Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 12/129/10. The contractual start date was in January 2014. The final report began editorial review in February 2016 and was accepted for publication in September 2016. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
At the time of the study, Antony Arthur was a member of the National Institute for Health Research Health Services and Delivery Research commissioning board and Jill Maben was a member of the National Institute for Health Research Health Services and Delivery Research researcher-led panel.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2017. This work was produced by Arthur et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction and background
Introduction
Our study set out to develop a training intervention for health-care assistants (HCAs) that could improve the relational care provided to older people in hospital. We examined whether or not such an intervention could be tested in a cluster randomised controlled trial. This chapter describes the context and background to the Can Health-care Assistant Training improve the relational care of older people? (CHAT) study. In this chapter we also consider the structure and role of the HCA workforce and the needs of the older people they care for. We describe how we use the term ‘relational care’ with reference to our study and briefly review previous attempts to evaluate interventions to improve the quality of relational care. Elsewhere in this report (see Chapter 2) we describe how the wider context of our study has changed over the period that the study was designed and conducted, particularly in relation to the Francis report1 and the Cavendish review. 2 The ways in which we drew on specific literature to influence the training intervention we developed and tested is presented in Chapter 5.
The care of older people in hospital
Those aged > 75 years now account for 24% of all hospital admissions, an increase of 57% over the previous decade, with the average hospital stay for this age group simultaneously decreasing from 15.2 to 9.4 days. 3 The quality of health care delivered to older people has come under increased scrutiny. A report by The King’s Fund cited 32 initiatives from statutory bodies, charities and campaign groups drawing attention to deficiencies in how older people are cared for. 4 The King’s Fund’s Point of Care programme was a response to a more general concern about ‘not getting the basics right’ in the care for older people. 5,6
In a NHS inpatient survey nearly one-fifth of respondents did not feel that they were always treated with respect and dignity. 7 Attitudes of staff is the second highest area of concern within complaints made to the NHS. 8 When the Care Quality Commission reviewed ‘the state of health and adult social care services’ in 2012, they found that many providers were ‘struggling in areas such as dignity and respect, nutrition, care and welfare’. 9 The devastating impact that deficiencies in care delivery can have on individuals can be seen in the Patients Association’s report10 of 13 cases of care failures.
Relational care
The focus of the CHAT study was the relational care provided to older people in hospital. Relational aspects of care include dignity, empathy and emotional support as distinct from functional or transactional aspects of care, such as access to services, waiting times, food and noise levels. 11 As most health-care interactions involve both transactional and relational elements, it follows that attempts to improve the quality of care have to go beyond methods that address only the transactional aspects of care and examine ‘how staff relate to patients, their mind sets, attitudes and feelings’. 12
In a synthesis of qualitative evidence of older patients’ and relatives’ experiences of hospital care,13 it was the relational aspects of care that affected whether care experiences were perceived as good or bad. Three themes that underscored older people’s understanding of relational care were identified: older people’s need for reciprocity (‘connect with me’), maintaining their identity (‘see who I am’) and sharing decision-making (‘include me’). Evidence from survey data is consistent with this. NHS patients responding to surveys report that emotional support, empathy and respect are the aspects of care that they consider most important. 14
For Nolan et al.,15 it is relationships ‘between patients, their families, staff from all disciplines, and the wider community’ that lie at the heart of health care. In shifting attention towards ‘relationship-centred’ care rather than person-centred care, emphasis is placed on care interactions (two-way) rather than on an oversimplified view of individual needs (one way). Although few would argue against patient-centred or relationship-centred care being of fundamental importance in how patients are cared for, there is a lack of clarity among staff at all levels as to what this actually means in practice. 16 Abstract concepts need to be operationalised in a way that is meaningful to staff at all levels.
In deconstructing ‘dignified care’, respectful communication was found to be a key element. 5 In a review of studies of physician–patient communication, physician qualities such as empathy, friendliness, courtesy and listening were associated with positive patient outcomes. 17 Hospital patients report that preservation of dignity requires respectful communication and forms of address18 and, for older patients in particular, the need for staff to show an interest in them, kindness, timeliness and attention to ‘the little things’. 19 In attempts to help health-care organisations focus on the experience of users, there have been occasional examples of organisations outside the public sector working with NHS organisations to develop ‘customer focus’, such as the work undertaken between Musgrove Park Hospital and John Lewis (Michelle Jennings, Musgrove Park Hospital Customer Care Programme Partnership with John Lewis, 2012, personal communication). Health-care staff are often uncomfortable with the notion of patients as consumers or customers,20 and acute health-care staff often hold the view that hospitals are not the best place of care for older patients, suggesting that care delivery is often provider led rather than user led.
Maintaining identity is a key element in how older people judge their interactions with paid carers,21 and both patients and their relatives comment on the importance of staff ‘seeing the person behind the patient’. 6 Life-story work is the process of gaining knowledge and information about an individual’s life that staff can use to enhance the care they provide and evidence for its clinical effectiveness is predominantly qualitative. 22 Although life-story work was originally developed for people with dementia, it is increasingly being used beyond dementia care settings and long-stay care settings. 23 In acute care settings, the challenge is for staff to get to know older patients over increasingly shorter patient stays in hospital.
The clinical support workforce
Nurses have often been targeted as both the source of the problem and the solution to concerns about loss of dignity for patients in hospital. 6 However, within the NHS, HCAs have become an increasingly important section of the workforce, particularly in relation to older people. The proportion of HCA time delivering direct and indirect patient care is approximately 60%, nearly twice that of registered nurses. 24
In England, there are approximately 130,000 HCAs employed in NHS hospital and community services. 25 Demographically, HCAs tend to differ from registered nurses, more closely resembling the ethnic diversity of the patient population they serve,24 and are likely to be a more ‘static’ part of the workforce. Over half (54.1%) are aged between 40 and 59 years, 15.8% are from ethnic minority backgrounds, 84.3% are female and most are on NHS pay band 2 (56.5%) or band 3 (36.0%). 25
The work of health-care assistants
The problems of invisibility, marginalisation and subordination of the ‘caring’ work of nurses,26 are likely to be replicated in HCAs whose work often gets little recognition, even from other staff (OS) groups. 27 Case studies28 and observational data29 suggest that HCA work in hospital is predominantly ‘bedside’ or involving routine technical tasks directly or indirectly related to patient care. Daykin and Clarke’s observational study30 of relationships between NHS hospital ward nurses and HCAs, identified a ‘strongly hierarchical’ organisation of care, with nurses having greater variety in their work, but often prevented from attending to patients by their responsibilities for administering medication and doing paperwork. HCA work by contrast tended to be concerned largely with physical aspects of care, often at the expense of negotiation or conversation with patients. In a survey of 1893 HCAs,31 when asked about the duties they performed, respondents reported talking to/reassuring patients and relatives (97%); making beds (86%); bathing patients (83%); telephone liaison with patients, relatives or other departments (83%); patient observations (82%); and feeding patients (79%).
Ethnographic observational data of HCAs working in dementia wards suggest that support in carrying out such a challenging role is drawn from the formation of close-knit groups of HCAs who are sometimes disconnected from the wider ward team,32 resulting in HCAs feeling alienated from the organisation in which they work. 33 Although the proximity to patients means that HCAs gather a lot of information about patients in their care, there are not always clear mechanisms to transfer knowledge from HCAs to nurses. 28,29 Schneider et al. 27 also found evidence of variable communication between HCAs and the wider ward team about patient care, with HCAs feeling ‘at risk’ if they stepped outside the boundaries of their role.
Health-care assistant skill development
Training for HCAs has hitherto been ad hoc, variable and marked by a tendency to focus on tasks and competencies, with little attention paid to relational care. Although investments in staffing and work environments are prerequisites for high-quality care,19,34 historically HCAs have been viewed as the ‘untrained workforce’, leading to an assumption that they are without training needs. 35 HCAs and nurses are largely in favour of more formal training for HCAs, although a blurring of role boundaries is of concern to both staff groups. 36 Among employing organisations there is a lack of consistency in HCA training and how HCAs interface with registered nurses. 37 Moreover, it appears that HCAs often lack confidence in pursuing the few training opportunities available to them. 24,27
Belatedly, and perhaps driven by economic imperatives, skill development of the support workforce has started to receive much greater attention. From an employer’s point of view, by developing the skills of HCAs and creating a better career pathway, there are economic benefits, as any increase in the proportion of the support workforce is ‘likely to be rewarded with significant financial returns’. 38 The Shape of Caring: A Review of the Future Education and Training of Registered Nurses and Care Assistants made a number of recommendations about the support workforce, specifically the need to value the care assistant role, widening access to enable HCAs who may wish to pursue a career in nursing and increasing the quality of education for HCAs. 39 The Council of Deans for Health40 have noted that, although there are an increasing number of initiatives in training and role development for HCAs, there are problems of variability in access and quality, poor communication between employers and education providers, and a workplace culture that often affords low priority to the personal development of HCAs.
Interventions to improve relational care
The following is not a systematic review of interventions to improve the quality of relational care. Interventions within the studies that we have identified all share a broad aim of seeking to improve relational care, person-centred or relationship-centred care and better communication or increased empathy on the part of health-care personnel looking after older people in hospital or care home settings. However, they are highly variable in the nature of the interventions studied and the target populations of those giving and receiving care. Many interventions that have been studied were designed to improve care for older people with dementia who make up a significant proportion of the older population in hospital and care homes.
Evaluations identified were typically small in scale and without a control group. Measurement of patient or resident outcomes was rare but one exception was a small study undertaken in a Dutch nursing home setting. 41 Nursing aids were individually trained to communicate effectively with residents by using positive speech and biographical statements. Although there were no direct effects of the intervention on the problem behaviours or psychopathology of residents, caregiver distress was reduced.
Bryan et al. 42 asked 157 participants in a course on communication to rate various aspects of their competence. The workshop package focused on the care worker’s own communication skills, ways to enhance these skills, different communication impairments, effects on interaction and practical ways to help. It included exercises, discussion and video material. Participants rated themselves before and after the workshop and reported an increase in confidence, reduced frustration and greater recognition of the need to allow more time to communicate with some individuals. Participants also felt that their attitudes towards and their ability to care for older people with communication difficulties had improved as a result of the training.
A review of 12 trials of interventions to enhance communication in dementia care in various care settings43 concluded that communication skills training in dementia care can improve quality of life and well-being of people with dementia and increase the quality of interactions between staff and people with dementia. The reviewers suggested that organisational features, such as incentives and ‘booster’ sessions for participants, might improve the sustainability of positive effects from communication interventions. In a Cochrane systematic review,44 some evidence was found that reminiscence therapy for people with dementia improves mood, cognition and staff knowledge of patient backgrounds and relieves caregiver strain, but trials are few and often small. When compared with communication skills training, a story-sharing intervention for nursing home residents and nurse aides improved mutuality and empathy. 45 A qualitative study of the introduction of a biographical approach to care in a general hospital setting found that relationships were strengthened between staff and patients and staff and relatives. 46
In a pilot study set in two nursing homes, nursing assistants received a multicomponent intervention to increase awareness of person-centred care using video-taped biographies of residents and video-tapes of resident–carer interactions. Following training, residents’ perceptions of relationship closeness were increased. Nursing assistants’ perceptions of satisfaction and closeness, and resident satisfaction also increased. 47 To determine the impact of a HCA education programme on the quality of care for older people living in a residential home in New Zealand a pre- and postintervention evaluation study was undertaken. The proportion of observations of resident care conducted after the training that were considered ‘appropriate and adequate’ increased. 48
Summary
Older people make up a large and increasing proportion of NHS hospital patients. There have been growing concerns about suboptimal standards of care that disproportionately affect older patients. Relational care can be understood as the way in which staff relate to patients as distinct from the transactional elements of care interactions. There is evidence that older people and their relatives judge their experience of hospital care in terms of how staff ‘connect with them’, help maintain their identity and involve them in decisions about their care. Although health-care staff are often uncomfortable with the notion of patients as ‘customers’, many of the things that older people believe are important (courtesy, respectful communication and attending to ‘the little things’) have a clear overlap with good customer care provided in non-health-care settings.
Health-care assistants deliver an increasing amount of the direct care of older patients in hospital. There is inconsistency in training and expectations, variability in roles and responsibilities within the ward setting and uncertainty about the interface between HCAs, the wider clinical team and visitors or relatives. Greater attention has recently been paid to the role of the HCA and their training needs. The evidence base for training interventions for HCA training in relational care is characterised by small-scale studies with a focus on dementia, and outcomes of acceptability rather than efficacy that are measured at caregiver level rather than the level of patients or care home residents.
Chapter 2 Methodological overview
Introduction
This chapter provides an overview of the CHAT study, its aims and the structure of the report. We describe the two phases of the CHAT study and how these relate to and inform each other. The methodological frameworks used in relation to each of the study elements are described and justified. We also report study oversight arrangements and how public and patient involvement informed the study from outset to completion.
Aims of the study
The original aims of the study were to:
-
understand the values-based training needs of HCAs in maintaining the dignity of, and affording respectful care to, older patients in acute NHS settings
-
develop a values-based training intervention for HCAs designed to address the needs of older patients for high-quality relational care
-
assess the feasibility of a cluster randomised controlled trial to compare the performance of the developed training intervention for HCAs with current training in improving the care of older patients in acute NHS settings.
Overview of study
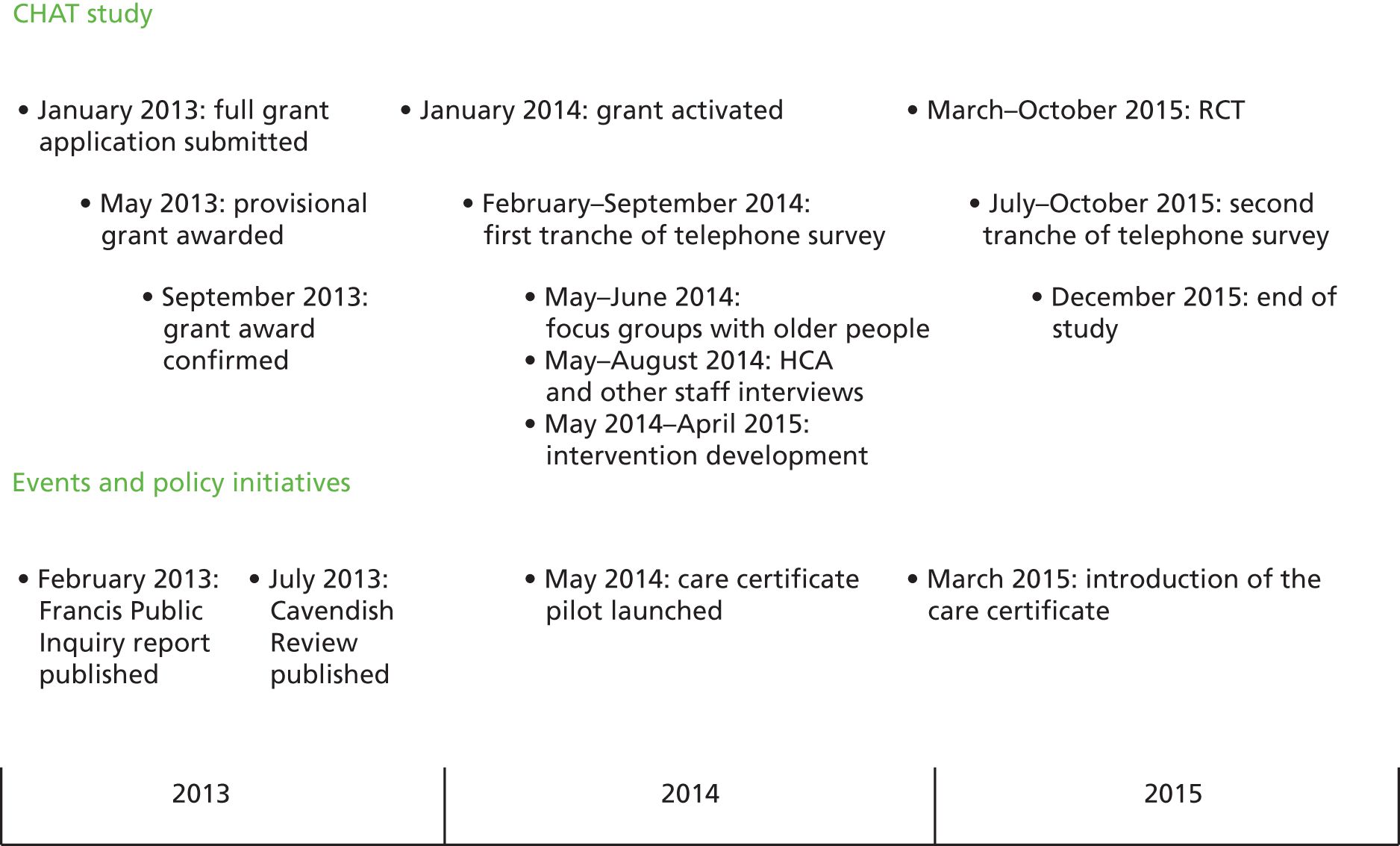
The study was conducted in two sequential phases across three study centres. Phase 1 (scoping and intervention development) was designed to address aims 1 and 2, and phase 2 (feasibility cluster randomised controlled trial and process evaluation) addressed aim 3. The overall study design is illustrated in Figure 1 and described in the following sections.
FIGURE 1.
Overview of CHAT study components and processes.

Phase 1
We conducted a telephone survey of all NHS trusts in England to understand what training as usual (TAU) looked like for HCAs caring for older people in hospitals in England. We wished to establish the structure, content and variability of HCA training and, in particular, training in providing relational care of older patients in hospital. Respondents to the survey were those responsible for HCA training within their trust. The methods and findings from the telephone survey are reported in detail in Chapter 3.
The qualitative component of phase 1 comprised focus groups of older people (or their carers) with recent experience of hospital care, together with interviews of HCAs and other hospital staff undertaken in each of the three study centres. These methods and findings are described and reported in Chapter 4. The purpose of these focus groups was to understand the care experiences of older people and their expectations of the training HCAs should receive. The purpose of the interviews with HCAs and members of staff who worked alongside them was to gain insights into staff perceptions of the challenges that HCAs face in caring for older people in hospital and to explore interviewees’ perceptions of training needs in this area of care.
A new training intervention for HCAs to improve the relational care of older people was developed as part of the study. The process of creating this training intervention, Older People’s Shoes™, is described in Chapter 5. The training intervention drew on several sources: the interviews conducted in phase 1, existing evidence from the literature, an expert panel and learning about customer care practices of four retail organisations.
Phase 2
The second phase of the CHAT study was a feasibility cluster randomised controlled trial and process evaluation. This compared TAU for HCAs with the new HCA training in relational care of older people, that is, the Older People’s Shoes intervention. The unit of randomisation was the hospital ward. Outcomes were assessed at the level of ward, HCA and patient. The purpose of the feasibility trial and the process evaluation was to determine the feasibility and viability of a definitive trial. Methods are described and findings reported in Chapter 6.
The process evaluation was conducted in parallel with the feasibility trial. This consisted of observations of the delivery of the intervention, follow-up interviews with trainers and HCA learners, and learners’ evaluation following training. The process evaluation is reported in Chapter 7.
Methodological frameworks
Owing to the nature of the study design and the range of methods used to address the aims, we drew on a number of methodological frameworks to inform our study. The HCA training intervention developed as part of this study and the feasibility testing of it as part of a trial was informed by the most recent guidance on the development and evaluation of complex interventions. 49 Of the four stages (or elements) of the process from development through to implementation of a complex intervention, the focus within our study was on development (phase 1 of the CHAT study) and feasibility/piloting (phase 2). Our aim was to follow this guidance when possible, up to but not including a definitive evaluation:
Best practice is to develop interventions systematically, using the best available evidence and appropriate theory, then to test them using a carefully phased approach, starting with a series of pilot studies targeted at each of the key uncertainties in the design, and moving on to an exploratory and then a definitive evaluation.
Medical Research Council,49 p. 8
In designing the feasibility study for a randomised controlled trial we used Kirkpatrick’s four-level evaluation model,50 and measured outcomes at each level: reaction (measured by course evaluation), learning (change in empathy and in stereotypical attitudes towards older people), transfer (observations of relational care delivery) and results (patient experience of the relational care they receive). The measurement of distal outcomes of health-care training is challenging. In the Older People’s Services and Workforce Interventions: a Synthesis of Evidence (OPSWISE) study for clinical support workforce developments,51 of the 76 papers identified, only two were reports of randomised controlled trials (Kuske et al. 52 and Clare et al. 53) and only one observed level 4 (care home resident) outcomes. 53
The Kirkpatrick training evaluation model has been criticised for a lack of attention to the environment in which trainee skills are practised. 54 This was in part addressed by the phase 2 process evaluation for which we drew on recently published guidance. 55 A range of methods was used to inform our understanding of the different contexts in which the training intervention was delivered, the process of intervention delivery and the mechanisms of impact.
The changing context of health-care assistant training
Between submission of the grant application for this study in January 2013 and the end of the study period in December 2015, the landscape of health-care delivery generally, and the care of older people and the work of HCAs specifically, underwent a number of changes. Our study needs to be understood in the light of certain events and reactions to those events, which occurred during this period (Figure 2).
FIGURE 2.
Policy-related events and CHAT study timeline.
In February 2013, the Francis report1 into the failings in care at Mid Staffordshire NHS Foundation Trust was published. A number of the findings of the public inquiry were particularly relevant to the present study. These included the observation that failings occurred predominantly on wards for older people’s care. The work and training of HCAs was also subject to scrutiny, with Francis highlighting the inconsistency between employers in how HCAs are trained and the lack of a common standard against which to assess competence. There was a clear acknowledgement that HCA work requires skill and training.
Francis recommended that ‘the aptitude and commitment of candidates for entry into nursing to provide compassionate basic hands-on care to patients should be tested by a minimum period of work experience, by aptitude testing and by nationally consistent practical training’. 1 This referred specifically to aspiring nurses and not to HCAs, but resulted in pre-nursing students being recruited as HCAs within a number of trusts during the survey period as part of the pre-nursing experience pilot. 56
Perhaps the most important outcome of the Francis report, with respect to this study, was that a review of training and recruitment of health and social care support workers was immediately recommended by the Secretary of State. The review, led by Camilla Cavendish, was published in July 2013. 2 The terms of reference for the review included recruitment, training, supervision, support and public confidence with respect to health and social care support workers. The recommendations of the review were guided by two principles: to try to reduce complexity and bureaucracy and to replicate what the best employers are already doing. Although the Cavendish review2 is a seminal work on health and social care support workers, it conveys only a broad picture with respect to the content of the training currently given to health and social care support workers. With respect to the NHS as an employer, Cavendish identified great diversity in training and support for HCAs, little correlation between pay and performance and insufficient supervision.
Cavendish proposed a Certificate of Fundamental Care known more widely as the ‘Care Certificate’. She asked that the Care Quality Commission require all new workers to have achieved this certificate before working unsupervised. Her review recommended that the Nursing and Midwifery Council should determine how best to draw elements of the practical nursing degree curriculum into the certificate. Health Education England, local education and training boards and employers were asked to have nursing students and HCAs complete the certificate together. Cavendish also recommended a rigorous system of quality assurance for training, which links funding to outcomes, so that money would not be wasted on ineffective courses.
The Care Certificate was piloted by 13 NHS trusts during the period May to September 2014 and was launched widely in March 2015. To be awarded the Care Certificate, an individual HCA needs to have been assessed in meeting 15 standards of care. 57 Of particular relevance to our study are the standards of ‘working in a person-centred way’, ‘communication’ and ‘privacy and dignity’.
Study management
The project was led by the University of East Anglia. At each of the other two centres there was a lead investigator. To co-ordinate work across the centres, weekly teleconferences were held involving the three members of research staff employed on the grant and the lead investigators. During the study period five project management group meetings and five steering group meetings were held. The project management group included all of the investigators, leads in each of the three trusts and the three research staff (one from each of the three academic institutions). Its remit was to manage and co-ordinate study activities across the three centres and ensure milestones were achieved. The remit of the steering group was to guide the study so that it maintained relevance to the wider community of stakeholders, to provide governance in terms of the conduct of the study, to monitor progress and to challenge the research team so that assumptions were questioned and methodological quality upheld.
The composition of the steering group altered slightly between phase 1 and phase 2 to comply with the National Institute for Health Research requirement of a 75 : 25 split between independent and non-independent members. 58 In both phases, independent members included representatives from the wider academic community, patients and the public, The King’s Fund, other NHS organisations and the Royal College of Nursing. In phase 2, steering group membership was extended to include an independent statistician, health economist and a HCA, and non-independent members were restricted to the lead investigator from each centre.
Public and patient involvement in the CHAT study
This was a complex study and our approach to public and patient involvement (PPI) was based on the principles that such involvement should be meaningful, respectful, relevant and collaborative. The complexity of the study was not simply because of the nature of the intervention but because of the complexity of the effect mechanism of which we wished to test the feasibility. For many interventions the person receiving the intervention is the target for the potential benefit. This is only partly true in our study where a training intervention was designed for HCAs to improve the relational care of older people in hospital. We took the view at the grant application stage that those whom this study would benefit were both HCAs (the proximal target group for our intervention) and older people who receive care in hospital and their visitors (the distal target group). This is consistent with the Kirkpatrick model for evaluating training interventions. 50 The voices of both these groups therefore needed not just to be heard but also to be at the heart of the content and delivery of the training intervention and, moreover, to inform the way in which staff and patient participants were recruited to the study. The overall purpose of PPI was, therefore, to ensure that both the intervention and the research process would be relevant and acceptable to staff, patients and their visitors.
Presubmission of the grant
Prior to the activation of the grant we worked with the Public and Patient Involvement in Research (PPIRes) group, an organisation hosted by the South Norfolk Clinical Commissioning Group. 59 The PPIRes group brings together volunteer members of the public to collaborate with researchers in local trusts and universities in Norfolk and Suffolk and to develop proposals from the initial idea through to dissemination. At the time of writing it has a panel of approximately 70 lay members. Prior to submission of the grant application we worked with the PPIRes co-ordinator to plan the PPI in the study and to invite panel members to be involved in the development of the application. Twenty-six volunteers responded and a summary of the study document was circulated via the PPIRes co-ordinator for review. The purpose of this was twofold: first, to get informal feedback from panel member views on the questions the study sought to address and on its proposed methods; and, second, to identify potential panel members who might wish to play a more active role should the study be funded. Views on the study were positive. A question was raised on whether or not the staff group should be extended beyond HCAs to OS. This highlighted the potential breadth of application for the intervention, but the focus of the commissioning brief prevented us from incorporating this suggestion. Some panel members expressed uncertainty as to the role of a HCA, and this was an early reminder of the need to check our assumptions about the ability of patients and relatives to distinguish members of the HCA workforce from other care staff. A discussion group was also organised in which all available documents were circulated in advance and six volunteers attended a 3-hour meeting to discuss the application in detail.
Recruitment and study documents
Prior to our application for ethics clearance to conduct phase 1 staff interviews and focus groups with older people, the PPIRes co-ordinator arranged a meeting (7 November 2013) of four panel members and the principal investigator. The purpose of the meeting was to review participant-facing study documents. Consent and participant information sheets based on NHS template documents were adapted in the light of detailed discussion at the meeting. Changes were made to simplify expression of interest forms and participant information sheets. The focus group prompt guide was also adapted, with suggestions made as to how to explain what we meant by relational care to focus group participants. At this point, two of the group became the PPI representatives for the CHAT study and remained so for the duration of the study period. Margaret McWilliams has been a PPIRes member for over 10 years. Her interest in this project stemmed from a carer perspective and a short hospital stay, which emphasised the importance of HCAs and how essential it was to be kept informed of what was going to happen as part of your daily routine. Margaret runs a hearing aid clinic for Norfolk Hearing Support Services where she speaks to many older people about their experiences. Janet Gray has been a PPIRes member for 2 years and is the carer of her parents and relatives who have experienced many hospital stays.
Focus groups
A later section of the report details our work with older people’s organisations to assist with raising awareness of, and recruitment to, the focus groups (see Chapter 4, Recruitment). In addition, we were keen for PPI representatives to play a key role in the conduct of the focus groups themselves. As our PPI representatives were based at one of the three study centres, local PPI representatives were recruited for this purpose at the other two centres. The contribution of the PPI representative was determined by their own preference and, therefore, varied at each centre. At one focus group, for example, a PPI representative chaired the discussion. At all three focus groups the PPI representative worked with the facilitator to welcome participants as they arrived, clarified facilitator topics and participant discussion as needed and alerted the facilitator to participants who indicated that they had a view to express but were reticent about joining in the discussion.
Intervention development
The process of intervention development is described fully in Chapter 5. The core intervention development team included our two PPIRes representatives together with a HCA from one of our partner trusts working on a ward caring for older people. Collectively, the PPI members worked to keep the focus on the needs of older users of hospital services and to ensure that the training intervention was designed with HCA learners firmly in mind. The group met on four occasions and formed a close knit team to produce what became the Older People’s Shoes training intervention. Roles inevitably became less demarcated and all team members became involved in all aspects of intervention development including structure, content, delivery, and proofreading training materials. We consider that the final product was substantially strengthened by this invaluable contribution. In addition, our HCA representative worked with researchers shortly prior to intervention delivery to ensure that activities were credible to reflect the work experience of HCAs in busy hospitals.
Study oversight
Details of the trial steering group are provided in Study Management. Membership of that group included our two PPIRes representatives as well as a HCA representative recruited via the Royal College of Nursing Health Practitioner Committee. The steering committee provided oversight to all aspects of the study. Our PPI and HCA representatives were vocal and enthusiastic members of this committee, providing sound and thoughtful advice at each stage of the research. They were also very supportive of the research team at points in the process when we hit challenges.
Feedback and reflection on the process of public and patient involvement in the CHAT study
For a relatively short project (2 years) we felt that both the process and outcome of PPI within the CHAT project was successful. We forged strong relationships over a short space of time. Soon after the study end point, the PPIRes co-ordinator conducted an informal meeting with our two PPI representatives to hear their views on the PPI process. Both PPI representatives commented on how much they had enjoyed being part of the team and that the experience had been rewarding. They felt their contribution was valued and they appreciated being included in communications beyond formal meetings. They felt that their views had been sought and respected by the steering group, with the chairperson of that group ensuring that they were actively involved in discussions. They were appreciative of travel arrangements for meetings being organised well in advance. Working alongside our HCA representatives had assisted them in understanding the nature of a HCA’s work, and, by extension, the focus of the study from both a user’s and a caregiver’s perspective.
Summary
The CHAT study was undertaken in centres in England and was conducted in two phases: (1) scoping and intervention development and (2) feasibility testing and process evaluation. In phase 1, data were collected in the form of a telephone survey of NHS hospital trusts, focus groups of older people and interviews with HCAs and staff working with HCAs. Following a process of intervention development, the second phase consisted of a feasibility cluster randomised controlled trial and process evaluation. The training intervention and feasibility testing was informed by guidance on the development and evaluation of complex interventions and the design of the feasibility study was informed by Kirkpatrick’s four-level evaluation model. 50 The study was managed by the principal investigator at the University of East Anglia and through regular team meetings with the other two centres. Governance arrangements included project management group meetings and five steering group meetings. The backdrop to the study was a rapidly changing landscape in terms of policy developments and initiatives relating to HCA work, most notably the publication of the Francis report,1 and the implementation of the Care Certificate following the Cavendish review. 2 PPI was central to each element of the study and was essential in ensuring that both the intervention and the research process were relevant and acceptable to staff, patients and their visitors.
Chapter 3 A national telephone survey of current provision of health-care assistant training in relational care for older people
Introduction
This chapter describes the methods and reports the findings of a telephone survey of acute NHS trusts in England to establish the structure, format and extent of training for HCAs in delivering relational care.
Telephone survey: methods
Purpose
The purpose of the telephone survey was to understand the current provision of HCA training, particularly with regard to relational care for older people. This would provide insight into how a new training intervention in relational care for HCAs could be effectively delivered within the context of current training provision in acute NHS hospitals. The objectives of the telephone survey were to understand (1) current training and support processes, (2) the extent of training content with respect to relational care and care specific to older people and (3) perceived challenges in delivering HCA training.
Sampling frame and eligibility
All NHS acute hospital trusts in England were eligible to take part. Trusts were identified from the Health and Social Care Information Centre,60 which places each trust into one of six categories (large, medium, small, multiservice, specialist and teaching). The one key contact at each trust eligible to take part in the telephone survey was a person with responsibility for designing, managing, delivering or overseeing the training of HCAs.
Recruitment
Recruitment to the telephone survey was carried out by four researchers employed on the study grant. The recruitment process is illustrated in Figure 3.
FIGURE 3.
Telephone survey recruitment process.
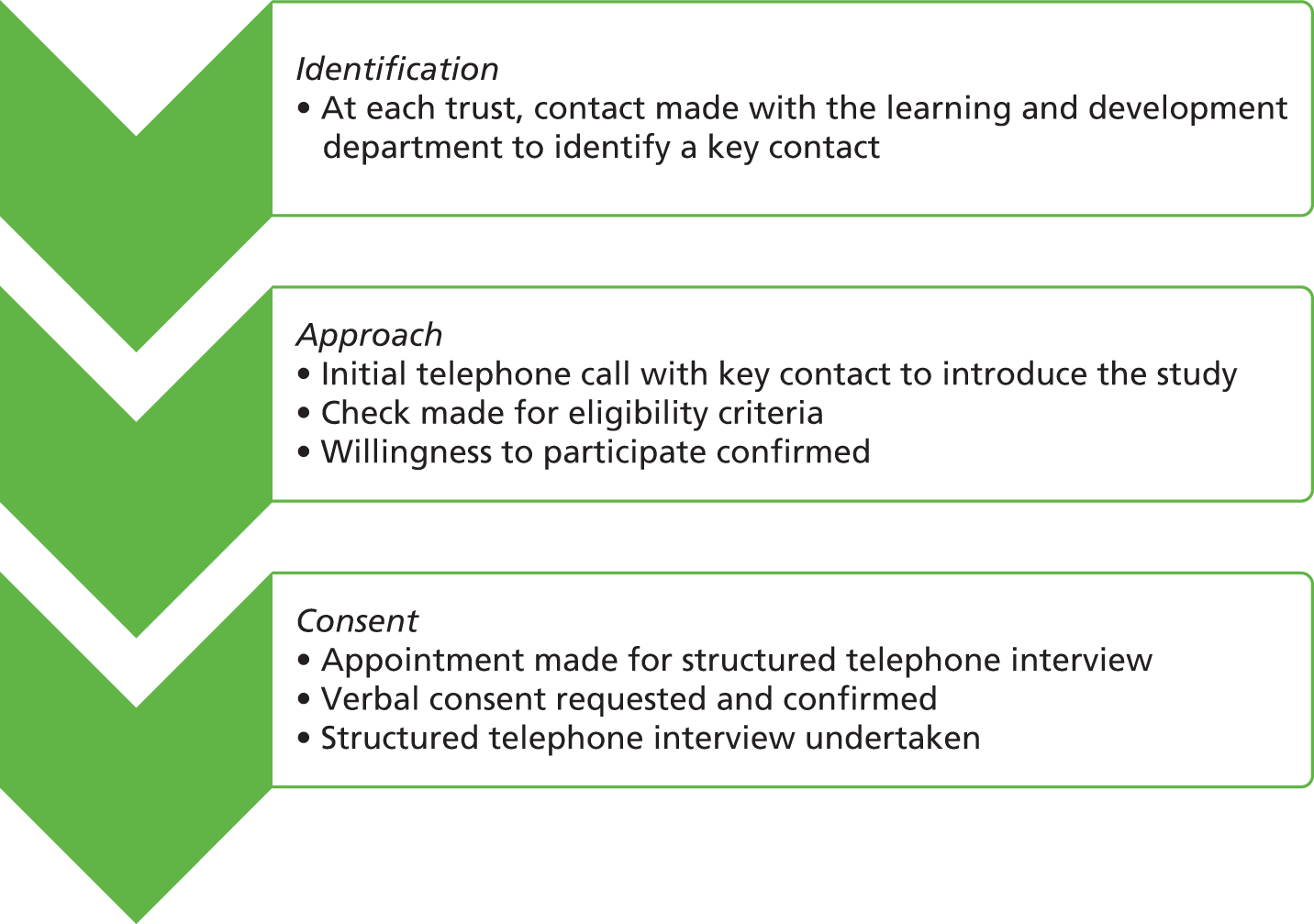
Identification
To identify the key contact, telephone contact was made with the learning and development department of the trust. When the researcher was unable to successfully identify the key contact for HCA training following five direct approaches to a trust over a minimum of a 3-week period, then no further approaches were made to the trust.
Approach
Once the key contact at a trust was identified, attempts were then made to establish contact with them and request their participation in a telephone interview. When the key contact responsible for HCA training was successfully identified but the researcher was unsuccessful in engaging in a two-way communication with this person (by either e-mail or telephone) following three direct approaches over a minimum 3-week period, no further attempts were made. When the key contact responsible for HCA training was successfully identified but within a minimum 3-week period the researcher was (1) unable to establish a mutually convenient time to conduct the telephone interview or (2) unsuccessful in completing the telephone interview at a minimum of two pre-agreed and mutually convenient times with the key contact, then no further contact was made.
Consent
Key contacts who were willing to take part were asked to identify a convenient date and time to take part in a structured telephone interview. Consent to participate and audio-record the structured telephone interview was requested and provided verbally.
Data collection
The survey was carried out over two periods: between February 2014 and September 2014, and then between July 2015 and October 2015. This was because of the early departure of a researcher at one centre and the period of time that elapsed before a replacement could be made.
Process
The structured telephone interviews followed a schedule designed to take approximately 30 minutes (see Appendix 1). It was scripted to ensure completeness but delivered in an unscripted, friendly and informal manner.
Content
Interview questions fell into three broad categories: (1) training and support processes, (2) content of HCA training and (3) challenges associated with training the HCA workforce.
We asked the key contact questions about what training a HCA starting work at that particular trust would receive with respect to duration, where it takes place and what is taught. We asked about ward-based training and support for new HCAs with respect to whether or not HCAs were supernumerary for any specific period or had support through formal mentoring or a less formal buddy system. We asked about training of long-standing members of the HCA workforce and whether or not there were differences in training for HCAs working in different clinical areas. We asked how long the training programme they had been describing had been in place with or without modification and whether or not there were any plans in place to develop HCA training at their trust. To explore whether or not any specific training was provided about the care of older people we asked one question verbatim: ‘in terms of the particular needs of older patients, which of those needs do you address in HCA training?’ No prompts were given. Telephone survey respondents were asked about what they saw as the challenges involved in training the HCA workforce. At the end of each structured telephone interview the researcher asked whether or not there was anything else in relation to HCA training that had not already been covered and that the participant wished to mention.
Data management, coding and analysis
Data were collected in a paper-based case report form and in audio files. Audio files were recorded using a portable digital voice recorder connected to a standard telephone. A unique identifier code was assigned to each trust. Audio data were uploaded and stored locally on secure servers. Structured telephone interview data were extracted from audio files and case report forms to a spreadsheet. Extracted data were anonymised and either coded for analysis or described accordingly. To categorise HCA training content, two researchers (CA and FN) coded data retrospectively using a shared template.
