Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 12/5002/04. The contractual start date was in June 2013. The final report began editorial review in February 2016 and was accepted for publication in June 2016. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2016. This work was produced by Bullock et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction
The focus of this research is NHS and university-based staff in knowledge brokering roles, how they link with knowledge and innovation, and how they transfer this to the health-care practitioner community. The transfer and mobilisation of knowledge from research into health-care delivery is a long-standing international challenge. 1–6 Sebba7 highlights the economic, moral and academic imperatives for investing resources in improving research use. Alongside the need to base decisions on evidence (moral imperative) and the increasing need to demonstrate impact of academic research (academic imperative), the economic imperative to ensure the best use of limited resources and minimise waste is a timely concern. In a time of unprecedented financial restrictions,8 health-care managers face the enormous challenge of purchasing and providing health care to an ageing population with increasing expectations. Management decisions about planning, commissioning and service delivery affect large populations and require large amounts of public money. Failure to inform practice with evidence limits the improvement of the effectiveness of health services, wastes money and potentially adds to the scale of preventable morbidity and mortality.
It is in this context that our study sought to find out how to get the best out of knowledge and innovation transfer (KIT) ‘agents’, that is, NHS practitioners in knowledge brokering or mobilisation roles.
Knowledge mobilisation
Gainforth et al. 9 defined knowledge mobilisation as ‘putting research in the hands of research users’, but the use of evidence is a complex, social and dynamic process. 10 To inform decision-making in practice, research evidence needs to be ‘available to those who may best use it, at the time it is needed . . . in a format that facilitates its uptake’ as well as ‘comprehensible to potential users and . . . relevant and usable in local contexts’. 11 In health care, this process and associated organisational change is widely recognised as complicated, messy, evolving and fraught with challenge. 12–14 For example, practitioners are alleged to lack the time, motivation and capacity to use evidence15,16 or are purported to be overwhelmed by the quantity of diverse evidence. 17–19 Research reports may lack relevance, can be opaque and verbose20 and it can be a long time before they are released. 21 Some argue that research output is dominated by a biomedical focus on drugs, tests and devices. Instead, Walshe and Davies22 suggest that the current ‘predominant concerns’ relate to ‘pathway and process redesign, safety and quality; organizational issues like coordination, integration and networking; workforce issues like training and skill mix; and patient issues like experience, education and empowerment’. Addressing these concerns may require alternative models of knowledge creation in order to close the knowledge–practice gap. 23,24
The policy context
There have been a number of efforts to build bridges between researchers, policy-makers and service providers, and there is growing interest in using collaborations to address the research–practice gap. 25,26 Some of these are institutional partnerships involving colocation of teams, shared resources and so forth, whereas others rely on key individuals to bridge. All aim to link knowledge and innovation producers and users through various means that may or may not include a formal knowledge broker or KIT agent. Our understanding of the work of these KIT agents remains poor, and examples of collaborations can provide insight into potential modes of and mechanisms for engagement.
Linking trusts and health boards to research teams through managers can help organisations to use research findings in their own settings, and enable them to set up service improvement projects to improve health and health-care outcomes. The review led by Sir Ian Carruthers, ‘Innovation, Health and Wealth: Accelerating Adoption and Diffusion in the NHS’,27 placed innovation at the top of the service agenda, setting out ambitious recommendations to encourage quicker transfer of new practice, ranging from infrastructure change to realignment of system incentives and promotion of high-impact initiatives. Central to the Carruthers report27 is the argument for ‘a more systematic delivery mechanism for diffusion and collaboration within the NHS by building strong cross boundary networks’. Although the proposals of the Carruthers report27 are clear – productive regional collaborations between academia, industry and the health sector to identify and spread innovation and so drive service improvement – its recommendations accommodate regional conditions. Capacity to access, understand and use research knowledge is emphasised to ‘bring about a major shift in culture within the NHS, and develop our people by “hard wiring” innovation into training and education for managers and clinicians’. The contents of this report complement these key policy themes.
Academic Health Science Collaborations, Partnerships and Networks
Following the Carruthers report,27 Academic Health Science Networks (AHSNs) have brought most NHS organisations in England into collaboration with universities. In England, 15 AHSNs were licensed in March 2013. AHSNs are tasked with aligning ‘education, clinical research, informatics, training and education and healthcare delivery’ and improving ‘patient and population health outcomes by translating research into practice and developing and implementing integrated health care systems’. 28 Like their predecessors, Academic Health Science Collaborations (AHSCs), the central aim of these collaborations is ‘knowledge mobilisation, rather than research production’. 22 As designated in ‘Innovation Health and Wealth’27 and the ‘Strategy for UK Life Sciences’,29 AHSNs are a systematic delivery mechanism for the adoption and spread of innovation at pace and scale through the NHS. The networks are designed to foster collaborations between academia, industry and health service, and shared aims include diffusing innovation, putting research into practice, and promoting economic growth. 30 They are expected to work closely with industry and funders to bring together researchers, managers, patient groups, planners and policy-makers.
Compared with England, infrastructure targeting knowledge mobilisation and innovation is not well funded in Wales. However, the sole AHSC in Wales has identified knowledge transfer as a priority. The AHSC formed three regional hubs – in the north, south-west and south-east of Wales. In their initial period, these hubs attracted small-scale funding from Health and Care Research Wales [formerly the National Institute for Social Care and Health Research (NISCHR)], but this ceased in 2014. The South East Wales Academic Health Science Partnership (SEWAHSP) became independent and continued to operate. SEWAHSP has two key objectives: (1) to increase the speed and quality of ‘translational’ research; and (2) to promote and support innovation in south-east Wales. 31 A national Task and Finish Group also made recommendations to Health and Care Research Wales on knowledge transfer policy. 32
Collaborations for Leadership in Applied Health Research and Care
Descriptive studies focused on how research does make it into practice point to the importance of close interpersonal relationships between researcher and user. 33–35 This has been built into interventions that seek to develop opportunities for both parties to link and engage. In England, these include programmes such as the National Institute for Health Research (NIHR)’s Collaborations for Leadership in Applied Health Research and Care (CLAHRCs), which were designed to address what Cooksey1 termed the ‘second gap in translation’, related to the failure of new ideas and tools to reach practice. CLAHRCs are serviced-led partnerships that aim to contract high-quality applied health research, implement findings and increase NHS capacity to engage in research. 36–39 In 2008, nine CLAHRCs were established and a second wave extended the CLAHRCs reach with tapered funding (from NIHR) for 13 CLAHRCs. This is an indicator of the perceived success of the programme.
The CLAHRCs are the most established and evaluated programmes in the UK. 39–46 The reports to date highlight similarities and differences between structural and content features of the CLAHRCs and point to early successes and challenges. For example, successes include strengthened networks and relationships;39,44,47 new organisational roles that ‘make sense to professionals’; collective action to improve practices;48 and creating a culture of reflection and learning. 47 More specific successes have also been reported. For example, the CLAHRC for Greater Manchester achieved success in improving patient services in chronic kidney disease. 41,49 Although such results demonstrate the impact of CLAHRCs and how the collaborations can change the approach of organisations for the better,39,50 it is very difficult to demonstrate a causal effect given the complexity of what they are and what they are trying to achieve. Walshe and Davies22 are more circumspect and conclude that ‘promising lessons’ can be distilled from the collaborations in England, which, among others, include ‘the development of organizational capacity in knowledge mobilisation’. Currie et al. 43 usefully summarise key areas of uncertainty for CLAHRCs, which include the problem of metrics. They note the following uncertainties:
The balance of activity between research and implementation; whether research should be clinically or implementation focused; appropriate metrics for CLAHRCs; whether CLAHRCs should orientate towards their academic or NHS partners; and whether CLAHRCs should focus upon individual behavioural or organizational/system level change.
They argue that the dominant approach is research focused, fixed on changing individual behaviour rather than ‘wider scale organizational and system level change’, as favoured by those from a social science tradition. 43
Knowledge brokers
Embedded within the concept of knowledge mobilisation are the roles of knowledge broker and boundary spanner. 51–53 Roles vary,42,54 but the essential feature is that they facilitate engagement between research and practice. 55 With the aim of improving the transfer of knowledge and innovation, knowledge brokers seek to close knowledge gaps and foster knowledge-responsive capacity and culture. 5,56–59
To facilitate knowledge mobilisation, many CLAHRCs used knowledge brokers, variously named. 22,60 For example, in the first round of CLAHRCs funding, the Cambridgeshire and Peterborough CLAHRC had a fellowship programme for clinicians, health- and social-care practitioners and managers to work alongside researchers; the Nottinghamshire, Derbyshire and Lincolnshire CLAHRC funded35 ‘diffusion fellows’ attached to their research projects. 61
The NIHR Service Delivery and Organisation (SDO) Management Fellowship programme provided another example, and one aimed exclusively at managers; an evaluation showed benefits from the interactions between the fellows, their NHS colleagues and research teams, but also revealed challenges in maximising those benefits for the workplace. 62 The NIHR SDO scheme was later merged with the NIHR Health Services Research programme to create the NIHR Health Services and Delivery Research (HSDR) programme.
As knowledge broker roles grew in number and type across the UK, an interest group formed in 2014 looking at fellows in the system. Several organisations, including the Health Foundation, NHS Education for Scotland, NHS Improving Quality, NIHR, and Universities UK, were involved in early data-gathering exercises to understand the characteristics of the wide range of fellows and fellowship programmes that exists across the health and care system. This exercise culminated in a 1-day event, ‘Fellows Connect’, bringing together quality improvement (QI) fellows from across the UK to share experiences. 63 At the same time, Berwick’s report on ‘Improving the safety of patients in England’ recommended a ‘national system of NHS Improvement Fellowships, to recognise the talent of staff and improvement capability and enable this to be available to other organisations’. 64 This resulted in the creation of an initiative called ‘Q for Quality’, led by the Health Foundation and supported and cofunded by NHS England, connecting people skilled in improvement across the UK. The Q initiative aims to grow to be a community of thousands of people: patient-facing front-line staff, managers, researchers, ‘patient leaders’, policy-makers and others in order to accelerate improvements to the quality of care. 65 Together, these recent developments illustrate the interest and also the investment by national organisations in the UK in maximising the potential of knowledge brokers to improve the quality and safety of health care for patients.
The aims and objectives of the study
The focus of this research is KIT ‘agents’ (NHS and university-based staff in knowledge brokering roles), how they link with evidence and innovation and how they transfer this to the health-care practitioner community. The study aimed to examine the work of KIT agents in practice in order to understand how the outcomes of their endeavours might be maximised. Our research questions are:
-
What are commonly shared expectations of the KIT agent role?
-
What, in practice, do KIT agents do?
-
What is their conception of KIT?
-
How do they see their role?
-
With whom do they link?
-
What are their principal activities?
-
-
How does the work of KIT agents impact on health-care practice?
-
How can KIT agents be best supported?
-
What are the barriers to, and enablers of, them meeting their objectives?
-
-
What measures can be used to assess the impact of KIT activity?
Our objectives were to:
-
map the innovation and knowledge transfer intentions of the new AHSNs and SEWAHSP
-
describe, and characterise, the roles of KIT agents and develop a typology of KIT agent roles
-
report the perceived impact of KIT agents on managers’ practice
-
investigate how KIT agents can be best supported
-
generate a set of impact measures for assessing innovation and knowledge transfer activities.
Concluding remarks
This chapter has established the importance of knowledge mobilisation in health care and provided the background policy context to the current position of initiatives designed to address the research–practice gap. We extend this in Chapter 2 by providing a summary of the literature on knowledge mobilisation.
Chapter 3 outlines the theoretical underpinnings, research study design and methods used. Chapter 4 explores the knowledge and innovation mobilisation intentions of the AHSNs in England and an Academic Health Science Partnership (AHSP) in Wales and introduces a suggested typology of the different forms that KIT roles may take.
The main reporting of the results begins in Chapter 5 with an overview of the case study KIT agents. They highlight content-specific knowledge transfer challenges, as well as generic mechanisms that support transfer. We commence the discussion of our findings in Chapter 6. We look across all the case studies to discuss common barriers and enablers reported by the KIT agents, and explore how they can be better supported in carrying out their role.
The focus of Chapter 7 is on assessing outcomes of knowledge brokering activity. It includes a report of the nominal group and also draws on the case study data and wider literature. In Chapter 8 we extend our discussion of outcomes by reviewing our findings through the lens of social marketing theory.
Last, Chapter 9 brings together the main conclusions and implications of the findings, positioning them within the wider literature and suggesting recommendations for future research.
Chapter 2 Learning from the literature
Introduction
A targeted review of literature was undertaken to identify existing KIT practices, attributes of the successful agents (knowledge brokers, boundary spanners) and outcomes. This assisted learning from previous evaluations, supported robust data analysis, informed the questions posed in the nominal group and provided a solid basis from which to consider the generalisability of findings.
Organised into six main sections, the review begins with a brief exploration of terminology from which we offer tentative definitions. We follow this with consideration of the models of knowledge transfer and mobilisation implicit in programmes designed to bridge the gap between research and health-care practice. We follow this with a section on the role of knowledge brokers or KIT agents and we identify factors shown to enable or impede knowledge transfer and mobilisation in the subsequent section. We follow this with a section summarising current knowledge on outcomes and impact of KIT programmes. The literature review concludes with a summary of main messages and an identification of further research needs.
Notes on the literature search
This review updates and builds on work previously carried out by Bullock et al. ;66 therefore, literature searches for the preparation of the current document were limited to publications post 2010. A broad search was carried out on Web of Science, PubMed, Ovid MEDLINE, Scopus, Cumulative Index to Nursing and Allied Health Literature (CINAHL) via EBSCOhost and Google Scholar™ (Google Inc., Mountain View, CA, USA) using appropriate forms of the terms, ‘knowledge AND transfer AND healthcare’, ‘knowledge’ AND (transfer OR translation OR mobili*ation) AND healthcare’, ‘innovation AND healthcare AND implementation’, knowledge AND (transfer OR exchange OR mobili*ation OR intermediatr* OR boundary spanners), ‘knowledge AND broker OR intermediary AND healthcare’, and ‘CLAHRC’. In addition, we sourced earlier papers from the citations of relevant papers and were vigilant for notifications of papers/reports as they were published. We complemented the electronic search by hand-searching two key journals (Implementation Science and Journal of Health Services Research and Policy) and searching the NIHR Journals Library of completed projects (www.journalslibrary.nihr.ac.uk). Grey literature relating to KIT policy in England and Wales was also reviewed (see Appendix 1).
Terminology
In our proposal we adopted the language of the funding call from NIHR (www.nets.nihr.ac.uk/_data/assets/pdf_file/0003/81786/CB-12-5002-04.pdf) and so refer to ‘KIT’. Lack of conceptual clarity around the theme has been noted in the literature67 and is not helped by a confusion of terms, which are ill defined and used interchangeably. 68 In this section, we draw on extant literature to develop tentative operational definitions of KIT. We did not seek to provide a comprehensive review of all terms and issues.
Knowing knowledge
Knowledge is perhaps the most easily grasped of our terms, but the most difficult to define. Some authors have classified knowledge according to the degree of analysis or inherent conceptual complexity. 69,70 Furthermore, literature on knowledge transfer is not narrowly limited to the transfer of facts to answer ‘how’ questions. Rather, although knowledge in this context is seen to include facts and information, importantly, it is also recognised as being about understanding. Knowledge in this sense can be both theoretical and practical, derived from education and experience. However, it is useful to illuminate the interpretation of terms, as they embody implicit assumptions about how knowledge may be transferred, exchanged and mobilised. The different terms used are associated with different concerns and values, and these have practical consequences. Conceptualising knowledge as empirical information, facts or data decontextualises and commodifies it as something that can be ‘moved around’. 4,71 Alavi and Leidner,72 writing about the conceptual foundations of knowledge management, describe the relationship between knowledge and values, experience and context. They explain how knowledge ‘originates and is applied in the minds of knowers’ and how in organisations ‘it often becomes embedded not only in documents or repositories but also in organizational routines, processes, practices and norms’. 72 This quotation raises the distinction between explicit knowledge, written and recorded in documents, and the implicit or tacit knowledge held by individuals, often without awareness of it and revealed in organisational customs.
Related to the tacit–explicit dimension of knowledge is whether it is understood as individual or social. 72 The distance between tacit (residing in the individual, difficult to transfer) and explicit knowledge (socially and organisationally located) underscores the challenge of identifying, articulating and transferring individually held knowledge. 73–76 Szulanski77 also describes how the ‘stickiness’ of knowledge can hamper its movement, and distinguishes different points at which stickiness is important, including initiation stickiness (which may be affected by competing priorities, for example) and implementation stickiness.
These issues are relevant to knowledge transfer and innovation, as they define what counts as knowledge, and influence how and if it can be transferred. A study of knowledge transfer necessarily gives greatest focus to explicit knowledge, and academic research in particular.
Knowledge and evidence
One issue that is particularly important in the health-care context is the relationship between knowledge and evidence. Knowledge and evidence are contested concepts. In health-care literature, knowledge is often synonymous with evidence and aligned with the principles of evidence-based medicine. Innvaer78 notes that a ‘call for evidence-based [decision-making] is also a call for the use of scientific methods in data collection and in the validation of information’. However, in health care, as well as evidence of effectiveness derived from traditional randomised controlled trials, evidence also needs to encompass feasibility, acceptability and appropriateness. 79
The implicit position of the NIHR,80 in relation to this field of inquiry, is complex. In the commissioning brief for this study, they noted the use of various terms and chose to adopt the term ‘innovation and knowledge transfer’. However, this did not appear to be associated with limited positivistic interpretation of research evidence, and, earlier, they recognised that ‘engagement with research is socially and organisationally situated and heavily dependent on local context’. In this interpretation, knowledge is socially situated, generated by a number of participants and methods81 and intertwined with practice. 82 It allows for the idea that knowledge can be coproduced and co-owned, and recognises the importance of tacit knowledge associated with organisational norms and customs. 72 Likewise, in the Promoting Action on Research Implementation in Health Services (PARiHS) framework,3 in addition to research, evidence includes ‘professional craft knowledge, patient preferences and experiences, and local information’. Harvey and Kitson83 have recently introduced the i-PARiHS (integrated PARiHS) framework. The ‘i’ stands for integrated and reflects how ‘evidence is incorporated within the broader concept of innovation to reflect the dynamic and iterative way in which knowledge to inform practice is generated and applied’. Neither of these definitions fit well with more formal definitions of evidence.
For clarity, we would prefer to hold the two terms as conceptually distinct, although connected, using the term ‘evidence’ to relate to a sort of knowledge defined by the way it was generated. Yet it is imperative that we use both terms as they are applied by the participants in the study in order to understand the terms and their significance from their perspective. Therefore, knowledge transfer will include forms of knowledge as relevant to participants, not simply the transfer of research findings from the positivist tradition.
The Research Supporting Practice in Education84 group at the Institute for Studies in Education, University of Toronto, has devised a potentially useful set of questions that help to clarify different aspects of knowledge and knowledge use. These questions are:
-
What knowledge (e.g. tacit, research, evidence, best practice)?
-
In whose interests (e.g. organisations, researchers, practitioners, knowledge brokers)?
-
For what purposes (e.g. change, influence, practice, decisions, empowerment)?
-
In what context (e.g. communities, workplaces, universities, boards)?
-
What techniques (e.g. guidelines, training and workshops, facilitation, communities of practice)?
-
With what impact (e.g. instrumental, conceptual, changing practice)?
Innovation
This study is interested in the transfer of innovation and knowledge. Therefore, we also need to give attention to ‘innovation’, a term that has increased in usage since publication of the Carruthers report,27 concerned with the adoption and diffusion of innovation in the NHS. This report places innovation at the top of the service agenda and sets out recommendations to encourage quicker transfer of new practice. 27
Carruthers’ definition of innovation built on Rogers’85 interpretation of innovation as a new idea, practice, or object but requiring that it is applied. According to Carruthers,27 innovation is ‘an idea, service or product, new to the NHS or applied in a way that is new to the NHS, which significantly improves the quality of health and care wherever it is applied’. Given the focus of our study on the benefits of innovation to patient care, this explicit inclusion of application in the definition seems helpful.
Alongside policy runs a literature looking at aspects of innovation in more detail. For example, Terwiesch and Ulrich52 have drawn a distinction between innovation that is ‘conceptual’ (new to a field) and innovation that is ‘contextual’ (new to an organisation). This is a potentially helpful distinction, allowing the term innovation to cover a range of ideas, services and products.
Implicit in the application of new ideas, services and products is a change in organisation and or individual behaviour. Birken et al. 86 explain that innovation implementation is a process in which organisational members become proficient in their use of a new practice. Walshe and Davies22 adopt a broad interpretation of innovation that encompasses both ‘clinical practice and service design’ and they explain that ‘service innovation means people at the front-line finding better ways of caring for patients’. Innovation in this sense may not involve formal and explicit knowledge transfer, unless these better ways are transferred outward to other colleagues and organisations. Walshe and Davies’22 perspective serves as a reminder that the focus of our study is anywhere in the health-care system that is relevant to managers’ ultimate role of improved care for patients within public service constraints, but with particular attention paid to the application of new ideas, services and products that are transferred into an organisation rather than those that emerge in an organic manner from within. It is also worth noting that while innovation can ‘go either way’ in terms of impact on care, most literature and policy appears to start from the assumption that innovation is good.
In terms of the application of innovation, Brockman and Morgan87 argue that knowledge transfer facilitates innovation, and Strach and Everett88 write that the ability to seek and maintain knowledge transfer capability facilitates a higher level of innovation. Radaelli et al. 89 found that individuals who share knowledge are also more likely to be engaged in creating and implementing innovations. This reflects a prevalent assumption that knowledge transfer is (or should be) a means to innovation. Knowledge is something you have; innovation is something you do. Innovation does not transfer, but knowledge about it does.
Transfer
The final element of KIT relates to transfer. This is a well-developed area of literature; in its commissioning brief, NIHR noted the multiplicity of terms. Prefaced by ‘knowledge’, ‘transfer’ is just one option of many. Others include ‘exchange’, ‘mobilisation’ ‘translation’, ‘management’, ‘mediation’, ‘dissemination’, ‘diffusion’, ‘utilisation’. Likewise, those working in roles to support this activity attract a variety of labels, including: ‘knowledge brokers’, ‘translators’, ‘boundary spanners’, ‘diffusion fellows’, ‘research navigators’, ‘research liaison officers’, and so forth. 13 There is both confusion of terms and confusion in the meaning of terms. 90 Knowledge translation, for example, can refer to the job of ‘translating’ lengthy and complex research reports into digests more suitable for busy practitioners; the translation of knowledge into action or practice arising from collaboration between researchers and practitioners;82,91 or the ‘transfer’ of research from one group to another with little interpretation or amendment. 7
Transfer needs to be understood in relation to definitions of knowledge and different models of KIT will prescribe the role for people and organisations responsible for enabling it.
Knowledge transfer models
Dominating policy-thinking and the biomedical research literature on knowledge transfer is a focus on the unidirectional linear flow of knowledge from one domain to the other. This transfer is intended to address an information deficit on the part of the practitioner. 92 However, it is deficient to assume that the production of the ‘right research’ will just get implemented by practitioners. 22 The process is not simply one of transference, that knowledge or innovation is something that can be parcelled up and distributed to ‘grateful recipients’. 81 The linear model, assuming a unidirectional flow of research-based knowledge19,56 and the term ‘knowledge transfer’ has been criticised for oversimplifying ‘the messy engagement of multiple players with diverse sources of knowledge’. 81 Knowledge flows not like water in a pipeline; rather, knowledge morphs and mutates as it is mobilised, being ‘personalised and recast’ by the decision-maker. 11
In an interactive model, both formal and informal links between researchers and research users are emphasised, and interpersonal and exchange relationships are seen as a means of bridging gaps. 33,35,93 Interactive or exchange models are also called ‘partnerships models’,94 ‘knowledge conduit models’,95 ‘linkage and exchange models’93 or ‘alliances, . . . collaborations, and coalitions’,96 as well as ‘mode two’45 and ‘integrative’13 or ‘integrated’ knowledge transfer. 97 Positive deviations is another term used to refer to the adoption of ‘unconventional methods’ to facilitate organisational change. 98
Partnerships in an interactive model come in a number of formats. 94,99,100 Davies et al. 90 suggested six archetypes of knowledge mobiliser: knowledge product pushers; brokers and intermediaries of their own research; brokers and intermediaries of wider research; evidence advocates (champions for evidence-informed practice); network fosterers (developing new ones and enhancing existing ones); and advancers of knowledge mobilisation (enhancing knowledge about KIT work). Within these archetypes, agents carry out three broad overlapping roles: developing and sharing research-based products, brokering and implementation. 90
There is a common expectation that the knowledge changes as a result of the interaction. Such coproduced knowledge demands a broad acceptance of what counts as evidence. 33,101,102 However, as noted earlier, this interpretation fails to fit with the idea of legitimate research evidence in evidence-based medicine. 102 A fuller discussion of linear and interactive models can be found elsewhere. 66
To address the commissioning brief, in this report we have adopted the term ‘KIT’ and we describe those supporting this activity as ‘KIT agents’. However, in our application of the term, we wish to include that sense of interaction and mobilisation, not the limited narrow notion of linear transfer.
The role of knowledge and innovation transfer agents
In this study we use ‘KIT agents’ to identify those people responsible for supporting the transfer and mobilisation of knowledge (broadly conceived) from one group to another. Potentially these groups have little contact with each other and perhaps little trust. 51,70,93,103,104 UK examples of KIT agents, to date, include knowledge transfer associates,105 secondees,106 improvement fellows or diffusion fellows in CLAHRCs, former SDO management fellows, and innovation leads in health boards in Wales. The role-holder seeks to create a link between the two groups, acting as a bridging agent,107 linkage agent108 or mediator. 7,109 Typically, and of interest to our project, the two groups are producers of knowledge (e.g. researchers, although not necessarily based in universities) and users of knowledge (health-care managers/practitioners/decision-makers). 110
The KIT agent roles vary. 42,54 Noting overlapping boundaries, Fisher111 distinguished four roles that grow in responsibility. She labelled the most limited role ‘information intermediary’, which focuses on helping practitioners to access information from multiple sources. The second he labelled ‘knowledge intermediary’, a role concerned with helping practitioners make sense of and apply information. The third was labelled ‘knowledge broker’, which, according to Fisher,111 is about improving knowledge use in decision-making. The most encompassing role is labelled ‘innovation broker’, which is about changing contexts to enable innovation. Fisher111 relates these four roles to the functions of knowledge brokering detailed by Michaels. 112 The six functions are (1) informing (disseminating content); (2) linking (expertise to need for a particular issue); (3) matchmaking (expertise to need across issues, disciplines); (4) focused collaboration (building collaborative relationships around an issue); (5) strategic collaboration (longer-term relationships); and (6) building institutions. These functions can be mapped against a continuum from linear dissemination to coproduction of knowledge and represent an increasing intensity of relationship between knowledge producers and users.
The limitations of the role of bridging agent, disseminating information between two organisations, have been highlighted by Soper et al. 39 and Long et al. ,104 suggesting that collaboration between organisations or groups is more effective. These authors maintain that bridging agents risk becoming gatekeepers or holders of knowledge and that this limits cross-collaboration and imposes pressure on the agent. Collaborative research partnerships were proposed as one mechanism to alleviate barriers to KIT. 15,17,21,22,113 We note that a proportion of the literature, particularly relating to collaboration programmes, refers to relationships between researchers and clinical practitioners114 with little on how managers interact with research,115 which may or may not be different from relationships between researchers and clinicians. Existing research14,66 suggests that in exploring how KIT works in practice, both organisations and individuals need to be taken into account. Enthusiastic individuals can be stonewalled by indifferent organisations, and organisations keen to learn and innovate can be hindered by reticent individuals, for example.
In this study, the essential feature is that KIT agents facilitate engagement between knowledge (broadly conceived) and practice,55 with the aim of improving the transfer and mobilisation of knowledge and innovation. Those in such a role can facilitate dialogue between research and practice,7,93 creating awareness of both sides’ interests and functions,116 and building relationships. 54,57,117 By encouraging greater involvement of decision-makers in knowledge production and knowledge producers in decision-making,117–119 and managing the ‘messy engagement of multiple players’,81 these KIT agents or knowledge brokers help to dismantle the cultural and language barriers between the two worlds. They do this by translating knowledge into appropriate language, highlighting its relevance to practice and emphasising the cross-applicability of each sides’ work. 11,57,116,117,120 More broadly, the role typically includes both ‘hard’ (obtaining and sharing diverse information) and ‘soft’ tasks (facilitating cross-group relationships, mentoring, coaching) to create a bridge across these knowledge gaps and foster a knowledge-responsive capacity and culture. 5,56–59
Managing the ‘messy’ process81 requires the broker to impose some form of structure on the process. There are a wide variety of models of knowledge transfer and mobilisation outlined in various fields of health-care literature. 117,121,122 Typically, methods include workshops or other professional development activities, written communication through print and electronic media and personal face-to-face contact, building linkage and exchange. 57,93,123 Through negotiation and understanding, the knowledge being mobilised across specialisations and organisations is reframed into a mutually agreed upon version. 124 In mobilising knowledge, the broker creates a new version, which Meyer125 labels ‘brokered knowledge’. Brokered knowledge is ‘knowledge made more robust, more accountable, more usable knowledge that ‘serves locally’ at a given time; knowledge that has been de- and reassembled’. 125
One further distinction relates to the location of the knowledge brokers; some are located within the organisation and others outside. Nyström et al. 126 suggested that locally based research and development (R&D) offices have the potential to act as KIT agents. An example of a separate organisation that supports knowledge mobilisation is the IRISS (Institute for Research and Innovation in Social Services), a charitable organisation working with social services in Scotland. For those individuals in knowledge brokering roles within organisations, some may work across departments, whereas the work of others may focus on teams within one department. This reflects an alternative classification of the brokering roles outlined by Gould and Fernandez. 127 They differentiated between brokers who work within their own community (‘co-ordinators’), those who work with a different community (‘itinerant brokers’ or ‘liaisons’), those who work with incoming exchanges (‘gatekeepers’) and those who work with outgoing exchanges (‘representatives’).
In concluding that approaches to knowledge brokering are varied and that a number of writers have grappled with distilling useful models, we note that when planning approaches and objectives, organisations make limited use of the theories and frameworks from the literature. 90 The KIT agent is defined by their work with producers and users of knowledge (in this case, managers/decision-makers) in helping to transfer and mobilise knowledge. The best way to do this is unknown and is a central question of this project.
Enabling knowledge and innovation transfer
There are a number of ways of organising the factors identified in the literature that enable KIT. Walker et al. 128 offer one classification and their four broad factors are:
-
context – factors in the external and internal environment
-
content – the changes being implemented (or knowledge being mobilised)
-
process – actions taken by the change agents
-
individual dispositions – attitudes, behaviours, reactions to change.
We use Walker et al. ’s128 classification as an organising framework. It can be related to other frameworks such as PARiHS. 129,130 In the PARiHS framework, successful implementation is represented as a function of the nature and type of evidence, the qualities of the context in which the evidence is being introduced and the way the process is facilitated. Both frameworks include a context factor; Walker et al. ’s128 ‘content’ can be mapped to ‘evidence’ in the PARiHS framework; and ‘facilitation’ in PARiHS seems to capture Walker et al. ’s128 ‘process’ and ‘individual dispositions’. The extended i-PARiHS framework131 incorporates the role of facilitation of an innovation with the recipients of the innovation in their ‘local, organisational and wider health system context’. We would map this to Walker et al. ’s128 ‘process’ factor.
Context factors
Macro-level context factors relating to the wider social, political and economic environment in which the health-care service, researchers, collaboration and KIT agents sit have been suggested to affect the success of KIT. 6,132 Factors in the external environment known to inhibit KIT include the rapid turnover of policies, ministers and civil servants. Major shifts in health care and other policy, singly and in combination, can have disruptive effects on knowledge transfer and mobilisation. 56
External context factors relating to funders or commissioners of research are a recognised, and under-researched, translational gap. 90 At an organisational level, short-term funding does not support sustainable partnerships. 94,133 Operating within a ‘closed system or fixed budget’,134 commissioners with shorter time horizons risk losing the insight that can arise from longer-term studies, and can be too preoccupied with immediate policy priorities, government targets and financial imperatives, all subject to change at short notice. 94 Thematic funding has also been suggested to engender fragmentation. 135 Restricted time and resources can also limit effective brokering or mobilisation. 15,93,134
Meso- or organisation-level context factors are often overlooked,4,136 but have a major impact. 134 A key factor in the internal context relates to the nature of the organisation – its attitude to research, to knowledge, to change – and the ability of the organisation to receive and process information. 113,137,138 In tune with Currie et al. ,43 Kitson et al. 3 reported that contexts that had ‘transformational leaders . . . learning organisations, and . . . feedback mechanisms’ were better able to implement evidence into practice. A similar conclusion was reached by others: when attempting to implement innovations, organisations face challenges such as professional barriers, inertia,139 misaligned incentives and competing priorities. 139,140 The supporting infrastructure needs ‘effective and inspiring institutional leadership’64,141 to create a ‘consistent and psychologically safe culture’. 134 An evaluation of CLAHRCs revealed a lack of emphasis on leadership (the ‘L’ in CLAHRCs) and concluded with an argument for the selection of leaders with a more systems-level approach who ‘have the capability to work across organisational and professional boundaries’. 43
King et al. 99 explain variation in outcomes and impact by differences in the ‘individual and organisational receptiveness’ or the state of preparedness of the workplace environment. The organisational value of using evidence may be limited. 100 The organisational culture needs to be adaptive142 or absorptive if it is to make use of knowledge, and increasing emphasis is given to organisational readiness. 18,82,138,143 The level of an organisation’s ‘absorptive capacity’144–147 is defined as ‘a firm’s ability to recognise the value of new information, assimilate it, and apply it to commercial ends’. 146 This ‘adaptive and responsive capacity’ is important to knowledge use in practice and is affected by the organisation’s ‘prior related knowledge, a readiness to change, trust between partners, flexible and adaptable work organisations and management support’. 145 Implementing innovations is demanding – cognitively, emotionally, physically, and spiritually. 139 If this capacity to learn, demand and generate new knowledge for the purposes of improvement is absent, then the impact of a KIT agent or knowledge broker is likely to be limited. Traynor et al. 148 concluded that the use of knowledge brokers had increased both individual capacity (improved knowledge searching, appraisal and application skills) and organisational capacity (management support and policies) of the target group.
Oborn149 indicates that ‘absorptive capacity is a strategic level capability which should be developed and nurtured by leadership teams’. Differences in hierarchical structures, leadership, power and professional cultures130 contribute to organisational receptiveness and cross-professional communication. 104,130,150 Cross-organisation and cross-discipline communication and collaboration are seen as vital. 134,150,151 However, Tasselli150 reported that professionals tend to be ‘embedded in distinctive professional cliques’.
Other studies have identified personal challenges for KIT agents around professional boundaries. 137 Career pathways and progression may be uncertain for KIT agents, particularly those in dedicated knowledge brokering roles. 133,137 Support, in the form of collective forums (i.e. communities of practice) and a physical home,137 help individuals to navigate the isolating aspect of the role. The provision of space benefits others; Dopson et al. 115 found that having access to ‘formative spaces’, removed from their organisational context, where managers could engage with knowledge, aided their appraisal of research. 115
Content factors
The work of some KIT agents entails the identification of the relevance of research to practice and the tailoring of findings to service need. Walker et al. 128 use the term ‘content factors’ to refer to the changes being implemented. It is perhaps more helpful to borrow from the PARiHS framework and include in the term issues around the nature of evidence or knowledge. Thus content factors can also relate to the nature and type of knowledge (explicit or tacit) that may be more or less readily transferred and mobilised, and to the type of evidence, varying from research findings to professional experience and local information. It concerns the social nature of knowledge and evidence; what counts, to whom and when.
Before knowledge or innovation can be implemented, the new evidence needs to be interpreted for the local context, integrated with existing knowledge and discussed. Arguably, decision-makers and researchers differ in their view of research;115,140 researchers look at the information for academic rigour, whereas decision-makers assess its local relevance. 140 At both the local and national level, new evidence may be supported or sidelined; it may address or be at odds with local needs;39,141,152 it may require change that is demanding (transformational and rapid) or the change may be incremental and require only fine-tuning. Relevance and benefit to the participants is an important enabler. 153 Decision-makers are more likely to engage if the project suits their needs. For example, an evaluation of the Québec Social Research Council (CQRS)’s partnership programme found that all respondents reported benefits to them as a reason for success. The research had relevance because it was linked to wider policy concerns (saliency). 154
Ross et al. 152 similarly found that decision-makers were more likely to engage with the research team when the research questions aligned with their interests, but also when they perceived their contribution to be essential to the success of the project (e.g. bringing local knowledge). Making a meaningful contribution drives practitioners. Bartunek et al. 75 suggested that short-term relationships, which focus on data collection, might result in the practitioners feeling exploited. Being able to help shape research questions is an important activity for some practitioners. 155
Competing agendas and priorities between partners can be a barrier to success156,157 and need acknowledging and managing. 114,155,156,158,159 Academics and commissioners alike have recognised deficiencies in the communication of research findings across boundaries. Researchers felt they should be involved more closely in the calls for research proposals; commissioners were more concerned that the users of research – policy colleagues and public service managers – should be involved more closely to ensure prioritisation of practical over academic concerns. 56 Commissioners found academics preoccupied with creating new knowledge suitable for publication in high-impact journals rather than policy-driven outputs. 56 Arguably, the ‘impact case studies’ that are a part of the Research Excellence Framework160 have gone some way to address this. However, a review of a sample of impact case studies indicated that impacts were relatively short term, often with limited direct impact on patient outcomes such as morbidity and mortality, and with limited consideration of the processes and interactions that may lead to indirect impact. 161 The time lag between identifying a demand for new knowledge and its synthesis for use in decision-making has also been noted, and decision-making time scales are short compared with research time scales. 162 Information relating to the ‘here and now’ is more likely to be used. 10
Process factors
In Walker et al. ’s128 model, process factors refer to actions undertaken by the change agents. In this sense, agents include all those parties involved in the process of change, not just the KIT agents themselves. Gagnon163 suggests that all parties should ‘plan for collaboration with an explicit description of roles and responsibilities and a commitment to regularly assessing its effectiveness’. The lack of clarity of brokering roles can limit success. 16,35,135,164 Against this, flexibility is also seen as important;66 brokerage roles may differ for different individuals127 or at different times. 165,166 Ross et al. 152 conclude that individual partnerships need to be flexible; one size does not fit all and finding the right person for a particular role is key.
