
| Denervation of spinal facet joint of thoracic vertebra NEC | V484 |
| Radiofrequency controlled thermal denervation of spinal facet joint of lumbar vertebra | V485 |
| Denervation of spinal facet joint of lumbar vertebra NEC | V486 |
| Unspecified denervation of spinal facet joint of vertebra | V489 |
| Manipulation of spine using traction | V501 |
| Other specified manipulation of spine | V508 |
| Unspecified manipulation of spine | V509 |
| Destruction of intervertebral disc NEC | V522 |
| Discography of intervertebral disc | V523 |
| Biopsy of lesion of intervertebral disc NEC | V524 |
| Other specified other operations on intervertebral disc | V528 |
| Other specified other operations on spine | V548 |
| One level of spine | V551 |
| Two levels of spine | V552 |
| Primary hemilaminectomy decompression of lumbar spine | V672 |
| Complex reconstruction of soft tissue of hand NEC | W024 |
| Osteotomy of multiple metatarsals | W032 |
| Total correction of claw toe | W033 |
| Localised fusion of joints of mid-foot and forefoot | W035 |
| Other specified complex reconstruction of forefoot | W038 |
| Implantation massive endoprosthetic replacement of bone | W052 |
| Attention to massive endoprosthesis of bone | W054 |
| Total excision of cervical rib | W061 |
| Total excision of rib NEC | W062 |
| Total excision of bone of foot NEC | W065 |
| Other specified total excision of bone | W068 |
| Unspecified total excision of bone | W069 |
| Excision of periarticular ectopic bone | W072 |
| Unspecified excision of ectopic bone | W079 |
| Excision of natural protuberance of bone | W081 |
| Excision of overgrowth of bone | W082 |
| Excision of excrescence of bone | W083 |
| Excision of fragment of bone | W084 |
| Partial excision of bone NEC | W085 |
| Excision of accessory ossicle | W087 |
| Other specified other excision of bone | W088 |
| Unspecified other excision of bone | W089 |
| Excision of lesion of bone NEC | W091 |
| Curettage of lesion of bone and graft HFQ | W092 |
| Curettage of lesion of bone NEC | W093 |
| Destruction of lesion of bone NEC | W094 |
| Curettage of tumour of bone NEC | W096 |
| Excision of tumour of bone | W097 |
| Angulation periarticular osteotomy and internal fixation NEC | W122 |
| Biosseus angulation periarticular osteotomy and external fixation HFQ | W123 |
| Other specified angulation periarticular division of bone | W128 |
| Displacement osteotomy | W132 |
| Relocation and derotation osteotomy | W134 |
| Other specified other periarticular division of bone | W138 |
| Unspecified other periarticular division of bone | W139 |
| Angulation diaphyseal osteotomy and internal fixation HFQ | W141 |
| Angulation diaphyseal osteotomy NEC | W143 |
| Rotation diaphyseal osteotomy and internal fixation HFQ | W144 |
| Osteotomy of neck of first metatarsal bone | W151 |
| Osteotomy of base of first metatarsal bone | W152 |
| Osteotomy of first metatarsal bone NEC | W153 |
| Osteotomy of head of metatarsal bone | W154 |
| Cuneiform osteotomy of proximal phalanx with resection of head of first metatarsal | W156 |
| Osteotomy of bone of foot and fixation HFQ | W157 |
| Other specified division of bone of foot | W158 |
| Unspecified division of bone of foot | W159 |
| Multiple osteotomy and internal fixation HFQ | W161 |
| Osteotomy and internal fixation NEC | W164 |
| Osteotomy and external fixation NEC | W165 |
| Other specified other division of bone | W168 |
| Unspecified other division of bone | W169 |
| Shortening of bone | W174 |
| Decompression of fourage of bone | W184 |
| Unspecified drainage of bone | W189 |
| Secondary open reduction of intra-articular fracture of bone | W233 |
| Secondary open reduction of fracture of bone and external fixation HFQ | W235 |
| Remanipulation of fracture of bone and skeletal traction NEC | W263 |
| Remanipulation of fracture of bone NEC | W264 |
| Application of internal fixation to bone NEC | W281 |
| Adjustment to internal fixation of bone NEC | W282 |
| Removal of internal fixation from bone NEC | W283 |
| Other specified other internal fixation of bone | W288 |
| Application of skeletal traction to bone NEC | W291 |
| Removal of skeletal traction from bone | W293 |
| Application of external fixation to bone NEC | W301 |
| Adjustment to external fixation of bone NEC | W302 |
| Removal of external fixation from bone NEC | W303 |
| Cancellous chip autograft of bone | W314 |
| Other specified other autograft of bone | W318 |
| Allograft of bone NEC | W322 |
| Open biopsy of lesion of bone | W331 |
| Debridement of bone NEC | W336 |
| Other specified other open operations on bone | W338 |
| Therapeutic drilling of bone NEC | W354 |
| Primary total prosthetic replacement of hip joint using cement | W371 |
| Primary total prosthetic replacement of hip joint not using cement | W381 |
| Primary total prosthetic replacement of hip joint NEC | W391 |
| Attention to total prosthetic replacement of hip joint NEC | W394 |
