Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 12/5002/19. The contractual start date was in September 2013. The final report began editorial review in April 2016 and was accepted for publication in January 2017. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Disclaimer
This report contains transcripts of interviews conducted in the course of the research and contains language that may offend some readers.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2017. This work was produced by Ferlie et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Study context and research objectives
This study analyses the early development of recently created English health-care organisations, namely Academic Health Science Networks (AHSNs), charged with accelerating the diffusion of health-improving and wealth-creating innovations across English health care. We will study how AHSNs approach their innovation diffusion and knowledge mobilisation tasks. We also take an agency perspective and explore the possible role of ‘knowledge leaders’ (KLs) in these regional sites.
The study responds to the Health Services and Delivery Research (HSDR) research brief 12/15002, ‘Research to Improve Knowledge Transfer and Innovation in Healthcare Delivery and Organisation’, which included relevant themes relating to increasing ‘research pull’ by health-care managers and promoting interactive and boundary spanning knowledge translation (KT).
The policy and organisational context
First, we outline the policy and organisational contexts before considering academic literatures that surfaced in our early protocol (although we develop our literature review in Chapter 3). The diagnosis at the policy level is that the UK NHS has been good at the invention of new treatments and products, but poor at their diffusion: ‘while the NHS is recognised as a world leader in invention, the spread of those inventions within the NHS has often been slow, and sometimes even the best of them fail to achieve widespread use’. 1
Accelerating the diffusion of promising innovations and more effective knowledge mobilisation across the health-care field has been a recurrent concern in recent English health policy (we review these policy texts more fully later). This policy-level concern has helped to create a new supporting institutional architecture for knowledge mobilisation, of which the AHSNs are an important part.
An emergent academic literature reflects on evolving UK health research policy. Walshe and Davies’ historical analysis of policy documents notes a shift from initial goals of knowledge production to later ones of ‘knowledge mobilisation’, which could embed the results of the research now produced more quickly into practice. 2
From the mid-2000s onwards, significant health and economic policy documents encouraged better translational research capacity at a macro level. The Cooksey Review outlined novel wealth generation goals for the health-care sector in addition to traditional health improvement goals. 3 It urged better system capacity in KT so that new scientific knowledge could flow ‘from bench to bedside’ speedily. The Cooksey Review’s characterisation of the so-called translation 2 gap – the long time taken for a promising innovation to roll out from pilot sites across the health-care field – is of particular interest here. 3
The Darzi Review4 further sought to support more rapid roll-out of evidence-based innovations in health care. It helped to invent a new organisational form (or, rather, imported it to England from well-known American sites, such as Johns Hopkins Medicine). It was stated that a ‘small’ number of leading edge and internationally competitive Academic Health Sciences Centres (AHSCs) would be created (only five in the first 2009 tranche) to bring together basic science, clinical practice and education and training and to stimulate more and speedier interactions between these three traditionally loosely coupled domains. 4
Further institutional change came with the first tranche of regionally based Collaborations for Leadership in Applied Health Research and Care (CLAHRCs) (2008) to encourage applied health research to improve patient outcomes across their areas. They should develop collaborations between NHS organisations and local universities and work to narrow the second translation gap. We review this important policy stream fully later.
And now Academic Health Science Networks . . .
A recent institutional change has been the Department of Health’s (DH’s)1 proposal to introduce – and then the decision to license (during 2013/14) – 15 AHSNs. AHSNs now cover all of England, unlike the AHSCs, which are concentrated in a few research-intensive universities. They broadly have a regional footprint with a population of 3 or 4 million. The foundational policy document was intriguingly called Innovation, Health, and Wealth, recognising the potential economic importance of the health-care sector and its contribution to science-led growth, as well as traditional health improvement goals. 1
This document saw AHSNs as part of a ‘delivery system’ for enhanced innovation. They would promote health-related goals: ‘their goal will be to improve patient and population health outcomes by translating research into practice and implementing integrated health care services. Working with AHSCs, they will identify high impact innovations and spread their use at pace and scale throughout the networks’ (p. 19). 1 They would also provide industry with a readily accessible NHS ‘lead customer’ and would ‘strengthen the collaboration between clinicians and other practitioners and the medical technology industry on which innovative product development so often depends’.
Briefly, AHSNs can be defined as small and multisectoral organisations that operate on a network basis, rather than as a hierarchy. They are organised as ‘managed networks’, which work to national policy objectives, and are monitored on their progress rather than more traditional tacit and professionally dominated clinical networks. 5
Academic Health Science Networks are membership-based organisations that receive some (relatively modest and time limited) NHS funding, but are also expected to generate subscriptions from their members. There is variation in their configurations and approaches, dependent on local circumstances, but all should promote both health and wealth objectives. They have a small management team, which would often include a non-executive part-time chairperson, a chief executive officer (CEO), a commercial director and support staff.
They have a catalytic and change management-orientated role in promoting the diffusion of innovations in complex multisectoral systems, including local universities, the NHS and private firms. They seek to contribute to broader culture change in making the NHS more open to industrial partners.
The academic and theoretical context
Any empirically grounded study of AHSNs should be informed by academic and theoretical literature so that it has a conceptual basis. We now draw on the literature review in our protocol to outline the initial academic emplacement of the study (www.nets.nihr.ac.uk/projects/hsdr/12500219), although our arguments are developed further in the full literature review later undertaken (see Chapter 3).
First, our protocol argued that the well-established diffusion of innovations literature6,7 needs consideration. Coleman et al. ’s6 classic early study of the diffusion of medical innovations (the timing of a clinician’s decision to prescribe a new antibiotic) highlighted the role of informal clinical networks in spreading knowledge about innovation. This study also found an important group of clinical ‘opinion leaders’ as influential in adoption decisions and explored their characteristics.
Rogers7 distinguishes the role of ‘early adopters’ as individuals well integrated into a local social system who act as the first port of call for advice and information about innovation. They play an important role in the ‘take-off’ stage of the diffusion of an innovation by spreading positive evaluations to colleagues. They draw on strong interpersonal networks and credibility to persuade others, and are also moderately more ‘cosmopolitan’ (e.g. attending more scientific conferences or having a national professional leadership role) than followers, while combining these attributes with strong local credibility. This perspective suggests that agency from credible opinion leaders may be important in innovation take-off.
A further issue concerns the long-term sustainability of health-care innovations. 8 Innovations may be adopted but later unadopted rather than undergo routinisation into everyday practice. A study of NHS service improvement, for example, noted pervasive ‘improvement evaporation’,9 with rapid reported improvements associated with short-term bursts of change management activity but followed by regression to the status quo. An implication is that longitudinal analyses of the career of innovations over time is required to assess any evaporation effects.
Second, the initial protocol suggested that literature on knowledge leadership in health-care organisations was important. Specifically, we built on two recently completed studies on the leadership of knowledge in health-care organisations previously undertaken by researchers on the proposal. Nicolini et al. 10 explored knowledge mobilisation practices undertaken by CEOs in the NHS trusts, using shadowing methods. Although the study sheds useful light on how information and knowledge enter these senior managers’ thinking, by its nature it offers limited evidence as regards how such knowledge is shared more widely. This current project extends this earlier study by retaining a focus on senior managerial agency, but examines the wider knowledge networks of what we originally termed AHSN very senior managers (VSMs), who could be either general managers or clinical–managerial hybrids.
More recently, Swan et al. ’s edition11 explores knowledge mobilisation processes in health care from a practice perspective. ‘Knowledge mobilisation’ is construed as a proactive process that involves efforts to transform practice through the circulation of knowledge within and across different practice domains. Knowledge is not a thing that people ‘have’, but it is what they ‘do’ and involves questions of who they are (or identity).
Dopson et al. 12 explored health-care managers’ accessing and use of management knowledge, rather than the more conventional focus on the implementation of guidelines by clinicians. Despite some calls for an evidence-based management movement that replicated evidence-based medicine (EBM), Dopson et al. 12,13 found few texts based on evidence-based management. Instead, radically different forms of management knowledge (such as business school faculty or management consultant-authored texts, often from American authors) were present. So, knowledge leadership may be exercised internationally, as influential texts may be written by international authors (often American) and imported. A second implication is that codified texts (such as bestselling books) could be important,14 in addition to local knowledge practices.
Dopson et al. 12 identified opportunities for local knowledge leadership within the health-care organisations studied. One important competence was brokering the movement of knowledge across distinct knowledge domains, epistemic boundaries and different institutions, encouraging its absorption by more than one organisation or profession. This finding is relevant to the AHSNs, as they too operate in a multisectoral and multiprofessional context.
Fischer et al. 14 ask how leaders influenced by research-based management knowledge mobilise such knowledge. The KLs found12 often had a strong desire for formal knowledge or a ‘will to know’, apparent throughout their personal biographies and over time. They might complete PhDs (Doctors of Philosophy degrees) in a related area or write and publish articles and books. These ‘KLs’ were not merely facilitators and translators of management knowledge, but rather personally deeply immersed in – and committed to – producing and diffusing such knowledge.
A third theoretical perspective explored in our protocol was that of ‘absorptive capacity’ (ABCA) drawn from the resource-based view of the firm in strategic management. The resource-based view sees the firm as a bundle of tangible and also intangible assets where a key intangible asset is the (variable) corporate ability to develop and exploit its fundamental knowledge base. 15 High ABCA may partly depend on well-positioned individuals who ‘stand at the interface of either the firm and the external environment or at the interface between subunits within the firm’16 as boundary spanners. In reading ABCA articles, we will explore how they conceive of agency.
Knowledge networks in health care and related settings were a fourth and final area of academic literature in our protocol. Within network-based organising, less formal, more interactive and interpersonal forms of communication and knowledge exchange across traditional boundaries assume greater prominence.
A generic management literature suggests that social and informal networks17 help staff to acquire and process knowledge in and across organisations. A recent study examined knowledge flows empirically in eight NHS managed networks5 (e.g. Managed Cancer Networks). The ASHNs are another example of the managed network form.
Strong interpersonal networks can potentially spread information and knowledge and build high ‘social capital’. Yet very dense networks also create closed cliques that stifle innovation, so one argument is that a network with more ‘weak ties’ may be more functional than one with fewer strong ones. 18 So, we shall be interested to map different networks in the AHSNs, to explore variation (how open/closed they are and how they evolve over time) and to explore any influence on innovation processes. We also noted that academic literature on knowledge flows in biotechnology clusters19 will be important.
Research aims and research questions
Following our early review of policy and academic literatures, our overall aims were defined in the initial protocol as follows:
-
to shed light on the dynamics of knowledge circulation, sharing and exchange that take place within and around newly formed AHSNs
-
to deepen understanding of the role of VSMs in triggering and instigating the knowledge mobilisation activities that are the core of the remit of the AHSNs
-
to explore how and why certain VSMs develop a strong engagement with knowledge exchange events and mobilisation strategies and how they have become ‘KLs’ within the research utilisation network instituted by the AHSN.
The specific research questions (RQs) are:
-
What role does ‘knowledge networking’ play both formally (in national and regional AHSN knowledge exchange fora) and informally (i.e. in VSMs’ professional and local networks) within knowledge mobilisation strategies and practices in AHSNs?
-
How is the ‘knowledge’ (in particular about knowledge mobilisation strategies and practices) discussed at these fora diffused by a group of engaged VSMs in their AHSNs?
-
Is there a subgroup of VSMs emerging who are highly engaged with such knowledge mobilisation events and who appear to act as KLs in their AHSNs?
-
If so, what explains such knowledge leadership behaviours?
We will report the results of the study by the various work packages (WPs) outlined in our protocol [note that there were some unavoidable amendments, as noted in our methods (see Chapter 2)]. Chapter 3 is the literature review, and this is followed by the findings from our policy-level interviews and texts presented in Chapter 4. In Chapters 5 and 6, we introduce the regional case studies and use social network analysis (SNA) to investigate the national and regional ‘knowledge networking’ supporting AHSNs at their early stage of development. Here, we highlight the role played by AHSN boards but also by other key actors as knowledge ‘brokers’. To build on this work, Chapter 7 explores the diffusion of this knowledge by AHSN senior managers, teams and stakeholders, and illustrates the models of knowledge mobilisation and innovation spread in action through an analysis of our ‘innovation tracers’. Finally, Chapter 8 sheds light on the role and activities of KLs.
Having outlined the policy, organisational and academic contexts of the study, we move on to specify further our research design in Chapter 2.
Chapter 2 Study design and research methodology
Introduction and overview
Overall, the study uses a mixed-methods design to study the early development of AHSNs, including an analysis of the wider health-care policy landscape, a SNA of knowledge networks, comparative case studies of the evolution of five AHSNs, including 10 ‘micro tracers’, and an examination of leadership dynamics. We used four types of research methods:
-
qualitative semi-structured interviews and case studies
-
SNA and accompanying surveys
-
observations of national and regional meetings and events
-
analysis of secondary documents (i.e. policy papers, AHSN official publications and website materials, board minutes and grey literature).
The project aim was to assess the early development of AHSNs and their specific knowledge exchange efforts; in addition, we aimed, to explore senior managers’ knowledge leadership strategies, specifically in relation to knowledge mobilisation. We tracked developments within five AHSNs, tracing their espoused knowledge mobilisation strategies and practices in use to meet health improvement and wealth creation policy objectives. Below, we provide an overview of our WPs, followed by a more detailed discussion of the methods used. A few approved adaptations from the original protocol are also described and the rationale for these is explained.
Research ethics and NHS governance
In advance of the study start date, we contacted the NHS Research Ethics Service (now located in the Health Research Authority) to establish whether or not NHS Research Ethics approval was required. An e-mail from the National Research Ethics Service (August 2013) confirmed that our study was not defined as ‘research’ for NHS purposes and that NHS Research Ethics Committee (REC) review would not be necessary because our study involved staff only and would not access patients or patient-sensitive data.
Our host university still required ethics review. We therefore submitted our research plans and early data collection materials to the King’s College London (KCL) REC, which granted full approval in November 2013 [reference REP(EM)/13/14-12]. Ethics permission from KCL was later extended to reflect a short (6-week) extension granted by the National Institute for Health Research (NIHR). Furthermore, as we progressed with the study and developed new materials (e.g. the SNA survey and interview protocols), we submitted these texts as ‘modifications’ to the KCL REC as supplementary documents, which were also granted approval.
Although the study was deemed to be low risk for NHS purposes, owing to the nature of the study (exploring networks with a wide geographic reach), we needed NHS governance permission across many NHS sites that we might visit to undertake face-to-face interviews. However, AHSNs invariably cut across large areas, with typically 10–30 NHS trusts and 5–25 Clinical Commissioning Groups (CCGs) per region, depending on local arrangements. To manage this complexity, we sought guidance from KCL’s local Research and Development (R&D) Governance Team located at Guy’s and St Thomas’s Foundation Trust (FT)/KCL Biomedical Research Centre (BRC). With support from this team, we applied for our study to be added to the NIHR Clinical Research Network (CRN) portfolio and completed relevant forms via the Integrated Research Application System. Site-specific access was granted, along with appropriate research passports for the researchers visiting NHS trusts when these were required locally. Only a very small number of NHS trusts did not provide governance permission and we were careful to avoid visiting these sites.
We had to deal with multiple NHS trust R&D offices and submit study accruals centrally, yet these were also sometimes requested by individual sites. In this way governance was highly complex in a network-based study of this kind and we often encountered duplication of processes (e.g. recruitment reporting). The Health Research Authority may now have simplified the NHS governance process for more recent similar studies; certainly we would welcome streamlined NHS permission systems, especially for low-risk studies involving staff and service evaluations.
We are especially grateful to the research and governance team based at Guy’s and St Thomas’s FT, who advised us throughout the course of this study.
Scoping work, site selection and policy analysis (work package 1, leading to work package 5)
First of all, we accessed the original prospecti from all 15 AHSNs, securing an initial overview of network objectives and their remit. Following our protocol, our sampling strategy was to ensure variation in our sample of five AHSNS, both geographically (rural/urban and north, midlands and south) and according to whether or not they had an AHSC at the time of licensing. We also wanted to include some regions with a well-developed health/biosciences capacity, given the strong policy and academic interest in regional innovation systems. In addition, there was a pragmatic consideration of which AHSNs would provide access for our 30-month study.
With our partner at Universities UK (UUK) and our Study Steering Committee (SSC) members, we discussed as a team which sites to approach. We were aware that AHSNs were being established in different ways post licensing: some were hosted by NHS trusts, others as companies limited by guarantee. We successfully achieved a balanced sample of five AHSNs following our selection rules, including a spread of AHSNs with different regional economies and hosting arrangements.
Policy interviews and documentary analysis (time points 1 and 2)
We first undertook desk research and reviewed relevant UK health, life sciences and economic policy documents (2003–15), including, but going well beyond, the core Innovation, Health and Wealth (IHW)1 text to trace the longer-term and broader policy trajectory.
Having undertaken this desk research and a literature review (see Chapter 3), we had identified several interesting papers on knowledge mobilisation, leadership and the triple helix model of knowledge production. However, we were also aware of the newness of AHSNs and some important knowledge gaps in the literature on issues such as knowledge leadership in the health sector. We therefore devised our time point 1 (T1) semi-structured policy interview schedule (see Appendix 1) to help us understand, in greater detail, the wider context of our study and policy background, including perspectives on barriers to public sector innovation. For example, we asked respondents to share their views on the perceived opportunities for AHSNs nationally and the leadership skills required for this kind of networked endeavour.
Through discussions with our policy partner (UUK) and reading of policy documents, we identified eight key individuals who had fed into central policy and AHSN development and/or with expertise in the NHS innovation landscape. We successfully recruited eight policy informants early in the study, who helped us to understand in detail the origins of IHW1 and the policy context. We later located additional life sciences, health policy and other government texts to help understand the longer-term evolution of this policy stream, and one of the team members constructed a chronological review highlighting the major developments over time, used as a reference point throughout the study (see Appendix 2). We found publications and strategic reviews going beyond the NHS and DH to include texts from the Her Majesty’s Treasury and Department for Business, Innovation and Skills (BIS), such as those analysing life sciences strategy or university–industry collaboration.
We returned to this WP towards the end of the study following our protocol and given our ambition to capture the development of AHSNs over time. We undertook further semi-structured policy interviews at time point 2 (T2), speaking with eight more respondents (four of whom contributed to a group discussion in the same policy-focused organisation). These later interviews (in 2016) focused on themes from our empirical analysis of prior material and were designed to ensure that the information captured was up to date (see Appendix 3). For example, questions picked up on newer policy developments in the health/life sciences field, such as the accelerated access review (AAR), and the longer-term impact of financial conditions on the health sector and process of NHS innovation adoption (a theme picked up during other qualitative interviews during the study). We also asked about AHSNs’ perceived effectiveness since their inception, thoughts about IHW1 5 years on and comments on recent regional developments in the health and life sciences sectors (e.g. devolution to Manchester; the emergence of MedCity in London).
Interviews lasted 45 minutes to 1 hour and were digitally recorded and professionally transcribed with informed consent (as with all of the interviews conducted during the study). Policy participants responded in an independent (rather than organisational) capacity and comments are not attributed. The transcripts were analysed by two researchers against a number of specified thematic areas, as outlined further below and in Chapter 5.
So, in all, we conducted discussions with 16 individuals. In these interviews we explored perceptions of regional variations that could affect the careers of AHSNs and extent to which knowledge mobilisation strategies were seen as emerging at AHSN level. We were especially interested in exploring the broadening of the NHS innovation landscape to include the stimulating of economic growth and how the rising growth agenda brought together the health and life sciences sectors and other important actors, such as universities, small and medium enterprises (SMEs) and large firms. Policy interviewees across both time points offered an overview from different perspectives – government, business/industry, academic and NHS policy.
For data analysis, we organised and then analysed T1 policy interview transcripts around the following thematic headings: (1) respondents’ perceptions of this health and economic policy stream; (2) reflections on challenges in innovation within the NHS; (3) recommendations on topics/authors to cover further (a section not reviewed here for reasons of space); (4) early thoughts about the nature of and regional contexts facing AHSNs, their opportunities and major challenge; and (5) preferred AHSN leadership styles, and reflections on their innovation and knowledge mobilisation models and approaches. For the T2 analysis, we cross-referenced the more recent empirical data against our earlier policy data analysis (T1) and data derived from the five AHSN case studies, creating newer themes such as on national and regional trends (e.g. central policy aimed at devolution in England).
In addition, access was granted to the ‘AHSN Network’, a national forum for all 15 managing directors (MDs)/CEOs hosted by ZPB Associates. Three meetings were attended by one researcher, plus one national Commercial Directors’ Forum. Informal discussions also took place around these meetings with persons from other AHSNs, which helped us to understand AHSN metric development and wealth creation strategies more broadly. Another researcher attended NHS Expo in 2015. These various sources informed our analysis throughout this report.
Literature review (work package 2)
The team originally proposed a literature review methodology based on the Chartered Association of Business Schools list of business management top ranked journals. We were encouraged by NIHR expert reviewers to amend this approach to a wider and ‘evidence-informed’ form of review. We then devised an alternative, more thematically focused, review methodology to identify high-quality and/or relevant papers from various disciplinary sources and to capture ‘grey literature’, such as commentary pieces about UK health policy.
A four-phase structured review method was devised. This approach was driven by our RQs and was intended to allow adequate coverage across a range of disciplines including inter alia, management, health care, business and political science. A consequence of broadening the search parameters – and steering away from the Chartered Association of Business Schools ranked journals – was that this WP expanded vastly, given the complexity of searching a dispersed literature base that also included journals of varying quality (see our later discussion of study limitations). We found – as have other health researchers20 – that it is most challenging to synthesise such social science, policy and health-care literatures without investing very significant resources, expertise and time. In the ABCA field, for example, there are a few very well-cited and enduring articles by key authors (e.g. Cohen and Levinthal;16 Zahra and George15) that are foundational texts. Where these articles take the form of theory development or a critical synthesis, the conventional health services research (HSR) notion of making a judgement about ‘high-quality evidence’ becomes problematic.
Phase 1: keyword terms and expert input
Working with an expert librarian, we first identified key terms from the conceptual framework outlined in the study protocol. To ensure validity, we e-mailed a provisional list of our search terms to nine academic experts, who contributed some further suggestions. The team next developed succinct Boolean word strings from this list (see Appendices 4 and 5).
Phase 2: data extraction and targeted search
An experimental search to test our keywords was then conducted, yielding > 4000 papers. This finding demonstrated that, because our themes were very broad in scope (e.g. leadership), the final search strategy should be broken down into manageable component parts. Our final data extraction strategy therefore developed iteratively, building on trial searches on major databases and discussions between two researchers and the librarian. We eventually decided to hone in on three theoretical angles to make the review more manageable:
-
networks and networking practices of top managers in knowledge-intensive settings/networked organisations and, more specifically, the potential agency of leaders (i.e. as brokers, KLs, or persons having ABCA or, conversely, displaying the ‘dark side’ of networks)
-
empirical studies not focusing on the role of individual leaders (agency), but providing macro- or middle-level insights about networks and collaborations, especially in the public sector, heath care or related knowledge-intensive settings (e.g. biotechnology, pharmaceutical)
-
academic and grey literature on knowledge mobilisation policy, including CLAHRCs, AHSCs and other NHS institutional architecture, plus academic health science systems abroad.
This final, three-pronged search strategy (what we refer to as ‘6a’, ‘6b’ and ‘6c’) was executed across four databases in the period January–February 2014:
-
ABI/INFORM®
-
ProQuest [including Applied Social Sciences Index and Abstracts, EconLit (American Economic Association’s electronic bibliography), International Bibliography of the Social Sciences, Worldwide Political Science Abstracts]
-
OvidSP [including MEDLINE, EMBASE, Health Management Information Consortium (HMIC) and Social Policy and Practice]
-
Web of Science.
Additional searches were also run on Google Scholar (Google Inc., Mountain View, CA, USA), Social Policy & Practice, HMIC and The King’s Fund database (reviewed for grey/policy literature). A separate yet interconnected hand-search of policy documents on life science and NHS innovation policy was undertaken to inform our policy analysis (repeated at different time intervals to keep knowledge up to date).
The results of the final search were limited to papers published in scholarly journals, conference proceedings, books and texts published in English from 1995 to 2014. All results (abstracts) were saved to EndNote X7 for Windows (Thomson Reuters, CA, USA) and duplicate entries were removed. Our review again captured > 4000 initial papers and required substantial reduction. We then developed inclusion and exclusion criteria to screen abstracts and remove irrelevant papers, of which there were many (see Appendices 6–9 for further details).
Phase 3: abstract selection and critical appraisal
An appraisal of a reduced number of abstracts was then conducted by paired researchers to build consensus about important conceptual and thematic areas and to provide some inter-rater reliability.
The detailed frameworks for selecting abstracts are provided in Appendices 7 and 8, but in Box 1 we outline the general guiding principles:
Applied SNA.
Formal and informal leadership within mandated networks.
Formal leaders’ personal networks (e.g. CEOs).
Leadership within informal networks (e.g. communities of practice, clusters).
Relevant high technology industries and regional clustering (e.g. science parks).
Knowledge spill-overs and university–industry knowledge transfer.
Triple helix of industry/university/government relations.
Collaborative knowledge production and strategies in health care.
NHS innovation (and barriers).
ABCA.
Open innovation.
Thematic exclusionsClinical/medical education/pedagogy.
Clinical decision-making.
Highly specialist clinical research (e.g. pharmacogenetics).
Local government programmes without a health/life sciences focus.
Health-care evaluations lacking a network/knowledge exchange focus.
Supply chain management and highly specialist management studies.
R&D networks lacking a health focus.
Industrial districts/clusters/regional innovation systems in less relevant industries and sector (e.g. food science, petrochemicals, banking and financial, automobiles).
Triple helix applied to developing economies without a high-level theoretical contribution.
Having gone through the relevance criteria above, we exported a manageable number of electronic abstracts to a Microsoft Excel® database (Microsoft Corporation, Redmond, WA, USA) to sift for quality. At this point we accessed full papers and organised references across nine key thematic areas (see Appendix 9). We then applied a scoring system to rate full papers (working in pairs), taking into account journal impact factor (1 year), methods, theory, interest/novelty and relevance (a 0–3 scale was applied across these dimensions, with 3 being high). Appling these indicative quality metrics helped to identify superior papers (around 4 to 15 papers, depending on the theme), which were generally those strong on theoretical explanation and empirical data presentation and relevant to our RQs. We were aware that certain journals (e.g. The Lancet) have high impact scores that can skew metricised results, and, therefore, also noted Google citation scores and ensured that relevance was retained as a key criterion for selecting papers.
We finally discussed relevant papers as a wider team, as well as how to organise the literature review write-up. A group of highly rated papers (n = 105) was selected for the report and these papers were clustered into the thematic areas already identified. We finally recorded some methodological reflections from this WP.
Phase 4: literature review and final write up
An original, descriptive draft of the literature review stood at nearly 30,000 words. For greater brevity, we moved to select > 60 full papers, with the researchers most involved in case writing choosing ‘higher priority’ articles they saw as having most relevance to the empirical analysis of the cases. This interactive selection process helped link underpinning theory and the empirical case material. These selected articles are discussed in this report, and the remaining 40 or so ‘lower priority’ articles were summarised in radically shortened form. As such, all the articles fully discussed have survived two tests of review: first, academic quality and, second, relevance to our cases. The length of the literature review has been radically reduced and in the latest revision has moved away from discussing individual papers to exploring overall key themes.
Reflections, limitations and conclusions
Some methodological observations on this work package
We made several observations during the data extraction phase. First, our evolving searches revealed that few papers connected major theoretical concepts – such as the ‘triple helix’, or ‘ABCA’ – with a specifically leadership/agency or ego-network focus, a point we discuss in more depth in our findings. Second, given the newness of AHSNs in 2013 (when our study commenced), there was a lack of literature available on this dimension of UK knowledge mobilisation policy (i.e. mandated networks for health innovation as opposed to research translation). This necessitated a review of emerging work on academic science-based organisational forms and policy, for example, searches on The King’s Fund database and a review of material on CLAHRCs and AHSCs as comparable topics. Third, our expert librarian indicated that it was extremely difficult to retrieve ‘a near perfect set of relevant references’ even with complex keyword/Boolean combinations; therefore, multiple databases needed to be searched with some flexibility – including a separate search run on Google Scholar – because databases have strengths and weaknesses and use different algorithms. We observe that a single ‘jackpot’ search strategy is unlikely to prove successful when dealing with a broad social science knowledge base and a spectrum of search variables, or when attempting to integrate social science and health-care databases. Our searches identified a large number of irrelevant results (ranging from 3000 to 4000+ abstracts), indicating the diversity of published material that is returned on extensive social science topics such as networks, innovation and leadership, even if Boolean search strings are applied systematically. Our solution to this issue was to break down our search strategy into thematic areas based on the questions in our study protocol and to conduct parallel searches using carefully constructed search strings. This made the review more manageable.
Indeed, a problem of systemic reviews is that important theoretical papers can be missed as a result of the search delimiters applied (e.g. date ranges). This was especially the case for the ‘6a’ search on leadership, networks and agency. We found Google Scholar useful for applying narrower search terms and less complex Boolean strings, here picking up on grey literature as well as highly cited journal articles.
We reflect that this literature review module was much more time-consuming than originally anticipated and the results were not easy to interpret. We adopted a protocol-driven review methodology at the outset to achieve inclusivity, breadth and depth. This is an approach stemming from a medical tradition but which fits less well within diffuse social science based fields, which we needed to draw on. With the benefit of hindsight, we would adopt a looser and more narrative approach moving from early exploratory readings and snowballing out from highly relevant, well-cited studies, with the flexibility to include newer articles and classic theoretical papers in a more inductive manner.
We conclude that pragmatic, narrative or ‘realist’ approaches may be suitable for such interdisciplinary literature reviews, rather than conventional systematic or highly structured methods. The various literatures that we identified varied markedly in terms of their empirical focus, methods and theoretical framing so they were difficult to ‘synthesise’. Our findings echo Greenhalgh and Peacock’s20 observations in their literature review of the diffusion of innovations in health-care organisations. We note that our review did not surface many relevant economic or service evaluations of specific health innovations and their impact as this angle was not part of our original brief.
During the course of our research we did identify a number of published internal AHSN reports providing evidence of the effectiveness of a number of innovations we studied (see Chapter 7). For reasons of anonymity we do not cite these papers in this report, but we observe that further research in this area may wish to incorporate a review of such available outputs where the innovations to be explored are known in advance or can be disclosed.
Social network analysis (work packages 3 and 4)
What is social network analysis and how can it be applied to our research questions?
Social network analysis is a theoretical perspective and methodology for mapping and understanding the relationships and structures of networks. 21 When studying such networks, we may be interested in ‘social capital’, or the personal network of contacts or resources individuals have access to,22 or, at a higher level, the relationships, partnerships and collaborations that create networked organisational systems. The method is well suited to analysing newly formed, complex or dynamic systems, such as AHSNs and associated regional innovation systems.
Technically, for analytical purposes, a ‘social network’ is seen as a set of ‘nodes’ connected by a set of ‘ties’. These nodes and ties can be represented visually in the form of network graphs or so-called sociograms. Nodes can be actors such as individuals, groups or organisations and are represented visually as points in a network graph. Ties are the connecting links or relations, describing the means through which nodes are interconnected, and are represented as lines in a network graph.
We applied SNA techniques to investigate AHSN knowledge mobilisation activity to support our research aim of tracking knowledge exchange circulations around newly formed AHSNs and to answer our first RQ: what role does ‘knowledge networking’ play in supporting the knowledge mobilisation strategies and practices of AHSNs? Specifically, in this report, SNA as a method is used to:
-
track the national and regional knowledge circulations emerging around AHSNs and generate comparative regional cases with accompanying metrics
-
study knowledge networking that supports wealth and health knowledge circulations, including the role of AHSN leadership in triggering these activities
-
identify a cohort of ‘knowledge brokers’ (individuals who are important for information sharing and the cross-fertilisation of knowledge because they connect otherwise disconnected parties) and ‘KLs’ – individuals who are perceived as highly knowledgeable about health-care innovation and who are effective at mobilising knowledge across geographic and sectoral boundaries.
Mapping knowledge mobilisation networks
We ran a large-scale SNA survey at two time periods to map knowledge circulations supporting population health improvement and wealth creation in the participating AHSNs. Two social network mapping surveys were run: the first (T1, April–November 2014) was launched towards the end of the AHSNs’ first year of licensing and ran for several months; the second was initiated a year later and was live for 1 month (T2, October–November 2015). The survey questions were developed in consultation with our SSC. The questionnaire was then piloted online and assessed through cognitive interviews with AHSN leadership teams and AHSN stakeholders in April 2014. Both surveys were web-hosted and AHSN communications teams provided help with their promotion through their newsletters and social media channels.
These data captured knowledge networks mobilised to support innovation since the AHSNs had been established and during their early life cycle. The T1 data focused on new innovative knowledge circulations ‘in the last 6 months’ (i.e. during the AHSNs’ early set up stage) that supported health improvement and wealth creation. The T2 data focused on connections made through AHSNs ‘in the last 12 months’ that had provided actionable knowledge to support wealth creation. For both surveys, we drew on the IHW definition of ‘innovation’, as per Table 1.
| Survey questions based on IHW definition of ‘innovation’ | ||||
|---|---|---|---|---|
| Innovation: health | ||||
| New ideas or research | New ideas or research for improving health | New products or services for improving health | Products or services | New application of existing idea, service or product |
| New ideas or research for creating wealth | New products or services for creating wealth | |||
| Innovation: wealth | ||||
The social network surveys featured a range of questions that allowed us to elicit a ‘network’ of individuals linked as knowledge sharing contacts. We asked further questions about the nature of the knowledge being mobilised through these networks and were subsequently able to investigate:
-
knowledge networks to support health improvement (Health-Net)
-
knowledge networks to support wealth creation (Wealth-Net)
-
‘strong tie’ networks of contacts who regularly exchanged knowledge and had known one another for 10 years or more (Old ties-Net)
-
knowledge networks leading to implementation (Implem-NET)
-
knowledge networks providing access to contacts (Broker-Net)
-
knowledge networks based on new ideas (Ideas-Net)
-
knowledge networks providing political influence or leverage (Power-Net)
-
knowledge networks providing trustworthy advice, guidance or information (Trust-Net).
Sampling strategy: identifying individuals as key knowledge contacts supporting health-care innovation
Traditionally, social network studies begin with a roster of names and researchers seek to plot connections between listed actors (‘nodes’) depending on the relation (or ‘ties’) of interest – in this case, the knowledge exchange. We immediately faced a challenge because knowledge circulations around AHSNs did not have a clear boundary, that is, they were cross-sector, cross-industry or cross-geography (regional, national and international) and encompassed a wide variety of individuals with different sets of expertise. Moreover, the key individuals active in these knowledge networks were largely unknown at the start of our research so it was not possible to assemble a roster of names.
Given the unknown parameters of AHSN knowledge-sharing networks and to avoid recruiting a list of ‘usual suspects’, we chose to design a survey tool that would evolve through a peer-driven sampling mechanism. We borrowed from network sampling methods used to uncover ‘linked’ individuals in hidden populations or where there are no clear sampling boundaries (i.e. respondent-driven or snowball sampling techniques commonly used, for example, in epidemiology and studies of drug users). 23–25 These sampling methods identify and recruit to the study a set of ‘seed’ individuals fitting the research parameters, who are asked to nominate other relevant individuals who are then recruited in turn. (See additional note on SNA design in Appendix 10.)
In this spirit, and to ensure that our sample was relevant to AHSNs, we began by inviting four VSMs in each of our five AHSN sites to complete the T1 social network survey (this same cohort also took part in the first wave of qualitative interviews). The survey included questions about the respondent and asked them to name up to five key contacts who had ‘over the past 6 months’ been ‘most active in circulating innovative knowledge’ defined as ‘to support new ideas or perspectives, new research, products or services for health improvement or wealth creation’.
We then invited to the survey the people nominated as key knowledge contacts by AHSN leaders. The survey was rolled out over a series of waves and halted at either a maximum of four waves or when sufficient saturation was reached (that is, when people were starting to be renamed and the structure of networking began to close in). Each wave of survey participants therefore consisted of the contacts named in the prior round. Importantly, this meant that the sample of individuals we derived for the knowledge sharing networks would be created via peer nominations and not constructed by our research team.
Social network data are usually collected in a systematised way; this is most often achieved using surveys, but it also takes place through structured interviews, whereby respondents are asked questions about their personal attributes, their contacts and the attributes of their contacts. Using a variety of survey questions, we elicited the names, job titles and employing organisation, industry, sector and professional expertise of a sample of individuals perceived by their peers as being important for knowledge circulation to support AHSNs. We also asked about the type of knowledge exchanged (and, for the T2 survey, included an additional question about if/how knowledge was implemented). We developed these survey questions and accompanying response categories with our SSC and through piloting with AHSNs and stakeholders. (See the SNA survey in Appendices 11 and 12.)
The final sample included AHSN leadership and core teams as well as wider stakeholders [general practitioners (GPs) and CCGs, academics, SMEs, bloggers, NHS trusts, local authorities, large corporations and government departments].
Response rates
The SNA survey yielded data on a total of 1016 individuals perceived as being key to knowledge mobilisation supporting health-care innovation linked to AHSNs (T1, n = 818; T2, n = 198).
At T1, we used a non-probability sampling technique based on peer referrals over several waves. The population was ‘hidden’ in the sense that we did not know (before the study) who were the key knowledge mobilisers supporting AHSN activity. The SNA helped us to identify these individuals and to map the structure of knowledge networking at national and regional levels. Response rates become difficult because we did not know the total size of the population and respondents were not selected from a sampling frame. Furthermore, we did not seek to recruit all nominated contacts (i.e. at the final wave we had to cease recruitment and, therefore, draw an artificial boundary). Our intention was thus to capture a subset of the knowledge circulations around AHSNs.
Given that we had a ready sample of names, we invited to the T2 survey everyone who participated and/or was nominated at T1 (resulting in a 24.2% response rate). The numbers for T2 were perhaps lower mainly because of attrition (bounced e-mails/turnover of roles) or respondent fatigue, but also because the survey was live for a much shorter time and we did not roll over subsequent waves (because the sample size was large to begin with). See Table 2 for more details.
| Time point | Respondents (n) |
|---|---|
| T1 | 818 |
| T2 | 198 |
| Total | 1016 |
Triangulation of data
From the SNA we derived a list of individuals perceived by their peers to be important to AHSN knowledge mobilisation. We conducted qualitative interviews with a subset of these individuals, in addition to the initial cohort of AHSN leaders who took part in the SNA and qualitative interviews. To help us to identify interviewees, we visualised the knowledge mobilisation networks for each AHSN region (see Chapters 5 and 6). This enabled us to see where individuals were located vis-à-vis each other in terms of their social networks (i.e. some individuals were positioned close to or distant from the AHSN and thus operated in distinct knowledge clusters, some were part of overlapping cliques, some were more peripheral). These relative social network positions were assessed to aid our selection, alongside a spreadsheet listing each person’s employing organisation, organisational role and sector.
For each AHSN region, we selected for interview individuals occupying different social positions and a range of organisational roles (see below for further detail).
Consulting the SNA visual and considering attribute data in tandem thus allowed us to select a diverse sample of interesting interviewees, including regional actors in senior and operational roles in the NHS, but also in academia, large firms and SMEs [see Time point 1 interviews with Academic Health Science Network senior managers and teams (work package 3) and Regional interviews with ‘knowledge contacts’ and stakeholders (work package 3)] and also most prominent national ‘KLs’ who were mobilising knowledge across regions (see Time point 2 interviews and ‘knowledge leaders’). We cross-checked the validity of the SNA survey nominations during our qualitative interviews by providing further opportunity to name other important knowledge mobilisers (see Appendices 13 and 14). Interim SNA results were also presented to AHSN boards and other stakeholders to ascertain whether or not findings resonated and we received a positive response to this feedback.
Social network analysis
The network data were analysed in UCINET (Analytic Technologies, Harvard, MA, USA)26 and Microsoft Excel. In this report, our analysis investigates the structure and composition of knowledge networks for each AHSN region, compares knowledge networking for health improvement with knowledge networking for wealth creation and identifies key players (such as central actors, and within- and cross-region brokers).
The main data set produced was a network of who exchanges knowledge with whom, the type of knowledge exchanged and attributes of knowledge contacts forming the network. We extracted several subnetworks from these data, for example to compare the structure and composition of AHSN region knowledge mobilisation networks and to investigate the relationship between different facets of these networks (trust, implementation, old contacts, etc.). (See the list of subnetworks in Appendix 10 and Chapter 6 for an exploration of results.)
The survey data required a large amount of cleaning before analysis. Notwithstanding the input errors and duplicate records, it was also necessary in many cases to match up and merge attribute data for consistency. For example, if a person is a survey respondent and also nominated as a knowledge contact, we would have two records for this person: one from the survey response and the second from his or her referrer. In these instances, we would keep the attribute data selected by the person themselves (i.e. their self-categorisation as a very senior leader, middle/clinical manager or non-manager) and their self-identification of professional expertise category. This was important only for the attribute data file and not for the relations data file (which need not be consistently matched between alters, i.e. person A can name person B as a knowledge contact but person B need not reciprocate).
Limitations
There are various limitations associated with SNA studies of this type. 27,28 We outline these below.
The very essence of SNA is based on exploring interdependency in linked samples; a network can be a network only if the nodes are connected, and social networks do not form randomly. There are inherent selection biases in the way people nominate contacts (i.e. choosing similar people/best friends, what can be referred to more technically as homophily, or overstating the status of contacts). 29 These are natural characteristics of the data itself and provide the network with shape and structure – the very things we are interested in capturing for our comparative analysis. Attempts were made to limit some kinds of selection biases, for example by not placing delimiters on nominations by sector, geography or hierarchy and allowing the sample to evolve through peer responses.
The data we collected represent only a subset of AHSN knowledge. There will, of course, have been many more knowledge exchanges, and it was impossible to capture all such activity, and so we do not intend the case networks to be generalisable. 28 Two subpoints become pertinent here: (1) our network sampling method yielded a convenience sample specific to the UK context and (2) the SNA data also provide temporal snapshots rather than dynamic images or understanding of process (we instead capture this through our qualitative elements).
We highlight that the AHSNs had different set-up stages, which affected the timing of our fieldwork, and these staggered starting points meant that the time taken to collect data varied between regions. Moreover, because we could not specify from the onset who would be invited to the survey, significant time was spent obtaining NHS governance permission to cover every NHS site in our five AHSN regions, plus additional NHS trusts and CCGs where the networks spanned across geographies. However, we believe that the data set SNA provides a good baseline that maps early knowledge mobilisation networks around the AHSNs and that will be useful for longitudinal and comparative research in the future.
It is also important to note that many standard inferential statistics do not apply because social network data violate case independency criteria as respondents are not sampled independently from their population (because they are linked samples). Instead, the metrics used in this report are based on permutation approaches, applied to calculate sampling distributions directly from observed networks using random assignment/matrix manipulation across thousands of trials under the assumption that null hypotheses are true (in other words, to calculate the likelihood that the observed network would have occurred by chance). We therefore avoid using these data to make predictions and focus instead on the different type of networking structures that emerged between AHSN regions and the differences between networks used to support health and wealth and to identify a cohort of key actors/KLs.
Qualitative data collection and analysis (work packages 3–5)
Time point 1 interviews with Academic Health Science Network senior managers and teams (work package 3)
The quantitative SNA WP was complemented by qualitative and case study-based work. This additional module was deemed necessary owing to the complexity of knowledge mobilisation (which occurs at multiple levels) in practice and so there was a need to capture the ‘doing’ of AHSN knowledge work as it happens, from understanding the early stages of setting up the networks, through to investigating the role of social networking and leadership in relation to innovation spread. Over the course of the study, we conducted a total of 135 qualitative interviews over various WPs. Below we provide more details.
First, we sampled four members from each of the AHSN senior leadership teams (in our protocol, termed VSMs following the term used in some earlier literature, although on the advice of our SSC we later dropped this term). Our sampling strategy at this stage was as follows: MD/CEO level, chairperson, commercial director and other senior figures (e.g. deputies or chief operating officer). These interviews were guided by broad themes coming from the literature review and our original study protocol. They lasted approximately 60 minutes, and were recorded and transcribed. In these interviews (n = 20), we specifically wanted to understand the processes and persons involved in the early establishment of the particular AHSN, any priorities for action and formal strategies devised since the AHSN had been established, and the nature of local interactions to support innovation spread within the NHS and wider regional health economy. Questions included asking senior leaders if there were any objectives that they personally wanted to see the AHSN achieve, and how they would describe the local health innovation system currently. (Please see Appendix 13 for the full protocol questions.)
With successful access to five AHSNs achieved, supplementary informal meetings with AHSN senior teams took place. These meetings confirmed access to the sites and two members of the research team were then designated as leads for each AHSN. The team undertook the collection of key AHSN-level documents (business plans, protocols, reports) and secured invitations to attend some local events and meetings to help understand the work of the AHSNs more broadly (e.g. innovation launches, joint meetings with other health or education groups). Observations and early meetings such as these were especially helpful for identifying ‘innovation tracers’ to follow during the study (see Chapter 7).
Regional interviews with ‘knowledge contacts’ and stakeholders (work package 3)
Further interviews were then undertaken with ‘knowledge contacts’ named in the SNA (see above) and triangulated with early VSM interview data. We first consulted SNA visuals to identify regional actors beyond AHSN core team members to include a wider set of AHSN stakeholders (e.g. industry and academia). Our sampling then moved beyond the SNA to pick up contacts mentioned during early qualitative interviews (e.g. important ‘go to’ persons for innovation, or those performing key roles within AHSN teams). We located persons, for example, involved in delivering AHSN projects and/or contributing to regional AHSN strategy (e.g. board members and AHSN programme managers/leads). Finally, we undertook some purposive sampling to ensure adequate representation from agencies that emerged as significant, such as heads of local enterprise partnerships (LEPs) and hospital and higher education institution (HEI) commercialisation leads. We did, however, impose a limiting sampling criterion: that ‘knowledge contacts’ had to be located within the AHSN region being studied because our emphasis in this stream of work was on local knowledge mobilisation and networks. These interviews explored topics such as the respondent’s involvement with the local AHSN, knowledge mobilisation, AHSN-led initiatives, perceptions of knowledge leadership and networking strategies. (See Appendix 14 for the interview schedule.)
Time point 2 interviews and ‘knowledge leaders’
Towards the end of the study (late 2015 onwards; T2), we undertook a small number of follow-up interviews with AHSN MDs/CEOs where possible (see Appendix 15 for the interview protocol). Owing to high turnover in AHSN leadership, however, such ‘catch-up’ interviews were not always possible. We explored with those MDs we could access persistent network leadership challenges, learning points, recent developments and perceptions of the evolution of their AHSN. There was also a final tranche of interviews undertaken in early 2016. These later interviews were extremely useful in gathering more recent data on the spread of some specific innovations, which had been initially explored in earlier interviews. Given the very early development of AHSNs at that stage (2014), spread/knowledge mobilisation data were necessarily not well developed and they were better picked up at the end of the study, suggesting the strength of a longitudinal approach.
An initial protocol aim was to identify 25 individuals who stood as prominent ‘KLs’ in the AHSN landscape for interview. We moved to a more operational definition of the concept of ‘knowledge leadership’, which we understood to be persons nominated by peers (in the quantitative SNA data) in three or more different AHSN regions. These people could be seen as having national, as opposed to regional, profiles. Our earlier WPs had explored within-region knowledge contacts and knowledge mobilisation and exchange efforts, but here we wanted to understand who was perceived as influential in a wider innovation landscape and how they operated to achieve their pan-regional impact or presence.
To progress this strand of work, we returned to our literature review, which suggested some characteristics of KLs. We used the literature review to inform the design of our interview questions for KLs (see Appendix 16). During the previous qualitative interviews with regional knowledge contacts, we had also asked respondents to identify persons considered as ‘KLs’ (see Appendix 14), along with why. This gave us an early qualitative data set about knowledge leadership characteristics to supplement our literature review.
We then analysed the aggregate data set of SNA survey results to identify pan-regional KLs using two criteria. The first was in-degree centrality index, which is based on the number of times a person was nominated as a key contact by their peers; the second criterion was the number of geographic regions that an individual was named in alongside the betweenness centrality index.
Using these methods, we could identify a small number of individuals (n = 14) whose reputation and influence spanned three or more AHSNs. From this point, we refer to them as ‘national knowledge mobilisation beacons’ (or ‘national beacons’ for short) to differentiate them from people identified as important regional actors who were often admired for their skills but who did not cut across regional boundaries to the same extent. A lead researcher undertook in-depth face-to-face or telephone interviews with these ‘beacons’, which explored their biographies, motivations, influence mechanisms and personal strategies of knowledge mobilisation. We also collected more ‘micro’ information about their daily activities, skills and professional outlook to understand the roots of their successful knowledge leadership behaviours. These interviews with ‘beacons’ therefore fulfilled our research objective to probe into the biography and attitudes of proactive KLs, exploring how they might be engendering a more knowledge-oriented culture in and around AHSNs and within the health-care field more widely.
Nevertheless, we should add that this cohort was a difficult group to recruit, given their seniority and the huge demands on their time. We successfully recruited 9 out of a possible 14 (another respondent indicated their willingness to take part, but could not do so within the period of the study). We also identified fewer pan-regional KLs than predicted in our original protocol. 25
All these qualitative interviews were audio-recorded and transcribed verbatim. The transcripts were coded thematically and analysed using an inductive procedure, with the support of NVivo 10 software (QSR International, Warrington, UK).
In total, we conducted 135 interviews across these various WPs (also including the AHSN case study tracers). More detail is provided in Table 3.
| Interviews | AHSN 1 | AHSN 2 | AHSN 3 | AHSN 4 | AHSN 5 | Total |
|---|---|---|---|---|---|---|
| AHSN senior managers (T1, T2) | 4 | 4 | 4 | 5 | 6 | 23 |
| Knowledge contacts | 13 | 15 | 14 | 14 | 9 | 65 |
| Knowledge mobilisation tracers | 7 | 5 | 4 | 3 | 3 | 22 |
| Policy interviews (T1, T2) | 16 | 16 | ||||
| KLs | 9 | 9 | ||||
| Total completed | 135 | |||||
Case studies of five Academic Health Science Networks (work package 5)
The qualitative modules also included five comparative cases of AHSNs. The design of the case study module reflected basic principles of organisational process analysis,30–32 which is a well-known school within management research. Process scholars are interested in how organisations as a whole evolve over time and how they achieve (generally intermediate) organisation-wide outcomes such as varying performance levels. There is often an interest in exploring the organisational correlates of high performance. Organisations are also seen as embedded in their wider contexts, which creates conditions of path dependence.
