Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 12/5001/45. The contractual start date was in June 2013. The final report began editorial review in June 2015 and was accepted for publication in November 2015. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Darren Flynn, Gary A Ford, Helen Rodgers and Richard G Thomson have been involved in marketing activity for COMPASS, a decision aid to support thrombolysis decision-making and risk communication, which may be made commercially available, including covering the costs of technical maintenance and updating of the information content. Helen Rodgers is president-elect of the British Association of Stroke Physicians and a member of the Intercollegiate Stroke Working Party. Gary A Ford’s previous institution has received research grants from Boehringer Ingelheim (manufacturer of Alteplase), and honoraria from Lundbeck for stroke-related activities. Gary A Ford has also received personal remuneration for educational and advisory work from Boehringer Ingelheim and Lundbeck; in addition, he is supported by a National Institute for Health Research Senior Investigator award.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2017. This work was produced by Thomson et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction
Overview of the research
This research involved the design and development of a discrete choice experiment (DCE) to explore the patient-related and clinician factors that influence clinical decision-making regarding the offer of intravenous thrombolysis for patients with acute ischaemic stroke. This chapter provides a synopsis of the context and the rationale for the study, including the study aims and details of the project team.
Context and rationale for the research
Stroke remains one of the leading causes of death and disability in the UK. 1 Thrombolysis with recombinant tissue plasminogen activator (rtPA) with alteplase is a cost-effective treatment for acute ischaemic stroke but unwarranted variation exists in use of thrombolysis in the UK, despite the existence of the National Stroke Strategy,1 National Institute for Health and Care Excellence (NICE) guidelines,2 treatment licensing criteria3 and a strong evidence base. 2,4–6 Since the expansion of ‘24/7’ hyperacute stroke services (i.e. services available 24 hours per day, 7 days per week), structural factors, such as access to treatment and computed tomography (CT) investigation, are less likely to explain this variation. Hence remaining variation is more likely to be accounted for by differences in clinical decision-making about offering thrombolysis, based on interpretation and understanding of patient variables, and on variables relating to the individual decision-makers (such as experience or attitude towards risk). The current study captured information on which patient and clinician factors influence clinicians’ willingness to offer intravenous thrombolysis to ischaemic stroke patients, as well as determining their impact on decision-making. By understanding how clinicians internally and externally negotiate the risks and benefits in different patients, we can optimise appropriate use of thrombolysis and better support risk communication, consent and decision-making with patients. Outcomes of the research will include benefits for service delivery by (1) translating learning into training and continuing professional development (CPD); (2) supporting the implementation of a decision support tool that has been developed to support decision-making in thrombolysis; and (3) informing the content and interpretation of audit and evaluation programmes.
Aims and objectives
This study aimed to identify the factors that contribute to variation in, and influence, clinicians’ decision-making about intravenous thrombolysis for acute ischaemic stroke, in order to inform programmes that seek to influence clinical behaviour and decision-making.
This study had four specific research objectives:
-
to determine which patient factors influence clinical decision-making about the offer of thrombolysis
-
to identify and quantify the trade-offs clinicians make regarding the decision to offer thrombolysis
-
to determine which clinical factors influence clinical decision-making about the offer of thrombolysis (e.g. clinician experience, setting, personality type)
-
to influence clinicians’ behaviour by translating learning into CPD activity, national clinical guidelines, supporting implementation of an existing thrombolysis decision support tool and informing clinical audit and evaluation programmes [e.g. Sentinel Stroke National Audit Programme (SSNAP)].
The study captured information on medical judgement and choice by undertaking a DCE. A DCE is an approach that facilitates the consideration of multiple factors in a decision, and therefore is an appropriate and valuable technique to explore the complex clinical decision of the offer of thrombolysis for patients with acute ischaemic stroke. This approach also allows for investigation of the impact of clinician factors, such as attitude to risk and level of experience, on decision-making. The DCE approach offers a means through which the nuances of decision-making, not easily accessed through other more traditional research methods, can be understood. DCEs have been increasingly adopted to examine decision-making in areas of health care including stroke rehabilitation. 7,8
This study involved two key components:
-
a five-stage iterative process to develop and design a clinically valid DCE
-
administration of the DCE.
Project team
The Project Management Group consisted of three stroke clinical researchers, one trainee stroke physician, two patient representatives (from the Stroke Association), two chartered psychologists, two health economists, an expert in shared decision-making and the project secretary. This group met on average once per month during the course of the project to discuss all aspects of the research.
An external advisory group met on three occasions during the course of the study. This group included the members of the Project Management Group and Professor Anthony Rudd (Professor of Stroke Medicine, King’s College London, who chaired the group), Ms Chucks Golding (patient representative), Dr Dean Shipsey (Emergency Medicine Consultant, Northumbria Healthcare NHS Trust), Ms Elizabeth Morris (Stroke Network Delivery Manager, NHS) and Professor Tim Coats (Professor of Emergency Medicine, University of Leicester). The function of the advisory group was to provide feedback and advice, and review progress on all aspects of the study.
Ethical approval
Ethical approval for this study was obtained from the Newcastle University Research Ethics Committee (reference 00720/2013). All potential participants were provided with information about the study and they had an opportunity to address questions to the researchers prior to participation. Individuals were informed that their participation was entirely voluntary and that they were free to withdraw at any time without reason. In the online DCE survey, an information screen preceded the survey, which included a brief study description, and participants were made aware that their consent was implied through completion of the survey. All personal identifiers were removed to protect confidentiality.
Structure of the report
Chapter 2 presents the background to the research in terms of an overview of the literature, including a summary of the literature on the clinical decision-making that has informed the design of the current study. Chapter 3 details the methods adopted in designing the study and the rationale for the use of a DCE. Chapter 3 also outlines the five-stage systematic process undertaken to design the DCE used in the current research, along with details on participant sampling, data management and the analysis. Chapter 4 describes the sample profile and the results of the DCE in terms of levels of patient and clinician factors that were identified as statistically significant predictors of thrombolysis decision-making. Chapter 5 discusses the results of the DCE in the context of the existing literature and offers recommendations for stroke training and further research. Finally, Chapter 6 summarises the conclusions that can be drawn from the research and offers suggestions for future work.
Chapter 2 Background
Stroke is a leading cause of death and disability; there are approximately 152,000 strokes in the UK every year and between 80% and 85% of these are ischaemic strokes. 9 Ischaemic strokes are caused by a blockage in a blood vessel supplying blood to the brain. This can halt blood flow, resulting in damage to the brain and a loss of function.
Context of the study: acute ischaemic stroke and intravenous thrombolysis
Intravenous thrombolysis using rtPA is an effective medical treatment for patients with acute ischaemic stroke. Despite its inclusion in national guidelines and evidence of its benefit in certain patient groups,5,6,10,11 it is underused, as recent estimates from SSNAP suggest that one in five patients eligible for intravenous thrombolysis does not receive it. 12,13 As thrombolytic treatment can reduce disability from stroke and resulting care costs,10 maximising its appropriate use is a health and economic priority.
Although there are national guidelines for treatment,2 the clinical decision regarding the offer of thrombolysis for patients is complex and multifactorial. The time-limited window for treatment (within 4.5 hours of symptom onset), the emergency context of the decision, potential difficulties in engaging patients and carers in decision-making and obtaining consent and the many clinical factors that might influence the balance between risk and benefit for individual patients further complicate the decision. 14 Early treatment of patients with acute ischaemic stroke with thrombolysis is associated with more favourable outcomes,15 yet there is a small but significant risk of adverse outcomes as a result of treatment. 16 Thrombolytic treatment may result in adverse effects, such as systemic bleeding, angioedema17 and symptomatic intracranial haemorrhage (sICH), which is the most disabling and potentially fatal complication, occurring in approximately 3–4% of patients. 12 By definition, sICH usually results in worse disability than would have occurred without thrombolytic treatment and in a small proportion of patients can be responsible for death. 18
Decision-making may be further complicated by areas of uncertainty in research evidence, typically where high-quality empirical data do not exist regarding the suitability of certain patients for thrombolysis, for example patients with dementia or older patients. 14,17 Given the recorded variation in thrombolysis treatment rates,19 the lack of expert consensus on several exclusion criteria for treatment (such as recent medical procedures and spontaneous improvement rate)20 and the ongoing debates regarding the efficacy of thrombolysis,21–26 it is important to understand factors which influence clinicians’ decisions about whether or not to give intravenous thrombolysis to patients with acute ischaemic strokes, using a method that reflects decision-making in practice. 27,28
Trial evidence and guidelines on intravenous thrombolysis
A meta-analysis of data from 6756 individual patient data combined from nine randomised trials was recently conducted to explore the effect of treatment delay, patient age and stroke severity on the effects of thrombolysis in acute stroke. 15 The analysis confirmed that thrombolysis increased the likelihood of a good outcome and that earlier treatment was associated with greater patient benefit and outcomes. 15 This work presented strong evidence of the benefit of thrombolysis (compared with placebo groups) up to 4.5 hours post symptom onset. Significantly, the analysis also revealed proportional treatment benefits that were similar irrespective of age or stroke severity. An increased risk of sICH was observed for the treatment group and was similar irrespective of treatment delay, age or stroke severity. However, those with more severe strokes had the greatest absolute risk of sICH.
The evidence underlying this meta-analysis was drawn from major clinical trials of thrombolysis (with alteplase) conducted since the 1990s: the European Cooperative Acute Stroke Study (ECASS) trials (ECASS-I, -II and -III),29,30 the National Institute of Neurological Disorders and Stroke (NINDS) trial,31 the Alteplase Thrombolysis for Acute Noninterventional Therapy in Ischaemic Stroke (ATLANTIS) trial32 and the Third International Stroke Trial (IST-3). 5
The first ECASS29 trial randomised over 600 patients presenting within 6 hours of symptom onset to placebo or treatment groups. Although no significant differences emerged between the groups, post-hoc analyses demonstrated that, if protocol violations were removed, results indicated a benefit of treatment with thrombolysis (improved functional and neurological outcomes for patients with moderate to severe neurological deficit).
In contrast to ECASS, NINDS31 randomised patients presenting within a shorter onset time: 3 hours from symptom onset. The NINDS study had two parts and two primary aims: the first tested if thrombolysis resulted in patient improvement in terms of an positive change of ≥ 4 points on the NIHSS (measuring neurological impairment) within 24 hours; and the second assessed whether or not there was a significant and consistent difference between the treatment and placebo groups in terms of the proportion of patients who recovered with minimal or no deficit 3 months post treatment (using a global statistic comprising four different outcome measures). 31 In part 1, no significant differences were observed, but post-hoc tests revealed improvement in the treatment group in most time periods, compared with placebo. In part 2, compared with the placebo group, thrombolysis was found to have a significant positive benefit on patient outcome measures. The NINDS trial concluded that, although an increased incidence of sICH was observed, treatment with intravenous thrombolysis within 3 hours of symptom onset improved patient outcomes at 3 months.
The second ECASS trial (ECASS-II30) again explored treatment with thrombolysis within an extended time window of up to 6 hours post symptom onset. The majority of enrolled patients were treated within the 3- to 6-hour time window and no significant differences emerged between the placebo and the treatment groups.
In the same period, the ATLANTIS32 trial explored the effect of administration of thrombolysis when symptom onset was between 3 and 5 hours. The results indicated no significant differences between the groups.
Following the completion of these trials, a pooled analysis of all trial data was conducted. 16 This revealed a significant positive effect of thrombolysis and highlighted the importance of treating patients as early as possible after symptom onset. A statistically significant treatment effect was present between 3 and 4.5 hours from symptom onset, but not between 4.5 and 6 hours. 16 It was concluded that patient outcomes are enhanced the earlier thrombolysis is administered, with a potential benefit after 3 hours, but with increased risk of adverse events.
The ECASS-III33 trial included over 800 patients randomised to treatment or placebo group within 3–4.5 hours of symptom onset. The trial confirmed the significant benefit of thrombolysis over placebo in terms of patient outcomes when treatment was administered within 3–4.5 hours post symptom onset. The results also found a higher risk of sICH in the treatment group.
Current UK NICE guidelines2 recommend intravenous thrombolysis with alteplase for treating patients with acute ischaemic stroke in adults if treatment is started as early as possible within 4.5 hours of the onset of stroke and when intracranial haemorrhage has been excluded by imaging techniques. The NICE Technology Appraisal Committee concluded that intravenous thrombolysis using alteplase, administered between 0 and 4.5 hours after the onset of stroke symptoms, was an effective treatment for acute ischaemic stroke. The treatment window was extended to 4.5 hours from the previous cut-off of 3 hours post symptom onset in 2012. 2,4
Although not submitted in time for the NICE review, the results of IST-35 have subsequently been published. The trial found that for every 1000 patients who receive thrombolytic treatment within 3 hours of stroke, approximately 100 more will survive alive and independent compared with 1000 patients not given thrombolytic treatment. Similarly, a benefit was also found for patients treated within 6 hours of stroke, but a smaller effect was observed in that approximately 50 more will be alive and independent compared with those not treated with thrombolysis. The trial also confirmed a benefit of treatment among patients aged > 80 years when treated within 3 hours of symptom onset. However, the benefit was not as strong when treating patients aged > 80 years closer to the 6-hour mark.
In a recent update to the Cochrane review on thrombolysis for acute ischaemic stroke,6,34 the authors concluded that thrombolytic treatment delivered < 3 hours after stroke symptom onset significantly reduced death or dependency at 3–6 months, but that at progressively later times to treatment, the benefit decreased, disappearing between 4.5 and 6 hours. It was also noted that the pooled trial data16 had demonstrated a significant reduction in death or dependency with treatment within 6 hours of symptom onset, but there was significant heterogeneity observed between trials.
Licensing criteria currently restrict treatment to patients aged ≤ 80 years, but most clinicians now treat patients aged > 80 years on the basis of recent trial evidence5 and recognition of the distinction between chronological and physiological age. The ECASS-III35 trial supported extension of the time window for treatment from 3 to 4.5 hours and the European licence time window was extended. 3 However, according to the Safe Implementation of Thrombolysis in Stroke-Monitoring (SITS-MOST) study, it is common for patients outside the licensing criteria to be treated,36 suggesting that different clinicians are satisfied with different levels of evidence and/or vary in their decision-making process regarding patient eligibility given the same evidence. Yet little is known about the source or drivers of this variation.
In recent years, there has been considerable debate between proponents of thrombolysis and those who question its efficacy. There have been arguments presented in prominent journals, such as the British Medical Journal,21,25 as well as papers targeted towards an emergency medicine audience. 24,26,37,38 These articles describe the evidence base for thrombolysis as uncertain and call for a reappraisal of the evidence, advocating the view that the risks of thrombolysis in acute stroke outweigh the potential benefits of treatment. These debates have also been the focus of recent media attention39 and, therefore, clinicians are likely to be aware of these ongoing issues.
As a result of these debates and public controversies surrounding other treatments, the Chief Medical Officer for England has called for an independent review of the safety and efficacy of medical treatments, and thrombolysis will be included in this Academy of Medical Sciences review. 39 An independent investigation of thrombolysis by the Medicines and Healthcare products Regulatory Agency has recently been published, confirming the benefit of thrombolysis for patients with acute ischaemic stroke. 39
The next section explores the factors that have been shown to influence clinical decision-making and factors that have been specifically implicated as influential in decision-making about thrombolysis.
Influences on clinical decision-making
There are myriad factors that may influence the clinical decision to offer intravenous thrombolysis. These factors may be considered in three broad categories: patient-related factors, clinician-related factors and environmental/systemic factors. This section will explore each of these influences.
Patient-related factors that can influence clinician decision-making
An international Delphi study conducted in 2007 sought to establish consensus on the relative contraindications for offering intravenous thrombolysis in acute ischaemic stroke. 20 Although agreement was reached on 12 of the 18 patient factors, there was a failure to reach consensus on factors such as stroke onset time to treatment, recent medical procedures, spontaneous improvement rate and blood pressure treatment (Table 1). 20 This study highlighted the variation between expert clinicians in their attitudes towards factors that influence decision-making about thrombolysis and underlined the degree to which ‘grey’ areas remain in the evidence base.
| Factors where consensus was reached | Factors where consensus was not reached |
|---|---|
| Previous stroke | Stroke onset to treatment time |
| Previous head trauma | Recent surgery |
| Recent gastrointestinal haemorrhage | Spontaneous improvement rate |
| Recent urinary tract haemorrhage | Blood pressure reduction |
| Stroke severity | Patient age |
| Systolic blood pressure | Recent arterial puncture |
| Diastolic blood pressure | |
| Platelet count | |
| Maximum serum glucose level | |
| Minimum serum glucose level | |
| International normalised ratio | |
| Activated partial thromboplastin time |
Studies have suggested that sex may have a population-level effect on thrombolysis administration, with evidence of the underutilisation of intravenous thrombolysis in women,40 although this may reflect a different age and presentation profile in women. 41 This is despite a pooled analysis of randomised controlled trials demonstrating that women are more likely than men to benefit from thrombolysis. 42,43 Research to assess and clarify the impact of sex on thrombolysis utilisation and outcomes using individual patient data collated from randomised trials is ongoing and should clarify this effect, if any. 15
Uncertainty exists regarding a number of patient factors, where there are ‘grey’ areas in the guidelines and/or research evidence. Patient factors, such as pre-stroke disability, stroke severity and comorbidities, can operate as a major influence on clinicians’ consideration of the potential risks and benefits of thrombolytic treatment. Research has explored whether or not pre-stroke disability was associated with negative outcomes of thrombolysis. 44 It was concluded that pre-stroke disability does not independently increase the risk of sICH after thrombolysis. However, higher modified Rankin Scale (mRS) scores (high scores indicating greater dependency on others for assistance with daily living) were associated with an increased risk of death at 3 months post treatment. Despite this, the authors state that as one-third of previously disabled patients can return to their pre-stroke dependency, these patients should not be excluded from treatment with intravenous thrombolysis.
Uncertainty also exists regarding minor strokes and self-limiting transient ischaemic attacks. Relatively minor symptoms may lead clinicians to believe that patients are not sufficiently impaired to warrant treatment, based on the perceived risk of treatment. Furthermore, the licensing criteria state that clinicians should exclude patients as eligible for treatment when there is a ‘minor neurological deficit or symptoms rapidly improving before start of infusion’45 and, thus, clinicians may withhold or delay thrombolysis where symptoms are mild or improving. 46 Many clinical trials excluded patients with low NIHSS scores (usually NIHSS score of ≤ 3–5), limiting the evidence base for such patients. However, a recent Austrian study found that those with a mild deficit (NIHSS score of ≤ 5) had significantly improved outcome with thrombolytic therapy, compared with matched cases who did not receive thrombolytic treatment. 47 A pooled analysis of individual patient data from stroke trials demonstrated better outcomes in patients with mild ischaemic stroke (NIHSS score of ≤ 4) treated with thrombolysis, although < 10% of enrolled patients had mild stroke. 15
Clinicians may also delay treatment or decision-making with thrombolysis if blood pressure is high (> 185/110 mmHg). Active blood pressure lowering is associated with an increased proportion of patients being treated with intravenous thrombolysis,48,49 compared with a conservative strategy, without a difference in sICH rate.
Clinician-related factors that can influence clinical decision-making
There is strong evidence that clinician-related factors can have a significant influence on medical decision-making. 50 Shamy et al. recently conducted a study which addressed the decision of administering intravenous thrombolysis for acute stroke. 51 In their online survey of 70 neurologists in Ontario, Canada, they found that respondents were less likely to administer thrombolysis to patients over the age of 80 years, to patients from nursing homes and to patients diagnosed with dementia. 51 Post-hoc analyses revealed that neurologists who consulted on more than 10 acute stroke cases per month were significantly less likely to treat large strokes and those with more than 10 years of clinical experience were significantly more likely to administer thrombolysis to patients with dementia.
Further clinician-centred influences on the consideration of thrombolysis have been postulated, and include factors such as concern about adverse effects, especially sICH, and uncertainty about effectiveness. 37,52 Recent academic debates regarding the efficacy of thrombolysis are also likely to impact on clinicians’ decision-making and might have influenced clinicians’ perception of the evidence base and confidence in the efficacy of thrombolysis. Attitude towards thrombolysis has been independently associated with willingness to administer thrombolysis,37 and clinicians’ interaction and involvement with their professional community and information-seeking behaviour can also influence medical decision-making. 53
In the wider literature on clinical decision-making, several factors, including clinicians’ age, sex, medical specialty and level of experience, have been shown to influence decision-making. For instance, level of experience54 and characteristics of clinicians (e.g. their medical specialty, age and ethnicity) can interactively influence decision-making. 55 A study examining variation in diagnostic decision-making in heart failure (a similarly complex decision characterised by high levels of uncertainty) found that clinician characteristics, such as grade or level of seniority, influence how evidence is weighted and used to inform a diagnostic decision. 56
Personality and individual values also differ among clinicians, potentially influencing decision-making. Research indicates that personality characteristics are associated with working in certain medical specialties57 and can predict the choice of person- or technique-oriented medical specialty. 58 Individuals can also differ in their approach to risk,59 and risk assessment is a routine component of clinicians’ everyday practice. The perception of risk can be influenced in many ways, such as through interaction with the patient and other clinicians and through the clinicians’ own attitudes towards risk. Personal attitude to risk has been explored in previous decision-making research, and a US-based study found that emergency medicine physicians’ scale scores correlated significantly with their rates of admission for patients with acute chest pain, in that individuals in the high-risk-taking group were less likely to admit patients after treatment than colleagues scoring as low risk takers. 59
Another relevant feature of clinical decision-making in practice is making decisions in uncertain circumstances, for instance when a diagnosis is unclear or when details about the patient’s history may be incomplete or unknown. A systematic review of the barriers to delivery of thrombolysis found that physician uncertainty about administering thrombolysis was a key barrier. 52 Gerrity et al. developed a scale to assess physicians’ affective reaction to uncertainty. 60,61 Research employing this measure found that it has been associated with decision-making. For instance, primary care providers with higher levels of anxiety about uncertainty were more likely to refer a chronic kidney disease patient to a nephrologist. 62
Clinicians are also vulnerable to the cognitive biases that affect us all. These are cognitive ‘rules of thumb’ that are based on experience and serve to reduce cognitive load. 54 While they are a mechanism by which rapid clinical decisions can be made in typical circumstances, they can also result in error and decision-making bias if adhered to rigidly in situations which are atypical. The availability bias is one which may influence the decision to offer intravenous thrombolysis. Availability may be described as the tendency for things to be judged as occurring more frequently, or as more likely to occur, if they can be readily brought to mind: that is, they are available and easily accessible in memory. This can lead to distortion in estimates of base rates (i.e. risk of sICH) and may lead clinicians to under- or overestimate the probability of a negative outcome of treatment. Even clinicians who are cognisant of the potential bearing of cognitive biases on clinical judgement and decision-making may still be susceptible. 63
Clinicians’ may also vary in their willingness to control blood pressure before administering thrombolysis, as this was not standardised during the trials which produced evidence about the efficacy of thrombolysis for stroke. A recent study48 found that active blood pressure lowering was associated with an increased proportion of patients treated with intravenous thrombolysis, compared with a conservative strategy, without a difference in sICH rate. However, it is unclear if all clinicians would be comfortable with actively trying to lower blood pressure before administering thrombolysis.
Taken together, this literature highlights the variation that can exist between clinicians, even when consulting on identical cases, and thus underscores the importance of examining both patient factors and clinician factors in a decision-making model.
Environmental/systemic factors that can influence clinical decision-making
Research suggests that the culture within a hospital or treatment centre can impact on decision-making and practice style. 64–66 A study conducted in the Netherlands found that several features of organisational culture were positively associated with rates of thrombolysis administration, including the availability of feedback on practice, a learning culture and clinical leadership. 67 Structural factors such as access to CT scanning might previously have had an influence on variation on intravenous thrombolysis rates in the UK; however, with the widespread implementation of ‘24/7’ hyperacute stroke services and the extension of telemedicine facilities,68 continuing variation is likely to reflect differences in clinical decision-making.
Summary and conclusions
It is clear that there are multifaceted influences on clinical decision-making more broadly and specifically on thrombolysis decision-making. It remains unclear which specific patient- and/or clinician-related factors influence the clinical decision to offer thrombolysis to patients, and especially their relative contributions to variation in treatment rates. In order to better understand clinical decision-making about intravenous thrombolysis, a study to explore factors influencing clinicians’ reasoning is warranted. Given the recorded variation in thrombolysis treatment rates, the lack of expert consensus on several exclusion criteria for treatment and the ongoing debates regarding the efficacy of thrombolysis, a robust method is required that facilitates an understanding of the preferences of clinicians who are making these decisions in a way that most closely reflects decision-making in practice. This study aimed to identify the factors that contribute to variation in, and influence, clinicians’ decision-making about offering intravenous thrombolysis to patients with acute ischaemic stroke.
Chapter 3 Research methodology
Rationale for a discrete choice experiment
A DCE is a method used to explore the relative importance of different factors in a decision-making process. Based on the principles of random utility theory and on Lancaster’s theory of demand,69,70 DCEs operate on the tenet that multiple factors/attributes influence decision-making and that all choices involve trade-offs. The DCE approach offers a means through which the nuances of decision-making, which are not easily accessed through other more traditional research methods, can be understood.