| Closed reduction of dislocated total prosthetic replacement of hip joint | W396 |
| Primary total prosthetic replacement of knee joint using cement | W401 |
| Primary total prosthetic replacement of joint using cement NEC | W431 |
| Primary total prosthetic replacement of joint not using cement NEC | W441 |
| Primary total prosthetic replacement of joint NEC | W451 |
| Other specified other total prosthetic replacement of other joint | W458 |
| Conversion to prosthetic replacement of head of femur not using cement | W472 |
| Primary prosthetic replacement of articulation of bone not using cement NEC | W531 |
| Attention to prosthetic replacement of articulation of bone NEC | W544 |
| Primary interposition arthroplasty of joint NEC | W562 |
| Primary excision arthroplasty of joint NEC | W572 |
| Primary resurfacing arthroplasty of joint | W581 |
| Unspecified other reconstruction of joint | W589 |
| Fusion of first metatarsophalangeal joint and excision of lesser metatarsophalangeal joint | W592 |
| Fusion of first metatarsophalangeal joint NEC | W593 |
| Fusion of interphalangeal joint of great toe | W594 |
| Fusion of interphalangeal joint of toe NEC | W595 |
| Revision of fusion of joint of toe | W596 |
| Primary arthrodesis and internal fixation of joint NEC | W621 |
| Primary arthrodesis and external fixation of joint NEC | W622 |
| Other specified other primary fusion of other joint | W628 |
| Unspecified other primary fusion of other joint | W629 |
| Revision of arthrodesis and internal fixation NEC | W631 |
| Other specified primary open reduction of traumatic dislocation of joint | W658 |
| Unspecified primary open reduction of traumatic dislocation of joint | W659 |
| Primary closed reduction of traumatic dislocation of joint and skeletal traction NEC | W662 |
| Other specified primary closed reduction of traumatic dislocation of joint | W668 |
| Unspecified primary closed reduction of traumatic dislocation of joint | W669 |
| Secondary open reduction of traumatic dislocation of joint NEC | W674 |
| Remanipulation of traumatic dislocation of joint | W676 |
| Other specified secondary reduction of traumatic dislocation of joint | W678 |
| Total synovectomy | W691 |
| Partial synovectomy | W693 |
| Open biopsy of synovial membrane of joint | W694 |
| Other specified open operations on synovial membrane of joint | W698 |
| Unspecified open operations on synovial membrane of joint | W699 |
| Open excision of semilunar cartilage NEC | W702 |
| Open excision of intra-articular osteophyte | W712 |
| Forage of joint | W713 |
| Other specified other open operations on intra-articular structure | W718 |
| Unspecified prosthetic reinforcement of ligament | W739 |
| Reconstruction of intra-articular ligament NEC | W742 |
| Reconstruction of extra-articular ligament NEC | W743 |
| Other specified other reconstruction of ligament | W748 |
| Unspecified other reconstruction of ligament | W749 |
| Open repair of multiple ligaments NEC | W751 |
| Open repair of intra-articular ligament NEC | W752 |
| Open repair of extra-articular ligament NEC | W753 |
| Other specified other open repair of ligament | W758 |
| Unspecified other open repair of ligament | W759 |
| Excision of ligament | W761 |
| Other specified other operations on ligament | W768 |
| Repair of capsule of joint for stabilisation of joint NEC | W771 |
| Transposition of muscle for stabilisation of joint | W772 |
| Blocking operations on joint using prosthesis for stabilisation of joint | W773 |
| Periarticular osteotomy for stabilisation of joint | W775 |
| Annular ligament reconstruction for stabilisation of joint | W776 |
| Transposition of ligament for stabilisation of joint | W777 |
| Other specified stabilising operations on joint | W778 |
| Unspecified stabilising operations on joint | W779 |
| Release of contracture of knee joint | W783 |
| Limited release of contracture of capsule of joint | W784 |
| Other specified release of contracture of joint | W788 |
| Soft tissue correction of hallux valgus | W791 |
| Excision of bunion NEC | W792 |
| Syndactylisation of lesser toes | W793 |
| Unspecified soft tissue operations on joint of toe | W799 |
| Open debridement and irrigation of joint | W801 |
| Open debridement of joint NEC | W802 |
| Open irrigation of joint NEC | W803 |
| Unspecified debridement and irrigation of joint | W809 |
| Excision of lesion of joint NEC | W811 |
| Open removal of loose body from joint | W812 |
| Drainage of joint | W813 |
| Incision of joint NEC | W814 |
| Exploration of joint NEC | W815 |
| Other specified other open operations on joint | W818 |
| Endoscopic total excision of semilunar cartilage | W821 |
| Endoscopic resection of semilunar cartilage NEC | W822 |
| Endoscopic repair of semilunar cartilage | W823 |
| Other specified therapeutic endoscopic operations on semilunar cartilage | W828 |