Agreeing roles, goals and expectations is a common recommendation. 16,41,42,152,155,163,167 Roles can take time to be established, and may take on different forms based on specific local organisations. 137,168 One reason given for the success of the CQRS’s partnership programme was that participants were expected to show measurable results. 141 Bullock et al. 62 found examples of interactions between the knowledge brokers and their managers that resulted in frustration because expectations had not been openly articulated. Additionally, individuals in the roles will embrace brokering and linking functions at different paces or not at all. In a study of hybrid physician–manager roles, the authors identified three different groups which they term ‘innovators’, ‘sceptics’ and the ‘late majority’ reflecting the different pace of role adoption. 48 Collaborative policy-setting has been suggested as a mechanism for ensuring needs-led evidence is produced, but it was noted that this method can be more time-consuming. 169
Collaborative partnerships seem to work best where there are effective links between researchers and practitioners. Communication and trust-building, and motivation and commitment by all the organisations involved in the CLAHRC partnerships have been shown to be central to making collaborations work. 36,49,50,58 Effective solutions cannot be ‘developed from the knowledge base in the absence of those who will apply the knowledge’. 170 The key to knowledge mobilisation impacting on organisational performance rests on ‘the transfer of knowledge to locations where it is needed and will be used’. 72 KIT agents typically act as a facilitator of this transfer, using guided interaction to support the uptake and use of knowledge. 171 Their work requires a ‘multi-level, multi-strategy approach’. 172 Current evidence suggests that there is benefit in gaining the bidirectional support of middle managers within organisations:173 ‘they may disseminate information vertically from top managers to front-line employees and from front-line employees to top managers, and horizontally, across top managers and across front-line employees’. 86
Building successful long-term, trusting partnerships between knowledge producers and knowledge users supports the use of research in informing decision-making. 174 However, this takes time and commitment. 137,152,156,159,175 Partnerships need people to attend meetings. 152,155 Bartunek et al. 75 suggest a number of physical links between the two communities – web-based discussion boards, practice-focused meetings and conferences. Baumbusch et al. 91 explain how project meetings were used to feed back emerging findings for practitioners to action, and for practitioners to provide context that would assist interpretation of the findings. Kislov et al. 40 describe such events and artefacts as ‘boundary objects’. Others also write of the importance of colocating the partners, which facilitates not only formal face-to-face meetings but also informal discussion ‘at the water cooler’. 137
Knowledge transfer and innovation carries costs. For example, the time required to develop the necessary skills and relationships with organisations takes people away from other tasks and, therefore, imposes financial costs91,113 for both employers and decision-makers. 152 Financial restrictions impede knowledge mobilisation;159 those in the roles are often unable to use their backfill because of organisational pressures. 106,176
Individual dispositions
Walker et al. ’s128 final area of concern relates to ‘individual dispositions’. This focuses on the KIT agents themselves, but needs to be located more broadly; KIT agents are limited by the context and the character and dispositions of their organisations and colleagues. Evidence suggests that other aspects influence their capacity to transfer knowledge and bring about innovation, not only factors to do with their disposition (e.g. patience and approachability). 148 This includes their role and seniority within the organisation and how they are perceived by others; for example,66 Soper et al. 44 note the importance of ‘understanding each other’s incentives and constraints’.
However, the skills and attitudes of the KIT agent or knowledge broker are a recurrent theme in the literature. Alongside excellent communication skills,176,177 they need to have a good understanding of both the research evidence and policy issues, and be able to transform that knowledge into something that is salient to their practitioner collaborators. 91,159 Platt178 warned of the risk of relying solely on ‘intermediaries’ who might not have the skills needed to interpret the evidence or be motivated by their own interests.
There is an argument that knowledge brokers in hybrid roles (e.g. clinical managers) may be best placed for mobilising both explicit and tacit knowledge because of their membership of multiple communities. 54 However, challenges may arise related to dimensions of their role and interorganisational factors. 179,180 For example, those in hybrid roles have been found to show preference to one aspect of the dual role over the other, to broker knowledge only within their professional sector, or to not be best placed to reach all levels of the organisation. 179,181–183
Mutual trust and respect are frequently reported as enablers. 74,91,114,155,158,175 The issues of trust and reciprocity feature prominently in the management literature on planned collaborations. 184,185 Other reported beneficial dispositions include clinical credibility, being known and having a good reputation60,186 and having good knowledge of the organisation’s culture. 187,188 For those from outside sectors, willingness to learn about the other community is stated rarely,75,188 but would seem to be essential.
For researchers to take part in interactive exchange models of knowledge mobilisation, it is likely that they need to have accepted a broad notion of ‘knowledge’. 75 Researchers’ ‘arrogance’ and power differentials can introduce problems. 175 Engagement with potential users of knowledge may be seen as signifying a lack of independence and objectivity in the work. 57 Concerns about academic rigour and violations to objectivity can be off-putting to academics – ‘if what is required is for researchers to do what policy-makers want them to do, then research may fail to fulfil one of its most important functions, namely to be objective, reliable and unbiased’. 189 Ross et al. 152 note that none of the researchers in their study identified this as an issue.
Measuring outcomes and impact
Knowledge brokering can be conceptualised as a set of complex social activities that are difficult to evaluate. Various studies have found it to be an effective strategy for knowledge mobilisation, but few are explicit about what aspects of the role are most effective. 190 Key questions are what types of brokering outcomes can and should be measured (e.g. increased evidence use, relationships and interactions between researchers and users, linkages and network, increases in capacity to use evidence) and how they can be adequately captured (e.g. via survey, interview, observation documentary analysis). 34
The ultimate test of success is the impact of the KIT agent on knowledge transfer, innovation and patient care. Kothari et al. 191 compared the take-up of research reports on breast cancer prevention between practitioners, some of whom had helped to prepare the report and others who had not. They reported that engaging practitioners in the discussion of findings and the preparation of the report improved their understanding of the limitations of the research and made them more likely to talk about using the research in future services. However, they also found that ‘interaction was not associated with increased utilisation of research findings in programs and policies within the time frame of [the] study’. Despite this, it remains important to discuss whether, and how, process measures can assist monitoring and assess their links to outcomes that are otherwise assumed.
The literature includes little on measurements of impact arising from research partnerships. Davies et al. 90 found learning from informal experience more useful than formal evaluations. One suggested solution to the difficulty of evaluating knowledge brokering is to design research within a clearly articulated theoretical framework, which provides a basis for later evaluation of outcomes. 192,193 PARiHS may be such a framework3 and realist evaluations using clearly defined frameworks are gaining recognition as valuable ways of examining and evaluating complex interventions. 60,194,195
Sustainability was found to be a priority for trainee KIT agents. 196 The NHS Institute for Innovation and Improvement’s sustainability model has developed a self-assessment tool, which encourages reflection in three domains: process, staff and organisation. Doyle et al. 197 concluded that the tool was potentially useful, but emphasised the need for capacity building and facilitation for it to be implemented meaningfully.
Demonstrating ways in which KIT agents facilitate desirable service outcomes is critical to many senior managers’ goodwill and willingness to ‘release’ staff to KIT agent roles, not least because there are costs for them. 66 Data gathering for impact assessment is a cost to collaborations, and there is clearly value in aligning (appropriate) approaches and measures sooner rather than later.
Concluding remarks
This chapter has explored the relevant international literature on KIT and mobilisation, highlighting it as a messy, complex, evolving and dynamic process. The use of ‘knowledge brokers’ (KIT agents in our study); people responsible for supporting the transfer and mobilisation of knowledge or innovation between producers (typically researchers) and users (health-care managers/practitioners/decision-makers), is a common approach to addressing the KIT challenge. The literature identifies enablers to developing successful partnerships between researchers and practitioners/decision-makers. These factors relate to context (external and internal, including policy shifts, fiscal restraint, absorptive capacity and leadership), content (e.g. the relevance of research and its match to local priorities), processes (e.g. expectations, flexibility, physical links) and individual dispositions (including extent of mutual trust and respect; KIT agents with the appropriate skills, attitudes and networks; and researcher acceptance of a broad interpretation of ‘knowledge’). The impact of collaborations and the activity of KIT agents/knowledge brokers is hard to measure, although there are some frameworks and tools worthy of further investigation.
Given the growing interest in using collaborations to address the research–practice gap,22 one evident conclusion is the need for further research. However, research about how partnerships between researchers and decision-makers facilitate knowledge exchange ‘is in its infancy’. 51 Oborn149 remarks that although collaborative engagement and reciprocal exchange ‘are increasingly common in health services ‘KT’ literature’, evaluation models ‘continue to focus on more linear and quantitative approaches’. This is insufficient for answering ‘which types of KT network is best?’. Oborn149 concludes that future research needs to contend with the possibility that ‘best practice’ may be socially constructed, rather than scientifically and objectively determined. Waring et al. 54 and Rycroft-Malone et al. 42 point to the need for more research on knowledge brokers. The impact of collaborations and the activity of KIT agents/knowledge brokers is difficult to assess and, despite the existence of some frameworks and tools, there is a need to apply and refine them in further research.
Chapter 3 Design and methods
The focus of this research was KIT agents (NHS and university-based staff in knowledge brokering roles) and the work they do in the knowledge mobilisation process with the health-care practitioner and management community. The study aimed to provide insight into the outcomes and impact of KIT agents’ knowledge brokering with NHS managers and clinicians.
The research used an in-depth qualitative case study approach, focused on a sample of KIT agents drawn from across England and Wales. Data were gathered from interviews, audio-diaries and observations. By examining cases (KIT agents) from a number of discrete initiatives designed to facilitate knowledge mobilisation, the study aimed to reveal how these endeavours worked in practice and how benefits can be maximised. To address one of the research questions, we used a consensus method in a meeting of experts (nominal group technique).
Study design
Theoretical frameworks
Within the case study design, data gathering was shaped by Kirkpatrick’s framework,198 which provides a useful structure for ensuring data collection beyond immediate reactions to an initiative and has been widely used in business and education. 199 The original Kirkpatrick framework comprises four levels. Level 1 is concerned with assessing the participants’ reactions to the activity; for example, did they think it was relevant to their needs? Level 2 relates to learning gains (knowledge acquired by the practitioners). Level 3 focuses on behaviour change as a consequence of participation (application of knowledge to practice). Level 4 is about impact (what difference changed behaviour makes). This framework fits well with social marketing theory and its focus on behaviour.
In earlier work,62 we modified the framework to address known limitations199,200 and to maximise its relevance to innovation and knowledge transfer in the NHS. These adaptations recognise that reactions, learning gains and behaviour change all contribute to outcomes and are themselves ‘impacts’; that these ‘impacts’ are linked to each other and are not arranged hierarchically; and that the processes and dynamics of initiatives (including motivations) and the wider context are important. 62
Our approach to data analysis is described later. In this, we drew on other classifications or frameworks in the literature, notably Walker et al. ’s128 work on factors affecting organisational change and the PARiHS framework. 201
To inform our understanding of the consequences and implications of our findings, we used social marketing theory. Social marketing is defined as ‘the systematic application of commercial marketing concepts and techniques to achieve specific behavioural goals relevant to the social good’. 202 It is focused on understanding (or having ‘insight’ into) why people (e.g. NHS managers) do what they do now (in relation to innovation and knowledge) and what ‘competition’ the new behaviour faces. Social marketing theory recognises that this may vary by subgroups and may require different kinds of support (‘segmentation and targeting’). These insights can be used for ‘creating attractive exchanges’,203 which can encourage the effective uptake of the new behaviour. Part of this is taking account of, and most likely modifying or adding an ‘offer’. 203 The strength of such an approach is that it starts with investigating KIT from the perspective of people who are being asked to do it. It seeks to understand the meaning they attach to it and the barriers to, and enablers of, doing it, without attempting to prejudge issues. The approach allows factors that challenge or enable KIT to be identified and context-specific solutions to be developed. Do different managers, clinicians, innovations, questions and health-care organisations require different activities or transfer pathways? What are the implications for practice? For example, managers with limited access to information technology and statistical support might find it impossible to apply modelling techniques, even if they know about them. The solution lies in improving hardware and support, not in communicating research findings differently. To give another example, to enhance knowledge mobilisation in a setting in which a KIT agent’s line manager expects them to ‘deliver’ without senior support may need a solution that focuses on the line manager and not the agent.
Advisory group
A project advisory group was established that comprised NHS managers, chief executives, representatives of the HSDR programme, academics with expertise in knowledge mobilisation (including from overseas), patient representatives and other partners. These are listed in Appendix 2 along with the main focus of each meeting.
Primary communication with the advisory group was by teleconference, preceded by an e-mailed agenda and supporting papers. Nine meetings were held over the course of the study. The advisory group helped to resolve practical issues and acted as a sounding board for sampling, data collection and analysis decisions. Most notable was its contribution to the discussions of early findings. Throughout the project, we presented drafts and questions to the advisory group members who used their knowledge and experience to inform our way forward. As a group, they provided a strategic voice for service users and service leaders. By facilitating the ongoing validation of research findings, the advisory group enhanced the credibility and relevance of the research project and contributed to early feedback of findings to stakeholder communities.
Patient and public involvement
As this project arose in response to a specific HSDR programme call for ‘research to improve knowledge transfer and innovation in health-care delivery and organisation’, patients and the public were not actively involved in identifying the research topic. 204 Public involvement was defined broadly in the call to include ‘local communities . . . members of the public, users of services, carers and minority ethnic groups as well as healthcare practitioners and managers’. 204 Our proposal was developed with the direct input of the research networks lead (de Pury), the director of an AHSP (Denman) and a health board manager (Howell). They made a significant contribution to prioritising and adding detail and contextual understanding to the objectives. Their views and opinion of their needs regarding innovation and knowledge transfer shaped the detail of the questions we asked.
Users are motivated to take part in research management when they feel they can make a contribution given their own expertise, experience and interest. For this reason, we focused our inclusion on patient representatives in the advisory group and the nominal group, in which discussion could be informed by their first-hand experience of services.
Data collection and sampling
We describe data collection methods in relation to three parts of the study: the initial mapping and typology development; the case studies; and the nominal group.
Mapping and typology development
For the national mapping of the KIT intentions of the networks (AHSNs and SEWAHSP) and the development of a typology of KIT agents we collected data from desk research and telephone interviews.
Desk research (June–August 2013)
The 15 AHSN prospectuses and business plan documents (versions submitted to NHS England for licensing in 2012) together with the SEWAHSP’s Five Year Strategy31 (July 2012) were reviewed to understand their interpretation of knowledge mobilisation and their planned approach and, in particular, their intentions to engage knowledge broker roles. The documents were scrutinised and searched for the terms ‘fellow’; ‘associate’; ‘lead’; ‘broker’; ‘agent’; ‘manager’; ‘boundary’; ‘transfer’; ‘exchange’; ‘span’; ‘connect’; ‘linkage’; ‘mobilise’; and ‘gap’.
Telephone interviews (November 2013–February 2014)
In order to supplement the initial mapping of knowledge mobilisation intentions, as set out in the documentation of the respective networks, the managing directors of the networks were approached by e-mail. The initial contact described the project’s aims and requested a 30-minute conversation, either in person or over the telephone, to understand their approaches to knowledge mobilisation. This was followed up with support staff to schedule the discussion and provide further background on the study’s aim and objectives. Interviews were conducted using a semistructured interview schedule (see Appendix 3).
Fourteen of the 16 network managing directors (including SEWAHSP) agreed to share their regional approach to knowledge mobilisation. Most managing directors stated that they were still in the planning and set-up stages of establishing their organisation and, therefore, could discuss their intentions around the use of KIT agents but not specific individuals. Eleven telephone and three face-to-face meetings were held between November 2013 and February 2014, ranging in length from 20 minutes to 1 hour. Twelve of the 14 discussions were held with the managing director and the other three were held with a named lead in the region. Two managing directors out of the 16 did not respond to multiple attempts to secure a discussion.
Appendix 4 summarises the main findings of the document review stage and the results are described in Chapter 4.
Case studies
Sampling
Using data from the intentions of the AHSNs and SEWAHSP, we purposively sampled five diverse sites, from which we selected case study KIT agents. The five networks were selected on the basis of:
-
stage of network development (e.g. ranging from de novo to well established)
-
diversity in regional research infrastructure (e.g. established links with CLAHRCs/no CLAHRCs; AHSCs/no AHSCs)
-
planned KIT roles in the region (e.g. part of the core team, secondments, fellowships)
-
geographical diversity (largely urban/rural and north/south representation)
-
willingness to engage with the project.
Our target population was KIT agents across England and Wales, that is, individuals who facilitate the mobilisation of knowledge to practice, knowledge brokers who link NHS managers/clinicians and the developers of knowledge and innovation. In the national mapping exercise we delineated definitions and expectations of the KIT agent role. From this, we drafted a typology of KIT agent roles, which we used to inform the identification of our individual case studies. In making our purposive selection of 13 KIT agents we actively sought variation of role, sampling within 4 of 15 AHSNs in place in 2013 and the first AHSP in Wales. We selected a number small enough to enable in-depth study of the work and impact of these KIT agents over time and yet provide good geographical coverage and system contrast. As a qualitative study, the sample size was necessarily small to enable richness and depth of data gathering and analysis. The specific innovations and knowledge that the agents helped to mobilise was diverse. This diversity enabled the detection of content-specific knowledge transfer challenges, as well as generic mechanisms that support transfer and mobilisation.
Data collection
Detailed case studies of KIT agents and their work were the source material for describing the roles of KIT agents, their linkages, relationships and engagement activities, and reporting the outcomes and perceived impact of their work on practice and management. They also provided data that enabled us to investigate how KIT agents can be best supported. We collected data from observation of KIT events/meetings; recurrent semistructured interviews with agents and interviews with their key Links (NHS managers/practitioners); and, when possible, audio-diaries kept by agents over 4 months.
Observations
We aimed to observe two or three activities of each case study agent. These were at the invitation of the KIT agent and included showcase events, reports to workplace colleagues, presentations of research and meetings to discuss progress on initiatives. These diverse, non-participant observations varied in length from relatively short meetings (< 2 hours) to 1-day events. Larger showcase events lasting 1 day were attended by two members of the research team; others were attended by one. Field notes were made, recording who was involved, what happened, reactions and reflections. These events also provided opportunities for informal discussion with people with whom the agent linked. We collected copies of any documentation used during the event.
Interviews
All interviews were audio-recorded and transcribed. An initial face-to-face lengthy interview was held with each of the case study agents. The schedule is presented in Appendix 5. In most cases, further interviews were conducted. These provided an opportunity to gain updates on specific activities and further explore outcomes and perceptions of impact. One agent withdrew from the study after the initial interview.
We had contact with agents’ line managers as part of arranging access and most agreed to a one-to-one interview, face to face or by telephone, depending on their preference (see Appendix 6 for the interview schedule).
We also conducted semistructured interviews with some of the key people with whom each agent linked. These Links were identified by the agents. Further details regarding the background of the Links are presented in Table 1, and it should be noted that these individuals do not represent the entire range of an agent’s network of contacts. The content of the interview varied depending on the nature and reason for the connection to the agent.
| Organisation | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Greenhills | Riverside | Moorlands | Wetlands | Homefields | |||||||||
| James | Grace | Sophie | Amy | Isabelle | Fran | Jessica | Holly | Daisy | Erin | Janice | Chloe | Molly | |
| Line manager | Chief executive | – | Chief executive | – | – | – | Managing director | – | Senior academic | – | Managing director | ||
| Link | Doctor | Doctor | Lead nurse | Associate medical director | Operational lead | Doctor | Regional lead | Quality director | – | Engineer | Clinical teacher | – | – |
| Link | Nurse | Board chairperson | Lead nurse | Effectiveness manager | – | Lead nurse | Director | Manager of services | – | Director | – | – | – |
| Link | Doctor | Development manager | Chief operating officer | – | – | – | – | – | – | – | – | – | – |
| Link | – | – | Assistant director | – | – | – | – | – | – | – | – | – | – |
Audio-diaries
Knowledge and innovation transfer agents were asked to keep diaries of activities and audio-recordings of their reflections on events and brokerage meetings. We explained the purpose of the audio-diaries and how to make recordings at our first face-to-face meeting. All those who agreed to take part were requested to record an audio-diary of their experiences (via a personal digital audio-recording device provided for participants or using their own digital recording equipment if they preferred). These solicited audio-diaries captured participants’ sense-making in action as they told their stories both to the researchers and to themselves205,206 and commented on outcomes and the potential impact that the role had on others. In order to enable participants to set the agenda for the content of their narratives, we gave them one principal request: ‘Please tell us about something that has happened in your role as a KIT agent since the last time you left a message’. However, we also included specific questions in subsequent requests to follow-up on earlier recordings. Participants were requested to record at least one short (2–3 minutes) diary entry per week, over a period of 4 months. However, despite regular prompts via text messaging or e-mail, contributions were highly variable.
Table 2 provides a summary of data collected from the case studies. Excluding set-up meetings, we conducted 50 interviews (23 with KIT agents, 22 with Links and five with line managers), 20 observations, and received 72 audio-diary entries (6 hours 20 minutes). This provided us with 46 hours of recorded data.
| Greenhills, agent (background) | Riverside, agent (background) | Moorlands, agent (background) | Wetlands, agent (background) | Homefields, agent (background) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| James (clinical) | Grace (clinical) | Sophie (clinical) | Amy (clinical) | Isabelle (non-clinical) | Fran (clinical) | Jessica (non-clinical) | Holly (clinical) | Daisy (clinical) | Erin (non-clinical) | Janice (clinical) | Chloe (clinical) | Molly (non-clinical) | |
| Observations, n | 3 | 3 | 4 | 2 | 1 | 1a | 2b | 3b | 2b | 1 | – | – | 3 |
| Agent interviews, n (minutes) | 2 (110) | 2 (86) | 2 (79) | 2 (120) | 1 (99) | 2 (112) | 4 (165)c | 3 (100)c | 2 (64) | 1 (111) | 1 (68) | 1 (55) | 2 (165) |
| Line manager interviews, n (minutes) | 1 (26) | – | 1 (56) | – | – | – | 1 (32) | Same LM | Same LM | – | 1 (50) | – | 1 (39) |
| Link interviews, n (minutes) | 3 (118) | 3 (135) | 4 (143) | 2 (79) | 1 (66) | 2 (107) | 2 (54) | 2 (57) | – | 2 (89) | 1 (53) | – | – |
| Audio-diary entries, n (minutes) | 10 (38) | 11 (113) | 4 (9) | 12 (115) | 5 (27) | 1 (e-mail: 10 pages) | 8 (24) | 18 (21) | 2 (8) | – | – | – | 2 (25) |
Nominal group
Sampling
A nominal group is a highly structured meeting of a panel of suitably experienced ‘experts’. 207 The size of the panel is typically 8–12 experts. Our group comprised a purposive sample of eight people from England, Scotland and Wales. Through consultation with our advisory group, we identified the roles we wanted represented (knowledge brokers, researchers/academics, network/policy leads, information scientists, patients/the public) and drew up a long list of potential members, informed by our knowledge of the field and the literature. To secure this group, we approached 28 individuals in two main waves. First, we approached 12 individuals and gained agreement from four. One of the 12 did not respond, but all others replied and suggested alternatives we might contact if they could not themselves attend. Second, we invited a further 16 people: five agreed, two did not respond and the remainder gave apologies. All those who replied were interested but were unable to make the date either because of other commitments or workload. In the event, one of the nine expected attendees could not attend because of a hospital appointment and another was ill on the day. As this was an academic working in the field, we felt justified in including a member of the research team in the group, although this was not our original plan.
Most members of the final panel of eight had dual roles. The group included three knowledge brokers, three researchers/academics, two network/policy leads, a senior information scientist and a patient and public involvement (PPI) specialist.
Data collection
The panel took place on 10 June 2015 (10.00 to 15.30), in Cardiff, and was facilitated by the project lead. In advance of the meeting, the panel members were given background information. It was explained that what counts as knowledge or evidence can be broadly interpreted, including not only the results of research but also the analysis and use of an organisation’s data as well as knowledge gained from experience and practice. ‘Knowledge mobilisation’ was described as a term used to refer to the use of knowledge to develop practice and services and inform decision-making. It was explained that the process of mobilising knowledge is not simple and linear; rather it is contingent on relationships and interactions. Knowledge brokers were described as having an important role to play in this process. While they may include a diverse group of individuals (clinical and non-clinical based in various locations including universities, libraries, public health settings, primary and secondary care settings, health boards and trusts), what they have in common is that they provide a two-way link between those who have or develop knowledge and those who use knowledge (practitioners).
The steps of the nominal group process were:
-
Silent generation of ideas in writing – the leader read aloud the question that the participants were to answer. This was clarified or modified as required following discussion. Each participant was then given a worksheet with the question written at the top and asked to take a few minutes to write down his or her ideas. Discussion was not permitted at this point.
-
‘Round-robin’ feedback of ideas – the leader asked each member to contribute one of his or her ideas summarised in a few words. These ideas were numbered and written on a flip chart so they were visible to all members. The process continued until no further ideas were forthcoming. Discussion was not permitted during this stage.
-
Serial discussion of ideas – each of the ideas on the board was discussed in turn. The objective of this discussion was to obtain clarity and to air points of view, but not to resolve differences of opinion.
-
Preliminary vote – the participants identified their top six items using a weighted voting system. The participants were given six voting cards (two 3-point cards; two 2-point cards; and two 1-point cards). They selected the six ‘most important’ items from the total list and wrote these on the 3-, 2- and 1-point cards, according to the level of importance that they assigned them (with 3 being the most important). Thus, each participant submitted six cards; on each card was written an item number and a ‘score’ (3 points; 2 points or 1 point). The cards were then collected and shuffled to maintain anonymity, and the votes read out and recorded on a tally chart that showed all the items and the votes allocated to each.
-
Discussion of preliminary vote – a brief discussion of the voting pattern was permitted. The purpose of the discussion was additional clarification, but pressure to change others’ votes was not permitted.
-
Final vote – step 4 was repeated.
Ethics and approvals
After seeking advice from a number of local, regional and national quarters [Cardiff University Research and Commercial Division and the Research Governance Officer, the NISCHR Clinical Research Centre, Aneurin Bevan R&D office and Queries National Research Ethics Service (NRES) Health Research Authority], it was confirmed that the project was deemed a service evaluation and, therefore, NHS research ethical approval was not required. Research ethics approval was then obtained from a Research Committee of Cardiff University (reference number 20/08/13) and the project registered on the Welsh portfolio (16/10/13; number 15479). Prior to fieldwork, we obtained any required approvals from the AHSNs and from the health board for each of the agents in Wales.
We prepared participant information sheets and consent forms (see Appendix 7) and sent these to all participants in advance of data gathering. Data were gathered in confidence and all individuals and places associated with the case studies were anonymised for analysis and presentation.
Data analysis
The data from the mapping were summarised and developed into a typology of KIT agents, which is reported in Chapter 4 and Appendix 4. The results of the nominal group are detailed in Chapter 7. In this section we explain the process of data analysis from the case studies. The analysis of the field notes and documents, the interview transcripts and audio-diary data were both deductive (based on a priori coding themes) and inductive (emerging from the data). Data from all these sources were managed in NVivo10 (QSR International, Melbourne, VIC, Australia).
The process entailed a thematic analysis using an adapted framework analysis approach. 208 This entailed developing a coding frame based on a priori themes derived from the research questions and wider literature supplemented by emergent themes identified through discussion with the research team and advisory group. We used Walker et al. ’s128 classification of factors influencing change as the basis of our analytic framework. This groups factors into four broad categories that we applied to our agents: context (factors in the external and internal environment); content (what knowledge or change was being transferred or implemented); processes (actions taken by the change agents); and individual dispositions (attitudes and behaviours of agents and reactions to change). It would have been appropriate to adopt an alternative model such as the PARiHS framework. 201 The overlap between these classifications has been shown (see Chapter 2, Enabling knowledge and innovation transfer). As the starting point for our analysis framework, Walker et al. ’s128 classification had utility. However, we extended this to include outcomes and impacts, conceptual definitions and descriptive codes for background and role. We used Kirkpatrick’s framework198 to report outcomes and impact in relation to reactions, learning gains and behaviour change. The coding frame is presented in Appendix 8.
The process of data coding was undertaken by three members of the research team. To ensure consistent application of the coding frame, on four separate occasions we independently coded several pages of transcript and then compared the coding. We debated and agreed any variation. This led to the addition of subthemes and further clarification or elaboration of codes.
The way we distributed transcripts between the coders facilitated greater sharing of the data such that it was rare for a researcher to code the interviews they had conducted. Team and advisory group discussion of the analysis helped to integrate themes and further summarise findings.
In reporting, we sought to analyse the work of individual agents, broadly within Walker et al. ’s128 classification, presenting a narrative of the agent and their work. These narratives drew directly from the agent and their Links’ accounts. Alongside this, we took a broader look across agents in order to draw out general findings and implications for how models of knowledge mobilisation can be helped to work in future.
Validation processes
We detail some of the strengths of the study in Chapter 8. Here we briefly detail the validation processes. Data, methodological and investigator triangulation209–211 were achieved through the use of multiple data sources, conducting both interviews and observations of the agent’s work, and having at least two members of the research team working with each case study. These steps provided a broader understanding of the agents and their work. Particularly important was the voice of others who linked with the agents. Representing a variety of relationships and interactions with the agents, these key informants provided their own perspectives on the value of the work of the agents. The observations were an additional means of corroborating and expanding on how the agents saw their work. Multiple team members’ involvement in the data gathering, analysis and reporting of each case study also allowed the work to be viewed from more than one standpoint.
Throughout the course of the project, a number of mechanisms helped us to discuss, validate and disseminate our emergent findings. We utilised a range of opportunities to discuss with stakeholders including health service managers and leaders (two of whom were included in our research team). Data were regularly presented to, and discussed with, the advisory group.
Another part of the validation process was through presentations to research workshops and conferences, notably the UK Knowledge Mobilisation Forum 2014 and 2015, the Health Services Research Network Symposium 2014 and 2015, a series of workshops and meetings to inform the knowledge mobilisation strategy for Wales, University Health Board Research and Development Conferences 2014 and 2015, and Fellows Connect meetings.
At the end of the fieldwork, we offered feedback to the agents and their network sites. These were taken up by two of the AHSNs (covering six agents) and the three sites in Wales. These meetings were discursive in nature and served to test out the validity or ‘truthfulness’ of our findings.
A final part of the verification process was achieved by drawing parallels with published studies in the field. Taken together, these validation mechanisms strengthen the transferability of our findings.
Caveats
No study is perfectly designed and no research runs exactly as planned. We briefly review each part of the study here; a more detailed discussion of study limitations is provided in Chapter 8.
We achieved our objective in the first mapping exercise and typology development on the basis of document review and discussion with 14 out of 16 leads. Ideally we would have liked to have spoken to all 16.
Although we recruited more than the expected 10–12 case study agents for this study, not all participated as fully as we hoped or in the way that we anticipated, and the number of data we have on each agent varies. Despite this, the number and quality of data we amassed made the job of systematic and thorough coding a time-consuming process. However, the variability means that we know more about the work of some agents and its effects than others, and we cannot make claims about the wider population of knowledge brokers. This is addressed to some extent by our process of validation, which increases our confidence in the trustworthiness and transferability of our findings. However, it is necessary to accept that analysis of interview data represents an account rather than observation of behaviour. We did not witness change in practitioners’ behaviour as a direct result of KIT agents’ activity. However, their accounts were largely corroborated from triangulating what agents claimed with the reflections of their Link interviewees and managers, and our observations of events.
From the nominal group we distilled important messages. However, the questions remain challenging, and there would be value in developing and extending the exercise to build on these initial findings.
Despite enormous effort and persistence, we were unable to complete one aspect of our study. We planned to run action learning sets with groups of knowledge brokers. These were designed partly as a means to ‘give back’ to our case study’s organisations, partly as a mechanism to disseminate early findings to stakeholders, and partly to learn more about the support needs of knowledge brokers. Case study agents, and those who participated in Link interviews, were invited to take part and invite others in their networks as appropriate. Invitations to attend the sessions were later made to a group of nurses engaged with knowledge mobilisation, public health staff with an interest in knowledge mobilisation, and R&D leads across Wales, without success. Although in most respects this omission does not distract from our main findings, we remain disappointed that despite considerable effort and interest from potential participants, commitments and other pressures prevented them from engaging with the activity.
Concluding remarks
This chapter has presented a detailed account of our research methods in studying the KIT role within the context of the AHSNs in England and the regional network in Wales. With several caveats noted, we next turn to our findings.
Chapter 4 Knowledge and innovation transfer intentions across networks
The development of the AHSNs in England took place over several stages, starting in 2011 with the publication of Innovation, Health and Wealth. 27 These new structures, tasked with supporting the identification, rapid adoption and spread of innovation and best practice across their regions, provided a unique opportunity to understand its intentions for individuals in KIT agent roles. At around the same time, AHSPs were developing in Wales. Of three regional hubs across Wales, the first to be established was in the south-east (SEWAHSP; others are in south-west and north Wales). Their intentions are to better engage NHS organisations in the formulation of R&D strategies to encourage clinical participation in R&D, and to accelerate research and innovation transfer and mobilisation. 32
This chapter presents the results of our review of early AHSN and SEWAHSP strategy documents and our subsequent telephone calls with network managing directors regarding their intentions for individuals in KIT agent roles. From these we present two snapshots in time: the first at prospectus (England) or strategy (Wales) stage, and the second during early network development in late 2013/early 2014.
We first provide a brief overview of the AHSN development stages to illustrate our study’s timing during network development (Table 3). We then proceed to the results of these two reviews. The methods for this phase are detailed in Chapter 3.
| Timeline | AHSN development |
|---|---|
| December 2011 | Innovation, Health and Wealth27 signalled a change in the innovation landscape in England, including the designation of AHSNs |
| June 2012 | The Department of Health invited expressions of interest from the NHS and partners to create AHSNs. This invitation outlined a core purpose of enabling the NHS and academia to work collaboratively with industry and to identify, adopt and spread innovation and best practice212 |
| September 2012 | AHSNs submitted their detailed network prospectus and draft business plans to NHS England |
| October 2012 | SEWAHSP’s Five Year Strategy launched31 |
| April 2013 | NHS England recommended that 15 AHSNs should be designated to cover the whole of England |
| May 2013 | NHS England confirmed the designation of 15 AHSNs |
| June–August 2013 | Snapshot 1: study team reviewed the AHSN prospectus documents and business plans and the SEWAHSP’s Five Year Strategy31 to understand their KIT role intentions |
| August 2013 | All AHSNs submitted a year 1 business plan |
| November 2013 | Final contracts were issued to all AHSNs for their ratification and signature in November 2013 |
| November 2013–February 2014 | Snapshot 2: study team conducted interviews with network managing directors to understand their plans for KIT roles |
| January 2014 | All 15 contracts returned and signed. England becomes the first country to fully implement a system of AHSNs universally |
| February–July 2014 | Selection and confirmation of case study sites |
| May 2014 –August 2015 | Data collection across sites |
Results
Snapshot 1: intentions of networks at prospectus or strategy stage
The AHSNs laid out their initial plans for their region in a prospectus document and accompanying business case in September 2012. Out of the 16 networks (15 AHSNs in England and one AHSP in Wales), the majority had plans in place to support KIT agents or to provide role support through training or buying time. The range of different approaches are summarised here and detailed in Appendix 4.
Intentions for specific knowledge and innovation transfer roles
Eight networks proposed a new or modified KIT role in the region often describing them as fellowships and/or secondments of various lengths, with or without protected time and targeting different clinical professionals, managers or academics, or all three. The stated objectives of these schemes include the creation and building of capacity and capability; to enable cross-fertilisation between the NHS, industry, voluntary sector and academia; to spread innovation at the local level; and to build an evaluation and learning culture.
Intentions for knowledge and innovation transfer role support
Four AHSNs proposed the development of a network to support service improvement leads or change practitioners through training programmes or buying staff time. One network proposed both a specific KIT role and role support through communities of practice. Looking across both types of KIT intentions – fellowship-like or network-like approaches – the following features were noted:
-
Content: the majority proposed a focus on improvement. Specific content areas included innovation, leadership, evaluation, change management, knowledge mobilisation and knowledge translation. We noted that several networks use more than one content area in their description and it is likely that the differing level of detail makes it difficult to discern what is included within the broad terms used.
-
Regional assets: several networks focus on building on their region’s existing structures, including working with local universities as well as NIHR bodies such as CLAHRCs and AHSCs.
Leveraging existing staff
Three of the 16 networks did not describe specific KIT roles. Two of these focused on leveraging the skills of existing staff, but it was unclear what support would be offered. The other network in this category deflected KIT role support to other organisations, for example, a NIHR body in the region had the remit to expand the research-active community and an educational body-led clinical improvement training.
Snapshot 2: intentions of each network as described by their leaders
We interviewed 14 representatives of the 16 networks to understand how their intentions for KIT roles were developing from the original prospectus. At this stage a number of general observations were made about the networks:
-
They were at different stages of development. This ranged from senior management teams in post with over 50 active projects to still recruiting for senior roles and agreeing priorities.
-
They started with different existing structures. This ranged from establishing completely new structures to inherited projects and staff from old structures (for example from Health Innovation and Education Clusters and CLAHRCs). One interviewee commented ‘We have spent the last 5 years building relationships’.
-
They had unique operational models. Models included a core network team providing central support along agreed themes; a separate organisational entity working alongside partners; and regional teams specialising in different aspects of the network’s clinical themes.
-
As a result of these differences, the operational challenges also differed. For example, some were challenged by the sheer size of their geographical footprint, others by trying to create partnerships when none had existed before, yet others by one dominant organisation in the network.
-
However, the core objective to drive improvement through innovation was common across all networks, and the influence of the growth agenda was common across all sites in England.
Role types
Different types of KIT agent roles were identified across the networks. Roles varied across a number of dimensions, including how the agent would be supported by the network, duration of the role and percentage of time spent on the role, number of agents in each organisation, and whether the role was focused on research and data gathering or on the implementation of research findings. Other features included whether the role was aimed at clinicians, managers, or both; the primary location – the NHS, university or industry; and the focus of the strategy delivered through the role – health, wealth or both. We also noted variation in relation to proposed training for agents: in knowledge brokering or improvement methodology; and bespoke or à la carte. The various roles are summarised in Table 4, and we note that a number of networks proposed more than one type of role.
| KIT role type | Roles (number of networks proposing role if more than one) | Key features |
|---|---|---|
| Roles with protected time and specific training programme | Trust innovation lead (three networks) | Nominated senior-level individual by organisation in network to receive training in improvement methods, leadership, strategy, data analysis and other areas. This will create a community of practice and they will endeavour to provide network support |
| Service improvement fellows | Working with the local CLAHRC to make their fellowship programme more widely available | |
| Local education and training board-funded professional fellowships | Fellows receive training through a regional centre for evidence-based practice leading to a 2-year MSc or 3-year PhD plus additional support for 1 year to embed into the organisation | |
| Roles with protected time, but individually determined training | Improvement fellows | Fellows based in partner organisations but supported for a specific period of time to work with the network core team on improvement project. They would be provided with peer support, IHI resources, data from local NHS providers and stable employment during the fellowship |
| Evaluation fellowships (two networks) | Fellows jointly supported by an AHSN and local education and training board. Fellowships for clinicians to act as knowledge leaders | |
| Secondments | Industry secondment | One post to be filled by an experienced manager from industry to deliver a number of clinical projects for the network. The post holder was expected to work between primary and secondary care to broker change |
| Commissioner secondment | Three senior commissioners seconded 1 day a week to local universities to bring NHS thinking to research, help academia develop a network of ideas and contacts, and learn about academic rigor, research and evaluation processes | |
| Operational lead with knowledge role | Operational directors | MSc-level qualified ‘academic managers’ who can operate in both a university and hospital setting. Expected to seek grant income but rewarded with job security |
| Executive-level leads | One lead per partner trust to have a role in locating innovations and presenting these to the network board. They would be provided with regional training | |
| Programme managers/hub team (two networks) | The network’s core team to provide objectivity and independence to advance projects. The core team comprises content experts and methodologists in data analysis, change management, and so forth. The methodologists will help to develop skills of individuals working in partner organisations | |
| Champions | Translators/local champions (two networks) | Innovation and research translation champions based in partner organisations and connecting with the network hub and national initiatives. Funding for their time will come from the partner organisation, not the network |
| Project-specific staff | Clinical and management project leads (two networks) | Front-line clinicians and managers to implement innovations in practice. The agents will provide support on a project-by-project basis. Funding for their time will come from the partner organisation, not the network. They may receive additional training or protected time depending on the project |
We note that fellowship or secondment roles and network building activity were still the main strategies for supporting KIT roles during early network formation. However, we found that most networks ‘have moved on from the prospectus’ (Managing director, network 750) focusing more on working with local organisations to deliver joint KIT support and less on introducing new training or protecting time. We also note the emergence of roles that are described as operational leaders with specific duties around promoting improvement and innovation. These differ from fellowships, as they are seen as more permanent members of the network team. Many network leaders describe these changes as a response to a funding shortfall and central policy changes.
