Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 09/1004/15. The contractual start date was in January 2012. The final report began editorial review in February 2016 and was accepted for publication in July 2016. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Nat Wright is a member of the National Institute for Health Research Health Technology Assessment programme mental, psychological and occupational health panel.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2017. This work was produced by Shaw et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction
Background
Prevalence of mental illness
In a large-scale study conducted for the Office for National Statistics (ONS) in 1997,1 > 90% of prisoners had one or more of the five psychiatric disorders studied [psychosis, neurosis, personality disorder (PD), hazardous drinking and drug dependence], with remand prisoners having higher rates of disorder than sentenced prisoners. More than half (59%) of men remanded, and 40% of men sentenced, had a neurotic disorder, with the corresponding figures for women being 76% and 63%, respectively. Rates of psychosis varied from 7% in the male sentenced population to 14% in female sentenced population. In addition, 78% of male remand prisoners and 50% of female remand prisoners had a PD. Levels of substance misuse were also high, with 51% of male remand, 43% of male sentenced, 41% of female sentenced and 54% of female remand prisoners being drug dependent in the year before prison. Over 50% of the men in the sample screened positive for hazardous drinking in the year before coming into prison; the analogous figure for female prisoners was 38%. 1
The ONS survey and other studies in England and Wales have shown that psychiatric comorbidity is the norm. 2–5 Between 12% and 15% of sentenced prisoners in the ONS study1 had four or five psychiatric disorders, and many prisoners present with complex psychiatric treatment needs,5 often confounded by issues of dual diagnosis, especially of personality or substance misuse disorders.
The high prevalence of mental disorder in prisons is not confined to England and Wales. In a large-scale systematic review of serious mental disorder in 23,000 prisoners in Western countries,6 approximately one in seven prisoners had either a psychotic illness or major depression, with approximately half of male prisoners and one-fifth of female prisoners having antisocial PD.
Compounding high levels of psychiatric morbidity, prison populations have high levels of suicidal and deliberate self-harming behaviours, with prisoners at a far greater risk of suicide than the general population. In the ONS study,1 around 24% of male and 40% of female prisoners had attempted suicide at some time in their lives. Twelve per cent of male remand and 23% of female remand prisoners reported having experienced suicidal thoughts in the week before interview (rates for sentenced prisoners were considerably lower); these figures rose to 35% and 50%, respectively, when measured over the past year. After a decade of the prison suicide rate in England and Wales reducing year on year, there has been a more recent trend of increasing numbers of suicide from around 2011, attributed by commentators on penal matters to increased population pressures and overcrowding, smaller budgets and significant deliberate reductions in staff numbers. 7
Diagnosis, treatment and care: the role of the prison in-reach team
Historically, Her Majesty’s Prison Service (HMPS), through the existence of the Prison Medical Service, latterly renamed the Prison Health Service, was responsible for the provision of the majority of health-care services for prisoners. Almost all services were provided in house, ranging from primary care for everyday physical complaints through to inpatient care for those with severe mental health problems. Staff, including doctors, prison health-care officers and qualified nurses were directly employed by HMPS. For decades, the development of multidisciplinary care in prisons lagged behind such initiatives in the NHS; for example, at a time when much mental health care in the wider community was being delivered by multidisciplinary community mental health teams (CMHTs), most care in prisons was dependent on input from visiting forensic psychiatrists, with little contribution from wider clinical disciplines. 8,9
In 1999, the NHS and HMPS formed a partnership to modernise the delivery of health care in prisons, acknowledging that the then current arrangements varied considerably in terms of organisation, delivery, quality, clinical effectiveness and links with the NHS. 10 One of the early areas targeted for reform was mental health provision and, in 2001, a specific strategy for mental health, Changing the Outlook, was published. 11
The strategy document reaffirmed that the existing delivery model did not meet prisoners’ needs and was ineffective and inflexible. It was acknowledged that most prisoners with mental health problems were not so ill as to require detention under mental health legislation and, if they were not in prison, would be receiving treatment in the community rather than as an inpatient. The strategy suggested a move away from the historically held assumption that prisoners with mental health problems should be located in prison health-care centres, towards supporting prisoners with mental health problems on ‘normal’ prison wings through the establishment of multidisciplinary mental health in-reach teams. Such teams were to be funded by local primary care trusts and provide specialist mental health services analogous to those provided by CMHTs. Although it was expected that all prisoners would eventually benefit from the introduction of in-reach teams, the early focus of the teams’ work was on those with severe mental illness (SMI), utilising the principles of the care programme approach (CPA),12 in particular to help ensure continuity of care between prison and community on release.
A national evaluation of prison in-reach services reported that, in spite of the new model of care, major challenges remained. 13 In particular, in-reach services struggled to effectively target their priority client group, those with SMI. Research demonstrated that in the month following reception into custody only one-quarter (25%) of those with current SMI were assessed by in-reach services and only 13% accepted into caseload. 14 An examination of the composition of in-reach caseloads identified that only 40% had SMI. Of the 60% with no diagnosis of SMI, 42% had PD, 32% had a common mental illness and 42% had neither. Those with no current diagnosis of SMI, PD or common mental illness exhibited high rates of previous contact with mental health services (lifetime 93%) and substance misuse (69%) before custody. 13
In a parallel study of the management of prisoners with SMI on in-reach caseloads, widespread disengagement from mental health services at the point of release from custody was identified. On examination of the prison in-reach case notes for 53 service users, the authors found evidence of discharge planning for only 27 (51%) individuals; fewer still, 20 (38%), had direct contact with their CMHT before release and, of those, only four (20%) had made contact with the CMHT at follow-up 1 month later. 15 Dyer and Biddle16 highlighted that functioning within the operational constraints of a prison often makes the task of planning and preparation for discharge challenging for in-reach services because of limited resources, functioning overcapacity in the delivery of treatment programmes and/or the sudden transfer of prisoners at short notice.
Transition: reoffending and post-release mortality, health and socioeconomic factors
The transition from institutional to community living is a vulnerable period, associated with a range of negative outcomes. Reoffending by released prisoners in England and Wales continues to be a challenge for the criminal justice system (CJS). In 2013, the reoffending rate of adults released from custody was 45.8%, a rate that has remained relatively static (45–49%) since 2004. Notably, adults who served sentences of < 12 months reoffended at a rate of 59.3%, compared with 34.7% for those who served determinate sentences of ≥ 12 months. 17
Several studies have shown that released prisoners with a history of mental illness and/or comorbid substance misuse, many of whom return to unstable environments characterised by socioeconomic disadvantage, are particularly vulnerable to relapse and reoffending. A large retrospective study in the USA found that prisoners with a diagnosis of SMI were more likely than those without to have experienced multiple prison terms in the 6 years before their index offence. For example, prisoners with a diagnosis of bipolar disorder were 3.3 times more likely to have had four or more previous prison terms than prisoners with no major psychiatric disorder. 18 In a further study of the same cohort, prisoners with comorbid SMI and substance misuse were more likely to have experienced multiple prison terms than those with a single such diagnosis. 19 Similar findings were reported in a study of parole violation in which a diagnosis of SMI was found to increase the likelihood of an individual breaking the terms of their parole; a comorbid diagnosis of substance use disorder increased that risk further. 20
Prison provides an opportunity for individuals with SMI to receive mental health treatment, including participation in programmes designed to reduce and control substance misuse. However, improvement is likely to be quickly jeopardised if, on release, the person does not engage with community services to enable treatment started during imprisonment to be continued. A failure to connect with community providers of mental health and substance misuse services has been linked to the high incidence of mortality in recently released prisoners. Farrell and Marsden21 found that newly released prisoners in England and Wales were at an acute risk of drug-related death in the first 2 weeks of leaving prison, with male and female prisoners, respectively, 29 and 69 times more likely to die of drug-related causes, relative to the general population, during their first week of release. This finding was confirmed in a later meta-analysis of drug-related deaths after release, which reported that drug-using prisoners had a three- to eightfold increased risk of drug-related death in the first 2 weeks post release compared with the subsequent 10 weeks, with risks remaining elevated through weeks 3 and 4. 22 Factors such as reduced tolerance to specific drugs, the high and variable potency of street drugs, and the temptation to engage in ‘celebratory’ drug-taking behaviour on release, were suggested explanations for these findings. Similar findings were reported in a systematic review and meta-analysis of all-cause and external mortality in released prisoners, identifying that released prisoners were at a substantially increased risk of death from all causes but from drugs, suicide and homicide in particular. 23
Studies of suicide by prisoners following release bring most sharply into focus how overwhelming transition can be for some. 24,25 A study of completed suicide by released prisoners found that age-adjusted standardised mortality rates were, compared with the general population, 8.3 times higher for men in the 12 months post release; the risk was even greater for women, at 35.8 times higher. Furthermore, 21% of those who completed suicide did so within 28 days post release, with just over half (51%) of deaths occurring within 4 months of release. 24 The authors conducted a subsequent study, identifying key risk factors for suicide by released prisoners. These included increasing age > 25 years, having a psychiatric diagnosis, previous contact with psychiatric services before custody, a history of alcohol misuse and a history of self-harm. Contact with prison mental health in-reach services while in custody and being recognised as ‘at risk’ of suicide while in prison were also relevant factors. The study authors reiterated the importance of improved release planning for those prisoners most at risk, to ensure immediate engagement with community mental health services, assertive follow-up and intensive post-release support. 25
Planning to prevent discontinuity of mental health and substance misuse treatment on release is critical, but addressing socioeconomic and psychological factors that might adversely impact on service engagement is also vital. Williamson26 listed multiple health and social care needs and factors that reflected the lifelong social disadvantage experienced by many prisoners, all or any of which may negatively influence the establishment of a stable routine lifestyle outside prison. For example, prisoners were more likely to have spent time as a child in local authority care, have a poor education and have a family history of CJS contact than those who had never been imprisoned. On release from prison, 42% had no fixed abode, 50% were not registered with a local general practitioner (GP) and 60% were unemployed. Despite this, it has also been reported that prisoners’ expectations of what life will be like following release may be unrealistically high or, equally damaging, the individual may be overwhelmed by concerns about how they are going to cope. In a longitudinal qualitative study of 40 prisoners, over one-quarter of whom self-reported a mental ill health problem, many prisoners’ aspirations before release were high with regard to finding work or going back into education, overcoming their drug and alcohol misuse and/or generally regaining some stability in the community. However, in the absence of co-ordinated service planning and advice, goals were often unrealistic and, therefore, difficult for the individual to achieve. Having family or peer support helped, but individuals without this support found their plans quickly fell through, negatively impacting on their ability to manage their housing arrangements and control drug and alcohol use, with reoffending once again becoming a coping mechanism. 27
A number of other studies have reported similar findings, noting that having a safe place to live, finding employment and maintaining mental and physical well-being are high priorities on release for prisoners, particularly as good mental and physical health is viewed as very important for securing employment. The prospect of relying on hostel accommodation and entering an environment in which the misuse of drugs and alcohol by others may be commonplace was a source of anxiety for soon to be released prisoners. In addition, the stigma attached to being identified as an ‘ex-offender’, with the associated disadvantages in terms of access to employment and other opportunities, provoked high levels of anxiety. 28,29
Integrating health and social care services to meet prisoners’ needs in a holistic way on release is therefore vital to successful community reintegration. Thus, effective release planning and resettlement requires not only continuity of health care but also measures designed to meet the economic and social needs of the prisoner.
The development of integrated health and social care services
More than 40 years ago, mental health-care policy moved away from the widespread provision of care in large psychiatric institutions towards delivering care in the community. Long-term care in hospital was viewed as untherapeutic, stigmatising and costly. 30–32 It was expected that providing care in the community would enable individuals with SMI to live with greater autonomy, have a better quality of life, and maximise community links and tenure. However, it became increasingly evident that the transition to community living was not always easy or straightforward, with many people needing proactive support with their illness not only from clinical services, but also from a range of social and community agencies.
Forerunners to critical time intervention: the case management and assertive community treatment models
Case management
To address this challenge of delivering effective and multifaceted community care, case management (CM), which was initially developed in the 1980s in the USA but took hold in the UK through the 1990s, required health and social care agencies to join together to form multidisciplinary multiagency teams. 33–37 The key aims of CM are to maintain client contact with mental health services, reduce the risk of rehospitalisation and, generally, improve the client’s functioning and ability to live independently, with all actions to be co-ordinated by a case manager. A review of CM summarised the case manager’s role as assessing a client’s needs, developing a care plan, arranging for that care to be provided, monitoring the quality of care and maintaining contact with the person. 38 Although initially likened to a ‘brokerage’ role for ensuring that the range of services the client needs are in place, the authors commented that the CM model had developed over time to include elements of clinical/therapeutic input by the case manager and the use of techniques to identify and work with the client’s strengths.
However, although CM was adopted widely by service providers, its efficacy in achieving its aims has been questioned. In a randomised controlled trial (RCT), patients under the care of a case manager generally fared better during the resettlement period than patients receiving standard care based on measures of social behaviour and social integration, deviant behaviour and improved mental state; however, the difference was only significant with regard to deviant behaviour. 39 A later systematic review and meta-analysis went on to show that CM clients were more likely to maintain contact with services, but with a greatly increased rate and length of hospitalisation compared with standard care. In addition, little improvement in other measures of clinical and social outcomes and mental state were achieved. 38
More recently, and with particular relevance to the current study, the efficacy of a low-intensity CM model on increasing contact between ex-prisoners and community primary care services was the subject of a RCT undertaken in Australia. 40 On release, prisoners were given their own personalised ‘passport’ detailing their health-care needs and listing the important contacts necessary to ensure physical and psychosocial needs were met and tasks such as securing accommodation and income were taken forward. The intervention involved following up participants by telephone on a weekly basis for the first 4 weeks post release. Research follow-up involved interviews at 1, 3 and 6 months post release. The authors concluded that, compared with treatment-as-usual (TAU) participants, those receiving the intervention were more likely to be in touch with primary care and mental health services at 6 months. 40
Assertive community treatment
Assertive community treatment (ACT), again developed in the USA, adopted a multidisciplinary team approach to jointly care for small caseloads of commonly high-need and high-risk clients. 41–43 In contrast to the CM model, ACT team members are not assigned specific clients but rather bring their discrete expertise, as required, to all clients under the care of the team.
Systematic reviews of ACT compared with standard care, hospital rehabilitation and CM have indicated that ACT is more successful in maintaining client contact with services, reducing the number of admissions and average days spent in hospital, maintaining stable accommodation, increasing days in employment and increasing rates of general client satisfaction compared with standard care. Data were not sufficient for reviews to make robust comparisons between ACT and hospital rehabilitation or CM. 44,45
Critical time intervention
Critical time intervention (CTI), a variant of ACT, was developed in the USA in the 1990s. CTI was designed as a structured but, unlike ACT, specifically time-limited (to a maximum of 9 months in original trials) intervention to prevent recurrent homelessness in transient individuals with SMI moving from hospital care to the community. 46–48 The intervention had two key components: first, to strengthen ties with service providers, family and friends; and, second, to provide practical and emotional support during transition from institution to the community.
To realise the first component, case managers made appointments with key service providers and accompanied clients to those appointments following discharge from hospital. The case manager ensured that clients had a named contact at each service and facilitated the formation of a relationship between the client and provider to better ensure continued engagement. The case manager also supported the client and his family in re-establishing their relationship; if the client’s family wished to be involved in providing care, the case manager helped them to better understand their relative’s illness, the difficulties they might encounter in their role as carer and ways to resolve those situations. To achieve the second component of the intervention, the case manager maintained close contact with the client, observing how they were adapting to living in the community, stepping in, if necessary, to provide practical help with the development of skills necessary to function independently. The case manager reviewed the extent to which their input was needed throughout the intervention period to the point when they judged they could withdraw without any disruption to engagement.
In an early trial, those in receipt of CTI had significantly fewer nights’ homelessness than the TAU group: 30 compared with 91 homeless nights, respectively. In addition, the strong ties with service providers that CTI put into place persisted after the intervention was withdrawn, with survival curves showing that, after 9 months of the intervention, the differences between the groups did not diminish. The authors noted that CTI could be used in any transition scenario, for example from prison to community, to better co-ordinate and augment existing processes in place to link individuals to other important services. 46
To examine this assertion, as well as the research described in this report, the CTI model is currently being trialled in the transition of two discrete populations leaving shelters for supported or independent housing: (1) individuals previously homeless and (2) women who have experienced domestic violence. 49 In addition, a trial using CTI at the point people first make contact with mental health services in order to put in place a comprehensive and enduring network from the start is under way. 50 These studies will, in due course, add to the body of evidence with respect to the transferability of the model to other scenarios.
Critical time intervention: prison to community feasibility trial by current authors
As previously outlined, many prisoners with mental illness reach the end of their time in custody without a clear plan of how to contact services in the community, or indeed what services they require and/or are available where they live. Staff working in prison are frequently hampered in planning care by having to do so at very short notice, for example when home detention monitoring is granted or if a remand prisoner is released unexpectedly following a routine court appearance. In addition, many prisoners are still held far away from their home area and this can bring problems for staff trying to contact and co-ordinate with a range of unfamiliar community services at great geographical distance from the prison, hampering their abilities to achieve a clear handover of responsibility to external providers. Owing to increased competitive tendering within the NHS, including offender health services, even when a prisoner is in custody within their home area, the prison mental care provider is increasingly likely to be a different NHS or private organisation from the community service; thus, referral processes can be as problematic as those undertaken remotely. 51
Although engaging with mental health services in order to ‘stay well’ might be understood as important by prisoners, research shows that other matters, such as housing, financial security and re-establishing relationships with family are often more highly prioritised on release, often to the expense of attending any appointments made with the CMHT or substance misuse services. 52 As a result, it was suggested that the CTI model could be usefully adapted to better plan for transition for this population. 53
In our earlier study, the CTI model was adapted and piloted for use with a male prisoner population. 54 Case managers were identified to proactively engage with prisoners with SMI before their release from prison in order to agree a discharge plan and provide practical help to ensure, as far as possible, that the prisoner’s most pressing needs on release could be met. In addition, their role was to proactively support the person and liaise in person with service providers following release to ensure that engagement and transfer of care to community services went smoothly. The original CTI model was adapted to better reflect the stages of transition for prisoners in England; the major change was that the post-release duration of the intervention was shortened to 6 weeks, recognising that 9 months would be cost prohibitive to deliver and reflecting the views of staff and service users involved that community services in the UK were generally superior to those in the USA. The adaptation of the original model also included a vastly increased input in the pre-release period, with early preparation of a detailed discharge plan that could be activated if unexpected discharge occurred, particularly likely in the case of remand prisoners.
The feasibility of implementing this intervention was tested. Sixty prisoners were recruited to the study, with 32 randomly allocated to the CTI arm and 28 to TAU. Of these, 23 were followed up 4–6 weeks post release. Participants assigned to the CTI group were more likely to be in touch with either mental health or substance abuse services, receiving their medication, registered with a GP and in receipt of benefits than TAU participants, although only the outcomes relating to being in receipt of medication and registered with a GP were statistically significant. There were no differences in terms of social support or housing.
The key aim of the pilot was to ascertain whether or not it was feasible to deliver CTI to prisoners with SMI during their transition to the community. We concluded that, because of the intensive pre-release input required by the case manager to identify prisoners’ needs and prepare community agencies to provide services, the case manager role was best carried out by someone based in prison and working with the in-reach team. Feedback from prisoners who received the intervention was positive and case managers reported that the intervention ‘felt like the right thing to do’. Although most differences in engagement and other outcome measures proved not to be statistically significant, the support provided by the case manager, particularly in the event of a delay in the start of community service provision, was thought to be valuable by staff and service users alike.
Although the feasibility trial involved a relatively small number of participants, the potential for the CTI model to improve transition for SMI prisoners merited a larger-scale study.
Rationale for current study
Managing transition for prisoners with SMI to the community has many similarities with the meeting of the health and social care needs of previously homeless individuals with SMI leaving hospital care. These similarities were the impetus for the development of the feasibility study in the prison population using CTI.
Our pilot to test the feasibility of delivering CTI within a prison setting with adult men with SMI was successful. A larger RCT was therefore undertaken to more rigorously test the utility of CTI for improving through-the-gate engagement of male prisoners with SMI with community mental health services and to examine the cost/benefits of this approach.
The primary objective was to establish whether or not CTI is clinically effective and cost-effective for released adult male prisoners with SMI in:
-
improving engagement with health and social care services
-
reducing mental health hospital admissions
-
reducing reoffending
-
increasing community tenure through reducing time in prison.
The secondary objectives were:
-
to establish the cost-effectiveness of CTI for this population
-
to develop service model manuals and training materials to support the implementation of CTI with criminal justice agencies, the NHS and relevant third-sector organisations
-
to facilitate and promote active service user, criminal justice, third-sector and health staff participation in the research work programme, thus encouraging greater engagement between the academic community of researchers, the practice community of health and justice staff, and users of criminal justice, community-based health-care and third-sector services.
Chapter 2 Quantitative methodology
Study design
The study was designed to evaluate CTI specifically adapted for male prisoners with SMI. It was designed as a parallel two-group RCT with 1 : 1 individual participant allocation to either CTI plus TAU (intervention group) or TAU alone (control group). The main trial was supplemented with (1) an economic evaluation examining the cost-effectiveness of providing CTI (see Chapter 6) and (2) a qualitative study to explore the views and experiences of participants and professionals involved in the study (see Chapter 4).
Ethics approval
Ethics approval for the study was granted by the research ethics committee (REC) for Wales in January 2012 (reference number 11/WA/0328). The National Offender Management Service research approval was given in February 2012 (reference number 184-11). The trial was registered with the International Standard Randomised Controlled Trial Number (reference number ISRCTN98067793). In addition, all required site-specific permissions and research governance approvals, that is the research and development (R&D) approvals, were obtained from the relevant NHS trusts.
Changes to protocol
The progress of this trial was severely impacted by recruitment shortfalls at the original sites and significant delays in obtaining a number of R&D approvals at new sites. We increased the number of sites involved from three to eight. A summary of the changes to the original protocol notified to the REC is given in Table 1. Approvals were also sought for another three prison establishments but, because of significant delays in obtaining these approvals, recruitment never commenced.
| Changes to protocol | Date |
|---|---|
| Increase of study sites from three to eight | 10 February 2014 |
| Use of the Operational Criteria Checklist for Psychotic and Affective Illness rather than the Structured Clinical Interview for Diagnostic and Statistical Manual of Mental Disorders-Fourth Edition Axis 1 disorders to record axis I mental health diagnosis | 10 February 2014 |
Increase of study sites from three to eight
The number of study sites was increased because of slow recruitment rates in the original three sites. This was mainly caused by potential participants failing to meet one or more of the eligibility criteria. The main reasons people were ineligible were (1) not likely to be released within the lifetime of the study and (2) not likely to be discharged to the local geographical area, thus unable to be followed up. One site, which had been the site with the largest recruitment in our feasibility study, was rerolled during this study, changing it from a category B remand local prison to a category C/D resettlement establishment. This meant that the prison started to take prisoners with longer sentences, so many were not likely to be released within the lifetime of the study. In one site, the original CTI manager left and the NHS trust was unable to recruit a replacement.
Research and development approval
For three of the trusts involved, it took approximately 6 months to obtain R&D approval and, in two cases, a complaint was lodged with the concerned trusts’ medical director in order to expedite matters. Complex commissioning and provider arrangements resulted in a lack of transparency as to where responsibilities lay; this required seeking multiple permissions from several provider organisations at single sites. In addition, retendering processes resulting in the award of contracts to new provider organisations impacted negatively on recruitment. In addition, two sites that had originally agreed to take part in the research pulled out before recruitment could begin, citing staffing shortages.
