Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 11/1024/06. The contractual start date was in March 2013. The final report began editorial review in March 2016 and was accepted for publication in September 2016. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2017. This work was produced by Völlm et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction
Forensic psychiatry is a subspecialty of psychiatry that operates at the interface between law and psychiatry. It is concerned with patients who have committed an often serious offence and may be detained in highly restrictive secure settings. The purpose of this detention is twofold: care for and treatment of the patient (i.e. to improve mental health and facilitate recovery) and protection of the public from harm from the offender (i.e. reduce the risk the patient poses). This dual function can cause tensions and dilemmas for the practitioner, who has potentially incompatible duties to the patient, to third parties and to the wider community. 1–4 These tensions remind us that the social and political context is crucial in medical decision-making generally, and even more so in the field of forensic psychiatry. For example, several authors have noted the current risk-aversive narrative in European and US societies, driving psychiatric practice to become more and more restrictive and potentially leading to increased lengths of stay (LoS) in forensic psychiatric settings. 5
Detention of mentally disordered offenders
The detention of mentally disordered offenders (MDOs) in the UK is regulated by a complex set of laws and regulations, of which mental health legislation, namely the Mental Health Act (MHA) of 1983,6 amended in 2007, is the most relevant. Unlike in other European legislations, which require reduced responsibility as a prerequisite for a person’s entry into the forensic psychiatric system, detention of MDOs in forensic settings in England and Wales is independent of criminal responsibility and determined solely on the basis of the person’s mental condition at the time of sentencing or transfer. The criteria for the detention of MDOs according to section 37 (hospital order: an order made by the court at the time of sentencing) of the MHA are, therefore, similar to those for non-offending patients under section 3 (admission for treatment) of the Act. MDOs may be detained if ‘the offender is suffering from a mental disorder . . . of a nature or degree which makes it appropriate for him to be detained in a hospital for medical treatment and appropriate medical treatment is available’. 6 Prisoners who are sentenced to a prison sentence can later be transferred to a forensic psychiatric facility, even years into their sentence,6 according to similar criteria. No further stipulation is made with regard to the nature or level of risk posed. The requirement of ‘appropriate treatment’ being ‘available’ has been interpreted as being met by very limited therapeutic input (e.g. nursing care only) or when a patient refuses to engage as long as the therapy is ‘available’. 7–9 There is no proviso that treatment offered has to be effective for the individual patient.
Detention in forensic care is generally not time-limited, and discharge depends on whether or not the individual is deemed to have made sufficient progress that they no longer present a risk. Discharge and transfer (e.g. to a less secure facility) is governed by a number of bodies (responsible clinician, hospital managers, mental health tribunals, Ministry of Justice) without further involvement of the sentencing court. The advantage of this framework is that it allows access to psychiatric care for those in need at any time. On the other hand, the fact that individuals with full criminal responsibility may be – and often are – held well beyond the time they would have been incarcerated had they received a prison sentence as a non-mentally-disordered individual, and the involvement of a political body in decision-making about discharge, are ethically problematic. 10
Services for mentally disordered offenders in the UK
Forensic psychiatric services may be provided in different levels of security – high, medium and low secure – as well as community forensic psychiatric services. High secure services cater for patients who ‘require treatment under conditions of high security on account of their dangerous, violent or criminal propensities’11 and ‘pose a grave and immediate danger’,12 medium secure services are for those presenting ‘a serious danger to the public’12 and low secure services are for those ‘who pose a significant danger to themselves and others’. In addition, ‘enhanced’ medium secure services are provided for women ‘who require enhanced levels of intervention and treatment . . . and for whom current medium secure services are not appropriate’. This tiered system has developed historically as described below; it allows – in theory – movement along a ‘treatment pathway’, where individuals move from more to less restrictive settings. Such provision in the least restrictive setting is essential not only for legal and ethical reasons but also for financial reasons. Forensic psychiatric services are high-cost, low-volume services: in England and Wales bed costs for high secure provision are approximately £275,000 per annum per patient; in medium secure care this figure is about £175,000. Forensic care consumes £1.2B per annum, 1% of the entire NHS and 10% of the mental health budget. 12–14
In the UK, the first forensic service was Broadmoor Hospital in Berkshire, which opened in 1863. Two other high secure hospitals opened in the 20th century: Rampton Hospital in Nottinghamshire in 1912, and Ashworth Hospital in Merseyside in 1990 (although this was formed through the merger of two existing services with a much longer history). Until the 1970s, these three high secure hospitals were the only provision for secure care in the UK. This brought with it challenges for rehabilitation, both because of the geographical distance of these services from patients’ home areas and due to the large gap in security between high secure care and general adult provision with nothing in between. Forensic service provision was, therefore, made subject to a review, and the Butler Committee15 subsequently recommended that smaller and more local ‘regional secure units’ (later to be known as medium secure units) be developed. The first such unit was opened at the end of the 1970s, and by the mid-1980s full national medium secure provision had been established. Medium secure beds are provided by the NHS but also (just under 50%) in the independent sector,16 which may provide for individuals with diagnoses/presentations for which there is insufficient capacity within NHS services.
Given these refigurations, it is not surprising that bed numbers in high and medium secure care have fluctuated, although, notably, the overall number of secure beds has risen. Security has also been tightened, partly due to specific concerns and high-profile inquiries (e.g. the Fallon Inquiry)17 and partly due to a less tolerant and more security-conscious attitude in society as a whole. Bed numbers in high secure care reached their peak in 1973 – before the introduction of medium secure services – with 2300 beds. By the beginning of the 1990s, there were 1700 high and 600 medium secure beds. 16 The latest figures are just under 800 beds in high secure care and just under 3200 for medium secure care. 12 A significant factor in the shift from high to medium secure care was the implementation of the ‘accelerated discharge programme’, as described below. 18
Management and commissioning of secure care
Arrangements for commissioning services for secure care have changed considerably over the years. 17 For high secure services, responsibility moved gradually from the Home Secretary to the Ministry of Health, which centrally managed the three high secure hospitals until the 1980s. From 1989 to 1996, this function was performed by the Special Hospitals Service Authority before full integration of the three ‘special’ hospitals into NHS trusts. The Department of Health11 maintains close oversight of these institutions, however, and issues the Directions on Safety and Security and visits by children to high-security psychiatric services. These Directions outline policies and procedures to be followed in running such hospitals (e.g. screening of visitors, possessions allowed in rooms, search procedures, mail monitoring). No equivalent document exists for medium secure care, although best practice is described in the Department of Health Best Practice Guidance. 19 The Quality Network for Forensic Mental Health Services, led by the Royal College of Psychiatrists College Centre for Quality Improvement, also issues Medium Secure Standards20 supported by NHS England, which are reviewed through self- and peer-review. These arrangements are voluntary, but most medium secure providers participate.
Each of the three high secure hospitals serves a defined catchment population for men diagnosed with a mental illness or personality disorder (PD). Only Rampton Hospital caters for women, patients with intellectual disabilities and deaf patients in high secure care. In addition, at the time of the study, services for individuals with so-called dangerous and severe PDs were operational at Rampton Hospital. These specialist services are national services. All NHS medium secure units cater for their catchment area’s mentally ill patients, although not all accept women, individuals with PDs or those with intellectual disabilities; for such patients, commissioners will identify other services, including those outside the catchment area or in the independent sector.
Secure care, like other ‘specialised services’, is commissioned by NHS England nationally (unlike other products that are commissioned through the 209 Clinical Commissioning Groups) through a complex set of arrangements. Secure care comes under the Mental Health National Programme of Care,21 which develops clinical strategies and expected outcomes for the services under its umbrella. Clinical advice on service specifications, commissioning policies, innovation and quality is provided to the National Programme of Care through topic-specific Clinical Reference Groups (relevant here is mainly the high and medium secure Clinical Reference Group, which feeds into the forensic pathway group, which was ‘formed to provide oversight for all secure services and to ensure consistency of approach and effective pathway planning’). 22 Clinical Reference Groups are constituted by clinicians, service users, commissioners and trust representatives. In addition to these structures, there are four regional teams that contract services informed by the specifications developed by the Clinical Reference Groups.
Treatment in secure care and outcomes
Forensic psychiatric services deal with individuals with complex histories, psychopathology and needs. More often than not, these patients have histories of emotional, physical and/or sexual abuse, neglect, deprivation and changes in caregivers. They frequently show early behavioural problems, substance abuse and offending. Their psychopathology is not easily assigned to just one of the International Classification of Diseases23 or Diagnostic and Statistical Manual of Mental Disorders24 categories; comorbidity between so-called serious mental illness (such as schizophrenia or bipolar disorder) and PDs is common. Given this complexity, it is not surprising that rigorous evidence of ‘what works’ in secure care is limited. 25 Interventions typically tackle a range of treatment needs, and may include pharmacological, individual and group psychological interventions to improve symptoms as well as to reduce risk (e.g. of violent and sexual offending). More than in other areas of psychiatry, the therapeutic milieu, with clear structures and boundaries, 24-hour nursing care, prosocial modelling, occupational activities, etc., plays a crucial role, and these more general aspects are almost impossible to disentangle from specific, time-limited psychological interventions. Despite these challenges, some evidence has emerged for the effectiveness of pharmacological interventions, psychoeducation and cognitive–behavioural approaches in high secure care, and reoffending rates following discharge from secure care are more favourable than those following release from prison (for a recent review see Fazel et al. 25).
Long stay in forensic settings
Concerns that a number of patients stay for too long in levels of security that are too high were first raised following studies in the 1990s, based on assessments by the patients’ own teams as well as independent multidisciplinary reviews, highlighting that between one-third and two-thirds of patients resident in high secure settings do not require that level of security (e.g. Maden et al. ,26 Reed,27 Pierzchniak et al. 28 and Thomas et al. 29). The inadequate provision of beds in less secure settings and inefficiencies in the system of transfer/discharge were thought to be significant factors in the delayed transfer of patients to more appropriate levels of security. The Tilt Report, commissioned to review the security at all three English high secure hospitals, also concluded that about one-third of the patients could be safely managed in lower levels of security. 30 These findings led to the establishment of a national ‘accelerated discharge programme’, which ran from 2002 to 2004 and led to the move of 400 patients and the reduction in high secure beds. At the same time, there were discussions regarding a need to open ‘long-stay’ services for some of these patients identified as requiring longer-term, but not necessarily high secure, care, and a small number of such wards were commissioned. Similar issues have been raised again in the recent high secure capacity review (E Kane, J Cattell, A Raza, C Duggan, R McDonald, University of Nottingham, 2015, unpublished report, available from the author on request only), with calls to independently review patients who fulfil certain criteria in relation to age and LoS.
There are three main methods to measure LoS. 31
-
Admission sample: all patients admitted during a particular period are included and their LoS calculated from admission to discharge.
-
Census sample: all patients resident in the setting of interest on a particular date. LoS is calculated from their date of admission to this point.
-
Discharge sample: including patients discharged during a particular period. LoS is calculated from their date of admission to this discharge date.
Most of the studies on LoS have used discharge samples (i.e. comparing cohorts with longer and shorter LoS to determine their different characteristics). This method has many advantages, including the relative ease with which such samples can be obtained, the calculation of ‘true’ LoS (completed care episodes) and the consistency of the legal and policy context at time of discharge. However, this method is less suited to predict factors that affect LoS, as there will be a number of confounders as a result of different admission criteria at the different times of admission in the cohort. Obviously, if one is interested in the characteristics and needs of patients who remain in the system and may have little prospect of discharge, then a census sample is the most suitable method, which is why this method was chosen for our study. The most significant drawback of this method is that it does not include completed care episodes and is, therefore, less suited to identifying factors predictive of LoS.
There is no accepted standard for LoS in either high or medium secure care. For medium secure care, the original guidance from government, based on the recommendations in the Glancy32 and Butler15 reports, suggested an upper limit of LoS of 2 years. However, a number of studies have demonstrated that this LoS is far exceeded in a large proportion of cases (see literature review in Chapter 4). For high secure care, earlier studies have identified an average LoS of about 8 years33 but, again, no shared standard exists as to from what LoS onwards individuals should be considered ‘long-stay patients’.
Length of stay in forensic psychiatric settings far exceeds that in general psychiatric services, although only a few studies have compared these two settings directly. A recent study,34 based on a 1-night census of a catchment area of a 1.2 million population in North London in 1999, found a median LoS of 79 days in non-forensic beds, whereas for forensic settings this figure was 1367 days. Of general psychiatric patients, 23.4% stayed for > 1 year and 17.9% stayed for > 5 years, whereas the corresponding figures for forensic patients were 81.2% and 39.1%, respectively. For high secure care, research in England has found an average LoS of about 8 years, and about 15% stay for ≥ 10 years. 35 International studies36 have found figures – at first glance – of comparable magnitude, with an average LoS of around 10 years, although these figures are based on the end point of discharge into the community, whereas in England the LoS in settings of different security levels have to be added up to calculate overall LoS in secure care.
Research identifying the factors associated with long stay and the characteristics and needs of those who stay in secure care for extended periods of time is limited, although some important insights have been gathered. One early study at Broadmoor Hospital33 identified severity of index offence as the most important factor for personality disordered patients, while for those with mental illness, psychopathology was a more relevant predictor of LoS. Studies in medium secure settings have identified severity of psychopathology, psychiatric history, seriousness of offending, patients being on ‘restriction orders’ (requiring Ministry of Justice permission for transfer), non-engagement in interventions, dependency needs and lack of step-down facilities as factors associated with long stay. 37–42 (See Chapter 4 for a full review of factors.)
Patients’ experiences
It is now widely accepted that obtaining the views of the recipients of health care is an essential element in the evaluation of mental health services. However, the evaluation of forensic mental health services is one area in which this principle has not been widely applied. A number of studies have explored the needs of service users in forensic settings from staff perspectives (e.g. Reed and Lyne43 and Jacques et al. 38). There has, however, been a shift away from using the views of professionals towards accessing and representing the views of recipients of care. 44
A considerable number of quantitative and qualitative studies, both UK based and international, have explored forensic patients’ experiences and perspectives relating to a range of topics surrounding their stay in forensic secure care. A substantial number of quantitative studies have used standardised measures to measure forensic patients’ perspectives on, for example, quality of life (e.g. Walker and Gudjonsson45 and Swinton et al. 46), service satisfaction (e.g. Ford et al. 47 and Bressington et al. 48) and recovery (e.g. Green et al. 49). The use of standardised measures to measure forensic patients’ satisfaction/quality of life/needs within services provides an opportunity to identify and prioritise patient-centred issues for future service development (e.g. Walker and Gudjonsson45). Data collected from these standardised measures can also generate estimates of resources required while representing an evidence-based approach to planning effective forensic psychiatric health care. 50
There has, however, been some scrutiny of studies using standardised measure questionnaires when exploring participants’ perspectives. For example, Rankin51 raised concerns with regard to studies using patient satisfaction surveys, which tend to favour the agenda of those asking the questions and often fail to account for what aspects of services those using the services are most satisfied and dissatisfied with. Swinton et al. 46 argued that it is important to explore patients’ subjective perspectives on what quality of life means to them without the use of standardised measures.
A number of qualitative studies have explored patient perspectives of secure care in relation to their social environment, including general experiences of and attitudes towards being in secure care (e.g. Ford et al. 47 and Yorston and Taylor52) and their time-use through participation in therapeutic and occupational activities. 53–56 In one interesting study, the perceptions of male offenders with psychosis of determinants of LoS in high secure care appear to have much in common with what one would expect in the wider community; patients in the sample tended to favour at least 5 years of detention in a secure hospital for a person with psychosis who had killed another, regardless of their mental state, but for minor property damage they felt that improvement in mental state should be the key determinant of discharge. 57 There is, however, little research explicitly exploring the views of long-stay patients on their experiences of care and desired service provision.
Nurses’ experiences
Mental health nursing is a complex and demanding task comprising different components such as supervision, forming therapeutic relationships, administering medication and maintaining a rehabilitative and social atmosphere on the wards. 58 According to Harrison et al. ,59 the profession is chosen by people who want to make a difference, seek opportunities for a patient-centred approach and are passionate about mental health. Owing to the long contact time and being the closest to patients – compared with other professions – nurses are the professional group engaging most in caring interactions and ensuring that patients’ treatment goals are met. 60,61
Forensic psychiatric nursing differs significantly from general psychiatric nursing for a number of reasons. 62 First, forensic psychiatric nurses face a dual obligation of ‘custody’ and ‘caring’. 63 Second, the patient group forensic psychiatric nurses work with is highly complex, as outlined earlier in this chapter. An additional challenge in working with patients in secure forensic settings is their often very long institutional stay. Life experience, empathy and clinical experience are the three identified key strengths in forensic psychiatric nursing. As secure services are highly restrictive for the individual, potentially impacting on their quality of life, providing a comfortable environment with sufficient recreational and educational opportunities, with an understanding of the different needs of each of the individual patients, is a priority64 and nurses can play an important role in this task. Their perceptions of long-stay patients and views on their care may, therefore, be of particular relevance, in addition to those of clinicians who hold overall responsibility for the patient’s care.
Carers’ experiences
The role of ‘forensic carer’ is difficult to define, but ‘at its core involves practical and emotional support provided to relatives across different secure settings. Forensic carers [carry] a significant emotional burden’. 65
A study by Amy et al. 66 found that a focus on carers had increased in general psychiatry, but had not done so to the same extent in forensic psychiatry. Consistent with this observation, very little information had been recorded about the experience of forensic carers until a recent report from the University of Central Lancashire. 65 This study was commissioned by the Scottish Forensic Quality Network and Support in Mind Scotland, and focused on forensic carers in Scotland. However, it can be reasonably assumed that their experience is similar to that of forensic carers in England.
The report relied on qualitative interviews with carers and identified some key themes. First, the emotional burden of carers is multilayered but is rarely addressed, so carers may effectively become incarcerated with their relative.
I can’t move on with my life, I feel like I’m stuck, I mean my job, I go to work but I don’t enjoy it and I can’t wait till the day is over, I don’t know if that’s because with my son or what but yeah I think it’s changed me as a person. I haven’t got any desires to go on holidays and do things, I feel I’ve changed quite a bit really . . .
Mother65
Many carers reported guilt and feeling responsible for their relatives’ behaviour while at the same time feeling powerless and helpless.
Issues regarding contact with their loved ones add to the stress experienced. Visiting their relative can be stressful and there appear to be inconsistencies across services where support for carers is concerned. Some staff were seen as being ‘empathetic and compassionate’ while others were perceived to ‘behave like prison wardens . . . you don’t experience courtesy’. Nevertheless, carers continue to visit, often travelling many miles, yet are never able to see their relative engaged in normal day-to-day activities or to meet the people they live with. Their loved ones’ experiences can feel like another world.
Carers also reported a lack of involvement in their relatives’ care and feeling that no one listened to their views or provided them with information, both generally and in relation to their relative’s care. Confidentiality seems to be one of the limiting factors in this context.
Although the study cited here noted that some improvements had been made, it was concluded that much still needs to be done. It is clear, therefore, that it is important to involve carers – as well as patients – in any service user input into research, including its interpretation and dissemination.
International perspective
Few papers have been published describing forensic psychiatric care in individual countries,18,67–69 and the literature on international comparisons is scarce. However, these comparisons are important, particularly as discussions regarding service reorganisation and cost improvements become more imperative worldwide. 70 International comparisons may stimulate national debate and improve the development of best practice.
A number of European Union (EU)-funded studies36,71,72 have begun comparing legal frameworks and service provisions in psychiatry, forensic psychiatry and prisons in a number of EU member states. Complex differences in patient populations, diagnoses, legal frameworks and service provision as well as cultural, political and public expectations lead to heterogeneity as to who is admitted to forensic care and how such care is provided. 36 Important differences between countries exist in the exclusion of individuals with certain conditions (e.g. PDs, substance abuse), the importance (or otherwise) of criminal responsibility in psychiatric (as opposed to criminal justice) disposal, whether or not transfer from prison to a psychiatric setting is possible after sentencing, etc.
Data from previous studies (e.g. Salize and Dressing36) indicate a wide variation in the number of forensic psychiatric patients per 100,000 inhabitants, but little is known about the LoS in relevant services, although the Netherlands and Germany have also reported an increase in LoS (e.g. Giesler73 and Nagtegaal et al. 74). Some countries have developed policies and services specifically for long-stay forensic populations, and these provisions are of particular interest to our study.
The research questions that arise from this literature are:
-
What is known about the LoS, characteristics and needs of long-stay patients, factors predictive of LoS and best practice in the care of these patients? (Literature review.)
-
What is the LoS profile of the current high and medium secure forensic psychiatric population in England? [Work package (WP) 1.]
-
How many long-stay patients are currently resident in high or medium secure care? (WP1.)
-
What are the characteristics, care pathways and mental health, psychosocial and service needs of these long-stay patients? (WP2.)
-
Which patient and non-patient factors are associated with long stay? (WP2.)
-
Are there different categories of long-stay patients with distinct needs and, if so, what are they? (WP2.)
-
What are the experiences of long-stay patients in forensic care? (WP3.)
-
What are the ethical and legal issues associated with long-stay secure forensic services? (WP4.)
-
Which service models could meet the needs of the different long-stay groups, improve resource use and quality of life of this patient group, and what are factors potentially impeding their implementation? (WP4.)
Chapter 2 Study aims and objectives
Overall aim
The overall aim of this project was to provide a comprehensive description of long-stay patients in high and medium secure settings in order to inform future service developments to improve the quality and cost-efficiency of care and management of such patients.
Objectives
Length of stay in secure care
We will identify:
-
the LoS profiles of the current high and medium secure population in England
-
the estimated number of long-stay patients in these settings according to our pre-defined criteria.
Characteristics and needs of long-stay patients
We will:
-
describe characteristics of long-stay patients, including sociodemographics, psychopathology, criminal history and risk
-
describe their care pathways and reasons for prolonged stay
-
describe their current and future mental health, psychosocial and service needs through file review and information from responsible clinicians
-
develop a categorisation of long-stay patients according to current presentation and future needs.
Patient experience of long stays
Using qualitative patient interviews we will identify:
-
patients’ perceptions of their treatment pathways, long-term needs and acceptable service provision to maximise their quality of life
-
effects of prolonged stay in secure settings on quality of life.
Service innovation
Using expert interviews, stakeholder consultation, workshops and a Delphi exercise we will:
-
describe existing service models for long-stay secure forensic psychiatric care in different European countries
-
describe essential and desirable characteristics of long-stay forensic units
-
explore the ethical and legal challenges of such care, drawing on the experience from other countries
-
explore the views of clinicians, managers, commissioners, policy-makers and other relevant professionals on long-stay forensic care
-
develop potential service models, identify potential hindrances regarding their implementation and make recommendations regarding implementation and evaluation, including economic evaluation.
In addition to these aims and objectives, it was felt that it would be helpful to thoroughly review the literature on long stay to inform our research and interpretation of findings.
Although not initially identified in the protocol, our service user reference group (SURG; see Chapter 11) identified the lack of perspective of carers of patients resident in secure settings. We therefore added carers as a group of stakeholders whose views would be explored.
Chapter 3 Research design and methods
Overview of study design
This study consisted of four WPs to address the research questions using a mixed-methods approach. In brief, we pursued the aims and objectives described above by:
-
undertaking a survey of units to identify the percentage of long-stay patients (WP1)
-
analysing their characteristics, treatment pathways and future needs using detailed case analyses and clinician questionnaires (WP2)
-
completing a series of qualitative interviews with patients (WP3)
-
conducting extensive consultation with stakeholders (senior clinicians and managers, including those with commissioning roles, clinical academics, legal professionals, commissioners and policy-makers) (WP4).
Table 1 gives an overview of the WPs, methods and their correspondence to the research questions. This chapter gives an overview of the methods employed; these methods are expanded on in Chapters 4–9.
| WP | Research questions | Methods |
|---|---|---|
| WP1: LoS in secure care | What is the LoS profile of the current high and medium secure forensic psychiatric population in England? How many long-stay patients are currently resident in high or medium secure care? |
Cross-sectional survey of patient population resident at selected units on 1 April 2013 Collection of basic patient characteristics through medical records Quantitative analysis |
| WP2: characteristics and needs of long-stay patients | What are the characteristics, care pathways and mental health, psychosocial and service needs of long-stay patients? Which patient and non-patient factors are associated with long stay? Are there different categories of long-stay patients with distinct needs and, if so, what are they? |
Detailed file-reviews of long-stay sample Consultant questionnaires Quantitative analysis, including logistic regression and cluster analysis |
| WP3: patient experience of long stay | What are the experiences of long-stay patients in forensic care? | Long-stay patient interviews Qualitative analysis |
| WP4: service innovation | What are the ethical and legal issues associated with long-stay in secure forensic services? Which service models could meet the needs of the different long-stay groups, improve resource use and quality of life of this patient group and what are factors potentially impeding their implementation? |
Description of international service models Stakeholder interviews Focus groups Workshops Delphi exercise |
Defining ‘long stay’
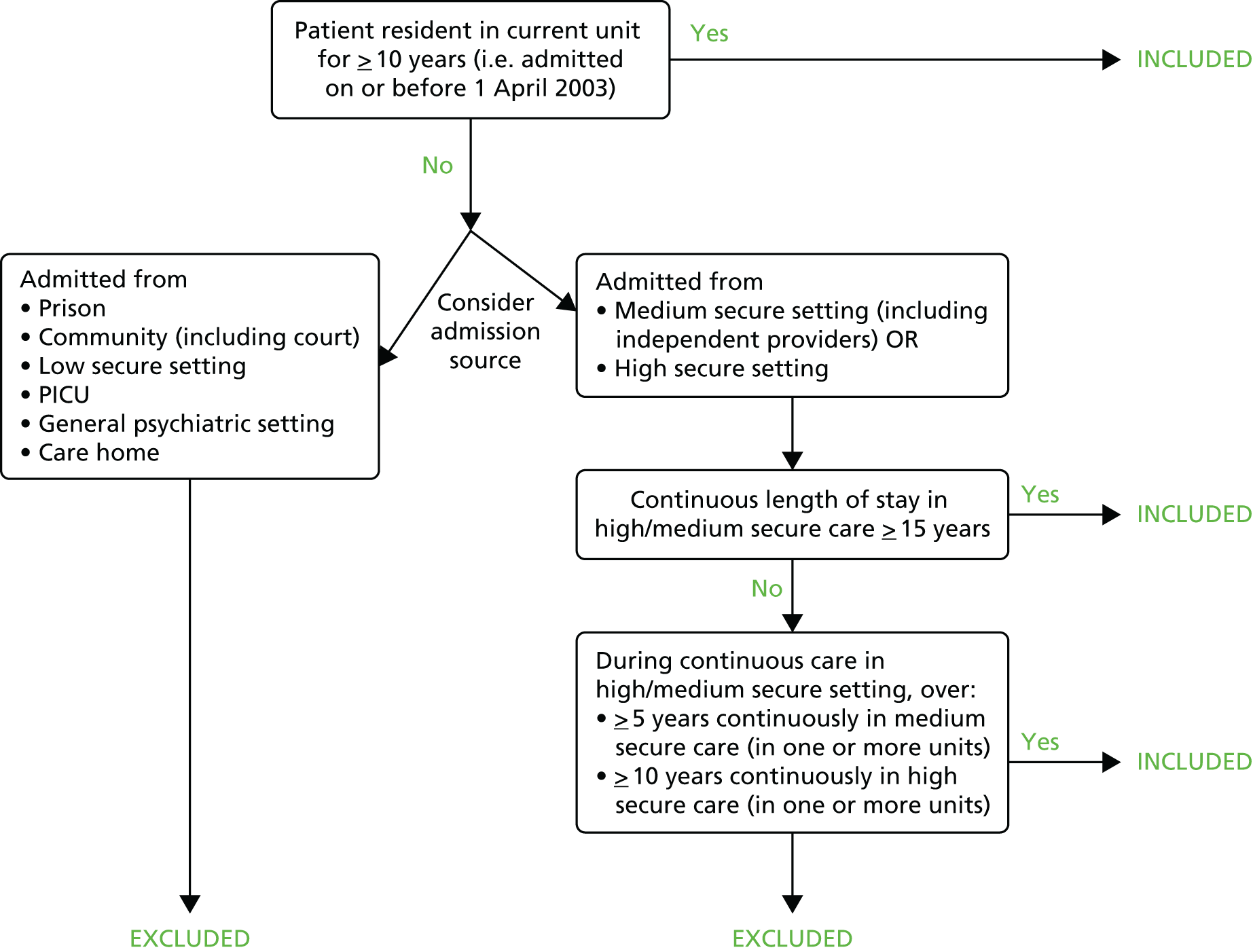
As outlined above, there is currently no accepted standard for LoS in either high or medium secure care. Our piloting data from one high secure care setting suggested that just over 15% of patients stayed for over 10 years. For medium secure care, the literature suggests that between 10% and 20% stay for ≥ 5 years. In the Netherlands, a country that has a designated long-stay service, at the time of the inception of the study, about 15% of the entire Dutch forensic population were staying in such services (although the cut-off point in years is lower there: 6 years). We therefore aimed to use a LoS cut-off point that would capture a similar proportion of patients. This decision was guided by the consideration that the population included should be large enough in size to provide meaningful conclusions for service developments (i.e. not so small that only a very limited number of patients would be included and not so large that a substantial proportion of patients would be captured). On balance, a cut-off point capturing around 15–20% of the population seemed appropriate. For allocation to ‘long-stay’ status, total time of continuous admission in high and/or medium secure care was taken into account, even if that time was spent in different units, according to the following criteria (Figures 1 and 2):
-
≥ 5 continuous years in medium secure care or
-
≥ 10 continuous years in high secure care or
-
a combination of the high and medium secure settings totalling ≥ 15 years of continuous secure care.
FIGURE 1.
Inclusion/exclusion criteria for long stay in medium secure care. PICU, psychiatric intensive care unit.
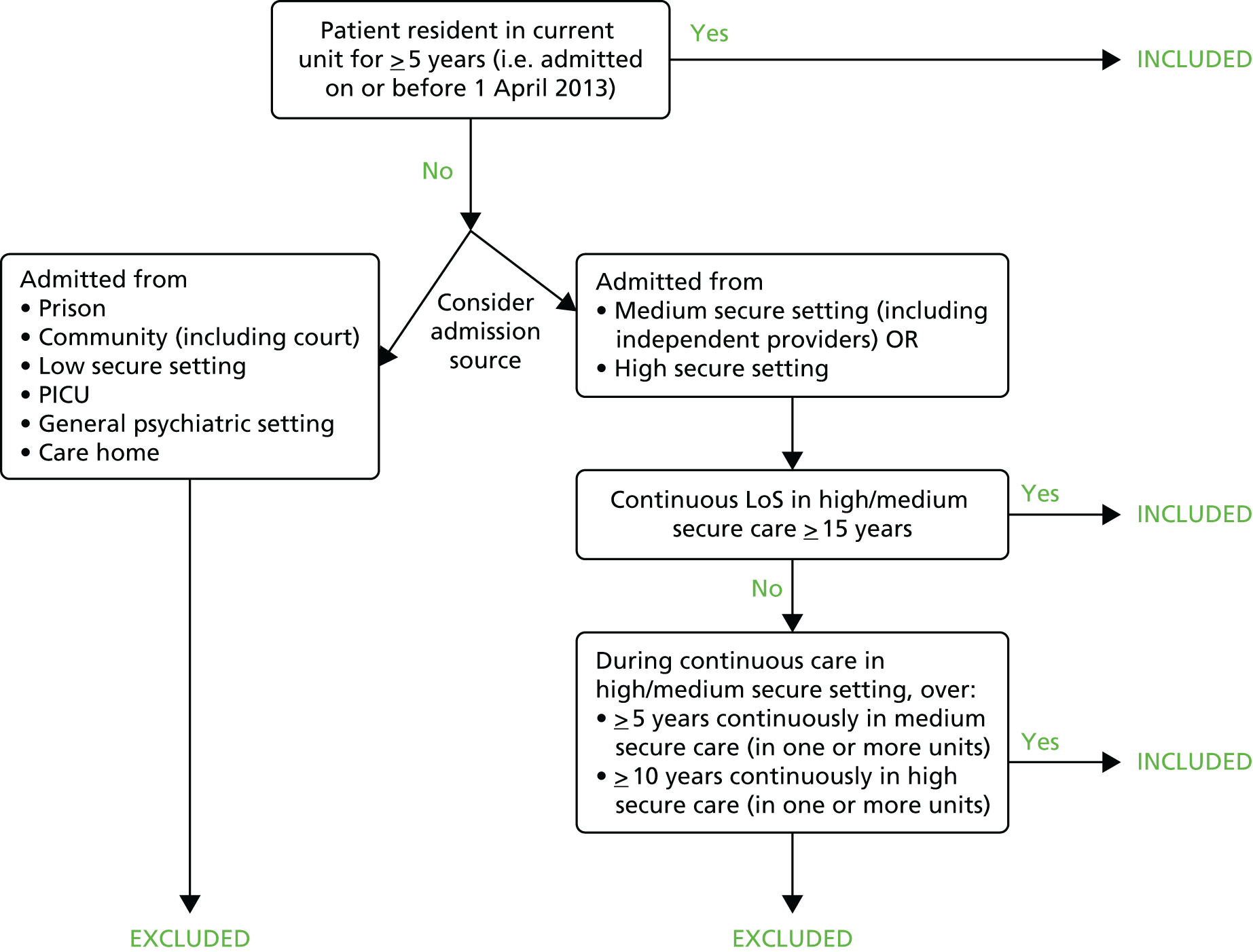
FIGURE 2.
Inclusion/exclusion criteria for long stay in high secure care. PICU, psychiatric intensive care unit.
Work packages
Work package 1 used a cross-sectional design to identify the LoS profile of the current high and medium secure population in England and to estimate the total number of long-stay patients. This consisted of collecting data on LoS (from admission to current setting to census date 1 April 2013) and basic patient characteristics (date of birth, gender, ethnicity, admission source, MHA section and type of current ward) of all patients resident on the census date at the three high secure hospitals and 23 medium secure units. When patients were admitted from other medium or high secure units, data were obtained on their total LoS in (medium/high) secure care to establish whether or not they fulfilled our inclusion criteria.
Work package 2 involved the collection of detailed data about the long-stay patients. To describe the characteristics of this population and identify their care pathways, we collected in-depth clinical, offending and risk data (in an anonymised form) using detailed file reviews and information from patients’ responsible clinicians. We also established factors associated with prolonged stay and developed subcategories of long-stay patients.
Work package 3 used semistructured interviews with a purposively sampled subset of long-stay patients, identified in WP2, to explore their perspectives and experiences of long stay, including their experiences of treatment pathways, strengths and weaknesses of current service provision, impact on quality of life, perceived reasons for long stay and long-term needs. An exploration of the concept of services specifically designed for long-stay patients was also included.
Work package 4 utilised a range of qualitative methods (e.g. semistructured interviews, focus groups) to describe existing service models for long-stay secure forensic psychiatric care internationally, to explore the views of key stakeholders on the issues of long stay, and to identify potential ethical, legal and practical challenges in the care of long-stay patients and in the implementation of potential changes to service provision, including specific services for long-stay patients. Potential service improvements for long-stay patients in the UK were drawn from the data from this WP as well as the patient interviews in WP3.
Sampling units
To use time efficiently, we devised a sampling strategy by unit rather than by patient. All three high secure units in England were included owing to the particular ethical challenges and resource implications of providing care in these facilities. There were approximately 57 medium secure units in England in the (then) 10 Strategic Health Authorities (regions), 34 in the NHS and 23 in the independent sector. A stratified cluster sampling frame was adopted with 23 medium secure units, comprising 14 NHS and 9 independent units, drawn according to sector, geographical region, size and specialisation (e.g. patient groups and designated purpose such as treatment, rehabilitation), with oversampling of units specialising in particular patient groups, including women and patients with intellectual disabilities. This sample represents approximately 40% of all medium secure units in England. One medium secure unit was included in regions with one to three units, two were included in regions with four or five units, three were included in regions with six or seven units, four were included in regions with eight or nine units and five were included in one region with 10 medium secure units. If there was a possible choice of units, taking into account geographical and provider mix, a unit was picked at random from those potentially eligible.
From the units initially approached, one independent provider unit could not be included as it had closed at the time of approach. We tried to replace this independent unit with another: the first one approached declined to participate without giving reasons; the next approached declined owing to potential resource implications. Of the NHS medium secure units initially approached, one declined because of potential conflict with their business interests, another declined because of concerns regarding the data collection procedure, and a third agreed to participate but there then followed excessive delays in communications. Two other medium secure units were recruited to replace these units. Replacement units were drawn from the same Strategic Health Authority region. To maintain the overall sampling approach, independent units were replaced by independent units and NHS units were replaced by NHS units. Table 2 lists the units finally included alongside the resulting patient numbers included in WP1 and WP2. One high secure unit participated in WP1 only.
| Region | Total number of units | Units included | NHS/independent | Patients, total (WP1) | Number of long-stay patients (WP2) |
|---|---|---|---|---|---|
| High secure hospitals | 3 | Ashworth | NHS | 190 | 41 |
| Broadmoor | NHS | 196 | N/A | ||
| Rampton | NHS | 329 | 75 | ||
| Total | 715 | 116 | |||
| Medium secure hospitals | |||||
| North East | 3 | Ridgeway | NHS | 77 | 19 |
| North West | 10 | Edenfield | NHS | 128 | 21 |
| Scott Clinic | NHS | 48 | 0 | ||
| Calderstones | NHS | 43 | 10 | ||
| The Spinney | Independent | 58 | 29 | ||
| Yorkshire | 4 | Humber Centre | NHS | 67 | 23 |
| Stockton Hall | Independent | 89 | 25 | ||
| East Midlands | 5 | Arnold Lodge | NHS | 84 | 11 |
| St Andrew’s Northampton | Independent | 151 | 16 | ||
| West Midlands | 5 | Reaside Clinic/Ardenleigh | NHS | 115 | 4 |
| St Andrew’s Birmingham | Independent | 25 | 2 | ||
| East of England | 9 | Norvic Clinic | NHS | 45 | 9 |
| Brockfield | NHS | 76 | 18 | ||
| Kneesworth House | Independent | 49 | 17 | ||
| St John’s House | Independent | 24 | 6 | ||
| London | 8 | North London Forensic Service | NHS | 143 | 25 |
| John Howard Centre | NHS | 130 | 19 | ||
| North London Clinic | Independent | 27 | 2 | ||
| South East | 6 | Hellingly | NHS | 40 | 3 |
| The Dene | Independent | 21 | 4 | ||
| South Central | 5 | Chadwick Lodge | Independent | 35 | 6 |
| South West | 2 | Fromeside | NHS | 67 | 14 |
| Langdon Hospital | NHS | 30 | 2 | ||
| Total | 57 | 23 | 14 NHS, 9 independent | 1572 | 285 |
Data collection
Work package 1
We collected data that were easily available through medical records departments for all patients resident in participating units on 1 April 2013. We identified a contact at each site and asked them to enter the relevant data into a Microsoft Excel® spreadsheet (Microsoft Corporation, Redmond, WA, USA) and return it to the research team in fully anonymised form. A unique identifier code was assigned to each patient at this point to allow their data to be tracked throughout the project. Units were paid administrative time for this task. From these data, we were able to identify long-stay patients for WP2.
Work package 2
To maintain anonymity, data for WP2 were collected by unit staff (e.g. trainee doctors, audit department staff, research nurses or Mental Health Research Network study officers where local arrangements had been made to that effect). The research team worked with a data collector at each site who was responsible for identifying long-stay patients and conducting subsequent file reviews. Any cases of uncertainty were fed back to the research team for discussion and final decision.
Once data collectors had been identified at each site and appropriately trained, they were given the list of identified long-stay patients at their unit (using the unique identifier code assigned during WP1) and asked to access all current and historical electronic and paper records for those patients. They then completed a data collection pro forma and returned this to the research team either electronically or by post. We achieved a 100% response rate for WP2. During the course of the study, several data collectors left their post and new ones had to be identified and retrained, causing delays to data collection. We paid units for staff time for this data collection.
Consultant questionnaires
For those long-stay patients still resident in the unit at the time of WP2 data collection, a questionnaire was given to the responsible clinician to ascertain their view of the patient’s security, dependency, treatment and political needs, both currently and for the future, and any potential reasons for their long stay. 64 Questionnaires were distributed by our local data collectors.
Work package 3
In WP3, a series of qualitative, semistructured interviews was conducted with a sample of 40 long-stay patients. The participants were purposively sampled from eight of the participating units (two high secure, three NHS medium and three independent medium). A topic guide was used and employed flexibly to explore participants’ views on the reasons for their long stay, their current situation and moving on. The interviews were digitally recorded and transcribed verbatim prior to analysis.
Work package 4
Work package 4 employed a number of methods of data collection, including semistructured interviews of international experts and experts from the UK (senior clinicians and managers, including those with commissioning roles, clinical academics, legal professionals, commissioners and policy-makers). In addition to these individual interviews, which were conducted mainly by telephone owing to the wide geographical spread of experts, focus groups were held at three different national/international forensic psychiatric conferences. Three focus groups were conducted with nursing staff in a high secure facility and three with carers of patients in high and medium secure settings. We also facilitated two workshops, one entitled ‘International service models for long-stay patients in forensic psychiatry’ held in October 2014 and the other called ‘Setting up databases in forensic psychiatric services – challenges and solutions’ held in October 2015 (see Appendices 16 and 17). Afternoon workshops at these events allowed for in-depth exploration of pertinent issues. Minutes were taken and their content was fed into Chapter 9 and the overall discussion. We also conducted a small Delphi survey on experts’ views on forensic psychiatric services for long-stay patients. Finally, we conducted an explorative comparative study of patient characteristics of long-stay patients in England and the Netherlands.
Data processing of quantitative data
The data we received for both WP1 and WP2 went through several stages of cleaning. Any missing data queries or inconsistencies were sent back to our contact person to be rectified. For WP2, this task was time-consuming because of the complexity of the data. The research team checked pro formas for inconsistencies, obvious errors and missing data, and any queries were clarified with the data collectors. In some cases this took several months, which caused delays to data collection and subsequent analysis. During this process, some issues arose concerning the interpretation of data, which needed clarification to keep the data consistent for all patients. These issues were discussed in the first instance with the data collector and were then taken back to the research team for further discussion. When decisions were reached they were recorded in one document entitled ‘Issues and decisions made about data entry’, which was circulated to all members of the research team and used during data entry to ensure consistency.
During this process, some discrepancies appeared between data received during WP1 and the data subsequently received as part of WP2 for the same patient (e.g. regarding admission source or MHA status). These were investigated by the WP2 data collector where possible. When WP1 information appeared correct following this process, WP2 data were corrected accordingly. However, most often the information collected during the file reviews in WP2 appeared correct. After careful consideration in the team as well at the Study Steering Committee (SSC), we decided nevertheless not to correct WP1 data in these cases. This was because we had more detailed information from patients’ files for long-stay patients only and correcting this information in WP1 for long-stay patients only would have introduced systematic bias. The only variable that was altered was long-stay status. If a patient was identified as a long-stay patient in WP1 but after further investigation during WP2 this turned out not to be the case, their long-stay status was changed in WP1.
Data analysis
Quantitative data analysis
Separate data files were created for WP1 and WP2. WP1 data analysis was performed using Stata 13. Significant within-cluster dependency was identified within the medium secure sample; therefore, a multilevel approach was taken. For the high secure sample this was not the case, and a fixed-effects model was therefore chosen.
For WP2, data were entered into a SPSS (Statistical Product and Service Solutions; version 21, IBM Corporation, Armonk, NY, USA) file. Descriptives were calculated for medium and high secure samples separately and differences between long-stay patients and non-long-stay patients were reported. Predictors for LoS were computed using multilevel binary logistic regression with MLWin software (version 2.35; Centre for Multilevel Modelling, Bristol, UK). Class analysis was performed using latent component analysis.
Qualitative data analysis
A thematic analysis was conducted using a framework approach75 to organise data into the topic guide’s main areas of enquiry. Within these areas, data were subject to open coding76 to identify categories that represented key issues discussed by participants. During this process, themes emerged within each of the areas.
Research approvals
Work packages 1 and 2 used routinely collected data only that were compiled by unit staff and transferred to the research team in a fully anonymised form. These WPs were deemed to constitute service evaluations as per confirmation by the research and development department of Nottinghamshire Healthcare NHS Trust, the host institution. Although, for consistency of data collection, it would have been preferable for our own researchers to collect the data at the different sites, the ethical and governance hurdles involved would have been prohibitive. Following a meeting with research and development staff at all collaborating sites at the beginning of the project, the process of data collection finally adopted was felt to be the most appropriate for this study. During these discussions some units raised concerns regarding the level of detail in WP2, in particular as some patients in secure settings have unique characteristics. We therefore removed a number of data fields or changed them to minimise the risk of patients being identifiable; this included, for example, the number of victims of homicide and dates of convictions. Units were offered the option to exclude certain high-profile patients if they felt that data could not be provided in a way that would exclude incidental identification. One high secure unit excluded one patient under this procedure.
Work package 3 involved patient interviews; this part of the study therefore required and received NHS Research Ethics Committee approval (REC reference 13/EM/0242). WP4 involved a mixture of research activities; the focus group with carers required and obtained separate NHS Research Ethics Committee approval (REC reference 15/em/0218), and research and development approval was obtained as required.
Project management
The study was hosted by Nottinghamshire Healthcare NHS Foundation Trust and supported by a Project Management Group (PMG), a SURG and a SSC. The individuals in these groups provided a wide range of knowledge, skills, experience and expertise including researchers and advisors with academic skills, but also those with lived experience in secure care, caring for someone in secure care, working in NHS hospitals, independent hospitals, third-sector organisations and prison settings, including senior managers and clinicians. To ensure that the research was relevant to all stakeholder groups, as well as academically sound, this collaboration between service users, clinicians and academics was crucial throughout the research process. Details of memberships of these groups can be found in Appendix 2.
The PMG and the SURG met quarterly, with the latter meeting more frequently at the early and later phases of the project. The SSC met biannually and was chaired by an independent senior academic, Barbara Barratt (Senior Lecturer in Health Economics at King’s College London). The role was originally held by Janet Parrott (Consultant Forensic Psychiatrist at Oxleas NHS Foundation Trust) but she stepped down from the position part way through the study to avoid potential conflict with her role at one of the recruiting trusts. The role of the SSC was to ensure that the protocol was followed, that deadlines were met and that the research was conducted ethically, as well as to provide advice and support to the research team with regard to any emerging challenges and the wider context for the interpretation of findings.
Chapter 4 Literature review on long stays in forensic settings
Searches
We carried out electronic searches of four databases (MEDLINE, EMBASE, PsycINFO and Cumulative Index to Nursing and Allied Health Literature) from 2000 to 9 November 2015 using the search strategy listed in Appendix 3. This search was overinclusive, yielding a total of 13,493 citations after duplicates were removed. These were screened, retaining those providing relevant information on any of the following in forensic inpatient settings:
-
definition or identification of long-stay patients
-
LoS profiles
-
factors predictive of LoS
-
characteristics or needs of long-stay patients
-
patients’ experiences of long-stay, including quality of life
-
service models for long-stay secure psychiatric care.
The reference list of each included document was checked for any additional relevant citations.
Study characteristics
A total of 38 documents (32 peer-reviewed journal papers, four reports and two theses) were included (Table 3). 12,26,28,29,33,34,37,39–42,57,74,76–99 Eleven countries were represented: the UK (n = 2212,26,28,29,33,34,37,39–42,77–80,82,84,86,87,89,92,97), the USA (n = 490,94,96,99), Ireland (n = 281,98), Germany [n = 293 (one of which was personal communication: Dönisch-Seidel, Ministerium für Gesundheit, Emanzipation, Pflege und Alter des Landes Nordrhein-Westfalen, 2013)], Croatia (n = 257,88), Australia (n = 185), Malaysia (n = 183), New Zealand (n = 195), Norway (n = 191), the Netherlands (n = 174) and Sweden (n = 176). The studies from the UK had samples drawn from high secure (n = 529,33,78,84,89), medium secure (n = 1426,37,39–42,77,79,80,82,86,87,92,97) and mixed secure (n = 312,28,34) settings. The Norwegian study was based in a ‘maximum’ secure setting. 91 The remaining 15 studies were of forensic samples in countries that do not differentiate security into levels in the same way. Thirty-two of the 38 studies had samples that were predominantly male (75% to 99% of sample) and four were all-male. 37,84,88,97 Two UK studies had samples drawn from a women’s medium secure unit. 40,87
| Study/report | Country | Security level | Sampling period | Study design | Sample size | Men in sample (%) |
|---|---|---|---|---|---|---|
| Andreasson et al.76 | Sweden | FS | 1999–2005 | Retrospective, admission sample | 125 | 81 |
| Brown and Fahy37 | UK | Medium | 2002–6 | Retrospective, discharge sample | 157 | 100 |
| Brown et al.77 | UK | Medium | 1983–97 | Census sample, inpatients on census day each year | 404 | 75 |
| Butwell et al.78 | UK | High | 1986–95 | Retrospective, resident sample (all patients resident in study period) | 3263 | 82 |
| Castro et al.79 | UK | Medium | 1995–8 | Retrospective, admission sample | 166 | 82 |
| Coid et al.80 | UK | Medium | 1988–94 | Retrospective, admission sample | 2608 | Mostly male |
| Davoren et al.81 | Ireland | FS | 2010–14 | Prospective, admission sample | 279 | 83 |
| Dell et al.33 | UK | High | 1972–4 | Retrospective, admission sample | 187 | Mostly male |
| Edwards et al.82 | UK | Medium | 1983–96 | Retrospective, admission sample | 225 | 85 |
| Fong et al.83 | Malaysia | FS | January–February 2007 | Cross-sectional, resident sample | 112 | 90 |
| German Ministry of Justicea | Germany | FS | December 2011 | Government statistics, census sample | 2097 | Mostly male |
| Glorney et al.84 | UK | High | 2000–1 | Retrospective admission sample | 63 | 100 |
| Green and Baglioni85 | Australia | FS | Census point | Census sample, survival analysis to census point | 670 | 82 |
| Kennedy et al.39 | UK | Medium | 1987–93 | Retrospective, admission sample | 31 | 87 |
| Knapp et al.86 | UK | Medium | 1994–8 | Retrospective, admission/discharge sample, all patients admitted and discharged between 1994 and 1998 | Mostly male | |
| Long and Dolley40 | UK | Medium | 2002–10 | Retrospective, admission sample | 70 | 0 |
| Long et al.87 | UK | Medium | Opening–2012 | Retrospective, discharge sample | 60 | 0 |
| Maden et al.26 | UK | Medium | 1980–94 | Longitudinal cohort; discharge sample; patients discharged from 1980 to 1994 and followed for 6.6 years | 234 | Mostly male |
| Margetić et al.57 | Croatia | FS | September–November 2011 | Subsample of patients resident | 52 | Mostly male |
| Margetić et al.88 | Croatia | FS | September–November 2011 | Retrospective, resident sample | 56 | 100 |
| McKenna41 | UK | Medium | Autumn 1994 | Retrospective, discharge sample | 100 | 84 |
| McKenna et al.89 | UK | High | 1995 | Retrospective, subsample of patients resident | 15 | 93 |
| Nagtegaal et al.74 | Netherlands | FS | 1990–2009 | Overview of LoS in forensic psychiatric hospitals in the Netherlands | Mostly male | |
| Noblin90 | USA | FS | 1999–2008 | Retrospective, resident sample | 767 | Mostly male |
| Pierzchniak et al.28 | UK | High and medium | 1995 | Retrospective, resident sample | 176 | 85 |
| Renkel and Rasmussen91 | Norway | ‘Maximum’ | 1987–2000 | Retrospective, admission sample | 82 | 99 |
| Ricketts et al.92 | UK | Medium | 1983–99 | Retrospective, admission sample | 504 | 82 |
| Ross et al.93 | Germany | FS | 2009–10 | Retrospective, resident sample | 137 | Mostly male |
| Rutherford and Duggan12 | UK | High and medium | 2006 | Government statistics, whole population of patients December 2004 | Mostly male | |
| Shah et al.42 | UK | Medium | 1999–2008 | Retrospective, discharge sample | 259 | 90 |
| Sharma et al.34 | UK | High and medium | November 1999 | Census study, patients resident one night | 185 | Mostly male |
| Silver94 | USA | FS | 1976–85 | Retrospective longitudinal study of insanity defendants admitted in study period | 6572 | Mostly male |
| Skipworth et al.95 | New Zealand | FS | 1976–2004 | Retrospective, admission/discharge sample, patients admitted in 1976, discharged in 2004 | 135 | 83 |
| Steadman et al.96 | USA | FS | 1971–6 | Retrospective, resident sample, insanity aquittees | 225 | 87 |
| Thomas et al.29 | UK | High | 2003 | Retrospective study, patients resident in 2003 | 1008 | 84 |
| Vitacco et al.99 | USA | FS | 2007–10 | Retrospective, discharge sample | 127 | 78 |
| Wilkes97 | UK | Medium | 2001–11 | Retrospective, discharge sample | 198 | 100 |
| Wright et al.98 | Ireland | FS | 1997–2003 | Retrospective, admission sample | 986 | 86 |
Definitions of ‘long stay’
We first identified the 10 studies in which a long-stay subgroup had been differentiated from a shorter-stay subgroup using a prospectively defined threshold. These studies date from 1987 to 2014, with samples covering the period from 1972 to 2011. Four countries were represented: the UK (n = 733,39,40,42,82,92,97), the USA (n = 199), Ireland (n = 198) and Germany (n = 193).
A threshold of 2 years was used in four studies of medium security in the UK10,39,42,97 and in one study of a forensic hospital in Ireland. 98 A similar threshold was used by Long and Dolley,40 also in the UK, who selected a threshold of 21.6 months based on a median split of their female medium secure sample. Thresholds of 2 years and additionally 5 years were used by Edwards et al. ,82 who observed that admission duration exceeded 5 years in > 10% of their UK medium secure sample. It would appear that in these cases the researchers were following the original guidance from government, based on the recommendations in the early Glancy32 and Butler15 reports that suggested an upper limit of a LoS of 2 years.
An earlier UK study of Broadmoor high secure patients by Dell et al. 33 used an 8-year threshold, the authors observing that 53% of those with a ‘psychopathic disorder’ and 42% of those with a ‘mental illness’ classification of the (then) MHA were ‘long-termers’ who were detained for > 8 years. A threshold of 10 years was used in Germany by Ross et al. ,93 who found that 15% of their sample had a LoS that exceeded 120 months.
In contrast, a much shorter threshold of 45 days was used by Vitacco et al. 99 to differentiate short-term from longer-term care in North America, although the authors note that this figure was chosen to align with the standard 45-day period used in forensic services in North America for initial inpatient assessment and that most individuals (approximately 75%) are committed for lengthier inpatient treatment.
It is difficult to draw any firm conclusions from these findings, other than to observe that although no shared standard exists as to the LoS beyond which individuals should be considered as ‘long-stay patients’, UK researchers tend to choose a threshold that aligns with the official LoS recommendations, even though a significant proportion of patients stay longer than the 2-year period recommended.
Length of stay in forensic settings
Figures on LoS of ‘long(er)-stay’ patients were given in 16 of the included studies (Table 4; only studies that give LoS figures separately for the whole sample and for a subsample of long-stay patients are shown). These were published between 1987 and 2015 with samples covering the period from 1972 to 2011. Five countries were represented: the UK (n = 1212,26,28,33,34,39–42,82,92,97), Germany (n = 193), the USA (n = 199), Malaysia (n = 183) and Ireland (n = 198). Thirteen studies supplied LoS as a mean value; only five provided medians, which are arguably a better measure of central dispersion for a variable that commonly has a non-normal (‘skewed’) distribution.
| Study | Country | Security level | Study period | Sample | LoS for whole sample | LoS for long-stay subgroup |
|---|---|---|---|---|---|---|
| Dell et al.33 | UK | High secure | 1972–4 | 187 patients admitted in study period | 44.4% had a LoS of > 8 years | |
| Edwards et al.82 | UK | Medium secure | 1983–96 | 225 patients admitted in study period | Mean 26 months (9 days to > 9 years) | 50% had a LoS of > 2 years 10% had a LoS of > 5 years |
| Fong et al.83 | Malaysia | Forensic | January–February 2007 | 112 patients resident in study period | Median 7 years (3 months to 47 years) | 34% had a LoS of > 10 years |
| Kennedy et al.39 | UK | Medium secure | 1987–93 | 31 patients admitted in study period | Mean 34.3 months for a LoS of > 2 years | |
| Long and Dolley40 | UK | Medium secure | 2002–10 | 70 female patients admitted in study period | Mean 29.9 months for a LoS of > 21.6 months | |
| Maden et al.26 | UK | Medium secure | 1980–94 | 234 patients discharged 1980 and 1994, 6.6 years’ follow-up | Mean 10 months | 9% had a LoS of > 2 years |
| McKenna41 | UK | Medium secure | 1994 | 100 discharged patients | Mean 30.1 weeks Median 15 weeks |
10% had a LoS of > 1.5 years 4% had a LoS of > 2 years |
| Pierzchniak et al.28 | UK | High and medium secure | 1995 | 176 patients resident in North London area | Mean 61.8 months | Mean 117.4 months (high secure subgroup) |
| Ricketts et al.92 | UK | Medium secure | 1983–99 | 504 patients admitted in study period | 13.1% had a LoS of > 2 years | |
| Ross et al.93 | Germany | FS | 2009–10 | 137 patients resident in study period | Mean 139.6 months for a LoS of > 10 years | |
| Rutherford and Duggan12 | UK | High and medium secure | 2004 | Whole population of patients December 2004 | 66% had a LoS of > 2 years 27% had a LoS of > 10 years 9% had a LoS of > 20 years 3% had a LoS of > 30 years |
|
| Shah et al.42 | UK | Medium secure | 1999–2008 | 259 discharged patients | Mean 749 days Median 428 days |
33.6% had a LoS of > 2 years 9.3% had a LoS of > 5 years |
| Sharma et al.34 | UK | High and medium secure | November 1999 | Census study of 185 patients resident one night in November 1999 | Mean 74.9 months Median 45 months |
39.1% had a LoS of > 5 years |
| Vitacco et al.99 | USA | FS | 2007–10 | 127 discharged patients | Mean 61.6 months | Mean 77.7 months for a LoS of > 45 days |
| Wilkes97 | UK | Medium secure | 2001–11 | 198 discharged male patients | Mean 25.2 months Median 21.2 months (6 to 136.5 months) |
45% had a LoS of > 2 years |
| Wright et al.98 | Ireland | FS | 1997–2003 | 986 patients admitted in study period | Mean 60 days | 3.4% had a LoS of 1–2 years 2.6% had a LoS of > 2 years |
It is clear that there is considerable variation in these figures, reflecting the heterogeneity of the samples (e.g. countries); for example, for medium secure samples the proportion with a LoS of > 2 years ranged from 2.6% to 66% (average of 27.9%).