Counts and percentages of non-missing data were used to describe categorical data, and means with their standard deviations (SDs) were used to describe continuous data. A key development in the interim between the two periods of time during which the survey was conducted was the introduction in March 2015 of the Care Certificate. To check for any bias that this may have caused, we compared trusts interviewed before and after the national launch of the Care Certificate, using unpaired t-tests for continuous variables and chi-squared tests for categorical variables. A similar process was used to examine non-response bias comparing trusts that took part with those who did not. For categorical variables, where one or more cells had expected cell counts of five or less, Fisher’s exact test was used. All data analysis was conducted in Stata version 14 (StataCorp LP, College Station, TX, USA).
Ethical considerations and ethics approvals
We were mindful that the care of older people in hospitals has been subject to recent criticism. 1 The telephone survey was undertaken at a time at which HCA training has been the focus of national attention. 2 This required our approach to both recruitment and the conduct of the telephone interview to be sensitive. Potential and actual participants were assured that the focus of the survey was to get a national picture of HCA training in acute NHS hospital trusts rather than identify particular failings. The researchers made it clear to the key contacts interviewed that individual trusts would not be identifiable in any reporting of survey findings.
Permission to undertake the telephone survey was provided by the Faculty of Medicine and Health Sciences Research Ethics Committee at the University of East Anglia on 19 December 2013 (reference number 2013/2014-19).
Telephone survey: findings
Sample
Of the 161 acute NHS trusts approached to take part in the survey, a total of 113 (70.2%) structured telephone interviews were completed (Table 1). Of those trusts that took part, the mean number of whole-time equivalent staff was 4646, and there was no evidence that size of staffing establishment differed between participating and non-participating trusts (p = 0.43). Across Health and Social Care Information Centre trust type (small, medium, large, multiservice, specialist or teaching) the proportion of trusts that responded did not vary (p = 0.94). Trusts were surveyed in one of two time periods over the study duration and the proportion participating was lower during the second period (56.9% vs. 80.9%; p < 0.001). Trusts approached in the second period included those that had not refused in the first period but were more difficult to establish contact with. The second period took place after many trusts had been involved in preparing for the introduction of the new Care Certificate that was officially launched in March 2015. Two-thirds (66.1%) of the key contacts at participating trusts were involved in the direct delivery of HCA training, whereas in the remainder the key contact had a more strategic role in HCA training.
| Trust, survey and respondent factors | Telephone survey completed | p-value | All trusts (N = 161) | |
|---|---|---|---|---|
| Yes (N = 113) | No (N = 48) | |||
| Staff WTE mean (SD) | 4645.6 (2710) | 4294.4 (2292) | 0.43a | 4540.9 (2590.4) |
| Trust type, n (%) | ||||
| Small | 27 (71.1) | 11 (29.0) | 0.94b | 38 |
| Medium | 26 (72.2) | 10 (27.8) | 36 | |
| Large | 25 (67.6) | 12 (32.4) | 37 | |
| Multiservice | 4 (80.0) | 1 (20.0) | 5 | |
| Specialist | 11 (61.1) | 7 (38.9) | 18 | |
| Teaching | 20 (74.1) | 7 (25.9) | 27 | |
| Survey period, n (%) | ||||
| Prior to Care Certificate | 72 (80.9) | 17 (19.1) | 0.001c | 89 |
| Following Care Certificate | 41 (56.9) | 31 (43.1) | 72 | |
| Role of contact in HCA training, n (%) | ||||
| Direct delivery | 74 (66.1) | |||
| Strategic planning | 38 (33.9) | |||
| Unknown | 1 | |||
Structure of health-care assistant induction training
Key contacts at just under half of participating trusts (50/110, 45.4%) reported induction programmes of 1 week or less, with the remainder having longer induction programmes and 1 in 10 having HCA programmes of between 2 and 3 weeks (Table 2). It was the norm for new HCAs to have a mentor or buddy (98/113, 86.8%), with only eight trust key contacts (7.1%) saying this was not the case. When respondents reported the type of mentor for those trusts with a system of mentoring or buddying, these were senior HCAs (n = 50, 46.3%), registered nurses (n = 16, 14.8%) or either (n = 17, 15.7%). New HCAs were accorded supernumerary status at most of the participating trusts (n = 81, 71.7%), the remainder reporting that new HCAs were not supernumerary or that supernumerary status was dependent on other factors. Many trusts indicated that the duration and type of support on wards was at the discretion of the ward manager. There was no evidence of differences between trusts surveyed at each time period with respect to how HCA induction was structured (analysis not shown).
| HCA induction variables | All trusts (N = 113), n (%) |
|---|---|
| Length of training (classroom based) | |
| < 1 week | 19 (17.3) |
| 1 week | 31 (28.1) |
| > 1 week to 2 weeks | 49 (44.6) |
| > 2 weeks to 3 weeks | 11 (10.0) |
| Missing | 3 |
| Mentor or buddy allocation | |
| Yes | 98 (86.8) |
| Informal | 6 (5.3) |
| No | 8 (7.1) |
| Do not know | 1 (0.9) |
| Mentor or buddy type | |
| Registered nurse | 16 (14.8) |
| Senior HCA or registered nurse | 17 (15.7) |
| Senior HCA | 50 (46.3) |
| Varies | 17 (15.7) |
| No mentor | 8 (7.4) |
| Missing | 5 |
| Supernumerary status | |
| Yes | 81 (71.7) |
| Varies/depends | 16 (14.2) |
| No | 16 (14.2) |
Content of health-care assistant induction training
One-third (n = 37, 32.7%) of trust key contacts reported content within their HCA training induction programme that we considered to be relational care (Table 3). When asked specifically about induction training that was related to the care of older people, 43 (38.1%) trust respondents referred to subject areas such as privacy, dignity and respect (n = 30, 27.3%) and communication skills (n = 24, 21.8%), all considered by the researchers to involve relational care. Only two respondents (1.8%) said that their trust covered the subject of ‘customer care’. Dementia care was reported as being included in HCA induction programmes by the majority of respondents (n = 94, 85.5%). Other training induction content relevant to older people and reported by survey respondents was nutrition and hydration (n = 31, 28.2%), falls (n = 25, 22.7%) and sensory/physical impairment (n = 23, 20.9%). Nearly one-third of respondents (n = 35, 31.5%) said that they made no distinction during induction training between the needs of older people and those of any age group. Nearly all trust respondents interviewed prior to the national launch of the Care Certificate reported plans to develop HCA training (56/57, 98.3%) compared with 73.7% (28/38) of trusts surveyed after the national launch (p < 0.001), suggesting changes were just starting to be introduced in the intervening period.
| Training content | All trusts (N = 113),a n (%) |
|---|---|
| Relational care (not age specific) | 37 (32.7) |
| Relating to older people | |
| Dementia | 94/110 (85.5) |
| Stroke | 3/110 (2.7) |
| Sensory/physical impairment | 23/110 (20.9) |
| End-of-life care | 15/110 (13.6) |
| Continence | 7/110 (6.4) |
| Falls | 25/110 (22.7) |
| Nutrition/hydration | 31/110 (28.2) |
| Skin care | 13/110 (11.8) |
| The ageing process | 7/112 (6.3) |
| Privacy, dignity and respect | 30/110 (27.3) |
| Communication | 24/110 (21.8) |
| Person-centred care, compassion | 19 (16.8) |
| Safeguarding, values and behaviours | 16 (14.2) |
| Customer care | 2 (1.8) |
| Relational care | 43 (38.1) |
| No age distinction made | 35/111 (31.5) |
Challenges of training health-care assistants
Reported challenges related to training HCAs were categorised under four headings: the wider context, resource limitations, ward engagement and HCA-related challenges (Table 4). The most frequently cited challenge for delivering training to the HCA workforce was getting staff released from wards to attend (n = 53, 46.9%). Whether this was because of a lack of ward manager engagement with HCA training delivered at trust level or simply because of a lack of staffing resource is not possible to determine from our data. However, many respondents unsurprisingly cited resource limitations as a challenge. Trust key contacts reported challenges of being limited not just in terms of funding but also in relation to the availability of assessors, mentors and training venues. The wider context of opportunities (or lack of opportunities) for HCAs to develop their role was highlighted by some, together with the difficulties associated with HCA training rarely recognised beyond an individual trust. The highly diverse nature of the HCAs in terms of their care experience and academic ability was the most cited challenge relating to members of the HCA workforce.
| Challenges | All trusts (N = 113), n (%) |
|---|---|
| Wider context | |
| Retention (HCAs leaving for nursing training or development opportunities) | 15 (13.3) |
| Lack of career progression for HCAs (no opportunities for HCAs to develop apart from through nursing training) | 16 (14.2) |
| Transferability of training (training not being accepted across trust/trusts) | 4 (3.5) |
| Lack of accreditation (HCA qualifications not nationally accredited) | 5 (4.4) |
| Ward engagement | |
| Release from ward (getting HCAs released from ward to attend training) | 53 (46.9) |
| Manager engagement (encouraging managers to engage with HCA training) | 17 (15.0) |
| Staff motivation (lack of motivation in existing staff to support and nurture new HCAs) | 10 (8.8) |
| HCA related | |
| Diversity in HCA recruits (differences in experience, academic qualifications, values) | 19 (16.8) |
| Computer skills (HCAs not always computer literate, making e-learning a problem) | 6 (5.3) |
| Numeracy and literacy problems | 8 (7.1) |
| Lack of confidence (HCA recruits lacking confidence/not feeling valued) | 3 (2.7) |
| Language problems (problems caused by English being a second language for some recruits) | 3 (2.7) |
Training beyond induction
The variability of the extent and nature of training after induction meant that insights into this area of HCA training were gleaned through open-ended questioning. Once the initial training/induction period was over, many trusts reported that HCAs had access to ongoing training, although the emphasis was on training newly employed personnel. Only one trust reported that they had received funding allowing them to put both new and existing HCA staff through the Care Certificate. One trainer suggested that restricted access to training affected the ability to retain good HCAs, thereby increasing HCA turnover and creating a ‘vicious circle’. Although many trusts reported having postinduction training available, this varied greatly in terms of structure, focus and content. The target group for this training also varied greatly between trusts. Some reported holding regular HCA study days covering an array of specialist skills; however, these sessions were rarely mandatory and tended to be at the discretion of ward managers. Owing to time and resource constraints some trusts had opted for an e-learning approach and offered packages in areas including dementia and end-of-life care.
One trust offered monthly open-access support worker sessions, which could be tailored to the needs of the individual, and another trust ran a weekly skills refresher day open to both registered nurses and HCAs. However, an ad hoc approach to training was the norm for most trusts. Many telephone survey respondents were unaware of the content of specialist training available to staff, as this was carried out on the ward by clinical trainers. Again, this training was governed by managerial requirements and limited by time constraints.
Summary
In a national survey of 113 of the 161 acute hospital trusts in England, which was designed to capture data on the current provision of HCA training, particularly relational care for older people, we found HCA induction to be highly variable, lasting between a few days and up to 3 weeks. One-third of interviewees reported content within their HCA training induction programme that we considered to be relational care. Only two respondents said that their trust covered the subject of ‘customer care’, whereas the majority reported the inclusion of dementia care in HCA induction programmes. The majority of new HCAs are provided with a mentor or buddy and 72% of trusts treat new HCAs as supernumerary. Reported challenges in training HCAs were related to resource limitations, engaging ward managers and the diverse nature of the HCA workforce. The most frequently cited challenge for delivering training to the HCA workforce was getting staff released from wards to attend. Emphasis was placed on induction but much less on ongoing training, which is typically devolved to ward managers. Older people’s needs are addressed in HCA training, but there was little evidence that relational care is seen as a priority within that.
Chapter 4 A qualitative investigation into the training needs of health-care assistants with respect to relational care of older people
Introduction
This chapter describes the methods and reports the findings of two components of the study: first, a series of focus groups with older people and carers with experience of hospital care to explore their expectations of the care provided by HCAs; and, second, qualitative interviews with HCAs and other NHS staff to identify the training needs and preferences for a training intervention to improve HCA relational care of older people.
Focus groups: methods
Purpose
To inform the content of the HCA training intervention we ran three focus groups (one in each centre) of older people and carers with experience of acute care. We wished to identify these groups’ experience of relational care as provided by HCAs. We wanted to understand the values-based training needs of HCAs in maintaining the dignity of, and affording respectful care to, older patients in acute NHS settings from the perspective of those they care for. Each focus group aimed to gather a broad range of perspectives from older people who had been an inpatient, or a carer of an inpatient, at an acute NHS trust. The purpose of focus groups is to explore people’s experiences, attitudes and feelings on a topic in a way that capitalises on group interaction. 61,62 Interaction enables participants to build on other people’s input and to ask questions of each other, as well as to re-evaluate and reconsider their own understanding of their specific experiences. 63
Setting and eligibility
Focus groups were carried out in non-clinical settings in venues that had disabled access and transport links. At each centre transport was arranged for participants who required it, and costs were reimbursed for others. Eligible participants were former hospital inpatients at any acute NHS trust aged ≥ 65 years or the carer of a former inpatient aged ≥ 65 years. Although not an eligibility criterion, we prioritised those whose experience of an inpatient stay was at least 3 months and no longer than 6 months prior to the focus group meeting on the basis that this would avoid any very raw emotions in a group setting, while maximising the chances of recall.
Recruitment
Identification
At each centre the recruitment strategy was adapted, when necessary, to reflect the local context and use existing networks. In centre 1, the team engaged a county-wide Older People’s Forum, which approved the study and passed on details of local branches. In centre 2, the research team worked with the national and local branches of Age UK. In centre 3, a number of outreach avenues were identified through local knowledge, networking and internet searches.
Approach
Potential focus group participants made expressions of interest by completing a form (see Appendix 2) that had been distributed in a variety of ways. In centre 1 the chairpersons of four local branches of a county-wide Older People’s Forum were sent details of the study and asked to circulate details at a meeting or by e-mail. The researchers also offered to present the study at a branch meeting, and two branches accepted this offer. In centre 2, advertisements were placed in two editions of the national Age UK newsletter and an item sent out with two local Age UK newsletters. The researcher attended a local event in an Age UK campaign and presented to a local Age UK Older People’s Advisory Group. In centre 3, the researcher presented the study to seven community organisations of older people and/or carers during previously convened meetings. In addition, an item appeared in the newsletter of one of these groups, and in that of two local Healthwatch groups.
In all centres the local researcher followed up written expressions of interest by telephone or e-mail depending on the potential participant’s preference. During these exchanges further explanation was given on the study and what participation would entail and a participant information sheet was provided (see Appendix 3). Exchanges were also used to check eligibility and to collect broad contextualising information about the potential participant, including whether they were an ex-patient or carer of one (or both) and, when relevant, time since last discharge from an inpatient stay, length of last stay and hospital attended. This information was gathered to allow purposive sampling of participants to include women and men, patients and carers, a range of ethnic groups and experiences in different hospitals. Additional information (including transportation requirements, mobility, capability and any other carer assistance required) was also collected at this stage and used to facilitate focus group attendance. At the point of recruitment it was explained to volunteers that sampling would take place at the end of the recruitment process, with the aim of getting a balance of men and women and patients and carers. When capacity to give informed consent was in doubt, volunteers were not selected to take part in the group.
Consent
During follow-up exchanges a judgement was made on the potential participant’s ability to provide informed consent. Verbal consent to participate was taken during these exchanges with potential participants once any questions had been answered. Four weeks before the focus group, letters were sent to all those who had expressed an interest in taking part. Those not purposely sampled for invitation to one of the focus groups were given a brief explanation as to why this was the case, informed that the number of expressions of interest had exceeded the number of places within the group and thanked for the interest they had shown in the study. Letters of invitation, which were provided to all selected participants, included details of the focus group. Consent forms were posted out 1 week ahead of the focus group to allow ample time for further consideration. Written consent was obtained at the focus group meeting, prior to the start of discussion and audio-recording.
Data collection
Process
Focus groups were designed to run for up to 2 hours and refreshments were provided. Ground rules were established before the discussion started (see Appendix 4). The interviews were audio-recorded and transcribed verbatim, and individual participants were identified by participant number. At each centre the focus group discussion was attended by two members of the research team and a PPI representative. Although the part they played varied between centres, PPI representatives played a bridging role between the research team and focus group participants. The roles and responsibilities of each facilitator were agreed beforehand. The participants were given gift vouchers to thank them for their time and effort.
Content
The discussion followed a topic guide (see Appendix 5). The focus group topics explored participants’ experiences and expectations of inpatient care, views on what ‘good care’ looked like, what training participants thought HCAs needed in order to improve their delivery of relational care and their recommendations on how good customer care from retail organisations might be applied to a ward setting. A summary is shown in Table 5.
| Areas explored | Questions askeda |
|---|---|
| What is important when an older person is first brought on to a new ward |
|
| What relational care looks like according to older patients and carers |
|
| Views on getting to know patients |
|
| Recommendation for training intervention |
|
| Experiences of relational care outside hospitals |
|
Data management, coding and analysis
An analysis of focus group transcript data was carried out in NVivo version 10 (QSR International, Warrington, UK). Data were initially coded in NVivo, using a framework of codes aligned to the broad themes suggested by topic guide, for example what people want when they arrive on a ward, examples of good relational care (in hospitals and in other settings) and what staff should know about individual older patients. This was followed by more detailed analysis using an inductive approach in which data within themes were examined and interpreted to draw out more refined themes and conceptual nuances.
Given that the purpose of the focus group was to inform the development of a training intervention for HCAs to improve their delivery of relational care, analysis focused on thematic content, and not behaviour or non-verbal data. 64 As focus groups are valuable for the interactions between participants, instances of consensus, contradiction and controversy were sought and used in presenting the findings. 61 Data were not analysed for differences between groups or along lines of sex or ethnicity. However, the relationship between patient and carer needs was examined.
Ethical considerations and ethics approvals
At the start of the focus group meeting, participants were reminded that data would be anonymised and kept confidential and were asked to maintain the anonymity and confidentiality of other participants. Thinking about and discussing experiences of and around hospital stay can be upsetting. At each focus group one member of the research team was given responsibility for looking after any participants should they be upset and wish to withdraw from the discussion. At the end of the discussion participants were provided with details of the local trust’s patient advice and liaison service should they wish to discuss their experiences further. Six months after the focus group, an update on the study was sent to all focus group participants, letting them know how their views were being used.
Permission to undertake the focus groups was provided by the Faculty of Medicine and Health Sciences Research Ethics Committee at the University of East Anglia on 19 December 2013 (reference number 2013/2014-19).
Interviews with health-care assistants and other staff: methods
Purpose
Semistructured one-to-one interviews with HCAs and OS (principally nursing staff) in the three centres were conducted to elicit their perspectives on what good relational care of older people looks like, what a training intervention for HCAs should contain and what style of training delivery was likely to be most effective. These interviews allowed us to understand the context of providing relational care to older patients, any barriers to training access or implementation of training and to investigate the perceived training needs of HCAs with respect to relational care.
Setting and eligibility
At each centre we worked with a partner acute NHS hospital trust. The three trusts were all teaching hospitals: one in London, one in a rural county and one in the Midlands. Wards caring for older people in the trusts were purposively sampled to reflect a wide range of HCA experience on different types of ward (health care of older people, general medical and orthopaedic). Our intention was to ensure that the training intervention developed would be relevant to HCAs with different levels and types of workplace experience. Eligible ‘OS’ were those who directly manage HCAs on recruited wards (ward managers and staff nurses), who work alongside HCAs on recruited wards (e.g. allied health professionals) or managers with responsibility at the division or trust level.
Recruitment
Identification
At each trust we worked with a senior member of nursing staff who identified which of their wards had a majority of older patients, and recommended the four most appropriate wards for a researcher to approach HCA interviewees (subject to the ward manager’s agreement). Participating ward managers were asked to suggest other relevant staff groups or individuals we might invite to interview.
Approach
The study was presented to ward managers on the four identified wards at one-to-one meetings with the local researcher. Once they had agreed to facilitate the study, it was presented more widely, initially at a handover meeting and, subsequently, during several visits to the ward. Researchers explained the study and what taking part would involve and answered any questions. Potential interviewees were left with a participant information sheet (see Appendix 6) and an expression of interest form to be completed if they were happy for the local researcher to contact them about participating in the study (see Appendix 7).
Consent
Verbal consent to take part in interviews was obtained after potential interviewees had had the opportunity to read the participant information sheet, and a time and date was then arranged for the interview. Written consent was taken immediately prior to the interview.
Data collection
Process
The interviews were audio-recorded with the interviewee’s permission. Audio files were transcribed verbatim. The transcripts were then anonymised and later pseudonymised. The interviews were carried out in a quiet room (e.g. empty day room or office) on trust premises.
Content
Rather than ask interviewees about views and experiences of a narrow definition of ‘relational care’, we asked a number of differently framed questions around ‘good care’ that would allow us to draw inferences about relational care and the role of HCAs in providing it. Interviews were designed to explore these perceptions of ‘good care’ and the training needs of HCAs with respect to relational care for older people.
We were keen to ensure that the training intervention (to be designed and feasibility tested in subsequent elements of the study) could be implemented in the ‘real world’. We therefore wanted to understand (1) what working on older people’s wards was like and (2) the difficulties in providing good relational care. We also wanted to know what support we could provide to HCAs through the intervention that would help them to provide relational care in challenging circumstances. We therefore asked about barriers to implementing training and what might be done at the point of delivery to facilitate implementation of training.
Topic guides for HCAs and OS were broadly similar (see Appendix 8), but recognised differences in their knowledge and experience. The areas explored and the key topics covered are presented in Table 6. Seven interviews across two of the three trusts were carried out after an imposed hiatus and the topic guides were modified slightly to get feedback on an early draft outline of the HCA training intervention.
| Areas explored | Key HCA interview topics | Key interview topics for other staff |
|---|---|---|
| What are HCAs and other staff members’ views on what ‘good care’ looks like? | What HCAs can do to make patients feel cared about | Examples of good care by a HCA |
| What HCAs can do to make being in, or having a relative in, hospital less distressing | What HCAs can do to make being in, or having a relative in, hospital less distressing | |
| Barriers to, and facilitators of, getting to know patients | Barriers to, and facilitators of, getting to know patients | |
| Personal experiences of good customer care (what providers did and what it felt like) | Personal experiences of good customer care (what providers did and what it felt like) | |
| Views on applying customer care lessons to an acute setting | Views on applying customer care lessons to an acute setting | |
| If you had an elderly relative in hospital, what would be most important to you about the way they were cared for? | ||
| HCAs training needs in relational care for older people | Work history | Challenges in caring for older people |
| Challenges in working as a HCA caring for older people | Thoughts on available training for HCAs/training gaps at the trust (including lack of training to address identified work challenges) | |
| Aspects of their role they feel most/least confident about | ||
| Training received at the trust and elsewhere (including most useful training; exploring any training on relating to patients or in dealing with identified work challenges) | ||
| Perceived training gaps | ||
| Recommendations for the delivery method, style and timing of a training intervention for HCAs | Difficulties in accessing training | Content and methods of any training previously recommended by HCAs |
| Content and methods of any memorable training | Recommended delivery style for HCA training on relational care | |
| Preferred training delivery style | ||
| Implementing any training on relational aspects of care | Barriers to, and facilitators of, implementing any training on relational aspects of care | Barriers to, and facilitators of, implementing any training on relational aspects of care |
| Problems in implementing trust’s HCA training policy | ||
| Later interviews only | ||
| Thoughts on draft outline of training intervention | Views on the purpose, topics, timing, structure, delivery, underpinning values and title of a draft outline | |
Data management, coding and analysis
The interview data from each trust were coded in NVivo by the local researcher using a coding framework developed from initial readings of the transcripts and agreed by the study team. This collaborative work to identify themes ensured validity and reliability of the analysis. The coding framework included broad themes specifically directed towards the aim of the study (to develop a training intervention for HCAs to improve relational care of older people). The analysis used both deductive and inductive approaches.
Examples of deductive themes were organisation- and patient-related challenges in HCAs’ work, the role of HCAs in relational care (categorised using the study team’s understanding of what relational care consisted of), experiences of good customer care and perceived gaps in training. Other themes were imposed to inform how we framed the intervention and managed practical arrangements, as well as giving important contextual data to help us interpret our findings on the feasibility of the intervention.
Following this process of deductive data extraction, a more detailed thematic analysis of the whole data set was then carried out in NVivo by one researcher, using an inductive approach and the constant comparative method in order to enhance analytical rigour65 and the credibility and ‘trustworthiness’ of the findings. 66 At this stage, subthemes such as ‘tensions inherent in HCAs’ work’ emerged from interviewees’ accounts.
The interview and analysis process was iterative. This meant that we were able to use findings from earlier interviews to inform subsequent interviews. For instance, we used early findings on ‘challenges in HCAs’ work’ to frame a question used in later interviews about whether or not interviewees thought such challenges could usefully be addressed in training.
Ethical considerations and ethics approvals
Ward managers agreed to participate in the study prior to fieldwork commencing. The research team was keen to ensure that ward staff were not under pressure from ward managers to take part in interviews. We therefore approached HCAs directly and made it clear that participation was voluntary. Verbal consent was taken at the initial approach and written consent immediately prior to the interview. All interviewees were free to refuse consent to being audio-recorded and to withdraw from the study at any time. Confidentiality and anonymity were assured.
Permission to undertake HCA and OS interviews was provided by the Faculty of Medicine and Health Sciences Research Ethics Committee at the University of East Anglia on 19 December 2013 (reference number 2013/2014-19) and from the research and development departments of each of the three participating NHS trusts.
Focus groups: findings
Sample
Thirty people were invited to participate in one of the three focus groups, of whom 29 attended (Table 7).
| Centre | Experience as (n) | Sex (n) | Total (N) | |||
|---|---|---|---|---|---|---|
| An older patient | A carer of an older patient | An older patient and carer | Male | Female | ||
| 1 | 5 | 4 | 2 | 3 | 8 | 11 |
| 2 | 8 | 1 | 0 | 2 | 7 | 9 |
| 3 | 3 | 6 | 0 | 2 | 7 | 9 |
Length of hospital stay ranged from 1 day to 4 weeks, and time since discharge ranged from 2 months to 3 years, although one carer had a friend in hospital at the time of the focus group. Participants drew on experience of care from 14 different hospitals. Focus group discussions were carried out in each centre between June and July 2014 and lasted an average of 1 hour and 45 minutes.
What is relational care?
Founded as it is on relationships and interaction, relational aspects of care can be discerned in terms of both how it makes patients and families feel ‘cared about’ and ‘feel in safe hands’ and what is required from staff in order to elicit that feeling. Attitudes, behaviours and communication styles were all implied. We asked focus group participants to tell us about experiences during a hospital stay when they had felt that they (as patients) or their family member or friend had been cared about. The findings presented here, which use pseudonyms, include comments from both patient and carer participants on what gave them a positive feeling of being cared for.
Five major themes emerged through our analysis of staff activities associated with effective relational care: building relationships, showing kindness and concern, noticing and being proactive, offering choice and individualising care and making patients and families feel welcome and secure. Our findings echo those from other studies of the importance placed by older patients and their families on the relational aspects of care. 11,13
In participants’ accounts, positive experiences of care hinged on relationships. Chatting to patients and getting to know them were important in building those relationships. A degree of mutual disclosure was also involved:
My father is very frail and doesn’t talk easily to people and will just keep himself to himself. But one day we went in to see him and he was chatting really happily with this health-care assistant, and they were having a laugh and he knew all about this health-care assistant’s life, he was another nice Jewish boy and whatever and blah, blah, blah. And it was just lovely, it was heart-warming.
Hannah, carer, centre 3
Staff showing kindness and concern was noted as important. An example was given of a HCA really going the extra mile in putting together a photo album for a patient who had great difficulty in communicating. Often these qualities were manifested in doing ‘little things’, such as charging a mobile phone, tending to a patient’s appearance or offering a cup of tea. These displays of good relational care played an important part in making patients feel cared about and secure in an alien environment:
[T]he most important thing to me was the kindness of the nurses. I couldn’t sleep and a nurse came round and she said ‘Are you OK?’ and I said ‘I’d love a cup of tea’ and she went and got me one. That was very important to me. It gave me a feeling of security, peace of mind and that sort of thing. It’s something I think most elderly people would value most, to have peace of mind because they’re away from their secure surroundings.
Evelyn, patient, centre 1
Participants in all three focus groups thought that ward staff should be proactive in noticing care needs and offering care. This was thought to be relevant for older people with communication difficulties or cognitive impairment but also to be applicable beyond that as older people often felt reluctant to ask for help:
[M]y mum would never ask anything anyway . . . So somebody to come and just talk and check on you regularly I think is really important.
Vera, carer, centre 1
It was also noted in all groups that one element of good relational care was offering choice and individualising care:
[T]he health-care assistant that was looking after my mum came to her in the morning, [. . .] and asked my mum ‘What do you want to happen as far as your care is concerned, like washing, dressing and stuff like that?’. Asked her what she actually wanted, and would she rather have her wash earlier or later? Did she want a shower, does she want a bath? She actually asked her what she wanted and what she preferred. [. . .] my mum really appreciated that.
Julia, carer, centre 3
Giving this kind of choice helped to incorporate familiar routines into an alien environment and gave patients a degree of self-determination. Talking over patients as if they were not there was given as a prime example of poor relational care. Such treatment was experienced as depersonalising. One person said it made her feel as if ‘you might as well not be there’. Another told of a friend’s distress and sense of being ‘demeaned’:
[O]n one occasion [. . .] the bed was being changed and there was a carer on both sides helping [my friend] because they couldn’t do it by themselves, and they talked over her, and just as they were leaving they said ‘Did you ever work?’ And in fact she was a very intelligent person who’d held down an important job in the National Health Service. And when I went in she said ‘They just didn’t relate to me in any way’. And she was almost in tears because she said ‘I know I’m old and it’s a long time ago, but at one point I was somebody’ [. . .] She was really upset by that because whether she’d worked or not was important, but she felt demeaned and I thought that was very sad.
Wendy, patient, centre 1
Carers valued being made to feel welcome and at home. They also wanted to be kept informed. Carers’ and patients’ feelings of comfort and support were intimately entwined. The treatment of one impacted on the feelings of the other:
I think it’s also very important when you’re a patient in hospital, lying there all day, waiting for the visiting time to start, that you’re confident that your family and your visitors feel confident enough to talk to the staff and find out if you’re OK, if anything else is going to crop up, so that everybody can work together and look after you as a team.
Sophia, patient, centre 1
One interviewee summed up a general view of relational care:
[B]y and large, it’s a matter of meeting that patient’s specific individual needs and engendering a relationship where the patient feels that he or she is being well looked after and has the confidence and the ability to rely on those who are around him or her.
David, carer, centre 3
There was a broad consensus among focus group participants of wanting patients to feel welcome, known, secure and ‘at home’, and there was an iterative relationship between the feelings of older patients and carers.
Experiences of relational care beyond health-care settings
As an alternative way to unpick what relational care looked like, we asked participants to talk about occasions outside health-care settings (e.g. shops, banks or restaurants) in which they had felt very well treated and what it was that had engendered such a feeling. There was a great deal of overlap in responses to this question and the question of relational care in hospital. Ingredients of relational care noted outside acute settings were a timely response and staff being kind, helpful and informative, knowing who you were, making you feel special, listening attentively and noticing your needs:
[W]hen you go out for lunch somewhere [. . .] when it really works and you feel really special and well treated is because they’re actually kind of noticing what’s going on all the time, noticing whether it’s time to come over and shift the plates rather than leave you there for ages. Noticing whether it’s the right moment and moving at the right time. So that observation but having the time to observe obviously and then to react accordingly and they’re quite busy of course in restaurants.
Vera, carer, centre 1
[In] Canada [. . .] you go into a shop, it’s ‘Good morning, how are you?’ and everything [. . .] which I think is most important because if you’re feeling down and you go into a shop and someone smiles at you, you feel so much better, you know.
Maureen, patient, centre 2
Although some participants voiced a wish that people should try to understand what it is like being old, this was not straightforward and a danger of being stereotyped was also acknowledged in one focus group:
I’m in a care home and we have people who are not very well trained. They do get training, particularly in all the things like infection control, and health and safety and so on and so forth, but it’s those other little things – them knowing how you think when you get older. And they think you’ve aged a lot more than you really have.
Mm.
And I sometimes sort of feel like turning round and saying ‘Look, I may be the age you can see on the care plan but I’m sorry, I don’t want to talk about that, I want to talk about something interesting, something out of the newspaper’. [. . .] they really do think we were – well we were born in the last World War. But we don’t always want to go around singing ‘Pack up your troubles in your old kit bag’!
Eileen, patient, centre 2
Not only did some participants complain of being stereotyped, but they felt they were dismissed, or even invisible, because of their age:
[. . .] I feel now they just see you as old.
They do, if they see you at all.
If they see you at all, they see you as old and dismissed.
[. . .]
There are some nice younger people.
Yes.
Yes, there is, there’s a lot of them they treat you with respect. But they’re just – you come across some that don’t, and it hurts sometimes because you think ‘I’m a human being still, even with my wrinkles and my ruddy arthritis and everything’, you know.
Avril and Joan, patients, centre 2
This feeling of being dismissed resonates with the depersonalisation that patients felt when staff talked over them as they carried out their tasks.
Patients’ and carers’ expectations of staff when first arriving on a ward
We asked participants what they felt they should be able to expect when they first arrived on a ward. This line of questioning was based on the assumption that ‘first impressions count’ and drew on research on older people’s experience in urgent care settings,67 which found that older people frequently experience a diminished sense of significance, a feeling that they do not matter, which the authors attributed in part to a lack of attention to older patients’ wider psychological and informational support needs. Our findings that patients and carers place great importance on being made to feel welcome and ‘at home’ suggest that these feelings need to be established early on:
A very good welcome. Make them feel comfortable. Make them feel valued. Make them feel like they’re in good hands. They are free to ask for whatever they feel will make them feel better.
Shola, carer, centre 3
A ‘good welcome’ included being greeted with a smile and being offered a warm drink, and staff introducing themselves. Being made to feel at home also included introductions to OS and their roles, being introduced to other patients in the bay, being orientated to the ward by being told or shown where things were and being informed about routines of the day, such as meal times and visiting times.
Patient and carer confidence and sense of ease was tied to feeling that staff made the effort to get to know a patient’s particular needs, such as whether or not they need glasses or a hearing aid, whether or not they had dementia, their dietary requirements and other preferences. One participant said:
Time at the beginning is really important because mum doesn’t understand, she’ll forget within 1 minute what you’ve said to her. And the carer needs to know specifically about her and what her needs are, otherwise she’s going to feel at sea and completely lost. So some time with somebody to get all the background.
Vera, carer, centre 1
What patients and carers want staff to know about them
Good relational care involves building relationships between staff and patients, and staff getting to know about patients’ individual care needs and preferences on arrival in a ward. With an average length of hospital stay of 9 days for an older person,3 we asked participants what they would wish or expect staff to know about a patient over this length of time. A positive experience on admission to a ward is crucial, but in the longer term participants want staff to know things about them that help to build a relationship and make them feel known as individuals. Such knowledge includes past occupation and something of their history, where they live, hobbies and interests and a bit about their family. Some participants pointed out that the relationship with staff members is stronger when information sharing is reciprocal:
I think it’s all part of the settling process, you know, if they could see one of these forms that you fill in, I think you get them from the Alzheimer’s Society, you look at it and you think ‘Oh, you know, he was in the RAF [Royal Air Force]’. ‘Oh you were in the RAF were you, [name]?’ and it perhaps just strikes a chord and he thinks ‘Oh, you know, they know something about me, I’m not just something that’s going to lay on a bed’.
Trish, carer, centre 1
Well I suppose generically whatever one needs to know in order to build a relationship. I’m not quite sure what the ingredients are. [. . .] It’s like when I go to the barber, you know, we talk about football or his children, my children, whatever it may be. Just those little details that sort of make the difference between a closer relationship and a more distant one.
David, carer, centre 3
I think it’s appropriate to have a little bit of background on the patient that would build a relationship [. . .] The children, the husband, just a little bit about the family. So that’s sort of starting the relationship, or the conversation. Then the nurse might also tell you a little bit about themselves so you have something in common to discuss about – as you said [David], about football and the rest of it – or something for discussion.
Gloria, carer, centre 3
Recommendations for health-care assistant training in relational care
Given the importance of relational care to focus group participants, the fact that not all of their experiences of this were positive and in acknowledgement of the fact that there is no standardised training for HCAs, there was strong support for HCA training in those aspects of relational care noted above: building relationships, kindness and compassion, being friendly and approachable, getting to know patients as people, finding out, noticing and expecting care needs, listening attentively [‘It’s listening and hearing isn’t it?’ (May, patient, centre 3)], individualising care, involving patients in decision-making and not depersonalising patients.
When asked about other areas of content they would wish to see in the training of HCAs, participants talked about communicating with people with dementia, doing stimulating activities with patients, ways of encouraging patients to eat and drink, not passing on work-related stress to patients and non-verbal communication. On this last point one participant said:
On the non-verbal, actually to be aware of body language and also bustle. If you’re bustling people are going to think OK, she’s in a hurry. If you can be kind of relaxed when you come to talk to the patient, it’s not just ‘How are you? Good morning’, it’s how you say it, not just what you say.
Vera, carer, centre 1
The focus groups threw around ideas about what the core messages of the training might be, and how to get those across. The first idea was that relational care was not an add-on task. Rather, it was something that could and should be woven through everyday care activities. As one participant put it:
I mean, when they’re actually doing observations with patients, taking temperatures and things like that, that’s the time they should be talking to the patient for 5 minutes. To just talk with the patient and, you know, get to know the patient a bit better.
Avril, patient, centre 2
The second idea was that it was important to understand what it is like to be an older person:
[R]emember that we are older (and I’m talking for myself now and probably for some other people) and we’re slower. And whereas somebody else can just sort of jump out of bed and that’s it, it takes me quite a time.
Anthea, patient, centre 1
The third idea regarded understanding what it is like to be an older person in hospital:
[U]nderstand the position that that person was in. [. . .] [T]hat person is in the hospital for a reason. They’re not in there because they’ve asked to go [. . .] they’re in there for a specific reason and I think it’s understanding that that person is in a totally strange environment, perhaps somewhat frightened (because most of us are frightened of the knife or whatever we’re in there for), and understanding that that person is totally out of the environment that they are used to being in, and it’s trying to get those person to make them feel at home, welcome and that they’re not on their own.
Clive, patient, centre 1
One noted aspect of being an older patient was how being dependent on staff for urgent needs created a feeling of powerlessness:
[W]hat I felt particularly was if only the person there could see how powerless these people feel when they’re so vulnerable and they’re in their beds. And have some understanding of that. Then they could be a lot more generous towards them I think.
May, patient, centre 3
This participant appears to be asking for staff to respond with empathy, a deep understanding or shared feeling, of what it must be like to need help and to have to rely on others to provide it. Other discussions raised the importance of HCAs understanding how difficult it is to lose one’s independence, a situation that arises both as a cause and as a result of an inpatient stay.