Role typology
Based on the findings from the review of the network intentions and the discussions with managing directors and alternates, we developed our classifications into a general typology of KIT roles. These ideal types are presented in Table 5. We then plotted these ideal types along a set of features related to level of support or training, role duration, full- or part-time, numbers in post, and extent of focus on research or implementation (Table 6).
| Type | Example |
|---|---|
| Type 1 | |
| ‘Dedicated KIT fellow’ (dedicated knowledge broker role with formal capabilities training) | Fellows nominated by each partner organisation in network receive training in support of becoming a KIT lead |
| Type 2 | |
| ‘Dedicated KIT lead’ (dedicated knowledge broker role with mentoring support) | Transformational leads with skills in evaluation and improvement methodology, and with access to peer network and core team. For example, improvement fellows |
| Type 3a | |
| ‘KIT within research role’ (service evaluator that includes KIT role) | Select group of academically oriented evaluators/researchers working on service change projects |
| Type 3b | |
| ‘KIT within role’ (operational leadership with supported/informal knowledge role) | Select group of academically oriented managers working on high-level service change projects (e.g. integration of services between primary and secondary care) |
| Type 4a | |
| ‘Project programme implementer’ (implementers on a project basis: integrated projects) | AHSN core team identifies and manages an integrated programme of projects and works alongside staff in partner organisations to roll out. Staff may be supported through other organisations (such as Strategic Clinical Networks) |
| Type 4b | |
| ‘Project implementer’ (implementers on a project basis: series of projects) | AHSN core team selects and manages a series of projects and works alongside staff in partner organisations to roll out, typically involved at the end of the project |
| Type 5 | |
| ‘Hobby project champion’ (informal project champions) | Clinician with ‘hobby project’ supported to develop their improvement/innovation and roll out to region |
High level of training provided  |
||||||
|---|---|---|---|---|---|---|
| Dedicated KIT fellow | Dedicated KIT lead | KIT within research role | KIT within role | Programme implementer | Project implementer | Hobby project champion |
Short duration of role  |
||||||
| Project implementer | KIT within research role | Dedicated KIT fellow | Hobby project champion | Dedicated KIT lead | Programme implementer | KIT within role |
Part-time KIT role  |
||||||
| KIT within role | Hobby project champion | KIT within research role | Project implementer | Programme implementer | Dedicated KIT lead | Dedicated KIT fellow |
Low numbers in post  |
||||||
| Dedicated KIT fellow | Dedicated KIT lead | KIT within research role | Programme implementer | KIT within role | Project implementer | Hobby project champion |
Research-focused role  |
||||||
| KIT within research role | Dedicated KIT lead | Hobby project champion | Project implementer | Programme implementer | KIT within role | Dedicated KIT fellow |
Case study sites
Our case study site selection was informed by the mapping exercise described in this chapter. Specifically, five networks were selected from the range of planned KIT roles described in the typology in Table 5, and also the different stages of network development (i.e. from a de novo network to an established partnership in research and innovation). The features of the five selected networks and their proposed KIT roles are summarised in Table 7.
| Stage of network development | Types of KIT rolesa | Regional infrastructure | Network operational models and challenges | Network approach to innovation/wealth creation |
|---|---|---|---|---|
| De novo network | Type 1: dedicated KIT fellow developed Type 2: dedicated KIT lead funded by network |
Integrated clinical research infrastructure | Partners have had to work together in the past | Main areas of activity will focus on the introduction of innovations into the NHS and innovations deriving from within the NHS and the facilitation of clinical trials |
| Established network with developed relationships with partners | Type 2: dedicated KIT lead Type 3b: KIT within role – operational leaders/academic managers |
Integrated CLAHRC, research networks, education and training | Network working alongside partners | Wealth creation applied across work |
| Early in terms of structures, but relationships are developed | Type 3b: KIT within role – core team has KIT roles; and innovation ambassadors Type 4b: project implementers on specific projects Type 5: hobby project champions – clinical |
Well-established CLAHRC Developing a regional centre for innovation and best practice |
Large geographical footprint with a couple of dominant players | Network core team roles to link with industry |
| Several projects under way and some staff in posts | Type 3a: KIT within research role Type 4a: project programme implementers |
Existing infrastructure not mapped to network region | Large, diverse region with core team being established | Enterprise and investment is core workstream |
| Newly established structures with several projects under way | Type 3b: KIT within role – core team has KIT roles Type 4b: project implementers on specific projects |
Network connected with clinical research infrastructure | Creating new collaborations. Funding challenges | Enterprise and investment is core workstream |
Concluding remarks
Two detailed snapshots have been presented in this chapter and Appendix 4 to address our project’s objective to map the KIT intentions of the networks. We have described KIT agent proposals including number and types of roles, as well as main features and existing structures to support roles. This stage served as our sampling frame for case study selection, as well as provided us with a starting point for understanding start-up conditions and the local context of the different networks.
Chapter 5 The case studies
In this chapter we provide short descriptions of each of the 13 case study KIT agents, their role and characteristics (dispositions), the context in which they worked, their focus (content), activities (processes) and who they work with (clients), and reported outcomes (using Kirkpatrick’s198 organisation of reactions, learning, behaviour and results). This information is summarised at the end of this chapter (see Table 8), and Chapter 6 provides a cross-case presentation of the findings.
James
The agent
James led a relatively new unit designed to improve services by supporting staff through the use of improvement methodologies, making space for innovation, and bringing organisations and people together for, in the terms of their website, ‘co-creating solutions’. A medical consultant by background, with significant experience in management and leadership roles, he directed the unit on a part-time basis. He was viewed by colleagues as a robust and charismatic leader who, in his own words, was prepared to cause ‘constructive disturbance’ and be the ‘grit’ in the system. Near to retirement, James saw the importance of building trusting relationships and viewed his role primarily as supporting coproduction, helping people to feel valued, enabling them to take ownership and to ‘grow their own stuff’. His skills were complemented by his team, who were recruited for their expertise in areas such as leadership, change management and patient safety.
Context
Although James characterised the internal organisational context as one of high-level support from the executive team, he nevertheless felt pressure to demonstrate his worth. Other challenges included handling territory sensitivities in relation to who provides change management training and not alienating staff wary of change. In contrast, however, he also described parts of the organisation as ‘open’ and ‘healthy’ as demonstrated by two teams agreeing to his observing them. James also alluded to challenges arising from the changing external context:
Demand has changed . . . A&Es [accident and emergency departments] were built for 25-year-olds with broken legs. The demand is now 85-year-olds with six conditions, dementia and frailty. A&E is a terrible place for them: no matter how you describe it, it is never going to work for these people. Or technology changes: well we used to do that with surgery, now we can do it with drugs. Or economics have changed: we used to have a million pounds to spend on this now we’ve only £750,000. So all those things tell you that improving is not going to deliver.
James
Content
James worked across various clinical and non-clinical work streams, including waiting lists and care in the community. This often involved cross-organisational working, for example with primary care, the local authority, charities and universities.
Activities
James deemed the leadership training the most important part of his and the unit’s work. The unit also provided staff training in QI methods. Other activities related to brokering meetings between organisations for developing improvement projects. James repeatedly highlighted the importance of bringing people together to discuss solutions to problems. An innovative element of their approach was the application of mathematical modelling.
Clients
James worked with clinical leaders and managers in his senior-level role, but also linked with others external to his organisation including patients.
Outcomes
James described how his initial attempt at developing an improvement culture ‘created a bit of hostility’. He revised his approach and talked about simply ‘having a conversation’, avoiding others feeling intimidated by the consequences.
Learning outcomes arose from leadership and QI training. James thought that the leadership training was ‘really nurturing a new breed of leaders’.
Changed behaviour was also linked to James’s work. He was seen as pivotal in challenging ‘silo’ thinking and working. One Link interviewee described his changed thinking thus:
Other people that are not working . . . in your field of practice . . . actually when you talk to them . . . they’ve got the wider vision, if you like, of the whole organisation . . . So I could be quite siloed really in dealing with older people, but it makes me think, well, what I’m doing for the older people now can actually be transferred to mental health services.
James’s Link
Tangible results from James’s work included joint research proposals, awards and QI projects linked to staff training. QI training was being embedded into appraisal systems, a step described by James as a mechanism for building capacity and critical mass. This was increasing the numbers of people engaging in projects, which in turn was leading to desired cultural change in the organisation. Although in the time scale of the research we cannot demonstrate the impact of James and his unit’s work, he felt that they were making strides in the right direction:
When I started this off I interviewed all the Execs [Executives] and they all said, ‘. . . but it will feel different, the organisation’ and, it does now. How much of that is related to us, how much of it isn’t, I don’t know. . . . And others are now looking to us to emulate the same thing.
James
Grace
The agent
Grace headed up a unit with a remit for improvement programmes and innovation. Clinically trained as a nurse, she had held a variety of roles in research and nurse education, and had developed a very strong network of contacts in the region as well as internationally. She had received training in Institute for Healthcare Improvement (IHI) methodologies and held a Master of Business Administration (MBA) degree. Her job was concerned with nurturing, guiding and developing clinical innovation and encouraging linkage. Grace explained that to develop trust and set up the conditions for learning, she needed to ensure that her approach was transparent, open and encouraged sharing. She was known for her ‘personal skills to make things happen and to bring people with her’ and ‘resilience’ to cope with obstacles (Link interviewee). Another Link described her hard-working approach and passion: ‘I know Grace is here till way past she should be in the evening . . . Grace is passionate. She believes in the cause’.
Context
Grace worked in a large NHS organisation located on the same site as a medical school. At the time of the study she was seeking a better physical home for the unit. Grace’s response to Greenhills-wide initiatives, such as the high profile patient flow programme, was similar to that of James: she saw them as both a challenge and an asset. She experienced some difficulties engaging with some members of the collaborative.
Content
She described her focus as on problems ‘that matter to patients’. Examples included electronic handovers, debriefing, the transforming theatres and scheduling programme, modernising health records, use of diagnostics, and patient pathways.
Activities
One of Grace’s chief activities was creating linkages and brokering relationships. One Link described her as a ‘key facilitator, gate keeper to the right people and the right departments and the right projects’. The role included information sharing and maximising ‘clinical innovation’. One Link reported, ‘Grace’s been very good at inviting me to various talks and every time I give a talk, people go ‘it’s amazing . . . why aren’t we doing more of this?’ Grace and her team tried ‘to bridge the gap’ between the NHS organisation and the university ‘and move from translation to transformation’. She supported staff in developing and progressing their ideas: ‘through to business cases, contracts, and negotiating intellectual property, patents, copyrights and all those good things’ (Grace). Another Link also described how she helped write funding applications and got letters of support.
Grace had established faculty meetings in which quality and safety improvement projects were shared. The meetings brought together people from ‘research, education, clinical innovation, improvement, service delivery all in one room’ and provided a network for those pursuing higher QI training. She herself was involved in providing improvement training to clinical teams and staff, although she sought to focus increasingly on the strategic mandate – embedding an improvement culture in the organisation – rather than actually doing the improvement projects.
A regular conference speaker, she engaged internationally with visits to or visitors from Sweden and the USA, for example. She presented on ‘the pragmatic approach to implementation and also the learning and the experience of our group’ (audio-diary).
Clients
Grace worked to bring together clinicians, academics and external stake holders (such as industry and the voluntary sector) with a view to solving problems.
Outcomes
Reactions were generally positive. Her narrative about her work with a group of junior doctors working on improvement projects expresses their enthusiasm and the energy they created:
We were all completely inspired by the positivity and the energy that was in the room. I had a couple of e-mails from some of the junior doctors afterwards, all fired up . . .
Grace
One form of tangible learning arose from the QI projects. She reported that ‘to date we have about 100 people who have gone through the second level of the programme’. She thought that capacity development was contributing to ‘sustainable change across the organisation’. The development of the QI faculty was described by a Link interviewee as one of her ‘greatest achievements’. In terms of results, one project – the placement of nasogastric tubes – had ‘significantly reduced the number of X-rays that patients were unnecessarily enduring’ (audio-diary) and had led to an award for the work. Another result related to bidding for and securing funding. She had success with the Health Foundation, for example.
Sophie
The agent
Sophie started her career in a front-line clinical role and, following completion of health-care management and leadership courses, worked her way up to a regional management position. She was well-known locally and had a wide-ranging knowledge of the organisation. At the time of interviewing, Sophie had been leading on all aspects of unscheduled care for 2.5 years. She reported directly to the chief operating officer. After 18 months in the position, she took on an improvement role addressing patient flow and length of stay. This part of her role initially took all her time, but after 1 year it had reduced to about 75% and was declining further.
She was described by Link interviewees as ‘responsive’, ‘tenacious’, and a problem-solving, ‘can-do’ person. While Sophie thought she was not good with the ‘softer’, ‘touchy-feely’ side of management, a Link interviewee described her supportive side:
When things aren’t going well, she will tell you and she would expect something to be done about it, but equally she’s highly complementary and supportive, very supportive.
Link
Context
The organisation in which Sophie was based serves a culturally and economically diverse population of 300,000 and employed > 8000 staff members. Problems pertinent to Sophie’s work included those arising from patients crossing authority boundaries and getting patients discharged into care homes. Despite this, emphasis on patient benefit provided a common motivator across organisations in the patch: ‘although the cultures are different across the organisations, they all want to do the best for their patients’ (Sophie). She was well supported by her line manager, who was in a senior position.
Content
The need for an improvement programme was prompted by a crisis in service delivery arising from high occupancy and delays in the system. Sophie’s focus was streamlining patient flow.
Activities
Sophie’s work addressed unscheduled care and patient flow in two district general and three community hospitals across the region. Sophie also mentored a clinician on secondment who supported the patient flow work.
Sophie was very hands-on: she held twice daily meetings with nursing teams at the two general hospitals, regular in-depth meetings with ward managers and the wider multidisciplinary team, and weekly ward ‘walk-arounds’, during which she spoke to staff and patients. She observed, ‘I’m in the thick of it with them. So I’m not a distant leader of this change I suppose’. She was in the process of gradually withdrawing to let the heads of nursing run the process and she was looking for suitable people to help with the role in the future.
At a team/management level Sophie gathered, brokered and disseminated information about performance from departments in an effort to challenge the culture around delays, encouraging them to be seen as ‘everybody’s responsibility’. Through sharing data she hoped to minimise silo working and to increase openness and visibility of performance – both good and bad.
She also shared relevant literature, including from outside health care (e.g. from business). Outside the organisation, Sophie regularly presented the organisation’s achievements at conferences and national programme events.
Clients
She linked with all tiers of medical staff at these hospitals, liaising with departmental managers, clinicians and nurses and other front-line staff. Sophie also linked with colleagues in other regions to manage patient flow.
Outcomes
Link interviewees valued Sophie as a sounding board and felt comfortable discussing options and decisions with her:
We work in a very stressful environment and . . . it’s highly valuable to have somebody that you feel comfortable approaching to get advice and somebody to just listen to you and she will help you to make your decisions really.
Link
Through Sophie, departments learned about each other’s performance. This had the effect of challenging the status quo:
It’s just challenging traditional practice, you know, historic practice and say ‘why do you do it like that?’
Link
Sophie was instrumental in creating a more target-driven atmosphere in which departmental performance levels were set and outcomes displayed on the intranet. Sophie met with teams regularly to review targets and set new challenges. She gave an example related to wait times: if the department meets a 12-hour target, they might be set the challenge of trying to average an 8-hour target the following month. As a result, tangible service improvements were noted in several departments; ambulance handover delays were reduced from ‘hundreds of hours delayed a month’ to 50 hours, and surgery cancellations were greatly reduced.
Amy
The agent
A nurse by background, Amy was on a 1-year secondment, working across patient safety projects but majoring on a specific sepsis project. She also facilitated several QI projects with partner organisations. One Link commented that Amy was ‘very active, very involved’ and had been ‘visible on the shop floor’. The agent was known as a good communicator, both verbally and in writing.
Context
Riverside covers a large urban area known for medical discovery, health-care innovation and education, yet also containing many socioeconomically deprived communities. At the network level, there was considerable variability within the partner organisations in terms of supportiveness. Other challenges included lack of resources to free up clinician’s time for improvement work and agents reported apparent confusion about overlapping mandates related to QI:
It’s become quite apparent that there are quite a few groups in the hospital whose job is QI – like clinical effectiveness, like quality improvement, safety patient groups, and what is everybody doing? They’re not joined up.
Amy
Amy described the immediate working environment as supportive. The three case study agents in Riverside used informal mechanisms from outside their department or line manager to make connections across the network and facilitate cross-fertilisation of ideas.
Content
Amy led an authority-wide QI project on sepsis.
Activities
She applied IHI QI methods, and a large part of her role involved improving measurement, specifically how data were collected, shared and applied to inform practice within the health authority. Amy worked with the information team to ‘build mortality tracking software’. This enabled staff to look at their own data in real time.
Amy was building capacity in the organisation by training and mentoring front-line clinicians in QI methods. This included delivering QI courses in various forms, leading learning sets, educating foundation doctors on sepsis during induction sessions and leading on training-the-trainer QI sessions. The mentoring involved regular meetings to discuss challenges, measurement approaches and QI tools, and to provide direct support where it was needed.
Amy also took on other duties including supporting the development of a health foundation bid and helping to co-ordinate a site visit for an international delegation. This aspect of the role helped to ensure that she was ‘taking some of the shared learning from one partner to another’.
Clients
Amy worked with front-line clinicians in her knowledge brokering role.
Outcomes
In relation specifically to the sepsis QI project, initially there was some negativity and resistance to the methods and approaches proposed as well as on selected measures from which to judge improvements. Unwilling to engage with the data presented, reactions from some senior clinicians had been defensive.
Despite this, others spoke of learning gains and a different way of thinking:
They’ve [Amy and the team] given us some really good feedback around what we need to be doing – how we can achieve our goal, how to approach things . . . They’ve kept us on a track . . . How it’s changed now is that the teams are really starting to think about using the QI methodology.
Link
The organisation had become more data driven, helped by the mortality tracking software that had contributed to driving improvement. She had been instrumental in improving processes around measuring and generating real-time data for sepsis.
Isabelle
The agent
Isabelle had a policy background and, after spending several years as both an in- and outpatient, now worked to improve patient engagement. She held two part-time jobs, but treated them both as full-time and admitted to working long hours to keep on top of both portfolios of work. Her KIT role was described as matchmaking across the network in terms of linking patients with those working clinically in a specific field and facilitating the involvement process. One Link thought that her personality, networking and influencing skills all contributed to her success in this role.
Context
Isabelle worked at Riverside alongside Amy.
Content
Isabelle’s main activity was to build on the insights gained from public engagement. She worked with people to help them make good use of the data that they had acquired.
Activities
Her role was facilitatory; she built relationships, connected people and provided advice on involving patients:
I use her as a network . . . So actually, you know, I need X group of patients. How do I get them? She’s quite linked in to all of those things . . . It saves me thinking about it.
Link
Isabelle reported spending the first few months in the role working out what currently happened around PPI in the network and building connections with key individuals. One Link described it as a ‘huge mapping exercise . . . across Riverside, nationally, globally’.
There was also a training and mentoring element to Isabelle’s work in order to build capacity for engagement. She was involved in planning both internal and external-facing events for the network related to patient involvement and contributed to bimonthly webinars.
Clients
Isabelle’s matchmaking role meant that she worked directly with patient groups, patient engagement leads and clinicians to improve patient engagement.
Outcomes
From her experiences of working with patient groups, reactions had been both negative (disruptive individuals with an agenda, difficult to recruit and engage) and positive (good access to people, worked well). Feedback on the learning set was said by Isabelle to be ‘overwhelmingly positive’.
She had developed learning about PPI and was known to ‘get people to think differently’ (Link). She had created learning communities, both online and in person, and learning sets.
In terms of tangible results, Isabelle, working with collaborators, had won an award at an ‘emerging leaders’ competition. Partner agencies had advanced their patient engagement strategies; for example, one had a patient and public engagement strategy.
A notable ‘movement’ around patient involvement could be detected by Links:
What’s happened is people have gone, ‘wow!’ ‘What an energising, exciting opportunity. We want to maintain this . . .’.
Link
Fran
The agent
Fran was a trainee doctor on a 1-year fellowship pursuing her interest in management and QI. For the last part of her fellowship she worked part-time. She reported to the medical director. Fran was credited with getting initiatives off the ground through her ‘enthusiasm’ and ‘commitment’ and by understanding the challenges of working on the front line. She was also approachable and diplomatic:
Very, very, very nice. So she’s very approachable and she is really good at not . . . treading on anyone’s toes. So she went about it in a really delicate way.
Link
Context
Fran worked at Riverside alongside Amy and Isabelle. She described the work environment as supportive, stating that ‘everyone who works there is really passionate and enthusiastic’ and ‘is really encouraging you’.
Content
Fran’s focus was on facilitating QI across a number of clinical areas. Examples included treatment escalation plans, falls prevention, patient safety and prescriptions at hospital discharge.
Activities
Her main activity was supporting clinicians in their own QI initiatives:
So I’ve been doing a lot of work with front line staff trying to get them to do quality improvement. So that’s for all junior doctors, non-medical allied health professionals. So I’m coaching them through smaller projects that they’re undertaking.
Fran
One Link interviewee explained how Fran had really helped her to progress her project, in part because of her understanding of the clinical setting:
In a way, it’s sort of access to supervision for me because she just asks the right questions . . . which is a luxury because nurses don’t get supervision.
Link
She taught QI methods, adapted QI training material for local audiences and professional groups, and also trained others to deliver courses after her departure. Over the course of the year, her role had shifted from supporting all the QI projects throughout the hospital to doing little direct support. That job had been taken on by Wendy in the clinical effectiveness unit.
She facilitated linkages, notably putting junior doctors in touch with a ‘tower block full of patient safety officers, the board, the audit team or the quality people’. She identified a notable achievement as ‘making sure we had buy-in from the exec team and getting them to board meetings’.
Links described how Fran helped them to become more aware of how and where to disseminate their QI projects:
So she’s really good at making you aware of what you can do with your quality improvement work. I didn’t even know that you could publish it or I didn’t know that, you know, there would be events at other hospitals where people would discuss it, and she’s kind of like opened my eyes.
Link
Fran had suggested that the Link should present her work at a regional event. She did, and won an award.
The agent also picked up a number of tasks that she described as ‘ad hoc’. Examples included writing up a pro forma for a team to adapt, developing e-learning on QI and looking up evidence in the literature. Fran also contributed to the development of the improvement advisor role in the network and set up a regional falls forum.
Clients
Fran primarily connected with front-line clinicians in her role, as well as facilitating linkages between these clinicians and hospital leaders (e.g. executive and board teams) as needed on specific QI projects.
Outcomes
Lack of interest was an initial reaction from some: Fran commented, ‘I was trying to coax them into using the improvement methodology . . . and . . . nobody was really that interested in . . . taking on that approach’.
Those she did work with developed learning in QI methods. Fran also spoke of her personal learning, which included better knowledge of hospital systems:
I think I understand structures of hospitals so much better – who does what – in a non-clinical sense actually more than clinical . . . I’ve learnt a lot about not being a doctor in sort of knowing what other people do with their time.
Fran
Fran’s role in training and mentoring front-line clinicians was credited with helping to drive projects further and faster, reaching outside the organisation through wider dissemination and helping to create change in the individuals themselves.
Tangible results included those she had helped to win awards and one trainee who gained a QI fellowship based on the training provided by Fran. The trainee stated that ‘the fellowship wouldn’t have happened without her influence’.
Jessica
The agent
Jessica was a practice-facing academic who worked between commissioners and researchers and created linkages between academics and practitioners. She had a long history of working on the region’s KIT strategy in the CLAHRC and now provided senior oversight of the organisation’s evidence review and evaluation work. For Jessica, the importance of context meant that it was not possible to simply apply KIT templates in a formulaic fashion. She described her role as fostering knowledge interaction and implementation, and supporting knowledge agents.
Jessica was pragmatic and perceptive. One thing she found challenging was the lack of organisational affiliation and not having a practitioner background.
Context
Moorlands covers a large geographical area with local variation in terms of demographics, political situations and drivers. The region had CLAHRC funding over 2008–13, but the network was relatively new at the time of the research. Projects were carried out across the region, in collaboration with a range of organisations, although relationships with industry were thought by the case study agents to be less well developed.
The KIT agents in Moorlands had relative autonomy to manage their roles within the context of national drivers and network guidelines. Although Moorlands cultivated a collaborative environment, the pressure to deliver was palpable. Faced with changing political drivers, funding uncertainty and organisational reconfiguration, a general lack of stability in the region was noted by the agents and influenced their thinking (i.e. only taking on projects that could be accomplished within a relatively short period). The agents’ line manager highlighted this uncertainty and emphasised the importance of demonstrating their contribution to improved patient care:
We’ve got to be able to demonstrate that we are a resource in support of improved patient care in partnership with our members, but I think it could all come to a crashing halt if we don’t do that. So I think this next period is critical. In terms of sustainability . . . I think the future is uncertain.
Line manager
Moorlands was transparent about its workings, posting on its website information about how projects were selected and commissioned and publishing outputs of recent projects.
Similar to other regions across the UK, the challenge of freeing up time from clinical or managerial roles to work on implementation was noted:
The hindrance is the extraordinary pressure under which the NHS is operating and the inability to lift one’s head in a senior management capacity above the parapet or as a middle management capacity. So it is the pure pragmatics of finding either the intellectual or physical capacity to implement change.
Line manager
A further challenge was noted by Jessica, who reported how eligibility restrictions caused problems when recruiting to roles that cross NHS–academic boundaries.
Content
A primary focus of Jessica’s work was commissioned and client-focused evidence-based reviews.
Activities
Her role involved dissemination of specialist knowledge to practitioner collaborators, as well as sharing tacit knowledge about the NHS environment with researchers, which helped them to gain access to NHS sites and recruitment participants. She had also contributed to the development of an integrated clinical academic pathway for a cohort of master and doctoral students who sought to develop a clinical academic career.
Jessica also provided support for others working in KIT roles. She counselled them about the problems they encountered and helped them to manage expectations. She encouraged other agents to adopt more reflective implementation practices.
Clients
Leading on evidence review and evaluation, Jessica worked with practitioners and academics.
Outcomes
Discussing the theoretical or more academic side of implementation with practitioners could sometimes be met with resistance: ‘unless you’re really lucky, the minute you start talking about the social science or theory of implementation it’s just like you can see like kind of the barriers go up’.
The evidence reviews were well received and informed future practice:
They have been excellent in producing the report for us in a relatively short period of time . . . and making sure that actually it would be a helpful product for us.
Link
Jessica expected her work to shift thinking and work practices:
If I’m doing my job properly they start talking about implementation, knowledge brokers and community of practice and it just becomes the norm to them.
Jessica
Holly
The agent
Holly had a nursing background and had held director-level positions within her profession, so was well-known and respected within the region. She worked 1 day per week as a KIT agent and the remaining time in one of Moorlands’ partner organisations. She was on the organisation’s executive group responsible for clinical programmes and provided the link between the board and what was happening at the coalface.
The agent’s communication skills, in what could sometimes be a difficult role (managing expectations with partners and promoting the Moorlands work to external organisations) were highlighted by her line manager. The benefit of successful implementation for patients was her key driver: ‘ultimately we want to just get this into practice for patients’.
Context
Holly worked in Moorlands alongside Jessica. One of her main challenges was getting practitioners to take time out of their clinical roles to engage in research and implementation. Other challenges arose from system reconfigurations and turnover of senior staff; relationships had to be rebuilt and alliances re-established: ‘You’ve got people on side and then the next minute they’ve gone’.
Content
Holly summarised what she thought the clinical professionals wanted: ‘they just want the practical help, you know . . . “It all sounds marvellous – how can we get these into practice to improve patient safety?” That’s what they want to know’.
Activities
Engaging with senior leaders and managers was a significant part of Holly’s role. Oversight of various network projects took up half of her time. This entailed early identification and resolution of issues. If a project encountered a delay then Holly convened a meeting with the project manager, the principal investigator and the practitioners involved. For the other part of her role, Holly provided a link between the NHS and academia. Through presentations and meetings, she brokered the benefits of using the network to both the clinical and academic sectors. She explained that the aim of these meetings was to ‘procure relationships and establish contacts with senior teams across the partner organisations’. Through her project management and linkage work, Holly was able to suggest personalised, appropriate contacts for people.
Her approach highlighted the need for organisations to be ‘on board’ and supportive of new interventions and innovations:
. . . more of the same is not the answer. We need to create a sustainable NHS and part of the way that we do that is to innovate and adopt and spread, and actually through coming on board with us and supporting implementation of new interventions.
Holly
Other activities included working with a colleague in a consultancy role to create a set of priorities for the region, focused on local pressure areas. She had also developed a brochure on capacity-building opportunities for organisations: ‘the short courses that we offer, research exchange placements, knowledge broker roles, PhD [doctor of philosophy] opportunities’.
Clients
Holly’s knowledge brokering role involved working with senior leaders and managers in NHS organisations, often connecting these individuals with academics.
Outcomes
Holly’s line manager noted that people were responsive to the brochure and other information/materials that she distributed. One Link interviewee expressed the value of the information that came from outside their own organisation; it was viewed as unbiased and, therefore, was more readily accepted. However, another Link interviewee highlighted that although the evidence reviews were useful, practitioners were busy and so the ‘easy one-liners’ were most useful. Yet for another Link, the simple dissemination of evidence or information was not enough. She valued personal communication as a source of new information.
As well as furthering individuals’ progress with their projects, Holly spoke of these linkages helping to form an interlinking ‘network of champions’ to help with ‘general implementation in change adoption improvement work’. It was through the implementation of new interventions that she anticipated improved quality of care and cost efficiencies, although Holly’s line manager acknowledged that these were slow and gradual changes: ‘we all know from experience you have to keep drip, drip, drip, drip all these things’.
Daisy
The agent
Originally trained as a nurse and experienced as a service improvement manager, Daisy was working as a research fellow, supporting implementation of the network projects as well as pursuing her own research. At the time of the study Daisy had only been in post for a few months. She initially found it difficult to balance the dual demands of the operation; support of research into practice, and researching that process (her own research). Later, she was assigned to a large, cross-organisational research project. She adopted a proactive approach; if she heard about a project that she felt she could contribute to or learn from, then she would request to take part in some way.
Context
Daisy worked in Moorlands alongside Jessica and Holly and noted their ‘strong team culture’. Although new in post, she was already aware of the uncertain future:
I am conscious, you know, everyone’s roles are being reviewed, that the environment that we’re working in might change, etc. etc. So I think I’ve got to, sort of, be realistic about what’s really, really important to deliver in the next, what, 3 to 6 months.
Daisy
Content
Daisy’s work aimed to improve thinking around the implementation and use of evidence. The review topics to which she contributed were suggested by practitioners and developed in line with their needs.
Activities
Daisy worked closely with project managers in organisations to understand the knowledge needs of users and areas in which implementation challenges exist. In a context described by her line manager as one in which clinical academics develop innovations but expect others to implement them, she saw Daisy’s role as being ‘about helping people think about their implementation and translation plans. Nudging them along the right way, or helping them develop networks’.
The complexity of the projects required a variety of methods rather than a set approach. Daisy’s methods were pragmatic but theoretically informed. She reported taking a systematic approach to the discussion of implementation with teams: ‘That’s when we really go through it in minute detail about the three areas of context, content and process’. Part of these discussions involved challenging teams to ascertain their current readiness and whether or not they were in a position of readiness for change. These steps were seen as ‘central to translation’ and the development of ‘a resource that will make a difference’.
Daisy also led on increasing the transparency of the network and its processes on their website.
Clients
Daisy worked with lead clinicians and others (e.g. project managers) proposing an improvement project within the network.
Outcomes
Importantly for organisations, the reviews were accessible and contained information that could be applied directly to aspects of their work. For example, one Link interviewee reported that the material was directly useful, and that employing the information given in presentations was ‘very easy to do’. Link interviewees observed that the reviews were not oversimplified and succeeded in covering all aspects relevant to the topic: ‘So, you know, depending on who you are and what your interest is there’s sort of something in there for everybody’.
By publishing on the website a flow chart with time scales and identifying relevant staff members, she had improved communication both inside and outside of the organisation.
Given her short time in post, it was difficult to identify changed behaviour or results. Daisy was aware that this was a more general difficulty: ‘It’s quite a hard role to demonstrate, I think, a clear impact’.
Erin
The agent
Erin was a PhD-level manager with a long history of working in the heath innovation infrastructure in her region. In her role she supported the commercialisation of new products and ideas, and split her time between NHS Innovations and the network.
She described herself as adaptable, loyal and hard-working, and was described by others as ‘approachable’ and accessible, with a friendly personality. She admitted that she could ‘adapt [her] personality dependent on who I’m speaking to’. Others saw her as motivated ‘to see that innovation developed for the benefit of patient care’.
Context
With a well-defined small geography, the largely rural region with an ageing population had high levels of deprivation and lower life expectancy than UK averages. Erin saw benefits arising from size and described herself as ‘lucky . . . it’s a small place. Everyone knows one another’. She reported that the board was ‘very, very powerful’, composed of NHS leaders supportive of the network’s ambitions, particularly in the wealth creation agenda. Not unlike other networks, political changes at the national level were front and centre on the agents’ minds, and they reported an uncertain future for the network. She reported close relationships between the local universities and clinical community, and a number of well-developed professional networks in the region.
Content
Erin led on the wealth creation agenda for the network, including developing service-level agreements, as well as monitoring due diligence and peer review of new products.
Activities
Erin operated at a senior-level in the organisation to create linkages and broker new relationships across organisations such as small and medium-sized enterprises (SMEs), local education partnerships and the Clinical Research Network. She facilitated the product development process by working closely with local staff to test and challenge their ideas before further resources were invested. She described this as ‘sense-checking’ and ‘idea health checking’ to determine ‘is it worth doing?’ and if so, whether or not a UK patent is appropriate. She described this as demystifying the patenting process.
Erin was supported by a team who provided more of the transactional activities, including working with partners to prepare them for board meetings and providing evidence and data to partners to support their market research, product development and business processes. The specific kinds of information were detailed as ‘potential sales volumes, how many hospital events . . . around the UK, how many cases that have happened, where there’s been patients that have been potentially injured’.
A Link interviewee described Erin’s contribution:
Erin was able to facilitate meetings and arrangements and we’re now in negotiation with the Health Authority about being a proper deliberate partner for them and looking at different ways of working with them.
Link
Erin reported working the wealth agenda at the national level with other commercial directors of networks.
Another key activity was developing funding bids and securing new contracts. Erin had been successful in securing matched funding, attracting notable amounts of European funding. She also delivered education and training, in particular related to the innovation and the intellectual property process.
Clients
Erin’s senior-level position within the network meant that she worked with senior leaders in the innovation space from across the various organisations in the network (e.g. SMEs, local education partnerships).
Outcomes
The support provided to local SMEs by Erin and her team was seen to be ‘really, really helpful . . . When we’ve been struggling to get decisions or struggling to get in front of the right people, they’ve always been useful on that front’. Brokering new relationships was allowing SMEs to engage at earlier stages of the development process with those in the health service who were the intended target for their new products.
The provision of data and information was also valued by local stakeholders. One Link interviewee commented: ‘We knew what we needed but we didn’t know where to get the information from. So that was Erin’s team that did that for us’. Having the relevant information enabled the Link to ‘negotiate better terms’.
In this way, Erin’s work was contributing to a shift in thinking around wealth agenda and a normalisation of innovation processes.
Janice
The agent
Janice was a clinical researcher with experience of conducting primary research, based at a local university. She divided her time between a knowledge mobilisation fellowship and completing her PhD. She worked as a clinician for several years before transitioning into a research role. She wanted practitioners to ‘feel that research is not an ivory tower’ thing undertaken by people ‘who are only in that for the paper’. She exhibited a belief in coproduction and believed in the need to engage service users if services are to improve.
Janice’s line manager described how she had ‘always been able to work independently,’ adding that Janice’s career path necessitated ‘a certain amount of resilience’ because ‘it’s not like there’s lots of handy signposts. You’re kind of making it up as you go along really’. She reflected that ‘a big part of what Janice does well is the fact that you can send her in to talk to anyone and she’ll do a good job and that she’ll leave a positive impression’. Another Link worked closely with Janice on her fellowship project and reflected that ‘Janice’s communication is really good . . . She’s really accommodating’. Janice described herself as ‘enthusiastic about every problem’ and ‘slightly relentless’.
Context
Janice worked in Wetlands alongside Erin. She commented that people were on ‘redundancy alert’ and awaiting the impact of the outcome of the general election (which was pending at the time of the interview in 2015).
In terms of internal context, Janice felt able to act with some autonomy and valued being based in a university rather than a hospital.
Content
The focus of Janice’s work was engaging with clinical staff and service users, specifically about maternity care.
Activities
Janice described what she did as ‘perhaps bringing a bit of reality into academia and a bit of academia into reality’. She collated and shared research evidence and information with the community of practitioners and service users depending on their needs. This involved working directly with the target audience to ‘decide which evidence the actual people want and which would be useful’. She used existing networks of mothers and babies to find out what their interests were and ‘how to explain research to them in a way that would make them want to be engaged with us’. She also presented to clinicians and attended local informal meetings to share the results of her work. In addition, Janice had a role in supporting fellowship applications.
Clients
Janice engaged with maternity clinical staff (e.g. midwives) and service users.
Outcomes
The Links responded positively to Janice.
Janice informed others of new research in the field as well as ‘the bigger picture of what’s going on at the hospital’. This Link was then able to share this learning with her patients: ‘So that’s been really beneficial in a very practical way for them. You know, just to inform and empower and allow them to know what their options are which has been really useful’.
One Link commented that ultimately she would expect to see ‘tangible outputs, resources for people to use in the future’.
Chloe
We have limited data on this case study as Chloe had to cease participation in the research.
The agent
Chloe was a lecturer at a local university, completing a PhD and working as a knowledge agent on a part-time basis. Originally trained as an allied health professional, she had many years’ experience, including management roles, and was recognised as a leader in her health professional community. Chloe described her role as one centred on engagement and increasing the two-way flow of knowledge between the university and the community.
Context
Chloe also worked in Wetlands.
Content
Chloe was a subject matter expert in her allied health field and engaged directly with practitioners in that field within the region to update their knowledge base.
Activities
Chloe’s role encompassed a number of related strands, notably identifying knowledge gaps, providing training in accessing and using evidence from research to inform practice, co-ordinating events and supporting colleagues to apply for fellowships and other funding in knowledge mobilisation.
Clients
Chloe worked with practitioners in the allied health field.
Outcomes
The training in using research evidence to inform practice was initiated and led by Chloe, and appeared to have resulted in learning gains and changed behaviour. Chloe reported that practitioners were increasingly incorporating evidence into their practice: ‘I’m seeing people and they’re saying, “actually . . . we ‘ve changed what we’re doing and we’re using the evidence”’. Chloe was able to look at available local data to see whether or not new evidence was being used in practice.
Molly
The agent
Molly was an experienced programme manager with a background in patient safety and QI. She was trained in improvement methodologies and applied IHI methods. As a member of the core network staff, her role was that of expert in patient safety and manager of a broad spectrum of the network’s activities.
Molly adopted a listening approach, believing in the importance of setting priorities for the work programme after hearing what the local population had to say. As a team leader, team-building was really important to Molly and she made an effort to work in the same office as other members of the team.
Context
The region this network site covers has a stable, older, population. Geography can be a challenge because other regional organisations have different boundaries than the Homefields network and the region itself is large. The region had an established CLAHRC with which they collaborated. The economic pressures were described by the line manager as ‘particularly acute here at the moment and much like other regions, our authority partners are struggling’. Despite the challenges, one observer noted a ‘very collaborative spirit’ in the region. The network benefited from strong, vocal, representative and engaged leadership from their board. Challenges also arose from the network having to shift its priorities according to central policy and funding decisions. For example, the patient safety agenda became one of the main programmes during the period with a budget and political importance attached to it.