Geographical variation
There was evidence of considerable geographical variation within the UK. For example, Coid et al. 80 studied 2608 patients admitted to medium secure settings in seven different regions between 1988 and 1994 and found that the mean LoS ranged from 25.0 months in one region (Mersey) to 59.1 months in another (North West Thames).
Gender variation
Three studies considered male and female patients separately. Each found that women tended to experience shorter LoS than men. In a prospective cohort study of 279 patients admitted between 2010 and 2014 to a forensic hospital in Ireland and followed up for a total of 66 months, Davoren et al. 81 found mean LoS figures of 304.3 days (median 60 days) for men and 202.6 days (median 24 days) for women. Edwards et al. 82 calculated LoS in a retrospective study of 225 patients consecutively admitted between 1983 and 1996 to a UK medium secure setting; for the 30 who were still inpatients at the end of October 1998, admission duration was calculated to that date. Eighteen patients had stayed > 5 years; only one (5.5%) of these was female, whereas 14.7% of the overall sample were women. In a census study of 607 forensic inpatients in Australia, Green and Baglioni85 obtained a mean LoS of 115 days (median 40 days) for men and 124 days (median 61 days) for women.
Change in length of stay over time
Findings are inconsistent regarding change in LoS over time. Butwell et al. 78 calculated LoS per episode, defined as from date of admission to discharge or census date (31 December 1995), whichever came first, and found no change from 1986 to 1995 in UK high secure hospitals. In contrast, Brown et al. 77 examined LoS over a 15-year period at a medium secure setting in the UK. The average LoS was calculated by taking the mean LoS of all inpatients on the same census day, rather than calculating the average on discharge, so that those patients who did not achieve discharge were included in the yearly average. They found an increase from 1992 to 1997. Ricketts et al. ,92 in a UK study of 504 medium secure patients admitted between 1983 and 1999, calculated the mean duration of admission for those who had been discharged. They found that the proportion staying longer than 2 years rose from 7% in 1983–7 to 16.2% in 1991–5, before falling to 12.3% in 1995–9.
Characteristics of long-stay patients in forensic settings
Twenty-four studies reported on differences between long(er)-stay and shorter-stay subgroups that were statistically significant using univariate analyses. These studies date from 1983 to 2015, with samples covering the period from 1971 to 2014, as shown in Tables 5 and 6. Nine countries were represented: the UK (n = 12), the USA (n = 4), Ireland (n = 2), Australia (n = 1), New Zealand (n = 1), Croatia (n = 1), Germany (n = 1), Malaysia (n = 1) and Sweden (n = 1). Ten studies took place in medium secure settings, two took place in high secure settings and 12 were in settings where such levels of security were not differentiated in this way.
| Factor | Number of studies | ||
|---|---|---|---|
| Sample at least 75% male | Female-only sample | All studies | |
| Demographics | |||
| Male | 2 | 0 | 2 |
| Older age on admission | 2 | 0 | 2 |
| White | 2 | 0 | 2 |
| Unemployed before admission | 2 | 0 | 2 |
| Female | 1 | 0 | 1 |
| Unmarried | 1 | 0 | 1 |
| No formal education | 1 | 0 | 1 |
| Not being a parent | 1 | 0 | 1 |
| Socially disadvantaged | 1 | 0 | 1 |
| Buddhism as a religion | 1 | 0 | 1 |
| Criminal history | |||
| History of violence | 4 | 0 | 4 |
| History of serious offences | 2 | 0 | 2 |
| Younger at first violent incident (according to HCR-20 H2) | 1 | 0 | 1 |
| Younger at first conviction | 1 | 0 | 1 |
| Younger when first sentenced | 1 | 0 | 1 |
| Longer total prison sentence duration | 1 | 0 | 1 |
| History of sexual offences | 1 | 0 | 1 |
| Index offence | |||
| Greater severity of index offence | 6 | 0 | 6 |
| Violent index offence | 4 | 1 | 5 |
| Murder or homicide as index offence | 4 | 0 | 4 |
| Arson as index offence | 0 | 1 | 1 |
| Index offence sexually motivated | 1 | 0 | 1 |
| Index offence apparently motiveless | 1 | 0 | 1 |
| Long prison sentence in conjunction with ‘diminished responsibility’ for index offence | 1 | 0 | 1 |
| MHA classification | |||
| Restriction order (MHA section 37/41) | 3 | 0 | 3 |
| Criminal MHA section | 2 | 0 | 2 |
| Hospital order (MHA section 37) | 1 | 0 | 1 |
| Transitional MHA section (e.g. transferred prisoner status as remand or sentenced) | 1 | 0 | 1 |
| Psychiatric history | |||
| Admitted from a high-security setting | 3 | 0 | 3 |
| Multiple previous inpatient admissions | 2 | 0 | 2 |
| Previous contact with child and adolescence psychiatric services | 1 | 0 | 1 |
| Younger when first admitted to forensic psychiatry | 1 | 0 | 1 |
| History of psychiatric treatment/longer psychiatric history | 1 | 0 | 1 |
| Time in another unit as an extracontractual referral | 1 | 0 | 1 |
| Not admitted from a high-security setting | 0 | 1 | 1 |
| Admitted from a general psychiatric inpatient unit or prison | 1 | 0 | 1 |
| Risk and current treatment | |||
| Breaches of security regulations/serious non-compliance with ward rules | 3 | 1 | 4 |
| History/risk of absconding | 2 | 0 | 2 |
| Greater number of adverse events during treatment | 1 | 1 | 2 |
| DUNDRUM-1 triage security scale (higher scores on most items) at pre-admission assessment | 1 | 0 | 1 |
| Seclusion needed following admission | 1 | 0 | 1 |
| Inappropriate behaviour during treatment | 1 | 0 | 1 |
| Violent behaviour during treatment | 1 | 0 | 1 |
| Threats during treatment | 1 | 0 | 1 |
| Lower therapy attendance | 0 | 1 | 1 |
| Conditional release failure | 1 | 0 | 1 |
| Diagnosis, symptoms and traits | |||
| Schizophrenia/other psychotic disorder/psychotic symptoms | 5 | 1 | 6 |
| Cognitive/organic deficit | 2 | 0 | 2 |
| Substance abuse | 2 | 0 | 2 |
| Higher overall symptomatology score (BPRS) | 0 | 2 | 2 |
| Comorbid medical illness | 1 | 0 | 1 |
| Severe mental impairment | 1 | 0 | 1 |
| Greater severity of primary diagnosisa | 1 | 0 | 1 |
| PD | 1 | 0 | 1 |
| Paranoid personality traits (MCMI-III) | 0 | 1 | 1 |
| Schizotypal personality traits (MCMI-III in last 6 months of stay) | 0 | 1 | 1 |
| Borderline personality traits (MCMI-III in last 6 months of stay) | 0 | 1 | 1 |
| Higher hostility, tension, excitement and motor hyperactivity scores (BPRS) | 0 | 1 | 1 |
| Higher psychological distress score (CANFOR) | 0 | 1 | 1 |
| Other | |||
| DUNDRUM-2 triage urgency scale (higher scores on most items) at pre-admission assessment | 1 | 0 | 1 |
| Factor | Number of studies | ||
|---|---|---|---|
| Sample at least 75% male | Female-only sample | All studies | |
| Demographics | |||
| Good ongoing contact with family | 3 | 0 | 3 |
| Black | 2 | 0 | 2 |
| Younger age on admission | 1 | 0 | 1 |
| Being a parent | 1 | 0 | 1 |
| Better professional qualifications | 1 | 0 | 1 |
| Better school qualifications | 1 | 0 | 1 |
| Migrated to current country of residence | 1 | 0 | 1 |
| Employed prior to first psychiatric diagnosis | 1 | 0 | 1 |
| Longer period of employment before admission | 1 | 0 | 1 |
| Criminal history | |||
| Admitted from the community | 1 | 0 | 1 |
| Legal status ‘sentenced’ on admission | 1 | 0 | 1 |
| Index offence | |||
| Criminal conviction | 2 | 0 | 2 |
| Not found criminally responsible for index offence | 1 | 0 | 1 |
| Severely violent index offence | 1 | 0 | 1 |
| Civil section (e.g. MHA section 3) | 1 | 0 | 1 |
| Psychiatric history | |||
| Past engagement in individual and group therapy | 0 | 1 | 1 |
| Risk and current treatment | |||
| Engagement in psychological therapies and/or group activities | 0 | 2 | 2 |
| Higher therapy attendance | 0 | 1 | 1 |
| Working in the hospital | 1 | 0 | 1 |
| Diagnosis, symptoms and traits | |||
| Affective disorder | 1 | 0 | 1 |
| Adjustment disorder | 1 | 0 | 1 |
| Psychotic disorder | 1 | 0 | 1 |
| Mood disorders | 1 | 0 | 1 |
| PD | 0 | 1 | 1 |
| PD (HCR-20) | 1 | 0 | 1 |
| Psychopathic disorder | 1 | 0 | 1 |
| Schizophrenia ‘in remission’ | 1 | 0 | 1 |
| Higher ‘co-operativeness’ trait score (TCI) | 1 | 0 | 1 |
| Higher ‘negative attitudes’ score (HCR-20) | 1 | 0 | 1 |
| Higher current GAF score | 1 | 0 | 1 |
| Other | |||
| Discharged to penal system | 1 | 0 | 1 |
A total of 60 characteristics were identified as being associated with a longer LoS. Some inconsistency might be anticipated, given the heterogeneity of studies and the different ways in which LoS was defined and samples were chosen. Nonetheless, a pattern emerges such that a longer LoS appears to be associated with a history of violent and/or serious offending, greater severity of index offence, greater psychopathology, being detained under a criminal section of the MHA (in the UK), being subject to ‘restriction orders’, being admitted from high security, being non-compliant with treatment and being older on admission. We found no evidence that LoS was related to medication dosage; for example, Renkel and Rasmussen91 found no differences in LoS between those on normal dosages and those on higher dosages of antipsychotic medication for a sample of 82 patients admitted between 1987 and 2000 to a Norwegian maximum security forensic setting.
A total of 31 characteristics were identified as being associated with a shorter LoS. These included having good ongoing contact with family members, being black, having a criminal conviction as an index offence and being engaged in treatment. It is interesting to note that one study reported a severely violent index offence as being associated with a shorter LoS. 42 The authors observed that although this finding might appear to have little face validity, their cohort contained a significant number of patients with no previous violence or convictions prior to the index offence and few or no previous psychiatric admissions. This, they suggest, may explain why a severely violent index offence is significantly associated with a shorter length of admission; they note that characteristics associated with long stay in medium security identified in their study are seldom associated with a severely violent index offence, and this can result in shorter admissions for severe violence.
Needs of long-stay patients
Three UK studies provided additional information on the ‘needs’ of patients currently receiving high secure care. Thomas et al. 29 focused on all patients resident in 2003 and Glorney et al. 84 reviewed the 63 male patients admitted between 2000 and 2001; both studies were of high secure samples and used the forensic version of the Camberwell Assessment of Need. Pierzchniak et al. 28 studied 176 high and medium secure patients resident in 1995 using a variety of measures. The key needs identified in these studies were:
-
risk reduction
-
daytime activities
-
physical health
-
treatment for alcohol misuse
-
treatment for drug problems
-
safety to others
-
safety to self (female patients)
-
psychotic symptoms/mental health recovery
-
therapeutic engagement
-
education
-
occupational
-
cultural and spiritual needs
-
care pathway management
-
treatment related to sex offences (male patients)
-
treatment to address arson issues (female patients)
-
psychological distress (female patients)
-
need for long-term 24-hour nurse-staffed accommodation, rather than long-term medium security.
Inspection of this list suggests considerable levels of disablement in these long-stay patients. It is therefore interesting to note the findings from a study by McKenna et al. ,89 who focused on a small sample of patients in a high security setting who were thought to no longer require conditions of maximum security but who did require long-stay medium secure care. When the needs of this group were compared with those of patients in a high-dependency rehabilitation unit, the rehabilitation patients were significantly more disabled on a variety of parameters.
Factors predictive of length of stay
This section focuses on factors that are predictive (rather than characteristic) of LoS. Although a considerable number of characteristics have been found to differentiate longer-stay forensic patients from those who experience shorter stays, many of these are confounded and so cannot be seen as uniquely predictive of LoS. We therefore concentrate here on the 10 studies that used more rigorous multivariate statistical techniques in an attempt to isolate the key predictive factors. These studies date from 1983 to 2014, with samples covering the period from 1971 to 2011. Seven countries were represented: the UK (n = 1), the USA (n = 4), Australia (n = 1), Croatia (n = 1), Germany (n = 1), Malaysia (n = 1) and Sweden (n = 1). The results are summarised in Boxes 1 and 2.
-
Male.
-
Not being a parent.
-
Unmarried.
-
Index offence severity (identified in three studies).
-
Index offence murder or homicide (identified in two studies).
-
Index offence violent (identified in two studies).
-
Schizophrenia/other psychotic disorder/psychotic symptoms (identified in two studies).
-
Cognitive/organic deficit.
-
Severity of primary diagnosis. b
-
Younger at first conviction.
-
Longer total prison sentence duration.
-
History of violence.
-
History of sexual offences.
-
History/risk of absconding during treatment.
-
Non-compliant with hospital treatment.
-
Conditional release failure.
In one study unless otherwise indicated.
Authors determined severity following the procedure outlined in National Institute of Mental Health. 100
-
Migrated to current country of residence.
-
Good ongoing contact with family.
-
Employment prior to first psychiatric diagnosis.
-
Length of time employed.
-
Mood disorders.
-
Co-operativeness trait (TCI).
TCI, Temperament and Character Inventory.
In one study unless otherwise indicated.
Having an index offence that was violent or resulted in death and having a psychotic or other serious mental disorder were the most commonly identified predictors of longer LoS, together with being male, certain factors relating to a history of serious offending and a poor compliance with treatment. In contrast, factors predictive of shorter LoS included being diagnosed with a mood disorder, having good ongoing contact with family members, spending a longer time in employment prior to admission and ‘co-operativeness’ as a personality trait.
Services for long-stay patients
The literature contains a considerable number of papers that comment generally on forensic services, both currently and in terms of future need. Much consideration has been given to the factors that contribute to increases in LoS in secure settings; for example, Brown et al. 77 observed that the high-profile reporting of inquiries into homicides by patients under psychiatric care from 1991 onwards may have both influenced the increased use of restriction orders and discouraged the discharge of forensic patients into the community. We found, however, no papers that described service models geared specifically to long-stay forensic patients.
Chapter 5 Cross-sectional survey of length of stay in high and medium secure care
Aims and objectives
The objectives of this part of the study were to identify:
-
the LoS profiles of the current high and medium secure population in England
-
the estimated number of long-stay patients in these settings.
Methods
Data collection
We used a cross-sectional design to identify the LoS profile of the current high and medium secure population in England. The data collected were based on information known to be readily available from administrative systems on the basis of a pilot trial conducted in two medium secure units and included:
-
date of admission to current unit
-
age
-
gender
-
ethnicity
-
admission source
-
current MHA section
-
type of current ward (in terms of diagnostic and stage of treatment specification).
Only individuals who were resident in the unit on the census date were included (i.e. individuals who were on trial leave were excluded). This was to prevent individuals from being counted twice, once in the unit from which they were on leave from and once as a patient at the unit where they currently resided.
For type of current ward, the categories were piloted with a number of units to ensure that they reflected the types of wards available (Table 7). The units were asked to assign their wards to one of the categories. From this we could identify the ward type for each patient. Although it was not possible to obtain diagnostic information on all patients owing to the different (or absent) recording of this information in the units, an approximation of the likely main clinical problem was possible through the diagnostic specification of the current ward.
| Specification according to diagnostic category | Specification according to stage of treatment |
|---|---|
| Mental illness | Admission/assessment |
| PD | Treatment |
| Comorbidity | High dependency |
| Intellectual disability | Long stay/slow stream |
| Neuropsychiatry | Pre-discharge/rehabilitation |
| Mixed diagnosis | Mixed assessment/treatment |
| Other diagnostic category | Other ward type |
| Cannot assign category | Cannot assign category |
It proved difficult to obtain information on the date on which patients were first admitted to (high or medium) secure care and hence to identify whether or not they fulfilled our long-stay criteria. For some patients, it was clear that they were long-stay patients based on their stay in the current unit alone. For those patients for whom this was not the case, we contacted the site to request access to admission history data if patients were admitted from a high or medium secure setting.
Data processing
The data were cleaned for errors and several variables were recorded for analysis. The patients were categorised into long-stay patients and non-long-stay patients. LoS categories for stay in current units were calculated: < 5 years, 5–10 years, 11–20 years, 21–30 years and ≥ 31 years. Age was transformed into an ordinal level age category variable (< 29 years, 30–39 years, 40–49 years, 50–59 years or ≥ 60 years) and ethnicity was collapsed into a broader ethnic class nominal variable (white, black, Asian, mixed or other). Admission source was collapsed into community (any non-secure psychiatric settings, including psychiatric intensive care units, non-institutional settings and police stations), low, medium and high secure settings, and prison. MHA section was categorised as civil/quasi-civil [section 2, 3, 37, 37(N), 41(5) or 47], hospital orders with restriction (section 37/41 or Criminal Procedure and Investigations Act101), prison transfer (section 47/49 or 48/49), presentencing (section 35, 36 or 38) and other. Despite the fact that those on a section 37 and section 47 will have committed an offence in order to obtain their section, we consider them here together with civil section on the basis of the similarities in the decision-making process regarding transfer and discharge. There were only a few cases of patients who were unfit to plead or insane; these were assigned to the section 37/41 category.
Data analysis
Data analysis was conducted separately for patients in high and medium secure settings.
Summary statistics was taken of all included variables.
Chi-squared tests, adjusting for unit variation in the case of medium secure patients, were conducted to determine bivariate associations between each of the variables with long-stay status. Variables with significant associations were subsequently entered simultaneously into logistic models. Nominal predictors were entered as dummy variables with modal categories chosen as references.
To examine the effects of variables on the likelihood of long-stay status, a multilevel approach was taken. Both samples potentially form a hierarchical structure with patients nested within the secure units in which they reside. There may be unit-level factors not measured in this study that may influence the duration of patients’ stays, and observations within units may, therefore, not be independent, as is typically assumed for generalised linear models. This was examined in both samples by applying the likelihood ratio test of unit-level variance for long-stay status alongside the intraclass correlation coefficient. The high secure sample did not show significant variation, and a normal fixed-effects model was therefore chosen for analysis. The medium secure sample did demonstrate significant within-cluster dependency. To allow for unit cluster correlation and residual dependencies, a multilevel approach was taken by incorporating a unit-level random effect into the model. The model was estimated using full maximum likelihood estimation.
Missing data were explored in Stata and addressed using multiple imputation for multilevel data using REALCOM-IMPUTE (Centre for Multilevel Modelling, University of Bristol). 102 Assuming missing at random mechanisms in both samples, an imputation model was built using long-stay status and other covariates to be used in the predictive model, with 10 data sets imputed.
Multicollinearity was assessed using variance inflation factors, model specification was assessed by examining the linear predicted and squared values, and outliers were checked using residual analysis. Anscombe residuals were screened for medium secure patients and standardised Pearson residuals in the high secure analysis, with those > 2.56 investigated. The medium secure residuals were checked from the fixed effects. Model fit and predictive accuracy was not assessed, owing to the multiply imputed estimation. Except where stated, all analyses were conducted in Stata 13 and statistical tests are two-tailed (α = 0.05).
Findings
Unit characteristics
The unit characteristics are shown in Table 8. About two-thirds of the units were NHS and just over one-third were independent provider units. The unit sizes (patient numbers) varied from small (≤ 50 patients) to larger units (over 100 patients). The units were spread geographically across England.
| Unit characteristic | Unit, n (%) |
|---|---|
| Provider type | |
| NHS | 14 (61) |
| Independent | 9 (39) |
| Unit sizea | |
| Small (≤ 50 patients) | 11 (48) |
| Medium (51–99 patients) | 7 (30) |
| Large (≥ 100 patients) | 5 (22) |
| English region | |
| North East | 1 (4) |
| North West | 4 (17) |
| Yorkshire and the Humber | 2 (9) |
| East Midlands | 2 (9) |
| West Midlands | 2 (9) |
| East of England | 4 (17) |
| London | 3 (13) |
| South East | 2 (9) |
| South Central | 1 (4) |
| South West | 2 (9) |
Prevalence of long stay
There were similar percentages of patients meeting our criteria for long stay in the high secure sample (22–26%); however, there was a much wider variation in the proportion of long-stay patients in the medium secure sample, from no patients to up to 50% of patients (Table 9).
| Unit name | Patients, total | Number (%) of long-stay patients |
|---|---|---|
| High secure hospitals | ||
| Ashworth | 190 | 41 (21.6) |
| Broadmoor | 196 | 52 (26.5) |
| Rampton | 329 | 75 (22.8) |
| Total | 715 | 168 (23.5) |
| Medium secure hospitals | ||
| Ridgeway | 77 | 19 (24.7) |
| Edenfield | 128 | 21 (16.4) |
| Scott Clinic | 48 | 0 (0) |
| Calderstones | 43 | 10 (23.3) |
| The Spinney | 58 | 29 (50.0) |
| Humber Centre | 67 | 23 (34.3) |
| Stockton Hall | 89 | 25 (28.1) |
| Arnold Lodge | 84 | 11 (13.1) |
| St Andrew’s Northampton | 151 | 16 (10.6) |
| Reaside Clinic/Ardenleigh | 115 | 4 (3.5) |
| St Andrew’s Birmingham | 25 | 2 (8.0) |
| Norvic Clinic | 45 | 9 (20.0) |
| Brockfield | 76 | 18 (23.7) |
| Kneesworth House | 49 | 17 (34.7) |
| St John’s House | 24 | 6 (25.0) |
| North London Forensic Service | 143 | 25 (17.5) |
| John Howard Centre | 130 | 19 (14.6) |
| North London Clinic | 27 | 2 (7.4) |
| Hellingly | 40 | 3 (7.5) |
| The Dene | 21 | 4 (19.5) |
| Chadwick Lodge | 35 | 6 (17.1) |
| Fromeside | 67 | 14 (20.1) |
| Langdon Hospital | 30 | 2 (6.7) |
| Total: 23 | 1572 | 285 (18.1) |
Current unit length of stay profile
For WP1, the information on patients’ LoS was available for their current unit only and, thus, does not constitute their total LoS in secure care. The summary descriptive statistics in Table 10 show a large variation in the LoS for both the high and the medium samples. The median LoS in high secure care was 1630 days (nearly 4.5 years), while in medium secure units it was 558 days (1.5 years). Both samples showed substantial variation in LoS, with interquartile ranges (IQRs) of 1910 and 835 days, respectively.
| LoS in current unit | High secure (n = 715) | Medium secure (n = 1572) | ||||
|---|---|---|---|---|---|---|
| Median (IQR) | Range | Mean (SD) | Median (IQR) | Range | Mean (SD) | |
| LoS (days) | 1630 (1910) | 14,322 | 2137 (2028) | 558 (835) | 7246 | 798 (876) |
| LoS (months) | 54 (62) | 470 | 70 (66) | 18 (27) | 238 | 26 (28) |
Breaking down LoS categories, groupings indicate slightly different distributions between the high and medium secure samples. The modal LoS category for both samples was under 5 years but, while the high secure sample showed greater range across the categories, the medium secure distribution demonstrated greater kurtosis. This is exemplified in Table 11.
| LoS in current unit | High secure (N = 715), n (%) | Medium secure (N = 1572), n (%) |
|---|---|---|
| LoS categories | ||
| < 5 years | 396 (55) | 1420 (90) |
| 5–10 years | 226 (32) | 134 (9) |
| 11– 20 years | 78 (11) | 18 (1) |
| 21–30 years | 10 (1) | 0 (–) |
| ≥ 31 years | 5 (< 1) | 0 (–) |
Comparisons of long-stay patients versus non-long-stay patients
In the high secure sample, significant differences were found between long-stay patients and non-long-stay patients in age category, MHA section, admission source and ward diagnostic category. The differences were non-significant for gender, ethnic class and ward pathway category.
The percentages for age categories showed that non-long-stay patients were generally younger, with decreasing frequency of cases across age groups. For MHA sections, although the proportions of civil/quasi-civil sections (including hospital orders without restrictions) in each group were broadly similar, at 18% and 20%, respectively, there were notably more long-stay patients on hospital orders with restrictions and fewer on prison transfer sections. Categories of admission source further differed between groups. Twenty-four per cent of long-stay patients were admitted from another high secure unit, whereas this was true of only 3% of non-long-stay patients. Similarly, 32% of long-stay patients came from a medium secure setting compared with 26% of non-long-stay patients. Conversely, the largest proportion of non-long-stay patients came from prison, whereas this was far less the case for long-stay patients. The two groups also differed in terms of the ward they resided on, although notable differences were seen only in intellectual disability wards, with a greater proportion of long-stay patients (14% and 6%, respectively) and PD wards, with fewer long-stay patients on such wards (29% and 38%, respectively). These differences are summarised in Table 12.
| Patient, pathways and MHA section factors | High secure | Medium secure | ||||
|---|---|---|---|---|---|---|
| Long-stay patients (N = 168) | Non-long-stay patients (N = 547) | χ2 (df) | Long-stay patients (N = 285) | Non-long-stay patients (N = 1287) | Adjusted χ2 (df)a | |
| Provider, n (%) | ||||||
| NHS | – | – | – | 178 (62) | 915 (71) | 1.19 (1) |
| Independent | 107 (38) | 372 (29) | ||||
| LoS in current unit (days), median (IQR) | 4294 (3756) | 1332 (1533) | – | 1560 (1778) | 438 (670) | – |
| LoS in current unit (months), median (IQR) | 141 (124) | 44 (50) | – | 51 (58) | 14 (22) | – |
| Age (years), mean (SD) | 45.43 (9.67) | 36.15 (9.72) | t(df) = –10.83 (713)** | 43.87 (11.74) | 34.68 (11.21) | t(df) = –3.45 (43)** |
| Age category (years), n (%) | ||||||
| 19–29 | 11 (6.5) | 163 (29.7) | 85.85 (4)** | 31 (10.9) | 509 (39.5) | 20.55 (4)** |
| 30–39 | 35 (20.8) | 189 (34.6) | 77 (27.0) | 373 (29.0) | ||
| 40–49 | 71 (42.3) | 141 (25.8) | 85 (29.8) | 270 (21.0) | ||
| 50–59 | 39 (23.2) | 45 (8.2) | 64 (22.5) | 99 (7.7) | ||
| ≥ 60 | 12 (7.1) | 9 (1.6) | 28 (9.8) | 36 (2.8) | ||
| Gender, n (%) | ||||||
| Male | 157 (93.5) | 514 (94.0) | 0.05 (1) | 240 (84.2) | 1049 (81.5) | 0.17 (1) |
| Female | 11 (6.5) | 33 (6.0) | 45 (15.8) | 238 (18.8) | ||
| Ethnic class, n (%)b | ||||||
| White | 128 (76.7) | 404 (75.0) | 2.18 (4) | 216 (77.8) | 808 (68.6) | 2.21 (4) |
| Black | 23 (13.8) | 75 (13.9) | 39 (14.1) | 208 (17.6) | ||
| Asian | 9 (5.4) | 22 (4.1) | 9 (3.2) | 81 (6.9) | ||
| Mixed | 6 (3.6) | 32 (5.9) | 12 (4.4) | 61 (5.2) | ||
| Other | 1 (< 1) | 6 (1.1) | 1 (< 1) | 20 (1.7) | ||
| MHA section, n (%) | ||||||
| Civil/quasi-civil | 30 (17.9) | 111 (20.3) | 42.70 (3)** | 81 (28.2) | 492 (38.2) | 9.76 (4)* |
| Hospital order with restrictions | 108 (64.3) | 205 (37.5) | 185 (64.9) | 516 (40.1) | ||
| Prison transfer | 30 (17.9) | 227 (41.5) | 19 (6.7) | 242 (18.8) | ||
| Pre sentencing | 0 | 4 (0.7) | 0 | 17 (1.3) | ||
| Other | 0 | 0 | 0 | 20 (1.6) | ||
| Admission source, n (%)c | ||||||
| Community | 4 (2.5) | 1 (< 1) | 97.26 (4)** | 12 (4.7) | 179 (15.3) | 40.89 (4)** |
| Prison | 65 (41.1) | 367 (70.3) | 46 (18.0) | 602 (51.3) | ||
| Low secure unit | 0 | 2 (< 1) | 8 (3.1) | 119 (10.1) | ||
| Medium secure unit | 51 (32.2) | 137 (26.2) | 118 (46.1) | 192 (16.4) | ||
| High secure unit | 38 (24.1) | 15 (2.9) | 72 (28.1) | 81 (6.9) | ||
| Ward diagnostic category, n (%) | ||||||
| Mental illness | 78 (46.4) | 245 (44.8) | 13.71 (3)** | 132 (46.3) | 472 (36.7) | 1.65 (3) |
| PD | 48 (28.6) | 209 (38.2) | 20 (7.0) | 80 (6.2) | ||
| Intellectual disabilities | 24 (14.3) | 34 (6.2) | 31 (10.9) | 143 (11.1) | ||
| Mixed/other | 18 (10.7) | 59 (10.9) | 102 (35.8) | 592 (46.0) | ||
| Ward pathway category, n (%) | ||||||
| Admission | 8 (4.8) | 46 (8.4) | 3.75 (4) | 9 (3.2) | 201 (15.6) | 10.18 (4)* |
| Treatment | 87 (51.8) | 294 (53.7) | 83 (20.1) | 382 (29.7) | ||
| High dependency | 26 (15.5) | 72 (13.2) | 1 (< 1) | 28 (2.2) | ||
| Slow/rehabilitation | 19 (11.3) | 61 (11.2) | 101 (35.4) | 221 (17.2) | ||
| Mixed/other | 28 (16.7) | 74 (13.5) | 91 (31.9) | 455 (35.4) | ||
In the medium secure sample, similar variables showed significant associations with long-stay status: age, age category, MHA section, admission source and ward pathway category, although not ward diagnostic category.
Age category showed a similar pattern for the medium secure sample as for the high secure sample, with non-long-stay patients being younger and the majority of long-stay patients being of middle age. Within MHA sections, there was a similar breakdown as in the high secure sample for the proportion on hospital orders with restrictions between long-stay patients (about two-thirds) and non-long-stay patients (about 40%). As in the high secure sample, long-stay patients were less likely to be on prison transfer sections. There were differences in admission source, with long-stay patients less likely than non-long-stay patients to come from community settings (5% vs. 15%), low secure units (3% vs. 10%) or prison (18% vs. 51%). They were instead more frequently admitted from high secure units (28% vs. 7%) or another medium secure unit (46% vs. 16%). Long-stay patients were more likely than non-long-stay patients to reside on slow stream/rehabilitation wards and less likely to be resident on admission wards.
Factors predicting long-stay status
The variables entered in the logistic model included age category, MHA section and admission source. For the high secure sample, ward diagnostic category was also entered, and for the medium secure sample, ward pathway category was also entered. For the high secure analysis, the categories ‘low secure unit’ from admission source, and ‘pre-sentencing’ and ‘other’ from the MHA section variables, were omitted, given the inadequate number of long-stay cases; the last two categories were also omitted from the medium secure analysis.
Mental Health Act sections were compared against ‘hospital order with restrictions’, admission source against prison entrants and ward diagnostic type against mental illness. Age category was treated as an ordinal variable, as the conditional distribution suggests a likely linear effect (Figures 3 and 4).
FIGURE 3.
Proportion of long-stay patients by age category (high secure sample).

FIGURE 4.
Proportion of long-stay patients by age category (medium secure sample).
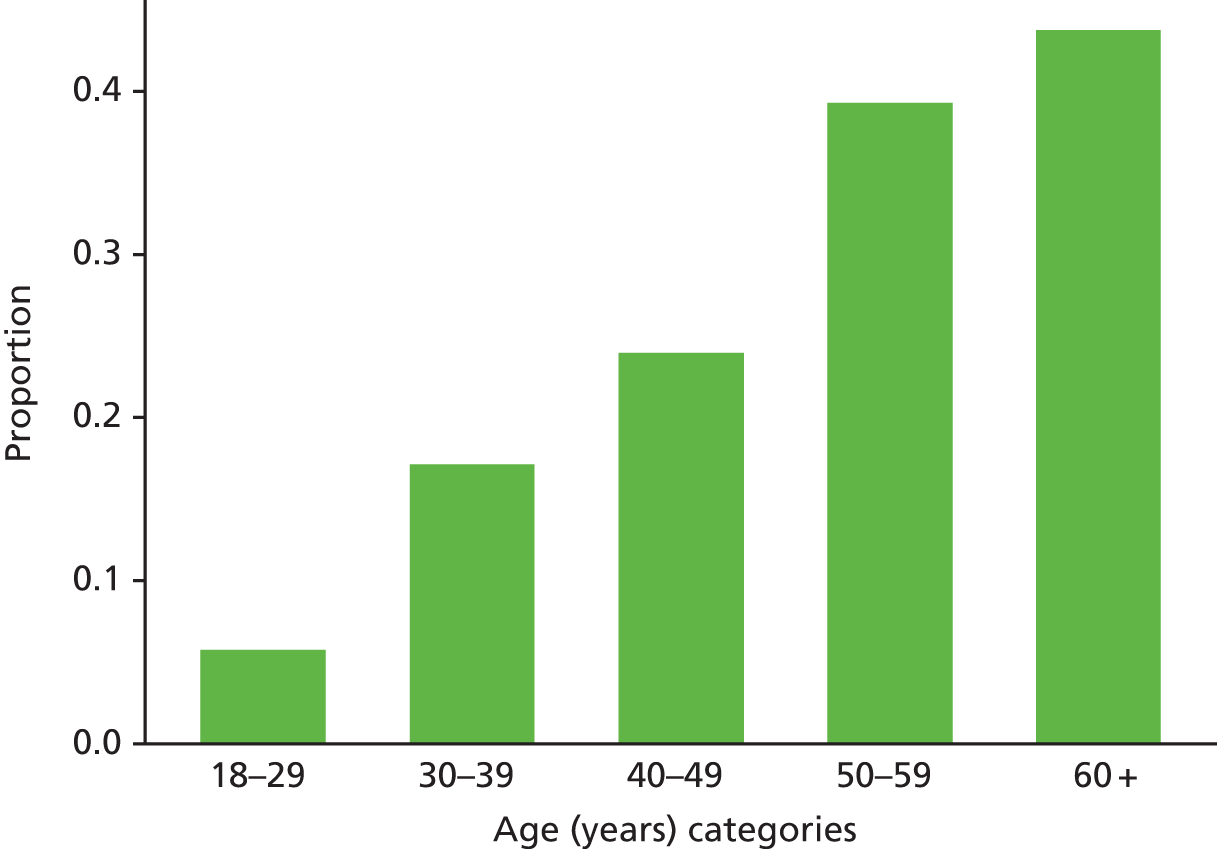
A non-imputed model was judged to be correctly specified (predicted values p < 0.001, squared values p = 0.324). Multicollinearity was not a concern, with a mean variance inflation factor of 1.04, well within usual recommendations (e.g. Hair et al. 103). The average variance increase owing to missing data was 0.003, suggesting that the missing data had only a small effect on the coefficients. Only 10 imputations were used for the missing data estimates, but the largest fraction of missing information was only 0.02, so this is unlikely to be a concern. Although model fit indices were unavailable for the multiply imputed analysis, the full model was a significant improvement on the constant-only model for long stay (F9,0 = 13.43; p < 0.001). Although a number of outliers were identified from individual imputations (n = 15–17), refitting separate models after their deletion did not meaningfully alter parameter estimates. Thus, leverage was assumed to be negligible, and all cases were retained for analysis.
High secure care
As expected, age category was a significant predictor of long-stay status, with each incremental age group having a 2.4 times increased odds of being classed as a long-stay patient (p < 0.001). Compared with patients admitted on section 37/41, other MHA section types significantly predicted reduced likelihood of long-stay status by over half. Those with a civil/quasi-civil section had 52% reduced odds [adjusted odds ratio (OR) = 0.472; p = 0.008] and patients on a prison transfer had 72% reduced odds (adjusted OR = 0.276; p < 0.001). Admission source was a significant predictor of increased likelihood of long stay only for previous high secure cases against prison admissions (adjusted OR = 7.617; p < 0.001), with both community (adjusted OR = 7.152; p = 0.085) and medium secure admissions (adjusted OR = 1.446; p = 0.141) being non-significant (Table 13). Diagnostic ward categorisation was a significant factor when comparing mental illness wards against intellectual disability-specified wards, with patients from the latter presenting with an increased likelihood of prolonged stay (adjusted OR = 2.857; p = 0.004). Patients on mixed-type wards also had an increased likelihood of long-stay status (adjusted OR = 1.144; p = 0.699) and those on PD wards had a reduced likelihood (adjusted OR = 0.914; p = 0.715), although both estimates were non-significant.
| Variable | Adjusted OR | Standard error | 95% CI | Significance |
|---|---|---|---|---|
| Age category | 2.409 | 0.259 | 1.951 to 2.976 | < 0.001 |
| MHA | ||||
| Hospital order with restrictions | 1.00 | 0.132 | 0.276 to 0.820 | 0.008 |
| Civil/quasi-civil | 0.476 | 0.076 | 0.160 to 0.475 | < 0.001 |
| Prison transfer | 0.276 | |||
| Admission source | ||||
| Prison | 1.00 | 8.160 | 0.764 to 66.939 | 0.085 |
| Community | 7.152 | 0.362 | 0.884 to 2.365 | 0.141 |
| Medium secure | 1.446 | 2.687 | 3.815 to 15.210 | < 0.001 |
| High secure | 7.617 | |||
| Ward diagnostic category | ||||
| Mental illness | 1.00 | 0.224 | 0.564 to 1.480 | 0.715 |
| PD | 0.914 | 1.052 | 1.388 to 5.882 | 0.004 |
| Intellectual disability | 2.857 | 0.399 | 0.577 to 2.269 | 0.699 |
| Mixed/other | 1.144 | |||
Medium secure care
An initial intercept only model was run to assess unit-level variation. The estimate for random unit variance was 0.469, which was more than twice its standard error (0.223), suggesting significant unit variation. The likelihood ratio test was significant (χ2 = 58.20; p < 0.001). The intraclass correlation coefficient indicated that 14% of the unexplained variance in long-stay status is a result of unobserved unit-level factors.
The model produced a better fit than the null hypothesis (F7, 0 = 31.89; p < 0.001), with an average variance increase = 0.003 and a fraction of missing information = 0.01, suggesting adequate imputation. Estimated level two variance remained significant at 0.52 (standard error = 0.24). Multicollinearity was not an issue (mean variance inflation factor = 1.09). Outliers (n = 29–31) did not appear to have a major leveraging effect and were retained. A single-level, non-imputed model was judged to be correctly specified (predicted values p < 0.001, squared values p = 0.780).
As shown in Table 14, age category was a significant predictor of long-stay status, with each incremental age group having 1.7 times increased odds of being classed as a long-stay patient (p < 0.001). Compared with patients sectioned on hospital orders with restrictions, those on civil/quasi-civil section had 39% reduced odds of being a long-stay patient (p = 0.006), and the odds were reduced by 74% for prison transfer patients (p < 0.001). Patients admitted from community settings were 35% less likely to be a long-stay patient, although this estimate was non-significant (p = 0.196). Patients arriving from high secure settings had 4.9 times the odds of being a long-stay patient (adjusted OR = 4.87; p < 0.001), 4.8 times if admitted from another medium secure service (adjusted OR = 4.812; p< 0.001), and the odds were reduced by 44% for those admitted from low secure settings, although this finding was not significant (adjusted OR = 0.559; p = 0.171). For ward pathway, patients had 60% reduced odds of long-stay status compared with those on mixed or other types of pathway if they were on admission wards (adjusted OR = 0.396; p = 0.024), and a non-significant, 22% reduction for treatment wards (adjusted OR = 0.781; p = 0.321), 65% reduction for high dependency wards (adjusted OR = 0.353; p = 0.334) and 1.6 times the odds for slow and rehabilitation pathways (adjusted OR = 1.573; p = 0.072).
| Variable | Adjusted OR | Standard error | 95% CI | Significance |
|---|---|---|---|---|
| Age category | 1.732 | 0.124 | 1.504 to 1.995 | < 0.001 |
| MHA | ||||
| Hospital order with restrictions | 1.00 | 0.109 | 0.426 to 0.866 | 0.006 |
| Civil/quasi-civil | 0.608 | 0.075 | 0.147 to 0.460 | < 0.001 |
| Prison transfer | 0.260 | |||
| Admission source | ||||
| Prison | 1.00 | 0.215 | 0.341 to 1.246 | 0.196 |
| Community | 0.652 | 0.311 | 0.420 to 1.749 | 0.171 |
| Low secure | 0.559 | 0.987 | 3.219 to 7.193 | < 0.001 |
| Medium secure | 4.812 | 1.150 | 3.071 to 7.743 | < 0.001 |
| High secure | 4.876 | |||
| Ward pathway category | ||||
| Mixed/other | 1.00 | 0.163 | 0.176 to 0.886 | 0.024 |
| Admission | 0.395 | 0.193 | 0.480 to 1.270 | 0.321 |
| Treatment | 0.781 | 0.380 | 0.42 to 2.918 | 0.334 |
| High dependency | 0.353 | 0.395 | 0.961 to 2.574 | 0.072 |
| Slow/rehabilitation | 1.573 | |||
| Between-unit variance | 0.469 | 0.223 | 0.185 to 1.191 | |
Extrapolation of total number of long-stay patients
For medium security, we extrapolated the overall number of long-stay patients in England using three different approaches, taking into account patient numbers in those units not included using publicly available sources to obtain this information. A list of all units, included and not included, with bed numbers and specifications is shown in Appendix 4.
-
We extrapolated the total long-stay patients by applying the average percentage of long-stay patients in all included units to non-included units and adding up both figures.
-
We took into account provider type (NHS or independent) by applying the different percentages of long-stay patients in NHS and in independent units found in our study to units not included.
-
Finally, we took into account diagnoses catered for, applying different percentages to units providing care to different patient groups.
We had also planned to take into account gender mix; however, this did not appear meaningful as the majority of units catered for both genders.
The findings are shown in Tables 15–17.
| Included units | Non-included units | |||
|---|---|---|---|---|
| Total patient numbers | Number of long-stay patients | Percentage of long-stay patients | Total patient numbers | Extrapolated number of long-stay patients |
| 1572 | 285 | 18.1% | 1520 | 275 |
| Provider type | Included units | Non-included units | |||
|---|---|---|---|---|---|
| Total patient numbers | Number of long-stay patients | Percentage of long-stay patients | Total patient numbers | Extrapolated number of long-stay patients | |
| NHS units | 1093 | 178 | 16.3 | 939 | 153 |
| Independent units | 479 | 107 | 22.3 | 581 | 130 |
| Total | 1572 | 285 | 1520 | 283 | |
| Provider type | Diagnosis | Included units | Non-included units | |||
|---|---|---|---|---|---|---|
| Total patient numbers | Number of long-stay patients | Percentage of long-stay patients | Total patient numbers | Extrapolated number of long-stay patients | ||
| NHS units | Mental illness only | 493 | 67 | 13.6 | 725 | 102 |
| Mental illness and PD | 283 | 40 | 14.1 | 16 | 2 | |
| Mental illness and intellectual disability | 0 | 0 | 0 | 145 | 27a | |
| Mental illness, PD and intellectual disability | 274 | 61 | 22.3 | 23 | 5 | |
| Intellectual disability only | 43 | 10 | 23.6 | 30 | 7 | |
| Independent units | Mental illness only | 25 | 2 | 8.0 | 216 | 17 |
| Mental illness and PD | 106 | 35 | 33.0 | 177 | 58 | |
| Mental illness and intellectual disability | 151 | 16 | 10.6 | 0 | 0 | |
| Mental illness, PD and intellectual disability | 173 | 48 | 27.7 | 158 | 44 | |
| Intellectual disability only | 24 | 6 | 25.0 | 30 | 8 | |
| Total | 1572 | 285 | 18 | 1520 | 270 | |
Discussion
This part of the study aimed to identify the prevalence and expected overall number of long-stay patients in English high and medium secure forensic care and the LoS profiles in these settings. We also compared long-stay patients with those not fulfilling our long-stay criteria on some sociodemographic and pathway variables, and identified predictors of long stay in our cross-sectional sample of patients resident in 23 medium and three high secure units on 1 April 2013. To our knowledge, this is the first national study addressing these issues in England.
The long-stay population
We identified a prevalence of long stay, according to our criteria, of 23.5% in high and of 18.1% in medium secure settings, although the percentage for the latter varied from 0% to 50%. Based on our prevalence figures, we estimate that there are about 560 long-stay patients in medium and just under 170 in high secure care in England. We will discuss the implications of this later on in this report.
There is limited research identifying how many patients stay for extended periods of time in high or medium secure hospitals in England, and comparisons are difficult to draw owing to the different cut-offs used. Additionally, most previous research employed discharge samples, described findings for single settings only, and only considered LoS for that setting rather than for the entire population of high/medium secure stay patients. Our study looked at all those resident at our census date, and hence their total LoS at the time of discharge will be higher than the average LoS identified here.
Dell et al. 33 found that 44.4% of patients had exceeded the average LoS of 8 years in their study at one high secure hospital. This would appear to be a higher figure than ours, although their study used a lower LoS cut-off point; in addition, the data of that study are now 20 years old and policy and pathways have changed, not least the accelerated discharge programme that has since taken place,30 targeting some of the residents in the Dell et al. 33 study. A study using a similar method to ours found that, combining all forensic care, 39.1% of patients in a London catchment area had stayed for > 5 years at their census date. The combination of different security levels and the time of this study (1999), again, limits the meaningfulness of any comparisons. Studies using our cut-off point of 5 years for LoS in medium secure care in England reported figures of 10%82 (based on an admission sample at one unit), 21%38 (based on a cross-sectional survey in one unit) and 9.3%42 (based on a discharge sample in one unit). Some of these figures seem lower than ours, which can be attributed to methodological factors as described above; it is also of note that the units in these studies were NHS rather than independent provider units; the one with the higher figure had opened a ward specifically addressing the needs of a long-stay group. Given the huge variation in prevalence in our study, it is clear that research in one single setting does not provide a useful national picture of LoS. In addition, taking into account continuous LoS in previous secure settings, as in our study, is likely to give a more meaningful estimate of the extent of the problem.
The large variation in prevalence of long stay for medium secure care is worth noting, from no cases to half of the patient population. One of the units included here had a ward set up specifically for those leaving high secure care as part of the accelerated discharge programme; therefore, a higher percentage of long-stay patients in this unit was expected. Variation may arise as a result of the different patient groups (e.g. those with PD or intellectual disabilities) catered for; some studies have also identified variation in admission rates by geographical location due to differences in social deprivation, ethnicity and the availability of low secure beds. 80 These factors are unlikely to fully account for the differences in long stay, particularly as we did not find some of them (e.g. ethnicity) to be associated with long-stay status. There are no national standards with regard to admission criteria for medium secure care beyond the patient being a ‘serious danger to the public’12 and it is possible (although this cannot be confirmed by our study) that individual units adopt their own (implicit or explicit) criteria, such as not admitting patients who have little prospect of moving on to less secure settings or of being discharged. Alternatively, it is possible that the interventions offered in units with a higher proportion of long-stay patients are less effective in allowing patients to move on.
For actual LoS (as opposed to the prevalence of long-stay cases), for this WP we were only able to use LoS in current unit; as expected, the median LoS was higher for high secure as opposed to medium secure care (54 vs. 18 months) and much higher for those identified as long-stay patients than for non-long-stay patients (141 vs. 44 months for high secure care and 51 vs. 14 months for medium secure care). No such data are available for high secure care, but for medium secure settings studies have identified broadly similar figures for LoS in the overall population, although our LoS figures are at the upper end of those reported in the literature,37,42,82 possibly reflecting an increase in LoS over time but, again, different methods and reporting make comparisons difficult.
Factors associated with length of stay
Our final model suggested that age category, MHA section, admission source and current ward type were independent predictors of long-stay status. Previous studies have produced somewhat conflicting findings with regard to associations between sociodemographic factors and LoS, although most have not found such a relationship. Two previous studies have identified that patients from black and minority ethnic (BME) groups had a shorter LoS than those from white ethnic groups,42,82 and studies that looked at gender differences have found shorter LoS in females (e.g. Davoren et al. 81). Notably, however, their longer-term outcomes seem to be worse. 104 We did not find any difference between long-stay patients and non-long-stay patients in terms of gender or ethnicity; the higher percentage of white ethnic class in long-stay patients in the medium secure setting failed to reach statistical significance. As expected, long-stay patients were older than non-long-stay patients in both high and medium secure care. The large number of older patients, with about one-third of the long-stay population aged over 50 years, has important implications for the service planning for this patient group.
In line with other research in individual settings,37,39,81 our national study has also identified an association between MHA and long-stay status in both medium and high secure patients, with significantly more patients in the long-stay groups on hospital orders with restrictions and fewer on prison transfers. This reflects the practical realities of this section in that it does not allow transfer (back) to prison for those who may (no longer) benefit from hospital treatment. In contrast with those civil sections (or quasi-civil sections, such as hospital orders without restrictions), these patients also require Ministry of Justice approval for moves to other secure settings, which is another reason for the delay in their transfer. These data on admission source additionally reflect potential challenges in the smooth transfer of this patient group along a pathway from more to less secure settings as identified by others (e.g. Tetley et al. 105 for PD patients). The observation that about two-thirds of the high and half of the medium secure long-stay group were admitted from the same or lower levels of security does suggest movement around rather than forward. These experiences can cause a significant amount of distress for patients and carers, as demonstrated elsewhere in this report (see Chapters 7 and 11).
A number of authors have suggested that a lack of secure services for patients with intellectual disabilities might contribute to these patients’ higher LoS (e.g. Alexander et al. 106), and most studies have found that severe mental illness was associated with longer and PD with shorter LoS (e.g. Shah et al. 42). We were not able to assess diagnosis in this part of the study, but diagnostic ward type can be used as a proxy for diagnosis and reflects these findings, although this is significant for high secure patients only.
Chapter 6 Characteristics and needs of long-stay forensic psychiatric patients
Aims and objectives
The key aims and objectives for this part of the project were to:
-
describe the characteristics of long-stay patients, including sociodemographics, psychopathology, criminal history and risk
-
describe their care pathways and the reasons for their prolonged stay
-
describe their current and future mental health, psychosocial and service needs through file review and information from responsible clinicians
-
develop a categorisation of long-stay patients according to their current presentation and future needs.
Methods
Data collection
Our long-stay sample was identified from data in WP1 as described in Chapter 3. A detailed data collection pro forma was developed with input from the PMG, the SURG and the SSC (see Appendix 5). A data collection training protocol was developed, which included a detailed guide to data collection, two exercises to assess understanding of the inclusion criteria and the documentation of criminal history. Following completion of training, a pilot pro forma was completed, which was reviewed by the study team with feedback given. Only if this seemed satisfactory were a further five pro formas completed for review, and then full data collection began if sufficient quality of data collection was achieved. Data collectors were encouraged to ask questions if they encountered any difficulties, and kept in regular contact with the research team, who provided supervisory input during this time.
For long-stay patients still resident in the unit at the time of WP2 data collection, their consultant was given a questionnaire to ascertain their views of the patient’s security, dependency, treatment and political needs based on the visual analogue scale developed by Shaw et al. 64 (see Appendix 6). To this questionnaire we added a question enquiring about the likelihood of patients needing lifelong care, either high or medium secure (scored from 0 to 10 with lower scores indicating higher likelihood). Our questionnaire also gave the option of indicating factors impeding the transfer of patients to less secure settings, using a list of pre-defined possible factors and rating from 0 to 5, with 5 indicating the highest relevance. The data collectors were responsible for distribution and were able to identify the relevant consultants based on patients’ unique identifier codes. The data collectors returned all completed anonymised questionnaires to the research team. We distributed 283 questionnaires, relating to those patients still in the same setting as our survey date in 2013, of which 169 were returned, a response rate of 60%.
Data processing
Following data cleaning and consistency checking, data were entered into a SPSS file and double-checked by at least one other researcher. It became apparent that some variables needed to go through a process of recategorisation for them to be more meaningfully statistically analysed and interpreted. Extensive discussions were held within the team regarding this process.
Examples of recategorisations include the introduction of LoS and age categories, categories of MHA sections (civil or quasi-civil, hospital orders with restrictions or prison transfers), categories of diagnoses (intellectual disabilities, mental illness, PD or mental illness + PD), category of offender (violent, sexual, mixed, other or non-offender) and severity of offending. To describe patients’ recent improvement or deterioration in risk, we labelled them as ‘improver’, ‘non-improver’ or ‘deteriorater’ based on the difference between the sum of their total clinical and risk items on the Historical Clinical Risk Management-20 (HCR-20)107 scale from 2013 (or from 2012 when 2013 scores were not available) and their scores from 2011 (or next most recent assessment).
The necessary recategorisations were allocated to members of the research team to be computed and new variables were created within the SPSS data set. These are documented in Appendix 7. Spot checks were done on all new entries to ensure the accuracy of this process.
Data analysis
A descriptive analysis was conducted using SPSS version 21 for the whole sample, and for patients currently in high and medium secure care separately. For categorical data, comparisons between patients in these two settings were completed using cross-tabulation and chi-squared tests. For continuous (‘scale’) data, comparisons were made using a non-parametric test (Mann–Whitney), because a number of variables deviated from an approximately normal distribution.
An analysis of factors that might predict LoS was carried out with MLWin software. The analysis was performed using multilevel binary logistic regression to account for unit variance (‘clustering effects’), setting ‘Unit’ at level 2 and ‘Patient’ at level 1. As commonly found in other studies, LoS in this sample was not normally distributed. Attempts to transform these data were of limited success, risking the possibility of violating the conditions for linear regression. We therefore chose to recode each patient’s LoS in continuous secure care as a binary variable based on a median-split, and to use this as the dependent variable in the logistic regressions. A number of potential predictive factors for LoS were identified from the literature and from our own study (see Appendix 8) and any that were not normally distributed were transformed to an approximately normal distribution before entering them into the regression. A separate regression was then performed for each potential factor to test its association with the binary LoS variable, allowing a shorter list of factors significantly associated with LoS to be obtained. This process was completed separately for patients currently residing in high and in medium secure care. Analyses of factors that might predict consultants’ views of patients’ need for lifelong secure care were carried out following a similar process.
For the pathway analysis, we described the percentages of patients moving into their current placement from each other type of placement and the average time spent in this previous placement, and continued this procedure for each previous placement identified.
To group patients into separate classes, latent class analysis108 was performed. The variables entered are shown in Appendix 9; the number of variables had to be reduced several times to this final set owing to the complexities of the resulting models. Estimation was performed using maximum likelihood with robust standard errors. The number of classes to be estimated was increased iteratively until the best-fitting model was used, in terms of both statistical and clinical criteria. The parsimony indices, the lowest Akaike information criterion and sample size-adjusted Bayesian information criterion, as well as the highest entropy, were examined. Higher entropy indicates a more accurate classification of individuals, with values > 0.8 suggesting adequate classification. 109 In addition, given the large number of categorical variables, the bootstrapped likelihood ratio test was used to help determine the number of classes to model. 110 A probability of < 0.05 for the test indicated that the model with more classes fitted significantly better than the model with fewer. The results from this model were subsequently screened for appropriate clinical interpretation before the final modelling solution was adopted.
