Notes
Article history
The research reported here is the product of a HS&DR Evidence Synthesis Centre, contracted to provide rapid evidence syntheses on issues of relevance to the health service, and to inform future HS&DR calls for new research around identified gaps in evidence. Other reviews by the Evidence Synthesis Centre are also available in the HS&DR journal. The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 13/05/12. The contractual start date was in October 2015. The final report began editorial review in May 2016 and was accepted for publication in September 2016. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2017. This work was produced by Baxter et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Background
Tuberculosis (TB) is an infectious disease, with latent infection estimated to affect at > 2 billion people worldwide. 1 Although approximately 95% of cases of TB occur in developing countries, the disease also exists in low-incidence countries, including the UK. 2 TB is known to disproportionately affect specific population groups, including socially disadvantaged people, immigrants and those with complex lifestyles (such as users of drugs or excessive alcohol). 3 Although levels of TB may be low in the UK, TB control strategies, including the use of contact-tracing investigations, remain important to control the level of the disease.
The priority of TB disease control programmes is the early identification and successful treatment of people with active infection to avoid further transmission. Strategies for TB control also include the efficient detection and treatment of latent infection to avoid further transmission. Approaches to identifying individuals with either active or latent infection include the screening of high-risk groups, active case finding and contact tracing. 4
The transmission of TB occurs via the inhalation of airborne particles from an infected person. 1 The tracing and screening of people who have had contact with an active case of TB is, therefore, a critical component in the control of transmission and the early detection of infection. 5 Contact tracing/investigation has three main objectives:6 first, to identify additional cases of active TB among contacts (to initiate treatment and avoid further transmission); second, to identify contacts with latent TB infection to offer them preventative treatment (to prevent their progression to active TB infection); and, third, to identify and treat the source of an outbreak. Contacts who show evidence of latent TB infection and who complete a course of prophylactic treatment may reduce their risk of progressing to active TB disease by 60–70%. 7 Investigation to identify contacts of an individual with active TB disease is, therefore, considered a key tool in the control of TB, to enable the early detection of infection and disease and to prevent secondary cases. 8
Research questions
-
What is the effectiveness and cost-effectiveness of specific interventions designed to improve TB contact tracing (such as use of community outreach workers/cultural facilitators, specific interviewing techniques, home/hostel/workplace visits, home/hostel/workplace screening and follow up of contacts) in specific population groups (such as migrants/homeless people)?
-
What is the acceptability, feasibility, appropriateness and meaningfulness of specific interventions designed to improve TB contact tracing in these population groups?
-
What are the barriers to, and facilitators of, delivery or uptake of contact tracing in these population groups?
-
What are the elements of the contact investigation pathway from interventions to impact, for TB contact tracing in wider population groups?
-
How might evidence from interventions for wider populations be applied to TB contact tracing in specific population groups, including the similarities and differences, and what elements of the pathway may be important for feasible, applicable and effective interventions?
Chapter 2 Review methods
The review used a two-stage process. We carried out initial mapping work to develop and refine the scope of the work. This was followed by two linked subreviews to identify and synthesise the most directly relevant evidence in this field.
Initial mapping work
An initial phase of mapping was used to broadly describe the published literature on contact tracing for TB in specific population groups, particularly that relevant to the NHS and similar health-care systems. We aimed to examine the potential volume of literature on contact tracing in specific populations to see if a full review of this evidence would be viable and provide potentially useful information. We used the term ‘specific population groups’ to mean any subgroups within whole populations (individuals or groups) who may be at higher risk of TB infection. This includes people described as ‘hard to reach’, those with drug or alcohol problems, homeless people, asylum seekers, immigrants, refugees, people from ethnic minorities and prisoners. The mapping exercise was intended to guide decisions regarding the focus of further review work in this area.
Mapping review search strategy
Targeted searches of key databases were undertaken using search terms in previous reviews, supplemented by the review protocol, and terms harvested from relevant evidence. We applied broad inclusion criteria and did not seek to distinguish between different potential purposes of contact tracing in TB prevention and management during the searching process or during the later stages of the review. The search focused on terms relating to people with TB, with terms relating to the intervention (contact tracing). Although we were primarily interested in finding literature on specific populations who may be at greater risk of TB, we did not use any search terms for particular subgroups. We felt that an a priori decision on terms relating to specific populations might have led to key groups being missed. Therefore, we used general population terms in the mapping review, with the aim of sifting out literature relating to subgroups from the retrieved citations.
The terms relating to contact tracing were harvested from the National Institute for Health and Care Excellence evidence review on TB9 and other relevant evidence. The search was limited to studies in the English language and in human populations, as a result of the restricted time scale for this work. Literature published between 2000 and 2015 was retrieved. It was expected that any significant earlier work would be included via review studies. The databases searched in October 2015 were MEDLINE via Ovid SP, EMBASE via Ovid SP, EconLit via Ovid SP, PsycINFO via Ovid SP, Social Policy and Practice via Ovid SP, Cumulative Index to Nursing and Allied Health Literature via EBSCOhost, Science and Social Science Citation Indices via Web of Science and The Cochrane Library via Wiley Online Library. We screened reference lists of included studies for relevant grey literature, and requested potentially relevant literature from topic advisors. The search terms used are provided in Appendix 1.
Mapping review sifting and identification of relevant literature
The search results were exported to a reference management database (EndNote version 7, Thomson Reuters, CA, USA) and the software deduplication process was applied. The database of citations was screened at title and abstract (when available) level initially by one reviewer, and blind second screening of the complete database was shared between two further reviewers. Potentially relevant studies on contact tracing were identified.
Full review methods
We incorporated the results of the mapping review into one of two subreviews. The full review encompassed a subreview of contact tracing in specific populations (including and extending the literature found in the mapping work) and a subreview of TB contact tracing in wider populations.
Search strategy
We re-examined the citations retrieved in the mapping review searches, and also extended the date of inclusion to 1995 onwards, in a second search in March 2016, thus examining over 20 years of research. In addition to conducting topic-based searching of electronic databases, we screened the reference lists of included studies.
Sifting and identification of relevant literature
The search results were exported to EndNote version 7 and the software deduplication process was applied. The database of citations was screened at title and abstract (when available) level initially by one reviewer, and blind second screening of the complete database was shared between two further reviewers, with approximately 95% agreement. Potentially relevant studies were coded as either ‘specific populations’ or ‘wider populations’.
Following this screening, all coded records were re-examined to identify literature relating to specific population groups (such as those described as hard to reach, people from ethnic minorities, substance abusers, homeless people, migrants, drug users or prisoners) versus papers that related to wider populations or that included wider populations as well as particular subgroups. We identified and excluded work carried out in countries of less relevance to the UK NHS [countries that are not members of the Organisation for Economic Co-operation and Development (OECD)].
Data extraction
We used a data extraction form developed from the team’s previous experience; this was piloted on several studies before the final version was established. Data in the included studies were systematically extracted to the form, encompassing first author and date, type of document, study design, country of origin, population, research methods, staff involved, measures used, results/data and main conclusions. See Appendices 2 and 3 for the completed data extraction tables.
Quality appraisal
We planned to select appropriate tools for quality appraisal based on the study designs that we found in the included literature. These included checklists such as those developed by Cochrane and the Critical Skills Appraisal Programme. 10,11 The literature that we found, however, was more limited than we had expected. The studies tended to be descriptive reports of contact investigations, either around the time that the investigation was carried out, or at a later point, when records completed at the time were retrospectively examined by the research team. This literature did not use the evaluative experimental or observational designs that are typically included in systematic reviews, and was not suitable for appraisal using established checklists. Criteria that might be used to assess quality, such as sample size, were not indicators of robustness, as a larger number investigated was not representative of a better-quality investigation (indeed, the reverse might be true). Other aspects that may be indicators of quality, such as sampling strategy or robustness of outcome measures, were also not applicable to this literature, which was dominated by descriptions of what happened during investigations with complex outcomes. The studies that we categorised as ‘qualitative’ referred to interviews with cases and contacts; however, qualitative data were not always provided. Although grey literature is typically considered to be of lower quality than peer-reviewed published papers, many of the reports and guidelines we identified were based on reviews of the literature (some of which were robust systematic reviews) and, therefore, was considered to not necessarily be weaker than the published studies. In the following synthesis, however, we have separated the reports and guidelines from the other studies, by describing them last in each section.
Given these assessment challenges, we considered whether or not and how to attempt to grade the identified literature on the basis of quality. We reached the conclusion that a quality criteria checklist approach was not feasible, as there were no clear indicators of quality and study methods were diverse. We therefore adopted an approach to quality appraisal whereby we highlighted those few studies of a stronger design, and any issues of particular concern during the narrative synthesis.
Approach to synthesis
The literature was divided into papers that focused on specific populations versus those that had a wider population focus; these groups of papers formed two subreviews. The content of the literature in each subreview was categorised by characteristics such as country and type of intervention. Narrative synthesis methods were used to provide an overview of the included studies within the two subreviews. The narrative included the exploration of similarities and differences between the subreviews, and highlighted data of importance for TB contact tracing in specific populations. In addition to the narrative, a logic model diagram was used to summarise the findings across the two subreviews. The purpose of the model was to integrate data from both reviews in the form of a pathway for contact-tracing investigations. The logic model diagram outlines key elements of the pathway, from initial decision-making regarding investigations to outcomes and impacts.
Inclusion criteria
-
The initial focus of the review was TB contact tracing in specific population groups; however, following the mapping phase of the work, we broadened the scope to also include TB contact tracing in any population. We considered ‘specific population groups’ as encompassing any subgroups within whole populations, including individuals or groups who may be at a higher risk of TB infection. This includes people described as ‘hard to reach’, those with drug or alcohol problems, homeless people, asylum seekers, immigrants, refugees, people from ethnic minorities and prisoners.
-
We defined contact tracing as any intervention or procedure for identifying and evaluating individuals who have been exposed to someone with active TB. We adopted broad criteria for the types of studies of interest, including those that aimed to evaluate outcomes following contact tracing investigations and also those describing or exploring the delivery of investigations. We aimed to focus on contact-tracing activities rather than screening, active case finding or other interventions to reduce infection and/or transmission. We recognised, however, that these distinctions may not be clear cut, and there may be overlap between these purposes. We therefore included any papers that included reference to contact tracing as part of a TB control strategy.
-
In relation to comparators, we included studies with any comparator and studies with no comparator. As we intended to produce an inclusive review, studies of any design, including experimental, observational, cross-sectional, qualitative and reviews, were eligible, together with grey literature in the form of reports and guidelines.
-
We included studies that reported any outcome related to contact-tracing activity.
Exclusion criteria
-
We excluded research that was published prior to 1995.
-
We excluded studies carried out in countries that are not members of the OECD. We intended to focus the review on low-TB-incidence countries that are most applicable to the UK.
-
We excluded studies that comprised discussion or opinion and those that did not relate to specific investigations.
-
We excluded conference abstracts, theses, letters to the editor and other commentaries.
Chapter 3 Results of the review
Results of the mapping work
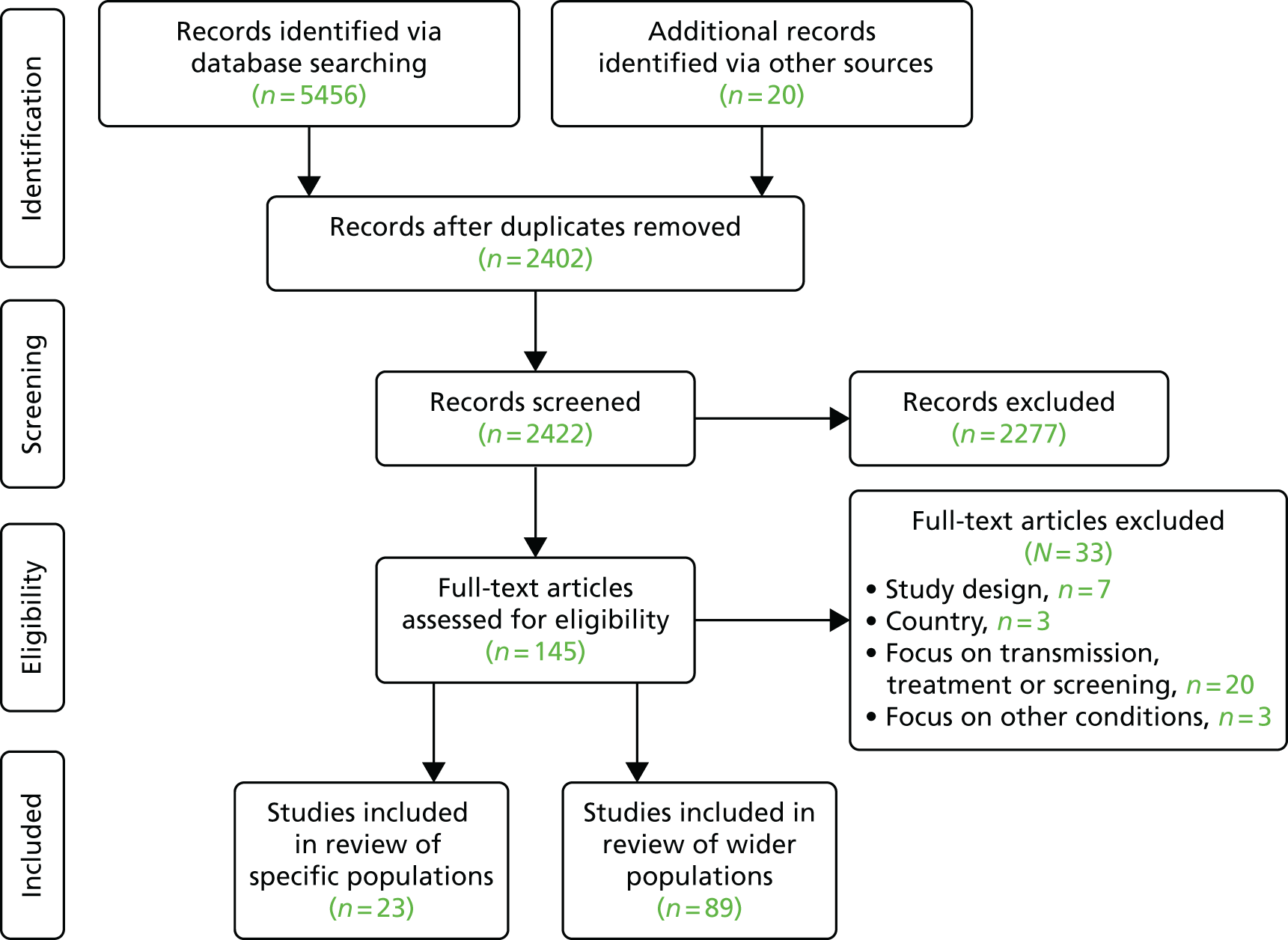
Searching the electronic databases identified 13 articles of relevance to a review of contact tracing in specific populations. Figure 1 provides an overview of the results of the mapping work.
FIGURE 1.
Results of the mapping work.

The mapping exercise indicated that there was unlikely to be a large number of research studies on contact tracing in specific populations and that the data identified were likely to derive from poor-quality studies. It was anticipated that the conclusions that might be drawn from a full review of this literature would be restricted by the limited numbers and quality of the available research studies. Therefore, following the mapping exercise, we proposed three potential options for further review work. These were presented for discussion with local and national policy-makers, topic experts, infectious disease and public health practitioners, specialists in the field and representatives of the review commissioners (the National Institute for Health Research Health Services and Delivery Research programme).
-
Widen the population inclusion criteria to TB contact tracing in any population (not just specific populations) and explore, in particular, implementation processes and feasibility. The mapping work indicated that there would be a substantive number of studies available to synthesise.
-
Examine contact tracing in specific populations for other conditions, drawing on data from existing systematic reviews. The other conditions included would need to be carefully considered to ensure that findings from these research studies would be applicable to TB, with careful documentation regarding the criteria for judging applicability. The review would aim to examine what may be learned from tracing in specific populations in other conditions and applied to contact tracing in TB.
-
The mapping exercise indicated that social network approaches, and use of community workers, may be promising approaches to TB contact tracing in specific populations. Further work could comprise a systematic review of these interventions in relevant conditions.
The three options presented seemed to offer different potential for adding to the knowledge base. The first option would have the advantage of keeping the focus on the condition and using instrumental lessons from the literature. However, coverage would be limited to approaches that have actually been implemented, and, based on the mapping review of interventions in specific populations, there may be a limited number of research studies and of poor quality. The second option would focus on the conceptual/theoretical contribution of the wider literature. It might offer innovative solutions from other populations and settings; however, it might be limited by heterogeneity in the nature of ‘contacts’ and issues of applicability. The third option might shed further light on the mechanisms and processes underpinning these promising interventions, and any issues of implementation reported in other conditions. However, differences in context and delivery may reduce its applicability to TB contact tracing.
Following consultation on the mapping review findings with topic experts in TB and public health, we received feedback that option 2 would have limited value because of the challenges inherent in applying findings from other conditions to contact tracing for TB. Topic experts expressed the opinion that, as a result of the relatively low transmissibility, the long and extremely variable incubation period and the limitations of existing diagnostic tests of infection and disease, among other issues, TB is sufficiently different from other infectious diseases for which contact tracing is conducted. These differences would severely limit the applicability of a review of contact tracing in other conditions to research and practice in the area of TB. Following feedback and discussion with the Health Services and Delivery Research team, the decision was made that further systematic review work would include contact tracing in wider populations, with a particular focus on what could be learned and applied to interventions for specific population groups. We therefore progressed to the implementation of option 1.
Results of the full review
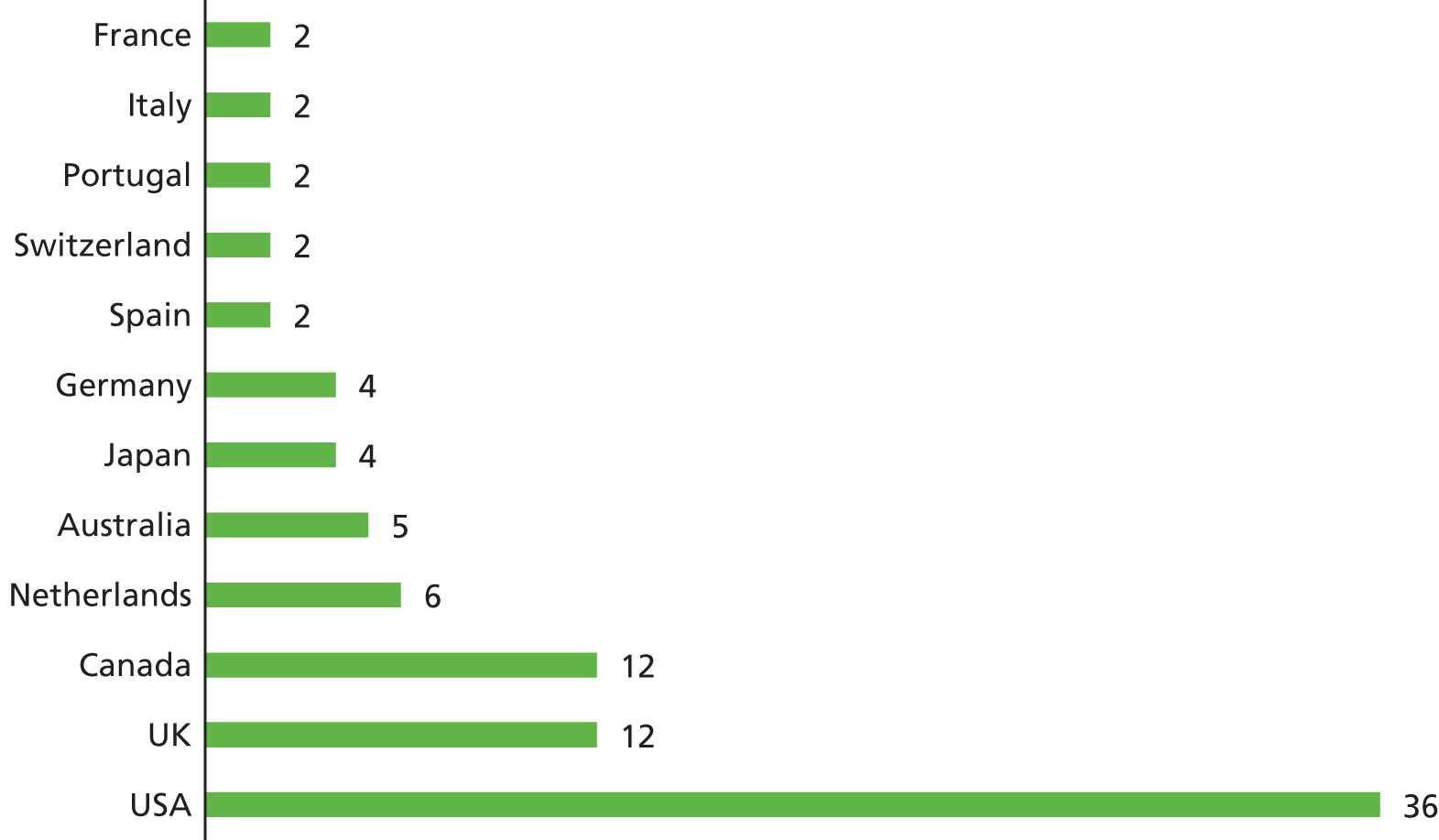
The searching of the electronic databases and the screening of reference lists identified 112 articles of relevance to a review of contact tracing. We identified an additional 10 papers relating to specific populations (further to the 13 papers found in the mapping exercise), giving a total of 23 papers. The remaining 89 papers related to wider populations. Figure 2 provides an overview of the inclusion process. Appendix 3 provides a list of papers excluded at full-text stage and the reasons for their exclusion.
FIGURE 2.
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) diagram illustrating the inclusion process.
Results of review of tuberculosis contact tracing in specific populations
Characteristics of the literature
We identified 23 papers with a focus on TB contact tracing in specific populations. 5,7,9,12–31 Sixteen of the papers originated from North America,5,7,12–25 five were from Europe26–30 and one was a systematic review from the UK,9 which formed the basis of national guidance. 31
Contact tracing was examined in five studies in migrants,18,26–29 four studies in drug users (one of which included homeless people),7,15,19,30 five studies in homeless people,12–14,21,24 one study in an ethnic minority group,25 one study in prisoners5 and one study predominantly in individuals with human immunodeficiency virus (HIV) who were described as ‘gay, transvestite or transsexual’. 23 One study16 reported a contact investigation involving customers of a bar who mostly ‘used alcohol excessively’, and five further papers9,17,20,22,31 described individuals who were ‘hard to reach’ or from a range of different population subgroups.
Quality of the literature
The quality of the available literature, as indicated by the proxy of study design, was generally low. We found one systematic review29 on rates of contact tracing in migrants versus local populations, one review18 on the cost-effectiveness of control strategies among immigrants and refugees, and an effectiveness and cost-effectiveness review of interventions among hard-to-reach groups that was an unpublished report. 9 One study26 used an evaluative design to examine the period prior to introduction of a community worker intervention, compared with the introduction period itself. Two studies19,20 reported that they included elements of qualitative methods (interviews), although neither provided qualitative data. The literature was dominated by studies that we term ‘descriptive accounts’ of the management of TB outbreaks, in which contact-tracing investigations had been employed. These papers provided narrative about how an investigation was carried out, and often provided data reporting the number of index cases and contacts that were identified. These data do not provide an indication of effectiveness, as each investigation will inevitably differ in terms of the number of contacts who should be approached, and identifying more contacts (rather than appropriately targeting) is not necessarily an optimal outcome. Table 1 provides an overview of the literature by study design.
| Study design | Study and year |
|---|---|
| Systematic review | Mulder et al., 200929 |
| Cost-effectiveness review | Rizzo et al., 20119 |
| Dasgupta and Menzies, 200518 | |
| Uncontrolled comparator design | Ospina et al., 201226 |
| Reported qualitative elements | Ashgar et al., 200919 |
| Wallace et al., 200320 | |
| Descriptive accounts of investigations | Bur et al., 20035 |
| McElroy et al., 20037 | |
| Li et al., 200312 | |
| Lofy et al., 200613 | |
| McElroy et al., 200314 | |
| Oeltmann et al., 200615 | |
| Kline et al., 199516 | |
| Malakmadze et al., 200517 | |
| Yun et al., 200321 | |
| Fitzpatrick et al., 200122 | |
| Sterling et al., 200023 | |
| Curtis et al., 200024 | |
| Cook et al., 201225 | |
| van Loenhout-Rooyacke et al., 200227 | |
| Mulder et al., 201128 | |
| de Vries and van Hest, 200630 | |
| Guidance | National Institute for Health and Care Excellence, 201231 |
Decision to instigate contact tracing and prioritisation of contacts
The included papers highlighted factors in the decision-making process that occur prior to, and during, contact-tracing investigations for specific populations. Factors that were described affected the degree and type of response following the identification of a case of active TB infection, including the prioritisation of contacts to trace. These factors were the infection level of the source case and perceived risk, the proportion of close contacts found to have active or latent infection, the estimated period of time for which the case had exhibited active TB, the potential locations of exposure, the potential intensity of exposure and the susceptibility of contacts. One study emphasised that the diversity of elements that need initial and ongoing consideration means that contact-tracing investigation methods need to be tailored to particular circumstances. 20
Types of contact-tracing investigations
The included studies provide a range of descriptive data related to contact-tracing investigations, and only one paper26 could be considered to be evaluating an investigation. Other papers reported strategies used during outbreaks and/or discussed the use of different strategies during the investigation. The strategies described can be broadly categorised into, first, those that targeted all members of a specific population; second, those that targeted individuals within a specific population; third, those that targeted the locations frequented by infected individuals and members of a specific population; and, finally, those that aimed to enhance the quality (efficiency/effectiveness) of contact investigations.
Population-based contact-tracing strategies
Three studies26,29,30 described population-based strategies. In relation to contact-tracing strategies targeting all members of a specific population, the authors described the use of local news/media to publicise an outbreak, and outlined how the media may be used to encourage those who may have been in contact with a case or those who may be exhibiting symptoms to come forward for testing. 29 Community meetings were suggested as useful way of publicising an outbreak or providing health information. 26 One paper30 recommended the use of mobile digital radiography units for the screening of groups such as people addicted to drugs and homeless people, in whom there was expected to be poor compliance with skin testing. The authors of this study provided data on the numbers examined during the outbreak, but did not give data that evaluate the use of the radiography unit versus methods of contact investigation. The study emphasised the overlap between the use of chest radiography during investigations and activities that could be considered population screening. Indeed, following the outbreak, a programme of mobile radiography screening for this population was reported to have been introduced. UK national guidance31 advocates the use of digital mobile radiography screening in settings where at-risk people congregate.
An unpublished report of a systematic review of interventions that aimed to identify people with TB, or raise awareness of TB among hard-to-reach populations,9 concluded that incentives to increase the take-up of the tuberculin skin test (TST) and enhance compliance with further investigation are effective and cost-effective in drug users and homeless populations. The authors recommended that an active approach to case finding, rather than contact tracing, may be more effective in hard-to-reach or at-risk populations. The report formed the basis of national guidelines. 31
Contact-tracing strategies targeting individuals
The literature frequently refers to ‘conventional contact tracing’, a term used to refer to an investigation method based on interviewing an index case and asking them to name individuals with whom they have been in contact. The conventional contact-tracing approach uses principles termed ‘stone in the pond’ or ‘concentric circles’ to refer to widening an investigation from only named close contacts to other contacts (usually described as casual or non-close). Several papers outlined the limitations of the conventional contact-tracing method, in particular a reluctance to name contacts19,23 and the perceived stigma in underpinning this reluctance. 9,29 It was highlighted that index cases may more freely reveal the names of household and workplace contacts than those of social contacts. 22
Three papers12–14 highlighted the limitations of conventional contact-naming approaches when investigating outbreaks centred on homeless shelters. One paper12 found that the number of contacts identified per homeless patient was significantly lower than that per non-homeless patients (median 1 vs. 4, p < 0.001; mean 2.7 vs. 4.8, p < 0.001). Homeless patients were four times more likely to have no contacts identified (p < 0.001). The study suggested that investigation methods other than conventional contact tracing should be used, with strategies focused on identifying the location of exposure rather than eliciting the names of contacts. The authors also suggested that conventional prioritisation systems for widening contacts may need to be revised, with being homeless at the time of diagnosis an indicator that prompt contact evaluation should be prioritised.
Another study13 reported similarly low numbers of contacts being named by homeless persons. In this investigation the median number of named contacts was 3.5 (mean 4.8) per index patient, and 14% of patients named no contacts. Rather than relying on patient contact naming, the authors of this investigation had used attendance records, when available, or staff recollections to prioritise TB screening. The prioritisation of locations for investigation was based on the number of infectious patients who visited each facility and the prevalence of positive TST results compared with other homeless sites. Contacts were prioritised for screening based on their cumulative number of exposed visits. It is important to note that although the methods outlined in this study were described as a contact investigation, they could also be considered to be population screening. The use of screening rather than contact investigation in specific populations was highlighted in the study by Curtis et al. 24 The authors recommended that routine screening should be considered in homeless shelters to overcome the limitations of the conventional contact-tracing approach.
Contact-tracing strategies focused on locations
Six papers7,16,17,19,22,25 emphasised that locations rather than individuals are the key to TB transmission in specific populations. The authors of these papers argued that contact-tracing investigations should, therefore, focus on identifying potential settings of transmission.
The use of a social network analysis approach (referred to as epidemiological investigation by some authors), which explores links between individuals (including the locations frequented), was described as valuable in populations of drug users, aboriginal communities and ‘hard-to-reach’ populations. Network analysis methods create diagrams that illustrate links between key individuals and their contacts, together with the types of activities in which cases and contacts engage. The authors of one paper outlining network methods19 reported that the limitations of conventional contact-naming methods could be overcome by investigation staff visiting and observing locations frequented by an index case. Of 187 contacts in their investigation, 49% were named and 10% were observed at a local ‘crack house’. The contacts that were identified by observation were eight times more likely to have positive skin-test results than those who were named [relative risk 7.8, 95% confidence interval (CI) 3.8 to 16.1].
A study describing a contact investigation that was focused on a neighbourhood bar16 reported that the index patient (a homeless person) named few contacts, but had spent most time in the bar. This index case proved to be highly infectious, with 14 linked cases of active TB and 27 cases of latent infection detected. The bar was the only site where there was any contact with the index patient for most of those who were found to be infected. The use of a network approach to investigation in another study17 echoed the importance of investigating potential locations for transmission. The construction of a social network diagram revealed several previously unrecognised locations of transmission, including a single-room occupancy hotel, homeless shelters, a bar and crack houses. Another study using social networks methods22 found that the majority of people identified with active TB disease were members of a single social network, and reported that the approach had been essential to identify this link.
Cook et al. 25 concluded from their discussion that methods including social network analysis, geographic information systems and genomics could improve the assessment of transmission, together with the prioritising of contacts. These methods were needed to overcome a key limitation of conventional contact-tracing approaches, which was described as not taking sufficient account of the differing social structure of different populations.
UK guidance31 recommends that investigations should be co-ordinated at places where an index case spends significant amounts of time, and where at-risk people congregate.
Elements that enhance the quality (efficiency/effectiveness) of contact-tracing investigations
A study5 outlining a contact investigation in both a prison and the community emphasised the importance of interagency working in carrying out an investigation. Another paper14 reported that at least half of the outbreak patients who were living in homeless shelters had spent time in prison or had visited the local sexually transmitted disease clinic in the prior 2-year period. The authors therefore suggested that TB control strategies would be enhanced by employing a joined-up approach to TB control among the relevant agencies.