There was a notable entrepreneurial spirit within the Homefield team, driven in part by their own funding uncertainty and evidenced by a long-term business model with sustainability as its goal. The organisational structure was purposely relatively flat, allowing a more flexible approach and giving individuals scope to experiment. The organisation was described by Molly as ‘complicated’, yet also ‘a really nice organisation to work in’.
Content
Integrating care from an individual patient point of view rather than integrating disease pathways was the priority. However, Molly also referred to traditional disease-specific projects such as strokes and diabetes.
Activities
The core network team, of which Molly was a key player, invested its time in an early listening exercise before determining the regional priorities. Molly used the term ‘honest-broker’ to describe the role of the network as it functioned as a conduit between various silos. Molly and the team were data driven and strove to connect new groups of people in the general field of patient safety.
Molly’s core role was project management and she led on the patient safety portfolio of activity. She worked across what she described as two types of projects, fact finding and field testing, and across different levels – macro and miso – in the system. She was concerned with how projects were prioritised and how the network achieved regional oversight of their activity, given the number of initiatives in the region. Molly looked to reduce duplication of improvement activity across the patch, and sought to link similar initiatives and to collaborate. She described a number of tools that were being created by the network, including a public-facing central repository of projects and a project management system. They were developing regional standardised, co-ordinated approaches in patient safety and patient feedback systems. Establishing the regional patient safety collaborative across all sectors (not just acute settings) became a significant part of Molly’s role during the study.
Molly was credited with co-ordinating a series of training sessions in IHI methodologies for a large cohort of practitioners. She also performed a range of roles in regional engagement events, from speaking at the event to co-ordinating registrations.
Clients
Molly worked with lead clinicians and others (e.g. project managers), proposing an improvement project within the network.
Outcomes
Responses to the honest broker role were positive. The line manager was ‘impressed’ with the QI training programme.
The organisation learned about the community’s priorities and regional improvement initiatives. Participants in training developed skills in QI methods.
Describing themselves as a listening organisation, Molly and her colleagues felt that they were contributing to a shift in culture.
Concluding remarks
This chapter has presented an overview of the 13 case study KIT agents (a summary is provided in Table 8). Selected for diversity, they highlight both content-specific knowledge transfer challenges as well as generic mechanisms that support knowledge mobilisation. These case studies provide an opportunity for comparison and cross-pollination of strategies and tactics, which are explored in the next chapter.
| Agent and organisation | Role and dispositions | Context | Content | Main activities (processes) | Outcomes | |||
|---|---|---|---|---|---|---|---|---|
| Reaction | Learning | Behaviour | Results | |||||
| James (Greenhills) NHS (within network) |
Medical background Unit Director Near retirement Charismatic leader who put grit in the system |
High-level support Pressure to demonstrate worth Some internal territorial sensitivities but also open Supported by executive External challenges from changing demographics, technological developments and economics |
Cross-organisational and clinical/non-clinical | Leadership and QI training Brokering |
Some hostility | Leadership, QI | Less siloed | Proposals, awards, projects QI in appraisal system Organisational cultural change? |
| Grace (Greenhills) NHS (within network) |
Nursing background with MBA Improvement unit lead One who makes things happen; passionate and resilient |
Large NHS organisation with medical school on site Seeking better physical location for unit Mixed views on Greenhills-wide initiatives |
Patient focused; clinical and non-clinical | Linkage and brokerage Information sharing Supporting innovation Funding bids Supporting QI: training and networking |
Positive | QI capacity development | Using QI methods | Successful funding bids Awards Results from QI projects |
| Sophie (Greenhills) NHS (within network) |
Clinical background with management and leadership training. Lead for improvement and unscheduled care Responsive, tenacious, can-do person |
Diversity across the region but patient focused Patient flow challenges Supportive line manager |
Patient flow | Hands-on daily meeting with nurse teams, regular meetings with ward managers and multidisciplinary team Disseminates performance data |
Comfortable | About performance | Shared ownership of problems | Achievement of targets Organisational cultural change? |
| Amy (Riverside) Network role within NHS host |
Nurse by background, on a 1-year secondment Patient safety projects, specifically sepsis Active, involved and visible |
Diversity across the region Variable support Overlapping mandates Lack of clinician time for QI Immediate team support |
QI sepsis project | Sepsis QI lead Improving measures, data collection Delivering QI training and mentoring Other supportive activity (funding bids, visits, events) |
Some defensive responses | Sepsis performance QI methods |
Using QI methods | More data driven Organisational cultural change? |
| Isabelle (Riverside) Network |
Policy background and past patient Linking patients with clinical researchers Hard-working with influencing skills Well networked |
As above | Patient engagement | Building relationships and connections Mapping PPI Training, mentoring, capacity building |
Generally positive, although examples of negative responses | Learning about patient engagement | Thinking differently | Improved PPI engagement (potentially) enhancing research and practice Award Strategies |
| Fran (Riverside) Network role within NHS host |
Trainee doctor on a 1-year fellowship QI facilitator Enthusiastic, committed, approachable and diplomatic |
As above | QI projects across clinical areas including escalation, falls, patient safety, prescriptions | Supporting QI projects Training, adapting materials Linking staff to other related support |
Some disinterest | QI methods Personal learning |
Using QI methods | Enhanced QI projects and dissemination Awards |
| Jessica (Moorlands) Network/CLAHRC |
Practice-facing academic Evidence review and evaluation Supporting knowledge agents Pragmatic and perceptive |
Large geographical area with variation New network with CLAHRC history Collaborative but challenged by uncertainty Transparent Lack of manager/clinician time for implementation |
Commissioned and client-focused evidence-based reviews | Leading on evidence review and evaluation Brokerage between practitioners and academics Supporting other KIT agents |
Resistance to theory Well-received reviews |
From specific reviews Researchers learning tacit knowledge about NHS Higher degree programme |
Shift in thinking; normalisation of KIT processes Changed behaviour in light of reviews (implied) |
Evidence reviews (as products) changing decisions (implied) |
| Holly (Moorlands) Network/CLAHRC |
Senior nurse by background, working 1 day per week in KIT role promoting Moorlands work Good communication skills |
As above Challenge of staff turnover |
Practical and patient focused | Engaging with senior leaders and managers Project oversight Brokerage between NHS and academia Priority setting Information on capacity building |
Responsive | How to progress projects Information on opportunities |
Better relationships Network of champions |
Implementation leading to improved care and cost efficiencies (implied) |
| Daisy (Moorlands) Network |
Nurse by background and experienced service improvement manager, working as a research fellow supporting implementation Proactive |
As above Strong team culture |
Use of evidence and implementation | Clarify user needs, contribute to evidence reviews and facilitate implementation Work on transparency |
Useful | How to implement Shared information on work of organisation |
Change arising from implementation (implied) | Early days |
| Erin (Wetlands) Network |
A manager with PhD, experience working with SMEs Intellectual property expertise Approachable, friendly, adaptable |
Small, largely rural region with areas of deprivation Powerful board Uncertain future Good local relationships |
Wealth creation agenda | Facilitating product development process Creating linkages and brokering new relationships Provision of data and information Funding bids Training related to innovation and Intellectual property processes |
Useful | Business development | Improved SME business planning and negotiations | Shift in thinking around wealth agenda; normalisation of innovation processes |
| Janice (Moorlands) University |
A clinically trained researcher on a knowledge mobilisation fellowship, independent, resilient, good communicator, relentless | As above On redundancy alert |
Clinician and user engagement, specifically maternity | Providing tailored information to practitioners and service users Creating linkages and brokering new relationships |
Positive | Learning tailored to local knowledge gaps | Changed behaviour in light of evidence (implied) | Improved use of research in practice |
| Chloe (Moorlands) University |
University lecturer and part-time knowledge agent Trained allied health professional |
As above | Subject matter expert in her allied health field | Identifying knowledge gaps Training in using research to inform practice Organising events Supporting fellowship applications |
No information | How to access and use knowledge | Changed behaviour in light of evidence (implied) | Improved use of evidence (implied) |
| Molly (Homefields) Network |
Programme manager with expertise in patient safety and QI Listening approach Team player |
Stable, older, population Established CLAHRC Mismatched boundaries Economic challenges Collaborative Strong leadership Entrepreneurial |
Patient safety | Project management and patient safety lead Co-ordinating QI training Sharing information about regional improvement initiatives Delivering regional events and engagement days |
Positive Impressed |
Community priorities Improvement initiatives QI methods |
Improved, co-ordinated projects | Listening – culture shift? |
Chapter 6 Cross-case findings: facilitating outcomes
In this chapter, we present details from the case studies to illuminate why the KIT agents acted as they did and were successful. Highlights of our findings are the importance of being proactive to define the KIT role, how individual dispositions outweighed technical knowledge in terms of enabling change and having the time and flexibility to develop the role.
Expectations of the knowledge and innovation transfer agent role
Knowledge and innovation transfer agents experienced multiple and sometimes conflicting expectations of their role. In this section we consider expectations from a number of perspectives, identifying the importance of actively defining and clarifying the role with line managers and Links and proactively planning for sustainability from the beginning by developing capacity within local teams.
Knowledge and innovation transfer agents’ expectations of their role
Knowledge and innovation transfer agents performed diverse roles and held many responsibilities that exemplify their boundary-spanning function. Their primary accomplishment was to link quite different communities and individuals. These linkages were made both within their organisation, across different departments or levels of management, and between organisations, notably linking academic and health services practitioners (managers and clinicians). They led change initiatives and challenged local practice by introducing and employing different knowledge sets (including both research-based and experiential knowledge). Another element of their role was building local capacity around KIT.
Role ambiguity and learning on the job was common across agents, but those who were well supported by line managers (e.g. James, Janice) were able to actively define their role, which played a part in their success. In several cases when the role was ill-defined or misunderstood, the agent took on work outside their scope or skill set, which could lead to feelings of anxiety and inadequacy. For example, Amy reflected in her audio-diary how she was being asked to take on too much:
So the meeting finished and I felt really anxious, really overwhelmed. My boss didn’t have time to hang around and catch up with me but I did speak to [Name] and I said that I felt really uncomfortable that I was going to be the core person trying to bring all this together, for lots of reasons . . . I felt way out of my depth, really uncomfortable in the job I was doing and really inadequate.
Amy
Another agent at Riverside, Fran, described how she took on work that ‘wasn’t actually meant for me’ and ended up doing a lot of the project rather than advising and coaching as was intended in the role. She reflected:
I wasn’t there as an extra pair of hands. I was there to improve their skills to do it.
Fran
Knowledge and innovation transfer agents expressed longer-term expectations for their role, including changing local culture, improving patient care, and improving relationships between academia and the NHS. For example, Sophie described how introducing a different format to ward meetings helped remove professional hierarchies, encouraging everyone to challenge each other. She felt that the process helped people to think differently and reflected that ‘the whole organisation feels different’. This suggests a way in which the KIT role could lead to a change in local culture.
Line managers’ expectations of knowledge and innovation transfer agents
Line managers had expectations that corresponded with all of the functional expectations held by agents. These included the centrality of building relationships as part of an engagement role, facilitating change and building capacity. Line managers also felt that the engagement role should ultimately lead to improved ways of doing things and improved patient care. However, this was viewed as a long-term goal as the role developed. James’s line manager described the first year as one to ‘raise awareness to have some warm feelings’ but expected beneficial outcomes arising from year 2 and beyond. He described these outcomes in terms of empowering others and building capacity: ‘. . . whether people feel that they are empowered to get on with changing their individual areas and whether they feel skilled’. He expected that such outcomes could be measured:
. . . and I think we can track some of those kinds of measures through.
James’s line manager
Other expectations about outcomes expressed by the line managers included the view that outcomes were delivered through a collective partnership and not held by one individual (Molly’s line manager) and that these roles do not necessarily generate financial savings, but recovering investment was a more appropriate framing around costs (James’s line manager). For this line manager, recovering investment meant that the KIT agent’s work would generate a level of savings within the organisation over time making the original investment cost neutral. However, measuring improvement or efficiency savings was described as challenging by Grace’s Link.
Links’ expectations of knowledge and innovation transfer agents
Links also expected KIT agents to make linkages between various parts of the organisation and individuals (e.g. between operational staff and the executive board) and to facilitate practice change. Uncertainty about the role and poor communication by the line manager were identified as problems. However, Links did not fault the agents for poor communication but rather reflected that they themselves needed to take time to find out more about the agent.
Knowledge and innovation transfer agents were also seen as experts by their colleagues, either based on their professional experience, subject expertise or experience in the specific organisation (e.g. the Links of Isabelle and Sophie). One of Amy’s Links expressed anxiety over the KIT role and had expectations that ‘they wouldn’t link in with our usual processes’. This hints at the importance of understanding and working within local contexts.
The knowledge and innovation transfer role: risks and sustainability
Knowledge and innovation transfer agent roles are seen as risky and lacking traditional forms of recognition in terms of progression and opportunities. Agents who left their clinical or managerial jobs to take on these roles expressed concern about future uncertainty:
I’m taking a bit of a personal risk, you know, I’ve dropped 70% of a job to be able to do this and at the end I have no, you know, I’ve got nothing lined up particularly. So I think there’s a real risk.
Janice
This agent went on to reflect that at the end of the fellowship she might end up back in a clinical role in which she would be ‘extremely restricted in how much [she] could do’. A related issue is the lack of a career trajectory as emphasised by Janice’s line manager: ‘the reality is that people don’t get promoted or don’t get career recognition on the basis of these things. Not yet anyway’.
We also found that academically oriented KIT agents were taking on a risk in moving away from traditional academic outputs and focusing on knowledge transfer and mobilisation. Jessica felt relatively secure in her current role, but expressed the lack of recognition from her university employers:
But then do my employers recognise that? Not a chance. I’m OK with my current [profession]. If my [profession] changes I will be in big trouble about that one.
Jessica
Another challenge for sustainability and attractiveness of these roles is that KIT work seemed to be undervalued and invisible compared with clinical duties. Fran’s Link reflected that the work of the KIT agent was something that was squeezed in alongside real (‘actual’) work: ‘I think it’s really about finding time to do this because obviously you’re doing it while you’re doing your actual work’. The invisibility of the role raised challenges around attribution and costing the role against organisational targets.
Agents on short-term fellowships (Amy and Fran) discussed having trouble finding a go-to person for a proper handover at the end of the fellowship. They felt personally responsible, but others felt it was an organisational responsibility. One of their Links suggested that there should be some kind of an agreement from the trust to fund the position after the fellowship: ‘maybe for sustainability that actually when you enter into that partnership within the organisation, . . . that there’s the agreement that they will support the sustainability once that fellow’s gone’. She likened this to the model adopted by some pharmaceutical companies who only invest in funding a short-term role when the organisation agrees to continuation funding.
Aware of these challenges (summarised in Table 9), many of our agents adopted proactive strategies including planning for hand-over from the onset by training others and developing capacity, pursuing other funding opportunities and focusing on demonstrating value.
| Factor | Enablers | Barriers |
|---|---|---|
| Expectations | Supportive line manager with shared expectations Agent able to actively define role and manage expectations |
Role not clearly communicated |
| Risk and sustainability | Planning for hand-over and developing capacity Organisation committment to sustainability Entrepreneurial mindset (e.g. seeking own funding, demonstrating value) |
Lack of career progression and recognition Undervaluing KIT work Invisible role |
Factors related to individual dispositions
Although technical knowledge is essential, many participants identified dispositional enablers as critical to the KIT role. These include outlook or attitude, having a supportive and skilled team, and the status of the individual. Links also described the importance of the agents’ leadership skills and interest in the change process.
Attitude and outlook
Six of our agents were described by their Links as having a can-do attitude and presenting as enthusiastic when working with front-line staff. One agent (James) reflected: ‘it’s about taking an attitude that this is possible rather than what’s difficult about it. To say, “this is the way forward, how do we overcome the problems” rather than be deterred by them’. This agent’s approach did not go unnoticed: one of his Links described it as ‘being solution focused, not talking about problems but talking about, “what are the issues here?”’.
In line with KIT agents’ own expectations, line managers expressed how a proactive approach to the role was a critical ingredient for success:
It’s doing the horizon scanning rather than waiting . . . Someone proactive, I suppose. Yeah . . . they need to have demonstrated that they can be proactive and will be.
Janice’s line manager
Fran, for example, described how in the first few months in post she had been proactive and met with different teams to define her projects.
Leading change, whether through innovation or implementing research, takes time and agents needed to be able to sustain their interest. One Link described Sophie as ‘tenacious’, adding that ‘it’s not been a 1-minute wonder. She’s sustained her interest in it’. Large system changes in particular required sustained attention.
The status of the agent
Agents with status in the organisation enabled engagement, especially with hard-to-reach groups such as consultants. One agent (James) reflected that being a senior doctor and directly accountable to the chief executive were two critical factors that facilitated his role. Another agent brought along a senior consultant when she facilitated a QI session with a group of challenging consultants. This approach proved useful and led to further reflections on the value of bringing together clinicians and managers:
So it was really useful for her [senior consultant] challenging them and making them think. So we’ve sort of reflected that where possible we need someone of that level, ideally a consultant peer in the room. Equally they’re all feeling quite frustrated that they have tried to get . . . quality improvement, but they feel they can get blocked by managers . . . So we’ve reflected that we really need some sort of senior manager in the room or they need to bring their managers.
Amy
The agent is unlikely to have the relevant status in all groups; one solution is to directly involve others (such as clinicians, managers) to complement the status of the agent.
Being known and having an established network of contacts within a region enables an agent’s capacity for brokerage. Chloe, for example, mentioned how she is often approached by members of her profession’s clinical network to provide the latest evidence on a subject because she is ‘well-known’ and knows who to contact within the network. Being well networked also helped agents gain buy-in from the ‘right’ individuals.
Leadership style
One of the qualities that KIT agents associated with good leadership was being a team player. Sophie’s line manager spoke of her leading from the front, saying ‘[Sophie] would pick a trolley up, you know, and help move a patient to a ward, if she was based on one of the sites at the tail end of the day’. Humility [e.g. ‘I demonstrate. I don’t always have the answer’ (Sophie)], creativity and celebrating success were valued. Another facet was a coaching or nurturing style:
You’ve got to make the conditions right, really, for people to share, to be transparent, trust and to learn. I think we all know that no one is perfect, but actually by working together and by applying improvement methodology you can really make change happen.
Grace audio-diaries
However, agents’ style differed and not all our agents felt they were always performing as a leader. Sophie’s style was perhaps less nurturing: ‘I don’t need that positive stroking to get me where I am and I sometimes struggle with other people requiring that’. What worked for one agent in one circumstance might not work for another in a different context. Factors related to individual dispositions are summarised in Table 10.
| Factors | Enablers |
|---|---|
| Attitude and outlook | Enthusiastic and positive Solutions focused Proactive Tenacious and persistent |
| Status of the agent | Experience valued by others (e.g. clinical, managerial) Seniority Being well-known and well networked |
| Leadership skills | Team player Suiting style to context (e.g. extent of nurturing) |
Organisational and network (meso) factors
Our study coincided with the initial stages of the AHSN and SEWAHSP development. Here, we explore the AHSN and SEWAHSP context as it relates to the KIT role and organisational factors facilitating or hindering KIT role success.
Network context
The agents in our study related to their host network in different ways:
-
employed and based in the network (n = 4)
-
based in network partner NHS organisation (n = 5)
-
joint appointment (n = 2)
-
employed by a university (n = 2).
Being employed by the network provided the agents with dedicated time away from their usual clinical or managerial duties to perform their knowledge brokering work. Agents reported a number of other enabling conditions including being based in a less hierarchical organisation with an entrepreneurial culture and having a peer group for knowledge exchange in their home network. However, the network-based role meant job insecurity in the long term; they needed to demonstrate their added value and secure longer-term funding. They were not performance managing those involved in change, so sometimes had limited influence and the networks were themselves complex organisations, as noted by Daisy:
So there’s something about the fact of what the AHSN does. They seem to be implementing or looking at issues at lots of different levels within health care. So, surprise, surprise, it’s even more complex and we’ll require a variety of methods, I think, rather than one approach.
Daisy
Agents also reported a competitive environment between the networks at a national level. For example, although directors received support from a national network of AHSNs, agents reported this support did not extend beyond the senior level.
Agents based in partner organisations reported similar enabling/hindering conditions and also felt they had to take the initiative to develop and articulate their role within their NHS organisation.
Agents on joint appointments were less susceptible to some of the challenges mentioned by those based in the networks but were faced with other issues around splitting their time and negotiating the different organisational practices. Molly remarked that ‘shared posts’ were a good idea but ‘a challenge for whoever fulfils the post because the two organisations are so different in terms of the way we work’.
Being based in a university gave KIT agents access to library resources including librarians providing literature reviews and training resources. Both our university-based KIT agents had a clinical background that they used to secure buy-in with their NHS-based clients. Chloe described this advantage as being able to say ‘I’ve done it’, which helped remove the barrier to being seen as external to the client’s clinical community.
Network characteristics
Case study networks were selected to cover four points of divergence as explained in the sampling section in Chapter 3. Here, we briefly explore our findings across the different categories of network characteristics.
Stage of network development
The stage of network development (ranging from de novo to well established) did not appear to influence the KIT agent’s activities; individuals reported spending their initial few months on building relationships and establishing links within their region, customising tools and approaches, and selecting their priority initiatives. This highlights how the role of a knowledge broker requires similar resources (e.g. time) regardless of the maturity of the organisation in which they are based.
Diversity in regional research infrastructure
The agents in our study reported mixed views of working with their regional research infrastructure (e.g. established links with CLAHRCs/no CLAHRC; AHSC/no AHSC). In one network (unnamed to preserve anonymity), the agent initially described their network as ‘lucky’ to have an established CLAHRC and that they were working together on a number of projects. However, over time, the same agent later reflected that they ‘don’t work collaboratively very well’ with the CLAHRC any more because of differences in personalities, organisational practices and views on implementation. Regarding their differing views on implementation, the agent reported:
[The CLAHRC has] a very academic approach to projects which means that they have 3 or 5 years trying to answer very specific questions. Whereas we have an approach that’s meant to be a very real-world interpretation with very rapid adoption and spread of what is determined as best practice and those two things don’t quite match.
Another agent reported that CLAHRCs and AHSNs have ‘come a long way but they haven’t been overly successful in taking other people with them.’ This demonstrates the challenge of harnessing the full potential of regional assets given the complex and challenging health-care landscape.
Planned knowledge and innovation transfer roles within the region
Our agents represent the range of different knowledge broker role arrangements (e.g. part of core team, secondments, fellowships). Interestingly, job security was seen as a challenge and risk for all regardless of whether or not they were employed as part of the network’s core team or on a fellowship. The difference was that for some the uncertainty related to the network’s 5-year term compared with those on a 1-year fellowship who were already transitioning to a new role before their fellowship ended.
Geography
As expected, KIT agents in regions with fewer organisations or smaller geographical footprints remarked that this was less of a challenge than in other regions. For example, these agents mentioned that engaging with their partners was easier because they only had a handful of clinical commissioning groups compared with another region with > 20. We did not observe any regional patterns in terms of north–south network characteristics.
Differences between England and Wales
There were several noteworthy differences between the network set-up across agents in England and Wales. Agents in Wales operated across a smaller geography in their network roles and the partnership, compared with AHSNs, did not operate as a separate entity. They were in more permanent posts (i.e. not on a short-term contract linked to the 5-year term of AHSNs). James reflected:
We’ve got it easier, much easier here but we’re local because we’re part of the organisation. Some of those relationships are already there. People are expected to relate to us and we’re expected to relate to them.
In England, the uncertainty around national priority areas and themes for the networks and the complexity of the AHSNs hindered agents in terms of long-term planning and general feelings of job security. Molly commented that ‘as the resource requirements are becoming clearer we’re still constantly adjusting it’. In general, agents did not feel that being external or independent as an AHSN was a disadvantage to knowledge brokering roles by positioning the network as a conduit between silos.
Regardless of how the individual related to their regional network and network characteristics, the KIT agents’ clients were based in health-care organisations faced with a resource-constrained environment. Indeed, there was resistance from both front-line practitioners unable to free up their time and also from management unable to see the immediate benefits of the knowledge work. We next consider resources to support KIT work, organisational leadership and organisational culture.
Resources to support knowledge and innovation transfer work
Time
Having the time and space for KIT work is described by agents and line managers alike as a key enabler. Indeed, ‘I think freeing people up for the time’ was James’s line manager’s response to a question about the most important thing that his organisation does to support KIT. Agents reported insufficient resources within their departments to provide backfill for clinicians/managers to be involved in KIT work. Jessica described it as ‘icing’ and the challenge is that clinicians and managers can get on with their practice without it: ‘you can eat cake without having icing on it, and research and evidence on daily practice is like icing’. The practitioners that KIT agents worked with were under pressure, to ‘deliver within the financial envelope, making sure that their targets are met’ (Holly). At Homefields (observation, 2 July 2014) we heard a reflection from a presenter that the clinical team had time for nothing other than delivering service; no time to review, evaluate, or improve.
The amount of time agents had for the KIT role was a limiting factor. Typically they were a small resource serving enormous organisations and could ‘only invest so much time in very few projects’ (Grace’s Link). Unsurprisingly, agents working on large-scale change projects found that the scale of those projects meant that they could only ‘skirt across’ the wider organisation (Sophie).
Physical space
Another manifestation of organisational resource was a physical home for those in KIT roles. Grace felt the lack of a physical space hampered her team’s ability to support improvement. This prevented her from initiating an open-door culture in which tools such as idea boards would be visible to all. She believed that visibility would contribute to creating ‘an energy which encourages and supports and nurtures a culture for improvement and innovation’.
Teams
Our Link interviewees highlighted the importance of the team who work closely with the agents and the role they play in supporting KIT activity. Often set up deliberately by the agent based on a project’s needs, the team could bring together complementary skills. Grace’s Link commented: ‘People matter. You also need a really great team and it needs to be people who are going to be essential to getting what you need done’. Another Link reflected on how the agent established a ‘fascinating’ team structure composed of groups with a specific remit:
You’ve got a process group, a mathematical modelling group, one focused on safety, one focused on leadership, and that gives real clarity to what support you can give.
James’s Link
In this way teams could exhibit the required skills and experience for their projects. We heard from another of James’s Links that beyond simply having relevant skills, the team were ‘approachable’ and people in the organisation felt that they could trust them.
Data
A number of challenges arose around data to support KIT work, including its collection, accuracy, sharing practices, beliefs and skills required to apply it. One meeting we observed centred entirely on the challenges of obtaining accurate and timely admissions data. Staff discussed the concerns with using mean length of stay, specifically its accuracy and meaningfulness, yet its use in practice continued and consequently the agent’s team had to ensure that those using the data actually understood the figures (Sophie observation, 7 October 2014).
A related issue is that performance data differ from the type of information KIT agents require to evaluate their efforts. To illustrate, James reflected in an audio-diary entry:
So I think one of the messages from me is how important data [are] for improvement and not performance data firstly, but the right data to understand the work. And we just don’t have that.
Organisational leadership and support
Agents reported that support from the executive boards and their line managers helped them to achieve desired change. Board and executive leader support were mentioned as enablers by several agents:
I think the exec[utive] leadership in that particular organisation is an enabler because it’s visible, it’s palpable . . . The chief exec is around all the time saying hello to people.
Isabelle
The change, certainly the change in attitude for the chief executives . . . and the support that they give is massive, and I can’t stress how important it is to have such a strategic board.
Erin
James outlined the importance of getting senior decision-makers interested and engaged at an early stage. He also emphasised the importance of developing leaders through targeted training programmes and reflected that his unit’s leadership programme was ‘probably the most important thing we’ve done’.
Molly’s line manager was inspired by some of the more innovative and entrepreneurial companies that provide their employees with freedom and he reflected ‘I think we’ve got to be in that space’. He created a relatively flat team structure and tried to avoid heavy top-down management.
Organisational culture and receptiveness
We heard from many agents that the organisational culture supports KIT work. One line manager (for James) described his guiding philosophy as valuing the input from grassroots: ‘. . . rather than feeling that we [Executives] are always right . . . the best value you can do is listen to your front-line staff who often know the best way of doing these things’. Another site (Homefields) very deliberately became a ‘listening’ organisation and used feedback from partners and the community to prioritise their work programmes. Agents reflected that organisations that do not listen to the needs of their stakeholders will erode trust and ‘set the relationship back’ which undermines the change programmes (James’s audio-diaries). One Link reported how Sophie helped to create a culture in which people were encouraged to question members of their team, from the doctors to the porters:
Well now everyone will challenge everyone, which is very healthy. It’s very, very, very well done.
Sophie
Aspects of the local culture that were described as unhelpful included a ‘very silo approach’, failure to cascade information from leads to the front line, and overlap of departmental missions leading to role confusion and duplication. Agents were challenged by the conflict between national and local policies. James, for example, described the ‘separate’ but overlapping initiatives:
People working on [improvement initiative] project internally and then there’s the national [improvement initiative] but they’re separate and we‘ve met quite a lot of resistance to trying to refocus the people internally, from one or two people who are quite senior.
James
Another challenge was described as ‘initiative-itis’ by the Moorlands line manager. Juggling different projects simultaneously without any additional resource was judged to be disabling for all concerned.
Interestingly, organisational culture was not seen as set in stone or immutable. James’s line manager spoke of redefining the executive team’s core values and introducing the improvement unit as part of an organisational ‘recalibration’. In Sophie’s site, the line manager explained how the creation of a space for professionals to meet and ask questions of each other had contributed to an organisational ethos that underscored the patient, as opposed to the professional hierarchy, as the central focus.
Organisational receptiveness, or lack thereof, influenced KIT agent activity. Jessica reflected that receptiveness towards researchers was ‘the greatest one that we’ve found’ when asked about barriers to KIT. Molly’s line manager summed up the idea of working with the willing:
People when they want it and embrace it, that’s where you get change happening. So, you know, if you look at some of the projects . . . where they’ve been successful is because the organisation wanted change and where they commissioned that piece of work, and that’s when they drive it. When they don’t want it, it’s just . . . it’s painfully, painfully difficult.
Molly’s line manager
Organisational enablers and barriers are summarised in Table 11.
| Factors | Enablers | Barriers |
|---|---|---|
| Network context and characteristics | Less hierarchical organisation Peer group support |
Job insecurity Competition between networks |
| Resources to support KIT | Time for practitioners to engage in KIT Time for KIT role Physical home Approachable KIT team with relevant skills Availability and usability of data |
Front-line staff having no time for anything other than service delivery |
| Organisational leadership | Board-level and line manager support Early engagement |
|
| Organisational culture and receptiveness | Listening Openness to challenge Receptive to research Working with the willing |
Professional silos Confusion between missions and ownership ‘Initiative-itis’ |
External (macro) factors
Constraints manifest at the meso level often emanated from pressures in the wider NHS context. We consider briefly the influence on the work of the KIT agents of national politics and the culture at the system level.
Politics
National policy drivers are seen as both enabling and constraining. A key barrier was frequent changes to national policy. Table 12 summarises policy changes in England and Wales alongside key network developments.
| Time period | Key national policy developments in England | Key national policy developments in Wales | Key network events in England and Wales |
|---|---|---|---|
| 2008–10 | 2008: the NHS published High Quality Care for All: NHS Next Stage Review Final Report 2008:213 confirmed the commitment of the Department of Health to developing a more systematic approach to spreading innovations and the creation of a network infrastructure to support research translation in the NHS. Key to this was investment in knowledge partnerships between universities and NHS organisations 2008: establishment of nine NIHR CLAHRCs 2009: establishment of 17 Health Innovation and Education Clusters |
2010: the Welsh Assembly Government published Economic Renewal – A New Direction,214 which included encouraging innovation through a R&D-intensive and knowledge-based economy as one of its five priorities for Wales | |
| 2011–12 | 2011: Strategy for UK Life Sciences published215 2011: Innovation, Health and Wealth27 signalled a change to the innovation landscape, including the designation of AHSNs |
2011: the Welsh Assembly Government published Together for Health: A Five Year Vision for the NHS in Wales216 | 2011: SEWAHSP’s Developing an Academic Health Science Partnership in SE Wales – An Outline Strategy217 published |
| 2012–13 | 2012: Health and Social Care Act218 | 2012: A Strategic Agenda for Science and Innovation in Wales219 was published laying out a plan for a step-change in Wales’ academic performance across the sciences 2013: Innovation for Wales220 published |
2012: AHSNs submitted their detailed network prospectus and draft business plans to NHS England 2012: SEWAHSP’s Five Year Strategy217 published laying out priorities for the period 2012–17 2013: licensing of 15 AHSNs in England |
Erin expressed concern about the consequences of political change:
HIECs [Health Innovation and Education Clusters] had just come into force. They’d just got up and running . . . If there’s a change in Government, will the AHSNs be scrapped?
Erin
A shortfall in central government funding for the networks was mentioned during the meetings and events we attended (e.g. Homefields observation, 2 July 2014). Delays in licensing meant network teams risked spreading themselves too thinly early on. During the course of our study we witnessed how the networks in England shifted their original plans as they responded to new programmes of work making them, as Molly observed, ‘incredibly chaotic’.
The different geographical boundaries introduced by recent national policies in England presented another barrier. For some agents the boundaries varied across different organisations within a region. The landscape that agents operated within was complex and constantly changing.
On the other hand, the political scene could be enabling, for example if the agent could position their work within an emerging priority. Jessica observed: ‘So, you know, politics can hinder but equally can be an amazing driver for something to happen both nationally or at a micro level’. Molly was able to take advantage of the patient safety initiative to grow her contribution.
System-level culture
The culture at the system level in the NHS also affected the KIT agents. The culture was characterised as one that was focused on short-term budgeting rather than better quality of care in the long run; dominated by command and control/hierarchical structures; driven by targets and performance instead of understanding patients and demands; and a relationship between primary and secondary care that was negative and competitive (James). Another agent (Sophie) drew attention to what she described as a ‘risk averse’ culture, which means that patients could not be discharged until the potential risks at home had been solved, yet they are running similar risks in the hospital on a daily basis. Table 13 presents a summary of external barriers and enablers.
| Factors | Enablers | Barriers |
|---|---|---|
| Politics | Initiative drivers | Pressures on the NHS Frequent policy change Funding shortfalls Delays in licensing Complexity of landscape and geographical boundaries |
| Culture at system level | Short-term budgeting Command-and-control culture Driven by targets Relationship between primary and secondary care Risk averse |
Content
Agents adapted their language and knowledge approaches to the local context and found some hooks by simplifying the process of knowledge mobilisation or by using metaphors to engage their clients.
Concepts and definitions
Language difficulties
Some agents reported that getting agreement over definitions was a challenge early on in their role. The message from the agents is that terms like knowledge transfer/translation/mobilisation are not useful in practice. Grace noted how they mean ‘a zillion different things to every individual person’. Another issue is that these terms are rooted in academia. Jessica talked about the unhelpful potential to ‘baffle them with the theoretical science’ and the need to use language that practitioners understand:
We had a particular . . . model of how we did translation, and it said that we were going . . . to use principles, organisational science and organisational learning. It was brilliant because it was just going to work because that was the mentality of the person that originally wrote it, without understanding actually the people who would be physically following that model are clinical academics and they had no idea what he was talking about and were particularly unreceptive. I think, yes, it was . . . rubbish.
Jessica
She went on to describe her approach:
We talked to them about being change agents because they understood that term in the NHS. We talked about being ambassadors. We talked to them about being like pieces in jigsaw puzzles, you know building bridges between people and groups. So . . . it’s about . . . trying to make it so it’s meaningful for the people that are having to do that work.
Jessica
Instead of using academic terminology, the KIT agents sought to use simplifying terms, choosing language that is rooted in an understanding of the local context, as Jessica described. They also used metaphors to convey what they do:
Getting people to light bulb moments.
Amy
Planting seeds of receptive thought and watering them.
Jessica
Few agents emphasised patient involvement in KIT. However, many felt that there was room to improve how patient input was solicited, and that insight gained from patients could translate into improvement (Isabelle). Speaking about ‘co-production’, James reflected that ‘If we are going to get co-production right we need to have a very different conversation between patients and professionals’. He criticised professionals for thinking ‘they have a right to own the knowledge they have got and share it out as they see fit’.
Innovation
Few agents in our study directly employed the term ‘innovation’ in their practice. James was one exception:
A new territory is innovation and that involves new narrative, new dialogue and new strategic dialogues and a new discourse. So it’s who do we need to sit down and talk to rethink how we deliver this, and re-engineer it completely. So start from scratch, say we’re no longer doing it like this anymore.
James
He described innovation as the result of bringing different ‘troops’ together to create a third troop. He was clear that innovation is transformative whereas improvement alone cannot deliver the necessary changes in the NHS. Grace and Erin were other exceptions. They both saw innovation more as a product that can be patented. For example, Grace, acknowledging that innovation ‘means lots of different things to lots of different people’, explained that it usually occurs when a clinical member of staff comes up with a novel process, technique or technology that requires intellectual property. When prompted if managers could come up with an innovation, Grace replied ‘Yeah, predominantly clinicians because it’s probably much more around people at the coal face who can actually see I’ve got a problem with how I cut open this wound or whatever else’. She differentiated an intellectual property-based innovation from improvements achieved through process changes like improved flow. These she saw as not having the potential to generate income or efficiency savings in the same way as a new technique or technology.
Similarly to Grace, innovation for Erin is grounded in intellectual property and new technology. Erin was at ease discussing the innovation process and ‘happy’ that the NHS had ‘ramped its game up with innovation’. National attention on innovation had helped her to put an infrastructure in place and she believed that most trusts were developing strategies in the area.
Project-level factors
Agents (Amy and Molly) mentioned a number of enabling factors at the project level, including starting from the beginning of a project rather than halfway through, setting clear boundaries for deliverables, timing (e.g. engaging with junior doctors once they had had a chance to settle in) and working on a tangible or visible change project. Also, having a shared set of outcomes with other professional groups working on the project was referenced as an enabler to keeping all parties engaged or accountable. Some agents mentioned logistics as a barrier in terms of travelling across their geography on certain projects.
Customising evidence
Tailoring emerged as a common strategy across agents. We found KIT agents focused on understanding the local context and the knowledge needs of their clients or partners. Janice described how she interviewed her clients to understand the context around use of evidence: ‘where the people do use evidence and how they use it and when they use it, and why they use it and what’s important to them about it’. She stressed the importance of understanding the content from their point of view so that ‘when we’re taking it back to them then we have a much better understanding about how it could be useful to them’.
Moorlands introduced evidence summaries as a tailored response to questions from their partners on topics not well evidenced in the academic literature. Daisy described a similar approach to the evidence summary work and emphasised the importance of context and knowing what was needed: ‘I think it’s just about having an awareness and understanding what’s going on in each of those trusts, what that person wants’. She explained that the role was not simply about producing the summaries but also the ‘pre-work’, which involved having a conversation with the individuals requesting the evidence to find out what practices were currently used, whether or not they have the capacity to act on the evidence and what other things they need to consider.
Despite customisation efforts, Links could still be challenged by the volume of information. One of Janice’s Links mentioned receiving 400 e-mails a day, and Holly’s Link referred to looking for one-liners to peak their interest. Table 14 shows a summary of content-related factors.
| Factors | Enablers |
|---|---|
| Concepts and definitions | Using meaningful language Avoiding academic language Understanding the local context Recognising that innovation will be interpreted differently |
| Project level | Agent involvement from the beginning of a project Clearly defined deliverables and project scope Knowing when to initiate a project Project visibility Engagement with others |
| Customisation | Understanding local context, needs and barriers |
Conducting knowledge and innovation transfer activities
This section explores the factors that helped or inhibited the KIT agents in carrying out their role. It is noteworthy that more than half of our sample of agents (n = 7) were applying QI methodologies, sometimes described as continuous improvement. This is in contrast to four who focused more on implementation of research knowledge and two on engagement. The importance of being able to engage others was a common observation across the agents. James commented, ‘most of this is about engagement’.