Findings
Patient characteristics, pathways and treatment
Our study generated a large number of detailed clinical data that are summarised in Table 18. We will not describe each finding in the text below, but rather highlight key aspects. We will do so under specific headings related to patient characteristics (e.g. sociodemographics, mental disorder) and service-related issues (e.g. admission source, pathways, treatment). We will describe findings for the overall sample as well as separately for patients currently residing in high and medium secure care and highlight significant differences between these two groups.
| Sociodemographic characteristic | Whole sample | High secure | Medium secure | Statistic | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | n | %,a mean (SD) | N | n | %,a mean (SD) | Rangeb | N | n | %,a mean (SD)b | Rangeb | ||
| Sex | ||||||||||||
| Male | 401 | 344 | 85.8 | 116 | 105 | 90.5 | 285 | 239 | 83.9 | χ2 = 3.88; p = 0.049 | ||
| Age | ||||||||||||
| Age in years, mean (SD) | 401 | 44.46 (11.26) | 116 | 45.60 (9.76) | 25–77 | 285 | 44.00 (11.79) | 20–82 | n.s. | |||
| Age group (years) | ||||||||||||
| 20–29 | 401 | 37 | 9.2 | 116 | 8 | 6.9 | 285 | 29 | 10.2 | n.s. | ||
| 30–39 | 401 | 102 | 25.4 | 116 | 23 | 19.8 | 285 | 79 | 27.7 | n.s. | ||
| 40–49 | 401 | 135 | 33.7 | 116 | 51 | 44.0 | 285 | 84 | 29.5 | n.s. | ||
| 50–59 | 401 | 90 | 22.4 | 116 | 26 | 22.4 | 285 | 64 | 22.5 | n.s. | ||
| ≥ 60 | 401 | 37 | 9.2 | 116 | 8 | 6.9 | 285 | 29 | 10.2 | n.s. | ||
| Ethnicity | ||||||||||||
| White | 401 | 313 | 78.6 | 116 | 95 | 81.9 | 282 | 218 | 77.3 | n.s. | ||
| Black | 401 | 45 | 11.3 | 116 | 10 | 8.6 | 282 | 35 | 12.4 | n.s. | ||
| Asian | 401 | 14 | 3.5 | 116 | 4 | 3.4 | 282 | 10 | 3.5 | n.s. | ||
| Mixed | 401 | 22 | 5.5 | 116 | 6 | 5.2 | 282 | 16 | 5.7 | n.s. | ||
| Other | 401 | 4 | 1.0 | 116 | 1 | 0.9 | 282 | 3 | 1.1 | n.s. | ||
| British | 399 | 377 | 94.4 | 116 | 108 | 93.1 | 283 | 269 | 95.1 | n.s. | ||
| Born in the UK | 397 | 364 | 91.7 | 116 | 107 | 92.2 | 281 | 257 | 91.5 | n.s. | ||
| Marital status | ||||||||||||
| Married | 385 | 11 | 2.9 | 106 | 4 | 3.8 | 279 | 7 | 2.5 | n.s. | ||
| Civil partnership | 385 | 0 | 0 | 106 | 0 | 0 | 279 | 0 | 0 | n.s. | ||
| In a relationship | 385 | 1 | 0.3 | 106 | 0 | 0 | 279 | 1 | 0.4 | n.s. | ||
| Divorced | 385 | 38 | 9.9 | 106 | 9 | 8.5 | 279 | 29 | 10.4 | n.s. | ||
| Widowed | 385 | 6 | 1.6 | 106 | 0 | 0 | 279 | 6 | 2.2 | n.s. | ||
| Never married | 385 | 329 | 85.5 | 106 | 93 | 87.7 | 279 | 236 | 84.6 | n.s. | ||
| Highest qualification | ||||||||||||
| No qualifications | 365 | 241 | 66.0 | 89 | 62 | 69.7 | 276 | 179 | 64.9 | n.s. | ||
| GCSEs | 365 | 79 | 21.6 | 89 | 18 | 20.2 | 276 | 61 | 22.1 | n.s. | ||
| A levels | 365 | 22 | 6.0 | 89 | 4 | 4.5 | 276 | 18 | 6.5 | n.s. | ||
| Bachelor’s or similar graduate degree | 365 | 4 | 1.1 | 89 | 1 | 1.1 | 276 | 3 | 1.1 | n.s. | ||
| Postgraduate degree or equivalent | 365 | 1 | 0.3 | 89 | 1 | 1.1 | 276 | 0 | 0 | n.s. | ||
| City & Guilds | 365 | 4 | 1.1 | 89 | 0 | 0 | 276 | 4 | 1.4 | n.s. | ||
| NVQs | 365 | 2 | 0.5 | 89 | 0 | 0 | 276 | 2 | 0.7 | n.s. | ||
| Other qualifications | 365 | 12 | 3.3 | 89 | 3 | 3.4 | 276 | 9 | 3.3 | n.s. | ||
| Ratio of no qualifications vs. the rest | 365 | 241 : 124 | 1.94 | 89 | 2.30 | 276 | 179 : 97 | 1.85 | n.s. | |||
| Employment status prior to admission | ||||||||||||
| Full-time employment | 333 | 40 | 12.0 | 83 | 15 | 18.1 | 250 | 25 | 10.0 | n.s. | ||
| Part-time employment (> 10 hours/week) | 333 | 9 | 2.7 | 83 | 1 | 1.2 | 250 | 8 | 3.2 | n.s. | ||
| Part-time employment (< 10 hours/week) | 333 | 3 | 0.9 | 83 | 1 | 1.2 | 250 | 2 | 0.8 | n.s. | ||
| Full-/part-time (hours unknown) | 333 | 16 | 4.8 | 83 | 12 | 14.5 | 250 | 4 | 1.6 | χ2 = 22.52; p < 0.001 | ||
| Full- or part-time education | 333 | 2 | 0.6 | 83 | 1 | 1.2 | 250 | 1 | 0.4 | n.s. | ||
| Voluntary work | 333 | 7 | 2.1 | 83 | 0 | 0 | 250 | 7 | 2.8 | n.s. | ||
| Unemployed | 333 | 247 | 74.2 | 83 | 46 | 55.4 | 250 | 201 | 80.4 | χ2 = 20.30; p < 0.001 | ||
| Other | 333 | 9 | 2.7 | 83 | 7 | 8.4 | 250 | 2 | 0.8 | n.s. | ||
| Ratio unemployed vs. the rest | 333 | 247 : 86 | 2.87 | 83 | 46 : 37 | 1.24 | 250 | 201 : 49 | 4.10 | χ2 = 20.30; p < 0.001 | ||
| Not been in community since 16 years | 356 | 23 | 6.5 | 99 | 16 | 16.2 | 257 | 7 | 2.7 | χ2 = 21.36; p < 0.001 | ||
| Ever full- or part-time employment for ≥ 6 months in the community | 346 | 136 | 39.3 | 86 | 27 | 31.4 | 260 | 109 | 41.9 | n.s. | ||
| HCR-20 | ||||||||||||
| HCR-20 relationship instability score, mean (SD) | 355 | 1.76 (0.51) | 107 | 1.86 (0.40) | 0–2 | 248 | 1.71 (0.54) | 0–2 | z = 2.60; p = 0.009 | |||
| HCR-20 lack of support score, mean (SD) | 368 | 1.26 (0.74) | 108 | 1.19 (0.81) | 0–2 | 260 | 1.29 (0.71) | 0–2 | n.s. | |||
| LoS | Whole sample | High secure | Medium secure | Statistic | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | n | %,a mean (SD) | N | n | %,a mean (SD) | Rangeb | N | n | %,a mean (SD) | Rangeb | ||
| LoS (months): continuous care | ||||||||||||
| Median (IQR) | 401 | 155.2 (136.4) | 116 | 183.6 (79.1) | 13.7–503.3 | 285 | 128.4 (145.5) | 60.2–651.0 | z = 5.21; p < 0.001 | |||
| Mean (SD) | 401 | 175.0 (103.9) | 116 | 203.6 (86.2) | 285 | 163.3 (108.3) | ||||||
| LoS (categories): continuous care | ||||||||||||
| 5–10 years | 401 | 144 | 35.9 | 116 | 7 | 6.0 | 285 | 137 | 48.1 | χ2 = 63.30; p < 0.001 | ||
| > 10–20 years | 401 | 178 | 44.4 | 116 | 86 | 74.1 | 285 | 92 | 32.3 | χ2 = 58.51; p < 0.001 | ||
| > 20–30 years | 401 | 53 | 13.2 | 116 | 13 | 11.2 | 285 | 40 | 14.0 | n.s. | ||
| > 30 years | 401 | 26 | 6.5 | 116 | 10 | 8.6 | 285 | 16 | 5.6 | n.s. | ||
| LoS (months): current unit | ||||||||||||
| Median (IQR) | 401 | 61.2 (78.5) | 116 | 140.0 (131.1) | 4.3–471.5 | 285 | 46.9 (53.9) | 1.2–238.5 | z = 9.47; p < 0.001 | |||
| Mean (SD) | 401 | 78.2 (70.4) | 116 | 139.5 (90.8) | 285 | 53.2 (38.5) | ||||||
| LoS (categories): current unit | ||||||||||||
| < 5 years | 400 | 191 | 47.8 | 116 | 29 | 25.0 | 284 | 162 | 57.0 | χ2 = 33.89; p < 0.001 | ||
| 5–10 years | 400 | 123 | 30.8 | 116 | 16 | 13.8 | 284 | 107 | 37.7 | χ2 = 22.06; p < 0.001 | ||
| > 10–20 years | 400 | 76 | 19.0 | 116 | 61 | 52.6 | 284 | 15 | 5.3 | χ2 = 119.8; p < 0.001 | ||
| > 20–30 years | 400 | 7 | 1.8 | 116 | 7 | 6.0 | 284 | 0 | 0 | n.s. | ||
| > 30 years | 400 | 3 | 0.8 | 116 | 3 | 2.6 | 284 | 0 | 0 | n.s. | ||
| Admission source | Whole sample | High secure | Medium secure | Statistic | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | n | %,a mean (SD) | N | n | %,a mean (SD) | N | n | %,a mean (SD) | ||
| To continuous care | ||||||||||
| Prison | 401 | 225 | 56.1 | 116 | 69 | 59.5 | 285 | 156 | 54.7 | n.s. |
| Low secure NHS | 401 | 35 | 8.7 | 116 | 9 | 7.8 | 285 | 26 | 9.1 | n.s. |
| Low secure private | 401 | 20 | 5.0 | 116 | 4 | 3.4 | 285 | 16 | 5.6 | n.s. |
| Other psychiatric setting | 401 | 48 | 12.0 | 116 | 16 | 13.8 | 285 | 32 | 11.2 | n.s. |
| Community | 401 | 64 | 16.0 | 116 | 15 | 12.9 | 285 | 49 | 17.2 | n.s. |
| Other | 401 | 9 | 2.2 | 116 | 3 | 2.6 | 285 | 6 | 2.1 | n.s. |
| To current unit | ||||||||||
| Prison | 401 | 79 | 19.7 | 116 | 45 | 38.8 | 285 | 34 | 11.9 | χ2 = 37.61; p < 0.001 |
| High secure setting | 401 | 97 | 24.2 | 116 | 23 | 19.8 | 285 | 74 | 26.0 | n.s. |
| Medium secure NHS | 401 | 71 | 17.7 | 116 | 30 | 25.9 | 285 | 41 | 14.4 | χ2 = 7.45; p = 0.006 |
| Medium secure private | 401 | 117 | 29.2 | 116 | 13 | 11.2 | 285 | 104 | 36.5 | χ2 = 25.51; p < 0.001 |
| Low secure NHS | 401 | 15 | 3.7 | 116 | 1 | 0.9 | 285 | 14 | 4.9 | n.s. |
| Low secure private | 401 | 5 | 1.2 | 116 | 1 | 0.9 | 285 | 4 | 1.4 | n.s. |
| Other psychiatric setting | 401 | 8 | 2.0 | 116 | 1 | 0.9 | 285 | 7 | 2.5 | n.s. |
| Community | 401 | 6 | 1.5 | 116 | 0 | 0 | 285 | 6 | 2.1 | n.s. |
| Other | 401 | 3 | 0.7 | 116 | 2 | 1.7 | 285 | 1 | 0.4 | n.s. |
| MHA classification | Whole sample | High secure | Medium secure | Statistic | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | n | %,a mean (SD) | N | n | %,a mean (SD) | N | n | %,a mean (SD) | ||
| MHA section on admission to continuous care | ||||||||||
| Section 2 | 400 | 6 | 1.5 | 116 | 1 | 0.9 | 284 | 5 | 1.8 | n.s. |
| Section 3 | 400 | 80 | 20.0 | 116 | 24 | 20.7 | 284 | 56 | 19.7 | n.s. |
| Section 35 | 400 | 6 | 1.5 | 116 | 2 | 1.7 | 284 | 4 | 1.4 | n.s. |
| Section 38 | 400 | 28 | 7.0 | 116 | 7 | 6.0 | 284 | 21 | 7.4 | n.s. |
| Section 48 | 400 | 4 | 1.0 | 116 | 1 | 0.9 | 284 | 3 | 1.1 | n.s. |
| Section 48/49 | 400 | 63 | 15.8 | 116 | 15 | 12.9 | 284 | 48 | 16.9 | n.s. |
| Section 37 hospital order | 400 | 20 | 5.0 | 116 | 3 | 2.6 | 284 | 17 | 6.0 | n.s. |
| Section 37/41 | 400 | 88 | 22.0 | 116 | 22 | 19.0 | 284 | 66 | 23.2 | n.s. |
| Section 47 | 400 | 5 | 1.3 | 116 | 1 | 0.9 | 284 | 4 | 1.4 | n.s. |
| Section 47/49 | 400 | 64 | 16.0 | 116 | 28 | 24.1 | 284 | 36 | 12.7 | χ2 = 8.05; p = 0.005 |
| Notional 37 | 400 | 4 | 1.0 | 116 | 1 | 0.9 | 284 | 3 | 1.1 | n.s. |
| CPIA | 400 | 5 | 1.3 | 116 | 2 | 1.7 | 284 | 3 | 1.1 | n.s. |
| Section 60/65 | 400 | 20 | 5.0 | 116 | 8 | 6.9 | 284 | 12 | 4.2 | n.s. |
| Other | 400 | 7 | 1.8 | 116 | 1 | 0.9 | 284 | 6 | 2.1 | n.s. |
| MHA section on admission to current unitb | ||||||||||
| Section 3 | 401 | 67 | 16.7 | 116 | 21 | 18.1 | 285 | 46 | 16.1 | n.s. |
| Section 35 | 401 | 3 | 0.7 | 116 | 3 | 2.6 | 285 | 0 | 0 | n.s. |
| Section 38 | 401 | 7 | 1.7 | 116 | 4 | 3.4 | 285 | 3 | 1.1 | n.s. |
| Section 48 | 401 | 1 | 0.2 | 116 | 0 | 0 | 285 | 1 | 0.4 | n.s. |
| Section 48/49 | 401 | 23 | 5.7 | 116 | 7 | 6.0 | 285 | 16 | 5.6 | n.s. |
| Section 37 hospital order | 401 | 26 | 6.5 | 116 | 4 | 3.4 | 285 | 22 | 7.7 | n.s. |
| Section 37/41 | 401 | 191 | 47.6 | 116 | 44 | 37.9 | 285 | 147 | 51.6 | χ2 = 6.16; p = 0.013 |
| Section 47 | 401 | 6 | 1.5 | 116 | 1 | 0.9 | 285 | 5 | 1.8 | n.s. |
| Section 47/49 | 401 | 46 | 11.5 | 116 | 24 | 20.7 | 285 | 22 | 7.7 | χ2 = 13.66; p < 0.001 |
| Notional 37 | 401 | 15 | 3.7 | 116 | 4 | 3.4 | 285 | 11 | 3.9 | n.s. |
| CPIA | 401 | 9 | 2.2 | 116 | 1 | 0.9 | 285 | 8 | 2.8 | n.s. |
| Section 60/65 | 401 | 3 | 0.7 | 116 | 3 | 2.6 | 285 | 0 | 0 | n.s. |
| Other | 401 | 4 | 1.0 | 116 | 0 | 0 | 285 | 4 | 1.4 | n.s. |
| Current MHA section (as of 1 April 2013)c | ||||||||||
| Section 3 | 401 | 57 | 14.2 | 116 | 14 | 12.1 | 285 | 43 | 15.1 | n.s. |
| Section 37 hospital order | 401 | 27 | 6.7 | 116 | 6 | 5.2 | 285 | 21 | 7.4 | n.s. |
| Section 37/41 | 401 | 242 | 60.3 | 116 | 68 | 58.6 | 285 | 174 | 61.1 | n.s. |
| Section 47 | 401 | 4 | 1.0 | 116 | 1 | 0.9 | 285 | 3 | 1.1 | n.s. |
| Section 47/49 | 401 | 36 | 9.0 | 116 | 17 | 14.7 | 285 | 19 | 6.7 | n.s. |
| Notional 37 | 401 | 21 | 5.2 | 116 | 6 | 5.2 | 285 | 15 | 5.3 | n.s. |
| CPIA | 401 | 13 | 3.2 | 116 | 4 | 3.4 | 285 | 9 | 3.2 | n.s. |
| Other | 401 | 1 | 0.2 | 116 | 0 | 0 | 285 | 1 | 0.4 | n.s. |
| Current MHA categories | ||||||||||
| Civil or quasi-civil | 400 | 110 | 27.5 | 116 | 27 | 23.3 | 284 | 83 | 29.2 | n.s. |
| Hospital order with restrictions | 400 | 254 | 63.5 | 116 | 72 | 62.1 | 284 | 182 | 64.1 | n.s. |
| Prison transfers | 400 | 36 | 9.0 | 116 | 17 | 14.7 | 284 | 19 | 6.7 | n.s. |
| Change in MHA section | ||||||||||
| Change in MHA section during continuous admission | 400 | 193 | 48.3 | 116 | 58 | 50.0 | 284 | 135 | 47.5 | n.s. |
| Treatment history | Whole sample | High secure | Medium secure | Statistic | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | n | %,a mean (SD) | N | n | %,a mean (SD) | Rangeb | N | n | %,a mean (SD)b | Rangeb | ||
| Age (years) first admitted to any inpatient psychiatric care, including secure care, mean (SD) | 389 | 21.78 (7.16) | 114 | 21.32 (6.59) | 7 to 40 | 275 | 21.97 (7.38) | 3 to 56 | n.s. | |||
| Any previous admissions to non-secure inpatient psychiatric care | 401 | 272 | 67.8 | 116 | 74 | 63.8 | 285 | 198 | 69.5 | n.s. | ||
| Number of previous admissions to non-secure psychiatric inpatient care | ||||||||||||
| Median (IQR) | 260 | 3.00 (4.00) | 77 | 2.00 (5.00) | 0 to 15 | 183 | 3.00 (3.00) | 0 to 56 | n.s. | |||
| Mean (SD) | 4.34 (5.01) | 3.82 (3.43) | 4.56 (5.54) | |||||||||
| Any previous admission to high, medium or low secure | 394 | 183 | 46.4 | 115 | 59 | 51.3 | 279 | 124 | 44.4 | n.s. | ||
| Any previous admission to low secure care | 393 | 79 | 20.1 | 114 | 18 | 15.8 | 279 | 61 | 21.9 | n.s. | ||
| Any previous admission to medium secure care | 396 | 121 | 30.6 | 116 | 32 | 27.6 | 280 | 89 | 31.8 | n.s. | ||
| Any previous admission to high secure care | 396 | 52 | 13.1 | 116 | 26 | 22.4 | 280 | 26 | 9.3 | χ2 = 12.39; p < 0.001 | ||
| Number of ward moves in the past 5 years | ||||||||||||
| Median (IQR) | 270 | 2.00 (2.00) | 90 | 2.00 (2.00) | 0 to 7 | 180 | 1.00 (2.00) | 0 to 9 | z = 1.97; p = 0.049 | |||
| Mean (SD) | 1.98 (1.73) | 2.19 (1.64) | 1.87 (1.78) | |||||||||
| Number of unit moves during current continuous care | ||||||||||||
| Median (IQR) | 401 | 1.00 (2.00) | 116 | 1.00 (2.00) | 0 to 6 | 285 | 1.00 (1.00) | 0 to 7 | z = 4.22; p < 0.001 | |||
| Mean (SD) | 1.43 (1.32) | 1.03 (1.18) | 1.59 (1.35) | |||||||||
| Mental disorder | Whole sample | High secure | Medium secure | Statistic | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | n | %,a mean (SD) | N | n | %,a mean (SD) | N | n | %,a mean (SD) | ||
| Current diagnosis | ||||||||||
| Dementia | 401 | 1 | 0.2 | 116 | 0 | 0 | 285 | 1 | 0.4 | n.s. |
| Brain injury | 401 | 10 | 2.5 | 116 | 5 | 4.3 | 285 | 5 | 1.8 | n.s. |
| Intellectual disability | 401 | 66 | 16.5 | 116 | 28 | 24.1 | 285 | 38 | 13.3 | χ2 = 7.00; p = 0.008 |
| Autism spectrum disorder | 400 | 10 | 2.5 | 116 | 4 | 3.4 | 284 | 6 | 2.1 | n.s. |
| Schizophrenia | 401 | 232 | 57.9 | 116 | 62 | 53.4 | 285 | 170 | 59.6 | n.s. |
| Schizoaffective disorder | 401 | 53 | 13.2 | 116 | 18 | 15.5 | 285 | 35 | 12.3 | n.s. |
| Other psychotic disorder | 400 | 12 | 3.0 | 116 | 3 | 2.6 | 284 | 9 | 3.2 | n.s. |
| Bipolar disorder | 401 | 13 | 3.2 | 116 | 5 | 4.3 | 285 | 8 | 2.8 | n.s. |
| Depression | 400 | 23 | 5.8 | 116 | 14 | 12.1 | 284 | 9 | 3.2 | χ2 = 12.03; p = 0.001 |
| PD | 398 | 186 | 46.7 | 114 | 57 | 50.0 | 284 | 129 | 45.4 | n.s. |
| Alcohol misuse/dependence | 400 | 18 | 4.5 | 116 | 2 | 1.7 | 284 | 16 | 5.6 | n.s. |
| Other substance misuse/dependence | 399 | 33 | 8.3 | 116 | 2 | 1.7 | 283 | 31 | 11.0 | χ2 = 9.94; p = 0.002 |
| Other significant mental disorders | 398 | 51 | 12.8 | 115 | 18 | 15.7 | 283 | 33 | 11.7 | n.s. |
| Diagnostic categories | ||||||||||
| Mental illness | 398 | 176 | 44.1 | 115 | 47 | 41.2 | 283 | 129 | 45.6 | n.s. |
| PD | 398 | 88 | 22.1 | 115 | 21 | 18.4 | 283 | 67 | 23.7 | n.s. |
| Mental illness + PD | 398 | 69 | 17.3 | 115 | 20 | 17.5 | 283 | 49 | 17.3 | n.s. |
| Intellectual disabilities | 398 | 64 | 16.1 | 115 | 26 | 22.8 | 283 | 38 | 13.4 | n.s. |
| Treatment-resistant schizophrenia | ||||||||||
| As % of whole sample | 401 | 76 | 19.0 | 116 | 25 | 21.6 | 285 | 51 | 17.9 | n.s. |
| As % of those who have schizophrenia | 232 | 76 | 32.8 | 62 | 25 | 40.3 | 170 | 51 | 30.0 | n.s. |
| PD types (as % of those with PD) | ||||||||||
| Paranoid | 186 | 13 | 7.0 | 57 | 6 | 10.5 | 129 | 7 | 5.4 | n.s. |
| Schizoid | 186 | 8 | 4.3 | 57 | 3 | 5.3 | 129 | 5 | 3.9 | n.s. |
| Schizotypal | 186 | 1 | 0.5 | 57 | 1 | 1.8 | 129 | 0 | 0 | n.s. |
| Antisocial | 186 | 127 | 68.3 | 57 | 45 | 78.9 | 129 | 82 | 63.6 | χ2 = 4.32; p = 0.038 |
| Borderline | 186 | 86 | 46.2 | 57 | 25 | 43.9 | 129 | 61 | 47.3 | n.s. |
| Histrionic | 186 | 2 | 1.1 | 57 | 2 | 3.5 | 129 | 0 | 0 | n.s. |
| Narcissistic | 186 | 10 | 5.4 | 57 | 3 | 5.3 | 129 | 7 | 5.4 | n.s. |
| Avoidant | 186 | 9 | 4.8 | 57 | 4 | 7.0 | 129 | 5 | 3.9 | n.s. |
| Dependent | 186 | 3 | 1.6 | 57 | 1 | 1.8 | 129 | 2 | 1.6 | n.s. |
| Obsessive–compulsive | 186 | 0 | 0 | 57 | 0 | 0 | 129 | 0 | 0 | n.s. |
| Mixed PD types (≥ 2) | 186 | 73 | 39.2 | 57 | 29 | 50.9 | 129 | 44 | 33.8 | χ2 = 4.83; p = 0.028 |
| Physical disorder | Whole sample | High secure | Medium secure | Statistic | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | n | %,a mean (SD) | N | n | %,a mean (SD) | N | n | %,a mean (SD) | ||
| Any physical health condition | 399 | 286 | 71.7 | 116 | 93 | 80.2 | 283 | 193 | 68.2 | χ2 = 5.81; p = 0.016 |
| High blood pressure | 399 | 46 | 11.5 | 116 | 16 | 13.8 | 283 | 30 | 10.6 | n.s. |
| Diabetes | 399 | 110 | 27.6 | 116 | 32 | 27.6 | 283 | 78 | 27.6 | n.s. |
| Heart disease | 399 | 18 | 4.5 | 116 | 8 | 6.9 | 283 | 10 | 3.5 | n.s. |
| Obesity | 399 | 149 | 37.3 | 116 | 61 | 52.6 | 283 | 88 | 31.1 | χ2 = 16.24; p < 0.001 |
| Cancer | 398 | 5 | 1.3 | 116 | 1 | 0.9 | 282 | 4 | 1.4 | n.s. |
| Epilepsy | 399 | 26 | 6.5 | 116 | 9 | 7.8 | 283 | 17 | 6.0 | n.s. |
| Disease of the respiratory system | 399 | 65 | 16.3 | 116 | 19 | 16.4 | 283 | 46 | 16.3 | n.s. |
| Disease of the gastrointestinal system | 399 | 21 | 5.3 | 116 | 11 | 9.5 | 283 | 10 | 3.5 | χ2 = 5.84; p = 0.016 |
| Disease of the musculoskeletal system | 399 | 16 | 4.0 | 116 | 5 | 4.3 | 283 | 11 | 3.9 | n.s. |
| Any other serious condition | 399 | 106 | 26.6 | 116 | 42 | 36.2 | 283 | 64 | 22.6 | χ2 = 7.79; p = 0.005 |
| Criminal history | Whole sample | High secure | Medium secure | Statistic | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | n | %,a mean (SD) | N | n | %,a mean (SD) | Rangeb | N | n | %,a mean (SD) | Rangeb | ||
| Category of offender | ||||||||||||
| Violent | 401 | 232 | 57.9 | 116 | 72 | 62.1 | 285 | 160 | 56.1 | n.s. | ||
| Sexual | 401 | 23 | 5.7 | 116 | 9 | 7.8 | 285 | 14 | 4.9 | n.s. | ||
| Mixed | 401 | 88 | 21.9 | 116 | 21 | 18.1 | 285 | 67 | 23.5 | n.s. | ||
| Other | 401 | 29 | 7.2 | 116 | 8 | 6.9 | 285 | 21 | 7.4 | n.s. | ||
| Non-offender | 401 | 29 | 7.2 | 116 | 6 | 5.2 | 285 | 23 | 8.1 | n.s. | ||
| Severity of offending | ||||||||||||
| Score 0 | 364 | 107 | 29.4 | 108 | 26 | 24.1 | 256 | 81 | 31.6 | n.s. | ||
| Score 1 | 364 | 147 | 40.4 | 108 | 43 | 39.8 | 256 | 104 | 40.6 | n.s. | ||
| Score 2 | 364 | 77 | 21.2 | 108 | 27 | 25.0 | 256 | 50 | 19.5 | n.s. | ||
| Score 3 | 364 | 33 | 9.1 | 108 | 12 | 11.1 | 256 | 21 | 8.2 | n.s. | ||
| Convictions | ||||||||||||
| Any convictions | 401 | 372 | 92.8 | 116 | 110 | 94.8 | 285 | 262 | 91.9 | n.s. | ||
| Age (years) at first conviction, mean (SD) | 365 | 19.99 (8.16) | 108 | 19.30 (7.77) | 10 to 56 | 257 | 20.29 (8.32) | 10 to 55 | n.s. | |||
| Custodial sentences | ||||||||||||
| Ever had a custodial sentence | 390 | 222 | 56.9 | 115 | 68 | 59.1 | 275 | 154 | 56.0 | n.s. | ||
| Age (years) at first custodial sentence, mean (SD) | 222 | 21.34 (4.98) | 68 | 21.32 (5.19) | 15 to 42 | 154 | 21.35 (4.90) | 14 to 43 | n.s. | |||
| Total number of offences | ||||||||||||
| Median (IQR) | 395 | 9.0 (20.0) | 116 | 12.5 (25.0) | 0 to 118 | 279 | 8.0 (18.0) | 0 to 130 | z = 2.52; p = 0.012 | |||
| Mean (SD) | 15.28 (18.81) | 18.28 (19.86) | 14.03 (18.25) | |||||||||
| Number of offences, mean (SD) | ||||||||||||
| Offences against the person | 366 | 3.30 (5.36) | 116 | 4.84 (8.55) | 0 to 82 | 280 | 2.67 (3.04) | 0 to 15 | z = 2.58; p = 0.010 | |||
| Sexual offences | 366 | 0.91 (2.36) | 116 | 0.91 (2.32) | 0 to 17 | 282 | 0.91 (2.38) | 0 to 20 | n.s. | |||
| Property offences | 366 | 2.85 (4.95) | 116 | 4.09 (6.06) | 0 to 33 | 279 | 2.33 (4.31) | 0 to 33 | z = 2.74; p = 0.006 | |||
| Theft and kindred offences | 366 | 4.29 (8.49) | 116 | 4.96 (7.98) | 0 to 35 | 279 | 4.01 (8.67) | 0 to 75 | n.s. | |||
| Fraud and kindred offences | 366 | 0.32 (1.79) | 116 | 0.24 (0.77) | 0 to 6 | 281 | 0.36 (2.07) | 0 to 26 | n.s. | |||
| Police/prison/court offences | 366 | 1.01 (2.57) | 116 | 1.09 (2.94) | 0 to 26 | 282 | 0.98 (2.40) | 0 to 21 | n.s. | |||
| Drug offences | 366 | 0.28 (1.00) | 116 | 0.10 (0.36) | 0 to 2 | 281 | 0.35 (1.17) | 0 to 9 | n.s. | |||
| Gun/offensive weapon offences | 366 | 0.42 (1.05) | 116 | 0.34 (0.72) | 0 to 3 | 282 | 0.45 (1.16) | 0 to 10 | n.s. | |||
| Public order offences | 366 | 0.66 (1.51) | 116 | 0.67 (1.77) | 0 to 16 | 280 | 0.65 (1.40) | 0 to 11 | n.s. | |||
| Vehicle/driving offences | 366 | 0.75 (2.81) | 116 | 0.95 (3.38) | 0 to 28 | 281 | 0.67 (2.54) | 0 to 29 | n.s. | |||
| Other offences | 366 | 0.49 (2.58) | 116 | 0.47 (2.13) | 0 to 14 | 282 | 0.50 (2.75) | 0 to 27 | n.s. | |||
| Most severe sentence for any offence | ||||||||||||
| Life sentence | 365 | 36 | 9.9 | 109 | 16 | 14.7 | 256 | 20 | 7.8 | n.s. | ||
| Hospital order | 365 | 276 | 75.6 | 109 | 80 | 73.4 | 256 | 196 | 76.6 | n.s. | ||
| Prison ≥ 10 years | 365 | 5 | 1.4 | 109 | 2 | 1.8 | 256 | 3 | 1.2 | n.s. | ||
| Prison 6–9 years | 365 | 10 | 2.7 | 109 | 3 | 2.8 | 256 | 7 | 2.7 | n.s. | ||
| Prison 4–5 years | 365 | 3 | 0.8 | 109 | 1 | 0.9 | 256 | 2 | 0.8 | n.s. | ||
| Prison 1–3 years | 365 | 11 | 3.0 | 109 | 3 | 2.8 | 256 | 8 | 3.1 | n.s. | ||
| Prison < 1 year | 365 | 4 | 1.1 | 109 | 0 | 0 | 256 | 4 | 1.6 | n.s. | ||
| Suspended sentence | 365 | 1 | 0.3 | 109 | 0 | 0 | 256 | 1 | 0.4 | n.s. | ||
| Community order | 365 | 3 | 0.8 | 109 | 1 | 0.9 | 256 | 2 | 0.8 | n.s. | ||
| Fine | 365 | 1 | 0.3 | 109 | 0 | 0 | 256 | 1 | 0.4 | n.s. | ||
| Conditional discharge | 365 | 2 | 0.5 | 109 | 0 | 0 | 256 | 2 | 0.8 | n.s. | ||
| Other sentence | 365 | 13 | 3.6 | 109 | 3 | 2.8 | 256 | 10 | 3.9 | n.s. | ||
| Arson convictions | ||||||||||||
| Any arson convictions | 400 | 79 | 19.8 | 115 | 31 | 27.0 | 285 | 48 | 16.8 | χ2 = 5.29; p = 0.021 | ||
| First offence | Whole sample | High secure | Medium secure | Statistic | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | n | %,a mean (SD) | N | n | %,a mean (SD) | Rangeb | N | n | %,a mean (SD) | Rangeb | ||
| Offence type of first conviction (as % of those with a conviction) | ||||||||||||
| Offence against the person | 366 | 130 | 35.5 | 108 | 34 | 31.5 | 258 | 96 | 37.2 | n.s. | ||
| Sexual offence | 366 | 33 | 9.0 | 108 | 12 | 11.1 | 258 | 21 | 8.1 | n.s. | ||
| Property offence | 366 | 94 | 25.7 | 108 | 42 | 38.9 | 258 | 52 | 20.2 | χ2 = 14.00; p < 0.001 | ||
| Theft and kindred offences | 366 | 128 | 35.0 | 108 | 46 | 42.6 | 258 | 82 | 31.8 | χ2 = 3.91; p = 0.048 | ||
| Fraud and kindred offences | 366 | 5 | 1.4 | 108 | 2 | 1.9 | 258 | 3 | 1.2 | n.s. | ||
| Police/prison/court offence | 366 | 7 | 1.9 | 108 | 1 | 0.9 | 258 | 6 | 2.3 | n.s. | ||
| Drug offence | 366 | 10 | 2.7 | 108 | 1 | 0.9 | 258 | 9 | 3.5 | n.s. | ||
| Gun/offensive weapon offence | 366 | 16 | 4.4 | 108 | 5 | 4.6 | 258 | 11 | 4.3 | n.s. | ||
| Public order offence | 366 | 15 | 4.1 | 108 | 4 | 3.7 | 258 | 11 | 4.3 | n.s. | ||
| Vehicle/driving offence | 366 | 21 | 5.7 | 108 | 6 | 5.6 | 258 | 15 | 5.8 | n.s. | ||
| Other offence | 366 | 7 | 1.9 | 108 | 1 | 0.9 | 258 | 6 | 2.3 | n.s. | ||
| Age (years) at first violent conviction | ||||||||||||
| Mean (SD) | 304 | 23.00 (8.45) | 90 | 21.80 (7.43) | 11 to 56 | 214 | 23.51 (8.81) | 11 to 56 | n.s. | |||
| Offence type of first violent conviction (as % of those with a violent conviction) | ||||||||||||
| Murder | 309 | 9 | 2.9 | 91 | 5 | 5.5 | 218 | 4 | 1.8 | n.s. | ||
| Attempted murder | 307 | 14 | 4.6 | 90 | 4 | 4.4 | 217 | 10 | 4.6 | n.s. | ||
| Manslaughter | 307 | 39 | 12.7 | 90 | 13 | 14.4 | 217 | 26 | 12.0 | n.s. | ||
| GBH | 307 | 61 | 19.9 | 90 | 11 | 12.2 | 217 | 50 | 23.0 | χ2 = 4.68; p = 0.031 | ||
| Robbery | 307 | 25 | 8.1 | 90 | 9 | 10.0 | 217 | 16 | 7.4 | n.s. | ||
| ABH | 307 | 69 | 22.5 | 90 | 22 | 24.4 | 217 | 47 | 21.7 | n.s. | ||
| Less serious violent conviction | 307 | 73 | 23.8 | 90 | 25 | 27.8 | 217 | 48 | 22.1 | n.s. | ||
| Other violent conviction | 307 | 34 | 11.1 | 90 | 10 | 11.1 | 217 | 24 | 11.1 | n.s. | ||
| Age (years) at first sexual conviction | ||||||||||||
| Mean (SD) | 109 | 22.88 (7.02) | 28 | 21.71 (7.26) | 10 to 47 | 81 | 23.28 (6.93) | 13 to 43 | n.s. | |||
| Offence type of first sexual conviction (as % of those with a sexual conviction) | ||||||||||||
| Rape | 110 | 24 | 21.8 | 28 | 4 | 14.3 | 82 | 20 | 24.4 | n.s. | ||
| Attempted rape | 109 | 8 | 7.3 | 28 | 1 | 3.6 | 81 | 7 | 8.6 | n.s. | ||
| Incest | 109 | 2 | 1.8 | 28 | 0 | 0 | 81 | 2 | 2.5 | n.s. | ||
| Indecent assault | 109 | 69 | 63.3 | 28 | 19 | 67.9 | 81 | 50 | 61.7 | n.s. | ||
| Indecent exposure | 109 | 1 | 0.9 | 28 | 1 | 3.6 | 81 | 0 | 0 | n.s. | ||
| Internet offence | 109 | 0 | 0 | 28 | 0 | 0 | 81 | 0 | 0 | n.s. | ||
| Other sexual conviction | 109 | 16 | 14.7 | 28 | 5 | 17.8 | 81 | 11 | 13.4 | n.s. | ||
| Sentence at first conviction (as % of those with a conviction) | ||||||||||||
| Life sentence | 346 | 3 | 0.9 | 106 | 2 | 1.9 | 240 | 1 | 0.4 | n.s. | ||
| Hospital order | 346 | 80 | 23.1 | 106 | 19 | 17.9 | 240 | 61 | 25.4 | n.s. | ||
| Prison ≥ 10 years | 346 | 0 | 0 | 106 | 0 | 0 | 240 | 0 | 0 | n.s. | ||
| Prison 6–9 years | 346 | 3 | 0.9 | 106 | 2 | 1.9 | 240 | 1 | 0.4 | n.s. | ||
| Prison 4–5 years | 346 | 2 | 0.6 | 106 | 0 | 0 | 240 | 2 | 0.8 | n.s. | ||
| Prison 1–3 years | 346 | 12 | 3.5 | 106 | 3 | 2.8 | 240 | 9 | 3.8 | n.s. | ||
| Prison < 1 year | 346 | 21 | 6.1 | 106 | 3 | 2.8 | 240 | 18 | 7.5 | n.s. | ||
| Suspended sentence | 346 | 9 | 2.6 | 106 | 1 | 0.9 | 240 | 8 | 3.3 | n.s. | ||
| Community order | 346 | 86 | 24.9 | 106 | 27 | 25.5 | 240 | 59 | 24.6 | n.s. | ||
| Fine | 346 | 40 | 11.6 | 106 | 17 | 16.0 | 240 | 23 | 9.6 | n.s. | ||
| Conditional discharge | 346 | 75 | 21.7 | 106 | 27 | 25.5 | 240 | 48 | 20.0 | n.s. | ||
| Other sentence | 346 | 15 | 4.3 | 106 | 5 | 4.7 | 240 | 10 | 4.2 | n.s. | ||
| Index offence | Whole sample | High secure | Medium secure | Statistic | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | n | %,a mean (SD) | N | n | %,a mean (SD) | N | n | %,a mean (SD) | ||
| No index offence | 401 | 66 | 16.5 | 116 | 19 | 16.4 | 285 | 47 | 16.5 | n.s. |
| Offence type of index offence (as % of those with an index offence) | ||||||||||
| Offence against the person | 334 | 232 | 69.5 | 97 | 70 | 72.2 | 237 | 162 | 68.4 | n.s. |
| Sexual offence | 334 | 78 | 23.4 | 97 | 16 | 16.5 | 237 | 62 | 26.2 | n.s. |
| Property offence | 334 | 66 | 19.8 | 97 | 25 | 25.8 | 237 | 41 | 17.3 | n.s. |
| Theft and kindred offences | 334 | 30 | 9.0 | 97 | 9 | 9.3 | 237 | 21 | 8.9 | n.s. |
| Fraud and kindred offences | 334 | 1 | 0.3 | 97 | 0 | 0 | 237 | 1 | 0.4 | n.s. |
| Police/prison/court offence | 334 | 6 | 1.8 | 97 | 2 | 2.1 | 237 | 4 | 1.7 | n.s. |
| Drug offence | 334 | 0 | 0 | 97 | 0 | 0 | 237 | 0 | 0 | n.s. |
| Gun/offensive weapon offence | 334 | 17 | 5.1 | 97 | 4 | 4.1 | 237 | 13 | 5.5 | n.s. |
| Public order offence | 334 | 7 | 2.1 | 97 | 2 | 2.1 | 237 | 5 | 2.1 | n.s. |
| Vehicle/driving offence | 334 | 4 | 1.2 | 97 | 0 | 0 | 237 | 4 | 1.7 | n.s. |
| Other offence | 334 | 4 | 1.2 | 97 | 1 | 1.0 | 237 | 3 | 1.3 | n.s. |
| Offence type of violent index offence (% of those who have a violent index offence) | ||||||||||
| Murder | 232 | 16 | 6.9 | 70 | 8 | 11.4 | 162 | 8 | 4.9 | n.s. |
| Attempted murder | 232 | 27 | 11.6 | 70 | 6 | 8.6 | 162 | 21 | 13.0 | n.s. |
| Manslaughter | 232 | 52 | 22.4 | 70 | 20 | 28.6 | 162 | 32 | 19.8 | n.s. |
| GBH | 232 | 64 | 27.6 | 70 | 14 | 20.0 | 162 | 50 | 30.9 | n.s. |
| Robbery | 232 | 21 | 9.1 | 70 | 6 | 8.6 | 162 | 15 | 9.3 | n.s. |
| ABH | 232 | 33 | 14.2 | 70 | 13 | 18.6 | 162 | 20 | 12.3 | n.s. |
| Less serious offence | 232 | 25 | 10.8 | 70 | 11 | 15.7 | 162 | 14 | 8.6 | n.s. |
| Other offence | 232 | 35 | 15.1 | 70 | 9 | 12.9 | 162 | 26 | 16.0 | n.s. |
| Offence type of sexual index offence (% of those who have a sexual index offence) | ||||||||||
| Rape | 78 | 24 | 30.8 | 16 | 4 | 25.0 | 62 | 20 | 32.3 | n.s. |
| Attempted rape | 78 | 14 | 17.9 | 16 | 0 | 0 | 62 | 14 | 22.6 | χ2 = 4.40; p = 0.036 |
| Incest | 78 | 0 | 0 | 16 | 0 | 0 | 62 | 0 | 0 | n.s. |
| Indecent assault | 78 | 48 | 61.5 | 16 | 11 | 68.8 | 62 | 37 | 59.7 | n.s. |
| Indecent exposure | 78 | 1 | 1.3 | 16 | 0 | 0 | 62 | 1 | 1.6 | n.s. |
| Internet offence | 78 | 0 | 0 | 16 | 0 | 0 | 62 | 0 | 0 | n.s. |
| Buggery | 78 | 6 | 7.7 | 16 | 3 | 18.8 | 62 | 3 | 4.8 | n.s. |
| Other sexual offence | 78 | 5 | 6.4 | 16 | 1 | 6.3 | 62 | 4 | 6.5 | n.s. |
| Sentence for index offenceb | ||||||||||
| Life sentence | 335 | 34 | 10.1 | 97 | 16 | 16.5 | 238 | 18 | 7.6 | n.s. |
| Hospital order | 335 | 249 | 74.3 | 97 | 67 | 69.1 | 238 | 182 | 76.5 | n.s. |
| Prison ≥ 10 years | 335 | 8 | 2.4 | 97 | 3 | 3.1 | 238 | 5 | 2.1 | n.s. |
| Prison 6–9 years | 335 | 10 | 3.0 | 97 | 4 | 4.1 | 238 | 6 | 2.5 | n.s. |
| Prison 4–5 years | 335 | 6 | 1.8 | 97 | 2 | 2.1 | 238 | 4 | 1.7 | n.s. |
| Prison 1–3 years | 335 | 8 | 2.4 | 97 | 2 | 2.1 | 238 | 6 | 2.5 | n.s. |
| Prison < 1 year | 335 | 4 | 1.2 | 97 | 1 | 1.0 | 238 | 3 | 1.3 | n.s. |
| Suspended sentence | 335 | 0 | 0 | 97 | 0 | 0 | 238 | 0 | 0 | n.s. |
| Community order | 335 | 2 | 0.6 | 97 | 0 | 0 | 238 | 2 | 0.8 | n.s. |
| Fine | 335 | 0 | 0 | 97 | 0 | 0 | 238 | 0 | 0 | n.s. |
| Conditional discharge | 335 | 0 | 0 | 97 | 0 | 0 | 238 | 0 | 0 | n.s. |
| Conviction | Whole sample | High secure | Medium secure | Statistic | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | n | %,a mean (SD) | N | n | %,a mean (SD) | N | n | %,a mean (SD) | ||
| Conviction for violent/sexual offence while in an institutional setting | 401 | 108 | 26.9 | 116 | 48 | 41.4 | 285 | 60 | 21.1 | χ2 = 17.31; p < 0.001 |
| Conviction for violent/sexual offence in an institutional setting in the last 5 years (as % of those committed such offences) | 108 | 34 | 31.5 | 48 | 15 | 31.3 | 60 | 19 | 31.7 | n.s. |
| Setting in which violent/sexual offence occurred as % of number of those with such an offence | ||||||||||
| Current unit | 108 | 39 | 36.1 | 48 | 25 | 52.1 | 60 | 14 | 23.3 | χ2 = 9.55; p = 0.002 |
| Current continuous admission but not current unit | 108 | 38 | 32.5 | 48 | 13 | 27.1 | 60 | 25 | 41.7 | n.s. |
| Prison setting | 108 | 10 | 9.3 | 48 | 7 | 14.6 | 60 | 3 | 5.0 | n.s. |
| Secure setting not during continuous admission | 108 | 15 | 13.9 | 48 | 5 | 10.4 | 60 | 10 | 16.7 | n.s. |
| Non-secure psychiatric setting | 108 | 17 | 15.7 | 48 | 6 | 12.5 | 60 | 11 | 18.3 | n.s. |
| Risk variable | Whole sample | High secure | Medium secure | Statistic | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | n | %,a mean (SD) | N | n | %,a mean (SD) | Rangeb | N | n | %,a mean (SD) | Rangeb | ||
| History of self-harm or suicidal behaviour | 401 | 256 | 63.8 | 116 | 81 | 69.8 | 285 | 175 | 61.4 | n.s. | ||
| Suicide attempts | ||||||||||||
| History of serious suicide attempts | 399 | 141 | 35.3 | 115 | 53 | 46.1 | 284 | 88 | 31.0 | χ2 = 8.17; p = 0.004 | ||
| Serious suicide attempts during current continuous admission | 399 | 57 | 14.3 | 114 | 22 | 19.3 | 285 | 35 | 12.3 | n.s. | ||
| Absconsion | ||||||||||||
| Attempted absconsion, ever | 399 | 148 | 37.1 | 116 | 39 | 33.6 | 283 | 109 | 38.5 | n.s. | ||
| Successful absonsion, ever | 399 | 159 | 39.8 | 116 | 43 | 37.1 | 283 | 116 | 40.8 | n.s. | ||
| Either in the last 5 years (out of ‘ever’) | 208 | 53 | 25.5 | 55 | 3 | 5.5 | 153 | 50 | 32.7 | χ2 = 15.79; p < 0.001 | ||
| Setting absconded from | ||||||||||||
| Current unit | 207 | 43 | 20.8 | 55 | 3 | 5.5 | 152 | 40 | 26.3 | χ2 = 10.68; p = 0.001 | ||
| Current continuous admission but not current unit | 207 | 83 | 40.1 | 55 | 24 | 43.6 | 152 | 59 | 38.8 | n.s. | ||
| Prison setting | 207 | 7 | 3.4 | 55 | 2 | 3.6 | 152 | 5 | 3.3 | n.s. | ||
| Secure setting not during continuous admission | 207 | 49 | 23.7 | 55 | 17 | 30.9 | 152 | 32 | 21.1 | n.s. | ||
| Non-secure psychiatric setting | 207 | 73 | 35.3 | 55 | 23 | 41.8 | 152 | 50 | 32.9 | n.s. | ||
| Hostage taking | ||||||||||||
| Attempted hostage taking | 401 | 17 | 4.2 | 116 | 6 | 5.2 | 285 | 11 | 3.9 | n.s. | ||
| Successful hostage taking | 401 | 11 | 2.7 | 116 | 3 | 2.6 | 285 | 8 | 2.8 | n.s. | ||
| Either in the last 5 years (out of ‘ever’) | 23 | 4 | 17.4 | 7 | 1 | 14.3 | 16 | 3 | 18.8 | n.s. | ||
| Setting for hostage taking | ||||||||||||
| Current unit | 22 | 3 | 13.6 | 7 | 2 | 28.6 | 15 | 1 | 6.7 | n.s. | ||
| Current continuous admission but not current unit | 22 | 13 | 59.1 | 7 | 3 | 42.9 | 15 | 10 | 66.7 | n.s. | ||
| Prison setting | 22 | 1 | 4.5 | 7 | 0 | 0 | 15 | 1 | 6.7 | n.s. | ||
| Secure setting not during continuous admission | 22 | 2 | 9.1 | 7 | 1 | 14.3 | 15 | 1 | 6.7 | n.s. | ||
| Non-secure psychiatric setting | 22 | 3 | 13.6 | 7 | 1 | 14.3 | 15 | 2 | 13.3 | n.s. | ||
| Other serious incidents, ever | ||||||||||||
| Attempted rooftop protest | 400 | 7 | 1.8 | 116 | 3 | 2.6 | 284 | 4 | 1.4 | n.s. | ||
| Successful rooftop protest | 400 | 6 | 1.5 | 116 | 2 | 1.7 | 284 | 4 | 1.4 | n.s. | ||
| Attempted room barricade | 400 | 41 | 10.3 | 116 | 17 | 14.7 | 284 | 24 | 8.5 | n.s. | ||
| Successful room barricade | 400 | 41 | 10.3 | 116 | 19 | 16.4 | 284 | 22 | 7.7 | χ2 = 6.67; p = 0.010 | ||
| Attempted fire setting | 400 | 79 | 19.8 | 116 | 29 | 25.0 | 284 | 50 | 17.6 | n.s. | ||
| Successful fire setting | 400 | 99 | 24.8 | 116 | 37 | 31.9 | 284 | 62 | 21.8 | χ2 = 4.48; p = 0.034 | ||
| Involved in a riot | 400 | 5 | 1.3 | 116 | 2 | 1.7 | 284 | 3 | 1.1 | n.s. | ||
| Involved in the possession of a weapon | 400 | 180 | 45.0 | 116 | 70 | 60.3 | 284 | 110 | 38.7 | χ2 = 15.54; p < 0.001 | ||
| Any serious incidents/seclusions | ||||||||||||
| In 2012–13 | 401 | 156 | 38.9 | 116 | 62 | 53.4 | 285 | 94 | 33.0 | χ2 = 14.53; p < 0.001 | ||
| In 2009–11 | 397 | 214 | 53.9 | 114 | 84 | 73.7 | 283 | 130 | 45.9 | χ2 = 25.18; p < 0.001 | ||
| Serious incidents/seclusions in the last 5 years | ||||||||||||
| Serious assault on staff | 397 | 102 | 25.7 | 114 | 48 | 42.1 | 283 | 54 | 19.1 | χ2 = 22.56; p < 0.001 | ||
| Serious physical assaults on others | 397 | 110 | 27.7 | 114 | 38 | 33.3 | 283 | 72 | 25.4 | n.s. | ||
| Serious deliberate self-harm | 397 | 46 | 11.6 | 114 | 18 | 15.8 | 283 | 28 | 9.9 | n.s. | ||
| Seclusion episodes | 397 | 176 | 44.3 | 114 | 77 | 67.5 | 283 | 99 | 35.0 | χ2 = 34.91; p < 0.001 | ||
| Any other incidents in the last 2 years | ||||||||||||
| Any other incidents in the last 2 years | 397 | 272 | 68.5 | 116 | 92 | 73.9 | 279 | 180 | 64.1 | χ2 = 8.86; p = 0.003 | ||
| Number of other incidents in the last 2 years | ||||||||||||
| Median (IQR) | 395 | 3.00 (18.00) | 116 | 4.00 (21.00) | 0–232c | 279 | 2.00 (17.00) | 0–307 | n.s. | |||
| Mean (SD) | 19.33 (41.69) | 18.66 (34.90) | 19.61 (44.27) | |||||||||
| HCR-20 total score | ||||||||||||
| Current (2013) score, mean (SD) | 202 | 27.01 (5.23) | 28 | 25.47 (4.23) | 18–34 | 174 | 27.26 (5.35) | 10–38 | z = 2.05; p = 0.041 | |||
| Current (2012) score, mean (SD) | 285 | 27.87 (5.36) | 65 | 28.23 (4.96) | 16–39 | 220 | 27.76 (5.48) | 10–39 | n.s. | |||
| HCR-20 history score | ||||||||||||
| Current (2013) score, mean (SD) | 202 | 15.47 (3.01) | 28 | 15.37 (3.43) | 9–20 | 174 | 15.49 (2.94) | 7–20 | n.s. | |||
| Current (2012) score, mean (SD) | 285 | 15.46 (3.01) | 65 | 16.28 (2.71) | 10–20 | 220 | 15.22 (3.05) | 6–20 | z = 2.53; p = 0.011 | |||
| HCR-20 clinic score | ||||||||||||
| Current (2013) score, mean (SD) | 202 | 5.63 (2.54) | 28 | 5.64 (2.42) | 0–10 | 174 | 5.63 (2.57) | 0–10 | n.s. | |||
| Current (2012) score, mean (SD) | 285 | 6.24 (2.61) | 65 | 6.49 (2.37) | 0–10 | 220 | 6.17 (2.68) | 0–19 | n.s. | |||
| HCR-20 risk management score | ||||||||||||
| Current (2013) score, mean (SD) | 202 | 5.92 (2.60) | 28 | 4.46 (2.35) | 0–10 | 174 | 6.15 (2.57) | 0–16 | z = 3.23; p = 0.001 | |||
| Current (2012) score, mean (SD) | 285 | 6.17 (2.49) | 65 | 5.46 (2.41) | 0–10 | 220 | 6.38 (2.48) | 0–14 | z = 2.52; p = 0.012 | |||
| Change in HCR-20 total score last 2 years | ||||||||||||
| Improver | 216 | 85 | 39.4 | 58 | 12 | 20.7 | 158 | 73 | 46.2 | χ2 = 11.57; p = 0.001 | ||
| Non-improver | 216 | 69 | 31.9 | 58 | 28 | 48.3 | 158 | 41 | 25.9 | χ2 = 9.73; p = 0.002 | ||
| Deteriorater | 216 | 62 | 28.7 | 58 | 18 | 31.0 | 158 | 44 | 27.8 | n.s. | ||
| Current management/treatment | Whole secure | High secure | Medium secure | Statistic | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | n | %,a mean (SD) | N | n | %,a mean (SD) | N | n | %,a mean (SD) | ||
| Current ward: diagnostic specification | ||||||||||
| Mental illness | 401 | 171 | 42.6 | 116 | 45 | 38.8 | 285 | 126 | 44.2 | n.s. |
| PD + DSPD | 401 | 53 | 13.2 | 116 | 28 | 24.1 | 285 | 25 | 8.8 | χ2 = 16.97; p < 0.001 |
| Comorbidity | 401 | 40 | 10.0 | 116 | 4 | 3.4 | 285 | 36 | 12.6 | χ2 = 7.74; p = 0.005 |
| Intellectual disability | 401 | 46 | 11.5 | 116 | 23 | 19.8 | 285 | 23 | 8.1 | χ2 = 11.22; p = 0.001 |
| Neuropsychiatry | 401 | 19 | 4.7 | 116 | 15 | 12.9 | 285 | 4 | 1.4 | χ2 = 24.27; p < 0.001 |
| Mixed | 401 | 70 | 17.5 | 116 | 1 | 0.9 | 285 | 69 | 24.2 | χ2 = 31.19; p < 0.001 |
| Other | 401 | 2 | 0.5 | 116 | 0 | 0 | 285 | 2 | 0.7 | n.s. |
| Current ward: treatment specification | ||||||||||
| Admission/assessment | 401 | 18 | 4.5 | 116 | 6 | 5.2 | 285 | 12 | 4.2 | n.s. |
| Treatment | 401 | 145 | 36.2 | 116 | 59 | 50.9 | 285 | 86 | 30.2 | χ2 = 15.28; p < 0.001 |
| High dependency | 401 | 13 | 3.2 | 116 | 12 | 10.3 | 285 | 1 | 0.4 | n.s. |
| Long stay/slow stream | 401 | 93 | 23.2 | 116 | 3 | 2.6 | 285 | 90 | 31.6 | χ2 = 38.90; p < 0.001 |
| Pre-discharge/rehabilitation | 401 | 21 | 5.2 | 116 | 8 | 6.9 | 285 | 13 | 4.6 | n.s. |
| Mixed | 401 | 100 | 24.9 | 116 | 24 | 20.7 | 285 | 76 | 26.7 | n.s. |
| Other | 401 | 11 | 2.7 | 116 | 4 | 3.4 | 285 | 7 | 2.5 | n.s. |
| Current monitoring | ||||||||||
| Telephone monitoring | N/A | 116 | 15 | 12.9 | N/A | |||||
| Mail monitoring | N/A | 116 | 24 | 20.7 | N/A | |||||
| Segregation | ||||||||||
| In 2012–13 | 400 | 10 | 2.5 | 115 | 9 | 7.8 | 285 | 1 | 0.4 | χ2 = 18.78; p < 0.001 |
| In 2009–11 | 399 | 6 | 1.5 | 114 | 6 | 5.3 | 285 | 0 | 0 | χ2 = 15.23; p < 0.001 |
| Medication | ||||||||||
| Psychotropic medication | 401 | 365 | 91.0 | 116 | 106 | 91.4 | 285 | 259 | 90.9 | |
| Depot | 400 | 70 | 17.5 | 116 | 19 | 16.4 | 284 | 51 | 18.0 | n.s. |
| Clozapine | 400 | 137 | 34.3 | 116 | 42 | 36.2 | 284 | 95 | 33.5 | n.s. |
| One drug class | 365 | 94 | 25.8 | 106 | 19 | 17.9 | 259 | 75 | 29.0 | n.s. |
| Two drug classes | 365 | 109 | 29.9 | 106 | 40 | 37.7 | 259 | 69 | 26.6 | n.s. |
| Three drug classes | 365 | 84 | 23.0 | 106 | 25 | 23.6 | 259 | 59 | 22.8 | n.s. |
| Four drug classes | 365 | 50 | 13.7 | 106 | 16 | 15.1 | 259 | 34 | 13.1 | n.s. |
| Five or more drug classes | 365 | 28 | 7.7 | 106 | 6 | 5.7 | 259 | 22 | 8.5 | n.s. |
| Non-compliance | 400 | 118 | 29.5 | 116 | 35 | 30.2 | 284 | 83 | 29.2 | n.s. |
| Psychological treatment | ||||||||||
| Currently receiving psychological treatment | 401 | 205 | 51.1 | 116 | 68 | 58.6 | 285 | 137 | 48.1 | n.s. |
| Contact with family/friends | Whole sample | High secure | Medium secure | Statistic | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | n | %,a mean (SD) | N | n | %,a mean (SD) | N | n | %,a mean (SD) | ||
| Contact with family in the last 2 years | 400 | 260 | 65.0 | 116 | 76 | 65.5 | 284 | 184 | 64.8 | n.s. |
| Contact with friends in the last 2 years | 401 | 21 | 5.2 | 116 | 4 | 3.4 | 285 | 17 | 6.0 | n.s. |
| Contact with both family and friends in last 2 years | 401 | 73 | 18.2 | 116 | 19 | 16.4 | 285 | 54 | 18.9 | n.s. |
| No contact with friends or family in last 2 years | 401 | 47 | 11.7 | 116 | 17 | 14.7 | 285 | 30 | 10.5 | n.s. |
| Whole sample | High secure | Medium secure | Statistic | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | n | %,a mean (SD) | N | n | %,a mean (SD) | N | n | %,a mean (SD) | ||
| Number of unsuccessful referrals to less secure settings in past 5 years | ||||||||||
| None | 295 | 198 | 67.1 | 66 | 38 | 57.6 | 229 | 160 | 69.9 | n.s. |
| One | 295 | 70 | 23.7 | 66 | 21 | 31.8 | 229 | 49 | 21.4 | n.s. |
| Two | 295 | 18 | 6.1 | 66 | 6 | 9.1 | 229 | 12 | 5.2 | n.s. |
| Three | 295 | 7 | 2.4 | 66 | 1 | 1.5 | 229 | 6 | 2.6 | n.s. |
| Four | 295 | 2 | 0.7 | 66 | 0 | 0 | 229 | 2 | 0.9 | n.s. |
| Number of tribunals in the last 5 years | ||||||||||
| Mean (SD) | 395 | 2.23 | 1.05 | 116 | 2.24 | 1.05 | 279 | 2.23 | 1.05 | n.s. |
| Type of need | Whole sample | High security | Medium security | Statistic | |||||
|---|---|---|---|---|---|---|---|---|---|
| n | Mean (SD)a | n | Mean (SD)a | Rangeb | n | Mean (SD)a | Rangeb | ||
| Security needsc | 169 | 4.83 (2.72) | 52 | 3.49 (2.44) | 0–9 | 117 | 5.42 (2.63) | 0–10 | χ2 = 4.22; p < 0.001 |
| Treatment needsc | 157 | 3.47 (2.27) | 40 | 2.95 (1.92) | 0–7.5 | 117 | 3.64 (2.35) | 0–9.5 | n.s. |
| Dependency needsc | 166 | 3.65 (2.31) | 49 | 3.40 (2.05) | 0–8.5 | 117 | 3.76 (2.41) | 0–10 | n.s. |
| Political needsc | |||||||||
| Median (IQR) | 167 | 8.0 (5.5) | 50 | 8.5 (4.5) | 1–10 | 117 | 8.0 (6.0) | 0–10 | n.s. |
| Mean (SD) | 167 | 6.82 (3.13) | 50 | 7.28 (2.71) | 1–10 | 117 | 6.62 (3.28) | 0–10 | n.s. |
| Need for lifelong secure cared | |||||||||
| Median (IQR) | 163 | 6.0 (6.0) | 47 | 3.0 (5.0) | 0.5–10 | 116 | 7.8 (4.5) | 0–10 | χ2 = 5.34; p < 0.001 |
| Mean (SD) | 6.08 (3.15) | 3.99 (2.84) | 6.92 (2.87) | ||||||
In Table 18, the mean [plus standard deviation (SD)] was used as the measure of central dispersion for continuous variables that were approximately normally distributed. The median (plus IQR) was additionally reported for continuous variables with a skewed distribution.