As summarised in Table 2, other methods to explore variation in clinicians’ decision-making about thrombolysis have weaknesses and are inappropriate to capture the nuances underlying complex decision-making processes. For this reason, the Delphi method cannot adequately address the research question, as it seeks to establish consensus among experts rather than explore the variation and differences in decision-making. Furthermore, a previous Delphi study20 aiming to reach consensus on the contraindications for thrombolytic treatment failed to achieve agreement on several indicators, further highlighting the variation that exists between clinicians in their decision-making when there is a lack of clinically applicable evidence. Similarly, although an ethnographic approach could provide rich observational qualitative data, such data give insights into the observable processes of decision-making rather than the implicit thought processes that shape those decisions. In addition, there are significant ethical and practical issues associated with undertaking observations in an emergency context. For instance, there would be difficulties in accessing an emotionally charged and sensitive situation and, coupled with the relative infrequency of this decision-making scenario, the researcher would need to be present for very long periods in order to access small numbers of decision-making events. Finally, insights from audit data are dependent on the extent, level of detail and completeness of the data set and may not be fit for purpose, and they cannot address the nuances of decision-making. For instance, the SITS-MOST database36 is limited to thrombolysed cases only and SSNAP does not collect information on all patient and clinician factors that could influence clinical decision-making.
| Method | Advantages | Disadvantages |
|---|---|---|
| Delphi study | Facilitates a group communication process to address a complex problem with the aim of achieving consensus | Focus is on achieving consensus rather than understanding variation in decision-making Delphi study has already been undertaken which demonstrated the need to better understand decision-making20 |
| Ethnography | Observation of real-time decision-making processes in actual clinical practice | Ethical and practical constraints around observing clinical decision-making in an emergency context Focus is usually on the observed behaviour rather than exploring the underpinning thought processes that shape the decision made56 Difficult to observe infrequent events |
| Audit | More straightforward to access and conduct | Focus on the decision outcome rather than the factors that shape decision-making, many of which will not be recorded in medical records Provides information on decisions made but does not capture trade-offs in decision-making Audit data have limitations such as the extent and completeness of the data set Analysis of audit data shows variation, but does not explain it with regard to decision-making71,72 |
| DCE | Unpacks the factors shaping decision-making and enables exploration of the trade-offs made and how these vary across a population of decision-makers | There may be challenges in explaining the method and the decision task to participants DCEs have been criticised on the grounds that participants might behave differently under test conditions from how they would behave in reality. However, DCE allows design of the choice set to mimic as closely as possible the decision of interest using vignettes designed with emphasis on clinical face/content validity to enhance external validity27 |
High levels of external validity have been demonstrated in DCEs in a number of areas in which DCEs have been applied, including in health, environment and transport settings. 73,74 For example, in a study of physicians’ prescribing decisions, stated preference responses to hypothetical scenarios were shown to align with revealed preference (i.e. preferences under simulated conditions aligned with actual behaviour). 74
In particular, data collected in DCEs are used to model choice (in this case of whether or not to offer thrombolysis) as a function of the attributes of the alternatives between which respondents are asked to choose (in our case the characteristics within the patient vignettes) and the characteristics of the decision-makers (the clinicians’ characteristics). This makes DCEs ideally suited to investigate which attributes described in the vignettes are important to clinicians when deciding to offer thrombolysis. Following testing, the preferred model can be chosen based on goodness-of-fit indicators such as Akaike and Bayesian information criteria. 27 Predicted probability analysis can investigate the probability of offering thrombolysis using clinically relevant values on the attribute levels. DCEs have been increasingly adopted to examine decision-making in areas of health care (e.g. to explore patient preferences for early stroke rehabilitation management8 and patient preferences for atrial fibrillation medication75), but none has examined the factors that influence clinicians’ decisions to offer thrombolysis.
Issues to consider in discrete choice experiment design and development
Traditionally, the design of a DCE is informed by literature review, expert opinion, theoretical arguments and/or qualitative work. However, there is no standard development process for a DCE, owing to the variable nature of the type of factors that may be included and the optimal presentation mode of choice sets or decision alternatives. As a result, the processes involved in the design of DCEs are often poorly described, with little or no detail reported regarding the procedures for selection of factors/levels in the final design. 76 In particular, there is a dearth of information on procedures undertaken to refine the number of factors and their associated levels and, when reported, this information has been characterised as ‘excessively brief’. 76
The International Society for Pharmacoeconomics and Outcomes Research (ISPOR) has published two reports on recommended research practice for DCEs. 77,78 These publications include advice on evidence-based factors and level selection, as well as a checklist for researchers to ensure best practice in the development, administration, analysis and reporting of DCEs. However, these guidelines do not offer a clear approach to DCE factor/level selection. Therefore, this research builds on these guidelines by offering a transparent approach to DCE development, which may be employed in other settings.
In the following section, we describe the multistage process undertaken to develop and conduct an online DCE to explore factors influencing clinical decision-making about intravenous thrombolysis in the treatment of acute ischaemic stroke. This process was guided by ISPOR recommendations for research practice, as well as recent published advice on the development and design process,7,76–78 to ensure optimal design of the DCE.
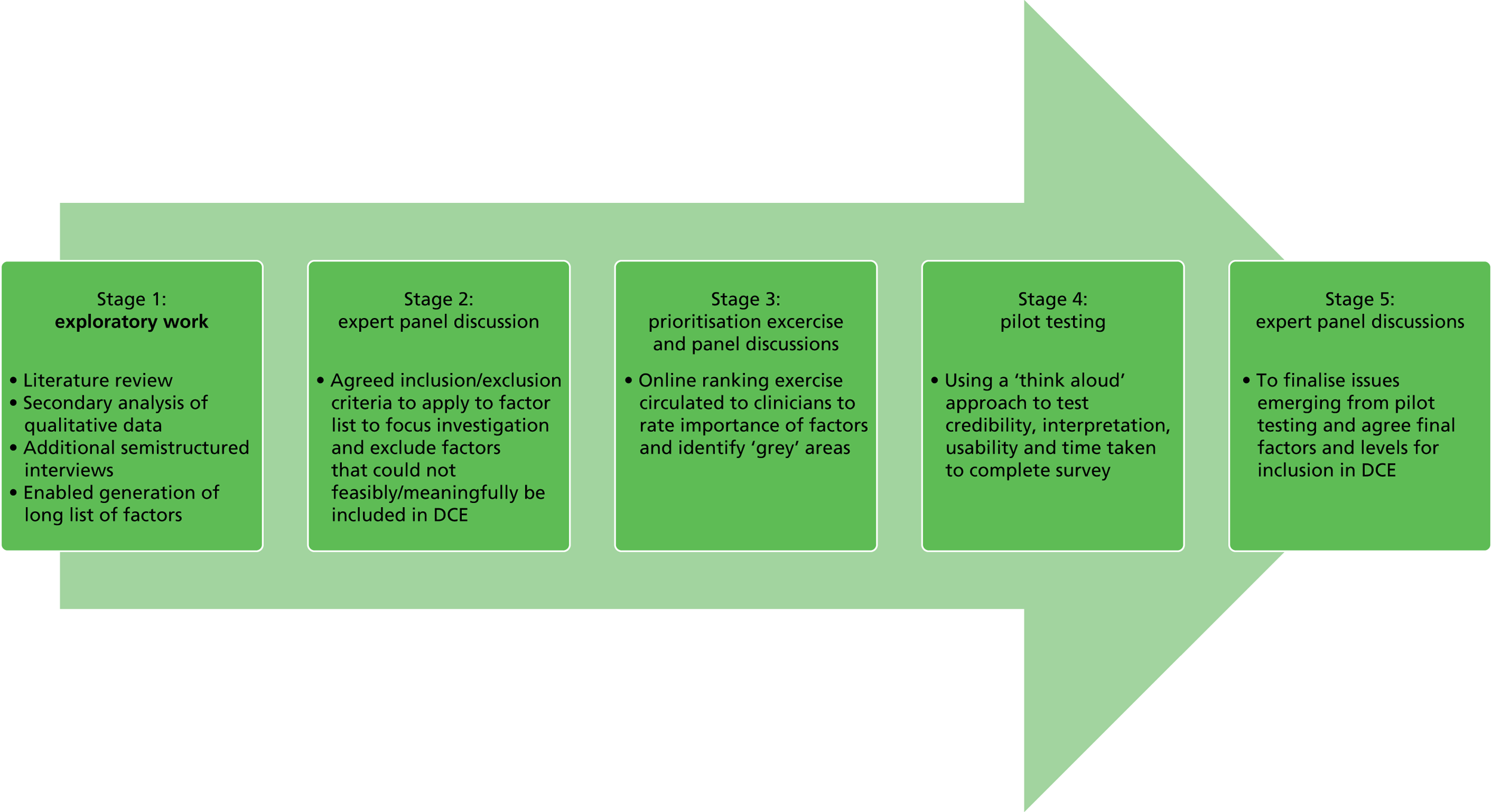
Overview of design process adopted in current study
The development process consisted of five iterative stages (Figure 1) in the development of an online DCE. We designed hypothetical patient vignettes to mimic as closely as possible the decision of interest. In contrast to the typical tabular approach to DCE presentation, vignette-style presentation was considered optimal for this study, as clinicians tend to be familiar (and probably more comfortable) with vignettes because these are regularly used in training and CPD. The decision of interest was a binary response to the hypothetical vignette (decision to offer thrombolysis or not), as this reflects routine clinical practice whereby clinicians are faced with one patient at a time and must decide whether or not to offer thrombolysis to that patient.
FIGURE 1.
Summary of the key stages of the DCE development process.
Stage 1: exploratory work
In the initial stages, we considered all factors that might be important for a clinician in decision-making, as omitting potentially important factors in the DCE may bias findings. 7 We drew on qualitative data collected in a previous research programme examining decision-making in acute stroke14 and on work to inform the development and testing of a computerised decision support tool for thrombolysis in acute stroke care. 79 This included qualitative interview data on the views and experiences of stroke clinicians about thrombolysis decision-making, ethnographic data collected through non-participant observation of thrombolysis decision-making discussions and data from the usability and feasibility testing of the decision support tool.
Relevant literature was also reviewed to help to identify further factors that have been documented to affect decision-making about thrombolysis and factors influencing clinical decision-making more broadly. 20,51,52,80–82
In addition, nine telephone-based semistructured interviews were conducted with stroke clinicians and leading experts in stroke research. The sampling strategy was purposive in order to capture the views of clinicians who had not contributed to the development and testing of a stroke thrombolysis decision support tool (Computerised Decision Aid for Stroke Thrombolysis; COMPASS), and targeted clinicians from hospitals in both the upper and lower quartiles of thrombolysis rates, based on figures from national audit reports. 19 These interviews aimed to identify any additional patient-related factors or levels that represented the borderline and/or difficult cases, in particular the nature of trade-offs made between influential factors and levels when making decisions about whether or not to offer thrombolysis.
Interviews were audio-recorded and transcribed verbatim and anonymised transcripts were then imported into QSR International’s NVivo 9 (Warrington, UK) to facilitate the coding and analysis of data. The resulting data set was coded thematically and analysed using a framework approach. 83 This qualitative analysis of interview data and review of secondary data sources from the Development and Assessment of Services for Hyperacute stroke (DASH) Programme Grant for Applied Research,14 alongside the literature review, facilitated the generation of a comprehensive list of 22 potentially influential patient-related factors on clinical decision-making regarding thrombolysis (Box 1).
-
SBP.
-
DBP.
-
Blood glucose level (BM).
-
Patient frailty.
-
Stroke severity (NIHSS score).
-
History of hypertension.
-
History of stroke.
-
Anticoagulation status/INR level.
-
Aspirin monotherapy.
-
A patient’s level of social support.
-
Major surgery in past 3 months.
-
Presence of diabetes at time of presentation.
-
Patient age.
-
Patient ethnicity.
-
Patient sex.
-
Socioeconomic status of patient.
-
Stroke onset time to treatment.
-
Recent infarction on CT/MRI scan.
-
Pre-stroke cognitive functioning/capacity/comprehension of risk information.
-
Pre-stroke dependency status.
-
Patient/relative values, knowledge and views on thrombolysis.
-
Comorbidities.
DBP, diastolic blood pressure; INR, international normalised ratio; MRI, magnetic resonance imaging; SBP, systolic blood pressure.
Stage 2: expert panel discussions – inclusion and exclusion criteria
Exploratory work commonly identifies too many factors/levels to include in DCEs and, owing to sample size constraints and the potential for respondent cognitive burden, it is often not practical or feasible to include all possible combinations that may influence decision-making. By including all potentially influential factors and levels of interest, the statistical power of a DCE to detect effects would be reduced, owing to the large number of possible combinations of levels and the inability of a small sample size to adequately assess all these various combinations. Methods are needed to select the most important factors and levels to include in a testable DCE. Although there are publications that provide generic advice,76,84 there is little agreement on the best approach to achieve this. A well-designed DCE has been described as ‘one that has sufficiently rich set of attributes and choice contexts, together with enough variation in the factor levels necessary to produce meaningful behavioural responses’. 27 Abiiro et al. 85 advise employing quantitative methods, such as ranking exercises, to support the process of selecting factors for inclusion to a manageable number.
In the first instance, the expert multidisciplinary panel in the current study (consisting of three stroke physicians who undertake clinical research, a trainee stroke physician, two patient representatives, two health psychologists, two health economists and an expert in shared decision-making) screened the list of factors in terms of whether they would be feasible or meaningful to include in a DCE, to be further scrutinised using a structured prioritisation exercise (SPE). Following discussions, a set of inclusion and exclusion criteria were agreed with reference to the study objectives (i.e. the study focus on decision-making in acute ischaemic stroke and not on diagnosis of acute stroke).
Removal of factors that could be considered as related to uncertainty regarding the diagnosis of acute ischaemic stroke
This was considered prudent based on the rationale that incorporating diagnostic uncertainty has methodological implications for the design of the patient vignettes and interpretation of results from the DCE. Given that a diagnosis of acute ischaemic stroke represents a gradient of certainty (and includes consideration of differential diagnoses such as transient ischaemic attack and stroke mimics), this does not lend itself well to the DCE framework. Furthermore, diagnostic uncertainty is outside the aims stated in the study protocol86 to explore factors influencing decisions to offer thrombolysis as opposed to what factors influence diagnosis.
Removal of redundant/uninformative questions from the structured prioritisation exercise
Questions were excluded if the panel agreed that the area of uncertainty on any factor had been clearly identified by the literature and/or qualitative data. For instance, a question regarding a patient’s pre-stroke status using the mRS was removed, as the panel were confident that most clinical variation in decision-making exists between mRS2 and mRS3.
Furthermore, factors were omitted that have been shown to have a population-level effect in research studies but were not considered by the expert panel (or were not identified in exploratory interviews) to be important for decision-making about thrombolysis at the individual patient level (e.g. patient’s current use of aspirin).
Stage 3: phase 1 – design of online structured prioritisation exercise
An online SPE was designed to ascertain the perceived relative importance of various patient-related factors for clinical decision-making about thrombolysis, as well as to help to identify the ‘grey’ areas and areas of uncertainty on specific factors. Questions were phrased to identify where uncertainty and ‘cut-offs’ existed on individual factors regarding the suitability of the patient for intravenous thrombolysis: for example,
Assuming all other indications point to thrombolysis, at what blood pressure levels [systolic and diastolic] would you no longer think it appropriate to offer intravenous thrombolysis?
Free-text boxes were provided after each question to capture any comments respondents had to provide more information about their response. The SPE was hosted on Qualtrics (www.qualtrics.com) and 30 stroke clinicians in the north-east of England were invited to participate. The rationale for limiting the sample to clinicians in this region was to avoid priming too many in the population who would be invited to participate in the main study. The SPE is included in this report as Appendix 2.
Stage 3: phase 2 – using the structured prioritisation exercise to inform selection of factors/levels
Based on the results from the exploratory work (Table 3), the SPE and expert panel discussions, the expert panel (n = 6) ranked each factor in order of priority for inclusion in the DCE (based on those which were perceived to have the greatest influence on thrombolysis decision-making), indicated how they would operationalise them and provided suggestions on possible levels for each patient-related factor (Table 4 provides the results). Results were then aggregated and fed back to the panel to inform the discussion on the selection of the final list of factors and levels for inclusion.
| Factor | Potential levels (‘grey’ areas) | Evidence | Rationale for inclusion/exclusion |
|---|---|---|---|
| (A) SBP | 180–184 mmHg 185–189 mmHg 190–194 mmHg |
Identified as upper cut-off points in the SPE Qualitative work indicated that was SBP was a highly influential factor Dirks et al.:20 Delphi study agreement of > 185/110 mmHg as cut-off Kent et al.:42 higher SBP = less benefit from thrombolysis NICE guidelines (2008)87 stated that SBP reduction to ≤ 185/110 mmHg should be considered in people who are candidates for thrombolysis |
Most important factors identified in SPE and a primary issue identified in qualitative exploratory work |
| (B) SBP control | SBP at decision time after attempt to reduce SBP at patient presentation (no attempt to reduce SBP made) |
The level at which a clinician would consider lowering SBP as a separate issue to at what level they are prepared to treat 11 out of 12 clinicians who responded to the SPE reported they would attempt to reduce SBP if necessary |
|
| (C) DBP | 100–104 mmHg 105–109 mmHg 110–114 mmHg 115–119 mmHg |
Delphi study20 agreement of 110 mmHg as cut-off | Ranked 3 out of 19 in SPE, indications of variation in acceptable upper level |
| (D) NIHSS score/stroke severity | Lower end: 0, 1, 2, 3 Upper end: > 25 |
Qualitative work identified NIHSS score of ≤ 3 as creating uncertainty around offer of thrombolysis; 4–25 = typical treatment zone; > 25 = higher risk and reported as cut-off for some SPE: clinicians commented that aphasia is more disabling than NIHSS suggests and this would be an important consideration (qualitative work indicated that NIHSS is not always considered to be reliable indicator of severity) |
Ranking in SPE table: 10 out of 19 Evidence for variance in acceptable lower and upper limit |
| (E) Pre-stroke cognitive status/capacity of patient | No cognitive impairment Moderate cognitive impairment Severe cognitive impairment |
Identified as an important factor by Shamy et al.51 Emerged as influential in qualitative findings (to varying degrees and depending on other factors including NIHSS, dependence on others for activities of daily living, impact on quality of life) SPE: severe cognitive impairment would influence decision-making of 64% of respondents; 27% reported no influence. Suggested that decision is influenced by the patient’s functional status |
Ranked 8 out of 19 in SPE Little previous research on this |
| (F) Patient’s pre-stroke dependency status (ADL) | Living independently/24-hour support with ADL (nursing home) Pre-stroke mRS score of > 2 |
Shamy et al.:51 clinicians less likely to offer thrombolysis to patients who were residents of nursing homes | Ranked 4 out of 19 in SPE |
| (G) Frailty | Based on reliance on others/presence of comorbidities or use of composite factor/absence or degrees of frailty | Major issue in qualitative work: clinicians concerned/nervous about treating very frail, elderly patients; concern regarding falls and potential underlying injuries SPE: 82% reported taking frailty into account when making thrombolysis decisions so this is clearly an important influential factor on decision-making |
Ranked 5 out of 19 in SPE table Difficulty operationalising gradient of frailty; could include as dichotomous variable: frail/not frail |
| (H) Patient age | General agreement on no upper limit Lower age limit 14–18 years |
Evidence indicates patients aged > 80 years receive similar benefit as those aged ≤ 80 years, particularly when treated earlier6 | Not considered important in SPE Some more likely to adhere to licence than others |
| (I) Anticoagulation status/INR level | < 1.6 < 1.7 < 1.8 |
Qualitative work found variation in acceptable levels (1.5–1.9) SPE indicated grey area was between 1.6 and 1.8 Recent evidence suggests thrombolysis when INR is ≤ 1.7 does not increase mortality risk/risk of bleeding;88 observational studies of bleeding risk among warfarin-treated patients receiving thrombolysis have been small and inconsistent89 |
Ranked 2 out of 19 in SPE May be possible to include within subset of patients |
| (J) Patient/relative preferences regarding thrombolysis | Patient lacking capacity and family not present (best interests) Relatives in favour of thrombolysis Relatives against thrombolysis |
Qualitative work: difficulty in communication risk/benefit information; concern patients/family did not fully understand/remember information under such stress. Some clinicians expressed discomfort making decision on behalf of patients when family members were not present Preferences of family/patients regarding thrombolysis cited as a barrier to optimal decision-making82 Review papers52,80 found evidence that delays in obtaining informed consent were considered to be a factor that delayed treatment delivery |
Ranked 6 out of 19 in SPE Challenging to operationalise in DCE |
| (K) Major surgery in past 3 months | Percutaneous coronary intervention (no time limit, < 1 week) Laparotomy for a perforated duodenal ulcer (SPE ‘grey’ areas: 2, 3, 4 weeks) |
Failure to reach agreement in Delphi exercise regarding time since previous surgery20 | Ranked 7 out of 19 in SPE Variation in acceptable times since major surgery |
| (L) Blood glucose level | 22–23.9 mmol/l 24–25.9 mmol/l 26–27.9 mmol/l |
SPE: variability among respondents; 25% said no upper limit Delphi study agreement of glucose levels 2.7–22 mmol/l20 |
Indications of variability between clinicians |
| (M) Willingness to treat to lower blood glucose level | Attempt has been made or has not yet been made to lower blood glucose | SPE: 66% would not seek to control blood glucose level before making thrombolysis decision | |
| (N) Presence of diabetes | History of type 2 diabetes No history of type 2 diabetes |
Patients with diabetes had better outcomes when treated with thrombolysis than controls with diabetes90 | Ranked 14 out of 19 in SPE |
| (O) Comorbidities | Qualitative work, e.g. undergoing cancer treatment, aneurysms | ||
| (P) Previous stroke | Moderate stroke NIHSS score of 7–12 (within previous 3 months) Severe stroke NIHSS score of ≥ 13 (within previous 3 months) |
Patients with previous stroke had better outcomes when treated with thrombolysis than controls with previous stroke90 | From SPE: previous severe stroke ranked as more important (ranking: 10) than previous mild stroke (13) |
| (Q) Time since onset of symptoms | 3∼4.5 hours > 4.5 and < 5–6 hours? |
Qualitative work: 4.5 hours was upper cut-off for most, but some clinicians were more willing to accept uncertainty around onset time | |
| (R) Level of social support | No/or minimal social support High level of social support |
All SPE respondents indicated that a patient’s level of social support would not impact on their decision-making about thrombolysis |
| Factor | Mean rank (SD)a | Median | Suggested levels |
|---|---|---|---|
| SBP | 1.67 (1.2) | 1 | 140 mmHg |
| 175 mmHg | |||
| 180 mmHg | |||
| 185 mmHg | |||
| 200 mmHg | |||
| Pre-stroke dependency status | 4 (2.6) | 4 | mRS1 |
| mRS2 | |||
| mRS3 | |||
| mRS4 | |||
| Pre-stroke cognitive status | 5.33 (2.6) | 5.5 | No impairment |
| Mild impairment | |||
| Moderate impairment | |||
| Severe impairment | |||
| NIHSS score/stroke severity | 6.5 (2.9) | 7 | NIHSS 2 |
| NIHSS 3 | |||
| NIHSS 5 | |||
| NIHSS 23 | |||
| NIHSS 25/26/27 | |||
| SBP (after reducing) | 6.6 (4.7) | 5 | 185 mmHg |
| 190 mmHg | |||
| 200 mmHg | |||
| INR/anticoagulation | 6.7 (2.7) | 5.5 | < 1.6 |
| < 1.7 | |||
| < 1.8 | |||
| 2 | |||
| DBP | 6.8 (5.2) | 6 | 100 mmHg |
| 110 mmHg | |||
| 115 mmHg | |||
| 120 mmHg | |||
| Frailty | 6.8 (3.9) | 7 | Composite measure using comorbidities, description of needs (i.e. walking stick), ‘patient you [do not] perceive as frail’ |
| Time since symptom onset | 7.8 (6.1) | 7 | < 1 hour |
| < 3 hours | |||
| 4 hours | |||
| 4 hours 15/20 minutes | |||
| Recent major surgery | 8.3 (3.6) | 7.5 | Percutaneous coronary intervention |
| Hip replacement | |||
| Laparotomy | |||
| Previous stroke | 9.2 (4.3) | 10.5 | Combine with stroke severity? |
| 2 weeks ago | |||
| 4 weeks ago | |||
| 3 months ago | |||
| Comorbidities | 9.8 (2.6) | 10 | Disability related |
| Chronic disease | |||
| Illness presenting bleeding risk | |||
| Blood glucose level (BM) | 10.8 (3.1) | 11 | 16/19 mmol/l |
| 22 mmol/l | |||
| 25 mmol/l | |||
| 27 mmol/l | |||
| Patient/relative preferences | 11.4 (2.6) | 12 | No family present |
| Family present and eager for patient to be treated | |||
| Family present and worried about bleeding risk | |||
| Willingness to treat blood glucose | 11.6 (3.7) | 11 | Option to treat before thrombolysis decision |
| Option to present already treated level | |||
| Patient age | 12.7 (5.7) | 14.5 | 62/68/75 years |
| 80/85 years | |||
| 95 years | |||
| Social support | 15 (3.1) | 16 | Indicator of dependency? |
| Use as part of frailty composite measure? | |||
| Presence of diabetes | 15.4 (2.4) | 16 | No history of diabetes |
| Patient has diabetes |
There was a need to compromise on the perceived importance of factors to ensure that concerns regarding sample size/design feasibility, ecological validity (i.e. ensuring that information presented is as consistent as possible with information that would be available in a real-life situation) and the potential impact of unconscious factors (e.g. patient ethnicity) were considered in the final factor selection process. Among the issues considered during these panel discussions were:
-
Ensuring clinical face validity. It was vital that patient information presented in vignettes was realistic and that factors and levels could plausibly occur together. Certain factor levels could not reasonably appear together meaningfully; therefore, some initial constraints were imposed on the design. For instance, a mRS score of 0 or 1 (indicating that the patient is able to carry out all usual duties and activities) was considered implausible for a patient described as having severe dementia. Vignette-style presentation was considered optimal, as clinicians tend to be familiar (and probably more comfortable) with vignettes because these are regularly used in training and CPD. Consequently, participating clinicians were unlikely to treat the exercise as a test and, thus, to behave differently from how they would in the real world. Similarly, vignettes (as opposed to a traditional tabular list of attributes and levels that are commonly used in DCEs) more closely reflect the way in which clinicians receive information about their patients, thereby increasing the realism of the decision task.