Other methods described to improve the efficiency/effectiveness of contact-tracing investigations in specific populations included the use of deoxyribonucleic acid (DNA) fingerprinting/molecular epidemiology. These additions to an investigation were described as valuable to permit the further analysis of relationships between cases, and for the establishment of clusters. The use of these technologies was described by authors of several studies as being an essential part of TB control strategies, as contacts could be infected by cases other than the presumed source. 16,29 In addition, DNA fingerprinting was recommended as useful for investigating cases once regular contact-tracing procedures had been completed. 27
The value of investigations having a focus on location rather than individuals was also echoed in a paper outlining the use of molecular epidemiology. 14 It suggested that DNA fingerprinting may offer a useful impetus to further question a patient regarding routine, contacts and places frequented, and thereby to uncover social networks in communities in which contact naming is challenging. 14 A paper describing the further investigation of a cluster of cases in a ‘hard-to-reach’ population17 found that, by using genotyping methods in addition to conventional contact tracing, an additional 98 contacts were identified who had been missed during routine contact investigation. The authors recommended that genotyping should be used alongside other methods of contact tracing, as it can aid the detection of unapparent transmission before an increase in incidence and, thus, help to identify clusters earlier. They highlighted, however, that to be successful, a policy of genotyping isolates from all (not just some) patients with culture-positive TB is required to identify clusters.
Three papers15,23,26 referred to the value of using community workers during contact investigations. One study26 evaluated a staff-based intervention that introduced trained community health workers in areas of high immigration. The workers were described as benefiting the contact-tracing process by acting as translators and cultural mediators, and also as facilitators during treatment. The study found a statistically significant increase in contact tracing coverage among immigrants during the intervention period, compared with the previous period of time (81.6% compared with 65%; p < 0.001). A second paper23 mentioned that community workers were used during contact tracing among ‘highly mobile’ communities. National guidance31 also recommended the use of peer educators when available and appropriate during investigations. One paper15 described the persistence and flexibility required by outreach workers investigating an outbreak among a group of illicit-drug users. Workers had to arrange meetings at times and locations convenient to the group, and spent many hours establishing trust in order to gain co-operation. The authors described how screenings could take place in various locations, including on street corners and in car parks. Often, outreach workers were successful only after spending hours driving around the community, searching for patients and contacts.
UK guidance31 highlights the need for partnership working between organisations in high-quality investigations.
Factors that can influence contact-tracing investigations
Sensitivity and specificity of tests
Three papers10,26,27 discussed the accuracy and feasibility of different testing tools used during investigations. The authors described potential issues of specificity with the TST, particularly from individuals in high-incidence TB countries. 29 A study13 describing an investigation in homeless shelters found that screening contacts with one sputum culture was as sensitive as chest radiography in detecting active TB disease (77% vs. 62%). The authors of one paper30 examining contact investigations in drug-addicted and homeless populations highlighted another factor influencing the success of investigations, namely the poor take-up of testing.
Systems and processes
The authors of two further papers18,19 mentioned other factors that could assist, or provide obstacles to, effective contact investigations. The factors that could assist included local expertise, local capability, communication, co-ordination, prompt action, and effective data management and infrastructure systems. 22 The obstacles described were perceived social stigma, the identification of additional contacts after the investigation had closed and failure to perform the initial evaluation owing to error or a lack of resources. 21
Social factors
One study outlined the need to customise investigations to individuals by taking into account language and cultural differences, and different settings. 20 This paper described challenges in conventional contact tracing in the foreign-born population (owing to the different languages spoken), in prison populations (because of the different systems between prisons and states) and in homeless people (as a result of the movement of individuals between shelters). To address these challenges, the authors recommended different agencies working together efficiently, accurate record-keeping in shelters and the use of photographs rather than relying on names when tracing contacts of homeless people. The work, however, provided few or no data to support these recommendations. A second paper24 highlighted that an index patient’s refusal to visit a hospital for the investigation of their symptoms could result in delay in instigating an investigation, and thereby increase the chance of disease transmission.
Outcomes and impacts following contact-tracing investigations
Study authors5,16,21 highlighted the issue of non-completion of treatment hindering successful outcomes from contact tracing. In one study,21 fewer than one-third of infected prisoner contacts completed treatment, and in another study5 only 44% of homeless people completed treatment. Kline et al. 16 reported that 19 of the 39 people with positive TSTs in their study attended follow-up appointments. Of these, 13 contacts refused prophylaxis or did not complete their treatment, with three individuals progressing to active TB within 2 years. The authors highlighted that chronic alcoholism may be a high-risk factor for progression to active disease, and that major efforts to ensure the completion of 6 months of isoniazid therapy are worthwhile in an alcohol-user population.
The outcomes most frequently reported by studies as indicating the effectiveness of contact-tracing investigations were, first, the number of contacts identified (yield), and, second, the number of positive skin test results. One study18 examined the cost-effectiveness of TB control strategies including screening and contact tracing. The authors concluded that contact tracing (particularly in ethnic minority communities) may be more cost-efficient and less intrusive than screening.
Main findings and implications from review of contact tracing in specific populations
The review found a small number of studies relating to contact investigation in specific populations. This is consistent with other related reviews, such as Rizzo et al. 9 and Fox et al. 32 The findings of the review suggested that methods that focus on locations rather than the individual naming of contacts, and approaches that draw on social network methods, may be of value. The provision of community health workers may also enhance the efficiency/effectiveness of investigations. The use of screening rather than contact investigation may be useful in a homeless population. The evidence base, however, is limited and underpinned by little empirical work. Although we identified a total of 23 papers across specific populations, the data are predominantly descriptive rather than evaluative. The following review of contact tracing, examining literature in wider populations, was carried out with the aim of providing additional insight into what may be learned and applied to contact tracing in specific populations.
Results of review of tuberculosis contact tracing in wider populations
Characteristics of the literature
We identified 891–3,6,8,32–115 papers that met our inclusion criteria for the review of wider populations. These studies originated from a variety of countries, with the greatest number from the USA and Canada (Figure 3). We excluded studies from countries that are not members of the OECD; therefore, the included literature is from contexts most applicable to the UK. Although these papers related to investigations in wider populations, some also included data relating to specific groups within their analysis, or mentioned elements of particular relevance to specific groups.
FIGURE 3.
Number of studies by country of origin.
Quality of the literature
As with the literature on contact tracing in specific populations, the quality of study design was generally low, with little empirical work evaluating contact-tracing methods. The majority of studies retrospectively examined either a group of investigations that had been completed in an area or investigations carried out over a particular time period (Figure 4). These papers scrutinised notes and patient records completed at the time, to describe and further examine the investigations. A second large group of studies ‘told the story’ of a single investigation, describing the process and outcomes, with data relating to the number of cases and contacts, and often outlining when issues and obstacles had been encountered.
FIGURE 4.
Number of studies by study design.
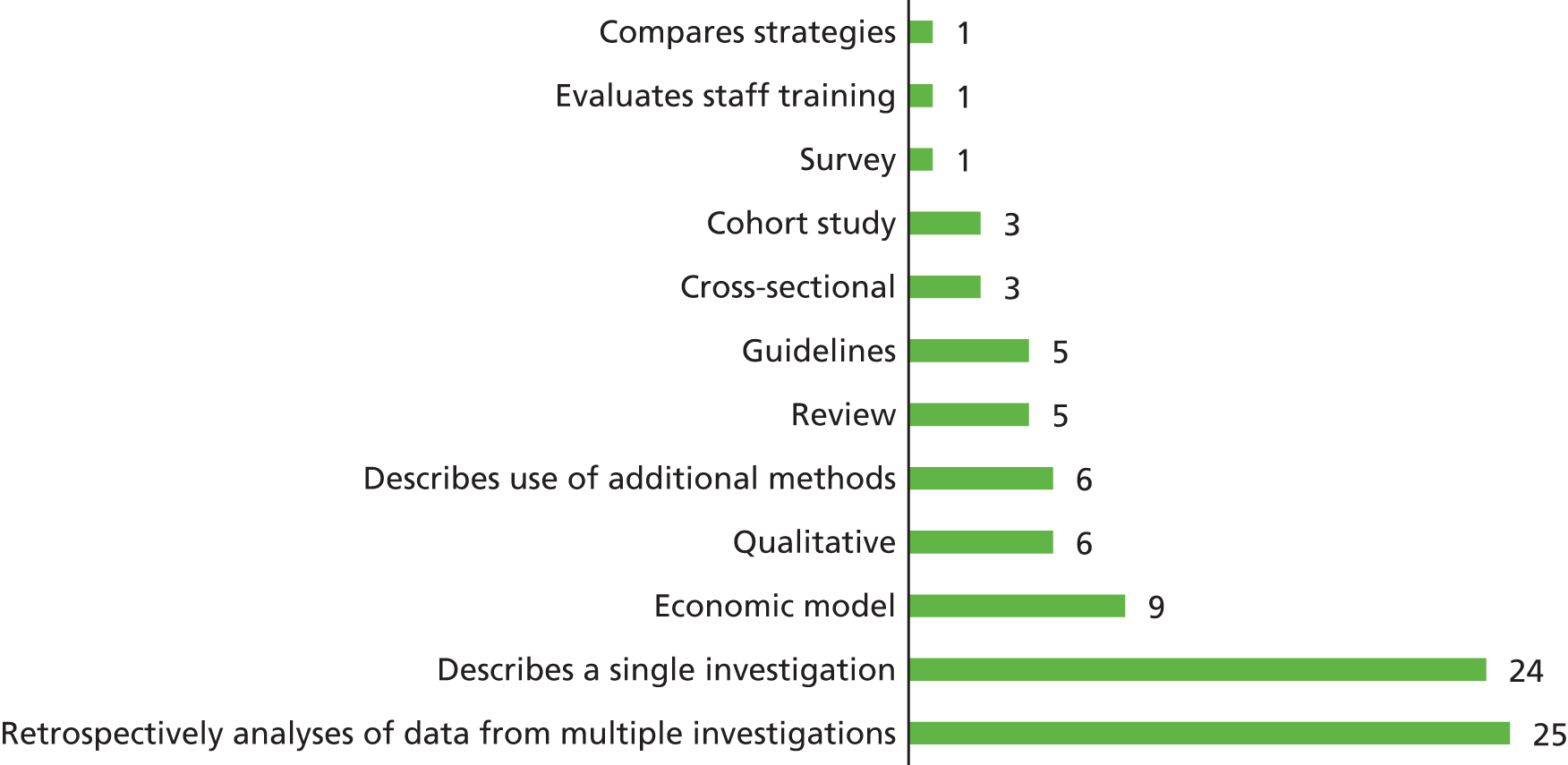
As we outlined in Chapter 2, owing to the diversity of designs, predominantly descriptive data and unclear quality indicators in the included literature, established quality appraisal tools, such as the risk-of-bias tool developed by The Cochrane Collaboration, were not suitable for use in this review. Instead, we used study design as a proxy for quality, and characterised study types during the narrative synthesis, highlighting any particular concerns regarding the quality of individual papers.
Integration and comparison of the specific population and wider population literature
We synthesised the elements of contact tracing described in the two subreviews using a logic model, which sets out the elements of the contact investigation pathway (Figure 5). We used this model to describe and compare data in the review of wider populations with those in the review of specific populations, and highlight data of particular relevance to contact tracing in specific populations.
FIGURE 5.
Logic model outlining elements of the contact-tracing pathway (bold = reported in specific population literature only). AFB, acid-fast bacillus; GPS, Global Positioning System; IGRA, interferon gamma release assay.
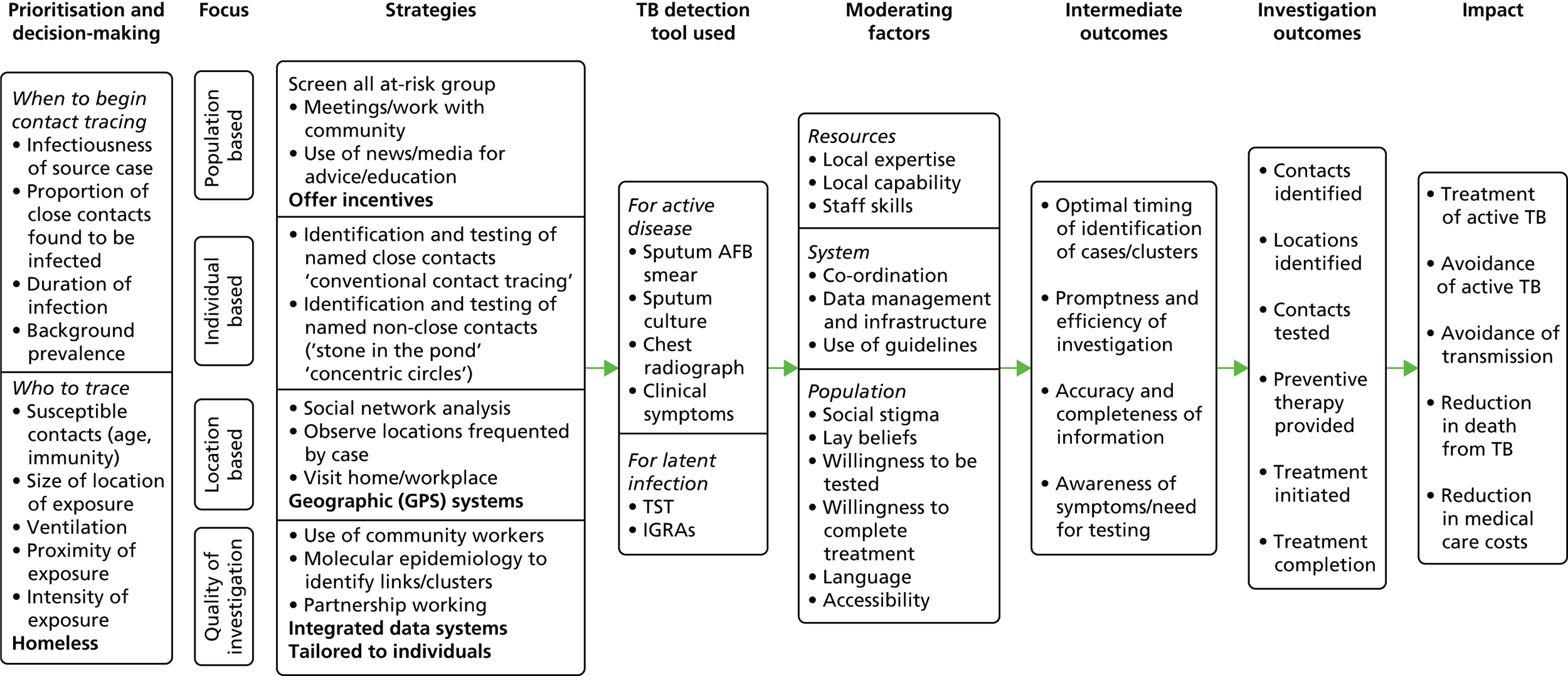
The elements of the model are drawn from the included literature. The elements of the model that are in standard typeface were referred to in both reviews; the elements of the model that are in bold typeface were described only with regard to specific populations.
The model pathway progresses from left to right. The first column details elements relating to prioritisation and decision-making required prior to commencing an investigation and during the investigation. The second column provides a categorisation of investigation activities, with the elements of these further itemised in the third column. Columns further to the right indicate the influence of TB detection and diagnosis tools used during investigations, followed by factors that may influence the process of an investigation and outcomes. The final columns detail outcomes that may be achieved during an investigation, and longer-term impacts that may result from contact-tracing investigations.
Prioritisation and decision-making
There was a high level of consensus in the literature regarding elements to consider when making decisions about when to instigate contact-tracing investigations, and then who should be prioritised for tracing and screening. The research studies included in the wider review echoed elements of prioritisation and decision-making that were described in the literature on contact tracing for specific populations. Authors described the need for a risk assessment approach36,60 based on the infection type, level and period of infection,71,87 the characteristics of contacts such as younger age or reduced immunity1,8,45,82,102 the duration of exposure and the proximity of exposure. 33,47,69,115 Elements relating to the specific environment also require consideration, such as the size of an area in which people congregate, together with the levels of ventilation in a location. 57,59,93
Several studies highlighted the importance of considering the background prevalence of TB in population subgroups, such as ethnic minority communities or those born overseas in TB-endemic countries. Having this information was described as a key element of decisions about when to commence or expand contact tracing, with some investigations reportedly expanded inappropriately when background prevalence had not been sufficiently taken into account. 32,44,62,89,94,95 The authors of one study95 highlighted that the ‘stone in the pond’ principle is useful only if accurate data regarding prevalence in specific communities (such as immigrants) are available.
Three papers68,83,92 outlined decision trees or tools for use when considering priorities for investigations. The first of these68 evaluated use of a decision tree for a set of 3162 contacts. The authors reported that the decision tree had a 9% sensitivity, 22% specificity and a false-negative rate of 7–10%. It was estimated that the use of the decision tree could lead to around a 20% reduction in the number of contacts investigated. The priorities for contact tracing detailed in the decision tree are if the index case has cavitary disease or if the total exposure of a contact per month is > 120 hours or if the contact is under the age of 15 years. If none of these criteria applies, then it is recommended that a case should be investigated only if the contact was exposed to a smear-positive case in their home or if the contact was exposed in a place where the ventilation was minimal. A second study83 also described the development of a checklist and decision tree. The tools were intended to be piloted, although it was reported that no suitable investigations were started during the period of the study and, therefore, the testing of the tools had not been carried out.
Mohr et al. 92 consulted experts to develop a decision-making tool for contact-tracing investigations following potential transmission to users of public transport. Nine elements were identified: symptoms of the index case; infectiousness of the index case; drug resistance pattern of index case; evidence of transmission to other contact person; the quality of contact between an index case and contact person (face to face/social interaction); the proximity of contact to case during exposure (more/less than 1 m); the duration of exposure (more/less than 8 hours); the susceptibility of the contact (< 5 years of age/HIV/substance abuse/other disease); and environmental factors (external ventilation present or not/with/without circulation).
Several sets of guidelines were identified during the review, which provide detailed recommendations regarding considerations of priority. 1,6,33–35,96 These guidelines confirm that priorities should be assigned to contacts (high/medium/low priority) based on, first, the likelihood of infection and, second, the potential hazards to the individual contact if he or she is infected (including the characteristics of the index patient, the characteristics of the contact and the intensity, frequency and duration of exposure).
Population-focused strategies
Four included studies40,41,47,65 described the use of media and information provision to reach populations during an investigation. A report of an investigation in a school40 described intense pressure from parents, which was addressed by holding information sessions, sending letters and factsheets to all parents and providing a central point of communication. A second investigation in a school41 found that it was important to counter public fears by providing simple, credible, accurate, consistent and timely information and letting the public know what action they could take. An investigation focused on a hospital47 set up a free telephone helpline, with press releases and media campaigns also used. A telephone helpline and information about TB symptoms/mode of transmission/availability of effective treatment were made freely available to the population of an area in which a public house was suspected to be a site of transmission. 65 The authors of another paper reporting an investigation around a public house97 described how several individuals had come forward as a result of awareness-raising activities among the local population. The authors suggested that targeted health education programmes may improve contact detection.
Papers in the specific populations review30,31 highlighted the potential overlap between contact tracing for population subgroups and population-screening activities. In the wider review we identified one study that compared the effectiveness of contact tracing versus population screening. 111 The paper supports the view that these interventions have areas of overlapping purposes. This UK study111 compared contact tracing among residents in a deprived area of London with the screening of all new entrants to the country. The authors concluded that tracing the contacts of individuals who had been identified with smear-negative pulmonary TB was significantly more effective in identifying individuals requiring intervention than the routine screening of all new entrants (7.7% of contacts of people with smear-negative pulmonary TB required full treatment or chemoprophylaxis vs. 3.1% of new entrants screened). This paper is particularly interesting with regard to specific populations, as it comments that in high-incidence areas contact tracing could be seen as a way of screening communities at particularly high risk, thus emphasising the overlap between these strategies. Another paper included in the wider review70 concluded, from its examination of contact tracing in a workplace setting, that the screening of all new employees from countries of high TB prevalence should be considered.
Individual-focused strategies
As found in the specific populations review, the literature in the wider populations review was dominated by reports of investigations which used ‘conventional contact tracing’ methods to identify individuals with possible active or latent infection. These investigations consisted of an index case being asked to name their close contacts, and ‘stone in the pond/concentric circles’ methods to widen the pool of contacts tested from close/family contacts to less close/casual contacts.
Several papers echoed the review of specific populations in describing the limitations of contact-tracing methods. Bock et al. 43 reported a study in which contacts were reinterviewed following the increase of an outbreak. Reinterviewing identified an additional 282 contacts from the original 61 contacts (19% of these had positive TSTs). It was concluded that contacts were originally missed because the normal daily connections between them were not recognised by investigators. In another study74 it was reported that although 67% of cases identified all of their contacts, 32% did not. The index case was less likely to identify contacts who were employed and those who were not a relative or cohabitant [odds ratio (OR) 4.82, 95% CI 1.71 to 13.54, and OR 0.22, 95% CI 0.10 to 0.47, respectively].
An area of frequent debate within the literature related to the expansion of investigations from close/household contacts to casual contacts. Some investigations prioritised only household contacts. 105 Others concluded that the screening of casual contacts was not cost-effective in low incidence areas,38 should be carried out only for smear-positive respiratory index cases102 or only for highly infectious cases,33 or that there should be only limited screening of casual contacts. 87 The authors of one study113 found that the screening of casual contacts was routinely omitted owing to limited resources. In contrast, the authors of another study97 argued that screening beyond close contacts must always be considered.
Although authors agreed that closeness was an important predictor of infection and should guide prioritisation of investigation,68,108 the definition of ‘close contact’ varied considerably32,113 and different authors used different categories. For example, one study39 defined a close contact as someone having < 4 hours’ exposure indoors or in a confined space, and a casual contact as someone with exposure other than close. Another study42 defined people who spent an estimated total of at least 40–100 hours with the index cases in the 3 months prior to diagnosis or during the infectious period as ‘close contacts’, and those who shared the same front door as the index case as ‘household contacts’. One study89 retrospectively examining a number of investigations reported that, in all of them, ‘household contacts’ were always defined as ‘close’. In other studies, ‘close contact’ was defined as exposure of > 6 hours per week and ‘occasional contact’ was defined as exposure of < 6 hours per week,48 or ‘close contact’ was defined as someone spending > 8 hours per week with the source case. 57 Another study44 reported that testing should be restricted to casual contacts having frequent (at least once per week) contact.
A review69 of published data relating to the likelihood of tuberculin reactions in casual contacts defined casual contacts as ‘persons sharing the same air, but having no direct contact with the index cases’. It concluded that the decision to extend a contact investigation to a group of casual contacts in a workplace or school should be based on the evidence of transmission from the index case to closer contacts, the number of hours of exposure and the likelihood of previous exposure in the population to be screened.
National guidelines tended to provide descriptive information regarding the categorisation of contacts. Guidelines from the USA34 defined close exposure as prolonged exposure in a small, poorly ventilated space or a congregate setting. Guidelines from the UK33 defined close contacts as people from the same household who shared kitchen facilities, and very close associates such as boyfriend or girlfriend or frequent visitors to the home. They noted, however, that contacts at work or in a hospital ward may be as close as a household contact. Guidance from Canada6 divided contacts into high priority (household contacts plus non-household contacts who are immunologically vulnerable), medium priority (close non-household contacts with daily or almost daily exposure, including those at school or at work) and low priority (casual contacts with lower amounts of exposure).
Two included documents6,51 suggested that recommendations for expanding investigations in general population groups may require further consideration in specific populations. The first of these51 carried out a descriptive literature review of contact investigation methods. They concluded that, although conventional strategies have given priority to household contacts, the importance of casual contacts and locations in contact tracing for high-risk or vulnerable groups is not always sufficiently recognised. It was recommended that the closeness of contact should be based on the amount of time an individual is exposed, rather than on environmental or social factors. The second document,6 comprising Canadian guidelines, included the statement that ‘the concentric circles approach does not take into account contacts who are vulnerable but may have had less exposure, and can be difficult to apply in congregate settings’. The guidelines recommended that the level of priority should be the primary consideration, with most effort put into tracing contacts who are most at risk of being infected and/or most at risk of developing active TB disease if infected.
Location-focused strategies
Three studies examined outbreaks among colleagues. 50,67,96 One paper,53 reporting a retrospective review of data from outbreaks across five states in the USA (which used a subset of data from another included study99), concluded that the potential for transmission of TB in the workplace needs further recognition. The study found inconsistent and limited recording of data collected during the investigations, and differences between the locations with regard to who was selected for screening and who was used as the primary source of information. Another study70 also concluded that the workplace can be an important site of transmission.
In a further investigation,96 coworkers had initially been classified as low priority; however, a high rate of infection found in high-priority cases (39%) led to the expansion of the investigation to low-priority contacts, and 15% of these subsequently had positive TSTs. Similarly, Duarte et al. 58 reported that expanding contact investigations to home and workplace visits increased the number of individuals screened and identified further patients with active and latent TB. Interviews identified 950 contacts (an estimate of 0.75 cases of infection per index patient identified); expanding the investigation to home and workplace visits helped to identify 2629 contacts (1.4 cases of infection per index patient). These results support the finding that locations such as the workplace can be important to consider in contact investigations.
A study65 from the UK examined the contact-tracing investigation surrounding an outbreak of TB in the south-west of England. The paper highlighted that few conventional household contacts were identified, but a significant number of secondary cases were detected from tracing contacts at a single public house location. An investigation in a village in Spain48 similarly found that few cases in the outbreak cluster appeared to have a close relationship, but many frequented some of the same bars. The authors of another study55 that highlighted the importance of bar locations concluded that contact investigation should examine the location itself and not focus on personal contacts. Although the bar in this study attracted a mixed clientele, it was located in a red light district and next door to a hostel for homeless people, so the conclusions are particularly relevant to investigations in specific populations.
In contrast to these papers, a retrospective analysis57 of 100 contact investigations carried out over a 5-year period in congregate settings (schools, workplaces, drug treatment centres, single-room hostels and other locations) found that transmission at congregate sites was uncommon (22% of investigations examined in this analysis), concluding that these investigations are resource intensive. The study recommended that decisions to perform testing at a congregate setting (not just among household contacts) should be based on the infectiousness of the source case, the size of the location, the level of crowding, the number of windows at the setting, the characteristics of contacts such as age and immune status, and the presence of case clusters.
Six papers2,39,52,66,76,91 outlined the benefits of a social network analysis approach to contact investigations. Findings from these studies build on the positive findings from the papers in specific populations reported previously. 16,17,19,22,25 Bailey et al. 39 described the development of network diagrams and calculation of reach, degree and ‘betweenness’ scores to examine relationships between an index case and contacts. The highest 20 scores and lowest 5 scores for each metric were used for prioritisation. The network diagram indicated that the index patient was directly linked to 56% and indirectly linked to 18% of secondary cases, and contacts prioritised using network analysis were more likely to have latent infection than non-prioritised contacts (OR 7.8, 95% CI 1.6 to 36.6). A similar study91 that explored an investigation, including contacts from a local community, a prison, a hospital and a school, concurred that the metrics calculated using social network methods enabled contacts with higher scores to be prioritised. Three contacts with high-ranking ‘betweenness’ scores were found to be links to the overall network. The authors concluded that network analysis provided a means to identify linkages among cases, quantify the magnitude of an outbreak and assist the prioritisation of contacts to screen. Gardy et al. 66 reported that social network analysis outperformed contact tracing in identifying a probable source case, as well as indicating several locations and persons who could be subsequently targeted for follow-up.
Another study52 supplemented routine investigation procedures with an interview to collect data on places of social aggregation for use in social network analysis. TB patients not linked via conventional contact tracing were linked by mutual contacts or places of social gathering. An association was found between TST results and being in the denser area of a person–place network (p < 0.01). The authors of a UK study2 reinterviewed patients using a social network enquiry approach. They found that associations detected previously tended to be family–friend relationships, whereas over half of the associations reported during the new interviews related to friends and socialising in public houses. Fourteen of the 43 epidemiological links were newly uncovered, although associations were not discernible for 45% of patients.
One included paper cautioned against the uncritical acceptance of studies advocating the use of social network analysis. 76 It found that betweenness scores (but not centrality scores) were useful for identifying contacts at greater risk of latent TB infection (significant association for contacts with higher betweenness score and latent TB infection, OR 2.12, 95% CI 1.14 to 3.96; p = 0.020). However, the complexity and time-consuming nature of the method reduces the potential for its incorporation into routine contact investigations. The study by Bailey et al. 39 also outlines potential issues of implementation. The authors reported that, although data required to perform network analyses are already routinely collected, they need to be organised into the proper format for analysis. Although the costs to carry out network analysis may be beyond some programmes, the authors recommended that principles such as pursuing repeatedly named contacts should be widely adopted.
Strategies to improve the quality (efficiency/effectiveness) of investigations
We identified only one paper that reported an intervention to improve the delivery of a conventional contact-tracing investigation. 67 Gerald et al. 67 examined existing contact-tracing protocols. They found considerable variance among field workers regarding their understanding of terms used in the protocols. There was also variance in understanding of the methods for eliciting information from index cases, and in the use of ‘concentric circles’ analysis. The authors developed standardised definitions and procedures as part of a new contact exposure and assessment worksheet. They also introduced training sessions to increase TB field worker adherence to the protocols. The quality of the training sessions was evaluated by self-reported questionnaires. Sessions were rated at a mean of 4.61, and the overall value of the training received was rated as 4.71 (on a scale of 1–5, with 5 meaning ‘excellent’). It was mentioned that ‘some further training was required when data entry errors and misunderstandings were identified’. 67
The review of specific populations had indicated the potential value of community health workers during investigations. In the wider review, one paper86 described the nurses’ perception that outreach workers would be of value.
One included study103 reported the linking of data from two different health-care data systems during a contact investigation based around a maternity ward (hospital-based electronic medical records to identify patients exposed to the index case, and an electronic immunisation registry to obtain contact information for exposed infants). There are limited data evaluating the impact of using the integrated system. However, the authors reported that the integrated system aided the identification, notification and evaluation of contacts, thereby reducing the resource burden required for the investigation. 103
A sizable group of papers focused on improving the quality of investigations via the use of epidemiological testing, predominantly with the aim of identifying clusters of cases. This echoes the specific population literature. These approaches were described as complementary strategies to contact tracing,80 and so they have been included in this review. The use of molecular epidemiology [referred to in the papers as DNA fingerprinting, genotyping, whole genome sequencing, spoligotyping, using IS6110-based restriction fragment length polymorphism (RFLP) analysis, mycobacterial interspersed repetitive unit 12 typing or 24 loci mycobacterial interspersed repetitive units variable number of tandem repeats] was described in nine papers42,46,55,61,66,78,80,114 in the review of wider populations.
Lambregts-van Weezenbeek et al. 80 reported that DNA fingerprinting can be useful to confirm suspected epidemiological links, to identify new links when transmission is not suspected and to identify when links between cases of TB are vague or with long periods in between. In their retrospective analysis of clusters over a 5-year period in the Netherlands, the authors found that DNA fingerprinting established an epidemiological link in 31% of clustered cases in which no link had been assumed or documented. Cluster feedback significantly improved the confirmation of documented epidemiological links (p < 0.001). In another study42 it was reported that DNA fingerprinting demonstrated that 30% of contacts with TB developed the disease at nearly the same time as, but not as a result of transmission from, the index case. The authors of a further study that used molecular epidemiology to examine an investigation at a workplace in Italy61 also reported that genotyping was important to establish linkages. Yeo et al. 114 examined public health data over a 4-year period and carried out additional genotyping. Genotyping by the research team identified up to 14 possible additional index cases. The authors described the contact investigations as extensive. The investigations had mostly been able to identify latent TB infection, but had been less successful in identifying the source cases.