To help HCA trainees to ‘get into older patients’ shoes’, participants recommended and supported the idea of role-play, using methods to ‘mimic’ the experience of conditions associated with ageing and having older patients contribute to the training.
Interviews with health-care assistants and other staff: findings
Sample
At each trust semistructured interviews were carried out with 10 HCAs (n = 30 in total) and eight other staff members (n = 24 total). The total number of semistructured interviews was 54. The majority of interviews were carried out between May and July 2014, with five HCA and two ‘OS’ interviews at two of the three trusts being held back until November 2014 to allow feedback on an early outline of the training intervention. The duration of the interviews ranged from 21 to 62 minutes, with a median length of 33 minutes.
Across the three study trusts the HCAs we spoke to had been working as HCAs for between 5 months and 15 years. Many of them had experience of paid and unpaid care work elsewhere prior to or concurrent with their work at the trust. ‘OS’ interviewed were matrons (n = 2), ward managers (n = 7), other nursing staff at bands 4–6 (n = 12), those with a role in HCA training (n = 2) and an allied health professional. Further details of the face-to-face interview samples are given below (Tables 8 and 9). In what follows we use ‘OS’ to denote all non-HCA interviews and interviewees and ‘staff’ to cover both groups of hospital staff.
| Trust | HCA, sex (n) | Range (median) length of service at trust (months) | |
|---|---|---|---|
| Female | Male | ||
| 1 | 10 | 0 | 5–186 (median 51) |
| 2 | 8 | 2 | 8–108 (median 24) |
| 3 | 8 | 2 | 5–180 (median 51) |
| All trusts | 26 | 4 | 5–186 (median 30.5) |
| Trust | Relationship with HCA (n) | ||
|---|---|---|---|
| Responsibility for HCA training or practice at above-ward level | Directly manage HCAs | Work alongside HCAs | |
| 1 | 0 | 6 | 2 |
| 2 | 2 | 3 | 3 |
| 3 | 2 | 5 | 1 |
| All trusts | 4 | 14 | 6 |
Experiences of health-care assistant training with respect to relational care at the three trusts
During the period in which the interviews were undertaken there was a 2- or 3-week mandatory induction programme for all HCAs joining each of the three trusts, although in one trust the induction training was being rolled out to long-standing staff. This meant that there was great diversity in the training HCAs at the trusts had received. In our interview sample 11 of the 30 HCAs had joined prior to the current induction programme being in place and said that they had received little or no training prior to starting work as a HCA. On the other hand, besides mandatory induction and update training, some of the HCA interviewees had undertaken training prior to or concurrently with their employment at the trust: six had nationally recognised qualifications in health care (National Vocational Qualification level 1–3), six had taken short courses in end-of-life care for patients and families run by a local hospice and seven had attended trust-based additional training on caring for people with dementia beyond the mandatory minimum.
Examples of topics covered in the current induction programmes across the three trusts that may be regarded as ‘relational care training’ were respect, privacy and dignity, compassion, communication, culturally sensitive care, palliative and end-of-life care and care of the confused older person. This training, perhaps through necessity, is far from extensive. In the trusts with the 2-week induction programme each of these topics were sessions lasting 60–90 minutes. The trust with the longer induction programme (trust 2) had some longer, more interactive sessions, including input from patients and a dementia charity.
It appeared, from a number of sources, that the level and style of the induction training in two of the trusts was largely theoretical. One interviewee felt that the induction training on topics related to relational care at their trust was focused on trust policies and expectations, rather than the practice of delivering relational care in a real-life setting.
Each trust had policies on ward-based supervision and ongoing assessment of competencies during the HCAs’ first year. However, difficulties in finding appropriate staff willing to mentor, supervise or sign off competencies for HCAs were mentioned in interviews at two of the trusts. There was a discrepancy between the competencies HCAs should have achieved within a year of starting work and the training gaps identified by staff interviewees. This meant that ward-based support often fell short of that required to facilitate the trust’s intended programme of training.
What is relational care for older people in acute care settings?
As in focus group discussions, interviews with hospital staff showed that relational care could be discerned through how it made patients and carers feel and what staff did to engender those feelings. In staff accounts, four key themes emerged as central to good relational care for older people in acute care: making patients and visitors feel welcome, seeing patients as people, getting to know patients and verbal and non-verbal communication (including noticing and reading non-verbal clues).
Making patients and visitors feel welcome
Staff making people feel welcome on the ward, through their demeanour and also through practical things such as greeting them, offering them a cup of tea or getting them a chair, was noted by staff as being part of relational care. Hospital staff felt a responsibility to look after visitors as well as patients, and recognised that visitors were highly sensitive to the atmosphere in the ward and used this as a measure of the care provided:
[F]irst impression really matters. Looking at the relatives of the patient come to visit them, they can say ‘Oh, the person I just met at the entrance was so nasty to me then how is he going to look after my relative very well?’.
Solomon, HCA, trust 3
[T]hat kind of welcoming – the right atmosphere I suppose is the word – just makes people feel better. And then I think the visitors that come in would then – it kind of gives the air that they’re not just there treating them really like patients, we are looking after them in a kind of holistic sense [. . .] And it reassures the relatives and the visitors that we’re friendly and are approachable.
Martha, OS, trust 1
People, not ‘old patients’
The HCAs and OS we interviewed noted that what has been termed as ‘seeing the person behind the patient’6 was an important part of relational care. For instance:
[Not] to think of them as an ‘old person’. Think – look behind that and think of them as a person. You know, still talk to them [as] normal.
Nancy, HCA, trust 2
[. . .] what can HCAs do to make a patient feel cared about?’ You know, rather than just sort of dealt with. You know, kind of connected to, I suppose, and known. [. . .] don’t treat them like a patient. When you go to them or whatever, you’re doing your washing or something, talk to them about stuff, like their family. Offer them a cup of tea. You talk about your life. And it’s like you’re interacting with them.
Shelby, HCA, trust 3
This last quotation also highlights the value of reciprocal disclosure in conversations with patients. Although seeing patients as people was seen as important, some HCAs struggled to achieve this, as this honest comment on the risk of objectifying patients reveals:
it is difficult to relate to them and sometimes you almost treat them as like – and it’s bad but you almost do treat them as objects as opposed to patients and people. And they’ve had lives.
Stephen, HCA, trust 2
Several staff interviewees mentioned that referring to patients as bed numbers was not good practice, although acknowledged that it was not uncommon.
Getting to know patients: individualising care and building relationships
Staff remarked how important it was to get to know patients, in order to be able to see the patient as a person, but also to provide personalised care and build relationships of trust and rapport. Interviewees gave numerous examples of methods they tried to use to get to know more about their patients, including talking to patients and family members, getting information from OS (informally and at handovers), patient-related paperwork (patient notes, special documents used for patients with dementia such as This Is Me, ‘specialing’ logs used for patients receiving one-to-one care, bedside notices), observing patients’ habits, routines and reactions and ward or hospital initiatives such as ‘patient unique’ (asking a patient, relative or staff to identify one unique thing about the patient that is shared at handover) or ‘patient stories’ (for which staff, including HCAs, interview a patient from another ward about their hospital experience and present that at a weekly across-ward meeting).
Noticing was identified as a core relational skill. Noticing, for example, a person’s needs, moods and capabilities. Knowing people helped HCAs to interpret what they noticed. All this helped them to deliver care that was responsive to the individual, as did involving patients in their care and asking permission before acting. The following story, in response to a request for an example of good care by a HCA, is a good illustration of these aspects of relational care:
[. . .] yesterday, I got one of my patients – she hasn’t had her hair washed for a long while, and the HCA was talking to her and then she noticed her hair was quite knotted, so she sat down and she said to her (she’s really terrified of having her hair washed) and she spoke to her. She said, ‘Would you like a shower?’ She said, ‘Yes’. And while they were in the shower, they were talking and I think maybe during that, they developed a relationship so the lady said, ‘I will have my hair washed now’. So she washed her hair, dried it and the lady was so happy. So I think that’s – well, that’s what it’s all about: making a difference . . . and trust.
Patience, OS, trust 3
The importance of communication in good relational care
Do you know, communication is such a massive issue on every level, with every complaint or anything I get in, it’s always about communication, about how someone’s been spoken to or the fact they’ve not been spoken to enough, so I don’t know if you can do something around communication [in the training intervention].
Janet, OS, trust 2
According to staff, there are many elements of good verbal communication. It involves the careful use of language, using names, not bay or bed numbers, respecting patients’ preferences for how they wish to be addressed, not talking down to patients or using diminutives or ‘elderspeak’ such as ‘love’, ‘darling’ and so on, and saying please and thank you. One’s tone of voice and taking enough time to speak and to listen such that patients felt ‘heard’ were seen as important. Some interviewees talked about the important skill of striking up a conversation and looking for conversation starters. Although communication is wider than conversations, interviewees spoke about how important conversation is as therapy, in building relationships, in exchanging information and for the patient to emerge as a person. However, staff often talked with regret about not having enough time to engage in conversations with patients.
Reading patients’ non-verbal clues was considered part of the art of noticing. Hence, noticing whether or not a patient is in the mood for talking was also a key communication skill:
[S]ome people like to talk, some people don’t necessarily like to talk but that don’t mean they don’t want you there, you know just be there, sit there with them, you know. Don’t necessarily have to talk to them. If you’re just there with them, get a magazine or something, that’s as good as sitting actually talking.
Kathleen, HCA, trust 2
Staff recognised that non-verbal communication is also important in making patients feel able to ask for help and instilling confidence that their needs will be met:
[I]if you’ve had a really bad day and it’s really hard to hide that sometimes, and you just sort of – you know, even if you just did this [exhausted sigh], and your patients are in that bay of six, and you’ve just lent on the side and gone like that, their confidence goes. [. . .] You’ve got to be really mindful about your body actions and what come out of your mouth in front of your patients.
Rosanna, OS, trust 1
What challenges do health-care assistants face in delivering relational care to older people?
Interviews with staff working on older people’s wards made it clear that working with older people means dealing with high levels of dependency (because of acuity, comorbidity, frailty, high risk and environmental/space issues). This reduces the amount of time HCAs can spend with individual patients, and the speed with which they can respond to patient needs and requests for help. HCAs frequently reported having to ration their time to meet the urgent care needs of several patients. This is made all the more difficult because physical and cognitive impairments associated with old age mean that patients take longer to perform actions and functions. Many interviewees felt that they do not have the time to give the care that they want to give to older patients, or to give an appropriately timely response, which they find distressing and demoralising:
[A]t the end of the day, in my book, every single person out there deserves exactly the same care, time, patience [. . .] staff who are running around like headless chickens – ‘cause we do look like headless chickens. [. . .] ‘cause you can’t slow down, because if you did, someone would suffer because of it. You can’t slow down. You’ve got to try and do everything you can do, the best you can do it, at the fastest speed possible. And that is rubbish, really, when you look at it like that. ‘Cause these aren’t loaves of bread that you’re pushing through a machine, is it?
Rosanna, OS, trust 1
However, interviewees also spoke of ways that they could provide good relational care while moving around the ward or carrying out tasks such as delivering food or helping patients with intimate care. This suggests that an important message in any relational care training should be that relational care can (and should) be woven into everyday activities and tasks and need not necessarily be an additional draw on limited time.
Our findings show that the working environment in older people’s wards is characterised by a number of tensions. Our interviewees described how it involves heavy work with frail people, maintaining patients’ dignity in undignified situations, promoting independence in a high-risk context and keeping patients calm and safe in a busy, noisy, unpredictable environment. In many cases the work involves a high level of communication need from people with hearing, visual and/or cognitive impairments, which makes communication difficult, caring for lonely, isolated and frightened patients in an environment alien to them and which they often fear and in a working environment where time is squeezed and working with vulnerable people who can behave violently and aggressively.
Almost without exception staff interviewees mentioned caring for patients with dementia, delirium or other cognitive impairment as extremely challenging. These patients can behave aggressively, violently or unpredictably. This work can be extremely draining and training does not always reflect the practical difficulties faced on the wards:
It’s very hard to give someone dignity when they’re stripping off and running around the ward and it’s very hard to deal with that so it doesn’t really prepare you but I don’t know whether a lot of in-house training, like sitting in a classroom is going to prepare you for trying to protect – like it’s all very good, like they’re like ‘oh close the curtains and the door and put a towel over them when you wash them’, blah, blah, but the person is trying to kick you and punch you at the same time, keeping them dignified is really difficult.
Rhona, HCA, trust 3
I think a lot of them find it – especially on a 12-hour shift with some of our patients it’s just draining – it’s the constant repetitiveness of it that they ask you a question, you explain to them, 5 seconds later they’ll ask that same question again because they just can’t hold the information you’ve given them so they’re asking you all day ‘where is my daughter, where is she?’.
Lucy, OS, trust 1
Accounts of the challenges involved in working on older people’s wards suggest the need for staff to be able to manage their own feelings of stress, tiredness, frustration, sadness, anger and fear. A few interviewees explicitly called for training on dealing with personal stress. Some interviewees also spoke about dealing with patients’ emotions and family members’ emotions. HCAs have a front-line presence on the ward and, particularly when registered staff numbers are depleted, are exposed to patients’ and relatives’ responses to a system that is understaffed and under strain. This means that HCAs often have to interact with family members seeking information who are sometimes pushy or angry, and not all HCAs in our survey felt sufficiently skilled in dealing with this task:
I think, personally, we need to do a training course on maybe how to communicate with relatives. I think that’s the hardest part of the day, because a lot of the time relatives do get quite angry, and a lot of the time they can’t always speak to the doctors ‘cause the doctors aren’t around.
Ellie, HCA, trust 1
We have already noted the important part that communication plays in relational care. We were given a strong message that training in communication skills would be extremely valuable. Interviewees talked about difficulties in communicating with patients with cognitive or sensory impairment or with non-English speakers and also in talking to patients and their relatives about bad news. As one HCA said:
I’ve been doing it long enough, but when you’re actually with somebody who has been told bad news, it’s difficult. It’s always trying to get the right words, and sometimes obviously the patient would like to talk to you and – [. . .] I would probably like a bit more [training on] how to say the right things without putting your foot in it if you know what I mean?
Hayley, HCA, trust 1
Recommendations for health-care assistant training in relational care
There was widespread, although not universal, support for additional HCA training in relational care. A few registered nurse interviewees believed that (any) HCA-specific training beyond mandatory requirements would make HCAs feel more valued. The aspects of relational care that hospital staff saw as most important in caring for older people in acute settings were making patients and visitors feel welcome, seeing patients as people, getting to know patients and verbal and non-verbal communication (including the art of noticing and reading non-verbal clues). HCAs and OS also identified a need for training in dealing with their own emotions and those of patients and relatives, in dealing with bad news and in caring for patients with dementia.
In terms of delivery, almost without exception, interviewees stressed that HCA training should be ‘practical’. There were many dimensions of practicality, for example not being ‘too theoretical’, practising skills, being relevant to the realities of life on a ward, role-modelling good practice, role-play and bringing situations ‘to life’. There was a strong belief that training should be interactive.
Consistent with focus group participants, staff interviewees thought it important to help HCAs to ‘get into older patients’ shoes’, to gain insight into the vulnerability and fears involved in being a patient. The value of ‘getting into older people’s shoes’ was about raising awareness of the challenges an older person in hospital might face and understanding how older patients might feel. There was strong support for using actual patients’ experiences in the training and for using age simulation suits and other types of simulation:
[W]hen I was at school we had like someone come with like different goggles on to check like with like tunnel vision and like blind in one eye and then we had to use a wheelchair and we had to go in the wheelchair and get from out the wheelchair to the toilet. Then we had like our legs strapped together and we did all things like that so we knew how it would be. I think that’d be good in that sort of thing ‘cause sometimes when a patient takes like 20 minutes to walk to the toilet you’re like ‘urgh!’ But then actually doing it yourself you sort of understand why it’s taking them so long.
Ailsa, HCA, trust 2
One interviewee talked about using imaginative journeys to understand what it is like being an older patient:
[T]ry to make us see the patient’s point of view. Like, try to make us, you know, understand that – you know? Like exchange roles with the patient. Yeah, like, say, ‘Imagine yourself. You’re in there’. Kind of take them on a journey to imagine that it’s you [. . .] How would you want to be cared for? So I think just taking them on that journey, to make them [. . .] imagine and travel in it and then they’re able to get inspired and deliver better than – or the best that they can deliver.
Aliya, HCA, trust 3
One HCA stressed that the training should explicitly recognise the important role that HCAs play:
Me, if I will train [a HCA], I think I need to explain [to] her how important the role of the health-care assistants for the patients. How can you make them comfortable, ‘cause they are vulnerable to come here because of what happen to them. So how can you look after them. How important your role is to that patient.
Jade, HCA, trust 1
We were advised by interviewees not to rely too heavily on e-learning because of difficulties in accessing computers, possible technical difficulties with trust computers, lack of information technology (IT) skills and because staff are rarely released from duty in order to do e-learning. Releasing staff for any training is always contingent on staff numbers and the demands of the ward at the time of training. It was clear from answers to our questions about access to training that, in order to maximise the chances of staff being released to attend training or attending training on off-duty days, training should be in blocks of a whole day. Prebooking bank staff to cover the work of HCAs who are attending a day’s training was also recommended.
Summary
Older people, and those who care for older people, broadly agreed on the ways that HCA training in relational care could improve the experiences of patients and HCAs. Older people and their carers stressed the importance of HCAs not stereotyping older people and that friendly, approachable staff who are good listeners make a huge difference to patient experience. HCAs and staff who work with and alongside them highlighted the need to learn how to have difficult conversations with patients and relatives and how to avoid projecting work-related stress. Both groups agreed that relational care needs to be incorporated into other physical care tasks and that care can be personal and individual only if the person being cared for is known as an individual rather than as a patient.
Older people and their carers, as well as care staff, felt strongly that, to be effective, HCA learning should be rooted in real patient experiences. Simulating the experience of being an older patient in hospital was considered a potentially powerful learning tool, but few HCAs had the opportunity to try this. HCAs wanted learning to build on the assets they bring to the care of older people. In practical terms, receiving training in a whole day better protected their learning needs, while e-learning alone was not a favoured approach.
Chapter 5 Intervention development
Introduction
Using our findings from the telephone survey, focus groups of older people and interviews with HCAs and OS (see Chapters 3 and 4), together with a range of other inputs, we designed a training intervention for HCAs to improve the relational care of older people in hospital. In this chapter we summarise the evidence and material (inputs) that informed the content, structure and format of the training; report the activities undertaken to turn the inputs into a deliverable and replicable training intervention (processes); and describe in detail the structure and content of the HCA training intervention (product). This product is the HCA training intervention, entitled Older People’s Shoes, tested as part of the feasibility pilot cluster randomised controlled trial. The feasibility trial is reported subsequently (see Chapter 6).
Intervention development: inputs
In developing the HCA training intervention we wanted to bring together our findings from phase 1 of the study with expertise of all kinds, both published sources and expert opinion, concerning the learning needs of HCAs with regard to relational care of older people, the teaching and learning approach best suited to meeting these needs, the educational methods that were likely to be feasible, acceptable and effective, and the design and format of teaching materials to be used in the training intervention.
Findings from focus groups of older people and staff interviews
We placed great weight on the views of older people, HCAs and OS as to the content, structure and style of our training intervention. An overview of our findings from our focus groups and staff interviews is reported in Chapter 4, Summary. These findings are summarised in Table 10 to illustrate the similarities (and occasional differences) between those receiving and those providing relational care in hospital settings.
| Findings from older people focus group discussions | Findings from one-to-one hospital staff interviews |
|---|---|
| Important messages for HCAs to hear | |
| Relational care should be woven through everyday activities and tasks | Relational care can and should be woven into everyday activities and tasks |
| Make patients and carers feel welcome, known, secure and ‘at home’ | Make patients and visitors feel welcome |
| Get to know patients as people (do not depersonalise people) | See the person not the ‘old patient’ (do not depersonalise people) |
| Get to know patients so that you can personalise care and build relationships | Get to know patients as people so that you can personalise care and build relationships |
| The art of noticing | The art of noticing |
| Little things mean a lot | Communication (verbal and non-verbal) |
| Be proactive in offering care, as older patients are often unable or reluctant to ask for help | Do not pass on work-related stress |
| Involve carers | |
| Old age brings challenges, but older people are all individuals – do not stereotype ‘old people’ | |
| Make patients feel ‘heard’ (legitimate/significant) by giving them a timely response and listening attentively | |
| Be friendly and approachable | |
| The importance of non-verbal communication | |
| Do not signal ‘busyness’ or pass on work-related stress | |
| Other training needs for HCAs working with older patients | |
| Communicating with people with cognitive impairments | Dealing with your own emotions |
| Doing stimulating activities with patients | Dealing with the emotions of patients and visitors |
| Ways of encouraging older patients to eat and drink | Difficult conversations |
| Caring for patients with cognitive impairments | |
| Training delivery style | |
Training should:
|
Training should:
|
Reviews of research evidence
Two reviews of current evidence were key in shaping the HCA training intervention, Older People’s Shoes. The first was a review and synthesis of qualitative evidence of older people’s and relatives’ experience of acute hospital care. 13 The second was a realist synthesis and review of the evidence for workforce development interventions to improve the skills and care standards of support workers in older people’s health and social care services. 51 As with the design of phase 1 of our own study, by using these two complementary reviews we were able to use evidence from two perspectives: (1) older patients and their relatives and (2) members of the clinical support workforce.
Bridges et al. 13 synthesised findings from 42 original studies and a systematic review that examined older people’s experience of acute care. The authors argued that, while technical aspects of care are often taken for granted, there are three aspects of relational care that, when adequately addressed, are associated with positive experiences of acute hospital care. The first, ‘connect with me’, relates to the relationship between the person providing care and the older patient and his or her relatives. A lack of a sense of reciprocity in the relationship makes people feel anxious and burdensome. The second, ‘see who I am’, illustrates the importance of care staff recognising and helping patients maintain their identity while an inpatient. The third, ‘include me’, refers to the importance of shared decision-making and the involvement of older people and their relatives in treatment and care. The desire for participation in decisions may vary, but the need to have an understanding of what is happening or planned is widely held but often not met, particularly for older patients. The authors conclude that the actions of individual care staff and the relationships they build with older people and their relatives have the potential to make a powerful difference.
The OPSWISE study51 was commissioned as part of the same funding call as the present study. Given the complementarity of the two studies, the study teams maintained close contact, including attending study steering meetings. Using realist principles, Rycroft-Malone et al. 51 identified a number of context–mechanism–outcome configurations (what works, in what context and in what way) from published evidence and stakeholder interviews. These eight configurations or explanations as to what elements of workforce development interventions work for the older person’s support workforce are (1) keep interventions close or ‘real’ to the work of the support worker, (2) pay attention to individual support worker’s starting point and role expectations, (3) tap into learners’ motivations, (4) develop interventions in the context of the organisation’s wider goals, (5) co-design training interventions using the right mix of people to reflect the complexity of the workforce, (6) get the right mix of people to deliver interventions to promote shared learning and improve cohesion, (7) take a planned approach that draws on theory and (8) ensure that interventions are comprehensive and multilayered to embed and spread impacts across organisations. The implications of these configurations are summarised in Box 1.
Workforce training interventions should:
-
reflect the reality of the support worker role
-
build on life skills and experiences individuals bring to the support worker role
-
use strategies and techniques to motivate individuals to engage with the intervention and wider development
-
align with organisational strategy
-
be designed with the right stakeholders from the outset
-
be delivered by a variety of stakeholders
-
be designed and delivered in a theory-driven and systematic way
-
be considered as complex programmes (or interventions) and context dependent
-
balance professional with emotional aspects of caring work.
Initiatives and tools to improve relational care
Although rarely evaluated, there have been a number of initiatives that have sought, explicitly or implicitly, to enhance the quality of relational care. Few, if any, are targeted at the care of older people exclusively, and those that were tended to specifically focus on the care of older people with dementia. We investigated the content of current initiatives that we were aware of in order to learn from existing tools, avoid overlap and be aware of where our own HCA training intervention was situated in the broader context of related interventions and initiatives.
The Setting, Ask, Gather, Empathy and Talk, Help, You, Me, End (SAGE & THYME) model was developed by clinical staff and a patient at University Hospital of South Manchester NHS Foundation Trust in 2006 to meet the 2004 National Institute for Health and Care Excellence’s guidance on ‘improving supportive and palliative care for adults with cancer’. 68 It was designed to be relevant to all grades of staff and to improve skills in how to listen and respond to patients and carers who are distressed or concerned. The title is a mnemonic guiding a health worker into and out of a conversation with someone in distress. Its approach is to encourage health workers to offer psychological support by holding back advice and prompt patients to consider their own solutions. It is taught using a foundation-level workshop by three facilitators using a mix of small-group work, lectures and rehearsals. It includes ‘live pause’ technique to facilitate direct feedback and discussion. There is evidence that these workshops have a positive effect on self-confidence, self-perception of competence and willingness to explore the emotional concerns of patients. 69
Barbara’s Story is part of a dementia awareness training initiative for hospital and community health staff developed by Guy’s and St Thomas’ NHS Foundation Trust. The initial Barbara’s Story film shows the experience of an older woman (Barbara) through her own eyes as she attends a hospital appointment and is admitted for investigations. The film was shown regularly from September 2012 to April 2013 and attendance was mandatory for all trust staff, with a total of 11,054 clinical and non-clinical staff attending during that time. Barbara’s Story was also embedded into the corporate induction programme for new trust staff. Subsequently, a second series of films was developed, which show Barbara’s health deteriorating and her receiving care in hospital and community settings. The films were shown from September 2013 to March 2014, with one new episode available each month. Staff are expected to gain an understanding of issues faced by patients with dementia in order to recognise the problems they face. Staff have reported that Barbara’s Story engaged them emotionally and prompted empathetic responses. 70 Reported changes included giving more time to patients, improved communication, giving more information and assisting patients who are looking lost or confused. 70
Active Caring for Everyone (ACE) is a programme developed at Worcestershire Acute NHS hospitals Trust designed to improve day-to-day interactions between staff and patients. As staff attitude accounts for a high proportion of patient or relative complaints in any NHS trust, the initiative includes a card carried by all staff and ‘shown’ if it is believed the care being delivered is falling below a certain standard and accompanied by the phrase ‘you didn’t play your ACE card’. It aims to show that each point of contact, no matter how small, can result in a positive patient experience, increase staff understanding of their own role and responsibilities in delivering high levels of customer service and recognise good customer service and actively seek ways to solve problems and handle concerns. There has been no external evaluation of this programme as far as we are aware.
A fairly common approach to increase empathy among health staff is to simulate the experience of disability and/or ageing. For this, some trusts have used equipment designed for this task or used more impromptu methods. Age simulation suits aim to get the wearer to experience the disabling effects of ageing on simple tasks, movement, orientation and energy levels. Training helps to highlight the importance of communication and limitation of the patient in the hospital environment (and others). An evaluation of a 2-day simulation training programme that included the use of an ageing suit found a significant increase in confidence across all staff grades, and staff reported spending more time getting to know patients. 71 Similar results of a rise in confidence and positive behaviour change are reported in an evaluation of a simulation-based educational programme to equip HCAs with non-technical skills to undertake their role safely and effectively. 72
Life-story work
Life-story work is considered to be an approach that can be used to transform how care staff think and feel about older people. 73 It is thought to be beneficial to older people, and the use of life-story instruments that capture important personal information about patients is increasingly encouraged by care organisations and patient groups. Older stakeholders and members of the steering committee also considered evaluation of routinely used life-story instruments important. Life-story instruments are known to have both advantages and disadvantages22 and these are summarised in Table 11. One of the disadvantages from our perspective is that they are often assumed to be relevant only for patients with a diagnosis of dementia. To help HCAs ‘see the person inside the patient’, we planned to develop and include a modified form of life-story work into our training intervention.
| Advantages of life-story instruments | Disadvantages of life-story instruments |
|---|---|
| Often used for people with dementia, but can be used for any patient | Difficult to find the time to complete |
| Patients and their families appreciate the time investment of staff | Staff worried about raising distressing memories |
| Enjoyable experience | Staff will need to listen to painful as well as pleasant memories |
| Interesting to read | Some information may lead to unease in relatives |
| Gives patient a history and helps staff to see the patient as an individual | Will oversimplify a life |
| Can change staff attitudes | For some staff knowing more will have no effect on the care they provide |
| Patients feel more valued | Ownership and consent need to be carefully considered. For example, what happens to the book after somebody dies? |
| Breaks down barriers (sharing lives) | Training for staff using these instruments is essential |
| Companionship (from sharing) | Management support required |
| Helps to orientate patients to their past | |
| Encourages meaningful conversation | |
| Could be used to improve mood/affirm value, for example activities based on knowledge | |
| Increased sociability and decreased aggression in some | |
| A ‘trigger’ for reality | |
| Greater understanding promotes better relationships | |
| Vehicle for improved communication | |
| Useful resource for patients moving to different wards |
A number of life-story instruments in common use were identified from internet searches and local knowledge. These were the Alzheimer’s Society’s This is Me,74 the Getting to Know Me book, based on original work by NHS Lanarkshire,75 the Getting to Know Me form from University Hospitals Coventry and Warwickshire NHS Trust76 and Worcestershire Acute Hospitals NHS Trust’s About Me – Lifestyle and Capabilities Booklet. 77 The areas covered in varying levels of detail include care preferences, physical ability to perform daily activities, communication impairment, mobility and relatives’ involvement in care. Something we were particularly interested in, because of our desire for our training to assist HCAs to engage with older people as people first and patients second, was the inclusion of items about personal history and particular preferences beyond those related to physical care. Items such as ‘my life so far’, past employment, live events, interests and hobbies were present in some of the instruments but, perhaps understandably, tended to be given lower priority than information required to perform physical care tasks.
Learning from customer care
Four large commercial/retail organisations agreed to speak with us prior to the development of the HCA training intervention. Our interest was in their approach to improving customer care provided by their staff, including training materials and modes of training delivery. Trainers from each of these organisations met us to provide insights that we expected would inform the content and delivery of our HCA training intervention.
The retail organisations involved were Boots Opticians, a company with 600 outlets in the UK, serving an older customer base; Aldi, a multinational company with approximately 400 supermarkets in the UK; Domestic & General, the leading UK domestic appliance care company providing protection plans for household appliances through telesales; and B&Q, a do-it-yourself store which has been recognised for its policy of actively promoting the employment of older staff.
Discussions with staff who had responsibility for customer service training in these organisations covered a range of topics, including any learning theories and principles used to underpin their training. Although commercial sensitivities prevent us from providing extensive detail and ascribing this to individual organisations, we learned about the use of neurolinguistic principles in training and the ways in which acronyms and mnemonics are used to reinforce key messages and encourage consistency in good customer service. Particularly important customer care learning points that were transferable to the health-care setting included how to make each contact count, the importance of active listening and the conscious actions of smiling and greeting customers. A list of key learning points that were drawn on for the HCA training intervention is given in Box 2.
Customer care training should include:
-
an understanding of the impact of good and bad practices in customer care
-
how to actively listen
-
why every interaction matters
-
why first impressions matter
-
the art of noticing
-
how to deal with challenging customers.
Intervention development: process
The process of developing the HCA training intervention overlapped with obtaining the inputs described above and, inevitably, the process itself yielded more information (or inputs) that informed the intervention. In this section we describe the series of events that were used to decide which materials to include and exclude, the frameworks drawn on to determine the most effective form of delivery and the process used to deliver the physical products described in Intervention development: product.
Panel of expert witnesses
Core members of the study team identified a number of national and international experts in relevant fields that would help us build the HCA training intervention. We invited these experts to provide ‘evidence’ by being informally interviewed by members of the study team that met on 8 September 2014. The members of the study team plus an experienced HCA from one of our partner NHS trusts formed a panel and each of the expert ‘witnesses’ (Table 12) were interviewed by the panel either by teleconference or skype™ (Microsoft Corporation, Redmond, WA, USA). All our experts were briefed prior to the panel about the study, the composition of the panel and our areas of interest. The specific areas of focus were policy, context, transmission, experience, evidence and content. The panel members used an informal checklist of areas to explore with each expert witness (Box 3).
| Name | Position | Area of expertise |
|---|---|---|
| Kirk Lower | Director of the Cambridgeshire and Peterborough and Norfolk and Suffolk Workforce Partnerships, Health Education East of England and National Project Lead for ‘Talent for Care’ | NHS education policy, workforce, bands 1–4 and project director for ‘Talent for Care’ |
| Liz McConnell | Lecturer in Interprofessional Practice, University of East Anglia | Mindfulness-based therapies, compassion-focused therapy, values-/attitudes-based education and learning (e.g. cultivating compassion) |
| Amanda Clarke | Professor of Nursing, Northumbria University | Methodological expertise includes engaging in life-story work with older adults |
| Jo Rycroft-Malone/Lynne Williams | Professor of Implementation and Health Services Research, Bangor University/Researcher on OPSWISE study | OPSWISE: Improving skills and care standards in the clinical support workforce: a realist synthesis of workforce development interventions. Evidence base for HCA training interventions |
| Jackie Bridges | Senior Lecturer, University of Southampton | Relational work of health-care professionals, particularly those working with older people. Identifying the modifiable factors that promote or inhibit relational work and developing and evaluating interventions aimed at manipulating these factors |
| Nick Napper | Lead Learning Advisor, Musgrove Academy, Musgrove Park Hospital | Training and induction for NHS staff, customer care issues within the NHS (experience of the John Lewis programme at Musgrove Park Hospital) |
| Kezia Scales | Postdoctoral Research Fellow, University of North Carolina | Ethnography of HCAs, emotional labour of HCAs and HCA culture/ethnography |
-
Could you describe your area of interest/expertise in the area of HCA workforce/training/older people (as appropriate)?
-
In your experience, what are the key components that are essential in training for HCAs with respect to relational care of older people/people with dementia?
-
How do we best support HCAs to enable change?
-
Can you tell us about any training intervention you know that supports people to provide relational care?
-
What issues, or problems, have you found in assessing/measuring relational/values-based care?
-
Can you tell us about the factors that promote or inhibit relational work?
-
Are you aware of other studies of the perceived/actual role of HCAs in respect to relational care?
-
Do you have any ideas/tips/best guesses/hunches for our intervention with HCAs?
-
Other spontaneous questions arising from the discussion.
-
What is your view of the nature of our intervention?
Thanks and concluding remarks, and a request for permission to make further contact if needed.
The key messages distilled by panel members from evidence provided by these expert witnesses were:
-
Values-based training is important but there are difficulties in providing training for established/existing HCAs as many trusts restrict training to new starters.
-
Be aware of barriers to training in the workplace, such as poor access to technology, lack of time, limited IT skills, attitudes of managers (‘HCAs do not need training’), the fact that HCAs themselves do not feel that they need training and the negative impact of the label ‘untrained workforce’.
-
HCAs need to be enabled to be self-aware, emotionally resilient and clear about their own self-compassion, but bear in mind that this may need to be handled with sensitivity and require adequate training of the trainer.
-
It is desirable to integrate ‘life-story work’ into everyday tasks and to encourage HCAs to ‘be a detective’ to find out things that highlight the individuality of each patient.
-
Recognise the lives and invaluable contribution of the HCAs themselves; adopt an assets-based approach (what strengths do HCAs bring?) rather than a deficit model (what skills are lacking?).
-
Small improvements can make a big difference.
-
Situate relational care within practical clinical care and, if using customer care practices, it is important to ensure that these are not superficial.
-
Be explicit and realistic about expectations and recognise the power that HCAs have ‘in the moment’, if not organisationally. HCAs are influential in patients’ and relatives’ experiences of care, yet this is seldom recognised and their contribution may remain invisible.
-
In terms of training design, learning should be participatory and interactive. Staff appreciate having a tailored training package but supervisor buy-in and post-training support are crucial.
-
Links to practice and use of real-life examples are important for authenticity.
Intervention development workshops
The development of the HCA training intervention was guided by members of the interdisciplinary study team comprising nurses, methodologists, education and social science researchers, together with a HCA and PPI representatives. Members of this group were based across the three centres and worked remotely but came together at eight intensive workshops, some residential, spread across the intervention development period of the study (Table 13).
| Workshop | Date | Content |
|---|---|---|
| 1 | 5 June 2014 | Broad themes for the training package were agreed from the initial sources of evidence and a learning design template was created |
| 2 | 8 and 9 September 2014 | Interviews of experts by panel. Content was organised into key themes and preliminary structure formed using storyboarding |
| 3 | 13 and 14 October 2014 | Themes were organised into three units; units were to run over 2 training days (one session per unit per training day) |
| 4 | 1 and 2 December 2014 | Learning outcomes and key messages were refined; learning design templates populated |
| 5 | 19 and 20 January 2015 | Materials and resources drawn together into the three units (six sessions) |
| 6 | 5 February 2015 | Test run of each session to check timings |
| 7 | 11 February 2015 | Review and refinement of units and sessions |
| 8 | 26 February 2015 | Review and refinement of units and sessions |
The purpose (and result) of these workshops was to refine the HCA training intervention and to set milestones in order to maintain progress as we worked through each stage of intervention development. The process drew on the group members’ familiarity with the data sources and other inputs, as well as with the experience that they collectively brought. HCAs and PPI members provided invaluable input ensuring the materials being developed were relevant to stakeholders. An example of how decision aids were used to process inputs from experts into the developing structure of the training intervention is provided below (Figure 4).
FIGURE 4.
An example of one of the decision tools used to inform structure and content with inputs.
Workshops were used to decide which elements of the inputs should be included in the HCA training intervention. All inputs were considered but not all were included. Some important points were not included in the training or were included minimally because they were considered to require specialist trainers (such as doing stimulating activities with patients) or dealt with a particular specialist need. For example, HCAs were very keen to acquire training that would help them to manage better dementia care but our remit and focus was on the relational care of older people. A small section on relational care and dementia was included, but attention remained on the needs of older people more generally.
Theoretical teaching and learning frameworks
The training intervention design process used a step-by-step approach to curriculum design (identifying what is to be learned), guided by instructional design frameworks (how it is to be learned). 78 The importance of using theoretical principles of instructional (pedagogical) design to develop educational interventions in health-care contexts is often overlooked, but it is essential to ensure that training builds on existing knowledge and values, harnesses intrinsic motivation and actively engages learners.