-
Ensuring sufficient information was present in vignettes. It was crucial to ensure that clinicians had sufficient information available to reach a decision about the offer of thrombolysis. It was decided that information on certain factors must be provided (as either variable or fixed factors) in the vignettes in order for clinicians to reach a decision and for the decision-making process to mimic real-life decisions as closely as possible. For instance, stroke severity score and the results of the CT scan were considered vital information. Factor order/placement in the vignette was decided based on the information that would be available to the clinician immediately and the typical order in which additional information may be obtained. The order of presentation of factors was also informed by work to develop the COMPASS decision support tool. 79
At this point, we also considered the relative frequency of various presentations of acute stroke. It was decided that relatively uncommon complications or patient characteristics (e.g. patient on warfarin or had recent surgery) would be excluded to ensure that vignettes included those factors that were more common to most patients (e.g. NIHSS score indicating stroke severity, patient age and patient sex). Data from Safe Implementation of Thrombolysis in Stroke (SITS) helped to inform this discussion. 91
-
Anticipated sample size and resulting design considerations. Although more levels can define the true relationship between factors and their influence on decision-making, there is an inherent trade-off between the number of factors and levels that can be included and the complexity of the design of the DCE. 27 Furthermore, there are important considerations regarding the maximum numbers of factors and levels a participant can process at one time, as well as issues regarding sample size. Owing to the limited size of the population of interest in the current study, restricting the number of variable factors and levels per factor was necessary to control the number of potential combinations in order to ensure that the DCE would have sufficient statistical power to detect important effects. The complexities and problems of performing sample size calculations for DCEs have been highlighted. 7 Optimal sample size requirements for the limited dependent variable models of the nature estimated in DCEs depend on knowledge of the true choice probabilities, which were not known prior to undertaking the research. 73
However, previous DCE studies have shown that robust choice models can be estimated from sample sizes of between 50 and 100 respondents. 92,93 Based on previous studies and estimates of the total number of clinicians treating acute stroke patients in the UK, a sample size of 150–200 was anticipated as achievable in the current study. This estimate represents approximately 35–47% of the 422 clinicians registered as ‘full members’ of the British Association of Stroke Physicians (BASP), although the proportion involved in thrombolysis decision-making was unknown. 94 Moreover, owing to the potential for cognitive burden, we judged that 12–16 hypothetical patient vignettes would be the upper limit of the number of decision vignettes that should be administered to each participant (and this would be tested in the piloting of the DCE in stage 4).
Factors that were deemed important to provide basic clinical information (but not included as variables in the DCE) were included as fixed factors in the design, meaning that they were described to respondents and held fixed in the choice context. The use of fixed factors helped to remove subjectivity around interpretation of additional issues, providing a common interpretation of such factors across respondents while retaining face validity. In the current study, blood glucose level was included as a fixed factor in each vignette, at a level of 6 mmol/l. An identical text description of a patient’s CT scan result was included in all vignettes to remove subjectivity around imaging interpretation and to minimise any uncertainty about diagnoses of acute ischaemic stroke.
Definitions were included to standardise the interpretation of factors and levels. For instance, the standard definitions for mRS scores95 used to assess pre-stroke dependency were presented in each vignette. Definitions were also provided to describe pre-stroke cognitive functioning and were operationalised based on the Global Deterioration Scale for the assessment of primary degenerative dementia. 96 The calculation for each level of stroke severity was described using the NIHSS97 to ensure consistent interpretation. These definitions are available in Table 3.
-
Consideration of explicit versus implicit influences on decision-making. The expert panel acknowledged the need to also consider implicit factors as having an impact on decision-making about thrombolysis. There is strong evidence that implicit factors can be influential in medical decision-making. 81 Therefore, the panel also considered factors that did not emerge from the exploratory work and SPE. For instance, there is a suggestion that sex may have a population-level effect on thrombolysis administration, with evidence of underutilisation of intravenous thrombolysis in women,40 although this may reflect a different age and presentation profile in women. 41 This suggestion comes despite a pooled analysis of randomised controlled trials demonstrating that women are more likely than men to benefit from thrombolysis. 42,43 The panel did not consider sex to be a conscious consideration at the individual, bedside level. Some factors may have an implicit effect on decision-making, such as ethnicity and social class. Panel discussions were focused on striking a balance between the inclusion of both implicit and explicit factors which may influence thrombolysis decision-making.
Consensus was reached during expert panel discussions on the factors and levels that were included in a pilot DCE.
Stage 4: pilot testing
A specialised software program, NGene (v1.1.1, Choice Metrics, Sydney, NSW, Australia; www.choice-metrics.com/), was used to generate a fractional factorial (d-efficient) design. This facilitated the generation of a design that was as balanced as possible, given the imposed constraints. A fractional factorial design was employed owing to the relatively large number of variable factors (nine) included in the final DCE, with number of levels varying from two to six on different factors. This allowed for the testing of a subset of possible combinations. The use of a blocked design allowed the number of vignettes presented to any one participant to be reduced to a number considered manageable in pilot testing to avoid overburdening participants. In each block, 13 hypothetical patient vignettes were presented to each participant.
The pilot testing of the initial DCE employed a ‘think-aloud’ approach that was guided by best practice guidelines. 98 This method asks participants to verbalise what they are thinking when responding to the survey. The aim of this pilot stage was to facilitate further testing of the credibility of the vignettes among the population of interest, examine participants’ understanding and interpretation of the task and questions, check the usability of the survey on different systems and browsers, and gauge how long the survey might take to complete.
Sixteen clinicians were invited to take part in pilot testing. Six agreed to take part and fully completed the pilot. Based on the results of pilot testing, some amendments were made. For instance, when two clinicians read that symptom onset began 4 hours and 15 minutes ago, they factored time to prepare the thrombolysis bolus into their decision-making (as the thrombolysis time window for treatment is up to 4.5 hours post symptom onset). Therefore, thrombolysis bolus preparation time was included as an additional fixed factor, stating that the treatment dose could be prepared within 5 minutes to address this.
The testing revealed that vignettes were credible, although a number of implausible combinations were suggested and added as constraints (i.e. excluded from the design). These included low NIHSS scores with aphasia combined with moderate/severe dementia. Three participants also commented that spacing should be larger within tables to improve readability. This was amended prior to the final testing of the survey by the expert panel. The pilot testing protocol is available in Appendix 3.
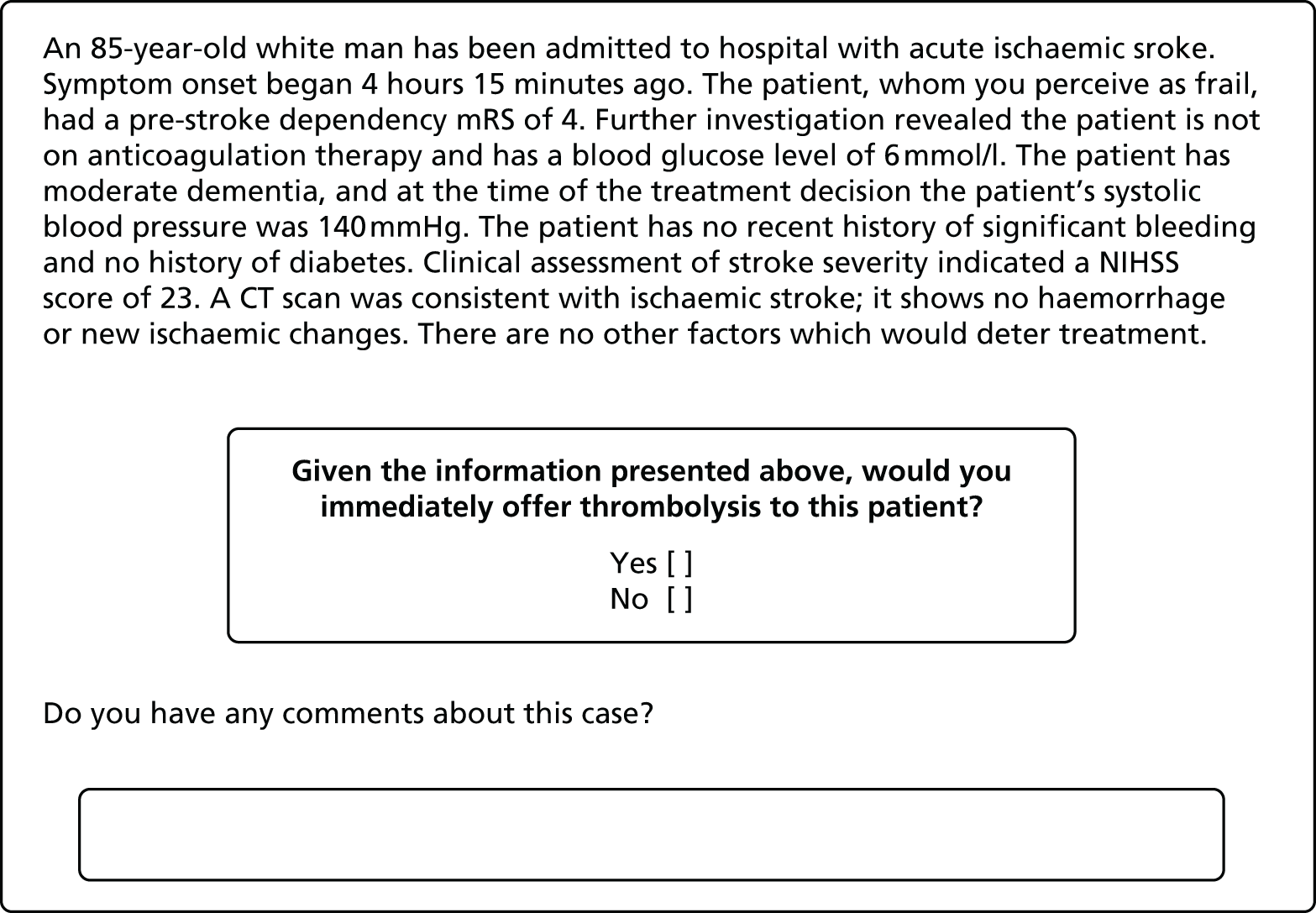
Stage 5: final expert panel discussions, key considerations and finalised discrete choice experiment design
Key considerations of the development of this online DCE were the size of the population of interest, the number of combinations of factor levels, respondent burden and likely response rate. It was crucial to consider these issues alongside the perceived importance of various factors and levels. Table 5 displays the fixed factors and levels included in the final survey and the rationale for their inclusion. Table 6 outlines the final variable factors and levels included in the final DCE and Table 7 provides the definitions used on various factors and levels. Based on our five-stage design process, we were confident that we had provided sufficient information to allow clinicians to reach a decision by using fixed and variable factors. The full survey is available in Appendix 4, and includes all demographic questions and scales used to collect information on clinician characteristics. A sample vignette is included in Figure 2. Optional free-text comment boxes were included after each vignette to allow participants to explain their decision-making and include comments as they felt necessary. These were included to assist with data interpretation.
| Factor | Rationale for inclusion | Fixed level | Rationale for level |
|---|---|---|---|
| Blood glucose level | Variable levels may result in diagnostic uncertainty | 6 mmol/l | Average blood glucose level based on SITS data of treated patients |
| CT scan text description | To avoid skill/subjectivity around interpretation of scans | CT scan was conducted and is consistent with ischaemic stroke; it shows no haemorrhage or new ischaemic changes | Decided not to include image owing to potential variability in CT image interpretation skill and subjectivity; difficulty finding scans to match multitude of various patient characteristics. Text description deemed most appropriate to remove diagnostic uncertainty |
| To ensure confirmation of diagnosis of acute ischaemic stroke | |||
| Anticoagulation status | Although it was deemed an influential factor, only a minority of stroke patients take an anticoagulant and therefore it was not included as variable factor | Patient is not on anticoagulation therapy | To avoid any issues surrounding INR levels that could complicate the decision to offer thrombolysis |
| Bleeding risk/recent surgery | Relevant for only a minority of patients. Challenging to operationalise variable and comparable levels in vignettes | No recent history of major bleeding | |
| Diabetes | Not ranked as important in vignettes | No history of diabetes | |
| Included as fixed factor for clinical validity | |||
| Patient consent/family assent | Assume either patient consent or family assent is available for treatment | ||
| Other/comorbidities | There are no other factors which would deter treatment | Owing to difficulty defining fully and generating comparable and feasible levels of comorbidities. Potential overlap with pre-stroke cognitive and pre-stroke dependency status | |
| Fixed factors included post-pilot testing (stage 4) | |||
| Handedness of patient | All patients are right-handed | To clarify and ensure that the deficits will be interpreted consistently across all level of stroke severity (NIHSS) | |
| Licensed dose bolus preparation time | Can be prepared for administration within 5 minutes | Pilot testing revealed that participants would factor in variable times in their decision-making and so stating this will help to control this potential error | |
| Factor | Levels | Rationale |
|---|---|---|
| 1. SBP | 140 mmHga 185 mmHg 200 mmHg |
Highest ranked factor in stage 3 phases 1 and 2 Levels include those across range from ‘safe to offer thrombolysis’ to ‘grey area’ to ‘outside the licensing guidelines’ |
| 2. Sex | Malea Female |
To increase clinical face validity To examine if sex has an unconscious influence on decision-making |
| 3. Age (years) | 68a 85 95 |
Included for purposes of ecological and face validity Evidence from exploratory work that some clinicians may take patient age into account and adhere to current licensing guidelines |
| 4. Frailty | You do not perceive as fraila You perceive as frail |
Very challenging to adequately define frailty owing to subjectivity in how clinicians view/consider it Aim was to trigger perception of frailty in patient and therefore the current phrasing was considered optimal to meet aim |
| 5. Time since symptom onset | 50 minutesa 2 hours 30 minutes 4 hours 15 minutes |
Potential greater benefit of very early treatment time (50 minutes) included to compare with mid-point in time window and rapidly approaching end of window (4 hours 15 minutes) |
| 6. Pre-stroke dependency (mRS score) | mRS1 mRS3 mRS4a |
Qualitative work suggested that mRS3 was the ‘grey’ area in dependency |
| 7. Pre-stroke cognitive functioning | No history of memory problemsa Moderate dementia Severe dementia |
Exploratory work suggested that dementia/cognitive functioning could influence decision to offer thrombolysis |
| 8. Ethnicity | Whitea Afro-Caribbean Asian |
Included as a factor that may have an implicit effect on decision-making Included as this is information that would be obvious in a typical decision |
| 9. NIHSS score (stroke severity) | NIHSS 2 (without aphasia)a NIHSS 2 (with aphasia) NIHSS 5 (without aphasia) NIHSS 5 (with aphasia) NIHSS 14 NIHSS 23 |
Presence or absence of aphasia deemed very important in previous stage and therefore was included at lower NIHSS scores (mild strokes) to assess whether it would influence decision-making NIHSS 14 included as it is SITS mean score (for treated patients) NIHSS 23 considered a severe stroke |
| Factor | Level | Definition |
|---|---|---|
| NIHSS score (stroke severity) | NIHSS 2 (with aphasia) | Mild-moderate aphasia (+1), LOC question (+1) |
| NIHSS 2 (without aphasia) | Right arm (drift +1), right leg (drift +1) | |
| NIHSS 5 (with aphasia) | Right leg (some effort against gravity +2), drift in right arm (+1), mild to moderate aphasia (+1), LOC question (+1) | |
| NIHSS 5 (without aphasia) | Right leg (some effort against gravity +2), right arm (no effort against gravity +3) | |
| NIHSS 14 | Face (partial paralysis +2), right arm (no movement +4), right leg (no movement +4), dysarthria (severe +2), sensory loss (severe to total +2) | |
| NIHSS 23 | LOC questions (+2), LOC commands (+1), best gaze (+1), facial palsy (+2), visual fields (complete hemianopia +2), no effort against gravity in right arm (+3), no movement in right leg (+4), sensory loss (severe to total +2), aphasia (severe +2), dysarthria (severe +2), extinction/inattention (+2) | |
| Pre-stroke cognitive functioning | Moderate dementia | Able to hold limited conversation but often requires prompting for daily routine. Forgetful of recent events and people’s names |
| Severe dementia | Cannot be left unsupervised. Wanders. No meaningful conversation. Unaware of time and place | |
| Pre-stroke dependency status (using mRS) | mRS1 | No significant disability. Able to carry out all usual duties and activities |
| mRS3 | Moderate disability. Requires some help, but able to walk without assistance | |
| mRS4 | Moderately severe disability. Unable to walk without assistance and unable to attend to own bodily needs without assistance |
FIGURE 2.
Sample patient vignette.
Further components of the online survey
The online survey also included questions and measurement scales to collect information on participant characteristics and traits (see Appendix 4 for the full survey). The following questions relating to the profile of respondents were collected prior to the decision scenarios: age, sex and medical specialty, level of experience (time in months) treating stroke patients, experience (time in months) administering intravenous thrombolysis and willingness to control blood pressure before administering thrombolysis. Participants were then randomly assigned to receive one of eight blocks of vignettes, where each block comprised 13 hypothetical patient vignettes. Following the presentation of the hypothetical vignettes, a series of additional questions and scales were included to gather information on clinician characteristics of interest that were hypothesised to influence thrombolysis decision-making. These are detailed below.
Institutional Culture Scale
For the purposes of the current research, in the absence of an available scale, a new scale was developed (from existing measures where possible) to gauge the culture of thrombolysis and stroke care, and the influence of colleagues at a respondent’s place of work. A six-item scale was collated to assess this dimension and Table 8 includes the items used for this purpose. Items were scored on a 6-point Likert-type scale from strongly disagree (1) to strongly agree (6). Factor analysis was conducted on this new scale and a one-factor solution was obtained, representing institutional culture of thrombolysis. The results of the complete results of the factor analysis are available in Appendix 5.
| Item | Adapted from |
|---|---|
| Most people whose opinion I value would approve of me treating a patient presenting with acute ischaemic stroke within the 4.5-hour time window with intravenous thrombolysis | Theoretical Domains Framework – social influences scale item99 |
| Prior to delivery of intravenous thrombolysis, clinicians are provided with adequate training to inform decision-making regarding the appropriate use of intravenous thrombolysis in the treatment of patients with acute ischaemic stroke | Theoretical Domains Framework – environmental influences and resources scale item99 |
| We encourage internal discussion of patient care adverse events | Practice Culture Scale66 |
| There is an identifiable practice style that we all try to adhere to | Practice Culture Scale66 |
| My unit strongly encourages me to thrombolyse patients who meet criteria for intravenous thrombolysis when presenting with acute ischaemic stroke | New item created for this study |
| My unit does not hold meetings regularly to discuss and review stroke service audit dataa | New item created for this study |
Attitude towards risk-taking
The risk-taking subscale of the Jackson Personality Inventory100 was employed. It is a six-item measure that has been previously used in clinical decision-making research59,101 and measures attitudes towards risk-taking. Scores were summed (reversed when appropriate) and, given that there were no missing data on scale responses, a final risk-taking raw score was computed for each individual.
Physician Reaction to Uncertainty scale
The Physician Reaction to Uncertainty scale was developed by Gerrity et al. 60,61 to assess the impact of affective uncertainty on clinicians. The scale has been widely used in medical decision-making research60–62,102 and was employed to understand how respondents react to and deal with uncertainty in their clinical practice regarding acute stroke care and decision-making about thrombolysis. Scores were summed (reversed when appropriate) and, given that there were no missing data on scale responses, a final raw score was computed for each respondent.
Questions relating to decision-making and experience of administering thrombolysis
Clinicians were also asked to state the recency of their last decision made about patient suitability for thrombolysis, how many patients they estimated they had thrombolysed in the past 12 months, how many were harmed as a result of treatment in the past 12 months and how recently a patient was harmed as a result of treatment with intravenous thrombolysis. These questions were aimed at assessing whether or not recency and regularity of thrombolysis decision-making, and recency and frequency of negative outcomes of thrombolysis, exerted an influence on decision-making about the offer of treatment. The recency of last decision about thrombolysis and recency of harmful outcome as a result of administration of thrombolytic treatment were transformed into total number of days for the purposes of the analyses.
Clinicians were also asked to state whether or not there was a formal acute stroke protocol for assessing patient eligibility for thrombolytic treatment at their site of practice. A 6-point Likert scale was also used to assess the impact of clinicians’ level of comfort treating a patient outside the licensing criteria on thrombolysis decisions. Two final questions (6-point Likert scales) in the survey asked clinicians to rate their level of comfort with communicating the risk/benefits of thrombolysis to patients (and/or family/carers) and their perception of the evidence base for thrombolysis (i.e. whether or not respondents believe that the evidence for treating acute stroke patients with intravenous thrombolysis is robust). Finally, participants were debriefed and thanked for their participation.
The responses to the questions on clinician characteristics were analysed using appropriate descriptive statistics.
Public/patient involvement in the research
Mr John Teah and Mr Stephen Simpson were the patient/public representatives on the Project Management Group and have been actively engaged with the planning and design of the research since the project began in June 2013. At least one patient representative attended each project management meeting, with both patient/public representatives present at the majority of meetings. Project materials, such as working document drafts and meeting agendas, were forwarded to all project management team members for comments or suggestions ahead of scheduled meetings. This ensured that all team members were clear on the topics for discussion and were provided with an opportunity to contribute on these topics. As members of the Project Management Group, Mr Teah and Mr Simpson were involved in:
-
advising on the design of the research
-
approving and supporting the ethics application and providing feedback on the draft application
-
providing feedback/input on drafts at all stages of the DCE development process and on drafts of papers, reports and conference posters
-
membership of the expert panel during study design discussions and ranking exercises
-
advice on the promotion of the online survey and dissemination of results via links with the Stroke Association
-
planning for the codelivery of research findings at dissemination events to non-specialist audiences.
Participant recruitment
We recruited clinicians via newsletter and e-mails sent through the professional associations of various medical specialties involved in stroke care in the UK. This included BASP, the Society for Acute Medicine, the College of Emergency Medicine, the British Geriatrics Society and the Association of British Neurologists. An invitation to participate was also sent to the SITS co-ordinators in the UK and a notice about the study was included as a news item on the SSNAP audit webpage. An invitation to participate, together with an information sheet and a link to the survey, was distributed via these routes. The invitation e-mail also stated that all respondents who finished the survey could be entered into an optional prize draw to win a tablet computer. Although sampling through BASP would capture the great majority of decision-makers on thrombolysis in the UK, we sought to extend our sample to take account of diversity in how services are delivered in the UK (e.g. in some cases emergency department specialist physicians may have independent responsibility for decision-making about thrombolysis) by also including other medical specialties with responsibilities for thrombolysis decision-making.
In order to ensure eligibility for participation in the survey, a screening question was first provided to participants asking if they were involved in the ‘final decision-making’ about the offer of thrombolysis for patients with acute ischaemic stroke. If they did not have a role in the final decision-making, they were screened out of the survey.
Data management and hosting of the online discrete choice experiment
The market research company (Accent, Edinburgh, UK; www.accent-mr.com/) converted the DCE design and survey into an online survey. The survey was live for 6 months from September 2014 to February 2015. Data were returned to the research team in an anonymised format and entered into Stata/IC13 for analysis (StataCorp LP, College Station, TX, USA).
Scripting error
On receipt of the data from the market research company, we identified that the programmers had made some errors in the final application of scripting the online survey. This was thoroughly investigated and we identified that, as a result, 10.3% of the vignettes included implausible combinations of patient characteristics (e.g. severe dementia with pre-stroke dependency of mRS1 and severe dementia with NIHSS 2 with aphasia). We therefore ran models both with and without the erroneous vignettes and found little difference in the results. We decided that our primary analysis would exclude the erroneous vignettes. All analyses reported are on this basis.
Analytical plan
An a priori data analysis plan was developed to prioritise predictors for inclusion in a hierarchical approach. To focus the enquiry, the expert panel ranked the variables (Figure 3 and Table 9). Models 1 and 2 specifically addressed study objectives 1 and 2 by examining which patient and clinician factors were statistically significant predictors of decision-making regarding the offer of thrombolysis. Model 3 was used to establish the additional variance explained by the remaining clinician factors.
FIGURE 3.
A priori data analysis plan for inclusion of predictors in the analytical model.
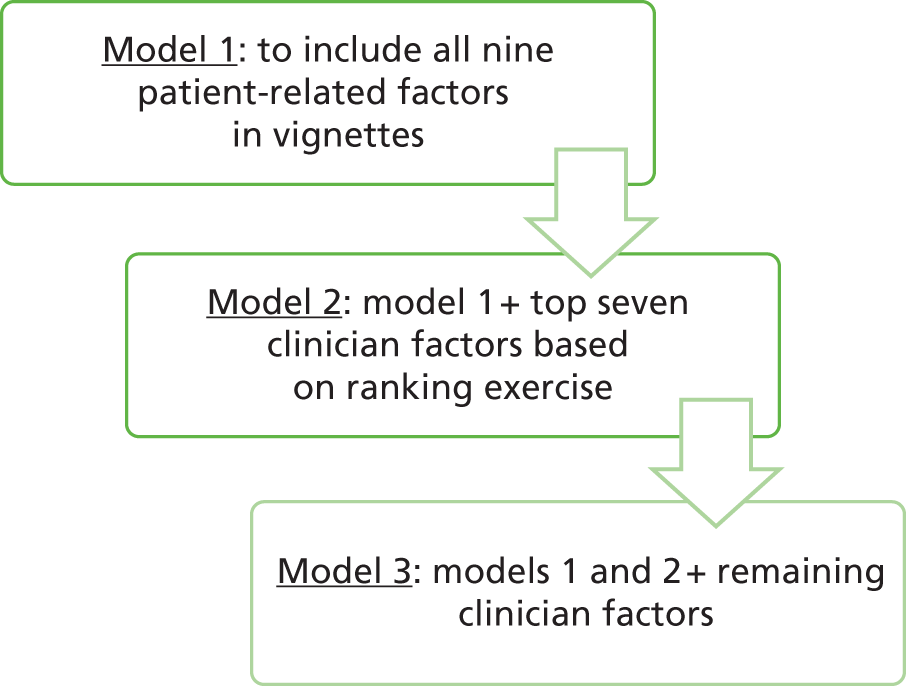
| Factor | Mean rank | SD | Median | Interquartile range | ||
|---|---|---|---|---|---|---|
| 1. Perception of evidence base | 3.3 | 2.5 | 3 | 7 | Model 2 variables | |
| 2. Attitude towards risk | 3.7 | 3.45 | 2 | 7 | ||
| 3. Comfort level treating patient outside licensing criteria/not treating a patient within criteria | 4 | 3.16 | 3 | 7 | ||
| 4. Number of patients harmed in past 12 months | 5.3 | 1.51 | 5 | 4 | ||
| 5. Physician reaction to uncertainty | 5.83 | 5.19 | 3 | 13 | ||
| 6. Time since most recent negative outcome of rtPA | 7.8 | 4.12 | 6 | 9 | ||
| 7. Number of patients thrombolysed in past 12 months | 8.3 | 3.21 | 8 | 11 | ||
| 8. Number of years’ experience | 9.3 | 5.75 | 11 | 14 | Model 3 variables | |
| 9. Medical specialty | 9.67 | 3.01 | 10 | 8 | ||
| 10. Willingness to control BP | 10.8 | 2.99 | 11 | 8 | ||
| 11. Perception of institutional culture | 11 | 4.86 | 10 | 13 | ||
| 12. Approximate thrombolysis rate | 11.2 | 3.66 | 12 | 10 | ||
| 13. Service configuration of hospital | 11.3 | 4.80 | 12 | 11 | ||
| 14. Confidence communicating risk information | 11.3 | 5.24 | 12 | 13 | ||
| 15. Recency of last rtPA decision | 11.8 | 3.43 | 11 | 10 | ||
| 16. Percentage of acute stroke patients thrombolysed of those assessed | 12.7 | 3.56 | 14 | 10 | ||
| 17. Location of hospital | 17.2 | 0.98 | 18 | 2 | ||
| 18. Availability of rtPA protocol | 17.2 | 2.32 | 18 | 7 | ||
| 19. Age | 18.7 | 1.03 | 19 | 3 | ||
| 20. Sex | 19.5 | .55 | 19 | 1 | ||
Analyses conducted on the data set
Appropriate summary statistics were used to describe the sociodemographic profile and other characteristics of the sample.