| Unspecified therapeutic endoscopic operations on semilunar cartilage | W829 |
| Endoscopic drilling of lesion of articular cartilage | W831 |
| Endoscopic shaving of articular cartilage | W833 |
| Endoscopic articular abrasion chondroplasty | W834 |
| Endoscopic articular thermal chondroplasty | W835 |
| Endoscopic excision of articular cartilage NEC | W836 |
| Other specified therapeutic endoscopic operations on other articular cartilage | W838 |
| Endoscopic repair of intra-articular ligament | W841 |
| Endoscopic division of synovial plica | W843 |
| Endoscopic decompression of joint | W844 |
| Endoscopic drilling of epiphysis for repair of articular cartilage | W845 |
| Endoscopic excision of synovial plica | W846 |
| Other specified therapeutic endoscopic operations on other joint structure | W848 |
| Unspecified therapeutic endoscopic operations on other joint structure | W849 |
| Endoscopic removal of loose body from knee joint | W851 |
| Endoscopic irrigation of knee joint | W852 |
| Other specified therapeutic endoscopic operations on cavity of knee joint | W858 |
| Unspecified therapeutic endoscopic operations on cavity of knee joint | W859 |
| Endoscopic removal of loose body from joint NEC | W861 |
| Other specified therapeutic endoscopic operations on cavity of other joint | W868 |
| Unspecified therapeutic endoscopic operations on cavity of other joint | W869 |
| Diagnostic endoscopic examination of knee joint and biopsy of lesion of knee joint | W871 |
| Other specified diagnostic endoscopic examination of knee joint | W878 |
| Unspecified diagnostic endoscopic examination of knee joint | W879 |
| Diagnostic endoscopic examination of joint and biopsy of lesion of joint NEC | W881 |
| Other specified diagnostic endoscopic examination of other joint | W888 |
| Unspecified diagnostic endoscopic examination of other joint | W889 |
| Endoscopic chondroplasty NEC | W891 |
| Unspecified other manipulation of joint | W919 |
| Replantation of thumb | X014 |
| Replantation of finger NEC | X015 |
| Replantation of toe | X023 |
| Amputation of phalanx of finger | X083 |
| Amputation of finger NEC | X084 |
| Other specified amputation of hand | X088 |
| Amputation of leg below knee | X095 |
| Amputation through metatarsal bones | X104 |
| Amputation of phalanx of toe | X112 |
| Other specified amputation of toe | X118 |
| Unspecified amputation of toe | X119 |
| Reamputation at higher level | X121 |
| Revision of coverage of amputation stump | X124 |
| Drainage of amputation stump | X125 |
| Other specified operations on amputation stump | X128 |
| Other specified operations for sexual transformation | X158 |
| Other specified correction of congenital deformity of hand | X218 |
| Primary osteotomy of pelvis for correction of congenital deformity of hip | X222 |
| Other specified primary correction of congenital deformity of foot | X248 |
| Unspecified primary correction of congenital deformity of foot | X249 |
| Osteotomy of body of os calcis | X251 |
| Wedge tarsectomy for correction of congenital deformity of foot | X252 |
| Other specified other correction of congenital deformity of foot | X258 |
| Release of syndactyly of toes | X272 |
| Correction of curly fifth toe | X274 |
| Other specified correction of minor congenital deformity of foot | X278 |
| Unspecified correction of minor congenital deformity of foot | X279 |
| Donation of bone marrow | X461 |
| Description | Code |
|---|---|
| Total mastectomy and excision of both pectoral muscles and part of chest wall | B271 |
| Total mastectomy and excision of pectoralis minor muscle | B273 |
| Total mastectomy NEC | B274 |
| Subcutaneous mastectomy | B275 |
| Skin sparing mastectomy | B276 |
| Other specified total excision of breast | B278 |
| Unspecified total excision of breast | B279 |
| Quadrantectomy of breast | B281 |
| Partial excision of breast NEC | B282 |
| Excision of lesion of breast NEC | B283 |
| Re-excision of breast margins | B284 |
| Wire-guided partial excision of breast | B285 |
| Excision of accessory breast tissue | B286 |
| Wire-guided excision of lesion of breast | B287 |
| Other specified other excision of breast | B288 |
| Unspecified other excision of breast | B289 |
| Revision of reconstruction of breast | B295 |
| Other specified reconstruction of breast | B298 |
| Unspecified reconstruction of breast | B299 |
| Insertion of prosthesis for breast | B301 |
| Revision of prosthesis for breast | B302 |
| Removal of prosthesis for breast | B303 |
| Renewal of prosthesis for breast | B304 |
| Other specified prosthesis for breast | B308 |
| Reduction mammoplasty | B311 |
| Augmentation mammoplasty | B312 |
| Mastopexy | B313 |
| Revision of mammoplasty | B314 |
| Other specified other plastic operations on breast | B318 |
| Percutaneous biopsy of lesion of breast | B321 |
| Biopsy of lesion of breast NEC | B322 |
| Wire-guided biopsy of lesion of breast | B323 |
| Other specified biopsy of breast | B328 |