Engaging others
Supporting and encouraging were key means by which the agents developed engagement:
I feel like my relationship with everybody I’ve worked with has been much more of a support motivator, providing clarity, positivity, holding hands, a lot of holding hands with people, coaching them, encouraging them. Sort of really saying, ‘you’re doing well, you’re doing well’. Saying to people, ‘you know the Board know you’re doing this and that’s really good’.
Fran
Amy was described as visible, attending every meeting and visiting front-line teams to help progress the project. She acknowledged the challenges the team were facing in terms of low morale as a result of a vacant unit lead role. One of her Links reported how she brought doctors and nurses together in the morning.
The importance of ‘going out to where people are’ and making them feel valued was echoed by Janice. She describes herself as ‘enthusiastic about every problem that’s put to me, because I think you have to be because . . . if you can’t be enthusiastic then you can’t expect anyone else to be’. The danger of having a charismatic individual leading the change is that they become the face of the improvement or innovation and their departure is a risk to the overall success of the initiative.
Several agents reflected that, although the tendency is to send e-mails or telephone, there is no substitute for face-to-face engagement. Isabelle mentioned scheduling quarterly visits to the trusts in her region as one method to ‘keep up the contacts and relationships’. Amy described how building relationships was central to getting clinicians to participate in training or capacity building. Another agent, Jessica, reflected that her efforts to meet with a project lead early on in the process contributed to them developing a productive relationship:
Even though it’s just like a 2-hour journey to it, I physically went and met the person . . . I had to wait I think an-hour-and-a-half . . . until he actually turned up . . . Even though it basically wiped out the day, it was a valuable thing to do because . . . we have developed a relationship.
Jessica
Our Link interviewees highlighted how being responsive to requests helped KIT agents achieve positive engagement. Ignoring or not paying attention to requests made by those involved in the change process inhibited success. One agent (James) described a situation in which a professional group requested a paper to go to them prior to publication but this request was not granted. James reflected on the consequences:
This feels like a common theme, that we don’t pay enough attention to what other people want and deliver on it when we say we will and this leads to a lack of trust.
James
Engagement facilitated further engagement: agents described an approach that encouraged front-line staff to come up with ideas which they then take forward. Such ownership enabled them to ‘take it forward in a much more meaningful way’ (Amy).
Challenging
Much in this section suggests that agents should be amenable, encouraging and responsive to requests (Table 15 provides a summary).
| Factors | Enablers |
|---|---|
| Engaging others | Supporting, encouraging, nurturing Enthusiasm Going out to where people are Face-to-face engagement Responsiveness Developing ownership |
| Challenging | Asking questions/being an irritant |
Such tactics seemed to facilitate engagement and from this position, practitioners could be encouraged to progress things themselves. However, there was also an argument for agents to adopt a more challenging stance, as some did (for example Sophie, James). James clearly articulated the tension between nurturing and challenging:
What we’ve got to be careful of we just don’t become part of the same fabric as everybody else because the whole point of this is that we’re an irritant to the system. We shouldn’t be in bed with the system. We should be poking it. Asking it difficult questions, saying, ‘why are you still doing this?’ So there’s something around how you manage that tension, if that makes sense.
James
Revisiting our knowledge and innovation transfer agent typology
Despite the variability in our sample, we found that agents expressed similar accounts of the enablers of (and barriers to) operating at the micro (individual), meso (organisational) and macro (political and system) levels. We also noted similarities in expectations for the role among agents. In addition, agents equally acknowledged and accepted the risk in taking on a KIT role compared with a traditional career path with known progression and recognition. Given our work in developing a typology for KIT agent roles, we were somewhat surprised by this degree of commonality, especially as our agents differed by level of seniority, length of time in post, amount of their time dedicated to KIT work and also in terms of the focus of their approach (e.g. service improvement, innovation, knowledge mobilisation). We found the frequency of linkage, engagement and knowledge management roles across all agents did not make it easy for us to apply the typology to differentiate our case study agents.
These findings demonstrate that, although roles vary, the enabling factors that help us to understand how KIT agents achieve desired outcomes could be applicable across a range of settings and contexts. We explore the factors associated with outcomes and impact in more detail in Chapter 8.
Concluding remarks
By looking across agents at the enablers of operating at various levels, this chapter shed light on the shared expectations of the role, how KIT agents might be supported and the influence of the organisation and wider political context on the role. Similar role expectations were held by agents, the Links and line manager in terms of what agents do (i.e. linking, engagement and knowledge management), but defining the role emerged as a key enabler as did shared expectations between the agent and their line manager. Key means of role support included funding not only for the agent but also for their Links (for example front-line staff) to facilitate their time on the project, line manager and team support, having a physical home and having access and the means to use data for improvement. The organisational and political context were seen as challenging to agents. Agents were not only addressing local barriers, such as the professional silos in their own organisations, but also navigating regional or national policies that resulted in further organisational instability and reduced resources, ultimately threatening KIT roles. However, we found that organisations with board-level support for knowledge mobilisation together with a culture of reflection (listening to the grassroots), openness to challenge and receptivity to research were enabling KIT agents to achieve desired outcomes.
Chapter 7 Assessing the outcomes of knowledge brokering activity
Introduction
The question that we explore in this chapter is how the outcomes of KIT agents’ activity might be assessed or measured. We do this in three ways. First, by working with a panel of experts (nominal group), we sought to identify a set of measures. Second, we turned again to our case study data to report how outcomes of our agents’ work were being identified, assessed or measured. Third, and finally, we looked to the wider literature to inform our conclusions.
Findings from the nominal group
The nominal group process is described in Chapter 3. The question for the nominal group was posed as ‘how do we assess or measure the success of the work of knowledge brokers?’. However, other questions needed to be considered prior to this question to establish a context for the main discussion. The five questions we discussed were:
-
With whom should knowledge brokers connect?
-
What outcomes should knowledge brokers try to achieve?
-
What should knowledge brokers do to contribute to the achievement of outcomes?
-
How can we measure the achievement of these outcomes?
-
What data do we need?
We now report the results of the five questions that were discussed.
Question 1: with whom should knowledge brokers connect?
The first question was amended slightly from ‘who do knowledge brokers serve?’ The panel agreed that our focus should be on the ideal (‘should’) rather than what might happen in practice (‘do’), and ‘connecting with’ was thought to be a better reflection than the more subservient and limited term ‘serve’.
A large number of responses (n = 30) were given to this question. Following discussion, items 24 and 30 were combined into item 17 prior to voting. The participants were given six voting cards (two 3-point cards, two 2-point cards and two 1-point cards). Thus, if all eight panel members used all their cards, a total of 96 voting points would be assigned. The results of the voting are displayed in Table 16. Each response was assigned a number reflecting the order in which it was suggested. The table is ordered by the results of the first round of voting. The two items that were combined (29 and 30) are marked with an oblique (/) and a dash (–) is recorded in the voting columns. In the first voting round, the item attracting most votes by some margin was ‘front-line clinicians’ (22 votes). The next highest number of votes was eight; five responses attracted seven or eight votes in the first round of voting. Nine responses attracted no votes.
| Item | Response | Vote (n) | |
|---|---|---|---|
| 1 | 2 | ||
| 1 | Front-line clinicians | 22 | 13 |
| 4 | Service users | 8 | 11 |
| 19 | Other knowledge brokers | 8 | 11 |
| 12 | Policy-makers | 8 | 6 |
| 18 | Managers | 7 | 7 |
| 22 | Everybody necessary | 7 | 6 |
| 10 | Organisation and development change agents | 6 | 9 |
| 5 | Researchers | 6 | 8 |
| 21 | Improvement agents – clinical governance, patient safety, etc. | 4 | 2 |
| 26 | The population | 3 | 5 |
| 7 | Those who are/may be at risk of knowledge deficit | 3 | 2 |
| 11 | Carers | 2 | 3 |
| 29 | Government and wider society | 2 | 3 |
| 15 | Those with knowledge that others should be aware of or have | 2 | 2 |
| 2 | Chief Executives/Leaders | 2 | 0 |
| 16 | Research networks | 2 | 0 |
| 20 | Potential future/next generation | 2 | 0 |
| 6 | Information analysts | 1 | 1 |
| 14 | National bodies | 1 | 0 |
| 9 | Students | 0 | 0 |
| 3 | National expectations | 0 | 3 |
| 27 | The media | 0 | 1 |
| 17 | Sponsoring bodies (e.g. Health Foundation, NISCHR) funders, commissioners | 0 | 0 |
| 13 | Educators | 0 | 0 |
| 8 | Industry | 0 | 0 |
| 23 | Knowledge brokers themselves | 0 | 0 |
| 25 | Communications team/social media | 0 | 0 |
| 28 | IT/technology support/website developer | 0 | 0 |
| 24 | Funders of knowledge brokers | – | – |
| 30 | Commissioners of knowledge broker activity | – | – |
| Total | 96 | 93 | |
The pattern of voting changed markedly between the voting rounds. Although ‘front-line clinicians’ still came out on top, the number of votes reduced from 22 to 13. Two items attracted the next highest number of votes (n = 11): service users and other knowledge brokers. In this second round of voting, two new items entered the top five: organisation and development change agents (nine votes) and researchers (eight votes).
We note that one panel member chose to not use three votes (hence vote 2 totals 93).
In summary, on the basis of two rounds of voting, the panel thought that knowledge brokers should connect with:
-
front-line clinicians
-
service users
-
other knowledge brokers
-
organisation and development change agents
-
researchers
-
managers
-
policy-makers
-
everybody necessary.
Question 2: what outcomes should knowledge brokers try to achieve?
The second question was amended slightly, to keep the focus on the ideal (‘should’). Forty responses to this question were provided. Item 33 was discussed and deleted prior to voting as it was a duplicate of item 11. The results of the voting are displayed in Table 17. Between the voting rounds there was some consolidation of voting; although there was no change to the top two ranked items, the votes were spread between fewer items (24 on the first vote; 15 on the second). In the first voting round, the two items attracting most votes by some margin were ‘safe, effective and efficient treatment and services’ (17 votes) and ‘better quality of life for population’ (16 votes). No other item attracted more than seven votes.
| Item | Response | Vote (n) | |
|---|---|---|---|
| 1 | 2 | ||
| 6 | Safe, effective and efficient treatment and services | 17 | 19 |
| 1 | Better quality of life for population | 16 | 16 |
| 18 | Service improvement | 7 | 3 |
| 7 | Build capacity and capability (in knowledge mobilisation, use of knowledge) | 6 | 16 |
| 31 | Increase research use and impact | 6 | 6 |
| 36 | Evidence of improvement | 5 | 7 |
| 3 | Informed decision-making/policy-making | 4 | 8 |
| 22 | Adoption, spread, scaling up at pace | 4 | 7 |
| 35 | Stronger economy | 3 | 3 |
| 20 | Avoiding duplication (between knowledge brokers) | 3 | 2 |
| 12 | Diversify the ownership of knowledge | 3 | 0 |
| 16 | Creating a culture supportive of change | 2 | 2 |
| 24 | Continued investment in knowledge creation, research | 2 | 2 |
| 28 | Organisational culture change | 2 | 2 |
| 10 | Behavioural change (individual) | 2 | 1 |
| 8 | Exploring and reflecting population need | 2 | 0 |
| 17 | Satisfied staff | 2 | 0 |
| 25 | Professional development for knowledge broker | 2 | 0 |
| 26 | Empowering critical engagement with evidence | 2 | 0 |
| 29 | Organisation learning, resilience | 2 | 0 |
| 11 | Best value, value for money | 1 | 2 |
| 5 | Empowerment | 1 | 0 |
| 9 | Organisational advantage | 1 | 0 |
| 19 | Communicating the limits of knowledge – risk, uncertainty | 1 | 0 |
| 13 | Horizon scanning | 0 | 0 |
| 14 | Prioritisation | 0 | 0 |
| 15 | Acknowledgement that knowledge mobilisation is integral | 0 | 0 |
| 2 | Increased knowledge | 0 | 0 |
| 4 | Challenging perspectives to achieve mutual comprehension | 0 | 0 |
| 21 | Knowledge of implementation science/best way to mobilise knowledge | 0 | 0 |
| 23 | Embedding routinely sharing of info | 0 | 0 |
| 27 | Making connections with reality ‘What we do’ | 0 | 0 |
| 30 | Kudos and social capital | 0 | 0 |
| 32 | Challenging knowledge hierarchies | 0 | 0 |
| 34 | Identify knowledge mobilisation champions | 0 | 0 |
| 37 | Enabling utilisation of different sorts of knowledge | 0 | 0 |
| 38 | Up, down, across, interprofessional: the acceptance of knowledge broker as the norm | 0 | 0 |
| 39 | Involvement of people who need to be involved | 0 | 0 |
| 40 | Focused attention/space | 0 | 0 |
| 33 | Value for money | _ | _ |
| Total | 96 | 96 | |
In the second round of voting these two items (i.e. ‘safe, effective and efficient treatment and services’ and ‘better quality of life for population’) pooled 19 and 16 votes, respectively, and were joined by ‘build capacity and capability (around knowledge mobilisation, use of knowledge)’ (16 votes). Four items were awarded 6–8 votes (‘informed decision-making/policy-making’; ‘adoption, spread, scaling up at pace’; ‘evidence of improvement’). No other item attracted more than three votes.
In summary, on the basis of two rounds of voting, the panel thought that knowledge brokers should try to achieve:
-
safe, efficient, effective treatment and services
-
better quality of life for the population
-
increased capacity and capability (around use of knowledge, knowledge mobilisation)
-
informed decision-making/policy-making
-
adoption, spread, scaling up at pace
-
evidence of improvement
-
increased research use and impact.
Question 3: what should knowledge brokers do to contribute to the achievement of outcomes?
The third question was amended (from ‘what do knowledge brokers do to achieve these outcomes?’) to keep the focus on the ideal (‘should’), and ‘contribute’ was added to recognise that knowledge brokers might be only a part of the process.
This question elicited 42 responses. On discussion, items 10, 13, 15, 20 and 21 were identified as personal skills or attributes and so seen as part of item 1 (‘personal skills and credibility to make connections – interpersonal, being present and known’). In addition, overlap between items 28 and 38 was noted. These were combined and, on further discussion, added to item 5 (‘motivating others to use knowledge’) prior to voting. The leadership part was added to item 12.
The results of the voting are displayed in Table 18. In the first voting round, the item attracting most votes by some margin was ‘personal skills and credibility to make connections (interpersonal), being present and known’ (22 votes). The next highest number of votes was for item 12 (‘teach, train, support, mentor, counsel, lead’). It is perhaps not surprising that these attracted most votes as they each included a number of elements.
| Item | Response | Vote (n) | |
|---|---|---|---|
| 1 | 2 | ||
| 1a | Personal skills and credibility to make connections (interpersonal), being present and known | 22 | 23 |
| 12a | Teach, train, support, mentor, counsel, lead | 13 | 17 |
| 5a | Motivate others to use knowledge | 9 | 17 |
| 3 | Facilitate access to knowledge, evidence, information (including published, tacit) | 6 | 12 |
| 4 | Engage and involve people | 5 | 3 |
| 34 | Think and work in systems | 5 | 2 |
| 24 | Be clear about scope – target what matters | 4 | 6 |
| 37 | Be ready to step outside the box and give an alternative perspective | 3 | 4 |
| 11 | Present knowledge in easily accessible formats at point of need | 3 | 3 |
| 27 | Collaborate | 3 | 1 |
| 16 | Use a range of communication methods to reach different groups | 3 | 1 |
| 26 | Organise and make sense of knowledge | 3 | 0 |
| 36 | Engage with the policy community | 2 | 1 |
| 7 | Mobilising networks to influence desired change | 2 | 0 |
| 9 | Know the key drivers for health improvement | 1 | 4 |
| 17 | Know your influencers, champions, potential blockers, early adopters | 1 | 0 |
| 31 | Have access to sources of knowledge | 1 | 0 |
| 33 | Practice what they preach, be the role model | 1 | 0 |
| 40 | Narrate, showcase others’ experiences | 1 | 0 |
| 15 | Act as translators between different groups and organisations | 0 | 1 |
| 35 | Invest time to build trusted relationships for giving/receiving information | 0 | 1 |
| 6 | Highlight relevance in research evidence, research synthesis | 0 | 0 |
| 8 | Facilitate or run experiential training events | 0 | 0 |
| 14 | Organise cross-professional information sharing events | 0 | 0 |
| 18 | Be willing to ask stupid questions | 0 | 0 |
| 19 | Save time for front-line staff | 0 | 0 |
| 22 | Be knowledgeable about measurement and evaluation | 0 | 0 |
| 23 | Celebrate success | 0 | 0 |
| 25 | Scrutinise all perspectives equally | 0 | 0 |
| 29 | Horizon scan, troubleshoot and plan, plan, plan | 0 | 0 |
| 30 | Demand the inclusion of knowledge mobilisation in organisational policy statements | 0 | 0 |
| 32 | Take people with you when brokering relationships | 0 | 0 |
| 40 | Advise individuals and teams | 0 | 0 |
| 41 | Facilitate dialogues | 0 | 0 |
| 42 | Identify resources | 0 | 0 |
| 10 | Listen well | – | – |
| 13 | Persist | – | – |
| 15 | Positivity and a ‘can-do’ attitude | – | – |
| 20 | Be flexible and adaptable | – | – |
| 21 | Respect your client | – | – |
| 28 | If appropriate, lead | – | – |
| 39 | To make what you do a priority for others | – | – |
| Total | 88 | 96 | |
In the second round, a further two items attracted notable numbers of votes: item 5 (‘motivating others to use knowledge’; 17 votes) and item 3 (‘facilitate access to knowledge, evidence, information’; 12 votes). No other item attracted more than six votes. We note that not all panel members chose to use all their votes in the first round (hence vote 1 totals 88).
In summary, on the basis of two rounds of voting, the panel thought that to contribute to the achievement of outcomes, knowledge brokers should:
-
use their personal skills and credibility to make connections
-
motivate and influence others
-
teach, train, support, mentor and lead
-
facilitate access to knowledge and evidence.
Questions 4 and 5: how can we measure (by proxy) the achievement of outcomes?
The panel decided to take the fourth and fifth questions together as they felt that discussion of ‘how to measure’ could not be separated from ‘what data’. Before suggesting responses, the panel commented on it being a highly complex question and that direct measures would be difficult to identify. They decided to allow for the inclusion of ‘proxy’ measures.
There was extensive discussion around the need to focus on one specific outcome when suggesting responses to this question. As a consequence, measures were suggested just for the most important item from question 2 (what outcomes should knowledge brokers try to achieve?); thus, the suggestions, and subsequent voting, were in relation to how we can measure the achievement of ‘safe, efficient, effective treatment and services’. In principle, the group could have repeated the exercise for the other main outcomes for question 2 [i.e. ‘better quality of life for population’, ‘build capacity and capability (around use of knowledge, knowledge mobilisation)’, ‘informed decision-making/policy-making’, ‘adoption, spread, scaling up at pace’, ‘evidence of improvement’, ‘increase research use and impact’]. However, this was not feasible in the time available. The important generic point of note was the need to relate the measure to specific intended outcomes.
Twenty-eight responses were given to ‘how can we measure the achievement of safe, efficient, effective treatment and services?’. On discussion, ‘of knowledge broker services’ was added to item 17 to clarify that these self-reported outcomes from ‘users’ were in reference specifically to the services provided by knowledge brokers. The results of the voting are displayed in Table 19. Three items pooled between 13 and 15 votes each. Four other items attracted between six and eight votes.
| Item | Response for safe, efficient, effective treatment and services | Vote 1 (n) |
|---|---|---|
| 2 | Mortality rates | 15 |
| 1 | Patient-reported outcome measures | 13 |
| 9 | Reduction in reportable adverse events | 13 |
| 5 | Baseline measures and plan–do–study–act (PDSA) cycles | 8 |
| 19 | Decrease in unwarranted variation | 7 |
| 21 | Achievement of targets | 6 |
| 22 | Case studies of change | 6 |
| 3 | Continued investment in research and evaluation | 4 |
| 8 | More evidence-based policies emerging | 4 |
| 25 | Cost-effectiveness (benefit?) comparison between knowledge broker and other improvement investments | 4 |
| 4 | Evidence of new working collaborations | 3 |
| 23 | Increased patient satisfaction in their interactions with clinicians | 3 |
| 11 | Continued investment in knowledge broker roles in organisations | 3 |
| 27 | Number of training sessions, contacts | 2 |
| 10 | Increased knowledge about knowledge mobilisation (capability, capacity) | 1 |
| 14 | Job description and CVs | 1 |
| 16 | PPI involvement in training and evidence use | 1 |
| 17a | Self-reported outcomes from ‘users’ of knowledge broker services | 1 |
| 18 | Increased awareness of research | 1 |
| 6 | Reach of knowledge broker within an organisation and within priority areas | 0 |
| 7 | Requests for knowledge broker input | 0 |
| 12 | Training awards gained, publications | 0 |
| 15 | Improved pace of change | 0 |
| 24 | Acquisition of new knowledge or new connection | 0 |
| 13 | Knowledge mobilisation in continuing professional development, revalidation, role profiles | 0 |
| 26 | Requests for knowledge summaries | 0 |
| 20 | Funding bids won | 0 |
| 28 | Contribution analysis of knowledge broker (formative evaluation) | 0 |
| Total | 96 | |
Considerable discussion followed the first round of voting and the group decided against a second round. Points of discussion included the following.
-
The challenge of causality: the work of knowledge brokers may only be indirectly related to impacts; for example, it is not possible to attribute causal links between their work and mortality rates. An attempt to relate their activity to impacts encounters too many confounding, intervening variables, making causal relationships untenable. Here we note that more discussion of the difference between more immediate ‘outcomes’ and wider ‘impacts’ might have refocused attention away from measures related to patient or population groups.
-
The value of case studies: in the context of indirect relationships between impacts and knowledge brokering activity, the panel highlighted the value of case studies.
-
The need to link specific goals to outcomes: again the panel emphasised the need for measures to be specific to intended outcomes. They rejected the idea of generic measures.
-
Who determines the knowledge broker role? Leading on from discussion of the need for measures to be specific to intended outcomes, the panel discussed how the work of knowledge brokers varies and is determined by whoever decides on the role specification.
-
Context and complexity: the complexity and relevance of context in determining the success or otherwise of knowledge brokering activity was raised – what works in one context might not work in another.
-
The unmeasurable: for example, influence – the panel recognised that an inherent risk in presenting responses to this question was that attention would necessarily focus on what might be ‘measurable’, which would ignore important ‘unmeasureables’.
This was an important discussion and resonated with findings from the case studies.
Insights from the case studies
To add further to our understanding of this assessment challenge, in this section we draw on relevant data from our case study KIT agents. Simply put, very few formal assessment measures were used by agents or their managers. None had formally developed metrics for the role. Agents referenced outputs, such as completing a strategy document, drafting implementation plans or completing a literature summary. Daisy, for example, described the creation of a community or network of champions as another deliverable. When asked how she judged success, Daisy reflected that it is difficult: ‘That’s a really, really interesting question because I’m really not sure’. In a similar fashion, James admitted that he ‘still did not know the answer to that question because I think there’s lots of dimensions to it’. He elaborated and added that in his opinion even the executives did not know what outcomes they expected from him and the team. Another agent, Grace, was quite vague and suggested that positive changes could be expected from having a consistent approach. Janice explained that she was going to ask the clinical community and the service user community what they value but she had yet to do that.
Despite an evident lack of clarity, we distilled a number of categories of measures, which we group according to Kirkpatrick’s evaluation levels: learning, behaviour and results.
Learning
Link interviewees highlighted the importance of the agents’ role in achieving increased capacity. This was sometimes spoken of in general terms, and sometimes more specifically, in relation to improvement methodologies. For example, one of the interviewees linked to Fran referred to the ‘growth’ she created in others. One of James’s Links described what he saw as the limited skill set in QI methodology, which ‘is ill-understood in the front line and very rarely utilised’. In his view, the number of people or projects using QI methodology was a good metric. An agent at Moorlands described how she planned to track downloads of their evidence reviews to understand spread of the product and seek qualitative data on how they were being used.
Behaviour
A number of agents watched for signs of cultural change within the organisation as a result of their role. They looked for changes in behaviours – people doing things differently. Chloe, for example, saw her success in terms of ‘evidence of people incorporating evidence and to put it into practice’. More rarely, agents mentioned specific behavioural change measures:
I’m looking for how well we’re doing at sepsis to get that looking better. That was our aim. That’s why I was brought in.
Amy
Implicit in Amy’s example is the importance of relating the measures to the intended outcomes. Erin provides another example of measures linked to intentions:
We’ve already attracted £600,000 worth of European monies . . . So I think really I’m probably the one individual . . . that is responsible for business development and bringing in, attracting in other contracts.
Erin
According to one of Isabelle’s Links, she saw that as the KIT role related to ‘influencing organisational strategy . . . influencing training and development,’ it should be measured by ‘how people change their behaviour or change what they’re doing as a result of interacting with her role’. Isabelle herself admitted to ‘struggling’ with measurement and drew attention to some of the easier-to-measure things such as ‘the number of people that are reaching out or the number of interactions that are going on’. Chloe saw her role as engagement and judged it appropriate to look at ‘the number of collaborative projects . . . between the university and the community’. Sophie also approached the question from an engagement perspective and referred to things that could be easily measured: ‘number of people willing to work with them’, ‘being invited to chair regional groups and lead on external reviews’. In a similar vein, Amy counted relationship building as a measure of success: ‘when I walk into the A&E department people say, ‘Hi Amy’, that they know who I am. They say hello to me’. Of course these quotations do not report anything about how such interactions change what people then do, a gap that was identified in the nominal group and by participants in Mansfield and Grunewald’s221 workshop.
Some agents spoke in terms of changed norms or ways of thinking:
The level of conversation that now starts with . . . ‘what about these patients, they’re delayed. How can we work together to change that part of it?’ It’s no longer the muddle. There’s still loads to do. This is probably 1 year of about a 5-year change process, but it’s . . . people are engaging all the time now.
Sophie
I was hoping to make . . . people kind of feel that research is not an ivory tower, people who are only in that for the paper, but there is a role for people to work together.
Janice
Results
At this level, measures would relate to improvements in organisational performance. These were rarely identified, although Sophie described outcome measures at this level:
I think the outcomes that have come out of this piece of work have been enormous and far reaching to the point of organisational reputation as well. So, you know, I can pull up umpteen graphs around our 4-hour, 8-hour, 12-hour, for months. I can look at the 15-minute handover. I can look at how many operations. So there’s those outcome measures but actually the fact that the whole organisation feels different. The fact that we are viewed very differently by . . . Government because we’re delivering on what we said we’d deliver on.
Sophie
Of course the risk associated with narrowly equating the impact of the KIT agents’ work with ‘results’ is that it underplays their contributions, and, as we have argued, learning and behaviour are also forms of impact.
We summarise these KIT agents’ suggestions in Table 20.
| Kirkpatrick level | Outcome or impact |
|---|---|
| Learning | Increased capacity (general or specific) |
| Behaviour | Cultural change/doing things differently Increased engagement or interaction Changed norms or ways of thinking |
| Results | Improved systems Improved organisational reputation |
Insights from the wider literature
To check out the wider applicability of our findings, we turned to the literature to explore publications directly related to some of the questions discussed in the nominal group and explored in the case study data.
NHS Education for Scotland has developed a ‘capability framework’ for their knowledge broker network. 222 This sets out the knowledge, skills, values and behaviours needed to ‘create a coordinated knowledge broker network . . . to support practitioners to apply knowledge in front-line practice, and to embed knowledge in healthcare improvement’. 222 The framework comprises five capability statements and 31 learning outcomes, subdivided into 81 (of which 25 are deemed core). The five capability statements relate to the knowledge broker network: building capacity and capability for using knowledge; co-ordinating and connecting; identifying knowledge needs and presenting knowledge; delivering and creating knowledge and embedding knowledge in health-care systems so that application of knowledge becomes routine; and exchanging and disseminating knowledge. There is notable overlap between the capabilities in the framework and the response of the nominal group to question 3 (what knowledge brokers should do). The responses attracting the most votes related to making connections, motivating and influencing, training and developing others and facilitating access of knowledge. These activities also closely resonate with our case study findings.
The Public Health Agency of Canada223 produced a ‘Knowledge Translation Planning Primer’. This is largely a ‘how to’ document, but it includes an appendix that sets out potential indicators for monitoring and evaluating the impact of knowledge products and services. Indicators of reach include recording number of copies distributed or downloads and referrals (e.g. web posts). Indicators of usefulness include user satisfaction data and product or service quality data (such as awards). The document includes a list of indicators that measure use, such as number of users using an information product to improve practice, but nothing is said about what data could be used for this indicator or how it might be collected. Similarly, suggestions of indicators that might measure collaboration and capacity building are suggested, such as number of instances of sharing knowledge at local, national or global level, but again, no detail is given about what data might be collected or how.
Mansfield and Grunewald221 report on the use of indicators for the monitoring and evaluation of knowledge management and knowledge brokering in international development. This report summarises the outcomes of a workshop event focused on the challenge of measuring the impact of knowledge brokering activity. In common with the outcomes from our nominal group and findings from the case studies, Mansfield and Grunewald221 report that measuring the impact of knowledge brokering work and ‘proving that this work had led to changes in knowledge attitudes, policy, practice and action’ faces ‘multiple challenges’. To trigger discussion at the workshop, participants were presented with 100 potential indicators. Most of these related to things that could be counted (e.g. number of user enquiries, number of knowledge products created and so forth) or percentages of staff who agreed or strongly agreed with various statements (e.g. ‘I feel encouraged to share my knowledge with colleagues’, ‘I am able to find the knowledge I need quickly and easily’). Other suggested indicators related to knowledge activities or success cases (e.g. number of staff able to provide an example of how knowledge activities have contributed to organisational performance, number of staff who believe their organisation is a learning organisation). Further indicators were grouped under headings such as policy and strategy (e.g. is there a knowledge brokering strategy?); human resources, training and development (e.g. percentage of staff inductions that make staff aware of knowledge brokering policy and processes); or finance/resource costs (e.g. number of examples of ‘where the organisation re-invented the wheel’).
Members of the workshop discussed the challenges of measuring impact. In accord with our findings, one participant commented, ‘while it is easy to measure activities, e.g. number of enquiries received/answered/followed up, it is extremely challenging to bridge the gap between how many people you reach with an activity and the impact that has had’, adding that ‘it is unfeasible to verify what people have said they will do’. Among their conclusions, Mansfield and Grunewald221 emphasise the importance of context, arguing that indicators should be tailored to context.
The project entitled ‘Supporting Policy In Health with Research: an Intervention Trial (SPIRIT)’224 hypothesises that an organisation’s response to something that catalyses knowledge use is shaped by its capacity to engage with research, and that research enrichment actions can support research use. The SPIRIT team proposes that a number of tools can be used to measure these three elements: capacity, research engagement actions and research use. They suggest an individual policy-maker’s capacity, research engagement actions and research use can be assessed using an online survey tool called ‘SEER’225 (Seeking, Engaging with and Evaluating Research). For assessing capacity at the organisation policy level, the team recommends ‘ORACLe’226 (Organisational Research Access, Culture and Leadership), which collects data from interviews and documentation. Finally, ‘SAGE’227 (Self-Assessment of Engagement with Evidence) is a tool that the team suggests can be used to measure research engagement actions and research use evidenced in policy documents. SAGE uses interview and documentation. The SPIRIT team argues that ‘together these tools provide detailed measures of each concept in the SPIRIT Action Framework and generate data to test the hypothesised relationships’. However, the reliability and validity of these tools has yet to be confirmed.
Tools have been produced by other organisations. For example, Research in Practice for Adults offers an organisational audit for evidence-informed practice, which supports a process of benchmarking and action planning. 228 The Community Impacts of Research Oriented Partnerships (CIROP) Measure229 is a questionnaire tool designed to collect data from community members on the impact of research partnerships. The Canadian Foundation for Healthcare Improvement has produced a self-assessment tool which asks ‘is research working for you?’230 This is another survey instrument comprising a set of statements that respondents rate on a five-point scale from strongly agree to strongly disagree. Dwan et al. 132 developed a self-report Likert scale evaluation tool containing six statements addressing three domains: effectiveness (in broadening knowledge and stimulating thinking; relevance (usability); and research receptivity (use in the past and next 12 months).
Although there are a number of tools in existence, measuring knowledge use and determining what approaches work is in its infancy. 91 Our study has usefully teased out some of the complexity of measuring the impact of knowledge brokering activity and underscored the need for measures to relate to specific activity. Our findings serve to consolidate prior work and lend weight to the call for more R&D in this area.
An approach to measuring outcomes of knowledge broker activity
In lieu of proposing a set of generic measures, we identify a set of principles to guide more specific measures of knowledge broker impact and then build on the work of Morton231 to suggest a framework for measuring outcomes of knowledge broker activity.
Principles
-
Distinguish between measuring what agents do and the effect of their actions on the behaviour of others.
-
Relate the measures to role specification and specific intended outcomes (rather than more distant population health improvements).
-
Do not try to claim causality: the work of knowledge brokers will be indirectly related to outcomes and confounded by other factors.
-
Take account of context: the success of knowledge broker activity will be facilitated and inhibited by local internal and wider external factors.
-
Tailor measures to specific circumstances.
-
Do not ignore the unmeasurable (e.g. a knowledge broker’s influence).
Framework
Drawing on experience of case study preparation for the Research Excellence Framework 2014,160 Morton231 developed a framework designed to explain and provide evidence of how research contributes to policy and practice. Based on logic modelling, the framework sets out a pathway from inputs and activities to change in practice and, finally, outcomes.
Morton231 acknowledges that the process of research utilisation is complex and that assessing research impact is challenging. In recognising the ‘context-specific and variable nature of impact’ she endorses the value of the case study approach. In addition to context challenges, she describes attribution as a key difficulty in the assessment of research impact; the results of research are integrated into practitioners’ existing beliefs and practices and moulded to particular circumstances, which makes it problematic to attribute outcomes to research in a causal fashion. Thus, her framework is based on the principle of research contribution.
Although Morton’s research contribution framework is intended to be used to assess research impact, and by contrast our focus is on the impact of knowledge brokers (which may be one factor in a research impact pathway), there is considerable value in considering the framework and adapting it in light of our research, to devise an approach to measuring outcomes of knowledge broker activity. We decided to use Morton’s231 framework to inform our own because it accords well with our proposed principles. Also, we note similarities with Kirkpatrick’s198 model of programme evaluation.
We set out our framework in Table 21. It is organised around five areas of contribution: inputs, activities, capacity development, behaviour and outcomes. In the second column we add a brief description about the concerns of each area, and in the subsequent three columns we provide example indicators, evidence and likely barriers to, and enablers of, the achievement of desired outcomes.
| Contribution | Description | Example Indicators | Example sources of evidence | Known barriers and enablers |
|---|---|---|---|---|
| Inputs | Human, financial, technical resources invested in knowledge brokerage Aims and intentions of the knowledge broker role |
Knowledge broker time, funding available | Accounts Job description |
Individual disposition, background of knowledge broker Context factors: internal organisation support |
| Activities | What knowledge brokers do and with whom | Meetings Collaborators and connections Presentations: seminars, conferences Research briefings Training |
Attendance records (and those not reached) User feedback/post-event evaluations (reactions) Observations Participant reflections |
Content factors: nature and relevance of change Process factors: networks and relationships Context factors: internal organisation support; organisational readiness |
| Capacity development | Development of practitioner and policy-makers’ knowledge and skills | Engagement with mentoring, training events and materials | Measures of learning gains Participant feedback Participant commitment to change |
Content factors: nature and relevance of change Process factors: networks and relationships Context factors: internal organisation support; organisational readiness |
| Behaviour | Changes to policy, practices (e.g. adoption and spread of named processes or products) | New practices, policy | Audit and Improvement projects Scores from self-assessment tools Citation in policy/strategy documents Case studies |
Content factors: nature and relevance of change Context factors: internal organisation support; organisational readiness |
| Outcomes | Better treatment or service | Less unwarranted variation Achievement of targets |
Policy and contextual analysis National or local indicators Investment |
External factors (e.g. government policy, national programmes) |
Concluding remarks
This chapter directly addresses research objective 5, which was concerned with generating a set of ‘impact’ measures for assessing KIT activities. Working with our nominal group, and informed by the literature, we sought to propose a set of measures for use in assessing the outcomes of knowledge mobilisation activity, and to explore the feasibility of these measures as part of our analysis of case studies. In our study proposal we described this goal as measuring impact. However, ‘impact’ is a problematic and somewhat limiting term if narrowly interpreted as effects on target populations (such as better health for patient groups). This unhelpfully diverts attention away from consideration of the more direct outcomes of KIT agents’ knowledge brokering activity. We have also suggested that reactions, learning and behaviour within the Kirkpatrick model can each be understood as a form of impact. Having said this, it is, nonetheless, easy to present a rationale for considering the questions we posed for the nominal group: it may help to determine what we might expect or hope for from knowledge brokers; it may help to identify how their work might be linked to organisational goals; having measures to demonstrate their value can help in the development of cases for further investment; it may assist in the identification of factors that help or hinder the achievement of outcomes. However, the nominal group raised critical and challenging questions, and we recognise that the exercise alone could not provide definitive answers. What it did achieve was progress towards answers, and we do not underestimate the value of clarifying the task through the identification of precursor questions and the discussion of issues related to causality, linking outcomes to intentions, the risk of overlooking the unmeasurable and the relevance of context.
These messages have been corroborated by others as demonstrated in our discussion of relevant literature, and our integration of findings from the case studies underscored the importance of relating the measures to intended outcomes. It also highlighted that very few formal assessment measures were employed by agents or their managers, and that there is a lack of distinction in practice between measuring what agents do and the effect of their actions on the behaviour of others.
What the nominal group suggested about the place of case studies might prove to be particularly valuable and is worthy of future investment. In the longer term, any measures would need to be validated; a significant amount of context-sensitive qualitative case study work would seem to be a necessary step in that process. This would provide data on what kinds of goals are agreed locally and reflections on the achievement of outcomes.
Chapter 8 A discussion of the findings from a social marketing perspective
Illuminating how KIT agents bring positive outcomes and impacts to health-care practice would allow future activities to be planned accordingly, and thus help to maximise their benefit. This section of the discussion, therefore, uses a social marketing framework to draw together key features within a ‘reusable’ single analytical framework that can be employed in planning and evaluating future KIT agent activities.
What is social marketing theory?
Social marketing attempts to apply techniques from commercial marketing to social outcomes. 232 It seeks to learn from commercial marketers’ success in changing behaviour and is an increasingly important aspect of the public health agenda in England and elsewhere. It has been applied with some success to health promotion and has been proposed as an effective technique to promote behaviour change in practitioners. 203 Although social marketing borrows heavily from commercial marketing, it faces a number of additional challenges that commercial marketing typically does not. Most relevant here is that social marketing frequently promotes an outcome that is uncertain and intangible, and where the benefits often accrue to third parties.
Social marketing theory is formed of a number of overlapping principles (Figure 1). Broadly these principles are:
FIGURE 1.
Principles of social marketing theory.