The data were modelled in a random utility theory framework using limited dependent variable modelling. The binary decision to offer thrombolysis was modelled as a function of the levels of the variable patient factors presented in the hypothetical vignettes and the characteristics of the decision-makers (the clinicians responding the survey).
Mixed-logit regression analyses were conducted on the data. This facilitated the examination of unobserved heterogeneity among respondents and accounted for the panel nature of the data. Further details on the mixed-logit regression and the rationale for its use are included in Appendix 6. The intercept [alternative specific constant (ASC) representing underlying preferences for treatment over no treatment, all else constant] and model parameters are assumed to be random and normally distributed (mean and standard deviations are reported). A positive coefficient for a level of a variable factor in the mixed-logit regression models, compared with the reference level of the factor, represents a driver of a decision to offer thrombolysis, whereas a negative coefficient represents an inhibiting influence on the decision to offer thrombolysis (i.e. more likely not to offer treatment). p-Values of < 0.05 indicate whether or not the coefficients are statistically significantly different from zero, and the odds ratios (95% confidence intervals) are presented to enable the magnitude/precisions of the effect to be assessed. Effects coding was used for all nine patient factors included in the DCE. Clinician factors were interacted with the ASC and then entered in the model. Further information on effects coding, and the theory and formulae underlying DCEs, is available in Appendix 6.
Independent covariates were interacted with the ASC to explore how preferences for offering treatment/not offering thrombolytic treatment differed depending on the covariates (i.e. characteristics of the decision-makers). Checks for multicollinearity were performed to ensure that predictor variables were not highly correlated with each other. The Project Management Group agreed that if this occurred, decisions on which variable to exclude/retain would be based on the criteria from the ranking exercise: that is those variables that are most amenable to change and useful in the context of CPD/learning.
Data can be obtained from the corresponding author.
External validity
We compared a number of patient vignettes included in the DCE with national patient data to assess the external validity of our findings. In consultation with SSNAP, six subsets of patient data were collated to compare decision-making about thrombolysis in the current study with real-world decision-making for UK patients admitted to hospital (or date of onset if already in hospital) between April 2013 and March 2015. Six patient vignettes were chosen as they represented the extremes of decision-making observed in the current study (high rates of offering and not offering thrombolysis, respectively) and were chosen to ensure that vignettes were sufficiently different so that no one patient would appear in more than one of the SSNAP data subsets.
However, SSNAP does not collect data for all patient factors examined in the current study (e.g. no information on blood pressure, frailty or pre-stroke cognitive function). Furthermore, certain categories of SSNAP data were extended to broaden the patient samples. For instance, decisions were made for the practical reason of avoiding limiting the patient samples so as to make them overly specific. Therefore, ranges were included for NIHSS score, patient age and onset to scan/decision time, and the vignette used in the study is representative of a patient in these categories. In addition, no restriction was placed on patient sex or ethnicity owing to the prohibitively small numbers that would have been observed in the patient data subsets.
Chapter 4 Results
Summary statistics for the sample
Table 10 presents a summary of the sociodemographic profile and other characteristics of the respondents (n = 138). Respondents had a mean age of 46 years (range 30–68 years). The majority were male (73.2%) and identified themselves as a stroke clinician. The average amount of experience treating acute ischaemic stroke patients and administering intravenous thrombolysis was 132 months (11 years; range 3 months to 38 years) and 76 months (6 years 4 months; range 3 months to 22 years), respectively. The average time taken to complete the online survey was 23 minutes.
| Variables | Mean (SD) | n (%) |
|---|---|---|
| Age | 45.83 (8.71) | |
| Male | 101 (73.2) | |
| Medical specialty | ||
| Stroke | 81 (58.7) | |
| A&E | 20 (14.5) | |
| Geriatric medicine | 17 (12.3) | |
| Neurology | 17 (12.3) | |
| Acute care | 3 (2.2) | |
| Grade/seniority | ||
| Consultant | 123 (89.1) | |
| Staff doctor | 6 (4.3) | |
| Specialty trainee | 7 (5.1) | |
| Other | 2 (1.4) | |
| Experience with treating acute ischaemic stroke (months) | 131.5 (99) | |
| Experience with administering thrombolysis (months) | 75.5 (43) | |
| Willing to control blood pressure (when applicable) before thrombolysis | 132 (95.7) | |
| Formal protocol is available for assessing patient eligibility for thrombolysis | 136 (98.6) | |
| Service configuration | ||
| Consultant led | 61 (44) | |
| Combined telemedicine and consultant led | 77 (56) | |
| Risk-taking scale score | –2.19 (5.33) | |
| Physicians’ Reaction to Uncertainty Scale score | 12.86 (9.39) | |
| Institutional Culture Scale score | 24.73 (5.24) | |
| Perception of the evidence base for thrombolysis | 4.67 (1.36) | |
| Confidence communicating benefits/risks of thrombolysis | 5.12 (1.02) | |
| Number of days since last thrombolysis decision made | 18 (38) | |
| Number of patients thrombolysed by respondents in past 12 months | 19 (15) | |
| Number of patients harmed as a result of thrombolysis in past 12 months | 0.8 (1.05) | |
| Days since patient was harmed as a result of thrombolysis | 408 (744) | |
Although no information is available on non-respondents to the online survey, the profile of the respondents is broadly representative of the population of medical professionals involved in acute stroke care in the UK. Based on data from the SSNAP acute organisation audit,103 the profile of the current sample in terms of medical specialty is proportionately representative of those involved in decision-making about thrombolysis; stroke clinicians are most often on thrombolysis rotas, followed in decreasing order by geriatricians/care of the elderly physicians, neurologists, and accident and emergency (A&E) and acute medicine physicians. Furthermore, the average age and sex split in the current sample is consistent with data from the Royal College of Physicians (RCP) 2012 census. 104 For example, there are more male consultants than female consultants in the specialties of stroke medicine, acute medicine, neurology and geriatric medicine (78%, 70%, 76% and 65%, respectively)104 and these proportions are reflected in the current sample. Similarly, the average age of respondents in the current sample is consistent with RCP census data.
Reliability analyses were conducted on the measurement scales employed in the survey. Following factor analysis, the Institutional Culture Scale developed specifically for this research demonstrated a one-factor solution. High scores on the scale represented a stronger institutional culture of thrombolysis. Respondents’ scores ranged from –1 to 29 and the internal consistency was high with Cronbach’s alpha of 0.84. On the Jackson Personality Inventory risk-taking subscale, scores ranged from –14 to 9, with higher scores indicating greater risk-taking. In the current study, the scale demonstrated good internal consistency of 0.76. Finally, on the Physician Reaction to Uncertainty Scale, scores ranged from –12 to 39, with higher scores indicating greater discomfort with uncertainty. In the current study, the scale demonstrated high internal consistency of 0.81.
Overview of decision-making about offer of intravenous thrombolysis
There was generic general preference not to offer treatment of intravenous thrombolysis to patients described in the hypothetical vignettes overall (Table 11).
| Decision | Frequency (%) |
|---|---|
| Offer thrombolysis | 504 (31.4) |
| Do not offer thrombolysis | 1103 (68.6) |
| Total | 1607 (100) |
In total, nine participants responded that they would not offer treatment to patients in all of the vignettes they were presented with. These participants were across a range of design blocks and included a range of medical specialties and experience levels; experience treating patients with intravenous thrombolysis among these participants ranged from 8 months to 10 years.
Discrete choice experiment regression results
All analyses were undertaken using Stata/IC13. Following adjustment of the data set (removal of implausible combinations of pre-stroke dependency of mRS1 and severe dementia, and of severe dementia and NIHSS 2 with aphasia), there were 1607 observations of discrete decisions about the offer of thrombolysis.
To control for any possible effects of block in the design, seven dummy variables were also included in the analyses (comparing each block with block 1) to control for potential differences between blocks. Where significant differences emerged, these are reported in the results tables.
Model 1: patient-related factors
The results of the mixed-logit analysis for model 1 are presented in Table 12. The ASC is negative and statistically significant, indicating a general preference not to offer intravenous thrombolysis, all else equal.
| Factor | Level | Coefficient | SE | p-value | Odds ratio (95% CI) |
|---|---|---|---|---|---|
| Patient age, mean (SD) | 68 | Reference | |||
| 85 | 0.71 (0.26) | 0.26 (0.33) | 0.005 (0.44) | 2.03 (1.23 to 3.35) | |
| 95 | –2.02 (0.71) | 0.66 (0.27) | 0.002 (0.01) | 0.13 (0.04 to 0.49) | |
| Patient ethnicity, mean (SD) | White | Reference | |||
| Asian | –0.46 (0.23) | 0.27 (0.28) | 0.09 (0.41) | 0.63 (0.37 to 1.08) | |
| Afro-Caribbean | 0.87 (0.09) | 0.33 (0.42) | 0.009 (0.82) | 2.39 (1.24 to 4.58) | |
| Patient sex, mean (SD) | Male | Reference | |||
| Female | –0.32 (0.01) | 0.44 (0.28) | 0.463 (0.97) | 0.73 (0.31 to 1.71) | |
| Time since symptom onset, mean (SD) | 50 minutes | Reference | |||
| 2 hours 30 minutes | 0.54 (0.61) | 0.25 (0.72) | 0.03 (0.40) | 1.72 (1.05 to 2.81) | |
| 4 hours 15 minutes | –1.54 (0.66) | 0.31 (0.32) | < 0.001 (0.04) | 0.21 (0.12 to 0.39) | |
| Patient frailty, mean (SD) | Not frail | Reference | |||
| Frail | –0.26 (0.34) | 0.19 (0.26) | 0.0179 (0.20) | 0.77 (0.53 to 1.12) | |
| Pre-stroke dependency (mRS score), mean (SD) | mRS1 | 0.80 (–3.01) | 1.05 (0.49) | 0.447 (< 0.001) | 2.23 (0.28 to 17.51) |
| mRS3 | 1.33 (0.39) | 0.42 (0.34) | 0.001 (0.24) | 3.78 (1.67 to 8.6) | |
| mRS4 | Reference | ||||
| Pre-stroke cognitive status, mean (SD) | No history of memory problems | Reference | |||
| Moderate dementia | 0.29 (1.30) | 0.31 (0.30) | 0.349 (< 0.001) | 1.34 (0.73 to 2.44) | |
| Severe dementia | –2.82 (0.11) | 0.60 (0.30) | < 0.001 (0.73) | 0.06 (0.02 to 0.19) | |
| SBP, mean (SD) | 140 mmHg | Reference | |||
| 185 mmHg | 1.17 (1.17) | 0.36 (0.33) | < 0.001 (< 0.001) | 3.22 (1.7 to 6.11) | |
| 200 mmHg | –5.19 (2.05) | 0.77 (0.42) | < 0.001 (< 0.001) | 0.01 (0.00 to 0.02) | |
| NIHSS score (stroke severity), mean (SD) | 2 (without aphasia) | Reference | |||
| 2 (with aphasia) | 0.15 (1.20) | 0.51 (0.53) | 0.761 (0.02) | 1.16 (0.43 to 3.14) | |
| 5 (without aphasia) | 1.48 (0.33) | 0.49 (0.59) | 0.002 (0.57) | 4.39 (1.69 to 11.38) | |
| 5 (with aphasia) | 0.65 (2.56) | 0.41 (0.60) | 0.111 (< 0.001) | 1.92 (0.86 to 4.28) | |
| 14 | 2.04 (0.39) | 0.60 (0.51) | 0.001 (0.45) | 7.69 (2.35 to 25.13) | |
| 23 | 1.38 (1.15) | 0.597 (0.52) | 0.021 (0.03) | 3.98 (1.23 to 12.84) | |
| ASC, mean (SD) | Decision to offer thrombolysis | –5.46 (2.07) | 1.03 (0.30) | < 0.001 (< 0.001) | 0.01 (0 to 0.03) |
| Block effects, mean | Block 6 | 1.82 | 0.9 | 0.042 | |
Compared with their reference categories (in brackets), four patient factors were statistically significant predictors of decisions not to offer thrombolysis: (1) patient age of 95 years (68 years); (2) stroke symptom onset time of 4 hours 15 minutes, proximal to the upper limit of 4.5 hours stipulated in the licensing criteria for thrombolysis (50 minutes); (3) patients with severe dementia (no history of memory problems); and (4) systolic blood pressure (SBP) values of 200 mmHg (140 mmHg).
There were also eight statistically significant predictors of decisions to offer thrombolysis (compared with reference levels in brackets): (1) patient age of 85 years (68 years); (2) Afro-Caribbean ethnicity (white); (3) stroke symptom onset time of 2 hours 30 minutes (50 minutes); (4) a pre-stroke dependency score of mRS3 (mRS4); and (5) SBP values of 185 mmHg (140 mmHg). Compared with the stroke severity reference category of NIHSS 2 (without aphasia), respondents were significantly more likely to offer thrombolysis to patients with scores of NIHSS 5 (without aphasia), NIHSS 14 and NIHSS 23.
The standard deviation for the ASC is statistically significant suggesting there was considerable heterogeneity among respondents in their thrombolysis decision-making. There was also substantial heterogeneity on several of the random effects coefficients (i.e. the patient factor levels), with nine standard deviations significant, indicating substantial variation between participants in their thrombolysis decisions as a function of differing levels of patient-related factors; or put differently, the response to or preferences in relation to particular attributes differed over clinicians.
Model 2: patient-related factors and prioritised clinician factors
Table 13 presents the results of the mixed-logit regression analysis for model 2, which includes the nine patient-related factors and seven clinician characteristics added to the model as a way to explore observed heterogeneity. These variables were prioritised for inclusion based on an a priori ranking exercise conducted by the expert panel (see Chapter 3, Analyses conducted on the data set). The clinician variables included were respondents’ perception of the evidence base for thrombolysis; Physician Reaction to Uncertainty Scale score; clinicians’ attitude towards risk score; the number of days since a patient was harmed as a result of treatment with thrombolysis; total number of patients thrombolysed in the past 12 months; comfort treating patients outside criteria; and number of patients harmed by thrombolysis in the past 12 months.
| Factor | Level | Coefficient | SE | p-value | Odds ratio (95% CI) |
|---|---|---|---|---|---|
| Patient age, mean (SD) | 68 | Reference | |||
| 85 | 2.99 (4.46) | 1.04 (1.17) | 0.004 (< 0.001) | 19.89 (2.58 to 152.7) | |
| 95 | –2.88 (2.95) | 1.24 (0.83) | 0.02 (< 0.001) | 0.06 (0 to 0.64) | |
| Patient ethnicity, mean (SD) | White | Reference | |||
| Asian | –0.32 (2.06) | 0.57 (0.58) | 0.57 (< 0.001) | 0.73 (0.24 to 2.22) | |
| Afro-Caribbean | 3.79 (2.78) | 1.15 (0.84) | 0.001 (0.001) | 44.42 (4.69 to 422.06) | |
| Patient sex, mean (SD) | Male | Reference | |||
| Female | 1.62 (2.21) | 1.07 (0.72) | 0.13 (0.002) | 5.05 (0.62 to 40.82) | |
| Time since symptom onset, mean (SD) | 50 minutes | Reference | |||
| 2 hours 30 minutes | 3.05 (0.91) | 0.85 (0.43) | < 0.001 (0.03) | 21.12 (4 to 111.1) | |
| 4 hours 15 minutes | –6.21 (3.72) | 1.65 (0.98) | < 0.001 (< 0.001) | 0 (0.01 to 0.05) | |
| Patient frailty, mean (SD) | Not frail | Reference | |||
| Frail | 0.01 (0.03) | 0.38 (0.35) | 0.98 (0.94) | 1.01 (0.48 to 2.14) | |
| Pre-stroke dependency (mRS score), mean (SD) | mRS1 | 3.08 (12.81) | 1.76 (3.28) | 0.08 (< 0.001) | 21.76 (0.69 to 685.31) |
| mRS3 | 3.51 (3.04) | 1.06 (0.88) | 0.001 (0.001) | 33.45 (4.11 to 271.11) | |
| mRS4 | Reference | ||||
| Pre-stroke cognitive status, mean (SD) | No history of memory problems | Reference | |||
| Moderate dementia | 2.87 (–1.81) | 0.99 (0.59) | 0.004 (0.002) | 17.64 (2.5 to 125.76) | |
| Severe dementia | –8.07 (5.42) | 1.97 (1.4) | < 0.001 (< 0.001) | 0.01 (0.01 to 0.02) | |
| SBP, mean (SD) | 140 mmHg | Reference | |||
| 185 mmHg | 4.64 (6.98) | 1.23 (1.79) | < 0.001 (< 0.001) | 103.54 (9.33 to 1158.2) | |
| 200 mmHg | –17.51 (9.11) | 4.1 (2.24) | < 0.001 (< 0.001) | 0 (0 to 0) | |
| NIHSS score (stroke severity), mean (SD) | 2 (without aphasia) | Reference | |||
| 2 (with aphasia) | –1.38 (3.82) | 1.05 (1.43) | 0.19 (0.01) | 0.25 (0.03 to 1.97) | |
| 5 (without aphasia) | 7.74 (2.41) | 2.22 (1.24) | < 0.01 (0.05) | 2298.5 (29.4 to 178,688) | |
| 5 (with aphasia) | 3.13 (11.84) | 1.17 (2.89) | 0.008 (< 0.001) | 22.87 (2.29 to 227.3) | |
| 14 | 6.98 (3.39) | 1.86 (1.11) | < 0.001 (0.002) | 1074.92 (28 to 41,386.5) | |
| 23 | 9.15 (0.37) | 2.7 (0.89) | 0.001 (0.68) | 9414.44 (43.6 to 2,047,889) | |
| Perception of evidence base | 0.55 | 0.29 | 0.053 | 1.73 (0.99 to 3.05) | |
| Number thrombolysed in past 12 months | 0.21 | 0.05 | < 0.001 | 1.23 (1.11 to 1.37) | |
| Physician reaction to uncertainty | 2.46 | 0.89 | 0.006 | 11.7 (2.01 to 67.71) | |
| Attitude towards risk | 0.06 | 0.07 | 0.35 | 1.06 (0.93 to 1.22) | |
| Number harmed by thrombolysis in past 12 months | –0.48 | 0.52 | 0.36 | 0.62 (0.22 to 1.72) | |
| Days since patient was harmed by thrombolysis | 0.01 | 0.001 | 0.48 | 1.01 (1 to 1.01) | |
| Comfort treating outside criteria | –0.78 | 0.34 | 0.02 | 0.46 (0.24 to 0.89) | |
| ASC, mean (SD) | Decision to offer thrombolysis | –26.99 (7.17) | 6.79 (1.82) | < 0.001 (< 0.001) | 0 (0 to 0) |
| Block effects, mean | Block 2 | 5.2 | 1.76 | 0.01 | |
| Block 3 | 3.93 | 1.76 | 0.03 | ||
| Block 5 | 6.81 | 2.16 | 0.01 | ||
| Block 7 | 6.48 | 2.07 | 0.01 | ||
| Block 8 | 4.91 | 1.89 | 0.01 | ||
Consistent with model 1, the ASC for model 2 is negative and statistically significant, indicating that there was a general preference not to offer intravenous thrombolysis. The standard deviation for the ASC for model 2 is also statistically significant, which indicates the presence of considerable heterogeneity among respondents regarding their thrombolysis decisions. There was also considerable heterogeneity for the random-effects coefficients (i.e. the levels of patient factors), with the standard deviations of 17 factor levels emerging as statistically significant.
The pattern of results obtained in model 2 is broadly consistent with that of model 1 (see Table 12). All of the statistically significant patient factor predictors of thrombolysis decisions from model 1 remained significant contributors to the model; however, an additional two patient factors were statistically significant predictors of decisions to offer thrombolysis: (1) moderate dementia and (2) NIHSS 5 (with aphasia).
Four of the seven clinician factors were statistically significant predictors of thrombolysis decisions. Respondents’ were significantly more likely to offer thrombolysis when they (1) perceived the evidence base for thrombolysis to robust; (2) had thrombolysed a high number of patients in the past 12 months; and (3) reported a higher level of discomfort with uncertainty (assessed by the Physicians’ Reaction to Uncertainty Scale). Finally, clinicians who reported being comfortable treating patients outside the licensing criteria were significantly less likely to offer thrombolysis.
Comparison of the Akaike and Bayesian information criteria established that model 2 was a better fit than both model 1 and model 3. The full results of model 3 are included in Appendix 7.
Predicted probabilities
The predicted probabilities of offering thrombolytic treatment to patients described in each vignette (based on model 1) are available in full in Appendix 8.
Predicted probabilities for decisions to offer thrombolysis ranged from 0% (vignette numbers 8, 10, 14, 18, 19, 27, 34, 39, 43, 47, 57, 59, 65, 68, 71, 87, 80, 96 and 97; total observed rate of offering thrombolysis = 0% to 23.1%) to 99.86% (vignette number 70; total observed rate of offering thrombolysis = 100%).
Based on the utility values (using the coefficients from model 1), the vignette in which respondents were most likely to offer thrombolysis was number 70, which included the following level specifications:
Age 95; female; white; 2 hours 30 minutes since symptom onset; no history of memory problems; pre-stroke mRS3; NIHSS 14; systolic blood pressure 140 mm/Hg; who you do not perceive as frail.
The vignette in which respondents were least likely to offer thrombolysis was number 39, which included the following specifications:
Age 85; male; white; 4 hours 15 minutes since symptom onset; moderate dementia; pre-stroke mRS4; NIHSS 2 (without aphasia); systolic blood pressure 200 mm/Hg; who you perceive as frail.
Qualitative comments and data interpretation
Of the 138 respondents, 96 individuals commented on at least one hypothetical patient vignette. In total, 497 free-text comments were provided by respondents as reasons why they would, or would not, offer thrombolysis to the hypothetical patients described in vignettes; for example:
The patient is already dependant, is at the edge of 4.5 hours and has a severe stroke. I would judge potential benefit of tpa as low and risk of haemorrhage relatively higher.
Male, neurologist, vignette 7, thrombolysis not offered
Against--Age of 85, MRS 3 (relative contraindication, in my opinion), high NIHSS. For- symptom onset <1 hr, BP 140, BM 6.
Male, stroke clinician, vignette 15, thrombolysis offered
To provide further insights into cognitive processes underpinning thrombolysis decisions, comments from respondents for variable patient factors are summarised below, along with direct quotes to illustrate key themes in these data.
Patient demographics (age, sex and ethnicity)
There were relatively few comments on patient sociodemographics (age, sex and ethnicity) as factors influencing decision-making for patient vignettes. Several respondents stated that patient age (independently) would not influence their decision-making about thrombolysis:
Age itself is not a barrier and within good time window to benefit; it rather depends on the breakdown of the NIHSS categories.
Male, stroke clinician, vignette 83, thrombolysis offered
Age alone not a reason NOT to [thrombo-] lyse.
Male, stroke clinician, vignette 72, thrombolysis offered
However, a large proportion of comments related to the interaction of patient age and onset time when making thrombolysis decisions, in particular with reference to patients aged > 80 years and evidence from IST-3:
I have been taught locally that due IST3 data suggesting benefit of rTPA after 3h in over 80s is minimal.
Female, neurologist, vignette 12, thrombolysis not offered
The IST3 trial did not show benefit in treating patients over 80yrs beyond 3 hours.
Male, stroke clinician, vignette 80, thrombolysis not offered
No respondents made any comments about patient sex. Only two comments explicitly referred to patient ethnicity in combination with other factors; specifically, the cultural background of Asian patients was mentioned in both instances as drivers of decisions to offer thrombolysis, with references to beliefs about cultural (familial) values and acceptability of palliative care in hospital:
Mobility and level of communication with family as well as participation in family life would be important. Some Asian elderly people can do actually better to what ADLs [activities of daily living] assessments are.
Female, stroke clinician, vignette 17, thrombolysis offered
IST-3 shows she could be safely treated; she is likely to be at home prior to this given her cultural background and would wish to remain so; leaving her with this stroke may mean she needed a PEG and/or institutional care which would not be in keeping with her culture?
Female, geriatric medicine physician, vignette 83, thrombolysis offered
Frailty
Patient frailty was not independently noted as a contraindication for treatment with thrombolysis, although frailty in combination with other patient factors such as mild stroke and moderate/severe dementia (and concomitant perception of increased bleeding risk) was frequently cited as a reason not to offer treatment.
Low NIHSS and high risk of bleeding as delayed presentation. Also frail. I feel the risk would be too high.
Male, geriatric medicine physician, vignette 39, thrombolysis not offered
The patient is frail, dependent with a MRS of 4 and has a low NIHSS.