| Unspecified biopsy of breast | B329 |
| Drainage of lesion of breast | B331 |
| Capsulotomy of breast | B332 |
| Exploration of breast | B333 |
| Other specified incision of breast | B338 |
| Subareolar excision of mammary duct | B341 |
| Excision of mammary duct NEC | B342 |
| Excision of lesion of mammary duct | B343 |
| Microdochotomy | B344 |
| Other specified operations on duct of breast | B348 |
| Unspecified operations on duct of breast | B349 |
| Excision of nipple | B352 |
| Extirpation of lesion of nipple | B353 |
| Plastic operations on nipple | B354 |
| Biopsy of lesion of nipple | B355 |
| Eversion of nipple | B356 |
| Other specified operations on nipple | B358 |
| Operations on nipple, unspecified | B359 |
| Tattooing of nipple | B364 |
| Unspecified reconstruction of nipple and areola | B369 |
| Reconstruction of breast using free deep inferior epigastric perforator flap | B393 |
| Unspecified destruction of lesion of breast | B409 |
| Block dissection of axillary lymph nodes | T852 |
| Excision or biopsy of axillary lymph node | T873 |
| Description | Code |
|---|---|
| Surgical removal of impacted wisdom tooth | F091 |
| Surgical removal of impacted tooth NEC | F092 |
| Surgical removal of wisdom tooth NEC | F093 |
| Surgical removal of tooth NEC | F094 |
| Surgical removal of retained root of tooth | F095 |
| Other specified surgical removal of tooth | F098 |
| Unspecified surgical removal of tooth | F099 |
| Full dental clearance | F101 |
| Upper dental clearance | F102 |
| Lower dental clearance | F103 |
| Extraction of multiple teeth NEC | F104 |
| Other specified simple extraction of tooth | F108 |
| Unspecified simple extraction of tooth | F109 |
| Augmentation of alveolar ridge using autobone graft | F112 |
| Endosseous implantation into jaw | F115 |
| Preprosthetic oral surgery, unspecified | F118 |
| Apicectomy of tooth | F121 |
| Root canal therapy to tooth | F122 |
| Drainage of abscess of alveolus of tooth | F161 |
| Surgical arrest of postoperative bleeding from tooth socket | F162 |
| Scaling of tooth | F164 |
| Application of fissure sealant | F165 |
| Other specified operations on tooth | F168 |
| Enucleation of dental cust of jaw | F181 |
| Marsupialisation of dental lesion of jaw | F182 |
| Other specified excision of dental lesion of jaw | F188 |
| Excision of dental lesion of jaw, unspecified | F189 |
| Excision of gingiva | F201 |
| Excision of lesion of gingiva | F202 |
| Biopsy of lesion of gingiva | F203 |
| Gingivoplasty | F204 |
| Other specified operation on gingiva | F208 |
| Operation on gingiva, unspecified | F222 |
| Description | Code |
|---|---|
| Partial excision of external ear | D012 |
| Excision of preauricular abnormality | D013 |
| Other specified excision of external ear | D018 |
| Excision of lesion of external ear | D021 |
| Other specified extirpation of lesion of external ear | D028 |
| Unspecified extirpation of lesion of external ear | D029 |
| Reconstruction of external ear using graft | D031 |
| Reconstruction of external ear NEC | D032 |
| Pinnaplasty | D033 |
| Meatoplasty of external ear | D034 |
| Other specified plastic operations on external ear | D038 |
| Drainage of haematoma of external ear | D041 |
| Drainage of abscess of external ear | D042 |
| Other specified drainage of external ear | D048 |
| Biopsy of lesion of external ear | D061 |
| Repair of lobe of external ear | D062 |
| Repair of external ear NEC | D063 |
| Other specified other operations on external ear | D068 |
| Irrigation of external auditory canal for removal of wax | D071 |
| Removal of wax from external auditory canal NEC | D072 |
| Removal of foreign body from external auditory canal | D073 |
| Other specified clearance of external auditory canal | D078 |
| Unspecified clearance of external auditory canal | D079 |
| Extirpation of lesion of external auditory canal | D081 |
| Drainage of external auditory canal | D083 |
| Irrigation of external auditory canal NEC | D085 |
| Other specified other operations on external auditory canal | D088 |
| Modified radical mastoidectomy | D102 |
| Cortical mastoidectomy | D103 |
| Simple mastoidectomy | D104 |
| Excision of lesion of mastoid | D105 |
| Revision of mastoidectomy | D106 |
| Unspecified exenteration of mastoid air cells | D109 |
| Atticotomy | D122 |
| Biopsy of mastoid | D123 |
| Exploration of mastoid | D124 |
| Atticoantrostomy | D127 |
| Other specified other operations on mastoid | D128 |
| Attention to fixtures for bone-anchored hearing prosthesis | D134 |
| Fitting of external hearing prosthesis to bone-anchored fixtures | D136 |
| Other specified attachment of bone-anchored hearing prosthesis | D138 |
| Tympanoplasty using graft | D141 |
| Tympanoplasty NEC | D142 |
| Revision of tympanoplasty | D143 |
| Combined approach tympanoplasty | D144 |
| Other specified repair of eardrum | D148 |
| Unspecified repair of eardrum | D149 |