The authors of one paper78 analysed data from an initiative to DNA fingerprint all new cases of TB during a 5-year period. Fingerprints were obtained and stored in a database and pattern matching software was used, with a network diagram approach also used and centrality scores calculated. DNA fingerprinting was reported to be valuable in identifying the size of outbreaks and in leading to recognition of the importance of location (bars) in understanding an outbreak. Contact investigation had identified only 12 links among 27 cases. The index case could not be linked to any other case, and half (51%) of cases could not be linked to another case via contact investigation. An analysis using the additional strategy found that around 80% of the patients could be linked by other people or places, and individuals were often linked by multiple places, providing several opportunities for infection.
One study compared DNA fingerprinting with whole sequence molecular epidemiology, with conventional contact tracing and social network analysis methods. 66 The authors reported that DNA fingerprinting had suggested that the outbreak had a single TB lineage, whereas more in-depth whole sequence molecular epidemiology revealed two lineages. Genotyping and contact tracing alone did not capture the true dynamics of the outbreak. Genome sequencing allowed the social network to be divided into subnetworks associated with specific genetic lineages of the disease. Genotyping was also reported to be valuable in excluding social relationships that could not have led to transmission according to the genomic data. This was described as greatly reducing the complexity of the network and aiding identification of index patients.
A study of particular relevance to specific populations46 highlighted that molecular epidemiological methods tended to identify non-household links. These methods also identified more individuals from precarious economic circumstances and social difficulties (p = 0.002) than conventional contact tracing. A second study of note for specific populations55 reported that conventional contact tracing is insufficient for the detection of chains of transmission in some harder-to-reach communities. The study found that 12 of 20 cases with confirmed recent transmission could be determined by DNA fingerprinting only. The authors highlighted that DNA fingerprinting not only provides important information regarding recent infection of one patient by another; it also allows structural weaknesses in an investigation to be identified.
Tuberculosis detection and diagnosis tools
Thirteen papers37,38,44,54,56,57,60,63,72,79,90,104,110 highlighted how the specific test used for screening for latent or active TB infection proved to be important during contact-tracing investigations. Four papers considered how the process of contact tracing could be influenced by the particular test. 37,38,57,104 In the first of these,37 the authors reported that the uptake and completion of chemoprophylaxis may be higher when latent TB infection is diagnosed with interferon gamma release assays (IGRAs) rather than TSTs. This finding was echoed in a second paper,104 which similarly found that contacts tested using IGRAs were more likely to complete screening.
One study of particular relevance to specific populations outlined the need for difference in the testing process for individuals in congregate settings versus other contacts. This investigation57 reported that testing should be carried out for high-risk groups as soon as possible, and again 10–12 weeks later. For other individuals, the authors recommended that testing was performed only once, at 10–12 weeks after exposure.
A further study38 described the effects of a change in policy regarding the follow-up of contacts. Previously, close contacts had been invited for follow-up annual radiological surveillance. Under the changed policy, close contacts were either discharged or referred to the chest clinic following their initial screening, with no annual follow-up. The study found that, compared with the results of the previous protocol, fewer contacts were unnecessarily screened. However, as a result of the new policy, referrals to the chest clinic increased, and the number of contacts given chemoprophylaxis also increased.
Nine further papers44,54,56,60,63,72,79,90,110 provided evaluations regarding the usefulness, effectiveness or cost-effectiveness of IGRAs [either QuantiFERON®-TB-Gold In-Tube (QFT-G) assay (Quest Diagnostics, NJ, USA) or the T-SPOT®. TB test (Oxford Diagnostic Laboratories, Oxford, UK)] instead of, or in addition to, TSTs. Borgen et al. 44 concluded that use of IGRAs could improve the positive predictive value of testing, and also enables TST for those with bacillus Calmette–Guérin (BCG) vaccination. Another study similarly concluded60 that IGRAs are more sensitive than TSTs in detecting latent TB infection. The authors of this literature review recommended that a positive TST should be followed by IGRAs, as IGRAs may be superior to TSTs in predicting latent infection becoming disease (although they recognised that this finding was not consistent across all of the literature). They also recommended that, when only a TST is used, a cut-off point for positivity must be decided regarding sensitivity versus specificity. The likelihood of infection and BCG status should be considered.
Other papers echo the superiority of IGRAs over TSTs for detecting latent TB infection. 54,56,72 Diel et al. 54 estimated that the use of IGRAs (either QFT-G or T-SPOT. TB) as a replacement for the TST would decrease the number of contacts to be investigated by approximately 70%. IGRAs were described as particularly useful for people who show tuberculin reactivity due to past BCG vaccination. 63 An economic modelling study from Canada cautions against the widespread use of QFT-G. 90 This study found that the most cost-effective strategy was to administer QFT-G in BCG-vaccinated contacts, and to reserve the TST for all others (at an incremental net monetary benefit cost of CA$3.70 per contact). The least cost-effective strategy was to administer QFT-G in all contacts (an incremental net monetary benefit cost of CA$11.50 per contact). Trieu et al. 110 similarly concluded that QFT-G was particularly useful for contacts from countries with BCG coverage; however, they also raised the issue of cost. The authors estimated that QFT-G was 16 times more expensive than TSTs. They also highlighted the need for field workers to be trained in taking blood samples, and that specimens needed to be transported to a laboratory for analysis within 16 hours of collection. In addition to people who are BCG vaccinated, the authors recommended the use of the test with people who are hard to follow up, such as homeless people, as the test requires only a single encounter.
The authors of another study79 constructed an economic model to compare high-resolution computed tomography with chest radiography (in combination with QFT or a TST) for the detection of active TB during contact investigations. The study found that a strategy that comprised QFT followed by high-resolution computed tomography yielded the greatest benefits at the lowest cost. High-resolution computed tomography, rather than chest radiography, was therefore recommended to evaluate and manage contacts with active TB infection.
Moderating factors
We grouped factors that could reportedly influence (or moderate) an investigation into those relating to available resources, those relating to systems and those relating to the population.
Resources
Studies described how contact investigations are complex, challenging and labour-intensive, and require the immediate availability of a large workforce. 41,64 Screening was described as costly, and diverted staff from other duties. 100 National standards in Canada6 outline the need for good organisation, and adequate staffing and resources.
One study43 described how the quality of an investigation was hampered by an inexperienced workforce. The authors reported that, as TB rates were historically low in the area, no specialised/experienced team was available to conduct contact tracing. Wilce et al. 113 found variability in levels of training received by staff involved in investigations. A qualitative study exploring the perceptions of patients with active TB and staff involved in contact investigations concluded that programmes may be enhanced by staff receiving training in listening and culturally appropriate interviewing techniques. 106 This need to train staff in interviewing techniques was echoed in a second study61 and further supported by Bock et al. ,43 who described how patients who were reinterviewed by ‘experienced interviewers’ named an additional 282 contacts who had not been identified in the first interview. Wilce et al. 113 described how, in one investigation, the content of the interview was typically left to the discretion of the interviewer.
An interesting finding regarding resources was described by Duarte et al. 58 This study compared investigations during two study periods (during the first period the investigation interview targeted close contacts; during the second period visits to home and workplace were also included) and found that, although there was an increase in workload, investigations including the assessment of locations could be carried out with the same resource.
Systems
The system-based elements that could impact on an investigation included the degree of communication and co-ordination between staff and between agencies. 77,106 One study50 described how the requirement for contact across different agencies had provided an additional complication to an investigation. The authors described how good communication among services was required to overcome this. This finding regarding working practices was echoed in another study, which reported that multidisciplinary team working is essential for effective management of an investigation. 65 A narrative overview of the literature51 concluded that there needs to be a focus on local capability and expertise, co-ordinated approaches, and strategies including the development of questionnaires and electronic data management. The importance of effective data management systems was also highlighted by Reichler et al. 99
As detailed in Results of review of tuberculosis contact tracing in wider populations, Characteristics of the literature, we identified several sets of guidelines during the review. 1,6,33–35 The provision of written policies and procedures for investigations was described as improving the efficiency and uniformity of investigations. 34 However, the included literature contained many references to inconsistency in use of guidelines, and a requirement for training and support to improve adherence and thereby increase the standard of contact-tracing investigations. 53,84,95,100,113
One study found inconsistent and limited recording of the data collected, and differences between who was selected for screening and who was used as the primary source of information. 53 Researchers who retrospectively analysed a TB data registry for children found limited documentation regarding the labelling of the level of closeness of contact among those screened. 112 They suspected that the labelling of close/not close had been made after the investigation was completed. Another study, which examined the decision-making of public health nurses during investigations, found evidence of the scaling up of an investigation from close to casual contacts, which was not required. Staff perceived the criteria for classification as being unhelpful/ambiguous, and there was reported difficulty in interpreting background population prevalence data. 95 The nurses tended to identify more contacts than just those at substantial risk of infection, with a perception that screening as many contacts as possible gave a more comprehensive view of the level of infectiousness of the index case. Staff expressed concerns regarding missing contacts and this omission then leading to further transmission.
Population
Moderating factors associated with the population related predominantly to the reported influence of perceived stigma among people with active TB, and also among contacts. A UK study explored the views of contacts who had attended for screening versus those who had not. 86 The findings highlighted the importance of working with a community to allay fears, educate and reduce the stigma. Fears regarding stigma, loss of employment or housing, and alienation or abandonment were described. 106 Another study similarly described reports of a fear of social discrimination. 55 In one investigation, perceived stigma had led the index case to claim that they were unemployed, which delayed the investigation of contacts at their workplace. 61
Three papers further described how the influence of lay beliefs could delay the initiation or course of an investigation. In one study,55 people with active disease reported irritation with the contact-tracing procedure, which they perceived to be intrusive. It was reported that more than one-quarter of patients identified with active TB had failed to seek medical attention. Those patients who did go to see a doctor delayed doing so for an average of 7 weeks after the onset of symptoms. Some cases reported trying to shield drinking partners from ‘bullying methods’ of the ‘health police’ by naming only contacts in more distant bars, or by naming more transient contacts such as neighbours.
Another study3 found that, although patients understood the concepts of airborne transmission and contact, prolonged contact was not thought to be required for infection. Modes of TB transmission were not always fully understood, with patients describing potential infection via airborne transmission, sharing utensils, consuming infected foods/drink and exchanging bodily fluids. The authors of another study106 echoed the importance of understanding lay beliefs in TB control strategies. They highlighted differences in understanding of the terms ‘contact’ and ‘at risk contact’; these were terms that could be vague or understood incorrectly. Some patients in this research were unclear about the purpose of naming contacts; it was not clear to them that the focus was not on getting the names but on finding the people who may have been infected. Patients reported preferring to inform contacts before they were contacted by the health department.
A failure to attend for screening could delay or limit the effectiveness of investigations, and one study described how non-attenders at screening appointments could be unaware of their missed appointment. 86 Reasons for people not attending testing included that their contact details were inaccurate, they shared houses where incoming post became mixed up, they had a limited understanding of the need for screening, they were unable to take time off work and they had childcare issues. The paper outlines a range of recommendations to aid the progress of contact investigations, including building good working relationships between TB services and general practitioners (GPs): sending letters to the patient to distribute to contacts: using outreach workers to trace contacts via home visits/telephone calls: walk-in appointments for screening; having testing sessions in GP surgeries rather than in hospitals; and using telephone text reminders.
Outcomes
The logic model depicts two columns relating to outcomes associated with contact investigations. These outcomes differ according to their place in the pathway, with the intermediate outcomes underpinning the investigation outcomes. Although the intermediate outcomes are of significance, as they help to explain the investigation outcomes, the investigation outcomes (number of contacts identified, and number tested and treated) were typically the focus of the literature.
Guidelines6,33 refer to the importance of indicators of effectiveness, timing of investigations, efficiency of processes and systems and accuracy of data recording. Few studies, however, provided data regarding these indicators. Wilce et al. 113 highlighted the variability in accuracy of information recorded and the need for improvement in this area. Only one paper97 referred to awareness raising as an outcome from an investigation.
Papers predominantly reported the number of contacts who were screened as a measure of the success of a contact investigation. The size of investigations varied substantially between studies, from those that had screened < 100–200 contacts41,61,65 to those that screened many thousands. 44,81 The number of contacts screened per index case also varied substantially; for example, in the Aissa et al. 36 study the mean number of contacts screened per case was 6 (with a range of 1–122). In another study45 the median number of contacts per case was 3 and the highest number was 150. Sprinson et al. 107 reported that the mean number of contacts per case was 10.5 (range 0–170). A further study estimated 102 contacts needed to be evaluated per prevalent case diagnosed (95% CI 90 to 115 contacts). 37
It is interesting to note that identifying high numbers of contacts appeared to be mostly reported as a positive outcome in the studies, despite the resource implications of increasing the size of the investigations. There was little reference to the appropriateness of the contacts being identified (apart from one study95 that described the inappropriate widening of investigations and another40 that described local pressure to expand an investigation). A study54 that reported the advantages of using IGRA testing described one benefit as being a reduction in the number of contacts requiring screening. Another study38 examining testing protocols similarly reported a reduction in inappropriate screening as a positive outcome.
Several studies reported that a proportion of index cases named no contacts. For example, Jereb et al. 73 found that 10% of index cases had no contacts listed. Sprinson et al. 107 reported that 11% of cases had no reported contacts. Data of particular importance to the consideration of specific populations are reported in two studies. Marks et al. 89 noted that fewer close contacts were identified by homeless people, men and Asian/Pacific islanders. No contacts were identified for 8% of index cases. Homelessness was significantly correlated with having no identified contacts (relative risk 1.3, 95% CI 1 to 1.5). Similarly, Reichler et al. 99 found that 13% of index cases had no contacts identified, and an additional 11% had no close contacts identified. Patients with no contacts listed were more likely to live in a homeless shelter (13% vs. 2%; p < 0.001).
Several studies highlighted the sizable numbers of contacts who might withdraw at different points during the process of screening and treatment. In one study,87 14.7% of contacts declined screening. In another study,57 83% of contacts were tested, 20% had latent infection, and 52% of these completed treatment. An even lower rate of 44% of contacts with latent infection completing treatment was reported in another paper. 73 An evaluation of a programme across one US state107 reported that 66% of contacts started treatment and 64.2% completed treatment. Around half chose to stop, 17% moved and for 17% the reason for non-completion was unknown. The study found that only 31% of areas investigated met the target of 85% treatment completion. Another study81 reported similar latent TB infection treatment completion rates of 67%, with 40% of contacts identified with latent TB infection either refusing or stopped treatment. One paper104 provided data of particular interest to consideration of specific populations, in reporting that contacts were less likely to complete screening if they were of working age, male, black or from the Indian subcontinent.
The Anger et al. 37 study concluded that contact screening is effective, even when completion rates for latent TB infection treatment are below ideal levels. The authors calculated the absolute risk reduction afforded by chemoprophylaxis initiation to be 1.1% (95% CI 0.6% to 1.9%), which equates to approximately 88 contacts needing to be treated to prevent one case of active TB (95% CI 53 to 164 contacts). Another study109 emphasised, however, how increasing treatment completion among contacts could substantially improve effectiveness. This study estimated that reducing loss to follow-up to a 10% level could lead to significant benefits in infection rates (5.4% prevented; p = 0.02).
Impacts
Two included papers71,75 used modelling methods to estimate the longer-term impact of contact-tracing investigation. The first of these71 developed a computational model using notification data during a 10-year period. The model indicated that conventional contact tracing using the ‘stone in the pond’/’concentric circles’ approach significantly reduced TB incidence (by 18.6%) and deaths (23.7%), compared with passive diagnosis only. The model indicated that around one-fifth of recently transmitted cases may be identified by contact tracing. The results of the model also relate to considerations regarding when to instigate contact tracing, as the model indicated that investigation of only smear-positive cases has a negative impact on effectiveness, rather than also including smear-negative cases (including both smear negative and smear positive reduces incidence avoidance to 10.4% and deaths to 13.2%).
A second study75 developed an agent-based simulation model of a TB epidemic. The model was used to compare household contact tracing with active case finding in the community. The model indicated that the maximum 5-year reduction in TB incidence achievable by household contact tracing was 10–15% (2–3% per year), although any impact would be lower with imperfect coverage or reduced sensitivity. The authors concluded that contact tracing can have substantial epidemiologic impact (up to 7% reduction in incidence per year), but only if it achieves relatively complete population coverage, is sustained over time and includes preventative therapy. They noted that contact-tracing evaluation should encompass the longer-term evaluation of latently infected contacts.
Six papers49,85,88,98,107,109 (five studies) provided cost-effectiveness data for contact-tracing investigations. The first of these107 estimated the cost of contact investigations during a single year in one US state to be US$4.8M. Two linked papers49,88 examined the cost-effectiveness of investigations following potential in-flight transmission. The first paper49 used an average cost-per-contact estimate of US$16.76, and calculated cost-effectiveness for a range of expenditures per contact (US$28, US$47, US$134 and US$164). The model indicated that every US$1 spent on investigations and treatment (contact tracing and also testing/treating TB disease and latent TB infection) resulted in more than US$1 of saving at moderate/high rates of infection and disease. However, low rates of infection and disease resulted in negative returns.
The second paper from the same team88 compared contact investigations instigated within 3 months (vs. within 6 months of the flight) and also investigation instigated only for those with sputum-positive TB by culture or nucleic acid amplification test, and sputum-smear-positive for acid-fast bacilli and cavitation on chest radiographs. The model indicated that introduction of the new protocol could result in an estimated 409 fewer contacts investigated (half the investigations), of whom 115 might test positive (three with active disease). The estimated risk for new protocol was 1.4–19% and for the old protocol was 1.1–24%. The estimated cost under the old protocol was US$222,000–1.3M, and under the new protocol was US$99,449–584,824. The authors concluded, therefore, that the new protocol (reducing the time period between exposure and investigation, and increasing the stringency of test results) would be more cost-efficient, while retaining an acceptable level of public health risk.
A study from Australia85 compared cost per case prevented in three scenarios: first, contact tracing as it had been carried out in 1991; second, a scenario in which the investigation was carried out adhering to guidelines in place at the time (1991); and finally a scenario in which up-to-date evidence-based guidelines were adhered to. The cost for contact investigations in 1991 was estimated at AU$309,065 per case prevented. During this period the study found that prevention was not considered a priority, and few infected contacts identified had received preventative therapy. The authors estimated that if guidelines in 1991 had been correctly followed the cost would have been reduced to AU$58,742 per case prevented. If current guidelines had been followed, the cost per additional case prevented was estimated at AU$3881. It was noted that lower referral rates, lower rates of preventative therapy and lower efficacy of preventative therapy than the rates used during the calculations would impact on these estimated costs.
Pisu et al. 98 in the USA carried out a cost-effectiveness analysis using a decision-analytic model to compare conventional ‘concentric circles’ contact tracing, with a contact priority model (using exposure hours, home and poorly ventilated environment). The aim was to explicitly categorise contacts as high risk and requiring testing, or low risk and not requiring testing. Conventional ‘concentric circles’ contact tracing was found to be more effective but more costly than a contact priority model. Savings would be made on the cost of TSTs; however, there would be higher costs from active disease. The ‘concentric circles’ approach was estimated to prevent one additional case of active disease for a cost of US$92,934 and one additional life-year at a cost of US$185,920. The estimated cost per 1000 contacts was US$339,896 for ‘concentric circles’ and US$294,596 for contact priority. There would be an estimated one or two additional cases of active disease per 3000 contacts if a contact-priority model, rather than conventional tracing model, was used.
Another study109 examined prioritisation models used mathematical modelling. Using the model it was estimated that targeting investigations by prioritising by age (children < 9 years old are traced first) and ethnicity (First Nation individuals traced first) could improve the effectiveness of contact tracing, compared with non-prioritisation (preventing 11% of cases over 20 years; p < 0.0001).
Authors of a study109 from Canada carried out a comparison of scenarios with and without contact tracing. The scenario involving no contact tracing indicated a higher average prevalence of TB infection than a scenario with contact tracing. The study found that the benefit of tracing the first 45% of contacts was greater than tracing the second 45%, indicating a diminishing return. In addition, in contrast to work described in regard to network analysis, this study found that prioritising contacts on the basis of the number of times they had been named had adverse outcomes. Furthermore, the work concluded that increasing the speed of the investigation (90% of contacts are tested within 30 days of diagnosis) did not lead to projected significant improvements in active cases or prevalence of infection.
Chapter 4 Discussion
What is the effectiveness and cost-effectiveness of specific interventions designed to improve tuberculosis contact tracing?
We identified a limited number of studies that permit the robust assessment of effectiveness and cost-effectiveness of different interventions. Of the 112 included papers, only one from the specific population review could be considered an evaluation of an intervention to improve the quality of investigations. 26 This study indicated that the addition of trained community workers improved the coverage of investigations. One study in the review of wider populations68 similarly described an intervention with staff to improve the conduct of investigations. Both of these papers provide very limited evaluation data but do suggest benefits from these interventions.
Although we identified several studies that reported the value of various strategies during investigations, there were few robust data to permit the identification of associations between strategies and outcomes. The main area of strength and consistency of findings was that location-based strategies might lead to identification of an increased number of contacts. Included research studies tended to report the influence of factors such as workforce and lay views and perceptions during investigations, rather than identifying interventions that might address these moderating factors. We also found few studies reporting intermediate outcomes in the pathway from investigations to impact. The studies predominantly reported data regarding the yield of investigations, rather than attempting to measure elements relating to the conduct of the investigation, or any effect on the target population’s knowledge, beliefs or behaviour.
The review of specific populations highlighted the overlap between screening, active case finding and contact tracing in approaches to TB control. 31 The use of screening in high-risk communities was advocated, particularly the use of mobile digital radiography with homeless people. 24,30,31 One study, however, concluded that contact tracing (particularly in ethnic communities) may be more cost-efficient and less intrusive than screening. 18 A second study (comparing contact tracing with the screening of immigrants)111 also concluded that contact tracing was more effective than large scale screening. The authors commented that contact tracing could be considered a form of screening, as contacts may be located in at-risk groups.
The types of outcomes reported by the majority of studies (number of contacts identified, number found to have active or latent infection) are problematic for comparing effectiveness between investigations and between studies, as differing contexts will impact these outcomes. For example (as reported in the studies), different index cases have very different numbers of contacts, and environmental factors influence rates of infection. Comparing these outcomes data between investigations is, therefore, of limited value. An indication of the effectiveness of the investigation processes may be determined if the numbers of contacts tested and the numbers who completed treatment as a proportion of the total number identified are provided; however, this information was rarely included.
The papers included in the review that used modelling methods to estimate effectiveness and cost-effectiveness indicated that contact tracing is an effective intervention. However, there are cautions that this may be only if contact tracing achieves relatively complete coverage of contacts, and includes the provision of preventative therapy to contacts. Both of these areas were highlighted in the review of specific populations as being challenging for investigations.
What is the acceptability, feasibility, appropriateness and meaningfulness of specific interventions designed to improve tuberculosis contact tracing in these population groups?
We identified no studies that provided data to answer this research question.
What are the barriers to, and facilitators of, delivery or uptake of contact tracing in these population groups?
We found a limited number of research studies examining barriers and facilitators. The use of IGRA testing rather than a TST was suggested to overcome barriers of loss to follow-up, although cost implications were highlighted. The use of financial incentives to increase number of contacts tested was described by one study in hard-to-reach populations. 8 The literature described the need for adequate resources and adequate systems for delivering investigations. The role of the fear of stigma and of population beliefs/understanding in determining uptake of contact tracing were common to investigations in both specific populations and wider groups.
What are the elements of the contact investigation pathway from interventions to impact for tuberculosis contact tracing in wider population groups?
We developed a logic model that details elements of the pathway relating to prioritisation and decision-making prior to and during investigations, investigation strategies, TB detection tools, moderating factors, intermediate outcomes, investigation outcomes and impact. The review of studies examining wider populations tended to echo the findings of the specific populations review, with most elements of the contact investigation pathway outlined being common to both.
How might evidence from interventions for wider populations be applied to tuberculosis contact tracing in specific population groups, including the similarities and differences, and what elements of the pathway may be important for feasible, applicable and effective interventions?
The literature on investigations for wider populations described a similar pathway to that in specific population groups. The recognised limitations of conventional investigation methods in wider populations, however, were amplified in specific populations. We constructed a logic model from the elements described in the included studies to explore the processes and systems that may influence the feasibility, applicability and effectiveness of contact investigations. This model sheds light on intermediary elements in the pathway from investigations to outcomes and impact that require consideration.
There was consensus across the two reviews that the initiation and scope of investigations should be determined by characteristics of the index case of active TB, features of locations of potential exposure and characteristics of potential contacts. One study in the review of specific populations highlighted that homelessness of a person found to have active TB should be a particular trigger for prioritising the commencement of contact investigations. 12 The wider populations literature emphasised the need to explore the likelihood, in the population to be screened, of previous exposure to TB infection. 69
Studies in the two reviews considered approaches to contact investigation that had a population, individual, location and/or increased quality focus. Reported intervention strategies did not differ between the reviews, although issues of cases identifying zero contacts, non-attendance at screening and failure to complete treatment or follow-up are particularly pertinent to specific populations.
In terms of population-based approaches, the value of using the media during investigations was described in both reviews, as was the need to work with local communities to provide information and reassurance.
The review of strategies used for specific populations was dominated by critique of the conventional contact-naming method. Papers in the wider review echoed these criticisms, highlighting that, more generally, the naming of contacts by people with active TB infection was problematic. 73 Papers in the wider review mirrored the specific population studies, in reporting that issues regarding contact naming are particularly apparent in specific groups, especially homeless people. 89
Whereas the specific populations review focused on the limitations of contact naming as part of conventional contact investigations, the wider review highlighted that conventional methods used to widen an investigation from close to less close contacts could also be problematic. The challenge when making decisions about expanding investigations related to unclear definitions of different categories of contact, with reports of investigation staff disregarding guidelines when widening investigations or being unsure of different classifications. 6,51 Of particular importance to the consideration of specific populations, one study noted that although casual contacts may be less important in wider populations, and therefore not included in investigations, they may be of particular importance for detecting transmission among harder-to-reach populations. 51
The review of contact tracing in specific populations emphasised the importance of investigating locations of transmission. This was echoed in the wider review, with bars/public houses featuring as key locations in studies. 65,97 The wider review also described the value of investigations at workplace locations. 53,58 Both reviews indicated the value of social network analysis approaches in mapping connections between cases and contacts. There was consensus regarding the importance of a location-based approach, rather than just tracing personal contacts. 55 Across the literature in both reviews there was an emphasis that the context will have a significant impact on the outcomes of an investigation and on the particular features of each investigation.
The use of molecular epidemiology to augment investigations was described in both reviews, with the added value of the method recognised for both specific populations and wider groups. Partnership working was reported as important to increase the efficiency/effectiveness of all investigations. The introduction of integrated data systems across organisations (such as prisons and local health services) was advocated in one specific populations study,103 and the importance of addressing individual needs (such as culture and language) was described in another. 20
Limitations
The nature of the included studies precluded the evaluation of the data using a meta-analysis. The limited quality of the literature, in particular the lack of experimental study designs and a single study that could be described as evaluative, meant that the use of established quality appraisal tools was not indicated. As the evidence as a whole was from studies with weak designs, it was not appropriate to compare the strength and volume of evidence for different aspects of contact tracing investigations. The purpose of the review was to provide a synthesis of the literature to inform future commissioning of research in the area. The inclusion of a diverse range of study designs permitted the examination of a substantial number of research studies that lie beyond the scope of many conventional systematic reviews.
We recognise that the English-language inclusion criterion will potentially have limited the number of studies included and the breadth of countries represented. The review, however, includes studies from 12 countries, which offers a valuable overview of the international literature. We acknowledge that there was no public and patient involvement in this work, which was intended to assist with developing future research strategy. We also acknowledge the degree of overlap between contact investigation and other forms of TB control strategies. There is the potential for relevant data to have been missed by our searches, which used terminology relating to contact tracing rather than other terminology, such as active case finding and screening. We believe that this potential limitation was mitigated to some extent by additional searching processes such as reference list screening.
Chapter 5 Conclusions
The review identified a substantive number of studies relating to contact investigations. The literature is predominantly descriptive, however, with little robust empirical work evaluating investigations in either specific or wider populations. Currently, studies that have used mathematical or economic modelling methods are the predominant means of examining the effectiveness of contact investigations and the outcomes of different strategies. Further studies are required if robust conclusions regarding the associations between different contact investigation methods and outcomes are to be made. The results of the review highlight the complexity of the pathway from initial decision-making to achieving long-term impact on the health of the population. The differing nature of the context of each investigation was emphasised throughout the literature, and is problematic when endeavouring to make comparisons between the effectiveness of different contact investigations.
The literature on investigations for specific populations has much concordance with that reporting research findings from wider population groups. The literature relating to both specific populations and wider groups highlights the limitations of conventional contact tracing approaches, in particular asking index patients to name contacts. The recognised limitations of conventional investigation methods may, however, be exacerbated in specific populations. The conventional methods of dividing contacts into groups of close versus casual contacts also require further consideration and clarification. Particularly for specific populations, casual contacts may be of most importance in transmission, and conventional prioritisation systems may need revising. The importance of considering contacts at locations of potential transmission was highlighted across both subreviews, although here again this strategy may be of particular importance for investigations in specific populations.
Currently, there are indicative studies to suggest that the quality of investigations may be enhanced by the use of additional testing such as molecular epidemiology. Few studies described how systems and processes during investigations may be optimised to overcome the range of moderating factors described in the literature. The examination of outcomes more closely relating to these systems and processes may help to address the limitations of the current evidence base examining the relative effectiveness of different contact-tracing strategies.
The limited nature of the evidence available should be fully recognised when considering the following implications for health care and research.
Implications for health care (in priority order)
-
Existing studies indicate the potential limitations of contact naming, with location-based methods recommended to establish a complete picture of contact networks. In particular, a location-based strategy may be a more effective approach for investigations in specific populations. This finding was based on studies that described contact investigations rather than evaluated interventions.
-
The available research studies suggest that contact investigations in specific populations may require greater prioritisation of investigation of casual contacts (non-household) than in other groups. This finding was based on studies that described investigations rather than evaluated interventions. One evaluative study suggested that employing community workers may assist in gaining participation from individuals in high-risk populations.
-
The results of the review suggest that an emphasis on the evaluation of processes undertaken during investigations, and also intermediate outcomes such as engaging with treatment, may provide valuable data regarding factors determining the effectiveness of investigations. Our logic model constructed from the data suggests the potential importance of these intermediary outcomes and elements of process; however, there were few data identified in the literature regarding these processes.
-
Available research indicates that it is important to consider adequate systems, process and resources including local expertise and skilled staff, sufficient workforce capacity, data management systems and effective co-ordination between agencies. This finding is based on descriptions and recommendations in the included literature rather than on empirical work. One evaluative study provided limited evidence that additional staff training may be beneficial.
-
Research studies suggest that use of mass media and other avenues for the provision of information and advice may be effective in improving communication with communities and individuals at risk during investigations. This finding is based on recommendations in the included literature rather than on empirical work.
Implications for research (in priority order)
-
A large proportion of the included literature describes investigations. Future studies should aim to adopt an evaluative approach, to increase the evidence base regarding associations between different contact investigation strategies and outcomes. We identified only two studies that could be considered to be evaluative.
-
Research studies should further explore the development of measures that can be used to compare the effectiveness of different contact investigations. The reporting of numbers of contacts identified during an investigation, or numbers who tested positive, has considerable limitations as a measure of success. Measures such as the number of contacts who are tested/complete treatment as a proportion of those who were identified can be more useful in gauging the effectiveness of investigation processes.