Male, geriatric medicine physician, vignette 16, thrombolysis not offered
Pre-stroke cognitive status
In vignettes where patients had moderate or severe dementia, many clinicians commented on the lack of evidence (and uncertainty) about the efficacy of thrombolysis and on increased bleeding risks, including concerns about the negative impact of severe dementia on the recovery process:
Evidence regarding safety of thrombolysis in dementia is lacking. Demented patient > 85 yrs may have microbleeds. Given mRS of 4, and reduced likelihood of benefit from late treatment, I would assume risk outweighs benefit.
Male, stroke clinician, vignette 7, thrombolysis not offered
Certainly not if moderate or severe small vessel changes on CT scan. If no such changes then perhaps: but severe dementia a very limiting factor to recovery.
Male, stroke clinician, vignette 71, thrombolysis not offered
I would perceive this frail patient at high risk of complications, although this may be balanced by the early time frame and significant motor deficit. I know that because of his dementia, he will find rehab difficult, so maybe thrombolysis is his best shot. I have easy rapid access to stroke physicians and this is the sort of case we would manage together.
Male, A&E physician, vignette 54, thrombolysis not offered
History of severe dementia would deter me from thrombolysis in this case.
Female, geriatric medicine physician, vignette 45, thrombolysis not offered
Systolic blood pressure
Comments about this patient factor related to both measured blood pressure values and blood pressure lowering. Regarding the latter, several clinicians would attempt to lower blood pressure (when it was above the licensing criteria cut-off of 185 mmHg) and then reassess the patients’ suitability for treatment, whereas others would offer treatment and simultaneously take steps to reduce SBP, although the importance of fully informing patients/family about the increased risk of bleeding in these circumstances was emphasised:
High BP but will treat and reassess.
Male, geriatrician, vignette 20, thrombolysis not offered
I would treat this BP first and if it came down easily I would lyse [thrombolyse] him with family assent.
Male, stroke clinician, vignette 53, thrombolysis not offered
After long discussion with patient and only when satisfied patient knows the risk. Would also simultaneously treat blood pressure.
Male, A&E physician, vignette 69, thrombolysis offered
There was also a subset of respondents who indicated they would actively monitor the patient’s blood pressure and delay treatment decisions until it was below the threshold stated in the licensing criteria. These considerations were influenced by onset time, and were mentioned in patient vignettes only when stroke symptom onset time was well within the 4.5 hours (i.e. either 50 minutes or 2 hours 30 minutes):
I would wait to see if the BP settled.
Male, stroke clinician, vignette 29, thrombolysis not offered
Might wait additional 15–30 minutes to check if SBP drops to criteria level before thrombolysis.
Male, stroke clinician, vignette 33, thrombolysis not offered
I would monitor SBP, ensure no pain, retention etc. but not pharmacologically lower immediately.
Male, geriatric medicine physician, vignette 22, thrombolysis not offered
Stroke severity score (National Institutes of Health Stroke Scale)
Respondents would be less willing to treat a patient with thrombolysis with mild stroke (NIHSS score of ≤ 5). NIHSS being ‘too low’ to warrant treatment was often cited by respondents as the primary reason underpinning their decisions not to offer thrombolysis to patients described in hypothetical vignettes. This may reflect the lack of a specific minimum NIHSS cut-off being stated in the licensing criteria and a lack of robust evidence for absolute benefit of treatment for very mild stroke:
NIHSS too low.
Female, geriatric medicine physician, vignette 30, thrombolysis not offered
Very mild stroke. No evidence substantial gains to be had from TPA.
Male, neurologist, vignette 13, thrombolysis not offered
However, some clinicians commented that low NIHSS with aphasia may influence their decision to offer treatment, as they considered aphasia a ‘significant deficit’ that would impact negatively on quality of life (which trumped low NIHSS scores).
Although NIH low, aphasia very disabling, potentially will mean significant change in social and functional status. Not bothered by age.
Female, geriatric medicine physician, vignette 30, thrombolysis offered
I don’t use age as a criteria - she has some dependency but not the severest level. This is not a mild stroke – aphasia if long lasting could make a big difference to her care requirements.
Male, stroke clinician, vignette 23, thrombolysis offered
At the higher NIHSS scores, even though respondents were cognisant that patients with high NIHSS scores were significantly more likely to have a poor outcome from thrombolysis, clinicians were more likely to offer treatment based on considerations that they had more to gain from treatment:
At higher risk of poorer outcome due to high NIHSS but time of onset within original NINDS 3 hour window so would thrombolyse.
Female, neurologist, vignette 21, thrombolysis offered
I would explain that the chances of a good outcome are lower than usual but she has had a very severe stroke and has little to lose.
Male, stroke clinician, vignette 35, thrombolysis offered
Severe Stroke. Little to lose from Rx[treatment].
Male, stroke clinician, vignette 60, thrombolysis offered
Pre-stroke dependency (modified Rankin Scale)
The influence of pre-stroke dependency on thrombolysis decision-making was variable. Patients’ pre-stroke dependency was described by some clinicians as a contraindication for treatment when the mRS score was 3 or 4. This may reflect modest inter-rater reliability of mRS assessments (κ < 0.5)105 and considerations about quality of life that may trump mRS assessments. Indeed, several clinicians commented that they would not rely on mRS alone in their assessment of quality-of-life gains from treatment and risk–benefit ratios for individual patients.
mrs = 3
Male, neurologist, vignette 59, thrombolysis not offered
MRS 4 risk > benefit
Male, neurologist, vignette 85, thrombolysis not offered
Too high level of dependency is primary reason for not thrombolysing
Male, A&E physician, vignette 27, thrombolysis not offered
mRS doesn’t tell the whole story so I would want to get a quick chat with family or carer to get a clearer picture of QOL. If appropriate based on this discussion I would lyse [thrombolyse]
Male, stroke clinician, vignette 35, thrombolysis offered
Symptom onset time
Early presentation/symptom onset time was a key driver of decisions to offer thrombolysis (which reflects robust evidence of increased benefit from earlier treatment) and other potential contraindications were traded off (such as severe stroke and mRS score of > 2) against the potential benefit of early treatment. In these cases clinicians were willing to give patients the ‘benefit of the doubt’, as such patients were considered to have ‘little to lose’.
This is a severe stroke with a very poor outcome. She has nothing to lose from treatment particularly as she can be treated early in time window.
Male, stroke clinician, vignette 15, thrombolysis offered
Very early presentation and therefore maximal likely benefit (& normal BP - probably less likely to bleed) in patient with significant speech defect probably will justify the treatment even with less than favourable premorbid state.
Male, stroke clinician, vignette 23, thrombolysis offered
With early presentation benefit probably outweigh concerns about premorbid state.
Male, stroke clinician, vignette 74, thrombolysis offered
However, when symptom onset was 4 hours 15 minutes (approaching the upper end of the treatment time window for thrombolysis) clinicians were reluctant to offer treatment in the context of other factors that would indicate a higher risk of bleeding/poor treatment outcome.
The time factor is important and it is 4 hours 15 minutes + the NIHSS of 2 would not persuade me to thrombolyse.
Male, stroke clinician, vignette 39, thrombolysis not offered
Time since symptom of onset is quite long and if true would decrease the likelihood of benefit from thrombolysis. Would discuss with consultant/seniors but my inclination would be not to thrombolyse.
Female, neurologist, vignette 35, thrombolysis not offered
Consult with colleagues or patient/family
There were many instances in which respondents would consult with colleagues in stroke medicine and/or engage the patient or family/carer in shared decision-making before making a final decision about thrombolysis, especially for cases at the extremes (grey zone) of the licensing criteria. Several respondents also expressed a wish to enquire further about the patient’s living status (nursing home or otherwise) in order to inform their thrombolysis decisions:
This is one I would discuss with a stroke physician. I would consider the patient to have high vascular fragility and at risk from complications. However, this patient has a significant disability. This is a case for shared decision making.
Male, A&E physician, vignette 23, thrombolysis not offered
Approaching the end of the longer 4.5 hour time window therefore I would discuss with consultant covering stroke whether their practice would be to thrombolyse or not.
Female, neurologist, vignette 50, thrombolysis not offered
I would discuss with family. She could be a good candidate but needs a best interest assessment given low NIHSS and high premorbid disability.
Female, neurologist, vignette 95, thrombolysis not offered
External validity
We compared a number of patient vignettes included in the DCE with national patient data. In consultation with SSNAP, six subsets of patient data were collated to compare decision-making about thrombolysis in this study with decision-making for UK patients admitted to hospital (or date of onset if already in hospital) between April 2013 and March 2015. Six vignettes were chosen as they represented vignettes at extremes of decision-making observed in the study (high rates of offering thrombolysis and high rates of not offering thrombolysis) and were purposively chosen to ensure no overlap between SSNAP data subsets (i.e. a patient from SSNAP database could qualify for inclusion in only one data subset).
Table 14 displays the features of the comparison between thrombolysis decisions made for patient vignettes in the DCE and SSNAP data subsets. For many of the data subsets, similar patterns are evident for treatment rates observed in practice in the UK and decision-making about the offer of thrombolysis in the current study. There is typically a lower treatment rate in practice than the rates of offering treatment in the current study; this was anticipated given that patients may be not be deemed eligible for treatment owing to other complications and comorbidities.
| Variable | Data subset 1 (vignette #70) | Data subset 2 (vignette #39) | Data subset 3 (vignette #10) | Data subset 4 (vignette #15) | Data subset 5 (vignette #83) | Data subset 6 (vignette #58) |
|---|---|---|---|---|---|---|
| Patient age range (years) | 90–100 | 80–90 | 63–73 | 80–90 | 90–100 | 63–73 |
| Patient sex | Male/female | Male/female | Male/female | Male/female | Male/female | Male/female |
| Onset to scan/decision time (hours:minutes) | 1:45 to 2:45 | 3:15 to 4:15 | 3:15 to 4:15 | 0:30 to 1:30 | 0:30 to 1:30 | 1:45 to 2:45 |
| Pre-stroke dependency (mRS score) | 3 | 4 | 4 | 3 | 4 | 4 |
| NIHSS score | 12–16 | 1–4 | 1–4 | 21–25 | 1–4 | 3–7 |
| Patient ethnicity | No restriction | No restriction | No restriction | No restriction | No restriction | No restriction |
| Total number of patients matching criteria in SSNAP | 51 | 36 | 11 | 68 | 6 | 19 |
| Number (%) of patients treated with thrombolysis in SSNAP | 18 (35.3) | 1 (2.7) | 0 (0) | 39 (57.4) | 0 (0) | 4 (21.1) |
| % who offered thrombolysis in current study | 100 | 0 | 0 | 100 | 69.2 | 39.1 |
Chapter 5 Discussion
Summary of key findings
This is the first DCE to explore patient- and clinician-related factors that influence the decision to offer intravenous thrombolysis to patients with acute ischaemic stroke. Analysis of the DCE data revealed a strong aggregate level preference not to offer thrombolytic treatment, which was expected given that the vignettes were specifically designed to elucidate the influence of factors on decisions related to the ‘grey’ areas of the current licensing criteria for treatment.
Levels of seven different patient-related medical and non-medical (sociodemographic) factors [patient age, patient ethnicity, stroke symptom onset time, pre-stroke dependency, SBP, stroke severity (NIHSS) and pre-stroke cognitive status] and four different clinician-related ‘psychosocial’ factors (perception of the evidence for thrombolysis, number of patients thrombolysed in the past 12 months, comfort with uncertainty and comfort with treating patients outside the licensing criteria) were significant predictors of an increased likelihood of decisions to offer or not offer thrombolysis (Table 15).
| Variables | Drivers (increased likelihood of offering thrombolysis) | Inhibitors (decreased likelihood of offering thrombolysis) |
|---|---|---|
| Patient age (years) | 85 (compared with 68) | 95 (compared with 68) |
| Patient ethnicity | Afro-Caribbean (compared with white) | |
| Stroke symptom onset time | 2 hours 30 minutes (compared with 50 minutes) | 4 hours 15 minutes (compared with 50 minute) |
| Pre-stroke dependency (mRS score) | 3 (compared with 4) | |
| SBP (mmHg) | 185 (compared with 140) | 200 (compared with 140) |
| Stroke severity (NIHSS score) | 5 (with and without aphasia), 14 and 23 (compared with NIHSS 2 without aphasia) | |
| Pre-stroke cognitive functioning | Moderate dementia (compared with no history of memory problems) | Severe dementia (compared with no history of memory problems) |
| Perceived robustness of the evidence base for thrombolysis | High | |
| Number of patients thrombolysed in the past 12 months | High | |
| Discomfort with uncertainty (physician reaction to uncertainty scale) | High discomfort with uncertainty | |
| Clinicians’ comfort with treating patients outside the licensing criteria | High comfort with treating patients outside the licensing criteria |
Interpretation of results in relation to the literature
Patient age
Patients aged 95 years were significantly less likely to be offered treatment than patients aged 68 years. Respondents were also significantly more likely to treat 85-year-olds than patients aged 68 years. The benefits of thrombolysis for older patients in terms of reduction in disability is at least as great as those for younger patients, despite an increased risk of sICH. Patients aged 85 years have more to gain from treatment than younger patients (irrespective of risk) and this would also reflect acceptance of IST-3 data that report benefit for patients aged > 80 years, in particular for those with onset to treatment time of < 3 hours (the cut-off stated in the licensing criteria and the upper age limit in trials) and increased recognition that chronological age does not necessarily equate to physiological age. 106 That respondents were more likely to treat 85-year-olds than 68-year-olds could indicate that, all things being equal, clinicians may be more willing to risk a potential negative outcome of thrombolysis in 85-year-old patients than in younger patients. Based on the results and qualitative data, it appears that clinicians are not disinclined to treat older patients until those patients reach higher ages (≈95 years). It may also indicate that clinicians are more likely to give the ‘benefit of the doubt’ to older patients and avoid denying treatment based on age. It is also feasible that a social desirability effect has been observed, whereby respondents may be overcompensating to avoid denying treatment based on age.
However, disinclination to treat patients aged 95 years may represent the upper limit of data from IST-3 or reflect clinical practice or experience (there are few patients who have been treated in this age range in routine practice). For instance, SITS data indicate that only approximately 10% of treated patients were older than 80 years106,107 and Stroke Improvement National Audit Programme data indicate that only 2.5% of the total number of patients who received thrombolysis between April 2010 and November 2011 were older than 90 years. 108
Time since symptom onset
Regarding the ‘time since symptom onset’ factor, consistent with expectations and strong evidence of increased benefit with earlier treatment,16 we identified a statistically significant decreased likelihood of offering treatment to patients who could be treated at 4 hours 15 minutes from symptom onset compared with 50 minutes from symptom onset. The former is at the extreme end of the licensing criteria, and, given the time dependency of the outcome, and that onset to treatment is estimated, would account for this time period being an inhibitor of decisions to offer treatment. Clinicians were significantly more likely to treat patients at 2 hours 30 minutes than at 50 minutes. This could indicate that clinicians have not been in this situation very often because acute stroke presentations typically occur later than this, and it may be that clinicians wait a short time in some borderline cases to see if the symptoms spontaneously improve.
This may indicate that some clinicians are willing to delay the final decision about thrombolysis if there are some factors which create uncertainty; for instance, in mild stroke when a patient’s symptoms are rapidly improving, the clinician may delay to see if symptoms resolve (per licensing guidelines45) or to potentially give blood pressure time to stabilise or to take more readings before making a final decision about the patient’s eligibility for thrombolytic treatment. 109–111 This is in spite of research which confirms that earlier treatment is associated with substantially more favourable outcomes,16 particularly when treatment occurs within the ‘golden hour’ (< 60 minutes from symptom onset),110 and that delaying treatment owing to perceived patient improvement or in the case of minor stroke could still risk significant disability or death. 111
Stroke severity score (National Institutes of Health Stroke Scale)
Respondents were significantly more likely to offer thrombolysis to patients with severe strokes (NIHSS 14 and NIHSS 23) and to not offer thrombolysis to patients with mild stroke. This finding reflects the lack of data on and uncertainty about the benefit of treatment of minor stroke and about poor outcomes for patients with severe strokes. There was significant heterogeneity among respondents on the influence of NIHSS 2 with aphasia and NIHSS 5 without aphasia. This implies that clinicians differ in their thresholds for treatment of minor stroke and may also differ when considering the gains in quality of life for individual patients with isolated language difficulties.
Patient ethnicity
Compared with white patients, Afro-Caribbean patients were significantly more likely to be offered treatment, although there was no effect for Asian ethnicity. This is contrary to US-based research which found that African American and minority patients were significantly less likely to receive thrombolytic treatment for acute ischaemic stroke. 112,113 Although efforts were made to exclude any diagnostic uncertainty, these findings may be related to a perception of increased diagnostic certainty of stroke, given the evidence of increased rates among this ethnic group. However, social desirability bias may help to account for the findings, with clinicians overcompensating to avoid being seen as denying treatment based on race.
Pre-stroke dependency (modified Rankin Scale)
Patients with pre-stroke dependency of mRS3 (moderate disability: requiring some help, but able to walk without assistance) were more likely to be offered treatment than those with mRS4 (moderately severe disability: unable to walk without assistance and unable to attend to own bodily needs without assistance), but mRS1 (no significant disability despite symptoms) was not significantly associated with thrombolysis decision-making. We would have expected that respondents would be more willing to treat patients with mRS1 than those with mRS4; however, the failure of this to reach significance may be due to an imbalance between the levels of pre-stroke dependency in the study. Vignettes including mRS1 were under-represented and therefore may have reduced the power to adequately compare these levels.
Pre-stroke cognitive status
Patients presenting with severe dementia were significantly less likely to be offered thrombolysis in models 1 and 2, with moderate dementia emerging as significant in model 2, indicating that clinicians were more likely to offer thrombolysis in these cases (compared with patients with no memory problems). Inspection of the standard deviations reveals significant variation between respondents on the influence of both moderate and severe dementia on thrombolysis decision-making. This again emphasises that clinicians are weighing up the pros and cons of treatment with reference to individual patient characteristics that are not part of the licensing criteria, although it may also reflect perceptions that dementia increases risk of sICH, which is contrary to research demonstrating no increased risk. 114 In the comment boxes after the vignettes, many respondents expressed that they would seek to discuss the risks and benefits of treatment with the patient’s family/carer or seek further information about living status/dependency level prior to making a final decision about the offer of treatment. It was also noted that patients with dementia may find recovery/rehabilitation more difficult and, therefore, in some instances, thrombolysis may be worth the risk in order to give the patient the best chance of regaining his or her pre-stroke quality of life.
Systolic blood pressure
Patients presenting with SBP of 200 mmHg were significantly less likely to be offered treatment than those presenting with SBP of 140 mmHg. Given that this level is outside the licensing criteria for treatment with thrombolysis, this is not surprising. However, results revealed that clinicians were more likely to offer thrombolytic treatment when SBP was 185 mmHg (compared with the reference category of 140 mmHg). This finding was surprising and no clear explanation was suggested for this in the comments. It may be that once clinicians make the decision to attempt to reduce blood pressure, the decision to treat with thrombolysis is reinforced. Thus, the decision to lower blood pressure may become interlinked with the decision to offer thrombolysis, increasing the likelihood of thrombolysis being offered if attempts are made to reduce blood pressure.
Clinician factors
Four of the seven clinician factors ranked a priori as potential significant influences on decision-making emerged as significant. There was a significant association found between the respondents’ perception of the evidence base and the offer of thrombolysis. Although the mean score for perception of the evidence was high, suggesting that the majority of respondents considered the evidence robust, those who perceived the evidence as more robust were more likely to offer treatment.
The Physician Reaction to Uncertainty scale60,61,102 has been demonstrated to influence diagnostic decision-making and, in the current study, higher discomfort with uncertainty was associated with increased likelihood of offering thrombolysis. This may indicate a preference for action over inaction in instances of high uncertainty, or what may be termed commission bias. 54 Commission bias is defined as the tendency towards action/intervention rather than inaction. 54 Given the high scores observed on the Institutional Culture Scale in the study, indicating a strong culture of administering thrombolysis in respondents’ institutions, clinicians may worry more about decisions not to treat and therefore those with higher levels of discomfort with uncertainty may be more willing to thrombolyse patients. Clinicians who experience high discomfort with uncertainty may be more likely to offer thrombolytic treatment to patients if it is perceived as the dominant or favoured position among colleagues or peers.
The results also indicated that clinicians who reported being more comfortable treating patients outside the licensing criteria were less likely to offer treatment in the current study; however, we do not have a clear explanation for this finding.
Finally, there was a significant association between clinicians’ experience of thrombolysis and the likelihood of offering thrombolysis in the current study. This may indicate that familiarity with administration of the treatment (and positive outcomes) increases likelihood of future use, and has important practical implications for how clinicians are supported when they begin involvement in decision-making about thrombolysis. Alternatively, it may simply represent the fact that those more likely to offer treatment in the DCE are more likely to offer treatment in practice, and therefore have higher reported treatment rates.
Strengths and limitations
A key strength of this study is the use of a systematically developed and clinically valid DCE embedded within an online survey. The DCE development process is clearly documented using a systematic, rigorous and iterative process involving a multidisciplinary team to derive the optimal number and type of factors, factor levels and associated operational definitions for inclusion in the DCE. It builds on ISPOR guidelines77,78 by proposing and providing explicit guidance on a five-stage process, which may be particularly beneficial when there is little or no previous research to guide DCE design in terms of optimal format for presenting choice sets and selection of factors for inclusion to maximise utility of the findings. This transparency in the development process of a DCE (process validity) to understand the decision of interest (decision to offer thrombolysis or not) as well as information used by clinicians in their decision-making and presentation of choice sets in a familiar format (patient vignettes), confers confidence in the rigour and reliability of our findings and applicability to the real-world (ecological validity). 28 Our exploratory work to inform the design of the DCE indicated that individual clinicians often varied in the cut-offs they employed for various factors in their decision-making about thrombolysis (e.g. blood pressure, pre-stroke dependency level). Given this variance, we aimed to explore and better elucidate these grey areas/areas of uncertainty in decision-making. Yet, as with most DCEs, a limitation is the fact that we had to exclude some factors to make the survey possible. However, this was counterbalanced to some degree by the inclusion of fixed factors, which allowed for the minimisation of extraneous influences on decision-making, insofar as this was possible.
Another strength of the analysis was our ability to account for both observed heterogeneity among respondents (via inclusion of clinician factors in the model) and unobserved variation (via the estimation of random parameters for the ASC and factor levels) using the mixed-logit regression.
Although we originally anticipated a sample size of 150–200 participants, our final sample (n = 138) represents a good response rate in terms of the total population of clinicians involved in the final decision-making regarding thrombolysis for acute ischaemic stroke patients in the UK (≈450–500). Furthermore, the RCP census data suggest that our sample is representative of the demographic profile of clinicians involved in stroke care in the UK. Observed response rates of clinicians involved in stroke care were also similar previous online studies in the field of stroke medicine115,116 and similar to response rates for other DCEs exploring clinical decision-making. 117–120
As no linear variables were included in the analysis, we could not perform analysis that was originally intended to investigate trade-offs in decision-making (marginal rates of substitution). The inclusion of factors such as age and SBP as linear variables was investigated but preliminary analysis revealed that their inclusion as linear would have masked the associations observed between various levels.
Key learning points and implications for research, training and practice
Our research offers an important contribution towards a deeper understanding of the factors that influence the decision to offer intravenous thrombolysis to patients with acute ischaemic stroke, in particular factors that influence decisions for patients who fall within the grey zone of the licensing criteria. The prohibitively long list of influential factors identified during stage 1 of the DCE development process underscores the need for further research to explore the influence, if any, of factors not explored in this study. For example, in acute stroke, patients on warfarin (and their associated anticoagulation/international normalised ratio status), recent surgery/bleeding and comorbidities are factors likely to influence thrombolysis decision-making and warrant future research.
As predicted based on SSNAP data,12,13,19 there was significant variation between clinicians in their decision-making about thrombolysis for ‘grey’ cases. Our findings indicate that factors underpinning this uncertainty in decision-making include medical factors, such as patients presenting with minor strokes, and those at the upper limit of the stroke treatment window (where there is insufficient evidence of the benefit of thrombolysis or where there may be uncertainty about the existing evidence). 17
The results also raise an important issue regarding the treatment of patients who would be deemed ineligible for treatment based on the current licensing criteria. For instance, several of the hypothetical patients described in the vignettes would be considered outside the licensing criteria and would thus be excluded from most major clinical trials (e.g. vignettes 11 and 23), and yet many participants in the study reported that they would offer treatment in these scenarios. The Medicines and Healthcare products Regulatory Agency, in their conclusions following the review of the evidence for thrombolysis,39 have cited several areas of the licensing criteria that should be reviewed to determine whether or not the product guidelines accurately reflect the data (e.g. age, the benefits/risks of thrombolysis in minor and major stroke). Clinicians make decisions about whether or not to give thrombolysis based on perceived risks and benefits of treatment for that individual. Participants in research studies are a clearly defined group who are not always representative of people with stroke. There are relative and absolute contraindications for intravenous thrombolysis and the questions asked by clinicians at the point of treatment decision-making are about the potential benefits and potential risks of treatment for an individual patient. Previous research has underlined that considerable variation can exist even among expert clinicians,20 and that experience and opinion (and probably other individual factors) rather than just the licensing criteria affect decision-making and the perception of a patient’s eligibility for treatment. The utility of decision support tools should be further explored to enable and support clinicians to make better decisions around patient eligibility for treatment. 79
The finding that respondents were less likely to treat milder strokes (NIHSS score of < 5) might reflect the lack of data/uncertainty around the benefit of treatment of minor stroke. It may be important to highlight language impairment after stroke as an important factor in reduced social participation and quality of life after stroke. 121–123
As reported by previous research,50,51 the personal values, attitudes and beliefs of clinicians may influence thrombolysis decision-making. Psychological and social factors are fundamental influencers of cognition and behaviour (decision-making) and therefore education around the interactional nature of medical and non-clinical influences on decision-making (biases) should form a part of clinical training. Research indicates that although clinicians working in acute settings acknowledge the importance and relevance of decision-making, there is little training or pursuit of theoretical learning on the topic. 124 Croskerry et al. have outlined the relevance of cognitive debiasing strategies for medical professionals and the importance of embedding such strategies in training and CPD to avoid cognitive errors. 63,125,126 Studies have found that cognitive biases associated with intuitive judgments may be remedied by analytical reasoning. 127,128 Thus, decision support tools that facilitate the mapping and visualisation of risk and benefit79,129 for individual patients may help to counteract intuitive-based biases or misperceptions, as well as assist in better communicating evidence to patients, family and carers. 130
Training and CPD should emphasise benefit of treating up to the 4.5-hour limit and the importance of treating early and not delaying decision-making, as research illustrates a great proportional benefit with early treatment when there are no contraindications for thrombolysis. 15,34 Finally, this study indicates that more experience of administering thrombolysis was associated with a greater likelihood of offering it. This is indicative of the importance of developing practical learning and increasing exposure to intravenous thrombolysis early in training to maximise appropriate delivery and build practitioner confidence and self-efficacy in the administration of intravenous thrombolysis. Similarly, familiarity with the evidence base for thrombolysis is crucial and should be a prerequisite for participation in thrombolysis rotas.