Although process research is not sectorally specific, it has been widely applied in UK and also in international studies to investigate processes of change in health-care organisations. 33 One of the research team has used these process methods in previous large-scale NHS-based organisational studies. 5 This process approach encourages us to generate a holistic understanding of the AHSN as a whole, over time and seen as embedded in a regional context. ‘Stronger’ case study designs are here seen as those that are comparative and longitudinal in nature rather than a single case, and as relating well to theory and conceptualisation as well as local empirics. These basic principles underpinned our approach to case study work.
We generated a basic template to organise the material in the same manner across the five cases to facilitate comparisons; thematic recognition and pattern recognition (see Appendix 17). The researchers engaged in the case study write-ups met face to face to present and discuss drafts of cases to encourage debate, critique and then movement to a more shared understanding. Long initial descriptive case reports were prepared, which were then radically shortened and made more consistent to fit with tight length constraints here.
As well as writing these macro-level cases, we also undertook two ‘micro’ studies of specific tracers in each case to reveal concrete knowledge mobilisation activity in action (see Chapter 7 and Appendix 17 for a list of interview questions). The tracers enabled us to explore each AHSN’s strategic approach to promoting innovation spread at pace and scale as enacted at the local level and over time (and thus help us assess the extent of knowledge mobilisation achieved in practice). We note that the tracers were selected in consultation with the AHSNs so there may be some positive bias, in that they may have been perceived as areas where the AHSN would be likely to make good progress.
Dissemination and engagement (work package 6)
Reflecting our study protocol, the team also engaged in numerous engagement activities during the study, as follows.
Interim face-to-face feedback was provided to all five participating AHSNs during the summer of 2015 at board/executive level. The findings were well received and validated demerging empirical findings (post-T1 SNA). The feedback from AHSN leaders subsequently informed the T2 SNA design. Presentations and short summaries were provided to the five sites.
A well-attended end of study event took place (2 June 2016 at UUK and organised in conjunction with UUK; see below for more details). Delegates were invited from industry, academic and NHS communities, and also included our SSC members. Members of AHSN teams were also invited (across the 15 nationally), and some AHSN sites had direct input, with AHSN leaders speaking on panels.
The team were made aware of various reports and studies about AHSNs/IHW that emerged in the period 2014–16, such as an Institute for Public Policy Research report, ‘Unleashing innovation across the NHS’,34 and a later project by RAND Europe – University of Manchester35 that evaluated IHW implementation. Contact was made with the latter research team and arrangements were discussed for co-operation between the studies, which the Manchester team may hopefully be able to take forward as their study will end at a later date than ours. Conversations with a relevant HSDR project team were also conducted early in the study (Professor Alison Bullock at Cardiff University, HSDR 12/5002/04).
Two members of the research team gave a well-attended seminar at Imperial College Health Partners in late 2015 to communicate academic thinking to this important grouping. Two researchers (Jean Ledger and Daniela D’Andreta) presented at the Health Services Research Network conference in 2015. From this event, links were made with NHS Improving Quality (NHS IQ) and The Health Foundation (the latter held a SNA event). Daniela D’Andreta also attended NHS Expo 2015.
The team presented a short summary of their research to the 15 AHSN leads in their national meeting in May 2016. The team presented a draft version of the policy chapter at the Organisational Behaviour in Health Care Conference at the University of Cardiff in April 2016.
Study Steering Committee and patient and public involvement
We are grateful for a very active SSC that met three times during the course of the project and provided very helpful advice. It was chaired by Professor James Barlow of Imperial College London, an expert in health-care innovation. Our members included an AHSN MD, a NHS director of research and innovation, a management school professor and two patient/public representatives.
Our patient and public involvement (PPI) representatives were recruited through the University of Warwick’s University/User Teaching and Research Action Partnership (UNTRAP) group, which organises service user involvement on research projects. We found the involvement of patient representatives useful for providing insights about how new health interventions and developments might be geared more towards patient benefit. One of our representatives was aware of other relevant knowledge exchange initiatives (e.g. digitech) linked to their local university and brought with them a breadth of knowledge owing to their engagement with the local health research community and patient experience.
Public engagement and partnership
For the purposes of this study, the greater emphasis was on public engagement and targeted dissemination involving communities interested in health innovation and the NHS; specifically, we sought to engage policy-makers, AHSN leaders, AHSN stakeholders, NHS employees, regional agencies and representatives of professional bodies (including industry).
Connectivity in this regard was made possible through a close and productive working relationship with UUK, with a senior dedicated person attached to the research team as an advisor. Our contact there was able to keep us in touch with contemporary policy developments in both the university and health-care sectors, as well as senior persons in the policy and health-care landscape. In addition, UUK hosts ‘HSR UK’, a professional network and series of events for the health delivery research community, which includes an annual symposium that we attended in 2015 to present our work.
We held a successful end of project conference at UUK in June 2016 to feed back results, which attracted interest and good attendance from senior AHSN staff and a number of other stakeholders from different communities (e.g. think tanks, academia, SMEs, consulting and Public Health England). The design of the day involved thematic sessions with presentations from the research team and responses from senior figures in the field to promote dialogue. We circulated our presentation slides to attendees after the event.
Variation against study protocol
In the initial protocol, we proposed attending an ‘AHSN forum’ to provide access to national-level events. Owing to developments beyond our control, and reflecting the fact that AHSNs were only just emerging and coming to fruition in 2013, which was the time of our study launch, this forum was no longer meeting. Instead, the team negotiated access to attend some meetings of a later national grouping of AHSN MD/CEOs, hosted by ZPB Associates, facilitated by a member of the SSC. We remain grateful for the permission from AHSN leaders to do so and also to the AHSN commercial directors who granted similar access to their national meetings.
Our SSC advised the research team that AHSN boards and executives would be especially interested in (1) how AHSNs compare; (2) what health/wealth networks look like visually; and (3) the regional and national picture. When the team engaged in face-to-face meetings with AHSNs, they reflected these helpful observations. Indeed, the end of study event has been expanded to include diverse stakeholders.
The May 2015 SSC supported the research team’s suggestion to undertake some qualitative interviews by telephone given the wide spread of actors across geographically dispersed AHSN regions to expedite the logistics of data collection.
Owing to various delays encountered, the NIHR kindly granted the team a no-cost, 6-week extension.
Summary of agreed changes to protocol
-
Agreement to observe national AHSN Network meetings in place of the ‘AHSN forum’, which was by then defunct (agreed at SSC, 5 May 2015 at University of Warwick).
-
Move to some telephone interviews to reduce long-distance fieldwork (agreed at same SSC).
Concluding remarks
Our study design is complex and covers a number of (interlinked) WPs. We now have doubts about our earlier decision to adopt a systematic review methodology, given the diffuse nature of the field we encountered. However, the triangulation of SNA and our qualitative data can be seen as a strength. The comparative and longitudinal nature of the case studies/tracers module can also be seen as a strength, enabling us to plot the spread of selected innovations over time. The set of 10 tracers is an interesting and distinctive database.
The design also enabled us to identify a small but interesting set of ‘knowledge beacons’ for interview. There was much interest found in the field about the study and also in the final conference, which helped stimulate active engagement. Finally, we have found it difficult to contain the mass of qualitative material we secured with the 50,000 word limit for final NIHR reports, which the editorial office has helpfully relaxed for the present draft.
Chapter 3 Literature review
Plan of the chapter
The aim of this study is to examine the early development and impact of five AHSNs and to deepen the understanding of how networking processes and knowledge leadership can support and accelerate health improvement and wealth creation. In this section we report the results of our structured literature review (WP 2, see also Chapter 2), which underpins the rest of the research. We start by examining three bodies of literature, which constitute the background of our research: work on promoting innovation and wealth creation at the intersection of industry, public sector and academic institutions; studies on how knowledge circulates in health care; and studies on how collaboration for innovation unfolds in the sector. We then move to an analysis of literature that is directly relevant to our study. First, we examine the literature on existing experiences such as AHSCs and CLAHRCs. These initiatives share some interesting common dimensions with AHSNs and for this reason they constitute relevant precedents that are worth considering. Second, we examine the research on managed networks as ways to govern innovation and quality improvement in health care. As we will see, these new developments require the deployment of new research methods, such as SNA, but also raise questions around ‘agency’, such as ‘where is the source of action in promoting and sustaining knowledge mobilisation and the diffusion of innovation?’. What is the role and contribution of leaders and managers in these initiatives? Finally, we turn our attention to the literature on the nature of leadership processes and forms supporting knowledge mobilisation in networked initiatives. In setting the scene, we also examine how the promotion of innovation and wealth creation occurs at the intersection of industrial, public sector and academic actors and institutions.
Literature review
One of the central remits of AHSNs is to deliver a step-change in identifying, developing and adopting innovations in the field of health care. The activities of AHSNs are predicated on partnership working and collaboration between the NHS, academia, the private sector and other partners. What models are available in the literature to make sense of this complex process of collaboration?
How to conceptualise the collaboration between NHS, academia, the private sector and other stakeholders?
Our review suggests that one of the most widespread ways to frame the issue is through the idea of ‘triple helix’ as conceptualised by Etzkowitz and Leydesdorff. 36 The basic ‘triple helix’ model suggests that innovations in many sectors are increasingly co-produced innovations that arise through the interaction between university, governmental agencies and business organisations. The ‘triple helix 3’ model is university centred: ‘the triple helix thesis states that the university can play an enhanced role in innovation in increasingly knowledge based societies’ (p. 109),36 unlike other models that privilege the state or the market. The university may itself be undergoing internal change with a new third mission of economic development, alongside research and teaching.
Triple helix 3 is consistent with strong trilateral networks and hybrids, which strongly involve universities. New organisational forms (such as technology transfer offices, spinouts and science parks) emerge across traditional boundaries. The evolution of the triple helix is not linear or predictable but, rather, is interactive, reflexive and emergent. The university is integral to the regional innovation systems that power economic growth. According to this model, the role of universities should shift towards acting as ‘incubators of incubators’. Etzkowitz,37 for example, argues that the contemporary university incubator model (e.g. technology transfer office, spinouts and the science park) builds on the classic venture capital firm but adds in the co-location of firms on green-field sites to encourage cross-fertilisation: ‘the university of the future will include an incubator as a regular feature along with classrooms, faculty offices and laboratories in each department or academic unit’ (p. 127). 37 The university is becoming more permeable and ‘outwards facing’, with more external alliances. By exploring ‘science city’ initiatives in regions searching to accelerate economic growth (e.g. Barcelona), Etzkowitz38,39 outlines transformations associated with the triple helix. First, there is no single dominant power within the triple helix but rather emergent, negotiated and cross-boundary development. Second, various organisational and ‘hybridising’ inventions are as important as physical devices in speeding innovation. These organisational forms include the entrepreneurial university, the innovative region (where Silicon Valley, CA, USA, and Route 128 in Boston, MA, USA, are cited as prime exemplars), the incubator, the science park, the venture capital firm and the knowledge intensive network.
The triple helix is not the only model used to conceptualised the collaboration between university, government and business. Fromhold-Eisebith and Werker40 discuss alternative academic literatures on the changing economic and social role of universities. As well as triple helix, they consider the new production of knowledge model, which is based on the distinction between mode 1 and mode 2 of knowledge production. Gibbons et al. ’s41 influential text argued that there was a long-term shift from so-called mode 1 to mode 2 knowledge production. Mode 1 includes the primacy of academic basic research, the strong agency of individual scientists, the importance of scientific peers, and a hierarchical and university-centred governance system. Mode 2, by contrast, exhibits transdisciplinary knowledge production, engagement from a wider range of sites, the formation of temporary knowledge networks and the production of applied knowledge for use within specific social and economic contexts. The message, therefore, is not only that to foster innovation one has to act at institutional and policy level, but also that other types of network-based forms are necessary to foster the mode 2 type of knowledge production. From this perspective, AHSNs are an early attempt to facilitate and foster, rather than to plan and govern, processes that fall within the new production of knowledge model. Schoonmaker and Carayannis42 propose a further model of the ‘quadruple helix/mode 3’ with an activated civil society. Carayannis and Campbell43 suggest that in a knowledge-orientated society, a ‘creative class’ of highly educated workers shapes a mode of public discourse that favours a future orientation, the production of knowledge and support for innovation as positive societal values. This notion of ‘civil society’ suggests the presence of ‘third-sector’ organisations lying between the state and the market not captured in the classic triple helix model.
One of the common themes of these models is that they shift attention from high-level policy interventions aimed at creating top-down institutional and economic change towards the promotion of specific networking and collaboration initiatives ‘on the ground’. For example, taking a perspective from economic geography, Fromhold-Eisebith and Werker40 review academic literature(s) on universities in the KT process. They explore cases in which university/regional knowledge flows have fallen short of expectations. Their message is that this happened because these initiatives remained at a traditional ‘policy’ level and did not consider or address the issues of networking and creating links within the system. In their words ‘we find that social network analysis and its theoretical basis, i.e., social network theory, will give more body to understanding knowledge transfer functions of universities’. 40
Learning from case studies of regional innovation and governance
Over the past decade or so, authors have utilised the triple helix and other models to examine the experience of regional efforts to promote innovation through collaboration and multilateral partnerships. Some have found, for example, that triple helix arenas are facilitated by intermediary organisations, including university incubators and industrial consortia. For example, Johnson’s44 study of PRECARN (‘PRE-Competitive Advanced Research Network’ – an industrial consortium in the field of intelligent systems) suggests that the network successfully acted as an intermediary organisation and was instrumental in the effort to lower the transaction costs associated with network-based working (e.g. acting as a mediator in case of dispute) and to generate new revenue streams for partners (p. 502). 44
Smith and Bagchi-Sen’s45 survey of the UK Oxfordshire biotechnology sector cluster explored the proposition that regional contexts for triple helices may vary. A metropolitan region, for example, may have greater scope and scale than smaller cluster-type regions. Labour market aspects of such regions, such as the availability of skilled labour, should be considered further. Although this region included a premier research-intensive university (Oxford), it played a less clear-cut role than triple helix theory would suggest. Leading universities operate in national and international networks as much as they do in regional ones. Their survey responses indicated that a strong role was also played by national funders and by extraterritorial linkages. The role of the university was more indirect (at least in firms not spun out by it) in helping to ensure the ready supply of skilled labour, as they found ‘that the role of Oxford University, a world centre for biomedical research, is secondary at the regional level rather than being dominant as might be expected and that the availability of skills, underplayed in traditional presentations of the model, is far more significant’ (p. 805). 45
Etzkowitz and Klofsten46 go a step further and question whether or not certain conditions can and should be replicated elsewhere. They do so on the basis of a study of the Swedish Linköping region. They wonder if the well-known US cases of Silicon Valley and Boston’s Route 128 reflect special historical circumstances that are difficult to replicate elsewhere, even in superficially promising locations: ‘Cambridge UK has generated a significant number of niche firms but has had difficulty in creating high growth firms, common in Silicon Valley’ (p. 244). 46
Goldstein and Glaser47 examined the governance of local and regional development in science parks developed from two research-intensive universities (University of North Carolina at Chapel Hill and Utrecht University). Drawing on political science work on ‘network governance’,48 they broaden the narrow focus on technology transfer in the current literature. Governance theory suggests that the direct command role of the nation state is declining as a broader range of policy actors develops from various sectors and tiers, including strong regions. Goldstein and Glaser47 distinguish between possible governance modes. The first, traditional, category is hierarchical governing. The second category shows movement to hierarchical governance in which non-governmental actors are more actively involved in collaborative decision-making, yet the final decision-making power still rests with the government actor (p. 161). 47 Third, ‘heterarchic’ governance reflects high interdependence and more equal power relations with more networks, public–private partnerships and co-management. Their two case studies were cautious and inconclusive (p. 172). 47 There was variation found in the governance mode, with Utrecht University showing greater heterarchy. Their lesson is that there is no ‘one model fits all’ solution on how to govern regional collaboratives and that one of the critical factors is aligning the mode of governance with expectations in the local institution and cultural norms (in their case, Utrecht’s heterarchic mode of governance was possible in view of the local political and cultural conditions that were absent in the USA). 47
Finally, some authors examined collaborations in a context more akin to that of the AHSNs. Feldman,49 for example, analysed the development of a science park in Linköping, Sweden, with a strong medical industrial sector. An interesting feature was the shift of innovation platform over time (pp. 1027–8). 49 The key growth point moved from being an incubator in a large bureaucratic firm to a small start-up. The shift depended on new strategies deployed by regional actors and wider changes to the administration and resources available to such actors. New actors (from the county and city councils and the local university) came into the field and constructed networks that made additional resources available. At the same time, these new actors were themselves experiencing internal policy and even ideological shifts (as in a growing ‘enterprise culture’ in the university).
In summary, the common theme emerging from these studies is that, although no ‘silver bullet’ exists, collaboration and triple helix effects at regional level are better served by initiatives run by agile, intermediary organisations with flexible mode of governance that can act as contained facilitators of processes, rather than trying to engineer and govern them. This in turn raises the issue of which types of agency and leadership processes are appropriate in such newly emerging organisational contexts. We return to these topics later in this review.
Understanding knowledge transfer, mobilisation and innovation in health care: theoretical framings
The topic of how knowledge and innovation circulate in health care, and how the process should be conceptualised, has attracted increasing attention among authors. This is reflected in a growing body of literature on the topic. Authors propose a variety of models and different ways of understanding the processes through which novel ideas, technologies and delivery practices are circulated and translated among those involved in health-care activities (including patients). Overall, the tendency is to abandon simplified ‘transfer’ linear models that see the process of the circulation of knowledge in terms of a rather mechanical sequence of production, transfer and utilisation. In their stead, authors favour more nuanced, ecological and socialised views. 11 This shift is usually signalled by the use of terms such as knowledge mobilisation rather than knowledge utilisation or knowledge transfer. The notion of mobilisation is seen as reflecting the fact that the circulation of knowledge and innovation in health care is dynamic, processual, moved by a number of diverging interests, and happens at different levels at the same time. 11
Different reviews of this literature on and mobilisation in health care exist (for a recent review see the introduction in Swan et al. , p. 201). 11 For example, Kitson50 presents a theoretical overview of social literature that is critical of received approaches to KT in the health-care sector in general and in the field of nursing in particular (the paper was published in an academic nursing journal). She argues that dominant KT models are too often linear and ‘machine like’, sitting badly with more organic models, perhaps drawing on more iterative organisation process work developing in management studies (e.g. Van de Ven et al. 51), and even complex adaptive systems (CASs) thinking. Her most general of five propositions states that ‘the (healthcare) system is best viewed as a complex, interactive, organic entity where experimentation, experiential learning and reflection are central to creating a culture of innovation, improvement and consequently effectiveness’ (p. 218). 50
Kitto et al. 52 seek to reconceptualise KT processes in health care, given what they see as the problem of the ‘vested interest’ of projects undertaken by KT specialists, which assume a goal of desired behaviour change, supported by the adoption of planned change models. They suggest that this framing is too rationalistic, individualistic and linear and argue for a new approach based on the sociology of KT: which is unburdened by the desire to demonstrate intervention successes ‘such an approach fully embraces the notion that “new” knowledges are generated in the activities between KT practitioners and the chosen communities in which they work, requiring an actively reflexive approach to KT intervention design and practice’ (p. 290). 52 They advocate a theoretical framing based on actor–network theory (ANT) and its tracing of associations and networks. They then apply their approach to the concrete analysis of a surgical safety checklist, of which some of the authors had strong professional knowledge, so that: ‘all aspects of the work to make connections between all contextual factors, newly introduced techniques of change (i.e. checklists, guidelines), KT practitioners and knowledge users are open to scrutiny’ (p. 296). 52
Nicolini et al. 53 presented a systematic literature review of health-care sector innovations based on knowledge management (KM) (a narrower phrase than that of ‘knowledge mobilisation’ used here). They identified three major themes in the literature. The first was an exploration of the ‘nature of knowing’ in the sector, which could be seen as typically fragmented and distributed. There seemed to be a proliferation of medical knowledge, information and data, which presented sectoral conditions of ‘knowledge overload’. There also seemed to be a preference for the use of local knowledge in the making of clinical decisions. The second theme covered a range of KM tools and techniques that could be used in the health-care sector, covering both ‘hard’ approaches (electronic libraries and repositories; data mining) and ‘soft’ social learning-based approaches, which Nicolini et al. 53 argued might fit the nature of the sector better. The third theme was an examination of what the literature saw as the enablers of and barriers to KM in the health-care sector (which they comment appeared similar to the literature on other sectors). Enablers included shared common values and culture, weaker power and status differences, and stronger interdisciplinarity. Barriers included overmanagement and interference from the political sphere, clinical managerial conflict, professional barriers and low levels of trust. They commented that, at the time of the review, some of the health-care literature appeared to present conditions of sectoral isolation from important concepts found in mainstream management literature, such as ‘social capital’ and ‘communities of practice’ (p. 258). 53
Best et al. 54 present a realist review of literature on large-scale transformation and innovation in health-care systems using CAS theory, previously developed in the health-care context by Plsek and Greenhalgh. 55 The literature on CAS is relevant in the present context, as it was developed to explain the behaviour of non-hierarchical and partially emergent organisations not unlike AHSNs. Best et al. 54 argue: ‘although CAS are complex and unpredictable, they are amenable to guided transformation by applying simple rules that are sufficiently flexible to allow for adaptation’ (p. 432). Their literature review enabled them to specify five such simple rules (and then middle-range propositions) as follows: (1) engage individuals at all levels in leading the change process (leadership should be both designated and distributed), (2) establish feedback loops, (3) attend to history (as change mechanisms are context sensitive), (4) engage physicians and (5) involve patients and families. They also called for more comparative case study analysis of change processes in health-care systems to build learning and a theoretical base.
Absorptive capacity and ‘dynamic capabilities’
A further promising approach to understand the process of knowledge mobilisation in health care is provided by the ABCA perspective. The approach, which is based on the resource-based view of strategic management, argues that firms even within the same sector (e.g. biotechnology firms) often generate distinctive collective competences (e.g. the ability to learn, absorb knowledge or change), which produce idiosyncratic profiles and positions in the marketplace. The firms’ assets include intangible elements (such as tacit knowledge) as well as traditional tangible elements (such as manufacturing plants). ‘ABCA’ constitutes one of these core competences. 56 Zahra and George15 define ‘ABCA’ as ‘a dynamic capability pertaining to knowledge creation and utilization that enhances a firm’s ability to gain and sustain a competitive advantage’ (p. 185). 15 They further distinguish between two dimensions of ‘potential’ ABCA (namely, acquisition and assimilation) and two of ‘realised’ ABCA (transformation and exploitation). The third transformation stage encompasses: ‘the firm’s capability to develop and refine the routines that facilitate combining existing knowledge and the newly acquired and assimilated knowledge’ (p. 190). 15 From this perspective routines and processes of the firm are seen as being of extreme significance for the capacity of organisations to learn and innovate. The third ‘transformation’ stage may be particularly interesting to study because it opens up the ‘black box’ of the firm at the critical stage of creative innovation. It is at this stage that the genesis of new competences may become apparent.
Agency and the role of the individual in knowledge mobilisation
Although the ABCA literature focuses on processes and routines, other scholars are more interested in the dimension of ‘agency’ in the process of knowledge mobilisation. Agency refers to the capacity of an entity to act in any given environment and more generally to particular source of action and change. In other terms, the literature asks where the agency is in the knowledge mobilisation process. Who or what has the capacity to make knowledge mobilisation happen?
The interest for the agential dimension of knowledge mobilisation has led to the identification of a number of specific roles that individuals play in promoting and sustaining knowledge creation and innovation diffusion. These roles are critical in our study as they provide the necessary concept by which to understand the role of managers and senior leaders in the activity of AHSNs:
-
Brokers: the idea of the broker refers to individuals who mobilise knowledge across professional, cultural and institutional boundaries, and is explored by authors such as Obstfeld. 57 He writes about the ‘tertuis iungens’ or the ‘third player’, or an entrepreneurial strategy connecting people who are disconnected (i.e. closing ‘structural holes’). This paper links to Burt’s work on brokerage, structural holes and innovation. 58 Long et al. 59 use SNA to explore if these individuals share characteristics (e.g. powerful, influential, well connected). Interestingly, there was empirically a mismatch between actual and perceived brokerage. Individuals with formal knowledge broker roles (i.e. formally designated directors and managers) were not necessarily the individuals who network members perceived as key in knowledge mobilisation.
-
Boundary spanners: Liu and Stuart60 investigate boundary spanning in a for-profit biotechnology and pharmaceutical research laboratory. They emphasise how innovation in the life sciences context arises in a context of porous organisational boundaries (such as between universities, research centres, private companies, spinouts and commercial laboratories). They paradoxically suggest that individuals in less central roles may find themselves in more central positions. They found that actively publishing researchers are much better connected to external (to the company) members of a knowledge-exchanging scientific community. Jones et al. 61 suggest a major role for the ‘knowledge champion’. This formulation places knowledge activists and change agents at the informational centre, where they provide regulative and communicative capacity. Such observations are pertinent to our study’s examination of ‘KLs’.
-
Institutional entrepreneurs: institutional entrepreneurship refers to the ‘activities of actors who have an interest in particular institutional arrangements and who leverage resources to create new institutions or to transform existing ones’ (p. 657). 62 Examining the conditions that facilitate institutional entrepreneurship in health care and encourage individuals that drive radical change. Lockett et al. 63 suggest that those individuals with limited structural legitimacy under prevailing institutional conditions (i.e. who are more peripheral and have limited access to resources) may be best placed to engender change, but least able to given prevailing conditions. Individuals with strong structural legitimacy, however, are most able to produce change but may be less willing to do and challenge the status quo if ‘privileged by existing institutional arrangements’ (p. 361). 63
-
Activists and champions: Käser and Miles64 argue that knowledge-intensive firms are increasingly relying on ‘knowledge activists’ to facilitate knowledge flows supporting innovation through effortful, creative and less formal means, such as obviating organisational hierarchies and building trust through communities of practice.
Overall, the literature we reviewed confirms the growing interest in non-linear views of the innovation processes that go beyond simple ‘technology push’ models to consider the operation of wider social–technical systems and the local enactment of knowledge exchange. It signals the importance of professional networks and interpersonal trust building that supports ‘knowledge driven innovation’ (p. 25). 64 The frameworks and theories in the literature also demonstrate the benefits of social science (including management)-based approaches to the study of KT processes, including important concepts such as situated learning (knowing rather than knowledge), communities of practice, ACBA and CASs.
Empirical studies of knowledge mobilisation
A number of papers offer more developed empirical views on the process of knowledge mobilisation, although still with a theoretical framing. Pope et al. 65 studied the introduction of treatment centres in the NHS as an organisational innovation after the 2000 NHS plan designed to reduce waiting lists for elective procedures (they studied eight different sites). They draw on a ‘negotiated order’ perspective to argue that there was great local variation in the way in which the innovation was instantiated locally, reflecting local systems of cultural meaning and interpretation. The implication is that other health-care innovations (including perhaps the case of AHSNs) could be constructed in very different fashions locally, reflecting local histories and meaning systems.
Greenhalgh et al. 66 used a multiple case study design (of four early adopter locales including both primary care and unscheduled care sites) to study the introduction of electronic patient records in the English NHS in the national Connecting for Health programme, informed by the diffusion of innovation theory. 67 These health-care innovations to information technology (IT) systems should be seen as involving both social and technical components rather than just operating as a simple ‘technology push’ (which is how policy discourse tended to cast them) so they were: ‘not plug in technologies. They are complex innovations that must be accepted by individual patients and staff and embedded in organizational and system levels and routines’ (p. 1043). 66 Although some early sites had strong leadership and ABCA, there could well be a need to build up such competences in later adopters.
Waldorff68 examined the local instantiation of a health-care innovation (a municipal health-care centre) in case studies from 18 local authorities in Denmark. The abstract concept was found to take different forms in different locales: ‘some municipalities conceptualised the centre as a building that is open for patients with chronic diseases to visit, while other municipalities created the centre as a collaborative network of local organizations which promote health for citizens in various places such as schools and workplaces’ (p. 219). 68 Theoretically, the paper drew on both institutional logics theory (as multiple logics were evident and co-existed in the broader municipal field) and ANT, with its interest in the translation process: “the concept of ‘translation’ from ANT enabled analysing the reform as a process in which local rationales of health care centres were constructed” (p. 230). 68
Other studies examined in depth the mechanisms and conditions of, and obstacles to, knowledge mobilisation in health care. For example, Gabbay and Le May’s69 well-cited ethnographic exploration of the social construction of evidence-based practice in two English primary care settings found that that the formal literature search/adoption model espoused in EBM models was not evident in these sites. There was a key role for professional networks (including opinion leaders) in spreading knowledge for primary care doctors, although nurses relied more on interactions within local teams. Pharmaceutical representatives and patients were also important sources of information. The authors presented a social constructionist model of learning and introduce the notion of ‘collective mindlines’ to describe how an especially adaptive mode of knowledge and understanding arises within professional communities of practice: ‘mindlines were therefore iteratively negotiated with a variety of key actors, often through a range of informal interactions in fluid communities of practice, interactions with and experience of patients and practice meetings. The result was day to day practice based on socially constituted knowledge’. 69
Their findings are echoed in Waring and Bishop’s70 ethnography of informal knowledge mobilisation and sharing activities in ‘the backstage’ of two NHS day surgery units. The study moved away from formal KM accounts to look at learning through informal ‘water cooler’ moments: ‘although these semi-private and casual situations constitute a potent vehicle for knowledge sharing, learning and the maintenance of organizational and occupational values based on privacy, trust and mutual understanding. They could also be seen as aligned with views on situated learning within COPs [communities of practice] or networks of practice’ (p. 326). 70 Waring and Bishop70 argue that the challenge is to try to align these informal processes with more formal patient safety and learning systems, but not in such a way that over formalisation drives out these more interpersonal ‘water cooler’ moments.
Currie and Suhomlinova’s71 well-cited paper explored limits to processes of knowledge sharing across various organisational and professional boundaries in a case study of an English academic health centre that sought to bring together the health and higher education sectors. Using a ‘neo-institutionalist’ framing, which distinctively is interested in organisational imitation or processes of field convergence across the health-care sector, they distinguished between three possible institutional and professional ‘boundaries’ that could influence knowledge-sharing processes: (1) between the higher education and health sectors, (2) between hospital medicine and primary care in the health sector and (3) between the different health-care professions. Strong institutional forces were found to segment knowledge and restrict its flow across these boundaries, allied to power inequalities. Hospital doctors remained dominant within the health sector. There appeared to be negative forces in operation driving academic professors and medical consultants further apart, as performance indicators and career-building strategies in higher education placed strong emphasis on publishing in top journals rather than engaging with local practice. These structural forces need to be taken into account in the policy domain: ‘in conclusion, we highlight cultural and political dimensions of knowledge sharing not hitherto recognised by policy makers’ (p. 26). 71 We comment that their use of the concept of an organisational and professional ‘boundary’ may be an important and helpful one. What creates these boundaries? Can knowledge move across them (as suggested in a mode 2 knowledge production framework), for example such as through the use of ‘boundary objects’ or ‘knowledge brokers’? Are these boundaries impermeable or semi-permeable?
Similar conclusions were arrived at by Kislov et al. 72 The authors explored KT processes in service improvement projects undertaken in four English general practices, in an initiative sponsored by Greater Manchester CLAHRC. They drew on community of practice (COP) theory73 to study knowledge flows in these settings, defining a COP as: ‘work related communities of individuals created over time through sustained collective pursuits of shared enterprises’ (p. 2). 72 Knowledge may flow easily within COPs, but ‘stick’ when it encounters a COP boundary. Kislov et al. 72 suggested that within the individual practices, interprofessional boundaries were not pronounced and teamwork was often good, but that boundaries were sometimes encountered between the practices and the specialist service improvement teams. In addition, communications between different general practices were sometimes poor. They concluded: ‘it is possible to view primary care organizations as a constellation of COPs united by a shared organizational culture and identity. As a result, constituent (multi professional) intra organizational COPs tend to become tighter than those (predominantly uniprofessional) networks of practice that cut across organizational boundaries in primary care’ (p. 10). 72 The configuration of COPs was found to have a significant influence on the KT process. They argued that a developmental approach to fostering such COPs was indicated, rather than a manipulative approach to try to create managed COPs for KM purposes, which would be unlikely to ‘stick’.
Finally, Jacobson et al. 74 presented a new model of KT in Canadian health care based on consulting activity from academic units to complement existing ‘interactive’ models. Given the increased attention on ‘impact’ and KT activity involving academics now being displayed in many academic settings, this model of highly applied working is of interest. They drew on three cases of projects undertaken by a health systems research and consulting unit working on mental health services and based at the University of Toronto. They concluded that ‘consulting appears to be an effective strategy for carrying out an interactive model of KT to enhance the use of research based knowledge in decision making environments’ (p. 317). 74
In summary, the literature sensitises us to the complexity of knowledge mobilisation and confirms the need to adopt a multilevel approach that is aware of how different values, interests and expectations shape knowledge and innovation flows in practice. There are also suggestions that stronger interactions between knowledge producers and consumers can aid knowledge mobilisation activities. 52,74,75 The literature adds a strong concern for the operation of ‘knowledge networks’, a topic that we discuss below. By contrast, there is much less attachment to formal hierarchy as an effective governance mode to support innovation. Finally, the literature suggests that we should search for novel disciplinary perspectives that cross conventional disciplinary boundaries (see, for example, Shaffique76).
Academic Health Science Networks: learning from previous experience
Academic Health Science Networks were established on the back of a number of previous national and international initiatives aimed at fostering the emergence of ‘systems for delivery of innovation’. 1 These initiatives included the AHSCs and the CLAHRCs. What lessons can be learnt from such previous experiences?
The experience of Academic Health Sciences Centres
Academic Health Sciences Centres are partnerships between universities and health-care providers focusing on research, clinical services, education and training. 77 They operate in a number of countries including Australia, Canada, the Republic of Ireland, Japan, the Netherlands, Qatar, Singapore, Sweden, the UK and the USA.
Ackerly et al. 78 studied the early development of these experiences and suggested that, in order to be successful, these organisations must strive to become leaders in what they describe as the increasingly globalised world of medicine (p. 1093). 78 Although adopting a global outlook is not without risks, they suggest that first movers and institutions that take the lead and offer themselves as leaders of international networks are likely to reap huge benefits. The authors add that, in order to perform in such a global leadership role, such organisations need to move towards a systems approach and become more integrated and inclusive. Dzau et al. 77 take a step further and suggest that, to transform health care, AHSCs should evolve further into Academic Health Science Systems. The idea is to establish organisations that can facilitate collaboration between multiple stakeholders involved in medical innovation. In their words: ‘we believe they [Academic Health Science Systems] can become models of horizontal integration of discovery and care delivery through reorganisation of their key structures and encouragement of cultural change that emphasises effective interfaces among academic departments, research organisations, and delivery systems, and by extending these interfaces to participate in more effective public–private partnerships’ (pp. 949–50). 77 The message is critical for the evolution of AHSNs because previous experience points towards the need for organisations to promote and govern relationships between stakeholders that normally see themselves as belonging to different worlds.
Studies of the development of AHSCs note an underlying variation in how the policy has been implemented in the UK and elsewhere. Ovseiko et al. 79 distinguish between two different organisational models in English AHSCs. One site (Imperial College London; the first AHSC) initially adopted an integrated model with a dean/CEO, whereas others that came on board worked with a joint partnership board. Ovseiko et al. ’s later commentary80 noted that the imperial AHSC later moved back to a confederal model and formed Imperial College Health Partners as a company limited by guarantee with internally generated multiyear funding. Governance models for AHSCs may therefore be tightly structured or looser affiliations between partners. 81 Ovseiko et al. 80 call for research on AHSCs and AHSNs to (1) assess the efficacy of different alignment mechanisms; (2) help formulate agreed success metrics; and (3) look at agency, notably leadership styles and to comment on their effectiveness (p. 11). 80
Authors such as Fish82 take a positive view on such variation. In a commentary on English AHSNs,82 the author argued for creative local variation between sites: ‘this approach to the delivery of innovations is mainly permissive: clear goals are set within a broad operating framework, leading much to be ascertained by local context’ (e18). 82 Success metrics could include (1) enhanced clinical outcomes, (2) improved innovation adoption times and (3) the creation of wealth. In achieving such goals, the ‘success of AHSNs depends on shared values, strong working partnerships, local leadership and energy and clarity on operational delivery, rather than one system of control or complex contractual arrangements’ (e18). 82
The literature on the evolution of AHSCs (and later of the emergence of AHSNs) is relatively small scale, but it suggests that variation in policy implementation can be seen as an opportunity as well as a source of complexity. This resonates with some of the studies reviewed in the section on the triple helix that suggest that replicating collaborative success in different geographic, historic and economic conditions requires flexibility rather than the top-down imposition of a pre-existing model. In terms of our research, the lesson of AHSCs for AHSNs is that variance should constitute a main focus of analysis.
The experience of Collaborations for Leadership in Applied Health Research and Care
A number of papers are also emerging that examine the experience of the CLAHRCs. A first group of papers examined the translation of the original policy in practice. Rowley et al. 83 consider one site operating with an explicit model of diffusion fellows that drew on social science-based literatures (organisational learning, situated learning and communities of practice). This approach had promising results, although many projects were at an early stage. Caldwell and Mays84 explored how the CLAHRC policy stream developed at macro (DH), meso (NIHR) and micro level. They looked at the mechanisms by which the CLAHRCs moved from a policy idea to a programme of implementation and analysed how the participants at each level framed their understanding of the policy and programme to determine the degree of congruence. They found ‘strong indications’ across the different levels of ‘a shared understanding’ with regard to the implementation of the policy and suggest that, ‘In effect, the programme as implemented matches the policy as envisioned’ (p. 42). 83
Although Caldwell and Mays84 found an overall coherence in the understanding of the original CLAHRCs policy intent, Oborn et al. 85 arrived at a different conclusion and found a substantial multiplicity in how the formal remit was implemented in practice. Oborn et al. 85 identify five archetypes drawn on by the original grouping of CLAHRCs. These were (1) involving a broad array of stakeholders in a multidisciplinary research process, (2) loosely autonomous research streams with designated knowledge brokers, (3) independent research and implementation activities, (4) collaborating through loose existing networks and (5) centrally controlled service improvement projects. They comment that there is no one best way but, rather, that ‘each type can be managed and led more or less effectively, present different challenges and are more suited to certain contexts’ (p. 17). 85 Importantly for this research, they suggest that ‘understanding and clarifying the organizing logic underpinning KT collaborations’85 is of great importance for two reasons: first, ‘clear organizing vision is important to enable leaders to unite multiple stakeholders and enable effective communication of common goals’ and second, ‘clear vision enables leaders to develop and articulate a clear strategy for achieving KT goals’ (p. 18). 85 The paper is relevant to our study as it suggests the need to triangulate the assertion made by managers with the analysis of actual instances of practice so that possible discrepancies may emerge.
Other authors also found variation in the implementation of the CLAHRCs. Currie et al. ,86 for example, registered differences between CLAHRCs and noted that NIHR allowed local variation between CLAHRCs as a learning opportunity. Different translational models were adopted in different sites, for example, with variation along the research/implementation spectrum. Across the set of CLAHRCs, however, they suggested that the dominant orientation was towards traditional and clinically oriented research. Many leaders were themselves senior clinical academics.
These studies – which mirror the findings on the evolution of AHSCs – have an important message for the present research. Variety of implementation should be expected and not necessarily connoted negatively. Indeed, a certain level of interpretive flexibility (i.e. the idea that innovation has slightly different meanings and interpretations for various groups located in different settings) is critical so that policy can be adapted to local contextual conditions.
Networks as forms of governance in the UK health service
We signalled the potential significance of regional governance arrangements to promote innovation earlier in this review. There is also an established literature on managed networks that have been promoted as a novel governance mode in UK public policy and applied in English health service settings. This reflects a policy turn from principles of market competition to network governance and collaboration, and became increasingly evident during the New Labour period (1997–2010). The use of this form of organisation for innovation and health improvement is also increasingly underpinned by a solid evidence base showing the capacity of networks to deliver results.
Harvey et al. ,87 for example, used a comparative case study-based approach to examine the correlates of high academic performance in four health-care research groups in one NHS region. They found that strong network connectedness was associated with high performance levels in elite health research groups. Their inductive model identified five factors behind this positive outcome: (1) strong strategic research leadership from a group director (so there was an individualistic element of leadership in this case), as well as specific ‘product champions’ lower down the hierarchy; (2) finding, rewarding and motivating talent; (3) strategies of related diversification; (4) strongly linked theory and practice; and (5) network connectedness, which could be seen as a key competence and which was placed in the centre of the visualisation of the model. The study corroborated the argument from the science policy literature (examined earlier) that there is a general shift proceeding in the dominant mode of knowledge production from an academically based and centralised mode 1 to a more dispersed, transdisciplinary and pluralist mode 2. The underpinning message is that networked organisations are the institutional form of choice to address the societal changes in a mode 2 knowledge production system.
The importance and operation of knowledge-orientated ‘managed’ networks in health-care settings was explored in several papers (e.g. Ferlie et al. 5). In a comparative case-based study, Addicott et al. 88 looked at the (early) evolution of the five Managed Cancer Networks set up across London in the early 2000s. One argument for such managed networks was that they should promote more effective knowledge mobilisation: ‘networks in health care were initially proposed inter alia as effective forums for sharing knowledge about ‘best practice’ and developing educational opportunities across organizational and professional boundaries’ (p. 95). 88 Empirically, the cases suggested the dominance of more policy-sensitive issues of structural reorganisation (especially the centralisation of specialist services) over KM. Of the five cases, however, one network appeared to be developing as a positive outlier, where there was a more developed focus on learning evident in the nursing subgroup and some of the clinical subgroups. These themes were picked up in a large-scale study of the evolution and impact of a set of eight managed health-care networks (four pairs drawn from different policy sectors, typically involving multiple players with different interests), all set up in the early 2000s. 5 The two Managed Cancer Networks studied were both assessed as higher performers. The argument was that, in order to make an impact, these networks would need first of all to develop competences within three different areas: (1) a move from vertical management to more lateral leadership, (2) stronger shared information and communication technologies (ICTs) and databases and (3) well-developed interorganisational learning.
Therefore, the emergence of managed networks as a novel governance mode in English health services raises different issues, one of which is how can we best study such forms of organising: an issue to which we now turn.
How to study networks and networked initiatives
The increasing attention on social networks and the recognition that they play a central role in the creation and diffusion of innovative knowledge has put social network theory and SNA, the methodological toolkit for studying social networks, on the research map in management and organisation studies. 89,90 Traditionally, this perspective was focused at the individual level of analysis (the personal or ‘ego-networks’ of managers) and prioritises competition and exploitation of opportunity over collaboration, and has spurred a wealth of subsequent management research. A typical example is the central notion of structural holes theory, which claims that individuals positioned at ‘gaps’ in a social networks are provided ‘structural advantage’ because they are better able to tap into heterogeneous sources of knowledge emanating from these fragmented networks, thus supporting their capacity to innovate. 91,92 More recently, however, the approach has been extended to broader social formations and is increasingly used to study and shed light on the dynamics of collaboratives and alliances. For example, Powell et al. 93 illustrated that the locus of innovation can be found in networks of learning and alliances, so it is not sufficient for firms to develop external networks, but social networks must offer some form of learning or new information in order to support innovation.
Social network analysis is increasingly used to examine innovation and improvement in health care. SNA is in fact particularly suitable to study phenomena that are dispersed, fluid and emergent. For example, Cunningham et al. ’s94 systematic review of literature on the structure of health professionals’ networks noted a growth of interest in network-based health-care delivery and in the use of SNA techniques to investigate them (given advances in computing capacity and SNA software). They accessed and rated published articles in this area using systematic methods. Of the 26 articles that survived their quality sift, 19 used SNA methods. They reviewed key concepts in the networks literature such as brokerage (bridging activity across conventional boundaries) and network density (how contained/intense a network is; it should be noted that highly dense networks might produce cliques). They observed that much existing literature has explored the structural features of such networks rather than making links to outcomes, and so recommend: ‘using multi methods approaches and exploiting advances in SNA . . . research should examine the relationships between professionals’ network structures and health outcomes in a range of different care settings’ (pp. 247–8). 94 Although their study operated at the micro level of service delivery, this recommendation could be applicable to macro-level health organisational research. How this might be done is demonstrated by a study by Lewis. 95 Here, power dynamics in the health policy-making process are explored within an Australian context. Respondents were asked to nominate influential actors in the policy field. Lewis found that ‘those who top the list are health academics, senior bureaucrats and people located in research institutes and NGOs [non-governmental organisations]. Most of the influential actors are medically trained and the vast majority of them are men’ (p. 2130). 95 These persons also had long standing interpersonal ties and were closely interconnected (e.g. serving on the same major committees). Importantly, SNA techniques were used to map and analyse underlying network structures. Although various clusters were discerned, two were of notable interest. First was a core block consisting of the minister, senior bureaucrats and medical deans (i.e. senior clinical academics who also had senior managerial roles). There was also a second and cohesive public health grouping. Overall, elite but invisible segments of medicine (as opposed to its institutionalised expression in visible interest groups) appeared to have regrouped and recaptured influence in the policy domain from what earlier on had been a challenging economist/management block.
In summary, with the growth of network-based forms of organisation in health care, SNA emerges as an important analytic technique. Network concepts and SNA techniques are a promising way to study initiatives such as AHSNs, in that they ‘provide novel and useful means for understanding the structures of influence which impact on the health policy process’ (p. 2135). 95 They may, therefore, shed light on the professional groups and actors that influence policy, but also on local processes of interpretation and implementation.
Bringing agency back into the study of networks and networked innovation
The increasing use of networked forms of organisation to govern and foster collaboration and innovation processes raises the important issue of ‘agency’. Where lies agency in innovation networks? Who or what has the capacity to make innovation happen? What types of leadership are appropriate for network forms of organisation?
In the UK health-care domain, Greenhalgh et al. 67 called for more research on the contribution of managers, knowledge workers and boundary spanners to the adoption and spread of innovation in health services organisations. NIHR-funded projects have since explored NHS managers’ use of evidence to support innovation. 10,12,96
Other research has sought to link social network structures and strategies with knowledge mobilisation. 97,98 Ferlie et al. 5 found a substantial move towards more lateral forms of leadership, often exercised by small multidisciplinary teams located at the centre of the NHS networks studied. Martin et al. 99 studied leadership in a comparative case study of cancer genetics pilots in the English NHS, highlighting dispersed leadership in achieving service change.
However, overall, relatively little is known about how the personal social networks and networking strategies of senior leaders impact knowledge mobilisation and innovation (especially health-care CEOs and boards). Questions about formal managerial leadership and agency in networks remain the ‘800 lb gorilla in the room’100 and in mandated networks, such as CLAHRCs and AHSNs, an understanding of leadership agency is still limited. Therefore, in the final section of this review, we examine the state of art of research on this topic.
Research on leadership, knowledge and networks for innovation
Knowledge-intensive networks tend to bring together a highly educated and professionalised work force potentially good for organisational learning, but also environments within which informal leaders emerge. As such, leadership may be distributed across a wider spectrum of individuals, organisational settings and hierarchies. 101 In complex organisational environments such as health care, leadership requires, first and foremost, the management of social relationships. Accordingly, informal ‘personal networks’ (i.e. friendship or support ties) are important, and research has shown that the maintenance of long-term relationships supports the flow of knowledge across organisational boundaries. 102 In the next four subsections we ask what types of leadership agency support knowledge-intensive innovation networks? What makes leadership effective in networked forms of organisation? In particular, we focus on the types of leadership agency that support knowledge-intensive innovation networks like AHSNs (such as in science, technology and health-care settings).
Models of networked leadership
Research on the agency of network members argues that the orchestration of innovation networks is the result of interplay between structure and agency (position in the network and effort, so to speak) rather than structural constraints and member inertia. 103 In clear terms, network position and networking strategies are often more important than formal roles and the authority associated with them. Zheng104 suggested that the structural components of social capital, including ego network size, structural holes, tie strength and centrality have a significant impact on innovation (see Glossary). This view is supported by research using interaction based-approaches to theorise leadership agency in network contexts, where power via formal roles cannot be taken for granted and individuals may lead in an informal capacity. Ohly et al. ,105 for example, suggest that, within networks, formal leaders are consulted more often for idea generation than for idea validation, and also that individuals with the same position in the hierarchy consult each other most often (leader–leader or follower–follower).
Of course, the emergent and rational nature of leadership in networked conditions also has its dark side. O’Toole and Meier106 show how individual network actors can work to bias the actions of the organisation in ways that are likely to benefit the select few. Other authors note that these homophilous tendencies (e.g. the tendency of individuals to associate and bond with similar people), replicate the characteristics of friendship networks and speculate that these interactions are less likely to provide novel ideas. Such dynamics could therefore hinder knowledge mobilisation.
The critical importance of leaders’ personal networks to foster collaboration
To the extent that leadership in networks requires first and foremost the management of social relationships, the nature and dynamics of the personal networks of formal leaders become of paramount importance. The focus here is on how formal and informal networks intersect, that is, how leaders’ personal friendships, prior networks and information/advice seeking outside the formal organisation influence decision-making and governance inside the organisation.
Research on this topic is mainly based on quantitative methods, statistical analysis, modelling and SNA. We found that attention was given to investigating the effects of network homophily and heterogeneity on knowledge mobilisation and innovation. Heterogeneous ties are those that exist between actors who are different in terms of their personal attributes and so are, theoretically, more likely to offer diversity in terms of resource or knowledge flow. Homophilous ties, by contrast, arise between like-minded and/or similar actors.
The extant research suggests that top managers use their homophilous friendship networks both for social support and to gain influence within their organisations, but may also use them to promote innovation. 107–109 Pre-existing networks are especially critical when leaders occupy new positions and in the early stages of the establishment of new organisations. This is because the maintenance of friendship ties between top executives allows them to connect to leaders of other firms, enabling the new organisation to quickly tap into a large network of sources of ideas and support. 110 There is also evidence of ‘rich social networks’ between senior managers being used for support and for the exchange of information, ideas and experiential knowledge. 111 This has implications for our project because it provides evidence that top managers use external and homophilous friendship networks for social support and to gain influence, but that the pursuit of these personal networking strategies goes hand in hand with the establishment of ties that can benefit the organisation. Thus, we need to remain sensitive to the pros and cons of homophilous networks; on the one hand, they may act as sources of support and speedy knowledge exchange for senior managers leading new organisations, but, on the other hand, they can emulate old friendship networks and therefore limit exposure to new ideas if senior networking remains too closed and clique based.