Use of Operational Criteria Checklist for Psychotic and Affective Illness rather than Structured Clinical Interview for Diagnostic and Statistical Manual of Mental Disorders-Fourth Edition Axis 1 disorders
Before data collection commenced, the use of the Structured Clinical Interview for Diagnostic and Statistical Manual of Mental Disorders-Fourth Edition Axis 1 disorders (SCID-I)55 by non-clinically trained researchers was reassessed because of concerns about the specialist knowledge required for its accurate completion. The use of the Operational Criteria Checklist for Psychotic and Affective Illness (OPCRIT)56 was agreed to solve this issue, as its completion is not as dependent on expert clinical assessment skills.
Other changes to protocol not requiring research ethics committee approval
Hospital admission
The number of days in hospital, including any detention under the Mental Health Act 1983,57 was collected via case notes at each follow-up. This varied from the original protocol in which we envisaged accessing Hospital Episode Statistics (HES), a nationally collated data source. Owing to slow recruitment rates and not being able to extend the study any further we are unable to use HES data in this report because recording lags in HES would have led to greater inaccuracies than collecting the data from individual notes.
Criminal justice contact and reconviction
In the original protocol, we planned to access Police National Computer (PNC) records to compare criminal justice contact and reconviction at 12 months post release from prison. As recruitment was slow and we could not extend the study, we were unable to use PNC data because recording lags would have made the available data incomplete. We will collect PNC data after this report is submitted, as this has been formally agreed with the Greater Manchester Police Service; this will form part of our subsequent publications, which will be available for the funders.
Community tenure
In the original protocol, we stated that we would calculate community tenure by subtracting days in hospital or custody from total time in the community. However, because of the inability to collect PNC data, we were unable to do this. However, this will form part of our subsequent publications, which will be available for the funders.
Definition of engagement with community mental health team
In the original protocol, we stated that engagement would be defined as (1) having an allocated care co-ordinator and care plan, (2) receiving appropriate medical treatment for mental health problems and (3) in regular, planned contact with their care co-ordinator. This was changed to (1) evidence of having an allocated care co-ordinator, (2) evidence of having a current care plan and (3) receiving medical treatment for mental health problems. Appropriate medical treatment was changed to medical treatment, as it was not possible for the researchers collecting the data via file records alone to make decisions about appropriateness. In addition, evidence of being in regular and planned contact was difficult to collect from file information alone, as it was very often not recorded. These changes were made before analysis and with the agreement of the Trial Steering Committee.
Sites
The study sought to recruit adult male prisoners with SMI. Originally, this was to be from three prison establishments (two in the north-west and one in the south of England) but, because of recruitment difficulties, this was subsequently expanded to include a further five prison establishments (two in the north-west and three in the south of England). Table 2 provides a brief description of the function of each site. Throughout the report, to maintain anonymity, prisons will be identified only by the letters A–H.
| Establishment | Type |
|---|---|
| A | Category B local prison accepting convicted and remand prisoners from local courts |
| B | Category A high-secure site, with a category B local function for convicted and remand prisoners |
| C | At the start of the project, this prison was a category B remand local prison, but during the course of the study became a category C/D resettlement establishment |
| D | Category B local prison accepting convicted and remand prisoners from local courts |
| E | Category C training prison holding convicted prisoners |
| F | Category B local prison accepting convicted and remand prisoners from local courts |
| G | Category B local prison accepting convicted and remand prisoners from local courts |
| H | Category B local prison accepting convicted and remand prisoners from local courts |
Participants
Inclusion criteria
Participants were considered for inclusion if they met all the following criteria:
-
were male
-
had SMI
-
were a service user of the prison mental health in-reach team
-
were able to give informed consent
-
were to be released from prison within the lifetime of the study
-
release would be to an agreed geographical area local to the prison.
Severe mental illness was defined as major depressive disorder, hypomania, bipolar disorder and/or any form of psychosis including schizophrenia, schizoaffective disorder and any other non-affective non-organic psychosis.
Exclusion criteria
Participants were excluded if they:
-
did not have SMI
-
were to be released outside the agreed geographical discharge area
-
posed security/safety issues that would compromise researcher/practitioner safety in prison or the community
-
were unable to give informed consent
-
had previously participated in the trial during an earlier period in custody.
Recruitment procedure
In all sites, the mental health in-reach team identified existing (at the start of the study in each site) and new (as the study continued) service users who fulfilled the inclusion criteria.
The in-reach team informed the service users of the proposed study and asked if they wished to learn more about it. If the service user expressed an interest, the in-reach team member, with the person’s permission, passed their name on to a member of the research team. A researcher then arranged a time to meet with the service user to describe the study. The potential participant was provided with all relevant clearly written information about the study and its implications. They had the opportunity to ask questions about the research and were given a minimum of 24 hours to decide if they would like to take part. Given the unique problems of gaining consent in custodial environments, careful emphasis was given to their rights to consent/not consent, including the right to withdraw at any time, without the need to give a reason for doing so, and free of any coercion or negative consequences to their mental health care or their progress in custody in general. If any concerns regarding capacity to give informed consent because of mental illness were raised, the researcher sought the opinion of the mental health in-reach team. The original signed and dated consent forms were held securely as part of the trial site file, with a copy held in the participant’s clinical records.
The likely release dates for unconvicted prisoners were predicted using the Sentencing Council Guidelines,58 based on the person’s index offence. Geographical discharge area for each prison was based on NHS R&D approval areas.
Randomisation
Eligible and consenting participants were randomised after baseline assessments were completed at the level of the individual participant to CTI or TAU by block randomisation, with randomly varying block sizes of two and four, stratified by prison. Randomisation was undertaken by the King’s College London Clinical Trials Unit, using an online system. Once the randomisation procedure had been completed, the outcome and further details about the allocated treatment were immediately communicated to the researcher and to the participant. Owing to the nature of the intervention, it was not possible to blind participants, researchers or CTI managers to the treatment allocation.
Intervention
Treatment as usual
Individuals in the control group received TAU. While still in prison, they were able to access primary care, secondary mental health and substance misuse services as would usually be the case. They also received support from criminal justice and any other third-sector organisations in the standard way.
South of England prisons (prisons C, F, G and H)
Treatment as usual at the south of England prisons was delivered by the prison mental health in-reach team and, when appropriate, other agencies. The in-reach teams aimed to complete a CPA meeting for each service user before release, inviting professionals from prison and community services. For sentenced prisoners, in-reach teams aimed to notify community teams in the relevant area of the date of release and provided them with contact details for further information as required. For remand prisoners, the teams checked HMPS and NHS information systems [Prison National Offender Management Information System (p-NOMIS; NOMS, London, UK) and SystmOne (tpp, Leeds, UK), respectively] to establish whether or not a person had been further remanded into custody and had returned to the prison following a court date. If they had not returned to custody, community teams would be notified. The extent to which this happened at each prison varied according to their resources.
At all four prisons, the in-reach teams were supported by probation officers and offender managers. In addition, a third-sector organisation provided resettlement support at prisons C, G and H; similar support was provided in conjunction with a different third-sector provider at prison C and H. A further third-sector provider provided resettlement support at prison F. One of these providers withdrew from prison H towards the end of the recruitment period.
At prison G, one NHS trust employed a criminal justice liaison nurse who followed patients from court to prison. Their main role was in planning for psychiatric hospitalisation if this was needed, but they also notified and provided information to CMHTs and GPs about released prisoners. Prison F was also eligible for this service, but the private health-care provider declined this input for the duration of this project.
North of England prisons (prisons A, B, D and E)
In prison A, the in-reach team took over care co-ordination responsibility while people were in custody. The CPA process was standardised and aimed to address all needs. Everyone on the in-reach caseload was assessed and reviewed under CPA every 6 months. If people were serving < 6 months, care co-ordination was not formally transferred and they kept contact with their CMHT. If they were not in receipt of any service in the community, in-reach tried to link them in before they left, usually 1 or 2 months before release. Staff from certain CMHTs came to the prison to complete assessments before release, but not all.
The in-reach team liaised with a range of CMHTs, community forensic mental health teams, assertive outreach services, the Personality Disorder Network, probation service, community drug and alcohol teams, homeless teams and third-sector organisations providing housing and social support. Some services, for example the Personality Disorder Network, could be accessed only from the community and, thus, no assessment process was possible pre release and service users had to attend appointments once in the community.
All mental health referrals from primary to secondary care went through a single point of access (SPA) referral system. SPA included brokering access to CMHTs, the crisis team, home intensive treatment team, adult psychology services and links to acute psychiatric wards but not to some more specialist services.
Once a service user was released, there was an expectation that the receiving community service, whether that be a new or previously involved service, would re-establish care co-ordination and follow-up the client within 7 days. Linking in with services is acknowledged to be more difficult with remand prisoners; however, the in-reach team sometimes attended court with clients.
In prison B, the in-reach team did not take over care co-ordination responsibility. Therefore, release preparation involved liaison with existing CMHTs or referring to a CMHT if the person had no contact with services before custody or has been discharged from caseload while in prison. Addressing needs, such as accommodation, was usually done by probation service staff and/or external CMHTs.
In prison D, the in-reach team assumed care co-ordination responsibility. Clients were referred to appropriate services in the community including CMHTs, drug and alcohol teams, and a range of third-sector providers. A third-sector organisation specialising in accommodation was based within the prison and the in-reach team liaised with them if needed. Service users were seen regularly leading up to, and including, the day of release. Some service users were accompanied to first community appointments on the day of release.
In prison E, the in-reach team held care co-ordination responsibilities. Release planning included needs-led liaison with services such as CMHTs, other mental health services, for example early intervention, complex care and/or criminal justice liaison teams, social services, drug and alcohol teams, rehabilitation units and accommodation services. The in-reach care remit ended at the gate, with no community activities or responsibilities.
Critical time intervention: adaptation for current randomised controlled trial
Critical time intervention is intensive CM at times of transition between the prison and community. CTI managers provide direct care where and when needed, for a limited time period. They commence their involvement with the service user in prison. For sentenced prisoners, this starts 4 weeks before discharge. For remand prisoners, or those with unpredictable dates of release, this work commences as soon as the person is on the caseload of the mental health team. The length of their involvement pre release is, therefore, ideally 4 weeks but may be shorter or longer in those with unpredictable release dates. In this adaptation of CTI, the period of contact post discharge was set at 6 weeks. The 6-week period of intervention was adopted because (1) the pilot study indicated that, by this stage, the service user would be engaged with the CMHT if that was going to occur at all; (2) it allowed a reasonable period post discharge in which adjustments to vital support systems, including accommodation and/or benefit entitlement/employment are most likely to be required; (3) to keep community caseloads low and workable for the CTI managers, some of whom were part-time; and (4) the adapted version of the intervention was heavily frontloaded with most of the vital liaison work being completed while the service user was still in prison.
The holistic intervention involved work with clients and clients’ families (when possible), as well as active liaison and joint working with relevant prison and community services. Five key areas were prioritised: (1) psychiatric treatment and medication management, (2) money management, (3) substance abuse treatment, (4) housing crisis management and (5) life-skills training. CTI is not prescriptive; it responds to the needs of each individual client. The intervention comprised four phases.
Phase 1 is conducted while the person is in prison. The CTI manager engages with the individual and develops a tailor-made discharge package based on a comprehensive assessment of the individual’s needs. This typically includes plans for engagement with community mental health treatment and addressing accommodation, financial and social support needs. The CTI manager and prisoner meet as often as required to make the discharge arrangements; pre-release contact is routinely twice weekly. In addition, the CTI manager liaises closely with community services to ensure their availability and suitability.
Phase 2 occurs immediately after release and focuses on providing very intensive personal support. In the first few weeks post discharge, the CTI manager maintains a high level of contact, including accompanying people to appointments to promote engagement and to help them establish relationships with community providers in order to facilitate the development of durable ties. The number of meetings/visits involved is directly influenced by the complexity of each person’s needs, but routinely involves up to 15 meetings per week for the first 2 weeks following discharge.
In phase 3, community services assume primary responsibility for the provision of support and services, and the CTI manager focuses on assessing whether or not the support system is adequate and functioning as planned. During this phase, the CTI manager encourages the individual to start to handle problems on their own. They meet less frequently but maintain regular contact in order to judge how the plan is working. The CTI manager remains ready to intervene if a crisis or potentially destabilising event arises. Again, the frequency of meetings is individually determined, but is typically at least weekly for 3 weeks.
In phase 4, care is fully transferred to community services in order to provide long-term support, thus work focuses on completing the transfer of care. This phase may typically consist of a meeting with the community care co-ordinator, service user and CTI manager, reviewing progress and agreeing future care. Throughout, the CTI manager will gradually reduce their role in delivering direct services to the individual. Their main function in this phase is to ensure that the most significant members of the ‘receiving’ support system meet together and, along with the individual, reach a consensus about the components of the ongoing system of support.
A manual for use by the CTI case manager was also developed to support their delivery of the intervention (see Chapter 5 and reproduced in full in Appendix 1).
Each CTI case manager received 2 days’ training on the manual, undertaken by the study’s principal investigator, a consultant forensic psychiatrist. The CTI case managers then received weekly CTI-specific supervision locally in addition to their normal clinical and/or line management supervision. In addition, group supervision was held by telephone, every 3 months, with the study principal investigator. The aim of the CTI supervision was to correct CM that was inconsistent with CTI principles and practices, provide guidance to assure that the approach was consistent with CTI principles and practices, and schedule case presentations for all new clients within a few weeks of enrolment into CTI.
All professionals who took part in this study in the role of CTI manager were qualified and experienced mental health clinicians; most were mental health nurses and one was a clinical psychologist. All had previous experience working in both prisons and either forensic community mental health services or intensive home treatment/assertive outreach teams. As such, they brought with them an extensive skill set, including existing motivational interviewing training; thus, the majority of training focused on describing the content of CTI as distinct from other ways of working in previous roles rather than clinical skills training per se.
Public and patient involvement
People with previous contact with criminal justice and mental health services were involved in study design and methods development, were Trial Steering Committee members and formed, alongside professionals, the working group which developed the intervention manual and training resources.
Data collection and management
Data were entered onto the online MACRO® (Elsevier, Amsterdam, the Netherlands) data entry system, which was hosted at the King’s College London Clinical Trials Unit. The system is compliant with good clinical practice guidelines,59 with a full audit trail, data entry and monitoring roles and formal database lock functionality.
To standardise recruitment/retention processes across the trial sites and maximise data quality, researchers were trained to use standard operating procedures for each stage of data collection. The database was designed to flag up data errors and a number of cross-checks were routinely performed as a means of ensuring that any data inconsistencies arising from either baseline assessment or follow-up were identified and resolved at the earliest opportunity.
Baseline assessment
At baseline all participants were seen by a member of the research team and the following data were collected:
-
OPCRIT+56 – the OPCRIT+ was used to obtain an Axis 1 diagnosis (Diagnostic and Statistical Manual of Mental Disorders-Fourth Edition55). OPCRIT+ is an electronic checklist of psychopathology items with algorithms for objective diagnosis of psychotic and affective disorders. Participants were asked about a range of mental health symptoms and responses entered into the OPCRIT database to produce a diagnosis. In its original format, OPCRIT data are designed to be gathered from case notes alone. 55 However, in a small pilot, it became apparent that there were frequently insufficient data in the notes alone to make a reliable diagnosis and, therefore, the case note data collection was supplemented by direct inquiry with the participant.
-
Structured Clinical Interview for Diagnostic and Statistical Manual of Mental Disorders-Fourth Edition Personality Disorders (SCID-II) – the SCID-II is a semistructured interview for the assessment of PD. The first part consists of eight open questions on the patient’s general behaviour, interpersonal relationships and self-reflective abilities. The second part has 140 items to be scored as 1 (absent), 2 (subthreshold) or 3 (threshold). 60 The full SCID-II interview was administered to all participants and any resulting diagnoses recorded.
-
The Michigan Alcohol Screening Test (MAST) – the MAST consists of 24 yes/no questions pertaining to lifetime use of alcohol. Each item is scored 0 or 1, with scores of ≥ 10 indicating evidence of having had a lifetime alcohol problem. 61
-
The Drug Abuse Screening Test (DAST) – the DAST is similar in design to the MAST. It consists of 20 yes/no questions, each scored 0 or 1. Scores of ≥ 11 indicate substantial problems with drug abuse. 62
-
Adapted Client Services Receipt Inventory – developed from the Client Services Receipt Inventory. 63 A pro forma was developed that enabled data on a specific range of services to be collected from health-care records by the research team.
All baseline assessments were conducted between October 2012 and July 2015.
Follow-up
Follow-up data collection was scheduled to take place at three time points: 6 weeks and 6 and 12 months post release from prison. The 6-week follow-up coincided approximately with the end of the intervention delivery phase and the 12-month follow-up was designed to inform the investigation of any longer-term effects of the intervention on study outcomes. All follow-up data were collected via file information from each participant’s care team in the community. All follow-up data were collected between November 2012 and October 2015.
Outcomes
Primary outcome
The primary outcome measure was engagement with mental health services at 6 weeks post release from prison. Engagement was defined as currently being in receipt of an appropriate level of mental health care, by virtue of (1) having an allocated care co-ordinator, (2) having a current care plan and (3) receiving medical treatment for mental health problems. To create the binary engagement variable, a score of 1 was assigned if all three of these were true, and a score of 0 assigned if any or all of these were not true (i.e. they did not have an allocated care co-ordinator, they did not have a current care plan or they were not receiving medical treatment for mental health problems).
Secondary outcomes
The secondary outcome measures were engagement, as defined above, with mental health services at 6 and 12 months.
Fidelity
Fidelity was assessed using an adapted version of the fidelity scale used in the Critical Time Intervention – Task Shifting study. 64 The adapted version took into account all changes to procedures from earlier CTI studies. The fidelity scale, included in this report as Appendix 2, was completed at eight time points during the intervention delivery phase.
Sample size
Original sample size justification
The original calculation for the research proposal, taking into account the attrition rate in the feasibility trial of 15%, required 100 participants randomised to each arm (CTI and TAU) to give 90% power to detect a difference at 6-week follow-up of 50% in the treatment group compared with 25% in the control group (or greater), at the conventional 5% significance level. Thus, 85 participants were required in each group at 6-week follow-up.
Revised sample size justification
Owing to slow recruitment rates, we checked our earlier assumptions after 120 participants had been randomised and found that the attrition rate was 9%. In addition, we also proposed reducing the statistical power available to detect a significant difference from 90% to 80%. The revised calculations are shown in Table 3. The number required for the primary outcome was 132.
| Power (%) | Attrition (%) | Number randomised | Number required for the primary outcome |
|---|---|---|---|
| 90 | 15 | 200 | 170 |
| 90 | 9 | 188 | 170 |
| 85 | 15 | 178 | 150 |
| 85 | 9 | 166 | 150 |
| 80 | 15 | 156 | 132 |
| 80 | 9 | 146 | 132 |
Statistical analysis
The analysis and reporting of this trial was undertaken in accordance with the Consolidated Standards of Reporting Trials (CONSORT) 2010 statement,65 showing attrition rates and loss to follow-up. All analyses were carried out using the intention-to-treat principle, with available data from all participants included in the analysis according to the group they were randomised to, including those who did not complete therapy. In addition, the report abides to Standard Protocol Items: Recommendations for Interventional Trials (SPIRIT) guidelines.
Analysis was conducted in Stata version 14 (StataCorp LP, College Station, TX, USA). The statistician was blinded to allocation groups until all analyses were performed.
Descriptive statistics within each randomised group are presented for baseline values. These include counts and percentages for binary and categorical variables and means and standard deviations, or medians with lower and upper quartiles, for continuous variables, along with minimum and maximum values and counts of missing values. There were no tests of statistical significance or confidence intervals (CIs) for differences between randomised groups on any baseline variables. Descriptive statistics were used to summarise assessments of feasibility and acceptability in terms of recruitment, dropouts and completeness of therapy.
The primary hypothesis for between-group differences in the primary outcome measure, engagement at 6 weeks, was analysed using a logistic regression model allowing for the site (prison in the north or south) and treatment assignment as fixed effects. Secondary outcome measures were analysed using the same modelling approach. The same models were used for the analysis of all the outcomes at 6 and 12 months. We report odds ratios and 95% CIs for all treatment effects.
Harms reporting
Definitions
Adverse event
An adverse event was defined as any untoward medical occurrence, unintended disease or injury or any untoward clinical signs (including an abnormal laboratory finding) in participants whether or not related to any research procedures or to the intervention.
Seriousness
Any adverse event will be regarded as serious if it:
-
results in death
-
is life-threatening
-
requires hospitalisation or prolongation of existing hospitalisation
-
results in persistent or significant disability or incapacity
-
consists of a congenital anomaly or birth defect.
An adverse event meeting any one of these criteria was considered as a serious adverse event (SAE).
Relationship
The expression ‘reasonable causal relationship’ means to convey, in general, that there is evidence or argument to suggest a causal relationship. The research team assessed the causal relationship between reported events and trial participation according to CONSORT65 guidance (see Appendix 3).
Reporting serious adverse events
In this study, SAEs were reported to the chief investigator (JS) regardless of relatedness within 24 hours of the principal investigator (or authorised delegate) becoming aware of the event. All SAEs deemed to have a causal relationship were reported to the Trial Steering Committee. Any non-SAEs (regardless of relatedness) were not reported in this study.
Data sharing and accessibility
Study data are handled in strict accordance with the University of Manchester’s data protection policy, which can be found at: www.dataprotection.manchester.ac.uk/ (accessed 10 October 2016).
As the data contain medical details, they will be kept securely for 10 years. Participant consent forms did not specifically allow for the sharing of anonymised data to third parties. Any request for access under the Data Protection Act 199866 or Freedom of Information Act 200067 would be referred to the University of Manchester’s records office for advice before disclosure. Please contact the corresponding author for more information.