The overarching theoretical basis for the design of the training package is derived from Carver’s framework79 for applying the principles of experiential education. This framework provided elements appropriate for the practical nature of a HCA’s role that could be applied throughout the development of the training intervention. Carver proposes four key elements to experiential education: (1) authenticity (activities being relevant to the participant’s role), (2) active learning (engaged and active learning activities), (3) draws on experiences (what happened to them, how it felt, how they reacted, what resulted, what they observed) and (4) provides mechanisms for connecting experience to future opportunity (learners reflect on their participation in activities or on their potential roles as community members to make experiences relevant to their future endeavours). Carver’s four key elements to experiential education and examples of how these were applied in developing the activities within the HCA training intervention are shown in Table 14.
| Element of experiential learning | Application to HCA training intervention |
|---|---|
| Authenticity | Activities are directly relevant to the HCA’s role in caring for older people in hospital |
| Active learning | Group exercises are embedded throughout to maintain HCA learner engagement and ensure learning is active rather than passive |
| Drawing on experience | HCA learners are encouraged to think about what happened to them in particular situations, how it felt, how they reacted, what resulted and what they observed |
| Provision of mechanisms for connecting experience to future opportunity | HCA learners are encouraged to reflect on their participation in learning activities to make their experiences relevant to their future work with older people |
When developing training interventions it is important to provide a pedagogical framework to ensure the materials and activities are structured for learning to take place optimally. Gagné’s model considers three important domains that impact on learning (affective, cognitive and psychomotor),80 making it particularly suited to a values-based training approach. Gagné’s original model has nine steps: (1) gain attention, (2) identify objective, (3) recall prior learning, (4) present stimulus, (5) guide learning, (6) elicit performance, (7) provide feedback, (8) assess performance and (9) enhance retention/transfer. The HCA training intervention was designed using an adapted version of this model to structure individual learning activities within each unit. A simpler model with a smaller number of steps was more appropriate for a short training programme. The following five steps were included in our pedagogical framework:
-
create learning goal
-
provide a trigger
-
present content or learning material
-
design some guided practice, simulation or reflection
-
reinforce key messages.
The intervention development group used design templates scaffolded by these five steps to ensure that each session contained the pedagogical elements as the training content and learning activities were developed. An example of how this framework was applied is illustrated in the following learning episode. One of the three units in our HCA training intervention was ‘Learning from customer care’ (details of all units are given in Intervention development: product). In this unit the (first) learning goal was to understand what is meant by ‘customer care’. The trigger activity was to ask the HCA learners ‘Think about the customer care you have experienced recently? What made this experience a good or bad one?’. The learning content presented by the trainer then covered the concepts of active listening, every interaction matters and the art of noticing. These were some of the learning points drawn from our retail partners. This was followed by asking HCAs to reflect on how these concepts might apply to their own practice. This learning activity is concluded by reinforcing the key message ‘good customer care can be provided by noticing customer cues, by listening to needs and by providing a consistent standard of care’.
Content development, review, production and editing
Having identified our theoretical and pedagogical frameworks, these were applied to each unit of the training and the units were developed using a learning design template. Learning objectives for each of the three units were generated. Each unit underwent a critical, in-depth, iterative quality review by the intervention development group and the steering committee, which included HCAs, PPI representatives and trust representatives from the three centres. During this phase, media assets such as still images and film clips were sourced, reviewed for relevance and appropriateness and formatted. Permissions were obtained to use any clips from other sources.
The course book for participants and a guide for trainers that elaborated on the intended delivery process for each stage were written and reviewed in detail by the intervention development group. Professional designers were used to produce the two manuals. The equipment required to support the training was purchased. This included age simulation suits (GERontologic Test suits, Niederstotzingen, Germany), pyjamas and utensils for role-play exercises, together with copyright licences. Slide presentations and a bespoke online learning site were also developed to support the trainers and HCAs who participated in the training.
Intervention development: product
The HCA training intervention was entitled Older People’s Shoes. This section describes (1) the structure and mode of delivery, (2) the content, (3) the materials that were produced to deliver Older People’s Shoes consistently across trainers and centres and (4) the ‘train-the-trainer’ process.
Structure and mode of delivery of Older People’s Shoes
Older People’s Shoes training comprised three units: (1) getting into older people’s shoes, (2) getting to know older people and (3) learning from customer care. Each unit was divided into two sessions, one per day, so learning on the first day was consolidated and built upon on the second day, approximately 1 week later. At the end of each session on day 1 HCA learners were asked to undertake brief individual work-based exercises prior to day 2. On day 2, each unit began with a brief discussion of these exercises so that learners could share from others’ experiences and learning. The structure and content of the 2 days are presented in Tables 15 and 16.
| Unit 1: session 1 – getting into older people’s shoes | |
|---|---|
| Learning goals | |
|
|
| Welcome to the ward | Trainers asked to ‘model’ a good welcome as HCA learners arrive |
| Group asked to think back to their first day on the ward | |
| Video clips of patients’ experience of hospital admission | |
| What it feels like to be a hospital patient | Video clips of patients reflecting on how it feels to be dependent on care staff followed by facilitated discussion |
| Empathy | Animation to illustrate the difference between sympathy and empathy |
| Guided discussion on the challenge of ‘not judging’ | |
| Learners view ‘Today is Monday’ video and comment on the way staff interact with patients | |
| Take-home exercise | Learners asked to identify a patient with a physical impairment and as part of their care engage in conversation as to how that impairment affects their life outside hospital and inside as a patient |
| Unit 2: session 2 – getting to know older people | |
| Learning goals | |
|
|
| Age and experience | Images and biographies of older people used to understand the interface between personal biography and social history |
| Challenges and benefits of ageing | Discussion-based exercise looking in depth at the life of Maud, a centenarian |
| ‘It helps to know’ | Quotations from older people used to explore how personal history gives older patients ‘personhood’ in hospital |
| Take-home exercise | Learners asked to identify an older patient in their care and attempt to find out a bit more about their lives when they were much younger |
| Unit 3: session 3 – learning from customer care | |
| Learning goals | |
|
|
| What is customer care? | Learners share examples of good and bad customer care in any setting. Trainer facilitates learners to make links with their own roles in delivering customer care |
| Exploring retail ‘customer care’ training | Customer care training from particular retail organisations is presented and discussed. Differences between ‘patients’ and ‘customers’ explored. HCAs reflect on the service they provide |
| Customer care in retail practice | Video presentation of good and bad customer care in a non-health-care setting |
| Take-home exercise | Learners asked to take note of one good and one bad experience of customer care practice to discuss in day 2 |
| Unit 1: session 4 – getting into older people’s shoes | |
|---|---|
| Learning goals | |
|
|
| Recap on session 1 | Facilitated discussion where learners discuss unit 1 take-home exercise |
| The ageing process and activities of daily living | Use of simulation suits to help learners experience some of the physical effects of older age. Simulation equipment includes restricted vision goggles, ear defenders, weighted jackets, and neck braces. Learners work in pairs with a list of specific tasks, for example walking across a room and negotiating obstacles |
| Hospital food and drink | Particular foods including ‘build-up’ drinks laid out and learners sample these both independently and receiving help |
| Discussion/reflection | Learners share their experiences of the simulation activities |
| Unit 2: session 5 – getting to know older people | |
| Learning goals | |
|
|
| Recap on session 2 | Facilitated discussion in which learners discuss unit 2 take-home exercise |
| What makes you you? | Exercise whereby learners match images of older people with a short biography. Learners asked to consider what personal and physical attributes ‘define’ them |
| What do you see? | Video and discussion about how ageing (‘the mask of ageing’) and being a patient works against the notion of ‘personhood’ |
| Getting to know older patients? | Practical tips on ways to get to know patients as people |
| Unit 3: session 6 – learning from customer care | |
| Learning goals | |
|
|
| Recap on session 3 | Facilitated discussion where learners discuss unit 3 take-home exercise |
| Managing the ‘difficult’ | Group discussion on why some patients are sometimes seen as ‘difficult’. Learners work in pairs to look at scenarios and consider what motivates certain behaviours |
| Dealing with anger | Learners introduced to four phases of anger. A short role-play exercise in which learners discover the cause of expressed anger in an older patient |
| Managing our own feelings | Group exercise and discussion on prioritising own care and underlining the importance of the well-being of the carer in relational care |
Each training day began at 09.00 with tea or coffee and introductions. Training was scheduled to finish at 16.20, with a 45-minute lunch break. The trainers were given guidance about approximately how long to spend on each section, and each session was allocated between 90 and 160 minutes of training time.
Training took place close to HCAs’ work places or in familiar training rooms. Rooms were laid out informally to foster a relaxed atmosphere. Rooms required computer and projection facilities and internet access; however, in case of technical problems, online materials were also available on a USB memory stick. It was important to look after the HCAs themselves during the training in case any aspect of the training caused any distress. This was done in a number of ways. The sessions were relaxed and interactive, HCAs were given time for reflection and could raise any concerns they had either within the group or individually with the trainer. The training was asset driven, affirming the importance of the HCA role in patient care, and the HCAs were shown how to access local support networks for any issues that may arise as a result of the training intervention.
Content of Older People’s Shoes
Unit 1: getting into older people’s shoes
This unit helps HCA learners to understand the challenges of being an older person in hospital. On day 1, HCAs are asked to remember their first day on the ward as a trigger to explore the importance of the HCA role in making parents and families feel welcome. Patients’ experiences are brought to life using talking-heads short film clips such as ‘Anna Brown describes her first few hours in A&E’ and narratives in which real older patients talk about their experiences (both good and bad) of hospital care. A discussion on empathy completes the unit on day 1, using an animation to show the difference between empathy and sympathy followed by a group discussion on examples of empathy identified in ‘Today is Monday’,81 a ‘fly-on-the-wall’ film shot with real care staff on a ward caring for older people with dementia.
On day 2 of the unit, experiential learning is provided through learners having the opportunity to use age-simulation suits. HCAs explore the sensory and physical restrictions experienced by older people as they age through the use of GERontologic Test suits, feeding each other with restricted vision and hearing, putting on pyjamas and doing up buttons.
Unit 2: getting to know older people
This unit challenges HCA learners to think about how hospitalisation can strip away much of what makes people individual and how stereotypical notions of ageing may lead care staff to make false or limiting assumptions about older people. Day 1 looks at how opportunities can be found to ‘discover the person behind the patient’ through rich life stories focusing on Hannah (aged 100 years), Nigel (aged 90 years) and Eva (aged 80 years). Their lives going back to 1910 are revealed through a Prezi-based (Prezi, Budapest, Hungary) visual storytelling activity, supplemented with still images of centenarians contributed by David Bailey. The unit ends on day 1 with an activity based on a discussion with real quotes from patients, HCAs and other ward staff as triggers, talking about the challenges and benefits of HCAs getting to know each of their patients.
Day 2 builds on the life-story work by starting to look at individuality and how becoming a patient can sometimes take away this individuality particularly, but not exclusively, those with difficulties in communicating. Relevant and anonymised quotes from qualitative interviews with HCAs are used as triggers for learning. Two film clips are used in this session, one to stimulate discussion about how not knowing or knowing an older person’s history can unintentionally affect how they are cared for, and the second to illustrate how knowing something about the life story of an older person with dementia might give important insights into their behaviour. The final part of this unit focuses on the ingredients needed to build a relationship and the importance of weaving relational care into everyday tasks to build stronger relationships with older people.
Unit 3: learning from customer care
This unit asks HCA learners to consider how some aspects of customer care provided in non-health settings can be applied to their work in the ward. Day 1 begins by asking the group to consider a time when they have experienced good and bad customer care and what made these experiences different and memorable. At this point the unit draws on some of the learning points gleaned from retail partners such as ‘active listening’, ‘every interaction matters’ and the ‘art of noticing’. These concepts are illustrated in a training film originally used by a travel agency to illustrate how dramatically an experience of a service can be enhanced positively or affected negatively by the attitude, interest and behaviour of front-line staff members. This is subsequently related to a facilitated discussion and the session finishes by asking HCAs to think about how these elements of customer care can be applied to patient care in the hospital setting.
Day 2 explores how being on the front line to patient care, in an environment which can be demanding and busy, means that HCAs often have to manage difficult situations such as dealing with angry patients and visitors. This session encourages peer-to-peer learning by facilitating discussion about strategies the HCAs themselves have found work for them as well as providing tips for building on these ideas.
Training materials
Successful delivery of the course to HCAs requires a complete training package comprising the trainee course book, an online support tool, the trainer guide and a train-the-trainer course. These four components of the training package are described below and are available on request from the principal investigator.
Trainee course book
The trainee course book (see Appendix 9) is a 43-page publication divided into six units (the three units delivered across 2 days). Learning goals, trigger questions, transcripts of film clips of service users shown in the sessions, and key ‘take-home’ messages are included in the course book. The course book is illustrated with images in both black and white and colour. Space is provided within the book for HCA learners to make notes during the sessions and for the ‘take-home’ exercises undertaken between day 1 and day 2.
Trainer guide
The trainer guide (see Appendix 10) takes the trainer through each unit of the training providing some rationale and background information for each unit, identifying the purpose and learning goals for each session, outlining learning activities, signposting to resources (e.g. slide numbers and media resources) and key messages for the sections. Three different icons are used to highlight where there is guided script for the trainer to use if required, sample answers to questions and activities, and suggested ways to handle particular situations that might arise. Indicative times for each element of the training are also given.
Online learning website
The online version of the Older People’s Shoes training was developed as a resource to support both the trainers and HCA trainees during the training and after the training had taken place. The structure of the site mirrored the course structure (and course book) to make navigation around the site intuitive and efficient. Simple hyperlinks and clear clickable tabs allowed the users (either the trainers or HCA learners) to navigate between the screens to see the course materials and activities. Film sequences were precisely clipped and embedded into the online site. This negated the need for users to have to play through a video clip to find the right section. Trainers and HCA learners were given a generic username and password (one for each type of user) to allow them to access the materials. An administrator area of the site allowed other categories of user to be added if necessary.
Slide presentations
Six slide presentations were developed in Microsoft PowerPoint® (Microsoft Corporation, Redmond, WA, USA) to support each unit of the course. Slides were used to reinforce learning goals and key messages and to provide on-screen quotes and images to support learning points. The slides were used as visual triggers for debate and reinforcement. Examples of slides are provided within excerpts from the trainer guide (see Appendix 10).
Training the trainer
Trainers were practice development nurses or nurses with responsibility for training HCAs and all were experienced educators involved in HCA training in their own trusts. Members of the research team ran ‘Train-the-trainer’ days at each centre. These training days consisted of a 1-day face-to-face session, with additional time on another day for the trainer to raise further questions about any aspect of the training. It was essential to spend time with the trainers explaining the context of the training, the findings from phase 1 of the CHAT study as well as going through each of the units of the training. A guide for researchers ‘training the trainer’ was provided (see Appendix 11).
Summary
We developed a HCA training intervention, Older People’s Shoes, through a process of synthesising evidence from data collected within phase 1 of the CHAT study, together with other inputs from recognised experts in relevant fields, existing evidence and, more specifically, life-story work and learning from retail sector organisations. We also investigated the content of current initiatives in order to learn from existing tools to avoid overlap and to situate our intervention in the broader context of related initiatives. Carver’s framework,79 which proposes four key elements to experiential education, provided a theoretical basis for the design of the training package. The product was refined through a series of intervention development workshops. Older People’s Shoes is a 2-day training course for HCAs caring for older people delivered by a trainer. Each day comprises three units: (1) getting into older people’s shoes, (2) getting to know older people and (3) learning from customer care. Learning from each unit on the first day was consolidated and built on day 2, approximately 1 week later. Materials created as part of the CHAT study and required to deliver the intervention include a trainee course book, a trainer guide and an online website.
Chapter 6 A pilot and feasibility cluster randomised controlled trial of a training intervention for health-care assistants
Introduction
This chapter reports the methods and findings of the pilot and feasibility cluster randomised controlled trial. It was registered as an International Standard Randomised Controlled Trial (ISRCTN10385799) on 29 December 2014. The protocol for our study has been published. 82
Feasibility trial: methods
Purpose
The main purpose of the feasibility cluster randomised trial was to assess the feasibility of a definitive trial to compare the newly developed HCA training package Older People’s Shoes in relational care with current training in improving the care of older patients in acute NHS settings. To inform the feasibility of a definitive trial83 (and then, if feasible, the design of such a trial), the following issues were explored:
-
the acceptability of the intervention to trainers and HCA trainees
-
the willingness of ward managers, HCAs and older patients to participate in a cluster randomised controlled trial
-
the willingness of ward managers for wards to be randomly allocated
-
the level of non-response and item non-response to outcomes at the level of ward, HCA and patient
-
the acceptability of outcome measures to participants
-
the ability to monitor levels of resource use and quality-of-life data
-
the variability within and between ward, HCA and patient
-
the appropriateness of ward as the unit of randomisation.
Design
A pilot cluster randomised controlled trial was conducted to compare Older People’s Shoes with ‘HCA TAU’. Clusters were wards within three acute NHS hospital trusts in England with outcomes observed at the level of the ward, HCA and patient (Figure 5). A brief description of these trusts was provided earlier (see Chapter 4, Setting and eligibility).
FIGURE 5.
The CHAT study pilot cluster randomised trial design and target recruitment. AGED, Age Group Evaluation and Description; AWES, Assessment of Work Environment Scale; EQ-5D-5L, EuroQol-5 Dimensions, five-level version; PEECH, Patient Evaluation of Emotional Care during Hospitalisation; QUIS, Quality of Interaction Scale; TEQ, Toronto Empathy Questionnaire.
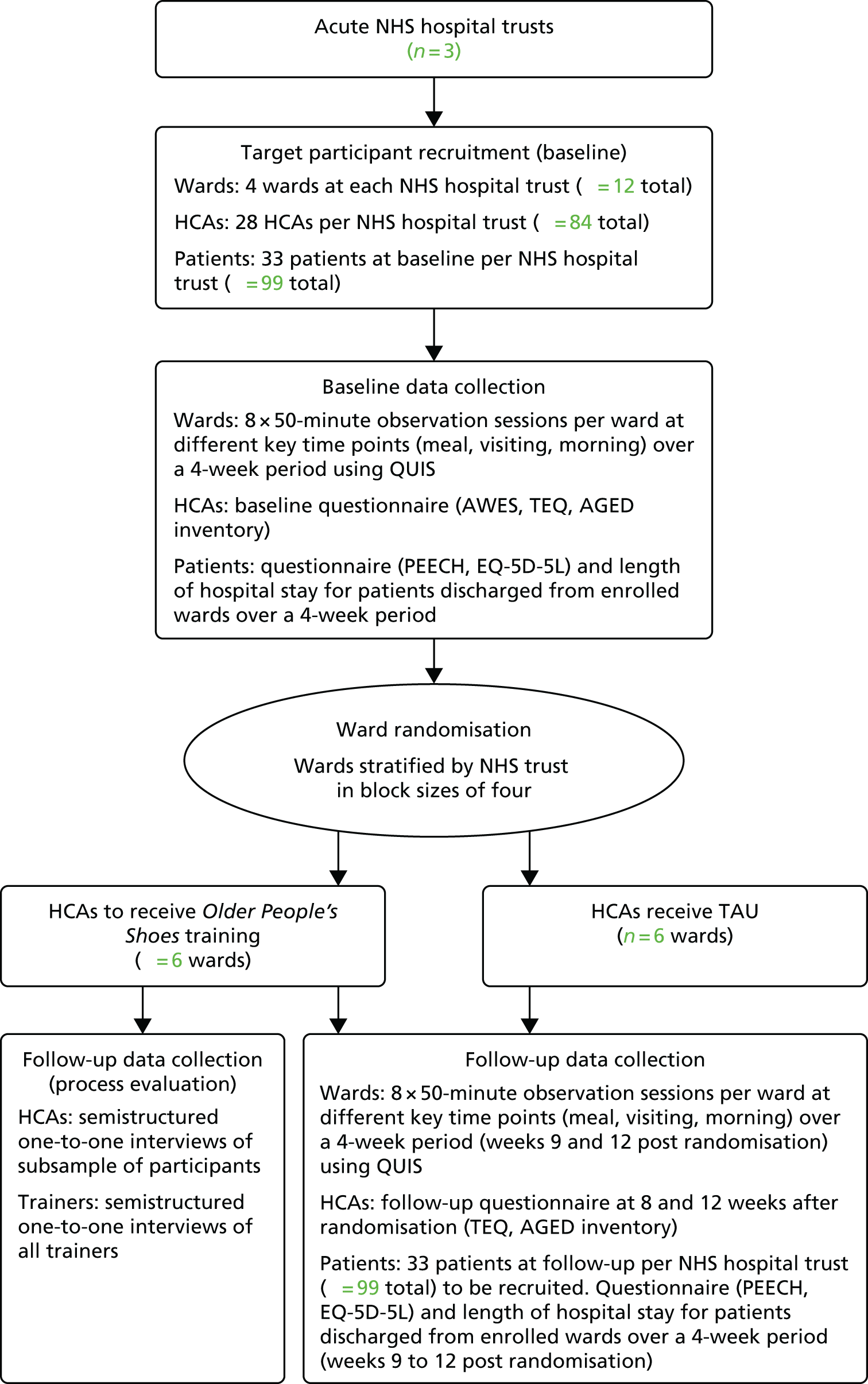
Eligibility
Wards
General medical, stroke or care of the elderly/older people wards were eligible to enter the trial. Specialist dementia wards and medical admissions units were excluded.
Health-care assistants
Health-care assistants employed full time or part time within enrolled wards were eligible to enter the trial. Those employed as bank staff and not part of the named staff on the ward roster were considered ineligible.
Patients
Patients were eligible if they were aged ≥ 70 years and discharged from an inpatient stay on an enrolled ward, during either the 4-week period prior to randomisation (baseline) or during weeks 9–12 post randomisation (follow-up). Patients transferred to another ward or hospital prior to discharge or considered by the nurse in charge not to have mental capacity (according to the Mental Capacity Act 200584) or to be in the final stages of a terminal illness were excluded.
Recruitment
Wards
The ward manager provided permission for ward participation. Recruitment of wards ceased once permission was given by ward managers of four eligible wards from each of three acute NHS hospital trusts (n = 12 wards in total).
Health-care assistants
Within each of the enrolled wards all HCAs were invited to take part in the study by a researcher employed on the grant. At a number of ward-based meetings during the 4-week baseline period, HCAs were given information about the study (see Appendix 12). Informed consent was obtained from all HCA participants.
Patients
The initial approach to patients was made on the enrolled ward a few days prior to their discharge. Older patients (aged ≥ 70 years) receiving inpatient care from the enrolled wards in the 4-week baseline period and the 4-week follow-up period were identified by a hospital-based research nurse in consultation with ward managers. Informed consent was obtained from all patient participants. The research nurse approached each of the identified patients, checked eligibility criteria, explained the study and provided the patient with a participant information sheet (see Appendix 13). If they agreed to receive a questionnaire after discharge from hospital, the research nurse asked them to sign a consent form. Patients who transferred to another ward prior to discharge or who were readmitted were subsequently excluded from analysis.
Baseline measures
Wards
To assess quality of interactions within a ward, the Quality of Interaction Scale (QUIS) observation tool was used by a trained observer at each hospital. 85 QUIS is an observational strategy in which individual interactions between patients and care staff are rated as positive social (interactions involving conversation and companionship), positive care (interactions during the appropriate delivery of care), neutral (indifferent, often very brief interactions), negative protective (keeping safe without explanation or reassurance) or negative restrictive (opposing or resisting patients’ freedom of action without good reason). Scores range between a minimum of one and a maximum of five, with higher scores indicating a more positive interaction. The interactions observed within each session were those that involved a patient and at least one HCA in a ward bay of between four and six patients. On Older People’s Shoes wards, interactions were included irrespective of whether or not the HCA involved in the interaction had received Older People’s Shoes training. In addition to rating, we recorded the duration, nature and number of staff involved in each interaction.
Ward observation sessions took place over a 4-week period prior to randomisation. Each observation session was conducted over a 50-minute period by one observer. The platform used for QuIS data collection was the Quality of Interactions Tool (QI Tool), a tablet-based interface developed by the University of Southampton that enables users to enter data in real time for subsequent wireless upload to an encrypted central database. Observations took place in the mornings, at mealtimes and during visiting periods. At each hospital a subsample of observational sessions was conducted using an additional observer to assess inter-rater reliability.
Health-care assistants
At baseline, HCAs received a self-completion questionnaire (see Appendix 14) containing the Assessment of Work Environment Scale (AWES),86,87 the Toronto Empathy Questionnaire (TEQ)88 and the Age Group Evaluation and Description (AGED) inventory. 89 The 34-item AWES measures HCA perception of the support provided in the work environment, in which the respondent rates each item on a 5-point scale. The total score was transposed to a scale of between 0 and 100, with higher scores indicating a more positive assessment of the work environment. The TEQ conceptualises empathy as an emotional process and contains 16 items, each a statement about empathetic responses to specific situations with which the HCA respondent is asked to rate on a 4-point scale their agreement. Minimum and maximum possible scores are 0 and 64, respectively, with higher scores indicating greater empathy. The AGED inventory measures the extent to which stereotypes about ageing are held by the respondent. It includes 28 semantic differentials relating to a specific age group (> 70 years) using a 7-point Likert scale. Each semantic differential is part of one of four AGED inventory dimensions relating to evaluative factors (goodness and positiveness dimensions) or evaluative factors (vitality and maturity dimensions). A mean score is calculated for each dimension, with a minimum possible score of 1 and maximum of 7, with higher scores indicating more positive attitudes to older age groups.
Patients
At 2 weeks after discharge from hospital, patients who consented to participate received a questionnaire (see Appendix 15) and prepaid addressed envelope. To assess the relational aspects of care experienced by patients, the Patient Evaluation of Emotional Care during Hospitalisation (PEECH)90,91 questionnaire was used. The PEECH was developed for use in acute hospital settings and contains 23 items and four subscales of levels of security, knowing, personal value and connection. Patients were asked to rate the extent (on a 4-point scale) to which hospital staff responded or behaved in particular situations. A mean score is calculated for each dimension, with a minimum possible score of zero and maximum of 3, with higher scores indicating a more positive evaluation of emotional care.
To assess quality of life, the self-report version of the EuroQol-5 Dimensions, five-level version (EQ-5D-5L™;92 EuroQol Research Foundation, Rotterdam, the Netherlands) was used. The EQ-5D-5L was developed by the EuroQol group and has two parts: a visual analogue scale/thermometer, in which participants are asked to rate their health on a 0 (worst health you can imagine) to 100 (best health you can imagine) scale and five questions that are used to provide a health profile/description. Here the five-level response format was used for the five dimension questions, on the grounds that it is more sensitive than the previous three-level version. 93 Once completed, the EQ-5D-5L provides a description of the participant’s health profile in relation to the level of problems (ranging from ‘no problems’ to ‘unable to do’) with regard to mobility, self-care, usual activities, pain and anxiety/depression. 92 This profile can subsequently be converted into a utility score (a scale in which death is equal to zero and full health equal to 1), when this was undertaken using a mapping approach based on the three-level version. 94 The resulting score is referred to as the EQ-5D-5L index value.
When undertaking a health technology assessment the National Institute for Health and Care Excellence recommends that the overall costs to the NHS and personal social services are estimated. 95 It is recognised that this can be a large undertaking and it is thereby acknowledged that one should concentrate on large cost drivers which are considered to be potentially related to the intervention in question. 96 With this in mind, we sought to estimate the hospital stay cost for each participant in the study. The research nurses at each centre were asked to record the number of days each participant spent (1) in hospital and (2) in the study ward within which they were consented.
Allocation of interventions
Stratified by NHS hospital trust, wards were randomly allocated by the Norwich Clinical Trials Unit. Each ward had an equal chance of receiving either Older People’s Shoes training for HCAs or TAU. Random allocation was generated via computer-written code using block sizes of four. To conceal allocation from those responsible for recruitment, randomisation took place immediately after baseline measures were completed and 4 weeks ahead of the start of the intervention (set-up period) to allow appropriate arrangements, including HCA staffing cover to be arranged.
Interventions
Older People’s Shoes training
Health-care assistants from wards randomised to Older People’s Shoes training (n = 6 wards, two wards per hospital) received the newly developed HCA training intervention that focuses on the relational care of older people. Full details of Older People’s Shoes training and the process of its development are provided in Chapter 5 and briefly summarised here.
Training was planned to take place during weeks 5–8 post randomisation after a 4-week set-up period. It comprises 2 training days, approximately 1 week apart, delivered to small groups of HCAs. Older People’s Shoes training is delivered by registered nurses, all of whom are employed at the local hospital trust in practice development or education and training roles. These trainers receive full training in the content and delivery of the Older People’s Shoes intervention from members of the research team.
Each unit is divided into two sessions, one per day, so that learning on the first day can be consolidated and developed during the second day. At the end of day 1, HCAs were asked to undertake brief individual work-based exercises prior to day 2. Additional materials were also available online with access restricted to HCAs allocated to the training intervention.
Training as usual
Health-care assistants from wards not randomised to the training intervention (n = 6 wards, two wards per trust) received ‘TAU’. This is typically restricted to periods of staff induction or focused on mandatory training requirements such as manual handling. HCAs from wards randomly allocated to this arm of the trial were not expected to receive training in relational care beyond any that might be experienced as part of the standard process within their employing NHS hospital trust.
Outcomes and other measures
Wards
Between weeks 9 and 12 of postrandomisation observation, sessions were conducted in the enrolled wards using identical methods to those used in the baseline period.
Health-care assistants
Health-care assistants were sent a follow-up questionnaire at weeks 9 and 12 post randomisation. The follow-up questionnaire included the TEQ and the AGED inventory. At follow-up, at both time points, the questionnaire included a question asking whether or not the average contact time with an older patient had changed since the start of the study. The response categories were not changed, increased/decreased by 1 minute or less, increased/decreased by 1 to 5 minutes or increased/decreased by more than 5 minutes.
Patients
Patients due to be discharged from enrolled wards between weeks 9 and 12 post randomisation were approached, recruited and administered questionnaires in an identical way to that used during the baseline period. The primary outcome was at the level of the patient (PEECH score).
Training costs
Levels of resource use associated with the training in relation to the intervention were recorded by the study team members who provided training to the HCA trainers. Unit costs (at 2013/14 financial year levels) were subsequently assigned to these training resource items.
Sample size
As the aim was to test feasibility and the study was a pilot cluster randomised controlled trial, it was not powered to determine superiority of HCA Older People’s Shoes training compared with HCA TAU.
Wards
Observations by a researcher employed on the grant were scheduled to take place on the four enrolled wards at each participating NHS hospital trust. For each ward, eight observational sessions were planned for the baseline period and eight during the follow-up period. Each observational session lasted 50 minutes.
Health-care assistants
All eligible HCAs were invited to take part. The numbers of HCAs employed on wards varies within, and between, NHS hospital trusts. We assumed that approximately 10 HCAs were employed on each enrolled ward and planned for an estimated recruitment of 70%, therefore expecting that 84 HCAs would be recruited (42 per arm).
Patients
It was expected that across all three NHS hospital trusts 100 patients would receive questionnaires during the 4-week baseline period and a further 100 patients would receive questionnaires during the 4-week follow-up period.
Data management
A data management plan was developed by the Norwich Clinical Trials Unit. Data were entered into a central database, password protected and accessible only to the principal investigator, members of the research staff and the database manager. Data entry was done via web pages created using Microsoft.NET technology (Microsoft Corporation, Redmond, WA, USA). All internet traffic was encrypted using standard secure sockets layer methodology. The data entry system validated data on entry to ensure that they were of the expected type (e.g. integers, dates) and within the expected range of values. The database was linked to an audit tool in which all data additions, modifications and deletions were recorded with date/time and user identifier.
Data analysis
Ward-level analysis
The QUIS score was analysed as a total mean rating for each observed session and the number of ratings per session. For the average QUIS score, analysis was based on a linear mixed-effects model. For the number of interactions per session a Poisson mixed-effects model was used and the results expressed as the ratio of average number of interactions between the Older People’s Shoes and TAU intervention. In these models the fixed effect was the allocation and the random effect was the ward. Owing to the small number of wards, this analysis was descriptive. The reliability of QUIS was calculated by examining the reliability for each two-way comparison of observers using a weighted kappa. A weighted kappa was used to account for the degree of similarity or difference between paired observer ratings. A complete agreement between observers would score 1, a difference of one category would score 0.9375, a difference of two categories would score 0.75, a difference of three categories would score 0.4375 and a difference of three categories would score zero. As the two-way comparisons were independent of each other, each two-way comparison was based on a different set of observations in different wards, they were combined using standard rules for meta-analysis of kappa statistics. We treated the analysis as exploratory because of the relatively small number of paired observation sessions. The number of interactions observed by each observer in a paired observation session is reported descriptively using summary statistics and graphically using a histogram of the absolute value of difference between the two observers.
Health-care assistant-level analysis
For the TEQ score and the four AGED inventory dimensions, linear mixed-effects models were used for each of these outcomes at both 8 weeks and 12 weeks. Intention-to-treat and per-protocol analyses were conducted. In these models the fixed effect was the allocation and the random effect was the ward. This accounts for the potential of dependence of HCA-level responses from HCAs within the same ward. In addition, the baseline value of the outcome was also included as a fixed effect in a sensitivity analysis. These models allowed the estimation of the parameters required, including the within- and between-ward variance as well as the intraclass correlation coefficient, for the planning of a future trial, including the HCA-level variation and between-ward variation. However, as suggested by recent research,97 these estimated parameters should be used with caution because of the uncertainty in the estimation. As the number of clusters was fewer than 15 per arm,98 this was also analysed as a total average per ward rating as well as the individual subtypes using a t-test as the assumptions of the mixed-effects model can be difficult to verify with a small number of clusters. Owing to the small number of wards this analysis was descriptive.
Patient-level analysis
All analysis was based on the intention-to-treat principle, including all recruited patients from within randomised wards. This excludes patients who were recruited in error or became ineligible. The total PEECH score was analysed using a linear mixed-effects model, with the fixed effect being the allocation and the random effect being the ward in order to account for the potential of dependence of patient-level responses from patients within the same ward. The four subscales were analysed using the same model. These models allowed for the estimation of the parameters required for the planning of future trials, including the patient-level variation and between-ward variation as well as the intraclass correlation coefficient, although, as with the HCA-level analysis, the same uncertainty in estimation should be taken into account. 97 Patient outcomes were also analysed as a total average, per ward, using t-tests as the assumptions of the mixed-effects model can be difficult to verify with a small number of clusters. 98
Cost and cost-effectiveness analysis
To assess the training costs we made the assumption that the costs associated with the development of the intervention (including the trainer manual and HCA course book; see Chapter 5, Training materials) would not need to be incurred again if the training intervention were to be rolled out more widely. We therefore considered this to be a sunk cost99 and did not include any associated costs for this, although subsequent costs associated with printing the trainer manual and HCA course book were included. The total cost of the training was estimated by summing the cost of training both the HCA trainers and the HCAs. Training costs were subsequently apportioned across the total number of HCAs who attended the training. In order to provide an estimate of annual patient throughput for these HCAs, and thereby estimate the cost per patient seen by a HCA, we summed the total number of patients screened in both the 4-week pre- and postrandomisation periods and multiplied this by 6.
Analyses were undertaken in order to estimate the mean interaction time and the mean cost of the interaction. The latter was costed in terms of the HCA cost per hour of patient contact, rather than per hour of employment, for which it was assumed that HCAs were involved in patient contacts 60% of the time. 29 Results are presented for both time periods (baseline and follow-up) and both trial arms (Older People’s Shoes and TAU), but as different participants were observed we did not seek to directly compare the times within each of these periods/groups. We assessed interaction/contact times from observed interactions and HCA self-report at follow-up of any changes to the time spent with older patients. Analyses were undertaken in order to estimate the frequency of each response at both times in each arm. In order to estimate the average change in contact time, an estimated mean time was assigned to each response category (e.g. 30 seconds for ‘1 minute or less’, 3 minutes for ‘1 to 5 minutes’) and these were weighted by the frequency of response in order to estimate the average change in contact time for HCAs in both arms of the study. A scenario analysis was subsequently undertaken to assess the potential impact of these reported changes in contact time. 99 Acknowledging that the same HCAs were asked the same question at both the 8- and 12-week follow-ups (and we did not want to bias results by including people twice), in order to provide what might be a conservative estimate, we used the lowest of two estimated differences in the reported mean change in contact time between the two arms of the study at the 8-week and 12-week follow-ups. The previously estimated unit cost per hour of HCA patient contact time was then assigned to the estimated mean change in contact time in order to estimate the potential change in cost per contact. Subsequently, to estimate the potential cost impact that any longer contact times might have for each HCA, we multiplied this estimated change in contact cost by the estimated number of patient interactions/contacts per hour and the number of hours a HCA would be estimated to work each year. Finally, to estimate the per patient cost of any change in contact time we divided the HCA cost by the number of patients each HCA was estimated to see each year (patient throughput).
As a feasibility study, analysis of EQ-5D-5L scores concentrated on completion rates with a view to considering whether or not the European Quality of Life visual analogue scale (EQ-VAS)/EQ-5D-5L index value provided an appropriate measure for this population and could be used in any future more definitive study. Results are presented for both time periods (baseline and follow-up) and both arms (Older People’s Shoes and TAU) but, because there are different participants in each of these periods and the group sizes are relatively small, we concentrated on the scores for all participants (overall). In addition, we compared the scores for participants in this study to age-adjusted population norms for the EQ-5D-5L. 100
Given the feasibility nature of the study, we sought to estimate the availability of data on both hospital and study ward length of stay. Analyses were undertaken to estimate the mean hospital stay and study ward cost. On the basis that most patients would be non-elective (e.g. stroke, exacerbation of chronic medical conditions, etc.) we assigned the previously estimated 101 non-elective inpatient excess bed-day cost to each day in hospital/study ward. This enabled the cost of each participant’s hospital and study ward stay to be estimated. Results are presented for both time periods (baseline and follow-up) and both arms (Older People’s Shoes and TAU) but, because there are different participants in each of these periods and the group sizes are relatively small, we do not make comparisons between these groups.
Ethical considerations and ethics approvals
For observational sessions, we attempted to be as unobtrusive as possible. No observation was made of interactions that occurred behind curtains. We alerted staff to our presence on the ward and explained the nature of the study. We spoke to individual patients in the ward bays that were being observed. If any patient or member of staff asked not to be observed we made no record of any interaction that included them. For HCAs and patients we went to great lengths to ensure that they were fully aware of what study participation would involve. We did not have access to named patient data. These were collected (and anonymised) by trust-employed research nurses.
A favourable ethical opinion for this study [CHAT (feasibility randomised controlled trial) Protocol v2 9.2.2015] was granted by Cambridge South Research Ethics Committee on 13 February 2015 (application number 15/EE/0025, Co-ordinated System for gaining Permission reference number 162616). The study was adopted onto the UK Clinical Research Network portfolio (study identifier UKCRN18280).
Feasibility trial: findings
Trial participation
Wards and health-care assistants
A total of 12 wards were enrolled into the study following agreement by ward managers. During the baseline period, 91 of the 96 planned observation sessions were successfully undertaken. There was a shortfall of five observation sessions as two wards were closed to visitors for a short time during the baseline period because of the presence of norovirus. The flow of HCA participants is reported in Figure 6. Of the 150 HCAs screened for eligibility, 134 fulfilled eligibility criteria and 112 agreed to take part in the study. Of the HCAs who consented to take part, 59 were based on wards randomly allocated to receive Older People’s Shoes training and 53 were based on wards allocated to receive TAU. Of the 59 who were allocated to receive Older People’s Shoes training, 45 successfully received the intervention. Baseline, first and second follow-up questionnaires were returned by, respectively, 40, 28 and 22 of those in the Older People’s Shoes arm and 32, 24 and 18 in the TAU arm. HCA recruitment took place between March and June 2015, with follow-up questionnaires sent out between June 2015 and October 2015.