A common consideration within this stream is that, because leadership networks become increasingly more homophilic with seniority, it may be very difficult for people at those levels, even with best intentions in mind, to avoid compromising effective governance at the expense of interpersonal ties. 112 In short, homophily has its own downside and the risk is that the same networking parts are reproduced and this can become a liability for initiatives that aim to establish new relationships and break down existing barriers.
Although homophilous ties offer one type of advantage, heterogeneous networks can benefit individuals and organisations in other ways. High-performing managers tend to rely most on selective but heterogeneous network ties for knowledge and innovation activities. 113 The compositional diversity offered by heterogeneous networks is crucial. A study of board member social networks found that the number of connections held is less important than the diversity of perspectives brought to the table through these ties; the latter provides a strategic context for decision-making that is the greater influence on corporate governance. 114 The degree of trust is an additional, important variable. 115 In other terms, firm performance is actually enhanced by CEOs seeking out contacts who are likely to offer perspectives on strategic issues that differ from their own (i.e. heterogeneous networks). 116 For example, a study of R&D expenditure found evidence of the clustering of innovation policy among firms whose directors have homogeneous networks. 117 This type of clustering may be encouraged in transitive network structures, in which friends of my friends are also my friends. Transitivity in manager social networks is important for idea generation but not validation. 118 There may be a further drawback to such structures if they result in powerful senior leadership cliques that stifle innovation. 86
Antecedent networks of leaders may have implications for networking and networking strategies, especially in terms of the alliance formation. 119 A study of academic spin-offs found that the prior social networks of the founders, especially the networks of the board’s chairperson, influenced board formation. 120,121 Examining an university–industry collaboration, Østergaard122 shows how engineers tend to use previous contacts rather than those provided by the formal collaboration. Müller et al. 123 make very similar observations, the key idea being that the way individuals seek knowledge is largely dependent on antecedents to the current situation, and previous actions and decisions.
To summarise, personal networks present a significant variable in determining the likelihood of effective innovation and collaboration. Homophilic networks offer opportunities for co-ordination117,124 and transitive networks,105 but are more susceptible to abuse and misuse. 121,125,126 Heterogeneous networks appear to enhance information processing, but rely heavily on diversity of their constituent parts. 114 However, both types of networks build on antecedent networks of leaders, especially when alliances come into play,127 thus bringing the environmental conditions within which networks exist to the fore.
How to lead mandated networks
In our review of existing research on leadership agency in knowledge and innovation networks we found that very little research has been published on formal leadership in mandated networks; studies on formal leaders in knowledge-intensive firms are much more common. As we noted above, questions about formal managerial leadership and agency in mandated networks remain the ‘800 lb gorilla in the room’. 100
Early research in this area tended to be exploratory. A qualitative study of leadership in four community care networks found that leadership in networks can be differentiated from that found in traditional hierarchical organisations because, in the former, membership is voluntary and egalitarian and often entails co-operation by organisations with different cultures and agendas, and network leaders often lack formal control over members and their actions. 128,129 A literature review of cross-sectoral interorganisational partnerships in health-care domains warned, in particular, that the form and functioning of a collaboration is contingent on its ‘strategic intent’ (the reason for its organising), which may change over time,130 especially given the probable internal epistemic plurality and network decentralisation of these collaborative forms. 131 Leadership processes and style should therefore align with the strategic intent according to the principle that forms should follow function.
More recently, the focus of research has turned towards how formal and informal leaders collaboratively shape the work of the network. Eglene et al. 109 explored leadership issues in four public knowledge network-based initiatives. They suggest that leadership style (charisma and adaptability), formal authority and perceived authority all affect networks’ ability to achieve substantive goals. Silvia and McGuire100 studied the differences between the behaviours of leaders when leading networks and when leading in traditional organisations, finding that when in network leadership mode these senior managers focused more on soft skills (‘people-oriented behaviours’) and less on hard skills (‘task-oriented behaviours’). Their findings are corroborated by Forno and Merlone,103 who argue that the skill sets required to lead networks are different from those needed to lead firms. The authors conceptualise leadership through the entrepreneurial agency of network members and argue that the orchestration of innovation networks involves collective interplay between structure and agency. In another study, Considine and Lewis132 found that formal leaders (political bureaucrats) in innovation networks recognise the potential leadership opportunities and role agency that their network positions offered to them in terms of decision-making, advice and ‘co-ordination of effort and relevant input across domains’. Brokerage potential was clearly understood as a role facilitating ‘strategic linkages’. The authors conclude that the leaders’ perceptions of their roles and associated agency accord with both the potential inherent in their network positions as well as actual activities known to increase the success of collaborative activity. 132
Studies on informal emergent leaders therefore suggest that one of the skills critical for leaders to operate in network conditions is a clear and accurate perception of the social system they operate in. In other words, how leaders understand and interpret their networks is paramount to their effectiveness. This point is argued quite strongly by Balkundi and Kilduff,133 who emphasise the importance of being aware of one’s own network position and the social structure one operates within. They suggest that networks are both actual structures of relationships that link individuals and cognitive structures in the minds of individuals (p. 434). 133 The (cognitive) perception of the state, and of personal organisational and interorganisational networks, leads individuals to pursue and maintain certain relationships, or to launch or avoid certain initiatives. Similarly, Cross and Sproull118 claim that social networks and cognitive motivation to realise network opportunities are linked to individual differences in personality. Finally, Long et al. 134 call for attention to be paid to the leaders’ self-perceptions in order to help explain differences in managers’ motivation to realise the potential benefits that exist in their social networks (i.e. social capital plus personality).
Other research involving the role of formal leaders in mandated networks has investigated the link between leadership and strategic intent in terms of the development and performance of mandated knowledge networks. Martin et al. 99 studied leadership and public–service networks (a comparative case study of cancer–genetics pilots in the English NHS) to highlight the importance of dispersed leadership in achieving change in a networked public–service setting. They argue that this dispersed model allows leaders to be effective in achieving change not only through the network’s formal structure, but also to facilitate complementary action in other organisational forms that coexist alongside the mandated network.
Last, in more recent studies, again relating to scientific research collaborations (CLAHRCs), there is evidence that the epistemological leanings of formal leaders combined with the antecedent conditions around the initial bid and senior team involved in this conception, influenced how the network evolved. 135 CLAHRC directors and senior teams actively built governance mechanisms into their organisational models that subsequently influenced how the network came to be shaped, co-ordinated and enacted. 135 These leaders have been conceived as ‘institutional entrepreneurs,’ possessing a demonstrable degree of creative licence, albeit with more credibility and privilege than enjoyed by leaders with traditional biomedical professional backgrounds. 86 This suggests that, despite various challenges, formal leaders of mandated networks do have sufficient agency in carving out a mission or vision for the network. However, although formal leadership plays a key role in agenda-setting for mandated networks, what is more important perhaps is how this is recognised and responded to by network members and how this mission subsequently shapes the actual programmes of work through which particular social network structures are constituted. 98 Similarly, Bond et al. 136 show how members’ social identification with the mandated network creates positive knowledge-transfer benefits for central organisations and symbolically affects network members’ perceptions of the network’s overall performance in light of knowledge-transfer benefits received, and as an antecedent to affective commitment to the network.
In summary, although some studies address the issue of the role, skill set and recommended conduct of those who aspire to guide or govern networked initiatives, a significant research gap exists around the actual experiences of formal leaders of mandated innovation networks such as AHSNs. In fact, relatively little is known about how the individual leadership competencies and personal networking strategies of formal leaders impact a network’s knowledge mobilisation and innovation activities. This evidence vacuum around how to lead mandated innovation networks has meant that there is no operational blueprint to accompany policy initiatives and learning is thus likely to be experiential, ‘on the job’ and subject to trial and error. More research is required to support leaders of mandated innovation networks who are tasked with engaging stakeholders without any formal power and influence, and often with limited resources.
Leadership and knowledge mobilisation
One of the main aims of the present research is to shed light on the process of knowledge mobilisation, here defined as ‘any attitude or action – joint or individual, observed or imputed – that prompts new and important knowledge to be created, elicited, shared and utilized in a way that ultimately brings a shift in thinking and collective outcomes’ (p. 2451). 137 As we have seen above, the literature considers a number of roles that different actors play in the process (institutional entrepreneurship, brokers, boundary spanners, knowledge activists, change agents and opinion leaders). However, less is known about how to trigger, stimulate, energise and govern such processes, all of which are tasks that we could subsume under the idea of ‘knowledge leadership’. We thus know little about whether or not formal leadership roles and informal knowledge leadership tend to overlap.
A recent exception is worth mentioning. Dopson et al. 12 identified processes of knowledge leadership among managers and clinical hybrids at different levels in the UK NHS and non-NHS health-care organisations. They found that an important competence was brokering the movement of knowledge across distinct knowledge domains, epistemic boundaries and institutions, which encouraged knowledge use by more than one organisation, unit or profession. According to the authors, ‘epistemic boundaries’ refer to boundaries between different knowledge domains and ways of knowing associated with, for example, different professional backgrounds, cultural provenance and research practices. In health care, epistemic boundaries can be found between administrators and clinicians12 as well as between different professional groupings with different research orientations and backgrounds. The researchers therefore go on to ask: how do leaders influenced by management research and ideas mobilise such knowledge into practice?14 The leaders they identified12 often had a strong desire for formal knowledge or a ‘will to know’, apparent throughout their personal biographies and developed over time. For example, KLs might complete PhDs or write and publish articles and books on a topic of special interest. However, these individuals were not merely facilitators and translators of formal management knowledge and research, but rather, personally deeply immersed in – and committed to – producing and diffusing knowledge to drive change in health-care organisations and systems.
In summary, an increasing number of authors are now focusing on formal and also emergent forms of network leadership, that is, how to lead the organisations that are charged with facilitating, brokering and supporting the development and mobilisation of innovations. However, almost no attention has been devoted to how to lead and facilitate these processes and we also know little about the role and characteristics of KLs in such settings.
Discussion and implications for the research
The literature review provides a number of valuable indications for our research. These include both the issue to be investigated and approaches and sensitising concepts that can be deployed to deepen our understanding of such issues. Among others, the following are worth noting.
Expect and study variance
The literature strongly suggests that we should take a non-linear approach to the study of the diffusion of health-care innovation that gets beyond a simple ‘technology push’ approach. At the organisational level, we should study the local implementation of AHSNs as they are represented in particular sites, as earlier studies attempted to do with the first tranche of CLAHRCs (evident in a cluster of papers in the policy stream). One of the critical messages emerging from our review is that the implementation of policies such as the one that established the AHSNs requires some form of local adaptation and translation. 138 Accordingly, variation is something to be expected and thematised in our study, and great care should be taken so that variation is not addressed in evaluative terms (as something negative or positive), but rather taken as a factor that needs to be understood and explained. It is worth adding that the literature also offers some sobering views on the possibility of replicating the success of one type of collaborative initiative across different contexts. Difficulties and challenges in policy implementation are therefore to be anticipated and treated as points of interest, as well as opportunities for learning.
Balance attention for process and agency
The literature review suggests that in distributed and non-hierarchical organisations, like the AHSNs, organisational routines and human agency have a central role. Accordingly, there is the need to balance the view of approaches – such as ABCA – with an attention to the roles of individuals in promoting and sustaining knowledge mobilisation and innovation diffusion. Understanding and clarifying the organising logic underpinning knowledge mobilisation processes and efforts is also critical. This for two reasons: first, ‘clear organizing vision is important to enable leaders to unite multiple stakeholders and enable effective communication of common goals’;85 and second, ‘clear vision enables leaders to develop and articulate a clear strategy for achieving KT goals’. 85 However, the literature also cautions about relying on the accounts of leaders and suggests the need to triangulate the assertion made by managers and other stakeholders with the analysis of actual instances of practice so that possible discrepancies may emerge.
Focus on the personal networks of managers and their cognitive dimension
As we have seen, the literature confirms our original intuition in our research proposal that network concepts and SNA techniques are a promising way to study initiatives such as the AHSNs. SNA promises, in fact, to provide novel and useful means for understanding the structures of influence that impact the implementation of policy process, but also knowledge mobilisation and innovation diffusion on the ground.
Attention should be paid to key concepts in SNA, such as homophily and heterogeneity, that encompass a formal exploration of network transitivity (how people ‘use’ friends of friends to carry out networking activities). Of particular interest is the impact of network heterogeneity among VSMs and emergent leaders, especially in terms of delineating the types of ties and attributes associated with knowledge and innovation mobilisation (i.e. what type of knowledge flows in heterogeneous networks compared with in homophilous networks?). Studies conceptualising activity in mandated networks as analogous to constellations139 suggest that a ‘small worlds’ analysis might be useful, by highlighting under what conditions networks might emerge and for what purpose (i.e. development of ideas, implementation). These nuances may bring us closer to understanding the characteristics of senior management alliances that are the locus of innovation. They may also help us to explore and comment on the dark side of networks and the capacity of homophily and other network processes to stifle innovation. The literature certainly alerts us to the reproduction of existing networking patterns that can constitute a hindrance for initiatives like AHSNs, as new possibilities and potentially valuable outliers may be unwittingly ignored or undervalued. In this sense attention to the cognitive dimension of networking – that is, exploring the perception of personal organisational and interorganisational networks – is critical as this may influence individuals to pursue (or avoid) certain relationships or initiatives.
Second, more is to be learnt about the brokering and absorption of knowledge across distinct knowledge domains, epistemic/professional communities and institutional boundaries, and associated leadership challenges. Our review of the literature revealed a sizable body of literature on knowledge brokers in both mandated networks and knowledge-intensive firms, alongside an additional category of papers on networked leadership. Attempts to tease out further the points of unification between these literatures will help to inform collaborative or membership forms of leadership that bring together a diversity of players across different sectors and industries in a wider knowledge economy.
What makes a (good) leader of a knowledge collaborative and/or a knowledge leader?
The literature also suggests that little research has been conducted to date on the networks and networking strategies of formal leaders of mandated networks charged with knowledge mobilisation and/or innovation remits. Interestingly, research has mostly focused on investigating the role and activities of informal (but not formal) leaders in knowledge-intensive networks, leaving space for inquiry into formal leadership and its influence. Topics for research, for example, are the skill sets of leaders and the extent to which these depend on whether they are leading networks or traditional organisations. We may also ask:
-
How do formal leaders of mandated networks perceive their network position?
-
How do other individuals perceive a leader’s power and influence?
-
Are formal leaders homophilous, or are they open and heterophilous in their networking?
-
What about the governance structures such as boards – are they closed and homophilous, or open and heterophilous?
-
Are the structures of an individual’s own personal network related to how innovative he/she is viewed as by others?
The literature review also revealed a dearth of studies on KLs as distinct from the leaders of collaborative or knowledge mobilisation initiatives. Indeed, there are plenty of indications in the literature that these roles may be distinct, although, occasionally, they may be played by the same individuals. This raises a number of further important issues:
-
What are the differences between network leaders and KLs?
-
What aspects of a person’s biography and career make a difference?
-
What makes a person an especially effective KL in the first place?
Finally, several strands of the literature – from studies of knowledge mobilisation from an ecological perspective11 to CASs,55 to the analysis of existing initiatives such as AHSC and CLAHRCs – indicate that knowledge mobilisation is a multilevel phenomenon that requires both vertical and horizontal connectivity. In this sense, the literature review invites us to explore not only knowledge leadership within given units and organisations, but also leadership across systems and initiatives. Questions in this vein include:
-
Are there KLs spanning the health-care economy?
-
Who are they?
-
What makes them different?
-
What practices and processes do they use or take advantage of?
Chapter 4 The policy landscape of health-care innovation and its evolution: the perceived role of Academic Health Science Networks
This chapter examines national-level life sciences, economic and health policy developments to help us understand how the mandate of regional-level AHSNs was constructed at a national level through analysis of key policy documents. We will also pick out implications for what were seen by policy interviewees as a preferred leadership style in the AHSNs and also those theories and models of knowledge mobilisation and innovation that were seen as helpful, as these issues relate directly to our lead RQs. Our protocol indicated that we wanted to explore this policy-related theme as one of our initial WPs. See Chapter 2 for further detail on T1 and T2 policy interviews.
We highlight a number of key findings. Our broader thematic analysis suggests a sustained change in the content of policy as well as in the processes of policy-making found in this field. There is first an increased policy-level expectation that publicly funded health-care agencies should pursue wealth creation objectives in addition to health improvement aims. We further suggest that, from a political science perspective, the health ‘policy-making community’140 appears at least in this policy stream to be broadening beyond the DH and influential health-care professional groups to include more economically orientated central departments and also commercial actors, now recast as policy partners.
Commentary on policy documents (2003–15): the NHS innovation challenge and progressing economic growth through the life sciences
We first comment on the key policy documents (2003–15) and their construction of a narrative about health-care innovation. The health-care sector (and the NHS) is here progressively construed as being of economic importance, with recent policy papers increasingly referring to wealth creation in conjunction with health improvement objectives. 1 This strand of policy appears consistent across governments, although post 2010 there is stronger reference to supply side incentives, such as tax concessions and deregulation.
Importantly, health-focused policy texts feature contributions from three central departments of state: not only the DH, but also the then Department of BIS141 (since reorganised, summer 2016) and Her Majesty’s Treasury. 3 Some DH papers1,142 are also open to economic objectives and the strategic role of the life sciences industry, complementing what might be seen as conventional health improvement aims: ‘the NHS has a crucial role in alleviating the burden of ill health, but it also has a wider role in contributing to economic growth, specifically growth in the life sciences industry for which it is the largest customer’ (p. 8). 1
Innovation, health and wealth: building an innovation architecture in the NHS
Innovation, Health and Wealth1 is now considered further as an important text. Economic and wealth creation policy objectives are again salient. It was argued that the NHS remained slow in the diffusion of effective innovations, reinforcing the findings of the earlier Cooksey Review3 and the ‘Next Stage Review’, the latter of which was led by a leading academic surgeon with extensive experience of health innovation. 4
The NHS innovation challenge was here framed in a wider context of global financial uncertainties and rising demands on public health systems. The NHS needed to become stronger at innovation, while also improving quality, productivity and efficiency. Eight broad themes were developed,1 each reinforcing the imperative of establishing a stronger NHS delivery system or ‘innovation architecture’. This architecture should support collaboration and address a ‘delivery’ deficit by various mechanisms – including new networked organisational forms – that is, the AHSNs. These networks should accelerate NHS innovation generation, adoption and spread and ensure better working across institutional boundaries and sectors:
We need a stronger relationship with the scientific and academic communities and industry to develop solutions to health care problems and get existing solutions spread at pace and scale in the NHS. We also need to develop much stronger knowledge exchange networks to spread best practice.
IHW (p. 19)1
Innovation, Health and Wealth1 further elaborated on the need for the NHS to become more business friendly and to provide industry with a focused point of access. The NHS to should act as a major lead customer, utilising new ideas, services and products better. There was a pledge to ‘declutter’ a complex innovation landscape in terms of too many agencies and bodies.
Global competitiveness and the UK health life sciences sector: policy continuity over time
The (re)positioning of domestic health policy to ensure that the UK remains competitive in global life sciences markets is another important national-level theme in policy texts. The Department of BIS,141 for instance, wants the UK to become ‘the global hub for life sciences’ (p. 6). 141 It argues:
. . . the industry is changing and the UK must adapt so we can compete in this challenging environment. The UK must capitalise on its strengths: its world class science and clinical research, talent base if pioneering life sciences researchers and the NHS, where discovery can be translated into results for patients. The race is on and we need to move quickly to ensure the UK is where innovation happens.
Department of BIS (p. 5)141
The explicit framing of the NHS as a driver of national and international industrial investment and growth, and its repositioning as an influential macro purchaser of innovation in an internationally competitive arena, is significant. There is evidence of a continued focus on NHS R&D and its connection to economic growth in the life sciences sector over a decade of policy-making and successive governments. Best Research for Best Health,142 for example, developed a NHS R&D strategy to ‘support the Government’s ambitions to improve the nation’s health and increase the nation’s wealth as set out in the ten-year Science and Innovation Investment Framework 2004–2014’. Policy was aimed at lightening bureaucratic processes and engendering a NHS research culture to make it the ideal hub for research investment. The Cooksey Review3 also aimed to close the ‘bench to bedside’ gap, with an emphasis on translational research architecture, leading to the emergence of AHSCs and CLAHRCs.
In 2011, the policy ambition of making the UK a leader in health-care innovation and the life sciences – and an attractive location for external investors and industry – was reiterated. The Department of BIS’s Strategy for UK Life Science141 is an emblematic example of a policy output focused on the life sciences sector and written from an economic perspective. The text sees the life sciences sector as a potential source of high skill and high-value jobs, but adds that a strong science base alone is not enough to ensure commercial success:
The UK has a high concentration of research excellence and pioneering clinicians. Evidence alone is not enough. The workforce needs to create value along the development pathway. People need to have the training to meet the needs of employers and the incentives to collaborate across disciplines and organizational boundaries.
Christensen et al. (p. 18)143
There is an argument made for more connections between private firms and UK universities. UK universities are seen as key knowledge assets and as highly productive in publication citation scores (as a marker of academic excellence), with the Oxford, Cambridge and London ‘triangle’ highlighted (p. 8). 141 Perhaps the Department of BIS’s core proposals lay in its attempts to create a globally competitive innovation ‘ecosystem’, arguing that ‘new ways of working between universities, hospitals and businesses need to be developed to place the UK at the forefront of medical research now and in the future’ (p. 8). 141 Such proposals are consistent with some of the papers on regional innovation systems surfaced in our literature review.
However, there is also a focus on implementation by developing system readiness for innovation adoption at scale. As one policy respondent explained:
[‘Innovation, Health and Wealth’] was a continuation of the Cooksey review from 2006 on life sciences and really looking at the funding mechanisms to unlock some of the potential that had been created by the AHSCs, so things like the biomedical catalyst, in fact the patent box. But what ‘Innovation, Health and Wealth’ did which I thought was incredibly clever was identify the T3 [translation 3] to T4 [translation 4] adoption and uptake gap.
We see here a focus on NHS-led entrepreneurialism derived from its strong clinical research base and service needs, with attention to the system’s ability to exploit a raft of new innovations, whether derived from within the NHS or external suppliers.
Interestingly, one earlier health policy text reviewed was somewhat divergent in its approach. The DH4 tried to move concepts of quality and innovation up the health policy agenda: ‘innovation must be central to the NHS’ (p. 55). 4 However, this text did not link strongly to the economic growth agenda, although it used a broader definition of ‘innovation’ beyond EBM: ‘too often, innovation has been defined narrowly, focussing solely on research, when in fact innovation is a broader concept, encompassing clinical practice and service design’ (p. 55). 4 Service redesign is here seen as an important capability for the NHS. We note the complexity for NHS organisations in meeting these overlapping objectives of service improvement, innovation adoption and wealth creation at the same time.
We now present our other empirical data – what respondents in interviews said about this policy stream – organised around the major themes already signalled.
Theme 1: perspectives on health care and life sciences innovation policy
Respondents’ views were generally well aligned with key arguments in the policy texts discussed above. They talked about this stream being on the long-term policy agenda since the early 2000s, but having now gained increasing importance, as reliance on mainstream efficiency measures is not sufficient to transform old NHS service delivery patterns at the pace and scale required through Quality, Innovation, Productivity and Prevention.
Respondents often stated that the NHS was good at inventing new treatments or products, but poor at spreading them. Scaling up innovation remained a challenge. Therefore, weakness in innovation diffusion was a long-term problem that had provoked various policy responses, now including the AHSNs:
. . . you could see AHSNs as just being the latest manifestation of a way of trying to address this issue of how do you reach the value, how do you address the very poor uptake of innovation . . .
Three concrete examples of the slow diffusion of even evidence-based innovative treatments in the NHS were given by respondents: novel anticoagulants, denosumab (a new drug for secondary bone cancers) and sofosbuvir (a radical new drug for hepatitis C). Some respondents reported frustration that pharmaceutical companies are bringing to market some evidence-based products with the potential to provide important health gains [and that have successfully gone through National Institute for Health and Care Excellence (NICE) appraisal], but that the NHS as a system is too slow to adopt them.
Interestingly, as explored later, some respondents noted a switch of interest from conventional incremental innovation to more radical, open or disruptive mode of innovation (Christensen143,144 was seen as a key author) promoting ‘. . . innovation in the radical sense of innovation, innovation outside a drugs, devices and software type innovation.’
Radical innovation included new service delivery modes, such as telemedicine or primary care polyclinics. The self-management of long-term conditions (LTCs) was cited as a significant area in which medical applications could transform service delivery. Concrete examples of science-led disruption were given:
Some of the new bio pharma technology is now disruptive because the science has got better . . . NOACs [new oral anticoagulants] are a case in point, they disrupt a pathway of care.
More radical innovation was advocated because traditional efficiency-based measures are insufficient to deal with the current challenges: ‘what would be achieved by simply making the system more efficient, dragging everyone up to the top decile or top quarter of performance?’ The argument was for bolder innovation, although we comment that reliance on disruptive technology to drive change143,144 may appear unfamiliar to a NHS system that has historically prized system stability and that has strict guidance around the procurement of new medicines and technology.
The strategic importance of the life sciences sector for economic recovery
The Department of BIS was seen as having its own economic policy priorities. One interviewee remarked: ‘BIS’s goal is to keep big pharma here’. Another argued: ‘we fell off the cliff last year because of Pfizer mainly [referring to the decision by Pfizer to close its manufacturing plant in Sandwich, East Kent, with the loss of highly skilled jobs] . . . they gave notice and they were out of the country in 12 weeks’. This relocation decision helped to make the retention of the biopharmaceuticals sector within the UK into a major policy issue.
Echoing the Department of BIS,141 respondents repeatedly emphasised the economic importance of the UK life sciences industry, with its big export market: ‘we probably have about 90,000 jobs in the UK . . . R and D investments are about 5 billion a year in the UK . . .’. However, successfully exporting products abroad was dependent on prior adoption at home by the ‘sluggish’ NHS; ‘. . . that market will ask “so does your home market buy it?”’.
In 2005/6, partly because of European directives, growing concern within the biopharmaceuticals field was reported about excessive regulatory obstacles to speedy recruitment into stage 3 clinical trials: ‘so all the big pharmas were basically saying “we have to go to the Far East or wherever to do our stage 3 clinical trials, because you do not do them any more”’. The new AHSC/AHSN configurations could, it was argued, deal with this gap in a legally sound way and provide industry with some reassurance about appropriate levels of regulation.
The recent creation of an Office for Life Sciences (OLS) (2014), explicitly linking the DH and the Department of BIS, appears to be an additional important change in the top-level institutional architecture which was generally welcomed by respondents, as it was seen as reflecting top-level political support for progressing the health and life sciences sectors within both ministries. One respondent argued that the then OLS minister:
. . . had transformed the environment because now we have the DoH and BIS talking to one another, and now we are seeing far more involvement from the Treasury as well. What I would be really interested in is seeing the next iteration which is where the Department of Work and Pensions starts getting involved.
Greater Department of Work and Pensions involvement in the future was seen as helpful because of issues of worklessness and keeping people healthier for longer in older age.
The OLS was, at the time of the study, physically based in the Department of BIS, although the minister spanned both departments (the Department of BIS and the OLS were subsequently reorganised in a summer 2016 reshuffle). Later policy advice (such as the interim report of the AAR145) also highlighted the need for greater integrated working across central government departments and a focus on ‘the growth potential around health and around life sciences in the UK’, as one respondent described it.
Health and wealth, or wealth versus health?
Respondents suggested that the health community had traditionally defined its contribution to economic growth rather minimally in terms of reducing rates of sickness at work (e.g. dealing with lower back pain) and supporting a productive workforce. Indeed, alignment or possible tension between health- and wealth-orientated policies was explored during interviews:
I think ‘Innovation, Health and Wealth’ is a moment of trying, of believing – as its title suggests – that there was a win/win situation between health gain and wealth gain. That somehow if we brought some of the large and small private sector players into a closer partnership with the NHS, if we managed to get translation right, that not only would the health outcomes of the British public improve but so would UK PLC [private limited company].
However, there was a risk that innovation and wealth creation would be ill received in the NHS or misunderstood:
So the intent behind IHW I think is very good. I think the idea that you can simultaneously improve health and improve wealth is a correct concept but it is not an easily marketable concept in the NHS for which the word wealth is synonymous with private sector profiteering.
Other respondents were more critical of the double-headed policy agenda:
. . . there is a policy divide that is submerged in IHW between a life sciences strategy on the one hand and a transforming health care strategy. They are not one and the same thing.
A more health improvement-orientated respondent gave a different view:
. . . of course, there is a wealth agenda in there, that is important, but fundamentally for me it is reducing variations in outcomes . . . to enable that, it is the acceleration of diffusion and uptake . . .
So, there was no consensus about whether or not the health and wealth streams could be readily aligned, particularly not in the early T1 interviews when AHSNs had only recently been licensed and not yet begun to bring their large remit of health/wealth enhancement into operational practice. Indeed, it may be too early to make a full assessment, especially given the complexities found in the health innovation landscape, which cuts across multiple institutional and community interests.
We also note that despite welcoming the aims of IHW – especially increased innovation adoption in the NHS – interviewees reflected that the policy was somewhat thin in terms of describing how AHSNs could achieve health improvement and wealth creation objectives together. Over the course of the study we witnessed AHSNs integrating these aspects through a learning process of discovery at local level. As one person noted:
I don’t think they [policy-makers] fully recognised that adoption of innovation is really hard and it’s really boring and I think the boring component is often overlooked . . . I think what Innovation, Health and Wealth failed to recognise is that the hard part needed to be done by roll up your sleeves operational people rather than leaders, and it needed to be done bottom up rather than top down.
Theme 2: achieving a co-ordinated innovation strategy for the NHS
Respondents also reflected on challenges faced in building a co-ordinated innovation strategy in the NHS. One problem is that there appears to be a recurrent pattern of rapid agency creation and then dismantling in this field. AHSNs1 built on the earlier AHSCs, set up just 3 years earlier. 4 The older Health Innovation and Education Clusters (HIECs) lasted only a short period of time. Smith146 recently recommended that the national service improvement agency NHS IQ (set up only in 2013) be abolished and some of its functions absorbed by the AHSNs.
Shortly after the establishment of AHSNs, NHS England147 proposed two new programmes to encourage radical health-care innovation further: innovation ‘Test Beds’ to host experiments alongside AHSCs and AHSNs; and ‘Vanguards’ trailing new care models (some 50 high-profile sites have now been established across England). In addition, ‘green-field’ sites in health and social care ‘new towns’ were to provide opportunities for radical service redesign.
It is perhaps for this reason that interviewees (in both this WP and the study more widely) were sometimes candid about the lack of joined-up innovation policy:
. . . the history is frankly of inconsistent funding, rapid institutional change and a reoccurrence of the sort of policy loop where institutions which seem to do a particular job are disestablished and then re-established with a different name.
. . . a very messy landscape of interlocking and overlapping institutions whose job it was to promote innovation.
The NHS was often seen as too short-termist, which created weaknesses in the innovation space. The long-term nature of the ‘innovation journey’51 was highlighted, including the development of a body of tacit knowledge as well as formal evidence perhaps taking place over a 20-year period:
. . . so what you have is a journey of an innovation or an idea which can take 20 years and often does, which includes the accumulation of evidence that it works but also the accumulation of knowhow about how to do it, and particularly complex innovations and service innovations that have multiple components.
Short-termism reflected intense operational management overload: ‘the pressures on the system, the incentives to do imminent things rather than longer term things. There are very few true incentives on people working in an NHS context to think long term, although the system as a whole has to . . .’. This pattern was evident in the innovation policy and regional development space too: ‘this whole thing of setting up institutions to do innovation and then killing them off again’. Frequent reorganisation eroded the organisational memory and core competences needed to foster a good innovative idea over the longer term. Overall, the picture was of a NHS innovation landscape that was ‘unnecessarily crowded’ and too often reinvented.
Rather, there was a need to align health policy better between different streams, including the financial regime (the present tariff-based system – Payment by Results – can pull activity into hospitals rather than away from them, undercutting innovation policy and models).
Consequences of agency short termism
Academic Health Science Networks have already been reviewed in their brief life. The review, chaired by Smith,146 restated their continuing, but subtly changed, role: ‘Their role should be: to support health systems to improve the health outcomes of their local communities and maximize the NHS’s contribution to economic growth by enabling and catalysing change through collaboration and the spread of innovation and best practice’ (p. 8). 146 The AHSNs should become ‘a single point of local access for improvement for commissioners and providers in their local areas’ and work with Strategic Clinical Networks (SCNs) (p. 7). 146 These shifts of mandate mid-way through the licence period had the potential to push AHSNs closer to NHS improvement partnerships and possibly away from industry.
Therefore, not only were AHSNs coexisting in a still cluttered innovation landscape, but, importantly, they were set up on only 5-year licences and their initial funding allocation was reduced shortly after set-up. Because the NHS field was seen as demonstrating rapid agency succession, there was a danger that the AHSNs would be perceived by stakeholders as of only momentary significance, at the same time at which AHSNs were trying to broker meaningful strategic partnerships (including with industry), as one respondent put it: ‘we will watch and we will play carefully with the AHSNs but we are not yet convinced that they are getting the traction in the system’. A respondent who was working closely with the local AHSN commented during a later interview:
So for me it’s all about giving them long enough to really show some significant downstream benefits, because I think that the signs are that they would come, but to judge them on 3 or 4 years’ performance I think would be dangerous.
In this respect, the message from the interim report of the AAR145 that the wholescale reorganisation of the AHSNs should be avoided is important and consistent with the views of most respondents.
Very early results from a national IHW evaluation35 suggest that AHSNs so far have been broadly well received and could be seen as a ‘high-visibility’ theme within the overall suite of IHW WPs, although concerns were also expressed about AHSNs’ broad focus. The need for AHSNs’ transition to self-generated funding in the future was seen as potentially deflecting them away from core innovation-spreading objectives.
Theme 3: commentary on Academic Health Science Networks – opportunities and challenges
We consider some positive features of the AHSNs reported to us in interviews and then some challenges. We note that some observations were made in the T1 period (early 2014) when AHSNs were very young. We incorporate later insights from T2 interviews and also comment elsewhere in the report on AHSN development over time.
A potentially important role in the health-care innovation ecosystem
Academic Health Science Networks were seen as potentially capable of acting as novel ‘learning networks’ and vehicles for facilitating collaboration within the wider health-care ecosystem. They could draw on good practice derived from the earlier experience of managed clinical networks, such as in cancer and cardiology, and fitted well with a stream of work nationally on research translation and KM. We observe that managed networks – with their emphasis on horizontal relations and collaboration – therefore remain an important development in the health-care field5 that have endured.
Academic Health Science Networks’ regional scale and outlook was seen as a helpful feature: ‘One of the things I see the AHSNs doing is helping the export wealth agenda and the inward investment wealth agenda. And I think the access to the health and social care network on a geographic footprint is very, very, important’.
Academic Health Science Networks also help to reinforce evidence-based knowledge and cutting-edge science in the NHS (e.g. genomics) and in health services redesign: ‘so part of the networks is as an organizational development vehicle, to get services out of acute and into primary care, embed the science, move the science in, and bring in the genomic centres, mobilise the genomics service’.
However, AHSNs will need time to effect the cultural change necessary across what are large regions:
. . . the main opportunity for them I think has to be about spreading innovation within the NHS or prising open a non-innovative culture . . . so how do you make the NHS more pro innovative at the same time as sending out signals which are all about standardisation. That is the issue, which is can you have standardisation and excellence, it is the ultimate conundrum.
There was widespread appreciation of the difficulties AHSNs were confronted with among those stakeholders closest to them, but also some lasting confusion about AHSNs’ remit among the more distant stakeholders. Respondents suggested a set of linked organisational concepts to characterise what AHSNs were engaged in. They used such terms as ‘learning and change networks’, ‘translation’, ‘knowledge-based organisations’ and ‘an organisational development vehicle’. Despite having communication and stakeholder engagement strategies, AHSNs’ multitudinous activities and brief could often confuse outsiders.
Finally, various respondents suggested that AHSNs could helpfully ‘loosen up’ an innovation-resistant NHS system: ‘prising open a non-innovative culture’. The NHS was slow to take up innovations, even those that were approved by NICE and that were evidence based and cost-effective. AHSNs could possibly market such innovations and stimulate interactions between producers and consumers, thereby promoting ‘a market place in ideas’:
. . . so one of the pervasive myths or ideas that bedevils the space of innovation is the idea that good ideas sell themselves: even the most well evidenced in the world which are probably pharmaceuticals, the companies that sell them spend more money on marketing than they do research. And nothing sells itself. So one of the problems is that the system is critically under resourced to allow people who might be potential users for innovation to find out about them.
Horizontal integration or back to hierarchy?
A few respondents explored early on (T1) whether the AHSNs were indeed ‘managed networks’ or whether they might revert to becoming hierarchical, regional vehicles, given a vacuum at that level. Top management’s desire for system stability could lead to AHSNs evolving in this quasi-hierarchical direction:
. . . there is also a tremendous pull back to hierarchy as a way of organizing things, partly because of time spans and incentives and partly because it is the default way of organising something when you have not thought about it very much, it is our default option . . .
These two models of vertical functioning (top-down led) and horizontal functioning (laterally based) had distinctive implications, leading to:
. . . those two different notions of what a AHSN might do, you might call them horizontal and vertical would be measured respectively by the tracking of particular innovations that they champion versus a broader social network analysis of the capacity of the system to pick up innovations and put them into practice.
However, during the period of this study – at least across the five case studies we tracked – a move back to hierarchism was not identified. AHSNs instead had a strongly regional, lateral focus, which reflected their membership and partners.
Ascertaining collective impact and commercial nous
The need for coherence and sharing across AHSNs was emphasised. The ‘network of networks’ was created during our study as a national forum for the 15 AHSNs, and we observed over time efforts to metricise AHSNs’ collective contribution on an agreed internetwork basis. One calculation reported to us from across the 15 AHSNs in an AHSN Networks document was that, since their formation, the AHSNs had leveraged £144M from various funding sources (both public and private sectors) and projected to save the NHS £54M. On these projections, AHSNs effectively recouped their running costs.
However, some private sector respondents and SME representatives felt that the AHSNs were still not commercial enough or delivering quickly enough given that the NHS remained recalcitrant to new products and ideas, and the adoption system was extremely complex for outsiders to navigate. Such comments were not necessarily a direct criticism of AHSNs per se, but rather suggested frustration with the pace of change. Respondents throughout the study – especially those close to or working within the NHS – expressed a deep knowledge of the internal problems experienced across the NHS innovation pathway. One commercial lead in a hospital described the situation thus:
[it is] very challenging to get through the decision making process in the NHS to get some ideas approved. And of course naturally as a hospital, they are traditionally risk-averse because all the training goes, it’s all about minimising risk and not taking risk, and of course when you’re in to the field of innovation, it’s actually about taking risks.
Academic Health Science Networks within their regional innovation systems
Respondents frequently characterised the different regional innovation systems within England and discussed them in a lively fashion, so there is a geographical lens in understanding the enactment of innovation policy within distinct regional contexts. AHSNs sat within these regional innovation ecosystems, which were difficult to reshape over the short term.
The distinction was often drawn by respondents between the so-called ‘golden triangle’ of top-tier universities and connected ecosystems and others. The extent to which other systems (notably Manchester) could carve out a strong presence or potential niche was discussed. A difference was also drawn between those AHSNs that were co-located with a pre-existing AHSC (generally seen as an advantage) and the others. Later on, as central government policy moved further towards localism and ‘city growth deals’,148 this geographical focus became even more apparent, for example through AHSNs’ closer working with LEPs, which appeared to be important in some of our case studies.
Additional regional tiers: ‘MedCity’ and ‘DevoManc’
Our T2 interviews examined what appears to be the further growth of a regional tier of governance in this field. A first example of a strongly regional perspective is MedCity, which focuses on London and the wider south-east (including Oxford and Cambridge: URL: www.medcityhq.com/). This brings together a number of key partners at the regional level of governance, such as academic institutions, industry and the Mayor of London’s office. Its website defines its core role as follows:
MedCity is a collaboration between the Mayor of London and the capital’s three Academic Health Science Centres – Imperial College Academic Health Science Centre, King’s Health Partners, and UCL [University College London] Partners.
MedCity
Launched in April 2014 to promote and grow the world-leading life sciences cluster of England’s greater south-east, it is promoting life sciences investment, entrepreneurship and industry in the region by:
Providing a single front door and concierge service for industry and investors looking for partners, infrastructure and expertise
Facilitating and supporting collaboration across all parts of the sector to turn innovations into commercial products and services
Fostering an environment that supports and encourages entrepreneurialism
Raising awareness globally of the region’s rich life sciences ecosystem.
MedCity
Indeed, there was a clear policy move enacted during the course of this research – under the post-2015 Conservative government, but building on earlier Coalition policies – towards regional devolution in England, most clearly symbolised by a ‘Northern Powerhouse’ in Manchester with a devolved health and social care budget of £6B, and a revised constitutional agreement with central government. Thus, we see evidence of greater policy attention on attracting business and foreign investment beyond the south-east to help rebalance the UK economy and stimulate growth across major cities in England. It was reported to us that the four northern AHSNs ‘are working together incredibly well’ as a significant cluster to take advantages of these opportunities as a collective grouping.
Theme 4: preferred Academic Health Science Network leadership style and knowledge mobilisation/diffusion of innovation models and approaches
Comments on Academic Health Science Network preferred leadership style
Respondents were asked about what they saw as a preferred leadership style for AHNSs. First, a cluster of responses distinguished between leading a more conventional setting such as a NHS FT and a network-based setting such as the AHSN, often referring to ‘soft power’-related concepts such as social capital and strong network-based relations (which might take time to build up). Examples of quotations include:
. . . well, the AHSNs have no powers . . . they are networks and the ability to build those networks would be crucial to the allegiance of those networks. The very fact of their existence proves nothing, so can they build the relations? So take someone like (admired network leader) at (AHSN X), he has invested huge amounts in relational capital or building relational capital inside that network. That is what he has been about, getting all these people involved.
An ability to work across three very different communities, NHS, academic and commercial, was seen as important:
. . . you have got to bring together three different types of philosophy, one of which is commercial, one of which is service provision and one of which is academic. And therefore the type of person you need in that role is someone who can work across all three. And those people are not easy to come by. The ASHNs have got some good people in place, in some of the places I have seen.
Another respondent suggested that:
. . . an openness and willingness to believe that industry collaboration can make a difference.
Second, their role was seen to be more an entrepreneurial and catalytic one than a conventional NHS service delivery role:
. . . we should be looking at them as being slightly more innovative, more start up like catalysts rather than NHS delivery. So I get worried and I have heard the analogy before that ‘well, NHS Chief Execs have two and a half years as well and why would you expect any different?’ Well, being in an ASHN should be one of the most exciting entrepreneurial roles out there and it should not be seen as being a Chief Executive of an NHS Trust.
Third, preferred leadership models were more distributed than highly individualistic in nature, although it was recognised that this model cut across the dominant model found in some NHS FTs. There were instead references to building small, mixed teams. A national-level respondent referred to attempts to twin NHS-based CEOs with a part-time non-executive chairperson from outside the NHS with new contacts and skills in early appointment processes; it was recognised that it was important to engage clinical leaders too. We add that AHSN commercial directors often brought in strong track records and contacts from the private sector too. One respondent favoured appointing a visionary scientifically credible leader but one balanced by a chief operating officer figure:
[Where visionary knowledge based leaders] were supported by a general manager who was not a Joan of Arc type but more much this distributive leadership model that basically stood behind that visionary and just made it all happen (i.e. project management tasks).
Fourth, and in addition to strong networking capability, effective AHSN leaders were seen as needing cognitive/scientific legitimacy. They needed either to be senior clinicians/clinical academics, or to be credible to such persons and create a shared sense of mission:
I am pretty convinced that you need clinical leadership actually. Or rather – people interpret that in different ways. The ability to work with senior clinicians and senior clinical academics it is pretty vital to have credibility with them. Secondly, building networks isn’t the same as managing organisations so the capacity to build good relations, to build relations and social capital when you have very weak formal levers or sources of power is I think important. And thirdly, a strong sense of mission or values or goals or ambitions or whatever it may be, that can coalesce these above the inevitable sectional interests . . .
Or again:
. . . the person who leads these must be credible, must be of the body of knowledge either, you know, nuclear physics, science, genomics, medicine, surgery, but they must be credible top scientists, top medics . . . when they call a meeting people turn up and their great skill is marshalling all the experts into brigades of expertise . . .
It was considered essential that AHSN leaders should be credible in their local health economies and know how to work the key institutions. One respondent argued that ‘good’ AHSN leaders:
. . . understand the health architecture around them, number one. Number two, that health architecture has probably got respect for those individuals so they are able to have a good peer to peer dialogue . . . Number 3, they understand . . . what it takes to make this a reality . . . and number 4, they are prepared to imagine what success could be.
There was a perceived need to energise the front-line level, in part by demonstrating early success so that partners would want to invest energy in the AHSN:
I think you need to have a leadership style that will ensure that there is an engagement from the bottom up. You need to make sure that you have three or four areas in which there is a consensus of what needs to be done. You need to identify what is the low hanging fruit. You certainly have to work with the leadership of all the organisations that are partners but . . . for that to work you need to find models of innovation or whatever the level of focus, it needs to come from the bottom up.
This quotation combines some of the key features picked out already, referring to:
. . . a dispersed leadership model that you needed to pull people together to work in a network way. They needed to have the skills to bring focus and clarity across quite a broad agenda, having a very acute political sense but also being a good analyst because you are dealing with people who like evidence, part of the thing that engages them. So it was and is quite a challenging set of leadership skills.
Long-term commitment was seen as important in helping the AHSNs bed down:
. . . you need to get away from the NHS’s 2 to 3 year time horizon, 2 years is quite a long time horizon in NHS terms, and someone needs to take responsibility for the development of innovations systematically over time and this happens but not very often . . . so to take some responsibility for the longer term.
Some respondents doubted if such continuity would be possible, given the high turnover of AHSN MDs, which was already apparent by 2016, in turn seen as a response to short-term strong performance pressures and an embedded pattern of constant agency turnover:
I do worry that the pressure that is being placed on them to perform in terms of delivery or metrics is too much because . . . measuring them and measuring their activity is difficult and that is why the metrics need to be made really simple and an understanding that they cannot do it all at once, and they can’t take on all the functionalities of the existing what is, but they can do one or two things really well.
Preferred innovation and knowledge mobilisation models in use
We also asked our respondents about which theories or models of knowledge mobilisation or innovation might be useful to AHSNs. Some health sector-specific authors (e.g. Professor Muir Grey’s work on KM; Lord Darzi’s work on a global innovation index; Professor David Fish’s article in The Lancet,82 which expressed concepts more widely in use in the AHSN community; and also the work of Professor Huw Davies and Professor Kieran Walshe) were mentioned. Leading American sources of advice [Mayo Clinic; Institute for Healthcare Improvement (IHI)] were mentioned by one respondent, as were some European ‘gurus’.
More generic management authors were also mentioned, as we explore below. One respondent clearly drew on industrial cluster theory, which somewhat privileges the ‘golden triangle’: ‘one of the lessons of Castells and Porter is actually you can’t do it everywhere’. So, Castells and Porter were here cited as influential authors.
Communities of practice literature – and its affinity with notions of learning networks – was also mentioned. One AHSN was reported as having launched a COP experiment as a diffusion vehicle. Social movement theory was mentioned by one respondent. There was some interest in the triple helix model of co-produced innovation, although it was seen as more descriptively valid when applied to the ‘golden triangle’ than in the other regions:
. . . it is emerging, it depends where you are. Because if you take London or the south east where you had pre existing (links), it is happening much quicker. It is harder for the guys where there was nothing in place before, really, it is harder for them. So I would say no, not yet, with the exception of London.
Some texts by Christiansen143,144 on disruptive modes of innovation were mentioned by a cluster of respondents and also seen as descriptively valid:
. . . a lot of the pharma technology is now disruptive because the science has got better. So a lot of the technology coming out of bio pharma is – the NOACs [new oral anticoagulants] are a case in point – they disrupt a pathway of care.
Interestingly, some respondents were thoughtful with regard to how Christiansen’s ideas143,144 might need to be adapted to the NHS context, such as the mediating role of professionals and also ‘user pull’:
. . . it is interesting because he thinks that somewhere some professional values kick in to make it possible for incumbent institutions in health care to transform themselves in ways – or he did – that was not possible in the private sector.
And again:
. . . if we look at how sectors transform the way in which demand is mobilised by users, which is why Christiansen is in part interesting, because what he says is that these generally develop out of underserved or underperforming areas and so forth, and that users drag these new forms of service into being.
Some were sceptical about the extent to which such models had really been absorbed by the NHS field. One respondent active in the formulation of the initial IHW policy text reflected:
And I realised that we had not really drawn on the knowledge transfer literature as explicitly as we should have done in the design work. Intuitively it was very closely aligned but looking at it now, I would have gone back and read some of the Huw Davies and Kieran [Walshe]’s work, much more explicitly influencing my thinking in what I was doing . . .
Rogers’7 diffusion of innovation model was seen as being absorbed by the NHS – ‘they kind of understand that’ – but other (even well-cited) texts were seen as less so:
. . . there is a bit of Rogers in there partially; Christensen is not absorbed at all . . . the communities of practice stuff is talked about a lot, but I would question how seriously it is taken . . .
Some AHSNs were seen as weak in this more conceptual area:
Does (the AHSN) have an implicit or explicit theory of innovation?
No is the short answer.
One think tank-based respondent was (perhaps unsurprisingly) most interested this area, suggesting two further streams of literature or models. The first was the organisational process model of a long-term ‘innovation journey’:
. . . there is no such thing as an actionable product without an actionable service to go with it. So what you have is a journey of an innovation or idea which can take 20 years and quite often does which includes the accumulation of evidence that it works but also the accumulation of knowhow about how to do it . . . it is institutional or tacit knowledge.
The second promising concept put forward was that of regional ‘ecosystems’ for innovation, where the NHS was seen as lagging behind high-growth private sector regions, such as Silicon Valley, where:
. . . there is a whole market infrastructure around people who rate, promote, publicise, all of the intermediary work that goes on to make an economy work. And you compare that to non-market innovations in a health-care context, even some of the market innovations, and the infrastructure in processes is just non existent in comparison.