Chapter 3 Quantitative results
Trial results
Recruitment
The NHS ethics and National Offender Management Service approvals were received by February 2012 but first recruitment did not commence until October 2012. Table 4 shows the recruitment issues at each site that contributed to delays and the number of participants randomised at each site.
| Prison | Delays in commencing | Recruitment | Reason for ending | Other problems | Number recruited | |
|---|---|---|---|---|---|---|
| Started | Ended | |||||
| A | Obtaining R&D approval took > 5 months. Once the CTI manager had been identified, there were delays in commencement because of training needs and commitments to a previous role. The CTI manager started delivery of the intervention in November 2012 | November 2012 | April 2013 | CTI manager became pregnant and could no longer work in the prison. Host service could not find suitable replacement | 3 | |
| B | Reaching an agreement on excess treatment costs. Permission from the prison took 3 months and was not received until 20 March 2012. As the prison is part of the high-secure estate, the lengthy vetting and induction process for researchers was started early but took until 29 October 2012 | November 2012 | May 2014 | Excess treatment cost money ended | Slow recruitment | 14 |
| C | Reaching an agreement on excess treatment costs. Identifying a suitable CTI manager, first person left post unexpectedly | October 2012 | July 2014 | Excess treatment cost money ended | Rerolled to a category C/D resettlement prison so recruitment slowed | 29 |
| D | R&D approval form was received quickly; however, there were subsequent delays negotiating information technology access for the CTI manager. We had to wait several months for an Information governance meeting for this to be approved. The induction meeting at the prison was cancelled on three occasions for the researchers and four times for the CTI manager | August 2013 | May 2014 | Excess treatment cost money ended | 7 | |
| E | First contact with R&D was made on 16 October 2012. After getting no response we involved the local research network for help, but eventually complained to the medical director. The R&D manager requested that we review in-reach caseload to assess for numbers eligible and report back before R&D would approve the study. This took us 5 months to gain access to the prison and the information required. Once data had been collected, we reapproached the R&D manager who had left and the new R&D manager requested that we start the application process again | February 2014 | May 2014 | Excess treatment cost money ended | 7 | |
| F | We had first meeting at the prison on 17 October 2012. Recruitment took 9 months to begin because of a new in-reach team setting up and lack of immediate support for the project because of staffing and resource concerns. There were also long delays in obtaining permission to follow up participants in one release catchment area. One R&D took > 6 months to receive. They required a local collaborator who held a contract with the trust; however, we were not informed of this until the application had been submitted. This meant it was rejected and we had to resubmit. The trust did not identify a suitable local collaborator within a reasonable time frame. Despite chasing up on a regular basis, approval was not received until July 2013 | July 2013 | May 2014 | Excess treatment cost money ended | 35 | |
| G | Initially informed approval needed from one NHS trust, which we obtained, but then they informed us we would need two additional approvals from other NHS trusts. This appeared to be a particular issue because of the complex commissioning arrangements for health care within the south of England. None of the trusts knew which should take the lead and, therefore, one of the applications was initially rejected because of resource concerns and the imminent retendering of the service. Permission was eventually granted after 6 months | February 2014 | April 2014 | Excess treatment cost money ended | 18 | |
| H | Site approached 5 months before the service provider was because of change (January 2014). It took until March to get access, assess caseload suitability and obtain backing from the health-care provider. So when the R&D application was submitted the existing trust had 2 months left before change over. This resulted in a lengthy disagreement between outgoing and incoming providers about who should issue approval. This meant that all required trust approvals were not in place until 20 May 2014 | June 2014 | July 2015 | No longer possible because of report deadline | 37 | |
| I | The prison originally agreed to participate but then informed us that they would have to withdraw owing to staffing issues. Agreement regarding their involvement was finally reached, but this caused significant delays and took approximately 6 months. There were then no eligible recruits so the study did not start | No participants identified as eligible | 0 | |||
| J | No participants identified as eligible | 0 | ||||
| K | No participants identified as eligible | 0 | ||||
Flow of participants in the trial
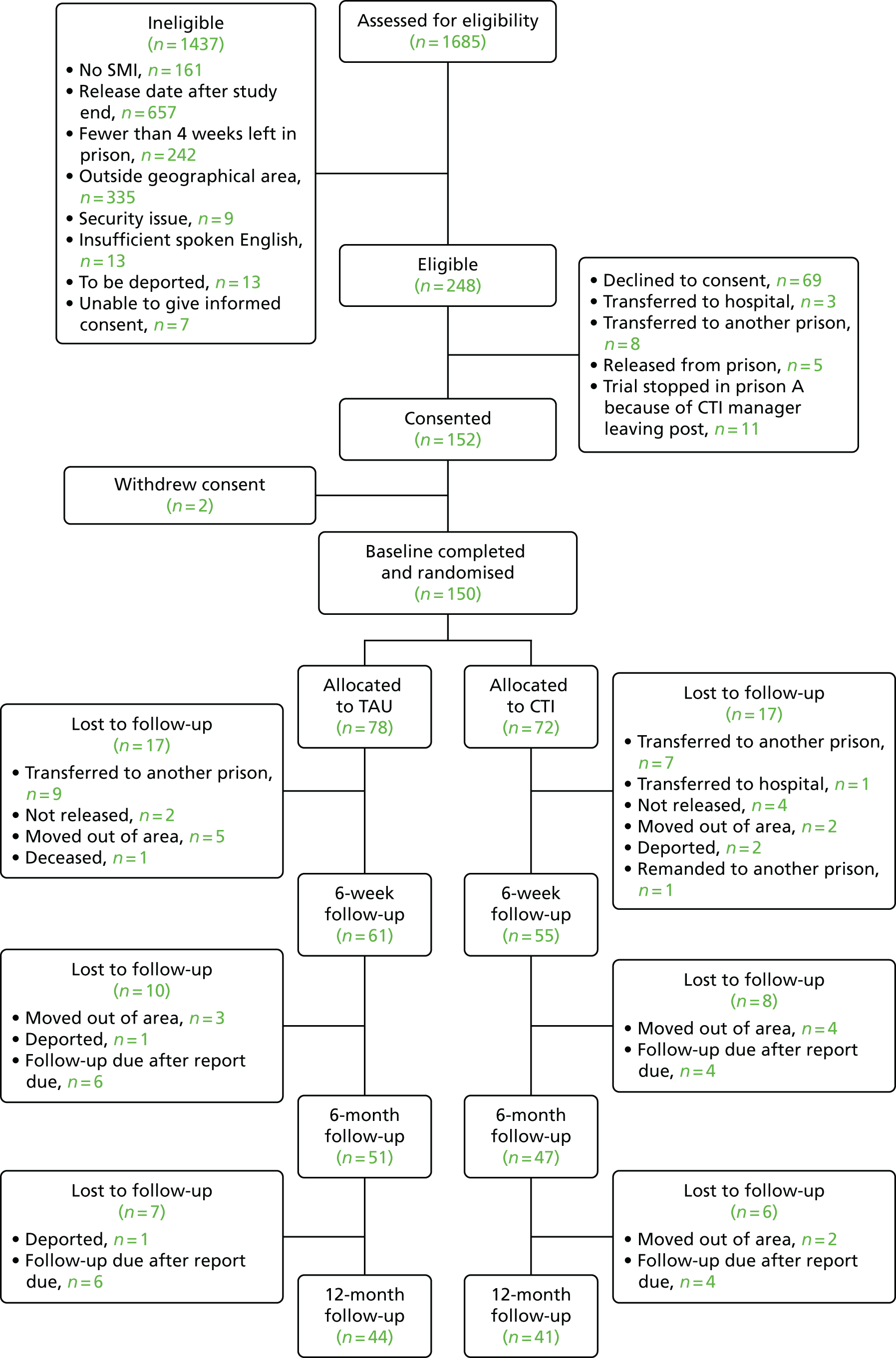
In total, 150 individuals were recruited to the trial, with 72 allocated to the intervention group and 78 to the TAU group. Figure 1 presents the CONSORT65 flow diagram for the trial and summarises participant throughput from eligibility screening and randomisation to completion of the 6-week, and 6- and 12-month follow-ups, as appropriate. The diagram also reports numbers of participants who declined, did not meet inclusion criteria, were excluded from the study, withdrew following randomisation or were lost to follow-up at the 6-week, or 6- and 12-month follow-up points.
FIGURE 1.
The CONSORT flow diagram.
Baseline comparability
Table 5 presents a summary of the baseline demographics to describe the sample and demonstrate the baseline comparability of the randomised groups.
| Characteristic | Trial arm | All (N = 150) | |
|---|---|---|---|
| CTI (N = 72) | TAU (N = 78) | ||
| Age (years), mean (SD) | 36.2 (9.5) | 36.5 (10.1) | 36.3 (9.8) |
| Ethnicity, n (%) | |||
| White | 35 (49) | 37 (47) | 72 (48) |
| Black and minority ethnic | 37 (51) | 41 (53) | 78 (52) |
| Marital status, n (%) | |||
| Single (including divorced/separated/widow) | 65 (90) | 69 (88) | 134 (89) |
| Married/partner | 7 (10) | 9 (12) | 16 (11) |
| Employment, n (%) | |||
| Unemployed/retired/benefits | 63 (88) | 71 (91) | 134 (89) |
| Employed/self-employed | 9 (12) | 7 (9) | 16 (11) |
| Living arrangements, n (%) | |||
| Alone | 56 (78) | 45 (58) | 101 (67) |
| With partner/children/family | 16 (22) | 33 (42) | 49 (33) |
| Accommodation, n (%) | |||
| House/flat | 34 (47) | 39 (50) | 73 (49) |
| Hostel/temporary accommodation | 21 (29) | 29 (37) | 50 (33) |
| Homeless/no fixed address | 17 (24) | 10 (13) | 27 (18) |
| Index offence, n (%) | |||
| Violent (including sexual offences and robbery) | 32 (44) | 38 (49) | 80 (53) |
| Non-violent (all others) | 40 (56) | 40 (51) | 70 (47) |
| Prisoner status, n (%) | |||
| Remand | 18 (25) | 28 (36) | 46 (31) |
| Convicted (unsentenced/sentenced) | 54 (75) | 50 (64) | 104 (69) |
| Time in prison current (months), mean (SD) | 12.4 (18.6) | 11.6 (19.7) | 12.0 (19.1) |
| Previous imprisonment, n (%) | |||
| Yes | 12 (17) | 14 (18) | 124 (83) |
| No | 60 (83) | 64 (82) | 26 (17) |
| Number of times in prison, mean (SD)a | 6.3 (5.7) | 7.9 (8.1) | 7.1 (7.1) |
| Axis I diagnosis (OPCRIT), n (%) | |||
| Schizophrenia | 51 (71) | 57 (73) | 108 (72) |
| Schizoaffective/schizophreniform disorder | 7 (10) | 5 (6) | 12 (8) |
| Psychosis | 3 (4) | 4 (5) | 7 (5) |
| Major depressive disorder | 9 (13) | 11 (14) | 20 (13) |
| Hypomanic episode | 0 (0) | 1 (1) | 1 (1) |
| None | 2 (3) | 0 (0) | 2 (1) |
| Axis II diagnosis (SCID-II), n (%) | |||
| Yes | 38 (53) | 42 (54) | 80 (53) |
| No | 34 (47) | 36 (46) | 70 (47) |
| Avoidant | 5 (7) | 7 (9) | 12 (8) |
| Dependent | 1 (1) | 2 (3) | 3 (2) |
| Obsessive–compulsive | 3 (4) | 3 (4) | 6 (4) |
| Passive-aggressive | 0 (0) | 8 (10) | 8 (5) |
| Depressive | 2 (3) | 11 (14) | 13 (9) |
| Paranoid | 6 (8) | 9 (12) | 15 (10) |
| Schizotypal | 0 (0) | 2 (3) | 2 (1) |
| Schizoid | 1 (1) | 4 (5) | 5 (3) |
| Histrionic | 1 (1) | 1 (1) | 2 (1) |
| Narcissistic | 1 (1) | 1 (1) | 2 (1) |
| Borderline | 10 (14) | 10 (13) | 20 (13) |
| Antisocial | 35 (49) | 38 (49) | 73 (49) |
| MAST | |||
| Total, mean (SD)b | 7.9 (5.7) | 6.3 (5.6) | 7.1 (5.7) |
| Cut-off points, n (%)b | |||
| ≤ 9 | 48 (68) | 61 (78) | 109 (73) |
| ≥ 10 | 23 (33) | 17 (22) | 40 (27) |
| DAST | |||
| Total, mean (SD)c | 13.8 (6.4) | 13.5 (6.9) | 13.6 (6.7) |
| Cut-off point, n (%)c | |||
| ≤ 10 | 23 (33) | 30 (39) | 53 (36) |
| ≥ 11 | 47 (67) | 46 (61) | 93 (64) |
The sample were all male, with broadly half (48%) from a white ethnic background and half (52%) from a black or minority ethnic background. The majority of the participants were single (89%), unemployed (89%) and living alone (67%). Nearly 20% of the sample said that they were homeless or had no fixed abode on arrival at prison. Proportionally more participants randomised to the CTI arm had been homeless. In relation to offending, half of the sample had committed a violent index offence. On average, participants had spent 1 year in prison at the point of baseline assessment and the majority (83%) had been in prison previously, with an average of seven previous prison terms.
In relation to mental health, all participants had an Axis I diagnosis, as determined by OPCRIT. 56 The most common primary diagnosis was schizophrenia, affecting 71% and 73% of the CTI and TAU groups, respectively. Overall, 13% of the sample was experiencing a major depressive disorder and 8% a schizoaffective/schizophreniform disorder. There were no significant differences across the intervention and TAU groups in terms of Axis I diagnoses.
In relation to Axis II diagnoses, 53% of the sample overall had at least one PD, as determined by the SCID-II assessment tool. The most common diagnosis was antisocial PD, identified in 49% of the sample overall. Thirteen per cent of the sample was identified as having borderline and 10% a paranoid PD.
In relation to drug and alcohol misuse, nearly 30% of the sample scored ≥ 10 on the MAST, indicating that they had had a severe drinking problem at some point in their life; more participants scoring over > 10 were randomised to the CTI group. In total, 64% of participants scored ≥ 11 on the DAST, indicating substantial problems with drug abuse. Table 6 presents a summary of the key service contact of the randomised groups.
| Characteristic | Trial arm, n (%) | All (N = 150), n (%) | |
|---|---|---|---|
| CTI (N = 72) | TAU (N = 78) | ||
| Previous mental health intervention, lifetime | |||
| Yes | 69 (96) | 77 (99) | 146 (97) |
| No | 3 (4) | 1 (1) | 4 (3) |
| Previous CMHT intervention | |||
| Yes | 59 (82) | 62 (79) | 121 (81) |
| No | 13 (18) | 16 (21) | 29 (19) |
| Mental health intervention in prison previously | |||
| Yes | 47 (68) | 48 (63) | 95 (66) |
| No | 22 (32) | 28 (37) | 50 (34) |
| Inpatient drug detox previously | |||
| Yes | 8 (11) | 10 (13) | 18 (12) |
| No | 64 (89) | 68 (87) | 132 (88) |
| Residential drug rehabilitation previously | |||
| Yes | 6 (8) | 9 (12) | 15 (10) |
| No | 66 (92) | 69 (88) | 135 (90) |
| Inpatient alcohol detox previously | |||
| Yes | 6 (8) | 5 (6) | 11 (7) |
| No | 66 (92) | 73 (94) | 139 (93) |
| Inpatient alcohol rehabilitation previously | |||
| Yes | 4 (6) | 6 (8) | 10 (7) |
| No | 68 (94) | 72 (92) | 140 (93) |
| First contact with mental health services (months) | |||
| < 12 | 8 (11) | 14 (18) | 22 (15) |
| > 12 | 64 (89) | 64 (82) | 128 (85) |
| Most recent contact with mental health services prior to imprisonment (months) | |||
| < 1 | 62 (86) | 59 (77) | 121 (81) |
| > 1 and < 6 | 3 (4) | 7 (9) | 10 (7) |
| ≥ 6 | 7 (10) | 11 (14) | 18 (12) |
| Most recent contact with mental health services prior to imprisonment (months) | |||
| < 1 | 62 (86) | 59 (77) | 121 (81) |
| > 1 and < 6 | 3 (4) | 7 (9) | 10 (7) |
| ≥ 6 | 7 (10) | 11 (14) | 18 (12) |
| Contact with mental health services on admission to prison | |||
| Yes | 33 (46) | 49 (63) | 82 (55) |
| No | 39 (54) | 29 (37) | 68 (45) |
| Mental health services treatment from GP on admission | |||
| Yes | 21 (29) | 27 (35) | 48 (32) |
| No | 51 (71) | 51 (65) | 102 (68) |
| Prescribed psychiatric medication on admission | |||
| Yes | 13 (18) | 10 (13) | 23 (15) |
| No | 59 (82) | 68 (87) | 127 (85) |
| Alcohol treatment on admission | |||
| Yes | 1 (1) | 3 (4) | 4 (3) |
| No | 67 (99) | 70 (96) | 137 (97) |
| Current psychological interventions (in prison) | |||
| Yes | 5 (7) | 7 (9) | 12 (8) |
| No or N/A | 67 (93) | 71 (91) | 138 (92) |
| Perceived current need for help with alcohol problem | |||
| Yes | 13 (18) | 12 (15) | 25 (17) |
| No | 59 (82) | 66 (85) | 125 (83) |
| Perceived current need for help with drug problem | |||
| Yes | 29 (40) | 19 (24) | 48 (32) |
| No | 43 (60) | 59 (76) | 102 (68) |
| Perceived current need for help with mental health problem | |||
| Yes | 55 (76) | 57 (73) | 112 (75) |
| No | 17 (24) | 21 (27) | 38 (25) |
With regard to dual diagnosis, less than half (42%; n = 63) of the sample had a diagnosis of a single Axis I condition alone. Eight (5%) had dual SMI and substance misuse issues, 56 (37%) had dual SMI and PD diagnoses and 23 (15%) had SMI, substance misuse and PD diagnoses.
In relation to contact with services at baseline, the vast majority (97%) had previously received a mental health intervention, with 81% receiving that from a CMHT. For the majority of participants (85%), their first contact with mental health services was > 12 months prior to baseline assessment, and their most recent contact was within the last month (81%). Around half (55%) of participants were in current contact with community mental health services on reception into custody and 32% were receiving support/treatment for mental health problems from their GP on reception. Few participants were receiving drug (15%) or alcohol (3%) treatment on reception. Very few participants were receiving any psychological interventions (8%) while in prison.
Primary outcome
The primary outcome measure was engagement with mental health services at 6 weeks post release from prison. Engagement was defined as a composite variable of (1) evidence of having an allocated care co-ordinator, (2) evidence of having a current care plan and (3) receiving medical treatment for mental health problems.
There were significant differences between the two groups with participants receiving CTI significantly more likely to be engaged with mental health services at 6 weeks; significantly more were likely to have a care co-ordinator in place, have evidence of a current care plan and be in receipt of medication (Table 7).
| Characteristic | Trial arm, n (%) | Analysis | |||||
|---|---|---|---|---|---|---|---|
| CTI (N = 55) | TAU (N = 61) | Odds ratio | Standard error | 95% CI | p-value | N | |
| Engagement with mental health services (care co-ordinator, care plan, medication) | |||||||
| Yes | 26 (53) | 14 (27) | 0.32 | 0.15 | 0.13 to 0.78 | 0.012 | 100 |
| No | 23 (47) | 37 (73) | |||||
| Care co-ordinator | |||||||
| Yes | 31 (56) | 17 (28) | 0.27 | 0.12 | 0.12 to 0.64 | 0.003 | 115 |
| No | 24 (44) | 43 (72) | |||||
| Current care plan | |||||||
| Yes | 30 (55) | 16 (27) | 0.27 | 0.12 | 0.11 to 0.63 | 0.002 | 115 |
| No | 25 (45) | 44 (73) | |||||
| Receiving medication | |||||||
| Yes | 45 (92) | 39 (75) | 0.27 | 0.17 | 0.08 to 0.90 | 0.033 | 101 |
| No | 4 (8) | 13 (25) | |||||
Secondary outcomes
At 6 weeks
In addition, at 6 weeks, data were also collected on a wider range of contact, service use and lifestyle variables. The only significant difference between the two groups was that those receiving CTI were more likely to be registered with a GP (Table 8).
| Characteristic | Trial arm, n (%) | Analysis | |||||
|---|---|---|---|---|---|---|---|
| CTI (N = 55) | TAU (N = 61) | Odds ratio | Standard error | 95% CI | p-value | N | |
| Planned contact | |||||||
| Yes | 16 (52) | 14 (82) | 2.04 | 1.74 | 0.38 to 10.85 | 0.403 | 48 |
| No | 15 (48) | 3 (18) | |||||
| Currently under CPA | |||||||
| Yes | 3 (5) | 5 (8) | 1.62 | 1.22 | 0.37 to 7.12 | 0.525 | 114 |
| No | 52 (95) | 54 (92) | |||||
| CPA arranged | |||||||
| Yes | 8 (15) | 4 (7) | 0.42 | 0.27 | 0.12 to 1.48 | 0.176 | 113 |
| No | 46 (85) | 55 (93) | |||||
| Medication compliant | |||||||
| Yes | 37 (84) | 33 (87) | 1.25a | 0.79 | 0.36 to 4.35 | 0.727 | 82 |
| No | 7 (16) | 5 (13) | |||||
| Registered with GP | |||||||
| Yes | 44 (90) | 40 (69) | 0.25 | 0.15 | 0.08 to 0.79 | 0.018 | 107 |
| No | 5 (10) | 18 (31) | |||||
| Hospitalisation | |||||||
| Yes | 1 (2) | 3 (5) | 2.79a | 3.28 | 0.28 to 27.93 | 0.383 | 114 |
| No | 53 (98) | 57 (95) | |||||
| Referral to drug and alcohol services | |||||||
| Yes | 11 (24) | 9 (18) | 0.69 | 0.35 | 0.26 to 1.88 | 0.470 | 96 |
| No | 35 (76) | 41 (82) | |||||
| Employment | |||||||
| Yes | 2 (5) | 1 (3) | 0.55 | 0.74 | 0.04 to 7.59 | 0.657 | 78 |
| No | 38 (95) | 37 (97) | |||||
| Contact with family | |||||||
| Yes | 34 (79) | 28 (78) | 0.92 | 0.52 | 0.30 to 2.79 | 0.878 | 66 |
| No | 9 (21) | 8 (22) | |||||
At 6 and 12 months
Outcomes for participants at 6 and 12 months are shown in Tables 9 and 10, respectively. A significant difference in engagement with mental health services at 6 months was maintained for the CTI group. There were no other significant differences between the groups at 6 or 12 months.
| Characteristic | Trial arm, n (%) | Analysis | |||||
|---|---|---|---|---|---|---|---|
| CTI (N = 47) | TAU (N = 51) | Odds ratio | Standard error | 95% CI | p-value | N | |
| Engagement with mental health services (care co-ordinator, care plan, medication) | |||||||
| Yes | 28 (74) | 21 (50) | 0.33 | 0.17 | 0.12 to 0.89 | 0.029 | 80 |
| No | 10 (26) | 21 (50) | |||||
| Care co-ordinator | |||||||
| Yes | 31 (66) | 24 (49) | 0.50 | 0.21 | 0.21 to 1.15 | 0.103 | 96 |
| No | 16 (34) | 25 (51) | |||||
| Planned contact | |||||||
| Yes | 11 (37) | 13 (54) | 2.04a | 1.15 | 0.68 to 6.16 | 0.205 | 54 |
| No | 19 (63) | 11 (46) | |||||
| Current care plan | |||||||
| Yes | 29 (64) | 23 (46) | 0.44 | 0.20 | 0.18 to 1.05 | 0.065 | 95 |
| No | 16 (36) | 27 (54) | |||||
| Currently under CPA | |||||||
| Yes | 18 (39) | 12 (24) | 0.49 | 0.22 | 0.20 to 1.18 | 0.112 | 96 |
| No | 28 (61) | 38 (76) | |||||
| CPA arranged | |||||||
| Yes | 7 (16) | 7 (14) | 0.84 | 0.52 | 0.25 to 2.80 | 0.781 | 95 |
| No | 38 (84) | 43 (86) | |||||
| Receiving medication | |||||||
| Yes | 36 (95) | 37 (84) | 0.27 | 0.23 | 0.05 to 1.41 | 0.120 | 82 |
| No | 2 (5) | 7 (16) | |||||
| Medication compliant | |||||||
| Yes | 31 (86) | 30 (83) | 0.81a | 0.53 | 0.22 to 2.95 | 0.745 | 72 |
| No | 5 (14) | 6 (17) | |||||
| Registered with GP | |||||||
| Yes | 39 (95) | 40 (85) | 0.29 | 0.24 | 0.06 to 1.47 | 0.134 | 88 |
| No | 2 (5) | 7 (15) | |||||
| Hospitalisation | |||||||
| Yes | 2 (4) | 3 (6) | 1.42 | 1.37 | 0.22 to 9.37 | 0.714 | 96 |
| No | 44 (96) | 47 (94) | |||||
| Referral to drug and alcohol services | |||||||
| Yes | 14 (36) | 11 (26) | 0.64 | 0.32 | 0.25 to 1.68 | 0.368 | 81 |
| No | 25 (64) | 31 (74) | |||||
| Employment | |||||||
| Yes | 2 (6) | 2 (6) | 1.03 | 1.06 | 0.14 to 7.79 | 0.978 | 71 |
| No | 34 (94) | 33 (94) | |||||
| Contact with family | |||||||
| Yes | 27 (77) | 28 (78) | 1.04a | 0.59 | 0.34 to 3.18 | 0.949 | 71 |
| No | 8 (23) | 8 (22) | |||||
| Characteristic | Trial arm, n (%) | Analysis | |||||
|---|---|---|---|---|---|---|---|
| CTI (N = 41) | TAU (N = 44) | Odds ratio | Standard error | 95% CI | p-value | N | |
| Engagement with mental health services (care co-ordinator, care plan, medication) | |||||||
| Yes | 19 (59) | 20 (71) | 1.70 | 0.95 | 0.56 to 5.11 | 0.347 | 60 |
| No | 13 (41) | 8 (29) | |||||
| Care co-ordinator | |||||||
| Yes | 27 (68) | 25 (58) | 0.67 | 0.31 | 0.27 to 1.65 | 0.382 | 83 |
| No | 13 (33) | 18 (42) | |||||
| Planned contact | |||||||
| Yes | 12 (44) | 7 (29) | 0.51a | 0.31 | 0.16 to 1.66 | 0.267 | 51 |
| No | 15 (56) | 17 (71) | |||||
| Current care plan | |||||||
| Yes | 19 (50) | 21 (50) | 1.01 | 0.45 | 0.42 to 2.44 | 0.990 | 80 |
| No | 19 (50) | 21 (50) | |||||
| Currently under CPA | |||||||
| Yes | 19 (48) | 8 (20) | 0.27 | 0.14 | 0.10 to 0.73 | 0.010 | 81 |
| No | 21 (53) | 33 (80) | |||||
| CPA arranged | |||||||
| Yes | 6 (15) | 5 (13) | 0.81 | 0.54 | 0.22 to 2.98 | 0.751 | 79 |
| No | 33 (85) | 35 (88) | |||||
| Receiving medication | |||||||
| Yes | 33 (97) | 27 (96) | 0.82a | 1.19 | 0.05 to 14.02 | 0.890 | 62 |
| No | 1 (3) | 1 (4) | |||||
| Medication compliant | |||||||
| Yes | 28 (85) | 20 (74) | 0.51 | 0.34 | 0.14 to 1.88 | 0.313 | 60 |
| No | 5 (15) | 7 (26) | |||||
| Hospitalisation | |||||||
| Yes | 1 (3) | 2 (5) | 2.05 | 2.54 | 0.18 to 23.37 | 0.564 | 80 |
| No | 38 (97) | 39 (95) | |||||
| Referral to drug and alcohol services | |||||||
| Yes | 8 (27) | 8 (27) | 1.06 | 0.63 | 0.33 to 3.43 | 0.925 | 60 |
| No | 22 (73) | 22 (73) | |||||
| Employment | |||||||
| Yes | 3 (10) | 1 (4) | 0.36a | 0.43 | 0.03 to 3.77 | 0.394 | 56 |
| No | 27 (90) | 25 (96) | |||||
| Contact with family | |||||||
| Yes | 23 (82) | 20 (83) | 1.09a | 0.81 | 0.25 to 4.68 | 0.911 | 52 |
| No | 5 (18) | 4 (17) | |||||
Issues with fidelity
The contact forms and progress notes of the CTI managers during the engagement and early linking phase provided little written evidence that there was communication with, and/or visits to, housing providers, family or CMHT at two time points (across different CTI managers) (Table 11). This activity may have happened, but was not being recorded adequately.
| Fidelity items | Rating average (range) |
|---|---|
| Components | |
| Engagement and early linking | 2.87 (1–4) |
| Intensive outreach | 3.12 (1–5) |
| Care plans | 3.5 (1–5) |
| Focused work | 5.00 (5) |
| Monitoring | 3.87 (1–5) |
| Cases closed | 4.00 (1–5) |
| 6-week post-release contact | 3.62 (1–5) |
| Structure | |
| Caseload size | 5.00 (5) |
| Quality | |
| Intake assessment | 5.00 (5) |
| Phase planning | 4.87 (4–5) |
| Cases closed | 2.87 (1–5) |
| CTI managers role with client | 4.12 (2–5) |
| Clinical supervision | 4.00 (1–5) |
| Organisational support | 4.75 (4–5) |
| Total fidelity score | 4.04 (3–4) |
Overall, intensive outreach was well implemented. However, one CTI manager had very limited contact with clients in the community.