FIGURE 6.
Flow of HCA participants through the feasibility trial.
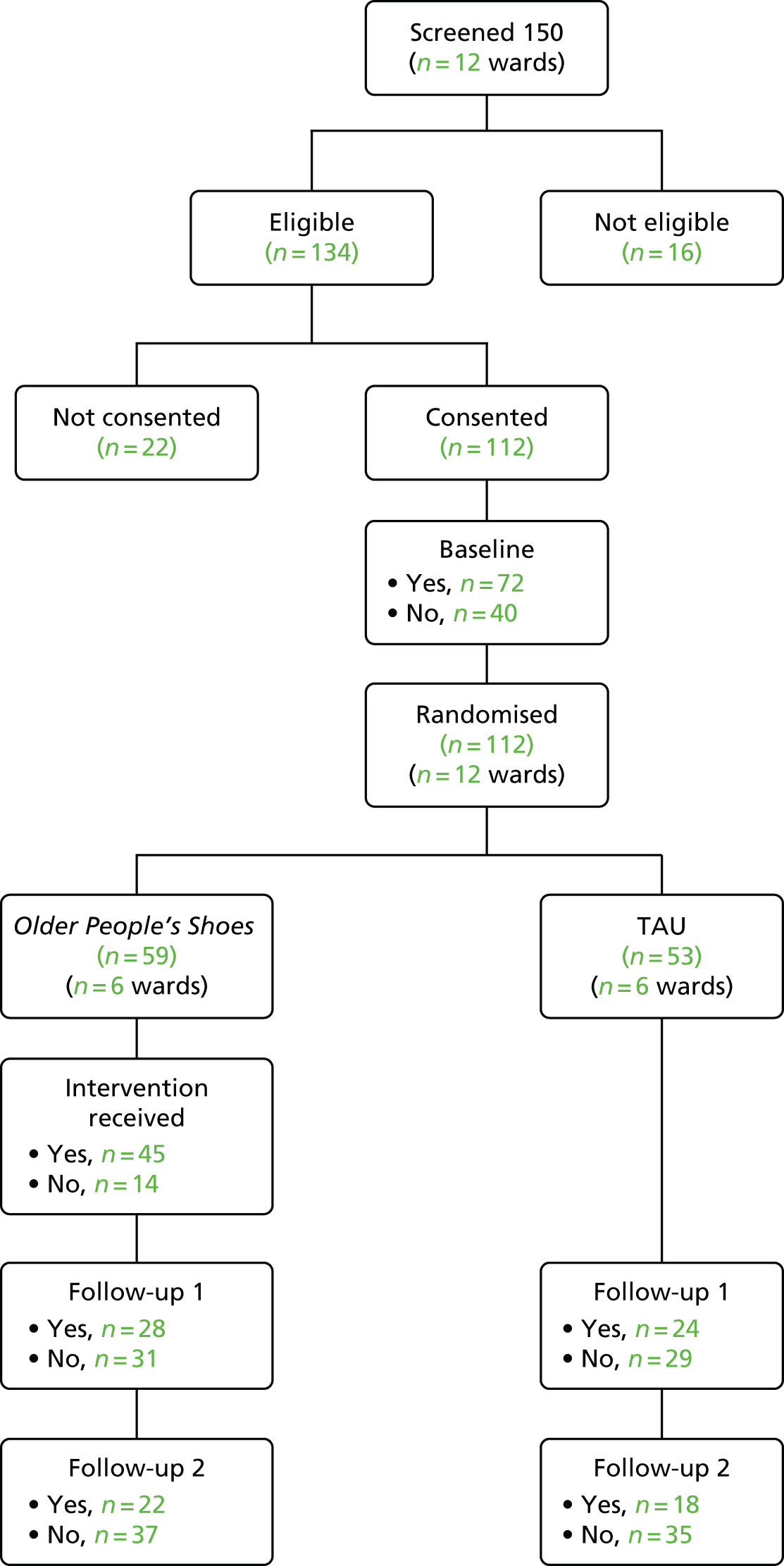
Patients
Patients were recruited to the trial during a 4-week period pre randomisation and during weeks 9 to 12 post randomisation. The flow of both groups of patients is reported in Figure 7. During the baseline period, 97 of 129 eligible patients agreed to take part in the study. Patients were recruited to the baseline period between March and July 2015. As some patients who were eligible at the point of consent subsequently became ineligible (e.g. because they were transferred to another ward, were not discharged or withdrew for health reasons), data from 40 Older People’s Shoes patients and 52 TAU patients were available at baseline. Of these patients, 23 in the Older People’s Shoes arm and and 27 in the TAU study arm returned a questionnaire.
FIGURE 7.
Flow of patients through the feasibility trial. a, Randomisation occurred after patients consented but it is displayed in this way to compare differences at baseline.
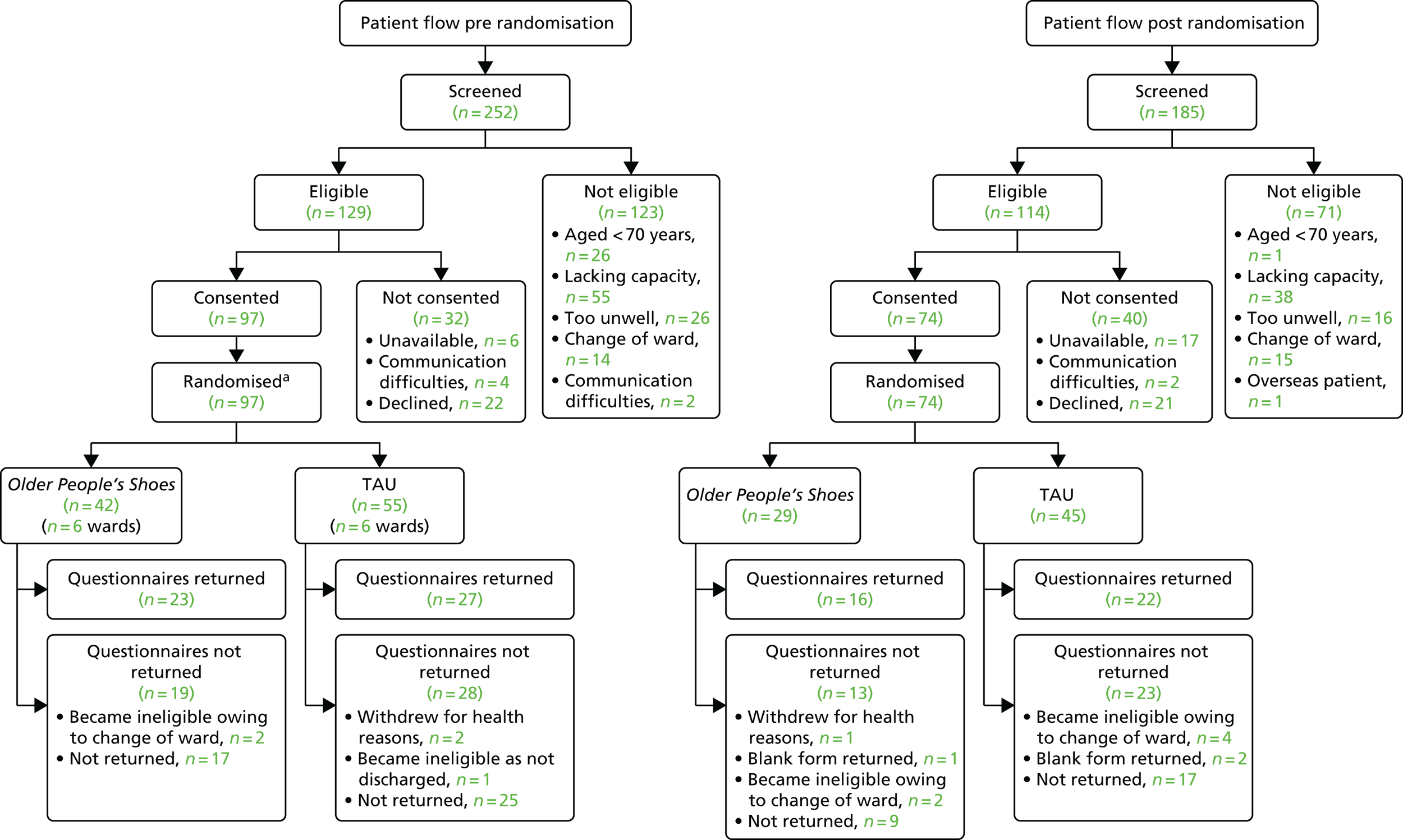
During the follow-up period, 74 of 114 eligible patients agreed to take part in the study, of whom 67 were eligible for inclusion in analysis (26 patients from Older People’s Shoes wards and 41 patients from TAU wards). Of these, 16 patients in the Older People’s Shoes arm and 22 patients in the TAU arm returned questionnaires. Patients were recruited for the follow-up period between June 2015 and October 2015.
Groups at baseline
Wards
Ward randomisation was stratified by hospital trust, with two wards at each trust allocated to each of the two trial arms. At baseline, the mean number of beds per ward was similar between the two arms of the trial. In total, 47 observation sessions took place across the six wards where HCAs were allocated to Older People’s Shoes training and 44 sessions on wards allocated to HCA TAU (Table 17). The mean QUIS interaction rating did not differ between the two arms of the trial (3.74 and 3.84, respectively): a score of 3 represents a ‘neutral’ rating and 4 indicates ‘positive care’. The number of interactions per session ranged between 1 and 31 in the Older People’s Shoes training arm of the study and between 1 and 27 in the TAU arm. The mean number of interactions per session was 8.23 (SD 7.07) in Older People’s Shoes wards and 7.34 (SD 5.44) in TAU wards.
| Ward and QUIS variables | Trial arm | |
|---|---|---|
| Older People’s Shoes (N = 6) | TAU (N = 6) | |
| Ward type | ||
| Health care for older people | 4 | 3 |
| General medicine | 1 | 1 |
| Acute medicine | – | 1 |
| Stroke | 1 | – |
| General medicine/endocrinology | – | 1 |
| Mean number of beds on ward (SD) | 29 (5.0) | 30 (5.9) |
| Sessions, n | 47 | 44 |
| QUIS interaction rating (score range 1–5), mean (SD) | 3.74 (0.55) | 3.84 (0.48) |
| Interactions per session, mean (SD) | 8.23 (7.07) | 7.34 (5.44) |
Health-care assistants
At baseline, HCA trial participants working on wards allocated to Older People’s Shoes training were broadly similar to those working on TAU wards in terms of sex and length of experience (Table 18). HCA trial participants were predominantly female (88.2%, 97/110), with just over half (55.3%, 57/103) having > 3 years’ experience as a HCA and 28.2% having ≥ 10 years’ experience. In both trial arms, HCA ratings of ward atmosphere, as measured by the AWES, were approximately two-thirds of the maximum score. HCA trial participants appeared to be well balanced between the two trial arms in terms of empathy (TEQ) scores, although in terms of attitudes towards older people (AGED inventory scores) HCAs working on TAU wards scored slightly higher in all four dimensions of the AGED inventory. In both groups the AGED inventory dimension of ‘goodness’ was where HCAs’ attitudes towards older people scored the highest and the dimension of ‘vitality’ scored the lowest.
| HCA variables | Trial arm | |
|---|---|---|
| Older People’s Shoes (N = 59)a | TAU (N = 53)a | |
| Female, n (%) | 52/58 (89.7) | 45/52 (86.5) |
| Length of experience, n (%) | ||
| < 1 year | 8/55 (14.6) | 10/48 (20.8) |
| 1 to 3 years | 15/55 (27.3) | 13/48 (27.1) |
| > 3 to < 10 years | 15/55 (27.3) | 13/48 (27.1) |
| ≥ 10 years | 17/55 (30.9) | 12/48 (25.0) |
| AWES (score range 0–100), mean (SD) | ||
| Total | 63.85 (14.74) | 68.39 (12.29) |
| TEQ (score range 0–64), mean (SD) | ||
| Total | 50.83 (6.88) | 47.88 (8.16) |
| AGED inventory (score range 1–7), mean (SD) | ||
| AGED goodness | 4.74 (0.81) | 4.93 (0.82) |
| AGED vitality | 3.56 (0.72) | 3.93 (0.72) |
| AGED maturity | 4.2 (0.73) | 4.59 (0.71) |
| AGED positivity | 3.99 (0.83) | 4.31 (0.86) |
Patients
Excluding patients who, following initial consent, became ineligible for inclusion in the study in the baseline period, 40 patients were discharged from Older People’s Shoes wards and 52 from TAU wards. Patient participants discharged from Older People’s Shoes wards tended to be younger, with a mean age of 80.6 years (SD 6.5 years), than those discharged from TAU wards, among whom the mean age was 83.6 years (SD 5.9 years) (Table 19). The proportion of patient participants who were female was much lower in Older People’s Shoes wards (29.6% vs. 76.6%) and their time spent on the study ward was shorter by approximately 1 day. At baseline, the 50 patients who returned questionnaires were broadly equivalent in terms of how they rated the relational care they received, as measured by total PEECH score and individual dimension scores.
| Patient variables | Trial arm | |||
|---|---|---|---|---|
| Older People’s Shoes (N = 40)a | TAU (N = 52)a | |||
| n with data available | Mean (SD) | n with data available | Mean (SD) | |
| Female, n (%) | 25 | 7 (28.0) | 46 | 36 (78.3) |
| Age (years) | 40 | 80.55 (6.49) | 52 | 83.64 (5.91) |
| Days in hospital | 36 | 6.64 (4.76) | 52 | 8.35 (9.62) |
| Days in study ward | 34 | 5.71 (4.46) | 52 | 6.87 (8.14) |
| PEECH scores (score range 0–3) | ||||
| Total | 20 | 2.24 (0.61) | 25 | 2.26 (0.55) |
| Security | 17 | 2.34 (0.63) | 25 | 2.43 (0.53) |
| Connection | 19 | 1.68 (1.09) | 25 | 1.51 (0.84) |
| Knowing | 22 | 2.39 (0.73) | 26 | 2.12 (0.88) |
| Person value | 19 | 2.39 (0.57) | 25 | 2.41 (0.6) |
Inter-rater reliability and Quality of Interaction Scale
Eight paired observation sessions were undertaken, within which a total of 40 interactions were observed independently by two observers. These took place across all centres, with observer pairs the same within, but not between, each centre. Weighted kappa statistics are reported in Table 20. Although the overall consistency of 0.61 [95% confidence interval (CI) 0.32 to 0.89] suggests moderate to substantial agreement overall,101 there was some evidence of heterogeneity between pairs (p = 0.057). In 34 of the interactions observed by both observers, there was agreement (Table 21). Where there was far less agreement was in the number of interactions recorded by each observer within a session. Of the eight sessions in which at least one interaction was observed, there was no difference in the number of interactions recorded by each observer in four sessions, but in one session 12 interactions were recorded by one observer compared with 29 by the paired observer (Figure 8).
| Paired observers | Kappa statistic | Standard error | Interactions (n) |
|---|---|---|---|
| 1 and 2 | 0.4632 | 0.2368 | 17 |
| 3 and 4 | 1.0000 | 0.2294 | 19 |
| 5 and 6 | 0.1111 | 0.3191 | 4 |
| Overall | 0.61a (95% CI 0.32 to 0.89) | 0.1464 | 40 |
| Observer pairs | Negative restrictive | Negative protective | Neutral | Positive care | Positive social |
|---|---|---|---|---|---|
| 1 vs. 2 | |||||
| Negative restrictive | 0 | 0 | 0 | 0 | 0 |
| Negative protective | 0 | 0 | 0 | 0 | 0 |
| Neutral | 0 | 0 | 1 | 0 | 0 |
| Positive care | 0 | 0 | 0 | 7 | 4 |
| Positive social | 0 | 0 | 0 | 2 | 3 |
| 3 vs. 4 | |||||
| Negative restrictive | 3 | 0 | 0 | 0 | 0 |
| Negative protective | 0 | 0 | 0 | 0 | 0 |
| Neutral | 0 | 0 | 3 | 0 | 0 |
| Positive care | 0 | 0 | 0 | 8 | 0 |
| Positive social | 0 | 0 | 0 | 0 | 5 |
| 5 vs. 6 | |||||
| Negative restrictive | 0 | 0 | 0 | 0 | 0 |
| Negative protective | 0 | 0 | 0 | 0 | 0 |
| Neutral | 0 | 0 | 2 | 0 | 1 |
| Positive care | 0 | 0 | 0 | 1 | 0 |
| Positive social | 0 | 0 | 0 | 0 | 0 |
FIGURE 8.
Histogram of the difference in the number of interactions observed per session between raters.
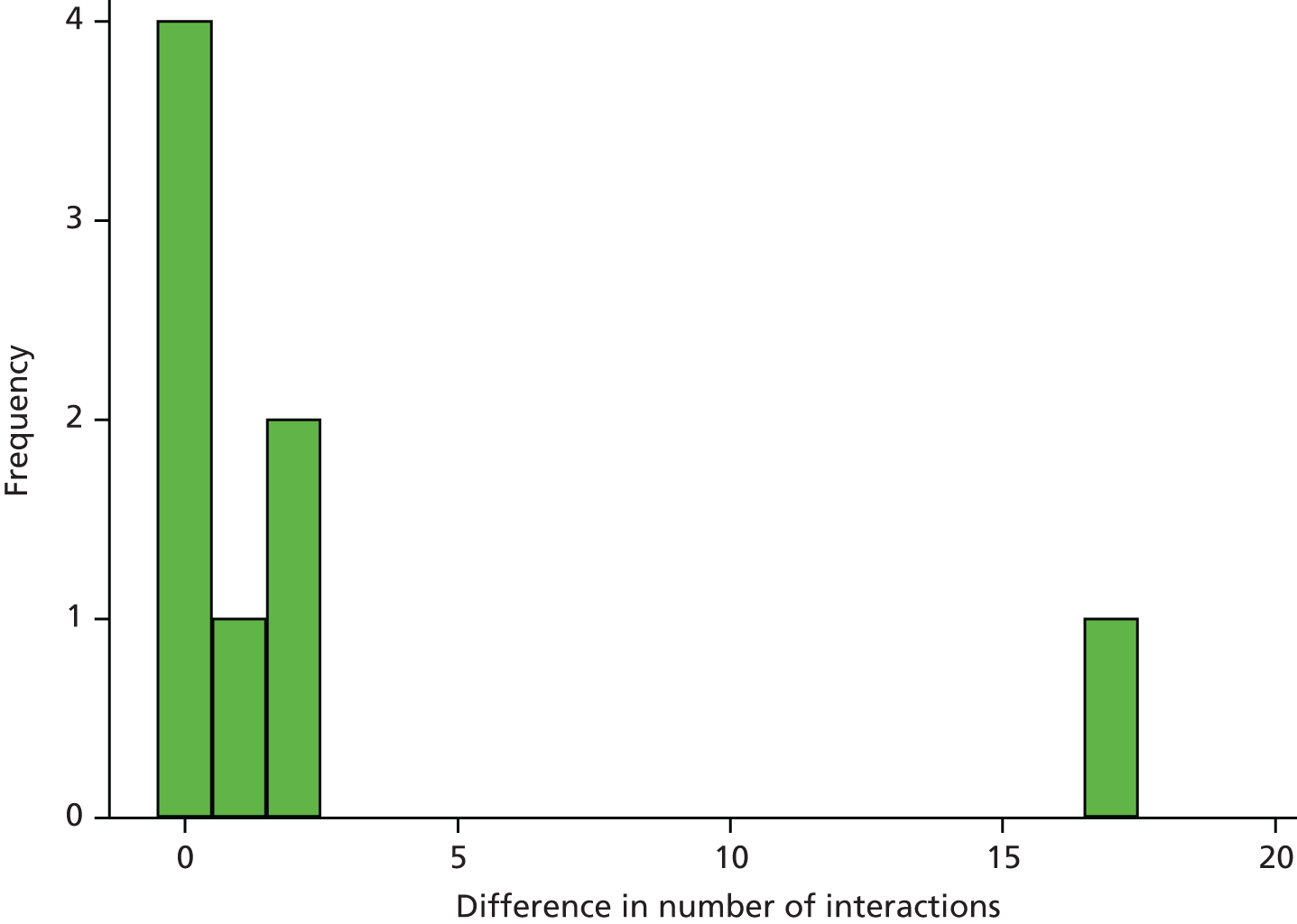
Outcomes and sensitivity analysis
Wards
At follow-up, as planned, a total of 96 observation sessions took place across the 12 wards, 48 sessions in each trial arm (Table 22). There was no evidence that mean interaction ratings differed between Older People’s Shoes and TAU wards. Although the number of interactions observed was higher in Older People’s Shoes wards, this was consistent with observations conducted during the baseline period (see Table 17). During the follow-up period the number of interactions per session ranged between 0 and 34 in the Older People’s Shoes training arm of the study and between 0 and 27 in the TAU arm.
| Factor | Trial arm, mean (SD) | Mean difference (Older People’s Shoes – TAU) | p-value | |
|---|---|---|---|---|
| Older People’s Shoes (n = 48) | TAU (n = 48) | |||
| Average rating | 3.98 (0.46) | 3.82 (0.58) | 0.02 (95% CI –0.20 to 0.25) | 0.832 |
| Average number of interactions | 8.48 (8.29) | 6.75 (6.12) | 1.19 (0.73, 1.95)a | 0.478 |
Health-care assistants
Intention-to-treat and per-protocol analyses of HCA outcomes at 8 weeks post randomisation are reported in Tables 23 and 24, respectively. After adjustment for baseline differences, the direction of effect was towards more positive TEQ and AGED inventory scores for HCAs working in Older People’s Shoes wards than for HCAs working in TAU wards. These findings demonstrate the potential differences that might be observed in a full trial. Intraclass correlation coefficients were calculated, but estimation lacked precision. 97 The findings from the intention-to-treat and per-protocol analyses were consistent. Sensitivity analysis using a cluster summary approach, the most robust method for cluster trials when the number of cluster is small (fewer than 15),98 is presented in Appendix 16. The findings from this sensitivity analysis are broadly in line with those from the linear mixed-effects model.
| Factor | Trial arm | Analysis | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Older People’s Shoes (N = 28)a | TAU (N = 24)a | Unadjustedb | Adjustedc | |||||||
| n | Mean score (SD) | n | Mean score (SD) | Mean difference in score (Older People’s Shoes – TAU) | p-value | ICC (95% CI)d | Mean difference in score (Older People’s Shoes – TAU) | p-value | ICC (95% CI)d | |
| TEQ | 26 | 49.10 (7.08) | 21 | 49.14 (6.61) | –0.04 (–3.91, 3.83) | 0.983 | 0.000 (0.00 to 0.21) | 1.70 (–1.17, 4.56) | 0.245 | 0.000 (0.00 to 0.23) |
| AGED goodness | 26 | 4.96 (0.85) | 22 | 4.87 (0.71) | 0.07 (–0.45, 0.58) | 0.806 | 0.113 (0.00 to 0.38) | 0.34 (–0.09, 0.77) | 0.120 | 0.000 (0.00 to 0.23) |
| AGED vitality | 27 | 3.75 (0.89) | 21 | 3.69 (0.6) | 0.05 (–0.38, 0.49) | 0.811 | 0.000 (0.00 to 0.19) | 0.08 (–0.36, 0.53) | 0.716 | 0.000 (0.00 to 0.24) |
| AGED maturity | 25 | 4.27 (0.8) | 22 | 4.3 (0.64) | –0.03 (–0.44, 0.38) | 0.869 | 0.000 (0.00 to 0.21) | 0.29 (–0.11, 0.68) | 0.157 | 0.000 (0.00 to 0.24) |
| AGED positivity | 26 | 4.3 (0.76) | 21 | 4.14 (0.67) | 0.16 (–0.25, 0.57) | 0.443 | 0.000 (0.00 to 0.20) | 0.35 (–0.10, 0.80) | 0.126 | 0.000 (0.00 to 0.24) |
| Factor | Trial arm | Analysis | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Older People’s Shoes (N = 26)a | TAU (N = 24)a | Unadjustedb | Adjustedc | |||||||
| n | Mean score (SD) | n | Mean score (SD) | Mean difference in score (Older People’s Shoes – TAU) | p-value | ICC (95% CI)d | Mean difference in score (Older People’s Shoes – TAU) | p-value | ICC (95% CI)d | |
| TEQ | 24 | 49.03 (7.38) | 21 | 49.14 (6.61) | –0.12 (–4.14, 3.91) | 0.954 | 0.000 (0.00 to 0.22) | –1.55 (–4.45, 1.35) | 0.294 | 0.000 (0.00 to 0.24) |
| AGED goodness | 24 | 5.04 (0.85) | 22 | 4.87 (0.71) | 0.14 (–0.36, 0.64) | 0.579 | 0.080 (0.00 to 0.34) | 0.37 (–0.06, 0.81) | 0.09 | 0.000 (0.00 to 0.23) |
| AGED Vitality | 25 | 3.76 (0.93) | 21 | 3.69 (0.6) | 0.06 (–0.39, 0.51) | 0.790 | 0.000 (0.00 to 0.20) | 0.09 (–0.36, 0.55) | 0.689 | 0.000 (0.00 to 0.25) |
| AGED maturity | 23 | 4.28 (0.84) | 22 | 4.3 (0.64) | –0.02 (–0.45, 0.40) | 0.914 | 0.000 (0.00 to 0.22) | 0.32 (–0.09, 0.72) | 0.124 | 0.000 (0.00 to 0.24) |
| AGED positivity | 24 | 4.3 (0.8) | 21 | 4.14 (0.67) | 0.16 (–0.26, 0.58) | 0.457 | 0.000 (0.00 to 0.21) | 0.37 (–0.10, 0.83) | 0.121 | 0.000 (0.00 to 0.25) |
At the second follow-up, 12 weeks post randomisation, 22 questionnaires were returned by HCAs from Older People’s Shoes wards (19 of whom received the intervention) and by 18 HCAs from TAU wards. Intention-to-treat and per-protocol analyses are reported in Tables 25 and 26, respectively. The direction of effect, in favour of Older People’s Shoes training, was similar to that observed at 8 weeks for the AGED inventory, but not for the TEQ. After baseline adjustment, the largest difference observed between trial arms in the intention-to-treat analysis was in the AGED goodness score when using either an intention-to-treat (mean difference 0.49, 95% CI 0.04 to 0.94; p = 0.032) or a per-protocol (mean difference 0.050, 95% CI 0.04 to 0.96; p = 0.032) approach to analysis. These statistically significant findings were not observed when using the cluster summary approach (see Appendix 17), for which the assumptions of the linear mixed-effects model were relaxed.
| Factor | Trial arm | Analysis | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Older People’s Shoes (N = 22)a | TAU (N = 18)a | Unadjustedb | Adjustedc | |||||||
| n | Mean score (SD) | n | Mean score (SD) | Mean difference in score (Older People’s Shoes – TAU) | p-value | ICC (95% CI)d | Mean difference in score (Older People’s Shoes – TAU) | p-value | ICC (95% CI)d | |
| TEQ | 21 | 51.57 (6.90) | 17 | 47.88 (7.52) | 3.73 (–0.87 to 8.33) | 0.112 | 0.020 (0.00 to 0.30) | –0.71 (–3.64 to 2.21) | 0.633 | 0.000 (0.00 to 0.29) |
| AGED goodness | 22 | 5.19 (0.86) | 17 | 4.75 (0.73) | 0.44 (–0.06 to 0.94) | 0.082 | 0.000 (0.00 to 0.25) | 0.49 (0.04 to 0.94) | 0.032 | 0.000 (0.00 to 0.30) |
| AGED vitality | 22 | 3.99 (0.6) | 18 | 3.77 (0.73) | 0.22 (–0.18 to 0.62) | 0.279 | 0.000 (0.00 to 0.25) | 0.18 (–0.35 to 0.71) | 0.505 | 0.114 (0.00 to 0.49) |
| AGED maturity | 22 | 4.53 (0.75) | 18 | 4.5 (0.63) | 0.03 (–0.41 to 0.48) | 0.883 | 0.040 (0.00 to 0.28) | 0.10 (–0.33 to 0.53) | 0.643 | 0.000 (0.00 to 0.29) |
| AGED positivity | 22 | 4.42 (0.73) | 18 | 4.21 (0.76) | 0.21 (–0.24 to 0.66) | 0.356 | 0.000 (0.00 to 0.25) | 0.18 (–0.31 to 0.67) | 0.475 | 0.000 (0.00 to 0.30) |
| Factor | Trial arm | Analysis | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Older People’s Shoes (N = 19)a | TAU (N = 18)a | Unadjustedb | Adjustedc | |||||||
| n | Mean score (SD) | n | Mean score (SD) | Mean difference in score (Older People’s Shoes – TAU) | p-value | ICC (95% CI)d | Mean difference in score (Older People’s Shoes – TAU) | p-value | ICC (95% CI)d | |
| TEQ | 18 | 50.75 (7.10) | 17 | 47.88 (7.52) | 2.87 (–1.84 to 7.57) | 0.233 | 0.000 (0.00 to 0.28) | –0.97 (–3.98 to 2.04) | 0.528 | 0.000 (0.00 to 0.30) |
| AGED goodness | 19 | 5.25 (0.86) | 17 | 4.75 (0.73) | 0.50 (–0.01 to 1.01) | 0.054 | 0.000 (0.00 to 0.28) | 0.50 (0.04 to 0.96) | 0.032 | 0.000 (0.00 to 0.30) |
| AGED vitality | 19 | 4.08 (0.57) | 18 | 3.77 (0.73) | 0.31 (–0.10 to 0.72) | 0.142 | 0.005 (0.00 to 0.27) | 0.27 (–0.24 to 0.78) | 0.302 | 0.085 (0.00 to 0.45) |
| AGED maturity | 19 | 4.56 (0.79) | 18 | 4.5 (0.63) | 0.06 (–0.41 to 0.54) | 0.789 | 0.037 (0.00 to 0.33) | 0.12 (–0.31 to 0.56) | 0.582 | 0.000 (0.00 to 0.30) |
| AGED positivity | 19 | 4.43 (0.78) | 18 | 4.21 (0.76) | 0.22 (–0.26 to 0.70) | 0.375 | 0.000 (0.00 to 0.27) | 0.18 (–0.33 to 0.69) | 0.482 | 0.000 (0.00 to 0.30) |
Patients
The outcomes for 26 patients from Older People’s Shoes wards and 41 patients from TAU wards recruited during the follow-up period (between weeks 9 and 12 post randomisation) are reported in Table 27. At baseline (see Table 19), recruited patients from TAU wards were older and more likely to be female. In contrast to the baseline period, the length of stay in hospital and on the study wards did not differ between patients from the two arms of the trial. Of those patients returning completed questionnaires, their report of the care they received as measured by PEECH score was similar between the two arms of the trial and similar to the care reported by those patients completing questionnaires during the baseline period. Based on completed questionnaires, there was also no significant difference between the mean quality-of-life scores in the two arms of the study, as measured by the EuroQol-5 Dimensions (EQ-5D). The results from the sensitivity analysis using the cluster summary approach are presented in (see Appendix 18) and are consistent with those using the linear mixed-effects model.
| Factor | Older People’s Shoes (N = 26) | TAU (N = 41) | Unadjusted (mixed effect) | ||||
|---|---|---|---|---|---|---|---|
| n | Mean (SD) | n | Mean (SD) | Mean difference (Older People’s Shoes – TAU) | p-value | ICC (95% CI)a | |
| Female, n (%) | 26 | 8 (31.0) | 40 | 31 (76.7) | |||
| Age (years) | 26 | 79.8 (6.52) | 41 | 84.0 (6.73) | |||
| Days in hospital | 26 | 6.31 (4.8) | 39 | 6.8 (5.75) | |||
| Days in study ward | 25 | 5.5 (4.6) | 39 | 5.5 (5.22) | |||
| PEECH scores (score range 0–3) | |||||||
| Total | 15 | 2.29 (0.42) | 15 | 2.37 (0.57) | –0.08 (–0.43, 0.26) | 0.640 | 0.000 (0.00 to 0.23) |
| Security | 14 | 2.44 (0.46) | 14 | 2.5 (0.58) | –0.06 (–0.42, 0.31) | 0.753 | 0.000 (0.00 to 0.25) |
| Connection | 16 | 1.5 (0.63) | 16 | 1.87 (0.87) | –0.38 (–0.93, 0.17) | 0.175 | 0.029 (0.00 to 0.27) |
| Knowing | 15 | 2.37 (0.67) | 15 | 2.3 (0.75) | 0.07 (–0.42, 0.56) | 0.790 | 0.000 (0.00 to 0.23) |
| Person value | 15 | 2.39 (0.42) | 16 | 2.45 (0.56) | –0.05 (–0.39, 0.29) | 0.761 | 0.000 (0.00 to 0.22) |
| EQ-5D-5L index value | 16 | 0.62 (0.21) | 22 | 0.50 (0.33) | 0.12 (–0.06, 0.30) | 0.280 | 0.015 (0.00 to 0.21) |
Training costs
The unit costs for staff are presented in Table 28. The levels of resource use associated with training both the HCA trainers and HCAs are described in Table 29 along with the associated unit costs for non-staff items. The total cost of all the resource items associated with the training was £36,816.58. When apportioned across the 45 HCAs who were trained (across the three centres), this was estimated to be equivalent to a cost of £818.20 per HCA. The total number of patients screened in the pre- and postrandomisation periods was 252 and 185, respectively. When summed and multiplied by 6, the annual patient throughput for the HCAs who were trained was thereby estimated to be 2622 patients. When the aforementioned total training costs were divided across this number of patients, this gave a cost of £14.04 per patient.
| Item | Estimated unit cost (£) |
|---|---|
| Trainer (train the trainer) (cost per hour of employment)a | 60.19 |
| Trainee/HCA trainer (cost per hour of employment)b | 38.10 |
| HCA (cost per hour of employment)c | 21.72 |
| Trainer support person (cost per hour of employment)d | 31.14 |
| HCA (cost per hour of patient contact time)c,e | 36.20 |
| Hospital admission (cost per day)f | 275.05 |
| Component part | Resources costed | Mean cost (per HCA trained)a |
|---|---|---|
| Training the trainer | Pre-course preparation by the trainer (8 hours at £60.19) (total £481.52) | £184.25 |
| Trainer time to prepare (1 hour at £60.19) and deliver the course (8 hours at £60.19), course ran three times (total £1625.13) | ||
| Trainee/HCA trainer course attendance time (8 hours at £38.10), two were trained at each of the three courses (total £1828.80) | ||
| Self-study (16 hours at £38.10 for each of the six trainees) (total £3657.60) | ||
| Post-training meeting for clarifications/checks (one trainer at £60.19 and two trainees at £38.10 each for 1.5 hours), ran three times (total £613.76) | ||
| Training material: trainer manual (£6.03 publication cost) and HCA course book (£6.03 publication cost) (one for the trainer and each of the six HCA trainers) (total £84.42) | ||
| Total cost: £8291.23 | ||
| Older People’s Shoes training sessions | HCA trainer time to prepare (2 hours at £38.10) and deliver the course (16 hours at £38.10), course ran eight times (total £5486.40) | £633.94 |
| Trainer support person (4 hours at £31.14 at each of the eight courses) (total £996.48) | ||
| HCA course receipt time (16 hours at £21.72) a total of 45 were trained across the eight courses (total £15,638.40) | ||
| Age-simulation suits (GERontologic Test suits), two (at £1000) at each of the three centres (total £6000) | ||
| Other consumables (to introduce the difficulty some older people have with certain activities),b three sets (total £132.72) | ||
| Training material: HCA course book (£6.03 publication cost), one for each of the 45 trained HCAs (total £271.35) | ||
| Total cost: £28,525.35 | ||
| Total | £36,816.58 | £818.20 |
Health-care assistant–patient contact time
Interactions took place within 179 of the 187 observation sessions conducted during baseline and follow-up periods. The end time of two of these sessions was not recorded. For one of these the end time for the last recorded interaction was after 50 minutes (the guideline time for each observation session), so the end time of this interaction was assumed to also be the end time for the session. For the other session the last observation recorded ended after 18 minutes and it was thus difficult to estimate the end time; therefore, we assumed that this session and another eight sessions (four in each arm at follow-up) in which no interactions took place (and, therefore, no start of end times were automatically recorded) lasted 50 minutes. Based on these data, the mean session length for the 187 observation sessions that took place was 50.92 minutes (Table 30). A total of 1441 timed interactions took place in these sessions. The mean interaction time was 2.85 minutes, which when costed at £36.20 (the assumed cost per hour of HCA patient contact time; see Table 28) gave a mean cost of £1.72 per interaction. HCA staff undertook the vast majority of interactions on their own (see Table 30). Nurses were the most common type of other staff involved (in 103 of the 1441 interactions), with other health professionals being the next most common (19 interactions). OS time in the interactions was not costed on the basis that it was relatively low. It should also be acknowledged that, although we do not seek to undertake formal comparisons between groups, there seems to be no suggestion that interaction resource use will be reduced after Older People’s Shoes training. Both the mean length of interactions and the mean number of OS involved were higher in the Older People’s Shoes arm post training.
| Time point | Arm | Sessions (n) | Interactions (n) | Mean session time (minutes) | Interactions per session (n) | Mean interaction time (minutes) | Mean cost of HCA interaction timea | Number of staff per interaction |
|---|---|---|---|---|---|---|---|---|
| Baseline | Older People’s Shoes | 47 | 387 | 51.50 | 8.2 | 2.88 | 1.74 | 1.13 |
| Baseline | TAU | 44 | 323 | 51.31 | 7.3 | 2.89 | 1.74 | 1.18 |
| Follow-up | Older People’s Shoes | 48 | 407 | 50.45 | 8.5 | 3.06 | 1.85 | 1.16 |
| Follow-up | TAU | 48 | 324 | 50.48 | 6.8 | 2.50 | 1.51 | 1.11 |
| Overall | 187 | 1441 | 50.92 | 7.7 | 2.85 | 1.72 | 1.15 | |
Consultation interaction times were also assessed by asking HCAs whether or not the average contact time with an older patient had changed since the start of the study as part of the follow-up questionnaire administered at 8 and 12 weeks post randomisation. This information was provided by fewer than half of the HCAs who were involved at the start of the study. Among those who did respond (Tables 31 and 32), there was certainly a trend towards an increased contact time rather than a decrease (of the 22 responses at the second follow-up only nine had not previously responded at the first follow-up). At 8 (and 12) weeks, the estimated mean change in contact time was 2.46 (2.89) minutes in the Older People’s Shoes arm, compared with 0.80 (1.53) minutes for TAU, a difference of 1.66 (1.36) minutes. After assigning the previously estimated unit cost of HCA patient contact time (£36.20 per hours) to these times, the implied extra cost per contact would be £1.00 per contact at 8 weeks and £0.82 at 12 weeks. Assuming that 7.7 contacts take place per hour (based on the mean number of interactions observed per session) this would equate to a cost equivalent to £6.32 per hour. We consider this to be a conservative estimate as individual patient bays were observed and there were likely to have been other unrecorded interactions occurring outside the observed bay. Assuming that HCAs work 1575 hours per year (as reported for a day ward nurse102), this would equate to an annual cost of £9949.98 per HCA. This is an estimate of the cost associated with the time that would need to be sacrificed from other activities if the HCA were to increase all patient contacts (in 1 year) by 1.36 minutes. On the assumption that each HCA might see 2622 patients per annum, this would equate to a per-patient cost of £3.79.
| Reported (category) change in interaction time (minutes) | Associated assumed mean change in interaction time (minutes) | Trial arm, number of responses | |
|---|---|---|---|
| Older People’s Shoes | TAU | ||
| Unchanged | 0 | 8 | 13 |
| Additional time | |||
| + ≤ 1 minute | 0.5 | 1 | 1 |
| + 1–5 minutes | 3 | 7 | 4 |
| + > 5 minutes | 6 | 9 | 3 |
| Decreased time | |||
| – ≤ 1 minute | –0.5 | 0 | 0 |
| – 1–5 minutes | –3 | 1 | 0 |
| – > 5 minutes | –6 | 1 | 2 |
| Not answered | 29 | 30 | |
| Requested | 56 | 53 | |
| Estimated mean change (minutes) | +2.46 | +0.80 | |
| Estimated change in HCA cost (£) | +1.05 | +0.34 | |
| Reported (category) change in interaction time (minutes) | Associated assumed mean change in interaction time (minutes) | Trial arm, number of responses | |
|---|---|---|---|
| Older People’s Shoes | TAU | ||
| Unchanged | 0 | 7 | 10 |
| Additional time | |||
| + ≤ 1 minute | 0.5 | 1 | 1 |
| + 1 to 5 minutes | 3 | 7 | 1 |
| + > 5 minutes | 6 | 7 | 5 |
| Decreased time | |||
| – ≤ 1 minute | –0.5 | 0 | |
| – 1 to 5 minutes | –3 | 0 | |
| – > 5 minutes | –6 | 0 | 1 |
| Not answered | 34 | 35 | |
| Requested | 56 | 53 | |
| Estimated mean change (minutes) | +2.89 | +1.53 | |
| Estimated change in HCA cost (£) | +1.23 | +0.65 | |
Quality of life using the EuroQol-5 Dimensions
The EQ-5D was sent to 159 of the 171 consented participants. Those who withdrew for health reasons (n = 3) or who became ineligible as a result of a change of ward (n = 8) or because they were not discharged (n = 1) were not sent the questionnaire. The details of the number of questionnaires returned and completed are given in Table 33. Overall, the response rate was just over 50% for both the EQ-VAS and EQ-5D-5L index value. For all participants, the resulting mean scores were 64.1 for the EQ-VAS and 0.606 for the EQ-5D-5L index value.
| Time point | Arm | Number consented | Number sent out | Responses (n) | Response (%) | Mean scores | Mean age of responders (years) | Sex of responders (% female) | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| EQ-VAS | EQ-5D-5L index value | EQ-VAS | EQ-5D-5L index value | EQ-VAS | EQ-5D-5L index value | EQ-VAS | EQ-5D-5L index value | EQ-VAS | EQ-5D-5L index value | ||||
| Baseline | Older People’s Shoes | 42 | 40 | 23 | 20 | 57.5 | 50.0 | 72.8 | 0.733 | 80.4 | 80.4 | 69.6 | 65.0 |
| Baseline | TAU | 55 | 52 | 22 | 24 | 42.3 | 46.2 | 56.3 | 0.590 | 82.8 | 82.4 | 95.5 | 91.7 |
| Follow-up | Older People’s Shoes | 29 | 26 | 16 | 16 | 61.5 | 61.5 | 64.9 | 0.616 | 79.8 | 79.8 | 37.5 | 58.3 |
| Follow-up | TAU | 45 | 41 | 21 | 21 | 51.2 | 51.2 | 62.0 | 0.496 | 83.7 | 83.6 | 76.2 | 75.0 |
| Overall | 171 | 159 | 82 | 81 | 51.6 | 50.9 | 64.1 | 0.606 | 81.8 | 81.7 | 72.0 | 71.6 | |
For those aged > 75 years, the population norms for the EQ-VAS are 72.90 for men and 74.07 for women, compared with 0.75 and 0.71 for the index value (based on the previous three-level version). As such, it can be seen that the participants in this study tended to have worse levels of health, according to the EQ-5D, than the population average for those with similar age or sex.