| Myringotomy with insertion of ventilation tube through tympanic membrane | D151 |
| Suction clearance of middle ear | D152 |
| Incision of eardrum NEC | D153 |
| Prosthetic replacement of ossicular chain | D161 |
| Graft replacement of ossicular chain | D162 |
| Other specified reconstruction of ossicular chain | D168 |
| Stapedectomy | D171 |
| Other specified other operations on ossicle of ear | D178 |
| Other operations on ossicle of ear, unspecified | D179 |
| Excision of lesion of middle ear | D191 |
| Destruction of lesion of middle ear | D192 |
| Biopsy of lesion of middle ear | D201 |
| Maintenance of ventilation tube through tympanic membrane | D202 |
| Removal of ventilation tube from tympanic membrane | D203 |
| Transtympanic injection to middle ear | D207 |
| Other specified other operations on middle ear | D208 |
| Other specified operations on Eustachian canal | D228 |
| Implantation of intracochlear prosthesis | D241 |
| Transtympanic electrocochleography | D245 |
| Examination of ear under anaesthetic | D282 |
| Other specified other operations on ear | D288 |
| Unspecified excision of nose | E019 |
| Reconstruction of nose NEC | E022 |
| Septorhinoplasty using implant | E023 |
| Septorhinoplasty using graft | E024 |
| Reduction rhinoplasty | E025 |
| Rhinoplasty NEC | E026 |
| Other specified plastic operations on nose | E028 |
| Unspecified plastic operations on nose | E029 |
| Submucous excision of septum of nose | E031 |
| Excision of lesion of septum of nose | E032 |
| Biopsy of lesion of septum of nose | E033 |
| Closure of perforation of septum of nose NEC | E034 |
| Septoplasty of nose NEC | E036 |
| Other specified operations on septum of nose | E038 |
| Unspecified operations on septum of nose | E039 |
| Submucous diathermy to turbinate of nose | E041 |
| Excision of turbinate of nose NEC | E042 |
| Biopsy of lesion of turbinate of nose | E045 |
| Cauterisation of turbinate of nose | E046 |
| Other specified operations on turbinate of nose | E048 |
| Cauterisation of internal nose | E051 |
| Ligation of artery of internal nose | E052 |
| Embolisation of artery of internal nose | E053 |
| Other specified surgical arrest of bleeding from internal nose | E058 |
| Packing of posterior cavity of nose NEC | E061 |
| Packing of anterior cavity of nose NEC | E062 |
| Removal of packing from cavity of nose | E063 |
| Balloon packing of cavity of nose | E064 |
| Other specified packing of cavity of nose | E068 |
| Unspecified packing of cavity of nose | E069 |
| Septorhinoplasty NEC | E073 |
| Polypectomy of internal nose | E081 |
| Extirpation of lesion of internal nose NEC | E082 |
| Division of adhesions of internal nose | E084 |
| Removal of foreign body from cavity of nose | E085 |
| Other specified other operations on internal nose | E088 |
| Excision of lesion of external nose | E091 |
| Destruction of lesion of external nose NEC | E092 |
| Suture of external nose | E093 |
| Shave of skin of nose | E094 |
| Biopsy of lesion of external nose | E095 |
| Laser destruction of lesion of external nose | E096 |
| Other specified operations on external nose | E098 |
| Biopsy of lesion of nose NEC | E101 |
| Other specified other operations on nose | E108 |
| Transantral neurectomy of Vidian nerve using sublabial approach | E124 |
| Other specified operations on maxillary antrum using sublabial approach | E128 |
| Excision of lesion of maxillary antrum | E132 |
| Intranasal antrostomy | E133 |
| Biopsy of lesion of maxillary antrum | E134 |
| Closure of fistula between maxillary antrum and mouth | E135 |
| Puncture of maxillary antrum | E136 |
| External frontoethmoidectomy | E141 |
| Intranasal ethmoidectomy | E142 |
| External ethmoidectomy | E143 |
| Transantral ethmoidectomy | E144 |
| Other specified operations on frontal sinus | E148 |
| Unspecified operations on frontal sinus | E149 |
| Other specified operations on sphenoid sinus | E158 |
| Excision of lesion of nasal sinus NEC | E172 |
| Biopsy of lesion of nasal sinus NEC | E173 |
| Other specified operations on unspecified nasal sinus | E178 |
| Unspecified operations on unspecified nasal sinus | E179 |
| Total adenoidectomy | E201 |
| Biopsy of adenoid | E202 |
| Unspecified repair of pharynx | E219 |
| Open excision of lesion of pharynx | E231 |
| Endoscopic extirpation of lesion of pharynx NEC | E242 |
| Other specified therapeutic endoscopic operations on pharynx | E248 |
| Unspecified therapeutic endoscopic operations on pharynx | E249 |
| Drainage of retropharyngeal abscess | E272 |
| Removal of foreign body from pharynx | E274 |
| Examination of pharynx under anaesthetic | E276 |
| Other specified other operations on pharynx | E278 |
| Vocal cord medialisation using implant | E335 |
| Other specified other open operations on larynx | E338 |
| Microtherapeutic endoscopic extirpation of lesion of larynx using laser | E341 |
| Microtherapeutic endoscopic resection of lesion of larynx NEC | E342 |