Care plans were well implemented for many, but there was limited evidence of creating care plans for clients at one site. Encouragingly, the rating for this item improved over time.
At one site, monitoring was rated as 1, based on the criterion that contact with the participants at the relevant phase should have been reducing but, because of the complex nature of the participants’ needs, contact with the CTI manager remained frequent.
Cases closed was rated low for some CTI managers, as many participants were still on the caseload after the 6-week (standard deviation ± 2 days) cut-off point.
Post-release contact at 6 weeks post release was rated low for one CTI manager because they had either lost contact with the client or the client had refused to continue to engage, before the 6-week point.
Closing cases, defined as making sure there was a clear transfer of care meeting with the client and services, was limited for some CTI managers and at different time points. Some CTI managers struggled to access other services’ information technology systems to ensure that notes were recorded or they were not part of a specific team and, therefore, again, had no access at certain clinical information technology systems.
When participants were engaged there was evidence that CTI managers were clear that care was ending but, for participants who struggled to engage, evidence of a clear ending was difficult to find.
Overall, clinical supervision was well implemented. However, for one CTI manager at one time point, no clinical supervision had been received and, for another, clinical supervision did not appear to be successful in correcting their use of inconsistent CTI principles, for example limited community contact.
Harms
In total, there were 10 SAEs during the trial, one leading to the death of a participant (see Figure 1) and nine resulting in periods of hospitalisation. Two were in the CTI group and seven were in the TAU group. None of the SAEs was deemed to have a causal relationship to participation in the trial.
Chapter 4 Trial participants’ and health professionals’ views and experiences of critical time intervention: a nested qualitative study
Introduction
Although still relatively uncommon, qualitative studies are increasingly used to complement RCTs of complex health-care interventions. 68 By exploring a range of stakeholder perspectives, qualitative research can provide an effective means of improving our understanding of key aspects of trial interventions and processes, such as the relationship between context and outcomes, thus providing insights that aid implementation. To gain a comprehensive picture of the perceptions and experiences of CTI, including barriers to, and facilitators of, its implementation, a nested qualitative study was conducted to explore trial participant and health professionals’ views and experiences of the intervention. The specific objectives of the qualitative study were to investigate:
-
trial participants’ previous and current experience of prison and through-the-gate support
-
trial participants’ views on the acceptability and experience of the intervention
-
health professionals’ experiences/views of CTI, with a particular focus on the barriers to, and facilitators of, implementation.
Although complementary, the two aspects of the study were conducted discretely and are thus reported separately. In the final section of the report, we examine similarities and differences between trial participants’ and health professionals’ perspectives, and comment on their implications for implementation.
Part 1: trial participants’ view and experiences
Methods
Recruitment and sampling
All trial participants were informed about the qualitative study at baseline and asked to give consent to being approached at a later time with a view to participating in this aspect of the study. Potential participants were purposively sampled to ensure maximum sample variation, specifically the inclusion of participants from each arm of the trial, both pre and post release, and across all sites. Consenting participants were first interviewed while still in prison and asked to give process consent to being invited for post-release follow-up interviews. Comprehensive contact details, including discharge addresses, telephone numbers (mobile and landline) and relative and friends’ contact details were taken to maximise the likely success of post-release contact.
Data collection
To provide insight into CTI from service users’ perspectives and to triangulate both health professionals’ views and quantitative findings, participants were interviewed at two time points: (1) within 3 weeks before release and (2) approximately 6–7 weeks post release. This allowed participants’ experiences and views to be tracked over time so that, alongside emergent perceptions and experiences, issues that were raised in the first (pre-release) interviews could be revisited 6 weeks post release.
For both (pre- and post-release) interviews, a semistructured interview schedule (see Appendix 4) was used to ensure consistency across interviews while allowing participants to raise issues that were important to them, but might not have been considered by the research team (Table 12). In addition, those who received the intervention were asked about frequency of contact with CTI managers, the support put in place by CTI managers, and to comment on what worked well and what did not. All interviews were conducted by GH and CS.
| Time of interview | Interview schedule items |
|---|---|
| Pre release | Previous experiences of support during release from prison (if applicable) |
| Issues/needs likely to be experienced on this release, for example health, substance misuse, housing, finances, employment and family | |
| Support from mainstream services intended to meet these issues/needs | |
| Receipt of treatment | |
| Views on available post-discharge support | |
| 6 weeks post release | Support needed in the community |
| Current well-being | |
| Current support received | |
| Receipt of treatment | |
| Views on support put in place | |
| Contact with the police | |
| Hospital admissions |
A total of 19 interviews were conducted with 14 participants: eight intervention recipients and six TAU recipients. Five people approached refused to take part in the interviews. Ten participants did not complete their post-release interview. This was either because they were uncontactable (n = 8) via the details taken pre release or because they refused to meet the researcher for interview when contacted (n = 2).
The majority of interviews (n = 15) were digitally recorded and documented using intelligent verbatim transcription. When prison establishments did not allow audio devices to be used, the researcher took brief notes during the interview and then expanded these immediately afterwards to minimise data loss and recall bias. Data were managed using NVivo version 10 (QSR International, Warrington, UK) software for qualitative analysis.
Data analysis
Data were analysed within a qualitative methodological framework. Owing to its systematic, rigorous and transparent approach, framework analysis has gained popularity in policy-related health services research. The framework approach allows for both deductive and inductive coding to be used concurrently, enabling important a priori themes or concepts to be combined with themes that emerge from the data. 69
The five key stages of this analytical process were as follows:
-
Familiarisation – two researchers (CS and CL) immersed themselves in the raw data by listening to recorded interviews, reading and rereading all interview transcripts and field notes, and making notes or ‘analytic memos’ on spontaneously arising topics of interest (inductive codes) as well as a priori (deductive) codes. One-quarter of the transcripts (n = 5) were also read by DE (qualitative supervisor) to ensure that all key codes were identified and that there were no significant omissions.
-
Identifying a thematic framework – developing the analytical thematic framework was an iterative process. A succession of analyses was conducted resulting in modification of the framework over time, based on resolution of the discrepancies between coders (CS and CL), indexing (coding using the themes and subthemes in the framework) and, subsequently, using the latest version of the framework to code across all transcripts. The first analytical framework drew on a priori issues based on the interview questions and phases of CTI (Box 1).
-
Indexing – this involved systematically applying the codes within the agreed analytical framework to code/recode all transcripts in the data set. CS and CL independently indexed the same five transcripts and met to discuss and agree codes and the coding framework. Coders, CS and CL, also met with the wider research team (JSh, JS, DE and AW) to further refine codes, for example subdividing complex or overlapping codes, ensuring that codes remained grounded in the original data. All data were then indexed by CS and checked for consistency by CL. Any disagreements were resolved by discussion and arriving at a consensus with the wider team.
-
Charting – data were entered into a framework matrix created by CS and CL. The matrix was a spreadsheet containing cells into which summarised data were entered. There were separate rows for each theme and separate columns for each group of interviewee, for example pre/post release and CTI/TAU. It also included participants’ direct quotations, providing a visual aid to improving organisation analysis and interpretation by establishing patterns within the data.
-
Mapping and interpretation – the matrix was then used to further refine codes into categories and to develop, define and discriminate concepts (themes and subthemes), ensuring that these encapsulated the full range of participants’ views. The data were finally reassigned to these themes producing interpretive concepts that describe and explain the final output of the data set.
-
Multiagency working and information sharing.
-
Establishing links with community services.
-
Accommodation.
-
Medication.
-
Money and benefits.
-
Substance misuse.
-
Employment, education and training.
-
Family relationships and social networks.
-
Physical health.
-
Life skills.
Qualitative findings part 1: participants’ views and experiences
Qualitative analyses were completed before analysis of the trial data to ensure that, although they could be used to interpret quantitative findings, the risk of introducing bias into the interpretation was minimised. Table 13 shows the five main themes that emerged from the data; the theme ‘support’ had three subthemes. In reporting, themes are illustrated with direct quotations. To protect confidentiality and maintain anonymity, quotations are identified only by timing of interview, pre/post release, and by group allocation, that is CTI or TAU.
| Theme | Subtheme |
|---|---|
| Uncertainty | |
| Support | Advocacy |
| Lack of continuity | |
| Reliance on others | |
| Accommodation | |
| Mental health and medication | |
| Stigma |
Theme 1: uncertainty
Conceptually, the ‘uncertainty’ theme reflected participants’ lack of clarity about post-release plans. Their accounts characterised the pre-release period as one during which they experienced increasing levels of stress, tension, worry and anxiety. Uncertainty about release dates is evident from this participant’s response to a specific query regarding his release date:
. . . about a month. But I’m going to court next week and it could be then. I don’t really know.
CTI, prison
This level of uncertainty made it virtually impossible to implement meaningful discharge planning:
I don’t know when I’ll actually be leaving and so I can’t tell people that and that means they can’t see where I can go because they [accommodation provider] won’t keep somewhere open waiting for me if I’m not actually going to be there.
TAU, prison
Among participants with previous experience of incarceration, the spectre of ‘release day’ loomed large. Instead of being a cause for celebration, their return to society was associated with anxiety about the likelihood of negative outcomes, as illustrated by this participant’s account of a previous release day, about how a lack of appropriate pre-release planning resulted in a ‘bad’ release day and ‘things going off track’ from the outset:
My brother picked me up and we had to go to bail hostel but we said we’d go for breakfast first. I felt agitated when I left, but my brother wasn’t there so if I’m honest I went for a beer, yeah. Just wanted to see what it was like.
CTI, prison
Indeed, some participants found their experiences so stressful that they considered reoffending in order to return to prison:
People get nervous when they’re going to go. You leave and you want to turn around and walk back in. Or do something to get back in. I don’t want to be like that though. You know, prison is tough, and the outside is tough too really. But I want to move on.
CTI, prison
In contrast, CTI appeared to have alleviated some participants’ uncertainty and associated anxiety for their upcoming release:
Most things were sorted and everyone knew when I was leaving so yeah I guess you could say ‘integrating’.
CTI, community
I found it easier with the CTI manager. I was getting help that didn’t get before and found everything less stressful. It’s a big help.
CTI, community
Theme 2: support
This theme also contained three related, but distinct, subthemes (‘advocacy’, ‘lack of continuity’ and ‘reliance on others’), each of which is explored in subsequent subsections.
In general, participants in the TAU group were more likely to characterise their current experiences as lacking in support. Those with previous experience of prison and expecting their upcoming release spoke candidly about services that, from their perspective, seemed to lack coherence or focus on the needs of prisoners and recently released individuals:
As far as I’m concerned I’m not in touch with any services. They come and ask questions then just go off and you don’t know who they’re speaking to or who you’re meant to speak to when you get released. That’s how it is, you might get a bit of information when you leave but it all seems to happen between them and not with us.
TAU, prison
No one helps with that [benefits] it’s down to you. You get the forms when you go and you sort that out when you can. Well like I’ve been saying, it’s rubbish isn’t it. There isn’t really any support. You just have to sort things yourself and try and work out whether people know you’re coming out or where you need to go. And it’s always like that.
TAU, prison
This contrasted sharply with participants in the intervention arm. CTI recipients predominantly reported receiving positive support from their CTI manager. Significantly, this support was available at various stages, including pre release:
I’ve been a bit stressed actually, and that support is good. With [CTI manager] I feel like I get seen more. Which I think I need before I go. Just to make sure.
CTI, prison
On the day of release:
[CTI manager] was there waiting outside the gate because I’d told her when I would be released. And she’d checked where we need to go so we could get the train and then the bus over to this hostel together. That was something I was worried about because I get so anxious about being on buses, being with other people in public. I think it would have been too overwhelming but [CTI manager] was there saying it’s OK.
CTI, community
And in the community:
I would have struggled to sort everything and go to appointments on my own as I’d forget.
CTI, community
Critical time intervention managers were also credited with trying to help people reintegrate into their communities:
I’ve been saying I want to get back into doing good activities and [CTI manager] gave me the details of some football teams for people who have problems like me. Like mental health problems or they’ve been in prison. So I want to start doing that. And he showed me how I can join a gym too.
CTI, community
According to this participant, immediate and ongoing support from the CTI manager both reduced the risk of reoffending and provided a realistic hope of a future outside prison:
Well just to say that this thing has been pretty good for me and it definitely has helped. [CTI manager] has helped me a lot and I reckon now I’ve been out this long I can keep it up. You know don’t you that I was in 8 years because of that one thing which was a long time and now I’m looking forward to staying out.
CTI, community
Advocacy
An emergent subtheme was the notion of advocacy. Participants reported that CTI managers, acting as advocates on their behalf, had been instrumental in improving access to services:
Yeah he’s [CTI manager] talked to them and I think he’s explained the situation that I keep getting told I don’t need help. And he said he’d refer me like normal but then he’d be able to come with me. And that’s going to make a difference isn’t it because it isn’t just a con coming to the office saying they need help, you’ve got someone who knows how things work saying this guy needs med[ication]s and needs to be seen that then they’re going to listen. You know what it’s like, when you get a probation officer they force the council to give you a hostel and the council knows they can’t say no to probation like they can say no to you.
CTI, prison
She arranged with probation to come here. She arranged when I could go to the community team. I think that kind of stuff, talking to people and making sure things get done.
CTI, community
Participants felt that advocacy was essential, as services rarely understood their needs:
But you and them don’t get it. You haven’t been in my position but you all think you know what I need. So it’s that too they won’t send you for the help you actually need.
TAU, prison
Lack of continuity
Participants in the TAU group frequently reported a lack of continuity both between and within services. This was most evident at the point of release:
. . . sometimes I don’t think they’ve realised you’ve gone. If you go from court not from prison sometimes you talk to the treatment team and no one has told them you’re out. Even if you want them to contact you they won’t know to.
TAU, prison
For this participant, who had been imprisoned several times, lack of continuity of care was directly correlated with reoffending and reimprisonment:
I get told I need this service or that service, then I go there and they change their mind. They’re always promising this and that and then it never happens does it. And that’s what always happens. I’ve been released so many times and this or that was meant to happen and it never does and I just end up back in here.
TAU, prison
The accounts of those receiving CTI suggested that the level of support and continuity of care compared favourably with previous incarcerations:
I think I’ve had a lot more help. I’m not sure whether that’s to do with your project but I think it might be. Things have gone a lot smoother than they ever have before. Like having that hostel and I had a CMHT worker visit me within a couple of weeks and make sure things were going fine, and seeing a doctor too.
CTI, community
Things have been more planned. Last time, I had that thing where I had loads of probation officers. My community team were pretty bad and they just gave me drugs, that was it. But this time it was more planned. I actually had one person who I needed to see and they were better at seeing me. [CTI manager] has seen me there [prison], seen me here [community], she can explain a lot more to them. She knows me better. And I don’t want to have to keep meeting new people but she was helpful being there.
CTI, community
Reliance on others (family relationships)
Participants reported receiving mostly practical compared with emotional support from family members. This was most apparent in relation to providing accommodation. However, this was often the source of tension as the individual transitioned back into their families and wider community:
My mum doesn’t like me drinking and we do argue about that and it’s none of her business. But I guess I do live there.
CTI, community
There have been some problems there and I have spent a few nights out as well. But that was in the first weeks and I’ve settled down a bit and got used to being with them again now so that hasn’t happened recently.
TAU, community
Participants in both arms of the trial reported reliance on their families for financial support. This was frequently needed because of delays in receiving benefits, which left individuals short of funds:
Yeah I’ll get some benefits but it isn’t much. And this is bad but I’ll have to rely on my mum won’t I? Because it takes a bit for benefits to come in. But it isn’t like I have rent or something, that’s when it’s more tough. Like I have friends who have flats or whatever and doing rent on benefits that’s what’s tough.
CTI, prison
Some participants found financial reliance on others very difficult. They reported that this was a source of embarrassment as well as signalling their lack of independence:
Yea that’s a problem. I’ve only just got my benefits back. My family can give me money, which I don’t like to do because that’s their money. I should be living by myself and I did used to. But they can help, they give me money for travel otherwise I can’t get nowhere.
CTI, community
Well, benefits obviously, but they don’t come in for about 5 or 6 week, I don’t think. That’s what I got told anyway. So I expect my family will give me a bit here and there. Yeah well it would be a problem. What am I going to do if I’ve got no money? I don’t thieve anymore, I stopped that years ago. And you know, it’s a bit embarrassing asking my little brother for money, puts on them a lot.
CTI, community
Financial dependence also served to reinforce a sense of ‘otherness’ and deviance in comparison with siblings who had not been to prison:
My brothers come round and they have jobs and the like and I’m the one who is staying with my mum. I’m the odd one out, the black sheep, and I’m the oldest too, I’ll just tell you that. They’ve all got houses, all got jobs, and I’m in prison.
CTI, community
Although families were cited as sources of practical and financial help and support, participants reported that they were ill equipped in terms of providing support with mental health problems:
My mum and dad do most things but maybe someone who knows more about the voices and mental health so they could talk to me and make sure things are going ok . . . to be honest, this whole mental thing is affecting that [family] because they’re getting stressed with it as well and it’s not good for our relationship.
TAU, community
Theme 3: accommodation
Accommodation (in particular uncertainty about accommodation on/post release) was an issue not only in its own right, but also one that impacted on other areas, as exemplified in earlier reports about support and reliance on others. Participants in both arms of the trial voiced concerns about both the availability and suitability of accommodation:
They [hostels] aren’t even that much better than prison. You can go out during the day I guess, but that’d happen on day release anyway. But the rooms aren’t good and you know the people here. They take drugs, they drink. Which I do too. But we shouldn’t be all together should we. Load of mad men all together. It’s not a good idea.
CTI, community
This was especially the case when accommodation had to be shared with others with similar problems, chiefly mental health and substance misuse:
I don’t like being around people with symptoms because it makes me worse. Like in the hostel, if you have someone who’s got symptoms it makes you worse and I don’t want to be around that.
CTI, prison
Participants felt that securing accommodation was a vital part of the resettlement process as lack of suitable accommodation was regarded as a key aspect of being able to access services:
Well because you leave and you need somewhere to sleep that first night out don’t you. And then that gives you a base to plan everything. You can’t be homeless and getting benefits and getting letters from people and your probation knowing how to see you. If you haven’t got that then you’ve got no hope.
TAU, prison
In addition, experience had taught them that a lack of accommodation increased their risk of reoffending and incarceration:
I’ve done this so many times and if you don’t have a hostel then that’s it you’ll be back in a week. That’s why I keep coming back, you don’t get somewhere to live you don’t have any chance.
TAU, prison
However, some participants reported that living in hostels had increased their access to services, some of which were available on site:
That’s the reason they put me here because the CMHT workers come here and they see everyone who needs to be seen rather than you having to go to them. It’s better. It means I don’t have to be going to their building and waiting around I can just come down from my room and see them.
CTI, community
Theme 4: mental health and medication
All participants talked about their mental health problems and symptoms. In particular, they talked about how poor mental health disrupted function and prevented them from working:
Because of my mental health, I don’t have to work. That is fair I think. I mean you can’t be working and thinking you’re hearing voices or something. That doesn’t work does it?
CTI, community
I can only really work when things aren’t too bad. There are days when I can’t get out of the house so then I can’t be in a job where they expect me in at the same time every day.
TAU, prison
Participants in both intervention and control groups talked about medication in relation to their mental health. Some individuals reflected on the positive impact of medication on their lives:
Well just medication to keep me on the level. Keep me grounded like. And that’s all really. I can cope pretty well with that.
CTI, community
Others felt that, without high levels of professional support, they would not be able to continue to take medication on a regular basis. Reinstitutionalisation, to either hospital or prison, appeared inevitable:
It’s going to start going downhill because you either don’t take your medication or when it runs out you stop and then there’s no going back. For me when that happens I’ll end up in prison or hospital.
TAU, prison
A more common theme in participants’ narratives was a sense of coercion in relation to medication:
They always think they know best. They’ll tell you ‘you need this or that drug’ and everything you think is wrong but I can sort myself out.
TAU, prison
Tablets for what they say is schizophrenia but I don’t always take them.
TAU, prison
Participants also protested about the unavailability of other treatment options, in particular a lack of psychological therapies:
They push me to keep taking these drugs and saying I can’t have this or that therapy or services. I don’t want that, drugs and psychiatrists, I want them to get me into counselling. I need counselling, that’s what would help me. Because I’ve been through so much, I don’t just need the drugs, I need someone to sit and listen to me and help me through this.