Hospital stay
Length of hospital and study ward stay were extracted for 97.5% of participants in the study (Table 34). Over all participants, the mean length of hospital stay was 7.3 days, compared with 5.9 days for the study ward. When a cost per bed-day of £275.05103 was assigned to each day in hospital/study ward, then the mean hospital stay cost was estimated to be £2017.62, compared with a study ward cost of £1635.82.
| Time point | Arm | Number consented | Number for whom data were requested | Number for whom data were obtained | Response rate (%) | Mean values (days) | Mean cost (£) | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Hospital length of stay | Study ward length of stay | Hospital length of stay | Study ward length of stay | Hospital length of stay | Study ward length of stay | Hospital length of stay | Study ward length of stay | ||||
| Baseline | Older People’s Shoes | 42 | 40 | 36 | 35 | 90.0 | 87.5 | 6.6 | 5.5 | 1826.02 | 1524.56 |
| Baseline | TAU | 55 | 52 | 52 | 52 | 100 | 100 | 8.3 | 6.9 | 2295.61 | 1888.32 |
| Follow-up | Older People’s Shoes | 29 | 26 | 26 | 26 | 100 | 100 | 6.3 | 5.3 | 1734.93 | 1459.88 |
| Follow-up | TAU | 45 | 41 | 41 | 39 | 100 | 95.1 | 7.3 | 5.5 | 2012.56 | 1516.30 |
| Overall | 171 | 159 | 155 | 155 | 97.5 | 97.5 | 7.3 | 5.9 | 2017.62 | 1635.82 | |
Summary
A pilot cluster randomised controlled trial was conducted on 12 wards in three NHS trusts to assess the feasibility of a definitive trial to compare the newly developed HCA training package (Older People’s Shoes) with ‘HCA TAU’. Clusters were wards within three acute NHS hospital trusts in England, with outcomes observed at the level of the ward, HCA and patient. Ward-level outcomes were observations of the quality of HCA and patient interactions using the QUIS. HCA outcomes were empathy (as measured by the TEQ) and attitudes towards older people (as measured by the AGED inventory). We measured patient-reported quality of life using the EQ-5D and patient-reported experience of care in hospital using the PEECH questionnaire. Twelve wards took part in the study and six were randomised to each arm of the trial (Older People’s Shoes or TAU). We conducted 91 observation sessions during the 4-week baseline period and a further 96 observation sessions between weeks 9 and 12 post randomisation. We recruited 112 HCAs, of whom 72 completed a baseline questionnaire, 52 completed the first follow-up questionnaire and 40 completed the second follow-up questionnaire. Of the 159 eligible patients recruited at baseline and follow-up period, 88 returned completed questionnaires. The total estimated cost of the training was £818.20 per HCA, equivalent to an estimated cost of £14.04 per patient.
Although not looking for evidence of effect, the direction of effect, at 8 weeks and to a lesser extent at 12 weeks, for HCAs was in favour of the Older People’s Shoes training intervention. There was no evidence that the mean interaction ratings differed between Older People’s Shoes and TAU wards. After adjustment for baseline differences, the direction of the effect was towards more positive TEQ and AGED inventory scores for HCAs working in Older People’s Shoes wards compared with TAU wards. Of those patients returning completed questionnaires, their report of the care they received (as measured by PEECH score) were similar between the two arms of the trial and to those patients completing questionnaires during the baseline period. Based on completed questionnaires, there was also no significant difference between the mean quality-of-life scores in the two arms of the study, as measured by the EQ-5D.
Chapter 7 Process evaluation of the intervention and trial process
Introduction
This chapter describes the methods and reports the findings of the process evaluation that was undertaken alongside and following the feasibility cluster randomised controlled trial. The process evaluation drew on a number of data sources to enhance our understanding of the delivery of the training intervention (Older People’s Shoes) and of the feasibility of a definitive trial.
Process evaluation: methods
Purpose
The aims of the process evaluation were to (1) understand the processes involved in implementing the HCA training intervention and the trial, in order to better assess the feasibility of a definitive randomised controlled trial, (2) learn what adjustments could be made (in either the intervention or the trial) to improve them and (3) gain some understanding of the potential impact of the intervention.
A number of different methods were used in the process evaluation. This enabled us to capture different types of data on different aspects of the trial and intervention and (when appropriate) to allow methodological triangulation. 104 The four research methods used were:
-
observations of all training sessions (‘course observations’) to capture ‘in the round’ process data for each training session and variation in delivery between centres
-
course evaluation forms from HCA learners attending Older People’s Shoes training to capture immediate impressions of the intervention and its predicted impact on practice
-
interviews with trainers to investigate trainers’ perceptions of Older People’s Shoes training, and their experience of delivering it
-
interviews with a sample of HCA learners to investigate perceptions of the training intervention in greater detail than was possible from evaluation forms, including reports of its impact on practice; and to explore experiences of participation in the trial.
Observations of training
All training intervention sessions were observed by at least one member of the local research team using a common template (excerpt in Appendix 19) that recorded deviations from the trainer guide, evidence of learning, the strength of the relational care focus, timing and practical issues arising. In vivo quotes were also captured. One member of the research team additionally observed the training intervention being delivered at each of the three centres to record differences in delivery between trainers and centres.
Course observation notes were analysed by researchers at each centre to draw out key messages for refining the intervention and to identify deviations from the course as prescribed. These findings were then collated and analysed thematically. Findings from observations were compared with other data in order to identify areas of congruence or divergence.
Evaluation forms from health-care assistants participating in the training intervention
At the end of each training day time was built in for all HCA learners to complete an anonymous evaluation form (see Appendix 20), which used closed and open-ended questions to ask for their views on the training as a whole and the different activities within it, the resources, perceived impacts and any expected changes in their practice. Descriptive statistics were used to analyse responses to closed questions. The responses to open-ended questions were analysed thematically.
Interviews with trainers who delivered Older People’s Shoes training
All trainers who delivered Older People’s Shoes training were provided with a participant information sheet (see Appendix 21) and invited to take part in an interview about their experience. Verbal consent to take part in interviews was obtained after potential interviewees had had the opportunity to read the participant information sheet and a time and date for the interview was then arranged as soon as practicable after all training had been delivered. Interviews took place during interviewees’ work time, in a private room on the ward or elsewhere on-site. Written consent was taken immediately prior to the interview. A topic guide was used (see Appendix 22), with interviews designed to take 30–45 minutes. These semistructured interviews explored their views of the training and support they received to deliver the intervention, the content of the training, any suggestions for improvement and the relevance and perceived impact of the intervention for HCAs. The interviews were audio-recorded, with the interviewee’s permission, and the audio files were transcribed verbatim. The transcripts were then anonymised.
Interviews with health-care assistants receiving Older People’s Shoes training
At the end of the follow-up period (to avoid differential treatment of HCAs in the two arms of the trial) a subsample of 12 HCAs who had participated in the training were provided with a participant information sheet (see Appendix 23) and invited to interview. This number was expected to represent around one-third of trainees. Of those HCA learners who gave initial consent to interview, purposive sampling was used to maximise variation of interviewees in terms of sex, length of experience as a HCA at the trust and (drawing on the course observations) observed levels of engagement in the training.
Procedures for consent, recording, transcription and anonymisation were the same as for trainers. A topic guide was used (see Appendix 24), with interviews designed to take 30–45 minutes. These semistructured interviews explored HCAs’ expectations of the training intervention, their experience of the intervention (including any suggestions for improvement), any impacts on their practice and their experience of participating in the trial.
Framework analysis was used in NVivo to manage all interview transcripts and analyse them thematically. Framework analysis is particularly useful for applied research designed to meet specific information needs while remaining true to the accounts of the interviewees. 105
Process evaluation: findings
Sample
In total, there were 25 sets of structured observations of the 2-day training intervention, which ran three times in centres 1 and 2 and twice in centre 3. All 16 days of training were observed by at least one researcher, with a second researcher observing one delivery of day 1 and one of day 2 at each centre. In addition, the researcher from centre 3 observed the delivery of day 1 training at centre 1 and of both training days at centre 2.
Across the three centres, 40 HCAs attended day 1 of the intervention and 41 attended day 2. There was a 100% response for evaluation forms for each of these days. All six trainers agreed to be interviewed. The interviews lasted an average of 35 minutes.
Twelve interviews were carried out with HCA learners. We had planned to recruit equal numbers across centres. However, because of delays in training delivery at one centre, HCA learners were drawn from two centres only. The interviews lasted an average of 35 minutes. Two HCA learner interviewees were men and 10 were women. Their length of experience as HCAs working at the trusts ranged from 5 months to 12 years. The median time in post was 22 months.
As different research tools (course observations, evaluation forms, interviews with trainers and interviews with HCA trainees) were used to capture and triangulate data in the process evaluation, there is necessarily some overlap in data from different sources. Therefore, we present the findings from the process evaluation data thematically, drawing on all relevant sources within each theme, rather than presenting findings from each data source in turn. This reflects the dual nature of the overall study, which comprised intervention development as well as a feasibility trial. The findings will be discussed under (1) findings related to the HCA training intervention and (2) findings related to the trial.
Findings related to the intervention
Overview of Older People’s Shoes training
Several HCAs remarked during the course of the training in evaluation form feedback that the training should be available to all HCAs and also to nurses. Our observations of the training, which included capturing ‘in the moment’ feedback from HCAs, showed that a number of basic elements of the intervention worked well. First, using trust-based trainers to deliver the training had several advantages. Their local situated knowledge appeared to give them credibility. Trainers’ use of examples from their own experience on the ward was well received. Second, giving HCAs time off the ward to reflect on their work, discuss difficulties and share good practice with fellow HCAs was regarded as a positive experience. Third, the assets-based approach appeared to make HCAs feel valued. Finally, the use of real patient experiences was reported to be eye-opening. HCAs engaged most with learning activities that involved active participation. In this respect the use of age simulation suits to experience some of the physiological and social aspects associated with ageing was a demonstrably powerful way for trainees to ‘get into older people’s shoes’. The training intervention would benefit from more physical activity, particularly on day 1. The feedback from HCAs was overwhelmingly positive (Tables 35 and 36).
| Comment | Centre |
|---|---|
| The most interesting course I have been on | 2 |
| [M]ore like a workshop than a course | 3 |
| Enjoyed how interactive the training was | 1 |
| They should do more of this type of study. It really helps the staff to reflect on their behaviour | 3 |
| Thank you, it’s great. HCAs are being recognised for their contribution | 3 |
| Comment | Centre |
|---|---|
| I’ve said to everyone on the ward, I recommend any health-care assistant going on that | 1 |
| It’s an amazing course, and my fellow HCAs that are bound to do the programme, I wish them all the best. And I think they will make use of it, just like me, and I pray that they will gain as much as they can, just like me. [. . .] [Then] I think every patient will get a better care | 3 |
| Ever since I’ve been on this course I haven’t stopped talking about it | 3 |
All HCAs reported enjoying the training and said it was relevant to their work with older people, with 90% (day 1) and 97.6% (on day 2) reporting the training as ‘very relevant’ (Table 37). On both days all responses indicated HCAs would recommend the training to fellow HCAs.
| Question | Day 1 (N = 40), n (%) | Day 2 (N = 41), n (%) |
|---|---|---|
| How much did you enjoy the Older People’s Shoes training today? | ||
| Not at all | 0 (0.0) | 0 (0.0) |
| Quite | 10 (25) | 4 (10) |
| A lot | 30 (75) | 36 (90) |
| Missing | – | 1 |
| How relevant do you think the training was to your work with older people? | ||
| Not relevant | 0 (0.0) | 0 (0.0) |
| Quite relevant | 4 (10) | 1 (2.4) |
| Very relevant | 36 (90) | 40 (97.6) |
| Has the training improved your understanding of what relational care is? | ||
| Not at all | 0 (0.0) | 0 (0.0) |
| Yes, a bit | 9 (23.1) | 9 (22.5) |
| Yes, a lot | 30 (76.9) | 31 (77.5) |
| Missing | 1 | 1 |
| Did you learn anything new? | ||
| No | 0 (0.0) | 0 (0.0) |
| A bit | 21 (52.5) | 15 (36.6) |
| A lot | 19 (47.5) | 26 (63.4) |
| Did it remind you about or underline anything you already knew? | ||
| Yes | 36 (92.3) | 39 (95.1) |
| No | 3 (7.7) | 2 (4.9) |
| Missing | 1 | – |
| Are you going to make any changes to the way you relate to older people on your ward as a result of this training? | ||
| Yes | 33 (84.6) | 36 (92.3) |
| No | 6 (15.4) | 3 (7.7) |
| Missing | 1 | 2 |
| Would you recommend this training to fellow HCAs? | ||
| Yes | 39 (100) | 40 (100) |
| No | 0 (0) | 0 (0) |
| Missing | 1 | 1 |
| Did you access the online resources? | ||
| Yes | – | 5 (15.1) |
| No | – | 28 (84.9) |
| Missing | – | 8 |
Our observations within and across training centres were invaluable for monitoring the fidelity of implementation. Appendix 25 lists deviations from fidelity and mitigating actions undertaken, and, for each, the proposed resolution prior to a definitive study. Although there were fidelity issues (related to navigating the computing equipment, practical issues such as time-keeping and use of resources, general delivery and deviation from the trainer manual), not all of these were negative. The trainers had a wealth of experience, and some of their innovations were evaluated as enhancing the training intervention as designed. In addition to the positive innovations noted above, course observations also allowed us to identify a number of other lessons for improving the intervention in terms of practicalities, delivery and training content. These are shown in Appendix 26.
Structure, style and delivery
Trainers and HCA learner interviewees reported that the 2-day structure worked well. One week’s gap between the days allowed for reflection and practice, which helped deeper learning. One HCA added that she felt that this was more sustainable for the ward than 2 consecutive days’ training. Trainers felt that the times allocated for each activity were broadly appropriate but some flexibility was required, and that trainers needed to impose time-keeping discipline. The pace was felt to be about right overall. However, HCAs said that where they felt the content was repetitive, or when the trainer was reading from the manual, the pace dragged but elsewhere they felt some activities were hurried because of lack of time. These views were supported by course observation data.
The assets-based approach to HCAs, encouraging peer-to-peer learning, drawing on trainers’ and HCAs’ experiences and using talking heads to bring real patients’ voices into the training were all felt to be valuable by trainers and by HCAs. Some HCA trainee interviewees reported that the practical ‘take-home’ exercises between training days helped to keep the learning alive. Observations showed that trainees, even if they did not manage to do the exercises, were able to draw on previous experience to reflect on the issues.
The evaluation forms indicated that HCAs enjoyed the variety of learning approaches, and that the intervention contained ‘not too much being “talked at” ’. They commented positively on being able to participate in discussions, the videos, the practical elements, the interactive approach and learning from others’ experiences. Many commented that the mix of elements was good, but several wanted more practical, physical activities. Trainers were praised for their inclusivity, their patience and their insights.
Training intervention content and resources
The evaluation form data demonstrate overall satisfaction with the content of the training. In interviews trainers spoke positively about the content and believed it relevant to the work of HCAs (and OS groups) caring for older people:
[W]hat I like about this is it really is nitty gritty detail from the relational care point of view.
Trainer, centre 2
With some provisos, HCA interviewees found that the content was relevant and had a good flow:
[A]nother thing that really struck home, when we did the practical sessions, was appreciating how vulnerable people are. I’ve never fully appreciated that [. . .] So to understand how vulnerable people are and how much [. . .] trust vulnerable people put into us, who are complete strangers.
HCA interviewee, centre 1
In response to the question on which part of the training had least impact on them, 30 of the 81 completed evaluation forms contained comments positively stating that it was all relevant/valuable/interesting/important:
All of this course was enjoyable and beneficial.
All made an impact.
All interesting and enlightening.
Every topic had something new to learn.
It was all equally relevant and important.
On evaluation forms and in interviews, opinion was often divided about particular activities. Although some said that the customer care activities had had the least impact, others rated them positively. The customer care unit (which included a training video used by Thomson travel agents) was the most contentious. A few HCAs were very positive about this unit:
The things that I enjoyed most was when we did the customer care [. . .] I’ve never seen anyone doing customer care in health care [. . .] you would think it’s bad to consider your patient as a customer. But when we did the training [. . .] in fact it is very important. It’s all around providing that service, and making the patient feel at ease and take out most of their worries, looking after the family [. . .] it made me think a lot, and it always stayed with me.
HCA interviewee, centre 3
But others (who had previously worked in the retail sector) thought that it did not fit well with the personal individual focus of the rest of the training intervention, that it had the ring of business, not care, to it, that it underplayed the level of care needed by older patients and that it neglected the lack of choice that patients had. One commented on the evaluation form:
Found it really hard to relate to the customer care, this job is way more rewarding and important than being a sales assistant.
Evaluation form, centre 2
There were elements of the training that could be improved in future. Some trainers and trainees felt day 1 to be too static, which was borne out by course observation notes. The relevance of some of the ‘getting to know older people’ activities to HCAs’ provision of relational care was felt to have been lost to some extent. Trainers and observers felt that much of the customer care unit did not work very well. This was partly attributed to the particular density of these sections of the manual and so it was difficult to keep delivery engaging. There was also a degree of repetition in the customer care activities. The negative comments on customer care suggest that this unit needed to be reframed somewhat, and better applied to bring out its relevance to the ward:
We kind of got the impression that they didn’t really understand why we were looking at customer care, because they were connecting it to retail [. . .] for some of them it was kind of they’d come out of the retail section previously because they didn’t like it.
Trainer, centre 1
The HCAs were asked about the course book and the e-learning resource. During training HCAs commented on the professional quality of the course book and appeared to read this as a signifier of the value that was being placed on them. On evaluation forms and in interviews the course book was reported as being informative, user-friendly, well written and visually engaging. Three HCA interviewees said they had used it to catch up on bits of the training they had missed and/or as a refresher. The course books allowed HCAs to read transcripts of videos and some of the slides, which some appeared to find helpful in the classroom.
On evaluation forms at the end of day 2 few trainees reported accessing the e-resource. Only five had done so by the end of the second day. Analysis of the use of the online resource during and in the months following the training confirmed that its use beyond the classroom was negligible. Four interviewees said they had used it either to revisit sections or to catch up on sections of the training they had missed. There was some support for including extended learning activities on the e-learning resource. All of those who reported using the e-resource were from the same centre, which suggests that this may be because of variability between centres in the signposting of the resource by trainers.
Self-reported impacts
Findings on self-reported impacts were drawn from evaluation form responses and interview data. A few HCAs commented that they thought the training would be most appropriate for new HCAs, but all found that they had learned new things on each day, including a greater understanding of what constitutes relational care. As well as new learning, 36 (92%) and 39 (95%) on day 1 and day 2, respectively, said that it had also underlined or reminded them about previous learning:
A lot of the time we know what to do but with workloads and lack of help it can easily become task orientated – so this course is a good reminder and I will always think about it when I feel I am falling into just wanting to get the task done.
Evaluation form, centre 1
On evaluation forms from day 1 and day 2, 33 (85%) and 36 (92%) of HCAs, respectively, reported that as a result of the training they planned to make changes to the way they related to older people on the ward. Their comments suggest expected behaviour changes predominantly in communicating better with patients (engaging them in conversation, listening more carefully, making efforts to get to know patients), trying to understand patients’ perspectives more, trying to take more time with patients (including not hurrying patients) and involving patients more in their care.
The majority of HCA interviewees were able to give examples of changes they had made since attending the training: not hurrying patients or talking to colleagues over patients’ heads, encouraging patients rather than telling them what to do, being more imaginative with presenting food and drink to patients, going back to patients they were unable to help immediately, doing people’s hair the way they liked it, taking opportunities to talk to patients and to find out more about them, listening to patients, making better connections with patients with dementia and involving relatives.
Health-care assistants also reported changes in attitudes. In interviews they told us that the training had helped them to see things from a patient’s point of view, better understand what it is like to be an older person and empathise with older patients. They spoke about realising ‘how important the person underneath is’, the value of a good welcome, how much older people had lived through and the effort and concentration many older people needed to do everyday tasks. They told us that the training had made them more reflective in their practice:
I’ve been here 5 years, it [the training] kind of looks at everything in a different perspective and you look at things wide open, ‘Oh actually maybe I need to consider this. I need to consider that’. Because the impact kind of keeps in your head.
HCA interviewee, centre 3
Six of the interviewees reported changes in the way they felt about their role: how important it was, what a difference they could make to people, how the recognition the training gave them made them feel more valued and, in one case, how the fact that such an intervention was being trialled made her see her work in the context of a wider community:
To see the effort that people around the country plus, you know, you guys of CHAT study putting in, making the experience of older people especially (who cannot speak for themselves) better. It’s really impressive. And it’s deeply touching that someone would sit down and think of them [. . .] You know, when you’re doing the work, sometimes you feel like it’s just you doing the work. But when you feel like there’s a wider community that’s in this, that’s what I wanted [. . .] It’s a really positive thing [. . .] To see that people are doing research that’s being paid for, you know, it makes me take pride in my work.
HCA interviewee, centre 3
There were inevitably challenges in implementing the training. Despite plans to take more time with patients (as reported in evaluation forms) lack of time was reported by half of the interviewees as making it more difficult to put what they had learned into practice. Given the busyness of the work, there was pressure to prioritise task-based care, and attitudes of OS played a part in this. One interviewee said that colleagues were sometimes antagonistic if they heard you ‘chatting’ to a patient, even while carrying out other tasks, and this was also raised in discussions during the training. HCAs felt torn between responsibilities to patients and to OS:
I always feel bad when I sit and talk to a patient because others are looking at me thinking ‘What are you doing?
HCA interviewee, centre 2
During the training another spoke about what she felt if she stopped doing tasks to chat to a patient:
[K]nowing you’re going to get ‘the look’, or ‘the tut’, and having to deal with that for another 10 hours. Giving you the silent treatment.
HCA interviewee, centre 2
Nevertheless, some HCA interviewees talked of ways in which, since the training, they used their time more imaginatively to provide relational care, such as talking to patients while doing essential care or tending to patients with better mobility first, so that one was less inclined to hurry patients who need more time. One HCA reflected:
I’ve learned to, kind of, time manage better really, I suppose is the way I’d look at it [. . .] I think there’s never going to be that time. But you learn to make the most of your free moments.
HCA interviewee, centre 1
Finally, we should note that the sheer physical, mental and emotional effort involved in the work of a HCA could make it difficult to deliver relational care. One HCA articulated this poignantly:
When I’m tired and frustrated it’s really difficult for me to be patient and everything. So despite the training I still have my limits [. . .] Of course I have to communicate well [. . .] and the training covered that. But sometimes I have nothing to say [. . .] [Sometimes] the best I can do is probably be silent and be polite. Just that.
HCA interviewee, centre 3
Although the intervention was not aimed at trainers, in interviews trainers told us that delivering the training intervention had impacted on them personally and professionally. Some planned to incorporate elements into current training. It had increased their own learning about relational care for older people and presented an opportunity to practice a new teaching style. Trainers also said that they enjoyed getting to know HCAs more and were left with a greater appreciation of their skills and dedication.
Support to trainers
Most trainers had experience of teaching topics that were coterminous with relational care and in training HCAs. However, trainers varied in the length and extent of experience they had in delivering day-long classroom-based group training. None of them had previously delivered anything as intensive, structured or prescribed as the Older People’s Shoes training intervention. This impacted on the confidence they felt in delivering the intervention and most admitted to a degree of stress involved. As one trainer put it:
[I]f I’d had time to [. . .] go through it half a dozen times and timing it, I would probably get it off to a tee. When you’re coming in stone cold, it’s almost quite prescriptive and it’s hard picking up anybody else’s material anyway.
Trainer, centre 2
In one centre, two trainers delivered the training on 3 of the 6 days, and in all centres the observing researcher also provided some practical help. Although three trainers felt one person could deliver it, they felt that two was optimal for a number of reasons. A second person was useful for helping with practicalities and meeting and greeting (demonstrating good relational care for trainees). A second trainer was also a good fail-safe in case of illness, as occurred at one centre.
Trainers had been asked to monitor the time spent on preparing to deliver the training intervention. They felt that a total of 3 days was needed to prepare adequately. From observations and interviews it was clear that trainers had a good understanding of relational care and also of the aims of the intervention, the values and key messages underpinning the intervention and the rationale behind the activities. They attributed this understanding to the train-the-trainer process and the trainer manual.
The formatting mechanisms used in the trainer manual (icons, emboldening, text boxes and pictures) were found helpful. However, in several places the manual was found to be too text dense. This could mean that the trainer risked losing the audience and having their ‘nose buried’ in the manual. Some trainers found it challenging to navigate between the manual, the slides and the online resource that contained the videos. It was suggested that embedding hyperlinks to the online resource into the PowerPoint slide could make this process easier.
Comparison of training across the centres demonstrated that trainers’ IT skills and their confidence in delivering training to groups in a classroom setting were important in shaping the delivery. When training was delivered by two trainers, this was useful for setting up IT, for transitioning between activities and for keeping the delivery dynamic. As much of the training was discussion based, the training intervention was designed to allow trainers some flexibility in facilitating the group and in drawing out the key messages from discussions. Trainers were also invited to draw on their own experiences in working with older people to contribute to discussions. However, this leeway had to be balanced with the need to include all activities in the training intervention. This balance was not always struck. One trainer who was particularly experienced and confident in delivering similar training tended to skip important introductions to activities and even activities themselves. On the other hand, those who were less confident sometimes got caught up in the trainer manual text, which meant that while they delivered information accurately, HCAs’ engagement diminished. We suggest a number of changes to address this problem: an optimal preparation time of 3 days; changes to the text in the trainer manual; and various changes to the train-the-trainer process (see Appendices 25 and 26).
Findings related to trial participation
Acceptability of participation in the trial
There was variation between centres and between wards in the arrangements made for releasing HCAs to attend the training. These variations reflected the notice period required by different wards and the notice that the study team was able to give the ward managers, whether or not there were existing staffing issues on the ward and ward managers’ preference and attitude to HCA training. The majority of ward managers were helpful in adjusting rosters to accommodate the training (despite the fact that in one centre the rosters had already been drawn up). However, on one ward, whose ward manager was sceptical that HCAs would turn up to training on a ‘study day’, all HCAs were rostered to an ‘off-duty’ day without promise of time in lieu or further encouragement to attend. Trainees attended under a variety of arrangements, which included the use of study days or release from duty for the hours of the training only or attending the training on an off-duty or annual leave day and then getting paid or given time off in lieu. Trainees’ willingness to attend under suboptimal conditions demonstrated a strong commitment to the training.
Acceptability of the measures used
Ward observations using the QUIS were acceptable to the HCAs interviewed for the process evaluation, although not all of them had experienced being observed. Some said that it felt a bit awkward initially but that they were reassured by speaking to the researcher. HCA interviewees found the length of the questionnaires acceptable. The questionnaires were distributed to HCAs on the ward by researchers (when possible) or via ward clerks or managers. For a number of practical reasons, including shift patterns and the absence or location of pigeonholes, there was inevitably some delay in some HCAs’ receipt of questionnaires. One HCA interviewee reported not receiving one questionnaire, which may have been experienced more widely. The AWES scale was not commented on by interviewees, which implied acceptability. One HCA (an ex-psychology student) felt that the role of HCAs made the TEQ particularly prone to desirability bias for this group. Several commented that they found the AGED inventory scale difficult to fill out because one could not generalise about ‘a typical 70 year old’.
Summary
The process evaluation was intended to (1) understand the processes involved in implementing the HCA training intervention and the trial, to assess the feasibility of a definitive randomised controlled trial, (2) learn what adjustments could be made (in either the intervention or the trial) to improve them and (3) gain some understanding of the potential impact of the intervention. Four different methods were used: (1) observations of all training sessions, (2) course evaluation forms from HCA learners attending Older People’s Shoes training, (3) interviews with trainers and (4) interviews with some HCA learners.
The following core elements were evaluated positively: using trust-based trainers to deliver the training, giving HCAs time off the ward to reflect on their work, discuss difficulties and share good practice with colleagues, taking an assets-based approach to HCAs and the use of real patient experiences. There was limited use of the online resource.
In course evaluation forms and at interviews HCAs receiving Older People’s Shoes training reported the training intervention to be a highly positive experience that was relevant to their work. In interviews, HCAs who had undertaken training also described changes to their approach to working with older people and in the way they thought about their work and older patients. The majority of HCA interviewees were able to give examples of changes they had made since attending the training.
Observations of intervention delivery suggested that although fidelity was generally good, there was an occasional tension with the need to avoid deviating from the trainer guide and the desire to ensure that training delivery was engaging. Trainers and HCA learner interviewees reported that the 2-day structure worked well and the practical and interactive elements with Older People’s Shoes were popular with HCA learners and trainers alike. Opinion was divided about particular activities, with the customer care unit the most contentious. Trainers enjoyed the experience, although some would have liked more time to prepare. Three trainers felt that one person could deliver the training, but two was optimal. In terms of feasibility issues, there was variation between centres and wards in the arrangements made for releasing HCAs to attend the training, but HCAs were keen to attend. Ward observations using the QUIS were acceptable to the HCAs interviewed and, although the questionnaires were acceptable, the need to ‘generalise’ in order to complete the AGED inventory scale was reported as difficult by some.
Chapter 8 Discussion and conclusions
Introduction
This chapter summarises findings from each component of the study in order to directly address the aims of the study. The feasibility questions specified in our protocol82 are addressed in turn. We examine our findings in the context of existing research and other evidence and draw conclusions in the light of what we have found.
Overview of findings
Training needs of health-care assistants for delivering relational care to older people
We aimed to understand the values-based training needs of HCAs in maintaining the dignity of, and affording respectful care to, older patients in acute NHS settings (study aim 1). This aim was addressed in the first phase of the study through (1) a telephone survey of NHS hospital trusts in England, (2) focus groups with older people and (3) semistructured interviews with HCAs and staff who work with HCAs.
To understand training needs, we needed to understand what training was currently given to HCAs working in acute hospitals. Key contacts were identified at each of the 113 trusts who took part in the national telephone survey and provided details of HCA training within their trust. Our findings suggest that induction training varies widely in terms of length, structure and content. Variability across and between trusts in how HCA training needs are met (or not) is a concern for policy-makers2,38,39,106 and one that the new Care Certificate has been designed to address. 57 Although the introduction of the Care Certificate took place midway through the time in which the survey was conducted, at this early stage there was no evidence from our survey that variability was diminishing.
We did not restrict the survey to questions about training that HCAs received at induction but aimed to glean a picture of HCA training for those in post as well as those newly appointed. We found that the greatest emphasis is placed on induction training, and the ongoing training of HCAs is typically devolved to ward managers through mentorship. The design of our survey did not enable us to pursue ward-level training beyond that known to the key contact at the participating trust. It became apparent that survey respondents who were employed at trust level were often unclear of the detail of such training. We cannot say whether or not postinduction training is adequate, but without trust-level oversight it is likely to be highly dependent on the motivation of individual ward managers. For survey respondents, the most frequently reported challenge was getting HCAs released from ward duties to undertake training. Others have noted that HCAs have been adversely affected in the past by a workplace culture that does not afford a particularly high priority to HCA training. 40
The prevalence of dementia among hospital patients aged ≥ 70 years is estimated to be 42%. 107 The nature of HCA work means that they will play a key part in managing challenging behaviour of older patients with dementia. Therefore, it was unsurprising, and welcome, that almost all trust respondents reported that HCA training included the care of patients with dementia. Aspects of training that could be considered to fall within our broad definition of ‘relational care’ were reported only by one-third of trust respondents. One-third of the trust contacts who participated in the survey stated that their HCA training did not distinguish between the needs of older people and patients of all ages. Although it is important that training should not stereotype older patients, there is a risk that this approach ignores the real challenges faced by older people when they are admitted to hospital. Calasanti108 refers to this as ‘age-blindness’, whereby age-associated bodily change and the marginal status of older people are overlooked.
Although older people’s needs are addressed in HCA training, we found no evidence from the telephone survey that relational care is considered a priority in such training. This was in contrast to our findings from the focus groups with older people with recent experience of being a patient in hospital. For older people and their relatives, their experience of hospital care often hinged on the quality of the relationships they had with staff who cared for them. Making connections at a personal level with staff transforms care for older people, allowing them to feel less like ‘patients’. Although this finding is not new,6,13,15,19 findings from our telephone survey would suggest that it does not currently explicitly inform the way HCA staff are trained to perform their role.
In interviews with HCAs and OS, participants were aware of the effect that poor communication can have on relationships with patients, although they were not always aware of the reticence some older people felt in asking for help. Staff identified a sense of conflict between the need for efficiency and the importance of providing good relational care. This is a finding supported in other literature,19,109 but evidence from our focus groups would suggest that older people acknowledge, and are sympathetic to, the pressure that care staff are under. HCAs were keen to learn how to have difficult conversations with patients and relatives and how to avoid projecting work-related stress. In our study older people and their relatives questioned whether or not staff were always aware of the sense of powerlessness older patients feel when they are in hospital. Pressures of time mean that HCA work is responsive to expressed need, but this is at the expense of attempts to meet needs, which older people are hesitant to voice.
Development of a health-care assistant training intervention
We aimed to develop a values-based training intervention for HCAs designed to address the needs of older patients for high-quality relational care (study aim 2). On the strength of our analysis of (1) HCA and OS interviews, (2) focus groups with older people and their relatives and (3) the telephone survey of hospital trusts in England, we established certain principles to guide the development of a relational care training intervention for HCAs:
-
Training should be connected to everyday practice to ensure credibility and allow learners to draw on experience and implement new skills.
-
Training should be interactive to retain learner interest, reflect the way HCAs work in teams and acknowledge the highly practical nature of their role.
-
Training should be assets based, whereby the starting point for learners is building on existing strengths rather than addressing weaknesses or deficits.
-
At the heart of training should be patient experiences conveyed using the words of patients wherever possible.
-
Web-based learning should be used as an adjunct to the training and not its primary mode of delivery.
-
Training should use novel experiential learning techniques to facilitate learners’ ability to consider the perspectives of older people in their care.
These principles were used to develop Older People’s Shoes, an intervention designed to meet the learning needs of HCAs working with older people. These principles were consistent with, and enhanced by, findings from the OPSWISE project,51 a realist synthesis of evidence to inform clinical support workforce developments. Through a series of intensive workshops and drawing on expertise within and outside health and education sectors we produced a 2-day training intervention for HCAs working with older people.
