Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 12/64/187. The contractual start date was in November 2013. The final report began editorial review in June 2016 and was accepted for publication in December 2016. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Jo Rycroft-Malone is a member of the National Institute for Health Research (NIHR) Journals Library Board and was a commissioned work stream board member of the Health Services and Delivery Research (HSDR) programme when this work was funded and, subsequently, was appointed as NIHR HSDR Programme Director, a role that she currently holds. Rebecca Crane receives royalties for mindfulness-based cognitive therapy Distinctive Features, Routledge 2009. She is a non-salaried co-director of Mindfulness Network Community Interest Company (CIC), a not-for-profit social enterprise offering continuing professional development services to mindfulness-based teachers. She directs the Centre for Mindfulness Research and Practice at Bangor University, which delivers professional training for mindfulness-based teachers. Willem Kuyken is the Director of the Oxford Mindfulness Centre, a research, training and education centre that is a collaboration between the University of Oxford and the not-for-profit charity the Oxford Mindfulness Foundation. Willem Kuyken donates all speaking or consultancy fees in full, and directly, to the Oxford Mindfulness Foundation. Until 2015, Willem Kuyken was the Director of the Mindfulness Network CIC, a small not-for-profit charity offering supervision to mindfulness teachers. He relinquished this role in 2015.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2017. This work was produced by Rycroft-Malone et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Background
Mental health problems affect some one in four people throughout their lifetimes, with as many as 10% of the population affected at any one time – this is > 6 million people in the UK. 1 Depression is a major public health problem that, like other chronic conditions, typically runs a relapsing and recurring course, producing substantial decrements in health and considerable human suffering. 2,3 After many years of decline, rates of suicide are rising and suicide is the leading cause of death in men aged 15–49 years. In terms of disability-adjusted life-years, the World Health Organization consistently lists depression in the top five disabling conditions4 and in terms of years lost to disability among the top two, and forecasts that this will worsen over time. 5 Although 23% of the total burden of disease is attributable to mental health problems, only 13% of NHS health expenditure is spent on mental health. 6 Health economic analyses of the cost of anxiety and depression in the UK suggest a cost of £17B or 1.5% of the UK gross domestic product. 6,7 A major factor contributing to the economic effects of depression is the reduced capacity that sufferers have to engage in work.
The last 50 years have seen a transformation in mental health with the development of a range of psychological treatments for depression that are effective and cost-effective,8,9 and significant advances in understanding and changes in public attitudes. 10 There has been a steady reduction in stigma around mental health and, mirroring this, government policies have called for ‘parity of esteem’; that is to say that physical and mental health should receive proportionate attention and funding. 11 The substantial health burden attributable to depression could be offset through making accessible evidence-based interventions that prevent depressive relapse among people at high risk of recurrent episodes. 12 Currently, the majority of depression is treated in primary care, and maintenance antidepressants are the mainstay approach to preventing relapse. To stay well, the National Institute for Health and Care Excellence (NICE) recommends that people with a history of recurrent depression continue antidepressants for at least 2 years. 13 However, there are many drivers for the use of psychosocial interventions that provide long-term protection against relapse. 14 The majority of patients express a preference for psychosocial approaches that can help them stay well in the long term and find that antidepressant medication can have unwanted side effects. The rates of adherence with medication regimes tend to be poor and in the perinatal period many women prefer an alternative to psychotropic medication. 14
Mindfulness-based cognitive therapy
To address this need, mindfulness-based cognitive therapy (MBCT) was developed as an intervention intended to teach people with a history of depression the skills to stay well in the long term. 15 MBCT is a group-based relapse prevention programme for people with a history of depression who wish to learn long-term skills for staying well. There are session-by-session guides for MBCT teachers16 and patients. 17 It combines systematic mindfulness training with elements from cognitive–behavioural therapy (CBT). It is taught in classes of 8–15 people over 8 weeks. Through the mindfulness course people learn new ways of responding that are more self-compassionate, nourishing and constructive. This is especially helpful at times of potential depressive relapse, when patients learn to recognise habitual ways of thinking and behaving that tend to increase the likelihood of relapse and can choose instead to respond adaptively.
A recent individual patient data meta-analysis of all randomised controlled trials of MBCT for recurrent depression (n = 1329) suggests that MBCT significantly reduces the rates of depressive relapse compared with those who did not receive MBCT over a 60-week follow-up (hazard ratio 0.69, 95% confidence interval 0.58 to 0.82). Furthermore, comparisons with active treatments suggest a reduced risk of depressive relapse within a 60-week follow-up period (hazard ratio 0.79, 95% confidence interval 0.64 to 0.97). 18 Usual care in these studies refers to normal health service provision in the nations in which the studies were conducted; the active comparisons were typically maintenance antidepressants. 19–21
Health economists have made the case that the modest cost of effective psychological treatments would be repaid in enhanced productivity, tax receipts and reduced disability benefits,7 to say nothing of the improvements in quality of life. Moreover, many chronic illnesses co-occur with depression, and there is a complex reciprocal relationship between the course of depression and physical conditions that affect both morbidity and mortality. 3,22–24 In terms of cost-effectiveness, MBCT is no more cost-effective than the current treatment of choice, maintenance antidepressants. 20,21 Beyond evidence from randomised trials, no implementation research to date has examined value for money;25 however, there is evidence of its acceptability to patients and referrers. 26,27 However, patients need to invest significant time in MBCT, both to attend the classes and undertake the mindfulness exercises and the group aspect of MBCT is a benefit for some, but a barrier for others. 28 The UK Network for Mindfulness-Based Teacher Training Organisations has set out good practice guidelines for training and supervision, and there is now a register of teachers who meet these guidelines. 29
NICE13 state that group-based MBCT has the strongest evidence base of all treatments designed specifically for this group and is expected to be effective for those who have had three or more episodes of depression.
This recommendation is mirrored by the Scottish Intercollegiate Guidelines Network (SIGN) guideline for the non-pharmaceutical management of depression in adults. 30
Yet in spite of this clear and compelling case for psychological treatments in the UK, they remain hard to access and there are marked geographical inequities in access; this reflects chronic underinvestment in mental health. There has also been a growing recognition that prevention, ideally earlier in life would be most likely to improve UK mental health. 10 A series of calls from patient groups, government policies and implementation drives have sought to ensure psychological treatments are available to those who would benefit and at stages in their lives that would have most impact. A recent task force concluded that:
The NHS needs a far more proactive and preventative approach to reduce the long term impact for people experiencing mental health problems and for their families, and to reduce costs for the NHS and emergency services.
Mental Health Taskforce. 10 Contains public sector information licensed under the Open Government Licence v3.0
National context for psychological therapies generally and mindfulness-based cognitive therapy specifically
Health care is devolved to each of the four UK nations, and within nations regions to organise care with a further degree of devolved autonomy. The key background for each of the four countries is summarised in Table 1.
| Country | Description | Key policy documents and guidelines |
|---|---|---|
| England | England has a population of 54 million. NHS England sets the priorities/direction for health and care. The budget to commission services is largely devolved to GPs and local CCGs. CCGs commission any service that meets NHS standards and costs, be they NHS hospitals, mental health trusts, social enterprises, charities or private sector health-care providers. Health and Wellbeing Boards ensure services work together | No Health without Mental Health11 is a cross-government mental health outcomes strategy for people of all ages (February 2011). It sets out a plan to improve people’s mental health and well-being and improve services for those with mental health problems. The strategy set six key objectives:
Five Year Forward View for Mental Health10 is a report from the independent Mental Health Taskforce to the NHS in England, which was published in February 2016. The taskforce was launched by NHS England and was independently chaired by Paul Farmer, Chief Executive of Mind A key feature of mental health delivery in the UK has been the large-scale roll-out of the IAPT programme.31 This has been a national investment in service delivery and therapist training to make evidence-based psychological therapies available for people with common mental health problems widely accessible in primary care. It includes extensive monitoring. Its primary focus has, until recently, been on CBT NICE published its last Depression: The Treatment and Management of Depression in Adults (Update) in 200913 |
| Northern Ireland | Northern Ireland has a population of 1.8 million. Health and social care is overseen by the Health and Social Care Board, but services are provided by six regional trusts that operate autonomously with their own budgets. Health and social care are provided in an integrated way | Service Framework for Mental Health and Wellbeing32 sets out 58 standards in relation to prevention, assessment, diagnosis, treatment and care of individuals and communities who have or at risk of developing mental health problems The Regional Mental Health Care Pathway33 launched in October 2014, commits health and social care services to deliver care that is more personalised and improves the experience of people with mental health problems, by adopting a more evidence-based/recovery-oriented approach to care across the system A Strategy for the Development of Psychological Therapy Services34 published in 2010. A strategy focused specifically on psychological therapies |
| Scotland | Scotland has a population of 5.4 million. NHS Scotland consists of 14 regional NHS boards delivering frontline health-care services. It also consists of seven special NHS boards and one public health body (Healthcare Improvement Scotland), supporting the regional boards. NHS boards in Scotland are all-purpose organisations: they plan, commission and deliver all NHS services | The Mental Health Strategy for Scotland 2012–201535 had seven key themes and 36 specific commitments that delivered over the period 2012–15 and that cover the full spectrum of mental health improvement, prevention, care, services and recovery The Mental Health (Scotland) Bill 201536 aims to enable people with mental health problems to access effective treatment quickly and easily The Mental Health in Scotland: A Guide to Delivering Evidence-Based Psychological Therapies in Scotland (The Matrix) (2011)37 is a guide to planning and delivering evidence-based psychological therapies within NHS boards in Scotland The SIGN30 is part of the public health body, Healthcare Improvement Scotland (and develops evidence-based clinical practice guidelines for the NHS in Scotland) The Doing Well By People with Depression programme (2006)38 was a 3-year initiative intended to build capacity to treat depression and to enhance access to sources of support. The programme presented an opportunity to try out ‘new’ approaches and to change existing ways of delivering interventions. Various sites included training in mindfulness-based approaches NHS Education for Scotland39 is a special health board responsible for education and training for those who work in NHS Scotland. It has been funding 8-week staff MBCT courses, CPD events and facilitated regular meetings between mindfulness leads Finally, Mindfulness Scotland40 is a charity that aims to contribute to the development of a more mindful and compassionate Scotland by working alongside the NHS and other public institutions. They offer a range of activities including teacher training and annual conferences |
| Wales | Wales has a population of approximately 3.1 million. NHS Wales (Welsh: GIG Cymru) is organised into seven local health boards. Each board is responsible for delivering all health-care services within its region | Together for Mental Health – A Strategy for Mental Health and Wellbeing in Wales41 is a 10-year strategy for improving the lives of people using mental health services, their carers and their families (October 2012). The main themes of Together for Mental Health are around promoting well-being and prevention, public partnership model, integration of care and joint working across sectors, and implementation. The Strategy is focused around six high-level outcomes and supported by a delivery plan. At the heart of the strategy is the Mental Health (Wales) Measure 2010,42 which places legal duties on health boards and local authorities to improve support for people with mental ill health |
With respect to MBCT specifically, two significant reports have drawn attention to the case for MBCT to be more widely available, arguing that for many it is an acceptable way for people with a substantial history of depression to learn skills to stay well in the long term. The Mental Health Foundation report included surveys of general practitioners (GPs) and the general public and recommended that MBCT be made more available through investment in training therapists, greater education of GPs so they know who and when to refer to mental health services and building capacity within the NHS to offer MBCT. 27 Five years later, the Mindfulness All Party Parliamentary Group (MAPPG) produced the Mindful Nation UK report43 that made four recommendations in the area of health:
-
MBCT should be commissioned in the NHS in line with NICE guidelines so that it is available to the 580,000 adults each year who will be at risk of recurrent depression. As a first step, MBCT should be available to 15% of this group by 2020, a total of 87,000 adults each year. This should be conditional on standard outcome monitoring of the progress of those receiving help.
-
Funding should be made available through the Improving Access to Psychological Therapies (IAPT) training programme to train 100 MBCT teachers per year for the next 5 years to supply a total of 1200 MBCT teachers in the NHS by 2020 in order to fulfil recommendation one.
-
Those living with both a long-term physical health condition and a history of recurrent depression should be given access to MBCT, especially those people who do not want to take antidepressant medication. This will require assessment of mental health needs within physical health-care services, and appropriate referral pathways being in place.
-
NICE should review the evidence for mindfulness-based interventions (MBIs) in the treatment of irritable bowel syndrome, cancer and chronic pain when revising their treatment guidelines.
The National Institute for Health Research Dissemination Centre in a 2016 highlight44 noted the following.
-
MBCT may provide an alternative for people with recurrent depression, especially those who have difficulty in adhering to maintenance antidepressant medication.
-
Patients who participated in MBCT, instead of antidepressants, had similar relapse rates to those who continued with antidepressants alone.
-
MBCT was no more cost-effective than antidepressants. However, costs were similar for patients receiving MBCT and those receiving antidepressants, as were outcomes, so from a cost perspective MBCT may be a reasonable alternative.
-
Both MBCT and CBT are intensive processes requiring significant commitment of time and effort. This will not suit everyone, and in particular interviews with study participants suggest that those with other health conditions found it difficult. MBCT is typically delivered in a group setting that, again, may not suit everyone.
-
However, there is currently no clear evidence about which patients might be more or less likely to benefit from cognitive therapies, so all patients should be considered for these therapies. It is important that patients know about all the different treatment options and what they involve before making a decision.
In line with the Medical Research Council Complex Interventions Framework and leading commentators,45 the next phase of work is to determine how MBCT can be implemented in ‘uncontrolled real world’ health-care settings. 46 Indeed, the 2009 NICE guideline13 recommended that provision of MBCT in the NHS be an implementation priority.
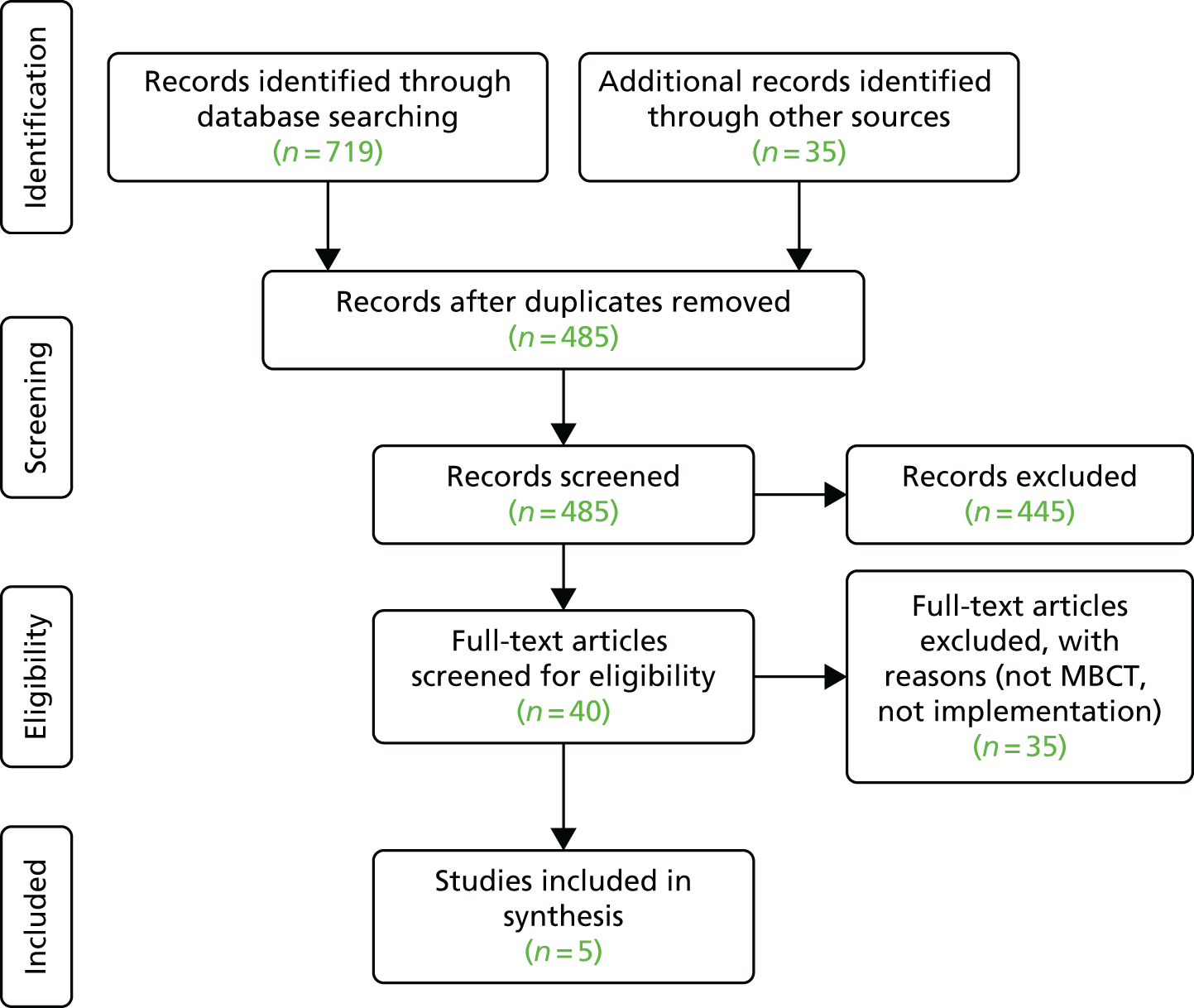
As an early step we conducted a high-level narrative review of the MBCT implementation literature (Figure 1). This included a search of MEDLINE, EMBASE and PsycINFO databases using the terms ‘Mindfulness,’ ‘Mindfulness-Based Cognitive Therapy’ and ‘MBCT’, with either ‘Implementation’, ‘Adoption’, ‘Diffusion’, ‘Dissemination’, ‘Evidence-based Practice’, ‘Knowledge transfer’, ‘Knowledge translation’, ‘Quality improvement’, ‘Translational research’ or ‘Research utilisation’. We also included literature identified by MBCT experts. We screened 485 papers and included 40 papers for full-text assessment. We excluded studies if they were not explicitly related to both MBCT and implementation issues.
The majority of the papers were reviews and opinion pieces. A consistent theme is that although the interest in MBCT is growing,48 implementation is patchy at best. 49–51 An analysis at the level of health-care systems suggests that MBCT might best be accommodated within contemporary systems of health-care delivery, such as stepped care that seeks to match the intensity of the intervention to the needs of individuals in a series of steps. 52 A conducive organisational context is noted as important,52–54 a theme consistent with implementation of other psychological treatments. 55 A number of commentators point to the value of starting implementation by offering MBCT to health-care professionals. 52,56 Identified barriers include a lack of agreed standards for MBCT training and teaching, limited access to training and supervision, and resources (time, staff, money.)50,52,54,56,57 Finally, a number of commentators note the need to fit MBCT to the implementation setting, meaning who is the population MBCT is intended for (client/patient population) and what is the context (health-care system and cultural). 52,54,56–63
There was a small set of primary research studies. The study that informed this work is described below as the feasibility work for this study. 64 A small-scale observational study identified implementers in primary care, provided pump priming funds and monitored impact over 8 months. 65 Although small (n = 5) and observational, this suggests that resourcing enthusiastic implementers can have some impact. A population-based analysis used Canadian health survey data to simulate the number of MBCT teachers needed to provide a sustainable service to people with recurrent depression. 66 They estimated that 4.2% of the population are candidates for MBCT. Estimating that it would be acceptable to some 20% of eligible people, they recommend one MBCT teacher per 100,000 population. Such analyses are prone to numerous methodological caveats,67 but are a starting point for considering staffing resources for mental health services wishing to offer MBCT.
Very limited work has asked people from diverse backgrounds about facilitators of and barriers to mental health care. 63,68–70 Minority groups typically face additional barriers in accessing mental health care, and the way this manifests with respect to access to MBCT has, as far as we are aware, not been researched. These commentaries are North American and the applicability to a UK context is as yet underexplored.
The largely opinion-based literature alongside a very small set of preliminary primary research studies suggests that the potential to create new knowledge in this study is significant.
Feasibility work
One of the few extant implementation studies was completed as a feasibility study for this project by two of the applicants. 64 This study asked to what extent MBCT has been implemented in the health service to date and what had facilitated implementation. It was based on (1) a stakeholder workshop (n = 57), (2) a postal survey (n = 103 responses) and (3) an overview of four services that had either partially or fully integrated MBCT services. The results suggested that accessibility across the UK is very limited. Eighty-one per cent of the postal survey respondents reported that the implementation of MBCT had not yet begun in their organisation. Where implementation had started, very few respondents reported a strategic and systematic approach to implementation. Instead, successful implementation was most frequently described as being due to ‘enthusiasts’ who had driven through change, but that these initiatives largely lacked organisational commitment or integration with other services. The authors note that the limited implementation of MBCT contributes to health inequalities and misses an opportunity to translate evidence into practice. This feasibility study was based on convenience samples and was largely descriptive. It also does not offer an explanation of why MBCT implementation to date is so patchy and inequitably distributed, nor does it offer recommendations for how MBCT might best be implemented – hence the need for this study.
Summary and research aims
Even if a psychosocial intervention has compelling aims, has been shown to work, is cost-effective and is recommended by a national advisory body, its value is determined by how widely available it is in the health service. Feasibility work completed in preparation for this study indicates that NHS provision of MBCT falls well short of that envisaged in national guidance. 64 A recent British Medical Journal editorial suggests that research is needed to answer the questions, ‘What are the facilitators and barriers to implementation of NICE’s recommendations for MBCT in the UK’s health services? Can this knowledge be used to develop an Implementation Plan for introducing MBCT consistently into NHS service delivery?’. 46 Moreover, NHS England has made ‘improving access to psychological therapies’ a priority in order to focus effort and resources on improving clinical services and health outcomes. The Parity of Esteem programme71 has ‘a national ambition by end March 2015 to increase access so that at least 15% of those with anxiety or depression have access to a clinically proven talking therapy services, and that those services will achieve 50% recovery rates’ (contains public sector information licensed under the Open Government Licence v3.0). Similar policy pledges in other UK countries aim at IAPT with a specific focus on prevention; for example, among the six high-level outcomes in the Welsh Strategy ‘Together for Mental Health’ one is ‘Access to, and the quality of preventative measures, early intervention and treatment services are improved and more people recover as a result’ (© Crown copyright 2012; contains public sector information licensed under the Open Government Licence v3.0). 41 There is a growing commitment among policy-makers, commissioners and those delivering services to ensuring that people with mental health problems receive the evidence-based treatments they need, for example as captured in the commitments of the Mental Health Strategy for Scotland 2012–201535 or the standards of the Service Framework for Mental Health and Wellbeing in Northern Ireland from 2011. 32 The MAPPG report pointed to the need for the 2009 NICE guideline13 to be implemented in the NHS and for more MBCT teachers to be trained. 43
This research will describe the current state of MBCT implementation across the UK and develop an explanatory framework of what is hindering and facilitating its progress. As such, this study does not seek to provide confirmatory evidence of clinical efficacy, but aims to fill a gap in the evidence about the implementation of a clinically effective psychological intervention. From this framework we will develop an implementation plan and related resources to promote wider access to and use of MBCT. The implementation plan will be a coherent framework and set of resources to support implementation of MBCT within the NHS, and will be freely accessible.
Specifically we will:
-
scope existing provision of MBCT in the health service across England, Northern Ireland, Scotland and Wales
-
develop an understanding of the perceived benefits and costs of embedding MBCT in mental health services
-
explore facilitators that have enabled services to deliver MBCT
-
explore barriers that have prevented MBCT being delivered in services
-
articulate the critical success factors for enhanced accessibility and the routine and successful use of MBCT as recommended by NICE
-
synthesise the evidence from these data sources and, in co-operation with stakeholders, develop an implementation plan and related resources that services can use to implement MBCT.
Chapter 2 Design and methods
Design
As outlined in Chapter 1, in this study our main aim was to investigate the implementation and accessibility of MBCT (a psychological therapy that has been shown to be clinically effective and cost-effective, and is recommended in NICE guidance) across the UK.
We conducted a two-phase qualitative, exploratory and explanatory study, which was conceptually underpinned by the Promoting Action on Research Implementation in Health Services (PARIHS) framework. In phase 1 we conducted interviews with participants from different regions across the UK about current provision of MBCT. In phase 2 we undertook a more in-depth study of MBCT implementation within 10 case studies. The study protocol has been previously published72 and can be found online.
Theoretical framework
The framework underpinning this study was PARIHS. 73 Co-developed by one of the investigators, PARIHS is a frequently used framework within a health service context as a guide for both implementation practice and research. It has been through a systematic process of development and refinement over a number of years. 74 PARIHS was developed as a means of understanding the complexities involved in the successful implementation of evidence into practice. Within PARIHS, successful implementation (SI) is represented as a function (f) of the nature and type of evidence (E) being implemented, the qualities of the context (C) in which it is being implemented and the process of facilitation (F) [SI = f(E,C,F)].
Promoting Action on Research Implementation in Health Services facilitates the mapping of factors that might need attention before, during and after implementation efforts, and, as such, it provided a conceptual map for the study. The framework was used as a heuristic to inform the development of data collection tools, and was also used in the analysis process.
Phase 1: interview study
In order to obtain an overview of whether or not and how MBCT is being delivered in the four countries of the UK, and to provide an overview of the factors that have facilitated and hindered the implementation of this intervention, we conducted interviews. Interviews have been described as a ‘conversation with a purpose’, providing a ‘flexible and adaptable way of finding things out’. 75 As we had a number of objectives to explore with interview participants, we used a semistructured interview approach that allowed us to explore specific topics, but also enabled the interviewer to probe further and gave participants the flexibility to include additional relevant information. Data collection methods are described in Methods.
Phase 2: case studies
As phase 1 provided an overview of MBCT implementation across the UK, in phase 2 we wanted to gain a more in-depth and contextually embedded understanding of MBCT implementation. As such, we used a case study approach. As an empirical enquiry, case studies provide an opportunity to explore and understand how and why (in this case) MBCT implementation was more or less successful within ‘its real life context’. 76 Furthermore, a case study is appropriate for when ‘a how or why question is being asked about a contemporary set of events over which the investigator has little or no control’. 77 In this study, MBCT accessibility and implementation was the phenomenon that we wanted to study in the real-life context of NHS health services and those delivering these services. We chose to study multiple cases because we speculated that the implementation of MBCT would be different depending on the context in which it was being implemented. Studying more than one case would enable the development of a more comprehensive account of MBCT implementation. As a research design, case studies are particularly appropriate for the inclusion of multiple data collection methods enabling description and explanation (see Data collection).
Patient and public involvement
We embedded patient and public involvement (PPI) throughout the conduct of this study, informed by INVOLVE, a national advisory group that supports active public involvement in NHS, public health and social care research, and the Mental Health Research Network’s approach to best practice. 78 Patients were involved in the development of the proposal, the creation of data collection tools, the analysis of phase 1 and phase 2 data, the creation of the implementation plan and the dissemination of findings.
The PPI group comprised four people with a history of recurrent depression, all of whom have accessed MBCT and who had varying views about MBCT, from the more positive to the more sceptical. Facilitated by AG, this group met four times during the study and had access to project materials throughout as they wished. At least one member of the PPI group also attended our monthly project management meetings and both of the advisory panel meetings.
Methods
Data collection
Data were collected between 4 December 2013 and 17 July 2015.
Phase 1
Semistructured audio-recorded interviews were undertaken with individual participants from all four UK countries, by telephone or face to face (as convenient), and were guided by an interview guide (see Appendices 1 and 2). The interview guide was broadly structured around the elements of evidence, context and facilitation (the main elements of the study’s conceptual framework), and was specifically designed to capture views and information about the accessibility of MBCT, the implementation of MBCT (including facilitators and barriers), and perceived costs and benefits. The schedule was used flexibly to enable participants to contribute additional information relevant to the research objectives. Phase 1 was descriptive in nature.
Sampling
Stakeholders of relevance to this study included commissioners, managers, MBCT practitioners and teachers, and people living with depression with experience of MBCT. To ensure geographical representation we sampled within the following NHS regions: England (North, Midlands, South and London), Wales, Scotland and Northern Ireland (see Chapter 3). Preparatory work involved securing the engagement of a key stakeholder within each of these regions, namely someone who had good knowledge of MBCT service delivery across the region. At the funding stage, the board asked that we randomly sample some of our participants to reduce the risk of positive accounts. Therefore, following interviews with key stakeholders within the regions we developed a list of potential participants that represented each of the groups described above in each area. We then randomly sampled from that list within each of the stakeholder groups (see Chapter 3, Sample).
Phase 2
The case studies were designed to enable a richer understanding of the implementation and accessibility of MBCT, building up an explanation from the findings of phase 1. A ‘case’ was defined as a NHS organisation in which NICE recommendations would indicate that MBCT provision should be accessible free at the point of delivery. Within each case, multiple qualitative methods (see below) were used concurrently and tailored accordingly, depending on the degree of uptake of MBCT with a case study site (see Chapter 4, Sample). As such, phase 2 was aimed at explanation, building on the description provided by phase 1. The methods used with the cases are described as follows.
Semistructured interviews
We conducted semistructured audio-recorded interviews in each site, these were our primary source of data. The interview schedules were initially informed by the findings of phase 1 so that we could test out the ideas that came from phase 1; however, in order to build up an explanation in phase 2, as data collection and familiarisation progressed, we revised the schedules to enable us to build up an explanation over cases. As such, the interview schedule evolved as we progressed with the case studies, to enable us to begin explanation building (see Appendices 1–3 for some examples). Interviews were mainly conducted face to face, but in a small number of instances where face to face was not possible, they were conducted by telephone. We stated in our protocol that we would interview up to 20 participants in each site, but as a result of reaching a point of data saturation, fewer than 20 were interviewed in some sites. A decision to stop data collection was reached by discussion between FG, HOG, JRM and WK.
We were interested in exploring some of the features of the framework that we developed from phase 1 data analysis (see Appendix 4), and, as such, questions about this were built into the schedule. Therefore, the schedule included questions relating to the MBCT implementation story, the mixture of factors that mediated the implementation of MBCT, including issues concerning the evidence base and the context of implementation.
Non-participant observation
We sought opportunities to observe naturally occurring meetings and events within each site. It was anticipated that this would provide an additional opportunity to gain insights into the context of service delivery in which MBCT may be being delivered. Observations, which were written up as field notes, were guided by drawing on a framework that included paying attention to space, actors, activities, objects, acts, time, events, goals and feelings. 79
Documentary analysis
A range of documents was collected to help contextualise and complement other data sources (see Appendix 5). We requested documents that may help us understand the implementation of MBCT in specific sites; as such, they differed across sites. Specifically, we asked for any strategy and/or policy documents about MBCT services, which would facilitate an understanding about where they were positioned within the structure of the organisation and pathways of care delivery. Additionally, we requested any meeting notes from MBCT planning meetings, business cases/proposals, service evaluations and any reports of relevance to MBCT. We were also open to the offer of relevant documents from site participants.
Context analysis
In order to gain an understanding of the broader context we gathered publicly available information about socioeconomics, ethnicity and mental health metrics (see Appendix 6). We also drew on site-specific, publicly available data, which is not referenced in order to maintain site anonymity. In combination with qualitative information gathered within sites, this enabled us to build up a description of each case (see Chapter 4, Case summaries).
The non-participant observations were conducted, and documents were gathered in order to confirm or refute claims made in the interviews.
Sampling
Sites
We purposively sampled 10 cases across England, Wales, Northern Ireland and Scotland, based on the extent of MBCT being embedded in service delivery. The number of sites was chosen during the funding process, as a reasonable number to ensure a spread of different levels of implementation and to ensure geographic coverage. Embeddedness was determined by strategy for MBCT delivery, trained staff delivering MBCT to minimum practice levels, referrers’ awareness of service, and an ongoing throughput of clients:
-
integrally embedded (four sites) – in which all the above criteria were reportedly in place at the time of discussions about accessing the case
-
partially embedded (four sites) – where strategy was less obvious and/or in the early stages of implementing it, delivery patchy and MBCT teachers were working in isolation
-
no or scarce MBCT implementation (two sites) – where there was an absence of delivery.
We also sampled to obtain some representation in relation to sociodemographic profile, prevalence of mental health problems, urban versus rural and the ethnic profile of the population served in each site.
Within sites
Within sites we used the following criteria to sample participants:
-
different stakeholders, including managers, MBCT teachers, referrers, practitioners, people living with depression and commissioners
-
ensuring we drew from participants across the organisation at macro, meso and micro levels
-
ensuring we were gathering a range of responses from those who were more and less disposed to the implementation of MBCT.
We worked with local collaborators to identify appropriate data collection opportunities and potential participants, but using the criteria above and taking care to ensure a balanced set of respondents. We did our best to ensure a balanced set of respondents by actively seeking out those people who were less positively disposed to MBCT.
Data analysis
Data were managed in Microsoft Word (2013, Microsoft Corporation, Redmond, WA, USA), Microsoft Excel (2013, Microsoft Corporation, Redmond, WA, USA) and ATLAS.ti (version 7.5.6, Scientific Software Development GmbH, Berlin, Germany). Audio-recorded data were fully transcribed. Hand-written field notes were converted into electronic text. All members of the research team were involved in the analysis process, which also included input from lay members (Table 2 shows who was involved in the analysis and at what points). This approach was useful for sense checking, building and refining explanations, and providing a further check on credibility.
| Stage | Activity | Who was involved |
|---|---|---|
| Familiarisation |
|
FG and HOG FG, HOG, JRM, WK, RC, AG and SM |
| Identifying the framework |
|
FG, HOG, JRM and WK PPI members FG, HOG, JRM, WK, RC, AG and SM JRM, WK, FG and HOG |
| Indexing |
|
FG and HOG |
| Charting |
|
FG, HOG, JRM and WK |
| Mapping and interpretation |
|
JRM, HOG, WK and FG FG, HOG, JRM, WK, RC, AG and SM, including PPI input Team (ongoing and not fully reported in this output) |
Data from both phases were analysed using a thematic approach informed by Ritchie and Spencer. 80 Phase 1 data analysis was nearly complete before we moved into data collection in phase 2. As such, the findings from phase 1 provided the basis of initial interview schedules for the case studies and a platform for initiating explanation building.
We used an iterative and combined inductive and deductive approach to analysis, which aimed to build, over time and data collection episodes, an increasingly explanatory account of what facilitates MBCT implementation in the UK NHS.
Use of the framework approach
We used the phases of the framework approach in the following way within each phase.
Case study analysis
The framework approach that was applied to data analysis in phase 1 facilitated the development of a conceptual map (see Figure 2) that enabled us to move to phase 2 data collection and analysis in a purposeful way (i.e. it provided an opportunity to seek further explanation, in contrast to more description).
To create a ‘case summary’, information was gathered from interview data and then observations and documents were checked to confirm or refute (refutation rarely occurred) statements made in the interviews. This was done by reading and reviewing documents and field notes against the coding frameworks developed from interview data.
Consistent with the comparative case study, each case was viewed as ‘whole’, in that data were analysed within it before being considered across sites. A pattern-matching logic based on explanation building was used. This strategy allowed for an iterative process of analysis reflecting the variety of data sources, and the potential insight each could offer in meeting the study objectives.
Ethical issues
Permission was granted from a NHS Research Ethics Committee (reference number 13/SW/0226) in August 2013. Once ethical approval was granted, we sought approval through local research and development governance processes [National Institute for Health Research Co-ordinated System for gaining NHS Permission (CSP) reference 134133 – accessibility and implementation in UK services of an effective depression relapse programme: mindfulness-based cognitive therapy (ASPIRE)]. Principles of good practice were adhered to throughout the study.
Confidentiality and anonymity
Each participant was assigned a unique numerical identifier following the data collection episodes. To ensure anonymity and confidentiality, role descriptions (e.g. teacher, manager, commissioner or service user) have been used to describe participants in this report. To ensure anonymity we have also assigned each participant in phase 1 a number, and each case in phase 2 a name (see Table 5).
Chapter 3 Phase 1 findings
Introduction
Over the next three chapters we report the findings of this study. In this chapter we report on the findings from semistructured interviews with a sample of participants from a cross section of regions in the UK. This account is a description of stakeholders’ perceptions about the extent of accessibility to MBCT, and the factors that have both facilitated and hindered its implementation. In Chapter 4 we provide a high-level description of each case site, before moving on to a cross-case explanatory account of the different factors and features of the implementation stories participants recounted to us. Our intention in reporting our findings in this way is that we build up an increasingly rich and explanatory account of the data.
Sample
Participants in phase 1 were drawn from 40 NHS sites. The balance of participation across the UK regions is seen in Figure 2.
FIGURE 2.
Map of phase 1 sample. Contains Ordnance Survey data © Crown copyright and database right 2010.

As described in our funded protocol,72 we sampled to ensure a variation of perspectives about MBCT. With the overall aim to interview up to 70 people, we wanted to make sure that data were collected from at least one key informant per region. In the first wave of data collection we therefore collected data from champions who were either clinicians (n = 27 MBCT teachers) or clinicians with a management role (n = 20). Next, and to ensure representativeness across other stakeholder groups, we created a sampling pool of a further 91 candidates, which included 39 managers, 23 commissioners, 16 service users and 13 referrers. We then randomly sampled (as requested by the funder) across this participant pool and interviewed seven managers, four commissioners, five referrers and five service users. Our total sample for phase 1 was 68 participants. In the interests of not revealing the identity of participants, we reference the region [England (South, London, Midlands, North), Scotland, Northern Ireland, Wales] rather than the trust or health board name.
Findings
The findings are reported below using the overarching structure offered by the PARIHS framework: evidence, context and facilitation. Overall, reports from participants showed that access to MBCT was patchy, even within the same region. There were no discernible patterns in the accounts of people between the different regions or between different types of participants, but where there were differences these are noted. However, MBCT teachers shared more information about activities, facilitators of and barriers to getting MBCT used in practice as they had been at the forefront of implementation efforts and, as such, we refer to these participants as implementers in the narrative that follows.
Types of evidence
National Institute for Health and Care Excellence: brand/badge – making a case
Participants often made positive reference to the fact that MBCT is recommended within NICE guidance. Those in the position of championing MBCT stated that the fact that it appeared in NICE guidance was helpful for making the case for commissioning MBCT and/or for convincing chief executives that they should be providing it within their service and allocating resources to it. The majority of MBCT teachers identified that the NICE badge helped by giving credibility to their efforts to raise awareness of and to support implementing the intervention. The NICE badge had also been used to secure funding for training. As NICE guidance is ‘based on evidence’ (teacher, North) and associated with ‘excellence’ (manager, London), implementers said that quoting it gave them ‘ground to stand on’ (teacher, South) if questioned about implementation activities. Furthermore, it was perceived that the NICE badge had ‘opened the door’ (teacher, South) and helped to progress implementation:
I would say another facilitator is the NICE guidelines. I mean that really sort of just opened the door I would say. I think without . . . just having MBCT in the NICE guidelines, just creates a legitimacy in people’s minds that . . . I don’t think we or others could have got nearly as far with this, you know without that, and without the other research that’s you know mushrooming now in mindfulness, and that we can refer to.
Teacher, South
Evidence fit with patient and practice
Although the NICE badge was viewed positively to help make the case, the fact that MBCT was part of NICE guidance was also referred to as a ‘double edge sword’ (teacher, South). Participants expressed challenges with applying MBCT in strict accordance with the NICE recommendation(s). As such, practitioners were adapting and adopting MBCT in flexible ways:
I guess in terms of MBCT, we don’t focus specifically on relapsing depression, so we’ve kind of opened it up a little bit more, where we accepts referrals for anxiety disorders . . . we’ve had to move away from this sort of strict MBCT recurring depression, because . . . I don’t know if we get enough referrals for that.
Teacher, Scotland
Some teachers welcomed the specificity of the recommendation and were trying to remain ‘faithful to the NICE guidelines and to the evidence base, so that if we are questioned, we are stood on very solid ground’ (teacher, London). Additionally, clinicians were sometimes asked to apply MBCT to other populations not included in NICE recommendations, in these cases the guidance was used to defend decisions not to widen the criteria:
. . . and I have a sort of mindfulness operational policy document [. . .], and I guess I’m keeping it quite strict to the NICE guidance in that there’s lots of requests for clients to come who have other challenges or difficulties, but the service is quite clear, that we’re only offering it to people with recurrent depression.
Teacher, South
However, there were examples from implementers of widening the NICE-recommended criteria to make it accessible to the sort of patients they were routinely seeing. In reality practitioners reported seeing patients who were more complex than those who were ‘currently well and have had three or more episodes of depression’ so that, if they ‘stuck tightly to the NICE guidelines’ (teacher, South), there would be limited opportunity for using MBCT. The inclusion criteria were widened because participants saw ‘applicability beyond’ (teacher, South) what NICE guidance recommended:
. . . we didn’t really have many people in the services who would meet that criteria. But there was a starting BDI [Beck Depression Inventory], Beck depression score of around 19 as opposed to about 10 as I think it is in the kind of original trials that are in NICE. But still sort of mildly, sort of mildly getting towards moderately depressed. But as time went on in secondary care, the group we are running, and you start to think well I can see how this might be helpful . . . that’s just how then it started to expand if you like . . . because you begin to the see the applicability beyond that group, even though you’re moving away from NICE guidelines.
Teacher, Midlands
After seeing some benefits to a wider population than those referred to within NICE recommendations, some questioned the relevance of NICE guidance. There was also a question about whether or not the evidence underpinning the guidelines may be out of date, particularly in the context of research emerging about the relevance of MBCT to other populations (e.g. from teachers from North, South and London).