Sociodemographics
The majority of patients were white, single, British and male with poor educational backgrounds. Their mean age was 44 years, but almost one-third of the sample were aged > 50 years. Just under 80% were of white ethnicity, with the largest other ethnicity group being black (11.3%). Approximately 86% had never been married and only 11 patients in the entire long-stay population were married at the time of the study. Two-thirds of the overall sample had no formal qualifications; however, for 22% (n = 79) their highest level of qualification was GCSE (General Certificate of Secondary Education) and 6% (n = 22) had achieved A levels. When last in the community, almost three-quarters of the sample (n = 247) were unemployed, but about one-fifth were in full- or part-time employment or education and 39% of the long-stay population (n = 136) had been in full- or part-time employment for a period of ≥ 6 months at some point in their lives.
No differences were observed between the high and medium secure sample of long-stay patients in terms of age, ethnicity, nationality, marital status or qualifications. However, significant differences were found in terms of their employment history; a lower proportion of the high secure sample than the medium secure patients (55% vs. 80%) were unemployed when last in the community, although more individuals in the high secure sample had also not been in the community since the age of 16 years (16% vs. 3%; χ2 = 21.36; p < 0.001).
Length of stay
The mean LoS in continuous care for the overall long-stay sample was 175 months, which equates to 14.5 years. Of the sample, 36% (n = 144) had a LoS of 5–10 years, 44% (n = 178) had a LoS of 11–20 years, 13% (n = 53) had a LoS of 21–30 years and 7% (n = 26) had a LoS of ≥ 31 years. The mean LoS in current unit was 78 months or 6.5 years; 48% (n = 191) had been in their current unit for < 5 years, 31% (n = 12) had been there for 5–10 years, 19% (n = 77) had been there for 11–20 years, 2% (n = 7) had been there for 21–30 years and 1% (n = 3) had been there for ≥ 31 years.
As expected, LoS in the high secure long-stay sample was found to be statistically significantly different from the medium secure long-stay sample, with a longer LoS in total (z = 5.21; p < 0.001) as well as in the current unit (z = 9.47; p < 0.001). About one-fifth of the patients (n = 79) had been in medium/high secure care for > 20 years, although no differences were found in these extreme long-stay patients between the high and medium secure groups, indicating that this group of patients can be found across both settings. Under 10% (n = 10) of the high secure sample had been resident in their current unit for > 30 years.
Pathways
Over half of the sample had been initially admitted to their current continuous secure admission from prison (56%, n = 225); 16% (n = 64) had been admitted from the community, 14% (n = 55) had been admitted from low secure care and 12% (n = 48) had been admitted from another psychiatric setting. With regard to admission to their current unit, nearly half (47%, n = 188) had been admitted from medium secure care (29% independent sector, 18% NHS), while 24% (n = 97) had been admitted from high secure care and 20% (n = 97) had been admitted from prison, with very low numbers admitted from other settings.
There were significant differences between those currently residing in high secure care and those in medium secure care in the percentage of patients admitted to their current unit from prison (39% vs. 12%; χ2 = 37.61; p < 0.001). The numbers of those admitted from NHS and independent medium secure care also varied significantly, with more patients in high secure care having been admitted to their current setting from a NHS medium secure unit (26% vs. 14%; χ2 = 7.45; p = 0.006) but more medium secure patients having been admitted from an independent medium secure unit (37% vs. 11%; χ2 = 35.51; p < 0.001). The variation in admission source to continuous medium/high secure care and admission to current unit demonstrates that a significant proportion of individuals do not remain in the setting to which they were originally admitted. This is not surprising given that patients typically move from a high to a medium secure setting as part of their treatment pathway. The complexity of pathways is further confirmed by our finding that, on average, patients experience 1.43 unit changes in their pathway, significantly more for those currently in medium secure care (1.59) than for those in high secure care (1.03; z = 4.22; p < 0.001).
The clinical pathways of long-stay patients were complex (Table 19 and see Figure 4 and Appendix 10). Only 41% of those currently resident in high secure care (n = 48) had stayed in a single high secure setting only. Similarly, only 23% of the total sample had been in one medium secure setting (n = 64) only. Thirteen patients had been in two high secure settings and one patient had been in three high secure settings. Sixty patients (15% of the total sample; 21% of the medium secure sample) had only ever been in medium security but had moved between three, four or five medium secure sites.
| High secure sample (N = 116) | Medium secure sample (N = 283) | Overall sample (N = 399) | |
|---|---|---|---|
| Current high secure setting only | 41% (n = 48) | 0 | 12% (n = 48) |
| Current medium secure setting only | 0 | 23% (n = 64) | 16% (n = 64) |
| Two settings | 33% (n = 38) | 30% (n = 86) | 31% (n = 124) |
| Three settings | 12% (n = 14) | 27% (n = 76) | 23% (n = 90) |
| Four settings | 9% (n = 11) | 12% (n = 34) | 11% (n = 45) |
| Five settings | 3% (n = 3) | 5% (n = 14) | 4% (n = 17) |
| Six settings | 0 | 2% (n = 6) | 2% (n = 6) |
| Seven settings | 1% (n = 1) | 1% (n = 4) | 1% (n = 5) |
| Four or more | 13% (n = 15) | 20% (n = 58) | 18% (n = 73) |
About one-third (31%) of the total sample (38 in high secure sample and 86 in medium secure sample) had been in two settings, 23% in three settings (14 in high secure sample and 76 in medium secure sample) and 18% in four or more settings (15 in high secure sample and 58 in medium secure sample). Many of these moves were from high to medium as well as from medium back up to high, but there were also moves between high and medium secure sites.
Mental Health Act sections
The most common MHA section on admission to continuous secure care in the whole sample was section 37/41, with 22%, followed by section 3 (20%) and section 47/49 (16%). Statistically significant differences between the high and medium secure long-stay patients were found in section 47/49, with a significantly larger proportion of patients in high secure care being admitted on this section (χ2 = 8.05; p = 0.005). This difference was also observed for admission to current unit, whereby 21% of the high secure sample and only 8% of the medium secure sample were admitted on a section 47/49 (χ2 = 13.66; p < 0.001). A larger proportion of patients in the medium secure sample were on a hospital order with restrictions (section 37/41) on admission to current unit (51.6% vs. 37.9%; χ2 = 6.16; p = 013). In relation to long stays, the most relevant section might be that at the current time. Here, it is relevant that the largest proportion in both samples was on a section 37/41 (about 60%) with the second largest group being on a section 3 (about 15%). Very few differences were observed between current high and medium secure patients in the current section and none was statistically significant.
Psychiatric treatment history
The mean age at first admission to any inpatient psychiatric service (secure or non-secure) in the overall sample was 22 years, with 68% (n = 272) of patients having had previous admissions to non-secure psychiatric inpatient care (mean number of previous admissions = 4). Of particular note is the high number of patients with previous admissions (i.e. prior to the current continuous care episode in secure care that may in itself include admissions to a number of consecutive units): 46% (n = 183) had previous admissions to secure psychiatric inpatient care (low, medium or high).
Few differences were found between our high and medium secure samples, although those currently residing in high secure care had a higher percentage of previous high secure admissions (22% vs. 9%; χ2 = 12.39; p < 0.001). Nearly two-thirds of the patients had a history of self-harm or suicidal behaviour, with no differences between the samples; 35.3% (n = 141) of the total sample had a history of serious suicide attempts. This figure was higher in the high secure sample: 46.1% compared with 31% of those in medium secure care (χ2 = 8.17; p = 0.004).
Current mental disorders
Looking at the broad categories of mental disorders, the most common type of primary diagnosis, at 44% (n = 176), was mental illness; for 22% (n = 88) this was PD, for 17% (n = 69) it was comorbid mental illness and PD and for 16% (n = 64) it was intellectual disability. The most prevalent single diagnosis was schizophrenia at 58% (n = 232), with 33% of these patients (n = 76) considered to be treatment resistant. The second most prevalent diagnosis was PD (47% of the total sample, n = 186), with the most prevalent type being antisocial (68% of those with a PD diagnosis, n = 127) followed by borderline PD (46%, n = 86). Over one-third of patients with PD (39%, n = 73) had a mixed diagnosis of two or more types. Thirteen per cent (n = 51) were considered to have current alcohol or other substance misuse issues or dependence.
There were no statistically significant differences in broad primary diagnostic categories, although more patients in high secure care were diagnosed with antisocial PD (79% vs. 44% of those with any PD; χ2 = 4.32; p = 0.038) or two or more PD types (51% vs. 34% of those with any PD; χ2 = 4.83; p = 0.028). Intellectual disability was also higher in high secure care (24% vs. 13%; χ2 = 7.00; p = 0.008).
Physical health
Almost three-quarters of our sample had a physical health condition (72%, n = 286), the most prevalent being obesity (37%, n = 149), diabetes (28%, n = 110) and diseases of the respiratory system (16%, n = 65); 27% (n = 106) had other serious physical health conditions not stipulated on the pro forma. The differences between high and medium secure were significant for any conditions (80% vs. 68%; χ2 = 5.81; p = 0.016), obesity (53% vs. 31%; χ2 = 16.24; p < 0.001), diseases of the gastrointestinal system (10% vs. 4%; χ2 = 5.84; p = 0.016) and other serious conditions (36% vs. 23%; χ2 = 7.79; p = 0.005).
Offending history
We collected detailed information on offending. In an attempt to aggregate information, we built broad categories of offending as well as a severity score comprising age at first conviction and number of previous serious and non-serious offences (see Appendix 7). Most individuals (just under 60%, n = 232) were classed as primarily violent offenders, while only a small number (6%, n = 23) were primarily sex offenders. However, just over 20% of the sample were both sexual and violent offenders, while about 7% (n = 29) were non-offenders (i.e. had never been convicted of any offences). The severity scores were mainly in the mid range (scores of 1 or 2) with 29% (n = 107) scoring 0 and 9% (n = 33) scoring 3. The mean age at first conviction was 20 years and 57% had previously had a custodial sentence (not including time on remand). There were no differences between the high and medium secure groups in terms of any of these general descriptors of offending.
Those currently in high secure care had a higher total number of offences (18 vs. 14; z = 2.52; p = 0.012). In terms of number of particular offences, those in high secure care had higher numbers of offences against the person (5 vs. 3; z = 2.58; p = 0.010) and property offences (3 vs. 2; z = 2.74; p = 0.006) but no differences were found for any of the other Police National Computer offence categories. Just under 20% (n = 79) of the total long-stay population had convictions for arson, higher in the high secure group (27% vs. 17%; χ2 = 5.29; p = 0.021).
Index offence
A significant proportion of patients (17%, n = 66) did not have any index offence. Of those with an index offence, for most this was an offence against the person (70%, n = 232), and the second most common category was a sexual offence (23%, n = 78). Of those with a violent index offence, for about 40% this was a homicide; for sexual index offences, the most common index offence was indecent assault, with 62%, followed by rape or attempted rape. With the exception of attempted rape (which was more common in the medium secure sample), there were no significant differences in any of the index offence variables between current high and medium secure patients.
Risk and institutional behaviour
We found that a large number of individuals had convictions for violent or sexual offences in institutional settings (27%, n = 108), with significantly higher figures for high secure care (41% vs. 21%; χ2 = 17.31; p < 0.001). About one-third of these convictions had occurred in the past 5 years.
A significant proportion of patients had at some point been involved in serious incidents in an institutional setting, such as absconsion (40%), room barricade (10%), hostage taking (4%), rooftop protest (2%) or rioting (1%). Just over one-quarter of patients had perpetrated a serious assault on a member of staff or on others, 10% had seriously self-harmed (requiring medical attention) and 44% had been in seclusion in the past 5 years. Nearly 70% had been involved in less serious incidents in the past 2 years. Some incident indices were higher in current high secure patients, including successful room barricade (16% vs. 8%; χ2 = 6.67; p = 0.010), serious assaults on staff (42% vs. 19%; χ2 = 22.56; p < 0.001) and seclusion episodes (68% vs. 35%; χ2 = 34.91; p < 0.001).
Maybe somewhat unexpectedly, the HCR-20 (total) scores were higher in the medium secure group than the high secure group (25 vs. 27; z = 2.05; p = 0.041), although there was a high percentage of missing data.
Current management and treatment
At the time of data collection, 43% (n = 171) of the long-stay patients resided on a mental illness ward, 13% (n = 53) were on a PD ward, 12% (n = 46) were on a ward for intellectually disabled individuals, 10% (n = 40) were on a comorbidity ward, 5% (n = 19) were on a neuropsychiatry ward, 17.5% (n = 70) were on a mixed ward and 1% (n = 2) were on a ward listed as ‘other’. Medium secure settings appeared to have more mixed wards (24% vs. 1% of patients on such wards; χ2 = 31.19; p < 0.001) and fewer wards specifically catering for those with a diagnosis of PD (24% vs. 9%; χ2 = 16.97; p < 0.001) or intellectual disability (20% vs. 8%; χ2 = 11.22; p < 0.001).
The majority of the long-stay sample were on a treatment or long stay/slow stream ward at the time of data collection (36% and 23%, respectively), with one-quarter being on a ward of mixed treatment stages (25%, n = 100). In medium secure units there were more patients on long-stay/slow-stream wards (32% vs. 3%; χ2 = 38.90; p < 0.001). Only small numbers were on an admission/assessment ward, a high-dependency ward or pre-discharge/rehabilitation wards.
In terms of specific interventions, over 90% in both groups were currently on psychotropic medication, with over one-third (34%, n = 137) being prescribed clozapine and 18% (n = 70) being on a depot. Of those prescribed psychotropic medication, 26% (n = 94) were prescribed only one drug class, 30% (n = 109) were prescribed two drug classes, 23% (n = 84) were prescribed three drug classes and 21% (n = 78) were prescribed four or more classes of drug. No significant differences were observed in prescribing between the high and medium secure samples. Just under one-third of patients in both groups had been non-compliant with their prescribed medication in the past 2 years.
Only half of the sample were currently receiving psychological treatment of any kind (51%, n = 205) (Table 20); 36.9% of the overall sample had been previously engaged in psychological therapy but were not currently, while 12% had never engaged in such interventions. Of those currently engaged, about three-quarters (73.1%) were judged as compliant, whereas one-quarter showed some evidence of non-compliance.
| Intervention and compliance | Whole sample, N/n (%) | High secure, N/n (%) | Medium secure, N/n (%) | Chi-squared statistic |
|---|---|---|---|---|
| Psychological interventions | ||||
| Current | 401/205 (51.1) | 116/68 (58.6) | 285/137 (48.1) | n.s. |
| Previous but not current | 401/148 (36.9) | 116/37 (31.9) | 285/111 (38.9) | n.s. |
| Never | 401/48 (12.0) | 116/11 (9.5) | 285/37 (13.0) | n.s. |
| Current compliance (of those in therapy) | ||||
| Fully compliant | 201/147 (73.1) | 67/51 (76.1) | 134/96 (71.6) | n.s. |
| Not compliant | 201/54 (26.7) | 67/16 (23.9) | 134/38 (28.4) | n.s. |
Table 21 shows a breakdown of the types of therapies; figures are shown for patients currently involved in these therapies as well as for those who had ever completed particular types of interventions. There was a wide range of therapies reported, although we have already reduced data by building categories of therapies. In relation to specific psychological models of intervention, cognitive–behavioural interventions were by far the most frequently mentioned, followed by dialectical–behavioural therapy. The figures for offence-related interventions were low.
| Type of intervention | Whole sample, N/n (%) | High secure, N/n (%) | Medium secure, N/n (%) |
|---|---|---|---|
| Offence-focused interventions | |||
| Violence reduction | 397/30 (7.5) | 116/8 (6.9) | 281/22 (7.7) |
| Sex offender treatment | 393/75 (18.7) | 114/24 (20.7) | 279/50 (17.5) |
| Other offending behaviour work | 398/17 (4.2) | 115/5 (4.3) | 283/12 (4.2) |
| Arson treatment | 401/17 (4.2) | 116/8 (6.9) | 285/9 (3.2) |
| Specific psychological interventions | |||
| Cognitive–behavioural interventions | 391/94 (23.4) | 114/47 (40.5) | 277/47 (16.5) |
| Cognitive–analytic therapy | 398/30 (7.5) | 116/10 (8.6) | 282/20 (7.0) |
| Dialectical–behaviour therapy | 395/39 (9.7) | 116/18 (15.5) | 279/21 (7.4) |
| Schema-focused therapy | 397/30 (7.5) | 116/14 (12.1) | 281/16 (5.6) |
| Psychodynamic-/psychoanalytic-based therapy | 397/6 (1.5) | 116/2 (1.7) | 281/4 (1.4) |
| Other therapy modalities | |||
| Art therapy | 395/40 (10.0) | 116/17 (14.7) | 279/23 (8.1) |
| Music therapy | 396/28 (7.0) | 116/17 (14.7) | 280/11 (3.9) |
| Family therapy | 399/1 (0.2) | 116/0 (0.0) | 283/1 (0.4) |
| Psychotherapy, not otherwise specified, and counselling | 394/72 (18.0) | 116/22 (19.0) | 278/50 (17.5) |
| Mindfulness/relaxation | 397/11 (2.7) | 115/2 (1.7) | 282/9 (3.2) |
| Other focused interventions | |||
| Preparation for therapy/motivational work | 398/23 (5.7) | 116/17 (14.7) | 282/6 (2.1) |
| Anger management | 401/53 (13.2) | 116/14 (12.1) | 285/39 (13.7) |
| Substance misuse-related therapy | 395/86 (21.4) | 116/20 (17.2) | 279/66 (23.2) |
| Trauma-related interventions | 399/4 (1.0) | 116/3 (2.6) | 283/1 (0.4) |
| Interpersonal/social skills | 395/73 (18.2) | 116/24 (20.7) | 279/49 (17.2) |
| Self-confidence and related | 396/12 (3.0) | 116/2 (1.7) | 280/10 (3.5) |
| Relapse prevention | 397/18 (4.5%) | 116/2 (1.7) | 285/16 (5.6) |
| Pre-discharge/transition | 398/1 (0.2) | 116/0 (0.0) | 282/1 (0.4) |
| Compassion-focused therapy | 399/2 (0.5) | 116/0 (0.0) | 283/2 (0.7) |
| Educational interventions | |||
| Mental health awareness/psychoeducation | 396/111 (27.6) | 114/31 (26.8) | 282/80 (28.1) |
| Non-specified interventions | |||
| Other treatment | 390/37 (9.2) | 115/15 (11.2) | 277/22 (7.7) |
Despite the high risk that the long-stay sample presents, only a relatively small proportion of patients currently in high secure care were on telephone or mail monitoring at the time of the study (13% and 21%, respectively). A very small group of only 16 patients had been managed in segregation in the past 5 years, although it should be noted that this is a relatively new practice and so current figures might be higher.
Family contact
The majority of patients were currently in contact with either family members (82.4%, n = 333) or friends (23.4%, n = 94); only 11.7% (n = 47) had not had any contact with either friends or family members in the past 2 years. For the majority of patients the contact involved actual visits. There were no significant differences in outside contacts between the high and medium secure groups.
Referrals and tribunals
Patients had an average of 2.23 tribunals in the past 5 years, with no significant differences between groups, suggesting probably a mix of automatic referrals (every 3 years) and patient applications.
About one-third of the overall sample had experienced unsuccessful referrals to settings of lower security in the past 5 years (32.9%, n = 95); this figure was somewhat higher for high secure patients (42.4%) than for medium secure patients (30.1%), although this difference did not reach statistical significance.
Factors associated with length of stay
Factors predictive of LoS are shown in Tables 22 and 23. A complex pattern of predictive factors emerged, suggesting that type of detention, diagnosis and offending history might be more important than recent intrainstitutional behaviour in longer LoS. This will be discussed in more detail later in this chapter (see Discussion).
| Factor | χ2 | p-value | Direction |
|---|---|---|---|
| Admission to current unit from high secure care | 4.19 | 0.041 | Longer LoS |
| Admission to current unit from medium secure care (any) | 4.40 | 0.036 | Shorter LoS |
| Section 3 on admission to continuous care | 4.98 | 0.026 | Shorter LoS |
| Section 3 on admission to current unit | 6.39 | 0.011 | Shorter LoS |
| Treatment resistant schizophrenia | 3.97 | 0.046 | Shorter LoS |
| Sentence for index offence was a hospital order | 4.22 | 0.040 | Longer LoS |
| Being on clozapine | 5.26 | 0.022 | Shorter LoS |
| Factor | χ2 | p-value | Direction |
|---|---|---|---|
| Admission to current unit from prison | 13.40 | < 0.001 | Shorter LoS |
| Admission to current unit from high secure care | 39.19 | < 0.001 | Longer LoS |
| Admission to current unit from medium secure care (any) | 4.17 | 0.041 | Shorter LoS |
| Admission to current unit from other source | 9.18 | 0.002 | Shorter LoS |
| MHA current: civil or quasi-civil | 5.63 | 0.018 | Shorter LoS |
| MHA current: prison transfer | 6.39 | 0.011 | Longer LoS |
| Type of offender: violent | 5.22 | 0.022 | Shorter LoS |
| Type of offender: mixed | 9.40 | 0.002 | Longer LoS |
| Ever custodial sentence | 7.00 | 0.008 | Longer LoS |
| Index offence sexual | 9.32 | 0.002 | Longer LoS |
| Violent or sexual convictions in institutional setting in past 5 years | 6.10 | 0.014 | Shorter LoS |
| Absconsion past 5 years | 11.73 | 0.001 | Shorter LoS |
| Absconded from current setting | 5.26 | 0.022 | Shorter LoS |
| Serious assaults on others past 5 years | 5.01 | 0.025 | Shorter LoS |
| Serious deliberate self-harm in past 5 years | 4.69 | 0.030 | Shorter LoS |
| Seclusion past 5 years | 11.03 | 0.001 | Shorter LoS |
| Being on two or more medications | 4.68 | 0.031 | Shorter LoS |
| Non-compliance with medication | 10.72 | 0.001 | Shorter LoS |
| Having no referrals to less secure settings in last 5 years | 14.19 | < 0.001 | Longer LoS |
| Number of ward moves in past 5 years (missing data = 105) | 8.11 | 0.004 | Shorter LoS |
| Current HCR-20 2012 (missing data = 65) | 10.04 | 0.002 | Shorter LoS |
Class analysis
Using latent class analysis as described in Methods, we fitted three different models as shown in Table 24. The four- and five-class models had approximately similar fit indices, but the five-class model appeared clinically more meaningful. The characteristics of patients in the different classes are also shown in Table 25. In this table, we indicate the variable category with the highest probability or the level of probability (for binary data) in each class. In addition, we highlight in bold those variable categories that had higher probabilities in a particular class, compared with the other classes, and make some further observations about class patterns.
| Model | AIC | BIC | Sample size-adjusted BIC | Entropy | Bootstrap LRT | Classes, n (%) |
|---|---|---|---|---|---|---|
| Three-class | 8309.303 | 8592.874 | 8367.586 | 0.865 | p < 0.001 |
|
| Four-class | 8212.854 | 8592.280 | 8290.838 | 0.875 | p < 0.001 |
|
| Five-class | 8193.292 | 8668.573 | 8290.977 | 0.874 | p < 0.001 |
|
| Variable | Class 1 | Class 2 | Class 3 | Class 4 | Class 5 |
|---|---|---|---|---|---|
| MHA section | Hospital order with restrictions | Hospital order with restrictions | Hospital order with restrictions | Civil/quasi-civil | Hospital order with restrictions |
| Current diagnosis | Mental illness | Intellectual disability | PD | Mental illness | Mental illness |
| Treatment resistant | High | Low | None | High | Low |
| Main offence type | Violent and sexual | Violent | Violent and sexual | None | Violent |
| Only sexual | Other | ||||
| Index offence sexual | High | None | High | None | None |
| Intrainstitutional convictions | Medium | High | Medium | None | Low |
| Recent serious self-harm | Low | Medium | Low | Medium | Low |
| Recent assaults | Low | High | Low | Medium | None |
| Recent seclusions | Medium | High | Low | High | Low |
| Physical health issues | High | High | High | High | High |
| Depot antipsychotic | Low | Low | Low | Low/medium | Low |
| Clozapine | Medium | Low/medium | None | Low/medium | Medium |
| More than two antipsychotics | Medium | High | None | Medium/high | Medium/high |
| Non-compliance | Low/medium | Medium/high | Low | Medium/high | Low |
| Current psychology | Medium | Medium/high | Medium/high | Medium | Medium |
| Contact with family and friends | None | Low | Medium/high | Low | Low |
| Unsuccessful referrals | Medium | Medium | Medium | Medium | Medium |
Class 1 (treatment resistant, unsettled, sex offender) represented patients with a primary diagnosis of mental illness with a high proportion of treatment-resistant schizophrenia and violent as well as sexual offending and presenting with ongoing challenging behaviour.
Class 2 (mixed diagnoses, violent, highly disturbed, non-compliant) included a high proportion of patients with intellectual disability with primarily violent offending and high levels of intrainstitutional behavioural problems and non-compliance.
Class 3 (personality disordered, mixed offender, currently settled) included the highest proportion of PD patients with violent and sexual offending but settled behaviour in the current setting.
Class 4 (treatment resistant, unsettled, civilly detained, non-violent offender, non-compliant) had the highest proportion of patients on civil or quasi-civil sections with a mixture of mental illness and PD, high levels of treatment resistance, other or no offending, non-compliance and ongoing disturbed behaviour.
Class 5 (treatment responsive, settled, violent offender) included almost inclusively violent offenders with mental illness, PD or both but low levels of treatment resistance and intrainstitutional behavioural disturbance.
Consultant views on current and future needs
The security, treatment and dependency needs of the long-stay population were rated on a scale of 0–10 by patients’ consultants, where a lower score indicates greater need. The distribution of scores can be found in Appendix 11; mean scores can be found in Table 18p. All domains of need were rated lower (indicating higher need) in the high secure sample than in the medium secure sample, although this difference reached statistical significance for security need only. Looking at the mean scores for the high and medium secure samples, and using the cut-off points suggested by Shaw et al. ,64 scores fell within the range expected for the current setting for security needs; for dependency need the mean score for the high secure group fell within the 0–3 bracket, indicating high dependency need, and for the medium secure sample it fell within the low dependency need range. For treatment need a cut-off point of 4 has been suggested to differentiate those with high need from those with low need; therefore, both of our samples showed high need in this domain while political need (cut-off point of 3) was within the low-need bracket in both groups. Looking at individual cases, however, within the high secure sample, 21 (40%) scored 4–7, placing them in the medium secure bracket, and 3 scored 8 or 9 (6%; low security). In the medium secure sample, 26 (22%) scored 8 or 9, indicating low security need, but 30 scored 0–3 (26%), indicating high security need.
Findings with regard to placement need in 2 and 5 years’ time are shown in Table 26. The majority of high secure patients were thought to still require high secure care in 2 years’ time and about 40% were thought to still require it in 5 years’ time. Consultants were more optimistic with regard to the progress of medium secure patients, with over 80% of patients expected to have moved to less secure settings in 5 years’ time, although only 12 patients were predicted to live independently in the community.
| Setting | Current high secure patients in 2 years’ time, n (%) | Current high secure patients in 5 years’ time, n (%) | Current medium secure patients in 2 years’ time, n (%) | Current medium secure patients in 5 years’ time, n (%) |
|---|---|---|---|---|
| Prison | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| High secure | 32 (71) | 17 (41) | 2 (2) | 1 (1) |
| Medium secure NHS | 6 (13) | 14 (33) | 27 (24) | 12 (11) |
| Medium secure private | 7 (16) | 9 (21) | 7 (6) | 6 (5) |
| Low secure NHS | 0 (0) | 1 (2) | 24 (21) | 18 (16) |
| Low secure private | 0 (0) | 0 (0) | 23 (21) | 18 (16) |
| Psychiatric intensive care unit (NHS) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Other psychiatric setting | 0 (0) | 1 (2) | 4 (4) | 5 (5) |
| Hostel | 0 (0) | 0 (0) | 6 (5) | 12 (11) |
| Community | 0 (0) | 0 (0) | 3 (3) | 12 (11) |
| Other residential setting | 0 (0) | 0 (0) | 1 (1) | 3 (3) |
| Supported accommodation | 0 (0) | 0 (0) | 14 (13) | 23 (21) |
| Other | 0 (0) | 0 (0) | 1 (1) | 1 (1) |
Consultants’ mean score for the likelihood of their patient requiring lifelong medium or high secure care was 6.1 (SD = 3.15), with the high secure sample displaying a significantly greater likelihood of requiring lifelong secure care than the medium secure sample (mean 4 vs. 6.9; χ2 = 5.34; p < 0.001). Sixty per cent of current high secure patients (n = 31) were scored 0–5, compared with only 32% (n = 37) of current medium secure patients, indicating a greater likelihood that high secure patients would need lifelong secure care. Extrapolating these figures onto all patients still present in secure care (i.e. taking into account responses extrapolated to non-responding responsible clinicians) indicates numbers of 58 for high secure care and 59 for medium secure care in units included in our study. However, one might want to consider that since our survey date in 2013, patients have not only moved on but others have ‘filled their places’ (i.e. have since become long-stay patients). Another way to extrapolate the total figures of patients needing lifelong secure care would therefore be to take the percentage of patients needing lifelong secure care and extrapolate this to total long-stay numbers. This estimation would result in 91 for medium secure care patients in our included units and in 88 for those in non-included medium secure units as well as 101 for patients in high secure care.
The main impediment to moving in the whole long-stay sample was felt to be psychopathology, with a mean score of 3.2 (out of a possible score of 5). The other key impeding factors were rated as follows: risk to others (mean = 3.0), personality traits (mean = 2.9), institutionalisation (mean = 2.6) and patient anxiety (mean = 2.3). Lack of suitable facilities (mean = 1.8) and media attention (mean = 0.9) were rated lowest. Psychopathology, risk, personality traits and patient anxiety were all rated as significantly higher in the high secure sample than in the medium secure sample.
Logistic regressions, with a median split of the likelihood for needing lifelong high/medium secure care, revealed only three variables significantly associated for high secure patients: number of ward moves in the past 5 years (more likely), violent offender type (less likely) and mixed offender (less likely). For medium secure patients, significant predictors were being on a depot (more likely) and three variables were associated with a lower likelihood of needed lifelong forensic care: absconsion in the past 5 years, being on clozapine and lack of family support.
Discussion
We gathered detailed information on patient characteristics and pathways of patients classed as ‘long-stay patients’ currently resident in high or medium secure care. Owing to the differences in methods in previous research, comparisons with such earlier work are not straightforward. In addition, secure care has undergone significant changes, a notable example being the Accelerated Discharge Programme in the early 2000s. Information on patient characteristics prior to this period is now likely to be obsolete. In putting our findings in the context of the wider literature we therefore draw particularly on Brown et al. ,37 Jacques et al. ,38 Shah et al. 42 and Wilkes. 97 We also refer to Knapp et al. ,86 Harty et al. ,18 Ricketts et al. 92 and Thomas et al. ,29 despite their study dates, owing to unique aspects of relevance (e.g. in terms of population studied or national coverage). The only recent study in the UK describing characteristics of a national medium secure sample105 is also of relevance, although it describes a discharge sample. These latter studies do not differentiate between long-stay patients and non-long-stay patients but inform about characteristics of patients in secure care more generally. Finally, a recent review of the literature on secure care, commissioned through the Department of Health Policy Research Programme,111 summarised research of relevance here. Space limitations do not permit a detailed comparison with previous research, but we will highlight the main differences and novel findings from our study.
Sociodemographic characteristics
We have commented on the literature on basic sociodemographic characteristics of long-stay patients in the previous chapter and this discussion will not be repeated here. In line with previous research, our findings suggest that our long-stay sample shares characteristics with general forensic samples that are suggestive of early disruptive lives with patients not having achieved stable relationships or employment. Others29,42,105 have described an over-representation of those from BME groups in general forensic samples, both high and medium secure. The percentage of patients from BME groups in our sample, in line with other long-stay studies,42,88 does not indicate over-representation, suggesting, maybe, that patients from BME groups are less likely to become long-stay patients, although longitudinal studies would be required to investigate differences in the pathways of patients from different ethnic backgrounds.
We found, maybe somewhat unexpectedly given their background, that a large number of patients were in contact with their families and/or others outside the secure setting. Given the cross-sectional nature of our study, it is not clear whether such contact is due to staying in or renewing contact with families. Clinical experience suggests that the latter contributes a significant proportion of family contact. It is also unclear how supportive these contacts are, although the high scores on the HCR-20 items ‘relationship instability’ and ‘lack of personal support’ suggest that, at least from a professional perspective, they are either not seen as supportive or limited in their impact. Given the protective nature of such contact,112 the extent of which has not been described before, our findings are nevertheless of importance in informing planning for patients’ recovery, but also place some responsibility on services to support carers and maximise the opportunities for meaningful interactions between patients and their families.
Admission and pathways
We have commented on admission source and current MHA section in the previous chapter. Analysing data of the long-stay patients in more detail confirmed that – in line with studies on general forensic populations29,105 – patients initially primarily entered the forensic psychiatric system via prison. In our study we were able to compare entry to secure care with admission to current unit, which revealed a significant shift from prison to other secure settings as admission source. Patients also changed MHA section over time, with many more being on a section 37/41 currently than at the point of admission to their current unit or on first admission. This suggests that, over time, patients move to a situation in which their legal position makes any positive moves more difficult to achieve, although these sections may also reflect ongoing psychopathology (with the involvement in incidents in secure care), which will also result in longer stays.
Through taking a whole-pathway approach, we were able to identify the number and sequence of consecutive high/medium secure placements. The significant percentage of patients making sideward moves suggests that the ideal pathway of moving from higher to lower levels of security is, in reality, not achieved for most patients. In fact, only 40 patients (10% of the total sample) experienced the desired pathway of a single move from high to medium secure care. This is not, of course, to say that all other movement is necessarily disadvantageous. In fact, some of the movements between high secure units are likely to have been triggered by ‘repatriation’ to patients’ home areas, which might have facilitated contact with family or friends. However, the complexity of pathways is striking and likely to be confusing for and frustrating to patients and carers, as well as inefficient and costly. In addition to the large number of different institutions patients stayed in during their current continuous secure care, we also found that a significant proportion had had previous admissions to secure care, suggesting that a whole life-span view is needed to understand the complex trajectories of this group.
This situation is further compounded by the significant proportion of unsuccessful referrals to less secure settings, in some cases repeatedly. A closer inspection of these cases might reveal unmet service needs. Inconsistencies in criteria applied to moving to less secure settings, differences in opinions between consultants in different services and delays in the assessment and transfer process are likely to contribute further to patients ‘getting stuck’, as others have identified previously. 113–115 Various suggestions have been made to improve this system, including paper-based assessments, single assessments and appeal panels, and these warrant further investigation. 116
Disorders and treatment
As expected, the largest group of disorder was mental illness, mainly schizophrenia, followed by PD. Unlike studies of general forensic populations, which found rates of PD of about one-third in medium secure care92,113 and between 40% and 50% in high secure care,18 our findings suggest higher rates of personality pathology in both levels of security. Other long-stay studies have also found a high percentage of primary or comorbid PD (e.g. Shah et al. 42), although PD has also consistently been associated with reduced LoS in discharge samples. For those who remain in secure care, however, personality pathology is likely to present a significant treatment need, in particular as personality dysfunction is likely to impact on other areas of function, such as relationships, motivation and engagement. 116 It is questionable whether this need is currently met sufficiently in medium secure settings. 114
A number of diagnostic groups warrant particular mention. We found a significant proportion of individuals with intellectual disabilities in our long-stay sample, although prevalence findings have to be interpreted cautiously owing to our deliberate oversampling of units catering to this group. Findings with regard to the impact of intellectual disabilities on LoS are inconsistent, with some authors concluding that those with intellectual disabilities stay longer117 and others reporting findings to the opposite effect. 118 Importantly, however, those with intellectual disabilities in high secure settings have been found to have a larger number of unmet needs than other patient groups, and these patients may not be able to move on because of a lack of facilities in less secure settings;29 this issue may be compounded by recent initiatives to close down institutions for patients with intellectual disabilities. 119 We found small numbers diagnosed with autistic spectrum disorders and, given recent research in secure settings, these figures might be an underestimation of the true extent of this pathology. 120 We relied on case notes for data collection, rather than applying diagnostic assessments ourselves; this might therefore be suggestive of undetected autistic spectrum disorders in the long-stay population. Self-harm is another area to highlight, and the high figures for self-harm and serious suicide attempts are of concern: one in seven had committed a serious suicide attempt during their current admission to secure care. This figure was higher in high secure care, as was the prevalence of depression, highlighting the need to be aware of psychopathology that is less related to risk and that might, therefore, receive less attention in secure settings.
As expected, psychopharmacological treatment was used in almost all cases. The high proportion of patients on clozapine might be reflective of treatment-resistant schizophrenia, although some studies have found that in high secure care up to one-fifth of patients were prescribed clozapine for the management of PD only. 115 Psychological treatment was less prevalent, although it is not clear if those not currently involved in such treatment were deemed to have completed all necessary interventions, if further interventions were not thought to be effective or if there were no further interventions owing to patient non-engagement. We did not analyse therapies delivered against offending history or psychopathology; therefore, it is not possible to judge the appropriateness of the interventions delivered. In addition, the extent of treatments received, particularly for previous interventions, might have been underestimated owing to difficulties in obtaining such information from file notes. It is of note, however, that others, using contemporaneous notes in a setting for those with dangerous and severe PDs, have also found that the therapy hours delivered fell short of what was expected, despite evidence of a link between hours of therapy and progress. 121 Even if the low rates for interventions found were purely due to difficulties in finding this information, this would nevertheless be a cause for concern, as this suggests that information might also be difficult for clinicians to utilise, in particular to pass on to new teams, resulting, possibly, in the often observed unnecessary repetition of treatments. 113 The number of different interventions mentioned on the pro formas was staggering, with idiosyncratic names used and similar names given for what appeared to be different interventions, and vice versa. It is clear that only a small number of these interventions will have an evidence base for their effectiveness.
Our findings suggest that it is crucial to pay particular attention to physical health, given the high number of patients with physical health issues, particularly in the high secure population. The prevalence rates identified in our study seem to be even higher than those in other studies, including one conducted at one of the high secure hospitals. 122 That study found rates of diabetes of 9%, while in our study the prevalence was about three times that. These discrepancies are, of course, likely to be at least partly related to the higher age of the participants in our sample; nevertheless, they are of serious concern.
Offending and risk
Consistent with other research,42,113 we found that just under two-thirds of our sample were primarily violent offenders and, in line with this, their index offence was also one of violence. The high percentages of sexual offences and arson as index offences in our long-stay patients are of note, and seem to be higher than those reported in the general forensic population, suggesting, maybe, a lack of effectiveness of interventions offered to these offenders or difficulties with moving such offenders on, or both. Those individuals, although they might be a high risk to others in the community, might be relatively settled within secure care and have therefore been identified as suitable for admission to dedicated long-stay services in countries with such services; research in those services has, consequently, found a disproportionately high number of sexual offenders. 73
There was some indication from the offending histories that those currently in high secure care might have more serious offending histories (e.g. they had higher numbers of overall and of violent offences). Nevertheless, most offending indicators did not differentiate between high and medium secure samples, and the HCR-20 scores, higher than in comparable general forensic groups in both samples,113 were even higher in those currently residing in medium secure care, suggesting, again, that the long-stay groups show more similarities than differences across settings.
Of particular significance is our finding of a high number of incidents within institutions, including convictions for serious offending. Few studies have thus far described incidents while in forensic care (e.g. Uppal et al. 123), although recent behaviour within institutions might arguably be at least as important as previous offending in determining future placement, in particular for those whose index offences are many years, sometimes decades, in the past. Others have found that need for seclusion81 and absonsion and aggression79 during admission are associated with longer LoS. Our findings also suggest that a significant proportion of patients remain unsettled and are, therefore, likely to require high staffing levels, access to seclusion facilities and similar measures for behavioural management in any future setting. There is, however, a group that has not engaged in intrainstitutional behavioural disturbance, and these patients might be manageable in a less highly staffed environment.
Factors predictive of length of stay
Describing factors predicting LoS was not the primary aim of this research, and our cross-sectional approach limits the interpretability of findings because all patients included were still on their care pathway. Nevertheless, comparing those with longer and shorter LoS in the long-stay group identified some relevant findings. Consistent with other research (e.g. Wilkes97), those admitted on and currently remaining on civil sections were in the shorter-stay group, while hospital order for index offence, mixed offending, previous custodial sentence, sexual index offence and admission from high secure care were associated with being in the longer-stay group. Not consistent with previous research, and somewhat unexpected, were findings indicating that more severe psychosis and – for those in medium secure care – intrainstitutional behaviour were more prevalent in the shorter-stay group. Given that the comparison group is one of longer LoS, this might mean that those staying for longer are more settled and could indicate a change over time in those indicators, although longitudinal studies would be required to confirm this hypothesis.
Needs and future predictions
Very similar to research that prompted the Accelerated Discharge Programme18 and needs assessments since then,64 we found that just under half of the high secure long-stay patients were judged to be more appropriately placed in less secure settings. For the medium secure sample, the picture was more mixed, with similar numbers being judged to be placed at too high and too low a level of security, a finding not previously reported. This may be related to a more challenging patient population being admitted to medium secure care over time, as has been suggested by, for example, Ricketts et al. 92 In line with previous research, the profiles for other needs areas were very similar for high and medium secure patients, indicating that this differentiation may not be helpful for a group with chronic, long-term needs. Our HCR-20 change scores indicated that about one-third of patients may still be on a trajectory of positive change. Nevertheless, according to consultants’ views, few are expected to reach the community within the next few years. The fact that none of the patients was predicted to be placed in prison in the future calls into question the likely success of recent policies favouring the placement of PD offenders in the prison system rather than in the health-care system, at least for this long-stay group. 124 Logistic regressions regarding the need for lifelong secure care did identify few predictors, indicating, maybe, that long-stay patients have very individual characteristics and needs and, thus, reasons for delays in their pathways.
Chapter 7 Qualitative investigation of the patient experience
Aims and objectives
The specific objectives of WP3 were:
-
to identify patients’ perceptions of their treatment pathways, long-term needs and acceptable service provision to maximise their quality of life
-
to investigate the effects of prolonged stay in secure settings on quality of life.
To add further depth to the exploration of long-stay patients’ experiences and perspectives of prolonged stay in secure care, a third objective was added:
-
to explore patients’ perceptions of the reasons for their prolonged stay in secure care, the effects of the prolonged stay on their daily life and their attitudes towards the future and moving on from secure care.
Methods
Overview of method and epistemological stance
Given the need for sensitive exploration of the experiences and perspectives of individuals who stay in secure settings for extended periods of time, WP3 employed a qualitative methodology. This involved a series of semistructured interviews with a purposive sample of long-stay forensic patients. Interviews were transcribed and subjected to a thematic analysis adopting a constructivist epistemological perspective. The constructivist position holds that the way people understand and perceive the world is constructed through their personal experiences, relationships and social interactions. In the context of the current research, we understand that the views participants hold about being a long-stay patient at any one time (i.e. the moment of interview) will have been shaped by prior events. By the same token, future events may be interpreted through the lens of that person’s construction of the social environment and/or may influence some reinterpretation. We elaborate on how this relates to our analysis and interpretation of the data in Discussion.
Ascertainment of study sample
A purposive sampling framework125 was used to recruit participants. This involved the application of formal sampling criteria for both site and participant selection to ensure that the sample exhibited the necessary range and diversity in terms of characteristics of potential relevance to the research question, thereby ensuring that different perspectives on the topic area and outcome of interest were captured. 126 Our initial target was to interview 30 long-stay patients, but we were open to the final sample size being inflated by the need to achieve data saturation and represent the key sampling criteria.
Sampling of sites
Work package 3 used unit-level data, obtained through WP2, to identify a subsample of sites from which to recruit a purposive sample of participants. To sample sites, we stratified all 23 units participating in WP2 by security level (high or medium secure units) and provider type (NHS or private).
Two high-security units participated in WP2, and both were automatically sampled. In relation to medium-security units, our target was to draw a sample of participants from six units (three NHS and three private), with the final sample purposively selected by applying the following secondary criteria:
-
Sites with small numbers of long-stay patients (< 10) were excluded because they provided an insufficiently large pool of patients from which to sample.
-
We purposively selected sites (at least one NHS and one private) with a population of female long-stay patients.
-
We ensured that different geographical regions were represented by ensuring that no single region contributed more than one site to the overall sample of high and medium secure sites.
The final sample of sites is shown in Table 27.
| Provider type | High security | Medium security |
|---|---|---|
| NHS | Ashworth Rampton |
Fromeside Humber North London Forensic Service |
| Independent | There are no independent high-security hospitals | St Andrew’s, Northampton Kneesworth House (Partnerships in Care) Stockton Hall (Partnerships in Care) |
Participant sampling procedure
Using an anonymised list of patients obtained through WP2, we stratified by two primary sampling criteria:
-
LoS [above or below the unit median length of (long) stay]
-
gender (where possible).
The final selection of participants was determined by applying secondary sampling criteria. Our aim was to achieve a sample in which the following characteristics were represented by at least one case at each site:
-
patients detained under MHA sections 37, 37/41, 47/49 and 3
-
patients aged ≤ 50 and > 50 years
-
white British and BME
-
clinical diagnosis of schizophrenia, PD and intellectual disability
-
index offence of major violence and sexual offences
-
offence history (one-off and repeat offenders)
-
admitted from each of prison, high and medium secure.
For the full rationale and description of participant and site sampling criteria, see Appendix 12.
Participant recruitment procedure
At each site, we selected up to 10 patients from the anonymised WP2 database of long-stay patients. We oversampled in anticipation of some attrition and refusal to participate. We then asked each patient’s responsible clinician for their agreement to approach the patient. If there were no clinical issues preventing this, we approached the patient’s named nurse, who gave the patient the information sheet and asked if they would be interested in participating in principle. The researcher liaised with the named nurse to arrange a time to visit the patient to gain his or her written informed consent and, if this was given, to conduct an interview. If the patient refused at either point, no further contact was made and they were not included in the study.
Interview method
Patients who consented to take part (participants) were interviewed using a semistructured approach. The interview topic guide was designed to reflect the main aims and objectives of the study. It was initially developed through a literature review and discussion within the PMG and the SURG, and then refined during the pilot interviews and early stages of the fieldwork (see Appendix 13).
Participants were asked an introductory question about how they came to be in the current unit, and were then asked a series of question exploring reasons for their long stay, their current situation and ‘moving on’. The researcher was free to vary the order and wording of the questions for the purposes of rapport and clarity of meaning. Probes and follow-up questions were used to achieve the necessary depth and self-reflection on the part of the respondent.
All interviews were conducted by a trained researcher (JH). Written informed consent was sought from all participants prior to the interview. Participants were given £10 payment for taking part in an interview.
Data analysis
All interviews were digitally recorded, transcribed verbatim and uploaded into NVivo analytical software (2014; QSR International, Warrington, UK). Each transcript was read line by line to achieve immersion in the data. A framework analysis approach127 was used to organise the data into the topic guide’s three main themes of enquiry, thereby accepting the key a priori structuring of the data implied by the main research objectives (reasons for long stays, current situation and moving on). We felt that this deductive approach was a pragmatic way to interpret and display our findings where ‘data is sifted, charted and sorted’128 in accordance with the main research objective of WP3 (Table 28 provides the analytical framework).
| Area of enquiry 1: reasons for long stays | Area of enquiry 2: current situation | Area of enquiry 3: moving on |
|---|---|---|
| 1a. Reasons for long stays 1b. Reasons for moving 1c. Reasons for not moving |
2a. Drawing comparisons: then and now 2b. Daily routine and occupation 2c. Relationships with staff 2d. Relationships with other patients |
3a. What ‘moving on’ looks like 3b. Reasons why ready to move on 3c. What could help them move on? 3d. What could stop them from moving on? 3e. Future units for long-stay patients |
Coding the data: an open coding approach
An open coding approach129 was used to identify categories that represented the key issues discussed by participants. After several transcripts were coded, a constant comparative method was used to group and merge common categories together. 130 When categories were revised or new categories were identified, previously coded transcripts were rechecked to ensure that these categories had not been missed and that a consistent approach to coding was employed throughout. During this process, themes emerged within each area of enquiry illustrating how participants made sense of their experiences in secure care. We used these themes to inform the next stage of analysis.
Narrative analysis: mapping individual stories
We used a narrative approach130,131 to further scrutinise the way in which each participant constructed their identity as a long-stay patient. According to Bal,132 there are three different levels of narrative research: the text, the fabula (the chronology of events) and the story. In the context of the long-stay patient narratives, the interview transcripts were the text, the three main areas of enquiry (which were arranged in chronological order) were the fabula, whereas the emergent themes helped to capture the manner in which the events were told, described and evaluated in telling the participant’s ‘story’.
Distinct patterns emerged in people’s stories concerning how they made sense of the past (reasons for long stays), present (current situation) and future (moving on). Informed by our constructivist position, we sought to understand these often very different perspectives on long stay in terms of how each participant appeared to construct an understanding of their chronology, current situation and trajectory. The similarities within and differences between participants’ stories ultimately resulted in the emergence of four long-stay stances, which are described in the final section of the findings that follow (see Stances on long-stay secure care).
Findings
Size and characteristics of the sample
Our initial target was to interview 30 participants. Given a time lapse between the collection of WP2 data and the implementation of WP3, we anticipated high levels of attrition (i.e. patients having left the unit) and that others would be unable or unwilling to participate. We therefore initially identified 10 purposively sampled cases at each site who we wished to invite for interview and notified the units concerned. In the event that a patient had left the unit, had died, was deemed not well enough to be interviewed or refused when asked, substitute cases were purposively sampled (where possible) to meet criteria under-represented in the sample. To achieve the representation of some sampling criteria (e.g. section 3 patients) we inflated our final sample, achieving a final total of 40 participant interviews.
To achieve this total, 124 cases were sampled. Of these, 35 had been discharged from the unit and two had died. In 11 cases the responsible clinician would not permit the patient to be interviewed, while a further 36 patients were approached but refused to provide informed consent.
Most of the 40 participants we interviewed were male (n = 34). Eleven participants were recruited from two NHS high secure units, 17 were recruited from three NHS medium secure units and 12 were recruited from three private medium secure units. Table 29 provides a summary of participants’ characteristics. (See Appendix 14 for full details.)
| Characteristic | Unit | ||
|---|---|---|---|
| High secure (two sites) (N = 11) | Medium secure NHS (three sites) (N = 17) | Medium secure independent (three sites) (N = 12) | |
| Age (years) | |||
| 21–30 | 1 | 4 | 1 |
| 31–40 | 4 | 2 | 2 |
| 41–50 | 5 | 6 | 8 |
| 51–60 | 1 | 2 | 1 |
| 61–70 | 2 | ||
| 71–80 | 1 | ||
| Gender | |||
| Male | 9 | 9 | 11 |
| Female | 2 | 2 | 1 |
| Ethnicity | |||
| White British | 8 | 12 | 12 |
| White Irish | 1 | 0 | 0 |
| White other | 1 | 0 | 0 |
| Black Caribbean | 1 | 1 | 0 |
| Black British | 4 | 0 | |
| Clinical diagnosis (primary) | |||
| Schizophrenia (other psychosis) | 5 | 8 | 6 |
| PD | 3 | 7 | 3 |
| Intellectual disability | 2 | 1 | 2 |
| PD and paedophilia | 1 | 1 | 1 |
| Index offence | |||
| Murder | 1 | 0 | 0 |
| Murder and rape | 0 | 1 | 0 |
| Manslaughter | 5 | 4 | 0 |
| GBH | 1 | 5 | 5 |
| GBH and sexual offence | 0 | 1 | 1 |
| Sexual offence | 1 | 3 | 2 |
| Property offence | 2 | 1 | 1 |
| Abduction | 0 | 1 | 0 |
| Attempted murder | 0 | 1 | 2 |
| None | 1 | 0 | 1 |
| Offence history | |||
| Repeat | 9 | 15 | 11 |
| One-off | 1 | 2 | 0 |
| Not applicable | 1 | 0 | 1 |
| MHA section | |||
| Section 37/41 | 7 | 14 | 6 |
| Section 47/49 | 2 | 3 | 1 |
| Section 37 | 1 (notional) | 0 | 2 |
| Section 3 | 1 | 0 | 3 |
| Admission source into current unit | |||
| Prison | 3 | 5 | 2 |
| High secure hospital | 3 | 9 | 5 |
| Medium secure hospital | 5 | 3 | 4 |
| Other psychiatric setting | 0 | 0 | 1 |
| Admission source into continuous care | |||
| Prison | 7 | 13 | 5 |
| Other psychiatric setting | 2 | 1 | 4 |
| Community | 1 | 3 | 3 |
| Children’s centre | 1 | 0 | 0 |
| LoS (current unit) | |||
| Median (years) | 13.2 | 3 | 3.2 |
| < median = 5 | < median = 8 | < median = 6 | |
| > median = 6 | > median = 9 | > median = 6 | |
| Overall LoS | |||
| Median (years) | 17.3 | 13.3 | 16.1 |
| < median = 5 | < median = 8 | < median = 7 | |
| > median = 6 | > median = 9 | > median = 5 | |
Interview findings
In this section we report the results of our analysis of the interview transcripts. We describe the key issues that participants talked about in the context of the analytical framework and present the themes that emerged from each main area of enquiry. We illustrate the ways in which participants constructed and made meaning of their reasons for long stays, their current situation and their potential to move on from secure care.