TAU, prison
Participants seemed to suggest that CTI was providing them with more support around mental health than previously:
All it was, yeah, was an injection. I’d go there, they’d do the injection then I’d go. No psychiatrist or no talking or anything. This time they reckon I’ll have a CPA in first 2 weeks so that’ll be better. I’m hoping everything goes right with the CPA. I needed support. For mental health mainly. And that’s been there this time. I feel very positive about the future now. It might not seem big to you or anyone else but [CTI manager] she’s been really helpful.
CTI, community
Theme 5: stigma
Participants’ accounts highlighted their feelings that the stigma of being an (ex)-offender permeated every aspect of their lives. They reported that stigma negatively impacted quality of life, hindered their job prospects and increased the risk of reincarceration:
There’s no chance of anyone employing me, is there? Why would they [employ me]? They’d find out I’ve been in prison and that’s it. Not even a chance.
TAU, prison
Almost 10 years in prison, I don’t have any chance of a job, do I?
CTI, community
A job isn’t an option with me being like I am and the history I’ve got.
TAU, prison
Participants reported that the stigma associated with being an offender not only impeded job prospects, it also had serious implications for access to their children:
I’m pretty gutted about this but I don’t know whether I can see my lad. That gets to me and I’m sad about that but maybe I just have to accept it. I don’t mean not think about him, I don’t want you to think that. But that I won’t be able to see him like I hoped. I’d have to go to court but I don’t think I can do that. I don’t know how I’d do that. And they’d see me wouldn’t they? Ex con[vict]. They aren’t going to like me are they?
CTI, community
Participants also reported self-imposed stigma in relation to mental illness, often keeping them from disclosing difficulties and from seeking mental health treatment in prison. This participant’s account typified the views of others. When asked about now receiving mental health support in prison, he replied:
Yeah, first time, in here, I always just kept it quiet, the voices and that, and self-medicated, because my idea of mental health and shrinks was that they’d put you in a straitjacket in a hospital and that would be it.
CTI, prison
It is noteworthy that the support this participant had been receiving from the CTI manager appeared to be changing his views of mental health treatment:
Yeah, they’re alright yeah. That guy who’s left seemed like he knew what he was doing, and that tall guy, dresses smart, he’s OK.
CTI, prison
Summary
There were commonalities and differences between participants in the CTI and TAU arms of the study. Commonalities were most apparent in participants’ reports of their reliance on others for practical help, particularly in terms of accommodation and financial support. The former was regarded as a potential source of tension within families, which had the potential to trigger reoffending. Financial reliance on families reinforced self-reported perceptions of being seen as ‘other’ and deviant. Embarrassment at needing financial help, particularly when received from siblings, increased the risk of reoffending. Both CTI and TAU participants stated that a lack of suitable accommodation had serious implications for reoffending. Similarly, not having a permanent address restricted access to benefits and services. Sharing accommodation with other (ex)-offenders and people with mental health and substance misuse problems increased participants’ vulnerability to resuming involvement with drugs and alcohol as well as putting their mental health at risk more generally. In both cases, participants indicated that this increased the risk of reoffending. Both groups of participants reported feeling coerced into taking psychotropic medication and expressed disappointment that there was a lack of access to psychological interventions. This, together with stigma, caused some participants not to disclose their mental health problems to professionals.
There were, however, differences between groups. Most notably, members of the CTI group who had experienced previous incarcerations reported less uncertainty and a sense that on this release care would be more integrated; this was linked to reduction in stress, anxiety and potential for reoffending. The CTI group also reported better continuity of care and improved access to services attributed, at least in part, to CTI managers advocating on their behalf. From these participants’ perspectives, there was a direct correlation between improved discharge planning, increased levels of support, greater continuity of care provided by CTI managers and a reduction in the likelihood of reoffending.
Part 2: health and care professionals’ views and experiences
Methods
Recruitment and sampling
To complement data from trial participants, three of the five CTI managers were recruited to participate in interviews. In addition, other health and care professionals, not delivering CTI but involved in supporting participants either in prison or in the community, were invited to take part. Although 12 were approached and agreed to participate in interviews, ultimately only five interviews were undertaken with professionals. The remainder were either unable to commit to a time for interview because of work pressures (n = 5) or did not respond when followed up (n = 2).
Data collection and analysis
Professionals were interviewed face to face at their place at work using a semistructured interview schedule (see Appendix 5), administered by GH and CS. This approach enabled the interviewer to focus on key areas of interest, specifically addressing the study aims and objectives. Table 14 provides an overview of the main topics covered by the interview schedule.
| Type of interview | Topic guide |
|---|---|
| Professionals | Discharge planning (pro/cons) |
| Multiagency working | |
| CTI (pros/cons) |
Adopting the approach described above regarding patient participants, interviews were digitally recorded, transcribed intelligent verbatim and analysed using framework analysis. The coding frame incorporating both a priori and emerging themes was developed and all transcripts.
Qualitative findings part 2: health and justice professionals’ views and experiences on critical time intervention
Two main and eight subthemes emerged from the data (Table 15). These will be presented using health and justice professionals’ verbatim quotations and, as with trial participants, quotations are assigned only to professional roles to preserve anonymity and confidentiality.
| Theme | Subtheme |
|---|---|
| Liaison | Collaborative care |
| Information sharing | |
| Gate keeping | |
| Resources | |
| Transition | Relationships/support |
| Accommodation | |
| Temptation/association | |
| Endings |
Theme 1: liaison
Health and justice professionals’ interviews highlighted the importance of liaison between individuals and agencies if interdisciplinary approaches were to prove effective. Within this overarching theme, there were four subthemes: collaborative care, information sharing, gate keeping and resource.
Collaborative care
Collaborative care is a key component of delivering person-centred care. Depending on the complexity of needs of the particular client, successful release planning might involve several agencies and services. However, the level of planning and interagency collaboration can vary greatly depending on geographical location:
There are 30 plus London boroughs I think? 32 or 36 something like that and there are prisoners from each of them, so therefore that means that we have to have in excess of 30 working relationships with different boroughs and with the various teams inside them, so that can be a bit challenging.
Consultant forensic psychiatrist
Although some services and agencies demonstrate high levels of collaboration, this was by no means universal, even when services espoused an interagency/multidisciplinary approach:
They’ll just get a letter to the GP and CMHT. There won’t be any chasing and whether it’s followed up, you don’t know.
CTI manager prison mental health nurse
Everything mental health related usually goes through the SPA first though. This is the gateway between primary and secondary care services. This doesn’t cover some specialist services though and generally includes CMHTs, the crisis team, home intensive treatment team, adult psychology services and links to acute psychiatric wards.
CTI manager (mental health nurse)
The collaborative care process also requires health and criminal justice organisations to work together, which is not always successfully achieved. This quotation illustrates health professionals’ frustration about their inability to deliver collaborative care when other agencies fail to consider the need for effective planning and collaboration to ensure that services are in place post release:
One of the difficulties we sometimes encounter is the prison service does not do ‘joined-up thinking’ and they are not involved really in the planning of the aftercare. Very often they will, for arbitrary reasons, transfer a prisoner to another prison with no notice whatsoever and that makes it very difficult then to follow up and ensure that services are following them and planning for their release.
Prison liaison specialist
Professionals’ perceptions of disjointed pre-release planning, resulting from little or no communication and interdisciplinary competition instead of teamwork, were reflected in their concerns about the potential for individuals to fall through the gaps between services:
There just tends to be a real lack of engagement. And you never, you know, you’re always slightly anxious whether actually they are going to pick that person up and are they going to see them. And, you know, and will they assertively try to see them rather than offer them an opt-in letter, you know.
Lead prison mental health nurse
I think the problem is endemic now with this notion of everybody has to compete where really it is not in anybody’s interest, it is all about the bottom line, it is not about the quality of care, you can tick boxes, you can go through any exercise and people look for ways to fake the results basically and that is not helping anybody at all. I think that they have got to get rid of this internal competition.
Prison liaison specialist
Despite these challenges, interviewees remained committed to working within the principles of collaborative care, acknowledging that the approach is essential for ensuring continuity of care between prison and community. However, they cited lack of resources as a major barrier to doing so:
[I]f we had the capacity then I think prison staff could actually go and visit community teams individually and present to them and try and sort of network and engage with them more and offer them, sort of, slots to come into the prison to spend time with the outreach team. I think that would work really well.
Lead prison mental health nurse
Information sharing
A lack of information sharing was identified as a major contributor to gaps in service between prison and community, as highlighted by these accounts of the impact on the referral process in general and medication in particular:
If you get that clear information with reasoning and detail on why this referral is being made that helps. But often it’s just a pro forma letter without very much detail and then you’re working out from an assessment whether this person is for the service and if they aren’t giving a full account you have to chase other people for more complete records.
Community psychiatric nurse
Sometimes medication information needs to be shared better between services (e.g. how much medication someone has been released with). Overmedication can be dangerous.
CTI manager (mental health nurse)
Lack of information sharing was sometimes because patients exercised their rights to withhold permission for information to be shared with other agencies:
[V]ery often a prisoner will not wish mental health services to communicate with their legal team and very often they forbid their legal team from talking to us which compromises their own future and safety.
Prison liaison specialist
However, there was also evidence of information not being shared because of professionals’ fear of breaching information governance rules, specifically the Data Protection Act 1998:66
They are highly fearful that they will pass on information that they shouldn’t, that they will do it by a means that is insecure.
Prison liaison specialist
As well as affecting care quality and patient safety, a lack of information sharing was perceived as having implications for public safety. This was particularly the case if individuals identified as being at high risk were falling through the gap between prison and community services:
We had a guy that was very high risk, he was, sort of, level 2 MAPPA [multiagency public protection arrangements], he’d served a long sentence, and there was difficulties pre release in terms of the community team saying they hadn’t received the referral and then sending it again and then they did receive it and then we assumed that they’d picked him up but then it looked like they hadn’t picked him up and, you know, who was taking responsibility?
Lead prison mental health nurse
Note that multiagency public protection arrangements (MAPPAs) are in place to ensure the successful management of violent and sexual offenders. MAPPA offenders are managed at one of three levels according to the extent of agency involvement needed and the number of different agencies involved. The great majority are managed at level 1 (ordinary agency management). This involves the sharing of information but does not require multiagency meetings. The others are managed at level 2 if an active multiagency approach is required (multiagency public protection meetings) and at level 3 if senior representatives of the relevant agencies with the authority to commit resources are also needed.
This case illustrated an important feature of CTI, namely the value of there being an individual well acquainted with all aspects of the client’s care at the centre of the collaborative care process. In this instance, CTI was able to ‘plug the gap’, thereby helping avert potentially serious consequences:
This was a CTI guy and it did get resolved. Otherwise, we wouldn’t have known anything about it, we certainly wouldn’t have been able to follow him up and it would have been very unclear who was going to follow him up and I think potentially things could have gone really horribly wrong there.
Lead prison mental health nurse
Gate keeping
Echoing trial participants’ views, staff spoke about difficulties of getting patients accepted to services as thresholds of clinical need/urgency were being raised and entry criteria becoming increasingly strict:
CMHTs are very selective and it’s difficult to get followed up.
CTI manager prison mental health nurse
If someone has been on the caseload in the past, we might accept them before they’re released because we can be fairly sure they meet our criteria, but if we have no knowledge of someone or we do but they’ve been discharged in the past then we’d need to arrange an assessment on release where we’d consider the notes from the prison team but also be making judgements about do they need to be accepted or can this be managed elsewhere.
Community psychiatric nurse
Somewhat counterintuitively, participants reported that there was no culture of gate keeping per se within services; rather the phenomenon was often because of individual practice:
I believe that by and large it is individuals rather that agencies that are perhaps more responsible for the gate keeping. It depends on sometimes the managers, of course, they tend to take the view that they are protecting a beleaguered staff which I find is not the best way of dealing with things.
Prison liaison specialist
Whether at individual or organisational level, the practice of gate keeping was perceived to be commonplace and firmly entrenched. This has implications for the implementation of CTI. The effectiveness of a CM model based on liaison with, and referral to, services will be reduced if, as a means of managing resources, thresholds continue to rise and entry criteria become more difficult to meet:
I think that there are certain cultures of gate keeping out there that will not be budged or not impressed by it [CTI] and not want to actually fall in with it.
Prison liaison specialist
Resources
Variations in through-the-gate services were perceived to be a result of resource issues. Some staff reported feeling increasingly overstretched and under pressure. In these circumstances, individuals described being unable to deliver the quality of care and support that they would like to offer:
I don’t mean to sound like we’re passing the buck or not wanting to engage, but everyone is under pressure, none of us have all the time to do what we’d ideally do or what might be strictly best practice, and I’m sure the prison teams or whoever else will tell you this too. There just isn’t the time to get all this done.
Community psychiatric nurse
Well, the in-reach team don’t have that much time for discharge planning really, because there’s 80 people on the caseload so they need seeing and there’s always people coming in who you have to treat as higher importance because you don’t know what you’re dealing with.
CTI manager prison mental health nurse
Service restrictions resulting from limited resources appeared to disproportionately affect availability of community services, especially in relation to the release planning process:
Certainly much more engagement from community teams prior to release. You very rarely find any community nurse, I understand that there’s pressure on them in terms of their time and they have large caseloads, but they very rarely come into visit prisoners whilst they’re with us and very rarely turn up as part of the CPA. And there just tends to be a real lack of engagement. And you never, you know, you’re always slightly anxious whether actually they are going to pick that person up and are they going to see them. And, you know, and will they assertively try to see them rather than offer them an opt-in letter, you know.
Lead prison mental health nurse
In this context, although perceiving CTI as having a potentially pivotal role in delivery of collaborative care, participants questioned whether or not the required resources would be made available:
Well, the major question is who’s going to pay for it isn’t it? When budgets are being cut I’m not sure who’s going to have the money to fund that and keep it going. But if someone is willing to then great, some extra help is something we’d all be open to.
Community psychiatric nurse
Theme 2: transition
Importance of relationships/support
Imprisonment is difficult for anyone; for those with mental health problems, it can be especially challenging and transition back to the community particularly difficult. Professionals expressed the view that having someone to support the client through this transition can mean the difference between success and failure:
A familiar face is massive. Seeing [the] same person really reduces anxiety. They feel supported and like they’re not going out on their own. Expecting clients to find their own way and meet all the new people can be a big ask, especially when they have a lot going on.
CTI manager (mental health nurse)
However, levels of release planning and resettlement support were reported to vary greatly, with some individuals having no support at all:
The people it works worst for I can say is people in prison who have no input and then they come out and no one knows who they are and what their situation is. They can be quite psychotic and have been for some time and no one has picked that up. I do wonder how in the prison atmosphere where you’re being monitored, how that is missed, but it does happen.
Community psychiatric nurse
If somebody is lucky enough to have a diligent care co-ordinator that will follow them in [to prison] then all well and good, things go swimmingly. When it doesn’t or if it is a difficult and perhaps unpleasant individual they may have a bumpier ride and they will get no service really because they will find themselves with nobody willing to particularly help them, or if you get someone who can draw a marvellous care plan but it is largely a work of fiction then they are worse than useless, they are dangerous in fact.
Prison liaison specialist
In the absence of effective through-the-gate care, it can fall to families, specifically parents, to provide the transitional support required. However, some individuals have never had good family relationships. Relationships with others might have deteriorated because of offending and imprisonment, resulting in:
. . . fractured family units because of that period of exclusion and being away from either the partners or from parents.
Community psychiatric nurse
Even where positive family relations exist, these may become strained in the early ‘post-honeymoon’ phase of resettlement:
One thing I might say is whether there’s maybe a honeymoon period after release and it’s after 6 weeks that the major problems start. That’s just a hunch but their families might be glad to have them back, maybe they can handle drugs and alcohol for a short while before that causes an issue too.
Community psychiatric nurse
Critical time intervention is aimed at bridging this service gap via liaison with appropriate services and supporting the service user through the initial engagement phase. This seamless plugging into services should also remove some of the pressure from families. Professionals involved in the release-planning process felt that CTI achieved this aim:
Well I mean it [CTI] sounds ideal in many ways because you have a tangible, physical link, a person you know before and who follows you out.
Prison liaison specialist
It’s exactly the kind of thing that’s going to fill that gap between what the prison teams do and what we do. And it’s targeting that first period where we might struggle to pick people up.
Community psychiatric nurse
Critical time intervention managers also saw the real benefits of the intervention:
CTI is a good extension of normal services and can help people more seamlessly into the community.
CTI manager (mental health nurse)
Well, release is a big thing for inmates. I think a lot of the time they are really lost. They don’t know what’s happening, and they don’t know how to go about it. CTI is really about helping them in that period.
CTI manager prison mental health nurse
Accommodation
Endorsing trial participants’ views, health professionals stated that securing suitable accommodation was arguably the number one priority for many released prisoners because it establishes a stable base from which to address other resettlement concerns:
If they’re going to be homeless then that’s a real problem. Services always insist on an address.
CTI manager prison mental health nurse
Professionals also linked a lack of accommodation with reoffending:
If someone is more or less sofa surfing then it’s a matter of time before they’re going to commit an offence.
Probation officer
Lack of accommodation was also linked to exacerbating mental health problems:
If you go out [of prison] to homelessness then how could you possibly look after your mental health? People need some form of stability there to enable mental health needs to be met.
Consultant forensic psychiatrist
Mental health isn’t always the priority for released prisoners, housing and money is. If these aren’t addressed properly then mental health states can be made worse.
CTI manager (mental health nurse)
In this context, interviewees reported that the process for housing applications was seriously flawed:
I think housing is the biggest problem and really that system works really badly. When someone’s released they need somewhere to sleep that same day. We’ve sat at the council with people until 8 p.m. just waiting to see if someone has a hostel that night or not. Where we’re working homelessness is a massive problem so these places can be quite full and I think people who’ve just come out of prison probably aren’t a priority. So that’s an issue, I think they should be processing applications before release and not just say when someone comes out they haven’t got any places.
CTI manager prison mental health nurse
In common with trial participants’ views and experiences, professionals also reported the need to advocate on behalf of clients for them to gain access to services:
Councils dismiss these people very quickly. If I go with them then I’ll say to them OK go to talk to the person, but I have to step in and explain the situation and then councils will do something. I think prisoners on their own will find it quite tricky and won’t get very far.
CTI manager prison mental health nurse
Finding suitable accommodation can also be hindered by certain licence restrictions:
If you’re working with some of the people with serious group offending, which is pretty common now, you can’t often go back to families or can’t often go back to local areas because they’ve got exclusions. Same goes for those who’ve sexually offended. They might have restrictions.
Probation officer
There were quite a lot of hostels contacted but there were conditions that he couldn’t live so close to places where children were.
CTI manager prison mental health nurse
As well as licence restrictions, a client’s reputation with housing services may be a major barrier to obtaining accommodation:
It is difficult unless they have some kind of working relationship with housing or if the prisoner hasn’t blotted their ticket basically.
Prison liaison specialist
He’d lived in so many hostels, and caused trouble and so he’s banned from a lot of them.
CTI manager prison mental health nurse
Temptation/associations
The initial period following release can be very important for people with substance misuse issues. Incarceration might have removed/reduced access to illegal substances and social networks associated with their drug or alcohol problems, but this access can be reinstated on release. Coupled with the stress of community reintegration, (ex)-offenders can quickly lose any progress made in prison:
. . . 6 weeks basically after coming out. I mean those can be 6 very busy weeks and very frustrating weeks and that’s when people become tempted to drink or drugs and they can start sliding back into bad old ways . . . once under the influence of their peers and the drugs and the alcohol how quickly things spiral out of control.
Prison liaison specialist
The risk of ‘sliding back into old ways’ was exacerbated by being allocated unsuitable accommodation:
For example, someone who’s got substance misuse issues and mental health issues placed in the hostel with other users and things like that and it can be setting them up to fail quite a lot.
Probation officer
They can take quite a slide down the social ladder in many ways and be at a disadvantage and in with other people that have exactly the same problems regarding drugs, alcohol etc. it [hostels] tends to be a ghetto basically, a dumping ground for people with mental health and alcohol problems.
Prison liaison specialist
Coupled with unsuitable accommodation, a lack of appropriate daytime activities was also seen as contributing to the potential return to old habits:
I think also if they have something productive it helps, they have a path to follow. Otherwise I think they end up just hanging around, they get bored. If they go to a hostel that’s full of drugs then they’ll fall into that trap.
CTI manager prison mental health nurse
Endings
Professionals recognised that the ending of any episode of care or therapeutic engagement needs to be prepared for and properly managed, and the same applies to CTI:
Yeah, I mean I think potentially for both the CTI manager and for the patients as well I think actually that disengagement process can be difficult. If you’ve worked with them for a, sort of, significant period of time, you might have been their care co-ordinator in prison or known them for a number of years and yeah, I think that disengagement can potentially be difficult.
Lead prison mental health nurse
Some staff felt there was potential to create dependence on CTI:
Maybe with patients, because of their character, they can actually become quite dependent. Every little thing they’ll be calling and in contact with you and maybe then when they get to 6 weeks they’ve got used to that and can’t do things for themselves.
CTI manager prison mental health nurse
Others felt that, if managed appropriately, disengagement need not be problematic:
If you were clear about the limits of what you’re doing I’m not sure that would be a big issue. Our clients are usually too high intensity for this but, if you think about IAPT [Improving Access to Psychological Therapies], it’s clear that that isn’t an open-ended service so if you’re clear then I think that would be OK.
Community psychiatric nurse
A member of the prison-based staff suggested that a step down in intensity might be more appropriate than a 6-week cut-off point:
In terms of the 6-week point, I mean obviously we’d like it to go on forever but I think being realistic I think 6 weeks is probably sufficient. It’s just . . . there would need to be something in place for the next point. I mean, it may well be that you have a person who is now quite capable of going to every appointment and doing things for themselves and a significant improvement in mental health but you could also have that person at 6 weeks who is nowhere near that.
Probation officer
This view point was endorsed by one of the CTI managers who felt that clarity and flexibility in terms of endings should reflect individual’s needs and varying contexts:
The CTI period should be flexible as people have different circumstances. Needs to be long enough but if too long then this can also create some dependence in the service user. You need to be really clear and open about disengagement.
CTI manager (mental health nurse)
Summary
Perhaps unsurprisingly, the emergent themes from professionals’ narratives indicated a preoccupation with liaison, specifically the extent to which collaborative care was being realised in everyday practice. Participants reported barriers to effective planning and delivery of services as linked to increasingly limited resources. This had led to the raising of thresholds for gaining access to services and more robust gate-keeping on the part of individuals, rather than necessarily being indicative of service culture.
Perceptions and experiences of CTI were positive. However, interviewees raised concerns about the availability of funding to roll out services, highlighting the considerable variation not only across the country, but also within localities such as London. Given that best practice suggests that service users should receive individualised care that is tailored to meet their discrete needs, participants wondered whether or not this was possible in the context of a manualised ‘Improving Access to Psychological Therapies-like’ approach to service, characterised by the delivery of a predetermined number of sessions, compared with a needs-led model, incorporating time to build and appropriately disengage from therapeutic relationships with CTI managers.
Supportive relationships, such as those provided by CTI managers alongside family and friends, were regarded as vital for effective transition from prison to the community. However, participants reported that these could not make up for shortcomings in more practical and essential aspects of care, specifically with regard to accommodation. In common with service users, professionals frequently complained about the lack of suitable accommodation, highlighting the increased risk of reoffending and exacerbation of mental illness within this vulnerable group caused by unsuitable housing.
Chapter 5 The case manager manual
To support the CTI case manager in the delivery of the intervention, the manual developed as part of the original CTI study46 was revised to reflect the adaptation of the intervention for use with the prison population included in this trial. A copy of the manual is included in Appendix 1.
The manual includes an introduction to the development and aims of the original CTI study; how the original model has been adapted, that is from a three- to four-stage intervention for mentally ill prisoners (see previous chapters); and the theoretical underpinning to the method(s) for interacting with service users and for developing good working relationships. The manual also presents some scenarios to stimulate reflection on situations the CTI case manager might encounter while interacting with the service user and practical advice in the form of ‘Notes’ (or tips) for consideration when planning or reviewing the mental health and social care that the service user needs.