| Microtherapeutic endoscopic destruction of lesion of larynx NEC | E343 |
| Other specified microtherapeutic endoscopic operations on larynx | E348 |
| Endoscopic resection of lesion of larynx | E352 |
| Endoscopic destruction of lesion of larynx | E353 |
| Endoscopic removal of foreign body from larynx | E355 |
| Other specified other therapeutic endoscopic operations on larynx | E358 |
| Injection into larynx | E381 |
| Other specified other operations on larynx | E388 |
| Closure of tracheostomy | E425 |
| Replacement of tracheostomy tube | E426 |
| Removal of tracheostomy tube | E427 |
| Unspecified exteriorisation of trachea | E429 |
| Closure of tracheocutaneous fistula | E435 |
| Diagnostic endoscopic examination of lower respiratory tract and biopsy of lesion of lower respiratory tract using rigid bronchoscope | E511 |
| Unspecified diagnostic endoscopic examination of lower respiratory tract using rigid bronchoscope | E519 |
| Bilateral dissection tonsillectomy | F341 |
| Bilateral guillotine tonsillectomy | F342 |
| Bilateral laser tonsillectomy | F343 |
| Bilateral excision of tonsil NEC | F344 |
| Excision of remnant of tonsil | F345 |
| Excision of lingual tonsil | F346 |
| Bilateral coblation tonsillectomy | F347 |
| Other specified excision of tonsil | F348 |
| Unspecified excision of tonsil | F349 |
| Destruction of tonsil | F361 |
| Biopsy of lesion of tonsil | F362 |
| Drainage of abscess of peritonsillar region | F363 |
| Removal of foreign body from tonsil | F364 |
| Other specified other operations on tonsil | F368 |
| Osteotomy of maxilla involving nasal complex | V103 |
| Description | Code |
|---|---|
| Insertion of encircling suture around perianal sphincter | H421 |
| Excision of mucosal prolapse of rectum NEC | H425 |
| Other specified perineal operations for prolapse of rectum | H428 |
| Examination of rectum under anaesthetic | H444 |
| Excision of polyp of anus | H481 |
| Excision of skin tag of anus | H482 |
| Excision of perianal wart | H483 |
| Other specified excision of lesion of anus | H488 |
| Unspecified excision of lesion of anus | H489 |
| Cauterisation of lesion of anus | H491 |
| Other specified destruction of lesion of anus | H498 |
| Anterior repair of anal sphincter | H502 |
| Other specified repair of anus | H508 |
| Unspecified repair of anus | H509 |
| Haemorrhoidectomy | H511 |
| Partial internal sphincterotomy for haemorrhoid | H512 |
| Stapled haemorrhoidectomy | H513 |
| Other specified excision of haemorrhoid | H518 |
| Unspecified excision of haemorrhoid | H519 |
| Cryotherapy to haemorrhoid | H521 |
| Injection of sclerosing substance into haemorrhoid | H523 |
| Rubber band ligation of haemorrhoid | H524 |
| Other specified destruction of haemorrhoid | H528 |
| Evacuation of perianal haematoma | H531 |
| Forced manual dilation of anus for haemorrhoid | H532 |
| Manual reduction of prolapsed haemorrhoid | H533 |
| Other specified other operations on haemorrhoid | H538 |
| Unspecified other operations on haemorrhoid | H539 |
| Anorectal stretch | H541 |
| Laying open of low anal fistula | H551 |
| Laying open of high anal fistula | H552 |
| Laying open of anal fistula NEC | H553 |
| Insertion of seton into high anal fistula and partial laying open of track HFQ | H554 |
| Probing of perineal fistula | H556 |
| Repair of anal fistula using plug | H557 |
| Other specified other operations on perianal region | H558 |
| Biopsy of lesion of anus | H561 |
| Lateral sphincterotomy of anus | H562 |
| Incision of septum of anus | H563 |
| Excision of anal fissure | H564 |
| Other specified other operations on anus | H568 |
| Unspecified other operations on anus | H569 |
| Drainage of ischiorectal abscess | H581 |
| Drainage of perianal abscess | H582 |
| Drainage of perirectal abscess | H583 |
| Other specified drainage through perineal region | H588 |
| Unspecified drainage through perineal region | H589 |
| Excision of pilonidal sinus and skin flap NEC | H592 |
| Excision of pilonidal sinus and suture HFQ | H594 |
| Other specified excision of pilonidal sinus | H598 |
| Unspecified excision of pilonidal sinus | H599 |
| Destruction of pilonidal sinus | H601 |
| Laying open of pilonidal sinus | H602 |
| Drainage of pilonidal sinus | H603 |
| Injection of radiocontrast substance into pilonidal sinus | H604 |
| Other specified other operations on pilonidal sinus | H608 |
| Description | Code |
|---|---|
| Excision of lesion of lip | F021 |
| Destruction of lesion of lip | F022 |
| Other specified extirpation of lesion of lip | F028 |
| Unspecified extirpation of lesion of lip | F029 |
| Revision of primary closure of cleft lip | F032 |
| Reconstruction of lip using skin flap | F042 |
| Other specified other reconstruction of lip | F048 |
| Excision of excess mucosa from lip | F051 |
| Suture of lip | F053 |
| Removal of suture from lip | F054 |
| Other specified other repair of lip | F058 |