Reasons for long stays
A majority of participants attributed their LoS in secure care to events prior to their admission, such as the severity of their index offence or their offence history; those who attributed their LoS to these factors believed that their LoS was justified and as expected. However, some recognised that their stay had been extended beyond what they had expected owing to their disruptive behaviour while in secure care. These explanations were commonly coupled with descriptions of factors that explicitly or implicitly presented as mitigation (e.g. acknowledgement that they were seriously unwell, were ‘on medication’ or were in a unit that did not meet their needs).
In contrast, other participants attributed their LoS to factors over which they had no control or responsibility. Sometimes these had to do with the structure or organisation of the treatment system, for example a change in their responsible clinician (and, therefore, changes to their treatment plans), a change in the system’s requirements for discharge or the absence of an appropriate facility for them to move into. Some acknowledged that their disruptive behaviour had been a factor in their long stay, but felt that the institution’s response to this had been disproportionate and/or reflected a risk-averse approach that restricted their progression.
I’ve been ticking all the boxes, you know [. . .] I just have, like, a few minor concerns . . . they’re trying to exploit it, exaggerate the situation, from these minor things, to make me look bad, you know.
NHS medium secure site B: participant 4
A number of patients attributed their moves to other units or wards to their engagement with therapies, treatment and staff, whereas others believed that they had moved because they had been disruptive and ‘acted out’ towards staff and other patients. In some cases, patients believed that they had moved simply because the wards/units had been refurbished.
Emerging theme 1: attribution
Participants’ accounts varied when explaining why they had stayed so long in secure care (which included why they had or had not moved units). Long stay was attributed to personal, interpersonal or structural factors. These attributing factors were, at times, dependent on the extent to which participants were aware of being unwell and/or the extent to which they were aware of the severity of their index offence and/or offence history.
Current situation
Participants described their current situation in secure care in the context of various topics such as their daily routine and their relationships with other patients and staff. They described not only how they felt about their current situation (their outlook) but also how they actually dealt with it (their approach).
Comparisons in physical environment
Those participants who had moved units while in secure care made comparisons between their current and previous units. Most participants who had moved down from high secure to medium secure units thought that their current units had less restrictive and more relaxed regimes. However, there were contrasting perspectives. Some perceived their medium secure units to be quite rule-bound. Others who had moved from medium to high secure units felt that they were receiving better treatment and that daily life was easier because they had less responsibility.
A majority of patients felt that being in hospital was a better option than prison, where many felt that they had not received appropriate care or treatment, but some felt that prison offered them greater scope than hospital to organise their own daily routine.
Daily routine and occupation
A large majority of patients described the importance of being proactive by having a routine or schedule, keeping busy and making the most of their time while in secure care. In some cases, patients who had leave (escorted or unescorted) explained how it was an important part of their daily routine. However, some felt that their daily routine was monotonous and described having ‘nothing to do’.
A number of occupational activities (e.g. woodwork, cooking, art, gym and educational courses) were mentioned by participants as ways for them to pass the time while in secure care. Some reported that valued activities had been stopped (as a result of incidents involving patients) or that, having undertaken the same activities for many years, they now chose not to engage. Some participants talked about taking up work either within the hospital (e.g. gardening, animal care) or outside the hospital (e.g. chef, bike repair shop), but some said that not enough of such opportunities were available.
A majority of participants explained how it was a change in their medication during their time in secure care that had improved their mental health. Furthermore, a large number of participants described how they found psychological therapies enjoyable and beneficial for their mental health by giving them the opportunity to talk about their index offence and past negative life experiences. In some cases, participants wished that they had been introduced to these psychological therapies earlier, as this may have resulted in them not staying as long in secure care:
I was young, I couldn’t cope, I didn’t realise, I’d lose my temper, I hadn’t learnt – I should, I ought to have been taught, I ought to have had psychology and then I would have learnt, I could have controlled myself.
NHS high secure site A: participant 2
There were other participants who felt that therapies were ineffective when they were just repeating the same therapies over again but still there were no changes to their current situation.
Relationships with staff
During their time in secure care, a large proportion of participants described how they now talked to staff more openly than they did when they were first admitted. They also described how they had become more familiar with staff, which resulted in them feeling that they could trust them. Some believed that it was also important that staff learnt to trust them by allowing them to take on more responsibility for their own care (such as being allowed leave). One participant described how his relationships with staff had helped him to progress:
Basically, just give him support, support him when he’s doing well [Yeah] try and play it down when he’s not doing too well, do you understand what I mean? So like, I then flourished.
NHS high secure site B: participant 4
However, not all participants had a good relationship with staff. Some described how there would always be ‘one or two who they just didn’t get on with’.
Relationships with other patients
Approximately half of the participants valued their friendships with other patients, as they allowed them to connect with others in similar situations to themselves. Some liked to give advice to other patients who had recently moved to their unit. However, some participants described how it was difficult to get on with other patients who were a lot younger than they were, citing a lack of common interests. Some participants felt that staff were often preoccupied with patients who were more unwell or less settled than they were. The patient dynamics within a ward could also be influenced by where patients had been admitted from:
. . . the people from high security, with more boundaries and restrictions, could understand the routine because we all came from high secure hospitals . . . the other ward people from the prison population haven’t had any sort of treatment and stuff.
NHS medium secure site A: participant 6
Some participants simply did not need or want to make friends with others. This was, at times, placed in the context of not being able to maintain previous friendships that had ended as a result of one patient moving to another unit.
Emerging theme 2: outlook
When describing how they felt about their current situation, some participants had a positive outlook, believing that their time in secure care had been helpful for their mental health, and said that they enjoyed being in their current unit/ward. Other patients had a negative outlook, feeling that their time in secure care had been pointless and ineffective. This outlook resonated through all aspects of their day-to-day life in secure care.
Emerging theme 3: approach
When describing how they coped with their current situation, participants took on either a proactive or a passive approach. The participants with a proactive approach were more likely to be self-motivated, take part in activities, engage with staff and other patients and seek to make the most of their current situation. The participants with a passive approach were more likely to lack motivation, not take part in activities and not engage with staff or other patients.
Moving on
What ‘moving on’ means
Most of the participants associated moving on with a physical movement such as moving to a lower secure setting or into the community. Some expressed the desire to one day have a house, a job and a family. Some participants described moving in relation to personal development, saying that for them it meant being able to start again by shaking off their offence history. However, some felt that they were never going to leave the secure care system and, as such, seemed indifferent to the prospect of moving on.
Being ready/not ready to move
Some participants felt that they had experienced a ‘turning point’ while being in secure care, whereby they had changed their behaviour and attitude and made progress as a result. Some gave more definitive reasons for why they were ready to move on, describing how there was no more treatment to do, that their LoS had exceeded their sentence and that they were no longer a danger to society. Some participants said that moving to a lower level of secure care would result in their becoming unwell again. In addition, some explicitly described how their prolonged LoS in secure care had left them dependent on the system.
What helps and stops you from ‘moving on’
Some participants felt that only they could help themselves to move on and stated the importance of being hopeful and wanting to better themselves. These participants described the importance of keeping well, displaying good behaviour, engaging with treatment and having family support. Some, however, felt that feeling comfortable and safe in their current unit undermined their motivation to move on. For example, one participant described being in conflict about whether or not they wanted to move on:
. . . because you feel more safer. It’s how you feel comfortable at the end that (influences) whether or not you could stay here or move on and face a bigger challenge and eventually out in the community.
NHS high secure site A: participant 3
Some participants felt that staff’s negative attitudes and perceptions could prevent them from moving on. For example, one participant described how the term ‘anxious’ is used by staff as a way to restrict patients:
. . . maybe people are anxious [. . .] But it seems like a favourite word they’ve got, not just in this service, but in every service I’ve seen, as well. [. . .] You get a lot more time added on . . .
NHS medium secure site A: participant 5
On a more practical level, two participants – one deaf and one in a wheelchair – were concerned about the availability of facilities that would cater for their specific needs.
Future units for long-stay patients
Some participants felt that specific long-stay units would be beneficial for patients who, like them, may be too high risk or too unwell to ever leave secure care. Some described this in the context of their current unit where they were progressing a lot slower than others, which meant that they could be with those similar to them. This participant described what she thought these units should look like:
Not cold and clinical but comfortable. [. . .] just where people can be like put out to grass really. And like, people could go there who were over 40 or been locked up like 20 years plus, like myself.
NHS high secure unit A: participant 6
When giving their views about alternative international models to long-stay units, most participants placed particular value on the idea of being able to take up work within the hospital. They felt that work did, or had potential to, add meaning and structure to their lives with or without any financial remuneration. However, there were some participants who felt that specific long-stay units would not be beneficial to any patient, but would simply exacerbate their dependency and reduce the likelihood of them ever leaving.
Emerging theme 4: readiness for change
When talking about the future and ‘moving on’, participants either felt ready or not ready to move on from secure care. This self-perceived readiness to ‘move on’ may or may not have been congruent with the views of others about whether or not they needed to be at their current unit. For example, some felt ready to move on from secure care but felt that their responsible clinician was holding them back, whereas some wanted to stay in their current unit even though they did not think that they needed to be there.
Stances on long-stay secure care
In this section, the themes presented in the previous section are used to illustrate patterns within and between participants’ narratives. This resulted in the emergence of four long-stay stances: (1) dynamic acceptance, (2) static acceptance, (3) dynamic resistance and (4) static resistance. Table 30 provides a summary of how each of the four themes related to the long-stay stances.
| Theme | Long-stay stance | |||
|---|---|---|---|---|
| Dynamic acceptance | Static acceptance | Dynamic resistance | Static resistance | |
| Attribution | Attributed reasons for long stay to being unwell and their own behaviour | Attributed reasons for long stay to their own behaviour alongside being on the wrong medication or being in a non-therapeutic environment | Attributed reasons for long stay to risk-averse factors that left them feeling unable to prove themselves to staff | Attributed reasons for long stay to interpersonal and structural factors that were out of their control |
| Outlook | Overall positive outlook towards being in secure care and believed that their mental health had improved while they had been in secure care | Overall positive outlook towards being in secure care and believed that their mental health had improved while they had been in secure care | Overall negative outlook towards being in secure care and felt bored, restricted and frustrated | Overall negative outlook towards being in secure care and felt bored, suffocated and a sense of pointlessness |
| Approach | All adopted a proactive approach, stressing the importance of keeping busy and making the most of their time by engaging in occupational activities and therapies | Most adopted a proactive approach with regard to occupational activities. Most were less willing to take part in therapies that they found ineffective | Most adopted a proactive approach by engaging in occupational activities and therapies that, although thought repetitive and pointless, would ultimately help them to move on | Most adopted a passive approach to daily life, choosing not to engage in any occupational activities or therapies |
| Readiness for change | Believed that they did not need to be in secure care and felt ready to move on to lower secure units | Believed that they were not ready to move on from their current unit | Believed that they did not need to be in their current unit but were stuck | Believed that they did not need to be in secure care but that they had no choice and so chose to stay in secure care |
Dynamic acceptance
I’m glad I came here; it’s helped me out.
NHS high secure site A: participant 2
Fourteen patients from the sample took a dynamic acceptance stance. They attributed their LoS in secure care to earlier disruptive behaviour and poor engagement. Those participants who had moved from high secure either down to medium secure units or to more independent wards within a unit believed that this was because of improvements to their mental health and, in turn, their behaviour. Three participants described how the worsening of their symptoms had led them to be transferred to higher levels of secure care; they all believed that this move had helped them to get better.
The participants who displayed dynamic acceptance had an overall positive outlook on their current situation and, to keep up with the progress they had made and to continue proving themselves to staff, these participants adopted a proactive approach by keeping busy and making the most of their time. Most participants who took this stance had gained ground or community leave, which they felt made their days more enjoyable. Aside from leave, most found psychological therapies effective and engaged in recreational activities on and off the ward.
These participants emphasised the importance of talking openly with staff on a regular basis, which they believed had helped them to progress. Most participants got on with other patients but also noted that differences between them and others could prove challenging in such close proximities. Some described how they were able to better manage conflict with other patients, having learnt to control their emotions, and, as such, tried to advise others to adopt a similar approach.
Participants who displayed dynamic acceptance did not feel that they needed to be at their current unit, explaining how they were ‘better’ and that there was no more treatment to do. They felt ready to move to lower levels of secure care with a vision that this would help them to rehabilitate back into the community. As such, a majority of these participants explained how they would be moving on to lower secure units soon. They felt that their chances of moving on could be jeopardised if they were to become unwell or if they were to break any rules. Most who took this stance were aware that the transition to other units would be difficult, as they would need to take on more responsibility for their own care while losing the support of the staff they had become familiar with.
An exception was one participant who felt that he did not need to be at his current unit as he had displayed continuous good behaviour but he believed that his chances were restricted by the limited availability of low secure services for deaf patients such as him.
Static acceptance
It’s an as you were situation you know, continue to stay here and have treatment here, after all where would I go if I wasn’t here? See what I mean?
NHS medium secure site A: participant 4
Twelve participants took a static acceptance stance. They not only attributed their LoS to the wrong diagnosis/medication but also felt that they were receiving inappropriate care and/or were in a non-therapeutic environment. Participants were likely to believe that they had moved units because the current unit was more suitable for their needs.
Unlike those with other long-stay stances, participants felt settled and comfortable in their current units, which, in turn, had an effect on their positive outlook towards their current situation, expressing the importance of living every day as it comes and not thinking too far into the future. For example, one participant explained how he preferred not to expect anything as his stay may keep being extended. Most adopted a proactive approach and emphasised the importance of keeping busy through routine and structure. With regard to psychological therapies, these participants were generally ‘fed up of going’, thought therapy was ineffective and expressed a reluctance to continue engagement.
Most felt that now, on their current ward, they had better relationships with other patients who they felt were similar to them. Most participants also got on well with staff, explaining how they felt understood and cared for and, as such, respected the rules that were put in place.
A majority of participants felt that they did not need to be at their current unit but at the same time felt safe and comfortable and therefore did not feel ready to move to a lower level of secure care, whereas some felt that they needed to be at the current level of security as they posed too much of a risk. All participants who took this stance wanted to stay in their current units and were not making an active attempt to progress or get out. They took the view that if they continued with what they were doing at their own pace with regard to their treatment and good behaviour then ‘maybe’ they could move on. A majority of these participants were, however, more frank about what could stop them from moving on, saying that they felt that nowhere else could be better.
Dynamic resistance
So here we have a situation where now I’ve got it all complete and still stuck.
Private medium secure site B: participant 2
Nine participants took a dynamic resistant stance. Those who took this stance attributed their long LoS to being embedded within a risk-averse secure care culture where they felt stigmatised and unable to shake off their offence history. This risk-averse attitude also played a part in their daily lives on the ward, where participants described how there were too many strict rules that they felt were put in place to make them fail and to keep them in secure care for longer. They also felt that their previous involvement in incidents was not dropped easily and was used against them when they were trying to make progress.
Those who exhibited dynamic resistance had an overall negative outlook on their current situation and most felt bored, restricted and frustrated, which, at times, led them to act out and become violent. Some even felt that their mental health had deteriorated and one participant had resorted to self-harm as a way to avoid harming others. Despite their negative outlook, those who took this stance adopted a proactive approach. However, these participants were more likely to think that taking part in both therapies and occupational activities was pointless and repetitive but had engaged as they thought that it would ultimately help them to move on.
Noted differences between them and other patients made it difficult for these participants to mix with others when they felt that everyone else was more unwell or worse behaved than they were. Most participants described getting on with staff but also felt that staff were overcautious and unnecessarily restrictive because of the patient’s offence history. For example, one participant expressed his frustration with being closely monitored while reading the newspaper because it could contain inappropriate content.
Participants felt ready to leave their current units as they felt that they had done what they were told to do and had made progress. However, they also felt stuck in secure care, which they usually associated with staff feeling that they had not made enough progress or that they were at risk of reoffending. In order for them to move on, those who took this stance felt that staff needed to trust them and, in turn, allow them to take on more responsibility, such as gaining more leave, to demonstrate that they could ‘exist within the community without causing any harm to any other person’ (private medium secure site B: participant 2).
Box 3 presents a case study of dynamic resistance.
Joe is a white British man in his early forties who has a PD. He was first admitted into medium secure services in 1993 for hostage taking. However, in 1999 he was moved to a high secure unit owing to increased risks. In 2010, he was transferred to a medium secure unit as a result of positive progress along the treatment pathway. To meet his rehabilitation needs in terms of community leave, he was transferred to his current medium secure unit in 2013. He is currently on a section 37/41.
Joe’s experiences of long stayWhen talking about previous units he had resided in, Joe explained how the previous move from his current medium secure unit up to a high secure setting had helped him to become better. He had been pleased to move back down to a medium secure setting as it proved that he had made progress. However, following this much anticipated move back down to his current medium secure unit, Joe felt that the unit did not offer as many opportunities as the high secure setting and that, in fact, he found the rules much stricter.
In his current unit, he likes to take part in various occupational activities and educational courses. Being proactive on a day-to-day basis is important to him as he likes structure and it is a good distraction from the monotony of the ward environment.
Aside from his proactive approach to daily life, Joe feels frustrated with the lack of progress he has made since moving back to his current medium secure unit. This mirrored his last tribunal, which he believed to be very critical towards ‘the way things had been done’ at the current unit. This he attributes to a constant change in his responsible clinician, which has resulted in him needing to start new care plans, repeat similar therapies and even lose leave that he had gained with previous responsible clinicians. As such, he explains the constant need to ‘start again’ by proving himself to the new responsible clinician.
Joe believes that prison was a much easier option than secure care because there were fewer rules and restrictions. He believes that this caused problems on wards that held a mixture of patients who had been admitted straight from prison and those who had been admitted straight from high secure care. Joe often found that those who had been admitted straight from prison were more disruptive; this often caused conflict and tension on the ward.
Joe feels ready to move to a lower level of secure care as he has made progress and ‘done a lot of work’. However, staff have told him that he is ‘not ready’. To move on Joe feels that he must ‘convince the clinical team’ by gaining their trust in order to prove himself. One way he thinks this could be achieved is by being given leave, which would not only test how responsible he can be but also give him hope that he will eventually move forward.
Static resistance
I’m not gonna get out so I might as well stay here.
NHS high secure site B: participant 3
Five participants took a static resistant stance. These participants believed that they did not need to be in secure care, that the severity of their index offence had been exaggerated (one completely denied committing their index offence) and as such treatment was unnecessary.
Participants who took this stance all shared a common belief that the secure care system worked against them and attributed their LoS to interpersonal and structural factors that were out of their control. For example, one participant felt that the reputation she had built up while being in secure care had restricted her from leaving the current unit. Another participant described having to undertake more treatment and therapies as a result of the hospital’s ‘goal posts’ moving.
Those who exhibited static resistance had the most negative outlook towards their current situation, describing feelings of boredom, suffocation and pointlessness. These participants adopted the most passive approach to daily life, and almost all expressed disinterest and lack of engagement in activities or therapies. These participants chose to keep to themselves and did not socialise with other patients. One participant felt marginalised and mocked by younger patients on the ward. Another expressed disgust at the offences that other patients had committed and therefore kept their distance.
Their relationships with staff were also poor. Some felt that staff put unnecessary restrictions in place and two participants described feeling targeted by certain members of staff whom they felt took pleasure in belittling them, for example by dictating when the patient could eat or make a telephone call.
These participants did not feel in control of their ability to move on from secure care. Three participants described previous experiences of thinking that they would be moving on, only to be knocked back. One stated how staff’s negative perceptions stopped her, whereas another was concerned that his age would prevent him from getting a job in the outside world and as such the ‘outside world won’t do what the system has done for him’. As a result, these participants believed that the possibility of ever leaving secure care was an impossible pursuit and, therefore, they chose to stay.
Box 4 presents a case study of static resistance.
Adam is a white British man in his late thirties who has a diagnosis of schizophrenia. He was transferred from prison to his current high secure unit in 1996 for a sexual offence, for which he is on a section 37. He has an extensive offence history, including sexual offences, offences against the person and public order offences.
In the past 5 years he has moved wards twice, the first time for a lack of progress and the second time for positive progress. He is currently engaging in various individual and group psychological therapies with which he has showed no signs of non-compliance.
Adam’s experiences of long stayAdam explained how he was too unwell to remember the events that took place when moving from prison to his current high secure unit. He believes that the reason he has stayed so long in secure care is because he refuses to leave. This was not always the case, however, as later in the interview Adam mentions how there had been several setbacks during his time in the unit. Referring to one time in particular, he explained how he had been due to move down to a lower level of secure care only to find out that the ‘goal posts had been moved’, resulting in him having to undergo more treatment and therapies. In the light of these setbacks, Adam described the process of moving on as ‘impossible’, as it is constantly ‘one step forwards and two steps back’.
Adam has moved wards several times but does not believe that this resulted from anything that he was personally responsible for and instead attributed these moves to ward refurbishments that had taken place. When asked how he felt about moving wards, he explained that this was just an inconvenience because he had to move his belongings.
With regard to his current situation, Adam described how secure care is similar to the outside world, where ‘every day is the same’. He considers his current ward as ‘low-stim’, which has been specifically laid out in such a way that patients do not become too excitable, and, as such, untoward incidents can be avoided. However, Adam is quite content with this environment as it means that he does not have to do anything and his days are usually spent sitting in his ‘usual spot’ listening to music and ‘keeping to himself’. As such, staff now ‘leave him alone’ and do not try to encourage him to engage in various activities on or off the ward.
Adam does not believe that he needs to be in secure care and instead would prefer to go back to prison, where life would be more laid back and he would have easy access to drugs. Owing to all of the previous ‘knock-backs’ that he has experienced since being in secure care, Adam now believes that he is ‘never going to get out’ and as such he might as well stay in the current unit. This has resulted him no longer attending any of his Care Programme Approaches or tribunals as he believes that they are pointless and will not lead to anything.
Discussion
Key findings
Our findings provide important insights into participants’ perspectives on long stay, with four key themes emerging from the data illustrating the extent to which participants (1) attributed their reasons for long stay to personal, interpersonal or structural factors, (2) held a positive or negative outlook, (3) adopted a proactive or passive approach and (4) felt ready to move on from secure care. How each participant positioned themselves in relation to these themes determined the patients’ overall stance in relation to long stay, with four distinct ‘stances’ emerging. In this section, we review these key findings, contextualise them in terms of the current literature and draw out their key implications. The limitations are discussed in Chapter 12, but we would like to draw attention to one limitation here: our study findings were generated by an analysis of data from a purposive sample of long-stay patients drawn from the populations at two high and six medium secure units across England. Although our sample has been purposively selected from within a larger epidemiologically-based study of secure hospitals, we cannot exclude the possibility that subjects drawn from other sites would have provided differing perspectives. Furthermore, we may be missing the perspectives of those patients whose responsible clinicians did not permit them to take part owing to their mental state (11 patients) or who were approached but refused to take part (36 patients). For example, referring to the data from WP2, 17 of these patients had a diagnosis of paranoid schizophrenia (five who were not permitted and 12 who refused) and 22 had been involved in one or more serious incidents in the past 5 years (six who were not permitted and 16 who refused). In addition, 15 were on clozapine (two who were not permitted and 13 who refused). These specific patient characteristics may not only provide explanations as to why we were unable to interview them but also indicate a group of patients whose experiences we were unable to capture as part of our sample.
Notwithstanding these limitations and the need for cautious interpretation that they imply, the study has generated the following key findings.
Acceptance, resistance and perceived locus of control
According to Scheff’s133 labelling theory, when an individual breaks a society’s unstated behavioural norms, he or she is compelled to accept the label through societal pressures and eventually come to internalise the characteristics of a psychiatric patient. Aside from societal labels, according to Scull134 psychiatric institutions also act as a form of control by defining normalcy and appropriate responses to diagnosed mental illness, such as the need to show ‘insight’ and comply with treatment. In our research, this was reflected in both of the acceptance long-stay stances. However, some individuals use their individual agency to reject or resist psychiatric care and the role of a psychiatric patient. 135 This resonates with the resistant long-stay stances.
It has been suggested that higher levels of personal recovery among patients are considered to be related to greater empowerment and lower internalised stigma. 136 This resonates with our own findings, which showed that recovery depended on the extent to which individuals attributed their health to their personal actions (internalised) or to environmental circumstances and powerful external agents (externalised); this is also known as a ‘health locus of control’ framework. 137 Participants who internalised their reasons for long stay (acceptance) believed in turn that their abilities to move on were determined by their own behaviour, whereas those who externalised their reasons for long stay (resistance) tended to believe that their abilities to move on from secure care were determined by factors largely out of their control.
Motivations to engage and readiness for change
The long-stay stances revealed patients who were actively trying to progress (dynamic) or were not trying to progress (static) while in secure care. This can be explained further in the context of Woods’138 ‘modes of adaption’, which illustrate motivation to change (the end result) and motivation to change in a particular way (means of that change). According to McMurran and Ward,139 difficulties may be not in the changes that offenders wish to seek (e.g. leaving secure care) but in the way in which they wish to seek these changes.
It was apparent that a conditional ‘tick-box culture’ of ‘doing what you need to do’ was considered key for some participants in being able to leave secure care. Participants who displayed ‘dynamic acceptance’ were motivated to engage in therapies with the hope of bettering themselves and to eventually move on; this is known as optimistic compliance. 138 Participants who displayed ‘dynamic resistance’ adopted an instrumental mode of adaptation, choosing to engage as a ‘means to and end’ by, for example, getting more leave or a ‘good report’ to aid their tribunal. Although those who displayed ‘dynamic resistance’ were engaging in therapies, they had also been involved in incidents of violence and disruption within the past 5 years that had led to them moving units (as opposed to those exhibiting a ‘dynamic acceptance’ stance, who had only been subject to a progressive move). This demonstrates how overly focusing on leaving secure care may hinder patients’ progression when they do not work through their troubles or address the reasons that they are in forensic care. 140
Jones141 argued why individuals tend to move between different adaptive modes as they go through the treatment process. Those who displayed ‘static resistance’ explained how they had built up their hopes too often in the past only to be disappointed by being ‘knocked back’, possibly as a result of some perceived rule change. This demonstrates how an initial instrumental approach to engagement could fall into a state of ‘intransience’, whereby participants come to reject therapeutic interventions through cynicism and indifference. A majority of these participants had stayed above median LoS both in continuous care and in their current units.
Similar to the ‘static resistance’ stance, those who adopted a ‘static acceptance’ stance were not actively trying to leave secure care. Data collected in WP2 show that over half of these participants had problems engaging with treatment and therapies. In addition, they tended to adopt a somewhat ‘ritualistic’ mode of adaption when engaging in occupational activities where there was little investment towards an end goal. Their desire to stay in their current unit, where they felt settled and comfortable, may be associated with previous negative experiences where they had either been kept in a unit where they were not receiving the right care or been moved to other units that they did not feel ready for. Unsurprisingly, participants who displayed static acceptance were more than likely to have been in secure care above the median overall LoS, which may have resulted in them becoming institutionalised, and thus dependent on the secure care system.
Perceptions of risky behaviour
For both dynamic and static acceptance stances, being open and talking to staff about issues they might have were key to patients staying well while in secure care. Those who exhibited ‘dynamic acceptance’ went on to further explain how staff had helped them to progress by teaching them to better manage their emotions and behaviour. In turn, they felt that staff had learnt to trust them and had their best interests at heart.
It has been suggested that professionals’ need to maintain safety and control can often result in a culture of control, which in turn leads to risk-averse, defensive practice and, ultimately, overcontrol. 142 For patients exhibiting resistant stances, restrictions put in place to prevent risky or disruptive behaviour could be seen as unnecessary ‘overcontrol’ and were ultimately the source of what caused them to become frustrated and act out. Differences in perceptions of risky behaviour resulted in dissonance not only between participants and staff but also with other patients. It was common for these participants to describe not being able to get on with other patients whom they perceived to be ‘madder’ or more disruptive.
The extent to which behaviour was perceived to be risky may have a negative impact not only on patients’ relationships with staff and other patients, but also on the way in which participants decided to manage this behaviour.
Being a long-stay patient in a non-long-stay environment
It has been suggested that the environment in a secure care setting can create barriers to participation in valued occupations. 53 Participants across all stances described what they perceived to be unnecessary restrictions when residing on wards with patients whom they felt were more unwell and higher risk then they were, for example not being able to go on escorted ground leave as staff’s time was taken up by needier patients, or activities being withdrawn as a result of specific incidents or general misuse. These restrictions were a particular issue for older participants who compared themselves to younger patients admitted onto the ward. 52 Some participants also described feeling ‘left out’ because they lacked common interests with younger patients on their ward. This was an exception for those who were residing on specific long-stay units/wards who described getting on with other patients who were of similar age and had similar needs to them; this may therefore contribute to a more settled ward environment.
Relevance and repetition of occupational activities and therapies
According to Stewart and Craik,143 patients in secure settings choose occupational activities based on their expectations of enjoyment and success, and associations with independence and normality. Although occupational activities were generally valued by all participants as a means of keeping them busy, they also felt that the activities on offer would not necessarily be something that they would find relevant or interesting outside secure care. Prolonged LoS may have further exacerbated participants’ frustrations when they felt that they were repeating the same activities over and over again.
Participants exhibiting all stances also expressed their frustrations with having to repeat therapies once they had moved to other units (even if they had moved as a result of positive progress). This may explain why some participants found therapies pointless and ineffective and why those with ‘static acceptance’ and ‘static resistance’ stances chose not to engage.
Familiarity and consistency when moving through secure care
Staff turnover caused problems for some patients, especially when they were trying to gain trust. This was a two-way trust, whereby patients described needing to trust staff while also needing to gain staff’s trust by proving that they were able to engage and behave well. For example, one patient felt stuck in his current medium secure unit because of a constant change in his responsible clinician who, rather than referring to the patient’s recent progress, would refer back to his index offence. However, it is also important to note that this participant thought that perhaps the high turnover in his responsible clinicians was due to a shortage of responsible clinicians specialising in PD, a diagnosis that most individuals with dynamic resistance had. According to Lewis and Appleby,144 psychiatrists often see patients with a PD as more difficult and less deserving of care than other patients. In addition, previous research suggests that medium secure units may be reluctant to accept personality-disordered patients, as the units lack the infrastructure to treat this patient group. 114
Chapter 8 International service models for long stay
Aims and objectives
The key aim of the international part of our study was to:
-
describe existing service models for long-stay secure forensic psychiatric care in different European countries.
To put findings into context, it was also important to:
-
assess the key differences in forensic psychiatric care related to legal frameworks and service provision.
We concentrated particularly on Germany and the Netherlands as the two countries with dedicated services for long-stay patients. In identifying service models across Europe we focused on their key characteristics and good practice but also on challenges in the implementation of such models.
An opportunity presented itself – through an international collaboration in another project – to conduct a study (with the support of a student) comparing the main characteristics of long-stay patients in the Dutch long-stay system with the characteristics of the long-stay population in our study. However, as this was not the main focus of our work, this study will be reported here only briefly.
Methods
Three principal methods were employed: a literature review, a written questionnaire followed by semistructured interviews with experts from 18 countries and a quantitative comparison of patient characteristics between the Netherlands and England. The literature review focused on system comparisons between the Netherlands, Germany and England with regard to the relevant legal frameworks; this information was complemented by interviews with experts from these countries. A larger number of country experts were interviewed specifically with regard to service provision for long-stay patients.
Literature review
A literature search was conducted in PsycINFO with a time frame of 2003–13. Owing to ongoing changes in legal frameworks and service provision, older literature was discounted; however, where relevant, we reviewed older publications identified in reference lists of included studies. The search terms included [(‘Dutch’) OR (‘TBS’)] AND (‘forensic’) AND (‘law’), [(‘German’) OR (‘Maßregelvollzug’)] AND (‘forensic’) AND (‘law’) and [(‘United Kingdom’) OR (‘England’)] AND (‘forensic’) AND (‘law’).
Interviewees
We approached experts associated with the EU-funded Cooperation in Science and Technology (COST) action IS1302 ‘Towards an EU research framework on forensic psychiatric care’ (www.cost.eu/COST_Actions/isch/Actions/IS1302). A national selection process is required to join this network, ensuring that all COST country representatives are leading clinicians or researchers with relevant expertise and a particular interest in long-term care. One country, Switzerland, was not a party to COST but was additionally recruited through the Forensic Section of the European Psychiatry Association owing to its long history of forensic psychiatry. Participating COST countries included Belgium, Croatia, UK, Finland, Germany, Ireland, Italy, Latvia, Lithuania (former Yugoslav Republic of) Macedonia, Poland, Portugal, Serbia, Slovenia, Spain and the Netherlands. Experts from Croatia and Macedonia were not available for interview but did complete the initial structured questionnaire.
Questionnaire and semistructured interviews
A written questionnaire was developed by the core group of the COST action, designed to provide context and prepare for and direct the subsequent semistructured interviews. This included topics such as legal frameworks, definitions and service characteristics for forensic patients. Semistructured interviews were conducted over the telephone. The interviews focused on similar themes but allowed more in-depth exploration of long-stay populations and services as well as of key challenges and hindrances in their implementation. The interviews were recorded with the consent of the participant and subsequently transcribed and analysed using thematic analysis.
Data analysis
Data analysis was conducted using thematic analysis to identify common themes, and was coded using NVivo software by one researcher, with 20% double-coded by the principal investigator. Data were analysed deductively via the use of coding determined by the themes explored in both the initial questionnaires and semistructured interviews. 145 All participants checked the full transcripts for accuracy of their statements before analysis. Only data from countries identified as having some type of long-stay service provision will be considered here; however, a full discussion of the data can be seen in a separately published paper. 146
Comparison study of patient characteristics
For this part of the study we carried out an exploratory comparison of the characteristics of the 401 long-stay patients identified in our study with 101 patients residing in long-stay terbeschikkingstelling (TBS; www.tbsnederland.nl) facilities in the Netherlands. These were randomly selected from the three long-stay TBS units and represented about 80% of the Dutch long-stay forensic population. Although the entry criterion for this service in terms of LoS is 6 years (i.e. shorter than the LoS for entry in our study), we felt that – given the overall shorter LoS in the Netherlands and the specific designation of the long-stay TBS service for patients who stay for excessive periods of time – this patient group presented the most useful comparator to inform any service developments in England. Extensive discussions took place with Dutch colleagues with regard to the interpretation of their variables to ensure comparability (e.g. of offence types). Data were compared for key sociodemographic, clinical and offending variables.
Findings
Legal frameworks and service provision in England and Wales, Germany and the Netherlands
Legal frameworks
For a full account of this comparison, see Edworthy et al. 146 In comparing the three countries, it is important to first note that England is unique in that it operates under common law, rather than civil law, as is the case in the other two countries. Each of the three countries has developed legislation that governs the detention and treatment of MDOs. In England and Wales, most of the relevant provisions are dealt with under specific mental health legislation, namely the MHA 1983 (amended in 2007), which covers both civil and criminal patients. However, in both Germany and the Netherlands the legislation relevant to MDOs is incorporated into criminal law: the German Criminal Code (Strafgesetzbuch)147 and the Dutch Penal Code, which introduced the measure of TBS in 1928. 148
An absence of, or at least a reduced, criminal responsibility is a prerequisite for entry into the forensic psychiatric system in Germany and the Netherlands (and in most other European countries), whereas in England and Wales, admission to forensic psychiatric care is independent of criminal responsibility and solely determined on the basis of the patient’s mental condition at the time of sentencing. Germany distinguishes between fully criminal responsible individuals, those with diminished responsibility and those with absent responsibility, whereas the Netherlands operates a sliding scale with five stages of responsibility. Although England also allows for a finding of ‘insanity’ and ‘diminished responsibility’ in separate legislation (the latter only for charges of murder), these concepts are unrelated to admission to forensic care. Therefore, even if found fully criminally responsible, individuals may be detained in the forensic system; transfer from prison to a psychiatric hospital is also possible later during a prison sentence, including at the very end of such a sentence, if the mental state of the offender warrants such transfer. This would not be possible in the other countries other than for emergency treatment; in such cases the offender would be transferred back to prison following this treatment and detention would not be allowed beyond the original sentence length.
Admission, review of detention, discharge
All three countries require the offender to suffer from a mental disorder in order to gain access to forensic psychiatric care, although none of the countries clearly defines such disorders. Exclusion criteria apply in England and Wales in that individuals with substance-related disorders only cannot be detained under mental health legislation. Until recent changes in the MHA, the Act in England and Wales included a ‘treatability clause’ for patients with PDs which stipulated that treatment had to be likely to ‘alleviate or prevent a deterioration of his condition’. In the current MHA, treatment has to only be ‘available’ but no requirement exists as to its effectiveness in a particular case. Germany and the Netherlands do not have exclusion criteria for any conditions resulting in a different case mix, with a higher number of individuals with substance-related disorders and PDs. Both the Netherlands and Germany make specific reference to risk as a criterion for detention, whereas in England detention in hospital merely has to be ‘appropriate’.
In England and Wales patients can apply for a review of their detention by a tribunal (consisting of a judge, an independent psychiatrist and a lay member) annually; if no application is made, the case is automatically reviewed every 3 years. In Germany detention is reviewed in all cases annually and in the Netherlands this happens every 2 years (although only every 6 years does the review include an independent psychiatric report). In both countries this review is conducted by the sentencing court, reflecting the ongoing involvement of the criminal justice system; in England, for individuals ‘sentenced’ to hospital instead of prison, such involvement ceases and decisions regarding treatment and discharge are primarily made by the responsible clinician (albeit with some role of the Ministry of Justice in cases of ‘restricted’ patients).
In all three countries detention must be terminated if criteria for the measure are no longer fulfilled and in all countries compulsory supervision following discharge is possible. Although there are some countries in Europe (Croatia, Italy, Portugal) where detention in hospital must not exceed the length of the sentence the individual would have been given had they been convicted as a non-MDO, in the three countries of interest here detention in forensic psychiatric care is potentially lifelong. The German constitutional court ruled, however, that the length of detention has to be proportionate to the index crime and that the longer detention lasts, the more the individual’s right to freedom weighs in relation to the protection of the public. 68
Service organisation
Service provision in England and Wales is described in Chapter 1. Unlike in England and Wales, in most German states the differing levels of security are encapsulated into one single service, allowing for much easier and quicker transfers. Services are delivered in forensic psychiatric hospitals with around 250–350 beds or smaller forensic departments of general psychiatric hospitals. However, owing to increasing patient numbers, more patients are treated in general psychiatric hospitals, which can cause severe security issues in addition to a lack of appropriate treatment provision. 71 Figures published by the German National Office for Statistics confirm an increase in forensic patient numbers by about 100% between 1998 and 2013. By the end of March 2013, there were 6652 patients detained under section 63 and 3819 under section 64 of the German Criminal Code (Strafgesetzbuch) (i.e. those treated for substance-related disorders). 149 Given that the population of Germany is just under 81 million, this represents about 13 people per 100,000 inhabitants.
Similar to the approach in Germany, TBS clinics in the Netherlands provide all levels of security within one hospital, including pre-discharge and community supervision. 67 According to research conducted by Petrila et al. ,5 there were 650 TBS beds in the Netherlands in 2001, which had increased to 2008 TBS beds in 2009, approximately 11.8 per 100,000 population. In recent years this trend has reversed again, with only 1564 beds in 2014, 9.2 per 100,000.
In both the Netherlands and Germany, forensic psychiatric care is funded through the Ministry of Justice. In Germany, bed costs are about €375 (about £300) and in the Netherlands bed costs are about €350 (about £275) per patient per day for the regular TBS system; both figures are considerably lower than those for England and Wales. This can be attributed largely to these countries’ far lower staffing levels, mainly for nursing staff.
Treatment and outcomes
Each of the three countries delivers treatment to MDOs to address their mental health problems and to lower their risk. English health care generally places a lot of emphasis on evidence-based practice [e.g. in the form of guidelines published by the National Institute for Health and Care Excellence (www.nice.org.uk)], while in the other two countries there appears to be less drive for standardisation and evidence-based treatment. In comparing the Dutch and the UK models of treatment philosophy, some authors67 have observed a more medical model in the UK with a paternalistic approach to decision-making, evidenced for example in the potential over-riding of a patient’s refusal to consent even if they have capacity. This contrasts with the opposite situation in Germany, where treatment must not be delivered against the will of the patient even if the patient lacks capacity.
In forensic psychiatric care, ultimately, the effectiveness of this care is to be judged by outcomes following discharge, in particular in relation to health outcomes, reoffending and social integration. A follow-up study of patients discharged from a medium secure hospital in England over a 20-year period showed relatively poor outcomes (although better than those following imprisonment), with 49% reconvicted, 38% readmitted to secure care, a mortality rate six times higher than that of the general population and very low numbers of people in paid work. 150 For 2-year reconviction rates, the figures were 25.1% for general offending and 6.5% for ‘grave’ offences. In the Netherlands, recidivism rates for discharged TBS patients have been steadily falling from 52% between 1974 and 1978 to 23% between 1994 and 1998. 67 A more recent study showed 2-year reoffending rates broadly similar to those in Davies et al. 151 for those discharged from TBS care between 2000 and 2010, with between 20% and 27% for general offending, 16% and 24% for serious offending and 4% and 8% for very serious offending. 151 In Germany readmission rates have fallen by 46% and recidivism rates by 74% between 1984 and 2003. 68 Although a full interpretation of these figures would require a more in-depth analysis of the underlying data, the heterogeneity of the outcomes further highlights the need for collaboration and harmonisation of approach towards the treatment of MDOs to provide a wider evidence base and to aid the development of best practice.
Long-stay service models across Europe: an exploration of definitions, service characteristics, good practice and challenges to implementation
Definition of long stay
Thirteen countries provided information on LoS in forensic care, including legal definitions of LoS, country-specific research and professional agreements as to what constitutes ‘long stay’. The Italian expert indicated that a LoS of over 4 years would be considered long in his country. Eight countries (Finland, Germany, Ireland, Latvia, Poland, Slovenia, Spain and Switzerland) indicated a typical LoS in forensic care of between 4 and 10 years, while Belgium, England and the Netherlands indicated that a LoS of over 10 years would not be unusual. Only the Netherlands indicated a legal definition of long stay for forensic psychiatric patients, which provides a cut-off point of 6 years.
Key characteristics of long-stay services
Some kind of special provision for long-stay patients was identified in six of the participating countries: England, France, Germany, Ireland, the Netherlands and Spain.
In the Netherlands, criteria for long-stay status are standardised by law under a separate TBS long-stay order. The criteria for this status are:
-
having been an inpatient in a forensic institution for at least 6 years
-
having been in two separate forensic hospitals
-
having completed relevant treatment programmes but with little discernible progress (or consistently refusing to participate in such programmes)
-
having no expected reduction in risk for the foreseeable future.
Individuals who fulfil these criteria can be given a long-stay TBS order and be transferred to a specific long-stay facility on application by their clinical team and following review by an independent national panel. There are currently about 112 such patients in the country who are cared for in two different facilities.
In the other countries specified long-stay treatment wards have been developed within forensic psychiatric hospitals but without any national laws or policies to govern these; therefore, the design of such services varies widely with no consistent pathways or agreed service specifications. Treatment in long-stay facilities generally was said to include general psychiatric and medical treatment, but with less focus on risk reduction and a greater focus on ‘well-being’ (Germany), ‘quality of life’ (England, Ireland and the Netherlands) and preparation for intensive rehabilitation and educational interventions (Spain). Key characteristics of long-stay care in the Netherlands included treatment to stabilise an individual’s mental state and providing optimal quality of life with as much autonomy as possible;152 the TBS long-stay system no longer measures risk formally (e.g. through the HCR-20, which is otherwise utilised in TBS care). Where specialised long-stay wards operate in Germany, it was felt fundamental for long-stay patients to be placed in an environment that is tailored to their needs to enhance their quality of life, provide as much freedom as possible and minimise risk. 73
Crucially, although individuals are expected to remain in long-stay care for long periods of time, potentially lifelong, the same review procedures of the need for detention as for non-long-stay patients, applied in all countries and all services, allowed people to move back into the mainstream system when this was felt to be appropriate.
A number of characteristics were noted of patients in need of long-stay services; the expert interviewed from France detailed ‘violent patients’, with other common characteristics between countries including ‘therapeutic non-responders’ (or treatment-resistance) and presenting a ‘danger to society’ (having committed violent crimes or presenting with continued violent behaviour). A study in Germany was identified that showed that patients considered to be ‘non-dischargeable’, and therefore long stay, were found to be significantly older, more likely to be sexual offenders and more likely to have a diagnosis of paraphilia, PDs or intellectual disabilities. 73
Good practice
Common themes of good practice identified in long-stay services in England, Germany, Ireland and the Netherlands included the promotion of ‘well-being’, ‘quality of life’ and ‘humane treatment’ for patients, as well as ‘protecting society’ and reducing overall costs. It was recognised that this patient group was one that got ‘stuck’ in the forensic system and there was greater emphasis on ‘maintenance’ of chronic, treatment-resistant patients and improving standards of living in what would otherwise be a highly restrictive environment, but with some expectation of progress in treatment. The importance of addressing quality of life in this service provision was recognised by all participants; however, it was acknowledged that this was difficult to measure.
A number of examples were given of what was considered good practice. In the Netherlands, there is a distinct difference in the language used in long-stay services. For example, there is ‘work’ rather than ‘treatment’ and ‘inhabitants’ rather than ‘patients’. The treatment goals of the Dutch service are to create as much autonomy as possible for the inhabitants and to give them as many real-life choices as they can to stimulate a sense of meaningfulness and belonging, which in turn improves social control and security. 152 The importance of a highly individualised approach in which pro-social behaviour is consistently reinforced, and a sense of group belonging is also emphasised. Relational security is relied on much more than physical security to create a safe environment for staff and patients. 152 There are freedoms that could not be expected in services in England, such as to keep pets and to engage in sexual relationships (with mainly long-term partners outside or inside the institution), although this is not a feature specific to the long-stay service.
In Germany, the Haina Vitos forensic psychiatric hospital was described as providing long-stay wards at each level of security (high, medium and low). The high secure ward is for patients with a high level of risk, who consistently refuse treatment and often show high levels of psychopathy. The medium secure ward is also for patients with a high level of risk but who are partially compliant, less volatile and easier to manage. The low secure ward is based on a farm in the hospital grounds where long-stay patients who are stable and relatively low risk live and work together in a community-like environment. 73 This grading allows for care given in the least restrictive setting; however, moves between levels of security can and typically do happen within days. Freedoms are available to patients similar to those described for the Dutch service.
The expert in England acknowledged that different services are available to different patient groups, with ‘low stimulus’, ‘homely environments’ for treatment-resistant populations and a ‘recovery-focused’ pathway for complex-diagnosis populations.
Outcomes
Outcomes for the long-stay population were described as more positive than was originally envisaged. Between 2010 and 2014, 38% of patients in the Dutch Long-term Forensic Psychiatric Care Pompefoundation were discharged, with many moving to lower levels of security and back to mainstream care, demonstrating that recovery and step-down can be achieved for the long-stay population (Bulten, Pompestichting, 2015, personal communication). Similarly, the interviewed expert in England acknowledged that a ‘recovery-focused’ long-stay pathway has been effective in terms of discharge rates: ‘we’ve actually found a success rate in discharging people who we thought we’d never discharge before’. In Germany a reduction has been described in the number of long-stay patients in complete confinement and increases in the number of long-stay patients with access to escorted leave, unescorted leave and leave outside the hospital grounds have been described. 73
Challenges to implementation
In Germany it was described that long-stay services had developed gradually over the past 20 years with little organisational reluctance or legal resistance, although it was acknowledged that some patients may challenge their detention should treatment no longer be provided. Experts in the Netherlands described difficulties in identifying criteria for admission, and even more so for discharge, when establishing long-stay services. In countries without separate, designated long-stay facilities, according to the experts interviewed (England, France, Ireland and Portugal), the term ‘long stay’ is not a widely used concept among practitioners, nor is it always considered a helpful categorisation. Opinions regarding the further development of specific long-stay services were mixed, with ideological and cost-related factors impeding further development, particularly with many countries in Europe being affected by austerity measures. Despite these apparent challenges, five countries expressed a clear need for long-stay service provisions, namely Belgium, Latvia, Serbia, Slovenia and Switzerland; however, only the expert from Slovenia was able to confirm that there are current plans to develop such services. Anticipated barriers to the set-up of future long-stay forensic services included institutional barriers, lack of finances and public attitudes towards MDOs. There were mixed views as to whether long-stay facilities were actually cheaper, and it was noted that the Dutch TBS service, originally cheaper than the mainstream TBS service, is now actually more expensive (€430 vs. €350/day) due to the higher staffing levels required to manage some of its patients.
Comparison study
As noted above, this comparison is reported only briefly here. Full data are available from the authors of this report on request and will be published in due course. A table with the main results is provided in Appendix 15. Dutch patients had a higher LoS in total, with nearly 40% having been an inpatient for > 20 years; they had also shown more changes in treatment settings, possibly partly a reflection of the requirement to have been treated in two different settings before being accepted into a long-stay facility. In both samples the majority of patients were male, unemployed, aged between 41 and 50 years and had never been married. However, Dutch patients were significantly older and more likely to have been married but less likely to have been employed previously. There were only two women in the long-stay sample in the Netherlands. Diagnoses of schizophrenia and at least one Axis II classification on the Diagnostic and Statistical Manual of Mental Disorders24 were highly prevalent among both cohorts, although the Dutch sample contained more PD patients and more patients with an autistic spectrum disorder. English patients were younger at first conviction and had more convicted offences, although in the Dutch sample there were almost twice as many individuals with a sexual index offence and the Dutch sample had higher HCR-20 scores (the last score before admission to the long-stay service).
Discussion
Significant differences in the legal and policy context between England, Germany and the Netherlands emerged in terms of both the legal frameworks governing forensic psychiatric care and how this care is designed and delivered. While the emphasis in England on the mental health needs (as opposed to the criminal responsibility) of the offender as an entry criterion for forensic services may, at first glance, seem in the best interest of the patient, significant ethical issues are raised as a result of the indeterminate nature of psychiatric detention, whereby fully criminally responsible individuals are incarcerated for longer than they would have been had they been given a custodial sentence as a non-MDO. In England and the Netherlands, a shift has been identified towards a greater concern for public protection as opposed to the individual offender’s right to freedom, leading to increasing LoS12 and a vast increase in forensic psychiatric beds,70 although this trend might be about to reverse. Germany, on the other hand, has witnessed a different trend; the pendulum appears to have swung back to an interest in individuals’ rights, with the introduction of the German Therapy Detention Act in 2011,153 which states that an institution must provide a therapeutic environment that places the least burden possible on the detained individual, and recent rulings have prohibited treatment against the will of the patient even if the patient lacks capacity. Both comparator countries offer significantly more individual freedoms to detained individuals than England, despite a recent focus in the latter on recovery principles. 154
Recent research has found a great deal of variation in outcomes internationally, with mortality rates varying between 289 and 2828 per 100,000 patient-years, readmission rates varying between 2926 and 16,641 per 100,000 patient-years and reconviction rates varying between 0 and 24,244 per 100,000 patient-years. 25 It is not clear how England compares in these outcomes internationally, although there is some indication that outcomes may be worse there than in other countries. 150 This may be due to ineffective treatment, although a more likely explanation might be the restrictive nature of services, reducing opportunities for patients to engage in varied prosocial activities, and policies (e.g. criminal records checks and offender registers) that make it more difficult for MDOs to adopt a new life after release.
Given the fundamental differences in forensic psychiatry between European countries, it is unsurprising that what constitutes a ‘long stay’ also varies widely across Europe, along with treatment philosophies, service provision and attitudes towards potential long-stay services. The Netherlands and Germany are highlighted as providing the most well-established long-stay services. The large number of individuals moving on from such services might suggest that patients become more willing to engage in risk reducing interventions when the (perceived) pressure to engage ceases. Although the Netherlands has a separate law for long stay, it is clear that such a legal framework is not necessary for services to be developed and these developments have taken place in a number of countries, with the aim of improving quality of life and the promotion of well-being forming the fundamental treatment philosophies.
There is currently no clarity regarding the resources required for long-stay services; however, it is likely that such services will require a different skills mix but will not necessarily be cheaper. A German discussion paper155 cautions that services treating long-term patients may not be less expensive and that increased resources may be required for physical health care, occupational therapy and educational staff and counselling, while fewer resources may be required for psychiatric and psychology staff. A number of countries have expressed the need to develop long-stay services in their countries; here international dialogue can be valuable in terms of sharing experiences and the development of best practice. In this context the comparison of patient samples, as performed here, will also be informative to judge whether or not service models will be applicable to the patient group in another country.
Chapter 9 Stakeholder perspectives
Aims and objectives
The objective of this part of the study was to explore the views of clinicians, managers, commissioners, policy-makers and other relevant professionals on long-stay forensic care and, in particular, to:
-
understand staff perceptions of the problems characterising long-term secure forensic care
-
develop possible strategies to address these issues
-
understand the factors that may impact on the development and implementation of a strategy for the management of long-stay forensic psychiatric patients
-
develop potential service models, identify potential hindrances regarding their implementation and make recommendations regarding implementation and evaluation, including economic evaluation.
Methods
Initially our plan was to use focus groups and interviews to explore these issues, but we also expanded our data collection to include site visits, as we explain further below.
Data collection
The approach for this part of the study was to use qualitative methods to explore the behaviours and attitudes of staff working in secure forensic psychiatric settings, as well as the way services are delivered. The interview questions and focus group discussions were designed to explore the ways in which service provision currently operated as well as views on possible alternatives to current provision.
We interviewed doctors (consultant forensic psychiatrists, n = 21), commissioning managers (n = 5), legal experts (n = 2) and others (an intellectual disability specialist, a policy lead from the National Offender Management Service and a former manager with experience of the Accelerated Discharge Programme) identified as part of the study. Doctors from 20 different facilities were interviewed, as our aim was to understand the range of types of services provided, and the differences and similarities between the facilities. We used a mix of face-to-face (n = 4) and telephone (n = 17) interviews, which were digitally recorded and transcribed verbatim. We used a combination of purposive and snowball sampling to recruit participants across a broad geographical area. Initially, we contacted psychiatrists who were members of an advisory group that informed commissioning decisions because we wanted to speak to individuals who, we hypothesised, would have a broad, as well as local, knowledge. Additionally, as our study was aimed at making recommendations for change, we hypothesised that these people would be well placed to comment on alternative models of service provision. We asked interviewees to recommend other suitable people to us and followed up their recommendations.
We also conducted focus groups to generate data on long stay in forensic settings in the UK and overseas. The focus group participants were recruited from international conferences on forensic psychiatry in 2014 and 2015. The study was advertised to conference participants in advance by the conference organisers as well as through leaflets at the conferences. Three focus groups were held with three, six and seven participants, respectively. The largest professional group of participants was (forensic) psychiatrists (n = 9, three of whom also had senior management duties); two participants were psychologists and five were from other professional backgrounds (one pharmacist, one social therapist, two researchers and one individual who worked for the regulatory body the Care Quality Commission).
As nursing staff spend most of their time immersed in the ward environment, it was important to capture their experiences and views. Resource constraints, in terms of both the research budget and nurses’ time, led to us using focus groups in one NHS trust to explore nurses’ views. The intention was also to allow nurses from one organisation to discuss their experiences with each other, in order to use dialogue as a way of prompting discussion and debate. Eleven participants were recruited and divided into three focus groups (with five, four and two participants). The uneven numbers across the groups was due to scheduling issues and last-minute cancellations as a result of other work demands.
We also spent 1 day in each of three ‘long-stay’ secure forensic facilities, where we visited wards and met and talked with staff. We held a focus group with staff at each site. At site 1, this involved two nurses and one psychiatrist. At site 2 the focus group members were two psychiatrists, one psychologist, one nurse and one nurse manager. At site 3 the group comprised three nurses, two psychiatrists and one psychologist group. When it was permitted to take recording equipment into the facility (in sites 2 and 3), we recorded these discussions and they were transcribed verbatim. When this was not possible, we made notes during the visit and elaborated on these as soon as we left the facility. The data collected also included notes relating to the layout and physical environment of the setting. We also made notes about the nature of the facilities more generally and the narratives that staff provided about them.
Data analysis
Initially, a small number of the interviews were coded thematically using NVivo software. We had identified issues from the literature and the project objectives that informed our interview schedules and we used these to inform our approach to coding data. To some extent our analysis was shaped by these prior themes and issues along lines similar to a framework approach. 75 However, we also identified new codes as part of the data analysis process. The focus group data and the data from the site visits were all coded using NVivo software. Emerging themes were discussed among team members, with disagreements resolved and queries clarified. This process continued during data collection and was used to modify the interview topic guide to incorporate new areas of investigation as the study progressed. The issues raised in interviews prompted us to organise site visits and also informed the site visits in terms of focus and areas of investigation as well as the coding of data from site visits. They also prompted us to identify additional interviewees who could shed further light on some of these issues.
Findings
Tensions and contradictions
Interviewees described places that embody inherent contradictions relating to the fact that residents are patients and, at the same time, offenders. The aim is to rehabilitate and ‘cure’ patients in a caring environment, but patients are detained against their will in a regime that applies pressure to comply with therapeutic interventions. A ‘recovery’-based approach to rehabilitation, in contrast to the traditional medical models of treating people with severe mental illness, aims to empower patients. Yet staff are charged with managing risk, which means that the extent to which they can empower patients is constrained. Furthermore, the recovery and rehabilitation model does not cater for the many patients who will never leave secure settings. 18 Staff emphasised the need to maintain hope, but hope was related to treatment and ‘cure’ in a context where this may not apply to a substantial minority of patients.