Overall, we conclude that respondents mentioned a number of authors, concepts and models, drawn from both the health-care sector and more generic business sectors (of course, both Porter and Christiansen have written both sectoral and generic texts). American authors from business schools and major American think tanks continue to exert a strong influence. Some were sceptical about the extent to which these texts had been absorbed by the AHSN field, and some AHSNs were seen as lacking a coherent model of innovation. Christiansen’s work143,144 on disruptive innovation was mentioned, as were ideas in relation to regional innovation systems/triple helix.
Overall conclusions
Our first conclusion of the policy module refers to policy content. We detect a cumulative policy stream about how the health-care sector can contribute to wealth generation as well as traditional goals of health improvement. Such policy discourse has survived various changes of government. At central departmental level, Her Majesty's Treasury and the Department of BIS have authored important policy documents, as has the DH, two of whose recent texts1,142 also strongly feature wealth improvement objectives. We suggest that ‘wealth AND health’ constitutes an important policy narrative.
Biopharmaceuticals is here construed as a research-intensive sector that could produce high-skill, high value-adding jobs in a stressed economy in which they are much needed. This economic/science focus then produces a cross-sectoral overlap of strategic themes and objectives, scattered across business, university and health sector-orientated policy documents. The creation of OLS was seen as a significant institutional development.
Second, the process of policy-making in this emergent health and life sciences ‘policy community’ deviates from the traditional analysis of the UK health policy community, as described by Ham,140 which narrowly centres on the DH and its close links with senior clinicians and medical bodies. The greater variety of players active in this health policy process is more consistent with the more recent network governance-based accounts of English public policy-making. 149,150 Our work may then be able to inform a current debate on whether or not the nature of the English health policy process is becoming more pluralist. 151
Our (admittedly early) analysis suggests that central economic departments have become important policy actors nationally in this policy stream alongside the DH, and the life sciences sector is increasingly construed as a key partner for government in health and economic policy. This policy field strongly includes industrial ‘peak organisations’ such as the Association of the British Pharmaceutical Industry, which appears influential in the contemporary policy community. There is also some early evidence of advice and involvement by ‘think tanks’ (notably The Young Foundation and Wellcome Foundation) as well as traditional DH civil servants. There is then some evidence of greater pluralism in this particular policy stream than in traditional models of the health policy-making process in Britain, reflecting an increase in the number of actors found and a broadening of policy networks.
There is some evidence of new levels of governance emerging below the national (English) level. The MedCity initiative, specifically, suggests a growing metropolitan and even supraregional level of co-ordination. Our study was too early to assess the impact of city-level devolution arrangements, but this theme should be followed up.
Theme 2 (achieving a co-ordinated innovation system) highlighted the danger of constant agency reorganisation, the multiple agencies still operating in this policy space and the danger that the remit of the AHSNs would not be clearly understood.
Theme 3 outlined some key opportunities and challenges that the AHSNs were seen to be facing.
Theme 4 outlined some leadership competences seen to be needed in AHSNs: a strength network and relationship building, a small team or distributed approach, vision and energy and also a strong cognitive authority were all highlighted as important. Some doubted that the AHSNs have a clear model of innovation and knowledge mobilisation. The work of Rogers7 on diffusion and of Christiansen143,144 on disruptive innovation, alongside triple helix theory, might be the most significant influences on the field.
Chapter 5 National knowledge networking supporting early stage Academic Health Science Network knowledge mobilisation: a macro picture
Introduction
Our first RQ focuses on the role of ‘knowledge networking’ to support the knowledge mobilisation strategies and practices of AHSNs, both nationally and regionally, with an emphasis on leadership. This chapter and Chapter 6 attempt to answer this question in part to present an analysis of knowledge networking and AHSN knowledge mobilisation at two levels: national (see Chapter 5) and local (see Chapter 6). Both chapters draw on our social network and qualitative interview data. Chapter 2 outlines these data in more detail. The social network survey and qualitative interview schedules can be found as appendices to this report (see Appendices 11 and 12 for SNA and Appendices 13–17 for qualitative interview questions).
In this chapter we provide a macro-level analysis of the knowledge networking taking place nationally within and around newly formed AHSNs. In the absence of the previously planned national AHSN knowledge exchange fora (see Chapter 2 for study adaptions), we explore the macro-level role of knowledge networks that evolved nationally across the UK to support knowledge mobilisation linked to the AHSN strategic remit around health improvement and wealth creation. We also identify who was involved in this early knowledge mobilisation and highlight the role of leadership in accessing and diffusing knowledge through networking by studying the networking activities of AHSN boards. Finally, we explore how knowledge generated through these national networks was implemented into practice by AHSNs and their stakeholders.
Insights from the literature
We develop the current literature on knowledge, networks and leadership in a number of ways.
To study knowledge mobilisation around AHSNs, we build on literatures on networked innovation systems (ecosystems, regional innovation systems, CASs) and networked leadership (distributed leadership, complex leadership). Here, the mobilisation of knowledge is conceptualised in these theories as being an interactive, collaborative and iterative process evolving through networks and network building among multiple actors. 50,152 A networked innovation systems perspective offers a broad framework through which to consider how leadership functions in national or region-wide knowledge-sharing networking and is a helpful lens through which to understand networked initiatives, such as AHSNs, which are tasked with responding to a ‘macro-level’ national policy challenge.
We thus develop these approaches using SNA to shed light on the importance of agency by highlighting the role of multiple actors (formal and informal leaders, i.e. AHSN boards and knowledge ‘brokers’) who together make a contribution to the national and regional knowledge-sharing system. In particular, the policy remit for AHSNs to deliver a step change in the adoption and spread of innovation around health improvement and wealth creation inevitably involves collaboration between NHS, academia, the private sector and other stakeholders. Capturing the structure (shape) and composition (distribution of actors and knowledge types) of knowledge networking around AHSNs can offer insights in to the highly complex nature of systems leadership as being relational and distributed because it emerges from the interaction and interdependencies among many individuals actors within these systems. 103,153
Where some previous SNA studies have focused on small/micro-scale knowledge networking (i.e. project teams, within and across firms), we attempt to capture here how such knowledge is mobilised at a national (macro) or regional level to support innovation across sectors and industries to satisfy a particular innovation remit or mandate. This reifies the importance of cross-sector hybrid networked organisational forms for transdisciplinary knowledge mobilisation involving a wider group of stakeholders (as highlighted in our literature review, i.e. triple helix, mode 2 and other). In this chapter we pay particular attention to the types of actors and types of knowledge being mobilised in the early stages of AHSN development to address the system-level challenges of health improvement and wealth creation.
We now provide a macro-level analysis of the knowledge networking found to be taking place nationally within and around newly formed AHSNs.
Early knowledge networking to support health and wealth
Key finding 1
At the early stages of AHSN development, different types of knowledge networks (with different contacts and connections) were mobilised to support health improvement and wealth creation.
Our previous chapter revealed different views in relation to the ‘double-headed’ policy agenda that sought to link health improvement with wealth creation as espoused through IHW. 1 In our interviews with AHSN leaders we found that some felt that health and wealth were interlinked in the sense that improvements could not be made in one area without addressing the other:
The AHSNs are one of the best things that was decided in Innovation, Health and Wealth, the idea of setting up 15 different entrepreneurial initiatives working on those two problems simultaneously.
AHSN chairperson
Still, not all AHSNs took the same approach: ‘We are about improving health and increasing wealth . . . and we view them as indistinguishable, but not all do’ (AHSN commercial director). Indeed, our next chapter on AHSN innovation tracers illustrates that, although AHSN innovation projects tended to serve ambitions to improve health and wealth, this activity tended to be led by one aspect with indirect outcomes in the other (see Chapter 6).
We were interested in the extent to which networks were activated, after the AHSNs had been established, to share knowledge to support health improvement and wealth creation. This networking would become integral to the unfolding of subsequent innovation projects on the ground. Our SNA revealed differences between knowledge networks supporting health improvement (Health-Net) and wealth creation (Wealth-Net) in terms of their structures and compositions (Table 4).
| Network characteristic | Knowledge network | |
|---|---|---|
| Health-Net (mature) | Wealth-Net (emergent) | |
| Composition | Strong ties: established relationships and contacts | Weak ties: new relationships and contacts |
| Structure | Diffuse, loosely structured. Regional and professional niches | Smaller and more tightly organised grouping |
| Knowledge function | ‘Multiplex’, feeding into different parts of innovation pathway | Ideas based and early stage innovation |
Wealth-Net presented, visually, as a more tightly organised structure (where individuals were mostly networking in a clustered group) than Health-Net, which had a more diffuse structure (where individuals were organised into regional and professional niches).
Networks supporting health improvement were largely based on old relationships and contacts (‘strong ties’). These networks also offered a more diverse range of knowledge-sharing functions, such as the exchange of new ideas and perspectives, the development of new products and services, and new research findings (i.e. they were ‘multiplex’ networks). This suggested that knowledge networks to support health were already well established and mature.
Networks used to share knowledge about wealth creation differed from knowledge networks supporting health improvement. Wealth creation networks comprised a smaller number of knowledge-sharing ties (65.6% relating to health improvement, compared with 34.4% of knowledge exchanges supporting wealth creation). Knowledge networks for wealth were also based on a high proportion of newly established relationships (i.e. with contacts met in the past 12 months). This was expected, given that the wealth creation challenge was newly emerging. Networks for wealth creation were mainly used for the discussion of new ideas or perspectives (rather than in relation to tangible products, services or research findings), so were not ‘multiplex’.
There was some overlap between the individuals appearing in Health-Net and Wealth-Net in the sense that some of the same people were sharing knowledge in both domains. Not all individuals were operating in both knowledge-sharing domains; however, 41% of individuals were named as knowledge contacts for either health improvement or wealth creation, but not both types of knowledge networking.
In summary, different networks were mobilised to support health improvement and wealth creation. Health-Net was loosely organised with a strong-tie base, with knowledge being shared to support different parts of the innovation pathway. Conversely, Wealth-Net was smaller, more tightly organised and based on mobilising weak ties to promote the exploration of ideas around this new challenge.
Creating a culture for collaboration: who was involved with knowledge mobilisation to support Academic Health Science Networks?
Key finding 2
Knowledge to support early-stage AHSN knowledge mobilisation mainly came from senior leaders and middle managers in the NHS, academia and industry, with a later growing involvement of individuals from other public sector domains and non-management roles.
Our social network survey peer-referral sampling strategy surfaced a national cohort of 818 individuals perceived as being key knowledge mobilisers supporting the AHSN remit at T1. The majority of these knowledge contacts were either very senior leaders (i.e. director, CEO, very senior clinician) or middle managers/clinical managers (45.5% and 42.3%, respectively), with a smaller proportion of non-managers (i.e. junior researchers, developers, trainee medics) also named (12.2%) (Figure 1).
FIGURE 1.
Important knowledge contacts by organisational role.
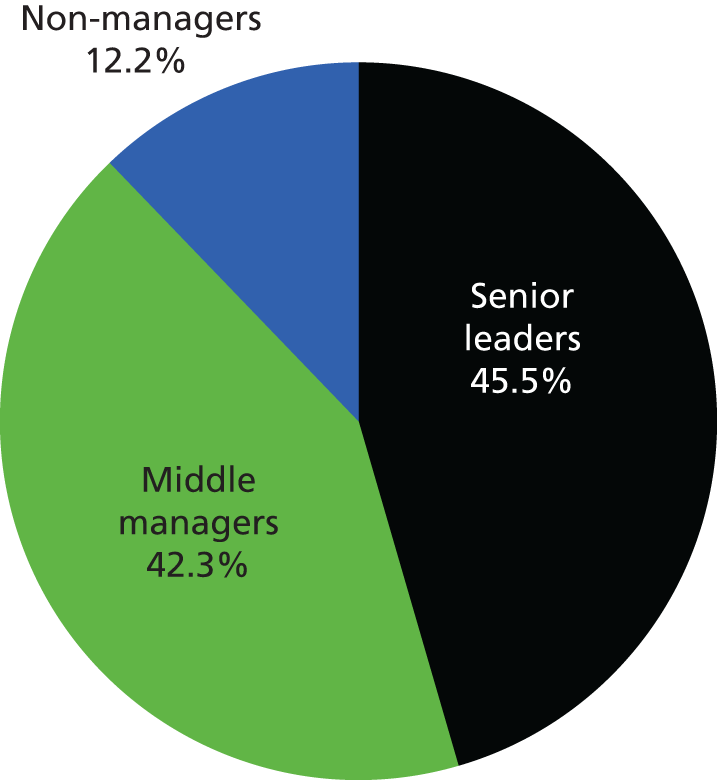
Looking at institutional composition, the NHS made up the largest component, at 41.5% (tenure from 3 months to 41 years, mean 9.4 years), followed by academia (26%), industry (19%; 9.6% from SMEs and 9.4% large commercial companies) and the third/not-for-profit sectors (8%), with smaller representation from central government (4.4%) and local authorities (1%) (Figure 2). This three-way network building and knowledge sharing across institutional boundaries was seen by many of our interviewees (AHSN leaders and stakeholders) as ‘the start of the blurring of the boundaries’, which would especially influence new connections between the NHS and SMEs.
FIGURE 2.
Important knowledge contacts by sector.
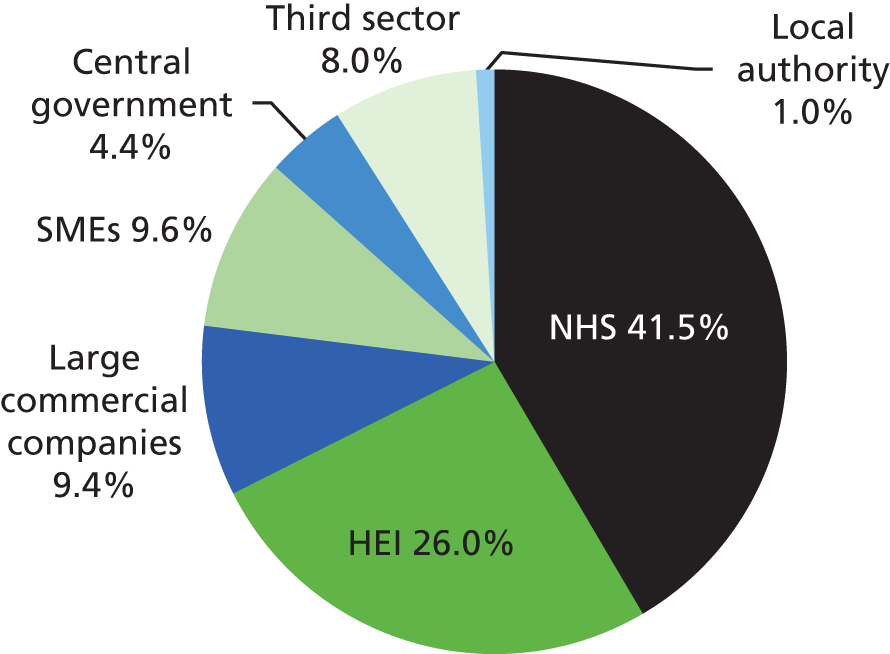
The professional expertise base of these key knowledge influencers was varied (Figure 3): 18.1% were experienced health-care managers, 16.4% were clinical and medical practitioners, 10% had experience in general business operations and management, 7.8% had skills in public health policy, 7.8% were skilled in digital health or health informatics, 7.7% had skills in commissioning and 5.6% had other, unclassified business expertise. In terms of research expertise, 14.4% were trained in clinical, medical or health sciences, 4.4% were biotechnology/life science researchers, 4% were pharmaceutical researchers and 3.8% were social scientists. Note that individuals often worked in more than one sector and had expertise across multiple disciplines (‘boundary spanners’) and were able to self-identify as such; thus, we provide percentages of the total number of selections across categories.
FIGURE 3.
Important knowledge contacts by professional expertise.

New contacts for wealth creation made through Academic Health Science Networks
We conducted a second national survey (late 2015) asking AHSN boards, core teams, members and stakeholders about the ‘new contacts’ they had ‘met at or through AHSNs over the past 12 months who had provided important actionable knowledge used to support regional economic growth and/or wealth creation’ aspects of the AHSN remit. We wanted to investigate how AHSNs had directly supported new networks to promote wealth creation with a focus on new contacts and new knowledge exchanges. Some 198 people responded to this survey, of whom 61% were VSMs/leaders, 29.5% were middle managers and 9.5% were identified as non-managers.
Who was mobilising knowledge to support wealth creation?
Nearly half of all new contacts nominated were VSMs/leaders [i.e. CEO/director-level persons (45.5%)], 33.2% were middle managers and a smaller percentage were non-managers (21.3%) (Figure 4). We note the diversification of contacts across organisational roles, especially the increased involvement of non-managers, compared with earlier data. Very senior leaders were regarded as being most knowledgeable across all types of knowledge (products, services, research), but were especially important for the creation of new ideas to support wealth creation. Knowledge sources for wealth were mainly from academic health industry bases, with a growth in industry and local authority contacts from our earlier survey [37.6% NHS, 27.8% industry (14.5% large commercial companies and 13.3% SMEs), 20% HEIs, 6.6% central government, 4.2% third sector and 3.8% local authority] (Figure 5). This is indicative of a ‘triple helix-style’ mode, with government-funded institutions (in this case the NHS and HEIs) and private industry playing a pivotal role in health-care market innovation and growth. 46
FIGURE 4.
Important knowledge contacts supporting wealth by organisational role.
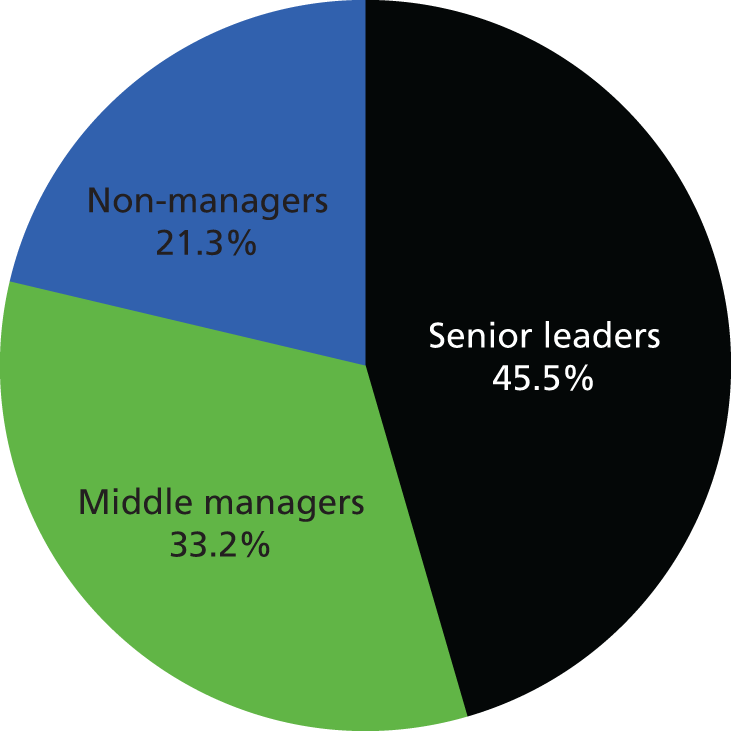
FIGURE 5.
Important knowledge contacts supporting wealth by sector.
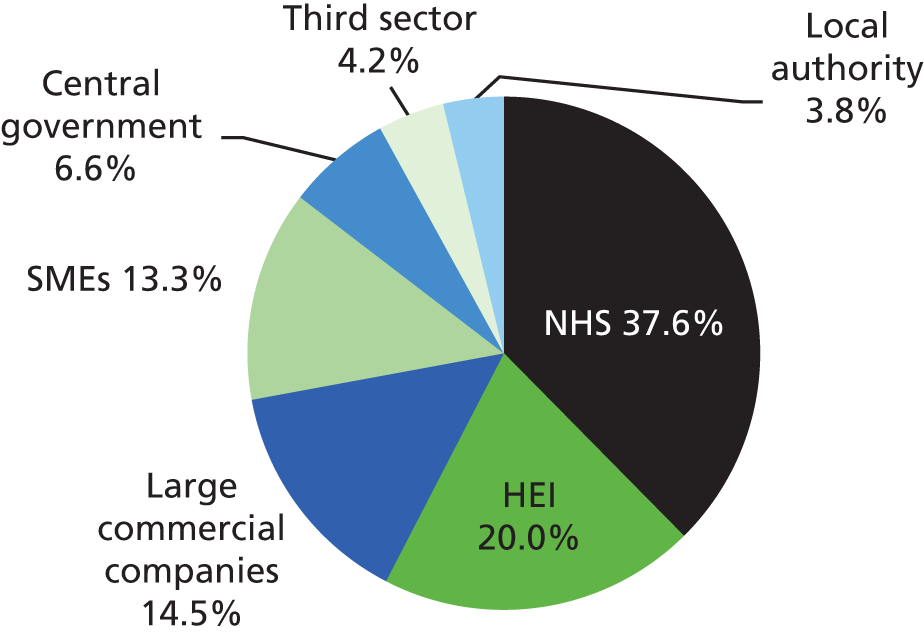
In our qualitative interviews, industry actors were signalled as being crucial to the success of AHSNs and significant work was under way to create new relationships in this area: ‘I think if we are successful and make a significant contribution to those two aspects of health and wealth, both of which I mean, . . . personally I think the NHS is just sunk basically without innovation, without industry playing a role and reducing some of those barriers’ (AHSN commercial director).
Academic Health Science Network board members and knowledge networking around wealth creation
Key finding 3
During the early development of the AHSNs, AHSN board members played an important role in triggering the circulation of knowledge to support activities at the core of the AHSN remit, especially for knowledge circulations relating to wealth creation.
We investigated the early role that AHSN leadership played in mobilising national networks for wealth creation. We highlight the knowledge mobilisation activity of AHSN board members in their formal networking capacity as a leadership collective. Figures 6 and 7 are visual sociograms depicting national knowledge circulations around health and wealth relevant to AHSNs in their initial development.
FIGURE 6.
National knowledge networking around health improvement (Health-NET).
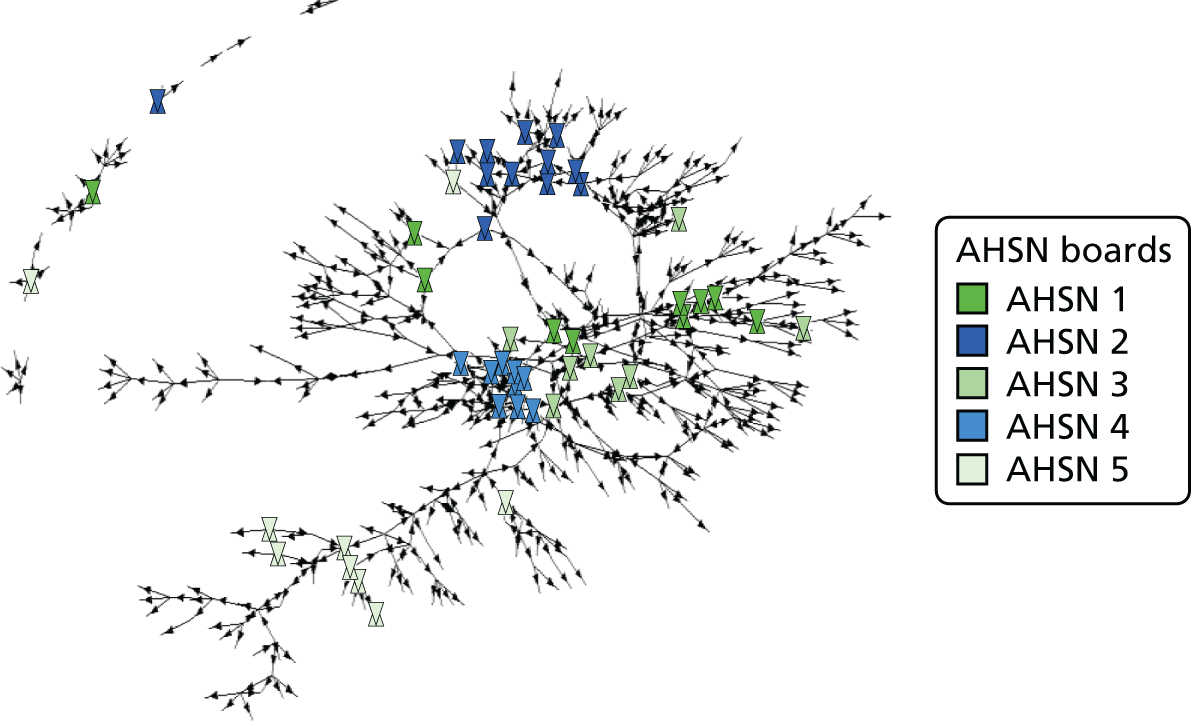
FIGURE 7.
National knowledge networking around wealth creation (Wealth-NET).
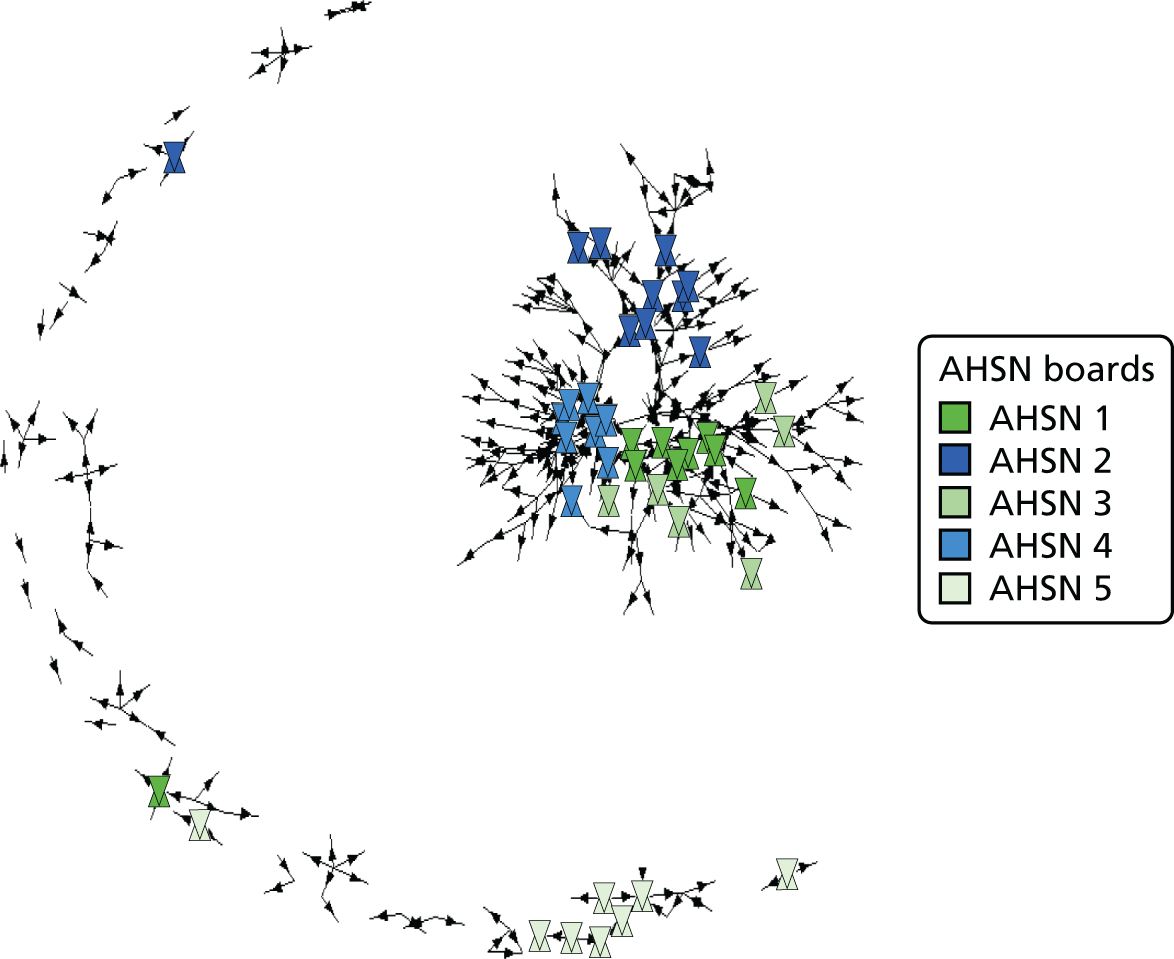
Individual knowledge contacts are represented as points in the sociograms (arrowheads and shapes) and the connecting lines between points represent knowledge exchanges between individuals. AHSN board members from each of our case regions are represented by shapes and smaller arrow heads represent other agents circulating knowledge in the knowledge mobilisation system. The positioning of individuals as points on a sociogram is determined ‘relationally’ by their knowledge-sharing relationships. The similar two individuals’ networks are (i.e. if they exchange the same type of knowledge with the same contacts), the closer together they will appear on the graph. AHSN board members that are positioned close together on the graph are therefore tapping in to similar knowledge contacts.
The network sociograms show that to access health-related knowledge, AHSN board members mostly networked within their own region (see scatter of AHSN leaders). For example, in Figure 6, AHSN 1 board members scatter most widely across the sociogram, a configuration that reveals that some board members are connecting with entirely different contacts from their colleagues; this is also suggestive of a geographically dispersed set of knowledge contacts (see Figure 7). In contrast, there is a much tighter configuration of board members for AHSN 4, who are tapping into the same knowledge sources as their regional colleagues.
The extent to which AHSN board members hold central positions in both sociograms indicates their centrality to national knowledge circulations related to the AHSN health/wealth remit. We see that the AHSNs with AHSCs (AHSNs 1, 3 and 4) appear as central and most tightly grouped (see also regional-level case studies in Chapter 6). AHSN 5 board members hold distinctly different positions from other AHSN leaders, suggesting that these individuals are mobilising knowledge separately. We also see this pattern to a much lesser extent for AHSN 2, whose leaders, although connecting with the dominant AHSC–AHSN grouping, position themselves at some distance and focus on within-region knowledge exchanges to support wealth creation.
Figure 6 reveals that AHSN board members are leading knowledge networking to support wealth creation by collectively networking with each other and similar sets of contacts. These shared interactions pull together some AHSN leaders into a more clustered display in the figure to provide a ‘critical mass’ of knowledge sharing around wealth creation. The centralised and clustered shape/structure of the network itself suggests a ‘problem-solving’ or strategising formation observed in other civic networks in mobilisation mode acting on behalf of collective and public interests. 154
Our interviews with AHSN commercial directors highlighted an ethos of national-level collaboration to promote national policy alongside regional competition:
So I think there’s a really good, healthy spirit of we’re all in this together and we want the whole movement to succeed, because if the whole movement doesn’t succeed what we’ll end up with is, is totally locally funded entities in the future . . . So I think it’s really important for us that the whole movement succeeds, not just us. And I think most of the 15 of us get that, so we do want to collaborate and we’ve collaborated with the Small Business Research Initiative and other AHSNs. But there’s also a bit of competition and, you know, I want us to be the best, you know, everyone does, don’t they?
National-level networking between AHSN leaders also supported on-the-job learning about network leadership: ‘So there are things I admire about a lot of the others and I’d like to, you know, openly pinch some of that and learn from them’.
Some AHSN commercial directors felt that monthly networking meetings with their counterparts from other regions were very helpful in formulating their own strategy around wealth:
. . . what was really helpful in terms of its formulation was conversations with other people doing my own job, other Commercial Directors from the other AHSNs. So we have monthly meetings which are a great opportunity in terms of, you know, checking how each other’s doing, sharing sort of best practice and ideas as well as, because in terms of what we’re here to deliver, you know, what does success look like because we’re such, we’re like a start-up organisation really ourselves, there’s a lot of debate about, well, how do we actually measure that, so there’s an ongoing debate around that and that sort of really sort of informed the strategy.
Commercial director
Opportunities for AHSN collaboration and networking were further evident at the national level, in the form of the AHSN Network and its meetings for CEOs/MDs, which we were invited to observe. Over time, there appeared to be an increasing emphasis on understanding AHSNs’ collective contribution and opportunities for joined-up working, such as by pooling ‘expertise and resources’. Certainly, at the national level, there was momentum for AHSNs to function as a collaborative movement, with alignment of AHSNs activities with NHS priorities and new initiatives that came on board after the inception of AHSNs (e.g. Vanguards, Patient Safety Collaboratives and Test Beds), as well as with small business research initiatives (SBRIs).
Academic Health Science Network knowledge networking and implementation into practice
Key finding 4
Early knowledge networking was more aligned with national policy and small local projects, whereas later knowledge networking to support wealth creation was being implemented through pan-regional initiatives.
Our qualitative interviews with AHSN leaders and stakeholders pointed to the need for knowledge mobilisation to be ‘practical’ and ‘operationalised’, not just academic or theoretical. The challenge for AHSNs was clear: ‘How do you prove the effect and the value of introducing A to B? You can’t, that is actually quite difficult’ (Director of AHSN Patient Safety Collaborative). One AHSN MD further highlights the complexity of the knowledge mobilisation process, which in his view, involves ‘joining up inputs across many fields or individuals to synthesise and develop ideas into reality at scale and pace’ (AHSN MD). Chapter 7 traces knowledge mobilisation and innovation processes at a more micro level and explores the problem of how to attribute the ‘success’ of collaborative innovation work. Here we use our SNA to explore how individuals put knowledge gained through networking into practice.
Early implementation of knowledge into practice
In our T1 survey we asked how knowledge gained through network contacts has or will be implemented (‘put into concrete action’). Examples of responses are provided below:
We are taking forward our ideas.
Using this to develop idea: currently in research stages and seeking funding as well as infrastructure.
Development of national tariff and outcome measurement.
Development of national policy and ground-breaking international access to treatment standards for access to effective care in mental health.
National policy on commissioning.
Developing innovative approaches across four AHSNs.
Used to develop industry engagement.
Development of IP [intellectual property] policy.
Extended the scope of existing work to capitalise on new participants or sectors.
To develop contacts and activity plans with proprietary suppliers of GP computer systems.
Action in progress to implement change (to inform commissioning cycle).
Drives government policy.
Self-published open-source meta-analysis to demonstrate that choice of technology is as important as choice of intervention.
Thinking incorporated into NHS Five Year Forward View.
In time I believe I will be able to put the knowledge gained into concrete action.
I will use it or support its use in the future as part of a planned event or programme of events.
I expect to be able to put this knowledge into concrete action in due course.
A small number of respondents described themselves as looking overseas for support with adoption and spread (i.e. ‘applying to expansion in export markets, especially USA’ and ‘corporate equity fundraising after NHS failure to adopt NICE recommended medical technology pushed as high impact innovation by NHS in Innovation Health & Wealth)’.
Our analysis revealed that much knowledge networking activity at T1 was in support of ‘planned’ implementation and/or implementation to feed into national policy initiatives, with few examples of concrete implementation of knowledge in to action.
Later-stage actionable knowledge to support Academic Health Science Network wealth creation activity
We later investigated (through our T2 social network survey) the wealth creation networks that had emerged as a result of AHSN networking and knowledge-sharing activity. The development of knowledge networking to support wealth creation was a particularly interesting avenue to explore given that our first survey had highlighted differences between networks of contacts being mobilised for health improvement and wealth creation and, importantly, that the latter were based on newly emerging relationships and, therefore, perhaps more likely to change over time.
Although recognising the difficulties of measuring ‘innovation’ given the presence of multiple collaborators and the need to take into account different stages of the innovation process, we tried to capture whether or not any actionable knowledge exchanges had resulted in tangible implementation or measurable outcomes. Respondents indicated that 58% of these knowledge exchanges to support wealth creation had so far led to non-tangible implementation (such as influencing one’s thinking, developing new ideas and supporting networking), and 42% had more concrete implementation outcomes such as the development, adoption or spread of an innovative product, service, initiative or programme.
We identified several outcomes from wealth-focused AHSN knowledge exchanges, some of which were already being measured (i.e. NHS efficiency savings, new income or funding), and others of which were happening but not yet being measured [i.e. the creation of new highly skilled jobs, revenues from patents/intellectual property (IP), formation of new companies or spinouts]. The difficulty of measuring outcomes for innovations reflects not only the early-stage capture of our own research project, but also the complexity of the innovation process. Some implementation activity was anticipated to take place in the future. One respondent commented that ‘thanks to the AHSN our team has fostered collaboration avenues around innovation and adoption, and conducted applied research into procurement and evaluation systems. We are still at the early stage of exploration and partnership development, but prospects look hopeful’. Other respondents provided specific examples of knowledge gained through AHSNs leading to innovation and implementation outcomes not yet measured, such as:
Design of an engagement programme for clinicians and SMEs, leading to new products for several SME participants. They are now working to sell to NHS and/or find venture capital funding to support further development.
Return on investment related to initial cost outlay for project for all CCGs in AHSN region (heath and social care costs).
Production of a region-wide data landscape tool that is already showing much interest from other AHSNs, NHS IQ and potentially NICE.
Developing a template for leaders to check their progress against known organisational changes to support safer, more effective and efficient care.
Development of technology that could lead to widespread adoption (currently being evaluated).
More effective treatments for patients, reduction in region’s social care costs.
New relationships and plans for a major overseas investment taken up by our university and an AHSN.
Appreciation of benefits working in partnership with GPs to harness better ways of working and efficiency gains in supporting people with diabetes mellitus through the community pharmacies.
This contact has connected us to some national experts to support Mental Health Crisis Care Vanguard applications using their expertise in modelling.
Deepening my university’s involvement with the EIT KIC [European Institute of Technology Knowledge and Innovation Community].
Being able to negotiate clinical and inter-organisational cultures, structures and sensitivities to discover opportunities with real potential.
We are using the intelligence and advice given by this contact to explore collaborative programme activities between our university and, potentially, NHS and third-sector organisations on workforce development, mental health and wellbeing.
Health-related open data usage in smart city approaches to infrastructure and service planning. We are currently at concept development and internal and external partner-development stages; but we are hopeful that our joint-working might lead to project and programme activities in the future.
Developing research project funding bid.
Working to potentially develop Community Interest Company locally.
Development of regional strategic plan for health innovation.
The interesting finding is that the knowledge being implemented at this later stage (emerging from AHSN introductions and activities) is more specific, joined-up, regional and strategic in content than the examples from our first survey, which were more about implementation that was generalist or planned or that fed into projects or policy.
Discussion and implications
This chapter has explored the role of national ‘knowledge networking’ to support AHSN knowledge mobilisation. We summarise the main findings in Box 2.
-
Leadership in formal structures supporting knowledge mobilisation is collective/distributed not individual (i.e. systems leadership).
-
Knowledge is mobilised as a form of ‘social capital’ through social networks.
-
Different network structures may affect capacity for implementation as well as what is implemented.
-
Building new networks around a policy ‘problem’ takes time and change is incremental.
Our approach to knowledge mobilisation and networking here, drawing on literature on networked innovation systems, illustrates that knowledge mobilised through networks is a type of ‘social capital’ resource, that is, a collective form of ‘capital that is captured through social relations’ providing instrumental gains for the wider collective community in this domain,22 at both national and regional levels. This knowledge develops as a relational resource and is generated through interaction between multiple actors and becomes part of the regional fabric in the same way as its infrastructure and assets. This process will inevitably create contextual differences between regions. 36 Building on our review of literature on knowledge, networks and leadership, we support the view that pro-innovation initiatives such as AHSNs, although responding to a top-down policy mandate, have then to navigate and position themselves as an ‘overlay’ to pre-existing knowledge networking structures.
Our research also provides an emerging example of ‘systems’ and ‘distributed’ forms of leadership to support innovation and change where multiple actors with a collective impetus for action interact across sectors and industries, so that knowledge mobilisation evolves from the bottom up to produce new modes of operating. 155 In particular, knowledge networking to support wealth creation appears to be a key strategic area for AHSNs with AHSN leaders already demonstrating concerted efforts in this area to support national policy. We note at our point of data capture, at the early stages of AHSN development, that national knowledge networking around wealth creation was largely ideas based, but we were able to identify some tangible outcomes from ‘actionable’ knowledge, particularly those linking to pan-regional initiatives.
This research also teases out points of note concerning ‘how’ AHSN stakeholders network to support innovation. Despite the ‘double-headed’ policy agenda positioning health and wealth as mutually reinforcing, in practice we found that, rather than health and wealth being tackled in total alignment, different knowledge networks were activated and built to support health improvement (established, old contacts/’strong ties’) and wealth creation (newer relationships/’weak ties’). This is important because if individual stakeholders network differently to support their health and wealth innovation work, targeted networking strategies may be more appropriate for AHSN knowledge mobilisation activity, and, indeed, some but not all AHSNs were cognisant of this. Alignment between health and wealth may be achieved incrementally, over time, as personal networking supporting health and wealth begins to overlap. Notwithstanding interests and inclinations, we emphasise that changes in networking practices take time and this may be at odds with the short-termism highlighted in our earlier policy chapter (see Chapter 4).
We also point to the dynamic nature of networks and networking in the sense that contacts, relationships and knowledge utilisation are evolving. Our SNA capture is based on networking ‘snapshots’. Looking at two such snapshots (earliest networking to support health and wealth innovation and then later networking to support wealth creation) we illustrate a change in who was involved in such knowledge networking and how knowledge mobilised through networks was being implemented by AHSN stakeholders. The next chapter in this report focuses more on innovation process, but future studies might be able to take a more longitudinal, in-depth approach to the study of networking practices when AHSN activity is further off the ground.
Chapter 6 Regional knowledge mobilisation systems: comparing Academic Health Science Networks
Introduction
To further investigate the role that ‘knowledge networking’ plays to support AHSN knowledge mobilisation, this chapter moves down to a regional level to consider the five AHSNs as studied within their local contexts. It draws on both the SNA material and the qualitative interviews with AHSN leaders and stakeholders to characterise the regional knowledge mobilisation systems that emerged and evolved. We provide a comparative analysis of the five case study AHSNs as knowledge mobilisation systems through a focus on their academic health science infrastructures, the ‘structure’ (shape) of their regional knowledge networks, the types of knowledge being shared through networking in each region and an exploration of knowledge leadership through identification of key knowledge ‘brokers’.
Insights from the literature
In this chapter we further develop the current literature on knowledge, networks and leadership as highlighted in the previous chapter (see Chapter 5). In particular, we study regional knowledge mobilisation systems through a comparative analysis of AHSNs, building on relevant literatures and theories emphasising the iterative, relational and collaborative dimensions of networks – such as networked innovation systems (ecosystems, regional innovation systems, CASs), networked leadership (distributed leadership, complex leadership, systems leadership) and the agency of actors in networks (i.e. AHSN boards and other knowledge ‘brokers’). In light of our literature review, we view these aspects of networking and interactions as structural components of ‘social capital’ that support knowledge mobilisation and innovation. 104
Where some previous SNA studies have focused on small-micro-scale knowledge networking (i.e. project teams, within and across firms), we attempt to capture here how such knowledge is mobilised at a national (macro) or regional level to support innovation across sectors and industries to satisfy a particular innovation remit or mandate. This reifies the importance of cross-sector hybrid networked organisational forms for transdisciplinary knowledge mobilisation involving a wider group of stakeholders (as highlighted in our literature review, i.e. triple helix, mode 2 and other). In this chapter we pay particular attention to the types of actors and types of knowledge being mobilised in the early stages of AHSN development to address the system-level challenges of health improvement and wealth creation.
We take this existing research as a broad framework through which to study, compare and contrast AHSNs as regional networked initiatives working under the same policy remit.
The five Academic Health Science Networks, their regional economies and academic health science infrastructures
In this chapter we provide a regionally based and comparative analysis of knowledge networking to characterise the knowledge mobilisation systems observed for each AHSN region. We first draw on our qualitative interviews with AHSN leaders and regional stakeholders and consultation of documents to provide an account of the five regional case study AHSNs in terms of their inherited infrastructure supporting academic health science innovation (from least to most developed).
Academic Health Science Network 1
Academic Health Science Network 1 is located in an urban setting with a mix of inner city and suburban areas and a growing population of about 3 million. The population displays substantial ethnic diversity, with some deprived areas alongside more prosperous locales. The patch includes medical schools in distinct subregions with some tensions reported between them. One medical school was part of an AHSC, linking it organically with large FTs. The AHSN also relates to many local authority councils and HEIs. Medical schools were influential in the (quick) preparation of the first bid, as bid writers tended to use ‘cues’ from the pre-existing regional infrastructure (e.g. AHSC, HIEC). Although it has a strong academic structure and some major NHS FTs, the AHSN region lacks a life sciences/science park infrastructure, which meant that wealth-creation activities developed slowly and often in an indirect way that was connected to bordering geographic areas.
Academic Health Science Network 5
Academic Health Science Network 5 covers a mixed and geographically extensive region, with some medium-sized urban centres and about 3 million total population. The region is seen as having a coherent ‘footprint’ in its health and social care economy. The footprint was described as a ‘complex institutional architecture’. The regional economy includes large firms (with a strong IT presence), an important SME sector and science park initiatives. The region has a traditionally powerful Russell Group university that includes a medical school with close links to a major acute hospital (this university was influential in the AHSN bid) and other post-1992 HEIs. A history of tensions between the Russell Group HEI and the post-1992 HEIs was reported. The region does not have an AHSC but did have an influential and well-regarded HIEC and now has a CLAHRC. Links between the AHSN and CLAHRC were still developing towards the end of our study.
The AHSN developed a wealth creation agenda, including both big firms and SMEs. It was co-operative with other AHSNs and with the life/health sciences sector and keen to develop regional growth through academic science. The AHSN leadership were challenged by working on a cross-regional basis, including with the powerful Russell Group university, while not being captured by it.
Academic Health Science Network 2
Academic Health Science Network 2 covers a large regional footprint with an urban–rural geography and a very diverse socioeconomic and demographic population of about 5 million, with considerable inconsistency and variation in health outcomes and health-care delivery.
The region’s assets are centres of clinical excellence, academic strength and industry capability through an engaged industry base that sits in geographic clusters. It has a CLAHRC, had three HIECs but no AHSC. The city hub is centred on a well-integrated partnership between a strong university and a leading university hospital, with an accompanying urban industry base (primarily SMEs) in medical and digital technology. In the north and south of the region, there are more HEIs (one with a medical school), trusts and CCGs working in innovative fields such as medical technology, diagnostics, digital health and bioscience alongside other science parks. Although described by AHSN leaders and stakeholders as being a ‘siloed’ region with ‘pockets of excellence’, the patch was not considered to have a fully joined-up academic health science infrastructure prior to the AHSN.
A challenge was dealing with regional silos, politicking, agenda setting and competition between the region’s geographies and institutions. The MD described how the AHSN worked hard to ‘create the conditions in which people can work together . . . and see the benefit of working together for the common good’ in what another AHSN leader described as ‘a ridiculously cluttered landscape . . . where we have to organically develop the right solutions and also have to be given the space to fail’.
Academic Health Science Network 4
Academic Health Science Network 4 is located in an asset-rich, knowledge-intensive region. A high-performing local university offers ready access to ‘bench science’ and translational expertise in health care and the life sciences, whereas regional universities train health-care professionals (doctors, nurses and allied health professionals). Life sciences, pharmaceutical and digital businesses are based in the geographical patch, ranging in size from smaller, nascent start-ups to larger corporations with international profiles (both health and non-health). There is a developing medical technology and diagnostics subsector with relevance for the AHSN. Industry–university commercialisation activities are supported by intermediary agencies, such as university technology offices and spinouts. As such, a pipeline of health research products and ‘competing technologies’ is potentially available to the AHSN, offering the possibility to transform health-care delivery both locally and further afield. The region was described as an important ‘centre for growth’ and particularly ‘exciting’ place to work.
Despite its placement in a thriving research and business-rich economy (which involves a number of universities and wide geographical footprint), there was a history of poor collaboration between NHS organisations that contributed to systemic fragmentation and poor co-ordination across sectoral boundaries, especially between some health-care providers. However, positive change in local relationships was reported over the study period and was attributed to various factors, such as effective AHSN leadership. This helped to reshape the local health economy via joined-up, systemic thinking about NHS sustainability and institutional collaboration.
Developing life sciences clusters, spinouts and entrepreneurial partnerships with industry was key (directly and through the LEP and SBRI), especially given regional strengths and opportunities, with an emphasis on collaboration to capitalise on the region’s knowledge assets. The long-term ambition was to be a strong competitor in the life sciences and biotechnology sector. Although there was a clear strategic case for capitalising on immediate assets and its thriving research community, the AHSN team was conscious of the need to avoid overlooking the needs of its wider population and membership.
Academic Health Science Network 3
This AHSN covers an urban conurbation with a stable yet diverse population of about 3 million residents with significant health inequalities. The region has a mature and reasonably joined-up academic health science infrastructure, coherent administrative geography and is home to HEIs and NHS trusts with a successful history of innovation, an AHSC, a CLAHRC, science parks and a NIHR innovation biomedical hub. The AHSN footprint maps coherently on to the existing NIHR CRN and is described by one senior leader as being on a journey to becoming a more integrated ‘complex adaptive ecosystem’.
The region has a strong academic health research base including several universities, an AHSC, a HIEC, a CLAHRC, a large medical school, a top-recruiting Comprehensive Local Research Network, a bio-innovation cluster, a NHS innovation hub, a health research and technology facility and several science parks. The region had recognised strengths in biopharmaceuticals, medical technology, clinical trials, implementation and adoption, and a health informatics intelligence infrastructure already in development.
The AHSN also received early formal commitment from the combined association of local authorities and the LEP to act as a delivery partner on economic growth and regeneration. SBRI was a further knowledge stream used around technology solutions.
The structure of Academic Health Science Network regional knowledge networking
Key finding 1
Different ‘structures’ of knowledge mobilisation systems emerged in each AHSN region. Connected and hybrid networking systems were found in regions with mature infrastructure, whereas loosely organised networking systems were found in regions with developing infrastructure.
Our policy chapter (see Chapter 4) illustrates a growing emphasis on the importance of ‘innovation architecture’ and ‘ecosystems’ based on cross-institutional collaboration to support the AHSN remit. In the previous chapter we looked at the composition of individuals involved in AHSN knowledge mobilisation across organisational hierarchies, sectors and professions (see Chapter 5). In this chapter we now use SNA to map the actual structure (or shape) of regional knowledge circulations that emerged during the early evolution of AHSNs. We describe these patterns below and draw attention to characteristics of each regional knowledge mobilisation system to highlight the different networking styles within AHSN regions during their early development.