Feasibility of a definitive cluster randomised controlled trial
We aimed to assess the feasibility of a cluster randomised controlled trial to compare the performance of the developed training intervention for HCAs with current training in improving the care of older patients in acute NHS settings (study aim 3). To address this aim we conducted a feasibility pilot cluster randomised controlled trial and a parallel process evaluation. In total, 12 wards (four from each partner NHS trust) were randomised to either HCA training in Older People’s Shoes or TAU. Although we did not seek to establish superiority of HCA training in Older People’s Shoes over TAU because of the feasibility study design, there was evidence that the direction of effect, after adjustment for baseline differences, was towards better HCA outcomes in the Older People’s Shoes arm of the trial. Feasibility was to be determined by the answers to a series of predefined questions (see Chapter 6, Purpose). These are dealt with in turn below.
Acceptability of the intervention to trainers and health-care assistant trainees
The level of uptake of the training intervention and findings from the process evaluation suggest that Older People’s Shoes was acceptable to trainers and HCA learners alike. For the intervention to be viable as a model of service delivery, it had to be acceptable to those delivering the training and those receiving training. For the training to have life beyond this study (or a definitive trial) it could not rely on research staff to deliver it. Hence, trust-based trainers were used to deliver Older People’s Shoes at each of the three centres. Trainers engaged with the process of learning how to deliver the training considered the experience rewarding and were impressed by the quality of the training materials. There was a balance to be struck between the need to deliver the training as prescribed (and written in the trainer guide) and the need for the training to be interactive and fully use the qualities and experience the trainers brought. Although the trainer guide was not intended to function as a script, there were times that the instructions held a level of detail that detracted from the trainer’s ability to engage with the learners.
Of the 59 HCA learners on wards randomly allocated to receive Older People’s Shoes training, 45 received at least one of the 2 days and 36 received both days of training. Evaluation forms reported high levels of satisfaction with the course and with those interviewed as part of the process evaluation. For HCA learners, the third unit that looked at customer care practices divided opinion the most, suggesting more work on explaining the relevance of this section may be warranted to trainers and learners alike.
Willingness of ward managers, health-care assistants and older patients to participate in a cluster randomised controlled trial
We did not interview ward managers about their experience of trial participation, so we can only infer their willingness to participate from the permission they gave for their ward to take part in the study. We successfully recruited 12 wards as planned to the study, with the permission of ward managers. This was facilitated by the relevant trust contact. We were not prevented from conducting ward observation sessions at any point other than when norovirus was present and the ward was closed to visitors.
The majority of the HCAs eligible to take part in the study did so. Of the 134 HCAs eligible to take part, 112 consented to participate (83.6%). This exceeded our target recruitment of 84 HCAs from an estimated 120 eligible (70% target). Ethical considerations prevented us from establishing reasons for not taking part. However, reaching all HCAs who were eligible was challenging, as many HCAs worked part-time or on night shifts so the opportunity to explain the study was not always available to us. During the baseline period, 97 out of 129 (75.2%) eligible patients agreed to take part and during the postrandomisation period 74 out of 114 (64.9%) eligible patients consented. This fell short of our target recruitment of 100 patients for each time period. As with HCAs we were unable to explore reasons for non-participation with patients. These patient recruitment figures are respectable given the frailty of this population of older hospitalised patients and a backdrop in declining participation more widely in studies of older people’s health. 110
Willingness of ward managers for wards to be randomly allocated
Ward managers were aware that involvement in the study included wards being randomised to Older People’s Shoes training or TAU. The advantage of the former was staff training to a section of the workforce often not catered for. However, there were disadvantages to being in this arm of the study in terms of the logistics of ensuring adequate staffing of the ward to release HCAs to attend training. Although we endeavoured to give wards as much notice as we could prior to delivering training, this still created problems for Older People’s Shoes wards to plan cover. HCA attendance at Older People’s Shoes training ranged from 44% (4/9) to 100% (10/10) among wards randomised to Older People’s Shoes.
Non-response and item non-response to outcomes at the level of ward, health-care assistant and patient
We successfully completed all ward observation sessions as planned (n = 96) during the follow-up period, but of the 96 sessions planned during the baseline period five could not be undertaken because of temporary ward closures when norovirus was present. This was an event that could not have been expected and occurred at a point in the baseline period that meant we were unable to reschedule the planned sessions.
For HCAs, completion of questionnaires was 72 out of 112 (64.2%) at baseline, 52 out of 112 (46.4%) at the first follow-up and 40 out of 112 (35.7%) at the second follow-up. Of those completing questionnaires at baseline, most HCAs completed all of the scales (AWES, 98.6%; TEQ, 100%; AGED goodness, 88.9%; AGED vitality, 90.3%; AGED maturity, 91.7%; and AGED positivity, 90.3%). For patients, across both time periods (prior to and 8 weeks after randomisation), a total of 159 eligible patients received questionnaires; 91questionnaires were returned (57.2%), three of which were blank. Of 88 non-blank questionnaires returned, the PEECH scale was completed in 75 (85.2%), the EQ-VAS was completed in 82 (93.2%) and the EQ-5D-5L was completed in 81 (92.0%).
Acceptability of outcome measures to participants
The interviews with HCAs conducted as part of the process evaluation suggested that any discomfort with being observed was short-lived and due to uncertainty about the purpose of the observations. We do not know if patients were uncomfortable when ward observation sessions were taking place, but an explanation was provided to each patient prior to each observation session. For the paired sessions there was a practical issue of finding space for two observers to conduct observations in bays of patients (in one participating trust four patients per bay was the norm and in the other two trusts ward bays consisted of six beds).
As reported in the previous section (see Non-response and item non-response to outcomes at the level of ward, health-care assistant and patient), the HCA questionnaire response rate was disappointing. That it declined steadily over the three time points suggests that the requirement to complete three questionnaires was too burdensome. Response was fairly similar in both arms of the trial, suggesting that the reason was not because of disappointment in not being allocated to receive Older People’s Shoes training. Disappointment in being allocated to the control arm of a trial is not uncommon. 111,112 Although we explained the importance of the questionnaire completion at the point of recruitment, this was possibly lost among the other information that needed to be absorbed at the point of recruitment. Those interviewed as part of the process evaluation generally enjoyed the experience of being in the trial, although we only sampled those in the Older People’s Shoes arm for interviews in this phase of the study. One interviewee did raise the difficulty of completing the AGED inventory and this is reflected in the lower rate of completion of AGED inventory items compared with the other scales.
Although a high portion of eligible patients consented (as reported in Non-response and item non-response to outcomes at the level of ward, health-care assistant and patient), this translated into returned questionnaires for just over half of the recruited sample. It is possible that the effort of completing a questionnaire was too great for patients shortly after being discharged from hospital. An alternative to this may be completing questionnaires with help on the wards prior to discharge. This approach is currently being used in a similar study with some success. 113
Ability to monitor levels of resource use and quality-of-life data
We were able to extract length of hospital stay data for nearly all patients who consented to take part. Quality of life, as measured by the EQ-5D, was available for approximately half of patients who consented to take part in the study and, therefore, it is difficult to make precise inferences about the health of recruited patient participants. This response rate was disappointing and lower than obtained in comparable studies. 92,114 However, this may be explained because among our participants health states were lower than in the general population standardised for age and sex. 100
The total training cost was £36,819. However, if the 45 HCAs who underwent Older People’s Shoes training were to provide care to 2622 patients per year, this would equate to a cost of £14.04 per patient seen. This might be considered a relatively cheap intervention at the patient level. This estimate needs to be treated with caution as estimates are based on screening for potentially eligible patients over an 8-week period in total and we cannot say with great certainty how many of these patients would have been cared for by the HCAs that were trained. Nonetheless, as the mean hospital stay cost is in the order of £2000, based on bed-day costs alone, this shows that these costs far outweigh both the per-patient cost of the Older People’s Shoes training (estimated to be between £10.00 and £20.00) and the per-patient cost of any change in contact time (estimated to be approximately £4.00).
Variability within and between the ward, health-care assistant and patient
Although HCAs appeared to be broadly similar in the two arms at baseline, there were differences in the male-to-female ratio and the mean age of patients. As the randomisation occurred at ward level and was stratified by NHS hospital trust, this suggests that there were real differences between wards. We calculated variability within and between wards for ward, HCA and patient outcomes. However, estimated intraclass correlation coefficients were insufficiently precise to be used to estimate sample size for a definitive trial. There is increasing evidence that pilot studies are rarely sufficiently powered to estimate an intraclass correlation coefficients with sufficient precision. 97
Appropriateness of ward as the unit of randomisation
Health-care assistants can, and do, work on more than one ward within the same hospital trust, and we were aware at the outset that this posed a risk of contamination between trial arms. To our knowledge, there was limited movement of HCAs between wards recruited to the study and this was partly because of our inclusion criteria that limited eligible HCAs to those named on a ward’s roster. The only alternative to randomisation at the ward level would be randomisation at the hospital level. This would reduce the risk of contamination, but the increased cost of such a trial design would be substantial and likely to make the study unviable.
Limitations of the research
Our study has a number of limitations that need to be taken into account when considering our findings.
-
The intention was for the telephone survey to be cross-sectional, but because of staff changes in the research team the national telephone survey was undertaken over two time periods with a gap of 9 months during which no telephone interviews were conducted. We were conscious of the changes that were occurring in terms of workforce policy and training, whereby HCAs were either the focus of those changes or likely to be affected by them. We tested for differences between the groups surveyed in each period. Apart from fewer plans to change HCA training among the second group of trust interviewees, we found no obvious differences.
-
Our telephone survey used a mix of closed and open-ended questions. Although this allowed us to capture the variability in how HCA training was reported as being provided, the open-ended questions meant that some post hoc interpretation and categorisation was required. To limit bias, all coded responses were conducted by at least two members of the research team.
-
Data from the focus groups relied on some of the participant older people or carers of older people to recollect experiences that had occurred > 1 year prior to the group discussion. Although recounted experiences in the shorter, rather than the longer, term are likely to be more detailed and ‘accurate’, it would have thrown up a number of ethical issues to have recruited participants where their experiences had been in the very recent past.
-
In our focus groups we went to great efforts to ensure participants understood that our focus was on the care provided by HCAs rather than other care staff. We expected that older people and the carers of older people might not always make the distinction between different grades and groups of staff when being cared for in hospital. We therefore took along examples of pictures of HCA uniforms from local hospitals. Even so, we were aware that the discussion within the groups often related to care staff in general (often nurses and HCAs) rather than HCAs specifically.
-
For the feasibility cluster randomised controlled trial, members of the research team recruited wards and relied on trust-based research nurses to recruit patients from within those wards. In general, research nurses work to targets of accrual to trials in which the randomisation is at the level of individual patient. This may explain why even after careful instruction and explanation, recruitment within wards was highly variable suggesting the focus was on achieving the total number of patients rather than the maximum number of eligible patients within recruited wards.
-
In conducting the QUIS observations it was not possible to determine which HCAs had undergone training within the wards allocated to Older People’s Shoes training. Although this is a strength, in that it avoids observer bias, it allows only for intention-to-treat analysis and not for per-protocol analysis.
-
To conduct the trial we required, and received, approval from trust-level directors of nursing and individual ward managers. However, commitment by ward managers to the study appeared to vary between and within the three trusts. This was apparent in the degree to which staff were encouraged to attend training (Older People’s Shoes wards) and complete questionnaires.
-
Our process evaluation did not extend to interviews with ward managers. It became apparent after the protocol was written that this was a group of stakeholders with a great deal to offer in terms of understanding the impact of the intervention and their own experience of involvement in the trial. Our distal outcomes (HCA behaviour and patient experience) were ambitious and ward managers may have provided useful insights at both the ward and trust level into the optimal work/care environment for the training intervention to positively influence those outcomes.
Implications for practice
Although the study conducted was predominantly methodological, it raises a number of implications for the training of HCAs:
-
‘Downward substitution’ within the health-care workforce is perhaps inevitable with increasing pressure to contain costs. Even if the size of the workforce does not change, the proportion of HCAs within it will grow. The work of HCAs is critical in improving the experience of older patients and their carers by delivering good relational care, but there is little relevant training available to them. Older People’s Shoes training which is grounded in evidence about HCAs’ everyday work can help them to deliver relational care in the challenging context in which they work.
-
Current training for HCAs in relational care is limited and variable particularly for existing (rather than new) staff. The Care Certificate includes dignity, communication and person-centred care. Relational care brings these aspects together into a coherent approach. Support for training in this area is imperative and greater oversight at the trust level is required beyond the induction of HCAs to ensure that efforts to equip the HCA workforce to provide relational care is not lost when responsibility is devolved to wards.
-
A number of factors (a degree of public distrust, the relative lack of investment and support by trusts for HCA training, staff hierarchies and restricted opportunities to come together as a section of the workforce) can make HCAs feel unsupported and unvalued. Training designed specifically around the needs of the HCA workforce but embraced by the wider system, can bring HCAs together to reflect and share good practice, boost morale and give HCAs a sense of value and purpose in their work.
-
The ‘front-line’ role of HCAs often exposes them to strong emotions (of anger, frustration, grief and despair) in patients and carers. Furthermore, their role often requires them to have ‘difficult conversations’. A lack of training in these areas leaves HCAs vulnerable and may result in a lack of appropriate support for patients and carers. Older People’s Shoes training allowed some exploration of these issues but further work is required in this area so that HCAs are given the skills to deal with these challenging situations and signposted to appropriate sources of support.
-
The demands of care on older people’s wards, in which patients have complex needs and comorbidities and need high levels of support with activities of daily living, can make it extremely difficult to create pockets of time through which to demonstrate relational care. Training needs to recognise this and help identify ways in which trainers can deliver good relational care while carrying out everyday care tasks.
-
Empathy is an important component of relational care. Training that deals with these concepts only in abstract form is unhelpful. Training that provides experiential learning and the opportunity to listen to older people’s accounts will help HCAs strengthen their relationships with patients to better understand their needs and feelings.
Recommendations for future research
In undertaking this work the need for research in the following areas became apparent:
-
Efforts to improve relational care in hospitals are often ward based, for which the unit is relatively easy to define and the notion of a ‘team’ is strong. In keeping with the remit of our study, and the commissioned call that this study was a part of, our focus was on HCA training. As ward teams are hierarchical in nature, with HCAs at the lower end of the hierarchical structure, there is an absence of evidence as to the relative benefits of HCA-specific compared with ward-targeted interventions.
-
Outcome measures that can detect improvements in relational care need further development. There are relatively few patient- and staff-reported/-observed outcomes. In our study the HCA outcome measures have been used predominantly, in North America. Certain items in these measures are likely to be culturally specific. The challenge is to identify measures that are simple, quick, unobtrusive, unburdensome, valid and suitable across staff groups.
-
Those who stand to benefit the most from good relational care in hospital and other care settings (and who are most at risk when that care is poor) are patients who are old, vulnerable, in poor health, who have complex needs and who are impaired physically and cognitively. Gaining access to samples who adequately represent this population is challenging and, although ethical concerns are paramount, their voice needs to be heard in studies of relational care. Studies are needed that examine creative ways of involving these patients that do not compromise ethics but can determine preferred methods of approach (timing, source or location), methods of data capture and the validity of proxy measures.
Conclusions
Based on our findings we draw the following conclusions:
-
Training of HCAs in delivering relational care is highly variable between employing NHS hospital trusts. Most training is received at induction and training thereafter tends to be devolved to ward-level mentorship. The needs of older people are addressed in HCA training, but training in relational care does not appear to be a priority. For those with trust-level responsibility for HCA training, getting staff to be released from ward duties is a challenge.
-
For older people and their relatives their experience of hospital care is shaped by the relationships that they have with the staff who care for them. They are aware of the competing demands placed on staff and the pressures they are under, but being in hospital can generate a feeling of powerlessness that often prevents older patients asking for help.
-
HCAs and OS are keen to extend their learning in relational care. Training should address HCA learning needs including having difficult conversations with patients and relatives and ways to manage, and not project, work-related stress. HCAs acknowledge that their work is more rewarding when they have greater knowledge about the lives of the people they care for.
-
A training intervention (Older People’s Shoes) was designed to meet the learning needs of HCAs in delivering high-quality relational care of older people. A transparent process of intervention development was undertaken. Structure and content were informed by the older people and their relatives, HCAs, staff working alongside HCAs, experts in relevant fields and learning theory.
-
The Older People’s Shoes training intervention was received positively by trainers and HCA learners and appears to meet a need, particularly for established HCAs, that is not met in other training provided by employing trusts.
-
The estimated per patient cost of a HCA receiving training in the Older People’s Shoes intervention is relatively small (£10.00–20.00) when considering the average cost of a hospital stay for patients from this population (approximately £2000).
-
Drawing on lessons from the present study, we propose that a definitive cluster randomised controlled trial of the Older People’s Shoes training intervention would be viable if the following methodological and contextual aspects were addressed.
-
As the focus on HCAs was considered a strength, greater awareness of this HCA intervention among ward managers and other ward staff members will reinforce messages about relational care in the workplace following intervention delivery. Ward manager involvement should extend beyond permission for ward participation.
-
Greater involvement of ward managers is likely to improve recruitment. Ward- and patient-level outcomes are relevant only if a high proportion (> 80%) of the HCAs within each ward are recruited and ‘treated as intended’ within the trial.
-
Greater commitment and recruitment may be secured with a ‘wait-list’ design, whereby all wards (and HCAs) recruited are confident of ultimately receiving the intervention.
-
Ward managers need to be confident that they can secure backfill for staff to be released for training. Although trusts supported the CHAT study, it was not always clear how funds agreed for backfill could be secured by ward managers.
-
HCAs are willing to participate, but are reluctant to complete questionnaires at three time points. The AGED inventory appears to be a discriminatory measure but completion is suboptimal.
-
More extensive training is needed for observers using the QUIS. When discrepancies occur between paired observers, this is typically when (and whether or not) one interaction ends and another begins rather than in the rating of the quality of the interaction.
-
The use of trust-based research nurses to recruit patients has the advantage of impartiality, as they are separate from both the research and ward teams. However, the additional layer this creates in communicating with a population that is already hard to access needs to be addressed.
-
Patients are willing to participate but questionnaire completion is burdensome. Methods of completion used by other studies to secure patient questionnaire completion (e.g. prior to discharge, using interviewers and/or proxies) need to be explored.
-
Acknowledgements
Many people have contributed to the successful completion of this research and we are very grateful to them all. We would particularly like to thank the following for their participation and support.
CHAT Intervention Development Workshop participants: Jackie Bridges, Amanda Clarke, Kirk Lower, Liz McConnell, Nick Napper, Kezia Scales and Lynne Williams.
CHAT study steering group members: Jo Cooper, Bev Fitzsimons, Tanis Hand, Nynke Hardy, Nicky Hayes, Corina Naughton, Jo Rycroft-Malone, Sagila Thiruthanikasalan and, our chairperson, Karen Spilsbury.
Organisations consulted with regard to customer care practice and training: Aldi Stores Limited, Domestic and General Services Limited, B&Q PLC and Boots Opticians.
Persons and organisations who kindly gave us permission to use and reproduce their images and materials including David Bailey, DIPEx, Patient Voices, Jackie Bridges and colleagues from City University, and the University of Nottingham.
The development of the training intervention would not have been possible without the members of community groups of older people and carers, HCAs and other hospital staff who took part in interviews as part of the CHAT study.
Grateful thanks also to our public and patient involvement PPIRes representatives, Margaret McWilliams and Janet Gray, and our HCA representatives, Patricia Annon and Sagila Thiruthanikasalan.
We are also grateful for the support of our partner NHS trusts, which, to protect the anonymity of the interviewees, we cannot name.
Contributions of authors
Antony Arthur (Professor of Nursing Science, principal investigator) was responsible for study concept, overall study design, application development, building and leading the study team, project governance, intervention development, overseeing data collection, data analyses and report writing.
Clare Aldus (Research Fellow, study manager) was responsible for day-to-day management of the study across centres and for managing research nurse activity, data collection, contributing to study design, intervention development, data analyses and drafting material for the report.
Sophie Sarre (Research Associate) contributed to study design and intervention development, conducted data collection, managed research nurse activity locally, carried out analysis of qualitative data from interviews, focus groups and process evaluation, led on the process evaluation design and drafted material for the report.
Jill Maben (Director, National Nursing Research Unit, coinvestigator) contributed to overall study design, managed the local research associate, contributed to data collection and intervention development, led on qualitative analysis and drafted material for the report.
Heather Wharrad (Professor of e-Learning and Health Informatics, coinvestigator) contributed to overall study design, managed local research associates, contributed to data collection, led on pedagogical and learning theory, managed training package production processes and drafted material for the report.
Justine Schneider (Professor of Mental Health and Social Care, coinvestigator) contributed to overall study design, intervention development, carried out a literature review and drafted material for the report.
Garry Barton (Reader in Health Economics, coinvestigator) contributed to the design of the economic evaluation, carried out health economic analyses and drafted material for the report.
Elaine Argyle (Senior Research Fellow) conducted data collection, managed research nurse activity locally and contributed to report writing.
Allan Clark (Senior Lecturer, statistician) contributed to study design, carried out statistical analyses and drafted material for the report.
Fiona Nouri (Research Assistant) contributed to telephone survey data collection, data analyses and drafted material for the report.
Caroline Nicholson (Research Fellow, co-investigator) contributed to overall study design, intervention development and report writing.
Publication
Arthur A, Maben J, Wharrad H, Aldus C, Sarre S, Schneider J, et al. Can Healthcare Assistant Training (CHAT) improve the relational care of older people? Study protocol for a pilot cluster randomised controlled trial. BMC Trials 2015;16:559.
Data sharing statement
Requests for access to anonymised data should be made to the corresponding author.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
References
- Francis R. Report of the Mid Staffordshire NHS Foundation Trust Public Inquiry. London: The Stationery Office; 2013.
- Cavendish C. Cavendish Review: An Independent Enquiry into Healthcare Assistants and Support Workers in the NHS and Social Care Setting. London: Department of Health; 2013.
- Hospital Episode Statistics: Admitted Patient Care, England – 2013–14. Leeds: Health and Social Care Information Centre; 2015.
- Cornwell J. The Care of Frail Older People with Complex Needs: Time for a Revolution. London: The King’s Fund; 2012.
- Tadd W, Hillman A, Calnan S, Calnan M, Bayer T, Read S. Dignity in Practice: An Exploration of the Care of Older Adults in Acute NHS Trusts. London: HMSO; 2011.
- Goodrich J, Cornwell J. Seeing the Person in the Patient: The Point of Care Review Paper. London: The King’s Fund; 2008.
- National NHS Patient Survey Programme: National Results from the 2014 Inpatient Survey. London: Care Quality Commission; 2015.
- Leatherman S, Sutherland K. The Quest for Quality: Refining the NHS Reforms. London: The Nuffield Trust; 2008.
- The State of Health Care and Adult Social Care in England: An Overview of Key Themes in Care in 2011/12. London: The Stationery Office; 2012.
- Stories from the Present, Lessons from the Future. Harrow: The Patients Association; 2012.
- Robert G, Cornwell J, Brearley S, Foot C, Goodrich J, Joule N, et al. What Matters to Patients? Developing the Evidence Base for Measuring and Improving Patient Experience. Coventry: NHS Institute for Innovation and Improvement; 2011.
- Cornwell J, Goodrich J. Challenges for improving patients’ experiences of health care. J Health Serv Res Po 2011;16:1-2. https://doi.org/10.1258/jhsrp.2010.010144.
- Bridges J, Flatley M, Meyer J. Older people’s and relatives’ experiences in acute care settings: systematic review and synthesis of qualitative studies. Int J Nurs Stud 2010;47:89-107. http://dx.doi.org/10.1016/j.ijnurstu.2009.09.009.
- Richards R, Coulter A. Is the NHS Becoming more Patient-Centred? Trends from the National Surveys of NHS Patients 2002–2007. Oxford: The Picker Institute; 2007.
- Nolan MR, Davies S, Brown J, Keady J, Nolan J. Beyond person-centred care: a new vision for gerontological nursing. J Clin Nurs 2004;13:45-53. http://dx.doi.org/10.1111/j.1365-2702.2004.00926.x.
- Gillespie R, Florin D, Gillam S. How is patient-centred care understood by the clinical, managerial and lay stakeholders responsible for promoting this agenda?. Health Expect 2004;7:142-8. http://dx.doi.org/10.1111/j.1369-7625.2004.00264.x.
- Beck RS, Daughtridge R, Sloane PD. Physician-patient communication in the primary care office: a systematic review. J Am Board Fam Pract 2002;15:25-38.
- Matiti MR, Trorey GM. Patients’ expectations of the maintenance of their dignity. J Clin Nurs 2008;17:2709-17. http://dx.doi.org/10.1111/j.1365-2702.2008.02365.x.
- Maben J, Adams M, Peccei R, Murrells T, Robert G. ‘Poppets and parcels’: the links between staff experience of work and acutely ill older peoples’ experience of hospital care. Int J Older People Nurs 2012;7:83-94. http://dx.doi.org/10.1111/j.1748-3743.2012.00326.x.
- Sturgeon D. ‘Have a nice day’: consumerism, compassion and health care. Br J Nurs 2010;19:1047-51. http://dx.doi.org/10.12968/bjon.2010.19.16.78198.
- Lloyd L, Calnan M, Cameron A, Seymour J, Smith R. Identity in the fourth age: perseverance, adaptation and maintaining dignity. Ageing Soc 2014;34:1-19. http://dx.doi.org/10.1017/S0144686X12000761.
- McKeown J, Clarke A, Ingleton C, Ryan T, Repper J. The use of life story work with people with dementia to enhance person-centred care. Int J Older People Nurs 2010;5:148-58. http://dx.doi.org/10.1111/j.1748-3743.2010.00219.x.
- Thompson R. Older People’s Mental Health Services: supporting and developing HCAs. Mental Health Practice 2007;10:30-4. https://doi.org/10.7748/mhp2007.07.10.10.30.c4317.
- Kessler I, Heron P. NHS modernisation and the role of HCAs. Br J Healthc Assistants 2010;4:318-20. https://doi.org/10.12968/bjha.2010.4.7.48906.
- Health and Social Care Information Centre . Healthcare Assistants by Level, AfC Band, Age Band, Ethnicity and Gender – Sept 13 2013. www.hscic.gov.uk/media/19430/Health-care-assistants-by-level-AfC-band-age-band-ethnicity-and-gender-Sept-2013/xls/ (accessed 2 January 2016).
- Maben J. The art of caring: invisible and subordinated? A response to Juliet Corbin: ‘is caring a lost art in nursing?’. Int J Nurs Stud 2008;45:335-8. http://dx.doi.org/10.1016/j.ijnurstu.2007.09.002.
- Schneider J, Scales K, Bailey S, Lloyd J. Challenging Care: The Role and Experience of Health Care Assistants in Dementia Wards. London: National Coordinating Centre for the Service Delivery and Organisation; 2010.
- Spilsbury K, Meyer J. Use, misuse and non-use of health care assistants: understanding the work of health care assistants in a hospital setting. J Nurs Manag 2004;12:411-18. http://dx.doi.org/10.1111/j.1365-2834.2004.00515.x.
- Kessler I, Heron P, Dopson S, Magee H, Swain D, Askham J. The Nature and Consequences of Support Workers in a Hospital Setting. London: NIHR Service Delivery and Organisation; 2010.
- Daykin N, Clarke B. ‘They’ll still get the bodily care’. Discourses of care and relationships between nurses and health care assistants in the NHS. Sociol Health Ill 2000;22:349-63. https://doi.org/10.1111/1467-9566.00208.
- Thornley C. A question of competence? Re-evaluating the roles of the nursing auxiliary and health care assistant in the NHS. J Clin Nurs 2000;9:451-8. https://doi.org/10.1046/j.1365-2702.2000.00398.x.
- Lloyd JV, Schneider J, Scales K, Bailey S, Jones R. Ingroup identity as an obstacle to effective multiprofessional and interprofessional teamwork: findings from an ethnographic study of healthcare assistants in dementia care. J Interprof Care 2011;25:345-51. http://dx.doi.org/10.3109/13561820.2011.567381.
- Schneider J. Research: support workers play vital role in dementia care. Br J Healthc Assistants 2010;4:498-501. https://doi.org/10.12968/bjha.2010.4.10.79076.
- Aiken LH, Sermeus W, Van den Heede K, Sloane DM, Busse R, McKee M, et al. Patient safety, satisfaction, and quality of hospital care: cross sectional surveys of nurses and patients in 12 countries in Europe and the United States. BMJ 2012;344. http://dx.doi.org/10.1136/bmj.e1717.
- Edwards M. The nurses’ aide: past and future necessity. J Adv Nurs 1997;26:237-45. https://doi.org/10.1046/j.1365-2648.1997.1997026237.x.
- Coffey A. Perceptions of training for care attendants employed in the care of older people. J Nurs Manag 2004;12:322-8. http://dx.doi.org/10.1111/j.1365-2834.2004.00442.x.
- Maben J, Griffiths P. Nurses in Society: Starting the Debate. London: National Nursing Research Unit; 2008.
- Skills for Health . The Healthcare Support Workforce: A Case for Ongoing Development and Investment 2015. www.skillsforhealth.org.uk/images/resource-section/reports/The Healthcare Support Workforce.pdf (accessed 1 January 2015).
- Health Education England . Shape of Caring: A Review of the Future Education and Training of Registered Nurses and Care Assistants 2015. www.hee.nhs.uk/sites/default/files/documents/2348-Shape-of-caring-review-FINAL.pdf (accessed 1 December 2015).
- The Council of Deans . Shaping the Future: Education and Training for Nurses and Care Assistants 2014. www.councilofdeans.org.uk/wp-content/uploads/2014/10/CoDH-Shape-of-Caring-Evidence-Response-20140917.pdf (accessed 1 December 2015).
- Sprangers S, Dijkstra K, Romijn-Luijten A. Communication skills training in a nursing home: effects of a brief intervention on residents and nursing aides. Clin Interv Aging 2015;10:311-19. http://dx.doi.org/10.2147/CIA.S73053.
- Bryan K, Axelrod L, Maxim J, Bell L, Jordan L. Working with older people with communication difficulties: an evaluation of care worker training. Aging Ment Health 2002;6:248-54. http://dx.doi.org/10.1080/13607860220142495.
- Eggenberger E, Heimerl K, Bennett MI. Communication skills training in dementia care: a systematic review of effectiveness, training content, and didactic methods in different care settings. Int Psychogeriatr 2013;25:345-58. http://dx.doi.org/10.1017/S1041610212001664.
- Woods B, Spector A, Jones C, Orrell M, Davies S. Reminiscence therapy for dementia. Cochrane Database Syst Rev 2005;2. https://doi.org/10.1002/14651858.cd001120.pub2.
- Heliker D, Nguyen HT. Story sharing: enhancing nurse aide-resident relationships in long-term care. Res Gerontol Nurs 2010;3:240-52. http://dx.doi.org/10.3928/19404921-20100303-01.
- Clarke A, Hanson EJ, Ross H. Seeing the person behind the patient: enhancing the care of older people using a biographical approach. J Clin Nurs 2003;12:697-706. https://doi.org/10.1046/j.1365-2702.2003.00784.x.
- Coleman CK, Medvene LJ, Van Haitsma K. A person-centered care intervention for geriatric certified nursing assistants. Gerontologist 2013;53:687-98. http://dx.doi.org/10.1093/geront/gns135.
- Smith B, Kerse N, Parsons M. Quality of residential care for older people: does education for healthcare assistants make a difference?. N Z Med J 2005;118.
- Developing and Evaluating Complex Interventions: New Guidance. London: Medical Research Council; 2008.
- Kirkpatrick DL, Kirkpatrick JD. Evaluating Training Programs. San Francisco, CA: Berrett-Koehler; 2006.
- Rycroft-Malone J, Burton CR, Williams L, Edwards S, Fisher D, Hall B, et al. Improving skills and care standards in the support workforce for older people: a realist synthesis of workforce development interventions. Health Serv Deliv Res 2015;4.
- Kuske B, Luck T, Hanns S, Matschinger H, Angermeyer MC, Behrens J, et al. Training in dementia care: a cluster-randomized controlled trial of a training program for nursing home staff in Germany. Int Psychogeriatr 2009;21:295-308. http://dx.doi.org/10.1017/S1041610208008387.
- Clare L, Whitaker R, Woods RT, Quinn C, Jelley H, Hoare Z, et al. AwareCare: a pilot randomized controlled trial of an awareness-based staff training intervention to improve quality of life for residents with severe dementia in long-term care settings. Int Psychogeriatr 2013;25:128-39. http://dx.doi.org/10.1017/S1041610212001226.
- Kaufman R, Keller J. Levels of evaluation: beyond Kirkpatrick. Hum Res Dev Quart 1994;5:371-80. https://doi.org/10.1002/hrdq.3920050408.
- Moore GF, Audrey S, Barker M, Bond L, Bonell C, Hardeman W, et al. Process evaluation of complex interventions: Medical Research Council guidance. BMJ 2015;350. https://doi.org/10.1136/bmj.h1258.
- Health Education England . Pre-Nursing Experience (Pilots) 2013. www.hee.nhs.uk/our-work/developing-our-workforce/nursing/pre-nursing-experience-pilots (accessed 20 January 2016).
- NHS Employers . Care Certificate 2015. www.nhsemployers.org/your-workforce/plan/education-and-training/care-certificate (accessed 22 January 2015).
- NIHR Health Services and Delivery Programme . Research Governance Guidelines: Study Steering Committee (SSC) or Trial Steering Committee (TSC) 2013. www.nets.nihr.ac.uk/__data/assets/pdf_file/0011/81992/ssc-guidance-may13.pdf (accessed 1 December 2013).
- Norfolk and Suffolk Primary and Community Care Research Office . Public and Patient Involvement in Research (PPIRes) n.d. http://nspccro.nihr.ac.uk/for-academics-and-nhs-staff/ppires (accessed 23 January 2016).
- Health and Social Care Information Centre . Data Files – Hospital Estates and Facilities Statistics 2014. http://hefs.hscic.gov.uk/DataFiles.asp (accessed 31 January 2014).
- Kitzinger J. Qualitative research. Introducing focus groups. BMJ 1995;311:299-302. https://doi.org/10.1136/bmj.311.7000.299.
- Morgan DL. Focus Groups as Qualitative Research. London: Sage; 1997.
- Barbour R, Flick U. The SAGE Handbook of Qualitative Data Analysis. London: Sage; 2013.
- Stewart D, Shamdasani P, Rook D. Focus Groups. Thousand Oaks, CA: Sage; 2007.
- Silverman D. Interpreting Qualitative Data. London: Sage; 2001.
- Lincoln Y, Guba E. Naturalistic Inquiry. London: Sage; 1985.
- Bridges J, Nugus P. Dignity and significance in urgent care: older people’s experiences. J Res Nurs 2010;15:43-5. https://doi.org/10.1177/1744987109353522.
- Improving Supportive and Palliative Care for Adults with Cancer. London: NICE; 2004.
- Connolly M, Perryman J, McKenna Y, Orford J, Thomson L, Shuttleworth J, et al. SAGE & THYME: a model for training health and social care professionals in patient-focussed support. Patient Educ Couns 2010;79:87-93. http://dx.doi.org/10.1016/j.pec.2009.06.004.
- Baillie L. An Evaluation of Barbara’s Story: Final Report 2015. www.btfn.org.uk/library/directory_listings/230/Barbaras story full report_January 2015.pdf (accessed 23 January 2016).
- Ross AJ, Anderson JE, Kodate N, Thomas L, Thompson K, Thomas B, et al. Simulation training for improving the quality of care for older people: an independent evaluation of an innovative programme for inter-professional education. BMJ Qual Saf 2013;22:495-50. http://dx.doi.org/10.1136/bmjqs-2012-000954.
- Lewis R, Kelly S, Whitfield M, McKenzie-Smith M, Strachan A. An Evaluation of a Simulation-Based Educational Programme to Equip HCAs With The Necessary Non-Technical Skills to Undertake Their Role Safely and Effectively, Specifically in Relation to the Measurement of Vital Signs 2013. www.shu.ac.uk/research/hsc/sites/shu.ac.uk/files/HCA evaluation project.pdf (accessed 2 January 2015).
- Spilsbury K, Brownlow R, Linklater L, Barr I. Promoting the Life Stories of Older People in Nursing Care Homes: A Collaborative Writing Project Between Student Nurses and Care Home Residents. York: Higher Education Academy; 2012.
- Alzheimer’s Society . This Is Me n.d. www.alzheimers.org.uk/thisisme (accessed 31 January 2015).
- NHS Lanarkshire . Getting to Know Me n.d. www.scottishcare.org/docs/037_280__gettingtoknowme_1369954145.pdf (accessed 31 January 2015).
- University Hospitals NHS Coventry and Warwickshire . Getting to Know Me 2013. www.uhcw.nhs.uk/clientfiles/File/Getting_to_know_me_form__1245__-_February_2013[1][1].pdf (accessed 31 January 2015).
- Worcestershire Acute Hospitals NHS Trust . About Me – Lifestyles and Capabilities Booklet n.d. www.worcsacute.nhs.uk/EasysiteWeb/getresource.axd?AssetID=75552&type=Full&servicetype=Attachment (accessed 31 January 2015).
- Kern D, Thomas P, Hughes M. Curriculum Development for Medical Education: A Six-Step Approach. Baltimore, MD: The Johns Hopkins University Press; 1998.
- Carver R. Theory for practice: a framework for thinking about experiential education. J Exp Educ 1996;19:8-13. https://doi.org/10.1177/105382599601900102.
- Gagné R. The Conditions of Learning. New York, NY: Holt, Rinehard & Winston; 1985.
- Gladman J, Harwood R, Foster P, Goldberg S, Davies O, Schneider J, et al. Today Is Monday – The Evidence Base Behind a Film About the Care of People With Dementia and Delirium in Hospital 2014. www.nottingham.ac.uk/mcop/documents/papers/issue13-mcop-issn2044-4230.pdf (accessed 15 March 2015).
- Arthur A, Maben J, Wharrad H, Aldus C, Sarre S, Schneider J, et al. Can Healthcare Assistant Training (CHAT) improve the relational care of older people? Study protocol for a pilot cluster randomised controlled trial. Trials 2015;16. http://dx.doi.org/10.1186/s13063-015-1077-3.
- NIHR Evaluation Trials and Studies Coordinating Centre . Glossary 2012. www.netscc.ac.uk/glossary/ (accessed 22 August 2012).
- Mental Capacity Act 2005. London: The Stationery Office; 2005.
- Dean R, Proudfoot R, Lindesay J. The quality of interactions scale (QUIS): development, reliability and use in the evaluation of two domus units. Int J Geriatr Psych 1993;8:819-26. https://doi.org/10.1002/gps.930081004.
- Nolan M, Grant G, Brown J, Nolan J. Assessing nurses’ work environment: old dilemmas, new solutions. Clin Effect Nurs 1998;2:145-54. https://doi.org/10.1016/S1361-9004(98)80011-3.
- Nolan M, Lundh U, Brown J. Changing aspects of nurses’ work environment: a comparison of perceptions in two hospitals in Sweden and the UK and implications for recruitment and retention of staff. Nurs Times Res 1999;4:221-33. https://doi.org/10.1177/136140969900400313.
- Spreng RN, McKinnon MC, Mar RA, Levine B. The Toronto Empathy Questionnaire: scale development and initial validation of a factor-analytic solution to multiple empathy measures. J Pers Assess 2009;91:62-71. http://dx.doi.org/10.1080/00223890802484381.