As part of the evaluation of the trial, the mental health professionals that had acted as CTI managers were surveyed informally on how helpful the manual had been in guiding the implementation of the intervention day to day. These comments were fed into an independent review of the manual undertaken by a small working group comprised of research team members, colleagues from prison in-reach teams not involved directly with the trial and experts by experience.
The working group met on three occasions, with meetings focusing on whether or not the contents of the manual were clear, relevant and, importantly, covered the range of issues related to community reintegration that the experts by experience had considered most important at the time prisoners had faced release and resettlement. Similarly, experienced prison in-reach colleagues on the working group were able to comment on whether or not the manual provided sufficient professional guidance to enable them to assume the case manager role. The group also agreed what kind of practical information for embedding the intervention into a service might be helpful and how to monitor that the intervention was being implemented as intended.
Chapter 6 Health economics evaluation
Introduction
The health economic component of the Critical time Intervention for Severely mentally ill Prisoners (CrISP) study aimed to measure and compare service use and costs between the two study groups. Further aims were to assess the link between costs and outcomes, and to identify predictors of cost over time.
Methods
The approach taken in the economic evaluation was similar to previous studies. The objective was to measure service use over time (pre and post intervention) using established methods. 63 Service use was measured for the 4 weeks before release and then in the periods up to 6 weeks and 6 and 12 months post release. Data were collected by researchers from case notes and records rather than directly from participants.
The first stage in the process was to clean the data and to identify any inconsistencies. This was followed by regrouping some of the service categories according to levels of use. Six categories of service use were collected: psychiatrist, psychologist, occupational therapist, mental health nurse, care co-ordinator and other. All other contacts were categorised into the following categories: other nurse, outpatient contacts, GP and social care. ‘Other nurse’ included contacts such as general, physical and mental health nurses, substance misuse workers and psychological therapy sessions. Outpatient included those other contacts that were based in hospitals (including the accident and emergency department). GP contacts were contacts in a primary care setting. Social care included social workers, housing officers, community support workers, counsellors and probation officers; it is acknowledged that the last two services are not strictly social care but the use of these was relatively low.
The second stage was to combine the service use data with appropriate unit cost information. These data were mainly derived from the annual compendium published by the Personal Social Services Research Unit at the University of Kent,70 with others coming from NHS Reference Costs 2012–2013. 71 Unit costs were multiplied by the number of contacts to calculate a cost per person. These total costs were averaged across all people for the different follow-up periods.
The unit cost of the intervention was based on the wages of the CTI managers for the time that they spent performing the intervention, plus a percentage increase to account for on costs and capital costs. This was then divided by the number of contacts a person in the CTI arm would typically have with their CTI manager (n = 41), identified earlier in the report. The assumption is that the entire CTI group received their full intended care and that, on average, there were 41 contacts per patient in the intervention group. The cost per contact was £65.23 and is applied at a flat rate for everyone in the intervention group based on when their contacts typically took place; therefore, information about intervention contacts was not extracted directly from case notes. This is because the case notes did not hold an accurate account of the number and length of CTI contacts participants were having, which is an important limitation of the data.
Results are presented separately for the different follow-up periods. Given that each covers a different length of time, the comparability of the data between time periods is problematic. In the tables we report the number and percentage of participants who had a particular service contact, the mean number of contacts among those actually using a service and the mean of cost across all participants. A total number of contacts (excluding inpatient days) and a total cost are also reported. (It is assumed that it may be positive for a participant to have more contacts with health services; however, inpatient contacts may indicate a poor outcome, therefore inclusion in the measure for average contacts per person would be counterintuitive.)
Results
In the 4-week period before release, about two-thirds of both groups had contacts with care co-ordinators, and around one-third had contacts with psychiatrists and mental health nurses (Table 16). People having contact with ‘other nurses’ and ‘mental health nurses’ were slightly higher in the TAU group than in the CTI group, with frequency of ‘other nurse’ being particularly high in the TAU group. Overall, total contacts per person using services were similar between the groups, at around five per person.
| Service | Group | |||||
|---|---|---|---|---|---|---|
| CTI | TAU | |||||
| n | % | Meana | n | % | Meana | |
| Psychiatrist | 26 | 36.6 | 1.81 | 27 | 34.6 | 1.44 |
| Psychologist | 3 | 4.2 | 1.67 | 4 | 5.1 | 1.75 |
| Occupational therapist | 1 | 1.4 | 1.00 | 0 | 0.0 | 0.00 |
| Mental health nurse | 27 | 38.0 | 2.82 | 31 | 39.7 | 2.19 |
| Care co-ordinator | 46 | 64.8 | 2.61 | 47 | 60.3 | 2.45 |
| Other nurse | 22 | 31.0 | 2.97 | 27 | 34.6 | 4.85 |
| Outpatient contact | 1 | 1.4 | 1.00 | 2 | 2.6 | 3.00 |
| GP | 13 | 18.3 | 1.31 | 8 | 10.3 | 1.13 |
| Social care contact | 4 | 5.6 | 1.50 | 3 | 3.8 | 1.00 |
| Psychiatric inpatient stay | 0 | 0.0 | 0.00 | 0 | 0.0 | 0.00 |
| Medical inpatient stay | 0 | 0.0 | 0.00 | 0 | 0.0 | 0.00 |
| Total | 71 | 78 | ||||
| Average contacts per patientb | 5.27 | 4.85 | ||||
The highest mean cost in both groups, after the cost of CTI, was for psychiatrist contacts, followed by care co-ordinators and other nurses (Table 17). Together, these services made up 76% of costs for both the CTI and TAU groups. The total for the CTI group was 12% higher than for the TAU group.
| Service | Group | |||
|---|---|---|---|---|
| CTI | TAU | |||
| Mean cost (£) | SD (£) | Mean cost (£) | SD (£) | |
| Psychiatrist | 74.39 | 127 | 56.19 | 91.9 |
| Psychologist | 5.01 | 27.7 | 6.38 | 30.7 |
| Occupational therapist | 0.26 | 2.2 | 0.00 | 0 |
| Mental health nurse | 28.70 | 65.1 | 23.37 | 43.3 |
| Care co-ordinator | 45.31 | 42.9 | 39.53 | 43.6 |
| CTI contacta | 521.84 | 0 | N/A | N/A |
| Other nurse | 25.30 | 73.6 | 45.03 | 212 |
| Outpatient contact | 1.58 | 13.3 | 8.64 | 64.7 |
| GP | 11.36 | 25.9 | 5.47 | 17.1 |
| Social care contact | 3.44 | 15 | 1.57 | 7.88 |
| Psychiatric inpatient stay | 0.00 | 0 | 0.00 | 0 |
| Medical inpatient stay | 0.00 | 0 | 0.00 | 0 |
| Total | 717.19 | 245 | 186.19 | 283 |
Table 18 shows the service use in the 6 weeks after release. The CTI group made more use of care co-ordinators and psychiatrists than the TAU group. The overall average contact (excluding inpatient services) was higher for the CTI group. When looking at inpatient care it can be seen that few were admitted. However, the number of days in hospital differed. CTI participants had more days admitted to medical wards and TAU participants had more days admitted to psychiatric wards.
| Service | Group | |||||
|---|---|---|---|---|---|---|
| CTI | TAU | |||||
| n | % | Meana | n | % | Meana | |
| Psychiatrist | 15 | 27.3 | 1.13 | 10 | 16.4 | 1.00 |
| Psychologist | 2 | 3.6 | 1.50 | 0 | 0.0 | 1.50 |
| Occupational therapist | 2 | 3.6 | 1.00 | 0 | 0.0 | 1.00 |
| Mental health nurse | 20 | 36.4 | 1.80 | 23 | 37.7 | 2.04 |
| Care co-ordinator | 27 | 49.1 | 2.15 | 13 | 12.3 | 2.69 |
| Other nurse | 2 | 3.6 | 3.00 | 1 | 1.6 | 2.00 |
| Outpatient contact | 1 | 1.8 | 1.00 | 0 | 0.0 | 0.00 |
| GP | 0 | 0.0 | 0.00 | 0 | 0.0 | 0.00 |
| Social care contact | 2 | 3.6 | 3.00 | 3 | 4.9 | 2.67 |
| Psychiatric inpatient stay | 0 | 0.0 | 0.00 | 2 | 3.3 | 26.00 |
| Medical inpatient stay | 1 | 1.8 | 31.00 | 1 | 1.6 | 1.00 |
| Total | 55 | 61 | ||||
| Average contacts per patientb | 2.58 | 1.52 | ||||
Even though very few participants were admitted to hospital, this care accounted for 77% of costs for the CTI group and 84% for the TAU group, excluding CTI costs (Table 19). Psychiatrist and care co-ordinator costs were around twice as much for the CTI group than for the TAU group.
| Service | Group | |||
|---|---|---|---|---|
| CTI | TAU | |||
| Mean cost (£) | SD (£) | Mean cost (£) | SD (£) | |
| Psychiatrist | 34.74 | 60.7 | 18.42 | 42 |
| Psychologist | 3.88 | 21.2 | 0.00 | 0 |
| Occupational therapist | 0.68 | 3.51 | 0.00 | 0 |
| Mental health nurse | 17.55 | 30.6 | 20.66 | 35.4 |
| Care co-ordinator | 28.27 | 33.6 | 15.38 | 37.4 |
| CTI contactsa | 2152.59 | 0 | N/A | N/A |
| Other nurse | 2.92 | 16 | 0.88 | 6.87 |
| Outpatient contact | 2.04 | 15.2 | 0.00 | 0 |
| GP | 0.00 | 0 | 0.00 | 0 |
| Social care contact | 4.43 | 24.4 | 5.34 | 25.2 |
| Psychiatric inpatient stay | 0.00 | 0 | 312.61 | 1891 |
| Medical inpatient stay | 345.70 | 2564 | 10.05 | 78.5 |
| Total | 2592.80 | 2579 | 383.35 | 1897 |
Critical time intervention contacts account for majority of the costs from release to the 6-week follow-up (see Table 19). This is because the majority of the intervention, in terms of contacts, is carried out in this time period. However, in reality, this cost would likely be more spread out across the follow-ups, as the work would be not be so concentrated in this period. Preparation work that does not involve actual patient contact would shift some of the cost before this period. Similarly, monitoring of patients in the final few months that does not typically result in regular face-to-face contact would also shift some of the costs to later in time. In addition, the single person with a 31-day stay in hospital is driving up the cost per person in the CTI arm as well as the intervention costs.
The period before the 6-month follow-up covers a period of 20 weeks. The number of people in the CTI arm having contacts with care co-ordinators was higher than at 6 weeks and the frequency of these contacts was also higher (Table 20). The TAU group had increased contact with mental health nurses compared with the 6-week follow-up point and also compared with the CTI group. The use of care co-ordinators was slightly higher in the CTI group at 6 months than in the TAU group. The average total service costs were again higher for the CTI group (Table 21). There is not a significant difference in the cost of mental health nurse contacts between the two groups because of the lower frequency of contacts.
| Service | Group | |||||
|---|---|---|---|---|---|---|
| CTI | TAU | |||||
| n | % | Meana | n | % | Meana | |
| Psychiatrist | 23 | 48.9 | 1.78 | 17 | 33.3 | 1.59 |
| Psychologist | 1 | 2.1 | 4.00 | 0 | 0.0 | 0.00 |
| Occupational therapist | 1 | 2.1 | 1.00 | 0 | 0.0 | 0.00 |
| Mental health nurse | 17 | 36.2 | 4.59 | 29 | 56.9 | 2.72 |
| Care co-ordinator | 27 | 57.4 | 4.96 | 23 | 45.1 | 3.39 |
| Other nurse | 3 | 6.4 | 1.33 | 5 | 9.8 | 1.40 |
| Outpatient contact | 0 | 0.0 | 0.00 | 1 | 2.0 | 24.00 |
| GP | 1 | 2.1 | 2.00 | 0 | 0.0 | 2.00 |
| Social care contact | 3 | 6.4 | 1.67 | 2 | 3.9 | 2.00 |
| Psychiatric inpatient stay | 0 | 0.0 | 0.00 | 2 | 3.9 | 9.00 |
| Medical inpatient stay | 1 | 2.1 | 31.00 | 0 | 0.0 | 0.00 |
| Total | 47 | 51 | ||||
| Average contacts per patientb | 5.745 | 4.294 | ||||
| Service | Group | |||
|---|---|---|---|---|
| CTI | TAU | |||
| Mean cost (£) | SD (£) | Mean cost (£) | SD (£) | |
| Psychiatrist | 98.03 | 125 | 59.50 | 104 |
| Psychologist | 6.05 | 41.5 | 0.00 | 0 |
| Occupational therapist | 0.39 | 2.71 | 0.00 | 0 |
| Mental health nurse | 44.49 | 108 | 41.53 | 73.6 |
| Care co-ordinator | 76.43 | 103 | 41.00 | 68.1 |
| CTI contactsa | 0 | 0 | N/A | N/A |
| Other nurse | 2.85 | 9.4 | 3.68 | 13.2 |
| Outpatient contact | 0.00 | 0 | 52.88 | 378 |
| GP | 2.02 | 13.8 | 0.00 | 0 |
| Social care contact | 4.33 | 17.5 | 3.19 | 17.9 |
| Psychiatric inpatient stay | 0.00 | 0 | 129.43 | 651 |
| Medical inpatient stay | 404.54 | 2773 | 0.00 | 0 |
| Total | 638.58 | 2761 | 331.22 | 1003 |
At the 12-month follow-up, the CTI group’s use of care co-ordinators remained similar to the previous follow-up and noticeably higher than for the TAU group (Table 22). The mean number of contacts with care co-ordinators was also far higher in the CTI group. Contacts with psychiatrists are slightly higher and more frequent in the CTI group. A higher number of the TAU group have contacts with mental health nurses; however, the frequency of these contacts is lower. Overall, the number of service contacts in the CTI group was about three times higher than in the TAU group.
| Service | Group | |||||
|---|---|---|---|---|---|---|
| CTI | TAU | |||||
| n | % | Meana | n | % | Meana | |
| Psychiatrist | 16 | 39.0 | 2.44 | 13 | 30.2 | 1.39 |
| Psychologist | 2 | 4.9 | 2.50 | 1 | 2.3 | 1.00 |
| Occupational therapist | 2 | 4.9 | 1.50 | 1 | 2.3 | 5.00 |
| Mental health nurse | 14 | 34.1 | 4.86 | 18 | 41.9 | 3.94 |
| Care co-ordinator | 21 | 51.2 | 5.33 | 17 | 39.5 | 2.88 |
| Other nurse | 2 | 4.9 | 7.00 | 3 | 7.0 | 2.33 |
| Outpatient contact | 0 | 0.0 | 0.00 | 0 | 0.0 | 0.00 |
| GP | 0 | 0.0 | 0.00 | 0 | 0.0 | 0.00 |
| Social care contact | 3 | 7.3 | 11.67 | 2 | 4.7 | 2.00 |
| Psychiatric inpatient stay | 0 | 0.0 | 0.00 | 1 | 2.3 | 12.00 |
| Medical inpatient stay | 0 | 0.0 | 0.00 | 1 | 2.3 | 3.00 |
| Total | 41 | 43 | ||||
| Average contacts per patientb | 6.732 | 3.604 | ||||
Table 23 shows that psychiatrists and care co-ordinators are the drivers of costs in the CTI arm. For the TAU group, inpatient care is the main cost driver. Overall, the costs are almost identical including mental health nurse contacts.
| Service | CTI | TAU | ||
|---|---|---|---|---|
| Mean cost (£) | SD (£) | Mean cost (£) | SD (£) | |
| Psychiatrist | 106.90 | 201 | 47.04 | 82.2 |
| Psychologist | 8.68 | 45.5 | 1.65 | 10.8 |
| Occupational therapist | 1.36 | 6.41 | 2.16 | 14.2 |
| Mental health nurse | 44.47 | 112 | 44.27 | 108 |
| Care co-ordinator | 73.24 | 95 | 30.55 | 44.8 |
| CTI contactsa | 0 | 0 | N/A | N/A |
| Other nurse | 9.15 | 47.4 | 4.36 | 21 |
| Outpatient contact | 0.00 | 0 | 0.00 | 0 |
| GP | 0.00 | 0 | 0.00 | 0 |
| Social care contact | 34.76 | 197 | 3.79 | 19.5 |
| Psychiatric inpatient stay | 0.00 | 0 | 102.34 | 671 |
| Medical inpatient stay | 0.00 | 0 | 42.79 | 280 |
| Total | 278.55 | 518 | 278.96 | 874 |
At each time point, excluding the 12-month follow-up, the mean costs are higher for the CTI group (Table 24). The cost per week is helpful when comparing between time periods. It can be seen that costs increase initially for both groups and then fall after the 6-week follow-up.
| Time point | Weeks covered | Group | |||||
|---|---|---|---|---|---|---|---|
| CTI | TAU | ||||||
| Total (£) | SD (£) | Per week (£) | Total (£) | SD (£) | Per week (£) | ||
| 4 weeks before release | 4 | 717.19 | 245 | 179.30 | 186.19 | 283 | 46.55 |
| 6-week follow-up | 6 | 2592.80 | 2579 | 432.13 | 349.02 | 1897 | 58.17 |
| 6-month follow-up | 20 | 638.58 | 2761 | 31.93 | 331.22 | 1003 | 16.56 |
| 12-month follow-up | 26 | 278.55 | 518 | 10.71 | 278.96 | 874 | 10.73 |
| Total year after release | 52 | 4418.59 | 5924 | 84.97 | 1445.96 | 2940 | 22.04 |
Without the imputed CTI intervention costs, the average service use costs in the intervention arm for the 4 weeks before release and the period from release to the 6-week follow-up are £195.35 (down from £717.19) and £440.21 (down from £2592.80), respectively. Both the service costs at 4 weeks before release and at the 6-week follow-up are not significantly different once CTI contacts are taken out, possibly because of the small sample size and high number of dropouts.
Service costs over the whole follow-up period in relation to age show large differences. For those participants aged 20–29 years the mean cost was £2432.94, for those aged 30–39 years it was £4521.58, for those aged 40–49 years it was £1647.20, and for those aged ≥ 50 years it was £2087.87. Participants with schizophrenia had mean costs of £3217.07, whereas for those with depression the cost was £1867.48. Participants who were diagnosed with schizophrenia complicated by a PD had average service costs of £3528.85. The remaining had an average cost of £2445.49. Those with schizophrenia complicated by alcohol or drug misuse had average costs of £3382.34 compared with £2735.07 for those without. Participants with an Axis II diagnosis had average costs of £3071.89 compared with £2546.88 for those without.
White participants’ costs were higher (£3523.04) than black (£2272.75) or Asian (£1953.12) participants’ costs. Perhaps not surprisingly, costs were substantially higher for participants who were unemployed (£3539.55) than for those in work (£1385.40).
Regression analysis performed on the cost data showed that service costs for unemployed participants were 1.5 times higher than for those who were in employment, and that costs for those not at work due to sickness (and those absent from work due to illness) were, similarly, 1.5 times higher than for those in employment. However, this relationship becomes insignificant when you exclude inpatient costs, suggesting that this relationship is driven by the inpatient costs, a service that relatively few people used. The cost breakdowns previously are for only the patients who had full service use information for the year, which totalled 84 participants. These costs also include the imputed cost of the intervention.
Combining the clinical effectiveness from the primary outcome measure, a difference of proportion of people engaged of 0.161 at 1-year follow-up and, costs, a difference of £2485.10 in favour of the CTI arm, gives a cost per additional person engaged of £15,426. To determine if this is cost-effective depends on society’s willingness to pay for an additional person to be engaged with mental health services at 1 year following release.
Summary
This chapter has reported on service use and costs for the two groups at different points in time. The CTI manager input was the most expensive element of costs for the intervention group and led to a major cost difference at the 6-week follow-up. However, costs were also higher at the other time points, with the exception of the final one at 12 months post release.
Aside from the intervention costs, it was also apparent that the CTI group had a greater level of service use than the control group. This is to be expected, given that the main aim of the intervention was to increase engagement and that, to a large extent, this was achieved. Increased engagement should lead to increased service use and costs.
We have briefly linked engagement to costs; however, we have not formally tested cost-effectiveness through cost-effectiveness acceptability curves in this chapter. As a result of the strong link between engagement and costs, to do so would have been less informative than having a clinical measure as a primary outcome. Future studies should consider using patient-reported outcomes, such as quality-adjusted life-years, in the economic evaluation.
Chapter 7 Discussion
Introduction
This chapter aims to bring together the discrete component parts of the study, discuss results, identify limitations and explore implications for service planning and delivery.
In Summary of main findings, findings related to the primary and secondary outcomes and other quantitative analyses are reviewed and discussed. In addition, the key findings of the qualitative and health economics aspects of the study are summarised.
In Strengths and limitations, the impact of the study is considered and challenges faced in securing the relevant permissions to conduct the trial are presented.
In Discussion and Recommendations for future research, we discuss the implications of this work for clinical practice and future RCTs in prison populations or at other points of transition within mental health services.
Summary of main findings
Achievement of the objectives of the study
The primary objective at the start of the trial was to establish whether or not CTI was clinically effective for released adult prisoners with SMI in:
-
improving engagement with health and social care services
-
reducing mental health hospital admissions
-
reducing reoffending
-
increasing community tenure through reducing time in prison.
The primary objective was partially met.
-
Those allocated to the CTI arm of the trial were more likely to be engaged with mental health services at the 6-week follow-up stage of the trial.
-
Those who received CTI were also more likely to be registered with a GP.
-
Continuing engagement with services was demonstrated for the CTI group at 6 months following release.
-
This advantage was not observed at the 12-month follow-up, although CTI participants were still more likely to be currently under CPA at this point.
As noted earlier, delays in recruitment led to us being unable to analyse the impact of CTI on hospital admission, reoffending and overall community tenure. This is considered further in Limitations.
The secondary objectives at the start of the trial were:
-
to establish the cost-effectiveness of CTI for this population
-
to develop a service delivery manual and training materials to support the implementation of CTI in vivo
-
to facilitate and promote active service user, CJS and NHS staff participation in the research programme, thus encouraging greater engagement between the academic and practice communities.
The study’s secondary objectives were achieved.
The health economic analysis consisted of a cost comparison between the two groups. The analysis indicated that:
-
participants receiving CTI incurred higher costs in relation to their service use than the TAU group before, and after, release
-
at each time point (except at the 12-month follow-up), the associated cost of service use by CTI participants was higher than those for the TAU group. Largely these costs were associated with psychiatrist and care co-ordinator contact
-
at no point during the course of the trial were costs incurred because of psychiatric inpatient hospitalisation for the CTI group. This positive outcome for the CTI group may reflect their increased contact with community services. Given that hospitalisation is by far the most expensive form of service provision, the increased service cost incurred by the CTI group may, over a longer time period, be cost-effective.
The main contributor to cost was that of the CTI managers. These costs were mostly incurred during the 6-week follow-up period. However, the use of other services was also generally increased. That costs were increased for the intervention group does not imply that the intervention is not cost-effective. If outcomes are improved by a sufficient amount then these extra costs would be acceptable. The outcomes described show that engagement was improved. We can assume that better engagement leads to more clinically effective treatment and, ultimately, improved well-being. We would argue that the increased costs would be justified. Ultimately, however, it is a value judgement whether or not this is a good use of funds.
A treatment intervention manual, with training materials included, was achieved. The manual was developed through a working group comprising prison- and community-based staff, experts by experience and researchers. The manual details the origins of CTI, outlines results of previous and current research, details the stages and content of the intervention to allow replication and includes skills training suggestions for staff. The establishment of the working group to participate in the development of the case manager manual also achieved our final secondary objective, that of encouraging engagement between researchers, practitioners and users of mental health services.