Talking about patient pathways, almost all doctors appeared to conceptualise the process in terms of an ‘admission, treatment, rehabilitation, cure’ trajectory, with little or no acceptance that not all patients would fit this model. An emphasis on treatment was common to almost all accounts, yet ‘wanting to help people’ implies that there is effective treatment. However, unlike in general hospitals where evidence-based medicine may be appropriate for patients who have, for example, broken their hip, in forensic psychiatric settings the evidence to guide practice may be much less clear. As one doctor described it, secure forensic psychiatry involves dealing ‘with patients . . . at the end of the distribution in terms of risk and complexity, algorithms don’t work very well . . . they tend to have broken the algorithm before they get here’ (psychiatrist ID8). Furthermore, with patients who are treatment resistant, the ‘admission, treatment, rehabilitation, cure’ trajectory is not so readily applicable.
Incentives
The incentives within the system were identified as acting as a barrier to the provision of care that would best meet patient needs. An emphasis on managing risk means that there are disincentives to take patients from other facilities that have higher levels of security. This means that although patients might be judged ready to ‘step down’, there are lengthy delays in patient transfers. Attitudes to risk were reported as varying between clinicians and also between sites. Differences in size, and hence in facilities, accounted for some of the variation in ability and willingness to accept patients, but attitudes to risk was an important factor.
We tended to take some patients which other RSUs [regional secure units] would not have done and would have referred to high security. I think in part that was a reflection of the size of this unit that we’ve always been one of the bigger medium secure units and therefore had a wider variety of ward environments, including for a number of years now a high-dependency ward. So I think that had something to do with that. I think also there’s an issue about custom and practice . . . If the custom is to do things a bit more slowly and a bit more risk-averse the chances of your length of stay will be higher.
Psychiatrist ID9
Furthermore, payment for capacity as opposed to hospitals being paid for their actual level of activity undertaken (‘money following patients’) might create incentives for providers to protect their bed base, rather than actively scrutinising the extent to which the setting and nature of care provided is the most suitable for the patient. At the same time, providers reported that they were active in seeking to discharge patients. They also described commissioners as scrutinising activity to ensure that patients were not being accommodated in higher levels of secure care than was necessary.
We’re already under a lot of scrutiny. We’ve got case managers monitoring all our patients and chasing them up. It’s us – the other way round – we’re going to commissioners saying we want your help to move these people out.
Clinical director, high secure hospital ID24
The funding arrangements for inpatient forensic psychiatry, which ensure that services are centrally commissioned, mean that community services are funded from a different budget. This is held by local Clinical Commissioning Groups and these arrangements were reported as creating a disincentive to develop community services and to engage in facilitating discharge into the community.
Because there’s a disincentive for CCGs [Clinical Commissioning Groups] to fund discharges now. Or to provide the adequate high support accommodation and clinical teams in the community.
FG Budapest
In some sites providers reported that commissioners set LoS targets to incentivise discharge, but such targets could be problematic for ‘long-stay’ patients. In one site commissioners colluded with a service provider to maintain the fiction that services were no different for this group of patients: ‘commissioners do not commission long-stay medium security. They do really, because the people are having it, but they don’t officially’ (ID3). Elsewhere, the explicit support from commissioners helped to lend legitimacy to such services.
The existing arrangements were also reported as creating little incentive for providers to innovate, particularly where this would threaten their existing bed base.
If a provider had, let’s, say 50 beds, what’s the incentive in reducing their 50 beds to 40 therefore their income by 20%? To develop this service for another provider to take over? There’s not! [Laughs.]
SB commissioner
Incentives to save money were seen as adversely impacting on the speed of transfers in a context in which receiving units were facing budgetary reductions. Such incentives had other consequences for patient care and patient trajectories, as illustrated in the following quotation:
They introduced this last year and the fact that you no longer need to be seen by the tribunal doctor unless you request it . . . it’s really important that when you go in there you’re been seen by someone who’s independent and can maybe just look at your notes and maybe just say ‘this guy doesn’t need to be kept in for much longer and who can then feed back to the other tribunal members’. And I think it’s obviously a money saving decision but I don’t think it’s serving the patients well.
Lawyer
Managing ‘long-stay’ patients
Despite the emphasis on treatment and ‘recovery’, staff also acknowledged that some patients were unlikely to leave in the short or medium term. To some extent this resulted in ‘complacency’ in relation to such patients, with resources being focused on demanding patients or on those for whom recovery was a more realistic goal.
If I feel that numbness or complacency’s creeping in, to try and shake it out and have a think about why that’s happening and what’s going on. But, yeah, I do suspect that that happens with long-stay patients when everyone is happy with it and the long-stay patients are quite happy with it as they don’t get challenged any further. They get challenged up to a functional point. It is almost tempting to leave it like that as it is quite comfortable.
Nurse RE FG: high secure hospital
The MHA requirement to offer ‘appropriate treatment’ is apparent in the concrete spaces of treatment rooms and embodied in the presence and practice of various health professionals whose rationale is to provide treatment. The absence of alternative provision for ‘long-stay’ patients who are unlikely to leave means that doctors focus on existing spaces and related practices, however deficient. At the same time, many do not see these as deficient.
We do offer appropriate treatment. So we have things like occupational therapy, integrated therapies, we offer adapted sex offender treatment programme, adapted fire setters programme . . . I think even if someone’s been there for 20 years you should still be trying to do something . . . Now I know you can get all sorts of interpretations of what offering appropriate treatment is but to my mind it has to be something a little bit more than just saying well there’s 24-hour nursing care. I know there have been High Court judgements that have said appropriateness in care, 24-hour nursing care, is appropriate treatment but I think that becomes just warehousing of people really.
Psychiatrist ID3
The phrase ‘warehousing’ was used often by psychiatrists who raised objections to the cessation of treatment. As the above quotation illustrates, for some psychiatrists active treatment should be continued regardless of how long the patient has been in the secure system, and approaches that limit ‘appropriate treatment’ to nursing care are unacceptable.
The ability to manage patients has to be seen in the context of broader social, historical and cultural factors that influence practice. Some doctors described historical changes imposed by the state that had reduced quality of life and access to spaces inside the hospital. These reinforced the isolated nature of the social space and reduced the number and diversity of participants who could contribute to its production. The boundaries between the hospital and the outside world had become less permeable as a result.
Following things like Fallon and the kind of reviews of security . . . football teams from outside used to come and play the patients and things like that and the community used to come in a lot more . . . and we don’t have any of that any more, nothing like that. It’s very isolated really and a bit more contained now here and a lot more secure in terms of that. But I think the patients felt more integrated, part of the world rather than very far removed. I think that’s certainly a quality of life issue.
Psychiatrist ID4
At the same time, others pointed to the positive influence of the state in disrupting the ‘old order’ and compelling staff to engage in a recovery-focused approach, despite the fact that the old asylum buildings in which many worked were not initially intended for this. Although doctors identified constraints arising from the nature of the buildings in which they worked, it was possible for changes to be made in these settings.
We work with an estate that’s 150 years old . . . I don’t know if the building would accommodate to changes . . . what we found in 2001 . . . there were a lot of people before the accelerated discharge programme about who the kind of assumptions had been made and in practice it wasn’t that hard to move many of them on.
Psychiatrist ID8
There also appeared to be a generational effect, with older psychiatrists suggesting that those who had trained more recently were more ‘evangelical’ in relation to treatment and ‘cure’ than previous generations.
. . . modern psychiatry . . . everybody who’s trained in mental health, nurses and doctors, has not had access to that whole literature from the sixties about what goes on in institutions. So they’re handicapped I think by not understanding that if you work in long-stay residential care life is different, you know, the way you talk about life and the way you organise your relationships, cure doesn’t make much sense. But care makes a lot of sense but care is complicated . . . some people can still find some work and fulfilment in their life, even if they’re detained for life in custody . . . it’s never about just warehousing . . . But you’re being honest and open with the person.
Psychiatrist ID17
. . . in the nineties [the] enthusiasm of people coming into forensic psychiatry to go along with the government agenda . . . there’s a kind of cohort of forensic psychiatrists who have been brought up and cut their clinical teeth during that period . . . people have different experience and they’ve been trained in different ways . . . but I think that one has sometimes . . . got to recognise . . . getting better doesn’t necessarily mean leaving hospital.
Psychiatrist ID18
Furthermore, the context in which patients are managed is one involving a range of stakeholders. This means that psychiatrists, and to some extent other staff, are attempting to take account of competing agendas and tensions, which makes life challenging.
There are a number of other stakeholders in a patient’s trajectory through secure care which have a bearing on this so it’s not just simply the consultant forensic psychiatrist making a decision about what happens, you have the Ministry of Justice, you have victim issues, you have a whole lot of factors like that . . . And even if they are not explicit in playing a role it would at least be in the mind of the person who is looking after the patient . . . I don’t think that psychiatrists are that interested in the effectiveness really to be perfectly honest. I think what they’re concerned about is risk . . . Our treatments are fairly feeble actually in their efficacy.
Psychiatrist ID22
The foregoing also highlights that individuals are not ‘empty vessels’, but bring various assumptions and attitudes to their practice. Patient perspectives are reported elsewhere in the report, but doctors reported that patients who ‘stepped down’ from high to medium secure hospitals brought expectations with them. In contrast to the high secure hospitals, most of the medium secure facilities we visited were located close to urban conurbations. Doctors reported that this meant that restrictions had to be imposed on patients. In high secure units with perimeter fences, patients may have access to grounds and outdoor areas in a way that is not possible in medium secure facilities.
For those who come from [high secure hospital] sometimes we’ve had a bit of a difficulty because they have high expectations and they think they’re just coming here and it’s a year and going into the community. When they know they have to stay longer they become a bit disillusioned but then leave issues while they’re roaming over the whole of [high secure hospital] it’s OK because it has got a perimeter fence but we don’t here. Our grounds are open . . . They come from a lot of leave within the grounds and then they go to the workshops and things like that just limiting them to the building.
Psychiatrist ID21
Furthermore, doctors reported that patients did not always conform to expectations, with some, for example, refusing to ‘step down’ to lower levels of security because this would mean losing their en-suite facilities. Additionally, some patients were reported as being anxious about ‘stepping down’ and preferring to remain in their existing location where they had good relationships with staff and/or other patients.
Changing the nature of service provision
Although staff provided accounts emphasising treatment, it appeared that their lived experience was, at times, at odds with the concrete buildings, guidelines and practices which characterised their daily working life. Patients did not readily conform to expectations in relation to recovery.
We still have sexual offenders who have predatory behaviour even on the ward. They need that kind of context of management and they need all the security. You can’t take them anywhere. They don’t engage in therapy. They don’t realise anything is wrong with them. And basically they’re just not changing.
Psychiatrist ID1
Additionally, in some sites, there was a growing recognition that mixing ‘long-stay’ and other patients was problematic. Some staff highlighted the deficiencies of the current approach that meant that the patients who may never leave ‘are still on their recovery ward so the gamut of therapy, groups, etc., would be the same despite the fact that it’s long-term care until physical health deteriorates and results in residential nursing home care . . . a 30- to 40-year job’ (psychiatrist ID11). Even when doctors acknowledged that there were likely to be patients who would never be discharged, they often felt uncomfortable explicitly discussing this situation with patients. Some suggested that norms did not allow such behaviours:
I sometimes want to say, ‘You know what? You’ve arrived and you’re not on a journey now’, and we’re not allowed to say that. It is seen as unprofessional or lazy or giving up, where, actually, it might be the most humane thing to say.
Psychiatrist ID23
Among commissioners there was a greater appetite for identifying patients who might never leave, as this quotation illustrates.
I was on one of the women’s wards a couple of weeks ago and there’s a woman there . . . She needs a secure environment because she is treatment resistant, to use a technical term, absolutely ‘mad as a hatter’, but doesn’t need . . . the level of security that you have in high secure . . . there are people in the long-term service who don’t need it, but there’s nowhere for them to go.
Commissioner ID13
Staff described how the impetus for thinking about alternative forms of practice was not a result of a sudden external policy directive, but rather a growing awareness that the needs of this group of patients were different in a way that had implications for care provision. Over time, this had prompted some doctors to reflect on their habitual behaviours and to question their validity. Some higher-profile patients had committed particular kinds of offences that made them targets for other patients in the hospital, who would gain status by threatening or assaulting them; this meant thinking about ‘collecting them together . . . keeping them safe and quality of life [being] . . . important aspects of their humane care’ (psychiatrist ID5). Existing provision that involved mixing the two groups of patients meant that those who did not progress might be unsettled by the high turnover, as well as being fearful of other potentially violent and disruptive patients. Having these two groups on one ward made it difficult to provide a context that was ‘more homely than sterile’ (psychiatrist ID9).
This was leading to changes in the way that wards were configured, as these doctors described.
It’s a smaller ward. It has accommodated the fact that it will have a group of higher-profile and longer-stay patients, there for an extended period of time . . . we shouldn’t have too many people coming in and moving off elsewhere . . . And not having the ward unsettled by too high a turnover I think is important . . . a lot of the patients say they prefer it here, they feel there, there’s less bullying there, they feel more relaxed there and their mental states have improved as a consequence of being there.
Psychiatrist ID8
A larger focus on sort of, ward-based activities, community activities, maybe cooking or plan of the day meetings, current affairs groups etc. So a real sense of a community . . . They’ve got their own lounge area, TV, the rooms are probably a little bigger. It’s got a different feel to the place.
Psychiatrist ID9
In these places, staff accounts emphasised improving the quality of life for patients and attempting to make it a more homely environment. At one site we visited, a nurse described travelling to another facility catering for ‘long-stay’ patients to learn from their experiences. There the visiting staff noticed that, although the professionals said that patients were not left to lie in their rooms all day (which was seen as part of the ethos of making the place more like home), various patients were sleeping on couches in the lounge during the day. The visiting staff resolved not to buy three-seater couches to prevent this from happening at their new facility. Here the emphasis was on quality of life and building a long-term community, although patients’ views about what constitutes a normal quality of life might be disregarded if they included daytime sleeping in this.
The extent to which patients in these types of ‘long-stay’ facilities could personalise their rooms differed across sites, as did the range of activities and facilities available to patients. Some patients in medium secure facilities had access to SkypeTM (Microsoft Corporation, Redmond, WA, USA) to enable them to keep in touch with relatives, and access to pornographic material was made available based on individual patient assessments. The emphasis and was on providing patients with a good quality of life and an existence that was as normal as possible, while implicitly, and occasionally explicitly, recognising that such patients would not be discharged. This is illustrated by the quotation below from a doctor, 1 month after starting on a new ‘long-stay’ ward.
On the current ward I’m on, they’re going to die there. I don’t have the option. They’ll only go to a care home. Well a hospital because I can’t send them to a care home . . . which is kind of depressing. It’s not a ward I’ve worked on before and I was looking forward to it but . . .
Focus group 2: psychiatrist ID3
This espoused ethos was based on a mostly implicit recognition of the fact that, rather than being temporary, this would be the patients’ home for many years, if not forever. Despite these aspirations, in practice patients were still subjected to the same procedures as those elsewhere in the facility. These include potential room searches, regulations on the limited number of items allowed in their rooms and the possibility of having to change room frequently in response to other patients’ needs. This approach severely limited the extent to which the ‘long-stay’ facilities could provide a homely environment.
There were further limits to ‘normality’; for example, sexual activity was not permitted. There is no national policy preventing this, but in the absence of such a policy staff are free to apply their own judgement. . The attitudes of staff in the settings we visited contrasted with those of staff in countries such as Germany and the Netherlands, where sexual activity is permitted between patients or between a patient and an outside partner. 156 Doctors explained that there was a need to protect vulnerable patients; they also highlighted the fact that many patients were sexual offenders, implying that they viewed a patient engaging in a sexual relationship as an obstacle to that patient’s recovery. 157 These responses may reflect the broader social and cultural context in which forensic units are situated (e.g. less liberal views regarding sexual relationships in the UK than in the Netherlands156) and they imply clear constraints on ‘normal’ living and quality of life. Furthermore, although spaces encouraging the development of a sense of community were seen in a positive light, the nature of the community’s residents meant that tensions between allowing freedoms and enforcing constraints required a delicate balance.
A few patients have used [the phrase] ‘the brotherhood’ and they feel like it’s ‘us’ against ‘them’ and we need to stand up together for our rights. I also am beginning to get the feeling that because they . . . are quite close to each other there might be an element of them not wanting to move off the ward because that comes with its own anxieties and they wouldn’t know if they’ll have the same friendships and groups that they have with us . . . we have had incidents where they have grouped up in communal areas and we thought that was extremely dangerous for staff because it’s quite possible to have 15 people . . . who know each other very well and if they decide to cause trouble there’s very little that anyone can do.
Psychiatrist ID19
Staff described patients who were not progressing and took us around spaces for such patients during our visits. They explained that the focus was on improved quality of life and reduced medical input, as such patients were unlikely to respond to treatment and equally unlikely to leave the secure setting. At the same time, they insisted that patients would move on.
Size is something that probably wasn’t determined scientifically but was a consequence of the ward that was available that was refurbished and the size is such that it is probably quite cheap to run . . . The therapeutic input has decreased a little in recent years . . . But you know at the end of the day, it’s not just a secure warehouse and it can’t be. It has to be an environment that enables people to move on.
Psychiatrist ID9
We’ve called it Enhanced Recovery Service . . . we want to maintain some realistic hope for some guys, but we’ve also got to make it pleasant and a good quality of life and optimising people’s recovery for some of those guys who aren’t going anywhere, and women, in the future.
Psychiatrist ID5
Doctors were opposed to the use of the phrase ‘long stay’ to denote spaces for patients who stayed for a long time and perhaps would never leave, as it implied failure. When we talked to psychiatrists and visited facilities for patients who were not progressing, we found that such facilities were variously named ‘slow-stream rehabilitation’, ‘enhanced recovery’ and ‘continuing care’. Medical input was reduced but there was a reluctance or refusal to accept that some of these patients would not be discharged. The use of specific language enabled the doctors involved in planning the use of these spaces to initiate a process of transforming them, while continuing to insist that such spaces were for transition and recovery.
For some patients, the nature of their offences may mean that they can never be released, even though this is not explicitly acknowledged. With regard to provision for permanent residents, most doctors had some knowledge of the system operating in the Netherlands and their views on this influenced the way in which they approached service change. The quotation below, from a doctor who was involved in thinking about new services at the time of the interview, illustrates this. This doctor was concerned that any long-stay service would not allow patients to move back into treatment, even though – as described in the previous chapter – the Dutch system allows this.
For the people who are not going to get to the community . . . I went over to Holland to look at their long-stay process, what I couldn’t really understand from them . . . How do you get back out of that? So we didn’t want to have a model whereby people were put into that. We wanted a model where, yes, you’re being managed long stay but any stage if they wanted to engage with the sort of normal process . . . it’s there, there’s no barrier at all . . . you’re not going to put someone through say the illness awareness group for the third time. They’re not going to just keep doing it, at one point you say, this person’s done this a couple of times, stop. No point having one-to-one psychology ad nauseam. So there will be a shift from [that to] long sort of chronic just quality of life stuff.
Psychiatrist ID15
When asked for their views on a system such as the service in the Netherlands, doctors provided a range of responses. One respondent suggested that ‘we learn from others, we actually pilot and develop a proof of concept model and just see what impact it actually has’, although, from a personal ethical perspective:
They would never say ‘I don’t think there’s any chance of you being discharged’ but would couch this in less threatening language such as ‘obviously you’ve been in hospital for x number of years, your discharge isn’t around the corner . . . maybe more opportunities for the kind of thing you’re interested in such as . . . whatever that is and that unit may be able to provide. Would they consider moving or having a period of time there just to see how it goes?’ I’d be more inclined to take that approach.
Psychiatrist ID1
Another was relatively supportive of such arrangements, suggesting that it would be better than existing provision with:
. . . people who are in units that are not designed for treatment-resistant individuals . . . and maintaining an absolutely hopeless degree of optimism . . . being required to repeat ad infinitum appropriate interventions which are destined in no way to be successful.
Psychiatrist ID2
Most, however, expressed caution about adopting a system based on that in the Netherlands. In addition to the perception that stopping treatment in that way amounted to ‘warehousing’ (psychiatrist ID3), the fear was expressed that labelling patients as ‘long stay’ would produce a particular ‘mindset’ (psychiatrist ID6) among the staff, with ‘a real risk of self-fulfilling prophecies’ (psychiatrist ID8). ‘I don’t really care what it’s called . . . I would be concerned about the mindset’ (psychiatrist ID6). The issue of ‘what it’s called’ appeared to be important to many doctors and, linked to this, clinicians’ responses suggested that many viewed such ‘warehousing’ as unethical.
To some extent, the process of putting plans into practice was a response to everyday problems and emergent issues. In one case, a facility was established to move patients from a high secure hospital who were unlikely to be released into the community but could be housed in a medium secure facility. In another example, a psychiatrist was aware of patients being placed hundreds of miles from home, which made it difficult and expensive for their ageing parents to visit. He described working with local commissioners and hospital staff, as well as allaying the fears of the local community, to develop a facility that would bring back patients located in various expensive placements far away from their families. This doctor and his team took the opportunity to visit other facilities in the planning stage to learn about and learn from what was happening elsewhere. In these cases, building a business case was important, as being able to provide services more cheaply was attractive to commissioners. In other cases, existing patients were relocated within the existing facility to create a stable long-stay environment in response to patients’ needs. It was also necessary to negotiate with and gain agreement from commissioners that these wards would be exempt from LoS targets in recognition of the nature of the patient population.
Even among doctors who conceptualised ‘long-term’ patients as a distinct group requiring a different approach from that for other patients, some reported barriers to change from external stakeholders. Despite the removal of the treatability test, various stakeholders did not view the cessation of active treatment as legitimate.
I think it depends where things go with level of care planning intervention, etc., with CQC [Care Quality Commission] expecting patients to have full therapeutic programmes which may not be appropriate for certain long-stay patients . . . sometimes their solicitors, the tribunal expect you to be doing just as intensive work with somebody who’s been in for 15 years as has been in for 1 year. And I think A – that’s unneeded and B – it’s not realistic. So I think there probably needs to be a mindset change there.
Psychiatrist ID12
Discussion
In terms of the problems characterising long-term secure forensic care, some of these can be understood as arising from the competing objectives of services as outlined above. On one level the received wisdom is that patients must be helped to recover. Yet experience suggests to staff that there are some patients for whom this will never be possible, at least in the sense of recovery being synonymous with cure and discharge. Some clinicians acknowledged that the needs of the two groups of patients (those who move through the system and those who do not) were different, but felt unable to state openly the implications for some patients. The accounts reflected conflict and ambiguity, with some clinicians describing the need to maintain hope and not accept that people will not move on, but seconds later outlining how patients who will never move on were managed within the system. A need to maintain hope is understandable in a context characterised by feelings of burnout and fatigue,158 as well as one in which professional identity is heavily bound up with treatment and ‘recovery’.
In addition to the conflicts created by the competing aims of the service, participants described incentive structures that often hampered their ability to deliver services in a way that best met the needs of the patients. Incentives were described as delaying discharges and stifling innovation. At the same time, some participants described service changes that were being initiated to provide care for ‘long-stay’ patients. The euphemisms for long or permanent stay appeared, in some cases, to be an attempt to disguise the potentially permanent nature of these facilities to make them more palatable to patients, but they also appeared to relate to an unwillingness on the part of staff to accept the implications of such facilities. In some cases, provider staff had worked with commissioners to navigate incentive structures in order to achieve this.
Participants also described a complex landscape in which a wide range of stakeholders participated. As part of this context, the history of policy in this area appeared to be influential in a number of ways. History also had implications for psychiatric practice, with different generations of forensic psychiatrists described as taking different approaches to clinical practice. Linked to this, the cultural context is one in which, for example, views regarding sexual relationships are less liberal in the UK than in the Netherlands. 156 This suggests that the development and implementation of a strategy for the management of long-stay forensic psychiatric patients must take into account the broader historical, social and cultural context in which the services are located. We return to this issue in Chapter 12.
In terms of possible strategies to address the issues we identified, there is an acceptance among most clinicians of the need to manage ‘long-stay’ patients differently, and the service changes we identified reflect this. However, these changes also make clinicians uncomfortable. It is also important to note that the changes emerged in a ‘bottom-up’ manner, which meant that they were not perceived as a threatening ‘top-down’ directive. In addition to tackling issues such as incentive structures, therefore, it is important to consider ‘softer’ factors such as professional identity and organisational culture. The development and implementation of a strategy for the management of long-stay forensic psychiatric patients needs to take these into account to avoid alienating clinicians.
Chapter 10 Survey of professionals
Method
This part of the project was originally planned as a Delphi exercise to ascertain consensus among a group of professionals regarding the need for a long-stay forensic psychiatric service in the UK and what such a service might look like. However, owing to a low response rate in the second round of the exercise, we were able to fully complete only one round. Because of this, we took the decision to present this work as a one-off professionals’ survey on the same topic. However, it is of note that the survey engaged senior commissioners and leaders in the field of forensic psychiatry. As such we felt that it was justified to present the findings here briefly, despite the lack of the consensus-forming step.
We developed the survey on elements of a long-stay service, based on characteristics of international service models of long-stay in forensic psychiatry, to assess whether or not these features could be applicable to the UK. The survey contained 53 statements across six sections; for each of these we asked participants to select their level of agreement. This survey was uploaded to SurveyMonkey® (Palo Alto, CA, USA) and the link was e-mailed to senior clinicians and managers from a number of high and medium secure services, as well to as a group of commissioners. We collated the responses received and report the findings below.
Participants
Sixty-three professionals were invited to take part in this survey, of whom 20 responded. Eighteen completed the full survey. Seventy-one per cent were male and 29% were female, with the majority (55%) aged between 41 and 50 years, 25% aged between 31 and 40 years and 20% aged between 51 and 60 years. Forty-eight per cent currently worked in a clinical setting, 29% worked in management, 14% worked in commissioning (including specialised commissioning) and 10% worked across both clinical and management roles. The majority of respondents (57%) worked in medium secure NHS units, while 10% worked in private medium secure units and 10% worked in high secure units. Other work settings included specialised commissioning, working across both medium and low security and working across all security levels. Years of experience working in forensic settings ranged from 7–32 years, with an average of 15 years.
Findings
The findings are shown in Table 31. The majority of participants agreed that there is a need for a separate secure long-stay service in forensic psychiatry, with 70% agreeing that the primary aim of this service should be to provide optimum quality of life as opposed to reducing risk. The majority also agreed that a key purpose of this service should be to provide a secure and stable living environment, with care rather than cure as the treatment philosophy. Suggestions for names of such a service included enhanced recovery, extended care, continuing care, forensic recovery service, ongoing treatment and slower-stream rehabilitation.
| Question | 1 (strongly disagree) | 2 | 3 | 4 | 5 (strongly agree) |
|---|---|---|---|---|---|
| Section A: purposes and aims of a long-stay service | |||||
| There is a need for a separate secure ‘long-stay’ service in forensic psychiatry | 5% | 15% | 15% | 45% | 20% |
| The primary aim for this service should be providing an optimum quality of life for patients as opposed to reducing risk | 0% | 20% | 10% | 45% | 25% |
| A key purpose of this service should be to provide a secure and stable living environment for those patients deemed to need long-term care | 0% | 0% | 10% | 55% | 35% |
| Care rather than cure should be the treatment approach/philosophy | 10% | 5% | 20% | 35% | 30% |
| This service should not be primarily aimed at reducing risk | 10% | 35% | 15% | 20% | 20% |
| This service should aim to give patients more autonomy than current secure services not designed for ‘long-stay’ | 15% | 10% | 20% | 45% | 10% |
| Section B: type of patient | |||||
| Patients should be considered for this service based on their LoS in continuous secure care | 25% | 35% | 15% | 20% | 5% |
| Patients who are deemed to need long-term care should be cared for in separate environments depending on their needs and presentation (i.e. separate ‘long-stay’ services would be needed for different subgroups within the ‘long-stay’ population) | 11% | 11% | 22% | 50% | 6% |
| Patients should be admitted to a ‘long-stay’ service on a voluntary basis only (i.e. they must agree to being admitted) | 38% | 31% | 25% | 0% | 6% |
| Patients must be willing and able to live socially with others in a community environment | 17% | 44% | 22% | 11% | 6% |
| Section C: characteristics of a long-stay service | |||||
| The ‘long-stay’ setting is understood to be the patients’ home for the foreseeable future and staff should understand and appreciate this | 0% | 22% | 11% | 44% | 22% |
| This service should be run according to the principles of a therapeutic community | 22% | 44% | 11% | 22% | 0% |
| This service will require less medical input than current secure services not designed for ‘long stay’ (i.e. a reduced number of psychiatrists) | 17% | 11% | 17% | 44% | 11% |
| This service will require less psychological input than current secure services not designed for ‘long stay’ (i.e. a reduced number of psychologists) | 6% | 33% | 22% | 33% | 6% |
| This service should have a higher number of occupational therapy staff and activity coordinators than current secure services not designed for ‘long stay’ | 0% | 6% | 17% | 44% | 33% |
| The importance of physical health should be emphasised and additional services made available due to the age of this population | 0% | 6% | 11% | 28% | 56% |
| This service should have a high secure perimeter but less internal physical and procedural security than current high/medium secure settings | 33% | 22% | 11% | 28% | 6% |
| Relational security should be emphasised and utilised more in a ‘long-stay’ service than in current high/medium secure settings | 17% | 33% | 22% | 22% | 6% |
| Policies and procedures should be more flexible in a service designed for long-term care than in current high/medium secure settings | 17% | 28% | 17% | 33% | 6% |
| This service should be exempt from routine measurements (e.g. HoNOS and HCR-20) | 22% | 39% | 17% | 11% | 11% |
| Section D: interventions | |||||
| This service should have less focus on formal psychological interventions than in current secure services not designed for ‘long stay’ | 6% | 17% | 28% | 50% | 0% |
| Occupational and vocational activities should be prioritised and made available for the majority of the day, more so than what is currently provided in secure services not designed for ‘long stay’ | 0% | 11% | 17% | 50% | 22% |
| Patients should not have to take part in risk reducing interventions | 44% | 28% | 17% | 11% | 0% |
| Staff should receive training on how to support patients in regaining their autonomy and this should be prioritised | 0% | 11% | 6% | 56% | 28% |
| Section E: challenges in setting up a long-stay service | |||||
| Commissioners may not want to support the development of ‘long-stay’ services | 0% | 28% | 22% | 33% | 17% |
| Staff may not want to work in a ‘long-stay’ service | 6% | 44% | 6% | 39% | 6% |
| Patients may not want to be transferred to a ‘long-stay’ service | 0% | 6% | 44% | 28% | 22% |
| Clinicians/service managers may not want to send patients to a ‘long-stay’ service | 17% | 33% | 11% | 22% | 17% |
| There may be reluctance from the government to support the development of ‘long-stay’ services | 0% | 28% | 28% | 33% | 11% |
| Public opinion may not be supportive of the development of ‘long-stay’ services | 17% | 44% | 33% | 6% | 0% |
| Section F: do you think a long-stay service will be . . . | 1 (much less expensive) | 2 (less) | 3 (the same cost) | 4 (more) | 5 (much more expensive) |
| 0% | 56% | 33% | 11% | 0% | |
| This service should be run under the remit of | |||||
| The Department of Health | 75% | ||||
| The Criminal Justice System | 25% | ||||
Responses were mixed regarding whether patients should be considered for this service based solely on their continuous LoS in secure care and participants did not believe that admission should be on an entirely voluntary basis. Nearly two-thirds believed the cut-off point for this service should be 5 years in secure care, with 75% agreeing that different cut-off points would be needed for those in high and medium security (those in high security needing a higher cut-off point). It was widely recognised that there are subgroups of long-stay patients requiring separate services, including sexual offenders, those with PDs, chronically psychotic/treatment-resistant patients, those with intellectual disabilities, and men and women.
The majority agreed the service should be seen as the patients’ home for the foreseeable future but did not think that it should be run according to the principles of a therapeutic community. Most agreed that this would require a reduced number of psychiatrists and an increased number of occupational therapists, but were split on whether or not the number of psychologists should also be reduced. The overwhelming majority agreed that there should be an increased focus on physical health care for this patient group. Responses regarding the type of security measures required were mixed, but most agreed that policies and procedures should be more flexible than those in current high and medium secure settings. Despite recognising the uniqueness of such a service, participants were uneasy with the idea of exempting it from routine measurements such as risk assessments.
Half of those who responded agreed that there should be less of a focus on formal psychological interventions, with nearly three-quarters agreeing that occupational and vocational activities should instead be prioritised for this patient group. Most disagreed with the idea that patients should not have to take part in risk reducing interventions. Over three-quarters agreed that it was important for staff to receive specialist training on how to work with this patient group and support patients in regaining their autonomy.
Responses were mixed regarding whether patients and different groups of professionals would support the development of such a service, but most agreed that the general public would be supportive. Most predicted that commissioners and the government would be concerned about costs and that patients and staff would be concerned about feelings of hopelessness. Over half of participants predicted that a long-stay service would cost less than current high and medium secure services and the overwhelming majority (94%) thought it should be run under the remit of the Department of Health (rather than Criminal Justice).
Other comments from the survey included:
There should not be an assumption that this patient group cannot progress with treatment, just that they may take longer to get there.
If the aim is care and not cure or treatment, then why do they sit within a forensic service and not a locked service outside of specialised commissioning?
Although reducing risk is not a primary aim it still needs to be a secondary aim of high importance.
The needs of this population are different and it is difficult to generalise answers. While ensuring quality of life is improved for this group, treatment should always be key regardless of degree and expectations, particularly as they are detained under the MHA.
Not a matter of ‘less’ psychological interventions, but more appropriate. Occupational and vocational activities should be tailored to patient need and ability.
There needs to be honest discussions with commissioners and politicians that, for some patients, their recovery will be relative and limited compared to others and for these people managing risk to others and quality of life is imperative. The views of patients and carers should be part of the discussion.
A long-stay environment is essentially a sound and desirable goal for certain individuals and these would need to be agreed with strict criteria. The concept needs thorough design and planning, taking into consideration the different needs of the client group as they will not fit neatly into a ‘box’.
Discussion
Our findings are limited by the small number of respondents and the lack of a formal consensus-building step. We therefore cannot rule out the possibility that the views presented here are ‘lone voices’ advocating a change in the current system of care for this group of patients. However, given the seniority of our respondents and the similarity of some of their views to those expressed in the in-depth interviews in Chapter 9, we feel that the opinions presented here are of relevance in informing the debate.
On the whole, the results of this survey show that professionals support the concept of a separate long-stay service within forensic psychiatry that focuses primarily on quality of life and increased autonomy in a settled and stable living environment with less formal treatment pressures, similar to that which is provided in both Dutch and German long-stay facilities. 73,152
Physical health, occupational activities and overall well-being should be prioritised for this patient group, and staff should be specially trained to support patient autonomy in a minimally restrictive environment that is likely to be the patient’s ‘home’ for the foreseeable future. 152 There are important areas of mixed responses from professionals, particularly regarding security measures and risk reduction, which were echoed in the stakeholder perspectives discussed in Chapter 9. There is no doubt that the safety of patients, staff and the public should still be of utmost importance; however, what is necessary and sufficient to achieve and monitor this seems more controversial.
Chapter 11 Service user reference group
This chapter describes the process of setting up, as well as the input of, the SURG for this study. In addition, it contains a brief summary of an additional study suggested by the SURG and not part of the original proposal exploring the perspectives of carers of those in long-term forensic care.
The service user reference group
Guidance from the funding body, empirical evidence159 and prior experience among members of the research team had reinforced the conviction that it would be beneficial to form an advisory group of service users and carers to help to shape the work. As a result, a SURG was formed; it met on 10 occasions throughout the research process and exerted a significant influence on the activities of the research team. The principal investigator and other members of the research team attended all SURG meetings, and SURG members also contributed to the research process in other ways.
Recruiting service user reference group members
The aim was to form a group that met the following criteria.
-
The group should be diverse within the frame of the research topic. We recruited people who had been forensic patients in the past, who were currently detained in a secure mental health setting, who cared for a family member using such services and who had prison experience.
-
Group members should be able to contribute in a group situation alongside academics. As it turned out, some members were highly educated and had prior experience of research, while others principally brought the voice of experience from their personal lives, and this helped researchers to see ‘the people behind the data’.
-
Group members needed the ability to broadly stay on task and help the researchers to focus their efforts to the best effect. This demanded the ability to challenge constructively and move on when necessary.
We recognise that the composition of the SURG as proposed here missed out the perspective of the ‘general population’; however, we felt that, on balance, ‘giving a voice’ to those marginalised patients in forensic settings was a priority for this study.
The patient and public involvement (PPI) lead (Peter Bates) contacted 100 organisations, including commissioners, providers, third sector, advocacy and involvement organisations drawn from a wider database of community groups. In addition, an advert was placed in a regular PPI bulletin that was circulated to 750 interested people in the region. Within the forensic community, consultant psychiatrists were invited to suggest names of patients they knew who might be interested in joining the group. Those who came forward were invited to an informal one-to-one meeting, which provided them with an opportunity to ask questions, discuss the research and talk about their personal experience. One participant expressed their commitment thus: ‘if we can make it work here, we can do it anywhere’.
Getting people together
Special consideration was given to enabling people using secure services to participate in the SURG, given the range of personal circumstances of the individuals concerned.
One person living in a secure setting wanted to participate while remaining anonymous. To comply with this request, one of the researchers took the agenda to the patient before each SURG meeting, and discussed the upcoming issues. The researcher then represented the patient’s views at the SURG meeting as best they could. Another detained patient in a secure setting was able to take part in the meetings via video link, although this took 6 months to organise. The video suite had to be booked, an escort was arranged and approval was obtained from the patient’s clinical team. It is to the individual’s credit that he repeatedly reminded staff about the meetings, encouraged them to check that arrangements were in place and was not discouraged by the lengthy preparations required. In future we aim to plan for these delays to ensure that everyone can start at the same time. At least one member of the group was unfamiliar with teleconferencing, and so had to get used to being on screen, especially in the room that was equipped with a voice-tracking zoom camera, and to the speaking protocols required.
Two members who attended the meetings in person were escorted by a member of their care team. This worked particularly well when the same member of staff regularly attended and was also able to contribute, although continuity was not always possible. The staff members’ perspectives were at times different from those of the SURG members, but this added to the debate rather than detracting from it. One member frequently asked his support staff member to sit in the background so that they would be discouraged from intervening in the meetings. There was also one carer in the group, the presence of whom added another dimension to the conversations. Two prospective members had permission from their care team to take unescorted leave and so bus, train and taxi travel arrangements were made, but the remote, rural location of their units made their participation impractical. The turnover of membership was probably higher in this SURG group than in other advisory groups, as people moved around the care system, adjusted to community life after institutional care and built a meaningful life for themselves, which sometimes meant that they favoured regular commitments over the very sporadic meetings of the SURG. Other members attended consistently in addition to contributing in other ways, as described further later in this chapter.
How the meetings were run
In consequence, the group was pleased with their attendance record. Service users attended the SURG meetings and their nominated representatives also attended the PMG and the SSC. Ten of the 12 project management meetings achieved PPI representation, 9 of the 10 SURG meetings planned at the outset took place, and all of the SSC meetings had service user representation. The average attendance at the SURG meetings was three or four service users plus the PPI lead. As one member declared, ‘I felt quite isolated when the project started, but not so towards the end’.
Prior to the forming of the SURG, one or two group members had some anxieties about the group, for example whether or not their views would be taken seriously and whether or not the research team was genuine about PPI. The facilitator wondered if reasonable adjustments needed to be made for service users regarding issues of trust or working with authority, and whether such issues might interfere with the running of the group. There were also considerable power differentials between SURG members on the one hand and the research team on the other, particularly as the principal investigator is also a forensic psychiatrist. 160 It was also possible that people would be inhibited as a result of how they felt about being associated with this sector. Both of these concerns turned out to be unfounded.
In the light of best practice advice,161 participation payments were offered to SURG members. Our assumption that this would motivate group members in straitened financial circumstances turned out to be unfounded, confirming experience elsewhere that many people are motivated to become involved in health research by altruism rather than by profit. 162,163 Additional negotiations were needed for people living in secure settings, to ensure that payments could be offered and accepted within those environments where patients do not always have access to money.
Chairing service user reference group meetings
During the 3-year life of the SURG three people took the chair, two of whom were service users. This new approach involved a part-time paid role being formed, the position being advertised, recruitment interviews being carried out by service users, and the postholder being employed for 4 hours per week to be worked flexibly, thus creating a model that could form a step-up opportunity for people wishing to return to employment. The role involved the following responsibilities.
-
Ensure that agendas and minutes are prepared and sent out in good time.
-
Chair SURG meetings.
-
Market SURG and recruit new members as necessary.
-
Stay in touch and offer low-level pastoral support to members.
-
Attend the PMG and other meetings to represent and report on SURG.
This was not entirely successful, for a variety of reasons. Such new ventures engage with a number of sensitive issues that emerge in the uncertain ground that lies between full-time and sessional work, tailored roles and equal opportunities, volunteering and paid work, competence and flexibility, and independence and accountability.
The chairperson was supported by the principal investigator, who regularly attended group meetings, listened carefully to views and provided a full report about the progress made by the research team. Indeed, one member remarked that the openness of the principal investigator was a refreshing contrast to the aloofness of some members of the care team they had previously encountered, and this contributed to the success of the SURG. An administrator also attended and took minutes, freeing up the chairperson to focus on the discussion and dynamics.
Over time, the SURG gradually shifted away from ‘student mode’, in which group members expected to listen to a detailed presentation from the researchers, to ‘inquiry mode’, in which the majority of the meeting was spent discussing issues and sharing experiences. There was a perceptible growth in the researchers’ ability to distil the complex issues that they faced into a clear question that could be briefly introduced, that connected with the lived experience of SURG members and that released their perspectives to shed light on the research. One researcher commented that the SURG had ‘really helped me to understand people’s experience – and the impact on carers was a huge eye-opener’.
The group met more frequently and with shorter agendas at the start of the project so that relationships could be established, and it helped to use a meeting space that was unoccupied before and after the meeting, so that people could arrive early or stay to chat. Informality and warmth characterised the tone of the meetings, so that people could disclose aspects of their story and chat informally over coffee or lunch. This was especially important for people who travelled long distances to attend the meetings or had few opportunities for interaction at other times.
Impact on the research
The SURG contributed to the research in a variety of ways, not all of which led to explicit, discernible changes. Indeed, it would be rather patronising to conduct an obsessive search for signs of the impact of the SURG when the work of the other external advisors is not similarly dissected. Nevertheless, there are a number of topics that can be safely reported.
Early discussions reviewed both the data collection pro forma used for collecting data drawn from file reviews and the topic guide that directed the interviews. In respect of the pro forma, SURG members felt that the focus on offending history, diagnosis and treatment neglected the contribution of quality of life issues such as meaningful daytime activities, continuing education, family contact and the quality of staff–patient relationships. This debate immediately highlighted the difficulties of capturing and coding such lifestyle issues, and raised their profile for the patient interviews that followed the desk review of casefiles.
Advice from the SURG also helped in preparing for the interviews; SURG members advised on the use of language, the phrasing of questions, and arrangements for the provision of support to interviewees. The SURG reminded researchers of the importance of collective views about the tribunal process, and helped to settle on language that was sensitive to the forensic patient population.
A recurring theme was the rationale for patient transfers between wards within secure facilities and between units. While the research team struggled to create a meaningful typology of the myriad of explicit and implicit therapeutic regimes, SURG members similarly wrestled with the sense of irrationality that often accompanies these unsettling moves: the feeling that people are moving around rather than moving forward. SURG members also talked about treatment dilemmas: programmes that were compulsory but not always relevant to the individual, the way in which some patients saw treatment compliance as an admission of guilt, the lack of an evidence base for treatments and the inuring effect of repeated exposure to unwanted therapy. When the researcher reported that some patients were reluctant to talk about the past or the future, SURG members helped with possible explanations of the cognitive or emotional processes that led to a focus on living day to day. These conversations shed light on the circumstances of long-stay patients, helped to prepare researchers for the interviews they were to undertake and changed the content of the interview topic guide. The SURG also recommended that interviewees be provided with information about the local advocacy service, in case the interview brought up issues that needed to be addressed.
Some very useful suggestions were made regarding the strategy for recruiting research participants. At the outset, the plan was to approach patients via the responsible clinician, but SURG members suggested that the named nurse would be a more appropriate person to provide information and encourage people to take part, and so it proved. SURG members felt validated when their advice was taken up and found to be effective.
At the outset, the research team had envisaged patient interviews being conducted by a researcher working alongside a SURG member. This was contentious, and the final decision to abandon this plan was influenced by the following issues:
-
All of the detained members of SURG were opposed to the plan. First, their experience of two-to-one interviews was in the context of managing dangerous incidents and so they felt that this could be intimidating. Second, they felt that patients would be unlikely to trust non-professionals with highly confidential information that could ruin their chances of a new start in the community. Third, there was a worry that SURG members may be unduly influenced by their own experiences, rather than fully attending to the experience of the patient.
-
One member of the academic team was opposed to the plan. Although one SURG member asserted that lived experience meant that ‘basically we will ask appropriate questions in an appropriate way’, the academic held the view that interview skills of creating rapport, detachment and critical self-awareness take many years to hone and the qualitative research process is much more sophisticated than ‘having a chat’. One of the SURG members had worked as a researcher prior to using forensic mental health services, but this did not resolve the conflict within the group.
-
Security issues on some sites meant that service user researchers might not have been granted access, especially those who had criminal convictions. One member wondered if these barriers to access were erected by prejudice rather than a result of a fair risk assessment.
This debate was vigorous and challenging to the SURG, and it is to their credit that they drew the debate to a conclusion, helped the overall research team to decide a way forward and accepted the outcome with equanimity, despite the fact that, for some, it contradicted their personal ambitions and established best practice within some parts of the research community. The outcome remained a cause of dissension throughout the project.
When a researcher was recruited to carry out these patient interviews, the SURG ensured that lived experience of mental health issues appeared as a desirable characteristic on the person specification, that the advertisement was circulated to patient groups and that a member of the SURG sat on the recruitment and appointment panel.
The SURG members helped to select the questions to ask of the vast quantitative data set, and to identify the themes and categories that were developed and validated in respect of the interview transcripts.
At the outset, the research proposal had neglected the perspective of family carers, and early in the life of the SURG this omission was raised by the carer in the group. As a result, a master’s student was engaged to complete a small study on this theme, although ultimately this student did not complete their thesis, and the focus groups were completed by the research team and a member of the SURG, as described in more detail in the second part of this chapter (see Carers study). The SURG highlighted that staff–carer relationships are not always warm; this is perhaps because staff need to be present while patients see their relatives, but because they feel that they are intruding they tend to withdraw to the side of the room, disengage from conversation and try to behave as if they are not there.
Finally, service users commented on a number of draft documents and helped to produce a lay summary of the findings of the research to provide feedback to the participants and general public.
Governance
The research study held itself accountable to a variety of stakeholders. First, an early presentation was given to the Patients’ Council at the nearest high-security hospital to establish a working relationship and win support. Second, an independent service user champion who has been recognised for his contribution to the improvement of secure care was appointed by the funding body to sit on the Study Steering Group. This helpfully connected the SURG with wider national and international programmes and service improvement initiatives that take a patient perspective. Third, the various meetings (SSC, PMG and SURG) were interlocked by overlapping the membership and running them all on the same day, with the SURG meeting happening first. This had both a practical and a symbolic value. In practical terms, it meant that a member of the SURG could simply stay on and attend the PMG that followed their own meeting, while members of the research team arrived early to contribute to the SURG. Presentations were adjusted for each audience, but the planning and preparation were streamlined. In symbolic terms, the SURG was seen to have an equal value and, indeed, started the day rather than being tagged on at the end.
‘Extracurricular’ activities
Quite independently of their SURG membership, members were involved in a significant array of activities beyond the research itself, which gave them a broader insight. These networks extended to national charities and professional bodies across Europe and to other policy and research initiatives. As the findings from the research become clear, SURG members will also harness these networks to support dissemination. Each SURG meeting included presentations about progress and often included discussion of research methods. In addition, two training events took place, one introducing SPSS software for the analysis of quantitative data and the other introducing NVivo, used to analyse interview transcripts. The SPSS training included one-to-one training with the SURG member. The training materials developed for these sessions are being reused with students. Participation in the SURG also enabled members to engage with a number of other activities, including co-authoring publications, conference attendances, presentations and a scientific mission, funded through a European project (COST action of forensic psychiatry), whereby the member of the SSC went to visit Dutch long-stay services. His experiences have been published on the Mind website (www.mind.org.uk).
Learning from the project
Four particular issues arose during the work of the SURG, which may have broader application in PPI work. First is the impact of participation on the individuals concerned. The SURG often talked about the irrationalities of the current system in which there is no obvious care pathway, unproven treatments are applied, and people spend many years undertaking activities that carry no value or meaning to them. Exposing these issues in conversation with the very people who are subject to such processes can cause frustration and distress, and it was a credit to SURG members that they were explored with honesty and resilience, and to researchers that they discussed such matters candidly.
Second, courageous conversations took place about the future. Patients must face the harsh realities of life, such as their lack of power compared with that of the clinical team and the tribunals, while holding on to hope about their stay. As one person put it, ‘it’s not until you fully recount these daily events that you realise how depressing, boring and inactive we really are. I found this quite upsetting’. This conversation was mirrored by discussions with staff about the effectiveness of their interventions, balancing the recognition of treatment resistance with clinical hope. One way to reduce the tension is to shrink aspirations until it is hard to imagine an alternative way of doing things, and yet one task of the SURG was to explore these very alternatives. For example, we found that patients in the Netherlands are able to make a home within a secure service, and recover a degree of control in a way that English patients are unlikely to think possible, meaning that they would be unlikely to spontaneously ask for this option in the service.
Third, the SURG touched on the variety of approaches to consent that play out in secure settings. In treatment reviews, the service has a duty of care to review everyone that is receiving a service at public expense – whether or not the person agrees to the process – while research ethics uphold the right of the patient to withdraw their participation. Again, research ethics demand sophisticated processes to ensure anonymity, while commissioners ask for extensive details of what is being purchased for each named individual without asking the patient’s permission for that information to be disclosed. Such differences may appear rational to an academic who has been schooled in these fine details, but to lay people and many patients it is hard to understand the reasons that some decisions are made by the patient and others are made by staff. Sometimes the community members of the SURG were more alert to these issues of power and control than the detained patients, who had adopted a laissez-faire survival strategy on this matter.
Fourth, although data were fully anonymised before they were sent from the treatment facility to the research team, there were some concerns that small sample sizes in the long-stay community could inadvertently lead to identity reattribution by patients or staff, and so SURG members were asked to sign a confidentiality commitment.
Conclusion
This report shows that the research has been sharpened through the contribution of the SURG. Researchers reported real value in the free-ranging discussions and the insights they gained from their participation in the group. As might be expected from other studies,164 SURG members reported that benefits arose from their participation. One member delighted in returning to an academic environment, while another found the simple experience of being believed and having others validate her own experience to be deeply significant.
Early experiments with appointing a service user to the paid role of chair for the SURG have improved our understanding of how this role might work in the future. The researchers’ commitment to supporting the SURG and making the most of the opportunity to glean views and experiences from group members paid dividends. Finally, and perhaps most significantly, the SURG demonstrated that security arrangements in forensic services are no barrier to meaningful involvement in research, as long as sufficient preparations and adjustments are made.
Several issues remain that may not be amenable to tidy answers. These include the challenges of critically discussing services with people who are currently immersed in them, negotiating consent with people who live in a tightly controlled environment and managing confidentiality in small communities. Our work has brought some of these issues to focus, but the task of resolving them must fall to others.
Carers study
Experiences of forensic carers: focus groups on support, involvement with care, and perspectives of the needs of long-stay patients in secure forensic hospital care
The SURG highlighted the need to hear the carer perspective on care provided to long-stay patients, which was absent from the original project proposal. The aims of the carer study were to understand carers’ experiences of long-stay patients in secure hospital care, to gauge their level of satisfaction and involvement with care, areas of possible improvement and their understanding of reasons for long stay, and to establish what services are available to support them. We provide here a short summary of the findings; a longer version will be published and is available from the authors on request.
A total of 18 carers were included, and 16 carers participated in the three focus groups: eight in the high secure group, four in a NHS medium secure setting and four in an independent medium to low secure setting. Although our line of enquiry for the main study was focused on high and medium care settings, we included one mixed (medium and low) setting on the assumption that carers of patients in this setting would have relevant experiences, given that the majority of patients in secure settings have had experiences of a number of institutions. In addition, we felt that it is the (perceived) long time an individual is detained rather than the specific type of setting that will be most pertinent to carers’ experiences. Two carers of relatives in high secure care provided written responses. A total of seven men and 11 women participated; 15 carers identified themselves as relatives and three identified themselves as befrienders (one of whom was a former employee of one of the hospitals) to predominantly male patients and one female patient currently or previously receiving secure inpatient forensic care. The range of LoS of patients, as identified by carers, was between 1 and 6 years. The question arises as to whether or not befrienders should be seen as carers.
Data analysis was conducted following a semantic approach to thematic analysis to identify common themes. Data were analysed both deductively, via the use of coding determined by the themes explored in the focus group questionnaire, and inductively (with themes that additionally emerged from focus group content). Coding was undertaken using NVivo qualitative data analysis software. The following themes emerged.
Satisfaction with and involvement in care
The majority described primarily negative experiences of patient care, their involvement therein and the support given to them as carers. Many carers described feeling ‘frustration and despair’, which appeared to lead to a lack of trust in staff and services. Lack of communication was another source of carer dissatisfaction.
Carers were frustrated with their lack of involvement and not feeling heard about patient care in an environment that sees professionals ‘come and go’:
He’s with that person for 6 months then they leave, then they coming again . . . and they start it over again, for about 5 years they’ve been doing this.
They considered themselves to be an important source of information, which, if tapped into, could enable more effective long-term recovery of their relative:
We have not felt involved or included in the care for our daughter, decisions have been made without our knowledge or consultation . . . Actually listening to the carers, parents, family, these are the people who know the patient more than any staff member, doctor or consultant will ever.
A number of carers felt like they had to ‘battle’ to be heard, particularly at Care Programme Approach meetings, which carers generally viewed as an unsupportive experience. Carers also stated that they were not given adequate information from services and, consequently, received most of their information from other carers. Some felt that confidentiality was sometimes used as an ‘excuse’ to not share information with carers: ‘I feel the hospital uses the issue of confidentiality as an excuse not to have to include you’.
A number of carers noted that they did not trust services.
I don’t have much trust in the service what’s been provided right the way through to be honest. I’m always questioning ‘is this true’, if the staff say something, is it true?
Carers raised particular concerns regarding physical health and disabilities. They felt that physical health was not taken seriously by staff in secure forensic environments, with concerns that increase in weight and decrease in overall physical health was occurring as a result of changes in medication, diet and routine, without the involvement of or communication to carers. Carers felt that patients with physical disabilities (such as blindness or deafness) were not given appropriate care, or even understanding, by care staff.
Befrienders did not describe the same frustration or despair; their relationship with patients was not regarded as an intimate or personal one, but one based on ‘mutual respect’, with confidentiality seemingly respected and more direct information given to them about what the patient’s future might look like.
Positive aspects and suggestions for improvement
More positive feedback was described with carers currently involved with low to medium secure services. Carers valued staff who they could see formed relationships with carers and patients early on, and who ‘see patients as people’, valuing their individual qualities and personalities, and involving carers in positive feedback. Other positive aspects involved being included as part of the patient’s daily routine in the hospital setting, and having the opportunity to see the living environment of their relative.
Improvement in communication between social workers, clinicians and care staff was considered integral to improving levels of support, as this would help to bring ‘trust’ back into the carer relationship. Peer support was considered a way forward, with one carer describing that it was important to feel part of a community.
Promoting structure was seen as important, but so was allowing ‘freedoms and responsibilities’ to improve quality of life. Carers thought that promoting a community spirit with the ‘outside world’, using education and practical skills (such as gardening or woodwork), should be encouraged, particularly in the restrictive forensic setting that creates an ‘unrealistic world’.
Carers felt that staff should receive more training in areas such as recovery, mental disorders, disabilities and complex needs, and in understanding the boundaries of their roles as custodians or caregivers.
Length of stay
Carers perceived reasons for LoS to be primarily service related, and these included mismanagement, paperwork, race, complex needs, finances and the complicated funding system. Some doubted that the hospital made enough effort to move patients on.
When you think about it our relatives are this hospital’s bread and butter so it’s in their interest to try and keep them here as long as possible and I think to a certain degree, that is what happens.
Perceptions of international long-stay services
With limited information on the Netherlands model provided to carers, opinions of a similar model in the UK were generally favourable, appreciating the trade-off of a longer stay over a highly restrictive environment. Some carers did express concerns about the potential consequences of a ‘long-term’ label or law, and whether such an approach would hinder rehabilitation, making it ‘even more difficult to get out’.
Chapter 12 Conclusions and implications for practice
The primary aims of this study were to establish the prevalence of long stays in high and medium secure settings in England, to describe the characteristics of long-stay patients and explore their experiences, and to engage with key stakeholders to identify their perspectives as well as the potential barriers in changing current provision for this patient group.
Key findings
Work package 1: survey of length of stay in high and medium secure care
-
It was found that 23.5% of those in high secure settings and 18.1% of those in medium secure settings in our sample were classed as ‘long-stay’ patients.