- Knox VJ, Gekoski WL, Kelly LE. The Age Group Evaluation and Description (AGED) Inventory: a new instrument for assessing stereotypes of and attitudes toward age groups. Int J Aging Hum Dev 1995;40:31-55. https://doi.org/10.2190/8CUC-4XK8-M33K-07YD.
- Murrells T, Robert G, Adams M, Morrow E, Maben J. Measuring relational aspects of hospital care in England with the ‘Patient Evaluation of Emotional Care during Hospitalisation’ (PEECH) survey questionnaire. BMJ Open 2013;3. http://dx.doi.org/10.1136/bmjopen-2012-002211.
- Williams AM, Kristjanson LJ. Emotional care experienced by hospitalised patients: development and testing of a measurement instrument. J Clin Nurs 2009;18:1069-77. http://dx.doi.org/10.1111/j.1365-2702.2008.02586.x.
- Herdman M, Gudex C, Lloyd A, Janssen M, Kind P, Parkin D, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res 2011;20:1727-36. http://dx.doi.org/10.1007/s11136-011-9903-x.
- Brooks R. EuroQol: the current state of play. Health Policy 1996;37:53-72. https://doi.org/10.1016/0168-8510(96)00822-6.
- van Hout B, Janssen MF, Feng YS, Kohlmann T, Busschbach J, Golicki D, et al. Interim scoring for the EQ-5D-5L: mapping the EQ-5D-5L to EQ-5D-3L value sets. Value Health 2012;15:708-15. http://dx.doi.org/10.1016/j.jval.2012.02.008.
- Guide to the Methods of Technology Appraisal 2013. London: NICE; 2013.
- Ramsey SD, Willke RJ, Glick H, Reed SD, Augustovski F, Jonsson B, et al. Cost-effectiveness analysis alongside clinical trials II-An ISPOR Good Research Practices Task Force report. Value Health 2015;18:161-72. http://dx.doi.org/10.1016/j.jval.2015.02.001.
- Eldridge SM, Costelloe CE, Kahan BC, Lancaster GA, Kerry SM. How big should the pilot study for my cluster randomised trial be?. Stat Methods Med Res 2016;25:1039-56. https://doi.org/10.1177/0962280215588242.
- Hayes RJ, Moulton LH. Cluster Randomised Trials. Boca Raton, FL: Taylor and Francis; 2009.
- Drummond MF, Sculpher MJ, Torrance GW, O’Brien BJ, Stoddart GL. Methods for the Economic Evaluation of Health Care Programmes. New York, NY: Oxford University Press; 2005.
- Kind P, Hardman G, Macran S. UK Population Norms for EQ-5D. York: University of York, Centre for Health Economics; 1999.
- Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics 1977;33:159-74. https://doi.org/10.2307/2529310.
- Curtis L. Unit Costs of Health and Social Care. Canterbury: PSSRU, University of Kent; 2014.
- Department of Health . National Schedule of Reference Costs 2013–14 2014. www.gov.uk/government/publications/nhs-reference-costs-2013-to-2014 (accessed 1 December 2015).
- Mason J. Qualitative Researching. London: Sage; 2001.
- Ritchie J, Spencer L, Bryman A, Burgess R. Analysing Qualitative Data. London: Routledge; 1994.
- The Council of Deans . Healthcare Support Workers in England: Five Proposals for Investing in Education and Development to Deliver High Quality, Effective and Compassionate Care 2013. www.educationandemployers.org/Data/Sites/8/codhhcsw5proposalsforinvestingineduc&devforhighqualitycare.pdf (accessed 1 December 2015).
- Sampson EL, Blanchard MR, Jones L, Tookman A, King M. Dementia in the acute hospital: prospective cohort study of prevalence and mortality. Br J Psychiatry 2009;195:61-6. http://dx.doi.org/10.1192/bjp.bp.108.055335.
- Calasanti T. A feminist confronts ageism. J Aging Stud 2008;22:152-7. https://doi.org/10.1016/j.jaging.2007.12.009.
- Parke B, Hunter KF. The care of older adults in hospital: if it’s common sense why isn’t it common practice?. J Clin Nurs 2014;23:1573-82. http://dx.doi.org/10.1111/jocn.12529.
- Gao L, Green E, Barnes LE, Brayne C, Matthews FE, Robinson L, et al. Changing non-participation in epidemiological studies of older people: evidence from the Cognitive Function and Ageing Study I and II. Age Ageing 2015;44:867-73. http://dx.doi.org/10.1093/ageing/afv101.
- Meinich Petersen S, Zoffmann V, Kjaergaard J, Graff Stensballe L, Greisen G. Disappointment and adherence among parents of newborns allocated to the control group: a qualitative study of a randomized clinical trial. Trials 2014;15. https://doi.org/10.1186/1745-6215-15-126.
- Skingley A, Bungay H, Clift S, Warden J. Experiences of being a control group: lessons from a UK-based randomized controlled trial of group singing as a health promotion initiative for older people. Health Promot Int 2014;29:751-8. http://dx.doi.org/10.1093/heapro/dat026.
- Bridges J, Griffiths P, Fuller A, Chable R, Yao G, Westwood G, et al. HS&Amp;DR – 13 07 48: Creating Learning Environments for Compassionate Care (CLECC): A Feasibility Study 2014. www.nets.nihr.ac.uk/projects/hsdr/130748 (accessed 1 December 2015).
- Barton GR, Sach TH, Avery AJ, Jenkinson C, Doherty M, Whynes DK, et al. A comparison of the performance of the EQ-5D and SF-6D for individuals aged > or = 45 years. Health Econ 2008;17:815-32. https://doi.org/10.1002/hec.1298.
Appendix 1 Structured telephone interview schedule
| Question number | Question |
|---|---|
| 1 | Please would you confirm for me your job title and describe your role in relation to the training of the HCA workforce at [name of trust]? |
| 2a | Could you describe what training a HCA starting work at your trust would receive? |
| Probes | How long does the initial training period last? |
| Is training mandatory or optional? | |
| Is training generic or HCA specific? | |
| Where does training take place? | |
| And what form does training take? | |
| 2b | Is there any ward-based training? |
| Probes | Is training mandatory or optional? |
| (If yes) What does that involve? | |
| Do you have any initiatives similar to the mentoring/preceptorship a newly qualified nurse might go through, or a less formal shadowing or buddy system? | |
| Who with? | |
| How long for? | |
| Are HCAs supernumerary during any or all of that ward-based training or support? | |
| How long does that go on for? | |
| 3a | After induction and initial training is there any further mandatory training? |
| 3b | Does that apply to all sections of the HCA workforce? |
| 3c | And what about optional training? |
| 4a | Are there differences in training (either at induction or later) for HCAs working in different clinical areas? |
| 4b | In terms of the particular needs of older patients, which of those needs do you address in HCA training? [no probes to be used for this section] |
| 5a | Is there any formal assessment of HCAs? |
| 5b | How is the assessment of HCAs managed? |
| 5c | What are the implications of passing or failing the assessment? |
| 5d | Do you assess the values of HCAs at any stage? (If asked, ‘i.e. compassion, empathy, cultural sensitivity, etc.’) |
| 6 | What (else) do you see as the challenges involved in training the HCA workforce? |
| 7 | Can you tell me how long the training programme you have been describing to me has been in place (with/without modifications)? |
| 7a | What impact (if any) has the introduction of the Care Certificate had on the training or assessment of HCAs at [the trust] |
| 7b | (If any impact mentioned) Does that apply equally to existing staff as well as new recruits? |
| 8 | Are there any plans in place to develop HCA training at [the trust]? |
| 9 | Is there anything you think is relevant to HCA training that I have not asked about? |
| 10 | If I need to clarify anything at a later date would it be OK to contact you again? |
Appendix 2 Focus group participant expression of interest form
Expression of interest form for older people’s focus group
Appendix 3 Focus group participant information sheet
We wish to invite 8–10 older people (aged 65 years or over) to join a focus group of those who have had direct or indirect experience of being cared for in hospital. By this we mean either as a patient or perhaps as a friend or relative of somebody who has been a hospital inpatient. To help you decide whether this is something you wish to consider this information sheet explains why the research is being conducted and what it would involve for you.
Study title
Can Health-care Assistant Training improve the relational care of older people? A development and feasibility study of a complex intervention.
What is the purpose of the study?
The study team are developing a short training course for health-care assistants who provide care for older people in hospital. The training needs of health-care assistants are often overlooked in spite of their increasing role in the direct care of older people. There has been increasing recognition of problems in the care of older people. We are particularly interested in the aspects of training such as dignity, empathy, and emotional support.
If I decide to take part now, can I change my mind later?
Yes. Your participation in our study is entirely voluntary. If you decide later, even during the focus group itself, that you do not wish to continue you are free to withdraw at any time without giving a reason.
What can I expect if I take part?
If you decide to take part you will be sent an invitation to a focus group to be held at [insert name of venue]. We will provide you with a date and time and give you as much notice as possible. When you attend for the focus group, a member of our team will be available to answer any questions about the study. If you are still happy to take part then we will ask you to complete and sign a consent form.
The focus group will last for approximately one and a half hours to two hours. It will be facilitated by a member of our team and there will be a note-taker present. The focus group will be recorded on a digital tape recorder. We are seeking the views of people like you on the care of older people in hospital with a particular emphasis on the work of HCAs. The discussion will be used in the development of a training course for HCAs working with older people in hospital.
We will provide light refreshments and travel costs will be reimbursed.
What are the possible risks/disadvantages of taking part?
The researcher will have experience of conducting focus groups to ensure participants are made to feel at ease. However, discussion about the care of older people may be upsetting if it directly or indirectly invokes a distressing experience. We only wish to hear the views that participants are comfortable in sharing within the group. If you find it difficult for any reason and would like to withdraw, you can do so at any time. However, anything that you have said within the group will be kept as part of the focus group data.
What are the possible benefits of taking part?
We cannot guarantee that the study will help you directly but we hope to learn from your experience and design of a training course that we anticipate will benefit health-care assistants and those they care for.
Will my taking part in the study be kept confidential?
We will keep your personal details (name, address and contact details) secure and this information will not be shared beyond members of the study team that you will meet. Everything you say/report is confidential unless you tell us something that indicates that you or someone else is at risk of harm. We would discuss this with you before telling anyone else. If we use quotes from the focus group discussion in any written reports, it will not be possible for individuals to be identified.
What if there is a problem?
If you are unhappy about the way the study is conducted you should contact (NAME).
Who is organising and funding the research?
The study is funded by the National Institute for Health Research via a research grant awarded to the University of East Anglia. The project is led by Professor Antony Arthur at the School of Nursing Sciences.
Further information and contact details?
[Details of centre-specific member of research team, researchers currently being recruited at each centre.]
Appendix 4 Focus group delivery guide
| Time frame (minutes) | What | Who | Where |
|---|---|---|---|
| 30 | Prior to the meeting ensure tables are arranged. Place name cards appropriately. Team interspersed around table. Try to ensure that more reticent participants are opposite the moderator so that they can be encouraged as required. Name cards should have names and patient or carer on both sides so that they can be seen by study team and by neighbouring participants (this may help to direct questions) | Team | Meeting room |
| 30 | Meet and greet (signpost people to loo and meeting room). Introduce yourself and your role for the day | Team | Reception |
| Take consent. Travel costs. Gift cards | Team | Reception and meeting room | |
| Try to ascertain any needs/special requirements | Team | ||
| Teas and coffees | Team | Meeting room | |
| 5 | Welcome and introduction | Moderator | |
| Map of room and broad note of who says what | Moderator | ||
| Introduction to focus group ground rules: everyone comfortable; OK to stretch legs/go to loo; permission to be tough regarding time; we want to hear from everyone; please be respectful of people’s views; group discussion; time out if needed; important that only one person speaks at any one time to facilitate transcription | Moderator | ||
| Introduce study. Check all consented. Permission to record | Moderator | ||
| 75 | Ask participants to tell us their name and whether their experience of hospital care was as a patient or a carer or both | Moderator | |
| Asking the main focus group questions | Moderator | ||
| Clarifying/probing/encouraging participation | Moderator | ||
| Time-keeping | Facilitator | ||
| Summarise main emerging points | Moderator | ||
| Check if all agree with summary | Moderator | ||
| 10 | Anything to add | Moderator | |
| Invitation to get in touch if want to add anything/ask any questions about focus group (give out researcher’s phone number) | Moderator | ||
| Thanks | Moderator | ||
| Thank you and signposting | Team | ||
| Hand out vouchers and travel expenses and get signed receipt | Team | ||
| X | Time for chat. Signpost to loo | Team | |
| Taxis, buses | Team | Reception |
Appendix 5 Focus group topic guide
This topic guide is based on that agreed by the team at Intervention Development Workshop Meeting 05062014 and used by King’s College London at their focus group on 6 June 2014. Sections of text shadowed in grey are sections which were omitted because of lack of time. It was agreed at Fieldwork Team Meeting 10062014 that all centres would omit these same sections if insufficient time to include them. The final question in this guide has been changed to reflect experience of King’s College London. It now asks specifically what single thing they would like to see included in the training.
Introductions (5 minutes)
Could we just go round the table and could you tell everyone your name, whether your recent inpatient experience was as a patient, a carer or both, and what hospital/hospitals that was in?
Settling in (10 minutes)
I’d like to start with a general question about what you think is important when an older person is first brought on to a new ward.
When an older person arrives on the ward, what should they be able to you expect from the staff who are caring for them?
In our discussion today we’d like to try and focus on the care you or your loved ones have received from HCAs.
[Specified team member to explain that HCAs are the people most likely to help patients with washing, dressing, getting to the toilet and so on]
Relational care
NOTE: at this point reiterate that what we are particularly trying to do is to develop training on kind and respectful care of older people in hospital
I’d like to take you back to when you/your loved one was in hospital. If you were the patient, can you take a minute to think about an instance when you felt really cared for by a HCA? And if you were visiting a family member, can you take a minute to think about an instance when you think the patient felt really cared for by a HCA . . .
Now, can you tell us what a member of staff did to make you feel that way? Or perhaps it was something they DID NOT do. (10 minutes)
And what about family members? What did staff do to make them feel cared about? (10 minutes)
[To patients only] What do you feel about the way members of their family were treated by staff on the ward? (5 minutes)
Seeing the person behind the patient (10 minutes)
The average length of stay in hospital for an older person is 11 days.
If that was you what kind of things would you expect the HCAs looking after you to know about you?
How would this help you feel cared for?
(If time) Can staff know too much do you think?
Training focus
It seems that the way you are treated in hospital can either make you feel ‘dealt with’ (in a negative way) or ‘cared for’. As you know, the aim of our study is to design a training package for HCAs working with older hospital inpatients to make sure we minimise ‘dealt with’ and maximise ‘cared for’ . . .
From your experience in hospital, what sort of things would you like to see included in our training? (10 minutes)
CLARIFY: Were there particular aspects of the way you were dealt with/cared for that you think HCAs should have had more training in?
We’ve been talking to HCAs and to ward sisters for this project. They told us things they think are important.
Specified team member to read through a list of prescribed examples supplemented by others that may have come up during the focus group and to prompt for comments at any that have not previously been mentioned. (10 minutes)
OK, now I’d like you to think about a time when you felt you were treated really well by an organisation (it may have been a shop, a bank, a restaurant, a hotel, an airline or whatever). (10 minutes)
What did the staff do to make you feel that way?
Is there anything we can learn from them that we could apply to staff working on wards?
[If time] What makes it easy to get help on a hospital ward?
What makes it difficult to get help?
Closing (10 minutes)
If you could choose just one thing we should include in the training we are developing, what would that be?
Thank you
Invitation to get in touch
Hand out patient advice and liaison service information for local trusts.
Appendix 6 Staff interview participant information sheet
Appendix 7 Staff interview expression of interest form
Appendix 8 Topic guide for staff member interviews
Welcome and introduction
Introduce yourself.
What the study’s about and aim of the study.
Details of the interview (duration; anonymity; confidentiality; audio recording).
Any questions?
Consent.
Work history
Just to give me a bit of background would you tell me . . .
How long have you been a HCA?
If you were working before you became a HCA, was there any aspect of your previous employment that helped prepare you for your work as a HCA in any way?
Has your HCA work always been in this trust?
Have you always worked in older people’s wards?
Training received
What training have you received since being a HCA at this trust?
Did you have to take that training or was any of that voluntary?
Are there any difficulties with accessing or doing any of the training?
What parts of the training have you found most useful in your work?
(If they mention compassion/dignity, etc., ask what that training consisted of and what form it took.)
(If they mention dementia/delirium training ask what that training consisted of and what form it took.)
* [If they haven’t mentioned this above] Have you had any training that deals with the way you relate to patients? Can you tell me more about that?
* Were there any particular training sessions that really stayed with you? (If so) Can you tell me a bit more about that?
I know the training consists of a mix of talks, DVDs, questionnaires, demonstrations, e-learning and so on.
* What style of delivery do you find helps you learn the best?
Sometimes it’s difficult to put all the training you have into practice, especially about getting to know patients and making them feel cared about.
Have you faced any barriers or difficulties in that respect?
What helps you to put your training into practice?
Is there anything else you’d like to say about training you’ve received?
Feelings about working as an health-care assistant
What do you find most challenging about your role as a HCA?
[If don’t mention challenges with patient group ask about that as a follow-up. If they ONLY mention patient group ask whether there are any other types of challenges (such as work relations or work conditions).]
What can HCAs do to make a patient feel cared about?
And what are the conditions necessary to achieve that?
And having a loved one is hospital can also be distressing for family members and friends. Is there anything HCAs can do to make them feel better?
Thinking about all the different patients that you see on the ward, do you think that you adapt the ways you care for them because they have different characteristics and backgrounds? [Probe on what the differences are and what the different approaches are.]
[Along with what you’ve just told me] Our interviews and other research have shown that working as a HCA involves a number of stressful situations – heavy work; challenges in the older patient group; upset families; dealing with distress, anger, death; staffing issues and so on.
Is that something that training could help with?
Have you come across any useful training around this?
Getting to know older people
How well do you tend to get to know the patients in the ward?
Do you think it would be helpful to know patients a bit better?
What helps you to get to know your patients?
[Prompt: Are there any tools you’ve come across that help? What about photos by the bedside?]
What gets in the way of getting to know older patients?
Customer care
*OK, now I’d like you to think about a time when you felt you were treated really well by an organisation (it may have been a shop, a bank, a restaurant, a hotel, an airline or whatever). What did the staff do to make you feel that way?
Is there anything we can learn from them that we could apply to health-care delivery?
Feedback on outline intervention training
-
The aim of this study is to develop and test some training for HCAs that focuses on ‘relational care’. This might be described as making people feel cared about; seeing the person behind the patient. We’ve talked to older patients and their carers, and we’ve also been using earlier interviews with HCAs and OS, to start to outline what that training package might look like. The interview we’ve just done will help with that. But it would be very helpful if I could take this opportunity to get your direct feedback on our ideas to date. Is that OK?
-
[Give them the handout (attached separately) and ask them to look at it. Ask what their general thoughts are? Ask about each element (title, topics, timing, etc.). Ask if they think there’s anything important missing.]
Would you be interested in going on training of that kind? (If not, why not?)
What about your colleagues; would they? (If not, why not?)
Ending
Thank you very much. I’ve finished my specific questions. Is there anything you’d like to add?
Appendix 9 Excerpts from trainee course book
Excerpt from unit 1
Excerpt from unit 2
Excerpt from unit 3
Appendix 10 Excerpts from trainer guide
Appendix 11 Guide for researchers training Older People’s Shoes trainers
Lunch and refreshments to be provided. The face-to-face training session should take place in a room that has an internet-enabled computer. A follow-up session which may be either face to face or remote will be offered so that any queries can be raised and resolved prior to HCA training sessions.
Training guide
| Section | Completed |
|---|---|
| Introduction |
|
| Research context |
|
| Background to the course |
|
| Relational care: what is it? |
|
| Rationale for developing HCA training in relational care |
|
| How the course developed |
|
| Underlying course values |
|
| Learning style |
|
| Teaching style |
|
| Course overview |
|
| Course materials |
|
| Online resource |
|
| PowerPoint files |
|
| HCA course book |
|
| Trainer guide |
|
| Content of the training course |
|
| Course overview |
|
| Before you start |
|
| Introduction |
|
| Day 1: unit 1 – getting into older people’s shoes |
|
| Day 1: unit 2 – getting to know older people |
|
| Day 1: unit 3 – learning from customer care |
|
| Take-home exercises |
|
| Day 2: unit 4 – getting into older people’s shoes |
|
| Day 2: unit 5 – getting to know older people |
|
| Day 2: unit 6 – learning from customer care |
|
| Closing section |
|
| In the case of technical problems? |
|
Training record for trainers providing health-care assistant training
| Section | Completed |
|---|---|
| Background to the course | |
| Relational care: what is it? | |
| Rationale for developing HCA training in relational care | |
| How the course was developed? | |
| Underlying course values | |
| Learning style | |
| Teaching style | |
| Ground rules | |
| How to use the training resources | |
| Online access to visual resources for trainers and HCAs | |
| PowerPoint resource files | |
| HCA course book | |
| Trainer guide | |
| Content of the training course | |
| Course overview | |
| Introduction | |
| Day 1: Unit 1 – getting into older people’s shoes | |
| Day 1: Unit 2 – getting to know older people | |
| Day 1: Unit 3 – learning from customer care | |
| Day 2: Unit 4 – getting into older people’s shoes | |
| Day 2: Unit 5 – getting to know older people | |
| Day 2: Unit 6 – learning from customer care | |
| In the case of technical problems? | |
Appendix 12 Health-care assistant trial participation information sheet
Appendix 13 Patient trial participant information sheet
Appendix 14 Health-care assistant questionnaire
Appendix 15 Patient questionnaire
Appendix 16 Sensitivity analysis for health-care assistant outcomes at 8 weeks using cluster summary approach (intention to treat)
| Outcome | Unadjusted | Adjusted | ||
|---|---|---|---|---|
| Mean difference (Older People’s Shoes – TAU) (95% CI) | p-value | Mean difference (Older People’s Shoes – TAU) (95% CI) | p-value | |
| TEQ | 0.44 (–5.08 to 5.96) | 0.8626 | –2.21 (–5.23 to 0.80) | 0.1332 |
| AGED goodness | 0.01 (–0.58 to 0.60) | 0.9713 | 0.11 (–0.47 to 0.68) | 0.6818 |
| AGED vitality | –0.03 (–0.56 to 0.51) | 0.9176 | 0.01 (–0.54 to 0.56) | 0.9647 |
| AGED maturity | –0.03 (–0.50 to 0.45) | 0.9064 | 0.28 (–0.15 to 0.70) | 0.1763 |
| AGED positivity | 0.08 (–0.33 to 0.49) | 0.6631 | –0.01 (–0.72 to 0.70) | 0.9736 |
Appendix 17 Sensitivity analysis for health-care assistant outcomes at 12 weeks using cluster summary approach (intention to treat)
| Outcome | Analysis | |||
|---|---|---|---|---|
| Unadjusted | Adjusted | |||
| Mean difference (Older People’s Shoes – TAU) (95% CI) | p-value | Mean difference (Older People’s Shoes – TAU) (95% CI) | p-value | |
| TEQ | 4.46 (–1.99 to 10.92) | 0.1544 | –0.19 (–3.81 to 3.43) | 0.9105 |
| AGED goodness | 0.28 (–0.45 to 1.01) | 0.4114 | –0.38 (–0.18 to 0.93) | 0.1603 |
| AGED vitality | 0.09 (–0.52 to 0.70) | 0.7542 | –0.09 (–0.52 to 0.70) | 0.7618 |
| AGED maturity | –0.03 (–0.60 to 0.55) | 0.9172 | 0.02 (–0.47 to 0.42) | 0.9027 |
| AGED positivity | 0.11 (–0.42 to 0.64) | 0.6513 | 0.07 (–0.27 to 0.41) | 0.6691 |
Appendix 18 Sensitivity analysis for patient outcomes using cluster summary approach (intention to treat)
| Outcome | Older People’s Shoes | TAU | Mean difference (Older People’s Shoes – TAU) (95% CI) | p-valuea |
|---|---|---|---|---|
| PEECH total | 2.40 (0.32) | 2.46 (0.31) | –0.06 (–0.67 to 0.55) | 0.820 |
| PEECH security | 2.56 (0.40) | 2.57 (0.32) | –0.01 (–0.71 to 0.69) | 0.971 |
| PEECH connection | 1.63 (0.32) | 1.96 (0.57) | –0.32 (–1.27 to 0.62) | 0.420 |
| PEECH knowing | 2.56 (0.38) | 2.44 (0.47) | 0.12 (–0.75 to 0.98) | 0.743 |
| PEECH person value | 2.50 (0.27) | 2.52 (0.29) | –0.03 (–0.58 to 0.53) | 0.910 |
| EQ-5D utility | 0.61 (0.19) | 0.46 (0.19) | 0.15 (–0.21 to 0.52) | 0.324 |
Appendix 19 Older People’s Shoes training intervention observation template
Observation grid: Older People’s Shoes
The aim of Older People’s Shoes is to improve the ‘relational care’ that HCAs provide for older inpatients. To this end we are interested in capturing observations about:
-
relational care
-
HCA learning
-
course delivery.
These observations are to help us improve the training as we go and for future development. They are also valuable data for our analysis and write-up of the study. In the observation grid please write comments and give examples. Please take down quotes from HCAs and mark with a Q in the margin.
Things to look out for re: relational care
Is the term ‘relational care’ problematic? What (other) words do HCAs use? (At what point) does the term relational care enter the vocabulary of the HCAs?
At what points in the course is relational care kept in clear focus? Where does it get lost? What makes relational care slip in/out of focus?
Things to look out for re: learning
Give examples of HCAs talking about examples of relational care/building on discussion points/missing the point/losing the thread.
Do participants seem clear about what relational care is? At what point(s) is a grasp of relational care achieved?
Which activities seem to work best in terms of learning? (Give examples of participant engagement – contributions to discussions; flip chart brain storming; ideas and anecdote sharing or obvious times/some participants where this is not happening.)
What conditions appear to help/hinder learning?
Things to look out for re: course delivery
Does the trainer appear to ‘get’ the point of the training? (e.g. do the key messages emerge for each activity? Does the trainer manage to bring discussions back to relational care? Would you expect the learning goals for each session to have been met?)
In order to facilitate learning we are aiming to make the tenor of the group participative and not didactic. Can you give evidence for this?
Does the trainer appear to uphold the assets-based values underpinning the training? (Give examples)
Fidelity of implementation – How closely does the trainer stick to the manual? In what respects? Please mark timings per activity on the grid below, where indicated.
Appendix 20 Older People’s Shoes health-care assistant learner evaluation form
Older People’s Shoes Evaluation questions for health-care assistants: day 2
Please help us by completing this form. For each question please circle the closest answer, and wherever you can please tell us more about your answer.
Appendix 21 Trainer interview participation information sheet
Appendix 22 Trainer interview topic guide
Topic guide for postintervention interviews with trainers who delivered the training
Thank you for agreeing to be interviewed. Your comments will help us to judge the acceptability and feasibility of the training, and could help us to improve the training. Just to remind you that anything you tell us will be treated in confidence, and all data will be anonymised. Do you have any questions about this interview before we begin?
Training and support to trainer
-
Did you feel confident that you understood the purpose of the Older People’s Shoes training programme?
-
[Recap on any feedback on the trainer manual already given by the respondent] Do you have any further suggestions on how could we can improve it to make it easier to use?
-
Did you feel confident in delivering the training programme? (If so what helped, if not what could we have done to support you more?)
-
Did you have previous experience of delivering something similar in terms of the style of learning used in Older People’s Shoes – 2-day, day-long, group size, interactive, peer-to-peer learning, shared discussion, reflection).
-
Did you have previous experience of delivering something similar in terms of the subject matter?
-
[Recap on pre-course training and support. This will include initial meeting to recruit trainers, Train-the-trainer sessions, any feedback after each day, all other e-mail/phone support]. Do you have any suggestions for improving the training or support you received in order to deliver the programme?
-
There was some practical input on the training days from the researcher(s) [and the other Practice Development Nurse] (setting up the room, putting up signs, welcoming participants, sorting out IT and catering, etc.). Do you think this course could be delivered without any additional help? (If not) what help do you think would be needed?
Course content
-
Were there sections or elements of the training programme that you felt didn’t work very well? Can you tell me more about that/those?
-
What sections or elements of the training programme did work well? Which bits do you feel the HCA trainees engaged with most?
-
Do you have any comments on the e-learning resource?
View of impacts on practice
-
What are your thoughts on the relevance of the training to HCAs working with older patients?
-
Do you know whether the training has had any impact on HCAs’ practice?
Suggested improvements
-
Are there any other steps you think we could take to improve it? (Prompts: title?/timetabling/number of days, gaps, rostering/support from research team/participants manual?, etc.)
-
Is there anything else you’d like to say about the training?
Thank you for your time.
Appendix 23 Health-care assistant learner interview participant information sheet
Appendix 24 Health-care assistant learner interview topic guide
Topic guide for postintervention interviews with health-care assistants who undertook the training
Thank you for agreeing to be interviewed. Your comments will help us to judge the acceptability and feasibility of the training, and could help us to improve the training. Just to remind you that anything you tell us will be treated in confidence, and all data will be anonymised. Do you have any questions about this interview before we begin?
Expectations
-
What were your thoughts about the Older People’s Shoes training before you came on the course?
-
What (if anything) did you hope to learn or practice during the training?
Course content and delivery
-
What did you enjoy the most?
-
Was there any of it you think we should cut?
-
Was there any topics you’d have liked more on?
-
Or anything else we should have covered?
-
The course included periods of watching and listening; reflection; discussion; sharing knowledge and experience; and doing. Do you feel the balance was about right? If not, what would you have wanted more/less of?
-
What about the timing of the course? Pace? Length of day? Number of days? Gap between days?
-
Have you accessed the e-learning at all? (If not) Why was that? (If yes) Between training days and/or since? Which elements did you look at? Was it easy to use? Was it useful?
View of impacts on practice
-
Overall what do you think you’ve gained from the course?
-
Has being on the course made any difference to the way you feel about older patients?
-
Has being on the course made any difference to the way you feel about your work?
-
Have you managed to put anything you learned into practice? (If so) Can you tell me more about that?
-
Has it been difficult to put any of it into practice? (If so) Can you tell me more about that?
Suggested improvements
-
We used the term ‘relational care’ in the training. Do you think that’s a useful term to describe what we were talking about? Is there a better term you can think of?
-
We’re looking at any ways we could improve the course if we run it again. Do you have any (other) suggestions? (Prompt if necessary re: what do you think of the title? Course book? Timetabling? Number of days? Gaps? Rostering? Did it cause you any difficulties attending the training?)
-
Is there anything else you’d like to say about the training?
Thank you for your time.
Appendix 25 Observed fidelity to training intervention
| Issue type | Observed in (order of site in delivering training) | Observed fidelity | Mitigating actions undertaken (if any) | Proposed resolution prior to definitive study |
|---|---|---|---|---|
| IT | All | Trainers varied in their ability to navigate the IT resources | Some help provided by researcher | Address in Train the Trainer (ensure all resources clearly explained, demonstrated and tested by trainer) Simplify resources (replace with ‘one-stop’ navigation; streamline Prezi presentation/replace with PowerPoint) |
| Practicalities | All | Timings for some sessions over-ran | Timetable refined between each cohort at first site, and between first and second site | Address in Train the Trainer (some flexibility acceptable, but allowing earlier units to over-run leaves inadequate time for later units) Amend trainer manual to flag time issue more clearly |
| First and second | Not all HCAs were good at returning on time after breaks | Trainer added punctuality request into ‘housekeeping’ | Amend trainer manual to include housekeeping (including punctuality) Adjust timetable slightly |
|
| Third | Not all resources (flip chart, hospital foods, pastoral care leaflets) were provided at earlier sessions | Researcher ensured all resources available at later sessions | Address in Train the Trainer (provide trainers with printable tick lists for resources for each session) | |
| Second | Poor sound and visual quality of videos due to IT and room issues | Ensure audio-visual equipment in training rooms is appropriate | ||
| Delivery | First and second | Diversion into grievances of HCAs sometimes waylaid discussions | Ways of managing given in feedback to trainer | Address in Train the Trainer (provide tactics to bring sessions back into focus) |
| Second | Modelling of welcome to HCAs was below optimal | Feedback given to trainer | Address in Train the Trainer (stress the importance of modelling a good welcome) | |
| Second and third | Insufficient direction on what to look for in video clips prior to viewing | Addressed in feedback from researcher | Address in Train the Trainer and amend trainer manual to make this more prominent | |
| Second | Take-home exercises and the benefits of their completion insufficiently explained | Address in Train the Trainer | ||
| Divergence from manual | Third | Not all HCAs signposted to online resource | Amend Train the Trainer and trainer manual to include | |
| Second and third | Introduction and wrap up for the whole training intervention (introduced after first day at first site) not always delivered/delivered in full | Trainers reminded to deliver introduction and wrap-up ‘scripts’ | Address in Train the Trainer (stress importance of introduction and wrap up for rationale and underlying values of the training) | |
| Second and third | ‘Set-up’ explanation (outlined in training manual), not always used at the start of each topic/activity | Address in Train the Trainer (stress importance of this for orientating learners to the activities and delineating different activities) | ||
| All | HCAs not always told that talking heads were real patients | Trainer reminded to point this out | Address in Train the Trainer (stress value of this to HCAs) | |
| First and third | Input from HCAs not always recorded on flipcharts where instructed | Trainer reminded of this | Address in Train the Trainer (Stress value of this in demonstrating the value placed on HCAs’ knowledge and contribution) | |
| Third | Some activities missed out, and the order of activities sometimes changed | These were pointed out to trainer | Ensure trainers have sufficient time to familiarise themselves with the training. Provide a one-page schematic for trainers to use as a road map of the structure of the training intervention | |
| Third | In unit 1.4.2 (‘Today Is Monday’ video clips) HCAs were encouraged to view the video critically, watching out for examples of poor as well as good practice | Consider amending trainer manual to include this prompt | ||
| Second | Trainer included a flipchart exercise after unit 2.3 (Maud’s biography illustrating challenges and benefits to old age) to summarise the points made. This seemed to work well | Consider adding to training intervention | ||
| Second | At unit 2.4 (benefit of getting to know patients) trainers added questions after each of the quotes and this worked well | Consider adding to training intervention | ||
| Second | At unit 2.4 HCAs gave examples of a variety of cultural issues important to some patients. Useful | Consider adding to training intervention | ||
| Second | Trainer used term ‘service user’ in place of ‘customer’ at places where patients referred to. Worked well | Consider adding to training intervention | ||
| All | Non-completion of take-home exercises | Trainers asked HCAs to draw on past experiences | Train the Trainer already suggests trainers to ask any HCAs who have not completed take-home exercises to draw on past experiences |
Appendix 26 Summary of lessons for improving the training intervention from course observations
| Issue type | Order of site in delivery of training | Lessons learned | Proposed resolution prior to definitive study |
|---|---|---|---|
| Practicalities | First and third | Location of training venue has implications for HCAs finding it and for getting materials there | Optimal training venue is close to wards, familiar to HCAs and has storage facility |
| All | Important to establish ground rules (e.g. giving everyone opportunities to speak, respecting others’ views, punctuality) | Amend trainer manual to include | |
| First and third | Lunch and coffee should both be earlier on day 1 | Amend timetable | |
| Second | Helpful to have flipchart sheets already prepared with titles and layout | Amend Train the Trainer to include in guidance and resource list | |
| Delivery | All | Some trainers were particularly good at holding aloft the key messages of the training (as outlined in Train the Trainer). It could be helpful to trainers to be given three memorable key messages | Amend Train the Trainer and trainer manual to include three punchy key messages |
| Second | Training run as a two-hander in site 1 worked well. Kept it dynamic. Useful for smooth transitions with IT | Consider using two trainers but also need to consider resource implications | |
| First | More guidance needed for trainer re: message of unit 1.4.1 (on empathic listening) and issue that may arise | Address in Train the Trainer (clarify message re: empathy/sympathy) and amend trainer manual re: guiding discussion | |
| Second | Less than optimal use of excellent examples given by trainees | Address in Train the Trainer (include guidance on using HCAs examples and referring back to HCA input) | |
| Second | Trainers did not always sufficiently probe or challenge HCAs’ responses | Address in Train the Trainer | |
| First and second | Some delivery very close to the text but insufficiently engaging | Address in Train the Trainer (include guidance on the need to balance fidelity to the message of the text with engaging delivery) | |
| First and second | Trainer’s expertise in managing discussions was variable | Address in Train the Trainer (include guidance on the use of prompts to discussion, managing group dynamics, allowing time for reflection, using open questions, keeping discussion focused on topic) | |
| Course content | Third | Need for greater clarity in the use of the term ‘relational care’ and its relationship to similar terms such as ‘relationship-/person-centred care’ | Consider amending Older People’s Shoes to include discussion on this |
| First | Relevance to HCAs provision of relational care needs to be clearer in unit 2 | Amend Older People’s Shoes to draw out relevance | |
| First and third | Trainers unsure how to run the activities in units 2.2 (Prezi on personal, social and historic timelines of older people), 6.3 (understanding ‘difficult’ patients and 6.4 (role-play on managing anger) | Amend trainer manual to include clearer instructions | |
| Third | Some older participants felt that unit 2.3 (Maud’s biography illustrating challenges and benefits to old age) presented older age in an overly negative way | Amend Older People’s Shoes to change balance between benefits and challenges of old age | |
| All | Units 3 and 6 (customer care) introduction too text-dense for optimal delivery | Amend trainer manual and HCA course book | |
| First | Units 3 and 6 (customer care) need tightening in terms of repetition | Amend Older People’s Shoes to excise repetition | |
| All | In unit 3.2 (discussions of own customer care experience) need to draw out ‘How did that make you feel?’ | Amend trainer manual and HCA course book to include this prompt | |
| First | Unit 3.3 (relevance of customer care to HCAs’ work on the ward) needs to have louder message re: its stated purpose | Amend Older People’s Shoes to draw out relevance |
List of abbreviations
- ACE
- Active Caring for Everyone
- AGED
- Age Group Evaluation and Description
- AWES
- Assessment of Work Environment Scale
- CHAT
- Can Health-care Assistant Training improve the relational care of older people?
- CI
- confidence interval
- EQ-5D
- EuroQol-5 Dimensions
- EQ-5D-5L
- EuroQol-5 Dimensions, five-level version
- EQ-VAS
- EuroQol visual analogue scale
- HCA
- health-care assistant
- IT
- information technology
- OPSWISE
- Older People’s Services and Workforce Interventions: a Synthesis of Evidence
- OS
- other staff
- PEECH
- Patient Evaluation of Emotional Care during Hospitalisation
- PPI
- public and patient involvement
- PPIRes
- Public and Patient Involvement in Research
- QUIS
- Quality of Interaction Scale
- SD
- standard deviation
- TAU
- training as usual
- TEQ
- Toronto Empathy Questionnaire