Qualitative study: service user and professionals’ view of the intervention
The quantitative results summarised were augmented by a strand of concurrent qualitative enquiry running throughout the life of the trial.
The comments received by the service users allocated to the CTI group were overwhelmingly positive. CTI participants reported:
-
reduced anxiety with respect to their impending release from prison
-
on the value of the CTI manager’s role linking with community services, which made contact and engagement easier and less daunting
-
on the CTI manager’s advocacy role, that is having someone who understood their needs, and how community providers operate to ensure appropriate transfer of care
-
receiving emotional support from the CTI manager, that is having someone they knew and trusted on both sides of the gate
-
an increased ability/wish to persevere with attending mental health/drug and alcohol service appointments, and maintaining treatment programmes that previously have fallen by the wayside
-
a continuing increase in self-confidence and self-reliance over time with regard to getting what they want from service providers
-
higher personal aspirations in relation to finding work, vocational training and/or education
-
improved relationships with peers and family members.
Staff who delivered CTI or staff who had observed the running of CTI within their service reflected on the barriers to, and facilitators of, successful delivery of the intervention, including the following:
-
Information sharing across service boundaries was seen as a barrier, taking a long time for CTI managers to establish; however, it could also facilitate care when it was functioning properly, contributing to averting potentially serious consequences.
-
The ability to spend more time with service users enabled CTI managers to establish rapport and facilitated continued engagement with them and other services.
-
Increasingly limited resources led to raising of thresholds for gaining access to community services, resulting in CTI managers spending increasing amounts of time negotiating access.
-
The time-limited nature of CTI was seen as a positive, but some felt that the 6-week cut-off point was too rigid and needed some flexibility to account for individual need.
-
There was a lack of suitable accommodation options for clients.
Strengths and limitations
Strengths
This research is the first RCT, worldwide, of CTI as a model for service delivery to support the transition of male prisoners with SMI back to community living. Prisoners have complex and comorbid mental health problems at rates significantly higher than the general population, and they frequently find themselves socially disadvantaged when resettling into the community life. Existing research has identified the problems that they face around gaining suitable accommodation and employment, and in repairing fractured family relationships. Their complex mental health needs make them unpopular patients in many community services both in terms of their clinical needs and their patterns of engagement, which can be chaotic and sporadic, influenced negatively by other lifestyle factors.
The study is also the first UK economic evaluation of delivering CTI as a high-intensity time-limited through-the-gate intervention for prisoners with SMI.
Limitations
Throughout the study we encountered numerous obstacles that challenged study set-up and recruitment. Our experiences provide evidence on the difficulties of obtaining research and ethics permissions and, when these systems fail, with implications for research in general. In addition, it also needs to be acknowledged that retendering and changes of provider, which are common throughout the NHS, including prison-based services, can effectively halt, or at least severely delay, ongoing research.
Delays in obtaining research and development permission from the prison estate
Negotiating access to the prison-based NHS and private health-care provider services presented the research team with several challenges that impacted negatively on the start of data collection. We experienced long delays in obtaining local R&D permission at prison sites which, in two instances, necessitated the escalation of the request to the medical director of the trust providing in-reach care to the establishment. In all instances of delay, all correct procedures had been followed by the research team.
In two establishments, following initial agreement, access was subsequently denied, with staff shortages stated as the reason. This meant that a large amount of work undertaken to gain permissions was wasted and the work had to start anew in additional sites.
As noted above, retendering processes resulted in providers changing midway through the study, leading to uncertainty regarding whether or not new governance permissions needed to be sought from the incoming provider. Retendering often led to fragmentation of service provision, with a number of statutory and third-sector services providing seemingly analogous or overlapping services, creating difficulties identifying precisely from which organisation(s) permission was required. This liaison with multiple organisations added both time and complexity to the permissions process and, in the case of third-sector providers, often placed the research team in the position of trying to educate providers about what they should require from us, as their own R&D procedures were non-existent.
Delays in adding additional sites because of excess treatment costs
All delivery of the intervention was covered by excess treatment costs. As already mentioned, as a result of slow recruitment, which was not expected by the feasibility trial, additional sites had to be added. In some cases, if the provider/commissioner was the same, it was possible to spread the excess treatment costs already agreed across sites. However, many of the new sites were run by a different provider/commissioner, meaning that new applications for excess treatment costs had to be submitted. This was a lengthy process in many sites, taking around 6–9 months, and, in some instances, our application for excess treatment costs was rejected because the provider/commissioner had not been included in the original grant application stage.
Issues accessing national data sources in a timely manner
First, it proved ultimately impossible, within the time scale of the project, to complete the additional analyses of the effect of CTI on rates of hospital admissions, reoffending and overall community tenure.
In relation to hospital admissions, the original plan was to obtain these data from the HES, which is a national database of bed usage. Owing to the delays to recruitment previously described, the end dates of recruitment and follow-up were later than stated in the original protocol. As a direct result, the time lag between a hospital stay being recorded locally and that information being notified to, and processed by, HES meant that HES data would be incomplete when we would have needed to gather it and, thus, would have led to inaccurate analyses. To counter this, each person’s individual care records were interrogated and any records of time as an inpatient were recorded locally.
Second, delayed recruitment also meant that it has not been possible to gather CJS contact and reoffending data as, again, the time lag between offences being committed and outcomes recorded on the PNC would have over-run the lifetime of the study.
Third, the inability to calculate impact on community tenure is directly related to not having access to days in hospital/reoffending data; these two variables were to be added together for each trial participant to obtain a measure of stay in the community. Although no longer within the scope of this report, the research team aims to pursue reoffending data outside the duration of this trial’s funding in order to subsequently report on any impact that CTI may have had on this post-release variable.
Economic evaluation
The health economic analyses consisted of a cost comparison between the two groups. A full evaluation would involve a synthesis of the cost and outcomes and, ideally, would involve a measure of quality-adjusted life-years; this was not feasible here because we had access only to data from notes rather than from patient-reported measures as would be required.
Fidelity to the intervention
The fidelity was assessed using an adapted version of the fidelity scale used in the Critical Time Intervention – Task Shifting study64 at eight time points over the course of the trial, which is a similar approach to other studies of CTI. However, a more reliable and detailed way to assess fidelity would have been for the CTI manager to complete a checklist per participant against core CTI principles. This would have allowed more detailed analysis of what each participant received, mapped against their needs.
There was variation in fidelity to the intervention across the different CTI managers. Low scores were not attributed to one person alone but across all CTI managers for different aspects (see Table 11). The study was not large enough to be able to evaluate the skills of those delivering the intervention against outcomes. However, the variation may be important to consider in terms of implementation issues, such as training, core competencies and information governance. For example, the researchers assessing fidelity rated items as low if there was no recorded evidence, although it is possible that an activity might have occurred but not have been recorded. This highlights the importance of maintaining clear and accurate records. In addition, cases closed at 6 weeks were generally among the lowest in terms of fidelity to the intervention; this may be an indication that, because of the complex nature of this group, full re-engagement with services by 6 weeks is difficult to achieve, or simply that it occurred but was not adequately evidenced in the records satisfactorily.
Discussion
Our trial showed significantly improved engagement with mental health services for the CTI group compared with TAU at 6 weeks. Recipients and staff spoke overwhelmingly in support of the intervention; recipients valued the additional support and the advocacy role adopted by the CTI manager, and staff appreciated the value of delivering a holistic package of care to difficult-to-engage patients with complex needs. However, at the final follow-up for this trial, 12 months post discharge, those who received CTI were no more likely to be engaged with services than the TAU group, the advantage lost somewhere between 6 and 12 months. We suggest that this loss of advantage may stem from several issues, relating to both individual patients and the response from services.
Our decision to adapt the CTI intensive post-discharge period from the original 9 months to 6 weeks was based on the findings of our pilot study, which indicated that, by 6 weeks, the service user should be engaged with the CMHT, if that was going to occur at all. This was sufficient time to address clinical and immediate accommodation and benefit entitlement/employment needs and, because the intervention was heavily frontloaded by work completed while the service user was still in prison, systems should be able to slot into place relatively rapidly after discharge. Importantly, the limited post-release support period kept community caseloads manageable for CTI managers, given the large number of people likely to be eligible for the intervention.
In addition, as noted earlier, it is known that in the first weeks and months following release from prison recently released individuals are particularly at risk of suicide and/or death due to accidental overdose. In a UK study, age-adjusted standardised mortality among men and women in the 12-month period following release from prison was 8.3 and 35.8 times higher, respectively, than in the general population. Crucially in the current context, 21% of those who completed suicide did so within 28 days post release, with just over half (51%) of deaths occurring within 4 months of release. 24 The study authors placed emphasis on the importance of improved release planning for those prisoners most at risk to ensure immediate engagement with community mental health services, assertive follow-up and intensive post-release support. 25 With regard to drug-related mortality, a meta-analysis reported that drug-using prisoners had a three- to eightfold increased risk of drug-related death in the first 2 weeks post release compared with the subsequent 10 weeks, with risks remaining elevated through weeks 3 and 4. 22 Recent Ministry of Justice statistics72 similarly identify the risk of reoffending in the immediate post-release period. Figures released in early 2016 show that 8.6% of prisoners released during 2013 were later convicted of a criminal offence committed within 18 days of release. Loss of engagement with services following the cessation of the intense phases of CTI is probably a result, at least in part, of the nature of the client group, who revert to their established pattern of engagement with the NHS. When not in prison, offenders have been demonstrated as having chaotic patterns of engagement with health-care services, with contact often crisis driven and characterised by heavy use of emergency care options, such as accident and emergency departments and ambulance services, rather than routine primary care. The essential nature of CTI is to offer intensive support for clients to engage with services and, in this study, post-release support was limited to 6 weeks of highly concentrated effort targeting a range of health and social care domains. The work is labour intensive, involving the CTI manager spending much more time with a client than would normally be the case in the community and, similarly, concentrating on needs other than those relating to the clinical treatment of SMI to an extent beyond standard CMHT involvement.
Routine contact with CMHTs is normally based on the presumption that patients choose to remain involved and that services are wholly non-coercive unless additional risks develop. Thus, a patient who by nature, evidenced by his or her history, finds it hard to remain in contact with services and starts to disengage, is likely, if this disengagement is not addressed robustly by CMHT staff very quickly, to fall out of contact. This leads, therefore logically, to consider the need for CMHTs to offer something other than routine care with CTI clients, in particular additional efforts in keeping someone in touch, above and beyond the efforts they would go to with their ‘normal’ clients.
Making additional efforts to keep in touch with CTI clients is a significant ask of CMHTs, who are routinely working with large caseloads and dealing with increasingly complex mental health issues in many clients, compared with years past when psychiatric inpatient beds were plentiful and admission much easier to arrange. When already facing these routine pressures, the request to be additionally proactive with CTI clients from prison will not be universally welcomed by CMHT staff.
Prins73 refers to offenders with mental disorders as ‘the unloved, the unlovely and the unloveable’, who are doubly stigmatised by mental illness and criminality. Our study sample, in line with offenders who have mental disorders more generally, had high levels of comorbid conditions and needs. Fewer than half of the participants (42%) had a straightforward diagnosis of a single SMI. Over one-third of the group (37%) had both SMI and PD, and 15% had SMI, PD and substance misuse diagnoses. This combination of chaotic engagement, multiple morbidity and criminality serves, very often, to make mentally disordered offenders ‘heart-sink patients’, described in general practice literature as patients who create ‘the feelings felt in the pit of your stomach when their names are seen on the morning’s appointment list’74 and/or those who ‘exasperate, defeat and overwhelm [clinicians] by their behaviour’. 75 Thus, individual practitioners who already feel beleaguered by the routine pressures they face with their standard caseload may not have the motivation to put in the work required to keep hold of CTI clients with multiple morbidities. That acknowledged, this is not an excuse for therapeutic nihilism; however difficult, this is a large group with needs that should be met by appropriate services. To do this, frontline staff need to feel suitably trained, working with adequate resources and supported in their clinical decision-making by managers and organisations. Providers and commissioners need to be honest and open about how they meet their duties and responsibilities to complex patients, acknowledging that it is likely that there will always be a subset of patients more resource intensive than others but that, by meeting needs holistically, people feel supported and lifestyle chaos and ultimately their needs overall reduce over time.
The second consideration is whether or not the reduction of the CTI post-discharge period to 6 weeks only, from the 9 months in the original trials, needs to be reconsidered. Logically, but ultimately untestable in this trial, long-term engagement with an appropriate mental health service is hypothesised to increase community tenure and reduce reoffending. Thus, is 6 weeks of intensive support insufficient to assure this long term?
As discussed, increasing the post-release period of CTI support would have implications for resources in the community, because of the large number of potentially eligible prisoner-patients. The intensive nature of CTI dictates small caseloads; thus, maintaining intensity is resource intensive. If the 9-month duration from the original trials was adopted, CTI community caseloads would increase in size and, in effect, would involve the running of a discrete service for this client group, running parallel to routine CMHT care.
Running parallel services is expensive and, in effect, serves merely to delay the inevitable transfer to routine CMHT care, given that the time-limited nature of CTI means that it must end at some point. The economic evaluation of this trial has clearly identified that CTI is more expensive than TAU, and the economic climate within the NHS is not one that would readily respond to increased costs over long periods of time. Parallel services for mentally disordered offenders are also at odds with the national policy of mainstreaming offender health care, rather than creating or maintaining ‘service silos’. We therefore do not believe that there are logical and economic arguments to advocate a 9-month post-discharge CTI intervention period, especially given that, within our model of 6 weeks of post-discharge support, much more work was tackled in the pre-discharge period than was the case in the early CTI trials. This therefore leads to the consideration that CMHTs may need to ‘do something different’ with this client group.
In the current and previous trials of CTI, only the actions of the CTI manager were ultimately determinable; no specific actions were prescribed from CMHT staff, for example in terms of frequency of ongoing contact and/or set contingency plans in response to likely disengagement. This raises the question of whether or not more consideration needs to be given to what CMHTs do when CTI intensive support has officially ended. We have commented throughout regarding the multiple clinical morbidities and measures of social exclusion experienced by this group, in particular their pattern of crisis-driven contact with health-care services. Knowing this, it is therefore reasonable to expect that, when ‘downgraded’ to the status of receiving routine CMHT support, with less frequent contact, an emphasis on personal autonomy and responsibility and continued engagement predicated on free choice, contact and engagement will wane.
If engagement is significantly improved when patients are given a period of very intensive support but that improvement is lost when their contact is with ‘routine’ community care, one solution may be to enhance the offering from CMHTs to these complex and, in terms of reoffending at least, high-risk patients, especially in terms of frequency of interventions/appointments and more robust efforts to be made to maintain contact when disengagement is likely. If ‘routine’ CMHTs cannot offer such intensity of contact and follow-up, should such patients be referred to assertive outreach teams, where they continue to exist, as standard? Assertive outreach teams’ core operating models are predicated on maintaining contact with complex clients, especially those who have proved difficult to keep in contact with routine community services. The difficulty is that assertive outreach teams are being phased out across the country in light of limited evidence of their superiority over standard CMHT on a number of outcomes. 38,45 This strengthens the argument that CMHTs simply have to come to terms with their role managing ‘difficult’ patients, as they are the only widely available and accessible service for people leaving prison.
Accepting that CMHTs are to be the main care provider in the community, then the transition between prison and community has to be handled effectively. CMHT staff will need CTI training and the time and resources to dedicate to their clients. This could be done by having CMHT staff who have reduced caseloads of only CTI clients, or giving all CMHT staff a small number of CTI clients along with a reduced ‘normal’ caseload. A further question is whether or not in-reach staff from outside the prison should follow people up and hand over care when they are in the community or if CMHT staff should take responsibility for CTI delivery while the person is still in prison, thus removing the need for a client to have two key workers within a relatively short period. This was a model we explored in our pilot study,54 choosing to adopt the former model for this trial, but a fuller examination of models is warranted in attempts to maximise resources and service delivery.
All of these options have significant resource implications in already overstretched NHS mental health services. However, the longer-term benefits across the health and justice domains may be large in terms of reducing reoffending and more sustained well-being. This requires further exploration.
Recommendations for future research
-
Completion of the examination of the impact of CTI on reoffending, hospitalisation and community tenure, as included within our original protocol but prevented by external events.
-
Adaptations of CTI for other prisoner groups. This could include women, young people and older adults, all of whom are likely to have discrete resettlement needs.
-
Examination of best mode of delivery, in particular evaluating prison in-reach staff maintaining time-limited contact with people in the community compared with CMHT staff assuming responsibility while the person is still in prison.
-
Further investigation of alternative holistic service models for offenders with mental disorders when leaving prison and serving sentences in the community, including both CTI-specific roles and required responses from standard mental health services. We would recommend a 360° qualitative exploration of how to provide better care for this group, consulting community service providers, commissioners, policy-makers and service users.
-
Adaptations of CTI at different points of transition would merit further exploration, for example as part of police custody-based mental health liaison and diversion services, and at transition between different mental health services, for example from inpatient care to home, child and adolescent to adult services.
Chapter 8 Conclusions
The CTI intervention, as delivered in this trial, was effective in ensuring engagement with services at 6 weeks. Furthermore, the difference between the intervention and the TAU group was maintained at 6 months; however, this advantage was lost by 12 months. We have discussed in previous chapters the factors we feel may have contributed to this.
Overall, staff and participants who were interviewed as part of the qualitative arm of the study were positive about CTI. Participants who received CTI generally reported an improved experience of transition back to the community, whereas case managers commented that CTI ‘feels like the right thing to do’.
Our economic analyses showed that the costs associated with the delivery of CTI are higher than the cost of TAU, and increase with the frequency and duration of contact between CTI participants and mental health professionals including CTI managers, psychiatrists, care co-ordinators and nursing professionals. However, this trial suggests that this may be beneficial in keeping people well and within the community. The possibility that this results in lower costs associated with longer-term inpatient care and a reduction in further periods of imprisonment or reoffending generally merits further consideration. It should be noted that other limitations in the cost data, for example the short time horizon and small number of service use categories collected, mean that we can draw only tentative economic conclusions.
Implications for health care
Critical time intervention achieved sustained engagement with mental health services in a difficult to care for, complex group whose normal pattern of contact with NHS services is chaotic and crisis driven. CTI was more expensive to deliver than TAU, but this does not take into account that in the real world TAU for this group is already more expensive than TAU for the wider population because of their heavy use of non-routine, emergency care options.
Critical time intervention achieved better contact with services for at least 6 months post prison discharge but the advantage was lost by 12 months. This has implications for community mental health services accepting CTI clients in terms of the likely need for them to adopt robust and proactive approaches to keeping patients engaged in the long term.
Acknowledgements
Contributions of authors
Jenny Shaw (Professor of Forensic Psychiatry/Consultant Forensic Psychiatrist) contributed to design of the study, overall interpretation of the findings and implications for service development and practice, and was a member of the study steering group.
Sarah Conover (Mental Health Researcher) contributed to design of the study, revising the report and final approval of the report to be published.
Dan Herman (Associate Professor of Clinical Epidemiology) contributed to design of the study, revising the report and final approval of the report to be published.
Manuela Jarrett (Researcher, Psychiatry) contributed to design of the study, revising the report and final approval of the report to be published.
Morven Leese (Reader, Psychiatry) contributed to design of the study, revising the report and final approval of the report to be published.
Paul McCrone (Professor of Health Economics) conducted the economic evaluation of the intervention, co-authored the relevant chapters of the report, contributed to design of the study, revising the report, final approval of the report to be published and was a member of the study steering group.
Caroline Murphy (Operations Director, King’s College London Clinical Trials Unit) contributed to design of the study, responsible for randomisation process, revising the report, final approval of the report to be published and member of the study steering group.
Jane Senior (Senior Research Fellow, Offender Health Research Network) contributed to design of the study, provided clinical guidance in the interpretation of the findings and implications for service development, revising the report, final approval of the report to be published, was also responsible for the review and revision of the case manager manual, and a member of the study steering group.
Ezra Susser (Professor of Epidemiology and Psychiatry) contributed to design of the study, revising the report and final approval of the report to be published.
Graham Thornicroft (Professor of Community Psychiatry) contributed to design of the study, revising the report, final approval of the report to be published and was a member of the study steering group.
Nat Wright (Spectrum Community Interest Company) contributed design of the study, revising the report, final approval of the report to be published and was a member of the study steering group.
Dawn Edge (Senior Lecturer, Psychology) authored Chapters 2 and 3, and was a member of the study steering group.
Richard Emsley (Senior Lecturer, Biostatistics) conducted the quantitative data analyses, co-authored Chapter 3 and was a member of the study steering group.
Charlotte Lennox (Research Fellow, Offender Health Research Network) interpreted the findings of the quantitative analyses, carried out the coding and analysis of the qualitative data, and co-authored Chapters 1–4, 7 and 8.
Alyson Williams (Research Fellow, Offender Health Research Network) wrote the introductory background sections to the report, undertook the initial compilation and formatting of the final report, and was also responsible for the review and revision of the case manager manual.
Henry Cust (Research Assistant) conducted the economic evaluation of the intervention and co-authored Chapter 6.
Gareth Hopkin (Research Assistant) was responsible for site set-up, collecting data, liaising with case managers and qualitative interviewing, and was a member of the study steering group.
Caroline Stevenson (Research Assistant) compiled the quantitative data for analysis, interpreted the findings of the quantitative analyses and carried out the transcription, coding and analysis of the qualitative data, and co-authored Chapter 4.
Case managers in the Critical time Intervention for Severely mentally ill Prisoners study
We would also like to thank the following individuals who were case managers, or managed the intervention at their locality: Sue Bell, Veronica Chincon, Naomi Humber, Theodora Machingura, John Martins and Kim Peacock.
Members of the Critical time Intervention for Severely mentally ill Prisoners study steering group
Philip Asherson, King’s College London; Paul Bebbington, University College London; Ian Cumming, Oxleas NHS Foundation Trust; Sean Duggan, Centre for Mental Health; Dawn Edge, University of Manchester; Richard Emsley, University of Manchester; Andrew Forrester, South London and Maudsley NHS Foundation Trust; Mari Harty, South West London and St George’s Mental Health NHS Trust; Gareth Hopkin, King’s College London; Paul McCrone, King’s College London; Caroline Murphy, King’s College London; Jenny Shaw, University of Manchester; Graham Thornicroft, King’s College London; Lucia Valmaggia, King’s College London; Loree Wilson, Make Your Way Community Interest Company, Sunderland; and Nat Wright, Transform Research Alliance, Spectrum Community Interest Company, Wakefield.
Members of the University of Manchester research team and working group for revision of Case manager manual
Alison Foreman, Lancashire Criminal Justice and Liaison and Diversion Team; William Harper, Merseycare NHS Trust; Charlotte Lennox, Research Fellow; Natasha Peniston, Volunteer; Jane Senior, Research Manager; Caroline Stevenson, Research Assistant; Dylan Stratton, Core Group Volunteer, Inspiring Change Manchester/Shelter; Alyson Williams, Research Fellow; and Nicola Worthington, Administrative Officer.
Data sharing statement
Participant consent forms did not specifically allow for the sharing of anonymised data to third parties. Any request for access would be referred to the University of Manchester’s records office for advice before disclosure. For further information about this study please contact the corresponding author.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
References
- Singleton N, Meltzer H, Gatward R, Coid J, Deasy D. Psychiatric Morbidity Among Prisoners: Summary Report. London: Office for National Statistics; 1998.
- Gunn J, Maden A, Swinton M. Mentally Disordered Prisoners. London: Institute of Psychiatry; 1991.
- Maden A, Taylor C, Brooke D, Gunn J. Mental Disorder in Remand Prisoners. London: Home Office; 1995.
- Birmingham L, Mason D, Grubin D. Prevalence of mental disorder in remand prisoners: consecutive case study. BMJ 1996;313:1521-4. https://doi.org/10.1136/bmj.313.7071.1521.