It became clear that a systems approach to understanding knowledge networking and leadership would be appropriate because ‘AHSN is different because it works from the bottom up and the 15 are all very different . . . Some people complain about that, I actually think it’s our strength. Because, you know, it’s not a template, it’s not one size fits all’ (AHSN commercial director). We summarise regional networking characteristics alongside regional infrastructure in Table 5.
| Pre-AHSN academic health science infrastructure (qualitative data) | ||||
|---|---|---|---|---|
| Developing | Mature | |||
| AHSN 1 | AHSN 5 | AHSN 2 | AHSN 4 | AHSN 3 |
| Strong academic infrastructure: AHSC, CLAHRC, HIEC, but weak life sciences and science park presence | Mixed industry presence (large companies, science park, SMEs), powerful HEI, CLAHRC, HIEC, no AHSC | Centres of excellence spread across region in silos (high-performing trusts and HEIs, HIECs, CLAHRC, science parks/SMEs). No AHSC | Asset-rich, knowledge-intensive region, history of innovation, leading HEI, spinouts push commercialisation from universities. Poor NHS collaboration. HEIC, no AHSC | Joined-up ecosystem, history of innovation. Strong academic health research and implementation base (including AHSC, HIEC, CLAHRC, bioinnovation clusters, technology facility, science parks) |
| Structure of knowledge networks emerging during AHSN’s early development (SNA) | ||||
| Loosely organised | Connected | Hybrid | ||
| AHSN1 | AHSN5 | AHSN2 | AHSN4 | AHSN3 |
| Loose structure: largest sized and geographically dispersed network | Loose structure: multiple, separate camps | Connected with small localised cliques | Connected: small and tight-knit, regional focus | Hybrid integrated: cliques and bridges |
Loosely organised knowledge mobilisation systems with developing academic health science infrastructure
Two AHSN regions had knowledge networking structures that were more loosely organised in the sense that individuals were less likely to be connected in tight groups (such as clusters or cliques) and more likely to be sharing knowledge across separate knowledge camps or to contacts who were themselves not connected.
The AHSN 1 region presented a loose knowledge network structure because of its large size (high number of contacts named), and also because these contacts were distributed across a wider geography beyond the AHSN region. AHSN 5 (like AHSN 1) presented a loosely structured knowledge network system with geographic dispersion. However, unlike AHSN 1, networks in the AHSN 5 region were organised into separate disconnected clusters.
Looser networks are more likely to have capacity for cross-fertilisation of new knowledge because there are more opportunities to ‘bridge’ disconnected groups and to tap into more diverse knowledge because they involve networking with contacts who are themselves not connected. These network structures also risk slower communication and information uptake, especially where knowledge is being shared across a wider geography and between disparate groups. 92 Loose structures are amenable to bringing in new contacts and, therefore, new knowledge, thereby providing more impetus for ‘radical innovation’ or culture change.
Connected and hybrid-type knowledge mobilisation systems with mature academic health science infrastructure
Highly connected networks are more likely to expedite knowledge diffusion. 92 Two AHSN regions presented as more connected (highly linked/tightly knited) systems (measuring higher on SNA cohesion metrics) and one AHSN region exhibited a hybrid form combining elements of connected and loosely organised network systems.
The two most connected knowledge networking systems were, however, connected in different ways. Knowledge networks in AHSN 2 were mostly connected within localised ‘cliques,’ reflecting the organisation of its infrastructure being concentrated in a ‘siloed’ institutional geography with ‘pockets of excellence’. Conversely, the asset-rich AHSN 4 also exhibited a connected system of knowledge networking but presented differently as a smaller and tight-knit structure, reflecting its smaller geography. Regional knowledge networks that are tightly connected and small in size are more likely to expedite knowledge diffusion across the region. They also have higher capacity for embedding this knowledge because individuals are already clustered into subgroups; however, because the network is so connected, knowledge sharing is less likely to ‘bridge’ disconnected groups (i.e. bridge ‘structural holes’, often the site of the cross-fertilisation of knowledge).
Finally, AHSN 3 presented as a hybrid integrated structure combining both cohesive clique-type structures and looser bridges spanning groups. Interviewees in this region frequently referred to it positively as an ‘ecosystem’, a structure that joined up regional health-care innovation activity. During qualitative interviews, several AHSN stakeholders described this structure as being integral to their involvement and enjoyment in AHSN activities in the sense that they felt part of the strategic work on regional health-care innovation. A NHS chief information officer describes how networks built to form small cohesive/clique-type groups (i.e. new teams or projects) contribute to wider strategic work:
It was to set up a start-up projects that jump start something bigger. So it is setting up eco systems . . . one of my clinicians has actually volunteered to go and work with that [digital] company for free on some of their other ideas. And the summary is, relationships that have been formed are symbiotic and mutually beneficial and there is an eco-system starting to form of relationships and understanding, which will bear fruit later on. But as with anything it is maturing and evolving, but there is mutual trust being built actually which is really, really interesting.
The type of knowledge being circulated by stakeholders through networking
Key finding 2
Stakeholders in all five AHSN regions perceived evidence, networks, governance, informatics and digital as key enablers of innovation. Disruptive innovation via service redesign/new care models and enhanced commissioning were seen as important mechanisms to improve patient outcomes and provide cost savings for the NHS.
Key finding 3
There were some differences in the actual content of the knowledge being shared by regional stakeholders; there was more focus on data/technology in AHSNs with more connected knowledge systems and developed infrastructure, whereas loosely organised knowledge systems with developing infrastructure were more focused on medicines.
Not only were the regional knowledge-sharing networks different in structure, but individuals within these networks were discussing different aspects of health-care innovation. Survey respondents were asked to provide up to five keywords to describe the innovative knowledge provided by their contact. We thematically coded these keyword entries into clinical domains and innovation enablers and then conducted a content analysis of the results to ascertain the top knowledge types in each AHSN region. Table 6 reflects the wider knowledge being mobilised by stakeholders in each region (knowledge about what), rather than the AHSNs themselves.
| Knowledge being circulated in region through personal networking by AHSNs and stakeholders (SNA) | ||||
|---|---|---|---|---|
| AHSN 1 | AHSN 5 | AHSN 2 | AHSN 4 | AHSN 3 |
| Key innovation enablers discussed | ||||
| Medicines optimisation, personalised medicine, safety, workforce education. Social media | Personalised medicine, patient experience, safety, telehealth and self-management. Social media, medical leadership | Medicines optimisation, clinical trials, leadership. Industry collaboration, inward investment | Big data, preventative medicine, diagnostics, imaging | Data sharing, procurement, technology and devices, SME. Citizen engagement |
| Key clinical domains discussed | ||||
| Palliative care, MSK disorders, diabetes mellitus, mental health, genomics and alcohol | Dementia, cancer and LTCs | LTCs, genomics | Diabetes mellitus, cancer, genomics and surgery | LTCs, CVD, dementia |
There were some commonalities. Respondents in all regions asserted the importance of change centred on the redesign of care pathways and/or new models of care (innovation that ‘disrupts’ existing practice), and enhanced commissioning channels both to improve patient outcomes and to provide cost savings for the NHS (this was also found for our policy interviews). Common innovation enablers were evidence, networks, governance, informatics and digital. We describe below the differences between knowledge circulations to support innovation found in each AHSN region.
Respondents in AHSN 1 were more focused on improving patient care through medicines optimisation, personalisation, safety and workforce education to address wealth creation indirectly. A range of clinical themes was important in this region, including palliative care, musculoskeletal (MSK) disorders, diabetes mellitus, mental health, genomics and alcohol. Emphasis was placed on primary care and community care, commissioning, social media and innovation culture and process.
Individuals in AHSN 2 shared knowledge about collaborating with industry and securing inward investment, pharmaceuticals, clinical trials, primary care, leadership, LTCs and genomics.
Discussions in the AHSN 3 region were largely about data sharing (open-source, electronic patient records) and SMEs (procurement, technology and devices). Interestingly, mentoring was important, as was citizen engagement. Key clinical themes discussed by knowledge contacts in this region were cardiovascular disease (CVD) and dementia.
Individuals in AHSN 4 were also focused on informatics, but more specifically ‘big data’, preventative medicine, diagnostics and imaging. The terms ‘clinical innovation adoption’, ‘life sciences’ and ‘biomedical’ were used more often in this region than in other regions. Key clinical themes discussed were diabetes mellitus, cancer, genomics and surgery.
Linking regional knowledge networking structures with the implementation of knowledge
Key finding 4
Academic Health Science Network regions with looser networking systems and developing infrastructure tended to draw on different sets of knowledge contacts to support health and wealth innovation and were also more likely to implement knowledge to support wealth creation from new contacts.
We wanted to explore how the connectivity of a region’s knowledge network was related to the implementation of knowledge (Table 7). Drawing on previous research on antecedent networks showing that it may be difficult for new (‘outsider’) knowledge sources and contacts to influence established groups in connected network structures,95 we investigated the effect of ‘old ties’ (in this case, close personal connections of over 10 years’ duration) on the implementation of health- and wealth-related knowledge.
| Key Indicator | Connected, developed (AHSNs 2 and 4) | Loose, developing (AHSNs 1 and 5) | Hybrid (AHSN 3) |
|---|---|---|---|
| Proportion of very new contacts (< 12 months) | Highest | Lowest | Median |
| Similar contacts used for health and wealth knowledge | High overlap | Low overlap | Median overlap |
| Implementation of health knowledge | Old contacts | Old contacts | Old contacts |
| Implementation of wealth knowledge | Old contacts | New contacts | Old contacts |
We found a greater degree of overlap between contacts used for health and wealth knowledge in AHSN regions presenting as more connected, developed, knowledge systems (i.e. the same individuals were contributing to both types of knowledge sharing and infrastructure was strong). We found more distinction between contacts used for health and wealth knowledge for AHSNs with looser knowledge systems with developing infrastructure. For all AHSNs, knowledge exchanges about health that led to implementation were more likely to originate from old contacts (> 10 years). Interestingly, newer contacts were more likely to support the implementation of knowledge in AHSNs with loosely linked networking systems.
This finding creates a challenge for AHSNs because, although strong ties and connected networks may benefit co-ordination, expedite the flow of tacit knowledge diffusion and thus support implementation,156 looser networks may support radical forms of knowledge mobilisation precisely because they are less reliant on pre-existing networks and practices and have more opportunities to broker new contacts. 91,157
Knowledge leadership and agency in networked systems: who are the key actors and institutions acting as knowledge brokers in each region?
Key finding 5
Senior leaders (including AHSN leadership) spanning NHS, HEI and industry backgrounds were most prominent as knowledge ‘brokers’ in AHSN regions with more connected or hybrid networking systems and developed infrastructure. Middle managers from NHS backgrounds were more prominent in regions with loosely organised networks and developing infrastructure.
Brokerage denotes a network position occupied by actors who connected otherwise disconnected parties. Knowledge brokers are important because they connect people and organisations that would otherwise be disconnected and thus can support the ‘absorption’ or circulation of innovative knowledge by linking people,57 while also being themselves privileged by these network positions (e.g. coming into contact with new knowledge by interacting with contacts who are themselves not connected).
We apply SNA to identify those individual actors and institutions that occupied key positions as brokers in each AHSN regional knowledge network (Table 8).
| Knowledge leadership and agency in networks: who were the regional knowledge brokers? (SNA) | |||||
|---|---|---|---|---|---|
| Structure of knowledge network | Loosely organised | Connected | Hybrid | ||
| AHSN 1 | AHSN 5 | AHSN 2 | AHSN 4 | AHSN 3 | |
| Brokers – key individuals and institutions | Middle managers. NHS | Some AHSN directors. NHS | AHSN directors and operational leads. HEIs and industry | AHSN directors and other very senior leaders. NHS, HEIs and industry | AHSN directors and other very senior leaders. NHS, HEIs and industry |
The first point of note from our SNA is that senior leaders (including AHSN leaders) were very prominent as ‘knowledge brokers’ in the connected and hybrid systems, whereas there was more visibility of middle managers alongside senior leaders in the loosely connected knowledge systems. In AHSN 2, we also found that AHSN operational leads were frequently nominated as key knowledge contacts within the region and occupied key broker positions in the network.
The second notable point is that both loosely organised systems were supported by knowledge brokering by individuals from NHS organisations (e.g. NHS trust directors and doctors, NHS England contacts, Health Education England director, CCG associates and GPs). One AHSN 1 director admitted that, despite the large size of their network (in terms of number of contacts), ‘I think there are lots of parts of the system we probably haven’t quite touched on in the right way yet’. Indeed, later emphasis was put on developing a broader range of targeted relationships: ‘looking a bit more laterally at skills that sit outside the health service, is a thing we’re keen on but we haven’t yet delivered on’. In particular, there was an emphasis on broadening the scope of networking to include academic partnerships with some ‘non-health universities and how we might use some of their skills’ (e.g. business schools and communications/new media departments).
The more connected and hybrid-style systems featured fewer NHS professionals occupying broker positions in the regional knowledge-sharing network. Academic and industry actors were the most visible knowledge contacts in AHSN 2 (e.g. a university vice chancellor, several academics/clinical academics, industry representatives and a SME entrepreneur), whereas the institutional composition for AHSNs 3 and 4 comprised more institutional ‘boundary spanners’ (individuals spanning multiple roles across NHS, life sciences research/HEI and commerce).
Individuals occupying broker positions in AHSN knowledge-sharing networks were described in our qualitative interviews as possessing the following capabilities:
-
Knowledge synthesis via boundary spanning: ‘experience working in and across different sectors’, ‘has a different perspective because she has worked elsewhere’, ‘a real champion for spreading innovation, they will look beyond their own programme to see how an organisation might also benefit from their other offerings’, ‘standing in another pair of shoes is always good, isn’t it?’.
-
Good network operators with a systems perspective: ‘ability to ‘focus other people’s attention’ and ‘very good at pulling things together from a neutral perspective’. Can achieve a critical mass by bringing subgroups of people with ‘bright minds’ and ‘enthusiasm’ together to ‘make things happen . . . without the financial envelope. That’s where networks come in’.
-
Personable character: ‘a critical friend’, ‘he will help you out, he will give you support’.
Discussion and implications
This chapter has compared the five regional AHSN knowledge mobilisation systems studied.
Our research suggests that regional knowledge networks to support health-care innovation emerge from antecedent relationships as well as existing academic health science infrastructure (top-down and bottom-up influences). Networked initiatives, such as AHSNs, with an innovation, change or improvement mandate that relies on knowledge mobilisation should therefore be understood as being situated within these differing contexts.
As we have seen, AHSN regions have variant structures of knowledge networking (connected, loose and hybrid integrated types) and AHSN leaders must navigate these networks to generate locally emergent models for knowledge mobilisation under the same policy mandate. Moreover, building new networks around a policy ‘problem’ takes time and change is incremental. These factors will influence how networks, knowledge mobilisation and leadership emerge from the ground up and create variant paths for innovation adoption and spread. Further research could investigate whether or not infrastructure and ‘old networks’ provide an advantage for some AHSNs or whether or not it means different innovation pathways. Chapter 7 explores the issue of path dependency, but other studies might tackle this issue at later stages of AHSN evolution when AHSN metrics and measures might be available for comparative analysis.
We also explored ‘agency’ and leadership in terms of the different actors contributing to knowledge networking. Our literature review highlighted the importance of knowledge ‘brokers’ for networking and the absorption and cross-fertilisation of knowledge. 57,91,92 Senior leaders (including AHSN leaders) with ‘boundary-spanning’ backgrounds (professional expertise spanning across NHS, HEI and industry) were most prominent as knowledge ‘brokers’ in AHSN regions with more connected or hybrid networking systems and developed infrastructure. Our qualitative research showed that these knowledge brokers were also able to take a systems perspective and operate well within networks in terms of being able to pull people and ideas together. This supports a broad, flexible conceptualisation of ‘knowledge leadership’ as operationalised both through the activities of official leaders who occupy formal roles and key network positions and through individuals in less visible and perhaps less senior organisational roles but who nonetheless occupy key network positions and are recognised as KLs by their peers.
Chapter 7 Processes of knowledge mobilisation and innovation spread in action: developing a typology
Introduction
In this chapter, we present a thematic analysis of knowledge mobilisation strategies for spreading innovations traced over the course of the study (two per AHSN site). These innovations reveal the role of AHSNs in selecting, supporting and mobilising health-care innovations across regional health economies. We present a range of approaches found within the AHSNs we studied and reflect on the role of individuals and AHSN teams in supporting knowledge mobilisation. We discuss four specific knowledge mobilisation strategies or ‘models’ and provide illustrative vignettes of the innovations that we tracked over time. The data presented below form part of a wider case study WP and draw on a range of qualitative interviews, field work observations and documentary analysis [such as supporting evidence, e.g. NICE Technology Assessments (TAs)], wherever possible. Later in the chapter we touch on issues surrounding innovation performance and measurement in AHSNs, before summarising our key findings and their implications.
We point out that AHSN leaders and members of their operational teams – specifically those with roles incorporating responsibilities for innovation adoption and spread – guided us to these innovation ‘tracers’. The concrete innovations we followed (n = 10) were therefore selected in dialogue with the AHSN managers interviewed during the early phase of the study and so these tracers were seen locally as innovations (although they may have already been adopted in other sites so were not necessarily inventions). These persons were asked to nominate streams of activity where issues related to processes of such innovation adoption would be apparent and also researchable, for example, innovations that had been particularly successful in their view or, conversely, those that illustrated systemic barriers to wider regional adoption in the NHS and local health economy. We were aware that these were early days (2014/15) and we (or the local AHSNs) were not in a position to make a full impact assessment of the success of specific innovations, either in terms of evaluating associated health improvement outcomes within specific populations or in terms of economic and efficiency gains at scale. Instead, we collected available information on the types of performance metrics and evidence important to AHSNs and used internally for mobilising selected innovations, remaining attentive to the issues encountered by AHSNs as they attempted to monitor the uptake and progress of selected innovations across local health-care geographies. Our main point of focus was therefore less on the substantive and technical content of the specific innovations we followed, and more on the processes used to mobilise these innovations within AHSNs and the key persons engaged in this type of activity.
Innovations within regional health systems: insights from the literature
In the two previous chapters we described variations between AHSN regions and compared the structures of knowledge exchange networks within this context. Now we look at more ‘micro’ data about specific innovations to identify some general approaches to innovation adoption and scale-up found across our sample of AHSNs.
Two observations are worth restating before examining the specific details of the knowledge mobilisation processes we identified. First, from the literature we recognise that knowledge mobilisation dynamics in health care are multilevel and influenced by individual, organisational and regional factors,11 as well as contemporary policy priorities. This observation was reinforced by the empirical data we collected during this study given that we found knowledge interactions arising between multiple organisations, institutions and agencies, both public and private (e.g. industry, local authorities, universities, national charities and NHS organisations).
Furthermore, local innovation pathways were being actively mediated by national and regional influences, such as the variety of technological and knowledge-intensive firms embedded within geographic regions. As discussed in our literature review, a regional innovation system perspective emphasises the spatial dimension of innovation adoption and the strategic relationships that arise between institutions – such as collaborations between knowledge producers (e.g. universities) and intermediary agencies (e.g. university spinouts) – all of which occur within a context of shifting regional and national innovation policy. 44 Regional innovation systems can be characterised as inward facing and distinctive (consider Silicon Valley or Route 128 in Boston), yet at the same time remain highly porous to global networks and markets. So even where technical innovation systems are responding to similar policy mandates regionally (as in the case of AHSNs), one would expect to find heterogeneity given that different clusters of innovation activity, knowledge assets and forms of investment are found within regional zones. 158 Indeed, attention to underpinning ‘micro-innovation systems’ is argued to help illuminate processes (such as local knowledge sharing and exchange, organisational practices) that support the functioning of larger regional and national innovation systems as a whole. 158 This view is closely related to concept of the triple helix, which relies on regional and national case studies to illustrate the workings of innovation systems from the ‘bottom up’. Etzkowitz and Klofsten,46 for example, discuss how ‘collective entrepreneurship’ between government, business and academic sectors drives ‘techno-economic’ change and growth within a region and emphasise a prominent role for the ‘entrepreneurial university’ (pp. 246–8),46 which provides the capacity and expertise for new innovations, transforming an innovation system from its traditional base through investment in niche areas of research expertise with the potential for commercialisation. 46
This leads on to a second point, namely that networks and networking practices support regional collaborative initiatives, which again highlights the relational nature of knowledge mobilisation. We found in our innovation ‘tracers’ that relationship building and investment in networks of contacts was paramount for enabling innovation spread and regional connectivity. Importantly, this included the NHS but also went beyond the NHS or any single institution or sector. As such, the vignettes outlined in this chapter provide a snapshot (as with our network analysis) of some of the ways in which AHSNs were found to be engaging in innovation-focused relationship building and knowledge mobilisation activities, in a manner that went beyond a linear product adoption pipeline within the NHS. Indeed, our case study data and tracers raised interesting questions about the types of innovations and system interventions that AHSNs can realistically prioritise and support (or should support), given restrictions around funding, local system capacity and delivery time scales, and also the types of targeted knowledge mobilisation mechanisms that might effectively bring about innovation adoption at ‘pace and scale’.
Finally, we briefly find it useful to refer back to the definitions of innovation that inform this study. A central concern in the literature and policy is how to define innovation, which can be a highly overused term. Rogers’ classic definition identifies innovation as a ‘an idea, practice, or object that is perceived as new by an individual or other unit of adoption’ (p. 12),7 so the key aspect is the perception of novelty. An invention may be old, but if it appears new to a recipient or a social system, then it is deemed innovative. IHW1 retained this emphasis on novelty in its view of health innovation as ‘An idea, service or product, new to the NHS or applied in a way that is new to the NHS, which significantly improves the quality of health and care wherever it is applied’. 1 When examining innovation tracers in practice, we referred back to this broad policy definition, but we also remained attentive to how innovation itself was conceived of and discussed by individuals involved with the AHSNs, in keeping with our research objectives.
We also take a processual approach to the study of the career of an innovation over time, building on Van de Ven et al. 51 who tracked the long-term evolution of a number of innovations in US work settings, including in the health-care sector. They found that their trajectories were often non-linear in nature rather than following a prescribed template, going through distinct periods and involving shifting groups of actors and leaders with different interests and visions.
Innovation selection and adoption approaches are far reaching within Academic Health Science Networks
Table 9 provides a brief overview of some the innovations that we encountered in AHSNs. The innovations varied by clinical domain and whether or not wealth creation/business or industry engagement was a predominant point of focus. Many AHSN innovations were addressing long-term and chronic conditions, as these were common NHS priorities for improving population health. AHSN innovations that had been prioritised for spread typically fell within specified work streams and thematic areas that had been agreed at the outset – such as mental health, digital technology, diabetes mellitus, wealth creation or cancer – usually in consultation with an AHSN board and/or membership committee or council. AHSNs were especially mindful of population health needs and local priorities (e.g. through accessing knowledge from an earlier Joint Strategic Needs Assessment), so innovations needed to fit with locally defined needs and recommendations as well as the concerns of a far-reaching range of AHSN stakeholders (local authorities, acute trusts, community providers, industry, charities, etc.). However, the innovations we observed varied qualitatively in terms of their content and approach, reflecting both contextual variations that had influenced their development and the different mobilisation strategies used by AHSNs.
| Thematic area | Wealth opportunities | Health improvement |
|---|---|---|
| Diabetes mellitus | Industry collaboration | Access to devices and improved self-management (NICE) |
| MSK | Wellness for work; some private sector engagement | Improved pain management and mobility |
| Diabetes mellitus | Industry collaboration | Improved patient knowledge |
| LTCs | Project funding (digitech) in primary care | Improved self-management |
| CVD/stroke | Industry–NHS joint working; cost savings | Improved clinical management (NICE) |
| SMEs | SME–NHS engagement/new products | Access to new devices |
| Diabetes mellitus | NHS–university (spinout) | Improved disease monitoring |
| CVD/stroke | Potential cost savings to NHS trusts | Improved recovery and clinical outcomes (NICE) |
| MSK | University–NHS–industry (clinical trials) | Access to new devices |
| Science park | Inwards investment; job creation | Health and life sciences research (long term) |
The meaning of ‘innovation’: ‘bottom-up’ versus ‘top-down’ initiatives for health and wealth
Academic Health Science Network leaders expressed an intent to support innovations that had actual potential to deliver improvements at scale and could be spread widely across health-care providers (NHS and non-NHS) to benefit patients: innovations that would ‘make a difference’. Two AHSN CEOs reflected as follows when discussing projects under consideration for adoption:
So I’ve said it’s got to be grand, it’s got to be definable innovation if it goes in to that programme.
VSM, AHSN 4
. . . you know, you have to have an acceptable failure rate. So my caution is, you know, it might go nowhere, but it is innovative. It’s got association with industry and it’s quite well circumscribed. My slight criticism is I’m not sure it’s quite ambitious enough.
VSM, AHSN 1
Another aspect of innovation selection was the extent to which AHSN leaders were prepared to take on risk, such as by seeing potential in novel medical technology products that may lack a well-established clinical evidence base, or more ambitious regional or systemic interventions, which could potentially bring about radical or ‘disruptive’ change in the local health-care system or economy. 144
However, variations in health-care practice across the NHS in an AHSN region were acknowledged to be a recalcitrant issue that needed addressing; therefore, an AHSN team might select NICE TAs that had patchy regional uptake. This approach was reflected in different stances towards innovation and the role of AHSNs:
. . . to me innovation in the NHS – and you may profoundly disagree – is not really what most academics consider innovation. It’s not really bringing out brand new ideas, projects, pieces of equipment. It’s much more making sure that established good practice is why, is disseminated widely.
VSM, AHSN2
Indeed, we observe that the very meaning of the term ‘innovation’ gave rise to varying opinions in our qualitative interviews – across AHSN core teams and the stakeholders who we interviewed in their capacity as AHSN ‘knowledge contacts’.
External observers, for example, did not often have in-depth knowledge of the innovations and activities that AHSNs were supporting, and this sometimes led to the impression that the focus of AHSNs was on high-tech devices, academic science and pharmaceutical products with broader applicability to the acute sector:
Because when we tend to think of innovation, now forgive me because this sounds really pathetic, we tend to think of a bit of kit, a bit of technology or a protocol or a way of behaving by a professional, we don’t think about innovation in a context and how it improves the health of a population, and I think that’s what’s missing for me.
Knowledge contact, AHSN 1
It was also pointed out that in a strained financial climate (such as in NHS trusts that were tasked with making very substantial efficiency savings), innovation was sometimes viewed culturally in the NHS as a ‘dirty word’, synonymous with ‘trying to save money’ rather than improving services.
However, our SNA (in particular, the T2 wealth survey) indicated that AHSN senior leaders were knowledgeable about a range of health-care innovations spanning research, service improvement and new products (including medicines but also medical technology devices). AHSN board members and wealth oversight committees in particular were contributing new contacts and ideas about wealth creation. This is likely to have contributed to greater pluralism and diversity in the types of innovations now being applied to local health-care economies in practice. In addition, an AHSN ethos towards preferred innovation types appeared to exert an influence on the overall approach taken – such as a strong leadership commitment to patient involvement, quality improvement, public health or regional economic prosperity and job creation.
Wealth creation projects were often linked to an imperative to make improvements in a regional health system, such as by adding capacity for service innovation in the NHS or promoting clinical research focused on large patient populations. Hence, wealth creation was not undertaken merely for the sake of wealth creation and economic growth per se or viewed in isolation from health; rather, it was inherently affiliated with health goals, as one MD explained: ‘The overarching criteria I guess for their selection are to do with either patient experience, patient benefit, so clinical benefit, or some kind of sort of value for money type, so financial benefit type metric, rather than wealth generation’.
Congruency with AHSN core programmes (some of which changed over time), local health needs, scale-up potential and fulfilment of AHSN licence objectives were typically cited as important reference points for innovation selection. Health-care innovations that appealed to AHSNs could be novel, niche and ‘bottom up’ (as in the case of new medical technology devices or treatments), or geared towards local NHS service improvements and change. Alternatively, ‘top-down’ innovations might be selected that already had established a solid evidence base (such as NICE TAs), but were suffering from inconsistent usage and uptake across the NHS.
Therefore, we found a variety of initiatives being supported, both directly and indirectly, by AHSNs and covering population health as well NHS efficiency and regional economic objectives. In fact, an innovation was unlikely to be selected for adoption and spread unless it could be justified in terms of both economic and financial viability (e.g. waste reduction, costs savings) and health gains. We now turn to the main types of innovation approaches and knowledge mobilisation strategies identified across our sites to explore these innovation dynamics in greater depth.
Knowledge mobilisation in practice: typology of four models for health innovation uptake and spread
Academic Health Science Networks were engaged in multiple types of knowledge mobilisation activities and thematic programmes, many of which overlapped with both health and wealth goals. Furthermore, AHSNs were intervening at different points of a long innovation journey, for example moving from early commercialisation and product development to NHS procurement, deployment and sustainable spread. We therefore conceptualise AHSN knowledge mobilisation strategies along a continuum ranging from more targeted initiatives to regional or systems-focused proposals (Figure 8). These strategies cover both knowledge ‘exploration’ processes (searching and discovering innovations and ideas) and knowledge ‘exploitation’ processes (using pre-existing understanding and practices) as outlined by Oborn et al. 85
FIGURE 8.
Typology of AHSN knowledge mobilisation strategies (four models).

We now describe four main ‘knowledge mobilisation models’ seen as ‘ideal types’ of knowledge mobilisation process directed at innovation adoption and spread within and across AHSNs, which we place in a general typology. These approaches frequently overlapped in practice but, nonetheless, had distinguishable features. The four models are:
-
investment in new products and ‘clinical entrepreneurship’ (co- or direct ownership/sponsorship)
-
improvement science and spread of evidence-based interventions (NHS change management and service improvement)
-
innovation networking and matchmaking (stakeholder events and industry/business interface)
-
cross-institutional regional brokerage and support for regional innovation systems (‘triple helix’ and regional economic growth).
Model 1: investment in new products and ‘clinical entrepreneurship’ (co- or direct ownership/sponsorship)
Academic Health Science Network core teams were engaged in actively ‘scouting’ for innovations within their regions. Many of the innovations we identified during our early data collection had originated locally, in research-intensive universities or small businesses (especially universities, spinouts or SMEs), usually with the involvement of a local clinician, academic or product champion who had developed the idea. The innovation might be a product (such as a medical technology device) or a treatment intervention.
One key type of activity found in AHSNs was therefore the mobilisation of health-care innovations by lending support to an interesting and important group of clinicians (who we term ‘clinical entrepreneurs’) and local innovators who had invested substantial time in developing a new product or service improvement idea, but who lacked the business skills or knowledge for commercialisation and/or scale-up across the NHS. Some individuals had commercial experience (e.g. they may have founded an associated company), yet, nevertheless, struggled to get their particular innovation rolled out across multiple NHS sites. So many promising innovations failed to gain traction within the NHS system and had remained dependent on the efforts of their original inventors to drive adoption. This issue did not appear to stem from only a lack of time on the part of clinicians or NHS managers; it was frequently noted that there was generally low capacity and expertise within NHS trusts – which acted independently – to successfully identify, commercialise and scale up ‘bottom-up’ innovations originating from within local services and the wider health economy. There was also the perception that it remained difficult to inculcate a genuinely innovative internal NHS culture with new ideas often remaining in silos, as one core AHSN team member explained:
So there was a lot of that, so things were happening in isolation or clinicians were saying, you know, over time we’ve developed this product because actually it’s better, you know, we’ve found that it works with patients, so it’s just become best practice. We recognise we could develop it but, you know, we’re working with this company, they’ve got the IP but we don’t really know what to do next.
Manager, AHSN 5
It was also observed that the ‘NHS mavericks’ and clinical entrepreneurs present in local health economies would benefit from training and support to help develop their innovations for use within the NHS. One AHSN, for example, had developed a short, intensive training course for clinicians (doctors, nurses and biomedical scientists) covering the basics of innovation development and topics such as marketisation, IP, regulation and manufacturing. The AHSN had offered funded places for a small cohort and drew in different knowledge agencies to develop the training programme, namely external industry experts, local educational providers, as well as levering the business expertise within the AHSN itself (several members of the AHSN had previous health and life sciences commercial experience). There was recognition that in order to create wider cultural impact across the NHS, such learning would need to extend its reach to NHS managers and ‘decision-makers’ in order to bring about greater understanding of innovation as a process; however, small-scale regional programmes provided a positive starting point.
Academic Health Science Networks were therefore directing different types of capital into the local health economy (e.g. financial, intellectual, social) to further promising products and ideas selected for their fit with AHSN clinical themes and license priorities. One hospital consultant involved in a diabetes mellitus innovation reflected as follows:
NHS mavericks by nature are not embraced, that’s always been the case, but you need your mavericks to make things happen . . . So where do the networks come in? The network might be able to harness that maverick power and say right, we’ll give it some structure so that you guys can play in a more bigger palace, a bigger field, and try and lead the change. You’ve done it where you are, can you now lead those changes across bigger areas, bigger patches, bigger networks, there’s mavericks who like that. That is where I think the network has got to play.
Knowledge contact, AHSN 5
Academic Health Science Network support for health innovation arose at different points along an innovation pathway, depending on how developed an innovation was. An innovation might require a high degree of AHSN sponsorship or ownership/co-ownership to get it off the ground. In such cases, AHSN-led open competitions, themed events and ‘scouting’ activities helped to identify local innovations and provide a point of entry for their progress across the NHS–industry interface. An AHSN could ‘pump prime’ an innovation or provide accelerator funding to move a product forward commercially or in terms of establishing its efficacy (e.g. cost-effectiveness, scale-up potential, etc.).
However, given our research interest in knowledge mobilisation as instigated by AHSNs, our tracers were especially attentive to examples of AHSNs supporting ‘roll-out’ and spread. We found AHSNs to be highly active in this space, selecting and pushing health-care innovations that had already secured some level of IP protection and/or research evidence base, but struggling to transform local services and provide benefits to patients at scale (i.e. beyond one or two NHS sites). Typically, such innovations were being promoted locally – and sometimes further afield – by clinical and academic entrepreneurs (‘clinical–academic hybrids’), in ways that were opportunistic and non-systematic. The spread of innovations was in this way highly reliant on an individual’s capacity to promote their particular product or idea through their professional network, but many such persons had full-time roles and limited resources (and time) to promote NHS uptake regionally. There was recognition of this challenge within AHSN teams:
. . . if you think that they used to talk about innovation taking 15 to 17 years to get in to the NHS, we’ve now got an innovation in, with this one, within months. It’s been a year and we’ve got three [Trusts] in, by the end of this financial year we intend to have the rest in. But the point is that there are system blocks that you have to overcome and I wouldn’t want to be a Trust trying to overcome those, or a clinician, if you’re a ground up, I wouldn’t want to be a clinician trying to overcome that.
AHSN 4
Vignettes 1 and 2 (Boxes 3 and 4) offer some concrete examples of innovations being mobilised by AHSNs and some of the processes and issues encountered when an innovation is pushed across the NHS by a network. The first innovation (vignette 1; see Box 3) is an example of a medical technology product – a diabetes mellitus-monitoring device – originally developed within the regional knowledge economy by an academic and further developed by a NHS clinical specialist. Like many other innovations that we traced (i.e. devices and service improvement innovations), the innovative technology in vignette 1 (see Box 3) had been developed over a significant time period (10+ years). Furthermore, there was a published research base emerging about its efficacy, which drew on different research methods [e.g. randomised controlled trials (RCTs)].
This innovation uses Bluetooth and mobile phone technology to support the clinical care of women with gestational diabetes mellitus. The number of women with this condition is rising and it presents a risk to maternal and fetal health. Traditional models of service delivery require in-hospital visits by patients and hardcopy patient data monitoring. Given that the condition is unpredictable and difficult to manage clinically, this model is not optimal. The project rested on an evidence base on digital health solutions for supporting both type 1 and type 2 diabetes mellitus management. This evidence base was growing to include published, peer-reviewed academic articles, including both RCT clinical trial data and qualitative evaluations capturing patient experience. A service evaluation was being undertaken in an early adopting NHS trust.
Stakeholders and partnersA collaboration between a medical consultant working in a local NHS trust and university academics developed a digital health solution to enable remote clinical management of pregnant women with diabetes mellitus, funded by the local BRC. Early prototyping developed a product to enable accurate, ‘real-time’ glucose-level monitoring in patients. This product utilised software in such a way that patients could send their blood glucose readings directly via Bluetooth technology and a smartphone to a secure NHS server, reducing the need for multiple visits to clinics and enabling better patient–doctor communication.
Clinical collaboration was deemed foundational to success because ‘the clinician [within a Trust] . . . feels guided and sort of reassured that somebody that understands what the technology is and what the clinical need is, has been involved in the design’.
Academic Health Science Network knowledge mobilisation strategy and contributionThe AHSN was praised for playing a ‘transformative’ role in spreading the innovation across multiple sites within a fragmented NHS landscape. The approach to mobilisation centred on clinical and professional networking at NHS trust level, and central AHSN project management to identify, support and monitor uptake. So a project management approach helped to manage spread across NHS trusts while AHSN clinical leadership promoted local understanding and lent professional credibility. A first stage was identifying a relevant contact person(s) at a NHS trust level to engage with, usually a clinical service lead and practitioner.
The AHSN provided funding for clinical support within NHS trusts that decided to adopt the innovation, promoting effective implementation and ensuring that there was ‘somebody on the ground while the roll out happened’. Direct involvement of a clinician who helped to develop the idea further contributed to regional spread, especially during initial meetings with trusts when possible changes to service delivery models were discussed.
This tracer reveals how a mix of tacit and explicit knowledge is helpful for innovation spread in the NHS in various respects. First, expert clinical knowledge provided reassurance to early adopters in NHS trusts. Second, explicit academic knowledge provided access to cutting-edge technology and built up a research evidence base. Third, an AHSN effectively combined tacit knowledge of NHS systems with commercial expertise to get the innovation through complex NHS approvals, such as procurement, contracting and tariffs. The amalgamation of these different knowledge bases within an AHSN supported knowledge mobilisation.
Illustrative quotations
. . . as straightforward as this project is in one sense, there are complications, OK. So the first thing that I would say is that getting engagement is a key thing, so making sure that we have our tools together, so we have a methodology that we follow which is clearly around we need to understand the local requirement and make sure that there’s a business case put together to enable [a] Trust to take it forward . . . then there’s another stage that takes place which is around the technical side of it, so we have a technical specification session which goes through actually, you know, this is how you work, OK, fine, we’ll we can change this for you but we can’t change this bit.
AHSN manager
. . . there had been a number of publications in exactly this sort of situation using new technology, some on the telephone, some of them, you know, computer, all different things, but all of them were single centre, none of them had been able to replicate it in a different centre. I think that is absolutely crucial in this sort of situation, in the complex way the NHS works, to be able to prove it at multiple centres.
Clinician
. . . what drives me, what gets me up . . . when I get on my bike or in the car in the morning, I drive past it [a hospital] and I can say actually in all of those rooms the patients are being observed and their risk of deterioration is evaluated using [an innovation] which my team and I designed.
Academic innovator
The AHSN prospectus highlighted MSK diseases as producing a heavy health burden for the population (e.g. arthritis). This tracer refers to an evidence-based programme for patients with chronic pain that integrates education, self-management and coping strategies. The innovation may reduce the need for surgery and help individuals return to work more quickly. It is highly consistent with NICE guidelines for MSK conditions and was selected by the AHSN as an early priority where high impact was possible given that the innovation had a strong evidence base (RCT, user experience) and associated outcome metrics. The aim was to roll out the innovation from a previously small number of sites. We collected interview data in the period July–December 2015. We note that mobilisation efforts were reported to have evolved in 2016.
Stakeholders and partnersThe range of partners is relatively contained. The innovation ‘inventor’ is a long-term change agent: a clinical academic who had been using interpersonal networks to spread the message but with mixed results. A private firm built an educational website to support spread. There was collaboration with a national charity to raise the profile of the innovation and clinical leadership from within the AHSN for a period of time.
Academic Health Science Network knowledge mobilisation strategy and contributionThe AHSN provided resource for (1) a programme-specific website; (2) dedicated programme management support and monitoring; and (3) pump priming financial support for extra health practitioner time in adopting sites.
Promotional and educational events were organised with key stakeholders, and a clinical leader, funded by the AHSN, wrote to NHS providers and CCGs about the innovation to encourage its wider adoption. An educational website was also built as an educational tool and to channel specific questions away from the inventor.
This strategy of ‘active diffusion’ sought to take demands off the inventor and provide collective scale-up capacity. The AHSN reported scale-up from 2 to 24 sites over a couple of years, including outside the region and into community and non-NHS settings.
There were small-scale and indirect links to wealth creation priorities as it was argued that the programme could improve productivity at work. However, there was debate about whether the programme should be commercialised or remain as a public good, free and accessible to the NHS. However, the AHSN experienced difficulties in getting CCGs to pay for the programme (even if adopted by providers), given local cost pressures. The innovation landscape remained fragmented and complex and the AHSN’s wish for cost-effectiveness and outcomes data was difficult to meet within routine clinics. It was reported that they were some ‘tensions’ around measurement, approach to spread and the major complexities to be navigated to get buy-in from the NHS, despite a solid evidence base and proven efficacy.
Illustrative quotations
We’ve no levers in the [AHSN], we’ve no, you know, financial levers to say if you don’t implement this you’re doing wrong here, you know, it’s costing us money . . . I think they struggle with that about who do we, who do we influence . . .
Academic innovator
[The inventor] is now starting to think about what is the model, what’s a sustainable model, and also how much can people adapt it locally without it losing what is it that makes it effective.
The medical technology innovation nevertheless had a long and protracted history around spread: the inventor had attempted to push the original technology into the NHS largely through using their personal and well-connected professional network and sheer determination. They reported a high degree of interest in the particular innovation at multiple levels over the years, including from senior health leaders, policy-makers and health-care professionals.
However, successive periods of NHS reforms had meant that ‘all the people that had been behind setting up the project had moved on . . . I mean a lot of people had given up then and, and I didn’t’.
With the advent of regional academic science infrastructure – an AHSN and also a BRC – real change arose when funding became available to renew work on the innovation and invest in its active diffusion in the NHS. At this point, a local clinical specialist approached the inventor (via their own professional network) to develop the technology further and produce a prototype product that could help respond to pressures arising within local clinical services.
The innovation was later picked out by an AHSN with a focus on scale up and spread. It handled issues such as the manufacture of the technology, NHS procurement and the promotion of technology to local NHS trusts and health professionals. It thus provided support for both the inventor and local clinical leadership to scale up the innovation by navigating ‘complexities’ within NHS contractual and supplier systems, as well as managing relationships with industry (who had potential to scale up production).
Of our 10 tracers, several touched on chronic LTCs, such as osteoarthritis or type 2 diabetes mellitus. In one AHSN, for example, there was a spectrum of AHSN interventions aimed at improving clinical outcomes for MSK patients and up-skilling local health professionals’ knowledge of MSK disorders as an illness. The AHSN reported training ‘over 200 GPs’ about how to deal more effectively with patients presenting MSK issues within 10-minute GP consultations and sponsored a second innovation, which we explored in depth, designed to enable better patient self-management and education as well as clinical outcomes (vignette 2; see Box 4).
Similar to the innovation described earlier, the MSK innovation had originated regionally within a HEI, led by a clinical academic. However, it ‘hadn’t been rolled out at all actually in this neck of the woods’, and in one local area the innovation had ‘died a death’, leading to a modified version being used. For this reason, innovation fidelity and NHS uptake were deemed problems for a very promising intervention.
The innovation highlighted dynamics around innovation ownership and scale-up as some tensions emerged around knowledge mobilisation at scale. The originator of the innovation had traditionally been the first port of call for early adopters and visited sites to promote uptake and to ‘get this thing out there on the streets’. The innovation had therefore been traditionally mobilised through a direct and highly personalised approach, such as through professional networking and ad hoc interest, a theme that recurs across our tracers. Consequently, the innovation had been applied in pockets of health-care practice without additional capacity to monitor innovation fidelity or sustainability.
The AHSN had a view to ‘get this going’ and ‘push the boundaries a little bit’. It was perceived as providing the ‘kudos’, ‘credibility’ and ‘push’ required to take forward implementation, offering a momentum previously lacking within local HEIs (whose interest in the innovation had been primarily research focused). Yet despite several evident successes, the AHSN had also struggled to promote regional adoption across the NHS as a result of prevailing cost pressures. This had resulted in a stronger community adoption focus and a focus on non-NHS providers.
We return to some common difficulties for knowledge mobilisation and innovation barriers later in the chapter (see Issues encountered and knowledge mobilisation barriers), but note the major challenges faced in both of these examples of an innovation that has already been mobilised locally on a small scale, but has struggled to gain acceptance across the NHS more widely (such as becoming incorporated in NHS provider or commissioning plans). This part of the spread process was found to take a huge amount of effort from persons knowledgeble about NHS decision-making processes and able to actively liaise between many organisational boundaries.
Therefore, we found that locally derived innovations that showed a great deal of promise for patient impact and for which there was evidence of efficacy (such as a high-quality research base of RCT standard, but also smaller pilot studies) were selected by AHSNs for wider adoption. Mobilisation processes that AHSNs engaged in included supplying expert knowledge about the NHS or innovation process, funding, project management support and capacity at service delivery level (e.g. through backfilled clinical posts). AHSN operational teams and middle managers also played a key role in promoting adoption across a larger number of NHS trusts by putting together NHS business plans and dealing with NHS supply procedures.
In the main, these types of innovations had been in existence for some time and stemmed from academic infrastructure and spinouts. They had been initiated by a key cluster of academic innovators and clinical entrepreneurs who were research active and highly motivated by goals of service change and modernisation in the NHS. However, these innovations had not necessarily been NICE endorsed (although they may have started the process), and were requiring further evaluation and research if they were to be rolled out across different contexts. As such, they were very much ‘bottom-up’ innovations endorsed and sponsored by AHSNs but requiring investment to realise their full potential.
Model 2: improvement science and spread of evidence based interventions (NHS change management and service improvement)
National Institute for Health and Care Excellence TAs were sometimes selected as an important area as AHSNs responded to a need for system-wide, sustainable spread of innovations that had already passed rigorous tests of economic and clinical efficacy. In this way they were addressing inconsistent usage of treatment guidelines and proven interventions and the challenge of ‘unwarranted regional variation’ in the NHS. The NICE TAs we observed addressed a variety of clinical areas such as diabetes mellitus, stroke, arthritis, nutrition, cancer and dementia.
Innovation, Health and Wealth1 promoted the wide-scale adoption of innovations that would strengthen NHS performance and add value and, above all, were replicable across settings (p. 9). Possibly for this reason, support of evidence-based and approved NICE TAs was viewed as an important inclusion by some AHSNs, in addition to their receptivity towards novel innovations originating within their regions.
This type of knowledge mobilisation had strong links with the theme of medicines optimisation at regional and pan-regional level and intranetwork knowledge sharing was important for knowledge mobilisation, such as co-operation with regional CLAHRCs (where present), SCNs and possibly other AHSNs. At the national level, we noted that AHSNs were discussing the NICE Implementation Collaborative, indicative of support for national partnership working.
Often the ‘knowledge contacts’ and inventors we spoke with about the health-care innovation landscape recognised the need for a positive and collaborative relationship with NICE and its associated programmes. However, there were also some frustrations mentioned about NHS evidential requirements for innovations, especially around medical technology and new technologies arising from smaller firms or spinouts, which lacked RCT-type trial capacity, as one product developer explained:
. . . the other barrier for us at the moment is the level of evidence required is, it’s almost in line with a new drug . . . we’re medtech but actually we’re not a medical device because we don’t actually provide any diagnostic or therapeutic impact, we’re effectively a better delivery mechanism . . . we know that there’s a great case for this and it fits perfectly with the NHS need to take some costs out of the system and to provide more support around mental health. . . . we’ve done some trials but they’ve been service trials, but we have evidence that it will improve the service delivery. What we don’t have and what I’m very keen for and what we asked the AHSNs was to have the clinical side of that trial.
Interestingly, the Five Year Forward View147 discussed the intention for the NHS to expedite the health innovation adoption pathway by supporting ‘lower cost RCTs’ and evaluations in cases in which full RCT trials were not feasible (p. 34). 147 There was also acknowledgement by the NHS that medical technology devices (as opposed to drug interventions) required support, for example through ‘operational pilots to generate evidence on the real world financial and operation impact on services’. 147 Nevertheless, in practice, we found that the resourcing of such trials was still difficult for innovators to leverage, even with AHSNs active in this space.
For AHSNs, sponsoring NICE TAs were a ‘win/win’ given that they were institutionally backed by the NHS and in an area where AHSN–industry collaboration was possible: ‘I’m getting a lot of requests to say can you help us with the uptake and reduction in variation in the NICE guidelines essentially . . . we’ve got best practice that’s been identified, you know, evidence based and we’ve got industry saying we’d like to engage with you on this, how do we work collectively to do that’.
However, some AHSNs had encountered resistance when attempting to mobilise NICE TAs in their regions:
I think people want different things from the AHSNs. So the commissioners don’t want us to get more NICE TAs used, they absolutely don’t want us to, they don’t want us to make them do that or persuade them to do it . . . Because they see it as NICE TAs are expensive.
AHSN 4
Three of our tracers focused on NICE TAs and covered clinical practice in CVD and stroke care, and diabetes mellitus (we present only two here for reasons of space; Boxes 5 and 6). They illustrate several core issues in the knowledge mobilisation of evidence-based interventions: (1) even where there is a convincing evidence base, regional and local knowledge mobilisation is particularly effortful, requiring boundary-spanning activities across organisations, sectors and networks and relationship building for maximum impact; passive dissemination is highly likely to be inadequate; (2) in a climate of severe financial restraint in the NHS at trust and commissioner levels, short-term cost drivers and concerns about decommissioning can present difficulties for the adoption of best practice within local health economies; and (3) changes or controversies in the evidence base at national level may slow down implementation and adoption processes at the local level.
Responding to NICE guidance in the clinical area of CVD, this AHSN programme aimed to implement at scale a pan-regional, standardised approach to improving patient outcomes for those at risk of an AF-related stroke. The AHSN built a data management system to demonstrate ‘opportunities’ and enhance and share capability for ‘seek and treat’ by identifying populations for anticoagulation.
Stakeholders and partnersThe programme involves collaboration with CCGs and NHS trusts, the wider regional academic health science system, pharmaceutical companies, other AHSNs and national networks. The AHSN was seeking academic partnerships in this area and had been approached by universities.