-
Interventions targeting local expertise and staff skills, workforce capacity, systems and processes (such as data management and co-ordination between agencies), and lay knowledge, beliefs and behaviour should be developed and evaluated, in order to address moderating factors reported in the literature. This is based on findings from qualitative studies, and recommendations from descriptive studies outlining contact investigations.
-
Researchers should include the measurement of intermediate indicators of effectiveness such as the timing of identification of cases/clusters, the promptness and efficiency of investigation, the accuracy and completeness of information and the awareness of symptoms/need for testing among contacts, when reporting investigations that have been undertaken. These factors were not reported in the literature, yet our logic model indicates that they may be important elements of the investigation pathway.
Acknowledgements
Contributions of authors
Susan Baxter (Research Fellow) led the study and took the lead in analysis and report writing.
Elizabeth Goyder (Professor of Public Health) led the development of the protocol and provided expertise and advice during the study.
Duncan Chambers (Research Fellow) contributed to the review processes.
Maxine Johnson (Research Fellow) contributed to the review processes.
Louise Preston (Information Specialist) developed the search strategy and carried out electronic database searching.
Andrew Booth (Reader) provided methodological input to the review processes.
Data sharing statement
All available data can be obtained by contacting the corresponding author.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
References
- Contact Investigations following Patient and Staff Exposure to Active Tuberculosis Infections: A Review of the Clinical Evidence and Guidelines. Ottowa, ON: Canadian Agency for Drugs and Technologies in Health; 2014.
- Jackson AD, Seagar AL, Reid ME, Doig C, Forbes KJ, Laurenson IF, et al. Characterising transmission of a tuberculosis genotype in Scotland: a qualitative approach to social network enquiry. Int J Tuberc Lung Dis 2009;13:486-93.
- Jackson AD, McMenamin J, Brewster N, Ahmed S, Reid ME. Knowledge of tuberculosis transmission among recently infected patients in Glasgow. Public Health 2008;122:1004-12. http://dx.doi.org/10.1016/j.puhe.2008.01.011.
- Begun M, Newall AT, Marks GB, Wood JG. Contact tracing of tuberculosis: a systematic review of transmission modelling studies. PLOS ONE 2013;8. http://dx.doi.org/10.1371/journal.pone.0072470.
- Bur S, Golub JE, Armstrong JA, Myers K, Johnson BH, Mazo D, et al. Evaluation of an extensive tuberculosis contact investigation in an urban community and jail. Int J Tuberc Lung Dis 2003;7:417-23.
- Rea E, Rivest P. Canadian Tuberculosis Standards. Ottowa, ON: Public Health Agency of Canada; 2014.
- McElroy PD, Rothenberg RB, Varghese R, Woodruff R, Minns GO, Muth SQ, et al. A network-informed approach to investigating a tuberculosis outbreak: implications for enhancing contact investigations. Int J Tuberc Lung Dis 2003;7:486-93.
- Verdier JE, Jan de Vlas S, Kidgell-Koppelaar ID, Richardus JH. Risk factors for tuberculosis in contact investigations in Rotterdam, the Netherlands. Infect Dis Rep 2012;4. http://dx.doi.org/10.4081/idr.2012.e26.
- Rizzo M, Martin A, Cliff-Matthews V, Jamal F, Lehmann A, Llewellyn A, et al. Evidence Review on the Effectiveness and Cost-effectiveness of Interventions Aimed at Identifying People with Tuberculosis and/or Raising Awareness of Tuberculosis among Hard-to-reach Groups. London: Matrix Evidence; 2011.
- The Cochrane Collaboration . Cochrane Handbook for Systematic Reviews of Interventions [version 5.1.0] 2011. handbook.cochrane.org (accessed 14 April 2016).
- Critical Skills Appraisal Programme (CASP) . Qualitative Research Checklist n.d. http://media.wix.com/ugd/dded87_29c5b002d99342f788c6ac670e49f274.pdf (accessed 21 November 2016).
- Li J, Driver CR, Munsiff SS, Fujiwara PI. Finding contacts of homeless tuberculosis patients in New York City. Int J Tuberc Lung Dis 2003;7:397-404.
- Lofy KH, McElroy PD, Lake L, Cowan LS, Diem LA, Goldberg SV, et al. Outbreak of tuberculosis in a homeless population involving multiple sites of transmission. Int J Tuberc Lung Dis 2006;10:683-9.
- McElroy PD, Southwick KL, Fortenberry ER, Levine EC, Diem LA, Woodley CL, et al. Outbreak of tuberculosis among homeless persons coinfected with human immunodeficiency virus. Clin Infect Dis 2003;36:1305-12. https://doi.org/10.1086/374836.
- Oeltmann JE, Oren E, Haddad MB, Lake Lk, Harrington TA, Ijaz K, et al. Tuberculosis outbreak in marijuana users, Seattle, Washington, 2004. Emerging Infect Dis 2006;12:1156-9. https://doi.org/10.3201/eid1207.051436.
- Kline SE, Hedemark LL, Davies SF. Outbreak of tuberculosis among regular patrons of a neighborhood bar. N Engl J Med 1995;333:222-7. http://dx.doi.org/10.1056/NEJM199507273330404.
- Malakmadze N, González IM, Oemig T, Isiadinso I, Rembert D, McCauley MM, et al. Unsuspected recent transmission of tuberculosis among high-risk groups: implications of universal tuberculosis genotyping in its detection. Clin Infect Dis 2005;40:366-73. http://dx.doi.org/10.1086/427112.
- Dasgupta K, Menzies D. Cost-effectiveness of tuberculosis control strategies among immigrants and refugees. Eur Respir J 2005;25:1107-16. http://dx.doi.org/10.1183/09031936.05.00074004.
- Asghar RJ, Patlan DE, Miner MC, Rhodes HD, Solages A, Katz DJ, et al. Limited utility of name-based tuberculosis contact investigations among persons using illicit drugs: results of an outbreak investigation. J Urban Health 2009;86:776-80. http://dx.doi.org/10.1007/s11524-009-9378-z.
- Wallace CE, Cruise P, Tyree AB, Shevick G. Approaches to contact investigations in Texas. Int J Tuberc Lung Dis 2003;7:358-62.
- Yun LW, Reves RR, Reichler MR, Bur S, Thompson V, Mangura B, et al. Outcomes of contact investigation among homeless persons with infectious tuberculosis. Int J Tuberc Lung Dis 2003;7:405-11.
- Fitzpatrick LK, Hardacker JA, Heirendt W, Agerton T, Streicher A, Melnyk H, et al. A preventable outbreak of tuberculosis investigated through an intricate social network. Clin Infect Dis 2001;33:1801-6. https://doi.org/10.1086/323671.
- Sterling TR, Thompson D, Stanley RL, McElroy PD, Madison A, Moore K, et al. A multi-state outbreak of tuberculosis among members of a highly mobile social network: implications for tuberculosis elimination. Int J Tuberc Lung Dis 2000;4:1066-73.
- Curtis AB, Ridzon R, Novick LF, Driscoll J, Blair D, Oxtoby M, et al. Analysis of Mycobacterium tuberculosis transmission patterns in a homeless shelter outbreak. Int J Tuberc Lung Dis 2000;4:308-13.
- Cook VJ, Shah L, Gardy J. Modern contact investigation methods for enhancing tuberculosis control in aboriginal communities. Int J Circumpolar Health 2012;71. http://dx.doi.org/10.3402/ijch.v71i0.18643.
- Ospina JE, Orcau A, Millet JP, Sánchez F, Casals M, Caylà JA. Community health workers improve contact tracing among immigrants with tuberculosis in Barcelona. BMC Public Health 2012;12. http://dx.doi.org/10.1186/1471-2458-12-158.
- van Loenhout-Rooyacke JH, Sebek MM, Verbeek AL. Contact tracing using DNA fingerprinting in an asylum seeker with pulmonary tuberculosis. Neth J Med 2002;60:281-4.
- Mulder C, van Deutekom H, Huisman EM, Meijer-Veldman W, Erkens CG, van Rest J, et al. Coverage and yield of tuberculosis contact investigations in the Netherlands. Int J Tuberc Lung Dis 2011;15:1630-7. http://dx.doi.org/10.5588/ijtld.11.0027.
- Mulder C, Klinkenberg E, Manissero D. Effectiveness of tuberculosis contact tracing among migrants and the foreign-born population. Euro Surveill 2009;14.
- de Vries G, van Hest RA. From contact investigation to tuberculosis screening of drug addicts and homeless persons in Rotterdam. Eur J Public Health 2006;16:133-6. http://dx.doi.org/10.1093/eurpub/cki203.
- Identifying and Managing Tuberculosis among Hard-to-reach Groups. London: National Institute for Health and Care Excellence; 2012.
- Fox GJ, Barry SE, Britton WJ, Marks GB. Contact investigation for tuberculosis: a systematic review and meta-analysis. Eur Respir J 2013;41:140-56. http://dx.doi.org/10.1183/09031936.00070812.
- Control and Prevention of Tuberculosis in the United Kingdom: Code of Practice. London: British Thoracic Society; 2000.
- National Tuberculosis Controllers Association . Guidelines for the investigation of contacts of persons with infectious tuberculosis: recommendations from the National Tuberculosis Controllers Association and CDC. MMWR Recomm Rep 2005;54:1-47.
- Tuberculosis Clinical Policies and Protocols. New York, NY: New York City Department of Health and Mental Hygiene; 2008.
- Aissa K, Madhi F, Ronsin N, Delarocque F, Lecuyer A, Decludt B, et al. Evaluation of a model for efficient screening of tuberculosis contact subjects. Am J Respir Crit Care Med 2008;177:1041-7. http://dx.doi.org/10.1164/rccm.200711-1756OC.
- Anger HA, Proops D, Harris TG, Li J, Kreiswirth BN, Shashkina E, et al. Active case finding and prevention of tuberculosis among a cohort of contacts exposed to infectious tuberculosis cases in New York City. Clin Infect Dis 2012;54:1287-95. http://dx.doi.org/10.1093/cid/cis029.
- Ansari S, Thomas S, Campbell IA, Furness L, Evans MR. Refined tuberculosis contact tracing in a low incidence area. Respir Med 1998;92:1127-31. https://doi.org/10.1016/S0954-6111(98)90406-1.
- Bailey WC, Gerald LB, Kimerling ME, Redden D, Brook N, Bruce F, et al. Predictive model to identify positive tuberculosis skin test results during contact investigations. JAMA 2002;287:996-1002. https://doi.org/10.1001/jama.287.8.996.
- Banner P. Tuberculosis contact tracing within a school environment: lessons for the future. NSW Public Health Bull 2013;24:27-8. http://dx.doi.org/10.1071/NB12096.
- Bargman C, Reeves R, Parker M, Belknap R, Bettridge J, Bedell D, et al. Transmission of Mycobacterium tuberculosis in a High School and School-Based Supervision of an Isoniazid-Rifapentine Regimen for Preventing Tuberculosis – Colorado, 2011–2012. Atlanta, GA: Centers for Disease Control and Prevention; 2013.
- Behr MA, Hopewell PC, Paz EA, Kawamura LM, Schecter GF, Small PM. Predictive value of contact investigation for identifying recent transmission of Mycobacterium tuberculosis. Am J Respir Crit Care Med 1998;158:465-9. http://dx.doi.org/10.1164/ajrccm.158.2.9801062.
- Bock NN, Mallory JP, Mobley N, DeVoe B, Taylor BB. Outbreak of tuberculosis associated with a floating card game in the rural south: lessons for tuberculosis contact investigations. Clin Infect Dis 1998;27:1221-6. https://doi.org/10.1086/514986.
- Borgen K, Koster B, Meijer H, Kuyvenhoven V, van der Sande M, Cobelens F. Evaluation of a large-scale tuberculosis contact investigation in the Netherlands. Eur Respir J 2008;32:419-25. http://dx.doi.org/10.1183/09031936.00136607.
- Borraccino A, Migliore E, Piccioni P, Baussano I, Carosso A, Bugiani M. Yield of tuberculosis contact investigation in a low-incidence country. J Infect 2014;68:448-54. http://dx.doi.org/10.1016/j.jinf.2013.12.005.
- Borrell S, Espanol M, Orcau A, Tudo G, March F, Cayla JA, et al. Factors associated with differences between conventional contact tracing and molecular epidemiology in study of tuberculosis transmission and analysis in the city of Barcelona, Spain. J Clin Microbiol 2009;47:198-204. https://doi.org/10.1128/JCM.00507-08.
- Carbonne A, Poirier C, Antoniotti G, Burnat C, Delacourt C, Orzechowski C, et al. Investigation of patient contacts of heath care workers with infectious tuberculosis: 6 cases in the Paris area. Int J Tuberc Lung Dis 2005;9:848-52.
- Castilla J, Palmera R, Navascués A, Abeti M, Guillermo A, Irisarri F, et al. Population-based contact investigation of a cluster of tuberculosis cases in a small village. Epidemiol Infect 2009;137:1426-35. http://dx.doi.org/10.1017/S0950268809002246.
- Coleman MS, Marienau KJ, Marano N, Marks SM, Cetron MS. Economics of United States tuberculosis airline contact investigation policies: a return on investment analysis. Travel Med Infect Dis 2014;12:63-71. http://dx.doi.org/10.1016/j.tmaid.2013.10.016.
- Collins J, Schlager S, Brasher E. Contact investigation of a case of active tuberculosis. Am J Infect Control 2004;32:38-43. http://dx.doi.org/10.1016/j.ajic.2003.05.004.
- Cook VJ, Shah L, Gardy J, Bourgeois AC. Recommendations on modern contact investigation methods for enhancing tuberculosis control. Int J Tuberc Lung Dis 2012;16:297-305. http://dx.doi.org/10.5588/ijtld.11.0350.
- Cook VJ, Sun SJ, Tapia J, Muth SQ, Argueello DF, Lewis BL, et al. Transmission network analysis in tuberculosis contact investigations. J Infect Dis 2007;196:1517-27. https://doi.org/10.1086/523109.
- Davidow AL, Mangura BT, Wolman MS, Bur S, Reves R, Thompson V, et al. Workplace contact investigations in the United States. Int J Tuberc Lung Dis 2003;7:446-52.
- Diel R, Loddenkemper R, Meywald-Walter K, Gottschalk R, Nienhaus A. Comparative performance of tuberculin skin test, QuantiFERON-TB-Gold In Tube assay, and T-SPOT.TB test in contact investigations for tuberculosis. Chest 2009;135:1010-18. http://dx.doi.org/10.1378/chest.08-2048.
- Diel R, Meywald-Walter K, Gottschalk R, Rüsch-Gerdes S, Niemann S. Ongoing outbreak of tuberculosis in a low-incidence community: a molecular-epidemiological evaluation. Int J Tuberc Lung Dis 2004;8:855-61.
- Diel R, Nienhaus A, Lange C, Meywald-Walter K, Forssbohm M, Schaberg T. Tuberculosis contact investigation with a new, specific blood test in a low-incidence population containing a high proportion of BCG-vaccinated persons. Respir Res 2006;7. http://dx.doi.org/10.1186/1465-9921-7-77.
- Driver CR, Balcewicz-Sablinska MK, Kim Z, Scholten J, Munsiff SS. Contact investigations in congregate settings, New York City. Int J Tuberc Lung Dis 2003;7:432-8.
- Duarte R, Neto M, Carvalho A, Barros H. Improving tuberculosis contact tracing: the role of evaluations in the home and workplace. Int J Tuberc Lung Dis 2012;16:55-9. http://dx.doi.org/10.5588/ijtld.10.0511.
- Edelson PJ, Phypers M. TB transmission on public transportation: a review of published studies and recommendations for contact tracing. Travel Med Infect Dis 2011;9:27-31. http://dx.doi.org/10.1016/j.tmaid.2010.11.001.
- Erkens CG, Kamphorst M, Abubakar I, Bothamley GH, Chemtob D, Haas W, et al. Tuberculosis contact investigation in low prevalence countries: a European consensus. Eur Respir J 2010;36:925-49. http://dx.doi.org/10.1183/09031936.00201609.
- Faccini M, Cantoni S, Ciconali G, Filipponi MT, Mainardi G, Marino AF, et al. Tuberculosis-related stigma leading to an incomplete contact investigation in a low-incidence country. Epidemiol Infect 2015;143:2841-8. http://dx.doi.org/10.1017/S095026881400394X.
- Forssman B, Gupta L, Mills K. A tuberculosis contact investigation involving two private nursing homes in inner western Sydney in 2004. NSW Public Health Bull 2006;17:44-7.
- Funayama K, Tsujimoto A, Mori M, Yamamoto H, Fujiwara K, Nishimura T, et al. Usefulness of QuantiFERON TB-2G in contact investigation of a tuberculosis outbreak in a university. Kekkaku 2005;80:527-34.
- Funk EA. Tuberculosis contact investigations in rural Alaska: a unique challenge. Int J Tuberc Lung Dis 2003;7:349-52.
- Gaber KA, Maggs A, Thould G, Goldman JM. An outbreak of tuberculosis in the South West of England related to a public house. Prim Care Respir J 2005;14:51-5. http://dx.doi.org/10.1016/j.pcrj.2004.06.005.
- Gardy JL, Johnston JC, Ho Sui SJ, Cook VJ, Shah L, Brodkin E, et al. Whole-genome sequencing and social-network analysis of a tuberculosis outbreak. N Engl J Med 2011;364:730-9. http://dx.doi.org/10.1056/NEJMoa1003176.
- Gerald LB, Bruce F, Brooks CM, Brook N, Kimerling ME, Windsor RA, et al. Standardizing contact investigation protocols. Int J Tuberc Lung Dis 2003;7:369-74.
- Gerald LB, Tang S, Bruce F, Redden D, Kimerling ME, Brook N, et al. A decision tree for tuberculosis contact investigation. Am J Respir Crit Care Med 2002;166:1122-7. http://dx.doi.org/10.1164/rccm.200202-124OC.
- Greenaway C, Palayew M, Menzies D. Yield of casual contact investigation by the hour. Int J Tuberc Lung Dis 2003;7:479-85.
- Gulati M, Liss DJ, Sparer JA, Slade MD, Holt EW, Rabinowitz PM. Risk factors for tuberculin skin test positivity in an industrial workforce results of a contact investigation. J Occup Environ Med 2005;47:1190-9. https://doi.org/10.1097/01.jom.0000183098.29627.47.
- Guzzetta G, Ajelli M, Yang Z, Mukasa LN, Patil N, Bates JH, et al. Effectiveness of contact investigations for tuberculosis control in Arkansas. J Theor Biol 2015;380:238-46. http://dx.doi.org/10.1016/j.jtbi.2015.05.031.
- Higuchi K, Harada N, Mori T, Sekiya Y. Use of QuantiFERON-TB Gold to investigate tuberculosis contacts in a high school. Respirology 2007;12:88-92. http://dx.doi.org/10.1111/j.1440-1843.2006.01000.x.
- Jereb J, Etkind SC, Joglar OT, Moore M, Taylor Z. Tuberculosis contact investigations: outcomes in selected areas of the United States, 1999. Int J Tuberc Lung Dis 2003;7:384-90.
- Josaphat J, Dias JG, Salvador S, Resende V, Duarte R. Tuberculosis: which patients do not identify their contacts?. Rev Port Pneumol 2014;20:242-7. http://dx.doi.org/10.1016/j.rppneu.2013.11.004.
- Kasaie P, Andrews JR, Kelton WD, Dowdy DW. Timing of tuberculosis transmission and the impact of household contact tracing. An agent-based simulation model. Am J Respir Crit Care Med 2014;189:845-52. http://dx.doi.org/10.1164/rccm.201310-1846OC.
- Kawatsu L, Izumi K, Uchimura K, Urakawa M, Ohkado A, Takahashi I. Can social network analysis assist in the prioritisation of contacts in a tuberculosis contact investigation?. Int J Tuberc Lung Dis 2015;19:1293-9. http://dx.doi.org/10.5588/ijtld.15.0378.
- Kettunen CM, Sunmonu Y, Hodgkinson AL, Verzumo M, Belding-Braun K, Vaccariello P, et al. Contact investigation of a case of active tuberculosis in the community. Am J Infect Control 2007;35:421-4. http://dx.doi.org/10.1016/j.ajic.2006.08.008.
- Klovdahl AS, Graviss EA, Yaganehdoost A, Ross MW, Wanger A, Adams GJ, et al. Networks and tuberculosis: an undetected community outbreak involving public places. Soc Sci Med 2001;52:681-94. https://doi.org/10.1016/S0277-9536(00)00170-2.
- Kowada A. Cost effectiveness of high resolution computed tomography with interferon-gamma release assay for tuberculosis contact investigation. Eur J Radiol 2013;82:1353-8. http://dx.doi.org/10.1016/j.ejrad.2013.02.017.
- Lambregts-van Weezenbeek CS, Sebek MM, van Gerven PJ, de Vries G, Verver S, Kalisvaart NA, et al. Tuberculosis contact investigation and DNA fingerprint surveillance in the Netherlands: 6 years’ experience with nation-wide cluster feedback and cluster monitoring. Int J Tuberc Lung Dis 2003;7:463-70.
- Langenskiold E, Herrmann FR, Luong BL, Rochat T, Janssens JP. Contact tracing for tuberculosis and treatment for latent infection in a low incidence country. Swiss Med Wkly 2008;138:78-84. http://dx.doi.org/2008/05/smw-11964.
- Lobato MN, Royce SE, Mohle-Boetani JC. Yield of source-case and contact investigations in identifying previously undiagnosed childhood tuberculosis. Int J Tuberc Lung Dis 2003;7:391-6.
- Logan S, Boutotte J, Wilce M, Etkind S. Using the CDC framework for program evaluation in public health to assess tuberculosis contact investigation programs. Int J Tuberc Lung Dis 2003;7:375-83.
- MacIntyre CR, Plant AJ. Impact of policy and practice on the effectiveness of contact screening for tuberculosis. Prev Med 1998;27:830-7. https://doi.org/10.1006/pmed.1998.0366.
- Macintyre CR, Plant AJ, Hendrie D. The cost-effectiveness of evidence-based guidelines and practice for screening and prevention of tuberculosis. Health Econ 2000;9:411-21. https://doi.org/10.1002/1099-1050(200007)9:5<411::AID-HEC524>3.0.CO;2-9.
- MacLellan J, Wallace K, Vacchelli E, Roe J, Davidson R, Abubakar I, et al. A multi-perspective service evaluation exploring tuberculosis contact screening attendance among adults at a North London hospital. J Pub Health 2016;38:e362-7. http://dx.doi.org/10.1093/pubmed/fdv129.
- Mandal P, Craxton R, Chalmers JD, Gilhooley S, Laurenson IF, McSparron C, et al. Contact tracing in pulmonary and non-pulmonary tuberculosis. QJM 2012;105:741-7. http://dx.doi.org/10.1093/qjmed/hcs045.
- Marienau KJ, Cramer EH, Coleman MS, Marano N, Cetron MS. Flight related tuberculosis contact investigations in the United States: comparative risk and economic analysis of alternate protocols. Travel Med Infect Dis 2014;12:54-62. http://dx.doi.org/10.1016/j.tmaid.2013.09.007.
- Marks SM, Taylor Z, Qualls NL, Shrestha-Kuwahara RJ, Wilce MA, Nguyen CH. Outcomes of contact investigations of infectious tuberculosis patients. Am J Respir Crit Care Med 2000;162:2033-8. http://dx.doi.org/10.1164/ajrccm.162.6.2004022.
- Marra F, Marra CA, Sadatsafavi M, Morán-Mendoza O, Cook V, Elwood RK, et al. Cost-effectiveness of a new interferon-based blood assay, QuantiFERON-TB Gold, in screening tuberculosis contacts. Int J Tuberc Lung Dis 2008;12:1414-24.
- Andre M, Ijaz K, Tillinghast JD, Krebs VE, Diem LA, Metchock B, et al. Transmission network analysis to complement routine tuberculosis contact investigations. Am J Public Health 2007;97:470-7. http://dx.doi.org/10.2105/AJPH.2005.071936.
- Mohr O, Hermes J, Schink SB, Askar M, Menucci D, Swaan C, et al. Development of a risk assessment tool for contact tracing people after contact with infectious patients while travelling by bus or other public ground transport: a Delphi consensus approach. BMJ Open 2013;3. http://dx.doi.org/10.1136/bmjopen-2013-002939.
- Muecke C, Isler M, Menzies D, Allard R, Tannenbaum TN, Brassard P. The use of environmental factors as adjuncts to traditional tuberculosis contact investigation. Int J Tuberc Lung Dis 2006;10:530-5.
- Mulder C, Erkens CG, Kouw PM, Huisman EM, Meijer-Veldman W, Borgdorff MW, et al. Missed opportunities in tuberculosis control in the Netherlands due to prioritization of contact investigations. Eur J Public Health 2012;22:177-82. http://dx.doi.org/10.1093/eurpub/ckr017.
- Mulder C, Harting J, Jansen N, Borgdorff MW, van Leth F. Adherence by Dutch public health nurses to the national guidelines for tuberculosis contact investigation. PLOS ONE 2012;7. http://dx.doi.org/10.1371/journal.pone.0049649.
- Munk E, Maltas G, Dorman S, Johnson B, Johnson S, Taylor K, et al. Workplace-based investigation of contacts of a patient with highly infectious tuberculosis – Maryland, District of Columbia, and Virginia, 2006. JAMA 2008;300:276-8. https://doi.org/10.1001/jama.300.3.276.
- Pettit S, Black A, Stenton C, Black N. Outbreak of tuberculosis at a Newcastle public house: the role and effectiveness of contact screening. Commun Dis Public Health 2002;5:48-53.
- Pisu M, Gerald J, Shamiyeh JE, Bailey WC, Gerald LB. Targeted tuberculosis contact investigation saves money without sacrificing health. J Public Health Manag Pract 2009;15:319-27. http://dx.doi.org/10.1097/PHH.0b013e31819c3ef2.
- Reichler MR, Reves R, Bur S, Thompson V, Mangura BT, Ford J, et al. Evaluation of investigations conducted to detect and prevent transmission of tuberculosis. JAMA 2002;287:991-5. https://doi.org/10.1001/jama.287.8.991.
- Rodriguez EM, Steinbart S, Shaulis G, Bur S, Dwyer DM. Pulmonary tuberculosis in a high school student and a broad contact investigation: lessons relearned. Md Med J 1996;45:1019-22.
- Ruben FL, Lynch DC. Tuberculosis control through contact investigation. Pa Med 1996;99:22-3.
- Rubilar M, Brochwicz-Lewinski MJ, Anderson M, Leitch AG. The outcome of contact procedures for tuberculosis in Edinburgh, Scotland 1982–1991. Respir Med 1995;89:113-20. https://doi.org/10.1016/0954-6111(95)90193-0.
- Sanderson JM, Proops DC, Trieu L, Santos E, Polsky B, Ahuja SD. Increasing the efficiency and yield of a tuberculosis contact investigation through electronic data systems matching. J Am Med Inform Assoc 2015;22:1089-93. http://dx.doi.org/10.1093/jamia/ocv029.
- Saunders MJ, Koh GC, Small AD, Dedicoat M. Predictors of contact tracing completion and outcomes in tuberculosis: a 21-year retrospective cohort study. Int J Tuberc Lung Dis 2014;18:640-6. http://dx.doi.org/10.5588/ijtld.13.0486.
- Shah NS, Yuen CM, Heo M, Tolman AW, Becerra MC. Yield of contact investigations in households of patients with drug-resistant tuberculosis: systematic review and meta-analysis. Clin Infect Dis 2014;58:381-91. http://dx.doi.org/10.1093/cid/cit643.
- Shrestha-Kuwahara R, Wilce M, DeLuca N, Taylor Z. Factors associated with identifying tuberculosis contacts. Int J Tuberc Lung Dis 2003;7:510-16.
- Sprinson JE, Flood J, Fan CS, Shaw TA, Pascopella L, Young JA, et al. Evaluation of tuberculosis contact investigations in California. Int J Tuberc Lung Dis 2003;7:363-8.
- Stoddart H, Noah N. Usefulness of screening large numbers of contacts for tuberculosis: questionnaire based review. BMJ 1997;315. https://doi.org/10.1136/bmj.315.7109.651.
- Tian Y, Osgood ND, Al-Azem A, Hoeppner VH. Evaluating the effectiveness of contact tracing on tuberculosis outcomes in Saskatchewan using individual-based modeling. Health Educ Behav 2013;40:98-110. http://dx.doi.org/10.1177/1090198113493910.
- Trieu L, Proops DC, Ahuja SD. Using QuantiFERON-TB Gold In-Tube for field-based tuberculosis contact investigations in congregate settings. J Public Health Manag Pract 2013;19:E11-13. http://dx.doi.org/10.1097/PHH.0b013e318268af0b.
- Underwood BR, White VL, Baker T, Law M, Moore-Gillon JC. Contact tracing and population screening for tuberculosis – who should be assessed?. J Public Health Med 2003;25:59-61.
- Ward LJ, Hughes SE, Grabau JC. The evaluation of school-based contact investigations in New York State, exclusive of New York City, 1997–2001. J Public Health Manag Pract 2004;10:308-15. https://doi.org/10.1097/00124784-200407000-00007.
- Wilce M, Shrestha-Kuwahara R, Taylor Z, Qualls N, Marks S. Tuberculosis contact investigation policies, practices, and challenges in 11 U.S. communities. J Public Health Manag Pract 2002;8:69-78. https://doi.org/10.1097/00124784-200211000-00010.
- Yeo IK, Tannenbaum T, Scott AN, Kozak R, Behr MA, Thibert L, et al. Contact investigation and genotyping to identify tuberculosis transmission to children. Pediatr Infect Dis J 2006;25:1037-43. https://doi.org/10.1097/01.inf.0000241101.12510.3c.
- Zangger E, Gehri M, Krähenbühl JD, Zuberbühler D, Zellweger JP. Epidemiological and economical impact of tuberculosis in an adolescent girl in Lausanne (Switzerland). Swiss Med Wkly 2001;131:418-21. http://dx.doi.org/2001/27/smw-09757.
Appendix 1 Sample MEDLINE search and results by database
Search strategy
-
contact tracing.ti,ab.
-
contact investigation*.ti,ab.
-
(case finding or case finding).ti,ab.
-
case detect*.ti,ab.
-
contact examin*.ti,ab.
-
contact screen*.ti,ab.
-
contact procedur*.ti,ab.
-
close contact*.ti,ab.
-
1 or 2 or 3 or 4 or 5 or 6 or 7 or 8
-
Tuberculosis/
-
TB.ti,ab.
-
tuberculosis.ti,ab.