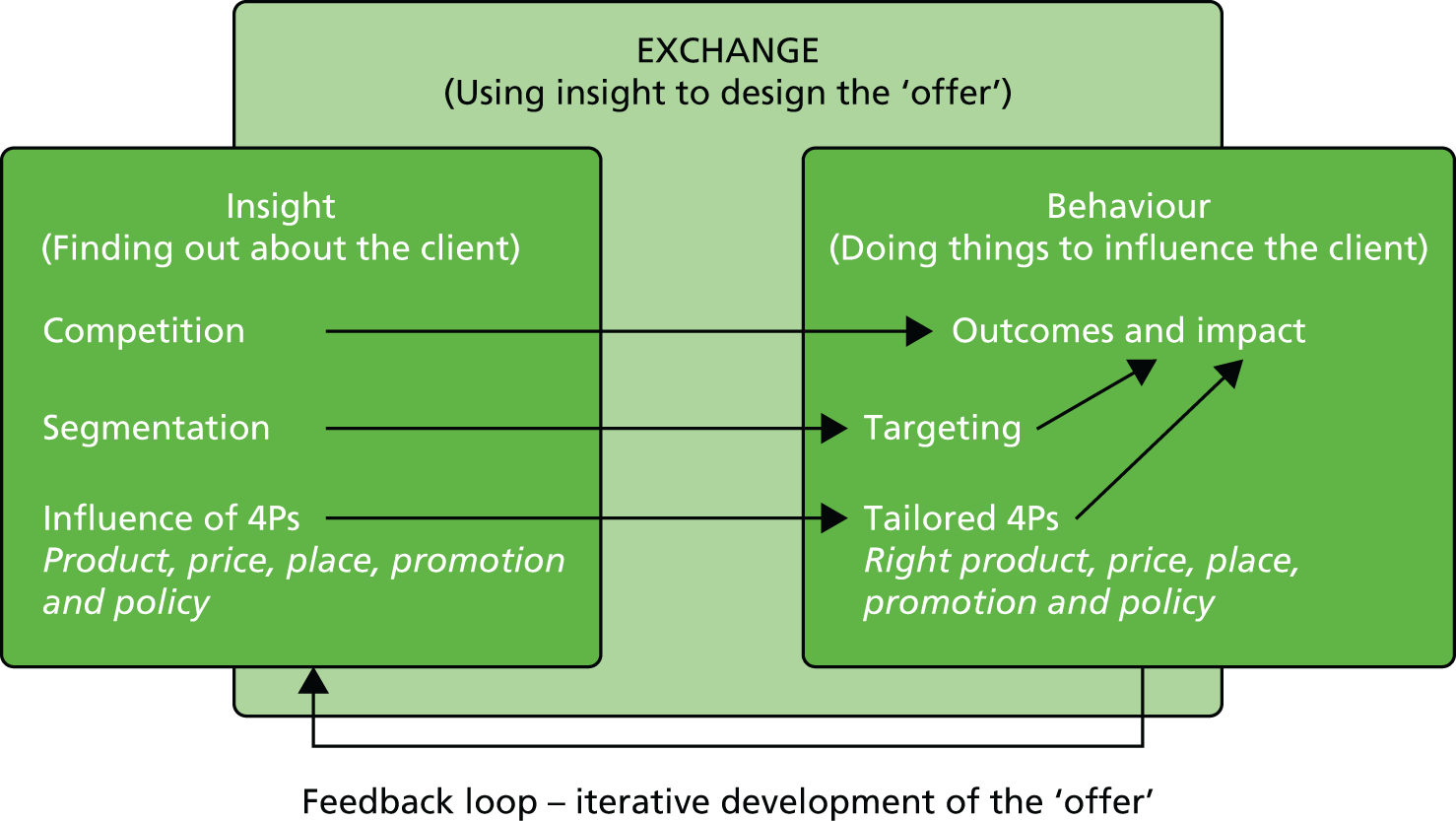
-
Know your client and their needs (customer insight).
-
Know the competition (including context) – what do people do now, why, what/who stops them doing something else?
-
Understand the importance of exchange – what do they want in exchange for a change in behaviour?
-
Segment and target – are there different groups within the market who require a different approach? Should they be approached differently?
-
Use the four ‘P’s of marketing to design interventions:
-
Product – how does what you do satisfy a need? This includes issues such as function, features, quality, variety, brand, credibility, wraparound services.
-
Price – most likely reducing costs in this context.
-
Place – how people can access the service – channels, locations, logistics.
-
Promotion – how the service is promoted, personal selling, peer to peer, social media etc. 233
-
Policy (an extra, ‘fifth P’) – how laws (smoking bans), fiscal arrangements (tax on tobacco and alcohol) and other levers (drug treatment services in prisons) available to governments can be used to encourage behaviour change.
-
The approach begins with generating ‘insights’ into actors’ current practices, beliefs, and preferences that influence their choices, which can then be used to develop more effective interventions. It is focused on understanding why people (e.g. NHS managers) do what they do now (in relation to innovation and knowledge) and what ‘competition’ the new behaviour faces (which can be informed by barriers identified in the literature). Social marketing theory recognises that this may vary by subgroups and may require different kinds of support (‘segmentation and targeting’). These insights can be used for ‘creating attractive exchanges’, which can encourage the effective uptake of the new behaviour. In commercial marketing the offer is characterised by what is called a ‘mix’ – product, price, place, and promotion. Social marketing differs from commercial marketing in that it takes account of the environment in which the actors operate and adds a fifth component to the ‘mix’: policy.
In this discussion, social marketing theory is used as an organising framework for linking outcomes and impact with processes, treating the KIT agent as the product or service. If the a priori categories are found to be relevant in the context of KIT agents, they may also be used to develop future programmes.
Applying social marketing theory to knowledge and innovation transfer agents
The earlier discussion (see Chapter 6) has demonstrated the importance of KIT agents developing insight. Although none of them expressed it in this way, they all referred to a set of behaviours designed to understand their client. ‘Listening’ was mentioned by KIT agents as part of the role, and Links saw this as a strength and something to look for in future KIT agents. Other studies of these roles have emphasised the importance of ‘soft skills’ such as listening and empathy. 177,234 Implicit here is that listening leads to something else: understanding. The extended period of interactions, working alongside practitioners within their organisations or projects, hearing of or experiencing organisational difficulties or individual and organisation aspirations, providing opportunities for practitioners to discuss issues and options in a ‘safe’ environment (‘giving permission’ to staff to step away from service provision to think more strategically), and understanding what motivates the client, are all relevant to developing insight.
The KIT agents discussed insights entirely in the context of adapting their offer to the specifics of the client. This is discussed in more detail below. Broadly, this sort of insight highlighted issues around how to talk about KIT (i.e. not using the terminology), how organisational features influenced clients (e.g. poor communication or co-ordination between levels within the organisation), attitudes towards home-grown or imported interventions, lack of time, issues around access to information, individual motivators and opportunities for change.
Social marketing focuses on behaviour change. Some argue that it is only behaviour change that counts, and factors such as changes in attitude or knowledge do not. Most of the KIT agents were seeking behaviour change at some level, but this did not always result in a measurable patient care outcome. Changes in knowledge and attitude are perhaps essential precursors to behaviour change, itself a potential precursor to improved outcomes. Within the time limits of the KIT support offered to an orgainsation, it is perhaps too much to expect consistent changes in behaviour, not least because achieving outcomes is likely to require some experimentation and adaptation for practice. However, the focus on behaviour change for improved outcomes is useful to keep. It has a number of benefits: (1) it provides motivation to participants; (2) it encourages an explicit articulation of how the pieces fit together and what needs to happen to exploit the potential; and (3) it provides intermediate measures on which to base feedback.
In order to articulate how the pieces fit together, and to develop an appropriate ‘offer’, it is necessary to understand the competition. This is a major purpose of gathering insight. Competition refers to anything that competes for an individual’s attention, willingness and ability to change, and therefore prevents new behaviour. It assumes that doing things differently comes at a cost – otherwise we would be doing it anyway. Impediments to change include habit, inertia, lack of awareness and/or belief in alternatives. Competition can be multifaceted and subject to external control. For instance, I might learn about QI methodology, but my boss (or I) might lack faith in its ability to help patients.
Although it was never referred to as ‘competition’ by the KIT agents, identifying and addressing competition was a major preoccupation of all them (what enabled, or inhibited, the impact of their work on Links’ ability to change their behaviour is covered in detail in Chapter 6). Between them, the KIT agents identified the following competition: lack of relevance of research and lack of access to research; pressures that limited the time available to acquire knowledge of new approaches, let alone the time to implement them; lack of specific skills (e.g. QI methodology, evaluation); lack of knowledge (e.g. knowing the market, potential solutions, helpful people or networks); lack of confidence to make changes; politics and territorialism; lack of alignment between different organisations within the area and between national and local progammes; reported lack of leadership support and guidance; lack of willingness to share practice and experience; and the sheer size of the task being undertaken coupled with the need to keep up with the job in hand.
Many of these factors are familiar issues in knowledge mobilisation literature. However, the experience reported in this study differs in a number of ways that are helpful in moving forwards. Chief among them is the KIT agents identifying what mattered to their clients (insight) and being empowered to devise a means of working with them that responded to those specifics and was not theoretical or generalised. Although general lists provide useful sensitisation to potential issues, social marketing theory would suggest it is the specifics that matter.
The specifics are used to develop an ‘exchange’ – ideally one in which ‘the benefits of change are so compelling and the costs so minimal that everyone will comply’. 235 A focus on exchange recognises that changing behaviour comes at a cost (financial, emotional, social, time, loss of preferred behaviour) and this requires some compensation commensurate with the cost. Again, insight is necessary to know what would be valued and motivating, as this will vary. The exchange is expressed through the ‘offer’, a combination of the marketing mix. It takes insight about the client – their needs and character – and considers how best to meet their needs with the least cost to them. KIT agents provide capacity, build capability and skill, support (listening, practical help, coaching), make local projects more visible to staff who might contribute to, or learn and make linkages within, the organisational hierarchy and with other people who can help (e.g. patent writers, manufacturers and researchers).
The product (here a service) is what is being offered to people. It is meant to meet a need, but could address a demand that is negative or non-existent. This is often the case in health promotion, for example, when men do not wish to receive advice on healthy eating236 and children do not decide whether or not they wear cycle helmets – their parents do. A distinctive feature of the KIT agents is how they developed their own product within this context. In some cases, they worked with people who did not want them and described themselves, for example, as ‘an irritant’, or with people who had not been asked if they wanted to work with a KIT agent (Amy and Fran). Although these scenarios are not ideal, the lessons learned from this experience are similar to those when the KIT agent was welcomed from the beginning.
Most of the KIT agents adapted their content to meet the specific needs and context of their clients. They worked with clients to help define and clarify the need and then address it. This explains the range of activities found in the study. They also reported adapting their services in other ways. They looked to make their services relevant, attractive and convenient to use. Part of this related to their use of language. A number of KIT agents reported adapting their way of talking about the work to make it salient to clients. This often meant avoiding the formal language of knowledge mobilisation and innovation – not ‘baffling’ practitioners with academic terminology, giving it a ‘pragmatic’ and relevant focus (perhaps at the expense of academic standards), ‘getting people to think’ and to ‘have ideas’. Although addressed in social marketing, the importance of language is perhaps better recognised in commercial marketing. Finlinson et al. ,237 for example, point out that if participants cannot relate to the terms (in their case relating to sexual identity), they will not make use of a sexual health programme. In social marketing the importance of how the topic is presented is often linked to peer education. For example, Stephenson et al. 238 report how school students described peer-led sex educators as ‘having greater relevant expertise and respect for pupils, holding more similar values about sex, [and] using familiar language’.
Those dealing with formal research evidence worked to tailor it for the needs of those who would use it, recognising that research papers are often not accessible and time pressures are likely to drive out thoughtful consideration. In other cases when clients were busy or distracted, KIT agents undertook tasks directly, preparing and sending out agendas for clients, for example, in order to keep things moving (however, these KIT agents stressed the importance of keeping ownership firmly with the client). Another KIT agent reported timing a specific piece of work to dovetail with the evolving execution of the client’s project, and others reported using a stepped approach to knowledge and skills development as client experience grew. Demonstrating the importance of understanding specific client groups, there are examples of KIT agents who used national programmes locally with success (e.g. patient flow), and others who worked with small local teams to ensure salience and ownership, and to increase the likelihood of diffusion across the host organisation. Again, this technique is used in health promotion, when target audiences are invited to help develop their own solutions to problems. A recent example is the Spanish arm of a European study to reduce childhood obesity. 239 The approach is also used with adults, particularly if formal services are absent. 240
Further themes relating to product (or service) that are employed in marketing are relevant and useful here, including the perceived quality of the product (and branding), its compatibility with existing products and the scope for personalisation. In terms of quality, there was an expectation that KIT agents should be competent in the area in which they gave support. This finding has been reported elsewhere. 60 We found that clinical and managerial experience was valued, as it was felt to give the KIT agent credibility and made them more difficult to dismiss. In some cases this was the direct experience of the problem being tackled, but was mostly about being able to understand the context in which clients operated. When KIT agents have direct experience of the issue at hand, it is a potential challenge to avoid superimposing their experience on the current problem their clients face, in order to ensure that clients take ownership of ideas and solutions.
In commercial marketing the idea of ‘homophily’ is considered helpful. This is the extent to which people in a relationship are similar in terms of demographic variables, attitudes, beliefs and values. Extending this, peer outreach that makes active use of social networks has been used successfully in public health241 and fits well with the observed preferences of health-care practitioners. 35,242–245 There were a number of examples of similar networks in the study. For example, Amy, Fran, James, Grace, Sophie, Holly, Daisy, Chloe and Janice all spoke of their clinical background and how it helped them to understand, but also to be taken seriously and listened to. This was generally confirmed by the Links.
Branding is also an issue in commercial marketing that may be relevant in the context of KIT agents. Each of the individuals was attached to a formal network organisation that may have enhanced credibility. In practice, this was little mentioned and the key influence on credibility seems to have been the individual’s reputation: it may be that this was taken for granted given their affiliation. Branded products were also used – IHI QI and Sepsis Six campaigns – providing shortcuts to interventions and support materials. This said, some sites complained of the difficulties of tying in its work with existing programmes. Branding would seem to require planning if it is to provide an advantage and the branded product must be adaptable to local needs.
One factor that seems crucial to success is the feedback function offered by KIT agents. The timeliness of feedback on performance, and recognition and appreciation was motivating to some people. Some Links mentioned prizes or awards for their work, others showed evidence of improvement with clear satisfaction. Others mentioned the KIT agents providing them with renewed confidence at times when they felt challenged. In a number of cases the KIT agent was also acting as the link between service staff and senior managers. Reporting success up and approval down was considered an important aspect of motivating staff and sustaining new behaviour.
Place or positioning is used to refer to where the service is offered and how. Many KIT agents commented on the importance of being ‘visible’, the need for face-to-face meetings in order to agree objectives and to build relationships. Being out and about and handy, sometimes even colocated with clients, all seem to have contributed to success. The importance of this is reflected in some comments from Links when they expressed frustration at the KIT agent being a shared resource and thus not always present. Another expressed a loss of the support once the relationship had come to an end, and another suggested more proactive client management as an improvement to an otherwise excellent service. One site also adopted what might be called a ‘pyramid approach’ of training the trainer. This was intended to embed the skills within the host trust and thus to reach a greater number of people.
In marketing, promotion refers to how the service is advertised and how people are encouraged to take part. This issue did not feature strongly in this study. However, when it did come up, this was often in relation to the KIT agent already being known and promoting their service personally through contacts and networks, or the agent’s line manager being well-known and connected, and offering the KIT agent’s services directly to potential clients. In some cases it fell to the KIT agent to find appropriate clients once the line manager had agreed to work with particular organisations. None of the KIT agents complained of lack of demand for their services, but understanding the best means of promotion in the context of KIT agents remains little understood. This may become more germane if services are expected to be revenue generating.
The other element in the social marketing mix is policy – a legal ban on smoking in public places, alongside fiscal measures and improved access to smoking cessation programmes, for example. In the context of a KIT agent, enabling policies were identified. Some spoke of the benefits of renewed policy interest in innovation and how the roles themselves, sponsored by research networks, fitted into the wider policy. Some KIT agents and Links talked about the increased emphasis on cost-saving or particular patient safety targets providing an impetus to do things differently. This element of social marketing brings attention to the macro and meso levels and prompts assessment of the likelihood of success and points to necessary changes. It encourages a more comprehensive assessment and planning of how the KIT agent might be expected to work, and highlighting of opportunities for change within the wider infrastructure (an element of competition). For example, one major barrier to change identified in a number of cases was the sheer pressure on the health-care system.
The final principles of social marketing relate to segmentation and targeting. These would encourage KIT agents to divide their potential clients into different groups and tailor their offer to each. One advantage of this is that it allows scarce resources to be concentrated where they are most likely to have an impact. If these groups are successful they can be used to support future efforts. Several KIT agents took this approach. They talked of working with the willing, not pushing projects that failed to get off the ground, and working with clients whose projects seemed viable. Over time, some were also able to build a portfolio of success stories to attract other clients.
To illustrate social marketing theory, we applied it to an example from the case study data, and this is presented in Appendix 9.
Strengths and limitations of social marketing theory
The strength of applying social marketing in this context is that it allows existing knowledge of real-life processes around KIT to be anticipated and addressed in planning. In turn, these expectations can be matched to outcomes in evaluation, and thus provide better insights into its relationship in practice. Third, social marketing theory offers KIT actors a structured means to identify likely causes of success and failure and to plan for them. We note here that our proposed framework for assessing the impact of KIT activity signals the need to recognise barriers to, and enablers of, the achievement of desired outcomes.
Social marketing theory’s comprehensive focus goes beyond identifying the shortcomings of non-adopters;246 rather, it seeks to understand and factor in their position and constraints. This seems to be missed by a number of critics247 who assume that lack of congruence between the social marketing ‘offer’ and the audience is a result of the theory rather than a weakness of a particular programme. However, understanding the client is fundamental to making social marketing work. 248 In our study, aspects of social marketing were used to interpret how KIT agents worked with clients in goal setting: participants identified local priorities and were supported to work towards them, rather than attempting to change basic beliefs. 249 This is not inevitable but requires conscious use.
Social marketing, like commercial marketing or social capital, is a tool that can be used towards different ends, for good or ill. One limitation is that the ‘principles’ of social marketing overlap and this can be distracting for people attempting to design programmes using the principles – which should be done first, segmentation or targeting, and when is promotion price? In practice, it matters less about being able to place something into a discrete category and more about having thought about the ‘principle’. Again, how the techniques are applied is not a theoretical question, but a moral one. There are other limitations. In our case, we used social marketing only to analyse the relationship between the KIT agent and their ‘client’, but the approach could have been to analyse the relationship between the KIT agent and their home organisation as well. This process might be usefully applied to the planning of future programmes.
Concluding remarks
This chapter has provided a necessarily brief discussion of the study’s findings to illustrate the potential utility of applying social marketing theory to the planning and evaluation of KIT agent posts. Analysis of the study through the lens of a social marketing framework has highlighted a number of key points that are associated with impact in the work of the KIT agents (objective 3) and also pinpoints key areas in which the KIT programme could be strengthened. Although these results were somewhat apparent without the use of this framework, it is the linking together of these ideas, with a focus on behaviour change, which is the major benefit of this approach. Social marketing theory helps explain why the KIT agents were able to support change and provides a useful checklist for future examples.
What social marketing theory does not do is bring attention back to supporting the KIT agents themselves, and this is important for future health-care practice. The role of KIT agent, variously named, is increasingly common in knowledge transfer and mobilisation programmes in health, and our study helps to illuminate what such a role can involve, how the agents can be made to be successful and what makes them vulnerable to disappointing results. Not only are the roles undertaken with some risk to the individual, but they could suffer dilution of effect as KIT agents look for funding and need to demonstrate worth. Yet they tend to be short-term posts with ambitious aims. The roles, and the people who occupy them, will need to be given time and support if they are expected to realise outcomes and impact rather than simply potential.
Chapter 9 Further discussion and conclusions
Introduction: our study’s contribution
The title of our project highlights our underlying aim to help NHS practitioners and managers to ‘get the most out of’ available knowledge and innovation for service improvement and patient benefit. This study is timely because of the increasing use of KIT roles by AHSNs and partnerships,60 and the relative lack of evidence for their effectiveness,94 although the literature on knowledge brokers has grown significantly in the last few years with the publication of evaluations of CLAHRCs39,42,44,60,245,250,251 and other initiatives. 90 The complexity of the role and the environment in which it is played out justifies the need for more research on knowledge brokers. 42,54 Our research contributes to that body of evidence. It focuses exclusively on this role as it operates within AHSNs and in England and partnerships in Wales to show how individual dispositions, processes and content contribute to desired outcomes. Oborn et al. 82 report that the journal Implementation Science ‘explicitly calls for papers which include more details around the context and developmental process of moving research knowledge into practice’. Our attention to context looking at common enablers and barriers as well as the specific features of the KIT activities in Chapter 6 moves in this direction.
There is a growing recognition that ‘research use is an intensely social and relational process’. 90 We build on these known relational aspects of knowledge mobilisation by highlighting the preparatory work undertaken by our case study agents, who build the relationships that are vital to knowledge uptake. For example, James focused on building trust with practitioners by visiting their sites and meeting their teams. Similarly, agents at Moorlands met with potential knowledge users to discuss not only their needs, but also their capacity to use knowledge. In both these cases, the agent(s) developed a relationship before starting the knowledge exchange phase. This finding suggests that achieving knowledge mobilisation goals from short-term fellowships might be particularly challenging, especially if the KIT agent is new to the organisation.
Our research finds that it is the generation of ‘insight’, as discussed in the previous chapter, which enabled KIT agents to develop more effective interventions. This finding advances our understanding of how best practice is socially constructed. 86 Agents need to develop an understanding of local context, by listening and building relationships, so that they can adapt their ‘offer’ to their clients of various forms of knowledge (i.e. organisational data, benchmarking, experiential and local knowledge, as well as research evidence). Research evidence is one of many other ways of knowing, a phenomenon described by Gabbay and May244 as ‘mindlines – collectively reinforced, internalised, tacit guidelines’. Our use of social marketing theory, a new contribution to this field, provides a framework for addressing key points and for maximising the contribution of research, by considering not only the competing forms of knowledge, but also its place, positioning and quality (among other factors).
The study’s strengths and limitations
Strengths
The qualitative approach taken with KIT agents and their clients (the professionals we have called Links for the purposes of the study) provided rich data on their real-life experiences. These data enabled us to better understand their role and the context of their practice. By setting the study in a complex, natural environment, we achieved high ecological validity. 252 Our engagement with agents typically extended over more than 1 year, from negotiating initial access to the final feedback discussions. This gives our experience of agents a longitudinal aspect, which was facilitated by the KIT agents’ audio-diaries. For agents who kept them, these audio-diaries captured their experiences and reflections after initial interviews and proved to be a valuable way of providing a more comprehensive coverage of their experiences. Data from the audio-diaries served to confirm and extend information gathered from interviews. We triangulated our data from agents with data from other sources: the observation of meetings and events; documentation research; and semistructured interviews with KIT agents’ line managers and Links. The validity of our findings was further strengthened by engaging nine case study agents in three networks in checking the analysis and interpretation of their case studies. Any bias as a result of the Hawthorne effect was reduced by conferring anonymity on the respondents.
The use of existing theoretical frameworks to guide study design, data gathering and analysis enhanced our consistent approach. These included the Kirkpatrick framework198 and Walker et al. ’s 128 classification of factors influencing change, and have been reported in Chapter 3. In data coding and analysis, we took measures to ensure internal consistency, and as a research team we regularly reviewed and discussed our interpretation of the data and periodically took data to the advisory group for discussion. Our advisory group was strengthened by the contribution of two service users who kept us focused on patient outcomes. Their feedback drew our attention to the lack of consistent approaches to patient engagement across the AHSNs (advisory group meeting on 4 February 2014), and helped us to understand why PPI did not feature prominently in most sites. The PPI advocate in the nominal group ensured that within that process the question ‘what does this mean for patients and the public?’ remained in the foreground. More by chance than design, the main focus of one case study agent (Isabelle) was to help others work out how to use insight from PPI.
Limitations
The degree to which individual KIT agents participated in the process was variable and, therefore, the number of data gathered for each differed in quantity. Some KIT agents gave several interviews, others only one. Participation in audio-diaries was relatively low. We asked diarists to submit a short recording (2–3 minutes) per week for 4 months. Four case study agents submitted no audio-diaries, although one of these did provide a written account. Of the nine who submitted audio-diaries, despite weekly reminders, the number of entries ranged from 2 to 18 and lasted 8–115 minutes. In terms of observations, some organised several but others were not able to co-ordinate a single observation within the time frame of the fieldwork. One KIT agent withdrew from the study after the first interview for personal reasons. Lack of time was an expressed concern of most of the participants, and was a key reason for not running the action learning sets as planned and set out in the original protocol. The varying degrees of commitment might reflect the way in which the KIT agents were recruited, that is, through senior staff at the network rather than directly. However, this method of recruitment was the preference of the AHSN leadership as the teams were in the early stages of setting up their networks.
Our access to the KIT agents’ network also varied. In total, five line managers of the KIT agents (one of these was line manager to three agents) and 22 Links were interviewed. In no case did anyone refuse to participate, but finding time to meet was very difficult. This is not surprising, given the challenges that the service faced at the time of our study, combined with the newness of the networks.
Despite notable disparity of data collection across agents, we have data from at least three of five sources (agent interviews and diaries, observations, line manager interview, Link interviews) for all agents apart from the one who withdrew from the study (Chloe). For 10 agents we collected data from at least four sources. We recognise that we had least data from Wetlands.
Another limitation of the study relates to the cross-sectional nature of data collection with regards to Links and line managers. Although efforts were made to follow up the KIT agents and use the audio-diaries to keep track of change, the line manager and Links were interviewed only once. It is likely, therefore, that the findings reflect how the process was working at the time for the line managers and Links. This ‘snapshot’ perspective was mitigated by the research design, which permitted a time lag between the initial interview with a KIT agent and their line manager/Links. When line managers attended feedback sessions, they were invited to offer further reflections. Links were not part of those meetings. Had resources permitted, it would have been helpful to reinterview the Links to provide additional insight on questions about sustainability. However, the study took longer to set up than planned for several reasons besides the participants’ lack of time. Reasons included delays in the establishment of AHSNs; reluctance on the part of some senior gatekeepers (KIT agents’ line managers or those above) to involve staff in the study; and a concern on the part of some KIT agents about the impact of them taking part in the research on their link organisations. Some were particularly concerned about anonymity. This led to an additional process of permission-seeking and negotiation. Delays within the AHSNs meant that some KIT agent programmes planned for inclusion in the study were not set up in time.
A further potential limitation of the study is the lack of ‘objective’ measurement of outcomes and impact. They tended to be self-reported and potential, rather than actual. Some line managers and Links gave relatively superficial appraisals of the agent and the role, focusing on personal characteristics in place of harder information about how they perform their role. We might have had more robust responses had we asked line managers and Links to comment on how they perceived social marketing concepts as fitting with the role. Instead we chose to use social marketing theory in our interpretation. We did this because the timing of our study meant that the networks were in the early stages of formation and we anticipated that our interviewees might struggle to interpret the agents’ work through a social marketing lens.
Although it was not the intention of the study to measure predefined outcomes, some will see it as a weakness. The study itself brings insight to the difficulty of objective measurement of outcomes and impact in two ways. First, data gathering and analysis were structured around an explicit and, therefore, transparent evaluation approach used in continuing professional development. 70 Second, one objective was designed to address the question of how success could be measured. This part of the study used the nominal group technique to develop group consensus. We also addressed this question with KIT agents and their line managers and Links during the interviews. Both sets of data highlight the difficulty in devising a set of generic measures and the risk that the application of a formal approach might not capture ‘softer’ outcomes such as enhanced relationships, capacity development and shifts in organisational culture. It is hard to measure the effect of the KIT agent, for example, who is the ‘grit’ in the system or the one who works across ‘silos’ to break down barriers. However, being mindful of such difficulties does not rule out the possibility that broad measures could be identified that might be evidenced using a combination of quantitative and less formal qualitative data, and tailored to particular circumstances. To this end we have proposed a set of principles and suggested a framework for measuring outcomes of knowledge broker activity.
With these limitations in mind, we report how the study has addressed the research questions.
How we addressed our research questions
What are the commonly shared expectations of the knowledge and innovation transfer agent role?
This question can be answered in two ways: the ways in which the expectations were shared by the agents in our study and, adopting the language of social marketing, how the KIT agents’ expectations were shared with their ‘clients’ – line managers and Links. In this study it appears that, despite variation in specifics, the broad expectation of the role was largely shared across both groups. In short, despite ambiguity at a detailed level, the role was about engaging with practitioners to help them develop their service in order to improve it for patients and, in some cases, also to save money. The focus of KIT agents’ work was on supporting and helping practitioners to develop, rather than doing things for them (although sometimes the former was a goal they were moving towards). The results of our nominal group exercise (see Chapter 7, Question 3: what should knowledge brokers do to contribute to the achievement of outcomes?) show that the group also agreed with role expectations around making connections, motivating and influencing others, teaching and training, and facilitating access to knowledge.
This result differs from earlier studies253 on research partnerships and knowledge brokers that showed a degree of mismatch in goals and expectations between parties. It may be that this is linked to the straightforward focus of the KIT agents in taking on the role within a network; in general, the KIT agents studied here appeared to be motivated to improve health-care provision rather than, say, explore career options. 66
The literature on intermediary roles in health groups their functions into three broad categories: ‘knowledge management’, ‘linkage and exchange’ and ‘capacity building’. 97,112 Our findings overlap with these three functional categories, but provide additional insight into the challenge of undertaking a KIT role and the necessity to define role expectations on an ongoing basis so that longer-term expectations are realistic. Others16,110,152,155,163 have also reported the importance of agreeing roles and expectations.
What, in practice, do the knowledge and innovation transfer agents do?
It was possible to answer this question in some depth and breadth because the sample was selected for maximum variation based on each network’s declared intentions for the roles. KIT agents were identified as such by network senior staff. In many cases the specifics of the role developed over time. Details are provided in Chapter 5, but the overall pattern of what the KIT agents did is summarised here.
Only one agent (Erin) focused directly on the growth agenda, although others included industrial partners in their engagements as a source of learning, and another agent (Grace) supported intellectual property development. Erin’s activities included providing market research, signposting people around the innovation systems, and linking people developing a service to commissioners. Two teams (Moorlands and Wetlands) were closest to more mainstream ideas of knowledge mobilisation7,54,57,93,108,117,168 and provided formal research evidence to clinical/management teams. Some teams (Greenhills, Riverside and Homefields) were responsible for introducing or developing approaches to health-care management, such as QI methodologies and PPI approaches, through formal training and support of topic-specific networks (e.g. leadership, new research, or evaluation approaches). Other KIT agents (e.g. Chloe, Amy, Fran) worked directly with practitioners on local projects. Most often these were related to QI. A number of KIT agents did more than one of these activities.
Recent studies of the CLAHRCs in England also found that mixed approaches to knowledge mobilisation were used by those in KIT roles. 60,179 These included service improvement, converting evidence into practical products, implementing national and/or local guidance into practice and mobilising local evidence. 60
Some KIT agents worked with people in different roles who focused on a single issue (e.g. patient safety). This meant that the agents thus linked not only with doctors but also with PPI leads, for example, in the case of Molly and Fran. Others worked with people around a particular project (e.g. doctors, nurses and managers addressing the issue of the deteriorating patient – Amy). Several linked academics and health-care practitioners, sometimes around a specific project (e.g. Jessica, James and Grace). Others dealt with non-NHS service providers or providers of services that were not NHS based (e.g. patent experts and antenatal groups – Isabelle and Janice). Most linked with multiple levels of organisations and, in some cases, provided links between levels of organisations for whom they did not work (e.g. Grace).
All the KIT agents were involved in bringing people to new knowledge with the intention of helping them to work differently (i.e. better). This was accomplished by providing that knowledge themselves, drawing people into an engagement in which they could acquire this knowledge from other people or documents, or signposting people to others from whom they could learn or who could learn from them.
Despite the difference in content of the KIT agents’ experiences, they shared a number of features. It is perhaps these features that differentiate the KIT agent approach from more traditional ‘information-deficit’ models254 of knowledge transfer and may in part account for their relative success in achieving desired outcomes. The KIT agents and Links reported a series of repeated and ongoing interactions, and the details of the actions taken were tailored to the needs of the Links (‘clients’). The importance of tailoring has been reported by others. 179 Repeated interaction also gave the KIT agents opportunities to provide feedback to Links and update their learning.
Building relationships was a critical part of KIT agents’ work. As one KIT agent put it, ‘you have to build relationships and there’s no substitute and knowledge transfer happens in the context of a relationship. It doesn’t happen in the middle of the ether’ (James). Rycroft-Malone et al. 60 also found that building relationships was a central ingredient in the success reported by knowledge brokers in CLAHRCs. Yet these relationships were typically intended to be finite. Most engagement aimed to embed knowledge, a set of skills, approaches, or set of contacts that would stay with the Link’s organisation beyond the interaction. In other words, the KIT agents entered the engagement with a view to the succession or termination of the engagement. While supporting Links in a practical way (teaching them about QI methodology, for example) they were consciously trying to extract themselves for more direct support (e.g. Erin, Isabelle, Fran) and develop the Links’ independence so they could continue the work when the KIT agent moved on. Many repeatedly reminded Links that this was their project, their data and their responsibility (Fran, Amy). A successful KIT agent is one that is no longer needed by specific Links at the end of their engagement with them.
How does the work of knowledge and innovation transfer agents impact on health-care practice?
Despite the recognised challenges of understanding what impact means and demonstrating it, we are able to point to a number of direct ways in which the work of KIT agents impacted on health-care practice (‘results’ in the Kirkpatrick framework). It is in no small measure problematic to do this, as discussed, but we are able to draw attention to the few specific projects with measurable outcomes to which agents contributed. These include working with a team to reduce ambulance handover time significantly (Sophie); and improvement in compliance with the sepsis care pathway that was reflected in mortality outcomes (Amy). Others reported a reduction in cancelled elective surgeries, reduced delays in patient flow, a reduction in the number of patient complaints, decreased infection control rates and a decrease in the number of patient falls. In these cases, the KIT agents worked with Links to gather data, analyse the problem, develop the intervention and measure its success. One team (Wetlands) was reported to have assisted the development and commissioning of a new rehabilitation centre (and a new approach to care). This has been described as providing quality care for patients and being cost-effective in an external evaluation. One of Sophie’s Links reported that by tracking patient flow to social workers, which was characterised by long wait times, they were able to secure more resources for these professionals.
A number of KIT agents also worked alongside practitioners to develop skills and organisational capability to improve care. One team (in Riverside) trained and supported audit staff in QI methodology. The team manager reported that the team had refocused their efforts, away from audit (counting) and towards improvement. They asked all staff who presented with an audit idea to consider it from an improvement perspective. The team offered training to staff to support them in this goal. Another Link (one of Janice’s) reported how useful she had found working with an academic team. This relationship gave her access to information about service provision, which she could then use with clients who were making choices about their own care.
Knowledge and innovation transfer agents and their Links also reported outcomes not directly related to health care, but showing potential for future practice. This included the development of research proposals and Links thinking differently about how to use feedback from patients to redesign the service. There were specific outcomes around improved capacity, including training staff in QI methodology and QI becoming part of the performance system.
How can knowledge and innovation transfer agents be best supported?
Our study provides useful pointers on how KIT agents can best be supported. Before considering this in more detail, we highlight some of the features of the role that make it unusual and potentially challenging. Similar to findings in previous studies,136,140,255 the roles are largely temporary, do not fit into a recognised career structure with progression and rewards, and do not always allow KIT agents to return to their original posts. Some KIT agents were working in, or with, organisations that did not employ them and over which they had no managerial control. Some reported a degree of disconnect with their employing organisation. A number of KIT agents also covered large geographical areas requiring travel, and were isolated. It is noteworthy that all bar one of the KIT agents in our study were women. This raises questions around whether or not knowledge brokering is a gendered role in health care. Alongside this, most of the KIT agent roles could be characterised as requiring some emotional labour,256 providing significant support to individuals and substantial effort to understand the needs of others and adapt to them. References to ‘hand holding’, managing hostility and the need for resilience were commonly mentioned and have been reported elsewhere. 178 Some KIT agents also felt underequipped for aspects of their roles, although this was not reported by their Links.
The KIT agents could benefit from better assistant support and a team approach: this addresses the implication of them wanting to engage with colleagues face to face, which is time-consuming and makes them unavailable to others at that time. Given the geography of some networks, travel time was not insignificant. Support from senior colleagues is essential, both directly and in helping the KIT agent keep their ‘clients’ motivated. Support from ‘the board’, ‘the exec team’ and similar was consistently mentioned as being of help, a finding echoed in the literature. 3,43,141 In most cases, but not all, in which there was more than one KIT agent in a network, individuals commented on the value of being able to draw on each other’s support (a finding similar to that reported by Chew et al. 137). This support did not necessarily relate to the specific content of the role (e.g. the details of the QI methodology), but was more often about managing a difficult relationship or issue and having the opportunity to express concern. Ensuring that KIT agents do not feel emotionally isolated is likely to be a useful support.
Flexibility with respect to how the KIT agent is managed is a related concern. The KIT agents were successful because they could be responsive and adapt their role and way of working to the needs of the Links, a finding echoed by Chew et al. 137 In most cases, this may have been necessitated by a lack of detailed planning about the role and work, but it seems to have worked well in these cases. KIT agents therefore require senior-level agreement to work flexibly and with a degree of independence to meet local needs while also actively engaging in their work. It appears that the role depends on a level of openness to the identification of projects. On paper this might look like excess capacity as the KIT agent is not recruited to do a specific job, and the potential for erroneous perception needs to be managed.
Timely training (e.g. within the first couple of months in post) was identified as a necessity for KIT agents who felt less confident in discharging some aspects of their role. For example, Fran and Amy both reported a sense of vulnerability at times as they were using approaches that were new to them and in some instances with people who had not sought their help. Others, however (e.g. James), embraced challenging others and being the ‘grit’ in the system.
What measures can be used to assess the impact of knowledge and innovation transfer activity?
This study suggests that generic measures, despite their attractiveness, would not adequately assess the impact of KIT activity, as KIT agents do a number of things towards different goals. Roles are difficult to measure and evaluate in the short term,137,168 and a generic measure is likely to be too non-specific to provide any meaningful measurement. Furthermore, KIT agents should be measured only against those things over which they have control (i.e. proximal to their work, rather than distal outcomes). Findings from the nominal group and interviews suggest ways forward. Like the KIT agent themselves, a system to measure results or impact most likely needs to be flexible. It needs to link processes to outcomes; specific actions linked to what the KIT agent and their clients agree they are trying to achieve, and the steps being taken towards it. Logic models170,257,258 might provide a useful tool for planning and evaluation. This process would have the additional benefit of requiring the active parties to articulate what they would like to achieve, how they would like the KIT agent to help, and the role of wider constraints, and to provide a basis for review.
Implications for effective knowledge brokering
Within the context of AHSNs and partnerships, our study of KIT agents suggests five important implications for knowledge brokering.
-
Individual dispositions such as listening and attitude, a proactive approach to both defining the role and the work, and status (i.e. a relevant background, notably clinical) were centrally important to KIT agent success. This suggests that screening, recruitment and HR processes related to these posts would benefit from a person specification reflective of these attributes. Seniority and visibility to the board, conditions we found linked to agent success, also need to be considered; if not held by the KIT agent, then they require senior management buy-in.
-
These roles take time and require flexibility on behalf of the organisation in order to develop and begin to see desired outcomes. Individuals in these posts are action-oriented through their repeated interactions with individuals across boundaries and their attention to the change process. This has implications for measurement and reveals that longer-term views to assessing the roles are necessary, which we note might be in tension with short-term fellowships. However, this is true across other successful change initiatives in which a requirement for time and space is recognised. A potential medium-term approach, as discussed by our nominal group, might entail the use of case studies. Case studies provide an in-depth, holistic understanding of events. They can be specific in focus and draw on various sources of data – quantitative and qualitative – to narrate the processes undertaken that led to desired outcomes and demonstrate the role of the knowledge broker within this. They can also highlight the challenges encountered (and overcome) and how things might be done differently in future (see Appendix 9).
-
The feelings of isolation reported by some of our KIT agents highlight the potential to connect those in these posts across the still relatively new structures. Learning from the experience of CLAHRCs in this regard would be a fruitful avenue to explore how national communities of practice could be developed within the context of competitive networks. Furthermore, Q, the initiative led by the Health Foundation is one such effort in terms of QI fellows that could include some KIT agents in their community.