-
There was significant variation in the percentage of long-stay patients in medium secure units, from 0% to 50% overall.
-
In NHS units the proportion of long-stay patients was 16.3%, and in independent units the proportion was 22.3%, although this difference was not statistically significant.
-
Extrapolating long-stay figures from our included units to the whole of the high/medium secure patient population in England, we estimate that there were approximately 730 forensic long-stay patients in high or medium secure services in England, with just under one-quarter residing in high secure care, at the time of our study.
-
Significant predictors of long-stay status were older age, admission source (with more long-stay patients being admitted from high or medium secure settings and fewer being admitted from prison) and current MHA section (with more patients on hospital orders with restrictions in the long-stay group).
-
Gender and ethnicity did not predict long-stay status.
Work package 2: characteristics and needs of long-stay patients
The characteristics of long-stay patients currently residing in high and medium secure care did not differ significantly for many characteristics; the following findings are based on an aggregated analysis of both groups unless otherwise stated.
-
The mean LoS in continuous high/medium secure care was 14.5 years, with just under one-fifth (19.7%) of patients having been resident for > 20 years. Those resident in high secure care had longer LoS, although there was no difference between settings in the percentage of extreme long-stay patients (> 20 years).
-
Whereas only 22% entered the forensic system on a section 37/41, 60.3% were on this section on our survey date. 56.1% of patients were first admitted to medium/high secure care from prison, although only 19.7% came from prison to their current unit.
-
Long-stay patients had complex pathways, with only a minority experiencing no moves or only one move along the treatment pathway.
-
There was a significant amount of movement across the same level of security, with 19.8% of high secure long-stay patients having been admitted from another high secure setting and 50.9% of those currently residing in medium secure care having come from another medium secure setting.
-
The majority of patients (67.8%) had previous admissions to general psychiatric care and 46.4% had previous admissions to secure care.
-
Nearly two-thirds (63.8%) had a history of self-harm and 35.3% had a history of serious suicide attempts. There was a significant difference in the percentage of serious suicide attempt histories between high and medium secure care (46.1% vs. 31%).
-
The most common diagnosis was schizophrenia (58%) but 46.7% had a PD.
-
Physical comorbidity was high, with 71.7% having any physical disorder, 27.6% being diagnosed with diabetes and 37.3% being diagnosed with obesity; significantly more patients in high secure care were obese (52.6% vs. 31.1%).
-
The majority of patients were primarily violent offenders (57.6%), whereas 5.7% were primarily sexual offenders, but for 21.9% both offence types were present. A significant proportion had no offending history (7.2%) or no index offence (16.5%). About one-fifth (19.8%) had previous convictions for arson.
-
A high proportion (23.4%) of patients had a sexual index offence.
-
Over one-quarter (26.9%) of patients had convictions for violent or sexual offences within institutions, with higher figures for those in high secure care (41.4% vs. 21.1%).
-
Levels of recent incidents and seclusions were high: 25.7% had committed a serious assault on staff within the past 5 years, 11.6% had seriously self-harmed and 44.3% had been secluded.
-
HCR-20 scores showed an average total score of 27 (with higher scores in medium secure care: 27.3 vs. 25.5); according to the HCR-20, about one-third of patients were still improving.
-
Only about half (51.1%) of the patients currently received formal psychological input, and completion rates for offending work were low.
-
The majority of patients (82.4%) had some form of contact with their families by letter, telephone or visits.
-
About one-third of the long-stay patients (32.9%) had had unsuccessful referrals to less secure care in the past 5 years.
-
We identified five clusters of patients with different characteristics within the long-stay sample.
-
According to the views of their responsible clinicians, about one-third of patients in high secure care might be placed in too high a level of security; for medium secure care about one-quarter each were judged to be detained in too high or too low a level of security.
-
None of the current long-stay patients in high secure care was judged by their responsible clinician to be able to reside in the community in 5 years’ time; for medium secure patients this was the case for 11% of patients.
-
Of the high secure patients 60% and of the medium secure sample 32% were judged to be likely to require lifelong high or medium secure care.
-
Patient factors (e.g. psychopathology) were judged to be more important than political or service provision factors in impeding movement to less secure settings.
-
No meaningful model could be derived for predictors of need for lifelong forensic care.
Work package 3: patient perspectives
Thematic analysis highlighted that patient’ perceptions of reasons for long-stay (internal/external), outlook towards secure care (positive/negative), approach (active/passive) and readiness to move differed. Four categories of ‘long-stay’ stances emerged.
-
Patients mainly attributed their LoS to events prior to admission, in particular their index offence, although they also recognised that their behaviour in secure care contributed to their LoS. Some patients saw the reasons for long stay primarily in ‘the system’.
-
When describing how they felt about their current situation, some patients described how the admission and care received had helped them in their mental health, but others felt that their time in secure care had been pointless and ineffective.
-
Patients with a proactive outlook engaged in a number of activities in the hope that this would lead to them moving on, while others expressed frustrations with the activities on offer and the perceived repetition of the same interventions without a clear goal or progress being made.
-
Although most patients aimed to move on, some either felt settled and comfortable in their current setting, and so did not wish to move, or had simply given up on achieving any move to less secure care.
Overall, four categories of long-stay ‘stances’ emerged: dynamic acceptance, static acceptance, dynamic resistance and static resistance. The dynamic/static distinction describes the extent to which patients actively wished to leave secure care; the acceptance/resistance dimension illustrates the extent to which they believed that the secure system helped them to move forward.
Work package 4: service innovation
-
Tensions were identified in staff trying to balance the aims of risk management and recovery.
-
Psychiatrists were reluctant to accept the reality of long stays and had a predominantly medical model of secure care: admission, treatment, rehabilitation, cure.
-
Other countries have successfully developed specific long-stay services, focusing on quality of life and maximising patient autonomy rather than focusing on risk-reducing interventions.
-
Stakeholders interviewed were reluctant to explore such models for fear of ‘warehousing’.
-
Existing funding arrangements act as barriers to system change, although some local initiatives have been created to cater for this patient group.
Implications for health care
Our research has provided, for the first time, evidence from a national, multicentre study that there are substantial numbers of long-stay patients with complex characteristics and pathways whose needs are not currently met by services provided. This patient group requires significant resources. Using the figures supplied from Rutherford and Duggan12 (£275,000 per annum per patient for high secure care and £175,000 for medium secure care) and using our figures of 168 long-stay patients in high secure and an estimated 560 long-stay patients in medium secure care, the care of these patients costs approximately £46.2M for the former group and £98M for the latter group. These figures are to be interpreted with caution, as they have been approximated from previous reports and are not based on a detailed economic analysis. If each of the high secure patients was to move to a medium secure setting, £16.8M could be saved per annum. If each of the medium secure patients moved to a low secure setting (assuming a cost of £150,000 per patient per annum), £14M could be saved per annum. Changes to the care of these patients, involving potentially quicker throughput or step-down, could therefore lead to substantial savings as well as improvements in the patients’ quality of life.
The evidence from our detailed file review in WP2 suggests that interventions offered have not resulted in sufficient changes to allow these patients to move on, and the distinction between high and medium secure care does not appear to be fully applicable to this group. At the same time, we found that there are significant obstacles to achieving system change (see Barriers to service change) and that the Dutch model is not easily adapted to the situation in England. This is partly because of the different patient groups served – the characteristics of patients in our study suggest that they continue to require high staffing levels as well as a secure and highly structured environment, although not necessarily high or medium secure care – and partly because of the reluctance of professionals to fully accept and articulate the issue of long stays. Without a national strategy, the needs of this group may not be met; the evidence suggests that the consideration of the following would be helpful in such a strategy:
-
agree on cut-off points for different settings
-
identify ways to improve the efficiency of pathways for this group
-
take a whole-pathway approach
-
explore interventions designed to reduce LoS
-
support the introduction and evaluation of pilot services for long-stay patients in forensic care.
The range of views expressed by different stakeholders suggests that in developing a national strategy for long-stay forensic patients, wide consultations including patients and carers are required to capture different perspectives and concerns.
Key elements of long-stay services
Overall considerations
It is not envisaged that a new legal framework would be required to introduce services for long-stay patients. Such services can be provided within existing frameworks, with patients being detained under their existing MHA sections, although consideration might be given to a voluntary move to any pilot schemes initially following clear and transparent information about the nature of the service. Services are likely to be regional rather than local, given patient numbers, although they might be developed within existing units. Careful consideration needs to be given to terminology, given the strong emotional reactions that the term ‘long stay’ seems to evoke in a range of stakeholders. Services are likely to be cost-neutral overall.
Our original intention was to develop a business case for an alternative service model. We decided not to do this for a number of reasons. As new models of provision need to be located within the overall system of care, the consideration of new models would require the collection of data on where patients are located currently and the costs of this. We were unable to do this, as the information is ‘commercial in confidence’. Even when providers were willing to give some indication of costs, they were less willing for this to be used in a report that would be placed in the public domain. Furthermore, they were keen to distinguish between notional ‘savings’, which would accrue if a small number of patients were relocated closer to friends and families, and ‘cash releasing’ savings, which would be realised only if larger-scale changes occurred. Linked to this, in a dynamic system of care, service change would need to maintain stability in the system. This means that such changes would require modelling to estimate the likely impacts of moving people and redistributing resources. Such a large-scale modelling exercise was beyond the scope of the study. In addition to these data-related concerns, although our research highlighted important issues that should be considered when designing care, it did not point to a single, well-described and agreed-on alternative model. We therefore outline below key service characteristics for this patient group as inferred from our study.
Physical requirements and procedures
Given the estimated overall numbers of long-stay patients currently in high and medium secure settings, and their characteristics, consideration could be given to whether or not these patients ought to be accommodated in dedicated services. Given their characteristics, as well as the views of patients, clinicians, service providers and other professionals, it would appear that the security levels of approximately medium secure care would be required for such services; however, relational security is likely to be of more relevance than physical security, as only a small proportion of patients in high secure care required post and mail monitoring, which would not be available in medium secure settings. Given the high number of incidents identified in our study, seclusion facilities need to be provided so that patients can remain in their known environment with the same staff at times when they become unsettled rather than having to move to a different setting.
Clinicians and patients expressed views that suggest that services should provide a stable environment on small wards with an emphasis on offering a ‘homely’ environment. This includes the selection of patients with similar needs. Our participants pointed out the importance of making the environment distinct from a hospital ward, for example by allowing patients to take ownership of the ward environment and, in particular, their own space (e.g. through decoration, furniture making). Given the substantial obstacles to achieving such an environment within existing structures, serious consideration needs to be given to developing a specific ‘long-stay’ service specification to allow more flexibility than current medium secure care contracts.
Some participants have suggested an external review of patients’ care and pathways to be undertaken at regular intervals (e.g. every 5 years).
Staffing
Our findings suggest that low staff turnover and minimising changes in key professional relationships are of particular importance in providing a stable and therapeutic environment for this patient group. Overall staffing levels are expected to be similar to those in current medium secure units, albeit with some differences in staff mix. Given the ageing and mulitmorbid patient group, physical health-care provision and health education are of greater importance than in mainstream forensic care. Psychology input is likely to be slightly less overall, and the psychological expertise required will be clinical forensic psychology. Occupational therapy and activity co-ordinators will be required to lead on quality of life and meaningful activities, and some of these activities can be delivered by unqualified staff. Given the concerns of some professionals about working with this patient group, staff training should be provided to develop the appropriate workforce and staff selected who wish to specifically work with this group.
Interventions/treatment
The patient characteristics identified in our study indicate that a full range of general medical and psychiatric care needs to be provided, owing to physical health-care needs and the high number of patients taking multiple medications, clozapine or depot medication, all requiring expert monitoring of effect and adverse reactions. Psychological and other therapeutic input needs to be tailored to individual need, and avoid repetition and offering interventions simply for the reason of ‘doing something’. The focus of psychology work is likely to be on motivation/engagement, as well as on maintaining hope and preventing self-harm/suicide. Work on life stories, identity, meaning and purpose was also suggested as an important focus. Patients indicated that they wish to be supported in their wish to move on but, equally, not to be put under any pressure to do so. The overall focus should be on quality of life.
In addition to formal interventions, ward-based activities and the provision of meaningful activity, including (paid) work and activities in the community outside the hospital, need to be supported as called for by both patients and carers in our study. Contact with family should be actively encouraged and flexible arrangements put in place for such contact, including extended and unsupervised visits and visits from the patient to their families. Relationships with other patients should also be actively supported, and peer-support workers and a buddy system might be beneficial.
Patients appreciated being given maximal opportunities to exercise autonomy and agency, and should be involved – along with their carers if so wished – not only in their own care but in the running of the ward overall to prevent dependency and institutionalisation. Carers (or befrienders) highlighted that they wished to be given opportunities to participate in the lives of their loved ones (e.g. by taking part in ward events, meals).
Moving on
Most stakeholders we interviewed expressed particular concerns regarding the inefficiencies of current service provision in terms of disjointed funding arrangements and the assessment process for pathway progression. Funding arrangements considering full episodes (from community to community) rather than care spells in one unit, the standardisation of care across services and joint admission assessments might go some way to increasing efficiency in service delivery. It might also be beneficial to adopt maximum flexibility in supporting patients when they move (e.g. several visits to their new unit, ensuring an overlap in staffing).
Barriers to service change
In terms of the barriers to service change, it is clear that current structures for incentives are not well aligned with the goals of ensuring that patients are in the most appropriate place to meet their needs. In addition, the emphasis on ‘cure’ and recovery makes it difficult for clinicians to conceptualise alternative models of care that do not have recovery as an aim. The historical context is one in which the younger generation of forensic psychiatrists is described as taking approaches to clinical practice, which acted as a barrier to change. Linked to this, clinicians emphasise treatment and appear resistant to a withdrawal of treatment in some cases, even when this has been shown to be ineffective in particular patients. Clinicians also mentioned the need to maintain hope, which they saw as being difficult in models of care that were not aimed at cure. Furthermore, in an environment in which regulatory bodies such as the Care Quality Commission (among other stakeholders) expects patients to receive treatment, there may be little support and legitimacy for alternative models aimed at, for example, maintaining quality of life for patients who are treatment resistant.
The cultural context is linked to this. For example, views regarding sexual relationships are less liberal in the UK than in the Netherlands. 156 Obtaining agreement for any proposed changes in the management of long-stay forensic psychiatric patients might be hampered, therefore, by the broader historical, social and cultural context in which services are located.
Ethical considerations
Forensic psychiatric services pose considerable ethical issues owing to the dual purpose of detention for the patient’s mental health as well as for the protection of the public. 165 Unlike in other areas of medicine, patients are detained against their will, and engagement in treatment is a requisite to moving on and regaining autonomy. These issues are compounded when patients stay in such services for a long period of time, potentially longer than necessary, and this must be a considerable concern. In addition, patients may be detained for longer than they would have been had they committed a similar offence and received a prison sentence as a non-mentally disordered individual; indeed, they may be detained, potentially for life, without ever having committed an offence at all. It is not surprising, therefore, that some patients and carers express frustration and hopelessness given their situation, particularly as treatments in forensic psychiatry are of questionable efficacy, pathways seem confusing and hence the patients’ ultimate release seems beyond reach.
Some authors have pointed out that some aspects of UK mental health law may not be compatible with the United Nations’ Convention on the Rights of Persons with Disabilities, which calls for non-discrimination of individuals with disabilities, including mental disorders. 166 Longer periods of detention of those with mental disorders and detention in the absence of diminished responsibility are certainly issues that could be argued to breach the principle of non-discrimination of those with mental disorders, although this is yet to be tested in court. Notably, other countries have adopted laws and policies that do not allow the length of detention in psychiatric care to exceed the equivalent prison sentence, and most other European countries would not allow patients with no index offence or with full responsibility to be detained in a forensic psychiatric setting or to be treated against their will even if they have capacity to consent but do not.
Considering ethical issues more broadly, the following principles are generally accepted in medical ethics: autonomy, beneficence, non-maleficence and justice. 165 It seems clear from the situation that long-stay patients in forensic settings find themselves in that all of these principles are seriously challenged. From an ethical point of view, it is, therefore, paramount that the services provided can be truly said to benefit the patient and allow as much autonomy as possible. The state has a responsibility, when making provision for the detention of individuals for the protection of others, to balance this with maximising individuals’ quality of life and normalising their life situation as far as possible under the circumstances. However, it is difficult to see how this is currently being achieved, particularly in light of the serious restrictions imposed on patients, including in crucial areas of life such as (family) relationships.
Strengths and limitations of our study
Our study has a number of strengths. First, we have provided, for the first time, a national picture of long stays in forensic settings, including both NHS and independent provider units. Second, we considered whole pathways in high/medium secure care rather than just admission to single units. Third, we collated very detailed information on patient and pathway characteristics. Fourth, we included comprehensive accounts from patients themselves as well as those of a range of key stakeholders, thereby generating important information to inform future service developments. Finally, we were able to include information on services in other countries.
A number of limitations need to be noted. First, we did not include all available units but rather took a sample of units spread by geographical location and size. In doing so, we oversampled units catering for female patients and those for patients with intellectual disabilities. As such, we might have overestimated the prevalence of patients with these characteristics. Although we did this with good reason, there are drawbacks to this approach, namely that we cannot determine whether or not these patient groups are over-represented in long-stay patients compared with those not staying for extended periods of time.
Second, given the large number of patients resident in included units, we were only able to identify – and thus use in comparisons between long-stay and non-long-stay patients – some basic characteristics, easily available from medical records departments, for all patients. We collected detailed information from file reviews for those identified as long-stay patients only, although this is consistent with our protocol and the stated aims of this research. We identified some discrepancies between WP1 data and the information collated in the later file reviews. We decided to not correct this information in WP1 subsequently to avoid introducing systematic bias. It is also of note that there appeared to be different agreements as to which patients are recorded towards unit caseloads (e.g. how trial leave patients are recorded), although we had detailed discussions with each unit to ensure a consistent approach to recording. Our file reviews were conducted by local collaborators rather than by our own research staff; using the latter would potentially have resulted in more consistent data recording, although we introduced measures to maximise consistency (e.g. through training exercises and regular communication with data collectors).
Third, our study findings regarding patient perceptions were generated by an analysis of data from a purposive sample of long-stay patients drawn from the populations at two high and six medium secure units across England. Although our sample was purposively selected from within a larger epidemiologically based study of secure hospitals, we cannot exclude the possibility that subjects drawn from other sites would have provided differing perspectives. Furthermore, we may be missing the perspectives of those patients whose responsible clinicians did not permit them to take part owing to their mental state (11 cases) or who were approached but refused to take part (36 cases). WP2 data of these patients indicate that these might have been mentally ill patients with ongoing challenging behaviour, which may explain why we were unable to interview them, but also that this was a group of patients whose experiences we were unable to fully capture within our sample.
Fourth, it is also of note that participants had been in secure care for prolonged periods of time and this sometimes made it difficult for them to recall the details of events that had occurred many years previously. Periods of mental ill-health also impacted on some patients’ abilities to recall past events. It is important to note that the extent to which participants were aware of being unwell and/or of their index offence may have varied and, therefore, affected their perceptions and experiences of secure care. However, our epistemological position dictated that we explore how participants constructed meaning based on their own personal lived experiences of long stays in secure care. It was neither appropriate nor our intention to make any judgement on the participants’ levels of insight.
Fifth, stakeholder perspectives were based on interviewees’ accounts rather than on direct observation of the settings and environments that were the focus of interviews. The latter would have allowed for a more in-depth appreciation of the atmosphere of these settings, the interactions of the key players within them and the subtleties of clinical decision-making. However, this was beyond the scope of our study.
Chapter 13 Recommendations for future research
Our study has added significantly to the knowledge base on long stays in high and medium secure forensic settings by providing further insight into the extent of the issue and the patients’ characteristics and needs, and by exploring the perspectives of all of those affected by long stays including patients, carers and professionals involved in the planning and delivery of services for this group. Our findings on potential inappropriate placement and future needs are in accordance with previous government reports,30 although it is now necessary to investigate how these issues can be effectively addressed and prevented in the future. As such, our research recommendations are as follows.
Recording of key information and outcomes
Our research has identified significant obstacles in obtaining the data needed for this study, as well as inconsistencies in the ways in which key information is recorded. Future investigations ought to prioritise:
-
engagement with stakeholders, including NHS England, with a view to agreeing a standardised way of recording key patient and service characteristics and meaningful outcome measures in forensic care to facilitate future research.
Predicting length of stay
Our research and the literature on factors associated with long stays have identified a number of characteristics of the long-stay population as well as factors predictive of long stays. Future research needs to:
-
use prospective designs to longitudinally follow up an admission cohort of high and medium secure patients to test the predictive validity of these factors with a view to developing instruments to predict LoS
-
follow up the current long-stay population to investigate which patients remain in the placement at the time of our study, aiming to retrospectively identify factors that contributed to different outcomes (remain vs. moved on).
In addition:
-
Smaller projects nested within a larger cohort, comparing particular subgroups (e.g. long-stay patients in high secure care who have moved on compared with those who have stayed, patients who moved forward but then had to be readmitted to a higher secure setting or long-stay patients compared with patients with an average LoS) will provide further insights into factors of relevance to LoS.
Patient experience
Our study concentrated on long-stay patients, although patient experiences might be similar for those staying in forensic settings for shorter periods of time. It is recommended that:
-
The themes identified (e.g. motivation to engage, attributions) are explored in a variety of forensic settings and with different patient groups in order to establish whether or not they are specifically relevant to prolonged stay.
-
An exploration of staff perspectives and experiences with secure care patients may help to offer further explanations behind the dissonance in perceptions, particularly of risk, but also to identify ways to improve the dialogue between staff and patients.
Current service provision
We have found significant variation in the percentage of long-stay patients within medium secure care, as well as inefficiencies in the forensic system as a whole. Some stakeholders suggested that patients may move on to low secure care but then ‘get stuck’ there. As such, future research could explore pathways in more detail, including low secure services:
-
Include low secure services with a view to describing patient characteristics and the care provided in these settings.
-
Explore the admission decisions, the interventions provided and the ward atmosphere, as well as the attitudes of senior management and clinical teams towards risk taking and moving on, to establish reasons for the wide variation of long stays in medium secure settings.
-
Describe existing services with high numbers of long-stay patients in more detail, and investigate the outcomes of such services, in comparison with non-long-stay provision, and including employing observational research approaches.
-
Utilise case series to describe patients with rare presentations in terms of diagnosis, offending or pathways to inform individualised interventions for such individuals.
-
Investigate in more detail the impact family contact might have on patients’ progress.
-
Identify inefficiencies, particularly through delay and repetition, and conduct an economic evaluation to quantify the economic impact of treatment interventions.
-
Compare pathways, staffing levels and outcomes of general forensic care in other European countries to identify why some countries are able to provide forensic care that is less resource intensive.
Interventions and future service provision
We have identified significant obstacles to service change in terms of both how services are organised and funded and stakeholders’ attitudes. To inform future service provision decisions, future studies using health economy methods as well as full engagement of all key stakeholders would be valuable to:
-
provide a full, clinical outcome and health economic evaluation of any commissioned long-stay services
-
develop and evaluate psychologically informed interventions, aiming at improving trust and engagement, for long-stay patients taking a static resistance stance
-
initiate and evaluate, in collaboration with interested service providers:
-
pilot projects for improved longer-term planning of pathways ensuring flexibility and enhanced co-operation between services
-
ward environments for the care of long-stay patients and their impact on progress and quality of life
-
-
develop and evaluate staff training programmes for those working with long-stay patients, focusing on engagement and quality of life in forensic care
-
explore how payment structures could be adapted to incentivise reduction in LoS and maximising quality of life.
Acknowledgements
First and foremost, our thanks go to all of the high and medium secure units that participated in the research, and particularly to the local data collectors who dedicated a lot of time and effort to this research. Similarly, we would like to thank all those who were interviewed or took part in focus groups (patients, carers and professionals alike) and gave their time to help us to understand their perspectives.
Contributions of authors
Birgit Völlm (Professor in Forensic Psychiatry and Consultant Forensic Psychiatrist) was the principal investigator. She undertook overall management and supervision of the project, was the major contributor to the development of the protocol and study design, supervised the data collection, contributed to the data analysis, was a main contributor to the data interpretation and synthesis and drafted the final report.
Rachel Edworthy (Research Assistant, Forensic Mental Health) was a research assistant for the entirety of the project; she set up agreements with the majority of participating units, was a major contributor to the development of the WP2 data collection pro forma, carried out data collection (including the survey of professionals and some expert and international interviews), data entry and data analysis, contributed to the organisation of workshops and the end-of-project conference, drafted parts of the report (Chapters 6, 8 and 10) and critically revised the report.
Jessica Holley (Research Fellow, Qualitative Research) was a research fellow for WP3 and was a major contributor to the development of the interview topic guide and the participant and site sampling criteria, conducted data collection (all patient interviews) and data analysis, contributed to the drafting of the report (Chapter 7) and critically revised the report.
Emily Talbot (Research Assistant, Forensic Mental Health) was a research assistant for WP2, initially providing maternity cover but staying with the project for further time after this; she supervised data collection and data entry, contributed to the organisation of workshops and contributed to the drafting of the report.
Shazmin Majid (Research Assistant, Forensic Mental Health) was a research assistant for WP2; she was a major contributor to data entry and analysis, carried out data collection and data analysis (nurses and carers focus groups), was a major contributor to the organisation of the end-of-project conference and contributed to the drafting of the report.
Conor Duggan (Emeritus Professor Forensic Mental Health) contributed to the protocol development, data interpretation and synthesis, and critically revised the report.
Tim Weaver (Associate Professor of Mental Health Research) was the research lead for WP3; he managed and supervised data collection and data analysis, contributed to data interpretation and synthesis, contributed to the drafting of the report (including Chapter 7) and critically revised the report.
Ruth McDonald (Professor of Health Science Research and Policy) was the research lead for WP4; she carried out data collection and data analysis (stakeholder interviews and focus groups), contributed to the data interpretation and synthesis, contributed to the drafting of the report (particularly Chapters 9, 12 and 13) and critically revised the report.
Acknowledgement of contributors
Shirley Mitchell (Head of Research and Innovation for Nottinghamshire Healthcare NHS Foundation Trust) provided continued support and a pragmatic approach for the duration of the project.
Laurie Hareduke (Data Analyst) conducted data analysis for WP1 and WP2 and contributed to the drafting of Chapter 5.
Nick Huband (Research Fellow) conducted data analysis for WP2 and the literature review, and contributed to the drafting of Chapter 4.
Boliang Guo (Statistician) provided advice and guidance for the WP1 and WP2 data analyses.
Peter Bates (PPI lead) supervised all PPI activities, recruited members for the SURG and contributed to the drafting of Chapter 11.
Vivek Furtado (Clinical Fellow) contributed to the development of the study design and led WP1 for the first part of the study.
Mike Harris (previous Executive Director of Forensic Services) provided support and guidance within Nottinghamshire Healthcare NHS Foundation Trust, particularly during the set-up phase.
Julie Hall (current Executive Director of Forensic Services) continued the support and guidance within Nottinghamshire Healthcare NHS Foundation Trust on the retirement of Mike Harris.
Peter Bartlett (Professor of Mental Health Law) provided advice and guidance from an ethical and legal standpoint throughout the project.
Jeremy Coid (Professor of Forensic Psychiatry) provided support and guidance on clinical and research matters.
Eddie Kane (Director, Centre for Health and Justice) provided guidance and advice from a policy perspective.
Dhanuja Senn (postgraduate student) conducted data collection and data analysis for the Netherlands/England long-stay patient comparison.
David Gardner (fourth year undergraduate student) conducted data analysis of the consultant questionnaires.
Data sharing statement
All available data can be obtained from the corresponding author of this report.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
References
- Appelbaum PS. The new preventive detention: psychiatry’s problematic responsibility for the control of violence. Am J Psychiatry 1988;145:779-85. http://dx.doi.org/10.1176/ajp.145.7.779.
- Boyd-Caine T. Protecting the Public? Detention and Release of Mentally Disordered Offenders. Oxford: Routledge; 2012.
- Carroll A, Lyall M, Forrester A. Clinical hopes and public fears in forensic mental health. J Forens Psychiatry Psychol 2004;15:407-25. http://dx.doi.org/10.1080/14789940410001703282.
- Forrester A. Preventive detention, public protection and mental health. J Forens Psychiatry 2002;13:329-44. http://dx.doi.org/10.1080/09585180210151248.
- Petrila J, de Ruiter C. The competing faces of mental health law: recovery and access versus the expanding use of preventative confinement. Amsterdam Law Forum 2011;3:59-68.
- Mental Health Act 1983 (as Amended by the Mental Health Act 2007). London: The Stationery Office; 1983.
- Baker E, Crighton J. Ex parte A: psychopathy, treatability and the law. J Forens Psychiatry 1995;6:101-19. http://dx.doi.org/10.1080/09585189508409879.
- Duggan C. To move or not to move – that is the question! Some reflections on the transfer of patients in the face of uncertainty. Psychol Crime Law 2007;13:113-21. http://dx.doi.org/10.1080/10683160600869874.
- Duggan C, Todd I, Middleton H. Treatment without Consent: An Investigation into the Workings of the Mental Health Act. Aldershot: Ashgate; 2007.
- Völlm B. Characteristics and Needs of Long-Stay Patients in High and Medium Secure Forensic Psychiatric Care: Implications for Service Organisation 2015.
- Department of Health . The High Security Psychiatric Services (Arrangements for Safety and Security) Directions 2013 2013. www.gov.uk/government/uploads/system/uploads/attachment_data/file/268545/HSH_Directions_Signed__2_.pdf (accessed March 2016).
- Rutherford M, Duggan S. Forensic Mental Health Services: facts and figures on current provision. Br J Forens Pract 2008;10:4-10. http://dx.doi.org/10.1108/14636646200800020.
- Guidance for Commissioners of Forensic Mental Health Services. London: Joint Commissioning Panel for Mental Health; 2013.
- McCrone P, Dhanasiri S, Patel A, Knapp M, Lawton-Smith S. Paying The Price: The Cost of Mental Health Care in England to 2026. London: The King’s Fund; 2008.
- Report of the Committee on Mentally Abnormal Offenders (Butler Report). London: Her Majesty’s Stationery Office; 1975.
- Gunn J, Taylor P. Forensic Psychiatry: Clinical, Legal And Ethical Issues. Boca Raton, FL: CRC Press; 2014.
- Department of Health . Report of the Committee of Inquiry into the Personality Disorder Unit, Ashworth Special Hospital (Fallon Inquiry) 1999. www.gov.uk/government/uploads/system/uploads/attachment_data/file/265696/4194.pdf (accessed 20 March 2016).
- Harty M, Shaw J, Thomas S, Dolan M, Davies L, Thornicroft G, et al. The security, clinical and social needs of patients in high security psychiatric hospitals in England. J Forens Psychiatry Psychol 2004;15:208-21. http://dx.doi.org/10.1080/14789940410001703967.
- Department of Health . Best Practice Guidance: Specification for Adult Medium-Secure Services 2007. www.rcpsych.ac.uk/pdf/Guidance%201.pdf (accessed March 2016).
- Do the Right Thing: How to Judge a Good Ward. Ten Standards for Adult In-patient Mental Healthcare. London: Royal College of Psychiatrists; 2011.
- NHS England . Mental Health National Programme of Care n.d. www.england.nhs.uk/commissioning/spec-services/npc-crg/group-c/.
- NHS England . C02 Adult Secure Services n.d. www.england.nhs.uk/commissioning/spec-services/npc-crg/group-c/c02/ (accessed 11 March 2016).
- World Health Organization . International Classification of Diseases n.d. www.who.int/classifications/icd/en/ (accessed 22 February 2017).
- American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders n.d. www.psychiatry.org/psychiatrists/practice/dsm (accessed 22 February 2017).
- Fazel S, Fimińska Z, Cocks C, Coid J. Patient outcomes following discharge from secure psychiatric hospitals: systematic review and meta-analysis. Br J Psychiatry 2016;208:17-25. http://dx.doi.org/10.1192/bjp.bp.114.149997.
- Maden A, Rutter S, McClintock C, Friendship C, Gunn J. Outcome of admission to a medium secure psychiatric unit. Br J Psychiatry 1999;175:313-16. http://dx.doi.org/10.1192/bjp.175.4.313.
- Reed J. The need for longer term psychiatric care in medium or low security. Crim Behav Ment Health 1997;7:201-12. http://dx.doi.org/10.1002/cbm.173.
- Pierzchniak P, Farnham F, de Taranto N, Bull D, Gill H, Bester P, et al. Assessing the needs of patients in secure settings: a multi-disciplinary approach. J Forens Psychiatry 1999;10:343-54. http://dx.doi.org/10.1080/09585189908403688.
- Thomas S, Leese M, Dolan M, Harty M, Shaw J, Middleton H, et al. The individual needs of patients in high secure psychiatric hospitals in England. J Forens Psychiatry Psychol 2004;15:222-43. http://dx.doi.org/10.1080/14789940410001702283.
- Tilt R, Perry B, Martin C, McGuire N, Preston M. Report of the Review of Security at the High Security Hospitals. London: Department of Health; 2000.
- Butwell M. Non Clinical Factors Associated With Length of Stay of Special (High Security) Hospital Patients 2004.
- Security in NHS Hospitals for the Mentally Ill and the Mentally Handicapped (Glancy Report). London: Department of Health and Social Security; 1974.
- Dell S, Robertson G, Parker E. Detention in Broadmoor. Factors in length of stay. Br J Psychiatry 1987;150:824-7. http://dx.doi.org/10.1192/bjp.150.6.824.
- Sharma A, Dunn W, O’Toole C, Kennedy HG. The virtual institution: cross-sectional length of stay in general adult and forensic psychiatry beds. Int J Ment Health Syst 2015;9. http://dx.doi.org/10.1186/s13033-015-0017-7.
- Edworthy R, Furtado V, Völlm B. Characteristics and Needs of Long Stay Patients in High and Medium Secure Forensic Psychiatric Care – Implications For Service Organisation n.d.
- Salize HJ, Dressing H. Placement and Treatment of Mentally Ill Offenders – Legislation and Practice in EU Member States. Mannheim: Central Institute of Mental Health; 2005.
- Brown K, Fahy T. Medium secure units: pathways of care and time to discharge over a four-year period in South London. J Forens Psychiatry Psychol 2009;20:268-77. http://dx.doi.org/10.1080/14789940802327291.
- Jacques J, Spencer SJ, Gilluley P. Long-term care needs in male medium security. Br J Forens Pract 2010;12:37-44. http://dx.doi.org/10.5042/bjfp.2010.0424.
- Kennedy J, Wilson C, Cope R. Long-stay patients in a regional secure unit. J Forens Psychiatry 1995 n.d.;6:541-51. http://dx.doi.org/10.1080/09585189508410782.
- Long CG, Dolley O. Factors predictive of length of stay for women in medium secure settings. J Psychiatr Ment Health Nurs 2012;19:870-4. http://dx.doi.org/10.1111/j.1365-2850.2011.01866.x.
- McKenna J. In-patient characteristics in a regional secure unit. Psychiatr Bull 1996;20:264-8. http://dx.doi.org/10.1192/pb.20.5.264.
- Shah A, Waldron G, Boast N, Coid JW, Ullrich S. Factors associated with length of admission at a medium secure forensic psychiatric unit. J Forens Psychiatry Psychol 2011;22:496-512. http://dx.doi.org/10.1080/14789949.2011.594902.
- Reed J, Lyne M. The quality of health care in prison: results of a year’s programme of semistructured inspections. BMJ 1997;315:1420-4. http://dx.doi.org/10.1136/bmj.315.7120.1420.
- Coffey M. Researching service user views in forensic mental health: a literature review. J Forens Psychiatry Psychol 2006;17:73-107. http://dx.doi.org/10.1080/14789940500431544.
- Walker J, Gudjonsson G. The Lancashire Quality of Life profile: data and experience with 58 detained mentally disordered offenders. Crim Behav Ment Health 2000;10:123-35. http://dx.doi.org/10.1002/cbm.350.
- Swinton M, Carlisle J, Oliver J. Quality of life for patients with a personality disorder – comparison of patients in two settings: an English special hospital and a Dutch TBS clinic. Crim Behav Ment Health 2001;11:131-43. http://dx.doi.org/10.1002/cbm.383.
- Ford K, Sweeney J, Farrington A. User views of a regional secure unit – findings from a patient satisfaction survey. Int J Psychiatr Nurs Res 1999;5:526-41.
- Bressington D, Stewart B, Beer D, MacInnes D. Levels of service user satisfaction in secure settings – a survey of the association between perceived social climate, perceived therapeutic relationship and satisfaction with forensic services. Int J Nurs Stud 2011;48:1349-56. http://dx.doi.org/10.1016/j.ijnurstu.2011.05.011.
- Green T, Batson A, Gudjonsson G. The development and initial validation of a service-user led measure for recovery of mentally disordered offenders. J Forens Psychiatry Psychol 2011;22:252-65. http://dx.doi.org/10.1080/14789949.2010.541271.
- O’Neill C, Heffernan P, Goggins R, Corcoran C, Linehan S, Duffy D, et al. Long-stay forensic psychiatric inpatients in the Republic of Ireland: aggregated needs assessment. Ir J Psychol Med 2003;20:119-25. http://dx.doi.org/10.1017/S0790966700007916.
- Rankin JM. ‘Patient satisfaction’: knowledge for ruling hospital reform – an institutional ethnography. Nurs Inq 2003;10:57-65. http://dx.doi.org/10.1046/j.1440-1800.2003.00156.x.
- Yorston G, Taylor PJ. Older patients in an English high security hospital: a qualitative study of the experiences and attitudes of patients aged 60 and over and their care staff in Broadmoor Hospital. J Forens Psychiatry Psychol 2009;20:255-67. http://dx.doi.org/10.1080/14789940802327259.
- Farnworth L, Nikitin L, Fossey E. Being in a secure forensic psychiatric unit: every day is the same, killing time or making the most of it. Br J Occup Ther 2004;67:430-8. http://dx.doi.org/10.1177/030802260406701003.
- Helbig K. Perceptions of meaningful activity amongst male patients in a high secure forensic addictive behaviours unit. Ment Health Occup Ther 2003;8:77-81.
- O’Connell M, Farnworth L, Hanson EC. Time use in forensic psychiatry: a naturalistic inquiry into two forensic patients in Australia. Int J Forensic Ment Health 2010;9:101-9. http://dx.doi.org/10.1080/14999013.2010.499558.
- Clarke C, Tapp J, Lord A, Moore E. Group-work for offender patients on sex offending in a high security hospital: investigating aspects of impact via qualitative analysis. J Sex Aggress 2013;19:50-65. http://dx.doi.org/10.1080/13552600.2011.595514.
- Margetić B, Ivanec D, Žarković Palijan T, Kovačević D. Offender patients’ opinions on placement in a forensic hospital. Crim Behav Ment Health 2012;22:360-8. http://dx.doi.org/10.1002/cbm.1848.
- Rask M, Hallberg IR. Forensic psychiatric nursing care – nurses apprehension of their responsibility and work content: a Swedish survey. J Psychiatr Ment Health Nurs 2000;7:163-77. http://dx.doi.org/10.1046/j.1365-2850.2000.00280.x.
- Harrison CA, Hauck Y, Hoffman R. Choosing and remaining in mental health nursing: perceptions of Western Australian nurses. Int J Ment Health Nurs 2014;23:561-9. http://dx.doi.org/10.1111/inm.12094.
- Caplan CA. Nursing staff and patient perceptions of the ward atmosphere in a maximum security forensic hospital. Arch Psychiatr Nurs 1993;7:23-9. http://dx.doi.org/10.1016/0883-9417(93)90019-S.
- Mason T. Forensic psychiatric nursing: a literature review and thematic analysis of role tensions. J Psychiatr Ment Health Nurs 2002;9:511-20. http://dx.doi.org/10.1046/j.1365-2850.2002.00521.x.
- Mason T, Lovell A, Coyle D. Forensic psychiatric nursing: skills and competencies: I role dimensions. J Psychiatr Ment Health Nurs 2008;15:118-30. http://dx.doi.org/10.1111/j.1365-2850.2007.01191.x.
- Peternelj-Taylor C. Forensic psychiatric nursing. The paradox of custody and caring. J Psychosoc Nurs Ment Health Serv 1999;37:9-11.
- Shaw J, Davies J, Morey H. An assessment of the security, dependency and treatment needs of all patients in secure services in a UK health region. J Forens Psychiatry 2010;12:610-37. http://dx.doi.org/10.1080/09585180127380.
- Ridley J, McKeown M, Machin K, Rosengard A, Little S, Briggs S, et al. Exploring Family Carer Involvement in Forensic Mental Health Services n.d. www.knowledge.scot.nhs.uk/media/8422527/exploring%20family%20carerinvolvement%20in%20forensic%20mh%20services%20-%20summary%20report.pdf (accessed 20 March 2016).
- Amy HM, Canning A, Séamus A. A survey exploring the provision of carer’s support in medium and high secure services in England and Wales. J Forens Psychiatry Psychol 2009;20:868-85. http://dx.doi.org/10.1080/14789940903174154.
- De Boer J, Gerrits J. Learning from Holland: the TBS system. Forens Psychiatry 2007;6:459-61. http://dx.doi.org/10.1016/j.mppsy.2007.08.008.
- Müller-Isberner R, Freese R, Jöckel D, Gonzalez Cabeza S. Forensic psychiatric assessment and treatment in Germany. Legal framework, recent developments, and current practice. Int J Law Psychiatry 2000;23:467-80. http://dx.doi.org/10.1016/S0160-2527(00)00056-X.
- Ogloff JR, Roesch R, Eaves D. International perspective on forensic mental health systems. Int J Law Psychiatry 2000;23:429-31. http://dx.doi.org/10.1016/S0160-2527(00)00062-5.
- Priebe S, Badesconyi A, Fioritti A, Hansson L, Kilian R, Torres-Gonzales F, et al. Reinstitutionalisation in mental health care: comparison of data on service provision from six European countries. BMJ 2005;330:123-6. http://dx.doi.org/10.1136/bmj.38296.611215.AE.
- Salize HJ, Dressing H, Peitz M. Compulsory Admission And Involuntary Treatment of Mentally Ill Patients – Legislation and Practice in EU-member States. Mannheim: Central Institute of Mental Health; 2002.
- Salize HJ, Dressing H, Kief C. Mentally Disordered Persons in European Prison Systems – Needs, Programmes and Outcome (EUPRIS). Mannheim: Central Institute of Mental Health; 2007.
- Giesler M. Long-Term Forensic Psychiatric Care (LFPC): Why, Who? How? 2012.
- Nagtegaal MH, van der Host RP, Schonberger HJM. Length of Stay in Forensic Psychiatric Hospitals: Numbers and Possible Explanations. The Hague: Boom Juridische Uitgevers; 2011.
- Ritchie J, Spencer L, Bryman A, Burgess RG. Analyzing Qualitative Data. London: Routledge; 1994.
- Andreasson H, Nyman M, Krona H, Meyer L, Anckarsäter H, Nilsson T, et al. Predictors of length of stay in forensic psychiatry: the influence of perceived risk of violence. Int J Law Psychiatry 2014;37:635-42. http://dx.doi.org/10.1016/j.ijlp.2014.02.038.
- Brown CS, Lloyd KR, Donovan M. Trends in admissions to a regional secure unit (1983–1997). Med Sci Law 2001;41:35-40.
- Butwell M, Jamieson E, Leese M, Taylor P. Trends in special (high-security) hospitals. 2: Residency and discharge episodes, 1986-1995. Br J Psychiatry 2000;176:260-5. http://dx.doi.org/10.1192/bjp.176.3.260.
- Castro M, Cockerton T, Birke S. From discharge to follow-up: a small-scale study of medium secure provision in the independent sector. Br J Forens Pract 2002;4:31-9. http://dx.doi.org/10.1108/14636646200200019.
- Coid J, Kahtan N, Gault S, Cook A, Jarman B. Medium secure forensic psychiatry services: comparison of seven English health regions. Br J Psychiatry 2001;178:55-61. http://dx.doi.org/10.1192/bjp.178.1.55.
- Davoren M, Byrne O, O’Connell P, O’Neill H, O’Reilly K, Kennedy HG. Factors affecting length of stay in forensic hospital setting: need for therapeutic security and course of admission. BMC Psychiatry 2015;15. http://dx.doi.org/10.1186/s12888-015-0686-4.
- Edwards J, Steed P, Murray K. Clinical and forensic outcome 2 years and 5 years after admission to a medium secure unit. J Forens Psychiatry 2002;13:68-87. http://dx.doi.org/10.1080/09585180210123294.
- Fong CL, Kar PC, Huei LT, Yan OL, Daud TIM, Zakaria H, et al. Factors influencing inpatient duration among insanity acquittees in a Malaysian mental institution. ASEAN J Psychiatry 2010;11:25-3.
- Glorney E, Perkins D, Adshead G, McGauley G, Murray K, Noak J, et al. Domains of need in a high secure hospital setting: a model for streamlining care and reducing length of stay. Int J Forensic Ment Health 2010;9:138-48. http://dx.doi.org/10.1080/14999013.2010.499552.
- Green B, Baglioni AJ. Length of stay, leave and re-offending by patients from a Queensland security patients hospital. Aust N Z J Psychiatry 1998;32:839-47. http://dx.doi.org/10.3109/00048679809073874.
- Knapp M, Healey A, Coid J, Hickey N, Raikou M, Mangalore R. An Economic Evaluation of Medium Secure Forensic Psychiatry Services. London: London School of Economics; 2007.
- Long C, Dolley O, Hollin C. Engagement in psychosocial treatment: its relationship to outcome and care pathway progress for women in medium-secure settings. Crim Behav Ment Health 2012;22:336-49. http://dx.doi.org/10.1002/cbm.1824.
- Margetić B, Margetić BA, Ivanec D. Can personality traits affect detention length in a forensic institution?. J Forensic Psychol Pract 2014;14:277-87. http://dx.doi.org/10.1080/15228932.2014.931127.
- McKenna J, Shaw J, Porceddu K, Ganley A, Skaife K, Davenport S. ‘Long-stay medium secure’ patients in special hospital. J Forens Psychiatry 1999;10:333-42. http://dx.doi.org/10.1080/09585189908403687.
- Noblin JL. Patient Length Of Stay: Predictive Variability Among Forensic and Civil Psychiatric Units and Populations 2011.
- Renkel S, Rasmussen K. Antipsychotic medication and length of stay at a psychiatric maximum-security unit in Norway (1987–2000). Nord J Psychiatry 2006;60:132-6. http://dx.doi.org/10.1080/08039480600583662.
- Ricketts D, Carnell H, Davies S, Kaul A, Duggan C. First admissions to a regional secure unit over a 16-year period: changes in demographic and service characteristics. J Forens Psychiatry 2001;12:78-89. http://dx.doi.org/10.1080/09585180121913.
- Ross T, Querengässer J, Fontao MI, Hoffmann K. Predicting discharge in forensic psychiatry: the legal and psychosocial factors associated with long and short stays in forensic psychiatric hospitals. Int J Law Psychiatry 2012;35:213-21. http://dx.doi.org/10.1016/j.ijlp.2012.02.011.
- Silver E. Punishment or treatment? Comparing the lengths of confinement of successful and unsuccessful insanity defendants. Law Hum Behav 1995;19:375-88. http://dx.doi.org/10.1007/BF01499138.
- Skipworth J, Brinded P, Chaplow D, Frampton C. Insanity acquittee outcomes in New Zealand. Aust N Z J Psychiatry 2006;40:1003-9. http://dx.doi.org/10.1111/j.1440-1614.2006.01924.x.
- Steadman HJ, Pasewark RA, Hawkins M, Kiser M, Bieber S. Hospitalization length of insanity acquittees. J Clin Psychol 1983;39:611-14. http://dx.doi.org/10.1002/1097-4679(198307)39:4<611::AID-JCLP2270390427>3.0.CO;2-Z.
- Wilkes VL. Predicting Length of Stay in a Male Medium Secure Psychiatric Hospital. Birmingham: University of Birmingham; 2012.
- Wright B, O’Neill C, Kennedy HG. Admissions to national forensic hospital 1997–2003. Ir J Psychol Med 2008;25:17-23. http://dx.doi.org/10.1017/S079096670001079X.
- Vitacco MJ, Vauter R, Erickson SK, Ragatz L. Evaluating conditional release in not guilty by reason of insanity acquittees: a prospective follow-up study in Virginia. Law Hum Behav 2014;38:346-56. http://dx.doi.org/10.1037/lhb0000071.
- Additions of Resident Patients at End of Year, State and County Mental Health Hospitals by Age and Diagnosis, by State, United States, 1983. Rockville, MD: Division of Biometry and Applied Sciences, Survey and Reports Branch; 1986.
- Criminal Procedure and Investigations Act 1996. London: The Stationery Office; 1996.
- Carpenter JR, Goldstein H, Kenwood MG. REALCOM-IMPUTE software for multilevel multiple imputation with mixed response types. J Stat Softw 2011;45:1-14. http://dx.doi.org/10.18637/jss.v045.i05.
- Hair JF, Anderson RE, Tatham RL, Black WC. Multivariate Data Analysis. New York, NY: Macmillan; 1995.
- Sahota S, Davies S, Duggan C, Clarke M, Huband N, Owen V. Women admitted to medium secure care: their admission characteristics and outcome as compared with men. Int J Forensic Ment Health 2010;9:110-17. http://dx.doi.org/10.1080/14999013.2010.499555.
- Tetley A, Jinks M, Huband N, Howells K, McMurran M. Barriers to and facilitators of treatment engagement for clients with personality disorder: a Delphi survey. Personal Ment Health 2012;6:97-110. http://dx.doi.org/10.1002/pmh.1176.
- Alexander R, Devapriam J, Michael D, McCarthy J, Chester V, Rai R, et al. ‘Why can’t they be in the community?’ A policy and practice analysis of transforming care for offenders with intellectual disability. Adv Ment Health Intellect Disabil 2015;9:139-48. http://dx.doi.org/10.1108/AMHID-02-2015-0011.
- Webster CD, Douglas KS, Eaves D, Hart SD. HCR–20: Assessing Risk for Violence (Version 2). Vancouver, BC: Simon Fraser University; 1997.
- Lazarsfeld PF, Henry NW, Anderson TW. Latent Structure Analysis. Boston, MA: Houghton Mifflin; 1968.
- Ramaswamy V, DeSarbo WS, Reibstein DJ, Robinson WT. An empirical pooling approach for estimating marketing mix elasticities with PIMS data. Marketing Science 1993;12:103-24. http://dx.doi.org/10.1287/mksc.12.1.103.
- Nylund KL, Asparouhov T, Muthén BO. Deciding on the number of classes in latent class analysis and growth mixture modeling: a Monte Carlo simulation study. Structural Equation Modeling 2007;14:535-69. http://dx.doi.org/10.1080/10705510701575396.
- Department of Health . Building the Evidence Base in Secure Forensic In-Patient Services in England (Including High, Medium and Low Secure Forensic Services) n.d. www.prp-ccf.org.uk/PRPFiles/SFR_April_2011/0060064%20SFR_Conor%20Duggan.pdf (accessed 20 March 2016).
- Robbé M. Protective Factors Validation of the Structured Assessment of Protective Factors for Violence Risk in Forensic Psychiatry 2014.
- Doyle M, Power LA, Coid J, Kallis C, Ullrich S, Shaw J. Predicting post-discharge community violence in England and Wales using the HCR-20V3. Int J Forensic Ment Health 2014;13:140-7. http://dx.doi.org/10.1080/14999013.2014.906517.
- Tetley AC, Evershed S, Krishnan G. Difficulties in the pathway from high to medium secure services for personality-disordered patients. J Forens Psychiatry Psychol 2010;21:189-201. http://dx.doi.org/10.1080/14789940903177066.
- Völlm BA, Chadwick K, Abdelrazek T, Smith J. Prescribing of psychotropic medication for personality disordered patients in secure forensic settings. J Forens Psychiatry Psychol 2012;23:200-16. http://dx.doi.org/10.1080/14789949.2012.655764.
- Olumoroti O, Forrester A, Wilson S, Dewhurst J. Mentally ill prisoners in need of urgent hospital transfer: appeal panels should resolve disputes to reduce delays. J Forens Psychiatry Psychol 2009;20:S5-S10. http://dx.doi.org/10.1080/14789940802710371.
- Reed S, Russell A, Xenitidis K, Murphy DG. People with learning disabilities in a low secure in-patient unit: comparison of offenders and non-offenders. Br J Psychiatry 2004;185:499-504. http://dx.doi.org/10.1192/bjp.185.6.499.
- Lunsky Y, White SE, Palucka AM, Weiss J, Bockus S, Gofine T. Clinical outcomes of a specialised inpatient unit for adults with mild to severe intellectual disability and mental illness. J Intellect Disabil Res 2010;54:60-9. http://dx.doi.org/10.1111/j.1365-2788.2009.01213.x.
- Hall J. A review of the factors that influence high, medium and low secure care pathways. Int J Care Pathw 2012;16:83-9. http://dx.doi.org/10.1258/jicp.2012.012005.
- Fazio RL, Pietz CA, Denney RL. An estimate of the prevalence of autism-spectrum disorders in an incarcerated population. Open Access J Forens Psychol 2012;4:69-80.
- Burns T, Fazel S, Fahy T, Fitzpatrick R, Rogers R, Sinclair J, et al. Dangerous severe personality disordered (DSPD) patients: characteristics and comparison with other high-risk offenders. Int J Forensic Ment Health 2011;10:127-36. http://dx.doi.org/10.1080/14999013.2011.577139.
- Cormac I, Ferriter M, Benning R, Saul C. Physical health and health risk factors in a population of long-stay psychiatric patients. The Psychiatrist 2005;29:18-20. http://dx.doi.org/10.1192/pb.29.1.18.
- Uppal G, McMurran M. Recorded incidents in a high-secure hospital: a descriptive analysis. Crim Behav Ment Health 2009;19:265-76. http://dx.doi.org/10.1002/cbm.741.
- No Health Without Mental Health: A Cross-Government Mental Health Outcomes Strategy for People of All Ages. London: HMG/Department of Health; 2011.
- Patton M, Patton M. Qualitative Designs and Data Collection. London: Sage; 1990.
- Creswell JW. Research Design: Qualitative, Quantitative, and Mixed Methods Approaches. Thousand Oaks, CA: Sage Publications; 2013.
- Ritchie J, Spencer L, Huberman AM, Miles MB. The Qualitative Researcher’s Companion. Thousand Oaks, CA: Sage Publications; 2002.
- Srivastava A, Thomson SB. Framework analysis: a qualitative methodology for applied policy research. JOAAG 2009;4:72-9.
- Glaser BG, Strauss AL. The Discovery of Grounded Theory: Strategies for Qualitative Research. New Brunswick, NJ: Transaction Publishers; 2009.
- Green J, Thorogood N. Qualitative Methods for Health Research. London: Sage; 2013.
- Sandelowski M. Telling stories: narrative approaches in qualitative research. Image J Nurs Sch 1991;23:161-6. http://dx.doi.org/10.1111/j.1547-5069.1991.tb00662.x.
- Bal M. Narratology: Introduction to the Theory of Narrative. Toronto, ON: University of Toronto Press; 2009.
- Scheff TJ. The labelling theory of mental illness. Am Sociol Rev 1974;39:444-52. http://dx.doi.org/10.2307/2094300.
- Scull A. The Insanity of Place/The Place of Insanity: Essays on the History of Psychiatry. Oxford: Routledge; 2006.
- Bowers L. The Social Nature of Mental Illness. Hove: Routledge; 2003.
- Livingston JD, Nijdam-Jones A, Brink J. A tale of two cultures: examining patient-centered care in a forensic mental health hospital. J Forens Psychiatry Psychol 2012;23:345-60. http://dx.doi.org/10.1080/14789949.2012.668214.
- Wallston KA, Wallston BS, DeVellis R. Development of the Multidimensional Health Locus of Control (MHLC) Scales. Health Educ Monogr 1978;6:160-70. http://dx.doi.org/10.1177/109019817800600107.
- Woods P. The Divided School. Oxford: Routledge; 2011.
- McMurran M, Ward T. Treatment readiness, treatment engagement and behaviour change. Crim Behav Ment Health 2010;20:75-8. http://dx.doi.org/10.1002/cbm.762.
- Hörberg U, Sjögren R, Dahlberg K. To be strategically struggling against resignation: the lived experience of being cared for in forensic psychiatric care. Issues Ment Health Nurs 2012;33:743-51. http://dx.doi.org/10.3109/01612840.2012.704623.
- Jones L, McMurran M. Motivating Offenders to Change: A Guide to Enhancing Engagement in Therapy. West Sussex: John Wiley and Sons Ltd; 2002.
- Langan J, Lindow V. Living with Risk: Mental Health Service User Involvement in Risk Assessment and Management. Bristol: Policy Press; 2004.
- Stewart P, Craik C. Occupation, mental illness and medium security: exploring time-use in forensic regional secure units. Br J Occup Ther 2007;70:416-25. http://dx.doi.org/10.1177/030802260707001002.
- Lewis G, Appleby L. Personality disorder: the patients psychiatrists dislike. Br J Psychiatry 1988;153:44-9. http://dx.doi.org/10.1192/bjp.153.1.44.
- Fereday J, Muir-Cochrane E. Demonstrating rigor using thematic analysis: a hybrid approach of inductive and deductive coding and theme development. Int J Qual Methods 2006;5:80-92.
- Edworthy R, Sampson S, Völlm B. Inpatient forensic-psychiatric care: legal frameworks and service provision in three European countries. Int J Law Psychiatry 2016;47:18-27. http://dx.doi.org/10.1016/j.ijlp.2016.02.027.
- Federal Ministry of Justice and Consumer Protection . German Criminal Code 2016. www.gesetze-im-internet.de/englisch_stgb/index.html (accessed 22 February 2017).