-
10 or 11 or 12
-
9 and 13
-
limit 14 to (English language and humans and yr=“1995 –Current”
Results by database
| First stage | Second stage |
|---|---|
| Cumulative Index to Nursing and Allied Health Literature via EBSCOhost: 332 | Cumulative Index to Nursing and Allied Health Literature via EBSCOhost: 39 |
| Science and Social Science Citation Indices via Web of Science: 581 | Science and Social Science Citation Indices via Web of Science: 32 |
| The Cochrane Library via Wiley Online Library: 33 | The Cochrane Library via Wiley Online Library: 8 |
| MEDLINE via Ovid SP: 1929 | MEDLINE via Ovid SP: 189 |
| EMBASE via Ovid SP: 2341 | EMBASE via Ovid SP: 175 |
| PsycINFO via Ovid SP: 35 | PsycINFO via Ovid SP: 37 |
| EconLit via Ovid SP: 3 | EconLit via Ovid SP: 0 |
| Social Policy and Practice via Ovid SP: 1 | Social Policy and Practice via Ovid SP: 1 |
Appendix 2 Extraction table for specific population studies
| Details of study | Methods | Results | Conclusions |
|---|---|---|---|
| Ashgar et al., 200919 | |||
| Type of document: journal article Study design: describes interviews with patients during a contact-tracing investigation, together with providing other routine data collected during the investigation Country: USA Population: 18 patients with TB living in a low-income area of Miami, FL, black non-Hispanic, frequented ‘crack house’, mostly HIV positive Quality comments: the data relate to the number of contacts identified and the test results, rather than qualitative data in the form of interview text |
Research methods: review of medical records and patient interviews Staff involved: N/A Measures used: TST and genotyping |
Results/data: patients were reluctant to name contacts. One patient attended a church and a dialysis centre Genotyping suggested more than one chain of transmission Repeated interviews resulted in an average of fives names per person. Skin tests were offered to observed persons at the crack house and at the named locations 9% of named contacts had positive TST results, 68% of observed contacts had positive TST results and 10–12% from the named locations had positive results. Observed contacts were 7.8% more likely than named contacts to have positive results. There was no difference in the likelihood of a positive result between named locations vs. named contacts |
Main conclusions: site visits and identification of observed contacts are likely to lead to a higher yield of contacts at risk of future TB than named contacts in this population |
| Bur et al., 20035 | |||
| Type of document: journal article Study design: report of a contact investigation Country: USA Setting: urban community with high rate of drug abuse and prison. An inmate who had spent time in prison and in the community Quality comments: the study provides general narrative about how the investigation was carried out, with the main data relating to numbers screened and test results |
Research methods: description of process and outcomes Staff involved: prison staff (required around 250 hours of staff time) and health department staff Measures used: TST and DNA fingerprinting |
Results/data: investigation used a ‘concentric circles’ approach, whereby evaluation was performed among closest contacts and those most at risk of progression to active disease. If the inner circle infection rate exceeds that expected for the population then investigation proceeds to wider circle (less exposure). All inmates housed with the case were initially screened; this was widened to all inmates Contact interviews elicited 10 names of the 67 contacts ultimately identified. Other community contacts were identified by observation of health staff while present in location carrying out screening. Community screening for a subset of inmates released resulted in only a 5% yield and was abandoned for other released inmates. A high proportion of infected contacts did not complete treatment (more than half of community and fewer than one-third of inmates) Eighteen cases identified, 11 in the community and six in prison. All named community contacts were TST positive. 41% of inmates housed with case were TST positive, 20% of all inmates Collaboration between health department and prison described as key to success. Also access to accurate records for inmates |
Main conclusions: observation in the community was an important means of identifying contacts There was a large proportion of infected contacts who did not complete treatment |
| Cook et al., 201225 | |||
| Type of document: journal article Study design: descriptive Country: Canada Population: Aboriginal communities Quality comments: few data to support a general description |
Research methods: descriptive only Staff involved: nurses/health-care workers Measures used: description |
Results/data: describes the limitations of conventional contact investigation, which relies on a person knowing all of their contacts and being willing to share names. There were issues with highly mobile persons, non-household environments, casual contacts, level of experience of workers in taking histories, resource shortages and long lists of contacts. In particular in Aboriginal communities there are issues of community isolation, language, cultural barriers and social stigma Describes the use of social network analysis (identifies how cases are connected to each other), geographic information systems (to visualise data involving distance and location) and genomics (such as DNA fingerprinting) to identify transmission events, individuals acting as spreaders and confirm relations between outbreaks |
Main conclusions: describes the limitations of interviewing and naming contact methods; suggests the potential of alternative/supplementary approaches |
| Curtis et al., 200024 | |||
| Type of document: journal article Study design: describes a contact investigation in a homeless shelter Country: USA Population: resident men of a homeless shelter, visitors and staff (n = 257) Quality comments: the study provides a general narrative about how the investigation was carried out, with the main data relating to numbers screened and test results |
Research methods: description of the investigation around 10 cases of TB Staff involved: unclear Measures used: TST, DNA fingerprinting, chest radiography and clinical assessment |
Results/data: 70% of shelter users and staff had a positive TST Seven of the 10 cases had identical DNA fingerprints; eight cases were considered related The believed source case was a long-term resident who had a previous history of TB and had been referred to hospital for a severe cough but had refused to go Environmental assessment revealed minimal ventilation, with the air handling unit and exhaust fans working poorly. Smoke tube testing showed that air at bed level moved little or travelled horizontally between beds |
Main conclusions: a high degree of suspicion of TB should be maintained Shelter users should be screened prior to admission Prompt screening should be implemented when cases are detected Efficient ventilation systems should be in place Additional effort should be made to treat the population |
| Dasgupta et al., 200518 | |||
| Type of document: journal article Study design: review and cost-effectiveness analysis Country: Canada Population: immigrants and refugees to low-incidence countries Quality comments: a reasonably robust review, although only one database was searched |
Research methods: search of MEDLINE and reference list screening Staff involved: N/A Measures used: any reported |
Results/data: in low-incidence countries the public health impact of TB in foreign-born persons is modest (estimates of 2%, 11% or 17% of active TB cases in general population that can be attributed to transmission from the foreign born). Reports evidence of the cost-effectiveness of contact-tracing programmes with CA$815 saving on hospital care per active case detected, and CA$600 of saving per active case prevented due to detection of latent infection | Main conclusions: global TB control would reduce the risk of TB among human migrants Contact tracing, particularly in ethnic communities, appears to be more effective and less intrusive than screening |
| de Vries and van Hest, 200630 | |||
| Type of document: journal article Study design: describes a contact investigation for a single case Country: the Netherlands Population: drug addicts and homeless persons/frequenters of homeless shelters, staff of mental health service Quality comments: the study provides a general narrative about how the investigation was carried out, with the main data relating to numbers screened and test results |
Research methods: description of the process and outcomes Staff involved: TB physician for mobile radiography; others unclear Measures used: TST, chest radiography and DNA fingerprinting |
Results/data: 20% of those examined using TST (staff and visitors to three homeless shelters and staff of mental health service) in first round had latent TB. A second round checked residents at the homeless shelters using TST or mobile digital radiography 507 persons were assessed, 127 using TST, with 28 (18 staff members and 10 shelter residents) found to have latent TB. 380 were examined by radiography, with six found to have active TB and four found to have latent TB Testing with DNA fingerprinting indicated that none of the other TB cases had the same DNA fingerprint as the original case. This finding underpinned the decision to reintroduce a screening programme for drug users/methadone users/homeless persons |
Main conclusions: the authors recommend the use of mobile radiography for difficult-to-reach TB groups. They describe the value of molecular technologies for recognising patterns. The overlap between contact investigation and screening was highlighted |
| Fitzpatrick et al., 200122 | |||
| Type of document: journal article Study design: description of an investigation Country: USA Population: a community in Indiana, described as a difficult-to-reach population. 31 patients with TB Quality comments: the study provides a general narrative about how the investigation was carried out, with the main data relating to numbers screened and test results. Although some interviews were carried out, there are no qualitative data |
Research methods: describes the process and outcomes of the contact investigation during an outbreak using social network methods. Retrospective review of records and interviews with patients who were still available Staff involved: public health nurses Measures used: TST and chest radiography |
Results/data: no source patient was identified who accounted for all of the outbreak cases. One potentially accounted for 71% (22) Only eight individuals initially provided the names of contacts with TB. Retrospective questioning revealed that 29 of known outbreak cases knew another case either indirectly or directly Transmission seemed to have occurred in congregate social settings (an apartment complex, a junkyard, a local bar, a liquor store). These were named by patients as locations of frequent social gathering to take drugs and alcohol Six persons with symptoms were not correctly diagnosed with TB. Health department personnel were not trained in TB control, resulting in persons being screened (named contacts and colleagues) who were not those at highest risk |
Main conclusions: the authors conclude that a social network approach would have been beneficial to identify contacts in similar social settings and halt the outbreak earlier, as there was a failure to consider unnamed contacts |
| Kline et al., 199516 | |||
| Type of document: journal article Study design: descriptive Country: USA Population: frequenters of a bar. The index patient was a homeless person (n = 97 contacts, including four staff and 93 customers). Most of the participants ‘used alcohol excessively’ Quality comments: the study provides general narrative about how the investigation was carried out, with the main data relating to numbers screened and test results |
Research methods: describes the contact investigation Staff involved: unclear Measures used: TST, chest radiography, clinical examination and RFLPs |
Results/data: the index patient supplied a few named contacts, but reported that most of the time he had been unwell had been spent at a bar and nearby rooming house. The investigation therefore targeted bar staff and customers. 14 cases of active TB and 27 latent infection were detected. In most cases the bar was the only site where there was any contact with the index patient Four people were later identified with active TB who had been missed by the investigation (they had been unwilling/unable to take part), and two further cases of active TB linked to bar frequenters were later identified RFLP fingerprinting proved useful to supplement the investigation by proving linkages between cases Of the 39 people with positive TSTs, 19 attended follow-up appointments. Of these, 13 contacts refused prophylaxis or did not complete their treatment. Three of these progressed to active TB. In addition, 13 other TST positive contacts did not attend for follow-up appointments for chest radiography and, of these, two cases progressed to active TB |
Main conclusions: the authors suggested that initial infection may progress to active disease more frequently in heavy alcohol users, although the high infectivity of the index patient may have been a significant factor Chronic alcoholism is a high-risk factor for progression to active disease and major efforts to ensure the completion of 6 months of isoniazid therapy are worthwhile |
| Li et al., 200312 | |||
| Type of document: journal article Study design: retrospective analysis of data Country: USA Population: homeless persons (n = 152 patients of 2988 patients investigated) Quality comments: the study provides a general narrative about how the investigation was carried out, with the main data relating to numbers screened, contacts identified and test results |
Research methods: TB cases identified from surveillance data 1997–9 Staff involved: not reported Measures used: bacteriologically confirmed cases of pulmonary TB |
Results/data: 48.8% of patients had four or more contacts identified, 38.7% had one to three contacts, and 12.5% had no contacts. The median number of contacts per patient was three (range 0–64). Homeless patients were more likely to be male, non-Hispanic black, US-born, unemployed, and alcohol or drug abusers, be infected with HIV and have mental illness. Homeless patients were more likely to have been lost to follow-up prior to treatment completion. The number of contacts identified per homeless patient was significantly lower than for non-homeless patients (median 1 vs. 4, p < 0.001; mean 2.7 vs. 4.8, p < 0.001). Homeless patients were four times more likely to have no contacts identified (p < 0.001) | Main conclusions: strategies for contact elicitation among homeless patients should be different from those applied to non-homeless patients Greater knowledge is needed of the barriers to contact identification and better approaches to contact investigation among homeless patients. Strategies focused on identifying the location of exposure rather than on eliciting names of contacts is one approach that may be useful among homeless patients Being homeless at the time of diagnosis should be used as an indicator for prioritising prompt contact evaluation |
| Lofy et al., 200613 | |||
| Type of document: journal article Study design: descriptive Country: USA Population: residents of homeless shelters (n = 1000 contacts at 10 shelters) Quality comments: the study provides a general narrative about how the investigation was carried out, with the main data relating to numbers screened and test results |
Research methods: describes the outbreak in 2002 and the contact investigation surrounding patients Staff involved: health department staff Measures used: TST and chest radiography |
Results/data: transmission occurred over a short period, in multiple settings, rather than in a single homeless facility A questionnaire was used to elicit the names of contacts and places where patients slept, worked, travelled, sought health care, ate, used drugs and spent time during their infectious period. Intake logs from facilities frequented by infectious patients were reviewed to quantify the time they spent in each facility while infectious Facilities visited by infectious patients were prioritised for TB screening based on the number of infectious patients who visited the facilities and the prevalence of positive TST results compared with other homeless sites When attendance records were available, these were used to identify clients who were in that location. If no records were available, staff were asked for the names of contacts. Contacts were prioritised for screening based on their cumulative number of exposed visits. Screening contacts with one sputum culture was as sensitive as chest radiography in detecting TB disease (77% vs. 62%) Network analysis and genotyping were used to explore and map clusters The median number of named contacts was 3.5 (mean 4.8) per patient. Six (14%) of index patients named no contacts. Sixty-nine per cent of contacts began treatment for latent infection |
Main conclusions: a comprehensive, resource-intensive approach is needed to control transmission in large TB outbreaks |
| Malakmadze et al., 200517 | |||
| Type of document: journal article Study design: descriptive Country: USA Population: Wisconsin (patients, n = 26; contacts, n = 292). Described as ‘hard to reach’ and having risk factors of alcohol abuse, crack cocaine use, homelessness and unemployment |
Research methods: patients were reinterviewed and the places patients frequented while they were infectious were visited to identify contacts. Genotyping was used and the findings compared with those of the original investigation Staff involved: unclear Measures used: TST, chest radiography, genotyping (spoligotyping, mycobacterial interspersed repetitive units and IS6110 RFLP) and epidemiological links |
Results/data: the new investigation revealed several previously unrecognised locations of transmission: a single-room occupancy hotel, two homeless shelters, a bar and two crack houses. Prior to the further investigation, epidemiologic links were known for 8 of the 26 patients. The investigation revealed 29 previously unsuspected epidemiologic links among 17 other patients. Epidemiologic links were identified for all cases but one. Using genotyping methods, an additional 98 contacts were identified who had been missed during routine contact investigation 95% of previously identified contacts had been tested; 16% of these were TST positive and 90% completed treatment. Of the 98 additional contacts identified, 31% were tested, 17% (5) were TST positive and two began treatment (three refused) |
Main conclusions: universal genotyping revealed unsuspected TB transmission and previously unrecognised sites of transmission A policy of genotyping isolates from all (not just some) patients with culture-positive TB is required to successfully identify clusters Genotyping should be used alongside other methods of contact tracing and can aid the detection of unapparent transmission before an increase in incidence, and thus will help to identify clusters earlier |
| McElroy et al., 200314 | |||
| Type of document: journal article Study design: description of an investigation Country: USA Population: an area with low incidence of TB; however, drug use and drug sharing is common among cases and contacts Quality comments: the main data relate to a description of how the network was established |
Research methods: describes the process and outcomes of the contact investigation during an outbreak using social network methods, including network questionnaire interviews Staff involved: unclear Measures used: TST, network questionnaire and DNA fingerprinting |
Results/data: network visualisation illustrated the complexity of interactions among the cases and contacts. The graph established (with two exceptions) the potential for contact between each case and at least one other case; a link to strip clubs was established as a connection among all cases | Main conclusions: the authors conclude that network analysis can clarify connections among cases and people with latent TB who would not be identified using traditional methods. Also that network analysis can identify patterns in behaviours in a group that may help to identify subgroups |
| McElroy et al., 20037 | |||
| Type of document: journal article Study design: retrospective review of data Country: USA Population: homeless shelter residents (n = 620) and shelter employees (n = 26) Quality comments: the study provides a general narrative about how the investigation was carried out, with the main data relating to numbers screened and test results |
Research methods: homeless shelter attendance and medical records 1999–2000 reviewed. Shelter attendance records, collected at nightly check-in, included name, age, ethnicity and specific dates of overnight stays. Dates spent in prison were obtained and employment records from labour agencies were examined Staff involved: radiologists, nurse, others unclear Measures used: TST, on-site chest radiography and DNA fingerprinting |
Results/data: duration of exposure was significantly associated with likelihood of infection Those spending 115–153 nights in the shelter had a 3.5 times greater risk of having a positive TST result than those spending fewer than 38 nights Of the 119 individuals identified with latent infection, 22% began the treatment course and 14% successfully completed it HIV co-infection is an important factor contributing to the clustering of TB cases At least half of the outbreak patients either had spent time in prison or had visited the local sexually transmitted disease clinic in the prior 2-year period. If testing had been carried out at these, infection might have been detected DNA fingerprinting may be useful to detect previously unrecognised links among cases. It may be a useful impetus to further question a patient regarding routine, contacts and places frequented to uncover social networks There is a need for improved strategies for ensuring the initiation and successful completion of treatment for latent infection among the homeless |
Main conclusions: earlier recognition of the homeless shelter as a main site of transmission might have been facilitated by the use of DNA fingerprinting |
| Mulder et al., 200929 | |||
| Type of document: journal article Study design: systematic review Country: the Netherlands and Sweden Population: migrants and those born abroad Quality comments: this systematic review was carried out to a reasonable standard |
Research methods: review of effectiveness of contact tracing for foreign born vs. natives exposed to a foreign-born case Staff involved: not reported Measures used: effectiveness measures included were coverage, TB yield, latent TB yield and contacts-to-index case ratio. The study considered transmission rates and outcomes for foreign born compared with native, European vs. non-European studies, and whether or not closeness of contact affected effectiveness |
Results/data: no papers using randomised design were found; 18 reported yield or coverage and were included in the review (six related to European Union coverage) The strategies and context of contact tracing across studies differed considerably. The setting, infectiousness of the source case, and media interest were influential factors. Six studies used the ‘stone in the pond’ principle, three used workplace contacts only, two studies screened only close contacts, one used only household contacts and for the remaining six the approach was unclear |
Main conclusions: foreign-born contacts have a higher median latent TB infection yield than local-born exposed to the same foreign-born case. This may be due to higher background rates in this population. Contact tracing may, therefore, be considered a form of screening Large variation between studies, and no difference in yield of infected contacts from foreign-born index cases vs. whole population index cases Different strategies are needed for different circumstances |
| Mulder et al., 201128 | |||
| Type of document: journal article Study design: analysis of records Country: the Netherlands Population: immigrants Quality comments: the main data relate to test results of those screened |
Research methods: data extracted from patient records Staff involved: N/A Measures used: number of contacts investigated |
Results/data: close contacts of immigrant patients were significantly less likely than Dutch patients to be screened for TB (89% vs. 93%) or infection (50% vs. 75%), although the yield for infection and disease was higher (1.5% vs. 0.4% and 13% vs. 10%, respectively) | Main conclusions: the effectiveness of contact tracing could be optimised by ensuring complete investigation in the immigrant population |
| National Institute for Health and Care Excellence, 201231 | |||
| Type of document: guidance Study design: guidance based on evidence reviews Country: UK Population: hard-to-reach groups Quality comments: guidelines based on commissioned high-quality reviews of the literature |
Research methods: based on reviews of evidence and expert consultation. Draws on Matrix Evidence report Staff involved: TB teams, public health units Measures used: any |
Results/data: the guidance recommends that teams should co-ordinate investigations at places where the index case spends a significant amount of time There should be partnership working between health and social care, voluntary, community and statutory organisations Peer educators should be involved when possible Digital mobile radiography units should be considered in places where there are large numbers of at-risk people Strain typing and social network analysis should be used to explore where transmission is occurring with a focus on active case finding in these settings People in contact with children who have active TB (close and wider contacts) should be traced to identify the source |
Main conclusions: investigation of locations is important Partnership working is required Use of peer educators can be valuable |
| Oeltmann et al., 200615 | |||
| Type of document: journal article Study design: descriptive Country: USA Population: illicit-drug users; mean age 22 years (patients, n = 11; contacts, n = 22) Quality comments: the study provides general narrative about how the investigation was carried out, with the main data relating to test results |
Research methods: describes the investigation Staff involved: outreach workers Measures used: TST, chest radiography |
Results/data: all reported frequent ‘hotboxing’, the practice of smoking marijuana with others in a vehicle with the windows closed so that exhaled smoke is repeatedly inhaled The risk of a positive TST result was 2.8 times greater among friends than among other contacts (95% CI 1.3 to 6.0) There was a reluctance to name contacts at risk and the locations that were frequented. Workers had to arrange meetings at times and locations convenient to the group. Outreach workers needed to establish trust in order to gain co-operation. Screenings took place in varying locations, including street corners and in car parks. Often outreach workers were successful only after spending hours driving throughout the community searching for patients and contacts |
Main conclusions: alternative strategies to name-based contact investigations are important |
| Ospina et al., 201226 | |||
| Type of document: journal article Study design: evaluation of an intervention Country: Spain Population: immigrant communities Quality comments: this is the only study that endeavours to evaluate an intervention using an uncontrolled ‘before and after’ design. The main data relate to numbers screened and test results. There are few data regarding the precise nature of the community worker intervention |
Research methods: compared the 2-year intervention period with the 2-year pre-intervention period Staff involved: community health workers trained in TB and psychosocial skills Measures used: number of TB cases detected |
Results/data: the increase in contact tracing coverage during the intervention period was statistically significant. Pre-intervention contact tracing was performed on 65%, compared with 81.6% during the intervention period (p < 0.001). Factors which were associated with contact tracing not being performed were being diagnosed in a hospital without contact tracing, being born in India/Pakistan/North Africa, having an unknown residence, being HIV infected and being homeless | Main conclusions: the authors recommend the use of community health workers to improve the effectiveness of contact tracing. They describe the key elements of the role as being interpreters, being intercultural mediators and undertaking community actions to reinforce patient response |
| Rizzo et al., 20119 | |||
| Type of document: report Study design: systematic review Country: UK Population: hard-to-reach groups Quality comments: systematic review that underpinned the NICE guidelines31 |
Research methods: review of the effectiveness and cost-effectiveness of identification and management of TB in hard-to-reach groups Staff involved: N/A Measures used: any |
Results/data: included 32 studies. Tracing household contacts of foreign-born cases appeared to be cost-effective but not for those who are not household contacts (evidence from two studies). The cost-effectiveness of active screening compared with passive case detection is uncertain. Using incentives to increase take-up of TSTs and further investigation is effective and cost-effective in drug users and homeless populations The use of peers can help to identify contacts among drug users and improve screening rates among homeless populations Concerns about death and stigma prevent many people being tested |
Main conclusions: in hard-to-reach or at-risk populations, an active approach to case finding is recommended The use of monetary incentives is recommended |
| Sterling et al., 200023 | |||
| Type of document: journal article Study design: description Country: USA Population: described as being highly mobile, predominantly young (median age 24 years), black, male, infected with HIV, and gay, transvestite or transsexual Quality comments: the study provides a general narrative about how the investigation was carried out, with the main data relating to numbers screened and test results |
Research methods: describes the management of a TB outbreak Staff involved: community workers, nurses Measures used: contacts identified, numbers tested |
Results/data: combined naming contacts with visits to the home of the source case. Also work-site screenings. Also included location-based screening at a nightclub frequented by source cases A community outreach worker was used to facilitate contacts with members of the community Community awareness was enhanced by distributing letters to clinics and placing flyers in clubs |
Main conclusions: only 14 of the 114 contacts (12%) were named by cases. Others were identified via location-based Screening or observation, or referrals from HIV clinics or community workers |
| van Loenhout-Rooyacke et al., 200227 | |||
| Type of document: journal article Study design: analysis of data Country: the Netherlands Population: asylum seekers. Contacts of a person found to have TB on entry compulsory TB screening Quality comments: data from an ongoing longitudinal study relating to numbers screened and test results |
Research methods: data from the DNA Fingerprinting Surveillance Project Staff involved: TB nurse Measures used: chest radiography, clinical symptoms |
Results/data: conventional tracing uses the ring principle (close contacts from same facilities or same procedures from native country screened first; if high infection rate then screen shelter employees/visitors/those moved to other shelters). Infection rate of 60% in first ring (five people) and 10.5% in second (among staff/visitors). Four cases among asylum seekers were later identified as originating from the index case Over a 2-year period regular contact tracing identified a suspected link between patients in 22% of cases. Using DNA fingerprinting techniques a definite link was made in 26% of cases and a probable link in a further 21% |
Main conclusions: DNA fingerprinting may detect the late transmission of infection after conventional contact tracing has been completed, and identifies links that are not found by regular contact tracing |
| Wallace et al., 200320 | |||
| Type of document: journal article Study design: description Country: USA Population: describes how practices may be customised to different populations including foreign born, prisoners, homeless Quality comments: the authors report carrying out interviews and group discussions with field workers and programme managers, although the data are purely descriptive |
Research methods: qualitative Staff involved: unclear Measures used: none |
Results/data: aspects such as culture, language, risk factors and different settings may lead to a requirement for different approaches to conventional contact tracing. Reports the use of different assessments in USA vs. Mexico (TSTs vs. symptom screening). Highlights investigations carried out by different agencies for inmates vs. their contacts outside the prison. Describes the use of photographs for contact investigation among the homeless, as nicknames and aliases may be used. Importance of registers in homeless shelters. Describes the use of TSTs screening of all residents in homeless shelters | Main conclusions: need for customised approach for different population groups |
| Yun et al., 200321 | |||
| Type of document: journal article Study design: description Country: USA Population: homeless Quality comments: the study provides general narrative about how the investigation was carried out, with the main data relating to numbers screened and test results |
Research methods: retrospective review of notes on investigations Staff involved: unclear Measures used: numbers screened and/or completed treatment |
Results/data: only 27 (44%) of 61 contacts completed treatment for latent TB infection. Contacts living in shelters were less likely to be contacted than non-shelter contacts. 18% of contacts were not evaluated | Main conclusions: there was a failure to identify contacts in some cases, although a large number of contacts were traced |
Appendix 3 Extraction table for wider population studies
| Detail of study | Methods | Results | Conclusions |
|---|---|---|---|
| Aissa et al., 200836 | |||
| Type of document: journal article Study design: cohort study Country: France Population: individuals over 15 living in the environment of a patient with pulmonary TB and who were culture-positive. Mean age 41.5 years; 325 index cases and 2009 contacts (1575 completed screening) Quality notes: provides statistical analysis to support conclusions |
Research methods: participants enrolled over an 18-month period for the first cohort and over a 12-month period for the second cohort. Aim to develop and evaluate a model for TB contact screening Staff involved: N/A Measures used: physical examination, TST and chest radiograph |
Results/data: the mean number of contacts per case was 6 (1–122). 98% were BCG vaccinated. Overall infection rate for contacts who completed screening was 27%, 1% active and 26% latent infection Risk of TB infection in a contact was significantly related to receiving free health care (p = 0.005; OR 2, 95% CI 1.2 to 3.2) and also the contact being a smoker (p = 0.021; OR 1.6, 95% CI 1.1 to 2.4). High incidence of TB in country of birth was significantly associated with risk of infection (p < 0.0001; OR 2.2, 95% CI 1.5 to 3.2) Risk of infection was strongly associated with number of hours spent with index case, closeness of contact (at night: p = 0.0009; OR 2.1, 95% CI 1.3 to 3.3) and being a first-degree relative (p = 0.001; OR 2.1, 95% CI 1.3 to 3.3). Infectiousness of index case also important |
Main conclusions: a number of risk factors are associated with likelihood of infection A significant proportion of infections may not be due to recent exposure |
| Anger et al., 201237 | |||
| Type of document: journal article Study design: cohort Country: USA Population: Contacts (n = 30,561) diagnosed as having active TB who had been identified during previous investigations of 5182 TB cases. Aged > 5 years. 1% HIV infected, 56% non-household exposure. 39% not USA born Quality notes: provides statistical analysis to support conclusions |
Research methods: TB registry in New York used to identify contacts during previous investigations over a 6-year period. Followed up, up to 4 years later Staff involved: N/A Measures used: TST, chest radiography for contacts with symptoms or positive TST results |
Results/data: 48% completion rate for chemoprophylaxis Latent TB infection was diagnosed in 79% of contacts who initiated chemoprophylaxis, and 61% who later completed treatment, and 39% who did not complete treatment Highlights the limitations of using the TST to diagnose latent TB infection (TST can produce false-positive results for individuals who have received the BCG vaccine). IGRAs may better prioritise chemoprophylaxis for those with greater risk of TB. In addition, uptake and completion of chemoprophylaxis may be higher when latent TB infection is diagnosed with IGRAs The absolute risk reduction afforded by chemoprophylaxis initiation was estimated to be 1.1% (95% CI 0.6% to 1.9%). This equates to approximately 88 contacts needing to be treated in order to prevent one case of TB (95% CI 53 to 164) |
Main conclusions: estimate of 102 contacts need to be evaluated per prevalent case diagnosed (95% CI 90 to 115) Contacts who completed chemoprophylaxis had the lowest incidence, although those who initiated and did not complete also had decreased incidence compared with contacts who did not initiate treatment Contact screening is therefore effective, even when completion rates are below ideal levels |
| Ansari et al., 199838 | |||
| Type of document: journal article Study design: before and after comparative Country: UK Population: residents of South Glamorgan (index cases, n = 103 + n = 103; close contacts, n = 611 + n = 732) Quality notes: provides descriptive statistics only to support conclusions |
Research methods: compared data from the TB contact tracing clinic, the Public Health Service Mycobacterium Reference Unit and the Consultant in Communicable Diseases Control, South Glamorgan Health Authority, at two time points: before and after a change to the contact-tracing protocol Staff involved: chest clinic staff Measures used: Heaf’s test and chest radiography |
Results/data: previously close contacts had been invited for follow-up annual radiological surveillance. In the changed policy close contacts were either discharged or referred to the chest clinic following their initial screening with no annual follow-up Close contacts defined as members of the same household sharing bathroom and kitchen facilities, and very close associates such as boyfriend/girlfriend or frequent visitors to the home of the index case 97% of contacts screened under both protocols, old protocol 23% considered unnecessary, new protocol 14% considered unnecessary. 1% of contacts screened were found to have disease and treated. 3% were given chemoprophylaxis and 22% were vaccinated with BCG Some lapses in adherence to the protocol were found: out of 707 contacts screened, 181 were casual contacts who need not have been screened Compared with the results of the previous protocol, fewer contacts were unnecessarily screened. However, referrals to the chest clinic increased, and the number given chemoprophylaxis |
Main conclusions: the revised protocol seemed to be as effective as the previous, more complex protocol Screening of casual contacts and contacts of extra-pulmonary TB cases is not cost-effective |
| Bailey et al., 200239 | |||
| Type of document: journal article Study design: retrospective analysis of data Country: USA Population: Oklahoma; n = 294 contacts for the index patient, a 23-year-old HIV-positive man who had been in prison five times; n = 1019 contacts for secondary cases Quality notes: some statistical analysis |
Research methods: reviewed available hospital admission charts, health department records, chest radiographs and prison records. Contact investigation data were taken from paper records. Used network visualisation and metrics to investigate the outbreak Staff involved: TB control staff Measures used: TST, genotyping closeness of relationship – reach, degree and betweenness |
Results/data: the strength of each patient–contact relationship was defined by the local TB control staff as close (> 4-hour exposure indoors or in a confined space), casual (exposure other than close) or undetermined (relationship strength not able to be characterised) 42% of contacts had a positive TST. With the exception of hospital, work and school contacts, all categories of contacts had positive TST rates exceeding 40% The network diagram indicated that the index patient was directly linked to 56% and indirectly linked to 18% of secondary cases Reach, degree and betweenness scores were calculated for relationships between the index case and contacts. The highest 20 scores and lowest 5 scores for each metric were used to prioritisation Contacts prioritised using network analysis were more likely to have latent infection than non-prioritised contacts (OR 7.8, 95% CI 1.6 to 36.6) |