-
The confusion at the level of the organisation related to who leads and supports QI should be addressed, because it is a challenge for KIT agents and possibly others. For example, we found one site where there was a quality department, an organisational development team, a research and innovation team and an audit team, as well as the KIT agent’s own team, all working within the same space. This led not only to confusion, but to duplication of effort, territorialism, frustration and wasted resources.
-
Multiple competencies are required around producing and using local data for improvement. These are not necessarily held by the KIT agent, but are required to support the change initiatives within KIT, whether QI, implementation or otherwise. Many agents saw this as their contribution – that is, supporting local teams to become ‘data driven’. This suggests that organisational capability in the use of data is central to these roles and requires investment not only in generating meaningful figures but training practitioners in its application to service improvement.
Future research
We suggest a number of areas for future research to further our understanding of the use of knowledge broker roles in health care.
There is a growing recognition that the knowledge brokering or boundary-spanning roles are held within a team rather than by an individual. 54,60,179 Future research might focus on how these roles are negotiated, maintained and transferred within a team setting and the related outcomes and impacts achieved. This could offer insights for leaders in setting up their teams (i.e. composition, HR implications, sustainability).
Another fruitful area of future inquiry might consider a longitudinal study of KIT roles to answer the following questions: are the perceived risks of taking on these roles (lack of career progression and recognition, time away from clinical or managerial duties) valid? What career options are available after leaving the KIT role? Are KIT agents lost in the system (i.e. do they return to clinical or management roles with limited potential to enact KIT after receiving training and support)? There is significant scope to follow up on agents who have been studied across a number of projects (not only this study but also within the CLAHRC evaluations and the SDO management fellows). This could also address the issue of sustainability. Specifically, what is the evidence that the results of KIT work are sustained?
Challenges related to career progression and recognition are exacerbated if the KIT role is the only component of the work. Those in hybrid roles (working in dual clinical–knowledge broker roles) may benefit from retaining membership and accountability within their profession. 181,259,260 However, further research is needed to understand how competing priorities can be managed successfully to ensure that the knowledge brokerage role is not squeezed. Such research could explore the differing challenges related to the career structure for nurses, doctors, academics and policy-makers.
Social marketing offers a new approach in this area, and insights from the theory might be included in question schedules for knowledge brokers, their line managers and Links. This would enable exploration of whether or not social marketing concepts guided KIT practice.
The emerging trend in the application of improvement approaches rather than approaches/tools typically described in knowledge mobilisation/transfer (e.g. use of guidelines, appraised evidence) deserves further attention. This trend might be explained in the UK through influential national training initiatives (for example 1000 Lives) and think tanks resourcing the improvement science discipline through fellowships, training and, most recently, the Q initiative (Health Foundation). The influence of the IHI approaches championed by Berwick has been made more visible in the UK via his recent report. 64 This is not to say that all our agents were applying improvement science per se, but even when they did use theoretical frameworks developed in the knowledge mobilisation literature, they did not describe them as such (see Chapter 6 for discussion on how KIT content was framed and tailored). The issue of QI and more traditional notions of research use coexisting within the context of the same policy and funding streams needs to be unpicked.
More work is clearly needed in understanding impacts and assessing how success is identified, credited or measured. The nominal group has started the debate on measures, while social marketing theory could provide a suitable theoretical framework for pushing this work forward.
The nominal group exercise raised the importance of knowledge brokers linking with service users (ranked second after front-line clinicians) and other knowledge brokers. However, we rarely observed our KIT agents interacting with either of these groups in our study. A select few of our KIT agents worked directly with service users (e.g. Isabelle, Janice) and even fewer mentioned linking with others in KIT agent roles. One proposition that has been posed is whether or not patients themselves can take on knowledge broker roles. 261
Finally, a comparative (country, sector, knowledge-based private sector) study of any similar roles which are deemed attractive and embedded merits consideration. It would be helpful for those in the health-care field to learn from other contexts in which the roles are not perceived as risky. This might also reveal lessons for continuing professional development and how to foster learning organisations.
Concluding remarks
The case studies in this research project show that KIT in organisations is still perceived as an add-on activity to clinical care, but is moving steadily towards being integrated into the fabric of organisations. It has its own confusing language and identity as a sphere of work, but its strong association with quality and continuous improvement strategies is helping in that respect.
Our sample of 13 KIT agents differed in their professional backgrounds, experience and expertise. Most had to ‘learn on the job.’ Some did not have a clearly defined or agreed-upon role. Nevertheless, they pursued similar goals to change the culture of their organisations, build capacity in KIT, improve the relationship between the NHS and higher education and, ultimately, improve patient care. To achieve these goals they frequently challenged the status quo, used a wide range of quality and continuous improvement methods to support colleagues in achieving change projects and co-ordinated activities within their organisations.
Historical, organisational and policy factors also exerted an influence. These factors related to the culture of organisations and the degree to which it supported new ways of working and was patient centred. The place of the KIT agent in the organisational structure appeared a less important factor if they were able to draw on senior-level support. The extent to which KIT agents could build on previous related work (e.g. CLAHRCs) featured less prominently than we had anticipated. Agents in regions with established CLAHRCs demonstrated that they learned from the collaboration’s experience, but we did not encounter them directly building on a CLAHRC’s existing work programme. Policy undoubtedly helped to drive change in KIT, but also hindered change by forcing the service to be driven by financial needs and targets.
The complexity and uniqueness of the KIT agents’ roles and the skills and qualities needed to manage them were striking to observe. They were clearly valued by those they supported for their expertise and qualities of leadership, flexibility, proactive approach and ‘can-do’ attitude. They were seen as making a difference. Yet some felt isolated and thought that the role was not always valued in their organisations. The role could be difficult in organisations with strong protected professional boundaries and staff averse to change. A common complaint was that there was not enough dedicated time or resources at their disposal to make the best of their role, which was often short term and lacking in career structure.
One over-riding conclusion is the need for further research on knowledge brokers. 42,54 Rycroft-Malone et al. 42 observe that ‘we know very little about how bringing the users and producers of research closer together might affect their capability to implement’, or what might work for whom, and in what context. 3 Linear approaches to evaluating what works best are arguably insufficient, and more interpretative approaches are needed. 82,262 The impact of the work of KIT agents/knowledge brokers is hard to measure, and although there are existing frameworks and tools, there is ample scope to explore this question in further studies.
In conclusion, the role of KIT agents is varied, complex, time-consuming and evolving. The stages they were at in achieving their objectives differed greatly on account of individual, local and policy-related factors. Given the sheer scale of the task and the environment in which they currently operate, the effectiveness of KIT agents needs a long-term view. They require senior-level commitment and support in organisations, training and networking opportunities with others in a similar role to share good practice and reduce isolation. Secondments should be long enough to allow them to achieve their objectives. A clearly defined career structure and succession planning will help to sustain the progress in KIT that is being realised.
In Appendix 10, we provide a summary of our findings in presentation format. This is designed to be shared with practitioner audiences of KIT agents/knowledge brokers, managers and others.
Acknowledgements
Acknowledgements and disclaimers
We would like to thank members of the project advisory group, the financial support of the NIHR and Elaine Russ for her administrative and organisational support with all aspects of the project.
Contributions of authors
Alison Bullock [Director, Cardiff University, Cardiff Unit for Research and Evaluation in Medical and Dental Education (CUREMeDE)] is the lead author and was involved in all aspects of the research study and reporting.
Emma Barnes (Research Associate, Cardiff University, CUREMeDE) was involved in all aspects of the research study and reporting.
Zoe Slote Morris (Researcher, Morris Buscher Associates) was involved in the design and data collection, and in the preparation of the report.
Jill Fairbank (Universities UK) was involved in the data collection and analysis, and in the preparation of the report.
John de Pury (Director, Universities UK) was involved in the design and data collection, and reviewed the report.
Rosamund Howell (Knowledge Mobilisation Lead, Aneurin Bevan University Health Board) was involved in research governance and in the preparation of the report.
Susan Denman (Wales Government) was involved in the study design. She was a contributing member of the advisory group and helped with the preparation of the report.
Data sharing statement
This is a qualitative study and, therefore, the data generated are not suitable for sharing beyond that contained within the report. Further information can be obtained from the corresponding author.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
References
- A Review of UK Health Research Funding: Sir D Cooksey. London: HM Treasury; 2006.
- Mitton C, Adair CE, McKenzie E, Patten SB, Waye Perry B. Knowledge transfer and exchange: review and synthesis of the literature. Milbank Q 2007;85:729-68. http://dx.doi.org/10.1111/j.1468-0009.2007.00506.x.
- Kitson AL, Rycroft-Malone J, Harvey G, McCormack B, Seers K, Titchen A. Evaluating the successful implementation of evidence into practice using the PARiHS framework: theoretical and practical challenges. Implement Sci 2008;3. http://dx.doi.org/10.1186/1748-5908-3-1.
- Ferlie E, Crilly T, Jashapara A, Peckham A. Knowledge mobilisation in healthcare: a critical review of health sector and generic management literature. Soc Sci Med 2012;74:1297-304. http://dx.doi.org/10.1016/j.socscimed.2011.11.042.
- Dagenais C, Somé TD, Boileau-Falardeau M, McSween-Cadieux E, Ridde V. Collaborative development and implementation of a knowledge brokering program to promote research use in Burkina Faso, West Africa. Glob Health Action 2015;8. http://dx.doi.org/10.3402/gha.v8.26004.
- Azimi A, Fattahi R, Asadi-Lari M. Knowledge translation status and barriers. J Med Libr Assoc 2015;103:96-9. http://dx.doi.org/10.3163/1536-5050.103.2.008.
- Sebba J. An exploratory review of the role of research mediators in social science. Evid Policy 2013;9:391-408. http://dx.doi.org/10.1332/174426413X662743.
- Ham C, Dixon A, Brooke B. Transforming the Delivery of Health and Social Care. The Case for Fundamental Change. London: The King’s Fund; 2012.
- Gainforth HL, Latimer-Cheung AE, Moore S, Athanasopoulos P, Martin Ginis KA. Using network analysis to understand knowledge mobilization in a community-based organization. Int J Behav Med 2015;22:292-300. http://dx.doi.org/10.1007/s12529-014-9430-6.
- Rushmer RK, Cheetham M, Cox L, Crosland A, Gray J, Hughes L, et al. Research utilisation and knowledge mobilisation in the commissioning and joint planning of public health interventions to reduce alcohol-related harms: a qualitative case design using a cocreation approach. Health Serv Deliv Res 2015;3.
- Sin C. The role of intermediaries in getting evidence into policy and practice: some useful lessons from examining consultancy–client relationships. Evid Policy 2008;4:85-103. http://dx.doi.org/10.1332/174426408783477828.
- Pearson A, Jordan Z, Munn Z. Translational science and evidence-based healthcare: a clarification and reconceptualization of how knowledge is generated and used in healthcare. Nurs Res Pract 2012;2012:1-6. http://dx.doi.org/10.1155/2012/792519.
- Graham ID, Logan J, Harrison MB, Straus SE, Tetroe J, Caswell W, et al. Lost in knowledge translation: time for a map?. J Contin Educ Health Prof 2006;26:13-24. http://dx.doi.org/10.1002/chp.47.
- Bottorff JL. Knowledge translation: where are the qualitative health researchers?. Qual Health Res 2015;25:1461-2. http://dx.doi.org/10.1177/1049732315611266.
- Evans BA, Snooks H, Howson H, Davies M. How hard can it be to include research evidence and evaluation in local health policy implementation? Results from a mixed methods study. Implement Sci 2013;8. http://dx.doi.org/10.1186/1748-5908-8-17.
- Karamitri I, Talias MA, Bellali T. Knowledge management practices in healthcare settings: a systematic review [published online ahead of print July 8 2015]. Int J Health Plann Manage 2015. http://dx.doi.org/10.1002/hpm.2303.
- Bhavnani SK, Warden M, Zheng K, Hill M, Athey BD. Researchers’ needs for resource discovery and collaboration tools: a qualitative investigation of translational scientists. J Med Internet Res 2012;14. http://dx.doi.org/10.2196/jmir.1905.
- Braithwaite J, Marks D, Taylor N. Harnessing implementation science to improve care quality and patient safety: a systematic review of targeted literature. Int J Qual Health Care 2014;26:321-9. http://dx.doi.org/10.1093/intqhc/mzu047.
- Blair M. Getting evidence into practice – implementation science for paediatricians. Arch Dis Child 2014;99:307-9. http://dx.doi.org/10.1136/archdischild-2012-303464.
- Waltz TJ, Powell BJ, Chinman MJ, Smith JL, Matthieu MM, Proctor EK, et al. Expert Recommendations for Implementing Change (ERIC): protocol for a mixed methods study. Implement Sci 2014;9. http://dx.doi.org/10.1186/1748-5908-9-39.
- Bulmer M, Bulmer M. Social Science and Social Policy. London: Allen and Unwin; 1986.
- Walshe K, Davies HT. Health research, development and innovation in England from 1988 to 2013: from research production to knowledge mobilization. J Health Serv Res Policy 2013;18:1-12. http://dx.doi.org/10.1177/1355819613502011.
- Marshall M, Pagel C, French C, Utley M, Allwood D, Fulop N, et al. Moving improvement research closer to practice: the Researcher-in-Residence model. BMJ Qual Saf 2014;23:801-5. http://dx.doi.org/10.1136/bmjqs-2013-002779.
- Estape ES, Mays MH, Harrigan R, Mayberry R. Incorporating translational research with clinical research to increase effectiveness in healthcare for better health. Clin Transl Med 2014;3. http://dx.doi.org/10.1186/2001-1326-3-20.
- Walter I, Davies H, Nutley S. Increasing research impact through partnerships: evidence from outside health care. J Health Serv Res Policy 2003;8:58-61. http://dx.doi.org/10.1258/135581903322405180.
- Baker R, Tang MY. The role of research in helping general practice commission efficient healthcare. London J Prim Care 2011;4:27-32. http://dx.doi.org/10.1080/17571472.2011.11493324.
- Innovation, Health and Wealth: Accelerating Adoption and Diffusion in the NHS. London: Department of Health; 2011.
- Academic Health Science Networks: Engaging with Innovation and Improvement. NHS Confederation; 2012.
- Bloor C, Sriskandarajah R, Croxford V, White H. Strategy for UK Life Sciences. London: Department for Business, Innovation and Skills and Office for Life Sciences; 2011.
- AHSN Network . History of AHSNs 2015. www.ahsnnetwork.com/about-academic-health-science-networks/history-of-ahsns/ (accessed 1 February 2016).
- Five Year Strategy. Cardiff: Cardiff University; 2012.
- Mobilising the Use of Research in Practice for Impacts on Health and Wealth – Recommendations of the AHSC Knowledge Transfer Task And Finish Group to NISCHR, Welsh Government. Cardiff: NISCHR AHSC; 2014.
- Lomas J. The in-between world of knowledge brokering. BMJ 2007;334:129-32. http://dx.doi.org/10.1136/bmj.39038.593380.AE.
- Ward V, House A, Hamer S. Developing a framework for transferring knowledge into action: a thematic analysis of the literature. J Health Serv Res Policy 2009;14:156-64. http://dx.doi.org/10.1258/jhsrp.2009.008120.
- Greenhalgh T, Robert G, Macfarlane F, Bate P, Kyriakidou O. Diffusion of innovations in service organizations: systematic review and recommendations. Milbank Q 2004;82:581-629. http://dx.doi.org/10.1111/j.0887-378X.2004.00325.x.
- Integrating Research into Practice: The CLAHRC Experience. NHS Confederation; 2012.
- Mawson S, Scholefield H. The National Institute for Health Research; collaboration for leadership in applied health research and care for South Yorkshire. J Res Nurs 2009;14:169-74. http://dx.doi.org/10.1177/1744987108101752.
- Thomson L, Schneider J, Wright N. Developing communities of practice to support the implementation of research into clinical practice. Leadersh Health Serv 2013;26:20-33. http://dx.doi.org/10.1108/17511871311291705.
- Soper B, Hinrichs S, Drabble S, Yaqub O, Marjanovic S, Hanney S, et al. Delivering the aims of the Collaborations for Leadership in Applied Health Research and Care: understanding their strategies and contributions. Health Serv Deliv Res 2015;3.
- Kislov R, Harvey G, Walshe K. Collaborations for leadership in applied health research and care: lessons from the theory of communities of practice. Implement Sci 2011;6. http://dx.doi.org/10.1186/1748-5908-6-64.
- Martin GP, McNicol S, Chew S. Towards a new paradigm in health research and practice? Collaborations for Leadership in Applied Health Research and Care. J Health Organ Manag 2013;27:193-208. http://dx.doi.org/10.1108/14777261311321770.
- Rycroft-Malone J, Wilkinson J, Burton CR, Harvey G, McCormack B, Graham I, et al. Collaborative action around implementation in Collaborations for Leadership in Applied Health Research and Care: towards a programme theory. J Health Serv Res Policy 2013;18:13-26. http://dx.doi.org/10.1177/1355819613498859.
- Currie G, Lockett A, El Enany N. From what we know to what we do: lessons learned from the translational CLAHRC initiative in England. J Health Serv Res Policy 2013;18:27-39. http://dx.doi.org/10.1177/1355819613500484.
- Soper B, Yaqub O, Hinrichs S, Marjanovich S, Drabble S, Hanney S, et al. CLAHRCs in practice: combined knowledge transfer and exchange strategies, cultural change, and experimentation. J Health Serv Res Policy 2013;18:53-64. http://dx.doi.org/10.1177/1355819613499903.
- Rycroft-Malone J, Wilkinson JE, Burton CR, Andrews G, Ariss S, Baker R, et al. Implementing health research through academic and clinical partnerships: a realistic evaluation of the Collaborations for Leadership in Applied Health Research and Care (CLAHRC). Implement Sci 2011;6. http://dx.doi.org/10.1186/1748-5908-6-74.
- Ling T, Soper B, Marjanovic S, Celia C, Yaqub O, Reding A, et al. Delivering the Aims of the CLAHRCs: Evaluating CLAHRCs’ Strategies and Contributions. Interim report Phase I. Santa Monica, CA: RAND Corporation; 2011.
- Spyridonidis D, Hendy J, Barlow J. Leadership for knowledge translation: the case of CLAHRCs. Qual Health Res 2015;25:1492-505. http://dx.doi.org/10.1177/1049732315583268.
- Spyridonidis D, Hendy J, Barlow J. Understanding hybrid roles: the role of identity processes amongst physicians. Public Admin 2015;93:395-411. http://dx.doi.org/10.1111/padm.12114.
- The CLAHRC Chronic Kidney Disease Collaborative: Improving Care for People with Chronic Kidney Disease: Report on Phase 1 of the CKD Collaborative. Manchester: NIHR CLAHRC; 2010.
- Gerrish K. Tapping the potential of the National Institute for Health Research Collaborations for Leadership in Applied Health Research and Care (CLAHRC) to develop research capacity and capability in nursing. J Res Nurs 2010;15:215-25. http://dx.doi.org/10.1177/1744987110363214.
- Dobbins M, Robeson P, Ciliska D, Hanna S, Cameron R, O’Mara L, et al. A description of a knowledge broker role implemented as part of a randomized controlled trial evaluating three knowledge translation strategies. Implement Sci 2009;4. http://dx.doi.org/10.1186/1748-5908-4-23.
- Terwiesch C, Ulrich K. Innovation Tournaments: Creating and Selecting Exceptional Opportunities. Boston, MA: Harvard Business Press; 2009.
- Hoens AM, Li LC. The knowledge broker’s ‘fit’ in the world of knowledge translation. Physiother Can 2014;66:223-7. http://dx.doi.org/10.3138/ptc.66.3.GEE.
- Waring J, Currie G, Crompton A, Bishop S. An exploratory study of knowledge brokering in hospital settings: facilitating knowledge sharing and learning for patient safety?. Soc Sci Med 2013;98:79-86. http://dx.doi.org/10.1016/j.socscimed.2013.08.037.
- Bornbaum CC, Kornas K, Peirson L, Rosella LC. Exploring the function and effectiveness of knowledge brokers as facilitators of knowledge translation in health-related settings: a systematic review and thematic analysis. Implement Sci 2015;10.
- Martin G, Currie G, Lockett A. Prospects for knowledge exchange in health policy and management: institutional and epistemic boundaries. J Health Serv Res Policy 2011;16:211-17. http://dx.doi.org/10.1258/jhsrp.2011.010132.
- Turnhout E, Stuiver M, Klostermann J, Harms B, Leeuwis C. New roles of science in society: different repertoires of knowledge brokering. Sci Publ Policy 2013;40:354-65. http://dx.doi.org/10.1093/scipol/scs114.
- Abdullah G, Rossy D, Ploeg J, Davies B, Higuchi K, Sikora L, et al. Measuring the effectiveness of mentoring as a knowledge translation intervention for implementing empirical evidence: a systematic review. Worldviews Evid Based Nurs 2014;11:284-300. http://dx.doi.org/10.1111/wvn.12060.
- Gagliardi AR, Webster F, Straus SE. Designing a knowledge translation mentorship program to support the implementation of evidence-based innovations. BMC Health Serv Res 2015;15. http://dx.doi.org/10.1186/s12913-015-0863-7.
- Rycroft-Malone J, Burton C, Wilkinson J, Harvey G, McCormack B, Baker R, et al. Collective action for knowledge mobilisation: a realist evaluation of the Collaborations for Leadership in Applied Health Research and Care. Health Serv Deliv Res 2015;3.
- Rowley E. Protocol for a qualitative study exploring the roles of ‘Diffusion Fellows’ in bridging the research to practice gap in the Nottinghamshire, Derbyshire and Lincolnshire Collaboration for Leadership in Applied Health Research and Care (CLAHRC-NDL). BMJ Open 2012;2. http://dx.doi.org/10.1136/bmjopen-2011-000604.
- Bullock A, Morris Z, Atwell C. A Formative Evaluation of the NIHR Service Delivery and Organisation (SDO) Management Fellowships. Final Report. Southampton: NIHR SDO programme; 2010.
- NHS Improving Quality . Launch of The Fellows Connect Programme 2015. www.nhsiq.nhs.uk/news-events/news/launch-of-the-fellows-connect-programme.aspx (accessed 21 December 2015).
- Berwick DM. A Promise to Learn – A Commitment to Act. Improving the Safety of Patients in England. London: Department of Health; 2013.
- The Health Foundation . Q Initiative 2015. www.health.org.uk/programmes/q-initiative (accessed 21 December 2015).
- Bullock A, Morris ZS, Atwell C. Collaboration between health services managers and researchers: making a difference?. J Health Serv Res Policy 2012;17:2-10. http://dx.doi.org/10.1258/jhsrp.2011.011099.
- Scott-Findlay S, Pollock C. Evidence, research, knowledge: a call for conceptual clarity. Worldviews Evid Based Nurs 2004;1:92-7. http://dx.doi.org/10.1111/j.1741-6787.2004.04021.x.
- Tetroe JM, Graham ID, Foy R, Robinson N, Eccles MP, Wensing M, et al. Health research funding agencies’ support and promotion of knowledge translation: an international study. Milbank Q 2008;86:125-55. http://dx.doi.org/10.1111/j.1468-0009.2007.00515.x.
- Crilly T, Jashapara A, Ferlie E. Research Utilisation & Knowledge Mobilisation: A Scoping Review of the Literature. Southampton: NIHR SDO programme; 2010.
- Greenhalgh T. What is this knowledge that we seek to ‘exchange’?. Milbank Q 2010;88:492-9. http://dx.doi.org/10.1111/j.1468-0009.2010.00610.x.
- Cornelissen E, Mitton C, Sheps S. Knowledge translation in the discourse of professional practice. Int J Evid Based Healthc 2011;9:184-8. http://dx.doi.org/10.1111/j.1744-1609.2011.00215.x.
- Alavi M, Leidner DE. Review: knowledge management and knowledge management systems: conceptual foundations and research issues. MIS Quarterly 2001;25:107-36. http://dx.doi.org/10.2307/3250961.
- Nonaka I, Takeuchi H. The Knowledge-Creating Company: How Japanese Companies Create the Dynamics of Innovation. New York, NY: Oxford University Press; 1995.
- Carlile PR. Transferring, translating, and transforming: an integrative framework for managing knowledge across boundaries. Organ Sci 2004;15:555-68. http://dx.doi.org/10.1287/orsc.1040.0094.
- Bartunek J, Trullen J, Bonet E, Sauquet A. Sharing and expanding academic and practitioner knowledge in health care. J Health Serv Res Policy 2003;8:62-8. http://dx.doi.org/10.1258/135581903322405199.
- Contandriopoulos D, Lemire M, Denis JL, Tremblay E. Knowledge exchange processes in organizations and policy arenas: a narrative systematic review of the literature. Milbank Q 2010;88:444-83. http://dx.doi.org/10.1111/j.1468-0009.2010.00608.x.
- Szulanski G. The process of knowledge transfer: a diachronic analysis of stickiness. Organ Behav Hum Decis Process 2000;82:9-27. http://dx.doi.org/10.1006/obhd.2000.2884.
- Innvaer S. The use of evidence in public governmental reports on health policy: an analysis of 17 Norwegian official reports (NOU). BMC Health Serv Res 2009;9. http://dx.doi.org/10.1186/1472-6963-9-177.
- Pearson A, Wiechula R, Court A, Lockwood C. A re-consideration of what constitutes ‘evidence’ in the healthcare professions. Nurs Sci Q 2007;20:85-8. http://dx.doi.org/10.1177/0894318406296306.
- SDO Management Fellowships - Evaluation of a Knowledge Mobilisation and Capacity Building Initiative. Southampton: University of Southampton; 2009.
- Davies H, Nutley S, Walter I. Why ‘knowledge transfer’ is misconceived for applied social research. J Health Serv Res Policy 2008;13:188-90. http://dx.doi.org/10.1258/jhsrp.2008.008055.
- Oborn E, Barrett M, Racko G. Knowledge translation in healthcare: incorporating theories of learning and knowledge from the management literature. J Health Organ Manag 2013;27:412-31. http://dx.doi.org/10.1108/JHOM-01-2012-0004.
- Harvey G, Kitson A. Necessary but not sufficient . . . comment on ‘Knowledge Mobilization in Healthcare Organizations: A View From the Resource-Based View of the Firm’. Int J Health Policy Manag 2015;4:865-8. http://dx.doi.org/10.15171/ijhpm.2015.159.
- Ontario Institute for Studies in Education (OISE) . What Is Knowledge Mobilization? 2013. www.oise.utoronto.ca/rspe/KM_Products/Terminology/index.html (accessed 4 November 2011).
- Rogers E. The Diffusion of Innovations. New York, NY: Free Press; 1995.
- Birken SA, Lee SY, Weiner BJ. Uncovering middle managers’ role in healthcare innovation implementation. Implement Sci 2012;7. http://dx.doi.org/10.1186/1748-5908-7-28.
- Brockman B, Morgan R. The role of existing knowledge in new product innovativeness and performance. Decis Sci 2003;34:385-419. http://dx.doi.org/10.1111/1540-5915.02326.
- Strach P, Everett A. Knowledge transfer within Japanese multinationals: building a theory. J Knowl Manag 2006;10:55-68. http://dx.doi.org/10.1108/13673270610650102.
- Radaelli G, Lettieri E, Mura M, Spiller N. Knowledge sharing and innovative work behaviour in healthcare: a micro-level investigation of direct and indirect effects. Creat Innov Manag 2014;23:400-14. http://dx.doi.org/10.1111/caim.12084.
- Davies HTO, Powell AE, Nutley SM. Mobilising knowledge to improve UK health care: learning from other countries and other sectors – a multimethod mapping study. Health Serv Deliv Res 2015;3.
- Baumbusch JL, Kirkham SR, Khan KB, McDonald H, Semeniuk P, Tan E, et al. Pursuing common agendas: a collaborative model for knowledge translation between research and practice in clinical settings. Res Nurs Health 2008;31:130-40. http://dx.doi.org/10.1002/nur.20242.
- Rashidian A, Eccles MP, Russell I. Falling on stony ground? A qualitative study of implementation of clinical guidelines’ prescribing recommendations in primary care. Health Policy 2008;85:148-61. http://dx.doi.org/10.1016/j.healthpol.2007.07.011.
- Ward V, House A, Hamer S. Knowledge brokering: the missing link in the evidence to action chain?. Evid Policy 2009;5:267-79. http://dx.doi.org/10.1332/174426409X463811.
- Mitchell P, Pirkis J, Hall J, Haas M. Partnerships for knowledge exchange in health services research, policy and practice. J Health Serv Res Policy 2009;14:104-11. http://dx.doi.org/10.1258/jhsrp.2008.008091.
- King G, Currie M, Smith L, Servais M, McDougall J. A framework of operating models for interdisciplinary research programs in clinical service organizations. Eval Program Plann 2008;31:160-73. http://dx.doi.org/10.1016/j.evalprogplan.2008.01.003.
- Currie M, King G, Rosenbaum P, Law M, Kertoy M, Specht J. A model of impacts of research partnerships in health and social services. Eval Program Plann 2005;28:400-12. http://dx.doi.org/10.1016/j.evalprogplan.2005.07.004.
- Fredericks S, Martorella G, Catallo C. Using knowledge translation as a framework for the design of a research protocol. Int J Nurs Pract 2015;21:157-63. http://dx.doi.org/10.1111/ijn.12338.
- Sustaining Community and Organizational Change: The Positive Deviance Approach. Hamilton, ON: McMaster University; 2014.
- King G, Servais M, Forchuk C, Chalmers H, Currie M, Law M, et al. Features and impacts of five multidisciplinary community-university research partnerships. Health Soc Care Community 2010;18:59-6.
- Marshall MN. Bridging the ivory towers and the swampy lowlands; increasing the impact of health services research on quality improvement. Int J Qual Health Care 2014;26:1-5. http://dx.doi.org/10.1093/intqhc/mzt076.
- Fitzgerald L, Harvey G. Translational networks in healthcare? Evidence on the design and initiation of organizational networks for knowledge mobilization. Soc Sci Med 2015;138:192-200. http://dx.doi.org/10.1016/j.socscimed.2015.06.015.
- Frenk J. Balancing relevance and excellence: organizational responses to link research with decision making. Soc Sci Med 1992;35:1397-404. http://dx.doi.org/10.1016/0277-9536(92)90043-P.
- Williams P. The competent boundary spanner. Public Adm 2002;80:103-24. http://dx.doi.org/10.1111/1467-9299.00296.
- Long JC, Cunningham FC, Braithwaite J. Bridges, brokers and boundary spanners in collaborative networks: a systematic review. BMC Health Serv Res 2013;13. http://dx.doi.org/10.1186/1472-6963-13-158.
- Harvey G, Fitzgerald L, Fielden S, McBride A, Waterman H, Bamford D, et al. The NIHR collaboration for leadership in applied health research and care (CLAHRC) for Greater Manchester: combining empirical, theoretical and experiential evidence to design and evaluate a large-scale implementation strategy. Implement Sci 2011;6. http://dx.doi.org/10.1186/1748-5908-6-96.
- Gerrish K, Piercy H. Capacity development for knowledge translation: evaluation of an experiential approach through secondment opportunities. Worldviews Evid Based Nurs 2014;11:209-16. http://dx.doi.org/10.1111/wvn.12038.
- Nutley S, Walter I, Davies H. Using Evidence: How Research Can Inform Public Services. Bristol: Policy Press; 2007.
- Oldham G, McLean R. Approaches to Knowledge-Brokering 1997. www.iisd.org/publications/pub.aspx?id=829 (accessed 21 December 2015).
- Holzmann V. A meta-analysis of brokering knowledge in project management. Int J Proj Manage 2013;31:2-13. http://dx.doi.org/10.1016/j.ijproman.2012.05.002.
- Dagenais C, Malo M, Robert É, Ouimet M, Berthelette D, Ridde V. Knowledge transfer on complex social interventions in public health: a scoping study. PLOS ONE 2013;8. http://dx.doi.org/10.1371/journal.pone.0080233.
- Fisher C. Knowledge Brokering and Intermediary Concepts: Analysis of E-Discussion on the Knowledge Brokers’ Forum. Brighton: Institute of Development Studies; 2010.
- Michaels S. Matching knowledge brokering strategies to environmental policy problems and settings. Environ Sci Policy 2009;12:994-1011. http://dx.doi.org/10.1016/j.envsci.2009.05.002.
- Ellen ME, Léon G, Bouchard G, Ouimet M, Grimshaw JM, Lavis JN. Barriers, facilitators and views about next steps to implementing supports for evidence-informed decision-making in health systems: a qualitative study. Implement Sci 2014;9. http://dx.doi.org/10.1186/s13012-014-0179-8.
- Baker EA, Homan S, Schonhoff R, Kreuter M. Principles of practice for academic/practice/community research partnerships. Am J Prev Med 1999;16:86-93. http://dx.doi.org/10.1016/S0749-3797(98)00149-4.
- Dopson S, Bennett C, Fitzgerald L, Ferlie E, Fischer M, Ledger J, et al. Health Care Managers’ Access and Use of Management Research. Southampton: NIHR SDO programme; 2013.
- Burt R. Structural holes and good ideas. Am J Sociol 2004;110:349-99. http://dx.doi.org/10.1086/421787.
- Morden A, Ong BN, Brooks L, Jinks C, Porcheret M, Edwards JJ, et al. Introducing evidence through research ‘push’: using theory and qualitative methods. Qual Health Res 2015;25:1560-75. http://dx.doi.org/10.1177/1049732315570120.
- Lomas J. Using ‘linkage and exchange’ to move research into policy at a Canadian foundation. Health Aff 2000;19:236-40. http://dx.doi.org/10.1377/hlthaff.19.3.236.
- Manns BJ. Evidence-based decision-making 7: knowledge translation. Methods Mol Biol 2015;1281:485-500. http://dx.doi.org/10.1007/978-1-4939-2428-8_29.
- Campbell D, Donald B, Moore G, Frew D. Evidence check: knowledge brokering to commission research reviews for policy. Evid Policy 2011;7:97-107. http://dx.doi.org/10.1332/174426411X553034.
- Prihodova L, Guerin S, Kernohan WG. Knowledge transfer and exchange frameworks in health and their applicability to palliative care: scoping review protocol. J Adv Nurs 2015;71:1717-25. http://dx.doi.org/10.1111/jan.12642.
- Moullin JC, Sabater-Hernández D, Fernandez-Llimos F, Benrimoj SI. A systematic review of implementation frameworks of innovations in healthcare and resulting generic implementation framework. Health Res Policy Syst 2015;13. http://dx.doi.org/10.1186/s12961-015-0005-z.
- Armstrong R, Waters E, Crockett B, Keleher H. The nature of evidence resources and knowledge translation for health promotion practitioners. Health Promot Int 2007;22:254-60. http://dx.doi.org/10.1093/heapro/dam017.
- Alin P, Taylor JE, Smeds R. Knowledge transformation in project networks: a speech act level cross-boundary analysis. Proj Manag J 2011;42:58-75. http://dx.doi.org/10.1002/pmj.20254.
- Meyer M. The rise of the knowledge broker. Sci Commun 2010;32:118-27. http://dx.doi.org/10.1177/1075547009359797.
- Nyström ME, Hansson J, Garvare R, Andersson-Bäck M. Locally based research and development units as knowledge brokers and change facilitators in health and social care of older people in Sweden. Evid Policy 2015;11:57-80. http://dx.doi.org/10.1332/174426514X14098428292539.
- Gould R, Fernandez R. Structures of mediation: a formal approach to brokerage in transaction networks. Sociol Methodol 1989;19:89-126. http://dx.doi.org/10.2307/270949.
- Walker HJ, Armenakis AA, Bernerth JB. Factors influencing organizational change efforts: an integrative investigation of change content, context, process and individual differences. J Organ Change Manag 2007;20:761-73. http://dx.doi.org/10.1108/09534810710831000.
- Kitson A, Harvey G, McCormack B. Enabling the implementation of evidence based practice: a conceptual framework. Qual in Health Care 1998;7:149-58. http://dx.doi.org/10.1136/qshc.7.3.149.
- Rycroft-Malone J, Seers K, Chandler J, Hawkes CA, Crichton N, Allen C, et al. The role of evidence, context, and facilitation in an implementation trial: implications for the development of the PARIHS framework. Implement Sci 2013;8. http://dx.doi.org/10.1186/1748-5908-8-28.
- Harvey G, Kitson AL, Harvey G, Kitson AL. Implementing Evidence-Based Practice in Healthcare: A Facilitation Guide. New York, NY: Routledge; 2015.
- Dwan KM, McInnes P, Mazumdar S. Measuring the success of facilitated engagement between knowledge producers and users: a validated scale. Evid Policy 2015;11:239-52. http://dx.doi.org/10.1332/174426414X14165029835102.
- Lightowler C, Knight C. Sustaining knowledge exchange and research impact in the social sciences and humanities: investing in knowledge broker roles in UK universities. Evid Policy 2013;9:317-34. http://dx.doi.org/10.1332/174426413X662644.
- Crilly T, Jashapara A, Trenholm S, Peckham A, Currie G, Ferlie E. Knowledge mobilisation in healthcare organisations: synthesising evidence and theory using perspectives of organisational form, resource based view of the firm and critical theory. NIHR SDO programme; 2013.
- van den Driessen Mareeuw F, Vaandrager L, Klerkx L, Naaldenberg J, Koelen M. Beyond bridging the know-do gap: a qualitative study of systemic interaction to foster knowledge exchange in the public health sector in The Netherlands. BMC Public Health 2015;15. http://dx.doi.org/10.1186/s12889-015-2271-7.
- Squires JE, Graham ID, Hutchinson AM, Linklater S, Brehaut JC, Curran J, et al. Understanding context in knowledge translation: a concept analysis study protocol. J Adv Nurs 2015;71:1146-55. http://dx.doi.org/10.1111/jan.12574.
- Chew S, Armstrong N, Martin G. Institutionalising knowledge brokering as a sustainable knowledge translation solution in healthcare: how can it work in practice?. Evid Policy 2013;9:335-51. http://dx.doi.org/10.1332/174426413X662734.
- Shea CM, Jacobs SR, Esserman DA, Bruce K, Weiner BJ. Organizational readiness for implementing change: a psychometric assessment of a new measure. Implement Sci 2014;9. http://dx.doi.org/10.1186/1748-5908-9-7.
- Shortell SM, Bennett CL, Byck GR. Assessing the impact of continuous quality improvement on clinical practice: what it will take to accelerate progress. Milbank Q 1998;76:593-624.
- Lomas J, Culyer T, McCutcheon C, McAuley L, Law S. Conceptualizing and Combining Evidence for Health System Guidance. Ottawa, ON: Canadian Health Services Research Foundation; 2005.
- Antil T, Desrochers M, Joubert P, Bouchard C. Implementation of an innovative grant programme to build partnerships between researchers, decision-makers and practitioners: the experience of the Quebec Social Research Council. J Health Serv Res Policy 2003;8:35-43. http://dx.doi.org/10.1258/135581903322405153.
- Heaton J, Day J, Britten N. Inside the ‘black box’ of a knowledge translation program in applied health research. Qual Health Res 2015;25:1477-91. http://dx.doi.org/10.1177/1049732315580104.
- Kislov R, Waterman H, Harvey G, Boaden R. Rethinking capacity building for knowledge mobilisation: developing multilevel capabilities in healthcare organisations. Implement Sci 2014;9. http://dx.doi.org/10.1186/s13012-014-0166-0.
- Inkpen A. Learning through joint ventures: a framework of knowledge acquisition. J Manage Stud 2000;37:1019-44. http://dx.doi.org/10.1111/1467-6486.00215.
- Parent R, Roy M, St-Jacques D. A systems-based dynamic knowledge transfer capacity model. J Knowl Manag 2007;11:81-93. http://dx.doi.org/10.1108/13673270710832181.
- Cohen WM, Levinthal DA. Absorptive capacity: a new perspective on learning and innovation. Admin Sci Quart 1990;53:128-52. http://dx.doi.org/10.2307/2393553.