Clinical judgement
As well as the NICE guidance, participants who were actively implementing MBCT talked about needing to bring in other types of evidence from their practice to delivery, implementation and evaluation activities. Some questioned the process of how trials and guidance are developed, emphasising that their own clinical judgement was equally important to delivering and evaluating a service:
. . . a reality with randomised control trials and who gets picked . . . how they’re done and who pays for it, and then guidelines being written, and yet there’s many treatments or many developments that are not there in the guidelines that are useful; there’s a way of having clinical judgement and being able to say why it’s useful, justify your decision, justify inviting somebody to the group.
Teacher, Scotland
Client feedback
Participants also reported supplementing trial evidence with client feedback to help with tailoring of the service locally, and as evaluative information to improve provision:
. . . our course has evolved partly from feedback from the participants, and from the facilitators, on what has worked and what hasn’t, and it actually is tailored to the needs of the local population rather than to you know university studies that may not entirely be the same in terms of population as ours.
Teacher, Scotland
Although participants expressed some challenges with collating feedback, partly because of being constrained by resources, there was evidence that some had used such information systematically by collating feedback and presenting it in a way that could help with evaluation:
We have an evaluation at the end with each of the clients and what I’ve been able to do is collect their own personal feedback from their perspective and collate in a kind of graph and actually it’s quite interesting because I’d noticed particular themes that were rising from that feedback.
Teacher, Midlands
In contrast to relying on anecdotal feedback, participants from 40 sites (19 including English IAPT services) reported including the collection of standardised information from clients/patients. Standard measures included the Patient Health Questionnaire (PHQ-9) for depression and the Generalised Anxiety Disorder-7 (GAD-7) pre and post intervention. The Center for Outcomes Research (CORE) measures seemed to be prevalent in secondary care settings, and the Hospital Anxiety and Depression Scale (HADS) used mostly in Scottish sites (see Appendix 8 for examples of measures used).
Mindfulness-based cognitive therapy: the intervention
The following sections describe findings related to the acceptability, accessibility and adaption of MBCT.
Acceptability
Participants often referred to an awareness of ‘mindfulness’ within their organisation and more generally within the community, owing to the increasing media attention. However, there was a perception that there was less awareness of what MBCT is as an intervention. Teachers reported that they had experienced challenges in educating managers about MBCT and what it entailed, and some managers interviewed also stated that they were not aware of the full extent of formal training, supervision, personal commitment and practical needs of MBCT:
. . . there’s MBCT and then there’s mindfulness, and I guess mindfulness feels easier to talk about. I’m aware in terms of formal MBCT training, that’s not something I think we as a service has engaged in.
Manager, Wales
There were some examples of scepticism in the data whereby teachers reported that in trying to inform managers and colleagues about the intervention it had been perceived as a ‘bit of luxury’ (teacher, Scotland) because of its preventative nature, with doubts expressed about what it entails:
There are staff and managers who think that you know you do an 8-week group as a participant and then you’re off. You know, you read the Green Book and then you can teach it. So you know that attitude is a barrier, and then convincing those people that they need to do quite a bit more, can be a challenge, and that this is a therapeutic intervention, it’s not just a bit of sitting on a cushion.
Teacher, South
Data also showed that there was some scepticism among commissioners; for example, that MBCT was viewed as a little ‘alternative’ (teacher, South) and only going to be accepted by people with a ‘particular world view’ (teacher, Scotland).
The media reporting had also been seen as providing advantages as well as disadvantages in that more and more people were hearing about ‘mindfulness’ and were wanting ‘to ride along with the wave’ (teacher, Scotland). In contrast, some managers said they were hearing about ‘mindfulness’ being used across different settings, and growing perceptions about it being some sort of panacea:
. . . we need to be slightly careful about what it is and what it isn’t . . . at the moment you would almost think it was a panacea sometimes . . . any age group . . . from school children to older adults . . . almost any setting . . . from primary schools to prisons, to hospitals . . . almost any condition from psychosis to depression . . . Now I’m happy to believe that’s true, but there’s a sceptical side of me.
Manager, Scotland
Accessibility
The majority of individuals accessed MBCT service by being a patient who was already known to the service, and who had previous interventions such as CBT, so they were being referred on from within the service (e.g. teachers and managers, South, London and Scotland). Others got referred by their GP (teachers, Midlands and Scotland), and data show that increasingly trusts and health boards were accepting self-referrals. There were some examples in our data of reports of GPs being less likely to refer straight to a MBCT service; for example:
I have to say our greatest referrals have been through primary care. We did do road shows to GPs, who were very receptive, but as far as referrals go, really quite poor in directly referring.
Teacher, South
Following on from referral, many sites took steps to ensure that suitable people got access and that those being referred to the service were appropriate. Those steps included an assessment usually over the telephone and an orientation or introductory session (teachers from South, London, Midlands, North and Wales). Although it was reported that demand had increased in some sites, the amount of people who fulfilled the criteria was relatively small (teacher, North); therefore, the screening and assessing process was essential to ensure that the correct people got access. Where a thorough screening and assessment had been made, it was reported that it was less likely that people dropped out (teachers, South).
To ensure that the service was accessible, implementers reported being flexible in their delivery, such as putting on evening sessions for clients who worked during the day. Such flexibility had been important to service users:
. . . we did have to wait a bit because we did want it to be an evening group and they had to wait until there were enough people who would be doing that . . . making it accessible to people who are employed is really important . . . whereas medical appointments, employers can be flexible . . . but to have 8 weeks . . . and because it takes at least half a day because of the length of the session . . . very few employers are happy for someone to use their worktime.
Service user, London
Waiting times varied across sites, and sometimes varied within the same site; as such, some participants expressed that access was a bit of a ‘post code lottery’ (manager, Midlands; teachers, Scotland). As a result of some sites only having one or two members of staff running MBCT groups, patients could be waiting at least 2 months or sometimes longer if the service only ran one or two groups a year. Service users reported waiting a couple of weeks (North) to over 1 year (South).
. . . it was probably 3 or 4 months to starting the 8-week course, from self-referral basically, but then there was another sort of 3 months before that to find the information to know I could self-refer . . . and then it was another 3 or 4 months of the XXXX [county] experience . . . so from the decision to do something about it, to actually starting the course, it was definitely 12 months, possibly longer I would say.
Service user, South
To facilitate access to the intervention, some sites chose to use the intervention as a ‘well-being’ intervention rather than a ‘therapy’ so that it could be viewed as a self-help intervention rather than one related to mental health. This strategy had also been used in several sites where courses were being made available to staff, for example:
I think it’s kind of just by chance we have taken it as being . . . sort of being pushed as a staff well-being thing. I think that’s been quite helpful because it gets, we’re getting people who are coming along and its part of them, you know it’s their own practice, rather than necessarily selling it as something you do to patients. So I think we’re getting people who are on board with their personal practice, rather than coming along just to be facilitators. That’s been quite helpful.
Teacher, Scotland
Adaptation
As outlined earlier, MBCT had often been adapted from what is stated within NICE guidance to reflect the local service needs. Some sites had an open to everyone approach in cases where it was felt that the client would benefit. Practitioners were delivering the intervention to different populations such as those with chronic pain, anxiety or stress and also adapting to include clients who were presenting as not currently well (teachers, South and London). Some teachers reported that if patients were in partial recovery and were well enough to engage in the course, then MBCT was offered and that if they adhered to the NICE recommendation many patients would not be able to access the service and groups would not be filled.
We’re much more open with who comes onto the course, so we’re not strictly seeing people who have had three or more episodes of depression and in recovery now. We have quite a mix, so we will have people who are still feeling somewhat depressed, but they might have had a CBT intervention. We’ve had people who have had anxiety problems and they’ve had interventions in the service. We have people who are in recovery following intervention, and we have people who are non-clinical as well.
Teacher, London
There were also examples of implementers branching out to diagnoses other than depression and anxiety, and tailoring the intervention to individuals, rather than at a group of people with the same diagnosis (teachers and managers, South and Midlands). This was done partially because they see the potential benefit of the intervention to these groups (teacher, Northern Ireland) and also because of pressures from the service to include more people (teachers, Northern Ireland and Midlands) and to ‘relieve some of the waiting times for the other services as well’ (teacher, Scotland).
Our data show that there were a number of models of delivery, from pure MBCT, as stated in NICE guidance, to hybrid MBCT/mindfulness-based stress reduction (MBSR) or MBCT/Compassionate Minds models. 81 Some practitioners reported that having the flexibility to switch from one model to the other, depending on their client group, was important and enabled responsiveness to client and local needs.
Context
Data show that context is a potentially powerful moderator of whether or not MBCT was available and accessible. The following sections identify the key contextual issues that emerged from discussions with stakeholders from across the UK regions.
Culture
Fit of mindfulness-based cognitive therapy in the current NHS
Pace
As described by participants, MBCT is not an intervention that provides ‘a quick fix’ (teachers, Wales). As such, it contrasts with the pace of health services in the UK, which resulted in a number of challenges reported by participants. Practitioners stated that within a pressurised, fast-moving NHS environment it was:
. . . quite a struggle . . . to deliver the programme in a mindful way, so like all the administration around it and so on, because the culture of IAPT and primary care therapy . . . tends to be therapy on roller skates, that’s the whole culture, its bums on seats, quickly in, quickly out, have we got to recovery, off we go, quick team meeting, you know, rush, rush, rush.
Teacher, South
Furthermore, it was reported that the pace of the environment presented challenges to upholding the integrity of the approach, with some feeling pressure to deliver the intervention in fewer than eight sessions, running larger and more diverse groups with less training and supervision, described by this participant as:
. . . a real tension between integrity and fast implementation. It was quite difficult to hold the line there, and really not be drawn into providing a level of service that just didn’t seem appropriate.
Teacher, Midlands
Medical model
In contrast to many interventions delivered within health services, MBCT is concerned with well-being ‘rather than about medicine, whereas the NHS mostly is about medical treatment . . .’ (teacher, South). Some accounts from commissioners also described the predominance of biomedical approaches:
GPs are interesting . . . they’re like many doctors, more inclined to prescribe medication than they are to recommend therapy. The NICE guidance points out that a combination of both talking therapy and prescription is likely to get the most sustained and reliable outcome, but they seem unwilling to do both.
Commissioner, South
A focus on physical health, the need for recovery, and a lack of understanding or awareness of the underpinnings of MBCT, resulted in frustration for some practitioners:
. . . the medics still don’t get it. [. . .] it’s not just another treatment that helps people cope with pain . . . Because you’re working in a context that’s based on a different personal physical paradigm, and they’re not even aware that they’re based on a paradigm . . . ‘oh can you give me some CDs [compact discs] so I can give them out to patients and use them like relaxation tapes’.
Teacher, South
Competing priorities
Commissioners described tensions between finances, in general ‘most things that we do is around potential saving that can be made . . .’ (teacher, London), and for mental health services in particular:
I’m trying to get more mental health funding from the CCG [Clinical Commissioning Group] because we feel that it’s underfunded . . . but of course that is a big challenge because of the big acute trusts swallowing up all the resources.
Referrer, London
Furthermore, a tension was described between the need to deliver outcomes at pace:
We’re required to move at a pace that’s more challenging and deliver savings that are more immediate, and I think that creates a conflict between us as commissioners and the provider.
Commissioner, South
Some accounts from managers also highlighted the difficulty of managing competing pressures of throughput and quality:
. . . the commissioners are only interested in whether we meet our targets or not . . . they are interested in numbers entering treatment and moving to recovery figures . . . they’re not really interested in the quality, as long as we get our 50% moving to recovery.
Manager, Midlands
It is possible that the tensions described by commissioners and managers led to a feeling by some practitioners that MBCT was not at the forefront of priorities:
I think that sometimes sort of the MBCT stuff gets pushed to the background sometimes. That’s certainly I think been the issue, not just with the therapists but the sort of more senior staff within the service.
Teacher, Midlands
Change in the NHS
Frequent changes, organisational complexity, ‘tradition’ and ‘hierarchies’ were mentioned by participants as a challenge for changing services of any kind, and for implementing MBCT in particular. Over half of our sample described the NHS to be in a constant state of flux; for example:
. . . a massive service structure as well, so change in their service structure, and we’re going through a period of flux of it, I think for them at the moment it’s not their priority to think about it.
Teacher, South
The type of changes that were noted by participants varied, but challenges included a ‘muddle’ of services working in isolation from each other within trusts (teacher, South), changes to regional service boundaries (manager, London), attempts to integrate service pathways via ‘internal reorganisation’ (teacher, South) whole teams being moved across trusts in an ‘amalgamation of services’ (teacher, South), primary care services being merged into IAPT since 2009 (teacher, South; manager, London) with some integrating MBCT from the start and some not.
Although described as a challenging implementation context, some also recognised the potential in this by, for example, seeing an opportunity to ‘use the chaos to embed MBCT’ (teacher, South) and enabling implementation to go forward ‘under the radar’ (teacher, South).
Resources
Our data show that MBCT work was frequently informally resourced. That is to say, it depended on the enthusiasm and commitment of individual people and the goodwill of senior managers. Frequently, it appeared to be not well embedded in budgets or in staff or organisational objectives. This meant that it was consistently at risk and that improvements in delivery achieved within a trust could easily be lost due to changes in personnel or changes in budgeting. The following sections describe findings that relate to different sorts of resources.
Human resources
Participants described a lack of dedicated human resource to deliver MBCT. In areas where MBCT was being implemented, implementers tended to be lone champions. Generally, a lack of qualified teachers was described, and where there were fully trained and accredited teachers it was rare that they were dedicated to delivering MBCT; these individuals were developing MBCT services in addition to their existing role and responsibilities.
Staffing and having enough qualified teachers was described as a ‘continual headache’ (teacher, South) in the majority of regions. It was reported that in sites where there was only one qualified teacher, champions relied on support to co-facilitate from individuals who had not been trained. Furthermore, the amount of human resources could vary within one organisation; for example, one region had three or four groups per year, but in other parts of the same trust groups were not running because of a lack of qualified teachers. This resulted in potentially fragile services where there was a perception that ‘if I was to leave tomorrow, essentially that mindfulness service would die with me’ (teacher, South).
In addition to teaching and delivery resource, practitioners delivering MBCT also reported that administration support was challenging, with many relying on goodwill: ‘. . . we have to buy her an awful lot of chocolate’, with none, or ‘little admin provision’ (teacher, Scotland).
Financial
The costs associated with setting up a MBCT service were acknowledged by many participants we spoke to: ‘if you want a good solid service that is delivered because it’s based in evidence . . . yeah it costs’ (teacher, South). This included the cost of training and continued supervision. This cost was set within the context of what was described by some commissioners, as a greater challenge of funding for mental health services and of under-resourcing more generally for health services:
. . . (what’s most pressing is) trying to find ways of increasing investment in mental health services because we know that generally they are under-resourced . . . and working within a very cash-limited environment.
Commissioner, South
This included balancing resources across different psychological interventions; for example, ‘carving out this job for this MBCT practitioner, meant there was less resource for our conventional services’ (teacher, London). As such, cost was described as a barrier to the implementation of MBCT.
The consequences of these funding challenges were that often practitioners had invested their own money in developing services by, for example, delivering it in their own time, paying for their own training and ongoing supervision, and paying for venues. Practitioners reported that they had made this investment by choice because of their interest and personal commitment to MBCT.
Time
Time manifested as an important resource factor for implementation. Frequently practitioners described the relationship between funding, staffing and time as a major implementation challenge because there was a lack of capacity and capability to be able to set up and maintain a new service. As such, they spoke about feeling the pressure to deliver something as quickly as possible with no funding and, as a consequence, had invested their ‘personal time to get it up and running’ (teacher, South). Additionally, there had been challenges, with some implementers being able to ring-fence the time for attending training sessions, some being able to take time ‘in lieu’ and others working in their own time because they were unable to secure managers’ agreement.
As described earlier, the need to deliver quickly was in conflict with a therapy that requires more than attendance at a short training course. Additionally, those delivering services described that it took time to embed a new MBCT service because of the need to develop appropriate links and raise awareness with referrers. Practitioners also described the nature of the intervention and time required to deliver MBCT groups, in contrast to other group interventions:
. . . the difference between running a mindfulness group and say running one of our stress management or move management groups, which are much, much quicker to prepare and deliver.
Teacher, South
Time was also described as a barrier to getting started or making a case for MBCT: ‘we haven’t put much effort into that, because it takes too much time [. . .] it’s just unbearably time consuming to get money’ (teacher, London). Additionally, participants described time as a barrier to conducting evaluative activity:
. . . a full time clinician has to see 25 patients a week . . . It doesn’t leave you much time to do anything else . . . that’s another reason why we’ve not been able to do any evaluation and audit of our course.
Teacher, London
Practical
Many implementers talked about practical resources being the major barrier to delivering MBCT groups. Adequate physical space, in the context of many NHS organisations reducing costs by selling buildings, a lack of money to hire rooms and challenges with finding appropriate rooms (for delivering the intervention), was a challenge. There were a number of consequences of a lack of appropriate space related to intervention accessibility and delivery (Table 3 shows a summary). In contrast, those services that had more developed services did have dedicated and free access to conduct group treatments.
| Challenge | Effect |
|---|---|
| Big enough | . . . it’s not big enough to have mats on the floor. So we do very little movement practice . . .Teacher, London |
| Conducive | Finding a room that can hold 15 people, most of them lying down undisturbed, a big challenge, a big challenge . . .Teacher, South |
| . . . we hadn’t been told that the only access to get to the toilet meant you had to walk through our group, you know, oh dear, so we were in the middle of the body scan the first week and suddenly the door opens and two people walk through . . .Teacher, South | |
| Accessibility: timing | I can’t do a group in the daytime because I can’t find the appropriate room for it . . .Teacher, Scotland |
Additionally, other resource challenges for implementers related to materials:
. . . just simple things like photocopying, you know getting CDs [compact discs] and stuff like that, you know. It’s those sorts of added costs in terms of resource that aren’t really factored in unfortunately.
Teacher, Midlands
Other practical resources such as mats, cushions, compact discs (CDs), etc., were often provided by the implementers as there was no funding for such equipment from trusts or health boards.
Money, money, money, money, oh my god, one year, in order to get CDs for the course, I had to dig up all the strawberry plants out of my garden, and sell them, and colleagues helped, and we had a cake and plant sale, and raised £400 and then bought our CDs for the courses. Getting mats, I’ve had to beg and borrow every March from senior management.
Teacher, North
Facilitation
Champions and championing
Implementation of MBCT appeared to be driven by ‘passionate’ champions who were ‘willing to go the extra mile’ (teacher, South), who invested a lot of personal time and effort into making it happen and who (it was reported) would ‘probably do it for free’ if they had to (teacher, North). As described above, implementers made personal and financial commitments to initiating and sustaining services. MBCT was reported to be a big part of their personal and professional life (teacher, South) and champions often talked about ‘embodying’ mindfulness (teachers, South and Midlands), and the importance of starting off with a personal practice (teachers, Midlands and North):
I believe in mindfulness, and I do the same thing whether it’s my NHS work or my private work. The message is basically the same . . . I’m kind of encouraging people to set up the practice and then practise themselves . . . the message is please don’t use it, unless you do it yourselves.
Teacher, North
Most implementers often worked alone in championing the intervention and, therefore, services grew from the ground up through the work of MBCT practitioner/teachers. This left services fragile with concerns that losing individuals would lead to services being stopped:
. . . the champion’s stepped aside now she’s still in the background but I have a worry and a concern when the champion’s moved ’cos we’re kind of I’ve only got 2 years to go before retirement my colleague is in that place as well so I have a worry about the loss of the service yeah.
Teacher, Midlands
Data show that these ‘champions’ had particular skills in pushing and driving implementation. Their stories show that they were constantly spreading the word and talking to others about how to implement and how to make MBCT more accessible. Additionally, the position or seniority of a champion was perceived to make a difference. For example, when the drive and enthusiasm came from GPs (teachers, Midlands, North and Scotland) or from a senior manager (teachers, South, Midlands and London) it helped to keep MBCT on the agenda at senior board meetings. Seniority also created and element of credibility, which had been facilitative:
. . . we created a new job that is explicitly the specialist care pathway lead for MBCT . . . it’s easier for me to get these things done because of the position I hold and it was easier for me to create a post and sort of empower this individual to do this project.
Manager, London
There were also examples of service users becoming champions and playing an important role in implementation activities, for example adapting course materials, setting up a service user website, co-facilitating groups or talking about their experiences at taster sessions.
Then this year or last year, October, November, we went on this time’s training course with XXXX [person] running it, and a guy called XXXX [person], another therapist, but were a lot more involved this time, because we weren’t participants. We told stories like I’m more or less telling you now, and at this time I’d made a list of hints and tips of things I’d learnt about leading a practice, which I sent to XXXX [person], and she said oh yeah, do a PowerPoint[® Microsoft Corporation, Redmond, WA, USA].
Service user, North
Although many participants reported that they were ‘lone’ champions within their service, being involved in a network of champions and being able to connect with other peers, from within and outside their service, who were ‘hugely enthusiastic and interested in mindfulness’ (teacher, South) had been helpful. Networks had been opportunities to share ideas and feedback so that they did not feel alone. Implementers reported creating new networks around them through graduate groups, local special interest groups, drop-in sessions and online peer support.
Strategies
The data showed us that implementation was mostly happening through ‘bottom-up’ initiatives and strategies, with some examples of a mixture of ‘bottom up’ and ‘top down’. This section describes factors that both hindered implementation and the strategies used to support or facilitate implementation.
Bottom up
Raising awareness
Earlier we described that knowledge and awareness of MBCT as an intervention varied within trusts. A frequently reported strategy for starting implementation activities was to raise awareness about what the intervention entailed. Practitioners ran introductory days, conferences, workshops and lunch time sessions where they introduced the ‘background and theory to MBCT, what it is’, why they do it and how it works. As such, attendees got to experience what the client would experience, which would then give them a better understanding of it as an intervention and in turn, more and appropriate referrals:
So people’s awareness of the therapy has been a bit of a barrier, but that’s shifting over time, again the more people who come to the staff groups, the more they get the approach and the more referrals you get. It has been a very, that’s been very clearly evidenced in the staff groups, high number of people from XXXX attending and we get the most referrals.
Teacher, London
To support the delivery of the workshops and taster sessions, implementers had invited individuals who could have an influence, or create a sense of credibility, for example a senior colleague who was willing to talk about how ‘mindfulness is now very much accepted within the NHS’:
I mean last year having XXXX [person] over, and having the Chief Scientific Officer for XXXX [country] speaking at the conference, is in a way a sign that mindfulness now is very much accepted within the NHS. I think it was probably a struggle at times to be accepted within a medical system because it doesn’t quite fit within a medical model, mindfulness, and I suppose there’s always that worry that it’s kind of associated with Buddhism and therefore, ‘oh is this acceptable?’.
Teacher, Scotland
Others had invited service users to share their real-life experience, and invited figureheads such as Mark Williams to be involved in training (teacher, North).
Practitioners also described constantly having conversations (teacher, London) and trying to ‘keep the flame burning, and continue to educate’ and ‘sell MBCT to the senior managers’ (teacher, Midlands) to align with service’s priorities. In contrast, one teacher reported that they found ‘convincing’ senior staff difficult and time-consuming, and that they would rather prioritise the time with mindfulness participants (teacher, North).
At an organisational level, some trusts/boards were raising awareness through disseminating leaflets, creating newsletters and building websites to advertise the service they are providing. One trust had web pages dedicated to help keep people informed and linked in, and included useful links and downloads to help patients and staff continue with practice. They had a web page dedicated to staff and another dedicated to service users, which was designed and maintained by a service user volunteer (North):
. . . we have two websites, one for service users, and one for teachers. Teachers obviously has a lot more detailed stuff on like practices and scripts and PDF and PowerPoint presentations that I’ve made. The service user one is mainly practices, but a lot of photos that I’ve found and things like that off YouTube [YouTube, LLC, San Bruno, CA, USA], video links, booklets, reunions, websites, and were using it now in sessions instead of CDs, were just giving a website link and they can download that practice for that week when they need it.
Service user, North
Relationships
Another strategy that implementers reported using was in building ‘good relationships’ (teacher, South) and ‘key alliances’ (teachers, Midlands) with senior management to enable good communication between them and to facilitate a shared understanding about priorities and service delivery, because if they were ‘on board’ they were influential decision-makers:
I think you need key people at all levels. So you need to have some key teachers, you need to have some key people in NHS management; you need to have some key people in commissioners. I don’t think you necessarily need everyone on board, but you need to have a few people that can help steer decisions and budgets . . . So I think you know there’s a long history of good relationship that allowed it to come to fruition.
Teacher, South
Some implementers had also been building relationships and collaborating with neighbouring universities to build on evidence, access training and supervision, help with evaluating services through doctor of philosophy (PhD) and master’s projects, and collaborating on new research into using MBCT in different populations. Other than universities, practitioners were building relationships with other organisations in order to help facilitate activities. One clinician had made connections with a third sector organisation in order to get sponsorship to complete their training (South) and another clinician had got in touch with a local venue to offer free spaces on their course to their staff if they were able to use the venue for free (Scotland).
Building a case
There were a number of examples of implementers writing business proposals/cases to share with management (Midlands and North). These included different strategies, for example developing their own training pathways and proposing that in-house training would be more cost-effective (Midlands), and developing an ‘apprenticeship model’ (South). Additionally, some implementers had been piloting the service and then using these to demonstrate impact and apply for funding (South, Midlands and Scotland). As described earlier, many implementers were also evaluating their service and using those figures to demonstrate impact to senior managers (South and Scotland).
Controlling scope and scale of implementation
Although some implementers were doing all of the above activities to build the profile and spread of MBCT as widely as possible, others had intentionally kept the growth and development of the service deliberately slow and ‘undercover’ (teachers, South). One said that they did not want to overstretch as ‘they already had a steady trickle so they didn’t want to push it any bigger as they wouldn’t be able to cope with the demand’ (teacher, South).
There was some evidence of working under the radar without management knowing about it so that they had a chance to develop skills before provision became formal. One person reported that it had been challenging to find the balance between ‘pushing it forward’ while also keeping the integrity of the intervention. In addition, keeping MBCT provision small meant for one person they were able to stay ‘hidden’ while ‘nobody is looking’ at them, and were then able to ‘duck a lot of the pressures’ (teacher, South).
Quality of teaching and provision
Assuring and sustaining the quality of teaching while rolling out services quickly and maintaining quality and integrity was a balance:
It’s a difficult one isn’t it because it’s a bit supply and demand. I suppose the demand for mindfulness has mushroomed, but the amount of people that fulfil the criteria for ethical practice is relatively small, and it’s how you can match supply and demand in that way . . .
Teacher, North
What participants referred to as training varied. Some training included graduating from university-based study and training, and others had been on a training pathway over an 18- to 24-month period. Some referred to other opportunities such as 5-day teacher training retreats (South and Midlands) to come out as fully qualified MBCT teachers, and going through an 8-week course as a participant, which as described would not meet the current minimum training and practice guidelines. There was also some concern expressed by teachers that buying the Green Book16 and then running mindfulness interventions was all that was expected. Some sites had actively discouraged such developments, by using national best practice guidelines, and by setting up training and supervision pathways.
The quality of teaching was also confounded by the fact that there are currently no official accreditation systems in place. In many accounts, practitioners were intent to abide by national teaching guidelines and explained that these are not a ‘set of techniques that you kind of pick off the shelf’ (teacher, South). Referred to by one participant as: ‘Purist theoretical model v. practical realities’ (teacher, South), there was also a tension expressed by managers in wanting to implement MBCT while adhering to quality standards and minimising costs:
It feels like a challenge in terms of mass roll out. I also wrestle a bit with this issue of professional standards in term of what you need in order to be able to discuss or deliver an idea or a concept . . . So I guess the point I’m making is about standards of proficiency, and that slightly worrying thing as a service lead, where you want to make a therapeutic idea or concept or modality as widely available as possible, but you also don’t want to fall short of the standards or training that are required, and that feels like a really live tension for me.
Manager, Wales
Some managers also expressed the challenge of understanding that those delivering services must practise mindfulness themselves and how this would be different from other treatment modalities, putting MBCT ‘in a very different league to other treatments’ (manager, South).
Service user interviewees were asked how they would know whether or not the MBCT practitioner was fully qualified. Some said that they would expect that in the NHS you would assume they abide by professional standards, but other accounts acknowledged that there were ‘blurry lines’ and ‘grey areas’ (teacher, South), and that they would not be able to tell (teachers, North and London).
Supervision
Supervision seemed to be a key element of maintaining and ensuring good quality service delivery. Often this happened informally from peer to peer, and in some cases using video and online forums. External supervision also functioned as an important aspect of implementation, by providing personal support, contact with national networks and guidance about developing local services based on experienced supervisors.
In sites with more embedded training pathways, supervision was part of maintaining the standards of service delivery:
. . . if you’re embedding something into the NHS it’s important to get all the clinical governance in place and all the standards in place that will protect it but also being very very mindful that we’re not going to dilute things; that we want things to be as authentic as possible and the other way to do that is to fit in with the standards and ensure that we’re supporting people through supervision.
Teacher, Midlands
Maintaining and sustaining
One of the ways many implementers maintained the service was by keeping staff and current and previous service users linked in, and providing support for them to maintain their practice. Implementers organised top-up days, drop-in sessions, silent meditation days and one had developed a special interest group to get more staff interested so that if one or two of the champions or trained staff left the service, there would be interest from others to keep it going.
Top down
In only a few examples, MBCT had been facilitated through a steer from board or commissioning levels, and where there was evidence of commitment and drive coming from senior levels of the organisation:
We’ve got lots of senior people I suppose who are right at the top of the organisation who are keen on it and I think that’s very significant.
Teacher, South
In one region in particular funding had been dedicated through a national programme to fund staff to do the teacher training (Scotland). In a different region and site, in a bid to reduce waiting times and reach targets, there was a steer from management level that they should all commit to doing groups and they included MBCT as one of the groups (teacher, Midlands). In another two sites, a dedicated role had been put in place to develop MBCT within the service; for example:
So my role is, my job title is Mindfulness Based Cognitive Therapy Clinical Lead for XXXX [trust]. So that involves overseeing developments within our health trust, which is a mixture of primary, involves secondary care and also IAPT services. So overseeing developments in terms of mindfulness based cognitive therapy across those areas. That involves training staff to deliver MBCT across a whole range of clinical areas, and then providing supervision, and sort of co-ordinating the delivery of MBCT groups within services.
Teacher, Midlands
Other implementers had referred to a lack of top-down push, and that leadership from higher levels of the organisation was hard to achieve. Without leadership from the top, traction was hard to achieve:
So essentially what you have is a lot of very busy overworked service leads, doing their best to think about both the strategy in their own organisations, but also know about how that might be made consistent . . . but all of us will respond to influences and dynamics and tendencies within our own organisation, and those don’t quite match . . . we haven’t had the kind of leadership that they’ve had in XXXX [country] to get that really clear consistent approach.
Manager, Wales
Summary
Findings from phase 1 show that accessibility to, and implementation of, MBCT is patchy across the UK, including within regions. Participants’ accounts came together to create a picture of MBCT implementation comprising of various components. The drive and commitment of implementers who, from the ground up, took on implementation activities and were met with more or less commitment from the top down. Their stories provided an account of their implementation journeys. NICE-badged evidence appeared to be both a catalyst (as a selling point) and restraint (target patient group). As such, different forms of evidence seemed to inform the adaptation and implementation of MBCT. The context comprised a number of features including resources and culture-mediated implementation by creating more or less favourable conditions for the intervention and for implementers’ activities. Stakeholders’ receptiveness, engagement and buy-in also influenced the potential of MBCT implementation.
These findings facilitated the development of a provisional conceptual map (Figure 3), which supported us in making the transition to phase 2. Phase 1 was concerned with description and phase 2 aimed for explanation. As such, the provisional map provided a way to design data collection tools and orient thinking in initial data analysis activity. This supported phase 2 data collection in being as rich as possible in terms of developing an in-depth explanatory account.
FIGURE 3.
Provisional conceptual map of MBCT implementation.
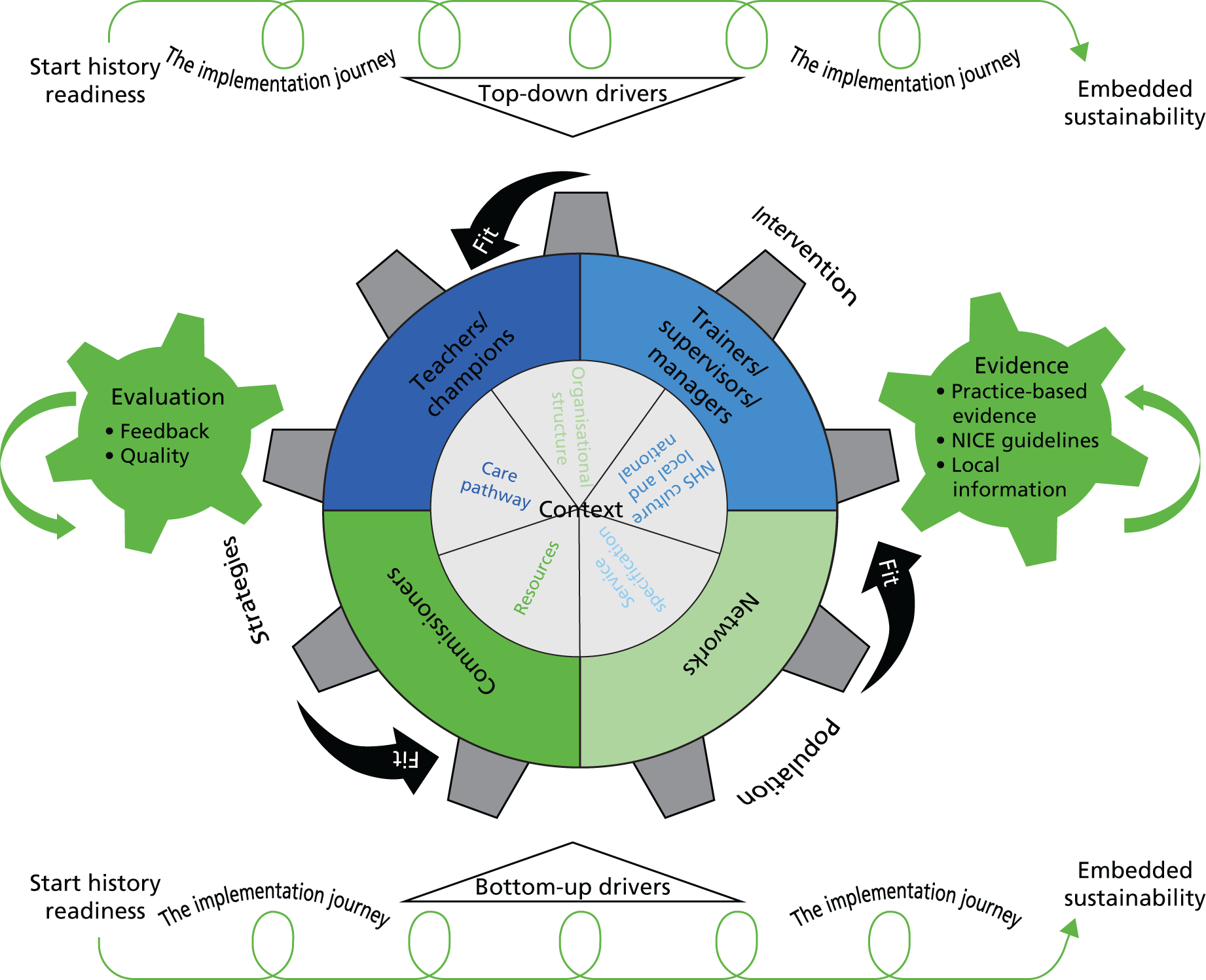
Chapter 4 Phase 2 findings: case study summaries
Introduction
In Chapters 4 and 5 we move from describing MBCT implementation in the NHS to developing an explanatory framework through case studies. In this chapter we first report the 10 case studies in the form of summaries (see Table 5) before moving to developing an explanatory framework in Chapter 5.
The case study summaries include some detail about the context of the site, an overview of MBCT delivery and training, and a timeline of implementation activities and events. The cases were purposively selected (see Chapter 2, Methods) to represent different levels of MBCT provision along a spectrum of embeddedness (see Table 4 for a description of embeddedness) and to represent provision across the UK. We sampled four cases where provision was embedded, four cases where provision was judged to be partially embedded and two cases that had no or scarce provision (see Table 6 for a description of each site’s level of provision). The criteria in Table 4 were used to sample and gain access to sites. Throughout the study it became clear that embeddedness was a challenging construct to define.
| Level of provision | Description |
|---|---|
| Embedded | Key features of best practice are present. For example:
|
| Partial | Absence of a compelling organisational strategy for implementation, MBCT teachers are working in isolation or the organisation has an explicit strategy but is at an early stage in implementing it |
| No or scarce | Absence of any MBCT provision free at the point of delivery or where delivery is partially or wholly funded by charging patients |
Case summaries
In the following we first provide case study names, a headline descriptor for each of the sites (Table 5), and outline the degree of perceived embeddedness for each case study (Table 6). In reality, when we entered the case studies, the embeddedness criteria were manifest in variable ways and contexts fluctuated during the life of the study. For example, one site (Elm) that had been identified as embedded experienced some challenges that resulted in withdrawal of MBCT provision. The remainder of this chapter offers a high-level summary of each of the 10 case studies under the headings of overview, context, and training and service delivery. These descriptions provide some context for the explanations in Chapter 5.
| Site label | Headline description |
|---|---|
| Oak | An accumulation of activities by a combination of stakeholders in a supportive context |
| Pine | All aboard: clinical, business and research elements coming together with the same agenda |
| Elm | Talents and perils of a single, primary implementer |
| Mangrove | Multiple implementers struggling to gain traction in a vast woodland |
| Bamboo | Fierce commitment to public services drives innovation and development on multiple fronts |
| Birch | Teething problems and turnover: getting there nonetheless |
| Hazel | A case of many trees within a large forest of competing priorities |
| Juniper | Volunteerism keeping it growing |
| Beech | Persevering through challenges and changes |
| Wisteria | Trying to find opportunities and developing in the midst of change and uncertainty |
| Level of embeddedness | Site rationale |
|---|---|
| Embedded MBCT implementation Key features of best practice are present. For example:
|
Oak
|
Pine
|
|
Elm
|
|
Mangrove
|
|
| Partial MBCT implementation Absence of a compelling organisational strategy for implementation, MBCT teachers are working in isolation or the organisation has an explicit strategy but is at an early stage in implementing it |
Bamboo
|
Birch
|
|
Hazel
|
|
Juniper
|
|
| No or scarce MBCT implementation Absence of any MBCT provision free at the point of delivery or where delivery is partially or wholly funded by charging patients |
Beech
|
Wisteria
|
Sample
Across the 10 case studies, we interviewed 127 participants and observed 16 events (which included supervision, special interest groups, service user sessions and teacher training sessions, and various meetings). Table 7 shows a breakdown of within-site data collection activity.
| Site | Total interviews | Teachers | Managers | Referrer/GP/commissioner | Service users | Observations |
|---|---|---|---|---|---|---|
| Elm | 20 | 6 | 6 | 2 | 6 | 7 |
| Pine | 17 | 5 | 8 | 2 | 2 | 2 |
| Oak | 20 | 6 | 9 | 2 | 3 | 4 |
| Mangrove | 7 | 3 | 2 | 2 | – | – |
| Beech | 9 | 4 | 4 | 1 | – | 1 |
| Juniper | 10 | 6 | 3 | – | 1 | – |
| Bamboo | 14 | 7 | 3 | 4 | – | 1 |
| Birch | 11 | 7 | 4 | – | – | 1 |
| Wisteria | 7 | 3 | 3 | – | 1 | – |
| Hazel | 12 | 7 | 4 | 1 | – | – |
| Total | 127 | 54 | 46 | 14 | 13 | 16 |
We also collected documents such as strategy papers, proposals, business plans and anything else that would help us understand the service and how they got to the point where they were (at the time of data collection) with respect to MBCT implementation (see Appendix 5 for a document list).
Case summaries
Oak
Overview
Oak had developed a strong network of implementers across all levels of the organisation over a 10-year period (Figure 4 shows a timeline of key junctures). Implementers made use of and developed facilitative contextual factors, including a supportive trust board and chief executive, and widespread grassroots interest in mindfulness from staff. Engaging staff through MBCT classes to promote staff well-being seemed to be key. Implementation was across services [adult, Child and Adolescent Mental Health Services (CAMHS) and recovery college] and levels of care (primary, secondary and tertiary). The development of an embedded training pathway and governance structure in year four, and the establishment of a Centre of Mindfulness in year six were key junctures.
FIGURE 4.
Oak timeline. CAMHS, Child and Adolescent Mental Health Services; CEO, chief executive officer.