Bringing about transformational change in the NHS involved lengthy negotiations, partnership building and trust. Collaborating with early adopters was seen as key, as the AHSN sought to make strategic region-wide change, so securing wider agreement from CCG board-level decision-makers was crucial, albeit time-consuming given limited staff resources.
Academic Health Science Network knowledge mobilisation strategy and contributionThe AHSN collaborated with the SCN, AHSC and CLAHRC to build on existing local evidence of clinical need, in reference to NICE guidance.
An AHSN dashboard compiled relevant data to provide prevalence metrics and cohort identification at practice level. The AHSN further contributed to a commissioning toolkit under a wider collaboration, which included another AHSN, the SCN, PHE and local authorities. A paper was produced for the regional heads of commissioning to outline complementary collaborative streams across the SCN and AHSN and urging them to ask CCGs to consider using both tools.
The opportunities for regional economic impact were anticipated through indirect cost savings such as reduced A&E admissions, reduced bed utilisation and reduced requirement for AF-related long-term rehabilitation and social care costs. The AHSN planned to use health economists to prepare return on investment projections to inform a region-wide business case for CCGs.
The innovation had captured the interest of pharmaceutical companies, which were invited to discuss joint working with the AHSN. The AHSN also actively sought to raise the national profile of AF service improvement and encourage wider adoption via the national AHSN Network.
Metrics to monitor impact included the number of patients transferred to NOACs and ultimately the reduction in avoidable strokes. The 5-year ambition was to make major improvements in the AF pathway (from appropriate prevalence attainment, through to innovations in diagnostics, optimising medicine management, and promoting self-care and self-management models) to bring about a reduction in AF-related strokes and indirect cost savings for the region.
Illustrative quotations
NICE guidelines on AF were coming out and we had seen the build-up to it . . . so we made that a clinical priority but when you start to engage with teams around how do we find these people, what choices do they have, what other options could they go onto, then you begin to have the conversation about well, actually, have we got the detection right, have we got the right diagnostic tools, is the pathway too long and it needs shortening.
AHSN team member
At the moment there is a traditional clinic anticoagulation system . . . so it’s a secondary care delivered service and yet people can monitor and indeed manage their anticoagulation at home like people manage their insulin at home. Why can’t they do that, it can, the technology is there that would enable it.
AHSN senior manager
This tracer centres on the use of national evidence-based guidance for using new technology in the NHS to avoid DVT and improve clinical outcomes in patients recovering from a stroke. The tracer formed part of a wider, evidence-based, national innovation adoption programme. NHS IQ had engaged with industry and purchased new technology ready to be rolled out at scale within NHS trusts.
The original evidence base for the innovation was a NIHR trial that had demonstrated improved patient outcomes and reduced mortality. However, in 2015, NICE guidance on the use of the new technology in immobile stroke patients shifted, affecting national adoption efforts and leading to a debate among clinical specialists and researchers (evidence was drawn from different clinical specialties that could have very different views).
Stakeholders and partnersThe intervention took the form of a multiagency and multinetwork improvement drive undertaken jointly between the local AHSN and SCN, with national support from NHS IQ. At the regional level, clinical leadership and expertise in the treatment of stroke existed within the SCN and specialist NHS stroke units. Clinical expertise on cardiovascular health resided within the AHSN, which had created an internal network to draw together clinical knowledge from the regional health economy.
Academic Health Science Network knowledge mobilisation strategy and contributionThe AHSN gathered baseline data on the utilisation of the innovation in stroke units (a central ‘dashboard’) for eligible patients to compare regional and national adoption rates. These data highlighted important variations across regional NHS trusts, raising questions about the enactment of best practice guidance in local hospitals. The AHSN was working to ‘understand in detail why is it that there’s variation here, what is going on, is it that you’ve not implemented the protocols properly, is there problems with supply or is it that you’re not recording the data, what is it?’.
The AHSN was actively going into trusts to support adoption, through a direct and networking approach. By co-ordinating expertise across the region – involving a mix of medical units, clinical stroke specialists and the SRN – the AHSN applied project management and networking approaches to help increase the adoption rates (by up to 50% in some trusts).
This innovation highlights how shifts in evidence-based recommendations at the national level can have local impact on service improvement plans. Indeed, there was a risk that NHS adoption processes could fail to keep up with rapidly evolving evidence and technology.
Illustrative quotations
I just plotted out utilisation modes, go against, you know, the information on Roger’s Curve and no surprise, it goes from zero to a hundred percent, but this is for [the new technology] . . . So you’ve got completely different uptake, and sometimes you see that in the same clinical service, you see two clinicians with a completely different uptake
AHSN senior manager
. . . we’ve now implemented this, we now need to go back in and understand in detail why is it that there’s variation here, what is going on, is it that you’ve not implemented the protocols properly, is there problems with supply or is it that you’re not recording the data, what is it? So that process is happening now and we expect, when we sign this up we expect people to be performing at this level.
AHSN manager
. . . you know, you can’t just purchase things and expect people to just use it, you know, I know as much as we would like the world to be like that, it isn’t . . . So, you know, it just doesn’t work. So the issue was about well how can we actually make this thing work?
AHSN manager
Interestingly, the attempted spread of NICE TAs by AHSNs had engendered a fair degree of multiagency working and opportunities for shared learning. The interventions were embedded within clinical systems; therefore, in many respects they were attempts at service quality improvement along established care pathways or, if more ambitious, regional attempts to reconfigure an entire treatment pathway to improve clinical outcomes and realise cost savings. Compared with some other innovations selected by AHSNs, NICE TAs tended to have clear, pre-established outcome metrics, and, therefore, performance measurement and impact assessment were altogether more straightforward.
Model 3: innovation networking and matchmaking (stakeholder events and industry/business engagement)
Early on, health improvement networks were found to be more mature in our SNA than wealth-orientated ones (as previously discussed in Chapter 5), indicating that AHSNs were tapping into previous networks of relationships and initiatives (largely NHS and academic contacts) to support innovation adoption and spread around health priorities. By contrast, the emergent wealth networks differed in their composition, suggesting that new contacts and relationships needed to be accessed to address their objective of wealth creation.
Our tracers illustrated the degree to which AHSNs needed to invest in relational and networking efforts across sectors and different parts of the NHS to support knowledge mobilisation, as indicated by one AHSN manager: ‘I think that we do have a great role in pushing the new technologies and all that type of stuff too, but we shouldn’t forget that actually it’s that forging the relationships and building the networks’.
So ‘managing’ and ‘brokering’ relationships for innovation was a core activity, one that frequently involved areas in which traditionally NHS engagement was perceived as poor or difficult to overcome, such as linkages to SMEs and industry:
. . . from a pharma point of view what has been interesting is that they have been allowed almost a different insight into the health-care market. So this is about them being seen as collaborators and partners. It is trying to change the relationship of pharma and health care. And I think that is our role as a knowledge broker to go they have a skill set. It was interesting because you get the health-care professionals in a room and they know their part of the pathway very well whereas pharma appreciate the whole pathway because of their interactions across all of the different pieces.
AHSN 2
Some AHSNs had invested resources mapping regional assets and businesses in the local economy early on, particularly in the health and life sciences and SMEs and spinouts, so they were acquiring knowledge on the key firms and partners within their regions and potentially how to connect them.
Some AHSNs that we observed were acting as innovation ‘matchmakers’ with the commercial sector, for example by creating spaces and forums where interested parties could meet, share knowledge and showcase new products and innovations. Knowledge mobilisation in this way centred around the practice of digital communications (websites, e-mail updates, newsletters, online platforms, etc.), events and behind-the-scenes knowledge brokering. To further support brokering with the commercial sector, events were organised by AHSNs targeted at specific health innovation subsectors such as the pharmaceutical, digital health and medical technology industries.
At the national level, we noted that building ‘a culture of partnership and collaboration’ was a collective objective for all AHSNs. In practice, we found this being promoted locally in the AHSNs we studied through inclusive governance structures (e.g. large membership councils and oversight committees with a direct influencing role) and an array of AHSN-hosted or jointly hosted events, sponsorship and leadership of collaborative efforts around service improvement.
Many of our tracers touched on these knowledge mobilisation strategies of network building, partnership and matchmaking (where individuals or groups were connected to progress particular innovations). Indeed, model 3 underpins many core AHSN activities.
To illustrate how AHSNs attempted to grow networks, we provide one example: a diabetes mellitus programme led by an AHSN. This aimed to create a cohort of ‘champions’ who were recruited to act as regional ‘change makers’ and then roll out improvements in diabetes mellitus care through their own professional networks. Several large pharmaceutical companies were involved, in addition to the third sector and local branch of Health Education England. Champions included individuals from primary care and CCGs, community pharmacists, hospital consultants and pharmaceutical representatives. Knowledge mobilisation in this case relied on the collective enthusiasm of champions; however, this meant that quantifying the overall impact of the programme was inherently problematic. However, in our qualitative interviews with champions, we found that improved knowledge mobilisation and self-confidence were considered important outcomes of the programme.
Vignette 5 (Box 7) illustrates how AHSNs were also engaging with SMEs during the course of the study. Very often, they were helping SMEs and other non-NHS organisations to negotiate NHS procedures in ways similar to model 1: ‘When I first got into post I put me and the SME in the middle and I drew lines out to all the people, all the organisations that I felt would be of use to my role and I made an effort to go out and explain to them what the AHSN was doing and what my role within the AHSN was doing’ (AHSN 3).
Some health-care innovations are largely university driven and grant funded at the early stage, after which market investors are unwilling to invest because innovation adoption into the NHS is difficult and procurement routes unclear. The AHSN aimed to investigate and repair this ‘broken bit of the pipeline’ in this tracer.
Stakeholders and partnersStakeholders were SMEs, inventors, trusts, CCGs and AHSN delivery partners (AHSC and innovation hub).
Academic Health Science Network knowledge mobilisation strategy and contributionThrough a series of events, communications and backing from its delivery partners, the AHSN positioned itself as the ‘first port of call’ for health-care businesses in the area with innovations that could benefit the NHS.
The AHSN drew on a US model for innovation adoption already embedded in translational work regionally. A comprehensive ‘support system’ for innovation adoption was supported by existing governance arrangements to join up assets across the region. AHSN leaders activated and mobilised their existing personal networks with known ‘experts’ with expertise in procurement, IP and commercialisation who could offer know-how and connections.
The AHSN supported SMEs and inventors to navigate NHS procurement and provided key information about clinical opinions, regulation, funding support and market analysis. The AHSN seed-corn funded several early-stage projects to achieve proof of concept to develop the solution to a point at which it could leverage additional funding. The AHSN was thus not simply brokering introductions on behalf of SMEs, but also empowering SMEs to be in a stronger selling position to challenge a ‘daunting’ and ‘risk-averse’ innovation culture.
Priority was given to local SMEs with innovations that matched the AHSN’s and wider NHS priorities, with eligibility also extended to ‘disruptive innovations’ originating from the wider UK and internationally – seen as vital to encourage new SMEs or companies to move into the region.
The AHSN began to scope out how prospective innovations might offer commercial opportunities; an idea explored was putting equity investment into some SMEs in the hope of future dividends. Targets were set around economic metrics such as number of SMEs supported, total investment generated, number of jobs created and percentage increase in NHS procurement spend in regional companies, but these were difficult to attribute directly to the AHSN.
This tracer demonstrates the importance of joining up existing regional resources through leveraging professional networks, and investment in improving the interface between SMEs, industry and the NHS. SMEs and industry often lacked substantive knowledge of NHS procurement – again a ‘problem’ perceived as of broad significance for innovation adoption. Yet the tracer also demonstrates that there was willingness by AHSNs to back early-stage but potentially game-changing, disruptive innovations if they could broker productive NHS–industry/SME relationships and make a strong business case for a particular innovation.
Model 4: cross-institutional, regional brokerage and support for regional innovation system development
The vision for AHSNs, set out in policy, was that they would serve as a ‘gateway’ between academia, industry and the NHS, and bring together disparate stakeholders from local authorities, the third sector and research communities (pp. 18–19). 1 AHSNs were tasked with disseminating impactful and effective innovations by working closely with other NHS innovation and research organisations (such as AHSCs). We found examples of cross-regional brokerage undertaken by AHSNs that brought together an array of non-NHS organisations. This type of intervention often built on antecedent networks (such as local HIECs or innovation hubs) or a member of an AHSN’s own professional network, especially in the early phases of the AHSNs. Compared with model 3, they show more prominent features associated with the concept of the ‘triple helix’ stream of literature (as discussed in Chapter 3) and were more university and/or growth focused.
One such ‘macro’ example is provided by vignette 6 (Box 8). The AHSN that we studied had funded an expert role to support the development of a life sciences cluster in the regional economy. The concept of a cluster was not in itself new and predated the AHSN. The AHSN provided a suitable ‘vehicle’ to take a concept further and helped to facilitate collaborative working with local partners – notably county councils, a strong regional university and LEPs. Across these partners, there was ‘strategic alignment’: for the AHSN, the concept of a life sciences cluster aligned with its wealth creation objectives (in this instance, the creation of new jobs locally and capacity building the life sciences); for external agencies, they had access to some funds and business support and expertise via the AHSN (the brokering of relationships and concept was led by an individual with academic and commercial experience and funded by the AHSN). In this way, innovations supported by an AHSN might extend beyond the NHS and have an especially strong economic, commercial or geographic focus in terms of investing in regional infrastructure for growth.
This innovation was a large-scale and macro-level tracer issue with two related foci: (1) a strategy to expand a regional life sciences cluster; and (2) within that, the associated redevelopment of a science park in a rural site, previously used by public sector research agencies with a long tradition of excellent scientific research, but now with spare capacity. A policy decision had recently been taken that a number of scientists would relocate to refurbished science labs out of the region so there was an economic concern regionally about the loss of well-paid science jobs in this area.
Stakeholders and partnersAn initial coalition of partners included the research and innovation division of the regional Russell Group university, a county council and LEP, and the AHSN (which undertook a review and proposed the idea of a regional life sciences cluster). This core grouping enrolled further support from leading scientists across the region, vice chancellors, a well-informed and sympathetic local MP and senior directors in the public research agencies currently on the science park site. Support was secured from government nationally. So a wide and disparate array of stakeholders was involved who came from various sectors and included political as well as administrative champions.
Academic Health Science Network knowledge mobilisation strategy and contributionThere was a strong concern to strengthen excellence in the life sciences regionally and in selected priority areas across the region. The region could then position itself to receive ‘refugees’ from what were portrayed as saturated science parks and clusters nationally (e.g. some of which had difficulties in getting planning permission for new science parks and expansion). This would stop the drain of its regional scientific talent to ‘golden triangle’ clusters and raise the identity and profile of the area to attract a significant number of firms, along with inward investment.
This tracer is the most ‘macro’ and strategic of the 10 studied and heavily focused on life science policy and wealth creation (in the form of a target to create > 2000 new jobs and attract £100M of investment within the 5 years). There are many players involved from different sectors, of which the AHSN is only one. The AHSN helped to build regional collaborations with other players (e.g. LEP, county council, a Russell Group university) and to write the initial vision. At an operational level, pump-priming money from the AHSN gave some resource to a well-established scientific group used to prepare successful bids for larger awards from prestigious outside funders.
Illustrative quotations
. . . what we’re really trying to do is create an infrastructure capable of (a) taking innovation from within our region and (b) attracting investors from outside who would wish to take advantage of the innovation capability in our universities and local companies.
Programme lead/consultant, AHSN 5
[AHSN funding] allowed us to go out and visit the main companies in the area, reach out to other organisations such as the neighbouring AHSNs, neighbouring institutions and of course the major UK-based institutions.
Programme lead/consultant, AHSN 5
Vignette 6 can be considered an outlier given the scale of the regional ambition and less immediate focus on population health, yet the brokering of strategic relationships across sectors and agencies (such as LEPs and councils) was a common activity in the AHSNs we studied.
An interesting feature of AHSN activity in this model was how networks were functioning as intermediary boundary-spanning vehicles by finding shared strategic interests across industry, universities and government agencies – in ways outlined by ‘triple helix’ theory (vignette 7; Box 9). Nevertheless, it was frequently boundary-spanning individuals with knowledge of each of the university, the NHS and commercial sectors in health care or life sciences who were able to effectively broker institutional relationships given their personal networks and knowledge. Agency within the triple helix, as well as institutional relations, therefore appears highly important.
The AHSN encouraged and helped fund a MSK research centre in a local university, working on research and treatment in such areas as new technologies and devices for elderly people with arthritis or fractures of the neck of femur. It was intended that the centre would work ‘across the university and with hospitals, industry partners and academics’ to deliver high-quality research, publications, learning and thought leadership, along with good patient outcomes. It would attract new inwards investment and create new science-based jobs. The MSK research team was seen as building on a good track record of academic/industry collaboration, led by very credible academics, and as having the potential to attract substantial inward investment (commercial trials) and create new science-related jobs within a new industrial cluster.
Stakeholders and partnersAt the core of the innovation lay a well-established research partnership involving orthopaedics and physiotherapy. The academics were supported by the AHSN, and also the LEP and a university with a strong presence in health sciences. The centre also had strong links with industrial partners (both large multinational firms and UK SMEs), built up in clinical trials in the medical devices area.
Academic Health Science Network knowledge mobilisation strategy and contributionThe academic team had been working together on clinical trials and publishing for a long period of time. The AHSN provided financial support, initial accelerator money and top-up money for a backfill appointment to release principal investigator time in a relatively pragmatic way, thus ensuring financial and time resources to grow an established academic collaboration. It acted as a broker, encouraging better links between the team and the LEP, for which this was a different sector from its usual field (creative industries and digital). The LEP provided important funding for a new laboratory in the institute and the university provided funding for substantive appointments and a cohort of PhDs. The case appears to be a good example of the triple helix model in action.
Illustrative quotations
We were saying well look at the context of the local economy, what the university needs, what the hospitals need, what could we do if we had some infrastructure around us and if we could get someone to buy in to that concept. And that was picked up by the university but also more importantly by [a member of the AHSN] who was working at the AHSN at that stage, and [they] came back to us and said well that’s interesting, that’s kind of what we’re doing. And [they] brought a new angle to it because we were very much in terms of research and improving technology, but [they] was saying well actually if you bring that money in, that’s wealth benefit.
Clinical academic
Our findings further suggest that local councils and other publicly funded innovation agencies may have been overlooked by triple helix theory given how strongly the concept emphasises the role of entrepreneurial universities in driving economic growth. Indeed, multiple external sources of external funding (e.g. such as from the European Union, local enterprises or industry) lent support to regional innovation in the health and life sciences, not simply HEI funding. Some of the AHSNs we studied were proving highly successful at leverage such funding streams within their regions (vignette 7; see Box 9).
Academic Health Science Network learning about knowledge mobilisation over time
Academic Health Science Networks should be seen as dynamic networks, with the implication that that their knowledge mobilisation strategies were also evolving over time. Some interviewees noted how at the outset of AHSNs they had perhaps been naive about innovation spread or attempted a more directive role aimed at diffusing high-impact innovations. Over time, greater cross-sector collaboration, matchmaking and regionally focused activities appeared prominent. There was less emphasis on direct AHSN ownership of innovations and a greater sense of matching local problems to promising innovations, some of which might more radically shape care pathways:
. . . we have moved away from pushing innovation to let’s work with our partners to define their needs and their challenges and then bring in industry, but not for the sake of bringing in industry but for the sake of solving the problems.
AHSN MD
There also appeared to be a growing understanding of effective approaches to knowledge mobilisation and the pervasive system challenges that needed addressing, such as NHS complex decision-making processes, along with issues around evaluation and evidence needed for innovation adoption, scale-up and replication:
I suppose joining the network it’s been quite a steep learning curve to go forget the traditional hierarchies that you’re used to and now start exploring and it doesn’t matter what position they are. And I suppose that’s, certainly I’ve been very conscious of in how I’ve approached things.
AHSN 2
In particular, negotiating NHS efficiency savings and engagement of CCGs was reported to have been difficult across the AHSNs that we studied and these efforts had not always worked out so well. AHSNs were also at times struggling to find a balance between target-led knowledge mobilisation strategies and the need to ensure wider membership coverage and stakeholder engagement which risked spreading their resources too thinly:
The one thing that I probably did not realise when I came into post, when I started looking at it, you know, this would be bought in an acute trust and you can see where products belong, probably sometimes better than the manufacturers and producers of them. But the most difficult people to get hold of, sit around the table with has been CCGs and it is the CCGs who really hold the purse strings to a lot of these products. . . . But the focus of the NHS at the moment especially with innovation is about saving money. Innovation has to demonstrate it can save money or else it’s just not going to get in there because there is no money to buy innovation.
AHSN 3
One of our principles is that of inclusivity. We have not yet spread our tentacles as it were as widely as we want to. But I think that’s important that we do that. However, there are an awful lot of organisations out there like CCGs, primary care, or acute trusts or mental health trusts or community trusts. I think pragmatically one has to try and get on board those that are most likely to come on board and do it as a sort of slowly incremental process.
AHSN 2
Knowledge mobilisation influences
. . . now we need to think slightly differently about the spread.
AHSN MD
Academic Health Science Networks in the early days were not drawing on explicit academic models or knowledge (e.g. from the social sciences) to support innovation adoption at pace and scale, although Rogers’s influential text7 was sometimes cited. Service improvement, collaborative and social movement methodologies also appeared to have had some influence (e.g. from Health Foundation and IHI texts), as one MD confirmed:
Yes, I don’t like diffusion, it sounds a bit passive but I know it’s in the textbooks. So I think we’d be open to a whole range of methodologies. . . . And I guess the two things which are most common that we’re looking at are the collaborative methodologies, so the breakthrough collaborative, but also then social movement.
AHSN 5
Academic Health Science Networks 1 and 2 showed more academic approaches to knowledge mobilisation, reflecting the influence of their local CLAHRCs. AHSN prospecti and documents outlined service improvement models, which included robust outcome measurement, better translational research capacity and evaluation and placed heavy emphasis on the academic base. Other sources sometimes viewed an AHSN in some ways as more linear – as a ‘downstream’ pipeline for the new science-/evidence-based innovations coming from an AHSC: ‘we have essentially defined a boundary between the two, they do the origination of technology and we do the spread of technology’.
However, our tracers illustrated that such a pipeline model often tended to have already been proven as ineffective in practice, with a long lag time for even locally developed innovations to enter health practice (empirically shown in our diabetes mellitus and MSK examples). The pipeline model was by itself too narrow and communicated badly with some stakeholders weary of a purely ‘academic science’ approach to spread.
Knowledge mobilisation based on ‘pushing’ evidence-based interventions and/or guidance (e.g. those originating from NICE) was apparent (as illustrated in model 3) and sat neatly with AHSN concerns to provide evidence of innovations that were impactful, effective and measurable (‘we are very data driven’). Yet in practice, service improvement and networking was often evolving through ‘bottom-up’ forms of collaboration and communication with stakeholders to create an ‘architecture’ for knowledge exchange and opportunities for ‘dialogue and learning’.
Academic Health Science Network 3 demonstrates the importance of tacit knowledge and antecedent networks for learning about knowledge mobilisation and innovation. Most AHSN directors in this site had previously worked together in some capacity within the region and so had a good understanding of each other’s roles, responsibilities and strengths. Some held other formal and informal roles spanning clinical, research and commercial engagement functions and so were boundary spanners and networkers. The directors spent much time out of the AHSN office at other sites – such as AHSC, university, NHS. In this sense, the leadership approach was distributed. This AHSN would align common assets and networks (e.g. leadership academy, improvement initiatives, along with a complex mix of a CRN, CLAHRC, AHSC, HIEC, clinical networks and local education and training boards) to deliver structured implementation, and used the official NHS Change Model to try to drive change. Networks in the region shared intelligence through ‘knowledge ambassadors’, which signalled a wider shared intention to develop an innovation system. The AHSN had identified three conditions for faster spread:
-
alignment of priorities for improvement
-
implementation using a disciplined improvement method for change [the AHSN enlisted a NHS innovation hub and a health research and technology facility (a translation of a US model), Advancing Quality Programme, university evaluations and the CLAHRC approach were referenced]
-
incentivisation.
Academic Health Science Network 4 referenced some academic literature reviews of innovation uptake, plus Rogers’ model. 7 During interviews, it emerged that the team was engaged with specialist university-based knowledge transfer agencies and tapping into HEI networks to widen its reach. A general AHSN knowledge mobilisation strategy was less easy to discern during the early period and ‘top-down’ adoption of evidence-based innovations was prioritised (model 2). Yet by the mid-licence period, the AHSN was exploring how to best to evaluate models of innovation adoption and capture its tacit knowledge and learning about effective innovation adoption drawn from examples within the region. There were indications that greater strategic thinking in this area was coming together. There was also more proactive engagement and co-ordination over time with other translational networks in the region (i.e. a CLAHRC, LEP and BRC).
Finally, in AHSN 5 various approaches were detected, which further developed through time. The AHSN prospectus had positioned the network as a ‘strategic space’, where learning and well-chosen risks would be encouraged across a large regional system. Some early thinking around assessing ‘system resilience’ as a concept did not survive, but ideas about an approach that was collaborative, multisectoral, and learning and change orientated did. Links with more basic academic work undertaken by the CLAHRC were still in development, even at a late stage. AHSN had staff, and also visited staff, from NHS IQ in search of ‘best practice’ ideas, such as social movement-based approaches including NHS Change Day (referenced in a presentation to the local Patient Safety Collaborative).
However, by 2016, it was clear that promising innovations needed extra push with ‘spread’. With help from an external consultancy, the AHSN (2016) produced a text outlining evidence-based guidelines on potential for ‘spread’, drawing on the basic work of Rogers7 and Greenhalgh et al. ,67 along with a structured process including a regional panel, for assessing spread potential. More internal resource was put into knowledge mobilisation work, as well as the directly clinically related programmes. The text was ‘road tested’ with members, bringing in local, tacit and experiential knowledge, and has been trialled with three or four programmes. It was reported that a dementia-related innovation in primary care was now spreading rapidly, previously having been ‘stuck’ (the target was for 75% or 80% of the practices in the region to adopt the innovation by 2018).
Issues encountered and knowledge mobilisation barriers
Every trust has their own financial instructions. They all have to follow public procurement roles. The only quick way to buy this at the moment is through supply chain.
AHSN 3
So I called NHS supply chain and said right, you know, the people that you have on the framework, it doesn’t work for us, we need another supplier and this is the supplier. We’ve done our market research, here it is and these are the reasons why they don’t have certain things that we need. And they said well I’m sorry but that’s tough because basically we won’t be going through that round again till 2017.
AHSN 4
Our tracers revealed a number of barriers to and enablers of innovation spread, yet complex NHS supply and procurement processes often stood out as common issues requiring much expertise and time to be negotiated for each innovation a AHSN took on board. In summary, the following issues repeatedly came up as impacting negatively on effective innovation spread:
-
NHS procurement and complex institutional architectures/processes
-
funding for sustainability
-
shifting evidence base/guidance (e.g. regulations, NICE)
-
low trust/cultural barriers (both industry and NHS)
-
time and resource restraints (e.g. for relationship building, sourcing innovations, supported implementation)
-
standardised metrification given diversity, attribution
-
engagement with clinical commissioners (‘product sell’, ‘battle’, lack of responsiveness).
Innovation and performance: the complexities of monitoring uptake, measuring success
In practice, the processes around innovation were often highly complex as AHSNs were attempting to find synergy and crossover between their health and wealth goals, ensuring that streams of activity and projects generated wealth but were also underpinned by clinical themes and core values (such as population health improvement). The tensions between the two sets of goals were not always easy to resolve. In many instances it was far from straightforward to manage an innovation process over the short term, especially where innovations were very early in development, or had a more large-scale or regional focus, meaning that potential returns on investment could take years or even decades to manifest (e.g. regional science park vignette). In the more triple helix-orientated vignettes (e.g. MSK group), an additional complication was the presence of multiple stakeholders within a regional network (e.g. AHSN, HEI, LEPS), each keen to attribute success for themselves but often with different indicators.
At the same time, AHSNs were under severe pressure to measure and demonstrate impact. Some necessarily crude indicators were being used in practice in the early days, such as the number of NHS trusts/primary care practices claiming to have adopted an AHSN sponsored innovation – such as a NICE TA – or, in the wealth creation domain, the number of new jobs or amount of internal investment claimed to have been secured.
As AHSNs progressed we observed greater co-ordinated attempts across AHSNs (at the national level) to demonstrate a collective impact through aggregating metrics and activities across the 15 networks. Metrics were being developed against core AHSN objectives, for example health improvement (e.g. the number of interventions resulting in patient benefit and/or fewer secondary care admissions); partnership and collaborative working (e.g. the number of organisations activity engaged in AHSN work streams and projects); adoption and diffusion (e.g. the number of sites adopting specific AHSN-sponsored innovations); and industry engagement (e.g. the number of introductions brokered by AHSNs between industry and the NHS). A publicly available impact report in 2015 also highlighted wealth creation achievements with SBRI involvement, for example > 100 contracts being awarded for new product development (The AHSN Network 2015; www.ahsnnetwork.com/wp-content/uploads/2014/12/AHSNs-impact-report-2015.pdf). Nevertheless, this important theme of success and performance measurement was still a complex and evolving area given the multifarious nature of the innovations and activities being supported by AHSNs in practice.
Discussion: key themes across the tracers
Key message 1
We have developed a four-category typology of AHSN approaches to innovation spread, which enables us to aggregate our 10 case study tracers within higher order categories and which we hope can inform future research into AHSNs. This typology enables us to model a wide variety of AHSN projects, which we found to occur at very different levels of analysis, from small scale and exploratory spinouts to larger regionally based or triple helix-style projects (Table 10).
| AHSN input | Types of mobilisation actions and activities |
|---|---|
| Direct ownership | Active incubation |
| Direct investments | |
| Project management | |
| Co-ownership and sponsorship | Existing innovations |
| Project management | |
| Additional funding | |
| Change management and scale up | |
| Matchmaking and providing spaces for matches to be identified | Web portals |
| Conferences and large engagement events | |
| Mapping of innovation stakeholders and regional assets | |
| Regional brokerage and support to regional innovation systems | Triple helix orientation |
| Support at systems level | |
| Improve fragmented innovation ecosystem |
Key message 2
Many of our tracers reveal the presence of a complex array of different stakeholders in different sectors (health, industry, higher education, science, local government). These actors may have distinct objectives, interests and success criteria. One role for the AHSN is to bring these different stakeholders together, but it should be recognised that it is only one of various actors in a crowded innovation landscape: one that may have influence but has little direct power. The degree to which stakeholders can be aligned depends on the nature of antecedent local networks as well as the AHSN’s actions (e.g. network building and brokering) and leadership strategies.
Key message 3
There appear to be conditions of ‘path dependency’ within regional innovation systems, whereby the AHSNs built on ‘what had worked’ (e.g. positive legacy of some HIECs or innovation hubs) and/or powerful stakeholders (e.g. AHSCs) or effective clinical entrepreneurs who were well networked in local systems. Some strategies or projects predated the AHSN but were inherited or recycled and taken further in terms of regional spread. Where AHSNs were in regions with established AHSCs, the pipeline or ‘science push’ model of knowledge mobilisation became more plausible (although still too narrow in practice). Path dependency theory suggests that regional trajectories may continue to differ over time.
Key message 4
As a result of key messages 1 and 2, linear or pipeline-led models of innovation diffusion were rarely present. Rather, innovation diffusion should be seen as an extended, unpredictable and negotiated process, involving a complex number of different actors, some of which had budgetary veto power (CCGs). Resource control was increasingly important in a cash-constrained NHS system. So evidence-based but (perceived) cost-increasing innovations (e.g. NHS TAs) could still struggle to become rolled out regionally.
Key message 5
The models – or rather practices – of knowledge mobilisation espoused by the AHSNs were often pragmatic. There was some evidence of more academic influence from Rogers’ theory of diffusion,7 and the work of the IHI and the Health Foundation also appeared to be important in some sites, so they can be seen as operating as institutional knowledge brokers. Some sites accessed nationally generated change management approaches sponsored by the then NHS IQ (NHS Change Model; NHS Change Day). Knowledge mobilisation models and practices (i.e. strategies for spread) were still under development and being ‘tested’ in practice.
Key message 6
Academic Health Science Networks were concerned to develop measurement and metrics to assess their local and national ‘impact’, and recently they have made progress nationally in this respect. The tracers indicate, however, that there will often be long time scales before full evidence of impact/results come through and that some realism is needed (especially for economic growth goals). Those projects that were quicker to get going may have predated the AHSN and had been selected by them early on as ‘low-hanging fruit’, that is, projects that could reasonably be expected to make good progress. However, for ‘the ideas that we (AHSN) supported, and if you like seed corn funded here today, our expected rate of return is literally year six or seven’.
Key message 7
There is an important role being played by local innovators and ‘clinical entrepreneurs’: individuals who develop ideas for service improvement and health improvement. Some of these individuals are brokering sectoral boundaries independently – across the NHS, industry and universities/university spinouts. However, such individuals may be ‘lost’ in a wider NHS system if their ideas are not picked up by intermediary agencies that offer the capacity to support the development of an innovation and its spread across an often fragmented NHS. Commercialisation and IP for innovations may be sought by some inventors but not all; indeed, a desire to push a specific innovation to a wider audience and further its development (and evidence base) for patient benefit was reported to be a strong motivator for clinical and academic entrepreneurs.
Chapter 8 Knowledge leadership and knowledge leaders at regional and national level
One of our RQs was to identify specific individuals who were perceived as being particularly involved in knowledge mobilisation within and across AHSNs and who were seen as critical for pursuing the health and wealth agendas. We were interested to understand who these people are, what they do, how they came to assume knowledge leadership roles and what explains their knowledge leadership behaviours. Knowledge leadership refers here to ‘any attitude or action – joint or individual, observed or imputed – that prompts new and important knowledge to be created, elicited, shared and utilized in a way that ultimately brings a shift in thinking and collective outcomes’. 137 (Please see Chapter 2 for more discussion of why this part of the original protocol needed to be adapted to the new conditions on the ground.)
To respond to these questions we proceed as described in Chapter 2 and build on (1) the results of the SNA survey, which included explicit questions on who in the AHSNs could be considered a KL; and (2) face-to-face or telephone interviews undertaken later with a small number of individuals (n = 9) whose reputation and influence, according to the results of our SNA, spanned different regions and AHSNs.
Insights from the literature
To better understand the characteristics that are important for persons leading innovation networks or in leadership roles in networked innovation settings, we first conducted a review of literature relating to leadership, knowledge and innovation networks (see Chapter 3). We found little on knowledge leadership in general and specifically on the formal and informal leaders of mandated innovation networks such as AHSNs. In addition, although an extensive literature exists on knowledge brokers and their role in promoting knowledge mobilisation, little is known about their individual leadership competencies and personal networking strategies.
In particular, we found that the existing literature on knowledge leadership is usually restricted to the organisational level and identifies generic behaviours that apply to managers and leaders of groups and small units. 159,160 Viitala,159 for example, suggests that knowledge leadership stems from orientation to learning, support of individual- and group-level processes, acting as a role model and creating a wider climate that supports learning. These behaviours are traditionally associated with leading teams and groups for innovation. 161 Little is known about the behaviour of individuals who need to animate broader and less structured networks such as the AHSNs.
More useful insights can be derived from the small body of literature on the leadership of networks. As discussed in Chapter 3, authors suggest that, in dispersed organisations and networks, leadership is derived from a combination of formal status, experience, power, being well connected and informal leadership. The last stems from perceived status and leaders being perceived by their peers as well connected across boundaries (i.e. geographies, sectors and hierarchies). The literature therefore warns against confusing formal authority and informal capacity to act as catalyst of knowledge mobilisation. Leaders of mandated networks are seen to have influence and authority but not necessarily knowledge leadership. This may require other characteristics, although what these are varies. As Mabey and Nicholds162 put it, in large networked organisations, knowledge leadership is unlikely to be ‘a manifestation of traditional “top-down” hierarchical mechanisms’ (p. 43). 162
Although the literature provides few indications of how and why certain individuals are perceived as playing a leadership role, it also suggests that much is to be gained if we cast our net widely and adopt an open view with regard to who could be considered a KL in an inherently loosely bounded initiative such as AHSNs.
Identifying local knowledge leadership
To explore the concept of knowledge leadership in AHSNs, we first used the survey of key knowledge contacts in the UK health-care innovation domain named through a peer referral sampling methodology (see Chapter 2).
In our social network survey we asked respondents to provide detail on the characteristics of their nominated knowledge contacts. This would provide some indications of who stood ‘out of the crowd’. The results are illustrated in Table 11. The top two categories across all AHSNs were ‘leader in their field’ (33.1%) and ‘an expert in their field’ (31.6%). This suggests that peer recognition of a person’s leadership quality as well as possessing specific expert knowledge are key prerequisites of being a KL. Being ‘well connected’ or ‘influential in their field’ were regarded as secondary characteristics (18.7% and 16.6%, respectively).
| Do you consider this person to be (please select all that apply) | Total across all sites |
|---|---|
| A leader in their field | 33.1% (n = 454) |
| An expert in their field | 31.6% (n = 433) |
| A well-connected person | 18.7% (n = 257) |
| Influential in their field | 16.6% (n = 227) |
| 100% (n = 1371) |
The perceived characteristics of knowledge contacts varied between AHSNs (Table 12 and Figure 9). We asked our survey respondents about the knowledge contacts they had named: Do you consider this person to be a leader in their field; an expert in their field; a well-connected person; influential in their field (please select all that apply)?
| Do you consider this person to be (please select all that apply) | AHSN 1 | AHSN 2 | AHSN 3 | AHSN 4 | AHSN 5 |
|---|---|---|---|---|---|
| A leader in their field? | 22.3% | 41.8% | 42.4% | 41.8% | 44.1% |
| An expert in their field? | 27.5% | 36.6% | 27.6% | 37.6% | 40.4% |
| A well-connected person? | 26.9% | 16.0% | 6.7% | 15.3% | 9.3% |
| Influential in their field? | 23.3% | 5.7% | 23.3% | 5.3% | 6.2% |
FIGURE 9.
Perceived characteristics of knowledge contacts (multiple responses allowed).

In all AHSN regions respondents were more likely to name as ‘important knowledge contacts’ for health-care innovation people who they perceived as ‘leaders’ and ‘experts’ in their field (except for AHSN 1 where respondents named contacts in relatively equal proportions across response categories). Discounting AHSN 1 and comparing the other regions, a knowledge contact’s ‘influence’ was most important in AHSN 3 (the region with an academic health science ‘ecosystem’ with a ‘hybrid’ knowledge network structure). Being ‘well connected’ seems to be an important characteristic of a knowledge contact in AHSNs 2 and 4 (regions with ‘connected’ knowledge network structures).
It is important to note that these findings reflect how individuals perceive their knowledge contacts, and are not necessarily accurate reflections of the nominated person’s leadership quality, expert status, personal networks or influence.
Attribution of knowledge leadership: who counts as knowledge leaders in Academic Health Science Network regions?
In the next stage we interviewed a sample of those who had completed the survey (knowledge contacts) (n = 65). Among other foci, in this phase we were interested to understand in more depth why our respondents had selected some individuals over others when identifying knowledge contacts: why was someone considered a leader? What expertise and influence mattered? To this end, a set of specific questions within the knowledge contact interview inquired directly about knowledge leadership issues. We asked in particular:
-
Whether or not within the particular AHSN region were there any individuals who acted as ‘KLs’ (i.e. ‘individuals highly engaged in the spread or adoption of health care innovations across organisational boundaries’)?
-
What did they do to attract the attention of the respondents?
-
What makes an individual effective in facilitating the circulation or adoption of health care innovations across organisational boundaries?
Findings
Apart from a small number of respondents who stated that they could not identify obvious KLs regionally, interviewees could identify specific individuals who in their view were especially engaged in the spread or adoption of health-care innovations and instrumental in making this happen. Individuals were attributed knowledge leadership for a number of reasons.
First, individuals were identified as KLs because they were at the top of their organisation. There was a sense that the combination of their social position and the qualities that allowed them to occupy the office in the first place enabled them to fulfil specific roles within the network; for example, this turned them into powerful gatekeepers and brokers. In the words of one of our informants:
They have traditional power because of the organisations that they are in and they have personal power as well because they are all charismatic individuals . . . It is an interesting thing about networks, isn’t it?
It is worth adding that some informants emphasised that occupying a formal position often is not enough and, indeed, innovation and transformation comes from individuals who ‘sit outside’ the formal structure. Formal position and leadership tended to reinforce each other.
Second, individuals were considered KLs due to their capacity to give access to material, cognitive and social resources. Most responses fell within this broad category. A small number of respondents associated KLs with the capacity to give access to material resources in terms of funds and money. KLs were thus recipients of large grants or individuals who had secured substantial investments. Much more attention, however, was given to the other two types of resources. Many respondents suggested that KLs were individuals who could provide access to critical knowledge and understanding. Particularly important were the span of knowledge (e.g. having a national outlook and a broad overview), breadth of skills (including business skills) and capacity to provide alternative views and act as carriers of new ideas. KLs were thus nominated because they had in-depth understanding of how the system worked; they ‘. . . look at things on a national basis’; they have experience and carry a historical memory; and ‘they have an ability to think outside the box’. By giving access to crucial knowledge and understanding, these individuals ‘helped [to] contextualise . . . where an AHSN can add value’.
Equally important was the sense that the nominated individuals could provide access to social resources in terms of contacts, access and relationship. KLs were thus especially well connected, in constant touch with other influential people, and provided valuable contacts:
. . . [He] has been instrumental in setting up a range of networks both locally, regionally and nationally.
. . . His network is extremely good and he has helped us to establish partnerships that otherwise we were struggling to do.
One recurrent characteristic was that these individual wore ‘multiple hats’ and thus could span different worlds and bridge local and national levels of activity:
He is managing to combine very rigorous world-class research with a local implementation.
They might have strong views and they might be able to offer them very eloquently but they are happy to listen to other views and to know how you could put them together.
Importantly, social brokering, that is, the capacity to provide a link between individuals and groups, was considered as a mean to an end. What made these individuals stand out was not so much having a vast and influential network as making this available as a resource for the AHSN:
If you want somebody to go and talk to local MPs [Members of Parliament], the Minister, well they’re always talking to them, they’re always on the bloody phone to them. So you have to recognise that he occupies a space that is much more than his job, just by the nature of who he is.
Third, many respondents suggested that KLs needed not only to be very well connected, but also accessible. Respondents often identified KLs as people who could act the ‘first port of call’ and who were able to provide support:
. . . it is those people who are interested in sharing and supporting others raise their grain rather than compete.
Not all respondents agreed on the last point. Some respondents told us that KLs were considered as such because of their distance and influence in spite of the absence of personal ties.
Fourth, several respondents associated KLs with specific personal qualities. These included empathy, ‘great personality’, capacity to engage with different public and charisma:
Now [this person] is charismatic in the extreme, he’s funny, he knows what he wants to do and I love working with him.
Other notable traits mentioned were visibility in the public sphere, credibility within their professional group, integrity and personal history and being considered a source of experience and wisdom. Communication capacity and an ability to transmit a vision or share passion were also mentioned as reasons for considering a specific individual as a KL:
[He] has the ability to engage very well and to sell the message and see it as an opportunity, and he will have particular traction with academics because he is one, he’ll have traction with the NHS because he works in the NHS and he has a delightful personality and he understands it.
Finally, individuals were considered KLs because of their capacity to make things happen or because of their effectiveness. Their leadership quality therefore stemmed from the results of their actions, which made them positive role models for what could be achieved:
She makes things happen and she’s constantly bringing learning from other programmes to the attention of whoever she happens to be speaking to, so I’d regard her as a good model and a very effective operator in that respect.
Interestingly, not only demonstrating effectiveness but being able to communicate it was associated with knowledge leadership. Effectiveness therefore derived not only from personal action, but also from the capacity to create narratives that allowed different stakeholders to find points of contacts and act together:
I think probably the most effective [KLs] are the ones who are able to tell a good story about why something is working.
The findings from the knowledge contact interviews are summarised in Figure 10.
FIGURE 10.
Findings from the knowledge contact interviews.
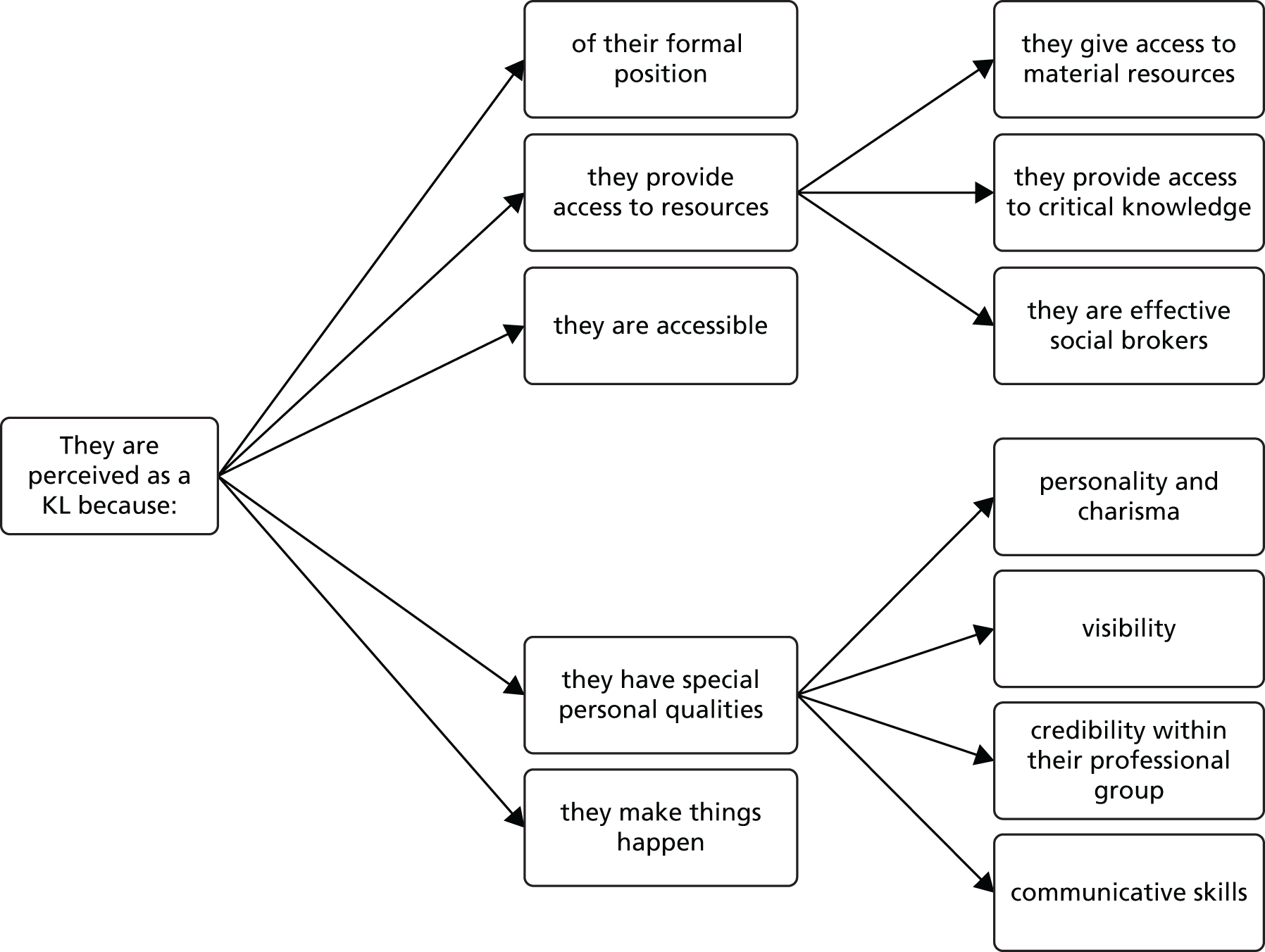
Discussion
Our findings align with the existing literature, which suggests that knowledge leadership in networks and collaboratives stem from a combination of formal status, experience and being well connected. Our findings also align with some of the existing literature on leadership. Leadership scholars suggest that in Western societies leadership is attributed according to five different sets of criteria or discourses. 163 These include position (where people operate makes individual leaders); personality (who the leaders are makes them so); process (it is what individuals do and how they do it that make them leaders); purpose (it is why leaders act that makes them leaders); and results (what people achieve connotes them as leaders). Each of these discourses of leadership focuses on and foregrounds some aspects over others. Not unexpectedly, all five discourses were utilised by our respondents, although a clear awareness exists that agency derived from status and leadership are two different things that may or may not go together. Some interesting novel aspects, however, emerge from our analysis:
-
Knowledge leadership is complex and derives from a combination of traditional traits (position and personal characteristics; personality and contacts; results and access). One-dimensional leaders who may thrive in traditional organisations are unlikely to be recognised as KLs in the context of a highly networked initiative such as AHSNs.
-
Different types of capital164 need to be carefully balanced. For example, structural capital (the capacity to establish connections between distant individuals and networks) needs to go hand in hand with cognitive capital (the capacity to create shared interpretation and narratives that enable effective communication across networks). Equally relational capital (the creation of network of trust reciprocity and obligations) need to be supported by symbolic capital (professional recognition, proven expertise). Carriers built out of one form of capital only are unlikely to be perceived, or be successful, as KLs.
-
Social and cognitive capitals are still prevalent, whereas access to material resources is mentioned and considered desirable but is not central. The finding aligns well with the rest of our research and the unequal difference from the health and wealth dimensions of the AHSNs’ agendas. The finding can be read in optimistic terms as a glass half full (the capacity to give access to material resources is considered as one of the traits of KLs) or in pessimistic terms as a glass that is half empty (this type of leadership is partly based on intangible assets).
-
Knowledge leadership requires a broad outlook and an in-depth understanding of the existing system of relations as one of their critical functions is to enable change or trigger innovation by creating new and novel links (they are enablers). However, they also need to be – and be perceived as being – rooted in a specific field of competence. Complete generalists are unlikely to thrive as KLs.
-
KLs are judged more for what they do and less by their prescribed status. KLs are therefore by definition not only doers but visible doers. Communication skills are therefore essential, although KLs must also demonstrate that they are able to make a difference.
In summary, our study suggests that in a large networked initiative knowledge leadership is likely to emerge as a property of horizontal network interactions, networking practices and networked effects. KLs appear less as heroic doers and more as enablers. Knowledge leadership itself appears less as a stable individual characteristic and more as a circulating function that certain individuals take on themselves for specific reasons and due to specific personal and biographical circumstances. What these reasons and circumstances might be was the object of the last steps of our research into KLs.