| Unspecified other repair of lip | F059 |
| Biopsy of lesion of lip | F062 |
| Shave of lip | F063 |
| Other specified other operations on lip | F068 |
| Unspecified other operations on lip | F069 |
| Facelift NEC | S012 |
| Brow lift NEC | S014 |
| Abdominoplasty | S021 |
| Thigh lift | S032 |
| Excision of redundant skin or fat of arm | S033 |
| Other specified plastic excision of skin of other site | S038 |
| Excision of sweat gland bearing skin of axilla | S041 |
| Excision of sweat gland bearing skin of groin | S042 |
| Excision of sweat gland bearing skin NEC | S043 |
| Other specified other excision of skin | S048 |
| Unspecified other excision of skin | S049 |
| Microscopically controlled excision of lesion of skin of head or neck using fresh tissue technique | S051 |
| Unspecified microscopically controlled excision of lesion of skin | S059 |
| Curettage and cauterisation of lesion of skin of head or neck | S081 |
| Curettage and cauterisation of lesion of skin NEC | S082 |
| Curettage of lesion of skin of head or neck NEC | S083 |
| Other specified curettage of lesion of skin | S088 |
| Unspecified curettage of lesion of skin | S089 |
| Laser destruction of lesion of skin of head or neck | S091 |
| Laser destruction of lesion of skin NEC | S092 |
| Photodestruction of lesion of skin of head or neck NEC | S093 |
| Other specified photodestruction of lesion of skin | S098 |
| Unspecified photodestruction of lesion of skin | S099 |
| Cauterisation of lesion of skin of head or neck NEC | S101 |
| Cryotherapy to lesion of skin of head or neck | S102 |
| Electrodessication of lesion of skin of head or neck | S105 |
| Other specified other destruction of lesion of skin of head or neck | S108 |
| Cauterisation of lesion of skin NEC | S111 |
| Cryotherapy to lesion of skin NEC | S112 |
| Electrodessication of lesion of skin NEC | S115 |
| Other specified other destruction of lesion of skin of other site | S118 |
| Other specified other distant flap of skin | S208 |
| Neurovascular island sensory flap of skin NEC | S222 |
| Z-plasty to head or neck | S231 |
| Z-plasty NEC | S232 |
| W-plasty NEC | S234 |
| Other specified flap operations to relax contracture of skin | S238 |
| Unspecified local flap of skin and muscle | S249 |
| Local fasciocutaneous subcutaneous pedicle flap NEC | S252 |
| Other specified local flap of skin and fascia | S258 |
| Local subcutaneous pedicle flap of skin to head or neck NEC | S265 |
| Other specified local subcutaneous pedicle flap of skin | S268 |
| Unspecified local subcutaneous pedicle flap of skin | S269 |
| Axial pattern local flap of skin NEC | S272 |
| Random pattern local flap of skin to head or neck NEC | S273 |
| Random pattern local flap of skin NEC | S274 |
| Local flap of skin to head or neck NEC | S275 |
| Other specified other local flap of skin | S278 |
| Unspecified other local flap of skin | S279 |
| Transfer of flap of skin to head or neck | S302 |
| Revision of flap of skin to head or neck | S303 |
| Meshed split autograft of skin to head or neck | S351 |
| Meshed split autograft of skin NEC | S352 |
| Split autograft of skin to head or neck NEC | S353 |
| Other specified split autograft of skin | S358 |
| Unspecified split autograft of skin | S359 |
| Full thickness autograft of skin to head or neck | S361 |
| Full thickness autograft of skin NEC | S362 |
| Composite autograft of skin NEC | S364 |
| Other specified other autograft of skin | S368 |
| Allograft of skin NEC | S372 |
| Unspecified other graft of skin | S379 |
| Other specified graft of other tissue to skin | S398 |
| Tape closure of skin NEC | S401 |
| Tissue adhesive closure of skin NEC | S402 |
| Tape closure of skin of head or neck | S403 |
| Tissue adhesive closure of skin of head or neck | S404 |
| Other specified other closure of skin | S408 |
| Unspecified other closure of skin | S409 |
| Primary suture of skin of head or neck NEC | S411 |
| Delayed primary suture of skin of head or neck | S412 |
| Other specified suture of skin of head or neck | S418 |
| Unspecified suture of skin of head or neck | S419 |
| Primary suture of skin NEC | S421 |
| Delayed primary suture of skin NEC | S422 |
| Secondary suture of skin NEC | S423 |
| Resuture of skin NEC | S424 |
| Unspecified suture of skin of other site | S429 |
| Removal of clip from skin NEC | S432 |
| Removal of suture from skin of head or neck | S433 |
| Removal of suture from skin NEC | S434 |
| Other specified removal of repair material from skin | S438 |
| Unspecified removal of repair material from skin | S439 |
| Removal of metal from skin of head or neck | S441 |
| Removal of metal from skin NEC | S442 |
| Removal of glass from skin of head or neck | S443 |
| Removal of glass from skin NEC | S444 |
| Removal of inorganic foreign body from skin of head or neck NEC | S445 |
| Removal of inorganic foreign body from skin NEC | S446 |