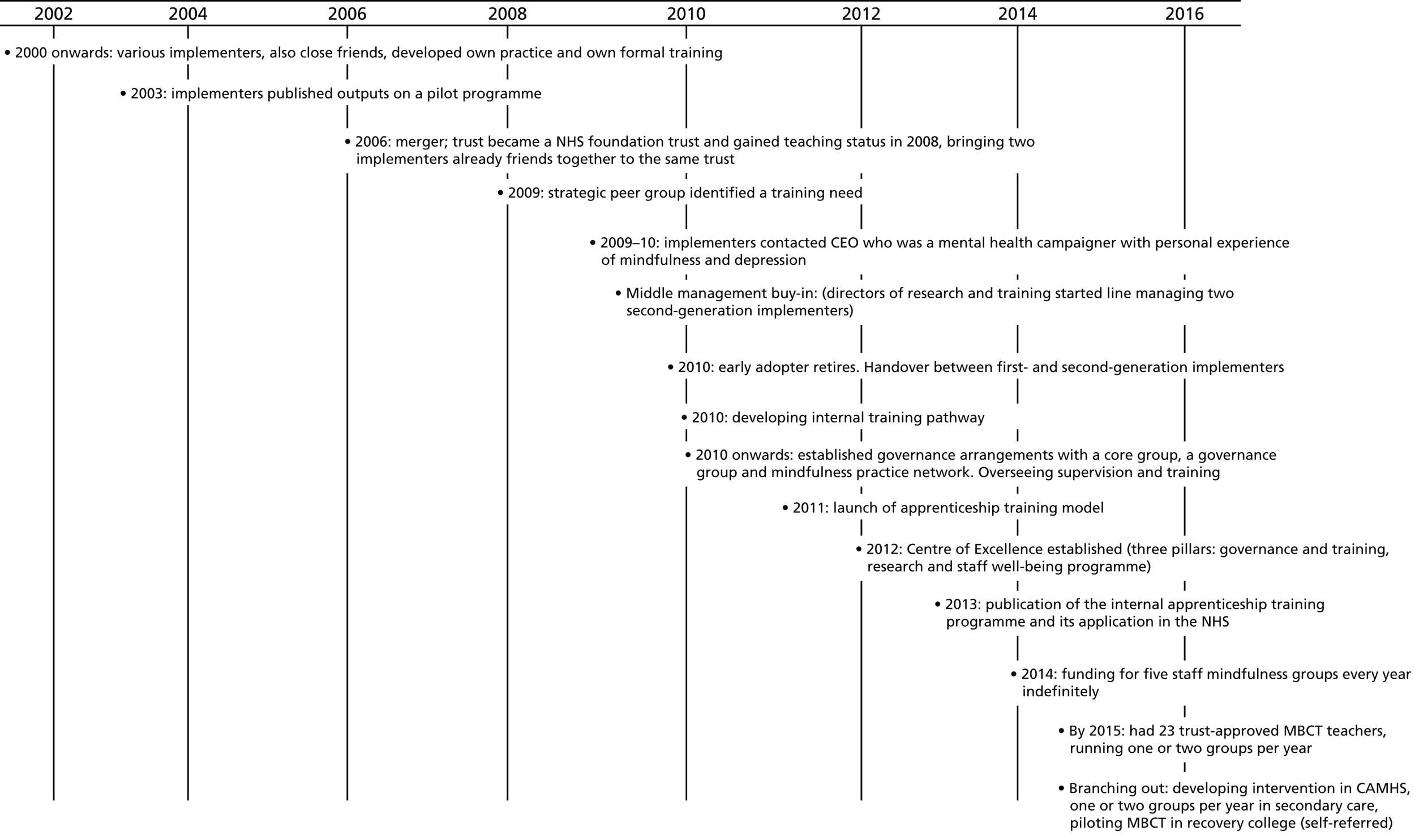
Context
This health-care organisation was established in 2006 and became an NHS foundation trust with teaching status in 2008. It provided mental health, learning disability and substance misuse services to a population of around 1.6 million people within a mix of urban and large rural areas across three local authorities. The trust merger in 2006 had implications for implementation as two early adopters located in different parts of the previously separate trusts were readily connected and had gradually built a reputation for mindfulness work since 2001. This also coincided with the national IAPT programme implemented in 2009, and the founding chief executive officer (CEO) being keen to champion MBCT.
Training and service provision
The main implementer had independently taken their training to teacher training retreat level 3 and regularly self-funded external supervision. The trust had established over the years a foundation teacher training programme with a 1-year supervised training pathway (including, among other elements, weekly supervision, eight ‘practice-ship’ modules, monthly seminars and trainees co-running MBCT with experienced teachers – especially in staff groups). This teacher training had been enabled through two teacher trainers who had been trained by the Centre for Mindfulness Research and Practice. They had a lot of experience in continuing professional development and they released a publication about their training pathway and its potential for wider application in the NHS. A hybrid of MBSR and MBCT was provided in both primary and secondary care settings. By the nature of provision in both primary and secondary care, services were provided to a mix of various populations outside the NICE remit, as well as being offered in many other services and including staff groups. By the time of our visit, this site had 23 trust-approved teachers (12 in secondary care, the rest in primary care and CAMHS).
There were an average of five staff mindfulness groups per year running for staff well-being (11 in the previous year), and the comprehensive research programme with numerous research publications focusing on the implementation of adapted mindfulness interventions with groups not traditionally offered MBCT.
Pine
Overview
In Pine there was a team including the local collaborator, clinical lead, senior academics as well as middle and senior management, who took a business-minded approach to implementation. A core group of two or three key implementers worked together on the implementation agenda, which included developing a range of implementation documents and activities in order to achieve a sustainable service. This included audit reports, strategy and governance papers for the training pathway (2010) business plans and strategy papers for IAPT and secondary care (around 2010–11), a CEO mission statement (2011), biannual reports since 2013, governance and operating guidelines (2013–14), values and strategy papers produced (2014), as well as sharing best practice through national networks since 2014 (Figure 5 shows a timeline of these key junctures).
FIGURE 5.
Pine timeline. APPG, All Party Parliamentary Group; LC, local collaborator; LD, learning disability; TTR2, teacher training retreat 2.
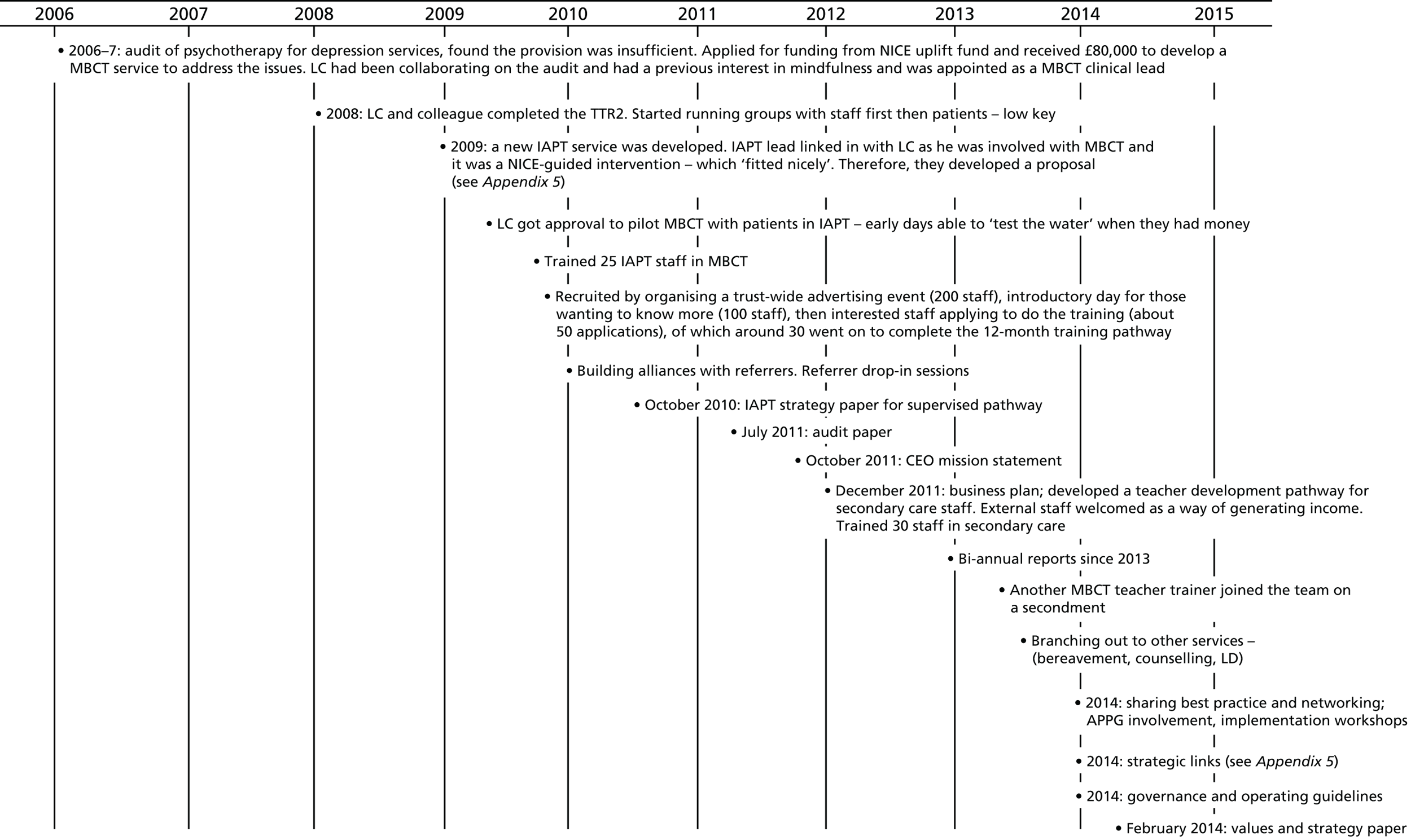
Reaching a critical mass of 30 trained MBCT teachers through an internal training pathway was a critical juncture and later in 2015 (after our site visit) a mindfulness centre of excellence had been established.
Context
Pine is a large provider of mental health, intellectual disability and community health-care services seeing about 190,000 people every year with 8800 staff. It had an annual budget/income of > £400M and was awarded foundation trust status in 2015. The trust provided services across the county for people with mental health needs, with needs relating to drug or alcohol dependency, mental and physical health services for people with intellectual disabilities and community physical health care. Implementers described an open culture, with stakeholders at different levels being supportive of MBCT. The CEO was a non-clinician, supporting and speaking out about experiencing mindfulness.
Training and service provision
Implementation comprised establishing an internal training pathway, which provided supervision in a 1.5-hour session every month in groups of two or three, a monthly peer supervision session and attendance four times a year at a 1-day silent retreat. This was all provided in house and in participants’ work time, and provided by the clinical lead with no external costs.
Pine recruited staff by a trust-wide advertising event (200 staff) and introductory day for those wanting to know more (100 staff), then interested staff applied to do the training (around 50 applications), of whom around 30 went on to complete the 12-month training pathway.
There were around 30 staff running MBCT groups across the trust (10 in IAPT) and an outwardly visible mindfulness centre of excellence had been established within the trust in 2015 (post site visit). MBCT (delivered as close to the manual as possible) was embedded within both secondary and IAPT services, and a mix of patients beyond the NICE remit were included. This entailed recurrent/remission and active levels of depression.
Elm
Overview
Elm’s implementation story began in 2000 when an early adopter started with a bottom-up approach using a lot of their own resources, autonomy and undercover strategies. After 6–7 years they started to receive some organisational (top-down) investment (Figure 6 shows a timeline of key events).
FIGURE 6.
Elm timeline. LC, local collaborator; PCT, primary care trust.

The site featured a mindfulness clinical lead (not funded) with a long-standing interest in mindfulness who had an experienced mentor helping them to develop teaching skills. This led to setting up a service for adults in 2007 after receiving NHS psychology service support and funding for five to six courses in adult services. In 2011, funding came from NHS health education for five staff courses. There was no other evidence of top-down support and investment.
At the time of data collection visits, a training pathway was currently on going and there were up to 30 MBCT teachers in five IAPT services. Following a critical juncture in early 2015 (after our site visit) when IAPT services made significant cuts, the training pathway and MBCT provision was stopped as it was deemed to be financially unviable.
Context
The services provided by the trust included community services such as health visiting, podiatry, sexual health and dentistry as well as inpatient and community mental health services. The trust covered the whole of the county footprint and employed around 7000 members of staff across > 400 sites. It provided health and well-being services for a population of around 1.4 million people.
During data collection we saw that the trust headquarters had instigated a ‘hot-desking’ environment in their offices in order to save building costs, and we observed a sitting group in this busy environment put together by a senior manager who was championing mindfulness (this person had left their post since the site visit).
Training and service provision
For many years an early adopter and current mindfulness clinical lead led pilot groups under the radar, using their own resources. The site reached critical juncture in 2007 when NHS psychology service support and funding enabled implementers to run six courses in adult services. In 2011, MBCT implementation plans developed for IAPT services and funding given for five 8-week courses for staff.
A 12-week teacher development programme including teacher trainee placement and supervision had been established, and they had recruited self-funding NHS professionals from other trusts. During our visit we found teachers struggling with demand and trying to keep up the throughput of training/supervision.
We found up to 30 teachers in five IAPT services actively delivering services across the county. MBCT was offered in several IAPT areas with accessible, adapted resources developed by implementers with the help of and for service users. Services were offered to a mix of populations (including staff groups) wider than the NICE guidance remit.
However, in the year following data collection the service faced pressures and changes in IAPT services; supervision was first halted and then later all MBCT provision and related training stopped.
Mangrove
Overview
In Mangrove, implementation of MBCT had started with three committed implementers working independently and with little official resources. This had resulted in them pursuing their own intentions in their own time. In this site there had been > 10 years (Figure 7) of grassroots service development with some ambition for an internal training pathway and centre of excellence, but as a result of different agendas and lack of middle-management buy-in, there were no obvious critical junctures that enabled MBCT to become embedded.
FIGURE 7.
Mangrove timeline. LC, local collaborator; MBA, mindfulness-based approach.
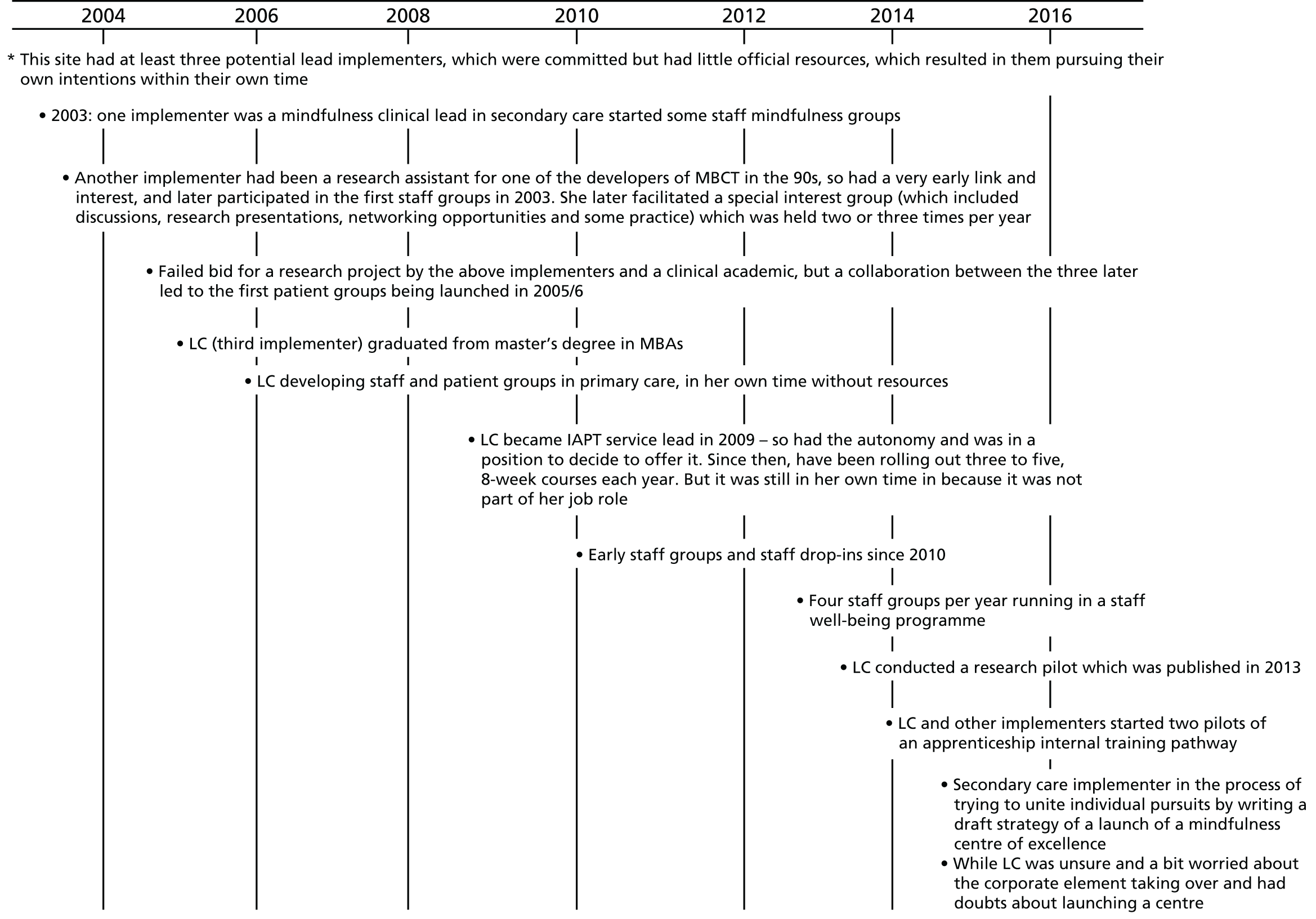
Context
This mental health trust provided the widest range of NHS mental health services in the UK, with 230 services including inpatient wards, outpatient and community services (foundation status since 2006). It had one of the largest mental health research and development portfolios in the UK through academic partnerships including various organisations.
Mangrove provided services to people living in four urban boroughs, comprising inpatient care for approximately 5300 people each year and > 45,000 patients in the community. The trust had about 4800 staff serving a local population of 1.1 million people.
Training and service provision
At the time of data collection, MBCT delivery had been developed in separate services by at least three implementers. This included secondary care services and Community Mental Health Teams (CMHTs), IAPT services, staff drop-ins and staff mindfulness groups offered across the trust, and some developments in specialist services (psychosis, cancer), as well as some mindfulness teaching at the local university. Within secondary care mental health services, MBCT groups had been offered by a psychiatrist teacher since 2005/6 with some IAPT populations referred, but also delivered to a mix of populations in CMHTs.
Mindfulness-based cognitive therapy was also offered (run by a service manager in their own time) within one of four IAPT services across the trust, with five groups per year currently offered depending on a waiting list. The type of group-based service included MBCT for depression, a MBCT/MBSR hybrid for long-term physical health conditions/medically unexplained symptoms (pain or fatigue), with a quarterly open follow-up offered to both.
Groups were a mix of presentations (option in care pathway and on website) applying loose criteria wider than the NICE remit (not currently in remission, some actively depressed, fatigue too, and generally more anxiety based than depression focused).
In terms of staff mindfulness and teacher training, the mindfulness clinical lead in secondary care started offering mindfulness to staff groups in 2003, conducted a research pilot that was published in 2013 and, with other implementers, started two apprenticeship pilots of an internal training route in 2014 and 2015 (with five places in each). This internal training pathway developed selectively in terms of recruitment and limited resources, with monthly drop-in sessions but insufficient funds/opportunities to expand.
Bamboo
Overview
In Bamboo implementation started around 2003 when an early adopter became a member of the advisory group of a national depression programme. This provided 3 years of funding to train NHS mental health practitioners in MBCT, and some leftover monies were then used to establish a national mindfulness teaching role for two implementers. These roles were crucial for the establishment of a small-scale national training pathway and also provided a regular network opportunity for implementers. There were six or seven implementers altogether, working across different services. In 2006, there was a country-wide strategy for depression published, and also around this time, seven teachers across two sectors (mix of primary and secondary care) received funding to run five MBCT groups per year. In 2008 and 2011 national guidance to deliver evidence-based interventions mentions MBCT for relapse prevention. A research and audit on mindfulness conducted by the local main university partner started in 2014, without significant external funding (Figure 8 shows a timeline of these key junctures). At the time of data collection the implementers were planning to progress from partially embedded provision to further embedding through the development of a training proposal, which would help ensure that more staff were trained to deliver MBCT groups.
FIGURE 8.
Bamboo timeline. MBA, mindfulness-based approach.
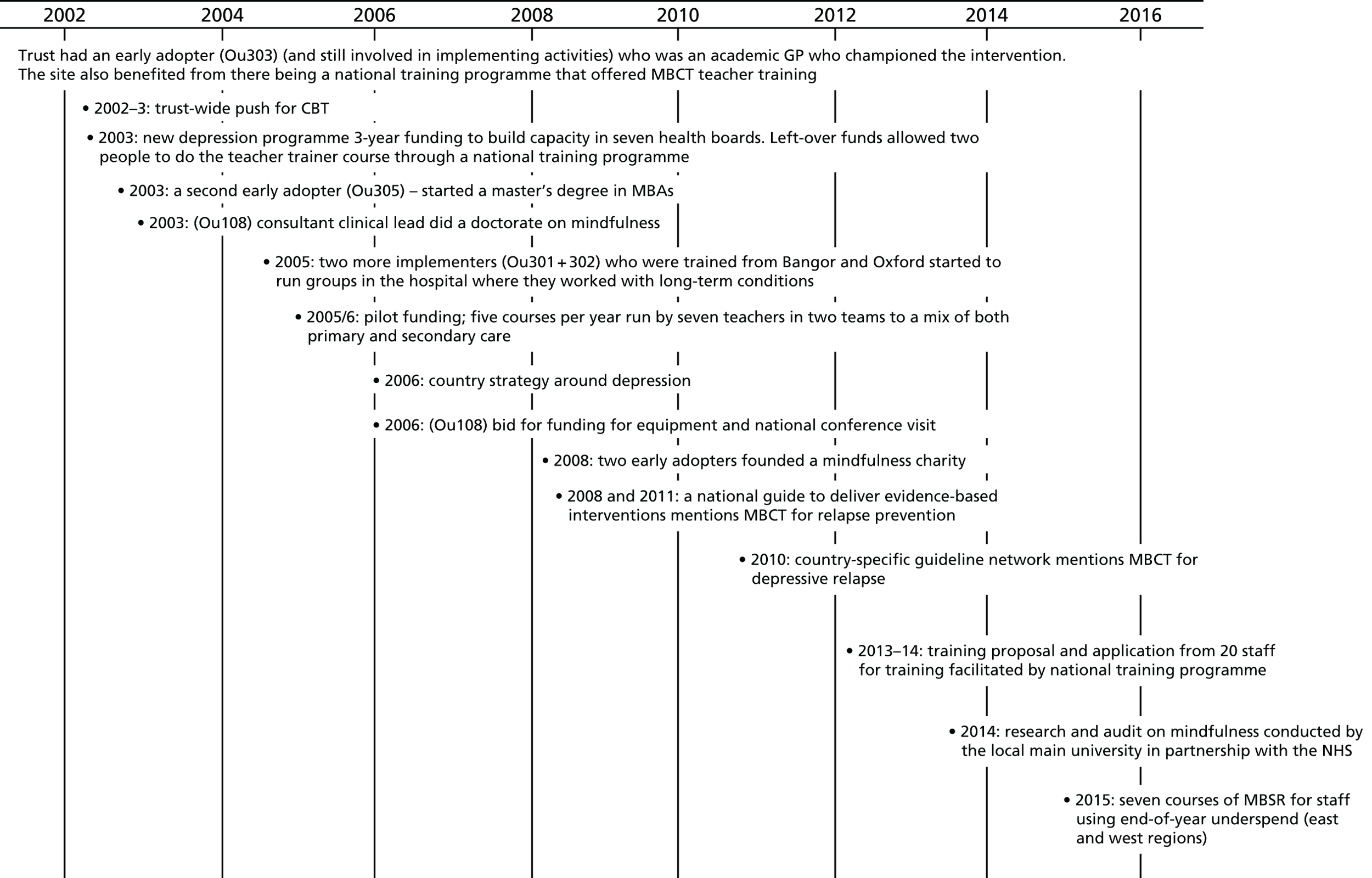
Context
Bamboo is an integrated health-care organisation that was formed in April 2006 by combining two smaller organisations. It served a population of 1,190,856, with 44,000 staff delivering services in the organisation as well as regionally and nationally.
There was a culture of a strong public service ethos, which included developing its own policies and systems, which had a slightly wider remit than the NICE guidelines. In terms of fit with organisation priorities, at the time of data collection MBCT was not recognised as a priority by middle and senior management. (Although since the site visit the overall lead for all psychological therapies across the site has asked for a strategy document for MBCT and a steering group for mindfulness interventions.)
Training and service provision
There were pockets of MBCT provision as a low-intensity intervention for depression across all adult mental health services, adhering closely to the original manual but with wider inclusion of patients including eating disorders/obsessive compulsive disorder and generally offered at the end of the care pathway.
As a consequence of the establishment of the national training pathway, a network was developed and met on a monthly basis which provided supervision and workshops as well as being an opportunity for people in the training pathway to connect. There was an annual teacher training attended by staff from both mental health (inpatient and community) as well as staff from the acute hospitals.
The service user service that started in 2006 also doubled up as opportunities for interested staff. Places were left for staff on all the MBCT groups, which had become an accepted route for training and also for staff wanting to develop mindfulness purely for personal reasons.
Two implementers secured one-off funding for courses in 2013–14 (including co-facilitating with trainees). The capacity within this service included seven MBCT teachers (one not yet ready to run groups) with a supervision group and practice maintenance group run in the evening (in their own time with no central funding).
In addition to mental health services, we also visited a specialist centre for complementary medicine (totally separate from mental health services but still a NHS facility delivering services free of charge), which also offered MBCT to patients with a wide range of physical and mental health conditions. Out of this wider network of stakeholders came the formation of a community interest charity offering teacher training to NHS and social care staff. Another source of teacher training was through a national NHS provider, which was not prescriptive to the MBCT manual and that allowed most national sites to work with either, both or hybrid MBCT/MBSR programmes.
Birch
Overview
Following the departure of an early adopter in this site, there was no evidence of a roll-out of MBCT services in Birch. The focus of recent activities had been mostly driven by external implementers (the previous early adopter) at the academic centre of excellence, and in developing the MBCT teacher training for staff.
There was evidence of some MBCT being delivered by a third sector consortium (commissioned by the health board), but there was uncertainty about how quality assurance was managed and whether or not the providers were appropriately trained to deliver MBCT.
This site experienced a critical juncture in 2012 (Figure 9) when the site received funding from local government to build capacity in psychological therapies. The psychological therapies lead in this site was part of a psychological training institute, which was a local initiative that made decisions about allocating and co-ordinating budgets around psychological therapy. The first wave of funding included a specific recommendation from the government to prioritise developing a range of options of psychological therapies. The decision was made by the psychological therapies lead and the psychological training institute to use this funding to fund the first cohort of MBCT trainees. They later received a second wave of funding, which funded a second cohort of trainees. Trainers and trainees reported that there was a lack of co-ordination between the commissioning of training and the transition from training to delivery. As a result of a lack of clarity about who was leading, implementation of the training proved challenging. Birch have since appointed a co-ordinator who leads in organising resources and supervision for trained staff.
FIGURE 9.
Birch timeline.
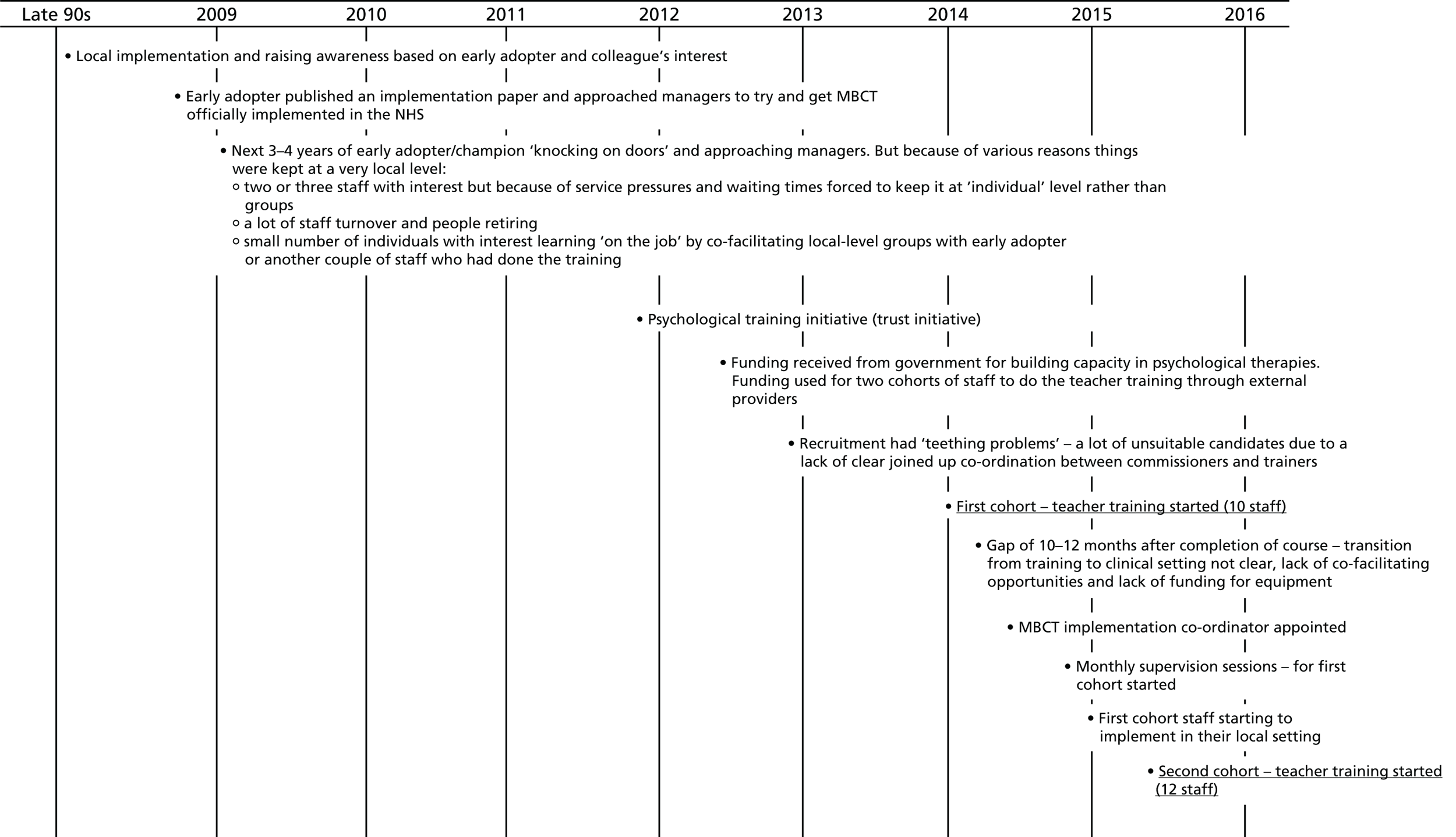
Context
This organisation was established in 2009 as a part of the devolved government reform programme for the NHS, which brought together a number of organisations with responsibility for delivering all NHS health-care services within a large geographical area. This large health board provides a full range of primary, community, mental health and acute hospital services for a population of around 687,000 people across the six counties. The site employed around 16,500 staff, and had a budget of around £1.3B.
The implementers stated that the contextual conditions for implementation were not supportive, with the organisation operating on short-term funding and people being rushed to hit targets. In this region of the UK, health is the responsibility of the devolved government, and initiatives such as IAPT is not in existence. There was not an explicit depression care pathway, which made it impossible to demonstrate and report impact of MBCT for particular populations.
Other relevant contextual factors described by implementers related to re-organisations and competing priorities, which meant that MBCT kept dropping down the priority list. Implementers told us that the board’s answer to that was to ‘squeeze’ MBCT delivery in with existing job roles, which was perceived to be unsustainable in the long run. Implementers had not managed to raise a high profile within the board to ensure their buy-in.
Training and service provision
At the time of our study, we found one official way to publicly access MBCT from within primary care. This was a health board-commissioned third sector consortium delivering MBCT groups. There was uncertainty about how quality assurance and good practice was managed. Managers within this service also described issues around appropriate referral as people who were currently well did not usually access their services. They therefore had varied and different populations accessing the service. We found implementers and emerging trainees operating across secondary care services, sporadically running groups or applying skills in one-to-one service delivery.
Between 2010 and 2015 implementers had two funding streams for psychological therapies, which enabled them to fund two cohorts of teachers trained in 2013–14 and 2014–15 (a total of 22 staff). With the first trained cohort there were a few difficulties in translating their training into practice. There was no funding or time being allocated to deliver MBCT in their individual services, and staff struggled to start anything up in their service. Following this they appointed an internal mindfulness co-ordinator to support the transition from training to delivery, and to organise practical and financial resources. This role was an add-on to the post-holder’s current role and existing workload, so no extra time was dedicated to it. At the time of our site visit we estimated that fewer than half of those in the first cohort were running groups, and the second cohort of staff were completing their training.
Hazel
Overview
In Hazel, there were individual, privately trained and personally funded practitioners who were not really aware of each other. They had personal interests in building their own skills and either a lack of experience or confidence to start teaching/supervising others within the trust.
For 5–6 years individual implementers ran workshops, taster sessions and staff groups, and in 2005 one implementer started a MBCT service for older adults, partly in their own time. Between 2006 and 2012 (Figure 10 shows a timeline) efforts appeared to be hindered by a trust merger, at which time competing priorities related to reorganisation and to a strategic focus on upskilling staff in other modalities other than MBCT. There were still pockets of activities across the trust but, as a result of a very pressurised context driven by targets, implementers reported feeling like they were hitting a brick wall, which resulted in them delivering what they could within their own local service.
FIGURE 10.
Hazel timeline.
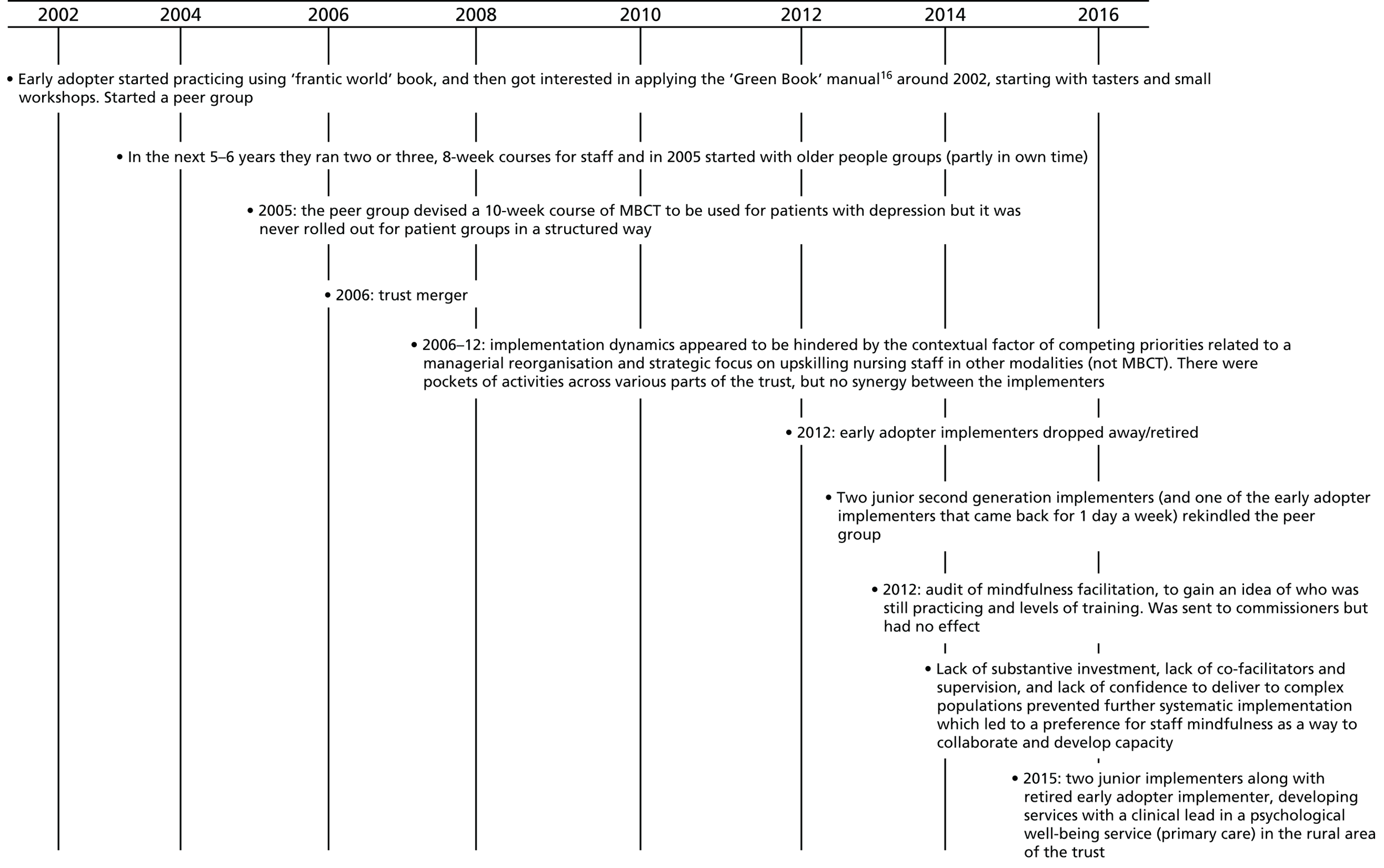
In 2012, there was an audit in the trust of mindfulness facilitation capacity in order to gain an idea of who was still practising and levels of training, which was jointly completed by a consultant psychologist, a psychologist and an occupational therapist. The results of the audit were sent to commissioners with no obvious outcome. Implementers expressed hopes for their new CEO, who had been recently appointed at the time of data collection (2014) and who had spoken at the first annual general meeting about their own history of depression and personal experience of mindfulness.
Context
This trust is one of the largest mental health and disability trusts in the UK. It was created in 2006 following the merger of three trusts covering a large geographical area totalling 2200 square miles, working from > 60 sites with a number of regional and national specialist services and a budget of > £300M. The organisation was authorised as a NHS foundation trust in 2009. It provided a wide range of mental health, learning disability and neurorehabilitation services to a population of 1.4 million people, across two UK counties.
Hazel had a long history of inpatient care in Victorian-built facilities and was in the process of shifting services into the community and investing in preventative and integrative care addressing multimorbidity and deprivation in suburban areas. Primary care services partly sat outside the trust and were provided by a third sector provider. Two senior managers had initiated a huge roll-out training programme of 1600 staff in 4200 days of training in six modalities including dialectical behavioural therapy, CBT for psychosis, Wellness Recovery Action Plan intervention and family therapy, but not MBCT.
Training and service provision
A number of MBCT practitioners had been trained but this had been predominantly through self-funding, with occasional pots of money being made available by immediate line managers. Clinicians with an interest/training in MBIs were based in various geographical areas, with pockets of services based in third sector IAPT, primary care, secondary care, specialist CBT services, well-being services (and recovery college), physical care and learning disabilities. Practitioners in these different services did not appear to know of the existence of each other within their own trust.
In terms of setting and referrals we found partially embedded islands of MBCT provision in eight different services (three primary care, four secondary care, one physical care), although this did vary from pure MBCT, as stated in NICE guidance, to hybrids of MBCT/MBSR or using elements of MBCT in one-to-one therapy. The population who were offered the MBCT group intervention fitted well with NICE guidance. A third sector IAPT service provider who had held a three-way contract in the previous 3 years between the trust, Clinical Commissioning Group (CCG) and local council provided MBCT, with the option for a stand-alone intervention, but the intervention was mainly offered after previous treatments.
In 2015 a peer group devised a 10-week course of MBCT to be used for patients with depression, but it was never rolled out for patients in a systematic way.
Juniper
Overview
A clinician with an interest in MBCT had been trying for a number of years to generate interest and apply for MBCT training, but had not been successful. In Juniper the only juncture that had experienced a positive impact happened in 2013 (Figure 11), when a fully trained (in MBIs) implementer joined the trust (on a voluntary basis) to focus on running MBCT groups. They facilitated five MBCT groups per year.
FIGURE 11.
Juniper timeline.

At the time of data collection Juniper had undergone a recent reorganisation and was commissioned to see a large number of people per month. This meant that clinicians were under a lot of pressure to cover more screening slots and were less able to facilitate groups and that individual and group waiting times increased. Clinicians reported that they were under-resourced to deal with the additional screening, the one-to-one and group work.
Context
This mental health foundation trust (since 2008) served a culturally and socially diverse metropolitan population of around 1.2 million and is one of the largest mental health foundation trusts in the country. The trust had > 4000 dedicated staff and operated from > 50 sites in a variety of settings, from community-based mental health teams through to acute wards and day centres.
We collected data in a NHS primary care psychological therapies service spread across three area teams (East/North, Central, South). MBCT implementation in this service began during the third wave of IAPT restructuring.
Training and service provision
A volunteer working full time in the East and North team was the only person running 8-week MBCT groups, and facilitated around five groups per year. This person was also working on adapting MBCT to be delivered to anyone who wanted it (e.g. those with bipolar depression, obsessive–compulsive disorder, stress, chronic fatigue, irritable bowel syndrome). Anyone who was interested in incorporating mindfulness in their own work was able to sit in on an 8-week MBCT course as a participant, and then introduce elements in their work if they believed it would be useful (working with the volunteer to adapt). The volunteer implementer would also help direct those who wanted to train further towards external teacher trainers. There were three clinicians who had adapted the classic 8-week MBCT approach by adding a compassionate-mind element to the MBCT manual and running two or three groups per year.
In terms of training, there were a variety of sources of training, two staff members were trained to a certain level, and core funding for five staff in each of the three teams was then released to receive an introduction to MBCT from a neighbouring university (5-day training for £650 each). There was a lack of clarity between training provider and manager about what the 5-day training would entail and the cost of it represented an issue as a 5-day course was a prerequisite for training (i.e. a personal/experiential practice development rather than developing nursing staff for professional service delivery, which is what the manager had envisaged). Those who had attended the 5-day course were expected to use the skills learned to introduce mindfulness into their work. There was also an internal CBT supervision group in which MBCT teachers were allowed to bring MBCT issues forward (some peer supervision).