Key learning points and implications for discrete choice experiment methods
Our study highlights the importance of an iterative design process for augmenting the clinical face validity of the choice task in terms of (1) mode of administration (paper-based or electronic); (2) identification and optimal selection of variable and fixed factors and associated levels to include in choice sets; (3) form of choice set presentation (textual vs. traditional tabular approach, and order of information presentation); and (4) the necessity of piloting to augment clinical face validity, and in turn external validity, and acceptance of choice sets by the target population, prior to the data collection phase.
Key advantages of hosting a DCE online include facilitating access to large numbers of participants who are geographically distributed; enabling respondents to complete a DCE survey at a time convenient for them; and the option of completing in multiple sessions in different locations by providing a save-and-return-later facility. Owing to the unpredictable working hours of clinicians in the NHS, it was important to include these options.
Recommendations for future research
The nature of DCEs demanded that only a subset of potentially influential factors on clinical decision-making could be explored in this research. Factors not investigated in this study warrant future research to understand their impact, if any, on the decision to offer intravenous thrombolysis. The long list of potential factors identified during stage 1 of the DCE development process underscores the range of patient factors that may act as potential influences on thrombolysis decision-making.
As no linear variables were included in the current analysis, we could not perform the analysis that was originally intended to investigate trade-offs that clinicians make in decision-making (marginal rates of substitution). The inclusion of factors such as age and SBP as linear variables was investigated but preliminary analysis revealed that their inclusion as linear would have masked the associations observed between various levels. Based on the qualitative results, it was clear that there were often multiple interacting factors influencing decision-making in individual cases and therefore future studies should seek to explore these trade-offs. In addition, exploring models accounting for attribute cut-offs may be a fruitful avenue for future research. 131
Further research is required in order to fully understand how clinician characteristics, beyond those examined here, may impact on decision-making, and the most effective interventions for addressing cognitive biases that may inhibit appropriate (and inappropriate) use of thrombolysis. Further work should explore the influence of decision support tools that utilise evidence-based graphical depictions of risk and benefit for individual patients on clinical decision-making and patient outcomes.
Strategy to translate findings into continuing professional development/learning and training
A range of dissemination activities are planned to ensure that the results of the research are translated into learning and will influence training and practice:
-
National Stroke Thrombolysis Masterclass for clinicians. An accredited CPD training event for clinicians involved in treatment of stroke patients took place on 16 October 2015 and an audience of approximately 120 attended. Results of the study were presented, along with an interactive discussion/voting session using patient vignettes from the research and results of decision-making from the study to generate discussion. Dissemination booklets were also provided to attendees.
-
Presentations at national and international conferences. Conferences targeted will include those on shared decision-making and evidence-based practice, health psychology, medical decision-making, stroke and emergency medicine. This will ensure that the results are disseminated widely to relevant medical specialties and research groups.
-
Dissemination event with the Stroke Association to present results to a public and patient audience.
-
Report to the Intercollegiate Stroke Working Party with summary of findings and recommendations for SSNAP audit data collection.
-
A summary report of the results will be forwarded for inclusion in the newsletters of the professional bodies through which we recruited participants and in the Stroke Association bulletin.
Chapter 6 Conclusions
-
This is the first DCE to explore factors that influence the decision to offer intravenous thrombolysis to patients with acute ischaemic stroke using vignettes specifically designed to elucidate the influence of factors on decisions related to ‘grey’ areas/areas of uncertainty in the licensing criteria/evidence.
-
This research has documented the iterative process of DCE design, an element lacking in most published DCE work in the field of clinical/medical decision-making.
-
Findings from this research indicate that statistically significant predictors of not offering thrombolysis are (reference categories in brackets) patient age of 95 years (68 years), SBP of 200 mmHg (140 mmHg), symptom onset time approaching the upper limit of the time window for treatment at 4 hours 15 minutes (50 minutes), and pre-existing severe dementia (no history of memory problems).
-
The analysis found statistically significant positive influences on decisions to offer thrombolysis which were in line with previous research or supported by qualitative comments from respondents (compared with reference categories in brackets): 2 hours 30 minutes since symptom onset time (50 minutes), pre-stroke dependency of mRS3 (mRS4), and NIHSS scores of 5 without aphasia, NIHSS 14 and NIHSS 23 (all compared with NIHSS 2 without aphasia).
-
Further statistically significant positive influences on decisions to offer thrombolysis were found but these were unexpected findings for which we do not have clear explanations: age 85 years, Afro-Caribbean ethnicity (white) and SBP of 185 mmHg.
-
There was evidence of significant heterogeneity among respondents in terms of overall decision-making and heterogeneity in terms of the influence of levels of patient factors on decision-making. Among the levels producing the most significant unobserved heterogeneity in decision-making were patient age of 95 years, SBP of 185 mmHg and 200 mmHg, moderate dementia and NIHSS 5 with aphasia.
-
Clinician-related factors also had a significant influence on thrombolysis decision-making (what the literature refers to as observed heterogeneity); those who perceived the evidence for thrombolysis as robust were more likely to offer thrombolytic treatment and those who reported higher rates of thrombolysing patients in the past 12 months were more likely to offer thrombolysis.
-
Two further clinician-related factors also influenced decision-making but require further research to clarify and explain these finding. First, clinicians who reported a higher discomfort with uncertainty were more likely to offer thrombolysis, perhaps indicating a preference for treatment over non-treatment in instances of uncertainty, potentially influenced by the strong institutional culture of thrombolysis observed. Second, the results indicate that clinicians who reported being more comfortable treating patients outside the licensing criteria were less likely to offer treatment in the current study; however, we do not have a clear explanation for this finding.
-
Training and CPD programmes for stroke care and intravenous thrombolysis should address the impact of non-medical influence on decision-making, impart cognitive debiasing strategies to optimise and support decision-making, and should ensure clinicians develop practical learning and self-efficacy in the administration of intravenous thrombolysis early in training and practice to maximise appropriate utilisation of the treatment.
-
The nature of DCEs demands that only a subset of potentially influential factors on clinical decision-making could be explored in this research. Factors not explored in this study warrant research to understand their impact, if any, on the decision to offer intravenous thrombolysis. Future work should seek to replicate these findings and further interrogate the results by considering how interactions may influence decision-making and explore trade-offs between various factors by including linear attribute. Furthermore, future research should explore the influence of decision support tools and/or graphical depictions of risk and benefit for individual patients on clinical decision-making and clinical outcomes.
Acknowledgements
We would like to express our thanks to Jan Fuller for her excellent administrative support. We are also grateful to the members of the project advisory group for their valuable advice throughout the study development process: Professor Tony Rudd, Ms Chucks Golding, Ms Elizabeth Morris and Dr Dean Shipsey. Gary A Ford is supported by a National Institute for Health Research Senior Investigator award.
Contributions of authors
Richard G Thomson (Professor of Epidemiology and Public Health) developed the study protocol and contributed to the study design, the data interpretation and the drafting of the report.
Aoife De Brún (research associate) contributed to the study design, managed the data collection, led on the data analysis, contributed to the data interpretation and led on the drafting of the report.
Darren Flynn (senior research associate) developed the study protocol and contributed to the study design, the data interpretation and the drafting of the report.
Laura Ternent (senior lecturer) developed the study protocol and contributed to the study design, the data analysis, the data interpretation and the drafting of the report.
Christopher I Price (honorary clinical senior lecturer and consultant stroke physician) developed the study protocol and contributed to the study design, the data interpretation and the drafting of the report.
Helen Rodgers (Clinical Professor of Stroke Care and consultant stroke physician) developed the study protocol and contributed to the study design, the data interpretation and the drafting of the report.
Gary A Ford (Chief Executive Officer of the Oxford Academic Health Science Network and consultant stroke physician; previously Jacobson Chair of Clinical Pharmacology) developed the study protocol and contributed to the study design, the data interpretation and the drafting of the report.
Matthew Rudd (associate clinical teacher and specialist trainee in geriatric and general internal medicine) contributed to the study design, the data interpretation and the drafting of the report.
Emily Lancsar (Associate Professor in Health Economics) developed the study protocol and contributed to the study design, the data analysis, the data interpretation and the drafting of the report.
Stephen Simpson (patient/public representative) contributed to the study design and the drafting of the report.
John Teah (patient/public representative) contributed to the study design and the drafting of the report.
Publications
Papers
De Brún A, Flynn D, Joyce K, Ternent L, Price C, Rodgers H, et al. Understanding clinicians’ decisions to offer intravenous thrombolytic treatment to patients with acute ischaemic stroke: a protocol for a discrete choice experiment. BMJ Open 2014;4:e005612.
De Brún A, Flynn D, Ternent L, Price CI, Rodgers H, Ford GA, et al. Factors that influence clinicians’ decisions to offer intravenous alteplase in acute ischemic stroke patients with uncertain treatment indication: Results of a discrete choice experiment. Int J Stroke 2017: in press. DOI: 10.1177/1747493017690755.
Conference presentations
De Brún A, Flynn D, Ternent L, Lancsar E, Price C, Rodgers H, et al. Understanding clinicians’ decisions to offer intravenous thrombolytic treatment to patients with acute ischaemic stroke: a discrete choice experiment. 7th National Institute for Health Research Stroke Research Network Annual Meeting, Newcastle, UK, 19–20 September 2013.
De Brún A, Flynn D, Ternent L, Price CI, Rodgers H, Rudd M, et al. Development process for a discrete choice experiment to explore variation in clinical decision-making about thrombolysis in acute ischaemic stroke. Division of Health Psychology Annual Conference 2014, York, UK, 10–12 September 2014.
De Brún A, Flynn D, Ternent L, Lancsar E, Price C, Rodgers H, et al. A discrete choice experiment to explore factors influencing decision-making about treatment of acute ischaemic stroke. Oral presentation at the ISDM-ISEHC Conference, Sydney, NSW, Australia, 19–22 July 2015.
De Brún A, Flynn D, Ternent L, Lancsar E, Price C, Rodgers H, et al. Factors that influence clinicians’ decision to offer intravenous thrombolysis for patients with acute ischaemic stroke. Poster presentation to the ISDM-ISEHC Conference, Sydney, NSW, Australia, July 2015.
De Brún A, Flynn D, Ternent L, Lancsar E, Price CI, Rudd M, et al. Patient factors that influence variation in clinical decision-making about thrombolysis in the treatment of acute ischaemic stroke: results of a discrete choice experiment. Poster presentation, UK Stroke Forum, Liverpool, UK, 1–3 December 2015.
Training/continuing professional development events
Presentation and interactive session at the Northern Deanery Neurology Specialist Registrar Training Day, The Royal Victoria Infirmary, Newcastle upon Tyne, UK, 15 October 2015.
Presentation and interactive session at the Reperfusion Masterclass, Royal York Hotel, York, UK, 16 October 2015.
Scheduled outputs and outputs in preparation
Papers
De Brún A, Flynn D, Ternent L, Lancsar E, Price CI, Rudd M, et al. A novel development and design process for selection of factors for inclusion in discrete choice experiments and optimal presentation of choice sets: case study exploring variation in clinical decision-making about thrombolysis in the treatment of acute ischaemic stroke. In preparation.
Data sharing statement
Data may be obtained on request from the corresponding author.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
References
- National Stroke Strategy. London: Department of Health; 2007.
- Alteplase for Treating Acute Ischaemic Stroke (Review of Technology Appraisal Guidance 122). London: NICE; 2012.
- Boehringer Ingelheim . Stroke. Boehringer Ingelheim Gains Approval of Extended 4.5 Hour Time-Window for Actilyse® in Acute Ischaemic Stroke for Majority of EU Countries 2011. www.boehringer-ingelheim.com/news/news_releases/press_releases/2011/04_november_2011_alteplase.html (accessed 26 July 2012).
- Alteplase for the Treatment of Acute Ischaemic Stroke. London: NICE; 2007.
- The Third International Stroke Trial (IST-3) collaborative group . The benefits and harms of intravenous thrombolysis with recombinant tissue plasminogen activator within 6 h of acute ischaemic stroke (The Third International Stroke Trial [IST-3]): a randomised controlled trial. Lancet 2012;379:2352-63. http://dx.doi.org/10.1016/S0140-6736(12)60768-5.
- Wardlaw JM, Murray V, Berge E, del Zoppo G, Sandercock P, Lindley RL, et al. Recombinant tissue plasminogen activator for acute ischaemic stroke: an updated systematic review and meta-analysis. Lancet 2012;379:2364-72. http://dx.doi.org/10.1016/S0140-6736(12)60738-7.
- Lancsar E, Louviere J. Conducting discrete choice experiments to inform healthcare decision making. PharmacoEconomics 2008;26:661-77. http://dx.doi.org/10.2165/00019053-200826080-00004.
- Laver K, Rehab M, Ratcliffe J, George S, Lester L, Walker R, et al. Early rehabilitation management after stroke: what do stroke patients prefer?. J Rehabil Med 2011;43:354-8. http://dx.doi.org/10.2340/16501977-0678.
- Townsend N, Wickramasinghe K, Bhatnagar P, Smolina K, Nichols M, Leal J, et al. Coronary Heart Disease Statistics 2012 Edition. London: British Heart Foundation; 2012.
- National Clinical Guideline for Stroke. London: RCP; 2012.
- Jauch EC, Saver JL, Adams HP, Bruno A, Demaerschalk BM, Khatri P, et al. Guidelines for the early management of patients with acute ischemic stroke a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2013;44:870-947. http://dx.doi.org/10.1161/STR.0b013e318284056a.
- SSNAP National Results Summary Report, Based on Stroke Patients Admitted to and/or Discharged from Hospital between April–June 2014. London: RCP; 2014.
- SSNAP National Results Summary Report, Based on Stroke Patients Admitted to and/or Discharged from Hospital between July–September 2014. London: RCP; 2015.
- Murtagh MJ, Watson DLB, Jenkings KN, Lie MLS, Mackintosh JE, Ford GA, et al. Situationally-sensitive knowledge translation and relational decision making in hyperacute stroke: a qualitative study. PLOS ONE 2012;7. http://dx.doi.org/10.1371/journal.pone.0037066.
- Emberson J, Lees KR, Lyden P, Blackwell L, Albers G, Bluhmki E, et al. Effect of treatment delay, age, and stroke severity on the effects of intravenous thrombolysis with alteplase for acute ischaemic stroke: a meta-analysis of individual patient data from randomised trials. Lancet 2014;384:1929-35. http://dx.doi.org/10.1016/S0140-6736(14)60584-5.
- Hacke W, Donnan G, Fieschi C, Kaste M, Von Kummer R, Broderick J, et al. Association of outcome with early stroke treatment: pooled analysis of ATLANTIS, ECASS, and NINDS rt-PA stroke trials. Lancet 2004;363:768-74. http://dx.doi.org/10.1016/S0140-6736(04)15692-4.
- Balami JS, Hadley G, Sutherland BA, Karbalai H, Buchan AM. The exact science of stroke thrombolysis and the quiet art of patient selection. Brain 2013;136:3528-53. http://dx.doi.org/10.1093/brain/awt201.
- Strbian D, Sairanen T, Meretoja A, Pitkäniemi J, Putaala J, Salonen O, et al. Patient outcomes from symptomatic intracerebral hemorrhage after stroke thrombolysis. Neurology 2011;77:341-8. http://dx.doi.org/10.1212/WNL.0b013e3182267b8c.
- SINAP: Latest Results January–December 2012. London: RCP; 2012.
- Dirks M, Niessen LW, Koudstaal PJ, Franke CL, van Oostenbrugge RJ, Dippel DW. Intravenous thrombolysis in acute ischaemic stroke: from trial exclusion criteria to clinical contraindications. An international Delphi study. J Neurol Neurosurg Psychiatry 2007;78:685-9. http://dx.doi.org/10.1136/jnnp.2006.102798.
- Alper BS, Malone-Moses M, McLellan JS, Prasad K, Manheimer E. Thrombolysis in acute ischaemic stroke: time for a rethink?. BMJ 2015;350. http://dx.doi.org/10.1136/bmj.h1075.
- Schellinger PD, Köhrmann M. 4.5-hour time window for intravenous thrombolysis with recombinant tissue-type plasminogen activator is established firmly. Stroke 2014;45:912-13. http://dx.doi.org/10.1161/STROKEAHA.113.002700.
- Wechsler LR. The 4.5-hour time window for intravenous thrombolysis with intravenous tissue-type plasminogen activator is not firmly established. Stroke 2014;45:914-15. http://dx.doi.org/10.1161/STROKEAHA.113.002701.
- Fatovich DM. Believing is seeing: stroke thrombolysis remains unproven after the third international stroke trial (IST-3). Emerg Med Australas 2012;24:477-9. http://dx.doi.org/10.1111/j.1742-6723.2012.01605.x.
- Brown SGA, Macdonald SPJ, Hankey GJ. Do risks outweigh benefits in thrombolysis for stroke?. BMJ 2013;347. http://dx.doi.org/10.1136/bmj.f5215.
- Hoffman JR, Cooper RJ. How is more negative evidence being used to support claims of benefit: the curious case of the third international stroke trial (IST-3). Emerg Med Australas 2012;24:473-6. http://dx.doi.org/10.1111/j.1742-6723.2012.01604.x.
- Ryan M, Gerard K, Amaya-Amaya M. Using Discrete Choice Experiments to Value Health and Health Care. Dordrecht: Springer; 2007.
- Lancsar E, Swait J. Reconceptualising the external validity of discrete choice experiments. PharmacoEconomics 2014;32:951-65. http://dx.doi.org/10.1007/s40273-014-0181-7.
- Hacke W, Kaste M, Fieschi C, Danilo T, Lesaffre E, von Kummer R, et al. Intravenous thrombolysis with recombinant tissue plasminogen activator for acute hemispheric stroke. JAMA 1995;274:1017-25. http://dx.doi.org/10.1001/jama.1995.03530130023023.
- Hacke W, Kaste M, Fieschi C, von Kummer R, Davalos A, Meier D, et al. Randomised double-blind placebo-controlled trial of thrombolytic therapy with intravenous alteplase in acute ischaemic stroke (ECASS II). Lancet 1998;352:1245-51. http://dx.doi.org/10.1016/S0140-6736(98)08020-9.
- The National Institute of Stroke Neurological Disorders rtPA Stroke Study Group . Tissue plasminogen activator for acute ischemic stroke. N Engl J Med 1995;333:1581-7. http://dx.doi.org/10.1056/NEJM199512143332401.
- Clark WM, Wissoman S, Hamandas JH, Albers GW, Madden KP, Hamilton S. Recombinant tissue-type plasminogen activator (Alteplase) for ischemic stroke 3 to 5 hours after symptom onset. The ATLANTIS Study: a randomized controlled trial. JAMA 1999;282:2019-26. http://dx.doi.org/10.1001/jama.282.21.2019.
- Hacke W, Kaste M, Bluhmki E, Brozman M, Dávalos A, Guidetti D, et al. Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med 2008;359:1317-29. http://dx.doi.org/10.1056/NEJMoa0804656.
- Wardlaw JM, Murray V, Berge E, del Zoppo GJ. Thrombolysis for acute ischemic stroke, update August 2014. Stroke 2014;45:e222-5. http://dx.doi.org/10.1161/STROKEAHA.114.007024.
- Bluhmki E, Chamorro Á, Dávalos A, Machnig T, Sauce C, Wahlgren N, et al. Stroke treatment with alteplase given 3.0–4.5 h after onset of acute ischaemic stroke (ECASS III): additional outcomes and subgroup analysis of a randomised controlled trial. Lancet Neurol 2009;8:1095-102. http://dx.doi.org/10.1016/S1474-4422(09)70264-9.
- Toni D, Lorenzano S, Puca E, Prencipe M. The SITS-MOST registry. Neurol Sci 2006;27:s260-2. http://dx.doi.org/10.1007/s10072-006-0632-9.
- Brown DL, Barsan WG, Lisabeth LD, Gallery ME, Morgenstern LB. Survey of emergency physicians about recombinant tissue plasminogen activator for acute ischemic stroke. Ann Emerg Med 2005;46:56-60. http://dx.doi.org/10.1016/j.annemergmed.2004.12.025.
- Scott PA, Xu Z, Meurer WJ, Frederiksen SM, Haan MN, Westfall MW, et al. Attitudes and beliefs of Michigan emergency physicians toward tissue plasminogen activator use in stroke: baseline survey results from the INcreasing Stroke Treatment through INteractive behavioral Change Tactic (INSTINCT) trial hospitals. Stroke 2010;41:2026-32. http://dx.doi.org/10.1161/STROKEAHA.110.581942.
- Medicines and Healthcare products Regulatory Agency . Alteplase for Treatment of Acute Ischaemic Stroke: Independent Review 2015. www.gov.uk/government/publications/alteplase-for-treatment-of-acute-ischaemic-stroke-independent-review (accessed 26 September 2015).
- Reeves MJ, Wilkins T, Lisabeth LD, Schwamm LH. Thrombolysis treatment for acute stroke: issues of efficacy and utilization in women. Womens Health 2011;7:383-90. http://dx.doi.org/10.2217/whe.11.31.
- de Ridder I, Dirks M, Niessen L, Dippel D. Unequal access to treatment with intravenous alteplase for women with acute ischemic stroke. Stroke 2013;44:2610-12. http://dx.doi.org/10.1161/STROKEAHA.113.002263.
- Kent DM, Selker HP, Ruthazer R, Bluhmki E, Hacke W. The stroke–thrombolytic predictive instrument a predictive instrument for intravenous thrombolysis in acute ischemic stroke. Stroke 2006;37:2957-62. http://dx.doi.org/10.1161/01.STR.0000249054.96644.c6.
- Kent DM, Price LL, Ringleb P, Hill MD, Selker HP. Sex-based differences in response to recombinant tissue plasminogen activator in acute ischemic stroke a pooled analysis of randomized clinical trials. Stroke 2005;36:62-5. http://dx.doi.org/10.1161/01.STR.0000150515.15576.29.
- Karlinski M, Kobayashi A, Czlonkowska A, Mikulik R, Vaclavik D, Brozman M, et al. Role of preexisting disability in patients treated with intravenous thrombolysis for ischemic stroke. Stroke 2014;45:770-5. http://dx.doi.org/10.1161/STROKEAHA.113.003744.
- electronic Medicines Compendium . Actilyse: Summary of Product Characteristics n.d. www.medicines.org.uk/emc/medicine/308 (accessed 1 June 2015).
- Yu AYX, Hill MD, Coutts SB. Should minor stroke patients be thrombolyzed? A focused review and future directions. Int J Stroke 2015;10:292-7. http://dx.doi.org/10.1111/ijs.12426.
- Greisenegger S, Seyfang L, Kiechl S, Lang W, Ferrari J. Thrombolysis in patients with mild stroke: results from the Austrian Stroke Unit Registry. Stroke 2014;45:765-9. http://dx.doi.org/10.1161/STROKEAHA.113.003827.
- Dirks M, Zonneveld TP, Dippel DWJ, Nederkoorn PJ, van de Beek D, van Oostenbrugge RJ, et al. Elevated pretreatment blood pressure and IV thrombolysis in stroke. Neurology 2015;84:1419-25. http://dx.doi.org/10.1212/WNL.0000000000001445.
- Potter JF, Robinson TG, Ford GA, Mistri A, James M, Chernova J, et al. Controlling hypertension and hypotension immediately post-stroke (CHHIPS): a randomised, placebo-controlled, double-blind pilot trial. Lancet Neurol 2009;8:48-56. http://dx.doi.org/10.1016/S1474-4422(08)70263-1.
- Flynn D, van Schaik P, van Wersch A, Douglass A, Cann P. Non-Medical Influences upon Medical Decision-Making and Referral Behavior: An Annotated Bibliography. Westport, CT: Praeger; 2003.
- Shamy MC, Jaigobin CS. The complexities of acute stroke decision-making: a survey of neurologists. Neurology 2013;81:1130-3. http://dx.doi.org/10.1212/WNL.0b013e3182a55ec7.
- Kwan J, Hand P, Sandercock P. A systematic review of barriers to delivery of thrombolysis for acute stroke. Age Ageing 2004;33:116-21. http://dx.doi.org/10.1093/ageing/afh064.
- Prosser H, Walley T. New drug uptake: qualitative comparison of high and low prescribing GPs’ attitudes and approach. Fam Prac 2003;20:583-91. http://dx.doi.org/10.1093/fampra/cmg516.
- Croskerry P. Achieving quality in clinical decision making: cognitive strategies and detection of bias. Acad Emerg Med 2002;9:1184-204. http://dx.doi.org/10.1111/j.1553-2712.2002.tb01574.x.
- McKinlay JB, Lin T, Freund K, Moskowitz M. The unexpected influence of physician attributes on clinical decisions: results of an experiment. J Health Soc Behavr 2002;43:92-106. http://dx.doi.org/10.2307/3090247.
- Hancock HC, Mason JM, Murphy JJ. Using the method of judgement analysis to address variations in diagnostic decision making. BMC Res Notes 2012;5. http://dx.doi.org/10.1186/1756-0500-5-139.
- Borges NJ, Osmon WR. Personality and medical specialty choice: technique orientation versus people orientation. J Vocat Behav 2001;58:22-35. http://dx.doi.org/10.1006/jvbe.2000.1761.