- Birmingham L. Screening prisoners for psychiatric illness: who benefits?. Psychiatr Bull 2001;25:462-4. https://doi.org/10.1192/pb.25.12.462.
- Fazel S, Danesh J. Serious mental disorder in 23000 prisoners: a systematic review of 62 surveys. Lancet 2002;359:545-50. https://doi.org/10.1016/S0140-6736(02)07740-1.
- Howard League for Penal Reform . Breaking Point: Understaffing and Overcrowding in Prisons. Research Briefing 2014. www.howardleague.org/publications-prisons/ (accessed February 2016).
- The Provision of Mental Health Care in Prisons. London: Prison Service; 1997.
- Birmingham L. The mental health of prisoners. Adv Psychiatr Treat 2003;9:191-20. https://doi.org/10.1192/apt.9.3.191.
- The Future Organisation of Prison Healthcare. London: Department of Health; 1999.
- Changing the Outlook: A Strategy for Developing and Modernising Mental Health Services in Prison. London: Department of Health; 2001.
- Care Programme Approach for People with a Mental Illness Referred to the Specialist Psychiatric Services. HC(90)23/LASSL(90)11. London: Department of Health; 1990.
- Offender Health Research Network . A National Evaluation of Prison Mental Health In-Reach Services: A Report to the National Institute of Health Research 2009. www.ohrn.nhs.uk (accessed August 2015).
- Senior J, Birmingham L, Harty MA, Hassan L, Hayes AJ, Kendall K, et al. Identification and management of prisoners with severe psychiatric illness by specialist mental health services. Psychol Med 2013;43:1511-20. http://dx.doi.org/10.1017/S0033291712002073.
- Lennox C, Senior J, King C, Hassan L, Clayton R, Thornicroft G, et al. The management of released prisoners with severe and enduring mental illness. J Forens Psychiatry Psychol 2012;23:67-75. https://doi.org/10.1080/14789949.2011.634921.
- Dyer W, Biddle P. Prison health discharge planning – evidence of an integrated care pathway or the end of the road?. Soc Policy Soc 2013;12:521-32. https://doi.org/10.1017/S1474746412000693.
- Proven Re-offending Statistics Quarterly Bulletin: January to December 2013, England and Wales. London: Ministry of Justice; 2015.
- Baillargeon J, Penn JV, Knight K, Harzke AJ, Baillargeon G, Becker EA. Risk of reincarceration among prisoners with co-occurring severe mental illness and substance use disorders. Adm Policy Ment Health 2010;37:367-74. http://dx.doi.org/10.1007/s10488-009-0252-9.
- Baillargeon J, Hoge SK, Penn JV. Addressing the challenge of community reentry among released inmates with serious mental illness. Am J Community Psychol 2010;46:361-75. http://dx.doi.org/10.1007/s10464-010-9345-6.
- Wilson JA, Wood PB. Dissecting the relationship between mental illness and return to incarceration. J Crim Justice 2014;42:527-37. https://doi.org/10.1016/j.jcrimjus.2014.09.005.
- Farrell M, Marsden J. Acute risk of drug-related death among newly released prisoners in England and Wales. Addiction 2008;103:251-5. http://dx.doi.org/10.1111/j.1360-0443.2007.02081.x.
- Merrall EL, Kariminia A, Binswanger IA, Hobbs MS, Farrell M, Marsden J, et al. Meta-analysis of drug-related deaths soon after release from prison. Addiction 2010;105:1545-54. http://dx.doi.org/10.1111/j.1360-0443.2010.02990.x.
- Zlodre J, Fazel S. All-cause and external mortality in released prisoners: systematic review and meta-analysis. Am J Public Health 2012;102:e67-75. http://dx.doi.org/10.2105/AJPH.2012.300764.
- Pratt D, Piper M, Appleby L, Webb R, Shaw J. Suicide in recently released prisoners: a population-based cohort study. Lancet 2006;368:119-23. http://dx.doi.org/10.1016/S0140-6736(06)69002-8.
- Pratt D, Appleby L, Piper M, Webb R, Shaw J. Suicide in recently released prisoners: a case-control study. Psychol Med 2010;40:827-35. http://dx.doi.org/10.1017/S0033291709991048.
- Williamson M. Primary care for offenders: what are the issues and what is to be done?. Qual Prim Care 2007;15:301-5.
- Hartfree YF, Dearden C, Pound E. High Hopes: Supporting Ex-Prisoners in Their Lives after Prison. London: Department for Work and Pensions; 2008.
- Binswanger IA, Nowels C, Corsi KF, Long J, Booth RE, Kutner J, et al. ‘From the prison door right to the sidewalk, everything went downhill’, a qualitative study of the health experiences of recently released inmates. Int J Law Psychiatry 2011;34:249-55. http://dx.doi.org/10.1016/j.ijlp.2011.07.002.
- Woodall J, Dixey R, South J. Prisoners’ perspectives on the transition from the prison to the community: implications for settings-based health promotion. Crit Public Health 2013;23:188-200. https://doi.org/10.1080/09581596.2012.732219.
- Powell E. Water Tower Speech, UK 1961. www.studymore.org.uk/powell.htm (accessed February 2016).
- Goffman E. Asylums: Essays on the Social Situation of Mental Patients and Other Inmates. London: Penguin; 1968.
- Wing JK, Brown GW. Institutionalism and Schizophrenia: A Comparative Study of Three Mental Hospitals. Cambridge: Cambridge University Press; 1970.
- Intagliata J. Improving the quality of community care for the chronically mentally disabled: the role of case management. Schizophr Bull 1982;8:655-74. https://doi.org/10.1093/schbul/8.4.655.
- Onyett S. Case Management in Mental Health. Cheltenham: Stanley Thornes; 1998.
- Burns T, Fioritti A, Holloway F, Malm U, Rössler W. Case management and assertive community treatment in Europe. Psychiatr Serv 2001;52:631-6. http://dx.doi.org/10.1176/appi.ps.52.5.631.
- Hangan C. Introduction of an intensive case management style of delivery for a new mental health service. Int J Ment Health Nurs 2006;15:157-62. http://dx.doi.org/10.1111/j.1447-0349.2006.00397.x.
- Smith L, Newton R. Systematic review of case management. Aust N Z J Psychiatry 2007;41:2-9. http://dx.doi.org/10.1080/00048670601039831.
- Marshall M, Gray A, Lockwood A, Green R. Case management for people with severe mental disorders (review). Cochrane Database Syst Rev 1998;2. https://doi.org/10.1002/14651858.cd000050.
- Marshall M, Lockwood A, Gath D. Social services case-management for long-term mental disorders: a randomised controlled trial. Lancet 1995;345:409-12. https://doi.org/10.1016/S0140-6736(95)90399-2.
- Kinner SA, Alati R, Longo M, Spittal MJ, Boyle FM, Williams GM, et al. Low-intensity case management increases contact with primary care in recently released prisoners: a single-blinded, multisite, randomised controlled trial. J Epidemiol Community Health 2016;70:683-8. http://dx.doi.org/10.1136/jech-2015-206565.
- Test MA, Stein LI. Practical guidelines for the community treatment of markedly impaired patients. Community Ment Health J 1976;12:72-8. https://doi.org/10.1007/BF01435740.
- Stein LI, Test MA. Alternative to mental hospital treatment. I. Conceptual model, treatment program, and clinical evaluation. Arch Gen Psychiatry 1980;37:392-7. https://doi.org/10.1001/archpsyc.1980.01780170034003.
- Bond GR, Drake RE, Mueser KT, Latimer E. Assertive community treatment for people with severe mental illness: critical ingredients and impact on patients. Dis Manage Health Outcomes 2001;9:141-59. https://doi.org/10.2165/00115677-200109030-00003.
- Mueser KT, Bond GR, Drake RE, Resnick SG. Models of community care for severe mental illness: a review of research on case management. Schizophr Bull 1998;24:37-74. https://doi.org/10.1093/oxfordjournals.schbul.a033314.
- Marshall M, Lockwood A. Assertive community treatment for people with severe mental disorders. Cochrane Database Syst Rev 1998;2. https://doi.org/10.1002/14651858.cd001089.
- Susser E, Valencia E, Conover S, Felix A, Tsai WY, Wyatt RJ. Preventing recurrent homelessness among mentally ill men: a ‘critical time’ intervention after discharge from a shelter. Am J Public Health 1997;87:256-62. https://doi.org/10.2105/AJPH.87.2.256.
- Herman D, Opler L, Felix A, Valencia E, Wyatt RJ, Susser E. A critical time intervention with mentally ill homeless men: impact on psychiatric symptoms. J Nerv Ment Dis 2000;188:135-40. https://doi.org/10.1097/00005053-200003000-00002.
- Lennon MC, McAllister W, Kuang L, Herman DB. Capturing intervention effects over time: reanalysis of a critical time intervention for homeless mentally ill men. Am J Public Health 2005;95:1760-6. http://dx.doi.org/10.2105/AJPH.2005.064402.
- Lako DA, de Vet R, Beijersbergen MD, Herman DB, van Hemert AM, Wolf JR. The effectiveness of critical time intervention for abused women and homeless people leaving Dutch shelters: study protocol of two randomised controlled trials. BMC Public Health 2013;13. http://dx.doi.org/10.1186/1471-2458-13-555.
- Carpinteiro da Silva TF, Lovisi G, Cavalcanti MT, Dahl C, Conover S, Valencia E, et al. Critical time intervention – task shifting: a new psychosocial intervention for people with severe mental illness in Latin America. Letter to editor. Rev Psiquiatr Clín 2013;40.
- Forrester A, Till A, Senior J, Shaw J. Competitive tendering and offender health services. Lancet Psychiatry 2015;2:859-61. http://dx.doi.org/10.1016/S2215-0366(15)00414-9.
- Bowen RA. Management of Mentally Disordered Prisoners: A Qualitative Study of the Early Stages of Custody 2008.
- Draine J, Herman DB. Critical time intervention for reentry from prison for persons with mental illness. Psychiatr Serv 2007;58:1577-81. http://dx.doi.org/10.1176/ps.2007.58.12.1577.
- Jarrett M, Thornicroft G, Forrester A, Harty M, Senior J, King C, et al. Continuity of care for recently released prisoners with mental illness: a pilot randomised controlled trial testing the feasibility of a critical time intervention. Epidemiol Psychiatr Sci 2012;21:187-93. http://dx.doi.org/10.1017/S2045796011000783.
- Diagnostic and Statistical Manual of Mental Disorders – Fourth Edition, Text Revision. Washington, DC: American Psychiatric Association; 2000.
- Rucker J, Newman S, Gray J, Gunasinghe C, Broadbent M, Brittain P, et al. OPCRIT+: an electronic system for psychiatric diagnosis and data collection in clinical and research settings. Br J Psychiatry 2011;199:151-5. http://dx.doi.org/10.1192/bjp.bp.110.082925.
- Mental Health Act 1983. London: The Stationery Office; 1983.
- The Sentencing Council for England and Wales . Sentencing Council Guidelines n.d. www.sentencingcouncil.org.uk/publications (accessed February 2016).
- MRC Guidelines for Good Clinical Practice in Clinical Trials. London: Medical Research Council; 1998.
- Spitzer RL, Williams JBW, Gibbon M, First MB. Structured Clinical Interview for DSM-III-R Axis II Disorders (SCID-II). Washington, DC: American Psychiatric Press; 1990.
- Selzer ML. The Michigan alcoholism screening test: the quest for a new diagnostic instrument. Am J Psychiatry 1971;127:1653-8. http://dx.doi.org/10.1176/ajp.127.12.1653.
- Skinner HA. The drug abuse screening test. Addict Behav 1982;7:363-71. https://doi.org/10.1016/0306-4603(82)90005-3.
- Beecham J, Knapp M, Thornicroft G. Measuring Mental Health Needs. London: Gaskell; 2001.
- da Silva TFC, Lovisi GM, Conover S. Developing an instrument for assessing fidelity to the intervention in the Critical Time Intervention – Task Shifting (CTI-TS) – preliminary report. Arch Psychiatr Psychotherapy 2014;1:55-62. https://doi.org/10.12740/APP/23279.
- Schulz KF, Altman DG, Moher D. CONSORT Group . CONSORT 2010 statement: updated guidelines for reporting parallel group randomized trials. BMJ 2010;340. https://doi.org/10.1136/bmj.c332.
- Data Protection Act 1998. London: The Stationery Office; 1998.
- Freedom of Information Act 2000. London: The Stationery Office; 2000.
- Lewin S, Glenton C, Oxman A. Use of qualitative methods alongside randomised controlled trials of complex healthcare interventions: methodological study. BMJ 2009;339. https://doi.org/10.1136/bmj.b3496.
- Ritchie J, Lewis J. Qualitative Research Practice: A Guide for Social Science Students and Researchers. London: Academic Press; 2003.
- Curtis L. Unit Costs of Health and Social Care 2014. Canterbury: Personal Social Services Research Unit, University of Kent; 2014.
- NHS Reference Costs 2012–2013. London: Department of Health; 2014.
- Barrat D. One in 12 Criminals Reoffends Just 18 days after Being Freed from Prison. The Telegraph 2016. www.telegraph.co.uk/news/uknews/crime/12097595/one-in-12-criminals-reoffends-just-18-days-after-being-freed-from-prison.html (accessed May 2016).
- Prins H. Offenders, Deviants or Patients?. London: Routledge; 2005.
- Ellis CG. Making dysphoria a happy experience. Br Med J 1986;293:317-18. https://doi.org/10.1136/bmj.293.6542.317.
- O’Dowd TC. Five years of heartsink patients in general practice. BMJ 1988;297:528-30. https://doi.org/10.1136/bmj.297.6647.528.
Appendix 1 Case manager manual
Appendix 2 Critical time intervention fidelity scale
| Components (compliance fidelity) | |
|---|---|
| Phase 1 (prison – 4 weeks prior to release) | Engagement and early linking |
|
|
| Phase 2 (release – 2 weeks post release) | Intensive outreach |
|
|
| Phases 1–3 | Three phases |
|
|
| Phases 1–3 | Focused |
|
|
| Phase 3 (3–6 weeks post release) | Monitoring |
|
|
| Closed cases | Time limited |
|
|
| 6 week post discharge | 6-week follow-up |
|
|
| Structure (context fidelity) | |
|---|---|
| Any phase | Caseload size |
| Caseload size is 18 standard caseload equivalents or fewer per worker | |
| Quality (competence fidelity) | |
|---|---|
| Phase 1 | Intake assessment |
|
|
| Any phase | Phase planning |
|
|
| Closed cases | Closing note |
|
|
| Phases 1 and 2 | CTI managers role with client |
|
|
| Not based on phase | Clinical supervision |
|
|
| Not based on phase | Organisational support |
|
|
Appendix 3 Harms reporting: Consolidated Standards of Reporting Trials – causal relationships’ definitions
The causal relationship between reported events and trial participation was assessed as follows.
| Relationship | Description |
|---|---|
| Unrelated | There is no evidence of any causal relationship |
| Unlikely | There is little evidence to suggest that there is a causal relationship (e.g. the event did not occur within a reasonable time after administration of the trial treatment/procedure). There is another reasonable explanation for the event (e.g. the participant’s clinical condition, other concomitant treatment) |
| Possible | There is some evidence to suggest a causal relationship (e.g. because the event occurs within a reasonable time after administration of the trial treatment/procedure). However, the influence of other factors may have contributed to the event (e.g. the participant’s clinical condition, other concomitant treatments) |
| Probable | There is evidence to suggest a causal relationship and the influence of other factors is unlikely |
| Definitely | There is clear evidence to suggest a causal relationship and other possible contributing factors can be ruled out |
Appendix 4 Interview schedules: intervention participants
Semistructured qualitative interview schedule: pre-release treatment-as-usual participant
-
How long to go until you are released?
-
Do you need help with anything when you are released?
-
Health.
-
Substance misuse.
-
Housing.
-
Finances.
-
Employment.
-
Family.
-
Are these things you feel you would need help with or are these things your care team have suggested would be helpful?
-
-
What responses to/support for these needs have you received?
-
Have you been put in contact with any services yet? If so,
-
Which ones?
-
Who organised this?
-
In what way?
-
If not, why not? (Services poor, hard to organise, not needed.)
-
-
Are you receiving any treatment at the moment? If so,
-
What?
-
Who organised this for you?
-
If on medication, what kind and will this continue when released? (If so, who will organise continuation?)
-
Are you taking the medication? If not, why not?
-
-
What do you think of the support you have received in preparing for release?
-
Is there anything that has been particularly good/helpful?
-
Is there anything that you feel should be improved?
-
Semistructured qualitative interview schedule: post-release treatment-as-usual participant
-
How long have you been released from prison?
-
When you were released did you feel you needed help with anything?
-
Health.
-
Substance misuse.
-
Housing.
-
Finances.
-
Employment.
-
Family.
-
-
How have things been going for you since you were released?
-
Health.
-
Substance misuse.
-
Housing.
-
Finances.
-
Employment.
-
Family.
-
-
What responses to/support for these needs have you received?
-
Are you in contact with any services at the moment? If so,
-
Which ones?
-
Who organised this?
-
In what way?
-
At what time point?
-
If not, why not? (Services poor, too hard to organise, not needed.)
-
-
Are you receiving any treatment at the moment? If so,
-
What?
-
Who organised this for you?
-
If on medication, what and did this continue from prison? (If so, who organised continuation?)
-
If not, who made the appointment/started the medication?
-
Are you taking the medication? If not, why not?
-
-
What do you think of the support you have received since release?
-
Is there anything that has been particularly good/helpful?
-
Is there anything that you feel should be improved?
-
-
Have you been in contact with the police since release?
-
If so, for what reason?
-
How many times?
-
-
Have you been in hospital since release?
-
How did this come about?
-
How many times?
-
Semistructured qualitative interview schedule: pre-release critical time intervention participant
-
How long to go until you are released?
-
Do you need help with anything when you are released?
-
Health.
-
Substance misuse.
-
Housing.
-
Finances.
-
Employment.
-
Family.
-
Are these things you feel you would need help with or are these things your care team have suggested would be helpful?
-
-
How often have you been seeing your CTI manager?
-
What have they been doing to address your problems/needs?
-
So far, has this been helpful?
-
What has been good?
-
What could be improved?
-
-
Have you been put in contact with any services yet? If so,
-
Which ones?
-
Who organised this?
-
In what way?
-
If not, why not? (Services poor, hard to organise, not needed.)
-
-
Are you receiving any treatment at the moment? If so,
-
What?
-
Who organised this for you?
-
If on medication, what kind and will this continue when released? (If so, who will organise this?)
-
Are you taking the medication? If not, why not?
-
-
Have you been in prison before? If so, how have you been finding the release process this time, compared with the previous time/s?
Semistructured qualitative interview schedule: post-release critical time intervention participant
-
How long have you been released from prison?
-
When you were released did you feel you needed help with anything?
-
Health.
-
Substance misuse.
-
Housing.
-
Finances.
-
Employment.
-
Family.
-
-
How have things been going for you since you were released?
-
Health.
-
Substance misuse.
-
Housing.
-
Finances.
-
Employment.
-
Family.
-
-
How often did you see your CTI manager before and after release?
-
What did they do to address your problems/needs?
-
Was this helpful?
-
What was good?
-
What could be improved?
-
-
Are you in contact with any services at the moment? If so,
-
Which ones?
-
Who organised this?
-
In what way?
-
At what time point?
-
If not, why not? (Services poor, too hard to organise, not needed.)
-
-
Are you receiving any treatment at the moment? If so,
-
What?
-
Who organised this for you?
-
If on medication, what and did this continue from prison? (If so, who organised continuation?)
-
If not, who made the appointment/started the medication?
-
Are you taking the medication? If not, why not?
-
-
Have you been in prison before? If so, how did you find the release process this time, compared with the previous time/s?
-
Have you been in contact with the police since release?
-
If so, for what reason?
-
How many times?
-
-
Have you been in hospital since release?
-
How did this come about?
-
How many times?
-
Critical time intervention participant qualitative matrix
| Pre-release TAU participant | Pre-release CTI participant | Post-release TAU participant | Post-release CTI participant | |
|---|---|---|---|---|
| Continuity of care | ||||
| Support/advocacy | ||||
| Uncertainty | ||||
| Coercion | ||||
| Loss/starting over | ||||
| Stable/suitable environment | ||||
| Reliance on others (family relationships) | ||||
| Established relationships/rapport | ||||
| Mental health | ||||
| Stigma/hopelessness |
Appendix 5 Interview schedules: health professionals
Semistructured qualitative interview schedule: community mental health staff
-
What is your professional role?
-
Can you talk me through the usual post-release process for patients coming out of prison?
-
How long before release do you liaise with prison mental health services?
-
Is this initiated by staff at the prison?
-
What are the common needs of patients on release?
-
What areas do they receive help with and who has responsibility for these? How do you provide help?
-
Is the process formally defined/standardised?
-
-
What organisations, if any, do you liaise with?
-
Are shared protocols held between all the relevant organisations?
-
Are roles and responsibilities formally defined?
-
-
What is the process for linking patients in with these services/organisations they may need contact with?
-
Is this a formal process or has it developed locally?
-
-
Is there a system for checking if patients attend appointments made for them?
-
Are there follow-up protocols?
-
Is there an agreed procedure if patients did not attend?
-
-
Which aspects of the release process work well?
-
Why?
-
-
Which areas of this process could be improved?
-
How?
-
Do you feel there are any gaps in the process that allow people to slip through the net?
-
-
Overall, how well would you say the release preparation and transition to community processes work?
-
What do you think of the CTI process?
-
Positives?
-
Negatives?
-
-
If CTI were to replace TAU do you think this would work?
-
If yes, why and what would be the benefits?
-
If no, why not and could changes be made to facilitate implementation?
-
-
What barriers to, and facilitators of, CTI have you come across?
Semistructured qualitative interview schedule: prison mental health staff
-
What is your professional role?
-
Can you talk me through the usual pre-release process for patients being discharged from prison?
-
How long before discharge does this begin?
-
How often are they seen?
-
What are the common needs of prisoners?
-
What areas do they receive help with and who has responsibility for these? How do you provide help?
-
After release, who is responsible for their care?
-
Is the process formally defined/standardised?
-
-
What organisations, if any, do you liaise with?
-
Are shared protocols held between all the relevant organisations?
-
Are roles and responsibilities formally defined?
-
-
What is the process for linking prisoners in with these services/organisations they may need contact with?
-
Is this a formal process or has it developed locally?
-
-
Which aspects of the release process work well?
-
Why?
-
-
Which areas of this process could be improved?
-
How?
-
Do you feel there are any gaps in the process that allow people to slip through the net?
-
-
Overall, how well would you say the pre-release preparation and transition to community processes work?
-
What do you think of the CTI process?
-
Positives?
-
Negatives?
-
-
If CTI were to replace TAU do you think this would work?
-
If yes, why and what would be the benefits?
-
If no, why not and could changes be made to facilitate implementation?
-
List of abbreviations
- ACT
- assertive community treatment
- CI
- confidence interval
- CJS
- criminal justice system
- CM
- case management
- CMHT
- community mental health team
- CONSORT
- Consolidated Standards of Reporting Trials
- CPA
- care programme approach
- CTI
- critical time intervention
- DAST
- Drug Abuse Screening Test
- GP
- general practitioner
- HES
- Hospital Episode Statistics
- HMPS
- Her Majesty’s Prison Service
- MAPPA
- multiagency public protection arrangements
- MAST
- Michigan Alcohol Screening Test
- ONS
- Office for National Statistics
- OPCRIT
- Operational Criteria Checklist for Psychotic and Affective Illness
- PD
- personality disorder
- PNC
- Police National Computer
- R&D
- research and development
- RCT
- randomised controlled trial
- REC
- research ethics committee
- SAE
- serious adverse event
- SCID-II
- Structured Clinical Interview for Diagnostic and Statistical Manual of Mental Disorders-Fourth Edition Personality Disorders
- SMI
- severe mental illness
- SPA
- single point of access
- TAU
- treatment as usual