Training levels varied; one clinician based in one team had developed an informal interest at university 15 years previously in a Buddhist centre and had then sporadically used mindfulness in one-to-one work. This person received no further training since and reported feeling like they were ‘learning on the job’.
Beech
Overview
In Beech the implementation journey began around 2006 (Figure 12) when an early adopter became interested in MBCT and personally funded their training in MBCT. This person led their first patient MBCT group in secondary care in 2007 with a co-facilitator, who at the time of data collection was Beech’s implementer. By 2009 they had two or three groups running per year, and by 2010 had developed an internal teacher training pathway. Beech had a juncture in 2012 when a trust merger happened and they adopted large waiting lists, which hindered implementation. Practitioners were diverted by a new manager to clear waiting lists for people needing individual therapy. This led to frustration by the early adopter who left the trust.
FIGURE 12.
Beech timeline. LC, local collaborator.
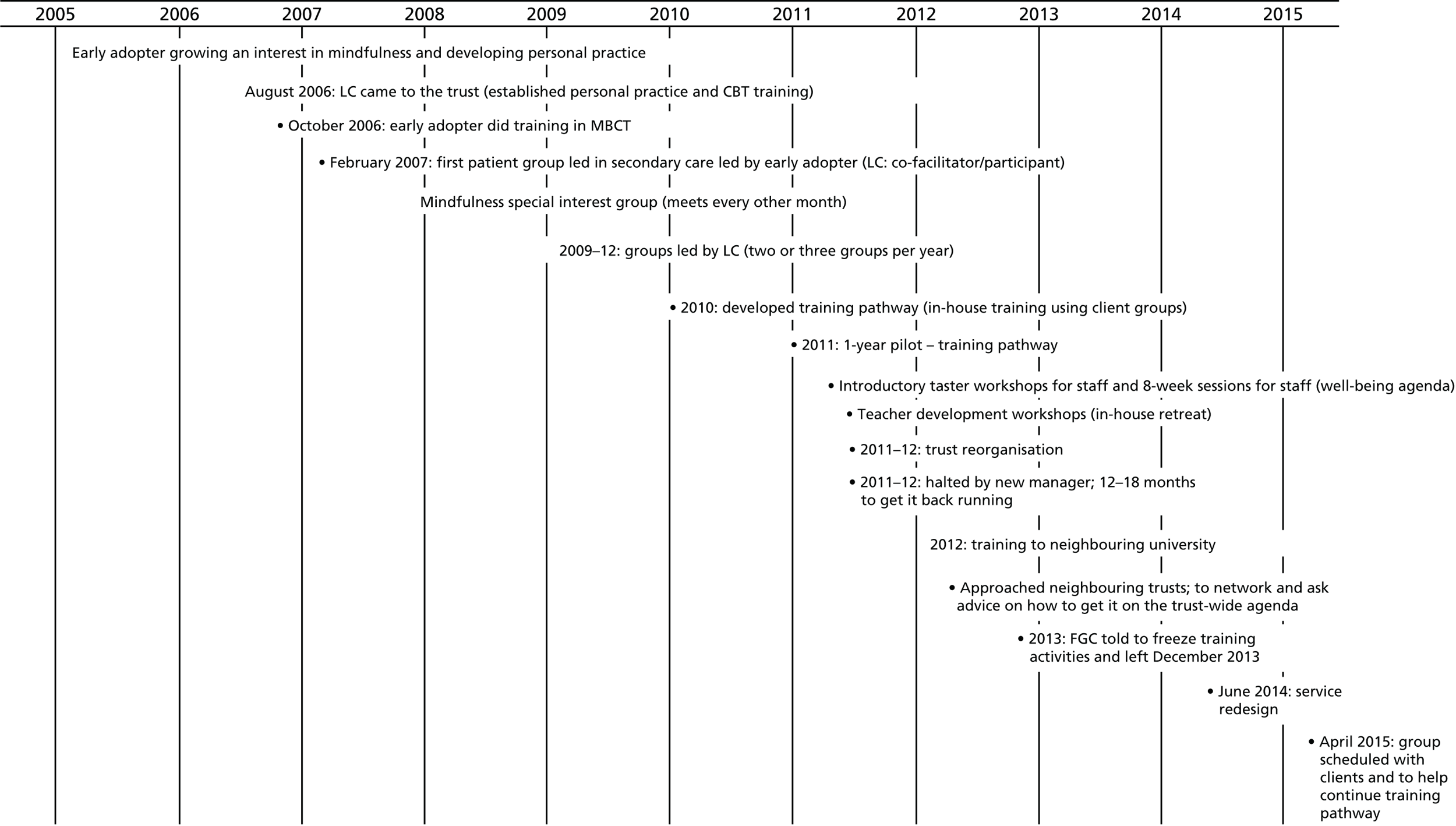
This left the remaining implementer struggling to do what they could with minimal support and resources. No MBCT 8-week groups had been delivered since December 2013. They experienced a secondary care service redesign in 2014, which meant that staff were assimilating to the new structure and new ways of working. A new MBCT group was scheduled to start in 2015 (post data collection).
Context
Beech was formed in 2006 and later integrated with community services from another trust in April 2012. The organisation aspired to obtain foundation trust status as soon as possible and was awaiting an inspection of services by the Care Quality Commission in 2016. It provided services from > 60 locations and employed > 4200 staff. Beech provided inpatient, community and day clinics, as well as specialist services, to a diverse population of about 1 million people living in a city/metropolitan borough.
A trust merger in 2012 meant that they adopted long waiting times. This was then followed by a redesign of the secondary care mental health services in 2014. A service manager indicated that with time, the service redesign could have positive implications for MBCT. This service redesign in secondary care meant that CMHTs were transformed into integrated practice units (IPUs), which are organised around ‘care clusters’. For example, IAPT is care cluster 1–2 sometimes 3 on border to site local collaborator’s own service based at 3–10 (anything but psychosis), IPU 10–17 is psychosis and IPU 18–21 is older adults, etc. This meant that the service ended up with different IPUs with different flows in of referrals with the following implications of the redesign on MBCT: (1) implementers would be able to target a particular group of patients more easily (i.e. to concentrate on care clusters 3–8), and (2) IPU interventions had to be NICE compliant so this would help the argument of providing MBCT.
Training and service provision
Internal training existed between 2010 and 2012, which was set up by the MBI-qualified early adopter. The trust merger interrupted the training pathway when a new manager was put in place and was presented with the task of tackling long waiting lists. The training pathway was put on hold, and later the early adopter was told to freeze all group intervention training and activity in order to focus on one-to-one interventions.
At the time of data collection we found services embedded in IAPT, where four or five of those who had completed the MBCT internal training pathway were actively involved in the delivery of group therapy. This was not MBCT groups as per the manual, but elements of MBCT were used in other group-based interventions.
Within secondary care mental health services between 2009 and 2012, two or three MBCT groups per year had been conducted by the local collaborator, carved into their current role. The first MBCT group since 2012 was scheduled to start in April 2015. The pre-course assessments and introduction session had just been set up and sessions were about to start following data collection.
Wisteria
Overview
It was very early days for this site in terms of their implementation journey (Figure 13). In Wisteria the implementer sat primarily within an occupational health department. This site featured MBCT (with a focus on stress in place of depression) for staff only. The main implementer was also raising awareness of MBCT within physical health through their part-time role in this context. This was a hospital-based service, and the implementer’s role in physical health comprised inpatient/outpatient with lots of group work (e.g. acceptance and commitment therapy). In addition to the role in physical health, the implementer came to the occupational health service with a remit of introducing group-based interventions.
FIGURE 13.
Wisteria timeline.

They had advertised for some staff to take part in a pilot group for staff in 2014, but had an overwhelming response of 197 applications within 3 days. Applications were reviewed and places offered on a first come first serve basis in accordance with information provided within the application form. Those who were not offered a place on the programme were later invited to a 1-day introduction to mindfulness workshop.
Context
The trust formed in 2007 after the merger of six trusts and was delivering integrated health and social care to around 340,000 people. The organisation had an annual budget of approximately £1B (spending about £3M each day) and employed 20,000 staff making it one of the largest trusts in the UK. The large number of staff was relevant in terms of implementation because as an occupational health department they were facing huge demands from staff with limited resources to implement and deliver MBCT to staff.
Training and service provision
The trust ran a pilot in 2014, and had an overwhelming response. The pilot attendees came from across departments and professional groups (no medics/not a lot of clinical staff – mainly nursing, management, human resources).
The curriculum followed the course content of manualised MBCT because some staff were experiencing depression due to stress. The timing of courses was an issue, with the pilot being offered in the evenings after work. Being a lone teacher also represented a challenge. At the time of data collection a second group orientation was planned.
Chapter 5 Phase 2: an explanatory account of mindfulness-based cognitive therapy implementation
Introduction
This chapter builds on the case studies to present cross-case study findings in the form of a number of explanations. As accounts were contextualised within a site’s own experience and evidence, a number of explanatory patterns emerged across cases. These cross-case explanations summarise the key features of the various multidimensional implementation stories of each site. Although these explanations may not fully capture the particular intricacies of a case’s implementation story, they do provide a theoretically transferable account to explain the how and why of MBCT implementation. Furthermore, as a check on face validity, these explanations were presented as part of our dissemination activity through a series of workshops (see Appendix 9), in which participants fed back on and reported resonating with our findings.
Implementation journey: a metaphor
Each site had its own implementation journey that was particular to them; however, each also faced similar conditions, including opportunities and challenges that mediated their progress. Each journey had a starting point, which varied in time point across sites. As such, some sites were further ahead than others by virtue of the fact that they had been on a longer journey, and/or had experienced different conditions, at different times along the way. For example, all sites were implementing within the same overarching context (i.e. a NHS facing challenging economic times). Some site participants reported that implementation had been easier before the financial crises, so that those who had started implementation earlier tended to make greater progress. Others stated that they started at a good time when IAPT was being launched, and had been looking for NICE guidance-based interventions to implement. Overall, however, as a consequence of the way MBCT has been recommended within NICE guidance (i.e. as a prevention intervention delivered at the end of a treatment pathway), and in a NHS context primary weighted towards treatment than well-being, the intervention was often not a straightforward fit into service pathways.
In all sites the progress made towards any level of MBCT implementation was a consequence of the work of one or more implementers. These MBCT teacher/practitioners often started off the implementation journey as lone enthusiasts, and had navigated their way through the local context by enacting their skills, characteristics, activities and experience. Lone enthusiasts struggled to build momentum on their own, and in sites where MBCT was more embedded, implementers had been successful in building support systems around themselves. More successful implementation happened when a site had a combination of different implementers, with a variety of seniority and skills, who were aligned around the same agenda. However, although data show that implementation started from the bottom up through the drive of local implementers, for implementation to be more successful this needed to be complemented by top-down organisational commitment and investment. Furthermore, a site’s context in the form of existing service pressures, drivers and priorities, and the availability of resources determined the pace and direction of implementation. As each site had its own implementation journey, no single factor or event was responsible for whether or not MBCT became accessible and used within a service; rather, there was an accumulation of factors over time that could lead to critical junctures or pivot points.
Explanations
The following sections present six interdependent explanations that constitute the implementation journey (Figure 14). They are interdependent in the sense that it is only in considering the interactions and relationships between them that we can build up a holistic picture of implementing MBCT in UK services.
FIGURE 14.
Implementation journey.
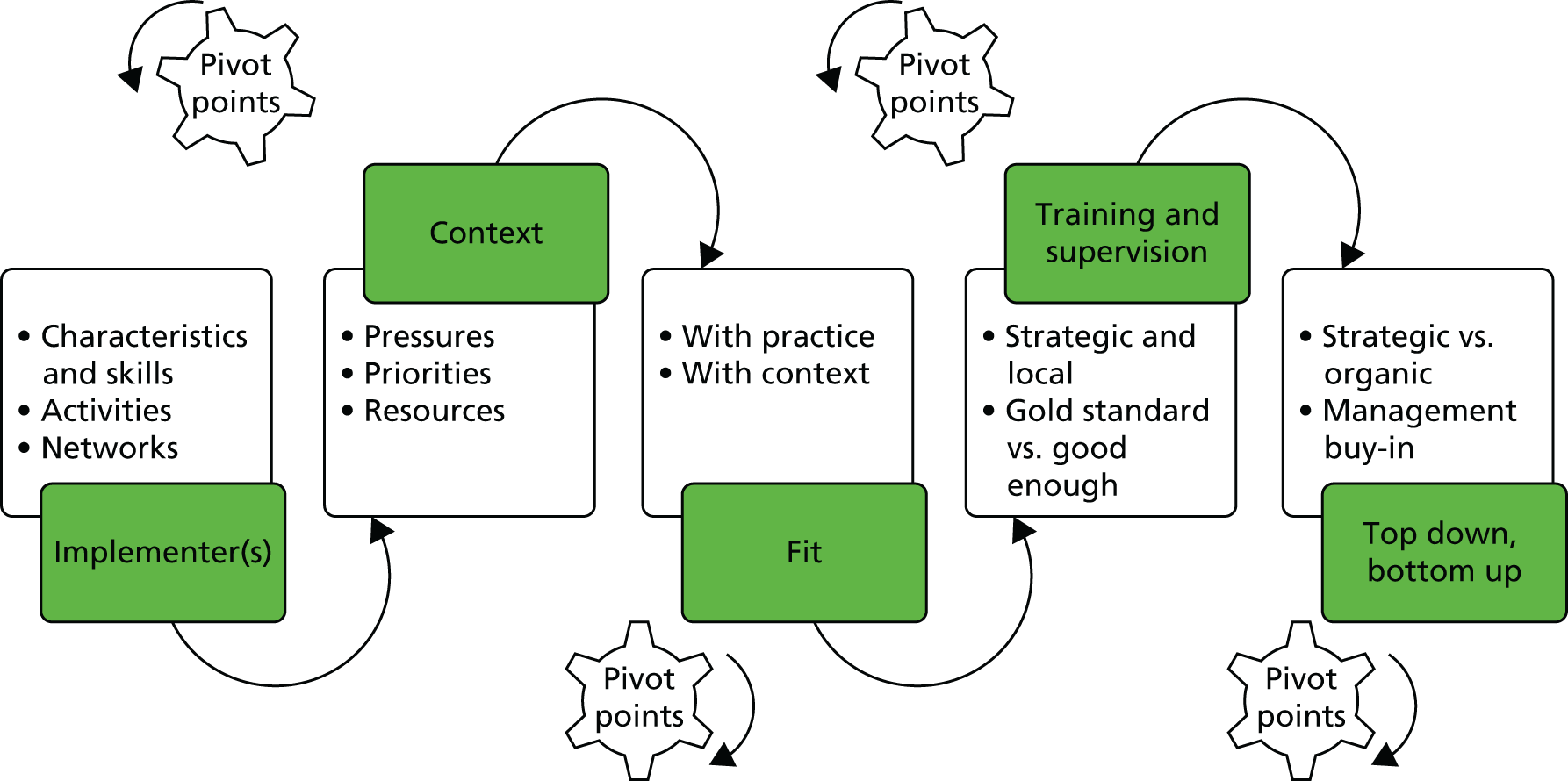
Although each site had their various starting points, heritage and opportunities to develop/implement MBCT over time, we were able to identify the following overarching explanations:
-
MBCT implementation relied on the presence of at least one person who drove and led implementation – the ‘implementer’. Implementation was more successful in some sites than others because of a combination of the implementer’s characteristics, skills and experience (e.g. commitment, drive, implementation skills, seniority); the networks she/he created, or was part of (multilevel, physical and interpersonal); and the context in which they were working.
-
The implementation context for MBCT presented possibilities and challenges to its application.
-
Successful implementation of MBCT was partly dependent on the degree of alignment between the intervention and NHS context, existing local service strategy, priorities and pathways, and efforts to adapt and make it fit.
-
The existence and quality of training and supervision was a function of the level of strategic priority and subsequent investment placed on MBCT implementation within an organisation. There was a tension between gold standard and ‘good enough’ teacher training models.
-
Implementation of MBCT was driven by a combination of bottom-up activity and top-down support and investment, the effect of which was enhanced by middle management and clinician buy-in.
-
A combination of factors led to pivot points in a site’s implementation journey, which were critical junctures where implementation either accelerated or was impeded.
The following sections unpack these explanations and in doing so we also draw out any site particularities, differences and commonalities to provide additional explanatory power and future potential learning. We revisit and elaborate further on the concept of implementation journey in Chapter 6 (see Implications).
Implementers
Mindfulness-based cognitive therapy implementation relied on the presence of at least one ‘implementer’, which was a person who drove and led implementation. Some sites were more successful than others in the implementation of MBCT because of a combination of different factors: the implementer’s characteristics, skills and experience (e.g. commitment, drive, implementation skills); the networks or activities they were part of or they created on multiple levels (physical and interpersonal); and the context in which they worked in (Figure 15, also see Context).
FIGURE 15.
Implementers.

Presence of implementer(s)
Our data are densely populated with examples of enthusiastic and passionate individuals who were acting as local leads and champions (implementers). The starting point for implementation in all sites was the presence of these implementers who acted as champions and change agents rather than a more strategic and/or commissioner-led initiation of MBCT within sites. The majority of these implementers were self-selected or had been nominated by their local team(s). Only one site (Pine) in this study had an official, designated and funded mindfulness lead role.
Most implementers had initially worked alone in driving forward the intervention and, as such, services had grown organically from the ground up. As each site was at a different stage in their implementation journey, correspondingly the presence of an implementer varied according to the starting point and history of the site in initiating MBCT. Implementers in Bamboo, Elm, Beech and Oak could be described as ‘early adopters’ in that they developed an interest, practice, research and championing activity before the intervention had been included in NICE guidance. Through the work of these early adopters and over time, there was a greater awareness and acceptance of MBIs in general, which paved the way for the potential of MBCT in particular in these sites. Some of these early adopters had been able to pass on a legacy to a second generation of implementers, who were equally committed to championing and leading the MBI agenda. In these cases MBCT had a greater chance of continuance (Elm, Oak, Mangrove, Hazel, Bamboo and Birch).
Implementer capacity varied across sites ranging from individuals working in isolation to those who worked as part of a small team committed to MBCT. For example, in Elm there had been a reliance on one implementer in a clinical lead role, and in other sites there were more implementers working at various levels of the organisation (Table 8).
| Site | Implementer capacity |
|---|---|
| Oak | Five implementers, who were also well known to each other and worked together from various regions of the trust. There was a range of board-level championing and good relationships between implementers and senior managers/directors |
| Pine | Two implementers who worked closely together, one who was at a senior level. An official MBCT lead role was created for the least senior implementer |
| Elm | Had an early adopter who mentored the second-generation implementer before retiring. The second implementer was the sole unofficial lead of MBCT. There was no top-down support for implementing MBCT |
| Mangrove | Three implementers who worked individually across different parts of the service, two were senior staff implementers. The activity of the three implementers did not appear to be co-ordinated because of time and resource constraints |
| Bamboo | All implementation activity was based around two implementers who were in relatively senior (but not board level) positions within their region, and a third implementer being a retired early adopter who was still running groups and providing supervision as an external teacher |
| Birch | Two early adopters left the trust to work in a HEI setting resulting in no implementer within the trust for a decade. Early adopters still actively pushing to get MBCT implemented in the trust, which resulted in two cohorts of teachers going through training. A member of staff from the first cohort was then identified as a MBCT co-ordinator |
| Hazel | Originally one early adopter and then two subsequent implementers who had retired. MBCT provision had been provided in eight different services within the trust, but each were unaware of the others. During the time of the visit, only staff mindfulness-based groups were being offered |
| Juniper | A sole implementer voluntarily running MBCT courses and led on the agenda within the trust on an honorary contract (i.e. not paid by the trust) |
| Beech | Implementation journey started off with an early adopter, then shortly joined by a second implementer after a couple of years, and both worked productively together. The early adopter left the service after the teacher training programme was scrapped and second-generation implementer was left as a lone implementer |
| Wisteria | Three implementers present at the time of visit; two working part time within the occupational health department and also as associate directors of the DClinPsy Programme at the local university. The third implementer was a lone MBCT teacher based in physical health in a part-time role |
Given the mainly self-selected nature of an implementer, it was perhaps unsurprising that individuals in sites where MBCT was less available did not have protected time or resources to undertake implementation-related activity; for example:
The way we’ve organised it so far is to identify a lead practitioner within the XXXX [trust] who has this as part of her remit, XXXX, but she’s had this sort of crowbarred into her ordinary job description and like a lot of psychotherapy training and treatments sometimes it just has to run on enthusiasm rather than organisation oomph if you know what I mean and some of the personal commitment that people bring is what keeps it going.
Head of psychological therapies, Birch206
Pressures have changed over time, everything is more rushed now so it’s very difficult to prepare, rush around and then lead a group. Managers have other pressures – relationship between manager and teacher becomes difficult – ‘leaves a sour taste’ – ‘I’m offering to deliver this service, in addition to my full working week, and you don’t give me the support that’s needed’.
Observation notes – peer supervision meeting, Elm
In contrast, in sites where MBCT was more embedded they had access to greater resources, including dedicated time to work on implementation activity:
. . . that’s just a combination of that network thing, just myself and XXXX [local collaborator] were friends personally and it was just having that connection and a willingness like XXXX [local collaborator] to give his time, his manager to allow him to give his time and my clinical director saying yeah let’s give it a go, not done it before but you’ve got some expertise coming in willing to help us, it fits what we’ve been commissioned to deliver so let’s go for it.
Clinical lead/manager within IAPT, Pine201
Implementer characteristics and skills
Data show that the characteristics and skills of an implementer were critical to role success, including their deployment of implementation-related activities.
It’s generally being conducted by enthusiasts . . . if you have experienced enthusiastic, committed, well trained, clever people, do almost anything, you know it’s gonna have a good outcome.
Associate medical director mental health, Bamboo201
Characteristics such as passion and dedication, role seniority and personal credibility, and implementation skills such as effective engagement and delivering activities were critical success factors, and were more evident in sites where MBCT was more embedded.
Consistent with findings described in Chapter 3, these implementers went over and above their professional roles because they were passionate about MBCT and to their own personal mindfulness practice; for example:
Because it needs the old grass roots as it were, it needs the people who are going to be delivering it to be the starting point in terms of their own personal interest and commitment to mindfulness and MBCT because without that of course there’s nothing; it doesn’t exist.
Mindfulness clinical lead, Pine101
However, although passion and commitment to the intervention was both the starting point and a driver, in sites where this was combined with other characteristics and implementation-specific skills such as engagement and communication (e.g. diplomacy, speaking the language), business sense (selling) and research (evaluation, demonstrating impact, intervention development), a greater chance of implementation success through mediating barriers and leveraging facilitators could be achieved:
. . . they don’t understand that there needs to be nuts and bolts to it with the costing and how they can go about influencing people. I think it’s that the skills that they need to understand what they need to do if they like and knowing where to go and who to speak to as well, that can be quite difficult and they have to be quite tenacious and not give up you know when they meet a barrier.
Research and innovation lead, Elm205
However, passion, enthusiasm and commitment were in themselves not enough for successful implementation. This had to be complemented by support from the organisation, particularly senior managers (see Top down, bottom up for more detail).
An implementer’s seniority or perceived credibility was also instrumental in enabling appropriate level decision-making, and in garnering support and resources. More progress was made in sites such as Oak, where implementers were in positions of authority and autonomy, and there was a cross-organisation network of implementers. In contrast, for example, in Birch, the sole implementer working in a clinical co-ordinator role was not in an appropriate position of authority, which resulted in ‘her hands being held behind her back a lot of the time’ (early adopter, Birch202). The level of authority also seemed to be associated with levels of confidence, with some implementers being more comfortable approaching and pitching their ideas to senior managers than others:
I think that’s where I fall down . . . I’d rather be working on a newsletter to encourage mindfulness participants, to stick with the practice, stay at it, get the benefits, rather than planning a presentation that’s going to make me knees knock in front of senior management, who are then going to ask me really hard questions about throughput . . .
Local collaborator and former mindfulness clinical lead, Elm101
This may have partly explained why MBCT had not progressed as far in some sites (e.g. Beech and Birch) or why activities were stopped (Elm) in contrast to other sites where there was both authority and confidence in a team of implementers (e.g. Oak and Pine).
Implementer activities
The implementation activities we heard about in phase 1 interviews were also reported by participants in phase 2 (see Chapter 3, Bottom up). Activities ranged from taster sessions/workshops to pitching the idea and making a case by using pilots and evaluations, and diversifying to generate income to sustain branching out to other services within the trust (Table 9). Within phase 2 data we saw that the range of activities corresponded with the degree of development of MBCT services. Sites where there was more embedded MBCT (e.g. Oak and Pine) had success in combining a number of strategies that involved different types of stakeholders in the organisation on a more continual basis, which seemed to have had a greater impact. However, it is difficult to disentangle whether or not their ability to be able to use a multistrategy approach was because these sites had a platform of greater organisational buy-in to delivering MBCT and, therefore, more resources (including financial and capacity) to support implementation activities (see Context for further details). This contrasted with sites where there was less evidence of MBCT delivery, which was arguably a function of a lack of organisation buy-in to MBCT and, as a consequence, less resource to support implementation activities, resulting in implementers working (often alone) within a strategic vacuum.
| Activities | Rationale and impact |
|---|---|
| Taster sessions, including workshops and short practice sessions | In the context of mindfulness either being not well known or misunderstood – to get stakeholders to ‘experience it and appreciate it’ (IAPT clinical lead, Pine201), and get buy-inThe way we sort of went about doing it, one was to do little tasters and stuff and immediately you get people in a room and you take them through a [mindfulness] practice you get at least 50% going golly I’d really like to do more of this . . . That really got people’s interestMindfulness clinical lead, Pine101 |
| This was a particularly helpful strategy for engaging referrers, commissioners and managers:Engage somebody at a senior level, and you know get them practicing, give them some experienceEarly adopter, Oak102It was a great session thanks and several Board members who were present were very interested in having a follow up sessionsDocument, e-mail between staff who co-ordinated a taster session to board members, Birch | |
| Incorporating into staff well-being agendas | Pitching mindfulness as a staff well-being initiative, and providing regular drop-in sessions to ensure continuity of provision and visibility:The head of HR came to see me to ask if there was something we could do for staff to help with sickness and so on and they had a small pot of money. So what we did we offered two things . . . one was mindfulness groups that staff could as a group book for their workforce and stress control and we’ve offered insomnia management training as well and what happened was we had departments contacting us saying could we have a mindfulness course. So with the pot of money we were able to go and offer these courses of training to groups of staff . . . They really saw it as something positive . . . to strengthen their resilience and we were quite actively promoting that and it worked really, really wellIAPT director Pine, IAPT regional service director, Pine208 |
| Combining different types of evidence to ‘make the case’, and combining the ‘hard science and the testimonials’ (external trainer Birch203) | Developing a range of documents such as business plans, audits, reports which draw on stakeholder appropriate evidence, such as. . . figures to answer service aims and targets, clear costing figures to managers who manage tight budgets, service user stories to reach hearts and minds . . . it’s the ability as a clinician to speak the language of the managers. So you meet with this group of clinicians and patients . . . mindfulness is great and everything, then you’ve got to translate that into management speak into pounds and sessions and productivity and they’re happy thenIAPT clinical lead, Pine201, Pine strategy paper 2011. . . participants starting the MBCT course measured as experiencing a severe level of depression. By the end of the course, scores on depression measures had improved by approximately 25%. 9/10 participants completed the 8 week course and all of these described the programme as being of significant benefitDocument, quarterly report, PineFacilitator shared Service User stories (none could attend today) The power of the Service User Voice. Not quite as effective when the LC is telling their story. Much more real and rich coming from the Service Users themselvesNotes, mindfulness awareness day staff, Elm, 29 September 2014 |
| Use of pilots and audits | To generate local evidence base for awareness, need and impact of MBCT:If I was rolling it out, I would encourage other services to run a pilot. Because what’s very difficult to argue with, is the resultsIAPT clinical lead, Pine201 |
| To increase the potential for local buy-in:. . . because our local evidence is not research it’s just service evaluation . . . it’s got more influence, local data hasn’t it. If you can take those sorts of graphs and shove them under a manager in the service and say ‘look this is the groups that’s running here, this is the results that it’s getting’. That is pretty. Whereas if you show them look this study here that was done in the States, or that was done in Oxford 5 years ago . . . ‘yeah yeah I’ve got research coming out of my ears, I’m not interested frankly’ . . . but if you show them a graph, this is the group that we did here with your customers and these are the results that we got. It’s got much more impact and immediacy and people respond to that much better in my experienceMindfulness clinical lead, Pine101 |
The issue of fit and intervention integrity (in relation to alignment with the way that MBCT is recommended within NICE guidance) are described in other sections (see Chapter 3, Evidence fit with patient and practice), and is further described by those in implementer roles. Implementers were giving themselves ‘the freedom to adapt’ (Oak101) in relation to the clients who were coming through the service:
I have a kind of stock phrase that guidance is guidance and it probably fits 70% possibly so you’ve got 30% play room and guidance isn’t fixed law that you must do this and the real life presentations of people don’t always fit the protocols so you need to have things that will cover a variety of different ways of people presenting. So it’s having wiggle room within the guidance, so the guidance gives you a sense of which direction to travel.
IAPT clinical lead, Pine201
There was also consideration of other factors such as additional research evidence that was emerging to inform current practice, which was also being weighed up:
Well if you’re strictly adhering to NICE guidance then it’s for relapse prevention in depression is the main index for people who’ve had three or more episodes but there was additional evidence coming in just about the time when our committee was meeting which was in 2010, so early papers in the Journal of Affective Disorders and several things since then about its effect in acute depression too, so symptomatic depression and that has been reinforced since . . . it was kind of helpful evidence for us because we wanted to show this as something that could be more effective across a broader range of things than just relapse prevention in depression.
Senior academic and clinician, Pine303
Networks
Lone implementers struggled to build momentum on their own, those who were more successful had greater levels of formal and informal support. Early adopters (particularly) had been lone champions working in environments and structures where MBIs and MBCT were not included as a service priority or at that time little was known about it. As such, they created and/or sought out informal structures and networks around themselves:
I guess meeting with other practitioners is also helpful because you can share ideas, and also share things that perhaps don’t always go according to plan, which is often more useful than positive ideas. You just feel like a community, so they’ll be people now that I know from other courses that work in other teams, and because I know them through the practice days etc. they’ll say oh you handle this, what would you do, would this person be suitable? So you’ve got all that informal, so it’s not only the formal structure, it’s the very informal structure.
Clinician, recently completed internal training, Pine103
This approach to seeking out and/or creating a supportive environment through informal and formal networks of various types, including virtual networks locally, regionally and nationally, resulted in implementers being able to share issues, learning, solutions and expertise (Table 10). We found that the more active, established and closer the networks (to the implementers) were, the stronger the support system.
Teachers there quite relaxed and format of the meeting was relaxed. Felt very informal and the teachers looked relaxed. A chance to for teachers to be re-assured and build on their confidence – ‘it’s ok, we’re dealing with the same thing’ or ‘that’s exactly how I feel’ type of feeling . . . This Peer Supervision session is a chance to learn about people’s challenges and use to arrange better for the future and learn how others overcame their obstacles.
Observation notes, peer supervision meeting, Elm
| Site | Internal/local networks | External/wider networks | Training and supervision networks |
|---|---|---|---|
| Oak | There was a social network and a professional network that coincided Practice-based interest group critical for developing, and supervision provided within governance arrangements Multilevel support system within the trust: clinicians, senior managers, directors and CEO Emphasis on the importance of local links with service users/communities and service providers |
Emphasis on the importance of university links and national networks. Research links Mindfulness practice network Involvement with the MAPPG |
Trust had a network of 23 trust approved teachers Weekly supervision arrangements |
| Pine | LC built a network of skilful people around him, people who knew how things worked in different levels of the organisation; someone who had the ‘ear of the’ managers, another who had experience of running a private business so knew how to build a financial case and manage income Multilevel support and engagement LC built an alliance with referrers |
Innovation network was established which was a collaboration of up to 150 active service users, the trust and the local university Strong research links with the local university Shared best practice through national networks |
A lot of formal and informal support and networks. Monthly supervision and peer supervision |
| Elm | Network of service user volunteers Awareness training offered to referrers and newsletters for practitioners and service users circulated regularly to keep people informed Not a strong relationship between implementer and managers Circulated newsletters to staff and service users |
Held mindfulness practice days and invited external speakers Online resources freely available |
Informal peer-led supervision every 6 weeks Offered training to neighbouring trusts and wider regional networks Ran development courses and awareness training for referrers and anyone interested in mindfulness |
| Mangrove | Combination of implementers – but they did not network that well together – they each have their own individual goals and interests which makes ‘buddying up’ more difficult (no common goal) One implementer organised special interest groups (business and not practice based) and staff drop-in sessions and yearly staff groups |
Link with professor at local university | Special interest group (peer support, 6–10 staff in different areas of trust but no shared project) Problem of cost and not having anybody trained up led to LC writing/piloting training pathway programme – started September 2013 with five hand-picked invited trainees (unfunded as a ‘gift’) |
| Bamboo | Services established in two out of the six regions within the trust Early implementer networked widely, and even though now retired, is still linked in with what is happening locally |
A network around a national training programme with a national network that meets three times a year to co-ordinate activities and share ideas Wide network of stakeholders came together to form a community interest charity offering teacher training (partially external to site) |
Signs of an emerging internal training pathway Links to a national training programme Supervision: implementers were mentored by retired early adopter Some peer supervision founded by two of the early adopters Supervision and maintenance group ran in the evening (in own time, no central funding) |
| Birch | In general within the trust there was not a ‘good flow of communication’ between stakeholders and it was difficult to network across the sites due to the large geographical spread. Took a while for co-ordinator to find out who they needed to speak to about resources and when they did, they were too junior to have an impact | Early adopter moved from the trust to the local university and still maintained a strong link with the trust through training and supervision arrangements Early adopter reached out to wider networks in the early days in order to build momentum (national mindfulness networks, research links with various universities and local MP) Third sector consortium commissioned to deliver MBCT for service user, but there were concerns (by LC) about the level of training providers had |
Training provided by the local university Supervision structures was not in place at the beginning but had been since improved with the help of a co-ordinator role. External supervision only Large rural geographical area, people not reaching supervision sessions (Birch103) |
| Hazel | Eight MBCT teachers were found in this trust but there was no connecting network between them. Some did not know of each other’s existence Evidence of a special interest group but very limited owing to staff changes – in a bit of a ‘lull’ since early adapter left |
Some teachers had links to a local Buddhist centre and a peer practice interest group met over many years but that did not offer supervision (since dissolved) | No visible structure to train trainers. Training and supervision mostly self-funded Staff attended courses outside the trust owing to own interest |
| Juniper | Implementer as an individual very active in trying to build a network of interested individuals, but still the only MBCT practitioner within the trust Implementer was very active in gathering the evidence and working with clinicians on adapting MBCT for various disciplines within the trust There is support in a sense that the implementer is allowed to do it and deliver it (for free) – but nothing further than that |
Very active in wider national mindfulness networks, but does not feel like there is a strong support system/network within the trust | Lone implementer offered advice and interested staff were allowed to sit in and co-facilitate groups, but if they wanted to pursue training they would have to find external training courses |
| Beech | Mindfulness Special Interest Group set up – but not well attended when observed. People talked about the difficulty of getting to it – would take 40 minutes to get across the city, then back again, so people do not have time to go and cannot justify that time when they could be spending those 80 minutes seeing patients No evidence of a multistakeholder support system |
Implementer had started to have conversations and tried to network with other more embedded sites, but because of other competing priorities and lack of resources not taken it any further; but some evidence of networking with the local university to deliver courses at the university | Site had developed an internal training and supervision pathway, but was halted because of reorganisation and waiting list targets |
| Wisteria | Manager within occupational health supportive of investment into prevention despite limited resources | LC involved in a practice peer group based on shared practice only (and some research interests, students) regularly within university | LC pays for own supervision every 4 weeks |
Often these networks would start with the local relationships and mentorships between MBCT and/or MBI exponents. Relationships and therefore networks took time to develop: those sites (e.g. Oak) that had more established provision had the time to build a range of networks such as a supportive network of colleagues and managers within the service; external networks of regional and national implementers; training and supervision networks; and research and development networks.
This paper outlines interventions that XXXX [Oak] can offer to partner organisations to introduce mindfulness in the workplace . . . this paper describes who we are, how mindfulness interventions can be offered to staff, the ways in which training would be evaluated and the costs.
Document, MBIs for staff, Oak
Furthermore, in more embedded sites there was a greater mix of formal networks such as supervision and special interest groups, and informal networks such as peer support:
I also started organising the Mindfulness Special Interest Group and I mean that’s something that’s grown very organically; so when it started off with three of us sitting and looking at a journal together and it’s grown so that we, normally do two or three events a year, sometimes we hold days, sometimes with internal speakers who’ve got some work to present and sometimes with external speakers.
Interest group facilitator staff mindfulness teacher, Mangrove102
Observational data of peer supervision sessions confirmed the importance of developing and sustaining implementer groups in the absence of formal supervision. For example, in Elm and Bamboo we observed a well-attended peer group of five MBCT teachers. We also observed a newly formed Mindfulness Special Interest Group in Beech that seemed to be less attended, due to the geographical dispersion of the various teams:
XXXX arrived saying she felt a bit guilty for coming but said they weren’t often held, only been once before. 2nd woman arrived, introduced herself . . . had travelled from XXXX, 35 minutes away.
Observation notes, Mindfulness Special Interest Group, Beech
Geography: the trust is quite spread out, seems that there’s more happening where the local collaborator is based. The further away from that, the more difficult it seems to be.
Field notes, Beech
I don’t think pretty much any of us go to the mindfulness groups (special interest group) and I would take a guess that we would all love to but when you’re talking about tolerated rather than encouraged we wouldn’t get any time to . . . it would be a whole half a day.
Clinician, Beech105
The opportunity to be part of a training and supervision network enabled a continuity of clinical support, as well as opportunities to learn from others’ experiences, which resulted in implementers feeling more networked. The closer the implementers were to the support system the further they moved away from being the lone enthusiast:
I think one of the things that they have done really well in [Pine], [local collaborator, Pine] has done really, really well, is trying to develop a network and he has tried to develop some benchmarks for practice, he has insisted that people come for supervision, he has insisted that people go through the training.
Consultant in psychological therapies, lead for depression service, academic, Pine204
Some successful implementers had also developed networks and links with universities. These links, which were strongest in sites where MBCT was more established (e.g. Pine, Oak) often started with audits, then built up to service evaluation, through to the development and evaluation of new MBIs. Additionally, closer links with universities had enabled research and development of new mindfulness-based courses (e.g. Pine, Birch, Mangrove and Juniper).
Context
The implementation context for MBCT presented possibilities and challenges to its application.
The implementation context for introducing MBCT was multilayered, including the broader NHS context, the country and/or regional context (see Chapter 1, National context for psychological therapies generally and mindfulness-based cognitive therapy specifically), and a site-specific context, and it was also multifaceted (Figure 16). Chapter 3 (see Evidence fit with patient and practice, also section on Fit later in this chapter) described how MBCT as a psychological therapy for keeping well ‘fits’ as an intervention into the pace and ethos of the NHS. Other general pressures, priorities and drivers within the service also presented implementation challenges. Additionally, access to resources including material and capacity, and capability for implementation acted as either facilitators or barriers. A misalignment of support, particularly from middle and senior managers within organisations presented challenges to the local MBCT implementers. These contextual factors were more or less evident in each site, their ability to work with them was a function of the multiple factors threaded throughout these explanations, and an accumulation of more facilitators than barriers to implementation (see Pivot points).
FIGURE 16.
Context.
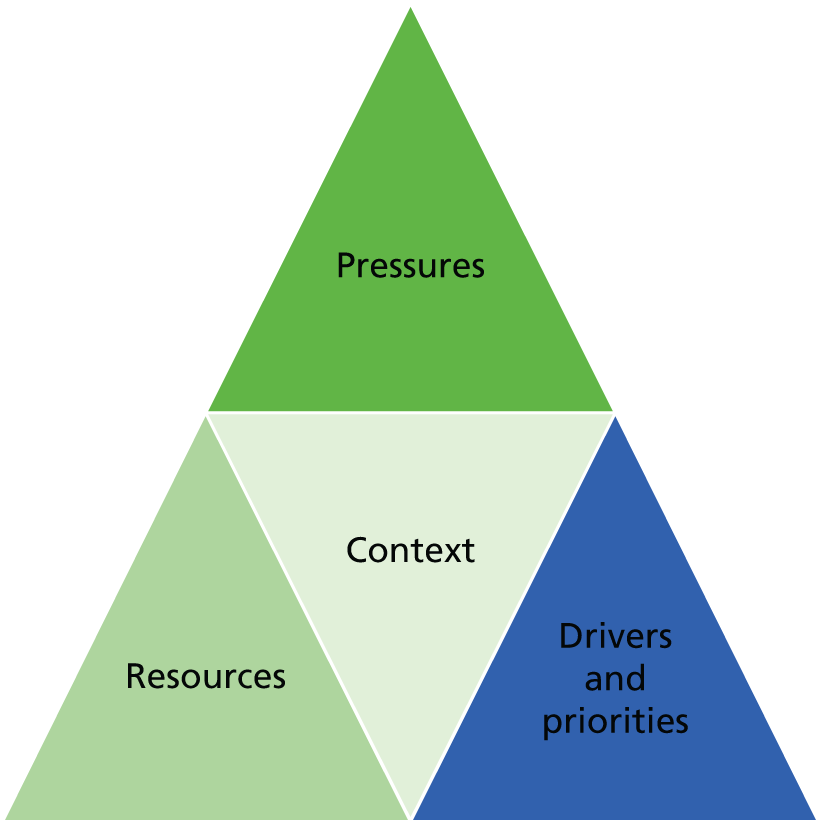
Service pressures
Findings from phase 1 described some of the challenges that the NHS context was presenting to the implementation of MBCT (see Chapter 3, Fit of mindfulness-based cognitive therapy in the current NHS). Case study Beech (and later on in Elm’s journey) shows patterns of similar challenges and provides some explanations as to why these issues challenged implementation efforts:
. . . because of the redesign of the psychology service told me to put all my training activities on hold and to not provide any further mindfulness training . . . because of the service redesign, I was told to freeze all of my training activities and I was diverted to clearing the waiting list for individual therapy.