Main conclusions: network analysis is useful in earlier detection of TB transmission and for prioritisation of contacts to complement standard contact investigation. It can be useful while awaiting genotyping results, which can take many months Data required to perform network analyses are already routinely collected and need to be organised into the proper format for analysis. Although the costs may be beyond some programmes, principles such as pursuing repeatedly named contacts could be adopted Decisions need to be made regarding how frequently network analysis should be used |
| Banner, 201340 | |||
| Type of document: journal article Study design: descriptive Country: Australia Population: primary school children/staff (n = 260 contacts) Quality notes: narrative description of the investigation |
Research methods: describes the methods used for investigation of one case (a teacher at the school) and outcomes Staff involved: TB co-ordinator at a chest clinic, public health unit director and head of local health service Measures used: TST and chest radiography |
Results/data: the children and staff who the teacher had most contact with were screened initially Information sent to parents of these children and an information session was given to staff by the co-ordinator. A second round of screening was carried out for those judged to be at medium risk Media involvement and parental pressure led to screening of a further low-risk group. 260 contacts screened, with 18 students and 7 teachers infected (12% of high-risk group, 5.5% of medium-risk group and 1.5% of low-risk group). None developed active disease |
Main conclusions: highlights the importance of holding information session for teachers, sending letters and factsheets to all parents and holding an open parents’ evening In addition, highlights the need for a central point of communication and for media departments to be alerted and updated |
| Bargman et al., 201341 | |||
| Type of document: report Study design: descriptive Country: USA Population: high school pupils and staff; n = 1249 contacts screened Quality notes: narrative description of the investigation |
Research methods: describes the investigation around one index case Staff involved: 81 staff from county and state health departments, two county medical reserve corps members, representatives from two schools of nursing, one school district representative, five nurses from four health departments, a clerk and two people from the Centers for Disease Control and Prevention. More than 885 person-hours for the screening and 890 hours for the treatment Measures used: TST and IGRA blood test |
Results/data: the investigation initially conducted in members of the household and teachers/students who shared at least two classes. It was later extended to all students and school personnel. Evaluation of all contacts with IGRA at the local laboratory was not feasible. A combined strategy using IGRA and TST was adopted. Those who were BCG vaccinated or who reported a positive TST were IGRA tested Local news media and internet social media reported the story and false information. Public meetings and meetings with news reporters were held to address concerns and perceptions about TB The index case later disclosed a number of non-school social contacts |
Main conclusions: the investigation was complex and labour-intensive and required immediate availability of a large workforce It is important to counter public fears by providing simple, credible, accurate, consistent and timely information about an event, and to let the public know what action they can take |
| Behr et al., 199847 | |||
| Type of document: journal article Study design: retrospective analysis of cases Country: USA Population: cases of TB in San Francisco, CA, between 1991 and 1996 with positive cultures who had been previously identified as contacts to active cases (n = 11,211 contacts) Quality notes: detailed description of links between cases and role of DNA fingerprinting |
Research methods: used DNA fingerprinting to further examine links between contacts and active cases. Routinely collected data from the TB registry were analysed Staff involved: disease control investigators Measures used: TST, and chest radiography for those with positive TST |
Results/data: people who spent an estimated total of at least 40–100 hours with the index cases in the 3 months prior to diagnosis or during the infectious period were considered to be ‘close contacts’ and those who shared the same front door with the index case were considered to be ‘household contacts’. For index cases with positive sputum smears, evaluation of extended family members and contacts at the school, place of work or social setting was initiated immediately, with further expansion dependent on numbers found with positive TSTs For index cases having negative smears but positive cultures, the initial investigation focused on close and household contacts, and the investigation was extended only if there was a higher-than-expected prevalence of positive TSTs in the inner circle. For culture-negative index cases, investigation was limited to close and household contacts. For index cases < 15 years of age, investigation was directed towards finding a possible source The study found that index and contact cases were infected with the same strain of TB in 38 instances (70%, 95% CI 56% to 82%); and 16 pairs (30%) were infected with unrelated strains. Unrelated infections were more common among foreign-born (risk ratio = 5.22; p < 0.001), particularly Asian (risk ratio = 3.89; p = 0.002) |
Main conclusions: DNA fingerprinting demonstrated that 30% of contacts with TB developed the disease at nearly the same time as, but not as a result of transmission from the index case. Contacts may have other risk factors for TB so the infection may have come from a source other than the index case. Contact tracing may be a useful way of identifying individuals at risk |
| Bock et al., 199843 | |||
| Type of document: journal article Study design: descriptive Country: USA Population: residents of a rural low-income county (n = 9 cases) Quality notes: narrative description of the investigation |
Research methods: describes an investigation surrounding an outbreak in 1996 Staff involved: Measures used: TST, and chest radiography for those with symptoms |
Results/data: initially 61 contacts were named by patients. When an outbreak was suspected, patients were reinterviewed by ‘experienced interviewers’, and patients, family and contacts were all interviewed, resulting in an additional 282 contacts; 19% of these had positive TSTs. Reinterview also established an illegal gambling group and other potential sites of infection such as bars and school Some contacts were missed because the normal daily connections between them were not recognised by investigators and social settings that were frequented were missed |
Main conclusions: illicit social connections were not identified as contacts. As TB rates were low in the area there was no specialised/experienced team. The follow-up investigation was delayed by 19 months as an outbreak was not initially suspected |
| Borgen et al., 200844 | |||
| Type of document: journal article Study design: descriptive Country: the Netherlands Population: supermarket employees and customers, 80 coworkers and estimated 23,700 inhabitants of the area around the supermarket (4.4 km2) Quality notes: narrative description of the investigation |
Research methods: describes the methods used for investigation of one case (an employee), and outcomes Staff involved: Measures used: TST – Mantoux method; chest radiography for older adults, those with BCG vaccination, TB or a positive TST |
Results/data: contacts were approached via letter to all households, locally distributed flyers, the internet and press releases. Invited to attend a local sports hall. A questionnaire was completed including demographics and frequency of visits 21,326 customers registered for screening; all but 56 of these were tested In total 15 cases of TB disease were identified by the contact investigation (12 of these were thought to be directly from the source case). 359 cases of latent infection were identified (34% of these were thought to be due to recent exposure). 114 individuals needed to be skin tested in order to identify one case |
Main conclusions: the investigation could have been improved by limiting testing to TST only and restricting it to frequent (at least once per week) customers Use of IGRA instead of or in addition to TST could have improved positive predictive value of testing and enables TST for those with BCG vaccination The optimal size of a contact investigation is setting specific, and depends not only on resources and logistics but also on background prevalence of latent TB infection |
| Borraccino et al., 201445 | |||
| Type of document: journal article Study design: retrospective data analysis Country: Italy Population: 833 TB cases and 4441 contacts in one region Quality notes: provides numbers investigated but no links with investigation method |
Research methods: analysis of registry data over a 6-year period Staff involved: N/A Measures used: TST – Mantoux method Those with symptoms or positive test also had clinical and radiographic examination |
Results/data: median number of contacts per case was 3; the highest number was 150. Those living in congregate settings showed a significantly higher number of contacts (risk ratio = 1.38, 95% CI 1.30–1.46). Homeless people and those not born in Italy had fewer contacts. Contacts aged > 35 years were more likely to be evaluated than those aged < 25 years (OR 1.45, 95% CI 1.05 to 1.94). Regular and household contacts were more easily evaluated | Main conclusions: more effort should be focused on younger TB contacts and those with results of sputum smear negative but sputum culture positive |
| Borrell et al., 200946 | |||
| Type of document: journal article Study design: retrospective data analysis. Compares conventional contact tracing with molecular epidemiology methods Country: Spain Population: residents of one city n = 892 cases (contact tracing carried out for 613), 5087 contacts Quality notes: some statistical analysis comparing the methods |
Research methods: analysed cases reported to the programme over a 2-year period Staff involved: N/A Measures used: smear positivity; IS6110-based RFLP analysis; mycobacterial interspersed repetitive unit 12 typing |
Results/data: 30% of contacts were household. Contact tracing was not performed in 31% of cases – 3.5% lack of consent, 4.5% logistic difficulties, 11.6% patient living alone, 11.6% lack of referral to study by GP A household link and individuals under age 15 years were most frequently identified by conventional contact tracing (predominantly mother–son). Molecular epidemiological methods tended to identify non-household links and identified more individuals from precarious economic circumstances and social difficulties (p = 0.002) |
Main conclusions: contacts identified via conventional tracing methods may differ from those identified using molecular epidemiological methods. Although household relationships are important, other links such as neighbourhood and leisure settings are relevant. In a sizeable proportion of cases identified the link with the source case was unknown |
| Canadian Agency for Drugs and Technologies, 20141 | |||
| Type of document: report Study design: review and guidelines Country: Canada Population: staff and patients in hospital Quality notes: systematic review underpinned the guidelines |
Research methods: systematic review Staff involved: unclear Measures used: TST |
Results/data: in one trial identified – age was the only predictor of latent TB infection (mean age 40 ± 9 vs. mean age 36 ± 9 years; p = 0.036). There was a low contagiousness of the index case to staff members. The review found little evidence relating to contact investigation in hospital settings | Main conclusions: guidelines regarding contact investigation in other settings may be applicable to a hospital setting, although recommendations are based on a low level of evidence |
| Carbonne et al., 200547 | |||
| Type of document: journal article Study design: descriptive Country: France Population: health-care workers and patients in Paris hospitals Quality notes: narrative description of the investigation |
Research methods: describes the methods used for the investigation of six cases of health-care workers with infectious TB Staff involved: crisis team including members of a hygiene unit, clinical wards, laboratories, occupational health service, risk management staff, regional centre, health authorities, trained staff for helpline Measures used: TST for children, chest radiography and medical observation |
Results/data: testing of patients was based on the degree of infectiousness of the worker, patient characteristics (lowered immunity, young children, those not BCG vaccinated), length of exposure and proximity Patients were notified by letter and GP was notified. Telephone helpline was set up. A press release and media campaign were used in some cases Number of contacts varied widely between cases No TB disease was identified; two potential latent cases had unclear links to the source case The methods used for the TST did not enable latent cases to be identified |
Main conclusions: the overall response rate was low. The use of a free telephone number was very valuable Different screening practices used made analysis of information difficult |
| Castilla et al., 200948 | |||
| Type of document: journal article Study design: descriptive Country: Spain Population: residents of a small village (n = 751) Quality notes: narrative description of the investigation |
Research methods: describes the investigation procedures for eight index cases Staff involved: Measures used: TST, medical consultation, and chest radiography for those with positive TST |
Results/data: initial contacts – family/friends/workmate or schoolmate. Investigation expanded to others living in the village in same age group (19–23 years). Summoned to medical consultation, interviewed and completed survey form including sociodemographics, health and disease, and public places frequented Close contact defined as exposure for > 6 hours per week, occasional contact as < 6 hours per week Close contact (friends/lived/work together) explained 24.7% of the cases detected. Sporadic contact explained 37.9%. Frequenting the same bars explained 33.3% of infections |
Main conclusions: the cases in the cluster appeared to have no close relationship but frequented some of the same bars |
| Coleman et al., 201449 | |||
| Type of document: journal article Study design: cost-effectiveness evaluation Country: USA Population: flight-related contacts Quality notes: economic model |
Research methods: a return on investment model was used Staff involved: N/A Measures used: treatment costs |
Results/data: the costs calculated included that for contact tracing and also for testing/treating TB disease and latent TB infection. The average cost per contact used in the model was US$16.76. Different states have different contact investigation processes and therefore a range of expenditures per contact was developed – US$28, US$47, US$134 and US$164 The model indicated that every US$1 spent on investigations and treatment resulted in more than US$1 of saving at moderate/high rates of infection and disease. Low rates of infection and disease resulted in negative returns |
Main conclusions: at moderate/high rates of infection contact investigation and treatment was cost-effective for flight-related contact A modified contact investigation procedure with sputum culture and smear positive or cavitation on chest radiograph (instead of and chest radiograph) was more cost-effective |
| Collins et al., 200450 | |||
| Type of document: journal article Study design: descriptive Country: USA Population: staff and patients of a veterans administration facility and local hospitals Quality notes: narrative description of the investigation |
Research methods: describes the methods used for investigation for one case Staff involved: infection control professional, three investigators, regional public health service administrator and two additional investigators from the department of public health Measures used: TST |
Results/data: used the ‘concentric circles’ approach to contact tracing. Skin testing performed at workplace of co-employees to facilitate compliance. Patients of the facility and ex-patients were sent letters requesting that they report for testing. The circle of contacts was expanded owing to potential contacts being compromised by additional health conditions. Initial testing and 3-month follow-up. Latent infection in 2% of coworkers, 2.4% of fellow patients, 46% of family members, 13% of closest contacts, 5% of contacts in congregate housing facility. Situation complicated by another family member identified with active TB Challenge in identifying symptoms of many contacts due to side effects of treatment for cancer. Changes in staffing rotas complicated identifying contacts |
Main conclusions: the extent of cross-facility contact complicated the investigation, and the importance of good communication among services was highlighted TB should be considered as a potential comorbidity in patients being treated for other diseases such as cancer |
| Cook et al., 200752 | |||
| Type of document: journal article Study design: analysis of existing patient data together with a questionnaire Country: USA/Canada Population: patients and contacts in three counties. TB patients, n = 87; contacts, n = 440; mean age 29 years Quality notes: predominantly narrative description of the investigation |
Research methods: used social network analysis methods. Supplemented routine investigation procedures with an interview to collect data on places of social aggregation over a 6-month period Staff involved: unclear Measures used: TST, molecular genotyping – spoligotyping, multiple interspersed repetitive units variable number tandem repeats, IS6110-based RFLP analysis |
Results/data: interviews with TB patients and contacts elicited 1056 places of social aggregation. TB patients not linked via conventional contact tracing were linked by mutual contacts or places of social aggregation For two of the counties few interconnections or common places were found, or groups connected by social network analysis were found not to be the same strain on genotyping. For the third county no association between TST positivity and densely connected contacts was found; however, places of social aggregation revealed a connected network. For this investigation an association between TST results and being in the denser area of a person–place network was found (p < 0.01) |
Main conclusions: network visualisations can provide evidence of the presence or absence of case clustering before genotype results are available in some instances (one of three investigations examined) |
| Cook et al., 201251 | |||
| Type of document: journal article Study design: descriptive review Country: Canada Population: any Quality notes: narrative review |
Research methods: provides an overview of the literature Staff involved: N/A Measures used: N/A |
Results/data: strategies for prioritisation have given priority to household contacts and those at greatest risk. Closeness of contact is based on amount of time rather than environmental or social factors. Extension of contact tracing often depends on number of TST positives compared with background rate. The influence of the infectious period and contact risk factors is unknown. Guidelines and recommendations vary. The limitations of contact tracing in high risk or vulnerable groups are highlighted, with importance of casual contacts and locations not always recognised. The completion of treatment remains a significant barrier. There are currently no guidelines for the use of social network analysis, geographic information systems genomics or genotyping. These may be of particular use in high-risk communities | Main conclusions: focus needs to be on development of questionnaires, electronic data management, local capability and expertise, co-ordinated approaches, strategies and evaluation |
| Davidow et al., 200353 | |||
| Type of document: journal article Study design: retrospective review of data Country: USA Population: employees of five workplace study sites (cases, n = 349; contacts, n = 724) Quality notes: narrative description of the investigation |
Research methods: analysis of case and contact records, including TB interview records, clinic charts and TB case reports Staff involved: unclear Measures used: TST |
Results/data: subset of data from the Reichler et al.99 study For smear-positive cases, workplace investigations were carried out alongside household and social contact investigations at all sites. For smear-negative cases, however, two sites conducted53 investigations conditional on the results of household and social investigations Over 30% of the investigations involved ≥ 20 contacts. The median number of contacts identified differed between smear-positive cases (9 contacts) and smear-negative cases (7 contacts; p < 0.04). 68% of cases were fully screened; of these 29% had a positive TST |
Main conclusions: the potential for transmission of TB in the workplace needs further recognition. There was inconsistent and limited recording of data collected during the investigations. There were also differences between the locations with regard to who was selected for screening and who was used as the primary source of information Standard guidelines for workplace investigations, written workplace investigation policies and standard data collection practices are needed |
| Diel et al., 200455 | |||
| Type of document: journal article Study design: examination of a cluster of cases during the study period Country: Germany Population: customers of a bar close to a red light district, next door to a hostel for homeless people – 38 patients (12 of no fixed abode) with four index cases, 421 contacts Quality notes: narrative description of the investigation |
Research methods: further examined the contact tracing investigation using DNA fingerprinting Staff involved: public health staff Measures used: TST and DNA fingerprinting |
Results/data: an average of 12.8 contacts per patient; five reported none Ten patients were not originally included in the investigation and were only identified as linked by DNA fingerprinting. There were reports of a fear of social discrimination and intentionally antisocial behaviour due to irritation over the contact-tracing procedure, which was perceived to be intrusive. Some of these cases reported trying to shield drinking partners from ‘bullying methods’ of the ‘health police’ by naming only contacts in more distant bars, or by naming their more transient contacts such as neighbours Persons who were presumed to be in close contact with eight of the patients showed no disease during the initial contact investigation, with some becoming ill after the investigation. Tracing of contacts was relevant for reaching a diagnosis only in two cases 40.1% of close contacts had positive TST results; 1.9% became ill Twelve of 20 cases with confirmed recent transmission could be determined only by DNA fingerprinting |
Main conclusions: only 40% of the 20 cases with epidemiologically confirmed recent transmission were included in the contact investigation Conventional contact tracing is insufficient for the detection of chains of transmission in some harder-to-reach communities. DNA fingerprinting can not only provide important information regarding recent infection of one patient by another; it also allows structural weaknesses in an investigation to be identified Contact investigation should examine the location itself and not focus on personal contacts and inflexible radiography screening schedules There should be a focus on informing the persons concerned about symptoms of disease and, if appropriate, conducting rapid screening by chest radiography or sputum analysis |
| Diel et al., 200656 | |||
| Type of document: journal article Study design: testing of contacts Country: Germany Population: contacts (n = 309) Quality notes: limited relevant data |
Research methods: compared the effectiveness of the two tests Staff involved: N/A Measures used: TST and QFT-G |
Results/data: QFT-G was unaffected by BCG vaccination status, unlike the TST | Main conclusions: in close contacts who were BCG-vaccinated, the QFT-G assay appeared to be a more specific indicator of latent TB infection than the TST |
| Diel et al., 200954 | |||
| Type of document: journal article Study design: testing of close contacts Country: Germany Population: close contacts (n = 182) Quality notes: limited relevant data |
Research methods: carried out testing using IGRAs Staff involved: N/A Measures used: QFT-G assay and the T-SPOT.TB test |
Results/data use of either IGRA as a replacement for the TST would decrease the number of latent TB infection suspects to be investigated by approximately 70% | Main conclusions: IGRAs are more accurate than TST |
| Driver et al., 200357 | |||
| Type of document: journal article Study design: retrospective analysis of investigations Country: USA Population: people in ‘congregate settings’ (schools (37% of investigations), workplaces (45% of investigations), drug treatment centres, single room hostels, other locations) n = 2740 contacts Quality notes: narrative description of the investigation |
Research methods: analysed 100 investigations over a 5-year period Staff involved: outreach staff Epidemiologist, screening, education and training staff, and a co-ordinator Measures used: TST and genetic testing; symptomatic contacts referred for chest radiography |
Results/data: testing carried out for high-risk groups as soon as possible and again 10–12 weeks later. For other testing was performed once (10–12 weeks after exposure) Decision to perform testing at a congregate setting (not just household) based on infectiousness of source case, size, crowding, windows of setting, characteristics of contacts such as age and immune status, and case clusters Use of written protocols, checklists and site-specific questionnaires. Contacts were notified by letter with plans for testing and educational materials included. Telephone reminders were used by schools. A health educator conducted group sessions on TB at sites Transmission classified as likely, possible, unlikely or unknown Exposure defined as number of hours per week the source case was at the site in the prior 3 months. Close contacts were defined generally as those spending > 8 hours per week with the source case 83% of contacts were tested, 20% were infected and 52% completed treatment Sites with likely infection compared with those unlikely tended to be those where the source case had a longer duration of cough (median 13 vs. 6 weeks; p = 0.01) cavitary lesions (84% vs. 44%; p = 0.01) Transmission defined as likely in 16%, possible in 7% and unlikely in 72% and could not be assessed in 5% |
Main conclusions: transmission at congregate sites was uncommon (22% of investigations) and is resource intensive. TSTs after most contacts would have converted should be considered in low-risk groups. Treatment completion rates were poor |
| Duarte et al., 201258 | |||
| Type of document: journal article Study design: comparison of data from two time periods (different strategies in use) Country: Portugal Population: residents of a metropolitan area (contacts in first period, n = 809; contacts in second period, n = 683) Quality notes: narrative description of the investigation |
Research methods: data on prevalence of infection among contacts compared 2001–3 and 2004–6 Staff involved: public health professionals and family doctors Measures used: TST, evaluation of symptoms, and chest radiography |
Results/data: during the first period the investigation interview targeted close contacts; during the second period visits to home and workplace were also included 67% of eligible contacts were screened in first period, 3% with active TB and 27% with latent TB. 83% completed therapy. Estimate 0.75 cases of infection per index patient identified In second period 87% of contacts were screened. Interviews identified 950 contacts; home and workplace visits helped to identify 2629 contacts. Estimate 1.4 cases of infection per index patient Although there was an increase in workload, resources did not change between the study periods |
Main conclusions: expanding contact investigations to home and workplace visits increased the number of individuals screened and identified further patients with active and latent TB |
| Edelson et al., 201159 | |||
| Type of document: journal article Study design: systematic review Country: Canada Population: travellers on public transport Quality notes: systematicreview |
Research methods: systematic review of literature on TB transmission among bus or train travellers Staff involved: N/A Measures used: evidence of infection |
Results/data: 12 documents were included. There was support for the possibility of TB transmission from active TB cases to co-travellers. In most reports exposure occurred daily over weeks or months. Ventilation was frequently reported to be poor The reports did not provide evidence regarding the precise risk to co-travellers or identify which may be at greatest risk |
Main conclusions: contact-tracing decisions should be based on proximity to index case, duration of exposure and other risk factors such as infectiousness of index case or susceptibility of contact |
| Erkens et al., 201060 | |||
| Type of document: journal article Study design: narrative review Country: the Netherlands Population: N/A Quality notes: descriptive overview of the literature |
Research methods: descriptive overview of the literature, expert consultation and recommendations Staff involved: N/A Measures used: N/A |
Results/data: key importance of establishing infectiousness of source case, the likelihood of infection among contacts and the risk of them developing TB Outdoors transmission is highly improbable. Room size, air circulation and ventilation are important factors in the dispersal of bacteria. Visits to potential transmission locations to estimate risk are recommended. Children < 5 years old are a main target of investigation IGRA tests more sensitive in detecting TB infection than TST. A positive TST should be followed by IGRA. Although neither are able to distinguish latent from active TB, some studies suggest that IGRAs superior to TSTs in predicting latent infection becoming disease, although this finding not consistent. Chest radiographs are usually normal in persons with latent infection The degree of exposure depends on intensity and duration. Contacts are classified into circles of priority groupings When only a TST is used, a cut-off point for positivity must be decided with decisions regarding sensitivity vs. specificity. Likelihood of infection and BCG status should be considered |
Main conclusions: a risk assessment approach is needed. Tests to identify latent TB have variable predictive value |
| Faccini et al., 201561 | |||
| Type of document: journal article Study design: descriptive Country: Italy Population: workers at a call centre (n = 107) Quality notes: narrative description of the investigation |
Research methods: describes methods used in an investigation for one case Staff involved: unclear Measures used: TST, clinical examination, chest radiography, pulmonary assessment, interferon gamma release assay if positive TST, genotyping |
Results/data: concentric methods approach used. A source case had been identified several years earlier; however, no contact investigation had been performed beyond family members. Perceived stigma had led the case to claim that they were unemployed | Main conclusions: TB-related stigma has major implications on TB control programmes as it can lead to the incomplete identification of contacts. Establishing trust and rapport between public and patients is important, with training in interviewing staff important Genotyping was important to establish linkages |
| Forssman et al., 200662 | |||
| Type of document: journal article Study design: descriptive Country: Australia Population: residents and staff of a nursing home Quality notes: narrative description of the investigation |
Research methods: description of an investigation for one case Staff involved: unclear Measures used: TST, chest radiography and clinical assessment if positive TST |
Results/data: no further cases of infection were found. The investigation highlighted that there was no policy in place regarding the screening of residents or staff in the district. Many staff were from TB-endemic countries and were TST positive | Main conclusions: highlights the need for TB screening |
| Fox et al., 201332 | |||
| Type of document: journal article Study design: systematic review and meta-analysis Country: Australia Population: any Quality notes: systematic review including a large number of studies |
Research methods: systematic review of studies reporting the prevalence of TB and annual incidence of TB among contacts of patients with TB Staff involved: N/A Measures used: any |
Results/data: 108 studies included from high-income countries. There was an average of 5.1 contacts per index case in high-income studies (95% CI 2.3 to 5 contacts) The definitions of household contact and close contact varied considerably In high-income settings the prevalence of TB among contacts was 3.3% (95% CI 27.6% to 42.7%) and of latent infection was 34.8% (95% CI 27.6% to 42.7%) The incidence is highest in the first year after contact, and remains above background incidence for at least 5 years after exposure. Children < 5 years of age and people living with HIV were particularly at risk Foreign-born contacts were significantly more likely to have latent infection than locally born contacts in high-income countries (OR 3.39, 95% CI 3.10 to 3.71; p < 0.0001) |
Main conclusions: contacts of TB are at a high risk of developing infection, particularly in the first year, although there is heterogeneity in reported prevalence. Many of the patterns of infection in contacts reflect that of the whole population. There is a need to demonstrate that contact tracing is more effective than case-finding alone |
| Funayama et al., 200563 | |||
| Type of document: journal article Study design: analysis of test results Country: Japan Population: university students (n = 462) Quality notes: limited data of relevance |
Research methods: compared QuantiFERON TB-2G (Qiagen Inc., Germantown, MD, USA) with TST Staff involved: N/A Measures used: QuantiFERON TB-2G and TST |
Results/data: in the non-close-contact group, the QuantiFERON TB-2G-positive rate was only 0.8%. In the TST group strong tuberculin reactions with erythema of ≥ 30 mm were seen in 18.2% in the (most likely due to the previous history of BCG vaccination) | Main conclusions: QuantiFERON TB-2G is a useful method for diagnosing TB infection, especially among individuals who show tuberculin reactivity due to past BCG vaccination |
| Funk, 200364 | |||
| Type of document: journal article Study design: descriptive Country: USA Population: Alaska natives Quality notes: narrative description of the investigation |
Research methods: describes the investigation of an outbreak in one region Staff involved: public health nurses Measures used: TST |
Results/data: describes the challenges of investigation in remote areas, including the interviewer being unfamiliar with the culture and being a non-native-language speaker Named contacts collected are not always screened. A workshop for health providers may be beneficial to improve investigations |
Main conclusions: contact investigations are challenging and labour intensive |
| Gaber et al., 200565 | |||
| Type of document: journal article Study design: descriptive Country: UK Population: locals who attended a house in south-west England including children (the public house had a playroom attached); n = 184 contacts Quality notes: narrative description of the investigation |
Research methods: description of the investigation Staff involved: consultant in communicable disease control, respiratory physician, microbiologist, TB nurse, communicable disease control nurse, hospital and ward managers Measures used: chest radiography Contacts who had symptoms or an abnormal radiograph were screened by the respiratory unit of the local district general hospital |
Results/data: the investigation centred on three avenues for contact tracing – the local public house, close-contacts and inpatient hospital staff and patients (as the index case was currently a patient) Staff and regular visitors to the public house were sent letters to attend screening, and all children were screened. Other potential contacts were also offered screening and letters were made available at the public house. The letter included education about TB symptoms, mode of transmission, the availability of effective treatment and details of a telephone helpline. Local GPs were kept informed. An open-access radiology service carried out the screening At the hospital patients who had > 8 hours’ contact and other close contacts with the index case were screened. The first seven patients who had undergone anaesthesia using the same ventilator after the index patient were also screened In total 15 contacts were treated for active TB and 13 were given chemoprophylaxis. DNA fingerprinting indicated all infections originated from a single source |
Main conclusions: despite identifying few conventional close household contacts, a significant number of secondary cases were detected from tracing contacts at a single location Multidisciplinary team working is essential for the effective management of an investigation |
| Gardy et al., 201166 | |||
| Type of document: journal article Study design: further analysis of a previous investigation using additional methods Country: Canada Population: residents of a community in British Columbia (n = 41 cases; included two children) Quality notes: narrative description of re-examination of the investigation |
Research methods: compares data and conclusions drawn from contact tracing, social network investigation, DNA fingerprinting and whole-genome sequencing approaches Staff involved: nurses and trained interviewers Measures used: social network questionnaire and laboratory-confirmed TB |
Results/data: the social network questionnaire was used subsequent to contact-tracing interviews with the cases. The ‘name generator’ questions related to drug and alcohol use; residential and travel history; places of social aggregation; and identification of contacts in the context of high-risk behaviours and locations. A single social network diagram was developed using software to characterise relationships between contacts During the contact investigation there was an emphasis on contacts of a paediatric case, in an effort to find the source of the child’s infection; however, a single source case could not be clearly identified. A social network approach using the social network questionnaire added to the investigation by revealing previously unreported social interactions and several locations frequented by infectious patients (two hotels, meal/community centres and crack houses) RFLP and 24 loci mycobacterial interspersed repetitive units variable number of tandem repeats whole-genome sequencing was carried out. This revealed two distinct TB lineages with 80% of contacts having both lineages. Social transmission networks were constructed to further examine relationships Genome sequencing allowed the social network to be divided into subnetworks associated with specific genetic lineages of the disease. It was also valuable in enabling removal of social relationships that could not have led to transmission according to the genomic data. This greatly reduced the complexity of the network and aided the identification of index patients |
Main conclusions: genotyping and contact tracing alone did not capture the true dynamics of the outbreak Social network analysis outperformed contact tracing in identifying a probable source case as well as several locations and persons who could be subsequently targeted for follow-up DNA fingerprinting had suggested that the outbreak had a single TB lineage, whereas more in-depth whole sequence molecular epidemiology revealed two lineages |
| Gerald et al., 200268 | |||
| Type of document: journal article Study design: describes the development and testing of a decision-support tool Country: USA Population: state of Alabama Quality notes: describes development and testing of the tool rather than usage |
Research methods: generalised estimating equations and classification and regression trees were used to develop a decision tree for predicting a positive TST result in contacts. The tree was tested in a set of 3162 contacts Staff involved: N/A Measures used: TST |