- Taber BJ, Hartung PJ, Borges NJ. Personality and values as predictors of medical specialty choice. J Vocat Behav 2011;78:202-9. http://dx.doi.org/10.1016/j.jvb.2010.09.006.
- Pearson SD, Goldman L, Orav ES, Guadagnoli E, Garcia TB, Johnson PA, et al. Triage decisions for emergency department patients with chest pain. J Gen Intern Med 1995;10:557-64. http://dx.doi.org/10.1007/BF02640365.
- Gerrity M, White K, DeVellis R, Dittus R. Physicians’ reactions to uncertainty: refining the constructs and scales. Motiv Emot 1995;19:175-91. http://dx.doi.org/10.1007/BF02250510.
- Gerrity MS, DeVellis RF, Earp JA. Physicians’ reactions to uncertainty in patient care: a new measure and new insights. Med Care 1990;28:724-36. http://dx.doi.org/10.1097/00005650-199008000-00005.
- Campbell K, Smith S, Hemmerich J, Stankus N, Fox C, Mold J, et al. Patient and provider determinants of nephrology referral in older adults with severe chronic kidney disease: a survey of provider decision making. BMC Nephrol 2011;12. http://dx.doi.org/10.1186/1471-2369-12-47.
- Croskerry P, Singhal G, Mamede S. Cognitive debiasing 2: impediments to and strategies for change. BMJ Qual Saf 2013;22:ii65-72. http://dx.doi.org/10.1136/bmjqs-2012-001713.
- Davies HTO, Nutley SM, Mannion R. Organisational culture and quality of health care. Qual Health Care 2000;9:111-19. http://dx.doi.org/10.1136/qhc.9.2.111.
- Scott T, Mannion R, Davies H, Marshall M. The quantitative measurement of organizational culture in health care: a review of the available instruments. Health Serv Res 2003;38:923-45. http://dx.doi.org/10.1111/1475-6773.00154.
- Shackelton R, Link C, Marceau L, McKinlay J. Does the culture of a medical practice affect the clinical management of diabetes by primary care providers?. J Health Serv Res Policy 2009;14:96-103. http://dx.doi.org/10.1258/jhsrp.2009.008124.
- van Wijngaarden JDH, Dirks M, Huijsman R, Niessen LW, Fabbricotti IN, Dippel DWJ, et al. Hospital rates of thrombolysis for acute ischemic stroke: the influence of organizational culture. Stroke 2009;40:3390-2. http://dx.doi.org/10.1161/STROKEAHA.109.559492.
- Moskowitz A, Chan Y-FY, Bruns J, Levine SR. Emergency physician and stroke specialist beliefs and expectations regarding telestroke. Stroke 2010;41:805-9. http://dx.doi.org/10.1161/STROKEAHA.109.574137.
- Ryan M, Gerard K. Using discrete choice experiments to value health care programmes: current practice and future research reflections. Appl Health Econ Health Policy 2003;2:55-64.
- Lancaster KJ. A new approach to consumer theory. J Polit Econ 1966;74:132-57. http://dx.doi.org/10.1086/259131.
- Royal College of Physicians . SINAP – Latest Results, January–March 2012 n.d. www.rcplondon.ac.uk/latest-results (accessed 5 March 2015).
- National Sentinel Stroke Clinical Audit 2010, Round 7. Public Report for England, Wales and Northern Ireland. London: RCP; 2011.
- Louviere JJ, Hensher DA, Swait JD. Stated Choice Methods Analysis and Application. Cambridge: Cambridge University Press; 2000.
- Mark T, Swait J. Using stated preference and revealed preference modelling to evaluate prescribing decisions. Health Econ 2004;13:563-73. http://dx.doi.org/10.1002/hec.845.
- Ghijben P, Lancsar E, Zavarsek S. Preferences for oral anticoagulants in atrial fibrillation: a best–best discrete choice experiment. PharmacoEconomics 2014;32:1115-27. http://dx.doi.org/10.1007/s40273-014-0188-0.
- Coast J, Al-Janabi H, Sutton EJ, Horrocks SA, Vosper AJ, Swancutt DR, et al. Using qualitative methods for attribute development for discrete choice experiments: issues and recommendations. Health Econ 2012;21:730-41. http://dx.doi.org/10.1002/hec.1739.
- Reed Johnson F, Lancsar E, Marshall D, Kilambi V, Mühlbacher A, Regier DA, et al. Constructing experimental designs for discrete-choice experiments: report of the ISPOR conjoint analysis experimental design good research practices task force. Value Health 2013;16:3-13. http://dx.doi.org/10.1016/j.jval.2012.08.2223.
- Bridges JF, Hauber AB, Marshall D, Lloyd A, Prosser LA, Regier DA, et al. Conjoint analysis applications in health – a checklist: a report of the ISPOR Good Research Practices for Conjoint Analysis Task Force. Value Health 2011;14:403-13. http://dx.doi.org/10.1016/j.jval.2010.11.013.
- Flynn D, Nesbitt D, Ford GA, McMeekin P, Rodgers H, Price C, et al. Development and testing of a computerised decision aid for thrombolysis in acute stroke care. BMC Med Inform Decis Mak 2015;15. http://dx.doi.org/10.1186/s12911-014-0127-1.
- Eissa A, Krass I, Bajorek B. Barriers to the utilization of thrombolysis for acute ischaemic stroke. J Clin Pharmacy Therapeutics 2012;37:399-40. http://dx.doi.org/10.1111/j.1365-2710.2011.01329.x.
- Flynn D. Non-Medical Influences upon Medical Decision-Making and Referral Behavior: An Annotated Bibliography. Westport, CT: Prager Publishers; 2003.
- Meurer WJ, Majersik JJ, Frederiksen SM, Kade AM, Sandretto AM, Scott PA. Provider perceptions of barriers to the emergency use of tPA for acute ischemic stroke: a qualitative study. BMC Emerg Med 2011;11. http://dx.doi.org/10.1186/1471-227X-11-5.
- Pope C, Ziebland S, Mays N. Analysing qualitative data. BMJ 2000;320:114-16. http://dx.doi.org/10.1136/bmj.320.7227.114.
- Coast J, Horrocks S. Developing attributes and levels for discrete choice experiments using qualitative methods. J Health Serv Res Policy 2007;12:25-30. http://dx.doi.org/10.1258/135581907779497602.
- Abiiro G, Leppert G, Mbera G, Robyn P, De Allegri M. Developing attributes and attribute-levels for a discrete choice experiment on micro health insurance in rural Malawi. BMC Health Serv Res 2014;14. http://dx.doi.org/10.1186/1472-6963-14-235.
- De Brún A, Flynn D, Joyce K, Ternent L, Price C, Rodgers H, et al. Understanding clinicians’ decisions to offer intravenous thrombolytic treatment to patients with acute ischaemic stroke: a protocol for a discrete choice experiment. BMJ Open 2014;4. http://dx.doi.org/10.1136/bmjopen-2014-005612.
- Stroke and Transient Ischaemic Attack in Over 16s: Diagnosis and Initial Management. London: NICE; 2008.
- Mazya MV, Lees KR, Markus R, Roine RO, Seet R, Wahlgren N, et al. Safety of intravenous thrombolysis for ischemic stroke in patients treated with warfarin. Ann Neurol 2013;74:266-74. http://dx.doi.org/10.1002/ana.23924.
- Xian Y, Liang L, Smith EE, Schwamm LH, Reeves MJ, Olson DM, et al. Risks of intracranial hemorrhage among patients with acute ischemic stroke receiving warfarin and treated with intravenous tissue plasminogen activator. JAMA 2012;307:2600-8. http://dx.doi.org/10.1001/jama.2012.6756.
- Mishra N, Ahmed N, Davalos A, Iversen H, Melo T, Soinne L, et al. Thrombolysis outcomes in acute ischemic stroke patients with prior stroke and diabetes mellitus. Neurology 2011;77:1866-72. http://dx.doi.org/10.1212/WNL.0b013e318238ee42.
- Lees KR, Ford GA, Muir KW, Ahmed N, Dyker AG, Atula S, et al. Thrombolytic therapy for acute stroke in the United Kingdom: experience from the safe implementation of thrombolysis in stroke (SITS) register. QJM 2008;101:863-9. http://dx.doi.org/10.1093/qjmed/hcn102.
- King M, Hall J, Lancsar E, Fiebig D, Hossain I, Louviere J, et al. Patient preferences for managing asthma: results from a discrete choice experiment. Health Econ 2007;16:703-17. http://dx.doi.org/10.1002/hec.1193.
- Ratcliffe J. Public preferences for the allocation of donor liver grafts for transplantation. Health Econ 2000;9:137-48. http://dx.doi.org/10.1002/(SICI)1099-1050(200003)9:2<137::AID-HEC489>3.0.CO;2-1.
- British Association of Stroke Physicians . BASP Autumn Newsletter 2014 n.d. www.basp.ac.uk/Portals/2/Newsletter%20Autumn&202014%20final%20282%29/pdf (accessed 12 January 2015).
- Van Swieten J, Koudstaal P, Visser M, Schouten H, Van Gijn J. Interobserver agreement for the assessment of handicap in stroke patients. Stroke 1988;19:604-7. http://dx.doi.org/10.1161/01.STR.19.5.604.
- Reisberg B, Ferris SH, de Leon MJ, Crook T. The Global Deterioration Scale for assessment of primary degenerative dementia. Am J Psychiatry 1982;139:1136-9. http://dx.doi.org/10.1176/ajp.139.9.1136.
- National Institutes of Health . National Institutes of Health Stroke Scale 2014. www.ninds.nih.gov/doctors/NIH_Stroke_Scale.pdf (accessed 3 November 2014).
- Willis GB. Cognitive Interviewing: A Tool for Improving Questionnaire Design. Thousand Oaks, CA: Sage; 2005.
- Huijg JM, Gebhardt WA, Crone MR, Dusseldorp E, Presseau J. Discriminant content validity of a theoretical domains framework questionnaire for use in implementation research. Implement Sci 2014;9. http://dx.doi.org/10.1186/1748-5908-9-11.
- Paunonen SV, Jackson DN. The Jackson Personality Inventory and the five-factor model of personality. J Res Pers 1996;30:42-59. http://dx.doi.org/10.1006/jrpe.1996.0003.
- Weissberg M, Sakai JT, Miyoshi TJ, Fryer GE. Medical student attitudes to risk taking and self-perceived influence on medical practice. Med Educ 2006;40:722-9. http://dx.doi.org/10.1111/j.1365-2929.2006.02531.x.
- Carney PA, Elmore JG, Abraham LA, Gerrity MS, Hendrick RE, Taplin SH, et al. Med Decis Making 2004;24:255-64. http://dx.doi.org/10.1177/0272989X04265480.
- SSNAP Acute Organisational Audit Report 2014. London: RCP; 2014.
- Census of Consultant Physicians and Medical Registrars in the UK 2012: Full Report. London: RCP; 2014.
- Quinn TJ, Dawson J, Walters MR, Lees KR. Reliability of the Modified Rankin Scale: a systematic review. Stroke 2009;40:3393-5. http://dx.doi.org/10.1161/STROKEAHA.109.557256.
- Ford GA, Ahmed N, Azevedo E, Grond M, Larrue V, Lindsberg PJ, et al. Intravenous alteplase for stroke in those older than 80 years old. Stroke 2010;41:2568-74. http://dx.doi.org/10.1161/STROKEAHA.110.581884.
- Mishra NK, Ahmed N, Andersen G, Egido JA, Lindsberg PJ, Ringleb PA, et al. Thrombolysis in very elderly people: controlled comparison of SITS International Stroke Thrombolysis Registry and Virtual International Stroke Trials Archive. BMJ 2010;341. http://dx.doi.org/10.1136/bmj.c6046.
- Bray BD, Campbell J, Hoffman A, Tyrrell PJ, Wolfe CDA, Rudd AG. Stroke thrombolysis in England: an age stratified analysis of practice and outcome. Age Ageing 2013;42:240-5. http://dx.doi.org/10.1093/ageing/afs167.
- Ferrari J, Knoflach M, Kiechl S, Willeit J, Matošević B, Seyfang L, et al. Stroke thrombolysis: having more time translates into delayed therapy: data from the Austrian Stroke Unit Registry. Stroke 2010;41:2001-4. http://dx.doi.org/10.1161/STROKEAHA.110.590372.
- Saver JL, Smith EE, Fonarow GC, Reeves MJ, Zhao X, Olson DM, et al. The golden hour and acute brain ischemia: presenting features and lytic therapy in over 30,000 patients arriving within 60 minutes of onset. Stroke 2010;41:1431-9. http://dx.doi.org/10.1161/STROKEAHA.110.583815.
- Barber PA, Zhang J, Demchuk AM, Hill MD, Buchan AM. Why are stroke patients excluded from TPA therapy? An analysis of patient eligibility. Neurology 2001;56:1015-20. http://dx.doi.org/10.1212/WNL.56.8.1015.
- Johnston S, Fung L, Gillum L, Smith W, Brass L, Lichtman J, et al. Utilization of intravenous tissue-type plasminogen activator for ischemic stroke at academic centers. The influence of ethnicity. Stroke 2001;32:1061-8. http://dx.doi.org/10.1161/01.STR.32.5.1061.
- Cruz-Flores S, Rabinstein A, Biller J, Elkind MSV, Griffith P, Gorelick PB, et al. Racial-ethnic disparities in stroke care: the American experience. A statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2011;42:2091-116. http://dx.doi.org/10.1161/STR.0b013e3182213e24.
- Alshekhlee A, Li CC, Chuang SY, Vora N, Edgell RC, Kitchener JM, et al. Does dementia increase risk of thrombolysis? A case–control study. Neurology 2011;76:1575-80. http://dx.doi.org/10.1212/WNL.0b013e3182190d37.
- Rankin AJ, Tran RT, Abdul-Rahim AH, Rankin AC, Lees KR. Clinically important atrial arrhythmia and stroke risk: a UK-wide online survey among stroke physicians and cardiologists. QJM 2014;107:895-902. http://dx.doi.org/10.1093/qjmed/hcu177.
- Brazzelli M, Shuler K, Quayyum Z, Hadley D, Muir K, McNamee P, et al. Clinical and imaging services for TIA and minor stroke: results of two surveys of practice across the UK. BMJ Open 2013;3. http://dx.doi.org/10.1136/bmjopen-2013-003359.
- Torbica A, Fattore G. Understanding the impact of economic evidence on clinical decision making: a discrete choice experiment in cardiology. Soc Sci Med 2010;70:1536-43. http://dx.doi.org/10.1016/j.socscimed.2009.12.030.
- Thrumurthy SG, Morris JJA, Mughal MM, Ward JB. Discrete-choice preference comparison between patients and doctors for the surgical management of oesophagogastric cancer. Br J Surg 2011;98:1124-31. http://dx.doi.org/10.1002/bjs.7537.
- de Bekker-Grob EW, Bliemer MCJ, Donkers B, Essink-Bot ML, Korfage IJ, Roobol MJ, et al. Patients’ and urologists’ preferences for prostate cancer treatment: a discrete choice experiment. Br J Cancer 2013;109:633-40. http://dx.doi.org/10.1038/bjc.2013.370.
- Foote C, Morton RL, Jardine M, Gallagher M, Brown M, Howard K, et al. COnsiderations of Nephrologists when SuggestIng Dialysis in Elderly patients with Renal failure (CONSIDER): a discrete choice experiment. Nephrol Dial Transplant 2014;29:2302-9. http://dx.doi.org/10.1093/ndt/gfu257.
- Pound P, Gompertz P, Ebrahim S. A patient-centred study of the consequences of stroke. Clin Rehabil 1998;12:255-64. http://dx.doi.org/10.1191/026921598666856867.
- Cruice M, Worrall L, Hickson L, Murison R. Finding a focus for quality of life with aphasia: social and emotional health, and psychological well-being. Aphasiology 2003;17:333-53. http://dx.doi.org/10.1080/02687030244000707.
- Bronwyn D, Tami H, Linda W, Louise H, Leanne T. Social participation for older people with aphasia: the impact of communication disability on friendships. Top Stroke Rehabil 2008;15:325-40. http://dx.doi.org/10.1310/tsr1504-325.
- Croskerry P. The theory and practice of clinical decision-making. Can J Anesth 2005;52:R1-8. http://dx.doi.org/10.1007/BF03023077.
- Croskerry P, Singhal G, Mamede S. Cognitive debiasing 1: origins of bias and theory of debiasing. BMJ Qual Saf 2013;22:ii58-64. http://dx.doi.org/10.1136/bmjqs-2012-001712.
- Croskerry P. Cognitive forcing strategies in clinical decisionmaking. Ann Emerg Med 2003;41:110-20. http://dx.doi.org/10.1067/mem.2003.22.
- Mamede S, Schmidt HG, Rikers RMJP, Custers EJFM, Splinter TAW, van Saase JLCM. Conscious thought beats deliberation without attention in diagnostic decision-making: at least when you are an expert. Psych Res 2010;74:586-92. http://dx.doi.org/10.1007/s00426-010-0281-8.
- Mamede S, Schmidt HG, Penaforte JC. Effects of reflective practice on the accuracy of medical diagnoses. Med Educ 2008;42:468-75. http://dx.doi.org/10.1111/j.1365-2923.2008.03030.x.
- Flynn D, McMeekin P, Ford GA, Rodgers H, Thomson RG. Development of a decision analytic model (DAM) to support decision-making and risk communication for thrombolytic treatment in acute stroke care. Cerebrovasc Dis 2011;31.
- Hawley ST, Zikmund-Fisher B, Ubel P, Jancovic A, Lucas T, Fagerlin A. The impact of the format of graphical presentation on health-related knowledge and treatment choices. Patient Educ Couns 2008;73:448-55. http://dx.doi.org/10.1016/j.pec.2008.07.023.
- Swait J, Adamowicz W. The influence of task complexity on consumer choice: a latent class model of decision strategy switching. J Consum Res 2001;28:135-48. http://dx.doi.org/10.1086/321952.
- Hutcheson GD, Sofroniou N. The Multivariate Social Scientist: Introductory Statistics using Generalized Linear Models. London: Sage; 1999.
- Comrey AL, Lee HB. A First Course in Factor Analysis. Psychology Press; 2013.
- Bech M, Gyrd-Hansen D. Effects coding in discrete choice experiments. Health Econ 2005;14:1079-83.
Appendix 1 Semistructured schedule for exploratory interviews regarding decision-making about thrombolysis
Appendix 2 Online structured prioritisation exercise
Appendix 3 Pilot testing protocol
Guidelines for interviewer:
-
Review questionnaire, determine appropriate probes for questions, list additional probes to encourage participants to engage in ‘thinking aloud’.
-
Before you begin interview/testing, explain process of interview to participant, using examples and exercises to communicate meaning of approach, i.e. how it operates in practice.
Script to guide interview:
-
Thank participant for taking part and for their time.
-
Briefly describe the aims and purpose of the research and why this pilot testing phase is important.
-
Explain how this testing differs from traditional interview/survey testing:
During this interview, you will be working your way through the online survey. However, this process differs from a typical interview or a survey testing session, as I’d like you to read instructions and questions aloud as you go, as well as think aloud, reporting your interpretations and reactions to questions, as well as what details and information you consider in reaching your answer to a question. Our goal with this approach is to get a better idea of how the questions are working and are being interpreted and this will help us to ensure there are not problems around questions being misleading, too vague or confusing. So, by speaking aloud your thought processes during the survey, we’ll be able to assess this. For this testing, we are not so much interested in your answer but rather your understanding of the questions and situations described and how you react and think through information to reach an answer.
At times I may stop and ask you more questions about certain questions or items and I may take occasional notes. Also, with your permission, it would be helpful to audio record the testing session.
Please keep in mind that I want to hear all of your opinions and reactions. Don’t hesitate to mention if a question is unclear or problematic for whatever reason.
Finally, the online survey should take no longer than 60 minutes to complete. Do you have any questions before we start?
Think-aloud practice exercise
To give you an idea of what the approach is like and help you adapt to it, we’ll just start with an example. I’ll go first with this one and then you can have a go.
-
How many windows are in your house or apartment?
-
How did you go about coming up with that answer?
-
How difficult was it to arrive at that answer?
Ask if there are any final questions before beginning survey. Remind participant again to think aloud and that interviewer will stay mostly silent during testing.
List of general probes:
-
In your own words, what is this question asking?
-
What does the term ‘x’ mean to you?
-
What do you consider when answering this question?
-
How did you arrive at your answer?
-
What did you consider in reaching your answer?
-
What time period did you consider in arriving at your answer?
-
When you’re asked about average, how did you arrive at an approximate rate? How difficult is this question to answer in terms of this question?
-
What made you hesitate in giving your answer?
-
Can you repeat what you’ve just read in your own words?
Appendix 4 Full online discrete choice experiment survey
Appendix 5 Factor analysis of Institutional Culture Scale
Factor analysis using principal component analysis (PCA) with orthogonal rotation (varimax) was conducted on the six-item scale. The Kaiser–Meyer–Olkin (KMO) measure verified the sampling adequacy for the analysis, KMO = 0.83, which suggests that the sample size is adequate for factor analysis. 132 Bartlett’s test of sphericity [χ2(15) = 338.95; p < 0.001] indicated that correlations between items were sufficiently large for PCA. An initial analysis was run to obtain eigenvalues for each component in the data. The results indicated that only one component had an eigenvalue of > 1 and explained 57.47% of the variance. Following inspection of the scree plot, the one component was confirmed and retained for the final analysis. Table 16 displays the factor loadings after varimax rotation. Factor loadings of > 0.55 are considered ‘good’ to ‘excellent’. 133 The one-component solution suggests that the items on the scale all measure institutional culture of thrombolysis. Reliability analysis was conducted and internal consistency was high, with Cronbach’s alpha of 0.84.
| Items | Rotated factor loadings |
|---|---|
| Most people whose opinion I value would approve of me treating a patient presenting with acute ischaemic stroke within the 4.5-hour time window with intravenous thrombolysis | 0.78 |
| Prior to delivery of intravenous thrombolysis, clinicians are provided with adequate training to inform decision-making regarding the appropriate use of intravenous thrombolysis in the treatment of patients with acute ischaemic stroke | 0.79 |
| We encourage internal discussion of patient care adverse events | 0.84 |
| There is an identifiable practice style that we all try to adhere to | 0.74 |
| My unit strongly encourages me to thrombolyse patients who meet criteria for intravenous thrombolysis when presenting with acute ischaemic stroke | 0.83 |
| My unit does not hold meetings regularly to discuss and review stroke service audit dataa | 0.52 |
| Scale reliability (α) | 0.84 |
Appendix 6 Further information on discrete choice experiment design and analysis
The DCE approach follows random utility theory, in which an individual, n, is assumed to choose the utility-maximising option i when presented with a choice set, Cn, containing alternative scenarios following:
where v is the systematic component, α refers to the ASC, β is related to the vector of coefficients, X is the vector of k attributes and εin relates to the random component (unobservable variation). A respondent is assumed to choose the scenario j among alternatives J if the utility derived from that alternative is greater than the utility from any other alternative in the choice set.
The model will estimate the probability of a chosen alternative, j, as a function of the attributes k. In the current study, the utility derived from the chosen option is described by:
Further details on discrete choice experiment analysis
The initial analysis employed the benchmark case of a conditional logit model (or clogit) which is based on three assumptions: (1) independence of irrelevant alternatives; (2) error terms are independent and identically distributed across observations; and (3) no preference heterogeneity (i.e. identical preferences across respondents). Alternative model specifications were also tested, including mixed logit and generalised multinomial logit models. Goodness-of-fit criteria, including Akaike and Bayesian information criteria, were used to determine the best model for the data.
Based on the data analysis plan, the objectives of the research, results of preliminary analyses, and Akaike and Baysian goodness-of-fit criteria, the mixed-effects logistic regression was deemed most appropriate. Mixed-logit regression models were optimal as they allow for the examination of unobserved preference heterogeneity: that is varying model estimates across individuals. Mixed-logit regression facilitated the examination of heterogeneity among respondents (which was expected) and relaxed the assumption of independence from irrelevant alternatives, which is an underlying assumption of the clogit model. The mixed-logit regression allowed for increased flexibility by specifying certain coefficients to be randomly distributed across individuals. Estimation by maximum simulated likelihood was undertaken using the user-written ‘mixlogit’ Stata programme (Arne Hole, Boston College Department of Economics, Boston, MA, USA). All estimation results reported were generated assuming the random parameters were normally distributed and using 250 Halton draws to simulate the likelihood functions to be maximised. There is an inherent trade-off between the number of Halton draws and the time taken to compute various models. It is suggested that an analysis build up models working from the default of 50, up to 100, 200, 250, 500 and up to 1000, if appropriate. However, given the number of random effects specified in the current study, it was not feasible to compute models with 500 or 1000 Halton draws and therefore 250 was set for each model.