Retired early adopter, Beech101
Data show a reiteration of the comments about the challenges of the fit of MBCT in the NHS, and we also heard (particularly from sites were there was less evidence of MBCT) about the importance of the presence of a culture of innovation for implementation of new initiatives to be more successful:
A lot of it is about culture to be honest isn’t it? It’s about the culture of an organisation and what’s open to your staff and how encouraged they are to innovate and implement and being given permission to do it and then support it.
Research and innovation lead, Elm205
In this example, the sole implementer in this service had found it challenging to sustain their implementation activities.
One contextual factor that explained some implementation challenges was that of frequent changes in service structures, with reorganisations affecting the availability of resources to run existing services:
. . . from a practical point of view I found that a lot of people in the trust have got heavy workloads, so all the things you hear in the media about pressure on the NHS with resources and staffing levels and things like this. So my experience is that a lot of the psychological therapists and clinical psychologists are so busy doing their normal job that reduces the time that they’ve got for innovation like reading research papers and introducing new treatments like MBCT.
Volunteer, Juniper103
Second, there were challenges in prioritising the investment needed to initiate a new service such as MBCT, when service priorities were frequently changing and resources were limited:
In common with many organisations [Birch] has, well the culture of a lot of organisations in an environment where there’s been a pressure to reduce cost, I mean our organisation isn’t unusual in that regard and I think then it becomes very difficult for managers to prioritise new investment, well not new investment in terms finances but kind of investment in changes in working practices because in a sense they are trying to run to keep up with doing what they were doing with maybe less than what they had . . . So I think the context is difficult.
Academic and dialectical behavioural therapy implementer, Birch204
In addition to the email below from [service manager], I spoke to [team manager] yesterday about the need to resource classes. [Team manager] has asked me to send her costings, but unfortunately she is of the opinion that the XXXX Government money can’t fund the equipment side of things, only the actual training.
Document, e-mail 2, co-ordinator to manager, Birch
An extreme example of service pressure impact was found in Elm where a considerable amount of work had been invested in MBCT teaching and teacher training, but was halted due to reorganisations, pressures from different targets and a retendering process for service provision:
So there’s been very big shifts on all the CBT therapists having a minimum of 25 contacts per week which used to be 15 so it’s a heck of a change in how the workforce are working. Very little preparation time, having to be very lean within the therapy hour that it’s 50 minutes so you have 10 minutes to write your notes up before the next person comes in . . . [it] became very very much forced by the summer of last year, summer 2014, and we were told at the time that it was necessary because we were being recommissioned if we didn’t succeed . . . And so they put the thumb screws on in early 2014 for us work on this 25 contacts per week to try and get the commissioning.
Local collaborator and former mindfulness clinical lead, Elm101
Furthermore, constant changes to personnel, particularly managers, meant that implementers, who relied on tapping into supportive networks (see Implementers), had found it difficult to know who to relate to when trying to make progress:
I guess the person behind the door is changing so much now that if you build an alliance with one person behind one door, you blink and that person has moved to another role, or has just been given three more roles as well as their role, and so there’s less opportunity to build those kinds of alliances with the higher management that ever before, because everybody at every level of the trust is so stretched.
Local collaborator and former mindfulness clinical lead, Elm101
The result of frequent changes to staff also helped to explain the stalling and fragility of implementation journeys in some sites. For example, in Beech an active early adopter facilitator left the service causing activity to halt for some time, and in Birch people were retiring and/or leaving, which left non-trained staff to run MBCT groups.
Drivers and priorities
At a national policy level, drivers around IAPT (although this specific political driver was of most relevance to English sites, see Chapter 1, National context for psychological therapies generally and mindfulness-based cognitive therapy specifically), widening access to psychological services, recovery and prevention, and health and social care integration have been positive drivers for MBCT implementation. Additionally, as described in Chapter 3, the inclusion of a recommendation within NICE guidance provided a lever for paying attention to its implementation. Furthermore, although it was perceived that the NHS is focused on medical rather than well-being interventions (see Chapter 3, Fit of mindfulness-based cognitive therapy in the current NHS), there was a sense that in some sites this emphasis had been shifting, which provided a positive context for offering low-intensity treatment options such as MBCT:
. . . the kind of conversations they were having 10 years ago are well you’re mentally ill and you’ll be mentally ill for all of your life and keep taking these tablets and keep coming back to see me and there’s this massive change in terms of actually no we don’t think that’s right; we’re not telling anybody that they should be forever in mental health services, it’s much more about that empowering, that collaborative relationship . . . We will assist you, we can help you, we can give you tools to do that.
Operational manager in adult mental health directorate, Pine202
Within the offer of low-intensity treatment options includes those that may be offered more cost-effectively as group options, such as MBCT. We explicitly asked participants whether or not cost-effectiveness was a motivator for facilitating implementation, and if they were collecting any cost-related evidence as part of implementation activities. Although there was a perception that ‘group work is more cost effective and efficient for a service than individual mindfulness sessions . . . that’s the evidence base on delivery of groups work . . . so I think it’s cost effective’ (talking therapy service lead, Oak211), cost(s) were not reported as an explicit driver, and evidence about costs of implementing MBCT within sites was not available.
In contrast to drivers, priorities that were often enacted through performance targets had presented challenges to MBCT implementation. One CEO described a ‘cocktail’ of competing priorities:
. . . we are struggling with year on year of historic disinvestment with escalating activity pressures due to the changing nature of urban boroughs, problems with staff, recruitment in terms of quality and all of those can add up to a pretty difficult cocktail when you’re trying to transform the way in which you work with people and do business.
CEO since 2013, Mangrove202
Such a context, which was commonly expressed across the sites engaged in this study, may leave little space or opportunity for prioritising interventions such as MBCT:
. . . although we’d celebrated getting mindfulness into the service operational plan as something that was routine across all services which felt like a real milestone last year, it felt with the shifting targets and the shifting landscape that nothing was safe, nothing was sacred and it all just became about targets.
Local collaborator and mindfulness clinical lead, Elm101
Professional Participant and very recently a service user; Attended a staff 8 week course. His manager not supportive at all – stopped the staff sessions because of financial cuts etc therefore competing priorities get the attention.
Observation notes, mindfulness awareness day for staff, Elm
Additionally, as a consequence of attempting to meet commissioners’ aims (as opposed to clinical aims, which were perceived to be at odds with each other in many participants’ accounts), there was evidence of expanding the target group of MBCT presenting a tension for the integrity of intervention delivery, as expressed by this psychological therapies consultant:
My original intention for our specialist depression service was to have groups for people solely with depression because that would be the NICE-recommended intervention and I think the whole thing has been a lesson really in how difficult it is to implement evidence based practice in an NHS setting because staff have their own views based on their own models and their own prejudices, like how things should be done . . . the difficulties with NHS practices is that there aren’t necessarily benchmarks for practice and because things are often operationally led by managers who are not clinicians rather led clinically led I think that can often be a point, and commissioners are the same . . . so what they commission may not necessarily be in context the best thing to do. I think what is always a concern to me is that MBCT is a highly effective intervention in certain groups and one of the dangers is that it can be so diluted that it ends up being used inappropriately but then it’s seen not to work and it’s the therapy that gets blamed for that rather than how the intervention is delivered
Consultant in psychological therapies, lead for depression service, academic, Pine204
A further consequence of not having MBCT embedded in service strategies (e.g. Beech, Hazel, Mangrove, Juniper and Wisteria) was that competing targets got priority. Additional activities, of which MBCT was one in those contexts, meant that they were happening ‘under the radar’, leading to more personal (rather than organisational investment) in implementation, a lack of support, and leading to patchy, unsustainable services (e.g. Elm, Mangrove and Hazel).
Hard to speak with managers. Introduced to 3 but they didn’t have time, they just said ‘XXXX [volunteer implementer] will tell you everything you need to know’. Same attitude was seen trust wide; Volunteer was passionate and so left to do everything. If XXXX [volunteer implementer] left, there would be no MBCT 8 week courses . . . Management have monthly meetings with different topics (raised by managers themselves) but apparently Mindfulness never seems to come up in those meetings.
Field note reflections, Juniper
Perhaps linked to the level of organisational commitment or priority around implementing MBCT, findings show that in sites where MBCT was more embedded there was evidence of a greater level of support, particularly from managers. The converse was the case; in sites where there was less evidence of MBCT, implementers had access to less support:
. . . my sense is our representation, psychology representation at senior management level and the kinds of forums where senior management sit isn’t there. We used to have an Associate Director of Psychology and that person I think did sit on the board possibly or one of the committees just down from the board and that was really important. That post went quite some time ago so there is no one now that holds that position and so I don’t know how far up the hierarchy the psychology influence goes. So that’s one possible explanation as to why there hasn’t been a top-down approach as well. It might be to do with the insufficient psychology representation at the very highest level.
Local collaborator, Beech102
The support from managers, aligned with organisational level buy-in (see Fit) led to a more supportive network and access to resources such as time during working hours to develop the service, and funding and time for training and implementation activities:
I think we’ve been very lucky in this trust that the number of elements combining to make it more possible . . . having a chief exec[utive] that was open to it, having a few people in the organisation that were keen for it to happen, a couple of consultants, [lead for depression service, academic, Pine204] helped to get it started . . . They’re all at different levels in the organisation but they’ve all got influence so I think that creates an environment in which it can happen . . . if you’ve got people in the organisation saying ‘yes we want this to happen’ this enables the people lower down.
Local collaborator, Pine101
Resources
Perhaps unsurprisingly given what has been described above and in other sections, the dedicated resources underpinning a commitment to MBCT were variable. Some sites had received some funding from a country-wide investment in psychological services (IAPT), but this had been relatively limited with respect to MBCT. As a result implementers had to make do and/or think creatively about resource use.
Having dedicated human resources greatly helped with the implementation of MBCT and with sustaining the service. Oak and Pine had part-time dedicated clinical lead roles (i.e. people were allowed the time and resources, which was enabling). A mindfulness clinical lead role existed informally in Mangrove and Elm; however, as there was no protected time or associated resources this meant that those implementers were having to do the majority of activities in their own time and under the radar. In Birch, the co-ordinator role had been recently established, but carved into existing workloads. In Juniper a lead role was filled with a person on an honorary contract, and in Bamboo the clinical lead role was also more on a voluntary rather than formal basis. In Beech there had also ‘never really been any recognised designated time’ (Beech102) for the implementer. As such, where MBCT was not part of an organisation’s strategy and plans, resource to deliver was scarce and, as described in previous sections (see Implementer and Chapter 3, Fit of mindfulness cognitive therapy in the current NHS), much of the burden then fell to those in championing positions.
There were examples of specific financial investments being made to kick-start or sustain implementation, including in Pine where £80,000 was allocated from a fund to increase access to NICE-recommended treatment for service users, and £68,000 from the regional authority was provided for training and a conference. In Oak the trust had invested in staff well-being (i.e. provision of mindfulness sessions) and in other sites (Bamboo and Birch) funding was available for training, although there was a sense of frustration in Birch that funding beyond training to support the delivery of the service was not in place:
I was hoping to bring this up with you next week, but I guess now is the best time as ever! There is a sense of frustration and despondency from some of the teachers that the go ahead to the funding of the basic resources for the Mindfulness classes has yet to be confirmed. Some were hoping to have run a course before Christmas but as funding for the venue, mates and books etc has not happened, delivering classes has not taken place. Whilst I understand that training more teachers is important, I also feel it is imperative that these practicalities are acknowledged as a very important part of service.
Document, e-mail from co-ordinator to service manager, Birch
Often research grants were helpful in progressing developments, most notably in Oak and Pine, which had strong links to local universities and good clinical academic capacity. However, in other sites, such as Elm, a lack of financial investment had a ‘detrimental effect’ on planning for the future:
There has not yet been a confirmation of the funding necessary to set up and run courses planned in 2012. This has previously been agreed by XXXX [manager] who will be leaving her post in the near future. The lack of confirmed funding is having a detrimental effect on future planning and perhaps to inform XXXX [different manager] of this problem.
MBCT practitioner meeting minutes, Elm
Given the patchy and usually short-term nature of resource allocation, some sites reported their success in and plans for income generation, which led to opportunities to fund and grow activities where resources had been scarce:
All of the investment has been a bit sort of sideways . . . So in terms of income we’ve been able to grow things on the basis of selling training places and that’s been very successful.
Training director, line manager of mindfulness clinical lead, Oak209
It’s been looking at using mindfulness as an income generator, because there’s huge pressures in terms of savings required annually, and mindfulness is very much in demand across all spheres of health and other organisations as well. So I think there is a demand for training, so that’s what I’ve been looking at more recently.
Head of psychological therapies, line manager of mindfulness clinical lead, Pine206
There is now a budget for overheads: XXXX [local collaborator] has generated income through offering the training courses. We can now request funding for CDs etc.
MBCT development meeting minutes, Elm
Fit
Successful implementation of MBCT was dependent on the degree of alignment between the intervention and NHS context, existing local service strategy, priorities and pathways, and efforts to adapt and make it fit.
Services that found creative ways to fit MBCT within their contexts were most likely to have successful and sustained implementation. This often meant using the NICE recommendations for MBCT as a starting point for making the case but then flexibility, adapting the MBCT programme to fit the local context and client groups (Figure 17). The degree of alignment of MBCT with other service initiatives (such as IAPT), management interests, resources and with a recovery ethos was often perceived to be a factor in implementation.
FIGURE 17.
Fit.
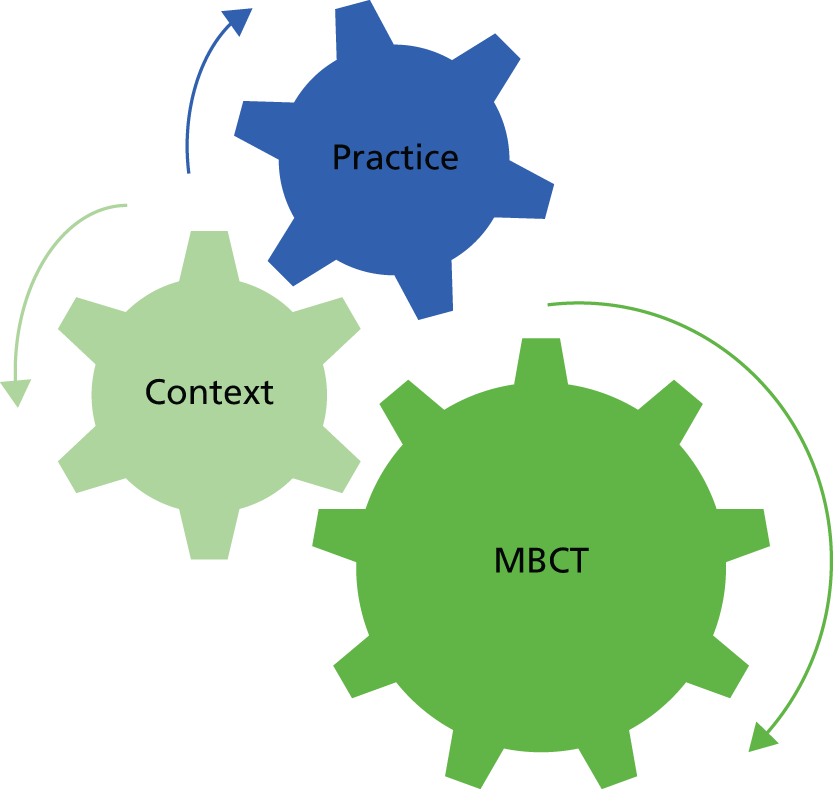
Table 11 provides a summary of some features of ‘fit’ that emerged from interview data and documentary evidence from sites.
| Site | Explanation 3: fit |
|---|---|
| Oak | Fit with local and trust culture and focus on mental health Fit with research interests/strategy Fit with executive interests to launch centre of excellence (clinical, staff, training) |
| Pine | Fit with research interests of senior clinical/academic psychiatrists Fit with IAPT rollout/group intervention remit run by the implementer’s former colleague Fit with culture based on empowerment service model |
| Elm | Fit of staff and patient mindfulness with rebranded Health & Wellbeing Trust’s focus on prevention NICE guidelines fit overall, but not with IAPT needs |
| Mangrove | Good fit/adaptation at various service levels but not across services Uneasy fit at trust level, preoccupied with managing stakeholders, revision of adult mental health pathway and divide between primary/secondary care Good fit with commissioning priorities around choice, prevention, parity |
| Bamboo | Non-ideal fit with country-specific performance targets that prioritise waiting times (struggling to meet these with scarcity of CBT therapists) Reasonable fit with site’s national guideline, SIGN 2015 guidelines,82 with wider remit for MBIs than NICE guidance Uneasy fit with health/social care integration agenda and focus on choice from range of therapies of deprived/multimorbid urban population |
| Birch | No fit with explicit depression pathway within integrated health-care organisation No fit with competing priorities (e.g. targets based around waiting times) Uneasy fit with geographical reach |
| Hazel | Non-fit with current reorganisation and huge training programme upskilling nursing staff in various modalities (not mindfulness) Uneasy fit with acute rather than preventative culture and CQUIN targeting NICE depression guidance perceived as low-intensity/primary care issue Some research in a learning disability context, but no fit with trust academic interest, which was predominantly pharmacological |
| Juniper | Fit with third wave of IAPT rollout and focus on group therapy Fit with mix of populations across range of modalities and IAPT stepped care model Fit with existing interest and enthusiasm of implementers |
| Beech | Fit with secondary care clusters and need for NICE compliance Uneasy fit with IAPT recovery model and competing adapted mindfulness group to target waiting lists |
| Wisteria | Fit of implementer coming to a lone role as psychologist in an occupational health environment with clear remit to introduce group-based interventions Good fit between occupational health and human resource agenda around prevention/sickness absence Uneasy fit of the intervention within a trust that has a reactive rather than proactive approach to health and well-being |
Evidence and fit with practice
Mindfulness-based cognitive therapy is not an intervention that provides ‘a quick fix’ (Commissioner, Wales) and, as such, in many cases it was perceived to be at odds with the pace and pressure of current health services. MBCT also aligns with a model of care that places people as active agents in their own recovery and promotes mental health and well-being, rather than a medical model. In NICE guidance, MBCT is included as a prevention intervention delivered further on in the treatment pathway to keep people well. As such, consistent with the findings from phase 1 (see Chapter 3), sites that were implementing MBCT had adapted the inclusion criteria stated in NICE guidance because they were seeing people who were not well:
Mindfulness is more of an exit strategy so within CAMHS in XXXX [town] MBCT hybrid is used as an exit strategy for young people who’ve had CBT or other kinds of 1 : 1 and the implementation there is much stronger because there’s a better fit between mindfulness and as an exit strategy.
Teacher trainer, Oak111
Adaptation of the intervention to service and population need was a frequently used implementation strategy (see Chapter 3, Adaptation). This included, for example, services trying to fit their offer to the needs of presenting clients:
I think the main focus is secondary care but it does vary and the clinical reality of working in NHS department somewhere is that you’re meeting a mixed group and this is true of any of empirical evidence applied to clinical issues; it’s interpreted with a view to the needs of the people who are presenting, so it’s interpreted slightly broadly according to clinical need . . . you know people are well, they’ve had two or more episodes of depression, in other areas it’s a more mixed group, primary care for example and there’s also the issue of client choice as well, and again in [Bamboo] which I know we started with giving people a choice, that mindfulness if it was something they felt they would find helpful.
National NHS training provider, Bamboo102
She mentioned the criteria had changed over the years to suit the demand. When they first started the NICE guidelines’ criteria was adhered to (3 or more episodes). Then in the past 2 years it’s been an anxiety and wellbeing course. And now with self-referrals in place it more of a preventative and wellbeing course.
Observation notes, peer supervision meeting, Elm
In Birch there was an uneasy fit due to pressures to adapt MBCT to a mix of patient populations. Added to this was the reliance on an external teacher, who in this site was the sole implementer and who wanted to ensure that MBCT was used in line with NICE guidance, which did not fit with other clinicians’ perspectives and current pressures in the trust.
So we were looking at the mix of population, what was needed, because the pure three or more episodes of depression, there weren’t enough people to have a class, so it was ‘what it was going to look like on the ground’ . . . there were lots of issues around the team not particularly wanting group work and there being pressure, waiting lists and them wanting this to be around more individual people on caseloads, they didn’t see the benefit of having groups at that point. So it was a bit of a challenge with only half the team on board.
External trainer/supervisor, Birch203
Fit and local context
Where there was a good fit between the aims of the MBCT intervention (recovery, keeping people well) and the organisation’s strategy, implementation had been more successful. For example, in Oak, mindfulness aligned with the CEO’s priorities:
. . . you have to decide which horse to back, you can’t do everything. For me mindfulness, equality, diversity and human rights and a few other, well the anti-stigma work . . . they were who I decided to prioritise on.
Retired CEO and campaigner, Oak212
Furthermore, MBIs ‘tied in nicely’ (board member, Oak213) with their research strategy and theme around ‘mood anxiety and mindfulness’. In this site, there was a cadre of clinical academics who were bridging the practice research boundaries to focus on mindfulness-related research as well as practice. Pine was another site where there was a strategic focus on mindfulness and on a ‘wellness and recovery ethos’ (mission statement document, Pine), and from that focus, the subsequent alignment of other agendas including resources and research to support the MBI agenda. As such, there was a number of senior people in the organisation who were supportive of the intervention (i.e. it was a good fit with their intention and mission):
. . . we’ve been very lucky with the board, and in fact our chief executive has led breathing spaces in her leadership briefings before, and she practises mindfulness and is very keen on it. In fact a lot of the senior directors are interested in it. So like I mentioned the finance director asked me to do a session for the finance department. The director that’s involved with staff well-being is very keen on developing it. There’s also another director who’s interested in sort of marketing it. So we’ve got lots of senior people I suppose who are right at the top of the organisation who are very keen on it and I think that’s very significant.
Mindfulness lead, Oak101
The opportunity that the early implementation of IAPT offered had also been seized on by Pine:
I think we were one of the first IAPT services to run mindfulness, there may have been others but I think we were one of the first IAPT services to do it [. . .] it fits what we’ve been commissioned to deliver so let’s go for it.
IAPT clinical lead, Pine201
In contrast, IAPT had been a barrier for others because ‘the IAPT menu does not have MBCT on it’ (former mindfulness clinical lead, Elm101). However, documentary evidence from November 2015 shows some changes to IAPT in which ‘mindfulness’ interventions are in the menu of services on offer,83 but does not detail the exact nature of the intervention to be offered (i.e. whether group or individual appointment). 84
Evidence from other sites showed a lack of, or poor fit between, the service delivery model and/or strategy/priorities of the organisation and the requirements of implementing MBCT. For example, in Hazel, MBCT was not a service modality that fitted a service reorganisation aimed at reducing costs alongside a focus on pharmacology rather than psychological therapies. Similarly, in Beech a service and organisational restructuring was focused on reducing waiting lists, which did not:
. . . fit within our recovery model. [. . .] From a service management point of view, as soon as somebody is below a certain point on their questionnaires they’re recovered and therefore you don’t need to carry on offering them treatment and obviously the ideal thing with MBCT is that it’s a relapse management prevention thing, so people should be relatively well going into it, which obviously doesn’t fit at all with that model of offering therapy . . . as the service works at the moment they get paid if somebody recovers on their figures, it’s not helpful, particularly to make sure they don’t come back, from a financial point of view. So to be offering them what is an expensive form of therapy when it’s not actually going to earn them [the trust] anything?
MBCT teacher, Beech105
Mindfulness-based cognitive therapy teacher training and supervision
The existence and quality of training and supervision was a function of the level of strategic priority and subsequent investment placed on MBCT implementation within an organisation. There was typically a tension between ‘gold standard’ and ‘good enough’ teacher training models.
The implementation journeys in all sites (irrespective of where they were in their journey) were ones of adaptation to local need, resource and capacity. Existence of MBCT training and supervision within sites was linked to the strategic priority and consequent financial investment (or lack of) that followed this, including the setting up of appropriate governance around service provision (Figure 18). As such, and consistent with findings that show a mixture of bottom-up and top-down driven implementation, our data show a varied picture of training and supervision arrangements, which ranged from one site that had developed their own ‘apprenticeship model’ of NHS MBCT teacher training (e.g. Oak). Some sites had a mixture of official and unofficial internal training and mentoring arrangements (e.g. Pine, Bamboo, Mangrove, Beech), whereas others had ad hoc to no formal arrangements (e.g. Hazel, Juniper). In Oak, implementers in senior roles had received external self-funded training, and three members of the core training team for one of the lead university-based training centres lived locally, a combination that then enabled them to develop the internal apprenticeship model as a collaboration between the trust and externally commissioned local teacher trainers.
FIGURE 18.
Training and supervision.

Data from implementers show the link between their interest in and motivation for maintaining and sustaining good-quality practice by ensuring a certain standard of training and supervision and successful service delivery (Table 12). For many this had resulted in a tension between striving towards a gold standard model of training and practice, and a pull from providers and commissioners who would seek a compromise towards a ‘good enough’ (Bamboo) model within current service pressures. There was pragmatic acknowledgement in successful sites of the bridge between meeting professional and personal needs through the ongoing good practice requirements for MBCT teaching. Successful sites provided most elements of the training pathway in house. The retreats were the element that was most likely to require self-funding and use of personal time.
| Site | 12-month training pathway (internal/combination/external)a | Funded (self-funded/partially funded/fully funded) | Staff delivering MBCT (also if known: number of trained mental health clinicians) | Retreatb | Supervisionc |
|---|---|---|---|---|---|
| Oak | Yes – internal Key implementers had invested in training with external providers and continued to receive external supervision and support. The implementers established an internal apprenticeship training programme and later a paper on its application in the NHS was published |
Fully funded (apart from retreat) | Yes – 23 staff They were recruited to do the training from within their mental health service |
CPD retreats encouraged in own time (self-funded) | Yes (weekly) Provided by internal supervisors (key implementers) No additional fee to staff |
| Pine | Yes – internal In 2010 the site established an internal training pathway. Previous to this, in 2008, MBCT lead in this site was funded (by the trust) to complete the TTR2 training at Bangor and continued to invest in external supervision and support |
Fully funded (apart from retreat) | Yes – 30 staff They were recruited to do the training from within their mental health service |
Guided day-long meditation retreat four times per year provided in house Longer self-funded retreats encouraged by lead but not compulsory |
Yes (monthly – partially in own time and partially in work time) MCBT teacher supervision for 1.5 hours every month in groups of two or three Monthly peer supervision sessions |
| Elm | Yes – internal (up until 2015) Early adopter and current implementer had invested in training with external providers and current implementer continued to receive external supervision and support from early adopter even after they had retired and left the service |
Fully funded | Combination We found around 30 teachers working within IAPT, therefore assuming they were trained in mental health This site also had service user volunteers helping to deliver courses, who were not trained in mental health |
Not provided as part of training pathway but staff were encouraged to do this in own time/own funding | Yes (monthly) – up until 2011 when it was stopped by new management. Then continued as peer supervision only More experienced implementers were providing peer support and peer-led supervisions every 6 weeks |
| Mangrove | Piloted an internal training pathway | Free for five hand-picked staff (pilot), but delivered in own time not work time | Three staff – unknown if all were trained mental health clinicians | Not part of training pathway | No |
| Bamboo | Combination Local charity training; mentoring model of co-facilitating National NHS provider training; approach not prescriptive to manual which allows most sites to work with either, both or hybrid MBCT/MBSR programmes |
Partially | Seven staff Unclear if all are trained in mental health. MBCT was being offered to a mix of mental health and physical conditions in a variety of settings |
Not part of training pathway | Yes (in own time) by internal and external providers |
| Birch | External provider – teacher training level 1 and supervision (provider offering three progressive levels but trust opting for level 1 and supervision) | Two cohorts trained by local university, funded by health board | Partially MBCT delivered by four or five from first training cohort MBCT delivered by third sector consortium (commissioned by trust). Level of mental health training unknown |
Not part of training pathway | Combination of internal and external providers Monthly supervision by external supervisor Also peer supervision groups No MBCT-specific supervision for third sector consortium staff |
| Hazel | No training pathway. Staff had attended courses through Bangor and Oxford (personal investment), but there was no structure to train teachers | Predominantly self-funded. Sporadic pots of money freed by immediate managers | Around eight mental health trained MBCT teachers working in isolation | No | Partially Some had self-paid, external supervision from Bangor |
| Juniper | No training pathway 15 members of staff received 5 days of MBCT introduction |
Funding released for introduction but this did not enable clinicians to reach minimum training standards | Yes. One volunteer provider. Trained in MBCT at Oxford Cognitive Therapy Centre. Completed a MSc in Mindfulness-Based Approaches at the Centre for Mindfulness Research and Practice, Bangor University | No | Not MBCT specific. Peer CBT and group intervention supervision. MBCT occasionally mentioned |
| Beech | Currently no training pathway A training pathway existed between 2010 and 2012 run by early adopter |
2010–12 training pathway was partially funded for staff, and took place partially in own time | One main provider of MBCT groups. Used to co-run training pathway with early adopter. (No groups currently running at time of visit.) Internally trained staff not currently running MBCT groups only elements in one-to-one work | No | Graduated from the 2010–12 cohorts were supervised on an ad hoc, non-formalised basis. At the time of visit none were delivering MBCT groups |
| Wisteria | No training pathway | N/A | One trained provider running MBCT groups for staff | No | No |
Strategic versus local solutions
Evidence of an organisation’s strategic investment in MBCT through training and supervision being part of the governance structure around provision was most obvious in Oak. In this site they had developed an ‘apprenticeship model’ of MBCT teacher training. In the context of ‘proper training because the trust governance spells it out’ (Oak112); implementers in this site had produced a set of publicly available governance criteria, organised nationally visible research and teaching conferences and practice days. The embedded nature of training and supervision was also obvious in an observation of a management meeting (with two research and training directors, and local collaborator) in which training was a standing agenda item. In this site, the embedding of training and supervision had been led by people with ‘passion and knowledge’:
. . . there’s something about the thoroughness and thoughtfulness that’s been put into the in-house training programme and how considered that’s been with [Oak101] and [Oak111] and [Oak112] who’ve, I suppose [Oak101] has led the training from a trust perspective but certainly they’re delivering the training . . . there’s a sense of people feeling confident in the quality of the training that they feel able to train in ways and feel safe.
Research lead, Oak101
This site through one of the leads was also well linked in with regional and national networks, including being involved in the UK network listing working party29 in the development of national standards for mindfulness-based approaches including MBCT:
I’m very involved in the UK Network Accreditation Working Party, I’m chairing it at the moment. My sense is that it needs to be held by the UK network, the accreditation process. What we do fits the good practice guidelines for people who want to train so we’re quite confident . . . So I think our training is a very high quality product within the mindfulness training world.
Teacher trainer, Oak111
In contrast to Oak’s approach and progress with embedding training in their service model, other sites had developed training organically, and without resource because of a lack of organisational buy-in. For example, in Mangrove they had piloted an internal training pathway on a ‘shoe-string’ (Mangrove102), in Hazel an implementer had ‘paid for supervision out of [their] own pocket’ (Hazel101) and in Birch at the start of their implementation journey people were ‘learning on the job’:
. . . they would have had to have done the 8-week course themselves with encouragement to keep up their own practice but in terms of the groups they would have joined a group as a participant/observer with clients before eventually co-facilitating and taking maybe a slightly lesser role with meditation practice . . . so it was a gradual thing.
MBCT teacher in NHS organisation, Birch107
In contexts where there was a lack of structure, capacity and resource there was also a challenge with access (physically and financially) to ongoing supervision and opportunities for co-facilitation (a feature of majority of training pathways or post-training guidelines, and of MBCT being adapted to fit different patient groups than those recommended in NICE guidance), which left those delivering services feeling ill-equipped:
So I did two groups but the difficulty has been having someone to run with them with really, so I haven’t done any groups since . . . I haven’t done one for a couple of years . . . the general message when I go to the special interest groups is don’t run them on your own it’s just too much and it is quite a lot on your own, to be doing every aspect of it isn’t ideal. So hence I haven’t done one since.
Clinical psychologist trained on internal pathway, Beech103
This less strategic approach to establishing and maintaining training and supervision was a function of a (mainly) bottom-up approach to establishing MBCT (see Chapter 3, Bottom up). As a consequence this had resulted in considerable personal, and often financial, investment by individuals attempting to introduce MBCT provision locally (see Implementers). All early adopters (apart from in Pine where there had been funding to initiate provision) started off with personal investment in training or supervision due to their personal interest and in the context of MBCT not being yet introduced to the NHS through NICE guidance. More embedded sites had later been met by top-down support for training pathways and supervision, which meant that the current trainees did not have to personally invest in the same way as those early adopters.
Gold standard versus good enough
Related to the findings described in Chapter 3 (see Quality of teaching and provision), there were also some tensions about maintaining the integrity of the intervention in NHS contexts that were time pressured and resource constrained. This ended up with some implementers negotiating and compromising on some elements of what was required in terms of training:
This [resourcing retreats] is a sticky point at the moment, the requirements for the best practice, so where people have to go and do retreats that can be quite a lot of time and that’s the bit where I end up negotiating with the service managers about we’ll pay for it or we’ll let people have time off and then you have to compromise with the staff to do that. It’s just unfortunately now, previously we would have funded everything but just at the moment there isn’t the money available.
IAPT clinical lead, Pine201
Arguably, the success that Oak had achieved with training and supervision was likely in part to be due to their approach in finding a middle road model by pragmatically meeting the standard of national guidance29 in the development of an affordable and timely teacher training pathway. Here they had developed what they perceived to be a quality, practice-based training provision that was fit for purpose:
4-year courses were just you know great but unfortunately unrealistically long and expensive for a lot of people. So we tried to develop something that kind of took down the middle road and met and would enable people to meet the good practice guidelines, so it was a year’s supervised training, and we put much more, it’s not actually linked to a university, it’s just our own sort of mindfulness centre training. So it’s got a much less academic kind of focus. There are some reflective pieces that people need to write. But the main emphasis is on people’s own practice. [. . .] sort of an apprenticeship model, so we get people fairly quickly into practicing leading practices in the workshops that we have and the seminar groups that we have.
Local collaborator and mindfulness clinical lead, Oak101
However, some implementers had not been prepared to compromise. For example, in Elm there was a lone implementer who was passionate about teacher training and had established an internal (to the service) training pathway, and had also started to generate income as an external training provider. As the organisation came under some scrutiny and reorganised, this person had been asked by senior management to ‘look at mindfulness provision and that it was impossible to support MBCT groups continuing with two CBT therapists providing the courses . . . we could either stop mindfulness provision or we could change what we were doing’.
I gave slightly different models but really felt that I had come into line with their needs, which was one teacher per group. So I was asked to attend a meeting . . . And the first thing they asked me was, ‘is there a light version of MBCT’, ‘is there something that’s shorter, less intensive, fewer hours and more easily provided without such stringent guidelines?. And I said well I said there’s lots of other people doing that, but I said ‘no, we’ve an NHS provider service, we provide as per the NICE guidelines and we’re working with people who have mental health problems and deserve the evidence based intervention . . . So I said I will not support the trust in delivering a light version of MBCT, so no’.
Local collaborator and mindfulness clinical lead, Elm101
In this site, MBCT was withdrawn from service delivery after we had finished data collection there.
Data show a fundamental tension with respect to the delivery of MBCT due to the links with Buddhist psychological frameworks. In an interview with a national teacher supervisor who was consulted by various implementers in the sites we visited, there was a lot of reference to the Buddhist background to MBIs. This participant expressed a belief that the delivery of mindfulness training (for patients) should be secular, but that ‘teachers need to have an understanding of the Buddhist foundations’ (Mangrove103). Furthermore, there was a clear expectation that to be a mindfulness teacher ‘you have to have an 8-week course and then I want you to practice for at least a year’ and that ‘Mindfulness supervision has to include looking at the teacher’s personal meditation practice as well as their work and their life and how well they all integrate, rather than just on the work itself’ (Mangrove103).
My concern with some of the applications I have seen so far is that they have been clear that whilst they have attended a (training) course they are not currently practising mindfulness regularly, if at all . . . Personal practice strongly supports and informs how we teach mindfulness . . . Maybe there could be an understanding that unless people can establish a reliable, regular personal practice during the course they will not be encouraged to teach through their work role until this is so?
Documents, e-mail from trainer and supervisor to service manager, Birch
Views about what mindfulness is, and what it should entail, had been challenging to implementation because of varying views about integrity and quality within the context of a resource constrained NHS, as this participant articulated:
. . . there’s an issue there in terms of challenge is about what’s the culture of mindfulness within the organisation, you know I think people can brand it, misunderstand it as just another form of relaxation treatment or something like that and ensuring the quality of the input is an issue . . . there is a certain sort of uniqueness to the adventure of mindfulness which is difficult to then quality assure. Speaking as somebody who’s been in involved in commissioning it as it were one of the things I have to marry up here is the gold standard mindfulness training that our local centre provides, versus working out the politics of financing all of that and for us to be happy with an imperfect but nevertheless good enough level of provision . . . reflects something about the sort of politics of interfacing with independent training providers and the sense of this being a very popular growing area of practice and presumably that must bring a certain market dynamic to the provision which might mean that what feels like pretty penniless NHS organisations are sort of struggling.
Head of psychological therapies, Birch206
Top down, bottom up
Implementation of MBCT was driven by a combination of bottom-up activity and top-down support and investment, the effect of which was enhanced by middle management and clinician buy-in.
The implementation journey of all sites, irrespective of their success, started with enthusiastic individuals who engaged in activities that drove the agenda (largely organically) from the ground up (see Implementers for an elaboration of the characteristics, activities, etc.). These implementers were able to achieve a certain amount, but in order for less piecemeal, more embedded and sustainable MBCT provision, bottom-up activity needed to be complemented by top-down support and investment (Figure 19). The experiences of Pine most vividly illustrated this bottom-up, top-down implementation dynamic:
I think what [Pine] has benefitted from over the last 7 years is that the leadership is committed to innovation . . . I think [CEO], there’s lots of evidence that [overall IAPT director, Pine203]’s given me ranging from using IT [information technology] to mindfulness to other bits and pieces, there’s a real drive within [CEO] for innovation and to try things differently to do things differently in different ways and there’s a connect there between the top and the bottom . . . if you want to integrate it it’s about getting both the key individuals on the ground and the connect with the real desire to be innovative and bring new things in at the top and get that connection between those two things.
Regional service director IAPT, Pine208
FIGURE 19.
Top down, bottom up.
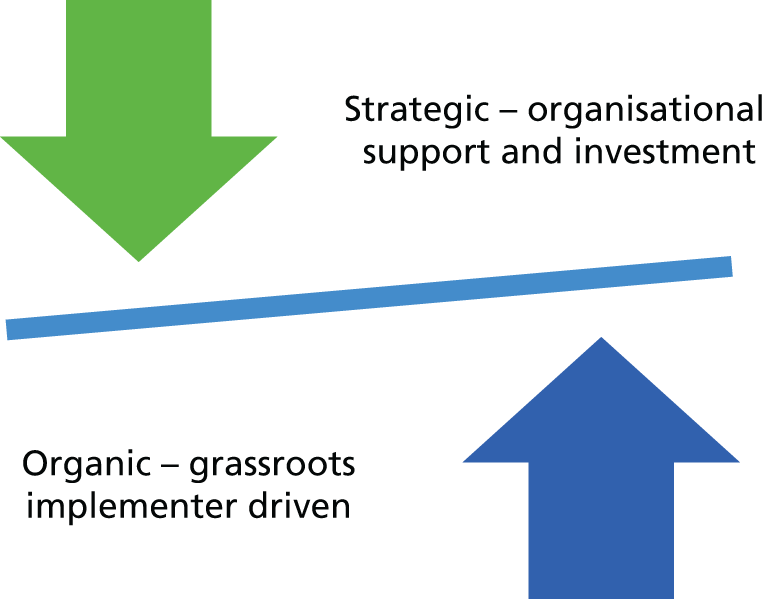
When bottom-up implementers were met with top-down support and investment it provided them with the autonomy to develop services in a more strategic way, and facilitated their implementation activities, including extending their scope for engagement across organisations:
I note with interest we have a planned session to help you both think through a strategy on mindfulness, and I have half an hour so I thought I would put some thoughts down now so we can reflect in advance, during and after the session. I have copied in XXXX [local service development] and XXXX [university department], and XXXX [executive sponsor] in order to encourage their contribution.
Document, thoughts, strategic, links 2014, CEO, Pine
Those implementers who were working in more senior positions (e.g. in Oak, Bamboo) had the authority to make decisions about provision themselves:
. . . but it’s also because we were both senior in the end and that makes a difference to the level of influence that you can have . . . if I’d been in a junior position I wouldn’t have been able to do anything.
Early adopter, Oak102
It’s been helpful being a consultant psychiatrist, because I can just do stuff, I don’t need to ask permission; I can say right this is what we’re doing [. . .].