From regional knowledge leaders to ‘national beacons’
To shed further light on KLs we identified individuals who according to our survey were ‘hyperconnected’ and highly influential not only within regions but also across them. We selected in particular individuals nominated as KLs with a 10% degree centrality score and who had been named in three or more AHSN regions (n = 14). In clearer terms, these were individuals considered as KLs in multiple parts of the country and had a national-level reputation, prestige and visibility. To differentiate them from the KLs discussed above, we call this selected group of individuals ‘national-level knowledge mobilisation beacons’ or ‘national beacons’ for short. National beacons are therefore interesting in that they are widely recognised as KLs and in a sense they constitute referent models worth investigating in depth. Our aim was not to investigate whether or not they were in fact ‘super-KLs’, but rather what led them to become so prominent in the public eye. So we interviewed them, focusing in particular on their biographies, what they do and what they did to become and remain influential and credible. We also asked them about the activities and skills that they considered central to enable them to act and be perceived as KLs.
Findings
Although for reasons of confidentiality we cannot report individual details of the national beacons, we provide an overview of the organisational roles of the 14 national beacons initially included in our list (Box 10). The job descriptions have been amended as necessary to avoid disclosure. In addition, only 10 of these 14 individuals responded to our invitation. Nine were interviewed, whereas another person indicated their willingness to take part, but could not do so given the time constraints of the study.
-
AHSN MD.
-
Innovation and improvement national specialist.
-
NHS FT chief executive.
-
Think tank director.
-
NHS FT manager with remit for innovation and improvement.
-
High-profile clinical academic.
-
Director of industry body.
-
AHSN manager at director level and national figure.
-
AHSN manager at director level and national figure.
-
Manager at director level of health-care collaborative.
-
Independent consultant and policy adviser.
-
Executive manager of health-care collaborative.
-
High-profile clinical academic.
-
AHSN programme director.
The list of organisational roles is consistent with our previous findings that KLs must combine institutional positions with other notable characteristics. Although all national beacons are high-profile individuals and, therefore, at the top of their professional games, only in some cases did they occupy top administrative positions (e.g. CEO of a FT, director of a think tank). There was a predominance of individuals with a long and at times very long tenure in the NHS or in public service, whereas members from industry were still a small minority. The small sample was almost equally divided between males and females. Finally, only 4 of the 14 nominated persons (and two of the nine interviewees) were directly involved in the activities of AHSNs. This is in itself an interesting finding, as it confirms that knowledge leadership and formal roles may and may not go hand in hand. For what concerns the individuals actually affiliated with AHSNs, we believe that the risk of biased answers was minimal. Our questions in fact were focused on personal journeys and managerial challenges rather than the AHSNs and their success.
Becoming and remaining national beacons
Although our respondents came from diverse backgrounds, had different personal stories and operated in different sectors (NHS, academia, government, industry), one common characteristic was that they all had non-linear careers that they described as ‘meandering’ or stated that they had ‘a very bizarre personal history’, using expressions such as ‘I’m slightly unusual’. (Note, the extracts from the interviews are not attributed to the respondents as this may identify them.) This comes in a time when linear careers were still the norm (all the national beacons were aged ≥ 45 years). The critical finding here is that the meandering career was one of the key explanations for their high connectivity. The travel through sectors and worlds had been used as an opportunity to accumulate social capital. In the words of one of the national beacons:
I think throughout your career, throughout your life time you amass a little black book of people, knowledge experts and maintaining that network and working with them, matrix management is a way it’s described, has enormous dividends.
The high number of referrals and connections captured by our survey were therefore the result of a long-term, slow, strategic work of accumulation rather than the outcome of, say, intense social media activity. According to our interviewees, the multiplicity of personal experiences allowed them to relate to and communicate with various publics and stakeholders. This in turn facilitated the establishment of new connections in what appears a self-reinforcing dynamic.
Another common characteristic of national beacons was that at different points in their careers these individuals, either by design or by chance, had occupied formal roles that gave them a broad overview of the entire system. Committees, panels and similar bodies were often mentioned. According to our informants, these personal experiences allowed them not only to multiply their contacts and become widely known, but also to grasp and understand the complexities of the issues they were grappling with. As one of our informants put it:
[this gives me] . . . an understanding of the landscape from a kind of a national perspective rather than from one hospital or one commissioning group or a local authority or one company. So I’ve kind of seen it from the bird’s eye if you like.
Given that we were dealing by definition with ‘hyperconnected’ individuals recognised as effective brokers of knowledge and innovation, it was not surprising to find that all of these individuals wore several hats and occupied several formal positions. One of the respondents interrupted our conversation saying: ‘I’d better pull up my CV because I have got quite a few other roles . . . Hang on a minute, let me just pull this up because you need this now, don’t you’. It was no surprise that these individuals had a very busy agenda, their work was highly fragmented and they spent considerable time in meetings. Two recurrent aspects mentioned by our informants, however, are worth noting.
First, all these individuals had strategically accepted roles on national bodies, boards, committees and panels that allowed them to nurture their bird’s eye view of the landscape and gave them access to a variety of contexts. As one of the national beacons put it:
. . . if I get invited to one of those [briefing] breakfasts I will move heaven and earth to be there because I think it is really, really key that you know, you’re sitting there and you’ve got people [from a wide variety of organisations].
Centrality and capacity to connect are the result of tactical work and are subject to maintenance.
Second, all the informants referred to the risks inherent in their role and the need to remain visibly grounded to a specific area of work and expertise. They referred to this in terms of ‘becoming famous for something concrete’. In this sense, they all carefully carved out enough time to pursue what they saw as their core activity (research, intervention, management). This was done both for personal reasons but also to prevent accusations of spreading themselves ‘too thin’.
How to connect worlds
One theme was the activities, tools and technologies that these individuals utilised in their brokering activities. As noted above, all these individuals devoted a significant part of their time to what they called ‘external facing activities’ and active networking. This was done often with a clear purpose:
I spend a lot of time on personal relationships with people in key roles. So I have always, I suppose in terms of my personal orientation I always try and be as helpful as I possibly can to people and help them in what they need to achieve and what I’ve found over the years is that if you’re helpful then people want to help you so there’s that sort of indirect reciprocation.
Contrary to existing stereotypes, however, the tools utilised to connect worlds were surprisingly low tech and often very ordinary. For example, although social media such as Twitter (Twitter, Inc., San Francisco, CA, USA), LinkedIn (LinkedIn Corporation, Mountain View, CA, USA) and blogs were used strategically by some (albeit not all) our informants, they were always mentioned as an addition to other activities that at least in their perceptions were considered primary. Among others, these activities included sitting on committees and interdisciplinary panels (as discussed above), talking at events and seminars, and publishing in academic journals and wide-circulation sector-specific periodicals (Health Service Journal and British Journal of Medicine were often mentioned).
One aspect that clearly emerged from our interview, however, was the (declared) importance of face-to-face personal communication. This aspect was repeated by all our informants and emphasised in different but consistent ways:
I tend to build networks through personal relationships with individuals.
I would say 70% of what we do . . . is face to face, about 30% is online digital. But that’s probably only been at that ratio probably in the last year, I think until recently we were about 90% face to face, 10%.
I do spend a lot of time on the phone, I talk to a lot of people, I meet a lot of people. I do a lot of public speaking and conference events. And I make myself very visible in those.
The rationale behind the choice of media and activities was a tacit understanding that the work of brokers is not that of diffusing information but rather establishing connections between people and initiatives that could benefit from each other. The effectiveness and reputation of brokers depends on the value added by the connections they make possible. As suggested by the last extract above, media and externally facing activities were often intentionally chosen because they gave access to different perspectives and understanding. These were opportunities not only to broadcast messages, but also to listen to the need and desires of groups and stakeholders so that significant connections could be established. This understanding was crystallised by one of our informants who emphasised that ‘. . . it’s more important to know the person than the policy. And often that’s a mistake that people make. They think the way to success is to learn and understand the policy and it’s not, it’s to learn and understand the people’.
Credibility and how to succeed as national beacons
When asked whether or not they perceived themselves as experts, networkers or ‘someone who gets things done’, our informants suggested that a critical skill to act as a national beacon is to balance all three aspects – but with a preference for the first two. Several informants refused to describe themselves as ‘experts’, although they all emphasised the need to remain grounded in a specific domain of activity as a way to retain credibility. This refusal to claim the role of expert is perhaps because they saw their roles as translators rather than imposers of powerful evidence or knowledge. As one of the respondents put it: ‘I would definitely say that I’m not an expert because expertise sounds quite a narrow thing but what I am quite good at is seeing the connections between things’.
One aspect that all beacons concurred on, however, was the need to be perceived as deliverers and as persons who add value through their networking activities:
I like making connections and thinking ah, this person could help that person and so I would, I think I am a connector and I hope that people see me as someone who gets things done and not just a load of hot air.
You’ve got to start with getting things done because, you know, your personal credibility, people’s willingness to invest in you comes from your ability to make things happen. Along with that then comes as a corollary thing such as, you know, your knowledge of your subject matter, your ability to build a network. I think if you start out solely to build a network, it can come across as very disingenuous.
The perceived effectiveness of national beacons was therefore a result of the skilled balancing act between strategically nurturing a variety or relationships that span across the health-care landscape; the capacity to expertly navigate this landscape thanks to existing social capital and direct experience of some of its ‘regions’; the capacity to recognise and align demands, offers and common interests; and the capacity to remain grounded in a specific domain of activity that would prevent these individual from being perceived as hollow or not authentic. In the words of one beacon: ‘I think that the danger is that if you spend too much networking and connecting that you’re not actually delivering grounded work that adds value, then all you’re doing is talking’.
Discussion
Zooming in on the biography and work activities of a small sample of national knowledge mobilisation beacons allowed us to further the understanding derived from our interviews with regional KLs. Among others, our findings suggest that:
-
Acting as KLs across regions and connecting part of the health-care landscape requires building on personal networks that are accumulated during an entire career. New connections thus build and expand existing ones.
-
Managing networking and knowledge leadership is a balancing act that requires one to remain grounded in a specific domain of activity and be perceived as adding value. Although KLs need to create narratives that allow people to find some common ground and work together, they also need to be seen as the authors and owners of those narratives. Alternatively, they may be perceived simply as a ‘gabber’ and lose credibility. In this sense, the traditional dichotomy between generalists and specialists do not apply to the individual as their perceived effectiveness depends on balancing the two.
-
Knowledge leadership is not the name of a set of abstract competencies as much the description of a specific type of concrete work. This work is conducted through a number of rather ordinary activities built on the principle that effective KLs are matchmakers rather than broadcasters and, therefore, their success is based on listening rather than talking.
-
The idea that KLs are hyperconnected thanks to the extensive use of social media is misplaced. In fact, knowledge leadership and cross-regional brokering is again the result of a careful mix of traditional and contemporary ways of communicating that are strategically chosen in view to the characteristics of the audience.
Chapter 9 Conclusion
Our overall research aims were (1) to explore AHSNs’ strategies and practices of knowledge mobilisation in their formative phase, when they were building health- and wealth-related networks to exchange knowledge about new ideas, products and services; and (2) to investigate how knowledge leadership took place and the characteristics of people perceived as KLs. We initially focused on AHSN VSMs as possible KLs, although in practice a broader set of people emerged. Our initial RQs, which operationalised our broader aims, were as follows:
-
What role does ‘knowledge networking’ play both formally (in national and regional AHSN knowledge exchange fora) and informally (i.e. in VSMs’ professional and local networks) within knowledge mobilisation strategies and practices in AHSNs?
-
How is ‘knowledge’ (in particular about knowledge mobilisation strategies and practices) discussed in these fora diffused by a group of VSMs in their AHSNs?
-
Is there a subgroup of VSMs emerging who are highly engaged with such knowledge mobilisation events and who appear to act as KLs in their AHSNs?
-
If so, what explains such knowledge leadership behaviours?
Chapter 2 outlined how the study adapted to developments in the field (e.g. a national forum changed its composition and we instead attended some national level network meetings); therefore, the majority of fieldwork took place at the regional level of AHSNs. In addition, the number of individuals we found exchanging knowledge and ideas (e.g. around health improvement and wealth creation) came in practice from a broader range of institutions than AHSNs and NHS organisations (e.g. including HEIs and LEPs). However, at the regional and local levels, AHSNs were experimenting with different knowledge mobilisation strategies to spread health-care innovations across NHS organisations within their region, so our core focus remained on understanding these practices and local knowledge leadership behaviours and networking within and around the five AHSNs we studied.
In this concluding chapter, we summarise our major findings in relation to our core themes and RQs and provide a summary table of the overall findings from all the earlier chapters (see Core study findings and Table 13). We then consider the study’s limitations and achievements (see Study Achievements and Limitations) and finally propose a future research agenda (see Future research agenda).
| Main findings | Corresponding chapter | Implications |
|---|---|---|
| We found a small body of literature addressing formal leadership of mandated networks. A greater focus of research is on informal roles in mandated networks (e.g. knowledge brokers) The concept of the ‘triple helix’, which explores knowledge society dynamics, is helpful for understanding collaborations arising between the public sector, universities and industry that drive regional innovation and economic growth |
Chapter 3, Literature review | There is scope to further understand how leaders’ informal and formal networks intersect in practice (i.e. networks both within and without organisational settings) Regional case studies that apply the concept of the triple helix to better understand health innovation in the UK could be useful. These might explore collaborations arising between government agencies, industry and universities to support the growth of health/life sciences clusters within regions |
| There is a discernible policy narrative around health improvement and wealth creation, with the UK health and life sciences sector seen as a vibrant economic growth area that intersects with the NHS. The health policy-making process also appears to be increasingly pluralist with a variety of actors involved in the policy-making process, beyond traditional groupings The innovation field in health care was depicted as an especially ‘crowded’ landscape by respondents. They also noted challenges for AHSNs leaders, such as frequent NHS reorganisation and expansion of their policy remit and brief |
Chapter 4, The policy landscape of health-care innovation and its evolution: the perceived role of Academic Health Science Networks | AHSNs may need to engage with economically orientated policy-makers and groupings as well as more traditional actors from the health-care sector The important macro national policy level and the micro level of the individual AHSN could usefully be connected at the middle level, where the existing AHSN ‘network of networks’ could play an important role Those at a distance from AHSNs may be confused by the number of agencies and initiatives aimed at supporting innovation in the NHS in a ‘crowded landscape’ ‘Mission creep’ and frequent reorganisation may cause problems for the AHSNs |
| Knowledge mobilisation in and around AHSNs was found to be collective/distributed rather than individually focused and reflecting levels of ‘social capital’ in each region Different types of network structures (Health-Net and Wealth-Net) may affect capacity for innovation implementation and also what is implemented AHSN board members were important in supporting knowledge circulation relating to wealth creation |
Chapter 5, National knowledge networking supporting early stage Academic Health Science Network knowledge mobilisation: a macro picture | There is no ‘one size fits all’ approach to networking as the health and wealth networks took very different forms Building networks around a new policy ‘problem’ (here an AHSN’s role in wealth improvement) takes time and effort AHSNs may need to place continuing special emphasis on building up their novel wealth-related networks Non-executive board members and chairpersons need to be chosen with care so that they can help widen existing health-orientated networks |
| We found regional variations when comparing knowledge networks around AHSNs, and between health and wealth networks. Antecedent networks and variations in the regional context (e.g. infrastructure, resources) are important for shaping the types of opportunities, knowledge exchanges and networks leveraged to support health-care innovation | Chapter 6, Regional knowledge mobilisation systems: comparing Academic Health Science Networks | Different ‘structures’ of knowledge mobilisation systems had emerged in each AHSN region. Connected and hybrid networking systems were found in regions with mature infrastructure, whereas loosely organised networking systems were found in regions with developing infrastructure These different network forms have distinctive advantages and disadvantages An awareness of key social network concepts might help network leaders to understand and then seek to develop their own regional networking processes in greater depth |
| The innovations and interventions supported by AHSNs were varied, although high-priority clinical themes were clearly evident across work programmes (e.g. diabetes mellitus). Four models of knowledge mobilisation were identified for spreading and scaling up innovations in AHSN regions: (1) investment in new products and ‘clinical entrepreneurship; (2) improvement science and spread of evidence-based interventions in the NHS; (3) innovation networking and matchmaking; (4) cross-institutional regional brokerage and support for regional innovation systems AHSNs were beginning to learn about more and less effective knowledge mobilisation strategies to support innovation spread within their local health economies. Their approaches often tended to be pragmatic rather than grounded in clear change models An embedded, linear pathway to innovation adoption and spread in the NHS was not identified in practice since multiple actors and organisations were involved in innovation processes |
Chapter 7, Processes of knowledge mobilisation and innovation spread in action: developing a typology | AHSNs may find our four-category typology of approaches to knowledge mobilisation helpful in developing their own strategies AHSNs can provide local capacity and resources to support an important group of innovators and clinical entrepreneurs to develop and scale up innovations across the NHS. AHSNs might well think about how they seek to engage and sustain this critical group Because AHSNs engage with a wide and diverse array of stakeholders, they may be well situated to understand how different institutional and organisational objectives can be aligned regionally to support local innovation processes (i.e. provide systems leadership and support for innovation) AHSNs may wish to reflect more on ‘what works’ and what does not in their strategies of knowledge diffusion and start to build an applied knowledge base. They may wish to access some change models (e.g. Rogers7) to inform their approach We suggest that innovations will often take the form of a complex and long ‘innovation journey’; this should be realistically recognised in the KPIs set for AHSNs |
| Our findings align with the existing literature which suggests that knowledge leadership in networks and collaboratives stem from a combination of formal status, experience and being well connected Knowledge leadership is complex and derives from a combination of traditional traits (position and personal characteristics; personality and contacts; results and access). One-dimensional leaders who may thrive in traditional organisations are unlikely to be recognised as KLs in the context of a highly networked initiative such as AHSNs Being a highly effective social broadcaster (e.g. via social media) or holding a formal organisational leadership position is not enough to be perceived, socially, as an effective KL Knowledge leadership requires a broad outlook and an in-depth understanding of the existing system of relations as one of their critical functions is to enable change or trigger innovation by creating new and novel links (they are enablers). However, they also need to be – and be perceived as being – rooted in a specific field of competence. Complete generalists are unlikely to thrive as KLs KLs are judged more for what they do and less by their prescribed status. KLs are therefore, by definition, not only doers, but visible doers. Communication skills are therefore essential, although KLs must also demonstrate being able to make a difference We further identified a small group of ‘national beacons’ active in the health-care field. These were individuals who were more widely recognised as having influence across AHSN regions and in health care more broadly. ‘Beacons’ had diverse career backgrounds, were highly connected (i.e. possessed high social capital) and often emphasised the importance of interpersonal networking and face-to-face communication Therefore, knowledge leadership was based on personal and professional networks built up organically during an entire career. Importantly, knowledge leadership appears to be a balancing act between specialisation (i.e. legitimacy and competency in an area of professional practice) and generalisation (i.e. possession of a broad outlook and understanding of local systems of relations) |
Chapter 8, Knowledge leadership and knowledge leaders at regional and national level | AHSNs may want to reflect on the implications of our research for the skills and competences that are needed in senior AHSN leaders and think through what it implies for selection to key posts AHSNs may wish to think about they can best identify and engage with a small but hyperconnected set of ‘national beacons’ |
Core study findings
Although the focus of the study broadened from an early emphasis on AHSN senior managers, our core themes of the strategies and practices of knowledge mobilisation and knowledge leadership endured. So what we have learnt?
Academic Health Science Network knowledge mobilisation strategies and practices
Our final report suggests some key messages around AHSN knowledge mobilisation. First, we highlight diversity in the pre-existing assets available to AHSNs that influences knowledge mobilisation strategies. These assets include the strength of inherited academic health sciences infrastructure (e.g. AHSC, BRC) and the relative development of science parks and clusters regionally, alongside other important NHS health networks (e.g. CLAHRCs). These inherited regional characteristics shape the development of regional innovation systems in the health-care field.
The SNA indicated that AHSNs had different types of knowledge networks: some were looser, whereas others were more tightly organised. Although there is no ‘one size fits all’ success formula, different types have their own advantages and disadvantages. For example, looser networking systems may draw in a wider variety of new contacts to support health improvement and wealth creation objectives, although the implementation of newly acquired knowledge may be effortful given that these networks are dispersed. Conversely, more tightly structured networks can expedite the implementation of new knowledge and innovations because of their interconnectedness but can be less open to new ideas and actors.
We further highlighted that AHSNs were engaged in a spectrum of knowledge mobilisation activities and presented a typology of four possible models, or ideal types. We emphasise the diversity of strategies found, reflecting the wide (and evolving) remit of AHSNs and the many stakeholders they interface with, which span public and private sector boundaries. AHSNs were involved in very different discussions about how to scale up a regional innovation in health care with other partners (e.g. with LEPs and HEIs) and supporting individuals and organisations (such as clinical entrepreneurs, local innovators and/or SMEs) to scale up promising innovations that had so far failed to be taken up widely in the NHS.
We reiterate the complexity of performance measurement for AHSNs given the various stakeholders involved in the health-care innovation process (e.g. AHSNs, LEPs, HEIs, NHS trusts), who may claim the attribution of any innovation success, according to their distinct key performance indicators. In addition, AHSNs had varied involvement and ownership levels in supporting the innovations we studied, which may affect the returns that can realistically be expected on them.
Academic Health Science Networks’ discussions of their approaches to knowledge mobilisation were primarily pragmatic and focused on meeting AHSN core objectives. There was some use of Rogers’ diffusion model7 and CLAHRC-related service and quality improvement approaches. Texts were used from IHI and NHS IQ on occasion. However, a theoretically well-developed and empirically grounded framework for knowledge mobilisation was generally lacking, although in one AHSN this work was being developed.
The practice of knowledge networking within and around Academic Health Science Networks
We identified two different types of emerging knowledge networks that contributed to AHSNs’ double-headed aims of health improvement and wealth creation. These two types of network differed in terms of the types of contacts and knowledge being exchanged.
Early knowledge exchanges and networking were more linked to the implementation of national policy and local projects. They were associated with pre-existing social ties and established relationships. In the later phases of our study, however, the knowledge being exchanged around wealth objectives suggested the emergence of new AHSN connections and activities, linked more to pan-regional developments and initiatives. Emergent wealth networks were in this way less mature and based on newer relationships and contacts than those focused on health improvement. AHSN board members were also playing an important role in bridging new contacts. We further note that, across the five AHSN regions, different network structures were found.
The construction of knowledge leadership
Among our key conclusions is that the body of literature on themes of the formal leadership of mandated networks and ‘knowledge leadership’ as a standalone concept is relatively small. An important empirical finding is that individuals in formal leadership positions (i.e. in networks or in organisations) may not necessarily be the most effective knowledge brokers, as leadership in a complex health system is likely to be dispersed. So we do not assume that the holding of formal authority by itself leads to effective knowledge mobilisation. Rather, although knowledge leadership may be performed by the formal leaders of mandated networks (as apparent in some of our AHSN case studies), it may also arise at different points within a wider system and be occupied by those with less formal role power.
We identified some attributes of individuals with perceived effectiveness as KLs within AHSN regions, including acting as powerful gatekeepers, matchmakers and brokers (this is likely to be easier for those with high levels of social capital accumulated over a career), and having access to materials and resources. KLs typically wear multiple hats and so draw on professional experience gained across different sectors and settings. In particular, they place importance on investing time in building strong interpersonal networks and are seen as good communicators, able to transmit their vision or passion widely. So we suggest that effective knowledge leadership involves well-developed relational capital (i.e. strong networks; high trust relationships), while at the same time personality traits (e.g. communication skills; drive) clearly have a role to play. Achieving a balance across different forms of capital (social, cognitive, material, symbolic) may be especially vital for cultivating knowledge leadership skills.
We also explored a subset of what we termed national knowledge ‘beacons’. These individuals were hyperconnected and influential beyond their own region. We thus differentiated them from AHSN-specific KLs and regional contacts. Many had long tenure in the NHS or public service; fewer came from private industry. Their generally non-linear careers helped to explain their high connectivity, as over time they had moved across sectors and professional communities and accumulated many contacts. These peer-nominated beacons were not necessarily directly involved in operational-level AHSN work, but had indirect influence with AHSN leaders and/or teams. These ‘beacons’ needed to be visibly rooted in a field of specialism to have the necessary legitimacy to ‘spread the gospel’ and their particular vision. Indeed, complete generalists, hyper-networkers or social media celebrities (perhaps with many Twitter followers but with no track record or specialist knowledge of the NHS) seemed less likely to be perceived as influential. Indeed, we found that beacons had built their professional network organically and used their professional positions actively to increase their influence; thus, these mechanisms at some point become self-reinforcing. This finding is different from the traditional SNA argument that one becomes important on account of structural positioning in networks because it instead stresses the role of activity and perceived influence.
Study achievements and limitations
We recognise that the study has some limitations as data collection (SNA surveys, interviews, observation and case studies – including of the mobilisation of specific innovations – see Chapter 7) proceeded over a relatively short time period (early 2014 to early 2016); therefore, it did not cover the entire 5-year licence period. We examined the early development and ‘forming’ phase of AHSNs, meaning that their concrete knowledge mobilisation strategies and practices emerged relatively late in the life of the study. We reiterate that the study was not intended as an impact evaluation of AHSNs against their licence objectives; the research protocol originally developed was in response to a call for greater understanding of knowledge exchange and leadership dynamics in the NHS, having noted an important gap about NHS senior leadership behaviours that might lend support to innovation. So it was beyond our brief to include an impact evaluation and indeed comment that this would be challenging at the national level and require substantial, longer-term resources (see Future research agenda). Our SNA captured snapshots of networking but only at two relatively close time points rather than over a more extensive period.
Achievements of the study include (1) early mapping of the types of networks emerging around AHSNs as mandated networks, with indications of how these networks may be developing over time (e.g. to include a wider pool of actors); (2) a contribution to the currently limited literature on knowledge leadership – both in health delivery research but also in management as a disciplinary field; (3) insights about regional innovation systems and potential opportunities for economic growth within them, which is arguably a topic of significance given economic shifts in knowledge economies internationally (e.g. the expansion of biomedical and life sciences sectors); (4) SNA that helpfully enabled us to identify the multiple actors operating in the health innovation landscape beyond central AHSN teams and to plot emerging wealth creation networks. Finally, we undertook a collection of 10 innovation tracers across a set of five different AHSNs on which is a good comparative data set about knowledge mobilisation practices and innovation pathways on which future studies may be able to build.
Future research agenda
As already mentioned, our study was not set up as an evaluation of AHSN impact, yet there was clearly a desire apparent in the policy and practice fields for such a study. Such a study would not be without methodological challenges in terms of unpicking causal processes around the careers of innovations in what is a highly complex organisational setting, and also in terms of the time lag that might be involved in making such an assessment and the sophistication of the indicators that are readily available. Nevertheless, we suggest that highest priority consideration should be given to such a study, in consultation with AHSNs and their members.
We further suggest that the wealth creation role of AHSNs should also be a high priority for future research; there is as yet a relatively contained volume of research on the wealth creation role of English health-care organisations – despite its rising importance in the policy domain which was apparent in Chapter 4 – as opposed to a more traditional health improvement and clinically orientated focus. For example, the SNA picked up some early evidence on the evolution of wealth networks but over a relatively short period of time. It would be useful to have more longitudinal survey data on the presence of SMEs and industry in these networks and how this is evolving. We found the health innovation landscape diverse, with different levels of innovation being developed in terms of scale and scope. So, large pharmaceutical companies had a presence and role to play alongside smaller start-ups and SMEs, which lacked substantial experience of navigating the NHS. Future research may wish to explore in more depth the consequences of such high diversity in terms of a pipeline of innovation relevant to the NHS and patient populations.
We have as yet very few English case studies of the operation of triple helix-style regional innovation systems, especially where the life and health sciences sector are rapidly developing; therefore, this is also a high-priority area in our view. New partnerships and strategic alliances may be forming between sectors and agencies that are novel and need to be explored.
In terms of what might be seen as longer-term research priorities, there are several further suggestions that flow from our other findings.
Chapter 4’s analysis of national policy around the health and life sciences suggested a broadening of the actors actively engaged as partners in the policy-making process – so possible movement beyond a traditional lobbying role for professional organisations and businesses to greater incorporation of a variety of stakeholders (including industry bodies) within the policy-making process. The role of the OLS was seen as significant, again reiterating the rapid changes under way in the wider institutional landscape. The chapter also raised the question of where national leadership for AHSN development and progress sits, since innovation policy risks remaining poorly integrated and disconnected. This policy stream could be an important candidate for more political science-informed research, which takes into account developments at both national and regional levels.
Chapter 7 began to explore the processes of knowledge mobilisation in relation to the scale-up of innovations selected by AHSNs from within their regions. A few authors and institutes were identified as having some influence on AHSN understandings of knowledge mobilisation (e.g. Rogers7), but this is an area where further work to understand the models in use would be helpful (beyond solely an AHSN or quality improvement focus).
Chapter 7’s other suggestion was that an important role was being played by a small but important group of clinical entrepreneurs and health inventors (including academic hybrids) in the health innovation process. This insight should be explored further: what roles do these individuals hold, what is their career trajectory and skill set? We noted that many innovators had a primary professional identity (e.g. nurse, doctor, engineer, academic), but had acquired a more entrepreneurial approach on the job and broadened their remit into other – often more commercial – arenas. Therefore, the active agency driving health-care innovation could be explored in greater depth, such as how and why individuals select specific problems for improvement and what sustains personal investment in a particular idea, product or service.
Finally, Chapter 8 suggested that there was a distinction to be drawn between actively managing and leading networks and enacting a knowledge leadership role that goes beyond formal role positions. KLs can help spread new ideas about innovation and knowledge mobilisation across health systems and beyond regional boundaries. Our idea of a national ‘knowledge beacon’ is an intriguing one, which could be explored empirically.
Generally speaking, these insights suggest the greater use of longitudinal rather than snapshot research designs, perhaps drawing on the present study as an early baseline. They also suggest that we need a greater awareness of systems-based approaches to the analysis of what are complex and regional innovation ecosystems.
Acknowledgements
We would like to acknowledge the assistance of Ray Phillips, Independent Libraries and Information Consultant, for help with the literature search, and Helena Silenzi, who provided part-time Research Assistant support, assisting with project management tasks, desk research and early data coding.
We would also like to thank members of the SSC and especially its chairperson, Professor James Barlow (Imperial College London), Dr Liz Mear (Chief Executive North West Coast AHSN), Professor Steve Smye (University of Leeds), Professor Maxine Robertson (Queen Mary, University of London), Mr Colin Tysall (PPI representative, UNTRAP) and Mr Andrew Entwistle (PPI representative, UNTRAP) for their support and advice, along with the five AHSNs that decided to participate and all those respondents who gave up their time to be interviewed.
We give thanks to the wider stakeholders (from different sectors involved in health innovation work) and the AHSN Network, all of whom generously gave of their time to participate in this study.
Finally, we would like to thank the anonymous reviewers for their comments on earlier drafts of the report.
Contributions of authors
Professor Ewan Ferlie (Principal Investigator) was responsible for data collection (policy interviews), data analysis, literature review and was co-ordinator for the report (lead author Chapter 4).
Professor Davide Nicolini (Co-investigator) was responsible for data collection (one site, KLs), data analysis, literature review and writing (lead author Chapter 8).
Dr Jean Ledger (Research Associate, Project Co-ordinator) was responsible for data collection (policy and three sites), literature review, data analysis and writing (lead author Chapter 7).
Dr Daniela D’Andreta (Research Fellow) was responsible for data collection (SNA lead and two sites), literature review, data analysis and writing (lead author Chapters 5 and 6).
Mr Dmitrijs Kravcenko (Part-time Research Assistant) was responsible for data collection (one site), literature review.
Mr John de Pury (Policy Advisor and Partner) was responsible for public engagement and dissemination strategy, feedback on analysis and was a SSC member and final event co-ordinator.
Data sharing statement
This is a mixed-methods study: the qualitative study and SNA component (driven by peer nomination) could identify participants. Therefore, the data generated are not suitable for sharing beyond those contained within the report. Further information can be obtained from the corresponding author.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
References
- Innovation, Health and Wealth. London: DH; 2011.
- Walshe K, Davies HT. Health research, development and innovation in England from 1988 to 2013: from research production to knowledge mobilization. J Health Serv Res Policy 2013;18:1-12. http://dx.doi.org/10.1177/1355819613502011.
- Cooksey D. A Review of UK Health Funding (Cooksey Review). London: HM Treasury; 2006.
- High Quality Care for All. London: DH; 2008.
- Ferlie E, Fitzgerald L, McGivern G, Dopson S, Bennett C. Public policy networks and ‘wicked problems’: a nascent solution?. Public Admin 2011;89:307-24. https://doi.org/10.1111/j.1467-9299.2010.01896.x.
- Coleman J, Katz E, Menzel H. Medical Innovation: A Diffusion Study. New York, NY: Bobbs-Merrill; 1966.
- Rogers E. Diffusion of Innovations. New York, NY: Free Press; 2003.
- Buchanan D, FitzGerald L, Buchanan D, FitzGerald L, Ketley D. The Sustainability and Spread of Organization Change. Abingdon: Routledge; 2007.
- Ham C, Kipping R, McLeod H. Redesigning work processes in health care: lessons from the National Health Service. Milbank Q 2003;81:415-39. https://doi.org/10.1111/1468-0009.t01-3-00062.
- Nicolini D, Powell J, Korica M. Keeping knowledgeable: how NHS chief executive officers mobilise knowledge and information in their daily work. Health Serv Deliv Res 2014;2.
- Swan J, Newell S, Nicolini D, Swan J, Newell S, Nicolini D. Mobilizing Knowledge in Health Care: Challenges for Management and Organization. Oxford: Oxford University Press; 2016.
- Dopson S, Bennett C, Fitzgerald L, Ferlie E, Fischer MD, Ledger J, et al. Health Care Managers Access and Use of Management Research. Final Project Report. Health Serv Deliv Res 2013. www.journalslibrary.nihr.ac.uk/programmes/hsdr/081808242/#/.
- Ferlie E, Ledger J, Dopson S, Fischer MD, Fitzgerald L, McGivern G, et al. The political economy of management knowledge: management texts in English healthcare organizations. Public Admin 2016;94:185-203. https://doi.org/10.1111/padm.12221.
- Fischer MD, Dopson S, Fitzgerald L, Bennett C, Ferlie E, Ledger J, et al. Knowledge leadership: mobilizing management research by becoming the knowledge object. Hum Relat 2016;69:1563-83. https://doi.org/10.1177/0018726715619686.
- Zahra SA, George G. Absorptive capacity: a review, reconceptualization, and extension. AMR 2002;27:185-203. http://dx.doi.org/10.5465/AMR.2002.6587995.
- Cohen WM, Levinthal DA. Absorptive capacity: a new perspective on learning and innovation. ASQ 1990;35:128-52. https://doi.org/10.2307/2393553.
- Brown JS, Duguid P. Organizational learning and communities-of-practice: toward a unified view of working, learning, and innovation. Org Science 1991;2:40-57. http://dx.doi.org/10.1287/orsc.2.1.40.
- Granovetter MS. The strength of weak ties. AMJ 1973;78:1360-80. https://doi.org/10.1086/225469.
- Owen-Smith J, Powell WW. Knowledge networks as channels and conduits: the effects of spillovers in the Boston biotechnology community. Org Science 2004;15:5-21. https://doi.org/10.1287/orsc.1030.0054.
- Greenhalgh T, Peacock R. Effectiveness and efficiency of search methods in systematic reviews of complex evidence: audit of primary sources. BMJ 2005;331:1064-5. https://doi.org/10.1136/bmj.38636.593461.68.
- Wellman B. Network analysis: some basic principles. Sociol Theory 1983;1:155-200. https://doi.org/10.2307/202050.
- Lin N. Building a network theory of social capital. Connections 1999;22:28-51.
- Coleman JS. Snowball sampling: problems and techniques of chain referral sampling. Hum Organ 1958;17:28-36. https://doi.org/10.17730/humo.17.4.q5604m676260q8n7.
- Goodman LA. Comment: on respondent-driven sampling and snowball sampling in hard-to-reach populations and snowball sampling not in hard-to-reach populations. Sociol Methodol 2011;41:347-53. https://doi.org/10.1111/j.1467-9531.2011.01242.x.
- Heckathorn DD. Respondent-driven sampling II: deriving valid population estimates from chain-referral samples of hidden populations. Soc Probl 2002;49:11-34. https://doi.org/10.1525/sp.2002.49.1.11.
- Borgatti SP, Everett MG, Freeman LC. Ucinet for Windows: Software for Social Network Analysis. Harvard, MA: Analytic Technologies; 2002.
- Wasserman S, Faust K. Social Network Analysis: Methods and Applications. Cambridge: Cambridge University Press; 1994.
- Heckathorn DD. Snowball versus respondent-driven sampling. Sociol Methodol 2011;41:355-66. http://dx.doi.org/10.1111/j.1467-9531.2011.01244.x.
- Seidel MD, Westphal JD. Research impact: how seemingly innocuous social cues in a CEO survey can lead to change in board of director network ties. Strategic Organ 2004;2:227-70. https://doi.org/10.1177/1476127004045252.
- Eisenhardt KM. Building theories from case study research. AMR 1989;14:532-50. http://dx.doi.org/10.5465/AMR.1989.4308385.
- Pettigrew AM. What is a processual analysis?. Scand J Management 1997;13:337-48. https://doi.org/10.1016/S0956-5221(97)00020-1.
- Langley A. Strategies for theorizing from process data. AMR 1999;24:691-710. http://dx.doi.org/10.5465/AMR.1999.2553248.
- Denis JL, Lamothe L, Langley A. The dynamics of collective leadership and strategic change in pluralistic organizations. AMJ 2001;44:809-37. https://doi.org/10.2307/3069417.
- Quilter-Pinner H, Muir R. Improved Circulation: Unleashing Innovation Across the NHS. London: Institute for Public Policy Research; 2015.
- Bienkowska-Gibbs T, Exley J, Saunders CL, Marjanovic S, Chataway J, MacLure C, et al. Evaluating the Role and Contribution of Innovation to Health and Wealth in the UK: A Review of Innovation, Health and Wealth: Phase 1 Final Report. Manchester: University of Manchester and RAND; 2016.
- Etzkowitz H, Leydesdorff L. The dynamics of innovation: from national systems and Mode 2 to a Triple Helix of university–industry–government relations. Res Policy 2000;29:109-23. https://doi.org/10.1016/S0048-7333(99)00055-4.
- Etzkowitz H. Incubation of incubators: innovation as a Triple Helix of university-industry-government networks. Sci Public Policy 2002;29:115-28. https://doi.org/10.3152/147154302781781056.
- Etzkowitz H. Innovation in innovation: the Triple Helix of university-industry-government relations. Soc Sci Inf 2003;42:293-337. https://doi.org/10.1177/05390184030423002.
- Etzkowitz H. The new visible hand: an assisted linear model of science and innovation policy. Sci Public Policy 2006;33:310-20. https://doi.org/10.3152/147154306781778911.
- Fromhold-Eisebith M, Werker C. Universities’ functions in knowledge transfer: a geographical perspective. Ann Reg Sci 2013;51:621-43. https://doi.org/10.1007/s00168-013-0559-z.
- Gibbons M, Limoges C, Nowotny H, Schwartzman S, Scott P, Trow M. The New Production of Knowledge: The Dynamics of Science and Research in Contemporary Societies. London: Sage; 1994.
- Schoonmaker MG, Carayannis EG. Mode 3: a proposed classification scheme for the knowledge economy and society. J Knowl Econ 2013;4:556-77. https://doi.org/10.1007/s13132-012-0097-4.
- Carayannis EG, Campbell DF. Mode 3 and Quadruple Helix: toward a 21st century fractal innovation ecosystem. Int J Technol Manag 2009;46:201-34. https://doi.org/10.1504/IJTM.2009.023374.
- Johnson WH. Roles, resources and benefits of intermediate organizations supporting Triple Helix collaborative R&D: the case of Precarn. Technovation 2008;28:495-50. https://doi.org/10.1016/j.technovation.2008.02.007.
- Smith HL, Bagchi-Sen S. Triple Helix and regional development: a perspective from Oxfordshire in the UK. Technol Anal Strateg 2010;22:805-18. https://doi.org/10.1080/09537325.2010.511143.
- Etzkowitz H, Klofsten M. The innovating region: toward a theory of knowledge-based regional development. R&Amp;D Manage 2005;35:243-55. https://doi.org/10.1111/j.1467-9310.2005.00387.x.
- Goldstein HA, Glaser K. Research universities as actors in the governance of local and regional development. J Technol Transf 2012;37:158-74. https://doi.org/10.1007/s10961-010-9193-4.
- Rhodes RAW. Understanding Governance. Buckingham: Open University Press; 1997.
- Feldman JM. The managerial equation and innovation platforms: the case of Linköping and Berzelius science park. Eur Planning Studies 2007;15:1027-45. https://doi.org/10.1080/09654310701448162.
- Kitson AL. The need for systems change: reflections on knowledge translation and organizational change. J Adv Nurs 2009;65:217-28. http://dx.doi.org/10.1111/j.1365-2648.2008.04864.x.
- Van de Ven A, Polley DE, Garud R, Venkataraman S. The Innovation Journey. Oxford: Oxford University Press; 1999.
- Kitto SC, Sargeant J, Reeves S, Silver I. Towards a sociology of knowledge translation: the importance of being dis-interested in knowledge translation. Adv Health Sci Educ Theory Pract 2012;17:289-99. http://dx.doi.org/10.1007/s10459-011-9303-6.
- Nicolini D, Powell J, Conville P, Martinez-Solano L. Managing knowledge in the healthcare sector. A review. Int J Mang Rev 2008;10:245-63. https://doi.org/10.1111/j.1468-2370.2007.00219.x.
- Best A, Greenhalgh T, Lewis S, Saul JE, Carroll S, Bitz J. Large-system transformation in health care: a realist review. Milbank Q 2012;90:421-56. http://dx.doi.org/10.1111/j.1468-0009.2012.00670.x.
- Plsek PE, Greenhalgh T. Complexity science: the challenge of complexity in health care. BMJ 2001;323:625-8. https://doi.org/10.1136/bmj.323.7313.625.
- Deeds DL, DeCarolis D, Coombs J. Dynamic capabilities and new product development in high technology ventures: an empirical analysis of new biotechnology firms. JBV 2000;15:211-29. https://doi.org/10.1016/s0883-9026(98)00013-5.
- Obstfeld D. Social networks, the tertius iungens orientation, and involvement in innovation. ASQ 2005;50:100-30. https://doi.org/10.2189/asqu.2005.50.1.100.
- Burt RS. Structural Holes: The Social Structure of Competition. Cambridge, MA: Harvard University Press; 2009.
- Long JC, Cunningham FC, Carswell P, Braithwaite J. Who are the key players in a new translational research network?. BMC Health Serv Res 2013;13. http://dx.doi.org/10.1186/1472-6963-13-338.
- Liu CC, Stuart TE. Boundary Spanning In a For-Profit Research Lab: An Exploration of the Interface Between Commerce and Academe. Cambridge, MA: Harvard Business School; 2010.
- Jones NB, Herschel RT, Moesel DD. Using ‘knowledge champions’ to facilitate knowledge management. J Knowledge Manag 2003;7:49-63. https://doi.org/10.1108/13673270310463617.
- Maguire S, Hardy C, Lawrence T. Institutional entrepreneurship in emerging fields: HIV/AIDS treatment advocacy in Canada. AMJ 2004;47:657-79. https://doi.org/10.2307/20159610.
- Lockett A, Currie G, Waring J, Finn R, Martin G. The role of institutional entrepreneurs in reforming healthcare. Soc Sci Med 2012;74:356-63. http://dx.doi.org/10.1016/j.socscimed.2011.02.031.
- Käser PA, Miles RE. Understanding knowledge activists’ successes and failures. Long Range Plann 2002;35:9-28. https://doi.org/10.1016/S0024-6301(02)00020-1.
- Pope C, Robert G, Bate P, Le May A, Gabbay J. Lost in translation: a multi-level case study of the metamorphosis of meanings and action in public sector organizational innovation. Public Admin 2006;84:59-7. https://doi.org/10.1111/j.0033-3298.2006.00493.x.
- Greenhalgh T, Stramer K, Bratan T, Byrne E, Mohammad Y, Russell J. Introduction of shared electronic records: multi-site case study using diffusion of innovation theory. BMJ 2008;337. http://dx.doi.org/10.1136/bmj.a1786.
- Greenhalgh T, Robert G, Macfarlane F, Bate P, Kyriakidou O. Diffusion of innovations in service organizations: systematic review and recommendations. Milbank Q 2004;82:581-629. https://doi.org/10.1111/j.0887-378X.2004.00325.x.
- Waldorff SB. Accounting for organizational innovations: mobilizing institutional logics in translation. SJM 2013;29:219-34. https://doi.org/10.1016/j.scaman.2013.03.010.
- Gabbay J, Le May A. Evidence based guidelines or collectively constructed ‘mindlines?’ Ethnographic study of knowledge management in primary care. BMJ 2004;329. https://doi.org/10.1136/bmj.329.7473.1013.
- Waring JJ, Bishop S. ‘Water cooler’ learning: knowledge sharing at the clinical ‘backstage’ and its contribution to patient safety. J Health Organ Manag 2010;24:325-42. http://dx.doi.org/10.1108/14777261011064968.
- Currie G, Suhomlinova O. The impact of institutional forces upon knowledge sharing in the UK NHS: the triumph of professional power and the inconsistency of policy. Public Admin 2006;84:1-30. https://doi.org/10.1111/j.0033-3298.2006.00491.x.
- Kislov R, Walshe K, Harvey G. Managing boundaries in primary care service improvement: a developmental approach to communities of practice. Implement Sci 2012;7. http://dx.doi.org/10.1186/1748-5908-7-97.
- Lave J, Wenger E. Situated Learning. Cambridge: Cambridge University Press; 1991.
- Jacobson N, Butterill D, Goering P. Consulting as a strategy for knowledge transfer. Milbank Q 2005;83:299-321. https://doi.org/10.1111/j.1468-0009.2005.00348.x.
- Harvey G, Fitzgerald L, Fielden S, McBride A, Waterman H, Bamford D, et al. The NIHR collaboration for leadership in applied health research and care (CLAHRC) for Greater Manchester: combining empirical, theoretical and experiential evidence to design and evaluate a large-scale implementation strategy. Implement Sci 2011;6:5908-16. https://doi.org/10.1186/1748-5908-6-96.
- Shafique M. Thinking inside the box? Intellectual structure of the knowledge base of innovation research (1988–2008). SMJ 2013;34:62-93. https://doi.org/10.1002/smj.2002.
- Dzau VJ, Ackerly DC, Sutton-Wallace P, Merson MH, Williams RS, Krishnan KR, et al. The role of academic health science systems in the transformation of medicine. Lancet 2010;375:949-53. http://dx.doi.org/10.1016/S0140-6736(09)61082-5.
- Ackerly DC, Udayakumar K, Taber R, Merson MH, Dzau VJ. Perspective: global medicine: opportunities and challenges for academic health science systems. Acad Med 2011;86:1093-9. https://doi.org/10.1097/ACM.0b013e318226b455.
- Ovseiko PV, Davies SM, Buchan AM. Organizational models of emerging academic health science centers in England. Acad Med 2010;85:1282-9. http://dx.doi.org/10.1097/ACM.0b013e3181e541bd.
- Ovseiko PV, Heitmueller A, Allen P, Davies SM, Wells G, Ford GA, et al. Improving accountability through alignment: the role of academic health science centres and networks in England. BMC Health Serv Res 2014;14. http://dx.doi.org/10.1186/1472-6963-14-24.
- French CE, Ferlie E, Fulop NJ. The international spread of Academic Health Science Centres: a scoping review and the case of policy transfer to England. Health Policy 2014;117:382-91. http://dx.doi.org/10.1016/j.healthpol.2014.07.005.
- Fish DR. Academic health sciences networks in England. Lancet 2013;381:e18-19. http://dx.doi.org/10.1016/S0140-6736(12)60866-6.
- Rowley E, Morriss R, Currie G, Schneider J. Research into practice: Collaboration for Leadership in Applied Health Research and Care (CLAHRC) for Nottinghamshire, Derbyshire, Lincolnshire (NDL). Implement Sci 2012;7. http://dx.doi.org/10.1186/1748-5908-7-40.
- Caldwell SE, Mays N. Studying policy implementation using a macro, meso and micro frame analysis: the case of the Collaboration for Leadership in Applied Health Research & Care (CLAHRC) programme nationally and in North West London. Health Res Policy Syst 2012;10. https://doi.org/10.1186/1478-4505-10-32.
- Oborn E, Barrett M, Prince K, Racko G. Balancing exploration and exploitation in transferring research into practice: a comparison of five knowledge translation entity archetypes. Implement Sci 2013;8. http://dx.doi.org/10.1186/1748-5908-8-104.
- Currie G, Lockett A, El Enany N. From what we know to what we do: lessons learned from the translational CLAHRC initiative in England. J Health Serv Res Policy 2013;18:27-39. http://dx.doi.org/10.1177/1355819613500484.
- Harvey J, Pettigrew A, Ferlie E. The determinants of research group performance: towards Mode 2?. JMS 2002;39:747-74. https://doi.org/10.1111/1467-6486.00310.
- Addicott R, McGivern G, Ferlie E. The distortion of a managerial technique? The case of clinical networks in UK health care. BJM 2007;18:93-105. https://doi.org/10.1111/j.1467-8551.2006.00494.x.
- Borgatti SP, Foster PC. The network paradigm in organizational research: a review and typology. J Manage 2003;29:991-1013. https://doi.org/10.1016/S0149-2063(03)00087-4.
- Borgatti SP, Cross R. A relational view of information seeking and learning in social networks. Manage Sci 2003;49:432-45. https://doi.org/10.1287/mnsc.49.4.432.14428.
- Burt RS. Structural holes and good ideas. AJS 2004;110:349-99. https://doi.org/10.1086/421787.
- Burt RS. Brokerage and Closure: An Introduction to Social Capital. Oxford: Oxford University Press; 2005.
- Powell WW, Koput KW, Smith-Doerr L. Interorganizational collaboration and the locus of innovation: networks of learning in biotechnology. ASQ 1996;41:116-45. https://doi.org/10.2307/2393988.
- Cunningham FC, Ranmuthugala G, Plumb J, Georgiou A, Westbrook JI, Braithwaite J. Health professional networks as a vector for improving healthcare quality and safety: a systematic review. BMJ Qual Saf 2012;21:239-49. http://dx.doi.org/10.1136/bmjqs-2011-000187.