| Removal of organic material from skin NEC | S454 |
| Removal of foreign body from skin of head or neck NEC | S455 |
| Removal of foreign body from skin NEC | S456 |
| Other specified removal of other substance from skin | S458 |
| Drainage of lesion of skin of head or neck | S471 |
| Drainage of lesion of skin NEC | S472 |
| Incision of lesion of skin of head or neck | S473 |
| Incision of lesion of skin NEC | S474 |
| Incision of skin of head or neck | S475 |
| Incision of skin NEC | S476 |
| Other specified opening of skin | S478 |
| Unspecified opening of skin | S479 |
| Adjustment to skin expander in subcutaneous tissue | S491 |
| Removal of skin expander from subcutaneous tissue of breast | S493 |
| Other specified attention to skin expander in subcutaneous tissue | S498 |
| Toilet to burnt skin of head or neck NEC | S543 |
| Debridement of burnt skin NEC | S551 |
| Removal of slough from burnt skin NEC | S552 |
| Cleansing and sterilisation of burnt skin NEC | S556 |
| Debridement of skin of head or neck NEC | S561 |
| Removal of slough from skin of head or neck NEC | S562 |
| Toilet to skin of head or neck NEC | S563 |
| Unspecified exploration of other skin of head or neck | S569 |
| Debridement of skin NEC | S571 |
| Removal of slough from skin NEC | S572 |
| Toilet of skin NEC | S573 |
| Cleansing and sterilisation of skin NEC | S576 |
| Dressing of skin using vacuum-assisted closure device NEC | S577 |
| Other specified exploration of other skin of other site | S578 |
| Unspecified exploration of other skin of other site | S579 |
| Larvae debridement therapy of skin NEC | S582 |
| Dermabrasion of skin of head or neck | S601 |
| Dermabrasion of skin NEC | S602 |
| Refashioning of scar NEC | S604 |
| Epilation NEC | S607 |
| Other specified other operations on skin | S608 |
| Liposuction of subcutaneous tissue NEC | S622 |
| Removal of inserted substance from subcutaneous tissue | S623 |
| Removal of pack from subcutaneous tissue | S624 |
| Removal of hormone implant from subcutaneous tissue | S625 |
| Other specified other operations on subcutaneous tissue | S628 |
| Excision of nail bed | S641 |
| Chemical destruction of nail bed | S642 |
| Destruction of nail bed NEC | S643 |
| Other specified extirpation of nail bed | S648 |
| Biopsy of lesion of nail bed | S661 |
| Repair of nail bed | S662 |
| Incision of nail bed | S663 |
| Other specified other operations on nail bed | S668 |
| Total excision of nail | S681 |
| Excision of wedge of nail | S682 |
| Partial excision of nail NEC | S683 |
| Other specified excision of nail | S688 |
| Unspecified excision of nail | S689 |
| Avulsion of nail | S701 |
| Removal of foreign body from nail | S703 |
| Other specified other operations on nail | S708 |
Glossary
- Attributable risk
- The difference in rate of a condition between an exposed population and an unexposed population.
- Hospital Episode Statistics
- An administrative database covering the main types of patient-level NHS hospital activity.
- Hospital Episode Statistics maternity tail
- In Hospital Episode Statistics, each episode related to delivery of a baby can capture details about the labour and delivery (e.g. parity, gestational age, birthweight) in supplementary data fields known as Hospital Episode Statistics ‘maternity tail’.
- Low birthweight
- A weight at birth of < 2500 g (5.5 lb) (World Health Organization definition).
- Multiparous
- The medical term used to describe a woman who has given birth before.
- Number needed to harm
- The number of patients who would have to undergo non-obstetric surgery for one of them to experience an adverse effect.
- Preterm
- Live birth before 37 weeks’ gestation (World Health Organization definition).
- Primiparous
- The medical term used to describe a woman who is giving birth for the first time.
- Relative risk
- A measure of association between a disease or condition and a factor under study.
- Spontaneous abortion
- A premature loss of a fetus up to 23 weeks of pregnancy and weighing up to 500 g (World Health Organization definition).
- Stillbirth
- A child that had issued forth from its mother after week 24 of pregnancy and which did not at any time, after being completely expelled from its mother, breathe or show any signs of life.
List of abbreviations
- ACOG
- American College of Obstetricians and Gynecologists
- CI
- confidence interval
- ENT
- ear, nose and throat
- HES
- Hospital Episode Statistics
- ICD-10
- International Classification of Diseases, Tenth Edition
- NIHR
- National Institute for Health Research
- NNH
- number needed to harm
- OPCS
- Office of Population, Censuses and Surveys’s Classification of Surgical Operations and Procedures
- OPCS-4
- Office of Population, Censuses and Surveys’s Classification of Surgical Operations and Procedures, version 4
- OR
- odds ratio
- RCM
- Royal College of Midwives
- RCOG
- Royal College of Obstetricians and Gynaecologists
- RR
- relative risk