Early adopter, Bamboo305
Without top-down drive and investment, data show that implementation only progressed as far as raising awareness at a local level, or the running of pilot groups under the radar, in one’s own time and in an organic (as opposed to planned and strategic) way:
I think there’s a lot of working beneath the radar that enabled it to get it to its stronger base and its foundations . . . and me being a CBT therapist . . . my role didn’t allow me to be part of the decision-making that happens in the trust.
Local collaborator and former mindfulness clinical lead, Elm101
Furthermore, and perhaps unsurprisingly, senior engagement was critical to ensure that resource followed strategy:
. . . what happened over recent years is having people in very senior positions and particularly having [professor] in post at [partner university] who are able to make higher-level strategic decisions and I think there does need to be buy-in at very senior levels and there does need to be strategic thinking about where limited resources can be put in terms of the different levels of development . . . The bottom up came first and I think that was essential definitely helpful because you can’t do it top down unless you’ve got people on the ground who’ve got a real heartfelt interest in this area.
Interest group co-ordinator, core staff teacher, Mangrove102
The connection between bottom-up with top-down buy-in and drive was facilitated and enhanced by middle management buy-in. Other findings show the value of partnership working to MBCT implementation (see Implementers), this extended to those in middle management positions, who were able to facilitate or, where this level of partnership working was lacking, impede service delivery:
Clinicians, well I’d hope that your management level, clinical lead level you’d have somebody with some, ‘cos it will stall otherwise if you haven’t got somebody who can drive it forward, so somebody at high level who’s willing to champion the cause who’s some experience of mindfulness and then identify two or three key players within your clinical team who are going to help you deliver that.
IAPT clinical lead, Oak201
It’s not the executives that need to be convinced much, the real barriers are encountered on the ever-changing and pressurized middle management [staff mindfulness service stopped in one area].
Field notes, debrief key learning, Elm
As the above evidence indicates, bottom-up implementation is unlikely to be successful without top-down buy-in and support; equally, data from Birch show that a top-down initiative without bottom-up co-ordination had failed to have traction. In this site there was a top-down initiative to fund two cohorts of MBCT teachers. However, there was a lack of co-ordination on the ground between the provision of training and putting that training into practice, including challenges with lack of supervision and trainees ending up not delivering MBCT or being delayed in getting a MBCT service set up.
Pivot points
A combination of factors led to pivot points in a site’s implementation journey, which were critical junctures in which implementation either accelerated or was impeded.
Over time, and depending on the respective starting points of sites, their resources and opportunities for implementation, some sites experienced different pivot point(s) (Figure 20). These pivot point(s) marked an accumulation of factors that enabled MBCT to become more embedded, or an accumulation of factors that resulted in MBCT provision ceasing, or failing to properly get off the ground (Table 13 shows a list of features that occurred in each site). As suggested earlier, the implementation journeys of each site evolved and the presence of pivot points during those journeys reflected this evolution or implementation life cycle. Some common features of pivot points that accelerated implementation included the coming together of adequate resources; an organisational structure (including investment) to deliver MBCT within services; a critical mass of MBCT teachers and practitioners; the development (and selling) of a compelling case informed by different forms of evidence; nationally badged guidance alongside evidence of local impact; and making visible the potential of MBCT through major events (see Explanatory framework).
FIGURE 20.
Pivot point. HH, high high; HL, high low; LH, low high; LL, low low.
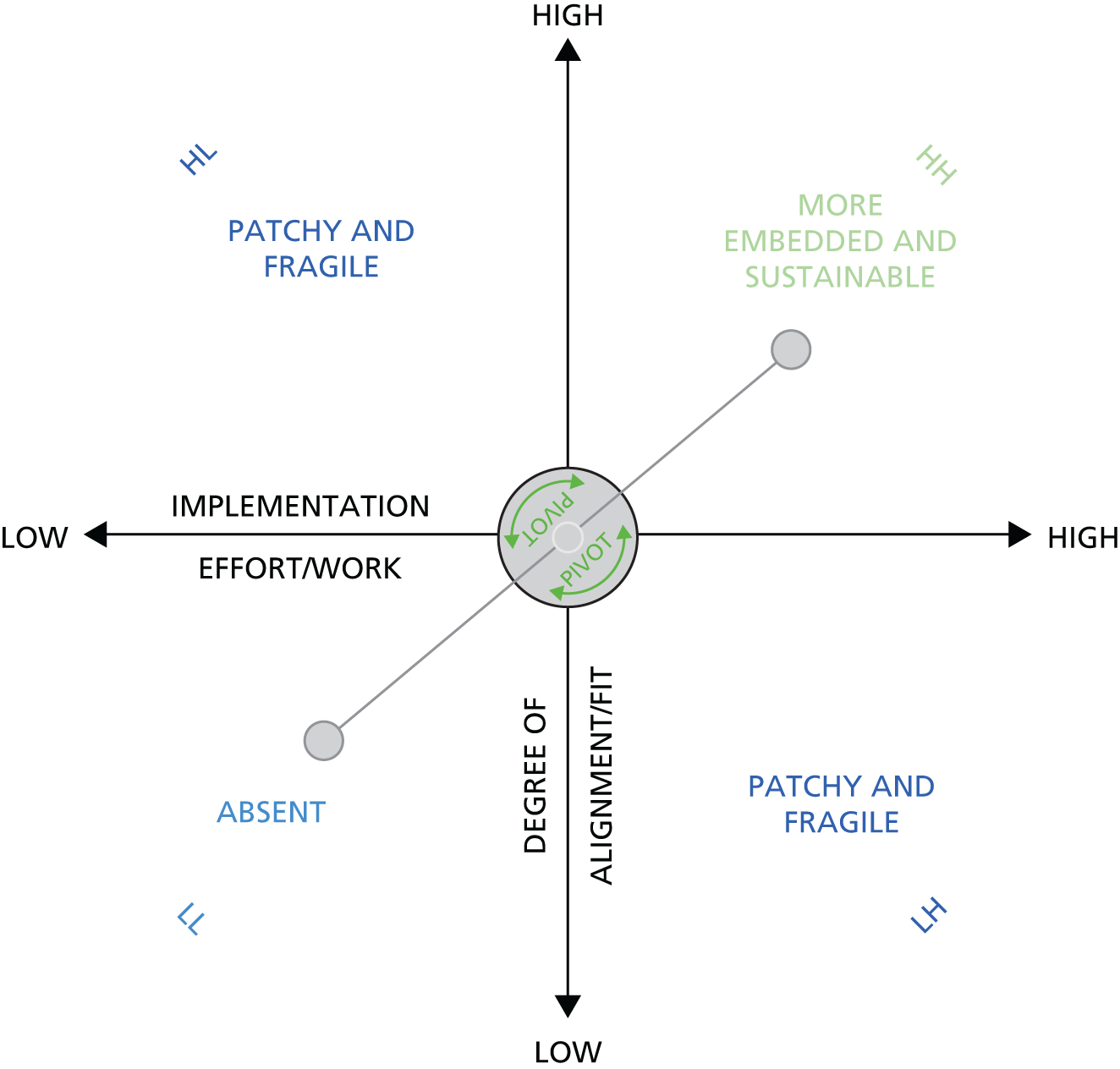
| Site | Accumulation of BU and TD events | Pivot point(s) |
|---|---|---|
| Oak |
|
Pivot point (upwards): establishing internal training pathway Pivot point (upwards): establishment of a centre of excellence with three pillars, governance and training, research and staff well-being |
| Pine |
|
Pivot point (upwards): employed a MBCT clinical lead Pivot point (upwards): 2011, reaching a critical mass of 30 trained MBCT teachers making it a sustainable service (through internal training pathway) Pivot point (upwards): 2015 Mindfulness Centre of Excellence |
| Elm |
|
Pivot point (upwards): in 2006 the commissioner funded five or six courses in adult services, and the funding was also used for teacher training. In 2011 funding came from executive management for a further five staff courses (TD) Pivot point (downwards): training pathway and MBCT provision stopped because it was not financially viable |
| Mangrove |
|
Mostly BU, but with some TD drive but implementers had different agendas Years of BU service development with some ambition for a centre of excellence, but because of different agendas progress not sustained. Lack of middle management buy-in No obvious pivot point evident |
| Bamboo |
|
Pivot point (upwards): adopter becoming a member of the advisory group of a national depression programme that provided 3 years of funding, and some leftover monies were used to establish a national mindfulness teaching role for two implementers (TD). These roles were crucial for the establishment of a small-scale national training pathway, and also provided regular network opportunities for implementers |
| Birch |
|
Pivot point (downwards): early adopters left the trust in 2002 leaving no-one in the trust as an implementer, apart from interested individuals introducing element in one-to-one work Pivot point (upwards): Psychological Training Institute (developed from a special interest group) had two funding streams for psychological therapies, which enabled them to fund two cohorts of MBCT teachers (TD) |
| Hazel |
|
Owing to a very pressurised context driven by targets and implementers ‘hitting brick walls’ (Hazel107), along with lack of resources, resulted in implementers delivering what they could within their own local service (BU) and, therefore, no obvious ‘pivot point’ |
| Juniper |
|
Pivot point (upwards): volunteer recruited on an honorary contract (not paid by the trust) to deliver MBCT groups within the trust |
| Beech |
|
Pivot point (downwards): reorganisation happened and the trust adopted large waiting lists and the early adopter was diverted by a new manager to clear waiting lists for individual therapy and felt frustrated and restricted Early adopter left the trust |
| Wisteria |
|
BU facilitation of MBCT for staff based in occupational health. Very early days and no pivot points evident |
Explanatory framework
Our findings come together in an explanatory framework (Figure 21). In this framework, an implementation journey is determined over time by a potentially creative tension between grassroots facilitation from implementers’ effort and work, and top-down organisational prioritisation of MBCT, through more or less strategic support and subsequent flow of resources, over time. The broader macro and meso context featured the absence or presence of IAPT, a focus on treatment rather than prevention and at which point in the care pathway MBCT was available to recipients. Each of these could be facilitative or hindering, depending on other factors. These features co-existed with service pressures and a pace of delivery that frequently appeared to be at odds with the implementation of MBCT, which requires space and time to deliver to an appropriate standard. The potential for sustainability in service provision was evident in services that had invested in developing training pathways.
FIGURE 21.
Explanatory framework. HH, high high; HL, high low; LH, low high; LL, low low.
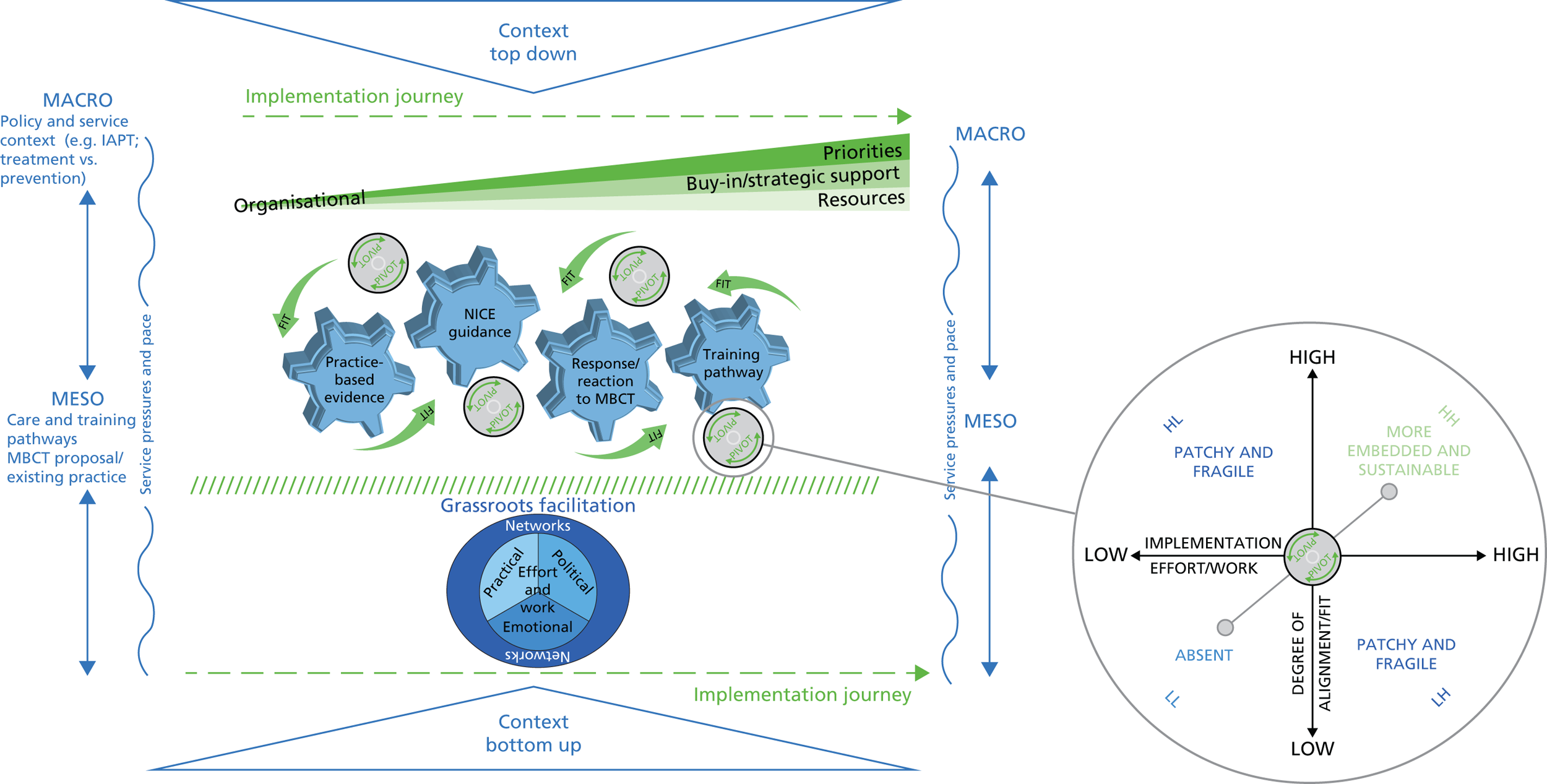
As such, implementation journeys could be enabled by a degree of alignment or fit between context, appropriately targeted grassroots implementation effort, working with different forms of evidence and responses/reactions to MBCT, and top-down factors. An accumulation of factors that were aligned resulted in some shift (positive or negative) in implementation progress. As outlined earlier, we conceptualise these as pivot points. Implementation success was explained by the degree of alignment (high–low) between the intervention and the context of implementation (e.g. MBCT implementation being challenged by NHS focused on treatment more than well-being, NHS fast paced – MBCT needs appropriate time, etc.) and the degree of implementation effort required (low–high).
Chapter 6 Discussion, conclusions and implications
In a British Medical Journal editorial in 2012 the question was asked: ‘What are the facilitators and barriers to the implementation of NICE’s recommendations for MBCT in the UK’s health services? Can this knowledge be used to develop an Implementation Plan for introducing MBCT consistently into NHS service delivery?’. 46 A more recent editorial noted that MBCT is at a crucial juncture as an exponentially growing body of research about its effectiveness, typically developed without reference to implementation has created an ‘implementation cliff’ that could lead to the field being caught in ‘implementation limbo’ and ‘stalling out’. 86 This study provides a body of knowledge and framework that can provide an implementation bridge into practice and policy. 87 In this chapter we also consider the findings in the context of some of the broader implementation research and MBCT literatures. We revisit each of our research aims in turn. We then consider the study’s strengths and limitations before drawing out implications for research and practice.
Discussion
We begin by summarising how our findings relate to the study’s research aims.
Revisiting the research aims
Scope existing provision of mindfulness-based cognitive therapy in the health service across England, Northern Ireland, Scotland and Wales
The first phase of our work involved 68 interviews with a range of stakeholders (MBCT teachers, managers, clinicians, commissioners, referrers and service users) in 40 NHS sites across all four UK nations. This covered primary and secondary care, and a range of different health and mental health services. Although the work was not designed to be a fully representative definitive survey, nonetheless a picture emerges suggesting that the provision of MBCT is becoming more widely available but that the access and format of MBCT provision across the NHS remains variable, even within the same region and site. NHS services have typically adapted MBCT to their context using a hybrid of MBCT/MBSR; indeed, 34 out of the 40 sites offered mindfulness-based services that did not fully match the recommendations in NICE guidance, including people who are currently depressed and those who have other physical/mental health conditions.
The integration of MBCT into care pathways was also highly variable, with some offering it at the end of the pathway for those who have received other treatments, others offering it to those on the waiting list for one-to-one therapy and others offering as an opt in/direct referral option within their service.
Since we started the work, from 2015 the NHS IAPT services workforce census started to collect data on numbers of MBCT trained teachers. The 2015 census reports that 256 IAPT staff self-identify as trained to teach MBCT, comprising 93% of whole-time equivalent staff and 2% of the IAPT workforce. Reporting by the CCG suggests that > 60% of CCGs had no trained MBCT staff. 88 The report points to the unreliability of these data, but it does highlight that less than half of the English NHS has no therapists trained to deliver MBCT in primary care IAPT services.
Although there appears to have been progress since our feasibility study,64 the accessibility of MBCT continues to be both limited and variable.
Develop an understanding of the perceived benefits and costs of embedding MBCT in mental health services. Explore barriers and facilitators that have prevented or enabled services to deliver MBCT. Articulate the critical success factors for enhanced accessibility and the routine and successful use of MBCT as recommended by National Institute for Health and Care Excellence
In the following sections we use the PARIHS framework6 elements to describe our findings and then give further consideration to our framework (see Figure 21) that helps to explain how MBCT becomes sustainably embedded in NHS services.
Context
The context for implementation comprised both macro (e.g. national policies, service priorities and culture) and meso (e.g. service specifications, care pathways) levels. A supportive implementation context tended to be linked to national policies, service priorities and crucially found a way to fit MBCT into existing services. For example, we found that there were marked differences in whether or not services adopted a medical model, well-being or recovery orientation. MBCT was more likely to flourish where implementers found a way to integrate MBCT with the prevailing orientation and service organisation, regardless of what the orientation and service organisation were. That is to say, it was not so much about certain contexts being more or less facilitative, but whether or not the implementers could match to, fit or align with what was there. This created tensions and helped to explain (to a certain extent) why there had been implementation challenges, as well as implementation successes.
Another key contextual factor was resourcing. This included building capacity in terms of MBCT teachers, accessing financial resources, time, as well as practical resources such as space, in which to offer MBCT. A similar tension was seen where implementers found ways to offer MBCT with limited resources.
There is a large and ever-growing body of literature and theory that supports the influence of context on implementation efforts. 89–91 Our findings help to explain that context does not simply act as a backdrop to action (i.e. as a set of obstacles or facilitators), but that is where implementation takes place. As the place and space of implementation, context can also create or produce implementation processes as well as be influenced by it. As such, there is a dynamic interaction between an intervention, its implementation and context. This then will play out differently from place to place. That is to say, it is contingent; what may provide helpful conditions in one place may constitute barriers in another. Embracing a more contingent and dynamic (and thereby uncertain) view of context is becoming of increasing interest to implementation researchers. 92
Evidence
Evidence was often important to implementation and took different forms. The NICE depression guideline was often cited as opening the door and creating legitimacy in people’s minds. Other types of evidence were often mentioned, most notably audits, evaluations and first-person accounts. There were several examples of pilots being used to build a case for implementation, and in the best cases as a platform from which to evolve and develop services further. Taken together, NICE, research and practice-based evidence played a crucial role in catalysing the potential for implementation (e.g. in selling the idea of MBCT) and in supporting implementation processes (e.g. using local evaluation information to demonstrate impact).
The idea that evidence in evidence-based practice constitutes more than research is consistent with the perspective of evidence represented in the PARIHS framework74 and the accounts of others. 90,93,94 These perspectives demonstrate that different types of evidence from different sources of knowledge are valued, and can both inform and impact on implementation processes. Communities of practice literatures, including the idea developed by Gabbay and Le May95 about clinical mind lines, show that evidence gets transformed and particularised by people, and with relevance to their contexts, including patient or client groups. This transformation makes research evidence relevant and applicable.
Facilitation
Mindfulness-based cognitive therapy implementation has been described as a grassroots movement. 43 Perhaps the most significant single theme in our data was the central role of the MBCT implementers, dedicated individuals who ‘championed’ implementation. Successful implementation was characterised by implementers who were dedicated, passionate, driven, credible and willing to go the extra mile. Over time, they cultivated new MBCT teachers who could become second-generation implementers, building capacity and ensuring succession planning. Several sites adopted a network approach, in which a set of implementers with diverse skills and different levels of the organisation worked collaboratively (e.g. Oak and Mangrove). Although dedicated implementers were crucial to successful implementation, there was also an inherent vulnerability in individuals (in isolation) being central to successful implementation, should they leave, burn out or fall out of favour with key stakeholders. We saw at least two examples of implementation reversing or services ceasing altogether where this happened.
Implementers were key to grassroots, bottom-up implementation. They (mainly) lacked formal designation as a champion or facilitator, but were a prominent feature in the data that characterised almost all the examples of successful implementation, particularly in the early stages of initiating MBCT in local contexts. Their role included raising awareness throughout the organisation of mindfulness and MBCT, often through taster sessions that provided an experiential opportunity to learn about MBCT. Another approach that was often very successful was starting with mindfulness staff groups that served to improve staff well-being, build understanding of mindfulness and develop capacity by identifying potential MBCT teachers (participation in a MBCT group is an early building block in training to become a MBCT teacher).
The crucial role of dedicated champions who act in facilitative roles in successful implementation is not unique to implementing MBCT. 96–98 In this literature facilitation is described as both a role and a process, which is consistent with findings from our data. Furthermore, implementers in our study demonstrated an array of skills, expertise and behaviours that are consistent with both enabling and more task-related conceptualisations of facilitation. 74 However, in addition there was evidence of a skilful ability to communicate mindfulness and MBCT to a range of stakeholders. We proposed that this is probably more unique given the nuances within the approach, the tensions with prevailing culture and the polarised views held by many key stakeholders about MBCT. For example, in the last few years the media has been characterised by overly positive representations of MBCT (e.g. as a panacea) and to a lesser extent by some overly negative representations (e.g. mindfulness as having many adverse effects). There are parallels with how views and behaviours around physical activity and diet have evolved in the last 50 years. 44
Successful implementation was also marked by skilful development of networks of teachers, managers and commissioners at every stage of the implementation journey. This took the form of supervision groups for MBCT teachers, implementation steering groups and links with universities.
Implementers steadily built a case for MBCT over time, often over many years, using a range of approaches. Implementers seemed to maximise engagement and impact when they combined a range of strategies and activities (tasters, staff mindfulness, mix of evidence, piloting/evaluating, adapting, managing expectations, reporting and demonstrating impact, branching out), which were tailored to match context (service need, culture) and audiences (across stakeholders and levels). An interesting and subtle feature of successful implementation was implementers who were able to match the scope and scale of implementation with capacity at any given time. The most effective implementers did what was manageable and effective, and did not over-reach. There was evidence of underambition and overambition associated with unsuccessful implementation. There is clearly great discernment required to know exactly what is needed and possible at any given time, where the pivot points might be and when to capitalise on these opportunities. Invariably there are times where opportunities are missed or there is over-reaching with some backlash, but effective implementers learned from and adapted their approach as the context changed, evidence came in and capacity changed (this is explored further in the explanatory framework set out below).
Perhaps one of the most substantive facilitators was the establishment of pathways to train MBCT teachers and then provide ongoing supervision and continuing professional development. This took time and the format varied in different settings, but this invariably marked successful implementation. Interestingly, many sites took responsibility for this internally, often combining access to external training with setting up training pathways themselves (e.g. Pine, Bamboo, Mangrove and Birch). There was almost invariably a tension between ‘gold standard’ training that met recognised good practice guidelines99 and ‘good enough’ training. 100 The characteristics of training and supervision pathways across our case studies are summarised in Chapter 5, Table 12. In many ways all the other implementation themes played out around training and supervision (context, evidence and key facets of facilitation). It is perhaps self-evident, but for any psychological therapy to be implemented sustainably it must provide a training pathway for practitioners who can deliver the intervention competently and in time go on to supervise and train others to do so.
Finally, our data were saturated with examples of implementation that could be characterised as top down and bottom up. The dedicated implementers generating a grassroots groundswell characterised bottom-up implementation. The analogy of water rising and first flowing into the obvious spaces and only later permeating into the less accessible spaces is helpful here. As already noted, MBCT implementation is most characterised by grassroots bottom-up approaches, as more people are offered a chance for tasters, those who find it interesting and helpful use it more and become part of the initial implementation ‘grassroots movement’. Later water might move into the less accessible spaces as implementers reach individuals and parts of the service that are more remote or where there are significant barriers. This of course relies on skilful communication and discernment, in terms of the content, pace and focuses of implementation. Top-down implementation was also key. It most typically came in later in the implementation process with organisational support being mobilised, greater alignment with organisational strategies and priorities, and securing the support of senior and key stakeholders. A typical example of this was working with the staff well-being directorate (e.g. human resources or occupational health) so that mindfulness was seen to be part of the organisation’s approach to staff well-being. When done skilfully this was a parallel part of the grassroots bottom-up process, as those passing through the staff programmes had the opportunity to benefit from high-quality mindfulness courses. Our most embedded sites were characterised by putting in place over time structures and processes that combined both bottom-up and top-down implementation facilitators. An obvious example is starting out with organic, grassroots training models, but over time embedding these into the organisations structures with governance and funding (e.g. Oak).
The interplay of top-down and bottom-up implementation had two interesting features. First, there were instructive examples of ‘middle management’ being pivotal (e.g. Elm). Although there can be both bottom-up and top-down drivers, middle managers can access levers of power that can be both enabling (e.g. Oak) or disabling (e.g. Elm). Not unrelated to this point, although typically top-down implementation marked middle and later stages of the implementation journey, there were examples of it being a key feature very early in implementation. In some cases the implementer started by engaging top levels of the organisation (e.g. Pine) and in others they were already engaged (e.g. in Oak the chief executive had a history of depression and used mindfulness, talking openly about this both within and outside the organisation). Nonetheless, more successful implementation seemed to be driven by a combination of top-down and bottom-up activities/factors with the balance shifting during the implementation journey.
Explanatory framework
In Chapter 5 we set out an explanatory framework (see Figure 21). We outline here what we regard as the three most important features of the framework; features that the implementation guidance will build from.
First, implementation is a process and a journey. We used, and ‘tested’ in our dissemination workshops, the metaphor of a team embarking on a bicycle journey as being an instructive way to bring the explanatory framework to life in a practical way (Figure 22).
FIGURE 22.
Cycling journey metaphor. HR, human resources; SH, stakeholder.

Success comprises a number of key elements.
First is the presence of an implementer with certain characteristics (e.g. commitment, drive, implementation skills) – the cyclist. Good implementers built networks, the team around the cyclist. MBCT implementation was more likely when the context (e.g. setting, culture, resources) was supportive of MBCT, and of the implementer’s activities; the cycling course that was available and/or selected was key, certain courses and terrain are more conducive than others. The section on implications for implementation practice expands on the cycling metaphor.
Second, an accumulation of top-down and bottom-up activities/factors led to pivot points (see Figure 20), which enabled implementation to develop further or not. These varied from case to case, but several commonalities emerged. Early phases were marked by implementers starting with grassroots, bottom-up approaches building a case, securing resources, accessing training in whatever ways were possible, creating networks and garnering support. A good example is Oak. Middle phases involved the creation of more stable training and supervision pathways, top-down support, and securing more stable resourcing and putting in place organisational structures and governance. In several cases a mindfulness centre was established (e.g. Oak and Pine). In some cases good practice was published, for example around internal NHS training pathways100 and supervision. 101 Later stages involved building capacity so that implementation was sustainable; often this involved developing second-generation implementers and sustainable business models so that implementation was less vulnerable to individuals leaving, a funding source drying up or an organisational reshuffle. A good example is Oak, where a mindfulness centre was created that straddled the NHS and local university, and included leads who worked together and provided leadership around MBCT training, governance and research.
Critical junctures that were evident in our findings included alignment of commitment by senior management, release or investment in resources, with the effort and energy of grassroots implementers; a nationally recognised evidence base to provide a compelling case and tool for implementers; capacity and capability in the development of a critical mass of MBCT teachers and deliverers, and a capability to provide teachers with training and support through internal training pathways; and critical mass, governance and training, research and engagement in policy enabling the establishment of centres of excellence.
A consistently successful cycling team shares many of the same features, with different key roles and functions identified and the team working together towards a shared aim. What emerges is that the influence of top-down and bottom-up influences depends on the context and stage of implementation. Generally speaking, implementation begins and is driven forwards with one or more key implementers implementing in a bottom-up way, ‘under the radar’ if necessary. However, for implementation to be sustainable in the long term, top-down support is needed, but this often comes in once much groundwork has been put in place. This mirrors what is seen in other implementation research both in health systems and also in education. 53,102,103
Third, evolutionary fitness provides a compelling analogy for successful implementation. Within an ecological view of implementation, there is an ebb and flow that develops and builds over time. Additionally, where there is attention to learning and evaluation, a greater fit or alignment between the intervention and context has the potential to develop over time. 104,105 In this study, where there was a good fit between the NHS context and the MBCT implementation, effective implementation was more likely. For example, where services’ orientation was matched with adaptations to MBCT, implementation was more likely to evolve successfully. Two contrasting examples were a service that focused on treatment of common mental health problems (anxiety and depression) compared with focusing on well-being. In each case the implementer skilfully matched the intervention to the organisation’s policies, orientation, targets and priorities (e.g. Elm and Birch). In some cases implementers took this further. They saw opportunities for innovation (niches that were unfilled). They built capacity that improved ‘fitness’ (adapting MBCT for patients on the waiting list; networks of teachers that met for supervision, links with universities in some cases). This capacity was then able to meet unmet needs and rather than surviving there were examples of thriving and flourishing as new innovations were developed, some of which evolved and strengthened the service (e.g. Pine, Birch, Mangrove and Juniper). This evolution included pivot points where stepwise upwards or downwards changes were possible (see Chapter 5, Table 13).
The explanatory framework could offer some suggestions about how and why different elements interact so that predictions can be made about the constellation of factors that make up implementation.
Study strengths and limitations
The findings need to be contextualised in terms of the study’s strengths and limitations.
This study is one of the largest and most systematic explorations of the implementation of a psychological therapy. We sampled purposively and from a random sample of a wide range of stakeholders. Data collection and analysis was theoretically driven and systematically conducted, including the perspectives of lay members of the wider team in these processes. The results converge on several themes and out of this emerged an explanatory framework. We developed from this a practical metaphor to inform implementation guidance. Our emerging descriptions and framework are grounded in a systematic approach, and we built in extensive review processes from the research team, PPI group and stakeholder groups.
Although we used purposive sampling and aimed to reach a broad constituency of stakeholders, inevitably individuals who were most invested in MBCT tended to be the most vocal research participants providing both positive and negative narratives. This may have introduced bias by providing an over-representation of their views and experiences. We tried to mitigate this potential through sampling a broad constituency, including sceptics and through looking for contradictory and disconfirming accounts in our data. Additionally, as stated in our published protocol, we actively sought through some random sampling and through purposively targeting those who were less well disposed to MBCT. The advisory group and PPI group were constituted intentionally to comprise advocates and sceptics, and they provided helpful counterpoints and checks on emerging accounts.
Our main source of data across both phases of the study was interviews. As such, there is the potential for self-reporting bias within this account. We attempted to mitigate this limitation by collecting other sources of data in observations and through the collection and analysis of documents. This provided an opportunity for data triangulation, although rarely did we find these sources of data contradicting accounts obtained through interviews.
Implementation research is still a ‘young’ and emerging field, which creates space for a range of epistemological positions, methods and analytic approaches. It creates a melting pot for researchers and practitioners with a variety of agendas and perspectives. This is both a strength and weakness. We, as best we could, used a systematic and transparent approach to articulating our questions and methods72 and outlining our analytic approach step by step in Chapters 1–4.
The authors had interests and affiliations both to the intervention (MBCT) and to the methodological approach (PARIHS). This was managed through (a) ensuring a range of views within the project advisory group, investigator group and PPI group; (b) sampling a range of voices, including sceptics; and (c) transparent declaration of interests.
Finally, even as the research was taking place, the context for the research was evolving, with NHS reorganisation and the publication of important new information. For example, in October 2015 the Mindful Nation UK was published setting out recommendations bearing directly on this work. 43 In the latter stage of the project, an initiative was announced to expand NHS IAPT services in England to other psychological therapies including MBCT, and in June 2016 NHS England made MBCT an IAPT mandated treatment. This changing landscape means the object of study was changing even as the study progressed. This creates fertile ground for this project to inform practice in a timely way.
Conclusions
Recently, several commentators have argued that MBCT implementation should be considered as integral to the development of the field86 and others that holding the ‘long view’ is most likely to support sustainable implementation. 15,43,106 Namely, implementation requires investing time and resources across the whole implementation journey. For example, often MBCT implementers had invested significantly in their own development as mindfulness practitioners and MBCT clinicians before starting to implement MBCT at a service/clinical level. This proved key in staying the course across implementation journeys lasting many years.
Capacity building is needed at individual and organisational levels, it cannot be rushed and takes time. Cultural change also requires time and discernment. Stepping up sustainable implementation requires clarity about the direction of travel and what will sustain developments in the long term. The data suggested that, to date, an evolutionary analogy works well: identifying niches, adapting and enhancing fitness. It is likely in the longer term that the same approach will lead to further developments. This study suggests a snap shot of this evolution, and perhaps a very early stage in that evolution. The long view may focus on the continued evolutionary development of mindfulness in a western context and the supports that might accelerate and catalyse that process. The context for MBCT and the MBCT intervention itself are in interaction; how they are influenced by and influence one another in the next 50 years will be an interesting evolution.
Integrated, sustainable mental health services that include not just the treatment of, but also the prevention of, depression will make a stepwise improvement to the public health problem of recurrent depression. 1,10 Moreover, such services would provide patients with access to a therapy that supports the development of skills that can support recovery in the long term,18 reduce suffering for patients and their families and reduce the costs for the NHS. 10 MBCT is fully aligned with an approach to integrated physical and mental health care, and emerging narratives that chronic physical health problems and mental health require preventative, well-being-oriented approaches whereby people are supported in taking responsibility for their long-term self-management and care with input from health-care services when and if required. Previous commentators have suggested that MBCT be accommodated within contemporary systems of health-care delivery, such as stepped care, that seek to match the intensity of intervention to the needs of individuals in a series of steps. 52 Lower intensity or self-help approaches (e.g. access to self-help resources such as applications, books, online courses) could be offered at earlier steps, with minimal practitioner support and more intensive teacher-led 8-week courses offered at later steps.
Implications
Our findings and conclusions highlight several implications for implementation of psychological therapies generally and MBCT specifically, and for implementation research.
Implications for future research
First, the explanatory framework and cycling metaphor will be used to develop implementation guidance. The next most obvious research question is ‘How effective is this implementation guidance in producing sustainable change and enhanced patient outcomes?’. A pragmatic cluster randomised implementation trial would be one way to answer this question. Such a trial might compare organisations randomised to using this implementation guidance with organisations delivering usual care, with patient access to MBCT in line with good practice guidelines as the primary outcome and recovery rates as a secondary outcome. A more naturalistic approach would be to seek to enhance implementation in different settings using our explanatory framework to predict how context, evidence and facilitation would interact to determine what supports sustainable implementation in each setting. NHS England is expanding patient choice within IAPT services to other NICE-recommended treatments. It has recently included MBCT as a mandated treatment choice and is including numbers of MBCT teachers in annual workforce censuses and is seeking to provide MBCT teacher training. National IAPT outcome monitoring includes recovery rates. The publication of the ASPIRE implementation guidance provides an extraordinary opportunity for a naturalistic study to examine whether or not this leads to greater access to MBCT and improved patient outcomes, especially in terms of recovery rates.
One theme emerging from our data was the tension between ‘good enough’ and ‘gold standard’ MBCT. An interesting approach would be to test the implementation guidance using the research approaches outlined above, titrating the quality of the MBCT teacher training and MBCT delivery with a cost–benefit analysis on MBCT’s acceptability, outcomes and costs.
Modelling implementation scenarios using health economic decision-making would enhance this work by providing guidance on, for example, the most cost-effective ways of sequencing treatments and workforce planning in terms of numbers of MBCT teachers needed in a given service. 1,25,66,107,108 Such work would be of value to service managers, policy-makers and commissioners. 87
The idea of alignment or fit in the context of an evolutionary and ecological view of implementation is beginning to emerge as a potentially useful framing. 86,87 In order for this idea to gain some traction, it needs further elucidation and then application.
Implications for implementation
Our final aim was to ‘Synthesise the evidence from these data sources, and in co-operation with stakeholders develop an Implementation Plan and related resources that services can use to implement MBCT’. By early 2017 we will release ASPIRE implementation guidance as a freely available online web resource. The implementation guidance builds from stakeholders’ suggestions collected during data collection (see Chapters 3 and 4) and our dissemination workshops (see Appendix 9). It uses the explanatory framework (see Figure 21) and cycling metaphor (see Figure 22) to provide a bridge to the implementation guidance.
The cycling metaphor is used to depict prerequisites (e.g. adequate preparation), facilitative conditions (e.g. road conditions/facilitative context), the key elements required for effective implementation (e.g. the cyclist, bicycle and support team) and the ways these relate to one another to create the conditions for successful implementation (see Figure 22).
The ideas that have emerged from our explanatory framework, particularly the idea of pivot points, might be a useful addition to the implementation research agenda. There is potential to test out this idea in future implementation research studies, and retrospectively apply it to existing data sets.
We saw that each site had its own journey that was unique, but that there were some common patterns in their experiences. Each journey had their own starting point (start of a cycling journey), which could explain why some sites were further along their journey than others in their implementation journey. Some simply had had more time (started the cycling journey earlier) and some started organically with an interested individual/group of individuals (riders) that gathered momentum over time. Others had started their journey at a time that was considered as a good or bad time (riding conditions were favourable). During the implementation ‘journeys’ that we saw, events/activities occurred that helped MBCT get further implemented in the service or things that hindered that progress and over the years the level of embeddedness could change, and that it could be very fragile, even if a site has had a lot of time (riders could be struggling uphill one moment, but could easily be descending the next, with many elements causing that to happen).
We saw that there was a need for an implementer or an individual with an interest (rider), but it was what those implementers did and/or how they did it that had an effect on implementation (skills and actions of the rider). We saw that lone enthusiasts struggled to build momentum on their own. More successful implementation happened when a site had a combination of different implementers, with a variety of seniority and skills, all working towards the same agenda. (A team of cyclists perform better than a single rider, they are all there to support each other, the more riders you have the more support you have, they take turns to be at the front, before falling back to let another member lead. )
We saw that there was a need for the implementer to guide the intervention (steer) so that it would fit the context in which they worked in, or stakeholders they worked with.
For successful implementation to happen we saw that there was a need for:
-
supportive context (roads that were suitable to ride on)
-
support for the intervention and the implementers activities (the tyres needed to be full of air and riders well-nourished).
Implementers had to engage in many activities to encourage a fit and to create the conditions for a ‘supportive context’. We saw that implementers seemed to maximise their impact when they combined a range of activities over time to try and gain that multilevel support system. [The bicycle chain; a combination of interlocking teeth (activities/strategies) that need to be driven around the cog and need oiling over time. ]
When there was a combination and the right tension of top-down and bottom-up drive, this drove forward implementation. (Think about the chain of the bicycle being driven by the pedals, and one pedal being ‘top-down’ activities, and the other pedal being ‘bottom-up’ activities, in order to go forward and build some speed you need both pushing and working together. )
Another important element of an implementation journey, particularly in relation to sustainability was the training pathway and supervision arrangements. (Success of a cyclist/team of cyclists would be dependent on whether or not they had a good training programme.)
In sites where MBCT was more embedded we saw a greater emphasis on quality, abiding to guidelines, and the importance of maintaining personal practice. (Illustrated by the idea of a cyclist and their fitness; if they have done the training and they keep up their training they are fit enough and have the stamina to succeed. )
As outlined earlier, a combination and accumulation of factors or events over a period of time influenced implementation, sometimes leading to a ‘pivot point’, which was a major event that led MBCT to be further embedded, or hindered the implementation of MBCT. [Similar to breaks (barriers) and gears (facilitators) on a bicycle. The more you break over time, you slow down and eventually stop. Changing gears enables the cyclist to move forward at the right speed, with more ease.]
We are using this metaphor to create a practical resource of relevance to different stakeholders. The plan will be split into two sections: ‘starting your journey’ and ‘developing and sustaining your service’. The first section will include essential resources and guidance for implementers thinking about implementing MBCT into their service, such as effective signposting to information around training, funding, networks and key publications. The second section will include resources to help implementers develop a more sustained service. This will include examples of successful implementation journeys (and lessons learnt from not so successful journeys) and implementation narratives with examples of ‘pivot points’. We will also provide templates and examples of business plans and proposals that successful implementers expressed were key to engaging with stakeholder at a higher level. It will have links to frequently asked questions along with suggested answers, and links to mentors and those experienced in the field.
The implementation guidance should have relevance to a broad audience and suitable to anyone wishing to implement MBCT in a NHS setting, such as clinicians or managers, but also include resources that might be relevant to commissioners. During our implementation workshops we collated ideas and suggestions from stakeholders on what they would find useful and would like to see included in the implementation plan, these are summarised in Appendix 9, and these will be incorporated into the development of the plan. There are exemplars of work to ensure that psychological therapies are accessible in settings and to populations from diverse backgrounds. 63,69 The proposed framework and implementation guidance provides for ensuring access and adaptations that ensure ‘fit’ and ‘evolution’.