Results/data: the decision tree developed had a 9% sensitivity and 22% specificity. It had a false-negative rate of 7–10%. It was estimated that use of the decision tree could enable around a 20% reduction in number of contacts investigated Priorities for contacts to be investigated are:
|
Main conclusions: decision trees can be developed to assist in prioritising contacts for investigation |
| Gerald et al., 200367 | |||
| Type of document: journal article Study design: development of protocols, standardised recording system and evaluation of an intervention for field workers Country: USA Population: TB field workers n = 6x small groups of 8–10 individuals Quality notes: an evaluative study, although very limited data regarding effectiveness |
Research methods: examination of existing protocols and development of revised versions via focus groups; also new sheet to record information The intervention was underpinned by social cognitive theory and the health belief model. It consisted of a workshop and computer-based module with individual supervisors allocated. It focused on interviewing skills and behaviour to improve efficiency and effectiveness, including skills work, use of motivational strategies during interviewing, training on new protocols and forms, and case scenarios. Follow-up monthly meetings in addition to workshops. The training took place over a 6-month period The protocols had been piloted in two areas Staff involved: TB field workers (registered nurses and disease intervention specialists who are college graduates with training in TB) Measures used: feedback from managers and staff; review of records |
Results/data: existing protocols required the investigation of those with close and prolonged contact; however, there was considerable variance among field workers regarding the meaning of these terms. There was also variance in understanding of methods for eliciting information and the use of ‘concentric circles’ analysis was apparent. There was a need to quantify information and standardise definitions using a new contact exposure and assessment worksheet The quality of the training sessions was rated at mean 4.61 and overall value of training was rated 4.71 (scale 1–5, 5 meaning excellent) Some further training was required when data entry errors and misunderstandings were identified |
Main conclusions: attention should be paid to precisely defining terms, protocols should be standardised and resources should be devoted to training to improve adherence to protocols |
| Greenaway et al., 200369 | |||
| Type of document: journal article Study design: review Country: Canada Population: divided into four groups (low/high background prevalence of TB) Quality notes: review of available data |
Research methods: reviewed published data relating to the likelihood of tuberculin reactions in casual contacts Staff involved: N/A Measures used: TST |
Results/data: casual contacts were defined as ‘persons sharing the same air, but having no direct contact with the index cases’. The hourly risk of infection reported among casual contacts ranged from 0.18% to 0.53%, and averaged 0.28% per hour Individuals exposed early in the course of the disease were less likely to have TB conversion than those exposed later in the course of disease Those with lower previous exposure to TB are more likely to be newly infected following a short duration of exposure (5 hours’ exposure for contacts from areas with low prevalence of TB will result in almost 50% likelihood of new infection vs. 200 hours’ exposure for individuals from countries with higher prevalence will result in 40% likelihood of new infection) Casual contacts with a high likelihood of previous exposure should undergo TSTs only if the initial index case was heavily contagious and/or the duration of contact was prolonged Casual contacts with a low likelihood of prior mycobacterial exposure should be tested following as little as 5–10 hours of exposure |
Main conclusions: the decision to extend a contact investigation to a group of casual contacts in a workplace or school should be based on
|
| Gulati et al., 200570 | |||
| Type of document: journal article Study design: descriptive Country: USA Population: employees of an industrial company described as having many foreign workers (n = 104). Index case was an immigrant from El Salvador who lived alone Quality notes: narrative description of the investigation |
Research methods: examined a contact investigation for one index case to identify levels of infection and factors associated with transmission Staff involved: occupational health medicine team – physician and industrial hygienist Measures used: TST |
Results/data: investigation included individual interviews and assessment of buildings and ventilation systems. The contact investigation was part of evaluation of the workplace for solvent and noise All 104 employees were recommended to be screened as the index case had worked in various areas; 97 completed screening. A screening questionnaire was developed and pilot tested that asked for information regarding risk factors for TB and symptoms Possible risk factors for transmission at the workplace were identified and ORs were calculated for an association with having a positive TST for each. Workplace risk factors included spending time in the lunchroom (OR 4.45, 95% CI 1.32 to 23.25; p = 0.004) and carpooling with the case (OR 5.54, 95% CI 1.32 to 23.24; p = 0.004) 37% were TST positive |
Main conclusions: the workplace can be an important site for transmission; screening should be considered for workplaces with large number of employees from high-prevalence countries |
| Guzzetta et al., 201571 | |||
| Type of document: journal article Study design: development of epidemiological model Country: USA Population: residents of one county Quality notes: modelling of data |
Research methods: development of a computational model using notification data during a 10-year period Staff involved: N/A Measures used: N/A |
Results/data: the model indicated that the contact-tracing programme (using a household contact, then school/work contact, then wider contact approach) significantly reduced TB incidence (by 18.6%) and deaths (23.7%), compared with passive diagnosis only The model indicated that around one-fifth of recently transmitted cases are identified by contact tracing Consideration of smear-positive cases only has a negative impact on effectiveness rather than also including smear-negative cases (reduces incidence avoidance to 10.4% and deaths to 13.2%) |
Main conclusions: a key aspect in success of the programme was investigation of contacts of smear-negative cases which nearly doubled the effectiveness. Although these cases have a lower rate of infectiousness, they contribute a substantial share to transmission rates |
| Higuchi et al., 200772 | |||
| Type of document: journal article Study design: cohort study Country: Japan Population: High school students (n = 349) Quality notes: limited data regarding accuracy of testing rather than other elements of an investigation |
Research methods: compared results from different testing methods and followed up participants over time Staff involved: N/A Measures used: TST, QFT-G and chest radiography |
Results/data: QFT-G appears more specific than TST as contacts with positive TST and negative QFT-G responses were not offered prophylaxis, and none developed TB during 3.5 years of follow-up | Main conclusions: the replacement of TSTs with QFT-G, or combined use of TSTs and QFT-G, may be more useful in diagnosing true infection |
| Jackson et al., 20083 | |||
| Type of document: journal article Study design: qualitative Country: UK Population: Residents of Greater Glasgow (patients, n = 21; next of kin, n = 3); aged 7–73 years Quality notes: provides some qualitative data to underpin conclusions |
Research methods: interviews Staff involved: N/A Measures used: N/A |
Results/data: patients with TB understood the cause of TB as a pathogen which was spread by person-to-person contact and could be influenced by level of immunity, social and environmental factors. Most patients believed that they had acquired TB from an unknown infected person and from a short period of contact time. Often public places were suggested as infection locations, particularly confined or crowded locations. Known TB contacts or stereotypical patients were always male, with female participants often described poor, ‘tramp’ individuals. Infection was often perceived to be a matter of bad luck or to have occurred when the immune system was weakened (such as when ill) | Main conclusions: most patients understood the concept of airborne transmission, and contact, but prolonged contact was not thought to be required. Modes of transmission described included airborne, sharing utensils, consumption of infected foods/drink and exchange of bodily fluids Aligning contact tracing with these lay beliefs may improve the approach |
| Jackson et al., 20092 | |||
| Type of document: journal article Study design: retrospective examination of surveillance data, interviews with nurses and patients Country: UK Population: most residents of one health board area. Social connections of 64 patients were investigated, 26 patients were interviewed Quality notes: mostly describes number of links. Interview aimed to uncover this information rather than provide qualitative data |
Research methods: social network enquiry approach using molecular epidemiology and staff/patient interviews to further analyse social connections in contact investigations over a previous 10-year period Staff involved: nurse specialists Measures used: IS6110 RFLP and spoligotyping |
Results/data: 43 epidemiological links between patients were identified, with 14 of these newly uncovered by interviewing patients Associations detected by previous surveillance review were family–friend relationships, whereas over half of associations reported during the new interviews related to friends and socialising in public houses. Sixteen sites of exposure were identified; 54% of patients frequented more than one of these sites Fourteen previously unidentified links were found. Associations were not discernible for 45% of patients |
Main conclusions: the use of a standardised interview schedule including social activities prior to diagnosis enables detection of time, place or person characteristics that link individuals |
| Jereb et al., 200373 | |||
| Type of document: journal article Study design: retrospective data analysis Country: USA Population: data from 29 states Quality notes: limited data presented |
Research methods: data from the Centers for Disease Control and Prevention Measures used: number of cases, number of contacts, number evaluated and number completed treatment |
Results/data: the number of cases, number of contacts and incidence varied widely between areas Evaluation was carried out for 83% of contacts; 44% completed treatment 10% of cases had no contacts listed |
Main conclusions: impact on prevention is limited by low number of infected contacts completing treatment |
| Joint Tuberculosis Committee of the British Thoracic Society, 200033 | |||
| Type of document: journal article Study design: review and guidelines Country: UK Population: any Quality notes: review of literature to underpin recommendations |
Research methods: review of literature Staff involved: N/A Measures used: any |
Results/data: contact tracing may be a method of assessing and screening a local population with a high incidence of TB Cases of TB occurring as part of an outbreak can be linked using molecular epidemiological or DNA fingerprinting techniques, provided that they are bacteriologically proven Close contacts – people from the same household sharing kitchen facilities and very close associates such as boyfriend/girlfriend or frequent visitors to the home. A contact at work or in a hospital ward may be as close as a household contact. It is important to examine lifestyle to identify locations of contact. Examination of casual contacts is necessary only if the index case is smear positive, there is notable infectiousness (> 10% of household contacts infected) or contacts are unusually susceptible Contacts should be investigated for the period of time during which the patient has had respiratory symptoms (if unknown, for 3 months preceding the first positive sputum smear or culture) For airline passengers the risk to fellow travellers is small. World Health Organization guidance recommends that contact tracing should be taken when:
If there is evidence of transmission screening of casual contacts with BCG vaccination be initiated |
Main conclusions: importance of location and period of exposure |
| Josaphat et al., 201474 | |||
| Type of document: journal article Study design: retrospective data analysis Country: Portugal Population: cases and contacts from one disease centre (n = 61 cases) Quality notes: identifies factors associated with being identified, some statistical analysis |
Research methods: review of case records over a 1-year period Staff involved: N/A Measures used: individual characteristics, numbers identified as contacts |
Results/data: 67% of cases identified all their contacts; 32% did not 23% of contacts were identified by the public health unit and 76% were identified by the index case Being employed and not being a relative or cohabitant were risk factors for not being identified by the index case (OR 4.82, 95% CI 1.71 to 13.54, and OR 0.22, 95% CI 0.10 to 0.47, respectively) Contacts identified by the index case tended to be younger (mean age 33 years vs. mean age 40 years; p = 0.001). Being a drug user was not a risk factor for not being identified |
Main conclusions: employed contacts may not be identified as readily as relatives and cohabitants by index cases |
| Kasaie et al., 201475 | |||
| Type of document: journal article Study design: simulation modelling Country: USA Population: 2000 households Quality notes: development of a epidemiological model |
Research methods: developed an agent-based simulation model of a TB epidemic. Compared household contact tracing with active case finding in the community Staff involved: N/A Measures used: incidence |
Results/data: the model indicated that the maximum 5-year reduction in TB incidence achievable by household contact tracing was 10–15% (2–3% per year), although impact would be lower with imperfect coverage or reduced sensitivity The model suggested that TB incidence might continue to decline for 2 years and would remain below baseline levels for > 15 years after a 5-year contact tracing intervention. The addition of preventative therapy nearly doubled the estimated impact |
Main conclusions: contact tracing can have substantial epidemiologic impact (up to 7% reduction in incidence per year) but only if it achieves relatively complete population coverage, is sustained over time, and includes preventative therapy. Short-term evaluations of contact tracing are likely to underestimate their long-term impact; therefore, contact-tracing evaluation should encompass longer-term evaluation of latently infected contacts |
| Kawatsu et al., 201576 | |||
| Type of document: journal article Study design: retrospective review of data Country: Japan Population: residents of Tokyo (patients, n = 8; contacts, n = 376) Quality notes: calculates degree of relationship scores used for network analysis |
Research methods: reviews data relating to an investigation for a TB outbreak surrounding one index case. Developed social network analysis matrices Staff involved: primary health centre nurse Measures used: TST |
Results/data: relationship score was calculated based on nature of contact [household, work (same room, same floor, same building, shares smoking room)] Two values for degree of contact and one value for betweenness centrality were calculated. The OR was calculated for the association between the likelihood of latent TB being diagnosed and contact relationship score at each percentile rank The OR was not significant for the degree of contact score and the likelihood of latent TB at any percentile rank. There was a significant association for contacts with higher betweenness score and latent TB infection (p = 0.020; OR 2.12, 95% CI 1.14 to 3.96 at the 40th percentile). For contacts with betweenness scores ≥ 90th percentile they were 3.66 times more likely to have latent TB infection diagnosed |
Main conclusions: betweenness scores (but not centrality scores) were useful to identify contacts who may be at greater risk of latent TB infection Social network analysis matrices can be useful during contact investigations; however, the complexity and time-consuming nature of the method at present reduces the potential for it to be incorporated into routine contact investigations |
| Kettunen et al., 200777 | |||
| Type of document: journal article Study design: descriptive Country: USA Population: residents of one state (n = 87) Quality notes: narrative description of the investigation |
Research methods: describes the approach used for investigation of one case Staff involved: public health nurse and infection control practitioner Measures used: TST |
Results/data: family members, friends and coworkers were tested. Only people who had spent time in the same residence on a routine basis were infected. The source case was believed to have had TB for some time before diagnosis. A pre-employment TST had been carried out but the patient denied symptoms of TB and a co-existing condition blurred the symptoms | Main conclusions: contact tracing requires diligence and effective communication |
| Klovdahl et al., 200178 | |||
| Type of document: journal article Study design: descriptive, further examination of contact investigations Country: USA Population: Houston, TX. Study focuses on 37 patients with active TB associated with an outbreak 1993–6 having identical DNA fingerprints. 70% identified themselves as gay, 10% identified as bisexual, and 70% reported that they had a positive HIV test Quality notes: narrative description of links between contacts |
Research methods: describes an initiative to DNA fingerprint all new cases of TB during a 5-year period. Fingerprints were obtained and stored in a database and pattern-matching software was used. Newly diagnosed patients were approached and interviewed using the Houston Myobacteria Active Surveillance Form Staff involved: research staff Measures used: DNA fingerprint |
Results/data: contact investigation had identified only 12 links among these 27 cases. The index case could not be linked to any other; half (51%) of cases could not be linked to another case 33 out of 34 of the cases could, however, be linked by location (44 bars/restaurants/cafes) A network diagram was constructed and centrality scores were calculated. About 80% of the patients were linked by other people or places, and individuals were often linked by multiple places providing several opportunities for infection. Based on the centrality scores, 6 of the top 10 most significant people/place elements in the network were locations, in particular bars |
Main conclusions: DNA fingerprinting identified the size of the outbreak and recognition of the importance of location (bars) was central to understanding of the outbreak. Contact-naming investigation had been unable to identify links in the transmission network |
| Kowada, 201379 | |||
| Type of document: journal article Study design: cost-effectiveness analysis Country: Japan Population: 20-year-old contacts in developed countries Quality notes: economic modelling |
Research methods: assessed the cost-effectiveness of the different assessment methods using Markov modelling Staff involved: N/A Measures used: high-resolution computed tomography, chest radiography, QFT-G, TST and cost-effectiveness |
Results/data: QFT-G followed by high-resolution computed tomography yielded the greatest benefit at the lowest cost (US$6308.65; 27.56045 quality-adjusted life-years) Cost-effectiveness was sensitive to BCG vaccination rate |
Main conclusions: a strategy with QFT-G followed by high-resolution computed tomography strategy yielded the greatest benefits at the lowest cost. High-resolution computed tomography instead of radiography is recommended |
| Lambregts et al., 200380 | |||
| Type of document: journal article Study design: investigation of the role of DNA fingerprinting and cluster monitoring to TB control Country: the Netherlands Population: national data Quality notes: outlines links established by using the method |
Research methods: retrospective analysis of clusters to establish the impact of establishing cluster links via DNA fingerprinting on contact investigations 1995–2000 Staff involved: project nurse Measures used: number of cases |
Results/data: DNA fingerprinting established an epidemiological link in 31% of clustered cases where no link had been assumed or documented. Cluster feedback significantly improved the confirmation of documented epidemiological links (p < 0.001) The additional information regarding cluster links seemed to have limited impact on contact investigations, however, with only 1% extended as a result of receiving cluster feedback |
Main conclusions: DNA fingerprinting and cluster monitoring can be useful to confirm suspected epidemiological links and to identify new links for which transmission is not suspected It may be useful where links between cases of TB are vague or with long periods in between It may be regarded as a complementary strategy to contact tracing, with both approaches required |
| Langenskiold et al., 200881 | |||
| Type of document: journal article Study design: retrospective analysis of data Country: Switzerland Population: patients and contacts from one hospital in Geneva, excluding those HIV-infected or children (n = 3582) Quality notes: describes brief characteristics of the data |
Research methods: medical record data examined from a 10-year period Staff involved: N/A Measures used: TST and chest radiography |
Results/data: there was an average of 4.3 contacts per index case. Being of foreign origin, level of exposure and contagiousness of the index case were predictive of latent infection. Treatment completion rate was 67%; 0.2% of those screened were found to have active disease and 36% to have latent TB | Main conclusions: contact-tracing effectiveness relies on improving therapy acceptance and completion rates |
| Lobato et al., 200382 | |||
| Type of document: journal article Study design: retrospective review of data Country: USA Population: children aged < 5 years resident in California (n = 164) Quality notes: brief description of characteristics of the data |
Research methods: review of patient records from 38 contact investigations Staff involved: TB programme staff Measures used: TST |
Results/data: 61% of contacts with a positive TST were started on treatment; no data for completion. Almost half of the investigations found two or more previously undiagnosed TB cases | Main conclusions: improved strategies are required for identifying young children with latent TB |
| Logan et al., 200383 | |||
| Type of document: journal article Study design: development of a tool for self-evaluation of investigations Country: USA Population: any Quality comments: describes the process of development but no evaluative data |
Research methods: used discussion and stakeholder engagement to develop tools and logic models based on the Centers for Disease Control and Prevention framework for developing evaluation tools Staff involved: nurse care managers and public health nurses Measures used: tool developed |
Results/data: the logic model outlines resources required, activities and outputs detailing the processes and required standards of a contact investigation. A self-evaluation questionnaire was developed from the models. The questionnaire was piloted to refine the questions A transmission risk assessment checklist was also developed to be used at initial visits to the TB case/suspect’s home, work or school, and other places A decision tree was also developed that illustrates the contact investigation process at the patient level, from determining the infectiousness of the TB case/suspect to screening close contacts for TB infection and disease The checklist and decision tree were intended to be piloted, although no suitable investigations were started during the period of the study |
Main conclusions: the paper refers to a number of tools that were developed; however, they are not provided within it. The focus of the paper is on using the framework for developing evaluation tools |
| MacIntyre et al., 199884 | |||
| Type of document: journal article Study design: retrospective analysis of data Country: Australia Population: Victoria (n = 1142 contacts screened in 1991) Quality notes: narrative description of the investigation |
Research methods: further examination of a contact investigation in 1991 Staff involved: unclear Measures used: TST and chest radiography |
Results/data: chest radiography was overused and was the sole screening tool for nearly 40% of contacts. 80% of repeat radiography was carried out following a normal initial study. TST was underused and had been carried out for only 60% of contacts. 22% of contacts had received preventative therapy | Main conclusions: the underuse of guidelines led to inefficiencies in the investigation |
| MacIntyre et al., 200085 | |||
| Type of document: journal article Study design: cost-effectiveness analysis Country: Australia Population: all Quality notes: used modelling methods to investigate a hypothetical scenario |
Research methods: compared contact tracing as it had been carried out, if guidelines had been followed, and a hypothetical model Staff involved: N/A Measures used: costs in terms of cases prevented, cases found and contacts traced |
Results/data: the cost for contact investigation during 1991 was estimated at AU$309,065 per case prevented. It was found that during this period prevention was not considered a priority, and few infected contacts identified received preventative therapy. The authors estimated that if guidelines had been correctly followed, the cost would have been AU$58,742 per case prevented. The cost of the hypothetical evidence-based model was estimated at AU$3881 per additional case prevented, although this would be impacted by lower referral rates, lower rates of preventative therapy and lower efficacy of preventative therapy than the rates used during the calculations | Main conclusions: case finding is expensive in all three models Clear programme aims, adherence to guidelines and high rates of preventative therapy are essential in order to achieve cost-effectiveness |
| MacLellan et al., 201586 | |||
| Type of document: journal article Study design: qualitative Country: UK Population: contacts referred to a TB screening clinic in north London. Contacts, n = 30; nurses, n = 8 Quality notes: includes qualitative data to underpin conclusions |
Research methods: questionnaires to contacts (half who attended half who did not) and interviews with clinic nurses Staff involved: specialist TB nurses and one nurse from the health protection unit Measures used: N/A |
Results/data: people reported attending owing to concern regarding the severity of the disease and worry regarding other vulnerable people. TB reportedly kept a secret Good working relationships with GPs were reported as important in prompting non-attenders to attend, although it was recognised that people in hard-to-reach populations may not have GPs Importance of working with a community to allay fears, educate and reduce the stigma The need for contact screening could cause fears of eviction in shared housing. Sending letters to the patient for them to distribute could be helpful Most non-attenders reported that they were unaware of their missed appointment. Reasons for not attending were given as contact details being inaccurate, living in shared houses with muddled incoming post, having limited understanding of the need for screening, being unable to take time off work and having childcare issues. Nurses highlighted the importance of outreach workers in tracing contacts via home visits/telephone calls Walk-in appointments could be inconvenient for people with limited time available; mornings and different days were reported as best. A GP surgery location was more convenient than a hospital. Use of SMS reminders was recommended Need for TB services to raise their profile, for leadership and resources for administration, community outreach, and core nursing staff |
Main conclusions: three core areas of awareness, hospital service delivery and leadership in the service were identified |
| Mandal et al., 201287 | |||
| Type of document: journal article Study design: retrospective data analysis Country: UK Population: patients of a clinic in Edinburgh aged > 18 years. Index cases, n = 275; contacts, n = 24 Quality notes: limited data |
Research methods: analysed data on screening episodes over a 3-year period Staff involved: Measures used: TST and QFT-G |
Results/data: the programme screens close contacts, household contacts and casual contacts (mostly workplace) 14.7% of contacts declined screening Contact tracing for non-pulmonary TB is as important as for pulmonary TB. Active TB was identified in 4.3% and latent TB was identified in 21.7% of contacts of non-pulmonary patients The number of casual contacts in the study was small; difficult to conclude if this group should be routinely screened or not. 21.2% of casual contacts were found to have active or latent disease |
Main conclusions: contact tracing should be carried out for non-pulmonary as well as pulmonary Screening of casual contacts could be limited to certain circumstances |
| Marienau et al., 201488 | |||
| Same study as Coleman et al. 201449 Type of document: journal article Study design: cost-effectiveness analysis Country: USA Population: flight-related contacts (n = 9284 contacts) Quality notes: cost-effectiveness analysis |
Research methods: economic analysis comparing a previous to a modified protocol for contact investigation for in-flight exposure. Data are from 2007–9 Staff involved: N/A Measures used: transmission risk and cost |
Results/data: the modified protocol changes the criteria for a contact investigation from within 6 months of the flight to within 3 months of the flight. Also, the criteria are changed to require sputum positive for TB by culture or nucleic acid amplification test and sputum smear positive for acid-fast bacilli and cavitation on chest radiography Applying the new protocol, it is estimated that 81 fewer potential cases and 409 fewer contacts would be investigated (half of the investigations), of whom 115 might test positive (three with active disease). The risk for new protocol is 1.4–19% and for old protocol is 1.1–24% Estimated cost under old protocol is US$222,000–1,300,000 and under new protocol is US$99,449–584,824 |
Main conclusions: the new protocol is more cost-efficient while retaining an acceptable level of public health risk |
| Marks et al., 200089 | |||
| Type of document: journal article Study design: retrospective data analysis Country: USA Population: data from metropolitan areas of more than 5000,000 residents. Sample of n = 1080 index cases and n = 6225 close contacts Quality notes: describes characteristics of the data |
Research methods: data reported to the Centers for Disease Control and Prevention Staff involved: public health nurses, outreach workers, TB programme personnel and health department staff Measures used: TST |
Results/data: median of 6 days to patient interview (mean of 22 days). Procedures differed between sites, including who supervised workers and what screening contacts received. All sites defined household contacts as close. 68% of patients identified were household contacts, 24% were non-household relatives, 21% were leisure contacts, 5% were coworkers and 17% were other types of close contacts. One-third of patients identified household contacts only The number and type of data on contacts varied. Risk factors for disease were often not recorded. There was a median of 4 (mean of 6) close contacts per patient. A home visit led to average two additional contacts (likely to be young children). Fewer close contacts were identified by homeless people, men and Asian/Pacific islanders. No contacts were identified for 8% (88). Homelessness was significantly correlated with having no identified contacts (RR 1.3, 95% CI 1 to 1.5) High TST conversion rates among foreign-born contacts may be the result of prior infection or boosting rather than of recent infection. This should be considered before expanding investigations |
Main conclusions: contact investigation could be improved by consistently defining a close contact and ensuring that patients list non-household as well as household close contacts Provision of targeted TB screening and access to care is needed for high-risk contacts |
| Marra et al., 200890 | |||
| Type of document: journal article Study design: cost-effectiveness analysis Country: Canada Population: drew data from a provincial population-based database and from published literature Quality notes: cost-effectiveness analysis |
Research methods: economic modelling using Markov model Staff involved: N/A Measures used: cost-effectiveness |
Results/data: the most cost-effective strategy was to administer QFT-G in BCG-vaccinated only contacts, and to reserve TSTs for all others Incremental net monetary benefit was CA$3.70 per contact for BCG vaccinated only. The least cost-effective strategy was QFT-G for all contacts (incremental net monetary benefit of CA$11.50 per contact) |
Main conclusions: QFT-G should be used in a targeted fashion |
| Andre et al., 200791 | |||
| Type of document: journal article Study design: examination of records relating to a cluster of cases, further interviewing of patients Country: USA Population: contacts from community, prison, hospital, school (n = 251). Total of 1039 contacts visualised Quality notes: calculated scores for relationship used in network analysis |
Research methods: describes use of network analysis to produce visualisations and calculate measures of importance in the transmission network Staff involved: TB control staff Measures used: TST, clinical observation |
Results/data: examined ‘reach’ ‘degree’ and ‘betweenness’ between the contacts in the network. 42% of contacts had a positive TST The diagram helped to link secondary cases with TB who were not named by the index patient. The majority of contacts could be linked to the index case; those who could not were investigated further The metrics calculated enabled contacts with higher scores to be prioritised. Three contacts with high ranking ‘betweenness’ scores were links to the overall network |
Main conclusions: network analysis provides a means to identify linkages among cases, to quantify the magnitude of an outbreak and to begin control measures before genotyping results are available. It also can assist prioritisation of contacts for screening |
| Mohr et al., 201392 | |||
| Type of document: journal article Study design: Delphi method Country: Germany Population: 23 topic experts involved Quality notes: describes development but not testing of the instrument |
Research methods: describes development of a decision-making instrument for contact tracing in TB and meningococcal disease after contact on public transport Staff involved: N/A Measures used: N/A |
Results/data: experts were asked to rate elements on a scale of low indication for contact tracing/neutral position/high indication for contact tracing. Nine elements for TB were identified:
|
Main conclusions: the tool may help rapid decision-making |
| Muecke et al., 200693 | |||
| Type of document: journal article Study design: descriptive Country: Canada Population: University students (n = 1144) Quality notes: narrative description of the investigation |
Research methods: describes the investigation around one index case and calculates the risk factors for a positive TST Staff involved: public health unit, occupational health Measures used: TST, observation of symptoms, chest radiography for those with positive TST, genotyping |
Results/data: used the ‘concentric circles’ approach. Began with family and close social contacts. Close social contact was defined as every day or every other day. Regular social contact was defined as twice a week. Investigation expanded as high number of positive TSTs to other students and university staff. Local media were used to contact people at three rave parties Duration of exposure based on number of hours of lectures attended with index case Size, type of ventilation and air changes per hour calculated for lecture rooms. Divided into more then or less than 300 m3 27.5% of students had positive TST results; three had active TB. 69% of close social contacts and family had positive TST results; three had active TB Majority of students shared only one course with index case. Those who were exposed for 3 hours per week over 12 weeks had an approximately fourfold greater risk of infection than those with less exposure. Main risk factors were > 35 hours’ exposure and smaller classroom (OR 6.6, 95% CI 1 to 44.9 and OR 5, 95% CI 1.4 to 10) |
Main conclusions: the hourly risk of infection together with ventilation measurements can be a useful element of contact investigations |
| Mulder et al., 201294 | |||
| Type of document: journal article Study design: retrospective analysis of data Country: the Netherlands Population: TB patients from the nationwide surveillance register 2006–7 (n = 904 patients); more than two-thirds were immigrant cases (half of these were asylum seekers or illegal residents) Quality notes: describes characteristics of the data |
Research methods: the study analysed factors associated with the likelihood of having contacts of an infected patient traced Staff involved: not reported Measures used: frequency of investigation, characteristics of index patient |
Results/data: contacts were investigated for 78% of cases Contacts were significantly less often investigated around immigrant index cases (OR 0.60, 95% CI 0.40 to 0.92) than around Dutch index cases. Contacts were significantly more often investigated for smear positive index cases (OR 3.52, 95% CI 2.23 to 5.55) and culture positive index cases (OR 2.71, 95% CI 1.76 to 4.16) than for smear negative and culture negative index cases, respectively. Contacts were significantly less often investigated around actively found index cases when compared with passively found index cases (OR 0.38, 95% CI 0.26 to 0.57) and around index cases who belonged to a risk group compared with index cases who did not (OR 0.44, 95% CI 0.30 to 0.65) |
Main conclusions: contacts of immigrant index cases were significantly less often investigated than contacts of Dutch index cases. By not investigating the contacts of immigrant patients, there is a risk of missing a significant number of infected and diseased contacts |
| Mulder et al., 201295 | |||
| Type of document: journal article Study design: qualitative Country: the Netherlands Population: public health nurses (n = 14) from different regions Quality notes: provides qualitative data to underpin conclusions |
Research methods: interviews; each participant was interviewed around the time a contact investigation had commenced, and then again after the investigation had been completed Staff involved: public health nurses Measures used: N/A |
Results/data: participants described identification as challenging, as index cases were not always able to recall or willing to share information Nurses tended to identify more contacts than just those at substantial risk of infection. There was a perception that as many as possible gave a more comprehensive view of the level of infectiousness of the index case. There were concerns regarding missing contacts and further transmission; those who were anxious or expected to cause conflicts were often classified as contacts even though the risk was low. Immunocompromised individuals were often not prioritised Assessing the level of infectiousness of immigrants was described as challenging owing to the high risk of infection in the country of origin. Native Dutch contacts were often included despite their limited exposure Half of nurses used the available prioritisation table. It was described as difficult due to limited ability to capture exposure locations, or the appearance of prioritising different groups could be problematic Terms such as daily, frequent or intensive were often used for level of exposure rather than terms in the guidelines. Nurses who were more experienced tended to use the table less Six investigations were appropriately scaled up and one was appropriately not scaled up. Seven were incorrectly scaled up to casual contacts. Guidelines regarding background prevalence in the community were ambiguous and, therefore, were often not used |
Main conclusions: staff did not always adhere to guidelines and tended to identify more individuals as contacts than recommended, and there was evidence of scaling up to casual contacts which was not required The criteria for classification could be perceived as unhelpful/ambiguous and there was difficulty interpreting background population prevalence data. The usefulness of the ‘stone in the pond’ principle requires accurate data regarding prevalence in specific communities (such as immigrants) |