Effects coding was used for the analysis. This refers to a way of using categorical predictor variables in estimation models. It is similar to dummy coding but uses ones, zeros and minus ones to represent information on factor levels. Effects coding facilitates reliable estimates of main effects and interaction effects (if included/required) and allows for estimation of all levels. 134
Appendix 7 Model 3: summary of mixed-effects logistic regression results
Table 17 displays the results of the analysis when all clinician variables are added as predictors to the model.
| Factor | Level | Coefficient | SE | p-value | Odds ratio (95% CI) |
|---|---|---|---|---|---|
| Patient age, mean (SD) | 68 | Reference | |||
| 85 | 1.3 (1.54) | 0.57 (0.57) | 0.02 (0.01) | 3.67 (1.21 to 11.15) | |
| 95 | –1.65 (0.15) | 1.15 (0.43) | 0.15 (0.01) | 0.19 (0.02 to 1.27) | |
| Patient ethnicity, mean (SD) | White | Reference | |||
| Asian | –0.81 (2.64) | 0.53 (0.82) | 0.13 (0.001) | 0.45 (0.16 to 1.27) | |
| Afro-Caribbean | 2.66 (0.03) | 0.97 (0.41) | 0.006 (0.94) | 14.34 (2.15 to 95.5) | |
| Patient sex, mean (SD) | Male | Reference | |||
| Female | 1.1 (0.23) | 0.98 (0.31) | 0.26 (0.46) | 3.0 (0.44 to 20.49) | |
| Time since symptom onset, mean (SD) | 50 minutes | Reference | |||
| 2 hours 30 minutes | 2.01 (2.2) | 0.71 (0.61) | 0.005 (< 0.001) | 7.48 (1.86 to 30.15) | |
| 4 hours 15 minutes | –3.27 (2.04) | 0.89 (0.54) | < 0.001 (< 0.001) | 0.04 (0.01 to 0.22) | |
| Patient frailty, mean (SD) | Not frail | Reference | |||
| Frail | –0.49 (0.1) | 0.39 (0.28) | 0.21 (0.72) | 0.61 (0.28 to 1.3) | |
| Pre-stroke dependency (mRS score), mean (SD) | mRS1 | 1.86 (3.77) | 1.74 (1.13) | 0.28 (0.001) | 6.42 (0.2 to 192.5) |
| mRS3 | 0.97 (2.69) | 0.55 (0.58) | 0.08 (< 0.001) | 2.65 (0.91 to 7.74) | |
| mRS4 | Reference | ||||
| Pre-stroke cognitive status, mean (SD) | No history of memory problems | Reference | |||
| Moderate dementia | 0.87 (2.43) | 0.5 (0.72) | 0.08 (0.001) | 2.39 (0.91 to 6.33) | |
| Severe dementia | –3.81 (2.2) | 1.14 (0.66) | 0.001 (0.001) | 0.02 (0 to 0.21) | |
| SBP, mean (SD) | 140 mmHg | Reference | |||
| 185 mmHg | 3.06 (2.5) | 0.88 (0.74) | 0.001 (0.001) | 21.24 (3.77 to 119.7) | |
| 200 mmHg | –9.89 (3.94) | 2.21 (0.94) | < 0.001 (< 0.001) | 0 (0 to 0) | |
| NIHSS score (stroke severity), mean (SD) | 2 (without aphasia) | Reference | |||
| 2 (with aphasia) | –0.83 (2.85) | 0.89 (0.89) | 0.35 (0.001) | 0.44 (0.08 to 2.48) | |
| 5 (without aphasia) | 3.24 (0.95) | 1.13 (0.77) | 0.004 (0.22) | 25.41 (2.79 to 231.6) | |
| 5 (with aphasia) | 2.3 (7.53) | 0.91 (1.92) | 0.01 (< 0.001) | 9.92 (1.68 to 58.79) | |
| 14 | 5.38 (0.71) | 1.63 (0.7) | 0.001 (0.32) | 216.2 (8.8 to 5318) | |
| 23 | 5.21 (1.5) | 1.67 (0.73) | 0.002 (0.04) | 182.5 (6.9 to 4793) | |
| Perception of evidence base | 0.55 | 0.29 | 0.056 | 1.73 (0.99 to 3.03) | |
| Number thrombolysed in past 12 months | 0.11 | 0.03 | < 0.001 | 1.11 (1.05 to 1.18) | |
| Physician reaction to uncertainty | 0.02 | 0.68 | 0.97 | 1.02 (0.27 to 3.83) | |
| Attitude towards risk | –0.03 | 0.07 | 0.67 | 0.97 (0.85 to 1.11) | |
| Number harmed by thrombolysis in past 12 months | –0.45 | 0.45 | 0.32 | 0.64 (0.26 to 1.55) | |
| Days since patient was harmed by thrombolysis | –0.001 | 0.001 | 0.31 | 1 (1 to 1) | |
| Comfort treating outside criteria | –0.53 | 0.23 | 0.02 | 0.59 (0.38 to 0.93) | |
| Experience administering thrombolysis (months) | –0.01 | 0.01 | 0.26 | 0.99 (0.97 to 1.01) | |
| Medical specialty (all compared stroke clinician) | 1.05 | 0.75 | 0.16 | 2.85 (0.65 to 12.4) | |
| Perception of institutional culture | 0.01 | 0.04 | 0.9 | 1.06 (0.9 to 1.11) | |
| Service configuration of hospital (combination telemed and consultant led compared with consultant led only) | 2.82 | 1.06 | 0.01 | 16.78 (2.1 to 133.9) | |
| Confidence communicating risk information | –0.24 | 0.34 | 0.47 | 0.78 (0.4 to 1.52) | |
| Recency of last tPA decision | –0.01 | 0.01 | 0.61 | 0.99 (0.81 to 1.01) | |
| Location: Midlands | 2.65 | 1.13 | 0.02 | 14.1 (1.5 to 128.5) | |
| Location: South | 2.99 | 1.16 | 0.01 | 20.1 (2.1 to 193.3) | |
| Location: London/Thames | 2.55 | 1.13 | 0.02 | 12.76 (1.4 to 116.8) | |
| Location: Northern Ireland | –12.39 | 3.45 | < 0.001 | 0 (0 to 0) | |
| Location: Scotland | 6.19 | 2.01 | 0.002 | 488.8 (9.5 to 25034) | |
| Location: Wales | 3.95 | 1.55 | 0.01 | 51.8 (2.5 to 1083) | |
| Location: Islands | –0.94 | 2.3 | 0.68 | 0.39 (0 to 34.8) | |
| Clinician age | 0.08 | 0.04 | 0.046 | 1.08 (1 to 1.2) | |
| Clinician sex (female) | 1.15 | 0.81 | 0.16 | 3.14 (0.6 to 15.3) | |
| ASC, mean (SD) | Decision to offer thrombolysis | –19.03 | 5.27 | < 0.001 | |
| Block effects, mean | Block 3 | 5.38 | 1.73 | < 0.01 | |
| Block 7 | 2.84 | 1.26 | 0.02 | ||
| Block 8 | 3.3 | 1.42 | 0.02 | ||
Appendix 8 Predicted probabilities of offering thrombolysis
| Vignette number | Block | Patient vignette details | Utility | Probability of treatment | % of respondents who offered treatment | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age | Sex | Ethnicity | Symptom onset time | Cognitive status | Dependency (mRS score) | NIHSS score | SBP | Frailty | |||||
| 1 | 7 | 95 | Female | White | 4 hours 15 minutes | No memory problems | mRS3 | 5 (with aphasia) | 140 mmHg | Not frail | 3.08 | 95.62 | 44.40 |
| 2 | 4 | 95 | Female | Afro-Caribbean | 2 hours 30 minutes | No memory problems | mRS3 | 2 (without aphasia) | 185 mmHg | Frail | –3.28 | 3.62 | 6 |
| 3 | 7 | 95 | Male | White | 50 minutes | Severe dementia | mRS3 | 14 | 140 mmHg | Frail | 1.79 | 85.75 | 55.60 |
| 5 | 4 | 85 | Female | White | 50 minutes | Moderate dementia | mRS1 | 14 | 185 mmHg | Not frail | 0.08 | 51.94 | 68.80 |
| 6 | 7 | 68 | Female | White | 2 hours 30 minutes | Moderate dementia | mRS4 | 5 (with aphasia) | 140 mmHg | Frail | –5.79 | 0.30 | 44.40 |
| 7 | 1 | 85 | Male | White | 4 hours 15 minutes | Moderate dementia | mRS4 | 23 | 140 mmHg | Frail | –3.07 | 4.43 | 20 |
| 8 | 7 | 85 | Female | White | 4 hours 15 minutes | Severe dementia | mRS3 | 2 (without aphasia) | 185 mmHg | Frail | –13.30 | 0.00 | 0 |
| 10 | 5 | 68 | Female | Afro-Caribbean | 4 hours 15 minutes | Severe dementia | mRS4 | 2 (without aphasia) | 140 mmHg | Frail | –16.07 | 0.00 | 0 |
| 11 | 8 | 95 | Male | White | 50 minutes | Severe dementia | mRS3 | 5 (with aphasia) | 140 mmHg | Frail | 0.41 | 60.01 | 30.80 |
| 12 | 2 | 85 | Female | White | 4 hours 15 minutes | No memory problems | mRS3 | 2 (with aphasia) | 200 mmHg | Frail | –8.46 | 0.02 | 9.10 |
| 13 | 1 | 85 | Female | Asian | 2 hours 30 minutes | Severe dementia | mRS3 | 2 (without aphasia) | 140 mmHg | Not frail | –7.90 | 0.04 | 15 |
| 14 | 8 | 95 | Male | White | 4 hours 15 minutes | Moderate dementia | mRS3 | 2 (without aphasia) | 200 mmHg | Not frail | –14.11 | 0.00 | 0 |
| 15 | 6 | 85 | Female | Asian | 50 minutes | No memory problems | mRS3 | 23 | 140 mmHg | Not frail | 5.00 | 99.33 | 100 |
| 16 | 4 | 95 | Male | Asian | 50 minutes | No memory problems | mRS4 | 2 (without aphasia) | 200 mmHg | Frail | –13.34 | 0.00 | 0 |
| 17 | 3 | 95 | Male | Asian | 2 hours 30 minutes | Moderate dementia | mRS3 | 14 | 140 mmHg | Not frail | 4.90 | 99.26 | 73.90 |
| 18 | 7 | 95 | Female | White | 50 minutes | Moderate dementia | mRS1 | 2 (without aphasia) | 200 mmHg | Not frail | –12.73 | 0.00 | 0 |
| 19 | 4 | 68 | Male | Afro-Caribbean | 2 hours 30 minutes | No memory problems | mRS4 | 2 (with aphasia) | 200 mmHg | Frail | –11.35 | 0.00 | 6.30 |
| 20 | 1 | 85 | Male | Afro-Caribbean | 50 minutes | No memory problems | mRS3 | 23 | 200 mmHg | Frail | –2.77 | 5.91 | 25 |
| 21 | 5 | 68 | Female | White | 2 hours 30 minutes | Moderate dementia | mRS3 | 23 | 185 mmHg | Frail | –4.45 | 1.15 | 69.20 |
| 22 | 7 | 85 | Male | Asian | 2 hours 30 minutes | No memory problems | mRS4 | 14 | 185 mmHg | Frail | –0.99 | 27.04 | 50 |
| 23 | 2 | 95 | Female | Afro-Caribbean | 50 minutes | Moderate dementia | mRS3 | 2 (with aphasia) | 140 mmHg | Frail | 3.65 | 97.46 | 54.50 |
| 24 | 5 | 68 | Male | White | 2 hours 30 minutes | Moderate dementia | mRS4 | 23 | 185 mmHg | Frail | –7.28 | 0.07 | 30.80 |
| 25 | 1 | 68 | Male | Afro-Caribbean | 4 hours 15 minutes | Moderate dementia | mRS4 | 23 | 140 mmHg | Frail | –5.23 | 0.53 | 45 |
| 27 | 6 | 68 | Male | White | 2 hours 30 minutes | Severe dementia | mRS4 | 5 (without aphasia) | 185 mmHg | Frail | –10.29 | 0.00 | 16.70 |
| 28 | 4 | 85 | Male | Afro-Caribbean | 2 hours 30 minutes | Severe dementia | mRS3 | 2 (without aphasia) | 185 mmHg | Frail | –9.30 | 0.01 | 6.30 |
| 29 | 6 | 85 | Female | Afro-Caribbean | 50 minutes | No memory problems | mRS3 | 5 (with aphasia) | 185 mmHg | Not frail | 2.74 | 93.93 | 54.20 |
| 30 | 1 | 95 | Female | Afro-Caribbean | 50 minutes | No memory problems | mRS3 | 2 (with aphasia) | 140 mmHg | Not frail | 6.40 | 99.83 | 70 |
| 32 | 2 | 68 | Female | White | 50 minutes | Moderate dementia | mRS4 | 14 | 140 mmHg | frail | –3.94 | 1.90 | 54.50 |
| 33 | 8 | 85 | Male | Afro-Caribbean | 2 hours 30 minutes | No memory problems | mRS3 | 23 | 200 mmHg | Not frail | –2.72 | 6.19 | 23.10 |
| 34 | 8 | 68 | Female | Asian | 50 minutes | Moderate dementia | mRS3 | 2 (without aphasia) | 200 mmHg | Not frail | –17.00 | 0.00 | 7.70 |
| 35 | 5 | 85 | Female | Asian | 4 hours 15 minutes | No memory problems | mRS3 | 23 | 140 mmHg | Frail | 1.94 | 87.47 | 84.60 |
| 36 | 7 | 85 | Male | Afro-Caribbean | 4 hours 15 minutes | Moderate dementia | mRS3 | 2 (with aphasia) | 200 mmHg | Not frail | –8.28 | 0.03 | 11.10 |
| 38 | 2 | 85 | Male | Asian | 2 hours 30 minutes | No memory problems | mRS4 | 5 (without aphasia) | 200 mmHg | Frail | –7.92 | 0.04 | 18.20 |
| 39 | 3 | 85 | Male | White | 4 hours 15 minutes | Moderate dementia | mRS4 | 2 (without aphasia) | 200 mmHg | Frail | –19.39 | 0.00 | 0 |
| 40 | 4 | 95 | Male | White | 4 hours 15 minutes | No memory problems | mRS3 | 14 | 200 mmHg | Frail | –4.62 | 0.97 | 0 |
| 41 | 7 | 95 | Male | White | 2 hours 30 minutes | Severe dementia | mRS3 | 5 (without aphasia) | 140 mmHg | Frail | 0.77 | 68.42 | 44.40 |
| 43 | 8 | 68 | Female | White | 2 hours 30 minutes | No memory problems | mRS4 | 2 (with aphasia) | 200 mmHg | Frail | –13.27 | 0.00 | 23.10 |
| 44 | 4 | 68 | Male | White | 2 hours 30 minutes | Severe dementia | mRS3 | 23 | 185 mmHg | Not frail | –6.41 | 0.16 | 37.50 |
| 45 | 5 | 68 | Female | Asian | 2 hours 30 minutes | Severe dementia | mRS3 | 5 (with aphasia) | 140 mmHg | Frail | –5.49 | 0.41 | 46.20 |
| 46 | 6 | 95 | Male | Asian | 4 hours 15 minutes | Severe dementia | mRS3 | 5 (with aphasia) | 140 mmHg | Not frail | –1.69 | 15.63 | 8.30 |
| 47 | 2 | 95 | Female | White | 4 hours 15 minutes | Moderate dementia | mRS1 | 2 (without aphasia) | 200 mmHg | Not frail | –15.28 | 0.00 | 0 |
| 48 | 2 | 85 | Female | White | 4 hours 15 minutes | Severe dementia | mRS3 | 5 (without aphasia) | 140 mmHg | Not frail | –2.75 | 6.00 | 18.20 |
| 49 | 2 | 95 | Female | White | 4 hours 15 minutes | Moderate dementia | mRS3 | 2 (with aphasia) | 140 mmHg | Not frail | 0.34 | 58.41 | 27.30 |
| 50 | 5 | 85 | Female | Asian | 4 hours 15 minutes | No memory problems | mRS3 | 14 | 185 mmHg | Frail | –0.26 | 43.63 | 61.50 |
| 51 | 7 | 85 | Female | White | 2 hours 30 minutes | Moderate dementia | mRS3 | 2 (without aphasia) | 185 mmHg | Frail | –8.11 | 0.03 | 11.10 |
| 52 | 3 | 68 | Male | White | 50 minutes | Moderate dementia | mRS3 | 23 | 200 mmHg | Frail | –9.72 | 0.01 | 17.40 |
| 53 | 5 | 95 | Male | Asian | 4 hours 15 minutes | No memory problems | mRS3 | 23 | 185 mmHg | Not frail | 1.54 | 82.38 | 53.80 |
| 54 | 2 | 85 | Male | White | 50 minutes | Severe dementia | mRS3 | 5 (without aphasia) | 185 mmHg | Frail | –2.93 | 5.07 | 18.20 |
| 55 | 6 | 68 | Female | Asian | 4 hours 15 minutes | Severe dementia | mRS3 | 23 | 140 mmHg | Frail | –6.85 | 0.11 | 45.80 |
| 56 | 6 | 85 | Female | Asian | 4 hours 15 minutes | No memory problems | mRS3 | 2 (with aphasia) | 200 mmHg | Frail | –8.51 | 0.02 | 4.20 |
| 57 | 5 | 68 | Female | Asian | 2 hours 30 minutes | Moderate dementia | mRS3 | 2 (with aphasia) | 200 mmHg | Frail | –12.11 | 0.00 | 15.40 |
| 58 | 3 | 68 | Male | Afro-Caribbean | 2 hours 30 minutes | Moderate dementia | mRS4 | 5 (with aphasia) | 185 mmHg | Frail | –6.73 | 0.12 | 39.10 |
| 59 | 1 | 68 | Female | Afro-Caribbean | 2 hours 30 minutes | Severe dementia | mRS3 | 2 (without aphasia) | 185 mmHg | Not frail | –12.87 | 0.00 | 0 |
| 60 | 6 | 68 | Female | Afro-Caribbean | 4 hours 15 minutes | Moderate dementia | mRS3 | 23 | 140 mmHg | Not frail | –1.90 | 13.02 | 95.80 |
| 61 | 4 | 68 | Female | White | 2 hours 30 minutes | Moderate dementia | mRS1 | 23 | 200 mmHg | Not frail | –10.84 | 0.00 | 0 |
| 62 | 5 | 68 | Female | Asian | 4 hours 15 minutes | No memory problems | mRS4 | 5 (without aphasia) | 185 mmHg | Frail | –7.72 | 0.04 | 23.10 |
| 65 | 4 | 68 | Male | White | 4 hours 15 minutes | Severe dementia | mRS3 | 5 (without aphasia) | 200 mmHg | Not frail | –14.77 | 0.00 | 0 |
| 66 | 5 | 68 | Female | Afro-Caribbean | 4 hours 15 minutes | No memory problems | mRS4 | 23 | 140 mmHg | Frail | –3.63 | 2.59 | 61.50 |
| 67 | 8 | 85 | Male | White | 50 minutes | Moderate dementia | mRS3 | 14 | 185 mmHg | Not frail | 1.25 | 77.74 | 69.20 |
| 68 | 6 | 95 | Male | White | 2 hours 30 minutes | No memory problems | mRS4 | 2 (without aphasia) | 200 mmHg | Frail | –13.75 | 0.00 | 0 |
| 69 | 3 | 95 | Female | White | 2 hours 30 minutes | No memory problems | mRS3 | 5 (with aphasia) | 185 mmHg | Frail | 1.80 | 85.85 | 52.20 |
| 70 | 2 | 95 | Female | White | 2 hours 30 minutes | No memory problems | mRS3 | 14 | 140 mmHg | Not frail | 6.56 | 99.86 | 100 |
| 71 | 3 | 68 | Male | Asian | 50 minutes | Severe dementia | mRS3 | 5 (without aphasia) | 200 mmHg | Not frail | –12.28 | 0.00 | 8.70 |
| 72 | 5 | 95 | Male | Afro-Caribbean | 50 minutes | Moderate dementia | mRS3 | 5 (with aphasia) | 140 mmHg | Frail | 4.79 | 99.17 | 76.90 |
| 73 | 2 | 95 | Female | White | 50 minutes | No memory problems | mRS3 | 2 (with aphasia) | 185 mmHg | Not frail | 2.27 | 90.67 | 54.50 |
| 74 | 2 | 85 | Male | Asian | 50 minutes | No memory problems | mRS4 | 2 (with aphasia) | 200 mmHg | Frail | –8.79 | 0.02 | 9.10 |
| 75 | 7 | 95 | Male | White | 50 minutes | Moderate dementia | mRS1 | 14 | 200 mmHg | Not frail | –4.34 | 1.28 | 16.70 |
| 76 | 3 | 95 | Female | White | 2 hours 30 minutes | No memory problems | mRS1 | 5 (with aphasia) | 200 mmHg | Not frail | –4.59 | 1.01 | 17.40 |
| 77 | 7 | 68 | Male | Asian | 50 minutes | Severe dementia | mRS3 | 14 | 185 mmHg | Not frail | –5.35 | 0.47 | 55.60 |
| 78 | 5 | 85 | Male | Asian | 50 minutes | No memory problems | mRS4 | 14 | 185 mmHg | Frail | –0.53 | 36.99 | 46.20 |
| 79 | 1 | 85 | Male | White | 4 hours 15 minutes | Moderate dementia | mRS4 | 5 (with aphasia) | 185 mmHg | Frail | –6.66 | 0.13 | 20 |
| 80 | 6 | 85 | Male | Asian | 4 hours 15 minutes | Severe dementia | mRS3 | 5 (without aphasia) | 185 mmHg | Frail | –5.53 | 58.71 | 12.50 |
| 81 | 7 | 68 | Female | Asian | 50 minutes | Moderate dementia | mRS4 | 2 (with aphasia) | 140 mmHg | Frail | –5.88 | 0.28 | 27.80 |
| 82 | 8 | 68 | Male | Afro-Caribbean | 50 minutes | Moderate dementia | mRS3 | 23 | 200 mmHg | Frail | –8.45 | 0.02 | 15.40 |
| 83 | 8 | 95 | Female | Asian | 50 minutes | No memory problems | mRS3 | 5 (without aphasia) | 140 mmHg | Not frail | 6.40 | 99.83 | 69.20 |
| 84 | 5 | 68 | Female | White | 50 minutes | No memory problems | mRS4 | 14 | 185 mmHg | Frail | –4.55 | 1.04 | 30.80 |
| 85 | 6 | 95 | Male | Asian | 4 hours 15 minutes | No memory problems | mRS4 | 5 (with aphasia) | 140 mmHg | Frail | –0.30 | 42.44 | 37.50 |
| 87 | 3 | 68 | Female | White | 2 hours 30 minutes | Moderate dementia | mRS3 | 5 (with aphasia) | 200 mmHg | Not frail | –11.04 | 0.00 | 8.70 |
| 88 | 3 | 95 | Male | Asian | 2 hours 30 minutes | Severe dementia | mRS3 | 5 (with aphasia) | 140 mmHg | Not frail | 0.40 | 59.89 | 34.80 |
| 89 | 1 | 95 | Male | Afro-Caribbean | 50 minutes | No memory problems | mRS3 | 5 (with aphasia) | 185 mmHg | Frail | 4.18 | 98.49 | 50 |
| 90 | 8 | 85 | Male | Afro-Caribbean | 50 minutes | Severe dementia | mRS3 | 2 (without aphasia) | 200 mmHg | Not frail | –14.70 | 0.00 | 0 |
| 91 | 8 | 68 | Female | Asian | 4 hours 15 minutes | Severe dementia | mRS3 | 5 (without aphasia) | 140 mmHg | Frail | –6.75 | 0.12 | 30.80 |
| 93 | 3 | 68 | Male | Asian | 50 minutes | Severe dementia | mRS4 | 23 | 140 mmHg | Frail | –7.12 | 0.08 | 39.10 |
| 94 | 8 | 68 | Female | Afro-Caribbean | 4 hours 15 minutes | No memory problems | mRS4 | 5 (with aphasia) | 185 mmHg | Frail | –7.22 | 0.07 | 61.50 |
| 95 | 2 | 85 | Female | Asian | 50 minutes | Moderate dementia | mRS4 | 2 (without aphasia) | 140 mmHg | Frail | –8.31 | 0.02 | 9.10 |
| 96 | 1 | 85 | Male | Afro-Caribbean | 4 hours 15 minutes | Moderate dementia | mRS4 | 2 (without aphasia) | 185 mmHg | Frail | –11.74 | 0.00 | 0 |
| 97 | 8 | 85 | Female | White | 2 hours 30 minutes | Moderate dementia | mRS3 | 2 (without aphasia) | 200 mmHg | Not frail | –13.97 | 0.00 | 7.70 |
| 98 | 6 | 95 | Male | Asian | 2 hours 30 minutes | No memory problems | mRS3 | 14 | 185 mmHg | Frail | 3.78 | 97.76 | 58.30 |
| 99 | 3 | 95 | Female | White | 2 hours 30 minutes | Moderate dementia | mRS3 | 2 (with aphasia) | 140 mmHg | Frail | 1.92 | 87.17 | 43.50 |
| 100 | 1 | 68 | Female | White | 50 minutes | No memory problems | mRS3 | 23 | 200 mmHg | Not frail | –7.61 | 0.05 | 15 |
| 101 | 2 | 95 | Male | Afro-Caribbean | 2 hours 30 minutes | Moderate dementia | mRS3 | 5 (with aphasia) | 140 mmHg | Not frail | 4.84 | 99.21 | 72.70 |
| 102 | 1 | 85 | Male | White | 50 minutes | Moderate dementia | mRS4 | 5 (without aphasia) | 185 mmHg | Frail | –3.28 | 3.61 | 35 |
| 103 | 7 | 95 | Female | Asian | 50 minutes | Severe dementia | mRS3 | 2 (without aphasia) | 140 mmHg | Frail | –6.65 | 0.13 | 5.60 |
| 104 | 6 | 85 | Male | Asian | 4 hours 15 minutes | No memory problems | mRS4 | 5 (with aphasia) | 185 mmHg | Frail | –4.47 | 1.13 | 29.20 |
List of abbreviations
- A&E
- accident and emergency
- ASC
- alternative specific constant
- ATLANTIS
- Alteplase Thrombolysis for Acute Noninterventional Therapy in Ischaemic Stroke
- BASP
- British Association of Stroke Physicians
- COMPASS
- Computerised Decision Aid for Stroke Thrombolysis
- CPD
- continuing professional development
- CT
- computed tomography
- DCE
- discrete choice experiment
- ECASS
- European Cooperative Acute Stroke Study
- ISPOR
- The International Society for Pharmacoeconomics and Outcomes Research
- IST-3
- Third International Stroke Trial
- mRS
- modified Rankin Scale
- NICE
- National Institute for Health and Care Excellence
- NIHSS
- National Institutes of Health Stroke Scale
- NINDS
- National Institute of Neurological Disorders and Stroke
- RCP
- Royal College of Physicians
- rtPA
- recombinant tissue plasminogen activator
- SBP
- systolic blood pressure
- sICH
- symptomatic intracranial haemorrhage
- SITS
- Safe Implementation of Thrombolysis in Stroke
- SITS-MOST
- Safe Implementation of Thrombolysis in Stroke-Monitoring Study
- SPE
- structured prioritisation exercise
- SSNAP
- Sentinel Stroke National Audit Programme