- Dutch Penal Code 1994. www.legislationline.org/documents/id/4693 (accessed 22 February 2017).
- Strafvollzugsstatistik 2013/2014. Wiesbaden: Statistisches Bundesamt, 2013/2014. Germany: Federal Statistical Office; 2014.
- Davies S, Clarke M, Hollin C, Duggan C. Long-term outcomes after discharge from medium secure care: a cause for concern. Br J Psychiatry 2007;191:70-4. http://dx.doi.org/10.1192/bjp.bp.106.029215.
- Wartna BS, Bregman IM, Schapers CE, Blom M, Boonmann C. Recidivecijfers per fpc. Eindrapport van het haalbaarheidsonderzoek naar het gebruik van recidivecijfers op het niveau van de afzonderlijke tbs-instellingen. Cahiers 2014–15. Den Haag: Wetenschappelijk Onderzoek – en Documentatiecentrum (WODC); n.d.
- Braun P. From Confinement to Staying in an Independent Living Unit: Going for Autonomy in Long-Term Forensic Psychiatric Care n.d.
- Federal Ministry of Justice and Consumer Protection . German Therapy Detention Act n.d. www.gesetze-im-internet.de/thug/.
- Grant A, Barker P. Psychiatric and Mental Health Nursing: The Craft of Caring. London: Hodder Arnold; 2009.
- Ergebnisse aus der Arbeitsgruppe Standards zur Unterbringung im Maßregelvollzug. Munich: Bundesarbeitsgemeinschaft der Träger Psychiatrischer Krankenhäuser; 2012.
- Tiwana R, McDonald S, Völlm B. Policies on sexual expression in forensic psychiatric settings in different European countries. Int J Ment Health Syst 2016;10. http://dx.doi.org/10.1186/s13033-016-0037-y.
- Brown SD, Reavey P, Kanyeredzi A, Batty R. Transformations of self and sexuality: psychologically modified experiences in the context of forensic mental health. Health 2014;18:240-60. http://dx.doi.org/10.1177/1363459313497606.
- Leiter MP, Harvie PL. Burnout among mental health workers: a review and a research agenda. Int J Soc Psychiatry 1996;42:90-101. http://dx.doi.org/10.1177/002076409604200203.
- Brett J, Staniszewska S, Mockford C, Herron-Marx S, Hughes J, Tysall C, et al. Mapping the impact of patient and public involvement on health and social care research: a systematic review. Health Expect 2014;17:637-50. http://dx.doi.org/10.1111/j.1369-7625.2012.00795.x.
- Grant A. Freedom and consent. Psychiatr Ment Health Nurs 2009;626.
- Budgeting for Involvement: Practical Advice on Budgeting for Actively Involving the Public in Research Studies. London: Eastleigh; 2013.
- Roca T, Bates P. Uncovering the values that motivate people in relation to payments for involvement in research. Mental Health and Social Inclusion 2014;18:17-20. http://dx.doi.org/10.1108/MHSI-02-2014-0005.
- McKeown M, Malihi-Shoja L, Hogarth R, Jones F, Holt K, Sullivan P, et al. The value of involvement from the perspective of service users and carers engaged in practitioner education: not just a cash nexus. Nurse Educ Today 2012;32:178-84. http://dx.doi.org/10.1016/j.nedt.2011.07.012.
- Ashcroft J, Wykes T, Taylor J, Crowther A, Szmukler G. Impact on the individual: what do patients and carers gain, lose and expect from being involved in research?. J Ment Health 2015;15:1-8.
- Völlm B, Bartlett P, McDonald R. Ethical issues of long-term forensic psychiatric care. Ethics Med Public Health 2016;2:36-44. http://dx.doi.org/10.1016/j.jemep.2016.01.005.
- Bartlett P. The United Nations Convention on the Rights of Persons with Disabilities and mental health law. Mod Law Rev 2012;75:752-78. http://dx.doi.org/10.1111/j.1468-2230.2012.00923.x.
- Moran P. The epidemiology of antisocial personality disorder. Soc Psychiatry Psychiatr Epidemiol 1999;34:231-42. http://dx.doi.org/10.1007/s001270050138.
- Coid J, Kahtan N, Gault S, Jarman B. Women admitted to secure forensic psychiatry services: I. Comparison of women and men. J Forens Psychiatry 2000;11:275-9. http://dx.doi.org/10.1080/09585180050142525.
- Long CG, Knight C, Bradley L, Thomas M. Effective therapeutic milieus in secure services for women: the service user perspective. J Ment Health 2012;21:567-78. http://dx.doi.org/10.3109/09638237.2012.734649.
Appendix 1 Group members
Collaborators
| Name | Role | Institution | Dates |
|---|---|---|---|
| Professor Birgit Völlm | Principal Investigator | University of Nottingham | March 2013–March 2016 |
| Professor Jeremy Coid | Professor of Forensic Psychiatry | Queen Mary University of London | March 2013–March 2016 |
| Dr Tim Weaver | Associate Professor, Mental Health Research | University of Middlesex | March 2013–March 2016 |
| Peter Bates (replaced Dr Julie Repper who did not start working on the project owing to other commitments) | Associate, National Development Team for Inclusion Associate Fellow, Institute of Mental Health |
University of Nottingham | March 2013–March 2016 |
| Dr Vivek Furtado | Clinical Senior Lecturer | Warwick University | March 2013–March 2016 |
| Dr Julie Hall (replaced Dr Mike Harris who retired from his post in April 2014) | Executive Director, Forensic Services | Nottinghamshire Healthcare NHS Foundation Trust | April 2014–March 2016 |
| Professor Ruth McDonald | Professor, Health Science Research and Policy | University of Manchester | March 2013–March 2016 |
| Professor Conor Duggan | Head of Research and Development | Partnerships in Care | March 2013–March 2016 |
| Professor Peter Bartlett | Professor Mental Health Law | University of Nottingham | March 2013–March 2016 |
| Professor Eddie Kane | Director, Centre for Health and Justice | University of Nottingham | March 2013–March 2016 |
Research staff
| Name | Role | Institution | Dates |
|---|---|---|---|
| Rachel Edworthy | Research Assistant | University of Nottingham | March 2013–March 2016 |
| Emily Talbot | Research Assistant | University of Nottingham | May 2014–September 2015 |
| Shazmin Majid | Research Assistant | University of Nottingham | January 2015–March 2016 |
| Jessica Holley | Research Assistant – WP3 | University of Middlesex | October 2014–March 2016 |
| Laurie Hareduke | Research Assistant – WP1 | Nottinghamshire Healthcare NHS Foundation Trust | January 2015–March 2016 |
Project Management Group
All collaborators plus the full-time research assistants listed above and a representative from the SURG formed the PMG.
Study Steering Committee
| Name | Role | Institution | Dates |
|---|---|---|---|
| Barbara Barrett (Chairperson) | Senior Lecturer in Health Economics | King’s College London | March 2013–March 2016 |
| Sue Bailey | Professor of Child and Adolescent Psychiatry | University of Central Lancashire | March 2013–March 2016 |
| Louise Thomson | Head of Research Support and Evaluation Unit | Institute of Mental Health | March 2013–March 2016 |
| Mike Doyle | Nurse Consultant for Clinical Risk | Greater Manchester West NHS Trust | March 2013–March 2016 |
| Graham Durcan | Associate Director, Criminal Justice Programme | Centre for Mental Health | March 2013–March 2016 |
| Quazi Haque | Medical Director | Partnerships in Care | March 2013–March 2016 |
| Georgina Vince (replaced Clare Hodson, National Offender Management Service representative from March 2013 to August 2015) | Lead Psychologist, High Security Close Supervision Centres | National Offender Management Service | October 2015–March 2016 |
| Lawrence Jones | Lead Psychologist, The Peaks Unit, Rampton Hospital | Nottinghamshire Healthcare NHS Foundation Trust | March 2013–March 2016 |
| Steve Sylvester (replaced Kath Murphy, Head of Specialised Commissioning from March 2013 to April 2015) | Head of Specialised Commissioning | NHS England | April 2015–March 2016 |
| Janet Parrott | Consultant Forensic Psychiatrist | Oxleas NHS Foundation Trust | March 2013–March 2016 |
| Ruth Sargent | Mental Health Programme of Care Lead | NHS England | March 2013–October 2014 |
| Sarah Skett (replaced Nick Benefield, Department of Health Advisor for PD from March 2013 to April 2014) | Joint Lead, Offender Personality Disorder Programme | NHS England | April 2014–March 2016 |
| Peter Braun | Lead Psychologist, Long-stay Care | Pompe Foundation, Netherlands | March 2013–March 2016 |
| Walter Schmidbauer (replaced Marco Giesler – Vita Hainos Hospital, Germany from March 2013 to December 2013) | Consultant Psychiatrist | Vita Hainos Hospital, Germany | January 2014–March 2016 |
| Molly Mattingly | Head of Learning Disabilities Programme | Mental Health Foundation | March 2013–March 2016 |
| Ian Callaghan | National Service User Lead, My Shared Pathway | Rethink | September 2013–March 2016 |
| Julie Luther | High Security Estate/PD Pathway Lead Psychologist | Her Majesty’s Prison Service | March 2013–March 2016 |
| Lewis Bradley (observer) | Assistant Programme Manager, Health Services and Delivery Research programme | University of Southampton | March 2013–March 2016 |
Service user reference group
| Name | Role/experience | Dates |
|---|---|---|
| Peter Bates (Chairperson) | PPI lead | March 2013–March 2016 |
| Sheena Foster | Carer | March 2013–March 2016 |
| John Shelton | Experience in forensic services | March 2013–March 2016 |
| CW | Remote member: Rampton Hospital (male) | October 2014–March 2016 |
| Anonymous | Remote member: Rampton Hospital (female) | October 2014–March 2016 |
| Richard | Experience in forensic services | July 2014–April 2015 |
| Luke | Experience in forensic services | October 2014–January 2015 |
| Simon | Experience of mental health issues in prison | July 2013–January 2015 |
| Claire | Carer for a person with PD. Chaired the PPI group | March 2013–April 2014 |
| Debbie | Experience of forensic services. Chaired the PPI group | April 2014–October 2014 |
| Denis | Experience of forensic services | January 2015–April 2015 |
Appendix 2 Literature search strategy – 9 November 2015
Electronic search strategies
MEDLINE
-
((patient? or inpatient) adj12 (admission? or discharg$ or transfer$)).ti,ab.
-
(discharge$ and plan$).ti,ab.
-
((stay? or treatment or admission or detention) adj2 (length? or duration or time or period)).ti,ab.
-
(hospital adj stay?).ti,ab.
-
(long adj stayer?).ti,ab. or hospital costs/
-
or/1-5
-
hospitalization/ and (psych$ or mental$).ti,ab.
-
(hospitali$ and (psych$ or mental$)).ti,ab.
-
hospitals, special/ and (psych$ or mental$).ti,ab.
-
hospitals, psychiatric/
-
forensic psychiatry/
-
criminals/
-
crime/
-
prisoners/
-
prisons/ or prison$.ti,ab.
-
((special adj hospital?) and (psych$ or mental$)).ti,ab.
-
((psychiatric or mental or forensic) adj (hospital? or institut$ or ward? or department? or unit?)).ti,ab.
-
(criminal? or offender?).ti,ab.
-
(criminal$ adj insan$).ti,ab.
-
(crime? or delinquen$ or convict?).ti,ab. or (TBS and forensic).ti,ab.
-
or/7-20
-
6 and 21
EMBASE
-
((patient? or inpatient) adj12 (admission? or discharg$ or transfer$)).ti,ab.
-
(discharge$ and plan$).ti,ab.
-
((stay? or treatment or admission or detention) adj2 (length? or duration or time or period)).ti,ab.
-
(hospital adj stay?).ti,ab.
-
(long adj stayer?).ti,ab. or hospital cost/
-
or/1-5
-
hospitalization/ and (psych$ or mental$).ti,ab.
-
(hospitali$ and (psych$ or mental$)).ti,ab.
-
hospitals, special/ and (psych$ or mental$).ti,ab.
-
hospitals, psychiatric/
-
forensic psychiatry/
-
criminals/
-
crime/
-
prisoners/
-
prisons/ or prison$.ti,ab.
-
((special adj hospital?) and (psych$ or mental$)).ti,ab.
-
((psychiatric or mental or forensic) adj (hospital? or institut$ or ward? or department? or unit?)).ti,ab.
-
(criminal? or offender?).ti,ab.
-
(criminal$ adj insan$).ti,ab.
-
(crime? or delinquen$ or convict?).ti,ab. or (TBS and forensic).ti,ab.
-
or/7-20
-
6 and 21
PsycINFO
-
((patient? or inpatient) adj12 (admission? or discharg$ or transfer$)).ti,ab.
-
(discharge$ and plan$).ti,ab.
-
((stay? or treatment or admission or detention) adj2 (length? or duration or time or period)).ti,ab.
-
hospital discharge/
-
hospital admission/
-
(hospital adj stay?).ti,ab.
-
(long adj stayer?).ti,ab.
-
or/1-7
-
hospitalization/ and (psych$ or mental$).ti,ab.
-
(hospitali$ and (psych$ or mental$)).ti,ab.
-
psychiatric units/
-
psychiatric hospitalization/
-
psychiatric hospital admission/
-
psychiatric hospital discharge/
-
mentally ill offenders/
-
forensic psychiatry/
-
psychiatric patient/
-
psychiatric hospitals/
-
criminals/
-
crime/
-
prisoners/
-
prisons/ or prison$.ti,ab.
-
((special adj hospital?) and (psych$ or mental$)).ti,ab.
-
((psychiatric or mental or forensic) adj (hospital? or institut$ or ward? or department? or unit?)).ti,ab.
-
(criminal? or offender?).ti,ab.
-
(criminal$ adj insan$).ti,ab.
-
(crime? or delinquen$ or convict?).ti,ab.
-
or/9-27
-
8 and 28
Cumulative Index to Nursing and Allied Health Literature
S1 TI ( ((patient? OR inpatient) N12 (admission? OR discharg* OR transfer*)) ) OR AB ( ((patient? OR inpatient) N12 (admission? OR discharg* OR transfer*)) )
S2 TI (discharg* N1 plan*) OR AB (discharg* N1 plan*)
S3 TI ( ((stay? OR treatment OR admission OR detention) N2 (length? OR duration OR time OR period)) ) OR AB ( ((stay? OR treatment OR admission OR detention) N2 (length? OR duration OR time OR period)) )
S4 (MH ‘Patient Admission’) OR (MH ‘Patient Discharge’) OR (MH ‘Discharge Planning’) OR (MH ‘Transfer, Discharge’) OR (MH ‘Length of Stay’)
S5 TI ( (hospital N2 stay?) OR (long N stayer?) ) OR AB ( (hospital N2 stay?) OR (long N stayer?) )
S6 S1 OR S2 OR S3 OR S4 OR S5
S7 ( (MH ‘Hospitalization’) AND (TI (psych* OR mental*) OR AB (psych* OR mental*)) ) OR ( (MH ‘Hospitals, Special’) AND (TI (psych* OR mental*) OR AB (psych* OR mental*)) ) OR ( (MH ‘Hospitals, Psychiatric’) OR (MH ‘Psychiatric Units’) OR (MH ‘Mentally Ill Offenders’) OR (MH ‘Involuntary Commitment’) OR (MH ‘Forensic Psychiatry’) OR (MH ‘Psychiatric Patients’) OR (MH ‘Crime’) OR (MH ‘Prisoners’) OR (MH ‘Correctional Health Services’) )
S8 TI prison* OR AB prison*
S9 TI ( hospitali* AND (psych* OR mental*) ) OR AB ( hospitali* AND (psych* OR mental*) ) OR TI ( ((special N hospital?) AND (psych* OR mental*)) ) OR AB ( ((special N hospital?) AND (psych* OR mental*)) ) OR TI ( (psychiatric OR mental OR forensic) N2 (hospital? OR institut* OR ward? OR department? OR unit?) ) OR AB ( (psychiatric OR mental OR forensic) N2 (hospital? OR institut* OR ward? OR department? OR unit?) ) OR TI ( (criminal? OR offender?) ) OR AB ( (criminal? OR offender?) ) OR TI (criminal* N insan*) OR AB (criminal* N insan*) OR TI ( (crime? OR delinquen* OR convict?) ) OR AB ( (crime? OR delinquen* OR convict?) )
S10 S7 OR S8 OR S9
S11 S6 AND S10
Appendix 3 List of all units, included and not included
Table 32 breaks down the included and excluded medium secure units in the study by region, gender and patient typology (mental health, intellectual disability, PD or combined). Numbers of long-stay patients per included medium secure units are also outlined.
| Region | Total number of units in region | Included units | Non-included units | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Units included | Gender of patients | MH patients (Y/N) | Intellectual disability patients (Y/N) | PD patients (Y/N) | Patients, total | Number of long-stay patients | Units not included | Gender of patients | MH patients (Y/N) | Intellectual disability patients (Y/N) | PD patients (Y/N) | Patients, total | ||
| North East | 3 | Ridgeway | Both | ✓ | ✓ | ✓ | 77 | 19 | Bamburgh Clinic | Male | ✓ | ✓ | 16 | |
| Kenneth Day Unit | Male | ✓ | 30 | |||||||||||
| North West | 9 | Edenfield Centre | Both | ✓ | 128 | 21 | Guild Lodge | Both | ✓ | 77 | ||||
| Scott Clinic | Both | ✓ | ✓ | 48 | 0 | Alpha Hospital Bury (now Cygnet) | Both | ✓ | ✓ | 39 | ||||
| Calderstones | Both | ✓ | 43 | 10 | Charles House Hospital | Both | ✓ | 24 | ||||||
| The Spinney | Male | ✓ | ✓ | 58 | 29 | St Mary’s Hospital | Male | ✓ | 16 | |||||
| Arbury Court | Female | ✓ | ✓ | 74 | ||||||||||
| Yorkshire | 4 | Stockton Hall | Both | ✓ | ✓ | ✓ | 89 | 25 | Newton Lodge (also known as The Yorkshire Centre for Forensic Psychiatry) | Both | ✓ | ✓ | 90 | |
| Humber Centre | Both | ✓ | ✓ | ✓ | 67 | 23 | Cheswold Park Hospital | Male | ✓ | ✓ | ✓ | 42 | ||
| East Midlands | 5 | Arnold Lodge | Both | ✓ | ✓ | 84 | 11 | Wathwood Hospital | Male | ✓ | 76 | |||
| St Andrew’s Northampton | Both | ✓ | ✓ | 151 | 16 | Calverton Hill | Both | ✓ | ✓ | ✓ | 64 | |||
| St Andrew’s Healthcare Nottingham | Male | ✓ | 30 | |||||||||||
| West Midlands | 4 | Raeside Clinic/Ardenleigh | Both | 115 | 4 | The Hatherton Centre | Male | ✓ | 45 | |||||
| St Andrew’s Birmingham | Male | ✓ | 25 | 2 | Janet Shaw Clinic (M&LSU) | Male | ✓ | 15 | ||||||
| East of England | 9 | Norvic Clinic | Both | ✓ | ✓ | 45 | 9 | Broadland Clinic | Male | ✓ | ✓ | 25 | ||
| Brockfield | Both | ✓ | ✓ | 76 | 18 | Eric Shepherd Forensic Services | Male | ✓ | ✓ | 30 | ||||
| Kneesworth House | Both | ✓ | ✓ | ✓ | 49 | 17 | Rowan House (Huntercombe Hospital) | Both | ✓ | 88 | ||||
| St John’s House | Both | ✓ | 24 | 6 | Cygnet Hospital Stevenage | Both | ✓ | 88 | ||||||
| Suttons Manor | Male | ✓ | ✓ | 26 | ||||||||||
| London | 7 | John Howard Centre | Both | ✓ | ✓ | ✓ | 130 | 19 | The Orchard | Female | ✓ | 45 | ||
| North London Forensic Service | Both | ✓ | 143 | 25 | Shaftesbury Clinic | Both | ✓ | 44 | ||||||
| North London Clinic | Male | ✓ | ✓ | 27 | 2 | Bridge House (comes up as River House) | Both | ✓ | 74 | |||||
| Regional Secure Unit (Three Bridges, Tony Hillis) | Male | ✓ | 80 (Tony Hillis Wing has amalgamated with this unit) | |||||||||||
| South East | 6 | The Dene | Both | ✓ | ✓ | 21 | 4 | Trevor Gibbens Unit | Both | ✓ | 55 | |||
| Hellingly Centre | Both | ✓ | 40 | 3 | Bracton Centre | Both | ✓ | 79 | ||||||
| Ashen Hill MSU (Amber Lodge) | Male | ✓ | ✓ | ✓ | 23 | |||||||||
| Farmfield Hospital | Male | ✓ | ✓ | ✓ | 52 | |||||||||
| South West | 2 | Langdon MSU | Both | ✓ | ✓ | 30 | 2 | |||||||
| Fromeside | Both | ✓ | 67 | 14 | ||||||||||
| South Central | 5 | Chadwick Lodge | Both | ✓ | ✓ | ✓ | 35 | 6 | Marlborough House | Male | ✓ | 28 | ||
| The Oxford Clinic | Male | ✓ | 32 | |||||||||||
| Ravenswood House | Male | ✓ | 75 | |||||||||||
| Thornford Park Hospital | Male | ✓ | ✓ | 38 | ||||||||||
| Totals | 54 | 23 (14 NHS and 9 independent) | 1572 | 285 | 31 units (19 NHS and 12 independent) | 1520 | ||||||||
Appendix 4 Work package 2 data collection pro forma
Appendix 5 Work package 2 consultant questionnaire
Appendix 6 Recategorisation of work package 2 variables
| Variable | Original categories | New categories | Comments |
|---|---|---|---|
| Unit name | Previously a string variable | Numerical category with 23 category, one for each of the participating units | |
| Age | Previously a continuous variable | 20–29 30–39 40–49 50–59 60+ years |
|
| Ethnicity | White British White Irish Any other white background Black/black British (Caribbean) Black/black British (African) Black/black British (any other black background) Chinese Asian or Asian British (Indian) Asian or Asian British (Pakistani) Asian or Asian British (Bangladeshi) Asian or Asian British (any other Asian background) Mixed (white and black Caribbean) Mixed (white and black African) Mixed (white and Asian) Mixed (any other mixed background) Not specified Other |
White Black Asian (including Chinese) Mixed Other Not specified |
|
| Has MHA section changed between entering continuous care and census date | No previous category | No Yes |
|
| Current MHA section | Section 2 Section 3 Section 35 Section 36 Section 38 Section 48 Section 48/49 Section 37 Hospital Order Section 37/41 Section 47 Prison Transfer Section 47/49 Notional 37 Section 41 (5) CPIA Section 60/65 Other |
Civil or quasi civil: S 3, 37, 37 (N), 47 Hospital orders with restrictions: S 37/41, CPIA Prison transfers: S 47/49 |
Only applicable to current section |
| LoS in continuous care (calculated in days) | No previous categories | 5+ years (2 April 2003–1 April 2008) from 1826 to 3652 days 10+ years (2 April 1993–1 April 2003) from 3653 to 7304 days 20+ years (2 April 1983–1 April 1993] from 7305 to 10,957 days 30+ years (anything before 1 March 1983) 10,958 plus days |
|
| LoS in current unit care (calculated in days) | No previous categories | 0–5 years (2 April 2008– 1 April 2013) up to 1825 days 5+ years (2 April 2003–1 March 2008] from 1826 to 3652 days 10+ years (2 April 1993–1 April 2003) from 3653 to 7304 days 20+ years (2 April 1983–1 April 1993] from 7305 to 10,957 days 30+ years (anything before 1 March 1983) 10,958 plus days |
|
| Ward moves | Current and previous wards: treatment and diagnostic specifications, dates from (month/year) and reasons for move | Whether their data are complete (yes/no) Number of ward moves in the last 5 years |
|
| Unit moves | Security level, date admitted and reasons for move | Number of ward moves For number of wards stayed on – plus 1 to this number |
|
| Diagnosis | A Active symptoms B No current symptoms but still receiving treatment C No current symptoms and not receiving treatment Diagnoses Dementia Brain injury Learning disability Autistic spectrum disorder Schizophrenia Schizoaffective disorder Other psychotic disorder Bipolar disorder Depression Personality disorder Alcohol misuse/dependence Substance misuse/dependence Other significant mental disorders |
For categories:
|
Only consider A and B (currently active diagnoses) |
| Personality Disorder | Yes or no overall | Yes/no for each type of PD:
|
|
| Offending | Age first conviction Number offences Number of offences Against the person Sex offences Property offences Theft and kindred offences Fraud and kindred offences Police/prison/court offences Drug offences Gun/offensive weapon offences Public order offences Vehicle/driving offences Other offences |
Violent offender:
|
|
| HCR-20 | Historical, clinical, risk management and total score for years 2004–13 | Category with numerical difference between the two scores (see right) Improver – any positive change (i.e. score down) Non-improver (same score) Deteriorater (any negative change, i.e. score up) |
Add up HCR R and C scores for 2013 (or 2012 if 2013 not available) and 2011 scores (or closest by) If scores only available for one year, improver category would be n/a |
| Medication | Current medication categories:
|
One drug class only Two drug classes Three drug classes Four drug classes Five or more drug classes |
|
| Current psychological interventions | Current psychological interventions:
|
Current psychological therapies: yes/no | |
| Serious incidents | Number of (per annum) Serious assaults on staff Serious assaults others Serious deliberate self-harm Seclusion episodes Other incidents in past 2 years |
Serious incident or seclusion 2012–13 (yes/no) 2009–11 (yes/no) Any incidents in past two years (yes/no) Number of other incidents in the last 2 years |
|
| Segregation (only for those who have been in high secure care from 2011 onwards) | Segregation option only for those who have spent time in HS from 2011. | Been in segregation in the last year (2012/13) (yes/no) Been in segregation in the last 5 years (yes/no) |
|
| Physical health | Current diagnosis of the following (yes/no):
|
Any serious physical medical condition (yes/no) | |
| Family/friend contact | Family letter contact Friends/acquaintances letter contact Family telephone contact Friends/acquaintances telephone contact Family visits Friends/acquaintances visits No contact with family No contact with friends/acquaintances |
Contact with family in the last 2 years (yes/no) Contact with friends in the last 2 years (yes/no) Contact with both family and friends in the last 2 years (yes/no) No contact with either family or friends in the last 2 years (yes/no) |
|
| Referrals | Year of referral Type of service referred to Outcome of referral |
Number of unsuccessful referrals in the past 5 years | |
| Tribunals | Year of tribunal Automatic or patient generated Outcome Extra stat recommendations (yes/no) |
Number of tribunals in the past 5 years |
Appendix 7 Work package 2 variables entered in binary logistic regressions
The following variables are based on our literature review and on our own findings.
Admission
-
Admission source to secure care: prison versus rest.
-
Admission to current unit: prison, high secure, medium secure (any), other.
Mental Health Act section
-
Section 3 on admission.
-
MHA current section (according to three categories).
Sociodemographic variables
-
Gender.
-
Ethnicity: white versus other.
-
Marital status: never married versus rest.
-
No qualifications versus rest.
-
Full-time/part-time employment ever.
Mental disorder
-
Diagnostic categories (our four categories).
-
Treatment resistant schizophrenia.
-
Diagnosis of antisocial PD.
Psychiatric history
-
Age first admitted to any in-patient psychiatric care.
-
Number of previous admissions to non-secure psychiatric care.
-
Any previous admissions to high, medium or low secure care.
-
Number of ward moves in past 5 years.
Criminal history
-
Type of offender.
-
Severity of offending.
-
Any convictions.
-
Age at first conviction.
-
Ever custodial sentence.
-
Age at first custodial sentence.
-
First offence against the person.
-
First sexual offence.
-
Age at first violent conviction.
-
Age at first sexual conviction.
-
First sentence hospital order.
-
Sexual index offence.
-
Index offence homicide.
-
Any arson convictions.
-
Sentence for index offence hospital order.
-
Violent or sexual convictions in institutional setting:
-
in past 5 years
-
in current unit.
-
Risk variables
-
History of deliberate self-harm.
-
History of serious suicide attempts.
-
Absconsion past 5 years.
-
Absconded from current setting.
-
Hostage taking/attempted past 5 years.
-
Serious assaults on staff past 5 years.
-
Serious assaults on others past 5 years.
-
Serious suicide attempts past 5 years.
-
Seclusion past 5 years.
-
Current HCR-20.
-
Change in HCR-20 past 2 years.
Physical disorder
-
Any serious physical health condition.
Treatment
-
Currently on mail monitoring (high secure only).
-
Currently on phone monitoring (high secure only).
-
Being on depot.
-
Being on clozapine.
-
Being on two or more different psychotropic medications.
-
Non-compliance with medication.
-
Currently receiving psychological treatment.
Other variables
-
No contact family or friends past 2 years.
-
I2b – lack of personal support.
-
Number of tribunals past 5 years.
-
No referrals past 5 years.
Appendix 8 Work package 2 variables entered in latent components analysis
Mental Health Act section
-
MHA current (according to three categories).
Mental disorder
-
Diagnostic categories (our four categories: intellectual disability, mental illness, PD, mental illness + PD).
-
Treatment resistant schizophrenia.
Criminal history
-
Category of offender (five categories).
-
Offence type of index offence: sexual index offence.
-
Violent or sexual convictions in institutional setting.
Risk variables
-
History of serious suicide attempts past 5 years.
-
Serious assaults on staff past 5 years.
-
Seclusion past 5 years.
Physical disorder
-
Any serious physical health condition.
Treatment
-
Being on a depot.
-
Being on clozapine.
-
Being on three or more different psychotropic medications.
-
Non-compliance with medication.
-
Currently receiving psychological treatment.
Other variables
-
Contact family or friends past 2 years.
-
Referrals past 5 years.
Appendix 9 Work package 2 pathway analysis
| Pathway | 1 (n = 112) | 2 (n = 124) | 3 (n = 90) | 4 (n = 45) | 5 (n = 17) | 6 (n = 6) | 7 (n = 5) |
|---|---|---|---|---|---|---|---|
| H only | 48 | ||||||
| M only | 64 | ||||||
| H–H | 13 | ||||||
| H–M | 40 | ||||||
| M–H | 25 | ||||||
| M–M | 46 | ||||||
| H–H–H | 1 | ||||||
| H–H–M | 8 | ||||||
| H–M–M | 16 | ||||||
| H–M–H | 3 | ||||||
| M–H–M | 8 | ||||||
| M–H–H | 4 | ||||||
| M–M–H | 6 | ||||||
| M–M–M | 44 | ||||||
| H–H–H–M | 2 | ||||||
| H–H–M–H | 1 | ||||||
| H–M–H–H | 1 | ||||||
| H–M–H–M | 3 | ||||||
| H–M–M–M | 8 | ||||||
| M–H–H–M | 3 | ||||||
| M–H–M–M | 6 | ||||||
| M–H–M–H | 3 | ||||||
| M–M–M–H | 5 | ||||||
| M–M–H–H | 1 | ||||||
| M–M–M–M | 12 | ||||||
| H–H–H–H–M | 1 | ||||||
| H–H–M–H–H | 1 | ||||||
| H–H–M–H–M | 3 | ||||||
| H–H–M–M–H | 1 | ||||||
| H–M–H–M–M | 1 | ||||||
| M–H–H–M–H | 1 | ||||||
| M–H–M–H–M | 1 | ||||||
| M–H–M–M–M | 4 | ||||||
| M–M–M–M–M | 4 | ||||||
| H–H–M–H–H–M | 1 | ||||||
| M–H–M–H–H–M | 1 | ||||||
| M–H–M–H–M–M | 1 | ||||||
| M–M–H–M–H–M | 2 | ||||||
| M–M–H–M–M–M | 1 | ||||||
| H–H–M–H–M–H–M | 1 | ||||||
| M–H–H–M–H–M–M | 1 | ||||||
| M–M–H–H–H–M–H | 1 | ||||||
| M–M–M–H–M–H–M | 1 | ||||||
| M–M–M–M–H–H–M | 1 |
Appendix 10 Work package 2 consultant questionnaire distribution of scores
FIGURE 5.
Distribution of overall security scores (item S4).
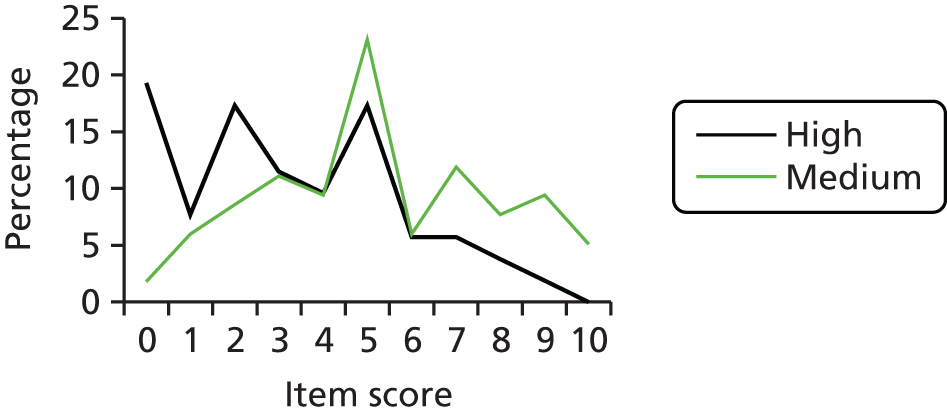
FIGURE 6.
Distribution of overall treatment scores (item T4).
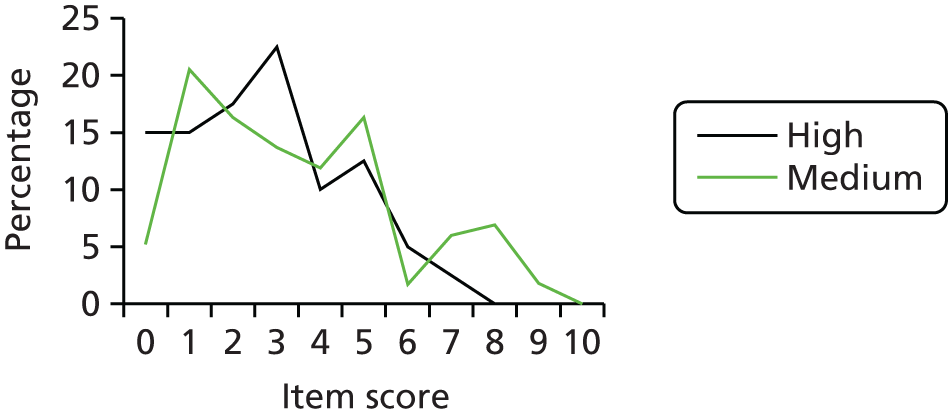
FIGURE 7.
Distribution of overall dependency scores (item D4).
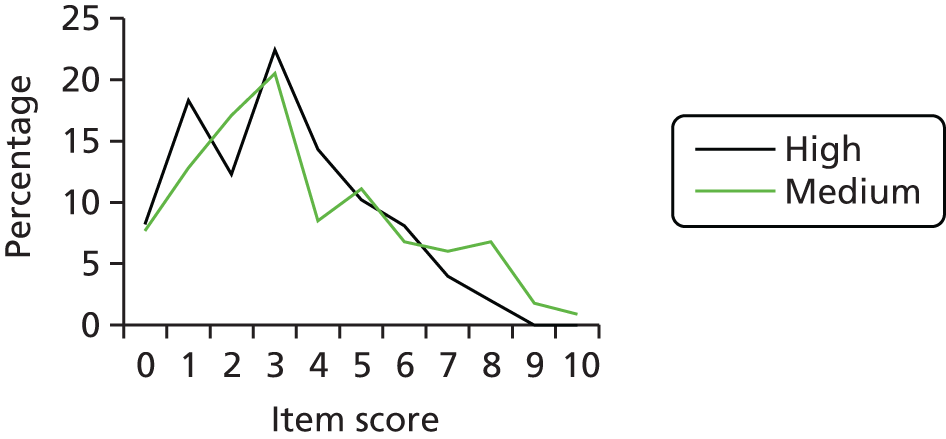
FIGURE 8.
Distribution of overall political scores (item P3).
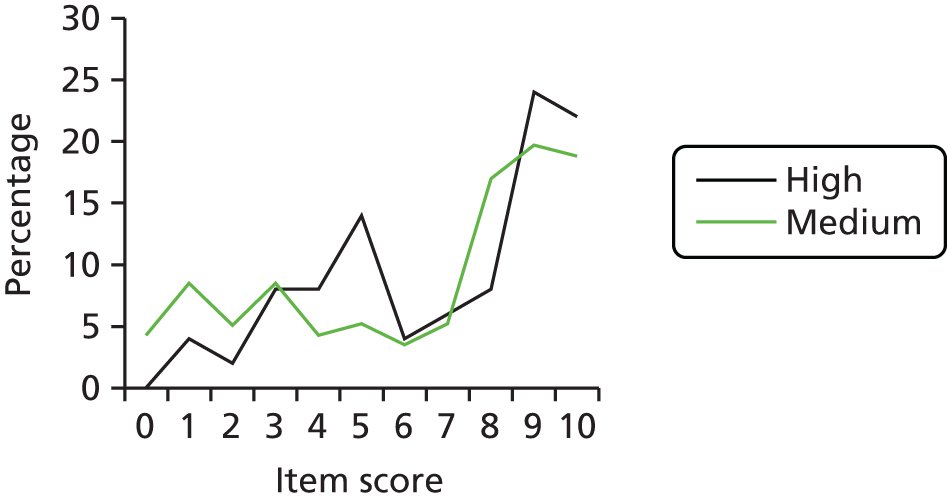
Appendix 11 Work package 3 participant and site sampling criteria
Site selection variables
Number of long-stay patients: the number of long-stay patients within each unit selected needed to be sufficient to generate a sample of subjects.
Geography: the geographical location of the units may impact on the long-stay patient population. For example, different regions may demonstrate variability in local bed availability, use of private sector beds, style of service provision and admission populations (Coid et al. 80). As such, we aimed to select sites from a range of UK regions.
Female long-stay patients: there is a higher proportion of male patients than female patients in medium and high secure forensic units in the UK and internationally. Male offenders may also remain hospitalised for a significantly longer period of time than female offenders (e.g. Moran167). Therefore, the largest proportion of our sample will be male. As such, it is important to select a minimum of one NHS high secure unit, one NHS medium secure unit and one private medium secure unit that has female long-stay patients.
Participant selection variables
The selection of participants at each site was informed by two primary variables.
-
Length of stay: it is important to capture different lengths of stay in medium and high secure units, as patients’ experiences may differ depending on their LoS. Participants were therefore divided into two categories (long-stay patients and long-long stay patients) on the basis of a median split.
-
Gender: in addition to the above rationale on female long-stay patients, the characteristics of female long-stay patients may differ significantly from those of men in secure services (Coid et al. 168; Long et al. ,169). Female long-stay patients are also more likely to be a minority within services, and so their experiences may differ from those of their male long-stay patient counterparts.
The selection of participants at each site was also determined by the following secondary variables.
-
MHA section: findings from WP2 indicated that a higher proportion of long-stay patients were likely to be on a hospital order with or without restrictions. Brown and Fahy37 suggested that people under a restriction order may have been convicted of more serious criminal acts and present a higher level of complexity and risk. We aimed to recruit patients on a section 37, 37/41 or 47/49. It was also important to recruit patients on a civil section (section 3) who had not been convicted of an offence and possibly had no offence history at all and, as such, might have had different treatment pathways and reasons for long stay.
-
Age: at least one case ≤ 50 years and > 50 years at each site. A number of empirical research studies have reported older age forensic patient population as > 60 years old (e.g. Yorston et al. , 200952; H Gordon, Broadmoor Hospital, 1990, unpublished report). We will use this cut-off point to sample patients above and below the age of 60 years.
-
Ethnicity: there is a higher proportion of white British long-stay patients within the high and medium secure units, although it is important that we represent experiences of long-stay patients from other ethnic groups. Patients’ ethnicity and culture may impact on their experiences of long-stay care. We aimed to sample a minimum of one non-white-British long-stay patient at each site.
-
Clinical diagnosis: patients’ clinical diagnosis could be related to their treatment pathway and their experiences of long-stay care. Some patients may have multiple diagnoses (i.e. primary and secondary) and comorbidities that may also impact on their treatment needs and experiences in long-stay care. As such, we aimed to include long-stay patients with a range of diagnoses in our sample, including those with schizophrenia (or other psychotic-related disorder), PD and intellectual disability. At least one diagnostic case needed to be sampled at each site.
-
Offence history/index offence: previous research suggests that patients with a less serious index offence (minor violence) are more likely to progress through secure care at a faster rate than those who have committed more serious offences (e.g. Long et al. 169). Whether the person has a history of offences or has just committed a one-off offence could also be relevant to their posed risks and, thus, their LoS in secure-care. In our sample we aimed to recruit participants with varied index offences including sexual offences, manslaughter, murder, grievous bodily harm and arson. We also tried to include one-off offenders and persistent offenders with a more diverse offending history. At least one index offence case was sampled at each site.
-
Admission source: previous research and the findings of our study suggests that admission source impacts on LoS (e.g. Kennedy et al. 39; Shah et al. 42). In one study, patients who had come from other secure hospitals accounted for the highest bed occupancy (McKenna et al. 41). Furthermore, patients’ experiences of transition between, for example, high to medium or medium to high services will impact on their quality of life. As noted in previous literature, not feeling fully prepared for this transition can impact on patients being able to ‘move on’ (Brown and Fahy37). We aimed to represent patients from a number of admission sources including prison, high, medium, low and other (community/outpatient unit), with at least one case sampled at each site.
Appendix 12 Work package 3 interview agenda and topic guide
Appendix 13 Work package 3 patient characteristics
| Participant | Age (years) | Gender | Ethnicity | Clinical diagnosis | Index offence | Offence history | MHA section | Admission source to current unit | Admission source continuous care | LoS current unit (years) | Overall LoS (years) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| NH1-1 | 53 | Female | White British | Schizophrenia | GBH | Repeat | 37/41 | Medium | Community | 5.3 | 22 |
| NH1-2 | 34 | Male | Black Caribbean | Intellectual disability | Manslaughter | One off | 37/41 | High | Psychiatric setting | 13.2 | 15.3 |
| NH1-3 | 46 | Male | White British | PD and paedophilia | Manslaughter | Repeat | 37/41 | High | Regional children’s centre | 14.4 | 30.1 |
| NH1-4 | 42 | Male | White other | PD | Triple manslaughter | Repeat | 47/49 | Prison | Prison | 17.7 | 17.7 |
| NH1-5 | 46 | Male | White British | Intellectual disability | Property offence | Repeat | 37/41 (recall) | Medium | Prison | 0.8 | 17.9 |
| NH1-6 | 40 | Female | White British | PD | Manslaughter | Repeat | 37/41 | High | Prison | 5.6 | 17.6 |
| NH2-1 | 35 | Male | White Irish | Schizophrenia | Murder | Repeat | 47/49 | Prison | Prison | 13.8 | 13.8 |
| NH2-2 | 26 | Male | White British | Schizophrenia | N/A | N/A | 3 | Unknown | Prison | 3.2 | 8.5 |
| NH2-3 | 45 | Male | White British | Schizophrenia | Rape | Repeat | 37 (N) | Prison | Prison | 14.9 | 14.9 |
| NH2-4 | 39 | Male | White British | PD | Manslaughter | Repeat | 37/41 | Medium | Psychiatric setting | 10.2 | 10.2 |
| NH2-5 | 41 | Male | White British | Schizoaffective disorder | Property offence | Repeat | 37/41 | Medium | Prison | 15.0 | 17.3 |
| PM1-1 | 33 | Female | White British | Schizophrenia | Attempted murder | Repeat | 37/41 | Prison | Community | 5.4 | 5.4 |
| PM1-2 | 46 | Male | White British | Schizophrenia | GBH | Repeat | 37/41 | High | Community | 2.1 | 19.6 |
| PM1-3 | 49 | Male | White British | Schizophrenia and paedophilia | N/A | N/A | 3 | High | Other psychiatric setting | 2.0 | 19.3 |
| PM2-1 | 50 | Male | White British | PD | Attempted murder | Repeat | 47/49 | Medium | Prison | 1.7 | 19.4 |
| PM2-2 | 65 | Male | White British | PD and paedophilia | GBH and sexual offence | Repeat | 37/41 | Unknown | Community | 1.7 | 30.2 |
| PM2-3 | 23 | Male | White British | PD | GBH | Repeat | 37/41 | Prison | Prison | 2.6 | 5.2 |
| PM3-1 | 50 | Male | White British | Schizophrenia | Sexual offence | Repeat | 3 | Medium | Other psychiatric setting | 3.9 | 5.8 |
| PM3-2 | 49 | Male | White British | Intellectual disability | Sexual offence | Repeat | 37 (notional) | High | Prison | 4.6 | 17.1 |
| PM3-3 | 46 | Male | White British | Schizophrenia | GBH | Repeat | 3 | Medium | Other psychiatric setting | 2.5 | 12.8 |
| PM3-4 | 45 | Male | White British | PD | GBH | Repeat | 37/41 | High | Prison | 8.3 | 10.7 |
| PM3-5 | 39 | Male | White British | Intellectual disability | Arson | Repeat | 37 | Medium | Prison | 8.6 | 8.6 |
| PM3-6 | 48 | Male | White British | Schizophrenia | GBH | Repeat | 37/41 | Other psychiatric setting | Other psychiatric setting | 4.2 | 7.5 |
| NM1-1 | 50 | Female | White British | Schizophrenia | Property offence | Repeat | 37/41 | High | Prison | 9.4 | 27.5 |
| NM1-2 | 72 | Male | White British | PD | Sexual offence | Repeat | 37/41 | High | Prison | 9.1 | 45.0 |
| NM1-3 | 60 | Male | White British | Schizophrenia | GBH | Repeat | 37/41 | Medium | Community | 5.5 | 28.7 |
| NM1-4 | 70 | Male | White British | PD | Manslaughter | One-off | 37/41 | High | Prison | 9.4 | 18.6 |
| NM1-5 | 29 | Male | White British | PD | GBH | Repeat | 37/41 | Prison | Prison | 7.1 | 8.3 |
| NM1-6 | 42 | Male | White British | PD | Abduction | Repeat | 37/41 | Medium | Prison | 0.9 | 21.4 |
| NM2-1 | 30 | Male | Black British | Schizophrenia | GBH | Repeat | 37/41 (recall) | Prison | Community | 5.3 | 5.3 |
| NM2-2 | 36 | Male | White British | Intellectual disability | Murder and rape | Repeat | 47/49 | High | Other psychiatric setting | 2.3 | 17.8 |
| NM2-3 | 47 | Male | Black Caribbean | PD | GBH and sexual offence | Repeat | 47/49 | High | Prison | 2.5 | 13.3 |
| NM2-4 | 50 | Male | Black British | PD | Sexual offence | Repeat | 47/49 | High | Prison | 0.3 | 11.1 |
| NM2-5 | 33 | Female | Black British | Schizophrenia | GBH | Repeat | 37/41 | Prison | Prison | 7.2 | 7.2 |
| NM3-1 | 50 | Male | Black British | Schizophrenia | Manslaughter | Repeat | 37/41 | High | Prison | ||
| NM3-2 | 64 | Male | White British | PD and paedophilia | Sexual offence | Repeat | 37/41 | High | Community | ||
| NM3-3 | 54 | Female | White British | Schizophrenia | GBH | Repeat | 37/41 | Medium | Prison | ||
| NM3-4 | 24 | Male | White British | Schizophrenia | Manslaughter | One-off | 37/41 | Prison | Prison | ||
| NM3-5 | 27 | Male | White British | PD | Manslaughter | Repeat | 37/41 | Prison | Prison | ||
| NM3-6 | 46 | Male | White British | Schizophrenia | Attempted murder | Repeat | 37/41 | High | Prison |
Appendix 14 Results of comparison study between England and the Netherlands
| Characteristic | UK (N = 401), n (%) | Netherlands (N = 102), n (%) | p-value |
|---|---|---|---|
| Sex | |||
| Male | 344 (85.8) | 100 (98.0) | 0.001*** |
| Female | 57 (14.2) | 2 (2.0) | |
| Age (years) | |||
| Mean (SD) | 44.5 (11.3) | 51.7 (8.9) | < 0.001*** |
| Median | 45.0 | 51.0 | |
| < 30 | 47 (11.7) | 0 (0.0) | < 0.001*** |
| 31–40 | 100 (24.9) | 8 (7.8) | |
| 41–50 | 145 (36.2) | 40 (39.2) | |
| 51–60 | 76 (19.0) | 36 (35.3) | |
| ≥ 61 | 33 (8.2) | 18 (17.6) | |
| Country of birtha | |||
| UK/Netherlands | 364 (90.8) | 70 (68.6) | < 0.001*** |
| Other/unknown | 36 (9.0) | 32 (31.4) | |
| Nationality | |||
| British/Dutch | 377 (94.0) | 97 (95.1) | 0.856 |
| Other/unknown | 24 (6.0) | 5 (4.9) | |
| Relationship status | |||
| Married/civil partnership | 11 (2.7) | 14 (13.7) | < 0.001*** |
| In a relationship but not married | 1 (0.2) | 7 (6.9) | |
| Divorced/separated | 38 (9.5) | 11 (10.8) | |
| Widowed | 6 (1.5) | 1 (1.0) | |
| Never married | 329 (82.0) | 64 (62.7) | |
| Other/unknown | 16 (4.0) | 5 (4.9) | |
| Employment status before admission | |||
| Employed | 86 (21.4) | 6 (5.9) | < 0.001*** |
| Unemployed/never worked | 270 (67.3) | 95 (93.1) | |
| Unknown | 45 (11.2) | 1 (1.0) | |
| LoS (years) | |||
| Mean (SD) | 14.1 (8.6) | 18.3 (6.4) | < 0.001*** |
| Median | 12.0 | 18.5 | |
| < 10 | 144 (35.9%) | 4 (3.9%) | < 0.001*** |
| 10–19 | 178 (44.4) | 58 (56.9) | |
| 20–29 | 53 (13.2) | 34 (33.3) | |
| ≥ 30 | 26 (6.5) | 6 (5.9) | |
| Number of units stayed in within current care episode | |||
| 1–2 | 236 (58.9) | 5 (4.9) | < 0.001*** |
| 3–4 | 137 (34.2) | 67 (65.7) | |
| ≥ 5 | 28 (7.0) | 30 (29.4) | |
| Current diagnosisb | |||
| Autism spectrum disorderc | 10 (2.5) | 22 (21.6) | < 0.001*** |
| Schizophreniad | 232 (57.9) | 40 (39.2) | < 0.005** |
| Other psychotic disordere | 12 (3.0) | 11 (10.8) | 0.001*** |
| Bipolar disorderd | 13 (3.2) | 7 (6.9) | 0.133 |
| Depressione | 23 (5.7) | 8 (7.8) | 0.001*** |
| Dementiad | 1 (0.2) | 8 (7.8) | 0.001*** |
| Schizoaffective disorderd | 53 (13.2) | 2 (2.0) | 0.002** |
| Axis II classificationb,f | |||
| 0 | 7 (1.7) | 23 (22.5) | < 0.001*** |
| 1 | 113 (28.2) | 55 (53.9) | |
| 2 | 53 (13.2) | 22 (21.6) | |
| ≥ 3 | 13 (3.2) | 2 (2.0) | |
| Substance abuse/dependence | |||
| Yes | 39 (9.7) | 6 (5.9) | 0.001*** |
| Possibly/previously | 128 (31.9) | 53 (52.0) | |
| No | 234 (58.4) | 43 (42.2) | |
| Most recent HCR-20 score | |||
| Historical scoreg | |||
| Mean (SD) | 15.7 (3.0) | 15.3 (2.6) | 0.164 |
| Median | 16.0 | 16.0 | |
| Clinical scoreh | |||
| Mean (SD) | 6.0 (2.6) | 5.8 (1.9) | 0.120 |
| Median | 6.0 | 6.0 | |
| Risk-management scoreg | |||
| Mean (SD) | 6.0 (2.5) | 9.2 (2.2) | < 0.001*** |
| Median | 6.0 | 10.0 | |
| Total scoreg | |||
| Mean (SD) | 27.7 (5.4) | 30.3 (3.9) | < 0.001*** |
| Median | 28.0 | 30.0 | |
| Total number of convictionsi | |||
| Mean (SD) | 11.1 (9.5) | 5.7 (5.3) | 0.761 |
| Median | 9.0 | 4.0 | |
| Age at first custodial sentence (years)j | |||
| Mean (SD) | 21.4 (5.1) | 23.9 (9.2) | 0.206 |
| Median | 20.0 | 21.0 | |
| Total number of offencesk | |||
| Mean (SD) | 22.3 (20.9) | 12.6 (23.1) | 0.389 |
| Median | 17.0 | 7.0 | |
| Age at first conviction (years)l | |||
| Mean (SD) | 17.3 (4.7) | 22.9 (8.7) | < 0.001*** |
| Median | 16.0 | 20.0 | |
| Most severe sentence everm | |||
| Imprisonment indefinitely or life sentence | 36 (9.0) | 1 (1.0) | < 0.001*** |
| Hospital order | 276 (68.8) | 19 (18.6) | |
| Prison ≥ 10 years | 5 (1.2) | 4 (3.9) | |
| Prison 6–9 years | 10 (2.5) | 6 (5.9) | |
| Prison 4–5 years | 3 (0.7) | 7 (6.9) | |
| Prison 1–3 years | 11 (2.7) | 39 (38.2) | |
| Prison < 1 year | 4 (1.0) | 17 (16.7) | |
| Community service | 3 (0.7) | 0 (0.0) | |
| Other sentence | 16 (3.2) | 0 (0.0) | |
| Suspended sentence | 1 (0.2) | 0 (0.0) | |
| Sentence for index offencen | |||
| Imprisonment indefinitely or life sentence | 34 (8.5) | 1 (1.0) | < 0.001*** |
| Hospital order | 249 (62.1) | 47 (46.1) | |
| Prison ≥ 10 years | 8 (2.0) | 4 (3.9) | |
| Prison 6–9 years | 10 (2.5) | 6 (5.9) | |
| Prison 4–5 years | 6 (1.5) | 4 (3.9) | |
| Prison 1–3 years | 8 (2.0) | 26 (25.5) | |
| Prison < 1 year | 4 (1.0) | 9 (8.8) | |
| Community service | 2 (0.5) | 0 (0.0) | |
| Other sentence | 14 (3.5) | 0 (0.0) | |
| Index offence typec | |||
| Violent offence | 232 (57.9) | 59 (57.8) | 0.029* |
| Sexual offence | 78 (19.5) | 42 (41.2) | < 0.001*** |
| Property offence | 66 (16.5) | 5 (4.9) | < 0.001*** |
| Theft and kindred offence | 30 (7.5) | 11 (10.8) | 0.585 |
| Fraud and kindred offence | 1 (0.2) | 1 (1.0) | 0.957 |
| Offence relating to police/courts/prison | 6 (1.5) | 2 (2.0) | 1.00 |
| Drug offence | 0 (0.0) | 0 (0.0) | – |
| Firearm/shotgun/offensive weapon | 17 (4.2) | 15 (14.7) | < 0.001*** |
| Public order offence | 7 (1.7) | 0 (0.0) | 0.306 |
| Other | 8 (2.0) | 5 (4.9) | 0.332 |
| First conviction typeo | |||
| Violent offence | 130 (32.4) | 39 (38.2) | 0.252 |
| Sexual offence | 33 (8.2) | 22 (21.6) | < 0.001*** |
| Property offence | 94 (23.4) | 2 (2.0) | < 0.001*** |
| Theft and kindred offences | 128 (31.9) | 31 (30.4) | 0.767 |
| Fraud and kindred offences | 5 (1.2) | 1 (1.0) | 1.00 |
| Offence relating to police/courts/prison | 7 (1.7) | 0 (0.0) | 0.354 |
| Drug offence | 10 (2.5) | 2 (2.0) | 1.00 |
| Firearm/shotgun/offensive weapon offence | 16 (4.0) | 2 (2.0) | 0.548 |
| Public order offence | 15 (3.7) | 4 (3.9) | 1.00 |
| Other | 28 (7.0) | 14 (13.7) | 0.027* |
| Previous convictionsp | |||
| Violent offence | 319 (79.6) | 71 (69.6) | 0.014* |
| Sexual offence | 110 (27.4) | 50 (49.0) | < 0.001*** |
| Property offence | 228 (56.9) | 13 (12.7) | < 0.001*** |
| Theft and kindred offences | 209 (52.1) | 56 (54.9) | 0.102 |
| Fraud and kindred offences | 44 (11.0) | 7 (6.9) | 0.491 |
| Offence relating to police/courts/prison | 126 (31.4) | 4 (3.9) | < 0.001*** |
| Drug offence | 50 (12.5) | 6 (5.9) | 0.194 |
| Firearm/shotgun/offensive weapon offence | 96 (23.9) | 21 (20.6) | 0.838 |
| Public order offence | 125 (31.2) | 8 (7.8) | < 0.001*** |
| Other | 93 (23.2) | 33 (32.4) | 0.001*** |
Appendix 15 Workshop 2014: international service models for long-stay patients in forensic psychiatry
Appendix 16 Workshop 2015: setting up databases in forensic psychiatric services
List of abbreviations
- BME
- black and minority ethnic
- COST
- Cooperation in Science and Technology
- EU
- European Union
- HCR-20
- Historical Clinical Risk Management-20
- IQR
- interquartile range
- LoS
- length of stay
- MDO
- mentally disordered offender
- MHA
- Mental Health Act
- OR
- odds ratio
- PD
- personality disorder
- PMG
- Project Management Group
- PPI
- patient and public involvement
- SD
- standard deviation
- SPSS
- Statistical Product and Service Solutions
- SSC
- Study Steering Committee
- SURG
- service user reference group
- TBS
- terbeschikkingstelling
- WP
- work package