- Ziam S, Landry R, Amara N. Supporting absorptive capacity for knowledge brokers: evidence of Canadian health organizations. Int J Innovat Tech Manag 2013;10:1-18.
- Traynor R, DeCorby K, Dobbins M. Knowledge brokering in public health: a tale of two studies. Public Health 2014;128:533-44. http://dx.doi.org/10.1016/j.puhe.2014.01.015.
- Oborn E. Facilitating implementation of the translational research pipeline in neurological rehabilitation. Curr Opin Neurol 2012;25:676-81. http://dx.doi.org/10.1097/WCO.0b013e32835a35f2.
- Tasselli S. Social networks and inter-professional knowledge transfer: the case of healthcare professionals. Organ Stud 2015;36:841-72. http://dx.doi.org/10.1177/0170840614556917.
- Bucknall T. Bridging the know-do gap in health care through integrated knowledge translation. Worldviews Evid Based Nurs 2012;9:193-4. http://dx.doi.org/10.1111/j.1741-6787.2012.00263.x.
- Ross S, Lavis J, Rodriguez C, Woodside J, Denis JL. Partnership experiences: involving decision-makers in the research process. J Health Serv Res Policy 2003;8:26-34. http://dx.doi.org/10.1258/135581903322405144.
- Valizadeh L, Zamanzadeh V, LakDizaji S, Nasiri KH, Mohammadian Roshan S, Maddah S, et al. The individual factors influencing knowledge transfer activities in nursing research. J Urmia Nurs Midwifery Fac 2015;13:99-107.
- Denis JL, Lehoux P, Hivon M, Champagne F. Creating a new articulation between research and practice through policy? The views and experiences of researchers and practitioners. J Health Serv Res Policy 2003;8:44-50. http://dx.doi.org/10.1258/135581903322405162.
- Garland AF, Plemmons D, Koontz L. Research–practice partnership in mental health: lessons from participants. Adm Policy Ment Health 2006;33:517-28. http://dx.doi.org/10.1007/s10488-006-0062-2.
- Nutley S, Walter I, Davies H. From knowing to doing: a framework for understanding the evidence-into-practice agenda. Evaluation 2003;9:125-48. http://dx.doi.org/10.1177/1356389003009002002.
- Boblin SL, Ireland S, Kirkpatrick H, Robertson K. Using Stake’s qualitative case study approach to explore implementation of evidence-based practice. Qual Health Res 2013;23:1267-75. http://dx.doi.org/10.1177/1049732313502128.
- Bowen S, Martens P. Need to Know Team . Demystifying knowledge translation: learning from the community. J Health Serv Res Policy 2005;10:203-11. http://dx.doi.org/10.1258/135581905774414213.
- Lyons R, Warner G, Langille L, Phillips S. Evidence in Action, Acting on Evidence: A Casebook of Health Services and Policy Research Knowledge Translation Stories. Ottawa, ON: Canadian Institutes of Health Research; 2006.
- Research Excellence Framework . Research Excellence Framework 2014 2014. www.ref.ac.uk/ (accessed 1 February 2016).
- Greenhalgh T, Fahy N. Research impact in the community-based health sciences: an analysis of 162 case studies from the 2014 UK Research Excellence Framework. BMC Med 2015;13:232-44. http://dx.doi.org/10.1186/s12916-015-0467-4.
- Ferri M, Dias S. Time, consensus and implementation: challenges for effective knowledge exchange. Addiction 2015;110:900-1. http://dx.doi.org/10.1111/add.12847.
- Gagnon ML. Moving knowledge to action through dissemination and exchange. J Clin Epidemiol 2011;64:25-31. http://dx.doi.org/10.1016/j.jclinepi.2009.08.013.
- Harvey G, Marshall RJ, Jordan Z, Kitson AL. Exploring the hidden barriers in knowledge translation: a case study within an academic community. Qual Health Res 2015;25:1506-17. http://dx.doi.org/10.1177/1049732315580300.
- Graf H. Gatekeepers in regional networks of innovation. Cambridge J Econ 2011;35:173-98. http://dx.doi.org/10.1093/cje/beq001.
- Visram S, Goodall D, Steven A. Exploring conceptualizations of knowledge translation, transfer and exchange across public health in one UK region: a qualitative mapping study. Public Health 2014;128:497-503. http://dx.doi.org/10.1016/j.puhe.2014.02.001.
- Dagenais C, Laurendeau MC, Briand-Lamarche M. Knowledge brokering in public health: a critical analysis of the results of a qualitative evaluation. Eval Program Plann 2015;53:10-7. http://dx.doi.org/10.1016/j.evalprogplan.2015.07.003.
- Seymour A, Rowley E. Collaboration for Leadership in Applied Health Research and Care East Midlands. Leicester: NIHR; 2014.
- Cooke J, Ariss S, Smith C, Read J. On-going collaborative priority-setting for research activity: a method of capacity building to reduce the research-practice translational gap. Health Res Policy Syst 2015;13. http://dx.doi.org/10.1186/s12961-015-0014-y.
- Armstrong K, Kendall E. Translating knowledge into practice and policy: the role of knowledge networks in primary health care. HIM J 2010;39:9-17. http://dx.doi.org/10.1177/183335831003900203.
- Berta W, Cranley L, Dearing JW, Dogherty EJ, Squires JE, Estabrooks CA. Why (we think) facilitation works: insights from organizational learning theory. Implement Sci 2015;10. http://dx.doi.org/10.1186/s13012-015-0323-0.
- Armstrong R, Waters E, Dobbins M, Anderson L, Moore L, Petticrew M, et al. Knowledge translation strategies to improve the use of evidence in public health decision making in local government: intervention design and implementation plan. Implement Sci 2013;8. http://dx.doi.org/10.1186/1748-5908-8-121.
- Beliveau J. Middle Managers’ Behavioral Exemplarity: A Sine Qua Non Condition for Knowledge Transfer n.d.;1:75-82.
- Ellen M, Brown A. Transferring research from researchers to knowledge users: the importance of relationships and getting them right. J Health Serv Res Policy 2016;21:134-6. http://dx.doi.org/10.1177/1355819615602030.
- Denis JL, Lomas J. Convergent evolution: the academic and policy roots of collaborative research. J Health Serv Res Policy 2003;8:1-6. http://dx.doi.org/10.1258/135581903322405108.
- Wright N. First-time knowledge brokers in health care: the experiences of nurses and allied health professionals of bridging the research-practice gap. Evid Policy 2013;9:557-70. http://dx.doi.org/10.1332/174426413X13836462527470.
- Lord L, Dowswell G, Hewison A. ‘The team for both sides?’ A qualitative study of change in heart failure services at three acute NHS Trusts. Health Soc Care Community 2015;23:121-30. http://dx.doi.org/10.1111/hsc.12118.
- Platt J. Research dissemination: a case study. Q J Soc Aff 1987;3:181-98.
- Kislov R, Hodgson D, Boaden R. Professionals as knowledge brokers: the limits of authority in healthcare collaboration. Public Admin 2015;94:472-89. http://dx.doi.org/10.1111/padm.12227.
- Burgess N, Strauss K, Currie G, Wood G. Organizational ambidexterity and the hybrid middle manager: the case of patient safety in UK hospitals. Hum Res Manage 2015;54:87-109. http://dx.doi.org/10.1002/hrm.21725.
- Burgess N, Currie G. The knowledge brokering role of the hybrid middle level manager: the case of healthcare. Br J Manage 2013;24:132-42. http://dx.doi.org/10.1111/1467-8551.12028.
- Currie G, Burgess N, Hayton JC. HR practices and knowledge brokering by hybrid middle managers in hospital settings: the influence of professional hierarchy. Hum Res Manage 2015;54:793-812. http://dx.doi.org/10.1002/hrm.21709.
- Currie G, White L. Inter-professional barriers and knowledge brokering in an organizational context: the case of healthcare. Organ Stud 2012;33:1333-61. http://dx.doi.org/10.1177/0170840612457617.
- Muthusamy SK, White MA. Learning and knowledge transfer in strategic alliances: a social exchange view. Organ Stud 2005;26. http://dx.doi.org/10.1177/0170840605050874.
- Widen-Wulff G, Ginman M. Explaining knowledge sharing in organizations through the dimensions of social capital. J Inform Sci 2004;30:448-58. http://dx.doi.org/10.1177/0165551504046997.
- Boari C, Riboldazzi F. How knowledge brokers emerge and evolve: the role of actors’ behaviour. Res Policy 2014;43:683-95. http://dx.doi.org/10.1016/j.respol.2014.01.007.
- Waterman H, Boaden R, Burey L, Howells B, Harvey G, Humphreys J, et al. Facilitating large-scale implementation of evidence based health care: insider accounts from a co-operative inquiry. BMC Health Serv Res 2015;15. http://dx.doi.org/10.1186/s12913-015-0722-6.
- Knott J, Weissert C. Linking Ideas to Policy: What Can Be Learned from Foundations’ Efforts to Inform Health Policymakers. East Lansing, MI: Institute for Public Policy and Social Research; 1996.
- Innvaer S, Vist G, Trommald M, Oxman A. Health policy-makers’ perceptions of their use of evidence: a systematic review. J Health Serv Res Policy 2002;7:239-44. http://dx.doi.org/10.1258/135581902320432778.
- Elueze IN. Evaluating the effectiveness of knowledge brokering in health research: a systematised review with some bibliometric information. Health Info Libr J 2015;32:168-81. http://dx.doi.org/10.1111/hir.12097.
- Kothari A, Birch S, Charles C. ‘Interaction’ and research utilisation in health policies and programs: does it work?. Health Policy 2005;71:117-25. http://dx.doi.org/10.1016/j.healthpol.2004.03.010.
- Eccles M, Grimshaw J, Walker A, Johnston M, Pitts N. Changing the behavior of healthcare professionals: the use of theory in promoting the uptake of research findings. J Clin Epidemiol 2005;58:107-12. http://dx.doi.org/10.1016/j.jclinepi.2004.09.002.
- Kitson A, Powell K, Hoon E, Newbury J, Wilson A, Beilby J. Knowledge translation within a population health study: how do you do it?. Implement Sci 2013;8. http://dx.doi.org/10.1186/1748-5908-8-54.
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 2008;337.
- Berwick DM. The science of improvement. JAMA 2008;299:1182-4. http://dx.doi.org/10.1001/jama.299.10.1182.
- Newman K, Van Eerd D, Powell BJ, Urquhart R, Cornelissen E, Chan V, et al. Identifying priorities in knowledge translation from the perspective of trainees: results from an online survey. Implement Sci 2015;10. http://dx.doi.org/10.1186/s13012-015-0282-5.
- Doyle C, Howe C, Woodcock T, Myron R, Phekoo K, McNicholas C, et al. Making change last: applying the NHS institute for innovation and improvement sustainability model to healthcare improvement. Implement Sci 2013;8. http://dx.doi.org/10.1186/1748-5908-8-127.
- Kirkpatrick D. Techniques for evaluating training programs. Training Dev J 1979;33:78-92.
- Bates R. A critical analysis of evaluation practice: the Kirkpatrick model and the principle of beneficence. Eval Program Plann 2004;27:341-7. http://dx.doi.org/10.1016/j.evalprogplan.2004.04.011.
- Richmond H. Beyond Kirkpatrick: an evaluation dilemma. Train J 2009:51-4.
- Rycroft-Malone J, Harvey G, Seers K, Kitson A, McCormack B, Titchen A. An exploration of the factors that influence the implementation of evidence into practice. J Clin Nurs 2004;13:913-24. http://dx.doi.org/10.1111/j.1365-2702.2004.01007.x.
- Changing Behaviour, Improving Outcomes: A New Social Marketing Strategy for Public Health. London: Department of Health; 2011.
- Morris ZS, Clarkson PJ. Does social marketing provide a framework for changing healthcare practice?. Health Policy 2009;91:135-41. http://dx.doi.org/10.1016/j.healthpol.2008.11.009.
- NIHR HSDR Programme. Research Brief (12/5002) . Call for Proposals: Research to Improve Knowledge Transfer and Innovation in Healthcare Delivery and Organisation 2012. www.nets.nihr.ac.uk/__data/assets/pdf_file/0005/81788/CB-12-5002-18.pdf (accessed 21 December 2015).
- Monrouxe L. Solicited audio diaries in longitudinal narrative research: a view from inside. Qual Res 2009;9:81-103. http://dx.doi.org/10.1177/1468794108098032.
- Bullock A, Monrouxe L, Atwell C. Working Paper 141: Evaluation of the London Deanery Training Course: Supervision Skills for Clinical Teachers. Cardiff: Cardiff School of Social Sciences Working Paper Series, Cardiff University; 2011.
- Jones J, Hunter D. Qualitative research: consensus methods for medical and health services research. BMJ 1995;311:376-80. http://dx.doi.org/10.1136/bmj.311.7001.376.
- Ritchie J, Spencer L, Bryman A, Burgess R. Analyzing Qualitative Research. London: Routledge; 1994.
- Patton M. Qualitative Evaluation and Research Methods. Thousand Oaks, CA: Sage Publications Ltd; 2001.
- Denzin N. Sociological Methods: A Sourcebook. Piscataway, NJ: Aldine Transaction; 2006.
- Lincoln Y, Guba E. Naturalistic Inquiry. Newbury Park, CA: Sage Publications Ltd; 1985.
- Academic Health Science Networks: Expressions of Interest. London: Department of Health; 2012.
- Department of Health . High Quality Care for All: NHS Next Stage Review Final Report 2008 2008. www.official-documents.gov.uk/document/cm74/7432/7432.pdf (accessed 14 November 2013).
- Economic Renewal – A New Direction. Cardiff: Welsh Assembly Government; 2010.
- Department for Business, Innovation and Skills . Strategy for UK Life Sciences 2011. www.gov.uk/government/uploads/system/uploads/attachment_data/file/32457/11-1429-strategy-for-uk-life-sciences.pdf (accessed 12 October 2015).
- Together for Health: A Five Year Vision for the NHS in Wales. Cardiff: Welsh Assembly Government; 2011.
- Developing an Academic Health Science Partnership in SE Wales – An Outline Strategy. Cardiff: SEWAHSP; 2011.
- Health and Social Care Act 2012. London: HMSO; 2012.
- Science for Wales – A Strategic Agenda for Science and Innovation in Wales. Cardiff: Welsh Assembly Government; 2012.
- Innovation for Wales. Cardiff: Welsh Assembly Government; 2014.
- Mansfield W, Grunewald P. The Use of Indicators for the Monitoring and Evaluation of Knowledge Management and Knowledge Brokering in International Development. Loughborough: Loughborough University Knowledge Services; 2013.
- A Capability Framework for NHS Scotland’s Knowledge Broker Network: Working Together to Translate Knowledge into Action to Improve Scotland’s Health and Care. Edinburgh: NHS Education for Scotland; 2012.
- Knowledge Translation Planning Primer. Ottawa, ON: Public Health Agency of Canada; 2012.
- Redman S, Turner T, Davies H, Williamson A, Haynes A, Brennan S, et al. The SPIRIT Action Framework: a structured approach to selecting and testing strategies to increase the use of research in policy. Soc Sci Med 2015;136–7:147-55. http://dx.doi.org/10.1016/j.socscimed.2015.05.009.
- The CIPHER Investigators . Supporting Policy In health with Research: an Intervention Trial (SPIRIT)-protocol for a stepped wedge trial. BMJ Open 2014;4. http://dx.doi.org/10.1136/bmjopen-2014-005293.
- Makkar SR, Turner T, Williamson A, Louviere J, Redman S, Haynes A, et al. The development of ORACLe: a measure of an organisation’s capacity to engage in evidence-informed health policy. Health Res Policy Syst 2016;14:1-18.
- Makkar SR, Brennan S, Turner T, Williamson A, Redman S, Green S. The development of SAGE: a tool to evaluate how policymakers engage with and use research in health policymaking. Res Eval 2016;25:315-28. http://dx.doi.org/10.1093/reseval/rvv044.
- Organisational Audit For Evidence-Informed Practice. Totnes, Devon: Research in Practice for Adults; 2012.
- King G, Servais M, Currie M, Kertoy M, Law M, Rosenbaum P, et al. The Community Impacts of Research Oriented Partnerships (The CIROP Measure) 2003. www.impactmeasure.org/files/CIROP_Measure_2006_08_Final.pdf (accessed 12 October 2016).
- Canadian Foundation for Healthcare Improvement . Is Research Working for You? A Self-Assessment Tool and Discussion Guide for Health Services Management and Policy Organizations 2014. www.cfhi-fcass.ca/PublicationsAndResources/ResourcesAndTools/SelfAssessmentTool.aspx (accessed 12 October 2016).
- Morton S. Progressing research impact assessment: a ‘contributions’ approach. Res Eval 2015;24:405-19. http://dx.doi.org/10.1093/reseval/rvv016.
- Hastings G. Social Marketing: Why Should the Devil Have All the Best Tunes?. Oxford: Butterworth–Heinemann; 2007.
- Gordon R. Re-thinking and re-tooling the social marketing mix. AMJ 2012;20:122-6. http://dx.doi.org/10.1016/j.ausmj.2011.10.005.
- Burchell H, Jenner EA. The role of the nurse in patient-focused care: models of competence and implications for education and training. Int J Nurs Stud 1996;33:67-75. http://dx.doi.org/10.1016/0020-7489(95)00071-2.
- Andreasen A. Marketing social marketing in the social change marketplace. J Public Policy Mark 2002;21:3-13. http://dx.doi.org/10.1509/jppm.21.1.3.17602.
- Gough B, Conner MT. Barriers to healthy eating amongst men: a qualitative analysis. Soc Sci Med 2006;62:387-95. http://dx.doi.org/10.1016/j.socscimed.2005.05.032.
- Finlinson HA, Colón HM, Robles RR, Soto M. Sexual identity formation and AIDS prevention: an exploratory study of non-gay-identified Puerto Rican MSM from working class neighborhoods. AIDS Behav 2006;10:531-9. http://dx.doi.org/10.1007/s10461-006-9107-5.
- Stephenson JM, Strange V, Forrest S, Oakley A, Copas A, Allen E, et al. Pupil-led sex education in England (RIPPLE study): cluster-randomised intervention trial. Lancet 2004;364:338-46. http://dx.doi.org/10.1016/S0140-6736(04)16722-6.
- Llauradó E A-MM, Tarro L, Papell-Garcia I, Puiggròs F, Arola L, Prades-Tena J, et al. A youth-led social marketing intervention to encourage healthy lifestyles, the EYTO (European Youth Tackling Obesity) project: a cluster randomised controlled trial in Catalonia, Spain. BMC Public Health 2015;15. http://dx.doi.org/10.1186/s12889-015-1920-1.
- Hays RB, Rebchook GM, Kegeles SM. The Mpowerment Project: community-building with young gay and bisexual men to prevent HIV1. Am J Community Psychol 2003;31:301-12. http://dx.doi.org/10.1023/A:1023966905973.
- Kelly JA, Amirkhanian YA, Kabakchieva E, Vassileva S, Vassilev B, McAuliffe TL, et al. Prevention of HIV and sexually transmitted diseases in high risk social networks of young Roma (Gypsy) men in Bulgaria: randomised controlled trial. BMJ 2006;333. http://dx.doi.org/10.1136/bmj.38992.478299.55.
- Grol R. Successes and failures in the implementation of evidence-based guidelines for clinical practice. Med Care 2001;39:II46-54. http://dx.doi.org/10.1097/00005650-200108002-00003.
- Mason A. New medicines in primary care: a review of influences on general practitioner prescribing. J Clin Pharm Ther 2008;33:1-10. http://dx.doi.org/10.1111/j.1365-2710.2008.00875.x.
- Gabbay J, May Al. Evidence based guidelines or collectively constructed ‘mindlines’? Ethnographic study of knowledge management in primary care. BMJ 2004;329. http://dx.doi.org/10.1136/bmj.329.7473.1013.
- Soper B, Hanney SR. Lessons from the evaluation of the UK’s NHS R&D implementation methods programme. Implement Sci 2007;2. http://dx.doi.org/10.1186/1748-5908-2-7.
- Grier S, Bryant CA. Social marketing in public health. Annu Rev Public Health 2005;26:319-39. http://dx.doi.org/10.1146/annurev.publhealth.26.021304.144610.
- Robinson M, Robertson S. The application of social marketing to promoting men’s health: a brief critique. Int J Mens Health 2010;9. http://dx.doi.org/10.3149/jmh.0901.50.
- Szmigin I, Bengry-Howell A, Griffin C, Hackley C, Mistral W. Social marketing, individual responsibility and the ‘culture of intoxication’. Eur J Mark 2011;45:759-7. http://dx.doi.org/10.1108/03090561111120028.
- Corner A, Randall A. Selling climate change? The limitations of social marketing as a strategy for climate change public engagement. Glob Environ Chang 2011;21:1005-14. http://dx.doi.org/10.1016/j.gloenvcha.2011.05.002.
- Scarbrough H, Newell S, Swan J, Powell J, Evans S, Marabelli M, et al. Networked Innovation in the Health Sector (NIHS): Comparative Evaluation of the Role of Collaborations for Leadership in Applied Health Research and Care (CLAHRC) 2014. www2.warwick.ac.uk/fac/soc/wbs/research/ikon/research/clahrc/ (accessed 9 October 2013).
- Oborn E, Barrett M, Prince K, Racko G. Balancing exploration and exploitation in transferring research into practice: a comparison of five knowledge translation entity archetypes. Implement Sci 2013;8. http://dx.doi.org/10.1186/1748-5908-8-104.
- Bonoma T. Case research in marketing: opportunities, problems, and a process. J Marketing Res 1985;22:199-208. http://dx.doi.org/10.2307/3151365.
- Levina N, Vaast E. The emergence of boundary spanning competence in practice: implications for implementation and use of information systems. MIS Quarterly 2005;29.
- Marteau T, Sowden A, Armstrong D, Donald A. Getting Research Findings into Practice. London: BMJ Publications; 1998.
- Currie LM, Desjardins KS, Stone PW, Lai TY, Schwartz E, Schnall R, et al. Near-miss and hazard reporting: promoting mindfulness in patient safety education. Stud Health Technol Inform 2007;129:285-90.
- Wharton A. The sociology of emotional labor. Annu Rev Sociol 2009;35:147-65. http://dx.doi.org/10.1146/annurev-soc-070308-115944.
- Pawson R, Tilley N. Realistic Evaluation. London: Sage; 1997.
- Logic Model Development Guide: Using Logic Models to Bring Together Planning, Evaluation, and Action. Battle Creek, MI: W.K. Kellogg Foundation; 2001.
- Fitzgerald L, Ferlie E. Professionals: back to the future?. Hum Relat 2000;53:713-39. http://dx.doi.org/10.1177/0018726700535005.
- Llewellyn S. ‘Two-way windows’: clinicians as medical managers. Organ Stud 2001;22:593-62. http://dx.doi.org/10.1177/0170840601224003.
- Burton C, Rycroft-Malone J. An untapped resource: patient and public involvement in implementation; ‘comment on ‘knowledge mobilization in healthcare organizations: a view from the resource-based view of the firm’. Int J Health Policy Manag 2015;4:845-7. http://dx.doi.org/10.15171/ijhpm.2015.150.
- D’Andreta D, Scarbrough H, Evans S. The enactment of knowledge translation: a study of the Collaborations for Leadership in Applied Health Research and Care initiative within the English National Health Service. J Health Serv Res Policy 2013;18:40-52. http://dx.doi.org/10.1177/1355819613499902.
Appendix 1 Literature search strategy
FIGURE 2.
Literature search strategy. a, Searches were carried out using appropriate configurations of the terms: Knowledge AND transfer/translation/mobilisation/exchange AND healthcare; Knowledge AND broker*/intermedia* AND healthcare; Knowledge AND implementation/evidence AND healthcare; b, exclusion criteria: not addressing knowledge mobilisation/knowledge brokerage (variously named), not health care, addressing organisational change or knowledge management (for example, patient records), not in the English language; and c, Implementation Science and Journal of Health Services Research and Policy.

Appendix 2 Advisory group members and meetings
Advisory group members
Sue Denman (Wales Government, Chairperson of Wales Knowledge Transfer Task and Finish Group).
Anita Kothari (overseas academic).
Jo Rycroft-Malone (academic).
Martin Marshall (academic).
Nick Mays (academic).
Lars Sundstrom [academic, SARTRE (Severnside Alliance for Translational Research) and West of England AHSN].
Wendy Warren (NHS manager).
Matt Westmore (NIHR HSDR programme).
Dot Williams (service user, Wales).
Edmond Brookes (service user, England).
Advisory group meetings
| Meeting | Date | Main focus |
|---|---|---|
| 1 | 20 September 2013 | Introductory meeting |
| 2 | 19 November 2013 | Critical feedback on the draft literature review; discuss understanding of the KIT agent role |
| 3 | 4 February 2014 | The draft typology and site selection criteria for potential case studies |
| 4 | 3 April 2014 | The typologies and dimensions developed to characterise the varying KIT agent roles and a discussion of the fieldwork process |
| 5 | 17 June 2014 | A series of vignettes based on the sites used to stimulate discussion of types of knowledge being brokered |
| 6 | 22 September 2014 | A series of adapted verbatim accounts from case study agents to stimulate discussion: brokerage of knowledge within organisations rather than across; KIT and QI and what type of knowledge is being brokered |
| 7 | 22 January 2015 | Measuring the impact of knowledge mobilisation |
| 8 | 21 May 2015 | Coding frame and approach to data analysis |
| 9 | 1 October 2015 | Writing up the case studies |
Appendix 3 Semistructured interview schedule for mapping exercise
-
Introductions.
-
Briefly describe project and respond to any questions.
-
Ask respondent to describe their local strategy for KIT.
-
Any significant changes in direction of travel with relation to KIT from prospectus document?
-
Ask about plans for KIT agents (who is involved in knowledge brokering and mobilisation schemes (specifically whether or not managers are included) and the types of activities planned.
-
-
Refer to points in spreadsheet for their network’s proposal regarding KIT agents – is this still planned? If so:
-
How many?
-
What are the main features of their role (expectations)?
-
What structures are in place?
-
How do they connect to CLAHRCs and other structures?
-
Can you refer us to KIT leads within your network?
-
Appendix 4 Summary of knowledge and innovation transfer intentions across Academic Health Science Networks and South East Wales Academic Health Science Partnership
| Network (randomised reference number) | Proposed KIT roles | Summary of proposal | Structures supporting KIT roles |
|---|---|---|---|
| 553 | Translators Core team has KIT roles |
Organisations in the regions to identify a ‘translator’ to champion innovation and research translation, and to act as a contact point for the central network team. Funding for their time will come from partner organisations, not from the network The network’s small core team who, as part of their role, support KIT through horizon scanning, identifying funding opportunities, offering business advice, creating collaborations and facilitating communications. Core team members have backgrounds in industry and academia, and expertise in grant application and translational research |
QI campaign in region |
| 307 | Fellowships Exchanges of staff across sectors |
A fellowship programme for senior NHS and social care staff from around the region released on 1 day per week, followed a taught curriculum on innovation involving local university departments. An apprentice model with health researchers and an action learning set The network aimed to expand and coordinate this approach within the regions to create capacity and capability for innovation |
CLAHRC fellowships in place since 2011 |
| 779 | New unit to support implementation and knowledge transfer | A highly flexible, bespoke and coproduced model of diffusion, building on both regional and national CLAHRC models. Opportunities for diffusion will be offered to clinicians, academics, managers and practitioners from the NHS, academia and industry A new unit with the capacity and capability to support adoption at a local level is proposed |
Building on CLAHRC learning |
| 296 | Fellowships | A suite of improvement capability programmes to support staff in the development of competencies in improvement science and change management methodology | Build on region’s academic programmes for clinicians interested in QI |
| 345 | Fellowship programme Secondments |
Integration of leaderships and improvement courses with fellowships and exchange schemes. Working with industry and relevant voluntary sector organisations to build on fellowship programmes Staff seconded across sectors to foster cross-fertilisation and innovation as well as gain appreciation of differences in cultures. Future leaders to be supported through a knowledge exchange programme with staff within organisations and between the NHS, industry and academic partners |
Integrate existing leadership and improvement courses. Build on fellowship programmes developed by the local trust and CLAHRC |
| 510 | Support existing staff | A critical mass of people who create innovation and increase competency and skills to deliver innovation will be supported. The network to capture what has already been achieved in supporting staff to do this and bring together best practice from existing programmes | |
| 839 | Support existing staff | Using the knowledge and experience of clinical staff to act as change agents to adopt and diffuse new practice across organisations | |
| 580 | Change practitioners’ community | Change practitioners to share experiences and to increase their skills in the processes of innovation and change management. The establishment of a common vocabulary across the network that will facilitate joint working and communication. This community will connect and share ideas through event programmes, best practice workshops and webinars. Peer-to-peer support systems encouraged and the possibility of a mentor programme developed | Peer-to-peer support systems Build on Health Innovation and Education Cluster |
| 667 | Fellowships for clinicians and managers to work on service improvement projects | Involve NHS clinicians in research by building on existing local NIHR fellowship schemes and the use of honorary university contracts. The research fellowships will enable NHS clinicians to spend time in the academic department undertaking service improvement projects. To be extended to NHS managers, those working across sectors or those providers working with local business schools | NIHR fellowship schemes exist/honorary university contracts collaborative learning networks |
| 762 | Network for service improvement leads | A team of trust innovation leads, experts in service improvement, will be centrally co-ordinated and supported. Support for service improvement: training and development of new innovation leads; sharing methods for achieving change across trusts and sectors; contributing to network communications; working with academic members to evaluate implementation efforts; contributing to the development of a positive culture for innovation. Innovation leads responsible for implementing AHSN plans and the spread of high-impact local or national innovations and NICE-guided innovations across the network. Grow researchers in under-represented professions to increase research use and variety of questions being asked | Closely linked to CLAHRC |
| 750 | Improvement fellows in each theme Community of local champions |
Improvement fellows working with each theme, supporting organisational and professional behaviour change through improvement science. Contributing to an evaluative and learning culture, providing a key link between research and education priorities A community of local champions leading innovation, including fellows who support the delivery of innovation and change in the priority areas across the AHSN. These fellowships may be part-funded by industry to encourage the cross-fertilisation of ideas |
|
| 299 | Fellowship programme | The fellows, on 12- to 18-month secondments, deliver health improvement, wealth creation and educational projects within the network’s programmes. They receive professional development through an accredited programme based on the Darzi Fellowship model | Region has AHSC and AHSN Quality and Evaluation Fellows |
| 341 | NIHR body to lead | The AHSN delivers research and innovation across partner organisations and workforce change via NIHR body investment. Expansion of research-active staff across the AHSN constituency and training for more NHS staff to engage in research | |
| 690 | Fellowships | Knowledge mobilisation fellowships, based on the NIHR model to strengthen NHS/research exchange at the middle management level | Work closely with CLAHRC |
| 699 | Communities of practice | A large number of clinicians, managers, patients, academics as associates recognised by time and title to build linked communities of practice at scale using peer-led learning to promote grassroots involvement | Secondments and joint appointments |
| 728 | Fellowship secondments | Development of strong cross-boundary networks, including secondments and fellowship opportunities. The theme leads are on part-time secondments |
Appendix 5 Semistructured interview schedule for knowledge and innovation transfer agents
1 Questions areas for first interviews
-
Exploration of role
-
– What do you do in the role?
-
– Who do you connect with? Who do you reach and how (interpersonal linkages between people or units). Who’s in the network? Patterns of network activity? Similar/different professional groups? Hierarchy, power?
-
– The quality of the relationships: trust, respect? Obligation and reciprocity? Do members of the network value cooperation? Trust one another? (this facilitates KT)
-
-
What time for the role? Training? Support?
-
Expected outcomes: shared vision and goals?
-
– What outcomes are expected from the role in general? From specific activities?
-
– How do you know if you are successful in the role? (what performance measures are used, if any?)
-
– From this, what’s your understanding of knowledge, innovation and transfer?
-
-
Exploration of barriers and enablers to KIT
2 Questions areas for follow-up interviews
The interview provides an opportunity to follow up on progress and tie up loose ends or clarify earlier comments. The interview will necessarily be tailored to the case study.
Topic areas might include:
-
Update on activities (including reference to specific projects, events, developments)
-
Judging ‘success’. What measurements are used (in terms of the KIT agent’s actions and/or related to specific projects)? What outcomes are important?
-
Staffing update including what next for the case study
-
Sustainability and future funding (in AHSNs this might link to money for patient safety)
-
Our next steps: feedback event; invoicing for the funds; collection of recorders
-
There may also be further events for us to observe or link interviews
-
Explore interest in joining an action learning set
-
Thank you for your participation.
Appendix 6 Semistructured interview schedule for line managers and knowledge and innovation transfer agent Links
-
What do you do in your role?
-
How do you connect with the case study(/ies)?
-
How would you describe the quality of that relationship?
-
What is the benefit/value of their work? How do they contribute to outcomes that are important to you? How do you judge the success of what they do?
-
How are your expected outcomes agreed?
-
Thinking of the future, is their work/role sustainable?
-
What are your thoughts on what helps or hinders the transfer and mobilisation of knowledge?
Appendix 7 Information sheets and consent forms
Information sheet for case study participants
Consent form for case study participants
Information sheet for Links/line managers
Consent form for Links/line managers
Appendix 8 Thematic analysis coding frame
| Node | Description | Subthemes |
|---|---|---|
| Background | Relevant background information about the KIT agent, their team and their working practices | Any relevant prior experience |
| Any existing networks that they brought with them to their KIT role | ||
| Their status within their organisation | ||
| How their team was set up/how their team operates | ||
| Other roles they may carry out | ||
| Time in their current post (length/allocated time if they have more than one role) | ||
| Where the agent is located (e.g. university, health board, over one or more offices, etc.) | ||
| Training | ||
| Sustainability/future of the agent’s role | ||
| Role | Information and perceptions of the agents’ role | Expectations |
| Support | ||
| Sustainability | ||
| Other | ||
| Conceptual/definitional | How the participant defines or demonstrates their understanding of ‘knowledge’ and ‘innovation’ | What is knowledge? |
| What is innovation? | ||
| Individual dispositions/qualities | The agent, line manager or Links’ personal understanding, receptivity and approach to KIT work | Leadership style |
| Values | ||
| Commitment/motivation | ||
| Context – internal | Factors within the organisation that influence KIT agents’ work, such as its culture and ethos, leadership and infrastructure (clear pathways and systems; whether linkage was encouraged or silo working dominated) | AHSN/(SEW)AHSP/UHB |
| The organisational culture of the workplaces/organisations that they are working with | ||
| Infrastructure support | ||
| Budgets/resources available for their work | ||
| Professional silos | ||
| Context – external | The influence of factors outside the organisation such as government policy, national programmes and other external factors on the KIT work | 1000 Lives Plus programme (Wales)/QI |
| Patient Safety (England) | ||
| HEE (England) | ||
| Health Foundation | ||
| Prudent Health (Wales) | ||
| CLAHRC (England) | ||
| Patient Flow (Wales) | ||
| Content | The content or focus of the evidence being translated | The nature of knowledge/innovation |
| Implementation | ||
| The intended target audience (e.g. managers, practitioners) | ||
| Its relevance to patients | ||
| New knowledge/innovation or maintenance of professional standards | ||
| Processes – what KIT activity? | Factors around the process of carrying out their KIT work | Facilitation/challenge |
| Linkages and brokerage | ||
| Information sharing/dissemination | ||
| Events | ||
| Meetings | ||
| Education and training | ||
| Mentoring or shadowing | ||
| Collecting, analysing and presenting data | ||
| Develop networks | ||
| Development of products (e.g. literature summaries, funding bids, etc.) | ||
| Implementation | ||
| Impact and outcomes (formal/informal) | The changes, outcomes or events that have occurred as a result of the KIT agents’ work | Action plans; policy development |
| Products (e.g. literature summaries, funding applications) | ||
| Training awards gained | ||
| Engagement via meetings/events | ||
| Developed networks for information sharing | ||
| Established new working collaborations | ||
| Enhanced existing relationships | ||
| Capacity development | ||
| Improved dissemination of knowledge and innovation (vague) | ||
| Implementation: examples of evidence of knowledge/innovation use, improved ways of doing things, targets achieved | ||
| Infrastructure changes | ||
| Micro | ||
| Meso | ||
| Macro | ||
| Personal impact on the KIT agent themselves | ||
| Organisational culture changes (e.g. receptiveness to research/change) | ||
| Barriers | Barriers to the KIT agents’ work | |
| Enablers | Enablers of the KIT agents’ work | |
| Key messages | Any key messages that emerge | |
| Other | ||
Appendix 9 A worked example of an application of social marketing theory
| Reported outcome(s) | Insights | Competition | Exchange | Segmentation and targeting | Intervention (product, place, price, promotion, policy) |
|---|---|---|---|---|---|
| Measurable improvements to implementation of the Sepsis Six patient care pathway that resulted in improved morbidity and mortality | Understanding what had been tried, what the barriers to change were, what the motivators were to change, recognised how the organisation wanted to do things for themselves and not ‘import solutions’, what was feasible for the organisation and how the team and organisation could be supported to develop and test an intervention. Recognised that the team needed support in running the project – planning meetings, gathering data, analysing and reporting. Helped the team generate insight, and design and test solutions | The service team lacked specific knowledge of how to address the problem, time to engage people to think about it, time and the capacity to run a project, and perhaps felt vulnerable and unsupported. Staff were also reluctant to take part in something new and challenging | Measures to reduce the cost to the project team included: helping to set a team; organise meetings; support data gathering, analysis and so forth; help build links with relevant national programmes Measures to increase the benefits to the project team: providing feedback on performance demonstrating to the project team that they were having an impact on patient care; helping to improve reporting within the trust hierarchy thus increasing project profile, feedback, etc. |
Chose a high-priority, narrowly focused issue. A hospital-wide intervention was specifically avoided Worked with medical director to identify, establish and support a team who were necessary or willing to take part Worked with a small team and local enthusiasts. Hoped that this team could spread good practice in time (home-grown solutions, tested in their trust). Focused primarily on activities that were necessary to achieve the task Provided a reporting conduit between the team and trust senior management team |
Product – tailored project support focused on client need (what they were trying to achieve, with what resources, from what position). This included QI methodology, project management previous relevant experience, and coming from a credible organisation Place – the KIT agent worked alongside the practitioners addressing the problem Price – the KIT agent reduced the cost of taking part in the project, and offered ‘free’ support in terms of planning, meeting, etc. Promotion – the KIT agent recruited people to the project directly with the medical director. Being a clinician with relevant experience helped Policy – sepsis management is a national priority |
Appendix 10 Summary of findings in presentation format
A series of slides have been designed for presentation to user groups including knowledge brokers, managers and other practitioners.
List of abbreviations
- A&E
- accident and emergency
- AHSC
- Academic Health Science Collaboration
- AHSN
- Academic Health Science Network
- AHSP
- Academic Health Science Partnership
- CLAHRC
- Collaboration for Leadership in Applied Health Research and Care
- CQRS
- Québec Social Research Council
- HSDR
- Health Services and Delivery Research
- IHI
- Institute for Healthcare Improvement
- i-PARiHS
- integrated Promoting Action on Research Implementation in Health Services
- KIT
- knowledge and innovation transfer
- MBA
- Master of Business Administration
- NIHR
- National Institute for Health Research
- NISCHR
- National Institute for Social Care and Health Research
- PARiHS
- Promoting Action on Research Implementation in Health Services
- PhD
- doctor of philosophy
- PPI
- patient and public involvement
- QI
- quality improvement
- R&D
- research and development
- SAGE
- Self-Assessment of enGagement with Evidence
- SDO
- Service Delivery and Organisation
- SEWAHSP
- South East Wales Academic Health Science Partnership
- SME
- small and medium-sized enterprise
- SPIRIT
- Supporting Policy in Health with Research: an Intervention Trial