- Lewis JM. Being around and knowing the players: networks of influence in health policy. Soc Sci Med 2006;62:2125-36. https://doi.org/10.1016/j.socscimed.2005.10.004.
- Swan J, Clarke A, Nicolini D, Powell J, Scarborough H, Roginski C, et al. Evidence in Management Decisions (EMD) – Advancing Knowledge Utilization in Healthcare Management. Final Report 2012.
- McGivern G, Dopson S. Inter-epistemic power and transforming knowledge objects in a biomedical network. Organ Stud 2010;31:1667-86. https://doi.org/10.1177/0170840610380808.
- D’Andreta D, Marabelli M, Newell S, Scarbrough H, Swan J. Dominant cognitive frames and the innovative power of social networks. Organ Stud 2016;37:293-321. https://doi.org/10.1177/0170840615613374.
- Martin GP, Currie G, Finn R. Leadership, service reform, and public-service networks: the case of cancer-genetics pilots in the English NHS. J Public Adm Res Theory 2009;19:769-94. https://doi.org/10.1093/jopart/mun016.
- Silvia C, McGuire M. Leading public sector networks: an empirical examination of integrative leadership behaviors. Leadersh Q 2010;21:264-77. https://doi.org/10.1016/j.leaqua.2010.01.006.
- Buchanan DA, Addicott R, Fitzgerald L, Ferlie E, Baeza JI. Nobody in charge: distributed change agency in healthcare. Hum Relat 2007;60:1065-90. https://doi.org/10.1177/0018726707081158.
- Bate P, Robert G, Dopson S, Mark A. Leading Health Care Organizations. Basingstoke: Palgrave Macmillan; 2003.
- Forno AD, Merlone U. Social entrepreneurship effects on the emergence of cooperation in networks. E:CO 2009;11:48-5.
- Zheng W. A social capital perspective of innovation from individuals to nations: where is empirical literature directing us?. Int J Mang Rev 2010;12:151-83. https://doi.org/10.1111/j.1468-2370.2008.00247.x.
- Ohly S, Kase R, Škerlavaj M. Networks for generating and for validating ideas: the social side of creativity. Innovation 2010;12:41-52. https://doi.org/10.5172/impp.12.1.41.
- O’Toole LJ, Meier KJ. Networking in the penumbra: public management, cooptative links, and distributional consequences. IPMJ 2006;9:271-94. https://doi.org/10.1080/10967490600899580.
- Howell JM, Boies K. Champions of technological innovation: the influence of contextual knowledge, role orientation, idea generation, and idea promotion on champion emergence. Leadersh Q 2004;15:123-43. https://doi.org/10.1016/j.leaqua.2003.12.008.
- Barrot C, Kuhlmann J, Popa A. Influence of personal communication networks on innovation adoption – using multi-agent simulations to project the launch of an innovative medical device. IJITM 2013;10. https://doi.org/10.1142/s021987701340021x.
- Eglene O, Dawes SS, Schneider CA. Authority and leadership patterns in public sector knowledge networks. Am Rev Public Adm 2007;37:91-113. https://doi.org/10.1177/0275074006290799.
- Westphal JD, Boivie S, Chng DHM. The strategic impetus for social network ties: reconstituting broken CEO friendship ties. SMJ 2006;27:425-45. https://doi.org/10.1002/smj.525.
- Tortoriello M, Reagans R, McEvily B. Bridging the knowledge gap: the influence of strong ties, network cohesion, and network range on the transfer of knowledge between organizational units. Org Science 2012;23:1024-39. https://doi.org/10.1287/orsc.1110.0688.
- Olk P, Elvira M. Friends and strategic agents: the role of friendship and discretion in negotiating strategic alliances. GOM 2001;26:124-64. https://doi.org/10.1177/1059601101262002.
- Alexiev AS, Jansen JJ, Van den Bosch FA, Volberda HW. Top management team advice seeking and exploratory innovation: the moderating role of TMT heterogeneity. JMS 2010;47:1343-64. https://doi.org/10.1111/j.1467-6486.2010.00919.x.
- Carpenter MA, Westphal JD. The strategic context of external network ties: examining the impact of director appointments on board involvement in strategic decision making. AMJ 2001;44:639-60. https://doi.org/10.2307/3069408.
- Neergaard H, Madsen H. Knowledge intensive entrepreneurship in a social capital perspective. JEC 2004;12:105-25. https://doi.org/10.1142/s0218495804000063.
- McDonald ML, Khanna P, Westphal JD. Getting them to think outside the circle: corporate governance, CEOs’ external advice networks, and firm performance. AMJ 2008;51:453-75. https://doi.org/10.5465/AMJ.2008.32625969.
- Liao CC, Chen J. Director networks and their similarity in R&D expenditure decision. IRJFE 2009;23:75-90.
- Cross R, Sproull L. More than an answer: information relationships for actionable knowledge. Org Science 2004;15:446-62. https://doi.org/10.1287/orsc.1040.0075.
- Fernández-Pérez V, del Mar Fuentes-Fuentes M, Bojica A. Strategic flexibility and change: the impact of social networks. JMO 2012;18:2-15. https://doi.org/10.1017/S1833367200001036.
- Clarysse B, Knockaert M, Lockett A. Outside board members in high tech start-ups. Small Bus Econ 2007;29:243-59. https://doi.org/10.1007/s11187-006-9033-y.
- McAdam M, Marlow S. A preliminary investigation into networking activities within the university incubator. IJEBR 2008;14:219-41. https://doi.org/10.1108/13552550810887390.
- Østergaard CR. Knowledge flows through social networks in a cluster: comparing university and industry links. SCED 2009;20:196-210. https://doi.org/10.1016/j.strueco.2008.10.003.
- Müller R, Glückler J, Aubry M, Shao J. Project management knowledge flows in networks of project managers and project management offices: a case study in the pharmaceutical industry. PMJ 2013;44:4-19. https://doi.org/10.1002/pmj.21326.
- Subrahmanyam A. Social networks and corporate governance. Eur Financial Mgt 2008;14:633-62. https://doi.org/10.1111/j.1468-036X.2007.00429.x.
- Kirchmaier T, Stathopoulos K. From Fiction to Fact: The Impact of CEO Social Networks. London: London School of Economics; 2008.
- McDonald ML, Westphal JD. A little help here? Board control, CEO identification with the corporate elite, and strategic help provided to CEOs at other firms. AMJ 2010;53:343-70. https://doi.org/10.5465/AMJ.2010.49389006.
- Bjørnåli ES, Gulbrandsen M. Exploring board formation and evolution of board composition in academic spin-offs. J Technol Transf 2010;35:92-112. https://doi.org/10.1007/s10961-009-9115-5.
- Alexander JA, Comfort ME, Weiner BJ, Bogue R. Leadership in collaborative community health partnerships. Nonprofit Manag Leadersh 2001;12:159-75. https://doi.org/10.1002/nml.12203.
- Head BW. Assessing network-based collaborations: effectiveness for whom?. PMR 2008;10:733-49. https://doi.org/10.1080/14719030802423087.
- Mitchell SM, Shortell SM. The governance and management of effective community health partnerships: a typology for research, policy, and practice. Milbank Q 2000;78:241-89.
- Scarbrough H, D’Andreta D, Evans S, Marabelli M, Newell S, Powell J, et al. Networked innovation in the health sector: comparative qualitative study of the role of Collaborations for Leadership in Applied Health Research and Care in translating research into practice. Health Serv Deliv Res 2014;2.
- Considine M, Lewis JM. Innovation and innovators inside government: from institutions to networks. Governance 2007;20:581-607. https://doi.org/10.1111/j.1468-0491.2007.00373.x.
- Balkundi P, Kilduff M. The ties that lead: a social network approach to leadership. Leadersh Q 2006;17:419-39. https://doi.org/10.1016/j.leaqua.2006.01.001.
- Long JC, Cunningham FC, Braithwaite J. Bridges, brokers and boundary spanners in collaborative networks: a systematic review. BMC Health Serv Res 2013;13. http://dx.doi.org/10.1186/1472-6963-13-158.
- D’Andreta D, Scarbrough H, Evans S. The enactment of knowledge translation: a study of the Collaborations for Leadership in Applied Health Research and Care initiative within the English National Health Service. J Health Serv Res Policy 2013;18:40-52. https://doi.org/10.1177/1355819613499902.
- Bond EU, Houston MB, Tang YE. Establishing a high-technology knowledge transfer network: the practical and symbolic roles of identification. Ind Market Manag 2008;37:641-52. https://doi.org/10.1016/j.indmarman.2008.04.012.
- Mabey C, Kulich C, Lorenzi-Cioldi F. Knowledge leadership in global scientific research. Int J Hum Resour Man 2012;23:2450-67. https://doi.org/10.1080/09585192.2012.668386.
- Spyridonidis D, Currie G, Heusinkveld S, Strauss K, Sturdy A. The translation of management knowledge: challenges, contributions and new directions. Int J Manag Rev 2016;18:231-5. https://doi.org/10.1111/ijmr.12110.
- Johannissson B. Personal networks in emerging knowledge-based firms: spatial and functional patterns. Entrep Reg Dev 1998;10:297-312. https://doi.org/10.1080/08985629800000017.
- Ham C. Health Policy in Britain. Basingstoke: Palgrave Macmillan; 2009.
- Strategy for UK Life Sciences. London: Department for Business, Innovation and Skills; 2011.
- Best Research for Best Health. London: DH; 2006.
- Christensen C. The Innovator’s Dilemma. Boston, MA: Harvard Business School Press; 1997.
- Christensen C, Grossman J, Hwang J. The Innovator’s Prescription. New York, NY: McGraw Hill; 2009.
- Accelerated Access Review Interim Report: Review of Innovative Medicines and Medical Technologies. Supported by the Wellcome Trust, London, for the Office of Life Sciences, London. London: Department for Business, Innovation and Skills, Department of Health and Office of Life Sciences; 2015.
- Review of Centrally Funded Improvement and Leadership Development Functions. Leeds: NHS England; 2015.
- Five Year Forward View. Leeds: NHS England; 2014.
- Unlocking Growth in Cities. London: Cabinet Office; 2011.
- Newman J. Modernising Governance. London: Sage; 2001.
- Rhodes RA. Understanding governance: ten years on. Organ Stud 2007;28:1243-64. https://doi.org/10.1177/0170840607076586.
- Alvarez-Rosete A, Mays N. Reconciling two conflicting tales of the English health policy process since 1997. British Politics 2008;3:183-20. https://doi.org/10.1057/bp.2008.2.
- Davies H, Nutley S, Walter I. Why ‘knowledge transfer’ is misconceived for applied social research. J Health Serv Res Policy 2008;13:188-90. http://dx.doi.org/10.1258/jhsrp.2008.008055.
- Osborn RN, Hunt JG, Jauch LR. Toward a contextual theory of leadership. Leadersh Q 2002;13:797-83. https://doi.org/10.1016/S1048-9843(02)00154-6.
- Baldassari D, Diani M. The Integrative power of civic networks. AJS 2007;113:735-80. https://doi.org/10.1086/521839.
- Uhl-Bien M, Marion R, McKelvey B. Complexity leadership theory: shifting leadership from the industrial age to the knowledge era. Leadersh Q 2007;18:298-31. https://doi.org/10.1016/j.leaqua.2007.04.002.
- Reagans R, McEvily B. Network structure and knowledge transfer: the effects of cohesion and range. ASQ 2003;48:240-67. https://doi.org/10.2307/3556658.
- Battilana J. The enabling role of social position in diverging from the institutional status quo: evidence from the UK National Health Service. Org Science 2011;22:817-34. https://doi.org/10.1287/orsc.1100.0574.
- Howells J, Archibugi D, Howells J, Michie J. Innovation Policy in a Global Economy. Cambridge: Cambridge University Press; 1999.
- Viitala R. Towards knowledge leadership. LODJ 2004;25:528-44. https://doi.org/10.1108/01437730410556761.
- Lakshman C. Organizational knowledge leadership: a grounded theory approach. LODJ 2007;28:51-75. https://doi.org/10.1108/01437730710718245.
- Edmondson AC. Teaming to Innovate. San Francisco, CA: Jossey-Bass; 2013.
- Mabey C, Nicholds A. Discourses of knowledge across global networks: what can be learnt about knowledge leadership from the ATLAS collaboration?. Int Bus Rev 2015;24:43-54. https://doi.org/10.1016/j.ibusrev.2014.05.007.
- Kempster S, Jackson B, Conroy M. Leadership as purpose: exploring the role of purpose in leadership practice. Leadership 2011;7:317-34. https://doi.org/10.1177/1742715011407384.
- Nahapiet J, Ghoshal S. Social capital, intellectual capital, and the organizational advantage. AMR 1998;23:242-66. http://dx.doi.org/10.5465/AMR.1998.533225.
- Von Krogh G, Nonaka I, Rechsteiner L. Leadership in organizational knowledge creation: a review and framework. J Manage Stud 2012;49:240-77. https://doi.org/10.1111/j.1467-6486.2010.00978.x.
- Wellman B. The community question: the intimate networks of East Yorkers. Am J Sociol 1979;84:1201-31. https://doi.org/10.1086/226906.
- Burt RS. Network items and the US general social survey. Social Networks 1984;6:293-339. https://doi.org/10.1016/0378-8733(84)90007-8.
- Fischer C. What do we mean by friend? An inductive study. Social Networks 1982;3:287-306. https://doi.org/10.1016/0378-8733(82)90004-1.
- Völker B, Flap H. The Survey on the Social Networks of the Dutch (SSND1): Data and Codebook. Utrecht: Utrecht University/ InterUniversity Centre for Social Science Theory and Methodology; 2002.
Appendix 1 Policy interview protocol (time point 1)
Appendix 2 Guiding policy questions: scoping review of documentation
-
What are the important/major life sciences and health innovation policies of the last 10 years?
-
What was the policy backdrop and ideas leading to the formation of AHSNs?
-
What key policy issues are important to consider when considering regional innovation (e.g. local funding sources)?
-
What is the government’s long-term strategy for higher education, health and research in the UK?
-
How does the UK compare in its policy and innovation track record (including R&D investment) to other European Union member states?
-
What do our interview data add to this timeline? What do people within the health innovation ‘policy network’ suggest should be added to this overview of key policies, ideas and events?
-
Is the policy the same/different across different governments?
-
Is there a long-term policy drift from health to wealth?
-
How is the knowledge mobilisation problem conceived? (Knowledge transfer/exchange – research, ideas and innovations.)
Appendix 3 Policy interview protocol (time point 2)
Appendix 4 Literature review key word terms (expert input)
| Team suggestions | Reviewer suggestions |
|---|---|
| Knowledge: | Reviewer 1: |
| Ideas | Utilisation |
| Innovations | Transfer |
| Translation | Reviewer 2: |
| Dissemination | Governance and surveillance |
| Mobilisation | Commercialisation |
| Diffusion | Spinout business engagement |
| Spread | Reviewer 3: |
| Exchange | Embeddedness |
| Sharing | Social position (in that where you are situated shapes how you see the world) |
| Leaders/leadership: | Sense-making, which to me is a key underplayed issue in knowledge mobilisation |
| Senior managers | Distributed/plural leadership |
| NHS | Specialisation |
| CEO or executive | Reviewer 4: |
| Director | Strong/weak ties |
| VSM | Bridging/linking ties |
| Network:* | Reachability |
| Ego-network* | Informal structure |
| Personal network* | Collaborative governance |
| Social network* | Network governance |
| Network position | Partnerships |
| Broker* | Dynamic capabilities |
| Closure | Innovators |
| Small world* | Knowledge economy |
| Social capital | Reviewer 5: |
| Structural holes | Transfer |
| Centrali* | Constraints |
| Heterogeneity | Expertise |
| Respondent driven sampling | Clinical directors |
| Snowball | Reviewer 6: |
| ERGM | Transfer |
| SNA | Knowledge utilisation |
| Hierarch* | Implementation science |
| Agent/agency: | ABCA |
| Power | Learning |
| Influence | Reviewer 7: |
| Strategies | Ideas: too vague |
| Practices | NHS: unspecific |
| Integration | Health/health care/health service: too broad |
| Engagement | Theories |
| Early adopters | Adoption |
| Entrepreneurship/entrepreneur | Tacit knowledge |
| ABCA | Practice-based knowledge |
| Expert | Hybrids |
| Professional | Clinicians |
| Network-based organisational forms: | Stakeholders |
| Innovation policy | Collaboration |
| Science policy | Inclusivity |
| Research policy | Life sciences |
| Health/health care/health service | SMEs |
| Health policy | Open innovation |
| UK NHS | Learning |
| CLAHRC | Reviewer 8 |
| AHSN | Social capital |
| AHSC | Knowledge transfer |
| Networked governance | Knowledge creation |
| R&D investment | Exploration |
| Regional economic growth | Exploitation |
| Wealth creation | Remove ‘information’ |
| Industry networks | Reviewer 9: |
| Triple helix | KLs |
| Science/scientific | University innovation units. I suspect universities have their own R&D networks involved in the AHSN |
| R&D | |
| Biotechnology | |
| Pharmaceutical | |
| Legal | |
| Boundaries/boundary spanning/barriers: | |
| Institutional | |
| Epistemic | |
| Non-spread | |
| Dark side (of social networks) | |
| Group-think | |
| Homophily | |
| Closure | |
| Cliques | |
| Resources | |
| Information | |
| Support | |
| Communities/communities of practice | |
| Social capital | |
| Cross-sectoral: | |
| Academic health centre (USA) | |
| Cluster | |
| Knowledge cluster | |
| Enterprise cluster | |
| Science cluster | |
| Science park | |
| Enterprise park | |
| LEP | |
| HIEC | |
| Welfare technology | |
| Innovation clinic |
Appendix 5 Literature review Boolean word strings
Search string strategy devised with librarian and based on key terms in relation to research questions
Who?
Early adopter* OR leader* OR entrepreneur* OR executive* OR director*
What about them?
Agency, social capital, absorptive capacity, institutional design, networks, knowledge transfer
Where/contexts?
‘institutional entrepreneurship’, ‘science parks’, ‘science AND cluster’, university collaborative, Triple Helix, ‘knowledge transfer partnership’. bio-tech, SME, ‘knowledge-intensive networks’, ‘knowledge-intensive firms’, Management, partnership, healthcare, innovation AND policy, university R&D
Appendix 6 Final search strategies used across databases
The text below provides notes, where appropriate, to explain tailored strategies.
| Database/resource | Search strategy | Iterations | Notes/comments |
|---|---|---|---|
| ABI/INFORM | AB,TI, SO(“Social network” OR “social network analysis” OR “ego-network” OR “ego network”) AND AB, TI, SO(CEO OR executive* OR leader* OR manager* OR CIO OR board OR elite OR director) AND ALL(Knowledge OR “innovation policy” OR “knowledge-intensive” OR “knowledge intensive” OR agen* OR “absorptive capacity” OR “early adopter” OR entrepren* OR “dark-side” OR “dark side” OR clique* OR power OR network*) Limited by: Source type: scholarly journals; working papers Language: English Subject: studies; social networks; knowledge management; leadership; social capital; decision making; organizational behavior; information sharing; research & development –r&d; corporate governance; innovations; organizational learning; knowledge; corporate culture; managers; models; organization theory; politics; social interaction; strategic management; boards of directors; business networking; collaboration; public administration; statistical analysis; multinational corporations; small & medium sized enterprises-sme; colleges & universities; executives Years: 1995–2014 |
6a | In the first line of the search, RP included suggestions from JL and added the phrase ‘social network analysis’. This was done because both the original wording and the suggested alternative produced similar results The source type was limited to exclude seemingly irrelevant or trivial returns from trade journals and newspapers. Subjects were chosen for a similar reasons: to limit irrelevant results |
| OvidSP | (‘Social network’ or ‘social network analysis’ or ‘ego-network’ or ‘ego network’).ti,ab. AND (CEO or executive* or leader* or manager* or CIO or board or elite or director).ti,ab. AND (knowledge OR “innovation policy” or “knowledge-intensive” or “knowledge intensive” or agen* or “absorptive capacity” or “early adopter” or entrepren* or “dark-side” or “dark side” or clique* or power).mp. Limited by: Languages: English Years: 1995–2014 Databases: MEDLINE HMIC Social Policy and Practice |
6a | Getting relevant results was an issue for this search. The abstract and title were selected for the first two areas to try to increase the chances of getting articles related to the keywords |
| ProQuest | AB,TI,SU(“Social network” OR “social network analysis” OR “ego-network” OR “ego network”) AND SU,TI,AB(CEO OR executive* OR leader* OR manager* OR CIO OR board OR elite OR director) AND ALL(knowledge OR “innovation policy” OR “knowledge-intensive” OR “knowledge intensive” OR agen* OR “absorptive capacity” OR “early adopter” OR entrepren* OR “dark-side” OR “dark side” OR clique* OR power) Limited by: Years: 1995–2014 Language: English Databases: Applied Social Sciences Index and Abstracts EconLit International Bibliography of the Social Sciences Social Services Abstracts Sociological Abstracts Worldwide Political Science Abstracts |
6a | |
| Web of Science | (TS=(“Social network” OR “social network analysis” OR “ego-network” OR “ego network”) AND TS=(CEO OR executive* OR leader* OR manager* OR CIO OR board OR elite OR director) AND TS=(“innovation policy” OR “knowledge-intensive” OR “knowledge intensive” OR agen* OR “absorptive capacity” OR “early adopter” OR entrepren* OR “dark-side” OR “dark side” OR clique* OR power)) Limited by: LANGUAGES=(ENGLISH) AND [excluding] WEB OF SCIENCE CATEGORIES=(ENERGY FUELS OR ENGINEERING MANUFACTURING OR COMPUTER SCIENCE INFORMATION SYSTEMS OR ETHNIC STUDIES OR FAMILY STUDIES OR COMPUTER SCIENCE ARTIFICIAL INTELLIGENCE OR GEOGRAPHY PHYSICAL OR ENGINEERING INDUSTRIAL OR LANGUAGE LINGUISTICS OR LINGUISTICS OR MATHEMATICS APPLIED OR SUBSTANCE ABUSE OR METEOROLOGY ATMOSPHERIC SCIENCES OR URBAN STUDIES OR ECOLOGY OR WOMEN S STUDIES OR PHYSICS APPLIED OR AGRICULTURAL ENGINEERING OR AGRICULTURE DAIRY ANIMAL SCIENCE OR ARCHAEOLOGY OR INFORMATION SCIENCE LIBRARY SCIENCE OR AUTOMATION CONTROL SYSTEMS OR COMPUTER SCIENCE HARDWARE ARCHITECTURE OR COMPUTER SCIENCE SOFTWARE ENGINEERING OR CONSTRUCTION BUILDING TECHNOLOGY OR TELECOMMUNICATIONS OR ENGINEERING ELECTRICAL ELECTRONIC OR VETERINARY SCIENCES OR MATHEMATICS INTERDISCIPLINARY APPLICATIONS OR WATER RESOURCES OR ZOOLOGY OR BIODIVERSITY CONSERVATION) Indexes: SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH Years: 1995–2014 |
6a | Limits were applied to exclude subjects that might increase the chances of irrelevant results |
| ABI/INFORM | AB,TI,SO((sharing OR network* OR collaborat* OR transfer OR exchange) AND (knowledge OR innovation)) AND AB,TI,SO(university OR academi* OR industry OR “knowledge intensive” OR government OR “public services” OR “public sector” OR scien* OR biotech OR pharma) AND AB,TI(“triple helix” OR “Triple Helix” OR health* OR NHS OR “NATIONAL HEALTH SERVICE” OR institutional architect* OR “absorptive capacity” OR “dark side” OR “dark-side” OR leader* OR “KTP”) Limited by: Source type: scholarly journals; working papers Language: English |
6b | |
| OvidSP |
HMIC
|
6b | The OvidSP databases were searched separately in this search so that I could either exploit their subject heading to improve the accuracy/relevance of results or so that I could exploit their relatively small sizes to look through results and exclude obvious irrelevancies |
| ProQuest | AB,TI,SU((sharing OR network* OR collaborat* OR transfer OR exchange) AND (knowledge OR innovation)) AND AB,TI(university OR academi* OR industry OR “knowledge intensive” OR government OR “public services” OR “public sector” OR scien* OR biotech OR pharma OR health*) AND AB,TI(“triple helix” OR “Triple Helix” OR NHS OR “NATIONAL HEALTH SERVICE” OR institutional architect* OR “absorptive capacity” OR “dark side” OR “dark-side” OR leader* OR “KTP”) Limited by: Language: English Database: International Bibliography of the Social Sciences; Applied Social Sciences Index and Abstracts; EconLit; Sociological Abstracts; Worldwide Political Science Abstracts; Social Services Abstracts Exclude: asia; china; japan; internet; developing countries; india |
6b | |
| Web of Science | TS=((sharing OR network* OR collaborat* OR transfer OR exchange) AND (knowledge OR innovation)) AND TS=(university OR academi* OR industry OR “knowledge intensive” OR government OR “public services” OR “public sector” OR scien* OR biotech OR pharma) AND TS=(“triple helix” OR “Triple Helix” OR health* OR NHS OR “NATIONAL HEALTH SERVICE” OR institutional architect* OR “absorptive capacity” OR “dark side” OR “dark-side” OR leader* OR “KTP”)) AND LANGUAGE: (English) Refined by: WEB OF SCIENCE CATEGORIES=(MANAGEMENT OR HEALTH CARE SCIENCES SERVICES OR BUSINESS) AND COUNTRIES/TERRITORIES=(USA OR ENGLAND OR CANADA OR NEW ZEALAND OR NETHERLANDS OR AUSTRALIA OR GERMANY OR SPAIN OR ITALY OR BELGIUM OR SWEDEN OR SWITZERLAND OR FRANCE OR NORWAY OR DENMARK OR FINLAND OR WALES OR SCOTLAND ) AND [excluding] WEB OF SCIENCE CATEGORIES=(COMPUTER SCIENCE SOFTWARE ENGINEERING OR COMPUTER SCIENCE THEORY METHODS OR ENGINEERING MANUFACTURING OR PLANNING DEVELOPMENT OR ENGINEERING INDUSTRIAL OR COMPUTER SCIENCE HARDWARE ARCHITECTURE OR INFORMATION SCIENCE LIBRARY SCIENCE OR NURSING SCI OR TELECOMMUNICATIONS OR NURSING SSCI OR WOMEN S STUDIES OR COMPUTER SCIENCE INFORMATION SYSTEMS OR CONSTRUCTION BUILDING TECHNOLOGY OR ENGINEERING MULTIDISCIPLINARY OR COMPUTER SCIENCE INTERDISCIPLINARY APPLICATIONS OR ENGINEERING ELECTRICAL ELECTRONIC OR INDUSTRIAL RELATIONS LABOR OR SPORT SCIENCES OR PUBLIC ENVIRONMENTAL OCCUPATIONAL HEALTH SCI OR BUSINESS FINANCE ) AND [excluding] DOCUMENT TYPES=(EDITORIAL MATERIAL OR REVIEW ) AND [excluding] WEB OF SCIENCE CATEGORIES=(MEDICINE LEGAL OR REHABILITATION OR ECONOMICS OR REHABILITATION SCI OR HOSPITALITY LEISURE SPORT TOURISM OR PUBLIC ENVIRONMENTAL OCCUPATIONAL HEALTH) Indexes: SCI-EXPANDED Years: 1995–2014 |
6b | Exclusion and refinements were made in order to increase relevancy and decrease the number of results |
| ABI/INFORM | ALL(“Academic Health Science Network” OR “AHSN” OR “Academic Health Science Centre” OR “AHSC” OR “Collaboration for Leadership in Applied Health Research and Care” OR “CLAHRC”) Limited by: Language: English Years: 1995–2014 |
6c | |
| OvidSP | (‘Academic Health Science Network’ or ‘Academic Health Science Centre’ or (‘Collaboration for Leadership in Applied Health Research and Care’) or ‘AHSN’ or ‘AHSC’ or ‘CLAHRC’).mp. limit 2 to english language limit 3 to yr=“1995 -Current” |
6c | |
| ProQuest | ALL(“Academic Health Science Network” OR “AHSN” OR “Academic Health Science Centre” OR “AHSC” OR “Collaboration for Leadership in Applied Health Research and Care” OR “CLAHRC”) Limited by: Language: English Years: 1995–2014 Database: International Bibliography of the Social Sciences; Applied Social Sciences Index and Abstracts; EconLit; Sociological Abstracts; Worldwide Political Science Abstracts; Social Services Abstracts |
6c | |
| Web of Science | TS=(“Academic Health Science Network” OR “AHSN” OR “Academic Health Science Centre” OR “AHSC” OR “Collaboration for Leadership in Applied Health Research and Care” OR “CLAHRC”) Limited by: Language: English Years: 1995–2014 |
6c | |
| Google search 1 | leader ceo manager agenc OR ceo OR director OR board OR manager OR knowledge OR innovation OR policy OR “knowledge intensive” OR “knowledge intensive” OR OR “Social network” | 6c | |
| Google search 2 | sharing OR network* OR collaborat* OR transfer OR exchange knowledge OR innovation university OR academi OR ‘ triple helix’ OR health ‘ triple helix’ -gene -collagen -peptide -nucleic -acid -“triple stranded” -DNA | 6c | Attempt to remove scientific genetic-based papers and focus on triple helix concept |
| Google search 3 | allintitle: “Academic Health Science Network” OR AHSC OR “Academic Health Science Centre” OR AHSC OR “Collaboration for Leadership in Applied Health Research and Care” OR CLAHRC allintitle: “academic health science” |
6c |
Appendix 7 ‘6a’ literature review framework (relevant papers given research questions)
| Contributing streams of literature: ontological framework | |||
|---|---|---|---|
| Network agency | |||
| Formal networks | Informal networks | ||
| Individual agency | Formal leadership | Formal leadership in mandated networks: What do we know about how managers, in particular top managers, lead formal networks? Literature on leading networked organisations. (Top manager/CEO networks, performance) |
Formal leaders’ personal networks: What do we know about how managers, in particular top managers, draw on their personal networks for leadership capabilities? (Antecedents to, and backstage performativity of, top manager/CEO networks – advice, support, trust, etc.) |
| Informal leadership | Emergent leadership in mandated networks: Innovation champions, knowledge brokers, diffusion fellows, entrepreneurs emerging in mandated networks. Nonaka KLs paper165 |
Emergent leadership and informal networks: Leadership via communities of practice, regional clusters, self-organised networks/innovation systems to overcome complexity/change48 |
|
6a leadership and network agency stream: research questions
-
What role do formal and informal leaders play in mobilising and circulating knowledge in networked organisations? How much agency do these KLs have?
-
What are the antecedent conditions under which leadership agency in knowledge networks happens or is hindered? In particular, what effect do formal leaders’ external connections (personal network) have on the networked organisation’s strategy/capacity for knowledge mobilisation?
-
How does the network organisation itself act as a knowledge leadership system?
Appendix 8 ‘6b’ and ‘6c’ literature review framework (relevant papers given research questions and study context)
| 6b, 6c: knowledge transfer in networks, policy and industry; NHS knowledge mobilisation, architecture and policy; relevance (included) | |
|---|---|
| Sectors and place | |
| High-technology industries or knowledge-intensive networks; innovation regions; innovation clusters and collaborations | Trust, power or leadership; high-tech case studies; knowledge transfer and social processes; networks and organisational learning; R&D consortia; management consulting; science parks SNA studies |
| Biotechnology and global/international pharmaceuticals | Biotechnology alliances Science entrepreneurial firms and knowledge exchange (KBIS) Biotechnology clustering and alliances |
| Universities and HEI research centres and partnerships | Knowledge or technology ‘spillovers’; social enterprises and knowledge transfer (e.g. HEIs and third sector); the ‘entrepreneurial university’ Commercialisation: UTTOs and patents and IP in HEIs ‘Collaborative knowledge production’ and collaborative strategies Intermediaries for diffusion of new technologies/innovations/knowledge |
Health settings, UK NHS and HSR in relation to:
|
Knowledge transfer and social processes; communities of practice (include key authors) ‘Knowledge networks’ or networks and ‘organisational learning’ AHSCs CLAHRCs Applied SNA studies Policy and health networks Public health (populations) innovation/networks/KTE Public sector innovation or health service innovativeness (including international examples, e.g. US medical centres); enterprise and innovation in the NHS International comparators on knowledge mobilisation and heath care Collaborative health networks and intersectoral collaboration in health for innovation (e.g. private, public and primary care) Social enterprises, innovation and health. Innovation with user input in health E-health/digital health innovation and networks Innovation barriers in health care (e.g. regulation) |
| Academic concepts | |
| ABCA | Applied to health-related fields (biotechnology and pharmaceutical) or leadership/agency Reviews and systematic reviews of key conceptual areas and literatures |
| Triple helix (theoretical papers; and applied to KIF settings or innovative technology and health) | Leading theoretical authors (e.g. Etzkowitz and Leydesdorff36); triple helix and HEIs/life sciences/SMEs Reviews and systematic reviews of key conceptual areas and literatures International examples from health-care sector HEI knowledge commercialisation: UTTOs; biotechnology and university alliances Private sector engagement in triple helix/partnerships, including SMEs |
| National and regional innovation policy and theory (macro and systems perspectives) | ‘Meta innovation’/regional innovation/’innovation zones’/entrepreneurial regions and ‘spinouts’ (e.g. regional science parks and cluster case studies) ‘Knowledge collaboratives’ and performance Regional economics ‘Open innovation’ (including international) ‘Disruptive innovations’ |
| Networks, network governance and power in network organisational forms | Power dynamics and ‘dark side’ of networks Trust in networks (KIF settings) Intraorganisational social capital |
| Agency and individuals (overlap with 6a) | |
| Knowledge ‘conveners’/’knowledge brokers’/’boundary spanners’ | Applied to health, networks, innovation or collaborations |
| Leadership | Concept of leadership applied to knowledge-intensive settings (e.g. HEIs); across HEIs and SMEs; health-care networks (e.g. CLAHRCs); network leadership Transformational leadership in HEIs, health-care settings or networks (e.g. ‘health-care entrepreneurs’) Research leaders (e.g. research directors) Distributed leadership and network forms/health/innovation |
| Policy literature | |
| Critical literature and analyses | For example, policy rhetoric |
| Systematic and ‘realist’ literature reviews | |
| ICT and KM in health care | |
| Translational medicine/research translation in health care | |
| Regional innovation systems and innovation theory literature | |
| Health-care innovation | |
| Relevant paper collections/conference paper collections (grey literature) | |
| Not relevant (in general, single case studies which are descriptive only: atheoretical and normative papers) | |
| HEIs | Research scholarship and HEIs |
| Non-KT/health/network focus | General health innovation programmes without specific KT, technology diffusion or network focus Local government and political science: without networks or health-related focus Health-care evaluations (no network or KTE focus) Local case studies (lack theoretical application) |
| Broad KM or knowledge exchange focus (lacking theory) | Community development and KM Researcher and research commissioner interactions |
| Narrow management literatures: performance/supply chain/R&D/operational management | Strategic management literature with narrow performance focus Supply chain management General papers on R&D or R&D networks Managerial effectiveness (no mention of networks or innovation) |
| Clinical/medical pedagogy; professional leadership; clinical CPD; strictly EBM or clinical focus | Learning and development in health care without network or agency focus Curricula and learning frameworks for health professionals EBM and clinical leadership for EBM Clinical leadership and uni-professional learning (e.g. nursing knowledge) Applied networks in health [e.g. Primary Research Care Networks (Primary Care Research Networks) with exclusive EBM focus (not new innovations or knowledge] Clinical decision-making Clinical pathways Specialist clinical and research areas (e.g. pharmacogenetics) Nursing/doctors and leadership Interprofessional education Epidemiological studies |
| Narrow ICT/KM literature | E-knowledge/web-based/digital networks or collaboratives/ICT |
| Low relevance: sectors and businesses | Non-relevant areas of public sector delivery or commercial sectors (non-health or social care) Industrial districts without health/bio/pharmaceutical focus and industrial policy Manufacturing and export/import sectors Petrochemical industry Food science Banking and financial sector Industrial clusters (automobile) |
| Cognitive frameworks | Cognitive or psychological studies (e.g. measures of ABCA) |
| Lacking theory | Normative leadership behaviour(s) and literature Generic biotechnology literature (not research-based or theorised) |
| Narrow or too broad policy guidance | Pharmaceutical policy Policy commentary (unless on innovation/life sciences policy) Global policy |
| Theoretical constructs not applied to networks/innovation | Foucauldian analyses/governmentality |
| Low-income countries and developing economies | Examples taken from comparable ‘knowledge economies’ (e.g. USA, Europe, Canada, Australia, New Zealand) Triple helix in developing economies |
| User involvement literature without health innovation focus | |
Appendix 9 Final literature search results table
| Databases/thematic domain | ABI/INFORM | ProQuest | Ovid | Web of Science | Google Scholar | Total (first reduction) | Total (second reduction) | Final eligible |
|---|---|---|---|---|---|---|---|---|
| 6a | 231 | 173 | 17 | 108 | (16,000+) | 529 | 295 | 59 |
| Leadership, networks and agency | (232) | (183) | (17) | (144) | (576) | |||
| 6b | 128 | 91 | 115 | 85 | (11,000+) | 419 | 235 | 193 |
| Knowledge transfer in health-care networks, policy and industry | (922) | (647) | (1030) | (731) | (3330) | |||
| 6c | 8 | 7 | 30 | 16 | (58) | 133 | 76 | |
| NHS knowledge mobilisation architecture and policy | (16) | (40) | (68) | (54) | (236) |
Appendix 10 Social network analysis sampling and design
Social network data are collected in a systematised way, most often using surveys but also through structured interviews – respondents are asked questions about their personal attributes, their contacts and the attributes of their contacts. Traditionally, social network studies begin with a roster of names and researchers seek to plot connections between listed actors depending on the ‘relation’ or ‘ties’ of interest.
We immediately faced a challenge because knowledge circulations around AHSNs did not have a clear boundary; that is, they were cross-sector, cross-industry, cross-geography (regional, national and international) and encompassed a wide variety of individuals with different sets of expertise. It was decided at the onset that a peer-driven sampling strategy would be most appropriate, rather than a researcher-led method.
To do this we began by inviting four VSMs in each of our five AHSN sites to complete the social network survey (this same cohort also took part in the first wave of qualitative interviews). The T1 survey included questions about the respondent and asked them to name up to five key contacts who had ‘over the past six months’ been ‘most active in circulating innovative knowledge’ defined as ‘new ideas or perspectives, new research, products or services for health improvement or wealth creation’.
The survey was then sent to each of the contacts named by the AHSN leaders (wave 1) and repeated for up to four waves with sufficient reach and compositional diversity to produce a saturation effect. We acknowledged that some social networks would be interlinked/overlapping in parts and this would induce clustering effects that would force the networks to ‘close in’. Delimiters were not placed on nominations and respondents could name contacts from any AHSN region and any sector from junior or senior positions. The question was broadly framed to test the compositional diversity of VSM networks beyond the NHS. This process allowed us to identify individuals key to mobilising knowledge circulations in the national and regional health-care innovation domain (as nominated by their peers).
Where the boundaries of a network are indeterminate and it is not clear who should be included as network members (as was the case in this study of AHSN networks), it is typical to use survey methods with an inbuilt ‘name generator’ question to elicit the names of individuals who will subsequently form part of the network and also to purposely delimit a respondent’s choice of contact nomination by specific criteria depending on research interest. In order to frame the data around our research interests, the name generator question was designed to incorporate some purposive bias, for example, limiting recall of contacts within certain contextual and time framed parameters166,167 and limiting recall of contacts around resource provision by prompting names of contacts who had provided specific types of knowledge. 168,169
The survey also included questions on the attributes of respondents and their contacts (such as employing sector, role, level of hierarchy, professional expertise), as well as tie characteristics to determine the nature of the knowledge that had been exchanged (new ideas or research relating to health-care improvement, knowledge about goods or services improving wealth creation); quality of interaction (length of time known contact, frequency of interaction); and the implicit resources embedded in relations (trust, political leverage, access to contacts). In addition, these ties can also be multiplex, that is, more than one type of knowledge exchange can exist between the same two actors.
Analysis
Subnetworks forming the SNA data set:
-
knowledge networks to support health improvement (Health-Net)
-
knowledge networks to support wealth creation (Wealth-Net)
-
strong tie networks of contacts who regularly exchanged knowledge and had known one another for 10 years or more (Old ties-Net)
-
knowledge networks leading to implementation (Implem-Net)
-
knowledge networks providing access to contacts (Broker-Net)
-
knowledge networks based on new ideas (Ideas-Net)
-
knowledge networks providing political influence or leverage (Power-Net)
-
knowledge networks providing trustworthy advice, guidance or information (Trust-Net).
It is important to note that many standard inferential statistics do not apply because social network data violate case independency criteria as respondents are not sampled independently from their population. Instead, metrics are based on permutation approaches, which are applied to calculate sampling distributions directly from observed networks using random assignment/matrix manipulation across thousands of trials under the assumption that null hypotheses are true (in other words, to calculate the likelihood that the observed network would have occurred by chance).
Appendix 11 Social network analysis survey (time point 1)
Appendix 12 Social network analysis survey (time point 2)
Appendix 13 Interview protocol: Academic Health Science Network very senior managers (time point 1)
Appendix 14 Interview protocol: regional knowledge contacts
Appendix 15 Interview protocol: Academic Health Science Network very senior managers (time point 2)
Appendix 16 Interview protocol: knowledge leadership and ‘national beacons’
Appendix 17 Case study protocol and interview schedule
Objectives of the ‘tracers’ case studies
-
Understand each AHSN’s strategic approach to promoting innovation spread at pace and scale at the local level (mobilisation in practice).
-
Understand how the AHSN deploys its strategy in practice.
-
Understand the nature of the relationship between the project and the AHSN and its development over time as an example of how AHSN strategy in practice has evolved/is evolving.
-
Understand how innovation adoption may relate to the contextual features of AHSNs (e.g. regional innovation economy investments, AHSC/non-AHSC, science park/pharmaceutical presence, etc.).
| Data collection | |
|---|---|
| Interviews | |
| Access and ethics | Prepare standard e-mail to gain access Use REC-approved study information sheet and consent form Comply with regulations for anonymous data collection and storage (e.g. data protection, REC submission) |
| Roles and position of the interviewees | Proposed interviewees
|
| n = 6–8 | |
| What information do we want to obtain from the different interviewees? |
|
| We use the questions in Appendix 1 (see below), but need to tailor the interview guide for each interviewee as each of them will have some but not all the pieces of the innovation ‘story’ (i.e. semi-structured interview format) | |
| Informal follow-up conversation | |
| n = 2–4 | Key informants will be contacted after 2–3 months to get a picture of the trajectory of the relationship between AHSN and project |
| Observation of critical project meeting(s) | If possible |
| n = 1–2 | We will observe one or two progress review meetings where the project is discussed by the AHSN management This will allow a more truthful picture of the actual dynamics between the project and AHSN |
| Documents | |
| What documents do we need? |
|
| Data analysis | |
| Cross-case comparison dimensions (provisional headings for case studies report) |
|
Appendix 18 Major conceptual areas identified through literature review reduction
-
ABCA in high-tech industries/health/HEIs.
-
Applied SNA: high tech and health.
-
Health and biomedical innovation transfer (biotechnology and pharmaceutical).
-
Health-care collaborations and networks: for knowledge transfer and exchange.
-
Innovation and knowledge mobilisation theories (including open innovation and disruptive innovations, diffusion models).
-
National and regional innovation systems.
-
Policy: health, growth and life sciences (UK).
-
Triple helix and HEI knowledge transfer.
-
Leadership, networks and agency.
Glossary
- Absorptive capacity
- A concept drawn from the resource-based view found within the strategic management literature that refers to the ability of an organisation collectively to sense, import and use external knowledge productively.
- Actor–network theory
- A school of thought within science and technology studies that treats non-human objects (such as computers) as part of complex networks of associations that produce and circulate scientific knowledge.
- Agency
- An action, activity or intervention undertaken by a person or persons that produces an effect; an agency-focused approach can be contrasted with a concern for underlying structure (i.e. structuralism).
- Boundary objects
- A term within science and technology studies that refers to objects that link different agents or communities (e.g. a shared protocol or information technology system). They have a common core, but other elements may be interpreted differently by different communities. Their presence allows disparate groups to collaborate on a common task.
- Communities of practice
- A term in the organisational studies literature that refers to a group of people who share a craft or profession and who develop a strong informal group identity through repeated interactions in the work setting.
- Complex adaptive systems
- A theoretical school that sees a social or organisational system – including some recent applications to health-care systems – as comprising many components that interact and evolve in an unpredictable and self-organising manner.
- Disruptive innovation
- A term that refers to a form of radical and non-incremental innovation that is often associated with the entry of incumbents into an established market and that typically offers cheaper, simpler and more accessible products.
- Episteme
- A philosophical term that refers to forms of science, knowledge or understanding.
- Epistemic boundaries
- A term in the science and technology studies literature that refers to barriers between different epistemes that stop the ready flow of some forms of knowledge.
- Evidence-based management
- An analogous movement now developing in some management literature, often taking evidence-based medicine as a positive role model.
- Evidence-based medicine
- A term in the clinical and health services research literatures that refers to a movement that has developed since the 1990s, which aims to ensure that clinical practice is informed by the results of well-conducted research.
- Institutional logics
- A concept within the neo-institutionalist school of organisational studies (see later definition), which focuses on how broader belief systems shape both the cognitions and behaviours of actors within organisations as they create ‘taken for granted’ rules of action.
- Knowledge leadership
- Refers to any attitude or action – joint or individual, observed or imputed – that prompts new and important knowledge to be created, elicited, shared and utilised in way that ultimately brings a shift in thinking and collective outcomes.
- Knowledge management
- The process of creating, using and managing knowledge collectively within an organisation. It may involve the use of specific knowledge management tools, technologies and techniques (such as an intranet). It often takes a relatively linear approach.
- Knowledge mobilisation
- A term found in the organisational and health services research literatures that refers to the processes involved in moving existing knowledge into active use; it is less linear and prescriptive that the alternative term of ‘knowledge management’.
- Knowledge translation
- Attempts to move formal knowledge – often of an innovative nature – into routine health care or other forms of practice.
- Neo-institutionalism
- A school of thought within organisational studies that argues that whole organisational fields (e.g. the health-care field) are prone to conditions of imitation and ready convergence.
- Network governance
- A school of thought in some political science literature that sees the current public policy process as involving a more extensive role for many actors going beyond the nation state; the role of the state now becomes more indirect in steering and shaping policy networks, rather than giving direct commands.
- Network homophily and heterogeneity
- Terms found within the social networks literature that refer to the extent to which a social network is characterised by a tendency of individuals to associate with or bond with similar individuals (homophily) as opposed to different types of individuals (heterogeneity).
- New production of knowledge model
- A model found in the science and technology literature that argues that there is a long-term shift in the form of knowledge being produced in contemporary societies away from mode 1 (university based; confined to single academic disciplines) to mode 2 (more pluralist; greater range of actors; more multi- and even trans-disciplinary research; greater emphasis on application and use).
- Open innovation
- A model of innovation on which the development of new (usually scientifically-based) products and paths to market is increasingly informed by a range of external actors beyond the historically important research units found within the core firm (e.g. moving beyond reliance on the internal research and development laboratories of large biopharmaceutical companies).
- Opinion leader
- A term in the diffusion of innovations literature that refers to a member of a professional body or network able to lead and influence the behaviour of other professional colleagues; related to the notion of a pro-innovation ‘champion’.
- Quadruple helix
- A more recent development of triple helix theory (see below), which adds the presence of an activated civil society as a fourth axis.
- Regional innovation system
- A concept in the science policy literature that examines the production of new knowledge in a territory that is larger than a city but smaller than a state. This geographically based system may encourage a collective learning process among the various actors involved.
- Situated learning
- A learning theory that suggests that learning takes place through socially embedded activity (e.g. in a workplace), rather than through more formal and cognitively orientated approaches to learning.
- Social capital
- A sociological concept that refers to patterns of social relations that have productive benefits.
- Sociogram
- A technique used within social network analysis that provides a graphic representation of the social links that a person has.
- Tertius iungers
- ‘The third who joins’; a concept in social network theory.
- Triple helix
- A concept from science and technology studies that refers to the interactive and emergent production of scientific and technological knowledge involving the ‘three aces’ of higher education institutions, business and government.
List of abbreviations
- AAR
- accelerated access review
- ABCA
- absorptive capacity
- AHSC
- Academic Health Sciences Centre
- AHSN
- Academic Health Science Network
- ANT
- actor–network theory
- BIS
- Business, Innovation and Skills
- BRC
- Biomedical Research Centre
- CAS
- complex adaptive system
- CCG
- Clinical Commissioning Group
- CEO
- chief executive officer
- CLAHRC
- Collaboration for Leadership in Applied Health Research and Care
- COP
- community of practice
- CRN
- Clinical Research Network
- CVD
- cardiovascular disease
- DH
- Department of Health
- EBM
- evidence-based medicine
- FT
- foundation trust
- GP
- general practitioner
- HEI
- higher education institution
- HIEC
- Health Innovation and Education Cluster
- HMIC
- Health Management Information Consortium
- HSDR
- Health Services and Delivery Research
- HSR
- health services research
- ICT
- information and communication technology
- IHI
- Institute for Healthcare Improvement
- IHW
- Innovation, Health and Wealth
- IP
- intellectual property
- IT
- information technology
- KCL
- King’s College London
- KL
- knowledge leader
- KM
- knowledge management
- KPI
- key performance indicator
- KT
- knowledge translation
- LEP
- local enterprise partnership
- LTC
- long-term condition
- MD
- managing director
- MSK
- musculoskeletal
- NHS IQ
- NHS Improving Quality
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health Research
- OLS
- Office for Life Sciences
- PhD
- Doctor of Philosophy
- PPI
- patient and public involvement
- R&D
- research and development
- RCT
- randomised controlled trial
- REC
- Research Ethics Committee
- RQ
- research question
- SBRI
- small business research initiative
- SCN
- Strategic Clinical Network
- SME
- small and medium-sized enterprise
- SNA
- social network analysis
- SSC
- Study Steering Committee
- T1
- time point 1
- T2
- time point 2
- TA
- Technology Assessment
- UNTRAP
- University/User Teaching and Research Action Partnership
- UUK
- Universities UK
- VSM
- very senior manager
- WP
- work package