| Munk et al., 200896 | |||
| Type of document: journal article Study design: descriptive Country: USA Population: residents and coworkers in Maryland (n = 287 contacts) Quality notes: narrative description of the investigation |
Research methods: description of the investigation surrounding one index case Staff involved: TB control staff Measures used: TST, chest radiography, sputum acid-fast bacilli smear for those with symptoms |
Results/data: household contacts, close social contacts, close workplace contacts and coworkers who travelled in a van with the index case were given high priority and evaluated within 7 days Family and social contacts with less duration of exposure and in more open environments were categorised as medium priority. Coworkers at sites of employment were classified as low priority High rate of infection in high priority cases (39%) led to expansion to low priority contacts. 15% of these had positive TSTs No cases of active TB were found. 71% of the medium or high priority cases with latent infection agreed to begin treatment, and 33% of low priority |
Main conclusions: the workplace can be an important location for contact investigations |
| National Tuberculosis Controllers Association, 200534 | |||
| Type of document: report Study design: guidelines Country: USA Population: all Quality notes: guidelines developed by expert consensus |
Research methods: outlines guidelines for contact investigation developed by an expert working group Staff involved: varying by area Measures used: any |
Results/data: although guidelines and standards are provided, unusually close exposure (prolonged exposure in a small, poorly ventilated space or a congregate setting) or exposure among particularly vulnerable populations at risk for TB disease such as children or immunocompromised individuals could justify starting an investigation that would normally not be conducted If contacts are likely to become unavailable then the investigation should receive a higher priority. Investigations may be affected by exaggerated concern regarding TB in a community and an investigation being demanded Outlines factors influencing prioritisation, including type of TB, level of infectiousness, age and HIV status Having written policies and procedures for investigations improves the efficiency and uniformity of investigations Establishing trust and consistent rapport between public health workers and patients is critical to gain full information and long-term co-operation during treatment. Workers should be trained in interview methods and tutored. Patients should be interviewed by persons who are fluent in their primary language or interpreters provided Provides recommendations for the content of interviews, a minimum of two of which is recommended Sites visits are required as they enable additional contacts to be identified and are the most reliable source of information regarding transmission settings. Details such as room sizes, ventilation systems and airflow patterns should be considered together with how often and how long the index patient was in each setting Data from the investigation should be recorded on standardised forms Priorities should be assigned to contacts and resources should be allocated to complete all investigative steps for high- and medium-priority contacts. Priorities are based on the likelihood of infection and the potential hazards to the individual contact if infected considering characteristics of the index patient, characteristics of the contact, and intensity, frequency and duration of exposure Provides detail on the contact interview content, decision-making for expanding investigations, involvement of the media and considerations for specific population settings |
Main conclusions: provides a comprehensive overview of contact-tracing procedures and decision-making considerations |
| New York City Department of Health and Mental Hygiene, 200835 | |||
| Type of document: guidance Study design: guidance Country: USA Population: city population Quality notes: details on basis for guidance not provided |
Research methods: description Staff involved: Measures used: N/A |
Results/data: provides definitions of terms Priorities for contact investigation based on both the characteristics of the known or suspected TB index patient and the characteristics of the contact Provides tables and flow charts for decisions to conduct or continue contact investigation. Provides a table outlining contacts most likely to be infected and contacts at high risk of developing TB once infected |
Main conclusions: provides flow charts to underpin decision-making during investigations |
| Pettit et al., 200297 | |||
| Type of document: journal article Study design: descriptive Country: UK Population: customers of a public house (cases, n = 12; contacts, n = 122) Quality notes: narrative description of the investigation |
Research methods: describes the investigation carried out Staff involved: unclear Measures used: TST, DNA fingerprinting |
Results/data: initial contact investigation focused on close contacts and revealed no further cases of infection. However, cases were later identified who all were customers of a public house where the presumed index case was a regular customer, and the investigation was extended to all staff/customers. 85 of 122 contacts were screened. The identification of regular patrons was extremely difficult. Two cases came to light as a result of health education/awareness raising One further case was identified by the investigation and two children were given preventative therapy (1.18% case detection rate) |
Main conclusions: transmission can occur between customers of a public house; therefore, extended contact screening beyond close contacts must be considered |
| Pisu et al., 200998 | |||
| Type of document: journal article Study design: cost-effectiveness analysis comparing conventional contact tracing with contact priority models Country: USA Population: residents of Alabama Quality notes: cost-effectiveness analysis |
Research methods: a cost-effectiveness analysis using a decision-analytic model comparing traditional ‘concentric circles’ contact tracing with a contact priority model Staff involved: N/A Measures used: TST and costs |
Results/data: the contact priority model uses a decision rule (exposure hours, home, poorly ventilated environment) to explicitly categorise contacts as high risk requiring testing or low risk not requiring testing The analysis used the total cost each model divided by outcomes (number of active TB cases, number of life-years attained) to calculate incremental cost-effectiveness ratios. A decision tree approach was used to model elements such as the likelihood of a TST being performed and Markov models were used to represent costs and outcomes Estimated cost of investigating a contact was US$250 Conventional ‘concentric circles’ contact tracing was found to be more effective but more costly than a contact priority model. Savings would be made on cost of TSTs; however, there would be higher costs from active disease in a contact priority model. The ‘concentric circles’ approach was estimated to prevent one additional case of active disease for a cost of US$92,934 and one additional life-year US$185,920. Estimated cost per 1000 contacts was US$339,896 for ‘concentric circles’ and US$294,596 for contact priority. There would be estimated one or two additional cases of active disease per 3000 contacts with a contact priority model |
Main conclusions: conventional ‘concentric circles’ contact tracing was found to be more effective but more costly than a contact priority model |
| Rea and Rivest, 20146 | |||
| Type of document: guidance (grey literature). Standards for contact follow-up and outbreak management in TB control (chapter 12 of TB standards) Study design: guidance referencing underpinning literature Country: Canada Population: any Quality notes: no details on process for developing guidance |
Research methods: descriptive Staff involved: public health/TB control authorities in collaboration with treating clinicians and other providers Measures used: N/A |
Results/data: only respiratory TB is infectiousness in most cases. Contact investigation should be carried out for both smear-negative and smear-positive cases. Source case investigation is recommended for children < 5 years old with a diagnosis of active TB Contact tracing should identify and treat any secondary cases and identify individuals with latent infection in order to offer preventative treatment Interviews should include questions about locations/activities of exposure and also specific named contacts. Prioritisation of contacts should be based on infectiousness of the source case, extent of exposure and vulnerability of those exposed Most effort should be put into contacts who are most at risk of being infected and/or most at risk of developing active TB disease if infected
TSTs and symptom assessment 8 weeks after exposure is recommended for non-household contacts. Household and high-priority contacts should be tested initially and again at 8 weeks. Two-step TSTs are not recommended. A history of BCG vaccination does not alter the interpretation of the TST result. A positive test is ≥ 5 mm, or an increase of at least 6 mm from previous test Elderly people in long-term care should not be tested with TST In homeless people and those with drug addictions, non-judgemental and supportive staff and use of incentives may help rates of participation. Interventions on site for a single session are likely to have more success. The primary focus should be on detection of secondary cases rather than assessment and treatment of latent TB |
Main conclusions: the concentric circles approach does not take into account contacts who are vulnerable but may have had less exposure, and can be difficult to apply in congregate settings. Level of priority should be considered DNA fingerprinting can be useful to confirm or disprove linkages. It can be useful in populations in whom contact investigation is challenging (such as the homeless) All cases should be asked about locations where they spend time. Social network analysis may be helpful School, workplace and other congregate setting investigations including homeless and other marginalised populations are best carried out on site Need for good organisation, adequate staffing and resources, clearly defined roles and responsibilities |
| Reichler et al., 200299 | |||
| Type of document: journal article Study design: retrospective review of records Country: USA Population: five areas of the USA with programmes perceived as the best, and best organised data. Patients aged over 14 years (n = 360) and contacts (n = 3824) Quality notes: describes characteristics of the data |
Research methods: data were analysed from contact investigations carried out in 1996 Staff involved: N/A Measures used: TST converters, numbers screened |
Results/data: close contact was defined differently in different areas. Closeness was not recorded in records for many contacts. For analysis, ‘close’ was defined as members, visitors or workers in the index case household or those who were friends or relatives Number of contacts was higher for patients who had both a positive smear and cavitary disease (median 8; p < 0.001). 13% of patients had no contacts identified; an additional 11% had no close contacts identified. Patients with no contacts were more likely to live in a homeless shelter (13% vs. 2%; p < 0.001). Only half of those patients with no contacts were recorded as being interviewed. Less than two-thirds of contacts completed screening |
Main conclusions: effective investigations require standard definitions of close contact and contact, definition of what constitutes exposure (duration, time, frequency, location), standard criteria for expanding investigations, development of effective data management systems and definition the extent of investigation needed in different settings |
| Rodriguez et al., 1996100 | |||
| Type of document: journal article Study design: descriptive Country: USA Population: high school students (close contacts, n = 122; non-close contacts, n = 1804) Quality notes: narrative description of the investigation |
Research methods: describes the investigation surrounding one case Staff involved: public health staff Measures used: TST, cost |
Results/data: positive TSTs were found among 2.5% of close contacts and 1.9% of non-close contacts. No other active TB case was identified The cost of TST screening was estimated to be US$36,507 |
Main conclusions: screening was costly and diverted staff from other duties. Existing guidance regarding expanding investigations should be followed |
| Ruben and Lynch, 1996101 | |||
| Type of document: journal article Study design: descriptive Country: USA Population: residents of Pittsburgh, PA Quality notes: narrative description of the investigations |
Research methods: describes the investigations carried out over a 1-year period Staff involved: NR Measures used: description only |
Results/data: unable to source the full text; the abstract refers to the challenges of carrying out contact-tracing investigations, although provides no further details | Main conclusions: the authors highlight the challenges in carrying out contact investigations |
| Rubilar et al., 1995102 | |||
| Type of document: journal article Study design: retrospective review of data Country: UK Population: residents of Edinburgh (cases of TB notified, n = 632; contacts, n = 3688) Quality notes: describes characteristics of the data |
Research methods: reviewed records of cases of TB notified 1982–91 (20% of records had been mislaid) Staff involved: NR Measures used: NR |
Results/data: 7.9% of those cases notified had been identified by contact tracing 1.4% of contacts screened had active TB and 1% had latent infection 54% of contacts with TB were under age 14 years, 34% were aged 15–44 years, 8% were aged 45–64 years and 4%) were aged over 65 years 84% of the cases among contacts were in contacts of patients with sputum smear-positive respiratory disease, and 98% of TB in contacts was detected within the first 3 months of screening Infection that may be detected later by ongoing radiography may be the result of infection from another source or reactivation of infection acquired from another source |
Main conclusions: screening of close contacts of all index cases other than smear-positive respiratory index cases was not recommended Screening of young people should be prioritised and carried out within the first 3 months |
| Sanderson et al., 2015103 | |||
| Type of document: journal article Study design: descriptive Country: USA Population: patients and staff on a maternity ward (n = 285) Quality notes: narrative description of the investigation |
Research methods: describes the contact investigation methods using electronic health data (electronic medical records and an immunisation register) Staff involved: hospital staff, Department of Health and mental hygiene staff Measures used: none |
Results/data: the linking of data from different electronic health systems reduced the resource burden required for the investigation. The identification, notification and evaluation of contacts was aided by the systems, and documented evidence of exposure assisted the focusing of those at greatest risk 100% of those potentially exposed were contacted The systems also identified current health-care providers who were contacted to distribute letters and guidelines |
Main conclusions: electronic health data are useful for enhancing contact investigations |
| Saunders et al., 2014104 | |||
| Type of document: journal article Study design: retrospective analysis of data Country: UK Population: data collected at a Birmingham hospital (n = 7365) Quality notes: describes characteristics of the data |
Research methods: analysed trends in data over a 20-year period (1990–2010) Staff involved: TB nursing service Measures used: screening completion rates, screening outcomes, number of contacts |
Results/data: 40.9% of contacts failed to complete screening. There was no evidence of a trend over the study period The number of contacts screened for each positive screening outcome was 15 for pulmonary TB and 45 for extrapulmonary TB Contacts were less likely to complete screening if they were of working age, male, black or from the Indian subcontinent Contacts tested using IGRAs were more likely to complete screening |
Main conclusions: work is required to increase screening completion rates and to increase screening for working age, black and Indian subcontinent populations |
| Shah et al., 2014105 | |||
| Type of document: journal article Study design: systematic review and meta-analysis Country: USA Population: patients with drug-resistant TB Quality notes: systematic review |
Research methods: calculated the reported yield of contact investigations Staff involved: N/A Measures used: number of household contacts |
Results/data: analysed data from 25 studies. The pooled yield was 7.8% for active TB and 47.2% for latent infection (there was significant heterogeneity; p < 0.0001). The majority of cases were identified in the first year | Main conclusions: there is a high yield of active and latent infection in household contacts of patients with drug-resistant TB |
| Shrestha-Kuwahara et al., 2003106 | |||
| Type of document: journal article Study design: qualitative Country: USA Population: pulmonary TB patients from the USA/Mexico (n = 54), programme staff (n = 18) Quality notes: provides qualitative data to underpin conclusions |
Research methods: focus groups Staff involved: contact investigation staff Measures used: N/A |
Results/data: patients reported providing contacts easily and willingly. On occasions, although they had given a large number of contacts only a few appeared in the records. Homeless people could only give street names of their friends and acknowledged that finding them was difficult when they had no place of residence Patients reported preferring to inform contacts themselves prior to the health department doing so Trust and good rapport were described as important, as well as good communication. Using interpreters or interpreters not being available could be challenges Differences in understanding of the term ‘contact’ and ‘at-risk contact’; term could be vague or understood incorrectly. Some patients were unclear about the purpose of needing names; it was not clear that the focus was not on getting the names but was on finding the people who may have been infected Fears regarding stigma, loss of employment or housing, and alienation or abandonment were described The timing of the investigation was when patients could be feeling ill and afraid and confused after diagnosis. Reinterviewing patients at a less stressful time could be helpful Staff reported need for training in counselling, improved systems of co-ordination between service providers and training in social and economic issues |
Main conclusions: programmes may be enhanced by staff training in listening, culturally appropriate interviewing techniques and reinterviewing patients after initial fears and confusion have reduced There seemed a mismatch between most patients reportedly giving contacts willingly and the small number of contacts recorded. There may be misconceptions regarding understanding of what a contact means; effective communication is needed |
| Sprinson et al., 2003107 | |||
| Type of document: journal article Study design: retrospective analysis of data Country: USA Population: California (n = 15,582 contacts) Quality notes: describes the characteristics of the data |
Research methods: analysis of programme management reports over 1 year to estimate effectiveness Staff involved: NR Measures used: TST, costs, contacts identified |
Results/data: 11% of cases had no contacts elicited. Mean number of contacts per case was 10.5 (range 0–170); 88.6% of contacts were evaluated, disease was found in 0.6% and latent infection was found in 24.1%. Of the 42 areas, 13 met the performance target of evaluating 95% of contacts 66% of contacts started treatment and 64.2% completed. Around half chose to stop, 17% moved and for 17% the reason was unknown. 31% of areas met the target of 85% treatment completion Investigations were estimated to have detected 81% of TB cases which might have been identifiable and estimated to have prevented 34.6% of future TB cases that might have occurred in the following 2 years Costs were estimated at US$4.8M |
Main conclusions: performance did not meet national objectives. Further data are required to evaluate performance |
| Stoddardt and Noah, 1997108 | |||
| Type of document: journal article Study design: survey of consultants in communicable disease control and medical officers of environmental health Country: UK Population: n = 732 contacts Quality notes: limited relevant data |
Research methods: survey sent to 155 districts. It requested information on the number of new cases of TB found in the preceding 3 years in which > 100 contacts had been screened Staff involved: NR Measures used: TST |
Results/data: 46% of districts reported at least one investigation which had screened > 100 contacts. Forty-four cases of TB were found in 18 of the 56 incidents, giving a detection rate of 0.375% | Main conclusions: the authors question the continued use of large-scale screening. Close contacts should be carefully defined, and only they should be screened |
| Tian et al., 2013109 | |||
| Type of document: journal article Study design: developed mathematical model of TB dynamics Country: Canada Population: province of Saskatchewan Quality notes: mathematical modelling |
Research methods: comparison of scenarios with and without contact tracing Staff involved: N/A Measures used: risk of infection |
Results/data: comparison of a scenario involving contact tracing and no contact tracing indicated a higher average prevalence of TB infection with no contact tracing. The benefit of tracing the first 45% of contacts was greater than tracing the second 45%, indicating a diminishing return Prioritising contacts on the basis of number of times that they have been named had adverse outcomes Increasing the speed of the investigation (90% of contacts are tested within 30 days of diagnosis) did not lead to projected significant improvement in active cases or prevalence of infection Reducing loss to follow-up to a 10% level could lead to significant benefits in infection rates (5.4% prevented; p = 0.02) Targeting investigations by prioritising by age (children aged < 9 years are traced first) and ethnicity (first nation individuals traced first) could improve the effectiveness compared with non-prioritisation (preventing 11% of cases over 20 years; p < 0.0001) |
Main conclusions: contact tracing leads to positive outcomes. Reducing loss to follow-up and targeting investigations may increase effectiveness |
| Trieu et al., 2013110 | |||
| Type of document: journal article Study design: descriptive Country: USA Population: HIV-infected index case, hotel resident and colleague contacts (n = 31) Quality notes: narrative description of the investigations |
Research methods: describes two investigations using IGRAs Staff involved: unclear Measures used: QFT-G IGRA |
Results/data: the study indicated that IGRAs can be used in congregate settings The drawbacks are increased cost compared with TSTs (16 times more) and requirement for staff trained in taking blood samples. Specimens also need to be received at a laboratory within 16 hours of collection Positive aspects of IGRA use are only a single encounter with a contact was needed and there were fewer false-positive results due to BCG or other bacteria present meaning fewer people were given prophylaxis treatment |
Main conclusions: use of IGRAs in the field is feasible It may be particularly preferred to TSTs in people hard to follow up and contacts who are BCG vaccinated |
| Underwood et al., 2003111 | |||
| Type of document: journal article Study design: retrospective data analysis to examine screening vs. contact-tracing approaches Country: UK Population: described as living in a socioeconomically deprived area (Tower Hamlets, London) (cases, n = 227; contacts, n = 643; new UK entrants screened, n = 332) Quality notes: compares data from two methods of screening rather than evaluating effectiveness of contact tracing |
Research methods: analysis of patient records and a TB database 1997–9. Compares new entry screening vs. contact tracing Staff involved: specialist TB nurses Measures used: number of cases detected, number screened |
Results/data: contact tracing of patients with both smear-negative pulmonary TB and non-pulmonary TB identified individuals with active and latent TB with combined prevalence similar in each group (7%) Contact tracing in cases of non-pulmonary disease is not recommended, but the results suggested that it may be at least as productive as the screening of new arrivals to the UK from high-incidence countries |
Main conclusions: a contact-tracing strategy is more effective than new entrant screening Contact tracing (even in cases of non-infectious TB) in high incidence areas could be seen as a way of screening extended families or communities at particularly high risk |
| Verdier et al., 20128 | |||
| Type of document: journal article Study design: retrospective analysis of data Country: the Netherlands Population: Rotterdam (n = 21,540 contacts) Quality notes: provides limited data |
Research methods: analysed data from contact investigations between 2001 and 2006 to identify risk factors for finding TB latent or active infection Staff involved: public health nurse Measures used: TST |
Results/data: ‘stone in the pond’ principle followed – close contacts, then regular contacts, then community contacts Residential or family relationships resulted in highest risk of infection, while work or education contact resulted in lower chance of transmission. Risk factors included older age of the patient and older age of the contact. Greater infection risk in community contacts was present if a large number of close contacts were infected |
Main conclusions: the risk factors match current guidelines – diagnosis of index patient, closeness of contact relationship, the age of patients and contacts and the number of infections of close contacts |
| Ward et al., 2004112 | |||
| Type of document: journal article Study design: retrospective analysis of data Country: USA Population: schools in New York state (n = 6990 contacts) Quality notes: describes characteristics of the data |
Research methods: analysed data from a TB registry for children aged 5–19 years 1997–2001 Staff involved: N/A Measures used: sputum smear, TST |
Results/data: each county used their own cut-off points in measuring millimetres of induration on the TST for determining if a contact was positive TST positivity among close and not-close contacts increased with increasing age of index cases (4.6% aged 5–9 years; 5.5% aged 15–19 years). The number of contacts tested increased with increasing children’s age. In very young children infection suggests recent transmission so the emphasis is on finding the index case. In older children transmission between children becomes more likely so there is greater focus on locating contacts In the first round of testing the mean number of close contacts per index case tested was 81 (range 0–725), and was significantly more than not-close contacts (p < 0.0001) Lower SES status of contacts was associated with greater TB risk (assessed by median income). Pupils at smaller schools were also at greater risk of being TST positive In one of the four regions not-close contacts unexpectedly had a higher rate of TST positivity than close contacts across the study as a whole (7.3% vs. 5.1%). In two regions close contacts had a higher rate of TST positivity than not-close (20% and 15.2% vs. 5.1%). The final region data did not differentiate between levels of contact 47.1% completed treatment (higher for this investigation than for the state as a whole) |
Main conclusions: many school investigations test more contacts than might be expected due to parental concern and public pressure (no data presented regarding this) Contact investigations may label close/not close after the investigation has been completed; there may be limited documentation regarding labelling It was often not recorded whether TST results for contacts were ‘negative’ or ‘not read’ |
| Wilce et al., 2002113 | |||
| Type of document: journal article Study design: qualitative and document analysis Country: USA Population: staff from 11 urban areas Quality notes: provides a range of descriptive data to underpin conclusions |
Research methods: interviews with staff and examination of policies and procedures Staff involved: various Measures used: N/A |
Results/data: all areas had policies in the form of documents or checklists. Policies varied widely in their content and comprehensiveness. Most described the main steps involved in a contact investigation, but specific actions within these were often not specified Review of medical records was only briefly mentioned in some policies; the time after diagnosis for an interview was often unclear; follow-up interviews were recommended in seven areas. The content of the interview was typically left to the discretion of the interviewer. Field visits were not required in four areas; policies typically provided few details on the procedure for visits. Checklists for assessing risk of transmission were typically available, although without accompanying instructions or space for recording findings Sites did not consistently define a ‘close’ contact. Information regarding risk factors such as HIV could be hard to obtain, although most sites had policies regarding immunocompromised persons Five sites referred to the ‘concentric circles’ approach (but provided little guidance on how to apply it). At six sites decisions regarding expansion were made by the worker responsible, at four sites they were made by a supervisor and at one site they were made during a meeting. Two sites routinely excluded casual contacts owing to limited resources Staffing models and training varied between sites. Data recording and data managements systems varied; also monitoring procedures Challenges reported related to communication barriers, structural barriers and patient-level barriers |
Main conclusions: there was generally inconsistency in guidelines, staffing and training across the different services. Comprehensive policies and support are required to improve the standard of contact-tracing investigations |
| Yeo et al., 2006114 | |||
| Type of document: journal article Study design: retrospective review of data Country: Canada Population: residents of Montreal under the age of 18 years (n = 66) Quality notes: describes characteristics of the data |
Research methods: examined public health data 1996–2000 and carried out additional genotyping Staff involved: N/A Measures used: number of cases and contacts, IS6110-based genotyping, and spoligotyping |
Results/data: 19 children were diagnosed after contact investigations of known adult cases No contact investigation had been carried out for eight children. For the remaining 39 children, a total of 616 contacts were identified. The median number of contacts per child was 9 (interquartile range 6–10 contacts) Four probable source cases were identified, all involving parents or other relatives. Genotyping by the research team identified up to 14 possible additional index cases. From the records available it was possible to identify a link to the children for only one of these additional cases |
Main conclusions: the contact investigations were extensive and had mostly been able to identify latent TB infection, but less successfully identified the source cases Genotyping indicated a substantial number of further sources of potential transmission |
| Zangger et al., 2001115 | |||
| Type of document: journal article Study design: descriptive Country: Switzerland Population: residents of Lausanne including family and school pupils and staff (n = 53) Quality notes: narrative description of the investigation |
Research methods: describes investigation around one source case (a 15-year-old girl) Staff involved: doctor, health officer, a nurse from the TB service Measures used: TST, chest radiography for those with positive TST, cost |
Results/data: three proximity groups:
Passing from one group to next reduced the rate of infection by 4 times. The compliance rate for treatment was 64% The cost of the investigation was over CHF24,000 The index case had arrived from Africa and had a positive test on arrival but no treatment |
Main conclusions: the distribution of cases confirms the importance of duration of contact and proximity of contact with the index case |
Appendix 4 Papers excluded at full-article stage
| Paper | Reason for exclusion |
|---|---|
| Abubakar I, Stagg HR, Cohen T, Mangtani P, Rodrigues LC, Pimpin L, et al. Controversies and unresolved issues in tuberculosis prevention and control: a low-burden-country perspective. J Infect Dis 2012;205(Suppl. 2):293–300 | Review of TB control strategies; does not refer to contact tracing |
| Armbruster B, Brandeau ML. Contact tracing to control infectious disease: when enough is enough. Health Care Manag Sci 2007;10:341–55 | Focus is on other conditions |
| Begun M, Marks GB, Wood JG, Newall AT. Contact tracing of tuberculosis: a systematic review of transmission modelling studies. PLOS ONE 2013;8:e72470 | Review of models, with emphasis on model development methods |
| Cardona M, Bek MD, Mills K, Isaacs D, Alperstein G. Transmission of tuberculosis from a seven-year-old child in a Sydney school. J Paediatr Child Health 1999;35:375–8 | Focus is on transmission rather than contact tracing |
| Chakhaia T, Magee MJ, Kempker RR, Gegia M, Goginashvili L, Nanava U, Blumberg HM. High utility of contact investigation for latent and active tuberculosis case detection among the contacts: a retrospective cohort study in Tbilisi, Georgia, 2010–2011. PLOS ONE 2014;9:e111773 | Non-OECD country |
| Classen CN, Warren R, Richardson M, Hauman JH, Gie RP, Ellis JHP, et al. Impact of social interactions in the community on the transmission of tuberculosis in a high incidence area. Thorax 1999;54:136–40 | Non-OECD country (South Africa) |
| Cook SA, Blair I, Tyers M. Outbreak of tuberculosis associated with a church. Commun Dis Public Health 2000;3:181–3 | Focus is on transmission rather than contact tracing |
| Crawford JT: Genotyping in contact investigations: a CDC perspective. Int J Tuberc Lung Dis 2003;7(Suppl. 3):453–7 | Discusses the use of genotyping; no data |
| Cronin WA, Golub JE, Lathan MJ, Mukasa LN, Hooper N, Razeq JH, et al. Molecular epidemiology of tuberculosis in a low- to moderate-incidence state: are contact investigations enough? Emerg Infect Dis 2002;8:1271–9 | Focus is on transmission rather than contact tracing |
| Dahle UR, Nordtvedt S, Winje BA, Mannsaaker T, Heldal E, Sandven P, et al. Tuberculosis in contacts need not indicate disease transmission. Thorax 2005;60:136–7 | Highlights that infection in contacts may be due to reactivation of disease rather than having a focus on contact tracing as an intervention |
| Dasgupta K, Schwartzman K, Marchand R, Tennenbaum TN, Brassard P, Menzies D. Comparison of cost-effectiveness of tuberculosis screening of close contacts and foreign-born populations. Am J Respir Crit Care Med 2000;162:2079–86 | Although mentions contact tracing, has a focus on screening of immigrants and the evaluation of two screening programmes |
| del Castillo Otero D, Penafiel Colas M, Alvarez Gutierrez F, Soto Campos JG, Calderon Osuna E, Toral Marin J, Sanchez Gomez J: Investigation of tuberculosis contacts in a nonhospital pneumology practice. Eur J Clin Microbiol Infect Dis 1999;18:790–5 | Focus is on transmission rather than contact tracing |
| Faccini M, Codecasa LR, Ciconali G, Cammarata S, Borriello CR, De Gioia C, et al. Tuberculosis outbreak in a primary school, Milan, Italy. Emerg Infect Dis 2013;19:485–7 | Focus is on transmission of infection |
| Kondo S, Ito M. Efficacy of tuberculosis contacts investigation and treatment, especially of preventative therapy in infants and young children. Tuberculosis 2003;78:677–82 | Focus is on diagnosis and treatment rather than contact tracing |
| LoBue PA, LeClair JJ, Moser KS. Contact investigation for cases of pulmonary Mycobacterium bovis. Int J Tuberc Lung Dis 2004;8:868–72 | Predominant focus on Mycobacterium bovis |
| Mandeville KL, Harris M, Thomas HL, Chow Y, Seng C. Using social networking sites for communicable disease control: innovative contact tracing or breach of confidentiality? Public Health Ethics 2014;7:47–50 | Focus is on other conditions |
| McElnay C, Thornley C, Armstrong R. A community and workplace outbreak of tuberculosis in Hawke’s Bay in 2002. N Z Med J 2004;117:U1019 | Refers to delays in contact tracing as a factor in the outbreak; however, focus is on infection rates and therapy |
| Migliore E, Borraccino A, Baussano I, Piccioni P, Carosso A, Bugiani M. Outcomes of a tuberculosis contact investigation programme in Italy. Eur Respir J 2012;40:1291–3 | Brief report duplicating information in Borraccino et al.45 paper |
| Mohle-Boetani JC, Flood J. Contact investigations and the continued commitment to control tuberculosis. JAMA 2002;287:1040–2 | Comment on other papers |
| Morrison J, Pai M, Hopewell D. Tuberculosis and latent tuberculosis infection in close contacts of people with pulmonary tuberculosis in low-income and middle-income countries: a systematic review and meta-analysis. Lancet Infect Dis 2008;8:359–68 | Focus is on the yield of investigations and argues for the need to carry out contact investigations in high-incidence countries |
| Ohno H, Ikegami Y, Kishida K, Yamamoto Y, Ikeda N, Taniguchi T, et al. A contact investigation of the transmission of Mycobacterium tuberculosis from a nurse working in a newborn nursery and maternity ward. J Infect Chemother 2008;14:66–71 | Predominant focus on numbers infected and treatment rather than the contact investigation |
| Reichler MR, Tapia J, Chavez-Lindell T, McAuley J, Thomas J, Yuan Y, Mangura B. Results of a prospective evaluation of tuberculosis (TB) contact investigations conducted in the United States and Canada. Am J Respir Crit Care Med 2009;179 | Conference abstract |
| Vella V, Racalbuto V, Guerra R, Marra C, Moll A, Mhlanga Z, et al. Household contact investigation of multidrug-resistant and extensively drug-resistant tuberculosis in a high HIV prevalence setting. Int J Tuberc Lung Dis 2011;15:1170–5 | Non-OECD country (South Africa) |
| Webb RM, Holcombe M, Pearson MM. Tuberculosis contact investigation in a rural state. Int J Tuberc Lung Dis 2003;7(Suppl. 3):353–7 | Describes the programme over 10 years in Mississippi, USA |
Glossary
- Active case finding
- Systematic screening for active tuberculosis.
- Active tuberculosis disease
- When a person has signs of disease that is caused by Mycobacterium tuberculosis or other members of the M. tuberculosis complex family in any part of the body, may be infectious and may spread tuberculosis bacteria to others.
- Contact
- An individual who is at risk of tuberculosis infection because they have been exposed to someone with active tuberculosis disease.
- Contact investigation
- A procedure for identifying and evaluating individuals who have been exposed to someone with active tuberculosis.
- Index case
- An individual with suspected or confirmed active tuberculosis disease who is reported to a tuberculosis infection control department, and is the case from whom the contact investigation begins.
- Latent tuberculosis infection
- When a person is infected with M. tuberculosis but does not have active tuberculosis.
- Positive skin reaction
- A tuberculin skin test reaction in a contact at a cut-off point designated during an investigation.
- Prophylaxis/prophylactic treatment
- The use of a drug for the prevention of active tuberculosis in someone thought to have latent infection.
- Skin test conversion
- A documented increase in reaction size on a tuberculosis skin test, indicative of recent tuberculosis infection.
- Source case
- A person with confirmed infectious tuberculosis who is responsible for transmitting tuberculosis infection to others. This individual may or may not be the index case.
- Specific population
- Any subgroup of the wider population containing individuals or groups who may be at higher risk of tuberculosis infection. This includes people described as ‘hard to reach’, those with drug or alcohol problems, homeless people, asylum seekers, immigrants, refugees, people from ethnic minorities and prisoners.
List of abbreviations
- BCG
- bacillus Calmette–Guérin
- CI
- confidence interval
- DNA
- deoxyribonucleic acid
- GP
- general practitioner
- HIV
- human immunodeficiency virus
- IGRA
- interferon gamma release assay
- OECD
- Organisation for Economic Co-operation and Development
- OR
- odds ratio
- QFT-G
- QuantiFERON®-TB Gold In-Tube
- RFLP
- restriction fragment length polymorphism
- TB
- tuberculosis
- TST
- tuberculin skin test