Finally, sharing best practice, consensus opinion and national good practice guidelines will likely support sustainable implementation. Appropriate governance frameworks, agreed good practice guidelines and UK register of MBCT teachers who meet these guidelines are still very recent developments. 43 There is much basic and applied research still to do. 109 Given that MBCT is still a relatively new psychological therapy this is very much a work in progress.
Acknowledgements
First, we would like to acknowledge the contribution and support of all the participants in our sites for their willingness to give their time and perspectives.
We would particularly like to recognise the local collaborators at each site who generously gave their time to support the researchers during the site visits, for providing feedback on case summaries and for participating in dissemination workshops.
We are very grateful to the members of our PPI group, Nigel Reed, Joanne Welsman, Stephanie Jibson, Paul Sharp and Faith Harris-Golesworthy. Each person was involved in different aspects of the project including in helping to design data collection tools, trialling data collection approaches, in analysis and in attending project meetings.
We would like to acknowledge the specific additional contribution of Nigel Reed, who contributed to regular project meetings and provided comments on draft versions of the final report, and co-wrote the lay summary to the report. Additionally, Paul Sharp gathered data on socioeconomics, ethnicity and mental health metrics about our sites.
Thank you to Nyree Hulme, who helped us with the formatting of the final report and the submission process.
Our thanks go to Val Moore (chairperson of the advisory group), Professor Anne Speckens, Andy Horwood, Dr David Crossley and Ruby Wax, who have acted as advisors to the research team and provided insight at critical points of the study.
Contributions of authors
Professor Jo Rycroft-Malone (Professor of Implementation and Health Services Research) was a co-principal investigator. She co-designed the study, co-led securing of funding, oversaw day-to-day project management, co-designed data collection tools and was involved in some phase 2 data collection activity. She also led, supervised and was actively engaged in data analysis for both phases of the project, co-led writing of the final report and approved the final report.
Dr Felix Gradinger (Research Officer) helped design PPI aspects of the project, is a named research fellow and was responsible for the operational day-to-day project management. He co-designed data collection tools, co-led data collection activities, co-led data coding and participated in analysis processes. He also co-designed and led PPI input into data analysis, supported and contributed to the dissemination workshops, drafted version 1 of Chapters 1 and 2, contributed to writing the final report and approved the final report.
Mrs Heledd O Griffiths (Research Support Officer) was responsible for the operational day-to-day project management, co-designed data collection tools, co-led data collection activities, co-led data coding, participated in analysis processes, and supported and contributed to the dissemination workshops. She also drafted version 1 of Chapter 4, contributed to the writing, and compiled and approved the final report.
Dr Rebecca Crane (Director, Centre for Mindfulness Research and Practice) was a co-applicant for this grant. She co-designed the study, supported the securing of funding, was involved in monthly project management meetings and supported access to sites for data collection purposes. She also participated in data analysis workshops, co-led dissemination workshops, wrote sections related to training pathways, commented on drafts of the final report and approved the final report.
Professor Andy Gibson (Associate Professor in PPI) was a co-applicant for this grant. He designed the PPI component of the project, supported the securing of funding and was involved in monthly project management meetings. He also supported PPI involvement in the development of data collection tools, participated in data analysis workshops, commented on a draft of the final report and approved final report.
Professor Stewart Mercer (Professor of Primary Care Research) was a co-applicant for this grant. He co-designed the study, supported the securing of funding and was involved in monthly project management meetings. He also supported access to sites for data collection purposes, participated in data analysis workshops, commented on drafts of the final report and approved the final report.
Professor Rob Anderson (Associate Professor of Health Economics and Evaluation) was the collaborator. He supervised Dr Gradinger at the University of Exeter in the latter part of the project and supported access to sites for data collection purposes. He also participated in a dissemination workshop, commented on drafts of the final report and approved the final report.
Professor Willem Kuyken (Professor of Clinical Psychology) was a co-principal investigator. He co-designed the study, co-led the securing of funding, oversaw day-to-day project management and co-designed data collection tools. He was also involved in data collection activity in phases 1 and 2, was actively engaged in data analysis for both phases of the project, co-led dissemination workshops, co-led writing of the final report and approved the final report.
Publication
Rycroft-Malone J, Anderson R, Crane RS, Gibson A, Gradinger F, Owen Griffiths H, et al. Accessibility and implementation in UK services of an effective depression relapse prevention programme – mindfulness-based cognitive therapy (MBCT): ASPIRE study protocol. Implement Sci 2014;9:62.
Data sharing statement
Data can be obtained by contacting the corresponding author.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
References
- Layard R, Clark DM. Thrive: The Power of Evidence-Based Psychological Therapies. London: Allen Lane; 2014.
- Collins PY, Patel V, Joestl SS, March D, Insel TR, Daar AS, et al. Grand challenges in global mental health. Nature 2011;475:27-30. http://dx.doi.org/10.1038/475027a.
- Derek R. Prevalence and clinical course of depression: a review. Clin Psychol Rev 2011;31:1117-25. http://dx.doi.org/10.1016/j.cpr.2011.07.004.
- Moussavi S, Chatterji S, Verdes E, Tandon A, Patel V, Ustun B. Depression, chronic diseases, and decrements in health: results from the World Health Surveys. Lancet 2007;370:851-8. https://doi.org/10.1016/S0140-6736(07)61415-9.
- Health Statistics and Information Systems: Disease Burden. Geneva: WHO; 2011.
- Layard R, Banerjee S, Bell S, Clark DM, Field S, Knapp M, et al. How Mental Illness Loses Out in the NHS. London: Centre for Economic Performance, London School of Economics and Political Science; 2012.
- Layard R. The case for psychological treatment centres. BMJ 2006;332:1030-2. https://doi.org/10.1136/bmj.332.7548.1030.
- Cuijpers P, Berking M, Andersson G, Quigley L, Kleiboer A, Dobson KS. A meta-analysis of cognitive–behavioural therapy for adult depression, alone and in comparison with other treatments. Can J Psychiatry 2013;58:376-85. https://doi.org/10.1177/070674371305800702.
- Cuijpers P, Smit F, Voordouw I, Kramer J. Outcome of cognitive behaviour therapy for minor depression in routine practice. Psychol Psychother 2005;78:179-88. http://dx.doi.org/10.1348/147608304X22391.
- Five Year Forward View for Mental Health. England: NHS England; 2016.
- No Health Without Mental Health. London: DH; 2011.
- Muñoz RF, Cuijpers P, Smit F, Barrera AZ, Leykin Y. Prevention of major depression. Annu Rev Clin Psychol 2010;6:181-212. http://dx.doi.org/10.1146/annurev-clinpsy-033109-132040.
- Depression: The Treatment and Management of Depression in Adults (Update). Clinical Guideline 90. London: NICE; 2009.
- Hunot VM, Horne R, Leese MN, Churchill RC. A cohort study of adherence to antidepressants in primary care: the influence of antidepressant concerns and treatment preferences. Prim Care Companion J Clin Psychiatry 2007;9:91-9. https://doi.org/10.4088/PCC.v09n0202.
- Williams JM, Kuyken W. Mindfulness-based cognitive therapy: a promising new approach to preventing depressive relapse. Br J Psychiatry 2012;200:359-60. http://dx.doi.org/10.1192/bjp.bp.111.104745.
- Segal ZV, Williams JMG, Teasdale JD. Mindfulness-Based Cognitive Therapy for Depression. New York, NY: Guilford Press; 2013.
- Williams JMG, Teasdale JD, Segal ZV, Kabat-Zinn J. The Mindful Way Through Depression: Freeing Yourself from Chronic Unhappiness. New York, NY: Guildford Press; 2007.
- Kuyken W, Warren F, Taylor RS, Whalley B, Crane C, Bondolfi G, et al. Efficacy and moderators of mindfulness-based cognitive therapy (MBCT) in prevention of depressive relapse: an individual patient data meta-analysis from randomized trials. JAMA Psychiatry 2016;73:565-74. https://doi.org/10.1001/jamapsychiatry.2016.0076.
- Segal ZV, Bieling P, Young T, MacQueen G, Cooke R, Martin L, et al. Antidepressant monotherapy vs sequential pharmacotherapy and mindfulness-based cognitive therapy, or placebo, for relapse prophylaxis in recurrent depression. Arch Gen Psychiatry 2010;67:1256-64. http://dx.doi.org/10.1001/archgenpsychiatry.2010.168.
- Kuyken W, Byford S, Taylor RS, Watkins E, Holden E, White K, et al. Mindfulness-based cognitive therapy to prevent relapse in recurrent depression. J Consult Clin Psychol 2008;76:966-78. http://dx.doi.org/10.1037/a0013786.
- Kuyken W, Hayes R, Barrett B, Byng R, Dalgleish T, Kessler D, et al. Effectiveness and cost-effectiveness of mindfulness-based cognitive therapy compared with maintenance antidepressant treatment in the prevention of depressive relapse or recurrence (PREVENT): a randomised controlled trial. Lancet 2015;386:63-7. http://dx.doi.org/10.1016/S0140-6736(14)62222-4.
- Cuijpers P, Smit F. Excess mortality in depression: a meta-analysis of community studies. J Affect Disord 2002;72:227-36. http://dx.doi.org/10.1016/S0165-0327(01)00413-X.
- Prince M, Patel V, Saxena S, Maj M, Maselko J, Phillips MR, et al. No health without mental health. Lancet 2007;370:859-77. https://doi.org/10.1016/S0140-6736(07)61238-0.
- Renn BN, Feliciano L, Segal DL. The bidirectional relationship of depression and diabetes: a systematic review. Clin Psychol Rev 2011;31:1239-46. http://dx.doi.org/10.1016/j.cpr.2011.08.001.
- Hoomans T, Severens JL, Evers SM, Ament AJ. Value for money in changing clinical practice: should decisions about guidelines and implementation strategies be made sequentially or simultaneously?. Med Decis Making 2009;29:207-16. http://dx.doi.org/10.1177/0272989X08327397.
- Allen M, Bromley A, Kuyken W, Sonnenberg SJ. Participants’ experiences of mindfulness-based cognitive therapy: ‘it changed me in just about every way possible’. Behav Cogn Psychother 2009;37:413-30. http://dx.doi.org/10.1017/S135246580999004X.
- Mindfulness Report. London: Mental Health Foundation; 2010.
- Malpass A, Carel H, Ridd M, Shaw A, Kessler D, Sharp D, et al. Transforming the perceptual situation: a meta-ethnography of qualitative work reporting patients’ experiences of mindfulness-based approaches. Mindfulness 2011;3:60-75. http://dx.doi.org/10.1007/s12671-011-0081-2.
- Mindfulness Teachers UK . UK Network for Mindfulness-Based Teacher Training Organisations; Setting Standards For Mindfulness-Based Teaching n.d. http://mindfulnessteachersuk.org.uk/#guidelines (accessed 13 October 2016).
- SIGN . Non-Pharmaceutical Management of Depression in Adults. A National Clinical Guideline 2010. www.sign.ac.uk/pdf/sign114.pdf (accessed 13 October 2016).
- IAPT Programme . Improving Access to Psychological Therapies (IAPT): Services for Depression and Anxiety n.d. www.iapt.nhs.uk (accessed 13 October 2016).
- Department of Health Social Services and Public Safety . Service Framework for Mental Health and Wellbeing 2011. www.scie.org.uk/publications/guides/guide30/files/northern_ireland_mental_health_and_wellbeing_service_framework.pdf?res=true (accessed 13 October 2016).
- Western Health and Social Care Trust . Adult Mental Health Service; Regional Mental Health Care Pathway n.d. www.westerntrust.hscni.net/services/2023.htm (accessed 13 October 2016).
- A Strategy for the Development of Psychological Therapies Services. Belfast: Department of Health; 2010.
- Scottish Government . Mental Health Strategy for Scotland: 2012–2015 2012. www.scotland.gov.uk/Publications/2012/08/9714 (accessed 13 October 2016).
- Scottish Parliament . Mental Health (Scotland) Bill 2015 n.d. www.parliament.scot/parliamentarybusiness/Bills/78451.aspx (accessed 13 October 2016).
- Mental Health in Scotland: A Guide to Delivering Evidence-Based Psychological Therapies in Scotland (The Matrix). Edinburgh: NHS Education for Scotland; 2011.
- The Doing Well By People With Depression National Evaluation Team (The Scottish Government) . National Evaluation Of The ‘Doing Well By People With Depression’ Programme 2006. www.gov.scot/Publications/2006/07/12090019/0 (accessed 13 October 2016).
- NHS Education for Scotland . NHS Education for Scotland: Quality Education for Healthier Scotland n.d. www.nes.scot.nhs.uk (accessed 13 October 2016).
- Mindfulness Scotland . Mindfulness Scotland: Enhancing the Well-Being of the People of Scotland n.d. www.mindfulnessscotland.org.uk/ (accessed 13 October 2016).
- Welsh Government . Together for Mental Health – A Strategy for Mental Health and Wellbeing in Wales 2013 n.d. http://gov.wales/docs/dhss/publications/121031tmhfinalen.pdf (accessed 13 October 2016).
- Mental Health (Wales) Measure 2010. Cardiff: Welsh Government; 2010.
- Mindful Nation UK. London: The Mindfulness Initiative; 2015.
- Rycroft-Malone J, Kuyken W. Preventing Depression With Mindfulness-Based Cognitive Therapy: From Evidence to Practice. Southampton: National Institute for Health Research Dissemination Centre; 2016.
- Abraham C, Michie S. A taxonomy of behavior change techniques used in interventions. Health Psychol 2008;27:379-87. http://dx.doi.org/10.1037/0278-6133.27.3.379.
- Kuyken W, Crane R, Dalgleish T. Does mindfulness based cognitive therapy prevent relapse of depression?. BMJ 2012;345. http://dx.doi.org/10.1136/bmj.e7194.
- Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JPA, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Ann Intern Med 2009;151:W65-94.
- Norcross JC, Pfund RA, Prochaska JO. Psychotherapy in 2022: a Delphi poll on its future. Prof Psychol Res Pr 2013;44. http://dx.doi.org/10.1037/a0034633.
- Fielding L. A clinicians’ guide to integrating mindfulness into evidence-based practice: a common elements approach. Diss Abstr Int B Sci Eng 2009;70.
- Crane RS, Kuyken W, Hastings RP, Rothwell N, Williams JM. Training teachers to deliver mindfulness-based interventions: learning from the UK experience. Mindfulness 2010;1:74-86. http://dx.doi.org/10.1007/s12671-010-0010-9.
- Paul HA. Review of therapy in the real world: effective treatments for challenging problems. Child Fam Behav Ther 2014;36:243-51. http://dx.doi.org/10.1080/07317107.2014.934166.
- Demarzo MM, Cebolla A, Garcia-Campayo J. The implementation of mindfulness in healthcare systems: a theoretical analysis. Gen Hosp Psychiatry 2015;37:166-71. http://dx.doi.org/10.1016/j.genhosppsych.2014.11.013.
- Durlak JA, DuPre EP. Implementation matters: a review of research on the influence of implementation on program outcomes and the factors affecting implementation. Am J Community Psychol 2008;41:327-50. http://dx.doi.org/10.1007/s10464-008-9165-0.
- Bhanji S. Is it time we turn towards ‘third wave’ therapies to treat depression in primary care? A review of the theory and evidence with implications for counselling psychologists. Couns Psychol Rev 2011;26:57-69.
- Dark F, Whiteford H, Ashkanasy NM, Harvey C, Crompton D, Newman E. Implementing cognitive therapies into routine psychosis care: organisational foundations. BMC Health Serv Res 2015;15. http://dx.doi.org/10.1186/s12913-015-0953-6.
- Clutton S. The implementation of a mindfulness group programme throughout the state of queensland. Asia Pac J Clin Oncol 2012;8. http://dx.doi.org/10.1111/ajco.12030.
- Edwards AR, Evans S, Aldao A, Haglin D, Ferrando SJ. Implementing a mindfulness-based stress reduction program in the community: lessons learned and suggestions for the future. Behav Ther 2014;37:13-7.
- Niemi M, Nguyen MTT, Falkenberg T. The contextual adaptation of a mindfulness intervention – a qualitative study in a semi-rural district in Vietnam. Eur J Integr Med 2010;2:186-7. http://dx.doi.org/10.1016/j.eujim.2010.09.032.
- Knobler HY, Abramowitz MZ. Novel psychotherapeutic methods and the role of mental health centers in their implementation. Harefuah 2011;150:659-87.
- Pons GB. Mindfulness-based stress reduction program: systemizing its implementation in a semirural public hospital in southern Chile. Psicoperspectivas 2011;10:221-42.
- Jacobsen P, Morris E, Johns L, Hodkinson K. Mindfulness groups for psychosis; key issues for implementation on an inpatient unit. Behav Cogn Psychother 2011;39:349-53. http://dx.doi.org/10.1017/S1352465810000639.
- Larkin H, Hardiman E, Weldon T, Kim H. Program characteristics as factors influencing the implementation of mindfulness meditation in substance abuse treatment agencies. J Relig Spiritual Soc Work Soc Thought 2012;31:311-27. http://dx.doi.org/10.1080/15426432.2012.716284.
- Dutton MA, Bermudez D, Matas A, Majid H, Myers NL. Mindfulness-based stress reduction for low-income, predominantly African American women with PTSD and a history of intimate partner violence. Cogn Behav Pract 2013;20:23-32. http://dx.doi.org/10.1016/j.cbpra.2011.08.003.
- Crane RS, Kuyken W. The implementation of mindfulness-based cognitive therapy: learning from the UK health service experience. Mindfulness 2012;10. http://dx.doi.org/10.1007/s12671-012-0121-6.
- Luchterhand C, Rakel D, Haq C, Grant L, Byars-Winston A, Tyska S, et al. Creating a culture of mindfulness in medicine. WMJ 2015;114:105-9.
- Patten SB, Meadows GM. Population-based service planning for implementation of MBCT: linking epidemiologic data to practice. Psychiatr Serv 2009;60:1540-2. http://dx.doi.org/10.1176/appi.ps.60.11.1540.
- Vale L, Thomas R, MacLennan G, Grimshaw J. Systematic review of economic evaluations and cost analyses of guideline implementation strategies. Eur J Health Econ 2007;8:111-21. http://dx.doi.org/10.1007/s10198-007-0043-8.
- Sobczak LR, West LM. Clinical considerations in using mindfulness- and acceptance-based approaches with diverse populations: addressing challenges in service delivery in diverse community settings. Cogn Behav Pract 2013;20:13-22.
- Fuchs C, Lee JK, Roemer L, Orsillo SM. Using mindfulness- and acceptance-based treatments with clients from nondominant cultural and/or marginalized backgrounds: clinical considerations, meta-analysis findings, and introduction to the special series. Cogn Behav Pract 2013;20:1-12. http://dx.doi.org/10.1016/j.cbpra.2011.12.004.
- Lawlor MS. Mindfulness in practice: considerations for implementation of mindfulness-based programming for adolescents in school contexts. New Dir Youth Dev 2014;2014:83-95. http://dx.doi.org/10.1002/yd.20098.
- Valuing Mental Health Equally With Physical Health or ‘Parity of Esteem’. 2013.
- Rycroft-Malone J, Anderson R, Crane RS, Gibson A, Gradinger F, Owen Griffiths H, et al. Accessibility and implementation in UK services of an effective depression relapse prevention programme – mindfulness-based cognitive therapy (MBCT): ASPIRE study protocol. Implement Sci 2014;9. http://dx.doi.org/10.1186/1748-5908-9-62.
- Rycroft-Malone J. The PARIHS framework – a framework for guiding the implementation of evidence-based practice. J Nurs Care Qual 2004;19:297-304. https://doi.org/10.1097/00001786-200410000-00002.
- Kitson AL, Rycroft-Malone J, Harvey G, McCormack B, Seers K, . Evaluating the successful implementation of evidence into practice using the PARiHS framework: theoretical and practical challenges. Implement Sci 2008;3. http://dx.doi.org/10.1186/1748-5908-3-1.
- Robson C. Real World Research: A Resource for Social Scientists and Practitioner-Researchers. Oxford: Blackwell; 1993.
- Yin RK. Case Study Research: Design and Methods. New York, NY: Sage Publications, Inc; 2008.
- Yin RK. Case Study Research: Design and Methods. London: Sage; 1994.
- National Institute for Health Research . INVOLVE: Mental Health Research Network – NIHR n.d. www.invo.org.uk/invodirect-org/nihr-mental-health-research-network/ (accessed 13 October 2016).
- Spradley JP. Participant Observation. New York, NY: Holt, Rinehart & Winston; 1980.
- Ritchie J, Spencer L, Bryman A, Burgess T. Analysing Qualitative Data. London: Routledge; 1994.
- The Compassionate Mind Foundation . About Us n.d. http://compassionatemind.co.uk/about-us (accessed 23 February 2017).
- Healthcare Improvement Scotland . Scottish Intercollegiate Guidelines Network (SIGN) 2015. www.sign.ac.uk/index.html (accessed 16 January 2017).
- Improving Access to Psychological Therapies Report, October 2015 Final, November 2015 Primary and Quarter 2 2015/16. Leeds: NHS Digital; 2015.
- Announcing Changes to IAPT Monthly Reports. Leeds: NHS Digital; 2015.
- Crane RS, Soulsby JG, Kuyken W, Williams JMG, Eames C. The Bangor, Exeter and Oxford Mindfulness-Based Interventions Teaching Assessment Criteria (MBI-TAC) For Assessing the Competence and Adherence of Mindfulness-Based Class-Based Teaching. Mindfulness Teachers UK; 2016.
- Dimidjian S, Segal ZV. Prospects for a clinical science of mindfulness-based intervention. Am Psychol 2015;70:593-620. http://dx.doi.org/10.1037/a0039589.
- Whitty CJ. What makes an academic paper useful for health policy?. BMC Med 2015;13. http://dx.doi.org/10.1186/s12916-015-0544-8.
- 2015 Adult IAPT Workforce Census Report. London: NHS England; 2016.
- Stetler CB, Ritchie JA, Rycroft-Malone J, Schultz AA, Charns MP. Institutionalizing evidence-based practice: an organizational case study using a model of strategic change. Implement Sci 2009;4. http://dx.doi.org/10.1186/1748-5908-4-78.
- Dopson S, Fitzgerald L. Knowledge to Action? Evidence-Based Health Care in Context. Oxford: Oxford University Press; 2005.
- Dixon-Woods M. Perspectives on Context: A Series of Short Essays Considering the Role of Context in Successful Quality Improvement. London: The Health Foundation; 2014.
- Chandler J, Rycroft-Malone J, Hawkes C, Noyes J. Application of simplified complexity theory concepts for healthcare social systems to explain the implementation of evidence into practice. J Adv Nurs 2016;72:461-80. http://dx.doi.org/10.1111/jan.12815.
- Nutley SM, Walter I, Davies HTO. Using Evidence. London: The Policy Press; 2007.
- Canadian Institute of Health Research . Knowledge Translation and Commercialization n.d. www.cihr-irsc.gc.ca/e/29529.html (accessed 13 October 2016).
- Gabbay J, Le May A. Practice-Based Evidence. Clinical Mindlines. Abingdon: Routledge; 2011.
- Harvey G, Kitson A. Implementing Evidence Based Practice in Health Care. A Facilitation Guide. Abingdon: Routledge; 2015.
- Berta W, Cranley L, Dearing JW, Dogherty EJ, Squires JE, Estabrooks CA. Why (we think) facilitation works: insights from organizational learning theory. Implement Sci 2015;10. http://dx.doi.org/10.1186/s13012-015-0323-0.
- Dogherty EJ, Harrison MB, Baker C, Graham ID. Following a natural experiment of guideline adaptation and early implementation: a mixed-methods study of facilitation. Implement Sci 2012;7. http://dx.doi.org/10.1186/1748-5908-7-9.
- Crane RS. The UK Good Practice Guidelines for Mindfulness-Based Teachers 2011. http://mindfulnessteachersuk.org.uk/ (accessed 2 February 2012).
- Marx R, Strauss C, Williamson C. Mindfulness apprenticeship: a new model of NHS-based MBCT teacher training. Mindfulness 2015;6. http://dx.doi.org/10.1007/s12671-013-0254-2.
- Evans A, Crane R, Cooper L, Mardula J, Wilks J, Surawy C, et al. A framework for supervision for mindfulness-based teachers: a space for embodied mutual inquiry. Mindfulness 2015;6:572-81. http://dx.doi.org/10.1007/s12671-014-0292-4.
- Grimshaw JM, Eccles MP, Lavis JN, Hill SJ, Squires JE. Knowledge translation of research findings. Implement Sci 2012;7. http://dx.doi.org/10.1186/1748-5908-7-50.
- Grol R, Grimshaw J. From best evidence to best practice: effective implementation of change in patients’ care. Lancet 2003;362:1225-30. https://doi.org/10.1016/S0140-6736(03)14546-1.
- Rycroft-Malone J, Burton C, Wilkinson J, Harvey G, McCormack B, Baker R, et al. Collective action for knowledge mobilisation: a realist evaluation of the Collaborations for Leadership in Applied Health Research and Care. Health Serv Deliv Res 2015;3.
- Rycroft-Malone J, Burton CR, Wilkinson J, Harvey G, McCormack B, Baker R, et al. Collective action for implementation: a realist evaluation of organisational collaboration in healthcare. Implement Sci 2016;11. http://dx.doi.org/10.1186/s13012-016-0380-z.
- Kuyken W. Taking the ‘Long View’ on Mindfulness and Mindfulness-Based Cognitive Therapy. Oxford: Oxford Mindfulness Centre, University of Oxford; 2016.
- Barrett B, Byford S, Knapp M. Evidence of cost-effective treatments for depression: a systematic review. J Affect Disord 2005;84:1-13. http://dx.doi.org/10.1016/j.jad.2004.10.003.
- Byford S, McCrone P, Barrett B. Developments in the quantity and quality of economic evaluations in mental health. Curr Opin Psychiatry 2003;16:703-7. http://dx.doi.org/10.1097/01.yco.0000097657.75497.bc.
- Davidson RJ. Mindfulness-based cognitive therapy and the prevention of depressive relapse: measures, mechanisms, and mediators. JAMA Psychiatry 2016;73:547-8. http://dx.doi.org/10.1001/jamapsychiatry.2016.0135.
- Smith BW, Dalen J, Wiggins K, Tooley E, Christopher P, Bernard J. The brief resilience scale: assessing the ability to bounce back. Int J Behav Med 2008;15:194-200. https://doi.org/10.1080/10705500802222972.
Appendix 1 Service user interview schedule: phases 1 and 2
Appendix 2 Stakeholder interview schedule: phase 1
Appendix 3 Stakeholder interview schedule: phase 2
Appendix 4 Phase 1 coding framework
| Domain | Subdomain | Example |
|---|---|---|
| Resources | Human resources | Staff, skills, training/supervision |
| Time | Delivering/developing services, training | |
| Financial | Core, additional | |
| Digital/IT/practical | Equipment, space | |
| Flexibility | In the system | |
| Intervention | Quality | Monitoring, sustaining, accreditation |
| Fit | Pathways, service | |
| Acceptability | Scepticism, knowledge | |
| Accessibility | Demand for service | |
| What is MBCT? | Core, peripheral, ethos | |
| Adaptation | Delivery, flexibility, integrity, dosage | |
| Context (service delivery; macro, meso, miso) | Structure | NHS (macro), service specific (meso), care pathways (micro); re-organisation |
| Business model | Short term, throughput, commissioning, targets | |
| Geography | Rural vs. urban | |
| Culture | Medical model | |
| Funding | ||
| Strategies | Bottom up/top down | Starting point, local strategies |
| Innovating | Experimenting with delivery pathways | |
| Selling/marketing | Taster sessions, raising awareness, publicity | |
| Champions | People, lobbying, commitment | |
| Evidence | NICE | Credibility, adaption, widening criteria |
| Different types of evidence | Practice-based evidence; feedback, evaluation | |
| Quality assurance | Measures | |
| Historic | Used as starting point | |
| Stakeholders | Network | Interest group, practice community |
| Relationships | Manager support | |
| Cost and benefit | From different perspectives | |
| Implementation plan |
Appendix 5 Documents collected on case study visits
| Document type | Document detail |
|---|---|
| Oak | |
| Strategies/plans/proposals | Oak_DocAnalysis_Mindfulness-basedIntervetnionsForStaff (outreach to other trusts) Oak_DocAnalysis_Staff Mindfulness Outreach_CC Oak_DocAnalysis_Staff Mindfulness Outreach_PPT Oak_DocAnalysis_Employee Recovery Project EMB paper (May 2013) |
| Evaluation, reports | Oak_DocAnalysis_EvaluationMBCTforSUandStaff_InterimReport2015 |
| Training and supervision | Oak_DocAnalysis_Flyer_FoundationalTraining/MasterClass2014/15 Oak_DocAnalysis_HandbookFoundationTraining2015 Oak_DocAnalysis_Training Group overview_Jan 2015 |
| Public/raising awareness | Oak_DocAnalysis_Upcoming events2014/15/16 Oak_DocAnalysis_TrustNewsletter2014 Oak_DocAnalysis_RecoveryCollegeProspectus Oak_DocAnalysis_TrustIntroductionDocument Oak_DocAnalysis_FlyerResearchDevelopmentEvents Oak_DocAnalysis_Research Magazine |
| Observations handouts | Oak_Obs_ResearchTeamMeeting Documents: agenda, last meeting notes, consort Oak_Obs_CAMHSMeeting Oak_Obs_StaffMindfulnessGroup Documents: CD, handout Oak_Obs_Network/GovernanceMeeting Documents: minutes, interim report 2015, post MBCT course questionnaire pack, draft questions for MBCT non-completers audit Oak_Obs_CoreGroupMeeting |
| Observation/field notes | Oak_Obs_ResearchTeamMeeting_ResearcherNotes Oak_Obs_CAMHSMeeting_ResearcherNotes Oak_Obs_Network/GovernanceMeeting_ResearcherNotes Oak_Obs_CoreGroupMeeting_ResearcherNotes |
| Other | Webpages Oak_DocAnalysis_MBCT referral criteria adapted for services |
| Pine | |
| Strategies/plans/proposals | Pine_DocAnalysis_SummaryDocForAPPG Pine_DocAnalysis_PPT_ImplementationWorkshop Pine_DocAnalysis_BusinessCaseProposal2014 Pine_DocAnalysis_CEO_Thoughts/StrategicLinks2014 Pine_DocAnalysis_ServiceStatergyOperatingGuidelines2013/14 Pine_DocAnalysis_StrategyPaper2010 Pine_DocAnalysis_StrategyPaper_22.7.11 Pine_DocAnalysis_IntegratingMBCTintoIAPT_Pitch2010 Pine_DocAnalysis_DraftOutlineBusinessCase2010 Pine_DocAnalysis_mission statement Pine_DocAnalysis_MBCTSecondaryCare:ProjectedClinicalActivity |
| Evaluation, reports | Pine_DocAnalysis_ReportToCommissioners2014 Pine_DocAnalysis_QuarterReportSecCare Pine_DocAnalysis_InstitueMentalHealthAnnualReport2014 Pine_DocAnalysis_ClinicalActivitySummary Pine_DocAnalysis_ResearchReport_MBCTinCommunitySetting Pine_DocAnalysis_DevelopmentSummary2014 Pine_DocAnalysis_MBCTReport2014 Pine_DocAnalysis_NICEReport12-13 |
| Training and supervision | Pine_DocAnalysis_MBCT Training 2014_PreliminaryWorkshopFlyer Pine_DocAnalysis_SupervisedPathwayDraftGuidelines2010 Pine_DocAnalysis_TrainingStratergyIAPT2010 Pine_DocAnalysis_Flyer_FoundationCourse2015 Pine_DocAnalysis_ApplicationUKNetworkMindfulnessTeachers&Trainers |
| Public/raising awareness | Pine_DocAnalysis_Flyer_ExperiencingMindfulness:AnIntroduction Pine_DocAnalysis_Mindfulness flyer_2011_BringingMBCTintoIAPTDay Pine_DocAnalysis_Flyer_MindfulnessAndMentalHealth Pine_DocAnalysis_RecoveryCollegeProspectus2014 Pine_DocAnalysis_Flyer_Conference2013 |
| Course materials | Pine_DocAnalysis_PPT_Introduction Pine_DocAnalysis_PPT_Week12/6 Pine_DocAnalysis_PPT_Module6 |
| Observation/field notes | Pine_Notes_HOG |
| Other | Pine_DocAnalysis_JobDes_MBCTClinicalLead Pine_DocAnalysis_JobDes_MindfulnessBasedAdvancedPractitioner Pine_DocAnalysis_Notes_ManagersMeeting10.11.10 Pine_DocAnalysis_PowerPoint_Masterclass |
| Elm | |
| Strategies/plans/proposals | Elm_DocAnalysis_4.12.14.MinutesMBCTDevelopmentMeeting Elm_DocAnalysis_ 7.8.13.MinutesMBCTDevelopmentMeeting Elm_DocAnalysis_5.06.13_ MinutesMBCTDevelopmentMeeting Elm_DocAnalysis_ServiceDevelopmentMeetingsAgendas_Email1 Elm_DocAnalysis_Service DevelopmentMeetingsAgendas_Email2 Elm_DocAnalysis_Service DevelopmentMeetingsAgendas_Email3 Elm_DocAnalysis_Minutes_RegionalNetwork(Various) Elm_DocAnalysis_MBCTPractitionersMeetingMinutes14.09.11 Elm_DocAnalysis_MBCTPractitionersMeetingMinutes25.06.14 Elm_DocAnalysis_RestructureConsultation2015 Elm_DocAnalysis_SummaryStrategicPlan14-15 Elm_DocAnalysis_PresentationProposalStep2-3_May2015 Elm_DocAnalysis_PresentationProposalStep2-3_UpdateJuly2015 Elm_DocAnalysis_ProposalTraining_2013 Elm_DocAnalysis_PlanningMeeting_19.04.14 Elm_DocAnalysis_MindfulnessDevelopmentMeeting21.07.2011 Elm_DocAnalysis_MindfulnessDevelopmentMeeting28.03.2012 Elm_DocAnalysis_MindfulnessSchoolProposal Elm_DocAnalysis_MindfulnessProvisionandFutureDevelopmentsNeeds_August2014 |
| Evaluation, reports | Elm_DocAnalysis_AnnualReport2011 Elm_DocAnalysis_StaffMindfulnessReport2014_ReductionSickness Elm_DocAnalysis_MappingIAPTJuly2014 Elm_DocAnalysis_ServiceEvaluationSummary |
| Training and supervision | Elm_DocAnalysis_NHSMindfulnessTrainingApplicationForm2014 Elm_DocAnalysis_TeacherDevelopmentCourseInfo_ExpressionInterest2014 Elm_DocAnalysis_RecommendedTrainingPathway2014 Elm_DocAnalysis_TeacherDevelopmentCourse_Outline2014 Elm_DocAnalysis_Training MBCT Therapist2013 Elm_DocAnalysis_UKTeacher_GPG2011 |
| Public/raising awareness | Elm_DocAnalysis_AwarenessWorkshopEvaluationForm Elm_DocAnalysis_AwarenessWorkshopHandout Elm_DocAnalysis_DayofMindfulnessPoster Elm_DocAnalysis_APPGPresentation2014 Elm_DocAnalysis_StaffWellbeingPresentation2014 Elm_DocAnalysis_TasterSessionHandouts1-11 Elm_DocAnalysis_SharingPracticePoster |
| Course materials | Elm_DocAnalysis_HandoutBooklistandWebsites Elm_DocAnalysis_HandoutDropinSessionHQ Elm_DocAnalysis_HandoutDropinSessionHQ_Data set Elm_DocAnalysis_HandoutSession1 Elm_DocAnalysis_HandoutSession1_Contract Elm_DocAnalysis_HandoutSession6 |
| Observation/field notes | Elm_ObservationNotes_Mindfulness Awareness Day Staff_29.09.14 Elm_Observation Notes_Peer Supervision Meeting_26.09.14 Elm_Observation Notes_Session 1_23.09.14 Elm_Observation Notes_Session 6_24.09.14 Elm_Observation Notes_Sitting Session at HQ_24.09.14 Elm_Observation Notes_Taster Session-Physio Department_30.09.14 |
| Other | Elm_DocAnalysis_MindfulnessSupervisionGroupMinutes(Various) Elm_DocAnalysis_MindfulnessSupervisionGroupMinutes_Email 2 Elm_DocAnalysis_Participant 243105_Chronology Elm_DocAnalysis_DocumentaryAnalysis1_Email Elm_DocAnalysis_JobDes_MBCT_Jan09 Elm_DocAnalysis_MindfulnessServiceUserVolunteerApplicationForm2014 |
| Mangrove | |
| Strategies/plans/proposals | Mangrove_DocAnalysis_CCG_GoverningBodyMeetings_12.03.15 Mangrove_DocAnalysis_CCG_CommissioningPack2013 Mangrove_DocAnalysis_CCG_CommissioningPresentation Mangrove_DocAnalysis_CCG_DataPack Mangrove_DocAnalysis_CCG April 2014 Talking Therapies engagement event presentation Mangrove_DocAnalysis_TrustPapers_March15 |
| Evaluation, reports | Mangrove_DocAnalysis_CQC_MonitoringReport_Oct14 Mangrove_DocAnalysis_Publication_StaffPilotPaper Mangrove_DocAnalysis_Publication_QuantPaperFollowUp Mangrove_DocAnalysis_Publication_QuantPaper |
| Public/raising awareness | Mangrove_DocAnalysis_SIGPresentation2013 Mangrove_DocAnalysis_StaffWellbeingFlyer Mangrove_DocAnalysis_TalkingTherapiesBrochure Mangrove_DocAnalysis_TrustAnnualConferenceProgramme2015 Mangrove_DocAnalysis_ServiceUserSupportGroupFlyer Mangrove_DocAnalysis_TrustNewsletter |
| Observation handouts | Mangrove_DocAnalysis_TrustAnnualConference2015Handouts |
| Other | Mangrove_DocAnalysis_ImplementerCV Mangrove_DocAnalysis_NewsPaperArticle Mangrove_DocAnalysis_JournalReview2011 Mangrove_DocAnalysis_MBCTWebPage |
| Bamboo | |
| Strategies/plans/proposals | Bamboo_DocAnalysis_MBCTPrimaryCareMentalHealthTeam_Proposal Bamboo_DocAnalysis_ProposalMindfulnessCoursesforStaff Bamboo_DocAnalysis_ROIforMindfulness Bamboo_DocAnalysis_Underspend bid for mindfulness Bamboo_DocAnalysis_DevelopingMBCT Report Bamboo_DocAnalysis_MentalHealthStratergy2011 Bamboo_DocAnalysis_UnderSpendRequest2014 |
| Evaluation, reports | Bamboo_DocAnalysis_Final Report Mindfulness_10062014 Bamboo_DocAnalysis_ MBCTforRecurrentDepressioninCommunitySetting_FinalReport Bamboo_DocAnalysis_Thesis_Evaluation Bamboo_DocAnalysis_PsychTherapiesReport Bamboo_DocAnalysis_PrimaryCareMentalHealthTeamReview Bamboo_DocAnalysis_Evaluation of MBCT_2014 Bamboo_DocAnalysis_Final Report Mindfulness_10062014 Bamboo_DocAnalysis_MentalHealthReport2006 Bamboo_DocAnalysis_CommitteeReport2013 |
| Training and supervision | Bamboo_DocAnalysis_Training Proposal 2013 MBCT Bamboo_DocAnalysis_TT application Bamboo_DocAnalysis_Training Pathway Bamboo_DocAnalysis_TeacherCompetencies Bamboo_DocAnalysis_TrainingProposalForm Bamboo_DocAnalysis_TeacherTrainingApplicationForm |
| Public/raising awareness | Bamboo_DocAnalysis_MBCTHandout Bamboo_DocAnalysis_ConferencePresentation Bamboo_DocAnalysis_WellbeingFlyer Bamboo_DocAnalysis_Newsletter_March2015 |
| Observation/field notes | Bamboo_ObservationNotes_PeerSupervisionGroup.31.03.15 |
| Other | Bamboo_DocAnalysis_SketchImplementation Map_2015 Bamboo_DocAnalysis_REFImpact Bamboo_DocAnalysis_PublicationOnMindfulness2006 Bamboo_DocAnalysis_ContextEmail by LocalCollaborator_13.03.15 Bamboo_DocAnalysis_ContextPowerPoint |
| Birch | |
| Strategies/plans/proposals | Birch_DocAnalysis_PsychologicalTherapiesImplementationPolicy Birch_DocAnalysis_MentalHealthPolicyPsychologicalTherapies2012 Birch_DocAnalysis_Email_CoordinatorNetworking Birch_DocAnalysis_Email_CoordinatorRole Birch_DocAnalysis_Email2_CoordinatorRole Birch_DocAnalysis_Email3_CoordinatorRole Birch_DocAnalysis_Email4_CoordinatorRole Birch_DocAnalysis_EmailASPIREPlan Birch_DocAnalysis_EmailInvoiceEquipment Birch_DocAnalysis_Email to Managers around funding |
| Evaluation, reports | Birch_DocAnalysis_MentalHealthAnnualReport2013 Birch_DocAnalysis_MBCTEvidencePaper |
| Training and supervision | Birch_DocAnalysis_Funding Application Birch_DocAnalysis_Email_GovernanceRouteforTeachers Birch_DocAnalysis_Email_GovernanceRouteforTeachers2 Birch_DocAnalysis_Email_GovernanceRouteforTeachersTL Birch_DocAnalysis_Email_SupervisionPracticalIssues Birch_DocAnalysis_Email2_SupervisionPracticalIssues Birch_DocAnalysis_Email3_SupervisionPracticalIssues Birch_DocAnalysis_Email4_SupervisionPracticalIssues Birch_DocAnalysis_Email_SupervisionLog Birch_DocAnalysis_EmailTrainingCandidates Birch_DocAnalysis_Launching Training_Email Birch_DocAnalysis_Launching Training_Flyer Birch_DocAnalysis_Email_MindfulnessTeacherDatabase |
| Public/raising awareness | Birch_DocAnalysis_Flyer_3rdSector Birch_DocAnalysis_3rdPartyConsortiumWebsite Birch_DocAnalysis_Email_TasterBoardMembers Birch_DocAnalysis_Email2_TasterBoardMembers Birch_DocAnalysis_Email_TasterChiefExec Birch_DocAnalysis_Email_DepMinisterVisit |
| Course materials | Birch_DocAnalysis_Email_OutcomeTools Birch_DocAnalysis_Email2_OutcomeTools |
| Observation/field notes | Birch_ObservationNotes_SupervisionGroup_15.6.15 |
| Other | Birch_DocAnalysis_MeetingMinutes.17.08.15 onwards Birch_DocAnalysis_MeetingMinutes.21.03.15 |
| Hazel | |
| Strategies/plans/proposals | Hazel_DocAnalysis_MentalHealthStratergy Hazel_DocAnalysis_CCG_CommissioningPack |
| Public/raising awareness | Hazel_DocAnalysis_CMHT_Patient Information Leaflet Hazel_DocAnalysis_CBT_Patient Information Leaflet Hazel_DocAnalysis_PsychologicalServices_Patient Information Leaflet Hazel_DocAnalysis_NewsletterSpring2014 Hazel_DocAnalysis_ConferencePresentation Hazel_DocAnalysis_MindfulnessFlyer2012 Hazel_DocAnalysis_ConferencePresentation_Mindfulness and Enduring Needs Hazel_DocAnalysis_ProspectusAutumnWinter 2014 Hazel_DocAnalysis_ProspectusSpringSummer 2014 Hazel_DocAnalysis_ReferrersLeaflet Hazel_DocAnalysis_WellbeingLeaflet Hazel_DocAnalysis_PsychologicalWellbeingServiceLeaflet Hazel_DocAnalysis_WellbeingGuide2013 Hazel_DocAnalysis_TalkingTherapiesLeaflet |
| Other | Hazel_DocAnalysis_OrgainisationChart Hazel_DocAnalysis_Publication_AcceptanceMindfulness Hazel_DocAnalysis_MentalHealthDirectory Hazel_DocAnalaysis_CommunityForumCommissioning |
| Juniper | |
| Public/raising awareness | Juniper_DocAnalysis_MHPatientInformationLeaflet |
| Observation/field notes | Juniper_FieldNotes_InitialReflections_HOG |
| Other | Juniper_DocAnalysis_LogofImplementerCollaborations |
| Juniper_DocAnalysis_EmailwithPrinciples24.4.15 | |
| Beech | |
| Training and supervision | Beech_DocAnalysis_TrainingPathway |
| Public/raising awareness | Beech_DocAnalysis_IAPTLeaflet |
| Observation/field notes | Beech_FieldNotes_InitialReflections_HOG |
| Beech_ObservationNotes_MSIG_16.3.15 | |
| Wisteria | |
| Strategies/plans/proposals | Wisteria_DocAnalysis_HealthWellBeingPositionPaper2015 |
| Public/raising awareness | Wisteria_DocAnalysis_HealthandWellbeingConference_Presentation |
| Observation/field notes | Wisteria_ObservationNotes_TasterSession27.04.15 |
| Observation handouts | Wistera_DocAnalysis_TasterSessionHandout27.04.15 |
| Wistera_DocAnalysis_TasterSessionHandout-EvaluationForm27.04.15 | |
Appendix 6 Socioeconomics, ethnicity and mental health metrics
Data were mostly gathered from: GOV.UK, URL: www.gov.uk/government/statistics (accessed 6 June 2016); Public Health England Community, Community Mental Health Profiles, URL: http://fingertips.phe.org.uk/profile-group/mental-health/profile/cmhp (accessed 6 June 2016); Nomis Official Labour Market Statistics, URL: www.nomisweb.co.uk/ (accessed 6 June 2016); StatsWales, URL: https://statswales.gov.wales/Catalogue (accessed 6 June 2016); Central Survey Unit Northern Ireland, URL: www.csu.nisra.gov.uk/ (accessed 6 June 2016); and the Scottish Government, URL: www.gov.scot/ (accessed 6 June 2016).
We also drew on publicly available data that are not referenced because they were site specific.
| Site | MBCT embedded? | Sociodemographics | % adults (aged ≥ 18 years) with depression | Rural (%) | ||||
|---|---|---|---|---|---|---|---|---|
| Age (years) | Estimated population by sex (%) | IMD rank | ||||||
| Mean | Median | Female | Male | |||||
| Elm | E | 40.7 | 40 | 50.75 | 49.25 | 79 | 14.18 | 27.3 significant rural |
| Pine | E | 34.8 | 30 | 49.58 | 50.42 | 18 | 10.53 | 0 predominantly urban |
| Mangrove | E | 34.6 | 32.8 | 42 | 8.51 | 0 predominantly urban | ||
| Oak | E | 41.1 | 43 | 51.61 | 48.39 | 109 | 13.38 | 44.13 significant rural |
| Birch | PE | 41.8 | 43 | 50.74 | 49.26 | N/A | N/A | N/A |
| Wisteria | NE | 37.19 | 35 | 51.69 | 48.31 | 2 | 19 | N/A |
| Bamboo | PE | N/A | N/A | 51.69 | 48.31 | N/A | N/A | 99.6 large urban areas, 0.4 accessible rural |
| Beech | NE | 36.8 | 34 | 49.97 | 50.03 | 42 | 10.45 | 0.75 predominantly urban |
| Juniper | PE | 39 | 39 | N/A | N/A | 60 | 11.14 | 4.77 predominantly urban (0.03, 9.51) |
| Hazel | PE | 42.8 | 45 | 51.17 | 48.83 | 91 | 15.67 | 79.56 predominantly rural |
| Site | 2011 census ethnic groups (%) | ||||
|---|---|---|---|---|---|
| White | Mixed/multiple ethnic groups | Asian/Asian British | Black/African/Caribbean/black British | Other ethnic group | |
| Elm | 92.3 | 1.1 | 6.1 | 0.3 | 0.2 |
| Pine | 87.8 | 3.1 | 5.7 | 2.7 | 0.6 |
| Mangrove | 55.1 | 7.0 | 10.5 | 25.0 | 2.5 |
| Oak | 93.5 | 1.9 | 3.2 | 0.9 | 0.5 |
| Birch | 97.5 | 0.7 | 1.3 | 0.2 | 0.3 |
| Wisteria | 96.8 | 0.5 | 2.2 | 0.4 | 0.2 |
| Bamboo | 96 | No data | 2.7 | No data | 1.3 |
| Beech | 73.8 | 2.6 | 16.3 | 5.6 | 1.7 |
| Juniper | 73.5 | 3.3 | 16.6 | 5.2 | 1.3 |
| Hazel | 98.4 | 0.5 | 0.8 | 0.1 | 0.1 |
Appendix 7 Phase 2 coding framework
| Domain | Subdomain |
|---|---|
| Engagement | On more than one level |
| The need to engage key people, tailor and pitch | |
| The role of evidence in convincing people | |
| Engage = function, form depending on audience (including appropriate evidence) | |
| Training | Pathways |
| Quality | |
| Personal engagement | |
| Intervention | Adaptation |
| Target group | |
| Response to | |
| Evidence | Different forms and how it’s used (e.g. in combination) |
| Facilitation | Champions; need for a combination of champions |
| Activities | |
| Strategies | |
| Networks (SH) | |
| Resources | Human resources |
| Practical | |
| Infrastructure (e.g. including space) | |
| Time | |
| Overarching/cross-cutting domains | |
| Context | |
| Fit | |
| Journey | |
| Top down/bottom up | |
Appendix 8 Type of outcome measures used
-
Qualitative feedback.
-
Patient Health Questionnaire-9 (PHQ-9).
-
Generalised Anxiety Disorder-7 (GAD-7).
-
Clinical Outcomes Routine Evaluation-10 (CORE-10; short measure of psychological distress).
-
World Health Organization Quality of Life (WHOQOL).
-
Warwick-Edinburgh Mental Wellbeing Scale (WEMWBS).
-
Self-Compassion Scale (SCS).
-
Mindful Attention Awareness Scale (MAAS).
-
Five Facet Mindfulness Questionnaire (FFMQ).
-
Freiburg Mindfulness Inventory (FMI).
-
Hospital Anxiety and Depression Scale (HADS).
-
Beck Depression Inventory (BDI).
-
Beck Anxiety Inventory (BAI).
-
Depression Anxiety Stress Scales (DASS).
-
Maslach Burnout Inventory (MBI).
-
Perceived Stress Scale.
-
Beck Hopelessness Scale.
-
Brief Resilience Scale: Smith et al. 110
-
Difficulties in Emotion Regulation Scale (DERS).
-
Cognitive and Affective Mindfulness Scale-Revised (CAMS-R).
-
Acceptance and Action Questionnaire (AAQ).
-
Scaled General Health Questionnaire-28 (GHQ-28).
-
Short Form questionnaire-36 items (SF-36).
Appendix 9 Implementation workshops and plan
Implementation workshop: implementing mindfulness-based cognitive therapy in the NHS
Three workshops were held:
-
South England – 23 February 2016, 10.00 to 16.00, Oxford Mindfulness Centre, Oxford.
-
Wales – 10 March 2016, 10.00 to 16.00, Reichel Hall, Bangor.
-
North of England – 22 April 2016, 10.00 to 16.00, Bolton Whites Hotel, Bolton.
These workshops were an opportunity to hear about the work carried out in the ASPIRE project, to share best practice and to contribute to the development of the implementation guidance.
These workshops were for stakeholders with an interest in and commitment to MBCT implementation in the NHS. The workshops aimed to:
-
update on the current status of MBCT implementation in the NHS
-
provide key lessons about what supports and hinders implementation
-
present case examples of successful implementation, including lessons where things were not successful
-
provide an opportunity to shape the implementation guidance.
The first two points were facilitated by Rebecca Crane and Willem Kuyken, and the third was facilitated by local implementers in the North of England region. Our hope is that the subsequent workshops would be delivered by local implementers when the implementation plan is produced in early 2017.
10.00: welcome housekeeping, practicalities and confidentiality.
Intentions for the day:
-
Share ASPIRE findings.
-
Interacting with the explanatory framework and bringing experience of MBCT implementation issues to the dialogue.
-
Co-create a way of relating to this material that is practically supportive to the implementation process in the workshop region specifically and the UK generally. Support implementers.
-
We expect that these workshops will be a live evolving process as they get offered around the UK.
10.05: mindfulness practice.
10.13 to 10.15: outline of the day.
10.15 to 10.30: introductions in small groups, name, where from, hopes for the day.
10.30: the ASPIRE project background and methodology – an overview.
10.40: questions and answers.
10.50: case studies. Each group given a different case study in the form of graph with bullet points and asked to discuss how can we understand the implementation journey in this setting? What facilitated and hindered implementation? What were the pivot points?
11.00: the ASPIRE findings – themes and explanatory findings. ‘Building a cycling team’.
11.30: coffee break.
11.45: questions and feedback.
12.00: case studies continued. Each group continues working with the case study and asked to discuss how can we understand the implementation journey in this setting using the ASPIRE findings? How did they engage with management and commissioners? What was their approach to training and supervision? Take each developmental stage for the case study as if it were happening right now. How might the framework be used to support and enable the next phase of implementation? Each group assigns a scribe who takes notes and is prepared to feedback to the large group.
12.30: lunch.
13.25: mindfulness practice.
13.30: presentations from each group.
14.00: application to local setting using goldfish bowl methodology (groups of four to six). How does the ASPIRE findings apply in my setting? What stage of implementation am I at? What milestones have and have not yet been reached? How does this help me understand what has happened so far and chart a way forwards? What will facilitate my work? What barriers might I expect to encounter? What are the risks, and how might I mitigate them? How will I engage with management and commissioners? What is my approach to training and supervision?
One person volunteers to be the focus of a learning exercise and three of four other people offer to listen to the problem:
-
Three-step breathing space.
-
Person describes their situation for 5 minutes, no interruptions.
-
Bell, with mindful pause.
-
Listeners ask questions (as succinct as possible), and the person in the goldfish bowl answers those questions as directly as possible. This will take 8–10 minutes, needs a central timer to call the time.
-
Bell, with mindful pause.
-
The focus person uses 5 minutes to reflect on their situation further, again no interruptions.
-
Bell, with mindful pause.
-
Finally, there is a quick round of all participants to gather – how was it for you, and what did you notice? 1 minute each would need another 5 minutes for this section.
14.30: feed back any general learning points to the large group.
14.45: coffee break.
15.00: small groups (four to six, different configurations to earlier groups, find someone you have not worked with before). What type of implementation guidance would be helpful to you and others?
15.15: feedback and discussion.
15.30: short sharing of key learning that participants will take back to their implementation context (pairs then whole group).
15.45: summary and close with mindfulness practice.
16.00: ending.
Use online survey to harvest feedback on the format and content of the workshop.
As we can see, the findings and emerging explanations from the ASPIRE project were presented in the form of a PowerPoint presentation, delegates were then asked to form groups to discuss case studies from the project and then asked to apply the emerging finding and explanations to their own site and reflect.
ASPIRE workshop: findings and emerging explanation, PowerPoint presentation
We had a range of stakeholders attending the workshops:
-
project co-investigators and members of project advisory panel
-
PPI representative
-
project local collaborators
-
NHS clinicians and managers (including IAPT managers)
-
implementers with a range of experiences and expertise
-
charity representatives.
Notes: HOG.
24 February 2016.
Exercise: what helps to understand the journey? Facilitators and barriers? Tipping points.
Elm case study
So much going on, but why no top-down buy in? Because they didn’t see it as financially viable. Why? Assuming Implementer failed to make a financial case. Not sure which measures they were using but that could have helped make a financial case.
Was the Implementer spread too thinly? Too ambitious, too passionate, the word ‘believe’ is quoted, could put people off.
Sudden change in 2006 – was this due to IAPT.
Too wide, too fast, too soon.
Not had a long term view.
Not a good fit here with Implementer Priorities and IAPT Priorities?
Top down culture not there.
Pine case study
Serendipity case.
Had 3 elements working in a team – seemed crucial – Business, Clinical and Academic.
Business element being a ‘double edged sword’.
Oak case study
Ripple of change in Culture.
Key dedicated mindfulness lead.
Mangrove case study
Isolation – not a trust priority- people feeling guilty for taking time out.
New CEO – meant there was a cultural shift from risk adverse to innovative.
Clear training guidelines needed.
XXXX (delegate A) commented on systematic approach to change, and whether or not there’s a resistance to a systematic approach.
How did people approach local change? What works best?
XXXX (delegate B) commented on the way that they managed change was to follow the trust’s project management framework, they had to in order to implement anything.
Importance of a team of expertise; someone who can build momentum bottom up but also someone who can write project management frameworks.
Important to grow a mass.
Some key learning from the group after the goldfish bowl exercise; what delegates reflected on that they need to do/keep in mind.
Highlight demand.
Identify gatekeepers.
Look for alternative route to access top down if one route is impossible.
Taking one step at a time.
Use the language of managers.
If knocking on doors, assure you are knocking on the correct one, who they need to talk to about this.
Long game, patience, being strategic.
Sphere of influence.
Tapping into resources (existing human resources).
ASPIRE workshopNotes: HOG.
10 March 2016.
Phase 2 analysis
Issue of TIME – Long view and time – riding waves . . . (riding hills!).
Learning from goldfish bowl exercise:
-
One member realised that there was more going on in her trust than first thought.
-
More roots (not at first visible).
-
Another was at a challenging ‘middle phase’ – flagging a little and hard to carry on the momentum – need to re-gather momentum.
-
One found the idea of ‘stepping back’ and letting someone else lead for a while (team cycling metaphor – drop back to the back of the team for a while, out of the windstream to recover) a difficult thing to do. Stepping back a little when you are a champion is difficult.
-
Dealing with the emotion of implementing – how people respond and deal with emotions, when things are not going well, because a champion is so personally involved, invested.
-
You’ll never get a ‘fully embedded’ site, it’s about accepting that the ‘sand’ is always shifting, and that people are swimming upstream even within in an ‘embedded’ site. It’s about accepting where you are on the journey, and being OK with that. Not being too ambitious, need to be realistic.
So it’s about having tools to support you ‘where you are now’ not tools to get you ‘fully embedded’. (Fully embedded will never exist, because of ever-changing context. It’s about getting more sustained, so that if the ‘sand’ shifts underneath, things are in place so that the service does not completely collapse.)
Implementation plan
We also asked workshop delegates to inform us of what they would like to see included in the final implementation plan.
Implementation plan suggestions/ideas
(Small group discussion.)
-
If we identified milestones that could be generalisable as steps needed to take to reach a sustainable service, and then resources attached to those milestones that would help achieve the milestone. For example:
-
Not cast in stone – has to be some flexibility.
-
Credibility and quality assured.
-
Not compulsory.
-
Disclaimers and inclusive.
-
Open resource.
-
A model to identify where you are and where you want to go or what you want to achieve.
-
MBCT specific – but making it fit.
-
User content – uploading stories and example.
-
Section on frequently asked questions.
-
Talking heads (project members).
-
Learning from others is key – hearing success stories.
-
Case summary vignettes in lay language.
-
‘Goldfish bowl’ exercise as a resource – link people to mentors.
-
Examples of documents so people do not have to re-invent.
-
Highlight what’s happening elsewhere internationally.
-
Get a group of senior ‘top-down’ people to review the toolkit.
-
Brief introduction for managers.
-
Short videos, on MBCT and on implementation, drawing on various people and expertise to capture widespread attention. (Outside authority.) [Mark Williams (commissioner), Ruby Wax, David Clark (NHS manager), service user/staff well-being member, politicians, Val Moore, ASPIRE project members. All speaking from different angles about MBCT and implementation.]
-
Theme of ‘adapting’ – discussion about the balance.
-
What research is already done on adapting?
-
List of outcome measures.
-
Documentary style outputs – media.
-
Support for implementers – list of mentors/networks.
-
Question and answer – blog style?
Workshop feedback
| Workshop 1: South of England region – Oxford | ||||||
|---|---|---|---|---|---|---|
| Very good | Good | Average | Fair | Poor | N/A | |
| Number of responses | 2 | 9 | 1 | 1 | 1 | – |
Comments:
It was slightly difficult to know from the course information if I was the right sort of person to be attending the event, as I am quite new to mindfulness teaching and by no means a service champion. However I did feel very welcome, and inspired by the day and hope I can take some of the ideas forward.
. . . little available and short notice for event.
| Workshop 2: Wales – Bangor | ||||||
|---|---|---|---|---|---|---|
| Very good | Good | Average | Fair | Poor | N/A | |
| Number of responses | 5 | 3 | 3 | 1 | – | – |
Comments:
It was enough. I was happy to attend for the full details of the projects outcomes and didn’t feel I needed more information prior to event.
The location of the venue was noted, although both myself and colleague struggles to find where this was on the university map.
| Workshop 3: North of England region – Greater Manchester | ||||||
|---|---|---|---|---|---|---|
| Very good | Good | Average | Fair | Poor | N/A | |
| Number of responses | 1 | 2 | 2 | 1 | 1 | – |
Comments:
While I received the course confirmation email I did not receive any further course details by email ie directions/post code, whether there was lunch etc. It was easy enough to find the basic info[rmation] of where to come to via the original web link though.
Little info[rmation] received before the day other than confirmation of attendance.
. . . no venue info[rmation] sent; I needed to try and find the original website where i had signed up, which was difficult. A quick email confirming venue would have been great.
Question 2: Centre for Mindfulness Research and Practice booking system
| Workshop 1: South of England region – Oxford | ||||||
|---|---|---|---|---|---|---|
| Very good | Good | Average | Fair | Poor | N/A | |
| Number of responses | 7 | 5 | 2 | – | – | – |
Comments:
I think there was a glitch with your system so it missed sending me confirmation, but this was resolved once i contacted admin[istration].
. . . easy!
| Workshop 2: Wales – Bangor | ||||||
|---|---|---|---|---|---|---|
| Very good | Good | Average | Fair | Poor | N/A | |
| Number of responses | 7 | 5 | – | – | – | – |
Comments:
Smooth, no issues.
An email confirmation a week before would have been helpful.
It was easy to book on the course.
| Workshop 3: North of England region – Greater Manchester | ||||||
|---|---|---|---|---|---|---|
| Very good | Good | Average | Fair | Poor | N/A | |
| Number of responses | 5 | 1 | 1 | – | – | – |
Comments:
Quite straight forward process.
Question 3: administrative team support
| Workshop 1: South of England region – Oxford | ||||||
|---|---|---|---|---|---|---|
| Very good | Good | Average | Fair | Poor | N/A | |
| Number of responses | 7 | 4 | – | 2 | – | 2 |
Comments:
Very helpful when I contacted re[garding] missing confirmation.
Helpful.
| Workshop 2: Wales – Bangor | ||||||
|---|---|---|---|---|---|---|
| Very good | Good | Average | Fair | Poor | N/A | |
| Number of responses | 6 | 4 | – | – | – | 2 |
Comments:
Had prompt response to any queries.
Attempts were made to contact the department and request further information regarding the location although it was not possible to speak to anyone with the knowledge.
| Workshop 3: North of England region – Greater Manchester | ||||||
|---|---|---|---|---|---|---|
| Very good | Good | Average | Fair | Poor | N/A | |
| Number of responses | 4 | 1 | – | – | – | 2 |
Comments: –
Question 4: course content| Workshop 1: South of England region – Oxford | ||||||
|---|---|---|---|---|---|---|
| Very good | Good | Average | Fair | Poor | N/A | |
| Number of responses | 7 | 6 | 1 | – | – | – |
Comments:
Actually excellent.
It was an inspiring day, hearing about the aspire research and the implementation. Personally I might have liked to have heard more about the practicalities of training teachers e.g. How training will be funded, how much should training be done ‘in house’, how much through external links? I liked the bottom up, top down discussions and thought how relevant and important it is to secure management/commissioner/government support.
. . . both informative and practical. Also very good for meeting others – both offering support and being supported.
. . . really thought provoking and inspiring.
| Workshop 2: Wales – Bangor | ||||||
|---|---|---|---|---|---|---|
| Very good | Good | Average | Fair | Poor | N/A | |
| Number of responses | 9 | 3 | – | – | – | – |
Comments:
Appreciated having the main themes presented. Helped me to understand the processes that often occur with implementation.
It was a very interesting day. I would like to hear more examples of how mindfulness is being applied in services in the NHS and the merits and limitations of theses adapted implementations, including in-house training of staff.
I did not know what to expect from the course, it was really helpful in considering the barriers in starting a mindfulness group and the factors that aid the maintenance of the group.
Excellent and confident regarding the implementation plan.
Although the course was more business-like than I had thought it would be, it was very interesting.
Really impressed by all the work that has been done.
| Workshop 3: North of England region – Greater Manchester | ||||||
|---|---|---|---|---|---|---|
| Very good | Good | Average | Fair | Poor | N/A | |
| Number of responses | 4 | 3 | – | – | – | – |
Comments:
Excellent day- all speakers were knowledgeable and engaging.
Question 5: course structure
| Workshop 1: South of England region – Oxford | ||||||
|---|---|---|---|---|---|---|
| Very good | Good | Average | Fair | Poor | N/A | |
| Number of responses | 5 | 7 | 2 | – | – | – |
Comments:
The day evolved as we went along and had probably been a bit over scheduled, nevertheless the structure worked extremely well.
I liked the presentations and the group discussions, also the opportunity to network. Free lunch was a nice gesture given that the day was free.
Good balance between information giving and practical implementation. Very open to contributions and ideas.
| Workshop 2: Wales – Bangor | |||||
|---|---|---|---|---|---|
| Very good | Good | Average | Fair | Poor | N/A |
| 8 | 4 | – | – | – | – |
Comments:
Liked the overview at the start, before breaking up into groups. Facilitators presence helpful to frame discussion and keep track.
A very clear structure, paced well throughout the day.
Great having the breathing spaces.
| Workshop 3: North of England region – Greater Manchester | ||||||
|---|---|---|---|---|---|---|
| Very good | Good | Average | Fair | Poor | N/A | |
| Number of responses | 5 | 2 | – | – | – | – |
Comments:
Great mix of experiential and powerpoint, lots of discussion and group group – lovely mix and very enjoyable. Great to have some thinking space.
Question 6: course materials
| Workshop 1: South of England region – Oxford | ||||||
|---|---|---|---|---|---|---|
| Very good | Good | Average | Fair | Poor | N/A | |
| Number of responses | 2 | 7 | 5 | – | – | – |
Comments:
. . . couldn’t read some of the powerpoint slides.
The first part of the workshop was about information giving but I found it difficult to follow the material as it was hard to read the board. Materials used (powerpoint) was too small. It might have helped if we were given a paper copy at the beginning to be able to follow what was being shared.
. . . will we have access to handouts?
| Workshop 2: Wales – Bangor | ||||||
|---|---|---|---|---|---|---|
| Very good | Good | Average | Fair | Poor | N/A | |
| Number of responses | 7 | 5 | – | – | – | – |
Comments
Fine. Not many materials needed in this instance.
Would have preferred to have a printed version of what Heledd read out as the research findings.
| Workshop 3: North of England region – Greater Manchester | ||||||
|---|---|---|---|---|---|---|
| Very good | Good | Average | Fair | Poor | N/A | |
| Number of responses | 4 | 3 | – | – | – | – |
Comments:
. . . could we have a copy of the slides?
Question 7: delivery methods
| Workshop 1: South of England region – Oxford | ||||||
|---|---|---|---|---|---|---|
| Very good | Good | Average | Fair | Poor | N/A | |
| Number of responses | 5 | 8 | 1 | – | – | – |
Comments:
The presentations, despite the complexity of the information, held the audience and communicated very effectively.
Well paced and clear.
| Workshop 2: Wales – Bangor | ||||||
|---|---|---|---|---|---|---|
| Very good | Good | Average | Fair | Poor | N/A | |
| Number of responses | 8 | 4 | – | – | – | – |
Comments:
Clear, effective presentations. Appreciated the ground exercises throughout the day.
| Workshop 3: North of England region – Greater Manchester | ||||||
|---|---|---|---|---|---|---|
| Very good | Good | Average | Fair | Poor | N/A | |
| Number of responses | 4 | 3 | – | – | – | – |
Comments:
Time to move around more – the chairs were not all that comfortable to sit on for the long periods we did. Loved the mindfulness exercises during the delivery, but maybe mindful movement would have helped me a lot.
Question 8: group participation
| Workshop 1: South of England region – Oxford | ||||||
|---|---|---|---|---|---|---|
| Very good | Good | Average | Fair | Poor | N/A | |
| Number of responses | 7 | 7 | – | – | – | – |
Comments: –
| Workshop 2: Wales – Bangor | ||||||
|---|---|---|---|---|---|---|
| Very good | Good | Average | Fair | Poor | N/A | |
| Number of responses | 10 | 2 | – | – | – | – |
Comments:
I could have participated more. The facilitators offered plenty of space to do this. The issue I had was that I felt the resume of how MBCT had come to be well established in our service missed out some key areas in terms of barriers and facilitators that I had witnessed in the process. I didn’t recognise my role within it as a practitioner paving the way in the early ears and felt inhibited to speak about this at this particular event. An example of this was how fragmented out teaching was in the early years, not supported by the different departments. The result was I was not involved to the extent I could have been. This came much later. Myself and my colleague now have a good working relationship and value the different strengths we have and the result is a service which is growing in terms of quality/consolidation. It was a disappointment to me that this did not come through within the Case Study.
It was really interesting to hear about experiences of others.
Thoroughly enjoyed the fish bowl exercise.
| Workshop 3: North of England region – Greater Manchester | ||||||
|---|---|---|---|---|---|---|
| Very good | Good | Average | Fair | Poor | N/A | |
| Number of responses | 5 | 2 | – | – | – | – |
Comments: –
Question 9: teaching skills| Workshop 1: South of England region – Oxford | ||||||
|---|---|---|---|---|---|---|
| Very good | Good | Average | Fair | Poor | N/A | |
| Number of responses | 5 | 7 | – | – | – | 2 |
Comments:
Light touch, just right, extremely effective.
The only comment I would make is that some of the presenters spoke extremely quietly and slightly monotone so at times it was hard to hear everything that they were sharing.
| Workshop 2: Wales – Bangor | ||||||
|---|---|---|---|---|---|---|
| Very good | Good | Average | Fair | Poor | N/A | |
| Number of responses | 9 | 2 | – | – | – | 1 |
Comments:
A variety of speakers and teachers is really helpful in keeping focused.
| Workshop 3: North of England region – Greater Manchester | ||||||
|---|---|---|---|---|---|---|
| Very good | Good | Average | Fair | Poor | N/A | |
| Number of responses | 4 | 3 | – | – | – | – |
Comments:
. . . can we get a list of all the websites and mailing lists that were mentioned at the end.
Question 10: teacher(s) knowledge/understanding
| Workshop 1: South of England region – Oxford | ||||||
|---|---|---|---|---|---|---|
| Very good | Good | Average | Fair | Poor | N/A | |
| Number of responses | 10 | 2 | 1 | – | – | 1 |
Comments:
All presenters were extremely knowledgeable and approachable.
| Workshop 2: Wales – Bangor | ||||||
|---|---|---|---|---|---|---|
| Very good | Good | Average | Fair | Poor | N/A | |
| Number of responses | 10 | 1 | – | – | – | 1 |
Comments: –
| Workshop 3: North of England region – Greater Manchester | ||||||
|---|---|---|---|---|---|---|
| Very good | Good | Average | Fair | Poor | N/A | |
| Number of responses | 6 | 1 | – | – | – | – |
Comments: –
Question 11: has anything been particularly meaningful for you?| Workshop 1: South of England region – Oxford | ||
|---|---|---|
| Yes | No | |
| Number of responses | 11 | 3 |
Comments: –
The extremely positive nature of the group interactions.
The workshop helped me clarify how I can contribute to the introduction of MBCT into my trust.
It was good to network with others and to gather some excellent ideas from others.
Very helpful to hear about the different ways in which MBIs have been implemented throughout the UK.
As mentioned, securing the top down support. Also the need to work together as a team, to be connected, and use each other’s strengths.
Fostering a sense of connection and knowing that other colleagues struggling with the same difficulties and looking forward to seeing the materials which will help us in putting our case at boardroom level etc and up to date research logged – we are so busy in our clinical roles that it is so difficult to make time for these kinds of things.
Has enabled to think about steps needed to build on current implementation of MBCT within my Trust and how I can be a part of those. Allowed useful networking to enable to take these forward.
. . . sharing forum, normalising, shared challenges, shared information, inspiration to keep going with service development.
Hearing the stories of implementation.
| Workshop 2: Wales – Bangor | ||
|---|---|---|
| Yes | No | |
| Number of responses | 12 | – |
Comments:
Valuable opportunity to have the results of the study and then how to use the research to help implement MBCT in the NHS.
The definition of themes that arise and how these repeat themselves.
It was good to have time to reflect on aspects of work, with other similar situations.
Being able to feel connected to others with similar challenges.
Feeling part of a wider community of practitioners delivering mindfulness in the NHS and hearing examples of how it’s been implemented in the different services over the whole time course, including the tipping points.
The importance of the structure and support when starting a course with a service.
Very useful to have information about various services in the UK.
Meeting like-minded people from other organisations – Group working.
The hard work and dedication of the team to get to this point.
My knowledge of mindfulness is currently minimal. This course has inspired me to increase my knowledge of it and I will be speaking with my manager to seek permission/funding to attend an 8 week course.
Dedication to promote mindfulness based CBT.
| Workshop 3: North of England region – Greater Manchester | ||
|---|---|---|
| Yes | No | |
| Number of responses | 7 | – |
Comments:
Thinking space, group discussions and gold fish bowl exercise.
. . . a small group exercise helped with a personal issue.
Now aware of the barriers against implementing MBCT – perhaps I was previously naive.
. . . interesting techniques for delivery – e.g. goldfish bowl. Interesting to gain a sense of wider implementation issues.
. . . a better understanding of how to implement & maintain Mindfulness within a service in the NHS.
Whole day, presentations, case studies, discussions all relevant and helpful.
. . . the models that we can use to bring in mindfulness to an organisation like the NHS will also be useful in bringing it in to a school or other work place.
Question 12: have there been any particular highlights?
| Workshop 1: South of England region – Oxford | ||
|---|---|---|
| Yes | No | |
| Number of responses | 9 | 5 |
Comments:
Opportunity to network with practitioners and colleagues.
Conversations with XXXX, XXXX and XXXX.
The way in which the research team managed a very complex set of interviews and extracted themes.
Reconnecting with colleagues from conferences etc, sharing ideas on how to involve other professions ie GPs and GP trainers etc I did realise that participating in the research and attending the day gave me a feeling of being supported and a sense of community which has been and is very sustaining.
Networking.
| Workshop 2: Wales – Bangor | ||
|---|---|---|
| Yes | No | |
| Number of responses | 9 | 3 |
Comments:
Interface with MBCT practitioners and researchers.
Meeting with other teachers. Being able to listen and be supportive, give encouragement, perhaps offer suggestions. I recognised many of the barriers they face through personal experience.
I enjoyed the analogies used to present the material.
Use of the mindfulness practices between exercises. Oh and the chocolate brownies!
The study itself is very fascinating and very applicable to helping understand the context and time course around implementation. The themes around the process were really interesting. Meeting other practitioners delivering courses was also beneficial.
Sharing information with others, networking and learning from others, as well as building an awareness of research findings. Hopefully this will aid our efforts in starting/expanding the use of mindfulness intervention at the Step 3 level.
The research was a big project and it will impact on so many lives.
I really appreciated the snippets of mindfulness throughout the day.
The finds of the interviews.
| Workshop 3: North of England region – Greater Manchester | ||
|---|---|---|
| Yes | No | |
| Number of responses | 5 | 1 |
Comments:
Hearing other’s professional and personal journeys into mindfulness. Able to meet others in the field – who are passionate about the subject.
. . . goldfish bowl task. food was fantastic, catering, location resources all great.
Heledd’s research and presentation.
. . . doing the gold fish bowl exercise.
Question 13: could anything be improved?
| Workshop 1: South of England region – Oxford | ||
|---|---|---|
| Yes | No | |
| Number of responses | 7 | 7 |
Comments: –
| Workshop 2: Wales – Bangor | ||
|---|---|---|
| Yes | No | |
| Number of responses | 1 | 11 |
Comments: –
| Workshop 3: North of England region – Greater Manchester | ||
|---|---|---|
| Yes | No | |
| Number of responses | 1 | 6 |
Comments: –
Question 14: any other comments?| Workshop 1: South of England region – Oxford | ||
|---|---|---|
| Yes | No | |
| Number of responses | 4 | 10 |
Comments:
An extremely successful day, if this is typical of the workshops then they will significantly help the project and help the participants themselves to move MBCT forward.
Thank you.
Time keeping . . . left little time for lunch . . . running late.
| Workshop 2: Wales – Bangor | ||
|---|---|---|
| Yes | No | |
| Number of responses | 3 | 9 |
Comments:
Follow up would be good.
It would be interesting in being part of a community of mindfulness practitioners that could share practice and research.
Thank you and look forward to continued working with the NHS and Universities.
| Workshop 3: North of England region – Greater Manchester | ||
|---|---|---|
| Yes | No | |
| Number of responses | 4 | 3 |
Comments:
I enjoyed the day. Information about implementation was very helpful.
. . . thanks for running this and to the ppn [Psychological Professions Network] for their support of the day.
Thank you for an excellent day.
I was late and missed part of the morning presentation. I was told that Heledd (?) the woman who gave the presentation would be able to share her slides with me. I am on XXXX Can you she email them to me or let me know if they will be posted on a website somewhere?
Question 15: overall, was the venue suitable for the event?
| Workshop 1: South of England region – Oxford | ||
|---|---|---|
| Yes | No | |
| Number of responses | 14 | – |
Comments: –
| Workshop 2: Wales – Bangor | ||
|---|---|---|
| Yes | No | |
| Number of responses | 12 | 0 |
Comments: –
| Workshop 3: North of England region – Greater Manchester | ||
|---|---|---|
| Yes | No | |
| Number of responses | 7 | 0 |
Comments: –
Question 16: teaching space| Workshop 1: South of England region – Oxford | ||||||
|---|---|---|---|---|---|---|
| Very good | Good | Average | Fair | Poor | N/A | |
| Number of responses | 8 | 6 | – | – | – | – |
Comments:
Light, airy, comfortable.
. . . was noisy when all small groups in same room.
Perhaps delegates can be asked to fill all the spaces at the opposite side from the entrance, leaving empty chairs near the entrance for the many latecomers?
| Workshop 2: Wales – Bangor | ||||||
|---|---|---|---|---|---|---|
| Very good | Good | Average | Fair | Poor | N/A | |
| Number of responses | 12 | – | – | – | – | – |
Comments: –
| Workshop 3: North of England region – Greater Manchester | ||||||
|---|---|---|---|---|---|---|
| Very good | Good | Average | Fair | Poor | N/A | |
| Number of responses | 5 | 2 | – | – | – | – |
Comments:
. . . room was cold initially.
Question 17: accommodation facilities
| Workshop 1: South of England region – Oxford | ||||||
|---|---|---|---|---|---|---|
| Very good | Good | Average | Fair | Poor | N/A | |
| Number of responses | 1 | 3 | – | – | – | 10 |
Comments:
Access to a couple more loos would have been good, and the locks on the doors were a bit odd.
| Workshop 2: Wales – Bangor | ||||||
|---|---|---|---|---|---|---|
| Very good | Good | Average | Fair | Poor | N/A | |
| Number of responses | 6 | 1 | – | – | – | 5 |
Comments: –
| Workshop 3: North of England region – Greater Manchester | ||||||
|---|---|---|---|---|---|---|
| Very good | Good | Average | Fair | Poor | N/A | |
| Number of responses | 5 | – | – | – | – | 2 |
Comments: –
Question 18: catering| Workshop 1: South of England region – Oxford | ||||||
|---|---|---|---|---|---|---|
| Very good | Good | Average | Fair | Poor | N/A | |
| Number of responses | 3 | 7 | 3 | – | 1 | – |
Comments:
Usual university food.
| Workshop 2: Wales – Bangor | ||||||
|---|---|---|---|---|---|---|
| Very good | Good | Average | Fair | Poor | N/A | |
| Number of responses | 11 | 1 | – | – | – | – |
Comments:
And the brownies to die for.
| Workshop 3: North of England region – Greater Manchester | ||||||
|---|---|---|---|---|---|---|
| Very good | Good | Average | Fair | Poor | N/A | |
| Number of responses | 7 | – | – | -– | – | – |
Comments: –
Glossary
- ATLAS.ti
- A computer program used to analyse qualitative data.
- Early adopter
- An implementer who had been in a site for a while before a second-generation implementer took over. An early adopter would have developed an interest in and practised, researched and championed mindfulness-based cognitive therapy before the intervention had been included in National Institute for Health and Care Excellence guidance.
- Facilitator/co-facilitator
- A facilitator is the lead person who co-ordinates mindfulness-based cognitive therapy groups. A co-facilitator helps the facilitator to run the groups. Co-facilitating with an experienced facilitator is often an intervention used at the end of a training pathway.
- Green Book
- Segal ZV, Williams JMG, Teasdale JD. Mindfulness-Based Cognitive Therapy for Depression. 2nd edn. New York, NY: Guilford Press; 2013. (The publication that describes the mindfulness-based cognitive therapy intervention.)
- Hybrid models
- When an implementer combines elements of compassion-focused therapy by The Compassionate Mind Foundation.
- Local collaborator
- The accessibility and implementation in UK services of an effective depression relapse programme: a mindfulness-based cognitive therapy project’s main informer and point of contact within the site.
- Maintenance group/drop-in session
- Usually held within a peer-group setting with other staff to discuss any issues and to support each other to maintain good practice guidelines.
- Mindfulness-based cognitive therapy teacher
- An individual trained to teach the mindfulness-based cognitive therapy programme.
- Personal practice
- Mindfulness-based cognitive therapy guidelines state that a teacher must have a commitment to a daily, personal, formal practice in order to teach and facilitate mindfulness-based cognitive therapy groups.
- Retreat
- An environment that supports the development of mindfulness practice, often of several consecutive days. This provides teachers with an opportunity to experience the kinds of processes that might arise for their participants and enables them to teach from their own ‘embodied experience’.
- Service user volunteer
- A service user who had previously been a patient but is now working alongside implementers as an advocate, sharing their experiences at taster sessions or helping to co-facilitate groups.
List of abbreviations
- ASPIRE
- accessibility and implementation in UK services of an effective depression relapse programme: mindfulness-based cognitive therapy
- CAMHS
- Child and Adolescent Mental Health Services
- CBT
- cognitive–behavioural therapy
- CCG
- Clinical Commissioning Group
- CD
- compact disc
- CEO
- chief executive officer
- CMHT
- Community Mental Health Team
- GP
- general practitioner
- IAPT
- Improving Access to Psychological Therapies
- IPU
- integrated practice unit
- MAPPG
- Mindfulness All Party Parliamentary Group
- MBCT
- mindfulness-based cognitive therapy
- MBI
- mindfulness-based intervention
- MBSR
- mindfulness-based stress reduction
- NICE
- National Institute for Health and Care Excellence
- PARIHS
- Promoting Action on Research Implementation in Health Services
- PPI
- patient and public involvement
- SIGN
- Scottish Intercollegiate Guidelines Network